Navigating Biological Variability in Lipidomics: From Experimental Design to Clinical Translation
Lipidomics, the large-scale study of lipid pathways and networks, is increasingly recognized for its role in precision health, with profiles often predicting disease onset years earlier than genetic markers.
Navigating Biological Variability in Lipidomics: From Experimental Design to Clinical Translation
Abstract
Lipidomics, the large-scale study of lipid pathways and networks, is increasingly recognized for its role in precision health, with profiles often predicting disease onset years earlier than genetic markers. However, the inherent biological variability of lipids—driven by circadian rhythms, diet, and individual metabolism—poses a significant challenge to data reproducibility and clinical interpretation. This article provides a comprehensive framework for researchers and drug development professionals to address this variability. We explore the foundational sources of lipid fluctuation, present advanced methodological approaches for robust data acquisition, detail statistical workflows for troubleshooting and normalization, and establish best practices for validating lipid-based biomarkers. By synthesizing the latest technological advances and analytical strategies, this guide aims to enhance the reliability and clinical applicability of lipidomic studies.
Understanding the Sources and Impact of Lipid Fluctuation
Frequently Asked Questions (FAQs)
FAQ 1: Why is a single time-point measurement insufficient for understanding lipid dynamics in my study? Lipid concentrations are highly dynamic and fluctuate in response to factors like circadian rhythm, dietary habits, and stress [1]. A single snapshot cannot capture these temporal patterns, which are crucial for understanding metabolic health and disease progression. Studies show that lipid profiles can reveal disease onset 3-5 years earlier than genetic markers, but this requires observing changes over time [2].
FAQ 2: What is the primary source of variability in lipidomics data, and how can I account for it? The major source of variability is biological (between-subject and within-subject), not technical. High-throughput LC-MS/MS studies demonstrate that biological variability significantly exceeds analytical batch-to-batch variability [3]. Accounting for this requires a study design that includes repeated measurements over time and the use of appropriate quality controls, such as National Institute of Standards and Technology (NIST) reference materials, to isolate technical noise from true biological signal [3] [1].
FAQ 3: Which lipid classes have the biggest impact on health and should be prioritized in longitudinal studies? Two major lipid classes have emerged as particularly significant:
- Phospholipids: Form the structural foundation of all cell membranes and determine cellular function. Their composition impacts how cells respond to hormones and medications, and abnormalities can precede insulin resistance by up to five years [2].
- Sphingolipids (particularly ceramides): Function as powerful signaling molecules that regulate inflammation, cell death, and metabolic processes. Elevated ceramide levels strongly predict cardiovascular events, and ceramide risk scores now outperform traditional cholesterol measurements in predicting heart attack risk [2].
FAQ 4: My lipidomics dataset has many missing values. How should I handle them before statistical analysis? The strategy depends on the nature of the missing data:
- Missing Not at Random (MNAR): If values are missing because they are below the detection limit, imputation with a percentage (e.g., half) of the lowest measured concentration for that lipid is often effective [1].
- Missing Completely at Random (MCAR) or at Random (MAR): k-nearest neighbors (kNN)-based imputation or random forest methods are generally recommended [1]. Before imputation, it is best practice to filter out lipid species with a high percentage of missing values (e.g., >35%) across samples [1].
Troubleshooting Guides
Issue 1: High Unwanted Variation in Lipidomics Data
Problem: Data is dominated by technical noise from batch effects or sample preparation inconsistencies, obscuring the biological signal.
Solution: Implement a rigorous quality control (QC) and normalization protocol.
- Step 1: Pre-acquisition Sample Preparation. Normalize sample aliquots based on cell count, protein amount, or volume before processing [1].
- Step 2: Use Quality Control Samples. Intersperse pooled QC samples (from all study samples) or commercial reference materials (e.g., NIST SRM 1950) throughout the analysis batch [3] [1].
- Step 3: Post-acquisition Normalization.
- With Internal Standards: Use software like ADViSELipidomics to normalize raw data against internal lipid standards, correcting for instrument response and lipid recovery efficiency to obtain absolute concentrations [4].
- Without Internal Standards: Apply statistical normalization methods (e.g., median, probabilistic quotient normalization) to remove batch effects [1].
Issue 2: Inability to Capture Cellular Heterogeneity
Problem: Bulk lipid analysis of tissues or cell populations averages the signal, masking crucial cell-to-cell differences.
Solution: Employ single-cell lipidomics or spatial lipidomics techniques.
- Step 1: Choose the Appropriate Technology. Utilize advanced mass spectrometry such as high-resolution Orbitrap or Fourier-transform ion cyclotron resonance (FT-ICR) MS for ultra-sensitive profiling of individual cells [5].
- Step 2: Incorporate Spatial Context. For tissue samples, apply Mass Spectrometry Imaging (MSI) techniques like MALDI-MSI or SIMS. This visualizes the distribution of lipids within a tissue, revealing spatial heterogeneity related to cellular function and disease pathology [5].
- Step 3: Data Integration. Combine single-cell lipidomic data with transcriptomic or proteomic data from the same cells to unravel lipid-mediated regulatory networks [5].
Issue 3: Interpreting Statistically Significant Lipid Lists
Problem: After statistical analysis, you have a list of differentially abundant lipids but struggle to extract biological meaning.
Solution: Follow a structured data analysis and interpretation workflow.
- Step 1: Robust Statistical Processing. Use tools in R or Python for hypothesis testing (e.g., t-tests, ANOVA with FDR correction) and dimensionality reduction (e.g., PCA, PLS-DA) to identify key lipid species [1].
- Step 2: Pathway and Enrichment Analysis. Input the significant lipid list into tools like MetaboAnalyst or LipidSig to identify enriched metabolic pathways (e.g., using Over-Representation Analysis) [6].
- Step 3: Biological Interpretation. Contextualize the results by cross-referencing with existing literature in databases like LIPID MAPS and PubMed. Generate testable hypotheses about the functional role of the altered lipids, for example, in membrane integrity or inflammatory signaling [6].
Experimental Protocols & Data Presentation
Standardized Protocol for Longitudinal Plasma Lipidomics
This protocol is designed for large-scale clinical studies to ensure high-throughput and reproducible measurement of the circulatory lipidome over time [3].
- Sample Collection: Collect fasted plasma samples in specialized tubes that prevent lipid oxidation at multiple time points from each participant.
- Sample Preparation (Semi-automated): Use a stable isotope dilution approach for robust and accurate quantification during the extraction process.
- Quality Control: Include the NIST plasma reference material as a QC in every batch to monitor analytical performance.
- LC-MS/MS Analysis: Apply a high-coverage hydrophilic interaction liquid chromatography (HILIC) method to separate a wide range of lipid classes. The MS should be operated in data-dependent acquisition (DDA) or targeted mode.
- Data Processing: Use software like LIQUID or LipidSearch for peak picking, lipid identification, and integration. Process the QC samples to assess between-batch reproducibility, aiming for a median coefficient of variation (CV) <15% [3].
Essential Research Reagent Solutions
Table 1: Key reagents and materials for robust lipidomics studies.
| Item | Function/Benefit |
|---|---|
| NIST SRM 1950 | Standardized reference material of human plasma; used to monitor batch-to-batch reproducibility and accuracy across longitudinal studies [3] [1]. |
| Stable Isotope-Labeled Internal Standards | Added to each sample prior to extraction; corrects for variations in sample preparation and MS ionization efficiency, enabling absolute quantification [3]. |
| Pooled QC Samples | A quality control created by mixing a small aliquot of every biological sample in the study; used to monitor instrument stability and for data normalization [1]. |
| LIPID MAPS Database | A curated database providing standardized lipid classification, structures, and nomenclature; essential for accurate lipid identification and reporting [5] [4]. |
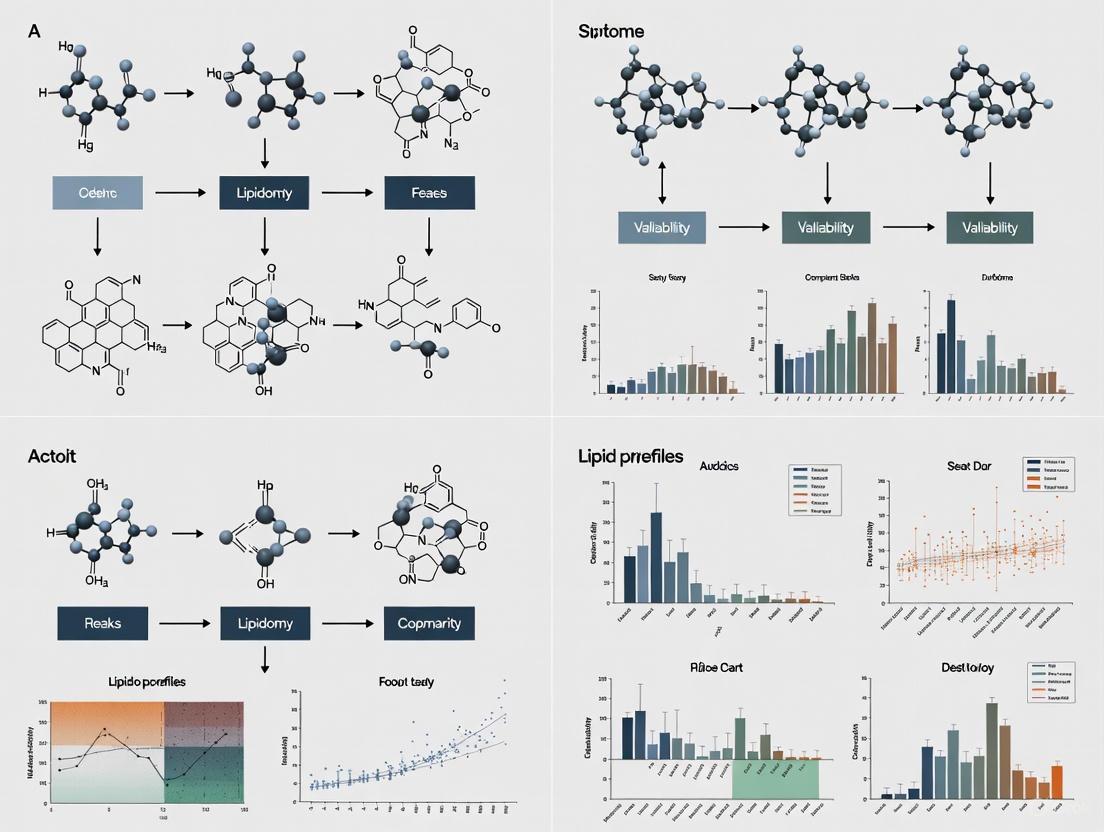
Workflow Visualization
Diagram 1: Longitudinal lipidomics workflow.
Diagram 2: Data analysis pipeline.
FAQs on Circadian Lipid Biology
What percentage of lipids show circadian rhythmicity?
Approximately 13% to 25% of the plasma lipidome demonstrates endogenous circadian regulation under controlled conditions [7] [8]. This rhythmicity spans multiple lipid classes, including glycerolipids, glycerophospholipids, and sphingolipids. At an individual level, the percentage of rhythmic lipids can range much higher—from 5% to 33% across different people—highlighting significant interindividual variation [7].
How consistent are lipid rhythms between individuals?
There is striking interindividual variability in lipid circadian rhythms. When comparing which specific lipid species are rhythmic between subjects, the median agreement is only about 20% [7]. The timing of peak concentrations (acrophase) for the same lipid can vary by up to 12 hours between individuals [7]. This suggests the existence of different circadian metabolic phenotypes in the population.
Does aging affect circadian lipid rhythms?
Yes, healthy aging significantly alters circadian lipid regulation. Middle-aged and older adults (average age ~58 years) exhibit:
- ~14% lower rhythm amplitude [8]
- ~2.1 hour earlier acrophase (peak timing) [8]
- Greater prevalence of combined sinusoidal and linear trends across constant routines (44/56 lipids in older vs. 18/58 in younger adults) [8]
These changes occur despite preservation of central circadian timing, suggesting peripheral clock alterations.
Troubleshooting Experimental Challenges
Challenge: High Variability in Lipid Measurements
Problem: Lipid measurements show unexpected variability, potentially obscuring circadian signals.
Solutions:
- Control sampling time: Collect samples at consistent circadian times across subjects [7] [8]
- Account for age effects: Stratify analyses by age group or include age as covariate [8]
- Use repeated measures: Collect multiple samples from the same individuals over time [9]
- Implement constant routines: For precise circadian assessment, use constant routine protocols that eliminate masking effects from sleep, posture, and feeding [8] [10]
Challenge: Discrepancies Between Group and Individual Rhythms
Problem: Lipids that appear arrhythmic in group-level analyses show clear rhythms at individual levels.
Solutions:
- Perform individual-level rhythm analysis in addition to group-level analyses [7] [11]
- Increase sampling frequency to better capture individual patterns [7]
- Cluster subjects based on rhythmicity patterns using consensus clustering with iterative feature selection [7]
Table 1: Circadian Lipid Rhythm Characteristics Across Studies
| Parameter | Young Adults | Older Adults | Interindividual Range | Citation |
|---|---|---|---|---|
| Rhythmic Lipids | 13-25% | ~25% (reduced amplitude) | 5-33% | [7] [8] |
| Amplitude Reduction | - | ~14% | - | [8] |
| Phase Advancement | - | ~2.1 hours | Up to 12 hours | [7] [8] |
| Interindividual Agreement | ~20% | - | - | [7] |
Table 2: Phase Response Curve Magnitudes for Lipids vs. Melatonin
| Analyte | Maximum Phase Shift (hours) | PRC Pattern vs. Melatonin | Citation |
|---|---|---|---|
| Melatonin | ~3.0 | Reference | [10] |
| Triglycerides | ~8.3 | Generally greater shifts | [10] |
| Albumin | ~7.1 | Similar timing | [10] |
| Total Cholesterol | ~7.2 | Offset by ~12 hours | [10] |
| HDL-C | ~4.6 | Offset by ~12 hours | [10] |
Experimental Protocols
Constant Routine Protocol for Endogenous Rhythm Assessment
The constant routine (CR) protocol is the gold standard for assessing endogenous circadian rhythms without environmental masking [8] [10].
Key Components:
- Duration: 27-55 hours of continuous wakefulness [8] [10]
- Posture: Maintain semi-recumbent position [8]
- Lighting: Constant dim light (<10 lux) to eliminate photic entrainment [10]
- Nutrition: Identical isocaloric snacks hourly to eliminate feeding-fasting effects [10]
- Sampling: Blood collection every 3-4 hours for lipidomic analysis [7] [8]
Applications: Isolates endogenously generated oscillations from evoked changes in lipid physiology [8].
Phase Response Curve Assessment Protocol
This protocol characterizes how lipid rhythms shift in response to zeitgebers like light and meals [10].
Procedure:
- Initial CR (CR1): Assess baseline circadian phase
- Intervention Day: 16-hour combined light (6.5h blue light) and meal exposure
- Systematic Variation: Schedule intervention at different circadian phases across participants
- Final CR (CR2): Assess phase shifts in lipid rhythms
Outcome: Generates phase response curves showing direction/magnitude of lipid rhythm shifts [10].
Visualization of Circadian Lipid Analysis
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function | Example Application |
|---|---|---|
| HPLC/MS Systems | Targeted lipidomics profiling of 260+ lipid species | Quantitative measurement of glycerolipids, glycerophospholipids, sphingolipids [7] |
| UPLC-QTOF-MS | Untargeted lipidomics with high resolution | Comprehensive skin surface lipid analysis [12] [13] |
| Constant Routine Facilities | Environmental control for circadian studies | Eliminating masking effects from light, feeding, activity [8] [10] |
| Cosinor Analysis Software | Statistical identification of circadian rhythms | Determining acrophase, amplitude, significance of rhythms [7] [8] |
| Deuterated Internal Standards | Absolute quantification of lipid species | Normalizing lipid measurements in complex mixtures [9] |
| AZ13705339 | AZ13705339, MF:C33H36FN7O3S, MW:629.7 g/mol | Chemical Reagent |
| Kif18A-IN-12 | Kif18A-IN-12, MF:C30H39F2N5O4S, MW:603.7 g/mol | Chemical Reagent |
Key Technical Recommendations
- Standardize sampling times across participants to minimize circadian variability [7] [9]
- Account for age effects in study design and statistical analysis [8]
- Consider individual metabolic phenotypes rather than assuming uniform rhythms [7]
- Use appropriate statistical methods (Cosinor, JTK_CYCLE) designed for circadian analysis [7] [8]
- For intervention studies, note that lipid rhythms may shift differently than melatonin rhythms [10]
Understanding and accounting for circadian regulation is essential for reducing variability and improving reproducibility in lipidomic studies.
Dietary and Metabolic Drivers of Short-Term Lipid Variability
Frequently Asked Questions (FAQs)
What are the primary biological factors that cause short-term lipid variability?
Short-term fluctuations in lipid levels are driven by several key biological and lifestyle factors. Dietary intake is a major driver; saturated fatty acids (SFA) from foods like milk, butter, cheese, and red meat increase LDL-C, while monounsaturated (MUFA) and polyunsaturated (PUFA) fatty acids from sources like olive oil and nuts lower LDL-C [14]. Carbohydrate quality also plays a significant role; low-quality carbohydrates, particularly simple sugars and fructose, promote hepatic de novo lipogenesis, leading to a robust increase in triglycerides (TG) [14]. Furthermore, non-fasting states, recent exercise, alcohol consumption, and circadian rhythms contribute to dynamic changes in the lipidome over short timeframes [15] [16].
How does short-term dietary fat intake specifically alter lipid profiles?
Short-term changes in dietary fat composition can rapidly influence circulating lipid levels. The table below summarizes the effects of different dietary fats on key lipoproteins [14]:
| Dietary Constituent | Major Food Sources | Effect on LDL-C | Effect on HDL-C | Effect on TGs |
|---|---|---|---|---|
| Saturated Fatty Acids (SFA) | Milk, butter, cheese, beef, pork, poultry, palm oil, coconut oil | Increase | Modest increase | Neutral |
| Monounsaturated Fatty Acids (MUFA) | Olive oil, canola oil, avocados, nuts, seeds | Decrease | Neutral | Neutral |
| Polyunsaturated Fatty Acids (PUFA) | Soybean oil, corn oil, sunflower oil, tofu, soybeans | Decrease | Neutral | Neutral |
| Trans Fatty Acids (TFA) | Naturally in meat/dairy; formed in hydrogenated oils | Increase | Decrease | Neutral |
| Dietary Cholesterol | Egg yolks, shrimp, beef, pork, poultry, cheese, butter | Modest increase (highly variable) | Neutral | Neutral |
Replacing SFA with PUFA in the diet not only lowers LDL-C but is also associated with a reduced risk of cardiovascular disease (CVD) [14]. Short-term high-fat feeding studies have specifically demonstrated its impact on postprandial lipemia, the temporary increase in blood triglycerides after a meal [17].
Why is understanding lipid variability critical for lipidomic study design and interpretation?
Accounting for lipid variability is essential for both the statistical power and biological validity of lipidomics research. High within-individual variance can severely attenuate observed effect sizes in association studies, requiring larger sample sizes to detect true relationships [9]. For instance, one study estimated that to detect a relative risk of 3.0 with high confidence, a case-control study would require a total of 1,000 participants to achieve 57% power, and 5,000 participants to achieve 99% power, after correcting for multiple comparisons [9].
Moreover, lipid variability is not just noise; it can be a meaningful clinical signal. Studies using electronic health records have shown that high variability in total cholesterol, LDL-C, and HDL-C—measured as the variation independent of the mean (VIM) from at least three measurements—is associated with an increased risk of incident cardiovascular disease, independent of traditional risk factors and mean lipid levels [18]. This underscores that fluctuating lipid levels may themselves be a pathophysiological risk marker.
What is the typical magnitude of lipid changes one can expect from short-term dietary interventions?
The average lipid response to dietary changes is relatively modest, typically in the range of ~10% reductions [14]. However, the response can vary significantly between individuals due to factors like genetics. For example, individuals with an apo E4 allele experience a more robust decrease in LDL-C in response to a reduction in dietary fat and cholesterol than those with other variants [14]. Clinical conditions also modulate this response, as the expected lipid-lowering effect of a low SFA diet is blunted in obese individuals [14]. This highlights the importance of personalized approaches and monitoring individual responses in both clinical and research settings.
Experimental Protocols
Protocol 1: Assessing the Impact of Short-Term Diet on the Plasma Lipidome
This protocol outlines a randomized crossover dietary intervention study to measure acute lipidomic changes.
1. Study Design:
- Design Type: Randomized, controlled, crossover trial.
- Participants: Recruit healthy participants or a cohort with a specific metabolic phenotype (e.g., insulin-sensitive vs. insulin-resistant) [16].
- Intervention Diets: Participants consume isoenergetic diets differing in macronutrient composition for a short term (e.g., 3 days) [17].
- High-Carbohydrate Diet: For example, 75% of total energy (TE) from carbohydrates, 10% TE from fat.
- High-Fat Diet: For example, 40% TE from fat, 45% TE from carbohydrates [17].
- Washout Period: A sufficient washout period (e.g., several days to weeks) is implemented between dietary phases to avoid carryover effects.
2. Sample Collection:
- Timeline: Collect fasting plasma samples before the diet (baseline) and at the end of the intervention period. To capture postprandial lipemia, collect additional samples at specific timepoints (e.g., 1, 2, 4, 6 hours) after a standardized test meal on the final day [17].
- Standardization: Control for pre-analytical variables by standardizing the blood draw time of day to account for circadian rhythms, and ensure consistent processing protocols (e.g., centrifugation speed/time, storage at -80°C) for all samples [15].
3. Lipidomic Profiling:
- Platform: Use a high-throughput quantitative lipidomics platform like the Lipidyzer, which combines liquid chromatography (LC) with a triple-quadrupole mass spectrometer (MS) and differential mobility separation (DMS) [16].
- Internal Standards: Spike all samples with a mix of deuterated internal standards immediately upon sample preparation to enable accurate quantification and control for extraction efficiency and instrument variance [16].
- Batch Randomization: Randomize samples across analytical batches to ensure that the factor of interest (diet) is not confounded with batch effects or measurement order [19].
- Quality Control (QC): Inject pooled QC samples (made from an aliquot of all samples) repeatedly at the beginning of the run, after every batch of experimental samples, and at the end to monitor and correct for instrumental drift [19].
4. Data Analysis:
- Preprocessing: Perform peak picking, alignment, and normalization. Use the QC samples for batch effect correction and signal drift compensation.
- Quantification: Calculate lipid species concentrations using the ratio of target compound peak areas to their assigned deuterated internal standard [9] [16].
- Statistical Analysis: Use paired t-tests or linear mixed models to identify lipid species and classes that are significantly altered between the two dietary regimens. Employ False Discovery Rate (FDR) correction for multiple testing.
Protocol 2: Quantifying Intra-Individual Lipid Variability from Longitudinal Data
This protocol describes how to calculate and interpret lipid variability from serial measurements, such as those from electronic health records (EHR) or dedicated longitudinal cohorts.
1. Data Source and Cohort Definition:
- Source: Identify individuals with at least three measurements of a lipid type (total cholesterol, LDL-C, HDL-C, or triglycerides) taken on different days over a defined period (e.g., 5 years) [18].
- Cohort: Define a baseline index date. Include individuals without prior cardiovascular disease at baseline to study variability as a risk factor for incident events [18].
2. Calculation of Lipid Variability:
- Metric: Use Variability Independent of the Mean (VIM). VIM is robust to the statistical issue of heteroscedasticity (where variability correlates with the mean level) and is uncorrelated with the mean measurement, providing a cleaner measure of fluctuation [18].
- Formula: VIM is calculated for each lipid type and each individual as:
VIM = k × SD / mean^x- Where
xis derived from fitting the power model:SD = constant × mean^x - And
kis a scaling factor to make VIM comparable to the SD:k = mean(mean^x)[18].
- Alternative Metrics: For sensitivity analyses, variability can also be assessed using the standard deviation (SD) or coefficient of variation (CV = SD/mean) [18].
