Lipid Metabolic Pathways in Hyperuricemia Patients with Diabetes: Molecular Mechanisms, Biomarkers, and Therapeutic Targeting
This article synthesizes current research on the intricate crosstalk between lipid metabolism and hyperuricemia in diabetic patients.
Lipid Metabolic Pathways in Hyperuricemia Patients with Diabetes: Molecular Mechanisms, Biomarkers, and Therapeutic Targeting
Abstract
This article synthesizes current research on the intricate crosstalk between lipid metabolism and hyperuricemia in diabetic patients. It explores foundational discoveries of specific dysregulated lipid species and pathways, such as glycerophospholipid and glycerolipid metabolism, identified via advanced lipidomics. The content delves into methodological approaches for analyzing these disruptions, examines the associated challenges in patient management and drug development, and evaluates emerging therapeutic strategies, including GLP-1 receptor agonists and novel small molecule inhibitors. Aimed at researchers and drug development professionals, this review provides a comprehensive framework for understanding the pathophysiological mechanisms and identifies promising targets for future biomarker discovery and precision medicine interventions in this complex comorbidity.
Unraveling the Core Lipid Pathways: Molecular Connections Between Hyperuricemia and Diabetic Dysregulation
Type 2 diabetes mellitus (T2DM) represents a complex metabolic disorder characterized by chronic hyperglycemia resulting from insulin resistance and impaired insulin secretion. Beyond its direct glycemic effects, T2DM frequently presents with a cluster of metabolic comorbidities, notably dyslipidemia and hyperuricemia, which independently and synergistically contribute to increased cardiovascular disease (CKD), chronic kidney disease (CKD), and microvascular complications [1] [2]. The co-occurrence of these conditions signifies a more advanced stage of metabolic dysregulation, warranting earlier and more aggressive intervention strategies [1].
The pathophysiological interplay between dyslipidemia and hyperuricemia in T2DM involves overlapping mechanisms including insulin resistance, chronic low-grade inflammation, oxidative stress, and endothelial dysfunction [1] [3]. In uncontrolled T2DM—typically defined by persistently elevated glycated hemoglobin (HbA1c) above target thresholds—these mechanisms are amplified, leading to accelerated vascular damage and a higher incidence of adverse renal and cardiovascular outcomes [1]. Understanding the epidemiological landscape and underlying biological pathways connecting these conditions is crucial for developing targeted therapeutic approaches for high-risk T2DM populations.
Epidemiological Landscape: Quantifying the Co-Occurrence
Prevalence Estimates and Population Risk
Epidemiological studies consistently demonstrate a strong association between dyslipidemia and hyperuricemia in T2DM populations, with significant variations across geographic regions and patient subgroups.
Table 1: Epidemiological Studies on Dyslipidemia and Hyperuricemia Co-Occurrence
| Study Population | Sample Size | Prevalence/Association | Key Findings | Citation |
|---|---|---|---|---|
| Uncontrolled T2DM (Romania) | 304 patients | 81.6% co-occurrence prevalence | RMRS significantly higher in co-occurrence group (median 16.9 vs. 10.0; p<0.001) | [1] [2] |
| General Population (Wuhu, China) | 298,891 participants | OR: 1.878 (95% CI: 1.835-1.922) | Dyslipidemia associated with 1.9x higher odds of hyperuricemia in multivariate analysis | [4] [5] |
| Hypertensive Chinese Population | 274 patients | Significant indirect effect via triglycerides | Hyperuricemia linked to T2DM through triglyceride mediation (coefficient=0.87, P=0.04) | [6] |
| Japanese vs. American Populations | 90,047 Japanese; 14,734 Americans | BMI cut-off for hyperuricemia: 23 kg/m² (Japan) vs. 27 kg/m² (U.S.) | Higher BMI associated with hyperuricemia risk in both populations, but at lower BMI thresholds in Japan | [7] |
The relationship between specific dyslipidemia subtypes and hyperuricemia reveals important patterns. In the large Wuhu population study, individuals with hypertriglyceridemia had 1.753 times higher odds (95% CI: 1.706-1.802), while those with mixed hyperlipidemia had 1.925 times higher odds (95% CI: 1.870-1.982) of hyperuricemia compared to those without dyslipidemia [4] [5]. This suggests that combined lipid abnormalities confer the greatest risk for elevated uric acid levels.
When examining lipid components, triglycerides demonstrate the strongest association with hyperuricemia. Individuals in the highest triglyceride quartile had 3.744 times higher odds of hyperuricemia (95% CI: 3.636-3.918) compared to those in the lowest quartile [4] [5]. Other significant lipid parameters included total cholesterol (OR: 1.518) and non-high-density lipoprotein cholesterol (OR: 1.775) in fully adjusted models.
Demographic and Clinical Risk Modifiers
The relationship between dyslipidemia and hyperuricemia in T2DM is further modulated by demographic and clinical factors:
Body Mass Index (BMI): A comparative study of Japanese and American populations revealed that while higher BMI was an independent risk factor for hyperuricemia in both populations, the BMI cut-off point above which hyperuricemia prevalence significantly increased was substantially lower in Japan (23 kg/m²) compared to the U.S. (27 kg/m²) [7]. This suggests ethnic variations in susceptibility to metabolic complications of obesity.
Hypertension: In hypertensive populations, the triad of hypertension, dyslipidemia, and hyperuricemia creates a particularly high-risk metabolic profile. Research indicates that hypertensive individuals with hyperuricemia demonstrate significantly higher triglyceride levels, which mediate diabetes risk in this population [6].
Diabetic Control Status: The Romanian study focusing specifically on uncontrolled T2DM (HbA1c ≥7%) found an exceptionally high co-occurrence rate of dyslipidemia and hyperuricemia (81.6%), suggesting that poor glycemic control exacerbates the clustering of these metabolic abnormalities [1] [2].
Pathophysiological Mechanisms and Signaling Pathways
The strong epidemiological association between dyslipidemia and hyperuricemia in T2DM is underpinned by several interconnected biological pathways.
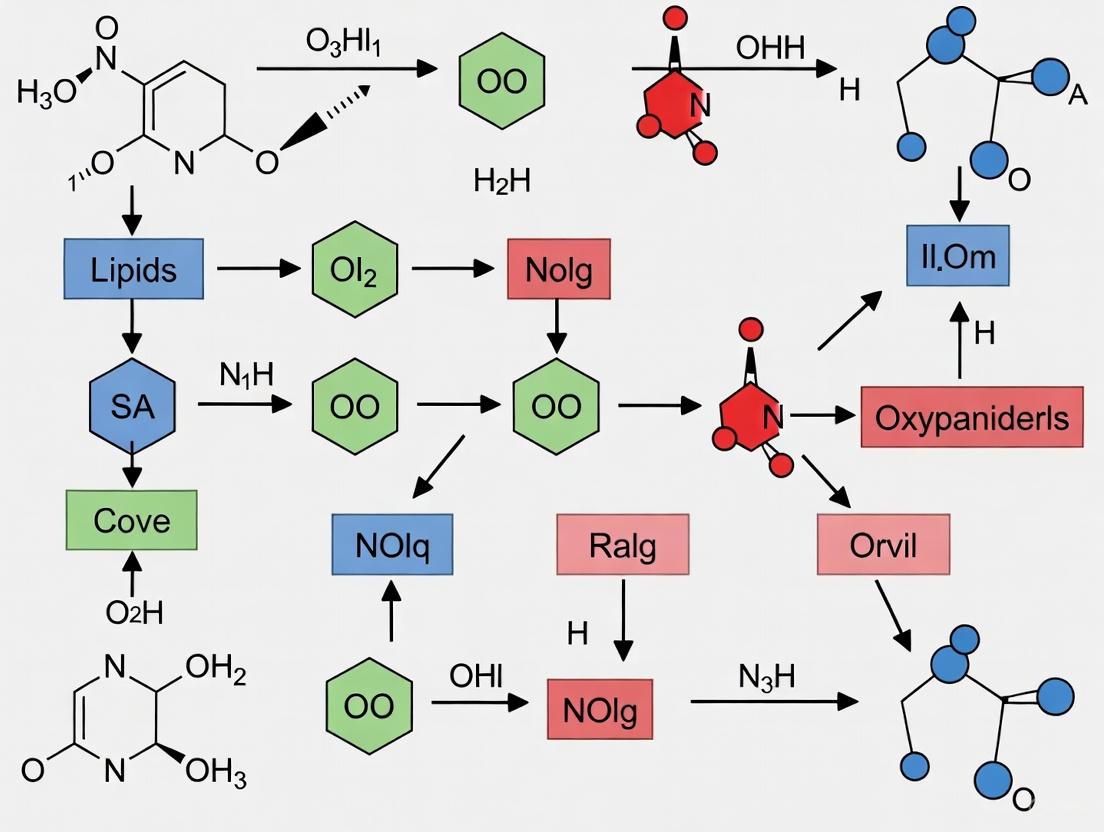
Integrated Metabolic Pathway
The following diagram illustrates the key pathophysiological mechanisms connecting dyslipidemia and hyperuricemia in T2DM:
Key Mechanistic Insights
Lipid Metabolism Disorders in Hyperuricemia
Advanced lipidomics approaches have revealed specific alterations in lipid metabolism associated with hyperuricemia. A multiomics study analyzing serum from 60 healthy individuals and 60 hyperuricemia patients identified 33 significantly upregulated lipid metabolites in hyperuricemia patients [8]. These metabolites were primarily involved in:
- Arachidonic acid metabolism
- Glycerophospholipid metabolism
- Linoleic acid metabolism
- GPI-anchor biosynthesis
- Alpha-linolenic acid metabolism
The study further established connections between specific immune factors and glycerophospholipid metabolism, including IL-10, CPT1, IL-6, SEP1, TGF-β1, Glu, TNF-α, and LD [8]. This suggests that hyperuricemia promotes a pro-inflammatory state that disrupts normal lipid metabolic pathways.
Triglyceride-Mediated Pathway to Diabetes
In hypertensive populations, triglycerides play a crucial mediating role between hyperuricemia and T2DM. Generalized structural equation modeling (GSEM) analysis revealed that while the direct effect of hyperuricemia on diabetes was not statistically significant (coefficient = -0.61, P=0.10), the indirect effect mediated by triglycerides was substantial (coefficient = 0.87, P=0.04) [6]. The path analysis demonstrated:
- Hyperuricemia → Elevated triglycerides (coefficient = 0.67, P=0.01)
- Elevated triglycerides → Increased diabetes risk (coefficient = 1.29, P<0.001)
This pathway underscores the importance of triglyceride metabolism as a mechanistic bridge between uric acid elevation and diabetes development in high-risk populations.
Uric Acid's Dual Role in Oxidative Stress
Uric acid exhibits a double-edged sword role in physiological and pathological contexts [3]. At normal levels, uric acid functions as a powerful antioxidant, effectively neutralizing singlet oxygen molecules, oxygen radicals, and peroxynitrite molecules due to its ability to provide electrons and act as a reducing agent [3]. However, when uric acid levels become elevated, it transforms into a pro-oxidant and pro-inflammatory molecule that exacerbates oxidative stress [3]. This paradoxical behavior contributes to the complex relationship between uric acid levels and metabolic dysfunction.
Research Methodologies and Experimental Approaches
Core Laboratory Techniques
Table 2: Essential Research Reagents and Methodologies
| Method/Reagent | Application | Technical Specifics | Research Utility |
|---|---|---|---|
| LC-MS/HPLC Lipidomics | Identification of differential lipid metabolites | UPLC system; Q-Exactive Plus MS; C18 column; positive/negative ion modes | Quantified 33 dysregulated lipids in hyperuricemia; identified 5 affected metabolic pathways [8] |
| ELISA Kits | Measurement of inflammatory cytokines & metabolic markers | Commercial kits for TNF-α, IL-6, CPT1, TGF-β1, etc.; microplate reader detection | Confirmed dysregulation of immune factors linked to glycerophospholipid metabolism [8] |
| Automatic Biochemical Analyzer | Standard lipid & uric acid profiling | Enzymatic colorimetric methods for TC, TG, HDL-C, LDL-C, SUA | Enabled large-scale epidemiological studies (n=298,891) with standardized measurements [4] [5] |
| Generalized Structural Equation Modeling (GSEM) | Mediation analysis of metabolic pathways | Bias-corrected bootstrapped CIs (5,000 resamples); adjustment for age, sex, BMI, medications | Quantified triglyceride mediation between HUA and T2DM (indirect effect: 0.87, P=0.04) [6] |
Analytical Workflows
The following diagram illustrates a standardized experimental workflow for investigating the dyslipidemia-hyperuricemia relationship in metabolic disease research:
Advanced Statistical Approaches
Contemporary research employs sophisticated statistical models to unravel the complex relationships between dyslipidemia and hyperuricemia:
Multivariable Logistic Regression: The large-scale Chinese study (n=298,891) employed binary logistic regression with sequential adjustment models (Model 1: unadjusted; Model 2: age and sex-adjusted; Model 3: fully adjusted for age, sex, smoking, drinking, obesity, hypertension, diabetes, and renal function parameters) to isolate the independent association between dyslipidemia and hyperuricemia [4] [5].
Risk Score Development: The Renal-Metabolic Risk Score (RMRS) was developed using standardized values of urea, TG/HDL ratio, and eGFR, with variable weights derived from logistic regression coefficients. The score was normalized to a 0-100 scale and demonstrated good discriminative performance (AUC: 0.78) for identifying T2DM patients with combined hyperuricemia and dyslipidemia [1] [2].
Mediation Analysis: The triglyceride mediation effect was tested using generalized structural equation modeling (GSEM) containing three paths: (i) hyperuricemia → triglycerides, (ii) triglycerides → T2DM, and (iii) hyperuricemia → T2DM, with adjustment for clinical covariates including renal function and medication use [6].
The robust epidemiological association between dyslipidemia and hyperuricemia in T2DM populations is supported by large-scale clinical evidence across diverse ethnic groups. The co-occurrence of these conditions, particularly in uncontrolled diabetes, identifies a high-risk subgroup requiring aggressive therapeutic management. The pathophysiological interplay involves complex mechanisms including shared metabolic pathways, inflammatory activation, and oxidative stress, with emerging evidence highlighting triglycerides as a key mediator in the hyperuricemia-diabetes relationship.
From a drug development perspective, these insights suggest that therapeutic strategies targeting both lipid metabolism and uric acid pathways may provide synergistic benefits for high-risk T2DM patients. Future research should focus on validating the RMRS in diverse populations, exploring the therapeutic potential of combined lipid- and urate-lowering approaches, and investigating specific molecular targets within the identified lipid metabolic pathways that link these two common metabolic disorders.
In the intricate landscape of metabolic disorders, the comorbidity of hyperuricemia and type 2 diabetes mellitus (T2DM) presents a significant clinical challenge, with dysregulated lipid metabolism serving as a crucial pathological link. Hyperuricemia, characterized by elevated serum uric acid levels, and T2DM, defined by impaired glucose regulation, frequently coexist, with epidemiological studies reporting a hyperuricemia prevalence of 21-32% among T2DM patients [9]. The interplay between these conditions is mediated substantially through perturbations in specific lipid classes, primarily triglycerides (TGs), phosphatidylethanolamines (PEs), and phosphatidylcholines (PCs). These lipids are not merely biomarkers but active participants in the pathophysiological processes, influencing insulin resistance, inflammatory responses, and metabolic homeostasis [10] [8] [11]. This review synthesizes current evidence on the roles of these three key lipid classes within the context of hyperuricemia and diabetes, providing researchers and drug development professionals with a comprehensive technical resource encompassing quantitative findings, methodological protocols, and visualized pathways.
Quantitative Profiling of Dysregulated Lipids
Advanced lipidomic technologies have revealed distinct alterations in triglyceride, phosphatidylethanolamine, and phosphatidylcholine profiles in patients with coexisting hyperuricemia and diabetes. These quantitative changes provide critical insights into the metabolic disturbances characterizing this comorbidity.
Table 1: Summary of Key Lipid Alterations in Hyperuricemia with Diabetes
| Lipid Class | Specific Lipid Species | Change Direction | Statistical Significance | Study Population | Citation |
|---|---|---|---|---|---|
| Triglycerides (TGs) | TG (16:0/18:1/18:2) and 12 other TGs | Significant upregulation | P < 0.001, FDR < 0.05 | DH vs. NGT (n=17/group) | [10] |
| Triglycerides | Overall TG levels | Significant elevation | P = 0.005 | Hypertensive diabetic patients (n=274) | [12] |
| Phosphatidylethanolamines (PEs) | PE (18:0/20:4) and 9 other PEs | Significant upregulation | P < 0.001, FDR < 0.05 | DH vs. NGT (n=17/group) | [10] |
| Phosphatidylcholines (PCs) | PC (36:1) and 6 other PCs | Significant upregulation | P < 0.001, FDR < 0.05 | DH vs. NGT (n=17/group) | [10] |
| Diacylglycerols (DAGs) | DAG (16:0/22:5), DAG (16:0/22:6), DAG (18:1/20:5), DAG (18:1/22:6) | Significant upregulation | P < 0.05 | Middle-aged/elderly Chinese (n=2247) | [11] |
Table 2: Mediation and Pathway Analysis of Dysregulated Lipids
| Analytical Approach | Key Finding | Effect Size/Impact | Citation |
|---|---|---|---|
| Generalized Structural Equation Modeling (GSEM) | Triglycerides mediate hyperuricemia-diabetes association | Indirect effect: coefficient = 0.87, P = 0.04 | [12] |
| Pathway Enrichment Analysis | Glycerophospholipid metabolism disturbance | Impact value = 0.199 | [10] |
| Pathway Enrichment Analysis | Glycerolipid metabolism disturbance | Impact value = 0.014 | [10] |
| Network Analysis | TAGs/PCs/DAGs module association with HUA risk | Positive association, P < 0.01 | [11] |
The magnitude of triglyceride dysregulation is particularly striking, with one study reporting that occasional smoking increased diabetes risk (OR=3.92, 95% CI: 1.00-15.35), while hyperuricemia was positively associated with elevated triglyceride levels (coefficient = 0.67, P=0.01), which subsequently increased DM risk (coefficient = 1.29, P < 0.001) [12]. The mediating role of triglycerides between hyperuricemia and diabetes underscores their central position in the metabolic cascade, explaining why although the direct effect of hyperuricemia on DM was not statistically significant (coefficient = -0.61, P=0.10), the indirect effect mediated by triglycerides was substantial (coefficient = 0.87, P=0.04) [12].
Methodological Framework for Lipid Analysis
Sample Preparation and Lipid Extraction
The accuracy of lipidomic profiling hinges on standardized sample preparation protocols. In studies of hyperuricemia and diabetes, the following methodology has been employed:
Sample Collection: Fasting venous blood samples (5 mL) are collected in EDTA-containing tubes or serum separation tubes [10] [8]. For plasma preparation, whole blood is immediately inverted for homogenization and centrifuged at 3,000 rpm for 10 minutes at 4°C [8]. The resulting plasma or serum is aliquoted and stored at -80°C until analysis.
Lipid Extraction: A modified methyl tert-butyl ether (MTBE) protocol is widely implemented [10] [11]. Briefly, 100 μL of plasma is mixed with 200 μL of 4°C water and 240 μL of pre-cooled methanol. After vortexing, 800 μL of MTBE is added, followed by sonication in a low-temperature water bath for 20 minutes and incubation at room temperature for 30 minutes [10]. The mixture is centrifuged at 14,000 g for 15 minutes at 10°C, and the upper organic phase is collected and dried under nitrogen gas [8]. The dried lipids are reconstituted in 200 μL of 90% isopropanol/acetonitrile for mass spectrometric analysis.
Lipid Quantification Using UHPLC-MS/MS
Ultra-high performance liquid chromatography coupled with tandem mass spectrometry (UHPLC-MS/MS) represents the gold standard for comprehensive lipid profiling:
Chromatographic Conditions: Separation is typically performed using a Waters ACQUITY UPLC BEH C18 column (2.1 mm × 100 mm, 1.7 μm particle size) maintained at 45°C [10] [8]. The mobile phase consists of:
- Phase A: 10 mM ammonium formate in acetonitrile:water (6:4 v/v)
- Phase B: 10 mM ammonium formate in acetonitrile:isopropanol (2:9 v/v) The gradient elution program runs from 30% mobile phase B (0-2 min) to 100% B (2-25 min), followed by re-equilibration [8].
Mass Spectrometry Parameters: Analysis is conducted using a SCIEX 5500 QTRAP or similar mass spectrometer with electrospray ionization [11]. Positive ion mode settings typically include: heater temperature 300°C, sheath gas flow rate 45 arb, spray voltage 3.0 kV, and capillary temperature 350°C. Negative ion mode uses a spray voltage of 2.5 kV [8]. Data acquisition employs both full scans (MS1, range 200-1800 m/z) and fragment scans (MS2) for structural identification.
Quality Control and Data Processing
Robust quality control measures are essential for reliable lipidomic data:
- Quality Control Samples: Pooled samples from all participants are prepared and analyzed every 10-15 experimental samples to monitor instrument stability [10] [11].
- Data Processing: Lipid identification and quantification are performed using specialized software (e.g., Analyst 1.6.3, MarkerView) [11]. Lipids with >20% missing data or coefficient of variation >30% in quality controls are typically excluded from further analysis [11].
- Statistical Analysis: Multivariate statistical approaches including principal component analysis (PCA) and orthogonal partial least squares-discriminant analysis (OPLS-DA) are employed to identify differentially abundant lipids [10]. Significant lipid species are determined using a combination of p-value (<0.05) and false discovery rate (FDR) correction (<0.05) to account for multiple testing [10].
Pathophysiological Pathways and Mechanisms
The dysregulated lipid classes participate in interconnected metabolic pathways that bridge hyperuricemia and diabetes pathophysiology. The following diagram illustrates key mechanistic relationships:
The mechanistic relationships illustrate how triglycerides, phosphatidylethanolamines, and phosphatidylcholines occupy central positions in the pathological network connecting hyperuricemia to diabetes. Hyperuricemia directly promotes elevations in all three lipid classes, with triglycerides demonstrating particularly strong association (coefficient = 0.67, P=0.01) [12]. These lipids subsequently contribute to diabetes development through multiple pathways: triglycerides directly increase diabetes risk (coefficient = 1.29, P<0.001) [12], while phosphatidylethanolamines and phosphatidylcholines primarily drive pro-inflammatory responses that exacerbate insulin resistance [8].
Notably, de novo lipogenesis—particularly involving 16:1n-7 fatty acids—strongly correlates with triglyceride and phosphatidylcholine elevations (Spearman correlation coefficients = 0.32-0.41, p<0.001) [11]. The adipokine retinol-binding protein 4 (RBP4) mediates approximately 5-14% of the lipid-hyperuricemia association, providing a molecular link between dyslipidemia and insulin resistance [11]. This creates a self-reinforcing cycle where insulin resistance impairs renal uric acid excretion, further elevating serum uric acid levels and perpetuating the metabolic disturbances [9].
Experimental Workflow for Lipidomic Analysis
The technical workflow for comprehensive lipid profiling in hyperuricemia-diabetes research involves multiple standardized steps from sample collection to data interpretation, as visualized below:
This standardized workflow ensures reproducible lipidomic profiling across studies. The MTBE-based extraction efficiently recovers a broad lipid spectrum, while the UHPLC-MS/MS platform provides the sensitivity and resolution needed to distinguish structurally similar lipid species [10] [11]. Critical quality control measures, including randomized sample analysis and regular quality control injections, minimize technical variability and enhance data reliability [11].
Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Lipidomic Studies
| Category | Specific Reagent/Equipment | Function/Application | Technical Notes |
|---|---|---|---|
| Chromatography | Waters ACQUITY UPLC BEH C18 Column (2.1×100mm, 1.7μm) | Lipid separation | Maintain at 45°C for optimal resolution [10] [8] |
| Mobile Phases | Ammonium formate in ACN/Hâ‚‚O (10mM) | Mobile phase A | Improves ionization efficiency [8] |
| Ammonium formate in ACN/IPA (10mM) | Mobile phase B | Facilitates elution of nonpolar lipids [8] | |
| Extraction Solvents | Methyl tert-butyl ether (MTBE) | Lipid extraction | Less toxic alternative to chloroform [10] [11] |
| HPLC-grade methanol | Protein precipitation | Pre-cooled to 4°C [8] | |
| Mass Spectrometry | SCIEX 5500 QTRAP Mass Spectrometer | Lipid detection & quantification | ESI source, positive/negative mode switching [11] |
| Internal Standards | Deuterated lipid standards | Quantification normalization | Species-specific for each lipid class [11] |
| Sample Preparation | Low-protein binding tubes | Sample storage | Prevents lipid adsorption [10] |
| Data Analysis | Analyst 1.6.3 Software | Data acquisition | Enables MS1 and MS2 data collection [11] |
The selection of appropriate reagents and equipment is critical for successful lipidomic profiling. The MTBE extraction method offers advantages over traditional chloroform-based methods, including higher recovery of polar lipids and formation of a upper organic phase that simplifies collection [10] [11]. The use of ammonium formate in mobile phases enhances ionization efficiency in mass spectrometry, improving detection sensitivity [8]. Deuterated internal standards are essential for accurate quantification, correcting for matrix effects and extraction efficiency variations [11].
The comprehensive profiling of triglycerides, phosphatidylethanolamines, and phosphatidylcholines in the context of hyperuricemia and diabetes has revealed their crucial roles as mediators, biomarkers, and potential therapeutic targets. The consistent upregulation of these lipid classes across multiple studies, their participation in key metabolic pathways, and their demonstrated mediation effects underscore the interconnected nature of purine, glucose, and lipid metabolism.
Future research directions should focus on several key areas: First, the development of targeted therapeutic approaches that simultaneously address hyperuricemia, dyslipidemia, and insulin resistance, potentially through agents that modulate glycerophospholipid and glycerolipid metabolism [9]. Second, the exploration of specific lipid species as precision medicine biomarkers for identifying high-risk individuals and monitoring intervention efficacy. Third, deeper investigation into the molecular mechanisms through which specific PE and PC species initiate and propagate inflammatory signaling in the context of hyperuricemia [8]. Finally, research into dietary and pharmacological interventions that specifically target the de novo lipogenesis pathway to reduce the production of atherogenic lipid species [11].
The integration of advanced lipidomics with other omics technologies and the application of causal inference methods like Mendelian randomization will further elucidate the complex relationships between these lipid classes and metabolic diseases, ultimately accelerating the development of effective interventions for patients with coexisting hyperuricemia and diabetes.
The coexistence of type 2 diabetes mellitus (T2DM) and hyperuricemia (HUA) represents a complex pathological condition characterized by concurrent disturbances in glucose and urate metabolism. The underlying pathophysiology is multifactorial, involving insulin resistance, oxidative stress, lipid metabolic dysfunction, and impaired renal urate excretion [9]. Epidemiological studies across diverse populations have consistently demonstrated a substantial prevalence of hyperuricemia among individuals with T2DM, ranging from 21% to 32% [9]. This comorbidity is typically associated with worsened insulin resistance, hypertension, dyslipidemia, and pronounced visceral obesity [9]. The bidirectional pathophysiological relationship between T2DM and HUA contributes to an increased risk of multisystem complications, with lipid metabolism disruptions serving as a central connecting pathway [13] [8] [9].
Recent advances in lipidomic technologies have enabled researchers to characterize specific alterations in glycerophospholipid and glycerolipid metabolism that occur in patients with concurrent diabetes and hyperuricemia [10]. These disruptions are not merely secondary phenomena but actively contribute to disease progression through multiple mechanisms, including inflammatory activation, mitochondrial dysfunction, and cellular signaling interference [8] [10]. Understanding these metabolic perturbations at a molecular level provides crucial insights for developing targeted therapeutic strategies aimed at interrupting this detrimental cycle.
Quantitative Lipidomic Profiling in Diabetic Hyperuricemia
Comprehensive lipidomic analyses reveal significant alterations in plasma lipid profiles among patients with diabetes mellitus combined with hyperuricemia (DH) compared to those with diabetes alone (DM) and healthy controls (NGT). Using ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS), researchers have identified 1,361 lipid molecules across 30 subclasses in patient plasma samples, demonstrating the extensive scope of metabolic disruption in this comorbidity [10].
Table 1: Significantly Altered Lipid Metabolites in DH Patients vs. Controls
| Lipid Class | Representative Molecules | Regulation Trend | Biological Impact |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) | Significantly upregulated | Energy storage, lipid droplet formation |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) | Significantly upregulated | Membrane structure, cellular signaling |
| Phosphatidylcholines (PCs) | PC(36:1) | Significantly upregulated | Membrane fluidity, lipid transport |
| Phosphatidylinositols (PIs) | Not specified | Downregulated | Cell signaling, membrane trafficking |
Multivariate statistical analyses including principal component analysis (PCA) and orthogonal partial least squares discriminant analysis (OPLS-DA) have confirmed distinct separation trends among DH, DM, and NGT groups, validating the unique lipidomic signature of the comorbid condition [10]. A total of 31 significantly altered lipid metabolites were pinpointed in the DH group compared to NGT controls, with 13 triglycerides, 10 phosphatidylethanolamines, and 7 phosphatidylcholines showing significant upregulation, while one phosphatidylinositol was downregulated [10].
The collective analysis of these metabolite groups revealed their enrichment in six major metabolic pathways, with glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) identified as the most significantly perturbed pathways in DH patients [10]. Furthermore, comparison of DH versus DM groups identified 12 differential lipids that were also predominantly enriched in these same core pathways, underscoring their central role in the pathophysiology of hyperuricemia complicating diabetes [10].
Table 2: Pathway Analysis of Lipid Metabolic Disruption in Diabetic Hyperuricemia
| Metabolic Pathway | Impact Value | Key Lipid Classes Involved | Biological Consequences |
|---|---|---|---|
| Glycerophospholipid Metabolism | 0.199 | PCs, PEs, PIs | Membrane integrity, inflammatory signaling |
| Glycerolipid Metabolism | 0.014 | TGs, DAGs | Energy homeostasis, lipid storage |
| Linoleic Acid Metabolism | Not specified | Fatty acid derivatives | Inflammatory mediator production |
| Arachidonic Acid Metabolism | Not specified | Eicosanoids | Pro-inflammatory signaling |
| Glycosylphosphatidylinositol (GPI)-anchor Biosynthesis | Not specified | GPI-anchored proteins | Membrane protein anchoring |
Additional studies involving Xinjiang patients with hyperuricemia have identified 33 significantly different lipid metabolites that were markedly upregulated and primarily involved in arachidonic acid metabolism, glycerophospholipid metabolism, linoleic acid metabolism, glycosylphosphatidylinositol (GPI)-anchor biosynthesis, and alpha-Linolenic acid metabolism pathways [8]. These lipid metabolites demonstrated significant correlations with immune factors including IL-10, CPT1, IL-6, SEP1, TGF-β1, Glu, TNF-α, and LD, suggesting intricate cross-talk between lipid disruption and inflammatory activation in hyperuricemia [8].
Experimental Models and Methodologies
Animal Model Development
To investigate the effects of high uric acid on glucolipid metabolism in diabetes, researchers have developed novel diabetic models of hyperuricemia and dyslipidemia in male Golden Syrian hamsters [13]. The selection of this animal model is strategic, as hamsters better reproduce hyperlipidemia patterns similar to human hepatic lipid metabolism and cholesteryl ester transfer protein activities compared to mice or rats [13].
The experimental design involved forty-two healthy male Golden Syrian hamsters (10 weeks old, 163 ± 7.43 g) obtained from Vital River Laboratory Animal Technology Company (Beijing, China) [13]. Diabetes was induced in thirty hamsters by intraperitoneal injection of streptozotocin (STZ) (30 mg/kg) once daily for 3 consecutive days [13]. After ten days, 24 hamsters with fasting blood glucose concentration (>12 mmol/L) were randomly divided into 4 groups (n = 6):
- DC group: standard diet
- DHF group: high-fat/cholesterol diet (HFCD)
- DHU group: PO treatment (intragastric potassium oxonate at 350 mg/kg and adenine at 150 mg/kg with 5% fructose water) with standard diet
- DHFU group: PO treatment with HFCD [13]
An additional twelve healthy hamsters were divided into two groups (n = 6): CHF group (HFCD) and C group (standard diet) as controls [13]. This comprehensive design enabled researchers to examine the individual and synergistic effects of hyperuricemia, dyslipidemia, and diabetes.
Analytical Techniques for Lipidomic Profiling
Ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) has emerged as the cornerstone technology for comprehensive lipidomic analysis in metabolic disorder research [10]. The detailed methodology encompasses several critical phases:
Sample Preparation and Lipid Extraction: Plasma samples (100 μL) are mixed with 200 μL of 4°C water, followed by addition of 240 μL of pre-cooled methanol [10]. After mixing, 800 μL of methyl tert-butyl ether (MTBE) is added, followed by 20 minutes of sonication in a low-temperature water bath and 30 minutes of standing at room temperature [10]. Centrifugation at 14,000 g for 15 minutes at 10°C separates the phases, with the upper organic phase collected and dried under nitrogen stream [10].
Chromatographic Separation: Sample separation employs a Waters ACQUITY UPLC BEH C18 column (2.1 mm i.d. × 100 mm length, 1.7 μm particle size) [10]. The mobile phase consists of:
- Phase A: 10 mM ammonium formate acetonitrile solution in water
- Phase B: 10 mM ammonium formate acetonitrile isopropanol solution [10]
The analysis uses a 3 μL injection volume, maintains a column temperature of 45°C, and a flow rate of 300 μL per minute [10].
Mass Spectrometric Analysis: Untargeted lipidomic analyses are performed using electrospray ionization mass spectrometers with Q active plus [10]. Positive ion mode source conditions include: heater temperature 300°C, sheath gas flow rate 45 ARB, auxiliary gas flow rate 15 ARB, sweep gas flow rate 1 ARB, spray voltage 3.0 kV, capillary temperature 350°C, and S-lens RF level 50% [10]. Negative ion mode parameters are similar with adjustments to spray voltage (2.5 kV) and S-lens RF level (60%) [10]. Data acquisition covers a scanning range of 200-1800 for MS1, with fragmentation patterns (MS2, HCD) collected to determine mass-to-charge ratios of lipid molecules and fragments [10].
Biochemical and Histopathological Assessments
Complementary to lipidomic profiling, comprehensive biochemical analyses are essential for correlating molecular findings with physiological manifestations. In animal studies, measurements include:
Serum Biochemical Parameters:
- Uric acid, glucose, triglyceride, and total cholesterol levels
- Liver xanthine oxidase activity
- Urea nitrogen and creatinine levels [13]
Molecular Markers:
- Plasminogen activator inhibitor-1 (PAI-1)
- Transforming growth factor-β (TGF-β) expressions
- Vascular endothelial growth factor (VEGF) [13]
Histopathological Examinations:
- Renal tissue analysis for glomerular mesangial cells and matrix proliferation
- Identification of protein casts and urate deposition
- Assessment of renal structural integrity [13]
Gut Microbiota Analysis:
- Fecal short-chain fatty acids content
- Relative abundance of specific bacterial taxa (e.g., Lieibacterium)
- Firmicutes to Bacteroidetes ratios [13]
These multidisciplinary approaches enable researchers to establish connections between lipid metabolic disruptions, organ damage, and systemic metabolic consequences in diabetic hyperuricemia.
