Navigating the Reproducibility Crisis in Lipidomic Biomarker Validation: From Foundational Challenges to Clinical Translation
Lipidomics has emerged as a powerful tool for discovering biomarkers that reflect real-time metabolic states in diseases ranging from cancer to inflammatory disorders.
Navigating the Reproducibility Crisis in Lipidomic Biomarker Validation: From Foundational Challenges to Clinical Translation
Abstract
Lipidomics has emerged as a powerful tool for discovering biomarkers that reflect real-time metabolic states in diseases ranging from cancer to inflammatory disorders. However, the translation of these discoveries into clinically validated diagnostics faces significant reproducibility challenges. This article explores the entire lipidomic biomarker pipeline, from foundational principles and methodological approaches in mass spectrometry to the critical troubleshooting of analytical variability and the rigorous validation required for clinical adoption. Aimed at researchers, scientists, and drug development professionals, it synthesizes current evidence on the sources of irreproducibility—including software discrepancies, pre-analytical variables, and a lack of standardized protocols—while highlighting advanced solutions such as machine learning and standardized workflows that are paving the way for more robust, clinically applicable lipidomic biomarkers.
The Promise and Peril of Lipidomic Biomarkers: Understanding the Fundamental Landscape
Lipids, once considered merely as passive structural components of cellular membranes, are now recognized as dynamic bioactive molecules that play critical roles in cellular signaling, metabolic regulation, and disease pathogenesis. The emergence of lipidomics—the large-scale study of lipid pathways and networks—has revealed the astonishing complexity of lipid-mediated processes, with thousands of distinct lipid species participating in sophisticated signaling cascades [1] [2].
This paradigm shift underscores lipids as active participants in health and disease, functioning as signaling hubs that regulate inflammation, metabolism, and immune responses [3] [2]. Understanding these dynamic roles is particularly crucial for advancing biomarker discovery and therapeutic development, though it presents significant challenges in validation and reproducibility that this technical support center aims to address.
Core Concepts: Lipid Signaling in Cellular Communication
Lipid Rafts as Signaling Platforms
What are lipid rafts? Lipid rafts are specialized, cholesterol- and sphingolipid-enriched microdomains within cellular membranes that create more ordered and less fluid environments than the surrounding membrane [4]. These dynamic structures serve as organizing platforms for signaling complexes and facilitate crucial cellular processes.
Table 1: Key Components of Lipid Rafts and Their Functions
| Component | Primary Function | Signaling Role |
|---|---|---|
| Cholesterol | Regulates membrane fluidity and stability | Maintains platform integrity for signaling assembly |
| Sphingolipids | Ensures tight packing and structural integrity | Forms ordered domains for receptor clustering |
| Gangliosides | Modulates cell signaling and adhesion | Serves as raft markers and signaling modulators |
| GPI-Anchored Proteins | Facilitates immune cell signaling | Links extracellular stimuli to intracellular responses |
| Transmembrane Proteins | Enables precise control of signaling events | Includes growth factor receptors and ion channels |
Lipid rafts are not static structures but exhibit dynamic fluidity within the fluid mosaic model of the cell membrane. Their ability to cluster or coalesce into larger domains in response to stimuli significantly influences cellular processes, including signal transduction and membrane trafficking [4]. For example, during immune activation, T-cell receptors accumulate in lipid rafts upon antigen binding, facilitating downstream signaling events essential for immune responses.
Bioactive Lipid Signaling in Immune Regulation
Lipids function as potent signaling molecules that regulate immune cell function and polarization. Macrophages, in particular, exhibit distinct lipid-driven metabolic reprogramming during polarization between pro-inflammatory M1 and anti-inflammatory M2 states [3].
M1 Macrophage Lipid Signaling:
- Increased glycolytic flux with glucose-6P diversion to pentose phosphate pathway for NADPH and ROS production
- Disruptions in TCA cycle leading to mitochondrial export of citrate and succinate
- Citrate conversion to acetyl-CoA for synthesis of acyl-CoA and phospholipids
- Free arachidonic acid release from phospholipids serving as substrate for pro-inflammatory eicosanoids [3]
M2 Macrophage Lipid Signaling:
- Dependence on oxidative phosphorylation with intact TCA cycle
- Functional glycolytic pathways supporting alternative activation
- CD36-mediated endocytosis of modified LDLs for membrane remodeling and energy production [3]
Figure 1: Lipid Raft Organization and Signaling Function. Lipid rafts serve as platforms that concentrate specific lipids and proteins to facilitate efficient signaling cascades.
Methodologies: Lipidomics Workflows and Protocols
Untargeted Lipidomics: LC-MS Workflow
Liquid chromatography-mass spectrometry (LC-MS) has become the analytical tool of choice for untargeted lipidomics due to its high sensitivity, convenient sample preparation, and broad coverage of lipid species [5].
Sample Preparation Protocol:
- Homogenization: Homogenize tissue samples or aliquot biological liquids
- Standard Addition: Add isotope-labeled internal standards as early as possible to enable normalization
- Stratified Randomization: Randomize samples in batches of 48-96 samples
- Blank Insertion: Insert blank extraction samples after every 23rd sample
- Lipid Extraction: Perform extraction in predetermined batches
- Centrifugation: Separate organic and aqueous phases by centrifugation
- Quality Control: Prepare QC samples by collecting aliquots from each sample into a pooled sample [5]
LC-MS Analysis Parameters:
- Chromatography: Reversed-Phase Bridged Ethyl Hybrid (BEH) C8 column
- Mass Detection: High-resolution mass spectrometer (e.g., Q-TOF instruments)
- Ionization Modes: Both positive and negative electrospray ionization modes
- QC Placement: Inject QC samples several times before initiating run, after each batch, and after completion [5]
Data Processing and Analysis
Data Conversion and Import:
- Convert centroid data to conventional mzXML format using ProteoWizard
- Organize files into folder structure reflecting study design
- Import into R environment using xcms Bioconductor package
- Group samples based on subfolder structure for peak alignment [5]
Statistical Analysis Framework:
- Univariate Methods: Student's t-test, ANOVA for analyzing lipid features independently
- Multivariate Methods: Principal Component Analysis (PCA) to identify relationship patterns
- Peak Alignment: Match MS peaks with similar m/z and retention times across samples [6]
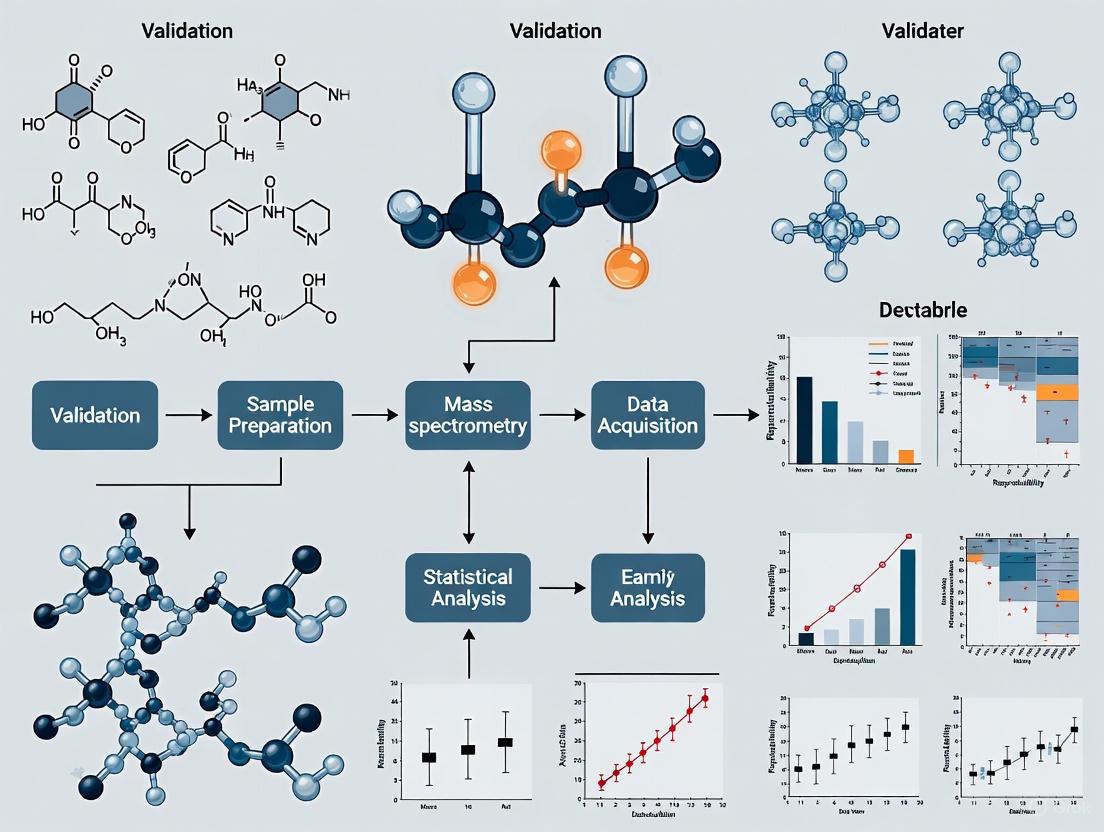
Figure 2: Untargeted Lipidomics Workflow. The comprehensive process from sample preparation to lipid identification ensures broad coverage of lipid species.
Research Reagent Solutions
Table 2: Essential Materials for Lipidomics Research
| Reagent/Equipment | Function | Application Notes |
|---|---|---|
| Isotope-Labeled Internal Standards | Normalization for experimental biases | Add early in sample preparation; select based on lipid classes of interest |
| C8 or C18 Reversed-Phase Columns | Chromatographic separation of lipids | Provides optimal separation for diverse lipid classes |
| Quality Control (QC) Samples | Monitor instrument stability and reproducibility | Prepare from pooled sample aliquots; inject throughout sequence |
| ProteoWizard Software | Convert MS data to mzXML format | Cross-platform tool for data standardization |
| xcms Bioconductor Package | Peak detection and alignment | Most widely used solution for MS data analysis |
| Lipid Maps Database | Lipid identification and classification | International standard for lipid nomenclature |
Troubleshooting Guides: Addressing Common Challenges
Biomarker Validation and Reproducibility
Issue: Low reproducibility across lipidomics platforms Problem: Different lipidomics platforms yield divergent outcomes from the same data, with agreement rates as low as 14-36% during validation [1].
Solutions:
- Standardize Pre-analytical Protocols:
- Implement consistent sample collection and processing procedures
- Use identical extraction buffers across comparisons
- Maintain consistent storage conditions (-80°C)
Harmonize Analytical Parameters:
- Standardize LC gradients and mobile phase compositions
- Calibrate mass spectrometers using reference standards
- Implement uniform data quality thresholds
Validate with Multiple Methods:
- Confirm identifications using MS/MS fragmentation patterns
- Cross-validate with orthogonal methods when possible
- Utilize shared reference materials for inter-laboratory comparisons
Issue: Batch effects in large-scale studies Problem: LC-MS batch effects persist even after normalization, confounding biological signals [5].
Solutions:
- Strategic Batch Design:
- Distribute samples among batches to enable within-batch comparisons
- Avoid confounding factors of interest with batch covariates
- Balance confounding factors between samples and controls
Quality Control Integration:
- Insert QC samples after every 10 experimental samples
- Inject blank samples at beginning and end of runs
- Monitor instrument stability through retention time drift
Advanced Normalization:
- Use internal standards for retention time correction
- Apply quality control-based robust spline correction
- Implement batch effect correction algorithms (ComBat, ARSyN)
Structural Characterization Challenges
Issue: Incomplete structural elucidation Problem: Typical high resolution and MS2 may be insufficient for complete structural characterization, particularly for lipid isomers [6].
Solutions:
- Advanced Fragmentation Techniques:
- Implement both HCD and CID fragmentation in tandem
- Utilize MS³ capabilities for complex isomers
- Combine positive and negative ion mode data
Chromatographic Optimization:
- Employ C30 reversed-phase columns for enhanced separation
- Optimize mobile phase modifiers for specific lipid classes
- Extend chromatographic gradients for complex mixtures
Complementary Techniques:
- Utilize chemical derivatization for double bond localization
- Incorporate ion mobility separation for isobaric species
- Apply 2D NMR for unequivocal structural assignment
FAQs: Lipidomics in Biomarker Research
Q1: What are the major challenges in translating lipidomic biomarkers to clinical practice?
A: The transition from research findings to approved lipid-based diagnostic tools faces several hurdles:
- Validation Complexity: Lipid changes are frequently subtle and context-dependent, requiring integration with clinical, genomic, and proteomic data [1]
- Regulatory Gaps: Incomplete regulatory frameworks for lipidomic biomarkers and lack of multi-center validation studies hinder clinical adoption [1]
- Standardization Issues: Biological variability, lipid structural diversity, and inconsistent sample processing exacerbate reproducibility problems [1] [2]
- Technical Limitations: Current platforms struggle with complete structural elucidation, particularly for lipid isomers and low-abundance species [6]
Q2: How can researchers improve reproducibility in lipid raft studies?
A: Enhancing reproducibility in lipid raft research requires:
- Cholesterol Modulation Controls: Include methyl-β-cyclodextrin treatments as positive controls for raft disruption
- Cross-Validation Methods: Combine multiple assessment techniques (e.g., detergent resistance, microscopy, functional assays)
- Standardized Isolation Protocols: Implement consistent detergent concentrations and centrifugation conditions
- Compositional Analysis: Regularly quantify cholesterol-to-phospholipid ratios in isolated raft fractions
Q3: What computational approaches are available for lipid nanoparticle design?
A: Computational methods are increasingly valuable for LNP optimization:
- Physics-Based Modeling: All-atom and coarse-grained molecular dynamics simulations capture lipid-RNA interactions and endosomal escape mechanisms [7]
- Constant pH Models: Scalable CpHMD models accurately reproduce apparent pKa values for different LNP formulations [7]
- Machine Learning: ML-driven approaches uncover complex patterns in LNP formulation and performance, though they require high-quality experimental datasets for training [7]
- Multiscale Frameworks: Integrative computational strategies bridge molecular properties with therapeutic efficacy across different length scales [7]
Q4: How do glycerophospholipid alterations contribute to neurodegenerative diseases?
A: Glycerophospholipids play active roles in neurodegeneration:
- Metabolic Dysregulation: In amyotrophic lateral sclerosis (ALS), glycerophospholipid alterations appear before motor symptom onset, suggesting early pathogenic involvement [8]
- Structural Consequences: Changes in glycerophospholipid composition affect membrane fluidity, protein function, and organelle integrity in neuronal tissues [8]
- Signaling Disruption: As precursors for bioactive lipids, glycerophospholipid imbalances perturb inflammatory signaling and cellular communication [8]
- Diagnostic Potential: Glycerophospholipid profiles in cerebrospinal fluid and blood show promise as biomarkers for early diagnosis and progression monitoring [8]
Lipidomics, a rapidly growing field of systems biology, offers an in-depth examination of lipid species and their dynamic changes in both healthy and diseased conditions [2]. This comprehensive analytical approach has emerged as a powerful tool for identifying novel biomarkers for a diverse range of clinical diseases and disorders, including metabolic disorders, cardiovascular diseases, neurodegenerative diseases, cancer, and inflammatory conditions [2]. Lipids are increasingly understood to be bioactive molecules that regulate critical biological processes including inflammation, metabolic homeostasis, and cellular signalling [2]. The technological improvements in chromatography, high-resolution mass spectrometry, and bioinformatics over recent years have made it possible to perform global lipidomics analyses, allowing the concomitant detection, identification, and relative quantification of hundreds of lipid species [9]. However, the routine integration of lipidomics into clinical practice and biomarker validation faces significant challenges related to inter-laboratory variability, data standardization, lack of defined procedures, and insufficient clinical validation [2]. This technical support center article addresses these reproducibility challenges by providing detailed troubleshooting guides and frequently asked questions to support researchers, scientists, and drug development professionals in implementing robust and reproducible lipidomics workflows.
Lipidomics Workflow: From Sample Preparation to Data Interpretation
The lipidomics workflow is a complex and intricate process that encompasses the interdisciplinary intersection of chemistry, biology, computer science, and medicine [10]. Each step is crucial not only for ensuring the accuracy and reliability of experimental results but also for deepening our understanding of lipid metabolic networks. The schematic below illustrates the comprehensive workflow from sample collection to final data interpretation, highlighting key stages where challenges frequently arise.
Troubleshooting Guides for Common Lipidomics Workflow Challenges
Pre-Analytical Phase: Sample Collection and Lipid Extraction
Problem: Inconsistent sample quality leading to unreliable results Solution: Implement standardized sample collection protocols. For plasma and serum samples, maintain consistent clotting times (30 minutes for serum), centrifugation conditions (2000 × g for 15 minutes at 4°C), and immediate storage at -80°C. Add antioxidant preservatives such as butylated hydroxytoluene (BHT, 0.01%) to prevent lipid oxidation during processing [9].
Problem: Incomplete or biased lipid extraction Solution: Use validated extraction methods with appropriate solvent systems. The Folch (chloroform:methanol 2:1 v/v) and Bligh & Dyer (chloroform:methanol:water 1:2:0.8 v/v/v) methods remain gold standards. Ensure consistent sample-to-solvent ratios (1:20 for Folch) and pH control. Include internal standards before extraction to monitor recovery and matrix effects [10].
Analytical Phase: Chromatographic Separation and Mass Spectrometry
Problem: Poor chromatographic separation leading to co-elution Solution: Optimize LC conditions based on lipid classes. For reversed-phase separation of non-polar lipids, use C8 or C18 columns with acetonitrile-isopropanol-water gradients. For comprehensive polar lipid analysis, employ hydrophilic interaction liquid chromatography. Maintain column temperature (45-55°C) for retention time stability [9].
Problem: Ion suppression and signal instability Solution: Implement quality control samples including pooled quality control (QC) samples, blank injections, and system suitability standards. Use internal standards for each major lipid class to correct for ion suppression. Monitor signal intensity drift (<20% RSD) and retention time shift (<0.1 min) throughout the analytical sequence [11].
Data Processing and Analysis: From Raw Data to Biological Interpretation
Problem: Inconsistent lipid identification across software platforms Solution: A critical study demonstrated that different lipidomics software platforms show alarmingly low agreement in lipid identifications, with just 14.0% identification agreement when analyzing identical LC-MS spectra using default settings [12]. To address this:
- Validate identifications across both positive and negative ionization modes
- Perform manual curation of MS/MS spectra and retention time alignment
- Use orthogonal identification criteria including accurate mass (<5 ppm error), MS/MS spectral matching, and retention time prediction models
- Implement consensus approaches across multiple software platforms [12]
Problem: Batch effects and technical variability Solution: Apply advanced normalization and batch correction methods. Use quality control-based correction algorithms such as LOESS (Locally Estimated Scatterplot Smoothing) and SERRF (Systematic Error Removal using Random Forest) [11]. Incorporate internal standards for each lipid class to correct for technical variation. Design analytical batches with balanced sample groups and regular QC injections (every 6-10 samples) [11].
Problem: Missing data points in lipidomic datasets Solution: Investigate the underlying causes of missingness before applying imputation. For data missing completely at random, use probabilistic imputation methods. For data missing not at random (due to biological absence or below detection limit), apply left-censored imputation approaches. Never apply imputation methods blindly without understanding the missingness mechanism [11].
Frequently Asked Questions (FAQs) on Lipidomics Workflows
Q1: What are the key differences between untargeted, targeted, and pseudo-targeted lipidomics approaches?
A1: The selection of an appropriate analytical strategy is crucial for successful lipidomics studies [10]. The table below compares the three main approaches:
| Parameter | Untargeted Lipidomics | Targeted Lipidomics | Pseudo-targeted Lipidomics |
|---|---|---|---|
| Objective | Comprehensive discovery of altered lipids [10] | Precise quantification of specific lipids [10] | High coverage with quantitative accuracy [10] |
| Workflow | Global profiling without prior bias [10] | Pre-defined lipid panel analysis [10] | Uses untargeted data to develop targeted methods [10] |
| MS Platform | Q-TOF, Orbitrap [10] | Triple quadrupole (QQQ) [10] | Combination of HRMS and QQQ [10] |
| Acquisition Mode | DDA, DIA [10] | MRM, PRM [10] | MRM with extended panels [10] |
| Quantitation | Relative quantification [10] | Absolute quantification [10] | Improved quantitative accuracy [10] |
| Applications | Biomarker discovery, pathway analysis [10] | Clinical validation, targeted assays [10] | Comprehensive metabolic characterization [10] |
Q2: How can we improve reproducibility in lipid identification across different laboratories?
A2: Improving reproducibility requires standardized workflows and cross-validation practices:
- Adopt Lipidomics Standards Initiative (LSI) guidelines for reporting lipidomics data [11]
- Use common reference materials and standardized protocols for sample preparation
- Implement system suitability tests with quality control standards before each batch
- Perform inter-laboratory cross-validation studies using standardized samples
- Apply data-driven outlier detection and machine learning approaches to identify problematic identifications [12]
Q3: What visualization tools are most effective for interpreting lipidomics data?
A3: Effective visualization is key in lipidomics for revealing patterns, trends, and potential outliers [11]. Recommended approaches include:
- Use violin plots or adjusted box plots instead of traditional bar charts to depict data distributions, especially for skewed data common in lipidomics [11]
- Employ specialized visualizations like lipid maps and fatty acyl-chain plots to reveal trends within lipid classes and fatty acid modifications [11]
- Implement dendrogram-heatmap combinations for interpreting quantitative bulk data and sample clustering patterns [11]
- Apply PCA and Uniform Manifold Approximation and Projection (UMAP) for unsupervised data exploration [11]
- Utilize volcano plots for visualizing significantly altered lipids in case-control studies [11]
Q4: What computational tools are available for lipidomics data processing and analysis?
A4: The field has developed comprehensive tools in both R and Python for statistical processing and visualization:
- R packages: ggpubr, tidyplots, ggplot2, ComplexHeatmap, ggtree, and mixOmics [11]
- Python libraries: seaborn and matplotlib for flexible and publication-ready visualizations [11]
- Lipid identification software: MS DIAL and Lipostar, though these show significant variability (only 14.0% identification agreement) requiring manual validation [12]
- Specialized resources: GitBook with complete code examples for lipidomics data analysis (https://laboratory-of-lipid-metabolism-a.gitbook.io/omics-data-visualization-in-r-and-python) [11]
Essential Research Reagents and Materials for Lipidomics
Table: Key Research Reagent Solutions for Lipidomics Workflows
| Reagent/Material | Function/Purpose | Application Notes |
|---|---|---|
| Internal Standards | Quantification normalization & recovery monitoring | Use isotopically labeled standards for each major lipid class; add before extraction [9] |
| Sample Preservation Reagents | Prevent lipid oxidation & degradation | BHT (0.01%), EDTA, nitrogen flushing for anaerobic storage [9] |
| Lipid Extraction Solvents | Lipid isolation from matrices | Chloroform:methanol (Folch), methyl-tert-butyl ether (MTBE) methods; HPLC grade with stabilizers [10] |
| Chromatography Columns | Lipid separation by class & molecular species | C18 for reversed-phase, HILIC for polar lipids; maintain temperature control [9] |
| Mobile Phase Additives | Enhance ionization & separation | Ammonium acetate/formate (5-10 mM), acetic/formic acid (0.1%); LC-MS grade [9] |
| Quality Control Materials | Monitor instrument performance & reproducibility | NIST SRM 1950 plasma, pooled study samples, custom QC pools [11] |
Data Processing Workflow: From Raw Spectra to Biological Insights
The computational workflow for lipidomics data involves multiple critical steps that transform raw spectral data into biologically meaningful information. The following diagram outlines the key stages and decision points in this process, emphasizing steps that impact reproducibility.
Future Perspectives: Addressing Reproducibility Challenges in Lipidomics
The lipidomics field continues to evolve with promising approaches to enhance reproducibility and clinical translation. Key developments include:
Artificial Intelligence and Machine Learning: Implementation of AI-driven annotation tools for improved lipid identification and reduced false positives [11]. Support vector machine regression combined with leave-one-out cross-validation has shown promise in detecting outliers and improving identification confidence [12].
Standardization Initiatives: The Lipidomics Standards Initiative (LSI) and Metabolomics Society guidelines provide frameworks for standardized reporting and methodology [11]. Adoption of these standards across laboratories is critical for comparability of results.
Integrated Multi-omics Approaches: Combining lipidomics with genomics, transcriptomics, and proteomics to validate findings through convergent evidence across biological layers [10]. This integrated approach helps distinguish true biological signals from technical artifacts.