3. Statistical Analysis for Association with Outcomes:
- Categorization: Group individuals into quintiles (Q1-Q5) based on their VIM value for a given lipid, with Q5 representing the highest variability [18].
- Outcomes: Follow participants for clinical outcomes like incident myocardial infarction (MI), stroke, or cardiovascular death.
- Modeling: Use Cox proportional hazards regression to investigate the association between lipid variability quintiles and the risk of incident CVD. Adjust for traditional risk factors, including baseline lipid level, sex, age, smoking status, hypertension, diabetes, and lipid-lowering medication use [18].
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential reagents and materials for conducting robust lipidomics studies focused on short-term variability.
| Item | Function/Application | Key Considerations |
|---|---|---|
| Deuterated Internal Standards | Enables absolute quantification of lipids; corrects for extraction efficiency and instrument variance. | Use a comprehensive mix covering major lipid classes (e.g., CE, TAG, DAG, PC, PE, SM, CER) [16]. Add to samples as early as possible in extraction. |
| Stable Isotope-Labeled Precursors | Tracks the incorporation of dietary components into complex lipids; studies de novo lipogenesis. | Use precursors like 13C-acetate or deuterated fatty acids in cell culture or animal models to trace metabolic flux. |
| Quality Control (QC) Pooled Plasma | Monitors instrument stability and reproducibility across batches; used for data normalization. | Create a large, homogeneous pool from an aliquot of all study samples. Analyze repeatedly throughout the analytical run [19]. |
| Structured Dietary Formulae | Provides precise control over macronutrient and fatty acid composition in intervention studies. | Macronutrient ratios (e.g., high-fat vs. high-carb) and specific fat sources (SFA, MUFA, PUFA) must be well-defined [14] [17]. |
| Automated Lipid Extraction Solvents | Isolates the lipid fraction from biological matrices like plasma or tissue. | Butanol:methanol or chloroform:methanol mixtures are common. Automated systems improve throughput and reproducibility [9] [19]. |
| Chromatography Columns | Separates complex lipid mixtures by class and species prior to mass spectrometry. | Reversed-phase (e.g., C8 or C18) columns are widely used in LC-MS for separating lipids by hydrophobicity [19]. |
| GUB03385 | GUB03385, MF:C198H322N60O52S, MW:4407 g/mol | Chemical Reagent |
| ON1231320 | ON1231320, MF:C22H15F2N5O3S, MW:467.4 g/mol | Chemical Reagent |
Distinguishing Biological Signal from Technical Noise in Cohort Studies
Frequently Asked Questions (FAQs)
1. What are the main sources of variability in lipidomic cohort studies? The total variability in lipidomic measurements comes from three main sources: between-individual variance (biological differences in "usual" lipid levels among subjects), within-individual variance (temporal fluctuations in lipid levels within the same person), and technical variance (variability introduced by laboratory procedures, sample processing, and instrumentation). In serum lipidomic studies, the combination of technical and within-individual variances accounts for most of the variability in 74% of lipid species, which can significantly attenuate observed effect sizes in epidemiological studies [9].
2. What sample size is typically required for robust lipidomic cohort studies? Lipidomic studies require substantial sample sizes to detect moderate effect sizes. For a true relative risk of 3.0 (comparing upper and lower quartiles) after Bonferroni correction for testing 918 lipid species (α = 5.45×10â»âµ), studies with 500, 1,000, and 5,000 total participants (1:1 case-control ratio) would have approximately 19%, 57%, and 99% power, respectively. The required sample size depends on the specific effect sizes you expect to detect and the number of lipid species being tested [9].
3. How can I minimize technical variability during sample preparation?
- Standardize extraction protocols: Use consistent, validated extraction methods like modified Bligh & Dyer (chloroform/methanol/water), modified Folch (chloroform/methanol), MTBE (methyl tert-butyl ether/methanol/water), or BUME (butanol/methanol) methods [20]
- Implement internal standards: Add appropriate deuterated internal standards during extraction to normalize for recovery and ionization efficiency [20]
- Control pre-analytical variables: Standardize sample collection, processing, and storage conditions across all samples to minimize batch effects [9] [21]
4. Which statistical approaches best distinguish biological signals from technical noise?
- For initial analysis: Use principal component analysis (PCA) to visualize data structure and identify outliers [6]
- For group comparisons: Apply t-tests (two groups) or ANOVA (multiple groups) with false discovery rate (FDR) correction for multiple testing [6]
- For classification: Employ multivariate methods like Partial Least Squares Discriminant Analysis (PLS-DA) or machine learning approaches (Random Forests, SVM) to handle highly correlated lipid data [6]
- For power considerations: Account for the moderate technical reliability of lipid measurements (median intraclass correlation coefficient = 0.79) when designing studies and interpreting results [9]
5. What computational tools are available for lipidomic data analysis? LipidSig provides a comprehensive web-based platform with data checking, differential expression analysis, enrichment analysis, and network visualization capabilities. Other tools include MS-DIAL for untargeted lipidomics data processing, LipidMatch for lipid identification, and MetaboAnalyst for pathway analysis [22] [6].
Quantitative Data on Lipidomic Variability
Table 1: Sources of Variance in Serum Lipidomic Measurements from the PLCO Cancer Screening Trial (n=693) [9]
| Variance Component | Proportion of Total Variance | Interpretation |
|---|---|---|
| Between-individual variance | Varies by lipid species | Represents true biological differences between subjects; optimal for detecting associations |
| Within-individual variance | Accounts for most variability in 74% of lipids | Temporal fluctuations within individuals; can attenuate observed effect sizes |
| Technical variance | Median ICC = 0.79 | Introduced by laboratory procedures; moderate reliability across measurements |
Table 2: Statistical Power for Lipidomic Case-Control Studies Based on Variance Components [9]
| Total Sample Size | Power to Detect RR=3.0* | Practical Interpretation |
|---|---|---|
| 500 (250 cases/250 controls) | 19% | Underpowered for most applications |
| 1,000 (500 cases/500 controls) | 57% | Moderate power for strong effects |
| 5,000 (2,500 cases/2,500 controls) | 99% | Well-powered for moderate to strong effects |
RR = Relative Risk comparing upper and lower quartiles, after Bonferroni correction for 918 tests (α = 5.45×10â»âµ)
Experimental Protocols for Minimizing Variability
Protocol 1: Standardized Sample Processing for Serum/Plasma Lipidomics
Materials:
- Serum collection tubes (SST)
- Pre-labeled cryovials for storage
- Internal standard mixture (SPLASH LipidoMix or equivalent)
- Extraction solvents (HPLC-grade methanol, methyl tert-butyl ether, water)
Procedure:
- Collect blood following standardized venipuncture procedures after consistent fasting status
- Process samples within 2 hours of collection: allow clotting (30 min), centrifuge (2000×g, 15 min, 4°C)
- Aliquot serum into cryovials, flash-freeze in liquid nitrogen, store at -80°C
- Thaw samples on ice immediately before extraction
- Add internal standards (normalized to protein content or fluid volume) prior to extraction [20] [9]
- Perform lipid extraction using validated methods (e.g., BUME: butanol/methanol 3:1 v/v followed by heptane/ethyl acetate 3:1 v/v with 1% acetic acid) [20]
- Evaporate organic phases under nitrogen and reconstitute in MS-compatible solvents
- Use randomized injection order with quality control samples (pooled reference samples) every 6-10 injections [9]
Protocol 2: Quality Control and Batch Effect Correction
Materials:
- Quality control (QC) samples: pooled from all study samples or commercial reference material
- Internal standards for retention time alignment
- Blank samples (extraction solvent only)
Procedure:
- Prepare QC samples identical to study samples
- Inject QC samples at beginning of sequence for system conditioning, then throughout analysis (every 6-10 samples)
- Monitor retention time drift: acceptable variation < 0.1 min over sequence
- Assess signal intensity: CV < 15-20% in QC samples for most lipid species
- Evaluate mass accuracy: < 5 ppm deviation for high-resolution instruments
- Apply batch correction algorithms (ComBat, LOESS normalization) if analyzing samples in multiple batches [6]
- Use signal filtering and noise reduction techniques to enhance data quality
- Perform systematic data quality assessment using tools like LipidQA or built-in instrument software [6]
Workflow Visualization
Workflow for Minimizing Technical Variability in Lipidomics
Research Reagent Solutions
Table 3: Essential Materials for Lipidomic Studies with Variability Control
| Reagent/Material | Function | Variability Control Application |
|---|---|---|
| Deuterated internal standards (SPLASH LipidoMix, Avanti Polar Lipids) | Quantification reference | Normalizes extraction efficiency and ionization variation; added prior to extraction [20] |
| Stable isotope-labeled lipids (e.g., D₃-16:0, ¹³C-18:0) | Method development and validation | Creates retention time databases; helps identify C=C positions in complex lipids [23] |
| Pooled reference material (NIST SRM 1950 or study-specific pools) | Quality control monitoring | Monitors technical performance across batches; identifies instrumental drift [9] |
| Standardized extraction kits (BUME, MTBE-based) | Lipid extraction | Provides consistent recovery across samples and batches; minimizes extraction bias [20] |
| Retention time markers (e.g., 1,3-dipentadecanoyl-2-oleoyl-glycerol) | Chromatographic alignment | Enables peak alignment across samples; corrects for retention time shifts [6] |
| Matrix-matched calibrators | Quantification | Compensates for matrix effects; improves accuracy of absolute quantification [21] |
Advanced Structural Resolution Protocol
Protocol 3: Determining C=C Positions in Complex Lipids
Background: Carbon-carbon double bond (C=C) positions in unsaturated complex lipids provide critical structural information but are challenging to determine with routine LC-MS/MS. Recent computational approaches now enable this without specialized instrumentation [23].
Materials:
- RAW264.7 macrophage cell line
- Stable isotope-labeled fatty acids (n-3, n-6, n-7, n-9, n-10 SIL-FAs)
- RPLC-MS/MS system with reverse-phase chromatography
- LC=CL computational tool (Lipid Data Analyzer extension)
Procedure:
- Supplement RAW264.7 cells with individual SIL-FAs for 24 hours
- Extract lipids using standardized protocols
- Analyze by RPLC-MS/MS with data-dependent acquisition
- Process data through LC=CL computational pipeline:
- Map retention times to reference database
- Use machine learning (cubic spline interpolation) for retention time alignment
- Automatically assign ω-positions based on established elution profiles
- Validate assignments using SIL-FA paired supplementation experiments [23]
Application: This approach revealed previously undetected C=C position specificity of cytosolic phospholipase Aâ‚‚ (cPLAâ‚‚), demonstrating how structural resolution can uncover novel biological insights that would be obscured by conventional lipidomics [23].
Advanced Structural Resolution Workflow
Scientific Foundation: Lipidomic Dynamics in Critical Illness
Critical illness triggers profound and dynamic alterations in the circulating lipidome, which are closely associated with patient outcomes and recovery trajectories. Research reveals that these changes are not random but follow specific temporal patterns that can inform prognostic stratification.
Key Lipidomic Patterns in Critical Illness
Table 1: Temporal Lipidomic Signatures in Critical Illness Trajectories
| Time Point | Resolving Patients (ICU <7 days) | Non-Resolving Patients (ICU ≥7 days/Late Death) | Early Non-Survivors (Death within 3 days) |
|---|---|---|---|
| 0 hours | Moderate reduction in most lipid species | Moderate reduction in most lipid species | Severe depletion of all lipid classes |
| 24 hours | Persistent suppression of most lipids | Ongoing lipid suppression | N/A |
| 72 hours | Continued lipid suppression | Selective increase in TAG, DAG, PE, and ceramides | N/A |
| Prognostic Value | Favorable outcome | Worse outcomes | Worst outcomes |
The previously reported survival benefit of early thawed plasma administration was associated with preserved lipid levels that related to favorable changes in coagulation and inflammation biomarkers in causal modelling [24]. Phosphatidylethanolamines (PE) were elevated in patients with persistent critical illness and PE levels were prognostic for worse outcomes not only in trauma but also in severe COVID-19 patients, showing a selective rise in systemic PE as a common prognostic feature of critical illness [24].
Lipidomic Pathways in Stress Response
The metabolic response to stress in critical illness unfolds across three distinct phases: acute, subacute, and chronic [25]. These phases involve significant endocrine and immune-inflammatory responses that lead to dramatic changes in cellular and mitochondrial functions, creating what is termed "anabolic resistance" that complicates metabolic recovery.
Methodological Framework: Lipidomic Analysis in Critical Care Research
Core Analytical Workflow
Table 2: Essential Methodologies for Critical Illness Lipidomics
| Methodological Component | Technical Specifications | Application in Critical Illness |
|---|---|---|
| Sample Collection | EDTA plasma; immediate processing or flash freezing; avoid freeze-thaw cycles | Trauma, sepsis, COVID-19 cohorts with known onset timing |
| Lipid Extraction | Modified Folch/Bligh & Dyer; MTBE; acidification for anionic lipids | High-throughput processing for critical care biobanks |
| LC-MS/MS Analysis | QTRAP platforms; C18 columns; DMS devices; polarity switching | Quantification of 800-1000+ lipid species across classes |
| Quality Control | Deuterated internal standards; pooled QC samples; batch correction | Monitoring technical variability in longitudinal studies |
| Data Processing | Peak alignment, annotation, missing value imputation, normalization | Handling heterogeneous ICU patient samples |
Liquid chromatography mass spectrometry (LC-MS) serves as the cornerstone technology for targeted lipidomic analysis in critical illness research. In comprehensive studies, this approach has enabled quantification of 996 lipids using internal standards, with quality control analysis showing a median relative standard deviation (RSD) of 4% for the lipid panel [24]. The representation typically spans 14 sub-classes, with triglyceride (TAG) being the most abundant lipid class identified in plasma, followed by phosphatidylethanolamine (PE), phosphatidylcholine (PC), and diacylglycerols (DAG) [24].
Experimental Protocol: Longitudinal Lipidome Profiling in ICU Patients
Protocol: Comprehensive Lipidomic Profiling in Critical Illness
Patient Stratification and Sampling
- Enroll critically ill patients with precise onset timing (e.g., severe trauma, sepsis with known infection time)
- Collect serial blood samples at admission (0h), 24h, and 72h
- Include healthy controls for baseline reference
- Process samples immediately: centrifuge at 4°C, aliquot, store at -80°C under argon atmosphere
Lipid Extraction and Preparation
- Use modified Bligh & Dyer or MTBE-based extraction
- Add antioxidant butylhydroxytoluene (BHT) for oxidation-sensitive lipids
- Include 54 deuterated internal standards for accurate quantification
- Employ automated butanol:methanol extraction for high-throughput processing
LC-MS/MS Analysis
- Platform: SCIEX QTRAP 5500 or Q Exactive HF-X with DMS device
- Chromatography: C18 column with binary gradient (water/acetonitrile to isopropanol/acetonitrile)
- Mass detection: MRM mode for targeted analysis, m/z 100-1350
- Polarity switching: Positive and negative electrospray modes
Data Processing and Normalization
- Use XCMS, MS-DIAL, or Lipid4DAnalyzer for peak alignment
- Apply quality control filters (RSD <30% in QC samples)
- Impute missing values using k-nearest neighbors (k=10)
- Normalize to internal standards and total protein content
This protocol enables robust quantification of lipidomic signatures that align with inflammatory patterns and outcomes in critical illness [24].
Troubleshooting Guide: Addressing Biological Variability in Lipidomic Studies
Frequently Asked Questions
Q1: How can we distinguish biological signals from technical variability in longitudinal critical care lipidomics?
A: Technical variability is moderate in lipidomics, with a median intraclass correlation coefficient of 0.79 [9]. However, the combination of technical and within-individual variances accounts for most of the variability in 74% of lipid species [9]. To address this:
- Implement rigorous quality control with blinded replicate samples
- Use multiple internal standards for each lipid class
- Apply batch correction algorithms like Combat
- Ensure sample randomization during extraction and analysis
- Calculate biological variance that sums between- and within-individual variances
Q2: What are the key considerations for sample handling in critical care lipidomics?
A: Sample processing is the most vital step in lipidomic workflow [26]. Specific challenges include:
- Circadian variations: Process samples at consistent times or record collection time
- Lipid degradation: Plasma concentration of lysophosphatidylcholine (LPC) increases when left at room temperature [26]
- Freeze-thaw effects: Particularly problematic for sphingosine, polyunsaturated fatty acids, and eicosanoids [26]
- Oxidation: Major concern for polyunsaturated fatty acids; use argon atmosphere and antioxidants
Q3: How much statistical power do we need for lipidomic studies in critical illness?
A: Epidemiologic studies examining associations between lipidomic profiles and disease require large sample sizes to detect moderate effect sizes [9]. For a true relative risk of 3 (comparing upper and lower quartiles) after Bonferroni correction:
- 500 participants: 19% power
- 1,000 participants: 57% power
- 5,000 participants: 99% power Always conduct power analysis during study design and consider pooled samples or repeated measurements to enhance power.
Q4: What lipid extraction method is most suitable for critical care samples?
A: The choice depends on lipid classes of interest:
- Folch/Bligh & Dyer: Good for global lipidomics
- MTBE-based: Better for high-throughput with less emulsion formation
- Acidified butanol: Optimal for lysophosphatidic acid extraction
- SPE methods: Useful for specific lipid class enrichment
Q5: How do we validate lipidomic biomarkers for clinical application in critical care?
A: Validation requires a multi-phase approach addressing pre-analytical, analytical, and post-analytical challenges [21]:
- Demonstrate reproducibility across platforms and laboratories
- Validate in independent cohorts with different critical illness etiologies
- Establish standard operating procedures for sample handling
- Integrate with clinical, genomic, and proteomic data
- Assess clinical utility through decision curve analysis
Advanced Technical Challenges and Solutions
Table 3: Troubleshooting Common Lipidomics Challenges in Critical Care Research
| Challenge | Root Cause | Solution | Preventive Measures |
|---|---|---|---|
| Low lipid recovery | Improper extraction solvent ratio; incomplete protein precipitation | Optimize chloroform:methanol:water ratio; use acidification for anionic lipids | Validate extraction efficiency with internal standards |
| Poor chromatographic separation | Column degradation; inappropriate gradient | Replace column; optimize mobile phase composition | Use guard columns; establish QC retention time markers |
| High background noise | Solvent impurities; column bleed | Use HPLC-grade solvents; condition columns properly | Implement blank injections; use high-purity reagents |
| Lipid oxidation | Polyunsaturated fatty acid degradation; metal ion catalysis | Add antioxidants; use argon atmosphere; chelating agents | Minimize sample processing time; store under inert gas |
| Inconsistent identification | Isomer separation limitations; software misannotation | Use ion mobility; manual validation; orthogonal fragmentation | Implement multi-platform validation; reference standards |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Critical Illness Lipidomics
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Deuterated internal standards | Quantification reference; extraction control | Include 54 standards across 9 subclasses; add before extraction |
| Butylhydroxytoluene (BHT) | Antioxidant protection | 0.1-0.01% in extraction solvents; prevents PUFA oxidation |
| Ammonium formate/acetate | Mobile phase additive; promotes ionization | 10 mM in water/acetonitrile and isopropanol/acetonitrile |
| Chloroform-methanol mixtures | Lipid extraction solvents | Folch (2:1) or Bligh & Dyer (1:2:0.8) ratios; toxic handling required |
| Methyl tert-butyl ether | Alternative extraction solvent | Less toxic; forms distinct upper organic phase |
| C18 chromatography columns | Lipid separation | 100-150mm length, 1.7-2.1μm particle size; 55°C temperature |
| Quality control plasma pools | Process monitoring | Create from leftover patient samples; run every 6-10 injections |
| Solid-phase extraction cartridges | Lipid class enrichment | Useful for phosphoinositides, sphingolipids, or oxylipins |
| Pyrimidyn 7 | Pyrimidyn 7, MF:C21H41N5, MW:363.6 g/mol | Chemical Reagent |
| GNE 2861 | GNE 2861, MF:C22H26N6O2, MW:406.5 g/mol | Chemical Reagent |
Lipid-Immune Signaling Networks in Critical Illness
The integration of lipidomic data with immune parameters reveals critical networks in sepsis and critical illness. Studies demonstrate that phosphatidylcholine (PC) levels correlate with monocytes, while cholesteryl ester (CE) and lysophosphatidylcholine (LPC) associate with complement proteins and CD8+ T cells [27]. These lipid-immune relationships differ significantly between younger and elderly patients, suggesting distinct pathophysiological mechanisms across age groups [27].
Risk stratification models incorporating six key lipids (LPC(19:0), PC(P-19:0), SM 32:3;2O(FA 16:3), PC(P-20:0), PC(O-18:1/20:3), CE(15:0)) and age have demonstrated accurate prediction of septic shock (AUC: 0.87 training, 0.82 validation) and mortality risk in elderly patients [27]. This highlights the translational potential of lipidomic signatures in critical care settings.
Advanced Analytical Techniques for Capturing Lipid Dynamics
Lipidomics provides critical insight into metabolic changes in health and disease, but traditional methods face challenges in sensitivity, lipid coverage, and annotation accuracy [28]. The integration of C30 reversed-phase chromatography with scheduled data-dependent acquisition (SDDA) addresses these limitations by significantly improving chromatographic separation and data acquisition efficiency.
Core Technological Advantages
- Enhanced Lipid Annotation: SDDA demonstrates a 2-fold increase in the number of lipids annotated compared to conventional DDA, with a 2-fold higher annotation confidence (Grade A and B) [28].
- Superior Separation: C30 stationary phases provide improved separation of complex lipid mixtures compared to traditional C18 columns, particularly for lipid isomers and isobaric species.
- Acquisition Efficiency: SDDA optimizes instrument time by triggering MS/MS scans only when precursors are eluting, increasing identification rates without compromising data quality.
