LncRNAs as Clinical Tools: From Discovery to Diagnostic Validation in Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) remains a leading cause of cancer-related mortality worldwide, largely due to late-stage diagnosis.
LncRNAs as Clinical Tools: From Discovery to Diagnostic Validation in Hepatocellular Carcinoma
Abstract
Hepatocellular carcinoma (HCC) remains a leading cause of cancer-related mortality worldwide, largely due to late-stage diagnosis. This comprehensive review examines the burgeoning role of long non-coding RNAs (lncRNAs) as biomarkers for HCC, addressing the complete validation pipeline from foundational discovery to clinical application. We explore the biological rationale for lncRNA involvement in hepatocarcinogenesis, methodological approaches for identification and verification, troubleshooting for analytical challenges, and rigorous validation against current clinical standards. For researchers and drug development professionals, this synthesis provides critical insights into how lncRNA biomarkers can revolutionize early detection, prognostic stratification, and personalized treatment strategies for HCC patients, ultimately aiming to improve dismal survival rates.
The Biological Landscape: Understanding LncRNA Roles in Hepatocellular Carcinoma Pathogenesis
HCC Clinical Burden and the Urgent Need for Improved Biomarkers
The Global Clinical Burden of Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) represents a significant global health challenge, characterized by poor prognosis, high recurrence rates, and limited responsiveness to current therapies. As the predominant form of primary liver cancer, HCC accounts for approximately 85-90% of all cases and stands as the third leading cause of cancer-related mortality worldwide [1] [2]. Epidemiological data reveal a concerning rise in HCC incidence, particularly in Western countries, where the age-adjusted rate has surged over the past three decades [3].
The pathogenesis of HCC involves complex biological processes including DNA damage, epigenetic modification, and oncogene mutation, with risk factors encompassing chronic hepatitis B (HBV) and C (HCV) infections, alcohol consumption, nonalcoholic fatty liver disease (NAFLD), and metabolic dysfunction-associated steatotic liver disease (MASLD) [1] [3]. While viral hepatitis has historically been the predominant cause, the burden of HCC is increasingly shifting toward non-viral aetiologies, such as ALD (alcohol-related liver disease) and MASLD [1].
Table 1: Current Challenges in HCC Clinical Management
| Challenge Area | Specific Limitations | Impact on Patient Outcomes |
|---|---|---|
| Early Detection | Limited sensitivity of ultrasound (~50%); high cost of MRI for routine surveillance [2] | Majority of patients diagnosed at advanced stages with limited curative options [4] |
| Diagnostic Biomarkers | AFP limitations in sensitivity and specificity [5] [2] | Missed early-stage diagnoses; reduced therapeutic window |
| Therapeutic Options | Low response rates to systemic therapies; drug resistance [6] [2] | Median overall survival remains limited even with treatment |
| Prognostic Prediction | Heterogeneity of HCC molecular profiles [2] | Suboptimal treatment outcomes for patients with atypical molecular profiles |
| Surveillance Access | Underuse of biannual ultrasound and AFP testing [1] | Delayed diagnosis in high-risk populations |
Limitations of Current Biomarkers and Diagnostic Modalities
The current landscape of HCC diagnosis relies on a combination of imaging techniques and serum biomarkers, each with significant limitations. While the National Comprehensive Cancer Network (NCCN) guidelines recommend semi-annual abdominal ultrasound and alpha-fetoprotein (AFP) screening for high-risk individuals, the diagnostic accuracy of ultrasound is only approximately 50%, and its sensitivity is limited for early lesions and tumor nodules [7] [2].
Alpha-fetoprotein (AFP) remains one of the most widely used biomarkers for HCC diagnosis, but its limitations in sensitivity and specificity are well-documented [5] [2]. Elevated AFP levels are not exclusive to HCC, as they can also occur in chronic liver conditions without malignancy, leading to false positives. Conversely, a significant proportion of HCC patients, particularly those with early-stage disease, do not exhibit elevated AFP levels, resulting in false negatives [5].
Other biomarkers such as glypican-3 (GPC3) and des-gamma-carboxy prothrombin (DCP) have shown promise but have not replaced AFP in clinical practice [5] [2]. The GALAD score (incorporating gender, age, AFP, AFP-L3, and PIVKA-II) and ASAP score (incorporating age, gender, AFP, and PIVKA-II) have demonstrated improved sensitivity for early-stage HCC screening, but their implementation faces challenges, particularly in developing countries due to limited availability of PIVKA-II and AFP-L3 testing [7].
Tissue biopsy, while providing definitive histological diagnosis, is invasive and carries risks including pain, bleeding, and potential intrahepatic metastasis from tumor cell detachment [2]. This limitation has accelerated the search for non-invasive alternatives, particularly liquid biopsy approaches that can provide valuable molecular information with minimal patient risk.
LncRNAs as Emerging Biomarkers in HCC
Long non-coding RNAs (lncRNAs) have emerged as critical regulators of gene expression in HCC, influencing tumorigenesis, metastasis, and therapy resistance through mechanisms such as miRNA sponging, chromatin remodeling, and protein interactions [6]. These RNA molecules, defined as transcripts longer than 200 nucleotides without protein-coding capacity, represent a promising frontier in biomarker discovery for precision diagnostics and targeted therapeutics [6] [3].
LncRNAs demonstrate several characteristics that make them ideal biomarker candidates. They exhibit high tissue specificity and can be detected in various body fluids, making them suitable for liquid biopsy applications [8] [2]. Their expression patterns show significant alterations in HCC compared to normal tissue, with specific lncRNAs associated with advanced tumor stages, metastasis, and poor prognosis [3] [9].
A meta-analysis of 40 studies evaluating 71 types of lncRNAs revealed that inconsistent expression levels of lncRNAs have positive statistical significance for prognostic prediction. Patients with elevated expression levels of oncogenic lncRNAs had a 1.25-fold higher risk of poor overall survival and a 1.66-fold higher risk of recurrence-free survival compared to patients with low expression levels [9].
Table 2: Promising LncRNA Biomarkers in HCC and Their Clinical Significance
| LncRNA | Expression in HCC | Prognostic Value | Proposed Mechanisms |
|---|---|---|---|
| HULC | Upregulated [9] | Poor OS [9] | Promotes phosphorylation of YB-1, activating downstream signaling pathways [9] |
| HOTAIR | Upregulated [9] | Poor OS [9] | Epigenetic regulation; promotes proliferation, migration, apoptosis resistance [3] |
| MEG3 | Downregulated [9] | Better OS when expressed [9] | Tumor suppressor function; induces cell cycle arrest and apoptosis [9] |
| NEAT1 | Upregulated [3] | Poor OS [3] | Regulates proliferation, migration, and apoptosis through multiple pathways [3] |
| H19 | Upregulated [3] | Poor OS [3] | Stimulates CDC42/PAK1 axis by down-regulating miRNA-15b [3] |
| DANCR | Upregulated [9] | Poor OS [9] | Promotes stemness and tumor progression [9] |
The regulatory role of lncRNAs in autophagy presents a particularly promising area for biomarker development. Autophagy plays a paradoxical role in HCC, acting as a tumor suppressor during initiation but promoting survival and progression in advanced stages [6]. LncRNAs have been shown to integrate into key signaling networks of autophagy (e.g., PI3K/AKT/mTOR, AMPK, Beclin-1), influencing drug resistance including resistance to first-line agents by altering autophagic flux and associated molecular pathways [6].
Experimental Protocols for LncRNA Biomarker Validation
Sample Collection and Processing
For lncRNA biomarker studies, collect paired tumor and adjacent non-tumor liver tissues (at least 2 cm away from tumor margin) from HCC patients undergoing surgical resection. Immediately snap-freeze tissue samples in liquid nitrogen and store at -80°C until RNA extraction. For liquid biopsy applications, collect peripheral blood in EDTA-containing tubes, process within 2 hours of collection to separate plasma, and store at -80°C in small aliquots to avoid freeze-thaw cycles [4] [2].
RNA Extraction and Quality Control
Extract total RNA from tissues or plasma using TRIzol reagent or specialized kits for biofluids. Treat samples with DNase I to remove genomic DNA contamination. Assess RNA quality and integrity using Agilent Bioanalyzer or similar systems, ensuring RNA Integrity Number (RIN) >7.0 for tissue samples. For plasma samples, concentrate circulating RNA using precipitation methods and verify the absence of hemolysis which can interfere with lncRNA detection [4] [9].
LncRNA Expression Profiling
For discovery phase studies, utilize next-generation sequencing (RNA-Seq) to identify differentially expressed lncRNAs. Prepare libraries using Illumina-compatible kits with ribosomal RNA depletion to enrich for non-coding RNAs. Sequence on Illumina platforms with minimum 30 million paired-end reads per sample. For validation studies, use quantitative real-time PCR (qRT-PCR) with SYBR Green or TaqMan chemistry. Design primers to span exon-exon junctions where applicable. Normalize expression data using stable reference genes (GAPDH, β-actin, or combination of multiple housekeeping genes) determined by stability algorithms [4] [9].
Functional Validation assays
| Assay Type | Key Reagents | Readout | Application in HCC LncRNA Studies |
|---|---|---|---|
| Gene Knockdown | siRNA or shRNA targeting specific lncRNAs; Lipofectamine RNAiMAX transfection reagent | qRT-PCR for knockdown efficiency; functional assays | Determine oncogenic function of upregulated lncRNAs [4] |
| Overexpression | lncRNA expression plasmids; Lipofectamine 3000 transfection reagent | qRT-PCR for overexpression efficiency; functional assays | Determine tumor suppressor function of downregulated lncRNAs [4] |
| Proliferation Assay | CCK-8 kit; colony formation assay reagents | Absorbance measurement; colony counting | Assess impact on HCC cell growth [4] |
| Migration/Invasion Assay | Transwell chambers with or without Matrigel coating | Cell counting after migration/invasion | Evaluate metastatic potential [4] |
| Xenograft Models | Immunodeficient mice (e.g., BALB/c nude mice) | Tumor growth measurement; immunohistochemistry | Validate in vivo tumorigenic effects [4] |
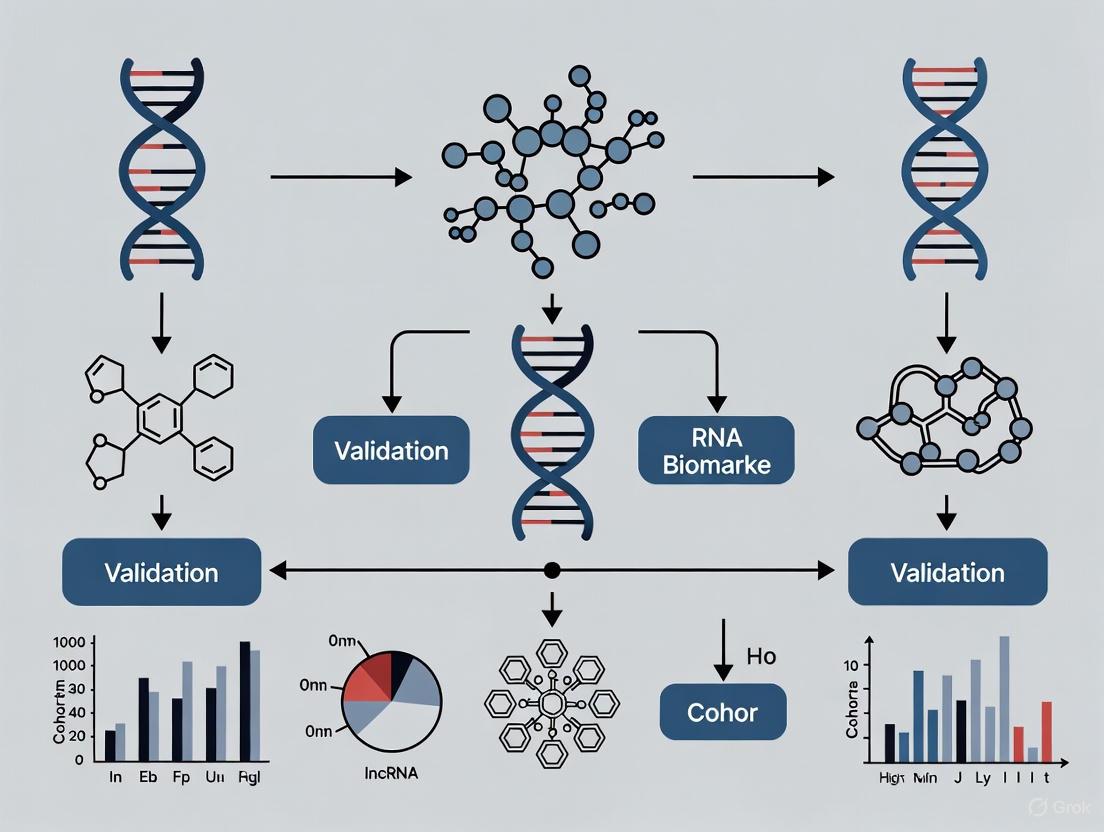
LncRNA Biomarker Discovery Workflow
Research Reagent Solutions for HCC LncRNA Studies
Table 4: Essential Research Reagents for HCC LncRNA Investigations
| Reagent Category | Specific Products | Application Notes |
|---|---|---|
| RNA Extraction | TRIzol Reagent, miRNeasy Mini Kit, Circulating RNA Extraction Kits | For tissue and biofluid samples; include DNase treatment [4] |
| RNA Quality Assessment | Agilent Bioanalyzer RNA Nano Kit, Qubit RNA Assay Kits | Essential for ensuring sample integrity before sequencing [4] |
| Library Preparation | Illumina TruSeq Stranded Total RNA Kit, KAPA RNA HyperPrep Kit | Use with RiboErase for ribosomal RNA depletion [4] [8] |
| qRT-PCR Reagents | SYBR Green Master Mix, TaqMan RNA-to-Ct Kits, Custom TaqMan Assays | Validate sequencing results; specific probe design for lncRNAs [9] |
| Cell Culture | HCC cell lines (HepG2, Huh7, PLC/PRF/5), Culture Media, FBS | Maintain under standard conditions for functional studies [4] |
| Transfection Reagents | Lipofectamine RNAiMAX, Lipofectamine 3000 | Optimize for each cell line; include appropriate controls [4] |
| Functional Assays | CCK-8 Kit, Matrigel Invasion Chambers, Annexin V Apoptosis Kit | Standardize protocols across experiments [4] |
Signaling Pathways in HCC Regulated by LncRNAs
LncRNA Regulatory Networks in HCC
The clinical burden of HCC continues to present significant challenges, necessitating innovative approaches to early detection, prognosis prediction, and treatment stratification. The limitations of current biomarkers and diagnostic modalities highlight the urgent need for more precise molecular tools. LncRNAs represent promising candidates that could address these deficiencies, offering high specificity, detectability in liquid biopsies, and functional relevance to HCC pathogenesis.
Future research directions should focus on validating lncRNA signatures in large, multi-center cohorts to establish standardized detection protocols and clinical cutoff values. The integration of lncRNA biomarkers with existing clinical parameters, imaging findings, and other molecular markers may further enhance their utility. Additionally, the development of targeted therapeutic approaches based on lncRNA mechanisms, such as antisense oligonucleotides, siRNAs, or CRISPR/Cas systems, represents an exciting frontier in HCC management that warrants further investigation [6].
As the field advances, the translation of lncRNA research from bench to bedside holds the potential to significantly improve outcomes for HCC patients through earlier detection, more accurate prognosis, and personalized treatment strategies tailored to individual molecular profiles.