Advanced Quality Control Systems: Development of real-time quality control feedback systems that monitor instrument performance and automatically flag analytical batches that deviate from predefined quality metrics [11].
Despite these advancements, the manual curation of lipid identifications remains essential. As one study emphasized, "manual curation of spectra and lipidomics software outputs is necessary to reduce identification errors caused by closely related lipids and co-elution issues" [12]. This human oversight, combined with technological improvements, represents the most promising path forward for reliable lipid biomarker discovery and validation.
Lipids are fundamental cellular components with diverse roles in structure, energy storage, and signaling. In clinical biomarker research, phospholipids (PLs) and sphingolipids (SLs) have emerged as particularly significant classes due to their involvement in critical pathological processes. Lipidomics, the large-scale study of lipid pathways and networks, has revealed that dysregulation of these lipids is implicated in a wide range of diseases, including cancer, neurodegenerative disorders, cardiovascular conditions, and osteoarthritis [13].
The transition of lipid research from basic science to clinical applications faces substantial challenges, particularly concerning reproducibility and validation. Understanding these challenges, along with established troubleshooting methodologies, is essential for advancing reliable biomarker discovery and implementation.
â–¼ Core Analytical Challenges in Lipidomics
A primary obstacle in lipid biomarker research is the concerning lack of reproducibility across analytical platforms. Key issues and their quantitative impacts are summarized below.
Table 1: Key Reproducibility Challenges in Lipid Identification
| Challenge Area | Specific Issue | Quantitative Impact | Proposed Solution |
|---|---|---|---|
| Software Inconsistency | Different software platforms (MS DIAL, Lipostar) analyzing identical LC-MS data | 14.0% identification agreement using default settings [14] [12] | Manual curation of spectra and software outputs |
| Fragmentation Data Use | Use of MS2 spectra for improved identification | Agreement increases to only 36.1% [14] [12] | Validation across positive and negative LC-MS modes |
| Retention Time Utilization | Underutilization of retention time (tR) data in software | Contributes to inconsistent peak identification and alignment [14] | Implement data-driven outlier detection and machine learning |
★ Featured Experimental Protocol: Validating Sphingolipid Biomarkers in Parkinson's Disease
The following detailed protocol is adapted from a study that identified and validated five sphingolipid metabolism-related genes (SMRGs) as potential biomarkers for Parkinson's Disease (PD) [15].
Objective
To identify and validate sphingolipid metabolism-related biomarkers for Parkinson's Disease using transcriptomic data and clinical samples.
Experimental Workflow
Step-by-Step Methodology
Data Acquisition and Preprocessing
- Source: PD-related transcriptome data were downloaded from the Gene Expression Omnibus (GEO) database.
- Samples: Utilize peripheral blood samples, which are more accessible than brain tissue and can reflect systemic physiological and pathological states. The study used datasets GSE100054 (10 PD vs. 9 healthy controls) and GSE99039 (205 PD vs. 233 healthy controls) [15].
- Gene List: A predefined list of 97 Sphingolipid Metabolism-Related Genes (SMRGs) was compiled from previous literature [15].
Identification of Differentially Expressed SMRGs
- Differential Analysis: Screen for Differentially Expressed Genes (DEGs) between PD and healthy control samples using the "limma" R package (version 3.52.4) with thresholds of |log2FC| ≥ 0.5 and adjusted p-value < 0.05 [15].
- Intersection Analysis: Obtain Differentially Expressed SMRGs (DE-SMRGs) by intersecting the list of DEGs with the list of SMRGs. The referenced study identified 14 DE-SMRGs [15].
- Functional Enrichment: Conduct functional enrichment analysis (e.g., Gene Ontology, KEGG pathways) on the DE-SMRGs using tools like the "clusterProfiler" R package (version 4.7.1) to identify involved biological processes (e.g., ceramide metabolic process) [15].
Biomarker Screening and Validation
- Protein-Protein Interaction (PPI) Network: Construct a PPI network using STRING database (version 11.5) with a confidence score threshold (e.g., 0.4). Analyze the network to identify hub genes using centrality measures like "Closeness." These hub genes (e.g., ARSB, ASAH1, GLB1, HEXB, PSAP) are defined as candidate biomarkers [15].
- Diagnostic Power Assessment: Evaluate the ability of each biomarker to distinguish PD from controls by drawing Receiver Operating Characteristic (ROC) curves and calculating the Area Under the Curve (AUC) using the "pROC" R package (version 1.18.0) [15].
- Expression Validation: Compare the expression levels of the candidate biomarkers between PD and controls in both the discovery and validation datasets (GSE100054 and GSE99039) [15].
Experimental Validation via qRT-PCR
- Technical Validation: Confirm the expression levels of the identified biomarkers (e.g., GLB1, ASAH1, PSAP) in independent clinical human samples using quantitative reverse transcription polymerase chain reaction (qRT-PCR). Consistency with bioinformatics analysis results strengthens the findings [15].
Mechanistic and Translational Exploration
- Immune Infiltration Analysis: Use algorithms like single sample gene set enrichment analysis (ssGSEA) to calculate the proportions of 28 immune cell types in PD versus control samples. Study correlations between biomarker expression and differential immune cells (e.g., macrophages) to explore immune-related mechanisms [15].
- Regulatory Network Construction: Predict targeted miRNAs of the biomarkers using databases like Starbase and construct an mRNA-miRNA regulatory network to reveal potential post-transcriptional regulation [15].
- Drug Prediction: Predict targeted drugs for the biomarkers that could be relevant for clinical treatment of PD (e.g., Chondroitin sulfate was predicted to target ARSB and HEXB simultaneously) [15].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for Sphingolipid Biomarker Research
| Item | Specification / Example | Function in Protocol |
|---|---|---|
| Transcriptomic Datasets | GEO Accession Numbers (e.g., GSE100054, GSE99039) | Provide raw gene expression data for differential analysis [15]. |
| SMRG Gene List | 97 predefined Sphingolipid Metabolism-Related Genes | Serves as a reference list for intersecting with DEGs [15]. |
| R Packages | "limma", "clusterProfiler", "pROC", "WGCNA" | Perform statistical analysis, enrichment analysis, ROC analysis, and co-expression network analysis [15] [16]. |
| PPI Database | STRING database | Provides protein interaction data to identify hub genes [15]. |
| qRT-PCR Reagents | Primers, reverse transcriptase, fluorescent dyes | Experimentally validate gene expression levels in clinical samples [15]. |
| ssGSEA Algorithm | - | Calculates immune cell infiltration scores from gene expression data [15] [16]. |
| miRNA Database | Starbase | Predicts miRNA-mRNA interactions for network construction [15]. |
| BOC-ARG(DI-Z)-OH | Boc-Arg(di-Z)-OH|Amino Acid Derivative | Boc-Arg(di-Z)-OH is a protected L-arginine derivative for peptide synthesis and proteinase inhibitor research. For Research Use Only. Not for human use. |
| Koumine (Standard) | Koumine (Standard), MF:C20H22N2O, MW:306.4 g/mol | Chemical Reagent |
â–¼ Sphingolipid Metabolism in Disease: Key Pathways
Sphingolipids are not just structural components; they are active signaling molecules. The balance between different sphingolipid species is crucial in determining cell fate, such as in cancer progression.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: Our lipidomics software identifies different lipid species from the same raw data file than my colleague's software. What is the root cause and how can we resolve this?
A: This is a documented reproducibility challenge. The root cause includes:
- Software-Specific Algorithms: Different platforms use proprietary algorithms for baseline correction, peak identification, and spectral alignment [14].
- Lipid Library Differences: Platforms may rely on different lipid databases (e.g., LipidBlast, LipidMAPS), leading to conflicting identifications [14].
- Solution: Do not rely solely on default "top hit" identifications. Implement a rigorous manual curation process for spectra. Validate identifications across both positive and negative LC-MS modes if possible. As a quality control step, consider using a machine learning-based outlier detection (e.g., support vector machine regression) to flag potential false positives [14] [12].
Q2: How can I determine if a detected lipid change is biologically relevant or just a statistical artifact?
A: To minimize false discoveries:
- Control for Multiplicity: When analyzing thousands of lipid species, use statistical corrections for multiple testing (e.g., False Discovery Rate - FDR) to control the number of false positives [17] [18].
- Account for Biological Variation: Use mixed-effects models if your study design includes multiple observations from the same subject (e.g., longitudinal samples, multiple tumors from one patient) to account for within-subject correlation. Ignoring this can inflate type I error and produce spurious results [17].
- Independent Validation: The most crucial step is to validate your findings in an independent set of samples or a separate cohort [18].
Q3: What is the evidence for phospholipids and sphingolipids as clinically useful biomarkers?
A: Growing evidence from lipidomic profiling supports their clinical relevance:
- Osteoarthritis (OA): Specific PL and SL species are significantly elevated in the serum of patients with early-stage OA (eOA), even before radiologic detection is possible. Serum levels were 3–12 times higher than in synovial fluid, suggesting a systemic response to the local joint disease [19].
- Parkinson's Disease (PD): Five sphingolipid metabolism-related genes (ARSB, ASAH1, GLB1, HEXB, PSAP) were identified as potential biomarkers, with validated expression changes in clinical human samples. These biomarkers are also linked to immune mechanisms like macrophage infiltration in PD [15].
- Cancer: Sphingolipid-related genes can be used to construct prognostic models for cancers like breast cancer. The ceramide/S1P "rheostat" is a key pathway where the balance between these opposing signals influences tumor cell proliferation, migration, and invasion [16].
Q4: How many lipid species should I expect to identify in a typical sample, and why does direct infusion give fewer IDs?
A:
- Expected Identifications: The number varies greatly by sample type, volume, and ion mode. For example, you might identify between 100 to 1,000 lipids in samples ranging from 1 million yeast cells to 80 µL of human plasma extract [20].
- Direct Infusion Limitations: LipidSearch and similar software are less accurate for direct infusion analysis of complex mixtures. This is because several overlapping precursor ions may be co-isolated and co-fragmented, leading to mixture MS2 spectra and lower identification accuracy and numbers. LC-MS separation is strongly recommended for complex samples [20].
Troubleshooting Guides
Guide: Addressing Software Disagreement in Lipid Identification
Problem: Different lipidomics software platforms (e.g., MS DIAL, Lipostar) provide conflicting lipid identifications from the same raw LC-MS dataset, leading to irreproducible results and hindering biomarker discovery.
Explanation: A 2024 study directly compared two popular open-access platforms, MS DIAL and Lipostar, processing identical LC-MS spectral files from a PANC-1 cell line lipid extract. The analysis revealed a critical lack of consensus between the software outputs [14].
Solutions:
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1. Quantify Disagreement | Process identical raw data with multiple software platforms and cross-reference the lists of identified lipids. | Benchmark the scale of the problem. In the referenced study, only 14.0% of lipid identifications agreed when using MS1 data with default settings. Agreement improved to 36.1% when using MS2 fragmentation data, but this remains a significant gap [14]. |
| 2. Mandate Manual Curation | Visually inspect MS2 spectra for top-hit identifications. Check for key fragment ions, signal-to-noise ratios, and co-elution of other compounds. | Software algorithms can be misled by closely related lipids or co-eluting species. Manual verification is the most effective way to reduce false positives. This is a required step, not an optional one [14] [12]. |
| 3. Validate Across Modes | Acquire and process data in both positive and negative ionization modes for your sample. | Many lipids ionize more efficiently in one mode. Confirming an identification in both modes dramatically increases confidence in the result [14]. |
| 4. Implement ML-Based QC | Use a data-driven outlier detection method, such as Support Vector Machine (SVM) regression with Leave-One-Out Cross-Validation (LOOCV). | This machine learning approach can flag lipid identifications with aberrant retention time behavior for further inspection, identifying potential false positives that may slip through initial processing [14]. |
Guide: Improving Analytical Reproducibility Across Batches and Labs
Problem: Lipidomic data suffers from batch effects, instrument variability, and a lack of standardized protocols, making it difficult to reproduce findings in different laboratories or at different times.
Explanation: Reproducibility is hampered by biological variability, lipid structural diversity, inconsistent sample processing, and a lack of defined procedures. One inter-laboratory comparison found only about 40% agreement in post-processed lipid features [14] [1].
Solutions:
| Step | Action | Rationale & Technical Details |
|---|---|---|
| 1. Plan the Sequence | Use a randomized injection order and include Quality Control (QC) samples—pooled from all samples—throughout the acquisition sequence. | A well-planned sequence with frequent QCs is essential for detecting and correcting for technical noise and systematic drift [11]. |
| 2. Apply Batch Correction | Use advanced algorithms like LOESS (Locally Estimated Scatterplot Smoothing) or SERRF (Systematic Error Removal using Random Forest) on the QC data. | These algorithms model and remove systematic technical variance from the entire dataset, significantly improving data quality and cross-batch comparability [11]. |
| 3. Handle Missing Data | Investigate the cause of missing values before applying imputation. Avoid blind imputation. | Values can be Missing Completely at Random (MCAR), at Random (MAR), or Not at Random (MNAR). The appropriate imputation method (e.g., k-nearest neighbors, minimum value) depends on the underlying cause [11]. |
| 4. Normalize Carefully | Prioritize pre-acquisition normalization using internal standards (e.g., deuterated lipids like the Avanti EquiSPLASH LIPIDOMIX standard). | This accounts for analytical response factors, extraction efficiency, and instrument variability. For post-acquisition, use standards-based normalization where possible [14] [11]. |
Frequently Asked Questions (FAQs)
Q1: Why do my lipid identifications differ so much when I use MS DIAL versus Lipostar, even with the same raw data?
A: The core issue lies in the proprietary algorithms, peak-picking logic, and default lipid libraries (e.g., LipidBlast, LipidMAPS) used by each platform. A 2024 benchmark study demonstrated that using default settings, the agreement between MS DIAL and Lipostar can be as low as 14.0% for MS1 data. Even with more confident MS2 data, agreement only reaches 36.1%. This highlights that software output is not ground truth and requires manual curation [14] [12].
Q2: What is the minimum validation required for a confident lipid identification?
A: Following the evolving guidelines of the Lipidomics Standards Initiative (LSI), a confident identification should include [14] [1]:
- MS1 Accurate Mass: Match within a specified ppm error (e.g., < 5 ppm).
- MS2 Spectral Match: MS2 spectrum should match a reference standard or library entry.
- Chromatographic Retention Time: Retention time should align with a authentic standard analyzed under identical LC conditions.
- Ionization Mode Confirmation: Where possible, validate the identification in both positive and negative ionization modes.
Q3: How can I effectively visualize and explore my lipidomics data to identify patterns and outliers?
A: Move beyond simple bar charts. The field is moving towards more informative visualizations [11]:
- Distribution Plots: Use box plots with jitter or violin plots to show the full data distribution.
- Volcano Plots: To visualize the relationship between p-values and fold-change for differential analysis.
- Lipid Maps & Acyl-Chain Plots: Specialized plots that reveal trends within lipid classes and fatty acyl-chain properties.
- Dendrogram-Heatmap Combinations: Powerful for visualizing sample clustering and lipid abundance patterns.
- PCA and UMAP: For unsupervised exploration to reveal sample groupings and potential outliers.
Q4: We have identified a promising lipid biomarker signature. What are the key steps to ensure it is robust and translatable?
A: Transitioning from a discovery signature to a validated biomarker requires rigorous steps [1] [21]:
- Independent Cohort Validation: Confirm the signature's performance in a completely separate, well-designed cohort that reflects the intended-use population.
- Multi-Center Validation: Demonstrate that the signature is reproducible across different clinical sites and analytical laboratories.
- Assay Development: Translate the lipidomic signature into a scalable, targeted, and CLIA-validated assay suitable for clinical settings.
- Integration with Clinical Data: Combine the lipid signature with established clinical variables or other omics data (e.g., proteomics) to improve diagnostic power, as demonstrated in a recent ovarian cancer study [22].
Experimental Protocols
Detailed Methodology: Cross-Platform Software Comparison
This protocol is adapted from a 2024 case study that quantified the reproducibility gap between lipidomics software [14].
1. Sample Preparation:
- Cell Line: Human pancreatic adenocarcinoma (PANC-1).
- Lipid Extraction: Modified Folch extraction using a chilled methanol/chloroform (1:2 v/v) solution, supplemented with 0.01% butylated hydroxytoluene (BHT) to prevent oxidation.
- Internal Standard: Add a quantitative MS internal standard (e.g., Avanti EquiSPLASH LIPIDOMIX) to a final concentration of 16 ng/mL.
2. LC-MS Analysis:
- Instrumentation: UPLC system coupled to a ZenoToF 7600 mass spectrometer (or equivalent high-resolution instrument).
- Column: Luna Omega 3 µm polar C18 (50 × 0.3 mm).
- Mobile Phase: A) 60:40 Acetonitrile/Water; B) 85:10:5 Isopropanol/Water/Acetonitrile. Both supplemented with 10 mM ammonium formate and 0.1% formic acid.
- Gradient:
0 – 0.5 min: 40% B0.5 – 5 min: Ramp to 99% B5 – 10 min: Hold at 99% B10 – 12.5 min: Re-equilibrate to 40% B12.5 – 15 min: Hold at 40% B
- Flow Rate: 8 µL/min.
- Injection Volume: 5 µL.
- Ionization Mode: Electrospray Ionization (ESI), positive mode.
3. Data Processing:
- Software Platforms: Process the identical set of raw spectral files (.wiff, .d, or other format) in both MS DIAL (v4.9 or newer) and Lipostar (v2.1 or newer).
- Settings: Use default parameters for each software initially to simulate a "out-of-the-box" experience for new users. Key settings should include:
- Mass Accuracy: 5 ppm (or as recommended for your instrument).
- Retention Time Tolerance: 0.1 min.
- Peak Width: Automatically detected.
- Identification Score Threshold: >80%.
- Output: Export the final aligned lipid identification tables from each software, including lipid name, formula, class, and aligned retention time.
4. Data Comparison:
- Lipid identifications are considered to be in agreement only if the lipid formula, lipid class, and aligned retention time (within a 5-second window) are identical between MS DIAL and Lipostar.
- Calculate the percentage agreement as:
(Number of Agreed Identifications / Total Number of Unique Identifications) * 100.
Protocol: Implementing a Data-Driven QC Step with Machine Learning
This protocol outlines the SVM-based outlier detection method described in the same 2024 study [14].
1. Input Data Preparation:
- From your lipidomics software output, create a .csv file containing the following columns for each putative lipid identification:
- Chemical formula of the parent molecule
- Lipid class
- Experimental retention time (tR)
- MS1 and MS2 identification status
- Pre-filtering: Exclude lipids with a retention time below 1 minute (or the time of your solvent front), as they have no meaningful column interaction.
2. Model Training and Prediction:
- Algorithm: Support Vector Machine (SVM) Regression.
- Validation: Use Leave-One-Out Cross-Validation (LOOCV).
- Dependent Variable: The experimental retention time (tR).
- Independent Variables: Features derived from the lipid's chemical structure and class that are predictive of tR.
- Process: The model is trained to predict the expected tR for each lipid based on its chemical properties. Lipids whose experimental tR is a significant outlier from the model's prediction are flagged for manual review.
Visualization of Workflows and Relationships
Lipid Identification Reproducibility Gap
Lipidomics Data Analysis & Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application | Key Details |
|---|---|---|
| Avanti EquiSPLASH LIPIDOMIX | A quantitative mass spectrometry internal standard containing a mixture of deuterated lipids across multiple classes. | Used for pre-acquisition normalization to account for extraction efficiency, instrument response, and matrix effects. Added prior to lipid extraction [14]. |
| Butylated Hydroxytoluene (BHT) | An antioxidant added to lipid extraction solvents. | Prevents oxidation of unsaturated lipids during the extraction and storage process, preserving the native lipid profile [14]. |
| Ammonium Formate / Formic Acid | Common mobile phase additives in LC-MS. | Ammonium formate promotes efficient ionization in ESI-MS. Formic acid helps with protonation in positive ion mode, improving signal for many lipid classes [14]. |
| QC Pooled Sample | A quality control sample created by pooling a small aliquot of every biological sample in the study. | Injected repeatedly throughout the LC-MS sequence to monitor instrument stability, correct for batch effects, and assess data quality [11]. |
| R and Python Scripts (GitBook) | Open-source code for statistical processing, normalization, and visualization of lipidomics data. | Provides standardized, reproducible workflows for data analysis, moving away from ad-hoc choices. Includes modules for batch correction (SERRF), PCA, and advanced plots [11]. |
| GW-406381 | GW-406381, CAS:537697-89-5, MF:C21H19N3O3S, MW:393.5 g/mol | Chemical Reagent |
| Isoscabertopin | Isoscabertopin, MF:C20H22O6, MW:358.4 g/mol | Chemical Reagent |
Diagnostic Lipidomic Signature for Pediatric Inflammatory Bowel Disease (IBD)
A 2024 study identified and validated a blood-based diagnostic lipidomic signature for pediatric inflammatory bowel disease (IBD) [23] [24]. This signature, comprising just two molecular lipids, demonstrated superior diagnostic performance compared to high-sensitivity C-reactive protein (hs-CRP) and performed comparably to fecal calprotectin, a standard marker of gastrointestinal inflammation [23].
Table 1: Diagnostic Performance of the Pediatric IBD Lipidomic Signature
| Biomarker | Lipid Species | Concentration Change in IBD | Comparison to hs-CRP | Comparison to Fecal Calprotectin |
|---|---|---|---|---|
| 2-Lipid Signature | Lactosyl ceramide (d18:1/16:0) | Increased | Improved diagnostic prediction | No substantial difference in performance |
| Phosphatidylcholine (18:0p/22:6) | Decreased | Adding hs-CRP to signature did not improve performance |
The study analyzed blood samples from a discovery cohort and validated the findings in an independent inception cohort, confirming the results in a third pediatric cohort [23] [24]. The signature's translation into a scalable blood test has the potential to support clinical decision-making by providing a reliable, easily obtained biomarker [23].
Detailed Experimental Protocol
The following workflow outlines the key experimental steps for identifying and validating the lipidomic signature, from cohort design to data analysis.
Key Methodological Details:
- Cohorts: The study used three independent pediatric cohorts: a discovery cohort (n=94), a validation cohort (n=117), and a confirmation cohort (n=263). All IBD patients were newly diagnosed and treatment-naïve, and were compared to age-comparable symptomatic non-IBD controls [23].
- Sample Preparation: Blood samples were collected, and plasma or serum was isolated. Proper pre-analytical handling is critical; samples should be immediately processed or frozen at -80°C to prevent enzymatic degradation of lipids, such as the generation of lysophospholipids [25]. Internal standards were likely added prior to lipid extraction for accurate quantification, as this is considered a best practice [25] [26].
- Lipid Extraction and Analysis: Lipids were extracted from plasma/serum. While the specific method was not detailed, common approaches include liquid-liquid extraction methods like Bligh & Dyer or MTBE-based protocols, which are considered the gold standard [25] [26]. Lipidomic analysis was performed using mass spectrometry-based techniques, likely liquid chromatography-mass spectrometry (LC-MS), which provides high sensitivity and specificity for lipid identification and quantification [23] [26].
- Data Processing and Statistical Analysis: Raw MS data were processed using software for peak identification, alignment, and quantification. The specific two-lipid signature was identified through statistical analysis comparing the lipid profiles of IBD patients and controls. Best practices for data analysis include handling missing values, normalization to correct for unwanted variation, and the use of multivariate statistics [27].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Lipidomics Biomarker Studies
| Item / Reagent | Function / Application | Key Considerations |
|---|---|---|
| Internal Standards (IS) | Corrects for variability in extraction and analysis; enables absolute quantification. | Use stable isotope-labeled IS for each lipid class of interest. Add prior to extraction [25] [26]. |
| Chloroform & Methanol | Primary solvents for biphasic liquid-liquid lipid extraction (e.g., Folch, Bligh & Dyer). | Chloroform is hazardous. MTBE is a less toxic alternative for some protocols [25] [26]. |
| Mass Spectrometer | Identification and quantification of individual lipid species. | LC-MS/MS systems are widely used. High mass resolution (>75,000) helps avoid overlaps [26]. |
| Chromatography Column | Separates lipid species by class or within class prior to MS detection. | Reversed-phase C18 columns are common for separating lipid species [28]. |
| Quality Control (QC) Samples | Monitors instrument performance and technical variability during sequence. | Use pooled samples from all study samples; essential for batch effect correction [27]. |
| Data Processing Software | Converts raw MS data into identified and quantified lipid species. | Platforms include MS DIAL, Lipostar. Manual curation of results is critical due to low inter-software reproducibility [28]. |
| Asatone | Asatone, MF:C24H32O8, MW:448.5 g/mol | Chemical Reagent |
| D-(+)-Cellotetraose | D-(+)-Cellotetraose, MF:C24H42O21, MW:666.6 g/mol | Chemical Reagent |
Lipidomic Biomarkers in Osteonecrosis
At the time of this writing, the provided search results do not contain specific information on successful lipidomic signatures for osteonecrosis. Research in this area may be emerging but is not captured in the current search. For this field, the general principles, challenges, and best practices outlined in this document serve as a foundational guide.