Method Performance Across Matrices
The C30-SDDA method has been rigorously validated across clinical blood matrices, with performance characteristics summarized below:
Table 1: C30-SDDA Performance Across Blood Matrices
| Matrix Type | Number of Lipids Annotated | Repeatability | Key Applications |
|---|---|---|---|
| Serum | >2000 lipid species | Highest | Primary for clinical diagnostics |
| EDTA-Plasma | Comprehensive coverage | High | Epidemiological studies |
| Dried Blood Spots (DBS) | Substantial coverage | Robust | Biobanking, remote sampling |
Troubleshooting Guide: Common Experimental Challenges
Chromatographic Issues
Problem: Peak broadening and reduced resolution in C30 separation
- Solution: Ensure proper column conditioning with gradual solvent transition; use longer gradient times for complex samples; maintain column temperature consistency (±2°C)
- Preventive measures: Implement guard columns, filter samples (0.2μm), and avoid pH extremes outside 2-8 range
Problem: Retention time drift affecting SDDA scheduling
- Solution: Implement robust system suitability tests using internal retention time markers; extend column equilibration time between runs; monitor pressure trends for early detection of column degradation
- Advanced tuning: Use quality control samples to update retention time windows in SDDA methods periodically
Mass Spectrometry Acquisition Problems
Problem: Insufficient MS/MS triggering in crowded chromatographic regions
- Solution: Adjust SDDA parameters to include dynamic exclusion with shorter durations; increase MS1 resolution for better precursor selection; implement intensity-based triggering thresholds
- Parameter optimization: Set maximum injection time to balance sensitivity and scan speed; use apex-triggering for optimal fragmentation spectra
Problem: Spectral quality issues affecting lipid identification
- Solution: Optimize collision energies based on lipid class; use lipid-class specific fragmentation rules; implement stepped collision energy for comprehensive fragmentation patterns
- Quality metrics: Monitor precursor isolation efficiency (>80%); ensure fragment ion accuracy (<5ppm)
Experimental Protocols
Sample Preparation for Blood Matrices
Serum/Plasma Lipid Extraction (Based on [28])
- Sample Volume: Use 10-50μL of serum or plasma per extraction
- Protein Precipitation: Add 500μL cold methanol, vortex 30 seconds, incubate at -20°C for 1 hour
- Lipid Extraction: Add 500μL methyl-tert-butyl ether, vortex 1 minute, sonicate 15 minutes
- Phase Separation: Add 125μL water, centrifuge at 14,000×g for 15 minutes
- Collection: Transfer upper organic phase to new tube, evaporate under nitrogen
- Reconstitution: Resuspend in 100μL 2-propanol/acetonitrile (60:40, v/v) for LC-MS analysis
Quality Control Measures:
- Include pooled quality control samples every 6-10 injections [3]
- Use internal standards covering major lipid classes for normalization
- Monitor extraction efficiency through reference materials
LC-MS Method Parameters
C30 Chromatographic Conditions:
- Column: C30 reversed-phase (150×2.1mm, 2.6μm)
- Temperature: 45°C
- Flow Rate: 0.4 mL/min
- Mobile Phase A: acetonitrile/water (60:40) with 10mM ammonium formate
- Mobile Phase B: 2-propanol/acetonitrile (90:10) with 10mM ammonium formate
- Gradient: 30-100% B over 60 minutes, 5-minute wash at 100% B, 10-minute re-equilibration
- Injection Volume: 5μL
SDDA Mass Spectrometry Parameters:
- MS1 Resolution: 120,000 @ m/z 200
- Scan Range: m/z 200-2000
- MS2 Resolution: 30,000 @ m/z 200
- Isolation Window: 1.2 m/z
- Maximum Injection Time: 100ms (MS1), 50ms (MS2)
- Collision Energies: Stepped 20, 30, 40eV
- Scheduling Window: ±1.5 minutes based on retention time
Signaling Pathways and Experimental Workflow
Figure 1: C30-SDDA Lipidomics Workflow from Sample to Biological Interpretation
Research Reagent Solutions
Table 2: Essential Materials for C30-SDDA Lipidomics
| Reagent/Material | Function/Purpose | Specifications/Alternatives |
|---|---|---|
| C30 UHPLC Column | Superior separation of lipid isomers | 150×2.1mm, 2.6μm particle size |
| Ammonium Formate | Mobile phase additive for improved ionization | LC-MS grade, 10mM concentration |
| MTBE | Lipid extraction solvent | High purity, low peroxide levels |
| Internal Standard Mix | Quantification normalization | SPLASH LipidoMix or equivalent |
| NIST Plasma SRM 1950 | Quality control and method validation | Metabolites in Frozen Human Plasma |
| Acetonitrile (LC-MS) | Mobile phase component | Optima LC/MS grade or equivalent |
| 2-Propanol (LC-MS) | Strong elution solvent | Optima LC/MS grade or equivalent |
Frequently Asked Questions
Q: Why does C30 chromatography provide better lipid separation than C18?
A: C30 stationary phases have higher hydrophobicity and greater shape selectivity, particularly beneficial for separating lipid isomers and isobaric species that co-elute on C18 columns. The longer alkyl chains provide enhanced retention and resolution of complex lipid mixtures.
Q: How does SDDA improve upon conventional DDA in lipidomics?
A: SDDA increases identification rates by 2-fold compared to conventional DDA by triggering MS/MS acquisition only when precursors are expected to elute, reducing redundant sequencing and increasing coverage of lower-abundance species [28].
Q: What is the evidence for addressing biological variability using this method?
A: Large-scale studies applying quantitative LC-MS/MS lipidomics to population cohorts have demonstrated that biological variability significantly exceeds analytical variability, with high individuality and sex specificity observed in circulatory lipidomes [3]. The robustness of C30-SDDA across batches (median reproducibility 8.5%) makes it suitable for detecting true biological variation.
Q: Can this method be applied to single-cell lipidomics?
A: While the current protocol is optimized for bulk analysis, the sensitivity enhancements of SDDA provide a foundation for adapting to single-cell applications. Emerging technologies in mass spectrometry are pushing sensitivity limits to enable single-cell lipid profiling [5].
Q: What are the key quality control measures for implementing this method?
A: Essential QC includes: regular analysis of reference materials (e.g., NIST plasma), monitoring retention time stability, evaluating peak shape and intensity, tracking internal standard performance, and assessing batch-to-batch reproducibility with quality control pools.
Lipids are fundamental biomolecules that serve as structural components of cell membranes, function as energy storage units, and play crucial roles in cellular signaling processes [29]. Consequently, dysregulated lipid metabolism is closely correlated with the occurrence and progression of pathological conditions, including diabetes, cancers, and neurodegenerative diseases [29]. However, a significant portion of the lipidome remains "dark" or "unmapped" due to analytical challenges in resolving structural isomers [29]. The structural complexity of lipids arises from variations in class, headgroup, fatty acyl chain composition, sn-position, and carbon-carbon double bond (C=C) location and geometry [30] [31]. In particular, C=C location isomers confer distinct biological functions and physical properties to lipids, yet they remain exceptionally challenging to characterize using conventional mass spectrometry approaches [29] [32].
Traditional collision-induced dissociation (CID) in tandem mass spectrometry (MS/MS) fails to generate diagnostic fragment ions for pinpointing C=C locations because cleavage of non-polar C–C bonds adjacent to a C=C bond is not favored [29]. This limitation represents a critical gap in lipidomic studies, especially when investigating biological variability where isomeric ratios may change in response to physiological or pathological stimuli [15]. The Paternò-Büchi (P-B) reaction has emerged as a powerful derivatization strategy that enables precise localization of C=C bonds in unsaturated lipids when coupled with MS/MS analysis [29] [30]. This technical support guide provides comprehensive troubleshooting and methodological support for researchers implementing P-B reactions in lipidomic studies, with particular emphasis on addressing biological variability in lipid isomer research.
The Scientist's Toolkit: Essential Reagents and Materials
Successful implementation of P-B reactions for lipid isomer analysis requires careful selection of reagents and materials. The table below summarizes key components and their functions in the experimental workflow.
Table 1: Essential Research Reagent Solutions for P-B Reaction Lipidomics
| Reagent/Material | Function | Examples & Notes |
|---|---|---|
| PB Reagents | Forms oxetane ring with C=C bonds via [2+2] photocycloaddition | Acetone (58 Da mass shift) [30], Benzophenone [29], 2-Acetylpyridine (2-AP) [29], 2′,4′,6′-Trifluoroacetophenone (triFAP) [29], Methyl Benzoylformate (MBF) with photocatalyst for visible-light activation [32] |
| Photocatalysts | Enables visible-light activation via triplet-energy transfer | Ir[dF(CF3)ppy]2(dtbbpy)PF6 (triplet energy ~60.1 kcal/mol) for use with MBF [32] |
| Light Sources | Activates carbonyl compounds to excited state | UV lamps (254 nm for aliphatic carbonyls) [33] [34], Visible light systems for photocatalytic approaches [32], Light Emitting Diodes (LEDs) [35] |
| Reaction Vessels | Container for photochemical reaction | Quartz cuvettes (transparent to UV) [29], Gas-tight round bottom flasks (prevent oxygen leakage) [29], Microreactors for online setups [29] |
| MS-Compatible Solvents | Medium for reaction and MS analysis | Acetonitrile, Methanol, Chloroform; Must be UV-transparent and minimize side reactions [29] |
| Internal Standards | Quality control and quantification | Deuterated lipid standards (e.g., Avanti EquiSPLASH LIPIDOMIX) [36] |
| Vilobelimab | Vilobelimab, CAS:2250440-41-4, MF:C43H60O6, MW:672.9 g/mol | Chemical Reagent |
| TJ-M2010-5 | TJ-M2010-5, CAS:1357471-57-8, MF:C23H26N4OS, MW:406.5 g/mol | Chemical Reagent |
Experimental Protocols: Key Methodologies for P-B Reaction in Lipidomics
Online RPLC-PB-MS/MS for Triacylglycerol Analysis
Objective: To separate and characterize triacylglycerol (TG) species from human plasma with confident C=C location assignment [37].
Protocol:
- Sample Preparation: Extract lipids from human plasma using modified Folch method with chloroform:methanol (2:1 v/v) supplemented with 0.01% butylated hydroxytoluene (BHT) to prevent oxidation [36].
- Chromatographic Separation:
- Column: Reversed-phase C18 column (e.g., 50 × 0.3 mm, 3 μm particles)
- Mobile Phase: A: 60:40 acetonitrile/water; B: 85:10:5 isopropanol/water/acetonitrile, both with 10 mM ammonium formate and 0.1% formic acid
- Gradient: 0-0.5 min (40% B), 0.5-5 min (99% B), 5-10 min (99% B), 10-12.5 min (40% B), 12.5-15 min (40% B)
- Flow Rate: 8 μL/min [37] [36]
- Online P-B Derivatization:
- Mix acetone (10% v/v) with column effluent via T-connector
- Use UV photochemical reactor (254 nm) with knitted polytetrafluoroethylene (PTFE) reactor coil
- Maintain reaction temperature at 20°C [37]
- Mass Spectrometry Analysis:
- Ionization: ESI in positive mode
- MS/MS: Select PB-modified lipids (original mass + 58 Da for acetone) for CID
- Identification: Look for diagnostic pair fragments (difference of 26 Da) indicating C=C location
- Limit of Identification: 50 nM [37]
Visible-Light Activated PCPI for Dual-Resolving of C=C Isomers
Objective: To simultaneously resolve both positional and geometric isomers of C=C bonds in bacterial and mouse brain lipids [32].
Protocol:
- Reaction System Setup:
- Carbonyl Substrate: Methyl benzoylformate (MBF, 10 mM)
- Photocatalyst: Ir[dF(CF3)ppy]2(dtbbpy)PF6 (0.5 mol%)
- Solvent: Acetonitrile
- Light Source: 455 nm blue LED lamp [32]
- Reaction Conditions:
- Incubate lipid extracts with reaction system for 10 minutes under light irradiation
- Maintain inert atmosphere with argon or nitrogen to prevent side reactions
- For offline derivatization, use quartz cuvettes as reaction vessels [32]
- LC-MS Analysis:
- Use reversed-phase LC with C18 column for separation
- Employ high-resolution mass spectrometer (e.g., Q-TOF) for detection
- Monitor both oxetane products (for C=C location) and isomerized lipids (for cis/trans configuration) [32]
- Data Interpretation:
- Positional Isomers: Identify via diagnostic fragments from oxetane ring cleavage in MS/MS
- Geometric Isomers: Determine by comparing LC patterns before and after photoisomerization; cis isomers show decreased peak areas while trans isomers increase [32]
Figure 1: Experimental Workflow for P-B Reaction in Lipidomics
Troubleshooting Guides: Addressing Common Experimental Challenges
Low Reaction Yield or Efficiency
Table 2: Troubleshooting Low P-B Reaction Efficiency
| Problem | Possible Causes | Solutions |
|---|---|---|
| Incomplete derivatization | Insufficient UV light intensity or inappropriate wavelength | Use quartz vessels for UV transparency at 254 nm; Ensure proper light source alignment; Consider visible-light photocatalytic system for improved efficiency [32] |
| Low product formation | Oxygen quenching of excited states | Degas solvents with argon/nitrogen; Use gas-tight reaction vessels; Maintain inert atmosphere throughout reaction [29] |
| Side reactions predominant | Prolonged reaction time or inappropriate solvent | Optimize reaction time (typically seconds to minutes in flow systems); Use non-polar solvents when possible; Test different PB reagents (acetone, benzophenone derivatives) [29] [34] |
| Poor MS response of products | Ionization suppression or inefficient fragmentation | Incorporate nanoESI for improved sensitivity; For free fatty acids, use double derivatization (PB reaction + carboxyl group labeling with DEEA) [30] |
Quantitative and Reproducibility Issues
Challenge: Inconsistent quantification of isomer ratios across batches or platforms.
Solutions:
- Internal Standards: Use deuterated lipid internal standards (e.g., Avanti EquiSPLASH LIPIDOMIX) added at the beginning of extraction to correct for technical variability [36].
- Quality Control Samples: Implement pooled quality control (QC) samples analyzed throughout the batch to monitor and correct for instrumental drift [15].
- Platform Validation: Validate identifications across both positive and negative LC-MS modes to reduce false positives caused by co-elution [36].
- Manual Curation: Manually inspect spectral outputs and software identifications; use data-driven outlier detection to flag potential misidentifications [36].
- Control Reaction Parameters: Standardize light intensity, reaction time, temperature, and PB reagent concentration across all samples [29].
Biological Sample-Specific Challenges
Challenge: Addressing biological variability while minimizing technical artifacts.
Solutions:
- Pre-analytical Standardization:
- Batch Design:
- Data Normalization:
Figure 2: Troubleshooting Common P-B Reaction Challenges
Frequently Asked Questions (FAQs)
Q1: What is the principle behind the Paternò-Büchi reaction for lipid C=C location analysis?
The P-B reaction is a photochemical [2+2] cycloaddition between an excited carbonyl compound (e.g., acetone) and a C=C bond in an unsaturated lipid, forming an oxetane ring. When this modified lipid is fragmented in MS/MS, the oxetane ring cleaves to produce a pair of diagnostic ions with a specific mass difference (e.g., 26 Da for acetone), which reveals the original location of the C=C bond in the fatty acyl chain [29] [30].
Q2: How can I minimize side reactions during P-B derivatization?
Key strategies include: (1) Using degassed solvents and maintaining an inert atmosphere to prevent oxidation; (2) Optimizing reaction time to avoid over-exposure to UV light; (3) Selecting appropriate PB reagents - aliphatic carbonyls like acetone generally produce fewer side products than aromatic carbonyls; (4) Implementing microreactors or flow systems to precisely control reaction parameters and minimize side product formation [29].
Q3: Can the P-B reaction distinguish between cis and trans geometric isomers?
Standard P-B reactions show limited capability for distinguishing cis/trans isomers. However, the recently developed photocycloaddition-photoisomerization (PCPI) reaction system using methyl benzoylformate with a photocatalyst under visible light can simultaneously resolve both C=C positions and geometric configurations. This system induces cis to trans isomerization, allowing identification by comparing LC patterns before and after the reaction [32].
Q4: What is the sensitivity and dynamic range of PB-MS/MS for lipid isomer analysis?
PB-MS/MS offers high sensitivity (sub-nM to nM detection limits) and a linear dynamic range spanning 2-3 orders of magnitude for profiling C=C location isomers. The limit of identification for triacylglycerol species in human plasma using online RPLC-PB-MS/MS is approximately 50 nM [29] [37].
Q5: How reproducible are lipid isomer ratio measurements using PB-MS/MS, and how does this help with biological variability studies?
The technique shows high precision with approximately 5% RSD for technical replicates. By measuring isomeric ratios rather than absolute abundances, the method further diminishes RSD from biological replicates, making it particularly valuable for detecting subtle but biologically relevant changes in isomer distributions in disease states [29].
Q6: What software tools are available for processing PB-MS/MS data, and how consistent are their results?
Common lipidomics software includes MS DIAL and Lipostar. However, studies show only 14.0% identification agreement between platforms using default settings with MS1 data, improving to 36.1% with MS2 spectra. This highlights the critical importance of manual curation and validation across multiple platforms and ionization modes to ensure reproducible lipid identifications [36].
The Paternò-Büchi reaction represents a powerful analytical tool that significantly advances our capability to resolve lipid C=C location isomers in complex biological systems. When properly implemented with appropriate troubleshooting and quality control measures, this methodology enables researchers to uncover previously inaccessible dimensions of lipid structural diversity. By integrating robust experimental protocols with careful consideration of biological variability sources, researchers can reliably apply PB-MS/MS to investigate lipid isomer dynamics in health and disease, ultimately contributing to more comprehensive lipidomic phenotyping and biomarker discovery.
Troubleshooting Guides
Table 1: Common Pre-analytical Errors and Corrective Actions
| Error Category | Specific Issue | Impact on Lipidomics Data | Corrective Action |
|---|---|---|---|
| Sample Collection | Incorrect collection tube (e.g., wrong anticoagulant) | Alters lipid classes; e.g., EDTA tubes affect lysophospholipids [38] | Standardize on K3EDTA tubes for plasma and validate tube type for your lipid panel [38] |
| Non-fasting state of participant | Introduces significant variability in triglyceride-rich lipids [15] | Implement strict fasting protocols (typically 10-12 hours) prior to blood collection [15] | |
| Hemolysis due to improper technique | Rupture of red blood cells releases lipids and interferes with accurate measurement | Train phlebotomists on proper technique; avoid excessive suction [39] | |
| Sample Handling & Storage | Intermediate storage at incorrect temperature | Degradation of unstable lipids (e.g., lipid mediators, lysophospholipids) [38] | Place plasma samples in ice water immediately after collection and freeze at -80°C within 2 hours [38] |
| Delayed processing of whole blood | Increased ex vivo generation of lysophospholipids and oxidation of fatty acids [40] | Process plasma (centrifugation, aliquoting) within 1-2 hours of draw [38] | |
| Improper long-term storage temperature | Lipid degradation over time, leading to inaccurate concentrations | Store samples at -70°C to -80°C; monitor freezer stability and avoid freeze-thaw cycles [9] [15] | |
| Sample Identification | Mislabeled specimen | Incorrect data attribution, rendering results useless and harmful | Label specimens at the patient's bedside using at least two unique identifiers [41] |
| Incomplete labeling on tube or form | Specimen rejection by laboratory, causing delays | Use barcoding systems where available and verify details against request form [41] |
Table 2: Statistical Implications of Pre-analytical Variability
| Variance Component | Description | Proportion of Total Variance (Median, from [9]) | Impact on Study Design |
|---|---|---|---|
| Technical Variance | Variability from laboratory procedures (e.g., analysis, processing) | Moderate (Median ICCTech = 0.79) [9] | High technical reliability reduces attenuation of observed effect sizes. |
| Within-Individual Variance | Biological variability over time within a single person | High (Combined with technical variance, accounts for most variability in 74% of lipids) [9] | A single measurement may poorly represent the "usual" lipid level, requiring larger sample sizes. |
| Between-Individual Variance | Variability of "usual" lipid levels among different subjects | Lower than other sources for many lipids [9] | This is the key variance for detecting associations; high between-individual variance is ideal. |
| Statistical Power Implication | For a true RR=3 with 500/1000/5000 total participants, power is only 19%/57%/99%, respectively [9]. |
Frequently Asked Questions (FAQs)
1. Why is standardizing pre-analytical protocols so critical in lipidomics research?
Pre-analytical sample handling has a major effect on the suitability of metabolites and lipids as biomarkers [38]. Errors introduced during collection, handling, and storage can lead to ex vivo distortions of lipid concentrations, meaning the measured levels do not reflect the true biological state [38]. Since most laboratory errors (61.9%-68.2%) occur in the pre-analytical phase [39], standardizing these protocols is the most effective way to ensure data reliability and quality.
2. What are the most unstable lipids, and how should they be handled?
Lipid mediators and certain lysophospholipids are particularly prone to rapid ex vivo generation or degradation [38] [40]. For these unstable analytes, meticulous processing is required. Recommendations include using ice-cold storage immediately after draw and adding enzyme inhibitors like 2,6-di-tert-butyl-4-methylphenol (BHT) to prevent oxidation during sample preparation [38] [15].
3. How does biological variability affect my lipidomics study's power, and how can I mitigate it?
Lipid levels are dynamic and influenced by factors like diet, circadian rhythm, and exercise [9] [15]. The combination of within-individual biological variability and technical variability accounts for most of the total variability for the majority of lipid species [9]. This "noise" attenuates the observed associations between lipids and diseases, drastically reducing statistical power. To mitigate this, use large sample sizes and, where feasible, collect multiple serial samples from participants to better estimate their "usual" lipid level [9].
4. What is "unwanted variation" (UV) in lipidomics, and how is it removed?
Unwanted Variation (UV) is any variation introduced into the data not due to the biological factors under study [15]. This includes variation from pre-analytical factors, analytical platforms, and data processing. The best strategy is to control for UV proactively through careful study design and standardized protocols [15]. Post-analytically, UV can be addressed using global normalization methods (e.g., SERRF, RUV-III) that leverage quality control samples run in each batch to correct for technical drift [15].
5. What are the minimum reporting standards for lipidomics data in publications?
To ensure reproducibility and data quality, journals are increasingly requiring detailed reporting. You should document:
- Sample Collection: Patient fasting status, blood draw tube, processing times and temperatures [40].
- Sample Storage: Long-term storage temperature and duration [40].
- Lipid Extraction: Exact protocol used (e.g., Folch, MTBE, BUME) [40].
- MS Analysis: Platform, identification strategies, and quantification methods (absolute is the "gold standard") [40].
- Data Processing: Software used and how missing values were handled [40].
Essential Workflow Diagrams
Pre-analytical Workflow for Plasma Lipidomics
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Pre-analytical Standardization
| Item | Function in Lipidomics | Key Considerations |
|---|---|---|
| K3EDTA Blood Collection Tubes | Standard anticoagulant for plasma preparation. Prevents coagulation while minimizing ex vivo lipid alterations [38]. | Preferred over serum for many lipidomic applications due to more controlled and rapid processing [38]. |
| BHT (2,6-di-tert-butyl-4-methylphenol) | Antioxidant added during sample preparation to inhibit lipid peroxidation and protect unsaturated fatty acids [38] [15]. | Critical for stabilizing oxidation-prone lipids. Concentration should be optimized and standardized across batches. |
| Deuterated Internal Standards (ISTDs) | Added to the sample before extraction to correct for losses during preparation and variability during MS analysis [9] [40]. | Should be selected to cover a broad range of lipid classes. Essential for accurate absolute quantification [40]. |
| MTBE or Chloroform/Methanol | Organic solvents for liquid-liquid extraction of lipids from plasma/serum (e.g., MTBE, Folch, or BUME methods) [15] [40]. | Different solvents have varying extraction efficiencies for different lipid classes. The chosen method must be consistent [40]. |
| Quality Control (QC) Pooled Plasma | A homogeneous sample from multiple donors, aliquoted and analyzed repeatedly throughout the analytical batch [9] [15]. | Used to monitor instrument performance, correct for batch effects, and perform post-acquisition normalization (e.g., with SERRF) [15]. |
| Gintemetostat | Gintemetostat, CAS:2604513-16-6, MF:C25H26F4N8O2, MW:546.5 g/mol | Chemical Reagent |
| taccalonolide AJ | taccalonolide AJ, MF:C34H44O14, MW:676.7 g/mol | Chemical Reagent |
Troubleshooting High-Throughput Lipidomics
Frequently Asked Questions (FAQs)
What is the typical number of lipids identified in different sample types, and why does it vary? The number of lipids identified depends heavily on the sample type, volume, and analysis mode. For instance, 1 million yeast cells or 80µL of human plasma extract can yield between 100 to 1000 lipids. The ion mode (positive or negative) also significantly impacts the results. In LC-MS/MS runs, the number of MS2 spectra acquired can range from 5,000 to over 10,000 in a 30-minute Top N experiment, directly influencing the number of lipid species identified and integrated [42].
How can I determine double bond position in lipids using high-throughput platforms? Routine MS-MS analysis alone cannot determine double bond position. This requires additional methodologies, such as:
- Using lipid standards to model retention time and identify likely candidates.
- Employing separate methods like hydrolysis followed by GC-MS.
- Implementing ion-molecule reactions (e.g., ozone-induced dissociation) or UVPD (photodissociation) [42].
Can I use direct infusion for complex lipid mixtures, and what are the drawbacks? While LipidSearch software supports identification from direct infusion (dd-MS2) data, it is not recommended for complex mixtures. Co-isolation of multiple precursor ions or isomers at the same m/z leads to mixed MS2 spectra, which reduces identification accuracy and typically results in a lower number of confidently identified species compared to LC-MS methods [42].
Why is there low agreement in lipid identifications between different software platforms? A key challenge is the lack of reproducibility between lipidomics software. A study processing identical LC-MS spectra in MS DIAL and Lipostar found only 14.0% identification agreement using default settings. Even when using fragmentation (MS2) data, agreement only rose to 36.1% [43]. This highlights the critical need for manual curation of results and validation across multiple analytical modes.
