Independent Prognostic lncRNA Biomarkers in HCC: From Multivariate Cox Validation to Clinical Translation
This article synthesizes current advancements in validating long non-coding RNA (lncRNA) biomarkers for hepatocellular carcinoma (HCC) prognosis using multivariate Cox regression models.
Independent Prognostic lncRNA Biomarkers in HCC: From Multivariate Cox Validation to Clinical Translation
Abstract
This article synthesizes current advancements in validating long non-coding RNA (lncRNA) biomarkers for hepatocellular carcinoma (HCC) prognosis using multivariate Cox regression models. It explores the foundational role of specific lncRNAs across biological processes like amino acid metabolism and ferroptosis, detailing rigorous methodologies for constructing multi-lncRNA signatures. The content addresses critical challenges in analytical optimization and troubleshooting, and emphasizes the necessity of robust validation through functional assays and clinical correlation. Aimed at researchers and drug development professionals, this review provides a comprehensive framework for developing clinically actionable lncRNA-based prognostic tools to guide personalized therapy and improve patient outcomes in HCC.
The Landscape of Prognostic lncRNAs in HCC: Core Biological Functions and Pathways
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most prevalent cancer worldwide and the fourth most common cause of cancer-related mortality [1]. As the predominant histological form of primary liver cancer, HCC constitutes more than 90% of total liver cancer cases worldwide, with its pathogenesis involving complex biological processes including DNA damage, epigenetic modification, and oncogene mutation [2] [3]. Over the past two decades, the role of long non-coding RNAs (lncRNAs)—RNA molecules longer than 200 nucleotides that lack protein-coding capacity—has received increasing attention in HCC research [2]. These molecules have emerged as crucial regulators of gene expression through multiple mechanisms: serving as signaling molecules that recruit transcription factors; acting as guiding molecules that direct chromatin-modifying enzymes to specific genomic locations; functioning as decoy molecules that sequester transcription factors or microRNAs; and working as scaffolding molecules that mediate the formation of multi-component complexes [3].
The investigation of lncRNAs in HCC has progressed from initial observations of dysregulated expression to sophisticated multivariate Cox regression analyses that validate their independent prognostic significance. This evolution has positioned lncRNAs as promising biomarkers for prognostic assessment and potential targets for therapeutic intervention. The functional characterization of these molecules reveals a complex regulatory network where specific lncRNAs can act either as oncogenes promoting tumor development or as tumor suppressors inhibiting carcinogenesis [4] [2]. This comparative analysis systematically examines the roles of dysregulated lncRNAs in HCC pathogenesis, focusing on their validated prognostic significance through multivariate Cox regression studies, with the aim of providing researchers and drug development professionals with a comprehensive resource for understanding this dynamic field.
Oncogenic lncRNAs in HCC: Mechanisms and Prognostic Value
Oncogenic lncRNAs demonstrate upregulated expression in HCC tissues and contribute to tumor development and progression through diverse molecular mechanisms. These molecules promote malignant phenotypes including uncontrolled cell proliferation, enhanced metastatic potential, evasion of apoptosis, and treatment resistance. Their elevated expression consistently correlates with advanced disease stage and poorer clinical outcomes, making them valuable prognostic indicators and potential therapeutic targets.
Table 1: Key Oncogenic lncRNAs in HCC and Their Prognostic Significance
| lncRNA Name | Expression in HCC | Molecular Mechanisms | Prognostic Value (Multivariate Cox Analysis) | Clinical Applications |
|---|---|---|---|---|
| LINC00152 | Upregulated [1] | Promotes cell proliferation through regulation of CCDN1 [1] | HR: 2.524; 95% CI: 1.661-4.015; P=0.001 for shorter OS [3] | Independent prognostic biomarker; potential therapeutic target |
| LINC01063 | Upregulated [5] | Regulates ferroptosis; promotes cell proliferation, migration, and invasion [5] | Part of 7-FRlncRNA signature predicting outcome [5] | Component of ferroptosis-related prognostic signature; oncogenic driver |
| UCA1 | Upregulated [1] | Promotes proliferation and inhibits apoptosis of HCC cells [1] | Combined with other lncRNAs improves diagnostic power [1] | Diagnostic biomarker, especially in combination panels |
| HOTAIR | Upregulated [4] | Competes with BRCA1 protein; regulated by mir-7 and mir-34a [4] | Associated with poor overall survival and disease-free survival [1] | Prognostic biomarker; promotes invasion and metastasis |
| H19 | Upregulated [2] | Stimulates CDC42/PAK1 axis by down-regulating miRNA-15b [2] | Contributes to HCC progression [2] | Oncogenic role; potential therapeutic target |
| ANRIL | Upregulated [4] | Enhances tumor growth in various cancers [4] | Positive correlation with poor prognosis in osteosarcoma [4] | Potential pan-cancer oncogenic marker |
| LINC01094 | Upregulated [3] | Not fully characterized | HR: 2.091; 95% CI: 1.447-3.021; P<0.001 for shorter OS [3] | Independent prognostic biomarker |
The functional validation of oncogenic lncRNAs extends beyond correlation studies to direct experimental demonstration of their cancer-promoting properties. For instance, LINC01063 was comprehensively validated as an oncogene in HCC through both in vitro and in vivo experiments. Knockdown of LINC01063 inhibited cell proliferation, disrupted colony formation ability, and reduced the migration and invasion capacities of HCC cells. In vivo studies using nude BALB/c mice injected with LINC01063-knockdown HCC cells exhibited reduced tumor growth compared to controls, providing direct evidence of its oncogenic function [5]. Similarly, H19 has been shown to affect proliferation, apoptosis, invasion, and metastasis of HCC cells through epigenetic modification, drug resistance, and regulation of downstream pathways [2].
The prognostic significance of these oncogenic lncRNAs has been rigorously validated through multivariate Cox regression analyses, confirming their independent value in predicting patient outcomes. For example, high pre-treatment expression of LINC00152 in tumor tissues independently predicted shorter overall survival (HR: 2.524; 95% CI: 1.661-4.015; P=0.001) in 63 HCC patients treated with curative surgical resection [3]. Similarly, LINC01094 expression was identified as an independent factor associated with shorter overall survival (HR: 2.091; 95% CI: 1.447-3.021; P<0.001) in 365 HCC patients [3]. These robust statistical analyses controlling for other clinical variables strengthen the case for incorporating these molecular markers into clinical prognostic assessment.
Figure 1: Mechanism of Action for Oncogenic lncRNAs in HCC. Oncogenic lncRNAs drive hepatocellular carcinoma progression through multiple molecular mechanisms including epigenetic regulation, miRNA sponging, and protein interactions, ultimately leading to enhanced proliferation, invasion, and treatment resistance.
Tumor-Suppressor lncRNAs in HCC: Protective Functions and Clinical Significance
Tumor-suppressor lncRNAs exhibit downregulated expression in HCC tissues and normally function to constrain malignant transformation and tumor progression. The loss of their protective activity through silencing or reduced expression removes critical brakes on cellular proliferation and creates a permissive environment for carcinogenesis. The restoration of their function represents a promising therapeutic strategy for HCC treatment.
Table 2: Key Tumor-Suppressor lncRNAs in HCC and Their Prognostic Significance
| lncRNA Name | Expression in HCC | Molecular Mechanisms | Prognostic Value (Multivariate Cox Analysis) | Clinical Applications |
|---|---|---|---|---|
| GAS5 | Downregulated [1] | Triggers CHOP and caspase-9 signal pathways; affects miR-32-5p/PTEN axis [4] [1] | Higher LINC00152 to GAS5 ratio correlated with increased mortality [1] | Tumor suppressor; inhibits cancer cell development and metastasis |
| LINC01146 | Downregulated [3] | Not fully characterized | HR: 0.38; 95% CI: 0.16-0.92; P=0.033 for longer OS [3] | Independent favorable prognostic biomarker |
| LINC01554 | Downregulated [3] | Not fully characterized | Low expression: HR: 2.507; 95% CI: 1.153-2.832; P=0.017 for shorter OS [3] | Independent prognostic biomarker |
| LASP1-AS | Downregulated [3] | Not fully characterized | Low expression: HR: 1.884; 95% CI: 1.427-2.841; P<0.0001 for shorter OS [3] | Independent prognostic biomarker |
| MEG3 | Downregulated [6] | Multiple tumor suppressor functions | Associated with tumor expansion, metastasis, prognosis [6] | Potential tumor suppressor lncRNA |
The molecular mechanisms of tumor-suppressor lncRNAs involve constraining key cancer-promoting pathways and activating cellular processes that inhibit malignant transformation. GAS5, for instance, has been demonstrated to inhibit invasion, migration, and proliferation of colorectal cancer HT-29 cells, and induces apoptosis in these cells [4]. In pancreatic carcinoma, overexpression of GAS5 prevents cancer cells from developing and metastasizing by affecting the miR-32-5p/PTEN axis [4]. This lncRNA represents a compelling example of a tumor suppressor with potential relevance across multiple cancer types, including HCC.
The prognostic significance of tumor-suppressor lncRNAs is evident in multivariate Cox regression analyses, where their reduced expression independently predicts unfavorable outcomes. For example, a low pre-treatment expression level of LINC01554 in tumor tissues was an independent predictor for shorter overall survival (HR: 2.507; 95% CI: 1.153-2.832; P=0.017) in 167 HCC patients treated with curative surgical resection [3]. Similarly, low expression of LASP1-AS independently predicted shorter overall survival in both training (HR: 1.884; 95% CI: 1.427-2.841; P<0.0001) and validation cohorts (HR: 3.539; 95% CI: 2.698-6.030; P<0.0001) encompassing 423 HCC patients [3]. These findings highlight the clinical importance of preserving the function of these protective lncRNAs.
The ratio between oncogenic and tumor-suppressor lncRNAs may provide even more powerful prognostic information than individual markers. One study found that a higher LINC00152 to GAS5 expression ratio significantly correlated with increased mortality risk, suggesting that the balance between competing lncRNA influences may critically determine disease outcome [1]. This ratio-based approach acknowledges the complex interplay within lncRNA networks and may offer enhanced prognostic precision.
Multivariate Cox Regression Studies: Validating lncRNA Prognostic Signatures
The application of multivariate Cox regression analysis has been instrumental in validating the independent prognostic value of lncRNA biomarkers in HCC, accounting for potential confounding factors such as age, sex, disease stage, and treatment modality. These rigorous statistical approaches have evolved from examining single lncRNAs to constructing multi-lncRNA signatures that offer superior predictive accuracy.
Table 3: Multivariate Cox Regression-Validated lncRNA Signatures in HCC
| lncRNA Signature | Number of lncRNAs | Study Cohort | Statistical Performance | Clinical Utility |
|---|---|---|---|---|
| Ferroptosis-Related Signature [5] | 7 FRlncRNAs | 365 HCC patients (TCGA) | AUC: 0.745 (1-year), 0.745 (2-year), 0.719 (3-year OS) | Predicts outcome and correlates with immunity and activated oncogene pathways |
| Five-lncRNA Signature [7] | 5 lncRNAs (RP11-325L7.2, DKFZP434L187, RP11-100L22.4, DLX2-AS1, RP11-104L21.3) | 167 early-stage HCC samples | Risk score was an independent prognostic factor for HCC | Prognosis prediction in early-stage HCC |
| Four-lncRNA Machine Learning Model [1] | 4 lncRNAs (LINC00152, LINC00853, UCA1, GAS5) | 52 HCC patients and 30 controls | 100% sensitivity, 97% specificity for HCC diagnosis | Diagnostic tool when integrated with conventional laboratory data |
| Plasma Exosomal lncRNA-derived 6-Gene Signature [8] | 6 genes (G6PD, KIF20A, NDRG1, ADH1C, RECQL4, MCM4) | 230 plasma exosomes and 831 HCC tissues | High prognostic accuracy in random survival forest model | Molecular subtyping, prognostic stratification, treatment response prediction |
| Four-lncRNA Prognostic Model [9] | 4 lncRNAs (DDX11-AS1, ZFPM2-AS1, AC016717.2, LINC00462) | 342 HCC patients (TCGA) | Reliably stratified patients into high-risk and low-risk groups (P<0.05) | Survival prediction based on risk score |
The integration of machine learning approaches with lncRNA biomarker analysis has enhanced the precision of prognostic stratification in HCC. One study demonstrated that a machine learning model integrating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters achieved 100% sensitivity and 97% specificity for HCC diagnosis, significantly outperforming individual lncRNAs which showed moderate diagnostic accuracy with sensitivity and specificity ranging from 60-83% and 53-67%, respectively [1]. This highlights the power of computational approaches to leverage lncRNA biomarkers for clinical application.
Ferroptosis-related lncRNA signatures represent a particularly innovative approach, leveraging the central role of ferroptosis in HCC development. One study established a prognostic signature comprising seven ferroptosis-related lncRNAs that effectively classified patients into low-risk and high-risk groups with significantly different prognosis [5]. The time-dependent receiver operating characteristic analysis yielded area under the curve values of 0.745, 0.745, and 0.719 for 1-, 2-, and 3-year overall survival, respectively, demonstrating robust predictive accuracy. Importantly, this signature also correlated with immune cell infiltration and expression of immune checkpoint genes, providing insights into the tumor microenvironment and potential implications for immunotherapy response [5].
Plasma exosomal lncRNAs offer a promising non-invasive approach for HCC management. One comprehensive study integrated transcriptomic data from 230 plasma exosomes and 831 HCC tissues to identify dysregulated plasma exosomal lncRNAs that form competitive endogenous RNA networks regulating 61 exosome-related genes [8]. Using unsupervised consensus clustering based on exosome-related gene expression profiles, HCC patients were stratified into three molecular subtypes with distinct survival outcomes, tumor microenvironments, and pathway activities. A subsequent random survival forest-derived 6-gene risk score demonstrated high prognostic accuracy and predicted differential treatment responses, with low-risk patients showing superior anti-PD-1 immunotherapy responses while high-risk patients exhibited increased sensitivity to DNA-damaging agents and sorafenib [8].
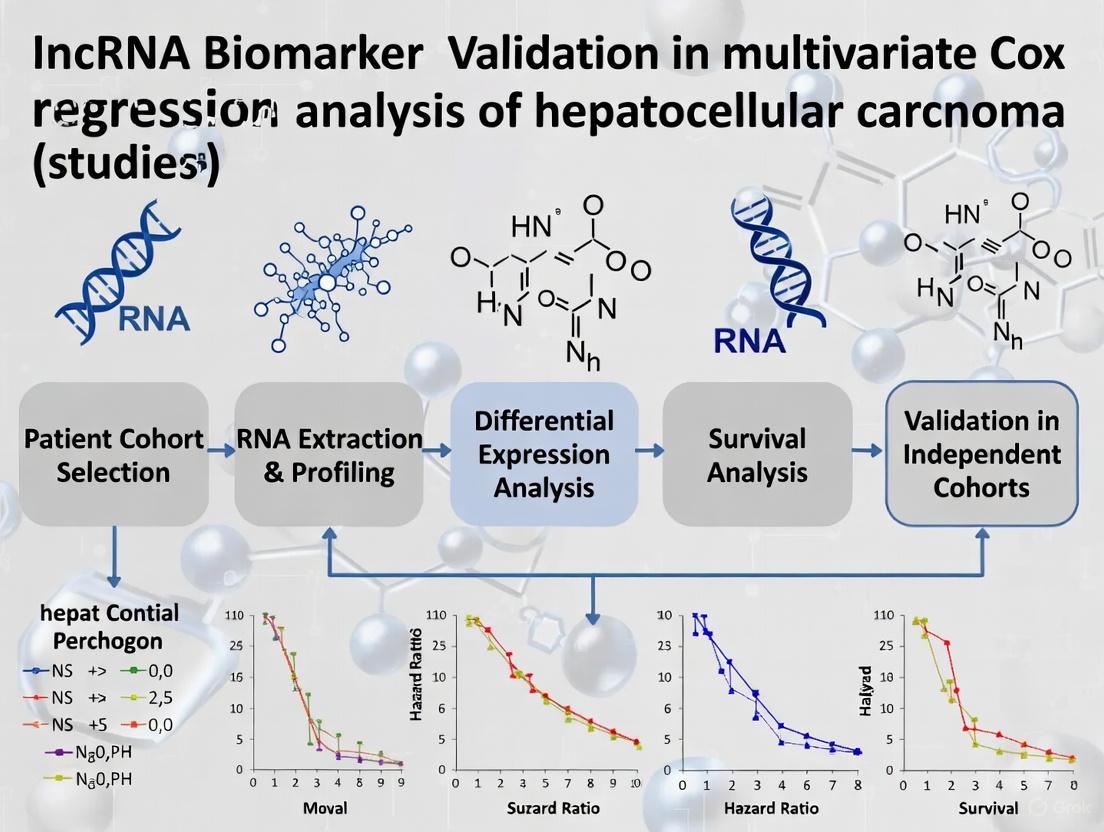
Figure 2: Workflow for Developing lncRNA-Based Prognostic Signatures in HCC. The standardized approach involves lncRNA profiling from patient samples, statistical analysis to identify prognostic candidates, signature construction using rigorous regression methods, risk model development, and validation in independent cohorts before clinical application.
Experimental Methodologies: Protocols for lncRNA Functional Characterization
The functional characterization of lncRNAs in HCC relies on standardized experimental protocols that validate their biological roles and clinical utility. These methodologies encompass approaches for lncRNA detection, quantification, functional manipulation, and mechanistic investigation.
lncRNA Detection and Quantification
Accurate measurement of lncRNA expression represents the foundation of HCC lncRNA research. The predominant methodology involves RNA isolation followed by reverse transcription quantitative real-time PCR. One study protocol detailed RNA isolation using the miRNeasy Mini Kit (QIAGEN) according to the manufacturer's protocol, followed by reverse transcription into complementary DNA using the RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) on a T100 thermal cycler (Bio-Rad) [1]. Quantitative real-time PCR was then performed using the PowerTrack SYBR Green Master Mix kit (Applied Biosystems) on a ViiA 7 real-time PCR system (Applied Biosystems), with the housekeeping gene GAPDH used for normalization of expression data [1]. Each reaction was typically performed in triplicate to ensure technical reproducibility, with the ΔΔCT method used for relative quantification and data analysis.
For large-scale lncRNA profiling, RNA sequencing represents the gold standard. Studies utilizing The Cancer Genome Atlas (TCGA) data typically process RNA-seq data downloaded as raw counts transformed to Transcripts Per Million values, followed by log2 transformation [8]. For microarray data from repositories such as GEO, data are used as provided by the authors after log2 transformation and quantile normalization [8]. Differential expression analysis typically employs packages such as DEseq and edgeR in R, with thresholds set at false discovery rate <0.05 and |log(fold change)|>1.3 [7].
Functional Validation Experiments
Functional characterization of candidate lncRNAs typically involves gain-of-function and loss-of-function studies in HCC cell lines. For instance, the oncogenic role of LINC01063 was validated through knockdown experiments that inhibited cell proliferation, disrupted colony formation ability, and reduced migration and invasion capacities of HCC cells [5]. In vivo validation was performed using nude BALB/c mice injected with LINC01063-knockdown HCC cells, which exhibited reduced tumor growth compared to controls [5]. These complementary approaches provide compelling evidence for the functional significance of lncRNAs in HCC pathogenesis.
The construction of competitive endogenous RNA networks represents a key methodology for elucidating lncRNA mechanistic actions. One comprehensive approach employed a multilevel strategy: first, miRNA binding sites of differentially expressed lncRNAs were predicted via the miRcode database; subsequently, the miRTarBase, TargetScan, and miRDB databases were integrated, retaining only miRNA-mRNA relationships supported by all three databases; finally, the intersection of target genes of differentially expressed lncRNAs and upregulated mRNAs in HCC tissues was used to define exosome-related genes, and a ternary regulatory network was constructed via Cytoscape [8]. This rigorous approach minimizes false positives and enhances the biological relevance of predicted interactions.
Table 4: Essential Research Reagents and Solutions for lncRNA Studies in HCC
| Reagent/Solution Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN) [1] | Total RNA extraction from tissues/cells | Preserves lncRNA integrity; removes contaminants |
| Reverse Transcription Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [1] | cDNA synthesis from RNA templates | Includes gDNA eraser; high efficiency for long transcripts |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems) [1] | Quantitative real-time PCR detection | Optimized for lncRNA detection; high sensitivity |
| PCR Systems | ViiA 7 real-time PCR system (Applied Biosystems) [1] | Real-time PCR amplification and detection | Multi-channel detection; high precision |
| Computational Tools | edgeR, DEseq [7] | Differential expression analysis | Handles count data; robust statistical framework |
| Pathway Analysis | clusterProfiler [8] | Functional enrichment analysis | GO/KEGG analysis; visualization capabilities |
| Network Visualization | Cytoscape [8] [9] | Biological network construction and visualization | Interactive interface; extensive plugin ecosystem |
| Survival Analysis | survival package in R [7] [9] | Cox regression and survival analysis | Handles time-to-event data; multivariate analysis |
Statistical Analysis and Model Validation
Robust statistical analysis is essential for validating the prognostic value of lncRNA biomarkers. Multivariate Cox regression analysis represents the gold standard for establishing independent prognostic significance while controlling for clinical covariates. Studies typically employ the survival package in R for this purpose [7]. For prognostic model development, multiple machine learning algorithms are often integrated, including CoxBoost, stepwise Cox, Lasso, Ridge, elastic net, survival support vector machines, generalized boosted regression models, supervised principal components, partial least squares Cox, and random survival forest, typically within a 10-fold cross-validation framework [8].