Frequently Asked Questions & Troubleshooting
Q1: Our lipidomics software outputs are inconsistent. How can we improve the confidence of our lipid identifications?
A: Inconsistent identification across different software platforms is a major challenge. One study found only 14-36% agreement between popular platforms like MS DIAL and Lipostar, even when using identical data [28].
- Multi-platform Validation: Process your data with more than one software tool and manually curate lipids that are consistently identified.
- Leverage Multiple Data Dimensions: Do not rely solely on mass-to-charge ratio (m/z). Use MS/MS fragmentation spectra and retention time (RT) matching to authentic standards, if available [25] [28].
- Manual Curation: Visually inspect MS2 spectra to confirm fragment ions match the proposed lipid structure and rule out co-eluting interferences [28].
- Follow Reporting Standards: Adhere to the Lipidomics Standards Initiative (LSI) guidelines for reporting lipid data, clearly stating the level of identification confidence [25].
Q2: We see high variability in our lipid measurements. What are the critical pre-analytical steps to control?
A: Pre-analytical factors are a primary source of variability.
- Sample Stability: Enzymatic activity continues after sampling. Immediately freeze samples in liquid nitrogen (tissues) or at -80°C (biofluids) [25] [26].
- Control Lipolysis: Lipids like lysophosphatidic acid (LPA) and sphingosine-1-phosphate (S1P) are generated artificially after blood draw. Special protocols, such as acidified Bligh & Dyer extraction, are required to preserve in vivo concentrations [25].
- Standardize Extraction: Add a cocktail of internal standards before the extraction step to account for recovery differences. Choose an extraction method (e.g., Folch, Bligh & Dyer, MTBE) appropriate for your lipid classes of interest, as recovery can vary [25] [26].
Q3: How should we handle missing values in our lipidomics dataset before statistical analysis?
A: Missing values are common, often because a lipid's abundance is below the limit of detection (LOD).
- Filter First: Remove lipid species with a high percentage of missing values (e.g., >35%) across all samples [27].
- Impute Intelligently: Use imputation methods suitable for the nature of the missingness. A common and effective strategy for values missing not at random (MNAR, e.g., below LOD) is to impute with a small constant value, such as a percentage of the minimum concentration for that lipid. For data missing at random, k-nearest neighbors (kNN) or random forest imputation are often recommended [27].
Q4: What are the biggest hurdles in translating a discovered lipidomic signature, like the pediatric IBD signature, into a clinically approved test?
A: The path from discovery to clinic is challenging [1] [2].
- Reproducibility and Standardization: The lack of standardized protocols across labs leads to inter-laboratory variability. Analytical techniques and results must be harmonized [1] [25] [2].
- Multi-Center Validation: A signature must be validated in large, independent, and multi-center cohorts that reflect the intended-use population. This is often lacking in early-stage studies [1].
- Regulatory Hurdles: The regulatory framework for complex lipidomic biomarkers is still evolving. Demonstrating analytical validity, clinical validity, and clinical utility to regulatory bodies like the FDA is a complex process [1]. Currently, very few lipid-based tests are FDA-approved.
Methodological Frameworks and Analytical Strategies for Robust Lipidomics
Lipidomics, the large-scale study of cellular lipids, faces significant challenges in biomarker validation and reproducibility. Selecting the appropriate analytical approach—untargeted or targeted lipidomics—is critical for generating reliable, translatable data in disease research and drug development. This guide provides technical support for navigating these methodologies within the context of biomarker reproducibility challenges.
Core Concepts: Untargeted vs. Targeted Lipidomics
What is the fundamental difference between untargeted and targeted lipidomics?
Untargeted and targeted lipidomics differ primarily in their scope and purpose. Untargeted lipidomics is a comprehensive, discovery-oriented approach that aims to identify and measure as many lipids as possible in a sample without bias. In contrast, targeted lipidomics is a focused, quantitative method that precisely measures a predefined set of lipids, often based on prior hypotheses or untargeted findings [29]. This fundamental distinction guides all subsequent experimental design choices.
When should I choose an untargeted versus a targeted approach?
The choice depends entirely on your research question and goals [29]. The following table summarizes the core characteristics of each approach:
| Feature | Untargeted Lipidomics | Targeted Lipidomics |
|---|---|---|
| Primary Goal | Hypothesis generation, novel biomarker discovery [29] [30] | Hypothesis testing, biomarker validation [29] [30] |
| Scope | Broad, unbiased profiling of known and unknown lipids [29] | Narrow, focused on specific, pre-defined lipids [29] |
| Quantification | Relative quantification (semi-quantitative) [31] [30] | Absolute quantification using internal standards [31] [29] |
| Throughput & Workflow | Complex data processing, time-consuming lipid identification [31] [29] | Streamlined, high-throughput, automated data processing [31] |
| Ideal Application | Exploratory studies, discovering novel lipid pathways [29] | Clinical diagnostics, therapeutic monitoring, validating findings [29] |
Methodologies and Experimental Protocols
What are the standard experimental workflows for untargeted and targeted lipidomics?
The workflows for both methodologies involve distinct steps from sample preparation to data analysis, each optimized for its specific goal.
Untargeted Lipidomics Workflow
- Sample Preparation: Lipids are extracted from biological matrices (e.g., plasma, tissue) using solvents like methyl tert-butyl ether (MTBE) or chloroform-methanol. This step aims for global metabolite extraction to maintain a representative profile of the entire lipidome [29] [32].
- Data Acquisition: Analysis is typically performed using Liquid Chromatography-Mass Spectrometry (LC-MS). High-resolution mass spectrometers (e.g., Time-of-Flight or Orbitrap) are preferred for their ability to distinguish between thousands of features. Data-Independent Acquisition (DIA) modes, such as SWATH, are often used to comprehensively fragment all ions in a sample, ensuring no data is missed [33] [29].
- Data Processing and Lipid Identification: This is a critical and complex step. Software tools (e.g., LipidView, LipidXplorer) are used to process the large datasets. They perform peak alignment, deconvolution, and identification by matching acquired mass-to-charge ratios and fragmentation patterns against lipid databases like LIPID MAPS [33] [1]. This process often requires manual validation due to lipid complexity and potential for misidentification [31].
Targeted Lipidomics Workflow
- Sample Preparation: Lipids are extracted with solvents, but a key difference is the addition of a mixture of stable, isotopically labeled internal standards specific to the lipid classes being targeted. These standards are crucial for correcting for variations in extraction and ionization efficiency, enabling absolute quantification [31] [29] [32].
- Data Acquisition: Analysis often uses LC coupled with triple quadrupole mass spectrometers. The instrument is operated in Multiple Reaction Monitoring (MRM) mode, which monitors specific precursor-to-product ion transitions for each target lipid. This method offers high sensitivity and specificity by filtering out much of the chemical noise [31] [32]. Some platforms, like the Lipidyzer, also use Differential Mobility Spectrometry (DMS) to add another dimension of separation for isomers and isobars [31].
- Data Processing and Quantification: Data processing is more straightforward. The peak areas for each target lipid are integrated and normalized against their corresponding internal standards. Concentrations are calculated using pre-established linear calibration curves, resulting in absolute quantitative data (e.g., nmol/g) [31] [34].
Technical Performance and Reproducibility
How do the precision and accuracy of these platforms compare, and what are the implications for biomarker validation?
Cross-platform comparisons reveal key performance differences that directly impact biomarker validation. A study comparing an untargeted LC-MS approach with the targeted Lipidyzer platform on mouse plasma found both could profile over 300 lipids [31]. The quantitative performance, however, showed notable differences:
| Performance Metric | Untargeted LC-MS | Targeted Lipidyzer |
|---|---|---|
| Intra-day Precision (Median CV) | 3.1% [31] | 4.7% [31] |
| Inter-day Precision (Median CV) | 10.6% [31] | 5.0% [31] |
| Technical Repeatability (Median CV) | 6.9% [31] | 4.7% [31] |
| Accuracy (Median % Deviation) | 6.9% [31] | 13.0% [31] |
These metrics highlight a critical trade-off: while the targeted platform demonstrated superior precision (repeatability), the untargeted platform showed slightly better accuracy in this specific comparison [31]. Reproducibility remains a major hurdle in lipidomics. One analysis found that different software platforms agreed on only 14-36% of lipid identifications from identical LC-MS data, underscoring the need for standardized protocols and rigorous validation, especially in untargeted studies [1].
Frequently Asked Questions (FAQs) and Troubleshooting
We often struggle with data reproducibility in our untargeted studies. What steps can we take to improve this?
Improving reproducibility in untargeted lipidomics requires a multi-faceted approach:
- Standardize Protocols: Implement and meticulously document standardized protocols for sample collection, extraction, and data acquisition across all samples and batches.
- Use Quality Controls: Incorporate pooled quality control (QC) samples throughout your batch run to monitor instrument stability and for data normalization.
- Leverage Multi-dimensional Separation: Techniques like Differential Mobility Spectrometry (DMS) can resolve isomeric and isobaric lipids that co-elute in standard LC, reducing misidentification and improving consistency [33].
- Adopt Robust Data Processing: Use validated software and consistently apply stringent filters for identification confidence (e.g., using MS/MS spectral matching) and blank subtraction.
How can we bridge the gap between biomarker discovery and validation?
The most effective strategy is an integrative one. Use untargeted lipidomics for the initial discovery phase to identify a broad list of lipid species that are differentially regulated in your condition of interest. Then, take the most promising candidate biomarkers and develop a targeted, MRM-based method for absolute quantification in a larger, independent cohort of samples [29] [1]. This sequential approach leverages the strengths of both platforms: the breadth of untargeted and the precision of targeted.
Our targeted method seems to be reaching a saturation point for very abundant lipids. How can we address this?
Signal saturation or plateauing at high concentrations, as observed for classes like TAG and CE in the Lipidyzer platform [31], can be mitigated by:
- Sample Dilution: The simplest solution is to dilute the sample and re-inject.
- Calibration Curve Range: Ensure your calibration curves cover the entire dynamic range of your samples. You may need to exclude the highest concentration point if it consistently causes plateauing [31].
- Alternative Ionization: Explore switching ionization modes (e.g., from positive to negative) if applicable, as different lipid classes can ionize with varying efficiencies.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table lists key reagents and materials critical for successful lipidomics experiments.
| Item | Function | Key Consideration |
|---|---|---|
| Stable Isotope-Labeled Internal Standards | Enables absolute quantification in targeted methods; corrects for extraction and ionization variability [31] [29]. | Crucial for accurate quantification. Should be added at the beginning of sample preparation. |
| Methyl tert-butyl ether (MTBE) | Solvent for lipid extraction; separates lipids from proteins and other biomolecules [29] [32]. | A common choice for robust, high-recovery lipid extraction. |
| LC Columns (C18, HILIC) | Separates lipid species by hydrophobicity (C18) or by lipid class based on polar head groups (HILIC) [29] [32]. | Column choice dictates lipid separation and coverage. |
| Mass Spectrometer (Q-TOF, Orbitrap, Triple Quad) | Identifies and quantifies lipids. Q-TOF/Orbitrap for high-res untargeted; Triple Quad for sensitive targeted MRM [31] [33] [29]. | Instrument selection is fundamental to the experimental design. |
| Lipid Identification Software | Processes complex MS data; identifies lipids by matching m/z and MS/MS spectra to databases [33] [1]. | Essential for untargeted data analysis. Database quality limits identification confidence. |
| Anemarsaponin E | Anemarsaponin E, MF:C46H78O19, MW:935.1 g/mol | Chemical Reagent |
| Ganoderenic acid E | Ganoderenic acid E, MF:C30H40O8, MW:528.6 g/mol | Chemical Reagent |
Navigating the challenges of lipidomic biomarker research requires a deliberate and informed choice between untargeted and targeted strategies. By understanding their complementary strengths and limitations—where untargeted lipidomics excels in unbiased discovery and targeted lipidomics provides the quantitative rigor needed for validation—researchers can design robust workflows. Adhering to rigorous protocols and adopting an integrative approach is paramount for overcoming reproducibility hurdles and translating lipidomic findings into clinically relevant biomarkers and therapeutic targets.
FAQs on Platform Performance and Reprodubility
1. Why do my lipid identifications vary significantly between different lipidomics software platforms when processing the same dataset?
Variations arise from differences in algorithmic processing, spectral libraries, and alignment methodologies inherent to each platform. A 2024 study directly comparing MS DIAL and Lipostar processing of identical LC-MS spectra found only 14.0% identification agreement using default settings [14]. Even when utilizing fragmentation data (MS2), agreement rose only to 36.1% [14]. Key sources of discrepancy include:
- Spectral Libraries: Platforms use different libraries (e.g., LipidBlast, LipidMAPS), leading to different matching results [14].
- Co-elution and Co-fragmentation: Closely related lipids or isobaric species eluting simultaneously can lead to misinterpreted MS2 spectra [14].
- Underutilization of Retention Time (tR): Many software tools do not fully leverage tR, a critical parameter for distinguishing isobaric lipids [14].
2. What steps can I take to improve confidence in lipid identifications and ensure reproducibility for biomarker validation?
A multi-layered validation strategy is essential to close the reproducibility gap [14].
- Manual Curation: Manually inspect spectral data, including peak shape and fragmentation patterns, to verify software-generated identifications [14].
- Multi-mode Chromatography: Validate identifications across both positive and negative LC-MS modes to confirm lipid class and acyl chain composition [35].
- Leverage Retention Time: Use experimentally derived or predicted retention times to support identifications and discriminate isobars [35].
- Implement Quality Controls: Use internal standards for normalization and monitor analytical precision. One protocol using internal standard normalization achieved relative standard deviations of 5-6% in serum analyses [36].
3. How can I optimize MS/MS fragmentation for confident annotation of phospholipid and sphingolipid classes?
Optimal collision energy is key to generating diagnostic fragment ions.
- For Phosphatidylcholines (PC) in negative ion mode, a collision energy ramp between 20–40 eV is suitable for generating diagnostic ions, including demethylated phosphocholine ions (e.g., m/z 168.0423) and carboxylate ions from fatty acyl chains [35].
- The negative ion mode is particularly valuable for identifying fatty acyl chains across phospholipid subclasses (PE, PI, PS, PG, PA) and can help determine their sn-1/sn-2 positions on the glycerol backbone based on carboxylate ion intensity ratios [35].
Troubleshooting Guides
Table 1: Troubleshooting Common Lipid Identification Issues
| Problem | Potential Cause | Recommended Solution |
|---|---|---|
| Low identification agreement between software platforms | Different default processing parameters and spectral libraries [14] | Manually curate outputs and align software settings where possible. Use a consensus approach from multiple platforms [14]. |
| Inconsistent retention times | Column degradation, mobile phase preparation errors, or gradient instability | Implement a rigorous column cleaning and testing schedule. Calibrate retention times using stable internal standards [36]. |
| Poor fragmentation spectra for low-abundance lipids | Insufficient precursor ion signal, improper collision energy [14] | Increase injection concentration if possible. Use stepped normalized collision energy to capture multiple fragment types [37]. |
| Poor reproducibility in quantitative results | Inconsistent sample preparation, instrument drift, lack of normalization | Use a simple, standardized extraction protocol (e.g., methanol/MTBE). Employ a suite of internal standards for normalization to achieve ~5-6% RSD [36]. |
Table 2: Quantitative Comparison of Software Identification Agreement
This table summarizes data from a case study processing identical LC-MS spectra with two software platforms [14].
| Comparison Metric | MS1 Data (Accurate Mass) | MS2 Data (Fragmentation) |
|---|---|---|
| Identification Agreement | 14.0% | 36.1% |
| Major Challenge | Inability to distinguish isobaric and co-eluting lipids without fragmentation data [14]. | Co-fragmentation of closely related lipids within the precursor ion selection window [14]. |
| Recommended Action | Require MS2 validation for all putative identifications, especially for biomarker candidates. | Perform manual curation of MS2 spectra and validate across positive and negative ionization modes [14]. |
Experimental Protocols for Enhanced Lipid Annotation
Protocol 1: Molecular Networking Coupled with Retention Time Prediction
This protocol provides a systematic approach for annotating phospholipids and sphingolipids by combining MS/MS spectral similarity with chromatographic behavior [35].
- Standard Acquisition: Analyze a mixture of 65 lipid standards to establish class-specific fragmentation patterns and define the relationship between lipid structure and retention time [35].
- Data Pre-processing: Convert LC-MS/MS data and perform feature detection (e.g., using MzMine 2) to align mass, retention time, and intensity data [35].
- Molecular Network Creation: Upload processed MS/MS data to the GNPS platform to generate a molecular network. Structurally similar lipids will cluster together based on spectral similarity [35].
- Annotation and Validation: Annotate unknown lipids within a cluster based on the annotated standard. Reinforce this annotation by comparing the experimental retention time of the unknown with the predicted retention time derived from the standard curve [35]. This method enabled the annotation of over 150 unique lipid species in a study on human corneal epithelial cells [35].
Protocol 2: A Reproducible Microscale Serum Lipidomics Workflow
This protocol is designed for high-throughput clinical applications with minimal sample consumption [36].
- Sample Extraction: Add 10 µL of serum to a simplified methanol/methyl tert-butyl ether (1:1, v/v) extraction solvent. Vortex and centrifuge to separate phases [36].
- Internal Standard Addition: Incorporate a ready-to-use internal standard mix (e.g., Avanti EquiSPLASH) at the extraction stage for normalization. A concentration of 16 ng/mL is typical [14] [36].
- LC-HRMS Analysis:
- Column: Use a reversed-phase column (e.g., Waters Acquity UPLC HSS T3, 1.8 µm, 2.1 × 100 mm).
- Gradient: Employ a water/acetonitrile (A) and isopropanol/acetonitrile (B) gradient with 10 mM ammonium formate/0.1% formic acid: 30% B to 60% B in 4.0 min, to 100% B at 9.0 min, hold until 15.0 min [36] [37].
- MS Parameters: Use a high-resolution mass spectrometer in both positive and negative ESI mode with data-dependent MS2 (ddMS2) at a resolution of 17,500 and stepped collision energies [37].
- Data Processing: Use a semi-automated script or software (e.g., Compound Discoverer) for feature alignment, normalization against internal standards, and statistical analysis [36] [37].
Workflow Visualization
This workflow highlights the necessity of using multiple software platforms and stringent manual validation steps to overcome reproducibility challenges in lipidomic biomarker discovery [14].
The Scientist's Toolkit
Table 3: Research Reagent Solutions
| Item | Function in the Experiment |
|---|---|
| Avanti EquiSPLASH LIPIDOMIX | A quantitative mass spectrometry internal standard; a mixture of deuterated lipids used for normalization and quality control [14]. |
| Methanol/MTBE (1:1, v/v) | A simplified extraction solvent protocol for simultaneous lipid and metabolite coverage from minimal serum volumes (e.g., 10 µL) [36]. |
| Ammonium Formate & Formic Acid | Mobile phase additives that enhance ionization efficiency and support the formation of [M+HCOO]â» adducts in negative ion mode for lipids like phosphatidylcholines [35] [37]. |
| Luna Omega Polar C18 / Acquity UPLC HSS T3 | Common UHPLC columns providing reversed-phase separation for complex lipid mixtures, crucial for resolving isobaric species [14] [37]. |
| LipidBlast, LipidMAPS, ALEX123 | Spectral libraries used by software platforms for matching accurate mass and MS/MS data; using multiple libraries can improve annotation coverage [14]. |
| m-PEG3-S-PEG1-C2-Boc | m-PEG3-S-PEG1-C2-Boc, MF:C16H32O6S, MW:352.5 g/mol |
| HKOCl-3 | HKOCl-3, MF:C26H14Cl2O6, MW:493.3 g/mol |
The Critical Role of Internal Standards and Quality Control in Lipid Quantification
Why are Internal Standards (IS) essential for accurate lipid quantification?
Internal Standards (IS) are chemically analogous compounds added to samples at a known concentration before lipid extraction. They are critical for accurate quantification because they correct for losses during sample preparation, matrix effects during ionization, and instrument variability.
| Function | Description | Impact on Data Quality |
|---|---|---|
| Recovery Correction | Accounts for losses during complex sample preparation steps (e.g., extraction, purification). | Improves accuracy of reported concentrations. |
| Ionization Correction | Compensates for signal suppression or enhancement caused by co-eluting compounds in the sample matrix (matrix effects). | Enhances precision and reliability of measurements. |
| Normalization | Serves as a reference point to normalize lipid species abundances, correcting for run-to-run instrument variability. | Allows for valid quantitative comparisons across large sample sets and batches. |
What are the consequences of poor Internal Standard selection or preparation?
Incorrect IS practices introduce significant errors and compromise data integrity.
| Common Error | Consequence |
|---|---|
| Incorrect IS Type | Using an IS from a different lipid class than the target analyte fails to correct for class-specific extraction efficiency and ionization. |
| Improper IS Amount | Adding too much IS can saturate the detector; adding too little fails to provide a robust signal above the noise for reliable normalization. |
| Inconsistent Addition | Failing to add the IS mixture at the same step (ideally before extraction) and with the same precision for every sample introduces uncontrolled variability. |
How should a pooled quality control (PQC) sample be used in a lipidomics study?
A Pooled Quality Control (PQC) sample is created by combining a small aliquot of every biological sample in a study. It is analyzed repeatedly throughout the batch to monitor analytical performance.
The following workflow visualizes the role of PQC and other quality controls in a typical lipid quantification experiment:
Key Uses of PQC:
- System Conditioning: The initial injections of the PQC condition the chromatographic system and column.
- Monitoring Stability: Interspersing the PQC throughout the batch (e.g., every 5-10 samples) allows you to monitor signal intensity, retention time, and peak shape stability over time.
- Data Quality Assessment: The PQC is used to perform Quality Control-based correction (like QC-RLSC) to remove non-biological, systematic drift from the data.
What quality control measures ensure data reproducibility across laboratories?
Inter-laboratory variability is a major challenge in lipidomics [14] [1]. Standardizing quality control practices is essential for reproducible biomarker discovery.
| QC Measure | Description | Role in Reproducibility |
|---|---|---|
| Surrogate QC (sQC) | A commercially available reference material (e.g., commercial pooled plasma) used as a long-term reference (LTR) across multiple batches and studies [38]. | Allows for performance benchmarking and data normalization over time and between different laboratories. |
| Long-Term Reference (LTR) | Aliquots of a stable, well-characterized sample pool analyzed in every batch alongside the PQC [38]. | Tracks analytical performance over weeks, months, or years, ensuring method robustness. |
| Blanks | Samples without biological matrix (e.g., solvent) processed alongside experimental samples. | Identifies background contamination and carryover. |
| Standard Operating Procedures (SOPs) | Documented, detailed protocols for every step from sample collection to data processing. | Minimizes introduction of pre-analytical and analytical variability, a key source of irreproducibility. |
Why do different software platforms report different lipids from the same data, and how can this be resolved?
A 2024 study directly comparing two popular platforms, MS DIAL and Lipostar, found alarmingly low identification agreement—only 14.0% using MS1 data and 36.1% even when using MS2 fragmentation data from identical LC-MS spectra [14].
Root Causes:
- Different Algorithms & Libraries: Platforms use unique algorithms for peak picking, alignment, and identification, and may rely on different lipid databases (e.g., LipidBlast, LipidMAPS) [14].
- Co-elution and Co-fragmentation: MS2 spectra can be contaminated by closely related lipids or isomers that are co-isolated and co-fragmented, leading to misidentification [14] [20].
- Underutilization of Retention Time: Many software tools do not fully leverage retention time (tR) information, a rich source of identification confidence [14].
Troubleshooting Guide: Follow this decision path to resolve conflicting software identifications:
Solutions:
- Mandatory Manual Curation: Do not rely on software "top hits." Visually inspect MS2 spectra to confirm fragment ions match the putative lipid identification [14].