Pathophysiological Mechanisms and Signaling Pathways
The disruption of glycerophospholipid and glycerolipid metabolism in diabetic hyperuricemia activates multiple interconnected pathophysiological mechanisms that accelerate disease progression. Uric acid-induced oxidative stress plays a central role in this process, directly impairing cellular function and promoting inflammatory signaling cascades [13] [9].
Experimental evidence indicates that high uric acid levels are closely associated with decreased antioxidant capacity and increased renal expression of pro-fibrotic factors including plasminogen activator inhibitor-1 (PAI-1) and transforming growth factor-β (TGF-β) [13]. These molecular changes manifest structurally as glomerular mesangial cells and matrix proliferation, protein casts, and urate deposition in renal tissues [13]. The synergistic effects of hyperuricemia and dyslipidemia on these parameters highlight the multifaceted nature of organ damage in this comorbidity.
The gut-kidney axis emerges as another significant mechanism in the pathophysiology of diabetic hyperuricemia. Studies demonstrate that high uric acid significantly alters the balance of intestinal flora in diabetic animals, characterized by increased acetic acid content, decreased butyric, propanoic, and isobutyric acid levels, and decreased Firmicutes to Bacteroidetes ratios [13]. These changes in microbial composition and metabolite production further influence host metabolism through effects on epithelial integrity, inflammation, and nutrient absorption [13].
At the cellular level, uric acid has been shown to contribute to diabetes progression by hindering islet beta cell survival rather than directly triggering the disease [14]. This mechanism complements the established understanding of insulin resistance in peripheral tissues, providing a more comprehensive picture of glucose homeostasis disruption in hyperuricemic states. Additionally, research indicates that thioredoxin-interacting protein reduces oxidative stress and counters HUA-induced insulin resistance, suggesting it as a potential therapeutic target [14].
The identification of specific lipid species that are upregulated in diabetic hyperuricemia, including triglycerides with specific fatty acid compositions (e.g., TG(16:0/18:1/18:2)) and phospholipids (e.g., PE(18:0/20:4)), provides molecular targets for understanding how lipid disruptions contribute to metabolic disease progression [10]. These lipids may directly interfere with insulin signaling pathways, promote ceramide accumulation, or serve as precursors for inflammatory mediators that sustain low-grade inflammation characteristic of both diabetes and hyperuricemia.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Lipidomic and Metabolic Studies
| Reagent/Material | Specific Application | Function in Research |
|---|---|---|
| Potassium Oxonate (PO) | Hyperuricemia induction in animal models | Competitive inhibitor of uricase to increase uric acid concentrations [13] |
| Streptozotocin (STZ) | Diabetes induction in animal models | Selective toxicity to pancreatic β-cells to impair insulin production [13] |
| High-Fat/Cholesterol Diet (HFCD) | Metabolic disorder induction | 15% fat, 0.5% cholesterol diet to induce dyslipidemia in animal models [13] |
| Methyl tert-butyl ether (MTBE) | Lipid extraction from biological samples | Organic solvent for efficient lipid separation from aqueous phases [8] [10] |
| Ammonium Formate | Mobile phase additive for LC-MS | Enhances ionization efficiency and improves chromatographic separation [10] |
| ACQUITY UPLC BEH C18 Column | Chromatographic separation | 2.1×100mm, 1.7μm particles for high-resolution lipid separation [10] |
| Q-Exactive Plus Mass Spectrometer | Untargeted lipidomic analysis | High-resolution mass detection with electrospray ionization capabilities [8] [10] |
| ELISA Kits for Cytokines | Inflammatory marker quantification | Measures TNF-α, IL-6, TGF-β1, IL-10 levels in patient/animal sera [8] |
| 3'-Hydroxy Simvastatin | 3'-Hydroxy Simvastatin, MF:C25H38O6, MW:434.6 g/mol | Chemical Reagent |
| 1,5,6-trihydroxy-3-methoxyxanthone | 1,5,6-trihydroxy-3-methoxyxanthone, CAS:50868-52-5, MF:C14H10O6, MW:274.22 g/mol | Chemical Reagent |
This comprehensive toolkit enables researchers to model the complex interplay between hyperuricemia, diabetes, and lipid metabolic disruptions, from whole-organism physiology to molecular-level mechanisms. The combination of these reagents and methodologies facilitates the development of translational research approaches that can bridge basic science discoveries with clinical applications.
The selection of appropriate animal models is particularly crucial in this field. While rodent models have traditionally been used, the hamster model offers distinct advantages for hyperlipidemia research due to similarities with human hepatic lipid metabolism and cholesteryl ester transfer protein activities [13]. Additionally, the effects of dietary cholesterol on blood lipid profiles in hamsters more closely mirror human responses compared to other rodent species [13].
Advanced mass spectrometry platforms represent another critical component, with the Q-Exactive Plus instrument providing the sensitivity, resolution, and mass accuracy necessary for comprehensive lipidome characterization [10]. The implementation of both positive and negative ionization modes enables detection of a broad spectrum of lipid classes with diverse chemical properties, from non-polar triglycerides to polar phospholipids [10].
The disruption of glycerophospholipid and glycerolipid metabolism represents a central pathological mechanism connecting hyperuricemia and diabetes, creating a mutually reinforcing cycle that accelerates metabolic deterioration and promotes end-organ damage. Through advanced lipidomic technologies, researchers have identified specific lipid species and metabolic pathways that are consistently altered in this comorbidity, providing both biomarkers for early detection and targets for therapeutic intervention.
The intricate interplay between uric acid metabolism, lipid homeostasis, and glucose regulation involves multiple organ systems and molecular networks, including inflammatory activation, oxidative stress, gut microbiota dysbiosis, and cellular signaling disruptions. The development of sophisticated animal models that recapitulate the human condition, combined with comprehensive analytical approaches, has enabled significant advances in understanding these complex relationships.
Future research directions should prioritize the development of "dual-action" therapeutic agents capable of simultaneously addressing hyperuricemia and diabetes through targeting of shared metabolic pathways [9]. Additionally, personalized management strategies based on individual metabolic phenotypes hold promise for improving outcomes in this complex patient population. The continued application of lipidomic technologies in longitudinal studies and clinical trials will further elucidate the temporal relationships between lipid disruptions and disease progression, potentially enabling earlier interventions to prevent the devastating consequences of these interconnected metabolic disorders.
Lipidomics, the large-scale study of lipid pathways and networks, is revolutionizing our understanding of complex metabolic diseases. In the context of comorbid diabetes mellitus (DM) and hyperuricemia (HUA), advanced lipidomic profiling is moving beyond single-molecule diagnostics to reveal specific lipid species and perturbed pathways that underlie this dangerous synergy. This whitepaper details the identification of definitive lipid biomarkers—including the triglycerides TG(16:0/18:1/18:2) and phosphatidylethanolamines PE(18:0/20:4)—and elucidates the glycerophospholipid and glycerolipid metabolism pathways as central hubs of the pathological interplay between hyperuricemia and diabetes, offering new avenues for targeted therapeutic strategies.
The coexistence of type 2 diabetes mellitus (T2DM) and hyperuricemia (HUA) represents a significant clinical challenge, driven by intertwined pathophysiological mechanisms including insulin resistance, oxidative stress, and systemic metabolic dysfunction [9]. Epidemiological studies reveal a substantial prevalence of HUA among individuals with T2DM, ranging from 21% to 32%, underscoring a shared metabolic burden that predisposes patients to higher risks of cardiovascular and renal complications [9]. While serum uric acid has traditionally been the focus in HUA management, it fails to capture the full spectrum of metabolic disarray. Lipidomics, a branch of metabolomics, provides a powerful framework to comprehensively characterize lipid metabolites, offering unprecedented insights into the specific molecular changes that occur when diabetes and hyperuricemia converge [10] [15]. This technical guide explores how lipidomic technologies are uncovering novel biomarkers and pathways, moving the field beyond uric acid toward a more integrated and mechanistic understanding of this complex comorbidity.
Key Lipid Biomarkers Identified in Comorbid DM and HUA
Advanced lipidomic profiling using techniques like UHPLC-MS/MS has enabled the precise identification of lipid species that are significantly altered in patients with coexisting diabetes and hyperuricemia (DH) compared to those with diabetes alone (DM) or healthy controls (NGT). The table below summarizes the most relevant lipid biomarkers identified in a recent clinical study [10].
Table 1: Significantly Altered Lipid Molecules in Patients with Diabetes Mellitus and Hyperuricemia (DH)
| Lipid Category | Specific Lipid Molecules | Trend in DH vs. NGT | Biological Relevance |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) and 12 other TGs | Significantly Upregulated | Key energy reservoirs; elevated levels indicate disrupted energy storage and lipid overload. |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) and 9 other PEs | Significantly Upregulated | Major constituents of cell membranes; influence membrane fluidity and cell signaling. |
| Phosphatidylcholines (PCs) | PC(36:1) and 6 other PCs | Significantly Upregulated | Essential for lipoprotein structure and lipid transport; alterations linked to insulin resistance. |
| Phosphatidylinositol (PI) | One unspecified PI | Significantly Downregulated | Precursor for second messengers; downregulation may disrupt intracellular signaling cascades. |
The study identified a total of 31 significantly altered lipid metabolites in the DH group compared to healthy controls, with a strong predominance of upregulated species [10]. A separate comparison between DH and DM-only groups further pinpointed 12 differential lipids, confirming that the lipidomic profile of the comorbid condition is distinct and not merely an extension of diabetes-related lipid disturbances [10]. The consistent upregulation of specific TGs like TG(16:0/18:1/18:2) underscores their potential role as central mediators in the disease process.
Disrupted Metabolic Pathways: A Systems Biology View
The identified differential lipid metabolites are not isolated entities; they are interconnected components of specific biological pathways. Pathway enrichment analysis using platforms like MetaboAnalyst 5.0 has revealed that these lipids are predominantly enriched in a limited number of core metabolic pathways, highlighting their systemic impact [10].
Table 2: Key Perturbed Lipid Metabolic Pathways in Diabetes with Hyperuricemia
| Metabolic Pathway | Impact Value | Key Lipid Classes Involved | Pathological Significance |
|---|---|---|---|
| Glycerophospholipid Metabolism | 0.199 | PEs, PCs, PI | Most significantly perturbed pathway; crucial for cell membrane integrity, signaling, and inflammation. |
| Glycerolipid Metabolism | 0.014 | TGs, DAGs | Central to energy homeostasis; dysregulation directly contributes to lipid accumulation and insulin resistance. |
The glycerophospholipid metabolism pathway, with the highest impact value, is critically involved in maintaining cellular membrane structure and function. Its disruption can affect insulin receptor signaling and promote inflammatory processes. Concurrently, abnormalities in glycerolipid metabolism, primarily involving triglycerides, reflect a fundamental disturbance in energy storage and utilization, a hallmark of both diabetes and hyperuricemia [10]. This pathway-centric view is supported by independent research in hyperuricemic populations, which also found significant enrichment in glycerophospholipid metabolism, affirming its central role in HUA-related lipid disorders [8] [16].
The following diagram illustrates the interconnected nature of these disrupted pathways and their relationship to the core pathophysiology of hyperuricemia and diabetes:
Diagram 1: Pathway Crosstalk in Hyperuricemia and Diabetes. This diagram maps the core pathophysiological drivers (HUA, DM) through intermediate mechanisms (insulin resistance, oxidative stress) to the dysregulation of key lipid metabolic pathways, resulting in the specific lipid biomarkers identified and culminating in exacerbated systemic metabolic dysfunction.
Detailed Experimental Protocol for Lipidomic Analysis
The discovery of these biomarkers relies on robust, sensitive, and reproducible lipidomic workflows. The following section details the standard protocol for plasma untargeted lipidomics, as applied in the cited research [10] [8].
Sample Collection and Pre-processing
- Blood Collection: Collect ~5 mL of fasting venous blood into sodium heparin or EDTA tubes.
- Plasma Separation: Centrifuge whole blood at 3,000 rpm for 10 minutes at room temperature to separate plasma.
- Aliquoting and Storage: Aliquot the upper plasma layer (e.g., 0.2 mL) into cryotubes and immediately store at -80°C until analysis.
- Quality Control (QC) Preparation: Pool equal volumes of plasma from all study samples to create a quality control (QC) sample, which is used to monitor instrumental performance throughout the analytical run.
Lipid Extraction
The following steps should be performed on ice or at 4°C using pre-cooled solvents to minimize lipid degradation [10] [8]:
- Thawing: Thaw plasma samples on ice.
- Aliquot: Transfer 100 μL of plasma into a 1.5 mL microcentrifuge tube.
- Protein Precipitation: Add 200 μL of ice-cold water and 240 μL of pre-cooled methanol. Vortex thoroughly.
- Liquid-Liquid Extraction: Add 800 μL of methyl tert-butyl ether (MTBE). Vortex vigorously for 1 minute and sonicate in a low-temperature water bath for 20 minutes.
- Phase Separation: Let the mixture stand at room temperature for 30 minutes, then centrifuge at 14,000 g at 10°C for 15 minutes.
- Organic Phase Collection: Carefully collect the upper organic phase.
- Drying and Reconstitution: Dry the organic extract under a gentle stream of nitrogen gas. Reconstitute the dried lipid residue in 100-200 μL of isopropanol/acetonitrile (e.g., 90:10 v/v) or a similar suitable solvent for MS analysis. Centrifuge again before injection to remove any insoluble material.
Instrumental Analysis: UHPLC-MS/MS Conditions
Chromatography (UHPLC)
- Column: Waters ACQUITY UPLC BEH C18 or CSH C18 (2.1 mm × 100 mm, 1.7 μm).
- Mobile Phase A: 10 mM ammonium formate in acetonitrile/water.
- Mobile Phase B: 10 mM ammonium formate in acetonitrile/isopropanol.
- Gradient Elution: Utilize a linear gradient from 30% B to 100% B over 20-25 minutes.
- Flow Rate: 0.3 mL/min.
- Column Temperature: 45°C.
- Injection Volume: 3-5 μL.
Mass Spectrometry (Tandem MS - Q-TOF)
- Ionization: Electrospray Ionization (ESI), operating in both positive and negative ion modes.
- Source Parameters:
- Sheath Gas Flow: 45 arb
- Auxiliary Gas Flow: 15 arb
- Spray Voltage: 3.0 kV (positive), 2.5 kV (negative)
- Capillary Temperature: 350°C
- Heater Temperature: 300-400°C
- Data Acquisition: Data-dependent acquisition (DDA) mode. A full MS1 scan (e.g., m/z 200-1800) is followed by MS2 scans of the top N most intense precursor ions using High-Energy Collisional Dissociation (HCD).
The following workflow diagram summarizes the key stages of this lipidomic analysis:
Diagram 2: Untargeted Lipidomics Workflow. The process from sample collection through lipid extraction, quality control, instrumental analysis, and data processing leading to biomarker identification and pathway analysis.
Data Processing and Statistical Analysis
- Peak Picking and Alignment: Process raw LC-MS data using software (e.g., MarkerLynx, MS-DIAL) to perform peak detection, alignment, and integration, generating a data matrix of m/z, retention time, and peak intensity.
- Multivariate Statistical Analysis: Import the data matrix into software like SIMCA-P.
- Principal Component Analysis (PCA): An unsupervised method to overview data clustering and identify outliers.
- Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA): A supervised method to maximize separation between pre-defined groups (e.g., DH vs. DM) and identify significant lipid features (Variables Important in Projection, VIP > 1.0).
- Biomarker Identification: Combine significant statistical results (VIP > 1.0 and p-value < 0.05 from univariate t-tests) with MS/MS spectral data to identify lipid structures by querying databases such as LIPID MAPS and HMDB.
- Pathway Analysis: Input the list of identified differential lipids into pathway analysis tools (e.g., MetaboAnalyst 5.0) to determine enriched metabolic pathways based on pathway impact and p-values.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists critical reagents and materials required to establish the described lipidomic workflow, based on the methodologies from the cited studies [10] [8] [16].
Table 3: Essential Research Reagent Solutions for Lipidomics
| Category / Item | Specific Example / Specification | Critical Function in Workflow |
|---|---|---|
| Chromatography Column | Waters ACQUITY UPLC BEH C18 / CSH C18 (2.1x100mm, 1.7μm) | High-resolution separation of complex lipid mixtures prior to MS detection. |
| Mass Spectrometry System | Q-Exactive Plus / Xevo G2-S Q-TOF (Orbitrap/Tof mass analyzer) | Provides high mass accuracy and resolution for precise lipid identification and structural elucidation via MS/MS. |
| Key Solvents | HPLC/LC-MS grade: Methanol, Acetonitrile, Isopropanol, MTBE, Water, Chloroform | Used for mobile phases and lipid extraction; high purity is critical to minimize background noise and ion suppression. |
| Additives for LC-MS | Ammonium Formate, Formic Acid | Volatile buffers and pH modifiers for mobile phases to enhance ionization efficiency and chromatographic separation. |
| Sample Preparation | Methyl-tert-butyl ether (MTBE), Nitrogen Evaporator, Low-Temperature Centrifuge, Vortex Mixer | Enables efficient liquid-liquid extraction of a broad lipidome, concentration of samples, and preparation for injection. |
| Data Analysis Software | SIMCA-P (Multivariate Stats), MS-DIAL / Lipostar (Lipid ID), MetaboAnalyst (Pathway Analysis) | Tools for statistical analysis, lipid annotation, and biological interpretation of high-dimensional lipidomic data. |
| Ethyl 3-oxoheptanoate | Ethyl 3-oxoheptanoate, CAS:7737-62-4, MF:C9H16O3, MW:172.22 g/mol | Chemical Reagent |
| D-Lactose monohydrate | D-Lactose monohydrate, CAS:5989-81-1, MF:C12H22O11.H2O, MW:360.31 g/mol | Chemical Reagent |
Lipidomics has unequivocally demonstrated that the pathophysiological interplay between diabetes and hyperuricemia is reflected in a distinct plasma lipid signature. The specific upregulation of lipids like TG(16:0/18:1/18:2) and PE(18:0/20:4), along with the central disruption of glycerophospholipid and glycerolipid metabolism, provides a molecular rationale for the exacerbated clinical outcomes observed in patients with this comorbidity. These findings move the field beyond uric acid, offering a new panel of potential biomarkers for early risk stratification, disease monitoring, and assessing therapeutic efficacy.
Future research must focus on the translational validation of these lipidomic signatures in larger, multi-center cohorts to establish standardized reference ranges and clinical cut-off values. Furthermore, integrating lipidomics with other omics data (genomics, proteomics) will paint a more complete picture of the regulatory networks at play. From a therapeutic perspective, these specific lipid pathways and species represent novel targets for the development of "dual-action" interventions designed to concurrently ameliorate hyperuricemia and improve glycemic and lipid control, ultimately paving the way for a more precise and effective management strategy for this complex metabolic syndrome.
Lipid metabolites serve as pivotal signaling molecules that orchestrate immune responses and modulate oxidative stress, creating a pathological bridge between metabolic dysfunction and chronic inflammation. In the context of hyperuricemia and diabetes, this interplay becomes increasingly complex, driving disease progression through well-defined immunometabolic pathways. This whitepaper synthesizes current evidence on how specific lipid classes—including fatty acids, phospholipids, and cholesterol—influence immune cell function, activate inflammatory signaling cascades, and exacerbate oxidative stress. We present comprehensive experimental data, detailed methodologies for investigating these relationships, and visualizations of key pathological mechanisms. Understanding these processes provides critical insights for developing targeted therapeutic interventions that disrupt the inflammatory bridge in patients with coexisting hyperuricemia and diabetes.
Lipid metabolism has evolved from being viewed primarily as an energy storage and structural framework to recognized as a sophisticated signaling network that actively directs immune cell differentiation, activation, and inflammatory potential. In metabolic diseases including hyperuricemia and diabetes, dysregulated lipid metabolism creates a pro-inflammatory milieu that accelerates tissue damage and disease progression [17] [18]. The "inflammatory bridge" concept describes how lipid metabolites activate immune responses and oxidative stress through three primary mechanisms: (1) direct receptor-mediated signaling, (2) modulation of membrane fluidity and lipid raft organization, and (3) generation of oxidative stress through lipid peroxidation.
The coexistence of hyperuricemia and diabetes represents a particularly aggressive metabolic phenotype characterized by amplified inflammatory responses. Epidemiological studies demonstrate that approximately 21-32% of patients with type 2 diabetes have concomitant hyperuricemia, creating a population with enhanced risk for renal and cardiovascular complications [9]. This clinical synergy stems from shared pathophysiological mechanisms, with disordered lipid metabolism serving as a central connector.
Core Mechanisms: Lipid-Mediated Immune and Oxidative Activation
Lipid Metabolites as Immune Signaling Molecules
Specific lipid classes function as potent signaling molecules that directly activate immune pathways:
Fatty Acids and Eicosanoids: Omega-6 polyunsaturated fatty acids (e.g., arachidonic acid) give rise to eicosanoid mediators (prostaglandins, leukotrienes) that promote pro-inflammatory macrophage polarization and enhance neutrophil recruitment [17]. In contrast, specialized pro-resolving mediators (SPMs) derived from omega-3 fatty acids orchestrate inflammation resolution.
Sphingolipids: The balance between ceramide and sphingosine-1-phosphate (S1P) determines immune cell fate. Ceramide promotes apoptosis and inflammatory activation, while S1P regulates lymphocyte egress from lymphoid organs and endothelial barrier function [17].
Phospholipids: Glycerophospholipids including phosphatidylcholines (PCs) and phosphatidylethanolamines (PEs) are remodeled to produce platelet-activating factor (PAF) and lysophosphatidic acid (LPA), which activate platelets and innate immune cells [10].
Table 1: Pro-inflammatory Lipid Mediators and Their Immune Functions
| Lipid Class | Specific Mediators | Immune Functions | Receptors/Signaling Pathways |
|---|---|---|---|
| Eicosanoids | PGEâ‚‚, LTBâ‚„ | Neutrophil chemotaxis, Vasodilation, Fever | GPCRs (EP, BLT receptors) |
| Sphingolipids | Ceramide, S1P | Apoptosis, Lymphocyte trafficking | Ceramide-activated protein kinases, S1PR1-5 |
| Phospholipids | PAF, LPA | Platelet activation, Monocyte adhesion | PAFR, LPAR1-6 |
| Oxidized Lipids | oxLDL, 4-HNE | Scavenger receptor activation, Protein adduction | CD36, TLR4, KEAP1-Nrf2 |
Membrane Lipid Composition and Immune Receptor Signaling
Beyond soluble mediators, lipids shape immune responses by influencing membrane properties:
Lipid Rafts: Cholesterol and sphingolipid-enriched microdomains serve as signaling platforms that concentrate immune receptors like the T-cell receptor (TCR) and B-cell receptor (BCR). Increased membrane cholesterol content lowers the activation threshold of T cells, promoting hyperactivation as observed in autoimmune conditions [17].
Metabolic Sensors: Nuclear receptors including peroxisome proliferator-activated receptors (PPARs) and liver X receptors (LXRs) function as lipid sensors that transcriptionally reprogram immune cell function. PPARγ promotes anti-inflammatory M2 macrophage polarization, while its inhibition favors pro-inflammatory M1 phenotypes [17] [18].
Lipid-Induced Oxidative Stress
Lipid overload and metabolism directly contribute to oxidative stress through multiple mechanisms:
Mitochondrial Dysfunction: Excess fatty acid oxidation increases electron transport chain activity, leading to electron leakage and superoxide production [19].
NADPH Oxidase Activation: Several lipid mediators directly activate NOX enzyme complexes, which deliberately produce superoxide for inflammatory signaling [19].
Lipid Peroxidation: Reactive oxygen species (ROS) attack polyunsaturated fatty acids in membranes, generating reactive aldehydes like 4-hydroxynonenal (4-HNE) and malondialdehyde (MDA) that amplify oxidative damage by modifying proteins and DNA [19].
In hyperuricemia, uric acid crystals themselves activate the NLRP3 inflammasome, further stimulating ROS production and creating a vicious cycle of inflammation and metabolic dysfunction [14].
Experimental Evidence: Lipidomic Signatures in Diabetes and Hyperuricemia
Distinct Lipidomic Profiles in Clinical Populations
Recent advances in lipidomics have enabled detailed characterization of lipid disturbances in metabolic diseases. A 2025 study employing UHPLC-MS/MS-based plasma untargeted lipidomic analysis revealed striking differences between patients with diabetes mellitus (DM), diabetes mellitus combined with hyperuricemia (DH), and healthy controls [10].
Table 2: Significantly Altered Lipid Species in Diabetes with Hyperuricemia (DH) vs. Healthy Controls
| Lipid Subclass | Specific Molecules | Change in DH | Proposed Pathological Role |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2), TG(16:0/18:1/20:4) | ↑ 1.5-2.3 fold | Energy storage, Lipotoxicity precursor |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4), PE(16:0/18:2) | ↑ 1.8-2.1 fold | Membrane fluidity, Inflammatory precursor |
| Phosphatidylcholines (PCs) | PC(36:1), PC(34:2) | ↑ 1.3-1.7 fold | Structural membrane lipid |
| Phosphatidylinositols (PIs) | PI(18:0/20:4) | ↓ 1.9 fold | Signaling precursor impairment |
This study identified 1,361 lipid molecules across 30 subclasses, with 31 significantly altered lipid metabolites in the DH group compared to healthy controls. Multivariate analyses revealed clear separation between groups, confirming distinct lipidomic profiles [10]. Pathway analysis demonstrated that glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) were the most significantly perturbed pathways in DH patients [10].
Experimental Protocol: UHPLC-MS/MS Lipidomics
For researchers investigating lipidomic profiles in metabolic diseases, the following methodology provides a robust approach [10]:
Sample Preparation:
- Collect 5 mL of fasting blood in EDTA tubes and centrifuge at 3,000 rpm for 10 minutes at room temperature.
- Aliquot 0.2 mL of plasma into 1.5 mL centrifuge tubes.
- Prepare quality control samples by pooling equal volumes from all samples.
- Store samples at -80°C until analysis.
- Thaw samples on ice and vortex thoroughly.
- Extract lipids using methyl tert-butyl ether (MTBE) method: Add 200 μL of 4°C water to 100 μL plasma, followed by 240 μL of pre-cooled methanol and 800 μL MTBE.
- Sonicate in a low-temperature water bath for 20 minutes, then stand at room temperature for 30 minutes.
- Centrifuge at 14,000 g for 15 minutes at 10°C.
- Collect upper organic phase and dry under nitrogen stream.
- Reconstitute in isopropanol for analysis.
UHPLC-MS/MS Conditions:
- Chromatography: Waters ACQUITY UPLC BEH C18 column (2.1 × 100 mm, 1.7 μm)
- Mobile Phase: A: 10 mM ammonium formate in acetonitrile/water; B: 10 mM ammonium formate in acetonitrile/isopropanol
- Gradient: Optimized linear gradient from 30% B to 100% B over 15 minutes
- Mass Spectrometry: High-resolution tandem mass spectrometry in both positive and negative electrospray ionization modes
- Data Processing: Use software such as LipidSearch, MS-DIAL, or XCMS for peak alignment, identification, and quantification
Statistical Analysis:
- Perform principal component analysis (PCA) and orthogonal partial least squares-discriminant analysis (OPLS-DA) to visualize group separation
- Identify significantly altered lipids using Student's t-test with false discovery rate (FDR) correction
- Conduct pathway analysis using MetaboAnalyst 5.0 or similar platforms
Figure 1: The Inflammatory Bridge Pathway in Hyperuricemia and Diabetes. Lipid metabolism dysregulation serves as a central node connecting hyperuricemia and diabetes to immune activation and oxidative stress, ultimately driving chronic inflammation and tissue damage.
Immunometabolic Reprogramming in Specific Immune Cells
Macrophage Polarization and Lipid Metabolism
Macrophages exhibit remarkable metabolic plasticity during polarization, with lipid metabolism playing a decisive role:
M1 Macrophages: Classically activated pro-inflammatory macrophages rely predominantly on glycolysis and exhibit disrupted TCA cycle with accumulation of succinate and citrate, which stabilizes HIF-1α and drives IL-1β production [18]. Fatty acid synthesis is increased in M1 macrophages, providing membranes for proliferation and organelles.
M2 Macrophages: Alternatively activated anti-inflammatory macrophages preferentially utilize oxidative phosphorylation and fatty acid oxidation (FAO) [18]. PPARγ and PPARδ activation promotes FAO and M2 polarization, facilitating inflammation resolution.
In hyperuricemia, uric acid crystals are phagocytosed by macrophages, activating the NLRP3 inflammasome and promoting IL-1β secretion, which represents a key link between hyperuricemia and inflammation [14].
T Cell Differentiation and Function
T cell subsets demonstrate distinct lipid metabolic programs that dictate their differentiation and functional capacities:
Effector T Cells: Upon activation, CD4+ and CD8+ T cells increase both glycolysis and fatty acid synthesis to support rapid proliferation and effector function [17].
Regulatory T Cells (Tregs): Tregs primarily rely on oxidative metabolism, particularly fatty acid oxidation, which supports their survival and suppressive function [17] [18].
Memory T Cells: Like Tregs, memory T cells depend on mitochondrial fatty acid oxidation for long-term persistence [17].
Cholesterol metabolism critically regulates T cell function by modulating membrane lipid raft composition and TCR signaling intensity. Increased cellular cholesterol content lowers the activation threshold of T cells, contributing to autoimmunity [17].
Figure 2: Lipid Metabolic Pathways in Macrophage Polarization. M1 and M2 macrophages utilize distinct lipid metabolic programs that drive their inflammatory versus anti-inflammatory functions.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for Immunometabolism Studies
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Lipid Extraction Solvents | Methyl tert-butyl ether (MTBE), Chloroform:methanol | Lipidomics sample preparation | MTBE method provides better phase separation than Folch |
| Chromatography Columns | Waters ACQUITY UPLC BEH C18 (1.7 μm) | Lipid separation prior to MS | Suitable for broad lipid classes; specialized columns needed for specific lipids |
| Mass Spectrometry Standards | SPLASH LIPIDOMIX, Avanti Polar Lipids standards | Lipid identification and quantification | Essential for both targeted and untargeted lipidomics |
| Metabolic Inhibitors | Etomoxir (CPT1 inhibitor), C75 (FASN inhibitor) | Manipulating lipid pathways in cells | Confirm specificity with rescue experiments |
| Immune Cell Markers | CD86 (M1), CD206 (M2), FOXP3 (Tregs) | Immune phenotyping by flow cytometry | Combine surface and intracellular staining for comprehensive profiling |
| ROS Detection Probes | H2DCFDA, MitoSOX, Amplex Red | Measuring oxidative stress | Use specific probes for different ROS types and compartments |
| Lipid Receptor Agonists/Antagonists | GW9662 (PPARγ antagonist), FTY720 (S1PR modulator) | Studying lipid signaling pathways | Titrate carefully due to potential off-target effects |
| Biliverdin hydrochloride | Biliverdin hydrochloride, CAS:55482-27-4, MF:C33H36Cl2N4O6, MW:655.6 g/mol | Chemical Reagent | Bench Chemicals |
| L-Histidine dihydrochloride | L-Histidine dihydrochloride, CAS:6027-02-7, MF:C6H11Cl2N3O2, MW:228.07 g/mol | Chemical Reagent | Bench Chemicals |
Therapeutic Implications and Future Directions
Targeting the inflammatory bridge represents a promising therapeutic strategy for patients with hyperuricemia and diabetes. Several approaches show particular promise:
PPARγ Agonists: Thiazolidinediones not only improve insulin sensitivity but also promote M2 macrophage polarization, potentially disrupting the inflammatory cascade [17] [18].
SGLT2 Inhibitors: Drugs like empagliflozin reduce both glucose and uric acid levels while demonstrating anti-inflammatory effects, representing a dual-action approach [9].
Specialized Pro-Resolving Mediators: Administration of resolvins, protectins, and maresins directly promotes inflammation resolution without immunosuppression [17].
NLRP3 Inflammasome Inhibitors: Targeting uric acid crystal-induced inflammation may break the cycle between hyperuricemia and metabolic dysfunction [14].
Future research should focus on tissue-specific lipidomic signatures, the gut-liver axis in lipid metabolism, and personalized approaches based on individual lipidomic profiles. The development of more specific inhibitors targeting key enzymes in lipid mediator synthesis (e.g., COX-2, SphK) may provide enhanced therapeutic efficacy with reduced side effects.
Lipid metabolites serve as essential connectors between metabolic diseases and immune dysfunction, creating an "inflammatory bridge" that propagates and amplifies tissue damage in hyperuricemia and diabetes. Through multiple mechanisms—including direct receptor activation, membrane reorganization, and oxidative stress generation—dysregulated lipid metabolism establishes a pro-inflammatory milieu that drives disease progression. Advanced lipidomic methodologies now enable detailed characterization of these disturbances, revealing specific lipid signatures and perturbed pathways. Therapeutic strategies that target these lipid-immune interfaces hold significant promise for interrupting the pathological cascade and improving outcomes in this high-risk patient population.
Advanced Analytical Techniques: Applying Lipidomics and Multi-Omics to Decipher Metabolic Dysfunction
Ultra-high-performance liquid chromatography coupled to tandem mass spectrometry (UHPLC-MS/MS) has become a cornerstone technique in modern lipidomics, enabling the precise separation, identification, and quantification of complex lipid mixtures from biological samples [20]. This technical guide details the established workflows from sample preparation to data acquisition, with a specific focus on applications in lipid metabolic pathway research for patients with diabetes mellitus (DM) and hyperuricemia (DH). Dysregulated lipid metabolism is a hallmark of metabolic diseases, and studies have revealed that patients with DH exhibit significant alterations in lipid species like triglycerides (TGs) and glycerophospholipids, alongside perturbations in key metabolic pathways such as glycerophospholipid metabolism [10]. The robustness of UHPLC-MS/MS allows researchers to uncover these critical disease-specific lipid signatures, providing a deeper understanding of the underlying pathophysiology [10] [21].
Core UHPLC-MS/MS Workflow in Lipidomics
The typical lipidomics workflow involves several critical and sequential steps to ensure data quality and reliability.
Sample Collection and Preparation
Proper sample preparation is the foundation for successful lipidomic analysis. For plasma or serum samples, fasting blood is collected and centrifuged to isolate the supernatant, which is then stored at -80°C until analysis [10] [21].
