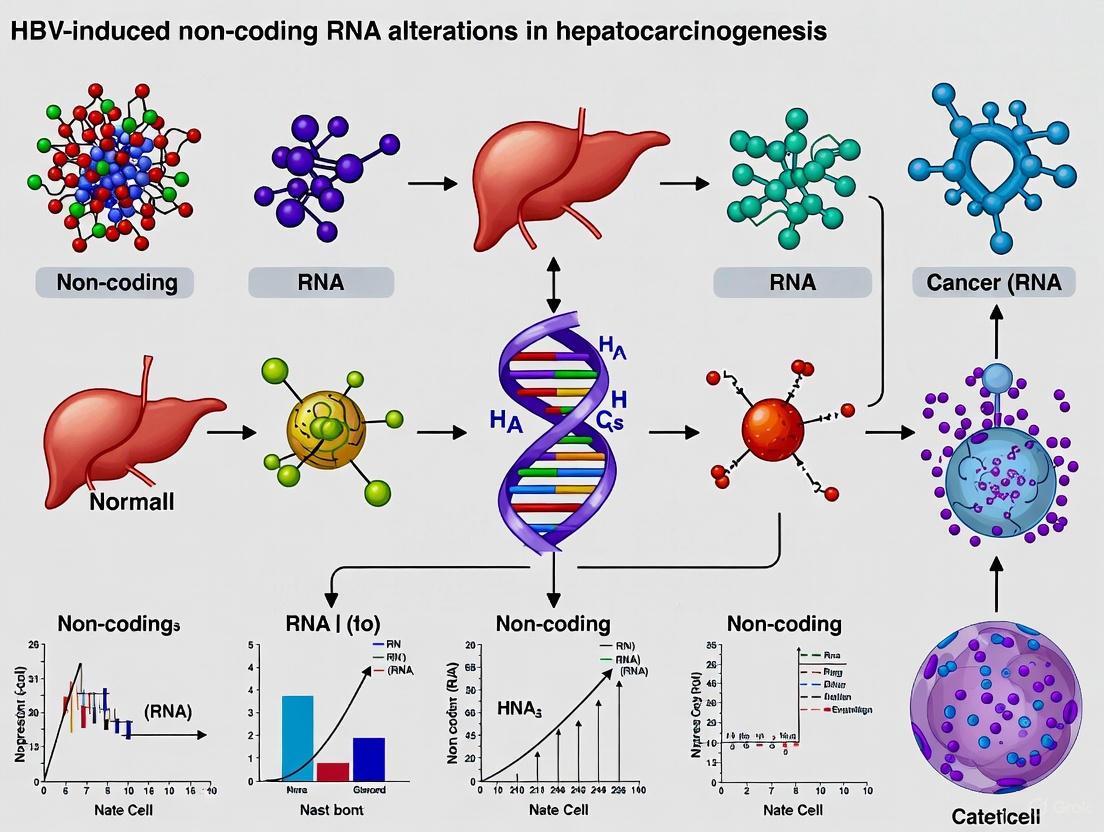
HBV-Induced Non-Coding RNA Alterations in Hepatocarcinogenesis: Mechanisms, Biomarkers, and Therapeutic Avenues
Hepatitis B virus (HBV) is a primary etiology of hepatocellular carcinoma (HCC), accounting for over half of all cases globally.
HBV-Induced Non-Coding RNA Alterations in Hepatocarcinogenesis: Mechanisms, Biomarkers, and Therapeutic Avenues
Abstract
Hepatitis B virus (HBV) is a primary etiology of hepatocellular carcinoma (HCC), accounting for over half of all cases globally. This review synthesizes current knowledge on the critical role of non-coding RNAs (ncRNAs)—including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—in HBV-driven hepatocarcinogenesis. We explore foundational mechanisms whereby the HBV X protein (HBx) dysregulates ncRNA expression, which in turn modulates key oncogenic pathways, the tumor microenvironment, and immune evasion. The article further assesses the methodological application of these ncRNAs as diagnostic and prognostic biomarkers and their potential as therapeutic targets. We address current challenges in clinical translation and compare emerging therapeutic strategies, including RNA interference and miRNA-based therapies, providing a comprehensive resource for researchers and drug development professionals aiming to advance the control of HBV-related HCC.
The Foundational Role of ncRNAs in HBV-Driven Liver Cancer
HBV Epidemiology and the Global Burden of HCC
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most commonly diagnosed cancer and the third leading cause of cancer-related mortality worldwide [1] [2]. Chronic hepatitis B virus (HBV) infection remains the predominant causative agent, responsible for approximately 50-55% of all HCC cases globally [3] [4]. Despite advances in vaccination and antiviral therapies, the absolute burden of HBV-related HCC continues to rise due to population growth and aging demographics [5] [3]. This whitepaper examines the current global epidemiology of HBV-driven HCC and explores the emerging role of non-coding RNAs (ncRNAs) as critical regulators in hepatocarcinogenesis, providing researchers and drug development professionals with a comprehensive overview of the field's current landscape and experimental approaches.
Global Epidemiological Profile of HBV-Related HCC
Current Burden and Regional Distribution
The global distribution of HBV-related HCC demonstrates significant geographical disparities, with the highest incidence rates concentrated in East Asia and sub-Saharan Africa, regions characterized by historically high rates of chronic HBV infection [4]. According to the most recent data from the Global Burden of Disease Study 2021, there were approximately 206,366 new cases and 181,194 deaths globally attributable to HBV-related liver cancer in 2021 [5]. When examining specific regions, the Western Pacific region bears the highest burden with 295,484 incident liver cancer cases reported in 2019, while the United States has experienced the greatest recent increase with a 41% rise in incident cases between 2010 and 2019 [4].
Table 1: Global Epidemiological Profile of HBV-Related HCC (2021)
| Metric | Global Value | Trend (1990-2021) | Regional Variations |
|---|---|---|---|
| New Cases | 206,366 | 120.2% increase in absolute numbers | Highest in Western Pacific region |
| Deaths | 181,194 | Significant increase in absolute numbers | Varies by SDI region |
| Age-Standardized Incidence Rate | 8.6 per 100,000 | Declining trend | Highest in middle SDI regions |
| Age-Standardized Death Rate | 8.0 per 100,000 | 21.7% decline in middle SDI countries | Lowest in low-middle SDI regions |
| DALYs | 191.5 per 100,000 | Declining trend after age standardization | Peaks in 85-89 age group |
Temporal Trends and Socioeconomic Correlations
Recent decades have witnessed notable shifts in the epidemiological patterns of HBV-related HCC. Between 1990 and 2021, the global age-standardized incidence rate (ASIR) and age-standardized prevalence rate (ASPR) showed an upward trajectory, while the age-standardized death rate (ASDR) demonstrated a significant decline, particularly in middle Socio-Demographic Index (SDI) countries where the ASDR dropped by 21.7% [5]. This decline in mortality rates is most pronounced among birth cohorts from the 1970s onward, reflecting the impact of widespread HBV vaccination programs implemented during this period [5].
A strong negative correlation exists between SDI, Universal Health Coverage (UHC), and liver cancer burden, highlighting the critical role of socioeconomic factors and healthcare access in disease management [5]. The number of deaths attributable to risk factors increased by 97.8% from 1990 to 2021, though projections indicate a potential 30.2% reduction in HBV-related liver cancer deaths globally by 2040 if current interventions are maintained and enhanced [5].
Table 2: HBV-Related HCC Trends in Selected Countries/Regions
| Country/Region | Trend Period | Key Trend | Postulated Reasons |
|---|---|---|---|
| United States | 2000-2020 | Peak in 2014 (11.5/100,000), decline to 9.4 by 2020 | Improved prevention/treatment of chronic liver disease [1] |
| Korea | 1999-2019 | Age-standardized incidence fell from 28.9 to 16.1 | HBV vaccination, antiviral agents, aging population [4] |
| Taiwan | 2001-2004 | Mortality dropped from 0.81 to 0.05/100,000 in ages 5-29 | Immunization campaign (1984) [4] |
| Global | 1990-2019 | HBV as primary cause decreased from >50% to 42% | Vaccination, antiviral treatments, rising NAFLD/ALD [4] |
Molecular Pathogenesis: HBV-Induced Non-Coding RNA Alterations
HBV Integration and Oncogenic Mechanisms
HBV promotes hepatocarcinogenesis through both direct and indirect mechanisms. HBV DNA integrates into the host genome during initial tumorigenesis, causing insertional mutagenesis of cancer-related genes and genomic instability [6]. The formation of extrachromosomal circular DNA (ecDNA), which is efficiently amplified to express viral genes and host oncogenes, represents another key oncogenic mechanism [6]. Viral proteins, particularly the regulatory HBV X (HBx) protein and modified preS/S envelope proteins, alter host cell gene expression profiles and drive malignant transformation [6].
The HBx protein plays a particularly significant role in epigenetic modifications during hepatocarcinogenesis by dysregulating non-coding RNA expression [7]. This protein functions as a weak oncogene or cofactor in hepatocarcinogenesis, with previous studies demonstrating that genetic alterations alone cannot account for the complexity of HBx-induced liver cancer development [7].
Non-Coding RNA Networks in HBV-Related HCC
Non-coding RNAs have emerged as critical regulatory molecules in HBV-induced hepatocellular carcinoma, with four main classes demonstrating significant roles in hepatocarcinogenesis.
MicroRNAs (miRNAs) in HBV-HCC
miRNAs represent a class of small endogenous ncRNAs approximately 21-25 nucleotides in length that regulate gene expression at the post-transcriptional level through binding to complementary sequences on target mRNAs [8]. In HBV-related HCC, global alteration of miRNA expression plays an important role in disease progression, with some miRNAs functioning as oncogenes and others as tumor suppressors [8].
Key oncogenic miRNAs upregulated in HBV-HCC include:
- miR-21: Regulated by HBx, targets PDCD4 and PTEN, and promotes tumor cell growth and survival [8]
- miR-221/miR-222: Upregulated by HBx, facilitate cell cycle progression and suppress apoptosis by targeting CXCL4/12 and transferrin receptor protein 1 (TFRC) respectively [8]
- miR-17-92 cluster: Includes miR-18a, miR-19a/b, and miR-92a, which contribute to proliferation, angiogenesis, and immune evasion by targeting ERα [8]
Tumor-suppressive miRNAs frequently downregulated in HBV-associated HCC include:
- miR-122: A liver-specific miRNA crucial for HBV infection, whose downregulation promotes tumor development, motility, and invasion through effects on anaerobic glycolysis and amino acid metabolism [8]
- miR-199a/b: Inhibits ROCK1/MLC and PI3K/Akt pathways via targeting Rho-associated coiled-coil kinase 1 (ROCK1), with low expression associated with poor overall survival [8]
- miR-125b: Inhibits angiogenesis by targeting VEGFA and induces cell-cycle arrest by directly targeting cyclin D2/E2 and IL-6-STAT3 signaling pathway [8]
Long Non-Coding RNAs (lncRNAs) in HBV-HCC
Long non-coding RNAs represent a diverse class of RNA molecules longer than 200 nucleotides that lack protein-coding capacity [8]. These molecules regulate gene expression through interactions with DNA, RNA, or proteins, influencing chromatin modification, transcriptional regulation, and post-transcriptional processing [8]. In HBV-related HCC, numerous lncRNAs have been identified as dysregulated and contributing to cancer initiation and progression.
Notable lncRNAs in HBV-related hepatocarcinogenesis include:
- HDAC2-AS2: A TGFβ-inducible lncRNA highly expressed in HBV-associated HCC tissues that promotes tumor growth by affecting the tumor microenvironment rather than through cell-autonomous effects [9]. This lncRNA is enriched in extracellular vesicles and facilitates cancer progression by suppressing cytotoxicity of intra-tumor CD8+ T cells through targeting and blocking cytosolic CDK9 [9].
- DREH: Frequently downregulated in HBV-associated HCC tissues, where it functions as a tumor suppressor and is inversely correlated with HBx mRNA expression [7]. Suppression of DREH expression promotes the proliferation of HCC cells both in vitro and in vivo [7].
- HULC: One of the most investigated lncRNAs in HBV-related HCC, though its specific mechanisms continue to be elucidated [8].
Experimental Approaches and Methodologies
Core Research Protocols
lncRNA Expression Profiling in HBV Models
Objective: To identify differentially expressed lncRNAs in response to HBV infection or HBx expression.
Methodology:
- Treat a panel of HCC cell lines with varying metastatic potential (e.g., HepG2, Huh7, MHCC97, PVTT) with TGFβ for 8 hours to simulate HBV-induced signaling [9]
- Extract total RNA and analyze using lncRNA microarray platforms
- Apply fold-change thresholds (≥2) and statistical significance (p ≤ 0.05) to identify differentially expressed lncRNAs [9]
- Validate candidates through comparison with public databases (e.g., TCGA via TANRIC) using less stringent thresholds (fold change ≥1.5, p ≤ 0.05) [9]
- Confirm top candidates through quantitative RT-PCR and RACE (rapid amplification of cDNA ends) assays for full-length transcript determination [9]
Functional Characterization of lncRNAs In Vitro and In Vivo
Objective: To determine the biological functions of specific lncRNAs in HBV-related HCC progression.
In Vitro Approaches:
- Gain-of-function: Clone lncRNA into expression vectors (e.g., pcDNA3.1) and transfert into liver cell lines [7]
- Loss-of-function: Design specific siRNAs targeting the lncRNA of interest and transfert into HBV-positive HCC cell lines [7]
- Functional assays:
In Vivo Approaches:
- Subcutaneous mouse models: Utilize immune-deficient nude mice for tumor formation studies with HBx-expressing cell lines [7]
- Orthotopic liver models: Employ immune-competent C57BL/6 wild-type mice to evaluate tumor growth in a more physiologically relevant microenvironment [9]
- Immune cell profiling: Is tumors and spleens for flow cytometric analysis of immune populations (CD8+ T cells, Tregs, macrophages) to assess tumor microenvironment modulation [9]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating ncRNAs in HBV-Related HCC
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Cell Lines | HepG2, Huh7, MHCC97, PVTT, HepG2.2.15 | In vitro modeling of HBV-HCC with varying metastatic potential | lncRNA screening, functional assays [9] [7] |
| Animal Models | BALB/c nude mice, C57BL/6 WT mice | In vivo tumor formation, tumor microenvironment studies | Subcutaneous, orthotopic models [9] [7] |
| Expression Vectors | pcDNA3.1-HBx, lncRNA clones | Forced expression of viral proteins or ncRNAs | Gain-of-function studies [7] |
| siRNA/shRNA | DREH siRNA, HDAC2-AS2 targeting | Knockdown of specific ncRNAs | Loss-of-function studies [9] [7] |
| TGFβ Pathway Modulators | SB431542 (inhibitor), Smad4 KO | TGFβ signaling manipulation | Mechanistic studies of lncRNA regulation [9] |
| (1-Azido-2-bromoethyl)cyclopentane | (1-Azido-2-bromoethyl)cyclopentane, CAS:2445791-41-1, MF:C7H12BrN3, MW:218.098 | Chemical Reagent | Bench Chemicals |
| 1-(3-Phenylpyrrolidin-1-yl)ethanone | 1-(3-Phenylpyrrolidin-1-yl)ethanone|C12H15NO|RUO | 1-(3-Phenylpyrrolidin-1-yl)ethanone is a pyrrolidine-based chemical reagent for non-human research. This product is For Research Use Only and is not intended for diagnostic or therapeutic use. | Bench Chemicals |
Signaling Pathways and Therapeutic Implications
Key Dysregulated Pathways in HBV-Related HCC
Multiple signaling pathways are dysregulated in HBV-related HCC, contributing to uncontrolled cell proliferation, metastasis, and recurrence. Beyond the frequently altered receptor tyrosine kinase (RTK) pathways, several other signaling cascades provide therapeutic potential for intervention.
The VEGF/VEGFR pathway represents one of the most prominent tumor-induced pro-angiogenic factors affecting HCC development, with VEGFA demonstrating 7-14% frequency of focal amplification in HCC [2]. Almost all approved tyrosine kinase inhibitors for advanced HCC involve VEGFR targets, making this pathway particularly relevant for therapeutic development [2].
The TGFβ signaling pathway plays critical roles during liver pathogenesis, including chronic HBV infection, liver cirrhosis, and tumorigenesis, contributing to a more immunotolerant microenvironment by upregulating functional RNAs and tumor-related signaling [9]. This pathway directly regulates several lncRNAs, including HDAC2-AS2, which is significantly upregulated in response to TGFβ stimulation in HCC cell lines [9].
Therapeutic Opportunities and Clinical Translation
Current therapeutic approaches for HBV-related HCC increasingly focus on combination therapies targeting both oncogenic signaling pathways and immune checkpoints. The success of the IMbrave150 trial, which combined atezolizumab (anti-PD-L1) with bevacizumab (anti-VEGF), demonstrated superiority over sorafenib in terms of overall survival, progression-free survival, and objective response rate, heralding a groundbreaking epoch in HCC treatment [2]. Similarly, the HIMALAYA trial led to FDA approval of durvalumab (anti-PD-L1) plus tremelimumab (anti-CTLA-4), achieving a 4-year overall survival rate of 25.2% for advanced HCC patients [2].
Emerging therapeutic strategies targeting ncRNAs in HBV-related HCC include:
- Antisense oligonucleotides designed to target and degrade oncogenic lncRNAs
- miRNA mimics to restore tumor-suppressive miRNA function
- Small molecule inhibitors targeting lncRNA-protein interactions
- Nanoparticle-based delivery systems for tissue-specific ncRNA modulation
The stability, detectability in bodily fluids, and disease-specific expression patterns render ncRNAs promising as non-invasive biomarkers for early detection, prognosis, and treatment response monitoring in HBV-related HCC [8]. Several ncRNAs, including HDAC2-AS2 and DREH, show strong associations with clinical outcomes and may eventually inform personalized treatment approaches [9] [7].
The global burden of HBV-related HCC remains substantial despite advances in vaccination and antiviral therapies, with significant regional disparities and complex molecular pathogenesis. Non-coding RNAs have emerged as critical regulators in HBV-induced hepatocarcinogenesis, functioning through diverse mechanisms including modulation of key signaling pathways, tumor microenvironment interactions, and immune system regulation. The continuing evolution of HBV-related HCC epidemiology, with declining viral etiologies but increasing absolute case numbers due to population aging and growth, underscores the ongoing importance of this field. Future research directions should focus on elucidating the precise mechanisms of ncRNA function in HBV-HCC, developing ncRNA-based biomarkers for clinical use, and exploring novel therapeutic approaches that target ncRNA networks in combination with existing modalities.
Non-coding RNAs (ncRNAs) have emerged as critical regulators of gene expression and key players in liver pathophysiology, particularly in HBV-induced hepatocarcinogenesis. Once considered "transcriptional noise," these molecules are now recognized as essential components of the epigenetic landscape that govern hepatocellular carcinoma (HCC) development and progression. This technical review comprehensively examines the three principal ncRNA classes—microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—focusing on their biogenesis, functional mechanisms, and intricate roles in HBV-related HCC. We highlight their regulatory networks, provide detailed experimental methodologies for their investigation, and discuss their emerging potential as diagnostic biomarkers and therapeutic targets, framing this discussion within the context of advancing hepatocarcinogenesis research.
Hepatocellular carcinoma represents a significant global health challenge, ranking as the sixth most common cancer worldwide and the third leading cause of cancer-related mortality [8]. Chronic hepatitis B virus (HBV) infection remains a predominant risk factor, contributing to approximately 80% of global HCC cases [8]. The pathogenesis of HBV-related HCC involves complex interactions between viral factors and host cellular machinery, with HBV integration, the HBx protein, and covalently closed circular DNA (cccDNA) serving as core drivers of oncogenic pathways [10].
In recent years, the discovery that approximately 70-90% of the human genome is transcribed into RNA, with only a minority encoding proteins, has revolutionized our understanding of gene regulation in health and disease [11]. Non-coding RNAs have emerged from being dismissed as "junk RNA" to being recognized as crucial epigenetic regulators in hepatocarcinogenesis. These molecules exhibit precise tissue-specific expression patterns and participate in virtually all aspects of cellular homeostasis, with their dysregulation contributing significantly to cancer hallmarks including sustained proliferation, evasion of growth suppressors, and activation of invasion and metastasis [8].
The stability, detectability in bodily fluids, and disease-specific expression patterns of ncRNAs render them promising biomarkers and therapeutic targets for HBV-related HCC [8]. This review systematically examines the three major ncRNA classes, their functional mechanisms in hepatic biology, and their specific roles in HBV-driven hepatocarcinogenesis, providing researchers with both theoretical frameworks and practical methodological guidance for investigating these complex regulatory molecules.
miRNA: Key Regulators in HBV-Related HCC
Biogenesis and Functional Mechanisms
MicroRNAs (miRNAs) represent a class of small endogenous ncRNAs approximately 21-25 nucleotides in length that regulate gene expression at the post-transcriptional level [8]. Their biogenesis involves multiple carefully regulated steps: miRNAs are first transcribed as primary transcripts (pri-miRNAs), which undergo nuclear processing by the Drosha enzyme to generate precursor miRNAs (pre-miRNAs). These precursors are exported to the cytoplasm, where they are cleaved by the Dicer enzyme to produce mature miRNAs. The mature miRNAs are subsequently assembled into the RNA-induced silencing complex (RISC), enabling them to bind to complementary sequences on target mRNAs, resulting in message degradation or translational inhibition [8].
Oncogenic and Tumor-Suppressive miRNAs in HBV-HCC
In HBV-related HCC, global alteration of miRNA expression plays a pivotal role in disease progression, with some miRNAs functioning as oncogenes and others as tumor suppressors [8]. The table below summarizes key dysregulated miRNAs in HBV-related HCC and their functional significance:
Table 1: Key miRNAs Dysregulated in HBV-Related Hepatocarcinogenesis
| miRNA | Expression in HBV-HCC | Primary Function | Key Validated Targets | Cellular Processes Affected |
|---|---|---|---|---|
| miR-21 | Upregulated | Oncogenic | PDCD4, PTEN | Cell growth, survival [8] |
| miR-221/222 | Upregulated | Oncogenic | CXCL4/12, TFRC | Cell cycle progression, apoptosis evasion [8] |
| miR-17-92 cluster | Upregulated | Oncogenic | ERα | Proliferation, angiogenesis, immune evasion [8] |
| miR-122 | Downregulated | Tumor-suppressive | Cyclin G1, PKM2, SLC7A1 | HBV replication, metabolism, tumor aggressiveness [8] [10] |
| miR-199a/b | Downregulated | Tumor-suppressive | ROCK1 | Cell motility, invasion, survival [8] |
| miR-125b | Downregulated | Tumor-suppressive | VEGFA, cyclin D2/E2 | Angiogenesis, cell-cycle arrest [8] |
| miR-101 | Downregulated | Tumor-suppressive | DNMT3A | DNA methylation patterns [8] |
The HBx protein significantly contributes to miRNA dysregulation in HBV-infected hepatocytes. For instance, HBx upregulates oncogenic miRNAs such as miR-21 while downregulating tumor-suppressive miRNAs including miR-101, miR-148a, and miR-152 [8]. This reprogramming of the miRNA landscape facilitates the creation of a cellular environment conducive to malignant transformation and tumor progression.
Experimental Protocols for miRNA Investigation
Protocol 1: Comprehensive miRNA Expression Profiling
- RNA Extraction: Use miRNeasy Mini Kit or similar, ensuring preservation of small RNAs. Include DNase I treatment to eliminate genomic DNA contamination.
- Quality Control: Verify RNA integrity using Agilent 2100 Bioanalyzer with RNA Integrity Number (RIN) >8.0 required for sequencing.
- Library Preparation: Employ QIAseq miRNA Library Kit or equivalent, incorporating unique molecular identifiers (UMIs) to correct for PCR biases.
- Sequencing: Perform on Illumina platforms with recommended depth of 10-15 million reads per sample for robust detection.
- Bioinformatic Analysis: Process raw data with tools such as miRDeep2 for novel miRNA prediction and edgeR or DESeq2 for differential expression analysis, implementing Benjamini-Hochberg correction for multiple testing (FDR <0.05).
Protocol 2: Functional Validation Using Antagomirs and Mimics
- Cell Culture: Utilize relevant HBV-infected hepatocyte models (HepG2.2.15, Huh7-HBV) and appropriate controls.
- Transfection: For miRNA inhibition, transfert with locked nucleic acid (LNA)-modified antagomirs at 25-50 nM concentration using lipid-based transfection reagents. For miRNA overexpression, use miRNA mimics at 30 nM.
- Phenotypic Assays:
- Proliferation: MTT assay at 24, 48, and 72 hours post-transfection.
- Apoptosis: Annexin V/PI staining with flow cytometry analysis at 48 hours.
- Migration/Invasion: Transwell assays with Matrigel coating for invasion assessment, fixed and stained at 24 hours.
- Target Validation: Dual-luciferase reporter assays with wild-type and mutant 3'UTR constructs of putative targets.
Figure 1: miRNA Biogenesis and Functional Mechanisms in HBV-HCC. The diagram illustrates the canonical miRNA maturation pathway and the dual regulatory roles of oncogenic and tumor-suppressive miRNAs in hepatocarcinogenesis, highlighting points of dysregulation by HBV/HBx.
lncRNAs: Architectural Regulators in Hepatic Pathobiology
Classification and Functional Diversity
Long non-coding RNAs (lncRNAs) represent a diverse class of RNA molecules longer than 200 nucleotides that lack protein-coding capability [8]. These molecules are transcribed by RNA polymerase II and typically undergo post-transcriptional modifications including 5' capping and 3' polyadenylation [8]. Based on genomic context and strand orientation, lncRNAs are classified into five major categories: intergenic (lincRNAs), intronic, bidirectional, sense, and antisense lncRNAs [11].
The functional mechanisms of lncRNAs are remarkably diverse and include: (1) Epigenetic silencing through interactions with polycomb-group proteins; (2) Transcriptional activation in cis or trans; (3) Regulation of alternative splicing; (4) Acting as competitive endogenous RNAs (ceRNAs) that sequester miRNAs; (5) Modulating protein stability; and (6) Serving as precursors for miRNAs [11].
Key lncRNAs in HBV-Related Hepatocarcinogenesis
The dysregulation of lncRNAs in HBV-related HCC impacts various cancer hallmarks including cellular proliferation, invasion, metastasis, angiogenesis, and immune evasion. The table below summarizes critically important lncRNAs in HBV-driven HCC:
Table 2: Functionally Significant lncRNAs in HBV-Related HCC
| lncRNA | Expression Pattern | Regulatory Mechanism | Functional Role in HCC | Molecular Targets/Pathways |
|---|---|---|---|---|
| HULC | Upregulated by HBx via CREB [12] | Epigenetic regulation, miRNA sponge | Promotes proliferation, tumor growth [8] [12] | miR-372, PRKACB, CREB phosphorylation [12] |
| HOTAIR | Upregulated by HBx via Plk1 [12] | PRC2 interaction, chromatin modification | Enhances proliferation, invasion [11] [13] [12] | SUZ12 degradation, epigenetic reprogramming [11] [12] |
| MALAT1 | Upregulated [12] | Alternative splicing regulation, molecular sponge | Promotes metastasis, cell cycle progression [11] [13] | SR proteins, cell cycle genes [11] |
| DREH | Downregulated by HBx [12] | Cytoskeletal regulation | Tumor suppressor, inhibits growth and invasion [12] | Vimentin filament structure [11] |
| HEIH | Upregulated [11] [12] | EZH2 interaction, epigenetic silencing | Promotes cell cycle progression [11] [12] | PRC2 complex, cell cycle regulators [11] |
| MVIH | Upregulated [12] | Angiogenesis regulation | Promotes tumor growth, microvascular invasion [12] | Angiogenesis factors [12] |
HBx employs sophisticated mechanisms to dysregulate lncRNA expression. For HOTAIR, HBx activates Plk1, which induces proteasomal degradation of SUZ12 (a PRC2 component) and ZNF198 (which stabilizes the LSD1/Co-REST/HDAC1 complex), resulting in chromatin modifications that activate HOTAIR transcription [12]. For HULC, HBx interacts with CREB to activate HULC promoter activity, while HULC reciprocally enhances CREB phosphorylation by inhibiting miR-372 and increasing expression of PRKACB, creating a positive feedback loop [12].
Experimental Framework for lncRNA Functional Characterization
Protocol 1: Comprehensive lncRNA Identification and Validation
- Transcriptome Sequencing: Perform strand-specific RNA-seq with ribosomal RNA depletion rather than polyA selection to capture non-polyadenylated lncRNAs.
- lncRNA Identification Pipeline:
- Assembly with StringTie or Cufflinks.
- Coding potential assessment using CPAT, CPC2, and PhyloCSF.
- Classification with FEELnc or lncRScan.
- Expression quantification via featureCounts or HTSeq.
- Experimental Validation:
- Cellular Localization: RNA-FISH with confocal microscopy, using U1 (nuclear) and GAPDH mRNA (cytoplasmic) as controls.
- RACE Assays: Determine transcript start and end sites using SMARTer RACE 5'/3' Kit.
- qRT-PCR Validation: Design exon-exon junction spanning primers; use standard curves for efficiency correction.
Protocol 2: Mechanism of Action Elucidation
- Epigenetic Regulation Studies:
- Chromatin Isolation by RNA Purification (ChIRP) with biotinylated tiling oligonucleotides.
- RNA Immunoprecipitation (RIP) for protein interaction partners (EZH2, LSD1).
- Follow with qPCR or sequencing to identify bound genomic regions.
- ceRNA Network Validation:
- Dual-luciferase reporter assays with wild-type and mutant miRNA response elements.
- AGO2-RIP to confirm direct miRNA binding.
- Correlation analysis of lncRNA and putative target mRNA expression in clinical samples.
- Functional Phenotyping:
- CRISPRi/a for endogenous transcriptional regulation.
- Orthotopic liver xenograft models for in vivo validation.
- Single-cell RNA-seq to assess tumor heterogeneity impacts.
Figure 2: Diverse Functional Mechanisms of lncRNAs in HBV-Related HCC. The diagram illustrates how lncRNAs operate through multiple distinct molecular mechanisms to influence critical cancer hallmarks, with HBV/HBx serving as a master regulator of lncRNA dysregulation.
circRNAs: Emerging Regulators in HBV-Driven HCC
Biogenesis and Unique Properties
Circular RNAs (circRNAs) constitute a novel class of ncRNAs characterized by their covalently closed continuous loop structure, which confers exceptional stability due to resistance to RNA exonuclease activity [14]. Most circRNAs are generated through a non-canonical splicing event called "back-splicing," where a downstream 5' splice site joins with an upstream 3' splice site, resulting in a circular configuration [14] [15]. Three primary circRNA subtypes have been identified: exonic circRNAs (ecRNAs), circular intronic RNAs (ciRNAs), and exon-intron circRNAs (EIciRNAs) [15].
The unique properties of circRNAs include: (1) High stability due to resistance to RNase R degradation; (2) Conservation across species; (3) Tissue-specific and developmentally regulated expression patterns; and (4) Specific subcellular localization signatures [14]. These characteristics make circRNAs particularly suitable as diagnostic biomarkers and potentially as therapeutic agents.
Functional Roles in HBV-Related HCC
While research on circRNAs in HBV-related HCC is less extensive than for miRNAs and lncRNAs, emerging evidence indicates they play significant roles in hepatocarcinogenesis through several mechanisms: (1) Acting as miRNA sponges to sequester miRNAs and derepress their target mRNAs; (2) Regulating transcription and splicing; (3) Interacting with proteins to modulate their functions; and (4) Occasionally serving as templates for protein translation [14] [15].
Notably, circRNAs participate in key signaling pathways dysregulated in HBV-HCC, including Wnt/β-catenin, PI3K/AKT, and MAPK pathways [14]. Their expression can be modulated by HBV infection, particularly through the action of HBx, which alters the host cell's splicing machinery and epigenetic landscape to favor the generation of specific circRNA profiles that support the viral life cycle and create a procarcinogenic microenvironment.
Methodologies for circRNA Investigation
Protocol 1: circRNA Discovery and Validation
- RNA Preparation: Extract total RNA using TRIzol with DNase I treatment. Divide each sample for linear RNA sequencing and circRNA analysis.
- RNase R Treatment: Treat 2-5 μg total RNA with 3 U/μg RNase R for 15-30 minutes at 37°C to enrich for circular RNAs by degrading linear RNAs.
- Library Construction and Sequencing: Use circRNA-specific protocols such as Circomics or circRNA-seq with random hexamer priming.
- Bioinformatic Identification:
- Map reads with STAR, BWA, or Bowtie2 using back-splice junction-aware algorithms.
- Utilize dedicated circRNA detection tools (CIRCexplorer2, CIRI2, find_circ) with multiple algorithm consensus recommended.
- Predict miRNA binding sites using TargetScan, miRanda, or RNAhybrid.
- Experimental Validation:
- Divergent Primer PCR: Design primers facing away from each other to specifically amplify back-splice junctions.
- Sanger Sequencing: Confirm back-splice junctions from PCR products.
- Northern Blotting: Use junction-specific probes to verify circular structure.
- RNA-FISH: Determine subcellular localization with junction-specific probes.
Protocol 2: Functional Characterization of circRNAs
- Loss-of-Function Approaches:
- Design siRNAs targeting back-splice junctions specifically.
- Utilize CRISPR/Cas13 systems for selective circRNA knockdown.
- Note: Traditional siRNA approaches may not effectively target circRNAs.
- Gain-of-Function Studies:
- Synthesize circRNA expression vectors containing flanking inverted repeat sequences.
- Use T4 ligation for in vitro circularization of RNA transcripts.
- Employ plasmid systems with permutationally designed complementary sequences.
- Interaction Mapping:
- Perform circRNA pulldown with biotinylated junction-specific probes.
- Conduct RNA immunoprecipitation (RIP) for protein interaction partners.
- Implement crosslinking and analysis of cDNAs (CRAC) for high-resolution interaction mapping.
The ncRNA Cross-Talk: Integrated Regulatory Networks in HBV-HCC
The three classes of ncRNAs do not function in isolation but rather form intricate regulatory networks that collectively drive HBV-related hepatocarcinogenesis. The most prominent interaction is the ceRNA network, where lncRNAs and circRNAs function as molecular sponges that sequester miRNAs, thereby derepressing miRNA target genes [11] [15]. For example, the lncRNA HULC acts as a ceRNA for miR-372, leading to increased expression of PRKACB and subsequent CREB phosphorylation, forming a positive feedback loop that promotes HCC progression [12].
Beyond ceRNA networks, additional layers of complexity exist: (1) miRNAs can regulate the expression of lncRNAs and circRNAs; (2) lncRNAs can serve as precursors for miRNAs; (3) Multiple ncRNA classes can coregulate common signaling pathways such as Wnt/β-catenin and PI3K/AKT; and (4) Epigenetic modifications of ncRNAs (e.g., m6A methylation) can influence their stability and function [15]. HBV infection, particularly through HBx, exploits these networks by systematically reprogramming the ncRNA landscape to create a cellular environment favorable for viral persistence and malignant transformation.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Reagents for ncRNA Investigation in HBV-HCC
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Cell Line Models | HepG2.2.15, HepAD38, Huh7-HBV | HBV replication studies, ncRNA functional validation | Confirm HBV replication competence regularly; use isogenic controls [10] |
| Animal Models | HBV-transgenic mice, Hydrodynamic injection models, Humanized liver mice | In vivo validation of ncRNA functions | Monitor HBV parameters; species-specific ncRNA differences [12] |
| qRT-PCR Assays | TaqMan Advanced miRNA assays, LNA-enhanced primers, Divergent primers for circRNAs | ncRNA expression quantification | Use appropriate normalization strategies; validate circRNA specificity [14] [15] |
| Sequencing Kits | Illumina Small RNA-Seq, SMARTer smRNA-Seq, ribosomal RNA depletion kits | ncRNA discovery and profiling | Select appropriate library prep based on ncRNA class; include RNase R for circRNAs [15] |
| Functional Tools | LNA gapmeRs, CRISPR/Cas13 systems, miRNA mimics/inhibitors | ncRNA gain/loss-of-function studies | Verify specificity of knockdown; use multiple approaches for confirmation [13] |
| Interaction Mapping | ChIRP, RAP-MS, Biotinylated miRNA pulldowns | ncRNA-mRNA/protein interaction mapping | Include stringent controls; validate interactions orthogonally [11] |
| (S)-2-Benzylaziridine-carboxylate | (S)-2-Benzylaziridine-carboxylate, CAS:1142923-78-1, MF:C17H17NO2, MW:267.328 | Chemical Reagent | Bench Chemicals |
| 2-(1,1-Difluoroethyl)-1,3-thiazole | 2-(1,1-Difluoroethyl)-1,3-thiazole, CAS:2580236-05-9, MF:C5H5F2NS, MW:149.16 | Chemical Reagent | Bench Chemicals |
The comprehensive investigation of ncRNAs in HBV-related HCC has revealed their critical importance as regulatory molecules, biomarkers, and potential therapeutic targets. miRNAs, lncRNAs, and circRNAs form sophisticated interactive networks that HBV exploits to establish persistent infection and drive hepatocarcinogenesis. Future research directions should include: (1) Systematic mapping of complete ncRNA interactomes in HBV-infected hepatocytes; (2) Elucidation of ncRNA functions in the tumor microenvironment and immune evasion; (3) Development of ncRNA-based therapeutics including antisense oligonucleotides and small molecule inhibitors; and (4) Exploration of ncRNA methylation modifications as regulatory mechanisms and therapeutic targets [15].
The integration of multi-omics approaches, advanced bioinformatics tools, and sophisticated experimental models will continue to unravel the complexity of ncRNA regulatory networks in hepatic biology. As our understanding deepens, the translation of ncRNA research into clinical applications holds significant promise for improving the diagnosis, prognosis, and treatment of HBV-related hepatocellular carcinoma, ultimately addressing a substantial global health burden.
Hepatitis B virus (HBV) infection represents a major global health burden and is a primary etiological factor in hepatocellular carcinoma (HCC). The HBV X protein (HBx) has emerged as a critical viral regulator that orchestrates extensive dysregulation of non-coding RNAs (ncRNAs), creating a permissive environment for hepatocarcinogenesis. This technical review comprehensively examines the molecular mechanisms through which HBx alters ncRNA expression and function, with particular focus on microRNAs (miRNAs) and long non-coding RNAs (lncRNAs). We synthesize current understanding of how HBx-mediated ncRNA aberrations impact key cellular processes including proliferation, apoptosis, metastasis, and immune evasion. The review also provides detailed experimental methodologies for investigating these mechanisms and discusses the translational potential of ncRNAs as biomarkers and therapeutic targets in HBV-associated HCC.
Hepatocellular carcinoma ranks as the third leading cause of cancer-related deaths worldwide, with chronic HBV infection contributing to approximately 80% of cases globally [16]. The molecular pathogenesis of HBV-associated HCC involves a complex interplay between viral factors and host cellular machinery, with the multifunctional HBx protein serving as a central orchestrator of oncogenic processes [17]. HBx, a 17 kDa regulatory protein encoded by the smallest open reading frame of the HBV genome, localizes to both cytoplasmic and nuclear compartments and functions as a transcriptional transactivator that influences both viral and host gene expression [18] [19].
Over the past decade, ncRNAs have emerged as crucial regulators of gene expression in both physiological and pathological states. These RNA molecules, which lack protein-coding capacity, include miRNAs (approximately 21-25 nucleotides), lncRNAs (>200 nucleotides), circular RNAs (circRNAs), and other specialized subtypes [16] [8]. In the context of HBV infection, HBx systematically dysregulates ncRNA networks to promote viral persistence and drive hepatocarcinogenesis through multiple mechanisms [19] [20]. This review delineates the precise molecular mechanisms of HBx-mediated ncRNA dysregulation and their functional consequences in HCC development.
HBx Protein: Structure and Multifunctional Roles
The HBx gene is located at nucleotide positions 1,060-1,838 in HBV genotypes B and C, with a promoter region at nt 1,060-1,373 and coding region at nt 1,374-1,835 [17]. The 154-amino acid HBx protein contains two primary functional domains: an amino-terminal negative regulatory domain (amino acids 1-50) and a carboxyl-terminal trans-activation domain (amino acids 52-148) [17]. The trans-activation domain further contains subdomains responsible for signal transduction activities (AA 58-119), nuclear trans-activation mechanisms (AA 120-140), and a C-terminal region crucial for protein stability [17].
HBx exhibits diverse subcellular localization patterns that correlate with its functional activities. Highly expressed HBx predominantly localizes to the cytoplasm, while lower expression levels favor nuclear distribution [17]. This dynamic localization enables HBx to interact with various cellular components and modulate numerous signaling pathways including MAPK, PI3K/AKT, JAK-STAT, NF-κB, and Wnt/β-catenin cascades [21] [17]. Through these interactions, HBx influences critical cellular processes such as apoptosis, DNA repair, cell cycle progression, oxidative stress response, and epigenetic regulation [17].
Table 1: Key Functional Roles of HBx in Hepatocarcinogenesis
| Pathway/Process | Effect of HBx | Functional Outcome |
|---|---|---|
| MAPK signaling | Enhancement of MAPK activation | Increased cell proliferation, apoptosis prevention, gene expression regulation |
| PI3K/AKT signaling | Stimulation of PI3K/AKT pathway | Apoptosis suppression, increased cell proliferation and survival |
| JAK-STAT signaling | Disruption of JAK-STAT system | Immunological suppression, increased cell survival and proliferation |
| NF-κB signaling | Activation of NF-κB pathway | Enhanced inflammation, immunological regulation, cell survival |
| Oxidative stress | Imbalance between ROS production and antioxidant defense | DNA damage, genomic instability, inflammation |
| Apoptosis and DNA repair | Inhibition of apoptosis and DNA repair mechanisms | Promoted cell survival, genomic instability |
| Epigenetic modification | Induction of DNA methylation, histone alterations, chromatin remodeling | Altered gene expression patterns and cellular responses |
Comprehensive Mechanisms of HBx-Mediated ncRNA Dysregulation
Direct Transcriptional Regulation
HBx modulates ncRNA expression by interacting with transcription factors and epigenetic regulators. Although HBx lacks a DNA-binding domain, it indirectly influences transcription by associating with key cellular factors including p53, c-Myc, nuclear factor kappa B (NF-κB), and survivin [19]. For instance, HBx represses miR-148a by inhibiting the tumor suppressor p53, leading to increased expression of hematopoietic pre-B-cell leukemia transcription factor-interacting protein (HPIP) and subsequent activation of Akt and ERK signaling pathways [19]. Similarly, HBx suppresses p53-mediated activation of miR-216b, which targets IGF2BP2 and facilitates downstream AKT/mTOR and MAPK/ERK signaling pathways [19].
Epigenetic Modifications
HBx extensively remodels the epigenetic landscape to alter ncRNA expression. A prominent mechanism involves DNA methylation, where HBx induces hypermethylation of miRNA promoter regions. This is exemplified by HBx-mediated epigenetic repression of miR-132 through DNA methylation, which enhances the Akt signaling pathway and promotes hepatoma cell growth [19]. Similarly, HBx inhibits miR-205 expression by promoting hypermethylation of its promoter region, contributing to aberrant lipid metabolism through overexpression of acyl-CoA synthetase long-chain family member 4 (ACSL4) [19] [20].
HBx also influences histone modifications and chromatin remodeling to regulate ncRNA accessibility. Through these epigenetic mechanisms, HBx can either activate or repress ncRNA expression depending on the specific context and target genes involved [19].
Regulation of ncRNA Processing Machinery
Beyond transcriptional control, HBx interferes with the maturation and processing of ncRNAs. HBx can inhibit key processing enzymes in the miRNA biogenesis pathway, including DROSHA and DICER complexes [18]. This disruption affects the conversion of primary miRNA transcripts (pri-miRNAs) to precursor miRNAs (pre-miRNAs) in the nucleus, as well as the subsequent processing of pre-miRNAs to mature miRNAs in the cytoplasm [18] [16]. By compromising these essential steps in miRNA biogenesis, HBx causes global alterations in miRNA expression patterns that favor viral persistence and oncogenesis.
miRNA Sponging and Competing Endogenous RNA Networks
HBx induces the expression of specific lncRNAs and circRNAs that function as competing endogenous RNAs (ceRNAs) or "miRNA sponges." These RNAs contain binding sites for specific miRNAs and sequester them, thereby preventing the miRNAs from interacting with their natural mRNA targets [10] [16]. For example, HBx-upregulated lncRNAs such as HULC can act as miRNA sponges to derepress oncogenic pathways. This ceRNA network represents a sophisticated layer of post-transcriptional regulation that amplifies the oncogenic effects of HBx through interconnected ncRNA interactions.
Quantitative Profiles of HBx-Dysregulated ncRNAs in HBV-HCC
The progression from asymptomatic HBV infection to HCC is characterized by accumulating dysregulation of ncRNAs. One study documented 37 dysregulated miRNAs in healthy controls, increasing to 77 in asymptomatic carriers, 101 in chronic hepatitis B, and 135 in acute liver failure [18]. Another investigation reported 79 dysregulated miRNAs in asymptomatic HBV carriers versus 203 in chronic HBV cases [18], highlighting the progressive nature of ncRNA alterations throughout disease progression.