- Cross-Mode Validation: Confirm identifications by analyzing samples in both positive and negative ionization modes where feasible [14].
- Leverage Retention Time: Use retention time models or databases to check if the lipid elutes at an expected time for the chromatographic method [14] [20].
- Data-Driven Outlier Detection: Employ machine learning approaches, such as Support Vector Machine (SVM) regression, to identify outlier identifications that may be false positives [14].
Experimental Protocol: Implementing a Robust QC Strategy for Targeted Lipid Quantification
This protocol outlines the key steps for integrating internal standards and quality controls into a targeted lipidomics workflow using UHPLC-MS/MS.
1. Materials and Reagents
- Internal Standard Mixture: A commercially available quantitative standard like the Avanti EquiSPLASH LIPIDOMIX, which contains deuterated lipids across multiple classes. Prepare a working solution in a suitable solvent like methanol or isopropanol.
- Surrogate QC (sQC): Commercially available reference plasma or a custom-made pool from a relevant biological matrix.
- Solvents: HPLC-grade or higher methanol, chloroform, isopropanol, acetonitrile, and water. Additives like ammonium formate/acetate and formic/acetic acid.
2. Sample Preparation with Internal Standards
- Thaw samples on ice and vortex.
- Aliquot a precise volume of each sample (e.g., 50 µL of plasma) into a clean glass tube.
- Add a precise volume of the Internal Standard mixture to every sample, blank, PQC, and sQC/LTR aliquot. Vortex thoroughly.
- Proceed with lipid extraction. A common method is a modified Folch extraction (using chloroform:methanol in a 2:1 ratio) or MTBE extraction [14]. After vortexing and centrifugation, collect the organic (lower) layer.
- Evaporate the organic solvent under a gentle stream of nitrogen or using a centrifugal evaporator.
- Reconstitute the dried lipid extract in a defined volume of a suitable LC-MS solvent (e.g., 1:1 isopropanol:acetonitrile). Vortex thoroughly and transfer to an LC vial.
3. LC-MS Analysis with In-Run QC
- Arrange the injection sequence to include:
- System Conditioning: 5-10 injections of PQC at the beginning.
- Batch: Samples analyzed in randomized order.
- QC Monitoring: A PQC injection after every 5-10 experimental samples.
- Long-Term Reference: An sQC/LTR injection in each batch.
- Blanks: Solvent blanks injected periodically to monitor carryover.
- Perform UHPLC-MS/MS analysis using your optimized method for targeted lipid quantification (e.g., reversed-phase C18 column, binary gradient, multiple reaction monitoring (MRM) on a triple quadrupole mass spectrometer).
4. Data Processing and QC Assessment
- Process raw data using your targeted analysis software (e.g., Skyline, MultiQuant).
- Calculate quantitative values for each target lipid by comparing the analyte response to the corresponding class-specific internal standard.
- Assess QC data: The peak areas and retention times of the internal standards in the PQC samples should have a relative standard deviation (%RSD) of <15-20% across the entire batch, confirming analytical stability.
The Scientist's Toolkit: Essential Research Reagent Solutions
| Reagent / Solution | Function |
|---|---|
| Deuterated Internal Standards (e.g., EquiSPLASH) | A mixture of stable isotope-labeled lipids across different classes for accurate, class-specific quantification [14]. |
| Pooled Quality Control (PQC) Sample | A pool of all study samples used to monitor and correct for analytical drift during a batch sequence. |
| Surrogate QC (sQC) / Long-Term Reference (LTR) | A commercially available or large-volume in-house pool used to track performance across multiple batches and studies [38]. |
| Stable Lipid Extraction Solvents (e.g., Chloroform:MeOH with BHT) | Solvents for efficient and reproducible lipid extraction. Butylated hydroxytoluene (BHT) is added as an antioxidant to prevent lipid degradation [14]. |
| Mobile Phase Additives (e.g., Ammonium Formate/Acetate) | Volatile salts and acids added to LC mobile phases to promote consistent analyte ionization and improve chromatographic separation. |
| MSA-2 dimer | MSA-2 dimer, MF:C29H28O8S2, MW:568.7 g/mol |
| Naph-EA-mal | Naph-EA-mal, MF:C22H21N3O4, MW:391.4 g/mol |
Lipidomics, the large-scale study of lipids in biological systems, has emerged as a powerful tool for identifying diagnostic and prognostic biomarkers for diseases ranging from cancer to cardiovascular disorders [13]. The integration of machine learning (ML) with lipidomic data, particularly using algorithms like Least Absolute Shrinkage and Selection Operator (LASSO) and Support Vector Machines (SVM), has significantly enhanced our ability to discover robust lipid signatures. However, this promising field faces substantial reproducibility challenges that can undermine biomarker validation. A critical study revealed that when identical LC-MS spectral data were processed through two popular lipidomics software platforms, MS DIAL and Lipostar, the agreement on lipid identifications was only 14.0% using default settings, increasing to just 36.1% even when fragmentation (MS2) data were utilized [14] [12]. This reproducibility gap represents a fundamental obstacle for researchers and drug development professionals seeking to translate lipidomic discoveries into clinically applicable biomarkers. This technical support guide addresses these challenges through targeted troubleshooting methodologies, experimental protocols, and best practices designed to enhance the reliability of ML-driven lipidomic biomarker identification.
Experimental Protocols & Workflows
Integrated Machine Learning-Lipidomics Workflow for Biomarker Discovery
The following diagram illustrates a robust experimental workflow that integrates lipidomic profiling with machine learning to enhance biomarker reproducibility:
Detailed Experimental Methodology
Sample Preparation and Lipidomics Profiling
- Sample Collection and QC: Collect biological samples (e.g., serum, plasma, tissues) following standardized protocols. For serum, collect venous blood after an appropriate fasting period, rapidly separate serum, and store immediately at -80°C to prevent lipid degradation [39] [40]. Implement a rigorous quality control (QC) strategy by pooling aliquots from each sample to create QC samples, which are analyzed intermittently throughout the LC-MS batch sequence to monitor instrument stability [41] [40].
- Lipid Extraction: Use modified Folch or Matyash extraction methods. For cells, employ a chilled methanol/chloroform (1:2 v/v) solution supplemented with 0.01% butylated hydroxytoluene (BHT) to prevent oxidation. Include an internal standard mixture (e.g., Avanti EquiSPLASH LIPIDOMIX) for quantitative accuracy [14] [40].
- LC-MS Data Acquisition: Utilize Ultra-High-Performance Liquid Chromatography coupled to mass spectrometry (UPLC-MS/MS). For comprehensive coverage, employ reversed-phase chromatography (e.g., C18 column) with a binary gradient using mobile phase A (acetonitrile/water with 10 mM ammonium formate) and phase B (isopropanol/acetonitrile with 10 mM ammonium formate) [41] [39]. Acquire data in both positive and negative ionization modes to maximize lipid coverage.
Data Preprocessing and Feature Selection
- Data Preprocessing: Convert raw data files (e.g., .raw, .d) to open formats (e.g., mzXML) using tools like ProteoWizard. Process data using software such as XCMS, MS-DIAL, or Lipostar for peak picking, alignment, retention time correction, and peak area extraction [39] [40]. Annotate lipids using databases (LIPID MAPS, LipidBlast) with a strict cutoff score (e.g., >0.3) [39].
- Lipidomic Data Matrix: The final dataset should comprise a matrix where rows represent samples, columns represent lipid species (features), and values represent peak intensities or concentrations. Include quality assurance steps: ensure >98% of lipid features in QC samples have a relative standard deviation (RSD) ≤30% [41].
- Feature Selection using ML Algorithms: Apply multiple feature selection methods to identify the most discriminatory lipid biomarkers:
- LASSO Regression: Implement with alpha=1 and set a random seed (e.g., set.seed(11)) for reproducibility. LASSO performs L1 regularization, shrinking less important coefficients to zero and selecting a parsimonious feature set [39] [42].
- SVM-Recursive Feature Elimination (SVM-RFE): Configure with 5-fold cross-validation. SVM-RFE recursively removes the least important features based on weight magnitude, optimizing model performance with a minimal feature set [43] [42].
- Random Forest: Execute with 2000 trees using Gini importance for feature ranking. Set random seed (e.g., set.seed(3)) [42].
- Boruta Algorithm: Run with parameters doTrace=2 and maxRuns=500 to identify all-relevant features by comparing original attributes with shadow features [42].
Machine Learning Model Building and Validation
- Data Splitting: Partition the dataset into training (70-80%) and testing (20-30%) sets. Use stratified splitting to maintain class distribution.
- Model Training: Train multiple classifiers on the selected features:
- Support Vector Machine (SVM): Utilize radial basis function kernel; optimize cost and gamma parameters via grid search.
- Random Forest (RF): Implement with 500-1000 trees; tune mtry parameter.
- Naive Bayes (NB): Apply with Gaussian kernel for continuous lipidomic data.
- K-Nearest Neighbors (KNN): Optimize the number of neighbors (k).
- Model Validation: Use 7-fold or 10-fold cross-validation on the training set to assess generalizability. Evaluate the final model on the held-out test set using Area Under the Receiver Operating Characteristic Curve (AUC), accuracy, sensitivity, and specificity. For example, a study on nonsyndromic cleft lip with palate (nsCLP) achieved an AUC of 0.95 using a Naive Bayes classifier with 35 lipid features [41]. Similarly, a KNN model for oral cancer diagnosis achieved an AUC of 0.978 using 13 metabolite features [39].
- Independent Validation Cohort: Validate the final lipid biomarker panel in an independent cohort using targeted lipidomics (e.g., Multiple Reaction Monitoring) to confirm diagnostic performance [41].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Our ML models achieve perfect training accuracy but perform poorly on the test set. What could be the cause and solution?
A: This indicates overfitting, commonly encountered with high-dimensional lipidomic data.
- Cause: Tree-based models (Random Forest, Decision Tree) are particularly prone to this. A study showed these models can achieve 100% training accuracy but testing accuracy below 0.8 [41].
- Solution:
- Apply Stronger Regularization: For LASSO, increase the penalty parameter (λ) to select fewer features.
- Ensemble Feature Selection: Use multiple feature selection methods (LASSO, RF, SVM-RFE) and select the consensus features. One study employed 8 feature evaluation methods combined with robust rank aggregation to identify stable biomarkers [41].
- Simplify the Model: Use Naive Bayes or Logistic Regression with L2 regularization, which are less prone to overfitting. The nsCLP study found Naive Bayes achieved the best performance without overfitting [41].
Q2: We get conflicting lipid identifications when using different software platforms. How can we improve identification confidence?
A: This is a widespread reproducibility challenge.
- Cause: Different software (MS DIAL vs. Lipostar) use distinct algorithms, lipid libraries, and alignment methodologies, leading to identification rates as low as 14-36% [14] [12].
- Solution:
- Manual Curation: Visually inspect MS2 spectra for top candidate lipids. Check for key fragment ions and neutral losses characteristic of lipid classes.
- Multi-Platform Validation: Process data through at least two software platforms and retain only consensus identifications.
- Retention Time Prediction: Utilize in-house retention time libraries or SVM-based prediction to flag outliers [14].
- Validate Identifications: Confirm lipid identities using purified standards when possible, especially for final biomarker candidates.
Q3: Our biomarker panel performs well in the discovery cohort but fails in the independent validation. What are the potential reasons?
A: This indicates lack of generalizability.
- Causes:
- Batch Effects: Technical variation between discovery and validation cohorts.
- Insufficient Sample Size: Discovery cohort too small, leading to non-representative feature selection.
- Biological Heterogeneity: Population differences between cohorts.
- Solutions:
- Batch Correction: Use ComBat or other batch correction algorithms.
- Sample Size Planning: Ensure adequate sample size (use power analysis). For lipidomics, >50 samples per group is recommended.
- Independent Validation Design: Validate in a truly independent cohort with similar demographic and clinical characteristics [41].
- Targeted Validation: Use targeted MRM-based lipidomics for validation rather than untargeted approach [41].
Troubleshooting Common Scenarios
Problem: Poor Model Performance (Low AUC) Even After Feature Selection
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| High Noise in Lipidomic Data | Check QC sample RSDs; >30% indicates issues | Improve peak picking parameters; apply more stringent blank subtraction |
| Non-Linear Relationships | Plot feature distributions; check for non-linear class boundaries | Use non-linear classifiers (SVM with RBF kernel, Random Forest) |
| Class Imbalance | Calculate class ratio in training set | Apply SMOTE oversampling or class weighting in algorithms |
Problem: Inconsistent Feature Selection Across Different Algorithms
| Observation | Implication | Action |
|---|---|---|
| Different features selected by LASSO vs. Random Forest | Method-dependent bias | Use ensemble feature selection; retain features identified by multiple methods |
| High correlation between selected features | Redundant biomarkers | Apply clustering on correlation matrix; select one representative per cluster |
| Biologically implausible lipids selected | Potential false positives | Incorporate prior biological knowledge; consult lipid databases |
Data Presentation & Visualization
Quantitative Performance of ML Algorithms in Lipidomics Studies
Table 1: Performance Metrics of Machine Learning Algorithms in Recent Lipidomics Biomarker Studies
| Disease Application | ML Algorithm | Feature Selection Method | Number of Features | Performance (AUC) | Reference |
|---|---|---|---|---|---|
| Nonsyndromic cleft lip with palate (nsCLP) | Naive Bayes | Ensemble (8 methods + RRA) | 35 | 0.95 | [41] |
| Oral cancer | K-Nearest Neighbors | LASSO | 13 | 0.978 | [39] |
| Aortic dissection | SVM, Random Forest | Boruta, LASSO, PPI | 2 (PLIN2, PLIN3) | Not specified | [42] |
| Diabetic kidney disease | Random Forest, SVM-RFE | LASSO | Not specified | Not specified | [43] |
Software Reproducibility Comparison
Table 2: Lipid Identification Reproducibility Across Software Platforms
| Software Comparison | Data Type | Identification Agreement | Key Challenges | Recommended Mitigation |
|---|---|---|---|---|
| MS DIAL vs. Lipostar | MS1 (default settings) | 14.0% | Different alignment algorithms and lipid libraries | Multi-platform validation, manual curation |
| MS DIAL vs. Lipostar | MS2 (fragmentation data) | 36.1% | Co-elution, closely related lipids | MS/MS validation, orthogonal separation |
| Any platform vs. manual curation | Mixed | Variable (often <50%) | Automated peak integration errors | Retention time prediction, outlier detection |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Essential Research Reagents and Computational Tools for ML-Lipidomics
| Category | Specific Product/Software | Function/Purpose | Key Considerations |
|---|---|---|---|
| Internal Standards | Avanti EquiSPLASH LIPIDOMIX | Quantitative accuracy across lipid classes | Ensure coverage of targeted lipid classes |
| Sample Preparation | Modified Folch reagent (CHCl3:MeOH 2:1) | Lipid extraction from biological samples | Add antioxidant (BHT) for oxidative protection |
| LC-MS Columns | Phenomenex Kinetex C18 (1.7μm, 2.1×100mm) | Lipid separation | Column chemistry affects retention of lipid classes |
| Data Processing | MS DIAL, Lipostar, XCMS | Peak picking, alignment, annotation | Reproducibility varies significantly between platforms |
| Feature Selection | glmnet (LASSO), randomForest, e1071 (SVM) | Dimensionality reduction, biomarker selection | Combine multiple methods for robust feature selection |
| Model Validation | caret R package | Cross-validation, parameter tuning | Implement stratified k-fold cross-validation |
| Lipid Databases | LIPID MAPS, LipidBlast | Lipid identification and annotation | Use for structural information and pathway mapping |
| Cinchonain IIb | Cinchonain IIb, MF:C39H32O15, MW:740.7 g/mol | Chemical Reagent | Bench Chemicals |
| Otophylloside O | Otophylloside O, MF:C56H84O20, MW:1077.3 g/mol | Chemical Reagent | Bench Chemicals |
Visualization of Reproducibility Challenges & Solutions
Software Validation Workflow for Robust Lipid Identification
The following diagram outlines a systematic approach to address lipid identification reproducibility:
Frequently Asked Questions (FAQs)
FAQ 1: Why is there such a major discrepancy in lipid identifications when I use different software platforms on the same dataset?
This is a common reproducibility challenge in lipidomics. A 2024 study directly compared two popular platforms, MS DIAL and Lipostar, processing identical LC-MS spectral data. When using default settings, the agreement on lipid identifications was only 14.0%. Even when using more reliable fragmentation (MS2) data, the agreement rose only to 36.1% [14]. These inconsistencies arise from differences in built-in algorithms for peak alignment, noise reduction, and the use of different lipid reference libraries (e.g., LipidBlast, LipidMAPS) [14].
FAQ 2: How can I improve confidence in my lipidomic biomarker identifications?
Beyond relying on software defaults, a multi-layered validation strategy is essential [14] [13]:
- Multi-Mode LC-MS: Validate identifications across both positive and negative ionization modes.
- Manual Curation: Visually inspect spectra to check for correct peak shape and isotope patterns.
- Leverage Retention Time: Use retention time (tR) as a quality control parameter; lipids with a tR below 1 minute (eluting with the solvent front) often have low identification confidence and should be treated with caution [14].
- Incorporate Machine Learning: Implement data-driven outlier detection, such as Support Vector Machine (SVM) regression, to flag potential false positives [14].
FAQ 3: What is the role of multi-omics integration in validating lipidomic biomarkers?
Integrating lipidomics with other omics data (e.g., genomics, transcriptomics, proteomics) is crucial for moving from a simple list of dysregulated lipids to a biologically meaningful context [13] [44]. This approach helps:
- Confirm Biological Relevance: By connecting a lipid biomarker to a corresponding change in a related gene or protein, you strengthen its biological plausibility.
- Reveal Underlying Mechanisms: Integration can uncover the molecular pathways and regulatory networks through which the lipid exerts its function [45].
- Improve Specificity: A multi-omics signature is often more robust and disease-specific than a lipid-only biomarker panel [44].
FAQ 4: What are the main computational strategies for integrating multi-omics data?
Integration strategies depend on how the data was generated. The table below summarizes the two primary approaches [46]:
Table: Multi-Omics Data Integration Strategies
| Integration Type | Data Source | Description | Example Tools |
|---|---|---|---|
| Matched (Vertical) | Different omics (e.g., RNA, protein) from the same cell. | The cell itself is used as an anchor to align the different data modalities. | Seurat v4, MOFA+, totalVI [46] |
| Unmatched (Diagonal) | Different omics from different cells (from the same or different studies). | A co-embedded space or manifold is created to find commonality between cells. | GLUE, Pamona, LIGER [46] |
Troubleshooting Guides
Issue: Low Reproducibility of Lipid Identifications Across Software
Problem: Your list of significant lipids changes drastically when the same raw data is processed with a different software package.
Solutions:
- Do Not Rely on Defaults: Treat software defaults as a starting point. Manually adjust parameters for peak picking, alignment, and noise reduction to match your instrument and sample type [14].
- Implement a Curation Pipeline: Develop a standard operating procedure (SOP) for your lab that mandates manual curation of all putative identifications, especially for potential biomarkers [14].
- Use Ensemble Feature Selection: When preparing data for machine learning, employ an ensemble feature selection strategy. This involves using multiple statistical and model-based methods to rank lipids, then aggregating the results to find the most robust candidates [41].
Issue: Isolating a Specific Lipid Biomarker Signature from a Complex Background
Problem: The biological signal from your candidate lipid biomarkers is weak or confounded by high biological variability and a complex matrix.
Solutions:
- Combine Untargeted and Targeted Workflows: Use an untargeted lipidomics discovery phase on a well-defined cohort to identify a wide range of candidate lipids. Then, validate the most promising candidates using targeted lipidomics (e.g., Multiple Reaction Monitoring - MRM) in a separate, independent validation cohort [41].
- Apply Robust Machine Learning Models: Use classification models to find the minimal panel of lipids that best predicts your condition of interest. Studies have shown that models like Naive Bayes can achieve high performance (AUC > 0.95) in classifying disease states based on lipidomic profiles [41].
Table: Quantitative Comparison of Lipidomics Software Agreement (2024 Study)
| Data Type | MS DIAL vs. Lipostar Identification Agreement | Key Factors Influencing Discrepancy |
|---|---|---|
| MS1 (Default Settings) | 14.0% | Different alignment algorithms, noise reduction, and library matching [14]. |
| MS2 (Fragmentation Data) | 36.1% | Co-elution of lipids, co-fragmentation, and different spectral libraries [14]. |
Experimental Protocols
Detailed Methodology: A Machine Learning-Driven Lipidomic Biomarker Discovery Pipeline
This protocol is adapted from a 2025 study that successfully identified a 3-lipid biomarker panel for prenatal diagnosis [41].
1. Sample Preparation and Untargeted Lipidomics (Discovery Phase)
- Lipid Extraction: Perform a modified Folch extraction using a chilled methanol/chloroform solution (1:2 v/v). Supplement with 0.01% butylated hydroxytoluene (BHT) to prevent oxidation [14].
- Internal Standard: Add a quantitative MS internal standard mixture (e.g., Avanti EquiSPLASH LIPIDOMIX) to enable relative quantification.
- LC-MS Analysis: Analyze samples using a reversed-phase UPLC system coupled to a high-resolution mass spectrometer (e.g., ZenoToF 7600). Operate in both positive and negative ionization modes. Use a binary gradient for separation [14] [41].
2. Data Processing and Machine Learning (Feature Selection)
- Software Processing: Process the raw spectral data (.raw files) using open-access software like MS DIAL or Lipostar. Export a list of aligned lipid features with their abundances [14].
- Stability Check: Ensure data quality by confirming that ≥98% of lipid features in quality control (QC) samples have a relative standard deviation (RSD) ≤30% [41].
- Ensemble Feature Selection:
- Apply eight different feature selection methods (e.g., based on fold change, p-value, variable importance in projection scores) to the dysregulated lipids.
- Use the Robust Rank Aggregation (RRA) algorithm to merge the results from all methods into a single, consensus-ranked list of the most important lipid features [41].
3. Model Training and Evaluation
- Train Classification Models: Input the top-ranked lipid features from the RRA list into seven different classification models (e.g., Naive Bayes, Support Vector Machine, Random Forest).
- Identify Top Model: Evaluate models using Area Under the Curve (AUC). The Naive Bayes classifier has been shown to be particularly effective for this type of data, achieving AUC values up to 0.95 without overfitting [41].
- Select Candidate Biomarkers: The lipids that contribute most to the performance of the best model are taken forward for validation.
4. Targeted Validation
- Method Translation: Develop a targeted, multiple-reaction monitoring (MRM) method on a triple quadrupole mass spectrometer for the candidate lipids.
- Independent Validation: Run the targeted method on a new, independent set of samples (the validation cohort) to confirm the diagnostic power of the biomarker panel [41].
Workflow: Lipidomic Biomarker Discovery
Workflow: Multi-Omics Integration for Context
The Scientist's Toolkit
Table: Essential Research Reagent Solutions for Lipidomic Biomarker Studies
| Reagent / Material | Function and Importance | Example / Specification |
|---|---|---|
| Quantitative Internal Standard | Enables relative quantification of lipids by correcting for instrument variability and matrix effects. | Avanti EquiSPLASH LIPIDOMIX (a mixture of deuterated lipids across several classes) [14]. |
| Antioxidant Supplement | Prevents oxidation of unsaturated lipids during extraction and storage, preserving the native lipid profile. | 0.01% Butylated Hydroxytoluene (BHT) [14]. |
| Chilled, HPLC-grade Solvents | Used for lipid extraction. Must be high-purity and chilled to maximize recovery and minimize degradation. | Modified Folch method: Methanol/Chloroform (1:2 v/v) [14]. |
| Chromatography Additives | Improves ionization efficiency and peak shape in LC-MS by controlling pH and promoting ion formation. | 10 mM Ammonium Formate and 0.1% Formic Acid in mobile phases [14]. |
| Reference Spectral Libraries | Essential for confident lipid identification by matching experimental MS2 spectra to reference data. | LipidBlast, LipidMAPS, ALEX123, METLIN [14]. |
| Gelomulide A | Gelomulide A, MF:C22H30O5, MW:374.5 g/mol | Chemical Reagent |
Identifying and Overcoming Critical Bottlenecks in Lipidomic Reproducibility
Frequently Asked Questions
Why do I get different lipid identifications when processing the same data with different software platforms? Even when using identical spectral data, different software platforms can yield vastly different results due to several factors. A 2024 study directly comparing MS DIAL and Lipostar found only 14.0% identification agreement when processing identical LC-MS spectra using default settings. This discrepancy stems from several technical factors [14] [47]:
- Different Algorithms and Libraries: Each platform uses proprietary algorithms for peak picking, alignment, and identification, and may rely on different lipid libraries (e.g., LipidBlast, LipidMAPS) [14] [48].
