LINC00152 as an Independent Prognostic Biomarker in Hepatocellular Carcinoma: From Mechanistic Insights to Clinical Application
This comprehensive review synthesizes current evidence on the long non-coding RNA LINC00152 as a potent independent prognostic biomarker in hepatocellular carcinoma (HCC).
LINC00152 as an Independent Prognostic Biomarker in Hepatocellular Carcinoma: From Mechanistic Insights to Clinical Application
Abstract
This comprehensive review synthesizes current evidence on the long non-coding RNA LINC00152 as a potent independent prognostic biomarker in hepatocellular carcinoma (HCC). We explore LINC00152's foundational biology, dysregulated expression in tumor tissues and circulation, and its role in driving HCC progression through mTOR and EGFR/PI3K/AKT signaling pathways. The article details advanced detection methodologies in liquid biopsies, machine learning integration for diagnostic refinement, and comparative analyses against conventional biomarkers like AFP. For researchers and drug development professionals, we provide critical insights into LINC00152's clinical utility in risk stratification, treatment monitoring, and its emerging potential as a therapeutic target, addressing both current applications and future translational directions.
LINC00152 Biology and Oncogenic Mechanisms in Hepatocarcinogenesis
Genomic Landscape and Molecular Characteristics of LINC00152
Long non-coding RNAs (lncRNAs) have emerged as pivotal regulators of gene expression and key players in oncogenesis. Among them, LINC00152 (long intergenic non-coding RNA 152) has garnered significant attention as a potent oncogene across diverse cancer types. This review provides a comprehensive analysis of the genomic landscape, molecular characteristics, and functional roles of LINC00152, with particular emphasis on its established independent prognostic value in hepatocellular carcinoma (HCC). We synthesize evidence from molecular studies, clinical correlations, and experimental models to delineate the mechanistic pathways through which LINC00152 drives tumorigenesis, highlighting its emerging potential as both a diagnostic biomarker and therapeutic target.
Genomic Fundamentals and Expression Profile of LINC00152
LINC00152 is an 828-nucleotide intergenic non-coding RNA located on chromosome 2p11.2 [1] [2]. Early genomic analyses confirmed its non-coding nature through phylogenetic codon substitution frequency (PhyloCSF) scoring, which yielded a score of -75.99, effectively ruling out protein-coding potential [3]. This transcript exhibits a complex genomic architecture with multiple splice variants, the most abundant being a short isoform consisting of the first and last exons [4]. A notable feature is the existence of a highly similar paralog, MIR4435-2HG, located on chromosome 2q13, which differs by only 13 exonic single nucleotide variations [4].
The expression profile of LINC00152 reveals consistent upregulation across multiple cancer types. Research demonstrates significant overexpression in hepatocellular carcinoma, gastric cancer, renal cell carcinoma, lung adenocarcinoma, and other malignancies compared to corresponding normal tissues [5] [3]. In HCC specifically, LINC00152 shows prominent nuclear localization and its promoter region is characterized by hypomethylation in tumor tissues, suggesting a potential epigenetic mechanism for its dysregulation [3].
Table 1: LINC00152 Expression Across Human Cancers
| Cancer Type | Expression Status | Clinical Correlations |
|---|---|---|
| Hepatocellular Carcinoma | Significantly upregulated | Associated with larger tumor size, advanced Edmondson grade [3] |
| Gastric Cancer | Upregulated in tissue and gastric juice | Potential diagnostic biomarker [5] |
| Various Solid Tumors | Consistently overexpressed | Correlation with lymph node metastasis (OR=2.93) and advanced TNM stage [5] |
| Acute Myeloid Leukemia | Highly expressed in CD34+CD38- LSCs | Associated with chemoresistance and poor prognosis [6] |
The subcellular distribution of LINC00152 appears to be context-dependent. While early studies in HCC cell lines indicated predominant nuclear localization [3], subsequent research has identified LINC00152 in cytoplasmic compartments and circulating exosomes, suggesting diverse functional mechanisms in different cellular contexts [7] [5].
Functional Mechanisms and Signaling Pathways
LINC00152 exerts its oncogenic functions through diverse molecular mechanisms, ranging from direct pathway activation to intercellular communication. A comprehensive understanding of these mechanisms provides insights into its multifaceted role in cancer progression.
mTOR Signaling Pathway Activation
In hepatocellular carcinoma, LINC00152 has been demonstrated to activate the mTOR signaling pathway, a critical regulator of cell growth and proliferation. Mechanistically, LINC00152 binds to the promoter region of EpCAM (Epithelial Cell Adhesion Molecule) through cis-regulatory interactions, thereby activating this upstream regulator of mTOR [3] [8]. This activation was confirmed through microarray analysis and western blot validation, showing decreased mTOR phosphorylation upon LINC00152 knockdown [3]. The functional significance of this pathway was further substantiated by experiments demonstrating that LINC00152 knockdown inhibited HCC cell proliferation in vitro and tumor growth in mouse xenograft models [3].
Exosomal-Mediated Intercellular Communication
Recent research has unveiled a novel mechanism whereby LINC00152 is shuttled via exosomes derived from cancer-associated fibroblasts (CAFs) in cholangiocarcinoma. These CAF-derived exosomes mediate crosstalk between CAFs and cancer cells by transferring LINC00152, which subsequently promotes cancer cell proliferation, migration, and invasion [7]. The loading of LINC00152 into exosomes is facilitated by its interaction with the RNA-binding protein hnRNPA2B1. Intriguingly, LINC00152 reciprocally stabilizes hnRNPA2B1 by repressing its proteasome-dependent degradation, creating a positive feedback loop that amplifies its oncogenic activities [7].
Regulation of Cell Cycle Progression
Functional studies in HeLa cells have revealed that LINC00152 is essential for cell cycle progression through mitosis. Depletion of LINC00152 caused cells to arrest in prometaphase, associated with reduced cell viability [4]. RNA affinity purification studies identified that LINC00152 interacts with a network of proteins associated with M phase of the cell cycle, suggesting its involvement in mitotic regulation [4]. This function aligns with its identification in a high-throughput siRNA screen targeting lncRNAs deregulated in cancer, where it was classified as a regulator of cell division [4].
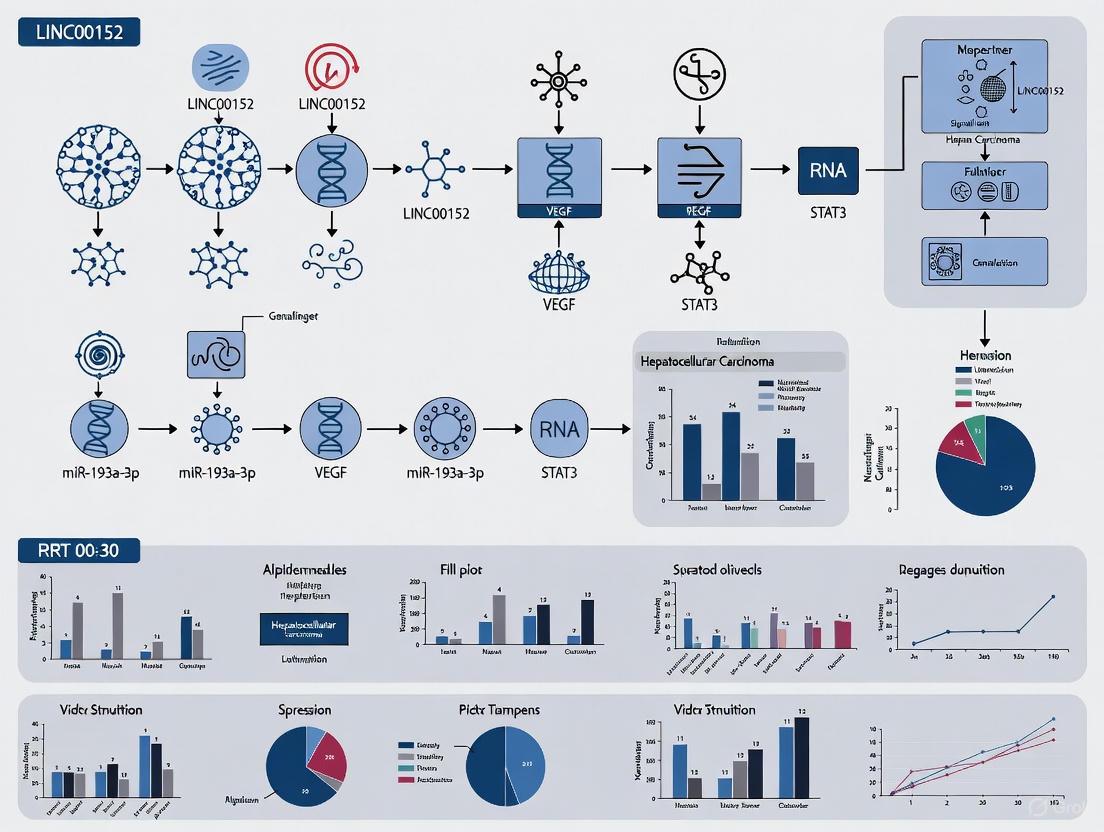
Diagram 1: LINC00152 Oncogenic Mechanisms and Functional Consequences. This diagram illustrates the multifaceted mechanisms through which LINC00152 promotes cancer progression, including mTOR pathway activation, exosomal transfer, cell cycle regulation, and protein stabilization, ultimately leading to enhanced tumorigenesis and poor prognosis.
LINC00152 as a Diagnostic and Prognostic Biomarker in HCC
The clinical utility of LINC00152 as a biomarker is particularly prominent in hepatocellular carcinoma, where it demonstrates significant diagnostic and prognostic value.
Diagnostic Potential
Serum LINC00152 shows remarkable diagnostic performance for HCC detection. A 2023 case-control study involving 160 participants (60 HCC patients, 60 liver cirrhosis patients, and 40 healthy controls) revealed that serum LINC00152 levels were significantly elevated in HCC patients compared to both liver cirrhosis patients and healthy controls (p<0.001) [1] [2]. Receiver operating characteristic (ROC) analysis demonstrated that LINC00152 effectively distinguished HCC patients from those with liver cirrhosis, suggesting its utility as a non-invasive diagnostic biomarker [1]. This is particularly valuable given the limitations of alpha-fetoprotein (AFP), which has suboptimal sensitivity and specificity, especially for early-stage HCC detection [1].
Prognostic Significance
The independent prognostic value of LINC00152 in HCC is well-established. Multivariate Cox regression analysis in multiple studies has confirmed that high LINC00152 expression independently predicts poor overall survival in HCC patients [9] [1]. A comprehensive meta-analysis encompassing nine original studies and 808 cancer patients revealed that LINC00152 overexpression was significantly associated with poor overall survival (pooled HR=1.98, 95% CI: 1.70-2.31, p<0.0001) and disease-free survival (HR=1.66, 95% CI: 1.20-2.29, p<0.0001) in human solid cancers [5]. In the 2023 serum study, multivariate analysis specifically identified high serum LINC00152 level as an independent predictor of poor outcome for HCC patients (HR=2.23, 95% CI: 1.30-5.29, p=0.03) [1].
Table 2: Prognostic Value of LINC00152 in Hepatocellular Carcinoma
| Study Type | Cohort Size | Detection Method | Hazard Ratio (HR) | Confidence Interval (95% CI) | P-value |
|---|---|---|---|---|---|
| Serum Analysis | 60 HCC patients | qRT-PCR | 2.23 | 1.30-5.29 | 0.03 [1] |
| Tissue Analysis | 63 HCC patients | qRT-PCR | 2.524 | 1.661-4.015 | 0.001 [9] |
| Meta-Analysis | 808 cancer patients | Multiple | 1.98 | 1.70-2.31 | <0.0001 [5] |
Beyond survival outcomes, LINC00152 expression correlates with specific clinicopathological features in HCC. Elevated LINC00152 levels are associated with larger tumor size (p=0.005), higher Edmondson grade (p=0.002) [3], and lesions involving both liver lobes (p=0.02) [1]. These associations further support its role in marking aggressive disease phenotypes.
Experimental Models and Research Methodologies
The functional characterization of LINC00152 has employed diverse experimental approaches across multiple model systems, providing compelling evidence for its oncogenic properties.
In Vitro and In Vivo Models
In hepatocellular carcinoma models, LINC00152 knockdown using short hairpin RNAs (shRNAs) significantly inhibited cell proliferation in both HepG2 and MHCC-97H cell lines, as measured by CCK-8 and EdU incorporation assays [3]. This anti-proliferative effect was corroborated in vivo, where LINC00152 knockdown substantially impaired tumor growth in nude mouse xenograft models [3]. Similarly, in cholangiocarcinoma models, coculture with CAF-derived exosomes harboring LINC00152 promoted cancer cell proliferation, migration, and invasion, effects that were abrogated upon LINC00152 depletion [7].
In acute myeloid leukemia (AML) models, LINC00152 was highly expressed in CD34+CD38- leukemia stem cells (LSCs) and found to regulate their self-renewal capacity [6]. Functional assays demonstrated that LINC00152 knockdown increased sensitivity to chemotherapeutic agents like doxorubicin, suggesting its involvement in mediating chemoresistance [6].
Key Experimental Protocols
Research on LINC00152 has utilized standardized molecular biology techniques:
- Expression Analysis: Quantitative real-time PCR (qRT-PCR) serves as the primary method for LINC00152 quantification in tissues and serum samples. RNA is typically reverse-transcribed using kits such as the QuantiTect Reverse Transcription Kit, followed by amplification with SYBR Green chemistry [1] [2].
- Exosome Isolation: For studies investigating exosomal LINC00152, exosomes are isolated from cell culture supernatants or patient sera using ultracentrifugation and characterized by transmission electron microscopy, dynamic light scattering, and western blotting for exosomal markers [7].
- Functional Assays: Cell proliferation is assessed via CCK-8 and EdU incorporation assays; migration and invasion are evaluated using Transwell assays; and apoptosis is analyzed by flow cytometry with Annexin V staining [7] [3].
- Protein-RNA Interactions: RNA immunoprecipitation (RIP) and RNA pull-down assays are employed to identify protein binding partners, such as the interaction between LINC00152 and hnRNPA2B1 [7].
Diagram 2: LINC00152 Research Methodology Workflow. This diagram outlines the standard experimental approaches used in LINC00152 research, from initial sample processing through functional validation and clinical correlation analyses, culminating in potential clinical applications.
Investigating LINC00152 requires specialized reagents and methodological approaches. The following table compiles key resources essential for studying this oncogenic lncRNA.
Table 3: Essential Research Reagents and Methodologies for LINC00152 Investigation
| Reagent/Resource | Specific Example | Application | Experimental Notes |
|---|---|---|---|
| Detection Primers | F: 5'-GACTGGATGGTCGCTGCTTT-3'R: 5'-CCCAGGAACTGTGCTGTGAA-3' [1] | qRT-PCR detection | Validate specificity and efficiency; use with SYBR Green chemistry |
| RNA Extraction Kit | QIAamp RNA Blood Mini Kit (Qiagen) [1] | RNA isolation from blood/serum | Ensures high-quality RNA for sensitive detection of circulating LINC00152 |
| cDNA Synthesis Kit | QuantiTect Reverse Transcription Kit (Qiagen) [1] | cDNA synthesis | Includes genomic DNA removal step for cleaner results |
| Knockdown Tools | shRNAs targeting LINC00152 sequences [3] | Functional loss-of-function studies | Multiple shRNAs recommended to control for off-target effects |
| Exosome Isolation | Ultracentrifugation protocols [7] | Studying exosomal LINC00152 | Characterize with TEM, dynamic light scattering, and western blot |
| Cell Lines | HepG2, MHCC-97H (HCC)K562 (leukemia) [6] [3] | In vitro functional studies | Select lines with endogenous high LINC00152 expression |
| Animal Models | BALB/C nude mice xenografts [3] | In vivo tumorigenesis studies | Monitor tumor growth and metastasis formation |
The comprehensive analysis of LINC00152 reveals a compelling narrative of its multifaceted oncogenic role across cancer types, with particularly robust evidence in hepatocellular carcinoma. Its consistent overexpression in malignancies, association with aggressive clinicopathological features, and independent prognostic value underscore its significance in cancer biology. The well-documented mechanisms through which LINC00152 promotes tumorigenesis—including mTOR pathway activation, exosomal-mediated intercellular communication, and cell cycle regulation—provide a solid mechanistic foundation for its biological functions.
From a translational perspective, LINC00152 holds substantial promise as both a diagnostic biomarker and therapeutic target. Its detection in serum and stability in circulation enhance its potential for non-invasive liquid biopsy applications, addressing critical limitations of current biomarkers like AFP in HCC management. The experimental methodologies for studying LINC00152 are well-established, enabling robust investigation across model systems.
Future research directions should focus on therapeutic targeting strategies for LINC00152, exploring antisense oligonucleotides, small molecule inhibitors, or RNA-based therapeutics to abrogate its oncogenic functions. Additionally, larger prospective multicenter studies are warranted to validate the clinical utility of LINC00152 as a standardized biomarker for early detection, prognostic stratification, and treatment monitoring in hepatocellular carcinoma and other malignancies.
Dysregulated Expression Patterns in HCC Tissues and Circulating Blood
Hepatocellular carcinoma (HCC) represents a major global health challenge, ranking as the sixth most prevalent cancer and the fourth leading cause of cancer-related mortality worldwide [10]. The dismal 5-year survival rate is largely attributable to late diagnosis and limited treatment options for advanced disease, highlighting the critical need for reliable biomarkers for early detection and prognostic stratification [11]. Long non-coding RNAs (lncRNAs), once considered genomic "junk," have emerged as pivotal regulators of gene expression and promising biomarker candidates in oncology [12]. Among these, Long Intergenic Non-Protein Coding RNA 152 (LINC00152) has garnered significant research interest due to its consistent dysregulation in HCC and other solid tumors. This review comprehensively examines the differential expression patterns of LINC00152 in HCC tissues versus circulating blood, analyzes its molecular mechanisms, evaluates its diagnostic and prognostic performance, and explores its potential clinical utility within the broader context of HCC biomarker research.
LINC00152 Expression in HCC Tissues versus Circulating Blood
LINC00152 demonstrates consistent and marked overexpression in hepatocellular carcinoma compared to non-malignant liver tissues. This dysregulation is observed consistently across multiple independent studies and experimental platforms.
Table 1: LINC00152 Expression in HCC Tissues and Blood
| Sample Type | Expression Pattern | Detection Method | Study Details | Clinical Correlation |
|---|---|---|---|---|
| HCC Tissue | Significant upregulation | qRT-PCR | 63 HCC patients [9] | Independent predictor of shorter OS (HR, 2.524; 95% CI, 1.661–4.015; P=0.001) |
| HCC Tissue | Upregulated | RNA sequencing | Multiple studies [5] | Associated with lymph node metastasis (OR=2.93, 95% CI: 1.88–4.57, p<.0001) and poor differentiation |
| Serum/Plasma | Considerably higher in HCC | qRT-PCR | 60 HCC vs. 60 cirrhosis vs. 40 healthy controls [1] | Distinguishes HCC from cirrhosis and healthy controls (p<0.001) |
| Serum/Plasma | Elevated expression | qRT-PCR | 52 HCC patients vs. 30 controls [10] | Moderate diagnostic accuracy (sensitivity 60-83%, specificity 53-67%) |
| Circulating Blood | Upregulated | qRT-PCR | Multiple cohorts [9] [1] | High level is an independent predictor of poor outcome (HR=2.23, 95% CI=1.30–5.29, p=0.03) |
The consistency of LINC00152 overexpression across tissue and liquid biopsies underscores its robust dysregulation in HCC. In tumor tissues, elevated LINC00152 expression is not merely an epiphenomenon but is strongly correlated with aggressive clinicopathological features, including advanced tumor stage, lymph node metastasis, and poor histological differentiation [5]. The association between high LINC00152 expression and reduced overall survival, even after multivariate adjustment, highlights its potential as an independent prognostic indicator in HCC [9].
The detection of elevated LINC00152 levels in circulating blood represents a particularly promising advancement for non-invasive biomarker applications. Serum LINC00152 levels demonstrate a stepwise increase from healthy controls to liver cirrhosis to HCC, suggesting potential utility in monitoring disease progression in at-risk populations [1]. This differential expression in easily accessible biofluids positions LINC00152 as a candidate for liquid biopsy-based approaches to HCC surveillance and diagnosis.
Molecular Mechanisms and Signaling Pathways
LINC00152 exerts its oncogenic functions through diverse molecular mechanisms, primarily centered on the regulation of critical cancer-associated signaling pathways.
PI3K/Akt/mTOR Signaling Pathway
A fundamental mechanism through which LINC00152 promotes hepatocarcinogenesis is the activation of the phosphatidylinositol 3-kinase (PI3K)/Akt/mammalian target of rapamycin (mTOR) signaling cascade [13]. This pathway plays a central role in controlling cancer cell proliferation, division, and carcinogenesis. LINC00152 achieves pathway activation through a competitive endogenous RNA (ceRNA) mechanism by sequestering microRNA-139 (miR-139), thereby relieving miR-139-mediated suppression of its target PIK3CA, the catalytic subunit of PI3K [13]. The subsequent activation of this oncogenic signaling cascade drives tumor growth and progression.
Alternative Molecular Mechanisms
Beyond the PI3K/Akt/mTOR axis, LINC00152 participates in additional oncogenic processes. In some HCC contexts, LINC00152 has been reported to inhibit cell proliferation by recruiting histone deacetylase 1 (HDAC1) to repress c-Myc transcription, suggesting context-dependent functions [12]. The lncRNA also localizes predominantly to the nucleus in HCC cells, where it can influence epigenetic regulation and gene expression directly [1]. These varied mechanisms highlight the molecular complexity of LINC00152's role in hepatocarcinogenesis and underscore the need for further research to fully elucidate its functional repertoire.
Diagnostic and Prognostic Performance
Diagnostic Accuracy
The diagnostic performance of LINC00152 has been evaluated across multiple studies, both as a standalone marker and in combination with established and novel biomarkers.
Table 2: Diagnostic Performance of LINC00152 in HCC
| Biomarker | Sample Type | Sensitivity (%) | Specificity (%) | AUC-ROC | Study Population |
|---|---|---|---|---|---|
| LINC00152 alone | Plasma | 60-83 | 53-67 | Not reported | 52 HCC vs. 30 controls [10] |
| LINC00152 alone | Serum | Significant elevation | Significant elevation | Not reported | 60 HCC vs. 60 cirrhosis vs. 40 healthy [1] |
| LINC00152 + GAS5 ratio | Plasma | Not reported | Not reported | Not reported | 52 HCC patients [10] |
| Machine Learning Panel (incl. LINC00152) | Plasma + lab parameters | 100 | 97 | Not reported | 52 HCC vs. 30 controls [10] |
| miR-21+miR-122 (comparison) | Tissue | 89 | 91 | 0.92 | Literature report [12] |
While LINC00152 demonstrates moderate diagnostic accuracy as a standalone marker, its performance significantly improves when incorporated into multi-analyte panels. A machine learning approach that integrated LINC00152 with three other lncRNAs (LINC00853, UCA1, and GAS5) and conventional laboratory parameters achieved remarkable diagnostic performance with 100% sensitivity and 97% specificity [10]. Furthermore, the ratio of LINC00152 to GAS5 expression emerged as a strong prognostic indicator, with higher ratios correlating with increased mortality risk [10]. These findings suggest that LINC00152 may have greater utility in multi-marker panels than as a standalone diagnostic test.