- Lipid Extraction: A liquid-liquid extraction is commonly performed to isolate lipids from the biological matrix. The methyl tert-butyl ether (MTBE)-based method is widely adopted for its high extraction yield, compatibility with a broad range of lipid classes, and lower toxicity compared to halogenated solvents [22]. Briefly, a sample aliquot (e.g., 100 μL of plasma) is mixed with methanol and MTBE, followed by sonication, incubation, and centrifugation. The upper organic phase containing the lipids is then collected and dried under a stream of nitrogen [10] [22].
- Quality Control (QC): To monitor analytical performance and ensure data reproducibility, a pooled quality control (PQC) sample is created by combining equal aliquots of all study samples. This PQC is injected at regular intervals throughout the acquisition sequence to assess instrument stability, signal drift, and precision [23] [24]. The use of commercial plasma as a surrogate for pooled study samples for long-term QC has also been evaluated [23].
Chromatographic Separation (UHPLC)
Chromatographic separation prior to mass spectrometry reduces ion suppression and enhances sensitivity by separating isobaric and isomeric lipids.
- Column: Reversed-phase chromatography on a C18 column (e.g., 100 mm x 2.1 mm, 1.7 μm particle size) is standard. The use of sub-2 μm fully porous or core-shell particles enables high resolution at elevated pressures [10] [22]. Charged Surface Hybrid (CSH) columns can further improve peak shape for acidic lipids [22].
- Mobile Phase and Gradient: A binary solvent system is typical. Mobile phase A is often water or an aqueous buffer with additives like ammonium formate or acetate, while mobile phase B is an organic solvent like acetonitrile-isopropanol mixture [10] [25]. The analysis uses a gradient elution, starting with a low percentage of B and ramping to over 95% B to elute the full range of lipids, from polar phospholipids to non-polar cholesteryl esters and triacylglycerols [25]. Advanced methods have successfully reduced total chromatographic run times to as little as 4-12 minutes while maintaining robust lipid coverage [22] [25].
Table 1: Typical UHPLC Gradient for Comprehensive Lipidomics
| Time (min) | Mobile Phase B (%) | Function |
|---|---|---|
| 0.0 | 35-40% | Initial condition, elution of lysophospholipids |
| 2.0 | 80% | Elution of phospholipids and sphingolipids |
| 7.0 | 100% | Elution of diacylglycerols and ceramides |
| 7 - 14 | 100% (Hold) | Elution of triacylglycerols and cholesteryl esters |
| 14 - 16 | 35-40% | Column re-equilibration |
Mass Spectrometric Detection (MS/MS)
MS detection provides the high sensitivity and specificity needed for lipid identification and quantification.
- Ionization Source: Electrospray Ionization (ESI) is the most prevalent soft ionization technique due to its efficiency in ionizing a wide range of lipid classes. It can be operated in both positive and negative ion modes to achieve comprehensive coverage of the lipidome [26].
- Mass Analyzers: High-resolution mass analyzers are preferred for untargeted lipidomics. Quadrupole Time-of-Flight (QTOF) and Orbitrap instruments deliver the high mass accuracy and resolution required to determine elemental compositions [10] [25]. For targeted quantification, triple quadrupole (QqQ) instruments operating in Selected Reaction Monitoring (SRM) or Multiple Reaction Monitoring (MRM) modes offer superior sensitivity and dynamic range [26].
- Data Acquisition Modes:
- Data-Dependent Acquisition (DDA): In this common untargeted approach, the instrument first performs an MS1 survey scan and then automatically selects the most abundant precursor ions for fragmentation (MS2), providing structural information [22].
- Data-Independent Acquisition (DIA): Methods like Sequential Window Acquisition of all Theoretical Mass Spectra (SWATH) fragment all ions within sequential isolation windows, capturing fragmentation data for all detectable analytes and allowing retrospective data mining [22].
- Ion Mobility Separation: The integration of Trapped Ion Mobility Spectrometry (TIMS) adds a fourth dimension of separation based on the ion's collision cross-section (CCS). This helps separate isomeric lipids and provides a CCS value, a physicochemical property that increases confidence in lipid identification [22].
The following diagram illustrates the logical workflow from sample to data, incorporating key decision points and outputs.
Application in Diabetes and Hyperuricemia Research
Applying this workflow to clinical research has proven highly effective. A case-control study comparing diabetic patients with and without hyperuricemia employed UHPLC-MS/MS-based untargeted lipidomics on plasma samples [10]. The study identified 1,361 lipid molecules across 30 subclasses. Multivariate analyses like Principal Component Analysis (PCA) and Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) revealed a clear separation between the DH, DM, and healthy control (NGT) groups, confirming distinct lipidomic profiles [10].
Specifically, 31 significantly altered lipid metabolites were pinpointed in the DH group compared to NGT controls. These included 13 triglycerides (TGs), 10 phosphatidylethanolamines (PEs), and 7 phosphatidylcholines (PCs) that were significantly upregulated [10]. Pathway analysis of these differential lipids, performed using platforms like MetaboAnalyst, identified glycerophospholipid metabolism and glycerolipid metabolism as the most significantly perturbed pathways in DH patients [10]. This insight directly links specific lipid class alterations to broader metabolic dysfunction.
Table 2: Key Lipid Classes and Research Reagents for UHPLC-MS/MS Lipidomics
| Lipid Class | Biological Relevance | Essential Research Reagents & Their Function |
|---|---|---|
| Phosphatidylcholines (PCs) | Major membrane phospholipids; significantly upregulated in DH [10]. | Internal Standards (e.g., PC(17:0/17:0)): Correct for extraction & ionization variance. Ammonium Formate: Mobile phase additive, improves ionization. |
| Phosphatidylethanolamines (PEs) | Membrane phospholipids; involved in cell signaling; altered in DH [10]. | Chloroform-Methanol (2:1): Classic Folch extraction solvent. C18 UHPLC Column: Separates lipid species by hydrophobicity. |
| Triglycerides (TGs) | Energy storage; strong association with insulin resistance and DH [10]. | MTBE: Less toxic, high-yield lipid extraction solvent. Isopropanol/Acetonitrile: Organic mobile phase for eluting non-polar lipids. |
| Sphingomyelins (SMs) | Structural components of membranes and myelin. | Deuterated Internal Standards (e.g., SM d18:1/18:1(d9)): Enable precise quantification. ESI Source: Soft ionization for intact lipid analysis. |
The relationship between the analytical findings and the resulting biological interpretation can be visualized as a pathway impact diagram.
Data Processing and Statistical Analysis
Raw data from UHPLC-MS/MS runs are processed using software tools like MZmine or vendor-specific packages for peak picking, alignment, and normalization [25] [10]. Following this, statistical analysis is critical for extracting biological insights.
- Normalization and Batch Correction: Data normalization is a critical step to correct for technical variance. This can be achieved using internal standards or advanced algorithms like Systematic Error Removal using Random Forest (SERRF) [24]. Batch effects can be corrected using techniques like LOESS regression based on data from pooled QC samples [24].
- Univariate and Multivariate Statistics: Differential lipids are initially screened using univariate tests (e.g., Student's t-test) and fold-change calculations [10]. Multivariate analyses such as PCA and OPLS-DA are then employed to visualize group separations and identify the lipid species most responsible for the variance [10] [21].
- Open-Source Workflows: To ensure reproducibility and transparency, there is a growing emphasis on using open-source programming languages like R and Python for statistical processing and visualization. These workflows facilitate the creation of diagnostic plots (PCA, QC trends), volcano plots, and advanced visualizations like lipid maps [24].
The UHPLC-MS/MS workflow, from rigorous sample preparation to sophisticated data acquisition and analysis, provides a powerful and versatile platform for comprehensive lipidomic profiling. Its application in studying complex metabolic diseases like diabetes with hyperuricemia has successfully identified distinct lipid signatures and implicated specific metabolic pathways in disease progression. As the field advances, the integration of techniques like ion mobility, the development of faster chromatographic methods, and the adoption of standardized, open-source data analysis workflows will further enhance the depth, speed, and reliability of lipidomics research, solidifying its role in biomarker discovery and mechanistic investigation.
Lipidomics, a specialized branch of metabolomics, has emerged as a powerful tool for characterizing the complete lipid profile within biological systems. This approach is particularly valuable for investigating complex metabolic disorders such as diabetes mellitus (DM) combined with hyperuricemia (HUA), where traditional clinical biomarkers provide limited insight into the underlying molecular mechanisms. Global health assessments indicate that hyperuricemia ranks as the second most prevalent metabolic disorder worldwide, following diabetes, with approximately 17.7% of participants in a major Chinese study meeting diagnostic criteria for HUA [10] [14]. The clinical intersection of these conditions is significant, with HUA prevalence among diabetic patients reported at 21.24% in China and 20.70% in North America [14]. This coexistence suggests shared pathophysiological pathways that can be effectively investigated through advanced lipidomic profiling.
The application of multivariate statistical models including Principal Component Analysis (PCA) and Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) has become increasingly crucial for extracting meaningful biological information from complex lipidomic datasets. These methods enable researchers to identify subtle alterations in lipid metabolism that precede clinical manifestations of disease, potentially enabling earlier intervention strategies [10] [27]. In the context of diabetes and hyperuricemia, lipidomic approaches have revealed significant disruptions in glycerophospholipid and glycerolipid metabolism pathways, providing new insights into the metabolic crosstalk between these conditions [10] [28]. This technical guide provides a comprehensive framework for applying PCA and OPLS-DA methodologies to differentiate lipidomic profiles in patient populations, with specific emphasis on the growing research domain of diabetes-hyperuricemia comorbidity.
Theoretical Foundations of Multivariate Statistical Models
Principal Component Analysis (PCA)
Principal Component Analysis represents an unsupervised multivariate statistical method that strategically employs orthogonal transformations to convert potentially correlated variables into a set of linearly uncorrelated variables called principal components [29]. This approach effectively compresses raw data into principal components that describe the most salient features of the original dataset, with PC1 capturing the most significant variance in the multidimensional data matrix, PC2 capturing the next most significant feature orthogonal to PC1, and so forth [29]. The primary strengths of PCA include its utility for data visualization, quality control assessment, and identification of major variation trends without incorporating prior knowledge of sample groups [29].
In practical omics applications, PCA serves two crucial functions. First, it acts as a quality control tool by visualizing biological replicates in PCA score plots, allowing researchers to assess whether samples cluster tightly (indicating good repeatability) or show unwanted dispersion or outliers [29]. The detection and removal of outlier samples is critical for preventing false positives or negatives in downstream statistical analysis. Second, PCA helps uncover the primary sources of variation in datasets, revealing which biological factors contribute most significantly to sample separation before applying more complex supervised methods [29]. This exploratory function makes PCA an essential first step in any lipidomic analysis workflow.
Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA)
Orthogonal Partial Least Squares-Discriminant Analysis represents a supervised discriminant analysis method that integrates orthogonal signal correction (OSC) with PLS-DA approaches [29]. This sophisticated algorithm decomposes the X matrix (variable matrix) into Y-related (predictive) and Y-unrelated (orthogonal) components, effectively separating biological variation of interest from structured noise unrelated to the class separation [29]. Unlike PCA, OPLS-DA incorporates class label information to maximize separation between predefined sample groups, making it particularly valuable for identifying differential variables in controlled experimental designs [29].
The key advantage of OPLS-DA lies in its enhanced interpretability compared to traditional PLS-DA. By filtering out variation unrelated to class separation, OPLS-DA provides clearer group distinctions and more straightforward biological interpretation [29] [27]. For instance, in studies where experimental conditions might be confounded by slight environmental variations (such as differences in light intensity among treated plants), OPLS-DA efficiently filters out such false positives, directing attention to metabolites of genuine biological interest [29]. This capability makes OPLS-DA particularly useful for analyzing spectral data to identify significant variables that distinguish patient groups based on lipidomic profiles [29].
Comparative Analysis of Multivariate Methods
Table 1: Comparison of Multivariate Analysis Methods for Lipidomic Data
| Feature | PCA | PLS-DA | OPLS-DA |
|---|---|---|---|
| Type | Unsupervised | Supervised | Supervised |
| Primary Advantages | Data visualization, evaluation of biological replicates, outlier detection | Identify differential metabolites, build classification models | Improves accuracy and reliability of differential analysis by removing orthogonal variation |
| Limitations | Unable to identify differential metabolites | May be affected by noise and non-experimental factors | Higher computational complexity, medium-high risk of overfitting |
| Best Applications | Exploratory analysis, quality control | Classification, biomarker discovery | Classification with clarity, analysis of complex data with structured noise |
| Overfitting Risk | Low | Medium | Medium–High |
The complementary nature of these methods typically necessitates a sequential analytical approach in lipidomic studies [29]. A standard workflow begins with PCA for data quality assessment and outlier detection, followed by PLS-DA or OPLS-DA for refined classification and mechanistic insights [29] [27]. This integrated approach leverages the strengths of each method while mitigating their individual limitations. For research specifically aimed at identifying key lipid biomarkers that differentiate patient groups, OPLS-DA has demonstrated particular utility due to its ability to separate predictive variation from orthogonal noise, resulting in more robust and interpretable models [29] [30].
Application to Lipidomic Profiling in Diabetes and Hyperuricemia
Experimental Design and Sample Preparation
The investigation of lipidomic profiles in patients with diabetes and hyperuricemia requires meticulous experimental design and sample preparation to ensure analytically robust results. In a recent study examining lipid metabolites in patients with diabetes mellitus combined with hyperuricemia (DH), researchers employed a matched case-control design with 17 patients each in the DH group, diabetes mellitus (DM) group, and healthy control (NGT) group [10]. Participants were permanent residents aged 18 years and above, matched 1:1 by sex and age, with fasting blood samples collected following a 12-hour fast [10]. Similar inclusion criteria (age range 30-70 years, multi-generational regional residence) and exclusion criteria (cardiovascular diseases, severe liver/kidney dysfunction, tumors, psychosis) were applied in a complementary study focusing specifically on hyperuricemia [8].
The sample processing protocol follows standardized procedures to maintain lipid integrity. Briefly, 5 mL of fasting venous blood is collected and centrifuged at 3,000 rpm for 10 minutes at room temperature to separate plasma or serum [10] [8]. The upper layer (0.2 mL plasma) is transferred to 1.5 mL centrifuge tubes, with quality control (QC) samples prepared by combining equal volumes from all samples [10]. For lipid extraction, 100 μL of plasma is mixed with 200 μL of 4°C water, followed by addition of 240 μL of pre-cooled methanol and 800 μL of methyl tert-butyl ether (MTBE) [10] [8]. After vortex mixing and 20 minutes of sonication in a low-temperature water bath, samples stand at room temperature for 30 minutes before centrifugation at 14,000 g for 15 minutes at 10°C [10]. The upper organic phase is collected and dried under nitrogen, then reconstituted in 100 μL of isopropanol or 200 μL of 90% isopropanol/acetonitrile for mass spectrometric analysis [10] [8].
Lipidomic Analysis Using UHPLC-MS/MS
Chromatographic separation represents a critical step in comprehensive lipidomic profiling. The methodology typically employs an ultra-high performance liquid chromatography (UHPLC) system with a Waters ACQUITY UPLC BEH C18 column (2.1 mm i.d. × 100 mm length, 1.7 μm particle size) maintained at 45°C [10] [8]. The mobile phase consists of A: 10 mM ammonium formate acetonitrile solution in water and B: 10 mM ammonium formate acetonitrile isopropanol solution [10]. The chromatography gradient starts at 30% mobile phase B (0-2 minutes), increasing to 100% (2-25 minutes), then returning to 30% (25-35 minutes) at a flow rate of 300 μL/minute with a 3 μL injection volume [10] [8].
Mass spectrometric detection is performed using tandem mass spectrometry (MS/MS) with electrospray ionization operating in both positive and negative modes. Typical source conditions include: heater temperature 300°C, sheath gas flow rate 45 arb, auxiliary gas flow rate 15 arb, sweep gas flow rate 1 arb, spray voltage 3.0 kV (positive) or 2.5 kV (negative), capillary temperature 350°C, and S-lens RF level 50-60% [10] [8]. Full scan MS1 data is collected over a mass range of 200-1800 m/z at resolution 70,000, followed by data-dependent acquisition of MS2 spectra (resolution 17,500) for the top 10 precursors [8]. This analytical approach enables identification of a comprehensive range of lipid molecules across multiple subclasses, with one study identifying 1,361 lipid molecules across 30 subclasses [10].
Data Processing and Multivariate Analysis
Following lipidomic data acquisition, multivariate statistical analysis is applied to extract biologically meaningful patterns. The process typically begins with PCA to assess data quality and identify any outliers or batch effects [29] [27]. QC samples are critical for evaluating analytical stability throughout the acquisition sequence. Once data quality is confirmed, OPLS-DA is employed to maximize separation between predefined patient groups (e.g., DH vs. DM vs. NGT) and identify lipid species that contribute most significantly to these distinctions [10] [29].
The statistical parameters for model validation include R²X (cumulative) and R²Y (cumulative), representing the fraction of variance in X and Y matrices explained by the model, and Q² (cumulative), indicating the predictive ability of the model calculated by cross-validation [29]. Permutation testing (typically 200-1000 permutations) is essential to guard against overfitting, with the resulting intercept values providing evidence of model robustness [29] [27]. Differential lipid molecules are typically selected based on a combination of variable importance in projection (VIP) scores from OPLS-DA (>1.0-1.5), statistical significance (p-value < 0.05 from univariate tests), and fold-change thresholds (>1.5-2.0) [10] [27].
Figure 1: Comprehensive Workflow for Lipidomic Analysis in Diabetes-Hyperuricemia Research
Key Research Findings in Diabetes-Hyperuricemia Lipidomics
Differential Lipid Signatures
Application of UHPLC-MS/MS-based lipidomic profiling combined with multivariate statistical analysis has revealed distinct lipid alterations in patients with diabetes and hyperuricemia. A comprehensive study identified 1,361 lipid molecules across 30 subclasses, with multivariate analyses (PCA and OPLS-DA) demonstrating significant separation trends among the DH, DM, and NGT groups, confirming distinct lipidomic profiles [10]. Specifically, researchers pinpointed 31 significantly altered lipid metabolites in the DH group compared to NGT controls, with the most relevant individual metabolites including 13 triglycerides (TGs) such as TG (16:0/18:1/18:2), 10 phosphatidylethanolamines (PEs) such as PE (18:0/20:4), and 7 phosphatidylcholines (PCs) including PC (36:1) that were significantly upregulated, while one phosphatidylinositol (PI) was downregulated [10].
A separate study focusing specifically on hyperuricemia patients identified 33 differential lipid metabolites that were significantly upregulated, with these lipid metabolites involved in arachidonic acid metabolism, glycerophospholipid metabolism, linoleic acid metabolism, glycosylphosphatidylinositol (GPI)-anchor biosynthesis, and alpha-linolenic acid metabolism pathways [8]. The consistent identification of glycerophospholipid metabolism disruptions across multiple studies suggests this pathway represents a central metabolic disturbance in the comorbidity of diabetes and hyperuricemia [10] [8].
Table 2: Significant Lipid Alterations in Diabetes with Hyperuricemia (DH) vs. Healthy Controls (NGT)
| Lipid Category | Specific Lipid Molecules | Regulation in DH | Biological Relevance |
|---|---|---|---|
| Triglycerides (TGs) | TG (16:0/18:1/18:2) and 12 other TGs | Significantly upregulated | Energy storage, lipid accumulation, insulin resistance |
| Phosphatidylethanolamines (PEs) | PE (18:0/20:4) and 9 other PEs | Significantly upregulated | Membrane fluidity, cellular signaling |
| Phosphatidylcholines (PCs) | PC (36:1) and 6 other PCs | Significantly upregulated | Membrane structure, lipoprotein assembly |
| Phosphatidylinositol (PI) | Not specified | Significantly downregulated | Cell signaling, insulin signaling pathway |
Perturbed Metabolic Pathways
Pathway analysis of differential lipid molecules using platforms such as MetaboAnalyst 5.0 has revealed their enrichment in specific metabolic pathways. In patients with combined diabetes and hyperuricemia, the collective analysis of differential metabolites revealed enrichment in six major metabolic pathways, with glycerophospholipid metabolism (impact value 0.199) and glycerolipid metabolism (impact value 0.014) identified as the most significantly perturbed pathways [10]. The comparison of DH versus DM groups identified 12 differential lipids that were also predominantly enriched in these same core pathways, underscoring their central role in the pathophysiology of hyperuricemia complicating diabetes [10].
Further investigation has revealed connections between these lipid metabolic pathways and immune-inflammatory responses. In hyperuricemia patients, specific immune factors including IL-10, CPT1, IL-6, SEP1, TGF-β1, Glu, TNF-α, and LD were associated with glycerophospholipid metabolism, suggesting integrated metabolic and immune dysregulation [8]. ELISA analyses confirmed significant differences in CPT1, TGF-β1, Glu, and LD levels between hyperuricemia patients and healthy controls, with levels of SEP1, IL-6, TGF-β1, Glu, and LD differing considerably between groups of the same ethnicity [8]. These findings suggest that specific lipid species may influence fatty acid oxidation and mitochondrial oxidative phosphorylation through the glycerophospholipid pathway, potentially reducing glycolysis rates and altering metabolic patterns in ways that promote disease progression [8].
Figure 2: Metabolic Pathways and Lipid Alterations in Diabetes-Hyperuricemia
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Lipidomic Studies
| Category | Specific Items | Function/Application | Examples from Literature |
|---|---|---|---|
| Sample Collection | Sodium heparin blood collection tubes, low-temperature centrifuge | Plasma separation, prevention of coagulation and degradation | Centrifugation at 3,000 rpm for 10 min at room temperature [10] [8] |
| Lipid Extraction | Methyl tert-butyl ether (MTBE), methanol, isopropanol, acetonitrile | Lipid extraction using MTBE/methanol/water method | 800 μL MTBE, 240 μL methanol, 200 μL water per 100 μL plasma [10] [8] |
| Chromatography | Waters ACQUITY UPLC BEH C18 column, ammonium formate | UHPLC separation of lipid classes | 2.1 mm i.d. × 100 mm, 1.7 μm particle size [10] |
| Mass Spectrometry | Q-Exactive Plus mass spectrometer, electrospray ionization source | Lipid identification and quantification | Resolution 70,000 (MS1), 17,500 (MS2), mass range 200-1800 m/z [8] |
| Immunoassays | ELISA kits for cytokines and metabolic factors | Validation of inflammatory and metabolic alterations | TNF-α, IL-6, CPT1, TGF-β1, Glu, LD measurements [8] |
| Data Analysis | MetaboAnalyst 5.0, SIMCA, R packages | Multivariate statistical analysis, pathway analysis | PCA, OPLS-DA, VIP selection, pathway impact calculations [10] [29] |
| DMT-dU-CE Phosphoramidite | DMT-dU-CE Phosphoramidite, CAS:289712-98-7, MF:C39H47N4O8P, MW:730.8 g/mol | Chemical Reagent | Bench Chemicals |
| Methyl 19-methyleicosanoate | Methyl 19-methyleicosanoate, CAS:95799-86-3, MF:C22H44O2, MW:340.6 g/mol | Chemical Reagent | Bench Chemicals |
Methodological Considerations and Best Practices
Experimental Design and Quality Control
Robust experimental design is paramount for generating reliable lipidomic data. Researchers should implement careful sample size calculations, proper matching of case and control groups, and randomization during sample processing and analysis [10] [8]. The inclusion of quality control samples prepared from pooled aliquots of all samples is essential for monitoring analytical performance throughout the acquisition sequence [10]. These QC samples should be injected at regular intervals (e.g., every 5-10 samples) to assess instrument stability, with tight clustering of QCs in PCA scores plots indicating good analytical reproducibility [29] [27].
Additional quality considerations include implementing blank samples (extraction without matrix) to monitor carryover and contamination, and using standard reference materials or internal standards where available to correct for extraction efficiency and matrix effects [27]. For studies comparing multiple groups, batch-to-batch variation should be minimized by randomizing samples across acquisition batches, with statistical correction methods applied if complete randomization is not feasible [29]. These rigorous quality control measures are particularly important when applying multivariate statistical methods like OPLS-DA, as technical artifacts can otherwise be misinterpreted as biological effects [29] [27].
Statistical Validation and Interpretation
The application of multivariate statistical models requires careful validation strategies to avoid overfitting and ensure biological relevance. For OPLS-DA models, internal cross-validation is crucial to assess predictive ability (Q² value) and prevent overfitting [29]. Permutation testing (typically 200-1000 permutations) provides further validation, where the class labels are randomly shuffled multiple times to create models that should theoretically have no predictive value [29] [27]. A valid original model should have significantly higher R² and Q² values compared to the permuted models, with the regression line of Q² versus correlation intercepting the vertical axis at or below zero [29].
The biological interpretation of multivariate models should integrate additional lines of evidence beyond statistical significance alone. Researchers should consider effect sizes (fold changes), analytical precision (coefficients of variation for quantified lipids), and prior biological knowledge about implicated lipid species and pathways [27]. For findings with potential translational significance, independent validation using alternative analytical methods (e.g., ELISA for inflammatory markers) or in separate patient cohorts strengthens the conclusions [8]. This multi-faceted approach to validation and interpretation ensures that identified lipid signatures reflect genuine biological phenomena rather than analytical artifacts or statistical noise.
The integration of multivariate statistical models with advanced lipidomic technologies has created unprecedented opportunities for understanding the complex metabolic interplay between diabetes and hyperuricemia. The consistent identification of glycerophospholipid and glycerolipid metabolism disruptions across multiple studies suggests these pathways represent promising therapeutic targets for managing the dual burden of these metabolic conditions [10] [28] [8]. Future research directions should include longitudinal studies to establish temporal relationships between lipid alterations and disease progression, integration with other omics datasets (genomics, proteomics) for comprehensive pathway mapping, and application of machine learning approaches to develop predictive models for patient stratification and treatment response [30].
From a methodological perspective, ongoing refinements in multivariate statistics include the development of robust versions of PCA and OPLS-DA that are less sensitive to outliers, integration of pathway topology information directly into the statistical models, and implementation of non-linear methods that can capture more complex relationships in lipidomic data [29] [27]. Additionally, standardized reporting frameworks for lipidomic studies would enhance reproducibility and meta-analysis across research groups [27]. As these methodological advances mature, lipidomic profiling combined with multivariate statistical analysis is poised to transition from a primarily research tool to clinical applications, potentially enabling earlier detection of at-risk individuals and personalized interventions targeting specific metabolic disturbances in diabetes and hyperuricemia.
In conclusion, PCA and OPLS-DA represent powerful multivariate statistical approaches that, when appropriately applied within rigorous experimental designs, can effectively differentiate lipidomic profiles in patients with diabetes and hyperuricemia. These methods have revealed specific lipid signatures and pathway disturbances that provide insight into the shared metabolic pathology of these conditions, offering promising directions for both basic research and clinical translation in metabolic disease therapeutics.
The integration of multi-omics data provides a powerful framework for elucidating complex molecular relationships in metabolic diseases. Within the context of lipid metabolic pathways in hyperuricemia patients with diabetes, correlating lipid profiles with immune markers offers particular promise for identifying novel mechanistic insights and therapeutic targets. Hyperuricemia, characterized by elevated serum uric acid (UA), frequently coexists with diabetes and lipid metabolism disorders, creating a complex pathological milieu that drives disease progression through intertwined metabolic and inflammatory pathways [14] [28] [31]. This technical guide outlines comprehensive methodologies for integrating lipidomic data with immune marker measurements and clinical parameters, providing researchers with structured approaches for investigating the crosstalk between metabolic dysregulation and immune response in hyperuricemia-diabetes comorbidity.
Biological Rationale and Established Associations
The Hyperuricemia-Diabetes-Lipid Metabolism Axis
Hyperuricemia represents a significant public health issue ranked second only to diabetes in prevalence, with substantial comorbidity between these conditions [14]. Research indicates that HUA prevalence among diabetic patients reaches 21.24% in China and 20.70% in North America, suggesting shared pathophysiological mechanisms [14]. The association between hyperuricemia and diabetes extends beyond coincidence, with HUA potentially increasing the risk of developing type 2 diabetes and contributing to diabetic complications [14]. Serum uric acid serves as the sole diagnostic marker for hyperuricemia and functions as both an antioxidant and a contributor to obesity-related insulin resistance [14].
At the molecular level, uric acid has been demonstrated to contribute to diabetes progression by impairing islet beta cell survival rather than directly triggering the disease [14]. Additionally, research in mouse models indicates that HUA promotes inflammation, impairs glucose uptake, disrupts insulin signaling, and accelerates diabetes progression [14]. The glucose transporter 9 (GLUT9) has emerged as a crucial mediator in this relationship, with elevated GLUT9 levels combined with impaired glycolysis from insulin resistance contributing to HUA pathogenesis [14].
Lipid-Immune Interactions in Hyperuricemia
A multi-omics study conducted on Xinjiang patients with hyperuricemia revealed significant disruptions in lipid metabolism correlated with immune alterations [31]. This research identified 33 significantly upregulated lipid metabolites in hyperuricemia patients involved in key metabolic pathways including arachidonic acid metabolism, glycerophospholipid metabolism, linoleic acid metabolism, glycosylphosphatidylinositol (GPI)-anchor biosynthesis, and alpha-Linolenic acid metabolism [31].
Crucially, this study established specific connections between lipid pathways and immune markers, demonstrating that IL-10, CPT1, IL-6, SEP1, TGF-β1, Glu, TNF-α, and LD were particularly associated with disturbances in glycerophospholipid metabolism [31]. These findings provide a compelling rationale for systematically investigating correlations between lipidomic profiles and immune markers in hyperuricemia patients with concurrent diabetes.
Methodological Framework for Integrated Omics Analysis
Core Analytical Workflow
The following diagram outlines the comprehensive workflow for integrating lipidomic, immune marker, and clinical data in hyperuricemia-diabetes research:
Lipidomics Experimental Protocols
Sample Preparation and Lipid Extraction
For reliable lipidomic profiling in hyperuricemia-diabetes research, consistent sample preparation is crucial:
Sample Collection: Collect venous blood after a 12-hour fast using sodium heparin tubes. Invert tubes immediately for homogenization and centrifuge at 3,000 rpm for 10 minutes at 4°C. Store plasma aliquots at -80°C until analysis [31].
Lipid Extraction MTBE Method: Utilize the methyl-tert-butyl ether (MTBE) extraction method for comprehensive lipid recovery:
- Combine 100 μL plasma with 240 μL precooled methanol and 200 μL water
- Vortex and add 800 μL MTBE
- Sonicate in a water bath at low temperatures for 20 minutes
- Incubate at room temperature for 30 minutes
- Centrifuge at 14,000 g for 15 minutes at 10°C
- Collect and dry organic phase under nitrogen
- Reconstitute in 200 μL of 90% isopropanol/acetonitrile
- Centrifuge at 14,000 g for 15 minutes at 10°C
- Transfer supernatant for LC-MS analysis [31]
Quality Control: Prepare quality control (QC) samples by combining equal volumes of all sample extracts. Analyze QC samples throughout the sequence to monitor instrument stability [31].
LC-MS Lipid Profiling
Liquid chromatography-mass spectrometry provides the foundation for comprehensive lipidomics:
Chromatography Conditions:
- Column: ACQUITY UPLC CSH C18 (Waters)
- Mobile Phase A: ACN/Hâ‚‚O (6:4 v/v) with 10 mM ammonium formate
- Mobile Phase B: ACN:IPA (2:9 v/v) with 10 mM isopropyl ammonium formate
- Gradient: 30% B (0-2 min) to 100% B (2-25 min), maintain 30% B (25-35 min)
- Flow Rate: 300 μL/min
- Injection Volume: 3 μL
- Column Temperature: 45°C [31]
Mass Spectrometry Parameters:
- Instrument: Q-Exactive Plus (Thermo Scientific)
- Ionization: Electrospray Ionization (ESI)
- Positive Mode: Spray voltage 3.0 kV, capillary temperature 350°C
- Negative Mode: Spray voltage 2.5 kV, capillary temperature 350°C
- Scan Range: 200-1800 m/z
- MS1 Resolution: 70,000
- Data Acquisition: Full scan followed by data-dependent MS/MS (top 10)
- MS2 Resolution: 17,500 [31]
Immune Marker Analysis
ELISA-Based Cytokine Quantification
For measuring immune markers IL-6, TNF-α, and TGF-β1 in hyperuricemia-diabetes studies:
Assay Principle: Utilize sandwich ELISA kits with pre-coated capture antibodies specific to each cytokine.
Procedure:
- Add 100 μL standards or samples to appropriate wells
- Incubate 2 hours at room temperature or overnight at 4°C
- Wash plates 3-4 times with wash buffer
- Add biotinylated detection antibody (100 μL/well)
- Incubate 1-2 hours at room temperature
- Wash plates and add streptavidin-HRP conjugate
- Incubate 30 minutes at room temperature
- Add substrate solution (TMB) and incubate 15-30 minutes
- Stop reaction with stop solution
- Read absorbance immediately at 450 nm [31]
Data Analysis: Calculate cytokine concentrations using standard curves generated with reference standards. Verify assay performance using quality control samples.
Multiplex Immunoassay Alternatives
For higher throughput analysis, multiplex platforms such as Meso Scale Discovery (MSD) or Luminex can simultaneously quantify multiple immune markers in small sample volumes, providing advantages for studies with limited sample availability.
Clinical Parameter Assessment
Essential clinical parameters for hyperuricemia-diabetes lipidomics studies include:
- Uric Acid Metabolism: Serum uric acid (enzymatic uricase method)
- Glucose Metabolism: Fasting blood glucose, HbA1c, insulin
- Lipid Profile: Total cholesterol, triglycerides, LDL-C, HDL-C, VLDL-C
- Renal Function: Creatinine, blood urea nitrogen (BUN), estimated glomerular filtration rate (eGFR)
- Liver Function: ALT, AST
- Inflammatory Markers: High-sensitivity C-reactive protein (hsCRP)
Data Integration and Analytical Approaches
Correlation Analysis Framework
Integrated analysis of lipidomic, immune marker, and clinical data requires a structured statistical approach:
Data Preprocessing: Normalize lipidomic data using QC-based approaches (e.g., LOESS, SERRF), log-transform where appropriate, and handle missing values using imputation methods suitable for mass spectrometry data.
Multivariate Statistics: Apply Principal Component Analysis (PCA) and Partial Least Squares-Discriminant Analysis (PLS-DA) to identify patterns separating patient groups based on combined omics profiles.
Correlation Networks: Construct integrated correlation networks using Spearman or Pearson correlation coefficients between significantly altered lipids, immune markers, and clinical parameters. Apply false discovery rate (FDR) correction for multiple testing.