- Handling of Complex Data: Issues like co-elution of lipids and the presence of closely related isomers are resolved differently by each software's data processing logic [14].
- Use of MS2 and Retention Time: The level of agreement improves when using fragmentation (MS2) data (up to 36.1%), but this is still low, highlighting inconsistent use of retention time (tR) and fragmentation patterns for confident identification [14].
How can I improve consistency and confidence in my lipid identifications? Improving confidence requires a multi-layered validation strategy that goes beyond default software outputs [14] [13] [49]:
- Mandatory Manual Curation: Always manually inspect spectral data and software outputs, checking peak shapes, co-elution, and the quality of MS/MS matches [14].
- Multi-Mode Validation: Acquire and validate data in both positive and negative ionization modes to cross-verify identifications [14].
- Leverage All Data Dimensions: Make full use of retention time, collision cross section (CCS) values from ion mobility spectrometry (IMS), and high-accuracy mass measurements as additional filters [48].
- Data-Driven Quality Control: Employ machine learning and statistical outlier detection methods to flag potentially false positive identifications [14] [11].
What is the difference between targeted and untargeted platforms, and how does this affect my results? The fundamental goals of these approaches lead to different outputs and inconsistencies [31]:
- Untargeted Platforms (e.g., LC-MS): Aim to detect all measurable lipids in a sample. They can identify a wider range of lipid classes but typically provide relative quantification (semi-quantitative) and require extensive, time-consuming data processing and validation [31].
- Targeted Platforms (e.g., Lipidyzer): Focus on the precise quantification of a pre-defined list of lipids. They are high-throughput, provide absolute quantification using internal standards, and have more straightforward data processing, but their coverage is limited to the included lipid classes and species [31]. A cross-platform comparison showed that while both approaches can detect a similar number of lipids (~340 in mouse plasma), they are also complementary. The untargeted LC-MS approach uniquely identified many ether-linked phosphatidylcholines (plasmalogens) and phosphatidylinositols, while the targeted Lipidyzer platform uniquely detected many free fatty acids and cholesteryl esters [31].
Are there standardized protocols or tools to harmonize results across laboratories? Yes, initiatives and tools are being developed to address reproducibility, though challenges remain [11] [50]:
- Community-Led Initiatives: The Lipidomics Standards Initiative (LSI) provides recommended procedures for quality controls, reporting checklists, and minimum reporting information to improve consistency across studies [14] [11].
- Standard Reference Materials (SRMs): The use of common materials, such as the NIST SRM 1950 – Metabolites in Frozen Human Plasma, allows laboratories to benchmark their performance and harmonize quantitation results across different platforms and methods [50].
- Statistical Workflows: Novel, code-based frameworks in R and Python are being published to standardize data processing, normalization, and visualization, promoting transparency and reproducibility [11].
Troubleshooting Guides
Problem: Low Overlap in Lipid Identifications Between Software
Issue: When you process your LC-MS data with two different software packages (e.g., MS DIAL and Lipostar), the list of identified lipids shows very little agreement.
Diagnosis Protocol:
- Check Identification Confidence Levels: Compare the levels of identification (e.g., MS1 only vs. MS/MS confirmed) between the two software outputs. Disagreements are most pronounced with MS1-only identifications [14].
- Compare Spectral Libraries: Investigate whether the two software platforms are using different lipid libraries for matching. A lipid present in one library but not the other will obviously lead to a discrepancy [14] [48].
- Analyze Retention Time Alignment: Check if the retention times for the same putative identification are aligned within a reasonable window (e.g., 5 seconds). Misalignment can cause the same peak to be assigned different identities [14].
Solution Strategy:
- Prioritize MS/MS Data: Configure software settings to rely on MS2 fragmentation spectra for identifications wherever possible. This increases the identification agreement to 36.1%, which, while still low, is a significant improvement over MS1-only [14].
- Implement a Cross-Platform Validation Workflow: Use one software's output as a discovery list and then verify each identification by manually checking the raw spectra in the other software or a third tool.
- Apply a Machine Learning Filter: As demonstrated in recent research, use a data-driven approach like Support Vector Machine (SVM) regression with leave-one-out cross-validation to identify and flag outlier identifications that are likely false positives [14].
Table 1: Quantitative Comparison of Software Identification Agreement from Identical LC-MS Data
| Comparison Metric | MS1 Identification Agreement | MS2 Identification Agreement |
|---|---|---|
| MS DIAL vs. Lipostar | 14.0% | 36.1% |
| Primary Cause of Discrepancy | Different peak picking and library matching algorithms | Different interpretation of fragmentation spectra and co-elution |
Problem: Translating Lipid Identifications to Clinically Validated Biomarkers
Issue: Lipid signatures discovered in initial experiments fail to validate in independent cohorts or across different analytical platforms, hindering clinical translation.
Diagnosis Protocol:
- Assess Reproducibility: Re-process your raw data using a different software platform. If the key biomarker candidates do not consistently appear, they are unlikely to validate externally [14] [13].
- Check for Platform Biases: Determine if your key lipid biomarkers are only detectable with a specific analytical method (e.g., untargeted LC-MS) and not with others (e.g., targeted platforms), limiting broad utility [31].
- Review Standardization: Check if your study follows LSI guidelines and uses appropriate quality controls and standard reference materials like NIST SRM 1950 to ensure analytical rigor [11] [50].
Solution Strategy:
- Multi-Software Consensus: Define your high-confidence biomarker list as only those lipids that are identified by more than one software platform or analytical method [31].
- Incorporate Advanced Quality Control: Use standardized R and Python scripts for robust data preprocessing, including batch effect correction, normalization using quality control samples, and handling of missing values to improve data quality and comparability [11].
- Independent Validation: Always validate potential biomarkers using a targeted, quantitative method on a separate instrument and a fresh set of patient samples [13] [49].
Table 2: Essential Research Reagents and Materials for Cross-Platform Lipidomics
| Reagent/Material | Function in Experimental Workflow |
|---|---|
| NIST SRM 1950 (Human Plasma) | A standardized reference material for inter-laboratory method harmonization and quality control [50]. |
| Deuterated Lipid Internal Standards (e.g., Avanti EquiSPLASH) | A mixture of isotopically labeled lipids added to samples prior to extraction to correct for losses and enable absolute or semi-quantitative analysis [14] [31]. |
| Standardized Lipid Libraries (e.g., LipidMAPS) | Curated databases of lipid structures and associated spectral data used for consistent identification across software tools [14] [48]. |
| QC Samples (Pooled from study samples) | Quality control samples injected at regular intervals throughout the analytical run to monitor instrument stability and correct for signal drift [11]. |
Experimental Protocols
Protocol: Cross-Platform Validation of Lipid Identifications
Objective: To establish a high-confidence lipid list by comparing and merging outputs from multiple lipidomics software platforms.
Materials:
- Raw LC-MS/MS data file (.raw, .d, etc.)
- Workstation with at least two lipidomics software packages installed (e.g., MS DIAL, Lipostar, Skyline, MZmine)
- Required lipid libraries for each software
Methodology:
- Data Processing: Process the identical raw data file in MS DIAL and Lipostar (or other platforms) using similar parameter settings (e.g., mass accuracy, retention time tolerance) and their default lipid libraries [14].
- Data Alignment: Export the resulting lipid identification lists, including lipid class, formula, retention time, and MS/MS confirmation status.
- Consensus Identification: Define a lipid as a "consensus identification" only if the following criteria are met across all platforms [14]:
- Lipid class and formula are identical.
- Aligned retention time is consistent within a 5-second window.
- Identification is supported by MS2 spectra in all platforms that reported it.
- Manual Curation: For lipids that are critical to your study (e.g., potential biomarkers), manually validate the identification by inspecting the raw MS/MS spectrum and comparing it to a reference spectrum from a database.
The following workflow diagram summarizes this cross-platform validation process:
Protocol: Data Preprocessing and Quality Control for Reproducible Lipidomics
Objective: To perform standardized data preprocessing and quality control to minimize technical variance and improve the reproducibility of lipidomics data.
Materials:
- Raw data files for all experimental and QC samples
- R or Python statistical environment with appropriate packages (e.g.,
MetaboAnalystR,lipID,pylbm)
Methodology:
- Peak Picking and Alignment: Use software (e.g., MS DIAL, MZmine) for peak detection, deisotoping, and retention time alignment across all samples [48] [49].
- Quality Control Based on QC Samples:
- Signal Stability: Plot the total ion chromatogram (TIC) or base peak intensity (BPI) of the QC samples. The signal should be stable throughout the run.
- PCA Outlier Detection: Perform Principal Component Analysis (PCA) on the entire dataset. QC samples should cluster tightly together, indicating system stability. Any experimental samples that fall outside the QC cloud are potential outliers [11].
- Data Normalization and Batch Correction:
- Normalization: Apply normalization to correct for overall sample concentration differences. This can be based on internal standards added during extraction, median intensity, or probabilistic quotient normalization [49] [11].
- Batch Correction: If data was acquired in multiple batches, use algorithms like LOESS, SERRF (Systematic Error Removal using Random Forest), or ComBat to remove batch effects [11].
- Missing Value Imputation: Investigate the nature of missing values. Impute values that are missing at random using methods like k-nearest neighbors (KNN) or minimum value imputation, but be cautious of non-random missingness, which may indicate true biological absence [11].
The following flowchart illustrates the key steps in this QC workflow:
In lipidomic biomarker research, the journey from sample collection to data generation is fraught with potential pitfalls. The pre-analytical phase—encompassing sample collection, processing, and storage—is the most significant source of variability, accounting for up to 80% of laboratory testing errors in clinical routine diagnostics [51] [52]. For lipidomics, this is particularly critical as lipids exhibit vastly different stabilities, ranging from very stable over several days to highly unstable within minutes after collection [51]. This variability directly challenges the reproducibility and validation of lipid biomarkers, making the standardization of pre-analytical procedures a cornerstone of reliable science. The following guide provides targeted troubleshooting advice to help researchers identify, avoid, and mitigate these pervasive pre-analytical variables.
FAQs and Troubleshooting Guides
Blood Collection & Handling
FAQ: What is the most critical step for ensuring blood sample quality for lipidomics?
Answer: The time and temperature management of whole blood before centrifugation is the most critical step. Whole blood is a "liquid tissue" containing trillions of metabolically active cells that continue to alter lipid concentrations ex vivo. The goal is to separate plasma from these cells as quickly and as cold as possible [51] [53].
Troubleshooting Guide: Unstable lipid species in plasma samples.
- Problem: Significant degradation of certain lipid classes (e.g., fatty acids, lysophospholipids) is observed, or high variability in lipid levels between samples processed at different times.
- Potential Cause: Prolonged exposure of whole blood to room temperature before centrifugation.
- Solution:
- Cool Immediately: Place blood collection tubes in wet ice or a refrigerated rack (4°C) immediately after draw [51] [53].
- Minimize Time to Centrifugation: Centrifuge within 2 hours of collection for comprehensive lipid profiling. If only robust lipid species are of interest, this window can be extended to 4 hours with continuous cooling [53].
- Validate Your Workflow: Use provided stability data to check if your lipids of interest are stable under your established pre-analytical conditions [53].
FAQ: Should I use serum or plasma for lipidomics analysis?
Answer: Both are acceptable, but the profiles are different, and the choice impacts protocol stability. Plasma, collected with anticoagulants like EDTA, is generally preferred for standardization because it allows for immediate cooling after draw. Serum generation requires a clotting time at room temperature (typically 30-60 minutes), which can introduce more variability for less stable lipids [51] [52]. The key is to be consistent within a study and never mix serum and plasma samples.
Sample Processing & Storage
FAQ: How do I choose the right blood collection tube?
Answer: The tube type can introduce chemical noise.
- Troubleshooting Guide: Suspicion of contaminating compounds in mass spectra.
- Problem: High background noise or unidentified peaks in chromatograms that interfere with lipid detection.
- Potential Cause: Leaching of plasticizers from tube walls or interfering compounds from tube additives (e.g., gels) [51] [52].
- Solution:
- Test Tubes Before Study: During the planning phase, test different tube brands and types (with/without gel separator) by analyzing blanks to check for interferences [51] [52].
- Avoid Gel Separators: Use tubes without polymer-based gel separators when possible, as the gel can improperly form or adsorb certain metabolites [51].
- Be Consistent: In multi-center studies, use the same brand and type of tube across all sites [52].
- Troubleshooting Guide: Suspicion of contaminating compounds in mass spectra.
FAQ: What are the best practices for long-term sample storage?
Answer: Proper storage is vital for preserving sample integrity over time.
- Troubleshooting Guide: Lipid degradation in samples after long-term storage.
- Problem: Deterioration of sample quality, evidenced by changes in lipid profiles or increased oxidation products after storage.
- Potential Causes: Inconsistent storage temperature, improper container, or multiple freeze-thaw cycles.
- Solution:
- Aliquot Samples: Store samples in multiple small-volume aliquots to avoid repeated freezing and thawing [52].
- Store at Ultra-Low Temperatures: Keep samples at -80°C or below for long-term preservation [52].
- Use Certified Vials: Ensure cryotubes and labels are certified to withstand ultra-low temperatures without cracking or label detachment [51].
- Standardize Thawing: Thaw samples on wet ice or in a refrigerator (4°C) and mix them accurately before analysis [52].
- Troubleshooting Guide: Lipid degradation in samples after long-term storage.
Data Quality & Analysis
FAQ: Why do my lipid identifications lack reproducibility when using different software?
Answer: This is a known, major challenge in the field. Different software platforms (e.g., MS DIAL, Lipostar) use distinct algorithms, libraries, and alignment methodologies, leading to inconsistent identifications even from identical raw data. One study found only 14-36% agreement between two common platforms [14].
Troubleshooting Guide: Inconsistent lipid identifications across software or laboratories.
- Problem: The same dataset yields different lipid lists when processed with different software.
- Potential Cause: Variability in software processing pipelines and a lack of manual curation.
- Solution:
- Manual Curation: Do not rely solely on automated "top-hit" identifications. Manually inspect spectra, particularly for potential biomarkers [14].
- Cross-Platform Validation: Confirm identifications across both positive and negative LC-MS modes if possible [14].
- Follow Community Standards: Adhere to guidelines from the Lipidomics Standards Initiative (LSI) for reporting and quality control [11] [14].
- Use Advanced QC: Implement data-driven quality control steps, such as machine learning-based outlier detection, to flag potential false positives [14].
The following tables consolidate key quantitative evidence on pre-analytical variable impacts to guide experimental design.
Table 1: Impact of Time and Temperature in EDTA Whole Blood on Lipid Stability [53]
| Exposure Condition | % of Stable Lipid Species (vs. baseline) | Most Affected Lipid Classes | Practical Recommendation |
|---|---|---|---|
| 2 hours at 4°C | >99.5% of metabolite features stable [51] | Minimal change | Ideal: Centrifuge within 2 hrs with immediate cooling |
| 2 hours at 21°C | ~90% of metabolite features stable [51] | Early signs of LPC, LPE, FA instability | Acceptable for many lipids, but not optimal |
| 4 hours at 4°C | >98% of lipid species stable | LPC, LPE, FA | Maximum limit for comprehensive profiling with cooling |
| 24 hours at 21°C | 78% of lipid species stable (325 of 417 species) | LPC, LPE, FA | Unacceptable for full profiling; use only if focused on "robust" lipids |
| 24 hours at 30°C | 69% of lipid species stable (288 of 417 species) | LPC, LPE, FA | Highly degraded; avoid |
Table 2: Common Pre-analytical Variables and Their Documented Effects [51] [52] [54]
| Variable | Documented Impact on Lipids | Recommended Best Practice |
|---|---|---|
| Fasting Status | Significant postprandial increases in triglycerides and other glycerolipids. | Standardize fasting for ≥12 hours before blood collection. |
| Time of Day | Diurnal variation in lipid metabolism and concentrations. | Collect samples in the morning (e.g., between 7-10 AM). |
| Physical Activity | Strenuous exercise can alter energy-related lipids and fatty acids. | Avoid unaccustomed, strenuous activity for 48 hours prior. |
| Tourniquet Use | Prolonged application can cause hemoconcentration, altering concentrations. | Limit tourniquet time to <1 minute. |
| Freeze-Thaw Cycles | Repeated cycles can degrade unstable lipids and promote oxidation. | Aliquot samples to avoid more than 1-2 freeze-thaw cycles. |
Experimental Workflows & Protocols
Standardized Workflow for Blood Plasma Lipidomics
The diagram below outlines a robust, standardized workflow for collecting blood plasma for lipidomics studies, integrating critical control points to minimize variability.
Key Protocol Details:
- Patient Preparation: Participants should fast for at least 12 hours and avoid unaccustomed strenuous exercise for 48 hours prior to blood collection. Samples should be taken in the morning to minimize diurnal variation [52].
- Centrifugation: A standard protocol is centrifugation at 4°C at 3100 g for 7 minutes to separate plasma from blood cells [53].
- Aliquoting and Storage: Immediately after centrifugation, the plasma supernatant should be aliquoted into pre-chilled cryotubes and flash-frozen in liquid nitrogen before transfer to a -80°C freezer for long-term storage [52].
Lipidomics Data Processing Workflow
A major source of post-analytical variability lies in data processing. The following workflow emphasizes steps to improve reproducibility in lipid identification and quantification.
Key Protocol Details:
- Software Processing: Use open-source platforms like MS DIAL or Lipostar with settings documented in a Standard Operating Procedure (SOP). Be aware that using default settings on different platforms can lead to identification agreement as low as 14% [14].
- Manual Curation: This is a non-negotiable step. Researchers must manually inspect spectra, check retention times, and verify fragment patterns for key lipids, especially potential biomarkers [14].
- Normalization: Use standards-based normalization to account for analytical variability. Advanced algorithms like LOESS or SERRF can be applied if quality control (QC) samples are embedded in the acquisition sequence [11].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials for Pre-Analytical Quality Control in Lipidomics
| Item | Function & Importance | Key Considerations |
|---|---|---|
| EDTA Blood Collection Tubes | Prevents clotting for plasma preparation; allows immediate cooling. | Test for contaminating compounds; avoid gel separators; use same brand across a study [51] [52]. |
| Internal Standards (IS) | Corrects for variability in extraction efficiency, matrix effects, and instrument response. | Use a comprehensive mixture (e.g., SPLASH LIPIDOMIX) covering multiple lipid classes, added at the start of extraction [53] [14]. |
| Quality Control (QC) Pool | Monitors analytical performance and stability throughout the LC-MS sequence. | Created by pooling a small aliquot of every experimental sample; analyzed repeatedly throughout the run to correct for instrumental drift [53] [11]. |
| Cryogenic Vials | For long-term storage of samples and extracts at -80°C. | Must be certified for ultra-low temperatures to prevent cracking and ensure sample integrity. Labels must withstand freezing without detaching [51] [52]. |
| Lipidomics Software (MS DIAL, Lipostar) | For processing raw MS data, identifying, and quantifying lipids. | Be aware of high inter-platform variability. Manual curation of results is essential. Follow Lipidomics Standards Initiative (LSI) guidelines [11] [14]. |
FAQs: Core Concepts and Challenges
What is chromatographic co-elution and why is it a critical problem in lipidomics? Chromatographic co-elution occurs when two or more compounds with similar chromatographic properties do not separate, appearing as a single or overlapping peak [55]. In lipidomics, this is a critical problem because closely related lipids can have nearly identical retention times, leading to misidentification and inaccurate quantification, which severely compromises biomarker validation and reproducibility [12].
How does co-elution directly impact the reproducibility of lipidomic biomarker studies? Co-elution is a significant source of the "reproducibility gap" in lipidomics. Different software platforms applied to identical spectral data can yield inconsistent identifications of co-eluted peaks. One study found only 14.0% identification agreement between two common open-access lipidomics platforms (MS DIAL and Lipostar) when using default settings on identical LC-MS spectra. Even with fragmentation data (MS2), agreement only reached 36.1% [12]. This variability is a major, underappreciated source of error for downstream users like bioinformaticians and clinicians.
What are the primary causes of peak tailing and peak splitting?
- Peak Tailing: Often results from void volumes caused by poorly installed fittings at the column head or an improper tubing cut, which creates a mixing chamber [56].
- Peak Splitting: If all peaks show splitting, the likely cause is a void in tubing connections or a scratched autosampler rotor. If only one peak is split, it typically indicates inadequate chromatographic separation of components [56].
My retention time is shifting. What is the likely culprit?
- Decreasing Retention Time: Often indicates a faulty aqueous pump. Purge the pump, clean the check valves, and replace consumables [56].
- Increasing Retention Time: Suggests an issue with the organic pump. Similar troubleshooting—purging, cleaning check valves, and replacing consumables—is recommended [56]. Note that run-to-run retention time variation of ±0.02-0.05 min is normal [56].
Troubleshooting Guide: Common HPLC Problems
The following table summarizes frequent issues, their potential causes, and solutions.
| Problem Observed | Likely Culprit | Recommended Troubleshooting Actions |
|---|---|---|
| Decreasing peak height, same area & retention time [56] | Column | Rinse column per manufacturer's instructions. If degradation continues, replace the column. Consider a guard column or sample clean-up step [56]. |
| Shifting retention time, same peak area [56] | Pump | For decreasing RT: Purge and service the aqueous pump (Pump A). For increasing RT: Purge and service the organic pump (Pump B). Check for leaks [56]. |
| Changing peak area and height [56] | Autosampler | Ensure the rinse phase is degassed. Prime and purge the metering pump to remove air bubbles [56]. |
| Extra peak in chromatogram [56] | Autosampler or Column | Perform blank injections. If the peak is wider, it may be a late-eluting compound from a previous run. Adjust the method to ensure all peaks elute. Adjust needle rinse parameters [56]. |
| Jagged baseline [56] | Multiple | Check for temperature fluctuations, dissolved air in the mobile phase, a dirty flow cell, or insufficient mobile phase mixing [56]. |
| Poor peak shape (tailing) [56] | Tubing/Connections | Inspect and re-make connections to eliminate voids. Ensure tubing is cut properly to a planar surface [56]. |
Advanced Solutions: Computational Peak Deconvolution
When chemical and technical solutions are insufficient, computational peak deconvolution is an effective strategy, especially for large datasets [55]. The following table compares two advanced methods.
| Method | Key Principle | Application Context | Key Advantage |
|---|---|---|---|
| Clustering-Based Separation [55] | Divides convolved fragments of chromatograms into groups of peaks with similar shapes. | Large datasets where the goal is to separate and compare peaks across many chromatograms. | Effectively separates overlapping peaks into distinct groups for quantitative analysis. |
| Functional Principal Component Analysis (FPCA) [55] | Detects sub-peaks with the greatest variability, providing a multidimensional peak representation. | Complex biological mixtures (e.g., metabolomics/lipidomics) in comparative studies. | Assesses the variability of individual compounds within the same peaks across different chromatograms, highlighting differences between experimental variants. |
Experimental Protocol: Computational Peak Separation Workflow
The following diagram and protocol outline a generalized methodology for separating co-eluted peaks in large chromatographic datasets, as applied in metabolomic and lipidomic studies [55].
Detailed Methodology:
- Data Pre-processing: Raw data from multiple chromatograms are first normalized by the sample mass. The baseline is removed, and retention time alignment is conducted to correct for run-to-run shifts [55].
- Peak Detection: Peaks are identified across all chromatograms in the dataset. This step can be performed without smoothing for simulated data, but real-world data typically requires noise reduction techniques [55].
- Identify Overlapping Peaks: Fragments of chromatograms containing suspected co-eluted compounds are isolated for further analysis [55].
- Apply Deconvolution Method:
- Method 1 (Clustering): Hierarchical clustering with bootstrap resampling is used to group similar peak shapes from across all chromatograms. The algorithm then defines separate peaks (e.g., one for a single compound, two for a double peak) by joining features from different clusters [55].
- Method 2 (FPCA): This method uses a set of basis functions (e.g., B-splines) to model the chromatographic peak. Functional Principal Component Analysis is applied to detect the sub-peaks (components) within the convolved signal that exhibit the greatest variability across samples, which is ideal for comparative studies [55].
- Output and Analysis: The result is a set of separated peaks, whose areas can be used as inputs for subsequent statistical analysis to identify significant differences between experimental groups and validate potential biomarkers [55].