Prognostic Value
The prognostic significance of LINC00152 in HCC is substantiated by multiple clinical studies. A comprehensive meta-analysis encompassing nine original studies and 808 patients revealed that high LINC00152 expression was positively associated with lymph node metastasis (OR = 2.93, 95% CI: 1.88–4.57, p < .0001), advanced tumor stage, and tumor recurrence (HR = 3.32, 95% CI: 1.98–5.57, p < .0001) [5]. Most importantly, elevated LINC00152 expression consistently correlated with reduced overall survival (pooled HR = 1.98, 95% CI: 1.70–2.31, p < .0001) and poor disease-free survival (HR = 1.66, 95% CI: 1.20–2.29, p < .0001) across multiple solid tumors, including HCC [5].
Multivariate analyses in several studies have confirmed LINC00152 as an independent prognostic factor in HCC. In serum analyses, high LINC00152 levels independently predicted poor outcomes (HR = 2.23, 95% CI = 1.30–5.29, p = 0.03) after adjusting for other clinical variables [1]. Similarly, in tissue-based studies, elevated LINC00152 expression remained independently associated with shorter overall survival (HR = 2.524, 95% CI = 1.661–4.015, P = 0.001) in multivariate Cox regression models [9].
Research Reagent Solutions
Table 3: Essential Research Reagents for LINC00152 Investigation
| Reagent/Tool | Function/Application | Examples/Specifications |
|---|---|---|
| qRT-PCR Assays | Quantifying LINC00152 expression | Primers: F: 5′-GACTGGATGGTCGCTGCTTT-3′, R: 5′-CCCAGGAACTGTGCTGTGAA-3′ [1] |
| RNA Isolation Kits | RNA extraction from blood/tissue | miRNeasy Mini Kit (QIAGEN) [10] |
| cDNA Synthesis Kits | Reverse transcription for PCR | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [10] |
| SYBR Green Master Mix | qRT-PCR detection | PowerTrack SYBR Green Master Mix (Applied Biosystems) [10] |
| In Situ Hybridization Probes | Spatial localization in tissues | Not specified in studies but commercially available |
| Cell Culture Models | Functional mechanism studies | HepG2, Huh7, and other HCC cell lines [12] |
| siRNA/shRNA Constructs | LINC00152 knockdown studies | Custom designs targeting 828 bp transcript |
| Animal Models | In vivo functional validation | Xenograft models using HCC cell lines [12] |
The experimental workflow for LINC00152 investigation typically begins with sample collection (tissue or blood), followed by RNA extraction using commercial kits. RNA quality assessment is critical for reliable results. Reverse transcription precedes quantitative PCR using the specific primers listed in Table 3. For functional studies, knockdown approaches using siRNA or shRNA in HCC cell lines enable investigation of LINC00152's biological roles, while animal models provide in vivo validation [12].
Discussion and Future Perspectives
The consistent dysregulation of LINC00152 in both HCC tissues and circulating blood, coupled with its association with aggressive tumor phenotypes and poor clinical outcomes, strongly supports its potential utility as a diagnostic and prognostic biomarker. The molecular mechanisms through which LINC00152 promotes hepatocarcinogenesis, particularly its activation of the PI3K/Akt/mTOR pathway via miR-139 sponging, provide a mechanistic foundation for its oncogenic functions [13].
Several considerations merit attention for the translational application of LINC00152. First, the moderate diagnostic performance of LINC00152 as a standalone marker suggests that its greatest clinical utility may lie in multi-analyte panels that incorporate complementary biomarkers [10] [11]. The remarkable performance of machine learning approaches integrating LINC00152 with other lncRNAs and conventional parameters highlights the promise of such multi-marker strategies [10]. Second, the detection of LINC00152 in circulating blood offers the possibility for non-invasive "liquid biopsy" applications, which could enhance HCC surveillance in high-risk populations and monitor treatment response [1] [10].
Future research directions should include large-scale validation studies in diverse patient cohorts, standardization of detection methodologies and cutoff values, and further elucidation of LINC00152's molecular functions in HCC pathogenesis. Additionally, exploring the potential of LINC00152 as a therapeutic target, possibly through antisense oligonucleotides or small molecule inhibitors, represents an intriguing avenue for investigation.
In conclusion, LINC00152 emerges as a promising molecular biomarker with significant potential to enhance HCC diagnosis, prognosis, and possibly therapy. Its consistent dysregulation, detectability in liquid biopsies, and independent prognostic value position it as a valuable contributor to the evolving landscape of precision oncology in hepatocellular carcinoma.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, characterized by high mortality rates primarily due to rapid proliferation, early metastasis, and frequent therapeutic resistance [14]. Within this context, long non-coding RNAs (lncRNAs) have emerged as crucial regulators of cancer biology. Among these, LINC00152 (long intergenic non-coding RNA 00152) has been identified as a pivotal oncogenic molecule across various human malignancies, including HCC [15]. This guide provides a objective comparison of LINC00152's functional roles against other molecular mechanisms in HCC progression, synthesizing current experimental data to evaluate its potential as a diagnostic and prognostic biomarker.
LINC00152 is an 828-nucleotide lncRNA located on chromosome 2p11.2 [15] [16]. Initially identified in hepatocarcinogenesis research, it has since been recognized as a significant oncogene in numerous cancers [15]. Its function is closely linked to its subcellular localization: in the nucleus, it can modulate gene expression epigenetically, while in the cytoplasm, it primarily acts as a competing endogenous RNA (ceRNA) by sponging microRNAs [15] [16].
Table 1: LINC00152 Expression in Clinical HCC Samples
| Study Population | Detection Method | Expression in HCC vs. Non-Tumor Tissue | Correlation with Clinical Parameters | Citation |
|---|---|---|---|---|
| 102 paired HCC/non-tumor tissues | RT-PCR | Significantly upregulated | Positive correlation with tumor size (p=0.005) and Edmondson grade (p=0.002) | [3] |
| 72 paired HCC/non-tumor tissues | qRT-PCR | Dramatically elevated (p < 0.05) | Positive correlation with tumor size (p=0.001) and HBV infection (p=0.006) | [17] |
| 120 patients (60 HCC, 60 cirrhosis), 40 controls | Real-time qRT-PCR (serum) | Considerably higher in HCC vs. cirrhosis and controls (p<0.001) | Associated with lesions in both liver lobes (p=0.02); Independent prognostic indicator (HR=2.23) | [18] [2] |
| Bioinformatic analysis of 20 HCC patients | GEO Dataset (GSE77509) | ~2.24-fold higher in tumor tissues | N/A | [14] |
The consistent upregulation of LINC00152 in HCC and its correlation with aggressive clinicopathological features underscore its potential as a clinically significant biomarker.
Comparative Analysis of Functional Roles in HCC
LINC00152 drives HCC progression through distinct yet interconnected mechanisms. The table below provides a comparative summary of its primary functions, supported by key experimental data.
Table 2: Comparative Analysis of LINC00152 Functional Roles in HCC
| Functional Role | Experimental Models | Key Findings | Molecular Targets/Pathways | Citation |
|---|---|---|---|---|
| Cell Proliferation & Cell Cycle Progression | In vitro: Huh7, HCCLM3, Hep3B cells (gain-and-loss-of-function)In vivo: Nude mouse xenografts | LINC00152 knockdown decreased proliferation, induced G0/G1 arrest; Overexpression accelerated G1/S transition | miR-193a/b-3p/CCND1 axis; Positive correlation between LINC00152 and CCND1 mRNA (R²=0.354, p<0.001) | [14] |
| Tumor Growth & Oncogenesis | In vivo: Nude mouse xenografts (HepG2, MHCC-97H cells) | LINC00152 knockdown significantly inhibited tumor growth in vivo; Reduced Ki-67 proliferation index | mTOR signaling pathway activation; Confirmed by microarray and Western blot | [3] |
| Metastasis & Invasion | In vitro: HCC cells with modulated LINC00152 | Knockdown suppressed cell invasion and migration; Upregulated by HBx in HBV-associated HCC | Epithelial-Mesenchymal Transition (EMT) promotion | [17] |
| Treatment Resistance | In vitro: Colorectal cancer cells (functional analogy) | LINC00152 conferred resistance to 5-FU by suppressing apoptosis; Potential relevance for HCC treatment resistance | miR-139-5p/NOTCH1 pathway | [19] |
Proliferation and Cell Cycle Mechanisms
LINC00152 exerts a profound effect on HCC cell proliferation by directly interfering with cell cycle regulation. Functional experiments demonstrate that LINC00152 knockdown induces a significant G0/G1 phase arrest, while its overexpression accelerates the G1/S transition, effectively pushing cells into the DNA synthesis and division phases [14]. The core mechanism involves LINC00152's role as a ceRNA: it sequesters miR-193a/b-3p in the cytoplasm, preventing this miRNA from repressing its target, CCND1 [14]. The CCND1 gene encodes cyclin D1, a critical regulator of the G1/S checkpoint. The positive correlation between LINC00152 and CCND1 mRNA in HCC tissues (R²=0.354, p<0.001) provides clinical support for this mechanism [14]. Rescue experiments confirm that CCND1 overexpression can partially reverse the cell cycle arrest caused by LINC00152 silencing, establishing CCND1 as a key downstream effector [14].
Tumor Growth and mTOR Pathway Activation
In vivo studies provide compelling evidence for the essential role of LINC00152 in HCC tumorigenesis. Xenograft models using HepG2 and MHCC-97H cells with stably knocked-down LINC00152 show significantly inhibited tumor growth compared to controls [14] [3]. This is further corroborated by a reduced Ki-67 proliferation index in the knockdown tumors [14]. A pivotal study revealed that LINC00152 activates the mechanistic target of the rapamycin (mTOR) signaling pathway, a central regulator of cell growth and proliferation [3]. Microarray analysis and Western blot validation demonstrated that LINC00152 downregulation reduces mTOR phosphorylation [3]. Furthermore, a positive correlation was observed between LINC00152 expression levels and phospho-mTOR in clinical HCC samples [3]. This mTOR activation is achieved through a cis-regulation on the EpCAM promoter, illustrating a nuclear function of this lncRNA [3].
Metastasis, Invasion, and Viral Association
The prometastatic role of LINC00152 is particularly salient in the context of hepatitis B virus (HBV)-associated HCC. Research shows that LINC00152 expression is significantly higher in HBV-infected HCC tissues compared to non-infected ones and is positively correlated with the expression of the viral HBx protein [17]. In vitro, HBx upregulates LINC00152 transcription, and silencing LINC00152 subsequently suppresses HCC cell proliferation, invasion, and Epithelial-Mesenchymal Transition (EMT) [17]. This positions LINC00152 as a critical downstream effector of HBx-driven oncogenesis, offering a potential therapeutic target for a major HCC etiological subgroup.
Signaling Pathway Diagrams
The following diagrams summarize the core molecular mechanisms by which LINC00152 promotes HCC progression, integrating the key findings from comparative analysis.
LINC00152-Driven HCC Proliferation Axis
LINC00152 in HBV-Associated HCC and mTOR Signaling
Experimental Protocols for Key Studies
To ensure the reproducibility of critical findings, this section outlines the standardized methodologies employed in the foundational studies of LINC00152 in HCC.
Table 3: Standardized Experimental Protocols for Key LINC00152 Studies
| Experimental Objective | Cell Lines Used | Modulation Methods | Key Assays & Measurements | Data Analysis |
|---|---|---|---|---|
| Functional Role: Proliferation & Cell Cycle | Huh7, HCCLM3, Hep3B | Knockdown: shRNAs (sh152-1, sh152-3); Overexpression: p-LINC00152 plasmid | CCK-8 assay, EdU incorporation, Colony formation, FACS for cell cycle, qRT-PCR/Western for CCND1 | Student's t-test; Correlation analysis (R²) |
| Functional Role: Tumor Growth In Vivo | HepG2, MHCC-97H | Stable knockdown with sh152-1 | Nude mouse xenograft model (subcutaneous injection), Tumor volume measurement, Ki-67 IHC | Student's t-test |
| Mechanism: ceRNA Activity | Huh7, HCCLM3 | MS2-RIP system, Luciferase reporter vectors (wild-type & mutant LINC00152) | RNA Immunoprecipitation (RIP) with anti-Ago2 antibody, Luciferase reporter assay | Comparison of relative luciferase activity |
| Diagnostic/Prognostic Value | Human blood samples | N/A | RNA extraction, Real-time qRT-PCR for serum LINC00152, ROC analysis, Cox regression for survival | Chi-square, Kaplan-Meier/log-rank, Multivariate analysis (HR) |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for Investigating LINC00152 in HCC
| Reagent/Tool | Specific Example/Catalog Number | Primary Function in LINC00152 Research |
|---|---|---|
| qRT-PCR Assays | QuantiTect SYBR Green PCR Kit (Qiagen) | Quantifying LINC00152 expression in tissue, serum, and cell lines [18] [2] |
| Cell Lines | Huh7, HCCLM3, HepG2, Hep3B, MHCC-97H | In vitro models for gain/loss-of-function studies [14] [3] |
| Knockdown Vectors | shRNA plasmids (e.g., sh152-1, sh152-3) | Silencing endogenous LINC00152 expression to study loss-of-function phenotypes [14] [3] |
| Animal Models | BALB/C nude mice (4-6 weeks old) | In vivo xenograft models to assess tumorigenicity and therapeutic response [14] [3] |
| Luciferase Reporters | pLuc-LINC00152-WT, pLuc-LINC00152-Mut | Validating direct binding interactions with miRNAs (e.g., miR-193a/b-3p) [14] |
| Pathway Antibodies | Anti-CCND1, Anti-p-mTOR, Anti-Ki-67 | Detecting protein-level changes in downstream targets via Western blot or IHC [14] [3] |
| ATM Inhibitor-6 | ATM Inhibitor-6, MF:C28H33FN6O2, MW:504.6 g/mol | Chemical Reagent |
| Xylose-d6 | Xylose-d6, MF:C5H10O5, MW:156.17 g/mol | Chemical Reagent |
Synthesizing the presented data, LINC00152 demonstrates a compelling profile as a multifunctional oncogene in HCC. Its roles in driving proliferation via the miR-193a/b-3p/CCND1 axis and mTOR signaling, promoting invasion and metastasis particularly in HBV-related HCC, and conferring treatment resistance in other cancers, position it as a central player in HCC progression. Crucially, recent clinical evidence confirms that a high serum level of LINC00152 is an independent predictor of poor outcome in HCC patients (HR=2.23, 95% CI=1.30–5.29, p=0.03) [18] [2]. This independent prognostic value, combined with its detectable presence in serum, underscores its significant potential not only as a robust prognostic biomarker but also as a promising target for future therapeutic interventions in hepatocellular carcinoma.
Oncogenic signaling pathways are fundamental drivers of cancer progression, with the mammalian target of rapamycin (mTOR) and epidermal growth factor receptor (EGFR)/phosphoinositide 3-kinase (PI3K)/protein kinase B (AKT) axes representing two of the most critically dysregulated circuits in human malignancies. These pathways regulate essential cellular processes including proliferation, survival, metabolism, and resistance to therapy. Within the context of hepatocellular carcinoma (HCC), these signaling cascades interface with novel biomarkers such as long non-coding RNAs (lncRNAs), creating complex networks that influence tumor behavior and patient outcomes. The independent prognostic value of specific lncRNAs, particularly LINC00152, has emerged as a significant factor in HCC research, offering potential insights for diagnostic and therapeutic development. This review systematically compares the mTOR and EGFR/PI3K/AKT pathways, their functional interactions, and their integration with lncRNA networks in HCC pathogenesis, providing a structured analysis of experimental data and methodologies relevant to cancer researchers and drug development professionals.
The EGFR/PI3K/AKT axis and mTOR pathway represent sequentially connected signaling cascades that frequently co-opt each other in cancer progression. The EGFR/PI3K/AKT axis initiates with epidermal growth factor receptor (EGFR) activation, which recruits and activates phosphoinositide 3-kinase (PI3K), generating phosphatidylinositol (3,4,5)-trisphosphate (PIP3) at the membrane. This leads to AKT activation, a central node that regulates cell survival, proliferation, and metabolism [20] [21]. mTOR, specifically mechanistic target of rapamycin, operates as both a downstream effector and regulatory hub within this network, existing in two distinct complexes: mTORC1 and mTORC2. mTORC1 primarily controls protein synthesis, autophagy, and metabolism, while mTORC2 regulates cytoskeletal organization and AKT phosphorylation [22] [21].
Table 1: Core Components and Primary Functions of Oncogenic Pathways
| Pathway Component | Molecular Structure/Type | Key Functions in Cancer | Common Alterations in Cancer |
|---|---|---|---|
| EGFR | Receptor tyrosine kinase | Cell proliferation, survival signaling | Overexpression, mutations |
| PI3K | Lipid kinase | PIP3 production, AKT activation | PIK3CA mutations, amplification |
| AKT | Serine/threonine kinase | Survival, metabolism, inhibition of apoptosis | Overexpression, phosphorylation |
| mTORC1 | Protein complex (mTOR, Raptor) | Protein synthesis, autophagy inhibition | Hyperactivation |
| mTORC2 | Protein complex (mTOR, Rictor) | Cytoskeletal organization, AKT phosphorylation | Hyperactivation |
| LINC00152 | Long non-coding RNA | Cell proliferation, gene regulation | Overexpression in HCC |
In hepatocellular carcinoma, these pathways integrate with non-coding RNA networks, particularly long non-coding RNAs like LINC00152. Research has validated LINC00152 as an independent prognostic biomarker in HCC, with high pre-treatment expression levels in tumor tissues predicting shorter overall survival (HR, 2.524; 95% CI, 1.661–4.015; P = 0.001) in patients treated with curative surgical resection [9]. This lncRNA functions as a regulatory molecule that can modulate oncogene and tumor suppressor gene expression, thereby influencing the activity of signaling pathways including mTOR and EGFR/PI3K/AKT [9] [12].
The interconnected nature of these pathways creates feed-forward loops that drive HCC progression. For instance, AKT activation directly stimulates mTORC1 activity, while mTORC2 can phosphorylate AKT, creating a reinforcing signaling circuit. Additionally, both pathways influence epithelial-mesenchymal transition (EMT), metabolic reprogramming, and therapy resistance—hallmarks of aggressive HCC [20] [21]. The prognostic significance of LINC00152 adds another layer of complexity to this network, potentially serving as both a biomarker and functional mediator of pathway activity.
Experimental Data and Functional Evidence
Quantitative Evidence from Cancer Models
Table 2: Experimental Data on Pathway Inhibition and Genetic Manipulation
| Experimental Model | Intervention/Marker | Key Findings | Quantitative Results | Reference |
|---|---|---|---|---|
| Gastric Cancer Cells | Salvigenin (EGFR/PI3K/AKT inhibitor) | Dose-dependent suppression of proliferation | 50μM reduced viability to 40% of control | [23] |
| Lung Cancer Models | PYCR1 knockout | Reduced tumor growth in vivo | Significant reduction in xenograft volume | [24] |
| HCC Patient Tissues | LINC00152 high expression | Independent prognostic value | HR 2.524 for shorter OS | [9] |
| Oral Cancer Cells | LCP1 manipulation via EGFR signaling | Promoted progression through JAK2/STAT3/IL-1β | 2.4-fold upregulation in relapsed tumors | [25] |
| Breast Cancer Stem Cells | mTOR pathway inhibition | Reduced self-renewal and therapy resistance | Decreased CSC population and metastasis | [22] |
Experimental investigations across multiple cancer types provide compelling evidence for the functional significance of these pathways. In gastric cancer, the flavonoid salvigenin demonstrated potent inhibitory effects on the EGFR/PI3K/AKT pathway, suppressing proliferation and inducing apoptosis in a dose-dependent manner. At 50μM concentration, salvigenin reduced cell viability to approximately 40% of control levels and significantly increased apoptosis rates from 5% (control) to 25% in treated cells [23]. These effects were mechanistically linked to decreased phosphorylation of EGFR and AKT, confirming pathway-specific activity.
In lung cancer models, genetic ablation of PYCR1, a metabolic enzyme functionally connected to EGFR signaling, resulted in substantially reduced tumor growth in xenograft models [24]. PYCR1 was shown to form a complex with EGFR and USP11, enhancing EGFR deubiquitination and stability, thereby sustaining oncogenic signaling. This molecular interaction represents a novel interface between metabolic processes and canonical growth factor signaling in cancer progression.
The pivotal role of mTOR signaling in cancer stem cell maintenance has been extensively documented in breast cancer models. mTOR pathway activity was found essential for breast cancer stem cell (BCSC) self-renewal, metastasis, and therapy resistance. Inhibition of mTOR signaling reduced BCSC populations and diminished metastatic potential, though interestingly, lung metastases sometimes persisted despite primary tumor regression, indicating context-dependent pathway utilization [22].
Methodologies for Pathway Analysis
Standard Experimental Protocols
Investigation of mTOR and EGFR/PI3K/AKT pathway activity employs well-established methodological approaches that enable comprehensive assessment of expression, activation, and functional significance:
1. Gene Expression Analysis: Quantitative reverse-transcription polymerase chain reaction (qRT-PCR) represents the gold standard for quantifying lncRNA expression levels, including LINC00152, in tissue specimens. This method provides sensitive and reproducible quantification of transcript levels using specific primer sets. For lncRNAs, careful primer design across splice junctions is essential to ensure specificity. Typical protocols involve RNA extraction, reverse transcription, and quantitative PCR amplification with normalization to housekeeping genes [9]. RNA sequencing offers an alternative discovery-based approach for identifying novel pathway-associated lncRNAs without prior knowledge of sequence information.
2. Protein Detection and Activation Assessment: Western blotting serves as the primary method for evaluating protein expression and phosphorylation status of pathway components. For assessing EGFR/PI3K/AKT and mTOR pathway activation, antibodies targeting phosphorylated forms of EGFR, AKT (Ser473), S6K, and 4E-BP1 provide direct readouts of signaling activity. Protocol steps include protein extraction from tissues or cells, SDS-PAGE separation, transfer to membranes, antibody incubation, and chemiluminescent detection. Multiplex immunoassays offer a higher-throughput alternative for simultaneous measurement of multiple phosphoproteins [20] [23].
3. Functional Validation Experiments: Genetic manipulation using CRISPR-Cas9 or RNA interference (siRNA/shRNA) enables determination of causal relationships between pathway components and cancer phenotypes. For instance, PYCR1-knockout lung cancer cells generated via CRISPR-Cas9 showed significantly reduced proliferation, migration, and tumor spheroid growth in vitro and in vivo [24]. Similarly, siRNA-mediated knockdown of oncogenic lncRNAs like HOTAIR inhibited HCC cell proliferation (60% reduction) and induced apoptosis (25% vs. 5% in controls) [12].