Table 2: Key HBx-Dysregulated miRNAs in HBV-Related HCC
| miRNA | Expression in HCC | Regulatory Mechanism | Validated Targets | Functional Consequences |
|---|---|---|---|---|
| miR-122 | Downregulated | Downregulated by IL-6 and TNF-α; inhibited by HBx via PPARγ interaction | CCL2, C/EBPα, c-myc, PKM2, SLC7A1 | Promotes tumor development, motility, invasion; alters anaerobic glycolysis and amino acid metabolism |
| miR-21 | Upregulated | Regulated by HBx | PDCD4, PTEN | Increased tumor cell growth and survival |
| miR-221/222 | Upregulated | Upregulated by HBx | CXCL4/12, TFRC | Facilitates cell cycle progression, suppresses apoptosis |
| let-7 family | Downregulated | Repressed via HBx-c-Myc-LIN28B axis | STAT3, ras, c-myc | Supports cell proliferation; double-negative feedback loop with c-Myc/LIN28B |
| miR-148a | Downregulated | HBx suppresses p53-mediated activation | HPIP | Activates AKT/ERK/FOXO4/ATF5 pathways; promotes proliferation, EMT, invasion |
| miR-216b | Downregulated | HBx suppresses p53-mediated activation | IGF2BP2 | Activates IGF2, AKT/mTOR, MAPK/ERK pathways; promotes proliferation, migration |
| miR-132 | Downregulated | HBx induces epigenetic repression via methylation | Akt signaling components | Facilitates hepatoma cell growth |
| miR-205 | Downregulated | HBx promotes promoter hypermethylation | ACSL4 | Causes lipogenesis dysregulation, cholesterol accumulation |
| miR-429 | Upregulated | Positively correlated with HBx expression | Rab18 | Induces lipogenesis dysregulation, promotes proliferation |
| miR-101 | Downregulated | Downregulated by HBx | DNMT3A | Induces aberrant DNA methylation |
Table 3: Key HBx-Dysregulated lncRNAs in HBV-Related HCC
| lncRNA | Expression in HCC | Regulatory Mechanism | Molecular Function | Pathogenic Role |
|---|---|---|---|---|
| HULC | Upregulated | Induced by HBx | miRNA sponge; chromatin modification | Promotes proliferation, invasion, metastasis |
| DLEU2 | Upregulated | Regulated by HBx | Chromatin regulation, transcription regulation | Enhances tumor formation |
| HOTAIR | Upregulated | Regulated by HBx | Chromatin regulation, cell cycle regulation | Constrains or enhances tumor formation |
| MALAT1 | Upregulated | Induced by HBx | Transcriptional and post-transcriptional regulation | Promotes proliferation, invasion |
Experimental Models and Methodologies for HBx-ncRNA Research
In Vitro Models and Cell Culture Systems
Hepatoma-Derived Cell Lines:
- HepG2.2.15: HepG2 cells stably transfected with HBV genome, supporting viral replication and serving as a model for chronic HBV infection [10].
- Huh7 and Hep3B: Widely used hepatoma cell lines for transfection studies with HBx expression vectors [10] [19].
- SMMC-7721: Used for HBx-induced epithelial-mesenchymal transition (EMT) studies, particularly through activation of c-Src [17].
Primary Human Hepatocytes:
- Isolated from liver tissues, these cells maintain hepatic functionality but are limited by gradual dedifferentiation in culture and variable support for HBV replication [21].
Advanced Ex Vivo Models
Liver Organoids:
- Developed from patient-derived liver tissues, organoids retain original tissue characteristics, undergo unlimited expansion, and can be differentiated into mature hepatocytes [21].
- Protocol for HBV Infection in Liver Organoids:
- Establish organoid cultures from human liver biopsy or surgical specimens in Matrigel-based 3D culture system.
- Maintain in expansion medium (Advanced DMEM/F12 supplemented with R-spondin-1, Noggin, EGF, Wnt3a, FGF10, HGF, Nicotinamide, and A83-01).
- Differentiate toward hepatocyte lineage by withdrawing Wnt3a and R-spondin while adding dexamethasone and ON-TARGETplus Human BMP7.
- Infect with natural HBV particles at multiplicity of infection (MOI) of 100-500 viral genomes per cell.
- Harvest samples at 3-14 days post-infection for ncRNA expression analysis [21].
Key Experimental Techniques
ncRNA Expression Profiling:
- Next-Generation Sequencing: Comprehensive identification of differentially expressed ncRNAs using RNA-seq protocols with ribosomal RNA depletion to enrich for ncRNA species.
- qRT-PCR Validation: TaqMan-based assays for specific miRNA quantification; stem-loop primers for mature miRNA detection.
Functional Characterization:
- Gain/Loss-of-Function Studies: HBx overexpression vectors (pcDNA3.1-HBx) and siRNA/shRNA-mediated knockdown for HBx and specific ncRNAs.
- Luciferase Reporter Assays: Validation of direct miRNA-mRNA interactions using pmiRGLO vectors containing wild-type or mutated 3'UTR sequences.
Epigenetic Analysis:
- Bisulfite Sequencing: Detection of DNA methylation patterns in miRNA promoter regions.
- Chromatin Immunoprecipitation (ChIP): Assessment of transcription factor binding and histone modifications at ncRNA loci.
Diagram 1: HBx-Mediated ncRNA Dysregulation Network. This diagram illustrates the multifaceted mechanisms through which HBx dysregulates ncRNA expression and the consequent pathological outcomes in HBV-associated HCC.
Signaling Pathway Integration in HBx-ncRNA Networks
HBx-dysregulated ncRNAs converge on several core signaling pathways that drive hepatocarcinogenesis. The Wnt/β-catenin pathway is activated in up to 50% of HCC cases, with β-catenin accumulation correlated with tumor progression and poor prognosis [21]. HBx-dysregulated miRNAs including miR-122 and miR-148a directly target components of this pathway, leading to constitutive activation.
The PI3K/AKT pathway represents another critical signaling cascade affected by HBx-ncRNA interactions. Multiple HBx-repressed miRNAs, including miR-122, miR-199a/b, and miR-216b, normally function to inhibit PI3K/AKT signaling [16] [19]. Their downregulation results in pathway hyperactivation, promoting cell survival and proliferation.
Additionally, HBx-dysregulated ncRNAs impact the Ras/Raf/MAPK pathway, JAK-STAT signaling, and NF-κB inflammatory cascades [21] [17]. These pathway alterations collectively establish an oncogenic signaling environment that facilitates HBV persistence and HCC development.
Diagram 2: HBx-ncRNA Pathway Integration in Hepatocarcinogenesis. This diagram illustrates how HBx-dysregulated ncRNAs converge on core signaling pathways to drive oncogenic processes in HBV-associated HCC.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating HBx-ncRNA Interactions
| Reagent Category | Specific Examples | Research Application | Experimental Notes |
|---|---|---|---|
| Cell Lines | HepG2.2.15, Huh7, Hep3B, SMMC-7721, PLC/PRF/5 | In vitro HBx-ncRNA functional studies | HepG2.2.15 stably supports HBV replication; other lines require HBx transfection |
| HBx Expression Vectors | pcDNA3.1-HBx, pSVL-HBx, lentiviral-HBx constructs | HBx overexpression studies | Include empty vector controls; monitor expression timing to avoid artificial effects |
| HBx Knockdown Tools | siRNA, shRNA against HBx | Loss-of-function studies | Multiple sequences recommended to control for off-target effects |
| ncRNA Modulation | miRNA mimics, inhibitors, lncRNA expression vectors, CRISPR-based ncRNA editing | Functional characterization of specific ncRNAs | Include appropriate scrambled controls; validate modulation efficiency |
| Reporter Systems | pmiRGLO, pGL3-based vectors with 3'UTRs | Validation of direct miRNA-mRNA interactions | Include mutant 3'UTR controls with disrupted miRNA binding sites |
| Epigenetic Reagents | 5-aza-2'-deoxycytidine (DNA methyltransferase inhibitor), Trichostatin A (HDAC inhibitor) | Epigenetic mechanism studies | Use combination approaches to distinguish methylation vs. acetylation effects |
| Antibodies | Anti-HBx, anti-p53, anti-acetylated histones, anti-methylated DNA | Protein detection, ChIP experiments | Validate specificity for ChIP-grade applications |
| Animal Models | HBV transgenic mice, hydrodynamic injection models, humanized liver mice | In vivo validation | Consider immune competence based on research question |
| 2,2-Dimethyl-4-oxopentanenitrile | 2,2-Dimethyl-4-oxopentanenitrile|CAS 33235-13-1 | Bench Chemicals | |
| 3-(2-Bromoethoxy)cyclopent-2-enone | 3-(2-Bromoethoxy)cyclopent-2-enone|CAS 42858-97-9 | 3-(2-Bromoethoxy)cyclopent-2-enone (CAS 42858-97-9) is a versatile cyclopentenone building block for organic synthesis. This product is For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Concluding Perspectives and Future Directions
The central role of HBx in dysregulating ncRNA networks represents a critical mechanism in HBV-associated hepatocarcinogenesis. Through multifaceted approaches including transcriptional regulation, epigenetic modification, processing interference, and sponge networks, HBx creates an extensive reprogramming of the cellular ncRNA landscape that drives oncogenic transformation. The progressive nature of ncRNA dysregulation throughout the HBV-HCC continuum underscores their potential as diagnostic biomarkers and therapeutic targets.
Future research directions should focus on elucidating the complete interactome of HBx with ncRNA regulatory networks, developing advanced animal models that recapitulate the human ncRNA environment, and exploring the therapeutic potential of ncRNA-based interventions. The convergence of multiple HBx-dysregulated ncRNAs on key signaling pathways suggests that combinatorial targeting approaches may yield enhanced efficacy. As technologies for ncRNA manipulation continue to advance, particularly in delivery and specificity, the translational potential of targeting HBx-ncRNA axes in HBV-associated HCC appears increasingly promising.
Understanding the intricate mechanisms of HBx-mediated ncRNA dysregulation will not only provide fundamental insights into hepatocarcinogenesis but also pave the way for novel diagnostic and therapeutic strategies against this devastating malignancy.
Non-coding RNAs (ncRNAs), once considered genomic "junk," are now recognized as pervasive regulators of cancer hallmarks, including sustained proliferation, evasion of apoptosis, and metastatic potential. In the specific context of hepatitis B virus (HBV)-induced hepatocarcinogenesis, viral components such as the HBx protein profoundly alter ncRNA expression profiles, rewiring core oncogenic signaling pathways. This whitepaper provides an in-depth analysis of the mechanisms by which microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) drive tumorigenesis. It further details state-of-the-art experimental methodologies for their investigation and discusses the burgeoning potential of ncRNAs as therapeutic targets and diagnostic biomarkers, framing these findings within the broader thesis of HBV-induced ncRNA alterations in liver cancer.
The central dogma of molecular biology, which posits a linear flow of information from DNA to RNA to protein, has been fundamentally challenged by the discovery that the vast majority of the human genome is transcribed into non-coding RNAs (ncRNAs) with no protein-coding capacity [22]. These ncRNAs are not mere transcriptional noise; they form an elaborate, hierarchical network that fine-tunes the flow of genetic information in eukaryotic cells [22]. The proportion of non-coding DNA correlates with organismal complexity, accounting for an astonishing 98.5% of the human genome [22], which suggests a critical role in regulating sophisticated biological processes.
In cancer, this regulatory network is profoundly disrupted. The prevailing somatic mutation theory, centered on protein-coding oncogenes and tumor suppressor genes, has been unable to fully explain the immense diversity and heterogeneity of genetic alterations observed within and across cancer types [22]. The ncRNA network offers a compelling explanation for these inconsistencies. Mutations that disrupt ncRNA function can perturb the higher-order states of equilibrium, known as attractor states, that correspond to stable gene-expression configurations of distinct cell types. Such perturbations can enable a state transition towards a neoplastic phenotype, representing a crux of tumorigenesis [22]. This review dissects the roles of key ncRNA classes—miRNAs, lncRNAs, and circRNAs—as drivers of core cancer hallmarks, with a specific focus on their alteration by HBV infection, a major global driver of hepatocellular carcinoma (HCC).
Classes and Functions of Oncogenic Non-Coding RNAs
ncRNAs are broadly categorized into housekeeping and regulatory types. The following sections focus on the regulatory ncRNAs most critically implicated in cancer.
Table 1: Major Classes of Regulatory Non-Coding RNAs in Cancer
| ncRNA Class | Size Range | Key Functions | Role in Cancer Hallmarks |
|---|---|---|---|
| MicroRNA (miRNA) | ~21-25 nt | Post-transcriptional gene silencing; translational repression [23]. | Dual role as oncogene ("oncomiR") or tumor suppressor [16] [24]. |
| Long Non-Coding RNA (lncRNA) | >200 nt | Chromatin modification; transcriptional regulation; protein scaffolding; molecular decoy [22] [24]. | Regulates proliferation, apoptosis, metastasis, and therapy resistance [25]. |
| Circular RNA (circRNA) | <100 nt - 4 kb | miRNA sponging; protein scaffolding; gene expression regulation [22]. | Acts as competitive endogenous RNA (ceRNA); often dysregulated in cancer [24]. |
MicroRNAs (miRNAs): Master Post-Transcriptional Regulators
MiRNAs are small, single-stranded RNAs that typically induce gene silencing by binding to complementary sequences on target messenger RNAs (mRNAs), leading to mRNA degradation or translational repression [23] [16]. Their biogenesis is a multi-step process involving transcription as primary miRNAs (pri-miRNAs), nuclear processing by Drosha into precursor miRNAs (pre-miRNAs), export to the cytoplasm, and final cleavage by Dicer into mature miRNAs, which are loaded into the RNA-induced silencing complex (RISC) [16] [25].
Long Non-Coding RNAs (lncRNAs): Versatile Epigenetic Architects
LncRNAs are defined as transcripts longer than 200 nucleotides that lack protein-coding potential. Their functional complexity stems from their ability to interact with DNA, RNA, and proteins [25]. They can act in cis (affecting neighboring genes) or in trans (affecting distant genes), influencing chromatin architecture, transcription, and mRNA stability [24]. Their large size and flexible conformation allow them to serve as scaffolds for protein complexes or as decoys that sequester miRNAs or proteins [22].
Circular RNAs (circRNAs): Stable Competitive Endogenous RNAs
CircRNAs are a more recently characterized class of ncRNAs that form covalently closed, continuous loops without a 5' cap or 3' poly-A tail, making them highly resistant to exonuclease degradation [24]. While some circRNAs function as protein sponges or scaffolds, a predominant mechanism is their role as competitive endogenous RNAs (ceRNAs) or "miRNA sponges," where they sequester miRNAs, thereby preventing them from binding to their target mRNAs [22] [24].
Mechanisms of Action in Cancer Hallmarks
Oncogenic ncRNAs exert their effects by rewiring critical intracellular signaling pathways that govern cell fate and behavior.
Driving Sustained Proliferation and Evading Apoptosis
ncRNAs directly target core cell cycle and apoptosis regulators. For instance, in HBV-related HCC, the miR-17-92 cluster is upregulated and promotes proliferation by targeting estrogen receptor alpha (ERα) [16]. Conversely, tumor-suppressive miRNAs like miR-199a/b are downregulated, leading to increased activity of the pro-survival PI3K/Akt and ROCK1/MLC pathways [16]. LncRNAs such as HOTAIR are overexpressed in colorectal cancer (CRC) and inhibit apoptosis while promoting cellular autophagy through the miR-93/autophagy-related 12 (ATG12) axis [25].
Activating Invasion and Metastasis
The process of metastasis, including epithelial-mesenchymal transition (EMT), is heavily influenced by ncRNAs. In HBV-HCC, downregulation of miR-30a-5p promotes EMT by increasing the expression of its target, SNAIL1, a key transcriptional repressor of epithelial genes [16]. The lncRNA HOTTIP is elevated in CRC and accelerates proliferation and migration, in part by stabilizing and promoting the expression of serum/glucocorticoid regulated kinase 1 (SGK1) [25].
Table 2: Selected Oncogenic ncRNAs and Their Mechanisms in HBV-HCC and Other Cancers
| ncRNA | Class | Expression in Cancer | Validated Target/Pathway | Functional Outcome |
|---|---|---|---|---|
| miR-21 | miRNA | Upregulated (by HBx) [16] | PDCD4, PTEN [16] | Increased cell growth & survival |
| miR-122 | miRNA | Downregulated [16] | PKM2, SLC7A1 [16] | Promoted motility, invasion, metabolic reprogramming |
| DLEU2 | lncRNA | Implicated in HCC [16] | Chromatin regulation [16] | Cell cycle dysregulation, tumor formation |
| KCNQ1OT1 | lncRNA | Overexpressed in CRC [25] | miR-216b-5p/ZNF146 axis [25] | Accelerated proliferation, migration, and invasion |
| circRNAs | circRNA | Variably dysregulated | miRNA sponging [22] [24] | Derepression of oncogenic miRNA targets |
Key Signaling Pathways Rewired by ncRNAs
- PI3K/Akt/mTOR Pathway: This critical pro-survival and proliferation pathway is frequently targeted. For example, miR-199a/b suppresses it by targeting ROCK1 in HCC [16], while miR-21 enhances its activity by inhibiting PTEN [23].
- Wnt/β-catenin Pathway: miRNAs such as miR-135a are involved in regulating this pathway, which is central to cell proliferation and stemness [16].
- p53 Pathway: The crucial tumor suppressor p53 is both regulated by and regulates a vast network of ncRNAs, forming complex feedback loops that are disrupted in cancer [23].
- MAPK/ERK Pathway: This growth-signaling pathway is modulated by ncRNAs like miR-155 and miR-135a, contributing to uncontrolled proliferation [23] [16].
Figure 1: HBV-Induced ncRNA Alterations Drive Oncogenic Hallmarks. The model shows how HBV, via the HBx protein, dysregulates ncRNA expression, which in turn rewires key cellular pathways to promote malignancy. Green arrows indicate activation/upregulation; red arrows indicate suppression/downregulation.
The HBV-ncRNA Axis in Hepatocarcinogenesis
Chronic HBV infection is a primary etiological factor for HCC, and its interplay with the host ncRNA landscape is a critical component of its oncogenicity. The HBV-encoded X protein (HBx) is a key viral factor that alters cellular ncRNA expression [16]. For instance, HBx upregulates oncogenic miR-21 and miR-221, while downregulating tumor-suppressive miR-122, miR-101, and miR-148a/152 [16].
Recent research reveals that HBV alone may not be sufficient to cause liver inflammation or cancer. Instead, HBV modulates the liver's immune and regenerative response to environmental carcinogens, such as diethylnitrosamine (DEN) [26]. In this model, HBV synergizes with the carcinogen to induce a specific inflammatory program driven by the IL-33/regulatory T cell (Treg) axis, which is required for liver carcinogenesis. This process involves increased DNA damage and release of the DAMP molecule HMGB1, activating the TLR4/TBK1/IRF3 pathway to drive IL-33 expression [26]. This creates a permissive microenvironment for the proliferation of ncRNA-dysregulated hepatocytes.
Experimental Protocols for ncRNA Research
Studying ncRNAs requires a combination of computational, molecular, and cellular biological techniques.
Protocol: Identifying and Validating ncRNA-RNA Interactions
This protocol outlines the key steps for confirming a predicted interaction between a ncRNA (e.g., a lncRNA or circRNA) and its target miRNA or mRNA.
In Silico Prediction:
- Objective: Generate a list of high-confidence candidate targets.
- Procedure: Use multiple bioinformatic algorithms to predict binding. For miRNA-mRNA interactions, use tools like TargetScan, miRDB, and miRTarBase. For lncRNA/circRNA-miRNA interactions, use tools like StarBase or CircInteractome. Intersect results from different algorithms to reduce false positives.
- Reagents: Publicly available databases and prediction software.
Expression Profiling and Correlation:
- Objective: Establish a biological context for the interaction.
- Procedure: Quantify the expression of the ncRNA and its putative target in matched normal and tumor tissues or cell lines (e.g., via RT-qPCR or RNA-Seq). A significant negative correlation between a miRNA and its target mRNA (or a positive correlation between a ceRNA and its target mRNA) provides preliminary supportive evidence.
- Reagents: TRIzol (RNA isolation), cDNA synthesis kits, SYBR Green RT-qPCR master mix, specific primers.
Functional Validation via Gain/Loss-of-Function:
- Objective: Determine the functional consequence of the interaction.
- Procedure: Transferd cells with:
- miRNA mimic (for overexpression) or miRNA inhibitor (for knockdown).
- siRNA/shRNA targeting a lncRNA or circRNA (for knockdown).
- Expression plasmid for a lncRNA or circRNA (for overexpression).
- Assess phenotypic changes using assays for proliferation (CCK-8, MTT), apoptosis (Annexin V/PI staining), and invasion (Transwell).
- Reagents: Lipofectamine or other transfection reagents, synthetic miRNAs/siRNAs, expression vectors, phenotypic assay kits.
Direct Interaction Validation:
- Objective: Provide biochemical evidence of a direct interaction.
- Procedure:
- Luciferase Reporter Assay: Clone the wild-type and mutant 3'UTR of the target mRNA (or the putative binding site in a lncRNA/circRNA) into a luciferase reporter plasmid. Cotransfect with the miRNA mimic or ncRNA expression vector. A decrease in luciferase activity for the wild-type, but not mutant, construct confirms direct binding.
- RNA Immunoprecipitation (RIP): Use antibodies against Argonaute2 (Ago2), a key component of RISC, to immunoprecipitate RNA-protein complexes. Detection of both the miRNA and its putative target mRNA/ceRNA in the precipitate confirms they are in the same complex.
- Biotinylated Pull-Down: Use a biotin-labeled miRNA or lncRNA/circRNA probe to pull down directly interacting RNAs from cell lysates. The coprecipitated RNAs are then identified by RT-qPCR or sequencing.
- Reagents: Luciferase reporter vectors, dual-luciferase assay kit, anti-Ago2 antibody, protein A/G beads, biotin labeling kit, streptavidin-coated magnetic beads.
Figure 2: Experimental Workflow for Validating ncRNA Interactions. The stepwise process begins with computational prediction and progresses through correlative, functional, and direct biochemical validation.
Table 3: Essential Reagents for ncRNA Functional Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| miRNA Mimics & Inhibitors | Chemically synthesized small RNAs to overexpress or block endogenous miRNA activity. | Validating the tumor-suppressive role of miR-199a by restoring its function in HCC cells [16]. |
| siRNA/shRNA against lncRNAs/circRNAs | RNAi-based tools for knocking down specific long and circular ncRNAs. | Investigating HOTAIR function by siRNA-mediated knockdown in CRC cells [25]. |
| CRISPR/Cas9 Systems | For genomic deletion or activation (CRISPRa) of ncRNA loci. | Creating stable knockout cell lines for a oncogenic lncRNA. |
| Luciferase Reporter Vectors (e.g., pmirGLO) | Validating direct binding between a ncRNA and its target sequence. | Confirming miR-30a-5p binding to the SNAIL1 3'UTR [16]. |
| Anti-Ago2 Antibody | For RNA Immunoprecipitation (RIP) to capture miRNA-mRNA complexes. | Identifying novel miRNA targets in a physiological setting. |
| Biotin-Labeled RNA Probes | For pull-down assays to identify proteins or RNA interacting with a specific ncRNA. | Finding the protein partners of a lncRNA like DLEU2 [16]. |
| RNA-Seq & Single-Cell RNA-Seq | High-throughput profiling of ncRNA expression and heterogeneity. | Discovering novel HBV-dependent circRNAs in liver tumors [27]. |
Clinical and Therapeutic Implications
The disease-specific expression, stability, and detectability of ncRNAs in bodily fluids (e.g., blood) make them highly promising non-invasive biomarkers for early diagnosis, prognosis, and monitoring treatment response [16] [24]. Furthermore, targeting ncRNAs offers a novel avenue for cancer therapy.
Several strategies are under active investigation:
- miRNA Therapeutics: Using antisense oligonucleotides (ASOs) to inhibit oncogenic miRNAs (Anti-miRs) or using miRNA mimics to restore tumor-suppressive miRNA function [28] [24]. The FDA approval of the siRNA therapeutic Patisiran (ONPATTRO) has paved the way for RNA-based drugs [28].
- Targeting the ncRNA Network: The complex interplay between different ncRNAs, where lncRNAs and circRNAs can act as ceRNAs, suggests that targeting key hubs in this network could have potent effects [24].
- Overcoming Therapy Resistance: ncRNAs are major players in resistance to chemotherapy, radiotherapy, targeted therapy, and immunotherapy. Targeting these ncRNAs could resensitize tumors to existing treatments [24]. For example, in HBV-HCC, targeting the IL-33 axis (upstream of ncRNA dysregulation) with pitavastatin was shown to suppress liver cancer development in mice and was associated with a reduced risk of hepatitis and HCC in patients [26].
Oncogenic ncRNAs are master regulators that drive the core hallmarks of cancer by rewiring essential signaling pathways. In HBV-induced hepatocarcinogenesis, the virus co-opts the host's ncRNA network, creating a permissive environment for the proliferation of dysregulated hepatocytes, evasion of cell death, and ultimate metastasis. The intricate network between miRNAs, lncRNAs, and circRNAs represents a complex regulatory layer that is only beginning to be understood. Future research, leveraging advanced single-cell technologies and sophisticated animal models, will be crucial to dissect this complexity. The translational potential is immense, offering a promising frontier for the development of novel ncRNA-based diagnostic biomarkers and targeted therapeutics to combat cancer.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most common cancer worldwide and the third leading cause of cancer-related deaths. A predominant etiological factor in HCC development is chronic hepatitis B virus (HBV) infection, which is responsible for a substantial proportion of liver cancer cases, particularly in developing countries. The molecular pathogenesis of HBV-related HCC involves complex interactions between viral factors and host cellular machinery, with the HBV-encoded X protein (HBx) playing a central oncogenic role. In recent years, non-coding RNAs (ncRNAs) have emerged as crucial regulators of gene expression and cellular homeostasis, with growing evidence demonstrating their significant involvement in hepatocarcinogenesis.
This technical guide focuses specifically on tumor-suppressive ncRNAs—a class of RNA molecules that function to inhibit tumor development and progression—within the context of HBV-induced hepatocellular carcinoma. We examine the mechanisms through which these protective RNAs are systematically inactivated during viral hepatocarcinogenesis, detail methodologies for their identification and validation, and discuss their potential therapeutic applications. The systematic inactivation of tumor-suppressive ncRNAs represents a critical pathway in HBV-mediated oncogenesis, creating permissive conditions for uncontrolled cell proliferation, evasion of apoptosis, and eventual malignant transformation.
Non-coding RNAs are functionally categorized as either oncogenic or tumor-suppressive based on their cellular targets and biological effects. Tumor-suppressive ncRNAs typically function to constrain cellular proliferation, promote differentiation, induce apoptosis, and maintain genomic stability. In the context of HBV infection, these protective RNAs are frequently downregulated or functionally inactivated through various virally-mediated mechanisms, thereby facilitating hepatocarcinogenesis.
The major classes of tumor-suppressive ncRNAs include microRNAs (miRNAs), small RNA molecules approximately 21-25 nucleotides in length that mediate post-transcriptional gene silencing, and long non-coding RNAs (lncRNAs), which exceed 200 nucleotides and regulate gene expression through diverse mechanisms including chromatin modification, transcriptional interference, and molecular scaffolding. Additionally, circular RNAs (circRNAs) have recently been identified as important regulators that can function as competitive endogenous RNAs (ceRNAs) to sequester miRNAs and prevent their interaction with target mRNAs.
HBV, particularly through its HBx protein, orchestrates a complex reprogramming of the host cellular environment that favors viral persistence and replication. This reprogramming frequently involves the systematic suppression of tumor-suppressive ncRNAs, which would otherwise function to constrain oncogenic signaling pathways and maintain cellular homeostasis. The resulting imbalance between oncogenic and tumor-suppressive ncRNAs creates a permissive environment for the accumulation of genetic and epigenetic alterations that drive the multi-step process of hepatocarcinogenesis.
Table 1: Major Classes of Tumor-Suppressive ncRNAs in HBV-Related HCC
| ncRNA Class | Size Range | Mechanisms of Action | Representative Examples |
|---|---|---|---|
| microRNAs (miRNAs) | 21-25 nucleotides | Post-transcriptional gene silencing via mRNA degradation or translational repression | miR-122, miR-101, miR-148a, miR-152, miR-199a/b |
| Long Non-coding RNAs (lncRNAs) | >200 nucleotides | Chromatin modification, transcriptional regulation, molecular scaffolding, protein stabilization | lncRNA-Dreh, MEG3, GAS5 |
| Circular RNAs (circRNAs) | Variable | miRNA sponging, protein sequestration, regulatory templates | cir-ITCH, CDR1as |
Mechanisms of Inactivation of Tumor-Suppressive ncRNAs
Epigenetic Silencing by HBx
The HBV-encoded HBx protein plays a pivotal role in orchestrating the epigenetic silencing of tumor-suppressive ncRNAs, primarily through the manipulation of DNA methylation patterns and histone modifications. HBx has been demonstrated to recruit DNA methyltransferases (DNMTs) to the promoter regions of specific tumor-suppressive miRNAs, resulting in their transcriptional repression through hypermethylation.
A well-characterized example of this mechanism involves miR-132, which undergoes HBx-mediated promoter hypermethylation, leading to its transcriptional silencing. This epigenetic inactivation relieves the miR-132-mediated inhibition of the AKT signaling pathway, thereby promoting hepatoma cell growth [19]. Similarly, miR-101 is downregulated by HBx through the induction of DNMT3A, resulting in aberrant DNA methylation patterns that contribute to HBV-related HCC pathogenesis [20] [16]. The HBx protein also facilitates the hypermethylation of the miR-205 promoter, further expanding the repertoire of tumor-suppressive miRNAs subjected to epigenetic silencing [19].
Beyond DNA methylation, HBx also influences histone modification patterns to suppress tumor-suppressive ncRNAs. HBx interacts with various histone-modifying enzymes and components of chromatin-remodeling complexes, including the polycomb repressive complex 2 (PRC2), to establish repressive chromatin marks at the genomic loci of tumor-suppressive lncRNAs. For instance, several lncRNAs, including HEIH, UCA1, HOTAIR, and LINC00152, are dysregulated in HBV-related HCC through interactions with EZH2, the catalytic subunit of PRC2 that mediates histone H3 lysine 27 trimethylation (H3K27me3) [11].
Transcriptional Repression
HBx mediates transcriptional repression of tumor-suppressive ncRNAs through both direct and indirect mechanisms. The protein can inhibit the transactivational function of p53, a critical tumor suppressor transcription factor that regulates the expression of numerous ncRNAs with tumor-suppressive properties. This interference disrupts the p53-mediated activation of key miRNAs, including miR-148a and miR-216b [19].
The suppression of miR-148a is particularly significant, as it leads to the increased expression of its target, hematopoietic pre-B cell leukemia transcription factor-interacting protein (HPIP). The elevated HPIP levels subsequently activate the AKT/ERK/FOXO4/ATF5/mTOR signaling pathways, promoting HCC cell proliferation, epithelial-mesenchymal transition (EMT), invasion, and metastasis [19]. Similarly, HBx-mediated repression of miR-216b results in the upregulation of insulin-like growth factor 2 mRNA-binding protein 2 (IGF2BP2), activating downstream IGF2, AKT/mTOR, and MAPK/ERK signaling pathways that drive cell proliferation, migration, and invasion [19].
HBx also influences the activity of other transcription factors involved in ncRNA expression. For example, HBx can modulate the expression and activity of c-Myc, which in turn regulates the let-7 family of tumor-suppressive miRNAs. The HBx-c-Myc-LIN28B axis mediates the repression of let-7 miRNAs, which normally function to suppress tumorigenesis by targeting STAT3, ras, and c-Myc itself, creating a double-negative feedback loop that promotes HCC development through enhanced cell proliferation [19].
miRNA Sponging via ceRNA Networks
The competitive endogenous RNA (ceRNA) hypothesis proposes that RNA transcripts can communicate with and regulate each other by competing for shared miRNA response elements. In HBV-related HCC, several virally-induced or upregulated lncRNAs function as molecular "sponges" that sequester tumor-suppressive miRNAs, preventing them from interacting with their natural mRNA targets.
A clearly elucidated example of this mechanism involves the lncRNA KCNQ1OT1/miR-335-5p/CDC7 axis. HBV core protein (HBc) significantly induces the expression of lncRNA KCNQ1OT1, which functions as a ceRNA to bind and sequester tumor-suppressive miR-335-5p. This sequestration diminishes miR-335-5p-mediated repression of its target, cell division cycle 7 (CDC7), leading to enhanced proliferation and migration of HCC cells [29]. CDC7, a key regulator of DNA replication initiation, is highly expressed in HCC and significantly correlated with poor survival rates, highlighting the oncogenic consequences of this ceRNA network.
Other lncRNAs, including Unigene56159, HULC, HBx-LINE1, UCA1, and ANRIL, have also been implicated in the development of HBV-related HCC by functioning as miRNA sponges that titrate tumor-suppressive miRNAs away from their legitimate targets [11]. This molecular sponge effect represents a sophisticated mechanism of tumor-suppressive ncRNA inactivation that operates at the post-transcriptional level.
Diagram 1: Mechanisms of Tumor-Suppressive ncRNA Inactivation in HBV-HCC. The diagram illustrates three primary mechanisms: epigenetic silencing through promoter hypermethylation, transcriptional repression via p53 inhibition, and miRNA sponging through ceRNA networks.
Identification and Analysis of Tumor-Suppressive ncRNAs
High-Throughput Sequencing Approaches
The comprehensive identification of tumor-suppressive ncRNAs in HBV-related HCC relies heavily on high-throughput sequencing technologies that provide unbiased profiles of ncRNA expression across the genome. RNA sequencing (RNA-Seq) enables the simultaneous detection and quantification of diverse ncRNA species, including both known and novel transcripts, in HBV-infected versus uninfected hepatocytes or in HCC tissues compared to adjacent non-tumorous liver tissues.
The standard workflow for ncRNA identification involves several key steps. First, total RNA extraction is performed from clinical specimens or cell culture models, followed by library preparation using protocols specifically optimized for different ncRNA classes. For miRNA sequencing, size selection strategies are typically employed to enrich for small RNA fragments. The prepared libraries are then subjected to high-throughput sequencing on platforms such as Illumina, generating millions of short sequence reads that are subsequently aligned to reference genomes using specialized tools like STAR or HISAT2. Differential expression analysis is conducted using software packages such as DESeq2, identifying ncRNAs that are significantly downregulated in HBV-HCC contexts—potential tumor-suppressive candidates worthy of further validation [29].
Beyond conventional RNA-Seq, more specialized approaches include small RNA-Seq for comprehensive miRNA profiling and single-cell RNA-Seq to resolve ncRNA expression patterns at the cellular level, enabling the identification of tumor-suppressive ncRNAs within specific cell subpopulations, including liver cancer stem cells (LCSCs) that play critical roles in HBV-related hepatocarcinogenesis [30].
Computational Prediction and Network Analysis
Bioinformatic approaches play an indispensable role in predicting the potential tumor-suppressive functions of candidate ncRNAs and elucidating their positions within broader regulatory networks. miRNA target prediction algorithms (e.g., TargetScan, miRDB) analyze sequence complementarity between miRNAs and putative mRNA targets, particularly focusing on seed region matches in 3' untranslated regions (3'UTRs). For lncRNAs functioning as ceRNAs, tools such as RNAhybrid can predict binding interactions with specific miRNAs, helping to construct potential ceRNA networks [29].
The construction of competing endogenous RNA (ceRNA) networks represents a powerful approach for identifying tumor-suppressive ncRNAs. This methodology begins with the identification of differentially expressed lncRNAs, miRNAs, and mRNAs from datasets such as The Cancer Genome Atlas (TCGA) HCC cohort. Potential interactions between these RNA species are predicted using databases like ENCORI/starBase, followed by the integration of these interactions into comprehensive regulatory networks using visualization tools such as Cytoscape. Within these networks, tumor-suppressive ncRNAs often occupy positions as hubs that regulate multiple oncogenic pathways [29].
Additional computational analyses include survival analysis using tools like GEPIA2 to correlate ncRNA expression levels with patient clinical outcomes, functional enrichment analysis (GO and KEGG) to identify biological processes and pathways potentially regulated by candidate ncRNAs, and epigenetic analysis to examine methylation patterns in promoter regions of downregulated ncRNAs.
Table 2: Experimental Approaches for Identifying Tumor-Suppressive ncRNAs
| Method Category | Specific Techniques | Key Applications | Representative Tools/Databases |
|---|---|---|---|
| High-Throughput Sequencing | RNA-Seq, small RNA-Seq, single-cell RNA-Seq | Genome-wide ncRNA expression profiling, identification of differentially expressed ncRNAs | DESeq2, STAR, HISAT2 |
| Computational Prediction | miRNA target prediction, ceRNA network analysis | Prediction of ncRNA-mRNA interactions, construction of regulatory networks | TargetScan, miRDB, RNAhybrid, ENCORI/starBase |
| Functional Validation | Luciferase reporter assays, knockdown/overexpression | Experimental verification of predicted interactions, functional characterization | Dual-luciferase systems, siRNA, CRISPRi |
| Phenotypic Analysis | CCK-8 assays, colony formation, wound healing assays | Assessment of ncRNA effects on proliferation, migration, tumorigenicity | Cell counting kits, migration assays |
Key Experimental Protocols for Functional Characterization
Luciferase Reporter Assays for Target Validation
The luciferase reporter assay represents a gold standard technique for experimentally validating predicted interactions between tumor-suppressive ncRNAs and their putative targets. This protocol involves several critical steps. First, vector construction is performed by cloning the wild-type 3'UTR sequence of the putative target gene downstream of a luciferase reporter gene (e.g., firefly luciferase) in an appropriate plasmid vector. Additionally, a mutant construct with altered sequences in the predicted ncRNA binding site is generated as a negative control.
For miRNA-target interactions, cell transfection is carried out by co-transfecting hepatoma cell lines (e.g., HepG2, Huh7) with the reporter construct and either a synthetic miRNA mimic (to restore tumor-suppressive miRNA function) or inhibitor (to further suppress endogenous miRNA activity). After 24-48 hours, luciferase activity measurement is performed using dual-luciferase reporter assay systems, with firefly luciferase values normalized to a co-transfected control (e.g., Renilla luciferase). A statistically significant reduction in luminescence in cells transfected with wild-type reporter and miRNA mimic compared to those with mutant reporter or control oligonucleotides confirms direct interaction [29].
For lncRNA-miRNA interactions, the protocol is modified by cloning fragments of the lncRNA containing predicted miRNA binding sites into the reporter vector. Co-transfection with miRNA mimics should similarly reduce luciferase activity if a direct interaction occurs. This approach has been successfully employed to validate interactions such as that between KCNQ1OT1 and miR-335-5p in HBV-related HCC models [29].
Functional Rescue Experiments
Functional rescue experiments provide critical evidence for establishing the tumor-suppressive activity of ncRNAs and their position within regulatory pathways. The standard methodology involves several stages. First, modulation of ncRNA expression is achieved through transfection of synthetic oligonucleotides (miRNA mimics or inhibitors) or viral-mediated delivery of expression constructs (for lncRNAs) into appropriate cell models, such as HBV-replicating hepatoma cells.
Subsequent phenotypic assessment is performed using various functional assays. Cell proliferation is typically measured via CCK-8 assays or colony formation assays, while migratory capacity is evaluated using wound healing assays or transwell migration assays. Apoptotic rates can be quantified through annexin V/propidium iodide staining followed by flow cytometry. For comprehensive rescue experiments, simultaneous modulation of both the ncRNA and its putative downstream target is performed to determine whether manipulating the target can reverse the phenotypic effects of ncRNA modulation.
A representative example of this approach demonstrated that miR-335-5p overexpression could reverse the promoting effects of KCNQ1OT1 on HCC proliferation and migration, while subsequent restoration of CDC7 (the miR-335-5p target) counteracted the suppressive effects of miR-335-5p, thereby confirming the functional position of this ncRNA within a specific oncogenic axis [29].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying Tumor-Suppressive ncRNAs
| Reagent Category | Specific Examples | Research Applications | Technical Considerations |
|---|---|---|---|
| Cell Line Models | HepG2, Huh7, SMMC-7721, HepG2.2.15, HBV-transfected cells | In vitro functional studies, viral replication models | Verify HBV replication status, authenticate regularly |
| Plasmid Constructs | pAAV-HBV1.2, HBx expression vectors, HBc expression vectors | HBV gene expression studies, mechanistic investigations | Include empty vector controls, verify protein expression |
| miRNA Manipulation | miRNA mimics, miRNA inhibitors, antagomirs | Functional gain/loss-of-function studies | Use appropriate scramble controls, optimize transfection conditions |
| Luciferase Reporters | psiCHECK-2, pGL3-based vectors | Target validation, interaction mapping | Include mutant controls, normalize transection efficiency |
| Antibodies | Anti-HBx, anti-CDC7, anti-DNMT3A, anti-EZH2 | Protein detection, mechanistic studies | Validate specificity, optimize working concentrations |
| Databases | TCGA, ENCORI/starBase, GEPIA2 | Bioinformatics analysis, clinical correlation | Use current versions, apply multiple testing corrections |
| 1-(3-nitrophenyl)-1H-tetrazol-5-ol | 1-(3-Nitrophenyl)-1H-tetrazol-5-ol | 1-(3-Nitrophenyl)-1H-tetrazol-5-ol is a high-purity chemical For Research Use Only (RUO). Explore its applications in medicinal chemistry and drug discovery. Not for human or veterinary use. | Bench Chemicals |
| 2-(bromomethyl)-4-chlorothiophene | 2-(Bromomethyl)-4-chlorothiophene|CAS 1400991-44-7 | 2-(Bromomethyl)-4-chlorothiophene (CAS 1400991-44-7). A versatile heterocyclic building block for research. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Therapeutic Implications and Future Perspectives
The systematic inactivation of tumor-suppressive ncRNAs in HBV-related HCC represents not only a key pathogenetic mechanism but also a promising therapeutic opportunity. Several strategic approaches have emerged for leveraging this knowledge for therapeutic benefit. ncRNA replacement therapy aims to restore the expression and function of tumor-suppressive ncRNAs that have been inactivated during hepatocarcinogenesis. For instance, synthetic mimics of tumor-suppressive miRNAs such as miR-122, miR-101, and miR-148a could potentially be delivered to HCC cells using viral or non-viral delivery systems to reestablish their growth-inhibitory effects.
The efficacy of this approach is supported by multiple preclinical studies. Restoration of miR-122 has been shown to sensitize hepatoma cell lines to chemotherapeutic agents like doxorubicin and oxaliplatin through suppression of the Wnt/β-catenin pathway and modulation of MDR1 expression [10]. Similarly, miR-101 supplementation could potentially counteract HBx-mediated epigenetic dysregulation by targeting DNMT3A, thereby restoring normal methylation patterns and expression of tumor suppressor genes [20] [16].
An alternative strategy involves targeting the inactivators of tumor-suppressive ncRNAs, such as oncogenic lncRNAs that function as miRNA sponges. Antisense oligonucleotides or small molecule inhibitors designed to disrupt the interaction between sponging lncRNAs (e.g., KCNQ1OT1) and their sequestered tumor-suppressive miRNAs (e.g., miR-335-5p) could potentially liberate these protective miRNAs to perform their normal regulatory functions [29]. Similarly, inhibitors of epigenetic modifiers such as EZH2 or DNMTs could reactivate silenced tumor-suppressive ncRNAs by reversing repressive chromatin marks.
The clinical translation of these approaches faces several challenges, including optimization of delivery vehicles for tissue-specific ncRNA delivery, minimization of off-target effects, and comprehensive safety profiling. However, the growing understanding of tumor-suppressive ncRNA inactivation mechanisms in HBV-HCC provides a strong foundation for the development of novel RNA-based therapeutics that could complement existing antiviral and anticancer strategies, potentially improving outcomes for patients with this aggressive malignancy.
Modulation of the Tumor Microenvironment and Immune Response by HBV-Related ncRNAs
Hepatocellular carcinoma (HCC) induced by chronic hepatitis B virus (HBV) infection represents a major global health burden, characterized by a complex tumor microenvironment (TME) that facilitates immune evasion and tumor progression. Emerging evidence has established that HBV-related non-coding RNAs (ncRNAs), including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), serve as master regulators of the tumor immune microenvironment (TIME). These ncRNAs modulate critical processes including immune cell recruitment, polarization, and function, thereby creating an immunosuppressive niche conducive to hepatocarcinogenesis. This technical review comprehensively synthesizes current mechanistic insights into how HBV-induced ncRNA alterations reprogram the hepatic immune landscape, with specific focus on their roles in regulating macrophage polarization, neutrophil activity, natural killer (NK) cell function, and myeloid-derived suppressor cell (MDSC) biology. We further provide detailed experimental methodologies for investigating ncRNA-TIME interactions and analyze the translational potential of these regulatory molecules as diagnostic biomarkers and therapeutic targets. The findings presented herein aim to provide researchers and drug development professionals with a comprehensive framework for advancing ncRNA-based immunotherapeutic strategies against HBV-related HCC.
Hepatocellular carcinoma ranks as the fifth most common malignancy globally and represents the third leading cause of cancer-related mortality [8] [31]. Chronic HBV infection constitutes a predominant risk factor, contributing to over half of all HCC cases worldwide and approximately 80% of cases in high-prevalence regions such as Southeast Asia and sub-Saharan Africa [8] [19]. The pathogenesis of HBV-related HCC involves a multistep process progressing through chronic inflammation, liver fibrosis, cirrhosis, and ultimately malignancy, driven by both viral factors (including the HBx protein, viral DNA integration, and covalently closed circular DNA [cccDNA]) and host determinants [10] [19].