Model performance is typically evaluated using the concordance index as the primary metric for prognostic models, with additional assessment via time-dependent receiver operating characteristic analysis calculating area under the curve values for 1-, 2-, and 3-year overall survival [5]. Risk scores are calculated using weighted formulae based on regression coefficients from multivariate Cox regression analysis, with patients subsequently stratified into high-risk and low-risk groups based on median risk score for survival comparison via Kaplan-Meier analysis with log-rank test [9].
The comprehensive analysis of dysregulated lncRNAs in HCC pathogenesis reveals a complex regulatory landscape with significant implications for clinical practice. The rigorous validation of both oncogenic and tumor-suppressor lncRNAs through multivariate Cox regression analyses provides a robust statistical foundation for their implementation as prognostic biomarkers. The development of multi-lncRNA signatures leveraging machine learning approaches demonstrates superior predictive accuracy compared to single lncRNA biomarkers, suggesting that combinatorial approaches may offer the most promising path toward clinical translation.
The therapeutic targeting of lncRNAs represents an emerging frontier in HCC management. Several strategies show promise, including the use of pHLIP-PNA to target solid tumors, with lncRNAs such as 91H, BCAR4, HULC, MALAT-1, TUG1, and UCA1 identified as oncogenic targets, while Loc285194 and MEG3 represent tumor suppressor candidates [4]. Advanced gene editing technologies such as TALEN or CRISPR/Cas9 methodologies are thought to enable detailed evaluation of lncRNA functions, potentially paving the way for therapeutic applications [4].
Future research directions should focus on validating lncRNA biomarkers in prospective clinical trials, standardizing detection methodologies for clinical implementation, and developing lncRNA-targeted therapeutics. The integration of lncRNA biomarkers with existing clinical parameters and imaging findings may facilitate personalized treatment approaches, ultimately improving the dismal survival statistics that currently characterize HCC. As our understanding of lncRNA biology in HCC continues to mature, these molecules hold exceptional promise for transforming the clinical management of this devastating malignancy.
Comparative Analysis of lncRNA Prognostic Models in Hepatocellular Carcinoma Across Key Biological Contexts
Hepatocellular carcinoma (HCC) remains a formidable global health challenge, ranking as the sixth most prevalent cancer and third leading cause of cancer-related deaths worldwide [10]. The disease often progresses asymptomatically in early stages, resulting in advanced presentation with limited therapeutic options and poor prognosis [10]. This clinical reality has driven extensive research into novel biomarkers for early detection, prognosis prediction, and treatment guidance. Long non-coding RNAs (lncRNAs), once considered "junk DNA," have emerged as crucial regulators of gene expression through transcriptional, post-transcriptional, and epigenetic mechanisms [10]. Their involvement in cancer initiation, progression, metastasis, immune escape, and drug resistance has positioned them as promising biomarkers and therapeutic targets [11].
The complex molecular landscape of HCC necessitates biomarker development within specific biological contexts that drive tumor progression. Key pathways including amino acid metabolism, ferroptosis, autophagy, and migrasome formation represent critical biological processes with distinct roles in hepatocarcinogenesis. Amino acids serve not only as building blocks for protein synthesis but also as key regulators of metabolic pathways and immune responses [12]. Ferroptosis, an iron-dependent form of programmed cell death characterized by lipid peroxidation, offers promising avenues for combating drug-resistant tumors [13]. Autophagy, a cellular degradation pathway essential for maintaining homeostasis, plays dual roles in tumor suppression and promotion depending on context [14]. More recently discovered, migrasomes—organelles that form during cell migration—facilitate intercellular communication and influence tumor microenvironment dynamics [15].
This review provides a comprehensive comparative analysis of lncRNA-based prognostic signatures derived from these four key biological contexts in HCC. By examining their construction methodologies, predictive performance, and clinical applicability, we aim to guide researchers and clinicians in selecting appropriate biomarker approaches for specific research and therapeutic objectives.
Comparative Performance of Biological Context-Specific lncRNA Signatures
Table 1: Comparative performance of lncRNA prognostic models across biological contexts in HCC
| Biological Context | Key lncRNAs in Signature | Patient Cohort | Predictive Performance (AUC) | Clinical Utility | Immune Response Prediction |
|---|---|---|---|---|---|
| Amino Acid Metabolism | 4-lncRNA signature (includes AL590681.1) | TCGA (n=340) | 1-year: ~0.753-year: ~0.725-year: NA | Prognostic stratification; enhanced cell activity confirmed functionally [10] | Correlates with immunosuppressive cell infiltration; anti-PD1 response prediction [10] |
| Migrasome Formation | LINC00839, MIR4435-2HG | TCGA (n=372) + external validation (n=100) | Consistent predictive accuracy across cohorts [11] | Prognostic stratification; promotes malignant behaviors and immune evasion [11] | Elevated immunosuppressive infiltration; immune checkpoint expression; ICI response prediction [11] |
| PANoptosis | Multiple lncRNAs (specific identities not highlighted) | TCGA + GEO databases | ROC and calibration curves confirm good predictive ability [16] | Prognostic stratification; distinguishes two molecular subtypes with different outcomes [16] | Cluster 1 subtype shows better prognosis and higher immune infiltration [16] |
| Ferroptosis | Not specifically developed in retrieved literature | Not applicable | Not applicable | Not applicable | Not applicable |
Table 2: Methodological approaches for lncRNA signature development across studies
| Development Phase | Amino Acid Metabolism Study [10] | Migrasome Formation Study [11] | PANoptosis Study [16] |
|---|---|---|---|
| Initial Gene Set | 374 AAM-related genes from MSigDB | 12 migrasome-related genes (TSPAN4, NDST1, CPQ, ITGAV) from GeneCards and literature | PANoptosis-related genes from published studies |
| lncRNA Identification | Pearson correlation (∣R∣ > 0.4, p < 0.05) | Pearson correlation (∣R∣ > 0.55, p < 0.001) | Correlation analysis with PANoptosis genes |
| Prognostic Filtering | Univariate Cox (p < 0.05) → 24 lncRNAs | Univariate Cox (p < 0.05) → 16 lncRNAs | Not explicitly detailed |
| Signature Refinement | LASSO + Multivariate Cox → 4-lncRNA model | LASSO-Cox with 1000x 10-fold CV → 2-lncRNA model | Lasso-Cox regression analysis |
| Validation Approach | Internal TCGA split (1:1 training:validation) | Internal TCGA split + external clinical cohort (n=100) | Internal validation with ROC and calibration curves |
Biological Contexts: Mechanisms and lncRNA Integration
Amino Acid Metabolism in HCC
Amino acids serve fundamental roles in cellular physiology beyond protein synthesis, including energy production, maintenance of redox balance, and activation of key signaling pathways such as mTOR [12]. In cancer cells, reprogramming of amino acid metabolism supports rapid proliferation and adaptation to metabolic stress. The branched-chain amino acids (BCAAs)—leucine, isoleucine, and valine—deserve particular attention as they account for 35% of essential amino acids in muscle and activate mTOR signaling, thereby promoting protein synthesis [12]. In HCC, dysregulated BCAA metabolism has been associated with cancer progression through multiple mechanisms. Alterations in circulating BCAA levels have been reported in cancer patients, with increased levels associated with higher pancreatic cancer risk [12]. The specific lncRNA AL590681.1, identified in the AAM-related signature, was experimentally validated to enhance HCC cell activity, confirming the functional relevance of this metabolic axis in hepatocarcinogenesis [10].
Ferroptosis Regulation in Cancer
Ferroptosis represents a unique iron-dependent form of programmed cell death characterized by glutathione depletion, GPX4 inactivation, and accumulation of lipid peroxides [13]. Morphologically, it features mitochondrial shrinkage, reduced cristae, and membrane rupture without the classic hallmarks of apoptosis. The core regulatory axis involves system Xc--mediated cystine uptake, glutathione synthesis, and GPX4 activity, which collectively protect against lethal lipid peroxidation [13]. Cancer cells with mesenchymal characteristics demonstrate particular vulnerability to ferroptosis induction due to their elevated polyunsaturated fatty acid incorporation into membrane phospholipids [13]. While the retrieved literature does not describe a specific ferroptosis-related lncRNA signature for HCC, the molecular machinery of ferroptosis offers rich opportunities for biomarker development, particularly given its established role in overcoming chemotherapy resistance in various cancers.
Autophagy in Cellular Stress Response
Autophagy constitutes an essential cellular degradation pathway that maintains homeostasis by recycling damaged organelles and proteins through lysosomal degradation [14]. This process becomes particularly crucial during metabolic stress, such as glucose starvation, where it helps sustain cellular energy production and survival. Recent research has elucidated that glucose starvation-induced autophagy involves distinct mechanisms compared to classic amino acid starvation-induced autophagy, with mitochondrial function playing a central regulatory role [14]. The Mec1-Atg9 phosphorylation axis has been identified as specifically required for energy stress-induced autophagy but not nitrogen starvation-induced autophagy, highlighting the pathway-specific nature of autophagy regulation [14]. While autophagy plays complex, context-dependent roles in cancer—sometimes suppressing and sometimes promoting tumor growth—its modulation represents a promising therapeutic avenue in HCC.
Migrasome Formation and Function
Migrasomes constitute a newly discovered class of extracellular vesicles that form during cell migration at the ends of retraction fibers [15]. These organelles facilitate long-distance communication by transporting various cargo molecules including proteins, lipids, and genetic material. Recent research has illuminated the intricate process of migrasome biogenesis, revealing that tubular endoplasmic reticulum extends through retraction fibers and incorporates into migrasomes through membrane contact sites, delivering cholesterol and calcium ions that promote migrasome growth, stability, and secretion [17]. In HCC, migrasome-related genes have been implicated in promoting invasion, metastasis, and immune evasion [11]. The functional validation of MIR4435-2HG from the migrasome-related lncRNA signature demonstrated its role in promoting proliferation, epithelial-mesenchymal transition, and PD-L1-mediated immune evasion, establishing a direct connection between migrasome biology and HCC progression [11].
Experimental Protocols for lncRNA Biomarker Development
Bioinformatics Analysis Pipeline
The development of context-specific lncRNA signatures follows a consistent bioinformatics workflow. Initial data acquisition typically involves retrieving HCC transcriptome data from TCGA-LIHC and normalizing expression values to transcripts per million [11]. For context-specific lncRNA identification, researchers first compile relevant gene sets—374 amino acid metabolism genes from MSigDB [10] or 12 migrasome-related genes from GeneCards and literature [11]. Pearson correlation analysis then identifies lncRNAs significantly co-expressed with these gene sets, with thresholds varying by study (∣R∣ > 0.4 [10] or ∣R∣ > 0.55 [11]). Prognostic filtration via univariate Cox regression identifies survival-associated lncRNAs, followed by dimensionality reduction using LASSO-Cox regression to construct the final multimarker signature [10] [11]. Model validation employs internal cohort splitting (typically 1:1 training:validation) and, in robust studies, external clinical cohorts [11]. Performance evaluation includes Kaplan-Meier survival analysis, time-dependent ROC curves, and calibration plots [10] [16].
Functional Validation Approaches
Table 3: Experimental methods for functional validation of prognostic lncRNAs
| Experimental Method | Key Reagents | Experimental Output | Application in HCC lncRNA Studies |
|---|---|---|---|
| Gene Knockdown | Lipofectamine 3000, specific shRNA/siRNA [10] [11] | Knockdown efficiency (RT-qPCR), phenotypic changes | Confirm role of AL590681.1 in HCC cell activity [10] and MIR4435-2HG in malignant behaviors [11] |
| Proliferation Assays | CCK-8 reagent, colony formation staining [10] | Cell viability, colony formation capacity | Assess impact of lncRNA modulation on HCC growth [10] |
| Gene Expression Analysis | RT-qPCR, specific primers [10] | Expression levels across cell lines | Determine AL590681.1 expression in various HCC cell lines [10] |
| Single-Cell Analysis | Single-cell RNA sequencing platforms | Cell type-specific expression patterns | Identify MIR4435-2HG enrichment in cancer-associated fibroblasts [11] |
Figure 1: Bioinformatics workflow for developing context-specific lncRNA signatures in HCC
Research Reagent Solutions for lncRNA Studies
Table 4: Essential research reagents for experimental validation of lncRNA biomarkers
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Transfection Reagents | Lipofectamine 3000 [10] [11] | lncRNA knockdown/overexpression | High efficiency, low cytotoxicity |
| Cell Culture Media | DMEM with 10% FBS [10] | HCC cell line maintenance | Standardized growth conditions |
| Detection Assays | CCK-8 assay [10] | Cell proliferation measurement | Sensitive, reproducible viability readout |
| RNA Analysis Tools | RT-qPCR reagents, specific primers [10] | lncRNA expression quantification | High specificity and sensitivity |
| Cell Lines | Hep-3B, Huh-1, Huh-7, HCCLM3 [10] | Functional validation studies | Represent HCC molecular heterogeneity |
This comprehensive analysis of lncRNA-based prognostic models across four key biological contexts reveals both the promises and challenges in translating these findings to clinical practice. The migrasome-related and amino acid metabolism-related signatures currently represent the most advanced approaches, with robust validation and demonstrated functional relevance to HCC pathogenesis. The migrasome-related model particularly stands out for its external validation and detailed mechanistic insights into immune evasion [11], while the amino acid metabolism signature benefits from the fundamental role of metabolic reprogramming in cancer [10] [12].
The absence of a well-developed ferroptosis-related lncRNA signature in the current literature represents a significant gap, given the established importance of ferroptosis in overcoming chemotherapy resistance [13]. Similarly, while autophagy plays crucial roles in HCC progression and treatment response [14], autophagy-focused lncRNA signatures remain underdeveloped. These gaps present valuable opportunities for future research.
For researchers and clinicians, selection of appropriate lncRNA biomarkers should consider specific clinical contexts and therapeutic intentions. The migrasome-related signature shows particular promise for immunotherapy guidance, while amino acid metabolism-related signatures may better inform metabolic targeting approaches. Future directions should focus on integrating multiple biological contexts into unified models, expanding external validation across diverse patient cohorts, and advancing functional studies to establish causal rather than correlative relationships between lncRNAs and HCC progression.
Systematic Identification of Candidate lncRNAs from Public Databases (e.g., TCGA-LIHC)
Hepatocellular carcinoma (HCC) remains a global health challenge with high mortality rates, largely due to late diagnosis and limited prognostic tools [18]. Long non-coding RNAs (lncRNAs), once considered "transcriptional noise," have emerged as crucial regulators of diverse cellular processes and promising biomarkers for cancer prognosis [18]. Public databases such as The Cancer Genome Atlas Liver Hepatocellular Carcinoma (TCGA-LIHC) repository provide extensive genomic datasets that enable researchers to systematically identify lncRNA signatures associated with HCC prognosis [19]. This guide objectively compares the performance of various computational and experimental approaches for lncRNA biomarker discovery within the context of multivariate Cox regression studies in HCC research.
Performance Comparison of Established lncRNA Signatures
Multiple research groups have developed different lncRNA signatures from TCGA-LIHC data, each demonstrating varying prognostic capabilities. The table below summarizes the performance characteristics of four prominent signatures:
Table 1: Performance Comparison of lncRNA Signatures from TCGA-LIHC
| Study & Signature Type | Number of lncRNAs | Validation Cohort | AUC (1/3/5-year) | Key lncRNAs Identified | HR (95% CI) |
|---|---|---|---|---|---|
| 11-lncRNA prognostic signature [19] | 11 | External GEO (n=203) | Up to 0.846 | GACAT3, AC010547.1, LINC01747 | 3.648 (2.238-5.945) |
| Costimulatory molecule-related 5-lncRNA signature [20] | 5 | Internal TCGA split | 0.735/0.706/0.742 (testing) | AC099850.3, BOK-AS1, NRAV | 2.78 (1.62-4.79) |
| 4-lncRNA early recurrence signature [21] | 4 | External cohort (n=24) | N/A (focused on recurrence) | AC108463.1, AF131217.1, TMCC1-AS1 | N/A |
| Migrasome-related 2-lncRNA signature [11] | 2 | Independent clinical cohort (n=100) | N/A | LINC00839, MIR4435-2HG | N/A |
The performance variation across these signatures highlights several critical aspects of lncRNA biomarker development. The 11-lncRNA signature demonstrated exceptional predictive power with an AUC reaching 0.846, suggesting high diagnostic accuracy [19]. Signatures derived from biologically relevant contexts, such as costimulatory molecules or migrasomes, show particular promise for understanding functional mechanisms in HCC progression [11] [20].
Table 2: Functional Validation Approaches for Candidate lncRNAs
| Functional Assay | Experimental Readout | Key Findings for Specific lncRNAs |
|---|---|---|
| CCK-8 and colony formation [19] [20] | Cell proliferation capacity | Silencing GACAT3 and AC099850.3 suppressed HCC cell proliferation |
| Transwell invasion and migration [19] | Metastatic potential | GACAT3 knockdown inhibited HCC cell invasion and migration |
| Quantitative RT-PCR [19] [1] | Expression levels in tissues/cell lines | GACAT3 highly expressed in HCC tissues; MIR4435-2HG associated with poor prognosis |
| Immune cell infiltration analysis [11] [21] | Tumor microenvironment composition | High-risk groups showed immunosuppressive cell infiltration and checkpoint expression |
Experimental Protocols for lncRNA Identification and Validation
Computational Identification from Public Databases
Data Acquisition and Preprocessing:
- Source HCC RNA-seq data and clinical information from TCGA-LIHC portal (https://portal.gdc.cancer.gov/) [19] [22]
- Normalize expression data to transcripts per million (TPM) or fragments per kilobase million (FPKM)
- Filter patients for complete clinical information, excluding those with survival <30 days [20]
Differential Expression Analysis:
- Identify differentially expressed lncRNAs (DElncRNAs) using "edgeR," "DESeq2," or "limma" R packages [19] [21]
- Apply thresholds of |log2 fold change| >2.0 and adjusted p-value <0.05 [19]
- For specialized signatures, perform co-expression analysis with relevant gene sets (e.g., migrasome-related genes, costimulatory molecules) using Pearson correlation (|r|>0.4-0.55, p<0.001) [11] [20]
Prognostic Model Construction:
- Conduct univariate Cox regression to identify OS-associated lncRNAs (p<0.05) [19]
- Apply machine learning algorithms: LASSO Cox regression with 10-fold cross-validation to prevent overfitting [19] [11] [21]
- Calculate risk score using the formula: Risk score = Σ(coefficientlncRNA × expressionlncRNA) [11]
- Validate signatures in internal testing sets and external cohorts (GEO, independent clinical samples) [19] [11]
Figure 1: Computational workflow for lncRNA signature identification from public databases.
Functional Validation of Candidate lncRNAs
Cell Culture and Transfection:
- Maintain HCC cell lines (e.g., MHCC-97H, HepG2, LM3) in DMEM with 10% FBS at 37°C with 5% CO₂ [19]
- Perform lncRNA silencing using siRNA or shRNA transfection with appropriate controls
Phenotypic Assays:
- Cell proliferation: Conduct CCK-8 assays and colony formation assays [19] [20]
- Invasion and migration: Perform Transwell assays with or without Matrigel coating [19]
- Apoptosis analysis: Utilize flow cytometry with Annexin V/PI staining
Molecular Analyses:
- RNA isolation and qRT-PCR: Extract total RNA using TRIzol, synthesize cDNA, and perform qPCR with SYBR Green [19] [1]
- Pathway analysis: Conduct Gene Set Enrichment Analysis (GSEA) on high- vs. low-risk groups [19]
Key Signaling Pathways and Biological Mechanisms
lncRNAs contribute to HCC progression through multiple interconnected signaling pathways and biological processes. The diagram below illustrates the primary mechanisms identified through functional studies:
Figure 2: Key mechanisms of lncRNAs in HCC pathogenesis and prognosis.
The multifunctional roles of lncRNAs in HCC pathogenesis include:
- Epigenetic regulation: Nuclear lncRNAs (e.g., HOTAIR) recruit chromatin-modifying enzymes to specific genomic loci, mediating DNA methylation and histone modifications [18]
- Post-transcriptional control: Cytoplasmic lncRNAs function as competing endogenous RNAs (ceRNAs) or miRNA sponges, affecting mRNA stability and translation [18]
- Immune modulation: Specific lncRNAs (e.g., MIR4435-2HG) promote immune evasion by regulating PD-L1 expression and establishing an immunosuppressive tumor microenvironment [11]
- Cell fate determination: lncRNAs influence key processes including proliferation (AC099850.3), epithelial-mesenchymal transition (GACAT3), and apoptosis [19] [20]
The Scientist's Toolkit: Essential Research Reagents and Databases
Table 3: Essential Resources for lncRNA Biomarker Discovery and Validation
| Resource Category | Specific Tools/Databases | Primary Function | Key Features |
|---|---|---|---|
| Public Databases | TCGA-LIHC [19] [22] | Genomic data repository | Clinical annotation, multi-omics data |
| GEO/SRA [19] [22] | Gene expression repository | Diverse studies, raw sequencing data | |
| GTEx [22] | Normal tissue reference | Tissue-specific expression patterns | |
| lncRNADisease v2.0/v3.0 [23] | LncRNA-disease associations | Experimentally validated interactions | |
| Computational Tools | "edgeR," "DESeq2," "limma" [19] [21] | Differential expression | Statistical analysis of RNA-seq data |
| "glmnet" (LASSO) [19] [11] | Feature selection | Regularized regression for biomarker selection | |
| "survival" R package [19] | Survival analysis | Cox regression, Kaplan-Meier curves | |
| GSEA software [19] | Pathway analysis | Biological mechanism exploration | |
| Experimental Reagents | HCC cell lines [19] | Functional validation | In vitro models (MHCC-97H, HepG2, LM3) |
| siRNA/shRNA [19] | Gene silencing | lncRNA knockdown studies | |
| qRT-PCR reagents [19] [1] | Expression validation | SYBR Green, target-specific primers | |
| Transwell assays [19] | Migration/invasion | Metastatic potential assessment | |
| Bombinin H-BO1 | Bombinin H-BO1, MF:C76H137N19O17, MW:1589.0 g/mol | Chemical Reagent | Bench Chemicals |
| Elemicin-d3 | Elemicin-d3, MF:C12H16O3, MW:211.27 g/mol | Chemical Reagent | Bench Chemicals |
Systematic identification of candidate lncRNAs from public databases like TCGA-LIHC has established robust prognostic signatures for hepatocellular carcinoma. The comparative analysis presented herein demonstrates that multivariate Cox regression models incorporating lncRNA expression data significantly enhance prognostic stratification beyond conventional clinical parameters. Future directions should focus on standardizing analytical pipelines, incorporating single-cell RNA-seq data for cellular resolution, and advancing functional studies to elucidate the mechanistic roles of candidate lncRNAs in HCC pathogenesis. The integration of computational biomarker discovery with experimental validation represents a powerful paradigm for advancing personalized oncology and identifying novel therapeutic targets.