Pathway Integration: Map correlated lipids and immune markers to known metabolic and signaling pathways using enrichment analysis tools such as LIPEA (Lipid Pathway Enrichment Analysis) and databases including LIPID MAPS and KEGG [32].
Experimental Findings and Data Representation
Key Lipid-Immune Correlations in Hyperuricemia
Table 1: Significant Lipid-Immune Marker Correlations in Hyperuricemia
| Lipid Class | Specific Lipid | Immune Marker | Correlation Direction | Proposed Mechanism |
|---|---|---|---|---|
| Glycerophospholipids | Phosphatidylcholines | IL-6, TGF-β1 | Positive [31] | Membrane remodeling & inflammatory signaling |
| Fatty Acids | Arachidonic acid | TNF-α, IL-6 | Positive [31] | Eicosanoid precursor metabolism |
| Glycerophospholipids | Phosphatidylethanolamines | IL-10 | Negative [31] | Anti-inflammatory resolution |
| Sphingolipids | Ceramides | TGF-β1 | Positive [31] | Insulin resistance & fibrosis signaling |
Methodological Comparison for Immune Marker Analysis
Table 2: Analytical Platforms for Immune Marker Quantification
| Platform | Sensitivity | Sample Volume | Multiplexing Capacity | Throughput | Best Use Cases |
|---|---|---|---|---|---|
| ELISA | High (pg/mL) | 50-100 μL | Single-plex | Moderate | Targeted validation |
| MSD | Very High (fg-pg/mL) | 25-50 μL | Medium-plex (10-plex) | High | Discovery studies |
| Luminex | Moderate-High | 25-50 μL | High-plex (up to 50-plex) | High | Screening studies |
| LC-MS/MS | High | 50-100 μL | Medium-plex | Moderate | Absolute quantification |
Mechanistic Insights and Pathway Mapping
Integrated Signaling Pathways in Hyperuricemia-Diabetes
The following diagram illustrates the key molecular relationships between lipid metabolism, immune markers, and clinical parameters in hyperuricemia with diabetes:
Molecular Mechanisms Linking Lipids and Inflammation
Research has elucidated several key mechanisms through which disrupted lipid metabolism influences immune responses in hyperuricemia-diabetes:
NLRP3 Inflammasome Activation: Uric acid crystals and certain lipid species activate the NLRP3 inflammasome, leading to caspase-1-mediated production of IL-1β and IL-18, which drive inflammatory responses [33].
Oxidative Stress Pathways: Hyperuricemia promotes reactive oxygen species (ROS) production through xanthine oxidase activity, while altered lipid metabolism further exacerbates oxidative stress, creating a pro-inflammatory environment that stimulates IL-6 and TNF-α production [28].
GSDMD-Mediated Pyroptosis: Recent evidence indicates that high intrahepatic UA levels induce gasdermin D (GSDMD)-mediated pyroptosis in hepatocytes via the NLRP3-Caspase-1-GSDMD pathway, contributing to hepatic inflammation in metabolic disorders [33].
Membrane Remodeling and Signaling: Dysregulated glycerophospholipid metabolism alters membrane composition, affecting fluidity, receptor function, and the production of lipid second messengers that modulate immune cell activation and cytokine production [31].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Integrated Omics Studies
| Category | Specific Product/Platform | Application Note | Key Feature |
|---|---|---|---|
| Lipid Extraction | MTBE/Methanol/Water System | Comprehensive lipid recovery from serum/plasma | Maintains lipid integrity [31] |
| LC-MS Platform | Q-Exactive Plus HRMS Orbitrap | Untargeted lipidomics with high mass accuracy | Enables structural elucidation [31] |
| Chromatography | ACQUITY UPLC CSH C18 Column | Separation of complex lipid mixtures | Enhanced lipidome coverage [31] |
| Immune Assays | ELISA Kits (IL-6, TNF-α, TGF-β1) | Quantitative immune marker analysis | High sensitivity & specificity [31] |
| Multiplex Assays | Meso Scale Discovery (MSD) | Simultaneous cytokine quantification | Reduced sample requirement [34] |
| Pathway Analysis | LIPEA (Lipid Pathway Enrichment) | Lipid pathway mapping from omics data | Database integration [32] |
| 2-Hydroxyl emodin-1-methyl ether | 2-Hydroxyl emodin-1-methyl ether, CAS:346434-45-5, MF:C16H12O6, MW:300.26 g/mol | Chemical Reagent | Bench Chemicals |
| 7-(6'R-Hydroxy-3',7'-dimethylocta-2',7'-dienyloxy)coumarin | 7-(6'R-Hydroxy-3',7'-dimethylocta-2',7'-dienyloxy)coumarin, CAS:118584-19-3, MF:C19H22O4, MW:314.4 g/mol | Chemical Reagent | Bench Chemicals |
The integration of lipidomics with immune marker analysis and clinical parameters provides a powerful multidimensional approach for investigating the complex interplay between metabolic dysregulation and inflammation in hyperuricemia patients with diabetes. The methodologies outlined in this technical guide—from standardized sample preparation and LC-MS analysis to advanced data integration strategies—offer researchers a comprehensive framework for uncovering novel mechanistic insights and identifying potential therapeutic targets in this complex metabolic-immune axis. As these integrated approaches continue to evolve, they hold significant promise for advancing our understanding of hyperuricemia-diabetes comorbidity and developing more effective, personalized treatment strategies.
Pathway analysis has become an indispensable methodology in modern metabolomics, enabling researchers to move beyond simple lists of differential metabolites toward meaningful biological interpretation. In the context of lipid metabolic pathways in hyperuricemia patients with diabetes, this approach allows for the systematic identification of perturbed biological pathways that underlie disease pathophysiology. MetaboAnalyst stands as a comprehensive web-based platform and R package specifically designed to address the computational challenges in metabolomics, offering a suite of statistical and functional analysis tools that transform raw spectral data into biological insights [35]. The platform supports the entire analytical workflow from data processing to pathway visualization, making it particularly valuable for researchers investigating complex metabolic disorders.
The integration of hyperuricemia and diabetes research represents a critical frontier in metabolic disease investigation. Epidemiological studies reveal that hyperuricemia affects approximately 17.7% of the Chinese population, with significantly higher prevalence in diabetic populations [10] [3]. Both conditions are characterized by profound lipid metabolism disruptions, creating a complex pathological interplay that pathway analysis can help elucidate. MetaboAnalyst provides the computational framework necessary to unravel these complex relationships through sophisticated statistical approaches and integration with curated metabolic databases.
Theoretical Foundations and Analytical Framework
Core Algorithms and Statistical Approaches
MetaboAnalyst employs a multi-faceted statistical framework for pathway analysis, combining both univariate and multivariate methods to ensure comprehensive coverage of metabolic perturbations. The platform's analytical pipeline begins with fold-change analysis and t-tests to identify individual metabolites showing significant alterations between experimental conditions [36]. These univariate methods are particularly valuable for initial feature selection, though they consider each metabolite independently without accounting for complex interdependencies.
For more sophisticated multidimensional analysis, MetaboAnalyst incorporates Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA), a supervised method that maximizes separation between predefined sample classes while filtering out variation unrelated to class discrimination [21]. The quality of OPLS-DA models is typically validated using R² and Q² values, with permutation testing to prevent overfitting. Additionally, the platform offers Sparse Partial Least Squares-Discriminant Analysis (sPLS-DA), which effectively reduces the number of variables in high-dimensional metabolomics data to produce robust, interpretable models [36]. The "sparseness" in sPLS-DA is controlled by adjusting the number of components and variables within each component, allowing researchers to focus on the most biologically relevant features.
The pathway analysis module itself primarily utilizes two complementary algorithms: Gene Set Enrichment Analysis (GSEA) and Over Representation Analysis (ORA). GSEA evaluates the distribution of all measured metabolites within a predefined pathway without applying arbitrary significance thresholds, making it particularly sensitive to subtle but coordinated changes across multiple pathway components. In contrast, ORA tests whether significantly altered metabolites (typically based on p-value and fold-change thresholds) are overrepresented in specific pathways compared to what would be expected by chance [35]. Both approaches calculate pathway impact scores that combine statistical significance with topological considerations, giving higher weight to metabolites that serve as key pathway hubs.
Data Requirements and Preparation
Proper data formatting is fundamental to successful pathway analysis in MetaboAnalyst. The platform supports multiple input formats, with specific requirements for each:
Table 1: MetaboAnalyst Input Data Formats for Pathway Analysis
| Format Type | Description | Use Case | Requirements |
|---|---|---|---|
| Compound Concentration Table | CSV table with quantified metabolite concentrations | Targeted metabolomics with identified compounds | Sample names in first column, followed by class labels, then numeric concentration values |
| Peak Intensity Table | CSV table with processed spectral peak intensities | Untargeted metabolomics with feature alignment | Unique feature names (m/z_retention time), missing values as empty or NA |
| MS/NMR Binned Spectra | CSV table with spectral bins | Chemometric analysis of raw spectral data | Consistent binning across all samples, proper normalization |
| mzTab 2.0-M | Standardized metabolomics data format | LC-MS/MS studies with metadata | Validated mzTab-M 2.0 files with complete metadata and small molecule tables |
For lipidomics studies in hyperuricemia-diabetes research, the compound concentration table is typically the most appropriate format, as it allows for direct investigation of specific lipid species and their pathway contextualization. Sample names must be unique and consist only of English letters, numbers, and underscores, with class labels immediately following sample names. Data values should contain only numeric, positive values without spaces (e.g., "1600" not "1 600") [37].
Data normalization is a critical preprocessing step that significantly impacts pathway analysis results. MetaboAnalyst offers multiple normalization options including sample-specific normalization (to constant sum, reference samples, or specific gravity), data transformation (log, cube root), and data scaling (mean-centered, unit-variance, Pareto scaling). For lipidomic data, which often exhibits heteroscedasticity, log transformation followed by Pareto scaling generally provides optimal results by reducing the influence of extreme values while preserving biological variation.
Practical Implementation for Hyperuricemia-Diabetes Lipidomics
Experimental Workflow and Protocol
Implementing pathway analysis for lipid metabolic pathways in hyperuricemia patients with diabetes requires a systematic approach from sample preparation to biological interpretation. The following protocol outlines the key experimental and computational steps:
Sample Collection and Preparation:
- Collect fasting blood samples from hyperuricemia-diabetes patients and appropriate controls (e.g., diabetes alone, hyperuricemia alone, healthy controls)
- Centrifuge at 3,000 rpm for 10 minutes at room temperature to separate plasma/serum
- Aliquot 0.2 mL of supernatant into sterile tubes and store at -80°C until analysis
- For lipid extraction, thaw samples on ice and vortex, then add 200 μL of 4°C water and 240 μL of pre-cooled methanol
- Add 800 μL of methyl tert-butyl ether (MTBE), sonicate in a low-temperature water bath for 20 minutes, and incubate at room temperature for 30 minutes
- Centrifuge at 14,000 g for 15 minutes at 10°C, collect the upper organic phase, and dry under nitrogen [10]
LC-MS/MS Lipidomic Analysis:
- Reconstitute dried lipids in 200 μL of 90% isopropanol/acetonitrile
- Separate lipids using UHPLC with a C18 column (2.1 × 100 mm, 1.7 μm) maintained at 45°C
- Use mobile phase A: 10 mM ammonium formate in acetonitrile/water (6:4 v/v) and mobile phase B: 10 mM ammonium formate in acetonitrile/isopropanol (2:9 v/v)
- Employ a gradient elution from 30% B to 100% B over 25 minutes at a flow rate of 300 μL/min
- Acquire mass spectra using Q-Exactive Plus Orbitrap mass spectrometer in positive and negative ionization modes
- Set spray voltage to 3.0 kV (positive) or 2.5 kV (negative), capillary temperature to 350°C, and scan range from 200-1800 m/z [8]
Data Processing and Pathway Analysis:
- Convert raw spectra to peak lists using vendor software or open-source tools like XCMS
- Export peak intensity table with features as rows and samples as columns
- Upload data to MetaboAnalyst web server (www.metaboanalyst.ca) or import into MetaboAnalystR
- Perform quality control, normalization, and missing value imputation
- Identify significant lipid features using fold-change analysis and statistical testing
- Execute pathway analysis using the integrated module
- Interpret results in the context of hyperuricemia-diabetes pathology
The following diagram illustrates the complete analytical workflow:
Research Reagent Solutions and Essential Materials
Table 2: Essential Research Reagents and Materials for Lipidomics in Hyperuricemia-Diabetes Research
| Reagent/Material | Specification | Function | Example Source |
|---|---|---|---|
| Methyl tert-butyl ether (MTBE) | HPLC grade, ≥99.9% | Lipid extraction solvent | Sigma-Aldrich, Cat# 34875 |
| Ammonium formate | LC-MS grade, ≥99.0% | Mobile phase additive for improved ionization | Thermo Fisher, Cat# 11574435 |
| UHPLC C18 Column | 2.1 × 100 mm, 1.7 μm | High-resolution chromatographic separation | Waters, ACQUITY UPLC BEH C18 |
| Quality Control Serum | Sigma human serum matrix | Inter-batch normalization and quality assurance | Sigma-Aldrich, Cat# H1388 |
| Reference Lipid Standards | SPLASH LIPIDOMIX | Quantification and identification of lipid species | Avanti Polar Lipids, Cat# 330707 |
| Potassium oxonate | ≥98% purity | Xanthine oxidase inhibitor for hyperuricemia modeling | Shanghai Aladdin, Cat# K2228616 |
Key Lipid Pathways in Hyperuricemia-Diabetes Pathology
Application of MetaboAnalyst pathway analysis to hyperuricemia-diabetes research has consistently identified several key lipid pathways that are centrally perturbed in this comorbidity. Recent studies have revealed that glycerophospholipid metabolism emerges as the most significantly altered pathway, with an impact value of 0.199, followed by glycerolipid metabolism (impact value: 0.014) [10]. These pathways are integral to membrane integrity, cell signaling, and energy storage, with their disruption contributing to insulin resistance and inflammatory responses characteristic of both conditions.
Specific lipid species demonstrating significant alterations include triglycerides (TGs) such as TG(16:0/18:1/18:2), phosphatidylethanolamines (PEs) including PE(18:0/20:4), and phosphatidylcholines (PCs) like PC(36:1), which are consistently upregulated in hyperuricemia-diabetes patients compared to controls [10]. Additionally, pathways involving linoleic acid metabolism, arachidonic acid metabolism, and glycosylphosphatidylinositol (GPI)-anchor biosynthesis show significant perturbations, reflecting the complex interplay between purine metabolism dysregulation and lipid homeostasis [8].
The following diagram illustrates the key interconnected pathways identified in hyperuricemia-diabetes research:
Advanced Applications and Integration Strategies
Multi-Omics Integration and Cross-Platform Analysis
MetaboAnalyst supports sophisticated multi-omics integration approaches that significantly enhance the biological interpretation of lipid pathways in hyperuricemia-diabetes research. The platform enables integrated pathway analysis combining metabolomic data with transcriptomic or proteomic datasets, allowing researchers to identify concordant pathway alterations across multiple biological layers. This capability is particularly valuable for distinguishing causal metabolic perturbations from compensatory mechanisms in complex disease states.
For advanced users, MetaboAnalystR provides programmatic access to these integration tools through R commands such as PerformIntegPathwayAnalysis() and PlotMultiOmics(). The typical workflow involves:
- Uploading pre-processed gene/protein and metabolite expression matrices
- Selecting appropriate reference databases (KEGG, Reactome, SMPDB)
- Specifying integration parameters (pathway overlap, joint visualization)
- Generating multi-omics pathway maps that highlight convergent biological processes
This integrated approach has revealed that alterations in glycine, serine, and threonine metabolism in hyperuricemia patients with hyperlipidemia may lead to chronic kidney disease, a common diabetic complication [21]. Similarly, disruptions in the phenylalanine, tyrosine, and tryptophan biosynthesis pathway show strong associations with fatty liver development in this patient population, providing potential mechanistic links between hyperuricemia and diabetes comorbidities.
MetaboAnalystR for High-Throughput and Reproducible Analysis
For research groups requiring high-throughput processing or implementing automated analysis pipelines, MetaboAnalystR offers a comprehensive R-based implementation of the web platform's capabilities. Installation requires R version >4.0 and can be accomplished using the devtools package:
Key functions for pathway analysis include:
InitDataObjects(): Initialize data object with appropriate data typeSetupCondDesign(): Set up experimental conditions and designCrossReference(): Perform metabolite set enrichment analysisMetaboliteSetEnrichment(): Execute mummichog algorithm for functional analysisNetworkExplorer(): Visualize results as metabolic networks
The package particularly excels in processing raw LC-MS/MS data through automated peak picking, alignment, and annotation workflows, significantly reducing manual processing time while improving reproducibility. For large-scale epidemiological studies of hyperuricemia-diabetes relationships, this computational efficiency enables rapid analysis of hundreds of samples while maintaining analytical consistency.
Biological Interpretation and Research Applications
Case Study: Pathway Analysis in Diabetes with Hyperuricemia
A recent investigation utilizing UHPLC-MS/MS-based plasma untargeted lipidomic analysis provides a compelling case study for MetaboAnalyst application in hyperuricemia-diabetes research. The study analyzed 17 patients with diabetes mellitus combined with hyperuricemia (DH), 17 with diabetes alone (DM), and 17 healthy controls with normal glucose tolerance (NGT) [10]. Multivariate analyses including PCA and OPLS-DA revealed clear separation trends among the three groups, confirming distinct lipidomic profiles associated with the comorbidity.
Pathway analysis of the 31 significantly altered lipid metabolites identified in DH patients revealed their enrichment in six major metabolic pathways, with glycerophospholipid metabolism and glycerolipid metabolism emerging as the most significantly perturbed [10]. The specific lipid alterations included 13 triglycerides (TGs), 10 phosphatidylethanolamines (PEs), and 7 phosphatidylcholines (PCs) that were significantly upregulated, while one phosphatidylinositol (PI) was downregulated. These findings suggest profound disruptions in membrane composition, signaling transduction, and energy storage mechanisms that potentially exacerbate both hyperglycemia and hyperuricemia pathophysiology.
Table 3: Significant Lipid Metabolite Alterations in Diabetes with Hyperuricemia
| Lipid Class | Representative Species | Regulation in DH | Potential Functional Impact |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) | Upregulated | Altered energy storage, hepatic steatosis |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) | Upregulated | Membrane fluidity changes, signaling disruption |
| Phosphatidylcholines (PCs) | PC(36:1) | Upregulated | VLDL assembly, lipid transport alterations |
| Phosphatidylinositol (PI) | PI(18:0/20:4) | Downregulated | Impaired insulin signaling transduction |
Clinical and Therapeutic Implications
The pathway insights generated through MetaboAnalyst analysis offer significant potential for clinical translation in hyperuricemia-diabetes management. The identification of specific disrupted lipid pathways provides a mechanistic foundation for developing targeted interventions that address both conditions simultaneously. For instance, the prominence of glycerophospholipid metabolism disturbances suggests potential therapeutic strategies focusing on membrane-stabilizing compounds or phospholipid-modulating agents.
Furthermore, the consistent observation that linoleic acid metabolism and arachidonic acid metabolism pathways are perturbed in hyperuricemia patients provides a molecular rationale for dietary interventions targeting polyunsaturated fatty acid intake [21] [8]. These pathway-centric insights move beyond conventional single-biomarker approaches to offer a systems-level understanding of the hyperuricemia-diabetes comorbidity, potentially informing more effective nutritional and pharmacological strategies that address the underlying metabolic network disruptions rather than isolated biochemical parameters.
MetaboAnalyst represents a powerful, accessible platform for conducting sophisticated pathway analysis in the context of lipid metabolic disruptions in hyperuricemia patients with diabetes. Its comprehensive analytical framework, spanning from basic statistical comparisons to advanced multi-omics integration, enables researchers to extract meaningful biological insights from complex lipidomic datasets. The consistent identification of glycerophospholipid metabolism, glycerolipid metabolism, and specific fatty acid metabolic pathways as centrally perturbed in this comorbidity highlights the value of pathway-centric approaches for understanding complex metabolic diseases. As lipidomics technologies continue to advance and reference databases expand, MetaboAnalyst is poised to remain an indispensable tool for unraveling the intricate relationships between purine metabolism, lipid homeostasis, and glucose regulation in metabolic syndrome and its related disorders.
The convergence of hyperuricemia and diabetes presents a significant clinical challenge, with growing evidence suggesting that dysregulated lipid metabolism serves as a critical pathological link between these conditions. Hyperuricemia, characterized by elevated serum uric acid levels, ranks as the second most prevalent metabolic disorder after diabetes [14]. Recent global research indicates the hyperuricemia prevalence in diabetic patients has reached 21.24% in China and 20.70% in North America [14], highlighting the substantial clinical overlap between these conditions. While conventional clinical lipid measurements provide limited insight, advanced lipidomics technologies now enable comprehensive profiling of hundreds to thousands of lipid species, revealing specific lipid signatures that may serve as sensitive biomarkers for disease detection, stratification, and prognosis [11] [38].
This technical guide examines the complete pipeline for developing diagnostic and prognostic scores from lipid signatures, with specific focus on applications in hyperuricemia patients with diabetes. We synthesize methodological approaches, analytical frameworks, and validation strategies to support researchers and drug development professionals in translating lipidomic data into clinically actionable tools.
Technical Foundations: Lipidomics Methodologies
Analytical Platforms and Workflows
Lipidomic analysis relies primarily on mass spectrometry (MS) platforms, with two predominant approaches: targeted (quantitative) and untargeted (discovery) lipidomics. The experimental workflow encompasses sample collection, preparation, chromatographic separation, mass spectrometric analysis, and data processing [39] [40].
Table 1: Comparison of Major MS-Based Lipidomics Platforms
| Platform Type | Key Features | Applications | Throughput |
|---|---|---|---|
| LC-MS/MS | High sensitivity and specificity; quantitative capability; requires sample preparation | Biomarker validation; clinical applications | Moderate (≥30 min/sample) |
| Direct MS (iEESI-MS) | Minimal sample preparation; high throughput; matrix interference resistance | Rapid diagnostic model development; intraoperative margin detection | High (≤1 min/sample) |
| MALDI-MSI | Spatial mapping of lipid distributions; tissue imaging | Tumor microenvironment analysis; pathological examination | Variable |
| GC-MS | Suitable for volatile lipids; requires derivatization | Fatty acid profiling; metabolic pathway analysis | Moderate |
For hyperuricemia and diabetes research, targeted lipidomic analysis using liquid chromatography-electrospray ionization mass spectrometry (LC-ESI-MS) has proven particularly valuable. This approach typically follows a standardized workflow: plasma samples are processed using modified methyl tert-butyl ether (MTBE) extraction protocols, followed by chromatographic separation using C8 or similar reverse-phase columns, with lipid species quantified using multiple reaction monitoring (MRM) or similar high-sensitivity detection modes [11].
Quality Control and Standardization
Robust lipidomic analysis requires rigorous quality control measures. Implementation of internal standards (e.g., SPLASH LIPIDOMIX Mass Spec Standard mixture) is essential for quantification accuracy [41]. Quality control samples should be analyzed throughout analytical batches to monitor instrument performance, with coefficients of variation <30% generally considered acceptable [11]. For clinical translation, standardization of pre-analytical variables (fasting status, sample processing protocols, storage conditions) is critical to minimize technical variability and ensure reproducible results across study populations.
Lipid Signatures in Hyperuricemia and Diabetic Populations
Hyperuricemia-Specific Lipid Alterations
Comprehensive lipidomic profiling has revealed distinct lipid signatures associated with hyperuricemia. A large-scale study of middle-aged and elderly Chinese individuals (n=2,247) identified 123 lipids significantly associated with uric acid levels after multivariable adjustment, with predominant alterations in glycerolipids (GLs) and glycerophospholipids (GPs) [11]. Specific lipid species showing the strongest positive associations with hyperuricemia risk included diacylglycerols (DAG (16:0/22:5), DAG (16:0/22:6), DAG (18:1/20:5), DAG (18:1/22:6)), phosphatidylcholine (PC (16:0/20:5)), and triacylglycerol (TAG (53:0)), while lysophosphatidylcholine (LPC (20:2)) was inversely associated with hyperuricemia risk [11].
Network analysis further revealed a coordinated dysregulation pattern, with a specific module enriched in triacylglycerols, phosphatidylcholines, and diacylglycerols showing positive association with hyperuricemia risk [11]. These lipid signatures were notably correlated with fatty acids in the de novo lipogenesis pathway, particularly 16:1n-7 (Spearman correlation coefficients = 0.32–0.41, p < 0.001), suggesting a mechanistic link between uric acid metabolism and endogenous lipid synthesis [11].
Diabetes-Related Lipid Perturbations
In diabetic populations, lipidomic studies have identified alterations in specific phospholipid species that may reflect underlying insulin resistance and metabolic dysfunction. Diabetes-associated phosphatidylcholines (PCs 16:0/16:1, 16:0/18:1 and 18:0/16:1) and phosphatidylethanolamine (PE 16:0/16:1) have been identified as potential markers, with these lipid species influenced by dietary patterns high in refined grains and low in fish, dairy, and soy products [11]. These findings highlight the complex interplay between genetic predisposition, lipid metabolism, and environmental factors in shaping diabetes-associated lipid signatures.
Integrated Lipid Signatures for Comorbid Hyperuricemia and Diabetes
The comorbid presence of hyperuricemia and diabetes appears to produce additive or synergistic effects on lipid metabolism. Studies comparing early-onset hyperuricemia (≤40 years) and gout patients have revealed more profound lipid alterations in younger patients, characterized by significant upregulation of phosphatidylethanolamines and downregulation of lysophosphatidylcholine plasmalogens/plasmanyls [41]. Multivariate statistical models based on these lipid signatures successfully differentiated early-onset hyperuricemia and gout groups from healthy controls with >95% accuracy, demonstrating the potential diagnostic utility of lipidomic profiling [41].
Table 2: Key Lipid Species Altered in Hyperuricemia and Diabetes
| Lipid Class | Specific Lipid Species | Direction of Change | Biological Relevance |
|---|---|---|---|
| Diacylglycerols (DAGs) | DAG (16:0/22:5), DAG (16:0/22:6), DAG (18:1/20:5), DAG (18:1/22:6) | ↑ in HUA | Insulin resistance; protein kinase C activation |
| Phosphatidylcholines (PCs) | PC (16:0/20:5) | ↑ in HUA | Membrane integrity; inflammation modulation |
| Lysophosphatidylcholines (LPCs) | LPC (20:2) | ↓ in HUA | Anti-inflammatory properties; insulin sensitivity |
| Triacylglycerols (TAGs) | TAG (53:0) | ↑ in HUA | Energy storage; cardiovascular risk |
| Phosphatidylethanolamines (PEs) | Multiple species | ↑ in early-onset HUA | Membrane fluidity; autophagy regulation |
| LPC Plasmalogens | Multiple species | ↓ in early-onset HUA | Antioxidant capacity; membrane protection |
Biomarker Development Pipeline
From Discovery to Validation
The transition from lipid signature discovery to validated biomarker requires a structured, multi-stage approach. Initial discovery phases typically employ untargeted lipidomics to identify differentially abundant lipid species between case and control groups. Promising candidates then advance through targeted validation in independent cohorts, with progressive refinement of biomarker panels based on performance metrics [39] [11].
For hyperuricemia and diabetes applications, study designs should account for potential confounders including body mass index, renal function, medication use (particularly urate-lowering and lipid-lowering therapies), and dietary patterns. The incorporation of stratification factors (e.g., early vs. late onset, presence of diabetes complications) enhances the clinical utility of resulting biomarker panels.
Statistical Analysis and Model Building
Robust statistical analysis is essential for developing lipid-based biomarker scores. Common approaches include:
- Univariate analysis: Identifying individual lipid species with significant case-control differences (false discovery rate correction for multiple testing)
- Multivariate methods: Partial least squares-discriminant analysis (PLS-DA), orthogonal PLS-DA to identify lipid combinations maximizing group separation
- Machine learning algorithms: Random Forest, support vector machines (SVM), LASSO regression for feature selection and model building [42]
For hyperuricemia applications, studies have successfully employed multivariate models combining 5-10 lipid species to achieve high classification accuracy (>95%) for distinguishing hyperuricemia patients from healthy controls [41]. Model performance should be rigorously assessed using receiver operating characteristic (ROC) analysis, with internal validation via bootstrapping or cross-validation and external validation in independent cohorts.
Integration with Clinical Variables
The highest diagnostic and prognostic utility typically emerges from integrating lipid signatures with established clinical parameters. For hyperuricemia and diabetes applications, relevant clinical variables include serum uric acid levels, HbA1c, HOMA-IR, renal function markers, and anthropometric measurements. Integrated models may demonstrate superior performance compared to either clinical or lipidomic data alone, potentially revealing novel pathophysiological insights into the relationship between hyperuricemia and diabetic complications.
Experimental Protocols for Lipid Biomarker Development
Sample Preparation Protocol for Plasma Lipidomics
Materials Required:
- EDTA plasma samples (fasting, 8-12 hours)
- HPLC-grade methanol, methyl tert-butyl ether (MTBE), isopropanol, water
- Internal standard mixture (e.g., SPLASH LIPIDOMIX or equivalent)
- Refrigerated centrifuge capable of 14,000×g
- Vortex mixer and analytical balance
Procedure:
- Thaw plasma samples on ice and vortex thoroughly
- Aliquot 50 μL plasma into 2-mL centrifuge tube
- Add 300 μL ice-cold methanol containing internal standards
- Vortex for 1 minute
- Add 1 mL MTBE, vortex for 1 minute, then shake gently for 1 hour
- Add 300 μL water to induce phase separation
- Centrifuge at 14,000×g for 15 minutes at 4°C
- Collect upper organic layer (lipid-containing) for analysis
- Dry under nitrogen or vacuum and reconstitute in appropriate solvent for MS analysis [39] [11]
Liquid Chromatography-Mass Spectrometry Analysis
Chromatographic Conditions:
- Column: BEH C8 (100 × 2.1 mm, 1.7 μm) or equivalent
- Mobile phase A: acetonitrile/water (60:40) with 10 mM ammonium acetate
- Mobile phase B: isopropanol/acetonitrile (90:10) with 10 mM ammonium acetate
- Flow rate: 0.26 mL/min
- Gradient: 32% B to 85% B over 14 minutes, then to 97% B
- Column temperature: 55°C
- Injection volume: 5 μL [39]
Mass Spectrometry Parameters:
- Ionization: Electrospray ionization (ESI) in positive and negative modes
- Resolution: ≥70,000 (for high-resolution instruments)
- Scan range: m/z 200-1200
- Source temperature: 300°C
- Sheath gas flow: Optimize for sensitivity
Figure 1: Lipid Biomarker Development Workflow
Diagnostic and Prognostic Applications
Diagnostic Score Development
Lipid-based diagnostic scores for hyperuricemia and diabetes integrate multiple lipid species into a single composite index. Development typically involves:
- Feature selection: Identifying the most informative lipid species through univariate and multivariate methods
- Weight assignment: Determining relative contributions of each lipid to the overall score
- Threshold establishment: Defining optimal cut-points for clinical classification
For hyperuricemia, a diagnostic score incorporating DAG (16:0/22:5), DAG (16:0/22:6), DAG (18:1/20:5), DAG (18:1/22:6), PC (16:0/20:5), TAG (53:0), and LPC (20:2) has demonstrated significant association with hyperuricemia risk (p < 0.05) [11]. Such scores may facilitate early identification of high-risk individuals before overt clinical manifestations develop.
Prognostic Applications
Beyond diagnosis, lipid signatures show promise for prognostic stratification in hyperuricemia and diabetes. Specific lipid patterns have been associated with:
- Disease progression from asymptomatic hyperuricemia to gout
- Development of diabetes complications (nephropathy, cardiovascular disease)
- Response to urate-lowering therapy [41]
Notably, lipidomic profiles in early-onset hyperuricemia (≤40 years) demonstrate more pronounced alterations compared to late-onset disease, suggesting potential utility for identifying aggressive disease subtypes requiring more intensive management [41].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for Lipid Biomarker Studies
| Category | Specific Products/Platforms | Application Notes |
|---|---|---|
| Internal Standards | SPLASH LIPIDOMIX Mass Spec Standard; Ceramide (d18:1-d7/15:0); Oleic acid-d9 | Quantification accuracy; sample recovery monitoring |
| Chromatography Columns | BEH C8 (100 × 2.1 mm, 1.7 μm); C18 columns for alternative separations | Glycerophospholipid and sphingolipid separation |
| Mass Spectrometry Platforms | SCIEX QTRAP systems; Thermo Q-Exactive Plus; Bruker timSTOF platforms | High-sensitivity lipid detection and quantification |
| Sample Preparation | Methyl tert-butyl ether (MTBE); methanol; ammonium acetate | Lipid extraction efficiency; compatibility with MS analysis |
| Data Processing Software | LipidSearch; MS-DIAL; XCMS; In-house pipelines | Peak alignment, identification, and quantification |
| Statistical Packages | R packages (ropls, mixOmics, caret); SIMCA-P; MetaboAnalyst | Multivariate analysis and model building |
| 5,7,2',6'-Tetrahydroxyflavone | 5,7,2',6'-Tetrahydroxyflavone, CAS:82475-00-1, MF:C15H10O6, MW:286.24 g/mol | Chemical Reagent |
| Tosufloxacin tosylate hydrate | Tosufloxacin tosylate hydrate, CAS:1400591-39-0, MF:C26H25F3N4O7S, MW:594.6 g/mol | Chemical Reagent |
Pathophysiological Context and Mechanistic Insights
Biological Pathways Linking Lipid Metabolism to Hyperuricemia and Diabetes
The observed lipid signatures in hyperuricemia and diabetes reflect alterations in several key biological pathways:
- De novo lipogenesis: Elevated DAGs and TAGS associated with hyperuricemia correlate with fatty acids in the DNL pathway [11]
- Phospholipid remodeling: Alterations in phosphatidylcholine and lysophosphatidylcholine species suggest disrupted membrane lipid homeostasis
- Inflammatory signaling: Specific lipid species may modulate NLRP3 inflammasome activation, creating a pro-inflammatory milieu that exacerbates insulin resistance [38]
- Oxidative stress response: Reduced lysophosphatidylcholine plasmalogens in early-onset hyperuricemia may impair antioxidant defenses [41]
Figure 2: Proposed Pathway Linking HUA and Diabetes via Lipids
Mediators and Modifiers of Lipid-Hyperuricemia Relationships
Emerging evidence suggests that the relationship between lipid dysregulation and hyperuricemia is partially mediated by adipokines, particularly retinol-binding protein 4 (RBP4), which has been linked to dyslipidemia and insulin resistance [11]. Mediation analyses indicate that RBP4 accounts for approximately 5-14% of the observed lipid-hyperuricemia associations [11].