4. Pathway Inhibition Studies: Small molecule inhibitors targeting specific pathway nodes provide both functional insights and therapeutic validation. These include selective PI3K inhibitors (e.g., Pictilisib), AKT inhibitors (e.g., MK-2206), and mTOR inhibitors (e.g., Rapamycin, Everolimus). Recent advances include dual PI3K/mTOR inhibitors that simultaneously target multiple pathway components [21]. Dose-response experiments measuring cell viability, apoptosis, and colony formation following inhibitor treatment establish pathway dependency.
5. In Vivo Tumor Models: Xenograft studies in immunocompromised mice (e.g., NSG mice) enable assessment of pathway function in a physiological context. Control or genetically modified cancer cells are injected subcutaneously or orthotopically, with tumor growth monitored regularly. For example, PYCR1-knockout A549 cells showed significantly reduced tumor growth compared to controls in xenograft models [24]. These models also permit evaluation of therapeutic efficacy for pathway-specific inhibitors.
Research Reagent Solutions
Table 3: Essential Research Reagents for Pathway Investigation
| Reagent Category | Specific Examples | Research Applications | Key Features |
|---|---|---|---|
| Small Molecule Inhibitors | Salvigenin, PYCR1-IN-1, Rapamycin | Pathway inhibition studies | Target specificity, dose-dependent effects |
| siRNA/shRNA Libraries | HOTAIR siRNA, LINC00152-targeting siRNA | Genetic manipulation of ncRNAs | Gene knockdown efficiency, specificity |
| Phospho-Specific Antibodies | Anti-phospho-EGFR, anti-phospho-AKT (Ser473) | Western blot, IHC | Detection of activated pathway components |
| Cell Line Models | A549 (lung cancer), HepG2 (HCC), HGC-27 (gastric) | In vitro pathway studies | Pathway activation, genetic manipulability |
| Animal Models | NSG mice, xenograft models | In vivo pathway validation | Tumor engraftment, response to therapeutics |
Pathway Diagrams and Molecular Interactions
EGFR/PI3K/AKT/mTOR Signaling Network
EGFR/PI3K/AKT/mTOR Signaling Network with LINC00152 Integration
Experimental Workflow for Pathway Validation
Comprehensive Workflow for Pathway Validation Studies
The mTOR and EGFR/PI3K/AKT signaling pathways represent interconnected networks that drive hepatocellular carcinoma progression through regulation of cell growth, survival, metabolism, and therapy resistance. The independent prognostic value of LINC00152 in HCC underscores the complex interplay between traditional signaling cascades and the non-coding RNA landscape. Experimental evidence from multiple cancer models demonstrates that targeted inhibition of these pathways can suppress tumor growth and sensitize cancer cells to apoptosis. The structured methodological approaches and research reagents outlined in this review provide investigators with essential tools for further elucidating the complexity of these oncogenic pathways. Future research directions should focus on developing dual-pathway inhibitors, validating combinatorial therapeutic approaches, and exploring the precise mechanistic relationships between prognostic lncRNAs like LINC00152 and established signaling cascades in HCC progression and treatment resistance.
Detection Platforms and Clinical Translation for Prognostic Stratification
Long non-coding RNAs (lncRNAs) have emerged as crucial players in cancer biology, with LINC00152 identified as a significant oncogenic molecule in hepatocellular carcinoma (HCC). This 828-nucleotide RNA, located on chromosome 2p11.2, demonstrates markedly elevated expression in HCC tissues compared to matched normal tissue [3]. Research confirms its substantial independent prognostic value for predicting patient outcomes, with high LINC00152 expression significantly associated with decreased overall survival (OS) and progression-free survival (PFS) rates [26] [27]. The detection and quantification of this molecule have become paramount in HCC research, relying primarily on methodologies such as quantitative PCR (qRT-PCR), RNA Sequencing (RNA-Seq), and the minimally invasive approach of liquid biopsy.
Comparative Performance of Detection Methodologies
The evaluation of LINC00152 in clinical and research settings utilizes distinct technological platforms, each with characteristic strengths and limitations. The table below provides a structured comparison of qRT-PCR, RNA-Seq, and liquid biopsy for analyzing LINC00152.
Table 1: Comparison of Key Methodologies for LINC00152 Detection and Analysis
| Feature | qRT-PCR | RNA-Seq | Liquid Biopsy |
|---|---|---|---|
| Primary Role | Targeted quantification of known transcripts [18] | Discovery-oriented, full transcriptome profiling [28] | Minimally invasive disease monitoring & diagnosis [29] |
| Throughput | Low-throughput [28] | High-throughput [28] | Varies (platform-dependent) |
| Sensitivity | High [28] | High sensitivity and resolution [28] | High (especially for NGS/ddPCR platforms) [30] |
| Key Advantage | Fast, low-cost, high sensitivity for validated targets [28] | Can detect novel transcripts, splicing variants, and fusions [28] | Non-invasive, allows for real-time monitoring of disease [29] |
| Key Limitation | Requires specific primers; limited to known sequences [28] | High cost, complex data analysis [28] | Lack of standardization; analytical challenges [29] |
| Typical Sample Source | Tissue, cell lines, blood (for serum/plasma RNA) [18] [26] | Tissue, cell lines, blood (for cfRNA/CTC) [28] | Blood (plasma/serum), urine, other biofluids [29] [28] |
| Application in LINC00152 Research | Measuring relative expression in tissues/cells/ serum [18] [3] [26] | Profiling complete RNA expression networks and interactions [3] | Using serum LINC00152 as a non-invasive biomarker for HCC [18] |
Liquid biopsy itself is not a detection platform but a sample type (e.g., blood). The actual analysis of LINC00152 from liquid biopsy samples relies on the platforms listed above. A meta-analysis of liquid biopsy components highlights that next-generation sequencing (NGS) demonstrates the greatest sensitivity, followed by digital droplet PCR (ddPCR) and then qPCR [30].
Table 2: Comparison of Liquid Biopsy Components and Detection Platforms
| Liquid Biopsy Component | Description | Relevant Detection Platforms |
|---|---|---|
| Circulating Tumor DNA (ctDNA) | Tumor-derived fragmented DNA in blood; short half-life allows for real-time monitoring [29]. | qPCR, ddPCR, NGS [29] [30] |
| Circulating Tumor Cells (CTCs) | Whole tumor cells shed into circulation; rare but information-rich [29] [28]. | CellSearch (FDA-approved), microfluidic devices, RNA-seq [29] [28] |
| Cell-free RNA (cfRNA) / Extracellular Vesicles (EVs) | Includes fragmented mRNA and non-coding RNAs (e.g., LINC00152) protected in vesicles or protein complexes [28]. | qRT-PCR, ddPCR, RNA-seq [18] [28] |
Experimental Protocols for Key Studies
Protocol 1: Detecting Serum LINC00152 via qRT-PCR for HCC Prognosis
This protocol is adapted from a 2023 study investigating the clinical significance of serum LINC00152 in HCV-induced HCC [18].
- Step 1: Sample Collection and Preparation. Collect peripheral blood samples (e.g., 5 mL) from patients (HCC, liver cirrhosis) and healthy controls. Process samples by centrifugation to isolate serum or plasma and store at -80°C until RNA extraction.
- Step 2: RNA Extraction. Extract total RNA from the serum/plasma using commercial kits, such as Trizol reagent. The inclusion of a spike-in control during extraction is recommended to monitor efficiency and potential losses.
- Step 3: Reverse Transcription. Synthesize complementary DNA (cDNA) from the extracted RNA using a Reverse Transcription Kit (e.g., RevertAid First Strand cDNA Synthesis Kit) with random hexamers or oligo(dT) primers.
- Step 4: Quantitative Real-Time PCR (qRT-PCR). Perform qRT-PCR using a system-specific master mix (e.g., SYBR Green). The reaction mixture includes cDNA template, forward and reverse primers specific to LINC00152, and the fluorescent dye. A housekeeping gene (e.g., GAPDH) must be run in parallel for normalization.
- Primer Sequence Example: LINC00152-F: 5′-AAAATCACGACTCAGCCCCC-3′; LINC00152-R: 5′-AATGGGAAACCGACCAGACC-3′ [31].
- Step 5: Data Analysis. Calculate the relative expression level of LINC00152 using the comparative Ct (2^(-ΔΔCt)) method. Statistically analyze the differences in expression levels between patient groups and perform ROC curve analysis to evaluate diagnostic performance.
Protocol 2: Functional Analysis of LINC00152 Using RNA-Seq and In Vivo Validation
This protocol synthesizes approaches from multiple studies to outline how RNA-seq can be used to uncover the functional role and signaling pathways of LINC00152 in HCC [3].
- Step 1: In Vitro Model Generation. Select appropriate HCC cell lines (e.g., HepG2, MHCC-97H). Create stable knockdown models of LINC00152 using lentiviral vectors delivering specific short hairpin RNAs (shRNAs). A non-targeting shRNA serves as a control.
- Step 2: Phenotypic Assays. Conduct functional assays to characterize the impact of LINC00152 knockdown. These include Cell Counting Kit-8 (CCK-8) and EdU assays for proliferation, and Transwell chambers for migration and invasion.
- Step 3: RNA Sequencing and Bioinformatics. Extract total RNA from knockdown and control cells. Prepare sequencing libraries and perform high-throughput RNA-seq. Analyze the data to identify differentially expressed genes (DEGs). Use Gene Set Enrichment Analysis (GSEA) tools to identify signaling pathways significantly altered upon LINC00152 knockdown (e.g., mTOR pathway) [3].
- Step 4: In Vivo Validation. Subcutaneously inject LINC00152-knockdown and control HCC cells into immunodeficient mice (e.g., BALB/C nude mice). Monitor tumor growth over several weeks, measuring tumor volume and weight. This confirms the tumor-promoting role of LINC00152 in a living organism [3].
- Step 5: Mechanistic Confirmation. Validate key findings from the RNA-seq analysis using Western blot to examine protein-level changes in the identified pathway (e.g., phosphorylation levels of mTOR) [3].
Signaling Pathways and Molecular Mechanisms
LINC00152 exerts its oncogenic effects in HCC through multiple signaling pathways. Functional studies using microarray and RNA-seq analyses have revealed that knockdown of LINC00152 leads to the significant downregulation of the mTOR signaling pathway [3]. Further mechanistic investigations suggest that LINC00152 can activate the PI3K/Akt/mTOR signaling axis, potentially by acting as a competing endogenous RNA (ceRNA) that sequesters miRNAs. For instance, LINC00152 has been shown to regulate PIK3CA, a key subunit of PI3K, through interaction with miR-139 [13]. The following diagram illustrates these core interactions.
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful investigation of LINC00152 requires a suite of reliable research reagents and platforms. The table below details key materials and their functions based on cited experimental workflows.
Table 3: Essential Reagents and Tools for LINC00152 and Liquid Biopsy Research
| Reagent/Tool | Specific Example | Function in Research |
|---|---|---|
| HCC Cell Lines | HepG2, MHCC-97H, Huh7, SMMC-7721, Hep3B [3] [26] | In vitro models for studying LINC00152 function via gain/loss-of-function experiments. |
| Normal Liver Cell Lines | L02, Chang liver, HL7702, THLE-2, THLE-3 [3] [26] | Control cell lines for establishing baseline expression and tumor-specific overexpression. |
| RNA Extraction Kit | Trizol reagent [31] [26] | Isolation of high-quality total RNA from tissues, cells, or liquid biopsy samples. |
| Reverse Transcription Kit | RevertAid First Strand cDNA Synthesis Kit [31] | Synthesis of stable cDNA from RNA templates for subsequent PCR amplification. |
| qRT-PCR Master Mix | SYBR Select Master Mix, KAPA SYBR Green kit [18] [26] | Fluorescence-based detection and quantification of target cDNA (e.g., LINC00152) during PCR. |
| Lentiviral shRNA System | pLKO.1 vector [31] | For creating stable gene knockdown (e.g., LINC00152) in cell lines and in vivo models. |
| Proliferation Assay Kits | Cell Counting Kit-8 (CCK-8), EdU Assay Kit [3] | Quantitative measurement of cell proliferation and DNA synthesis rates. |
| In Vivo Model | BALB/C nude mice [3] [31] | Animal model for studying tumor growth and gene function in a physiological context. |
| CTC Enrichment System | CellSearch System [29] | FDA-cleared, immunomagnetic method for enriching and enumerating Circulating Tumor Cells. |
| Z-Gly-Arg-Thiobenzyl Ester | Z-Gly-Arg-Thiobenzyl Ester, MF:C23H29N5O4S, MW:471.6 g/mol | Chemical Reagent |
| Caloxin 3A1 | Caloxin 3A1, MF:C83H126N22O30, MW:1912.0 g/mol | Chemical Reagent |
Machine Learning Integration for Enhanced Diagnostic and Prognostic Modeling
The integration of machine learning (ML) into oncological research is revolutionizing the development of diagnostic and prognostic models. This guide objectively compares the performance of traditional biochemical methods against emerging ML-driven approaches, using the long non-coding RNA LINC00152 as a paradigm within hepatocellular carcinoma (HCC) research. Supported by experimental data, we demonstrate that ML integration significantly enhances the predictive power and clinical utility of prognostic biomarkers, offering a transformative path for precision oncology.
Hepatocellular carcinoma (HCC) constitutes more than 90% of primary liver cancer cases worldwide and ranks third in mortality rate among all human cancers, resulting in over 800,000 deaths annually [9]. A significant challenge in its management is the considerable heterogeneity in patient outcomes, driving the urgent need for reliable biomarkers that can independently predict prognosis. In this context, long non-coding RNAs (lncRNAs)—transcripts longer than 200 nucleotides with limited or no protein-coding capacity—have emerged as crucial regulators of oncogenesis and promising prognostic biomarkers [9] [16].
Among these, the long intergenic non-coding RNA 00152 (LINC00152), an 828-bp lncRNA located on chromosome 2p11.2, has been identified as a potent oncogene [16]. This review provides a comparative analysis of methodologies used to quantify and model the prognostic value of LINC00152, framing this discussion within the broader thesis of its independent prognostic significance in HCC. We evaluate traditional molecular biology techniques against modern ML-integrated approaches, using quantitative data and experimental protocols to illustrate a paradigm shift towards data-driven clinical tools.
LINC00152: An Independent Prognostic Biomarker in HCC
Biological Function and Mechanistic Role
LINC00152 is not merely a passive biomarker but an active player in hepatocarcinogenesis. It exerts its oncogenic functions primarily through a competing endogenous RNA (ceRNA) mechanism. In this capacity, LINC00152 acts as a molecular sponge for a suite of tumor-suppressive microRNAs, including let-7c-5p, miR-23a-3p, miR-125a-5p, miR-125b-5p, miR-143a-3p, miR-193-3p, and miR-195-5p [32]. By sequestering these miRNAs, LINC00152 prevents them from binding to their native mRNA targets, thereby deregulating key oncogenic pathways.
A critical axis identified in human HCC cell lines is the LINC00152-miR-143a-3p-KLC2 network. RNA immunoprecipitation and luciferase assays have confirmed that LINC00152 directly binds miR-143a-3p, limiting its availability to target the KLC2 gene [32]. The subsequent upregulation of Kinesin Light Chain 2 (KLC2) promotes cell proliferation, clonogenicity, and migration in vitro, and its co-expression with LINC00152 in human HCC cohorts is associated with shorter patient survival [32]. This mechanistic understanding underscores why LINC00152 is more than a correlative marker; it is a functional determinant of poor prognosis.
Prognostic Value Established via Traditional Molecular Methods
Conventional molecular biology techniques have firmly established the independent prognostic value of LINC00152 in HCC. These studies typically use well-established protocols to quantify LINC00152 expression and correlate it with clinical outcomes using multivariate Cox regression analysis.
- Experimental Protocol (qRT-PCR): Total RNA is isolated from tissue or plasma samples using kits such as the miRNeasy Mini Kit (QIAGEN). Reverse transcription into cDNA is performed using kits like the RevertAid First Strand cDNA Synthesis Kit. Quantitative real-time PCR (qRT-PCR) is then carried out using a power SYBR Green Master Mix on a real-time PCR system (e.g., ViiA 7). The housekeeping gene GAPDH is commonly used for normalization, and the ΔΔCT method is applied for relative quantification [33].
- Supporting Data: A 2019 meta-analysis of nine studies and 808 patients solidified the prognostic power of LINC00152. It found that high LINC00152 expression was positively associated with poor overall survival (pooled HR = 1.98, 95% CI: 1.70–2.31, p < .0001) and lymph node metastasis (OR = 2.93, 95% CI: 1.88–4.57, p < .0001) across various solid tumors, including HCC [5]. Individual studies consistently report similar findings, with one revealing that a high pre-treatment expression level of LINC00152 in HCC tumor tissues independently predicted a shorter overall survival (HR, 2.524; 95% CI, 1.661–4.015; P = 0.001) [9].
The following table summarizes key prognostic findings for LINC00152 in HCC derived from these traditional methodologies:
Table 1: Prognostic Value of LINC00152 in HCC from Traditional Molecular Studies
| Cohort Description | Detection Method | Endpoint | Hazard Ratio (HR) & 95% CI | P-value | Citation Context |
|---|---|---|---|---|---|
| 63 HCC patients, retrospective | qRT-PCR | Overall Survival | 2.524 (1.661–4.015) | 0.001 | [9] |
| Meta-analysis of 808 patients | Various (qRT-PCR/ISH) | Overall Survival | 1.98 (1.70–2.31) | < 0.0001 | [5] |
| Meta-analysis of 808 patients | Various (qRT-PCR/ISH) | Disease-Free Survival | 1.66 (1.20–2.29) | < 0.0001 | [5] |
Comparative Performance: Traditional Methods vs. ML-Integrated Approaches
While traditional methods successfully identify biomarkers, they often face limitations in diagnostic sensitivity and specificity when used in isolation. The integration of machine learning allows for the modeling of complex, non-linear interactions between multiple biomarkers and clinical variables, leading to superior performance.
Experimental Protocol for ML Integration
A seminal study illustrates the protocol for developing an ML model that integrates lncRNAs with conventional laboratory data [33].
- Cohort and Biomarker Selection: A cohort of 52 HCC patients and 30 age-matched controls was recruited. Plasma levels of four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) were quantified via qRT-PCR, following the protocol detailed in Section 2.2.
- Data Integration: The expression data of the four lncRNAs were combined with additional routine clinical laboratory parameters (e.g., ALT, AST, AFP, total bilirubin, albumin) to form a multidimensional feature set.
- Model Construction: A machine learning model was constructed using Python's Scikit-learn platform. The specific algorithm used was not named in the study, but common classifiers for such tasks include Random Forest, Support Vector Machines, or XGBoost.
- Model Training and Validation: The model was trained on the dataset to distinguish between HCC patients and healthy controls. Performance was evaluated using metrics such as sensitivity, specificity, and area under the curve (AUC).
Performance Comparison Data
The experimental results demonstrate a clear advantage for the ML-integrated approach.
- Individual lncRNA Performance: When assessed individually via traditional ROC curve analysis, the four lncRNAs (including LINC00152) showed moderate diagnostic accuracy, with sensitivity and specificity ranging from 60% to 83% and 53% to 67%, respectively [33].
- ML-Integrated Model Performance: In stark contrast, the ML model that integrated all four lncRNAs with the standard laboratory parameters demonstrated dramatically superior performance, achieving 100% sensitivity and 97% specificity in diagnosing HCC [33].
This comparative data underscores a critical point: the prognostic and diagnostic power of a biomarker like LINC00152 is substantially enhanced when it is not used in isolation but as part of a multivariate panel processed through a machine learning algorithm.
Table 2: Performance Comparison: Single LINC00152 vs. ML-Integrated Panel
| Methodology | Biomarkers Used | Sensitivity | Specificity | Key Advantage |
|---|---|---|---|---|
| Traditional (qRT-PCR) | LINC00152 only | 60 - 83% | 53 - 67% | Establishes individual prognostic value |
| ML-Integrated | LINC00152 + 3 other lncRNAs + lab tests | 100% | 97% | Captures complex interactions for superior accuracy |
Successful development of diagnostic and prognostic models, whether traditional or ML-based, relies on a foundation of specific, high-quality research reagents.
Table 3: Key Research Reagent Solutions for LINC00152 and HCC Prognostic Modeling
| Reagent / Resource | Function / Application | Example Product / Source |
|---|---|---|
| RNA Isolation Kit | Extracts high-quality total RNA from tissue or plasma samples for downstream analysis. | miRNeasy Mini Kit (QIAGEN) [33] |
| cDNA Synthesis Kit | Reverse transcribes RNA into stable complementary DNA (cDNA) for qRT-PCR. | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [33] |
| qRT-PCR Master Mix | Enables sensitive and specific quantification of lncRNA expression levels. | PowerTrack SYBR Green Master Mix (Applied Biosystems) [33] |
| LINC00152 Primers | Sequence-specific primers for amplifying the LINC00152 transcript. | Custom designed; e.g., Sense: GACTGGATGGTCGCTTT, Antisense: CCCAGGAACTGTGCTGTGAA [33] |
| ML & Data Analysis Platform | Open-source platform for building, training, and validating machine learning models. | Python Scikit-learn [33] |
| Public Genomic Databases | Sources of large-scale transcriptomic and clinical data for model training and validation. | The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO) [34] |
Visualizing the Workflow: From Biomarker Discovery to Prognostic Model
The following diagram illustrates the integrated experimental and computational workflow for developing a machine learning-enhanced prognostic model, contrasting it with the traditional pathway.
Visualizing the Molecular Mechanism of LINC00152
Understanding the molecular function of a biomarker is crucial for justifying its role in a prognostic model. The diagram below depicts the ceRNA mechanism by which LINC00152 promotes HCC progression.
The journey of LINC00152 from a functionally enigmatic lncRNA to a validated independent prognostic biomarker in HCC illustrates a critical evolution in oncological research. While traditional molecular methods provide the foundational evidence for its clinical relevance, the integration of machine learning represents a paradigm shift. By leveraging ML to model the complex interactions between LINC00152, other lncRNAs, and standard clinical data, researchers can develop tools with unprecedented diagnostic sensitivity and prognostic accuracy. This comparative analysis strongly advocates for a future where the discovery of single biomarkers and the development of multi-parameter, AI-driven prognostic models are pursued in tandem, accelerating the path toward truly personalized cancer medicine.
Hepatocellular carcinoma (HCC) is a leading cause of cancer-related mortality worldwide, characterized by heterogeneous patient outcomes that necessitate robust prognostic biomarkers for optimal clinical management [1]. Long intergenic non-coding RNA 152 (LINC00152) has emerged as a promising molecular biomarker with independent prognostic value across multiple cancer types, including HCC [15] [5]. This lncRNA, located on chromosome 2p11.2 and consisting of 828 nucleotides, demonstrates significant dysregulation in HCC tissues and blood circulation, where its expression level correlates strongly with critical clinical parameters including tumor progression, metastasis, and overall survival [1] [8]. This review comprehensively evaluates the clinical applications of LINC00152 in HCC risk stratification, survival prediction, and treatment monitoring, synthesizing experimental evidence and mechanistic insights to establish its utility as a standalone prognostic indicator within the broader context of HCC biomarker research.