Building a Robust Prognostic Model: From Statistical Analysis to Signature Development
In the field of hepatocellular carcinoma (HCC) research, the validation of long non-coding RNA (lncRNA) biomarkers requires robust statistical workflows that can handle high-dimensional genomic data while ensuring model reliability and clinical interpretability. The integration of univariate screening, LASSO-penalized Cox regression, and multivariate Cox analysis has emerged as a powerful framework for identifying stable prognostic signatures from thousands of candidate lncRNAs. This comparative guide examines the performance, implementation, and practical application of these methodological approaches within the context of lncRNA biomarker validation for HCC prognosis and therapeutic development.
Methodological Comparison and Experimental Performance
Core Methodologies and Comparative Performance
The statistical workflow for lncRNA biomarker validation typically follows a sequential approach that balances variable screening intensity with model stability. The table below summarizes the key characteristics and performance metrics of each methodological stage based on recent HCC studies.
Table 1: Performance comparison of statistical methods in lncRNA-HCC studies
| Methodological Stage | Key Characteristics | Typical Variable Reduction | Reported C-index (HCC Studies) | Primary Advantages | Key Limitations |
|---|---|---|---|---|---|
| Univariate Screening | Initial filter based on univariate Cox p-values or correlation coefficients | 80-95% reduction (e.g., 191 to 16 lncRNAs) [11] | 0.60-0.68 (alone) [11] | Computational efficiency; removes obvious noise | Ignores multivariate relationships; potential false negatives |
| LASSO-Cox Regression | L1-penalization with cross-validation; automated variable selection | 70-90% further reduction (e.g., 16 to 2-8 lncRNAs) [11] | 0.65-0.75 [24] [11] | Handles high-dimensional data; prevents overfitting; creates sparse models | May exclude correlated predictors; sensitivity to hyperparameter tuning |
| Multivariate Cox Regression | Final model refinement with selected variables | Fixed number of predictors (typically 2-10 lncRNAs) | 0.70-0.85 (in final models) [10] [11] | Provides interpretable hazard ratios; clinical familiarity | Requires limited predictors; assumes proportional hazards |
Experimental Data from Recent HCC Studies
Recent investigations applying this statistical workflow to lncRNA biomarker discovery in HCC demonstrate consistent patterns of performance:
A migrasome-related lncRNA study utilized this sequential approach, beginning with 191 candidate MRlncRNAs identified through correlation analysis. Univariate Cox screening reduced these to 16 significant candidates, with subsequent LASSO-Cox regression further refining the signature to just two lncRNAs (LINC00839 and MIR4435-2HG). The final multivariate Cox model achieved a C-index of 0.72 in the validation cohort, effectively stratifying patients into distinct prognostic groups (p < 0.001) [11].
An amino acid metabolism-related lncRNA study in HCC applied a similar workflow, identifying 24 prognostic AAM-related lncRNAs through univariate analysis before employing LASSO-Cox to develop a 4-lncRNA risk signature. The resulting model showed significant predictive power for overall survival (p < 0.001) and demonstrated clinical utility for immunotherapy response prediction [10].
Research on elderly glioma patients provided comparative data, showing that LASSO-Cox models with five variables demonstrated superior predictive performance (higher C-index) compared to full Cox models with four variables, highlighting the value of penalized regression even after initial variable screening [24].
Experimental Protocols and Implementation
Standardized Workflow for lncRNA Biomarker Validation
The following diagram illustrates the complete statistical workflow for lncRNA biomarker development and validation in HCC studies, integrating the three methodological components:
Detailed Methodological Protocols
Univariate Screening Protocol
The initial screening phase focuses on reducing dimensionality while retaining potentially significant lncRNAs:
Expression Filtering: Begin with normalization of lncRNA expression data (typically TPM or FPKM) and removal of lowly expressed transcripts (e.g., those with zero counts in >80% of samples) [11].
Correlation Analysis: Calculate Pearson correlation coefficients between candidate lncRNAs and reference gene sets (e.g., migrasome-related genes, amino acid metabolism genes). Apply thresholds of |correlation coefficient| > 0.4-0.55 with p < 0.001 to identify biologically relevant lncRNAs [10] [11].
Univariate Cox Regression: Perform survival analysis for each candidate lncRNA using Cox proportional hazards models. Retain transcripts with p-values < 0.05 for further analysis. This typically reduces the candidate pool by 80-95% while preserving potentially significant predictors [11].
LASSO-Cox Regression Implementation
The LASSO-Cox regression provides the critical variable selection mechanism:
Parameter Tuning: Implement 10-fold cross-validation to determine the optimal penalty parameter (λ). Both λ.min (value that gives minimum mean cross-validated error) and λ.1se (most regularized model within one standard error of the minimum) are commonly used, with λ.1se preferred for more parsimonious models [25] [11].
Model Training: Fit the LASSO-Cox model using the remaining lncRNAs after univariate screening. The L1 penalty shrinks coefficients of less relevant variables to exactly zero, automatically performing variable selection. The optimization follows:
(\hat{\beta}(lasso) = \underset{\beta}{\text{argmax }} l(\beta) - \lambda || \beta ||_1)
where (l(\beta)) is the log-partial likelihood and (|| \beta ||_1) is the L1-norm penalty [26] [25].
Iteration and Stability: Repeat the LASSO procedure multiple times (e.g., 1000 iterations) with different random seeds to ensure selection stability. Retain only those lncRNAs consistently selected across iterations for the final model [11].
Multivariate Cox Model Development
The final stage refines the prognostic model:
Proportional Hazards Assumption: Verify the proportional hazards assumption for each selected lncRNA using Schoenfeld residuals before final model construction.
Model Optimization: Enter the LASSO-selected lncRNAs into a multivariate Cox proportional hazards model alongside key clinical variables (e.g., age, stage, tumor size) to adjust for potential confounders.
Risk Score Calculation: Compute individual risk scores using the formula:
(Riskscore = \sum{i} Coefficient{MRlncRNAsi} \times Expression{MRlncRNAs_i})
Stratify patients into high-risk and low-risk groups using the median risk score as cutoff [11].
Successful implementation of this statistical workflow requires both biological and computational resources. The following table details essential research reagents and their applications in lncRNA biomarker validation for HCC.
Table 2: Essential research reagents and computational tools for lncRNA biomarker validation
| Category | Specific Resource | Application in Workflow | Key Features/Considerations |
|---|---|---|---|
| Data Sources | TCGA-LIHC Database | Primary source of lncRNA expression and clinical data | Includes 372 LIHC tumors and 50 normal tissues; provides survival outcomes [10] [11] |
| Molecular Databases | GeneCards | Identification of reference gene sets (e.g., migrasome-related genes) | Provides comprehensive gene annotation; enables biological context [11] |
| Statistical Software | R Statistical Environment | Implementation of all statistical analyses | Essential packages: survival, glmnet, timeROC, caret [26] [11] |
| Specialized R Packages | glmnet | LASSO-Cox regression implementation | Handles high-dimensional data; efficient cross-validation [26] [25] |
| Visualization Tools | ggplot2, survminer | Creation of publication-quality figures | Kaplan-Meier curves, ROC plots, risk stratification visualizations [10] [11] |
| Validation Tools | timeROC | Time-dependent ROC analysis | Evaluates prognostic accuracy at 1, 3, and 5 years [11] |
The integrated statistical workflow combining univariate screening, LASSO-Cox regression, and multivariate Cox analysis represents a robust methodology for lncRNA biomarker validation in HCC research. Experimental data from recent studies consistently demonstrates that this approach effectively handles high-dimensional genomic data while producing clinically interpretable prognostic signatures. The sequential application of these methods balances statistical rigor with practical implementation, enabling researchers to distill complex lncRNA expression patterns into stable, clinically relevant biomarkers. As HCC research continues to evolve toward more personalized therapeutic approaches, this statistical framework provides a validated foundation for translating lncRNA discoveries into meaningful prognostic tools and potential therapeutic targets.
Constructing Multi-lncRNA Prognostic Signatures and Calculating Risk Scores
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most common cancer worldwide and the third leading cause of cancer-related mortality [10] [27]. The disease exhibits considerable genetic and phenotypic heterogeneity, making accurate prognosis prediction particularly challenging [28]. Traditional clinicopathological factors often provide insufficient prognostic information, driving the search for more precise molecular biomarkers. Within this context, long non-coding RNAs (lncRNAs)—transcripts longer than 200 nucleotides with limited protein-coding potential—have emerged as crucial regulators of gene expression and promising biomarker candidates [1] [3].
The construction of multi-lncRNA prognostic signatures represents a paradigm shift in HCC prognosis prediction, moving beyond single-marker approaches to integrated models that better reflect the molecular complexity of the disease. These signatures leverage the power of high-throughput sequencing technologies and sophisticated statistical methods to generate risk scores that stratify patients according to their clinical outcomes [29] [7]. This comparative guide examines the methodology, performance, and clinical applicability of various multi-lncRNA signatures currently advancing the field of HCC research and drug development.
Comparative Analysis of Multi-lncRNA Prognostic Signatures
Table 1: Comprehensive Comparison of Multi-lncRNA Prognostic Signatures in HCC
| Signature Focus | Specific lncRNAs Identified | Patient Cohort Size | Performance (AUC) | Key Clinical Applications |
|---|---|---|---|---|
| Inflammatory Response [28] | AC145207.5, POLH-AS1, AL928654.1, MKLN1-AS, AL031985.3, PRRT3-AS1, AC023157.2 | 369 HCC samples from TCGA | Not specified | Prognosis prediction, immune targeted therapy guidance |
| Cuproptosis-Related [30] | AL590705.3, SPRY4-AS1, AC135050.5, AL031985.3 | Not specified | 1-year: 0.715 | Prognosis prediction, immunotherapy response assessment |
| Amino Acid Metabolism [10] | 4-lncRNA signature (including AL590681.1) | 340 HCC samples (170 training/170 validation) | Not specified | Prognosis prediction, immunotherapy response, cell proliferation assessment |
| Five-lncRNA Signature [7] | RP11-325L7.2, DKFZP434L187, RP11-100L22.4, DLX2-AS1, RP11-104L21.3 | 167 early-stage HCC samples | Not specified | Early-stage prognosis prediction, understanding HCC development mechanisms |
| Disulfidptosis-Related [27] | AC016717.2, AC124798.1, AL031985.3 | 369 HCC cases (185 training/184 validation) | 1-year: 0.756, 3-year: 0.695, 5-year: 0.701 | Prognosis prediction, immune function analysis, drug sensitivity assessment |
Table 2: Analytical Comparison of Signature Performance and Clinical Value
| Signature Type | Statistical Strength | Biological Relevance | Therapeutic Guidance Potential | Validation Rigor |
|---|---|---|---|---|
| Inflammatory Response | Multivariate Cox regression with LASSO | Direct link to tumor microenvironment | High for immune-targeted therapies | Internal validation with TCGA data |
| Cuproptosis-Related | Superior to traditional clinical factors (age, gender, stage) | Connection to copper-induced cell death | Promising for immunotherapy selection | ROC analysis demonstrating outperformance of conventional factors |
| Amino Acid Metabolism | Significant risk stratification (p < 0.05) | Addresses metabolic reprogramming in cancer | Identified responders to anti-PD1 treatment | Experimental validation in HCC cell lines |
| Five-lncRNA Signature | Independent prognostic factor across subgroups | Multiple cancer pathways identified | Limited direct therapeutic guidance | Validation across age, sex, and alcohol consumption subgroups |
| Disulfidptosis-Related | Strong time-dependent ROC performance | Links novel cell death mechanism to HCC | Drug sensitivity predictions provided | Training and validation cohort approach |
Core Methodological Framework: From Data to Risk Score
The construction of multi-lncRNA prognostic signatures follows a systematic workflow that integrates bioinformatics, statistical modeling, and clinical validation. The standard methodology encompasses several critical phases that ensure the robustness and clinical applicability of the resulting risk scores.
Data Acquisition and Preprocessing
The foundation of any robust lncRNA signature begins with comprehensive data acquisition. Researchers typically obtain RNA sequencing data and corresponding clinical information from large-scale repositories such as The Cancer Genome Atlas (TCGA) Liver Hepatocellular Carcinoma (LIHC) dataset [28] [10] [7]. To ensure data quality, stringent preprocessing is applied, including the removal of samples with survival times of less than 30 days to avoid perioperative mortality bias [10] [31]. The remaining samples are typically randomly divided into training and validation cohorts, often in a 1:1 ratio, to enable internal validation of the derived signature [10] [27].
Identification of Relevant lncRNAs
The identification of biologically relevant lncRNAs represents a critical step in signature development. Two primary approaches dominate current methodologies:
Pathway-focused identification links lncRNAs to specific biological processes by retrieving relevant gene sets from databases such as the Molecular Signatures Database (MSigDB) [28] [10]. For example, in developing an inflammatory response-related signature, researchers identified 154 inflammatory response-related differentially expressed genes (DEGs) between HCC and noncancerous liver tissues (36 upregulated and 118 downregulated) [28]. Similarly, amino acid metabolism-related signatures began with 374 genes associated with amino acid metabolism pathways [10].
Correlation-based filtering applies Pearson correlation analysis to identify lncRNAs significantly correlated with the target genes. Standard thresholds include |correlation coefficient| > 0.4-0.5 with statistical significance of P < 0.05 [28] [10] [27]. This process typically identifies hundreds to thousands of candidate lncRNAs, which are subsequently refined through differential expression analysis comparing tumor versus normal tissues or poor versus good prognosis samples [7].
Signature Construction and Risk Score Calculation
The core analytical phase employs sophisticated statistical approaches to distill the candidate lncRNAs into a focused prognostic signature:
Univariate Cox regression analysis serves as the initial filter, identifying lncRNAs significantly associated with overall survival (OS) or recurrence-free survival (RFS) at a significance threshold of typically P < 0.05 [28] [7]. This step might identify dozens of potentially significant lncRNAs—for instance, 62 inflammatory response-related lncRNAs were identified in one study [28].
LASSO (Least Absolute Shrinkage and Selection Operator) regression addresses the risk of overfitting by penalizing the magnitude of coefficients, effectively reducing the number of lncRNAs in the signature while preserving the most prognostically relevant ones [28] [30] [32].
Multivariate Cox proportional hazards regression finally establishes the independent prognostic value of each selected lncRNA, generating weighted coefficients that reflect their relative contribution to the prognostic model [28] [7] [27].
The risk score formula represents the culmination of this analytical process, taking the form of a linear combination: [ \text{Risk Score} = \sum{i=1}^{n} (\text{coefficient}i \times \text{expression level of lncRNA}_i) ] where ( n ) represents the number of lncRNAs in the final signature, typically ranging from 3-9 lncRNAs [28] [30] [27]. Patients are then stratified into high-risk and low-risk groups based on the median risk score for subsequent survival analysis and clinical correlation studies.
Experimental Validation and Functional Analysis
Assessment of Prognostic Performance
Rigorous validation constitutes an essential component of signature development, employing multiple analytical approaches to assess prognostic performance:
Kaplan-Meier survival analysis consistently demonstrates significant separation between high-risk and low-risk groups across multiple studies, with high-risk patients exhibiting poorer overall survival (p < 0.05) [28] [30] [10]. For example, the disulfidptosis-related lncRNA signature showed clear stratification, with high-risk patients experiencing significantly worse survival outcomes [27].
Time-dependent receiver operating characteristic (ROC) analysis quantifies the predictive accuracy of the risk scores at clinically relevant timepoints. The disulfidptosis-related signature achieved AUCs of 0.756, 0.695, and 0.701 for 1-, 3-, and 5-year survival, respectively [27]. Similarly, the cuproptosis-related lncRNA signature demonstrated an AUC of 0.715 for overall survival, outperforming traditional clinical factors such as age (AUC=0.531), gender (AUC=0.509), and stage (AUC=0.671) [30].
Decision curve analysis (DCA) provides clinical utility assessment by quantifying the net benefits of using the lncRNA signatures for prognostic decision-making compared to traditional approaches [28].
Exploration of Biological Mechanisms and Immune Microenvironment
Advanced bioinformatic analyses elucidate the potential biological mechanisms underlying the prognostic signatures:
Gene Set Enrichment Analysis (GSEA) identifies signaling pathways preferentially enriched in high-risk versus low-risk groups. For inflammatory response-related signatures, pathways including the PI3K-AKT signaling pathway, NOD-like receptor signaling pathway, focal adhesion, TNF signaling pathway, and NF-kappa B signaling pathway were significantly enriched [28]. Similarly, amino acid metabolism-related signatures revealed expected enrichments in metabolic pathways alongside cancer-related pathways [10].
Immune microenvironment analysis leverages algorithms such as CIBERSORT, QUANTISEQ, MCPCOUNTER, XCELL, EPIC, and TIMER to quantify immune cell infiltration [28] [10]. Studies consistently reveal distinct immune profiles between risk groups, with high-risk patients typically exhibiting increased immunosuppressive cell populations and altered immune function. For instance, the inflammatory response-related signature identified significant differences in cytolytic activity, MHC class I, type I INF response, type II INF response, inflammation-promoting, and T cell coinhibition between risk groups [28].
Immune checkpoint analysis demonstrates clinical relevance by revealing differential expression of checkpoint molecules between risk groups. High-risk patients in the inflammatory response-related signature study showed elevated expression of HHLA2, NRP1, CD276, TNFRSF9, TNFSF4, CD80, and VTCN1, suggesting potential responsiveness to immune checkpoint inhibitors [28].
Table 3: Essential Research Resources for lncRNA Signature Development
| Resource Category | Specific Tools & Databases | Primary Function | Key Features |
|---|---|---|---|
| Data Resources | TCGA-LIHC, ICGC-LIRI-JP | Provide transcriptomic and clinical data | Annotated HCC cohorts with survival data |
| Pathway Databases | Molecular Signatures Database (MSigDB) | Curated gene sets for biological pathways | Pathway-specific gene collections |
| Analytical Tools | R packages: limma, survival, survminer, GSVA, clusterProfiler | Statistical analysis and visualization | Specialized packages for bioinformatic analysis |
| Experimental Validation | miRNeasy Mini Kit, RevertAid cDNA Synthesis Kit, PowerTrack SYBR Green Master Mix | lncRNA quantification from patient samples | RNA extraction, cDNA synthesis, qRT-PCR |
| Cell Line Models | THLE2, Hep-3B, Huh-1, Huh-7, HCCLM3 | Functional validation of signature lncRNAs | Representative HCC and normal liver cells |
Pathway Integration and Biological Significance
The biological relevance of multi-lncRNA signatures extends beyond statistical association to encompass direct involvement in critical cancer pathways. The diagram below illustrates how different lncRNA classes interface with key hepatocellular carcinoma processes:
The development of multi-lncRNA prognostic signatures represents a significant advancement in hepatocellular carcinoma management, offering superior prognostic stratification compared to conventional clinical parameters. These signatures successfully integrate complex biological pathways—including inflammatory response, cuproptosis, amino acid metabolism, and disulfidptosis—into clinically applicable risk scores that inform both prognosis and therapeutic selection.
The consistent methodological framework underlying these signatures, combining high-throughput data analysis with rigorous statistical modeling, ensures robust performance across diverse patient populations. Furthermore, the ability of these signatures to reflect the tumor immune microenvironment positions them as valuable tools for guiding immunotherapy decisions in an era of increasing personalized medicine.
As validation efforts expand and functional characterization deepens, multi-lncRNA signatures are poised to transition from research tools to clinical applications, ultimately fulfilling their potential to improve risk stratification, treatment selection, and clinical outcomes for hepatocellular carcinoma patients worldwide.
In the field of hepatocellular carcinoma (HCC) research, the validation of long non-coding RNA (lncRNA) biomarkers relies on robust statistical methods to assess their prognostic performance. Among these, Kaplan-Meier (KM) survival analysis and time-dependent Receiver Operating Characteristic (ROC) curves serve as fundamental tools for evaluating the ability of biomarkers to stratify patient risk and predict survival outcomes. While KM analysis visually represents survival probability differences between groups over time, time-dependent ROC curves provide a dynamic measure of a biomarker's discriminatory accuracy at specific clinical follow-up points. These methodologies are particularly crucial in lncRNA biomarker studies where researchers aim to translate molecular signatures into clinically applicable prognostic tools. This guide provides an objective comparison of methodological approaches and software implementations for these analytical techniques within the context of multivariate Cox regression studies in HCC research.
Analytical Framework for lncRNA Biomarker Validation
Kaplan-Meier Survival Analysis in HCC lncRNA Studies
Kaplan-Meier estimation is a non-parametric statistic used to estimate survival functions from time-to-event data, commonly employed to visualize differences in survival outcomes between patient groups stratified by lncRNA expression levels. In typical HCC biomarker studies, patients are categorized into high-risk and low-risk groups based on lncRNA expression thresholds, and KM curves are generated to compare overall survival (OS) or recurrence-free survival (RFS) between these groups. The statistical significance of observed differences is typically assessed using the log-rank test.