LncRNA Biogenesis, Classification, and Functional Mechanisms in Oncogenesis
Long non-coding RNAs (lncRNAs), defined as transcripts longer than 200 nucleotides with limited or no protein-coding capacity, have emerged as critical regulators of gene expression in both physiological and pathological processes. Their roles in oncogenesis, particularly in hepatocellular carcinoma (HCC), are rapidly being elucidated. This application note provides a comprehensive overview of lncRNA biogenesis, classification systems, and diverse functional mechanisms, with specific emphasis on their utility as biomarkers in HCC cohorts. We summarize current experimental protocols for lncRNA investigation and present visualized signaling pathways to facilitate research in this evolving field, offering a structured framework for biomarker validation in HCC research programs.
Once considered "transcriptional noise," lncRNAs are now recognized as functional RNA molecules transcribed by RNA polymerase II (and less commonly, Pol I and Pol III) that play crucial roles in regulating gene expression at epigenetic, transcriptional, and post-transcriptional levels [10] [11]. The human genome encodes thousands of lncRNAs, which exhibit stronger cell-type, tissue, and spatial-temporal specificity compared to protein-coding genes, making them particularly attractive as tissue-specific biomarkers and therapeutic targets [10] [11]. In hepatocellular carcinoma (HCC), the third leading cause of cancer-related death worldwide, lncRNAs have demonstrated significant clinical potential for early detection, prognosis prediction, and therapeutic monitoring [12] [13] [14].
LncRNA Biogenesis and Classification
Molecular Biogenesis
LncRNA biogenesis shares similarities with mRNA processing but also exhibits distinct characteristics. Most lncRNAs are transcribed by RNA polymerase II, harboring a 5' methyl-cytosine cap and 3' poly(A) tail, and undergo splicing similar to mRNAs [10] [11]. However, they can also be processed through noncanonical mechanisms:
- Cleavage by RNase P: Mature 3' end formation through recognition and cleavage of tRNA-like structures (e.g., MALAT1, Menβ) [10]
- snoRNP complex capping: Enhanced stability through capping by snoRNA-protein complexes at both ends [10]
- Circular RNA formation: Generation of circular structures through back-splicing that protect against degradation [10] [11]
The biogenesis of lncRNAs is regulated by various epigenetic modifications and regulators. For instance, H3K56 acetylation and the chromatin remodeler SWI/SNF promote antisense lncRNA transcription, while the chromatin assembly factor complex CAF-1 represses this process [10]. Additionally, degradation pathways mediated by exosomes with Nrd1-Nab3-Sen1 and TRAMP complexes in the nucleus or by Xrn1 in the cytoplasm tightly control lncRNA homeostasis [10].
Classification Systems
LncRNAs can be classified based on various characteristics, with genomic position relative to protein-coding genes serving as a primary organizational framework:
Table 1: LncRNA Classification Based on Genomic Context
| Classification Type | Genomic Relationship | Example |
|---|---|---|
| Sense | Overlaps exons of protein-coding gene on same strand | - |
| Antisense | Overlaps exons of protein-coding gene on opposite strand | XIST [10] |
| Bidirectional | Promoter located within 1 kb of protein-coding gene promoter on opposite strand | - |
| Intronic | Transcribed entirely from within an intron | - |
| Intergenic (lincRNA) | Located between protein-coding genes | HOTAIR [10] |
Functional Mechanisms of LncRNAs in Oncogenesis
LncRNAs employ diverse molecular mechanisms to regulate gene expression, which can be categorized into five primary modes of action:
In HCC, these mechanisms translate into specific pathological functions through multiple dimensions:
Epigenetic Regulation
LncRNAs can recruit chromatin-modifying complexes to specific genomic loci, thereby influencing gene expression patterns. For example, they can guide polycomb repressive complex 2 (PRC2) to gene promoters, leading to repressive histone methylation (H3K27me3) through the histone-methyl transferase subunit EZH2 [15]. Conversely, they can recruit activating complexes such as the mixed-lineage leukemia (MLL) histone methyltransferase complex to induce activating chromatin marks (H3K4me3) [15].
Transcriptional and Post-transcriptional Regulation
In the nucleus, lncRNAs can directly interact with DNA to form R-loops (DNA-RNA hybrids) that prevent DNA methyltransferase action and promote open chromatin configurations, facilitating transcription factor binding [15]. As enhancer RNAs (eRNAs) transcribed from enhancer regions, they can promote chromatin looping and gene activation [15]. In the cytoplasm, lncRNAs affect mRNA translation, stability, and turnover through interactions with 5'UTR or 3'UTR regions [15].
Competing Endogenous RNA (ceRNA) Mechanism
One of the most widely studied mechanisms involves lncRNAs acting as molecular sponges for microRNAs. By sequestering miRNAs through sequence-complementarity interactions, lncRNAs prevent miRNA-induced silencing complex (RISC) formation and subsequent mRNA destabilization, thereby allowing target mRNA expression [10] [15]. This ceRNA network represents a critical layer of post-transcriptional regulation frequently dysregulated in cancer.
HCC-Specific Functional Roles
In hepatocellular carcinoma, lncRNAs contribute to multiple aspects of tumor pathogenesis:
- EMT and Metastasis: LncRNA-ATB promotes metastasis by upregulating ZEB1 and ZEB2, thereby stimulating EMT [16]. HOTAIR promotes metastasis of various cancers, including HCC, through TGF-β signaling [16] [15].
- Metabolic Reprogramming: Under energy stress, lncRNA NBR2 activates AMPK through direct binding, and its knockdown leads to metabolic dysregulation [16]. LINKA regulates HIF-1α phosphorylation, maintaining its stability and activating transcriptional programs in cancer metabolism [16].
- Immune Evasion: Lnc-EGFR promotes immune escape in HCC by stimulating Treg cell differentiation [16]. NKILA enhances T cell sensitivity to activation-induced cell death by inhibiting the NF-κB pathway [16].
LncRNAs as Biomarkers in Hepatocellular Carcinoma
The dysregulation of specific lncRNAs in HCC tissues and circulation offers promising opportunities for biomarker development, particularly for early detection and prognosis prediction:
Table 2: Clinically Relevant lncRNAs in Hepatocellular Carcinoma
| LncRNA | Expression in HCC | Clinical Utility | Mechanism/Association | Reference |
|---|---|---|---|---|
| HULC | Upregulated | Diagnostic biomarker detectable in blood | Highly specific up-regulated lncRNA in HCC | [17] [14] |
| MALAT1 | Upregulated | Predicts tumor recurrence | Associated with recurrence after liver transplantation | [17] |
| HEIH | Upregulated | Independent prognostic factor | Regulates cell cycle; powerful predictor of recurrence | [13] |
| *Seven-lncRNA Signature | Upregulated | Prognostic prediction | Associated with Jab1/CSN5; predicts worse survival | [18] |
| RP11-731F5.2 | Upregulated | HCC risk and liver damage biomarker | Potential biomarker for HCC risk in CHC patients | [14] |
| KCNQ1OT1 | Upregulated | Liver damage biomarker | Noninvasive biomarker for liver damage in HCV infection | [14] |
| SNHG6 | Upregulated | Prognostic indicator | Correlated with Jab1/CSN5; predicts shorter overall survival | [18] |
*The seven-lncRNA signature includes SNHG6, CTD3065J16.9, LINC01604, CTD3025N20.3, KB-1460A1.5, RP13-582O9.7, and RP11-29520.2 [18]
Liquid biopsy approaches for lncRNA detection offer particular promise for HCC management. Plasma lncRNAs such as HULC and RP11-731F5.2 represent potential biomarkers for HCC risk in patients with chronic hepatitis C (CHC), while RP11-731F5.2 and KCNQ1OT1 may serve as noninvasive biomarkers for liver damage due to HCV infection [14]. These circulating biomarkers address critical clinical challenges associated with tissue biopsies, including invasiveness, sampling variability, and tumor heterogeneity [14].
Experimental Protocols for LncRNA Investigation
LncRNA Expression Profiling Using Microarray
Principle: Comprehensive detection of differentially expressed lncRNAs between HCC and matched non-tumor liver tissues.
Protocol:
- Sample Preparation: Extract total RNA from frozen tissue blocks using TRIzol reagent or mirVana RNA Isolation Kit. Assess RNA quality using NanoDrop spectrophotometer and agarose gel electrophoresis [13] [17].
- rRNA Removal and Labeling: Purify RNA from 1 µg total RNA after rRNA removal (mRNA-ONLY Eukaryotic mRNA Isolation Kit). Amplify and transcribe each sample into fluorescent cRNA using random priming method along the entire transcript length without 3' bias [17].
- Microarray Hybridization: Hybridize labeled cRNAs onto Human LncRNA Array (8×60 K, Arraystar). Wash slides and scan arrays using Agilent Scanner G2505B [13] [17].
- Data Analysis: Analyze acquired array images using Agilent Feature Extraction software. Perform quantile normalization and subsequent data processing using GeneSpring GX software. Identify differentially expressed lncRNAs through fold change filtering (Fold Change ≥2.0 or ≤0.5), paired t-test (p<0.05), and multiple hypothesis testing (FDR<0.05) [17].
Validation by Quantitative Real-Time PCR (qRT-PCR)
Principle: Confirm microarray results and quantify specific lncRNA expression in patient samples.
Protocol:
- RNA Extraction: Isolate total RNA from 500 μL plasma sample using Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit. Treat RNA samples with Turbo DNase to remove genomic DNA contamination [14].
- Reverse Transcription: Reverse transcribe RNA to cDNA using High-Capacity cDNA Reverse Transcription Kit [13] [14].
- qRT-PCR: Perform qRT-PCR using Power SYBR Green PCR Master Mix with StepOne Plus System. Use the following conditions: initial denaturation at 95°C for 2 min, followed by 40 cycles of 95°C for 15 sec and 62°C for 1 min [14].
- Data Analysis: Calculate lncRNA expression level using the 2−ΔΔCt method with β-actin as an internal reference. Confirm assay specificity by dissociation melting curve and polyacrylamide gel electrophoresis. Analyze samples in triplicate with no-template controls [13] [14].
Bioinformatic Analysis
Co-expression Network Construction: Build lncRNA-mRNA co-expression networks based on correlation between differentially expressed lncRNAs and mRNAs. Represent down-regulated lncRNAs as red ellipses, down-regulated mRNAs as green diamonds, up-regulated lncRNAs as blue ellipses, and up-regulated mRNAs as black diamonds. Use solid lines for positive correlations and dotted lines for negative correlations [17].
Functional Enrichment Analysis: Upload differentially regulated mRNAs to the Database for Annotation, Visualization and Integrated Discovery (DAVID) to analyze coding gene enrichment. Perform Gene Ontology (GO) and pathway analysis to determine the roles of differentially expressed mRNAs in biological pathways [17].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Reagents for LncRNA Research
| Reagent/Kit | Manufacturer | Function |
|---|---|---|
| mirVana RNA Isolation Kit | Applied Biosystems | Total RNA extraction from tissue samples |
| Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit | Norgen Biotek Corp. | RNA isolation from plasma/serum samples |
| Turbo DNase | Life Technologies Corp. | Genomic DNA contamination removal |
| High-Capacity cDNA Reverse Transcription Kit | Thermo Fisher Scientific | cDNA synthesis from RNA templates |
| Power SYBR Green PCR Master Mix | Thermo Fisher Scientific | qRT-PCR detection |
| Human LncRNA Array v2.0 (8×60 K) | Arraystar | Genome-wide lncRNA expression profiling |
| Propiverine Hydrochloride | Propiverine Hydrochloride, CAS:54556-98-8, MF:C23H30ClNO3, MW:403.9 g/mol | Chemical Reagent |
| Bassianolide | Bassianolide | Bassianolide, a cyclodepsipeptide fromBeauveria bassiana. For Research Use Only (RUO). Not for human or veterinary diagnosis or therapeutic use. |
LncRNAs represent a crucial layer of gene regulation with profound implications for hepatocellular carcinoma pathogenesis. Their diverse biogenesis pathways, classification systems, and functional mechanisms underscore their potential as biomarkers and therapeutic targets. The experimental protocols outlined in this application note provide a foundation for investigating lncRNAs in HCC cohorts, with particular emphasis on biomarker validation. As research continues to evolve, lncRNA-based signatures are poised to enhance early detection, prognostic stratification, and therapeutic monitoring in hepatocellular carcinoma, ultimately improving patient outcomes in this lethal malignancy.
Long non-coding RNAs (lncRNAs) have emerged as pivotal regulators of gene expression in hepatocellular carcinoma (HCC), operating through complex competing endogenous RNA (ceRNA) networks and signaling pathway modulation. This application note provides a comprehensive framework for investigating lncRNA-mediated ceRNA regulatory networks in HCC biomarker validation cohorts. We detail standardized methodologies for ceRNA network construction, experimental validation of lncRNA functions, and integration of multi-omics data to establish clinically relevant prognostic signatures. The protocols emphasize the quantification of lncRNA-miRNA-mRNA interactions, functional assessment of lncRNAs in HCC progression, and clinical translation of lncRNA biomarkers for precision oncology applications. Implementation of these standardized approaches will enhance reproducibility in lncRNA research and accelerate the development of lncRNA-based diagnostic and therapeutic strategies for HCC.
The competing endogenous RNA (ceRNA) hypothesis represents a transformative framework for understanding post-transcriptional regulation in hepatocellular carcinoma. This mechanism involves a sophisticated RNA language where long non-coding RNAs (lncRNAs), circular RNAs, and pseudogenes communicate through shared microRNA response elements (MREs) [19]. In HCC, these regulatory networks have been shown to govern critical oncogenic and tumor-suppressive pathways, contributing to the disease's characteristic heterogeneity and therapeutic resistance [20] [21]. The lncRNAs function as molecular sponges that sequester microRNAs (miRNAs), thereby attenuating the degradation or inhibition of miRNAs to their downstream protein-coding target genes [19]. This dynamic regulation enables a previously unrecognized layer of control over gene expression that is particularly relevant in cancer pathophysiology.
Advances in transcriptomic profiling have revealed that over 60% of the human transcriptome consists of non-coding RNAs, with lncRNAs representing a substantial proportion [20]. In HCC, specific lncRNAs including HOTAIR, MALAT1, and HOTTIP demonstrate aberrant expression and participate in extensive ceRNA crosstalk [20] [22] [23]. The tissue-specific expression patterns of lncRNAs make them particularly attractive as biomarkers and therapeutic targets. The construction and validation of ceRNA networks require integrated approaches combining bioinformatics predictions with experimental validation, which will be detailed in subsequent sections of this application note.
Application Note: ceRNA Network Construction and Validation
Computational Identification of ceRNA Networks
The systematic construction of lncRNA-mediated ceRNA networks begins with comprehensive transcriptomic data acquisition from HCC patient cohorts. The following protocol outlines the standardized workflow for ceRNA network construction:
Table 1: Primary Data Sources for ceRNA Network Construction
| Data Type | Source | Sample Size | Accession |
|---|---|---|---|
| RNA-seq | TCGA-LIHC | 374 HCC, 50 normal | TCGA Data Portal |
| miRNA-seq | TCGA-LIHC | 424 tumor specimens | TCGA Data Portal |
| Clinical data | TCGA-LIHC | 361 HCC tissues | TCGA Data Portal |
Step 1: Differential Expression Analysis
- Obtain raw RNA-seq, miRNA-seq, and clinical data from The Cancer Genome Atlas (TCGA) Liver Hepatocellular Carcinoma (LIHC) dataset [22] [24]. Normalize expression data to transcripts per million (TPM) or fragments per kilobase million (FPKM) to enable cross-sample comparisons.
- Identify differentially expressed lncRNAs (DElncRNAs), miRNAs (DEmiRNAs), and mRNAs (DEmRNAs) using DESeq2 or edgeR packages in R [24]. Apply thresholds of |log2(fold change)| > 2 and false discovery rate (FDR) < 0.05 for coding genes, and |log2(fold change)| > 4 with FDR < 0.01 for lncRNAs to account for their generally lower expression levels [22].