The tumor immune microenvironment of HCC is a highly intricate ecosystem comprising diverse cellular and non-cellular components that dynamically interact to either suppress or promote tumor progression [31]. Cellular constituents include innate and adaptive immune cells (macrophages, neutrophils, MDSCs, NK cells, dendritic cells, T cells, and B cells), alongside stromal elements such as cancer-associated fibroblasts (CAFs), hepatic stellate cells (HSCs), and vascular cells [31]. Non-cellular components encompass the extracellular matrix and a plethora of soluble factors including cytokines, chemokines, and growth factors [31]. In HBV-related HCC, this microenvironment typically evolves toward an immunosuppressive state that facilitates immune evasion and tumor progression.
Non-coding RNAs have emerged as pivotal regulators of gene expression and cellular function in both physiological and pathological contexts. These RNAs, which lack protein-coding capacity, constitute approximately 98% of the human transcriptome [31] and are broadly classified based on molecular structure and size into linear RNAs (including miRNAs and lncRNAs) and circRNAs [31]. HBV infection, particularly through the action of the HBx protein, significantly alters the expression landscape of host ncRNAs, which in turn modulate various hallmarks of cancer, including sustained proliferation, evasion of growth suppression, activation of invasion and metastasis, and immune evasion [8] [19] [20]. The stability, detectability in bodily fluids, and disease-specific expression patterns render these ncRNAs promising biomarkers and therapeutic targets for HBV-related HCC [8].
HBV-Induced Alterations in ncRNA Expression
The HBV-encoded X protein (HBx) serves as a master regulator of host ncRNA expression, driving extensive reprogramming of the transcriptional landscape in infected hepatocytes. HBx modulates ncRNA expression through multiple mechanisms, including direct transcriptional activation, epigenetic modifications, and interaction with key transcription factors and signaling pathways [19] [20]. Through its interaction with various transcription factors such as p53, c-Myc, survivin, and nuclear factor kappa B (NF-κB), as well as its activation of cytoplasmic signaling pathways including mitogen-activated protein kinase (MAPK) pathways, HBx transactivates both viral and cellular genes, resulting in widespread dysregulation of ncRNA networks [19]. Furthermore, HBx can induce epigenetic modifications such as DNA methylation and histone alterations, leading to sustained changes in ncRNA expression patterns that contribute to hepatocarcinogenesis [19] [20].
Table 1: Key HBV-Dysregulated ncRNAs in Hepatocellular Carcinoma
| ncRNA | Expression in HBV-HCC | Regulated by HBx | Primary Functions in HCC | Impact on TIME |
|---|---|---|---|---|
| miR-122 | Downregulated [8] [10] | Yes (via IL-6 and TNF-α) [8] | Tumor suppressor; regulates metabolism [8] | Inhibits neutrophil recruitment via CCL2 [31] |
| miR-28-5p | Downregulated [31] | Not specified | Regulates IL-34/FAK/ERK1/2 signaling [31] | Promotes TAM recruitment and infiltration [31] |
| miR-223 | Downregulated [31] | Not specified | Modulates neutrophil maturation [31] | Attenuates neutrophil activation [31] |
| HULC | Upregulated [8] [32] | Yes [32] | Promotes proliferation, metastasis [8] | Modulates immune cell function via HBx/STAT3 axis [32] |
| HOTAIR | Upregulated [32] [31] | Yes [32] | Promotes transcription and replication [32] | Recruits MDSCs via CCL2 [31] |
| LINC00662 | Upregulated [31] | Not specified | Sponges miR-15a/16/107 [31] | Promotes M2 macrophage polarization [31] |
| circASAP1 | Upregulated [31] | Not specified | Sponges miR-326/miR-532-5p [31] | Promotes TAM infiltration via CSF-1 [31] |
| circUHRF1 | Upregulated [31] | Not specified | Sponges miR-449c-5p [31] | Induces NK-cell exhaustion [31] |
The table above summarizes key ncRNAs dysregulated in HBV-related HCC and their documented impacts on the tumor immune microenvironment. This dysregulation pattern represents a critical mechanism through which HBV remodels the hepatic landscape to favor immune evasion and tumor progression.
Mechanisms of ncRNA-Mediated Immune Regulation in HBV-HCC
Regulation of Innate Immune Cells
Macrophages and Tumor-Associated Macrophages (TAMs)
Macrophages constitute a major component of the innate immune cell population within the TIME and exhibit remarkable plasticity in response to microenvironmental cues [31]. In HCC, TAMs predominantly display an M2-polarized phenotype, characterized by anti-inflammatory, pro-angiogenic, and pro-tumorigenic functions [31]. HBV-related ncRNAs extensively regulate both the recruitment and polarization of TAMs through diverse molecular mechanisms.
The downregulation of miR-28-5p in HCC leads to enhanced expression of interleukin-34 (IL-34), resulting in activation of FAK and ERK1/2 signaling pathways in macrophages, ultimately promoting their recruitment and infiltration into HCC tumor sites [31]. Similarly, circASAP1, which is significantly upregulated in HCC cells, functions as a competitive endogenous RNA (ceRNA) by sponging miR-326 and miR-532-5p, thereby alleviating their repression of CSF-1 expression [31]. CSF-1 serves as a potent chemoattractant, survival, and differentiation factor for macrophages, and its upregulation enhances TAM infiltration into the tumor bed, contributing to HCC growth and metastasis [31].
Multiple lncRNAs have been implicated in regulating macrophage polarization. LINC00662 promotes M2 macrophage polarization through a paracrine mechanism by acting as a ceRNA for miR-15a/16/107 to stimulate WNT3A expression and secretion from HCC cells [31]. Similarly, lncRNA PART1 facilitates M2 polarization through the miR-372-3p/TLR4 axis, promoting HCC cell proliferation, epithelial-mesenchymal transition (EMT), and metastasis [31]. lncRNA TUC339 is upregulated in HCC and promotes macrophage activation, M2 polarization, and pro-tumorigenic activities, although its precise molecular targets require further elucidation [31].
Diagram 1: ncRNA-Mediated Regulation of Macrophages in HBV-HCC. This diagram illustrates how HBV-induced ncRNA alterations regulate TAM recruitment and M2 polarization through multiple molecular pathways.
Natural Killer (NK) Cells
NK cells serve as critical effectors of innate antitumor immunity, capable of directly recognizing and eliminating malignant cells without prior sensitization. HBV-related ncRNAs modulate NK cell function through various mechanisms, ultimately leading to impaired cytotoxic activity and immune evasion.
The upregulation of miR-561-5p in HCC inhibits the infiltration and activation of CX3CR1+ NK cells by targeting CX3CL1 and downstream STAT3 signaling, thereby promoting pulmonary metastasis [31]. circUHRF1, which is elevated in HCC, induces NK cell exhaustion and dysfunction by sponging miR-449c-5p, leading to subsequent upregulation of TIM-3, a well-characterized immune checkpoint molecule [31]. This mechanism contributes to immune evasion and resistance to anti-PD-1 immunotherapy [31].
Conversely, several tumor-suppressive ncRNAs enhance NK cell-mediated antitumor immunity. lncRNA GAS5, which is downregulated in HCC, enhances the killing capacity of NK cells by modulating the miR-544/RUNX3 axis [31]. Similarly, circRNA hsacirc0007456 and circRNA ARSP91 strengthen NK cell cytotoxicity through regulation of miR-6852-3p/ICAM-1 and ULBP1 pathways, respectively, thereby enhancing innate immune surveillance and suppressing HCC proliferation [31].
Myeloid-Derived Suppressor Cells (MDSCs) and Neutrophils
MDSCs represent a heterogeneous population of immature myeloid cells with potent immunosuppressive capabilities. lncRNA HOTAIR, which is upregulated in HBV-related HCC, promotes the recruitment of MDSCs through CCL2-dependent mechanisms, thereby fostering tumor growth and metastasis [31].
Neutrophils play dual roles in tumor immunity, exhibiting both pro-tumor and antitumor activities depending on their activation state and microenvironmental cues. miR-223, which is downregulated in HCC, attenuates neutrophil maturation and activation, thereby limiting their antitumor functions [31]. Similarly, the downregulation of miR-122, a liver-specific miRNA, reduces recruitment of neutrophils to the tumor site via CCL2 regulation, indirectly facilitating tumor progression [31].
Regulation of Adaptive Immunity and Immune Checkpoints
While the search results provided limited specific information on ncRNA regulation of adaptive immunity in HBV-HCC, several mechanisms can be inferred from general HCC biology. ncRNAs likely modulate T cell function through regulation of antigen presentation, T cell activation, and differentiation of T helper cell subsets. Additionally, ncRNAs may influence immune checkpoint expression, including PD-1, PD-L1, CTLA-4, and TIM-3, thereby contributing to T cell exhaustion, a hallmark of HBV-related HCC.
Table 2: ncRNA-Mediated Regulation of Innate Immune Cells in HBV-HCC TIME
| Immune Cell | Regulating ncRNA | Expression | Molecular Target/Pathway | Functional Outcome |
|---|---|---|---|---|
| Macrophages | miR-28-5p | Downregulated | IL-34/FAK/ERK1/2 | Promotes TAM recruitment [31] |
| circASAP1 | Upregulated | miR-326/miR-532-5p/CSF-1 | Promotes TAM infiltration [31] | |
| LINC00662 | Upregulated | miR-15a/16/107/WNT3A | Promotes M2 polarization [31] | |
| PART1 | Upregulated | miR-372-3p/TLR4 | Promotes M2 polarization [31] | |
| NK Cells | miR-561-5p | Upregulated | CX3CL1/CX3CR1/STAT3 | Inhibits NK-cell infiltration [31] |
| circUHRF1 | Upregulated | miR-449c-5p/TIM-3 | Induces NK-cell exhaustion [31] | |
| GAS5 | Downregulated | miR-544/RUNX3 | Enhances NK cytotoxicity [31] | |
| hsacirc0007456 | Downregulated | miR-6852-3p/ICAM-1 | Strengthens NK cytotoxicity [31] | |
| MDSCs | HOTAIR | Upregulated | CCL2 | Promotes MDSC recruitment [31] |
| Neutrophils | miR-223 | Downregulated | Not specified | Attenuates neutrophil activation [31] |
| miR-122 | Downregulated | CCL2 | Inhibits neutrophil recruitment [31] |
Experimental Approaches for Investigating ncRNA-TIME Interactions
Methodologies for ncRNA Profiling and Functional Validation
Comprehensive analysis of ncRNA-TIME interactions requires an integrated experimental approach combining high-throughput screening techniques with mechanistic functional studies. The following protocols outline key methodologies for identifying and validating ncRNA functions in the context of HBV-related HCC.
Protocol 1: High-Throughput ncRNA Screening in HBV-Infected Hepatocytes
Objective: To identify differentially expressed ncRNAs in HBV-infected hepatocytes and their correlation with immune regulatory gene signatures.
Materials and Reagents:
- Human hepatocyte cell lines (Huh7, HepG2, HepG2.2.15)
- HBV infection system or HBx-expression vectors
- TRIzol reagent for RNA extraction
- miRNA and lncRNA microarrays or next-generation sequencing kits
- qRT-PCR reagents (primers, reverse transcriptase, SYBR Green)
- Bioinformatics software (DESeq2, EdgeR, miRBase, NONCODE databases)
Procedure:
- Establish HBV infection models: Infect Huh7 or HepG2 cells with HBV or transfect with HBx-expression vectors; include appropriate controls.
- RNA extraction: Isolate total RNA at multiple time points (24h, 48h, 72h) post-infection/transfection using TRIzol reagent.
- ncRNA profiling: Perform miRNA and lncRNA microarray analysis or next-generation sequencing according to manufacturer protocols.
- Bioinformatics analysis: Identify differentially expressed ncRNAs (fold change >2, p-value <0.05) and perform pathway enrichment analysis using KEGG and GO databases.
- Validation: Confirm expression changes of selected ncRNAs using qRT-PCR with specific primers.
- Correlation with immune signatures: Correlate ncRNA expression with RNA-seq data of immune-related genes to identify potential regulatory networks.
Expected Outcomes: Identification of HBV-regulated ncRNAs potentially involved in immune modulation, with verification of expression patterns in primary HCC samples.
Protocol 2: Functional Validation of ncRNA in Immune Cell Recruitment and Polarization
Objective: To determine the functional role of specific ncRNAs in regulating immune cell behavior in the HCC microenvironment.
Materials and Reagents:
- ncRNA overexpression vectors (lentiviral systems) or siRNA/shRNA for knockdown
- Human monocyte cell line (THP-1) for macrophage differentiation
- Primary human NK cells or NK cell lines (NK-92)
- Transwell migration chambers
- Flow cytometry antibodies (CD68, CD163, CD86, CD11b, CD33, CD15)
- ELISA kits for cytokine detection (IL-10, TGF-β, IL-12, IFN-γ)
- Co-culture system (immune cells with hepatocytes/HCC cells)
Procedure:
- Modify ncRNA expression: Stably transduce HCC cells with ncRNA overexpression or knockdown constructs using lentiviral systems.
- Conditioned media collection: Harvest culture supernatants from modified HCC cells after 48 hours.
- Immune cell treatment:
- Differentiate THP-1 monocytes to macrophages using PMA
- Treat differentiated macrophages with conditioned media for 48 hours
- Culture NK cells with conditioned media for 24 hours
- Migration assay: Seed immune cells in Transwell inserts and measure migration toward conditioned media from ncRNA-modified HCC cells.
- Phenotypic analysis: Analyze macrophage polarization markers (CD68, CD163 for M2; CD86 for M1) and NK cell activation markers (CD69, NKG2D) by flow cytometry.
- Functional assays:
- Measure phagocytic activity of macrophages using fluorescent beads
- Assess NK cell cytotoxicity against K562 target cells
- Quantify cytokine production by ELISA
- Mechanistic studies: Perform RNA immunoprecipitation (RIP) and luciferase reporter assays to validate direct targets of ncRNAs.
Expected Outcomes: Determination of how specific ncRNAs alter immune cell recruitment, polarization, and effector functions, along with elucidation of underlying molecular mechanisms.
Table 3: Essential Research Reagents for Investigating ncRNA-TIME in HBV-HCC
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Cell Models | HepG2.2.15 (HBV-integrated), Huh7-HBx, Primary human hepatocytes | In vitro modeling of HBV infection | HepG2.2.15 naturally produces HBV particles; Huh7-HBx allows HBx-specific studies [10] |
| Immune Cells | THP-1 (monocytes), NK-92 (NK cells), Primary MDSCs, Neutrophils | Study immune cell-ncRNA interactions | Primary cells better reflect physiological responses but have limited expansion capacity [31] |
| ncRNA Modulation | Lentiviral shRNA, miRNA mimics/inhibitors, CRISPRa/i systems | Functional gain/loss-of-function studies | Include appropriate scrambled controls; verify efficiency via qRT-PCR [31] [20] |
| Analysis Tools | Flow cytometry antibodies (CD markers, checkpoint proteins), ELISA kits (cytokines), Transwell chambers | Assess immune cell phenotype and function | Multiplex panels enable comprehensive immune profiling; Transwell assays quantify migration [31] |
| Molecular Assays | RIP kits, Luciferase reporter vectors, ChIP assays | Mechanism of action studies | RIP validates direct ncRNA-protein interactions; Luciferase reporters confirm target regulation [19] [20] |
Clinical Translation and Therapeutic Perspectives
The intricate involvement of ncRNAs in modulating the TIME of HBV-related HCC presents compelling opportunities for clinical translation in diagnostics, prognostication, and therapeutics. The stability of ncRNAs in circulating biofluids renders them particularly attractive as non-invasive biomarkers for early detection, disease monitoring, and treatment response assessment [8] [31].
From a therapeutic standpoint, multiple strategies targeting oncogenic ncRNAs or restoring tumor-suppressive ncRNAs are under investigation. Antisense oligonucleotides (ASOs) and locked nucleic acids (LNAs) can be designed to inhibit oncogenic ncRNAs, while ncRNA mimics or expression vectors can restore tumor-suppressive functions [8]. The successful clinical translation of these approaches will require optimization of delivery systems to ensure sufficient targeting of both tumor cells and relevant immune populations within the TIME.
Furthermore, combining ncRNA-targeting therapies with existing immunotherapies (such as immune checkpoint inhibitors) represents a promising strategy to overcome resistance mechanisms and enhance antitumor immune responses in HBV-related HCC [31]. As our understanding of ncRNA networks in the HBV-HCC TIME continues to expand, these molecular insights will undoubtedly catalyze the development of novel immunotherapeutic strategies with improved efficacy and precision.
HBV-related ncRNAs serve as master regulators of the tumor immune microenvironment in hepatocellular carcinoma, orchestrating complex interactions between malignant hepatocytes and diverse immune cell populations. Through mechanisms including miRNA sponging, regulation of cytokine signaling, and modulation of critical immune pathways, these ncRNAs shape an immunosuppressive landscape that facilitates immune evasion and tumor progression. The comprehensive experimental frameworks and technical resources outlined in this review provide researchers with robust methodologies for elucidating the precise functions of ncRNAs in the HBV-HCC TIME. As the field advances, the translational potential of targeting ncRNA-TIME axes offers promising avenues for developing novel diagnostic, prognostic, and therapeutic strategies against this devastating malignancy. Future research should focus on delineating the complex ncRNA regulatory networks operating within specific immune cell subsets and exploring combinatorial approaches that simultaneously target multiple nodes of these networks for enhanced therapeutic efficacy.
From Bench to Bedside: Diagnostic and Therapeutic Applications of ncRNAs
Non-coding RNAs as Non-Invasive Biomarkers for Early Detection and Prognosis of HBV-HCC
Hepatocellular carcinoma (HCC) related to chronic hepatitis B virus (HBV) infection remains a significant global health challenge characterized by high mortality and poor prognosis. Recent advances have revealed that non-coding RNAs (ncRNAs), including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), play critical regulatory roles in HBV-induced oncogenesis. These molecules exhibit remarkable stability in bodily fluids and disease-specific expression patterns, rendering them highly promising as non-invasive biomarkers for early detection and prognosis of HBV-HCC. This technical review comprehensively examines the types, mechanisms, and clinical applicability of HBV-related ncRNAs, emphasizing their dual roles as oncogenes and tumor suppressors. We further provide detailed experimental methodologies for ncRNA analysis and data visualization of key signaling pathways, offering researchers a comprehensive resource for advancing biomarker development and therapeutic targeting in HBV-HCC.
Hepatocellular carcinoma (HCC) ranks as the sixth most prevalent cancer worldwide and the third leading cause of cancer-related mortality [16] [20]. Chronic hepatitis B virus (HBV) infection impacts more than 296 million individuals globally, placing them at heightened risk for severe liver conditions including cirrhosis and HCC [16]. In developing regions such as China and Africa, chronic HBV infection serves as the predominant factor contributing to HCC, accounting for approximately 80% of cases globally [16] [33]. Despite advancements in diagnostic techniques and treatment modalities, the 5-year survival rate for HCC remains dismal at approximately 5-6%, underscoring the urgent need for improved early detection methods and prognostic tools [34].
The molecular pathogenesis of HBV-related HCC involves complex interactions between viral factors and host cellular machinery. The HBV-encoded X protein (HBx) plays a particularly significant role in hepatocarcinogenesis by modulating host gene expression and signaling pathways [20] [19]. HBx lacks DNA-binding capacity but functions as a transactivator by interacting with various transcription factors and epigenetic regulators, ultimately leading to aberrant expression of both protein-coding genes and non-coding RNAs [19].
Non-coding RNAs, once considered "transcriptional noise," have emerged as crucial regulators of gene expression in health and disease. The human genome encodes a vast repertoire of ncRNAs that far exceeds the number of protein-coding genes [35]. In the context of HBV-HCC, ncRNAs have demonstrated immense potential as non-invasive biomarkers due to their stability in bodily fluids, disease-specific expression patterns, and critical roles in oncogenic processes [16] [8]. This whitepaper provides a comprehensive technical resource for researchers investigating ncRNAs as biomarkers for HBV-HCC, with particular emphasis on their molecular mechanisms, clinical applicability, and experimental analysis.
Molecular Alterations of ncRNAs in HBV-Hepatocarcinogenesis
HBV-Driven Epigenetic Alterations and ncRNA Dysregulation
The HBV X protein (HBx) serves as a key orchestrator of ncRNA dysregulation in hepatocarcinogenesis. HBx mediates both genetic alterations in tumor suppressor genes and oncogenes as well as epigenetic aberrations in HCC pathogens [19]. Through interactions with various transcription factors and signaling pathways, HBx modulates the expression of numerous ncRNAs, effectively reprogramming the cellular transcriptome to favor oncogenic transformation [20].
HBx employs multiple mechanisms to regulate ncRNA expression. It can inhibit tumor suppressor miRNAs through promoter hypermethylation, as demonstrated for miR-132, miR-205, and others [19]. Alternatively, HBx can activate transcription factors such as c-Myc and nuclear factor kappa B, which in turn regulate the expression of both miRNAs and lncRNAs [19]. The resulting ncRNA dysregulation affects fundamental cellular processes including proliferation, apoptosis, metabolism, and immune evasion, collectively driving hepatocarcinogenesis.
Functional Classification of HBV-Related ncRNAs
HBV-related ncRNAs can be functionally categorized based on their roles in hepatocarcinogenesis:
- Oncogenic ncRNAs: Promote tumor development and progression (e.g., miR-21, HULC, circMET)
- Tumor-suppressive ncRNAs: Inhibit tumorigenic processes (e.g., miR-122, GAS5, miR-199a/b)
- Context-dependent ncRNAs: Exhibit dual functions depending on cellular context (e.g., miR-222)
The following sections detail specific ncRNA classes with biomarker potential for HBV-HCC, emphasizing their mechanisms of action and regulation by HBV/HBx.
ncRNA Classes as Biomarkers for HBV-HCC
MicroRNAs (miRNAs)
miRNAs are small endogenous ncRNAs approximately 21-25 nucleotides in length that regulate gene expression at the post-transcriptional level by binding to complementary sequences on target mRNAs, resulting in message degradation or translational inhibition [16] [8]. The biogenesis of miRNAs involves multiple steps including transcription, nuclear processing by Drosha, export to cytoplasm, cleavage by Dicer, and assembly into the RNA-induced silencing complex (RISC) [16].
Table 1: Oncogenic and Tumor-Suppressive miRNAs in HBV-HCC
| miRNA | Expression in HBV-HCC | Regulation by HBx | Target Genes/Pathways | Biological Functions |
|---|---|---|---|---|
| miR-21 | Upregulated | Activated | PDCD4, PTEN | Promotes cell growth and survival [16] |
| miR-221/222 | Upregulated | Activated | CXCL4/12, TFRC | Facilitates cell cycle progression, suppresses apoptosis [16] |
| miR-17-92 cluster | Upregulated | Activated | ERα | Promotes proliferation, angiogenesis, immune evasion [16] |
| miR-122 | Downregulated | Suppressed | PKM2, SLC7A1 | Loss promotes tumor development, motility, and invasion; regulates metabolism [16] [8] |
| miR-199a/b | Downregulated | Suppressed | ROCK1, PI3K/Akt | Inhibits proliferation pathways; low expression associated with poor survival [16] |
| miR-101 | Downregulated | Suppressed | DNMT3A | Induces aberrant DNA methylation in HCC [16] [20] |
| miR-148a | Downregulated | Suppressed via p53 inhibition | HPIP, AKT/ERK/FOXO4/ATF5 | Repressed expression promotes EMT and invasion [16] [19] |
| let-7 family | Downregulated | Repressed | STAT3, ras, c-myc | Suppression supports cell proliferation [19] |
HBx regulates multiple miRNAs through diverse mechanisms. For instance, HBx downregulates tumor-suppressive miR-148a by inhibiting p53-mediated activation, which in turn increases expression of hematopoietic pre-B-cell leukemia transcription factor-interacting protein (HPIP) and activates oncogenic signaling pathways [19]. Similarly, HBx induces epigenetic repression of miR-132 through promoter methylation, facilitating Akt signaling and hepatoma cell growth [19]. HBx also dysregulates lipid metabolism through miRNA manipulation, such as via the HBx/miR-429/Rab18 pathway and through miR-205 downregulation, both contributing to abnormal lipid metabolism and proliferation of hepatoma cells [20] [19].
Long Non-Coding RNAs (lncRNAs)
LncRNAs represent a diverse class of RNA molecules longer than 200 nucleotides that lack protein-coding capability [16] [8]. They are transcribed by RNA polymerase II and undergo typical post-transcriptional modifications including 5' capping and 3' polyadenylation [16]. LncRNAs exhibit diverse regulatory mechanisms including chromatin modification, transcriptional regulation, post-transcriptional processing, and serving as molecular scaffolds [8].
Table 2: Dysregulated lncRNAs in HBV-HCC with Diagnostic Utility
| lncRNA | Expression in HBV-HCC | Potential Diagnostic Performance | Biological Functions | Clinical Significance |
|---|---|---|---|---|
| HULC | Upregulated | N/A | Promotes proliferation, invasion, metastasis, angiogenesis, immune evasion [8] | One of the most investigated lncRNAs in HBV-HCC [8] |
| HOTAIR | Upregulated | N/A | Chromatin regulation, transcription regulation, cell cycle control [16] | Associated with poor overall survival [36] |
| LINC00152 | Upregulated | 83% sensitivity, 53% specificity [36] | Promotes cell proliferation through CCDN1 regulation [36] | Higher LINC00152:GAS5 ratio correlates with increased mortality [36] |
| UCA1 | Upregulated | 60% sensitivity, 67% specificity [36] | Promotes proliferation and apoptosis resistance [36] | Used in diagnostic panels |
| LINC00853 | Downregulated | 63% sensitivity, 67% specificity [36] | N/A | Used in diagnostic panels |
| GAS5 | Downregulated | 60% sensitivity, 63% specificity [36] | Triggers CHOP and caspase-9 pathways, inhibits proliferation, activates apoptosis [36] | Tumor suppressor; lower expression associated with poor prognosis [36] |
| NEAT1 | Upregulated | N/A | Binds to miR-155, interferes with Tim-3 expression | Regulates CD8+ T cell apoptosis and cytolytic activity [35] |
LncRNA expression profiling in HBV-HCC has revealed significant dysregulation patterns. A microarray-based study identified 659 lncRNAs differentially expressed between HCC and non-tumor tissues, with 171 significantly downregulated and 488 upregulated in HCC tissues [34]. These findings highlight the extensive reprogramming of the non-coding transcriptome in HBV-driven hepatocarcinogenesis and support the potential of lncRNAs as diagnostic biomarkers.
Circular RNAs (circRNAs)
CircRNAs are a novel class of lncRNAs characterized by a stable closed-loop structure produced by back-splicing, which confers resistance to RNA exonuclease-mediated degradation [35]. They exhibit high abundance, diversity, sequence conservation, stability, tissue specificity, and tumor stage-dependent characteristics [35].
CircRNAs function primarily as microRNA sponges that sequester miRNAs and prevent them from binding to their target mRNAs [16]. For example, circMET acts as an oncogenic circRNA in HCC by functioning through the miR-30-5p/Snail/dipeptidyl peptidase-4 (DPP4) axis [35]. CircMET expression is detrimental to CD8+ T cell infiltration into tumors, and targeting this axis can enhance response to anti-PD1 immunotherapy [35].
The unique stability of circRNAs due to their circular structure makes them particularly attractive as non-invasive biomarkers for early detection and monitoring of HBV-HCC progression.
Quantitative Diagnostic and Prognostic Performance
Individual ncRNA Diagnostic Performance
Studies have quantified the diagnostic accuracy of individual ncRNAs for detecting HBV-HCC:
Table 3: Diagnostic Performance of Individual ncRNAs in HBV-HCC
| Biomarker | Sensitivity (%) | Specificity (%) | AUC | Sample Type | Reference |
|---|---|---|---|---|---|
| LINC00152 | 83 | 53 | N/A | Plasma | [36] |
| UCA1 | 60 | 67 | N/A | Plasma | [36] |
| LINC00853 | 63 | 67 | N/A | Plasma | [36] |
| GAS5 | 60 | 63 | N/A | Plasma | [36] |
| AFP | ~66* | N/A | N/A | Serum | [36] |
*Approximately two-thirds of HCC patients exhibit elevated AFP levels [36]
While individual ncRNAs show moderate diagnostic accuracy, their performance generally surpasses that of traditional biomarkers like alpha-fetoprotein (AFP), which is elevated in only approximately two-thirds of HCC patients [36].
Multi-Marker Panels and Machine Learning Approaches
Combining multiple ncRNAs into diagnostic panels significantly enhances detection performance. A study integrating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters using a machine learning algorithm achieved 100% sensitivity and 97% specificity for HCC detection, far surpassing the performance of individual markers [36].
Machine learning models have also been successfully applied to prognostic prediction in HBV-HCC. One study developed a prognostic model using a machine learning algorithm that identified body mass index (BMI), albumin (ALB) levels, surgical resection method (SRM), and AJCC stage as key predictors [37]. The model achieved a C-index of 0.736 and accurately predicted 1-, 3-, and 5-year survival rates with AUC values of 0.843, 0.797, and 0.758, respectively [37].
Another study focused on predicting recurrence in HBV-HCC patients with low platelet-albumin-bilirubin (PALBI) scores after interventional therapy identified age, aspartate aminotransferase (AST), and prothrombin time activity (PTA) as key predictors [33]. The resulting nomogram effectively stratified patients into high and low recurrence risk groups, demonstrating excellent discrimination and clinical utility [33].
Random forest algorithms have shown particular utility in analyzing prognostic factors in HCC diagnosis, with studies identifying Milan criteria, BCLC classification, and albumin levels as variables with the greatest impact on patient prognosis [38].
Experimental Protocols for ncRNA Analysis
Sample Collection and RNA Isolation
Protocol for Plasma Collection and RNA Isolation:
- Sample Collection: Collect whole blood in EDTA-containing tubes. Process samples within 2 hours of collection by centrifugation at 1,900 × g for 10 minutes at 4°C. Transfer the supernatant (plasma) to fresh tubes and centrifuge again at 16,000 × g for 10 minutes to remove remaining cells and debris [36].
- RNA Isolation: Extract total RNA using the miRNeasy Mini Kit (QIAGEN, cat no. 217004) according to the manufacturer's protocol. Elute RNA in 100 μL of nuclease-free water [36].
- Quality Control: Determine RNA yield using a NanoDrop 2000 spectrophotometer (Thermo Scientific). Assess RNA integrity by agarose gel electrophoresis with ethidium bromide staining [34].
Reverse Transcription and Quantitative PCR
Protocol for cDNA Synthesis and qRT-PCR:
- Reverse Transcription: Use the RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, cat no. K1622). Perform reactions in a GeneAmp PCR System 9700 (Applied Biosystems) using 0.5 μg RNA in a 10 μL reaction volume with the following conditions: 37°C for 15 minutes followed by heat inactivation at 85°C for 5 seconds [36].
- Quantitative PCR: Perform qRT-PCR using PowerTrack SYBR Green Master Mix (Applied Biosystems, cat no. A46012) on a ViiA 7 real-time PCR system (Applied Biosystems). Use 1 μL of diluted cDNA in a 10 μL reaction volume with the following cycling conditions: 95°C for 10 minutes; 40 cycles of 95°C for 10 seconds, 60°C for 30 seconds [36].
- Data Analysis: Normalize expression data using the housekeeping gene GAPDH. Calculate relative expression using the ΔΔCT method. Perform each reaction in triplicate for statistical reliability [36].
Microarray Analysis for lncRNA Profiling
Protocol for lncRNA Microarray:
- RNA Labeling: Label 200 ng of total RNA using the LowInput Quick-Amp Labeling Kit, One-Color (Agilent, p/n 5190-2305) [34].
- Array Hybridization: Hybridize labeled RNA on Gene Expression Hybridization Kit (Agilent, p/n 5188-4242) using Agilent human lncRNA arrays containing 46,506 human lncRNAs probes and 30,656 human mRNAs probes [34].
- Signal Detection and Analysis: Detect hybridization signals using the Microarray Scanner (Agilent, p/n G2505C). Analyze scanned images with Feature Extraction Software (Agilent) [34].
Signaling Pathways and Molecular Mechanisms
HBx Regulation of ncRNA in Hepatocarcinogenesis
The HBV X protein (HBx) serves as a central orchestrator of ncRNA dysregulation in HBV-related HCC through multiple molecular mechanisms. The following diagram illustrates key pathways through which HBx regulates ncRNA expression and function:
HBx modulates ncRNA expression through three primary mechanisms: (1) epigenetic modifications including DNA methylation that represses tumor-suppressive miRNAs like miR-132 and miR-205; (2) activation of transcription factors including c-Myc and nuclear factor kappa B that induce expression of oncogenic miRNAs and lncRNAs; and (3) inhibition of tumor suppressor p53, which normally activates miR-148a and miR-216b [20] [19]. Additionally, HBx drives metabolic reprogramming through pathways such as the HBx/miR-429/Rab18 axis, resulting in abnormal lipid metabolism that supports hepatoma cell proliferation [20] [19].
ncRNA Regulation of Immune Microenvironment in HBV-HCC
The tumor immune microenvironment plays a crucial role in HBV-HCC progression and therapy response. ncRNAs significantly influence immune cell function through diverse mechanisms:
Multiple ncRNAs regulate CD8+ T cell function in the HBV-HCC microenvironment. Lnc-Tim3 binds directly to the Tim-3 immune checkpoint protein and blocks interaction with Bat3, inhibiting downstream Lck/NFAT1/AP-1 signaling and exacerbating CD8+ T cell exhaustion [35]. NEAT1 interferes with Tim-3 expression by binding to miR-155, and its downregulation enhances CD8+ T cell cytolytic activity [35]. CircMET functions through the miR-30-5p/Snail/DPP4 axis to reduce CD8+ T cell infiltration into tumors [35]. Targeting these ncRNA-mediated immune regulatory pathways represents a promising approach to enhance immunotherapy efficacy in HBV-HCC.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for ncRNA Studies in HBV-HCC
| Reagent/Category | Specific Product/Example | Application in ncRNA Research | Technical Notes |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN, 217004) | Total RNA extraction from plasma/serum/tissues | Maintains small RNA fraction including miRNAs |
| cDNA Synthesis Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, K1622) | Reverse transcription for qRT-PCR analysis | Use random hexamers and oligo-dT for comprehensive coverage |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems, A46012) | Quantitative real-time PCR for ncRNA detection | Provides high sensitivity for low-abundance targets |
| Microarray Platforms | Agilent human lncRNA array (46,506 lncRNA probes) | Genome-wide lncRNA expression profiling | Includes 30,656 mRNA probes for integrated analysis |
| PCR Instruments | ViiA 7 Real-Time PCR System (Applied Biosystems) | High-throughput ncRNA quantification | Enables multiplexing for validation studies |
| Reference Genes | GAPDH, U6, 18S rRNA | Normalization of ncRNA expression data | Validate stability in specific experimental conditions |
| Machine Learning Algorithms | Random Forest, XGBoost, SVM | Development of diagnostic/prognostic models | Random Forest shows high accuracy for biomarker panels [38] |
| Statistical Analysis Tools | R software (v4.4.1), SPSS (v26.0) | Statistical analysis and model validation | R provides comprehensive packages for ncRNA analysis |
| 1-Methyl-2-(oxetan-3-yl)piperazine | 1-Methyl-2-(oxetan-3-yl)piperazine, CAS:1895314-91-6, MF:C8H16N2O, MW:156.229 | Chemical Reagent | Bench Chemicals |
| 5-Carboxy-2-(5-tetrazolyl)-pyridine | 5-Carboxy-2-(5-tetrazolyl)-pyridine | 5-Carboxy-2-(5-tetrazolyl)-pyridine is a high-purity heterocyclic compound for research use only (RUO). Explore its applications in pharmaceutical development and material science. | Bench Chemicals |
Non-coding RNAs have emerged as powerful molecular regulators and promising biomarkers in HBV-related hepatocellular carcinoma. Their stability in circulation, disease-specific expression patterns, and critical roles in hepatocarcinogenesis render them ideal candidates for non-invasive diagnostic and prognostic applications. The integration of ncRNA biomarkers into multi-parameter panels, enhanced by machine learning algorithms, demonstrates superior performance compared to traditional biomarkers like AFP alone.
Future research directions should focus on validating ncRNA biomarkers in large, multicenter prospective cohorts to establish standardized detection protocols and clinical cutoff values. Additionally, exploring the therapeutic potential of ncRNAs through antisense oligonucleotides or small molecule inhibitors may yield novel treatment strategies for HBV-HCC. As our understanding of the complex ncRNA regulatory networks in HBV-induced hepatocarcinogenesis deepens, these molecules are poised to revolutionize early detection, prognosis prediction, and personalized treatment approaches for this devastating malignancy.
Leveraging ncRNA Signatures for Patient Stratification and Personalized Medicine
The molecular pathogenesis of hepatitis B virus (HBV)-related hepatocellular carcinoma (HCC) involves complex alterations in non-coding RNA (ncRNA) networks that drive hepatocarcinogenesis. Recent advances in ncRNA biology have revealed their exceptional potential as biomarkers for patient stratification and therapeutic targets. This technical guide comprehensively outlines the current landscape of HBV-induced ncRNA aberrations, detailing experimental methodologies for their investigation, visualization of associated signaling pathways, and translation of these findings into personalized medicine approaches for HBV-HCC management. We synthesize evidence from cutting-edge research to provide a framework for leveraging ncRNA signatures in clinical decision-making and drug development.
HBV-related HCC represents a major global health challenge, accounting for approximately 80% of HCC cases worldwide and causing significant cancer-related mortality [16]. The persistence of covalently closed circular DNA (cccDNA) and viral integration into the host genome establish a permissive environment for hepatocarcinogenesis, largely mediated through the regulatory functions of the HBV X protein (HBx) [19]. HBx acts as a master regulator of ncRNA expression, inducing epigenetic modifications that alter cellular processes including proliferation, apoptosis, immune evasion, and metastasis [19] [39].
Non-coding RNAs, particularly microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), have emerged as critical players in HBV-associated HCC pathogenesis. These molecules demonstrate disease-specific expression patterns, stability in bodily fluids, and remarkable tissue specificity, rendering them ideal candidates for diagnostic biomarkers and therapeutic targets [16] [8]. The following sections provide a comprehensive technical overview of validated ncRNA biomarkers, their mechanisms of action, experimental approaches for their investigation, and their clinical applications in patient stratification and personalized treatment regimens.
HBV-Regulated ncRNA Signatures and Functional Mechanisms
Key miRNA Alterations in HBV-HCC
HBx-mediated dysregulation of miRNA expression represents a fundamental mechanism in HBV-driven hepatocarcinogenesis. These alterations can be categorized into oncogenic miRNAs (oncomiRs) that are upregulated and tumor-suppressive miRNAs that are downregulated in HBV-HCC.
Table 1: Oncogenic miRNAs Upregulated in HBV-HCC
| miRNA | Regulation by HBx | Target Pathways/Genes | Biological Functions |
|---|---|---|---|
| miR-21 | Upregulated [16] | PDCD4, PTEN [16] | Promotes tumor cell growth and survival [16] |
| miR-221/222 | Upregulated [16] | CXCL4/12, TFRC [16] | Facilitates cell cycle progression, suppresses apoptosis [16] |
| miR-17-92 cluster | Upregulated [16] | ERα [16] | Promotes proliferation, angiogenesis, immune evasion [16] |
| miR-210-3p | Upregulated [16] | HIF-1α, FGF1 [16] | Enhances tumor survival under hypoxic conditions [16] |
| miR-96 | Upregulated [16] | GPM6A [16] | Promotes proliferation and growth [16] |
Table 2: Tumor-Suppressive miRNAs Downregulated in HBV-HCC
| miRNA | Regulation by HBx | Target Pathways/Genes | Biological Functions |
|---|---|---|---|
| miR-122 | Downregulated by IL-6, TNF-α [16] | PKM2, SLC7A1 [16] | Loss promotes tumor development, motility, invasion; regulates metabolism [16] |
| miR-199a/b | Downregulated [16] | ROCK1, PI3K/Akt [16] | Inhibits ROCK1/MLC and PI3K/Akt pathways; low expression linked to poor survival [16] |
| miR-125b | Downregulated [16] | VEGFA, cyclin D2/E2, IL-6-Stat3 [16] | Inhibits angiogenesis, induces cell-cycle arrest [16] |
| miR-101 | Downregulated [16] | DNMT3A [16] | Induces aberrant DNA methylation [16] |
| miR-148a/152 | Downregulated [16] | HPIP, RIZ1 via DNMT1 [16] | Represses AKT/ERK/FOXO4/ATF5 pathway [16] |
| miR-30a-5p | Downregulated [16] | SNAIL1 [16] | Influences EMT dynamics [16] |
| let-7a | Downregulated [19] | STAT3, ras, c-myc [19] | Suppression supports cell proliferation [19] |
| miR-216b | Downregulated via p53 inhibition [19] | IGF2BP2 [19] | Reduced levels induce proliferation, migration, invasion [19] |
| miR-205 | Downregulated via promoter hypermethylation [19] | ACSL4 [19] | Downregulation enhances lipogenesis and proliferation [19] |
The let-7 family repression exemplifies the complex regulatory networks in HBV-HCC. HBx establishes a double-negative feedback loop between c-Myc/LIN28B and let-7, wherein HBx activates c-Myc and LIN28B, which subsequently repress let-7 expression, ultimately promoting hepatocarcinogenesis through dysregulation of STAT3, ras, and c-Myc signaling [19].
Long Non-Coding RNA Signatures in HBV-HCC
LncRNAs represent a diverse class of RNA molecules longer than 200 nucleotides that regulate gene expression through interactions with DNA, RNA, and proteins. These molecules exert their effects through chromatin modification, transcriptional regulation, and post-transcriptional processing [8]. In HBV-related HCC, lncRNAs are frequently dysregulated, impacting cellular proliferation, invasion, metastasis, angiogenesis, and immune evasion [8] [40].
Prominent examples include HULC, one of the most extensively investigated lncRNAs in HBV-HCC, along with DLEU2 and HOTAIR, which are implicated in chromatin regulation, transcription, and cell cycle control [16] [8]. These lncRNAs frequently function as competitive endogenous RNAs (ceRNAs) by "sponging" miRNAs, thereby infringing on their regulatory capacity and modulating the expression of miRNA target genes [16].
Experimental Protocols for ncRNA Investigation
Core Methodologies for ncRNA Profiling and Validation
Cell Culture and Transfection
Human podocytes or hepatocyte cell lines are cultured in RPMI 1640 medium supplemented with 10% fetal bovine serum and 1% penicillin/streptomycin at 37°C with 5% CO2 [41]. For HBx expression studies, plasmids encoding the HBx gene (pHBx) and corresponding negative control plasmids are constructed and purified. Cells are seeded onto 6-well plates at a density of 5 × 10^4 cells/cm^2 and transfected at approximately 70% confluence using Lipofectamine 3000 according to manufacturer instructions [41]. Experimental groups typically include:
- Control group (no treatment)
- Empty plasmid group (transfected with empty plasmid)
- HBx group (transfected with pHBx plasmid)
- HBx + miRNA mimic/inhibitor group (co-transfected with pHBx and ncRNA modulator)
Transfection efficiency is assessed using quantitative PCR to detect expression levels of specific genes associated with the plasmid vectors and ncRNA modulators [41].
RNA Extraction and Quantitative Real-Time PCR
Total RNA is extracted using TRIzon Reagent and purified using UltraPure RNA Kit [41]. Reverse transcription is performed with Evo M-MLV RT Premix. Quantitative PCR is conducted using SYBR Green Pro Taq HS qPCR Kit on a CFX Connect Real-Time PCR system with the following cycling conditions: 95°C for 2 minutes, followed by 40 cycles at 95°C for 3 seconds, 60°C for 30 seconds, and 70°C for 10 seconds [41]. A melting curve analysis is performed post-amplification. The internal reference for miRNAs is typically U6, while GAPDH serves as reference for mRNAs. Gene expression is quantified using the 2^-ΔΔCT method [41].
Functional Validation Assays
ROS Level Determination Cells are washed with PBS and incubated with 10 µM DCFDA from ROS ELISA Kit for 30 minutes at 37°C in darkness [41]. After incubation, cells are washed, lysed, and centrifuged at 12,000×g for 15 minutes at 4°C. Supernatants are transferred to a 96-well plate and fluorescence measured at 450 nm using a microplate reader [41].
LDH Level Determination Cell lysates are centrifuged at 12,000×g for 15 minutes at 4°C [41]. Supernatants are transferred to a 96-well plate according to LDH ELISA Kit protocol. Absorbance is measured at 450 nm to assess cellular damage [41].
Cell Viability Assessment (MTT Assay) Cells are seeded in a 96-well plate at 5,000 cells per well [41]. After treatment, 20 µl MTT solution is added and incubated for 4 hours at 37°C. Medium is removed and 150 µl DMSO added to dissolve formazan crystals. Absorbance is measured at 490 nm [41].
Western Blot Analysis Cells are lysed with enhanced RIPA buffer containing PMSF [41]. Protein concentrations are determined using BCA Kit. Proteins are separated by SDS-PAGE and transferred to PVDF membranes. Membranes are blocked with 5% milk and incubated with primary antibodies overnight at 4°C, followed by HRP-conjugated secondary antibodies. Chemiluminescent detection is performed using ECL kit, and band intensity quantified using ImageJ [41].
Advanced Technical Approaches
Single-Cell RNA Sequencing (scRNA-seq)
scRNA-seq enables resolution of transcriptomic landscapes at cellular level, identifying distinct subclusters associated with disease progression [41]. This approach is particularly valuable for understanding tumor heterogeneity and identifying rare cell populations contributing to HBV-HCC pathogenesis.