The accuracy of KM analysis depends heavily on proper methodology implementation. Recent methodological research has demonstrated that reconstructed individual-level patient data (IPD) from published KM curves can generate hazard ratio (HR) estimates with a high degree of similarity to originally reported values, with mean absolute percentage differences of approximately 2.85% [33]. This approach is particularly valuable for meta-analyses when original datasets are inaccessible.
Table 1: Key Performance Metrics for Kaplan-Meier Analysis in HCC lncRNA Studies
| Metric | Definition | Interpretation in HCC Context | Typical Values in lncRNA Studies |
|---|---|---|---|
| Hazard Ratio (HR) | Ratio of hazard rates between groups | Measure of effect size for lncRNA biomarker | Values >1 indicate increased risk with high lncRNA expression [3] |
| Log-rank P-value | Significance of survival difference | Statistical significance of lncRNA stratification | P < 0.05 considered significant [27] [11] |
| Median Survival | Time until 50% of group experiences event | Clinical relevance of risk stratification | Often reported separately for high/low risk groups [11] |
| Censoring Rate | Proportion of patients with incomplete follow-up | Data completeness indicator | Varies by study; affects statistical power |
Time-Dependent ROC Curve Methodology
Traditional ROC analysis evaluates diagnostic accuracy at a single time point, but this approach is insufficient for survival data where disease status changes over time. Time-dependent ROC curves address this limitation by evaluating a marker's classification accuracy at specific time points during follow-up [34]. Three primary definitions exist for time-dependent sensitivity and specificity:
- Cumulative/Dynamic (C/D): Cases are defined as individuals experiencing the event before time t, while controls are those event-free at time t [34]. This approach is most clinically intuitive for determining prognosis at a specific time point.
- Incident/Dynamic (I/D): Cases are defined as individuals with an event at exactly time t, while controls are those event-free at time t [34]. This method is more appropriate for evaluating early detection capabilities.
- Incident/Static (I/S): Cases are individuals with an event at time t, while controls are a fixed set of individuals who remain event-free throughout the study [34].
For HCC studies with lncRNA biomarkers, the C/D approach is most commonly employed as it aligns with clinical decision-making at specific time horizons (e.g., 1-, 3-, and 5-year survival) [34].
Table 2: Time-Dependent ROC Curve Definitions and Applications
| Definition Type | Case Definition | Control Definition | Appropriate Use Cases in HCC |
|---|---|---|---|
| Cumulative/Dynamic (C/D) | T ≤ t | T > t | Prognostic assessment at fixed time points (1, 3, 5 years) |
| Incident/Dynamic (I/D) | T = t | T > t | Early detection capability evaluation |
| Incident/Static (I/S) | T = t | T > t* for all t* | Fixed control group comparisons |
Experimental Protocols for Method Validation
Protocol 1: IPD Reconstruction from Published KM Curves
The reconstruction of individual-level survival data from published KM curves enables validation and meta-analysis of lncRNA biomarkers in HCC research. This process involves two critical steps [33]:
- Digitization Step: Extract coordinates from KM survival curve images using specialized software. Tools such as CurveSnap, ScanIt, or the R Shiny application IPDfromKM can be employed for this purpose. To ensure accuracy: preprocess images to eliminate unwanted regions, draw two guidelines parallel to the axes to specify coordinate information, and use semi-automated or automated programs to reduce noise and errors [33].
- Reconstruction Step: Apply an iterative algorithm to generate IPD from the extracted coordinates. The algorithm proposed by Guyot et al. and enhanced by Liu et al. is recommended. This algorithm requires the number of patients at risk at different time points and the corresponding time points as reported in the published paper to ensure accurate reconstruction. The IPDfromKM R package automatically adjusts coordinates to maintain the non-increasing trend of KM survival curves over time [33].
Validation studies using this methodology have demonstrated reconstructed hazard ratios with less than 5% difference from originally reported values in most cases, confirming the reliability of this approach for secondary analyses and meta-analyses [33].
Protocol 2: Time-Dependent ROC Analysis for lncRNA Biomarkers
Implementing time-dependent ROC analysis for lncRNA biomarkers in HCC involves the following workflow [34]:
- Data Preparation: Organize dataset with time-to-event (overall survival or recurrence-free survival), event indicator (censoring status), and lncRNA expression values (often as a continuous risk score derived from a multivariate model).
- Time Point Selection: Identify clinically relevant time points for evaluation (typically 1, 3, and 5 years based on HCC clinical guidelines).
- Method Selection: Choose the appropriate time-dependent ROC definition (C/D recommended for prognostic assessment in HCC).
- Estimation Procedure: Calculate time-dependent sensitivity and specificity using inverse probability of censoring weights (IPCW) or cumulative sensitivity/dynamic specificity approaches.
- AUC Calculation: Compute the area under the time-dependent ROC curve at each selected time point using non-parametric or semi-parametric estimators.
- Visualization: Plot ROC curves at each time point and create AUC-over-time graphs to visualize discriminatory performance trends.
This protocol allows researchers to quantify how the prognostic accuracy of lncRNA biomarkers evolves throughout the disease course, providing insights beyond single-time-point assessments.
Software Comparison for Analysis Implementation
Kaplan-Meier Analysis Software Tools
Several software platforms support Kaplan-Meier survival analysis with varying capabilities:
Table 3: Software Solutions for Kaplan-Meier Survival Analysis
| Software | Key Features | KM Curve Digitization | IPD Reconstruction | License |
|---|---|---|---|---|
| R Survival Package | Comprehensive survival analysis, log-rank tests, multivariate Cox models | No | Through IPDfromKM package [33] | Open source |
| IPDfromKM R Package | Specialized in reconstructing IPD from KM curves, automatic coordinate modification | Yes | Yes, primary function [33] | Open source |
| MedCalc | User-friendly interface, log-rank tests, hazard ratio calculations | No | No | Commercial |
| NCSS | Complete survival analysis module, multiple comparison tests | No | No | Commercial |
ROC Analysis Software Comparison
Various software tools offer ROC analysis capabilities with different strengths for time-dependent applications:
Table 4: Software Solutions for ROC Curve Analysis
| Software | Time-Dependent ROC | AUC Comparison | Clinical Utility Features | License |
|---|---|---|---|---|
| R timeROC Package | Yes, comprehensive implementations | DeLong method, bootstrapping | Limited | Open source |
| MedCalc | Limited | DeLong et al. method, Hanley & McNeil | Cost analysis, optimal threshold determination [35] | Commercial |
| NCSS | Limited | DeLong et al., Hanley & McNeil | Partial AUC, multiple curve comparisons [36] | Commercial |
| XLSTAT | No | DeLong, Hanley & McNeil, Sen | Decision plots, cost analysis [37] | Commercial |
| Metz ROC Software | Limited specialized research tools | Multiple methods including PROPROC | Focused on radiology applications [38] | Free academic |
Visualizing Analytical Workflows
Workflow for lncRNA Biomarker Validation in HCC
Time-Dependent ROC Framework for Survival Data
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 5: Essential Research Reagents and Computational Tools for lncRNA Biomarker Studies
| Item Category | Specific Examples | Function in Research Workflow |
|---|---|---|
| Data Sources | TCGA-LIHC dataset [27] [11] | Provides standardized HCC transcriptomic and clinical data for model development |
| lncRNA Detection Methods | RNA sequencing, qRT-PCR, ISH [3] | Quantifies lncRNA expression levels in tissue or blood samples |
| Statistical Software | R packages: survival, timeROC, IPDfromKM [33] [34] | Implements survival analysis and time-dependent ROC methodology |
| Commercial Analysis Tools | MedCalc, NCSS, XLSTAT [35] [36] [37] | Provides user-friendly interfaces for ROC and survival analysis |
| Validation Cohorts | Institutional HCC patient cohorts [11] | Enables external validation of lncRNA biomarker signatures |
| BChE-IN-30 | BChE-IN-30, MF:C23H39N3O3S, MW:437.6 g/mol | Chemical Reagent |
| Antibiofilm agent-2 | Antibiofilm agent-2, MF:C17H21NO5, MW:319.4 g/mol | Chemical Reagent |
The integration of Kaplan-Meier survival analysis and time-dependent ROC curves provides a robust framework for assessing the prognostic performance of lncRNA biomarkers in HCC research. While KM analysis offers intuitive visualization of survival differences between risk groups, time-dependent ROC curves deliver a dynamic perspective on biomarker discrimination accuracy at clinically relevant time points. The methodological protocols and software comparisons presented in this guide offer researchers practical resources for implementing these analyses. As lncRNA biomarker research advances, proper application of these performance assessment tools will be crucial for translating molecular discoveries into clinically applicable prognostic signatures that can ultimately improve HCC patient management through personalized risk stratification.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most prevalent cancer and the third leading cause of cancer-related deaths worldwide [10] [11]. Despite advances in diagnostic techniques and therapeutic options, the prognosis for HCC patients remains unsatisfactory, with a 5-year survival rate of approximately 18% and a recurrence rate as high as 80% [39]. The high heterogeneity of HCC results in substantially different clinical outcomes among patients with similar clinical stages, complicating treatment decisions and prognostic predictions [40] [39]. This clinical challenge has driven the search for more precise prognostic tools that can stratify patients according to their individual risk profiles.
The integration of long non-coding RNAs (lncRNAs) into prognostic nomograms represents a promising approach to address this clinical need. LncRNAs are non-protein-coding transcripts longer than 200 nucleotides that play crucial roles in regulating gene expression through various mechanisms, including transcriptional, post-transcriptional, and epigenetic regulation [10] [41]. In HCC, specific lncRNAs have been implicated in tumor initiation, progression, metastasis, immune escape, and drug resistance [10] [42]. The altered expression of these lncRNAs in tumor tissues and blood circulation of HCC patients has positioned them as potential biomarkers for predicting prognosis [3]. The development of lncRNA-based nomograms that integrate molecular biomarkers with clinical parameters represents a significant advancement in personalized medicine for HCC, enabling more accurate survival predictions and tailored treatment strategies.
Methodological Framework: Constructing lncRNA-Based Prognostic Models
Data Acquisition and Preprocessing
The construction of robust lncRNA-based prognostic models begins with comprehensive data acquisition from publicly available databases. The Cancer Genome Atlas (TCGA) Liver Hepatocellular Carcinoma (TCGA-LIHC) dataset serves as the primary resource for transcriptome expression data and corresponding clinical information [10] [11]. Researchers typically apply specific filtration criteria to ensure data quality, excluding patients with overall survival of less than 30 days to avoid bias from short-term mortality events [10]. Additional validation datasets may be sourced from the Gene Expression Omnibus (GEO) database or institutional patient cohorts to ensure model robustness [42] [43].
The process continues with the identification of lncRNAs related to specific biological processes or structures relevant to HCC pathogenesis. For amino acid metabolism-related lncRNAs, researchers retrieve gene sets from the Molecular Signature Database (MSigDB) and calculate Pearson correlations between these genes and lncRNA expression levels [10]. Similarly, for migrasome-related lncRNAs, a predefined set of migrasome-related genes is obtained from the GeneCards database, and correlation analysis identifies associated lncRNAs [11]. These approaches ensure that the selected lncRNAs have biological relevance to cancer pathways.
Statistical Modeling and Validation
The core analytical workflow employs multiple statistical techniques to identify prognostic lncRNA signatures. Univariate Cox regression analysis serves as the initial filter to identify lncRNAs significantly associated with overall survival [10] [42] [11]. This is followed by LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression with 10-fold cross-validation to prevent overfitting and select the most relevant lncRNAs [10] [11] [43]. Finally, multivariate Cox regression analysis establishes the final prognostic model, assigning coefficients to each lncRNA based on their relative contribution to survival prediction [10] [41] [43].
The general formula for calculating the risk score is: [ Riskscore = \sum{i}(Coefficient{lncRNAi} \times Expression{lncRNA_i}) ]
Patients are stratified into high-risk and low-risk groups based on the median risk score [10] [42] [41]. The model's performance is evaluated using Kaplan-Meier survival analysis with log-rank tests to compare survival between risk groups, and time-dependent receiver operating characteristic (ROC) curve analysis to assess predictive accuracy at 1, 3, and 5 years [10] [42] [41]. Both internal validation (through random splitting of datasets) and external validation (using independent cohorts) are essential to demonstrate model generalizability [42] [11] [43].
Table 1: Key Statistical Methods in lncRNA Prognostic Model Development
| Method | Purpose | Key Parameters |
|---|---|---|
| Univariate Cox Analysis | Initial screening of survival-associated lncRNAs | P-value < 0.05 for significance |
| LASSO-Cox Regression | Variable selection and overfitting prevention | 10-fold cross-validation; optimal lambda value |
| Multivariate Cox Analysis | Final model construction with coefficient assignment | Hazard ratios (HR) with confidence intervals |
| Kaplan-Meier Analysis | Survival comparison between risk groups | Log-rank P-value < 0.05 for significance |
| Time-dependent ROC | Predictive accuracy assessment | Area under curve (AUC) at 1, 3, 5 years |
Nomogram Construction and Evaluation
The final step involves integrating the lncRNA signature with clinical parameters into a nomogram for individualized prognosis prediction. The nomogram assigns points for each variable based on multivariate Cox regression coefficients, allowing clinicians to calculate total points corresponding to predicted survival probabilities at 1, 3, and 5 years [40] [39]. The nomogram's performance is evaluated using calibration curves to assess agreement between predicted and observed outcomes, concordance index (C-index) to measure predictive discrimination, and decision curve analysis (DCA) to evaluate clinical usefulness [44] [40] [39].
Diagram 1: Comprehensive Workflow for Developing lncRNA-Based Prognostic Nomograms. This diagram illustrates the multi-step process from data acquisition to clinical application, highlighting key statistical modeling and validation procedures.
Comparative Analysis of lncRNA Signatures in HCC Prognostication
Performance Metrics of Established lncRNA Signatures
Multiple studies have developed lncRNA-based prognostic signatures with varying numbers of lncRNA components. The performance of these signatures demonstrates consistent predictive value across different HCC patient populations.
Table 2: Comparison of lncRNA Signatures for HCC Prognosis Prediction
| Study Focus | Number of lncRNAs | AUC Values | Key lncRNAs Identified | Clinical Utility |
|---|---|---|---|---|
| Amino Acid Metabolism-Related [10] | 4 | 3-year: ~0.75 | AL590681.1 (key functional gene) | Predicts immunotherapy response; high-risk group shows more immunosuppressive cells |
| Migrasome-Related [11] | 2 | 3-year: >0.70 | LINC00839, MIR4435-2HG | Stratifies immunotherapy responders; MIR4435-2HG promotes immune evasion via PD-L1 |
| General Prognostic [41] | 6 | 5-year: 0.727 | CBR3-AS1, SPACA6P-AS, AP005131.2 | Independent of age, ER status; correlates with immune cell infiltration |
| Head & Neck Cancer [43] | 8 | 3-year: 0.740 5-year: 0.706 | MIR4435-2HG, LINC02541, MIR9-3HG | Validated in external cohort (n=102); superior to clinical factors alone |
The 4-lncRNA amino acid metabolism-related signature developed by researchers incorporates AL590681.1, which was functionally validated to enhance HCC cell activity [10]. Patients in the high-risk group demonstrated significantly lower overall survival rates and exhibited more immunosuppressive immune cell infiltration, expressing immune checkpoints including CD276, CTLA4, and TIGIT [10]. Importantly, the high-risk group showed better survival prospects with anti-PD1 treatment, indicating the model's value in predicting immunotherapy response.
The migrasome-related 2-lncRNA signature (LINC00839 and MIR4435-2HG) effectively stratified HCC patients by prognosis and immunotherapy responsiveness [11]. Functional validation revealed that MIR4435-2HG promotes malignant behaviors and immune evasion by regulating epithelial-mesenchymal transition (EMT) and PD-L1 expression [11]. Single-cell analysis showed its enrichment in cancer-associated fibroblasts, suggesting a role in tumor-stroma crosstalk and immune suppression.
Comparison with Traditional Staging Systems
Traditional staging systems for HCC, including the Barcelona Clinic Liver Cancer (BCLC) staging, American Joint Committee on Cancer (AJCC) TNM staging, and International Staging System (ISS) for multiple myeloma, have provided foundational prognostic frameworks but demonstrate limitations in capturing tumor heterogeneity [40] [39]. The integration of lncRNA signatures with these established systems significantly enhances prognostic accuracy.
In multiple myeloma, nomograms incorporating lactate dehydrogenase (LDH), albumin, and cytogenetic abnormalities demonstrated superior prognostic predictive ability compared to the International Staging System alone [40]. Similarly, for advanced non-small-cell lung cancer, nomogram models based on basic clinical features and routine lab testing exhibited cross-study robustness with integrated area under the ROC curve values ranging from 0.723 to 0.83 across validation cohorts [45].
For colorectal cancer patients not receiving primary site surgery but undergoing chemotherapy, nomograms integrating age, marital status, primary site, grade, histology, T stage, M stage, tumor size, and CEA levels demonstrated excellent predictability with time-dependent AUCs exceeding 0.7, providing greater clinical benefit than traditional TNM staging [44].
Experimental Protocols for lncRNA Validation
Functional Characterization of Prognostic lncRNAs
The transition from bioinformatic identification to clinical application requires experimental validation of lncRNA function in HCC progression. The standard protocol begins with cell culture of various HCC cell lines (e.g., Hep-3B, Huh-1, Huh-7, HCCLM3) alongside normal liver cells (THLE2) as controls [10]. Cells are maintained in DMEM or RPMI 1640 medium supplemented with 10% fetal bovine serum at 37°C with 5% CO₂ [10] [42].
Gene expression analysis via real-time quantitative PCR (RT-qPCR) follows, using TRIzol for RNA extraction, cDNA synthesis kits for reverse transcription, and SYBR Green Master Mix for quantitative PCR [10] [42]. The 2–ΔΔCt method normalizes relative expression levels to internal controls like GAPDH [42]. For functional assessment, RNA interference using lncRNA-specific short hairpin RNA (shRNA) or siRNA is transfected into HCC cells using Lipofectamine 3000 reagent [10] [42].
Phenotypic assays then evaluate the functional consequences of lncRNA modulation. The CCK-8 assay assesses cell viability at 48 hours post-transfection [10]. Colony formation assays evaluate long-term growth potential by plating 1000 transfected cells per well in six-well plates, followed by 14-day incubation, paraformaldehyde fixation, and crystal violet staining [10]. Migration assays using Transwell or wound-healing approaches further characterize the lncRNA's role in metastatic potential [11].
Diagram 2: Experimental Workflow for Functional Validation of Prognostic lncRNAs. This diagram outlines the comprehensive process from initial bioinformatic discovery through in vitro and in vivo mechanistic studies to establish clinical relevance.
Immune Microenvironment and Therapeutic Response Assessment
Given the importance of immunotherapy in HCC treatment, evaluating the impact of lncRNAs on the tumor immune microenvironment represents a critical component of functional validation. Computational algorithms including single-sample gene set enrichment analysis (ssGSEA) and quanTIseq deconvolution analyze immune cell infiltration using RNA-seq data from bulk tumors [10] [42]. These methods quantify the abundance of various immune cell types, including cytotoxic T cells, natural killer cells, macrophages, and myeloid-derived suppressor cells, in high-risk versus low-risk patient groups.
The Tumor Immune Dysfunction and Exclusion (TIDE) framework evaluates the potential for immune escape mechanisms by integrating gene expression profiles related to T-cell dysfunction and exclusion [10]. This algorithm predicts responses to immune checkpoint inhibitors, with high TIDE scores indicating non-response and low scores suggesting potential therapeutic benefit [10]. Additionally, Subclass Mapping (SubMap) identifies similar molecular subtypes across datasets to predict immunotherapy responses [10].
Experimental validation includes flow cytometry to quantify immune cell populations in vitro and in animal models, and immunohistochemistry of patient tissues to validate computational predictions [11]. For immune checkpoint analysis, ELISA and western blotting measure protein expression levels of PD-1, PD-L1, CTLA4, and other checkpoints following lncRNA modulation [11].
Research Reagent Solutions for lncRNA Studies
Table 3: Essential Research Reagents for lncRNA Biomarker Development
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Cell Lines | THLE2 (normal), Hep-3B, Huh-1, Huh-7, HCCLM3, NCI-H929 (MM) | Functional validation of lncRNAs across cancer types | Authenticate regularly; use low passages |
| Gene Modulation | LncRNA-specific shRNA/siRNA, Lipofectamine 3000, lentiviral constructs | Loss-of-function and gain-of-function studies | Include scrambled controls; verify efficiency (48-72h) |
| Expression Analysis | TRIzol, cDNA synthesis kits, SYBR Green Master Mix, specific primers | Quantification of lncRNA expression | Normalize to GAPDH/β-actin; use 2–ΔΔCt method |
| Functional Assays | CCK-8 reagent, crystal violet, Transwell chambers, matrigel | Phenotypic characterization (viability, migration) | Include appropriate controls; optimize cell numbers |
| Immune Analysis | Flow cytometry antibodies, ELISA kits, IHC antibodies | Tumor microenvironment and immune checkpoint assessment | Multi-color panel design; isotype controls |
Clinical Translation and Path Forward
The integration of lncRNA biomarkers into prognostic nomograms represents a significant advancement in personalized oncology. The consistent demonstration that lncRNA signatures serve as independent prognostic factors across multiple cancer types underscores their clinical potential [10] [41] [11]. The transition from traditional staging systems to molecularly informed prognostic tools addresses the critical challenge of tumor heterogeneity, enabling more precise risk stratification.