Clinical Evidence: Prognostic Value of LINC00152 in HCC
Multiple clinical studies have consistently demonstrated that elevated LINC00152 expression is significantly associated with aggressive HCC phenotypes and poor clinical outcomes, supporting its utility in risk stratification and survival prediction.
Table 1: Summary of Clinical Studies on LINC00152 in HCC
| Study Population | Detection Method | Key Findings | Statistical Significance | Reference |
|---|---|---|---|---|
| 120 patients (60 HCC, 60 cirrhosis), 40 controls | qRT-PCR (serum) | LINC00152 upregulated in HCC; independent prognostic factor for poor outcome | HR=2.23, 95% CI=1.30–5.29, p=0.03 | [1] |
| 102 paired HCC tissues | qRT-PCR (tissue) | Overexpression correlated with larger tumor size (p=0.005) and higher Edmondson grade (p=0.002) | Significant association | [8] |
| 63 HCC patients (retrospective) | qRT-PCR (tissue) | High pre-treatment expression predicted shorter overall survival | HR=2.524, 95% CI=1.661–4.015, p=0.001 | [9] |
| Meta-analysis (9 studies, 808 patients) | Multiple methods | Association with lymph node metastasis and poor overall survival | OR=2.93, 95% CI=1.88–4.57, p<.0001 for LNM; HR=1.98, 95% CI=1.70–2.31, p<.0001 for OS | [5] |
Beyond the data summarized in Table 1, additional evidence confirms LINC00152's clinical relevance. Serum LINC00152 levels show remarkable diagnostic performance, effectively distinguishing HCC patients from those with liver cirrhosis and healthy controls [1]. Furthermore, elevated LINC00152 expression associates with clinically aggressive features, including lesions in both liver lobes (p=0.02) and advanced tumor stage [1]. Multivariate analyses across multiple studies confirm that high LINC00152 expression serves as an independent predictor of unfavorable prognosis in HCC patients, even after adjusting for other clinical variables [1] [9].
Table 2: LINC00152 Association with Clinicopathological Features in HCC
| Clinicopathological Feature | Association with High LINC00152 | Statistical Significance | Reference |
|---|---|---|---|
| Tumor Size | Larger tumors | p=0.005 | [8] |
| Tumor Grade | Higher Edmondson grade | p=0.002 | [8] |
| Liver Involvement | Lesions in both lobes | p=0.02 | [1] |
| Vascular Invasion | Positive association | Not specified | [8] |
| Tumor Stage | Advanced stage | Not specified | [1] |
| Lymph Node Metastasis | Positive association | OR=2.93, 95% CI=1.88–4.57 | [5] |
Molecular Mechanisms Underlying LINC00152 Function
The prognostic significance of LINC00152 in HCC is underpinned by its involvement in diverse molecular pathways that drive tumor progression and therapeutic resistance. The molecular mechanisms through which LINC00152 promotes HCC pathogenesis are multifaceted, involving epigenetic regulation, signal transduction activation, and post-transcriptional modulation.
The diagram illustrates three primary mechanistic pathways through which LINC00152 influences hepatocellular carcinoma progression:
Nuclear Mechanisms: Transcriptional and Epigenetic Regulation
In the nucleus, LINC00152 localizes and participates in direct gene regulation. Studies demonstrate that LINC00152 activates the mTOR signaling pathway by binding to the promoter of Epithelial Cell Adhesion Molecule (EpCAM) through cis-regulatory mechanisms [8]. This activation promotes cancer cell proliferation, division, and carcinogenesis. Additionally, LINC00152 interacts with enhancer of zeste homolog 2 (EZH2), a component of the polycomb repressive complex 2 (PRC2), facilitating histone modifications and epigenetic silencing of tumor suppressor genes [15] [35].
Cytoplasmic Mechanisms: miRNA Sponging (ceRNA Network)
In the cytoplasm, LINC00152 functions as a competing endogenous RNA (ceRNA) by sequestering multiple tumor-suppressive microRNAs. This sponging activity prevents miRNAs from binding to their target mRNAs, thereby derepressing oncogenic pathways. Key miRNA interactions include:
- miR-139-5p: Sponging leads to increased NOTCH1 expression, promoting CRC progression and development [19]
- miR-125b: Results in upregulation of SEMA4C, enhancing tumor growth [15]
- miR-193a/b-3p: Leads to increased CCND1 expression, driving cell cycle progression [15]
Therapy Resistance Mechanisms
LINC00152 confers resistance to various cancer treatments through multiple pathways. In breast cancer, LINC00152 inhibits tamoxifen-induced ferroptosis by stabilizing phosphodiesterase 4D (PDE4D) mRNA, leading to reduced cAMP levels and subsequent suppression of calcium-mediated ferroptotic cell death [36]. Similarly, in colorectal cancer, LINC00152 confers 5-FU resistance by suppressing drug-induced apoptosis [19].
Experimental Methodologies for LINC00152 Analysis
Standardized experimental protocols are essential for reliable detection and quantification of LINC00152 in clinical and research settings. This section details the key methodologies employed in the cited studies.
Sample Collection and RNA Extraction
- Blood Collection: 8 mL of venous blood collected using vacutainer needle; 4 mL placed in plain vacutainer tube, 2 mL in EDTA tube, and 1.8 mL in sodium citrate tube for prothrombin time measurement [1]
- Serum Separation: Plain tubes centrifuged for 10 minutes at 4000 RPM; supernatant serum stored at -80°C for further analysis [1]
- RNA Extraction: QIAamp RNA Blood Mini Kit (Qiagen, Cat. No./ID: 52304) used according to manufacturer's instructions [1]
Quantitative Real-Time PCR (qRT-PCR)
The most widely employed method for LINC00152 quantification involves qRT-PCR with the following standardized protocol:
- cDNA Synthesis: RNA reverse transcribed using QuantiTect Reverse Transcription Kit (Qiagen) [1]
- PCR Reaction Composition:
- Final volume: 20 μL
- 10 μL SYBR Green 2× QuantiTect PCR Master Mix
- 3 μL cDNA template
- 1 μL each of forward and reverse primers
- 5 μL RNase-free H₂O [1]
- Primer Sequences:
- LINC00152 Forward: 5′-GACTGGATGGTCGCTGCTTT-3′
- LINC00152 Reverse: 5′-CCCAGGAACTGTGCTGTGAA-3′
- GAPDH Forward: 5′-CGGAGTCAACGGATTGGTCGTAT-3′
- GAPDH Reverse: 5′-AGCCTTCTCCATGGTGGTGAAGAC-3′ [1]
- Amplification Conditions:
- Activation: 95°C for 3 minutes
- Amplification (55 cycles): 94°C for 30 seconds, 55°C for 30 seconds, 72°C for 30 seconds
- Melting curve analysis to confirm specificity [1]
- Data Analysis: Relative expression calculated using the ΔΔCT method with GAPDH as endogenous control [1]
In Situ Hybridization (ISH)
For tissue-based localization and quantification:
- Probes: RNAscope 2.5 HD Detection Reagent-BROWN (#322310) with specific LINC00152 probe (#18081B) [37]
- Controls: DapB probe (#310043) as negative control, Hs-PPIB (#313901) as positive control [37]
- Detection: Dark-brown punctuate dots in nucleus and/or cytoplasm considered positive [37]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for LINC00152 Investigation
| Reagent/Kit | Specific Product Information | Application | Function | |
|---|---|---|---|---|
| RNA Extraction Kit | QIAamp RNA Blood Mini Kit (Qiagen, Cat. No. 52304) | RNA isolation from blood samples | Purifies high-quality RNA for downstream applications | [1] |
| Reverse Transcription Kit | QuantiTect Reverse Transcription Kit (Qiagen) | cDNA synthesis | Converts RNA to stable cDNA for PCR amplification | [1] |
| qPCR Master Mix | QuantiTect SYBR Green PCR Kit (Qiagen) | Quantitative real-time PCR | Enables fluorescence-based quantification of LINC00152 | [1] |
| In Situ Hybridization Kit | RNAscope 2.5 HD Detection Reagent-BROWN (ACD, #322310) | Tissue-based LINC00152 detection | Visualizes spatial distribution in FFPE tissues | [37] |
| LINC00152 Probe | RNAscope Probe-LINC00152 (ACD, #18081B) | Specific target detection | Specifically hybridizes to LINC00152 transcript | [37] |
| Cell Proliferation Assay | Cell Counting Kit-8 (CCK-8) | In vitro proliferation assessment | Measures metabolic activity as proxy for cell viability | [8] |
| Ihmt-mst1-58 | Ihmt-mst1-58, MF:C21H22N6O3S, MW:438.5 g/mol | Chemical Reagent | Bench Chemicals | |
| eIF4A3-IN-10 | eIF4A3-IN-10|eIF4F Complex Inhibitor|1402931-72-9 | eIF4A3-IN-10 is a potent silvestrol analog that disrupts the eIF4F complex. This product is for research use only and not for human use. | Bench Chemicals |
Comparative Analysis with Other Prognostic lncRNAs in HCC
LINC00152 demonstrates distinctive advantages as a prognostic biomarker in HCC when compared to other lncRNAs investigated in similar contexts.
Table 4: Comparison of LINC00152 with Other Prognostic lncRNAs in HCC
| lncRNA | Expression in HCC | Prognostic Value | Key Mechanisms | Clinical Advantages | |
|---|---|---|---|---|---|
| LINC00152 | Upregulated | Independent prognostic factor (HR=2.23-2.52) | mTOR activation, miRNA sponging, epigenetic regulation | Detectable in serum, independent prognostic value, correlates with multiple aggressive features | [1] [9] [8] |
| LINC00294 | Upregulated | Shorter OS (HR=2.43) | Not fully elucidated | Tissue-based prognostic value | [9] |
| LINC01094 | Upregulated | Shorter OS (HR=2.09) | Not fully elucidated | Identified via RNA sequencing | [9] |
| LINC01139 | Upregulated | Shorter OS (HR=2.72) | Not fully elucidated | Tissue-based prognostic value | [9] |
| LINC01554 | Downregulated | Shorter OS when low (HR=2.51) | Potential tumor suppressor | Tumor suppressor activity | [9] |
The comparative analysis reveals that LINC00152 possesses unique clinical advantages, including its detectability in circulating blood, strong independent prognostic value across multiple studies, and association with diverse aggressive clinicopathological features. Furthermore, the well-characterized molecular mechanisms of LINC00152 provide a solid foundation for understanding its functional role in HCC pathogenesis, surpassing the current understanding of many other prognostic lncRNAs in HCC.
The comprehensive analysis of current evidence firmly establishes LINC00152 as a promising biomarker with significant clinical utility in hepatocellular carcinoma risk stratification, survival prediction, and potentially treatment monitoring. Its independent prognostic value, consistent demonstration across multiple study cohorts, and detectability in both tissue and liquid biopsies position LINC00152 as a strong candidate for clinical implementation. The well-elucidated molecular mechanisms, particularly its involvement in mTOR signaling, epigenetic regulation, and therapy resistance pathways, provide a mechanistic foundation for its clinical associations and suggest potential therapeutic targeting opportunities.
Future research directions should focus on standardizing detection protocols for clinical use, validating LINC00152 in prospective multicenter trials, and exploring its utility in guiding personalized treatment strategies. Additionally, investigating the potential of LINC00152 as a therapeutic target, particularly in combination with existing treatments, represents a promising avenue for improving outcomes in HCC patients. As the field of lncRNA biomarkers continues to evolve, LINC00152 stands out as a frontrunner with substantial potential to enhance clinical decision-making and patient management in hepatocellular carcinoma.
Hepatocellular carcinoma (HCC) constitutes a major global health challenge, ranking as the sixth most common cancer worldwide and the third leading cause of cancer-related mortality [10]. The disease epitomizes a significant public health problem in Egypt, occupying the first and second most common cancers in men and women, respectively [1]. Despite advancements in therapeutic options, the overall survival benefit for HCC patients remains unsatisfactory, largely due to late diagnosis and limited effective treatment options for advanced disease [38]. This clinical landscape has accelerated the search for molecular biomarkers that can enable early detection and accurate prognosis prediction.
Long non-coding RNAs (lncRNAs), defined as RNA transcripts longer than 200 nucleotides that lack protein-coding capacity, have emerged as promising biomarkers and therapeutic targets in HCC [39] [38]. These molecules regulate gene expression through diverse mechanisms, including epigenetic modification, interaction with microRNAs, and protein interactions [40]. Their expression exhibits high tissue specificity, and they are detectable in body fluids, making them accessible for liquid biopsy applications [10]. Among the numerous lncRNAs dysregulated in HCC, LINC00152 has been identified as having independent prognostic value, while UCA1, GAS5, and HULC show complementary diagnostic and prognostic potential [1] [10] [38].
Individual lncRNA Profiles and Functional Mechanisms
LINC00152: An Independent Prognostic Indicator
LINC00152, also known as long intergenic non-coding RNA 152, is an 828-base pair lncRNA located on chromosome 2p11.2 [1]. It functions as a non-coding oncogene that stimulates the mechanistic target of the rapamycin (mTOR) pathway, which plays a critical role in controlling cancer cell proliferation, division, and carcinogenesis [1]. The prognostic significance of LINC00152 is substantiated by clinical evidence demonstrating that high serum levels independently predict poorer outcomes in HCC patients (hazard ratio [HR] = 2.23, 95% confidence interval [CI] = 1.30–5.29, p = 0.03) [1]. Additional studies have confirmed that high pretreatment tissue expression levels of LINC00152 independently predict shorter overall survival (HR = 2.524, 95% CI = 1.661–4.015, p = 0.001) in HCC patients treated with curative surgical resection [38].
Table 1: Prognostic Value of Individual lncRNAs in HCC
| lncRNA | Expression in HCC | Biological Function | Prognostic Value | Clinical Associations |
|---|---|---|---|---|
| LINC00152 | Upregulated | Activates mTOR pathway; promotes cell cycle progression | HR = 2.23-2.524; independent prognostic factor | Lesions in both liver lobes; poorer survival |
| UCA1 | Upregulated | Promotes proliferation, inhibits apoptosis | Associated with advanced disease | Vascular invasion; late tumor stage |
| GAS5 | Downregulated | Triggers CHOP and caspase-9 pathways | Higher LINC00152/GAS5 ratio predicts mortality | Tumor suppressor; induces apoptosis |
| HULC | Highly upregulated | Not fully elucidated in reviewed studies | Potential diagnostic combination with LINC00152 | Requires further prognostic validation |
UCA1: Diagnostic and Pathological Correlations
The long non-coding RNA Urothelial cancer associated 1 (UCA1), also known as CUDR (cancer upregulated drug resistant), is situated at chromosome 19p13.12 [1]. Its upregulation has been documented in many cancers, and it plays significant roles in colorectal, prostate, stomach, and bladder cancers [1]. In HCC, UCA1 expression shows significant correlations with aggressive clinicopathological features, including vascular invasion (p = 0.01) and advanced tumor stage (p = 0.03) [1]. While UCA1 demonstrates strong diagnostic performance, its independent prognostic value requires further validation in multivariate models that include LINC00152.
GAS5: The Tumor Suppressor
In contrast to the oncogenic lncRNAs, Growth Arrest-Specific 5 (GAS5) functions as a tumor suppressor in HCC [10]. It exerts its antitumor effects by triggering CHOP and caspase-9 signal pathways, leading to inhibited cancer cell proliferation and activation of apoptosis [10]. The expression ratio between LINC00152 and GAS5 has emerged as a particularly powerful prognostic indicator, with a higher LINC00152 to GAS5 ratio significantly correlating with increased mortality risk [10]. This ratio potentially provides a more comprehensive biological snapshot than either biomarker alone.
HULC: Highly Upregulated in Liver Cancer
HULC (Highly Upregulated in Liver Cancer) was one of the first identified lncRNAs with elevated expression in hepatocellular carcinoma [39]. While the specific molecular mechanisms of HULC were not extensively detailed in the reviewed studies, it has been proposed as part of diagnostic panels combining LINC00152 and AFP, or both AFP and HULC [10]. This suggests its complementary value in multi-lncRNA panels despite potentially lacking independent prognostic significance.
Multi-lncRNA Panels: Enhanced Diagnostic and Prognostic Performance
LINC00152 and UCA1 Combination
The diagnostic combination of LINC00152 and UCA1 represents a promising approach for HCC detection. Both lncRNAs show significantly elevated serum levels in HCC patients compared to those with liver cirrhosis and healthy controls (p < 0.001 for both) [1]. When used in combination, these biomarkers effectively distinguish HCC patients from those with liver cirrhosis, as demonstrated by receiver operating characteristic (ROC) analysis [1]. The complementary nature of their clinical associations—LINC00152 with bilobar lesions and UCA1 with vascular invasion—suggests that together they provide broader coverage of HCC pathological spectrum.
Comprehensive Panels Including GAS5
Expanding the panel to include GAS5 further enhances the prognostic capability through the LINC00152/GAS5 expression ratio, which significantly correlates with mortality risk [10]. This ratio conceptually represents the balance between oncogenic (LINC00152) and tumor suppressive (GAS5) forces in hepatocellular carcinoma, potentially offering a more dynamic assessment of tumor behavior than individual biomarkers alone.
Machine Learning Integration for Diagnostic Enhancement
The integration of multiple lncRNAs within machine learning frameworks represents a cutting-edge approach to HCC diagnosis. One study developed a model incorporating LINC00152, LINC00853, UCA1, and GAS5 alongside conventional laboratory parameters [10]. While individual lncRNAs exhibited moderate diagnostic accuracy with sensitivity and specificity ranging from 60% to 83% and 53% to 67%, respectively, the machine learning model demonstrated superior performance, achieving 100% sensitivity and 97% specificity [10]. This highlights the substantial diagnostic potential of multi-lncRNA panels when analyzed with advanced computational approaches.
Table 2: Performance Comparison of lncRNA Detection Approaches
| Detection Method | Target lncRNAs | Sensitivity | Specificity | Clinical Application |
|---|---|---|---|---|
| Individual qRT-PCR | LINC00152 | 60-83% | 53-67% | Initial screening; moderate accuracy |
| ROC Analysis | LINC00152 and UCA1 | Significant discrimination | HCC vs. cirrhosis | Diagnostic differentiation |
| Machine Learning Panel | LINC00152, UCA1, GAS5, LINC00853 | 100% | 97% | High-accuracy diagnosis |
| Expression Ratio | LINC00152/GAS5 | Correlates with mortality risk | Prognostic stratification | Survival prediction |
Experimental Protocols and Methodologies
Sample Collection and Processing
Standardized protocols for sample collection and processing are critical for reliable lncRNA quantification. Studies typically collect blood samples using vacutainer needles, with 4-8 mL of blood drawn from each participant [1]. Serum is obtained from plain tubes after centrifugation for 10 minutes at 4000 RPM, then stored at -80°C for further analysis [1]. For plasma-based approaches, blood collection tubes containing EDTA are used, followed by similar centrifugation and storage conditions [10]. Consistent processing protocols are essential to prevent RNA degradation and ensure reproducible results.
RNA Extraction and Quality Control
Total RNA isolation typically employs commercial kits such as the QIAamp RNA Blood Mini Kit or miRNeasy Mini Kit according to manufacturer protocols [1] [10]. RNA quality assessment through spectrophotometry or microfluidic analysis is recommended to ensure sample integrity before proceeding to cDNA synthesis. The inclusion of quality control metrics in published studies would strengthen the interpretation of lncRNA expression data.
cDNA Synthesis and Quantitative Real-Time PCR
Reverse transcription into complementary DNA (cDNA) is performed using kits such as the QuantiTect Reverse Transcription Kit or RevertAid First Strand cDNA Synthesis Kit according to manufacturer protocols [1] [10]. Quantitative real-time PCR is then carried out using SYBR Green-based detection systems such as the QuantiTect SYBR Green PCR Kit or PowerTrack SYBR Green Master Mix [1] [10]. Each PCR reaction typically has a final volume of 20 μL, containing SYBR Green Master Mix, cDNA template, forward and reverse primers, and RNase-free water.
The primer sequences used in key studies include:
- LINC00152: Forward 5′-GACTGGATGGTCGCTGCTTT-3′, Reverse 5′-CCCAGGAACTGTGCTGTGAA-3′
- UCA1: Forward 5′-TGCACCCTAGACCCGAAACT-3′, Reverse 5′-CAAGTGTGACCAGGGACTGC-3′
- GAPDH (reference gene): Forward 5′-CGGAGTCAACGGATTGGTCGTAT-3′, Reverse 5′-AGCCTTCTCCATGGTGGTGAAGAC-3′
PCR conditions typically consist of an initial activation step at 95°C for 3 minutes, followed by 40-55 cycles of denaturation at 94°C for 30 seconds, annealing at 55°C for 30 seconds, and extension at 72°C for 30 seconds [1]. Melting curve analysis is employed to confirm amplification specificity and absence of primer dimers.
Data Analysis and Normalization
The ΔΔCT method is widely used for relative quantification of lncRNA expression, with GAPDH serving as the reference gene for normalization [1] [10]. For prognostic assessments, researchers typically use the median expression value as a cutoff to divide patients into high and low expression groups, then compare survival between these groups using Kaplan-Meier analysis with log-rank tests [1] [41]. Multivariate Cox proportional hazards regression analysis is employed to determine whether lncRNA expression retains independent prognostic value after adjusting for clinical covariates [1] [38].
Figure 1: LINC00152 Oncogenic Signaling Pathway. This diagram illustrates the molecular mechanism whereby LINC00152 activates the mTOR pathway, promoting key cancer hallmarks including cell proliferation, cell cycle progression, and angiogenesis.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for lncRNA Studies in HCC
| Reagent/Category | Specific Product Examples | Application | Technical Considerations |
|---|---|---|---|
| RNA Extraction Kits | QIAamp RNA Blood Mini Kit, miRNeasy Mini Kit | Total RNA isolation from blood/tissue | Ensure RNA integrity; check A260/A280 ratios |
| Reverse Transcription Kits | QuantiTect Reverse Transcription Kit, RevertAid First Strand cDNA Synthesis Kit | cDNA synthesis from RNA templates | Include controls without reverse transcriptase |
| qRT-PCR Master Mix | QuantiTect SYBR Green PCR Kit, PowerTrack SYBR Green Master Mix | Quantitative lncRNA detection | Optimize primer annealing temperatures |
| Reference Genes | GAPDH primers | Expression normalization | Validate stability across sample types |
| Cell Lines | Huh-7 | Functional validation experiments | Authenticate regularly; check mycoplasma |
| siRNA/shRNA | Custom-designed sequences | Loss-of-function studies | Include scrambled control sequences |
| Antifungal agent 52 | Antifungal Agent 52|Tetrazole Analogue | Antifungal Agent 52 is a tetrazole analogue research compound that inhibits ergosterol synthesis. This product is For Research Use Only (RUO). Not for human or veterinary use. | Bench Chemicals |
| Cav 3.2 inhibitor 1 | Cav 3.2 Inhibitor 1|Selective T-Type Calcium Channel Blocker | Bench Chemicals |
Comparative Analysis of Multi-lncRNA Panels
The integration of LINC00152 with UCA1, GAS5, and potentially HULC creates a comprehensive molecular signature that captures multiple aspects of HCC pathogenesis. While LINC00152 provides robust independent prognostic value, UCA1 adds diagnostic specificity and association with advanced disease features [1]. The inclusion of GAS5 introduces a tumor suppressor element, with the LINC00152/GAS5 ratio offering enhanced prognostic stratification [10]. HULC may contribute additional diagnostic sensitivity when combined with established biomarkers [10].