Machine Learning Integration
Machine learning algorithms analyze high-dimensional genomic data to enhance precision of target identification [41] [42]. These approaches facilitate discovery of intricate molecular interactions underlying HBV-HCC and enable development of predictive models for patient stratification.
Visualization of ncRNA Regulatory Networks in HBV-HCC
HBx-miRNA Regulatory Network in Hepatocarcinogenesis
HBx-miRNA Regulatory Network: This diagram illustrates HBx-mediated regulation of oncogenic (red) and tumor-suppressive (blue) miRNAs and their contributions to key cancer hallmarks (green).
Experimental Workflow for ncRNA Signature Validation
ncRNA Validation Workflow: This diagram outlines the comprehensive experimental pipeline for ncRNA signature identification and validation, from initial cell culture to final biomarker signature development.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for ncRNA Studies in HBV-HCC
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Culture | Human podocytes, hepatocyte cell lines (Huh-7, MHCC97H) [41] [42] | In vitro modeling of HBV-HCC pathogenesis |
| Transfection Reagents | Lipofectamine 3000 [41] | Delivery of expression plasmids and ncRNA modulators |
| Expression Plasmids | pHBx (HBx encoding plasmid) [41] | HBx protein expression in cellular models |
| RNA Extraction | TRIzon Reagent, UltraPure RNA Kit [41] | High-quality RNA isolation for downstream applications |
| Reverse Transcription | Evo M-MLV RT Premix [41] | cDNA synthesis for qPCR analysis |
| qPCR Kits | SYBR Green Pro Taq HS qPCR Kit [41] | Quantitative gene expression analysis |
| Functional Assay Kits | ROS ELISA Kit, LDH ELISA Kit, MTT solution [41] | Assessment of oxidative stress, cytotoxicity, and viability |
| Western Blot | Primary antibodies (CRIM1, GAPDH), HRP-conjugated secondary antibodies [41] | Protein expression validation |
| scRNA-seq Platforms | 10X Genomics, Smart-seq2 [41] | Single-cell transcriptomic profiling |
| Machine Learning Tools | LASSO-Cox regression, random forest [42] | Predictive model development and biomarker selection |
| 1-butyl-1H-1,2,3-triazol-4-amine | 1-Butyl-1H-1,2,3-triazol-4-amine|RUO | 1-Butyl-1H-1,2,3-triazol-4-amine is a versatile chemical scaffold for drug discovery research. This product is for Research Use Only. Not for human or veterinary use. |
| 4-(Benzyloxy)benzene-1-sulfinicacid | 4-(Benzyloxy)benzene-1-sulfinicacid, CAS:740053-31-0, MF:C13H12O3S, MW:248.3 | Chemical Reagent |
Clinical Translation and Therapeutic Applications
ncRNA-Based Patient Stratification
The development of dual tissue mRNA and serum protein signatures represents a promising approach for risk stratification in HCC patients. Recent research has identified five biomarkers (AKR1B10, ANXA2, COL15A1, SPARCL1, and SPINK1) that demonstrate consistent prognostic value across multiple cohorts [42]. These biomarkers exhibit significant positive correlation between serum levels and tissue protein expression (R > 0.8, p < 0.001), enabling non-invasive monitoring through serum testing [42].
Machine learning approaches applied to these biomarker signatures can effectively stratify patients into distinct risk categories. High-risk HCC identified through these signatures demonstrates poor response to sorafenib and transarterial chemoembolization (TACE) but increased sensitivity to agent ABT-263 in silico, in vitro, and in vivo [42]. This stratification capability enables more personalized treatment selection based on individual molecular profiles.
RNA-Targeted Therapeutic Approaches
Emerging RNA-targeted therapies show considerable promise for HBV functional cure. Two leading approaches include:
Imdusiran (AB-729): A GalNAc-conjugated small interfering RNA (siRNA) that silences all HBV transcripts and may stimulate immune responses [43]. In Phase II trials (IM-PROVE II), combination therapy with imdusiran followed by therapeutic vaccination (VTP-300) and low-dose nivolumab resulted in functional cure in 2 of 13 patients (15%), evidenced by sustained HBsAg loss and anti-HBs seroconversion [43].
Bepirovirsen (GSK3228836): A modified antisense oligonucleotide (ASO) that binds and degrades HBV RNA, reducing antigen production [43]. Phase IIa trials demonstrate effective HBsAg reduction with a favorable safety profile characterized mainly by mild injection site reactions and transient ALT elevations [43].
These RNA-targeted approaches function by reducing viral antigen load, potentially reversing T-cell exhaustion and enabling immune reconstitution—a critical component for achieving functional cure [43].
The integration of ncRNA signatures into HBV-HCC research and clinical practice offers unprecedented opportunities for patient stratification and personalized medicine. The documented alterations in miRNA and lncRNA expression patterns, coupled with advanced detection methodologies and analytical approaches, provide a robust foundation for refining prognostic prediction and therapeutic selection.
Future developments in this field will likely focus on several key areas: (1) standardization of ncRNA detection methodologies across platforms; (2) validation of multi-analyte signatures in diverse patient populations; (3) integration of ncRNA profiling with other molecular data types (genomic, proteomic); and (4) development of ncRNA-targeted therapeutics for precision intervention. As these advancements mature, ncRNA-based stratification approaches promise to transform clinical management of HBV-HCC, enabling truly personalized treatment strategies based on individual molecular profiles.
The landscape of cancer therapeutics has been revolutionized by the growing understanding of non-coding RNAs (ncRNAs) and their profound roles in oncogenesis. Within the specific context of hepatitis B virus (HBV)-induced hepatocellular carcinoma (HCC), the dysregulation of ncRNAs by viral proteins, particularly the HBV X (HBx) protein, creates a unique oncogenic network that drives hepatocarcinogenesis. This whitepaper provides an in-depth technical guide for researchers and drug development professionals on leveraging antisense oligonucleotide (ASO) and small interfering RNA (siRNA) strategies to target these pathogenic ncRNAs. We detail the molecular mechanisms, present structured quantitative data, outline robust experimental protocols, and visualize key signaling pathways and workflows. The content is rigorously framed within the context of HBV-induced ncRNA alterations, offering a targeted blueprint for advancing therapeutic interventions in HBV-related HCC.
Hepatocellular carcinoma (HCC) is a major global health burden, with chronic HBV infection being a leading etiological factor, particularly in Asia [20]. The molecular pathogenesis is complex, wherein the HBx protein encoded by HBV plays a pivotal carcinogenic role by dysregulating host cell processes, including apoptosis, DNA damage repair, and cell cycle regulation [20]. A critical mechanism of HBx-mediated hepatocarcinogenesis is its extensive interaction with the host's ncRNA network.
Non-coding RNAs, including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), are no longer considered "transcriptional noise" but are recognized as pervasive regulators of cancer hallmarks such as proliferation, invasion, metastasis, and therapy resistance [44] [24]. In HBV-related HCC, HBx systematically alters the expression of numerous ncRNAs. For instance, HBx downregulates tumor-suppressive miRNAs like miR-148a and miR-101, while upregulating oncogenic species such as miR-21 and miR-429 [20]. These altered ncRNAs form a dense, interactive network that rewires critical signaling pathways (e.g., STAT3, mTOR, AKT), promotes metabolic reprogramming towards glycolysis, aggravates liver inflammation and fibrosis, and fosters an immunosuppressive tumor microenvironment [20] [45]. This HBx-ncRNA axis represents a compelling therapeutic frontier. Targeting these oncogenic ncRNAs using sequence-specific modalities like ASOs and siRNAs offers a promising strategy to dismantle key nodes of this pathogenic network and potentially reverse or halt the progression of HBV-related HCC.
Therapeutic Targeting Strategies: ASOs and siRNAs
Antisense Oligonucleotides (ASOs)
ASOs are short, synthetic, single-stranded oligonucleotides (typically 18–30 nucleotides in length) designed to be complementary to a target RNA sequence through Watson-Crick base pairing [46]. Their primary mechanisms of action include:
- RNase H1-Dependent Cleavage: "Gapmer" ASOs contain a central block of DNA nucleotides flanked by modified RNA nucleotides. The DNA-RNA hybrid formed with the target RNA recruits RNase H1, which cleaves the target RNA, leading to its degradation [46].
- Steric Hindrance: ASOs designed with high-affinity chemistry can bind to target RNAs without inducing degradation, thereby physically blocking the access of ribosomal complexes or splicing machinery. This can inhibit translation or modulate alternative splicing [46].
ASOs can be engineered to target oncogenic ncRNAs directly or to inhibit the expression of protein-coding mRNAs that are dysregulated by these ncRNAs.
Small Interfering RNAs (siRNAs)
siRNAs are synthetic double-stranded RNA molecules (typically 21–23 bp) that harness the endogenous RNA interference (RNAi) pathway. Upon introduction into the cell, the siRNA duplex is loaded into the RNA-induced silencing complex (RISC). The guide strand then directs RISC to a perfectly complementary mRNA sequence, resulting in the catalytic cleavage and degradation of the target mRNA [46]. While siRNAs are predominantly used to target protein-coding mRNAs, they can be strategically deployed to degrade pre-miRNAs or lncRNAs by designing sequences complementary to their functional regions.
Approved Nucleic Acid Therapeutics
The clinical validation of ASO and siRNA drugs underscores their therapeutic potential. The following table summarizes key approved nucleic acid therapeutics, illustrating their indications, mechanisms, and delivery strategies.
Table 1: Approved Nucleic Acid Therapeutics (as of 2025) [47] [46]
| Drug Name | Type | Approval Year | Indication | Primary Target | Key Delivery Strategy |
|---|---|---|---|---|---|
| Spinraza (Nusinersen) | ASO | 2016 | Spinal Muscular Atrophy | SMN2 pre-mRNA | Intrathecal injection |
| Tegsedi (Inotersen) | ASO | 2018 | Hereditary ATTR Amyloidosis | Transthyretin (TTR) mRNA | Subcutaneous injection |
| Onpattro (Patisiran) | siRNA | 2018 | Hereditary ATTR Amyloidosis | TTR mRNA | Lipid Nanoparticles (LNPs) |
| Givlaari (Givosiran) | siRNA | 2019 | Acute Hepatic Porphyria | Aminolevulinic Acid Synthase 1 mRNA | GalNAc-conjugate |
| Oxlumo (Lumasiran) | siRNA | 2020 | Primary Hyperoxaluria Type 1 | Hydroxyacid Oxidase 1 (HAO1) mRNA | GalNAc-conjugate |
| Leqvio (Inclisiran) | siRNA | 2021 | Hypercholesterolemia | PCSK9 mRNA | GalNAc-conjugate |
| Amvuttra (Vutrisiran) | siRNA | 2022 | Hereditary ATTR Amyloidosis | TTR mRNA | GalNAc-conjugate |
Application in Targeting HBV-Related Oncogenic ncRNAs
The following table outlines specific examples of dysregulated ncRNAs in HBV-HCC and proposes potential ASO/siRNA strategies for their targeting.
Table 2: Targeting HBV-Related Oncogenic ncRNAs with ASOs and siRNAs [20] [45]
| Dysregulated ncRNA | Role in HBV-HCC | Associated Pathway/Target | Proposed ASO/siRNA Strategy |
|---|---|---|---|
| miR-21 | OncomiR, upregulated by HBx; suppresses apoptosis and IL-12 [20]. | PDCD4, IL-12 | ASO (Anti-miR-21) to inhibit its oncogenic function. |
| miR-429 | OncomiR, upregulated by HBx; promotes lipid metabolism and proliferation [20]. | Rab18 | siRNA against pre-miR-429 or ASO to block its activity. |
| LincR-Cer2-5'AS | LncRNA regulating immune cell migration in TIME [45]. | GATA-3 | Gapmer ASO for RNase H1-mediated degradation. |
| Lnc-LFAR1 | Promotes liver fibrosis and inflammation via NF-ĸB and TGF-β/Smad [45]. | Smad2/3 | siRNA pool targeting multiple exons of the lncRNA transcript. |
| miR-132 | Upregulated in CHB and HCC; transcriptionally inhibited by HBx via methylation [20]. | p300, AKT | Strategy context-dependent: restoration or inhibition. |
| miR-148a | Tumor suppressor; downregulated by HBx; negatively regulates HPIP/mTOR [20]. | HPIP | miRNA mimic (double-stranded RNA functioning like siRNA) to restore its function. |
Experimental Protocols for Preclinical Development
Protocol 1: In Vitro Screening of Candidate ASOs/siRNAs
Objective: To identify the most potent ASO or siRNA sequence for degrading a target oncogenic ncRNA in cultured hepatoma cells (e.g., HepG2.2.15, Huh-7).
Materials:
- Cells: Relevant HBV-positive and HBV-negative hepatoma cell lines.
- Oligonucleotides: A library of 3-5 candidate ASOs (e.g., Gapmers with 2'-MOE or LNA modifications) or siRNAs targeting different regions of the target ncRNA, along with scrambled negative control oligonucleotides.
- Transfection Reagent: Lipid-based transfection reagent (e.g., Lipofectamine RNAiMAX, Lipofectamine 3000).
- RNA Isolation & Analysis: RNA extraction kit (TRIzol), Reverse Transcription kit, Real-Time PCR System, primers for target ncRNA and control genes (e.g., GAPDH, U6).
- Viability Assay: Cell Titer-Glo or MTT assay kit.
Methodology:
- Cell Seeding: Seed cells in 24-well or 96-well plates to reach 60-70% confluency at the time of transfection.
- Oligonucleotide Complex Formation:
- Dilute ASO/siRNA stocks to a working concentration series (e.g., 1 nM, 10 nM, 50 nM, 100 nM) in a serum-free medium.
- Dilute the transfection reagent separately in the same medium.
- Combine the diluted oligonucleotides with the diluted transfection reagent (e.g., 1:1 ratio), incubate for 15-20 minutes at room temperature to form complexes.
- Transfection: Add the complexes to the cells. Include a negative control (scrambled oligonucleotide) and a mock transfection control (reagent only).
- Incubation: Incubate cells for 24-72 hours at 37°C, 5% CO₂.
- Efficacy Analysis (qRT-PCR):
- Harvest cells 48 hours post-transfection for RNA isolation.
- Perform reverse transcription using ncRNA-specific stem-loop primers (for miRNAs) or random hexamers (for lncRNAs).
- Conduct quantitative real-time PCR (qPCR) to measure the remaining levels of the target ncRNA. Normalize to housekeeping genes (U6 for miRNAs, GAPDH for lncRNAs).
- Calculate percentage knockdown relative to the negative control.
- Specificity & Off-Target Assessment:
- Perform RNA sequencing or a qPCR array on the top-performing ASO/siRNA candidates to profile genome-wide expression changes and identify potential off-target effects [48].
- Functional Phenotyping:
- At 72 hours post-transfection, perform functional assays such as Cell Titer-Glo for viability, Caspase-Glo for apoptosis, and transwell migration/invasion assays.
Protocol 2: In Vivo Efficacy Testing in an HBV-HCC Mouse Model
Objective: To evaluate the efficacy and tolerability of the lead ASO/siRNA candidate in a preclinical mouse model of HBV-related HCC.
Materials:
- Animals: Immunodeficient mice (e.g., NOD/SCID) engrafted with HBV-positive human hepatoma cells, or hydrodynamic injection-based HBV-HCC mouse models.
- Oligonucleotide: Lead ASO/siRNA candidate and scrambled control.
- Delivery Vehicle: For unmodified ASOs/siRNAs, use invivo-jetPEI or similar in vivo transfection reagent. For advanced delivery, use GalNAc-conjugated siRNAs or lipid nanoparticles (LNPs).
- Administration Equipment: Syringes, 29-30G needles for subcutaneous (GalNAc) or intravenous (LNP) injection.
- Monitoring Equipment: In vivo imaging system (IVIS) if using luciferase-labeled cells, ultrasound machine for tumor monitoring.
- Histology Reagents: Formalin, paraffin, antibodies for immunohistochemistry (IHC).
Methodology:
- Model Establishment: Establish the HBV-HCC model and randomize mice into treatment and control groups (n=5-10 per group) once tumors are palpable (~50-100 mm³).
- Dosing Regimen:
- Group 1: Lead ASO/siRNA (e.g., 5-10 mg/kg for ASOs, 1-3 mg/kg for siRNAs).
- Group 2: Scrambled control oligonucleotide (same dose and schedule).
- Group 3: Vehicle control (e.g., PBS).
- Administer via subcutaneous (GalNAc-siRNA) or intravenous (LNP) injection twice weekly for 3-4 weeks.
- Long-Term Monitoring:
- Measure tumor dimensions 2-3 times per week using calipers and calculate tumor volume (Volume = (Length × Width²)/2).
- Monitor mouse body weight as an indicator of systemic toxicity.
- Terminal Analysis:
- At the end of the study, euthanize mice and harvest tumors and major organs (liver, kidney, spleen).
- Tumor Analysis: Weigh tumors. Divide each tumor for multiple analyses: snap-freeze for RNA/protein extraction (to confirm target knockdown via qRT-PCR and Western blot), and fix in formalin for histology (H&E staining, IHC for proliferation-Ki67, apoptosis-cleaved caspase-3).
- Toxicity Assessment: Process organ tissues for H&E staining to evaluate histopathological changes. Analyze serum for liver enzymes (ALT, AST) and renal function markers (BUN, Creatinine).
Visualization of Mechanisms and Workflows
Diagram: HBx-ncRNA Oncogenic Network and Therapeutic Intervention
This diagram illustrates the key pathogenic interactions between the HBV-derived HBx protein and host ncRNAs in hepatocarcinogenesis, and the points of intervention for ASO and siRNA therapeutics.
Diagram Title: HBx-ncRNA Network and ASO/siRNA Intervention
Diagram: ASO and siRNA Mechanisms of Action
This diagram details the distinct molecular mechanisms of RNase H1-active ASOs and siRNA-based therapeutics within the cell.
Diagram Title: ASO and siRNA Molecular Mechanisms
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs critical reagents and their applications for conducting research on targeting ncRNAs in HBV-HCC.
Table 3: Research Reagent Solutions for ncRNA Targeting Studies
| Reagent / Material | Function / Application | Example Use-Case |
|---|---|---|
| GalNAc-Conjugated siRNAs | Targeted delivery to hepatocytes via the asialoglycoprotein receptor (ASGPR); enables subcutaneous administration with high liver uptake [46]. | In vivo testing of siRNA efficacy in mouse models of HBV-HCC with reduced off-target exposure. |
| Lipid Nanoparticles (LNPs) | Encapsulates and protects nucleic acids; facilitates efficient cellular uptake and endosomal escape, especially for intravenous delivery [46]. | Delivery of large or unmodified siRNA/ASO constructs for in vivo studies. |
| Locked Nucleic Acid (LNA) | A high-affinity RNA nucleotide analog used in ASOs ("LNA-Gapmers") to dramatically increase binding strength and biostability [47] [44]. | Designing potent ASOs against highly structured or challenging ncRNA targets (e.g., specific lncRNAs). |
| 2'-MOE Modification | (2'-O-methoxyethyl) modification increases nuclease resistance and binding affinity to RNA, used in the flanking regions of Gapmer ASOs [46]. | Improving the pharmacokinetic and safety profiles of ASOs for in vivo applications. |
| Phosphorothioate Backbone | Replaces non-bridging oxygen with sulfur in the oligonucleotide backbone, enhancing resistance to nucleases and binding to plasma proteins for improved tissue distribution [46]. | A standard modification for first-generation ASOs and a component of most modern oligonucleotide designs. |
| HepG2.2.15 Cell Line | A widely used human hepatoma cell line that is stably transfected with HBV, enabling in vitro study of HBV replication and virus-host interactions [20]. | Screening ASO/siRNA candidates in a context that mimics chronic HBV infection. |
| In Vivo Imaging System | Enables non-invasive, longitudinal monitoring of tumor growth and metastasis in live animals, often using bioluminescence (luciferase) [44]. | Tracking the efficacy of anti-ncRNA therapy on tumor burden over time in a single cohort of mice. |
| 6-Bromo-1,3-benzodioxole-5-thiol | 6-Bromo-1,3-benzodioxole-5-thiol | 6-Bromo-1,3-benzodioxole-5-thiol is a key synthetic intermediate for developing kinase inhibitors in anticancer research. For Research Use Only. Not for human or veterinary use. |
| 4-Chloro-2-methyl-8-nitroquinoline | 4-Chloro-2-methyl-8-nitroquinoline|CAS 56983-07-4 | 4-Chloro-2-methyl-8-nitroquinoline (CAS 56983-07-4) is a high-purity chemical building block for pharmaceutical and organic synthesis research. For Research Use Only. Not for human use. |
Targeting oncogenic ncRNAs with ASOs and siRNAs presents a powerful and rational therapeutic strategy for combating HBV-induced hepatocellular carcinoma. The ability to design sequence-specific agents that can dismantle key nodes in the HBx-dysregulated ncRNA network offers hope for addressing a significant unmet medical need. While challenges remain—including optimizing delivery efficiency, minimizing off-target effects, and ensuring long-term safety—the rapid pace of innovation in oligonucleotide chemistry, delivery platforms (such as GalNAc and LNPs), and our understanding of ncRNA biology is steadily overcoming these hurdles. The integration of robust preclinical protocols, detailed in this guide, will accelerate the transition of these promising therapies from the bench to the clinic. As the field progresses, future work will likely focus on combination therapies that simultaneously target multiple ncRNAs or pair ncRNA-targeting agents with existing modalities, ultimately paving the way for more effective and personalized treatments for HBV-related HCC.
Restoration of Tumor-Suppressive ncRNA Function as a Therapeutic Modality
The dysregulation of non-coding RNAs (ncRNAs) is a hallmark of hepatitis B virus (HBV)-induced hepatocarcinogenesis. The restoration of tumor-suppressive ncRNA function has emerged as a promising therapeutic modality in the fight against hepatocellular carcinoma (HCC). This whitepaper details the mechanistic basis for ncRNA dysregulation in HBV-associated HCC and synthesizes current strategies for reactivating these molecular safeguards. We provide a technical guide encompassing key experimental protocols for validating ncRNA function, a curated toolkit of research reagents, and data visualization to aid researchers and drug development professionals in translating these concepts into viable therapeutic candidates.
Hepatocellular carcinoma (HCC) is a leading cause of cancer-related mortality worldwide, with chronic HBV infection being a major etiological risk factor [49] [50]. While only 1.5% of the human genome codes for proteins, the vast majority is transcribed into non-coding RNAs (ncRNAs), which are now recognized as pivotal regulators of gene expression and cellular homeostasis [51]. The ncRNAs, including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), govern critical processes such as cell proliferation, migration, apoptosis, and epigenetic regulation.
In HBV-related HCC, the viral proteins HBsAg and HBx orchestrate a profound reprogramming of the host cell's transcriptome, leading to widespread dysregulation of ncRNAs [49] [50]. This occurs through several key mechanisms:
- Viral Protein Intervention: HBV-encoded HBsAg activates the NF-κB pathway, inducing oncogenic lncRNAs like LINC00665, which drives hepatocarcinogenesis by promoting cell proliferation, migration, and colony formation while inhibiting apoptosis [49].
- Epigenetic Alterations: The HBx protein mediates extensive epigenetic modifications, including aberrant DNA methylation, histone modifications, and alterations to the covalent closed circular DNA (cccDNA) minichromosome, leading to the silencing of tumor-suppressive ncRNAs and activation of oncogenic ones [50] [51].
- Genetic Alterations: Copy number variations (CNVs) in HCC frequently affect genomic regions rich in ncRNAs, leading to their amplification or deletion. For instance, lncRNAs with copy number gain were found to be upregulated in over 50% of HCC tumor tissues [51].
The restoration of tumor-suppressive ncRNA function represents a novel and powerful therapeutic modality aimed at counteracting these HBV-induced alterations and reversing the oncogenic phenotype.
Core Mechanisms and Therapeutic Strategies
The following table summarizes the primary classes of tumor-suppressive ncRNAs, their mechanisms of action, and the consequences of their dysregulation in HBV-HCC.
Table 1: Tumor-Suppressive ncRNAs in HBV-Induced Hepatocarcinogenesis
| ncRNA Class | Example | Expression in HCC | Mechanism of Action | Therapeutic Restoration Strategy |
|---|---|---|---|---|
| miRNA | miR-122 [51] | Downregulated | Essential for liver homeostasis; loss promotes carcinogenesis. | miRNA mimics delivered via lipid nanoparticles (LNPs) [52]. |
| miRNA | miR-144/451a [51] | Downregulated (silenced by EZH2/H3K27me3) | Tumor suppressive activity. | Demethylating agents; miRNA mimics. |
| miRNA | miR-1 [51] | Downregulated (promoter hypermethylation) | Tumor suppressive activity. | DNA methyltransferase inhibitors (e.g., 5-azacytidine) [51]. |
| lncRNA | SRHC [51] | Downregulated (promoter hypermethylation) | Tumor suppressive activity. | Demethylating agents; saRNA-mediated activation. |
| lncRNA | TSLNC8 [51] | Downregulated (frequent deletion) | Tumor suppressor; frequently deleted. | Gene delivery systems (e.g., viral vectors, PNPs). |
| circRNA | circTRIM33-12 [51] | Downregulated | Independent risk factor for poor survival. | RNA delivery platforms (e.g., engineered EVs). |
Signaling Pathways in HBV-Mediated ncRNA Dysregulation
The diagram below illustrates the core pathway through which HBV components dysregulate ncRNA expression to drive hepatocarcinogenesis, highlighting key points for therapeutic intervention.
Experimental Protocols for Validating ncRNA Function
Robust experimental validation is crucial for establishing the tumor-suppressive function of an ncRNA and its potential as a therapeutic target. Below are detailed protocols for key functional assays.
Protocol: CRISPR Interference (CRISPRi)-Based Knockdown of Oncogenic ncRNA
This protocol is adapted from studies investigating the oncogenic lncRNA LINC00665 [49].
1. sgRNA Design and Vector Construction:
- Design: Design 3-5 sgRNAs targeting the promoter region or specific exons of the target oncogenic lncRNA (e.g., LINC00665). Use online tools (e.g., CRISPick) to minimize off-target effects.
- Cloning: Clone the sgRNA sequences into a lentiviral vector containing a catalytically dead Cas9 (dCas9) fused to a KRAB repressor domain (e.g., pLV hU6-sgRNA hUbC-dCas9-KRAB-T2a-Puro).
2. Lentivirus Production and Cell Transduction:
- Production: Co-transfect HEK-293T cells with the sgRNA/dCas9-KRAB lentiviral vector and packaging plasmids (psPAX2 and pMD2.G) using a transfection reagent like polyethylenimine (PEI). Harvest the virus-containing supernatant at 48 and 72 hours post-transfection.
- Transduction: Transduce target HCC cell lines (e.g., HepG2, Huh7) with the lentiviral supernatant in the presence of 8 µg/mL polybrene. Select stable pools with 1-2 µg/mL puromycin for 5-7 days.
3. Functional Validation Assays:
- qRT-PCR: Confirm knockdown efficiency by extracting total RNA and performing quantitative reverse transcription PCR (qRT-PCR). Normalize lncRNA expression to a housekeeping gene like GAPDH.
- Proliferation Assay: Seed 2,000-5,000 cells per well in a 96-well plate. Assess cell viability daily for 5 days using a colorimetric assay like MTT or CCK-8. Measure absorbance at 450 nm.
- Colony Formation Assay: Seed 500-1,000 cells in a 6-well plate and culture for 10-14 days. Fix colonies with methanol, stain with 0.1% crystal violet, and count manually or with imaging software.
- Apoptosis Assay: Induce apoptosis (e.g., with 1µM Staurosporine for 6 hours). Harvest cells and stain with Annexin V-FITC and Propidium Iodide (PI). Analyze using flow cytometry within 1 hour.
Protocol: Restoration of Tumor-Suppressive miRNA Using Synthetic Mimics
This protocol is based on strategies for restoring miRNAs like miR-122 and miR-1 [52] [51].
1. miRNA Mimic Transfection:
- Design: Use commercially available synthetic, double-stranded RNA molecules (miRNA mimics) designed to mimic the mature sequence of the endogenous tumor-suppressive miRNA (e.g., miR-122).
- Transfection: Seed HCC cells to achieve 50-70% confluency at transfection. Using a lipid-based transfection reagent, complex with 25-50 nM of the miRNA mimic. Include a negative control mimic (scrambled sequence). Change media 6-8 hours post-transfection.
2. Downstream Functional and Molecular Analysis:
- qRT-PCR: Validate mimic uptake and function 48 hours post-transfection by measuring the levels of the mature miRNA and its known target mRNAs.
- Western Blotting: Harvest protein 72-96 hours post-transfection. Analyze the expression of protein targets (e.g., Cyclin G1 for miR-122) using specific antibodies.
- Migration/Invasion Assay: Use a transwell chamber with an 8µm pore membrane. For invasion, coat the membrane with Matrigel. Seed 50,000-100,000 transfected cells in the upper chamber in serum-free media. Use media with 10% FBS as a chemoattractant in the lower chamber. After 24-48 hours, fix, stain, and count cells that have migrated/invaded.
- In Vivo Validation: Subcutaneously inject 1-5 million mimic-transfected HCC cells into immunodeficient mice (e.g., NOD/SCID). Alternatively, systemically administer miRNA mimics formulated in lipid nanoparticles (LNPs) to tumor-bearing mice. Monitor tumor volume twice weekly for 4-6 weeks.
The Scientist's Toolkit: Research Reagent Solutions
Successful research in this field relies on a suite of specialized reagents and tools. The following table catalogs essential solutions.
Table 2: Key Research Reagent Solutions for ncRNA Functional Studies
| Reagent/Tool Category | Specific Example | Function & Application | Key Considerations |
|---|---|---|---|
| Gene Silencing | CRISPRi (dCas9-KRAB) [49] | Targeted transcriptional repression of oncogenic lncRNAs. | High specificity; allows for stable, long-term knockdown. |
| Gene Silencing | siRNA / shRNA | Knockdown of specific mRNA or ncRNA targets. | shRNA allows for stable integration; siRNA for transient knockdown. |
| Gene Activation | Small Activating RNA (saRNA) [52] | Targeted transcriptional activation of tumor-suppressive genes/ncRNAs. | MTL-CEBPA is a clinical-stage example for HCC. |
| Delivery Vectors | Lipid Nanoparticles (LNPs) [52] | In vitro and in vivo delivery of RNA payloads (siRNA, miRNA, mRNA). | Protects RNA, enhances cellular uptake; clinically validated. |
| Delivery Vectors | Polymer Nanoparticles (PNPs) [52] | Delivery of nucleic acids (e.g., p53 mRNA); can be engineered for targeted release. | Biocompatible and customizable polymer chemistry. |
| Delivery Vectors | Lentiviral Vectors [49] | Stable integration of genetic constructs (e.g., shRNA, dCas9). | Enables creation of stable cell lines; biosafety level 2 required. |
| Chemical Inhibitors/Activators | 5-Azacytidine (DNA methyltransferase inhibitor) [51] | Reactivates epigenetically silenced tumor-suppressive ncRNAs. | Can have global, off-target effects on the epigenome. |
| Chemical Inhibitors/Activators | HDAC Inhibitors (e.g., Trichostatin A) [51] | Increases histone acetylation, reactivating silenced ncRNAs. | Can have global, off-target effects on the epigenome. |
| Analytical Tools | ncRNA Databases (e.g., miRBase, LNCRNAwiki) [53] | Annotation, prediction, and functional information on ncRNAs. | Essential for target identification and mechanistic hypothesis. |
| Tert-butyl 2-(azetidin-3-yl)acetate | Tert-butyl 2-(azetidin-3-yl)acetate|Research Chemical | Bench Chemicals | |
| 1,3-Bis(2-methylbut-3-yn-2-yl)urea | 1,3-Bis(2-methylbut-3-yn-2-yl)urea|CAS 63989-51-5 | Bench Chemicals |
Visualization of a Therapeutic Restoration Workflow
The DOT script below outlines a generalized experimental workflow for developing a therapeutic strategy based on restoring a tumor-suppressive ncRNA, from target identification to in vivo validation.
MicroRNA (miRNA)-based therapeutics represent a promising frontier in the treatment of chronic viral infections and their associated complications. This technical guide explores the therapeutic potential of miR-29b-1-5p, a recently characterized miRNA that targets the hepatitis B virus (HBV) entry receptor, sodium-taurocholate cotransporting polypeptide (NTCP). We examine the molecular mechanisms through which miR-29b-1-5p mediates its antiviral effects, present comprehensive quantitative data from key studies, and detail experimental protocols for investigating this pathway. The content is framed within the broader context of HBV-induced non-coding RNA alterations in hepatocarcinogenesis, providing researchers and drug development professionals with a foundational resource for developing novel miRNA-based interventions for HBV and its associated hepatocellular carcinoma (HCC).
Chronic hepatitis B virus (HBV) infection remains a significant global health burden, affecting more than 250 million individuals worldwide and representing a primary etiology for hepatocellular carcinoma (HCC) [54] [55] [56]. HBV drives hepatocarcinogenesis through multiple mechanisms, including viral DNA integration, chronic inflammation, and expression of viral proteins such as HBx that extensively modulate the host epigenetic landscape [56] [57]. The covalently closed circular DNA (cccDNA) persistence in host nuclei establishes a stable viral reservoir that current nucleoside analog therapies cannot eliminate, creating a need for novel therapeutic approaches that target earlier stages of the viral lifecycle [54] [56].
The discovery of NTCP as the functional entry receptor for HBV has opened new avenues for therapeutic intervention [54] [55]. NTCP, a transmembrane bile acid transporter encoded by the SLC10A1 gene, serves as the critical portal for HBV and hepatitis D virus entry into hepatocytes [54]. Inhibition of NTCP function presents a strategic approach to prevent de novo infection and limit viral spread within the liver. Among emerging strategies, miRNA-based therapeutics offer a promising approach for targeted gene regulation, with several miRNAs identified as regulators of pathways relevant to HBV infection and HCC pathogenesis [58] [57].
The miR-29 family, consisting of miR-29a, miR-29b, and miR-29c, has drawn significant research interest due to its diverse roles in cellular processes and disease pathogenesis [59]. While initially regarded as a passenger strand, recent evidence has established miR-29b-1-5p as a functionally significant miRNA with distinct biological activities, including a newly discovered role in regulating NTCP expression and inhibiting HBV infection [54] [55] [60]. This guide comprehensively explores the therapeutic targeting of NTCP by miR-29b-1-5p within the framework of HBV-induced non-coding RNA alterations in hepatocarcinogenesis.
Molecular Mechanisms of miR-29b-1-5p in NTCP Inhibition and HBV Entry Blockade
Biogenesis and Functional Switching of miR-29b-1-5p
The miR-29b-1-5p originates from the miR-29b-1 gene locus on human chromosome 7q32.3 [59]. In conventional miRNA biogenesis, one strand of the miRNA duplex (the guide strand) is preferentially incorporated into the RNA-induced silencing complex (RISC), while the passenger strand (denoted with -5p) is typically degraded. However, recent evidence demonstrates that miR-29b-1-5p undergoes an arm-switching mechanism during maturation, shifting from its traditional passenger status to become a functionally dominant miRNA in specific biological contexts, including hepatic function and aging [60].
This functional switching represents a critical regulatory mechanism that expands the miRNA regulatory network beyond conventional guide strand dominance. In the case of miR-29b-1-5p, this switching appears to be influenced by cellular context and environmental factors, including interferon stimulation and possibly HBV infection itself [54] [60]. The mature miR-29b-1-5p sequence contains distinct nucleotide compositions that differentiate it from other miR-29 family members and contribute to its unique target specificity and functional profile.
Mechanism of NTCP Post-Transcriptional Regulation
miR-29b-1-5p exerts its antiviral function through direct interaction with the 3'-untranslated region (3'-UTR) of NTCP mRNA. Bioinformatics analyses using TargetScanHuman have identified two potential binding sites for miR-29b-1-5p within the NTCP 3'-UTR, with one site exhibiting particularly high complementarity featuring an 11-nucleotide consecutive complementary sequence [54] [55].
The mechanistic pathway through which miR-29b-1-5p mediates its antiviral effects can be visualized as follows:
Figure 1: miR-29b-1-5p Antiviral Mechanism Pathway. This diagram illustrates the sequence of molecular events from interferon stimulation to HBV inhibition.
Upon binding to the NTCP 3'-UTR, miR-29b-1-5p facilitates mRNA degradation and translational repression, resulting in significantly reduced NTCP transcript and protein levels [54]. This post-transcriptional regulation effectively diminishes the availability of functional NTCP receptors on hepatocyte surfaces, thereby limiting HBV entry opportunities. The specificity of this interaction has been confirmed through mutagenesis experiments, wherein mutations in the seed binding sites abolished miR-29b-1-5p-mediated repression of NTCP [54] [55].
Broader Context in HBV-Induced Non-Coding RNA Alterations
The regulation of NTCP by miR-29b-1-5p represents just one example of the extensive interplay between HBV infection and the host non-coding RNA landscape. HBV, particularly through its HBx protein, actively modulates host miRNA expression patterns to create a favorable environment for viral persistence and replication [57]. These HBV-induced non-coding RNA alterations contribute significantly to hepatocarcinogenesis by dysregulating critical cellular pathways involved in proliferation, apoptosis, and immune evasion.
The miR-29 family demonstrates context-dependent roles in HCC pathogenesis, with reported tumor-suppressive and oncogenic functions depending on cellular conditions and targets [59]. This functional duality highlights the complexity of miRNA networks in liver disease and emphasizes the importance of understanding specific miRNA-mRNA interactions rather than making broad functional categorizations.
Recent investigations have yielded substantial quantitative evidence supporting the therapeutic potential of miR-29b-1-5p against HBV. The following table summarizes key experimental findings from foundational studies:
Table 1: Quantitative Summary of miR-29b-1-5p Antiviral Effects
| Experimental Parameter | Experimental System | Effect Size | Statistical Significance | Reference |
|---|---|---|---|---|
| NTCP mRNA reduction | Primary Human Hepatocytes | Significant reduction | p < 0.01 | [54] [55] |
| Luciferase reporter activity | NTCP 3'-UTR reporter assay | 37.3 ± 6.0% decrease | p = 0.0234 | [54] [55] |
| HBV DNA copies | PHH infection model | Remarkable reduction | p = 0.0003 | [54] [55] |
| HBV pgRNA levels | PHH infection model | Significant inhibition | p = 0.0160 | [54] [55] |
| Rescue with NTCP overexpression | PHH with NTCP complementation | Abrogated antiviral effect | Not significant | [54] [55] |
The robustness of these findings is strengthened by the use of primary human hepatocytes (PHHs), considered the gold standard for HBV studies and antiviral therapeutic evaluations [54] [55]. The specificity of the miR-29b-1-5p effect was further demonstrated through rescue experiments, where NTCP overexpression abolished the antiviral activity, confirming that NTCP targeting is the primary mechanism of action rather than secondary immune activation or off-target effects [54].
Additional context for miRNA-mediated NTCP regulation comes from studies of miR-6126, another interferon-induced miRNA that similarly targets NTCP and demonstrates antiviral activity [61]. This pattern suggests that interferon response may employ a multi-miRNA strategy to regulate HBV entry, with miR-29b-1-5p representing a particularly potent candidate for therapeutic development.
Experimental Protocols for Investigating miR-29b-1-5p and NTCP Interactions
miRNA Expression Profiling and Induction Protocols
Protocol 1: Interferon-Induced miRNA Profiling in Primary Human Hepatocytes
- Cell Culture: Maintain two distinct lots of PHHs in appropriate hepatocyte culture medium supplemented with 10% FBS, penicillin (100 U/mL), streptomycin (100 µg/mL), and non-essential amino acids.
- Interferon Treatment: Treat PHHs with IFN-α analog (e.g., CDM-3008) at determined optimal concentrations. Include untreated controls.
- RNA Isolation: At 24-48 hours post-treatment, lyse cells in TRIzol reagent and isolate total RNA following manufacturer's protocol. Further purify RNA using RNeasy MinElute Cleanup Kit.
- miRNA Microarray: Label RNA using FlashTag Biotin HSR RNA Labeling Kit and hybridize to Affymetrix GeneChip miRNA 2.0 Array or equivalent platform.
- Data Analysis: Identify differentially expressed miRNAs using appropriate software, applying filters of fold change > 1.5 and p < 0.05 (t-test). Validate key findings (e.g., miR-29b-1-5p) with miRNA-specific quantitative PCR [54] [55].
Protocol 2: Functional Validation of miRNA Targets
- Target Prediction: Use computational tools (TargetScanHuman, miRDB) to identify potential miRNA-mRNA interactions, focusing on 3'-UTR complementarity.
- Luciferase Reporter Assay:
- Clone wild-type and mutated NTCP 3'-UTR sequences downstream of luciferase gene in appropriate vectors.
- Co-transfect HepG2 or HEK293T cells with reporter constructs and miRNA mimics (50 nM miR-29b-1-5p or control).
- Measure luciferase activity 24-48 hours post-transfection using dual-luciferase reporter assay system.
- Normalize firefly luciferase activity to Renilla luciferase control [54] [55].
The experimental workflow for investigating miR-29b-1-5p antiviral activity proceeds through defined stages:
Figure 2: Experimental Workflow for miRNA Functional Analysis. This diagram outlines the sequential approach for validating miRNA targets and antiviral effects.
Antiviral Efficacy Assessment in Infection Models
Protocol 3: HBV Infection Assay in miRNA-Modified Hepatocytes
- miRNA Transfection: Transfect PHHs with synthetic miR-29b-1-5p mimics (50 nM) or control miRNAs using appropriate transfection reagent. Optimize conditions for minimal cytotoxicity.
- Infection: Four days post-transfection, infect hepatocytes with HBV (multiplicity of infection to be determined based on viral stock).
- Monitoring: Collect culture supernatants and cell lysates at various time points (e.g., 3, 7, 14 days post-infection).
- Analysis:
Protocol 4: Rescue Experiment with NTCP Overexpression
- Vector Construction: Generate NTCP expression vector lacking the 3'-UTR to avoid miR-29b-1-5p regulation.
- Co-transfection: Transfect PHHs with miR-29b-1-5p mimics together with NTCP expression vector or empty control.
- Infection and Analysis: Perform HBV infection as in Protocol 3 and assess viral parameters to determine if NTCP complementation restores HBV susceptibility [54] [55].
The investigation of miR-29b-1-5p and NTCP interactions requires specific experimental systems and reagents. The following table details essential resources for this research area:
Table 2: Essential Research Reagents for miR-29b-1-5p and NTCP Studies
| Reagent/Resource | Specifications | Research Application | Key Considerations |
|---|---|---|---|
| Primary Human Hepatocytes (PHHs) | Multiple donors, fresh or cryopreserved | Gold standard for HBV infection studies; physiological NTCP expression | Donor variability requires multiple lots; limited expansion capacity |
| HepG2-NTCP Cells | HepG2 stably overexpressing NTCP | HBV entry studies; more accessible than PHHs | Limited response to anti-NTCP miRNAs if NTCP lacks 3'-UTR |
| miR-29b-1-5p Mimics | Synthetic RNAs mimicking mature miR-29b-1-5p | Gain-of-function studies | Chemical modifications enhance stability and reduce off-target effects |
| miR-29b-1-5p Inhibitors | Antagomirs or sponge constructs | Loss-of-function studies | Specificity validation essential to exclude effects on related miRNAs |
| NTCP 3'-UTR Reporter | Luciferase vector with NTCP 3'-UTR insert | Direct target validation | Must include mutation controls for binding specificity |
| IFN-α Analogs (e.g., CDM-3008) | Specific formulations as reported | Induction of endogenous miR-29b-1-5p | Concentration optimization required for different cell systems |
| HBV Viral Stocks | Genotype-specific, titered preparations | Infection models | Safety considerations; biosafety level 2+ requirements |
| NTCP Antibodies | Validated for Western blot, immunofluorescence | NTCP protein quantification | Specificity validation crucial due to transmembrane nature |
Discussion and Future Perspectives
The characterization of miR-29b-1-5p as a regulator of NTCP expression represents a significant advancement in the field of miRNA-based antiviral therapeutics. This discovery not only identifies a potential therapeutic candidate but also illuminates a natural mechanism of viral entry control that could be harnessed for clinical benefit. The interferon inducibility of miR-29b-1-5p suggests it may contribute to the antiviral effects of interferon therapy, potentially serving as both a therapeutic agent and a biomarker of treatment response [54] [55].
Several considerations must be addressed in the translational development of miR-29b-1-5p-based therapies. Delivery efficiency to hepatocytes remains a primary challenge, though recent advances in lipid nanoparticles and GalNAc-conjugated siRNAs provide promising delivery platforms that could be adapted for miRNA therapeutics. The potential for off-target effects necessitates comprehensive toxicology studies, though the natural occurrence of this miRNA and its induction during interferon therapy suggest favorable tolerability.
The dualistic nature of miR-29 family members in cancer pathogenesis warrants careful evaluation. While miR-29b-1-5p demonstrates antiviral effects through NTCP inhibition, other miR-29 family members have reported both tumor-suppressive and promoting activities in different contexts [59]. For instance, miR-29a has been shown to promote HBx-induced hepatocarcinogenesis by suppressing PTEN and activating AKT signaling, while also demonstrating tumor-suppressive effects in non-HBV contexts by activating apoptosis [59]. This functional complexity underscores the importance of understanding specific miRNA-mRNA interactions and cellular contexts in therapeutic development.