For clinical implementation, several considerations require attention. First, standardization of lncRNA detection methodologies is essential, whether through RNA sequencing, RT-qPCR, or emerging technologies like digital droplet PCR [3]. Second, the development of clinically feasible workflows that can integrate lncRNA assessment into routine diagnostic pathways must be prioritized. Third, prospective validation in multi-center trials remains necessary to establish generalizability across diverse patient populations.
The potential applications of lncRNA-based nomograms extend beyond prognosis prediction to therapeutic guidance. The ability of certain lncRNA signatures to predict response to immunotherapy [10] [11] and chemotherapy [42] positions them as valuable tools for treatment selection. As functional studies continue to elucidate the mechanistic roles of specific lncRNAs in HCC pathogenesis, these molecular insights may reveal novel therapeutic targets, completing the transition from prognostic biomarker to therapeutic target.
The ongoing refinement of lncRNA-based nomograms through the integration of additional molecular features, including mutations, epigenetic alterations, and proteomic signatures, will further enhance their predictive accuracy. As these tools evolve, they hold the promise of fundamentally transforming HCC management from population-level estimates to individualized risk-adaptive management, ultimately improving patient outcomes in this challenging malignancy.
Overcoming Analytical Hurdles: Ensuring Model Accuracy and Clinical Relevance
In the development of prognostic long non-coding RNA (lncRNA) signatures for hepatocellular carcinoma (HCC), a major challenge is the high-dimensionality of genomic data where the number of potential predictor lncRNAs vastly exceeds the number of patient samples. This creates a significant risk of overfitting, where models perform well on training data but fail to generalize to new datasets. This guide examines how the combined application of LASSO (Least Absolute Shrinkage and Selection Operator) regression and cross-validation has become the methodological standard for addressing this critical issue, enabling the creation of robust, clinically applicable prognostic models in HCC research.
The Overfitting Challenge in HCC lncRNA Research
Hepatocellular carcinoma exhibits profound molecular heterogeneity, with tumor progression influenced by complex interactions between tumor cells and the immune microenvironment [46]. In this context, lncRNAs have emerged as promising prognostic biomarkers and therapeutic targets due to their diverse regulatory functions and roles in HCC development and progression [46]. However, transcriptomic analyses typically involve thousands of lncRNA candidates, while most HCC studies contain only hundreds of patient samples—a classic high-dimensionality problem that predisposes models to overfitting.
Table 1: Data Dimensionality Challenges in Recent HCC lncRNA Studies
| Study Focus | Initial LncRNA Candidates | Final Signature Size | Analytical Approach |
|---|---|---|---|
| CD8 T-cell Exhaustion-associated LncRNAs [46] | Not specified | 5 lncRNAs | LASSO + Multivariate Cox |
| Amino Acid Metabolism-related LncRNAs [10] | 24 prognostic lncRNAs | 4 lncRNAs | LASSO + Multivariate Cox |
| PANoptosis-related LncRNAs [47] | 547 candidate lncRNAs | 5 lncRNAs | WGCNA + LASSO + Cox |
| Ferroptosis-related LncRNAs [48] | Not specified | 7 lncRNAs | LASSO Cox Regression |
| Cuproptosis-related LncRNAs [49] | 509 candidate lncRNAs | 3 lncRNAs | LASSO Cox Regression |
Without proper regularization, models may identify lncRNAs that appear significant due to random variations in the training data rather than true biological associations. This creates clinically dangerous situations where prognostic signatures fail validation in independent cohorts or diverse patient populations, potentially misguiding treatment decisions.
LASSO Regression: Mathematical Foundation and Implementation
Core Mechanism and Penalization
LASSO regression addresses overfitting by applying an L1-norm penalty that shrinks coefficient estimates toward zero, effectively performing continuous feature selection. The method minimizes the following objective function:
RSS(β) + λ‖β‖â‚
Where RSS(β) is the residual sum of squares, β represents the coefficient vector, and λ is the tuning parameter controlling the strength of penalization. The L1-penalty has the special property that it can force some coefficients to exactly zero, thereby selecting a parsimonious model [50].
Integration with Survival Analysis
In HCC prognostic studies, LASSO is typically integrated with Cox proportional hazards models. The risk score for each patient is calculated as:
Risk Score = ∑(coefficient_lncRNA_i × expression_lncRNA_i)
For instance, in developing a PANoptosis-related lncRNA signature, researchers applied LASSO Cox regression to identify five key lncRNAs (AL442125.2, MIR4435-2HG, AC026412.3, LINC01224, and AC026356.1) from 105 candidate lncRNAs identified through weighted gene co-expression network analysis (WGCNA) [47].
Figure 1: LASSO Regression Workflow for LncRNA Signature Development
Cross-Validation: Optimizing Model Generalizability
The Role of k-Fold Cross-Validation
Cross-validation works synergistically with LASSO to determine the optimal value of the penalty parameter λ. The most common approach—10-fold cross-validation—randomly partitions the dataset into 10 subsets, using 9 for model training and 1 for validation, rotating this process until all subsets have served as validation data [8].
Table 2: Cross-Validation Implementation in Recent HCC Studies
| Study | CV Type | Implementation Details | Primary Outcome |
|---|---|---|---|
| Plasma Exosomal LncRNA Signature [8] | 10-fold cross-validation | Integrated with 10 machine learning algorithms; 118 model configurations tested | Identified random survival forest as optimal approach |
| Immune-Related LncRNA Signature [50] | 10-fold cross-validation | Applied to LASSO Cox model via glmnet package; optimal λ at minimum partial likelihood deviance | Selected 2-lncRNA signature (PRRT3-AS1, AL031985.3) |
| Hypoxia-Related LncRNA Signature [51] | 1,000-round cross-validation | Tuning parameter selection for minimum partial likelihood deviance | Established 3-lncRNA prognostic signature |
Determining the Optimal Penalty Parameter
The optimal λ value is typically selected through one of two criteria: the λ that minimizes the cross-validated partial likelihood deviance (λmin) or the largest λ within one standard error of the minimum (λ1se). The latter approach produces a more sparse model while maintaining comparable predictive performance [51].
Experimental Protocols and Methodological Standards
Standardized Analytical Pipeline
The integration of LASSO with cross-validation follows a well-established protocol in HCC lncRNA research:
- Data Preprocessing: Quality control, normalization, and batch effect correction using limma R package [52]
- Candidate LncRNA Identification: Filtering via Pearson correlation (|R| > 0.4, p < 0.001) with biological processes of interest [46] [10]
- Initial Prognostic Screening: Univariate Cox regression (p < 0.05) to identify survival-associated lncRNAs [50]
- LASSO Application: Implementation via glmnet R package with 10-fold cross-validation for λ optimization [50] [47]
- Multivariate Cox Regression: Final model development using lncRNAs selected by LASSO [46] [10]
- Model Validation: Performance assessment in internal validation sets and external independent cohorts [47] [48]
Validation Frameworks
Beyond cross-validation during model development, rigorous validation includes:
- Temporal Validation: Splitting TCGA-LIHC data into training/test sets (typically 7:3 ratio) [47]
- External Validation: Application to independent cohorts (ICGC, GEO datasets) [8] [47]
- Clinical Validation: Correlation with established clinical parameters and survival outcomes [1] [48]
Figure 2: Comprehensive Validation Framework for HCC LncRNA Signatures
Comparative Performance of LASSO-Based Signatures
Table 3: Predictive Performance of LASSO-Derived LncRNA Signatures in HCC
| Signature Type | 1-Year AUC | 3-Year AUC | 5-Year AUC | Independent Validation |
|---|---|---|---|---|
| Cuproptosis-Related LncRNAs [49] | 0.759 | 0.668 | 0.674 | Experimental validation in HCC cell lines |
| Hypoxia-Related LncRNAs [51] | 0.805 | 0.672 | 0.630 | Test set consistency confirmed |
| Ferroptosis-Related LncRNAs [48] | 0.745 | 0.745 | 0.719 | Testing set verification |
| CD8 T-cell Exhaustion LncRNAs [46] | Strong prognostic performance reported | Independent predictor of overall survival | Not specified | Functional validation for AL158166.1 |
| Amino Acid Metabolism LncRNAs [10] | Not specified | Not specified | Not specified | Drug sensitivity analysis performed |
The performance metrics demonstrate that LASSO-derived signatures maintain predictive accuracy across multiple timepoints while using substantially fewer lncRNAs than initial candidate pools. This balance between model complexity and predictive power is a direct result of effective overfitting control.
Table 4: Key Research Reagent Solutions for HCC LncRNA Studies
| Resource Category | Specific Tools | Application in lncRNA Research |
|---|---|---|
| Data Sources | TCGA-LIHC, GEO, ICGC | Provide transcriptomic data and clinical annotations for model development and validation [46] [52] [8] |
| Computational Packages | glmnet, survival, timeROC (R packages) | Implement LASSO Cox regression, survival analysis, and time-dependent ROC curves [46] [50] [47] |
| Validation Algorithms | TIDE, CIBERSORT, ESTIMATE | Assess tumor immune microenvironment, immunotherapy response prediction [46] [10] [8] |
| Experimental Validation | RT-qPCR, CCK-8 assay, Transwell assay | Confirm lncRNA expression and functional roles in HCC progression [10] [49] [48] |
| Pathway Analysis | clusterProfiler, GSEA, GSVA | Functional enrichment analysis of lncRNA signatures [46] [8] [47] |
The integration of LASSO regression with cross-validation represents a methodological cornerstone in HCC lncRNA biomarker research, effectively addressing the critical challenge of overfitting in high-dimensional genomic data. This approach enables the development of parsimonious prognostic signatures that maintain robust performance across validation cohorts, facilitating their potential translation into clinical practice. As the field advances toward multi-omic integration and more complex model architectures, these foundational regularization techniques will remain essential for generating biologically meaningful and clinically applicable prognostic tools in hepatocellular carcinoma.
Data Preprocessing and Normalization Strategies for Reliable lncRNA Quantification
The validation of long non-coding RNA (lncRNA) biomarkers in hepatocellular carcinoma (HCC) research represents a promising frontier in precision oncology. However, the accurate quantification of lncRNAs presents unique computational challenges that distinguish them from protein-coding genes. LncRNAs exhibit lower expression levels, less accurate annotation, and higher tissue specificity compared to protein-coding genes, necessitating specialized preprocessing and normalization approaches [53]. In the context of multivariate Cox regression for HCC survival studies, where models incorporate multiple clinical variables to predict patient outcomes, unreliable lncRNA quantification can significantly compromise prognostic signature validity and clinical utility.
This guide objectively compares current normalization methodologies and preprocessing pipelines, evaluating their performance specifically for lncRNA quantification in HCC biomarker research. By synthesizing evidence from recent studies and experimental benchmarks, we provide researchers with evidence-based recommendations to enhance the reliability of their lncRNA biomarkers in multivariate survival analyses.
Understanding lncRNA-Specific Quantification Challenges
The accurate detection and quantification of lncRNAs are fundamentally challenged by several biological and technical factors that must be addressed during data preprocessing:
Annotation instability: LncRNA annotations undergo continuous evolution and expansion, unlike the relatively stable annotations of protein-coding genes. According to GENCODE, the human genome contains over 19,000 lncRNAs, with this annotation continuously evolving [53].
Low expression abundance: LncRNAs typically display lower expression levels compared to protein-coding genes, placing them closer to the detection limit of sequencing technologies and making their quantification more susceptible to technical noise [53].
High cell type specificity: LncRNAs exhibit remarkably high tissue and cell type specificity, which, while biologically significant, complicates their detection across diverse sample types and conditions [53].
These challenges are particularly problematic for HCC prognostic model development, where false positives or inaccurate quantification can lead to poorly predictive multivariate Cox regression models and unreliable clinical biomarkers.
Normalization Methods: Comparative Performance Evaluation
Comprehensive Comparison of Normalization Techniques
Normalization methods perform differently depending on the research context, data types, and analytical goals. The table below summarizes the performance characteristics of major normalization methods for lncRNA quantification:
Table 1: Comparative Performance of Normalization Methods in lncRNA Studies
| Normalization Method | Technical Approach | Best Use Cases | Performance Evidence | Limitations |
|---|---|---|---|---|
| Quantile Normalization (QN) | Makes distribution of gene expression identical across samples [54] | Cross-platform integration (microarray + RNA-seq) [55] | Effective for supervised learning with mixed platforms [55] | Requires reference distribution; performance suffers at extremes [55] |
| Trimmed Mean of M-values (TMM) | Uses weighted trimmed mean of log expression ratios [54] [56] | Between-sample normalization within same platform [54] | Robust for differential expression analysis [56] | Assumes most genes not differentially expressed [54] |
| Transcripts Per Million (TPM) | Accounts for sequencing depth and transcript length [54] | Within-sample comparisons [54] | Sum of TPMs consistent across samples [54] | Requires within-dataset normalization for between-sample comparisons [54] |
| Binning-By-Gene (BBG) | Allocates expressions into bins based on rank [57] | Learning gene expression relationships | Significantly enhances learning of biological attributes [57] | Novel method with limited testing across diverse datasets |
| Training Distribution Matching (TDM) | Normalizes RNA-seq to target distribution of array data [55] | Machine learning applications with cross-platform data | Performs well with moderate RNA-seq in training sets [55] | Specialized for specific cross-platform applications |
| FPKM/RPKM | Accounts for sequencing depth and gene length [54] | Within-sample comparisons [54] | Standard for single-sample normalization [54] | Problematic for between-sample comparisons [54] |
Experimental Evidence for Normalization Method Performance
Several experimental studies have directly compared normalization methods in contexts relevant to lncRNA biomarker discovery:
In cross-platform integration studies, Quantile normalization, Nonparanormal normalization (NPN), and Training Distribution Matching (TDM) all demonstrated capability to maintain model performance when combining microarray and RNA-seq data. These methods allowed effective training of subtype classifiers even with varying proportions of RNA-seq data in the training sets, with QN performing particularly well except at extreme cases (0% or 100% RNA-seq data) [55].
For bulk RNA-seq analyses, a comprehensive comparison of five normalization methods (TMM, Upper Quartile, Median, Quantile, and PoissonSeq) revealed that normalization choice significantly impacts differential expression results. The study proposed a universal workflow for selecting optimal normalization using control genes, method sensitivity/specificity, and classification errors [56].
The novel Binning-By-Gene normalization method developed for the GeneRAIN model addressed specific biases in standard z-score normalization, where genes with low mean expression but high variance could dominate high rank positions. BBG equalized the probability of each gene occupying any rank position, significantly enhancing the model's efficiency in learning gene biological attributes (p = 0.007) [57].
Preprocessing Pipelines: Profound Impact on lncRNA Detection
Pipeline Performance Benchmarking
The choice of preprocessing pipeline significantly impacts lncRNA detection sensitivity. A comprehensive benchmarking of scRNA-seq preprocessing pipelines revealed striking differences in lncRNA detection:
Table 2: Preprocessing Pipeline Comparison for lncRNA Detection
| Preprocessing Pipeline | Base Methodology | lncRNA Detection Performance | Resource Requirements | Integration with Downstream Analysis |
|---|---|---|---|---|
| Kallisto-Bustools | Pseudoalignment [53] | Superior - detects significantly more highly-expressed lncRNAs [53] | Fast running times, less memory-intensive [53] | ELATUS framework for functional lncRNA identification [53] |
| Cell Ranger | STAR-based alignment [53] | Moderate - misses many highly-expressed lncRNAs [53] | Standard resource requirements | Standard 10x Genomics workflow [53] |
| Salmon-Alevin | Pseudoalignment with selective alignment [53] | Moderate - similar to Cell Ranger [53] | Fast running times, less memory-intensive [53] | Compatible with standard downstream tools |
| STARsolo | STAR-based alignment [53] | Moderate - similar to Cell Ranger [53] | Higher memory requirements | Compatible with standard downstream tools |
The performance differences remained significant even when controlling for expression levels, indicating that detection disparities were not merely due to the generally lower expression of lncRNAs [53]. This has crucial implications for HCC biomarker studies, where missing biologically relevant lncRNAs could lead to incomplete prognostic signatures.
Specialized Workflows for lncRNA Analysis
The ELATUS framework was specifically developed to address the limitations of standard preprocessing pipelines for lncRNA detection. By combining the pseudoaligner Kallisto with selective functional filtering, ELATUS enhances detection of functional lncRNAs from scRNA-seq data, demonstrating higher concordance with ATAC-seq profiles than standard methods [53].
The framework's superior performance is particularly evident with inaccurate reference annotations, which characterizes lncRNA annotations. In one validation, ELATUS identified AL121895.1, a previously undocumented cis-repressor lncRNA in triple-negative breast cancer cells, whose role was unnoticed by traditional methodologies [53].
For multi-omics integration, the lncRNACNVIntegrateR package provides a specialized framework for correlating lncRNA expression with copy number variations (CNVs). This R package integrates transcriptomic data, CNV profiles, and clinical information from matched samples, providing a complete pipeline for data preprocessing, lncRNA-CNV correlation analysis, and identification of CNV-driven prognostic signatures [58].
Experimental Protocols for Key Methodologies
Cross-Platform Normalization Validation Protocol
The experimental protocol for validating cross-platform normalization methods involved:
Dataset Preparation: BRCA and GBM datasets from TCGA were used with varying numbers of RNA-seq samples added to microarray training sets [55].
Normalization Application: Seven normalization approaches were tested: LOG, NPN, QN, QN (CN), QN-Z, TDM, and z-scoring, plus untransformed data as a negative control [55].
Model Training: Three classifiers (LASSO logistic regression, linear SVM, and random forest) were trained to predict subtypes or mutation status [55].
Performance Assessment: Kappa statistics were used to assess performance on holdout sets composed entirely of microarray or RNA-seq data [55].
Pathway Analysis: Pathway-Level Information Extractor (PLIER) was used to identify pathways significantly associated with latent variables in mixed-platform data [55].
This protocol demonstrated that QN, TDM, and NPN all performed well when moderate amounts of RNA-seq data were incorporated into training sets, maintaining performance on both microarray and RNA-seq holdout sets [55].
lncRNA Signature Development for HCC Prognosis
The standard protocol for developing lncRNA prognostic signatures in HCC involves:
Data Acquisition: RNA-sequencing data and clinical information for HCC patients obtained from TCGA [19] [20] [51].
LncRNA Identification: Differential expression analysis between tumor and normal tissues to identify dysregulated lncRNAs [19].
Prognostic Filtering: Univariate Cox regression to identify survival-associated lncRNAs [19] [20].
Signature Construction: LASSO Cox regression with 1000-fold cross-validation to prevent overfitting, followed by multivariate Cox regression to build prognostic signatures [19] [20].
Model Validation: Risk score calculation and division of patients into high- and low-risk groups based on median risk score, followed by Kaplan-Meier survival analysis and time-dependent ROC curve assessment [19] [20].
Functional Analysis: Gene set enrichment analysis (GSEA) to identify pathways enriched in different risk groups [19] [51].
This protocol has been successfully applied to develop various HCC prognostic signatures, including costimulatory molecule-related lncRNAs [20] and hypoxia-related lncRNAs [51], with risk scores serving as independent prognostic factors in multivariate Cox regression.
Integrated Workflow for Reliable lncRNA Quantification
The diagram below illustrates a comprehensive workflow for lncRNA preprocessing and normalization, integrating the most effective methods identified through performance benchmarking:
Figure 1: Comprehensive Workflow for Reliable lncRNA Quantification in HCC Studies
The Scientist's Toolkit: Essential Research Reagents and Computational Solutions
Table 3: Essential Research Resources for lncRNA Quantification Studies
| Resource Category | Specific Tool/Resource | Primary Function | Application Context |
|---|---|---|---|
| Computational Packages | lncRNACNVIntegrateR [58] | Multi-omics data integration | Correlating lncRNA expression with CNV profiles |
| ELATUS [53] | Enhanced lncRNA detection from scRNA-seq | Identification of functional lncRNAs | |
| edgeR/DESeq2 [56] | Differential expression analysis | Identifying differentially expressed lncRNAs | |
| Normalization Methods | Quantile Normalization [55] [54] | Cross-platform data integration | Combining microarray and RNA-seq data |
| TMM [54] [56] | Between-sample normalization | RNA-seq studies with same platform | |
| Binning-By-Gene [57] | Bias reduction in representation learning | Deep learning applications with expression data | |
| Data Resources | TCGA-LIHC [19] [20] [51] | Clinical and molecular HCC data | Prognostic signature development and validation |
| GENCODE [53] | Comprehensive lncRNA annotation | Reference for lncRNA identification | |
| lncRNADisease/MNDR [23] | Experimentally validated LDAs | Benchmarking and validation |
Based on comprehensive performance benchmarking and experimental evidence, we recommend the following strategies for reliable lncRNA quantification in HCC biomarker studies:
For single-cell RNA-seq studies, implement the Kallisto-Bustools preprocessing pipeline within the ELATUS framework to maximize detection of functional lncRNAs that would be missed by standard alignment-based methods [53].
For cross-platform integration of microarray and RNA-seq data, apply Quantile Normalization, which has demonstrated robust performance for supervised learning with mixed platform training sets [55].
For multivariate Cox regression in HCC, employ rigorous preprocessing and normalization specifically optimized for lncRNAs' characteristics, as this significantly impacts the prognostic power of resulting biomarkers [19] [20] [51].
For novel lncRNA discovery, utilize the Binning-By-Gene normalization method to reduce bias in representation learning, enabling more comprehensive capture of biological information [57].
The integration of these specialized preprocessing and normalization strategies addresses the unique challenges of lncRNA quantification, ultimately enhancing the reliability and clinical utility of lncRNA biomarkers in HCC multivariate survival models. As lncRNA research continues to evolve, continued refinement of these computational approaches will be essential for translating molecular discoveries into clinically actionable biomarkers.