How does biological variability impact the design of lipidomics studies? Lipid levels exhibit biological (within-individual) and technical variability. A large serum lipidomics study found that for 74% of lipid species, the combination of technical and within-individual variance accounted for most of the total variability [9]. This variability attenuates the observed relative risks in association studies, requiring larger sample sizes for robust power.
Table 1: Statistical Power in Lipidomics Epidemiological Studies (True RR=3, α=5.45x10â»âµ) [9]
| Total Study Participants | Case-Control Ratio | Estimated Statistical Power |
|---|---|---|
| 500 | 1:1 | 19% |
| 1,000 | 1:1 | 57% |
| 5,000 | 1:1 | 99% |
Troubleshooting Common Experimental Issues
Problem: Inconsistent or Irreproducible Results Across Batches
- Potential Cause: Uncontrolled biological and technical variability introduced during sample collection, handling, storage, and preparation [44] [9].
- Solutions:
- Standardize Protocols: Implement and strictly adhere to harmonized experimental protocols for sample processing [45].
- Use Internal Standards: Employ well-defined, chemically pure synthetic lipid standards for accurate quantification and identification. This is crucial for correcting instrument response variations [45] [42].
- Batch Correction: Apply statistical techniques like ComBat or LOESS normalization during data preprocessing to adjust for variability between analytical runs [6].
Problem: Low Confidence in Lipid Identifications
- Potential Cause: Misidentifications, improper annotation, and over-reporting due to software inconsistencies or co-elution of isobaric lipids [45] [43].
- Solutions:
- Multi-Platform Validation: Cross-check identifications using multiple software platforms and manual curation of spectra [43].
- Quality Control Scoring: Implement a lipidomics scoring system that awards points for different layers of analytical information (e.g., MS, chromatography, ion mobility) to abstract structural evidence into a quality score [46].
- Leverage Retention Time: Use retention time modeling and data-driven outlier detection (e.g., using support vector machine regression) to flag potentially false positive identifications [43].
Problem: Low Signal-to-Noise or High Background
- Potential Cause: Inefficient lipid extraction, sample contamination, or ion suppression from co-eluting compounds [47].
- Solutions:
- Optimize Extraction: Choose an extraction method suited to your lipid classes. The MTBE method offers easier handling and is better for glycerophospholipids and ceramides, while chloroform-based methods (Folch, Bligh & Dyer) are superior for saturated fatty acids and plasmalogens [47].
- Use High-Purity Solvents: Avoid plasticizers by using glassware where possible and ensure solvent purity to reduce chemical noise [48].
- Clean-Up Samples: Utilize solid-phase extraction (SPE) to purify specific lipid classes and remove interfering contaminants [48].
Experimental Protocols for Addressing Biological Variability
Protocol: Sample Collection and Preparation to Minimize Pre-Analytical Variability
Principle: The goal is to preserve the in-vivo lipid profile by halting enzymatic and chemical degradation immediately upon sample collection [47].
Materials:
- Cryogenic vials
- Liquid nitrogen
- Pre-chilled solvents (e.g., Methanol, Chloroform, or MTBE)
- Glass homogenizers (e.g., Potter-Elvehjem) or bead mills
- Internal standard mixture (e.g., Avanti EquiSPLASH LIPIDOMIX) [43]
Procedure:
- Rapid Sampling & Stabilization: Flash-freeze tissue samples immediately in liquid nitrogen. For biofluids, process plasma/serum within 30 minutes or use additives to inhibit enzymes like lipases [47].
- Homogenization: For tissues, use shear-force-based grinding in a pre-chilled solvent with a Potter-Elvehjem homogenizer or a bead mill. This ensures equal solvent accessibility to all tissue parts [47].
- Lipid Extraction: a. Weigh the frozen tissue or aliquot biofluid. b. Add a mixture of internal standards to account for extraction efficiency and instrument variability [9] [43]. c. Perform a two-phase liquid-liquid extraction. The MTBE method is recommended for its safety and efficiency [47]: * Add MTBE/Methanol/Water in a ratio of 5:1.5:1.25 (v/v/v). * Vortex and centrifuge to separate phases. * Collect the upper organic (MTBE) phase containing the lipids.
- Storage: Evaporate solvents under nitrogen and reconstitute in a suitable MS-compatible solvent. Store extracts at -80°C, minimizing freeze-thaw cycles [47].
Protocol: Data Acquisition and Preprocessing for High-Throughput Workflows
Principle: Ensure consistent, high-quality data acquisition and preprocess raw data to correct for technical noise and alignment issues before statistical analysis [6].
Materials:
- UPLC system with C18 reversed-phase columns (e.g., 50-100 Ã… pore size)
- High-resolution mass spectrometer (e.g., Q-TOF, Orbitrap, or ZenoTOF)
- Data processing software (e.g., MS-DIAL, LipidSearch, Lipostar)
Procedure:
- Chromatographic Separation: Use a binary gradient with solvents like (A) acetonitrile/water and (B) isopropanol/acetonitrile, both supplemented with 10 mM ammonium formate. A typical microflow gradient runs for 15 minutes [43].
- Mass Spectrometry: Operate the MS in data-dependent acquisition (DDA) mode, switching between full MS and MS2 scans. Acquire data in both positive and negative electrospray ionization modes to maximize lipid coverage [43].
- Data Preprocessing: a. Peak Picking & Alignment: Use software to identify lipid peaks and align their retention times across all samples. b. Noise Reduction & Normalization: Apply signal filtering and normalize data to internal standards and/or total lipid content to correct for instrument drift. c. Batch Effect Correction: Use statistical tools like ComBat to remove systematic technical variation between different processing batches [6]. d. Imputation: For lipids with missing values (e.g., present in some samples but not others), use methods like k-nearest neighbors (KNN) to impute missing data, ensuring a complete data matrix for statistical testing [9] [48].
Visual Workflows and Pathways
Lipidomics Quality Assurance Workflow
Addressing Variability in Lipid Analysis
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Robust Lipidomics
| Reagent / Material | Function & Rationale | Example Product / Composition |
|---|---|---|
| Internal Standards (Quantitative) | Enables absolute quantification by correcting for extraction efficiency and instrument response variance. Critical for data reproducibility. | Avanti EquiSPLASH LIPIDOMIX; a mixture of deuterated lipids across multiple classes [43]. |
| Internal Standards (Qualitative) | Aids in the confident identification of lipid structures by providing a reference for fragmentation patterns and retention time. | Chemically pure synthetic lipid standards from providers like Avanti Polar Lipids [45]. |
| Extraction Solvents | To efficiently isolate lipids from the biological matrix while minimizing degradation and contamination. | MTBE (safer, easier handling), Chloroform-Methanol (classical Folch/Bligh & Dyer), Butanol-Methanol (BUME, for automation) [47]. |
| Antioxidants | Prevents oxidation of unsaturated lipids during extraction and storage, which can create artifacts and skew results. | Butylated Hydroxytoluene (BHT) [43]. |
| LC-MS Grade Solvents & Additives | Provides high-purity mobile phases to reduce chemical noise, improve ionization efficiency, and prevent instrument contamination. | Acetonitrile, Isopropanol, Water, Ammonium Formate, Formic Acid [43]. |
| Tdp-43-IN-1 | Tdp-43-IN-1, MF:C20H17F2N5OS, MW:413.4 g/mol | Chemical Reagent |
| R-10015 | R-10015, MF:C20H19ClN6O2, MW:410.9 g/mol | Chemical Reagent |
Lipid metabolism is not static; it undergoes dynamic changes influenced by development, environment, and interventions. The Developmental Origins of Health and Disease paradigm suggests that prenatal, perinatal, and postnatal influences result in long-term physiological and metabolic changes that can contribute to later-life disease risk [49]. Longitudinal lipidomic studies are essential for capturing these dynamic processes, moving beyond single-timepoint snapshots to reveal meaningful biological trends. However, this approach introduces significant methodological challenges, primarily concerning biological variability and technical consistency across timepoints. This technical support center provides targeted guidance for researchers navigating these complexities to generate robust, reproducible data on lipid metabolism throughout critical life stages.
Essential Research Reagent Solutions
The following reagents and materials are fundamental for ensuring reproducibility and accuracy in longitudinal lipidomic profiling.
Table 1: Key Research Reagents for Longitudinal Lipidomics
| Item | Function | Example/Specification |
|---|---|---|
| Internal Standards | Correct for extraction efficiency and instrument variability; essential for data normalization across batches. | Commercially available stable isotope-labeled lipid mixtures [49]. |
| Solvent System | Lipid extraction from biological matrices. | Butanol:Methanol (1:1) with 10 mM Ammonium Formate [49]. |
| Passivation Solution | Prevents peak tailing and absorption of acidic phospholipids to instrument surfaces. | 0.5% Phosphoric Acid in 90% Acetonitrile [49]. |
| UHPLC Solvents | Mobile phases for chromatographic separation. | Solvent A: 50% H2O/30% Acetonitrile/20% Isopropanol with 10 mM Ammonium Formate. Solvent B: 1% H2O/9% Acetonitrile/90% Isopropanol with 10 mM Ammonium Formate [49]. |
| Quality Control (QC) Pools | Monitor instrumental stability and data quality throughout the acquisition sequence. | Pooled Plasma QC (PQC) from study samples; Technical QC (TQC) from pooled PQC extracts [49]. |
Frequently Asked Questions (FAQs) & Troubleshooting
Study Design & Sampling
Q1: What is the optimal frequency and timing for sample collection in a early-life lipidomics study?
A: The schedule should capture key developmental transitions. The Barwon Infant Study (BIS) provides a robust framework, with sampling at critical developmental windows: birth (cord serum), 6 months, 12 months, and 4 years [49]. For adult or intervention studies, align timepoints with expected biological shifts, such as pre-/post-intervention and multiple follow-ups. Consistency in the time-of-day for collection is critical to minimize diurnal variation.
Q2: How can we account for high inter-individual variability in longitudinal lipidomics?
A: Employ a paired sample design where each subject serves as their own control. Analyze serial samples from the same individual across timepoints. This design powerfully isolates temporal trends from baseline inter-individual differences. Statistically, use methods like Generalized Estimating Equations (GEE) that are designed to model within-subject correlation [50].
Lipid Extraction & Analysis
Q3: How many lipid species can we typically expect to measure in human plasma, and what affects this number?
A: The number varies based on sample volume and analytical depth. Using UHPLC-MS/MS, targeted methods can measure 776 distinct lipid features across 39 lipid classes from 10 µL of human plasma [49]. Broader discovery-based methods may detect 100-1000+ lipids, influenced by sample type, extraction efficiency, and MS/MS data acquisition parameters [42].
Q4: What is the recommended QC strategy to ensure data stability in a long-running study?
A: Implement a rigorous QC protocol. Inject a Pooled QC (PQC) sample every 10-20 study samples to monitor instrument performance and correct for signal drift [49]. Include a Technical QC (TQC) at the same frequency to isolate technical variation from biological variation. Visually inspect PQC data in Principal Component Analysis (PCA) to identify and exclude analytical batches with significant drift.
Q5: We observe peak tailing for acidic phospholipids. How can this be resolved?
A: Peak tailing is often due to adsorption to active metal surfaces in the UHPLC system. Passivate the instrument prior to each batch by running 0.5% phosphoric acid in 90% acetonitrile for 2 hours, followed by a thorough flush with 85% H2O/15% acetonitrile before the sample run [49].
Data Analysis & Statistics
Q6: What statistical methods are suitable for identifying significant lipid-environment interactions in longitudinal data?
A: Standard linear models are invalid due to within-subject correlation. Penalized Generalized Estimating Equations (PGEE) within the GEE framework are advanced methods developed specifically for this purpose. They can handle high-dimensional data (where lipids >> samples) and select significant main and interaction effects while accounting for the longitudinal correlation structure [50].
Q7: Can direct infusion (shotgun lipidomics) be used for longitudinal studies?
A: While faster, direct infusion is not recommended for complex mixtures in longitudinal designs. Liquid chromatography (LC) separation prior to MS analysis is superior because it reduces ion suppression and co-isolation of isomeric lipids, which can lead to inaccurate identification and quantification. LC-MS/MS provides more reliable data for tracking subtle changes over time [42].
Detailed Experimental Protocol: A Population-Based Longitudinal Workflow
The following protocol is adapted from a comprehensive population study investigating the ontogeny of lipid metabolism from pregnancy into early childhood [49].
Table 2: Detailed Longitudinal Lipidomics Experimental Protocol
| Step | Procedure | Critical Parameters |
|---|---|---|
| 1. Sample Collection | Collect serial samples (e.g., maternal serum, cord serum, child plasma) at predetermined timepoints. | Centrifuge blood samples within 2 hours of collection. Aliquot and immediately store serum/plasma at -80°C. Maintain consistent processing protocols across all timepoints. |
| 2. Lipid Extraction | Mix 10 µL of plasma with 100 µL of pre-cooled Butanol:Methanol (1:1) containing 10 mM Ammonium Formate and a mixture of internal standards. | Vortex thoroughly. Sonicate for 1 hour. Centrifuge at 14,000× g for 10 minutes at 20°C. Transfer supernatant to MS vials with glass inserts. |
| 3. UHPLC-MS/MS Analysis | Inject 1 µL onto a dual-column UHPLC system (e.g., ZORBAX Eclipse Plus C18 columns). Use a 12.9-minute stepped linear gradient with Solvents A and B. | Thermostat columns at 45°C. Use a dual-column setup to increase throughput. Employ dynamic scheduled Multiple Reaction Monitoring (MRM) in both positive and negative ion modes. |
| 4. Quality Control | Inject one Pooled QC (PQC) and one Technical QC (TQC) for every 20 study samples. | Use PQC to monitor overall process stability and TQC to monitor instrumental variation. Track retention time and peak area stability in QCs throughout the sequence. |
| 5. Data Processing | Integrate lipid peaks using appropriate software (e.g., LipidSearch, TraceFinder). | Normalize lipid species intensities using the internal standards added prior to extraction. Perform batch correction if necessary using the PQC data. |
Visualizing the Workflow: From Sample to Insight
The following diagram illustrates the complete integrated workflow for a longitudinal lipidomics study, from initial design to final data interpretation.
Data Analysis Pathway
After data acquisition and preprocessing, the analysis phase involves specific steps to model changes over time and identify significant effects.
Statistical Workflows and Data Processing for Robust Lipidomics
Implementing FAIR Data Principles with R and Python Lipidomics Toolkits
Frequently Asked Questions (FAQs)
Q1: What are the FAIR data principles and why are they critical for lipidomics? The FAIR data principles are a set of guiding rules to make data Findable, Accessible, Interoperable, and Reusable [51]. In lipidomics, adhering to these principles is essential for ensuring that complex datasets are transparent, reproducible, and can be effectively shared and integrated across research groups and computational platforms [52]. This is particularly important for studies investigating biological variability, as it allows for the precise tracking of how data was processed to distinguish true biological signal from technical noise.
Q2: My lipidomics data is highly skewed. Which R/Python visualization tools should I use instead of traditional bar charts? For skewed lipidomics data, traditional bar charts can be misleading. It is recommended to use:
- Violin plots or box plots with jitter to show the full data distribution.
- Adjusted box plots that use medcouple-based whisker definitions for a more robust representation of asymmetric distributions [52].
In R, you can use
ggpubrandggplot2to create these plots. In Python, theseabornandmatplotliblibraries are recommended for generating publication-ready visualizations [52] [1].
Q3: How should I handle missing values in my lipidomics dataset before statistical analysis? The strategy for handling missing values should be based on their likely cause:
- Missing Not at Random (MNAR): Often due to abundances falling below the detection limit. A common and often optimal method is imputation with a percentage (e.g., half) of the lowest concentration for that lipid [1].
- Missing Completely at Random (MCAR) or Missing at Random (MAR): k-Nearest Neighbors (kNN)-based imputation or Random Forest methods have been shown to perform well [1]. Before imputation, it is a best practice to filter out lipid species with an excessively high proportion of missing values (e.g., >35%) [1].
Q4: What is the benefit of a modular R/Python workflow over a fully automated online platform? While automated platforms like MetaboAnalyst are user-friendly, modular R/Python workflows prioritized in recent guidelines offer greater flexibility and transparency [52] [1]. They avoid "black box" processing and allow researchers to understand, customize, and document each step of the analysis—from normalization and imputation to advanced visualization. This is a key requirement for implementing FAIR principles and for rigorous investigation of biological variability [52].
Troubleshooting Guides
Issue 1: Inconsistent Lipid Identification Across Analysis Batches
Problem: Lipid species identifiers or concentrations are not consistent when the same sample is run in different batches, complicating the analysis of biological variability.
Solution:
- Pre-Acquisition Planning: Incorporate Quality Control (QC) samples into your sequence. These can be a pool of all study samples or a standard reference material like NIST SRM 1950 [1].
- Post-Acquisition Correction: Use the QC samples to perform batch effect correction.
- In R/Python, algorithms like LOESS (Locally Estimated Scatterplot Smoothing) or SERRF (Systematic Error Removal using Random Forest) can be applied to correct for systematic drift [52] [1].
- Follow the data normalization workflows provided in the associated GitBook, which use
mixOmicsin R and analogous Python libraries [52].
Prevention:
- Always plan your acquisition sequence according to guidelines from the Lipidomics Standards Initiative (LSI) and the Metabolomics Society [52].
- Use a standardized sample preparation protocol, such as a stable isotope dilution approach, to minimize technical variability from the start [3].
Issue 2: Low Statistical Power to Detect Biologically Relevant Changes
Problem: A pilot study fails to find significant associations, potentially because the study is underpowered to detect changes against a background of high biological and technical variability.
Solution: Understanding the sources of variance in your data is the first step. Research has shown that for many lipid species, the combination of technical and within-individual variance accounts for most of the total variability [9].
Table: Power Analysis for Lipidomics Case-Control Studies
| Total Study Participants (1:1 Case-Control Ratio) | Estimated Power to Detect a Relative Risk of 3.0* | Key Considerations |
|---|---|---|
| 500 | 19% | Highly underpowered for most lipidomic studies. |
| 1,000 | 57% | Moderate power; suitable only for effects with large effect sizes. |
| 5,000 | 99% | Well-powered to detect moderate effect sizes. |
| Note: Assumes a Bonferroni-corrected significance threshold for 918 lipid species (α = 5.45e-5). Based on variance estimates from [9]. | ||
| Py-MPB-amino-C3-PBD | Py-MPB-amino-C3-PBD, MF:C41H44N8O6, MW:744.8 g/mol | Chemical Reagent |
Recommendations:
- Increase Sample Size: Power calculations strongly suggest that large sample sizes (in the thousands) are often needed to detect moderate effect sizes robustly [9].
- Utilize Serial Measurements: If feasible, collect multiple samples per individual to better estimate and account for within-individual variability.
- Focus on High-Reliability Lipids: Prioritize lipid species with a higher technical intraclass correlation coefficient (ICC), as these provide more reliable measurements [9].
Issue 3: Creating Non-FAIR (Irreproducible) Data Analysis Scripts
Problem: Custom R/Python scripts are disorganized, lack documentation, and use hard-coded paths, making it impossible for others (or yourself in the future) to reproduce the results.
Solution: Adopt a reproducible research workflow.
- Use Version Control: Initialize a Git repository for your analysis project and commit code changes frequently.
- Structure Your Project: Use a standard project structure (e.g., separate folders for
data/raw,data/processed,scripts,output/figures). - Leverage Dynamic Reporting: Use RMarkdown (R) or Jupyter Notebooks (Python) to interweave code, results, and textual explanations. This ensures the connection between the data, analysis, and output is transparent.
- Document Dependencies: Use tools like
renv(R) orvirtualenv/conda(Python) to record the specific versions of packages used, ensuring the analysis environment can be recreated.
Prevention:
- Follow the modular and documented R/Python workflows provided in the
GitBookthat accompanies the "Best Practices and Tools" guideline [52] [1]. This resource is designed specifically to promote transparent and reusable analysis in lipidomics.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table: Key Reagents for Robust Quantitative Lipidomics
| Item | Function in Lipidomics Workflow |
|---|---|
| NIST SRM 1950 (Standard Reference Material) | A standardized human plasma sample used as a quality control (QC) to monitor instrument performance, correct for batch effects, and assess inter-laboratory reproducibility [3] [1]. |
| Stable Isotope-Labeled Internal Standards | Deuterated or otherwise isotopically labeled lipid standards added to each sample during extraction to correct for losses during preparation, matrix effects, and instrument response variability, enabling accurate quantification [3]. |
| Blinded Replicate QC Samples | Aliquots from a pooled sample placed randomly in the analysis sequence as unknowns. Used to precisely quantify the technical variance of the entire measurement process [9]. |
| Specialized Sample Collection Tubes | Tubes designed to prevent lipid oxidation or degradation during blood sample collection and storage, preserving the integrity of the lipidome from the moment of sampling [2]. |
Experimental Protocol: Quantifying Biological vs. Technical Variability
This protocol is designed to systematically assess the different sources of variability in a lipidomics study, which is a prerequisite for designing sufficiently powered experiments.
Objective: To decompose the total variance of each lipid species into its between-individual, within-individual, and technical components.
Materials and Samples:
- Serial Blood Samples: Collected from each participant in a cohort at multiple time points (e.g., baseline, 1 year, 5 years) [9].
- Blinded Replicate QC Samples: Multiple aliquots from a pooled serum sample [9].
- Stable Isotope Internal Standards for quantification [3].
Methodology:
- Sample Preparation and Analysis:
- Data Processing:
- Process raw files using a targeted or untargeted lipidomics platform.
- Apply a predefined filter to remove lipid species with >50% missing values. For lipids with 1-50% missing values, impute with the lowest observed concentration (for MNAR) [9].
- Log-transform the concentration data for each of the remaining lipid species.
- Variance Component Analysis:
- For each lipid species, use a linear mixed model to decompose the total variance (( \sigma^2_{Total} )) as follows:
- ( \sigma^2_{Total} = \sigma^2_{Between} + \sigma^2_{Within} + \sigma^2_{Technical} )
- ( \sigma^2_{Between} ): Variance of the "usual" lipid level among different subjects.
- ( \sigma^2_{Within} ): Variance over time within the same individual.
- ( \sigma^2_{Technical} ): Variance introduced by the laboratory measurement process (estimated from the blinded replicate QCs) [9].
- For each lipid species, use a linear mixed model to decompose the total variance (( \sigma^2_{Total} )) as follows:
- Calculation of Key Metrics:
- Calculate the Technical Intraclass Correlation Coefficient (ICC~Tech~) for each lipid: ( ICC_{Tech} = \sigma^2_{Between} / (\sigma^2_{Between} + \sigma^2_{Within} + \sigma^2_{Technical}) ). A higher ICC~Tech~ indicates better measurement reliability [9].
- Use the variance components to perform power calculations for future case-control studies, as illustrated in the troubleshooting guide above.
Quantifying Lipidomics Variability
Workflow Visualization: FAIR-Compliant Data Analysis
The following diagram outlines the logical workflow for a FAIR-compliant lipidomics data analysis, integrating the tools and principles discussed.
FAIR Lipidomics Analysis Workflow
Best Practices for Batch Effect Correction, Normalization, and Missing Value Imputation
Frequently Asked Questions
Q1: What are the most effective methods for correcting batch effects in large-scale lipidomics studies? The optimal method can depend on your experimental design. For studies where biological groups are completely confounded with batch (e.g., all controls in one batch, all cases in another), ratio-based scaling using a common reference material is highly effective. This method scales the absolute feature values of study samples relative to those of a reference material profiled in each batch [53]. For other scenarios, machine learning approaches like SERRF (Systematic Error Removal using Random Forest), which uses quality control (QC) samples, have been shown to outperform many traditional methods by modeling nonlinear drifts and correlations between compounds [54] [52].
Q2: My data has many missing values. Should I impute them, and if so, which method should I use? Yes, imputation is generally recommended, but the choice of method should be guided by the nature of the missingness [1].