Future research directions should include:
- Comprehensive assessment of miR-29b-1-5p's effect on bile acid metabolism given NTCP's physiological role in bile acid uptake
- Investigation of potential resistance mechanisms through viral or host adaptation
- Exploration of combination therapies with existing antivirals to target multiple stages of the HBV lifecycle
- Development of optimized delivery systems for hepatic targeting of miRNA therapeutics
The progression of miR-29b-1-5p from basic research to clinical application will require coordinated efforts across multiple disciplines, but the compelling preclinical evidence positions it as a promising candidate in the growing arsenal of miRNA-based therapeutics for viral hepatitis and associated hepatocarcinogenesis.
The development of non-coding RNA (ncRNA) therapeutics for hepatocellular carcinoma (HCC) represents a paradigm shift in precision oncology, particularly for hepatitis B virus (HBV)-induced hepatocarcinogenesis. The liver's unique physiology—characterized by fenestrated endothelium, robust blood supply, and role in first-pass metabolism—makes it exceptionally suitable for nucleic acid-based therapies [62]. These anatomical advantages facilitate enhanced uptake and delivery of therapeutic agents, positioning the liver at the forefront of ncRNA therapeutic development.
HBV infection remodels the hepatic ncRNA landscape, driving oncogenesis through dysregulation of microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) [16] [8]. These molecular alterations present compelling therapeutic targets, yet the clinical translation of ncRNA-based interventions faces substantial delivery challenges. This technical guide examines current targeted delivery strategies, their experimental validation, and emerging solutions to overcome biological barriers for effective ncRNA delivery in HBV-related HCC.
ncRNA Alterations in HBV-Induced Hepatocarcinogenesis
HBV infection orchestrates extensive reprogramming of the hepatic ncRNA landscape, creating a molecular environment conducive to malignant transformation. The HBV-encoded X protein (HBx) plays a pivotal role in modulating ncRNA expression, which subsequently affects critical cellular processes including proliferation, apoptosis, and immune evasion [16].
Dysregulated miRNA Networks in HBV-HCC
miRNAs undergo significant expression alterations in HBV-related HCC, functioning as either oncogenic drivers or tumor suppressors:
- Oncogenic miRNAs: miR-21, upregulated by HBx, targets tumor suppressors PDCD4 and PTEN to promote cell growth and survival. The miR-17-92 cluster facilitates proliferation, angiogenesis, and immune evasion by targeting ERα [16] [8].
- Tumor-suppressive miRNAs: miR-122, a liver-abundant miRNA, is significantly downregulated in HCC and regulates metabolic pathways through targets including pyruvate kinase M2 (PKM2). miR-199a/b inhibits ROCK1/MLC and PI3K/Akt pathways, with its low expression correlating with poor survival [16] [8].
Table 1: Key Dysregulated miRNAs in HBV-Related HCC
| miRNA | Expression in HCC | Regulation by HBV | Validated Targets | Functional Impact |
|---|---|---|---|---|
| miR-21 | Upregulated | HBx-induced | PDCD4, PTEN | Promotes growth, survival |
| miR-122 | Downregulated | Suppressed by IL-6, TNF-α | PKM2, SLC7A1 | Regulates metabolism; loss promotes invasion |
| miR-199a/b | Downregulated | HBx-mediated suppression | ROCK1 | Inhibits PI3K/Akt pathway; prognostic marker |
| miR-221/222 | Upregulated | HBx-induced | CXCL4/12, TFRC | Cell cycle progression, anti-apoptosis |
| miR-17-92 cluster | Upregulated | HBx-induced | ERα | Angiogenesis, immune evasion |
Functional Roles of lncRNAs and circRNAs
Long non-coding RNAs contribute to HBV hepatocarcinogenesis through diverse mechanisms. Highly Upregulated in Liver Cancer (HULC) promotes proliferation and metastasis by acting as a competing endogenous RNA (ceRNA) [8]. The liver-specific lncRNA FAM99B exhibits significant downregulation in HCC tissues and functions as a tumor suppressor by interacting with DDX21 to inhibit ribosome biogenesis [63].
Circular RNAs participate in oncogenic networks primarily through miRNA sponging, sequestering tumor-suppressive miRNAs and preventing their interaction with target mRNAs [16].
Targeted Delivery Platforms for Hepatic ncRNA Therapeutics
GalNAc-Conjugation Technology
N-acetylgalactosamine (GalNAc) conjugation represents the most advanced targeted delivery platform for hepatic ncRNA therapeutics. This approach exploits the asialoglycoprotein receptor (ASGPR), which is highly expressed on hepatocytes, enabling receptor-mediated endocytosis of conjugated therapeutics [64] [65].
Mechanical Advantage: GalNAc conjugation facilitates efficient cellular uptake and endosomal escape, achieving productive gene silencing at substantially lower doses compared to untargeted approaches [65]. The technology has been successfully applied to both siRNA and ASO therapeutics, with multiple GalNAc-conjugated drugs receiving FDA approval [65].
Clinical Validation: The efficacy of GalNAc-conjugated lncRNA therapeutics has been demonstrated in preclinical HCC models. GalNAc-conjugated FAM99B truncation (GalNAc-FAM99B65-146) significantly inhibited growth and metastasis of orthotopic HCC xenografts, establishing proof-of-concept for lncRNA replacement therapy [63].
Lipid-Based Nanoparticle Systems
Lipid nanoparticles (LNPs) represent another prominent delivery platform, with clinical validation achieved through approved siRNA therapeutics like patisiran [64] [65]. Modern LNP formulations have been optimized for hepatic delivery through careful modulation of:
- Ionizable cationic lipid composition - affects endosomal escape efficiency
- Polyethylene glycol (PEG) lipids - influences pharmacokinetics and opsonization
- Particle size (typically 80-100 nm) - facilitates hepatic sinusoid traversal [62] [64]
Current research focuses on enhancing LNP tropism for specific liver cell populations, including hepatocytes and hepatic stellate cells, through surface ligand decoration [64].
Emerging and Alternative Delivery Platforms
Viral Vectors: Adeno-associated virus (AAV) vectors provide efficient gene transfer to hepatocytes, with several serotypes demonstrating preferential hepatic tropism. AAV-mediated delivery of pri-miRNA backbones has entered clinical trials for Huntington disease, establishing precedent for ncRNA delivery [65].
Exosome-Based Delivery: Naturally occurring exosomes represent promising delivery vehicles due to inherent biocompatibility, low immunogenicity, and natural cargo-loading mechanisms. Exosomal ncRNAs have been shown to reflect tissue-specific gene expression changes in HCC, highlighting their potential as both biomarkers and therapeutic vehicles [66].
Table 2: Comparison of Hepatic Delivery Platforms for ncRNA Therapeutics
| Delivery Platform | Mechanism of Delivery | Key Advantages | Clinical Status | Notable Examples |
|---|---|---|---|---|
| GalNAc Conjugates | ASGPR-mediated endocytosis | Excellent hepatocyte specificity, proven clinical success | Multiple FDA-approved drugs | Inclisiran, Golodirsen |
| Lipid Nanoparticles (LNPs) | Endocytosis/fusion | High payload capacity, proven siRNA delivery | FDA-approved (Patisiran) | COVID-19 mRNA vaccines |
| AAV Vectors | Viral transduction | Long-term expression, high transduction efficiency | Clinical trials for ncRNA delivery | rAAV5-miHTT (NCT04120493) |
| Exosomes | Natural vesicle fusion | Native trafficking, low immunogenicity | Preclinical development | MSC-derived exosomes |
| Polymeric Nanoparticles | Endocytosis | Tunable properties, biodegradable | Preclinical development | PLGA-based systems |
Experimental Workflows for Delivery System Evaluation
In Vitro Characterization Pipeline
Comprehensive in vitro assessment establishes the foundational characteristics of delivery systems prior to biological evaluation:
Physicochemical Characterization:
- Dynamic light scattering for particle size and polydispersity index
- Zeta potential measurement for surface charge
- Electron microscopy for morphological analysis
- Stability assessment in physiological buffers and serum
Cell-Based Assays:
- Uptake efficiency in hepatocyte models (primary hepatocytes, HepG2, Huh7)
- Cytotoxicity profiling (CCK-8, LDH release)
- Endosomal escape quantification using pH-sensitive dyes
- Target engagement validation (qRT-PCR, Western blot)
In Vivo Validation in Preclinical HCC Models
Robust in vivo evaluation employs orthotopic and genetically engineered mouse models that recapitulate HBV-related hepatocarcinogenesis:
Therapeutic Efficacy Assessment:
- Orthotopic xenograft models for metastasis evaluation
- Hydrodynamic injection-based HBV persistence models
- DEN-induced carcinogenesis in HBV-expressing mice [26]
- Tumor burden quantification through bioluminescent imaging and histology
Biodistribution and Safety Profiling:
- Fluorescent or radioactive labeling for tissue distribution studies
- Plasma pharmacokinetics and clearance rates
- Immune activation assessment (cytokine release, liver enzymes)
- Histopathological examination of major organs
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Hepatic ncRNA Delivery Studies
| Reagent/Category | Specific Examples | Experimental Function | Key Considerations |
|---|---|---|---|
| Hepatocyte Models | Primary human hepatocytes, HepG2, Huh7, HepaRG | In vitro uptake and efficacy screening | Metabolic competence, ASGPR expression |
| HBV Persistence Models | pAAV-HBV1.2 vector, HepG2.2.15 | HBV-specific ncRNA function studies | Viral gene expression kinetics |
| Delivery Components | Ionizable lipids (DLin-MC3-DMA), GalNAc ligands, PEG lipids | Delivery system formulation | Structure-activity relationships |
| ncRNA Modifications | 2'-O-methyl, 2'-fluoro, phosphorothioate, LNA | RNA stability and potency enhancement | Impact on RISC loading and immunogenicity |
| Analytical Tools | Dynamic light scattering, qRT-PCR, RNA sequencing | System characterization and efficacy assessment | Sensitivity and quantification standards |
| In Vivo Models | DEN-treated mice, hydrodynamic injection, orthotopic xenografts | Preclinical therapeutic evaluation | Model relevance to human HCC pathogenesis |
| 4-(2,5-Dichlorophenoxy)benzoic acid | 4-(2,5-Dichlorophenoxy)benzoic Acid|High-Quality RUO | Bench Chemicals |
Technical Protocols: Key Methodological Approaches
GalNAc-Conjugated lncRNA Therapeutic Protocol
Based on the pioneering work with FAM99B, the following protocol details GalNAc-conjugated lncRNA development:
Step 1: Identification of Functional lncRNA Domain
- Perform 5' and 3' RACE to determine full-length sequence
- Generate truncation mutants through serial deletion
- Test tumor-suppressive activity in vitro (CCK-8, colony formation, migration assays)
- Identify minimal functional domain (e.g., FAM99B65-146) [63]
Step 2: Chemical Synthesis and Conjugation
- Synthesize RNA using phosphoramidite chemistry with 2'-O-methyl modifications
- Incorporate phosphorothioate linkages for nuclease resistance
- Conjugate trivalent GalNAc ligand via solid-supported synthesis
- Purify by HPLC and characterize by mass spectrometry [65]
Step 3: In Vivo Efficacy Testing
- Establish orthotopic HCC xenografts via intrahepatic injection of luciferase-expressing Huh7 cells
- Administer GalNAc-conjugated lncRNA truncation (1-10 mg/kg) via subcutaneous injection
- Monitor tumor growth and metastasis via bioluminescent imaging
- Terminate study at 6-8 weeks for histological analysis [63]
LNP-formulated miRNA Mimic/AntagomiR Protocol
Step 1: RNA Design and Modification
- For miRNA mimics: design duplex with guide strand identical to mature miRNA
- For antagomiRs: employ complete LNA or 2'-O-methoxyethyl modification
- Incorporate phosphorothioate backbone for enhanced stability
- Pre-anneal strands in appropriate buffer [64]
Step 2: LNP Formulation
- Prepare lipid mixture (ionizable cationic lipid:phosphatidylcholine:cholesterol:PEG-lipid)
- Employ microfluidic mixing for precise nanoparticle formation
- Dialyze against PBS to remove ethanol and establish pH gradient
- Characterize size (80-100 nm), PDI (<0.2), and RNA encapsulation efficiency (>90%) [64]
Step 3: In Vivo Delivery and Assessment
- Administer via intravenous injection (0.5-3 mg/kg RNA dose)
- Assess biodistribution using fluorescently labeled RNA
- Evaluate target engagement via qRT-PCR of cognate mRNA targets
- Monitor therapeutic efficacy in relevant HCC models [62]
Targeted delivery vectors for ncRNA therapeutics have revolutionized our approach to treating HBV-induced hepatocellular carcinoma. GalNAc conjugation technology has emerged as the leading platform for hepatocyte-specific delivery, with LNP systems providing complementary capabilities for broader hepatic distribution. The continued refinement of these platforms, coupled with emerging technologies such as exosomal delivery and selective ORGAN targeting, promises to expand the therapeutic landscape for liver cancer.
The integration of ncRNA therapeutics with conventional treatments—including immune checkpoint inhibitors and tyrosine kinase inhibitors—represents a promising strategy to overcome resistance mechanisms and improve patient outcomes [62]. As delivery technologies mature and our understanding of HBV-related ncRNA networks deepens, the clinical impact of these targeted therapeutic approaches will undoubtedly grow, ultimately transforming the management of hepatocellular carcinoma.
Navigating Challenges and Optimizing ncRNA-Based Strategies
Addressing Off-Target Effects and Ensuring Specificity in ncRNA Therapeutics
The therapeutic targeting of non-coding RNAs (ncRNAs) represents a transformative approach for treating diseases ranging from cancers to viral infections, including Hepatitis B Virus (HBV)-induced hepatocellular carcinoma (HCC) [65] [24]. Unlike proteins, ncRNAs—particularly microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—offer a unique therapeutic opportunity through complementary base-pairing recognition, potentially making "undruggable" targets accessible [47]. However, this very mechanism of action also presents the foremost challenge in ncRNA therapeutic development: off-target effects that can compromise efficacy and safety [67].
In the context of HBV-induced hepatocarcinogenesis, the dysregulation of ncRNAs creates a complex network of interactions that drive disease progression [8]. HBV infection significantly alters the expression of numerous ncRNAs; for instance, the viral HBx protein upregulates oncogenic miRNAs like miR-21 and represses tumor-suppressive miRNAs such as miR-122 and miR-199a/b [8]. Therapeutic interventions in this environment must achieve precise targeting despite the inherent promiscuity of RNA interactions, the sequence similarities among related ncRNAs, and the potential for immune activation [67]. This technical guide examines the mechanisms of off-target effects in ncRNA therapeutics and provides detailed methodologies for ensuring specificity, with particular emphasis on applications in HBV-HCC research.
Mechanisms of Off-Target Effects
Understanding the molecular origins of off-target effects is fundamental to designing specific ncRNA therapeutics. These unintended effects arise through several well-characterized mechanisms that vary between different ncRNA therapeutic platforms.
Seed Sequence-Mediated Off-Targeting
The seed sequence (nucleotides 2-8 of the guide strand) plays a predominant role in miRNA and siRNA off-target effects [67]. This region mediates imperfect complementarity to unintended mRNA targets, leading to translational repression or mRNA degradation of transcripts with only partial sequence similarity to the intended target. In HBV-HCC, where specific miRNA dysregulation drives oncogenic pathways (e.g., miR-21 targeting PDCD4 and PTEN), therapeutic miRNAs must be designed to avoid inadvertently regulating other critical pathways through seed sequence homology [8].
Immune Activation
Double-stranded RNA (dsRNA) therapeutics can activate pattern recognition receptors, including Toll-like receptors (TLRs) and RIG-I-like receptors, triggering interferon responses and inflammatory cytokine production [67]. This not only causes toxicity but can also alter the expression of numerous genes indirectly. In the context of liver disease, where inflammation already plays a crucial role in disease progression, such immune activation poses significant safety concerns.
Saturation of Endogenous RNAi Machinery
High concentrations of exogenous RNAi compounds can overwhelm cellular processing machinery, including Exportin-5 and RISC components [67]. This saturation effect disrupts the natural miRNA regulatory network, potentially affecting hundreds of endogenous miRNA targets. Given the extensive miRNA dysregulation already present in HBV-HCC, this represents a particularly relevant concern for therapeutic development.
Table 1: Major Types of Off-Target Effects in ncRNA Therapeutics
| Mechanism | Molecular Basis | Primary Impact | Relevant ncRNA Types |
|---|---|---|---|
| Seed Sequence-Mediated | Partial complementarity to unintended mRNAs via nucleotides 2-8 | Repression of transcripts with seed matches | siRNA, miRNA mimics |
| Immune Activation | Recognition by TLRs, RIG-I, and other pattern recognition receptors | Interferon response, inflammatory cytokine release | dsRNA, siRNA |
| RISC Saturation | Competition with endogenous miRNAs for loading into RISC | Disruption of natural miRNA regulatory networks | siRNA, miRNA inhibitors |
| Sequence Similarity | Homology to non-targeted ncRNAs or mRNAs | Modulation of related but unintended RNA targets | All oligonucleotide-based therapeutics |
Computational Design Strategies for Enhanced Specificity
Rational design represents the first line of defense against off-target effects. Multiple computational approaches can significantly reduce the potential for off-target interactions during the therapeutic design phase.
Bioinformatics Screening
Comprehensive in silico screening against transcriptome databases is essential for identifying potential off-target interactions. The following protocol outlines a thorough bioinformatics workflow:
Protocol: Bioinformatics Screening for Off-Target Prediction
- Sequence Alignment: Perform BLAST or similar alignment of the proposed therapeutic sequence against the complete human transcriptome (RefSeq, Ensembl).
- Seed Region Analysis: Specifically identify transcripts with complementarity to nucleotides 2-8 of the guide strand.
- Mismatch Tolerance Mapping: Evaluate potential targets with up to 3 mismatches, giving particular weight to mismatches outside the seed region.
- Free Energy Calculations: Calculate hybridization energies for both intended and potential off-targets using tools like RNAcofold.
- Conservation Analysis: Assess sequence conservation across species for predicted off-target sites to evaluate potential clinical relevance.
This approach is particularly valuable in HBV-HCC research, where the transcriptomic landscape includes both human and viral RNA elements that must be considered in therapeutic design [8].
Algorithm-Guided Design
Specialized algorithms incorporating thermodynamic properties and sequence accessibility significantly improve target specificity. Key considerations include:
- Introducing asymmetric destabilization at the 5' end of the sense strand to promote correct RISC loading
- Avoiding GC-rich sequences that increase promiscuous binding
- Incorporating chemical modification patterns that reduce seed-mediated binding while maintaining on-target activity
Table 2: Key Research Reagent Solutions for Specificity Assessment
| Reagent/Category | Specific Examples | Function in Specificity Research |
|---|---|---|
| Bioinformatics Tools | BLAST, RNAcofold, siRNA design algorithms | Prediction of potential off-target interactions during design phase |
| Chemical Modifications | 2'-O-methyl, 2'-F, 2'-MOE, LNA, GalNAc conjugates | Enhanced nuclease resistance, cellular uptake, and target specificity |
| Screening Libraries | Genome-wide siRNA libraries, miRNA mimics and inhibitors | Systematic assessment of off-target potential across transcriptome |
| Detection Assays | RNA-seq, pSILAC, RISC immunoprecipitation | Comprehensive identification of off-target effects and RISC loading |
| Delivery Systems | Lipid nanoparticles, GalNAc conjugates, AAV vectors | Tissue-specific delivery to reduce exposure in non-target tissues |
Chemical Modification Strategies
Chemical modifications to oligonucleotide therapeutics represent a powerful approach to enhance specificity while improving pharmacological properties.
Backbone and Sugar Modifications
Phosphorothioate (PS) backbones increase nuclease resistance and plasma protein binding, extending half-life [65]. 2'-Sugar modifications (2'-O-methyl, 2'-fluoro, 2'-O-methoxyethyl) enhance binding affinity and reduce immune recognition [65] [47]. These modifications can be strategically placed to direct productive RISC loading while minimizing off-target interactions.
Position-Specific Modification
The specific placement of chemical modifications significantly influences specificity:
- Seed region modifications (e.g., 2'-O-methyl at positions 2-8) reduce seed-mediated off-target effects while largely preserving perfect-match on-target activity
- Asymmetric modifications between sense and antisense strands promote preferential RISC loading of the guide strand
- Terminal stabilizations at 5' and 3' ends protect against exonucleases without compromising RISC functionality
The following diagram illustrates a chemically modified siRNA with strategic enhancements for reduced off-target effects:
Experimental Validation of Specificity
Robust experimental validation is essential to confirm computational predictions and verify therapeutic specificity before clinical advancement.
Transcriptomic Profiling
RNA sequencing provides the most comprehensive approach for identifying off-target effects at the transcriptome level. The following protocol details best practices for transcriptomic profiling of ncRNA therapeutics:
Protocol: RNA-Seq for Off-Target Detection
Treatment Conditions:
- Therapeutic ncRNA at multiple concentrations (including clinically relevant doses)
- Scrambled control sequence
- Untreated controls
- Time points: 24h and 72h post-transfection
Library Preparation:
- Use ribosomal RNA depletion rather than poly-A selection to capture non-coding transcripts
- Employ strand-specific protocols to determine directionality
- Aim for 40-50 million reads per sample
Bioinformatics Analysis:
- Map reads to reference genome (e.g., GRCh38) using Spliced Transcripts Alignment to a Reference (STAR)
- Quantify transcript expression with tools like Salmon or featureCounts
- Identify differentially expressed genes (DEGs) using DESeq2 or edgeR (FDR < 0.1, fold change > 1.5)
- Perform pathway enrichment analysis on DEGs using GO, KEGG, and Reactome databases
In HBV-HCC models, this analysis should include both human and HBV transcripts to fully capture potential off-target effects [8].
Proteomic Approaches
Pulsed stable isotope labeling with amino acids in cell culture (pSILAC) provides direct measurement of changes in protein synthesis rates, complementing transcriptomic data [67]. This method is particularly valuable for detecting off-target effects that occur through translational repression without mRNA degradation.
RISC Loading Analysis
Immunoprecipitation of Ago2 followed by sequencing of bound RNAs directly identifies which transcripts are being targeted by the RISC complex after therapeutic administration. This approach provides the most direct evidence of actual engagement between the therapeutic and its targets.
The following workflow diagram integrates these experimental approaches for comprehensive specificity validation:
Specificity Considerations in HBV-Induced HCC
The molecular environment of HBV-induced hepatocarcinogenesis presents unique challenges and considerations for ncRNA therapeutic specificity.
HBV-Related ncRNA Networks
HBV infection dramatically alters the ncRNA landscape through multiple mechanisms. The HBx viral protein directly modulates host ncRNA expression, including upregulation of oncogenic miR-21 and repression of tumor-suppressive miR-122 [8]. Additionally, HBV DNA integration into the host genome can disrupt ncRNA genes and regulatory regions. Therapeutic design must account for this altered landscape, targeting key hubs in the HBV-HCC ncRNA network while avoiding further destabilization of the regulatory system.
Tissue-Specific Delivery
The liver-specific delivery of ncRNA therapeutics represents both a challenge and an opportunity for HBV-HCC treatment. N-acetylgalactosamine (GalNAc) conjugation enables targeted delivery to hepatocytes through binding to asialoglycoprotein receptors [65] [68]. This approach minimizes exposure to non-target tissues, effectively reducing systemic off-target effects. Current FDA-approved RNA therapeutics like givosiran and inclisiran demonstrate the clinical viability of this strategy [65] [47].
Combination Approaches
The complexity of HBV-HCC ncRNA networks suggests that combination therapies targeting multiple nodes may be more effective than single-target approaches. However, this strategy requires careful optimization to avoid synergistic off-target effects. Rational combination design should target functionally related ncRNAs with non-overlapping off-target profiles.
Table 3: Clinically Approved ncRNA Therapeutics and Their Specificity Features
| Therapeutic | Type | Target | Specificity Enhancements | Indication |
|---|---|---|---|---|
| Patisiran (Onpattro) | siRNA | Transthyretin (TTR) | LNP delivery, 2'-F/2'-O-Me modifications | hATTR amyloidosis |
| Givosiran (Givlaari) | siRNA | ALAS1 | GalNAc conjugation, tissue-specific delivery | Acute hepatic porphyria |
| Lumasiran (Oxlumo) | siRNA | HAO1 | GalNAc conjugation, seed region optimization | Primary hyperoxaluria type 1 |
| Inclisiran (Leqvio) | siRNA | PCSK9 | GalNAc conjugation, enhanced metabolic stability | Hypercholesterolemia |
Emerging Technologies and Future Directions
Novel approaches to enhance ncRNA therapeutic specificity continue to emerge, offering promising solutions to current limitations.
RNA-Targeting Chimeras
Ribonuclease targeting chimeras (RIBOTAC) represent a innovative approach that recruits endogenous RNases to degrade specific RNA targets [47]. This technology utilizes small molecules that bind both the target RNA and RNase L, directing localized RNA degradation with high specificity. While still in early development, RIBOTACs offer the potential for enhanced specificity through small molecule recognition of structural RNA elements.
CRISPR-Based Approaches
CRISPR-Cas13 systems provide an alternative mechanism for targeted RNA degradation with different specificity constraints than RNAi-based approaches [47]. The requirement for protospacer adjacent motifs (PAMs) in some Cas13 variants naturally constrains targetable sequences, while the use of single guide RNAs (sgRNAs) with full complementarity to targets may reduce seed-mediated off-target effects.
Advanced Screening Platforms
High-throughput screening technologies continue to evolve, with genome-wide CRISPR screens now enabling systematic identification of genetic modifiers of ncRNA therapeutic efficacy and specificity. These approaches can identify synthetic lethal interactions and pathway dependencies that inform both target selection and combination therapy design.
The strategic addressing of off-target effects remains the critical path for advancing ncRNA therapeutics from laboratory tools to reliable medicines. For HBV-induced hepatocellular carcinoma, where the ncRNA network is extensively rewired, specificity is not merely a technical consideration but a fundamental requirement for therapeutic success. Through integrated application of computational design, chemical modification, robust experimental validation, and tissue-specific delivery, researchers can develop ncRNA therapeutics with the precision needed to target HBV-HCC pathogenesis while sparing normal cellular functions. As these technologies mature, they offer the promise of transforming the treatment landscape for this devastating malignancy.
Overcoming Stability and Pharmacokinetic Hurdles of RNA Molecules In Vivo
The therapeutic potential of RNA molecules extends from targeting traditionally "undruggable" proteins to modulating disease-causing genes in hepatitis B virus (HBV)-induced hepatocellular carcinoma (HCC) [69]. However, the clinical application of RNA therapeutics faces significant challenges related to stability and pharmacokinetics. Native RNA molecules are rapidly degraded by nucleases, exhibit low affinity for plasma proteins resulting in rapid clearance, and cannot efficiently cross cell membranes for intracellular delivery [70]. Understanding and overcoming these biological barriers is essential for developing effective RNA-based treatments for HBV-related hepatocarcinogenesis, where non-coding RNAs (ncRNAs) play critical regulatory roles [16]. This technical guide examines current strategies to enhance RNA stability and pharmacokinetic properties, with specific application to HBV-HCC research and therapy.
Core Challenges for RNA Therapeutics In Vivo
Stability and Degradation
RNA instability presents a fundamental challenge for therapeutic development. RNA is prone to both chemical degradation and physical instability in biological systems [71]. Key factors affecting RNA stability include:
- Length: Longer RNA transcripts demonstrate negatively correlated stability profiles [71].
- Structural elements: Integrity of the 5' cap and 3' poly-A tail significantly impacts stability [71].
- Environmental conditions: pH, buffering species, temperature, and divalent cation concentration all influence degradation rates [71].
- Nucleases: Ubiquitous ribonucleases in plasma and tissues rapidly degrade unmodified RNA [70].
The activation energy for mRNA degradation has been measured at approximately 31.5 kcal/mol normalized per phosphodiester backbone, highlighting the inherent thermodynamic instability of these molecules [71].
Pharmacokinetic Barriers
RNA therapeutics face multiple pharmacokinetic barriers that limit their clinical utility:
Absorption: Most RNA therapeutics require parenteral administration (intravenous or subcutaneous) due to poor bioavailability from other routes [70]. Bioavailability after subcutaneous administration is typically low to intermediate, primarily due to nucleolytic degradation at the administration site [70].
Distribution: The molecular size and highly negatively-charged backbone of RNA therapeutics result in limited tissue distribution and a low volume of distribution [70]. Efficient delivery to target organs, particularly the liver in HBV-HCC therapy, requires specialized formulation approaches.
Metabolism and Excretion: Nucleases metabolize RNA therapeutics to shortened chains, though the metabolic ratio is relatively low compared to small molecule drugs [70]. Consequently, most RNA therapeutics are excreted predominantly in their intact form [70].
Table 1: Key Pharmacokinetic Properties of Representative RNA Therapeutics
| Drug | Type | Administration Route | Primary Modifications | Target Indication |
|---|---|---|---|---|
| Nusinersen | ASO | Intrathecal | 2'-O-MOE, PS linkage | Spinal muscular atrophy [70] |
| Patisiran | siRNA | IV | LNP formulation | Hereditary transthyretin-mediated amyloidosis [70] |
| Inclisiran | siRNA | SC | 2'-F, 2'-OMe, PS linkage, GalNAc | Primary hypercholesterolemia [70] |
| Eteplirsen | ASO | IV | PMO | Duchenne muscular dystrophy[ccitation:2] |
Strategic Solutions for Enhanced Stability and PK Properties
Chemical Modifications
Strategic chemical modifications to the RNA structure represent the primary approach for enhancing stability and pharmacokinetics:
Sugar moiety modifications: The 2'-carbon position of ribose is most frequently modified, with 2'-O-methyl (2'-O-Me), 2'-fluoro (2'-F), and 2'-O-methoxyethyl (2'-O-MOE) modifications conferring nuclease resistance and extending half-life [70].
Backbone modifications: Phosphorothioate (PS) linkages, where a non-bridging oxygen is substituted with sulfur, provide resistance to nuclease degradation and enhance tissue uptake [70].
Morpholino oligomers: Phosphorodiamidate morpholino oligomers (PMO) contain modified morpholine rings connected by phosphorodiamidate linkages, conferring extensive enzymatic resistance [70].
Table 2: RNA Chemical Modifications and Their Functional Impacts
| Modification Type | Representative Examples | Primary Benefits | Clinical Examples |
|---|---|---|---|
| Sugar Modifications | 2'-O-Me, 2'-F, 2'-O-MOE | Nuclease resistance, increased binding affinity | Givosiran, Lumasiran [70] |
| Backbone Modifications | Phosphorothioate (PS) | Nuclease resistance, protein binding, tissue uptake | Mipomersen, Inotersen [70] |
| Conjugate Chemistry | GalNAc | Targeted liver delivery | Givosiran, Inclisiran [70] |
| Structural Scaffold | PMO | Enzymatic resistance, neutral backbone | Eteplirsen, Golodirsen [70] |
Advanced Delivery Systems
Formulation strategies significantly enhance the delivery and efficacy of RNA therapeutics:
Lipid Nanoparticles (LNPs): Patisiran, the first FDA-approved siRNA drug, utilizes an LNP system comprising four lipid excipients (including DLin-MC3-DMA and PEG2000-C-DMG) for circulation stability and effective liver uptake [70].
Ligand Conjugates: N-acetylgalactosamine (GalNAc) conjugates facilitate targeted delivery to hepatocytes through asialoglycoprotein receptor-mediated endocytosis, as demonstrated by givosiran, lumasiran, and inclisiran [70].
Experimental Protocols for Stability and PK Assessment
RNA Stability Assessment Protocol
Objective: Quantify RNA integrity under various conditions to guide formulation development.
Materials:
- Purified RNA therapeutic (synthesized with desired modifications)
- Appropriate buffer systems (e.g., citrate, phosphate, Tris) across pH range
- Differential Scanning Calorimeter (DSC)
- Circular Dichroism Spectrometer
- Thermal cycler or controlled temperature water baths
- Agarose or polyacrylamide gel electrophoresis system
- RNA staining solution (e.g., SYBR Gold)
Methodology:
- Sample Preparation:
- Prepare RNA solutions at multiple concentrations (e.g., 0.1-1.0 mg/mL) in selected buffers.
- Aliquot samples into nuclease-free containers.
Temperature Stability Studies:
- Incubate samples at controlled temperatures (4°C, 25°C, 37°C, 55°C).
- Remove aliquots at predetermined time points (0, 1, 3, 7, 14, 28 days).
- Analyze integrity by gel electrophoresis and quantify degradation bands.
Thermodynamic Analysis:
- Using DSC, determine the onset temperature of melting (Tm).
- Calculate activation energy for degradation using Arrhenius equation from data collected at multiple temperatures.
Structural Integrity Assessment:
- Use circular dichroism to monitor changes in secondary structure under different conditions.
- Correlate structural changes with functional activity when possible.
Data Analysis:
- Plot percentage of intact RNA versus time to determine degradation kinetics.
- Compare stability across different buffer compositions, pH values, and RNA modifications [71].
Pharmacokinetic Evaluation Protocol
Objective: Characterize absorption, distribution, metabolism, and excretion of RNA therapeutics in preclinical models.
Materials:
- Radiolabeled or fluorescently tagged RNA construct
- Appropriate animal model (typically rodent)
- Liquid chromatography-tandem mass spectrometry (LC-MS/MS) system
- Tissue homogenization equipment
- Scintillation counter or fluorescence detector
- Surgical equipment for blood and tissue collection
Methodology:
- Dose Administration:
- Administer RNA therapeutic via relevant routes (IV, SC) at therapeutically relevant doses.
- Include both single-dose and multiple-dose regimens when appropriate.
Sample Collection:
- Collect blood/serum/plasma at predetermined time points post-dose (e.g., 5 min, 15 min, 30 min, 1, 2, 4, 8, 12, 24, 48, 72 hours).
- At terminal time points, collect tissues of interest (liver, kidney, spleen, etc.).
Bioanalysis:
- Extract RNA from biological matrices using appropriate methods.
- Quantify intact RNA and major metabolites using specific assays (e.g., hybridization ELISA, LC-MS/MS).
- For tissue distribution studies, quantify drug levels in homogenized tissues.
Data Analysis:
- Calculate standard PK parameters: Cmax, Tmax, AUC, half-life, clearance, volume of distribution.
- Determine absolute bioavailability for non-IV routes.
- Assess tissue distribution patterns and accumulation [70].
Application to HBV-Induced Hepatocarcinogenesis
In HBV-related HCC, ncRNAs including miRNAs, lncRNAs, and circRNAs play critical regulatory roles in tumor progression, making them attractive therapeutic targets [16]. Successful targeting requires overcoming the stability and delivery challenges specific to the liver microenvironment:
- Oncogenic miRNAs: miR-21, regulated by HBx, is consistently upregulated in HBV-HCC and targets tumor suppressors PDCD4 and PTEN [16].
- Tumor-suppressive miRNAs: miR-122, a liver-specific miRNA, is downregulated in HCC and affects metabolic pathways including anaerobic glycolysis by targeting pyruvate kinase M2 (PKM2) [16].
- Therapeutic restoration: For tumor-suppressive miRNAs like miR-122, chemical modifications (2'-F, 2'-O-Me, PS backbone) enhance stability in circulation and facilitate delivery to hepatocytes.
Diagram 1: HBV Modulation of ncRNAs in Hepatocarcinogenesis
Research Reagent Solutions
Table 3: Essential Research Reagents for RNA Therapeutic Development
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Stabilizing Excipients | Sucrose, trehalose, PEG | Protect RNA against degradation during storage and delivery [71] |
| Buffer Systems | Citrate, phosphate, Tris | Maintain optimal pH for RNA stability [71] |
| Delivery Vehicles | LNPs, GalNAc conjugates, polymers | Enhance cellular uptake and targeted delivery [70] |
| Analytical Tools | DSC, CD spectroscopy, LC-MS/MS | Characterize RNA stability and pharmacokinetics [71] |
| Modification Enzymes | Capping enzymes, poly-A polymerases | Generate 5' cap and 3' poly-A tail for enhanced stability [70] |
| Nuclease Inhibitors | RNase inhibitors, antisera | Prevent degradation during experimental procedures [70] |
Diagram 2: RNA Therapeutic Optimization Strategy
Overcoming the stability and pharmacokinetic challenges of RNA molecules requires integrated strategies combining chemical modifications, advanced delivery systems, and optimized formulations. The application of these approaches to HBV-induced hepatocarcinogenesis enables targeting of critical ncRNAs involved in disease progression. As RNA therapeutic technology continues to evolve, with advancements in computational design, screening methodologies, and delivery platforms, the potential for effective RNA-based treatments for HBV-HCC and other liver diseases continues to expand.
Strategies to Counteract Viral Heterogeneity and Treatment Resistance
Viral heterogeneity presents a formidable challenge in the treatment of chronic hepatitis B virus (HBV) infection and the prevention of HBV-associated hepatocellular carcinoma (HCC). This technical review comprehensively examines the mechanisms by which HBV diversity, particularly through non-coding RNA (ncRNA) alterations, drives treatment resistance and hepatocarcinogenesis. We synthesize current research on viral evolution, host-virus interactions, and emerging therapeutic strategies designed to overcome resistance barriers. The analysis specifically focuses on HBV-induced ncRNA aberrations as both drivers of heterogeneity and potential therapeutic targets, providing a framework for developing next-generation antiviral interventions that maintain efficacy across diverse viral populations and host environments.
Chronic hepatitis B virus infection affects approximately 296 million people globally and represents a primary etiology of hepatocellular carcinoma, accounting for over 80% of cases in high-prevalence regions [16] [19]. The remarkable genetic diversity of HBV, stemming from its error-prone reverse transcriptase and high replication rate, facilitates rapid evolution under selective pressure from antiviral therapies and host immune responses [72]. This heterogeneity manifests through multiple mechanisms: the emergence of resistance mutations to direct-acting antivirals (DAAs), viral integration into the host genome leading to insertional mutagenesis, and profound alterations to the host cellular environment through viral proteins, particularly the HBV X protein (HBx) [20] [6].
The HBx protein serves as a central orchestrator of HBV-induced hepatocarcinogenesis, functioning as a multifunctional oncoprotein that localizes to both cytoplasm and nucleus [19]. HBx transactivates viral and cellular promoters by interacting with various transcription factors and modulating cytoplasmic signaling pathways associated with cell growth and survival, including nuclear factor kappa B (NF-κB) and mitogen-activated protein kinase (MAPK) pathways [19]. Crucially, HBx achieves these effects largely through systematic manipulation of the host's non-coding RNA landscape, creating an environment conducive to viral persistence and malignant transformation.
Recent evidence further suggests that environmental co-factors significantly influence HBV pathogenicity. A 2025 study demonstrated that HBV alone does not cause liver inflammation or cancer in mouse models but dramatically augments carcinogen-induced hepatocarcinogenesis through modulation of the immune response, specifically via the IL-33/regulatory T cell axis [26]. This highlights the complex interplay between viral factors, host pathways, and environmental exposures in driving heterogenous disease outcomes.
HBV-Induced Non-Coding RNA Alterations in Hepatocarcinogenesis
Types and Functions of HBV-Related Non-Coding RNAs
Non-coding RNAs constitute approximately 90% of the human genome and have emerged as critical regulators in HBV-associated HCC pathogenesis [16] [19]. These RNAs are broadly categorized by size and function, with key classes including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), circular RNAs (circRNAs), and small nucleolar RNAs (snoRNAs). HBV, particularly through HBx, systematically dysregulates these ncRNAs to create a favorable environment for viral persistence and oncogenic progression [16].
Table 1: Major Classes of Non-Coding RNAs in HBV-Hepatocarcinogenesis
| ncRNA Class | Size Range | Primary Functions | Role in HBV-HCC | Key Examples |
|---|---|---|---|---|
| miRNAs | 19-25 nucleotides | Post-transcriptional gene regulation via mRNA targeting | Oncogenic or tumor suppressive functions; extensively modulated by HBx | miR-21, miR-122, let-7a, miR-148a [16] [19] |
| lncRNAs | >200 nucleotides | Chromatin modification, transcriptional regulation, molecular sponges | Promoted by HBx to influence proliferation, metastasis | KCNQ1OT1, DLEU2, HOTAIR [16] [29] |
| circRNAs | Variable | miRNA sponges, protein decoys, regulators of transcription | Modulate HBV-related signaling pathways | Numerous circRNAs implicated in immune regulation [16] |
| snoRNAs | 60-300 nucleotides | Guide chemical modifications of other RNAs | Dysregulated in HBV-HCC; potential biomarkers | SNORD31, SNORD17 [16] |
Mechanisms of HBx-Mediated ncRNA Dysregulation
HBx employs multiple sophisticated mechanisms to hijack the host's ncRNA network. These mechanisms include:
Transcriptional Regulation: HBx modulates ncRNA expression by interacting with transcription factors such as p53, c-Myc, survivin, and NF-κB [19]. For instance, HBx inhibits p53-mediated activation of miR-148a and miR-216b, thereby activating downstream oncogenic pathways including AKT/ERK/FOXO4/ATF5 and IGF2BP2 signaling [19].
Epigenetic Manipulation: HBx induces epigenetic repression of tumor-suppressive miRNAs through promoter hypermethylation. This mechanism has been demonstrated for miR-132 and miR-205, where DNA methyltransferase activation leads to their silencing [19].
ceRNA Network Disruption: HBx upregulates specific lncRNAs that function as competing endogenous RNAs (ceRNAs), effectively "sponging" tumor-suppressive miRNAs and preventing them from binding their natural mRNA targets. A 2025 study identified the KCNQ1OT1/miR-335-5p/CDC7 axis as a key pathway promoted by HBV core protein (HBc) that drives HCC proliferation and migration [29].
Post-transcriptional Regulation: HBx influences miRNA biogenesis pathways and stability, as seen with the HBx-mediated downregulation of miR-101, which subsequently leads to increased DNA methyltransferase 3A (DNMT3A) expression and aberrant DNA methylation patterns [19].
Experimental Approaches for Investigating ncRNA in HBV Pathogenesis
Core Methodologies for ncRNA Network Analysis
Table 2: Essential Experimental Protocols for HBV-ncRNA Research
| Methodology | Application | Key Steps | Technical Considerations |
|---|---|---|---|
| ceRNA Network Construction | Identify lncRNA-miRNA-mRNA interactions | 1. Download HCC and normal tissue data from TCGA2. Identify differentially expressed genes using DESeq23. Classify into lncRNA, miRNA, mRNA using GDCRNATools4. Predict interactions via ENCORI/starBase5. Visualize network with Cytoscape | Ensure rigorous statistical thresholds (FDR <0.05, log2FC >1) to minimize false positives [29] |
| Luciferase Reporter Assay | Validate predicted miRNA-mRNA interactions | 1. Clone wild-type and mutant 3'UTR sequences into reporter vector2. Co-transfect with miRNA mimics/inhibitors3. Measure luciferase activity 24-48h post-transfection | Include multiple negative controls; confirm specificity with mutant constructs [29] |
| Functional Validation | Assess phenotypic impact of ncRNAs | 1. Modulate ncRNA expression (overexpression/knockdown)2. Conduct CCK-8 and colony formation assays for proliferation3. Perform wound healing and Transwell assays for migration4. Analyze apoptosis via flow cytometry | Use multiple cell lines (e.g., HepG2, HepG2.215, SMMC-7721) to confirm findings [29] |
| HBV Protein-specific Effects | Determine viral components responsible | 1. Transfect cells with HBV whole genome or individual protein plasmids (HBx, HBs, HBc)2. Measure ncRNA and target gene expression via qRT-PCR and Western blot3. Correlate with functional phenotypes | Include empty vector controls; verify protein expression [29] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating HBV-ncRNA Interactions
| Reagent/Cell Line | Specifications | Research Application | Key Findings Enabled |
|---|---|---|---|
| HepG2.215 | Human hepatocellular carcinoma cells stably transfected with HBV genome (RRID: CVCL_L855) | Model of persistent HBV infection; assess viral-ncRNA interactions | Confirmed HBV-induced alterations to lncRNA and miRNA expression profiles [29] |
| pAAV-HBV1.2 Vector | AAV vector containing 1.2x length HBV genome | Establish HBV persistence in mouse models via hydrodynamic injection | Demonstrated that HBV alone doesn't cause cancer but amplifies carcinogen effects [26] |
| HBx, HBs, HBc Plasmids | Recombinant plasmids expressing individual HBV proteins | Dissect specific viral protein contributions to ncRNA dysregulation | Identified HBc as inducer of KCNQ1OT1/miR-335-5p/CDC7 axis [29] |
| γ-Secretase Inhibitors | Small molecule inhibitors (e.g., LY411575) | Increase surface BCMA expression by preventing cleavage | Enhanced BCMA-targeted CAR-T efficacy; applicable to other membrane proteins [73] |
Figure 1: HBV-Induced ncRNA Alterations Drive Treatment Resistance and Hepatocarcinogenesis. HBV proteins, particularly HBx and HBc, systematically dysregulate non-coding RNA networks, activating multiple oncogenic pathways that culminate in treatment resistance and hepatocellular carcinoma development.
Strategic Approaches to Overcome Viral Heterogeneity and Resistance
Targeting the Genetic Basis of Antiviral Resistance
The emergence of resistance mutations represents a fundamental challenge in HBV therapy. Several factors influence resistance development, including:
Genetic Barrier to Resistance: Defined as the number of mutations required for resistance development. DAAs typically have lower genetic barriers compared to host-targeted antivirals (HTAs) [72]. For instance, resistance to lamivudine (3TC) and emtricitabine (FTC) can emerge through a single M184V substitution in HIV reverse transcriptase, conferring 300-600 fold reduction in potency [72].