Essential Research Reagent Solutions
The table below lists key materials and their functions for conducting reliable chromatographic separations in lipidomics.
| Item | Function / Application |
|---|---|
| Guard Column [56] | A short column placed before the analytical column to protect it from particulate matter and chemically irreversibly adsorbed components, extending its lifetime. |
| Degassed Solvents [56] | Mobile phase that has been degassed to prevent air bubbles from forming in the system, which can cause unstable baselines and erratic pump operation. |
| B-spline Functions [55] | Mathematical functions used in computational deconvolution methods (like FPCA) to generate and model the shapes of chromatographic peaks and their underlying components. |
| MS DIAL / Lipostar [12] | Open-access lipidomics software platforms used for feature identification and quantification; requires cross-validation and manual curation to improve reproducibility. |
| Bidirectional EMG Function [55] | A mathematical model (Exponentially Modified Gaussian) used in advanced peak deconvolution algorithms to describe and separate overlapping chromatographic peaks. |
Frequently Asked Questions (FAQs) on Lipidomics Standards
1. What is the Lipidomics Standards Initiative (LSI) and why is it important? The Lipidomics Standards Initiative (LSI) is a community-wide effort that aims to create guidelines for the major lipidomics workflows. Its importance lies in providing a common language for researchers, which is essential for the successful progress of lipidomics. These standards enable reproducibility, facilitate data comparison across different laboratories, and provide the interface to interlink with other disciplines like proteomics and metabolomics [57] [58].
2. Which parts of the lipidomics workflow does the LSI cover? The LSI guidelines cover the entire lipidomics workflow. This includes detailed recommendations on how to [57] [58]:
- Collect and store samples (pre-analytics)
- Extract lipids from samples
- Execute the mass spectrometry (MS) analysis
- Perform data processing, which encompasses lipid identification, deconvolution, annotation, quantification, and quality control evaluation
- Report the final data The guidelines also cover the validation of analytical methods themselves [57].
3. I'm getting different results when using different software on the same data. Is this normal? Yes, this is a recognized and significant challenge in the field. Studies have shown that even when using identical LC-MS spectral data, different open-access software platforms (like MS DIAL and Lipostar) can show very low agreement in lipid identification—as low as 14% using default settings. This "reproducibility gap" underscores the critical need for manual curation of software outputs and validation across different LC-MS modes to reduce false positives [12].
4. What are the main categories of lipids used in lipidomics classification? The widely accepted classification system, established by the LIPID MAPS consortium, categorizes lipids into eight key categories [1] [10]:
- Fatty Acyls (FA)
- Glycerolipids (GL)
- Glycerophospholipids (GP)
- Sphingolipids (SP)
- Sterol Lipids (ST)
- Prenol Lipids (PR)
- Saccharolipids (SL)
- Polyketides (PK)
5. What is the difference between untargeted and targeted lipidomics? The choice of strategy depends on your research goal, and the LSI provides context for applying each [1] [10].
- Untargeted Lipidomics: An exploratory approach aiming to comprehensively detect and measure as many lipids as possible in a sample, without prior bias. It is ideal for discovering novel lipid biomarkers and is typically performed using high-resolution mass spectrometry (HRMS) [1] [10].
- Targeted Lipidomics: A focused approach for the precise identification and accurate quantification of a predefined set of lipid molecules. It is used to validate potential biomarkers discovered in untargeted screens and employs techniques like multiple reaction monitoring (MRM) for high sensitivity and accuracy [1] [10].
Troubleshooting Common Lipidomics Challenges
The following table outlines common issues encountered during lipidomics workflows, their potential impact on biomarker validation, and evidence-based solutions guided by standardization principles.
Table 1: Troubleshooting Guide for Lipidomics Experiments
| Challenge | Impact on Reproducibility & Biomarker Validation | Recommended Best Practices & Solutions |
|---|---|---|
| Low Inter-Software Agreement [12] | Leads to inconsistent lipid identification from identical data; undermines the reliability of discovered biomarkers. | - Validate identifications across both positive and negative LC-MS modes.- Manually curate spectral matches and software outputs.- Supplement with data-driven outlier detection and machine learning validation. |
| Pre-analytical Variability [57] [59] | Sample collection and storage inconsistencies introduce artifacts, affecting data quality and cross-study comparisons. | - Strictly adhere to LSI guidelines for sample collection and storage [57] [59].- Implement standardized protocols across all samples in a study.- Use quality controls (QCs) to monitor pre-analytical variations. |
| Inconsistent Data Reporting [57] [58] | Makes it difficult to reproduce studies or integrate datasets from different laboratories. | - Follow the LSI reporting guidelines for data and metadata [57] [58].- Report absolute quantitative values where possible, not just relative changes.- Provide detailed methodology following published best practice papers [59]. |
| Complexity of Lipid Metabolism & Structural Diversity [1] [60] | Subtle, context-dependent lipid changes can be missed or misinterpreted, reducing biomarker specificity. | - Employ a pseudo-targeted approach to combine the coverage of untargeted with the accuracy of targeted methods [1] [10].- Integrate lipidomic data with other omics data (genomics, proteomics) for a systems biology context [1] [60]. |
Standardized Experimental Protocols for Lipidomics
Protocol: Comprehensive Lipidomics Workflow Based on LSI Best Practices
This protocol provides a generalized workflow for MS-based lipidomics, integrating key steps highlighted by the Lipidomics Standards Initiative [57] [59] and applied research [1] [10].
Principle: To ensure the quality and reproducibility of lipidomics data, the entire process—from sample handling to data reporting—must be standardized.
Procedure:
- Sample Collection and Storage (Pre-analytics):
- Adhere to specific LSI-recommended protocols for your sample type (e.g., plasma, tissue) concerning collection tubes, anticoagulants, and immediate processing steps [57] [59].
- Flash-freeze samples (e.g., in liquid nitrogen) and store at -80°C or lower to preserve lipid integrity. Avoid multiple freeze-thaw cycles [59].
Lipid Extraction:
- Use standardized extraction methods (e.g., Folch, Bligh & Dyer, or MTBE-based methods) that have been validated for comprehensive lipid recovery [57] [59].
- Include internal standards (IS) for various lipid classes at the beginning of extraction to correct for losses during preparation and ion suppression in MS.
MS Analysis and Data Acquisition:
- For Untargeted Screening: Use High-Resolution Mass Spectrometry (HRMS) like Q-TOF or Orbitrap instruments coupled with liquid chromatography (LC). Data-Independent Acquisition (DIA) or Data-Dependent Acquisition (DDA) modes can be employed for comprehensive profiling [1] [10].
- For Targeted Validation: Use triple quadrupole (QQQ) or similar instruments in Multiple Reaction Monitoring (MRM) mode for highly sensitive and accurate quantification of specific lipids [1] [10].
Data Processing and Quality Control:
- Process raw data using lipidomics software (e.g., MS-DIAL, Lipostar, etc.). Be aware of the potential for low inter-software agreement [12].
- Implement a rigorous quality control (QC) strategy. This includes analyzing pooled quality control samples (a mixture of all samples) throughout the analytical sequence to monitor instrument stability and data quality [57] [59].
Lipid Identification and Quantification:
- Identify lipids using a combination of accurate mass, MS/MS spectral matching against reference libraries (e.g., LIPID MAPS), and retention time information when available [12] [59].
- Quantify lipids by comparing the signal intensity of the lipid species to the signal of the corresponding class-specific internal standard. Report data as absolute concentrations (e.g., pmol/µg protein) whenever possible to enhance reproducibility [58].
Data Reporting:
Protocol: Cross-Platform Validation of Lipid Identifications
This protocol directly addresses the critical challenge of software-related irreproducibility in biomarker discovery [12].
Principle: To minimize false positive identifications by leveraging multiple software platforms and manual validation.
Procedure:
- Process your identical LC-MS/MS (MS2) data set with at least two different software platforms (e.g., MS DIAL and Lipostar).
- Cross-reference the lists of identified lipids from all platforms. Give higher confidence to lipid species that are identified by multiple software tools.
- For lipids that are identified by only one platform, or for key biomarker candidates, perform manual validation:
- Visually inspect the raw MS/MS spectra.
- Confirm the presence of diagnostic fragment ions specific to the putative lipid class and fatty acyl chains.
- Check the chromatographic peak shape and retention time for consistency.
- Utilize emerging machine learning-based tools to assist in spectral annotation and outlier detection [12].
Research Reagent Solutions
The following table lists essential materials and reagents used in standardized lipidomics workflows, with their critical functions.
Table 2: Key Research Reagents for Lipidomics Workflows
| Reagent / Material | Function in the Workflow |
|---|---|
| Internal Standards (IS) Mix | A cocktail of stable isotope-labeled or non-natural lipid analogs. Added at extraction start, they correct for analyte loss, matrix effects, and enable accurate quantification [59]. |
| LIPID MAPS Database | The central, curated reference database for lipid structures, nomenclature, and mass spectra. Essential for correct lipid identification and annotation according to international standards [57] [1]. |
| Quality Control (QC) Pooled Sample | A pooled mixture of a small aliquot of every sample in the study. Analyzed repeatedly throughout the MS sequence, it monitors instrument performance, signal drift, and data quality [57] [59]. |
| Standard Reference Material (SRM) | Certified materials with known lipid concentrations (e.g., NIST SRM 1950 plasma). Used to validate and benchmark entire analytical methods for accuracy and precision [60]. |
| Chromatography Columns | Reverse-phase (e.g., C18) columns are standard for separating lipid species by their hydrophobicity. Column chemistry and performance are critical for resolving complex lipid mixtures [12] [59]. |
A significant challenge in lipidomics is the translation of research findings into clinically validated biomarkers. Promising lipid signatures often fail to be replicated across different laboratories and studies, with one analysis noting that prominent software platforms agree on as little as 14–36% of lipid identifications when processing identical LC-MS data [13]. This lack of reproducibility stems largely from bioinformatics hurdles and the dependence on proprietary, platform-specific data processing tools. This technical support center addresses these specific data processing bottlenecks, providing actionable guides and FAQs to help researchers achieve more consistent, reliable, and platform-independent results in their lipidomics workflows.
Troubleshooting Guides & FAQs
Frequently Asked Questions (FAQs)
Q1: Why do my lipid identifications vary when I use different software packages on the same dataset?
This is a common issue driven by several factors:
- Divergent Algorithms: Different software uses unique algorithms for peak picking, spectral deconvolution, and library matching. For instance, some tools may prioritize different fragments or use varying mass tolerance windows [13].
- Inconsistent Libraries: Each software often relies on its own built-in lipid library, which can have differences in coverage, fragmentation rules, and accepted nomenclature [61].
- Solution: To mitigate this, use tools that leverage large, standardized libraries or allow for the import of custom, platform-independent libraries. When reporting results, always specify the software, version, and database used to ensure transparency [62] [11].
Q2: How can I handle missing values in my lipidomics dataset without introducing bias?
Missing values are pervasive in lipidomics and can arise for technical (e.g., below detection limit) or biological reasons.
- Diagnosis First: Before imputation, investigate the pattern of missingness. Values can be Missing Completely at Random (MCAR), Missing at Random (MAR), or Missing Not at Random (MNAR), which often indicates the analyte concentration is below the instrument's detection limit [63].
- Tailored Imputation: There is no single best method for all situations. Common strategies include:
- k-Nearest Neighbors (kNN) or Random Forest imputation for MCAR/MAR data.
- Imputation by a constant value (e.g., a percentage of the minimum measured value) for MNAR data, which is common for low-abundance lipids [63].
- Best Practice: Always document the method and percentage of values imputed, and consider performing a sensitivity analysis to ensure your conclusions are robust [11] [63].
Q3: My data shows strong batch effects. How can I correct for this?
Batch effects are systematic technical variations that can obscure biological signals.
- Prevention: Incorporate a randomized run order and use Quality Control (QC) samples throughout your acquisition sequence. These can be pooled samples from the study set or commercial reference materials like NIST SRM 1950 [63] [38].
- Correction: Use QC-based normalization algorithms. Effective methods include:
- LOESS (Locally Estimated Scatterplot Smoothing) regression.
- SERRF (Systematic Error Removal using Random Forest), which uses QC samples to model and correct systematic drift [11].
- Visualization: Always plot QC metrics (e.g., PCA, total ion chromatogram) before and after correction to assess the effectiveness of the normalization [11].
Q4: What are the key steps for ensuring my lipidomics analysis is reproducible and platform-independent?
- Standardized Protocols: Adhere to guidelines from the Lipidomics Standards Initiative (LSI) and the Metabolomics Society for sample preparation, data acquisition, and reporting [11].
- Open-Source Tools & Scripting: Utilize flexible, script-based environments like R or Python for data processing. This makes the entire analysis transparent and reproducible, moving away from "black box" commercial software [11] [63].
- Data Sharing: Deposit raw and processed data in public repositories like the Metabolomics Workbench to enable independent verification and meta-analysis [61].
The table below summarizes common software tools, highlighting how they address platform independence and reproducibility.
Table 1: Overview of Common Lipidomics Data Processing Software
| Software | Primary Use | Key Features | Platform Independence & Reproducibility |
|---|---|---|---|
| LipidIN [62] | Untargeted Lipidomics | 168.5-million lipid fragmentation library; AI-based retention time prediction; Reverse lipidomics fingerprint regeneration. | Designed as a "flash platform-independent" framework. Aims to overcome instrument-specific variability. |
| LipidSearch [61] | Untargeted/Targeted | Automated identification/quantification; Tailored for Thermo Orbitrap instruments. | Platform-dependent (optimized for specific vendors). Limited transparency in proprietary algorithms. |
| MS-DIAL [13] | Untargeted Metabolomics/Lipidomics | Comprehensive identification; Supports various data formats. | High flexibility with vendor-neutral data format support, but identification consistency can be low compared to other tools. |
| LipidMatch [61] | Lipid Identification | Rule-based for HR-MS/MS; Customizable workflows. | High degree of user control and flexibility, promoting reproducibility through customizable, documented rules. |
| R/Python Workflows [11] [63] | Statistical Analysis & Visualization | Modular, script-based; Access to vast packages (e.g., ggplot2, seaborn). |
Highest level of reproducibility and transparency. Code-based workflows ensure exact methods are documented and shareable. |
Experimental Workflow for Robust Lipid Identification
The following diagram outlines a generalized workflow for LC-MS-based lipidomics, integrating steps to enhance reproducibility and cross-platform consistency.
Lipidomics Workflow for Reproducibility
Detailed Methodologies for Key Steps
Step 1: Sample Preparation & Data Acquisition [40] [38]
- Sample Collection: Use flash-freezing and store at -80°C to prevent lipid degradation.
- Lipid Extraction: Employ standardized methods like liquid-liquid extraction (e.g., chloroform-methanol mixtures) or solid-phase extraction.
- Internal Standards: Add a mixture of stable isotope-labeled lipid internal standards before extraction to correct for losses during preparation and ionization variability during MS analysis.
- Quality Control (QC) Samples: Prepare a pooled QC sample by combining a small aliquot of every biological sample in the study. Inject the QC repeatedly at the beginning of the run to condition the system and then at regular intervals throughout the acquisition sequence to monitor instrument stability.
Step 2: Data Conversion & Preprocessing [62] [11] [63]
- Conversion: Use tools like MSConvert (ProteoWizard) to convert proprietary raw data files into an open, vendor-neutral format like .mzML or .mzXML. This is a critical first step for platform-independent analysis.
- Preprocessing: This includes peak picking, alignment across samples, and isotope deconvolution. This can be done within tools like MS-DIAL or via custom scripts in R/Python.
Step 3: Lipid Identification & Validation [62] [13]
- Spectral Library Matching: Compare experimental MS/MS spectra against large, curated databases like LIPID MAPS or the 168.5-million spectrum hierarchical library in LipidIN. Use a scoring threshold (e.g., cosine score > 0.7) to assign identities.
- Retention Time (RT) Validation: Use relative retention time (RRT) rules to reduce false positives. Advanced tools like LipidIN employ AI models that learn the relationship between lipid structure (e.g., carbon chain length, double bonds) and RT. Key rules include:
- Equivalent Carbon Number (ECN): For lipids with the same double bond equivalents (DBEs), RT follows a predictable polynomial trend with carbon number.
- Intra-subclass Unsaturation Parallelism (IUP): The fitted trends for different DBEs within a subclass are parallel.
Step 4: Data Analysis & Reporting [11] [63]
- Statistical Analysis: After rigorous normalization and imputation, perform univariate (t-tests, ANOVA) and multivariate (PCA, PLS-DA) analyses to identify differentially abundant lipids.
- Data Deposition: Share raw and processed data in public repositories like the Metabolomics Workbench to adhere to FAIR (Findable, Accessible, Interoperable, Reusable) data principles and enable validation.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for Reproducible Lipidomics
| Item | Function | Consideration for Reproducibility |
|---|---|---|
| Internal Standard Mix | Corrects for variability in extraction, ionization, and analysis. | Use a comprehensive set of isotopically labeled lipids covering multiple classes. Essential for accurate quantification. |
| NIST SRM 1950 | Standard Reference Material of human plasma. | Used as a long-term reference or surrogate QC to harmonize measurements across labs and instruments [38]. |
| Pooled QC Sample | Monitors instrument performance and technical variation throughout a run. | Created from a pool of all study samples; critical for batch effect correction using algorithms like LOESS or SERRF [11] [63]. |
| Solvents & Reagents | Lipid extraction and mobile phase preparation. | Use high-purity, LC-MS grade solvents to minimize background noise and ion suppression. |
| Open Data Formats | Vendor-neutral data files (.mzML). | Enables data analysis with any software tool, ensuring long-term accessibility and platform independence [62]. |
From Discovery to Clinic: Validation Frameworks and Comparative Effectiveness
FAQs on Lipidomic Biomarker Validation
Q1: Why is validation across independent cohorts non-negotiable for clinical lipidomics? Validation in independent cohorts is essential to ensure that a lipidomic signature is robust and not a false positive finding specific to the original study population. It tests the generalizability of the biomarker across different demographics, clinical sites, and sample handling protocols. A biomarker that fails this step lacks the clinical credibility for diagnostic use. For instance, a signature for pediatric inflammatory bowel disease (IBD) was first identified in a discovery cohort (AUC=0.87) and then validated in a separate cohort (AUC=0.85), confirming its diagnostic potential beyond the initial patient group [21].
Q2: Our team identified a promising lipid panel. What are the key steps to validate it? A rigorous validation strategy involves several key steps:
- Secure an Independent Cohort: Obtain samples from a completely separate group of patients and controls, ideally from a different clinical center. This cohort should reflect the intended-use population.
- Blinded Analysis: Perform lipidomic analysis without knowledge of the patients' clinical diagnoses to prevent bias.
- Statistical Validation: Apply the pre-defined model (e.g., the specific lipids and their weights) from your discovery phase to the new cohort. Evaluate its performance using metrics like the Area Under the Curve (AUC) to confirm diagnostic accuracy [21].
- Benchmarking: Compare the performance of your lipidomic signature against established clinical biomarkers, such as high-sensitivity C-reactive protein (hsCRP) or fecal calprotectin [21].
Q3: We validated our signature, but its performance dropped significantly in the new cohort. What are common causes? A drop in performance often points to issues with reproducibility or overfitting. Common pitfalls include:
- Overfitting the Initial Model: The discovery model may have been too complex, incorporating noise specific to that dataset rather than a true biological signal. Using simpler models with fewer lipids can improve generalizability [64].
- Pre-analytical Variability: Differences in sample collection, processing, and storage between cohorts can alter lipid profiles [12].
- Software Discrepancies: Different lipidomics software platforms can inconsistently identify and quantify the same lipids from identical data. One study found only 14.0% identification agreement between two common platforms. Validating across positive and negative LC-MS modes and manual curation of spectra are crucial to mitigate this [12].
- Cohort Heterogeneity: The new cohort may have different underlying demographics, comorbidities, or disease subtypes that affect the lipidome.
Troubleshooting Guide: Experimental Protocols
Issue: Inconsistent lipid identification between different analysis software. This is a major source of irreproducibility, where the same raw data yields different lipid lists depending on the software used [12].
Protocol to Improve Reproducibility:
- Cross-Platform Validation: Analyze a representative subset of your samples using two different software platforms (e.g., MS-DIAL and Lipostar). Compare the identified lipid species for consistency [12].
- Leverage Multiple Data Acquisition Modes: If possible, collect data in both positive and negative ionization modes. A lipid identified confidently in both modes is more reliable than one identified in only one [12].
- Manual Curation: Do not rely solely on automated software outputs. Manually inspect the MS2 fragmentation spectra for your key biomarker candidates to verify the identification.
- Incorporate Machine Learning: Use support vector machine (SVM) regression combined with leave-one-out cross-validation on your spectral outputs as a data-driven method to identify and filter out outlier identifications [12].
Issue: Designing a validation study for a cardiovascular disease (CVD) lipidomic risk score. The goal is to prove the score predicts risk in a population distinct from the one in which it was developed.
Step-by-Step Validation Protocol:
- Cohort Selection: Partner with a consortium that manages a large, longitudinal clinical trial or population study with archived plasma samples and documented cardiovascular outcomes. The LIPID trial or the Western Norway Coronary Angiography Cohort are examples used in previous studies [64].
- Sample Preparation:
- Use a standardized, high-throughput protocol (e.g., 96-well plate format) for lipid extraction [64].
- Spike samples with a known set of internal standards (ITSD) for precise quantification.
- Randomize samples from the validation cohort alongside quality control (QC) pools to monitor instrument performance.
- LC-MS/MS Analysis:
- Use a targeted LC-MS/MS method focused on the specific lipids in your risk score (e.g., ceramides and phosphatidylcholines for the CERT2 score) [64].
- The method should be optimized for high throughput and precision, not necessarily for discovering new lipids.
- Data Analysis and Model Application:
- Quantify the target lipids using your established pipeline.
- Apply the exact mathematical formula of your risk score from the discovery phase to the new lipid concentration data. Do not re-train the model on the new data.
- Statistically compare the risk score's ability to predict CVD events (e.g., using hazard ratios) against traditional models based only on cholesterol levels [64].
Quantitative Data from Key Validation Studies
The table below summarizes data from published studies that successfully validated lipidomic signatures, demonstrating the process and its impact.
| Lipidomic Signature / Score | Discovery Cohort Performance (AUC) | Independent Validation Cohort Performance (AUC) | Key Validated Lipids (Examples) | Outcome |
|---|---|---|---|---|
| Pediatric IBD Signature [21] | 0.87 (IBD vs controls) | 0.85 (IBD vs controls) | LacCer(d18:1/16:0), PC(18:0p/22:6) | Outperformed hsCRP (AUC=0.73); performance comparable to fecal calprotectin. |
| CERT2 (CVD Risk Score) [64] | N/A (Hazard Ratio: 1.44) | HR: 1.47 (LIPID trial)HR: 1.69 (KAROLA study) | Ceramides, Phosphatidylcholines | Significantly predicted cardiovascular mortality across three independent cohorts. |
| CVD/Statin Response Model [64] | Validated via intra-trial cross-validation | Improved prediction over traditional risk factors alone | PI(36:2), PC(38:4) | A ratio of these lipids was predictive of statin treatment benefit, independent of cholesterol changes. |
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function in Lipidomics Validation |
|---|---|
| Stable Isotope-Labeled Internal Standards (ITSD) | Added to every sample before extraction to correct for losses during preparation and variations in instrument response, enabling precise quantification [64]. |
| Standard Reference Material (SRM) | A well-characterized control sample (e.g., from NIST) used to benchmark instrument performance and ensure data quality across multiple validation batches [64]. |
| Quality Control (QC) Pool | A representative pool of all study samples, analyzed repeatedly throughout the batch sequence to monitor and correct for instrumental drift over time. |
| 96-well Plate Extraction Platform | Enables high-throughput, semi-automated lipid extraction from small volumes of plasma or serum, which is critical for processing large validation cohorts efficiently [64]. |
Lipidomic Biomarker Validation Workflow
The following diagram outlines the critical path for developing and validating a clinically credible lipidomic biomarker, from discovery to implementation.
Multi-Cohort Validation Strategy
This diagram illustrates the essential process of testing a biomarker signature across multiple, separate patient groups to ensure its reliability.
Frequently Asked Questions (FAQs)
Q1: What are the most critical performance metrics for benchmarking a new lipidomic biomarker, and which should be prioritized?