- For values Missing Not at Random (MNAR), often caused by abundances falling below the detection limit, half-minimum (hm) imputation (replacing with a percentage of the lowest detected value) or Quantile Regression Imputation of Left-Censored data (QRILC) are considered optimal [1] [55].
- For values Missing Completely at Random (MCAR) or at Random (MAR), k-Nearest Neighbors (kNN) and Random Forest (RF) imputation are consistently strong performers [1] [55]. Tools like ImpLiMet can help you systematically select the best imputation method for your specific dataset [56].
Q3: How can I visually assess if my batch correction was successful? Use unsupervised clustering methods like PCA (Principal Component Analysis) or t-SNE (t-distributed Stochastic Neighbor Embedding).
- Before correction: Samples typically cluster primarily by their batch identifier.
- After successful correction: Samples should cluster by their biological group, and the distinct clusters by batch should be diminished [53] [57]. Quantitative metrics like the Average Silhouette Width (ASW) or kBET (k-nearest neighbour Batch Effect Test) can provide a numerical assessment of the correction's success [57].
Q4: Can batch correction accidentally remove true biological signal? Yes, this is a significant risk, particularly if the study design is confounded (when batch and biological group are perfectly mixed) and an inappropriate correction method is used [53]. Some methods, like SERRF, have also been observed in some cases to inadvertently mask treatment-related variance [58]. It is crucial to validate the results of any batch correction using both visual and quantitative methods to ensure biological variation is preserved.
Q5: How do I choose between the many normalization methods available? The best method can vary by data type. Recent evaluations in multi-omics temporal studies identified Probabilistic Quotient Normalization (PQN) and LOESS regression on QC samples (LoessQC) as top performers for metabolomics and lipidomics data. For proteomics data, PQN, Median normalization, and LOESS were found to be effective [58]. The key is to avoid applying normalization automatically; the choice should be informed by the data's properties and the biological question [52].
Troubleshooting Guides
Issue 1: Poor Separation of Biological Groups After Batch Correction Problem: After applying batch correction, your samples still do not cluster well by the biological condition of interest in a PCA plot. Solutions:
- Re-evaluate Method Choice: Your chosen method might be over-correcting or be unsuitable for your study design. Try a different algorithm. Ratio-based methods are robust in confounded designs [53].
- Check for Confounding: If your batch and biological group are perfectly mixed, most standard correction methods will fail. If possible, redesign the experiment to include biological groups in each batch. If not, a reference-material-based ratio method is strongly advised [53].
- Inspect Preprocessing: Ensure that prior steps like peak picking and alignment were performed correctly. Batch effects should be addressed as early as possible in the preprocessing stage [59].
Issue 2: Introducing Bias During Missing Value Imputation Problem: After imputation, the statistical analysis reveals many false positives or the data structure appears distorted. Solutions:
- Investigate Cause of Missingness: Apply different imputation methods to features suspected of being MNAR (e.g., low-abundance lipids) versus MCAR/MAR. Using a single method for all missing values can introduce bias [1].
- Use Structured Tools: Implement a tool like ImpLiMet, which runs a grid search across multiple imputation methods and missingness patterns to recommend the optimal solution for your dataset [56].
- Filter High-MV Features: Prior to imputation, filter out lipids or metabolites with a very high percentage (e.g., >35%) of missing values, as these cannot be reliably imputed [1].
Issue 3: Inconsistent Results After Normalization Problem: Normalization leads to high technical variance or does not improve the consistency of Quality Control (QC) samples. Solutions:
- Leverage QC Samples: Use machine learning-driven normalization methods like SERRF, which are specifically designed to use the profiles of pooled QC samples to model and remove complex, nonlinear technical variations across a run sequence [54].
- Align Method with Data Type: Apply the normalization methods that have been benchmarked as best for your specific omics data type (e.g., PQN for metabolomics/lipidomics) [58].
- Validate with Metrics: Assess the improvement by calculating the Relative Standard Deviation (RSD) of your QC samples before and after normalization. A successful normalization will significantly reduce the RSD of these samples [60].
Method Comparison Tables
Table 1: Comparison of Batch Effect Correction Algorithms (BECAs)
| Method | Principle | Best For | Strengths | Limitations |
|---|---|---|---|---|
| Ratio-Based (e.g., Ratio-G) | Scales data using a common reference sample analyzed in each batch [53]. | Confounded study designs; multi-omics integration [53]. | Handles severe confounding; conceptually simple [53]. | Requires analysis of reference material in every batch [53]. |
| SERRF | Machine learning (Random Forest) using QC samples to model systematic error [54]. | Large-scale studies; complex, nonlinear technical drifts [54]. | Models correlations between compounds; handles p >> n data; robust to outliers [54]. |
Risk of over-correction or masking biological variance in some cases [58]. |
| ComBat | Empirical Bayes framework to adjust for known batch effects [57]. | Balanced designs with known batch labels [57]. | Widely used and simple to apply [57]. | Assumes linear effects; poor performance with confounded designs [53]. |
| LOESS on QCs | Local regression on QC data to model and correct intensity drift [58]. | Instrumental drift over time [58]. | Effective for gradual temporal drift [58]. | Less effective for sudden batch-to-batch jumps [54]. |
Table 2: Comparison of Missing Value Imputation Methods
| Method | Mechanism | Best for Missingness Type | Performance Notes |
|---|---|---|---|
| k-Nearest Neighbors (kNN) | Imputes based on average from k most similar samples [1] [55]. |
MCAR, MAR [1] | Robust performer; recommended in multiple reviews [1] [55]. |
| Random Forest (RF) | Machine learning model predicting missing values using other features [1] [55]. | MCAR, MAR [1] | Often outperforms kNN; handles complex feature interactions [1] [55]. |
| Half-Minimum (hm) | Replaces missing values with a fixed value (e.g., 1/2 minimum) for each feature [55]. | MNAR [1] [55] | Simple and effective for values below detection limit [1] [55]. |
| Quantile Regression (QRILC) | Imputes based on quantile regression assuming a Gaussian distribution [1]. | MNAR [1] | Good for left-censored data (below detection limit) [1]. |
Experimental Workflows and Decision Pathways
Diagram 1: A comprehensive workflow for processing lipidomics data, integrating decisions for batch effect correction and missing value imputation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Robust Lipidomics
| Item | Function | Application in Troubleshooting |
|---|---|---|
| Pooled Quality Control (QC) Sample | A pool of all study samples analyzed repeatedly throughout the batch run [54]. | Essential for monitoring technical variance, normalizing with SERRF/LOESS, and assessing correction quality [54] [52]. |
| Reference Materials (e.g., NIST SRM 1950) | Commercially available standardized reference material from an authoritative source (e.g., National Institute of Standards and Technology) [1]. | Used for inter-laboratory comparison, normalization, and as a common denominator in ratio-based batch correction [1] [52]. |
| Internal Standards (IS) | Stable isotope-labeled lipid analogs added to every sample during extraction [1]. | Corrects for variation in sample preparation, extraction efficiency, and matrix effects; used in IS-based normalization [1]. |
| Extraction Quality Controls (EQCs) | Control samples used to monitor variability introduced during the sample preparation and extraction process [60]. | Helps distinguish variability from extraction versus analysis, allowing for more targeted troubleshooting and batch correction [60]. |
| Blank Samples | Solvent-only samples processed alongside biological samples [1]. | Identifies background contamination and instrumental carry-over, which can be a source of noise and missing values [1]. |
Frequently Asked Questions (FAQs)
Q1: What are the key visualization tools for interpreting lipidomics data in a biological context? Several advanced tools facilitate the biological interpretation of complex lipidomics data. LipidSig 2.0 is a comprehensive web-based platform that provides a full workflow, from data preprocessing to differential expression, enrichment, and network analysis. It automatically assigns 29 distinct lipid characteristics, such as fatty acid chain properties and cellular localization, to help link data to biological context [61]. For a more structural perspective, Lipidome Projector uses a shallow neural network to embed lipid structures into a 2D or 3D vector space, allowing researchers to visualize entire lipidomes as scatterplots where structurally similar lipids are positioned near each other. This enables exploratory analysis and quantitative comparison based on lipid structures [62].
Q2: Why are all the data points on my volcano plot grey, and why is the legend incorrect?
This issue, often encountered in tools like nf-core/differentialabundance, typically arises from a problem in the data annotation step. The most common cause is a mismatch between the data and the gene annotation file (GTF). The pipeline may fail to correctly map the differential expression status (e.g., "UP," "DOWN," "NO") to the data points if the expected identifier column (e.g., "gene_name") is not present or correctly specified in your input file [63]. To troubleshoot, verify that the column names in your dataset match the feature name columns specified by the software's parameters (e.g., --features_name_col).
Q3: How can I use standard reference materials for quality control in lipid quantitation? LipidQC is a specialized tool designed for this purpose. It provides a semi-automated process to visually compare your experimental concentration measurements (nmol/mL) of lipid species from NIST Standard Reference Material (SRM) 1950 against benchmark consensus mean concentrations and their uncertainties. These benchmarks are derived from the NIST Lipidomics Interlaboratory Comparison Exercise, which aggregated data from 31 different laboratories. This comparison allows you to assess the accuracy and harmonize the results of your lipidomics workflow against a community standard [64].
Q4: My lipidomics software offers only basic statistics. How can I perform more sophisticated analyses? Many dedicated lipidomics software packages, such as LipidSearch, focus on identification and basic relative quantitation, providing only fundamental statistics like mean, standard deviation, and p-values. The standard procedure for advanced statistical analysis and custom visualization is to export the results table. The data, typically in a format like Microsoft Excel, can then be imported into specialized statistical programming environments (e.g., R or Python) for sophisticated downstream analysis, including the creation of custom volcano plots, PCA, and complex statistical modeling [42].
Troubleshooting Guides
Troubleshooting Volcano Plot Annotations
Problem: A volcano plot renders with all data points in grey, a legend showing "unselected rows," and no hover labels, even though a static PNG version appears correct.
Diagnosis: This is a data annotation issue, not a visual rendering problem. The interactive plot cannot associate the correct "Differential Status" (upregulated, downregulated, non-significant) with the data points.
Solution:
- Step 1: Verify your input data file contains a column that clearly indicates the differential expression status for each feature (e.g., a column named "diffexpressed" with values "UP", "DOWN", "NO").
- Step 2: Ensure the software is correctly instructed on which column to use for this information. This may require checking and specifying command-line parameters like
--differential_feature_name_column[63]. - Step 3: Confirm that the annotation file (e.g., GTF file) used by the pipeline is compatible with your dataset and contains the necessary feature identifiers.
Troubleshooting Lipid Scatter Plots in Vector Space
Problem: A lipidome scatterplot in a tool like Lipidome Projector shows unexpected clustering or does not separate lipid classes effectively.
Diagnosis: The issue could lie in the input data parsing or the constraints applied to handle structural ambiguity.
Solution:
- Step 1: Check Lipid Name Parsing. The tool uses Goslin to parse lipid names. Ensure your lipid nomenclature is standardized and recognized by Goslin. Parsing failures can lead to lipids being excluded or incorrectly mapped [62].
- Step 2: Review Constraints File. Mass spectrometry often identifies lipids at a summary level (e.g., "PC 36:2"), which can correspond to multiple structural isomers. Lipidome Projector uses a constraints file (listing allowed fatty acyls and long-chain bases for your organism) to filter implausible isomers. An incomplete or incorrect constraints file can result in a non-representative average vector for the lipid, distorting its position on the plot [62].
- Step 3: Validate Data Integrity. Check for and handle any missing values or extreme outliers in your abundance data that could skew the visualization.
Experimental Protocols
Protocol: Using LipidQC for Method Validation
This protocol allows you to benchmark your lipidomics workflow against community-derived reference values [64].
1. Principle: LipidQC performs a visual comparison of experimentally determined lipid concentrations in NIST SRM 1950 against consensus mean concentrations established by the NIST Lipidomics Interlaboratory Comparison Exercise.
2. Materials and Reagents:
- NIST SRM 1950 "Metabolites in Frozen Human Plasma"
- Your standard lipid extraction kit or reagents (e.g., Bligh-Dyer reagents)
- LipidQC software (downloadable)
- LC-MS/MS or DI-MS instrument platform
3. Procedure:
- Step 1: Sample Preparation. Extract lipids from a defined volume of NIST SRM 1950 (e.g., 25-30 µL of plasma) using your established method (e.g., Bligh-Dyer extraction).
- Step 2: Data Acquisition. Analyze the lipid extract using your standard MS platform and acquisition method (either LC-MS or direct infusion).
- Step 3: Data Processing. Process the raw data with your usual software to obtain a table of lipid species and their calculated concentrations in nmol/mL.
- Step 4: Data Input into LipidQC. Format your concentration data according to LipidQC requirements. The software supports various nomenclature styles (sum composition, fatty acid position level).
- Step 5: Visualization and Analysis. Run LipidQC to generate plots comparing your measured values against the NIST consensus means. The tool will automatically sum isomeric species for appropriate comparison.
4. Data Interpretation: Examine the generated plots for systematic biases. Consistent over- or under-estimation across multiple lipid classes may indicate a need to optimize your extraction efficiency, instrument calibration, or response factors.
Protocol: Creating a Custom Volcano Plot in R
This protocol provides a step-by-step method for generating a publication-quality volcano plot from differential lipid expression results [65].
1. Materials and Software:
- R and RStudio
- R packages:
tidyverse(includesggplot2,dplyr),ggrepel,RColorBrewer - Input data: A CSV file with columns for lipid identifier, p-value, and log2 fold change.
2. Procedure:
- Step 1: Set Up Script and Load Data.
- Step 2: Define Differential Expression Status.
- Step 3: Create a Basic Volcano Plot with Thresholds.
- Step 4: Customize and Annotate.
- Step 5: Export the Plot.
Lipidomics Quality Control Workflow
The following diagram illustrates the integrated workflow for using advanced visualizations in lipidomics QC, from raw data to biological insight.
LipidQC Validation Protocol
This diagram details the specific steps for the LipidQC method validation protocol.
Research Reagent Solutions
Table 1: Essential Reagents and Software for Lipidomics QC and Visualization
| Item Name | Function / Purpose | Key Details / Application Notes |
|---|---|---|
| NIST SRM 1950 | Matrix-matched quality control material for harmonizing lipid quantitation across platforms and laboratories. | Frozen human plasma; provides community consensus mean concentrations for hundreds of lipid species for method benchmarking [64]. |
| LipidSig 2.0 | Web-based platform for comprehensive lipidomic analysis and characteristic insight integration. | Automatically assigns 29 lipid characteristics; performs differential expression, enrichment, and network analysis [61]. |
| Lipidome Projector | Web-based software for visualizing lipidomes as 2D/3D scatterplots based on structural similarity. | Uses a pre-computed lipid vector space; allows interactive exploration of lipid abundance and structure [62]. |
| Goslin Parser | A grammar for standardizing lipid nomenclature across different databases and software tools. | Critical for ensuring accurate lipid name recognition and matching in tools like LipidSig and Lipidome Projector [61] [62]. |
| LipidQC | Software for visual comparison of experimental lipid concentrations against NIST consensus benchmarks. | A semi-automated tool for method validation; supports data from various LC-MS and direct infusion platforms [64]. |
| R/tidyverse & ggrepel | Open-source programming environment and packages for custom statistical analysis and visualization. | Used for creating customized plots (e.g., volcano plots) and performing analyses beyond built-in software functions [65]. |
Machine Learning for Anomaly Detection and Drift Correction in Large Datasets
Core Concepts: Anomalies, Drift, and Lipidomics
This section answers fundamental questions about the key concepts and their specific relevance to your lipidomics research.
What is an anomaly in the context of data analysis?
An anomaly is a data pattern that does not conform to expected, normal behavior. In machine learning (ML), anomalies are broadly categorized into three types [66] [67]:
- Point Anomalies: A single, unusual data instance. Example: A sudden, inexplicable spike in the intensity of a specific lipid species in a single sample.
- Contextual Anomalies: A data point that is anomalous only in a specific context. Example: A low concentration of a particular lipid might be normal in one tissue type but anomalous in another.
- Collective Anomalies: A collection of related data points that, as a group, are anomalous, even if individual points are not. Example: A subtle but consistent shift in the ratios of multiple lipids within a pathway across several samples.
How does "drift" relate to anomalies and data quality?
Drift, or concept drift, refers to a change in the underlying statistical properties of the data over time. In lipidomics, this can manifest as batch effects or shifts introduced by instrumental drift, reagent lots, or subtle changes in sample preparation protocols [68] [69]. While not always an anomaly itself, uncorrected drift can:
- Create artificial patterns that obscure true biological signals.
- Be misinterpreted as a biological discovery, leading to false positives.
- Reduce the power of ML models to detect true anomalies and biomarkers. Correcting for drift is therefore a critical pre-processing step to ensure data integrity.
Why are these concepts critical in lipidomic studies?
Lipidomics data is particularly susceptible to technical variability, which can confound the detection of true biological signals [69] [70].
- Biological Variability: High inherent biological variability in human studies can mask disease-specific lipid signatures [68].
- Technical Variability: "Latent variables" such as genetics, sample preparation, and tissue heterogeneity contribute to a lack of agreement across studies, hampering reproducibility and meta-analysis [68].
- Biomarker Discovery: Without proper correction for these sources of variation, ML models may learn technical artifacts instead of genuine biological patterns, resulting in biomarkers that fail to validate in independent cohorts [71] [70].
Troubleshooting ML Workflows
This section provides solutions to common problems encountered when implementing ML for anomaly and drift detection.
How do I handle a high rate of false positives from my anomaly detection model?
A high false positive rate often stems from a poorly defined "normal" baseline or low-quality data [67].
- Solution 1: Refine Your Baseline: Re-examine your definition of "normal" to ensure it accounts for all known biological and technical contexts (e.g., time of day, diet, sample batch). Incorporate these contexts into a contextual anomaly detection model [66] [67].
- Solution 2: Improve Data Quality: Ensure the data used for training is clean and representative. Focus on monitoring data streams with the highest impact on core research metrics [67].
- Solution 3: Tune Alert Thresholds: Set clear, meaningful alert thresholds that trigger specific actions. Implement feedback loops where experts validate anomalies to fine-tune the detection logic over time [67].
My model performance degraded on new data. What should I do?
This is a classic sign of model drift, where the relationships the model learned are no longer valid, or data drift, where the input data's statistical properties have changed [72].
- Solution 1: Monitor for Drift: Continuously monitor model performance and input data for signs of drift. Implement systems to detect when data distributions shift from the training set [67] [72].
- Solution 2: Retrain the Model: ML models are not "set-and-forget." They require periodic retraining on new, representative data to adapt to changing patterns. This is a core component of a continuous learning framework [73] [67].
- Solution 3: Review Data Pipelines: Investigate if changes in sample collection, instrumentation, or reagents have introduced new technical variability that needs to be corrected [69].
The "black box" nature of my model is a concern for scientific review. How can I add transparency?
The lack of transparency in complex ML models can erode trust and hinder clinical or scientific adoption [72].
- Solution: Implement Explainable AI (XAI): Invest in and use XAI techniques to improve the interpretability of your models. This allows you and reviewers to understand which features (e.g., specific lipid ions) the model is using to make a decision, which is crucial for biological validation and regulatory compliance [72].
Experimental Protocols & Methodologies
This section provides detailed workflows for key experiments and analyses.
Protocol: Surrogate Variable Analysis (SVA) for Drift Correction
This protocol is designed to automatically estimate and correct for unmeasured technical confounders (e.g., sample processing date, operator) and biological latent variables (e.g., cell type composition) in your dataset [68].
Principle: SVA estimates "surrogate variables" (SVs) from the data's correlation structure. These SVs represent the space spanned by unmeasured latent variables. By including them as covariates in downstream models, their effect can be removed, improving inter-study agreement and biomarker reproducibility [68].
Workflow:
- Input: A normalized, pre-processed data matrix (e.g., lipid peak intensities) with samples as columns and features as rows.
- Software: Implementable in R. The
svapackage is a standard tool [74]. - Estimation: Use the
svaseq()function (for count data) orsva()function to estimate the surrogate variables. The number of SVs can be determined empirically or based on the data structure. - Correction: Include the estimated SVs as covariates in your differential expression or biomarker discovery model (e.g., in a linear model with
limma). - Output: A corrected dataset where the influence of the latent variables has been statistically accounted for.
Protocol: Untargeted Lipidomics for Biomarker Discovery with ML
This protocol outlines a multi-omic ML approach for robust biomarker discovery, as demonstrated in ovarian cancer research [71].
Objective: To identify a proof-of-concept multi-omic model (lipids + proteins) for distinguishing early-stage disease from controls within a clinically complex, symptomatic population [71].
Workflow:
- Cohort Design: Assemble two independent cohorts designed to reflect the target population (e.g., including cancer, benign conditions, and healthy controls) [71].
- Data Acquisition:
- Data Pre-processing: Process raw LC-MS spectra for peak picking, alignment, and annotation. Normalize and scale the data [74].
- Feature Selection: Identify significantly altered lipid and protein features across cohorts.
- ML Modeling:
- Evaluation: Assess model performance using Area Under the Curve (AUC) and other classification metrics.
The logical flow of this experimental design is summarized in the diagram below.
Multi-omic Biomarker Discovery Workflow
The Scientist's Toolkit
This section details essential reagents, software, and algorithms used in the featured experiments and the broader field.
Research Reagent Solutions
| Item | Function/Description | Example from Literature |
|---|---|---|
| Commercial Plasma | Serves as a long-term reference or Surrogate Quality Control (sQC) to monitor and correct for analytical variation across batches in targeted lipidomics [69]. | Used as a pooled quality control (PQC) sample to evaluate analytical performance in lipidomics [69]. |
| Frozen Serum Samples | The primary biospecimen for discovering circulating lipid biomarkers. Sourced from clinically annotated biobanks [71]. | Used from biobanks (e.g., University of Colorado Gynecologic Tissue and Fluid Bank) to profile lipid alterations in ovarian cancer [71]. |
| Internal Standards | Isotopically labeled lipid analogs added to samples to correct for variability in sample preparation and instrument response during MS analysis. | Critical for quantification in targeted lipidomics using UHPLC-MS/MS [69]. |
Key Machine Learning Algorithms & Tools
| Algorithm/Tool | Use-Case | Key Reference / Performance |
|---|---|---|
| XGBoost | A powerful gradient-boosting classifier for structured/tabular data. | Achieved 0.99 accuracy and perfect detection (1.00) of normal traffic and drift in a wireless network DT study, outperforming other models [75]. |
| Random Forest | An ensemble learning method for classification and regression. | Achieved high accuracy (0.98) in anomaly detection, second only to XGBoost in a comparative study [75]. |
| Surrogate Variable Analysis (SVA) | A statistical method for correcting unknown and known batch effects and latent confounders. | Demonstrated to improve agreement across multiple sclerosis and Parkinson's disease microarray studies, facilitating biomarker discovery [68]. |
| MetaboAnalystR | An R package for comprehensive metabolomics data analysis, from raw spectral processing to functional interpretation. | Provides an auto-optimized LC-MS spectral processing workflow and functional analysis modules [74]. |
| Explainable AI (XAI) | A suite of techniques to interpret and explain the output of ML models. | Recommended solution to the "black box" problem, critical for building trust and meeting regulatory standards in healthcare and science [72]. |
FAQs: Addressing Common Challenges
What are the first signs that my dataset might need drift correction?
Early signs include:
- Poor Inter-Study Concordance: Your top biomarkers from one cohort or batch do not replicate in another, despite addressing the same biological question [68].
- Batch Clustering in PCA: Principal Component Analysis shows strong clustering of samples by processing date or batch, rather than by the biological groups of interest.
- Deteriorating Model Performance: An ML model that was previously accurate begins to perform poorly on new, incoming data [67] [72].
I have a limited sample size. How can I improve my ML model's robustness?
- Leverage Public Data: Use public compendia of data to pre-train models or to validate findings, applying correction methods like SVA to improve agreement [68].
- Multi-Omic Integration: Combining multiple data types (e.g., lipids with proteins) can provide a more robust signal, as demonstrated in ovarian cancer detection, improving performance even with limited samples [71].