Mutation Type and Frequency: Transition mutations (AG, CT) occur more frequently than transversion mutations, affecting how rapidly resistant variants emerge [72].
Pharmacological Factors: Suboptimal drug exposure due to poor pharmacokinetics or inadequate adherence creates selective pressure for resistance emergence. Maintaining consistent viral suppression is critical to prevent resistant variant selection [72].
Strategic solutions include developing combination therapies targeting multiple viral proteins simultaneously, designing antivirals with higher genetic barriers, and implementing resistance testing before treatment initiation to guide therapeutic selection.
Novel Therapeutic Platforms Addressing Heterogeneity
Combination Therapies to Modulate Antigen Expression
Overcoming antigenic heterogeneity is crucial for both immune-mediated therapies and antiviral approaches. Several combination strategies show promise:
Protease Inhibition: γ-secretase inhibitors (GSIs) prevent cleavage of target antigens like BCMA, increasing their surface density and enhancing CAR-T cell efficacy. A phase 1 clinical trial demonstrated that GSI combined with BCMA CAR-T cells was well-tolerated and increased target antigen density in vivo [73].
Signaling Pathway Modulation: ALK inhibitors prevent internalization and degradation of ALK in neuroblastomas, increasing surface expression and enhancing CAR-T cell cytotoxicity against tumors with low baseline ALK expression [73].
Epigenetic Reactivation: Demethylating agents like 5-Azacytidine (5-AZA) can reactivate epigenetically silenced genes, restoring expression of target antigens such as CD123 and CD70 on AML cells [73].
Advanced Cellular Engineering Strategies
Innovative approaches in cellular engineering offer promising avenues to address viral and tumor heterogeneity:
Multi-Targeting CAR-T Cells: Engineering T cells with multiple antigen receptors or tandem CARs that can recognize several targets simultaneously, reducing the likelihood of escape through antigen loss [73].
CAR Structure Optimization: Modifying CAR structures to enhance sensitivity to low-density antigens through affinity tuning, incorporation of costimulatory domains, and prevention of CAR downregulation [73].
Trogocytosis Mitigation: Implementing strategies to reduce trogocytosis (transfer of antigens from tumor cells to CAR-T cells), which contributes to fratricide and T cell exhaustion. Approaches include using low-affinity CARs, modifying cholesterol metabolism, and targeting the ATF3-CH25H regulatory axis [73].
Figure 2: Strategic Framework for Overcoming Viral Heterogeneity and Treatment Resistance. Multiple complementary approaches address distinct resistance mechanisms to achieve broad antigen coverage and sustained treatment response.
Targeting the HBV-ncRNA Axis for Therapeutic Advantage
The intricate relationship between HBV and host nc networks presents unique therapeutic opportunities:
miRNA-Based Therapeutics: Synthetic miRNA mimics (for tumor-suppressive miRNAs) and antagomirs (for oncogenic miRNAs) offer potential to restore normal regulatory networks. For instance, miR-122 supplementation could counteract HBx-mediated suppression, while anti-miR-21 oligonucleotides could reduce its oncogenic activity [16] [19].
LncRNA Targeting: Specifically designed antisense oligonucleotides (ASOs) or small interfering RNAs (siRNAs) can target oncogenic lncRNAs upregulated in HBV-HCC, such as KCNQ1OT1 [29].
Nanoparticle Delivery Systems: Lipid-based or polymeric nanoparticles can enhance delivery of ncRNA-targeting therapeutics to hepatocytes, improving efficacy while reducing off-target effects.
Combinatorial ncRNA Approaches: Simultaneously targeting multiple nodes in dysregulated ncRNA networks, such as combining KCNQ1OT1 inhibition with miR-335-5p restoration [29].
The formidable challenge of viral heterogeneity and treatment resistance in HBV-associated hepatocarcinogenesis demands innovative approaches that target both viral and host factors. The emerging understanding of HBV-induced ncRNA alterations provides a sophisticated framework for developing next-generation therapeutics that address the fundamental mechanisms driving resistance.
Future research directions should prioritize several key areas: First, comprehensive mapping of HBV-ncRNA interaction networks across different disease stages and viral genotypes to identify conserved vulnerabilities. Second, development of advanced delivery systems that enable efficient targeting of ncRNAs in hepatocytes. Third, exploration of combination strategies that simultaneously address multiple resistance mechanisms, such as combining DAAs with ncRNA-targeting approaches and immunomodulators.
The recent identification of pitavastatin as an IL-33 inhibitor that can suppress HBV-plus-carcinogen-induced liver cancer in mouse models offers promise for repurposing existing medications to prevent HCC in HBV carriers [26]. Similarly, the delineation of specific axes like KCNQ1OT1/miR-335-5p/CDC7 provides novel therapeutic targets for intervention [29].
As we advance our understanding of viral heterogeneity and host-virus interactions, the integration of ncRNA-targeting strategies with conventional antivirals and emerging immunotherapies holds significant potential to overcome treatment resistance and improve outcomes for patients with chronic HBV infection and HBV-associated hepatocellular carcinoma.
The management of chronic Hepatitis B Virus (HBV) infection, particularly in individuals co-infected with HIV, represents a significant clinical challenge. The pursuit of a functional cure, characterized by sustained HBsAg loss, has emerged as the cornerstone of modern HBV therapy [74]. This whitepaper examines the critical intersection of finite treatment strategies for HBV, informed by co-infection models and the growing understanding of HBV-induced hepatocarcinogenesis. Emerging evidence reveals that HBV promotes hepatocellular carcinoma (HCC) through complex mechanisms involving viral proteins and non-coding RNA (ncRNA) networks that alter host gene expression and immune responses [16] [9] [29]. Within the context of HIV-HBV co-infection, where accelerated liver disease progression occurs, optimizing finite treatment requires careful consideration of antiviral selection, monitoring parameters, and novel therapeutic targets. This review synthesizes current guidelines, mathematical modeling insights, and molecular mechanisms to provide a comprehensive framework for developing effective finite treatment regimens against the backdrop of HBV-driven oncogenic pathways.
Chronic HBV infection remains a substantial global health burden, affecting approximately 350 million individuals worldwide and significantly increasing the risk for cirrhosis and hepatocellular carcinoma (HCC) [6]. In HIV-co-infected individuals, the challenge is magnified, with increased HBV viremia, decreased spontaneous clearance, and accelerated progression to end-stage liver disease compared to HBV mono-infection [75]. The 2025 guidelines from the Canadian Association for the Study of the Liver (CASL) and the Association of Medical Microbiology and Infectious Disease (AMMI) Canada emphasize a patient-centered approach with expanded treatment indications and refined diagnostic protocols [76].
The paradigm of HBV management is shifting from indefinite viral suppression toward finite treatment regimens aiming for functional cure. This transition is particularly relevant in co-infected individuals, where long-term multidrug therapy poses challenges of cumulative toxicity, drug interactions, and adherence issues. Simultaneously, research into HBV-associated hepatocarcinogenesis has revealed the pivotal role of non-coding RNAs—including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—in mediating HBV-driven oncogenic transformation [16]. These ncRNAs function as critical regulators of gene expression, influencing key cancer hallmarks including proliferation, apoptosis, immune evasion, and metastasis.
Table 1: Key Challenges in HIV-HBV Co-infection Management
| Challenge | Clinical Impact | Guideline Recommendation |
|---|---|---|
| Accelerated Disease Progression | Increased risk of cirrhosis and HCC | Expanded treatment criteria regardless of ALT levels [76] |
| Altered Serological Patterns | Decreased HBeAg clearance, occult infections | Comprehensive serological profiling and HBV DNA monitoring [75] |
| ART Selection Constraints | Need for dual HBV/HIV activity | TAF, TDF, or ETV as first-line with fully suppressive ART [76] [75] |
| NcRNA-Mediated Hepatocarcinogenesis | Enhanced tumor progression via immune modulation | Research focus on novel biomarkers and therapeutic targets [16] [9] |
HBV-Induced ncRNA Alterations in Hepatocarcinogenesis
The mechanistic link between chronic HBV infection and hepatocellular carcinoma involves sophisticated reprogramming of the host's non-coding RNA landscape. HBV proteins, particularly the HBx protein and core/capsid protein (HBc), dysregulate multiple ncRNA networks that collectively promote oncogenic transformation.
MicroRNA Dysregulation in HBV-HCC
MicroRNAs serve as critical mediators of HBV-induced hepatocarcinogenesis, with distinct profiles functioning as either oncogenes or tumor suppressors. Key dysregulated miRNAs include:
- Oncogenic miRNAs: miR-21, regulated by HBx, targets tumor suppressors PDCD4 and PTEN; miR-221/222 promote cell cycle progression and inhibit apoptosis; the miR-17-92 cluster enhances proliferation, angiogenesis, and immune evasion [16].
- Tumor-Suppressive miRNAs: miR-122, a liver-specific miRNA crucial for metabolic regulation, is downregulated in HCC; miR-199a/b inhibits ROCK1 and PI3K/Akt pathways; miR-125b targets VEGFA to inhibit angiogenesis; miR-101, downregulated by HBx, modulates DNA methylation patterns by targeting DNMT3A [16].
Long Non-Coding RNA Networks in HBV-Associated HCC
LncRNAs have emerged as central players in HBV-driven HCC, functioning through complex regulatory mechanisms:
- HDAC2-AS2: This TGFβ-inducible lncRNA is significantly upregulated in HBV-associated HCC tissues and correlates with poor survival. HBV infection increases TGFβ secretion, which in turn upregulates HDAC2-AS2 expression. Tumor-derived extracellular vesicles enriched with HDAC2-AS2 suppress CD8+ T cell cytotoxicity by blocking cytosolic translocation of CDK9, leading to T cell exhaustion and impaired antitumor immunity [9].
- KCNQ1OT1: This lncRNA functions as a competing endogenous RNA (ceRNA) by binding to miR-335-5p, thereby upregulating cell division cycle 7 (CDC7)—a key regulator of DNA replication and cell cycle progression. HBV core protein significantly induces the KCNQ1OT1/miR-335-5p/CDC7 axis, promoting HCC proliferation and migration [29].
Figure 1: HBV-Induced ncRNA Networks in Hepatocarcinogenesis. HBV proteins activate TGFβ signaling, which upregulates oncogenic lncRNAs HDAC2-AS2 and KCNQ1OT1. These lncRNAs promote HCC through immune evasion (via CD8+ T cell suppression) and enhanced cell proliferation (via CDC7 activation).
Environmental Carcinogens and HBV Synergy in HCC Development
Notably, HBV alone may not be sufficient to induce hepatocarcinogenesis. Recent research demonstrates that HBV alters the liver's response to environmental carcinogens, such as diethylnitrosamine (DEN), by modulating the immune microenvironment. HBV synergizes with carcinogens to upregulate interleukin-33 (IL-33), which activates regulatory T cells (Tregs) and suppresses CD8+ T cell function, creating a permissive environment for cancer development [26]. This mechanism highlights the importance of considering environmental exposures in managing HBV-infected individuals, particularly in the context of finite treatment strategies.
Finite Treatment Strategies in HIV-HBV Co-infection
Current Treatment Guidelines and Regimen Selection
The 2025 guidelines from leading hepatology organizations reflect a trend toward earlier and broader treatment initiation. Key recommendations include:
- Expanded Treatment Indications: Treatment is now recommended for HBeAg-positive patients over 40 years with normal ALT and HBV DNA >2,000 IU/mL (formerly immune tolerant), and for HBeAg-negative patients over 40 years with normal ALT and HBV DNA >2,000 IU/mL to reduce HCC risk [76].
- First-Line Therapies: Tenofovir alafenamide (TAF), tenofovir disoproxil fumarate (TDF), or entecavir (ETV) are recommended as first-line monotherapy for HBV mono-infection. In HIV-HBV co-infection, ART regimens must include drugs with dual activity against both viruses [76] [75].
- Treatment Monitoring: Quantitative HBV DNA testing every 6 months during NA therapy confirms adherence and efficacy, while quantitative HBsAg measurement every 1-2 years helps monitor treatment response and functional cure potential [76].
Table 2: Finite Treatment Endpoints and Monitoring Parameters in HIV-HBV Co-infection
| Treatment Goal | Virological Marker | Monitoring Frequency | Special Considerations in Co-infection |
|---|---|---|---|
| Viral Suppression | HBV DNA <20 IU/mL | Every 3-6 months during treatment; more frequently if adherence concerns | Must maintain ART with anti-HBV activity regardless of HBV DNA level |
| HBeAg Seroconversion | HBeAg loss, anti-HBe appearance | Every 6-12 months | Delayed seroconversion in co-infection; longer treatment duration often needed |
| Functional Cure | HBsAg loss with or without anti-HBs development | Annually if HBsAg positive; confirm sustained response if HBsAg loss occurs | Rare in co-infection; should not guide ART decisions |
| Immune Reconstitution | CD4+ count, HIV RNA | According to HIV monitoring guidelines | HBV flare risk during immune recovery; requires close monitoring |
Mathematical Modeling Insights for Treatment Optimization
Mathematical modeling of HIV-HBV co-infection dynamics provides valuable insights for optimizing finite treatment strategies. A 2025 integer-order co-infection model evaluated the cost-effectiveness of various control strategies, including:
- HIV protection controls (education, PrEP, harm reduction)
- HBV vaccination
- HIV treatment (ART)
- HBV treatment (antivirals)
The model demonstrated that implementing all control strategies simultaneously had the greatest impact on reducing co-infection prevalence. However, cost-effectiveness analysis identified strategy 4—combining HIV protection controls with HBV treatment—as the most cost-effective approach [77]. This finding supports integrated prevention and treatment programs rather than isolated interventions.
Novel Biomarkers for Guiding Finite Therapy
Emerging biomarkers beyond traditional virological markers show promise for personalizing finite treatment approaches:
- Quantitative HBsAg (qHBsAg): Useful for predicting functional cure and guiding treatment cessation decisions [74].
- HBV RNA and HBcrAg: These novel markers reflect transcriptional activity of covalently closed circular DNA (cccDNA) and may help identify patients who can safely discontinue therapy [74].
- NcRNA Profiles: Specific miRNA and lncRNA signatures associated with HBV integration and HCC risk may help stratify patients for more intensive monitoring or extended treatment duration [16] [9] [29].
Experimental Approaches and Research Reagents
Key Methodologies for Investigating HBV-ncRNA Interactions
Advanced experimental techniques are essential for delineating the complex relationships between HBV infection, ncRNA dysregulation, and treatment outcomes:
Extracellular Vesicle (EV) Isolation and Characterization [9]:
- Differential ultracentrifugation to isolate EVs from cell culture supernatants or patient serum
- Nanoparticle tracking analysis to determine EV size distribution and concentration
- Transmission electron microscopy for EV morphology validation
- Western blotting for EV markers (CD63, CD81, TSG101) and absence of contaminants (calnexin)
Functional Analyses of ncRNAs in HBV-HCC [29]:
- Luciferase reporter assays to validate direct binding between lncRNAs and miRNAs
- RNA immunoprecipitation (RIP) to confirm RNA-protein interactions
- Colony formation and cell counting kit-8 (CCK-8) assays to assess proliferation
- Wound healing and Transwell assays to evaluate migration and invasion
- Orthotopic and subcutaneous mouse models to investigate tumor growth and immune responses in vivo
Comprehensive ncRNA Profiling [29]:
- RNA sequencing to identify differentially expressed lncRNAs, miRNAs, and mRNAs
- Quantitative RT-PCR with specific primers for validation
- Rapid amplification of cDNA ends (RACE) to determine full-length transcript sequences
- Database mining (TCGA, ENCORI/starBase) for clinical correlation analysis
Table 3: Essential Research Reagents for HBV-ncRNA Studies
| Reagent/Cell Line | Key Characteristics | Experimental Applications |
|---|---|---|
| HepG2.2.15 | Stable integration of double-copy HBV genome | Studying HBV replication and viral protein effects on ncRNA expression [9] [29] |
| HepG2-NTCP | Expresses sodium taurocholate cotransporting polypeptide | Permissive for HBV infection; modeling natural viral entry [9] |
| pAAV-HBV1.2 Vector | Delivers HBV genome to hepatocytes via hydrodynamic injection | Establishing persistent HBV gene expression in mouse models [26] |
| HBV Protein Plasmids | HBx, HBs, HBc recombinant plasmids | Dissecting specific viral protein contributions to ncRNA dysregulation [29] |
| TGFβ Pathway Modulators | SB431542 (inhibitor), Smad4 knockout constructs | Investigating TGFβ signaling in lncRNA regulation [9] |
| CD8+ T Cell Isolation Kits | Magnetic bead-based separation | Studying tumor immune microenvironment and T cell exhaustion mechanisms [9] |
Figure 2: Experimental Workflow for Investigating HBV-ncRNA Interactions in Hepatocarcinogenesis. A systematic approach combining bioinformatics, in vitro validation, animal models, and mechanistic studies enables comprehensive characterization of ncRNA functions in HBV-driven HCC.
The optimization of finite treatment regimens for HIV-HBV co-infection requires a multifaceted approach that integrates conventional antiviral strategies with emerging insights into HBV pathogenesis and the viral manipulation of host ncRNA networks. The evolving treatment paradigm emphasizes expanded indications for therapy, carefully monitored treatment cessation in select patients, and the pursuit of functional cure.
Future directions in the field should focus on:
- Validating ncRNA Biomarkers: Prospective studies to establish clinical utility of specific miRNA and lncRNA signatures for predicting treatment response and HCC risk in co-infected individuals.
- Developing ncRNA-Targeted Therapies: Exploring antisense oligonucleotides, small molecule inhibitors, or RNA-based therapeutics that disrupt oncogenic ncRNA networks in HBV-associated HCC.
- Personalizing Treatment Duration: Integrating novel biomarkers (HBV RNA, HBcrAg, qHBsAg) with ncRNA profiles to identify optimal candidates for finite therapy.
- Combination Immunotherapies: Leveraging insights from HBV-ncRNA-immune interactions to develop rational combinations of antivirals, immune checkpoint inhibitors, and ncRNA-targeting agents.
The intricate relationship between HBV infection and ncRNA dysregulation represents both a challenge and an opportunity. As our understanding of these mechanisms deepens, so too does our potential to develop more effective finite treatment strategies that address not only viral suppression but also the underlying oncogenic processes that drive long-term morbidity in HIV-HBV co-infected individuals.
The intricate relationship between Hepatitis B Virus (HBV)-induced alterations in non-coding RNA (ncRNA) expression and the progression to hepatocellular carcinoma (HCC) represents a pivotal area for therapeutic innovation. This whitepaper delineates a novel combinatorial framework that simultaneously targets viral-induced ncRNA dysregulation, reverses immune exhaustion, and modulates critical metabolic pathways. We provide a technical exploration of how integrating ncRNA-directed therapies—including strategies against viral miRNAs like HBV-miR-3 and host long non-coding RNAs (lncRNAs)—with immunomodulators such as Treg-targeting agents and repurposed statins can disrupt the hepatic inflammation–fibrosis–cancer axis. Supported by recent preclinical and clinical data, including quantitative evidence for statin efficacy, this guide outlines a multi-pronged strategy to achieve a functional cure for chronic HBV and prevent hepatocarcinogenesis, presenting detailed methodologies and key reagents for the research community.
Chronic Hepatitis B Virus (HBV) infection remains a monumental global health challenge, affecting an estimated 254 million individuals worldwide and serving as a primary etiological driver for hepatocellular carcinoma (HCC) [78] [79]. The pathogenesis of HBV-related HCC is a multi-factorial process fueled by persistent viral infection, chronic hepatic inflammation, and profound alterations in the host genomic and transcriptomic landscape. Central to this process is the virus's ability to hijack host cellular machinery through its encoded proteins and, as recently discovered, through its own non-coding RNAs.
HBV-miR-3, a virus-encoded miRNA, has been identified as a key oncogenic driver by directly targeting the cholesterol efflux regulator ABCA1, leading to intracellular cholesterol accumulation and promoting a pro-proliferative phenotype in hepatocytes [80]. Concurrently, host-derived long non-coding RNAs (lncRNAs) undergo significant dysregulation as a consequence of chronic viral infection. HBV, particularly through its HBx protein, manipulates the expression of numerous lncRNAs, which in turn govern critical cancer-associated pathways such as Wnt/β-catenin and PI3K/Akt/mTOR [40] [81]. These lncRNAs, including well-characterized examples like HULC, H19, and NEAT1, function as molecular scaffolds, decoys, and sponges, exerting pleiotropic effects on cell cycle control, apoptosis, and invasion [81].
The immunological milieu of the chronically infected liver is characterized by T cell exhaustion and the dominance of immunosuppressive elements, particularly Regulatory T Cells (Tregs). These Foxp3+ Tregs are recruited to the liver microenvironment, where they potently suppress antiviral effector responses, facilitating viral persistence and creating conditions favorable for malignant transformation [78]. This triad of ncRNA dysregulation, immune dysfunction, and metabolic alteration forms the rational basis for a combinatorial therapeutic approach. Targeting a single axis is likely insufficient to dismantle the robust, multi-layered pathogenesis of HBV-induced HCC; instead, a synchronized attack on all three fronts holds the promise of achieving durable viral control and preventing cancer.
Core Therapeutic Pillars: Mechanisms and Targets
Non-coding RNA (ncRNA) Therapeutics
The ncRNA landscape in HBV-infected hepatocytes offers a rich repository of therapeutic targets. Strategies can be categorized based on the origin and function of the target ncRNA.
- Targeting Viral miRNA (e.g., HBV-miR-3): This conserved viral miRNA is derived from the stem of a hairpin structure within the HBsAg coding region. Its primary oncogenic mechanism involves the direct suppression of the ABCA1 transporter mRNA. The subsequent intracellular accumulation of cholesterol and lipid droplets drives hepatocyte proliferation and colony formation in vitro [80]. Therapeutic inhibition of HBV-miR-3 using antisense oligonucleotides (ASOs) or antagomirs can de-repress ABCA1, thereby normalizing cholesterol flux and mitigating its pro-oncogenic effects.
- Targeting Host-Derived Long Non-Coding RNAs (lncRNAs): The expression of host lncRNAs is profoundly altered by HBV infection, often via the transcriptional transactivator function of the HBx protein. These lncRNAs can be targeted therapeutically using siRNAs or ASOs to knock down oncogenic species or, alternatively, through mimic constructs to restore the function of tumor-suppressive lncRNAs. For instance:
- H19: Promotes HCC cell proliferation by acting as a molecular sponge for miR-15b, thereby activating the CDC42/PAK1 axis [81].
- Linc-RoR: Functions as a competitive endogenous RNA (ceRNA) for the tumor suppressor miR-145, leading to the upregulation of downstream targets like HIF-1α and driving glycolysis and cell proliferation [81].
- LncRNA-p21: Forms a positive feedback loop with HIF-1α to accelerate glycolytic metabolism in HCC cells under hypoxia [81].
Immunomodulators
The goal of immunomodulation in chronic HBV is to break the state of immune tolerance and reinvigorate exhausted antiviral responses.
- Targeting Regulatory T Cells (Tregs): The enrichment of Foxp3+ Tregs in the liver is a hallmark of chronic HBV infection. Two primary strategies are under investigation:
- Reducing Treg Frequency: Depleting Tregs using anti-CD25 antibodies or other cytotoxic agents.
- Inhibiting Treg Function: Blocking key immunosuppressive cytokines (e.g., IL-10, TGF-β) or critical functional receptors like the IL-33 receptor (ST2). Recent evidence demonstrates that the IL-33/ST2 axis is pivotal for Treg-mediated immunosuppression in HBV-related carcinogenesis, and its disruption enhances intrahepatic CD8+ T cell cytotoxicity [26].
- Immune Checkpoint Inhibitors (ICIs): Antibodies targeting co-inhibitory receptors such as PD-1, CTLA-4, and Tim-3 can reverse the exhausted phenotype of HBV-specific T cells, potentially restoring their capacity to clear infected and transformed hepatocytes [82].
- Therapeutic Vaccines: These agents are designed to elicit robust, antigen-specific T and B cell responses against HBV antigens (e.g., HBsAg, HBcAg), aiming to achieve immune control over the virus [79].
Repurposed Statins
Statins, HMG-CoA reductase inhibitors, exhibit pleiotropic effects beyond cholesterol reduction that are highly relevant to HBV-induced hepatocarcinogenesis. The protective effects of statins, particularly lipophilic statins (e.g., atorvastatin, simvastatin, pitavastatin), are mediated through multiple mechanisms:
- Inhibition of Viral Replication: Statins disrupt the cholesterol biosynthesis pathway, depriving HBV of essential lipids for viral envelope formation and secretion. Atorvastatin has been shown to accelerate the reduction of HBV DNA viral load when combined with tenofovir [83].
- Targeting the HBV-miR-3-ABCA1 Axis: By lowering intracellular cholesterol, statins directly counter the oncogenic phenotype induced by HBV-miR-3. Simvastatin, atorvastatin, and fluvastatin can inhibit HBV-miR-3-induced proliferation and colony formation in hepatoma cells [80].
- Suppression of Pro-Carcinogenic Signaling: Pitavastatin has been identified as a potent inhibitor of IL-33 expression. Given that the IL-33/Treg axis is required for liver cancer development in the context of HBV and environmental carcinogens, statin use correlates with a significantly reduced risk of hepatitis and HCC in patients [26] [84].
Table 1: Quantitative Evidence for Statin Efficacy in Chronic Viral Hepatitis (Meta-Analysis Data)
| Adverse Event | Hazard Ratio (HR) with Statin Use | P-value | Number of Studies (Participants) | Notes |
|---|---|---|---|---|
| Hepatocellular Carcinoma (HCC) | 0.56 | < 0.001 | 11 (~450,000) | Lipophilic statins particularly effective (HR=0.56) [84] |
| All-Cause Mortality | 0.63 | < 0.001 | 6 (~150,000) | Consistent protective association [84] |
| Cirrhosis | 0.54 | < 0.001 | 4 (~580,000) | Indicates potential for preventing disease progression [84] |
| Cirrhosis Decompensation | 0.54 | < 0.001 | 4 (~580,000) | [84] |
Table 2: Key ncRNA Targets in HBV-Related HCC and Their Functions
| ncRNA Name | Type | Expression in HCC | Primary Function/Mechanism | Therapeutic Approach |
|---|---|---|---|---|
| HBV-miR-3 | Viral miRNA | Upregulated | Suppresses ABCA1, causing cholesterol accumulation and proliferation [80] | Antisense Oligonucleotides (ASOs) |
| H19 | Host lncRNA | Upregulated | Sponges miR-15b, activates CDC42/PAK1 axis [81] | siRNA, ASO |
| Linc-RoR | Host lncRNA | Upregulated | Sponges miR-145, upregulates HIF-1α, promotes glycolysis [81] | siRNA, ASO |
| NEAT1 | Host lncRNA | Upregulated | Regulates paraspeckle formation, promotes cell proliferation [81] | siRNA |
| HULC | Host lncRNA | Upregulated | Highly upregulated in liver cancer, functions as a miRNA sponge [40] | siRNA |
Experimental Protocols for Key Investigations
Protocol 1: Validating ncRNA-Target Interactions
Objective: To confirm that a candidate ncRNA (e.g., HBV-miR-3) directly binds to and regulates a predicted target mRNA (e.g., ABCA1).
Methodology:
- Plasmid Constructs:
- Clone the wild-type 3'-Untranslated Region (UTR) of the target gene (ABCA1) containing the predicted miRNA response element (MRE) downstream of a luciferase reporter gene (e.g., in psiCHECK-2 vector) to create pWT-ABCA1-UTR.
- Generate a mutant control plasmid (pMut-ABCA1-UTR) by deleting the 8-nt seed region of the MRE using site-directed mutagenesis [80].
- Cell Culture and Transfection:
- Culture human hepatoma cell lines (e.g., Huh7, HepG2) in DMEM with 10% FBS.
- Co-transfect cells in 24-well plates using a lipofectamine reagent. Each transfection should include:
- Group 1: 300 ng pWT-ABCA1-UTR + 300 ng HBV-miR-3 expression plasmid (pHBV-miR-3).
- Group 2: 300 ng pWT-ABCA1-UTR + 300 ng empty vector control.
- Group 3: 300 ng pMut-ABCA1-UTR + 300 ng pHBV-miR-3.
- Group 4: 300 ng pMut-ABCA1-UTR + 300 ng empty vector [80].
- Luciferase Assay:
- 48 hours post-transfection, lyse cells and measure Firefly and Renilla luciferase activities using a dual-luciferase reporter assay system.
- Normalize Renilla luciferase activity (from the reporter) to Firefly luciferase activity (internal control). Plot data as Relative Luciferase Units (RLU).
- Interpretation: A significant reduction in RLU only in Group 1 (WT UTR + miRNA) confirms specific, sequence-dependent repression.
Protocol 2: Assessing Combination EfficacyIn Vivo
Objective: To evaluate the synergistic effect of an ncRNA therapy, an immunomodulator, and a statin in an HBV-related HCC mouse model.
Methodology:
- Animal Model Generation:
- Treatment Groups:
- Group A: Vehicle control
- Group B: ncRNA inhibitor (e.g., ASO against HBV-miR-3/H19) alone
- Group C: Immunomodulator (e.g., anti-ST2 antibody) alone
- Group D: Statin (e.g., Pitavastatin, 10 mg/kg/d in diet) alone
- Group E: Triple combination (B + C + D)
- Endpoint Analysis (8-12 months post-infection):
- Tumor Burden: Count and weigh macroscopic liver tumors.
- Proliferation Index: Perform immunohistochemistry (IHC) for PCNA to quantify proliferating hepatocytes.
- Immune Profiling: Analyze intrahepatic lymphocytes by flow cytometry for CD8+ T cells (CD3+CD8+), Tregs (CD4+CD25+Foxp3+), and exhaustion markers (PD-1, Tim-3).
- Viral Parameters: Measure serum HBsAg and intrahepatic HBV DNA and cccDNA levels.
Visualization of Core Signaling Pathways
The following diagram integrates the key pathological mechanisms and therapeutic targets discussed, illustrating how HBV infection drives hepatocarcinogenesis and how the combinatorial therapy intervenes.
Diagram Title: HBV Hepatocarcinogenesis and Combination Therapy
This diagram illustrates the central pathways through which HBV infection promotes liver cancer. The model shows how HBV proteins and viral miRNAs drive ncRNA dysregulation and cholesterol accumulation, while also activating the IL-33/Treg axis to cause immune dysfunction. The combination therapeutic strategy (blue inhibitors) simultaneously targets these multiple pathways to block the progression to HCC.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Investigating Combination Therapies
| Reagent / Tool | Category | Function in Research | Example Source / Model |
|---|---|---|---|
| pAAV-HBV1.2 Plasmid | In Vivo Model | Enables hydrodynamic transfection in mice to establish persistent HBV gene expression, mimicking chronic infection [26]. | Addgene, academic labs |
| Huh7 & HepG2 Cell Lines | In Vitro Model | Human hepatoma cell lines; standard for in vitro studies of HBV replication, ncRNA function, and drug screening [80]. | ATCC, NCCS |
| psiCHECK-2 Vector | Molecular Biology | Dual-luciferase reporter plasmid for validating direct ncRNA-mRNA interactions via 3'UTR cloning [80]. | Promega |
| Lipophilic Statins | Small Molecule Inhibitor | Research-grade Pitavastatin, Atorvastatin, Simvastatin for investigating antiviral and chemopreventive effects in vitro and in vivo [80] [26] [84]. | Sigma-Aldrich, TCI |
| Anti-ST2 Antibody | Immunomodulator | Monoclonal antibody for blocking the IL-33/ST2 signaling axis in vivo, thereby inhibiting Treg-mediated immunosuppression [26]. | Bio X Cell, R&D Systems |
| Anti-miR-3 ASO | ncRNA Therapeutic | Antisense oligonucleotide designed to specifically inhibit and degrade the viral HBV-miR-3 [80]. | Custom synthesis (e.g., IDT) |
| Diethylnitrosamine (DEN) | Carcinogen | Used in mouse models to provide the "second hit" of genotoxic stress, synergizing with HBV to induce robust HCC tumorigenesis [26]. | Sigma-Aldrich |
The integration of ncRNA-targeting agents, immunomodulators, and statins constitutes a paradigm shift in the approach to treating chronic HBV and preventing its oncogenic sequelae. This multi-target strategy acknowledges and confronts the inherent complexity of the virus-host interaction. By concurrently dismantling viral support networks (via ncRNA inhibition), reinvigorating host immune surveillance (via Treg disruption and checkpoint inhibition), and normalizing dysregulated metabolic pathways (via statins), this approach offers a path to durable viral control that transcends the limitations of monotherapies.
Future work must prioritize the optimization of delivery vehicles—particularly lipid nanoparticles or viral vectors capable of targeting these novel agents specifically to hepatocytes—to maximize efficacy and minimize off-target effects. Furthermore, the identification of robust biomarkers, such as serum levels of HBV-miR-3 or specific lncRNA signatures, will be crucial for patient stratification and monitoring treatment response. The promising clinical and preclinical data supporting the efficacy of statins in this context provide a strong rationale for their immediate investigation in prospective clinical trials as part of combination regimens. Ultimately, the systematic deconstruction of the HBV-induced hepatocarcinogenic network through rational combination therapy heralds a new era in the management of this global health challenge, moving us closer to the ultimate goal of a functional cure.
Hepatitis B virus-related hepatocellular carcinoma (HBV-HCC) represents a significant global health challenge, accounting for over 50% of HCC cases worldwide and exhibiting distinct molecular pathogenesis driven by viral integration and chronic inflammation [74] [16]. The complex interplay between HBV and host liver cells creates a unique carcinogenic environment characterized by non-coding RNA alterations, epigenetic modifications, and immune response dysregulation that fundamentally influence therapeutic outcomes. In this context, precisely defining clinical endpoints becomes paramount for accurately evaluating novel interventions targeting the intricate molecular pathways of HBV-induced hepatocarcinogenesis.
Clinical endpoints serve as targeted outcomes that are statistically analyzed to determine the efficacy and safety of investigational therapies [85]. For HBV-HCC trials, endpoints must capture not only antitumor effects but also antiviral activity and alterations in the underlying liver disease landscape. The 2025 European Association for the Study of the Liver (EASL) guidelines mark a shift toward biomarker-led, finite, and personalised therapy, with functional cure defined as sustained HBsAg loss emerging as a key therapeutic goal [74]. This evolution in treatment paradigms necessitates increasingly sophisticated endpoint frameworks that can accommodate both traditional oncological metrics and HBV-specific virological outcomes.
Endpoint Classification in HBV-HCC Clinical Trials
Primary Endpoints
Primary endpoints form the cornerstone of clinical trial design, serving as the main data evaluated for regulatory approval and determining whether a study meets its primary objectives [85]. In HBV-HCC trials, selection of appropriate primary endpoints depends heavily on the study phase, therapeutic mechanism, and patient population.
Overall Survival (OS): remains the gold standard for phase 3 trials, measuring the time from randomization to death from any cause. While objectively measured and clinically meaningful, OS requires large sample sizes and extended follow-up periods, and may be confounded by subsequent therapies in HBV-HCC where multiple treatment lines exist.
Progression-Free Survival (PFS): captures the time from treatment initiation to disease progression or death, providing earlier assessment of treatment effect than OS. For HBV-HCC, PFS must be carefully defined to account for both hepatic functional reserve and tumor burden, particularly in patients with underlying cirrhosis.
Time to Progression (TTP): focuses specifically on disease progression, excluding mortality unrelated to HCC progression. This endpoint is particularly relevant in HBV-HCC populations with compromised liver function where non-HCC-related mortality may occur.
Objective Response Rate (ORR): defined as the proportion of patients with a predefined reduction in tumor burden, typically assessed via RECIST criteria or modified RECIST for HCC. ORR is especially valuable for early-phase trials screening for initial signals of antitumor activity.
Table 1: Primary Endpoint Considerations for HBV-HCC Clinical Trials
| Endpoint | Definition | Advantages | Limitations in HBV-HCC |
|---|---|---|---|
| Overall Survival | Time from randomization to death from any cause | Gold standard, unambiguous, clinically meaningful | Long follow-up needed; may be confounded by sequential therapies and liver dysfunction |
| Progression-Free Survival | Time to disease progression or death | Captures drug activity; earlier readout than OS | Potential subjectivity in progression assessment; composite nature includes non-HCC deaths |
| Time to Progression | Time to disease progression only | Focuses purely on antitumor effect | Excludes mortality; may miss clinical deterioration from liver dysfunction |
| Objective Response Rate | Proportion with tumor size reduction | Early activity signal; valuable for single-arm trials | May not correlate with survival; challenging with irregular HCC lesions |
Secondary and Exploratory Endpoints
Secondary endpoints provide supportive information about a therapy's effect on the primary endpoint or demonstrate additional effects on the disease [85]. In HBV-HCC trials, these often include:
- Disease Control Rate (DCR): combining complete response, partial response, and stable disease
- Duration of Response (DOR): measuring the sustainability of antitumor effects
- Time to Symptomatic Progression: capturing patient-reported outcomes
- Virological Response Metrics: including HBV DNA suppression, HBeAg seroconversion, and HBsAg reduction
Exploratory endpoints in HBV-HCC trials are increasingly focusing on non-coding RNA biomarkers and other molecular correlates that may inform mechanisms of response and resistance [16]. These include changes in circulating microRNA profiles, long non-coding RNA expression patterns, and viral integration sites that influence hepatocarcinogenesis.
Biomarker-Driven Endpoints and the Role of Non-Coding RNAs
Emerging Biomarker Endpoints in HBV-HCC
The complex molecular pathogenesis of HBV-HCC creates unique opportunities for biomarker-driven endpoints that reflect underlying disease biology. Non-coding RNAs (ncRNAs), including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), have emerged as critical regulators in HBV-induced oncogenesis and promising biomarkers for clinical trial endpoints [16].
These ncRNAs modulate various cancer hallmarks including sustained proliferation, evasion of growth suppressors, and activation of invasion and metastasis through precise regulation of target genes and associated cellular processes [16]. Their stability, detectability in bodily fluids, and disease-specific expression patterns render them promising biomarkers for diagnostic, prognostic, and predictive endpoints in HBV-HCC trials.
Table 2: Key Non-Coding RNA Biomarkers in HBV-HCC Pathogenesis
| ncRNA Category | Specific Examples | Regulatory Role in HBV-HCC | Potential Endpoint Application |
|---|---|---|---|
| Oncogenic miRNAs | miR-21, miR-221, miR-222 | Upregulated by HBx; targets PTEN, PDCD4, TFRC; promotes proliferation | Pharmacodynamic biomarkers for targeted therapies |
| Tumor-Suppressor miRNAs | miR-122, miR-199a/b, miR-125b | Downregulated by HBx; modulates metabolism, apoptosis, stemness | Biomarkers of therapeutic response and disease monitoring |
| Long Non-Coding RNAs | DLEU2, HOTAIR | Chromatin regulation, transcription, cell cycle control | Predictive biomarkers for treatment selection |
| Circular RNAs | Various circRNAs | miRNA spongeing; regulation of oncogenic pathways | Early detection biomarkers and minimal residual disease monitoring |
Quantitative Biomarker Assessment Methodologies
Accurate quantification of biomarker endpoints requires standardized methodologies. For ncRNA profiling in HBV-HCC trials, the following protocols are recommended:
RNA Extraction and Quality Control
- Obtain PBMCs or plasma samples using standardized collection tubes
- Extract total RNA using silica-membrane based kits with DNase treatment
- Assess RNA quality using Bioanalyzer (RIN >7.0 required)
- Quantify RNA using fluorometric methods
Reverse Transcription and Quantitative PCR
- Perform reverse transcription using stem-loop primers for miRNAs or random hexamers for other ncRNAs
- Conduct qPCR using TaqMan assays with specific primer-probe sets
- Use exogenous spike-in controls (e.g., cel-miR-39) for normalization
- Calculate expression using the 2^(-ΔΔCt) method relative to stable endogenous controls (e.g., RNU44, RNU48)
Next-Generation Sequencing Profiling
- Prepare libraries using kits specifically designed for small RNA or total RNA
- Sequence on platforms with minimum 20 million reads per sample
- Align reads to reference genomes using specialized algorithms (e.g., STAR, Bowtie)
- Identify differentially expressed ncRNAs using statistical packages (e.g., DESeq2, edgeR)
Validation and Adjudication of Endpoints in HBV-HCC
Endpoint Adjudication Processes
Independent endpoint adjudication is critical for systematic classification of clinical outcomes in clinical trials in an unbiased way [86]. For HBV-HCC trials, this process requires specialized expertise in both oncology and hepatology.
Imaging Endpoint Adjudication
- Utilize central imaging laboratories with radiologists specialized in HCC
- Implement standardized imaging protocols across trial sites
- Apply consistent response criteria (RECIST 1.1, mRECIST) with predefined definitions of progression
- Ensure blinded sequential review of imaging studies
Clinical Event Committee (CEC) Operations
- Establish multidisciplinary CECs including hepatologists, oncologists, and pathologists
- Develop predefined event definitions incorporating both oncological and hepatic considerations
- Implement blinded review processes with standardized case report forms
- Determine causality assessment for adverse events relative to both anticancer and antiviral effects
Statistical Considerations for Endpoint Validation
Endpoint validation requires rigorous statistical approaches tailored to the unique characteristics of HBV-HCC:
- Sample Size Calculation: must account for expected dropout rates due to liver dysfunction and competing risks of death from liver failure
- Stratification Factors: should include baseline liver function (Child-Pugh class), HCC stage (BCLC), and virological status (HBeAg, HBV DNA)
- Analysis Methods: should incorporate time-to-event analyses with appropriate handling of censoring and competing risks
Integrated Endpoint Framework for HBV-HCC Trials
The multifactorial nature of HBV-HCC necessitates an integrated endpoint framework that captures the complex interplay between antiviral activity, antitumor effect, and hepatic preservation. The following visualization illustrates the key relationships between different endpoint categories in HBV-HCC trials:
Diagram 1: Integrated Endpoint Framework for HBV-HCC Trials. This diagram illustrates the interrelationships between different endpoint categories and their connection to disease biology and clinical decision-making.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for HBV-HCC Endpoint Assessment
| Category | Specific Tool/Platform | Application in Endpoint Assessment | Key Features |
|---|---|---|---|
| Serological Biomarkers | ARCHITECT i2000SR Analyzer | High-throughput measurement of AFP, PIVKA-II, LG2m | CE-marked assays; automated processing; high reproducibility [87] |
| Nucleic Acid Detection | Droplet Digital PCR | Absolute quantification of HBV DNA and ncRNAs | High sensitivity; minimal sample requirement; absolute quantification without standards |
| ncRNA Profiling | TaqMan Advanced miRNA Assays | Specific detection of miRNA biomarkers | Stem-loop primers for mature miRNAs; high specificity; compatible with standard real-time PCR |
| Multiplex Immunoassays | Luminex xMAP Technology | Simultaneous measurement of cytokine profiles and immune markers | High-plex capability; low sample volume; custom panel configuration |
| Next-Generation Sequencing | Illumina NovaSeq Series | Comprehensive ncRNA transcriptome profiling | High sequencing depth; single-nucleotide resolution; discovery-based approach |
| Cell Separation | Ficoll-Paque Density Gradient Medium | Isolation of PBMCs for splicing signature analysis | High cell viability recovery; minimal activation; compatible with downstream molecular analyses [88] |
The evolving landscape of HBV-HCC trial endpoints reflects advances in both hepatology and oncology. Future developments will likely include:
- Standardized ncRNA biomarker panels validated across diverse patient populations
- Integrated composite endpoints that simultaneously capture virological, oncological, and functional outcomes
- Digital pathology endpoints incorporating artificial intelligence for objective response assessment
- Liquid biopsy endpoints utilizing circulating tumor DNA and ncRNAs for minimal residual disease monitoring
The 2025 EASL guidelines emphasizing biomarker-led, finite, and personalised therapy underscore the critical importance of well-defined endpoints that reflect the unique molecular pathogenesis of HBV-HCC [74]. As novel therapies targeting specific ncRNA pathways emerge, the endpoint framework must continue to evolve to accurately capture their clinical utility. By implementing rigorous endpoint definitions that account for both the oncological and virological dimensions of HBV-HCC, clinical trials can more effectively benchmark success and accelerate the development of transformative therapies for this complex malignancy.
Validation and Comparative Analysis of Emerging ncRNA Therapeutics
This technical guide provides a comprehensive overview of preclinical models for Hepatitis B virus-associated Hepatocellular Carcinoma (HBV-HCC), with a specific focus on their application in studying non-coding RNA (ncRNA) alterations in hepatocarcinogenesis. We detail established in vitro and in vivo methodologies, experimental protocols, and key reagent solutions to facilitate robust preclinical validation of HBV-HCC mechanisms and therapeutic interventions. The content emphasizes the crucial role of HBx-mediated ncRNA aberrations in driving hepatocarcinogenesis through multiple signaling pathways, providing researchers with validated tools to advance drug discovery and mechanistic studies.
Hepatocellular carcinoma (HCC) represents the sixth most commonly diagnosed cancer and the third leading cause of cancer-related deaths globally, with Hepatitis B virus (HBV) infection accounting for more than half of all cases worldwide [89] [19]. The prevalence of liver cancer continues to increase, with predictions of 56.4% more fatalities by 2040, creating a significant global health burden [89]. HBV-associated hepatocarcinogenesis involves complex mechanisms wherein the virus-encoded X protein (HBx) plays a pivotal oncogenic role by inducing genetic and epigenetic alterations, particularly in non-coding RNA networks [20] [19].