When evaluating a new lipidomic biomarker, a combination of metrics provides the most complete picture of its diagnostic potential. No single metric should be used in isolation. The most critical metrics, along with their interpretation, are summarized in the table below.
Table 1: Key Performance Metrics for Biomarker Benchmarking
| Metric | Definition | Interpretation & Benchmarking Value |
|---|---|---|
| AUC | Area Under the receiver operating characteristic Curve. Measures the overall ability to distinguish between classes. | Ranges from 0.5 (useless) to 1.0 (perfect). An AUC > 0.9 is considered excellent, while > 0.8 is good [65]. |
| Specificity | The proportion of true negatives correctly identified. | Measures how well the biomarker avoids false alarms in healthy or control populations. A high value (e.g., > 0.90) is crucial for diagnostic tests [65]. |
| Sensitivity | The proportion of true positives correctly identified. | Measures the ability to correctly identify individuals with the disease. A high value is vital for screening or ruling out disease [65]. |
| Diagnostic Odds Ratio (DOR) | The ratio of the odds of positivity in disease relative to the odds of positivity in non-disease. | A single indicator of test performance. Higher values indicate better discriminatory performance. Can be exceptionally high (e.g., 395) for top-tier biomarkers [65]. |
For benchmarking, the AUC provides the best single measure of overall performance. However, the choice between prioritizing sensitivity or specificity depends on the biomarker's intended clinical use. For instance, a screening biomarker may prioritize high sensitivity to avoid missing cases, while a confirmatory diagnostic test requires high specificity to prevent false positives [66] [65].
Q2: Our lipidomic biomarker shows a statistically significant difference between groups (p < 0.05), but classification accuracy is poor. Why is this happening, and how can we improve it?
A statistically significant p-value in a between-group hypothesis test does not guarantee successful classification for individual subjects. This is a common point of failure in biomarker development [66].
- Reason: A low p-value indicates that the group means are likely different, but it does not account for the overlap in distributions between the groups. If the distributions of the lipid species in the diseased and healthy groups have wide variances and significant overlap, the classification error rate (
P_ERROR) can approach 50% (random guessing) even with a very low p-value [66]. - Solution:
- Focus on Classification Metrics: Shift the focus from p-values to metrics like
P_ERROR, AUC, sensitivity, and specificity from the start. - Employ Robust Model Selection: Use feature selection algorithms like LASSO (Least Absolute Shrinkage and Selection Operator) or Elastic Net to eliminate non-predictive lipid features and prevent overfitting. These methods help build a more robust and generalizable model by selecting only the most relevant variables [67] [66].
- Validate with Care: Ensure cross-validation is performed correctly to avoid overly optimistic performance estimates [66].
- Focus on Classification Metrics: Shift the focus from p-values to metrics like
Q3: What are the major technical challenges specific to lipidomic biomarker validation that can impact metrics like AUC and specificity?
Lipidomics faces unique analytical challenges that directly threaten the reproducibility and reliability of performance metrics.
Table 2: Key Challenges in Lipidomic Biomarker Validation
| Challenge Category | Specific Issue | Impact on Performance Metrics |
|---|---|---|
| Analytical & Data Quality | Low reproducibility across platforms and laboratories. Agreement rates between different lipidomics software can be as low as 14-36% [1]. | Inflates variability, reduces observed AUC, and compromises specificity when deployed in different settings. |
| Lack of standardized protocols for sample processing, data acquisition, and analysis [2] [1]. | Introduces bias, making benchmarks unreliable and hindering cross-study comparisons. | |
| Biological & Clinical | High biological variability and the subtle, context-dependent nature of lipid changes [1]. | Can mask true biomarker signals, leading to lower than expected sensitivity and specificity. |
| Insufficient clinical validation in large, diverse, multi-center cohorts [2] [68]. | Results in biomarkers that fail to generalize, with performance metrics (AUC, specificity) dropping significantly in new populations. |
Q4: How can we establish that our lipidomic biomarker is reliable for longitudinal monitoring of treatment response?
A biomarker that distinguishes groups at a single time point may not be useful for tracking change over time. To be a valid monitoring biomarker, you must establish its test-retest reliability [66].
- Measure Reliability: Quantify the stability of the lipid measurement in a clinically stable individual over a short period. This is not assessed by linear correlation but by the Intraclass Correlation Coefficient (ICC). It is critical to select the appropriate version of the ICC for your study design [66].
- Link to Clinical Change: Demonstrate that changes in the lipid biomarker level correlate with clinically assessed improvement or deterioration. A biomarker that is a trait of the disease (e.g., a risk factor) but does not change with clinical status will fail as a monitoring tool [66].
Troubleshooting Guides
Problem: Inconsistent AUC and Specificity Across Validation Cohorts
This is a classic sign of a biomarker or model that has not generalized beyond the discovery cohort.
- Possible Cause 1: Overfitting. The model is too complex and has learned noise from the discovery dataset rather than the true biological signal.
- Solution: Implement rigorous feature selection (e.g., LASSO, Elastic Net) during model development to reduce the number of lipid variables. Use a nested cross-validation strategy to ensure the feature selection process is contained within the training loop and does not leak information into the validation set [67] [66].
- Possible Cause 2: Cohort Differences. Differences in patient demographics, sample collection protocols, or analytical platforms between the discovery and validation cohorts.
- Solution: Adopt standardized operating procedures (SOPs) for pre-analytical sample processing. Use batch correction algorithms during data analysis. Prioritize biomarkers validated through multi-modal data fusion approaches, which integrate data from multiple sources to create more robust models [69].
- Possible Cause 3: Underpowered Studies. The initial discovery study had a sample size that was too small to provide a reliable estimate of performance.
- Solution: Perform sample size calculations based on the target performance metrics (e.g., the width of the confidence interval for AUC) before starting validation studies. The sample sizes required for reliable biomarker evaluation are often much larger than those computed for simple hypothesis testing [66].
Problem: Poor Specificity When Differentiating Between Related Diseases
Your lipid biomarker may be detecting a general state of metabolic dysregulation or inflammation common to several conditions, rather than a disease-specific signal.
- Possible Cause: Lack of Disease Specificity. The lipid signature is associated with a broad pathological process (e.g., inflammation, cell proliferation) and is not unique to the target disease.
- Solution:
- Incorporate Multi-Omics Data: Move beyond a single-omics view. Integrate your lipidomics data with proteomic or genomic data to build a more specific multi-omics biomarker panel. This can capture the unique molecular fingerprint of the disease more accurately [69] [70] [10].
- Benchmark Against Established Biomarkers: Validate your new lipidomic panel in a head-to-head comparison with existing clinical biomarkers. For example, in a field like Alzheimer's disease, benchmark against core biomarkers like p-tau217 (which has an AUC of 0.99 and specificity of 0.94) or the Aβ42/p-tau181 ratio (AUC of 0.93) to establish comparative utility [65].
- Refine the Panel: Use model selection techniques to find a combination of lipid species that maximizes specificity for the target disease against the most clinically relevant differential diagnoses.
- Solution:
Experimental Workflow for Validation
The following diagram outlines a rigorous, multi-stage workflow for the development and validation of a lipidomic biomarker, designed to address common reproducibility challenges.
Diagram: Lipidomic Biomarker Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Lipidomic Biomarker Research
| Tool / Technology | Function in Biomarker Workflow | Key Considerations |
|---|---|---|
| High-Resolution Mass Spectrometry (HRMS) | The core platform for untargeted and targeted lipid identification and quantification. Offers exceptional sensitivity and resolution [1] [10]. | Orbitrap and Q-TOF systems are widely used. Crucial for detecting low-abundance lipid species. |
| Liquid Chromatography (e.g., UPLC) | Separates complex lipid mixtures prior to MS analysis, reducing ion suppression and improving quantification accuracy [1] [10]. | UPLC-QQQ-MS is the gold standard for targeted quantification due to high sensitivity and stability [10]. |
| Multiplex Immunoassays (e.g., MSD U-PLEX) | Validates specific lipid-associated proteins or pathways in a high-throughput manner. Allows custom panel design [68]. | More sensitive and cost-effective for validating multiple protein biomarkers simultaneously compared to running multiple ELISAs [68]. |
| AI/Bioinformatics Software | For data processing, lipid identification, and building predictive models. Tools like MS2Lipid can predict lipid subclasses with high accuracy [1]. | Essential for handling high-dimensional data. Machine learning frameworks are needed to integrate multi-omics data and improve predictive power [69] [70] [1]. |
| Standardized Reference Materials | Used for instrument calibration and to enable inter-laboratory comparison of results. | Critical for addressing reproducibility challenges. The lack of such standards is a major hurdle in the field [2] [1]. |
Core Concepts and Importance
Why are cross-platform and inter-laboratory comparisons essential for lipidomic biomarker research? These comparisons are critical for assessing whether lipidomic biomarkers discovered in research settings maintain their accuracy and reliability across different measurement technologies, laboratories, and sample types. They test the real-world robustness of biomarkers by identifying and quantifying technical variability that can obscure true biological signals. Successful validation across platforms significantly increases confidence in a biomarker's clinical potential [71] [13].
The fundamental challenge is that platform-specific technical biases can introduce more variance than the actual biological differences caused by disease status. For example, a recent multi-platform proteomics study in Parkinson's disease found that while a few proteins like DDC showed consistent dysregulation, the overall reproducibility of findings across different technologies was limited. This highlights that platform selection itself is a major source of variability that must be carefully evaluated [71].
Troubleshooting Common Experimental Issues
FAQ: Why do my lipid identification results differ when using different LC-MS platforms or software?
- Problem: Lipidomics software platforms (like MS DIAL and Lipostar) frequently disagree on lipid identifications, with studies reporting agreement rates as low as 14–36% even when analyzing identical LC-MS data with default settings [13].
- Solution:
- Standardize Reference Materials: Use a common, well-characterized quality control sample across all platforms and batches, such as the NIST SRM 1950 – Metabolites in Frozen Human Plasma [72] [50].
- Harmonize Identification Criteria: Establish and document consistent post-analysis filtering criteria across platforms, including mass error tolerance, isotopic pattern quality, and MS/MS spectral match scores [5].
- Cross-Validate with Standards: Whenever possible, confirm identities using authentic chemical standards for the lipid species of interest.
FAQ: How can I determine if inconsistent results are due to platform technical differences or true biological variability?
- Problem: It is challenging to disentangle technical artifacts from genuine biological effects, especially when working with diverse sample types (e.g., CSF, plasma, urine) or patient populations [71].
- Solution:
- Implement a Study Design with Balanced Batches: Distribute samples from different experimental groups (e.g., disease vs. control) evenly across measurement batches and platforms. This prevents confounding of the biological factor of interest with batch or platform covariates [5].
- Perform Orthogonal Validation: Measure a subset of key lipid biomarkers using a different, independent technology (e.g., NMR if MS was used initially) to confirm the initial findings [71] [64].
- Use a Data-Driven Reference Approach: Employ stably expressed internal standards or "housekeeping" lipids as references to create contingency tables and normalize data, which can help eliminate platform-specific biases and make results more comparable [73].
FAQ: What is the best way to handle data when different laboratories report results in varying units or formats?
- Problem: Lack of standardized data reporting leads to difficulties in pooling data for meta-analysis or comparing findings across studies.
- Solution:
- Adopt Community Standards: Follow the LIPID MAPS classification, nomenclature, and shorthand notation for reporting lipid structures to ensure consistency and clarity [13] [50].
- Implement Rigorous Data Validation Checks: The table below outlines essential data quality checks to perform before cross-platform or inter-laboratory data integration.
| Quality Check Type | Purpose | Implementation Example |
|---|---|---|
| Accuracy Validation | Confirm data correctness | Cross-check values for a pooled QC sample across all platforms [74]. |
| Completeness Check | Detect missing data | Automatically scan data tables for gaps in key lipid measurements [74]. |
| Format Consistency | Standardize data presentation | Validate all files against a predefined template for decimal separators, units, and column headers [74]. |
| Cross-Platform Sync | Ensure alignment across tools | Compare timestamps and synchronized values for the same sample measured on different systems [74]. |
Standardized Experimental Protocols
Protocol for an Inter-Laboratory Lipid Comparison Study
This protocol is adapted from the NIST harmonization study [72] [50] and best practices in untargeted lipidomics [5].
1. Sample Preparation and Distribution
- Central QC Material: A central reference material (e.g., NIST SRM 1950) is aliquoted and distributed to all participating laboratories.
- Internal Standards: Provide a standardized mix of isotope-labeled internal standards (ITS) to all labs to be spiked into every sample during the lipid extraction process. This corrects for variability in extraction efficiency and instrument response [5] [64].
- Blinded Samples: Include blinded biological samples (e.g., from case/control cohorts) alongside the QC materials to assess performance on real study samples.
2. Lipid Extraction and LC-MS Analysis
- Stratified Randomization: Samples should be randomized within and across analytical batches to avoid bias from instrument drift.
- Blank Samples: Insert blank extraction samples (empty tubes without tissue) after every set of experimental samples to monitor and subtract background contamination [5].
- Pooled QC Samples: Create a pooled Quality Control (QC) sample from an aliquot of all experimental samples. This QC should be injected repeatedly at the beginning of the run to condition the column, after every batch of samples, and at the end of the run to monitor instrument stability [5].
3. Data Processing and Analysis
- Consensus Lipid Identification: Each laboratory processes its raw data using its preferred software, but applies a common set of consensus identification criteria for reporting.
- Consensus Concentration Estimation: For lipids measured by multiple laboratories, a consensus value (e.g., median of means) is calculated. The associated uncertainty (e.g., coefficient of dispersion) is reported to quantify inter-laboratory variability [72] [50].
The following workflow diagram illustrates the core steps of a cross-platform validation study.
Protocol for a Single-Laboratory Cross-Platform Validation
For a single lab comparing two platforms (e.g., two different LC-MS instruments or kits):
1. Sample Set Design
- Select a balanced set of samples representing the biological range of interest (e.g., 10 disease, 10 control).
- Include technical replicates to assess intra-platform reproducibility.
2. Cross-Platform Analysis
- Analyze all samples on both platforms in a randomized order.
- Ensure sample preparation is identical up to the point of injection or platform-specific protocol steps.
3. Data Integration and Comparison
- Perform correlation analysis of effect sizes (e.g., fold-change) for lipids quantified on both platforms.
- Identify consistently dysregulated lipid species that show the same direction and significance of change regardless of the platform used [71].
The Scientist's Toolkit: Essential Research Reagents and Materials
The table below lists key materials required for robust cross-platform and inter-laboratory lipidomics studies.
| Item | Function & Importance |
|---|---|
| NIST SRM 1950 | A certified human plasma reference material for inter-laboratory quality control and harmonization. It provides community-wide benchmark values for hundreds of lipids [72] [50]. |
| Isotope-Labeled Internal Standards (ITS) | A mixture of stable isotope-labeled lipid standards spiked into samples before extraction. They normalize for losses during sample preparation and analytical variability, enabling accurate quantification [5] [64]. |
| Pooled Quality Control (QC) Sample | A homogeneous sample created by combining small aliquots of all study samples. It is used to monitor instrument stability, batch effects, and analytical reproducibility throughout the data acquisition sequence [5]. |
| Blank Extraction Solvents | High-purity solvents processed through the entire extraction and analysis workflow without any biological sample. They are critical for identifying and filtering out background signals and contaminants [5]. |
| Standardized Data Reporting Template | A pre-defined template (e.g., based on LIPID MAPS nomenclature) that ensures all laboratories report lipid identities, intensities, and associated metadata in a consistent format for seamless data integration [13] [50]. |
Interpreting Results and Statistical Validation
Key Metrics for Assessing Robustness
When analyzing the results of a cross-platform comparison, focus on these quantitative metrics:
- Correlation of Effect Sizes: Calculate the correlation coefficient (e.g., Spearman's Ï) between the effect sizes (e.g., log2 fold-change) of lipids measured on both platforms. A significant positive correlation indicates general concordance in identifying the direction and relative magnitude of changes [71].
- Overlap of Significant Hits: Determine the percentage of significantly dysregulated lipids (e.g., FDR < 0.05) that are replicated across platforms. The number of consistently validated biomarkers is often small but more reliable [71].
- Classification Performance: If the goal is diagnostic classification, train a model on data from one platform and test its performance on data from the other platform. This tests the real-world translational potential of the biomarker signature [73] [64].
The following diagram outlines the logical decision process for evaluating cross-platform validation outcomes.
Diagnosing Inflammatory Bowel Disease (IBD) in pediatric patients presents unique clinical challenges. Children often present with more extensive and aggressive disease compared to adults, and symptoms frequently overlap with many other gastrointestinal conditions, leading to diagnostic delays [75]. Approximately 25% of IBD cases are diagnosed before the age of 20, with incidence rates rising globally, particularly in newly industrialized regions [75]. The absence of a robust, non-invasive diagnostic test for screening pediatric patients with gastrointestinal symptoms often translates into delayed diagnosis, which is associated with disease complications, surgery, and poorer long-term outcomes [21].
Current biomarkers have significant limitations. While C-reactive protein (CRP) is the most studied blood-based marker, it shows poor performance in ulcerative colitis (UC), and a substantial portion of Crohn's disease (CD) patients do not mount a significant CRP response [21]. Fecal calprotectin (FC) is a recognized marker of gastrointestinal inflammation but suffers from variable specificity in children and poor patient acceptance due to the nature of sample collection [21] [76]. Consequently, there is an urgent need for a reliable, easily obtained biomarker to support clinical decision-making and shorten the diagnostic delay for pediatric IBD [21] [75].
Lipidomics, the large-scale study of molecular lipids in biological systems, has emerged as a promising approach for biomarker discovery. Lipids are involved in vital cellular processes, including cell signaling, energy storage, and structural membrane integrity, and altered lipid metabolism has been implicated in inflammatory disorders, including IBD [21] [13]. This case study examines the identification and validation of a specific blood-based diagnostic lipidomic signature for pediatric IBD, focusing on the experimental workflows, key findings, and troubleshooting the reproducibility challenges inherent in translating such discoveries into clinically applicable tools.
The Identified Lipidomic Signature and Its Performance
Core Lipid Biomarkers
Through a comprehensive lipidomic analysis of blood samples from treatment-naïve pediatric patients across multiple independent cohorts, a diagnostic signature comprising two key lipids was identified and validated [21].
Table 1: Core Lipidomic Signature for Pediatric IBD Diagnosis
| Lipid Abbreviation | Full Lipid Name | Chemical Category | Direction of Change in IBD | Proposed Biological Relevance |
|---|---|---|---|---|
| LacCer(d18:1/16:0) | Lactosylceramide (d18:1/16:0) | Sphingolipid | Increased | Sphingolipids like ceramides are potent signaling molecules regulating inflammation, cell death, and metabolic processes [77]. |
| PC(18:0p/22:6) | Plasmalogen Phosphatidylcholine (18:0p/22:6) | Glycerophospholipid (Ether-linked) | Decreased | Plasmalogen PCs are phospholipids with antioxidant properties and are key structural components of cell membranes [21] [13]. |
The discovery and validation process involved analyzing cohorts of incident treatment-naïve pediatric patients, confirming that this two-lipid signature is consistently dysregulated in pediatric IBD compared to symptomatic non-IBD controls [21].
Diagnostic Performance vs. Established Biomarkers
The diagnostic performance of this lipidomic signature was rigorously evaluated against high-sensitivity CRP (hsCRP) and, in a subset of patients, against fecal calprotectin.
Table 2: Diagnostic Performance Comparison in Validation Cohort
| Diagnostic Method | Condition | Area Under the Curve (AUC) | 95% Confidence Interval | Statistical Comparison |
|---|---|---|---|---|
| Lipidomic Signature | IBD vs. Controls | 0.85 | 0.77 - 0.92 | Significantly higher than hsCRP (p < 0.001) [21] |
| High-Sensitivity CRP (hsCRP) | IBD vs. Controls | 0.73 | 0.63 - 0.82 | Reference [21] |
| Lipidomic Signature | Crohn's Disease vs. Controls | 0.84 | 0.74 - 0.92 | Nominally higher than hsCRP (p = 0.10) [21] |
| Lipidomic Signature | Ulcerative Colitis vs. Controls | 0.76 | 0.63 - 0.87 | Data compared to hsCRP [21] |
The study concluded that the lipidomic signature improved diagnostic prediction compared to hsCRP. Furthermore, adding hsCRP to the lipidomic signature did not enhance its performance, indicating that the lipid markers capture robust, independent diagnostic information [21]. In patients who provided stool samples, the diagnostic performance of the lipidomic signature and fecal calprotectin did not differ substantially, suggesting the blood-based lipid test could be a viable alternative to fecal testing [21].
Experimental Workflow & Protocol
The validation of the lipidomic signature followed a multi-stage process, from sample preparation to data analysis. The workflow below outlines the key stages, which are detailed in the subsequent sections.
Sample Collection and Pre-Analytical Processing
Protocol: Blood samples should be collected after a recommended fasting period. Blood is drawn into specialized tubes containing EDTA or other appropriate anticoagulants for plasma separation. For serum, blood is collected in clot-activating tubes. Following collection, samples must be centrifuged under standardized conditions (e.g., 2,000-3,000 x g for 10-15 minutes at 4°C) to separate plasma/serum from cellular components. The supernatant is then aliquoted into cryovials and immediately snap-frozen on dry ice or liquid nitrogen before storage at -80°C to prevent lipid degradation [77] [78].
Troubleshooting FAQ:
- Q: We observe high variability in lipid levels between replicates from the same cohort. What could be the cause?
A: Inconsistent pre-analytical handling is a major source of variability. Ensure strict standardization of [13] [79]:
- Fasting Status: Confirm and record patient fasting duration uniformly.
- Sample Processing Time: Minimize and standardize the time between blood draw and centrifugation/freezing.
- Storage Conditions: Avoid repeated freeze-thaw cycles. Aliquoting samples is critical.
Lipid Extraction Methodology
Protocol: The modified methyl-tert-butyl ether (MTBE) extraction method is widely used for its high recovery of diverse lipid classes [78]. Briefly:
- Aliquot a precise volume of plasma/serum (e.g., 50-100 µL) into a glass tube.
- Add a mixture of methanol and internal standard mixture (IS). The IS are stable isotope-labeled lipid analogs added to correct for extraction efficiency and instrument variability.
- Vortex thoroughly.
- Add a volume of MTBE, typically 4-5 times the volume of the methanol/sample mixture.
- Shake or sonicate the mixture to form a single phase.
- Add a volume of water to induce phase separation (upper organic MTBE layer containing lipids, lower aqueous layer).
- Centrifuge to complete phase separation.
- Collect the upper organic layer and evaporate to dryness under a gentle stream of nitrogen gas.
- Reconstitute the dried lipid extract in a suitable solvent mixture (e.g., isopropanol/acetonitrile) for LC-MS analysis [80] [78].
Troubleshooting FAQ:
- Q: Our lipid recovery is low or inconsistent for certain lipid classes. How can we improve this?
A: [78]
- Internal Standards: Use a comprehensive suite of internal standards covering all major lipid classes (e.g., PCs, Cer, SM, TGs) to accurately quantify recovery.
- Extraction Efficiency: Test and validate your extraction protocol (e.g., Bligh & Dyer vs. MTBE) for your specific sample matrix to ensure it is optimal for the lipid classes of interest.
- Matrix Effects: The presence of non-lipid components can suppress or enhance ionization. Cleanup steps or more selective extraction techniques may be necessary.
Liquid Chromatography-Tandem Mass Spectrometry (LC-MS/MS) Analysis
Protocol: A multiplexed normal phase liquid chromatography-hydrophilic interaction chromatography (NPLC-HILIC) multiple reaction monitoring (MRM) method is highly effective for quantifying a wide range of lipid classes in a single run [80].
- Chromatography: Use a suitable HILIC column (e.g., 2.1 x 150 mm, 2.7 µm) with a binary gradient. Mobile phase A is often acetonitrile/water, and phase B is isopropanol/acetonitrile, both with volatile buffers like ammonium formate or acetate. The gradient elutes lipids by class based on the polarity of their head groups.
- Mass Spectrometry: Operate a triple quadrupole (QQQ) mass spectrometer in scheduled MRM mode. Nitrogen is used as the collision gas. Optimize MS parameters for each lipid class, including Declustering Potential (DP) and Collision Energy (CE). Both positive and negative ionization modes are required for comprehensive coverage [80] [81].
- Quantification: Use lipid class-based calibration curves with authentic standards to interpolate lipid concentrations. Utilizing multiple MS/MS product ions per lipid species improves confidence in identification and can help determine relative abundances of isomers [80].