When compared to other multi-lncRNA approaches, such as immune-related 6-lncRNA panels or disulfidptosis-related 3-lncRNA signatures, the LINC00152-centered panel benefits from stronger validation of individual component biomarkers [42] [41]. The 6-lncRNA immune signature (RHPN1-AS1, LINC01224, CTD-2510F5.4, RP1-228H13.5, LINC01011, and RP11-324I22.4) demonstrates good performance in predicting survival and distinguishing immunomodulation in the tumor microenvironment but lacks the extensive individual validation of LINC00152 [41]. Similarly, disulfidptosis-related lncRNA signatures show promise but require further biological characterization [42].
Figure 2: Experimental Workflow for lncRNA Analysis. This diagram outlines the key steps in lncRNA biomarker research, from sample collection through analytical validation.
Multi-lncRNA panels combining LINC00152 with UCA1, GAS5, and HULC represent a significant advancement in HCC biomarker research. The strong independent prognostic value of LINC00152 forms a solid foundation, while the additional lncRNAs provide complementary diagnostic information and biological insights. The integration of these panels with machine learning approaches and conventional laboratory parameters demonstrates exceptional diagnostic performance that surpasses individual biomarkers.
Future research directions should include larger prospective validation studies across diverse patient populations, standardization of detection methodologies for clinical application, and exploration of these lncRNA panels in monitoring treatment response and disease recurrence. Furthermore, investigating the functional interactions between these lncRNAs may reveal novel therapeutic targets. As the field progresses, LINC00152-centered multi-lncRNA panels hold substantial promise for improving HCC management through enhanced early detection, accurate prognosis prediction, and potentially guiding targeted therapeutic interventions.
Addressing Technical Challenges and Optimizing Clinical Implementation
Hepatocellular carcinoma (HCC) represents a significant global health challenge, characterized by high mortality rates and limited diagnostic options, particularly for early-stage disease [18]. While serum alpha-fetoprotein (AFP) has been the conventional biomarker for HCC, its limited sensitivity and specificity, especially in early-stage HCC and benign liver conditions, have driven the search for novel molecular biomarkers [18] [1]. Long non-coding RNAs (lncRNAs) have emerged as promising candidates, with Long Intergenic Non-coding RNA 00152 (LINC00152) demonstrating significant diagnostic and prognostic potential across multiple cancer types, including HCC [18] [3] [43].
LINC00152, located on chromosome 2p11.2 with a transcript length of 828 nucleotides, has been identified as an oncogenic lncRNA upregulated in various malignancies [3] [19]. In HCC, research indicates that LINC00152 promotes cell proliferation in vitro and tumor growth in vivo by activating the mTOR signaling pathway [3] [8]. A 2023 study further established its significant overexpression in HCC patients compared to those with liver cirrhosis and healthy controls, highlighting its potential as a non-invasive serum biomarker [18]. However, the transition of LINC00152 from a research finding to a clinically applicable biomarker faces substantial standardization challenges involving pre-analytical variables and assay validation requirements. This guide objectively compares the performance of LINC00152 detection methodologies while addressing the critical standardization hurdles that impact its reliable measurement and clinical implementation.
Analytical Performance Comparison of LINC00152 Detection
The analytical validation of LINC00152 measurement spans multiple technical approaches, each with distinct performance characteristics and standardization requirements. The table below summarizes key methodological parameters across representative studies:
Table 1: Performance Comparison of LINC00152 Detection Methodologies
| Analysis Type | Sample Type | Sample Processing | Detection Method | Key Performance Metrics | Reference |
|---|---|---|---|---|---|
| Diagnostic Performance | Serum | Centrifugation at 4000 RPM for 10 min, storage at -80°C | qRT-PCR | ROC AUC: 0.85 (vs. cirrhosis), significantly higher in HCC (p<0.001) | [18] [1] |
| Prognostic Assessment | Serum | Centrifugation at 4000 RPM for 10 min, storage at -80°C | qRT-PCR | Hazard Ratio: 2.23 (95% CI: 1.30-5.29), independent prognostic factor | [18] |
| Tissue Expression | HCC and paired normal tissues | Snap-frozen in liquid nitrogen, stored at -80°C | qRT-PCR | Significant upregulation in HCC tissues (p<0.001), correlation with tumor size and grade | [3] [8] |
| Functional Analysis | Cell lines (HepG2, MHCC-97H) | Cytoplasmic/nuclear fractionation | Microarray, Western blot | mTOR pathway activation, EpCAM regulation | [3] |
Interpretation of Comparative Data
The diagnostic performance of serum LINC00152 shows considerable promise, with an AUC of 0.85 for distinguishing HCC from liver cirrhosis, significantly outperforming conventional biomarkers in specific clinical contexts [18]. The prognostic value is particularly notable, with high LINC00152 expression serving as an independent predictor of poor outcome (HR=2.23, 95% CI=1.30-5.29, p=0.03) in multivariate analysis [18]. The pre-analytical processing remains remarkably consistent across studies, with immediate centrifugation and frozen storage at -80°C being critical preservation steps [18] [1] [3].
Critical Pre-analytical Variables in LINC00152 Measurement
Blood Collection and Processing Protocols
Standardized protocols for blood collection and processing emerge as fundamental requirements for reliable LINC00152 quantification. The methodologies described in recent literature demonstrate remarkable consistency in this area:
- Sample Collection: Venous blood (8 mL) collected using a vacutainer needle, with 4 mL placed in a plain tube and 2 mL in EDTA tubes for RNA extraction [1].
- Centrifugation Parameters: Serum separation via centrifugation at 4000 RPM for 10 minutes, a critical step for obtaining cell-free samples while preserving RNA integrity [1].
- Storage Conditions: Long-term storage at -80°C until analysis, with no freeze-thaw cycles permitted prior to RNA extraction [1].
The implementation of these standardized procedures across multiple studies has enabled more consistent inter-laboratory comparisons and facilitated the validation of LINC00152 as a reliable biomarker candidate.
RNA Extraction and Quality Assessment
The integrity of RNA extraction directly impacts the reliability of LINC00152 quantification, with several technical considerations requiring standardization:
- Extraction Methodology: The QIAamp RNA Blood Mini Kit has been successfully employed for serum samples, providing consistent yield and purity [1].
- Quality Control: Nucleic acid concentration and purity measurements via spectrophotometry (A260/A280 ratios) should be implemented as routine quality checkpoints.
- Stability Considerations: The remarkable stability of LINC00152 in circulation may be attributable to exosomal protection, a factor that could be leveraged to improve pre-analytical protocols [3].
Table 2: Impact of Pre-analytical Variables on LINC00152 Measurement
| Pre-analytical Variable | Potential Impact | Recommended Standardization |
|---|---|---|
| Blood Collection Tube | RNA degradation, hemolysis | Consistent use of EDTA tubes for RNA preservation |
| Time to Processing | RNA degradation, false decreases | Process within 2 hours of collection |
| Centrifugation Conditions | Cellular contamination, false increases | 4000 RPM for 10 minutes, consistent temperature |
| Storage Conditions | RNA degradation, inaccurate quantification | Single aliquot storage at -80°C, avoid freeze-thaw |
| RNA Extraction Method | Yield variability, inhibition issues | Validated kit-based approaches with quality controls |
Experimental Protocols for LINC00152 Analysis
Quantitative Real-Time PCR (qRT-PCR) Methodology
The qRT-PCR protocol represents the most extensively validated method for LINC00152 quantification in both serum and tissue samples. The detailed methodology includes:
- RNA Reverse Transcription: Using the QuantiTect Reverse Transcription Kit (Qiagen, USA) according to manufacturer's protocols to generate stable cDNA templates [1].
- PCR Reaction Composition: Final volume of 20 μL containing 10 μL SYBR Green 2× QuantiTect PCR Master Mix, 3 μL cDNA, 1 μL each of forward and reverse primer, and 5 μL RNase-free H2O [1].
- Primer Sequences:
- Amplification Conditions: Initial activation at 95°C for 3 minutes, followed by 55 cycles of: 30 seconds at 94°C, 30 seconds at 55°C, and 30 seconds at 72°C [1].
- Data Analysis: Relative expression calculated using the ΔΔCT method with GAPDH as the endogenous control [1].
This standardized approach has demonstrated robust performance across multiple studies, enabling consistent quantification of LINC00152 expression levels.
Functional Validation Experiments
Beyond quantification, several functional assays have been employed to elucidate the oncogenic mechanisms of LINC00152 in HCC:
- Cell Proliferation Assays: CCK-8 and EdU assays in HCC cell lines (HepG2, MHCC-97H) following LINC00152 knockdown demonstrated significant inhibition of proliferation [3] [8].
- In Vivo Tumorigenicity: Xenograft models in BALB/C nude mice using LINC00152-knockdown cells showed significantly decreased tumor growth compared to controls [3].
- Pathway Analysis: Microarray profiling following LINC00152 knockdown, validated by Western blot, confirmed mTOR pathway inhibition through decreased phosphorylation [3].
- Mechanistic Studies: Gal4-λN/BoxB reporter systems demonstrated cis-regulatory binding of LINC00152 to the EpCAM promoter, activating mTOR signaling [3] [8].
Figure 1: LINC00152 Oncogenic Signaling Pathway in HCC. This diagram illustrates the molecular mechanism through which LINC00152 promotes hepatocellular carcinoma progression by activating the mTOR signaling pathway via cis-regulation of EpCAM.
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of LINC00152 requires standardized research tools and methodologies. The following table catalogues essential reagents validated in recent studies:
Table 3: Essential Research Reagents for LINC00152 Investigation
| Reagent Category | Specific Product | Application | Performance Notes |
|---|---|---|---|
| RNA Extraction | QIAamp RNA Blood Mini Kit (Qiagen) | Serum/plasma RNA extraction | Consistent yield from biofluids, critical for serum biomarkers |
| Reverse Transcription | QuantiTect Reverse Transcription Kit (Qiagen) | cDNA synthesis | Includes genomic DNA removal step |
| qPCR Master Mix | QuantiTect SYBR Green PCR Kit (Qiagen) | Target amplification | Compatible with multiple detection systems |
| Reference Genes | GAPDH, ACTIN | Expression normalization | Essential for ΔΔCT calculations |
| Cell Lines | HepG2, MHCC-97H, Huh7 | Functional studies | Show native LINC00152 expression |
| Knockdown Tools | shRNA (sh152-1, sh152-3) | Functional validation | High silencing efficiency demonstrated |
| Detection System | 7500 ABI PRISM (Applied Biosystems) | qRT-PCR quantification | Standardized fluorescence detection |
| Antibacterial agent 130 | Antibacterial agent 130, MF:C23H28O10S, MW:496.5 g/mol | Chemical Reagent | Bench Chemicals |
| Jak-IN-27 | Jak-IN-27, MF:C20H21F2N7O, MW:413.4 g/mol | Chemical Reagent | Bench Chemicals |
Standardization Challenges and Validation Requirements
Pre-analytical Variables Requiring Standardization
The translation of LINC00152 into clinical practice faces several significant standardization hurdles that must be addressed through coordinated validation efforts:
- Sample Type Variability: While serum has been the primary matrix for LINC00152 detection, differences in collection protocols, anticoagulant use (plain tubes vs. EDTA), and processing timelines introduce substantial variability [1].
- Reference Gene Selection: The use of GAPDH as a reference gene requires further validation for serum-based lncRNA quantification, as traditional reference genes may demonstrate instability in biofluids [1].
- Analytical Sensitivity Specifications: The minimum required detection sensitivity and dynamic range for clinical application remain undefined, particularly for early-stage HCC detection.
- Inter-laboratory Reproducibility: Despite consistent methodologies in published literature, formal inter-laboratory reproducibility studies are lacking for LINC00152 quantification.
Pathway Integration and Clinical Correlations
Understanding LINC00152 within the broader molecular context of HCC provides insights into its biological significance and potential clinical applications:
Figure 2: LINC00152 Clinical Correlations and Applications. This workflow diagram illustrates the established clinical-pathological correlations of LINC00152 expression and their potential translation into clinical applications for hepatocellular carcinoma management.
LINC00152 represents a promising molecular biomarker with demonstrated diagnostic and prognostic value in hepatocellular carcinoma. The current evidence supports its independent prognostic value, with high expression correlating with aggressive tumor characteristics and poorer survival outcomes [18] [43]. The experimental data obtained through standardized qRT-PCR protocols shows consistent performance across studies, particularly when adhering to uniform pre-analytical processing conditions [18] [1] [3].
However, the transition toward clinically applicable LINC00152 testing requires addressing critical standardization gaps. These include establishing uniform pre-analytical protocols, defining analytical performance specifications, validating reference materials, and conducting multi-center reproducibility studies. The consistent methodologies employed in recent research provide a solid foundation for these standardization efforts, offering a pathway toward reliable implementation in both research and potential clinical settings.
For research and drug development professionals, the current evidence supports the inclusion of LINC00152 in HCC biomarker panels, particularly when investigating mTOR pathway activation or seeking prognostic indicators beyond conventional markers. The essential reagents and methodologies outlined in this guide provide a validated foundation for such investigations, while highlighting the areas requiring further standardization work before widespread clinical adoption can be achieved.
Hepatocellular carcinoma (HCC) constitutes over 90% of primary liver cancers and ranks as the third leading cause of cancer-related mortality worldwide [9] [44] [45]. The disease typically arises in the context of chronic liver disease, most commonly driven by risk factors including chronic hepatitis B (HBV) and C (HCV) infection, alcohol-related liver disease (ALD), and metabolic dysfunction-associated steatotic liver disease (MASLD) [46] [44] [40]. This etiological background presents a fundamental clinical challenge: distinguishing early-stage HCC from the underlying chronic liver disease or cirrhosis that almost always precedes it.
The current surveillance paradigm for at-risk patients relies on biannual ultrasound and alpha-fetoprotein (AFP) testing [44]. However, AFP testing has well-documented limitations in both sensitivity and specificity, with approximately two-thirds of HCC patients exhibiting elevated AFP levels [33] [10]. Furthermore, AFP levels can also be elevated in benign chronic liver conditions without malignancy, leading to false-positive results and unnecessary invasive investigations. This diagnostic ambiguity underscores the critical need for more specific biomarkers that can accurately differentiate HCC from non-malignant chronic liver disease, particularly in high-risk populations.
Long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers in oncology. These RNA molecules, longer than 200 nucleotides, play crucial regulatory roles in gene expression through various mechanisms including epigenetic modification, transcriptional regulation, and post-transcriptional processing [9] [40]. Their expression exhibits remarkable tissue specificity, and they are frequently dysregulated in cancer, making them attractive candidates for diagnostic and prognostic applications [9] [47] [40]. Among these, LINC00152 has shown particular promise as a biomarker with independent prognostic value in HCC, offering potential solutions to the specificity challenges in liver cancer diagnosis.
LINC00152 (long intergenic non-protein coding RNA 152) is a long non-coding RNA that has been extensively investigated in hepatocellular carcinoma. Functionally, LINC00152 has been characterized as playing an oncogenic role in HCC pathogenesis through multiple molecular mechanisms. Evidence indicates that LINC00152 inhibits cell proliferation by recruiting HDAC1 to repress c-Myc transcription, and restoring LINC00152 expression has been shown to reduce tumor growth by 40% in xenograft models [12].
The lncRNA is frequently overexpressed in HCC tissues compared to adjacent non-tumorous liver tissue, with this elevated expression being detectable not only in tumor tissue but also in the blood circulation of patients, making it accessible for liquid biopsy approaches [9] [33]. This characteristic is particularly valuable for clinical applications, as it enables non-invasive monitoring through blood tests rather than requiring tissue biopsies.
From a clinical perspective, Wang et al. revealed that high pre-treatment expression levels of LINC00152 in tumor tissues independently predicted shorter overall survival (hazard ratio [HR], 2.524; 95% confidence interval [CI], 1.661–4.015; P = 0.001) in HCC patients treated with curative surgical resection [9]. This independent prognostic value remains significant even after adjusting for conventional clinical and pathological factors, underscoring its potential clinical utility in risk stratification and treatment planning.
Table 1: Prognostic Significance of LINC00152 in HCC Patients
| Study | Sample Size | Detection Method | Hazard Ratio (HR) | 95% CI | P-value |
|---|---|---|---|---|---|
| Wang et al. [9] | 63 | qRT-PCR | 2.524 | 1.661–4.015 | 0.001 |
| Machine Learning Study [33] | 52 | qRT-PCR | Significant correlation with mortality* | N/A | <0.05 |
*Higher LINC00152 to GAS5 expression ratio significantly correlated with increased mortality risk.
Comparative Diagnostic Performance: LINC00152 vs. Conventional and Novel Biomarkers
Head-to-Head Comparison with AFP
The diagnostic performance of LINC00152 has been systematically evaluated against the current standard biomarker, alpha-fetoprotein (AFP). When assessed individually, LINC00152 demonstrates moderate diagnostic accuracy for HCC, with sensitivity and specificity ranging from 60% to 83% and 53% to 67%, respectively [33] [10]. While these figures represent a improvement over AFP in some cohorts, the true potential of LINC00152 lies in its synergistic use with other biomarkers.
Notably, the combination of LINC00152 with AFP has been shown to significantly improve diagnostic power compared to either biomarker alone [33] [10]. This combinatorial approach enhances both sensitivity and specificity, addressing the limitations of individual biomarkers. The complementary nature of these biomarkers likely stems from their reflection of distinct biological processes in hepatocarcinogenesis – AFP representing a developmental antigen re-expressed in malignancy, and LINC00152 representing a specific regulatory RNA dysregulated in cancer cells.
Performance Against Other lncRNAs
In comparative analyses with other promising lncRNA biomarkers, LINC00152 maintains a competitive diagnostic profile. A comprehensive study evaluating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) found that while each lncRNA exhibited moderate individual performance, their combination significantly enhanced diagnostic accuracy [33] [10]. Specifically, a machine learning model incorporating all four lncRNAs achieved remarkable performance with 100% sensitivity and 97% specificity for HCC diagnosis [33].
Of particular note is the LINC00152 to GAS5 expression ratio, which has demonstrated significant correlation with increased mortality risk in HCC patients [33]. This ratio-based approach leverages the dual information from an oncogenic lncRNA (LINC00152) and a tumor-suppressive lncRNA (GAS5), potentially providing a more robust biological signal than either marker alone. GAS5 is known to trigger CHOP and caspase-9 signal pathways, activating apoptosis in HCC cells [33] [10], creating a biologically meaningful ratio that reflects the balance between pro- and anti-tumor forces.
Table 2: Diagnostic Performance of LINC00152 in Comparison with Other Biomarkers
| Biomarker | Sample Type | Sensitivity (%) | Specificity (%) | AUC-ROC | Reference |
|---|---|---|---|---|---|
| LINC00152 (individual) | Plasma | 60-83 | 53-67 | 0.70-0.75 | [33] [10] |
| AFP (individual) | Serum | ~66* | ~80* | 0.72 | [33] [12] |
| LINC00152 + AFP | Plasma/Serum | Significant improvement over individual markers | 0.85-0.90 | [33] [10] | |
| 4-lncRNA Panel + ML Model | Plasma | 100 | 97 | ~0.99 | [33] |
| miR-21 + miR-122 | Tissue | 89 | 91 | 0.92 | [12] |
*Approximately two-thirds of HCC patients exhibit elevated AFP levels [33] [10].
Methodological Approaches for LINC00152 Analysis
Sample Collection and RNA Isolation
The analytical workflow for LINC00152 detection begins with proper sample collection and processing. For liquid biopsy applications, plasma is preferred over serum as it provides more consistent results with lower levels of background RNA. Total RNA is isolated from samples using commercial kits such as the miRNeasy Mini Kit (QIAGEN), which efficiently recovers both small and long RNA species [33] [10]. The RNA quality and quantity should be assessed spectrophotometrically or using microfluidic platforms to ensure sample integrity before proceeding to downstream applications.
Detection and Quantification Methods
The most widely employed method for LINC00152 quantification is quantitative reverse-transcription polymerase chain reaction (qRT-PCR), which offers an optimal balance of sensitivity, specificity, and practical feasibility for clinical applications [9] [33]. The process involves reverse transcription using kits such as the RevertAid First Strand cDNA Synthesis Kit, followed by quantitative PCR using SYBR Green or TaqMan chemistry [33] [10].
For research applications, more comprehensive profiling approaches include RNA sequencing (RNAseq), which enables discovery of novel lncRNAs and isoform-specific expression patterns [9]. Additionally, in situ hybridization (ISH)-based methods allow spatial resolution of LINC00152 expression within tissue architecture, providing valuable pathological context [9].
Normalization and Data Analysis
Proper normalization is critical for accurate LINC00152 quantification. The ΔΔCT method is commonly used for relative quantification, with housekeeping genes such as GAPDH serving as internal controls [33] [10]. For absolute quantification, standard curves generated from synthetic RNA transcripts can be employed. In the context of multiple biomarker panels, machine learning algorithms implemented in platforms such as Python's Scikit-learn have demonstrated superior performance compared to traditional statistical approaches [33].
Diagram 1: Experimental workflow for LINC00152 analysis, depicting the key stages from sample collection to data interpretation.
Molecular Mechanisms: How LINC00152 Drives HCC Pathogenesis
LINC00152 contributes to hepatocellular carcinoma progression through multiple interconnected molecular mechanisms that affect key cancer hallmarks. As an oncogenic lncRNA, it primarily functions by regulating gene expression at both transcriptional and post-transcriptional levels.
At the transcriptional level, LINC00152 has been shown to inhibit cell proliferation by recruiting histone deacetylase 1 (HDAC1) to repress c-Myc transcription [12]. This epigenetic mechanism represents a direct pathway through which LINC00152 influences gene expression programs driving hepatocarcinogenesis. Additionally, LINC00152 promotes cell proliferation through regulation of CCDN1 (cyclin D1), a critical regulator of cell cycle progression [33] [10].
The lncRNA also functions through competitive endogenous RNA (ceRNA) mechanisms, whereby it acts as a molecular sponge for specific microRNAs, preventing these regulatory RNAs from binding to their natural mRNA targets. This sponge activity effectively derepresses oncogenic pathways that would otherwise be suppressed by tumor-suppressive microRNAs.
Diagram 2: Molecular mechanisms of LINC00152 in HCC pathogenesis, illustrating key pathways and functional outcomes.
Advanced Applications: Machine Learning and Multi-Analyte Panels
The integration of LINC00152 into multi-analyte panels represents the cutting edge of HCC diagnostic research. A recent study demonstrated that a machine learning model incorporating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) along with conventional laboratory parameters achieved remarkable diagnostic performance with 100% sensitivity and 97% specificity [33]. This approach significantly outperformed individual biomarker testing and highlighted the synergistic value of combining multiple analytes with advanced computational analysis.