- Perform hierarchical clustering analysis using the pheatmap R package (v0.7.4) to visualize expression patterns across HCC and normal adjacent tissues [24].
Step 2: ceRNA Network Construction
- Identify potential miRNA response elements (MREs) in lncRNAs using miRcode database and miRNA-target interactions using miRDB, miRTarBase, and TargetScan databases [22] [25].
- Establish lncRNA-miRNA-mRNA regulatory axes based on significant negative correlations between lncRNAs and miRNAs (Pearson correlation coefficient < -0.5, p < 0.05), and positive correlations between lncRNAs and potential mRNA targets (Pearson correlation coefficient > 0.6, p < 0.05) [22] [24].
- Construct the ceRNA network using Cytoscape (v3.8.0 or higher) with edge and nodal gene information to visualize interaction networks [22].
Step 3: Functional and Pathway Enrichment Analysis
- Perform Gene Ontology (GO) enrichment analysis including biological processes, cellular components, and molecular functions using the clusterProfiler R package [22] [26].
- Conduct Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis to identify significantly enriched pathways, with particular attention to HCC-relevant pathways such as PPAR signaling, retinol metabolism, cell cycle regulation, and cancer pathways [24].
- Adjust p-values for multiple testing using Benjamini-Hochberg method with FDR < 0.05 considered statistically significant.
Figure 1: ceRNA Network Mechanism. LncRNAs function as miRNA sponges through microRNA Response Elements (MREs), preventing miRNA-mediated inhibition of target mRNAs.
Experimental Validation of ceRNA Interactions
Functional validation is essential to confirm bioinformatically predicted ceRNA interactions. The following protocol details the experimental approaches for validating key network components:
Step 1: Cell Culture and Transfection
- Maintain HCC cell lines (HEP3B, HEPG2, Huh7) in Dulbecco's Modified Eagle Medium supplemented with 10% fetal bovine serum at 37°C in 5% CO₂ [26].
- Design and obtain lncRNA-specific siRNAs, miRNA mimics, and miRNA inhibitors from commercial suppliers (e.g., GenePharm) [22].
- Transfect HCC cells using lipofectamine 3000 according to manufacturer's protocol with optimal transfection conditions determined empirically for each cell line [22]. Include appropriate negative controls (scrambled siRNA) and positive controls.
Step 2: Functional Assays for ceRNA Validation
- Cell Viability Assessment: Perform Cell Counting Kit-8 (CCK-8) assays at 24, 48, and 72 hours post-transfection to measure cell viability changes following lncRNA modulation [22].
- Proliferation, Migration, and Invasion Assays: Conduct colony formation assays, wound healing assays, and Transwell invasion assays to evaluate malignant phenotypes [26].
- Gene Expression Analysis: Extract total RNA using TRIzol reagent and synthesize cDNA using reverse transcription kits. Perform quantitative RT-PCR with SYBR Green protocols using primer sets designed for target lncRNAs, miRNAs, and mRNAs [22] [26].
- Luciferase Reporter Assays: Clone wild-type and mutant lncRNA sequences into psiCHECK-2 vector downstream of Renilla luciferase gene. Co-transfect with miRNA mimics or inhibitors into HCC cells. Measure firefly and Renilla luciferase activities 48 hours post-transfection using dual-luciferase reporter assay system [19].
Table 2: Key Functional Assays for ceRNA Validation
| Assay Type | Purpose | Readout | Interpretation |
|---|---|---|---|
| CCK-8 | Cell viability | Optical density at 450nm | Decreased viability with tumor-suppressive lncRNAs |
| qRT-PCR | Expression quantification | Ct values | Confirm co-expression relationships |
| Luciferase reporter | Direct binding validation | Luminescence intensity | Reduced luminescence indicates binding |
| Wound healing | Migration capability | Wound closure rate | Increased migration with oncogenic lncRNAs |
| Transwell | Invasion capacity | Cell count per field | Enhanced invasion with metastasis-promoting lncRNAs |
Application Note: Prognostic Signature Development
Construction of lncRNA-Based Prognostic Models
The development of robust lncRNA signatures for HCC prognosis requires rigorous statistical approaches and validation in independent cohorts. The following protocol outlines the standardized methodology:
Step 1: Identification of Prognosis-Associated lncRNAs
- Extract clinical outcome data (overall survival, disease-free survival) from TCGA-LIHC and merge with lncRNA expression matrices [27] [26].
- Perform univariate Cox regression analysis to identify lncRNAs significantly associated with survival (p < 0.05). For studies focusing on specific biological processes (e.g., disulfidptosis, migrasome formation), include only lncRNAs correlated with relevant genes (Pearson R > 0.4, p < 0.001) [27] [26].
- Apply Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression with 10-fold cross-validation using the glmnet R package to select the most prognostic lncRNAs while preventing overfitting [27] [26].
Step 2: Risk Score Model Construction
- Calculate risk scores for each patient using the formula: Risk score = Σ (ExplncRNA × coeflncRNA), where ExplncRNA represents the expression level of each prognostic lncRNA and coeflncRNA represents its regression coefficient derived from multivariate Cox analysis [27] [26].
- Dichotomize patients into high-risk and low-risk groups using the median risk score as the cutoff value.
- Validate the prognostic model in training/testing sets through random splitting of the cohort (typically 50:50 or 70:30 ratio) and in independent validation cohorts when available [27].
Step 3: Model Performance Assessment
- Evaluate the predictive performance of the risk score using time-dependent receiver operating characteristic (ROC) curve analysis at 1, 3, and 5 years using the timeROC R package [27] [26].
- Perform Kaplan-Meier survival analysis with log-rank tests to compare survival distributions between high-risk and low-risk groups.
- Conduct univariate and multivariate Cox regression analyses to determine whether the lncRNA signature serves as an independent prognostic factor after adjusting for clinical variables (age, gender, tumor stage, grade) [27].
Figure 2: Prognostic Signature Development Workflow. Integration of transcriptomic and clinical data for construction and validation of lncRNA-based prognostic models.
Integration with Tumor Microenvironment and Therapy Response
Advanced prognostic models incorporate tumor microenvironment features and therapy response predictors to enhance clinical utility:
Step 1: Immune Microenvironment Characterization
- Estimate immune cell infiltration abundances using CIBERSORT, EPIC, MCP-COUNTER, or similar deconvolution algorithms to analyze the composition of 22 immune cell types in HCC tissues [27] [22].
- Analyze correlations between risk scores and immune cell infiltration levels, immune checkpoint expression (PD-L1, CTLA-4, etc.), and immunosuppressive features [27].
- Evaluate the tumor immune dysfunction and exclusion (TIDE) score to predict immunotherapy response potential in high-risk versus low-risk groups [27] [26].
Step 2: Therapeutic Sensitivity Prediction
- Calculate half-maximal inhibitory concentration (IC50) values for common HCC therapeutics (sorafenib, 5-fluorouracil, doxorubicin) using the pRRophetic R package to identify differential drug sensitivities between risk groups [26].
- Correlate lncRNA expression with drug response data to identify potential resistance mechanisms.
- Develop nomograms incorporating the lncRNA signature and clinical parameters to predict individual patient survival probabilities at 1, 3, and 5 years [27] [26].
Table 3: Representative Prognostic lncRNA Signatures in HCC
| Signature Type | Key lncRNAs | Cohort Size | Performance (AUC) | Clinical Utility |
|---|---|---|---|---|
| Migrasome-related | LINC00839, MIR4435-2HG | TCGA + 100 validation | 1-year: 0.82, 3-year: 0.79 | Predicts immunotherapy response |
| Disulfidptosis-related | TMCC1-AS1 | 374 TCGA | 1-year: 0.75, 3-year: 0.72 | Identifies sorafenib-sensitive patients |
| Diagnostic | RP11-486O12.2, LINC01093 | 361 HCC, 50 normal | 0.992 (SVM model) | Early detection biomarker |
| ceRNA network | HOTTIP | 424 TCGA | Significant in multivariate analysis | Guides targeted therapy |
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for lncRNA-ceRNA Research
| Reagent/Resource | Function/Application | Example Products/Sources |
|---|---|---|
| siRNA and miRNA modulators | lncRNA knockdown and miRNA manipulation | GenePharm, Dharmacon |
| Lipofectamine 3000 | Nucleic acid delivery into HCC cells | Thermo Fisher Scientific |
| CCK-8 assay | Cell viability and proliferation measurement | Dojindo Molecular Technologies |
| TRIzol reagent | RNA extraction from cells and tissues | Thermo Fisher Scientific |
| SYBR Green kits | qRT-PCR quantification of lncRNAs | Takara Bio |
| Luciferase reporter vectors | Validation of miRNA-lncRNA interactions | Promega psiCHECK-2 |
| TCGA-LIHC dataset | Primary transcriptomic and clinical data | The Cancer Genome Atlas |
| CIBERSORT algorithm | Immune cell infiltration analysis | https://cibersort.stanford.edu/ |
| Cytoscape software | ceRNA network visualization | Cytoscape Consortium |
| glmnet R package | LASSO Cox regression analysis | CRAN repository |
| Rosiglitazone-d3 | Rosiglitazone-d3 | Stable Isotope | For Research Use | Rosiglitazone-d3, a deuterated internal standard. Essential for accurate LC-MS/MS quantification in metabolism studies. For Research Use Only. Not for human use. |
| 4-Methoxy-2,3,6-trimethylbenzyl bromide | 4-Methoxy-2,3,6-trimethylbenzyl bromide, CAS:69877-88-9, MF:C11H15BrO, MW:243.14 g/mol | Chemical Reagent |
Concluding Remarks
The systematic investigation of lncRNA-mediated ceRNA networks represents a transformative approach for understanding HCC pathophysiology and developing novel biomarkers. The protocols detailed in this application note provide a standardized framework for constructing and validating ceRNA networks, developing prognostic signatures, and translating lncRNA discoveries into clinical applications. Implementation of these methodologies will enhance reproducibility across studies and accelerate the validation of lncRNA biomarkers in HCC cohorts. Future directions should focus on single-cell resolution of ceRNA networks, integration with epigenetic regulation, and development of lncRNA-targeted therapeutics to ultimately improve outcomes for HCC patients through precision oncology approaches.
Tissue-Specific Expression Patterns and Epigenetic Regulation in HCC
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, ranking as the sixth most diagnosed cancer and the third leading cause of cancer death worldwide [28]. Its complex pathogenesis and significant heterogeneity present substantial challenges for early detection and effective treatment. Current screening methods, which primarily rely on abdominal ultrasound and serum alpha-fetoprotein (AFP) testing, demonstrate limited sensitivity of only 47-63% for early-stage HCC detection [28]. The 5-year survival rate for HCC remains dismal at approximately 18%, highlighting the urgent need for improved diagnostic and prognostic biomarkers [28].
The investigation of tissue-specific expression patterns and epigenetic regulation in HCC represents a promising frontier for addressing these clinical challenges. This application note explores how integrating gene expression profiling with epigenetic analyses, particularly focusing on long non-coding RNAs (lncRNAs), can enhance biomarker discovery and validation in HCC cohorts. The content is structured to provide researchers with both theoretical frameworks and practical methodologies for advancing HCC biomarker research.
Tissue-Specific Gene Expression Patterns in HCC
Gene expression profiling has revealed distinctive molecular patterns that distinguish HCC from non-tumor liver tissues and other liver malignancies. cDNA microarray studies analyzing over 200 samples, including 102 primary HCC specimens, have demonstrated that HCC tissues exhibit consistent and distinctive gene expression signatures readily distinguishable from both nontumor liver tissues and tumors metastatic to the liver [29].
Key Dysregulated Protein-Coding Genes
Analysis of differentially expressed genes in HCC has identified several consistently dysregulated protein-coding genes with potential functional significance in hepatocarcinogenesis. The table below summarizes key upregulated and downregulated genes identified through microarray and RNA sequencing studies:
Table 1: Key Dysregulated Protein-Coding Genes in HCC
| Gene Symbol | Gene Name | Expression in HCC | Proposed Functional Role in HCC |
|---|---|---|---|
| GYS1 | Glycogen Synthase 1 | Upregulated | Disulfidptosis-related gene [26] |
| SLC7A11 | Solute Carrier Family 7 Member 11 | Upregulated | Disulfidptosis-related gene [26] |
| GALECTIN-3 | Galectin-3 | Upregulated | Cell growth and adhesion [30] |
| SGK | Serum/Glucocorticoid Regulated Kinase 1 | Upregulated | Cell proliferation signaling [30] |
| eIF-4A, -4B, -3 | Eukaryotic Initiation Factors | Upregulated | Translation initiation [30] |
| FGFR | Fibroblast Growth Factor Receptor | Upregulated | Growth factor signaling [30] |
| RPL35A | Ribosomal Protein L35A | Upregulated | Protein synthesis [30] |
| Nip3 | Nineteen kD Interacting Protein-3 | Downregulated | Apoptosis regulation [30] |
| DECORIN | Decorin | Downregulated | Matrix organization and growth inhibition [30] |
| IGFBP-3 | Insulin-like Growth Factor Binding Protein-3 | Downregulated | Growth factor modulation [30] |
The expression patterns vary significantly among HCC samples and show association with specific phenotypic and genotypic characteristics, including growth rate, vascular invasion, and p53 overexpression [29]. This heterogeneity underscores the importance of comprehensive molecular profiling for accurate HCC classification and personalized treatment approaches.
Epigenetic Regulation Mechanisms in HCC
Epigenetic mechanisms play central roles in HCC pathogenesis, offering dynamic and potentially reversible regulatory processes that contribute to tumor initiation and progression. The major epigenetic alterations in HCC encompass DNA methylation, histone modifications, and non-coding RNA regulation.
DNA Methylation Alterations
DNA methylation patterns in HCC are characterized by two principal phenomena: global hypomethylation and focal hypermethylation of specific gene promoters. These alterations are mediated through dysregulation of DNA methyltransferases (DNMTs) and ten-eleven translocation (TET) family enzymes [28].
Table 2: DNA Methylation Alterations in HCC
| Methylation Type | Key Regulatory Enzymes | Affected Genomic Regions/Genes | Functional Consequences |
|---|---|---|---|
| Global Hypomethylation | DNMT1 ↓, DNMT3b ↓, TET1 ↓, TET2 ↓ | Repetitive elements, oncogene promoters | Genomic instability, oncogene activation (e.g., C/EBPβ) [28] |
| Focal Hypermethylation | DNMT1 ↑, DNMT3b ↑ | Tumor suppressor gene promoters | Silencing of CDKN2A, RASSF1A, APC, SOCS1, GSTP1, HIC1 [28] [31] |
| Enhancer Hypomethylation | TET1 ↓, TET2 ↓ | Enhancer regions (e.g., C/EBPβ) | Transcriptional activation of oncogenes [28] |
The extent of genomic demethylation correlates with advanced disease states, including higher histopathological grades and larger tumor sizes, suggesting a role in HCC progression rather than initiation [28]. Approximately 230 hypomethylated gene promoters that are overexpressed have been reported to enhance HCC development and progression [28].
Histone Modifications
Post-translational modifications of histone proteins, including acetylation, methylation, phosphorylation, and ubiquitination, significantly alter chromatin structure and gene expression in HCC [28] [31]. The balance between histone acetyltransferases (HATs) and histone deacetylases (HDACs) is frequently disrupted in HCC, with HDAC overexpression leading to chromatin condensation and silencing of tumor suppressor genes [32] [31]. Similarly, histone methyltransferases such as EZH2 are often upregulated in HCC, contributing to transcriptional repression of tumor suppressor genes [31].
Non-Coding RNA Networks
Long non-coding RNAs have emerged as crucial regulators of epigenetic processes in HCC, functioning through diverse mechanisms including chromatin modification, transcriptional regulation, and post-transcriptional processing.