In the pursuit of reliable long non-coding RNA (lncRNA) biomarkers for hepatocellular carcinoma (HCC), researchers face a formidable obstacle: cohort heterogeneity. This variability in patient characteristics—including age, sex, disease etiology, tumor stage, and comorbidity profiles—introduces confounding effects that can compromise the validity of multivariate Cox regression analyses used to establish prognostic significance. The insidious nature of HCC, with its frequently late-stage diagnosis and complex multifactorial pathogenesis, exacerbates these challenges, often resulting in biomarkers that demonstrate promising performance in initial discovery cohorts but fail to validate in broader clinical populations [10] [59].
The consequences of unaddressed heterogeneity are profound. A brain imaging study demonstrated that population diversity substantially impacts predictive accuracy and pattern stability, with performance decay particularly evident in models applied to demographically dissimilar subpopulations [60]. Similarly, in therapeutic research, heterogeneity of treatment effect (HTE) analyses reveal that interventions often exert markedly different effects across patient subgroups, necessitating sophisticated approaches to identify these variations [61] [62]. For lncRNA biomarker validation in HCC, where the goal is to establish independent prognostic value beyond standard clinical parameters, navigating this heterogeneity is not merely a statistical concern but a fundamental requirement for clinical translation.
This guide examines systematic approaches for identifying, measuring, and addressing cohort heterogeneity in HCC lncRNA studies, providing researchers with methodological frameworks to enhance the robustness and generalizability of their findings.
Quantifying Heterogeneity: Measurement Approaches and Diagnostic Tools
Propensity Score Framework for Diversity Assessment
The propensity score framework offers a powerful approach to quantify population diversity by consolidating multiple covariates into a composite confound index. Originally developed for treatment assignment probability estimation, this method encapsulates mixed covariates into a single dimension of variation, enabling researchers to stratify cohorts along a spectrum of similarity [60]. Participants with proximal propensity scores share similar constellations of covariates, while larger differences indicate substantial population stratification. In practice, this involves:
- Model Construction: Developing a statistical model (typically logistic regression) to estimate the probability of group membership based on relevant clinical covariates
- Stratification: Dividing the cohort into subgroups based on propensity score quantiles
- Heterogeneity Assessment: Evaluating lncRNA biomarker performance across propensity strata to identify differential effects
Application of this approach in neuroimaging cohorts has revealed that predictive performance decays systematically as diversity between training and testing populations increases, with brain patterns derived from heterogeneous cohorts showing preferential instability in regions of the default mode network [60].
Heterogeneity of Treatment Effect (HTE) Analysis
HTE analysis provides a structured framework for examining how treatment effects—or in this context, biomarker performance—vary across patient subgroups. A review of 150 prospective cohort studies revealed that 58% reported some measure of HTE, with higher rates in high-impact journals, pharmacological studies, and recent publications [61]. Key considerations for HTE analysis in lncRNA biomarker studies include:
- Prespecification: Defining subgroup hypotheses before analysis to reduce false discovery
- Interaction Testing: Formally evaluating whether the biomarker-outcome relationship differs across patient characteristics
- Multi-dimensional Assessment: Examining heterogeneity across multiple covariates simultaneously rather than in isolation
Unfortunately, only 31% of studies reporting HTE used formal interaction tests, highlighting an area for methodological improvement [61].
Table 1: Diagnostic Approaches for Detecting Cohort Heterogeneity
| Method | Key Principle | Application in HCC lncRNA Studies | Statistical Requirements |
|---|---|---|---|
| Propensity Score Stratification | Creates a composite confound index from multiple covariates | Identify patient subgroups with similar clinical backgrounds for stratified validation | Sufficient sample size across strata; balance diagnostics |
| Interaction Testing | Formally tests whether biomarker effects differ across patient subgroups | Determine if lncRNA prognostic value is modified by specific clinical variables | Adequate power for detecting effect modification; adjustment for multiple testing |
| Variance Inflation Analysis | Quantifies how much heterogeneity inflates variance estimates | Assess instability in hazard ratio estimates from multivariate Cox models | Careful specification of covariance structure; bootstrapping for confidence intervals |
| Leave-One-Subgroup-Out Cross-Validation | Systematically excludes patient subgroups during validation | Evaluate generalizability of lncRNA signatures across clinical sites or patient demographics | Multiple conceptually similar subgroups; careful subgroup definition |
Methodological Strategies for Confounding Control
Study Design Approaches
Strategic study design offers the first line of defense against confounding by clinical variables. Several approaches have emerged as particularly valuable in HCC lncRNA research:
Stratified Recruitment and Randomization When assembling HCC cohorts, researchers can implement stratified recruitment to ensure balanced representation across key clinical variables known to influence prognosis, including liver function (Child-Pugh class), tumor burden (BCLC stage), and etiology (viral vs. non-viral) [10] [20]. In biomarker validation studies, this involves predefining stratification factors and ensuring proportional representation across these strata. The TCGA-LIHC dataset, frequently used in lncRNA biomarker discovery, exemplifies this approach with careful documentation of clinical parameters enabling post-hoc stratification [10] [20] [11].
Cohort Splitting with Propensity Matching For retrospective studies using existing datasets, propensity score matching creates balanced comparison groups by matching patients with similar clinical profiles across different biomarker expression levels [60]. This method has demonstrated utility in mitigating confounding in neuroimaging studies and can be similarly applied to HCC lncRNA research. The procedure involves:
- Estimating propensity scores based on relevant clinical covariates
- Matching high- and low-lncRNA expression patients using algorithms (e.g., nearest-neighbor, optimal matching)
- Assessing balance diagnostics to ensure adequate covariate balance post-matching
- Proceeding with multivariate Cox regression in the matched cohort
Analytical Approaches
When design-based approaches are insufficient, statistical methods offer additional tools for addressing confounding:
Multivariate Regression with Targeted Covariate Adjustment The workhorse method for addressing confounding in lncRNA biomarker studies remains multivariate Cox proportional hazards regression. Successful implementation requires careful selection of adjustment variables based on prior knowledge of prognostic factors in HCC. As demonstrated in multiple lncRNA signature studies, typical adjustment covariates include age, sex, tumor stage, grade, and liver function indicators [10] [20] [11]. The critical consideration is distinguishing true confounders (variables associated with both the lncRNA biomarker and survival) from mediators (variables on the causal pathway) to avoid overadjustment.
Stratified Analysis and Subgroup Validation Formal subgroup analysis allows researchers to test whether lncRNA biomarkers maintain prognostic performance across clinically relevant patient subsets. This approach aligns with the growing recognition of HCC molecular heterogeneity and the potential for biomarker performance to vary across etiological subtypes [59] [3]. In practice, this involves testing for significant interaction effects between the lncRNA biomarker and patient characteristics, then reporting stratum-specific hazard ratios with appropriate acknowledgment of reduced statistical power in subgroups.
Regularization Methods for High-Dimensional Confounding When facing numerous potential confounders relative to sample size, regularization methods like LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression can selectively retain important confounding variables while shrinking others toward zero [10] [20] [11]. This approach has been widely employed in developing multi-lncRNA prognostic signatures for HCC, simultaneously performing variable selection and coefficient estimation to optimize predictive performance while managing multicollinearity.
Table 2: Comparison of Statistical Methods for Addressing Confounding in HCC lncRNA Studies
| Method | Mechanism | Advantages | Limitations | Representative Applications in HCC |
|---|---|---|---|---|
| Multivariate Cox Regression | Simultaneously models biomarker and clinical variables | Familiar to clinicians; direct hazard ratio interpretation | Collinearity with highly correlated covariates; requires correct model specification | Most lncRNA prognostic studies [10] [20] [3] |
| Propensity Score Stratification | Adjusts for composite confound index | Handles multiple confounders simultaneously; intuitive stratification | Requires sufficient sample size within strata; different methods can yield different results | Brain imaging classification across diverse cohorts [60] |
| LASSO Regularization | Selects variables while shrinking coefficients | Automatic variable selection; handles high-dimensional data | Complex interpretation; selected variables can be unstable | Construction of multi-lncRNA prognostic signatures [10] [11] [63] |
| Interaction Testing | Formally evaluates effect modification | Identifies heterogeneous biomarker effects; enables personalized prognosis | Reduced power; multiple testing concerns | HTE analysis in cohort studies [61] |
Experimental Protocols for Robust lncRNA Biomarker Validation
Protocol 1: Propensity-Adjusted Biomarker Validation
Objective: To validate the independent prognostic value of a lncRNA biomarker while accounting for multiple clinical confounders through propensity score methods.
Methodology:
- Cohort Assembly: Retrieve HCC patient data with lncRNA expression profiles and clinical annotations from TCGA or institutional cohorts [10] [20]
- Propensity Model Development: Construct a logistic regression model estimating the probability of high versus low lncRNA expression based on clinical covariates (age, sex, stage, grade, etiology)
- Stratification: Divide the cohort into quintiles based on propensity scores
- Stratum-Specific Analysis: Perform Cox regression within each propensity quintile to assess the lncRNA-survival association
- Overall Assessment: Pool stratum-specific estimates using random-effects meta-analysis
- Sensitivity Analysis: Compare results with traditional multivariate Cox regression
Interpretation: Consistent hazard ratios across propensity strata strengthen evidence for independent prognostic value, while variation suggests effect modification by clinical factors.
Protocol 2: Heterogeneity of Prognostic Effect (HPE) Assessment
Objective: To systematically evaluate whether lncRNA prognostic performance varies across clinically relevant patient subgroups.
Methodology:
- Pre-specification of Subgroups: Define clinically meaningful subgroups based on established HCC classifications (e.g., BCLC stage, Child-Pugh class, viral status)
- Subgroup Analysis: Perform Cox regression within each subgroup, estimating subgroup-specific hazard ratios
- Interaction Testing: Introduce interaction terms between lncRNA expression and subgroup indicators in a global model
- Multiple Testing Correction: Apply false discovery rate correction to interaction p-values
- Visualization: Forest plots displaying subgroup-specific effects with confidence intervals
Interpretation: Statistically significant interaction terms indicate heterogeneous prognostic effects, suggesting context-dependent biomarker utility.
Visualization of Methodological Approaches
Diagram 1: Comprehensive workflow for addressing cohort heterogeneity in lncRNA biomarker validation studies
Research Reagent Solutions for HCC lncRNA Studies
Table 3: Essential Research Reagents and Resources for HCC lncRNA Biomarker Validation
| Reagent/Resource | Function | Example Applications | Technical Considerations |
|---|---|---|---|
| TCGA-LIHC Dataset | Provides transcriptomic data with clinical annotations | lncRNA discovery; multivariate adjustment; validation | Includes 377 HCC samples; requires careful preprocessing [10] [20] |
| Molecular Signature Database (MSigDB) | Curated gene sets for functional analysis | Identify metabolism, pyroptosis, or migrasome-related lncRNAs | v7.5 contains 374 amino acid metabolism genes [10] |
| TIDE Algorithm | Computational framework for immunotherapy response prediction | Evaluate association between lncRNA signatures and immunotherapy response | High scores indicate immune evasion; predicts anti-PD1 response [10] |
| CIBERSORT | Algorithm for estimating immune cell infiltration | Characterize tumor immune microenvironment in high- vs low-risk groups | Revealed Treg and M2 macrophage differences in pyroptosis study [63] |
| LASSO Regression | Regularization method for variable selection | Construct multi-lncRNA prognostic signatures with high-dimensional data | Implemented with 10-fold cross-validation; repeated 1000x for stability [11] |
| Propensity Score Package | Statistical tools for propensity score estimation and matching | Balance clinical covariates between high and low lncRNA expression groups | R package "MatchIt" commonly used; requires balance diagnostics [60] |
Navigating cohort heterogeneity represents both a challenge and an opportunity in HCC lncRNA biomarker research. The strategies outlined in this guide—from propensity-based approaches to formal heterogeneity assessment—provide methodological rigor necessary for developing clinically useful prognostic tools. As the field advances, researchers must move beyond simply adjusting for confounders toward explicitly characterizing and reporting context-dependent biomarker performance. This transparency will accelerate the translation of lncRNA biomarkers from statistical associations to clinically actionable tools that improve personalized prognosis and treatment selection for HCC patients.
The integration of robust study design, appropriate statistical adjustment, and comprehensive sensitivity analysis represents the path forward for lncRNA biomarker validation. By embracing rather than ignoring cohort heterogeneity, researchers can develop prognostic signatures that not only achieve statistical significance but also demonstrate clinical utility across the diverse patient populations encountered in real-world HCC management.
Leveraging Machine Learning Algorithms to Enhance Predictive Performance
The integration of machine learning (ML) algorithms with long non-coding RNA (lncRNA) biomarkers is revolutionizing prognostic prediction in hepatocellular carcinoma (HCC). This comparison guide objectively evaluates the performance of diverse ML approaches in developing multivariate Cox regression models for HCC survival prediction. By analyzing experimental data from recent studies, we demonstrate how ML-enhanced lncRNA signatures significantly outperform traditional statistical methods in stratification accuracy, prognostic value, and clinical utility. The synthesized evidence indicates that ML algorithms, particularly when combined with lncRNA biomarkers, offer powerful tools for personalized HCC management and therapeutic decision-making.
Hepatocellular carcinoma represents a significant global health challenge, ranking as the sixth most prevalent cancer and the third leading cause of cancer-related deaths worldwide [64] [11]. The disease's heterogeneous nature and variable treatment response have intensified the search for robust prognostic biomarkers, with long non-coding RNAs emerging as promising candidates due to their crucial roles in regulating gene expression, chromatin remodeling, and post-transcriptional modifications [11]. The convergence of lncRNA research with advanced machine learning algorithms has created unprecedented opportunities for developing precise prognostic models that can stratify patients based on their survival probability.
Machine learning approaches enhance prognostic modeling in HCC by identifying complex, nonlinear relationships within high-dimensional transcriptomic data that conventional statistical methods often miss. These algorithms can process vast amounts of lncRNA expression data alongside clinical variables to construct predictive signatures that reliably estimate overall survival (OS) and disease-free survival (DFS) [65] [1]. Furthermore, ML techniques excel at feature selection—distilling dozens of potential lncRNA biomarkers into parsimonious signatures with maximal prognostic value while minimizing overfitting [66]. This capability is particularly valuable in clinical contexts where simplicity and interpretability are essential for implementation.
Performance Comparison of Machine Learning Algorithms
Algorithm Efficacy in Prognostic Signature Development
Table 1: Performance Comparison of ML Algorithms in HCC Prognostic Modeling
| Algorithm | Study Context | Prediction Target | Key Performance Metrics | Advantages |
|---|---|---|---|---|
| LASSO-Cox | MRlncRNA signature [11] | Overall survival | AUC: 0.72-0.75 (1-3 years); C-index: 0.65-0.68 | Automatic feature selection, handles multicollinearity |
| SVM-RFE | MCC genes [65] | HCC diagnosis | AUC: 0.879-1.0 across datasets | Effective for high-dimensional data, robust to outliers |
| Random Forest | Clinical predictors [66] | HCC detection | Accuracy: 98.9%, Sensitivity: 90.5%, Specificity: 99.8% | Handles nonlinear relationships, provides feature importance |
| StepCox + Ridge | Advanced HCC [64] | Overall survival | C-index: 0.65-0.68; AUC: 0.72-0.75 (1-3 years) | Combines feature selection with regularization |
| RF-RFE | MCC genes [65] | HCC diagnosis | Slightly lower than SVM-RFE | Robust to noise, minimal parameter tuning |
Comparative Performance of lncRNA Signatures
Table 2: Performance of ML-Derived lncRNA Signatures in HCC Prognostication
| lncRNA Signature | Number of lncRNAs | Validation Cohort | Survival Stratification | Independent Prognostic Value |
|---|---|---|---|---|
| MRlncRNA [11] | 2 (LINC00839, MIR4435-2HG) | TCGA + clinical (n=100) | Significant (p<0.05) | Yes, across subgroups |
| Four-lncRNA panel [1] | 4 (LINC00152, LINC00853, UCA1, GAS5) | Clinical cohort (n=52) | 100% sensitivity, 97% specificity | Combined with conventional markers |
| NETs-related [67] | 6 (including GAS5) | TCGA-OV + clinical | Significant (p<0.05) | Yes, independent of clinical factors |
The performance evaluation reveals several key trends. First, ensemble methods like Random Forest demonstrate exceptional discriminatory power in detection tasks, achieving up to 99.8% specificity in identifying HCC cases from clinical data [66]. Second, regularization techniques such as LASSO-Cox and Ridge regression provide balanced performance in survival prediction, with time-dependent AUC values maintaining 0.72-0.75 across 1-3 years [64] [11]. Third, recursive feature elimination methods, particularly SVM-RFE, show superior gene selection capabilities for diagnostic applications, achieving perfect AUC (1.0) in TCGA data while maintaining generalizability to external datasets (AUC: 0.879-0.95) [65].
Notably, the number of lncRNAs required for robust prognostication varies significantly, with some studies achieving effective stratification with only two lncRNAs [11], while others incorporate six or more [67]. This variation highlights how ML algorithms can identify minimally redundant yet maximally informative biomarker combinations tailored to specific clinical contexts.
Experimental Protocols and Methodologies
Data Acquisition and Preprocessing
The foundational step in developing ML-enhanced prognostic models involves systematic data acquisition and rigorous preprocessing. Most studies utilize RNA-seq data from public repositories such as The Cancer Genome Atlas (TCGA), which provides transcriptomic profiles and corresponding clinical information for hundreds of HCC patients [65] [11]. For lncRNA-specific profiling, some researchers employ mining approaches to re-annotate microarray data from Gene Expression Omnibus (GEO) datasets, effectively extracting lncRNA expression values from platforms not originally designed for non-coding RNA analysis [68]. Additional data sources include clinical cohorts with paired lncRNA measurement and outcome data, which serve crucial roles in external validation [1] [67].
Data preprocessing typically involves normalization to correct for technical variability, with methods varying by platform. For RNA-seq data, transcripts per million (TPM) normalization is commonly employed [11], while microarray data often undergoes Guanine Cytosine Robust Multi-Array Average (GCRMA) normalization [68]. Quality control measures include filtering genes with low counts, removing outliers, and correcting for batch effects. For survival analysis, patients with insufficient follow-up (typically <30 days) are often excluded to avoid immortal time bias [65] [67]. The resulting dataset is typically partitioned into training and testing cohorts, with common splits ranging from 50:50 to 70:30, ensuring sufficient samples in both sets for model development and validation.
ML-Enhanced lncRNA Signature Development Workflow
Feature Selection and Model Construction
Feature selection represents the most crucial phase in developing prognostic lncRNA signatures, with studies employing multi-stage approaches to identify optimal biomarker combinations. The process typically begins with univariate Cox regression analysis to identify lncRNAs significantly associated with overall survival (p<0.05 or more stringent thresholds) [11] [69]. Some studies incorporate additional filtering steps, such as assessing proportional hazards assumptions using Schoenfeld residuals and excluding genes that violate these assumptions [65].
The refined candidate lncRNAs then undergo advanced ML-based feature selection. LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression is particularly prominent, applying L1 regularization to shrink coefficients of less informative features to zero, thereby selecting a parsimonious set of prognostic biomarkers [67] [11]. Alternative approaches include Support Vector Machine-Recursive Feature Elimination (SVM-RFE) and Random Forest-RFE, which iteratively remove the least important features based on model performance [65]. For studies incorporating clinical variables, methods like random forest feature importance and information gain algorithms help identify the most predictive factors [66].
Model construction typically employs multivariate Cox proportional hazards regression with the selected features. The resulting model generates a risk score formula based on the expression levels of signature lncRNAs weighted by their regression coefficients [11] [69]. Patients are stratified into high-risk and low-risk groups using the median risk score or optimal cutoff determined by maximally selected rank statistics. The prognostic performance is evaluated using Kaplan-Meier survival analysis, time-dependent receiver operating characteristic (ROC) curves, and concordance index (C-index) calculations [65] [64].
Validation Strategies and Clinical Application
Rigorous validation is essential to demonstrate clinical utility and generalizability of ML-derived lncRNA signatures. Internal validation typically involves bootstrap resampling or k-fold cross-validation within the training dataset [65] [66]. More robust approaches employ completely independent validation cohorts, either from held-out portions of the original dataset or external populations [11]. Some studies further enhance validation through geographical or temporal external cohorts, which test model performance across different healthcare settings or time periods [1].
The clinical application phase evaluates the signature's utility in realistic scenarios. This includes assessing whether the lncRNA signature provides prognostic value independent of established clinical parameters like AJCC stage, tumor grade, and liver function through multivariate Cox regression [65] [11]. Some studies additionally perform stratification analyses to determine if the signature maintains predictive power across different patient subgroups based on age, gender, or disease characteristics [65]. For signatures intended to guide therapy, researchers may evaluate their association with treatment response or perform in vitro experiments to confirm functional roles of identified lncRNAs [67] [11].
Table 3: Essential Research Reagents and Computational Tools for ML-lncRNA Studies
| Category | Specific Tools/Reagents | Function/Application | Examples from Literature |
|---|---|---|---|
| Data Sources | TCGA-LIHC, GEO datasets | Provide transcriptomic and clinical data | GSE39582, GSE17538 [68] |
| LncRNA Annotation | GENCODE, ENSEMBL | LncRNA identification and classification | GENCODE release 19 [68] |
| Computational Tools | R/Bioconductor, Perl, Python | Data processing and analysis | edgeR, limma, glmnet [65] |
| ML Algorithms | SVM-RFE, RF-RFE, LASSO | Feature selection and model building | LASSO-Cox regression [67] [11] |
| Survival Analysis | survival R package, timeROC | Prognostic model evaluation | Kaplan-Meier, Cox regression [65] |
| Experimental Validation | qRT-PCR reagents, cell lines | Confirmatory biological experiments | A2780, SKOV3 [67] |
The integration of machine learning algorithms with lncRNA biomarker research has substantially advanced prognostic prediction in hepatocellular carcinoma. The experimental data synthesized in this comparison guide demonstrates that ML-enhanced approaches consistently outperform traditional statistical methods in developing multivariate Cox regression models for HCC survival prediction. The most successful implementations combine robust feature selection techniques like LASSO or SVM-RFE with rigorous validation protocols, yielding lncRNA signatures with independent prognostic value across diverse patient populations.