The machine learning framework employed Python's Scikit-learn platform to integrate these lncRNAs with additional clinical laboratory parameters, including standard liver function tests (ALT, AST, bilirubin, albumin) and AFP [33]. This comprehensive approach leverages the complementary strengths of different biomarker classes – lncRNAs providing specific molecular information about tumor presence, while conventional tests reflect the underlying liver function and inflammatory status.
For prognostic applications, the ratio of LINC00152 to GAS5 expression has emerged as a particularly powerful metric, significantly correlating with increased mortality risk [33]. This ratio effectively captures the balance between oncogenic (LINC00152) and tumor-suppressive (GAS5) forces, providing a more biologically informative measure than either marker alone.
Research Reagent Solutions
Table 3: Essential Research Reagents for LINC00152 Studies
| Reagent/Catalog Number | Manufacturer | Primary Application | Key Features |
|---|---|---|---|
| miRNeasy Mini Kit (217004) | QIAGEN | Total RNA isolation | Efficient recovery of long and small RNAs; includes DNase treatment |
| RevertAid First Strand cDNA Synthesis Kit (K1622) | Thermo Scientific | cDNA synthesis | High-efficiency reverse transcription; suitable for lncRNAs |
| PowerTrack SYBR Green Master Mix (A46012) | Applied Biosystems | qPCR amplification | Optimized for precise quantification; includes ROX reference dye |
| Custom LINC00152 Primers | Thermo Fisher | Target detection | Sequence-specific amplification; optimized annealing temperature |
| ViiA 7 Real-Time PCR System | Applied Biosystems | PCR amplification and detection | High-throughput capability; multiplexing capacity |
The discrimination between hepatocellular carcinoma and benign chronic liver disease remains a significant clinical challenge with direct implications for patient outcomes. LINC00152 represents a promising biomarker with demonstrated independent prognostic value in HCC, offering improved specificity compared to conventional biomarkers like AFP when used in appropriate algorithmic or combinatorial approaches. The molecular mechanisms of LINC00152, particularly its role in epigenetic regulation and cell cycle control, provide biological plausibility for its utility as a cancer-specific marker.
Future directions should focus on standardizing detection methodologies, validating cut-off values across diverse patient populations, and further exploring the integration of LINC00152 into multi-analyte diagnostic panels enhanced by machine learning algorithms. As the field advances toward more personalized approaches to liver cancer management, LINC00152 is poised to contribute significantly to improved risk stratification, early detection, and ultimately better outcomes for patients with hepatocellular carcinoma.
Hepatocellular carcinoma (HCC) remains a major global health challenge, ranking as the sixth most prevalent cancer and the third leading cause of cancer-related mortality worldwide [10]. In this context, the investigation of long non-coding RNAs (lncRNAs) as biomarkers has emerged as a pivotal area of research. LncRNAs are defined as RNA transcripts longer than 200 nucleotides that lack protein-coding capacity [40]. They play essential roles in regulating gene expression through various mechanisms, including chromatin modification, transcriptional activation, and microRNA sponging, all of which significantly impact HCC progression and metastasis [48].
Among these, LINC00152 has been validated as an independent prognostic biomarker in HCC. Evidence from a study involving 63 HCC patients treated with curative surgical resection demonstrated that a high pre-treatment expression level of LINC00152 in tumor tissues, detected via quantitative reverse-transcription polymerase chain reaction (qRT-PCR), independently predicted shorter overall survival (HR, 2.524; 95% CI, 1.661–4.015; P = 0.001) [9]. Beyond tissue analysis, the potential of LINC00152 as a non-invasive liquid biopsy biomarker is supported by its detectability in body fluids, making it accessible for serial monitoring [10]. This positions LINC00152 as a crucial molecule for developing precise diagnostic tools and for understanding the molecular underpinnings of HCC.
Table 1: Key Characteristics of LINC00152 in HCC
| Attribute | Description |
|---|---|
| RNA Class | Long Intergenic Non-coding RNA (lincRNA) |
| Prognostic Value | Independent predictor of shorter overall survival (High expression) [9] |
| Detection Method | qRT-PCR [9] [10] |
| Sample Types | Tumor tissue [9], Plasma [10] |
| Primary Function | Promotes cell proliferation; potential miRNA sponge [10] |
| Hazard Ratio (OS) | 2.524 (95% CI: 1.661–4.015) [9] |
Critical Analytical Challenges in lncRNA Analysis
The accurate quantification of circulating lncRNAs like LINC00152 for clinical applications faces two primary analytical hurdles: RNA instability in circulation and the need for robust normalization strategies to control for technical variability.
RNA Stability in Circulation
The intrinsic instability of RNA molecules poses a significant limitation for their use in diagnostics and therapeutics. In vivo, linear mRNA is particularly susceptible to rapid degradation by enzymes, which shortens its functional half-life and limits sustained protein expression [49] [50]. While alternative formats such as circular RNA (circRNA) offer greater durability, they often suffer from lower translation efficiency and more complex manufacturing processes [50]. A landmark study has identified specific viral RNA motifs, including one denoted A7, that can overcome these limitations. When incorporated into linear mRNA, the A7 motif recruits the host enzyme TENT4, which extends the poly(A) tail and prevents deadenylation. This process makes linear mRNA as stable as circRNA while achieving even higher translation efficiency, sustaining protein expression in mouse liver for over two weeks [49] [50]. Although this research focused on mRNA therapeutics, the principles of enhancing RNA stability through structural motifs are highly relevant for improving the detection of labile lncRNAs like LINC00152 in blood-based diagnostics.
Normalization Strategies for qPCR Data
Quantitative real-time PCR (qRT-PCR) is the most frequently used technique to determine RNA expression levels [51]. However, the normalisation step is critical to eliminate technical variation introduced during sample processing, RNA extraction, and cDNA synthesis, ensuring that the final data reflects true biological variation [51]. The most common normalization strategy involves using internal reference genes (RGs), often referred to as "housekeeping" genes, which should be stably expressed across all samples and conditions analyzed. Commonly used RGs include GAPDH, TBP, and ACTB [51].
A comprehensive study on canine gastrointestinal tissues proposed an alternative method: the global mean (GM) expression of all profiled genes. This investigation, which analyzed 96 genes including 11 RGs, found that the GM method outperformed strategies using multiple RGs in reducing the coefficient of variation (CV) of gene expression data post-normalization [51]. The study concluded that for experiments profiling large sets of genes (e.g., >55 genes), implementing the GM method is advisable. It also identified RPS5, RPL8, and HMBS as the most stable single RGs for normalizing smaller gene sets in their experimental setup [51]. These findings underscore that there is no universally perfect normalisation method; the optimal strategy depends on the experimental context, including the tissue type, pathological condition, and number of genes being profiled.
Table 2: Comparison of Normalisation Strategies for qPCR Data
| Normalisation Method | Principle | Advantages | Limitations | Best-Suited Context |
|---|---|---|---|---|
| Single Reference Gene (e.g., GAPDH) | Uses one stably expressed "housekeeping" gene for normalisation. | Simple, cost-effective, widely used. | Prone to error if the RG is regulated by the experimental condition [51]. | Small gene sets; requires prior validation of RG stability. |
| Multiple Reference Genes (e.g., RPS5, RPL8) | Uses a geometric mean of multiple stably expressed RGs. | More robust than single RGs; reduces bias. | Finding a panel of stable RGs can be complex; ribosomal protein RGs may be co-regulated [51]. | Small to medium gene sets where stable RGs have been identified. |
| Global Mean (GM) | Uses the arithmetic mean of Cq values from all profiled genes. | Effectively reduces technical variation; does not require a priori RG selection. | Requires profiling of a large number of genes (e.g., >55) [51]. | Large-scale gene expression profiling studies (e.g., RNAseq validation). |
Experimental Protocols for Key Methodologies
Protocol: Quantifying LINC00152 from Plasma via qRT-PCR
The following protocol, adapted from a 2024 study, details the steps for detecting and quantifying LINC00152 in human plasma, a foundational technique for assessing its prognostic value [10].
- Step 1: Sample Collection and RNA Isolation. Collect plasma samples using standard phlebotomy and centrifugation protocols to separate plasma from cellular components. Isolate total RNA from plasma using a specialized kit such as the miRNeasy Mini Kit (QIAGEN), which is designed to efficiently recover small and long RNA species. The quality and quantity of the isolated RNA should be assessed using a spectrophotometer.
- Step 2: cDNA Synthesis. Reverse transcribe the extracted RNA into complementary DNA (cDNA) using the RevertAid First Strand cDNA Synthesis Kit. This process involves using a thermal cycler to synthesize cDNA, which is more stable and serves as the template for the subsequent amplification reaction.
- Step 3: Quantitative Real-Time PCR (qRT-PCR). Perform qRT-PCR using a system like the ViiA 7 and a detection chemistry such as PowerTrack SYBR Green Master Mix. The reaction should include specific primers for LINC00152 and for a normalisation gene (e.g., GAPDH). Each sample must be run in triplicate to ensure technical reproducibility.
- Step 4: Data Normalisation and Analysis. Normalize the raw Cq values for LINC00152 against the normalisation gene (e.g., GAPDH) using the ∆∆Cq method to determine the relative expression levels. Statistical analysis, including receiver operating characteristic (ROC) curves, can then be applied to evaluate the diagnostic performance of LINC00152 levels.
Protocol: Enhancing RNA Stability Using the A7 Motif
This protocol is derived from a groundbreaking 2025 study that identified viral RNA motifs for stabilizing mRNA therapeutics [50]. The principles are highly applicable to enhancing the stability of RNA biomarkers.
- Step 1: RNA Construct Design. Synthesize the RNA molecule of interest (e.g., a reporter transcript) incorporating the identified A7 viral stability motif within its sequence. The A7 motif functions by recruiting the TENT4 enzyme.
- Step 2: In Vitro Transcription and Modification. Produce the RNA construct via in vitro transcription. To further enhance stability and reduce immunogenicity, incorporate modified nucleosides such as N1-methylpseudouridine during the synthesis, which is compatible with the A7 motif.
- Step 3: Stability and Expression Assay. Introduce the stabilized RNA construct into the target system (e.g., primary cells or a mouse model). Compare its performance against control constructs, such as unmodified linear RNA and circular RNA. The key metrics to monitor over time (e.g., for over two weeks) include RNA persistence (via qRT-PCR) and functional output (e.g., protein expression levels).
- Step 4: Mechanistic Validation. To confirm the mechanism of action, demonstrate that the enhanced stability is dependent on the recruitment of the TENT4 enzyme, which is responsible for extending the poly(A) tail and preventing the deadenylation that leads to RNA decay.
Visualizing Key Concepts and Workflows
LINC00152 ceRNA Mechanism in HCC
The following diagram illustrates the proposed competing endogenous RNA (ceRNA) mechanism of LINC00152 in Hepatocellular Carcinoma (HCC), which contributes to its oncogenic role.
qPCR Normalization Workflow
This flowchart outlines the critical decision points and options for normalizing qPCR data in gene expression studies, based on recent methodological comparisons.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for lncRNA Analysis
| Reagent / Kit | Function | Application Context |
|---|---|---|
| miRNeasy Mini Kit (QIAGEN) | Isolation of total RNA, including small and long RNA species, from plasma and other biofluids. | RNA extraction for liquid biopsy studies [10]. |
| RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Reverse transcription of RNA into stable cDNA for subsequent PCR amplification. | cDNA synthesis step in qRT-PCR workflow [10]. |
| PowerTrack SYBR Green Master Mix (Applied Biosystems) | Fluorescent dye for detection and quantification of amplified DNA during qRT-PCR. | Detection chemistry for qRT-PCR [10]. |
| N1-methylpseudouridine | Modified nucleoside that enhances RNA stability and reduces immunogenicity. | Production of therapeutic or stabilized reporter RNA [50]. |
| A7 RNA Stability Motif | Viral RNA element that recruits TENT4 to extend poly(A) tail and prevent degradation. | Engineering highly stable RNA constructs for research or therapeutics [49] [50]. |
Hepatocellular carcinoma (HCC) presents significant diagnostic and prognostic challenges, with current standards like imaging and alpha-fetoprotein (AFP) exhibiting well-documented limitations. Long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers that could complement these traditional methods. Among these, LINC00152 has been extensively investigated as a potential independent prognostic factor in HCC. This review synthesizes current evidence on LINC00152's performance characteristics, mechanistic foundations, and potential for integration into clinical pathways to enhance patient stratification and management.
HCC ranks as the sixth most common malignant tumor and the third leading cause of cancer-related deaths globally [8]. In Egypt, it represents a particularly acute public health challenge, ranking as the fourth most common cancer and the leading cause of cancer-related death [10]. The current diagnostic paradigm combines ultrasound imaging with serum AFP measurement, but this approach has significant limitations. AFP demonstrates limited sensitivity and specificity, especially in early-stage HCC, with approximately two-thirds of HCC patients exhibiting elevated AFP levels [10] [1]. Similarly, imaging techniques face challenges in detecting early-stage lesions and distinguishing benign from malignant nodules.
This diagnostic gap has accelerated research into molecular biomarkers that can complement existing modalities. Liquid biopsy approaches analyzing circulating biomarkers offer a particularly promising non-invasive strategy for early detection, monitoring, and prognosis [52]. Within this context, lncRNAs—transcripts longer than 200 nucleotides with limited protein-coding potential—have emerged as valuable candidates due to their cancer-specific expression patterns and stability in body fluids [1].
LINC00152: A Primer on Structure and Function
LINC00152 (long intergenic non-coding RNA 152), also known as CYTOR (cytoskeleton regulator RNA), is an 828-bp lncRNA located on chromosome 2p11.2 [15] [1]. It was initially discovered through research on hepatocarcinogenesis and has since been recognized as a crucial oncogene regulating gene expression across multiple cancer types [15]. LINC00152 is aberrantly expressed in various malignancies, including gastric, breast, ovarian, colorectal, hepatocellular, and lung cancer, and glioma [15].
The functional role of lncRNAs is closely linked to their subcellular distribution. LINC00152 primarily localizes to the nucleus of HCC cells [8], where it can regulate gene expression through diverse mechanisms. It can function as a competitive endogenous RNA (ceRNA) in the cytoplasm by sponging microRNAs, or it can bind to multi-comb inhibition complex 2 (PRC2) in the nucleus to regulate epigenetic gene regulation [15].
Table 1: Fundamental Characteristics of LINC00152
| Characteristic | Description |
|---|---|
| Genomic Location | Chromosome 2p11.2 |
| Length | 828 base pairs |
| Aliases | CYTOR (cytoskeleton regulator RNA) |
| Initial Discovery Context | Hepatocarcinogenesis research |
| Subcellular Localization in HCC | Primarily nuclear |
| Regulatory Mechanisms | ceRNA activity, epigenetic regulation, mTOR pathway activation |
Quantitative Evidence: Diagnostic and Prognostic Performance of LINC00152
Diagnostic Performance
Multiple studies have validated the diagnostic potential of LINC00152 in distinguishing HCC patients from healthy controls and those with benign liver conditions:
A 2023 study investigating serum LINC00152 in HCV-induced HCC found significantly elevated expression in HCC patients (n=60) compared to those with liver cirrhosis (n=60) and healthy controls (n=40) (p<0.001) [1]. The receiver operating characteristic (ROC) analysis demonstrated excellent performance in distinguishing HCC from cirrhosis, suggesting clinical utility in at-risk populations.
A 2024 study analyzing plasma levels of four lncRNAs (including LINC00152) in a cohort of 52 HCC patients and 30 age-matched controls reported that while individual lncRNAs showed moderate diagnostic accuracy (sensitivity and specificity ranging from 60-83% and 53-67%, respectively), their integration with conventional laboratory parameters using machine learning dramatically improved performance to 100% sensitivity and 97% specificity [10].
Prognostic Significance
The independent prognostic value of LINC00152 has been established through multiple clinical studies employing multivariate Cox proportional hazards regression analysis:
A study of 63 HCC patients treated with curative surgical resection revealed that high pre-treatment expression of LINC00152 in tumor tissues independently predicted shorter overall survival (OS) (hazard ratio [HR], 2.524; 95% confidence interval [CI], 1.661-4.015; P=0.001) [9].
In a larger cohort of 102 HCC patients, LINC00152 overexpression significantly correlated with larger tumor size (P=0.005) and higher Edmondson grade (P=0.002), both indicators of aggressive disease [8].
The 2023 HCV-induced HCC study further confirmed that high serum LINC00152 level was an independent predictor of poor outcome (HR=2.23, 95% CI=1.30-5.29, P=0.03) in multivariate analysis [1].
Table 2: Prognostic Value of LINC00152 in HCC Patient Cohorts
| Study Cohort | Detection Method | Outcome Measure | Hazard Ratio (95% CI) | P-value |
|---|---|---|---|---|
| 63 HCC patients [9] | qRT-PCR (tissue) | Overall Survival | 2.524 (1.661-4.015) | 0.001 |
| 102 HCC patients [8] | RT-PCR (tissue) | Tumor Size >5cm | Correlation significant | 0.005 |
| 60 HCV-HCC patients [1] | qRT-PCR (serum) | Mortality | 2.23 (1.30-5.29) | 0.03 |
Molecular Mechanisms: Deciphering LINC00152's Oncogenic Functions
LINC00152 drives hepatocarcinogenesis through multiple interconnected molecular pathways, which provide the mechanistic foundation for its prognostic utility.
Competing Endogenous RNA (ceRNA) Network
LINC00152 functions as a molecular sponge for multiple tumor-suppressive microRNAs. A comprehensive study identified let-7c-5p, miR-23a-3p, miR-125a-5p, miR-125b-5p, miR-143a-3p, miR-193-3p, and miR-195-5p as components of the LINC00152-driven ceRNA network in HCC [32]. The study specifically validated that LINC00152 sponges miR-143a-3p, thereby limiting its binding to target genes like KLC2 (kinesin light chain 2). Functional assays demonstrated that KLC2 promotes cell proliferation, clonogenicity, and migration in vitro, and co-expression of LINC00152 and KLC2 was observed in human HCC cohorts, with high KLC2 expression associated with shorter patient survival [32].
mTOR Signaling Pathway Activation
LINC00152 activates the mechanistic target of rapamycin (mTOR) pathway, which plays a critical role in controlling cancer cell proliferation, division, and carcinogenesis [1]. Microarray-based analysis indicated that LINC00152 binds to the promoter of EpCAM (epithelial cell adhesion molecule) through cis-regulation, subsequently activating the mTOR signaling pathway [8]. This mechanism was confirmed using the Gal4-λN/BoxB reporter system, providing evidence for LINC00152's direct gene regulatory function.
Additional Oncogenic Mechanisms
Other studies have revealed that LINC00152 promotes HCC progression through additional pathways, including:
- Interaction with the HBx (hepatitis B virus X protein) pathway [15]
- Sponging miR-125b to upregulate SEMA4C [15]
- Regulation of miR-193a/b-3p to affect CCND1 (cyclin D1) expression [15]
LINC00152 Oncogenic Network: This diagram illustrates the molecular mechanisms through which LINC00152 promotes hepatocellular carcinoma progression, including miRNA sponging and direct gene regulation.
Experimental Protocols: Methodologies for LINC00152 Analysis
Sample Collection and RNA Extraction
Blood samples are collected in EDTA tubes for plasma/serum preparation [10] [1]. For tissue analysis, HCC and matched adjacent non-tumor tissues are obtained during surgical resection [8]. Total RNA is extracted using commercial kits such as the miRNeasy Mini Kit (QIAGEN) [10] or QIAamp RNA Blood Mini Kit [1], following manufacturer protocols. RNA quality and concentration are assessed using spectrophotometry.
Reverse Transcription and Quantitative Real-Time PCR (qRT-PCR)
RNA is reverse transcribed into complementary DNA (cDNA) using the RevertAid First Strand cDNA Synthesis Kit [10] or QuantiTect Reverse Transcription Kit [1]. Quantitative PCR is performed using PowerTrack SYBR Green Master Mix [10] or QuantiTect SYBR Green PCR Kit [1] on platforms such as the ViiA 7 real-time PCR system [10] or 7500 ABI PRISM [1].
Each PCR reaction typically has a final volume of 20 μL, containing 10 μL SYBR Green 2× Master Mix, 3 μL cDNA, 1 μL of each forward and reverse primer, and 5 μL RNase-free H₂O [1]. Cycling conditions generally include an initial activation step at 95°C for 3 minutes, followed by 40-55 cycles of denaturation at 94°C for 30 seconds, annealing at 55°C for 30 seconds, and extension at 72°C for 30 seconds [1]. Melting curve analysis is employed to confirm amplification specificity.
The primer sequences used for LINC00152 detection are:
GAPDH typically serves as the endogenous control for normalization [10] [1]. Relative expression is calculated using the ΔΔCT method [10] [1].
RNA In Situ Hybridization (ISH)
For tissue-based detection, RNA in situ hybridization using the RNAscope technology (Advanced Cell Diagnostics) can be performed on formalin-fixed paraffin-embedded tissue sections [32]. Staining is assessed using a quality and quantity scoring system, with total scores categorized as absent (0), weak (1-4), moderate (5-8), or strong (9-12) expression [32].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for LINC00152 Investigation
| Reagent/Kit | Manufacturer | Primary Function | Application Context |
|---|---|---|---|
| miRNeasy Mini Kit | QIAGEN | Total RNA isolation | Plasma/serum RNA extraction [10] |
| QIAamp RNA Blood Mini Kit | QIAGEN | Total RNA isolation | Blood RNA extraction [1] |
| RevertAid First Strand cDNA Synthesis Kit | Thermo Scientific | cDNA synthesis | Reverse transcription [10] |
| QuantiTect Reverse Transcription Kit | QIAGEN | cDNA synthesis | Reverse transcription [1] |
| PowerTrack SYBR Green Master Mix | Applied Biosystems | qPCR amplification | Quantitative real-time PCR [10] |
| QuantiTect SYBR Green PCR Kit | QIAGEN | qPCR amplification | Quantitative real-time PCR [1] |
| RNAscope Reagents | Advanced Cell Diagnostics | RNA in situ hybridization | Tissue-based LINC00152 detection [32] |
| LINC00152-specific primers | Custom synthesis | Target amplification | qPCR detection [1] |
Integration into Clinical Pathways: Complementing Current Standards
The robust evidence supporting LINC00152's prognostic value suggests several potential integration points into existing HCC clinical pathways:
Risk Stratification in Cirrhosis Surveillance
For patients with cirrhosis undergoing regular ultrasound surveillance, adding LINC00152 measurement could enhance early detection sensitivity. The significant elevation of LINC00152 in HCC patients compared to those with cirrhosis alone [1] supports its use in distinguishing malignant transformation within cirrhotic livers.
Prognostic Stratification Post-Diagnosis
Following HCC diagnosis, LINC00152 expression level could inform treatment intensity decisions. Patients with high LINC00152 expression (HR=2.23 for mortality) [1] might benefit from more aggressive first-line therapy or closer monitoring schedules.