Table 3: Mechanistic Roles of Key lncRNAs in HCC Epigenetic Regulation
| lncRNA | Expression in HCC | Epigenetic Mechanism | Functional Outcome |
|---|---|---|---|
| HULC | Upregulated | Acts as miRNA sponge; promotes phosphorylation of YB-1 | Oncogenic mRNA translation [9] [31] |
| HOTAIR | Upregulated | Interacts with chromatin modifiers | Transcriptional repression; poor prognosis [9] [31] |
| MALAT1 | Upregulated | Regulates alternative splicing; sponges miRNAs | Promotes aggressive tumor phenotypes [33] [31] |
| GAS5 | Downregulated | Triggers CHOP and caspase-9 pathways | Tumor suppressor; induces apoptosis [33] |
| LINC00152 | Upregulated | Promotes cell proliferation via CCDN1 regulation | Oncogenic function [33] [34] |
| TMCC1-AS1 | Upregulated | Disulfidptosis-related mechanism | Promotes proliferation, migration, invasion [26] |
Experimental Protocols for lncRNA Biomarker Validation
This section provides detailed methodologies for key experiments in lncRNA biomarker discovery and validation, specifically framed within HCC cohort studies.
Tissue Collection and RNA Isolation Protocol
Objective: To obtain high-quality RNA samples from HCC and matched non-tumor liver tissues for lncRNA expression analysis.
Materials:
- RNase-free tubes and pipette tips
- Liquid nitrogen storage system
- RNeasy Mini Kit (QIAGEN) or equivalent
- miRNeasy Mini Kit (QIAGEN) for simultaneous miRNA isolation
- β-mercaptoethanol
- 70% ethanol (molecular grade)
- RNase-free DNase set
- Nanodrop spectrophotometer or equivalent
- Bioanalyzer system (Agilent) or equivalent
Procedure:
- Collect tissue specimens (approximately 0.5-1 cm³) during surgical resection
- Immediately snap-freeze in liquid nitrogen within 30 minutes of resection
- Store at -80°C until processing
- Divide each specimen into three equal slices for (a) RNA extraction, (b) genomic DNA isolation, and (c) histological examination
- Homogenize tissue samples in RLT buffer with β-mercaptoethanol using a rotor-stator homogenizer
- Isolate total RNA following manufacturer's protocol, including on-column DNase digestion
- Assess RNA quality using Bioanalyzer (RIN >7.0 required for sequencing)
- Quantify RNA concentration using Nanodrop spectrophotometer
- Store RNA at -80°C for downstream applications
Quality Control Measures:
- Independent histological review by two pathologists for all samples
- RNA integrity number (RIN) assessment
- Absorbance ratios (A260/280 >1.8, A260/230 >2.0)
- Confirmation of absence of genomic DNA contamination
lncRNA Expression Profiling by Quantitative RT-PCR
Objective: To quantitatively measure specific lncRNA expression levels in HCC tissue and plasma samples.
Materials:
- Total RNA samples (100-500 ng)
- Reverse transcription kit (RevertAid First Strand cDNA Synthesis Kit)
- PowerTrack SYBR Green Master Mix
- Gene-specific primers for target lncRNAs
- Housekeeping gene primers (GAPDH, β-actin)
- 96-well or 384-well reaction plates
- Real-time PCR system (ViiA 7 or equivalent)
Procedure:
- Synthesize cDNA using 500 ng total RNA according to manufacturer's protocol
- Design primers to span exon-exon junctions where applicable
- Prepare qRT-PCR reactions in triplicate with the following components:
- 10 μL SYBR Green Master Mix
- 1 μL forward primer (10 μM)
- 1 μL reverse primer (10 μM)
- 8 μL nuclease-free water
- 5 μL cDNA (1:10 dilution)
- Run qRT-PCR with the following cycling conditions:
- Initial denaturation: 95°C for 10 minutes
- 40 cycles of:
- Denaturation: 95°C for 15 seconds
- Annealing/extension: 60°C for 60 seconds
- Melt curve analysis: 60-95°C with 0.3°C increments
- Analyze data using the ΔΔCT method for relative quantification
- Normalize to housekeeping genes (GAPDH or β-actin)
Validation Requirements:
- Primer efficiency between 90-110%
- Melt curve showing single amplification product
- Correlation coefficient of standard curve >0.98
- Inter-assay and intra-assay CV <10%
Disulfidptosis-Related lncRNA Signature Construction
Objective: To construct a prognostic lncRNA signature based on disulfidptosis-related mechanisms for HCC patient stratification.
Materials:
- RNA sequencing data from HCC cohorts (e.g., TCGA)
- Clinical follow-up data (overall survival, recurrence-free survival)
- R statistical environment with "glmnet," "survival," and "survminer" packages
- List of disulfidptosis-related genes (GYS1, LRPPRC, NCKAP1, NDUFA11, NDUFS1, NUBPL, OXSM, RPN1, SLC3A2, SLC7A11)
Procedure:
- Retrieve RNA-seq transcriptome data and clinical information from TCGA database
- Identify disulfidptosis-related lncRNAs (DRLs) by Pearson correlation analysis (R > 0.4, p < 0.001)
- Perform univariate Cox regression analysis to identify prognostic DRLs (p < 0.001)
- Divide dataset into training and testing sets (typically 70:30 ratio)
- Apply LASSO Cox regression with 10-fold cross-validation to identify most prognostic DRLs
- Construct risk score model using formula: Risk score = Σ [Exp (lncRNA) × coef (lncRNA)]
- Stratify patients into high-risk and low-risk groups using median risk score as cutoff
- Validate signature in testing set and entire cohort using Kaplan-Meier analysis and ROC curves
Statistical Considerations:
- Multivariate Cox regression to adjust for clinical covariates
- Time-dependent ROC analysis for predictive accuracy
- C-index calculation for model performance
- Calibration plots for nomogram validation
Signaling Pathways and Molecular Interactions
The CCL21/CCR7 axis represents a critical signaling pathway in HCC with context-dependent roles in tumor progression and treatment response. The following diagram illustrates the dual functions of this pathway in HCC pathogenesis:
Diagram 1: Dual Roles of CCR7 Signaling in Hepatocellular Carcinoma. The diagram illustrates how CCR7 expression in tumor cells promotes EMT and sorafenib resistance, while stromal CCR7 activation promotes anti-tumor immunity and enhances immunotherapy response.
The paradoxical role of CCR7 signaling highlights the complexity of the HCC tumor microenvironment and emphasizes the importance of cell-type-specific analysis when evaluating potential therapeutic targets.
Research Reagent Solutions
The table below provides essential research reagents and their applications for investigating tissue-specific expression patterns and epigenetic regulation in HCC:
Table 4: Essential Research Reagents for HCC Epigenetic and Expression Studies
| Reagent/Category | Specific Examples | Primary Research Application | Key Considerations |
|---|---|---|---|
| RNA Isolation Kits | RNeasy Mini Kit (QIAGEN), miRNeasy Mini Kit (QIAGEN) | Total RNA and miRNA isolation from tissues and plasma | Assess RNA integrity (RIN >7.0); include DNase treatment [29] [33] |
| cDNA Synthesis Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Reverse transcription for qRT-PCR applications | Use random hexamers for lncRNA applications [33] |
| qRT-PCR Reagents | PowerTrack SYBR Green Master Mix (Applied Biosystems) | lncRNA expression quantification by qRT-PCR | Optimize primer concentrations; include melt curve analysis [33] |
| Microarray Platforms | cDNA microarrays (~17,400 genes) | Genome-wide expression profiling | >1.5-fold intensity over background; 3-fold change cutoff [29] |
| Epigenetic Inhibitors | DNMT inhibitors (5-azacytidine, decitabine), HDAC inhibitors (vorinostat, belinostat) | Experimental modulation of epigenetic states | Combination approaches with immunotherapy show promise [31] |
| Cell Culture Models | HCC cell lines (HEP3B, HEPG2, HCCLM3, MHCC97H) | In vitro functional validation studies | CRISPR-Cas9 knockout (e.g., CCR7) for mechanistic studies [35] [26] |
| Immunohistochemistry Reagents | Anti-CCR7 antibodies, CD34 staining, p53 antibodies | Protein expression validation in tissue microarrays | Independent pathological review recommended [29] [35] |
| Bioinformatics Tools | TCGA data analysis, Pearson correlation, LASSO Cox regression | Prognostic signature development and validation | R packages: "glmnet," "survival," "clusterProfiler" [26] |
The integration of tissue-specific expression patterns with epigenetic regulatory mechanisms provides powerful insights for lncRNA biomarker validation in HCC cohorts. The distinctive gene expression signatures characteristic of HCC, combined with specific epigenetic alterations such as DNA methylation changes, histone modifications, and lncRNA dysregulation, offer promising avenues for improved diagnosis, prognosis, and treatment stratification. The experimental protocols and analytical frameworks presented in this application note provide researchers with comprehensive methodologies for advancing this field. Future directions should focus on validating these findings in large-scale clinical trials and developing integrated multi-omics approaches for personalized HCC management.
From Sequencing to Signatures: Methodological Approaches for LncRNA Biomarker Development
Hepatocellular carcinoma (HCC) presents a significant global health challenge, characterized by high mortality rates often due to late diagnosis. Long non-coding RNAs (lncRNAs) have emerged as crucial regulatory molecules in carcinogenesis, offering immense potential as diagnostic and prognostic biomarkers. However, the high-dimensional nature of transcriptomic data, where the number of features (genes) vastly exceeds the number of patient samples, creates substantial analytical challenges. This application note details how three key machine learning algorithms—LASSO regression, Random Forests, and Support Vector Machine (SVM) classification—are being deployed to address these challenges and validate lncRNA biomarkers in HCC cohorts.
Machine Learning Application Notes
LASSO (Least Absolute Shrinkage and Selection Operator) Regression
Application Context: LASSO regression is predominantly used for feature selection and the construction of prognostic signatures in high-dimensional genomic data. Its ability to penalize regression coefficients drives unnecessary features to zero, effectively selecting a parsimonious set of biomarkers with the strongest prognostic power [36] [37].
Key Protocols and Findings:
- Prognostic Signature Development: A standard protocol involves extracting lncRNA expression data from cohorts such as The Cancer Genome Atlas (TCGA-LIHC). Following correlation analysis to identify lncRNAs associated with a biological process of interest (e.g., ferroptosis, disulfidptosis), univariate Cox regression is performed to select candidates with significant survival correlation. LASSO-penalized Cox regression is then applied for final feature selection [36] [37]. For instance, this method was used to develop a 7-ferroptosis-related lncRNA signature and a 3-disulfidptosis-related lncRNA signature, both of which independently stratified patients into high- and low-risk groups with distinct overall survival outcomes [36] [37].
- Validation Workflow: The cohort is typically split into training and testing sets. The model is built on the training set, and its prognostic performance is validated on the testing set using Kaplan-Meier survival analysis and time-dependent Receiver Operating Characteristic (ROC) analysis. Area Under the Curve (AUC) values for 1-, 3-, and 5-year survival are calculated to quantify predictive accuracy [37].
- Integration with Clinical Variables: A critical final step involves performing univariate and multivariate Cox regression analyses that include the LASSO-derived risk score and standard clinical variables (e.g., TNM stage, Child-Pugh grade). This confirms the risk score's value as an independent prognostic factor [38].
Table 1: Exemplary LASSO Regression Applications in HCC lncRNA Research
| Study Focus | Selected lncRNAs | Cohort | Performance (AUC) | Key Outcome |
|---|---|---|---|---|
| Ferroptosis-related Signature [36] | 7-lncRNA signature (incl. LINC01063) | TCGA (n=365) | 1-year: 0.745, 3-year: 0.719 | Signature correlated with immunity; LINC01063 validated as oncogene |
| Disulfidptosis-related Signature [37] | AC016717.2, AC124798.1, AL031985.3 | TCGA (n=369) | 1-year: 0.756, 3-year: 0.695, 5-year: 0.701 | High-risk group linked to poor OS and distinct immune function |
| Immune-related Signature [38] | 8-lncRNA signature (incl. HHLA3, LINC01232) | TCGA (n=377) | Training: 0.827, All samples: 0.757 | Riskscore was an independent prognostic factor |
Random Forests
Application Context: Random Forests, an ensemble learning method, are primarily used for classifying cancer samples (e.g., tumor vs. normal) and ranking feature importance. Their robustness against overfitting makes them suitable for analyzing complex, non-linear relationships in transcriptomic data [39] [40].
Key Protocols and Findings:
- Biomarker Discovery and Diagnostic Panels: A common protocol involves identifying differentially expressed genes (DEGs) from public repositories like TCGA and GEO. Multiple machine learning algorithms, including Random Forests, are then trained and evaluated on these DEGs to identify a minimal set of feature genes with high diagnostic power [39]. One study applied 109 combinations of 12 machine learning algorithms and identified Random Forests as particularly effective in pinpointing key feature genes for HCC [39].
- Model Comparison and Validation: The performance of different models is compared using metrics like accuracy and AUC from ROC analysis via cross-validation. The optimal model, which may be a combination of several algorithms, is selected based on the highest average AUC across training and testing cohorts [39] [33].
- Liquid Biopsy Analysis: Random Forests can be applied to plasma-derived lncRNA data. One study integrated the expression of four lncRNAs (LINC00152, LINC00853, UCA1, GAS5) with standard laboratory parameters in a machine learning model, achieving superior diagnostic performance (100% sensitivity, 97% specificity) compared to individual lncRNAs [33].
The following workflow diagram illustrates the typical process for biomarker discovery and validation using these machine learning techniques.
SVM (Support Vector Machine) Classification
Application Context: SVM classifiers are powerful tools for high-dimensional classification tasks, such as distinguishing HCC tumors from normal tissues or predicting cancer subtypes based on lncRNA expression profiles. SVM works by finding the optimal hyperplane that maximally separates different classes of samples [40].
Key Protocols and Findings:
- Diagnostic Classification: SVMs can be trained on lncRNA expression data to create a classifier for HCC. The input is a matrix where rows represent patients and columns represent the expression levels of selected lncRNAs. The model learns to assign new samples to "HCC" or "normal" categories with high accuracy [40].
- Integration with Artificial Intelligence (AI): AI-powered approaches, including SVMs, are increasingly used to analyze complex RNA expression patterns from liquid biopsies. These models offer a non-invasive and highly sensitive method for early cancer screening, outperforming traditional diagnostic methods [40].
- Multi-Omics Data Integration: Advanced applications involve using SVMs and other AI models to integrate multi-omics data (e.g., RNA-seq with genomic and proteomic profiles). This generates comprehensive diagnostic signatures that improve early detection rates and minimize false positives [40].
Table 2: Comparison of Machine Learning Applications in HCC lncRNA Studies
| Algorithm | Primary Role | Key Strengths | Common Validation Metrics |
|---|---|---|---|
| LASSO Regression | Feature selection & Prognostic modeling | Prevents overfitting, produces interpretable models, handles high-dimensional data | Hazard Ratio (HR), C-index, Time-dependent AUC |
| Random Forests | Classification & Feature importance ranking | Robust to outliers and non-linear relationships, provides feature importance scores | Accuracy, AUC, Sensitivity, Specificity |
| SVM Classification | Sample classification & Diagnostic modeling | Effective in high-dimensional spaces, versatile with different kernel functions | Accuracy, AUC, Precision, Recall |
Experimental Protocols
Protocol: Developing a LASSO-Derived Prognostic lncRNA Signature
Objective: To identify a minimal set of lncRNAs with independent prognostic value and construct a risk score model for HCC patients.
Materials and Reagents:
- Data Source: Transcriptomic data (RNA-seq or microarray) and matched clinical data (survival time, status, TNM stage, etc.) for an HCC cohort (e.g., from TCGA).