Dietary factors also significantly modify these relationships. Reduced rank regression analyses have identified that increased aquatic product consumption correlates with both elevated hyperuricemia risk and higher levels of HUA-associated lipids, while high dairy intake is associated with lower levels of HUA-associated lipids [11]. These findings highlight the potential for dietary interventions to modulate lipid metabolism in ways that may impact hyperuricemia and diabetes risk.
Lipidomics represents a powerful approach for developing diagnostic and prognostic scores in hyperuricemia and diabetes. The systematic application of mass spectrometry-based lipid profiling, coupled with robust statistical modeling, can yield biomarker panels with potential clinical utility for early detection, risk stratification, and therapeutic monitoring. Future directions in this field include:
- Integration with other omics technologies (genomics, proteomics) to develop multi-dimensional biomarker panels
- Large-scale validation across diverse populations to establish generalizability
- Standardization of analytical and reporting frameworks to facilitate clinical translation
- Elucidation of causal relationships through Mendelian randomization and intervention studies
As lipidomic technologies continue to advance and large-scale epidemiologic studies accumulate, lipid-based biomarkers are poised to play an increasingly important role in precision medicine approaches for hyperuricemia and diabetes management.
Challenges and Solutions: Navigating Complexities in Patient Stratification and Drug Discovery
Lipid-lowering therapies, particularly HMGCR inhibitors (statins) and PCSK9 inhibitors, represent cornerstone interventions for managing cardiovascular risk in diabetic populations. However, emerging evidence reveals a paradoxical relationship between these therapies and uric acid metabolism, presenting complex clinical management challenges in hyperuricemic patients with diabetes. This whitepaper synthesizes current research findings demonstrating that HMGCR inhibitors may elevate gout risk despite their anti-inflammatory properties, while PCSK9 inhibitors appear to increase serum urate levels through mechanisms potentially involving triglyceride mediation and inflammatory pathways. Through systematic analysis of genetic studies, molecular investigations, and clinical data, we elucidate the intricate pathways governing these paradoxical effects and provide comprehensive experimental frameworks for continued investigation in this critical area of metabolic research.
The management of cardiovascular risk in patients with diabetes and metabolic syndrome necessitates aggressive lipid-lowering therapy, with HMGCR inhibitors (statins) and PCSK9 inhibitors representing first-line and advanced options, respectively. Concurrently, hyperuricemia and gout represent significant comorbid conditions in this population, with complex pathophysiological intersections between lipid and purine metabolism. Hyperuricemia prevalence exceeds 4% in developed nations, with over 7 million new cases emerging globally annually, creating substantial healthcare burden through inflammatory arthritis, chronic kidney disease, and cardiovascular complications [43].
The paradoxical relationship between lipid-lowering therapies and urate homeostasis presents a significant clinical and research challenge. While dyslipidemia increases gout risk and serum urate levels, specific lipid-lowering agents appear to exert unanticipated effects on urate metabolism and gout incidence. Mendelian randomization studies reveal that genetic proxies for HMGCR inhibition correlate with increased gout risk, while PCSK9 inhibition associates with elevated serum urate levels [43]. This review comprehensively examines the mechanistic basis for these paradoxical effects, focusing on the intersection with diabetes pathophysiology and implications for drug development and clinical management.
Causal Effects of Lipid-Lowering Drugs on Urate and Gout
Table 1: Mendelian Randomization Analysis of Lipid-Lowering Drug Effects on Urate and Gout
| Drug Target | Outcome | Effect Size (OR [95% CI]) | P-value | Method |
|---|---|---|---|---|
| HMGCR inhibitors | Gout risk | 1.25 [1.03, 1.46] | 0.0436 | IVW |
| PCSK9 inhibitors | Urate levels | 1.06 [1.01, 1.10] | 0.0167 | IVW |
| NPC1L1 inhibitors | Gout risk | Not significant | >0.05 | IVW |
| NPC1L1 inhibitors | Urate levels | Not significant | >0.05 | IVW |
Table 2: Clinical Associations Between Uric Acid, Lipid Parameters, and Diabetes
| Association | Population | Effect Size | P-value | Mediation |
|---|---|---|---|---|
| Hyperuricemia → Triglycerides | Hypertensive Chinese | Coefficient = 0.67 | 0.01 | Triglycerides mediate HU-T2DM link |
| Triglycerides → T2DM risk | Hypertensive Chinese | Coefficient = 1.29 | <0.001 | |
| UHR → AAC scores | NHANES 2013-2014 | β = 0.53 | <0.001 | Diabetes mediates 7.5% of association |
| SUA → PCSK9 levels | Chinese women | Positive correlation | <0.05 | Mediated by triglycerides and inflammation |
Pathophysiological Framework
The relationship between lipid metabolism, glucose homeostasis, and uric acid regulation involves complex, interconnected pathways. The following diagram illustrates the central paradox and established mechanistic relationships:
HMGCR Inhibitors: The Gout Risk Paradox
Mechanistic Insights
HMGCR inhibitors demonstrate a complex duality in urate-related pathophysiology. While genetic evidence indicates increased gout risk, experimental models reveal potent anti-inflammatory mechanisms that might theoretically protect against gout flares. This paradox centers on the NLRP3 inflammasome, a multiprotein complex that activates interleukin-1β (IL-1β), a key mediator in monosodium urate (MSU) crystal-induced inflammation [44].
Statins suppress MSU crystal-induced NLRP3 inflammasome activation through PPAR-γ dependent pathways. In THP-1 human monocytic cells, atorvastatin, simvastatin, and mevastatin significantly increased PPAR-γ expression and activity while reducing NLRP3, caspase-1, and IL-1β expression at both mRNA and protein levels [44]. The critical role of PPAR-γ was confirmed through siRNA knockdown experiments, wherein PPAR-γ deficiency attenuated the inhibitory effects of statins on NLRP3 inflammasome activation.
Simultaneously, statins demonstrate antioxidant properties through reduction of intracellular reactive oxygen species (ROS) generation stimulated by MSU crystals. This effect was partially dependent on PPAR-γ signaling, as demonstrated by transfection experiments with PPAR-γ siRNA [44].
Experimental Protocols for HMGCR Investigation
In Vitro Assessment of NLRP3 Inflammasome Inhibition
Cell Culture: Maintain human monocytic THP-1 cells in RPMI-1640 medium supplemented with 10% fetal bovine serum, 2 mM L-glutamine, 100 U/mL penicillin, and 100 μg/mL streptomycin at 37°C in 5% CO₂.
Differentiation and Treatment:
- Differentiate THP-1 monocytes into macrophages using 100 nM phorbol 12-myristate 13-acetate (PMA) for 48 hours
- Pre-treat cells with HMGCR inhibitors (atorvastatin, simvastatin, mevastatin) at concentrations of 5-10 μM for 24 hours
- Stimulate with MSU crystals (0.3 mg/mL) for various timepoints depending on assay
Molecular Analysis:
- Quantitative RT-PCR: Isolate RNA using TRIzol reagent, synthesize cDNA, and perform qPCR for PPAR-γ, NLRP3, caspase-1, and IL-1β using appropriate primers and cycling conditions
- Western Blotting: Extract proteins, separate by SDS-PAGE, transfer to PVDF membranes, and probe with antibodies against target proteins
- PPAR-γ Activity Assay: Measure transcriptional activity using PPAR-γ responsive luciferase reporter systems
- ROS Measurement: Assess intracellular ROS using Hâ‚‚DCF-DA fluorescence with flow cytometry analysis
Gene Silencing Approach
PPAR-γ Knockdown:
- Transfert THP-1 cells with PPAR-γ siRNA or non-targeting control siRNA using appropriate transfection reagents
- Incubate for 24-48 hours to achieve efficient protein knockdown
- Verify knockdown efficiency through Western blot analysis
- Proceed with statin treatment and MSU crystal stimulation as described above
PCSK9 Inhibitors: Urate Elevation Mechanisms
Pathways and Mediators
PCSK9 inhibition associates with elevated serum urate levels through complex mechanisms potentially involving lipid mediation and inflammatory pathways. Unlike HMGCR inhibitors, PCSK9 inhibitors demonstrate no significant direct association with clinical gout risk in Mendelian randomization studies, but show consistent effects on serum urate elevation [43].
The triglyceride mediation pathway represents a significant mechanism in the relationship between uric acid and metabolic disorders. In hypertensive Chinese populations, hyperuricemia shows a positive association with elevated triglyceride levels (coefficient = 0.67, P=0.01), which subsequently increases diabetes risk (coefficient = 1.29, P<0.001) [45] [6]. This mediation effect is particularly relevant given the high prevalence of combined dyslipidemia and hyperuricemia in uncontrolled type 2 diabetes, exceeding 80% in some hospitalized populations [2].
Sex-specific associations between uric acid and PCSK9 further complicate this relationship. Serum uric acid levels and hyperuricemia show positive associations with serum PCSK9 levels in Chinese women but not men, with these associations partially mediated by metabolic factors (particularly triglycerides) and inflammation [46]. This sexual dimorphism may reflect hormonal influences on both urate metabolism and lipid regulation.
PCSK9 Experimental Methodology
Epidemiological Assessment of PCSK9-Urate Relationships
Study Population Selection:
- Recruit large cohort (n>2,500) with balanced sex distribution
- Apply strict exclusion criteria: acute/chronic kidney disease, inflammatory conditions, severe hepatic/renal insufficiency, pregnancy
- Collect comprehensive demographic, clinical, and medication data
Laboratory Measurements:
- Serum PCSK9: Quantify using commercial ELISA kits according to manufacturer protocols
- Lipid Profile: Measure triglycerides, total cholesterol, HDL-C, and calculated LDL-C
- Uric Acid: Determine serum uric acid using uricase method
- Inflammatory Markers: Assess white blood cell count, neutrophil count, high-sensitivity C-reactive protein
Statistical Analysis:
- Perform multiple linear regression to assess association between SUA and PCSK9
- Conduct logistic regression to evaluate hyperuricemia-PCSK9 relationship
- Implement mediation analysis to quantify role of triglycerides and inflammation
- Conduct sex-stratified analyses to identify gender-specific effects
Integrated Metabolic Pathways in Diabetes and Hyperuricemia
The Cholesterol-Uric Acid Interface
The intricate relationship between cholesterol metabolism and uric acid homeostasis involves multiple interconnected pathways. In hyperuricemic conditions, adenosine and inosine (major purine metabolites) upregulate HMGCR expression by activating adenosine Aâ‚‚A receptor via the Srebp-2/Creb axis [47]. This mechanism directly links purine metabolism to cholesterol biosynthesis regulation.
Simultaneously, taurine deficiency contributes to cholesterol metabolism dysfunction in hyperuricemia. Taurine administration in hyperuricemic mice significantly reduces cholesterol elevation by inhibiting adenosine Aâ‚‚A receptor, providing a potential therapeutic approach for comorbid hypercholesterolemia and hyperuricemia [47].
The following diagram illustrates the integrated metabolic pathways connecting lipid regulation, uric acid metabolism, and diabetic pathophysiology:
Composite Biomarkers and Risk Stratification
The uric acid to HDL-cholesterol ratio (UHR) emerges as a significant composite biomarker capturing both oxidative stress and metabolic dysfunction. In cross-sectional studies, each one-unit increase in logâ‚‚-transformed UHR associated with a 0.53 increase in abdominal aortic calcification (AAC) scores and 43% higher AAC risk [48]. Diabetes mediated 7.5% of the association between UHR and AAC scores, and 14% of the association between UHR and severe AAC risk [48].
For clinical risk stratification, the Renal-Metabolic Risk Score (RMRS) integrates renal and lipid parameters to identify patients with combined dyslipidemia and hyperuricemia. In uncontrolled type 2 diabetes populations, RMRS demonstrated good discrimination (AUC=0.78) for identifying co-occurrence, with prevalence increasing from 64.5% in the first quartile to 96.1% in the fourth quartile [2].
Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating Lipid-Urate Pathways
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Cell Lines | THP-1 human monocytic cells | In vitro inflammation studies | Differentiate into macrophages for NLRP3 inflammasome research |
| Molecular Biology Tools | PPAR-γ siRNA, SREBP-2 antibodies | Gene expression modulation | Pathway inhibition and protein detection |
| Induction Agents | MSU crystals (0.3 mg/mL), PMA | Disease modeling | Induce gout-like inflammation and cell differentiation |
| Detection Assays | H₂DCF-DA, IL-1β ELISA, caspase-1 kits | Phenotypic measurement | Quantify ROS, cytokines, and inflammasome activation |
| Animal Models | Hyperuricemic mice models | In vivo validation | Study cholesterol metabolism and therapeutic interventions |
| Clinical Measures | PCSK9 ELISA, uricase method, lipid panels | Human studies | Quantify biomarkers in patient samples |
The paradoxical effects of lipid-lowering drugs on urate metabolism and gout risk represent a significant challenge in managing diabetic patients with comorbid hyperuricemia. HMGCR inhibitors demonstrate complex duality, increasing gout risk while simultaneously exerting anti-inflammatory effects through PPAR-γ-mediated suppression of the NLRP3 inflammasome. PCSK9 inhibitors consistently associate with elevated serum urate levels, potentially through triglyceride-mediated pathways and sex-specific mechanisms.
Future research should prioritize prospective clinical studies examining the net clinical impact of these therapies in high-risk populations with combined dyslipidemia and hyperuricemia, particularly in the context of diabetes progression and cardiovascular outcomes. Elucidation of the precise molecular mechanisms underlying these paradoxical effects will enable development of targeted therapies that optimize both lipid and urate management, ultimately improving cardiovascular and metabolic outcomes in this complex patient population.
The Cardiovascular-Kidney-Metabolic (CKM) syndrome represents a complex interplay among metabolic risk factors, chronic kidney disease, and cardiovascular disease, creating significant challenges for risk stratification and therapeutic management. This whitepaper examines the development and validation of the Renal–Metabolic Risk Score (RMRS), a novel tool integrating renal and lipid parameters to identify patients with uncontrolled type 2 diabetes at heightened risk for combined hyperuricemia and dyslipidemia. We present comprehensive data on the pathophysiological foundations, methodological frameworks, and clinical applications of RMRS, with particular emphasis on its utility in guiding targeted interventions for researchers and drug development professionals working at the intersection of lipid metabolism and hyperuricemia in diabetes.
The coexistence of type 2 diabetes (T2D), hyperuricemia (HUA), and dyslipidemia represents a particularly challenging clinical scenario characterized by compounded metabolic risk. Epidemiological studies across diverse populations have consistently demonstrated a substantial prevalence of hyperuricemia among individuals with T2D, ranging from 21% to 32% [9]. This convergence is not coincidental but stems from shared pathophysiological mechanisms including insulin resistance, oxidative stress, and endothelial dysfunction [2] [9].
The Cardiovascular-Kidney-Metabolic (CKM) syndrome framework formally recognizes the interconnections among obesity, diabetes, chronic kidney disease, and cardiovascular disease [49] [50]. Within this framework, serum uric acid (SUA) has emerged as both a biomarker and potential mediator of metabolic and vascular injury. Mendelian randomization studies have confirmed that elevated SUA demonstrates a potential risk effect on stage 4 of CKM syndrome, including ischemic heart disease (OR = 1.090, 95% CI: 1.003-1.184) and peripheral artery disease (OR = 1.174, 95% CI: 1.058-1.303) [49] [50].
The Renal–Metabolic Risk Score (RMRS) was developed to address the critical need for simple, clinically applicable tools that integrate both renal and metabolic parameters to identify high-risk patients in resource-limited settings [2] [51]. Unlike traditional biomarkers, RMRS captures the intertwined nature of renal clearance and lipid metabolism dysregulation in uncontrolled T2D, providing a more integrative metabolic–renal perspective for early risk stratification.
Pathophysiological Framework: Unraveling the Metabolic Crosstalk
Uric Acid as a Metabolic Mediator
Uric acid, the end product of purine catabolism in humans, has evolved beyond its role in gout pathogenesis to be recognized as an active contributor to metabolic dysregulation. Humans have higher SUA levels (3 to 10 times) compared to other mammals due to the loss of uricase activity during evolution, potentially providing an advantage in regulating blood pressure under low-salt diets and offering protection against oxidative stress [50]. However, in the context of modern metabolic diseases, this evolutionary adaptation becomes detrimental.
The pathophysiological mechanisms linking hyperuricemia to metabolic syndrome include:
- Insulin Resistance: SUA impairs insulin signaling through stimulation of oxidative stress and inflammatory pathways [9]
- Endothelial Dysfunction: Uric acid reduces nitric oxide bioavailability in endothelial cells, promoting vasoconstriction and hypertension [2]
- Renal Dysfunction: Impaired uric acid excretion creates a vicious cycle further exacerbating renal impairment [50]
- Inflammatory Activation: SUA activates the NLRP3 inflammasome, promoting IL-1β production and systemic inflammation [9]
Bidirectional Relationship Between Hyperuricemia and Dyslipidemia
The relationship between hyperuricemia and dyslipidemia is particularly relevant to RMRS development. Dyslipidemia in T2D typically presents as hypertriglyceridemia, reduced HDL-C, and a predominance of small dense LDL particles [2]. The triglyceride-to-LDL cholesterol ratio (TG/LDL) incorporated into RMRS reflects this distinctive dyslipidemic pattern, which shares underlying mechanisms with hyperuricemia, including insulin resistance and chronic low-grade inflammation [2].
Table 1: Epidemiological Evidence for Uric Acid-Metabolic Syndrome Association
| Study Population | Number of Studies | Mean UA Increase in MetS (mg/dL) | 95% CI | p-value |
|---|---|---|---|---|
| Overall | 43 (56 groups) | 0.57 | 0.54-0.61 | <0.00001 |
| Men with MetS | 17 studies | 0.53 | 0.45-0.62 | <0.00001 |
| Women with MetS | 15 studies | 0.57 | 0.48-0.66 | <0.00001 |
Source: Systematic review and meta-analysis of 91,845 subjects with MetS and 259,931 controls [52]
Development and Validation of the Renal–Metabolic Risk Score (RMRS)
Study Design and Population
The RMRS was developed through a retrospective, observational cohort study including 253 adults with uncontrolled T2D (HbA1c ≥ 7%) admitted to Bihor County Emergency Hospital, Oradea, Romania, between 2022-2023 [2] [51]. The study population demonstrated a high prevalence (81.6%) of dyslipidemia and hyperuricemia co-occurrence, highlighting the clinical significance of this comorbidity in uncontrolled T2D [2].
Table 2: Baseline Characteristics of RMRS Development Cohort
| Parameter | Co-occurrence Group (n=247) | No Co-occurrence Group (n=57) | p-value |
|---|---|---|---|
| Age (years) | 66.90 ± 10.99 | 66.33 ± 11.51 | 0.737 |
| Gender (Male) | 54.3% | 47.4% | 0.429 |
| Provenance (Rural) | 55.9% | 56.1% | 1.000 |
| Lipid-lowering therapy use | Significantly higher | Lower | <0.001 |
| Antihypertensive therapy use | Significantly higher | Lower | 0.040 |
RMRS Calculation and Components
The RMRS was calculated from standardized values of serum urea and TG/HDL ratio, with variable weights derived from logistic regression coefficients. The score was normalized to a 0–100 scale using the following approach [2]:
- Serum Urea: Reflects renal function and nitrogen turnover
- TG/HDL Ratio: Captures atherogenic dyslipidemia pattern
- Regression Coefficients: Used to weight each parameter based on strength of association
- Normalization: Transformation to 0-100 scale for clinical utility
The selection of these specific parameters was based on their complementary reflection of renal and metabolic health, routine availability in clinical practice, and low cost—making the score particularly suitable for resource-limited settings [51].
Performance Characteristics
Validation studies demonstrated that RMRS was significantly higher in the dyslipidemia-hyperuricemia co-occurrence group compared to others (median 16.9 vs. 10.0; p < 0.001) [2]. Receiver operating characteristic (ROC) analysis showed an area under the curve (AUC) of 0.78, indicating good discrimination ability for identifying combined metabolic risk [2].
Quartile analysis demonstrated a monotonic gradient in co-occurrence prevalence from 64.5% in Q1 to 96.1% in Q4, confirming the score's ability to stratify patients across a risk spectrum [2]. This gradient relationship supports the clinical utility of RMRS for identifying degrees of risk rather than merely a binary classification.
Comparative Analysis of Uric Acid-Based Risk Assessment Tools
The RMRS represents one of several approaches to assessing metabolic risk through uric acid-related parameters. Comparative analysis with other biomarkers provides context for its specific utility.
Table 3: Comparison of Uric Acid-Based Metabolic Risk Assessment Tools
| Assessment Tool | Components | Target Population | AUC/Performance | Key Advantages |
|---|---|---|---|---|
| RMRS [2] [51] | Serum urea, TG/HDL ratio | Uncontrolled T2D | AUC = 0.78 | Integrates renal & lipid parameters; uses routine labs |
| SUA/Cr Ratio [53] | Serum uric acid, Creatinine | General population without diabetes | Cut-off: 7.02 for MetS | Normalizes UA to renal function |
| SUA Alone [52] | Serum uric acid only | General population | 0.57 mg/dL higher in MetS | Simple; widely available |
| Multivariable MR [49] [50] | Genetic instruments for SUA | General population for causal inference | OR = 1.09-1.17 for CVD | Establishes causality; less confounding |
The serum uric acid to creatinine ratio (SUA/Cr) has also demonstrated utility in predicting insulin resistance, β-cell function, and metabolic syndrome incidence in normal Korean adults, with optimal cut-off values of approximately 7.0 for predicting MetS risk [53]. However, unlike RMRS, this ratio does not incorporate lipid parameters, potentially limiting its sensitivity to the full spectrum of metabolic dysregulation in diabetes.
Methodological Protocols for RMRS Implementation
Laboratory Assessment Protocol
Specimen Collection and Processing:
- Collect blood samples after overnight fast (12 hours)
- Process samples within 2 hours of collection
- Use standardized tubes for serum separation
- Store at -80°C if batch analysis required
Analytical Methods:
- Serum uric acid: Enzymatic colorimetric method (uricase)
- Lipid profile: Enzymatic methods for TG, HDL-C, LDL-C
- Serum urea: Kinetic UV assay with urease and glutamate dehydrogenase
- Serum creatinine: Modified Jaffe method traceable to isotope dilution mass spectrometry
Quality Control:
- Implement internal quality control with two levels daily
- Participate in external quality assurance programs
- Calibrate instruments according to manufacturer specifications
RMRS Calculation Protocol
The standardized protocol for RMRS calculation involves the following steps:
- Parameter Measurement: Obtain serum urea and lipid profile results
- TG/HDL Ratio Calculation: Divide triglyceride value by HDL cholesterol value
- Standardization: Convert raw values to z-scores based on population reference
- Weighted Summation: Apply regression-derived coefficients to each parameter
- Normalization: Transform final score to 0-100 scale using linear transformation
Specific regression coefficients and transformation parameters are detailed in the original validation study [2] and require validation in local populations before clinical implementation.
Signaling Pathways and Pathophysiological Mechanisms
Diagram 1: Pathophysiological Pathways in Renal-Metabolic Syndrome. This diagram illustrates the key mechanisms connecting insulin resistance, hyperuricemia, dyslipidemia, and renal dysfunction in CKM syndrome. Critical vicious cycles amplify metabolic risk, particularly between renal dysfunction and reduced uric acid excretion.
Research Reagent Solutions and Methodological Toolkit
Table 4: Essential Research Reagents for Renal-Metabolic Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Uric Acid Assays | Uricase-based colorimetric kits; Electrochemiluminescence Immunoassay (Roche) | SUA quantification | Cross-validate with mass spectrometry; monitor hemolysis interference |
| Lipid Profile Kits | Enzymatic triglyceride, HDL-C, and LDL-C assays | Dyslipidemia characterization | Standardize fasting samples; use direct LDL-C methods for accuracy |
| Renal Function Markers | Jaffe creatinine assays; Urease-based urea kits | Renal status assessment | Standardize to IDMS for creatinine; account for muscle mass variations |
| Genetic Analysis Tools | GWAS arrays; PCR-based genotyping | Mendelian randomization studies | Use validated instruments for uric acid and renal traits |
| Cell Culture Models | Human proximal tubular cells; Adipocyte lines | Mechanistic pathway studies | Consider species differences in urate handling |
| Animal Models | Uricase knockout mice; db/db diabetic mice | Therapeutic intervention testing | Monitor renal function longitudinally |
| Collagen proline hydroxylase inhibitor | Collagen proline hydroxylase inhibitor, CAS:223666-07-7, MF:C18H18N4O4, MW:354.4 g/mol | Chemical Reagent | Bench Chemicals |
| Carmoxirole hydrochloride | Carmoxirole hydrochloride, CAS:115092-85-8, MF:C24H27ClN2O2, MW:410.9 g/mol | Chemical Reagent | Bench Chemicals |
Experimental Workflow for RMRS Validation
Diagram 2: RMRS Development and Validation Workflow. This sequential methodology outlines the key stages in deriving and validating the Renal-Metabolic Risk Score, from initial cohort identification through to clinical implementation.
Therapeutic Implications and Future Research Directions
Targeted Pharmacological Approaches
Mendelian randomization drug targeting analyses have identified lesinurad (targeting SLC22A11 and SLC22A12) as a validated therapy for ischemic heart disease in the context of hyperuricemia [49] [50]. This finding exemplifies the potential for uric acid-related therapeutic targets in CKM syndrome.
Additional pharmacological considerations include:
- SGLT2 Inhibitors: Empagliflozin reduces SUA by promoting renal urate excretion and demonstrates renoprotective effects in diabetic nephropathy [9]
- Dual-Action Agents: Future drug development should prioritize agents addressing both hyperglycemia and hyperuricemia through shared pathways [9]
- Personalized Approaches: RMRS may help identify patients most likely to benefit from urate-lowering therapy beyond gout management
Research Agenda
Future research on RMRS and renal-metabolic risk stratification should prioritize:
- External Validation: Multicenter studies in diverse ethnic and clinical populations
- Longitudinal Outcomes: Association with hard endpoints (ESRD, CVD events, mortality)
- Interventional Trials: Testing RMRS-guided treatment escalation strategies
- Omics Integration: Incorporation of genomic, proteomic, and metabolomic data
- Digital Health Applications: Development of electronic health record-integrated calculators
The Renal–Metabolic Risk Score represents a significant advancement in addressing compounded metabolic risk through the integration of routinely available renal and lipid parameters. For researchers and drug development professionals, RMRS offers a validated methodology for patient stratification that reflects the intertwined pathophysiology of hyperuricemia, dyslipidemia, and renal dysfunction in uncontrolled type 2 diabetes. Future efforts should focus on validating this score in broader populations, exploring its utility in guiding targeted therapies, and developing more comprehensive risk assessment tools that incorporate emerging biomarkers and genetic data. As our understanding of the CKM syndrome evolves, tools like RMRS will be increasingly essential for designing precision medicine approaches to complex metabolic disease.
The development of therapeutic inhibitors for metabolic diseases, particularly in type 2 diabetes (T2DM), has been complicated by the unintended consequence of inducing or exacerbating hyperuricemia. This whitepaper examines the molecular interplay between lipid metabolism, drug mechanisms, and serum uric acid (SUA) elevation, with a focus on identifying therapeutic strategies that circumvent this adverse effect. We synthesize evidence from clinical trials, lipidomics studies, and molecular pharmacology to provide a comprehensive framework for developing next-generation inhibitors without hyperuricemic consequences. Particular emphasis is placed on sodium-glucose cotransporter-2 (SGLT2) inhibitors as a model for compounds that concurrently improve glycemic control and lower SUA through novel mechanisms.
Hyperuricemia, characterized by serum urate levels exceeding 7.0 mg/dL in men or 6.0 mg/dL in women, represents a significant comorbidity in patients with metabolic disorders [54]. The global prevalence of hyperuricemia shows considerable variation, ranging from 2.6% to 36% across different populations, with approximately 21% of U.S. adults affected [3] [54]. This condition arises from either uric acid overproduction or, more commonly (in 90% of cases), underexcretion by the kidneys [54]. The delicate balance of urate homeostasis is governed by multiple transporter systems, including URAT1, GLUT9, and ABCG2, which become perturbed by several pharmacological interventions [3] [54].
The clinical significance of drug-induced hyperuricemia extends beyond gout risk to encompass broader cardiometabolic consequences. Hyperuricemia is increasingly recognized as an independent risk factor for hypertension, chronic kidney disease (CKD), cardiovascular diseases, and metabolic syndrome [55]. Mendelian randomization studies have established causal relationships specifically between hyperuricemia, gout, and kidney disease, though associations with other cardiometabolic conditions remain controversial [3]. Understanding the mechanisms through which therapeutics influence urate metabolism is therefore paramount for drug development programs targeting metabolic diseases, particularly in populations with pre-existing hyperuricemia risk factors.
Molecular Interplay: Lipid Metabolism and Uric Acid Homeostasis
Integrated Pathways in Hyperuricemic Patients
The biochemical interface between lipid metabolism and uric acid homeostasis represents a critical nexus for understanding drug-induced hyperuricemia. Recent lipidomics studies have revealed that hyperuricemia is characterized by distinct alterations in lipid metabolic pathways, particularly glycerophospholipid metabolism, arachidonic acid metabolism, and glycosylphosphatidylinositol (GPI)-anchor biosynthesis [8] [16]. These pathways influence urate metabolism through several mechanisms, including modulation of inflammatory responses, alteration of membrane transporter function, and generation of pro-oxidant environments that promote urate crystal formation.
Uric acid possesses dualistic redox properties, functioning as an antioxidant at physiological levels but transforming into a pro-oxidant molecule when levels are elevated [3]. In hyperuricemic states, urate mediates innate immune responses through the release of inflammatory mediators and activation of the renin-angiotensin system, creating a pro-inflammatory milieu that further disrupts metabolic homeostasis [3]. This inflammatory cascade promotes insulin resistance and dyslipidemia, establishing a vicious cycle wherein lipid metabolic disturbances exacerbate hyperuricemia and vice versa.
Table 1: Key Lipid Pathways Altered in Hyperuricemia
| Metabolic Pathway | Key Alterations | Relationship to Uric Acid |
|---|---|---|
| Glycerophospholipid Metabolism | Increased phosphatidylcholines, phosphatidylethanolamines | Correlates with inflammatory markers (IL-6, TGF-β1) |
| Arachidonic Acid Metabolism | Elevated eicosanoid precursors | Promotes pro-inflammatory state |
| Linoleic Acid Metabolism | Oxidized metabolites | Linked to oxidative stress |
| GPI-Anchor Biosynthesis | Modified membrane anchors | Alters cell surface protein function |
| Sphingolipid Metabolism | Ceramide accumulation | Promotes insulin resistance |
The identification of these disrupted pathways provides both biomarkers for monitoring drug effects and potential targets for therapeutic intervention. Lipidomics approaches have revealed 33 significantly upregulated lipid metabolites in patients with hyperuricemia, primarily involved in the five pathways listed in Table 1 [8]. These lipid metabolites demonstrate significant correlations with immune factors including TNF-α, IL-6, TGF-β1, and CPT1, suggesting an interface between lipid dysregulation and inflammation in hyperuricemia pathogenesis [8].
Signaling Network Integration
The diagram below illustrates the core signaling pathways connecting lipid metabolism, inflammatory responses, and uric acid homeostasis, highlighting potential targets for therapeutic inhibition without hyperuricemic consequences:
Problematic Therapeutics: Drugs with Hyperuricemic Consequences
Several established drug classes unexpectedly induce or exacerbate hyperuricemia through diverse mechanisms, creating significant clinical challenges in managing patients with metabolic diseases.
Diuretics
Thiazide and loop diuretics produce a dose-dependent increase in serum urate levels, with nearly 80% increased relative risk of gout [54]. The hyperuricemic effect occurs primarily through reduced extracellular fluid volume, which enhances urate reabsorption in the proximal tubule, and direct interference with urate transporter function [54]. This presents a significant therapeutic dilemma as diuretics remain first-line agents for hypertension, which frequently coexists with hyperuricemia and gout.
Immunosuppressants
Cyclosporine, a calcineurin inhibitor used in transplant recipients, induces hyperuricemia in approximately 80% of patients, with gout developing in 10-15% [56]. The mechanism involves decreased renal urate clearance through altered tubular function, particularly in the context of concurrent diuretic use and renal impairment commonly seen in transplant populations.
Anti-Tuberculosis Agents
Pyrazinamide and ethambutol both increase serum urate concentrations by competitively inhibiting urate secretion in the renal tubules [56]. Pyrazinamide's structural similarity to uric acid enables it to compete for renal tubular secretion sites, while ethambutol appears to decrease urate clearance through less well-defined mechanisms.
Nicotinic Acid
High-dose niacin or nicotinic acid, used for dyslipidemia management, consistently increases uric acid levels by approximately 10% through stimulation of purine biosynthesis and possible reduction in renal urate excretion [56]. The effect appears dose-dependent and can precipitate acute gout in susceptible individuals.
Table 2: Medications with Hyperuricemic Effects and Proposed Mechanisms
| Drug Class | Specific Agents | Primary Mechanism | Magnitude of Effect |
|---|---|---|---|
| Diuretics | Thiazides, Furosemide | Reduced renal excretion; volume contraction | ~80% increased gout risk |
| Immunosuppressants | Cyclosporine, Tacrolimus | Decreased renal urate clearance | 80% develop hyperuricemia |
| Anti-tuberculosis | Pyrazinamide, Ethambutol | Inhibits renal tubular secretion | SUA increase 2-4 mg/dL |
| Lipid-lowering | Nicotinic acid | Increased purine synthesis | ~10% SUA increase |
| Cytotoxic | Chemotherapy agents | Tumor lysis; purine release | Variable, potentially severe |
Promising Alternatives: SGLT2 Inhibitors as Urate-Lowering Therapeutics
Sodium-glucose cotransporter-2 (SGLT2) inhibitors represent a paradigm shift in managing metabolic diseases while concurrently reducing uric acid levels, offering a unique therapeutic profile that contrasts with many conventional agents.
Mechanisms of Urate Reduction
SGLT2 inhibitors lower serum urate through multiple convergent mechanisms. By inducing a state of "starvation mimicry" amid nutrient surplus, these inhibitors decrease flux through the pentose phosphate pathway, thereby attenuating purine and urate synthesis [57]. Additionally, they promote renal urate excretion through complex transporter interactions, potentially involving inhibition of URAT1 and GLUT9 [57] [58]. The net effect is a reduction in both urate production and enhanced elimination.
These drugs also downregulate xanthine oxidase activity via enhancement of the SIRT-1 signaling pathway, further decreasing uric acid generation [58]. By promoting glycosuria, SGLT2 inhibitors create an osmotic diuresis that differs fundamentally from traditional diuretics, as it does not promote volume contraction sufficient to trigger compensatory urate reabsorption [58].