The HBx protein, a 154-amino acid multifunctional oncoprotein, localizes to both cytoplasm and nucleus and facilitates hepatocarcinogenesis through trans-activation of viral and cellular genes [19]. Accumulating evidence demonstrates that HBx regulates ncRNA expression, which subsequently modulates critical cellular processes including proliferation, apoptosis, epithelial-mesenchymal transition (EMT), and metastasis [20] [19]. Non-coding RNAs, which constitute approximately 90% of the human genome, include microRNAs (miRNAs, 19-25 nt), long non-coding RNAs (lncRNAs, 200 nt to 100 kb), and other small ncRNAs that regulate gene expression without encoding proteins [20] [19]. These HBx-mediated ncRNA aberrations represent promising diagnostic biomarkers and therapeutic targets for HBV-HCC.
In Vitro HBV-HCC Models
Established Cell Lines and Their Applications
In vitro models provide controlled systems for investigating HCC pathophysiology, screening therapeutic compounds, and studying pharmacokinetic and pharmacodynamic responses [89]. The table below summarizes key human and murine HCC cell lines used in HBV-HCC research:
Table 1: Characterized Cell Lines for HBV-HCC Research
| Cell Line | Origin | Key Characteristics | Applications in HBV-HCC |
|---|---|---|---|
| HepG2 | Human hepatoblastoma | Non-tumorigenic, HBV replication incompetent | Baseline hepatocyte biology [89] |
| HepG2.2.15 | HepG2 derived | Stably transfected with HBV genome; produces viral particles | HBV replication, viral-host interactions, drug screening [89] |
| Huh-7 | Human HCC | Well-differentiated, tumorigenic | HCC pathogenesis, drug metabolism studies [89] |
| Hep3B | Human HCC | HBV integration, produces HBsAg | HBx functional studies, apoptosis mechanisms [89] |
| PLC/PRF/5 | Human HCC | Contains integrated HBV DNA, expresses HBsAg | Viral integration studies, antigen expression [89] |
| HepaRG | Human hepatic progenitor | Differentiates into hepatocyte-like cells | HBV infection studies, differentiation therapy [89] |
Experimental Protocols for In Vitro Manipulation
HBx Gene Transfection Protocol
Purpose: To introduce HBx gene into HCC cell lines for studying its oncogenic functions and ncRNA regulation.
Materials:
- HBx expression plasmid (pcDNA3.1-HBx)
- Lipofectamine 3000 transfection reagent
- Opti-MEM reduced serum media
- Appropriate cell culture media and supplements
Procedure:
- Seed HCC cells (e.g., HepG2 or Huh-7) in 6-well plates at 60-70% confluence
- Incubate for 24 hours at 37°C, 5% CO₂
- For each well, prepare two tubes:
- Tube A: Dilute 2.5 μg DNA in 125 μL Opti-MEM, add 5 μL P3000 reagent
- Tube B: Dilute 7.5 μL Lipofectamine 3000 in 125 μL Opti-MEM
- Combine tubes A and B, incubate 15 minutes at room temperature
- Add DNA-lipid complex dropwise to cells with 1.85 mL fresh media
- Assay for gene expression after 24-72 hours
- Validate transfection efficiency via Western blot (HBx detection) and qRT-PCR (HBx mRNA)
miRNA Expression Profiling Protocol
Purpose: To identify differentially expressed miRNAs in HBx-transfected cells versus controls.
Materials:
- miRNeasy Mini Kit (RNA extraction)
- miScript Reverse Transcription Kit
- miScript miRNA PCR Array
- Quantitative PCR instrument
Procedure:
- Extract total RNA including small RNAs from HBx-expressing and control cells
- Synthesize cDNA using miScript Reverse Transcription Kit with RNA template
- Perform qPCR with miScript SYBR Green PCR Kit and miRNA-specific primers
- Use U6 snRNA as endogenous control for normalization
- Analyze data using the 2^(-ΔΔCt) method to calculate fold changes
- Validate significantly dysregulated miRNAs using miRNA inhibitors/mimics
In Vivo HBV-HCC Models
Murine Models of HBV-HCC
Animal models, particularly murine systems, are fundamental for understanding HBV-HCC disease progression, evaluating therapeutic efficacy, and conducting preclinical safety studies [89]. These models replicate various aspects of human hepatocarcinogenesis, from inflammation-driven carcinogenesis to genetic manipulation approaches.
Table 2: In Vivo Models for HBV-HCC Research
| Model Type | Induction Method | Key Features | Advantages | Limitations |
|---|---|---|---|---|
| Hydrodynamic Transfection | HBx plasmid injection via tail vein | HBx expression in hepatocytes | Rapid implementation, cost-effective | Transient HBx expression [89] |
| Transgenic Mice | Liver-specific HBx expression | Spontaneous tumor development | Stable HBx expression, progressive disease | May lack full immune response [89] |
| Xenograft Models | Implantation of human HCC cells | Tumor formation in immunodeficient mice | Reproducible tumor growth, human context | Lack intact immune system [89] |
| Patient-Derived Xenografts (PDX) | Implantation of patient tumor tissue | Preserves tumor heterogeneity | Clinically relevant, personalized medicine approach | Expensive, requires immunosuppressed mice [89] |
| CClâ‚„-Induced Cirrhosis-HCC | Repeated CClâ‚„ injections | Liver fibrosis progressing to HCC | Models inflammation-fibrosis-carcinoma sequence | Non-viral etiology [89] |
| DEN-Induced HCC | Single diethylnitrosamine injection | Rapid tumor development | Synchronized carcinogenesis, high penetrance | Primarily genotoxic, not viral etiology [89] |
Experimental Protocols for In Vivo Studies
Hydrodynamic Transfection of HBx
Purpose: To deliver HBx gene into mouse hepatocytes for studying HBx-mediated hepatocarcinogenesis and ncRNA alterations.
Materials:
- Endotoxin-free HBx expression plasmid
- Physiological saline (0.9% NaCl)
- 1mL syringes with 27G needles
- Animal warming chamber
Procedure:
- Prepare HBx plasmid DNA solution in physiological saline (10μg DNA in 1.8-2.0mL saline per mouse)
- Heat mice in warming chamber (37°C) for 3-5 minutes to dilate tail veins
- Restrain mouse and identify lateral tail vein
- Inject DNA solution rapidly (within 5-7 seconds) into tail vein
- Monitor mice for immediate adverse reactions
- Sacrifice at predetermined timepoints for tissue collection
- Analyze liver tissues for HBx expression, histopathology, and ncRNA profiling
Tissue Processing and Analysis Protocol
Purpose: To evaluate tumor development, histopathological changes, and molecular alterations in liver tissues.
Materials:
- Formalin solution (10% neutral buffered)
- Paraffin embedding system
- Hematoxylin and eosin (H&E) stains
- RNA preservation solution (RNAlater)
- Antibodies for immunohistochemistry (IHC)
Procedure:
- Harvest liver tissues and divide for various analyses:
- Fix portion in formalin for histology
- Preserve portion in RNAlater for RNA studies
- Flash-freeze portion in liquid nitrogen for protein studies
- Process fixed tissues through graded alcohols, xylene, and paraffin embedding
- Section tissues at 4-5μm thickness
- Perform H&E staining for histopathological evaluation
- Conduct IHC for HBx, proliferation markers (Ki-67), and HCC biomarkers
- Extract RNA from preserved tissues for ncRNA expression profiling
- Analyze results with appropriate statistical methods
Key Signaling Pathways in HBx-Mediated Hepatocarcinogenesis
The HBx protein facilitates hepatocarcinogenesis through interaction with various non-coding RNAs and subsequent modulation of critical signaling pathways. The diagram below illustrates the major signaling networks involved in HBx-mediated hepatocarcinogenesis via non-coding RNA alterations:
HBx-ncRNA Signaling Network: This diagram illustrates how HBx protein regulates non-coding RNAs to activate multiple oncogenic signaling pathways in hepatocarcinogenesis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for HBV-HCC Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| HBx Detection | Anti-HBx antibodies (monoclonal/polyclonal) | Immunodetection in Western blot, IHC, immunofluorescence |
| ncRNA Analysis | miRNA mimics/inhibitors, lncRNA overexpression/knockdown constructs | Functional studies of ncRNAs in HBx-mediated hepatocarcinogenesis |
| qRT-PCR Assays | TaqMan miRNA assays, SYBR Green master mixes | Quantification of miRNA and other ncRNA expression levels |
| Cell Culture | HepG2.2.15, Huh-7, Hep3B, HepaRG cells | In vitro modeling of HBV-HCC pathogenesis and drug screening |
| Animal Models | Immunodeficient mice (NSG, NOG), transgenic HBx mice | In vivo preclinical validation of therapeutic candidates |
| Pathway Inhibitors | STAT3 inhibitors (Stattic), AKT inhibitors (MK-2206), MEK inhibitors (trametinib) | Target validation and combination therapy studies |
| Histopathology | H&E staining kits, IHC detection systems | Morphological assessment and protein localization in tissues |
| RNA Sequencing | Small RNA library prep kits, stranded total RNA library prep | Genome-wide discovery of dysregulated ncRNAs |
Advanced Model Systems: Organoids and PDX
Recent advancements in preclinical models include the development of patient-derived organoids and xenografts (PDX) that better preserve tumor heterogeneity and microenvironmental interactions [89]. HBV-HCC organoids can be established from patient tumors and maintain genomic and phenotypic characteristics of the original tissue, providing valuable platforms for drug screening and personalized medicine approaches [89].
The experimental workflow for establishing HBV-HCC organoids involves:
- Collection of fresh tumor tissues from HBV-HCC patients
- Tissue digestion and isolation of epithelial cells
- Embedding in extracellular matrix (e.g., Matrigel)
- Culture with defined growth factors and signaling inhibitors
- Expansion and cryopreservation for biobanking
- Validation through genomic profiling and histology
These advanced models enable high-throughput drug screening and study of tumor-stroma interactions in a more physiologically relevant context than traditional 2D cultures, bridging the gap between conventional cell lines and in vivo models.
Preclinical validation from cell lines to animal models remains essential for advancing our understanding of HBV-HCC pathogenesis and developing novel therapeutic strategies. The integration of ncRNA biology into these model systems has revealed critical mechanisms of HBx-mediated hepatocarcinogenesis, providing new opportunities for diagnostic biomarker discovery and targeted interventions. By employing appropriate in vitro and in vivo models with standardized protocols, researchers can effectively translate basic findings into clinical applications, ultimately addressing the significant global health burden of HBV-associated hepatocellular carcinoma.
Comparative Analysis of Different ncRNA Classes as Therapeutic Targets
Hepatitis B virus (HBV)-induced hepatocellular carcinoma (HCC) represents a major global health challenge, accounting for approximately 80% of HCC cases worldwide. The pathogenesis involves complex interactions between viral factors and host cellular machinery, with non-coding RNAs (ncRNAs) emerging as critical regulators in hepatocarcinogenesis. This review provides a comprehensive comparative analysis of microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) as therapeutic targets in HBV-related HCC. We examine their distinct biogenesis pathways, molecular mechanisms, and functional roles in viral persistence, immune evasion, and tumor progression. The analysis incorporates recent advances in ncRNA-based therapeutic strategies, experimental methodologies for target validation, and the development of targeted delivery systems. Our comparative assessment reveals that while each ncRNA class presents unique therapeutic opportunities, lncRNAs offer particularly promising targets due to their high tissue specificity and central regulatory functions. However, effective clinical translation requires overcoming challenges in delivery efficiency, specificity, and safety profiles. This analysis provides a framework for researchers and drug development professionals to prioritize and optimize ncRNA-targeting strategies for HBV-induced hepatocarcinogenesis.
HBV-induced hepatocarcinogenesis involves a multistep process driven by both viral and host factors, with an estimated 296 million people chronically infected worldwide at risk of developing HCC [16] [56]. The HBV-encoded X protein (HBx) plays a central role in initiating and promoting tumorigenesis through multiple mechanisms, including alteration of host gene expression, impairment of DNA repair, and induction of epigenetic modifications [90] [19]. Emerging evidence indicates that ncRNAs, which constitute approximately 90% of the human transcriptome, serve as critical effectors in HBV-related HCC pathogenesis [16] [19].
NcRNAs were initially considered transcriptional "noise" but are now recognized as essential regulators of gene expression at transcriptional, post-transcriptional, and epigenetic levels. Their involvement in virtually all aspects of cellular homeostasis and disease processes has positioned them as attractive therapeutic targets [81]. In HBV-induced HCC, the expression profiles of numerous ncRNAs are significantly altered, either driving or suppressing tumorigenic processes through complex interactive networks [91] [90]. The stability of certain ncRNAs in bodily fluids and their disease-specific expression patterns further enhance their potential as biomarkers for early detection and prognostic assessment [16] [92].
This review systematically compares the three principal ncRNA classes—miRNAs, lncRNAs, and circRNAs—as therapeutic targets in HBV-induced HCC, with emphasis on their molecular mechanisms, experimental approaches for functional characterization, and translational applications. By synthesizing recent advances in this rapidly evolving field, we aim to provide researchers and drug development professionals with a comprehensive resource for developing ncRNA-targeted therapies against HBV-associated hepatocellular carcinoma.
ncRNA Classes in HBV-Induced Hepatocarcinogenesis
MicroRNAs (miRNAs)
MiRNAs are small endogenous ncRNAs approximately 21-25 nucleotides in length that regulate gene expression at the post-transcriptional level. Their biogenesis involves multiple coordinated steps: initial transcription as primary miRNAs (pri-miRNAs), nuclear processing by Drosha to generate precursor miRNAs (pre-miRNAs), export to the cytoplasm, and final cleavage by Dicer to produce mature miRNAs. The mature miRNAs are then incorporated into the RNA-induced silencing complex (RISC), enabling them to bind complementary sequences on target mRNAs, typically resulting in mRNA degradation or translational repression [16].
In HBV-related HCC, miRNAs demonstrate diverse roles, functioning as either oncogenes or tumor suppressors. The HBx protein significantly influences miRNA expression patterns, contributing to hepatocarcinogenesis through multiple mechanisms:
Oncogenic miRNAs frequently show upregulated expression in HBV-HCC. For instance, miR-21, regulated by HBx, targets tumor suppressors PDCD4 and PTEN, promoting tumor cell growth and survival [16]. Similarly, miR-221 and miR-222 are commonly upregulated by HBx and facilitate cell cycle progression while suppressing apoptosis [16]. The miR-17-92 cluster, including miR-18a, miR-19a/b, and miR-92a, demonstrates oncogenic properties by promoting proliferation, angiogenesis, and immune evasion [16].
Tumor-suppressive miRNAs often show downregulation in HBV-associated HCC. miR-122, a liver-specific miRNA crucial for HBV infection, is downregulated by inflammatory cytokines IL-6 and TNF-α, and its loss promotes tumor development, motility, and invasion [16] [90]. Similarly, miR-199a/b inhibits the ROCK1/MLC and PI3K/Akt pathways, with low expression associated with poor overall survival [16]. HBx-mediated downregulation of miR-101 induces aberrant DNA methylation by targeting DNMT3A, while miR-125b inhibits angiogenesis by targeting VEGFA and induces cell-cycle arrest [16].
Table 1: Key miRNAs in HBV-Related HCC and Their Therapeutic Potential
| miRNA | Expression in HCC | Regulated by HBx | Target Genes/Pathways | Primary Functions | Therapeutic Potential |
|---|---|---|---|---|---|
| miR-21 | Upregulated | Yes | PDCD4, PTEN | Promotes cell growth, survival | Antagomir inhibition |
| miR-221/222 | Upregulated | Yes | CXCL4/12, TFRC | Cell cycle progression, anti-apoptosis | Antagomir inhibition |
| miR-122 | Downregulated | Indirectly | PKM2, SLC7A1 | Suppresses tumor development, metabolism | Mimic restoration |
| miR-199a/b | Downregulated | Yes | ROCK1, PI3K/Akt | Inhibits proliferation, promotes apoptosis | Mimic restoration |
| miR-101 | Downregulated | Yes | DNMT3A | Regulates DNA methylation | Mimic restoration |
| let-7a | Downregulated | Yes | STAT3, c-myc | Suppresses proliferation | Mimic restoration |
| miR-148a | Downregulated | Yes | HPIP, AKT/ERK/FOXO4/ATF5 | Inhibits proliferation, EMT | Mimic restoration |
Long Non-Coding RNAs (lncRNAs)
LncRNAs represent a diverse class of RNA molecules longer than 200 nucleotides that lack protein-coding capacity. Transcribed by RNA polymerase II, they undergo typical post-transcriptional modifications including 5' capping and 3' polyadenylation [16]. LncRNAs exhibit high tissue specificity and can be classified based on their genomic location relative to protein-coding genes, including intergenic lncRNAs, antisense lncRNAs, intronic lncRNAs, and enhancer RNAs [81]. Their functional mechanisms are exceptionally diverse, encompassing interactions with DNA, RNA, and proteins to regulate chromatin modification, transcription, mRNA stability, and post-translational modifications [16] [81].
In HBV-related HCC, numerous lncRNAs demonstrate altered expression and contribute significantly to disease pathogenesis:
Oncogenic lncRNAs such as HULC (highly upregulated in liver cancer) show elevated expression in HCC tissues. Its expression is promoted by HBx in conjunction with CREB, leading to downregulation of the neighboring tumor suppressor p18 and subsequent promotion of hepatocellular proliferation [92]. HOTAIR, another well-characterized oncogenic lncRNA, interacts with polo-like kinase 1 (Plk1) and participates in carcinogenic epigenetic reprogramming related to HBV replication and HBx function [92]. A novel lncRNA, HDAC2-AS2, was recently identified as playing a critical role in HCC immune evasion. It is secreted via extracellular vesicles into the tumor microenvironment, where it enters immune cells and interacts with CDK9 protein, leading to CD8+ T cell dysfunction characterized by increased exhaustion and apoptosis [93].
Tumor-suppressive lncRNAs frequently show reduced expression in HBV-HCC. MEG3 demonstrates tumor-suppressive functions, and its downregulation correlates with liver fibrosis in chronic hepatitis B patients [92]. Similarly, Dreh (downregulated expression by HBx) inhibits tumor growth and metastasis in HBx-mediated hepatocarcinogenesis by binding to vimentin and suppressing its expression [92].
Table 2: Key lncRNAs in HBV-Related HCC and Their Therapeutic Potential
| lncRNA | Expression in HCC | Regulated by HBx | Molecular Mechanisms | Primary Functions | Therapeutic Potential |
|---|---|---|---|---|---|
| HULC | Upregulated | Yes | Downregulates p18; epigenetic regulation | Promotes proliferation | siRNA/ASO inhibition |
| HOTAIR | Upregulated | Yes | Interacts with Plk1; epigenetic reprogramming | Promotes viral replication, tumor growth | siRNA/ASO inhibition |
| HDAC2-AS2 | Upregulated | TGF-β signaling | Binds CDK9; impairs CD8+ T cell function | Immune evasion | ASO inhibition; biomarker |
| DLEU2 | Upregulated | Yes | Recruited to cccDNA; displaces EZH2 | Activates viral transcription | siRNA inhibition |
| MEG3 | Downregulated | Yes | Multiple signaling pathways | Tumor suppression | Ectopic expression |
| Dreh | Downregulated | Yes | Binds vimentin; inhibits expression | Suppresses metastasis | Ectopic expression |
| H19 | Upregulated | Yes | miRNA sponge; regulates CDC42/PAK1 | Promotes proliferation | siRNA/ASO inhibition |
Circular RNAs (circRNAs)
CircRNAs constitute a unique class of lncRNAs characterized by covalently closed continuous loops without 5' caps or 3' poly(A) tails. This circular structure confers exceptional resistance to RNA exonucleases, resulting in enhanced stability and longer half-lives compared to linear RNAs [16]. CircRNAs primarily function as competitive endogenous RNAs (ceRNAs) that sequester miRNAs, thereby preventing them from binding to their target mRNAs. This "sponge" mechanism allows circRNAs to indirectly regulate gene expression by modulating miRNA activity [16].
In HBV-related HCC, circRNAs participate in various aspects of disease progression, including proliferation, invasion, and metastasis, through regulation of multiple signaling pathways and target genes [90]. While specific circRNAs in HBV-related HCC were not extensively detailed in the available search results, their general functional mechanisms and structural stability position them as promising therapeutic targets and biomarkers for HCC.
Comparative Therapeutic Targeting Strategies
miRNA-Targeted Approaches
Therapeutic strategies targeting miRNAs primarily involve either restoration of tumor-suppressive miRNAs or inhibition of oncogenic miRNAs. For miRNA restoration, synthetic miRNA mimics are designed to reconstitute the function of downregulated tumor-suppressive miRNAs. These molecules duplicate the seed region of endogenous miRNAs and are incorporated into RISC to target oncogenic mRNAs. For miRNA inhibition, several approaches have been developed:
- Antagomirs: Chemically modified antisense oligonucleotides complementary to specific miRNA sequences that silence target miRNAs through stable binding and sequestration [16].
- Locked Nucleic Acids (LNAs): High-affinity RNA analogs with a bridged ribose ring that confers enhanced stability and binding affinity to target miRNAs [16].
- miRNA Sponges: Ectopically expressed transcripts containing multiple tandem binding sites for a miRNA family that competitively absorb miRNAs, preventing them from interacting with endogenous targets [16].
The advantages of miRNA-targeted therapies include their relatively small size, which facilitates delivery, and their ability to simultaneously regulate multiple genes within related pathways. However, challenges remain in achieving sufficient tissue specificity and minimizing off-target effects [16] [90].
lncRNA-Targeted Approaches
lncRNAs present unique opportunities and challenges as therapeutic targets due to their complex secondary structures, tissue-specific expression, and diverse mechanisms of action. Primary strategies for targeting lncRNAs include:
- Antisense Oligonucleotides (ASOs): Chemically modified single-stranded DNA analogs that bind complementary lncRNA sequences through Watson-Crick base pairing, triggering RNase H-mediated degradation of the target lncRNA [94] [81].
- RNA Interference (RNAi): Synthetic small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) that direct sequence-specific degradation of complementary lncRNA transcripts through the RISC pathway [81].
- Small Molecule Inhibitors: Compounds designed to disrupt specific structural domains or protein interactions of functional lncRNAs [81].
- CRISPR-Based Approaches: CRISPR/Cas9 systems for genomic deletion of lncRNA genes or CRISPR interference (CRISPRi) for transcriptional repression without DNA cleavage [92] [81].
A significant advance in lncRNA therapeutics involves nanoparticle-based delivery systems. Nanoparticles protect lncRNA molecules from degradation and enable precise targeted delivery to enhance therapeutic efficacy while reducing systemic toxicity [94]. For example, lipid-based nanoparticles can encapsulate ASOs or siRNAs targeting oncogenic lncRNAs, while functionalization with targeting ligands (e.g., galactose for hepatocyte-specific delivery) improves specificity [94].
circRNA-Targeted Approaches
Therapeutic targeting of circRNAs is less developed compared to other ncRNA classes but holds significant potential due to their exceptional stability and specific expression patterns. Primary strategies include:
- RNAi and ASOs: Designed to target back-splice junction sequences unique to circRNAs, enabling specific discrimination from linear RNA isoforms.
- circRNA Expression Vectors: Engineered circular RNA molecules that function as super-sponges for oncogenic miRNAs, with enhanced stability compared to linear sponges.
The closed circular structure of circRNAs presents both challenges and opportunities for therapeutic development, as the unique back-splice junctions provide highly specific targeting sequences but also complicate efficient degradation by conventional oligonucleotide therapies [16].
Table 3: Comparative Analysis of ncRNA-Targeted Therapeutic Approaches
| Parameter | miRNAs | lncRNAs | circRNAs |
|---|---|---|---|
| Primary Targeting Strategy | Mimics (for tumor suppressors); Antagomirs/ASOs (for oncogenes) | ASOs, RNAi, CRISPR-based approaches, small molecules | Back-splice junction targeting ASOs, expression vectors |
| Delivery Challenges | Moderate (small size advantageous) | High (large molecular weight, complex structure) | Moderate (unique junctions enable specificity) |
| Stability of Targeting Agents | Moderate to high | Moderate (ASOs) to low (RNAi) | High (targeting agents can be designed for stability) |
| Tissue Specificity | Moderate (some tissue-specific isoforms) | High (frequently tissue-specific) | Moderate to high (often tissue-specific) |
| Therapeutic Specificity | Moderate (target multiple genes) | High (specific isoforms targetable) | High (unique back-splice junctions) |
| Clinical Stage | Advanced (multiple in clinical trials) | Early to mid-stage (preclinical and early clinical) | Early stage (primarily preclinical) |
| Key Advantages | Multi-gene targeting; well-established design rules | High specificity; diverse mechanisms targetable | Exceptional stability; unique targeting sequences |
| Major Limitations | Off-target effects; redundant functions | Delivery challenges; complex structure-function relationships | Emerging field; limited functional characterization |
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing ncRNA research and therapeutic development requires a comprehensive toolkit of reagents, technologies, and methodologies. The following resources represent essential components for investigating ncRNAs in HBV-related HCC:
Table 4: Essential Research Reagents and Methodologies for ncRNA Research
| Reagent/Methodology | Function/Application | Key Considerations |
|---|---|---|
| RNA-seq | Comprehensive profiling of ncRNA expression; identification of novel ncRNAs | Enables unbiased detection of known and novel transcripts; specialized libraries required for circRNAs |
| Single-cell RNA-seq | Analysis of ncRNA expression at single-cell resolution; identification of cell-type specific expression | Reveals heterogeneity in tumor and immune cells; computationally intensive |
| CRISPR/Cas9 Screening | Functional screening for ncRNA involvement in specific phenotypes; target validation | Enables genome-wide loss-of-function studies; gRNA design critical for non-coding regions |
| ASOs and siRNAs | Functional validation of ncRNA targets; therapeutic development | Chemical modifications enhance stability and reduce immunogenicity; delivery optimization required |
| Nanoparticle Delivery Systems | In vitro and in vivo delivery of ncRNA-targeting therapeutics; improves biodistribution | Lipid nanoparticles most common; surface functionalization enhances tissue specificity |
| RNA Immunoprecipitation (RIP) | Identification of proteins bound to specific ncRNAs | Antibody quality critical; appropriate controls essential for specificity |
| Chromatin Isolation by RNA Purification (ChIRP) | Genome-wide mapping of lncRNA binding sites | Requires design of multiple antisense oligonucleotides; validation essential |
| Extracellular Vesicle Isolation Kits | Isolation of ncRNAs circulating in biofluids; biomarker development | Multiple methods available (ultracentrifugation, precipitation, size exclusion); purity varies |
| Luciferase Reporter Assays | Validation of miRNA-mRNA and ceRNA interactions | Vector design critical; appropriate normalization controls essential |
Experimental Workflows for ncRNA Functional Characterization
A standardized approach to ncRNA functional characterization involves sequential phases of discovery, validation, and mechanistic investigation. The following diagram illustrates a comprehensive workflow for identifying and validating therapeutic ncRNA targets in HBV-related HCC:
Diagram 1: Experimental Workflow for ncRNA Target Identification and Validation. This comprehensive workflow outlines the key stages in identifying and validating therapeutic ncRNA targets, from initial discovery through clinical translation.
Molecular Mechanisms of ncRNAs in HBV-Related HCC
The following diagram illustrates the complex molecular networks through which different ncRNA classes function in HBV-related hepatocarcinogenesis, highlighting potential therapeutic intervention points:
Diagram 2: Molecular Networks of ncRNAs in HBV-Related HCC. This diagram illustrates the complex regulatory networks between different ncRNA classes and their collective impact on cellular processes driving hepatocarcinogenesis, highlighting potential therapeutic intervention points.
The comparative analysis of ncRNA classes as therapeutic targets in HBV-induced HCC reveals distinct advantages and challenges for each category. miRNAs offer the advantage of relatively straightforward therapeutic design and multi-gene targeting capabilities but face challenges with specificity and off-target effects. lncRNAs provide exceptional tissue specificity and diverse mechanistic opportunities but present significant delivery challenges due to their size and structural complexity. circRNAs offer unique targeting opportunities through their back-splice junctions and exceptional stability but require further fundamental characterization of their biological functions.
Future directions in ncRNA-targeted therapies should focus on several key areas:
- Advanced Delivery Systems: Development of cell-type-specific delivery platforms, particularly nanoparticles functionalized with targeting ligands, will be essential for clinical translation.
- Combination Therapies: Strategic combinations of ncRNA-targeting agents with conventional antivirals, immunotherapies, or chemotherapy may yield synergistic effects.
- Biomarker Integration: Implementation of ncRNA biomarkers for patient stratification and treatment monitoring will enable more personalized therapeutic approaches.
- Innovative Targeting Platforms: Continued development of CRISPR-based technologies and small molecule inhibitors will expand the ncRNA therapeutic toolbox.
The growing understanding of ncRNA biology in HBV-induced hepatocarcinogenesis, coupled with advances in oligonucleotide therapeutics and delivery technologies, positions ncRNA-targeted approaches as promising components of comprehensive therapeutic strategies against this devastating malignancy. As research progresses, the rational design of ncRNA-based therapies informed by comparative analyses of their unique properties will accelerate the development of effective treatments for HBV-related HCC.
The therapeutic landscape for chronic Hepatitis B Virus (HBV) infection is undergoing a profound transformation, moving beyond viral suppression toward the achievable goal of a functional cure. This shift is largely driven by the emergence of small nucleic acid therapeutics, including small interfering RNAs (siRNAs) and antisense oligonucleotides (ASOs), which directly target viral transcripts and address the limitations of existing nucleos(t)ide analog therapies [95]. The pursuit of a functional cure, defined as sustained loss of hepatitis B surface antigen (HBsAg) with or without seroconversion, represents a paradigm shift in clinical management [95]. This whitepaper provides a technical analysis of the clinical trial landscape for these innovative modalities, framing their development within the context of HBV-induced non-coding RNA alterations that drive hepatocarcinogenesis. For researchers and drug development professionals, understanding the interplay between these therapeutic mechanisms and the underlying molecular pathology of HBV is crucial for designing next-generation clinical trials and combination regimens.
Table 1: Key Characteristics of Nucleic Acid Therapeutics in HBV
| Therapeutic Class | Mechanism of Action | Primary Molecular Target | Key Advantage in HBV |
|---|---|---|---|
| siRNA | RNA interference; degradation of complementary mRNA sequences [46] | All HBV transcripts (via targeting of conserved regions) [95] | Potently reduces HBsAg production from both cccDNA and integrated DNA [96] |
| ASO | RNase H1-dependent cleavage or steric hindrance of target RNA [46] | Specific HBV mRNA sequences | Can be designed to modulate splicing or inhibit translation [46] |
| Nucleic Acid Polymers (NAPs) | Information not covered in search results | Information not covered in search results | Information not covered in search results |
The HBV Genome and the Basis for Nucleic Acid Drug Design
The design of siRNA and ASO therapies is predicated on the unique structure and replication strategy of the HBV genome. The HBV genome is a compact, approximately 3200-nucleotide, partially double-stranded DNA molecule with four overlapping open reading frames (S, C, P, and X) [95]. Upon infection, the viral DNA is converted in the host nucleus into a stable covalently closed circular DNA (cccDNA) episome, which serves as the persistent transcriptional template for all viral RNAs [95].
A critical feature for drug design is that all HBV transcripts—the 3.5 kb preC/C mRNA, 2.4 kb PreS1 mRNA, 2.1 kb PreS2/S mRNA, and 0.7 kb X mRNA—share a common polyadenylation signal [95]. Consequently, strategically designed siRNAs or ASOs targeting this shared region can, in theory, trigger the degradation of multiple viral mRNAs simultaneously, thereby inhibiting the production of various viral proteins, including HBsAg [95]. Furthermore, because HBsAg can be produced from integrated HBV DNA fragments in the host genome—a source not affected by current NAs—the ability of nucleic acid therapies to target these transcripts is a fundamental component of their therapeutic promise [95].
Current Clinical Trial Landscape and Therapeutic Candidates
The clinical pipeline for siRNA and ASO therapies in HBV is robust, with several candidates demonstrating significant reductions in viral antigens in clinical trials. A key advancement has been the widespread adoption of GalNAc (N-acetylgalactosamine) conjugation for hepatocyte-specific delivery. This approach leverages the asialoglycoprotein receptor (ASGPR), which is highly expressed on hepatocytes, enabling efficient targeted delivery and reducing off-target effects [97].
Promising preclinical data for the GalNAc-conjugated siRNA RBD1016 illustrates the potential of this platform. In mouse models of HBV, RBD1016, which targets the HBx transcript, achieved substantial reductions in HBsAg (∼3.22 log) and HBV DNA (∼3.40 log) [96]. Notably, repeated dosing led to seroconversion—the production of anti-HBs antibodies—which is a key marker of a functional cure [96]. The effects were durable, lasting over 6 months, supporting infrequent dosing regimens in humans [96].
Table 2: Select Nucleic Acid Therapeutics in Development for HBV
| Therapeutic Candidate | Class | Delivery Platform | Key Preclinical/Clinical Findings | Development Status (as of 2025) |
|---|---|---|---|---|
| RBD1016 | siRNA | GalNAc-conjugate | >3 log HBsAg reduction; induced seroconversion in mouse models [96] | Preclinical/Phase 1 |
| ALN-BCAT-001 | siRNA | GalNAc-conjugate | In development for hepatocellular carcinoma [97] | Phase 1 |
| Patisiran (Onpattro) | siRNA | Lipid Nanoparticle (LNP) | First approved siRNA drug (for hATTR amyloidosis) [46] | Approved (non-HBV) |
| Givosiran (Givlaari) | siRNA | GalNAc-conjugate | Approved for Acute Hepatic Porphyria [97] | Approved (non-HBV) |
Methodologies for Evaluating siRNA and ASO Therapeutics
The development and evaluation of siRNA and ASO therapies require specialized in vitro and in vivo models, along with specific analytical techniques to assess pharmacokinetics and pharmacodynamics.
Key Experimental Models and Workflows
In Vitro Models:
- HepG2 Cell Lines: Engineered to express HBV genes or support HBV replication, these are used for initial screening of siRNA/ASO potency against viral transcripts and antigens (e.g., HBsAg, HBeAg) [96].
- High-Throughput Screening (HTS): Automated systems are employed to test libraries of siRNA or ASO sequences for optimal target binding and efficacy [46].
In Vivo Models:
- AAV-HBV Mouse Model: Mice are transduced with an adeno-associated virus (AAV) carrying the HBV genome. This model results in high levels of viremia and antigenemia, useful for assessing the ability of candidates to knock down antigens in a de novo infection context [96].
- HBV Transgenic Mouse Model: Mice genetically engineered to carry the entire HBV genome. This model mimics chronic infection and is critical for evaluating the durability of response and the potential for seroconversion after treatment [96].
Diagram 1: Experimental workflow for siRNA/ASO development.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Nucleic Acid Therapeutic Research
| Reagent / Material | Function in R&D | Technical Notes |
|---|---|---|
| GalNAc Conjugates | Targets therapeutics to hepatocytes via ASGPR-mediated endocytosis [97] | Industry standard for liver-targeting; improves therapeutic index and enables subcutaneous dosing. |
| Chemically Modified Nucleotides | Enhances stability against nucleases, increases binding affinity, and reduces immunogenicity [46] | Common modifications: 2'-O-methyl, 2'-fluoro, phosphorothioate backbone. |
| LC-MS/MS Systems | Quantifies oligonucleotide drug concentrations in plasma and tissue homogenates (Pharmacokinetics) [97] | Crucial for understanding tissue distribution and half-life; LLOQ can reach sub-ng/ml. |
| Stem-loop RT-qPCR | Highly sensitive detection and quantification of oligonucleotide therapeutics and their metabolites [97] | Offers higher sensitivity than LC-MS but lower specificity for distinguishing parent drug from metabolites. |
Connecting Therapeutics to HBV-Induced Non-Coding RNA Alterations
The rationale for nucleic acid therapies extends beyond direct antiviral activity to the correction of profound HBV-induced disruptions in the host's non-coding RNA (ncRNA) network, a key driver of hepatocarcinogenesis. The HBx protein is a central player in this process, acting as a master regulator of ncRNA expression [20] [19] [16].
HBx exerts widespread epigenetic control, often by dysregulating microRNAs (miRNAs). For instance, HBx can:
- Downregulate tumor-suppressive miRNAs like miR-148a and miR-101, leading to increased cell proliferation and aberrant DNA methylation [19] [16].
- Upregulate oncogenic miRNAs like miR-21, which inhibits apoptosis and supports tumor cell survival [16].
This HBx-mediated rewiring of the ncRNA landscape facilitates all hallmarks of cancer, including sustained proliferation, evasion of immune destruction, and activation of invasion and metastasis [20] [16]. The diagram below illustrates this complex network.
Diagram 2: HBx-ncRNA network in hepatocarcinogenesis.
By drastically reducing the viral load and HBsAg, siRNA and ASO therapies indirectly reduce the levels of HBx, potentially restoring the balance of the ncRNA network. This immune re-engagement is critical for achieving a functional cure and may also have a profound impact on preventing or delaying HBV-related hepatocarcinogenesis [96].
The future of nucleic acid therapies for HBV lies in rational combination regimens. The most promising strategy involves combining siRNA or ASO therapies, which directly reduce viral antigen burden, with immunomodulators—such as therapeutic vaccines or immune checkpoint inhibitors—to reverse T-cell exhaustion and enable the host immune system to clear the infection [96]. Furthermore, the integration of artificial intelligence in drug discovery is accelerating the design of more potent and stable oligonucleotide sequences, predicting target accessibility, and optimizing chemical modifications for improved safety and efficacy profiles [98].
In conclusion, the clinical trial landscape for siRNA and ASO therapies in HBV is defined by a clear trajectory toward achieving a functional cure. These modalities offer a direct mechanism to address the persistent antigenemia that drives both immune dysfunction and HBx-mediated oncogenic signaling. For researchers and clinicians, the evolving understanding of HBV-related ncRNA biology provides not only a rationale for these therapies but also a roadmap for developing next-generation combinations that target both the virus and the host-level pathological mechanisms, ultimately aiming to cure chronic HBV and prevent its devastating sequelae.
The therapeutic landscape for hepatitis B virus (HBV)-induced hepatocellular carcinoma (HCC) is undergoing a significant transformation, moving from conventional antivirals and immunotherapies to sophisticated RNA-based approaches. Non-coding RNA (ncRNA) therapies represent a emerging class of treatments with unique mechanistic advantages that address key limitations of existing modalities. This whitepaper provides a technical comparison of these therapeutic classes, detailing their mechanisms, synergistic potential, and practical experimental approaches for research and development. Within the specific context of HBV hepatocarcinogenesis, where viral proteins like HBx orchestrate extensive alterations to the host ncRNA landscape, targeting these ncRNAs offers novel opportunities for disrupting tumor-promoting pathways and overcoming treatment resistance. The integration of ncRNA therapies with established antivirals and immunotherapies presents a promising strategic direction for achieving durable responses in this difficult-to-treat malignancy.
HBV-related hepatocarcinogenesis represents a complex interplay between viral persistence, host immune responses, and accumulating genetic and epigenetic alterations. The HBx protein, a key viral regulatory protein, plays a central role in reprogramming the host cellular environment by directly influencing the expression and function of numerous ncRNAs [20]. This altered ncRNA landscape contributes significantly to tumor initiation, progression, and therapy resistance by modulating key processes including immune evasion, epigenetic regulation, and metabolic reprogramming [99] [20].
Conventional direct-acting antivirals (DAAs) for HBV primarily target viral replication but exhibit limited efficacy against established HCC and often fail to fully reverse virus-induced ncRNA alterations. Meanwhile, immunotherapies, particularly immune checkpoint inhibitors (ICIs), have demonstrated remarkable success in subsets of HCC patients but face significant challenges including primary and acquired resistance mechanisms [100] [101]. ncRNA therapies represent a paradigm shift by targeting the master regulators of gene expression that underlie both viral persistence and malignant transformation, offering potential solutions to these therapeutic limitations.
Comparative Mechanism Analysis
Table 1: Comparative Mechanisms of Therapeutic Classes in HBV-HCC
| Therapeutic Class | Specific Examples | Primary Molecular Targets | Key Mechanisms in HBV-HCC | Major Limitations |
|---|---|---|---|---|
| Direct-Acting Antivirals (DAAs) | Nucleos(t)ide analogs | Viral reverse transcriptase/DNA polymerase | Suppress viral replication; reduce viral load [102] | Do not target integrated HBV DNA; limited impact on established ncRNA alterations [20] |
| Immunotherapies | PD-1/PD-L1 inhibitors (nivolumab, pembrolizumab); CTLA-4 inhibitors (ipilimumab) | Immune checkpoint proteins | Reinvigorate exhausted T-cells; restore antitumor immunity [101] | High resistance rates; immune-related adverse events; immunosuppressive TME [100] [101] |
| ncRNA Therapeutics | miRNA mimics/inhibitors; siRNA; ASOs; lncRNA modulators | Specific ncRNAs and their downstream targets | Reverse HBx-induced ncRNA alterations; modulate TME; target multiple oncogenic pathways simultaneously [99] [100] [103] | Delivery challenges; potential off-target effects; stability issues [99] [103] |
The HBx protein drives extensive reprogramming of the ncRNA network in hepatocytes, which in turn facilitates hepatocarcinogenesis through multiple interconnected pathways. HBx has been shown to dysregulate specific miRNAs including miR-122, miR-101, miR-145, and miR-148a, contributing to abnormal lipid metabolism, epigenetic dysregulation, and enhanced proliferative signaling [20]. These HBx-induced ncRNA alterations create a cellular environment permissive for malignant transformation and represent critical therapeutic targets for ncRNA-based interventions.
Table 2: Key HBx-ncRNA Interactions in Hepatocarcinogenesis
| ncRNA | Regulation by HBx | Functional Consequences | Experimental Evidence |
|---|---|---|---|
| miR-122 | Downregulation | Increased CCL2 expression; loss of tumor suppression [20] | In vitro models of HBV infection; patient tissue analysis [20] |
| miR-101 | Downregulation | DNMT3A upregulation; aberrant DNA methylation [20] | HBx transfection models; clinical correlation studies [20] |
| miR-145 | Downregulation | CUL5 derepression; enhanced cell proliferation [20] | HBx expression systems; functional assays [20] |
| miR-148a | Downregulation via p53 inhibition | HPIP/mTOR pathway activation; EMT promotion [20] | p53 pathway analysis; EMT marker assessment [20] |
| LncRNAs | Multiple lncRNAs dysregulated | Chromatin remodeling; transcriptional reprogramming [99] [20] | RNA-seq; chromatin interaction studies [99] |
Quantitative Efficacy Comparison
Table 3: Therapeutic Efficacy Metrics Across Modalities
| Therapeutic Approach | Response Rate in Advanced HCC | Impact on Tumor Microenvironment | Effect on HBV Replication | Durability of Response |
|---|---|---|---|---|
| Direct-Acting Antivirals | Not applicable as monotherapy | Minimal direct impact | High suppression | Requires continuous therapy |
| ICI Monotherapy | 15-20% [104] [101] | Moderate (reduces T-cell exhaustion) | No direct effect | Variable; can be long-lasting in responders |
| ICI Combinations | 30-35% (e.g., atezolizumab+bevacizumab) [101] | Significant (vascular normalization + immune activation) | No direct effect | Improved versus monotherapy |
| ncRNA Therapeutics | Preclinical data only | Potentially comprehensive (multiple cell types) | Potential dual antiviral/antitumor effect | Theoretical potential for sustained effect |
Clinical trials have established benchmark efficacy data for existing modalities. The HIMALAYA trial demonstrated a 36-month overall survival rate of 30.7% with tremelimumab plus durvalumab compared to 20.2% with sorafenib alone in unresectable HCC [104]. The IMbrave150 trial established atezolizumab plus bevacizumab as a standard-of-care with significantly improved survival over sorafenib [101]. While these represent substantial advances, a significant proportion of patients remain non-responsive, highlighting the need for novel approaches like ncRNA therapeutics that address the fundamental drivers of resistance.
Synergistic Potential and Combinatorial Approaches
The convergence of ncRNA therapies with existing treatment modalities creates multiple synergistic opportunities in HBV-HCC. The diagram below illustrates key synergistic mechanisms between ncRNA therapies and established treatments:
Synergistic Therapy Mechanisms
Specific synergistic mechanisms include:
Overcoming ICI Resistance: ncRNAs can modulate the tumor immune microenvironment by targeting immunosuppressive cells including myeloid-derived suppressor cells (MDSCs) and tumor-associated macrophages (TAMs) [100]. For example, miR-449c has been implicated in regulating MDSC function, suggesting its potential for enhancing ICI efficacy [100].
Multi-Targeting Oncogenic Pathways: ncRNA therapies can simultaneously target multiple HBx-driven pathways. For instance, miR-148a restoration can inhibit HPIP-mediated mTOR signaling and epithelial-mesenchymal transition (EMT), addressing both tumor growth and metastasis [20].
Epigenetic Reprogramming: LncRNAs such as HOTAIR and MALAT1, which are frequently dysregulated in HCC, can be targeted to reverse epigenetic alterations that maintain the malignant state [99] [103].
Experimental Protocols and Methodologies
Comprehensive ncRNA Profiling in HBV-HCC Models
Objective: To identify and validate HBx-induced ncRNA alterations in relevant experimental models.
Workflow:
- Model Establishment: Utilize HBx-expressing cell lines (HepG2-HBx, Huh7-HBx) or primary human hepatocytes with HBV infection; include appropriate controls [20].
- RNA Extraction: Employ miRNeasy kits or similar with quality control (RIN >8.0).