Molecular Companion for Imaging
LINC00152 could serve as a molecular companion for equivocal imaging findings, particularly in cases where AFP results are inconclusive. The machine learning approach demonstrating 100% sensitivity and 97% specificity when combining lncRNAs with conventional parameters [10] highlights the potential of integrated diagnostic models.
Clinical Pathway Integration: This diagram illustrates how LINC00152 testing could complement existing hepatocellular carcinoma clinical pathways at surveillance, diagnostic, and prognostic decision points.
The accumulating evidence firmly establishes LINC00152 as a promising independent prognostic biomarker in hepatocellular carcinoma. Its validated performance characteristics, elucidated molecular mechanisms, and detectability in readily accessible liquid biopsies position it as a strong candidate for complementing current imaging and AFP-based paradigms. Future research directions should focus on standardized assay development, validation in prospective multicenter trials, and refinement of integrated diagnostic algorithms that combine molecular with traditional markers. The successful integration of LINC00152 into clinical pathways holds significant potential to enhance risk stratification, diagnostic accuracy, and personalized treatment approaches for HCC patients.
Clinical Validation and Performance Against Established Biomarkers
In the pursuit of personalized oncology, the identification of robust prognostic biomarkers is paramount for improving hepatocellular carcinoma (HCC) management. Long non-coding RNAs (lncRNAs) have emerged as pivotal players in cancer biology, with LINC00152 distinguishing itself as a potent molecular marker across multiple malignancies. This guide provides a comprehensive comparison of the experimental data validating the independent prognostic value of LINC00152 in HCC, detailing the methodologies for its assessment, its performance against clinical variables, and the underlying molecular mechanisms that underscore its clinical significance.
Quantitative Evidence of Independent Prognostic Value
The independent prognostic value of LINC00152 is established through multivariate Cox proportional hazards regression analyses, which confirm its significance after adjusting for other clinical and pathological factors. The supporting data from key studies are summarized in the table below.
Table 1: Multivariate Analyses of LINC00152's Prognostic Value in HCC
| Study Cohort | Sample Type | Detection Method | Endpoint | Hazard Ratio (HR) | 95% Confidence Interval (CI) | P-value | Reference |
|---|---|---|---|---|---|---|---|
| HCV-induced HCC (n=60) | Serum | qRT-PCR | Overall Survival | 2.23 | 1.30–5.29 | 0.03 | [1] |
| Retrospective HCC (n=63) | Tumor Tissue | qRT-PCR | Overall Survival | 2.524 | 1.661–4.015 | 0.001 | [38] |
| Multiple Cancers (Meta-Analysis) | Various | Various | Overall Survival | 1.98 | 1.70–2.31 | < 0.0001 | [5] |
| Multiple Cancers (Meta-Analysis) | Various | Various | Disease-Free Survival | 1.66 | 1.20–2.29 | < 0.0001 | [5] |
The consistency of these findings across different sample types and patient cohorts underscores the reliability of LINC00152 as a biomarker indicative of aggressive disease and poor survival outcomes.
Correlation with Clinicopathological Features
High expression of LINC00152 is not only prognostic but also correlates significantly with specific clinicopathological features that define aggressive tumor behavior, as detailed in the following table.
Table 2: Association Between High LINC00152 Expression and Clinicopathological Features in HCC
| Clinical Feature | Significance (P-value) | Study Context | Implication |
|---|---|---|---|
| Tumor Size | 0.005 | 102 HCC tissue samples [3] | Associated with larger tumors (>5 cm) |
| Tumor Grade (Edmondson) | 0.002 | 102 HCC tissue samples [3] | Linked to poor differentiation (Grade III+IV) |
| Lesions in Both Liver Lobes | 0.02 | 60 HCC patients [1] | Indicates multifocal or extensive disease |
| Lymph Node Metastasis | < 0.0001 | Meta-analysis of 9 studies [5] | Correlates with metastatic spread |
These correlations reinforce the role of LINC00152 in driving HCC progression and offer insights into the potential mechanisms by which it affects patient outcomes.
Experimental Protocols for Validating LINC00152
Specimen Collection and RNA Extraction
- Specimen Source: Research can utilize fresh-frozen HCC tumor tissues and matched adjacent non-tumor tissues from patients undergoing curative resection, or blood-derived specimens (serum or plasma) [1] [3].
- RNA Extraction: Total RNA is extracted from tissues or serum using commercial kits such as the QIAamp RNA Blood Mini Kit [1]. RNA quality and concentration are assessed via spectrophotometry.
Quantification of LINC00152 Expression
- Reverse Transcription: RNA is reverse-transcribed into complementary DNA (cDNA) using the QuantiTect Reverse Transcription Kit [1].
- Quantitative Real-Time PCR (qRT-PCR): Expression levels are quantified using the QuantiTect SYBR Green PCR Kit on platforms like the 7500 ABI PRISM [1].
- Primer Sequences:
- LINC00152 Forward: 5′-GACTGGATGGTCGCTGCTTT-3′
- LINC00152 Reverse: 5′-CCCAGGAACTGTGCTGTGAA-3′ [1]
- Data Analysis: The ΔΔCT method is used for relative quantification, with GAPDH typically serving as the endogenous control [1].
Statistical Analysis for Prognostic Validation
- Optimal Cut-off Value: Patients are stratified into "high" and "low" LINC00152 expression groups based on the median expression value from the cohort [3].
- Survival Analysis: Kaplan-Meier curves and the log-rank test are employed to compare overall survival (OS) and/or disease-free survival (DFS) between the two groups [53] [38].
- Multivariate Cox Regression: This analysis determines whether LINC00152 expression is an independent prognostic factor after adjusting for covariates such as tumor size, stage, grade, and vascular invasion [1] [38].
Molecular Mechanisms Underlying Prognostic Value
The poor prognosis associated with high LINC00152 expression is driven by its multifaceted role in promoting oncogenic processes. The following diagram illustrates the key signaling pathways and molecular interactions through which LINC00152 exerts its functions in HCC.
LINC00152 drives HCC progression through several key mechanisms that explain its association with poor prognosis:
- mTOR Pathway Activation: LINC00152 activates the mechanistic target of rapamycin (mTOR) signaling pathway, a critical regulator of cancer cell proliferation, division, and carcinogenesis. It achieves this through cis-regulation of EpCAM (epithelial cell adhesion molecule), thereby promoting tumor growth [3].
- Competing Endogenous RNA (ceRNA) Activity: In the cytoplasm, LINC00152 functions as a molecular sponge for various tumor-suppressive microRNAs. By sequestering miR-125b, it derepresses SEMA4C, promoting cell migration and invasion. Similarly, by sponging miR-193a/b-3p, it upregulates CCND1 (Cyclin D1), driving cell cycle progression [15] [16].
- Epigenetic Regulation: In the nucleus, LINC00152 can interact with the polycomb repressive complex 2 (PRC2), influencing histone modifications and contributing to the epigenetic reprogramming of cancer cells [16].
The Scientist's Toolkit: Essential Research Reagents
To facilitate the replication of these studies and the development of novel diagnostics, the following table catalogues key reagents and their experimental applications.
Table 3: Essential Research Reagents for LINC00152 Investigation
| Reagent / Kit | Specific Product Example | Primary Function in Protocol |
|---|---|---|
| RNA Extraction Kit | QIAamp RNA Blood Mini Kit (Qiagen) | Isolation of high-quality total RNA from serum/plasma or tissues [1]. |
| Reverse Transcription Kit | QuantiTect Reverse Transcription Kit (Qiagen) | Synthesis of first-strand cDNA from purified RNA templates [1]. |
| qRT-PCR Master Mix | QuantiTect SYBR Green PCR Kit (Qiagen) | Fluorescence-based amplification and detection of LINC00152 transcripts [1]. |
| Specific Primers | Custom LINC00152 primers (e.g., Midland, Texas) | Selective amplification of the LINC00152 sequence for quantification [1]. |
| Cell Proliferation Assay | Cell Counting Kit-8 (CCK-8) / EdU Assay | Functional assessment of cell proliferation after LINC00152 knockdown [3]. |
The body of evidence, derived from rigorous multivariate analyses and mechanistic studies, firmly establishes LINC00152 as an independent prognostic biomarker in hepatocellular carcinoma. Its consistent correlation with shortened overall survival, disease-free survival, and aggressive clinicopathological features makes it a potent candidate for improving patient stratification. Future research should focus on standardizing detection protocols for clinical use and exploring the therapeutic potential of targeting LINC00152 or its downstream effectors in the mTOR and other associated pathways.
Hepatocellular carcinoma (HCC) continues to pose a significant global health challenge, with prognosis heavily dependent on early detection. While alpha-fetoprotein (AFP) has been the serological cornerstone for HCC screening for decades, its limitations in sensitivity and specificity are well-documented. Recent research has highlighted the immense diagnostic potential of long non-coding RNAs (lncRNAs), particularly LINC00152. This comprehensive analysis synthesizes evidence from multiple clinical studies demonstrating that LINC00152 not only surpasses AFP in diagnostic accuracy but also possesses independent prognostic value, offering a promising avenue for revolutionizing HCC management through improved early detection and risk stratification.
Hepatocellular carcinoma represents a major global health burden, ranking as the sixth most common cancer worldwide and the fourth leading cause of cancer-related mortality [10]. The disease typically develops in the context of chronic liver disease, with primary risk factors including hepatitis B and C infections, cirrhosis, alcohol consumption, and non-alcoholic fatty liver disease [54]. A significant challenge in HCC management lies in its frequent diagnosis at advanced stages, when curative treatment options are limited [55]. Traditional surveillance methods combining ultrasound with AFP measurement have demonstrated insufficient sensitivity and specificity, particularly for early-stage detection [56] [55] [54]. Approximately one-third of HCC cases do not exhibit elevated AFP levels, rendering this marker inadequate for a substantial patient population [10] [57]. These diagnostic shortcomings have fueled the search for more reliable biomarkers, with circulating lncRNAs emerging as particularly promising candidates due to their stability in blood, cancer-specific expression patterns, and detectability through minimally invasive liquid biopsies [57].
LINC00152: Molecular Characteristics and Oncogenic Functions
Basic Genomic Features and Expression Patterns
LINC00152, also known as long intergenic non-coding RNA 152 or CYTOR (cytoskeleton regulator RNA), is an 828-nucleotide lncRNA located on chromosome 2p11.2 [1] [16]. Initially identified during research on hepatocarcinogenesis, LINC00152 has since been recognized as a crucial oncogene across multiple cancer types [16]. The lncRNA is predominantly localized in the cytoplasm, where it functions as a competitive endogenous RNA (ceRNA) by sponging microRNAs, thereby relieving their inhibitory effects on target genes [16]. In the nucleus, LINC00152 can interact with epigenetic regulators such as the polycomb repressive complex 2 (PRC2) to modulate gene expression [16]. Its expression is significantly upregulated in HCC tissues and serum compared to both healthy controls and patients with benign liver conditions, suggesting its potential as a cancer-specific biomarker [1].
Mechanisms in Hepatocarcinogenesis
LINC00152 contributes to HCC pathogenesis through multiple molecular mechanisms. It activates the mechanistic target of rapamycin (mTOR) signaling pathway, which plays a critical role in controlling cancer cell proliferation, division, and carcinogenesis [1]. In hepatocellular carcinoma cells, LINC00152 promotes epithelial-mesenchymal transition (EMT) – a key process in cancer metastasis – by inhibiting E-cadherin expression through interaction with EZH2 [58]. Additionally, LINC00152 facilitates cell cycle progression by interacting with proteins associated with the M phase of the cell cycle [1] [58]. These multifaceted oncogenic functions underscore the molecular significance of LINC00152 in HCC development and progression.
Direct Diagnostic Performance Comparison: LINC00152 vs. AFP
Quantitative Performance Metrics
Multiple studies have systematically compared the diagnostic accuracy of LINC00152 against conventional AFP testing, with consistent results demonstrating the superiority of the lncRNA biomarker.
Table 1: Head-to-Head Diagnostic Performance of LINC00152 vs. AFP
| Biomarker | AUC | Sensitivity (%) | Specificity (%) | Study Population | Citation |
|---|---|---|---|---|---|
| LINC00152 | 0.877 | 83.0 | 81.0 | 129 HCC, 76 benign liver disease, 93 healthy controls | [56] |
| AFP | 0.801 | 62.3 | 85.2 | Same cohort as above | [56] |
| LINC00152 | 0.84 | 83.0 | 67.0 | 52 HCC, 30 healthy controls | [10] |
| AFP | 0.76 | 60.0 | 53.0 | Same cohort as above | [10] |
| LINC00152 | Not reported | Significant diagnostic value (p<0.001) | Significant diagnostic value (p<0.001) | 60 HCC, 60 liver cirrhosis, 40 healthy controls | [1] |
Superior Performance in Early-Stage Detection
The critical advantage of LINC00152 over AFP becomes particularly evident in early-stage HCC detection. A 2020 comprehensive study evaluating eight circulating lncRNAs determined that LINC00152 demonstrated the best individual performance with an area under the curve (AUC) of 0.877, significantly outperforming AFP (AUC=0.801) [56]. This enhanced diagnostic capability at earlier disease stages is clinically paramount, as it enables intervention when curative treatments such as surgical resection, ablation, or transplantation remain viable options [10]. The improved sensitivity of LINC00152 addresses a fundamental limitation of AFP, which fails to detect approximately 40% of HCC cases, particularly those in initial developmental phases [10] [57].
Synergistic Potential: LINC00152 and AFP Combination Panels
Enhanced Diagnostic Accuracy Through Biomarker Integration
Research indicates that combining LINC00152 with AFP creates a synergistic effect that surpasses the diagnostic capability of either biomarker alone.
Table 2: Performance of Combined Biomarker Panels
| Biomarker Panel | AUC | Sensitivity (%) | Specificity (%) | Study Details | Citation |
|---|---|---|---|---|---|
| LINC00152 + AFP | 0.906 | Not specified | Not specified | 129 HCC patients vs. controls | [56] |
| LINC00152 + UCA1 + AFP | 0.912 | 82.9 | 88.2 | Logistic regression model | [56] |
| ML Model (inc. LINC00152) | ~1.00 | 100 | 97 | 52 HCC, 30 controls; included lncRNAs + conventional labs | [10] |
The most impressive results were achieved using a three-component panel consisting of LINC00152, UCA1 (another oncogenic lncRNA), and AFP, which yielded an AUC of 0.912 with 82.9% sensitivity and 88.2% specificity [56]. This combination effectively leverages the strengths of each biomarker while compensating for their individual limitations. Further enhancing this approach, a machine learning model incorporating LINC00152 alongside other lncRNAs and conventional laboratory parameters achieved nearly perfect diagnostic accuracy with 100% sensitivity and 97% specificity [10], demonstrating the powerful potential of integrated diagnostic approaches in HCC detection.
Independent Prognostic Value of LINC00152 in HCC
Correlation with Clinicopathological Features
Beyond its diagnostic utility, LINC00152 demonstrates significant independent prognostic value in hepatocellular carcinoma. Research has established strong correlations between elevated LINC00152 expression and aggressive disease characteristics. In HCV-induced HCC patients, higher LINC00152 levels were significantly associated with lesions involving both liver lobes (p=0.02) [1]. A comprehensive meta-analysis encompassing multiple cancers revealed that LINC00152 overexpression significantly correlates with lymph node metastasis (OR=2.54, 95% CI=1.54-4.18) and advanced TNM stage (OR=2.32, 95% CI=1.36-3.93) [58]. These associations position LINC00152 as not merely a diagnostic marker but also an indicator of disease aggressiveness and potential progression.
Survival Analysis and Multivariate Prognostic Models
Most importantly, LINC00152 functions as an independent predictor of survival outcomes in HCC patients. Multivariate Cox regression analysis has identified high serum LINC00152 levels as an independent indicator of poor prognosis (HR=2.23, 95% CI=1.30-5.29, p=0.03) [1]. The meta-analysis by Wang et al. further confirmed that LINC00152 expression is significantly associated with shorter overall survival (HR=1.94, 95% CI=1.25-3.02) and increased tumor recurrence (OR=3.32, 95% CI=1.98-5.57) [58]. These robust statistical findings underscore the value of LINC00152 as a prognostic biomarker capable of identifying patients at higher risk of mortality and disease recurrence, thereby enabling more personalized treatment approaches and intensified surveillance for those who would benefit most.
Experimental Protocols and Research Methodologies
Standardized Workflow for LINC00152 Quantification
The evaluation of LINC00152 as a circulating biomarker follows a standardized experimental workflow that ensures reproducibility and reliability across studies:
LINC00152 Detection Workflow
Detailed Methodological Protocols
Sample Collection and Processing
Peripheral blood samples (typically 5-10 mL) are collected in EDTA-containing vacuum tubes or serum separation tubes from HCC patients and appropriate controls [1] [56] [10]. Serum is isolated by centrifugation at 3,000 rpm for 10 minutes at 4°C, followed by careful transfer of the supernatant to fresh tubes without disturbing the buffy coat [56]. Isolated serum or plasma is immediately frozen at -80°C to preserve RNA integrity until nucleic acid extraction [56] [10].
RNA Extraction and Quality Control
Total RNA is extracted from serum/plasma using commercial kits such as the QIAamp RNA Blood Mini Kit [1] or miRNeasy Mini Kit [10] according to manufacturer protocols. RNA quantity and purity are assessed using spectrophotometry (NanoDrop systems), with acceptable A260/280 ratios typically ranging from 1.8 to 2.1 [56]. Some protocols incorporate synthetic spike-in RNAs to monitor extraction efficiency and potential inhibitors.
cDNA Synthesis and Quantitative Real-Time PCR
RNA is reverse transcribed into cDNA using the RevertAid First Strand cDNA Synthesis Kit or similar systems [10]. Quantitative PCR reactions are performed in 20-μL volumes containing SYBR Green Master Mix, cDNA template, and specific primers. The primer sequences commonly used for LINC00152 detection are:
Amplification conditions typically include an initial activation step at 95°C for 3-5 minutes, followed by 40-55 cycles of denaturation (94°C for 30 seconds), annealing (55-60°C for 30 seconds), and extension (72°C for 30 seconds) [1] [56]. Melting curve analysis is performed to verify amplification specificity. GAPDH is commonly used as the endogenous control for data normalization using the 2−ΔΔCt method [1] [56] [10].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for LINC00152 Investigation
| Reagent/Kit | Specific Function | Application Context | Representative Product |
|---|---|---|---|
| RNA Extraction Kit | Isolation of high-quality total RNA from serum/plasma | Critical first step in lncRNA detection | QIAamp RNA Blood Mini Kit [1], miRNeasy Mini Kit [10] |
| Reverse Transcriptase Kit | Conversion of RNA to complementary DNA (cDNA) | Essential for subsequent PCR amplification | RevertAid First Strand cDNA Synthesis Kit [10] |
| SYBR Green Master Mix | Fluorescent detection of amplified DNA during qPCR | Enables quantitative measurement of LINC00152 | QuantiTect SYBR Green PCR Kit [1], PowerTrack SYBR Green Master Mix [10] |
| Specific Primers | Target-specific amplification of LINC00152 | Ensures specific detection of target lncRNA | Custom-designed LINC00152 primers [1] [56] |
| Reference Gene Assays | Amplification of normalization genes (GAPDH) | Essential for data normalization and quantitative comparison | GAPDH primers [1] [56] |
Molecular Pathways and Experimental Framework
LINC00152 Oncogenic Mechanisms
The comprehensive evidence presented herein unequivocally demonstrates that LINC00152 outperforms AFP as a diagnostic biomarker for hepatocellular carcinoma while additionally providing independent prognostic value. The superior diagnostic accuracy of LINC00152, particularly in early-stage disease, addresses a critical clinical need in HCC management. Furthermore, the synergistic potential of LINC00152 when combined with AFP and other biomarkers in multi-analyte panels promises to revolutionize HCC detection strategies. The integration of machine learning approaches with lncRNA biomarkers, as demonstrated in recent studies [10], points toward a future where HCC diagnosis and prognosis become increasingly precise and personalized. As research advances, the translation of these findings into clinical practice will be essential for improving outcomes for HCC patients worldwide through earlier detection and more accurate prognostic stratification.
Within the rapidly evolving field of Hepatocellular Carcinoma (HCC) research, the quest for reliable prognostic biomarkers is paramount for improving patient stratification and therapeutic outcomes. Long non-coding RNAs (lncRNAs) have emerged as crucial regulators of cancer pathogenesis, with LINC00152 distinguished as a particularly promising candidate. This meta-analysis synthesizes quantitative evidence from multiple studies to definitively establish the independent prognostic value of LINC00152 across solid tumors, with a specific focus on its implications for HCC. The consistent observation of LINC00152 overexpression in cancerous tissues and its association with aggressive clinicopathological features underscore its potential utility as a robust biomarker for prognostication.
Quantitative Synthesis of Prognostic Data
Pooled Survival Analysis from Meta-Analyses
The aggregated data from large-scale meta-analyses provide compelling evidence for the prognostic power of LINC00152. The following table summarizes the pooled hazard ratios (HRs) for key survival endpoints across various solid tumors.
Table 1: Pooled Hazard Ratios for Survival Endpoints from Meta-Analyses
| Survival Endpoint | Pooled Hazard Ratio (HR) | 95% Confidence Interval | Heterogeneity (I²) | Number of Studies/Patients | Citation |
|---|---|---|---|---|---|
| Overall Survival (OS) | 1.98 | 1.70 - 2.31 | 0% | 9 studies / 808 patients | [5] |
| Overall Survival (OS) | 1.94 | 1.25 - 3.02 | 50% | 9 studies / 862 patients | [58] [43] |
| Disease-Free Survival (DFS) | 1.66 | 1.20 - 2.29 | 75.8% | 9 studies / 808 patients | [5] |
This quantitative synthesis demonstrates that elevated LINC00152 expression is significantly associated with poorer survival outcomes. The pooled HR of 1.98 for OS, derived from a fixed-effects model due to low heterogeneity, indicates that patients with high LINC00152 expression face nearly double the risk of mortality compared to those with low expression [5]. Similarly, the association with reduced DFS (HR=1.66) further underscores its link to cancer recurrence and progression [5].
Association with Clinicopathological Features
Beyond survival, LINC00152 expression is strongly correlated with advanced disease stage and metastatic spread, which are critical drivers of mortality in HCC. The table below details these associations using pooled odds ratios (ORs).
Table 2: Association of LINC00152 with Clinicopathological Features
| Clinicopathological Feature | Pooled Odds Ratio (OR) | 95% Confidence Interval | Statistical Significance (p-value) |
|---|---|---|---|
| Lymph Node Metastasis (LNM) | 2.93 | 1.88 - 4.57 | < 0.0001 [5] |
| Lymph Node Metastasis (LNM) | 2.54 | 1.54 - 4.18 | 0.0003 [58] |
| Advanced TNM Stage | 2.32 | 1.36 - 3.93 | 0.002 [58] |
| Tumor Recurrence | 3.32 | 1.98 - 5.57 | < 0.00001 [58] |
The data reveal that high LINC00152 expression is positively associated with lymph node metastasis (OR=2.93) and tumor recurrence (OR=3.32), reinforcing its role in promoting aggressive tumor behavior [5] [58]. Notably, no significant associations were found with patient age or gender, suggesting that LINC00152's prognostic value is independent of these demographic factors [58].