- Simple Models: Start with simpler, more interpretable models (e.g., Regularized Logistic Regression) which can perform well and are less prone to overfitting with smaller sample sizes.
How do I choose between rule-based, statistical, and ML-based anomaly detection?
The choice depends on your data environment [67]:
- Rule-Based Systems: Best for predictable, well-understood problems with simple thresholds (e.g., "alert if pressure > X"). They don't scale well for complex, dynamic data [67].
- Statistical Methods: Useful for stable, structured datasets with consistent trends (e.g., Z-scores). They struggle with seasonality and multiple correlated variables [67].
- Machine Learning Models: Ideal for large-scale, dynamic systems where "normal" is complex and multi-dimensional (e.g., sensor data from a bioreactor, LC-MS drift patterns). They adapt to changing patterns and detect subtle contextual anomalies [66] [67].
Developing a Lipid Re-programming Score (LRS) for Clinical Risk Stratification
Frequently Asked Questions (FAQs)
Q1: What is a Lipid Re-programming Score (LRS), and what is its primary clinical utility? A Lipid Re-programming Score (LRS) is a quantitative risk assessment tool derived from mass spectrometry-based lipidomic profiling. It uses machine learning to integrate the levels of multiple lipid species into a single score that predicts an individual's disease risk. Its primary clinical utility lies in enhancing risk stratification, particularly for individuals falling into the "intermediate-risk" category where traditional clinical tools are often indecisive. For example, one study demonstrated that an LRS significantly improved the prediction of cardiovascular events over the traditional Framingham Risk Score, with a net reclassification improvement of 0.36, allowing for better triage of patients for further interventions like coronary artery calcium scoring [76].
Q2: My lipidomic data shows high variability across sample batches. What are the major sources of this variability? The total variability in lipidomic measurements can be decomposed into three main components [9]:
- Between-individual variance (( \sigma^2_B )): Represents the true, stable biological differences in "usual" lipid levels among subjects in a population.
- Within-individual variance (( \sigma^2_W )): Arises from temporal fluctuations within an individual due to factors like diet, circadian rhythm, and recent meals.
- Technical variance (( \sigma^2_T )): Introduced by laboratory procedures, including sample collection, storage, processing, and instrumental analysis. For a majority (74%) of lipid species, the combination of technical and within-individual variance accounts for most of the total variability. Therefore, a single measurement may not reliably represent an individual's long-term lipid level, potentially attenuating observed associations with clinical outcomes [9].
Q3: How does biological individuality impact LRS development, and how can this be addressed? Lipidomes exhibit high individuality and sex specificity. Studies show that biological variability per lipid species is significantly higher than batch-to-batch analytical variability, and within-subject variance can sometimes be substantial [3] [77]. One study found that for some phospholipids, within-subject variance was up to 1.3-fold higher than between-subject variance over a single day with meal intake [77]. This high individuality is a key prerequisite for using lipidomics for personalized metabolic health monitoring but must be accounted for in study design by ensuring consistent sample collection times and considering sex as a biological variable [3].
Q4: What is the recommended sample size for a lipidomic epidemiological study aiming to develop an LRS? The required sample size depends on the expected effect size and the number of lipid species tested. One power analysis indicated that to detect a true relative risk of 3.0 (comparing upper and lower quartiles) with a Bonferroni-corrected significance threshold of ( \alpha = 5.45 \times 10^{-5} ) (for 918 lipids), a study would need [9]:
- 500 total participants for 19% power
- 1,000 total participants for 57% power
- 5,000 total participants for 99% power This underscores that studies examining lipidomic-disease associations require large sample sizes to detect moderate effect sizes reliably.
Q5: Can I use direct infusion (infusion) for sample analysis in LRS development? While technically possible, it is not recommended for complex lipid mixtures. In direct infusion, several overlapping precursor ions may be co-isolated, resulting in mixed MS2 spectra. This leads to less accurate identification and typically a lower number of lipid species being confidently identified compared to LC-MS/MS methods. LipidSearch software itself advises against using infusion analysis for complex mixtures [42].
Troubleshooting Guides
Table 1: Common Lipidomic Experimental Issues and Solutions
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Sample Preparation & Analysis | Low number of lipids identified. | Sample type/volume insufficient, suboptimal extraction conditions, incorrect ion mode selection [42]. | Optimize sample input (e.g., use 80µL human plasma); validate extraction protocol; acquire data in both positive and negative ion modes. |
| High technical variability between batches. | Inconsistent sample processing, instrumental drift, lack of quality controls [9]. | Implement a semi-automated sample prep protocol; use a stable isotope dilution approach; analyze quality control samples (e.g., NIST plasma) in every batch [3]. | |
| Data Acquisition & Processing | Poor identification from direct infusion data. | Co-isolation of multiple precursor ions leading to mixed MS2 spectra [42]. | Switch to LC-MS/MS for superior separation and cleaner spectra. |
| Inconsistent lipid quantification, especially for TGs. | Varying response factors for TG species with different numbers of double bonds [42]. | Use lipid standards to model and apply an average response factor for correction [42]. | |
| Biological Interpretation | High within-subject variability obscures biological signal. | Natural circadian rhythms, recent meal intake, lifestyle factors [9] [77]. | Standardize sample collection times (e.g., always fasted); implement dietary standardization before sampling [77]. |
| LRS model fails to validate in an external cohort. | Overfitting during model development; cohort-specific biases (diet, ethnicity); unaccounted for batch effects. | Use rigorous cross-validation and penalized regression (e.g., LASSO/ridge); collect detailed patient metadata; harmonize protocols across study sites. |
Protocol: Estimating Biological and Technical Variability in Lipidomic Studies
To reliably develop an LRS, you must first quantify the different sources of variability in your lipidomic data. Here is a detailed protocol based on established methodologies [9].
Objective: To decompose the total variance of each lipid species into between-individual, within-individual, and technical components.
Materials:
- Samples: Serum or plasma samples from a minimum of 50-70 participants.
- Study Design: Each participant should provide serial blood samples (e.g., at baseline and a second sample 1-5 years later) to estimate within-individual variance.
- Quality Control (QC): Prepare blinded replicate QC samples from a pool of sera (e.g., 4-12 replicates per participant from a small subset) to estimate technical variance [9].
Experimental Workflow:
- Sample Collection and Storage: Collect non-fasting or standardized fasting blood samples. Process serum/plasma aliquots and store at -70°C or below in a single biorepository to minimize pre-analytical variance.
- Sample Analysis: Analyze all samples (including serial samples and blinded QCs) in randomized batches alongside the participant samples. The QCs should be placed at the beginning and end of each batch to monitor drift.
- Lipidomics Profiling: Use a quantitative LC-MS/MS platform. The example below used Metabolon's Complex Lipid Panel on a Sciex SelexION 5500 QTRAP platform, measuring 918 lipid species across 15 classes [9].
- Data Preprocessing: Exclude lipid species with >50% missing values. For lipids with 1-50% missingness, impute with the lowest observed concentration. Log-transform the data to stabilize variance.
Statistical Analysis: Using a linear mixed-effects model, the total variance (( \sigma^2_{Total} )) for each lipid is decomposed as: ( \sigma^2_{Total} = \sigma^2_B + \sigma^2_W + \sigma^2_T ) [9] Where:
- ( \sigma^2_B ) = Between-individual variance
- ( \sigma^2_W ) = Within-individual variance
- ( \sigma^2_T ) = Technical variance
Calculate the Technical Intraclass Correlation Coefficient (ICC~Tech~) as: ( ICC_{Tech} = \frac{\sigma^2_B}{\sigma^2_B + \sigma^2_W + \sigma^2_T} ) A high ICC~Tech~ indicates that most variability is due to true biological differences between individuals, which is ideal for association studies.
Protocol: Developing and Validating a Lipid Re-programming Score (LRS)
This protocol outlines the key steps for constructing a robust LRS, mirroring the successful approach used in cardiovascular risk prediction [76].
Objective: To create a machine-learning model that integrates lipid species into a single score for clinical risk stratification.
Materials:
- Cohort Data: A large, well-phenotyped cohort with lipidomic data and prospective clinical outcome data (e.g., AusDiab, n=10,339) [76].
- Validation Cohorts: At least one external cohort for validation (e.g., Busselton Health Study, n=4,492) [76].
Methodology:
- Cohort Partitioning: Split the primary cohort into a training set (e.g., ~60%) and a testing set (~40%).
- Feature Selection and Model Training: In the training set:
- Use ridge regression or LASSO Cox regression to select the most predictive lipid species and build the model, thereby reducing overfitting [76] [78].
- The final LRS is a linear combination of the selected lipid species, weighted by their regression coefficients.
- ( LRS = \sum_{i=1}^{n} \beta_i \cdot Exp_i )
- Where ( \beta_i ) is the coefficient and ( Exp_i ) is the expression level of each prognostic lipid [78].
- Model Validation:
- Internal Validation: Test the LRS on the held-out test set from the primary cohort.
- External Validation: Apply the exact same model (lipids and coefficients) to the independent validation cohort(s).
- Performance Benchmarking:
- Compare the LRS against established clinical risk scores (e.g., Framingham Risk Score) using discrimination metrics like the Area Under the Curve (AUC).
- Assess Net Reclassification Improvement (NRI) to determine how well the LRS correctly reclassifies individuals, especially those at intermediate risk, into higher or lower-risk categories [76].
Table 2: Key Lipid Classes and Species with High Biological Variance
This table summarizes lipid classes and species known to exhibit significant biological variability, which must be considered in LRS development [9] [77].
| Lipid Class | Example Species (or characteristics) | Key Variability Considerations | Association with Dynamic Processes |
|---|---|---|---|
| Phosphatidylethanolamines (PE) | PE (m/z 716, 714, 740, 742, 744) | Show consistent time-dependent increases post-meal; within-subject variance can be high [77]. | Dietary incorporation, circadian rhythms [77]. |
| Phosphatidylcholines (PC) | PC (m/z 520) | Some species show significant temporal variation; major membrane components [77]. | Membrane synthesis, lipoprotein metabolism. |
| Triacylglycerols (TAG) | Various (518 species measured) | High within-individual variability; composition is highly influenced by diet [9]. | Energy storage, postprandial metabolism. |
| Sphingomyelins (SM) | --- | Show prominent sex differences, with higher concentrations often found in females [3]. | Structural components of lipoproteins and membranes. |
| Ether-linked Phospholipids | --- | Show prominent sex differences, with higher concentrations often found in females [3]. | Cell signaling, antioxidant properties. |
Table 3: Performance Metrics of an LRS in Cardiovascular Risk Prediction
Data from a study developing an LRS to augment the Framingham Risk Score (FRS) for primary prevention of cardiovascular disease [76].
| Cohort | Sample Size | Primary Outcome | AUC (FRS alone) | AUC (FRS + LRS) | Net Reclassification Improvement (NRI) |
|---|---|---|---|---|---|
| AusDiab (Development) | 10,339 | CVD Events | Baseline | +0.114 (p<0.001) | 0.36 (95% CI: 0.21-0.51) |
| Busselton (Validation) | 4,492 | CVD Events | Baseline | +0.077 (p<0.001) | 0.33 (95% CI: 0.15-0.49) |
| BioHEART (Validation) | 994 | Coronary Artery Calcium | 0.74 | 0.76 (p<1.0×10â»âµ) | Not Reported |
Visualized Workflows and Pathways
Lipid Reprogramming Score Development Workflow
Lipid Metabolic Pathways in Disease Reprogramming
The Scientist's Toolkit: Key Reagents & Materials
Table 4: Essential Research Reagents for Robust LRS Development
| Reagent / Material | Function / Purpose | Technical Notes |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Enables absolute quantification of lipid species by correcting for instrumental and procedural variability [3]. | Use a comprehensive mix covering major lipid classes. Critical for achieving median between-batch reproducibility of <10% [3]. |
| Reference Material (e.g., NIST Plasma) | Serves as a long-term quality control to monitor batch-to-batch analytical variability and instrument performance [3]. | Analyze in every batch. The median %RSD for QC samples should be significantly lower than the biological variability. |
| Automated Sample Preparation System | Minimizes technical variance and improves throughput and reproducibility of lipid extraction [3]. | Platforms that support a butanol:methanol extraction method are widely used [9]. |
| LC-MS/MS System with High Resolution | Identifies and quantifies a wide panel of lipid species (e.g., 700+) across a wide dynamic range [3]. | The Sciex SelexION 5500 QTRAP or similar platforms are commonly employed for targeted and discovery lipidomics [9]. |
| Bioinformatics Software (e.g., LipidSearch) | Processes raw MS data to identify lipid species from MS2 spectra and perform relative quantification [42]. | For more sophisticated statistics, export data to R or Python environments [42]. |
Biomarker Validation and Comparative Analysis with Other Omics
Troubleshooting Guides
Lipid Identification and Reproducibility
Problem: Inconsistent lipid identification across different software platforms.
- Potential Cause: Different algorithms, lipid libraries, and alignment methodologies used by software platforms [43].
- Solution: Implement a multi-step verification process:
- Process data through multiple software platforms (e.g., MS DIAL, Lipostar) and compare outputs [43]
- Perform manual curation of spectra and lipid identifications [43]
- Utilize both positive and negative LC-MS modes for validation [43]
- Incorporate retention time data and machine learning approaches (e.g., Support Vector Machine regression) for outlier detection [43]
Problem: Low inter-laboratory reproducibility for lipidomic biomarkers.
- Potential Cause: Lack of standardized protocols and analytical variability between batches [21] [43].
- Solution:
Biological Variability and Clinical Translation
Problem: Accounting for biological variability in lipidomic studies.
- Potential Cause: High individuality and sex specificity of circulatory lipidome [3].
- Solution:
- Ensure sample sizes are sufficient to detect signals above biological variability [3]
- Stratify analyses by sex and other demographic factors [3]
- Collect multiple time points from the same individuals where possible [3]
- Demonstrate that biological variability significantly exceeds analytical variability [3]
Problem: Translating research findings to clinically applicable biomarkers.
- Potential Cause: Insufficient clinical validation and understanding of Context of Use (COU) [21] [79].
- Solution:
Frequently Asked Questions (FAQs)
Q: What are the key steps for validating a lipidomic biomarker? A: The validation process requires addressing pre-analytical, analytical, and post-analytical stages [21]:
- Pre-analytical: Standardize sample collection, handling, and storage protocols
- Analytical: Demonstrate assay precision, accuracy, and reproducibility across batches
- Clinical: Validate the biomarker's performance in relevant populations and settings
- Regulatory: Submit evidence to regulatory bodies like FDA with clear Context of Use [79]
Q: What is the typical reproducibility expected for lipidomic measurements? A: In well-controlled studies using quantitative LC-MS/MS approaches, median between-batch reproducibility of 8.5% can be achieved across 13 independent batches comprising over 1,000 samples [3]. However, software platform agreement can be much lower (14-36%), highlighting the need for manual curation [43].
Q: Can published literature alone qualify a biomarker with regulators? A: Published literature can support qualification, but additional analytical and clinical validation data are typically needed, depending on the proposed Context of Use [79].
Q: What are the most promising lipid classes for biomarker development? A: Phospholipids and sphingolipids (particularly ceramides) have emerged as significant for human health, with ceramide risk scores outperforming traditional cholesterol measurements in predicting cardiovascular events [2].
Q: How can we address the challenge of inter-laboratory variability? A: Key strategies include [21] [43]:
- Adopting Lipidomics Standards Initiative guidelines
- Using common reference materials across laboratories
- Implementing standardized data processing and curation protocols
- Conducting multi-center validation studies
Table 1: Software Reproducibility in Lipid Identification
| Comparison Metric | MS1 Data (%) | MS2 Data (%) | Analysis Conditions |
|---|---|---|---|
| Identification Agreement Between Platforms | 14.0 | 36.1 | Default settings, identical LC-MS spectra [43] |
| Post-processed Feature Agreement | ~40 | N/A | Inter-laboratory comparison [43] |
Table 2: Analytical Performance in Clinical Lipidomics
| Performance Metric | Result | Study Context |
|---|---|---|
| Between-batch Reproducibility | 8.5% (median) | 1,086 plasma samples, 13 batches [3] |
| Biological Variability | Significantly higher than analytical variability | Population study of 364 individuals [3] |
| Predictive Accuracy Improvement | 42% greater vs. genetic-based risk | Comprehensive Lipid Risk Assessment algorithm [2] |
Table 3: Lipid Biomarker Validation Success Factors
| Factor | Minimum Standard | Optimal Practice |
|---|---|---|
| Sample Size | Sufficient to detect above biological variability | Large-scale cohorts (n>1000) with multiple time points [3] |
| Analytical Precision | <15% between-batch variability | <10% with quality control materials [3] |
| Software Verification | Single platform with default settings | Multiple platforms with manual curation [43] |
| Clinical Validation | Single cohort retrospective | Multiple independent cohorts, prospective validation [21] |
Experimental Protocols
Targeted Lipidomics Workflow for Biomarker Validation
Targeted Lipidomics Workflow
Detailed Methodology from Clinical Study [80]:
Sample Preparation:
- Collect 400 μL of serum and add to 2 mL tube
- Add 1 mL of lipid extraction solution and internal standard mixture
- Vortex for 2 minutes, sonicate for 10 minutes in 4°C water bath
- Add 500 μL water, vortex for 1 minute
- Centrifuge at 15,000 rpm for 10 minutes
- Collect 500 μL supernatant and dry under nitrogen gas
- Reconstitute in 100 μL mobile phase B
LC-MS/MS Conditions:
- Platform: UPLC-MS/MS (Triple Quad 6500+)
- Columns: CSH C18 (2.6 μm; 2.1 × 100 mm) and Luna NH2 (3 μm; 2.0 × 100 mm)
- Ion Source Conditions:
- Positive mode: ISVF 5200 V, source temperature 350°C
- Negative mode: ISVF -4500 V, source temperature 350°C
- Data Acquisition: Multiple reaction monitoring (MRM)
Multi-omics Integration Protocol
Procedure for Integrating Lipidomics with Other Omics Data [21] [81]:
- Generate lipidomic profiles using LC-MS/MS as described above
- Collect genomic (DNA sequencing), transcriptomic (RNA sequencing), and proteomic (mass spectrometry) data from same samples
- Apply batch correction and normalization across all omics datasets
- Use multivariate statistical methods (PCA, PLS-DA) for initial data exploration [82]
- Implement machine learning frameworks for biomarker panel identification
- Validate integrated biomarkers in independent cohorts
Signaling Pathways and Regulatory Framework
Biomarker Validation Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for Lipid Biomarker Studies
| Reagent/Material | Function | Example Specification |
|---|---|---|
| Internal Standards | Quantification reference | Avanti EquiSPLASH LIPIDOMIX (deuterated lipids) [43] |
| Lipid Extraction Solvent | Lipid isolation | Methanol/chloroform (1:2 v/v) with 0.01% BHT [43] |
| LC Columns | Lipid separation | Kinetex C18 (2.6 μm, 2.1 × 100 mm) [80] |
| Mobile Phase Additives | Chromatography optimization | 10 mM ammonium formate + 0.1% formic acid [43] |
| Quality Control Materials | Batch monitoring | NIST plasma reference material [3] |
| Sample Collection Tubes | Sample integrity | Specialized tubes preventing lipid oxidation [2] |
Advanced Statistical Methods for Lipidomics
Multivariate Analysis Pipeline [82]:
- Data Preprocessing:
- Log2 transformation and median-centering
- Data filtering (e.g., signal present in ≥75% of samples)
- Normalization to internal standards
Exploratory Analysis:
- Principal Component Analysis (PCA) for data structure visualization
- Partial Least Squares Discriminant Analysis (PLS-DA) for group separation
Feature Selection:
- LASSO (Least Absolute Shrinkage and Selection Operator)
- Support Vector Machine Recursive Feature Elimination (SVM-RFE) [80]
Validation:
- Leave-one-out cross-validation
- Independent cohort testing
- Receiver Operating Characteristic (ROC) analysis
Machine Learning Integration:
- MS2Lipid: AI model with 97.4% accuracy in predicting lipid subclasses [21]
- Support Vector Machine regression for outlier detection in retention time data [43]
- Comprehensive Lipid Risk Assessment algorithms for clinical prediction [2]
For decades, genomics has dominated the precision medicine landscape, offering insights into genetic predispositions for various diseases. However, a fundamental shift is occurring in predictive healthcare. Lipidomics, the large-scale study of lipid molecules, is emerging as a powerful alternative that can reveal real-time physiological changes and disease processes years before clinical symptoms appear. This technical support center provides researchers and drug development professionals with essential methodologies and troubleshooting guidance for implementing lipidomic approaches in early disease prediction, with particular emphasis on addressing the critical challenge of biological variability in lipidomic studies.
Frequently Asked Questions (FAQs)
Q1: What is the core advantage of lipidomics over genomics for early disease prediction?
While genomics identifies static genetic predispositions, lipidomics captures dynamic, functional changes in metabolism that more directly reflect active disease processes. Lipid profiles can reveal physiological alterations 3-5 years earlier than genetic markers alone, providing a crucial window for intervention [2]. Lipids serve as both structural components and signaling molecules, with patterns that reflect current metabolic health, inflammation status, and disease progression more directly than genetic markers [2].
Q2: What are the two most impactful lipid classes for health monitoring?
Phospholipids and sphingolipids have emerged as particularly significant for human health assessment [2]:
- Phospholipids form the structural foundation of all cell membranes and determine cellular function. Their composition directly impacts how cells respond to hormones, neurotransmitters, and medications, with abnormalities preceding insulin resistance by up to five years [2].
- Sphingolipids, particularly ceramides, function as powerful signaling molecules that regulate inflammation, cell death, and metabolic processes. Elevated ceramide levels strongly predict cardiovascular events and correlate with insulin resistance, with ceramide risk scores now outperforming traditional cholesterol measurements in predicting heart attack risk [2].
Q3: How does biological variability impact lipidomic study design?
Biological variability presents a significant challenge in lipidomics research. Studies have shown that the combination of technical and within-individual variances accounts for most of the variability in 74% of lipid species [9]. This variability arises from both external factors (diet, medication, time of day) and internal factors (age, sex, circadian rhythm) [9]. For an average true relative risk of 3 with correction for multiple comparisons, studies require approximately 1,000 total participants to achieve 57% power, highlighting the need for larger sample sizes in lipidomic epidemiology [9].
Q4: What are the key methodological considerations for ensuring lipidomic data quality?
High-quality lipidomic studies require:
- Standardized sample collection protocols (fasting status, collection tubes that prevent oxidation)
- Use of stable isotope internal standards for quantification
- Incorporation of quality control materials like National Institute of Standards and Technology (NIST) reference plasma
- Batch-to-batch reproducibility monitoring (targeting <10% variability)
- Validation across multiple analytical platforms [83] [9] [3]
Comparative Performance Analysis: Lipidomics vs. Genomics
Table 1: Quantitative Comparison of Predictive Performance in Early Disease Detection
| Performance Metric | Lipidomics Approach | Genomics Approach | Clinical Implications |
|---|---|---|---|
| Prediction Timeline | 3-5 years earlier than genetic markers [2] | Limited to lifetime risk assessment | Critical window for preventive interventions |
| Cardiovascular Event Reduction | 37% reduction with lipid-based interventions (LIPID-HEART trial) [2] | 19% reduction with gene-based assessments [2] | Nearly double the preventive efficacy |
| Alzheimer's Progression | 28% slowing of cognitive decline with custom lipid supplements [2] | Limited success with genetic approaches [2] | First meaningful intervention for early-stage patients |
| Metabolic Syndrome Improvement | 43% greater improvement in insulin sensitivity [2] | Standard improvement based on genetic risk | More responsive to therapeutic modifications |
| Cost-Effectiveness (QALY) | ~$3,200 per quality-adjusted life year gained [2] | ~$12,700 per QALY gained [2] | 4x more cost-effective for healthcare systems |
Table 2: Variability Components in Lipidomic Measurements Across Major Lipid Classes
| Lipid Class | Between-Individual Variance (%) | Within-Individual Variance (%) | Technical Variance (%) | Interpretation for Study Design |
|---|---|---|---|---|
| Sphingomyelins (SM) | 65-75% [3] | 15-25% | 8-12% | High individuality enables smaller cohort sizes |
| Phosphatidylcholines (PC) | 55-70% | 20-30% | 8-12% | Good for cross-sectional analyses |
| Triacylglycerols (TAG) | 45-60% | 30-40% | 8-12% | Requires multiple measurements per subject |
| Diacylglycerols (DAG) | 50-65% | 25-35% | 8-12% | Moderate reliability for single measurements |
| Ceramides (CER) | 60-75% [3] | 15-25% | 8-12% | Excellent biomarker candidates due to high individuality |
Troubleshooting Guides
Issue 1: High Within-Subject Variability in Lipid Measurements
Problem: Lipid species show significant fluctuation within the same individual across timepoints, reducing statistical power.