- Library Preparation and Sequencing:
- Small RNA-seq for miRNAs using Illumina platforms.
- Ribosomal RNA depletion for lncRNA/circRNA analysis.
- Bioinformatic Analysis:
- Alignment to combined human/HBV reference genome.
- Differential expression analysis (DESeq2, edgeR).
- Coding potential assessment (CPC, PhyloCSF).
- Integration with public datasets (TCGA-LIHC, GEO).
- Functional Validation:
- CRISPR-based ncRNA modulation (knockout/activation).
- qRT-PCR confirmation (TaqMan assays for miRNAs).
- In situ hybridization for spatial localization.
The following diagram illustrates the key experimental workflow for ncRNA profiling and functional validation:
Experimental Workflow for ncRNA Profiling
Functional Validation of Candidate ncRNAs
Protocol for miRNA Gain/Loss-of-Function Studies:
- Design of miRNA Modulators:
- miRNA mimics: Double-stranded RNA molecules mimicking mature miRNA.
- miRNA inhibitors: Single-stranded antisense oligonucleotides (ASOs) with chemical modifications (2'-O-methyl, LNA).
- Transfection Optimization:
- Test multiple transfection reagents (lipofectamine RNAiMAX, DharmaFECT).
- Optimize concentrations (typically 10-50 nM for mimics/inhibitors).
- Include fluorescent controls to assess efficiency.
- Functional Assays:
- Proliferation: MTT, colony formation.
- Apoptosis: Annexin V/PI staining.
- Migration/Invasion: Transwell assays.
- Target Validation:
- 3'UTR reporter assays (psiCHECK-2 vectors).
- Western blot of predicted targets.
- RIP-seq for Ago2-bound targets.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for HBV-ncRNA Studies
| Reagent Category | Specific Examples | Application | Technical Notes |
|---|---|---|---|
| HBV/HBx Models | HepG2.2.15 cells; HepAD38 system; HBx-expressing lentiviruses | Modeling HBV persistence and HBx effects | Confirm HBx expression by Western (17 kDa band) and functionality [20] |
| ncRNA Modulation | LNA-modified antisense oligonucleotides; miRNA mimics; CRISPR-activation/inhibition systems | Functional studies of specific ncRNAs | Include appropriate scrambled/negative controls; optimize delivery [103] |
| Sequencing Kits | Illumina Small RNA-seq; SMARTer smRNA-seq; ribosomal depletion kits | ncRNA profiling | Use spike-in controls for normalization; sufficient biological replicates (n≥3) [99] |
| Delivery Systems | Lipid nanoparticles (LNPs); GalNAc conjugates; polymer-based nanoparticles | Therapeutic testing of ncRNA candidates | Characterize size (70-150 nm), PDI (<0.3), and encapsulation efficiency (>80%) [103] |
| Immune Monitoring | Multiplex cytokine assays; flow cytometry panels (CD8, CD4, PD-1, CTLA-4); MHC multimers | Assessing immunotherapy interactions | Include functional assays (IFN-γ ELISpot) for T-cell activity [100] [101] |
Advanced delivery systems are particularly critical for translational applications. Current approaches include lipid nanoparticles (LNPs), N-acetylgalactosamine (GalNAc) conjugates for hepatocyte-specific targeting, cell-derived membrane nanocarriers, and polymer-based systems [103]. Each platform offers distinct advantages in terms of payload capacity, targeting efficiency, and immunogenicity profile.
The integration of ncRNA therapies into the therapeutic arsenal for HBV-induced HCC represents a promising frontier in oncology and virology. The unique ability of ncRNA-based approaches to simultaneously target multiple aspects of HBV-induced hepatocarcinogenesis - including viral persistence, immune evasion, and oncogenic signaling - positions them as ideal candidates for combination regimens with existing antivirals and immunotherapies. The documented role of HBx in systematically reprogramming the host ncRNA landscape provides a strong mechanistic rationale for targeting these regulatory molecules.
Future development in this field will require advances in several key areas: (1) improved delivery systems with enhanced hepatocyte specificity and reduced immunogenicity; (2) comprehensive biomarker strategies to identify patients most likely to benefit from specific ncRNA therapies; and (3) sophisticated combination regimens that leverage the synergistic potential between ncRNA-targeting approaches and established treatment modalities. As our understanding of the complex interactions between HBV infection and the host ncRNA network deepens, particularly through single-cell and spatial transcriptomics approaches, the precision and efficacy of ncRNA-based therapeutic interventions will continue to improve, offering new hope for patients with this challenging malignancy.
The Role of Novel Biomarkers (HBV RNA, HBcrAg) in Validating Therapeutic Efficacy
The pursuit of a functional cure for chronic hepatitis B (CHB), defined as sustained loss of hepatitis B surface antigen (HBsAg), represents the central challenge in viral hepatitis therapeutics worldwide [79]. With over 250 million people living with chronic HBV infection and current nucleos(t)ide analog (NA) therapy rarely achieving HBsAg loss, the development of novel therapeutic strategies demands equally advanced biomarkers for evaluating treatment efficacy [105] [79]. The limitations of traditional biomarkers—HBV DNA for viral replication and HBsAg for antigen load—have become increasingly apparent as they cannot directly assess the transcriptional activity of the persistent viral reservoir within hepatocytes [105].
In this context, serum HBV RNA and hepatitis B core-related antigen (HBcrAg) have emerged as crucial novel biomarkers that provide unprecedented insights into the intrahepatic viral reservoir status [105]. These biomarkers directly reflect the activity of covalently closed circular DNA (cccDNA), the stable minichromosome responsible for viral persistence, and offer superior predictive value for treatment outcomes [105]. Furthermore, their significance is magnified when framed within the growing understanding of HBV-induced non-coding RNA alterations in hepatocarcinogenesis, as they represent measurable serum indicators of complex viral-host interactions that drive liver disease progression toward hepatocellular carcinoma (HCC) [32] [19].
This technical guide comprehensively examines the role of HBV RNA and HBcrAg in validating therapeutic efficacy for diverse audiences of researchers, scientists, and drug development professionals. We present structured experimental data, detailed methodologies, and mechanistic insights to facilitate the implementation of these biomarkers in both clinical trials and basic research settings.
The Biological and Clinical Significance of Novel HBV Biomarkers
Serum HBV RNA: Composition and Origins
Serum HBV RNA exists as a complex mixture of viral transcripts with distinct molecular origins and clinical implications [105]. The predominant forms include:
- Full-length pregenomic RNA (pgRNA): A 3.5 kb transcript directly from cccDNA containing complete coding region with polyadenylated tail [105]
- 3′-Truncated pgRNA: Lacks the 3′ polyadenylated tail due to incomplete template degradation; proportion increases during long-term NA therapy [105]
- pgRNA splicing variants: At least 20 distinct secreted isoforms generated through aberrant host cell splicing mechanisms [105]
- HBx transcripts: Generally present at low levels, including full-length or truncated HBx open reading frames [105]
- HBV-human chimeric RNAs: Recently detected in serum samples from CHB patients with integrated HBV DNA [105]
Critically, serum HBV RNA originates directly from cccDNA templates, making it a more precise indicator of intrahepatic cccDNA levels and transcriptional activity compared to traditional biomarkers [105]. During NA therapy, which suppresses reverse transcription but not transcription from cccDNA, HBV RNA becomes particularly valuable as it reflects ongoing cccDNA activity despite DNA suppression [105].
Hepatitis B Core-Related Antigen (HBcrAg): Components and Significance
HBcrAg represents a composite biomarker that immunologically detects several viral proteins sharing common antigenic determinants [105]:
- HBV core antigen (HBcAg)
- Hepatitis B e antigen (HBeAg)
- A truncated core protein (p22cr)
Like HBV RNA, HBcrAg shows a strong correlation with intrahepatic cccDNA levels and transcriptional activity [105]. It provides complementary information to HBV RNA as it reflects both viral replication (via cccDNA activity) and translation of core-related proteins [105]. This dual nature makes it particularly valuable for monitoring patients across different phases of CHB natural history and during antiviral therapy.
Integration with Non-Coding RNA Alterations in Hepatocarcinogenesis
The significance of these novel biomarkers extends beyond viral monitoring to encompass the oncogenic transformation processes in HBV-related HCC. Hepatitis B virus X protein (HBx)-mediated aberrations in non-coding RNAs create a molecular environment conducive to hepatocarcinogenesis [19]. Long non-coding RNAs (lncRNAs) such as DLEU2, HOTAIR, and HULC facilitate HBV replication and progression to HCC through complex regulatory mechanisms [32].
Table 1: HBV-Related Non-Coding RNAs in Hepatocarcinogenesis
| Non-Coding RNA | Regulation by HBx | Molecular Mechanism | Role in HCC |
|---|---|---|---|
| DLEU2 | Upregulated | Binds HBx or EZH2; displaces EZH2 from viral chromatin | Enhances viral transcription and replication [32] |
| HOTAIR | Upregulated | Elevates activities of HBV promoters via cccDNA-bound SP1 modulation | Promotes HBV transcription and replication [32] |
| HULC | Upregulated | Activates HBx/STAT3/miR-539/APOBEC3B axis; forms HAT1/HULC/HBc complex on cccDNA | Enhances HBV replication and cancer progression [32] |
| PCNAP1 | Upregulated | Enhances PCNA through sponging miR-154; PCNA interacts with HBV cccDNA | Promotes HBV replication via miR-154/PCNA/HBV cccDNA axis [32] |
| HOTTIP | Induced by HBV | Restrains HBV replication via CREB1/HOTTIP/HOXA13 axis | Suppresses HBV replication, contributing to persistent infection [32] |
HBV RNA and HBcrAg serve as detectable serum manifestations of these underlying ncRNA-regulated processes, providing accessible windows into the molecular events driving hepatocarcinogenesis. Their quantification in clinical settings offers potential for early intervention before overt malignancy develops.
Quantitative Assessment and Clinical Validation
Detection Methodologies and Technical Considerations
Accurate quantification of serum HBV RNA requires sophisticated molecular techniques, each with distinct advantages and limitations [105]:
- RT-qPCR (Reverse Transcription Quantitative PCR): Most widely used; targets conserved regions (X, preC/C, or S); cannot differentiate RNA isoforms; high sensitivity [105]
- RT-droplet digital PCR: Enables absolute quantification with potential for isoform differentiation; uses microfluidic partitioning [105]
- SAT (Fluorescence-based Nucleic Acid Isothermal Amplification Testing): Operational simplicity; eliminates DNase treatment; cannot differentiate isoforms [105]
- RACE (Rapid Amplification of cDNA Ends): Selectively amplifies polyadenylated transcripts; cannot detect truncated RNAs lacking polyA tail [105]
For HBcrAg detection, chemiluminescence enzyme immunoassay (CLEIA) is the standard methodology, providing high sensitivity and reproducibility across a broad dynamic range [105].
Table 2: Analytical Performance of Novel HBV Biomarker Assays
| Parameter | Serum HBV RNA | HBcrAg |
|---|---|---|
| Detection Method | RT-qPCR, RT-ddPCR, SAT | CLEIA |
| Detection Limit | 50 copies/mL (varies by assay) | <3 log U/mL (high-sensitivity assays) |
| Dynamic Range | 1-8 log copies/mL | 3-7 log U/mL |
| Isoform Differentiation | Limited with standard methods | Not applicable |
| Correlation with Intrahepatic cccDNA | r = 0.25-0.89 [105] | Strong correlation demonstrated [105] |
| Effect of NA Therapy | Unaffected (transcription not inhibited) | Gradual decline reflects cccDNA reduction |
Clinical Validation and Predictive Value
Substantial clinical evidence supports the utility of both biomarkers in predicting treatment outcomes across different therapeutic contexts:
HBV RNA Predictive Value: In children with low-level viremia (LLV) receiving entecavir therapy, higher HBV RNA levels at week 48 emerged as an independent risk factor for non-virological response (adjusted odds ratio: 5.86; 95% CI: 1.40-24.62; P = 0.016) [106]. Although HBV RNA alone was slightly less predictive than HBV DNA (AUC: 0.76 vs. 0.80), the combination of both markers significantly improved prediction accuracy (AUC: 0.82; P < 0.05 vs. single markers) [106].
HBcrAg Predictive Value: HBcrAg demonstrates strong prognostic value for spontaneous HBeAg seroconversion, virological response to therapy, and HCC risk stratification [105]. Patients with elevated baseline HBcrAg levels show reduced likelihood of achieving functional cure with current therapies, informing patient selection for clinical trials of novel agents [105].
The 2025 Canadian Association for the Study of the Liver (CASL) guidelines explicitly recognize the importance of these novel biomarkers, noting that "future testing algorithms will likely involve a combination of standard and new biomarker assays providing results that may provide a scoring system" [76].
Experimental Protocols for Biomarker Implementation
Protocol 1: Serum HBV RNA Quantification via RT-qPCR
Principle: This method detects total serum HBV pgRNA through reverse transcription followed by quantitative PCR amplification [105].
Sample Preparation:
- Collect 5-10 mL of venous blood in serum separation tubes
- Allow clotting for 30 minutes at room temperature
- Centrifuge at 1,500-2,000 × g for 10 minutes
- Aliquot serum into nuclease-free tubes and store at -80°C until analysis
- Avoid repeated freeze-thaw cycles (maximum 2 cycles)
RNA Extraction:
- Use commercial viral RNA extraction kits (e.g., QIAamp Viral RNA Mini Kit)
- Include DNase treatment step to eliminate contaminating HBV DNA
- Elute RNA in 30-50 μL nuclease-free water
- Determine RNA purity spectrophotometrically (A260/A280 ratio >1.8)
Reverse Transcription:
- Use gene-specific primers targeting conserved regions of HBV pgRNA
- Employ reverse transcriptase with high processivity (e.g., SuperScript IV)
- Include negative controls without reverse transcriptase to monitor DNA contamination
- Reaction conditions: 50°C for 30 minutes, 80°C for 10 minutes
Quantitative PCR:
- Design TaqMan probes spanning splice junctions of pgRNA to enhance specificity
- Target regions: PreC/C or 5' end of pgRNA to ensure full-length transcript detection
- Use standard curve with known copy numbers of in vitro transcribed HBV RNA
- Cycling conditions: 95°C for 3 minutes, followed by 45 cycles of 95°C for 15s and 60°C for 1 minute
- Include internal control to monitor extraction efficiency
Data Analysis:
- Calculate copy numbers using standard curve method
- Express results as log10 copies/mL
- Establish assay detection limit using serial dilutions (typically 50-100 copies/mL)
- Implement quality control criteria including inter-assay coefficient of variation <15%
Protocol 2: HBcrAg Quantification via CLEIA
Principle: HBcrAg is measured using a two-step immunoassay with monoclonal antibodies recognizing denatured HBeAg, HBcAg, and p22cr [105].
Sample Preparation:
- Collect serum samples as described in Protocol 1
- Pretreatment with detergent-containing buffer to denature core-related antigens and expose epitopes
- Heat treatment at 60°C for 30 minutes to dissociate immune complexes
Immunoassay Procedure:
- Incubate pretreated samples with magnetic particles coated with anti-HBcAg/HBeAg monoclonal antibodies
- Wash to remove unbound materials
- Add F(ab')2 fragments of monoclonal antibodies conjugated with alkaline phosphatase
- Incubate and wash to remove unbound conjugates
- Add chemiluminescent substrate (e.g., CDP-Star)
- Measure chemiluminescence intensity with luminometer
Calibration and Quantification:
- Use calibrators with known HBcrAg concentrations (3-7 log U/mL)
- Construct standard curve from calibrator readings
- Calculate sample concentrations from standard curve
- Report results as log U/mL
Quality Assurance:
- Include internal quality control samples at low, medium, and high concentrations
- Participate in external proficiency testing programs
- Validate assay performance characteristics regularly
Biomarker Applications in Therapeutic Development
Clinical Trial Endpoints and Patient Stratification
The development of novel antiviral agents targeting distinct aspects of the HBV life cycle necessitates sophisticated biomarkers for early efficacy assessment [79]. HBV RNA and HBcrAg provide critical insights for several therapeutic classes:
- RNA interference therapeutics: Monitor rapid declines in HBV RNA and HBcrAg reflecting reduced viral transcription [79]
- Core protein allosteric modulators (CpAMs): Assess impact on pgRNA packaging and reverse transcription through HBV RNA reductions [79]
- HBV entry inhibitors (e.g., bulevirtide): Evaluate prevention of new infection through delayed biomarker responses [79]
- Immunomodulators: Detect immune-mediated clearance of infected hepatocytes through complex biomarker kinetics [79]
Recent clinical guidelines have begun formalizing the role of these biomarkers in treatment decision-making. The 2025 CASL/AMMI Canada guidelines recommend quantitative measurement of HBsAg every one to two years to monitor treatment response and in determining functional cure, while acknowledging that new biomarkers associated with cccDNA transcriptional activity require further research on clinical utility and cost-effectiveness [76].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Novel HBV Biomarker Studies
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Nucleic Acid Extraction Kits | QIAamp Viral RNA Mini Kit, MagMAX Viral RNA Isolation Kit | Isolation of serum HBV RNA | Include DNase treatment step; monitor extraction efficiency with internal controls [106] |
| HBV RNA Standards | In vitro transcribed pgRNA, WHO international standard (when available) | Assay calibration and quantification | Ensure integrity of RNA standards; store in single-use aliquots at -80°C [105] |
| RT-qPCR Reagents | SuperScript IV One-Step RT-PCR System, TaqMan RNA-to-Ct 1-Step Kit | HBV RNA detection and quantification | Optimize primer/probe combinations; validate against DNA contamination [106] |
| HBcrAg Assay Kits | Lumipulse G HBcrAg assay, Luminulse G HBcrAg - NEXT | HBcrAg quantification | Standardize pretreatment conditions; establish laboratory-specific reference ranges [105] |
| Reference Materials | WHO international standards for HBV DNA, panel samples with known cccDNA levels | Assay validation and standardization | Use commutable materials; participate in proficiency testing programs [105] |
Pathway Diagrams and Molecular Relationships
Diagram 1: Molecular Relationships Between Novel Biomarkers and Hepatocarcinogenesis. This diagram illustrates how serum HBV RNA and HBcrAg originate from cccDNA transcriptional activity and serve as predictors of HCC risk, while being modulated by HBV-induced non-coding RNA alterations.
Diagram 2: Experimental Workflows for Novel Biomarker Assessment. This diagram outlines the sequential steps for quantifying serum HBV RNA (yellow) and HBcrAg (green), highlighting key methodological considerations for research implementation.
The integration of HBV RNA and HBcrAg into the standard assessment armamentarium for CHB represents a paradigm shift in therapeutic monitoring and drug development. These biomarkers provide critical insights into cccDNA activity—the primary barrier to HBV cure—that cannot be gleaned from conventional markers alone [105]. Their utility extends beyond mere viral monitoring to encompass risk stratification for hepatocarcinogenesis, connecting serum virological profiles with the underlying molecular pathology of HBV-driven HCC [32] [19].
For the research community, several priority areas demand attention:
Standardization of Assay Platforms: International collaboration is needed to establish reference materials, standardized protocols, and uniform reporting units across platforms [105]
Isoform-Specific Detection: Technological innovations enabling differentiation of HBV RNA isoforms would provide deeper insights into the relative contributions of cccDNA versus integrated DNA to the serum RNA pool [105]
Integration with ncRNA Profiling: Combining serum biomarker quantification with analysis of HCC-associated ncRNAs in tissue and liquid biopsies could enhance early detection of malignant transformation [16]
Regulatory Qualification: Formal qualification of these biomarkers as drug development tools by regulatory agencies would accelerate their adoption in clinical trial contexts [76]
As novel therapeutic strategies progress through clinical development—including RNA interference agents, core protein modulators, and immunotherapeutic approaches—HBV RNA and HBcrAg will play increasingly vital roles in guiding combination therapies and identifying responder populations [79]. The ongoing refinement of these biomarkers and their interpretation within the framework of HBV-induced ncRNA alterations will undoubtedly enhance our capacity to achieve durable functional cure and prevent HCC development in the millions living with chronic HBV infection worldwide.
The pursuit of a functional cure for chronic Hepatitis B Virus (HBV) infection, defined as sustained loss of hepatitis B surface antigen (HBsAg) after treatment cessation, represents one of the most pressing challenges in hepatology [79]. Despite the availability of effective nucleos(t)ide analogs that suppress viral replication, these treatments rarely achieve HBsAg seroclearance, with an annual clearance rate of only approximately 1% [79]. The persistence of HBV covalently closed circular DNA (cccDNA) and high viral antigen loads that exhaust HBV-specific immunity create significant barriers to cure [79]. Within this complex virological and immunological landscape, HBV-induced alterations in non-coding RNAs (ncRNAs) have emerged as critical drivers of hepatocarcinogenesis, presenting both challenges and therapeutic opportunities [16] [8].
Research paradigms from HIV management and oncology offer valuable conceptual frameworks and methodological approaches for advancing the HBV cure agenda. The successful transformation of HIV from a fatal diagnosis to a manageable chronic condition through combination antiretroviral therapy demonstrated the power of targeted antiviral strategies and meticulous care coordination [107]. Similarly, innovations in cancer immunotherapy, particularly immune checkpoint inhibitors, have revealed mechanisms for reversing T-cell exhaustion—a phenomenon directly relevant to the impaired immune responses in chronic HBV [108]. This whitepaper examines how these cross-disciplinary insights can accelerate the development of ncRNA-targeted therapeutic strategies for HBV-related hepatocellular carcinoma (HCC), with a specific focus on diagnostic biomarkers, therapeutic targeting, and clinical trial design.
Table 1: Key Parallels Between HIV, Cancer, and HBV Research
| Research Domain | Core Concept | Application to HBV/HCC |
|---|---|---|
| HIV Management | Treatment cascade analytics | Tracking patient progression from diagnosis to cure [107] |
| HIV Management | Combination antiretroviral therapy | Multi-targeted approach for HBV functional cure [79] |
| Cancer Immunotherapy | Immune checkpoint inhibition | Reversing T-cell exhaustion in chronic HBV [108] |
| Cancer Biomarker Development | Molecular profiling for personalized therapy | ncRNA signatures for HBV-HCC stratification [16] [8] |
HIV Research: Lessons for Enhancing HBV Care Continuum and Therapeutic Strategies
Treatment Cascade Analytics for HBV Cure Monitoring
The HIV treatment cascade model has revolutionized patient care by systematically tracking outcomes from diagnosis through viral suppression. Application of this framework to HBV care has demonstrated remarkable potential for improving cure rates. A 2023 study partnering with the Connecticut Department of Health applied this model to hepatitis C treatment, achieving a 73% cure rate across 11 clinics—approaching the WHO target of 80% [107]. The cascade analysis identified specific disparities, revealing that women and patients with poorly controlled HIV were less likely to initiate hepatitis C treatment, thereby highlighting populations needing targeted intervention [107].
This methodology can be directly adapted to HBV functional cure programs by establishing monitoring systems that track patient progression through critical stages: initial diagnosis, linkage to care, appropriate treatment initiation, adherence monitoring, and ultimately HBsAg seroclearance. The granular data obtained through such tracking enables clinics to identify very specific barriers to cure at each stage of the patient journey and implement tailored interventions to overcome these obstacles.
Combination Therapy Principles from Antiretroviral Regimens
The fundamental principle of combination therapy that transformed HIV management—simultaneously targeting multiple viral replication pathways—now directly informs next-generation HBV therapeutic strategies. Current HBV drug development focuses on combining direct-acting antivirals with immunomodulators to achieve synergistic effects [79]. This approach recognizes that effective viral control requires both suppression of replication and restoration of host immune responses.
promising combination strategies include RNA interference (RNAi) therapeutics that target viral transcripts alongside immune stimulators. For instance, the antisense oligonucleotide Bepirovirsen incorporates dual mechanisms:它ä¸ä»…é™è§£ç—…毒RNA,还通过Tollæ ·å—体8 (TLR8)刺激å…ç–«å应 [109]. Similarly, RNAi agents like VIR-2218 (siRNA) and AB-729 (RNAi therapeutic) are being evaluated in combination with pegylated interferon and other immune modulators to achieve sustained HBsAg reduction [109] [79]. This multi-pronged approach mirrors the combination antiretroviral regimens that successfully contain HIV replication while preventing resistance emergence.
Oncology Research: Immunotherapy and ncRNA Therapeutics for HBV-Related HCC
Immune Checkpoint Inhibition for Reversing T-Cell Exhaustion
Oncology's breakthrough in immune checkpoint inhibition offers a crucial framework for addressing the dysfunctional immune responses in chronic HBV and HBV-related HCC. HIV research has similarly revealed that inadequate immune surveillance contributes to hepatocarcinogenesis, particularly in patients with low CD4+ cell counts [108]. Immune checkpoint inhibitors (ICIs) developed in oncology can potentially reverse the T-cell exhaustion characteristic of chronic viral infections, though their application in HIV/HBV co-infection requires careful consideration.
Notably, HIV-infected patients have historically been excluded from many cancer clinical trials, particularly those involving immunotherapies, leaving a significant evidence gap regarding ICI safety and efficacy in this population [108]. However, emerging data suggest that properly selected HIV-positive patients can achieve comparable outcomes to HIV-negative individuals when treated with agents like sorafenib for HCC [108]. This underscores the need to reconsider exclusion criteria that have limited patient access to life-prolonging therapies and restricted our understanding of ICI effects in co-infected populations.
ncRNA-Targeted Therapeutics for HBV-Induced Hepatocarcinogenesis
The oncology field has pioneered RNA-based therapeutics that can be directly applied to HBV-related HCC. Non-coding RNAs, particularly microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), play critical regulatory roles in HBV-induced oncogenesis and represent promising therapeutic targets [16] [8]. These molecules function as either oncogenes or tumor suppressors, modulating key cancer hallmarks including proliferation, invasion, metastasis, angiogenesis, and immune evasion [16].
Table 2: Key ncRNAs in HBV-Related HCC and Their Therapeutic Implications
| ncRNA | Expression in HBV-HCC | Function | Target/Mechanism | Therapeutic Approach |
|---|---|---|---|---|
| miR-21 | Upregulated | Oncogenic | Targets PDCD4 & PTEN [16] | Anti-miR (inhibition) |
| miR-221 | Upregulated | Oncogenic | Targets CXCL4/12; promotes cell cycle [16] | Anti-miR (inhibition) |
| miR-122 | Downregulated | Tumor suppressive | Regulates metabolism (PKM2, SLC7A1) [16] | miRNA replacement |
| miR-199a/b | Downregulated | Tumor suppressive | Inhibits ROCK1/MLC & PI3K/Akt [16] | miRNA replacement |
| HULC | Upregulated | Oncogenic | Acts as miRNA sponge; promotes proliferation [8] | RNAi-based targeting |
The stability and detectability of ncRNAs in bodily fluids further enhances their clinical utility as non-invasive biomarkers for early detection, prognosis, and treatment monitoring [16] [8]. For instance, miRNA expression deregulation occurs early in HBV-associated multistep hepatocarcinogenesis, with changes accumulating through progression from chronic hepatitis to cirrhosis to HCC [110]. Specific miRNAs like miR-221 show gradient expression alterations across disease stages—downregulated in acute HBV infection, normally expressed in chronic infection, and upregulated in HCC—suggesting their potential as biomarkers for tracking disease progression [111].
Experimental Models and Methodologies for Investigating ncRNAs in HBV-Related HCC
Cell Models for HBV-Related Hepatocarcinogenesis
Robust experimental models are essential for delineating the functional roles of ncRNAs in HBV-related HCC. Established cell systems include the human HepG2 hepatoblastoma cell line (virus-free model), HepG2 cells transfected with a 1.3-fold full-length HBV genome (acute infection model), and HepG2.2.15 cells stably transfected with a complete HBV genome (chronic infection model) [111]. These models enable researchers to investigate stage-specific ncRNA alterations and their contributions to malignant transformation.
Comparative miRNA profiling across these cell models has revealed distinct expression patterns during acute versus chronic HBV infection. One study identified 77 differentially expressed miRNAs during acute infection and 48 during chronic infection, with 25 miRNAs in common between both phases [111]. Among these, 14 showed coherent expression changes (1 upregulated, 13 downregulated), while 11 demonstrated inverse patterns, suggesting complex temporal regulation of ncRNA networks during HBV infection [111].
Methodologies for ncRNA Profiling and Functional Validation
Comprehensive ncRNA analysis requires integrated methodological approaches spanning discovery, validation, and functional characterization. Key techniques include:
- Microarray Profiling: High-throughput screening using mammalian miRNA arrays containing probes for hundreds of human mature miRNAs enables discovery-phase identification of differentially expressed ncRNAs [111].
- Real-time RT-qPCR: Targeted quantification of candidate miRNAs (e.g., miR-10b, miR-21, miR-122, miR-145, miR-199b, miR-221, miR-224) in clinical samples validates expression patterns and correlates findings with pathological features [110].
- Functional Manipulation: Gain-of-function (miRNA mimics, lncRNA expression vectors) and loss-of-function (anti-miRs, siRNA, CRISPR-based approaches) experiments establish causal relationships between ncRNAs and malignant phenotypes [62].
- Mechanistic Studies: RNA immunoprecipitation, luciferase reporter assays, and rescue experiments elucidate molecular mechanisms of action, including miRNA-mRNA interactions and pathway regulation [16].
Table 3: Key Research Reagent Solutions for HBV-related ncRNA Studies
| Reagent/Resource | Function/Application | Examples/Specifications |
|---|---|---|
| Cell Models | In vitro study of HBV-ncRNA interactions | HepG2 (HBV-negative), HepG2.HBV (acute infection model), HepG2.2.15 (chronic infection model) [111] |
| Profiling Platforms | Genome-wide ncRNA expression analysis | Mammalian miRNA arrays (924 probes); Custom miRNA arrays (435 human miRNA probes) [111] |
| Functional Validation Tools | Gain/loss-of-function studies | miRNA mimics, inhibitors (anti-miRs), siRNA, CRISPR-based systems [62] |
| Delivery Systems | Therapeutic ncRNA delivery | Lipid nanoparticles, GalNAc conjugates, viral vectors [62] |
| Animal Models | In vivo therapeutic efficacy testing | Humanized liver mice, immunocompetent HBV mouse models [62] |
Integrated Therapeutic Roadmap: Combining Insights for HBV Functional Cure
The convergence of insights from HIV management, cancer immunotherapy, and ncRNA biology creates a powerful integrated framework for advancing HBV functional cure strategies. This multidisciplinary approach suggests several key strategic priorities:
First, combination therapies should simultaneously target multiple aspects of the HBV life cycle and host immune response. Promising regimens might include direct-acting antivirals (entry inhibitors, RNAi therapeutics, capsid assembly modulators) combined with immunomodulators (TLR agonists, immune checkpoint inhibitors, therapeutic vaccines) [79]. The HIV experience demonstrates that strategic combination therapy can overcome the limitations of monotherapies and prevent resistance emergence.
Second, ncRNA-based therapeutics offer precise mechanisms for targeting specific pathogenic pathways in HBV-related HCC. miRNA replacement therapy using tumor-suppressive miRNAs (e.g., miR-122, miR-199a/b) or anti-miR approaches against oncogenic miRNAs (e.g., miR-21, miR-221) can potentially reverse the malignant phenotype [16] [62]. The development of efficient, liver-targeted delivery systems, such as GalNAc-conjugated siRNAs that specifically target hepatocytes, represents a critical enabling technology for this approach [62].
Third, comprehensive patient monitoring systems modeled after the HIV treatment cascade should be implemented to track progression through the entire care continuum—from diagnosis to functional cure. These systems enable identification of specific attrition points and implementation of targeted interventions to maintain patients in care and optimize treatment outcomes [107].
Finally, inclusive clinical trial designs that enroll appropriately selected HIV/HBV co-infected patients are needed to generate robust safety and efficacy data across diverse patient populations. Historical exclusion of these patients from clinical trials has created significant evidence gaps and limited access to novel therapeutics [108].
The path to HBV functional cure requires continued collaboration across virology, oncology, immunology, and RNA biology. By building on the foundational lessons from HIV and cancer research while leveraging growing understanding of ncRNA networks in hepatocarcinogenesis, the scientific community can accelerate progress toward eliminating HBV as a global health threat.
Conclusion
The intricate network of HBV-induced ncRNA alterations represents a cornerstone of hepatocarcinogenesis, offering profound insights into the disease's molecular underpinnings. From foundational discovery to therapeutic application, ncRNAs have proven to be pivotal as drivers of tumorigenesis, sensitive biomarkers, and promising therapeutic targets. The path forward requires a concerted effort to translate these discoveries into clinical practice by optimizing delivery systems, validating efficacy in robust clinical trials, and developing combinatorial strategies that target both viral and host ncRNA pathways. Future research must prioritize understanding the crosstalk between different ncRNA species and exploiting the unique immunological context of HBV infection. By doing so, the scientific community can move closer to achieving the dual goals of a functional cure for chronic HBV and effective prevention and treatment for HBV-related hepatocellular carcinoma.
References
- 1. Trends in Incidence of Hepatocellular Carcinoma Between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178839/]
- 2. Hepatocellular carcinoma: signaling pathways and ... [https://www.nature.com/articles/s41392-024-02075-w]
- 3. Global, regional, and national burden of liver cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598365/]
- 4. Changing etiology and epidemiology of hepatocellular ... [https://www.e-jlc.org/journal/view.php?number=557]
- 5. Global epidemiology of liver cancer burden due to hepatitis ... [https://pubmed.ncbi.nlm.nih.gov/41173651/]
- 6. Hepatitis B virus integration and hepatocarcinogenesis [https://www.sciencedirect.com/science/article/pii/S2542568425000509]
- 7. Downregulated long non-coding RNA DREH promotes cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5530050/]
- 8. Non-coding RNAs as key regulators in hepatitis B virus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12230020/]
- 9. HBV-associated hepatocellular carcinomas inhibit ... [https://www.nature.com/articles/s41467-025-57367-8]
- 10. Perspectives on NcRNAs in HBV/cccDNA-driven HCC ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12182653/]
- 11. Long non‑coding RNAs in HBV‑related hepatocellular ... [https://www.spandidos-publications.com/10.3892/ijo.2019.4909]
- 12. Long Non-Coding RNAs in Hepatitis B Virus-Related ... [https://www.mdpi.com/1422-0067/18/12/2505]
- 13. LincRNA-miR interactions in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s00210-025-04285-7]
- 14. Circular RNAs in hepatitis B virus-induced hepatocellular ... [https://www.sciencedirect.com/science/article/pii/S2352304225000947]
- 15. Non-coding RNA methylation modifications in hepatocellular ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-023-01357-0]
- 16. Non-coding RNAs as key regulators in hepatitis B virus- ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1602252/full]
- 17. The oncogenic role of hepatitis B virus X gene in ... [https://www.explorationpub.com/Journals/etat/Article/1002209]
- 18. The Multiple Roles of Hepatitis B Virus X Protein (HBx ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7412373/]
- 19. Hepatitis B virus X protein-mediated non-coding RNA ... [https://www.nature.com/articles/emm2016177]
- 20. Mechanism of HBx carcinogenesis interaction with non-coding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10517716/]
- 21. HBV-related hepatocarcinogenesis: the role of signalling ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-019-5916-6]
- 22. The Primary Role of Noncoding RNA in the Pathogenesis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294578/]
- 23. The Role of Non-Coding RNAs in the Regulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388849/]
- 24. Targeting non-coding RNAs to overcome cancer therapy ... [https://www.nature.com/articles/s41392-022-00975-3]
- 25. Non-Coding RNAs in Colorectal Cancer: Their Functions ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.783079/full]
- 26. Hepatitis B virus promotes liver cancer by modulating the ... [https://www.nature.com/articles/s41467-025-60894-z]
- 27. Decoding the molecular and genomic landscape of ... [https://www.nature.com/articles/s44355-025-00038-8]
- 28. The roles and mechanisms of coding and noncoding RNA ... [https://www.nature.com/articles/s12276-024-01307-x]
- 29. Hepatitis B virus core/capsid protein induces hepatocellular ... [https://tcr.amegroups.org/article/view/101438/html]
- 30. Insight into the mechanisms regulating liver cancer stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11555838/]
- 31. Role of Noncoding RNAs in the Tumor Immune Microenvironment of Hepatocellular Carcinoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10037505/]
- 32. Long noncoding RNAs in hepatitis B virus replication and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9280728/]
- 33. Machine learning-based model for predicting tumor ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1409443/full]
- 34. LncRNAs expression signatures of hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4033470/]
- 35. Non-coding RNAs in hepatocellular carcinoma: Insights ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.985815/full]
- 36. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 37. Machine Learning Prognostic Model for Post-Radical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11847427/]
- 38. Prognostic Factors for Mortality in Hepatocellular ... [https://www.mdpi.com/2075-4418/14/4/406]
- 39. Hepatitis B virus X protein-mediated non-coding RNA ... [https://pubmed.ncbi.nlm.nih.gov/28186085/]
- 40. Current progress and role of lncRNAs in HBV infection ... [https://www.sciencedirect.com/science/article/pii/S2352304225003678]
- 41. Identification of novel therapeutic targets in hepatitis-B ... [https://www.nature.com/articles/s41598-025-03625-0]
- 42. Dual tissue mRNA and serum protein signatures improve ... [https://www.nature.com/articles/s41698-025-01142-x]
- 43. Strategies to Achieve Functional Cure in HBV [https://link.springer.com/article/10.1007/s11901-025-00710-w]
- 44. Non-coding RNAs and potential therapeutic targeting in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC7856203/]
- 45. The HBV-induced non-coding RNAs alterations in ... [https://www.techscience.com/biocell/v47n1/49930/html]
- 46. Landscape of small nucleic acid therapeutics [https://www.nature.com/articles/s41392-024-02112-8]
- 47. Noncoding RNAs Emerging as Drugs or Drug Targets [https://pmc.ncbi.nlm.nih.gov/articles/PMC9573214/]
- 48. Off-target effects of oligonucleotides and approaches ... [https://www.sciencedirect.com/science/article/pii/S2472555225000474]
- 49. Hepatitis B Virus-Encoded HBsAg Contributes to Hepatocarcinogenesis by Inducing the Oncogenic Long Noncoding RNA LINC00665 through the NF-κB Pathway - PubMed [https://pubmed.ncbi.nlm.nih.gov/35993712/]
- 50. Hepatitis B virus X protein mediated epigenetic alterations in the pathogenesis of hepatocellular carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/35648301/]
- 51. The Mechanism Underlying the ncRNA Dysregulation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.847728/full]
- 52. RNA nanotherapeutics for hepatocellular carcinoma treatment [https://pmc.ncbi.nlm.nih.gov/articles/PMC11700867/]
- 53. Decoding the Non-coding: Tools and Databases Unveiling the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11249652/]
- 54. miRNA-29b-1-5p mediates an antiviral activity by targeting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229319/]
- 55. miRNA-29b-1-5p mediates an antiviral activity by targeting ... [https://www.nature.com/articles/s41598-025-09655-y]
- 56. HBVâ€Induced Carcinogenesis: Mechanisms, Correlation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11669079/]
- 57. Frontiers | The Epigenetic Modulation of Cancer and Immune Pathways in Hepatitis B Virus-Associated Hepatocellular Carcinoma: The Influence of HBx and miRNA Dysregulation [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2021.661204/full]
- 58. MicroRNA and liver cancer [https://www.oaepublish.com/articles/cdr.2019.110]
- 59. New Insights into the Role of miR-29a in Hepatocellular Carcinoma: Implications in Mechanisms and Theragnostics - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8003318/]
- 60. Novel role of miR-29b-1-5p expression - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8935397/]
- 61. Pegylated interferon therapy-related microRNA-6126 ... [https://www.sciencedirect.com/science/article/abs/pii/S0378111922008885]
- 62. Harnessing non-coding RNA therapeutics for ... [https://www.sciencedirect.com/science/article/abs/pii/S0163725825001688]
- 63. The liver-specific long noncoding RNA FAM99B inhibits ... [https://www.nature.com/articles/s41419-025-07401-w]
- 64. RNA Therapeutics: Delivery Problems and Solutions—A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567017/]
- 65. Noncoding RNA therapeutics — challenges and potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8212082/]
- 66. Integrative analysis of exosomal ncRNAs and their regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11992429/]
- 67. Editorial focus: understanding off-target effects as the key to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6902517/]
- 68. Regulatory guidelines and preclinical tools to study the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8957368/]
- 69. Advancements in clinical RNA therapeutics: Present ... [https://www.sciencedirect.com/science/article/pii/S2666379124002477]
- 70. Clinical Pharmacokinetics of Approved RNA Therapeutics - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9821128/]
- 71. Factors Affecting Stability of RNA – Temperature, Length, ... [https://www.sciencedirect.com/science/article/pii/S0022354923004987]
- 72. Strategies and efforts in circumventing the emergence of ... [https://www.nature.com/articles/s44259-025-00125-z]
- 73. Strategies to Overcome Antigen Heterogeneity in CAR-T ... [https://www.mdpi.com/2073-4409/14/5/320]
- 74. Chronic Hepatitis B in 2025: Diagnosis, Treatment and ... [https://www.sciencedirect.com/science/article/pii/S1470211825002453]
- 75. Prevention and Management of Hepatitis B Virus Infection ... [https://www.hivguidelines.org/guideline/hiv-hbv/]
- 76. The Management of Chronic Hepatitis B: 2025 Guidelines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12269321/]
- 77. HIV/AIDS and HBV co-infection with optimal control ... [https://www.nature.com/articles/s41598-024-83442-z]
- 78. The role of immune regulation in HBV infection and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949809/]
- 79. Drug development for chronic hepatitis B functional cure [https://pmc.ncbi.nlm.nih.gov/articles/PMC12038417/]
- 80. HBV-miR-3 induces hepatic cholesterol accumulation by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12391803/]
- 81. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 82. The interplay between hepatitis B virus and antitumor ... [https://link.springer.com/article/10.1007/s10238-025-01928-0]
- 83. Atorvastatin Rapidly Reduces Hepatitis B Viral Load in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9303483/]
- 84. Statins exposure and adverse events in participants with ... [https://www.nature.com/articles/s44355-025-00020-4]
- 85. Endpoint - NCATS Toolkit [https://toolkit.ncats.nih.gov/glossary/endpoint/]
- 86. Clinical Endpoint Classification [https://domsccr.stanford.edu/research-capabilities/clinical-event-adjudication-committee/]
- 87. Combining serologic biomarkers with the PAGE B score ... [https://www.nature.com/articles/s41598-025-16059-5]
- 88. Alternative splicing immune signature for detecting HBV ... [https://www.sciencedirect.com/science/article/pii/S2405580825003930]
- 89. Preclinical human and murine models of hepatocellular ... [https://www.sciencedirect.com/science/article/abs/pii/S2210740124001396]
- 90. Mechanism of HBx carcinogenesis interaction with non- ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1249198/full]
- 91. The HBV-induced non-coding RNAs alterations in ... [https://www.sciencedirect.com/org/science/article/pii/S0327954522001566]
- 92. 长链éžç¼–ç RNA在HBV感染和è‚细胞癌进展ä¸çš„当å‰è¿›å±•å’Œä½œç”¨ [https://www.ebiotrade.com/newsf/2025-10/20251015151317318.htm]
- 93. lncRNA在è‚细胞癌ä¸çš„æ½œåœ¨ç”Ÿç‰©æ ‡å¿—ç‰©å’Œæ²»ç–—é¶ç‚¹åº”ç”¨ç ”ç©¶ [https://www.zhihuiya.com/news/info_7889.html]
- 94. 基于纳米颗粒和长链éžç¼–ç RNAé¶å‘治疗è‚ç™Œçš„ç ”ç©¶è¿›å±• [http://www.bnujournal.com/article/doi/10.12202/j.0476-0301.2024166]
- 95. Small nucleic acid drugs-the dawn of functional cure of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511008/]
- 96. siRNA approaches in HBV: From antigen reduction to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12538891/]
- 97. Translational and clinical development of therapeutic siRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12477600/]
- 98. Artificial intelligence in the development of small nucleic ... [https://www.sciencedirect.com/science/article/pii/S1359644625002016]
- 99. Unraveling the advances of non-coding RNAs on the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131439/]
- 100. Noncoding RNAs as an emerging resistance mechanism to ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1268745/full]
- 101. synergies among immune checkpoints, TKIs, and chemotherapy [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-025-01739-6]
- 102. Overview of host-directed antiviral targets for future ... [https://www.sciencedirect.com/science/article/pii/S2211383525001431]
- 103. Role of non-coding RNA through nanomedicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579740/]
- 104. The Evolving Role of Combination Systemic Therapies in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9666801/]
- 105. Emerging Serum Biomarkers for Chronic Hepatitis B [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422880/]
- 106. Serum hepatitis B virus RNA in low-level viremia of chronic ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-025-02712-y]
- 107. Using Lessons from HIV to Treat Hepatitis C [https://medicine.yale.edu/news-article/using-lessons-from-hiv-to-treat-hepatitis-c/]
- 108. Hepatocellular cancer therapy in patients with HIV infection [https://pmc.ncbi.nlm.nih.gov/articles/PMC8220238/]
- 109. Hepatitis B Virus Pipeline Drugs Report 2025 [https://www.theglobeandmail.com/investing/markets/markets-news/GetNews/34928260/hepatitis-b-virus-pipeline-drugs-report-2025-unveiling-drug-development-progress-clinical-advances-pharma-strategies-and-market-evolution/]
- 110. Deregulation of microRNA expression occurs early and ... [https://www.sciencedirect.com/science/article/abs/pii/S0168827810009256]
- 111. Hepatitis B virus and hepatocellular carcinoma at the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3160541/]