Clinical Efficacy Data
Substantial clinical evidence supports the urate-lowering effects of SGLT2 inhibitors across diverse patient populations:
Table 3: Clinical Efficacy of SGLT2 Inhibitors on Uric Acid Parameters
| Study Design | Population | Urate Reduction | Gout Risk Reduction | Citation |
|---|---|---|---|---|
| Systematic Review & Meta-analysis | T2DM, HF, CKD | 0.6-1.5 mg/dL | 30-50% | [57] |
| Updated Meta-analysis | With/without T2DM | - | 32-37% hyperuricemic events | [58] |
| Multicenter Retrospective Cohort | DM, HF, CKD | 4.5% overall; 10% with baseline elevation | Not assessed | [59] |
| JACC Review | Diabetes, Heart Failure | 0.6-1.5 mg/dL | 30-50% | [57] |
The urate-lowering effect appears most pronounced in patients with elevated baseline levels (10% reduction) and those with heart failure (9% reduction) [59]. Multivariate analysis has identified the combination of diabetes and heart failure as an independent predictor of response to SGLT2 inhibitors, with an odds ratio of 2.2 (95% CI: 1.2-4.04) [59].
Experimental Approaches: Methodologies for Evaluating Uric Acid Effects
Lipidomics Workflow for Hyperuricemia Research
Comprehensive assessment of drug effects on urate metabolism requires integrated methodological approaches. The following experimental workflow outlines key procedures for evaluating potential hyperuricemic consequences of novel inhibitors:
Detailed Methodological Protocols
Lipidomics Analysis Using UPLC-Q-TOF/MS
Sample Preparation: Collect serum or plasma samples following standard venipuncture procedures. Centrifuge whole blood at 3,000 rpm for 10 minutes at 4°C to separate serum. Aliquot 80 μL serum into 1.5 mL Eppendorf tubes and add 320 μL of chilled chloroform/methanol (3:1, v/v) solution. Vortex for 60 seconds to ensure complete mixing, then centrifuge at 14,000 rpm for 10 minutes at 4°C. Carefully collect 80 μL of the organic phase (lower chloroform layer) and dry under a gentle stream of nitrogen at room temperature. Reconstitute the lipid extract in 100 μL of acetonitrile/isopropanol (1:1, v/v) and centrifuge at 13,000 rpm for 10 minutes prior to analysis [16].
Chromatographic Conditions: Utilize an ACQUITY UPLC CSH C18 column (2.1 × 100 mm, 1.7 μm) maintained at 45°C. Employ a binary mobile phase system consisting of (A) 0.1% formic acid in water and (B) acetonitrile with 0.1% formic acid. Apply the following gradient elution program: 0-1 min: 99% A; 1-10 min: linear gradient to 2% A; 10-13 min: maintain at 99% A. Set the flow rate to 0.2 mL/min with an injection volume of 3 μL [16].
Mass Spectrometry Parameters: Operate the Q-TOF mass spectrometer in both positive and negative electrospray ionization modes. Set the capillary voltage to 3.0 kV and cone voltage to 28 V. Maintain the source temperature at 100°C with desolvation temperatures of 450°C (positive mode) or 400°C (negative mode). Use cone gas flows of 20 L/h (positive) or 50 L/h (negative). Acquire data over a mass range of m/z 200-1800 with a scan time of 0.5 seconds [16].
Biochemical Validation assays
Inflammatory Marker Analysis: Quantify serum levels of IL-6, TNF-α, TGF-β1, and IL-10 using validated ELISA kits according to manufacturer protocols. Briefly, coat 96-well plates with capture antibodies overnight at 4°C. Block plates with 1% BSA for 1 hour at room temperature. Incubate with standards and samples for 2 hours, followed by detection antibody for 1 hour. Develop with streptavidin-HRP and TMB substrate, then measure absorbance at 450 nm with correction at 570 nm [8].
Uric Acid Transport assays: Assess inhibitor effects on urate transporter function using transfected HEK293 cells expressing human URAT1, GLUT9, or ABCG2. Measure radiolabeled urate uptake or efflux over time in the presence of varying drug concentrations. Calculate IC50 values through nonlinear regression analysis of concentration-response curves [57] [58].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Hyperuricemia-Drug Interaction Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| UPLC-MS Systems | ACQUITY UPLC CSH C18 Columns, Q-Exactive Plus Mass Spectrometer | Lipidomics profiling | Separation and identification of lipid species |
| Cell-Based Transport Models | HEK293 cells expressing URAT1, GLUT9, ABCG2 | Transporter inhibition studies | Assessment of drug effects on urate flux |
| Animal Models | Potassium oxonate-induced hyperuricemic rats | In vivo efficacy and safety testing | Evaluation of urate-lowering without side effects |
| ELISA Kits | Human IL-6, TNF-α, TGF-β1, IL-10, CPT1 assays | Inflammatory marker quantification | Assessment of metabolic inflammation |
| Biochemical Assay Kits | Uric acid, creatinine, triglyceride kits | Metabolic parameter measurement | Evaluation of renal function and lipid metabolism |
| Specialized Reagents | Formic acid, ammonium formate, HPLC-grade solvents | Mobile phase preparation | Optimal chromatographic separation |
| Lofexidine Hydrochloride | Lofexidine Hydrochloride, CAS:21498-08-8, MF:C11H13Cl3N2O, MW:295.6 g/mol | Chemical Reagent | Bench Chemicals |
The pursuit of therapeutic inhibitors without hyperuricemic consequences represents a critical frontier in metabolic drug development. The evidence synthesized in this whitepaper demonstrates that thoughtful targeting of specific pathways, particularly through SGLT2 inhibition, can simultaneously address glycemic control, lipid metabolism, and urate homeostasis. The integrated experimental approaches outlined herein provide a robust framework for screening novel compounds for hyperuricemic liability early in development pipelines.
Future research directions should prioritize the development of more sophisticated in silico models predicting urate transporter interactions, expanded lipidomic panels specifically validated for hyperuricemia assessment, and longer-term clinical studies evaluating the cardiovascular and renal benefits of urate-sparing therapeutic strategies. As our understanding of the intricate connections between lipid metabolism and urate homeostasis deepens, so too will our capacity to design precision therapeutics that circumvent the historical challenge of drug-induced hyperuricemia.
The comorbidity of hyperuricemia and type 2 diabetes mellitus (T2DM) represents a significant clinical challenge characterized by interconnected pathophysiological pathways involving purine and lipid metabolism. This whitepaper synthesizes current evidence on the metabolic crosstalk between these conditions and provides a comprehensive framework for developing optimized therapeutic regimens combining urate-lowering and lipid-modifying agents. Through analysis of emerging clinical data, lipidomic studies, and pharmacological mechanisms, we demonstrate that targeted combination approaches—particularly those incorporating SGLT2 inhibitors, febuxostat, and strategic lipid management—offer superior outcomes for this complex patient population. The integration of advanced drug delivery systems and personalized medicine principles presents promising avenues for future therapeutic development in this evolving field of metabolic medicine.
Hyperuricemia (HUA) and type 2 diabetes mellitus (T2DM) frequently coexist in clinical practice, creating a complex pathological state with bidirectional relationships that significantly impact patient outcomes. Epidemiological studies across diverse populations consistently demonstrate a substantial prevalence of hyperuricemia among individuals with T2DM, ranging from 21% to 32% [9]. This comorbidity is typically associated with worsened insulin resistance, hypertension, dyslipidemia, and pronounced visceral obesity, creating a metabolic triad that accelerates end-organ damage [9]. The underlying pathophysiology is multifactorial, involving insulin resistance, oxidative stress, lipid metabolic dysfunction, and impaired renal urate excretion [9].
Recent research has identified novel biomarkers that reflect this metabolic interplay. The uric acid-to-high-density lipoprotein cholesterol ratio (UHR) has emerged as a composite indicator capturing both oxidative stress and metabolic dysfunction, with studies demonstrating significant positive correlations between UHR and abdominal aortic calcification scores [60]. Similarly, the triglyceride-glucose (TyG) index serves as a reliable marker for insulin resistance and has shown stronger correlation with multi-vessel coronary artery disease compared to uric acid alone [61]. These integrated biomarkers highlight the interconnected nature of uric acid metabolism, glucose homeostasis, and lipid regulation.
Pathophysiological Framework: Molecular Mechanisms and Metabolic Crosstalk
Bidirectional Relationship Between Uric Acid and Insulin Resistance
The relationship between hyperuricemia and diabetes is fundamentally bidirectional. Hyperuricemia exacerbates insulin resistance and β-cell dysfunction through multiple mechanisms, primarily by impairing renal uric acid excretion and activating oxidative stress (e.g., via the NF-κB pathway) and inflammatory cascades [9]. Uric acid acts as an important endogenous "damage-associated molecular pattern" (DAMP) molecule that can induce renal tubular epithelial cell damage, activate the local renin-angiotensin system (RAS) in the kidneys, promote oxidative stress, and trigger the release of pro-inflammatory factors (such as IL-1β, TNF-α) [62].
Conversely, insulin resistance promotes hyperuricemia through reduced renal urate excretion. Insulin stimulates renal urate reabsorption via URAT1 and other transporters, creating a vicious cycle where hyperinsulinemia leads to elevated serum uric acid levels, which in turn worsens insulin sensitivity [9]. This metabolic crosstalk creates a self-perpetuating cycle that accelerates the progression of both conditions and their associated complications.
Lipid Metabolism Dysregulation in Combined Disease States
Advanced lipidomic analyses have revealed distinctive lipid perturbation patterns in patients with coexisting diabetes and hyperuricemia. Using UHPLC-MS/MS-based untargeted lipidomic analysis, researchers identified 1,361 lipid molecules across 30 subclasses, with significant alterations in patients with both conditions compared to those with diabetes alone or healthy controls [10].
Table 1: Significantly Altered Lipid Metabolites in Diabetes with Hyperuricemia
| Lipid Class | Representative Molecules | Change Direction | Metabolic Pathway Association |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) | Significantly upregulated | Glycerolipid metabolism |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) | Significantly upregulated | Glycerophospholipid metabolism |
| Phosphatidylcholines (PCs) | PC(36:1) | Significantly upregulated | Glycerophospholipid metabolism |
| Phosphatidylinositol (PI) | Not specified | Downregulated | Inositol phosphate metabolism |
The collective analysis of these metabolite groups revealed their enrichment in six major metabolic pathways, with glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) identified as the most significantly perturbed pathways in patients with combined diabetes and hyperuricemia [10]. These findings provide a molecular basis for the lipid abnormalities observed in this patient population and highlight potential therapeutic targets for intervention.
Current Therapeutic Landscape: Evidence-Based Combination Approaches
Pharmacological Agents with Dual Benefits
Several pharmacological classes demonstrate beneficial effects on both uric acid metabolism and lipid parameters, making them particularly valuable for patients with coexisting conditions:
SGLT2 Inhibitors
SGLT2 inhibitors represent a cornerstone therapy for this patient population due to their pleiotropic benefits. A recent multicenter retrospective cohort study demonstrated that SGLT2 inhibitors significantly reduced uric acid levels by 4.5% overall (p=0.006), with the most pronounced reduction observed in patients with baseline elevated UA (10%, p=0.001) and those with heart failure (9%, p=0.001) [59]. The mechanism of action involves enhanced urinary excretion of uric acid through modulation of renal transporters, distinct from conventional urate-lowering therapies. Multivariate analysis confirmed diabetes & heart failure as an independent predictor of response (OR = 2.2, 95% CI: 1.2–4.04) [59].
Xanthine Oxidase Inhibitors
Febuxostat, a selective xanthine oxidase inhibitor, has demonstrated significant renoprotective effects in patients with diabetic kidney disease (DKD) and hyperuricemia. A meta-analysis of 17 randomized controlled trials involving 1,300 patients showed that febuxostat significantly improved multiple renal parameters compared to control groups [62].
Table 2: Efficacy of Febuxostat in Diabetic Kidney Disease with Hyperuricemia
| Outcome Measure | Effect Size | Statistical Significance | Clinical Implications |
|---|---|---|---|
| Overall effective rate | RR = 1.24, 95%CI: 1.17–1.32 | Z = 7.17, P < 0.001 | Superior clinical response |
| Serum uric acid (SUA) | Significant reduction | P < 0.001 | Effective urate lowering |
| Urinary albumin-to-creatinine ratio (UACR) | Significant reduction | P < 0.001 | Improved renal parameter |
| Estimated glomerular filtration rate (eGFR) | Significant improvement | P < 0.001 | Renal function preservation |
Beyond its urate-lowering effects, febuxostat exhibits additional benefits including potential anti-inflammatory, antioxidant, and endothelial function-improving properties that may contribute to its therapeutic effects on lipid metabolism and cardiovascular risk [62].
Drug Interaction Considerations in Combination Therapy
The complexity of managing coexisting diabetes and hyperuricemia necessitates careful attention to potential drug interactions. A prescription screening study identified ten significant drug interactions in patients receiving combined therapy, consisting of 8 moderate (80%), 1 major (10%), and 1 minor (10%) interactions [63]. The most frequently prescribed medications included metformin (82%), glimepiride (76%), and allopurinol (88%), with moderate interactions identified primarily between antidiabetic drugs and non-steroidal anti-inflammatory drugs (NSAIDs) [63]. These findings highlight the importance of comprehensive medication review and appropriate monitoring when implementing combination regimens.
Experimental Models and Methodological Approaches
Lipidomic Profiling Techniques
The application of advanced lipidomics has been instrumental in characterizing metabolic perturbations in patients with combined diabetes and hyperuricemia. The standard experimental workflow for comprehensive lipid profiling involves:
Sample Preparation Protocol:
- Collection of 5 mL fasting morning blood with centrifugation at 3,000 rpm for 10 minutes at room temperature
- Aliquoting of 0.2 mL plasma into 1.5 mL centrifuge tubes
- Protein precipitation using pre-cooled methanol
- Lipid extraction with methyl tert-butyl ether (MTBE)
- Sonication in low-temperature water bath for 20 minutes
- Standing at room temperature for 30 minutes
- Centrifugation at 14,000 g for 15 minutes at 10°C
- Collection of upper organic phase and drying under nitrogen [10]
UHPLC-MS/MS Analysis Conditions:
- Chromatography: Waters ACQUITY UPLC BEH C18 column (2.1 mm × 100 mm, 1.7 μm particle size)
- Mobile Phase: A: 10 mM ammonium formate acetonitrile solution in water; B: 10 mM ammonium formate acetonitrile isopropanol solution
- Mass Spectrometry: Untargeted analysis using tandem mass spectrometry with appropriate ionization sources
- Data Processing: Multivariate statistical analysis including principal component analysis (PCA) and orthogonal partial least squares discriminant analysis (OPLS-DA) [10]
This methodological approach enables the identification and quantification of hundreds of lipid species simultaneously, providing comprehensive insights into alterations in lipid metabolic pathways.
Assessment of Metabolic and Vascular Outcomes
Integrated biomarker approaches are essential for evaluating therapeutic efficacy in this complex patient population. Key methodological considerations include:
Uric Acid to HDL Cholesterol Ratio (UHR):
- Calculation: UHR = UA (mg/dL)/HDL (mg/dL)
- Analytical Methods: Uric acid measured via timed endpoint technique; HDL cholesterol measured after elimination of non-HDL cholesterol by adding magnesium/dextran sulfate
- Clinical Utility: Significant positive correlations observed between UHR and abdominal aortic calcification scores (β: 0.53, 95% CI: 0.31–0.75) [60]
Triglyceride-Glucose (TyG) Index:
- Calculation: TyG index = ln[FPG(mg/dl) × TG(mg/dl)/2]
- Cut-off Values: Optimal TyG index cutoff value of 9.33 for predicting cardiovascular risk
- Predictive Value: Demonstrated higher predictive value for multi-vessel CAD compared to uric acid alone in feature importance analysis using XGBoost model [61]
Visualization of Key Pathways and Relationships
Metabolic Crosstalk in Diabetes and Hyperuricemia
Therapeutic Targeting Strategy
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Tools for Investigating Lipid-Uric Acid Interactions
| Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Lipidomic Analysis Platforms | UHPLC-MS/MS with C18 columns | Comprehensive lipid profiling | Enables identification of 1,361+ lipid molecules across 30 subclasses [10] |
| Metabolic Pathway Analysis | MetaboAnalyst 5.0 | Identification of perturbed metabolic pathways | Key for revealing glycerophospholipid and glycerolipid metabolism alterations [10] |
| Insulin Resistance Assessment | TyG index = ln[FPG(mg/dl)×TG(mg/dl)/2] | Surrogate marker of insulin resistance | Strong predictor of multi-vessel CAD; cutoff >9.33 [61] |
| Integrated Biomarkers | Uric acid to HDL ratio (UHR) | Assessment of metabolic dysfunction | Correlates with vascular calcification; calculated as UA(mg/dL)/HDL(mg/dL) [60] |
| Statistical and ML Approaches | XGBoost, LASSO, multivariate regression | Identification of risk factors and predictors | Feature importance analysis for multi-vessel CAD prediction [61] [64] |
| Advanced Drug Delivery Systems | Lipid-based nanoparticles, stimuli-responsive hydrogels | Enhanced therapeutic targeting | Improves bioavailability and enables targeted delivery to inflamed tissues [65] |
Future Directions and Translational Perspectives
The management of combined hyperuricemia and diabetes is evolving toward precision medicine approaches that account for individual variations in metabolic phenotypes, genetic predispositions, and therapeutic responses. Future research directions should prioritize:
Advanced Drug Delivery Systems (DDS): Emerging DDS platforms including lipid-based, polymer-based, and stimuli-responsive systems offer transformative potential for managing hyperuricemia in diabetic patients. These systems significantly enhance therapeutic outcomes by improving drug solubility, enabling targeted delivery, providing sustained release, facilitating synergistic drug co-delivery, and responding to pathological microenvironments [65]. Specifically, nanotechnology approaches such as nonionic surfactant-based niosomes encapsulating allopurinol have achieved 82% drug release within 24 h and significantly reduced SU levels in MSU crystal-induced gout models, outperforming free drug formulations [65].
Integrated Biomarker Development: The combination of uric acid levels with lipid parameters (such as UHR) and insulin resistance markers (TyG index) provides a more comprehensive assessment of metabolic risk than any single parameter alone. Future studies should validate these integrated biomarkers for risk stratification and treatment monitoring in larger, diverse populations.
Personalized Combination Therapies: Based on current evidence, optimal therapeutic regimens should be tailored to individual patient characteristics. For patients with diabetic kidney disease and hyperuricemia, febuxostat demonstrates significant renoprotective effects [62]. For those with cardiovascular comorbidities, SGLT2 inhibitors offer dual benefits on both uric acid metabolism and cardiovascular outcomes [59]. The development of predictive algorithms incorporating clinical, biochemical, and genetic factors will enable more precise targeting of combination therapies.
The continued integration of basic science discoveries with clinical applications will be essential for advancing the management of this complex metabolic intersection. Interdisciplinary collaboration among researchers, clinicians, and drug development professionals remains critical to translate these innovations into tangible improvements in patient outcomes.
Precision medicine represents a transformative paradigm in healthcare, moving beyond universal treatment strategies to approaches tailored to an individual's unique genetic makeup, molecular profile, and lifestyle. For complex metabolic diseases such as diabetes mellitus (DM) combined with hyperuricemia (HU), this approach is particularly pertinent. These conditions frequently coexist and exhibit significant heterogeneity in underlying pathophysiology and treatment response. This technical guide explores the integration of genetic and lipidomic profiling to dissect this heterogeneity, focusing on the distinct lipid metabolic pathways dysregulated in hyperuricemic diabetic patients. We provide detailed methodologies for lipidomic analysis, visualize key disrupted pathways, and catalog essential research tools to advance the development of targeted, effective therapeutic strategies for this patient population.
Diabetes and hyperuricemia are major public health issues that are increasingly prevalent worldwide, often occurring together as interconnected metabolic disorders [66]. Hyperuricemia, characterized by elevated serum uric acid (SUA) levels, is a significant comorbidity of diabetes; studies indicate that its prevalence is higher in diabetic populations than in non-diabetic populations [10]. Epidemiological data reveal that the risk of developing diabetes increases by 17% for every 1 mg/dL increase in serum uric acid, underscoring a robust correlation between these conditions [10] [66]. Both diseases are characterized by profound metabolic disturbances, with dyslipidemia being a common feature. However, conventional clinical biomarkers often fail to capture the full spectrum of lipid abnormalities, creating a critical need for advanced profiling techniques to elucidate the specific molecular bridges between health and disease in this comorbid state [67].
Genetic Foundations for Personalized Treatment
A core tenet of precision medicine is understanding the genetic predispositions that influence disease susceptibility and treatment response.
Genetic Susceptibility and Pharmacogenomics
Large-scale genomics studies have identified nearly 80 susceptibility loci for type 2 diabetes (T2D), providing a foundational knowledge base for personalized risk assessment [68]. Pharmacogenomic research has revealed that genetic variations account for approximately 34% of the variability in patient response to metformin, a first-line therapy for T2D [68]. Key genes involved in metformin pharmacokinetics and pharmacodynamics include those encoding organic cation transporters (OCTs), which influence drug absorption and tissue distribution. Understanding these genetic factors enables the stratification of patients into subgroups more likely to benefit from specific treatments, thereby optimizing therapeutic efficacy and minimizing adverse effects.
Genetic Insights into Hyperuricemia
The genetic underpinnings of hyperuricemia offer another layer for personalization. Research has highlighted the role of urate transporters, such as urate transporter 1 (URAT1) and glucose transporter 9 (GLUT9), in regulating serum uric acid levels [14]. Furthermore, the evolutionary loss of the uricase enzyme in humans has been postulated as a "thrifty gene" that may have conferred a survival advantage in the past but now predisposes individuals to higher uric acid and glucose levels, contributing to the diabetes-hyperuricemia link [66]. Mendelian randomization studies help distinguish causal relationships from mere associations, providing a powerful tool for validating therapeutic targets [3] [66].
Table 1: Key Genetic Factors Influencing Diabetes and Hyperuricemia
| Gene/Region | Function/Association | Potential Clinical Utility |
|---|---|---|
| OCT1/OCT2 | Transport of metformin; influences pharmacokinetics and response [68] | Predict metformin efficacy and risk of side effects |
| GLUT9 (SLC2A9) | Urate transport; linked to serum uric acid levels [14] | Identify patients with genetic predisposition to hyperuricemia |
| URAT1 (SLC22A12) | Renal reabsorption of uric acid [3] | Target for uricosuric drugs; patient stratification |
| Uricase Pseudogene | Loss of function increases serum uric acid [66] | Understanding evolutionary basis for comorbidity |
| NLRP3 Inflammasome | Modulator between urate and insulin resistance; implicated in inflammation [66] | Novel therapeutic target for both conditions |
Lipidomic Profiling in Diabetes and Hyperuricemia
Lipidomics, a branch of metabolomics, provides a comprehensive analysis of lipid species within a biological system. It is an effective tool for characterizing the specific lipid perturbations that precede and accompany complex metabolic diseases [10] [69].
Distinct Lipidomic Signatures in Comorbid Patients
Untargeted lipidomic studies using UHPLC-MS/MS have revealed significantly altered plasma lipid profiles in patients with combined diabetes and hyperuricemia (DH) compared to those with diabetes alone or healthy controls. One study identified 1,361 lipid molecules across 30 subclasses in patient plasma, demonstrating the power of this approach [10]. Multivariate analyses confirmed a significant separation trend among these groups. Specifically, the DH group showed 31 significantly altered lipid metabolites compared to healthy controls. Among the most relevant were:
- 13 Triglycerides (TGs) (e.g., TG (16:0/18:1/18:2)) were significantly upregulated.
- 10 Phosphatidylethanolamines (PEs) (e.g., PE (18:0/20:4)) were significantly upregulated.
- 7 Phosphatidylcholines (PCs) (e.g., PC (36:1)) were significantly upregulated.
- 1 Phosphatidylinositol (PI) was downregulated [10].
This distinct signature indicates a profound disruption in specific lipid metabolic pathways, which can serve as both biomarkers and guides to underlying pathophysiology.
Dysregulated Metabolic Pathways
Pathway analysis of these differential lipids reveals their enrichment in core metabolic processes. The most significantly perturbed pathways in DH patients are glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) [10]. The central role of these pathways is further underscored by the fact that the comparison between DH and DM groups also identified differential lipids enriched in the same core pathways. This positions glycerophospholipid and glycerolipid metabolism as critical hubs in the pathophysiology of hyperuricemia complicating diabetes.
The following diagram illustrates the key lipid metabolic pathways found to be disrupted in patients with combined diabetes and hyperuricemia, based on lipidomic profiling data.
Diagram 1: Disrupted Lipid Pathways in Diabetic Hyperuricemia. This diagram integrates lipidomic findings with established pathological mechanisms, showing how dysregulated glycerolipid and glycerophospholipid metabolism contribute to insulin resistance and β-cell dysfunction. Abbreviations: TG: Triglyceride; DAG: Diacylglycerol; PC: Phosphatidylcholine; PE: Phosphatidylethanolamine; PI: Phosphatidylinositol.
Integrated Precision Medicine Workflow
Implementing precision medicine for diabetic hyperuricemic patients requires a systematic, multi-omics workflow. The following diagram outlines a proposed pipeline from patient stratification to treatment monitoring.
Diagram 2: Integrated Precision Medicine Workflow. This pipeline illustrates the cyclical process of using multi-omics data to develop, apply, and refine personalized treatment strategies for patients with diabetes and hyperuricemia. Abbreviations: DH: Diabetes with Hyperuricemia; DM: Diabetes Mellitus; NGT: Normal Glucose Tolerance.
Experimental Protocols for Lipidomic Analysis
Robust and reproducible lipidomic profiling is fundamental to this precision approach. Below is a detailed protocol for plasma untargeted lipidomics based on UHPLC-MS/MS.
Sample Collection and Pre-processing
- Collection: Collect fasting blood samples (e.g., 5 mL) into appropriate anticoagulant tubes.
- Plasma Separation: Centrifuge at 3,000 rpm for 10 minutes at room temperature. Aliquot the upper plasma layer (e.g., 0.2 mL) into cryotubes.
- Storage: Store all samples at -80°C until analysis. Create quality control (QC) samples by pooling equal volumes from all experimental samples.
- Lipid Extraction: Employ a methyl tert-butyl ether (MTBE)-based extraction:
- Thaw samples on ice.
- Pipette 100 μL of plasma into a 1.5 mL microcentrifuge tube.
- Add 200 μL of 4°C water and vortex.
- Add 240 μL of pre-cooled methanol and vortex.
- Add 800 μL of MTBE, vortex, and sonicate in a low-temperature water bath for 20 minutes.
- Let the mixture stand at room temperature for 30 minutes.
- Centrifuge at 14,000 g for 15 minutes at 10°C.
- Collect the upper organic phase and dry under a gentle stream of nitrogen.
- Reconstitute the dried lipid extract in a suitable solvent (e.g., 100 μL isopropanol) for LC-MS analysis [10].
UHPLC-MS/MS Analysis Conditions
- Chromatography:
- Column: Use a reversed-phase column, e.g., Waters ACQUITY UPLC BEH C18 (2.1 mm × 100 mm, 1.7 μm).
- Mobile Phase: A: 10 mM ammonium formate in acetonitrile:water; B: 10 mM ammonium formate in acetonitrile:isopropanol.
- Gradient: Implement a linear gradient from high A to high B over a runtime of 10-20 minutes.
- Temperature: Column oven set to 45-55°C.
- Injection Volume: Typically 1-5 μL [10].
- Mass Spectrometry:
- Ionization: Use electrospray ionization (ESI) in both positive and negative ion modes.
- Scan Mode: Data-Dependent Acquisition (DDA) or Data-Independent Acquisition (DIA) for untargeted profiling.
- Scan Range: m/z 150-1500.
- Collision Energies: Use stepped collision energies for improved fragmentation data.
Data Processing and Analysis
- Peak Picking and Alignment: Use software platforms like MS-DIAL, Lipostar, or XCMS for raw data conversion, peak detection, alignment, and lipid identification against databases (e.g., LIPID MAPS).
- Statistical Analysis:
- Univariate: Student's t-test, ANOVA with post-hoc testing.
- Multivariate: Principal Component Analysis (PCA) for quality control; Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) to identify group-separating lipid species.
- Fold Change (FC): Calculate to determine the magnitude of lipid alterations.
- Pathway Analysis: Input significantly altered lipids (e.g., p < 0.05, FC > 1.5) into platforms like MetaboAnalyst 5.0 to identify enriched metabolic pathways (e.g., glycerophospholipid metabolism) [10].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the precision medicine workflow relies on a suite of specialized reagents, instruments, and software.
Table 2: Key Research Reagent Solutions for Precision Medicine Studies
| Category / Item | Specific Example | Function / Application |
|---|---|---|
| Sample Preparation | Methyl tert-butyl ether (MTBE) / Methanol | Lipid extraction from plasma/serum [10] |
| Ammonium formate / Acetonitrile / Isopropanol | Mobile phase additives for UHPLC separation [10] | |
| Chromatography | Waters ACQUITY UPLC BEH C18 Column (1.7 μm) | High-resolution separation of complex lipid mixtures [10] |
| Mass Spectrometry | Quadrupole-Time of Flight (Q-TOF) or Orbitrap Mass Spectrometer | High-sensitivity and high-resolution lipid detection and identification [10] [69] |
| Data Analysis Software | MS-DIAL, Lipostar, XCMS | Untargeted lipidomic data processing, peak alignment, and lipid annotation [69] |
| Bioinformatics Tools | MetaboAnalyst 5.0 | Statistical and pathway analysis of lipidomic data [10] |
| Genetic Analysis | Next-Generation Sequencing (NGS) Systems | Whole genome/exome sequencing for variant discovery [70] |
| Cell & Animal Models | Urate Oxidase Knockout (Uox-KO) Mice | Genetically modified model for studying hyperuricemia and its metabolic effects [66] |
The integration of genetic and lipidomic profiling provides an unprecedented opportunity to redefine how we diagnose and treat patients with diabetes and hyperuricemia. The identification of distinct lipidomic signatures, such as the upregulation of specific TGs, PEs, and PCs, and the pinpointing of glycerophospholipid metabolism as a critically perturbed pathway, offers concrete targets for therapeutic intervention [10]. The future of this field lies in the continued integration of multi-omics data (genomics, lipidomics, microbiomics) through advanced computational and artificial intelligence (AI) models [67] [69] [68]. Machine learning frameworks, such as MS2Lipid, are already demonstrating high accuracy in predicting lipid subclasses, which will accelerate biomarker discovery [69]. Future research must focus on large-scale, multi-center validation studies to translate these lipidomic biomarkers and genetic signatures into clinically approved diagnostic tools and targeted therapies, ultimately enabling a new era of personalized metabolic medicine.
Evaluating Emerging Targets and Therapies: From Preclinical Models to Clinical Translation
The interplay between lipid metabolic pathways and metabolic diseases presents a fertile ground for therapeutic innovation. This whitepaper provides a technical evaluation of three key regulatory nodes—Monoacylglycerol Lipase (MAGL), Carnitine Palmitoyltransferase 1 (CPT1), and Cluster of Differentiation 36 (CD36)—in the context of dysregulated lipid metabolism. Within the specific pathophysiology of hyperuricemia coexisting with diabetes, these targets offer promising avenues for intervention by modulating lipid storage, mitochondrial oxidation, and cellular lipid uptake. We present a detailed analysis of target biology, validated experimental approaches, and essential research tools to facilitate rigorous investigation and drug development.
Target Biological Rationale and Mechanisms
Monoacylglycerol Lipase (MAGL)
Biological Function and Significance: MAGL is a serine hydrolase that catalyzes the hydrolysis of monoacylglycerols (MAGs) into free fatty acids (FFAs) and glycerol. This reaction represents the final step in the breakdown of triglycerides [71] [72]. MAGL is a critical regulator in the convergence of metabolic and signaling pathways. It terminates the signaling of the endocannabinoid 2-arachidonoylglycerol (2-AG) and controls the release of fatty acids, notably arachidonic acid, which serve as precursors for pro-inflammatory eicosanoids [71]. In the context of diabetic hyperuricemia, inhibition of MAGL may concurrently reduce inflammatory tone and modulate lipid intermediates that contribute to insulin resistance.
Carnitine Palmitoyltransferase 1 (CPT1)
Biological Function and Significance: CPT1 is an outer mitochondrial membrane enzyme that acts as the rate-limiting step for the import and subsequent β-oxidation of long-chain fatty acids. It catalyzes the transfer of an acyl group from acyl-CoA to carnitine, forming acyl-carnitine [73] [74]. Recent research has identified Mitochondrial Carrier Homolog 2 (MTCH2) as a key regulatory protein that interacts directly with CPT1, modulating its sensitivity to its allosteric inhibitor, malonyl-CoA [73]. In states of nutrient excess, such as diabetes, malonyl-CoA levels are elevated, which normally suppresses CPT1 activity and leads to lipid accumulation. Enhancing CPT1 activity or reducing its inhibition presents a strategy to increase mitochondrial fatty acid oxidation (FAO), thereby alleviating ectopic lipid deposition and lipotoxicity in tissues such as the liver and skeletal muscle [73] [74].
CD36 (Fatty Acid Translocase)
Biological Function and Significance: CD36 is a multifunctional transmembrane scavenger receptor that facilitates the cellular uptake of long-chain fatty acids and modified lipoproteins (e.g., oxidized LDL) [75] [76] [77]. Its expression is upregulated by high-fat diets, leptin, and insulin, and it is present in key metabolic tissues including adipocytes, myocytes, hepatocytes, and pancreatic β-cells [75] [77]. CD36 serves not only as a transporter but also as a signaling receptor. Its activation can initiate pathways involving Src family kinases and MAPK, contributing to inflammatory responses, oxidative stress, and insulin resistance [76] [77]. In diabetic complications, elevated CD36-mediated lipid uptake promotes ectopic lipid deposition, ceramide accumulation, and cellular dysfunction, making it a prime target for mitigating lipotoxicity [77] [74].
Table 1: Core Functional Roles of MAGL, CPT1, and CD36
| Target | Primary Location | Core Metabolic Function | Key Regulatory Factors |
|---|---|---|---|
| MAGL | Cytoplasm | Hydrolyzes monoacylglycerols (e.g., 2-AG) to FFA and glycerol; regulates endocannabinoid signaling | Dietary fat intake; endocannabinoid tone |
| CPT1 | Mitochondrial Outer Membrane | Rate-limiting enzyme for long-chain fatty acid import into mitochondria for β-oxidation | Malonyl-CoA inhibition; MTCH2 interaction; AMPK activation [73] [74] |
| CD36 | Plasma Membrane / Mitochondria | Facilitates cellular uptake of long-chain FAs and modified lipoproteins; functions as a signaling receptor | High-fat diet, insulin, leptin; PPARγ activation [75] [77] |
Experimental Analysis and Methodologies
Research on these targets yields quantitative data on expression, activity, and metabolic impact across different physiological and pathological states.