- Software: R statistical software with packages:
glmnet(for LASSO),survival(for Cox regression),timeROC(for ROC analysis),caret(for data partitioning).
Procedure:
- Data Preprocessing and lncRNA Filtering: Annotate the transcriptome data to separate lncRNAs. Normalize expression data (e.g., TPM for RNA-seq). Filter out lowly expressed lncRNAs.
- Identify Phenotype-Related lncRNAs: Perform correlation analysis (e.g., Pearson) between a list of genes of interest (e.g., ferroptosis-related genes) and all lncRNAs. Retain lncRNAs with |correlation coefficient| > 0.4-0.5 and P < 0.001 [36] [38].
- Univariate Cox Regression: For each candidate lncRNA from Step 2, fit a univariate Cox proportional hazards model with overall survival. Retain lncRNAs with P < 0.05 for further analysis.
- LASSO-Cox Regression: Input the expression matrix of significant lncRNAs from Step 3 into the LASSO-Cox algorithm. Use 10-fold cross-validation to determine the optimal penalty parameter (λ) that minimizes the partial likelihood deviance. The lncRNAs with non-zero coefficients at the optimal λ are selected for the final signature.
- Calculate Risk Score: For each patient, compute a risk score using the formula:
Riskscore = Σ (Coefficient_lincRNA_i × Expression_lincRNA_i). - Stratify Patients: Dichotomize patients into high-risk and low-risk groups using the median risk score as the cutoff.
- Validate the Model:
- Split Data: Randomly divide the cohort into training and testing sets (e.g., 1:1 ratio).
- Assess Prognostic Power: Perform Kaplan-Meier survival analysis with log-rank test to compare survival curves between risk groups in both sets.
- Evaluate Accuracy: Generate time-dependent ROC curves for 1, 3, and 5-year overall survival and calculate AUC values.
- Test Independence: Conduct univariate and multivariate Cox regression analyses including the risk score and key clinical variables to confirm the score is an independent prognostic factor.
Protocol: Building a Random Forest/SVM Diagnostic Classifier
Objective: To integrate multiple lncRNA biomarkers into a machine learning model for highly accurate diagnosis of HCC.
Materials and Reagents:
- Sample Data: Plasma or tissue expression levels of target lncRNAs from HCC patients and healthy controls.
- Software: Python's Scikit-learn library or R with
randomForestande1071(for SVM) packages.
Procedure:
- Data Collection and Preparation: Quantify lncRNA expression (e.g., by qRT-PCR) in patient and control samples. Normalize expression values (e.g., using the ΔΔCT method relative to a housekeeping gene like GAPDH). Assemble a dataset with expression values and class labels (e.g., "HCC" or "Control") [33].
- Feature Selection (Optional but Recommended): Use statistical tests (e.g., Mann-Whitney U test) or other feature selection methods to identify the most differentially expressed lncRNAs between groups.
- Model Training and Selection:
- Split Data: Partition the dataset into training (e.g., 70-80%) and hold-out testing (e.g., 20-30%) sets.
- Train Multiple Models: Train multiple classifiers (e.g., Random Forest, SVM, others) on the training set. For Random Forest, tune parameters like the number of trees. For SVM, tune the cost parameter and kernel (e.g., linear, radial basis function).
- Evaluate and Compare: Use k-fold cross-validation (e.g., 10-fold) on the training set to estimate model performance. Compare models based on average accuracy, AUC, sensitivity, and specificity.
- Final Model Validation: Apply the best-performing model to the held-out test set. Report final performance metrics (sensitivity, specificity, accuracy, AUC) to estimate real-world diagnostic performance [33].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for lncRNA Biomarker Validation
| Reagent / Resource | Function and Application | Example Specifications |
|---|---|---|
| RNA Extraction Kit | Isolate high-quality total RNA from tissue or plasma samples for downstream expression analysis. | miRNeasy Mini Kit (QIAGEN) [33] |
| cDNA Synthesis Kit | Reverse transcribe RNA into stable complementary DNA (cDNA) for qRT-PCR amplification. | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [33] |
| qRT-PCR Master Mix | Quantify the relative expression levels of target lncRNAs with high sensitivity and specificity. | PowerTrack SYBR Green Master Mix (Applied Biosystems) [33] |
| Public Genomic Database | Source for transcriptomic and clinical data to discover and validate lncRNA biomarkers. | The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO) [36] [39] |
| R / Python Software | Platforms for statistical analysis, data visualization, and implementing machine learning algorithms. | R packages: glmnet, randomForest, survival, caret. Python: scikit-learn [39] [38] |
| Pirlimycin | Pirlimycin, CAS:78822-40-9, MF:C17H31ClN2O5S, MW:411.0 g/mol | Chemical Reagent |
| 3,4-Dimethoxyphenol | 3,4-Dimethoxyphenol, CAS:2033-89-8, MF:C8H10O3, MW:154.16 g/mol | Chemical Reagent |
Pathway and Workflow Visualizations
The following diagram illustrates the functional roles and regulatory impact of validated lncRNA biomarkers in the context of HCC biology, showing how they influence key cancer hallmarks.
Clinical Translation: Validation Frameworks and Performance Assessment Against Current Standards
This application note provides a detailed protocol for the validation of long non-coding RNA (lncRNA) biomarkers in hepatocellular carcinoma (HCC) using independent cohorts from The Cancer Genome Atlas (TCGA) and the International Cancer Genome Consortium (ICGC). We outline standardized methodologies for multi-omics analysis, prognostic model construction, and experimental validation to ensure reproducible and clinically translatable results for researchers and drug development professionals.
Hepatocellular carcinoma represents a significant global health challenge, characterized by poor prognosis and limited treatment options, particularly in advanced stages. The discovery and validation of lncRNAs as biomarkers for diagnosis, prognosis, and therapeutic prediction have emerged as a promising frontier in HCC research. However, the transition from discovery to clinical application requires rigorous validation across independent patient cohorts. This protocol details a standardized framework for lncRNA biomarker validation using TCGA and ICGC datasets, supplemented by experimental approaches, to establish robust, clinically relevant signatures within the context of HCC biomarker research.
Material and Methods
Data Acquisition and Preprocessing
Required Resources:
- TCGA-LIHC Dataset: RNA-seq data, clinical information, and survival data for 369 tumor and 50 normal adjacent tissues.
- ICGC LIRI-JP Dataset: Independent validation cohort containing 231-243 HCC samples with corresponding clinical annotations.
- GEO Datasets: Accession numbers GSE54236 (81 tumor, 80 normal) and GSE104310 (12 tumor, 8 normal) for additional validation.
Protocol:
- Data Download: Retrieve RNA-sequencing data (raw counts and FPKM) from TCGA data portal and ICGC database. Corresponding clinical and survival data should be obtained from UCSC Xena browser.
- Data Normalization: Convert FPKM values to transcripts per million and apply log2(x+1) transformation to normalize the data distribution.
- Quality Control: Remove genes with >20% missing values and impute remaining missing values using weighted K-nearest neighbor algorithm (K=10).
- Cohort Definition: Ensure patients have complete information on survival time, survival status, and TNM stage for subsequent survival analysis.
Identification of Prognosis-Associated LncRNAs
Protocol:
- Differential Expression Analysis: Perform analysis using "edgeR" package for TCGA data and "limma" package for GEO datasets with threshold of |log2(fold change)| >1 and adjusted p-value <0.05.
- Univariate Cox Regression: Identify lncRNAs significantly associated with overall survival (p<0.05).
- LASSO-Cox Regression: Conduct least absolute shrinkage and selection operator regression with 10-fold cross-validation repeated 1000 times to select most prognostic features while preventing overfitting.
- Multivariate Cox Analysis: Construct final prognostic model using genes satisfying proportional hazards assumption (p>0.05) and variance inflation factor <2.
Prognostic Model Construction and Validation
Protocol:
- Risk Score Calculation: Compute risk score using formula: Risk score = Σ (Coefficient~i~ × Expression~i~)
- Patient Stratification: Divide patients into high-risk and low-risk groups using optimal cut-off value determined by X-tile software or median risk score.
- Survival Analysis: Perform Kaplan-Meier analysis with log-rank test to compare overall survival between risk groups.
- Time-dependent ROC Analysis: Evaluate predictive performance of signature at 1, 3, and 5 years using "timeROC" package.
- Independent Validation: Apply identical risk score formula and cut-off values to independent ICGC cohort to verify robustness.
Experimental Validation Using Clinical Samples
Required Resources:
- Plasma/serum samples from HCC patients and healthy controls
- RNA extraction kit (e.g., Plasma/Serum Circulating and Exosomal RNA Purimentation Mini Kit)
- DNase treatment reagents
- Reverse transcription kit (e.g., High-Capacity cDNA Reverse Transcription Kit)
- Real-time PCR system and SYBR Green Master Mix
Protocol:
- Sample Collection: Collect plasma from peripheral blood centrifuged at 704× g for 10 minutes. Store at -70°C until use.
- RNA Extraction: Isolate total RNA from 500μL plasma using specialized kits for circulating RNA.
- DNAse Treatment: Treat RNA samples with Turbo DNase to remove genomic DNA contamination.
- cDNA Synthesis: Reverse transcribe RNA to cDNA using High-Capacity cDNA Reverse Transcription Kit.
- RT-qPCR Analysis: Perform quantitative PCR with Power SYBR Green PCR Master Mix using following conditions: initial denaturation at 95°C for 2 min, followed by 40 cycles of 95°C for 15 sec and 62°C for 1 min.
- Data Analysis: Calculate lncRNA expression using 2−ΔΔCt method with β-actin as internal reference.
Key Experimental Protocols
LncRNA Detection in Plasma/Serum Samples
Principle: This protocol enables sensitive detection of circulating lncRNAs as non-invasive biomarkers for HCC diagnosis and prognosis assessment.
Detailed Procedure:
- Patient Cohort Selection: Recruit three participant groups: HCC patients, chronic hepatitis C (CHC) patients who developed HCC within 5-year follow-up (HCCpos), CHC patients who did not develop HCC (HCCneg), and healthy blood donors as control group (CG). Balance groups for age and sex.
- Sample Preparation: Collect peripheral blood in EDTA tubes and centrifuge at 704× g for 10 minutes within 2 hours of collection. Aliquot plasma and store at -70°C.
- RNA Isolation: Use commercial plasma/serum circulating RNA purification kits according to manufacturer's protocol. Include DNase treatment step to eliminate genomic DNA contamination.
- Quality Assessment: Verify RNA integrity using polyacrylamide gel electrophoresis. Ensure A260/A280 ratio between 1.8-2.0.
- Reverse Transcription: Use High-Capacity cDNA Reverse Transcription Kit with random primers in 20μL reaction volume.
- Quantitative PCR: Perform in triplicate using SYBR Green chemistry with the following cycling parameters:
- Initial denaturation: 95°C for 2 minutes
- 40 cycles of: 95°C for 15 seconds, 62°C for 1 minute
- Melting curve analysis: 60-95°C with 0.3°C increments
- Data Analysis: Calculate expression using 2−ΔΔCt method with β-actin as reference gene. Include no-template controls in each run.
Functional Validation of Candidate LncRNAs
Principle: Establish biological relevance of identified lncRNAs through in vitro functional assays.
Detailed Procedure:
- Gene Knockdown: Design and transfert siRNA or ASO targeting candidate lncRNAs (e.g., MIR4435-2HG) into HCC cell lines using appropriate transfection reagents.
- Proliferation Assay: Assess cell viability using MTT or CCK-8 assays at 24, 48, and 72 hours post-transfection.
- Migration and Invasion Assays: Perform transwell migration and Matrigel invasion assays 48 hours post-transfection. Quantify cells that migrate through 8μm pores.
- EMT Marker Analysis: Evaluate epithelial-mesenchymal transition by Western blotting for E-cadherin, N-cadherin, and vimentin.
- Immune Evasion Assessment: Measure PD-L1 expression changes post-knockdown using flow cytometry or Western blot.
Data Analysis and Interpretation
Statistical Considerations
Protocol:
- Survival Analysis: Use Kaplan-Meier method with log-rank test to compare overall survival between risk groups.
- ROC Analysis: Generate time-dependent receiver operating characteristic curves at 1, 3, and 5 years to evaluate predictive accuracy.
- Multivariate Cox Regression: Assess independent prognostic value of lncRNA signature after adjusting for clinical variables (age, gender, stage, grade).
- Calibration: Plot calibration curves to evaluate agreement between predicted and observed survival probabilities.
Validation Metrics and Reporting
Protocol:
- Performance Metrics: Report hazard ratios (HR) with 95% confidence intervals, p-values, and area under curve (AUC) values for all validation cohorts.
- Clinical Utility: Evaluate net reclassification improvement and integrated discrimination improvement when adding lncRNA signature to established clinical predictors.
- Reproducibility: Assess consistency of risk stratification across multiple independent cohorts.
Representative Results and Applications
Table 1: Clinically Validated lncRNAs with Independent Prognostic Value in HCC
| LncRNA | Expression in HCC | Sample Type | Cohort Size | HR (95% CI) | P-value | Function |
|---|---|---|---|---|---|---|
| LINC00152 | High | Tissue | 63 | 2.524 (1.661-4.015) | 0.001 | Promotes proliferation |
| LINC01146 | High | Tissue | 85 | 0.38 (0.16-0.92) | 0.033 | Tumor suppressor |
| HOXC13-AS | High | Tissue | 197 | 2.894 (1.183-4.223) | 0.015 | Promotes recurrence |
| LASP1-AS | Low | Tissue | 423 | 3.539 (2.698-6.030) | <0.0001 | Tumor suppressor |
| ELMO1-AS1 | High | Tissue | 222 | 0.430 (0.225-0.824) | 0.011 | Tumor suppressor |
| HULC | High | Plasma | 41 HCC, 22 CG | - | <0.05 | Diagnostic biomarker |
| RP11-731F5.2 | High | Plasma | 41 HCC, 22 CG | - | <0.05 | HCC risk assessment |
Table 2: Multi-Gene Signature Performance in Independent Validation Cohorts
| Signature Type | Genes Included | Training Cohort (TCGA) | Validation Cohort (ICGC) | Clinical Application |
|---|---|---|---|---|
| Glycolysis-Associated Multiomics Prognostic Model | 19 glycolysis-associated genes | 363 patients, p<0.001 | Significant OS difference, p=0.003 | Stratifies patients into risk groups |
| Six-Gene Expression Signature | PZP, HMMR, LCAT, GRAMD1C, LPL, ANGPTL1 | 339 patients | 231 patients, independent prognostic factor | Predicts OS and progression-free interval |
| Angiogenesis-Related Signature | EFNA3, EGF, MMP3, AURKB | 371 patients, AUC 0.76 at 0.5 years | 243 patients, AUC 0.79 at 1 year | Predicts OS and recurrence |
| Migrasome-Related lncRNA Signature | LINC00839, MIR4435-2HG | 372 patients | 100 patients in external cohort | Predicts immunotherapy response |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for lncRNA Biomarker Studies
| Reagent/Category | Specific Examples | Function/Application | Protocol Notes | |||
|---|---|---|---|---|---|---|
| RNA Extraction Kits | Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) | Isolation of circulating lncRNAs from biofluids | Use 500μL plasma input; include DNase treatment | |||
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | cDNA synthesis from low-input RNA samples | Use random primers; minimum 10ng RNA input | |||
| qPCR Reagents | Power SYBR Green PCR Master Mix (Thermo Fisher) | Quantitative detection of lncRNA expression | Run in triplicate; include dissociation curve | |||
| Bioinformatics Tools | edgeR, limma R packages | Differential expression analysis | FDR <0.05, | log2FC | >1 | |
| Survival Analysis Packages | survival, survminer, timeROC R packages | Prognostic model development and validation | Kaplan-Meier curves with log-rank test | |||
| Functional Validation Reagents | siRNA, ASO against target lncRNAs | Loss-of-function studies | Optimize transfection efficiency for each cell line | |||
| Clinical Validation Cohorts | TCGA-LIHC, ICGC LIRI-JP | Independent validation of biomarkers | Ensure consistent preprocessing across cohorts | |||
| Atraric Acid | Methyl 2,4-dihydroxy-3,6-dimethylbenzoate|CAS 4707-47-5 | Methyl 2,4-dihydroxy-3,6-dimethylbenzoate (Atraric Acid). High-purity grade for antiandrogen, fragrance, and organic synthesis research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
Troubleshooting and Technical Notes
- Low RNA Yield from Plasma: Pre-centrifuge plasma at 12,000× g for 10 minutes to remove debris before RNA extraction.