Future developments in this field will likely focus on multi-omics integration, combining lncRNA expression with genomic, proteomic, and radiomic data to create more comprehensive prognostic models [64] [11]. Additionally, as single-cell sequencing technologies mature, ML algorithms will be essential for deciphering cell-type-specific lncRNA signatures and their implications for tumor heterogeneity and treatment response. The clinical translation of these models will require standardized analytical protocols and prospective validation in multicenter trials, but the current evidence strongly supports their potential to revolutionize personalized management of hepatocellular carcinoma.
From Statistical Significance to Clinical Utility: Rigorous Validation and Functional Insights
In the field of hepatocellular carcinoma (HCC) research, particularly in the development of long non-coding RNA (lncRNA) prognostic signatures, rigorous validation methodologies are paramount to ensure clinical translatability. The hierarchical validation framework, encompassing both internal cross-validation and external independent cohort testing, provides a structured approach to evaluate model performance and generalizability. This systematic validation process is especially crucial for multivariate Cox regression models that incorporate lncRNA biomarkers, as it helps mitigate overfitting and optimism bias commonly encountered with high-dimensional omics data [48] [70].
The transition from internal to external validation represents a critical pathway from model development to clinical implementation. Internal validation techniques, including various cross-validation strategies, provide initial performance estimates using the development dataset, while external validation assesses model transportability to entirely independent populations [70] [71]. For lncRNA-based signatures in HCC, this hierarchical approach is essential given the molecular heterogeneity of the disease and the complex interactions between lncRNAs and key cancer pathways such as ferroptosis, epithelial-mesenchymal transition (EMT), and immune regulation [48] [72] [73].
Internal Cross-Validation: Methodologies and Performance Assessment
Technical Approaches and Implementation Frameworks
Internal cross-validation encompasses several methodological approaches, each with distinct advantages and limitations in the context of lncRNA biomarker development for HCC. A recent benchmark simulation study directly compared common internal validation strategies for high-dimensional time-to-event data, providing evidence-based recommendations for prognostic model development [70].
Table 1: Comparison of Internal Validation Methods for High-Dimensional Time-to-Event Data
| Validation Method | Optimal Sample Size | Key Advantages | Key Limitations | Reported AUC Stability |
|---|---|---|---|---|
| Train-Test Split | N > 500 | Simple implementation | High performance instability, inefficient data use | Unstable across replicates |
| Bootstrap | N > 1000 | Comprehensive data usage | Over-optimistic without correction | Over-optimistic with conventional methods |
| K-fold Cross-validation | N > 100 | Balanced bias-variance tradeoff | Performance fluctuations with small N | Most stable across sample sizes |
| Nested Cross-validation | N > 100 | Optimizes hyperparameters, reduces bias | Computationally intensive, complex implementation | Fluctuates by regularization method |
The experimental protocol for implementing these validation strategies typically begins with random division of the development cohort, followed by application of the selected cross-validation technique. For instance, in developing a ferroptosis-related lncRNA signature for HCC, researchers typically first divide 365 patients from The Cancer Genome Atlas (TCGA) into training and testing sets (e.g., 184 vs 181 patients) [48]. Feature selection via univariate Cox regression followed by Least Absolute Shrinkage and Selection Operator (LASSO) regression is performed exclusively on the training set, with the final model validated on the held-out test set [48] [74].
K-fold cross-validation, particularly with 5-10 folds, has demonstrated superior stability for internal validation of Cox penalized regression models in high-dimensional settings compared to train-test splits or bootstrap approaches [70]. This method involves partitioning the dataset into k equally sized folds, with each fold serving as a validation set once while the remaining k-1 folds form the training set. The process is repeated until each fold has been used for validation, with performance metrics aggregated across all iterations [70] [71].
Performance Metrics and Statistical Considerations
The evaluation of internal validation performance employs multiple statistical metrics to comprehensively assess model discrimination, calibration, and clinical utility. For lncRNA-based prognostic signatures in HCC, time-dependent receiver operating characteristic (ROC) analysis typically reports area under the curve (AUC) values at 1-, 2-, and 3-year overall survival intervals [48]. High-performing signatures, such as the 7-ferroptosis-related lncRNA model, demonstrate AUC values of 0.745, 0.745, and 0.719 for these timepoints respectively [48].
Additional metrics include the C-index for discrimination, integrated Brier score for calibration, and decision curve analysis for clinical utility [70] [71]. The proportional hazards assumption must be verified for Cox models, and optimism correction should be applied to adjust for overfitting [75]. For high-dimensional settings where the number of features (p) exceeds the number of samples (n), penalized regression methods like LASSO, Ridge, or Elastic Net are essential to prevent model overfitting [48] [70] [74].
External Independent Cohort Testing: Validation Across Populations
Methodological Standards and Cohort Considerations
External validation represents the gold standard for assessing model generalizability to independent populations not represented in the development cohort. This critical step involves applying the fully specified model (including predetermined coefficients and risk thresholds) to entirely independent datasets, ideally from different institutions or geographical regions [75] [71]. The TRIPOD-AI and PROBAST-AI guidelines provide comprehensive frameworks for reporting and assessing prediction model studies, emphasizing the importance of external validation [71].
Table 2: External Validation Performance of HCC Prognostic Models
| Model Type | Development Cohort | External Validation Cohort | Key Performance Metrics | Reference |
|---|---|---|---|---|
| 7-FRlncRNA Signature | TCGA (n=365) | Not specified | AUC: 0.719 (3-year OS) | [48] |
| NETs/Immune Gene Model | TCGA (n=368) | GSE14520 (n=221) | Consistent risk stratification | [75] |
| EMT/Anoikis Signature | TCGA (n=360) | ICGC-LIPI-JP (n=232) | Independent prognostic factor | [73] |
| Machine Learning HCC Risk | Single-center (n=736) | Temporal validation (n=315) | AUC: 0.979 | [74] |
For lncRNA biomarkers in HCC, successful external validation requires careful consideration of several factors. The validation cohort should be sufficiently large (typically >100 events based on Riley's criteria) and represent the target patient population [71]. Technical validation of lncRNA measurement is crucial, with quantitative reverse-transcription polymerase chain reaction (qRT-PCR) representing the most common method for verifying expression levels in independent samples [72]. For example, in the validation of ferroptosis-related lncRNAs, LINC01063 was confirmed as an oncogene through both in vitro and in vivo experiments following computational identification [48].
Advanced External Validation Designs
More robust external validation strategies have emerged to better estimate real-world performance. Leave-source-out cross-validation is particularly valuable when multi-source data are available, as it provides more realistic performance estimates for deployment to new institutions compared to standard K-fold approaches [76]. This method involves iteratively leaving out all samples from one source (e.g., hospital) for validation while training on the remaining sources.
Temporal validation, where the model is tested on subsequent patients from the same institution, and geographical validation, using patients from different regions or countries, represent particularly rigorous forms of external validation [71]. For instance, a machine learning-based HCC risk prediction model developed at Beijing Ditan Hospital maintained an AUC of 0.979 when validated on a temporal validation cohort from the same institution [74]. Similarly, a prognostic model based on neutrophil extracellular traps (NETs) and immune-related genes demonstrated robust performance when validated on the GSE14520 dataset from a different geographical population [75].
Comparative Performance Analysis Across Validation Stages
Performance Metrics Across Validation Hierarchies
The transition from internal to external validation typically reveals a decrease in model performance, with the magnitude of this decrease serving as an indicator of model robustness. For instance, machine learning models for HCC risk prediction in patients with hepatitis B virus-related compensated advanced chronic liver disease demonstrated minimal performance degradation from internal to external validation, with AUCs maintained above 0.97 [74]. In contrast, models developed on smaller sample sizes or with less feature selection rigor typically exhibit more substantial performance decreases during external validation.
Table 3: Representative Performance Metrics Across Validation Stages for HCC Prognostic Models
| Model Characteristics | Internal Validation Performance | External Validation Performance | Performance Degradation |
|---|---|---|---|
| 7-FRlncRNA (Cox Model) | 1-year AUC: 0.745, 3-year AUC: 0.719 | 3-year AUC: ~0.719 (testing set) | Minimal |
| NETs/Immune Gene Model | Significant risk stratification in TCGA | Maintained stratification in GEO | Minimal |
| Machine Learning (RF) | Derivation AUC: 0.824±0.008 | External AUC: 0.801 (0.774-0.827) | Moderate |
| Cox vs. RSF for DM-HCC | 3-month AUC: 0.746 (Cox), 0.745 (RSF) | 12-month AUC: 0.729 (Cox), 0.718 (RSF) | Minimal for Cox |
Comparative studies between traditional Cox regression and machine learning approaches provide insights into model performance across validation stages. One analysis of distant metastatic HCC patients found that both Cox regression and Random Survival Forest models maintained robust performance in external validation, with Cox regression exhibiting superior temporal stability at longer prediction horizons (12-month Brier score: 0.125 for Cox vs. higher for RSF) [77]. This suggests that while machine learning approaches may capture complex nonlinear relationships, Cox models maintain advantages in stability and interpretability for clinical applications.
Methodological Recommendations for lncRNA Biomarker Studies
Based on current evidence, specific methodological recommendations emerge for lncRNA biomarker development in HCC. For internal validation, k-fold cross-validation (5-10 folds) is preferred over train-test splits or bootstrap methods, particularly for sample sizes between 100-500 patients [70]. LASSO regularization should be incorporated during feature selection to enhance model sparsity and interpretability [48] [74]. For external validation, prospective collection of independent cohorts from multiple institutions is ideal, with careful attention to standardized lncRNA measurement protocols [72].
The sample size for both development and validation cohorts should follow Riley's criteria, targeting a minimum of 20 events per predictor parameter to limit overfitting [71]. For lncRNA signatures with 7-10 features, this typically requires several hundred patients. Additionally, reporting should adhere to TRIPOD-AI guidelines, including comprehensive discrimination, calibration, and clinical utility metrics [71].
Table 4: Essential Research Reagents and Resources for lncRNA Biomarker Validation
| Reagent/Resource | Specific Examples | Primary Function | Application Context |
|---|---|---|---|
| Data Sources | TCGA-LIHC, ICGC-LIRI-JP, GEO (GSE14520) | Provide transcriptomic and clinical data | Model development & validation |
| Ferroptosis Databases | FerrDb (382 FRGs) | Identify ferroptosis-related genes | FRlncRNA signature development |
| Immune Gene Sets | ImmPort (1793 IRGs) | Identify immune-related genes | Tumor microenvironment analysis |
| lncRNA Detection | qRT-PCR, RNA-seq, ISH | Quantify lncRNA expression | Experimental validation |
| Functional Validation | CCK-8 assay, Transwell, colony formation | Assess oncogenic functions in vitro | Mechanistic studies (e.g., LINC01063) |
| In Vivo Models | Nude BALB/c mice xenografts | Evaluate tumor growth in vivo | Preclinical validation |
| Bioinformatics Tools | DESeq2, WGCNA, glmnet, GSVA | Differential expression, co-expression, penalized regression | Computational analysis |
| Validation Frameworks | TRIPOD-AI, PROBAST-AI | Reporting guidelines for prediction models | Study design & reporting |
Hierarchical validation represents an indispensable framework for developing robust lncRNA-based prognostic signatures in hepatocellular carcinoma. The evidence from recent studies demonstrates that rigorous internal validation using k-fold cross-validation, followed by comprehensive external validation in independent cohorts, produces models with superior generalizability and clinical potential. The consistent performance of well-validated signatures across diverse patient populations underscores their potential utility in personalized HCC management.
Future directions in lncRNA biomarker validation should emphasize prospective multi-center studies, standardized measurement protocols, and integration with established clinical variables. Additionally, as single-cell sequencing technologies advance, validation frameworks must adapt to accommodate increasingly complex data structures while maintaining methodological rigor [73]. Through continued adherence to robust hierarchical validation principles, lncRNA biomarkers hold significant promise for improving risk stratification and treatment personalization in hepatocellular carcinoma.
In the evolving landscape of hepatocellular carcinoma (HCC) research, long non-coding RNAs (lncRNAs) have emerged as promising prognostic biomarkers. However, their clinical utility remains uncertain unless they provide predictive value beyond established clinical factors. This comparison guide objectively evaluates the performance of lncRNA-based prognostic models against conventional staging systems and clinical parameters, focusing on their independent predictive value in multivariate Cox regression analyses. The validation of lncRNAs within the rigorous framework of multivariate analysis represents a critical step in translational oncology, enabling researchers to distinguish truly independent biomarkers from those merely correlated with established prognostic factors.
Established Prognostic Factors in HCC: The Benchmark
Before assessing lncRNAs' independent value, one must understand the established prognostic factors they must outperform. Conventional HCC staging incorporates tumor burden, liver function, and patient performance status.
Table 1: Established Prognostic Factors and Staging Systems in HCC
| Prognostic Factor Category | Specific Parameters | Role in Prognostication |
|---|---|---|
| Tumor Burden | Tumor size, tumor number, vascular invasion, metastasis | Directly correlates with disease progression and treatment options; often the strongest prognostic factor [78] [79]. |
| Liver Function | Child-Pugh class (CPC), Albumin-Bilirubin (ALBI) score, presence of ascites/encephalopathy | Determines the liver's functional reserve and ability to tolerate treatments [80] [79]. |
| Overall Health & Inflammation | Patient performance status (e.g., ECOG), systemic inflammation indicators (e.g., NLR, CRP) [81] | Reflects the patient's overall condition and ability to withstand cancer and its treatment. |
The Barcelona Clinic Liver Cancer (BCLC) system, which integrates many of these factors, is widely used but has demonstrated variable performance, with pooled C-indices at external validation reported around 0.646–0.703 [79]. Other established models like the CLIP and JIS scores also show moderate performance, with pooled C-indices below 0.7 [78]. This performance gap establishes the benchmark against which novel lncRNA biomarkers must be measured.
LncRNA Biomarkers: From Single Markers to Multi-Gene Signatures
Single LncRNA Biomarkers
Evidence from numerous studies confirms that individual lncRNAs hold significant prognostic value. A meta-analysis of 40 studies found that elevated levels of detrimental lncRNAs were associated with a 1.25-fold higher risk of poor overall survival (OS) and a 1.66-fold higher risk of poor recurrence-free survival (RFS) [59].
Table 2: Selected Single LncRNAs with Independent Prognostic Value in HCC
| LncRNA | Expression in HCC | Adjusted Hazard Ratio (HR) for Overall Survival | Multivariate Cox Regression P-value |
|---|---|---|---|
| LINC00152 | High | HR: 2.524 (95% CI: 1.661–4.015) | 0.001 [3] |
| HOXC13-AS | High | HR: 2.894 (95% CI: 1.183–4.223) | 0.015 [3] |
| LASP1-AS | Low | HR: 3.539 (95% CI: 2.698–6.030) | < 0.0001 [3] |
| GAS5-AS1 | High | HR: 0.370 (95% CI: 0.153–0.898) | 0.028 [3] |
Multi-LncRNA Signature Models
To improve predictive power, researchers have developed prognostic signatures combining multiple lncRNAs. These models are typically constructed using Cox regression coupled with machine learning techniques like LASSO (Least Absolute Shrinkage and Selection Operator) to prevent overfitting.
Table 3: Comparison of Multi-LncRNA Prognostic Signatures in HCC
| LncRNA Signature Type | Specific LncRNAs in Model | Performance (Area Under Curve - AUC) | Independent Prognostic Value Confirmed by Multivariate Analysis |
|---|---|---|---|
| Amino Acid Metabolism-Related [10] | 4-lncRNA signature (incl. AL590681.1) | Not specified | Yes (P-value for risk score < 0.05) |
| Disulfidptosis-Related [27] | 3-lncRNA signature (AC016717.2, AC124798.1, AL031985.3) | 1-year: 0.756, 3-year: 0.695, 5-year: 0.701 | Yes |
| Migrasome-Related [11] | 2-lncRNA signature (LINC00839, MIR4435-2HG) | Not specified | Yes |
These multi-lncRNA signatures consistently demonstrate that the risk score derived from the model is an independent prognostic factor, even after adjusting for critical clinical variables such as age, TNM stage, and tumor grade [10] [27] [11].
Experimental Protocols for Validation
Core Methodology for Establishing Independent Prognostic Value
The standard protocol for validating the independent prognostic value of lncRNAs involves a structured, multi-step process confirmed across multiple studies [10] [27] [11]:
Key Analytical Techniques
Multivariate Cox Proportional Hazards Regression: This is the definitive statistical test for independent prognostic value. The model includes the lncRNA-based risk score alongside established clinical factors (e.g., age, gender, TNM stage, BCLC stage, Child-Pugh class). A significant P-value (typically < 0.05) for the risk score confirms its independent value [10] [3].
LASSO (Least Absolute Shrinkage and Selection Operator) Regression: Employed during model construction to reduce overfitting and select the most relevant lncRNAs from a larger candidate pool by penalizing the absolute size of regression coefficients [27] [11].
Time-Dependent Receiver Operating Characteristic (ROC) Analysis: Evaluates the model's predictive accuracy for survival at specific time points (e.g., 1, 3, 5 years). The Area Under the Curve (AUC) quantifies discrimination ability, with values above 0.7 considered good [27].
Nomogram Construction: Integrates the lncRNA signature with significant clinical factors into a visual predictive tool, allowing for individualized probability estimation of survival [27].
Table 4: Key Research Reagent Solutions for lncRNA Biomarker Validation
| Reagent/Resource | Function in Validation Pipeline | Examples/Specifications |
|---|---|---|
| TCGA-LIHC Dataset | Primary source for transcriptomic data and clinical correlations for hypothesis generation and discovery [10] [27] [11]. | Available via NIH GDC Portal; contains RNA-seq and clinical data for 373+ HCC patients. |
| qRT-PCR Assays | Gold standard for quantifying lncRNA expression in patient tissues or plasma for experimental validation [1]. | Use SYBR Green or TaqMan chemistry; GAPDH or β-actin as reference genes for normalization. |
| Lipofectamine Transfection Reagents | For in vitro functional validation studies (e.g., knockdown) to investigate lncRNA mechanism of action [10]. | Lipofectamine 3000 for siRNA/shRNA delivery into HCC cell lines. |
| CCK-8 Assay Kit | To assess cell viability and proliferation after lncRNA modulation in functional studies [10]. | Colorimetric assay based on WST-8 reagent. |
| R/Bioconductor Packages | Open-source software for statistical analysis, model building, and visualization. | "survival" (Cox regression), "glmnet" (LASSO), "timeROC" (ROC analysis), "rms" (nomograms). |
The transition from discovering differentially expressed lncRNAs to validating their independent prognostic value represents a critical milestone in HCC biomarker research. The evidence confirms that rigorously validated lncRNA signatures, particularly those based on biological mechanisms like amino acid metabolism, disulfidptosis, or migrasome function, can provide prognostic information that complements and potentially refines established staging systems. For researchers and drug developers, these biomarkers offer promising tools for enhancing patient stratification in clinical trials and moving toward more personalized treatment approaches. Future progress will depend on standardizing detection methods and moving these biomarkers into prospective clinical validation studies.
In the evolving landscape of hepatocellular carcinoma (HCC) research, long non-coding RNA (lncRNA) signatures derived from multivariate Cox regression analyses have emerged as powerful prognostic tools. Beyond predicting survival, these risk scores are increasingly recognized for their intimate connections with tumor immunity. This guide provides a comparative analysis of how different lncRNA-based risk models correlate with the tumor microenvironment (TME), immune cell infiltration, and immune checkpoint expression, offering researchers a framework for evaluating and selecting appropriate models for immunotherapy response prediction.