Solution:
- Implement controlled pre-sampling conditions (12-hour fasting, consistent time of day) [9]
- Collect multiple serial samples per participant when possible
- Use standardized sampling tubes that prevent lipid oxidation [2]
- Consider within-individual variance when calculating statistical power
- Apply mol% normalization to account for total lipid concentration variations [9]
Validation Protocol:
- Collect baseline and 1-year follow-up samples from 10% of cohort
- Calculate intraclass correlation coefficients for key lipid species
- Exclude lipids with ICC <0.4 from single-timepoint analyses
- Adjust statistical models incorporating variance components
Issue 2: Inconsistent Results Across Analytical Platforms
Problem: Different laboratories report divergent lipidomic profiles from identical samples.
Solution:
- Adopt reference materials from NIST for inter-laboratory calibration [3]
- Implement the International Lipidomics Standards Initiative (2024) protocols [2]
- Use multiple reaction monitoring (MRM) modes for targeted quantification [9]
- Participate in ring trials with other laboratories to harmonize methods
- Report lipid species using LIPID MAPs classification and nomenclature [83]
Quality Control Workflow:
Diagram 1: Lipidomics quality control workflow
Issue 3: Low Statistical Power in Epidemiologic Studies
Problem: Inadequate sample size leads to inability to detect clinically relevant associations.
Solution:
- Conduct power analysis incorporating variance components before study initiation
- For case-control studies, aim for minimum 500 participants per group to detect moderate effects [9]
- Use Bonferroni correction for multiple comparisons (α = 0.05/number of lipids)
- Prioritize lipid species with higher between-individual variability for biomarker discovery [9]
- Collaborate with consortia to achieve sufficient sample sizes
Power Calculation Method:
- Estimate variance components from pilot data
- Calculate attenuation factors for each lipid species
- Determine minimum detectable relative risk for planned sample size
- Adjust for multiple testing using false discovery rate methods
Experimental Protocols
Protocol 1: Comprehensive Lipid Profiling for Biomarker Discovery
Objective: Quantify 700+ lipid species across multiple classes with high reproducibility.
Materials:
- Serum or plasma samples (fasting recommended)
- Automated butanol:methanol extraction system
- Deuterated internal standards for each lipid class
- LC-MS/MS system with SelexION 5500 QTRAP or equivalent
- HILIC (hydrophilic interaction liquid chromatography) column
Procedure:
- Sample Preparation:
- Add 50μL serum to 950μL butanol:methanol (1:1) containing internal standards
- Vortex for 10 seconds, incubate at 25°C for 10 minutes
- Centrifuge at 14,000g for 5 minutes
- Transfer supernatant to MS vials
LC-MS/MS Analysis:
- Column temperature: 45°C
- Mobile phase A: acetonitrile/water (95:5) with 10mM ammonium acetate
- Mobile phase B: acetonitrile/water (50:50) with 10mM ammonium acetate
- Gradient: 0-2min 0% B, 2-15min 0-40% B, 15-20min 40-100% B
- Flow rate: 0.4mL/min, injection volume: 5μL
Data Processing:
- Quantify lipids by peak area ratios to internal standards
- Perform background subtraction using process blanks
- Express concentrations as mol% of total lipid class
- Apply quality filters: CV < 20% in quality control samples
Troubleshooting:
- Poor peak resolution: Condition column with 50 injections of reference plasma
- Low signal: Check ionization source cleanliness, increase injection volume
- High background: Extend equilibration time, use higher purity solvents
Protocol 2: Longitudinal Lipid Variability Assessment
Objective: Characterize within-individual vs. between-individual variability.
Materials:
- Serial blood samples from same participants (1-5 year intervals)
- 72 blinded replicate quality control samples
- Automated liquid handling system for consistency
- Batch randomization software
Procedure:
- Sample Organization:
- Place serial samples from same participant consecutively in analysis queue
- Randomize quality control samples at beginning and end of each batch
- Include 5% reference samples across all batches
Variability Calculation:
- For each lipid, decompose total variance into: σ²Total = σ²Between + σ²Within + σ²Technical
- Calculate technical intraclass correlation coefficient: ICCTech = σ²Between/σ²Total
- Determine biological ICC: ICCBiological = σ²Between/(σ²Between + σ²Within)
Power Estimation:
- Use variance components to calculate attenuation factors
- Project sample sizes needed for 80% power at α = 5.45×10â»âµ (Bonferroni correction)
Research Reagent Solutions
Table 3: Essential Materials for Robust Lipidomics Research
| Reagent/Material | Function | Specifications | Quality Control Parameters |
|---|---|---|---|
| Deuterated Internal Standards | Quantification reference | Coverage of 15+ lipid classes | Isotopic purity >98%, concentration verified by GC-MS |
| NIST SRM 1950 | Inter-laboratory standardization | Certified reference plasma | Between-batch CV <10% for targeted lipids |
| Butanol:MeOH (1:1) | Lipid extraction | LC-MS grade, 0.22μm filtered | Peroxide-free, stored under nitrogen |
| HILIC Chromatography Column | Lipid separation | 2.1×100mm, 1.7μm particles | Peak symmetry 0.8-1.2 for lysophospholipids |
| Quality Control Pooled Plasma | Batch monitoring | 100+ donor pool, gender-balanced | Storage at -80°C, freeze-thaw cycles <3 |
| Automated Liquid Handler | Sample preparation | 96-well format capability | Volume accuracy ±1%, precision CV <3% |
Lipid Signaling Pathways in Disease Prediction
Diagram 2: Predictive lipid pathways in disease development
The integration of lipidomics into early disease prediction requires careful attention to biological variability, methodological standardization, and appropriate statistical approaches. By implementing the troubleshooting guides, experimental protocols, and quality control measures outlined in this technical support resource, researchers can leverage the superior predictive power of lipidomics while addressing its unique methodological challenges. The future of lipidomics in precision medicine will depend on continued refinement of standardized protocols, multi-omics integration, and large-scale validation studies to translate lipid biomarkers into clinically actionable tools.
Experimental Protocols for Lipid Biomarker Validation
Sample Collection and Preprocessing for Pediatric Studies
Patient Population Considerations:
- Age-Specific Protocols: For children under 5 years, diagnosis relies on clinical criteria as spirometry is not feasible. Include at least 3 documented episodes of bronchial obstruction with improvement following short-acting beta-agonists [84].
- Sample Collection: Collect morning fasting venous blood using heparin anticoagulant tubes. Centrifuge at 3,000 rpm for 10 minutes at 4°C. Aliquot plasma into cryopreservation tubes and store at -80°C to avoid freeze-thaw cycles [85].
- Ethical Compliance: Obtain written informed consent from all parents or guardians. Study protocols must be approved by the institutional bioethics committee in accordance with the Declaration of Helsinki [84].
Quality Control Procedures:
- Pooled QC Samples: Create quality control samples by pooling 20 μL from each sample. Run 10 QC samples initially to equilibrate the instrument, then inject one QC sample every 10 test samples to monitor system stability [85].
- Sample Preparation: Thaw plasma samples at room temperature. Precipitate proteins using 120 μL cold precipitant (dichloromethane/methanol, 3:1, v/v) per 40 μL plasma. Vortex for 1 minute, stand at room temperature for 10 minutes, then store at -20°C overnight. Centrifuge at 4,000 rpm for 30 minutes at 4°C [85].
Targeted Lipidomics Using LC-MS/MS
Chromatography Conditions:
- Column: Reversed-phase ACQUITY UPLC HSS T3 column (100 mm × 2.1 mm, 1.8 μm) maintained at 40°C [85].
- Mobile Phase: Solvent A (water with 0.1% formic acid) and Solvent B (acetonitrile with 0.1% formic acid) at 0.4 mL/min flow rate [85].
- Gradient Elution: 0-1 min (99% A), 1-3 min (1%-15% B), 3-6 min (15%-50% B), 6-9 min (50%-95% B), 9-10 min (95% B), 10.1-12 min (99% A) [85].
Mass Spectrometry Parameters:
- Ionization Modes: Operate in both positive and negative ion modes for comprehensive lipid coverage [85].
- Mass Range: 50-1,200 Da with 0.2s scan time [85].
- MS/MS Fragmentation: Fragment all precursor ions at 20-40 eV with 0.2s scan time [85].
- Quantification Approach: Use external calibration curves for quantifiable lipids and pseudo-quantitation based on predicted retention time and similar internal standards for remaining compounds [86].
Troubleshooting Common Experimental Challenges
Addressing Biological Variability in Pediatric Populations
FAQ: How can we account for high biological variability in childhood asthma studies?
Answer: Implement stratified recruitment based on asthma phenotypes and control for key covariates:
- Asthma Phenotyping: Clearly define patient groups using standardized criteria. The study group should include children with asthma and IgE-dependent allergy, while the control group consists of children without asthma or IgE-dependent allergy [84].
- Covariate Control: Document and control for age, sex, BMI, medication use, and comorbid allergic conditions. These factors significantly influence lipid profiles [84] [86].
- Sample Size Considerations: For pilot studies, aim for minimum 10-15 participants per group. Larger cohorts (n=997) provide greater statistical power for detecting subtle lipid changes [84] [86].
FAQ: What statistical methods effectively handle lipidomic data with high variability?
Answer: Employ a combination of univariate and multivariate approaches:
- Data Preprocessing: Apply log2 transformation and median-centering to mitigate nonlinearity and scale differences [82].
- Multivariate Analysis: Use Principal Component Analysis (PCA) and Partial Least Squares Discriminant Analysis (PLS-DA) for pattern recognition and dimensionality reduction [82].
- Validation Methods: Perform univariate and multivariate receiver operating characteristic (ROC) curve analysis. Combined indicators often demonstrate greater sensitivity and specificity than individual variables [84].
Technical Reproducibility in Lipid Measurement
FAQ: How can we improve reproducibility in ceramide and phosphatidylserine quantification?
Answer: Standardize sample processing and analytical conditions:
- Internal Standards: Use stable isotope-labeled internal standards for both ceramide and phosphatidylserine classes to correct for extraction and ionization efficiency variations [86].
- Extraction Consistency: Maintain consistent solvent ratios, timing, and temperature during lipid extraction. The dichloromethane/methanol (3:1, v/v) precipitant provides reliable protein removal while preserving lipid integrity [85].
- Instrument Calibration: Perform regular mass calibration and system suitability tests using reference standards [84].
FAQ: What quality controls ensure reliable lipidomic data?
Answer: Implement a comprehensive QC protocol:
- Process Blanks: Include extraction blanks to monitor contamination.
- Pooled QC Samples: Analyze every 10th sample to track instrument performance drift [85].
- Reference Materials: Use standardized reference materials when available. The International Lipidomics Standards Initiative aims to establish reference materials and protocols [2].
Table 1: Troubleshooting Guide for Common Lipidomics Challenges
| Problem | Possible Cause | Solution |
|---|---|---|
| High variability in lipid measurements | Inconsistent sample processing | Standardize extraction protocols; use internal standards |
| Poor chromatographic separation | Column degradation or mobile phase issues | Replace column; freshly prepare mobile phases |
| Low signal intensity | Ion suppression or inefficient ionization | Optimize LC gradient; improve sample cleanup |
| Inconsistent identification | Mass accuracy drift | Regular mass calibration; system suitability tests |
| Batch effects | Instrument drift over time | Randomize sample analysis; include pooled QC samples |
Biomarker Validation and Data Interpretation
Analytical Validation of Lipid Biomarkers
FAQ: What validation steps confirm biomarker reliability?
Answer: Conduct comprehensive analytical validation:
- Linearity and Range: Establish calibration curves for each lipid species across physiological concentrations [86].
- Precision and Accuracy: Determine intra-day and inter-day variability using QC samples. Acceptable precision is typically <15% CV [86].
- Specificity: Confirm identity through MS/MS fragmentation patterns and retention time matching with authentic standards when available [85].
FAQ: How do we address confounding factors in childhood asthma biomarker studies?
Answer: Account for major asthma risk factors that influence lipid metabolism:
- Genetic Factors: Consider ORMDL3 genotype status, as functional SNPs in this sphingolipid regulator gene significantly impact ceramide levels [86] [87].
- Vitamin D Levels: Measure circulating 25(OH)D levels, as vitamin D status modifies sphingolipid metabolism and asthma risk [86].
- Gut Microbiome: Assess gut microbial maturity, as bacterial sphingolipids can enter host metabolic pathways [86].
Biological Interpretation of Lipid Changes
FAQ: How do we interpret the biological significance of altered ceramide and phosphatidylserine levels?
Answer: Contextualize findings within known asthma pathobiology:
- Ceramide Signaling: Elevated ceramides promote apoptosis, reactive oxygen species generation, and neutrophil recruitment - key features of severe asthma [87].
- Sphingolipid Metabolism: Note that different sphingolipid classes have distinct associations; ceramide elevations correlate with asthma risk factors, while recycling sphingolipids associate with asthma phenotypes [86].
- Membrane Dynamics: Phosphatidylserine and other phospholipids influence membrane fluidity, receptor function, and cellular signaling in airway cells [88].
Table 2: Key Lipid Biomarkers in Childhood Asthma and Their Clinical Correlations
| Lipid Class | Specific Biomarker | Asthma Association | Clinical Utility |
|---|---|---|---|
| Sphingolipids | Ceramide (d16:0/27:2) | Negatively correlates with asthma severity [88] | Potential severity marker |
| Sphingolipids | Sphingosine-1-phosphate | Associated with asthma risk factors [86] | Mechanistic biomarker |
| Phosphatidylcholines | PC 40:4 | Combined with serotonin ratio distinguishes asthma [84] | Diagnostic biomarker |
| Phosphatidylethanolamines | PE (38:1) | Distinguishes asthmatic patients from healthy controls [88] | Diagnostic potential |
| Phosphatidylethanolamines | PE (20:0/18:1) | Positively correlates with asthma severity and IgE [88] | Severity and allergy marker |
Research Reagent Solutions
Table 3: Essential Research Reagents for Asthma Lipidomics
| Reagent/Kit | Manufacturer | Function | Application Notes |
|---|---|---|---|
| AbsoluteIDQ p180 Kit | Biocrates Life Sciences AG | Targeted metabolomics analysis | Quantifies 188 metabolites including lipids [84] |
| ACQUITY UPLC HSS T3 Column | Waters | Chromatographic separation | 100 mm × 2.1 mm, 1.8 μm particle size [85] |
| Atopic Polycheck 30-I Panel | Biocheck | Allergen-specific IgE detection | Confirms IgE-dependent allergy status [84] |
| DiaSorin Liaison 25(OH)D Assay | DiaSorin | Vitamin D quantification | Important covariate in sphingolipid studies [86] |
| CM-H2DCFDA | ThermoFisher | Reactive oxygen species detection | Links ceramide to oxidative stress [87] |
Advanced Methodological Considerations
Multivariate Data Analysis in Lipidomics
FAQ: Are PCA and PLS-DA appropriate for analyzing lipidomic data despite biological variability?
Answer: Yes, with proper implementation:
- Established Methods: PCA and PLS-DA are well-validated tools for pattern recognition in high-dimensional lipidomic data, despite their linear nature [82].
- Data Treatment: Apply appropriate data transformations (log2 transformation, median-centering) to meet analysis assumptions and mitigate nonlinearity [82].
- Complementary Approaches: Integrate multivariate methods with univariate statistical testing (moderated t-tests with FDR correction) and biological validation for robust conclusions [82].
Integrating Lipidomics with Other Data Types
FAQ: How can we integrate lipidomic data with genetic and clinical variables?
Answer: Employ integrated analysis frameworks:
- Mediation Analysis: Test whether ceramides mediate the relationship between ORMDL3 genotypes and asthma outcomes [86].
- Interaction Testing: Examine whether lipid biomarkers interact with environmental factors like vitamin D status in predicting asthma [86].
- Multi-Omic Integration: Combine lipidomic data with genetic, transcriptomic, and microbiome data for comprehensive pathway analysis [86].
Integrating lipidomics with genomics and microbiome data represents a powerful strategy in systems biology. While genomics provides a blueprint of potential biological outcomes, and microbiome analysis reveals the complex ecosystem of commensal organisms, lipidomics delivers a functional readout of metabolic activity and cellular state. This tripartite integration offers unprecedented insights into physiological and pathological processes, from understanding host-microbe interactions to unraveling complex disease mechanisms [89] [90].
Lipids constitute approximately 70% of plasma metabolites and serve as crucial components of cell membranes, energy storage molecules, and signaling mediators [90]. The lipidome reflects real-time metabolic changes, providing a snapshot of cellular activity that complements genetic predisposition revealed by genomics and community structure shown by microbiome analysis. This multi-omics approach enables researchers to build comprehensive models of biological systems by connecting genetic determinants, microbial influences, and functional metabolic outcomes [91] [92].
Key Research Reagent Solutions
Table 1: Essential Research Reagents and Kits for Multi-Omics Studies
| Reagent/Kits | Primary Function | Application Notes |
|---|---|---|
| Zymo ZR-96 MagBead Kit | DNA extraction for microbiome studies | Includes mechanical lysis step; ideal for low-biomass samples like skin swabs [89] |
| D-Squame Standard Sampling Discs | Skin tape stripping for lipid collection | 22mm diameter; used with standardized pressure pen (225 g/cm²) for consistent sampling [89] |
| Deuterated Internal Standards | Lipid quantification reference | Added during lipid extraction for precise absolute quantification via mass spectrometry [9] |
| HotStar Taq Master Mix Kit | 16S rRNA gene amplification | Used with BSA and MgClâ‚‚ supplements to enhance amplification in low-biomass samples [89] |
| Butanol:methanol extraction solvent | Comprehensive lipid extraction | Automated method for broad-spectrum lipid recovery from biological samples [9] |
Troubleshooting Common Multi-Omics Integration Challenges
FAQ 1: Our integrated analysis shows poor correlation between genomic variants, microbiome composition, and lipid profiles. What could explain this discrepancy?
Answer: Discrepancies between omics layers are common and often reflect biological reality rather than technical failure. Consider these factors:
- Temporal dynamics: Lipid levels can fluctuate significantly within hours after meals, while microbiome and genomic signals are more stable [77]. One study showed that within-subject variance for certain phosphatidylethanolamine and phosphatidylcholine species can be up to 1.3-fold higher than between-subject variance over a single day with standardized meals [77].
- Regulatory complexity: mRNA and protein expression often diverge due to post-transcriptional regulation, and similarly, microbial presence doesn't always translate to functional metabolic output [93].
- Technical considerations: Ensure proper normalization across modalities. RNA-seq is often normalized by library size, proteomics by TMT ratios, and lipidomics by internal standards - if not harmonized, one modality can dominate integrated analyses [93].
Solution: Implement biology-aware integration approaches:
- Map all measurements to a temporal axis when possible
- Use integration tools like MOFA+ or DIABLO that explicitly model shared and unique variation across modalities
- Focus on pathway-level coherence rather than individual feature correlations [93]
FAQ 2: How can we account for the high biological variability in lipidomic measurements when integrating with more stable genomic and microbiome data?
Answer: Biological variability in lipidomics is a significant challenge that requires specific experimental and analytical strategies:
- Implement longitudinal sampling: Collect multiple samples across time points to distinguish true biological signals from transient fluctuations. Research shows that collecting samples at consistent times (accounting for circadian rhythms) and relative to meals significantly improves data quality [77].
- Increase sample size: Epidemiological studies examining lipidomic-disease associations require large sample sizes to detect moderate effect sizes. One study estimated that for an average true relative risk of 3, a study with 500, 1,000, and 5,000 total participants would have 19%, 57%, and 99% power, respectively [9].
- Control pre-analytical variables: Standardize fasting status, time of day, and sample processing protocols across all subjects. Studies show that 74% of lipid species have technical and within-individual variances accounting for most of their total variability [9].
Solution: Include quality control samples and technical replicates to quantify and account for technical versus biological variance. Use mixed-effects models that can separate within-subject from between-subject variation [9] [77].
FAQ 3: Our multi-omics integration produces clusters driven primarily by one data type (e.g., genomics) while ignoring patterns in lipidomics. How can we achieve balanced integration?
Answer: This common problem typically stems from three issues:
- Unmatched samples across omics layers: When different omics data come from different sample sets, integration becomes forced and biased [93].
- Improper normalization: If data types are not brought to comparable scales, high-variance modalities will dominate [93].
- Resolution mismatch: Attempting to integrate bulk lipidomics with single-cell genomics or microbiome data without accounting for compositional differences [93].
Solution:
- Create a sample matching matrix to ensure true sample overlap across modalities
- Apply cross-modal normalization (quantile normalization, log transformation, or CLR) before integration
- Use integration-aware tools that weight modalities separately rather than simple concatenation followed by PCA [93]
Table 2: Quantitative Lipid Variability Metrics from Epidemiological Studies
| Variability Type | Median Value | Implications for Study Design |
|---|---|---|
| Technical Variance (ICC~Tech~) | 0.79 [9] | Moderate reliability; requires technical replicates for low-abundance lipids |
| Lipid Species with High Technical + Within-Individual Variance | 74% [9] | Single measurements insufficient for these species; longitudinal sampling needed |
| Power for Detection (RR=3) with 1,000 participants | 57% [9] | Large sample sizes required for moderate effect sizes after multiple testing correction |
| Within-subject vs Between-subject Variance Ratio | Up to 1.3-fold higher [77] | Within-individual changes can exceed population-level differences in controlled settings |
Experimental Workflows for Robust Multi-Omics Integration
Integrated Sample Collection Protocol
Sample Collection for Skin Microbiome-Lipidomics Studies:
- Microbiome sampling: Swab a 5×5cm skin area for 30 seconds with a sterile flock swab dipped in phosphate buffered saline (PBS). Rotate swab between thumb and forefinger while rubbing back forth in a cross-wise manner [89].
- Lipidomics sampling: Apply D-Squame tape (22mm diameter) to skin surface using standardized pressure pen (225 g/cm²). Collect 4 consecutive tapes from the same spot [89].
- Storage: Place swab heads in sterile microcentrifuge tubes and tape strips in D-Squame storage cards. Store all samples at -80°C until analysis [89].
Critical Considerations:
- Collect samples before any washing or product application
- For temporal studies, standardize collection times relative to meals and circadian rhythms
- Process paired samples from the same subjects simultaneously to minimize batch effects [89] [77]
Lipidomics Methodologies for Multi-Omics Integration
Untargeted Lipidomics:
- Purpose: Comprehensive discovery of lipid alterations across conditions
- Platform: High-resolution mass spectrometry (Q-TOF, Orbitrap)
- Data acquisition: Data-dependent acquisition (DDA) or data-independent acquisition (DIA)
- Application: Ideal for initial biomarker discovery and hypothesis generation [90]
Targeted Lipidomics:
- Purpose: Precise quantification of specific lipid panels
- Platform: Triple quadrupole mass spectrometry (UPLC-QQQ MS) with multiple reaction monitoring (MRM)
- Application: Validation of findings from untargeted approaches; high-precision clinical biomarker applications [90]
Pseudotargeted Lipidomics:
- Purpose: Balances coverage and quantification accuracy
- Approach: Uses information from untargeted analysis to develop targeted methods for broader coverage
- Application: Ideal for complex disease studies requiring both discovery and validation [90]
Multi-Omics Integration Workflow
Analytical Framework for Robust Integration
Addressing Biological Variability in Study Design
Lipid Variability Sources
Data Processing and Normalization Strategies
Cross-Modal Normalization Protocol:
- Within-modality processing:
- Lipidomics: Normalize using internal standards, then log-transform
- Microbiome: 16S rRNA sequencing data processed through standard QIIME2 pipeline
- Genomics: Standard variant calling and quality control pipelines
Between-modality harmonization:
Feature selection:
- Apply biology-aware filters (remove mitochondrial genes, unannotated peaks)
- Focus on features with known biological relevance to the system
- For lipidomics, prefer high-confidence, consistently detected lipid species [93]
Successful integration of lipidomics with genomics and microbiome data requires addressing both technical and biological challenges. By implementing standardized protocols, accounting for biological variability, and using appropriate analytical frameworks, researchers can unlock the full potential of multi-omics approaches to advance understanding of complex biological systems and disease mechanisms.