- Inconsistent RT-qPCR Results: Normalize using multiple reference genes and include inter-run calibrators.
- Batch Effects in Multi-Cohort Analysis: Apply ComBat or other batch correction algorithms when integrating datasets.
- Overfitting in Model Development: Use repeated LASSO with cross-validation and validate in completely independent cohorts.
- Functional Validation Challenges: Use multiple siRNA sequences and rescue experiments to confirm specificity.
This application note provides a comprehensive framework for rigorous validation of lncRNA biomarkers in HCC using TCGA, ICGC, and multi-center study designs. The standardized protocols for bioinformatic analysis, experimental validation, and clinical correlation enable researchers to generate robust, reproducible data with potential for clinical translation. Independent cohort validation remains essential for establishing the clinical utility of lncRNA signatures in HCC diagnosis, prognosis, and treatment selection.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most prevalent malignancy worldwide and the third leading cause of cancer-related mortality [39] [33]. The insidious onset of HCC often results in late-stage diagnosis, contributing to poor prognosis despite therapeutic advances [39]. Conventional serum biomarkers such as alpha-fetoprotein (AFP) demonstrate limited diagnostic accuracy, with suboptimal sensitivity and specificity that hinder early detection efforts [41] [42]. Within this diagnostic landscape, long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers with the potential to revolutionize HCC detection and prognosis.
LncRNAs are transcripts longer than 200 nucleotides with limited protein-coding capacity that regulate gene expression at transcriptional, post-transcriptional, and epigenetic levels [43] [44]. Their dysregulation has been intimately linked to hepatocarcinogenesis, with specific expression patterns correlating with tumor development, progression, and metastasis [9] [45]. Crucially, lncRNAs are remarkably stable in blood circulation and other body fluids, making them exceptionally suitable for liquid biopsy applications [14] [41]. This stability, combined with their disease-specific expression patterns, positions lncRNAs as ideal candidates for developing non-invasive diagnostic tools.
The evaluation of lncRNA diagnostic performance relies heavily on rigorous statistical measures, particularly receiver operating characteristic (ROC) curves, sensitivity, specificity, and the area under the curve (AUC) values. These metrics provide standardized frameworks for assessing biomarker efficacy, enabling direct comparison between novel lncRNA signatures and established diagnostic methods. This application note details the experimental protocols and analytical frameworks required for proper validation of lncRNA biomarkers in HCC cohorts, with emphasis on quantitative accuracy assessment through ROC analysis.
Performance Metrics of lncRNA Biomarkers in HCC
Table 1: Diagnostic Performance of Individual lncRNA Biomarkers for HCC Detection
| lncRNA | Sample Type | Sensitivity (%) | Specificity (%) | AUC | Reference |
|---|---|---|---|---|---|
| LINC00152 | Plasma | 83 | 67 | 0.79 | [33] |
| UCA1 | Plasma | 60 | 53 | 0.72 | [33] |
| GAS5 | Plasma | 63 | 60 | 0.70 | [33] |
| LINC00853 | Plasma | 77 | 63 | 0.75 | [33] |
| HULC | Plasma | Reported in panels | Reported in panels | 0.76 | [14] |
| RP11-731F5.2 | Plasma | Reported in panels | Reported in panels | 0.81 | [14] |
Table 2: Multi-lncRNA Signatures and Machine Learning Models for HCC Diagnosis
| Biomarker Panel/Model | Sensitivity (%) | Specificity (%) | AUC | Components | Reference |
|---|---|---|---|---|---|
| 4-lncRNA ML Model | 100 | 97 | 0.99 | LINC00152, UCA1, GAS5, LINC00853 + clinical parameters | [33] |
| SVM Model (HBV-HCC) | 95.7 | 100 | 0.96 | 9-lncRNA signature including AL356056.2, TRIM52-AS1 | [43] |
| Random Forest (HBV-HCC) | 94.3 | 86.5 | 0.90 | 9-lncRNA signature including AL356056.2, TRIM52-AS1 | [43] |
| 3-lncRNA Panel | Data not specified | Data not specified | 0.89 | PTENP1, LSINCT-5, UCA1 | [41] |
Table 3: Prognostic lncRNA Signatures for HCC Patient Stratification
| lncRNA Signature | Clinical Application | Risk Groups | HR (High vs. Low Risk) | Reference |
|---|---|---|---|---|
| 7-lncRNA Ferroptosis-Related | Overall Survival Prediction | High-risk vs. Low-risk | 1-year AUC: 0.75, 3-year AUC: 0.72 | [42] |
| 4-lncRNA Amino Acid Metabolism-Related | Overall Survival Prediction | High-risk vs. Low-risk | Significant separation (p<0.05) | [44] |
| 7-lncRNA ceRNA-based | Overall Survival Prediction | High-risk vs. Low-risk | Significant separation (p<0.05) | [46] |
The quantitative performance of lncRNAs as HCC biomarkers varies from moderate for individual markers to exceptional for multi-lncRNA panels enhanced by machine learning algorithms. Individual lncRNAs such as LINC00152 demonstrate respectable diagnostic potential with sensitivity of 83% and specificity of 67% (AUC=0.79) [33]. Similarly, LINC00853 shows sensitivity of 77% with specificity of 63% (AUC=0.75) [33]. The real diagnostic power emerges when these markers are combined into panels or incorporated into machine learning models. A four-lncRNA panel (LINC00152, UCA1, GAS5, LINC00853) integrated with standard clinical parameters through machine learning achieved remarkable performance with 100% sensitivity and 97% specificity [33]. Similar enhancements were observed in HBV-related HCC, where a support vector machine model utilizing a 9-lncRNA signature achieved an AUC of 0.96 with 95.7% sensitivity and 100% specificity [43].
Beyond diagnosis, lncRNA signatures show significant prognostic value. A 7-lncRNA ferroptosis-related signature effectively stratified HCC patients into high-risk and low-risk groups with distinct overall survival outcomes, achieving AUC values of 0.745, 0.745, and 0.719 for 1-, 2-, and 3-year survival prediction, respectively [42]. Similarly, amino acid metabolism-related lncRNA signatures and ceRNA-based models have demonstrated robust prognostic capabilities for HCC patient stratification [44] [46].
Experimental Protocols for lncRNA Biomarker Validation
Sample Collection and RNA Extraction
Principle: Proper sample collection and RNA isolation are critical for obtaining high-quality lncRNA samples from blood or tissues. Circulating lncRNAs exhibit remarkable stability in blood, making them suitable for liquid biopsy applications [41].
Protocol:
- Plasma Separation: Collect peripheral blood in EDTA tubes and centrifuge at 704-800 × g for 10 minutes at 4°C to separate plasma from cellular components [14] [33].
- RNA Extraction: Isolate total RNA from 500 μL plasma using commercial kits (e.g., miRNeasy Mini Kit, QIAGEN; or Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit, Norgen Biotek) according to manufacturer protocols [14] [33].
- DNAse Treatment: Treat RNA samples with Turbo DNase to remove genomic DNA contamination [14].
- Quality Assessment: Evaluate RNA quality and concentration using spectrophotometry (NanoDrop) or bioanalyzer systems.
Technical Notes:
- Consistent processing time (within 2 hours of collection) minimizes RNA degradation.
- Aliquot samples to avoid repeated freeze-thaw cycles.
- Include positive and negative controls in each extraction batch.
cDNA Synthesis and Quantitative Real-Time PCR
Principle: Reverse transcription followed by quantitative PCR enables specific and sensitive detection of lncRNA expression levels.
Protocol:
- cDNA Synthesis: Convert 500 ng-1 μg total RNA to cDNA using High-Capacity cDNA Reverse Transcription Kit with random hexamers or gene-specific primers [14] [33].
- qRT-PCR Setup: Prepare reactions with Power SYBR Green Master Mix, cDNA template, and specific primers (Table 4).
- Amplification Parameters: Use the following cycling conditions: initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 60-62°C for 1 minute [14] [33].
- Melting Curve Analysis: Include a dissociation step (60-95°C) to verify amplification specificity.
Table 4: Essential Research Reagent Solutions for lncRNA Biomarker Studies
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN), Norgen Plasma/Serum Kit | Isolation of high-quality lncRNAs from plasma, serum, or tissues | Select kits optimized for circulating RNA; includes DNase treatment |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | Conversion of RNA to cDNA | Use random hexamers for unbiased representation |
| qPCR Master Mixes | Power SYBR Green Master Mix, PowerTrack SYBR Green Master Mix | Fluorescence-based detection of lncRNA amplification | SYBR Green is cost-effective for multiple targets; validate specificity with melting curves |
| Reference Genes | β-actin, GAPDH | Normalization of lncRNA expression levels | Validate stability in your experimental system; avoid genes affected by pathological conditions |
| Primer Sets | Custom-designed lncRNA-specific primers | Specific amplification of target lncRNAs | Design primers spanning exon-exon junctions when possible; verify specificity with BLAST |
| Commercial Assays | RevertAid First Strand cDNA Synthesis Kit | cDNA synthesis | Follow manufacturer's protocols for optimal results |
Data Normalization and Expression Quantification
Principle: Accurate normalization is essential for reliable lncRNA quantification and cross-sample comparison.
Protocol:
- Reference Gene Selection: Use stable reference genes (β-actin or GAPDH) for normalization [14] [33].
- Cycle Threshold Determination: Set threshold in exponential phase of amplification plots.
- Relative Quantification: Calculate expression using the 2^(-ΔΔCt) method [14].
- Quality Control: Run samples in triplicate with no-template controls; exclude assays with amplification in negative controls or poor efficiency.
Technical Notes:
- Validate reference gene stability under experimental conditions.
- Assay efficiency should be 90-110% for reliable 2^(-ΔΔCt) calculation.
- Implement inter-plate calibrators for multi-plate experiments.
ROC Curve Analysis and Statistical Validation
Diagnostic Accuracy Assessment
Principle: ROC curve analysis evaluates the discriminatory power of lncRNA biomarkers by plotting sensitivity against 1-specificity across all possible cutoff points.
Protocol:
- Data Preparation: Compile normalized lncRNA expression values with clinical diagnosis (HCC vs. control) for all samples.
- ROC Curve Generation: Use statistical software (R package "pROC," GraphPad Prism, or Python Scikit-learn) to generate ROC curves [39] [43].
- AUC Calculation: Determine AUC as a measure of overall diagnostic accuracy.
- Optimal Cutoff Selection: Identify the point on the ROC curve maximizing both sensitivity and specificity (Youden's index).
- Performance Metrics Calculation:
- Sensitivity = True Positives / (True Positives + False Negatives)
- Specificity = True Negatives / (True Negatives + False Positives)
- Positive Predictive Value = True Positives / (True Positives + False Positives)
- Negative Predictive Value = True Negatives / (True Negatives + False Negatives)
Technical Notes:
- For multi-lncRNA panels, use logistic regression or machine learning algorithms to generate composite scores.
- Apply cross-validation (leave-one-out or k-fold) to minimize overfitting.
- Compare AUC values between novel biomarkers and established standards (e.g., AFP) using DeLong's test.
Machine Learning Integration for Enhanced Diagnostics
Principle: Machine learning algorithms can integrate multiple lncRNA biomarkers with clinical parameters to improve diagnostic and prognostic accuracy.
Protocol:
- Feature Selection: Identify the most informative lncRNAs using random forest, LASSO regression, or stepwise selection [39] [43].
- Model Training: Utilize algorithms such as support vector machines (SVM), random forests, or generalized linear models with cross-validation [39] [43] [33].
- Model Validation: Assess performance on independent validation cohorts using ROC analysis.
- Clinical Implementation: Develop user-friendly tools (nomograms, online calculators) for clinical translation.
Figure 1: Experimental Workflow for lncRNA Biomarker Validation in HCC
The rigorous assessment of diagnostic accuracy through ROC curves, sensitivity, specificity, and AUC values provides an essential framework for validating lncRNA biomarkers in hepatocellular carcinoma. Individual lncRNAs show moderate diagnostic performance, but their true potential emerges when combined into multi-marker panels and enhanced through machine learning approaches. The experimental protocols outlined herein provide a standardized methodology for lncRNA biomarker development, from sample processing through statistical validation. As research in this field advances, lncRNA biomarkers promise to significantly improve early detection, prognostic stratification, and personalized treatment approaches for HCC patients, ultimately addressing critical unmet needs in oncology clinical practice.
Within the framework of a thesis on long non-coding RNA (lncRNA) biomarker validation in hepatocellular carcinoma (HCC), the statistical confirmation of a biomarker's independent prognostic value is a critical step. This protocol details the application of the multivariate Cox proportional hazards regression model to validate the association between lncRNA expression levels and key clinical endpoints: Overall Survival (OS) and Recurrence-Free Survival (RFS). This methodology allows researchers to determine whether a candidate lncRNA is an independent predictor of patient survival, after statistically adjusting for other established clinical and pathological factors [47] [48].
Key Concepts and Definitions
- Overall Survival (OS): The time from a defined starting point (e.g., diagnosis or start of treatment) until death from any cause [49].
- Recurrence-Free Survival (RFS): The time from a defined starting point (e.g., curative surgical resection) until the recurrence of the cancer [50] [51].
- Censoring: A fundamental aspect of survival data where the event of interest (death or recurrence) has not been observed for some patients by the end of the study follow-up period. These patients are "right-censored," meaning their true survival time is unknown but is at least as long as the last follow-up time [48] [49].
- Hazard Ratio (HR): The primary effect size estimate from a Cox model. It represents the relative increase (HR >1) or decrease (HR <1) in the instantaneous risk of the event (e.g., death) associated with a one-unit change in a predictor variable [47] [48].
Experimental Workflow and Data Analysis Protocol
The following diagram outlines the comprehensive workflow for prognostic validation, from cohort definition through to final interpretation.
Data Collection and Variable Coding
The first phase involves meticulous preparation of the dataset, where each variable must be correctly defined and coded.
Dependent Variables (Outcomes):
Independent Variables (Predictors/Covariates):
- lncRNA Expression: Can be analyzed as a continuous variable (e.g., ∆Ct values from RT-qPCR) or dichotomized into "high" vs. "low" expression groups based on a predefined cutoff (e.g., median) [51] [33].
- Clinical Covariates: These are factors known to influence prognosis and must be included for adjustment. They can be:
Statistical Analysis Protocol
The analysis proceeds in a stepwise manner to build a robust statistical model.
- Univariate Analysis: Perform a separate Cox regression for each variable of interest (including the lncRNA and all clinical covariates). This provides an initial, unadjusted assessment of each factor's relationship with survival [47] [52].
- Multivariate Analysis: Construct a Cox regression model that includes the lncRNA expression level along with clinically relevant covariates identified from the univariate analysis or the literature. This determines the independent effect of the lncRNA on survival after accounting for other factors [47] [50] [48].