Comparative Analysis of lncRNA Risk Models in HCC
Table 1: Comparison of lncRNA Risk Score Models in Hepatocellular Carcinoma
| Model Type | Key lncRNAs Identified | Immune Correlations Demonstrated | Prognostic Performance (AUC) | Primary Data Source |
|---|---|---|---|---|
| Hypoxia-Related Signature [51] | 3 lncRNAs | Immune cell infiltration, immune checkpoints, m6A-related genes | 1-year: 0.805, 3-year: 0.672, 5-year: 0.630 | TCGA-LIHC (N=374) |
| General Prognostic Signature [19] | 11 lncRNAs including AC010547.1, GACAT3, LINC01747 | Validated via GSEA but limited explicit immune correlation | Up to 0.846 | TCGA (N=371) |
| Coagulation-Related lncRNAs (CRLs) [82] | EWSAT1, LINC00645, LINC00901, LINC02962 | Immunosuppressive TME genes (CD96, IDO1, IL10, KDR, LAG3, TGFB1, TIGIT) | Not specified | TCGA (CRC focus) |
Table 2: Immune System Correlations of Hypoxia-Related lncRNA Signature in HCC
| Immune Parameter Category | Specific Correlations Identified | Analytical Methods Used | Research Implications |
|---|---|---|---|
| Immune Cell Infiltration | Significant differences in immune cell populations between risk groups | CIBERSORT-ABS, XCELL, EPIC, MCPcounter, TIMER, QUANTISEQ, CIBERSORT | High-risk group shows immunosuppressive TME |
| Immune Checkpoints | Correlation with checkpoint expression levels | Differential expression analysis | Potential for predicting immunotherapy response |
| m6A-Related Genes | Association with m6A mRNA modifications | Correlation analysis | Links epitranscriptomics with tumor immunity |
| Immune-Related Pathways | Enriched in high-risk group | Gene Set Enrichment Analysis (GSEA) | Identifies potential resistance mechanisms |
Experimental Protocols for Key Methodologies
Protocol 1: Construction of lncRNA-Based Risk Models
- Data Acquisition: Obtain RNA-sequencing data and clinical information from TCGA or GEO databases [19] [51]
- LncRNA Identification: Differentiate lncRNAs from mRNAs using gene transfer annotation files from Ensembl
- Feature Selection:
- Perform univariate Cox regression to identify survival-associated lncRNAs (p < 0.05)
- Apply LASSO Cox regression with 1000-round cross-validation to prevent overfitting
- Conduct multivariate Cox regression to compute final coefficients [19]
- Risk Score Calculation: Use the formula: Risk score = Σ(coefficient × lncRNA expression) [51]
- Validation: Split cohorts into training and test sets (typically 1:1 or 7:3 ratios) and validate in external datasets [19]
Protocol 2: Immune Correlation Analysis
- Immune Cell Infiltration Quantification:
- Immune Checkpoint Analysis: Extract expression data of key checkpoints (PD-1, PD-L1, CTLA-4, LAG-3, TIM-3, TIGIT) from RNA-seq data [84] [51]
- Functional Enrichment:
- Perform Gene Set Enrichment Analysis (GSEA) using MSigDB collections
- Conduct GO and KEGG pathway analysis via "clusterProfiler" R package [51]
- Tumor Mutational Burden Calculation: Process mutation data in "maf" format using "maftools" R package [83]
Visualizing the Workflow: From lncRNA Signature to Immune Correlation
Table 3: Key Research Reagent Solutions for lncRNA-Immunity Studies
| Reagent/Resource Category | Specific Examples | Research Application | Key Providers/Sources |
|---|---|---|---|
| Bioinformatics Databases | TCGA, GEO, MSigDB, GENCODE | Data mining and lncRNA annotation | NIH, Broad Institute, EMBL-EBI |
| Analysis Packages | "edgeR", "limma", "glmnet", "survival", "clusterProfiler" | Differential expression, survival analysis, enrichment | Bioconductor, CRAN |
| Immune Deconvolution Tools | CIBERSORT, EPIC, MCP-counter, TIMER, XCELL | Immune cell infiltration quantification | Academic developers |
| Validation Reagents | siRNA constructs, qPCR primers, apoptosis kits | Functional validation of lncRNA targets | Commercial suppliers (RiboBio, Solarbio) |
| Cell Culture Resources | HCC cell lines (MHCC-97H, HepG2, MHCC-LM3), culture media | In vitro functional studies | Cell banks (ATCC, Chinese Academy of Sciences) |
Discussion: Clinical Implications and Research Applications
The integration of lncRNA risk scores with tumor immunity parameters represents a significant advancement in personalized cancer therapy. The hypoxia-related lncRNA signature demonstrates particular promise, as hypoxia is a known driver of immunosuppression in the TME [51]. These models enable researchers to stratify patients not only by prognosis but also by likelihood of responding to immunotherapies.
The differential expression of immune checkpoints across risk groups provides a mechanistic basis for combining lncRNA signatures with existing immunotherapy biomarkers. Furthermore, the association between risk scores and m6A-related genes establishes a connection between epitranscriptomic modifications and anti-tumor immunity [51].
For drug development professionals, these models offer insights into novel therapeutic targets. The functional validation of lncRNAs like GACAT3, which promotes HCC cell proliferation, invasion, and migration, highlights potential targets for therapeutic intervention [19].
Future Directions
Future research should focus on validating these signatures in prospective clinical trials and integrating them with existing immunotherapy biomarkers. The development of standardized protocols for assessing lncRNA-immune correlations will be essential for clinical translation. Additionally, exploring the mechanistic roles of specific lncRNAs in modulating immune responses may uncover novel immunotherapeutic strategies for HCC patients who currently have limited treatment options.
Within the rapidly advancing field of lncRNA biomarker discovery in hepatocellular carcinoma (HCC), the identification of prognostic signatures through multivariate Cox regression is becoming increasingly common. However, the transition from a statistical association to a biologically validated target requires rigorous functional validation. This guide objectively compares the core experimental approaches—in vitro and in vivo knockdown and overexpression experiments—that researchers employ to provide causal evidence for lncRNA function in HCC progression. By comparing the protocols, applications, and limitations of these methods side-by-side, we provide a framework for evaluating the experimental data that underpins claims of lncRNA relevance.
The following table summarizes the key characteristics, strengths, and limitations of the primary functional validation techniques.
| Experimental Approach | Primary Objectives | Typical Readouts/Assays | Key Strengths | Inherent Limitations |
|---|---|---|---|---|
In Vitro Knockdown |
Assess necessity of lncRNA for malignant cellular phenotypes [10] [11] |
- CCK-8/CellTiter-Glo for viability [85] [10]- Colony formation for clonogenicity [85] [10]- Wound healing/Transwell for migration & invasion [85] [86] [11]- Flow cytometry for apoptosis/cell cycle | - High-throughput capability- Precise control of experimental conditions- Mechanistic insights via downstream molecular analysis- Lower cost relative to in vivo studies |
- May not reflect complex tumor microenvironment (TME)- Simplified model lacking systemic physiology |
In Vitro Overexpression |
Assess sufficiency of lncRNA to drive oncogenic phenotypes [86] |
- Same as above, confirming phenotype induction | - Establishes causal role in transformation- Useful for studying tumor suppressor lncRNAs |
- May result in non-physiological expression levels |
In Vivo Knockdown/Overexpression |
Validate tumorigenic role within a physiological system, including TME and metastasis [86] [87] | - Tumor volume/weight- Bioluminescent imaging- Metastasis burden (e.g., liver/lung nodules)- Immunohistochemistry (IHC) for proliferation (Ki-67), apoptosis, etc. | - Models full complexity of tumor-stroma-immune interactions- Provides critical preclinical data for therapeutic development | - Technically demanding, time-consuming, and expensive- Ethical considerations regarding animal use |
Detailed Methodological Protocols
In VitroFunctional Assays
A. Gene Perturbation Techniques
- Knockdown: Typically achieved by transfecting
lncRNA-specific small interfering RNAs (siRNA) or short hairpin RNAs (shRNA) into HCC cell lines (e.g., Huh-7, Hep3B, HCCLM3) using lipid-based reagents like Lipofectamine 3000 [10] [11]. At least two to three non-overlappingsiRNAsare recommended to control for off-target effects, with efficiency validated by quantitative RT-PCR (qRT-PCR) 48 hours post-transfection [86]. - Overexpression: Full-length
lncRNAcDNA is cloned into plasmid or lentiviral vectors under a strong promoter (e.g., CMV). Stable overexpression cell lines are then generated via lentiviral transduction followed by antibiotic selection (e.g., puromycin) [85].
B. Phenotypic Characterization Workflows
- Cell Viability and Proliferation:
- CCK-8 Assay: Cells are seeded in 96-well plates after transfection. At designated time points, CCK-8 reagent is added, and the absorbance at 450 nm is measured with a microplate reader. The signal correlates with the number of viable cells [85] [10].
- Colony Formation Assay: A low density of cells (500-1000 cells/well) is seeded in 6- or 12-well plates and cultured for 1-2 weeks. Colonies are fixed, stained with crystal violet, and counted manually or with imaging software to assess clonogenic survival [85] [10].
- Migration and Invasion:
- Wound Healing Assay: A scratch is made in a confluent cell monolayer. Images are taken at the scratch edges immediately and after 24-48 hours. The rate of gap closure is quantified [86].
- Transwell Assay: For migration, cells are seeded in the upper chamber of a Transwell insert with a porous membrane. For invasion, the membrane is coated with Matrigel. Serum-containing medium is used as a chemoattractant in the lower chamber. Cells that migrate/invade to the underside of the membrane are fixed, stained, and counted [85] [86].
In VivoFunctional Validation
A. Animal Models
- Xenograft Models: Immunodeficient mice (e.g., NOD/SCID) are the standard host. HCC cells with stable
lncRNAknockdown or overexpression are injected subcutaneously into the flanks or, more relevantly, into the liver (orthotopic model) to better mimic the tumor microenvironment [86] [87]. - Study Design: Critical parameters include the choice of species, strain, gender, and age. The number of animals per group must be statistically justified, and appropriate control groups (e.g., scrambled
shRNAor empty vector) are mandatory [87].
B. Tumorigenicity and Metastasis Analysis
- Tumor Growth Monitoring: Subcutaneous tumor dimensions are measured regularly with calipers, and volume is calculated. Orthotopic tumor growth is often tracked via bioluminescent imaging if luciferase-expressing cells are used [86].
- Endpoint Analyses: At sacrifice, tumors are weighed. Tissues are processed for histology. Immunohistochemistry (IHC) is performed on tumor sections for markers like Ki-67 (proliferation), cleaved caspase-3 (apoptosis), or CD31 (angiogenesis). Metastasis is assessed by examining distant organs (e.g., lungs, liver) for nodules [86].
Supporting Data from HCClncRNAStudies
The following table compiles quantitative functional data for specific lncRNAs from recent HCC studies, demonstrating the application of these experimental paradigms.
lncRNA Name |
Experimental Perturbation | Key In Vitro Phenotypic Change |
Key In Vivo Phenotypic Change |
Proposed Mechanism/Pathway |
|---|---|---|---|---|
| AL590681.1 [10] | Knockdown (siRNA) |
- ↓ Cell viability (CCK-8)- ↓ Colony formation | Not Reported | Associated with amino acid metabolism |
| MIR4435-2HG [11] | Knockdown (shRNA) |
- ↓ Proliferation- ↓ Migration- ↓ EMT phenotype- ↓ PD-L1 expression | - ↓ Tumor growth- ↓ Immune evasion | Promotes EMT and PD-L1-mediated immune evasion |
| PAQR3 (P6-55 peptide) [85] | Overexpression (Peptide) | - ↓ Colon cancer cell viability- ↓ Colony formation- ↓ Migration (Transwell) | - ↓ Tumor growth in xenograft models | Suppresses PI3K-AKT signaling pathway |
| Prioritized Tip EC Genes (e.g., CD93, TCF4) [86] | Knockdown (siRNA in HUVECs) |
- ↓ Migration (Wound Healing)- ↓ Proliferation (³H-Thymidine) | Impaired vessel sprouting (in vivo angiogenesis models) | Regulation of angiogenesis |
The Scientist's Toolkit: Essential Research Reagents
This table details key reagents and their functions essential for conducting successful functional validation experiments.
| Reagent / Material | Critical Function in Experiments | Example Products / Methods |
|---|---|---|
siRNA / shRNA |
Induces transient or stable lncRNA knockdown by targeting its transcript for degradation. |
Custom-designed sequences; Lentiviral shRNA particles for stable lines [10] [86]. |
| Lentiviral Vectors | Enables highly efficient and stable gene delivery for both overexpression and knockdown in a wide range of cell types, including primary cells. | Third-generation packaging systems (psPAX2, pMD2.G) [85]. |
| Lipofectamine Reagents | Lipid-based transfection reagents for delivering siRNA or plasmid DNA into cells in vitro. |
Lipofectamine 3000 [10]. |
| CCK-8 Reagent | A tetrazolium salt-based solution used for colorimetric, non-radioactive quantification of cell viability and proliferation. | Glpbio GK10001; Dojindo CK04 [85]. |
| Transwell Inserts | Permeable supports used to assay cell migration and invasion through a porous membrane, with or without Matrigel coating. | Corning Costar inserts; BD BioCoat Matrigel [85]. |
| Matrigel | A basement membrane matrix extract used to coat Transwell inserts for invasion assays and to support the growth of xenograft tumors. | Corning Matrigel [85]. |
| qRT-PCR Kits | Essential for validating the efficiency of lncRNA knockdown or overexpression by precisely measuring transcript levels. |
TaqMan assays; SYBR Green master mixes [10]. |
Visualizing Key Signaling Pathways in HCC
The PI3K-AKT pathway is a frequently validated downstream mechanism of functional lncRNAs. For instance, PAQR3 exerts its tumor-suppressive effects by binding to the PI3K catalytic subunit P110α, inhibiting AKT phosphorylation and downstream signaling [85].
Functional validation through in vitro and in vivo experiments is the cornerstone that transforms a computationally derived lncRNA signature into a biologically credible target. While in vitro knockdown/overexpression studies provide a high-throughput platform for initial phenotypic and mechanistic screening, in vivo models remain indispensable for confirming the functional relevance of a lncRNA within the complex pathophysiology of HCC. A robust validation pipeline strategically employs both paradigms, moving from cell-based assays to animal models to build a compelling case for a lncRNA's role in tumorigenesis. This rigorous, multi-step process is critical for identifying the most promising lncRNA candidates for further development as biomarkers or therapeutic targets.
Conclusion
The validation of lncRNA biomarkers through multivariate Cox regression represents a paradigm shift in prognosticating hepatocellular carcinoma. This synthesis demonstrates that robust, multi-lncRNA signatures, grounded in specific biological pathways and rigorously validated, hold immense potential as independent prognostic tools. Future directions must focus on standardizing analytical pipelines, advancing functional mechanistic studies, and transitioning these biomarkers into clinical trials. The ultimate goal is their integration into routine practice, enabling precise risk stratification, prediction of immunotherapy response, and the development of novel lncRNA-targeted therapies, thereby moving closer to truly personalized care for HCC patients.
References
- 1. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 2. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 3. Long non-coding RNA-based single and combination ... [https://link.springer.com/article/10.1007/s12672-025-03309-1]
- 4. Tumor suppressor and oncogenic role of long non-coding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7103751/]
- 5. Identification and validation of a ferroptosis-related long ... [https://pubmed.ncbi.nlm.nih.gov/40672083/]
- 6. The dual role of LncRNAs in hepatocellular carcinoma [https://www.sciencedirect.com/science/article/pii/S2949752324000311]
- 7. A five lncRNA signature for prognosis prediction in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6522922/]
- 8. Plasma exosomal lncRNA-related signatures define ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1663943/full]
- 9. An lncRNA Model for Predicting the Prognosis of ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.749313/full]
- 10. Amino acid metabolism-related LncRNAs as prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12545943/]
- 11. A migrasome-related lncRNA signature predicts prognosis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581122/full]
- 12. Amino acid metabolism in health and disease [https://www.nature.com/articles/s41392-023-01569-3]
- 13. Ferroptosis in cancer: revealing the multifaceted functions of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12271051/]
- 14. 基础医å¦é™¢æ˜“èªè¯¾é¢˜ç»„PNASæ示葡è„糖饥饿诱导自噬å‘生的 ... [http://www.news.zju.edu.cn/2025/0217/c777a3016186/pagem.htm]
- 15. Shedding light on the cell biology and diverse ... [https://pubmed.ncbi.nlm.nih.gov/40437622/]
- 16. 基于生物信æ¯å¦è¯†åˆ«è‚细胞癌ä¸çš„PANoptosis相关lncRNAs并 ... [http://www.chinagene.cn/CN/10.16288/j.yczz.24-208]
- 17. JCB丨陈扬团队æ示管状内质网通过远端定å‘ä¿¡å·ä¼ 导调控 ... [https://www.163.com/dy/article/KF2B3AAI0532HZIO.html]
- 18. Long non-coding RNAs in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC5583571/]
- 19. Identification and Validation of a Prognostic lncRNA Signature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7298074/]
- 20. Identification of a novel prognostic signature for HCC and ... [https://www.nature.com/articles/s41598-022-13792-z]
- 21. Combining a machine-learning derived 4-lncRNA signature ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-023-09194-8]
- 22. RNA-Seq and scRNA-Seq Public : a Comparative Review Databases [https://bigomics.ch/blog/ultimate-guide-to-public-rnaseq-and-sc-rna-seq-databases/]
- 23. Decoding potential lncRNA and disease associations ... [https://www.nature.com/articles/s41598-025-16177-0]
- 24. Variable screening and model construction for prognosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11422072/]
- 25. Lasso-Cox Regression for Variable Selection in Survival ... [https://www.serdarbalci.com/jsurvival/articles/09-lassocox-comprehensive.html]
- 26. Prognosis of lasso-like penalized Cox models with tumor ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-022-10117-1]
- 27. A novel disulfidptosis-related lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582836/]
- 28. Inflammatory Response-Related Long Non-Coding RNA Signature Predicts the Prognosis of Hepatocellular Carcinoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8947866/]
- 29. Integrating AI and RNA biomarkers in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512311/]
- 30. Cuproptosis-Related lncRNA Risk Model for ... [https://pubmed.ncbi.nlm.nih.gov/41196839/]
- 31. Expression levels of lncRNAs are prognostic for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7269992/]
- 32. Construction of an HCC recurrence model based on the ... [https://www.sciencedirect.com/science/article/pii/S216225312100281X]
- 33. Reconstructing patient level survival data from published ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409465/]
- 34. Time-dependent ROC curve analysis in medical research [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-017-0332-6]
- 35. ROC curves in MedCalc [https://www.medcalc.org/en/features/roccurves.php]
- 36. ROC Curves | NCSS Statistical Software [https://www.ncss.com/software/ncss/roc-curves-ncss/]
- 37. ROC curves | Statistical Software for Excel [https://www.xlstat.com/solutions/features/roc-curves]
- 38. Metz ROC Software - Radiology - The University of Chicago [https://radiology.uchicago.edu/research/metz-roc-software]
- 39. Development and validation of a nomogram for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583323/]
- 40. Application of clinical nomograms to predicting overall ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.958325/full]
- 41. The nomogram based on the 6-lncRNA model can promote ... [https://www.nature.com/articles/s41598-021-00364-w]
- 42. Identification and evaluation of a six-lncRNA prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11147969/]
- 43. Identification of a nomogram based on an 8-lncRNA ... [https://www.aging-us.com/article/104014/text]
- 44. Development and validation of nomograms for predicting ... [https://www.nature.com/articles/s41598-025-96526-1]
- 45. Development and Validation of a Nomogram Prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6452590/]
- 46. CD8 T cell exhaustion-associated LncRNA signature reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508406/]
- 47. Identification and validation of PANoptosis-related ... [https://www.nature.com/articles/s41598-025-90498-y]
- 48. Identification and validation of a ferroptosis-related long non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261030/]
- 49. Bioinformatics prediction and experimental verification ... [https://www.sciencedirect.com/science/article/pii/S2405580823000833]
- 50. Development and Validation of an Immune-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7500314/]
- 51. Identification and Validation of Hypoxia-Related lncRNA ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.744113/full]
- 52. Creation of an innovative diagnostic framework for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1485421/full]
- 53. Uncovering functional lncRNAs by scRNA-seq with ELATUS [https://www.nature.com/articles/s41467-024-54005-7]
- 54. RNA-Seq Normalization: Methods and Stages [https://bigomics.ch/blog/why-how-normalize-rna-seq-data/]
- 55. Cross-platform normalization enables machine learning ... [https://www.nature.com/articles/s42003-023-04588-6]
- 56. The Impact of Normalization Methods on RNA-Seq Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4484837/]
- 57. GeneRAIN: multifaceted representation of genes via deep ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03749-6]
- 58. LncRNACNVIntegrateR: a novel framework for correlating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535741/]
- 59. lncRNAs as prognostic molecular biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5601763/]
- 60. Population heterogeneity in clinical cohorts affects the ... [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3001627]
- 61. Reporting of heterogeneity of treatment effect in cohort ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5767059/]
- 62. Explaining heterogeneity of individual treatment causal ... [https://www.sciencedirect.com/science/article/pii/S0933365721000737]
- 63. Screening prognostic markers for hepatocellular carcinoma ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05299-9]
- 64. Performance of AI-based machine learning models for ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1719479/full]
- 65. Machine learning-based identification of diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12393733/]
- 66. Minimal clinical predictors enable machine learning ... [https://www.nature.com/articles/s41598-025-22927-x]
- 67. Assessment of lncRNA biomarkers based on NETs for ... [https://www.nature.com/articles/s41598-025-97548-5]
- 68. LncRNA profile study reveals a seven-lncRNA signature ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-020-00187-3]
- 69. A long non-coding RNA signature for predicting survival in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5955136/]
- 70. Internal validation strategy for high dimensional prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451366/]
- 71. Construction and validation of a risk prediction model for ... [https://www.nature.com/articles/s41598-025-24478-7]
- 72. Long non-coding RNA-based single and combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405140/]
- 73. Identification of prognostic biomarkers related to epithelial ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1600546/full]
- 74. Machine learning-based hepatocellular carcinoma risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504168/]
- 75. A reliable prognostic model for hepatocellular carcinoma ... [https://www.nature.com/articles/s41598-025-01335-1]
- 76. Empirical investigation of multi-source cross-validation in ... [https://www.sciencedirect.com/science/article/pii/S0010482524013568]
- 77. Comparison of machine learning and Cox regression ... [https://www.sciencedirect.com/science/article/pii/S2589845025000570]
- 78. Systematic review and meta-analysis of validated ... [https://www.sciencedirect.com/science/article/pii/S0748798321007381]
- 79. Prognostication and risk factor stratification for survival of ... [https://www.nature.com/articles/s41598-023-37277-9]
- 80. Prognostic Factors for Mortality in Hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10888215/]
- 81. Predictive value of biomarkers for lenvatinib in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368414/]
- 82. Editorial: LncRNAs in tumor microenvironment: its role ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1560928/full]
- 83. Migrasome-related LncRNA features predict immune ... [https://www.nature.com/articles/s41598-025-24226-x]
- 84. Checkpoint molecules on infiltrating immune cells in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9441912/]
- 85. Transcriptomic and Functional Validation Reveals PAQR3/P6 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292340/]
- 86. Prioritization and functional validation of target genes from ... [https://www.nature.com/articles/s42003-023-05006-7]
- 87. Identifying and validating novel targets with in vivo disease ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644607001481]