Table 2: Key Quantitative Findings from Experimental Studies
| Target | Experimental Context | Key Quantitative Findings | Significance / Outcome |
|---|---|---|---|
| CD36 | HFD (65% fat) in obese vs. lean humans [75] | HFD increased skeletal muscle CD36 levels in obese individuals but not in lean subjects. | Suggests a dysregulated response to lipid overload in obesity, exacerbating lipid accumulation. |
| CD36 | In vitro macrophages treated with ox-LDL or TG [76] | Silencing CD36 significantly attenuated lipid-droplet formation in macrophages. | Directly links CD36 to foam cell formation, a key event in atherogenesis. |
| MTCH2/CPT1 | siRNA knockdown of MTCH2 in human adipocytes [73] | Knockdown increased cAMP-stimulated mitochondrial respiration and maximal respiratory capacity. | Identifies MTCH2 as a negative regulator of energy expenditure by controlling CPT1-mediated FA influx. |
| CPT1 | Fasting in murine β-cells [74] | PLIN5 upregulation facilitates FA release from LDs and transport into mitochondria via CPT1 for β-oxidation. | Highlights the physiological role of CPT1 in providing energy to sustain β-cell function during fasting. |
Detailed Experimental Protocols
Protocol 1: Assessing CD36-Mediated Lipid Uptake and Foam Cell Formation In Vitro [76]
This protocol is crucial for evaluating the role of CD36 in atherogenic dyslipidemia and for screening potential inhibitors.
- Cell Culture: Maintain macrophages (e.g., THP-1 derived or primary murine peritoneal macrophages) in standard culture conditions.
- Treatment and Intervention:
- Lipid Loading: Treat macrophages with a gradient of glyceryl trioleate (TG) or oxidized low-density lipoprotein (ox-LDL) for 24-48 hours to induce lipid-droplet formation (LDF).
- Genetic Knockdown: Transfect cells with siRNA targeting CD36 or a non-targeting control siRNA prior to lipid loading.
- Pharmacological Inhibition: Co-incubate cells with potential therapeutic agents (e.g., dapagliflozin, alirocumab) during lipid loading.
- Output Measurements:
- Lipid Droplet Quantification: Fix cells and stain with LipidTOX (neutral lipid stain) or Oil Red O. Quantify lipid droplet number and area per cell using high-content imaging or spectrophotometry.
- Molecular Analysis: By western blot, measure protein expression levels of CD36, ANGPTL4, PPARγ, and components of the Fyn/Src/MAPK signaling pathway.
- Inflammatory Markers: Quantify secretion of proinflammatory cytokines (e.g., TNF-α, IL-6) in the supernatant via ELISA.
- Lipoprotein Lipase Activity (LPLa): Assess LPLa using a fluorometric or colorimetric assay kit.
Protocol 2: Evaluating CPT1 Activity and Mitochondrial FA Oxidation via MTCH2 Interaction [73]
This protocol outlines a functional screen to identify regulators of mitochondrial metabolism in adipocytes, with a focus on the MTCH2-CPT1 axis.
- Cell Model: Use human multipotent adipose-derived stem (hMADS) cells differentiated into white or beige adipocytes.
- Genetic Manipulation: Perform a siRNA-based functional screen. Transfect adipocytes with siRNA libraries targeting candidates (e.g., MTCH2) or non-targeting control.
- Metabolic Phenotyping: Utilize a Seahorse XF Analyzer to measure real-time mitochondrial respiration.
- Basal Respiration: Measure oxygen consumption rate (OCR) under baseline conditions.
- Stimulated Respiration: Inject dibutyryl-cAMP (a stable cAMP analog) to stimulate mitochondrial function and record OCR.
- Proton Leak: Inject oligomycin to inhibit ATP synthase and measure OCR attributable to proton leak.
- Maximal Respiration: Inject FCCP, a chemical uncoupler, to induce maximal OCR.
- Mechanistic Follow-up:
- Gene Expression: Analyze transcript levels of MTCH2, CPT1, and other FAO genes (e.g., PPARα) via qPCR.
- Protein Interaction: Validate direct physical interaction between MTCH2 and CPT1 using co-immunoprecipitation (Co-IP) in adipocyte lysates.
- CPT1 Activity Assay: Measure CPT1 enzyme activity spectrophotometrically by monitoring the conversion of palmitoyl-CoA to palmitoyl-carnitine in the presence of varying malonyl-CoA concentrations to assess inhibitor sensitivity.
Pathway Visualization and Workflows
The following diagrams, generated with Graphviz DOT language, illustrate the core signaling pathways and experimental logic for these targets.
CD36 Signaling in Metabolic Dysfunction
Diagram 1: CD36 signaling in metabolic dysfunction.
MTCH2-CPT1 Axis Regulating Mitochondrial Oxidation
Diagram 2: MTCH2-CPT1 axis regulates mitochondrial oxidation.
Integrated MAGL, CD36, and CPT1 Workflow
Diagram 3: Integrated lipid metabolism and target interplay.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Target Investigation
| Reagent / Tool | Specific Example | Primary Function in Research |
|---|---|---|
| siRNA/shRNA | ON-TARGETplus siRNA pools (e.g., for MTCH2, CD36) [73] | Targeted knockdown of gene expression to validate target function in vitro and in vivo. |
| Specific Agonists/Antagonists | GLP-1 receptor agonists; Dapagliflozin; Alirocumab [76] | Pharmacological tools to modulate interconnected pathways and assess therapeutic potential. |
| Antibodies for Western Blot/IF | Anti-CD36 [76]; Anti-CPT1; Anti-PLIN5 [74]; Anti-MTCH2 [73] | Detection of protein expression, subcellular localization, and post-translational modifications. |
| Metabolic Assay Kits | Seahorse XF Palmitate Oxidation Stress Test Kit; CPT1 Activity Assay Kit | Direct measurement of mitochondrial fatty acid oxidation rates and CPT1 enzymatic activity. |
| Lipid Staining Dyes | LipidTOX (HCS); Oil Red O [76] | Visualization and quantification of neutral lipid content and lipid droplet dynamics in cells. |
| Animal Models | db/db mice on HFD [76]; Diet-Induced Obese (DIO) mice | Preclinical models for studying metabolic syndrome, diabetes, and target efficacy in a whole-organism context. |
Integrated Therapeutic Implications
The concurrent targeting of MAGL, CPT1, and CD36 addresses complementary facets of dysregulated lipid metabolism. MAGL inhibition may reduce the provision of fatty acid precursors for inflammatory mediators and modulate endocannabinoid tone. Strategies to enhance CPT1 activity, potentially via disrupting its interaction with MTCH2, promote energy expenditure and reduce ectopic lipid storage. CD36 inhibition directly limits the initial cellular uptake of excess lipids, mitigating the cascade of lipotoxicity and inflammation. In the complex pathophysiology of hyperuricemia and diabetes, where lipid derangements and inflammation are paramount, a multi-target approach holds significant promise for restoring metabolic homeostasis and preventing end-organ damage.
Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) represent a transformative class of therapeutics that extend far beyond their initial application as glucose-lowering agents. This whitepaper delineates the integrated mechanisms through which GLP-1 RAs concomitantly regulate glucose and lipid homeostasis, with particular relevance to the complex pathophysiology of patients with diabetes and hyperuricemia. We synthesize evidence from foundational science, clinical trials, and emerging research to elucidate how these agents modulate metabolic pathways at cellular, tissue, and systemic levels. The analysis is framed within the context of cardiorenal metabolic syndrome, where dysregulated lipid metabolism and hyperuricemia frequently intersect with diabetes, driving progressive disease. For the research and development community, we provide detailed experimental methodologies, key reagent solutions, and visual schematics of critical pathways to facilitate advanced investigation and therapeutic innovation.
The global burden of diabetes mellitus continues to escalate, affecting over 422 million individuals currently, with projections indicating a rise to 783 million by 2045 [78]. This epidemic is compounded by the frequent co-occurrence of lipid metabolism disorders and hyperuricemia, creating a pathological triad that accelerates cardiovascular, renal, and metabolic (CKM) syndrome [78] [14]. Hyperuricemia, characterized by elevated serum uric acid levels, ranks as the second most prevalent metabolic disorder after diabetes and exhibits a complex, bidirectional relationship with both insulin resistance and dyslipidemia [14].
GLP-1 receptor agonists have emerged as pivotal agents addressing this metabolic convergence. Initially developed for glycemic control, their therapeutic profile has expanded to encompass robust effects on lipid metabolism, cardiovascular protection, and potential uric acid modulation [79] [80]. This whitepaper examines the dual-action benefits of GLP-1 RAs on glucose and lipid homeostasis, with specific consideration of the underlying mechanisms that position these agents as comprehensive metabolic modulators in complex patient phenotypes, including those with hyperuricemia and diabetes.
Molecular Mechanisms and Signaling Pathways
Core Signaling Cascades
The therapeutic efficacy of GLP-1 RAs stems from their activation of the GLP-1 receptor (GLP-1R), a class B G protein-coupled receptor (GPCR) widely expressed in pancreatic islets, brain, cardiovascular tissues, kidneys, liver, and gastrointestinal tract [81] [79]. Upon agonist binding, GLP-1R initiates multiple intracellular signaling pathways with distinct temporal and spatial characteristics:
- Primary cAMP/PKA Pathway: Gαs-mediated activation of adenylyl cyclase leads to cyclic adenosine monophosphate (cAMP) accumulation and protein kinase A (PKA) activation. This canonical pathway phosphorylates downstream targets, including the transcription factor CREB (cAMP response element-binding protein), which translocates to the nucleus and induces expression of cytoprotective genes [79].
- PI3K/Akt Survival Pathway: Parallel to cAMP signaling, GLP-1 receptor activation stimulates the phosphatidylinositol 3-kinase (PI3K)/Akt pathway, a critical mediator of cell survival and metabolic regulation. Activated Akt phosphorylates multiple substrates, including inhibition of glycogen synthase kinase-3β (GSK-3β), which enhances insulin signaling and prevents tau hyperphosphorylation [79].
- β-Arrestin-Mediated Signaling: β-arrestin-2 plays a concentration-dependent role, serving as a negative regulator at physiological concentrations but becoming essential for sustained extracellular signal-regulated kinase (ERK) activation and CREB phosphorylation at therapeutic GLP-1 RA concentrations [79].
- Wnt/β-Catenin Signaling: GLP-1 receptor activation engages the Wnt/β-catenin signaling cascade through PKA-mediated inhibition of GSK-3β, stabilizing β-catenin and enabling nuclear translocation of genes that promote tissue regeneration and β-cell proliferation [79].
Integrated Pathway Visualization
The following diagram illustrates the coordinated signaling mechanisms through which GLP-1 receptor activation regulates glucose and lipid metabolism across key metabolic tissues:
Experimental Approaches for Investigating GLP-1 RA Mechanisms
Core Methodologies for Metabolic Research
Elucidating the dual-action benefits of GLP-1 RAs requires integrated experimental approaches spanning molecular, cellular, and physiological levels. The following table summarizes key methodologies cited in foundational research:
Table 1: Experimental Protocols for Investigating GLP-1 RA Mechanisms
| Research Objective | Experimental Model | Key Protocol Components | Outcome Measures |
|---|---|---|---|
| GLP-1R Signaling Pathways | Clonal cell lines (e.g., β-cells, hepatocytes), Human islets [81] [79] | - Receptor binding assays- cAMP quantification (ELISA)- Western blot (pAkt, pERK, pCREB)- Gene silencing (siRNA) | - cAMP accumulation- Kinase phosphorylation- Target gene expression |
| Hepatic Lipid Metabolism | in vivo: Ob/ob mice, high-fat diet modelsin vitro: Human hepatocytes (HepG2) [80] | - Lipidomics (LC-MS)- Gene expression (qPCR: SREBP-1c, PPARγ)- Oil Red O staining- Autophagy flux assays | - Triglyceride content- Lipid droplet formation- Autophagy markers (LC3-II) |
| Adipose Tissue Function | Primary adipocytes, Animal models [80] | - Glucose uptake assays- Lipolysis measurements (glycerol release)- Thermogenesis (UCP1 expression)- Adipokine profiling | - Fatty acid oxidation- Adipocyte differentiation- Insulin sensitivity |
| Cardiovascular Protection | Animal models of atherosclerosis, Ischemia-reperfusion [82] | - Echocardiography- Histological plaque analysis- Isolated heart perfusion (Langendorff)- Vascular reactivity | - Plaque area/stability- Cardiac function- Endothelial function |
| Clinical Translation | RCTs in T2DM/obesity populations [78] [82] | - Hyperinsulinemic-euglycemic clamps- Stable isotope tracers- MRI/MRS for organ fat- Biobanking for biomarkers | - Insulin sensitivity- Lipoprotein kinetics- Ectopic fat deposition |
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for GLP-1 RA Investigations
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| GLP-1 Receptor Agonists | Exendin-4, Liraglutide, Semaglutide [81] [79] | In vitro and in vivo mechanistic studies | GLP-1R activation with varying pharmacokinetics |
| Cell Culture Models | INS-1 (β-cells), HepG2 (hepatocytes), 3T3-L1 (adipocytes) [80] | Tissue-specific metabolic assays | Representative cellular systems for metabolic research |
| Signal Transduction Inhibitors | H-89 (PKA), LY294002 (PI3K), U0126 (MEK) [79] | Pathway mapping and validation | Selective inhibition of specific signaling branches |
| Antibodies for Detection | Anti-GLP-1R, pCREB, pAkt, UCP1, SREBP-1 [79] [80] | Western blot, IHC, flow cytometry | Detection of receptor expression and pathway activation |
| Metabolic Assay Kits | cAMP ELISA, Lipolysis assay, Glucose uptake kits [80] | Quantification of metabolic endpoints | Standardized measurement of key metabolic parameters |
| Animal Models | ob/ob mice, Zucker diabetic fatty rats, High-fat diet models [80] | In vivo efficacy and metabolism studies | Pathophysiologically relevant models of metabolic disease |
GLP-1 RA Effects on Glucose Homeostasis
Pancreatic Mechanisms
GLP-1 RAs enhance glucose-dependent insulin secretion from pancreatic β-cells through multiple mechanisms. By activating the cAMP/PKA pathway, they promote closure of ATP-sensitive K+ channels and opening of voltage-dependent Ca2+ channels, facilitating insulin exocytosis [81] [79]. Simultaneously, they suppress glucagon secretion from pancreatic α-cells, particularly during hyperglycemic conditions, thereby reducing hepatic glucose production [83]. Beyond acute effects, GLP-1 RAs provide long-term β-cell support by stimulating proliferation through ERK1/2 and PI3K/Akt pathways, while inhibiting apoptosis by downregulating pro-apoptotic signals and enhancing resistance to endoplasmic reticulum stress [79] [84].
Extrapancreatic Mechanisms
The glucose-regulating effects extend beyond the pancreas through multiple extrapancreatic pathways. GLP-1 RAs delay gastric emptying and reduce postprandial glucose excursions through direct action on gastric smooth muscle and neural regulation via the vagus nerve [83] [85]. In the central nervous system, they enhance satiety and reduce food intake by acting on receptors in the hypothalamus and brainstem, contributing to weight loss and improved metabolic status [81] [85]. They also enhance glucose disposal in peripheral tissues, with studies showing improved insulin sensitivity in muscle and adipose tissue through both direct receptor-mediated effects and indirect weight loss-mediated benefits [82] [85].
GLP-1 RA Effects on Lipid Homeostasis
Hepatic Lipid Metabolism
The liver represents a critical target for GLP-1 RA-mediated lipid regulation. These agents reduce hepatic steatosis through multiple mechanisms, including downregulation of sterol regulatory element-binding protein-1c (SREBP-1c), a master transcription factor for lipogenesis [80]. Concurrently, they enhance fatty acid β-oxidation by upregulating peroxisome proliferator-activated receptor-α (PPARα) and its coactivator PGC-1α [82] [80]. GLP-1 RAs also promote autophagy and lysosomal lipid degradation through the transcription factor EB (TFEB)-mediated pathway, providing an alternative mechanism for lipid clearance [80]. Additionally, they improve hepatic insulin sensitivity, thereby reducing hyperinsulinemia-driven lipogenesis and promoting a metabolic shift toward reduced lipid accumulation [82].
Adipose Tissue Regulation
GLP-1 RAs exert multifaceted effects on adipose tissue function and distribution. They promote lipolysis in white adipose tissue through both direct receptor activation and centrally-mediated sympathetic nervous system stimulation [83] [80]. They also enhance adipose tissue browning by inducing expression of fibronectin type III domain-containing protein 5 (FNDC5) and uncoupling protein 1 (UCP1) via the cAMP/CREB pathway, increasing energy expenditure [80]. GLP-1 RAs inhibit preadipocyte differentiation and reduce lipid storage capacity by downregulating key adipogenic transcription factors including CCAAT/enhancer binding protein α (C/EBPα) and PPARγ [80]. Furthermore, they modulate adipokine secretion, increasing adiponectin production while reducing pro-inflammatory cytokines, thereby improving systemic insulin sensitivity [83].
Cholesterol and Lipoprotein Metabolism
Beyond triglyceride metabolism, GLP-1 RAs favorably influence cholesterol homeostasis. They enhance reverse cholesterol transport by upregulating ATP-binding cassette transporter A1 (ABCA1) mRNA expression, mediating increased cholesterol efflux from macrophages [80]. Clinical studies consistently demonstrate significant reductions in LDL-cholesterol, triglycerides, and apolipoprotein B levels, with increases in HDL-cholesterol, contributing to improved cardiovascular outcomes [82] [85].
Clinical Evidence and Quantitative Outcomes
Metabolic Efficacy in Clinical Trials
Robust clinical evidence supports the dual metabolic benefits of GLP-1 RAs. The following table synthesizes key efficacy data from major clinical trials and meta-analyses:
Table 3: Clinical Efficacy of GLP-1 Receptor Agonists on Glucose and Lipid Parameters
| GLP-1 RA | HbA1c Reduction (%) | Body Weight Reduction (kg) | LDL-C Reduction (%) | Triglyceride Reduction (%) | Cardiovascular Risk Reduction (HR for MACE) |
|---|---|---|---|---|---|
| Liraglutide | 1.1 - 1.6 [85] | 2.0 - 3.6 [85] | 4.6 - 9.9 [82] | 10.2 - 15.6 [82] | 0.87 [82] |
| Semaglutide (SC) | 1.5 - 1.8 [79] | 4.3 - 6.9 [79] | 8.0 - 15.0 [82] | 12.0 - 20.0 [82] | 0.74 [82] |
| Dulaglutide | 1.4 - 1.6 [85] | 1.4 - 3.0 [85] | 6.5 - 11.0 [82] | 9.5 - 14.8 [82] | 0.88 [82] |
| Tirzepatide | 1.9 - 2.6 [83] | 7.6 - 12.9 [83] | 10.2 - 18.5 [82] | 17.4 - 28.5 [82] | 0.80 [82] |
Cardiometabolic Protection in Hyperuricemic Context
Emerging evidence suggests that GLP-1 RAs may provide particular benefits in patients with concurrent diabetes and hyperuricemia. This population experiences heightened risks for cardiovascular-renal complications driven by interconnected pathophysiological pathways [14]. The lipid-improving effects of GLP-1 RAs are particularly relevant given the association between hyperuricemia, atherogenic dyslipidemia, and non-alcoholic fatty liver disease (NAFLD) [14] [80]. Additionally, the weight loss and insulin-sensitizing effects of GLP-1 RAs may indirectly influence uric acid metabolism through reduced insulin resistance, which promotes renal urate reabsorption [14].
Future Directions and Therapeutic Innovations
The therapeutic landscape of GLP-1-based therapies continues to evolve with several promising frontiers. Next-generation multi-agonists targeting complementary metabolic pathways represent a paradigm shift, with dual GLP-1/GIP receptor agonists (e.g., tirzepatide) and triple GLP-1/GIP/glucagon receptor agonists (e.g., retatrutide) demonstrating superior efficacy for both glycemic control and lipid metabolism compared to selective GLP-1 RAs [81] [79]. Novel formulations and delivery systems, including oral GLP-1 RAs with absorption-enhancing technology (e.g., semaglutide with SNAC), ultralong-acting injectables, implantable pumps, and noninvasive systems, aim to enhance bioavailability, reduce dosing frequency, and improve patient compliance [78] [79]. Research is also expanding into potential direct effects on uric acid metabolism, with investigations exploring whether GLP-1 RAs influence urate transporters (e.g., GLUT9) or inflammatory pathways linking hyperuricemia to insulin resistance [14].
GLP-1 receptor agonists represent a transformative therapeutic class that integrates glucose and lipid regulatory mechanisms through multifaceted pathways. Their capacity to simultaneously address hyperglycemia, dyslipidemia, and associated metabolic disturbances positions them as comprehensive agents for managing complex cardiorenal metabolic disease, particularly in challenging phenotypes such as patients with diabetes and hyperuricemia. The continued evolution of this drug class—through optimized receptor targeting, innovative delivery systems, and combination approaches—promises to further enhance their therapeutic potential. For the research and development community, understanding these integrated mechanisms provides a foundation for developing next-generation therapies that target the root causes of metabolic disease constellations.
Sodium-glucose cotransporter-2 (SGLT2) inhibitors represent a paradigm shift in the management of hyperuricemia in patients with type 2 diabetes (T2D), offering dual cardiorenal protection alongside urate-lowering benefits. Unlike traditional urate-lowering therapies (ULTs) that primarily target uric acid production or excretion, SGLT2 inhibitors modulate interconnected metabolic pathways, addressing hyperuricemia within the broader context of cardiovascular-kidney-metabolic (CKM) syndrome. This whitepaper synthesizes evidence from recent clinical trials, real-world studies, and mechanistic investigations to evaluate the comparative efficacy of SGLT2 inhibitors against conventional ULTs. We place particular emphasis on the lipid metabolic perturbations characteristic of the diabetes-hyperuricemia phenotype, providing detailed experimental protocols and analytical frameworks to guide future research and drug development. The analysis reveals that SGLT2 inhibitors not only significantly reduce serum urate levels but also demonstrably lower gout incidence and recurrent flare rates, while concurrently improving cardiovascular and renal outcomes—benefits not consistently observed with traditional ULTs.
The comorbidity of type 2 diabetes mellitus (T2DM) and hyperuricemia (HUA) represents a complex pathological condition characterized by concurrent disturbances in glucose, urate, and lipid metabolism [9]. The underlying pathophysiology is multifactorial, involving insulin resistance, oxidative stress, lipid metabolic dysfunction, and impaired renal urate excretion [9]. Epidemiological studies consistently demonstrate a substantial prevalence of hyperuricemia among individuals with T2DM, ranging from 21% to 32% across diverse populations [9]. This coexistence is not coincidental but rooted in shared pathophysiological mechanisms, including insulin resistance-mediated reduced renal uric acid excretion and activation of inflammatory pathways such as NF-κB [9].
Lipidomic analyses reveal that patients with combined diabetes and hyperuricemia (DH) exhibit significantly altered plasma lipid profiles compared to those with diabetes alone or healthy controls [10]. These alterations are characterized by upregulated triglycerides (TGs), phosphatidylethanolamines (PEs), and phosphatidylcholines (PCs), with enrichment primarily in glycerophospholipid metabolism and glycerolipid metabolism pathways [10]. These disturbed lipid pathways contribute to a pro-inflammatory milieu, exacerbating insulin resistance and creating a vicious cycle that promotes both hyperglycemia and hyperuricemia. Understanding these interconnected metabolic disturbances is crucial for evaluating therapeutic agents that claim benefits beyond mere glucose or urate reduction.
Mechanisms of Action: Contrasting Physiological Targets
Traditional Urate-Lowering Therapies (ULTs)
Traditional ULTs operate through two primary mechanisms:
- Xanthine Oxidase Inhibition (Allopurinol, Febuxostat): Block the conversion of hypoxanthine to xanthine and xanthine to uric acid in the purine catabolism pathway, thereby reducing uric acid production [86].
- Uricosuric Agents (Probenecid, Benzbromarone): Inhibit urate reabsorption transporters in the renal proximal tubule, primarily URAT1, thereby enhancing renal uric acid excretion [86].
These agents provide a targeted approach to urate reduction but generally lack significant effects on glucose metabolism, cardiovascular outcomes, or the underlying lipid perturbations in DH patients.
SGLT2 Inhibitors: A Pleiotropic Approach
SGLT2 inhibitors demonstrate a multi-mechanistic approach to urate reduction and metabolic improvement:
- Enhanced Urinary Urate Excretion: SGLT2 inhibition induces glucosuria, which is correlated with increased urate excretion potentially via GLUT9 and other transporters [58]. The diuretic effect of SGLT2 inhibitors may also contribute to increased uric acid clearance [87] [86].
- Modulation of Renal Transporters: Evidence suggests SGLT2 inhibitors may regulate additional renal transporters to reduce urate reabsorption, possibly through indirect effects on URAT1 [87] [86].
- Metabolic Pathway Modulation: SGLT2 inhibitors may inhibit purine synthesis via the pentose phosphate pathway while enhancing UA elimination [87].
- Anti-inflammatory Effects: These drugs demonstrate anti-inflammatory properties, including inhibition of the NLRP3 inflammasome activation, potentially through increased circulating hydroxybutyrate levels [88]. This mechanism may explain the reduced incidence of gout flares shortly after initiation, contrary to the "mobilization flares" common with traditional ULTs [86].
Table 1: Comparative Mechanisms of Action
| Therapy Class | Primary Mechanism | Effect on Serum Urate | Metabolic Effects | Anti-inflammatory Properties |
|---|---|---|---|---|
| XOI (Allopurinol) | Xanthine oxidase inhibition | ~30-40% reduction | Minimal direct effects | Limited |
| Uricosurics | URAT1 inhibition | ~20-35% reduction | Minimal direct effects | Limited |
| SGLT2 Inhibitors | Multiple: glucosuria-induced uricosuria, transporter modulation | ~10-15% reduction | Improved glycemic control, weight reduction, blood pressure lowering | Significant: NLRP3 inflammasome inhibition, reduced cytokine production |
Quantitative Efficacy Assessment: Clinical and Real-World Evidence
Serum Uric Acid Reduction
SGLT2 Inhibitors demonstrate consistent urate-lowering effects across multiple studies:
- A meta-analysis of 51 RCTs showed SGLT2 inhibitors significantly reduced SUA levels compared to placebo [MD = -32.14 μmol/L, 95% CI (-35.96 to -28.31); P < 0.001] [87].
- Subgroup analysis revealed differences among specific agents: empagliflozin achieved the greatest reduction [MD = -45.61 μmol/L], while sotagliflozin had the least effect [MD = -13.72 μmol/L] [87].
- A multicenter retrospective study (n=454) found SGLT2 inhibitors significantly reduced UA levels by 4.5% (p=0.006), with the most pronounced reduction in patients with baseline elevated UA (10%, p=0.001) and those with HF (9%, p=0.001) [89].
Traditional ULTs typically produce greater absolute urate reduction but lack the pleiotropic benefits:
- Xanthine oxidase inhibitors typically reduce serum urate by 30-40% with appropriate dose titration.
- Uricosuric agents generally provide 20-35% reduction in serum urate levels.
Table 2: Comparative Efficacy on Gout-Related Outcomes
| Outcome Measure | SGLT2 Inhibitors | Traditional ULTs | Study Details |
|---|---|---|---|
| Incident Gout Risk | HR 0.62 (95% CI, 0.48-0.80) vs. sulfonylureas [90] | Established prevention with adequate dose titration | Population-based cohort (n=34,604) |
| Recurrent Gout Flares | RR 0.66 (95% CI: 0.57, 0.75) vs. DPP-4 inhibitors [91] | ~50-75% reduction with maintained urate lowering [91] | Gout patients with T2D (n=8,150) |
| Gout-Primary Hospitalizations/ED Visits | RR 0.52 (95% CI: 0.32, 0.84) [91] | Limited data on healthcare utilization | |
| Time to Effect | Relatively rapid effect (weeks to months) [86] | Requires months of sustained therapy | |
| Cardiovascular Benefits | Significant reduction in MACE and HF hospitalizations [90] [91] | Limited or neutral effects (FDA warning for febuxostat) [87] |
Cardiometabolic and Renal Outcomes
The cardiometabolic benefits of SGLT2 inhibitors represent a crucial differentiator:
- In a population-based cohort study, SGLT2i use was associated with lower risk of major adverse cardiovascular events (HR 0.87, 95% CI: 0.77-0.98) and heart failure hospitalization (HR 0.53, 95% CI: 0.38-0.76) compared to sulfonylureas [90].
- A systematic review and meta-regression found SGLT2 inhibitors lowered the risk of developing clinically relevant hyperuricemic events by 32-37% in patients with and without T2DM [58].
- For patients with chronic heart failure and hyperuricemia, dapagliflozin significantly reduced uric acid levels, enhanced cardiac function, and decreased cardiovascular mortality and hospitalization risk [88].
Traditional ULTs have not demonstrated consistent cardiorenal benefits, with febuxostat carrying an FDA warning for cardiovascular mortality risk [87].
Experimental Protocols for Investigating Lipid Metabolic Pathways in DH
Lipidomic Profiling Protocol
Objective: To characterize lipid metabolic perturbations in diabetes with hyperuricemia (DH) and evaluate therapeutic interventions.
Sample Preparation:
- Collection: Collect 5 mL fasting morning blood in EDTA tubes from DH patients, diabetes-only controls, and healthy subjects.
- Processing: Centrifuge at 3,000 rpm for 10 minutes at room temperature to isolate plasma.
- Storage: Aliquot 0.2 mL supernatant into 1.5 mL centrifuge tubes; store at -80°C [10].
Lipid Extraction:
- Thaw samples on ice and vortex.
- Combine 100 μL plasma with 200 μL 4°C water.
- Add 240 μL pre-cooled methanol and mix.
- Add 800 μL methyl tert-butyl ether (MTBE); sonicate 20 minutes in low-temperature water bath.
- Stand 30 minutes at room temperature; centrifuge at 14,000 g for 15 minutes at 10°C.
- Collect upper organic phase; dry under nitrogen [10].
UHPLC-MS/MS Analysis:
- Chromatography: Waters ACQUITY UPLC BEH C18 column (2.1 mm × 100 mm, 1.7 μm).
- Mobile Phase: A: 10 mM ammonium formate acetonitrile solution in water; B: 10 mM ammonium formate acetonitrile isopropanol solution.
- Gradient: 0-2 min, 60% B; 2-2.5 min, 60-85% B; 2.5-13 min, 85-100% B; 13-15 min, 100% B; 15-15.1 min, 100-60% B; 15.1-17 min, 60% B.
- Flow Rate: 0.3 mL/min; column temperature: 50°C; injection volume: 2 μL [10].
Data Processing and Statistical Analysis:
- Identification: Identify lipid molecules using tandem mass spectrometry and database matching.
- Multivariate Analysis: Perform PCA and OPLS-DA to visualize group separations.
- Differential Analysis: Apply Student's t-test and fold-change (FC) to identify significantly altered lipids.
- Pathway Analysis: Use MetaboAnalyst 5.0 to identify enriched metabolic pathways [10].
Clinical Trial Design for Comparative Efficacy
Target Trial Emulation Framework (adapted from [90] [91]):
Eligibility Criteria:
- Adults ≥18 years with T2D and hyperuricemia (SUA >6.0 mg/dL women, >7.0 mg/dL men)
- Exclusion: Active gout flare, history of cancer, recent ULT changes
Treatment Strategies:
- Intervention: SGLT2 inhibitor (empagliflozin 10-25 mg/d, dapagliflozin 10 mg/d)
- Comparator: Traditional ULT (allopurinol 300 mg/d) or alternative glucose-lowering agent
Outcome Assessment:
- Primary: Percentage change in SUA from baseline
- Secondary: Gout flare rates (defined by ED visit/hospitalization with primary gout diagnosis plus medication dispensing within 7 days), cardiovascular events, lipid parameters
Statistical Analysis:
- Use propensity score matching or overlap weighting to address confounding
- Employ Poisson regression for recurrent flare counts, Cox models for time-to-event outcomes
Diagram 1: Experimental workflow for comparative efficacy study
Analytical Framework: The Scientist's Toolkit
Essential Research Reagents and Platforms
Table 3: Key Research Reagents and Platforms
| Item | Function/Application | Example Specifications |
|---|---|---|
| UHPLC-MS/MS System | Untargeted lipidomic profiling; quantification of lipid species | Waters ACQUITY UPLC BEH C18 column (2.1 mm × 100 mm, 1.7 μm); electrospray ionization |
| Lipid Extraction Solvents | Comprehensive lipid extraction from plasma/serum | Methyl tert-butyl ether (MTBE), methanol, water in 8:2:2.5 ratio (v/v/v) |
| Internal Standards | Quantification normalization; quality control | Stable isotope-labeled lipid standards (e.g., d7-cholesterol, 13C-labeled fatty acids) |
| MetaboAnalyst Platform | Pathway analysis and visualization of lipidomic data | Version 5.0; incorporates lipid pathway databases (KEGG, Lipid Maps) |
| Cohort Database Platforms | Real-world evidence generation; target trial emulation | Population Data BC, UK Biobank, All of Us Research Program |
| Statistical Software | Advanced statistical analysis of clinical and omics data | R, Python (scikit-learn, statsmodels), SPSS, Stata |
Pathway Visualization: Lipid Metabolism in Diabetes-Hyperuricemia
Diagram 2: Metabolic crosstalk and SGLT2 inhibitor mechanisms in DH
Discussion and Future Research Directions
The evidence synthesized in this whitepaper positions SGLT2 inhibitors as multifaceted therapeutic agents that address hyperuricemia within the broader context of CKM syndrome. While traditional ULTs provide more potent absolute urate reduction, SGLT2 inhibitors offer the distinct advantage of concurrently addressing multiple cardiometabolic risk factors, including the perturbed glycerophospholipid and glycerolipid metabolism pathways characteristic of DH patients [10].
The clinical implications are substantial, particularly for the management of T2D patients with comorbid hyperuricemia or gout. SGLT2 inhibitors provide a dual-purpose therapeutic option that addresses both glycemic control and hyperuricemia while simultaneously reducing cardiovascular and renal risk. This is especially relevant given that hyperuricemia in T2D is associated with an increased risk of diabetic complications, including nephropathy, adverse cardiac events, and peripheral vascular disease [10].
Future research should prioritize several key areas:
- Mechanistic Studies: Further elucidation of the molecular pathways linking SGLT2 inhibition to lipid metabolism and inflammatory responses.