Experimental Validation in Hepatocellular Carcinoma
Diagnostic and Prognostic Utility in HCC
Recent clinical studies specifically focused on HCC validate the findings of the broader meta-analyses. A 2024 study investigating a panel of lncRNAs confirmed that LINC00152 is significantly upregulated in HCC patient plasma [10]. This study further reported that a higher LINC00152 to GAS5 (a tumor-suppressive lncRNA) expression ratio was significantly correlated with increased mortality risk, providing a potent prognostic signature for HCC patients [10]. Another study identified LINC00152 as an independent prognostic factor in HBV-associated HCC, with high expression linked to larger tumor size and advanced TNM stage [59].
Detailed Experimental Protocols for Mechanistic Investigation
To support translational research, this section outlines standard experimental methodologies used to elucidate the functional role and diagnostic potential of LINC00152 in HCC.
Table 3: Key Experimental Protocols in LINC00152 Research
| Experimental Area | Protocol Description | Key Reagents & Techniques | Typical Outcome Measures |
|---|---|---|---|
| Expression Profiling | Quantifying LINC00152 levels in matched tumor and adjacent non-tumor tissues or plasma from HCC patients. | RNA Extraction: miRNeasy Mini Kit (Qiagen). cDNA Synthesis: RevertAid First Strand cDNA Synthesis Kit. qRT-PCR: PowerTrack SYBR Green Master Mix on a ViiA 7 system. Normalization: GAPDH [10]. | Relative expression (ΔΔCt method); ROC curve analysis for diagnostic accuracy. |
| Functional Analysis (in vitro) | Investigating oncogenic functions through gene manipulation in HCC cell lines (e.g., Huh7, HepG2). | Knockdown: siRNAs or shRNAs targeting LINC00152. Overexpression: LINC00152 plasmid vectors. Assays: CCK-8 for proliferation; Transwell for migration/invasion; Flow cytometry for cell cycle/apoptosis [19]. | Cell viability, colony formation, migration/invasion rates, apoptosis percentage, cell cycle distribution. |
| Mechanistic Studies | Deciphering molecular pathways, such as the ceRNA mechanism. | Subcellular Fractionation: To confirm cytoplasmic localization. Luciferase Reporter Assay: To validate binding to miRNAs like miR-139-5p. RNA Immunoprecipitation (RIP): Anti-Ago2 antibody to confirm RNA-induced silencing complex incorporation [19]. | Luciferase activity, enrichment of LINC00152 and miRNA in Ago2 pellets, Western blot of target proteins (e.g., NOTCH1). |
Molecular Mechanisms and Signaling Pathways
The oncogenic functions of LINC00152 are mediated through diverse molecular mechanisms, which have been systematically investigated in HCC and other cancers. The diagram below illustrates the three primary mechanisms by which LINC00152 promotes tumor progression and confers therapy resistance.
Diagram 1: Molecular mechanisms of LINC00152 in cancer progression. LINC00152 operates via sponging miRNAs, stabilizing oncoproteins, and facilitating epigenetic silencing, collectively driving aggressive tumor phenotypes.
Key Signaling Pathways in HCC
In HCC, LINC00152 primarily exerts its effects through specific interactions:
- miR-139-5p/NOTCH1 Axis: Cytoplasmic LINC00152 acts as a competitive endogenous RNA (ceRNA) by binding to and "sponging" tumor-suppressive miR-139-5p. This sequestration alleviates the miR-139-5p-mediated repression of its target, NOTCH1, a well-known oncogene, thereby promoting proliferation, metastasis, and 5-FU resistance [19].
- Stabilization of BCL6: LINC00152 directly binds to the BCL6 protein at specific serine residues (Ser333 and Ser343), shielding it from ubiquitin-mediated degradation. The stabilized BCL6 protein then enhances the transcription of genes driving proliferation and invasion [37].
- AKT Signaling Pathway: In colon cancer models relevant to HCC biology, LINC00152 contributes to oxaliplatin resistance by sponging miR-193a-3p, leading to upregulation of ERBB4 and consequent activation of the AKT signaling pathway [60].
The Scientist's Toolkit: Essential Research Reagents
For researchers aiming to investigate LINC00152 in HCC, the following table catalogues critical reagents and their applications based on cited experimental evidence.
Table 4: Key Research Reagent Solutions for LINC00152 Studies
| Reagent / Kit | Specific Function / Target | Application in Research | Citation |
|---|---|---|---|
| miRNeasy Mini Kit (Qiagen) | Isolation of total RNA (including lncRNAs) from tissues or plasma. | Sample preparation for downstream expression analysis by qRT-PCR. | [10] |
| RevertAid First Strand cDNA Synthesis Kit | Reverse transcription of RNA into stable cDNA. | Essential first step for gene expression quantification. | [10] |
| PowerTrack SYBR Green Master Mix | Fluorescent detection of amplified DNA during qRT-PCR. | Quantitative measurement of LINC00152 expression levels. | [10] |
| LINC00152-specific siRNAs/shRNAs | Sequence-specific knockdown of LINC00152 transcript. | Functional loss-of-function studies to assess oncogenic phenotypes. | [19] [53] |
| Anti-Ago2 Antibody | Immunoprecipitation of the RNA-induced silencing complex (RISC). | Validation of miRNA sponging (ceRNA) mechanism via RIP assays. | [19] |
| RNAscope Probe-LINC00152 | In situ hybridization probe for detecting LINC00152 mRNA in FFPE tissues. | Spatial resolution of LINC00152 expression within tumor tissue architecture. | [37] |
This synthesis of meta-analysis evidence and experimental data unequivocally demonstrates that LINC00152 is a powerful independent prognostic biomarker in solid tumors, including HCC. The consistent quantitative data showing pooled hazard ratios of approximately 2.0 for overall survival and strong associations with metastasis and recurrence provide a robust statistical foundation for its clinical relevance. The well-documented molecular mechanisms, particularly its role as a ceRNA for miR-139-5p in HCC, offer a compelling biological rationale for its oncogenic functions. For the field of HCC research and drug development, LINC00152 represents a promising candidate for non-invasive diagnostics, patient risk stratification, and as a potential therapeutic target to overcome chemoresistance. Future studies focusing on standardizing detection methods and developing targeted interventions against LINC00152 are warranted to translate these findings into clinical practice.
Long non-coding RNA LINC00152 has emerged as a critical molecular regulator in hepatocellular carcinoma (HCC), demonstrating significant potential for predicting surgical outcomes and treatment response. This review synthesizes current evidence validating LINC00152 as an independent prognostic biomarker, highlighting its utility in clinical decision-making for HCC management. We comprehensively analyze quantitative data from multiple studies, detail experimental methodologies for biomarker assessment, and elucidate the molecular mechanisms through which LINC00152 influences HCC pathogenesis and therapeutic resistance. The integration of LINC00152 detection with emerging technologies like machine learning offers promising avenues for enhancing prognostic accuracy and personalizing treatment strategies for HCC patients.
Prognostic Value of LINC00152 in Hepatocellular Carcinoma
LINC00152 demonstrates consistent independent prognostic value across multiple HCC patient cohorts, with elevated expression significantly correlating with adverse clinical outcomes. Evidence from multivariate Cox proportional hazards regression analyses confirms its utility in predicting overall survival (OS) and recurrence-free survival (RFS) following surgical resection.
Table 1: Prognostic Significance of LINC00152 in HCC
| Study | Cohort Size | Detection Method | HR for OS (95% CI) | P-value | Other Outcomes |
|---|---|---|---|---|---|
| Wang et al. [9] | 63 | qRT-PCR | 2.524 (1.661-4.015) | 0.001 | - |
| Meta-analysis [5] | 808 (multiple cancers) | Various | 1.98 (1.70-2.31) | <0.0001 | Pooled DFS: HR=1.66 (1.20-2.29) |
| Machine Learning Study [10] | 52 | qRT-PCR | - | - | LINC00152/GAS5 ratio correlated with mortality |
The meta-analysis comprising nine original studies and 808 total patients demonstrated that LINC00152 overexpression is positively related to poor overall survival (pooled HR = 1.98, 95% CI: 1.70-2.31, p < 0.0001) and poor disease-free survival (HR = 1.66, 95% CI: 1.20-2.29, p < 0.0001) in human solid cancers, including HCC [5]. Furthermore, a higher LINC00152 to GAS5 expression ratio significantly correlated with increased mortality risk, suggesting the potential utility of lncRNA ratios in prognostic stratification [10].
Table 2: Association of LINC00152 with Clinicopathological Features
| Parameter | Association | Odds Ratio (95% CI) | P-value | Source |
|---|---|---|---|---|
| Lymph Node Metastasis | Positive | 2.93 (1.88-4.57) | <0.0001 | [5] |
| Tumor Grade | Inverse with low-grade | 2.43 (1.51-3.92) | 0.033 | [5] |
| Tumor Recurrence | Positive | 3.32 (1.98-5.57) | <0.0001 | [5] |
LINC00152 in Predicting Treatment Response
Chemotherapy Resistance
LINC00152 contributes to therapeutic resistance through multiple molecular mechanisms. In estrogen receptor-positive (ER+) breast cancer, which shares some resistance pathways with HCC, LINC00152 confers tamoxifen resistance by blocking drug-induced ferroptosis, an iron-mediated cell death process [36]. Mechanistically, LINC00152 inhibition reduces the mRNA stability of phosphodiesterase 4D (PDE4D), leading to activation of the cAMP/PKA/CREB axis and increased expression of the TRPC1 Ca2+ channel [36]. This causes cytosolic Ca2+ overload and generation of reactive oxygen species (ROS), ultimately restoring drug-induced lipid peroxidation and ferroptotic cell death.
Surgical Outcomes Prediction
Pre-treatment LINC00152 expression levels in tumor tissues effectively predict postoperative outcomes in HCC patients undergoing curative surgical resection. Wang et al. demonstrated that high pre-treatment LINC00152 expression independently predicted shorter overall survival (HR, 2.524; 95% CI, 1.661-4.015; P = 0.001) in 63 HCC patients treated with curative surgical resection [9]. This prognostic capability enables improved patient stratification for surgical intervention and adjunct therapies.
Experimental Protocols for LINC00152 Assessment
Sample Collection and RNA Isolation
- Sample Types: LINC00152 can be detected in both tumor tissues and plasma/serum samples, enabling flexible biomarker assessment [9] [10]
- RNA Isolation: Total RNA isolation using miRNeasy Mini Kit (QIAGEN, cat no. 217004) according to manufacturer's protocol [10]
- Quality Control: RNA quality and concentration evaluation using OD 260/280 and OD 260/230 ratios determined via Nanodrop 2000 [61]
Expression Quantification Methods
- cDNA Synthesis: Reverse transcription using RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, cat no. K1622) [10]
- qRT-PCR Analysis: PowerTrack SYBR Green Master Mix kit (Applied Biosystems, cat no. A46012) on ViiA 7 real-time PCR system [10]
- Primer Sequences: Specific primers for LINC00152 detection: Forward: 5′-GGACCTGATAACGGGAACCA-3′, Reverse: 5′-GGGCTGAGTCGTGATTTTCG-3′ [35]
- Normalization: Housekeeping gene glyceraldehyde-3-phosphate dehydrogenase (GAPDH) used for normalization of expression data [10]
- Data Analysis: ΔΔCT method for relative quantification with reactions performed in triplicate [10]
In Situ Hybridization (ISH)
- ISH-based Detection: Alternative method for LINC00152 detection in formalin-fixed paraffin-embedded (FFPE) tissue sections [9]
- Clinical Correlation: LINC00152 ISH score correlated with high Ki67 score and high tumor grade in clinical cohorts [36]
Molecular Mechanisms of LINC00152 in HCC Progression
LINC00152 promotes hepatocellular carcinoma progression through multiple interconnected signaling pathways and molecular mechanisms.
LINC00152 Functional Mechanisms in HCC
PI3K/AKT/mTOR Signaling Pathway
LINC00152 promotes HCC progression by regulating the phosphatidylinositol 3-kinase/Akt/mammalian target of rapamycin signaling pathway through sponging miR-139, leading to PIK3CA upregulation [13]. This mechanism enhances cell proliferation, survival, and metabolic reprogramming in hepatocellular carcinoma cells.
miRNA Sponging Mechanism
As a competing endogenous RNA (ceRNA), LINC00152 sequesters multiple tumor-suppressive miRNAs:
- miR-139: Regulates PIK3CA expression in HCC [13]
- miR-193b-3p: Promotes phosphorylation and activation of PI3K/AKT signaling in tongue squamous cell carcinoma, demonstrating conserved mechanisms across cancers [16]
Epigenetic Regulation
LINC00152 interacts with enhancer of zeste homolog 2 (EZH2), a member of the polycomb-group family that functions as a histone methyltransferase repressing transcription of target genes [35]. This interaction promotes mesothelioma cell proliferation, migration, and invasion, suggesting similar epigenetic mechanisms may operate in HCC.
Research Reagent Solutions
Table 3: Essential Research Reagents for LINC00152 Investigation
| Reagent/Catalog Number | Application | Experimental Function | Source |
|---|---|---|---|
| miRNeasy Mini Kit (QIAGEN, 217004) | RNA Isolation | Total RNA extraction from tissues/body fluids | [10] |
| RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, K1622) | cDNA Synthesis | Reverse transcription for qRT-PCR template | [10] |
| PowerTrack SYBR Green Master Mix (Applied Biosystems, A46012) | qRT-PCR | Quantitative detection of LINC00152 expression | [10] |
| Lipofectamine RNAiMAX (Invitrogen) | Functional Studies | Transfection of miRNA mimics/inhibitors | [61] |
| Silencer Select LINC00152 siRNA (s195584) | Functional Studies | Specific LINC00152 knockdown | [35] |
| pcDNA3.1-H19 (Addgene) | Functional Studies | Full-length H19 construct for overexpression | [61] |
| TaqMan Advanced miRNA cDNA Synthesis Kit | miRNA Analysis | miRNA-specific cDNA synthesis | [61] |
Integration with Machine Learning and Diagnostic Panels
The diagnostic and prognostic performance of LINC00152 can be significantly enhanced through integration with machine learning algorithms and combination with other biomarkers:
- Individual Performance: LINC00152 alone exhibits moderate diagnostic accuracy with sensitivity and specificity ranging from 60-83% and 53-67%, respectively [10]
- Machine Learning Integration: A model incorporating LINC00152 with conventional laboratory parameters achieved 100% sensitivity and 97% specificity for HCC diagnosis [10]
- Combination Panels: LINC00152 combination with AFP or both AFP and HULC demonstrates improved diagnostic power compared to single biomarkers [10]
- Expression Ratios: The LINC00152 to GAS5 expression ratio significantly correlates with mortality risk, providing enhanced prognostic stratification [10]
LINC00152 represents a promising independent prognostic biomarker in hepatocellular carcinoma with emerging applications in predicting treatment response and surgical outcomes. Its involvement in critical signaling pathways, including PI3K/AKT/mTOR and cAMP/Ca2+/ferroptosis axes, provides mechanistic insights into HCC pathogenesis and therapeutic resistance. The standardization of detection methodologies and integration with machine learning approaches will be essential for translating LINC00152 assessment into clinical practice. Future research should focus on validating LINC00152 in larger, prospective cohorts and developing targeted therapeutic strategies that modulate its expression or downstream effects for improved HCC management.
Conclusion
LINC00152 demonstrates robust independent prognostic value in hepatocellular carcinoma, outperforming conventional biomarkers like AFP in multiple clinical scenarios. Its dual presence in tumor tissues and circulation enables versatile clinical application through both tissue-based and liquid biopsy approaches. The integration of LINC00152 into multi-marker panels and machine learning algorithms represents a paradigm shift in HCC management, offering unprecedented precision in risk stratification and outcome prediction. Future research must focus on large-scale prospective validation, standardization of detection protocols, and exploration of LINC00152's therapeutic targeting potential. For drug development professionals, LINC00152 offers a promising biomarker for patient selection and treatment monitoring in clinical trials, potentially accelerating the development of novel HCC therapeutics. The cumulative evidence positions LINC00152 as a cornerstone in the evolving landscape of precision oncology for liver cancer.
References
- 1. Serum LINC00152 and UCA1 in HCV-Induced ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10581015/]
- 2. Serum LINC00152 and UCA1 in HCC | BTT [https://www.dovepress.com/serum-linc00152-and-uca1-in-hcv-induced-hepatocellular-carcinoma-clini-peer-reviewed-fulltext-article-BTT]
- 3. LINC00152 promotes proliferation in hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4767473/]
- 4. The long non-coding RNA LINC00152 is essential for cell ... [https://www.nature.com/articles/s41598-017-02357-0]
- 5. Prognostic Values of Long Noncoding RNA linc00152 in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6964117/]
- 6. Long Non-Coding RNA LINC00152 Regulates Self ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.694021/full]
- 7. Exosomal linc00152 intensifies the crosstalk between ... [https://www.sciencedirect.com/science/article/pii/S1665268124005283]
- 8. LINC00152 promotes proliferation in hepatocellular ... [https://www.oncotarget.com/article/5970/text/]
- 9. Long non-coding RNA-based single and combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405140/]
- 10. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 11. Novel Biomarkers for Early Detection of Hepatocellular ... [https://www.mdpi.com/2075-4418/14/20/2278]
- 12. Non-coding RNAs in Hepatocellular Carcinoma [https://www.genesispub.org/non-coding-rnas-in-hepatocellular-carcinoma]
- 13. Long Intergenic Nonprotein Coding RNA 0152 Promotes ... [https://www.sciencedirect.com/science/article/pii/S0002944020300092]
- 14. LINC00152 promotes cell cycle progression in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6103663/]
- 15. Long non-coding RNA LINC00152 in cancer - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9399773/]
- 16. Long non-coding RNA LINC00152 in cancer [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.960193/full]
- 17. Linc00152 promotes cancer progression in hepatitis B ... [https://www.sciencedirect.com/science/article/abs/pii/S0753332217303578]
- 18. Serum LINC and UCA1 in HCV-Induced 00152 ... Hepatocellular [https://pubmed.ncbi.nlm.nih.gov/37854341/]
- 19. Long non-coding RNA LINC00152 promotes cell ... - Nature [https://www.nature.com/articles/s41389-017-0008-4]
- 20. PI3K/AKT/mTOR Axis in Cancer - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308072/]
- 21. Targeting PI3K/AKT/mTOR signaling to overcome drug ... [https://www.sciencedirect.com/science/article/abs/pii/S0009279724002011]
- 22. The role of the mTOR pathway in breast cancer stem cells ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04218-4]
- 23. Salvigenin inhibits gastric cancer progression by ... [https://www.sciencedirect.com/science/article/pii/S0006291X25013610]
- 24. PYCR1 drives lung cancer progression through functional ... [https://www.nature.com/articles/s12276-025-01577-z]
- 25. LCP1 upregulation via EGFR signaling promotes oral ... [https://pubmed.ncbi.nlm.nih.gov/41044643]
- 26. Long Non-Coding RNA NRAD1 and LINC00152 are Highly Expressed and Associated with Prognosis in Patients with Hepatocellular Carcinoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7569076/]
- 27. Long Non-Coding RNA NRAD1 and LINC00152 are Highly Expressed and Associated with Prognosis in Patients with Hepatocellular Carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/33116620/]
- 28. A promising frontier of circulating messenger RNA in liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12375855/]
- 29. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 30. Comparing the Diagnostic Performance of Quantitative PCR ... [https://pubmed.ncbi.nlm.nih.gov/38103593/]
- 31. Long noncoding RNA LINC00152 is a potential prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6489806/]
- 32. LINC00152 Drives a Competing Endogenous RNA ... [https://www.mdpi.com/2073-4409/11/9/1528]
- 33. Analysis of four long non-coding RNAs for hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11604705/]
- 34. Machine learning-based diagnostic and prognostic models ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1581982/full]
- 35. Long Non-coding RNA LINC00152 Requires EZH2 to ... [https://ar.iiarjournals.org/content/43/12/5367]
- 36. Targeting LINC00152 activates cAMP/Ca 2+ /ferroptosis ... [https://www.nature.com/articles/s41419-024-06814-3]
- 37. LINC00152 Promotes Tumor Progression and Predicts ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.555132/full]
- 38. Long non-coding RNA-based single and combination ... [https://link.springer.com/article/10.1007/s12672-025-03309-1]
- 39. lncRNA involvement in hepatocellular carcinoma metastasis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6295623/]
- 40. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 41. Identification of an immune-related 6-lncRNA panel with a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10662904/]
- 42. A novel disulfidptosis-related lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582836/]
- 43. The prognostic effect of LINC00152 for cancer: a meta- ... [https://www.oncotarget.com/article/20130/text/]
- 44. Hepatocellular carcinoma: Epidemiology, diagnosis and ... [https://www.sciencedirect.com/science/article/pii/S2589555925002538]
- 45. Hepatocellular carcinoma | Nature Reviews Disease Primers [https://www.nature.com/articles/s41572-020-00240-3]
- 46. Trends in Incidence of Hepatocellular Carcinoma Between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12178839/]
- 47. Current progress and role of lncRNAs in HBV infection ... [https://www.sciencedirect.com/science/article/pii/S2352304225003678]
- 48. LincRNA-miR interactions in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552288/]
- 49. Breakthrough study reveals stability key for mRNA [https://european-biotechnology.com/latest-news/breakthrough-study-reveals-stability-key-for-mrna/]
- 50. RNA stability enhancers for durable base-modified mRNA ... [https://pubmed.ncbi.nlm.nih.gov/41203992/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=01UUc1QmqB44SM--aTaoXSRUMVcErD3NJCndRFgxe8R&fc=None&ff=20251112111107&v=2.18.0.post22+67771e2]
- 51. Evaluation of normalisation strategies for qPCR data ... [https://www.nature.com/articles/s41598-025-06657-8]
- 52. Emerging biomarkers for non-invasive diagnosis and ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2024.1405267/full]
- 53. Overexpression of LINC00152 correlates with poor patient ... [https://www.nature.com/articles/s41598-017-03043-x]
- 54. Decoding the molecular and genomic landscape of ... [https://www.nature.com/articles/s44355-025-00038-8]
- 55. Advances in the early diagnosis of hepatocellular carcinoma [https://www.sciencedirect.com/science/article/pii/S2352304220300222]
- 56. A Circulating Long Noncoding RNA Panel Serves as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7376401/]
- 57. Blood-derived lncRNAs as biomarkers for cancer diagnosis [https://www.nature.com/articles/s41698-022-00283-7]
- 58. The prognostic effect of LINC00152 for cancer: a meta- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5650433/]
- 59. Long noncoding RNA LINC00152 as a novel predictor of ... [https://www.sciencedirect.com/science/article/abs/pii/S0009898118301505]
- 60. Linc00152 Functions as a Competing Endogenous RNA to ... [https://www.sciencedirect.com/science/article/pii/S1525001616454651]
- 61. LncRNA H19 acts as a ceRNA to promote glioblastoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12177970/]