Troubleshooting FAQ:
- Q: We are getting poor chromatographic separation or peak shape for certain lipids. What should we check?
A: [78]
- Column Condition: Ensure the LC column is not degraded. Flush and re-condition the column according to the manufacturer's instructions.
- Solvent Quality: Use only high-purity, LC-MS grade solvents and additives.
- Sample Cleanliness: If the sample is too complex or dirty, consider optimizing the lipid extraction or introducing a solid-phase extraction (SPE) cleanup step.
- Q: How do we address in-source fragmentation that leads to misidentification?
A: In-source fragmentation is a known challenge. To ensure selectivity and confident identification [80]:
- Chromatographic Separation: Ensure that the precursor ion and its in-source fragment are chromatographically resolved.
- Multiple Ions: Monitor multiple MRM transitions (precursor > product ion) for a single lipid species.
- Standard Verification: Confirm fragmentation patterns and retention times using authentic lipid standards when available.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for Lipidomic Biomarker Validation
| Item Category | Specific Examples / Functions | Critical Role in the Workflow |
|---|---|---|
| Internal Standards (IS) | Stable isotope-labeled lipids (e.g., PC(13:0/13:0), Cer(d18:1/17:0), SM(d18:1/12:0), TG(17:0/17:0/17:0)) | Essential for precise quantification. They correct for variations in sample preparation, matrix effects, and instrument performance [80] [78]. |
| Authentic Lipid Standards | Unlabeled pure lipid standards for various classes (e.g., LacCer, PC plasmalogens from Avanti Polar Lipids) | Used to optimize MS parameters, construct calibration curves for absolute quantification, and confirm retention times [80] [78]. |
| LC-MS Grade Solvents | Methanol, Acetonitrile, Isopropanol, Chloroform, MTBE, Water | High-purity solvents are critical to minimize background noise, prevent ion suppression, and ensure system stability [78]. |
| Volatile Buffers | Ammonium Formate, Ammonium Acetate | Added to mobile phases to promote efficient ionization of lipids during MS analysis, improving sensitivity and reproducibility [78]. |
| Quality Control (QC) Material | Commercially available reference plasma (e.g., NIST SRM 1950) or a pooled sample from your study | Pooled QC samples are analyzed intermittently throughout the batch to monitor instrument stability, data quality, and reproducibility [80] [79]. |
Navigating Reproducibility Challenges
A core challenge in lipidomics is the transition from a discovery-level finding to a validated, reproducible assay suitable for clinical application. The following diagram and text outline the major hurdles and proposed solutions.
Pre-analytical Variability: Biological variability and inconsistencies in sample collection, processing, and storage are significant sources of irreproducibility. Lipids are dynamic and can degrade or change with handling [13].
- Solution: Implement and document Standard Operating Procedures (SOPs) for every pre-analytical step, from patient preparation (e.g., fasting) to long-term storage at -80°C. Using a consistent sample matrix (e.g., plasma vs. serum) is also critical [79].
Lack of Analytical Standardization: Differences in lipid extraction methods, LC-MS platforms, and data processing software can lead to laboratories reporting divergent results from the same sample. Agreement rates between common software platforms can be as low as 14-36% [13].
- Solution: Follow FDA Bioanalytical Method Validation Guidance principles where applicable [80]. Key steps include:
- Method Qualification: Determine and report on key parameters such as limit of detection (LOD), linear dynamic range, intra- and inter-batch accuracy and precision, and carry-over [80] [79].
- Cross-Lab Validation: Participate in inter-laboratory studies and use standardized reference materials like NIST SRM 1950 plasma to benchmark performance [80].
Data Processing and Reporting Complexity: The vast amount of data generated in lipidomics requires robust bioinformatics, and a lack of transparent reporting makes it difficult to reproduce findings.
- Solution: Adopt emerging reporting standards, such as the Lipidomics Reporting Checklist (LRC), to ensure all critical methodological information is shared [78]. Utilize validated bioinformatics pipelines and make raw data available when possible.
The validation of a blood-based lipidomic signature comprising LacCer(d18:1/16:0) and PC(18:0p/22:6) represents a significant advance in the quest for a non-invasive diagnostic test for pediatric IBD. This case study underscores that the path to a clinically useful biomarker requires not only the identification of dysregulated molecules but also a rigorous, standardized, and reproducible validation process that actively troubleshoots technical and analytical challenges.
Future efforts will focus on the transition of this validated lipidomic signature into a scalable, cost-effective diagnostic blood test. This will require large-scale multi-center validation studies and the development of simplified, high-throughput analytical platforms that can be integrated into clinical laboratory workflows. Overcoming the reproducibility challenges detailed here is paramount to realizing the potential of lipidomics in supporting clinical decision-making and improving outcomes for children with IBD.
Frequently Asked Questions (FAQs)
Q1: What are the most critical factors for ensuring reproducibility in lipidomic biomarker identification?
The most critical factors involve addressing significant inconsistencies in data analysis software and implementing robust validation protocols. Studies show that even when using identical spectral data, different software platforms can yield highly inconsistent results. For instance, a 2024 study found only 14.0% identification agreement between two popular platforms, MS DIAL and Lipostar, using default settings. Agreement improves to 36.1% when using fragmentation (MS2) data, but this still highlights a substantial reproducibility gap [12] [14]. Key factors include:
- Multi-platform Validation: Cross-validating findings using more than one software platform.
- Manual Curation: Manually inspecting and curating software outputs to reduce false positives.
- Comprehensive MS Modes: Using both positive and negative LC-MS modes for validation.
- Data-Driven QC: Employing machine learning approaches, like support vector machine regression, for outlier detection [14].
Q2: What regulatory aspects should be considered early in assay development?
Prioritizing regulatory requirements from the outset is essential for a smooth transition from research to clinically approved diagnostics.
- Early Framework Establishment: For assays intended for FDA approval (e.g., under CLIA), adopt an ISO 13485 phase-gated development process from the start. This ensures all necessary documentation is in place for regulatory submission [82].
- Component Testing: Regulatory agencies typically require validation studies that include multiple lots of critical assay components (e.g., enzymes, primers) to demonstrate consistency and reliability [82].
- Design Control: Consider the final product's workflow (e.g., cartridge design, point-of-care test) during the initial Research Use Only (RUO) phase to avoid costly re-engineering later [82].
Q3: How can assay scalability and reproducibility be improved during scale-up?
Scalability and reproducibility are challenged by manual workflows, human error, and supply chain instability. Solutions include:
- Automation: Implementing precise, automated liquid handling systems to ensure consistent droplet sizes, minimize human error, and enable traceability for audits [83].
- Assay Miniaturization: Scaling down reaction volumes conserves valuable and expensive reagents and precious clinical samples, leading to significant cost savings without compromising performance [83].
- Supply Chain Strategy: Engaging with reputable suppliers early in the design process and auditing their capabilities for consistent, high-quality ingredients and inventory management is crucial to avoid manufacturing delays [82].
Q4: What are common pitfalls in interpreting lipid mass spectrometry data for mammalian samples?
A major pitfall is the reporting of lipid species that are unlikely to exist in mammalian samples. Due to the vast structural diversity and high similarity of lipids, misidentification is common. Biologists must adhere to established protocols and apply critical judgment when interpreting data, focusing on major lipid classes like phospholipids, glycerolipids, and sphingolipids to avoid incorrect biological conclusions [84].
Troubleshooting Guides
Troubleshooting HPLC Issues in Lipidomics
High-Performance Liquid Chromatography (HPLC) is a core component of LC-MS workflows. The table below summarizes common issues and their solutions.
| Problem | Possible Causes | Recommended Solutions |
|---|---|---|
| Retention Time Drift | Poor temperature control, incorrect mobile phase composition, poor column equilibration, change in flow rate [85] | Use a thermostat column oven, prepare fresh mobile phase, increase column equilibration time, reset and test flow rate [85] |
| Baseline Noise | System leak, incorrect mobile phase, air bubbles in system, contaminated detector cell [85] | Check and tighten loose fittings, check mobile phase preparation and miscibility, degas mobile phase and purge system, clean detector flow cell [85] |
| Broad Peaks | Changed mobile phase composition, leaks, low flow rate, column overloading, contaminated guard/column [85] | Prepare fresh mobile phase, check for leaks and tighten fittings, increase flow rate, decrease injection volume, replace guard column/column [85] |
| Peak Tailing | Long flow path, prolonged analyte retention, blocked column, active sites on column [85] | Use shorter/narrower tubing, modify mobile phase composition or use a different column, flush or replace column, change column [85] |
| High Back Pressure | Column blockage, flow rate too high, injector blockage, mobile phase precipitation [85] | Backflush or replace column, lower flow rate, flush injector, flush system and prepare fresh mobile phase [85] |
Troubleshooting Software & Data Reproducibility
Inconsistent lipid identification across software platforms is a major challenge. The following workflow provides a systematic method to improve confidence in your results.
Steps for Multi-Platform Lipid Identification:
- Process Data in Parallel: Analyze your raw LC-MS data with at least two different software platforms (e.g., MS DIAL and Lipostar) [12] [14].
- Cross-Reference Results: Compile the lists of putative lipid identifications from all platforms.
- Check for Agreement: Identify lipids where the software platforms agree on both the lipid class and molecular formula. These can be considered higher-confidence identifications [14].
- Apply Rigorous Filters to Discrepant Identifications: For lipids identified by only one platform, or where there is conflict, apply additional manual checks:
- Manual Curation: Visually inspect the MS1 and MS2 spectra for quality and matching.
- Retention Time Plausibility: Check if the retention time is consistent with the putative lipid identity.
- Biological Plausibility: Consult literature to confirm the lipid is known to be present in your sample type (e.g., mammalian systems) [84].
Experimental Protocols & Workflows
Protocol: LC-MS-Based Untargeted Lipidomics
This protocol outlines a standard workflow for untargeted lipidomics, adapted from recent methodologies [14].
1. Sample Preparation
- Lipid Extraction: Use a modified Folch extraction. Add a chilled solution of methanol/chloroform (1:2 v/v) to your cell pellet or tissue homogenate. Supplement with 0.01% butylated hydroxytoluene (BHT) to prevent lipid oxidation [14].
- Internal Standard Addition: Add a quantitative mass spectrometry internal standard mixture (e.g., Avanti EquiSPLASH LIPIDOMIX) to the extract for later quantification. Dilute the sample to an appropriate concentration (e.g., 280 cells/µL) [14].
2. Liquid Chromatography (LC) Separation
- Column: Use a polar C18 column (e.g., Luna Omega 3 µm, 50 × 0.3 mm) for microflow separation [14].
- Mobile Phase:
- Eluent A: 60:40 acetonitrile/water
- Eluent B: 85:10:5 isopropanol/water/acetonitrile
- Supplement both eluents with 10 mM ammonium formate and 0.1% formic acid [14].
- Gradient:
- 0 – 0.5 min: 40% B
- 0.5 – 5 min: ramp to 99% B
- 5 – 10 min: hold at 99% B
- 10 – 12.5 min: return to 40% B
- 12.5 – 15 min: re-equilibrate at 40% B [14].
- Flow Rate: 8 µL/min [14].
- Injection Volume: 5 µL [14].
3. Mass Spectrometry (MS) Data Acquisition
- Instrument: Couple the LC system to a high-resolution mass spectrometer (e.g., ZenoToF 7600) [14].
- Ionization Mode: Operate in both positive and negative ionization modes to maximize lipid coverage [12] [14].
- Data Acquisition: Use data-dependent acquisition (DDA) to collect both MS1 (precursor) and MS2 (fragmentation) spectra.
Protocol: A Scalable Automated NGS Clean-up Workflow
This protocol demonstrates how automation can enhance scalability and reproducibility in next-generation sequencing (NGS) workflows, which are often integrated with biomarker discovery.
Workflow Diagram for Automated NGS Preparation:
Steps:
- Transfer: The I.DOT Liquid Handler automatically and precisely transfers the NGS library reaction mixture using non-contact dispensing. This minimizes reagent use and prevents cross-contamination [83].
- Clean-Up: The mixture is processed using the G.PURE NGS Clean-Up Device to remove enzymes, salts, and other impurities [83].
- Elution: The purified DNA library is eluted in a ready-to-sequence buffer.
- Scalability: This automated bundle allows for the processing of thousands of samples daily with significant miniaturization, conserving reagents and ensuring consistent, high-quality results [83].
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function & Rationale |
|---|---|
| Quantitative Internal Standards (e.g., EquiSPLASH) | A mixture of deuterated lipids added to the sample before extraction. It corrects for variability in extraction efficiency and ionization efficiency during MS analysis, enabling accurate quantification [14]. |
| Chilled Methanol/Chloroform | Organic solvent mixture used in Folch extraction for efficient and broad-range lipid extraction from biological matrices [14]. |
| Butylated Hydroxytoluene (BHT) | An antioxidant added to lipid extraction solvents to prevent the oxidation of unsaturated lipids, preserving the sample's native lipid profile [14]. |
| Ammonium Formate & Formic Acid | Mobile phase additives in LC-MS. They promote the formation of [M+H]+ or [M-H]- ions, enhancing ionization efficiency and stabilizing the chromatographic baseline [14]. |
| High-Purity HPLC Grade Solvents | Essential for preparing mobile phases to minimize baseline noise, ghost peaks, and system contamination that can interfere with detecting low-abundance lipids [85]. |
Conclusion
The journey to reliable and clinically impactful lipidomic biomarkers is fraught with reproducibility challenges, yet also rich with opportunity. A synthesis of the evidence reveals that overcoming these hurdles requires a multi-faceted approach: rigorous standardization from pre-analytical steps to data processing, the strategic integration of machine learning for robust feature selection, and mandatory validation across independent cohorts and platforms. The future of lipidomics in precision health depends on the field's collective ability to close the reproducibility gap. This will involve developing more consistent software algorithms, establishing universal standards, and creating integrated workflows that seamlessly connect lipidomic discoveries with proteomic and genomic data. By systematically addressing these challenges, lipidomic biomarkers can fully realize their potential to provide earlier, more accurate diagnostics and drive the development of personalized therapeutic strategies across a wide spectrum of human diseases.
References
- 1. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/abs/pii/S0009898125005777]
- 2. Exploring lipidomics in biomarker discovery [https://pubmed.ncbi.nlm.nih.gov/41197707/]
- 3. Bioactive lipid signaling and lipidomics in macrophage ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1550500/full]
- 4. Lipid rafts: novel therapeutic targets for metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12004566/]
- 5. The Hitchhiker's Guide to Untargeted Lipidomics Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8624948/]
- 6. Lipidomics Workflows [https://www.thermofisher.com/us/en/home/industrial/mass-spectrometry/mass-spectrometry-learning-center/mass-spectrometry-applications-area/metabolomics-mass-spectrometry/lipidomics-workflows.html]
- 7. Challenges and opportunities in computational studies for ... [https://www.nature.com/articles/s44386-025-00024-3]
- 8. Glycerophospholipids in ALS: insights into disease ... [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-025-00876-3]
- 9. Lipidomics in Biomarker Research [https://link.springer.com/chapter/10.1007/164_2021_517]
- 10. The strategic role of lipidomics in biomarker identification ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1546512/full]
- 11. Streamlining Lipidomics: Novel Statistical Workflows and ... [https://www.chromatographyonline.com/view/streamlining-lipidomics-novel-statistical-workflows-and-visualization-in-r-and-python]
- 12. Challenges in Lipidomics Biomarker Identification [https://pubmed.ncbi.nlm.nih.gov/39195557/]
- 13. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/pii/S0009898125005777?dgcid=rss_sd_all]
- 14. Challenges in Lipidomics Biomarker Identification [https://pmc.ncbi.nlm.nih.gov/articles/PMC11356033/]
- 15. Exploring sphingolipid metabolism-related biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12173885/]
- 16. Exploring the role of sphingolipid-related genes in clinical ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1116839/full]
- 17. Biomarker Validation: Common Data Analysis Concerns [https://pmc.ncbi.nlm.nih.gov/articles/PMC4122484/]
- 18. Biomarker Discovery and Validation: Statistical Considerations [https://pmc.ncbi.nlm.nih.gov/articles/PMC8012218/]
- 19. Serum phospholipids and sphingolipids are linked to early ... [https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-025-03537-4]
- 20. LipidSearch Software Support-Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/mass-spectrometry-support-center/liquid-chromatography-mass-spectrometry-software-support/lipidsearch-software-support/lipidsearch-software-support-troubleshooting.html]
- 21. Identification and validation of a blood- based diagnostic ... [https://www.nature.com/articles/s41467-024-48763-7]
- 22. Utilizing Serum-Derived Lipidomics with Protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12409608/]
- 23. Identification and validation of a blood- based diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11148148/]
- 24. based diagnostic lipidomic signature of pediatric ... [https://pubmed.ncbi.nlm.nih.gov/38830848/]
- 25. Recommendations for good practice in MS-based lipidomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC8585648/]
- 26. Lipidomics: Techniques, applications, and outcomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5085849/]
- 27. Best practices and tools in R and Python for statistical ... [https://www.nature.com/articles/s41467-025-63751-1]
- 28. Challenges in Lipidomics Biomarker Identification [https://www.mdpi.com/2218-1989/14/8/461]
- 29. Untargeted vs. Targeted Lipidomics—Understanding the ... [https://lipidomics.creative-proteomics.com/resource/untargeted-vs-targeted-lipidomics-understanding-the-differences.htm]
- 30. Targeted vs Untargeted Metabolomics [https://www.metabolon.com/blog/targeted-vs-untargeted-metabolomics/]
- 31. Cross-Platform Comparison of Untargeted and Targeted ... [https://www.nature.com/articles/s41598-018-35807-4]
- 32. Targeted lipidomics analysis of possible molecular ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1531524/full]
- 33. Untargeted Lipidomics [https://sciex.com/applications/biomedical-and-omics-research/lipidomics/untargeted-lipidomics]
- 34. Targeted lipidomics analysis of possible molecular ... [https://pubmed.ncbi.nlm.nih.gov/39850562/]
- 35. Lipid Annotation by Combination of UHPLC-HRMS (MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7345884/]
- 36. Rapid and reproducible LC-HRMS for combined lipidomics ... [https://www.sciencedirect.com/science/article/pii/S0026265X25032254]
- 37. Serum untargeted lipidomics by UHPLC-ESI-HRMS aids the ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-022-09427-1]
- 38. Analytical quality control in targeted lipidomics [https://www.sciencedirect.com/science/article/pii/S0003267025006191]
- 39. Identification of novel serum lipid metabolism potential ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13561-x]
- 40. Steps Required to Interpret Lipidomics Data [https://www.metwarebio.com/how-to-interpret-lipidomics-data-a-step-by-step-guide/]
- 41. Combining lipidomics and machine learning to identify lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12128965/]
- 42. Identification of novel lipid metabolism-related biomarkers ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1681989/full]
- 43. Lipidomics reveals potential biomarkers and ... [https://www.sciencedirect.com/science/article/pii/S2589936825000106]
- 44. Multi-omics Data Integration, Interpretation, and Its Application [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]
- 45. Integrated multi-omics analysis identifies lipid metabolism ... [https://www.nature.com/articles/s41598-025-13703-y]
- 46. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 47. Challenges in Lipidomics Biomarker Identification [https://cris.bgu.ac.il/en/publications/challenges-in-lipidomics-biomarker-identification-avoiding-the-pi]
- 48. Evaluating Software Tools for Lipid Identification from Ion ... [https://www.mdpi.com/1420-3049/28/8/3483]
- 49. How to Interpret Lipidomics Data: A Step-by-Step Guide [https://lipidomics.creative-proteomics.com/resource/how-to-interpret-lipidomics-data-a-step-by-step-guide.htm]
- 50. Harmonizing lipidomics: NIST interlaboratory comparison ... [https://www.sciencedirect.com/science/article/pii/S0022227520335549]
- 51. From bedside to bench—practical considerations to avoid pre-analytical pitfalls and assess sample quality for high-resolution metabolomics and lipidomics analyses of body fluids | Analytical and Bioanalytical Chemistry [https://link.springer.com/article/10.1007/s00216-021-03450-0]
- 52. From bedside to bench—practical considerations to avoid pre ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8410705/]
- 53. Ex vivo instability of lipids in whole blood: preanalytical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10208886/]
- 54. Pre and post analytical errors in lipid determination [https://link.springer.com/article/10.1007/BF02868405]
- 55. Separation of Chromatographic Co-Eluted Compounds by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8065729/]
- 56. Diagnosing Chromatography Problems & Troubleshooting [https://www.ssi.shimadzu.com/service-support/faq/liquid-chromatography/knowledge-base/diagnosing-chromatography-problems-troubleshooting/index.html]
- 57. Lipidomics Standards Initiative (LSI) [https://lipidomicssociety.org/interest_groups/lipidomics-standards-initiative-lsi/]
- 58. Lipidomics Standards Initiative (LSI) – Page 2 [https://lipidomicssociety.org/interest_groups/lipidomics-standards-initiative-lsi/2/]
- 59. Recommendations for good practice in MS-based lipidomics [https://pubmed.ncbi.nlm.nih.gov/34662536/]
- 60. Next-Generation Lipidomics: Analyzing Cellular Lipid ... [https://www.azolifesciences.com/article/Next-Generation-Lipidomics-Analyzing-Cellular-Lipid-Profiles-for-Disease-Biomarkers.aspx]
- 61. Common Lipidomics Databases and Software [https://www.metwarebio.com/common-lipidomics-databases-and-software/]
- 62. LipidIN: a comprehensive repository for flash platform ... [https://www.nature.com/articles/s41467-025-59683-5]
- 63. Best practices and tools in R and Python for statistical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12485147/]
- 64. Clinical lipidomics: realizing the potential of lipid profiling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8528718/]
- 65. Evaluation of the diagnostic efficacy of core biomarkers in ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1667402/full]
- 66. Biomarkers in Clinical Practice: Challenges & Opportunities [https://esmed.org/biomarkers-in-clinical-practice-challenges-opportunities/]
- 67. Benchmarking feature projection methods in radiomics [https://www.nature.com/articles/s41598-025-16070-w]
- 68. Beyond ELISA: the future of biomarker validation [https://www.drugtargetreview.com/article/154316/beyond-elisa-the-future-of-biomarker-validation/]
- 69. Applications and challenges of biomarker-based predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399543/]
- 70. Challenges and Future Trends in Biomarker Analysis for ... [https://blog.crownbio.com/challenges-and-future-trends-in-biomarker-analysis-for-clinical-research-whats-ahead-in-2025]
- 71. Multi-platform proteomics profiling of CSF, Plasma, and Urine ... [https://pubmed.ncbi.nlm.nih.gov/41040736/]
- 72. NIST interlaboratory comparison exercise for lipidomics using ... [https://pubmed.ncbi.nlm.nih.gov/28986437/]
- 73. Multiplatform biomarker identification using a data-driven ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-019-3140-7]
- 74. Guide To Cross-Platform Competitor Data Validation [https://metricswatch.com/insights/guide-to-cross-platform-competitor-data-validation]
- 75. Inflammatory bowel disease in paediatrics: Navigating the old ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12476641/]
- 76. Performance of fecal S100A12 as a novel non-invasive ... [https://www.sciencedirect.com/science/article/pii/S0021755723000402]
- 77. Up-to-Date Look at Lipids Role in Precision Health (2025) [https://www.laboratoriosrubio.com/en/lipidomics-precision-health/]
- 78. Enhanced lipidomics workflows for plasma and ... [https://www.sciencedirect.com/science/article/abs/pii/S0039914025003376]
- 79. Method Validation – lipidomicstandards.org [https://lipidomicstandards.org/method-validation/]
- 80. Validation of a multiplexed and targeted lipidomics assay ... [https://pubmed.ncbi.nlm.nih.gov/35489416/]
- 81. The strategic role of lipidomics in biomarker identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483926/]
- 82. Scaling Up Assays: 4 tips to help avoid the most common ... [https://blog.biosearchtech.com/mastering-assay-scale-up-4-tips]
- 83. 5 Key Challenges of Molecular Assay Development & How ... [https://dispendix.com/blog/5-key-challenges-of-molecular-assay-development-how-to-overcome-them]
- 84. Pitfalls in Lipid Mass Spectrometry of Mammalian Samples [https://lipidomicssociety.org/2024/07/03/pitfalls-in-lipid-mass-spectrometry-of-mammalian-samples-a-brief-guide-for-biologists/]
- 85. HPLC Troubleshooting Guide [https://scioninstruments.com/us/blog/hplc-troubleshooting-guide-2/]