Key recommendations:
- Design studies with matched samples across all omics modalities
- Account for temporal dynamics in lipid measurements through standardized collection times
- Use integration methods that balance contributions from different data types
- Report both shared and modality-specific signals in integrated analyses [93]
- Validate findings across multiple cohorts to address biological variability [9]
Troubleshooting Guides
Addressing Biological Variability in Lipidomic Studies
Problem: High biological variability is obscuring disease-specific lipid signatures.
Biological variability, particularly between individuals and sexes, is a fundamental characteristic of the circulatory lipidome that can complicate the identification of robust diagnostic biomarkers [3].
Possible Cause: High inter-individual lipidome differences exceeding analytical variability.
- Suggested Solution: Implement a repeated-measures sampling design. As demonstrated in a study of 364 individuals sampled at three time points, biological variability is significantly higher than batch-to-batch analytical variability (8.5% median reproducibility). Focus on establishing an individual's stable lipidome baseline rather than relying solely on population-wide cross-sectional comparisons [3].
Possible Cause: Unaccounted-for sex-specific lipid differences.
- Suggested Solution: Stratify analysis by sex during study design and data analysis. Significant sex differences exist, with sphingomyelins and ether-linked phospholipids present at significantly higher concentrations in female plasma. Failing to account for this can confound disease-related findings [3].
Possible Cause: Inadequate sample size for robust statistical power.
- Suggested Solution: Perform a power calculation prior to study initiation. The high individuality of the lipidome necessitates larger cohorts to distinguish true disease effects from natural variation. Utilize high-throughput LC-MS/MS methods capable of processing over 1,000 samples to achieve the necessary statistical power [3].
Problem: Lipid-based diagnostic model performance is not reproducible in validation cohorts.
- Possible Cause: Suboptimal data preprocessing and analytical workflows for high-dimensional lipidomics data.
- Suggested Solution: Adopt a standardized data analysis pipeline. This should include:
- Data Preprocessing: Log2 transformation and median-centering of data to mitigate nonlinearity and scale differences [82].
- Multivariate Analysis: Use Principal Component Analysis (PCA) and Partial Least Squares Discriminant Analysis (PLS-DA) as established exploratory tools for visualizing variance and grouping in high-dimensional data [82].
- Statistical Validation: Follow multivariate analysis with rigorous univariate testing (e.g., moderated t-tests with False Discovery Rate (FDR) correction) and biological validation to ensure findings are both statistically and biologically significant [82].
- Suggested Solution: Adopt a standardized data analysis pipeline. This should include:
Cost-Effectiveness and Implementation Challenges
Problem: The cost-effectiveness of a lipid-based diagnostic intervention is uncertain for health system adoption.
Possible Cause: Intervention costs are high relative to the quality-of-life gains.
- Suggested Solution: Structure the intervention for efficiency. A within-trial analysis of a family-based cardiovascular risk reduction program demonstrated cost-effectiveness. The intervention cost Int$157.5 per person more than usual care but gained 0.014 incremental Quality-Adjusted Life Years (QALYs), resulting in an Incremental Cost-Effectiveness Ratio (ICER) of Int$11,352 per QALY, which is considered cost-effective at a threshold of three times the GDP per capita [95].
Possible Cause: Inefficient allocation of resources within the intervention.
- Suggested Solution: Utilize a cost-by-outcomes table to identify the most efficient targets. The PROLIFIC trial showed varying incremental costs per unit reduction in different risk factors [95]:
- Systolic Blood Pressure: Int$28.5 per unit reduction
- Fasting Plasma Glucose: Int$26.9 per unit reduction
- HbA1c: Int$130.8 per unit reduction
- Total Cholesterol: Int$178.7 per unit reduction
- Focusing on outcomes with lower cost per unit reduction can optimize the intervention's overall cost-effectiveness [95].
- Suggested Solution: Utilize a cost-by-outcomes table to identify the most efficient targets. The PROLIFIC trial showed varying incremental costs per unit reduction in different risk factors [95]:
Frequently Asked Questions (FAQs)
Q: What are the key lipid classes that have the biggest impact on health and should be prioritized in diagnostic panels? A: While comprehensive profiling is valuable, two lipid classes have a major impact on health. Phospholipids form the structural foundation of all cell membranes and their composition directly impacts cellular function and response; abnormalities can precede insulin resistance by up to five years. Sphingolipids, particularly ceramides, are powerful signaling molecules that regulate inflammation and cell death; elevated ceramide levels strongly predict cardiovascular events and correlate with insulin resistance, with ceramide risk scores now outperforming traditional cholesterol measurements for heart attack prediction [2].
Q: How does the clinical utility of lipid-based diagnostics compare to genetic testing? A: Lipid-based profiling offers distinct advantages for near-term clinical utility. Lipid profiles reflect real-time physiological status and are highly modifiable, allowing for quick monitoring of intervention effects. A 2024 trial (RESPOND) showed lipid-focused personalized treatments yielded a 43% greater improvement in insulin sensitivity than genetic-based approaches. Furthermore, lipid-centric prevention programs have demonstrated superior cost-effectiveness, at approximately $3,200 per quality-adjusted life year gained compared to $12,700 for genetic-based programs [2].
Q: What is the evidence that lipid-based interventions actually improve patient outcomes? A: Robust clinical trials demonstrate significant outcome improvements. The LIPID-HEART trial (2024) showed personalized interventions based on detailed lipid profiles reduced cardiovascular events by 37% compared to standard care, significantly outperforming gene-based risk assessments (19% reduction). In neurodegenerative disease, the BRAIN-LIPID study demonstrated that custom lipid supplements slowed cognitive decline in early Alzheimer's patients by 28% [2].
Data Presentation
Cost-Effectiveness of Lipid-Based Interventions
Table: Incremental Cost-Effectiveness of a Family-Based Cardiovascular Risk Reduction Intervention over Two Years (PROLIFIC Trial) [95]
| Parameter | Intervention Group | Usual Care Group | Incremental Difference |
|---|---|---|---|
| Total Cost per Person | Int$ 381.6 | Int$ 224.1 | Int$ 157.5 |
| Quality-Adjusted Life Years (QALYs) | 0.0166 | 0.0027 | 0.014 |
| ICER (Cost per QALY Gained) | Int$ 11,352 |
Table: Incremental Cost per Unit Reduction in Key Risk Factors [95]
| Risk Factor | Incremental Cost per Unit Reduction |
|---|---|
| Systolic Blood Pressure | Int$ 28.5 |
| Fasting Plasma Glucose | Int$ 26.9 |
| Waist Circumference | Int$ 39.8 |
| HbA1c | Int$ 130.8 |
| Total Cholesterol | Int$ 178.7 |
Analytical Performance in Lipidomics
Table: Key Metrics for Robust Quantitative LC-MS/MS Lipidomics [3]
| Performance Metric | Specification | Importance for Diagnostic Utility |
|---|---|---|
| Between-Batch Reproducibility | Median of 8.5% | Ensures measured differences are biological, not technical. |
| Lipid Coverage | 782 lipid species across 22 classes | Provides a comprehensive view of the lipidome. |
| Concentration Range | Six orders of magnitude | Allows simultaneous quantification of abundant and rare lipids. |
| Biological vs. Analytical Variability | Biological variability significantly higher | Prerequisite for detecting physiologically relevant changes. |
Experimental Protocols
Protocol: High-Throughput Quantitative Lipidomics for Clinical Biomarker Discovery
This protocol is designed to ensure robust and reproducible measurement of circulatory lipids in large-scale studies, minimizing analytical variability to better resolve biological variability [3].
Key Materials:
- Stable isotope-labeled internal standard mixture (for stable isotope dilution)
- National Institute of Standards and Technology (NIST) plasma reference material
- Semiautomated sample preparation platform
- LC-MS/MS system with HILIC (Hydrophilic Interaction Liquid Chromatography) capability
Procedure:
- Sample Collection and Preparation: Collect fasted plasma samples. Use a semiautomated platform for sample preparation to minimize human error. Employ a stable isotope dilution approach for accurate quantification [3].
- Quality Control Integration: Alternate the analysis of every set of patient samples with an analysis of the NIST plasma reference material. This serves as a continuous between-batch quality control to monitor instrument performance and reproducibility over time (e.g., across 13 independent batches) [3].
- LC-MS/MS Analysis: Analyze samples using a HILIC-based LC-MS/MS method. This methodology allows for the robust measurement of a wide panel of lipids (e.g., 782 species) across a very wide concentration range [3].
- Data Processing and Validation: Process raw data. The between-batch reproducibility should be calculated (target <15%) using the quality control data. Confirm that the biological variability observed in the study samples is significantly higher than the analytical variability, ensuring data quality [3].
Protocol: Multivariate Data Analysis for Lipidomic Data
This protocol outlines a standardized workflow for the statistical analysis of high-dimensional lipidomics data, crucial for identifying robust diagnostic signatures amidst biological noise [82].
Procedure:
- Data Preprocessing: Apply log2 transformation and median-centering to the lipid abundance data. This helps mitigate nonlinearity and scale differences, making the data more suitable for linear multivariate analysis. Visually inspect distribution plots to confirm effective normalization [82].
- Exploratory Analysis with PCA: Perform Principal Component Analysis (PCA) on the preprocessed data. Use this to visualize the overall distribution of samples, identify potential outliers, and observe natural groupings based on treatment, disease state, or individual [82].
- Supervised Modeling with PLS-DA: Perform Partial Least Squares Discriminant Analysis (PLS-DA) to maximize the separation between pre-defined groups (e.g., diseased vs. healthy). This helps identify the lipid species that contribute most to the class separation [82].
- Univariate Statistical Validation: Follow the multivariate analysis with rigorous univariate testing. Perform moderated t-tests on individual lipid species across comparison groups, applying a False Discovery Rate (FDR) correction for multiple comparisons (e.g., p < 0.01). Combine this with fold-change analysis (e.g., >1.5) [82].
- Biological Interpretation: Integrate the results from the multivariate and univariate analyses to generate a list of statistically significant, differentially abundant lipids. Interpret these findings in the context of known biological pathways (e.g., fatty acid synthesis, phospholipid metabolism) for functional validation [82].
Workflow and Pathway Visualizations
High-Throughput Lipidomics Workflow
Variability vs Clinical Utility
The Scientist's Toolkit
Table: Essential Research Reagent Solutions for Robust Lipidomics
| Reagent / Material | Function | Application Note |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Enables precise absolute quantification of lipid species via mass spectrometry by correcting for sample loss and ion suppression. | Use a comprehensive mixture spanning multiple lipid classes for accurate quantification across the entire lipidome [3]. |
| NIST Plasma Reference Material | Serves as a consistent quality control material across batches to monitor and ensure analytical reproducibility. | Analyze alternating with study samples in every batch to track performance; target <15% between-batch variability [3]. |
| Specialized LC-MS/MS Lipidomics Platforms | High-resolution mass spectrometry systems for identifying and quantifying thousands of lipid species. | Platforms like the ZenoTOF 7600 system with EAD technology enable detailed structural characterization [96]. |
| Multivariate Data Analysis Software | Software packages for performing PCA, PLS-DA, and other statistical analyses on high-dimensional lipidomics data. | Essential for dimensionality reduction, pattern recognition, and identifying lipid signatures amidst biological variability [82]. |
Conclusion
Effectively addressing biological variability is not a barrier but a gateway to unlocking the full potential of lipidomics in precision medicine. By adopting a holistic approach that integrates rigorous experimental design, advanced analytical techniques, robust statistical workflows, and stringent validation, researchers can transform lipid variability from a source of noise into a rich source of biological insight. The future of lipidomics lies in embracing this complexity—leveraging AI-driven annotation, continuous monitoring technologies, and standardized multi-omics integration to develop dynamic, personalized lipid models. These advances will cement lipidomics as an indispensable tool for early disease detection, understanding disease mechanisms, and developing targeted therapies, ultimately leading to more predictive and personalized healthcare.
References
- 1. Best practices and tools in R and Python for statistical ... [https://www.nature.com/articles/s41467-025-63751-1]
- 2. Up-to-Date Look at Lipids Role in Precision Health (2025) [https://www.laboratoriosrubio.com/en/lipidomics-precision-health/]
- 3. Clinical lipidomics reveals high individuality and sex ... [https://www.sciencedirect.com/science/article/pii/S0022227525000409]
- 4. ADViSELipidomics: a workflow for analyzing lipidomics data [https://pmc.ncbi.nlm.nih.gov/articles/PMC9750127/]
- 5. Unravelling lipid heterogeneity: Advances in single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270072/]
- 6. How to Interpret Lipidomics Data: A Step-by-Step Guide [https://lipidomics.creative-proteomics.com/resource/how-to-interpret-lipidomics-data-a-step-by-step-guide.htm]
- 7. Extensive diversity in circadian regulation of plasma lipids and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3761633/]
- 8. Age-related changes in circadian regulation of the human ... [https://www.nature.com/articles/s42003-023-05102-8]
- 9. Sources of Variability in Serum Lipidomic Measurements ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10144665/]
- 10. Circadian lipid and hepatic protein rhythms shift with a ... [https://www.nature.com/articles/s41467-022-28308-6]
- 11. Investigating the effects of circadian rhythm on the human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541903/]
- 12. Circadian Rhythms of Skin Surface Lipids and ... [https://www.mdpi.com/2079-7737/13/12/1031]
- 13. Circadian Rhythms of Skin Surface Lipids and Physiological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11673904/]
- 14. The Effect of Diet on Cardiovascular Disease and Lipid ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK570127/]
- 15. Challenges and opportunities for prevention and removal ... [https://www.sciencedirect.com/science/article/abs/pii/S0163782722000327]
- 16. Dynamic lipidome alterations associated with human ... [https://www.nature.com/articles/s42255-023-00880-1]
- 17. Postprandial lipemia after short-term variation in dietary fat ... [https://www.sciencedirect.com/science/article/abs/pii/S002604950016682X]
- 18. Variability in Lipid Levels and Risk for Cardiovascular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10111433/]
- 19. The Hitchhiker's Guide to Untargeted Lipidomics Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8624948/]
- 20. Lipidomics: Techniques, applications, and outcomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5085849/]
- 21. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/abs/pii/S0009898125005777]
- 22. FAQ - LipidSig 2.0 [https://lipidsig.bioinfomics.org/FAQ/]
- 23. Computationally unmasking each fatty acyl C=C position in ... [https://www.nature.com/articles/s41467-025-61911-x]
- 24. Lipidomic signatures align with inflammatory patterns and ... [https://www.nature.com/articles/s41467-022-34420-4]
- 25. The metabolic response to stress in critical illness [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554859/]
- 26. A concise review on lipidomics analysis in biological samples [https://pmc.ncbi.nlm.nih.gov/articles/PMC8923307/]
- 27. Plasma lipidomic signatures reveal age-associated ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1659425/full]
- 28. Scheduled data - dependent MS provides enhanced... acquisition [https://pubmed.ncbi.nlm.nih.gov/40825638/]
- 29. Deep lipidomic profiling enabled by the Paternò-Büchi ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267025008505]
- 30. Review of Recent Advances in Lipid Analysis of Biological ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8623600/]
- 31. Incorporation of the Paternò–Büchi reaction into mass ... [https://hammer.purdue.edu/articles/thesis/Incorporation_of_the_Patern_B_chi_reaction_into_mass_spectrometry-based_systems_for_lipid_structural_characterization/11327954]
- 32. Dual-resolving of positional and geometric isomers of C=C ... [https://www.nature.com/articles/s41467-022-30249-z]
- 33. The Paternò-Büchi reaction—Mechanisms and application ... [https://www.sciencedirect.com/science/article/pii/S1389556717300886]
- 34. Oxetane Synthesis through the Paternò-Büchi Reaction [https://pmc.ncbi.nlm.nih.gov/articles/PMC6269742/]
- 35. Paternò–Büchi reaction [https://en.wikipedia.org/wiki/Patern%C3%B2%E2%80%93B%C3%BCchi_reaction]
- 36. Challenges in Lipidomics Biomarker Identification [https://www.mdpi.com/2218-1989/14/8/461]
- 37. Structural elucidation of triacylglycerol using online acetone ... [https://pubmed.ncbi.nlm.nih.gov/32761025/]
- 38. Pre-analytical sample handling standardization for reliable ... [https://pubmed.ncbi.nlm.nih.gov/36872954/]
- 39. Specimen integrity: How errors occur and the role ... [https://www.cardinalhealth.com/en/product-solutions/medical/laboratory-products/specimen-collection/specimen-integrity-resources/specimen-integrity-how-errors-occur.html]
- 40. Reporting of lipidomics data should be standardized [https://www.sciencedirect.com/science/article/abs/pii/S1388198117300379]
- 41. Errors with specimen and sample collection process [https://stateclaims.ie/learning-events/errors-with-specimen-and-sample-collection-process]
- 42. LipidSearch Software Support-Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/mass-spectrometry-support-center/liquid-chromatography-mass-spectrometry-software-support/lipidsearch-software-support/lipidsearch-software-support-troubleshooting.html]
- 43. Challenges in Lipidomics Biomarker Identification [https://pmc.ncbi.nlm.nih.gov/articles/PMC11356033/]
- 44. Challenges and opportunities for prevention and removal ... [https://pubmed.ncbi.nlm.nih.gov/35780914/]
- 45. Lipidomics in biomedical research: chance and challenges [https://www.ddw-online.com/lipidomics-in-biomedical-research-chance-and-challenges-12719-202108/]
- 46. Introduction of a lipidomics scoring system for data quality ... [https://www.sciencedirect.com/science/article/pii/S002222752500077X]
- 47. Lipidomics from sample preparation to data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC7118050/]
- 48. Steps Required to Interpret Lipidomics Data [https://www.metwarebio.com/how-to-interpret-lipidomics-data-a-step-by-step-guide/]
- 49. Ontogeny of circulating lipid metabolism in pregnancy and early... [https://elifesciences.org/articles/72779]
- 50. Penalized Variable Selection for Lipid–Environment Interactions in... [https://www.mdpi.com/2073-4425/10/12/1002]
- 51. FAIR data principles: What you need to know [https://tiledb.com/blog/fair-data-principles-explained]
- 52. Streamlining Lipidomics: Novel Statistical Workflows and ... [https://www.chromatographyonline.com/view/streamlining-lipidomics-novel-statistical-workflows-and-visualization-in-r-and-python]
- 53. Correcting batch effects in large-scale multiomics studies ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-023-03047-z]
- 54. Systematic Error Removal Using Random Forest for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9652764/]
- 55. Comparison of imputation and imputation-free methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8769695/]
- 56. Imputation for Lipidomics and Metabolomics (ImpLiMet) [https://pubmed.ncbi.nlm.nih.gov/39867531/]
- 57. Why You Must Correct Batch Effects in Transcriptomics Data? [https://www.metwarebio.com/transcriptomics-batch-effect-correction/]
- 58. Evaluation of normalization strategies for mass ... [https://pubmed.ncbi.nlm.nih.gov/40593232/]
- 59. Addressing the batch effect issue for LC/MS metabolomics ... [https://www.nature.com/articles/s41598-020-70850-0]
- 60. Enhancing statistical power and data reliability in Lipidomics [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25026943]
- 61. LipidSig 2.0: integrating lipid characteristic insights into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11223864/]
- 62. Lipidome visualisation, comparison, and analysis in a vector ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12058142/]
- 63. Missing colour and hover labels in interactive report ... [https://github.com/nf-core/differentialabundance/issues/270]
- 64. LipidQC: Method Validation Tool for Visual Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11493136/]
- 65. Volcano plots in R: easy step-by-step tutorial [https://biostatsquid.com/volcano-plots-r-tutorial/]
- 66. Anomaly Detection in Manufacturing: The 2025 Ultimate Guide [https://f7i.ai/blog/the-definitive-guide-to-anomaly-detection-in-manufacturing-2025]
- 67. Anomaly Detection in Machine Learning [https://spd.tech/machine-learning/anomaly-detection-with-machine-learning/]
- 68. Increasing Consistency of Disease Biomarker Prediction Across... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3989170/]
- 69. Analytical quality control in targeted lipidomics [https://www.sciencedirect.com/science/article/pii/S0003267025006191]
- 70. Cancer biomarker discovery is improved by accounting for variability ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-016-1050-9]
- 71. Utilizing Serum-Derived Lipidomics with Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409608/]
- 72. 9 AI problems in 2025: Common challenges and solutions [https://lumenalta.com/insights/ai-problems-9-common-challenges-and-solutions]
- 73. AI Troubleshooting Guide 2025 [https://www.rapidinnovation.io/post/ai-agents-for-technical-troubleshooting]
- 74. MetaboAnalyst [https://www.metaboanalyst.ca/docs/RTutorial.xhtml]
- 75. Anomaly detection using machine learning and adopted ... [https://www.nature.com/articles/s41598-025-02759-5]
- 76. Lipidomic Risk Score to Enhance Cardiovascular ... [https://pubmed.ncbi.nlm.nih.gov/39048275/]
- 77. Discovering and validating between-subject variations in ... [https://www.nature.com/articles/srep19139]
- 78. Lipid metabolism-related gene signature predicts ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1021678/full]
- 79. Biomarker Qualification Program Submission Frequently ... [https://www.fda.gov/drugs/biomarker-qualification-program/biomarker-qualification-program-submission-frequently-asked-questions]
- 80. Clinical serum lipidomic profiling revealed potential lipid ... [https://www.nature.com/articles/s41598-024-66157-z]
- 81. Biomarker discovery and validation: Bridging research and ... [https://www.abcam.com/en-us/knowledge-center/immunology-and-infectious-disease/biomarker-discovery-and-validation]
- 82. Multivariate Data Analysis Methods and Their Application in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12280249/]
- 83. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/pii/S0009898125005777?dgcid=rss_sd_all]
- 84. Biomarker Discovery in Childhood Asthma: A Pilot Study of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207927/]
- 85. Plasma lipids, amino acids, and their metabolic pathways ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1549431/full]
- 86. Sphingolipid classes and the interrelationship with pediatric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11175620/]
- 87. CERAMIDE IN APOPTOSIS AND OXIDATIVE STRESS IN ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8081742/]
- 88. Lipid metabolism and identification of biomarkers in ... [https://www.sciencedirect.com/science/article/pii/S1388198120302456]
- 89. Microbiome and lipidomic analysis reveal the interplay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11043602/]
- 90. The strategic role of lipidomics in biomarker identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483926/]
- 91. From Omics to Multi-Omics: A Review of Advantages and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11675490/]
- 92. Integration of lipidomics and metabolomics for in-depth ... [https://www.sciencedirect.com/science/article/abs/pii/S1673852719302000]
- 93. Why Multi-Omics Data Integration Often Fails [https://www4.accurascience.com/blogs_44_0.html]
- 94. Ten quick tips for avoiding pitfalls in multi-omics data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10325053/]
- 95. Within-Trial Cost-Effectiveness Analysis of a Family-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12315683/]
- 96. Lipidomics: Bring Your Research To a New Level [https://sciex.com/applications/biomedical-and-omics-research/lipidomics]