- Model Assumption Check: The Cox model relies on the proportional hazards (PH) assumption, meaning the hazard ratio for any factor is constant over time. This must be verified using statistical tests or graphical methods (e.g., Schoenfeld residuals) [47].
- Model Performance: Assess the model's predictive accuracy using the concordance index (C-index), which is analogous to the Area Under the ROC Curve for survival data. A C-index of 0.837, for example, indicates strong predictive ability [50].
Data Presentation and Interpretation
The results of the Cox regression analysis are typically presented in a table format, as illustrated below with examples from HCC and other cancer studies.
Table 1: Exemplary Multivariate Cox Regression Analysis for Overall Survival in a Hypothetical HCC Cohort
| Covariate | Category / Unit | Coefficient | Hazard Ratio (HR) | 95% CI for HR | P-value |
|---|---|---|---|---|---|
| LINC00152 | High vs. Low Expression | 0.926 | 2.524 | (1.661 – 4.015) | 0.001 |
| HOXC13-AS [51] | High vs. Low Expression | 1.063 | 2.894 | (1.183 – 4.223) | 0.015 |
| LASP1-AS [51] | Low vs. High Expression | -0.633 | 0.531 | (0.352 – 0.801) | 0.002 |
| Age | >70 vs. ≤70 years | 0.584 | 1.793 | (1.15 – 2.79) | 0.009 |
| Tumor Grade | II vs. I | 0.885 | 2.423 | (1.40 – 4.19) | <0.001 |
| III vs. I | 0.885 | 2.423 | (1.40 – 4.18) | <0.001 | |
| Tumor Stage | Per 1-stage increase | 0.731 | 2.077 | (1.82 – 2.37) | <0.001 |
| Molecular Subtype | Triple Negative vs. Other | 0.746 | 2.109 | (1.45 – 3.07) | <0.001 |
Interpretation Guide
- Hazard Ratio (HR): An HR of 2.524 for high LINC00152 expression means that the risk of death is about 2.5 times higher in patients with high expression compared to those with low expression, after adjusting for all other factors in the model [47] [51].
- Confidence Interval (95% CI): An interval that does not include 1.0 (e.g., 1.66 - 4.02) indicates a statistically significant association at the 5% level.
- P-value: A p-value less than 0.05 is typically considered statistically significant, suggesting the association is unlikely due to chance.
The Scientist's Toolkit
Table 2: Essential Research Reagent Solutions for lncRNA Prognostic Validation Studies
| Item | Function / Application | Specific Examples from Literature |
|---|---|---|
| RNA Isolation Kit | For extraction of total RNA, including lncRNAs, from plasma, serum, or tissue samples. | Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) [14]; miRNeasy Mini Kit (QIAGEN) [33]. |
| cDNA Synthesis Kit | Reverse transcription of RNA into stable cDNA for subsequent PCR amplification. | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) [14]; RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [33]. |
| qRT-PCR Master Mix | For quantitative real-time PCR to precisely measure lncRNA expression levels. | Power SYBR Green PCR Master Mix (Thermo Fisher) [14]; PowerTrack SYBR Green Master Mix (Applied Biosystems) [33]. |
| Reference Genes | Endogenous controls for normalization of lncRNA expression data to account for technical variability. | β-actin [14]; GAPDH [33]. |
| Statistical Software | To perform the Cox regression analysis, generate Kaplan-Meier curves, and calculate statistics. | R with "survival" package [48]; SPSS; SAS; Stata; GraphPad [14]. |
Signaling Pathways and Logical Relationships
The prognostic power of a lncRNA is often rooted in its biological function. The following diagram illustrates a generalized signaling logic by which an oncogenic lncRNA might influence HCC survival pathways, thereby providing a mechanistic basis for its prognostic value.
Within the context of hepatocellular carcinoma (HCC) biomarker validation, a central question is whether single biomarkers or multi-lncRNA panels offer superior clinical utility. Long non-coding RNAs (lncRNAs) have emerged as promising biomarkers due to their roles in carcinogenesis and their detectability in biological fluids, facilitating liquid biopsy approaches [14]. This application note provides a comparative analysis of single and combination lncRNA biomarkers, detailing their prognostic performance, experimental protocols for validation, and integration into predictive models.
Performance Comparison of Single and Combination LncRNA Biomarkers
Prognostic Value of Single lncRNA Biomarkers in HCC Tissues
Multiple studies have validated the independent prognostic significance of individual lncRNAs in HCC patient tissues using multivariate Cox regression analysis. The table below summarizes key single lncRNA biomarkers associated with overall survival (OS) and recurrence-free survival (RFS).
Table 1: Single lncRNA Biomarkers with Independent Prognostic Value in HCC
| LncRNA Name | Expression in Tumor | Hazard Ratio (HR) for OS | 95% CI | P-value | Cohort Size (n) | Detection Method |
|---|---|---|---|---|---|---|
| LINC00152 [51] | High | 2.524 | 1.661–4.015 | 0.001 | 63 | qRT-PCR |
| LINC00294 [51] | High | 2.434 | 1.143–3.185 | 0.021 | 94 | ISH |
| LINC01094 [51] | High | 2.091 | 1.447–3.021 | <0.001 | 365 | RNAseq |
| LINC01146 [51] | High | 0.38 | 0.16–0.92 | 0.033 | 85 | qRT-PCR |
| HOXC13-AS [51] | High | 2.894 | 1.183–4.223 | 0.015 | 197 | qRT-PCR |
| LASP1-AS [51] | Low | 1.884 (Training) | 1.427–2.841 | <0.0001 | 423 (total) | qRT-PCR |
| ELMO1-AS1 [51] | High | 0.518 (Training) | 0.277–0.968 | 0.039 | 222 (total) | qRT-PCR |
| FOXP4-AS1 [51] | High | 2.712 (Training) | 1.140–6.450 | 0.024 | 121 (total) | qRT-PCR |
| GAS5 [33] | Low | N/A | N/A | N/A | 52 | qRT-PCR |
Enhanced Diagnostic and Prognostic Performance of Combination Panels
Combination lncRNA panels demonstrate significantly improved performance characteristics compared to single lncRNA biomarkers, as evidenced by higher sensitivity, specificity, and area under the curve (AUC) values in receiver operating characteristic (ROC) analyses.
Table 2: Performance of Combination LncRNA Biomarker Panels in HCC
| Biomarker Panel Composition | Sample Type | Performance Metrics | Clinical Application | Reference |
|---|---|---|---|---|
| 4-lncRNA Panel (LINC00152, LINC00853, UCA1, GAS5) + conventional lab data | Plasma | 100% Sensitivity, 97% Specificity (Machine Learning Model) | HCC Diagnosis | [33] |
| 2-lncRNA Panel (HULC, RP11-731F5.2) | Plasma | Potential for HCC risk assessment in Chronic Hepatitis C patients | Early Diagnosis / Risk Stratification | [14] |
| 14-RNA Model (8 immune-related lncRNAs + 6 mRNAs) | Tissue (TCGA) | Training set AUC: 0.827; All samples AUC: 0.757 | Survival Prognosis | [38] |
| 20-Pair DE-irlncRNA signature | Tissue (TCGA) | Effective prognosis prediction for HNSCC | Survival Prognosis | [53] |
| mRNA-lncRNA Panel (SMC1B, CELSR3, FEZF1-AS1, LINC01305) | Tissue & Blood | Tissue AUC: 0.9659 (SCC), 0.9636 (ADC); Blood AUC: 0.9320 | Cervical Cancer Diagnosis | [54] |
Experimental Protocols for LncRNA Biomarker Validation
Sample Collection and RNA Isolation
Protocol for Plasma/Serum Collection and RNA Extraction
- Sample Collection: Collect peripheral blood in serum separator tubes (e.g., BD gold-top tubes) [55]. Centrifuge at 704 × g (RCF) for 10 minutes to separate plasma/serum [14]. For plasma, use EDTA or heparin tubes followed by centrifugation at 3,000 rpm for 10 minutes [54].
- Storage: Immediately aliquot and store samples at -70°C until RNA extraction.
- RNA Isolation: Use commercial kits specifically designed for liquid biopsies:
- DNAse Treatment: Treat RNA samples with Turbo DNase (Life Technologies) to remove genomic DNA contamination [14].
- Quality Assessment: Measure RNA concentration and purity using spectrophotometry (e.g., SpectraMax QuickDrop). Acceptable 260/280 ratios are >1.7, with most samples >1.9 [55].
cDNA Synthesis and Quantitative Real-Time PCR (qRT-PCR)
Standardized qRT-PCR Protocol for LncRNA Quantification
- Reverse Transcription:
qRT-PCR Setup:
- Reaction Mix: Power SYBR Green PCR Master Mix (Thermo Fisher) [14] or PowerTrack SYBR Green Master Mix (Applied Biosystems) [33].
- Primer Design: Customize exon-spanning primers against human lncRNAs. Pre-dry primers in 96-well plates for high-throughput studies [55].
- Internal Control: Use reference genes (β-actin [55] [14] or GAPDH [33]) for normalization.
- Platform: Use real-time PCR systems (e.g., LightCycler 96 [Roche] [55], ViiA 7 [Applied Biosystems] [33], or StepOne Plus [Applied Biosystems] [14]).
- Reaction Conditions: Initial denaturation at 95°C for 2 min, followed by 40 cycles of 95°C for 15 sec and 62°C for 1 min [14].
- Technical Replication: Perform all reactions in triplicate with no-template controls.
Data Analysis:
Statistical Analysis and Model Building
Protocol for Biomarker Validation and Model Development
- Data Preprocessing:
Differential Expression Analysis:
Performance Assessment:
Predictive Model Construction:
- For combination panels: Use binomial regression with DR diagnosis as response variable and lncRNA expression as predictors [55].
- For prognostic models: Use Cox regression analysis with survival data [51] [38].
- Machine Learning Approaches: Implement algorithms like Random Forest, Support Vector Machine, or XGBoost using Python's Scikit-learn platform [33].
- Apply train/validation/test splitting (e.g., 60/20/20) with stratified sampling to ensure balanced outcome distribution [56].
- Use 10-fold cross-validation for model tuning and avoid overfitting.
Nomogram Construction:
- Incorporate riskscore and clinical variables (e.g., TNM stage, Child-Pugh classification) using regplot package in R to predict patient survival [38].
Signaling Pathways and Molecular Mechanisms
LncRNAs regulate HCC progression through multiple mechanisms, including immune modulation, and can function as signaling molecules, guiding molecules, decoy molecules, or scaffolding molecules [51].
Experimental Workflow for Biomarker Validation
The complete workflow for lncRNA biomarker validation encompasses sample collection, molecular analysis, and computational modeling.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for LncRNA Biomarker Studies
| Reagent Category | Specific Product Examples | Primary Function | Application Notes |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN), Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) | High-quality RNA extraction from limited samples | Optimized for low-concentration circulating RNA |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit (Applied Biosystems), RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | cDNA synthesis from RNA templates | Include DNAse treatment step to remove genomic DNA |
| qPCR Master Mixes | Power SYBR Green PCR Master Mix (Thermo Fisher), PowerTrack SYBR Green Master Mix (Applied Biosystems) | Fluorescence-based detection of amplified products | SYBR Green suitable for well-annotated targets |
| Reference Genes | β-actin, GAPDH | Internal controls for normalization | Validate stability across sample types |
| Primer Design Tools | Custom exon-spanning primers (Thermo Fisher) | Specific amplification of target lncRNAs | Avoid genomic amplification and ensure specificity |
| qPCR Platforms | LightCycler 96 (Roche), ViiA 7 (Applied Biosystems) | Accurate quantification of gene expression | Enable high-throughput screening capabilities |
Long non-coding RNAs (lncRNAs) have emerged as pivotal regulators in hepatocellular carcinoma (HCC), influencing tumor initiation, progression, and therapeutic response. These molecules, defined as RNA transcripts longer than 200 nucleotides with limited or no protein-coding capacity, demonstrate differential expression patterns across diverse cancers, affecting their growth and survival potential [57] [33]. In HCC, lncRNAs modulate gene expression at epigenetic, transcriptional, and post-transcriptional levels, actively participating in pathological and physiological processes [57]. The emerging roles of lncRNAs extend to shaping the immune microenvironment, influencing immune cell infiltration, cytokine profiles, and immune checkpoint expression, thereby affecting the tumor's immunogenicity and response to immunotherapies [58]. This application note explores the predictive biomarker potential of specific lncRNAs in HCC, detailing their correlation with treatment response and utility as therapeutic targets, complete with validated experimental protocols for research applications.
Clinically Relevant lncRNAs in HCC: Expression and Diagnostic Performance
Comprehensive profiling studies have identified hundreds of dysregulated lncRNAs in HCC tissues compared with normal tissues [59]. The table below summarizes key lncRNAs with documented diagnostic and prognostic significance in hepatocellular carcinoma.
Table 1: Key lncRNAs with Demonstrated Clinical Relevance in HCC
| LncRNA Name | Expression in HCC | Biological Function | Clinical Correlation | Prognostic Value |
|---|---|---|---|---|
| HULC | Upregulated [60] [57] | Promotes angiogenesis via SPHK1; induces autophagy [57] | Positively correlates with Edmondson grade & HBV infection [57] | Potential plasma biomarker [57] |
| MALAT1 | Upregulated [60] [61] | Promotes aggressive tumor phenotypes & progression [33] | Higher sensitivity than AFP for HCC detection [61] | Associated with poor prognosis [33] |
| HOTAIR | Upregulated [60] [61] | Epigenetically suppresses miR-122 [61] | Discriminates HCC from cirrhosis [61] | Poor overall & disease-free survival [33] |
| H19 | Upregulated [60] [33] | Promotes proliferation, invasion, angiogenesis [33] | Linked to HCC progression [33] | Poor prognosis [33] |
| GAS5 | Downregulated [33] | Inhibits proliferation, activates apoptosis via CHOP/caspase-9 [33] | Lower expression in HCC patients [33] | Tumor suppressive function |
| LINC00152 | Upregulated [33] | Promotes cell proliferation via CCDN1 regulation [33] | Higher plasma levels in HCC patients [33] | Diagnostic biomarker potential |
| SLC1A5-AS | Upregulated [62] | Enhances glutamine uptake, promotes growth & metastasis [62] | Associated with poor prognosis [62] | Potential therapeutic target |
Recent advances demonstrate that integrating multiple lncRNAs into diagnostic panels significantly enhances detection accuracy. A 2024 study quantified plasma levels of four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) and developed a machine learning model that integrated these lncRNAs with conventional laboratory parameters, achieving 100% sensitivity and 97% specificity for HCC diagnosis, substantially outperforming individual lncRNAs or AFP alone [33].
Table 2: Diagnostic Performance of Individual lncRNAs vs. Combined Model
| Biomarker | Sensitivity (%) | Specificity (%) | Notes | Reference |
|---|---|---|---|---|
| LINC00152 | 60-83 | 53-67 | Moderate diagnostic accuracy | [33] |
| LINC00853 | 60-83 | 53-67 | Moderate diagnostic accuracy | [33] |
| UCA1 | 60-83 | 53-67 | Moderate diagnostic accuracy | [33] |
| GAS5 | 60-83 | 53-67 | Moderate diagnostic accuracy | [33] |
| AFP | ~66 | Varies | Traditional standard | [33] |
| ML Model (lncRNA Panel + Clinical) | 100 | 97 | Superior performance | [33] |
LncRNAs as Predictive Biomarkers for Treatment Response
Correlation with Conventional Therapies
LncRNA expression profiles correlate significantly with treatment response in HCC. For instance, lncRNAs such as PVT1 and SNHG7 are associated with HCC metastasis and recurrence. One study identified these lncRNAs through comparison of expression profiles between early recurrence HCC tissues with metastasis and late recurrence HCC tissues without metastasis. Functional validation through loss-of-function assays confirmed that knockdown of SNHG7 and PVT1 impaired HCC cell invasion, suggesting their potential as biomarkers for predicting aggressive disease and treatment resistance [59].