- Head-to-Head Trials: Direct comparative trials of SGLT2 inhibitors versus traditional ULTs, with comprehensive lipidomic profiling.
- Biomarker Development: Identification of lipid species that predict treatment response and cardiovascular risk reduction.
- Combination Therapies: Investigation of synergistic effects between SGLT2 inhibitors and traditional ULTs in refractory hyperuricemia.
The development of "dual-action" agents capable of simultaneously modulating glucose, urate, and lipid homeostasis represents the future of metabolic syndrome management [9]. SGLT2 inhibitors provide a foundational template for this approach, demonstrating that targeting interconnected metabolic pathways can yield benefits beyond singular parameter reduction.
SGLT2 inhibitors represent a significant advancement in the management of hyperuricemia in patients with type 2 diabetes, offering a favorable efficacy and safety profile alongside pleiotropic cardiorenal benefits. While traditional ULTs remain essential for patients with severe hyperuricemia or tophaceous gout, SGLT2 inhibitors provide a comprehensive metabolic intervention that addresses the interconnected pathways of glucose, urate, and lipid metabolism. Their demonstrated ability to reduce serum urate levels, prevent gout flares, and improve cardiovascular outcomes positions them as valuable therapeutic options, particularly for T2D patients with CKM syndrome. Future research integrating deep phenotyping and lipidomic profiling will further refine their place in the therapeutic armamentarium against metabolic diseases.
The Uric Acid to HDL-Cholesterol Ratio (UHR) has emerged as a novel, integrative biomarker with significant prognostic utility for cardiovascular risk assessment, particularly in complex metabolic patients. This technical review synthesizes evidence from recent population-based studies demonstrating that UHR effectively predicts all-cause mortality, cardiovascular mortality, and incident cardiovascular disease in patients with gout, metabolic dysfunction-associated steatotic liver disease (MASLD), and the general population. The underlying pathophysiology links lipid metabolic pathways and hyperuricemia, creating a synergistic pro-inflammatory state that accelerates atherosclerosis. We provide detailed methodological protocols for UHR validation, standardized analytical workflows, and practical frameworks for implementing this biomarker in clinical research and therapeutic development for diabetic populations with hyperuricemia.
Cardiovascular disease (CVD) remains a leading cause of global mortality, with its pathogenesis intricately linked to metabolic dysregulation. In patients with concurrent type 2 diabetes mellitus (T2DM) and hyperuricemia (HUA)—a comorbidity affecting 21-32% of diabetic populations—the need for refined risk stratification tools is particularly pressing [9]. The Uric Acid to HDL-Cholesterol Ratio (UHR) represents an innovative composite biomarker that integrates two crucial metabolic pathways: purine metabolism (represented by uric acid) and reverse cholesterol transport (represented by HDL cholesterol).
Uric acid, the final product of purine metabolism, contributes to atherosclerosis by oxidizing low-density lipoprotein cholesterol (LDL-C) and damaging vascular walls [92]. Conversely, high-density lipoprotein cholesterol (HDL-c) offers cardioprotective benefits through its antioxidant and anti-inflammatory properties [92]. Independently, both components have demonstrated limited predictive accuracy due to comorbidities affecting kidney function and lipid metabolism [92]. The UHR biomarker addresses this limitation by capturing the balance between pro-atherogenic and anti-atherogenic factors, providing a more systematic risk evaluation system that reflects underlying inflammatory and metabolic status [92] [93].
Pathophysiological Framework: Linking Hyperuricemia, Lipid Metabolism, and Cardiovascular Risk
The relationship between hyperuricemia and disrupted lipid metabolism creates a pathological synergy that accelerates cardiovascular disease progression in diabetic patients. The mechanistic interplay involves several interconnected pathways:
Bidirectional Metabolic Crosstalk
The comorbidity of T2DM and HUA represents a complex pathological condition characterized by concurrent disturbances in glucose and urate metabolism. The underlying pathophysiology is multifactorial, involving insulin resistance, oxidative stress, lipid metabolic dysfunction, and impaired renal urate excretion [9]. Hyperuricemia exacerbates insulin resistance and β-cell dysfunction by impairing renal uric acid excretion and activating oxidative stress (e.g., via the NF-κB pathway) and inflammatory cascades [9]. This metabolic crosstalk establishes a vicious cycle where hyperuricemia promotes endothelial dysfunction while reduced HDL functionality diminishes vascular protection.
Pro-Inflammatory and Pro-Atherogenic Pathways
Elevated uric acid contributes to atherosclerosis through multiple mechanisms: oxidation of LDL cholesterol, vascular smooth muscle proliferation, and stimulation of inflammatory cytokines [92]. Simultaneously, dysfunctional HDL in metabolic diseases loses its cardioprotective capacities, including reverse cholesterol transport, anti-inflammatory, and antioxidant functions [92] [93]. The UHR quantitatively captures this imbalance, with higher values indicating a dominance of pro-atherogenic over atheroprotective forces.
Diagram: Pathophysiological Pathways Linking Hyperuricemia and Lipid Metabolism in Cardiovascular Risk
Clinical Validation: Population Studies and Mortality Associations
Recent large-scale epidemiological studies have robustly validated the prognostic value of UHR for cardiovascular outcomes across diverse populations. The following table synthesizes key findings from major studies conducted between 2024-2025.
Table 1: Clinical Validation Studies of UHR for Cardiovascular Risk Assessment
| Study Population | Sample Size | Follow-up Duration | Key Findings on UHR | Statistical Significance |
|---|---|---|---|---|
| Gout Patients [92] | 1,479 | 2007-2018 | Q3 quartile (14-19%) had highest all-cause mortality (HR: 1.44) and cardiovascular mortality (HR: 1.73) | P < 0.001; 95% CI: 1.05-1.97 (all-cause), 1.04-2.87 (CVD) |
| General Population (CVD Incidence) [93] | 6,370 | 2001-2018 | Strong association with CVD incidence; Q4 (>19%) showed 11% CVD rate vs. Q1 (4.7%) | P < 0.001; progressive increase across quartiles |
| MASLD Patients [94] | 4,280 | 1999-2018 | 1-SD increase associated with 18% higher all-cause mortality | HR: 1.18; 95% CI: 1.07-1.30; P < 0.001 |
| General Population (Dyslipidemia) [93] | 4,117 | 2001-2018 | Significant positive association with dyslipidemia after adjustment | OR: 11.65; 95% CI: 8.995-15.17 |
Nonlinear Relationships and Threshold Effects
Restricted cubic spline analyses across multiple studies have revealed important nonlinear dynamics in UHR-mortality relationships:
- U-shaped association with all-cause mortality in gout patients, with significantly increased risk above a threshold of 21.6% (HR: 1.68, 95% CI: 1.26-2.24) [92]
- Linear positive correlation with cardiovascular mortality in the same population (HR: 1.40, 95% CI: 1.05-1.86) [92]
- Nonlinear relationships with CVD incidence in the general population, indicating potential threshold effects [93]
These pattern variations highlight the context-dependent nature of UHR interpretation and the importance of population-specific risk stratification.
Methodological Framework: Experimental Protocols for UHR Validation
Standardized UHR Calculation and Measurement
The UHR is calculated using the formula: UHR (%) = (UA [mg/dL] ÷ HDL [mg/dL]) × 100 [93]. Proper measurement requires strict adherence to standardized protocols:
Table 2: Analytical Methods for UHR Component Measurement
| Analyte | Measurement Method | Sample Processing | Quality Control |
|---|---|---|---|
| Serum Uric Acid (UA) | Timed endpoint method using uricase enzyme reaction on DxC800 automated chemistry analyzer [94] | Fasting blood samples collected in early morning; enzymatic oxidation to allantoin and hydrogen peroxide | Adherence to Westgard rules; CLIA 1988 standards; photometric quantification at 520 nm [93] |
| HDL Cholesterol | Direct immunoassay with magnesium sulfate/dextran solution precipitation [94] | Enzymatic hydrolysis of cholesterol esters; chromogen formation with 4-AAP and HSDA | NHANES QA/QC protocols; photometric detection at 600 nm; precipitation of non-HDL fractions [93] |
Covariate Assessment and Statistical Adjustment
Robust UHR validation requires comprehensive covariate assessment to account for potential confounders:
- Demographic factors: Age, gender, race/ethnicity [92] [93]
- Anthropometric measures: Body mass index (BMI), waist circumference [93]
- Lifestyle factors: Smoking status (never, former, current), alcohol consumption (never, former, current) [93]
- Comorbidities: Diabetes, hypertension, cancer, cardiovascular disease history [92] [94]
- Laboratory parameters: Liver enzymes (ALT, AST), renal function (creatinine), additional lipid profiles [92]
Statistical analyses should employ appropriate techniques for complex survey designs, including sample weighting, stratification, and clustering to ensure population representativeness [93] [94]. Recommended analytical approaches include Cox proportional hazards models for mortality outcomes, multivariate logistic regression for binary outcomes, and restricted cubic spline modeling for nonlinear relationship detection [92] [93].
Diagram: UHR Validation Study Design and Analytical Workflow
Research Implementation: Practical Toolkit for UHR Integration
Essential Research Reagents and Analytical Solutions
Table 3: Research Reagent Solutions for UHR Biomarker Studies
| Reagent/Category | Specific Examples | Research Function | Technical Considerations |
|---|---|---|---|
| Uric Acid Assay Kits | Uricase-based timed endpoint methods; 4-AAP and DCHBS chromogenic systems | Enzymatic quantification of serum uric acid via peroxidase-coupled reaction | Linear range: 1-20 mg/dL; interference from ascorbic acid, hemoglobin [94] |
| HDL Cholesterol Kits | Direct immunoassay kits with magnesium sulfate/dextran precipitation | Homogeneous measurement without separation steps | Standardized against CDC reference methods; non-HDL complex precipitation [93] |
| Automated Chemistry Analyzers | DxC800 series and comparable platforms | High-throughput simultaneous UA and HDL-C measurement | Integration with laboratory information systems; calibration verification [94] |
| Quality Control Materials | Commercial serum pools; NIST-traceable reference materials | Monitoring analytical performance across batches | Three-level controls (normal, borderline, abnormal); Westgard rule application [93] |
Data Standardization and Integration Protocols
The integration of UHR into clinical research requires addressing several methodological challenges:
- Structured data abstraction from electronic health records using standardized terminology [95]
- Cross-platform normalization to account for inter-laboratory methodological variations [95]
- Missing data protocols including multiple imputation techniques or random forest approaches for UHR component estimation [92]
- Longitudinal tracking of UHR trajectories rather than single measurements for dynamic risk assessment
The Uric Acid to HDL-Cholesterol Ratio represents a clinically actionable integrative biomarker that reflects the intersection of purine metabolism, lipid pathways, and inflammatory signaling. Validation across multiple large populations confirms its utility for cardiovascular risk stratification, particularly in complex patients with concurrent hyperuricemia and diabetes. Implementation in research settings requires strict adherence to standardized measurement protocols, appropriate statistical handling of nonlinear relationships, and consideration of population-specific thresholds.
Future research should prioritize randomized controlled trials evaluating UHR-guided therapeutic interventions, exploration of genetic determinants of UHR variability, and development of standardized reference materials for assay harmonization. Integration of UHR with omics technologies and digital health platforms represents a promising frontier for personalized cardiovascular risk assessment in metabolic disease populations.
The convergence of incretin-based therapies and microRNA (miRNA) biology is poised to redefine the therapeutic landscape for metabolic diseases, particularly in the complex interplay between diabetes, hyperuricemia, and lipid metabolic pathways. GLP-1R/GIPR dual agonists exemplify the shift toward multi-targeted therapeutics, demonstrating unprecedented efficacy in glycemic control and weight management. Parallelly, miRNA-based therapeutics offer a novel approach for precisely modulating the gene regulatory networks underlying diabetic complications. This whitepaper synthesizes current evidence and delineates the integrated future of these modalities, detailing molecular mechanisms, experimental methodologies, and their synergistic potential for creating personalized, mechanism-driven treatments for cardiorenal-metabolic diseases.
The management of type 2 diabetes (T2DM) and its comorbidities is undergoing a paradigm shift from simple glycemic control to a holistic approach that addresses intertwined pathophysiological pathways. The coexistence of metabolic disorders—including dyslipidemia, hyperuricemia, and insulin resistance—creates a vicious cycle that accelerates the progression of cardiorenal diseases [96]. Within this framework, two innovative therapeutic classes have emerged:
- GLP-1R/GIPR Dual Agonists: These represent the pinnacle of peptide engineering, leveraging the complementary actions of multiple incretin hormones to achieve superior metabolic outcomes.
- miRNA-Based Therapeutics: These agents target the post-transcriptional regulators of gene expression, offering a platform to intervene in the complex pathogenesis of diabetic complications.
The integration of these strategies is particularly pertinent for patients with hyperuricemia, a condition frequently associated with uncontrolled T2DM and lipid dysregulation, which reflects underlying renal and metabolic stress [51].
GLP-1R/GIPR Dual Agonists: Mechanism and Clinical Promise
Molecular Pharmacology and Signaling
Tirzepatide, the first-in-class dual GLP-1R and GIPR agonist, possesses a unique imbalanced affinity, with a five-fold weaker affinity for GLP-1R compared to the native peptide and a higher affinity for GIPR [97]. This specific profile drives a distinct and potent downstream signaling cascade. Upon receptor engagement, the primary signaling pathway involves Gs-mediated activation of adenylyl cyclase, leading to intracellular cyclic adenosine monophosphate (cAMP) accumulation. This canonical pathway activates protein kinase A (PKA) and the exchange protein directly activated by cAMP (Epac) [98] [79]. Beyond this, dual agonists engage parallel survival pathways, including PI3K/Akt, which inhibits glycogen synthase kinase-3β (GSK-3β) to enhance insulin signaling and provide cytoprotection [79]. Recent evidence also highlights the role of the Wnt/β-catenin signaling cascade, which is engaged via PKA-mediated inhibition of GSK-3β, thereby promoting tissue regeneration and β-cell proliferation [98] [79].
A critical aspect of their mechanism is the concentration-dependent role of β-arrestin-2. At pharmacological concentrations, β-arrestin-2 is essential for sustained extracellular signal-regulated kinase (ERK) activation and CREB phosphorylation, which promotes pancreatic β-cell survival [79]. Furthermore, emerging research on tirzepatide reveals unintended interactions with β-adrenoceptors (β-ARs) in cardiomyocytes. Molecular dynamics simulations indicate that TZPD binds with high affinity to β3-ARs, and in hyperglycemic or senescent cardiac cells, it decreases activated β3-ARs and protein kinase G (PKG) levels, normalizing depressed cAMP and cGMP and improving glucose uptake independent of its primary receptors [99]. This pleiotropic signaling underlines the multifaceted cardioprotective effects of these agents.
Quantitative Clinical Efficacy and Safety Profile
The therapeutic efficacy of dual agonists is demonstrated by robust outcomes from clinical trials, summarized in Table 1.
Table 1: Clinical Efficacy and Safety Profile of GLP-1R/GIPR Dual Agonists
| Parameter | Efficacy/Safety Outcome | Comparative Context |
|---|---|---|
| HbA1c Reduction | Superior reduction vs. conventional antidiabetics or selective GLP-1RAs [97] | |
| Weight Loss | Substantial weight loss, superior to mono-agonists [97] | Up to 22-24% with next-generation combinations (e.g., CagriSema) [79] |
| Cardiovascular Risk | Reduces major adverse cardiovascular events (MACE) [97] | Approx. 12% reduction vs. placebo for GLP-1RAs [97] |
| Renal Outcomes | Significant reduction in renal disease score, less glomerular filtration rate (GFR) decline [97] | |
| Common AEs | Gastrointestinal intolerance (nausea, vomiting, diarrhea) [97] | Affects up to half of patients; can lead to discontinuation [97] |
| Serious AEs | Potential risk of acute kidney injury (from dehydration), thyroid C-cell tumorigenesis (contraindicated in at-risk patients), acute pancreatitis, diabetic retinopathy [97] | Risk of acute pancreatitis appears higher in obese patients on long-term, high-dose therapy [97] |
Detailed Experimental Protocol: Assessing Dual Agonist Action in Cardiac Cells
Objective: To elucidate the direct cardioprotective effects and unintended receptor interactions of a dual agonist (e.g., Tirzepatide) in a model of hyperglycemia-induced cardiac dysfunction.
- Cell Line: H9c2 cardiomyocytes (embryonic rat heart cell line) [99].
- Treatment Groups:
- Control: Normal glucose medium (e.g., 5.5 mM glucose).
- Hyperglycemia (HG) Group: High glucose medium (e.g., 33 mM glucose for 48 hours).
- HG + TZPD Group: High glucose medium with Tirzepatide intervention.
- β3-ARs Overexpressed (β3OE) Group: H9c2 cells overexpressing β3-ARs, subjected to HG with/without TZPD [99].
- Methodologies:
- Western Blotting: Quantify protein levels of GLP-1R, GIP-R, β1/β2/β3-ARs, PKG, IRS-1, and GLUT4.
- cAMP/cGMP ELISA: Measure second messenger production in the presence or absence of specific receptor antagonists.
- Molecular Dynamics Simulations: Study the binding affinity and interaction of TZPD with GLP-1R, GIP-R, and β-ARs.
- Immunofluorescence Microscopy: Visualize the translocation of GLUT4 to the sarcolemma.
- Calcium Imaging: Assess the regulation of intracellular Ca2+ handling using fluorescent dyes (e.g., Fura-2AM) [99].
- Key Outcome Measures: Normalization of cAMP/cGMP levels, reduction in activated β3-ARs and PKG, increased GLUT4 translocation and protein levels, and improved cellular Ca2+ regulation.
miRNA-Based Therapeutics: Precision Targeting of Complications
miRNAs as Circulating Biomarkers and Therapeutic Targets
MicroRNAs are small non-coding RNAs that post-transcriptionally regulate gene expression. Their dysregulation is implicated in the metabolic memory phenomenon, whereby the effects of hyperglycemia persist long after glucose normalization, driving the progression of vascular complications [100]. A systematic review identified 79 miRNAs differentially expressed in diabetic complications, with miRNA-126, miRNA-192, and others reported across multiple studies [100]. These miRNAs represent promising circulating biomarkers for early diagnosis and prognostic assessment.
Table 2: Key miRNA Signatures in Diabetic Complications
| Complication | Dysregulated miRNAs | Predicted Target Genes (Examples) | Associated Pathways |
|---|---|---|---|
| Diabetic Cardiomyopathy (DC) | hsa-miR-126-3p, hsa-miR-133a-3p, hsa-miR-1-3p [100] | PTPN9, PLXNB2, ITGA6 (miR-126-3p) [100] | Angiogenesis, cardiomyocyte viability |
| Diabetic Retinopathy (DR) | hsa-miR-15a-3p, hsa-miR-320a, hsa-miR-200a-3p [100] | RNF13, ZNF654 (miR-15a-3p) [100] | Apoptosis, vascular permeability |
| Diabetic Nephropathy (DN) | hsa-miR-192, hsa-miR-21 [100] | Fibrosis, inflammation | |
| Shared Across Complications | miRNA-126, miRNA-192 [100] | Endothelial dysfunction, oxidative stress |
KEGG pathway enrichment analysis of these miRNAs reveals involvement in 103 distinct pathways, encompassing chronic inflammation, endoplasmic reticulum stress, and vascular endothelial dysfunction [100]. This provides a roadmap for targeting interconnected pathological processes.
Experimental Protocol: miRNA Profiling and Functional Validation
Objective: To identify and validate the functional role of a specific miRNA in a model of diabetic complication.
- Step 1: Patient Selection and miRNA Profiling
- Cohort: Recruit patients with T2DM, stratified by complication status (e.g., nephropathy, retinopathy) and matched controls.
- Sample Type: Blood specimens (plasma or serum) [100].
- Profiling Technique: Next-generation sequencing (NGS) or RT-qPCR panels to identify differentially expressed miRNAs.
- Step 2: Bioinformatic Analysis
- Target Prediction: Use algorithms from DIANA-microT-CDS and TargetScan to predict miRNA target genes. Select genes predicted by both tools to improve accuracy [100].
- Pathway Enrichment: Perform KEGG pathway analysis using tools like miRPathDB to identify biological pathways significantly enriched for the predicted target genes [100].
- Step 3: In Vitro Functional Validation
- Cell Model: Use relevant cell lines (e.g., renal mesangial cells for DN, retinal endothelial cells for DR).
- Gain/Loss-of-Function: Transfect cells with miRNA mimics (to overexpress) or inhibitors (antagomiRs) to modulate miRNA levels.
- Functional Assays:
- Luciferase Reporter Assay: Clone the wild-type and mutated 3'UTR of a predicted target gene into a reporter vector to confirm direct binding.
- Western Blotting/qPCR: Assess the impact on target gene expression at the protein and mRNA levels.
- Phenotypic Assays: Measure cell proliferation, apoptosis, migration, and inflammation in response to miRNA modulation.
Integrated Future: Combining Agonists and miRNA Therapeutics
The true future potential lies in the synergistic combination of dual agonists and miRNA therapeutics. This approach can target multiple layers of disease pathology: dual agonists provide systemic metabolic optimization, while miRNA-based drugs can be designed to fine-tune tissue-specific responses or mitigate off-target effects. For instance, an antagomiR targeting a miRNA that promotes hepatic lipid synthesis could complement the weight loss and lipid-lowering effects of tirzepatide. Furthermore, miRNA signatures can serve as pharmacogenetic biomarkers to predict individual response to dual agonist therapy, paving the way for truly personalized treatment regimens [97] [100].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Dual Agonists and miRNA Therapeutics
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Tirzepatide (TZPD) | Dual GLP-1R/GIPR agonist for in vitro and in vivo studies | Investigating direct cardiac effects in H9c2 cells under hyperglycemia [99] |
| GLP-1R Antagonists (e.g., Exendin(9-39)) | Pharmacological blockade of GLP-1R | Mechanistic studies to isolate GIPR-specific effects in dual agonism [99] |
| β3-ARs Agonists/Antagonists | Tools to probe unintended receptor interactions | Studying TZPD's modulation of β-adrenergic signaling in cardiomyocytes [99] |
| miRNA Mimics & AntagomiRs | Chemically modified RNAs for miRNA overexpression or inhibition | Functional validation of miRNA targets in disease-relevant cell models [100] |
| cAMP/GMP ELISA Kits | Quantify second messenger levels in cell lysates | Measuring proximal GLP-1R/GIPR and β-AR signaling activity [99] |
| GLUT4 Translocation Assay | Detect GLUT4 movement to the plasma membrane | Assessing insulin-independent glucose uptake mechanisms [99] |
| DIANA-microT-CDS / TargetScan | In silico prediction of miRNA target genes | Identifying putative mRNA targets of a dysregulated miRNA [100] |
Visualizing Signaling and Workflows
Dual Agonist Pleiotropic Signaling
miRNA Discovery & Validation Workflow
The concurrent development of GLP-1R/GIPR dual agonists and miRNA-based therapeutics marks a pivotal advancement in metabolic disease management. Dual agonists offer powerful, multi-system benefits, while miRNAs provide the granularity needed for precision medicine. Future research must focus on integrating these approaches, using miRNA biomarkers for patient stratification, and developing combinatorial therapies that simultaneously correct systemic metabolism and tissue-specific pathophysiological pathways. This integrated strategy holds the promise of not only managing but potentially reversing the progression of diabesity and its devastating complications.
Conclusion
The intricate interplay between lipid metabolic pathways and hyperuricemia in diabetes represents a critical pathophysiological axis with significant diagnostic and therapeutic implications. Key findings confirm that specific disruptions in glycerophospholipid and glycerolipid metabolism, identifiable through advanced lipidomics, are central to this comorbidity. The development of integrated biomarkers, such as the UHR and RMRS, offers practical tools for risk stratification, while emerging therapeutic strategies—including GLP-1-based therapies and novel small molecule inhibitors—hold promise for multi-targeted intervention. Future research must prioritize longitudinal studies to validate these lipid species as clinical biomarkers, further elucidate the causal mechanisms through Mendelian randomization, and accelerate the development of dual-action therapeutics that concurrently address hyperglycemia, dyslipidemia, and hyperuricemia. This integrated approach is essential for advancing personalized medicine and improving outcomes for patients with these interconnected metabolic disorders.
References
- 1. Interrelationship Between Dyslipidemia and Hyperuricemia in... [https://www.mdpi.com/2227-9032/13/20/2605]
- 2. Interrelationship Between Dyslipidemia and Hyperuricemia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562356/]
- 3. Hyperuricemia and its related diseases: mechanisms and ... [https://www.nature.com/articles/s41392-024-01916-y]
- 4. Dyslipidemia and hyperuricemia: a cross-sectional study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10759755/]
- 5. and Dyslipidemia : a cross-sectional study of residents... hyperuricemia [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-023-01528-7]
- 6. Frontiers | Triglycerides as a mediator in the hyperuricemia -diabetes... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1645766/full]
- 7. Different Risk for Hypertension, Diabetes, Dyslipidemia , and... [https://pubmed.ncbi.nlm.nih.gov/30081468/]
- 8. The effect of lipid metabolism disorder on patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10598229/]
- 9. Revisiting the metabolic crosstalk between type 2 diabetes ... [https://www.sciencedirect.com/science/article/abs/pii/S0925443925004521]
- 10. UHPLC-MS/MS-based plasma untargeted lipidomic ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1656458/full]
- 11. Associations of Plasma Lipidomic Profiles with Uric Acid ... [https://link.springer.com/article/10.1007/s43657-024-00157-x]
- 12. Triglycerides as a mediator in the hyperuricemia-diabetes link [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462057/]
- 13. Evaluation of the Effects of High Uric Acid on Glucolipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12474470/]
- 14. The link between hyperuricemia and diabetes: insights from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11842261/]
- 15. Exploring lipidomics in biomarker discovery [https://pubmed.ncbi.nlm.nih.gov/41197707/]
- 16. Lipidomics coupled with pathway analysis characterizes ... [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-019-1054-z]
- 17. Immunocyte lipid metabolic reprogramming: a novel pathway ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631377/]
- 18. Metabolic regulation of the immune system in health and ... [https://www.nature.com/articles/s41392-024-01954-6]
- 19. The Interplay Between Oxidative Stress and Lipid ... [https://www.mdpi.com/1422-0067/26/17/8544]
- 20. Recent Advances in Liquid Chromatography–Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204688/]
- 21. Metabolic pathway analysis of hyperuricaemia patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9805114/]
- 22. Development and application of a fast ultra-high ... [https://www.sciencedirect.com/science/article/pii/S002196732200317X]
- 23. Analytical quality control in targeted lipidomics [https://www.sciencedirect.com/science/article/pii/S0003267025006191]
- 24. Streamlining Lipidomics: Novel Statistical Workflows and ... [https://www.chromatographyonline.com/view/streamlining-lipidomics-novel-statistical-workflows-and-visualization-in-r-and-python]
- 25. Ultrahigh-Performance Liquid Chromatography–Mass ... [https://www.chromatographyonline.com/view/ultrahigh-performance-liquid-chromatography-mass-spectrometry-lipidomics-2]
- 26. Mass Spectrometry in Analytical Lipidomics [https://www.spectroscopyonline.com/view/mass-spectrometry-analytical-lipidomics-1]
- 27. Multivariate Data Analysis Methods and Their Application in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12280249/]
- 28. Metabolic crosstalk and therapeutic interplay between ... [https://www.sciencedirect.com/science/article/pii/S0168822725002189]
- 29. PCA vs PLS-DA vs OPLS-DA: Which One to Choose for ... [https://www.metwarebio.com/metabolomic-analyses-comparison-of-pca-pls-da-and-opls-da/]
- 30. Integrating lipidomics and machine learning to characterize ... [https://www.sciencedirect.com/science/article/pii/S003257912500481X]
- 31. The effect of lipid metabolism disorder on patients with ... [https://www.nature.com/articles/s41598-023-45564-8]
- 32. The strategic role of lipidomics in biomarker identification ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1546512/full]
- 33. High uric acid exacerbates nonalcoholic steatohepatitis ... [https://www.sciencedirect.com/science/article/pii/S002192582502099X]
- 34. Higher uric acid associated with elevated IL‑6 and IL‑1β levels ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12316710/]
- 35. MetaboAnalyst: a web server for metabolomic data analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2703878/]
- 36. Statistical Analysis [https://www.metaboanalyst.ca/resources/vignettes/Statistical_Analysis_Module.html]
- 37. Data Formats [https://www.metaboanalyst.ca/docs/Format.xhtml]
- 38. Lipid Biomarkers and Cardiometabolic Diseases: Critical ... [https://www.mdpi.com/2218-1989/15/2/108]
- 39. Plasma Lipidomics Identifies Unique Lipid Signatures and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8581228/]
- 40. Direct MS Enabled Discovery of Lipid Signatures with ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708525005394]
- 41. Alterations in lipidome profiles distinguish early-onset ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10693150/]
- 42. Identification of novel lipid metabolism-related biomarkers ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1681989/full]
- 43. Associations between lipid-lowering drugs and urate and ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1398023/full]
- 44. HMG-CoA Reductase Inhibitors Suppress Monosodium ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10145217/]
- 45. Triglycerides as a mediator in the hyperuricemia-diabetes ... [https://pubmed.ncbi.nlm.nih.gov/41019336/]
- 46. Mediation effect of metabolic factors and inflammation on ... [https://www.sciencedirect.com/science/article/abs/pii/S1933287424001843]
- 47. Taurine alleviates dysfunction of cholesterol metabolism ... [https://www.sciencedirect.com/science/article/pii/S0022227525000069]
- 48. Diabetes mediates the association between uric acid to ... [https://www.nature.com/articles/s41598-025-19388-7]
- 49. Serum uric acid, renal status, cardiovascular-kidney ... [https://pubmed.ncbi.nlm.nih.gov/40809993/]
- 50. Serum uric acid, renal status, cardiovascular-kidney ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344259/]
- 51. Integrating Renal and Metabolic Parameters into a Derived ... [https://www.mdpi.com/1648-9144/61/11/2042]
- 52. Association between metabolic syndrome and uric acid [https://www.nature.com/articles/s41598-022-22025-2]
- 53. Serum uric acid to creatinine ratio as a predictor of insulin ... [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-025-01860-0]
- 54. Hyperuricemia - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK459218/]
- 55. Asymptomatic Hyperuricemia – A silent activator of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7075706/]
- 56. Drug-induced gout [https://www.sciencedirect.com/science/article/abs/pii/S095035790580295X]
- 57. Hyperuricemia and Gout Reduction by SGLT2 Inhibitors in ... [https://pubmed.ncbi.nlm.nih.gov/38199714/]
- 58. Reducing hyperuricemic events with SGLT2 inhibitors [https://www.sciencedirect.com/science/article/abs/pii/S2530016424001472]
- 59. Revealing the hidden impact of SGLT2 inhibitors on uric ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1667438/full]
- 60. Diabetes mediates the association between uric acid to high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511334/]
- 61. The role of insulin resistance in the relationship between ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1660317/full]
- 62. Evaluation of febuxostat in treating diabetic kidney disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597919/]
- 63. Prescription Screening for Drug Interaction Identification in ... [https://journal-jps.com/new/index.php/jps/article/view/894]
- 64. Assessment of drug induced hyperuricemia and gout risk ... [https://www.nature.com/articles/s41598-025-06114-6]
- 65. Advances in drug delivery systems for the management of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521190/]
- 66. The Management of Diabetes with Hyperuricemia: Can We Hit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10757772/]
- 67. Metabolic phenotypes: Molecular bridges between health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615335/]
- 68. Advancements in precision medicine: multi-omics ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1506767/full]
- 69. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/pii/S0009898125005777?dgcid=rss_sd_all]
- 70. Transform diabetes care with precision medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10616361/]
- 71. Unraveling the complexities of diet induced obesity and ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01837-y]
- 72. Mitochondrial and cellular mechanisms for managing lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4116787/]
- 73. MTCH2 modulates CPT1 activity to regulate lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494973/]
- 74. Lipid droplet dynamics in type 2 diabetes and its complications [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-025-02747-8]
- 75. FAT/CD36 Participation in Human Skeletal Muscle Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9821548/]
- 76. CD36 serves as a signaling receptor and Free Fatty Acid ... [https://pubmed.ncbi.nlm.nih.gov/40990667/]
- 77. The Multifunctionality of CD36 in Diabetes Mellitus and Its ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7465275/]
- 78. Current Perspectives on GLP-1 Agonists in Contemporary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12511252/]
- 79. Emerging Frontiers in GLP-1 Therapeutics [https://www.mdpi.com/1999-4923/17/8/1036]
- 80. Glucagon-Like Peptide-1: New Regulator in Lipid Metabolism [https://www.e-dmj.org/journal/view.php?number=2843]
- 81. Glucagon-like peptide-1 receptor: mechanisms and ... [https://www.nature.com/articles/s41392-024-01931-z]
- 82. GLP-1 receptor agonists synergistic effects of metabolic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1614726/full]
- 83. Mechanisms of action and therapeutic applications of GLP ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2024.1431292/full]
- 84. Mechanistic Pathways and Clinical Implications of GLP-1 ... [https://www.mdpi.com/1422-0067/25/17/9351]
- 85. Glucagon-Like Peptide-1 Receptor Agonists - StatPearls - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK551568/]
- 86. SGLT-2 inhibitors: Diabetes and CKD and CHF (and gout?) ... [https://www.ccjm.org/content/91/7/392]
- 87. Serum uric acid reduction through SGLT2 inhibitors [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1551390/full]
- 88. Dual benefits of sodium-glucose cotransporter 2 inhibitors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11752429/]
- 89. Revealing the hidden impact of SGLT2 inhibitors on uric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580082/]
- 90. Sodium-Glucose Cotransporter-2 Inhibitors vs Sulfonylureas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11019449/]
- 91. Comparative effectiveness of sodium-glucose cotransporter-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11921103/]
- 92. Association of serum uric acid to high-density lipoprotein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12628874/]
- 93. Association between the uric acid-to-HDL-cholesterol ratio ... [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-025-02551-4]
- 94. Serum uric acid to high-density lipoprotein cholesterol ratio ... [https://www.nature.com/articles/s41598-025-94651-5]
- 95. Overcoming challenges to integrating biomarker data into ... [https://cotahealthcare.com/news/tech-developments/overcoming-challenges-to-integrating-biomarker-data-into-clinical-trials/]
- 96. Role of metabolic conditions in cardiorenal diseases [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1701084/full]
- 97. Deliberating the striking effect of dual GLP-1R and GIPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596976/]
- 98. Engineered GLP-1R-targeting nanoplatforms: multimodal ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03677-4]
- 99. The dual GLP-1 and GIP receptor agonist tirzapetide provides ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-025-02828-z]
- 100. Discovering diabetes complications-related microRNAs [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079836/]