Predictive Value for Immunotherapy Response
The tumor immune microenvironment plays a crucial role in determining responses to immune checkpoint inhibitors (ICIs), and lncRNAs are critical modulators of this environment [58]. Specific lncRNAs influence immune cell function and immune checkpoint expression:
- NEAT1: Upregulated in peripheral blood mononuclear cells (PBMCs) of HCC patients, where it promotes CD8+ T cell apoptosis and reduces cytolytic activity through the miR-155/Tim-3 pathway. Downregulation of NEAT1 enhances CD8+ T cell cytotoxicity against HCC cells, indicating its potential as a biomarker for predicting and improving immunotherapy outcomes [58].
- Lnc-Tim3: Binds directly to Tim-3, preventing its interaction with Bat3 and subsequently inhibiting T cell receptor signaling. This mechanism contributes to T cell exhaustion in the HCC microenvironment, potentially affecting response to anti-PD-1/PD-L1 therapies [58].
These findings highlight the potential of lncRNAs as predictive biomarkers for immunotherapy response, although clinical validation in large cohorts is ongoing.
LncRNAs as Therapeutic Targets: Mechanisms and Approaches
Targeting Oncogenic lncRNAs
Therapeutic silencing of oncogenic lncRNAs represents a promising strategy for HCC treatment:
- HULC: Promotes HCC progression through multiple mechanisms, including autophagy induction. Ectopic HULC decreases P62 expression and increases LC3 at the transcriptional level, activating LC3 through Sirt1 and increasing expression of autophagy-related genes (becline-1), ultimately accelerating malignant progression of hepatoma cells [57].
- SLC1A5-AS: This hypoxia-induced lncRNA exhibits significantly elevated expression in HCC tissue and is associated with poor prognosis. Functional studies reveal that SLC1A5-AS promotes invasion and metastasis by enhancing glutamine metabolism. Mechanistically, SLC1A5-AS directly binds with myeloid zinc finger 1 (MZF1), acting as a transcriptional repressor and diminishing its binding to the SLC1A5 promoter region, thereby increasing ASCT2 expression and glutamine uptake [62]. Targeting SLC1A5-AS/MZF1, in conjunction with ASCT2 inhibitor treatment, represents a potential therapeutic strategy for HCC.
Activating Tumor-Suppressive lncRNAs
Reactivating tumor-suppressive lncRNAs presents an alternative therapeutic approach:
- GAS5: This tumor-suppressive lncRNA is downregulated in HCC and triggers CHOP and caspase-9 signal pathways, inhibiting cancer cell proliferation and activating apoptosis [33].
- MEG3: Another tumor-suppressive lncRNA downregulated in HCC, particularly in HBV-associated cases, playing a role in inhibiting cell growth and promoting apoptosis [57].
Experimental Protocols for lncRNA Biomarker Validation
Protocol 1: Plasma-Based lncRNA Quantification for Diagnostic Applications
Objective: To quantify lncRNA expression levels in plasma samples for HCC diagnosis and prognosis prediction.
Materials and Reagents:
- miRNeasy Mini Kit (QIAGEN, cat no. 217004) [33]
- RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, cat no. K1622) [33]
- PowerTrack SYBR Green Master Mix kit (Applied Biosystems, cat no. A46012) [33]
- Primers for target lncRNAs (e.g., LINC00152, LINC00853, UCA1, GAS5) and housekeeping gene GAPDH [33]
Procedure:
- Sample Collection and Preparation: Collect plasma from whole blood in EDTA tubes by centrifugation at 2,000 × g for 10 minutes at 4°C. Store at -80°C until RNA extraction.
- RNA Isolation: Extract total RNA using the miRNeasy Mini Kit according to manufacturer's protocol. Include DNase treatment to remove genomic DNA contamination.
- cDNA Synthesis: Perform reverse transcription using 1 μg of total RNA and the RevertAid First Strand cDNA Synthesis Kit on a thermal cycler.
- Quantitative Real-Time PCR: Set up reactions in triplicate using PowerTrack SYBR Green Master Mix on a real-time PCR system. Use the following cycling conditions: 95°C for 2 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 30 sec.
- Data Analysis: Calculate relative expression using the 2−ΔΔCT method with GAPDH for normalization. For machine learning integration, normalize lncRNA expression values and combine with clinical parameters (AFP, ALT, AST) for model construction.
Applications: This protocol can be used for early HCC detection, prognosis assessment, and treatment response monitoring through liquid biopsy.
Protocol 2: Functional Validation of lncRNAs in HCC Progression
Objective: To investigate the functional role of candidate lncRNAs in HCC cell invasion and metastasis.
Materials and Reagents:
- HCC cell lines (e.g., HuH1, Huh-7) [59] [62]
- siRNA targeting lncRNAs and negative control siRNA [59]
- RNAiMAX transfection reagent (Invitrogen) [59]
- TRIzol reagent for RNA extraction [59]
- Transwell chambers (Corning, 8.0-μm pores) [59]
- Matrigel (Sigma-Aldrich) for invasion assays [59]
Procedure:
- Cell Culture and Transfection: Culture HCC cells in appropriate medium (e.g., Dulbecco's modified Eagle's medium with 10% fetal bovine serum). Transfect cells with lncRNA-specific siRNAs or negative control using RNAiMAX according to manufacturer's instructions.
- Knockdown Efficiency Validation: Harvest cells 48 hours post-transfection. Extract RNA using TRIzol reagent and perform qRT-PCR to confirm lncRNA knockdown.
- Invasion Assay: Coat Transwell chambers with Matrigel. Seed 1 × 10^5 transfected cells in 300 μL medium containing 1% FBS in the upper chamber. Add 700 μL medium with 10% FBS to the lower chamber. Incubate for 24 hours.
- Analysis: Fix cells that invaded through the membrane with methanol, stain with 0.1% crystal violet, and image using an inverted microscope. Quantify cell invasion by counting cells in multiple fields.
Applications: This protocol allows functional characterization of lncRNAs involved in HCC metastasis and can be used to validate potential therapeutic targets.
Visualization of Key lncRNA Mechanisms in HCC
The following diagrams illustrate critical mechanistic pathways through which lncRNAs contribute to hepatocellular carcinoma progression and treatment response.
Diagram 1: Key Mechanistic Pathways of lncRNAs in HCC Progression. This diagram illustrates three critical pathways: HULC promotes autophagy and angiogenesis through miRNA sponging and SPHK1 upregulation; SLC1A5-AS enhances glutamine metabolism and metastasis by interfering with MZF1-mediated repression of SLC1A5; NEAT1 regulates T cell function through the miR-155/Tim-3 axis, contributing to immune evasion.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for lncRNA Studies in HCC
| Reagent/Catalog Number | Function/Application | Key Protocols |
|---|---|---|
| miRNeasy Mini Kit (QIAGEN, 217004) | Total RNA isolation from plasma, tissues, and cells | Plasma-based lncRNA quantification [33] |
| RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, K1622) | Reverse transcription for cDNA synthesis | lncRNA expression analysis [33] |
| PowerTrack SYBR Green Master Mix (Applied Biosystems, A46012) | qRT-PCR detection of lncRNAs | lncRNA quantification [33] |
| RNAiMAX Transfection Reagent (Invitrogen) | Delivery of siRNAs into HCC cells | Functional validation [59] |
| Transwell Chambers (Corning, 8.0-μm pores) | Cell migration and invasion assays | Metastasis studies [59] |
| Matrigel (Sigma-Aldrich) | Extracellular matrix for invasion assays | Metastasis studies [59] |
| TRIzol Reagent | RNA extraction from cell lines | lncRNA expression validation [59] |
LncRNAs demonstrate significant potential as predictive biomarkers and therapeutic targets in hepatocellular carcinoma. Their differential expression patterns correlate with disease progression, treatment response, and survival outcomes. The integration of multiple lncRNAs into diagnostic panels, particularly when combined with machine learning approaches and conventional biomarkers, enhances detection accuracy significantly. From a therapeutic perspective, targeting oncogenic lncRNAs like HULC, MALAT1, and SLC1A5-AS or restoring tumor-suppressive lncRNAs like GAS5 represents a promising strategy for HCC management. Furthermore, the role of lncRNAs in modulating the immune microenvironment suggests their potential as biomarkers for predicting immunotherapy response. As research progresses, lncRNA-based approaches are poised to contribute substantially to personalized medicine for HCC patients, enabling more accurate diagnosis, prognosis prediction, and targeted therapeutic interventions.
Conclusion
The validation of lncRNA biomarkers in hepatocellular carcinoma represents a paradigm shift in molecular diagnostics, offering unprecedented opportunities for early detection and personalized management. Through rigorous foundational research, methodological innovation, analytical optimization, and comprehensive clinical validation, lncRNAs have demonstrated significant potential to supplement or surpass current standards like AFP. Promising biomarkers such as ZFAS1, LINC00152, and multi-lncRNA signatures show robust diagnostic and prognostic capabilities, particularly when integrated with machine learning approaches. Future directions must focus on large-scale prospective trials, standardization of detection methodologies, exploration of lncRNA therapeutic targeting, and development of point-of-care testing platforms. As this field matures, lncRNA-based strategies are poised to fundamentally improve HCC patient outcomes through earlier intervention and more precise prognostic stratification.
References
- 1. Hepatocellular carcinoma: Epidemiology, diagnosis and ... [https://www.sciencedirect.com/science/article/pii/S2589555925002538]
- 2. Biomarkers for diagnosis and therapeutic options in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02101-z]
- 3. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 4. Identification and Validation of Novel Biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7545743/]
- 5. Biomarker discovery in hepatocellular carcinoma (HCC) for ... [https://www.sciencedirect.com/science/article/abs/pii/S1359610124000674]
- 6. Long non-coding RNAs and autophagy: dual drivers of ... [https://www.nature.com/articles/s41420-025-02667-7]
- 7. Serum-biomarker-based population screening model for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11889663/]
- 8. Discovery and Validation of Clinically Relevant Long Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405614/]
- 9. lncRNAs as prognostic molecular biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5601763/]
- 10. Long non-coding RNAs: Biogenesis, functions, and clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8637188/]
- 11. Long non-coding RNAs: definitions, functions, challenges ... [https://www.nature.com/articles/s41580-022-00566-8]
- 12. Long non-coding RNA-based single and combination ... [https://pubmed.ncbi.nlm.nih.gov/40892177/]
- 13. LncRNAs expression signatures of hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4033470/]
- 14. lncRNAs as Biomarkers of Hepatocellular Carcinoma Risk ... [https://www.mdpi.com/1467-3045/47/5/348]
- 15. Involvement of lncRNAs in cancer cells migration, invasion ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-023-02741-x]
- 16. Emerging roles of lncRNA in cancer and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6682721/]
- 17. The Long Noncoding RNA Expression Profile of ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0101707]
- 18. Identification of a seven-long non-coding RNA signature ... [https://www.nature.com/articles/s41420-021-00560-7]
- 19. The role of lncRNA-mediated ceRNA regulatory networks ... [https://www.nature.com/articles/s41420-022-01061-x]
- 20. LincRNA-miR interactions in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552288/]
- 21. The role of lncRNA-mediated ceRNA regulatory networks ... [https://www.sciencedirect.com/science/article/pii/S2468054024000015]
- 22. Comprehensive analysis of lncRNA-mediated ceRNA ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.1042928/full]
- 23. Comprehensive analysis of lncRNA-mediated ceRNA ... [https://pubmed.ncbi.nlm.nih.gov/36338699/]
- 24. Identification of diagnostic long non‑coding RNA biomarkers in... [https://www.spandidos-publications.com/mmr/20/2/1121]
- 25. Construction of an lncRNA-mediated ceRNA network to ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0317710]
- 26. Integrating bioinformatics and experimental validation to unveil... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-023-03208-x]
- 27. Frontiers | A migrasome-related lncRNA signature predicts prognosis... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581122/full]
- 28. The epigenetic basis of hepatocellular carcinoma [https://www.nature.com/articles/s41416-025-02969-8]
- 29. Gene Expression Patterns in Human Liver Cancers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC117615/]
- 30. Gene Expression Profile Analysis in Human Hepatocellular ... [https://www.sciencedirect.com/science/article/pii/S1016847823151193]
- 31. Epigenetic drivers of liver cancer: unraveling mechanisms ... [https://ecancer.org/en/news/26640-epigenetic-drivers-of-liver-cancer-unraveling-mechanisms-behind-hepatocellular-carcinoma]
- 32. Epigenetic Regulation Through Histone Deacetylation [https://pubmed.ncbi.nlm.nih.gov/40940750/]
- 33. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 34. Long non-coding RNA-based single and combination ... [https://link.springer.com/article/10.1007/s12672-025-03309-1]
- 35. Differential expression pattern of CC chemokine receptor 7 ... [https://www.nature.com/articles/s41392-025-02308-6]
- 36. Identification and validation of a ferroptosis-related long ... [https://pubmed.ncbi.nlm.nih.gov/40672083/]
- 37. A novel disulfidptosis-related lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582836/]
- 38. Potential role of immune-related LncRNAs in prognosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399479/]
- 39. Identification and validation of feature genes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12558189/]
- 40. Integrating AI and RNA biomarkers in cancer: advances in ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02434-2]
- 41. Blood-derived lncRNAs as biomarkers for cancer diagnosis [https://www.nature.com/articles/s41698-022-00283-7]
- 42. Identification and validation of a ferroptosis-related long non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261030/]
- 43. Potential lncRNA Biomarkers for HBV-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8536424/]
- 44. Amino acid metabolism-related LncRNAs as prognostic ... [https://link.springer.com/article/10.1007/s12672-025-03789-1]
- 45. Non-coding RNAs in Hepatocellular Carcinoma [https://www.genesispub.org/non-coding-rnas-in-hepatocellular-carcinoma]
- 46. Identification of lncRNA biomarkers in hepatocellular ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.832952/full]
- 47. Survival Analysis Part II: Multivariate data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2394368/]
- 48. Use of the Cox regression analysis in thoracic surgical research [https://jtd.amegroups.org/article/view/22276/html]
- 49. Survival Analysis Part I: Basic concepts and first analyses [https://pmc.ncbi.nlm.nih.gov/articles/PMC2394262/]
- 50. Leveraging survival analysis and machine learning for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11779859/]
- 51. Long non-coding RNA-based single and combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405140/]
- 52. Survival Analysis by Kaplan–Meier Curves and Cox ... [https://bio-protocol.org/exchange/minidetail?id=9055140&type=30]
- 53. A new marker constructed from immune-related lncRNA pairs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10433616/]
- 54. A novel non-invasive mRNA-lncRNA biomarker panel for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12426746/]
- 55. Use of serum long non-coding RNA expression panel as a ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2025.1523997/full]
- 56. Long non-coding RNAs as a biomarker for homologous ... [https://www.nature.com/articles/s42003-025-08836-9]
- 57. The role of long non-coding RNA in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC10929815/]
- 58. Frontiers | Long non-coding rnas as key modulators of the immune microenvironment in hepatocellular carcinoma: implications for Immunotherapy [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1523190/full]
- 59. A comprehensive genomeâ€wide analysis of long noncoding RNA expression profile in hepatocellular carcinoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5727245/]
- 60. Progress and Prospects of Long Noncoding RNAs (lncRNAs) in Hepatocellular Carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/25968300/]
- 61. Detection and validity of long non-coding RNAs HOST2, ... [https://www.sciencedirect.com/science/article/pii/S2773044124000937]
- 62. LncRNA SLC1A5-AS/MZF1/ASCT2 Axis Contributes to Malignant Progression of Hepatocellular Carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/38058065/]