Non-Coding RNA Dysregulation in the Hepatocellular Carcinoma Tumor Microenvironment: Mechanisms, Biomarkers, and Therapeutic Avenues
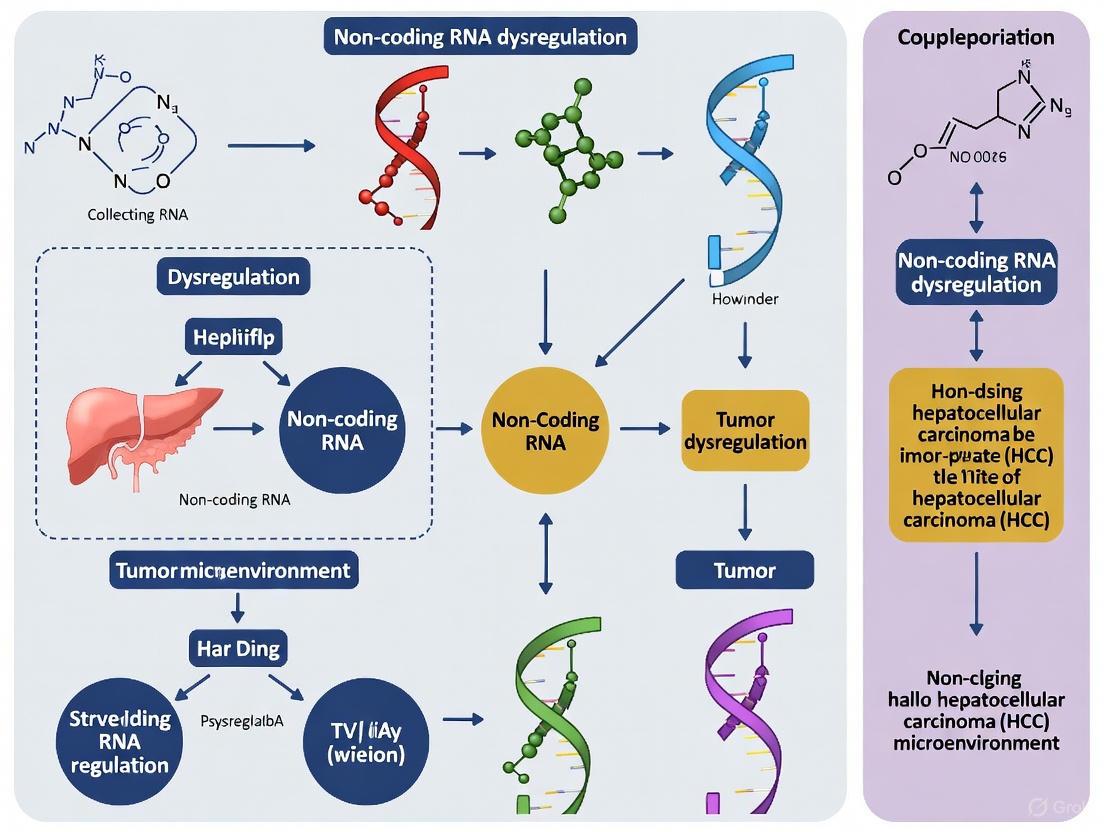
This article comprehensively explores the critical roles of non-coding RNAs (ncRNAs)—including miRNAs, lncRNAs, and circRNAs—in reshaping the hepatocellular carcinoma (HCC) tumor microenvironment (TME).
Non-Coding RNA Dysregulation in the Hepatocellular Carcinoma Tumor Microenvironment: Mechanisms, Biomarkers, and Therapeutic Avenues
Abstract
This article comprehensively explores the critical roles of non-coding RNAs (ncRNAs)—including miRNAs, lncRNAs, and circRNAs—in reshaping the hepatocellular carcinoma (HCC) tumor microenvironment (TME). It details the foundational mechanisms by which dysregulated ncRNAs influence key processes such as metabolic reprogramming, immune evasion, and metastasis. The scope extends to methodological advances in targeting ncRNAs, troubleshooting delivery and specificity challenges, and validating ncRNAs as prognostic biomarkers and predictors of immunotherapy response. Aimed at researchers and drug development professionals, this review synthesizes current knowledge to highlight the significant potential of ncRNA-based strategies in improving HCC diagnosis and therapy.
The Landscape of ncRNA Dysregulation in HCC: Core Players and Microenvironmental Crosstalk
Non-coding RNAs (ncRNAs) have emerged as critical regulators of gene expression and central players in cellular physiology and disease. Once dismissed as transcriptional "noise," these RNA molecules are now recognized for their roles in fine-tuning nearly every aspect of cell biology [1] [2]. In the context of cancer, and particularly in the complex ecosystem of the hepatocellular carcinoma (HCC) tumor microenvironment (TME), the dysregulation of ncRNAs contributes significantly to tumor progression, immune evasion, and therapeutic resistance [3] [4]. This review provides a comprehensive technical guide to three principal ncRNA classes—microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—focusing on their biogenesis, molecular functions, and specific roles in shaping the HCC TME to inform future research and therapeutic development.
miRNA: Biogenesis and Functional Mechanisms
Canonical Biogenesis Pathway
MicroRNAs (miRNAs) are small non-coding RNAs approximately 22-23 nucleotides in length that function as key post-transcriptional regulators of gene expression [5]. Their biogenesis begins with RNA Polymerase II/III transcription of primary miRNA (pri-miRNA) transcripts, which can be several kilobases long and contain one or more hairpin structures [6] [5]. In the nucleus, the microprocessor complex—comprising the RNase III enzyme Drosha and its cofactor DGCR8—cleaves the pri-miRNA to release a ~60-90 nucleotide precursor miRNA (pre-miRNA) featuring a 2-nucleotide 3' overhang [6] [7]. Exportin-5 then transports the pre-miRNA to the cytoplasm in a Ran-GTP-dependent manner, where the RNase III enzyme Dicer cleaves off the terminal loop to generate an unstable miRNA:miRNA* duplex of approximately 19-22 nucleotides [6] [5].
One strand of this duplex (the guide strand) is selectively loaded into an Argonaute (AGO) protein to form the core of the RNA-induced silencing complex (RISC), while the passenger strand is typically degraded [6] [5]. Strand selection depends on thermodynamic stability, with the strand possessing lower 5' stability often being preferentially selected [5]. The mature RISC complex uses the miRNA as a guide to identify complementary mRNA targets through base pairing, primarily between the miRNA "seed region" (nucleotides 2-8) and sequences in the 3' untranslated region (3' UTR) of target mRNAs [6].
Non-Canonical Biogenesis Pathways
Several non-canonical miRNA biogenesis pathways bypass elements of the canonical pathway. Mirtrons represent one well-characterized class of non-canonical miRNAs that are processed from introns during mRNA splicing, independent of Drosha/DGCR8 processing [5]. These short intronic RNAs fold into pre-miRNA-like structures that are directly exported by Exportin-1 and processed by Dicer in the cytoplasm [5]. Another non-canonical pathway involves 7-methylguanosine (m7G)-capped pre-miRNAs that are transcribed as short hairpin RNAs and exported via Exportin-1 without Drosha cleavage, exhibiting strong 3p strand bias due to the 5' cap preventing 5p strand loading into Argonaute [5]. Additionally, some Dicer-independent miRNAs are processed by Drosha from endogenous short hairpin RNA (shRNA) transcripts and require AGO2 for their cytoplasmic maturation [5].
Mechanisms of Gene Regulation
miRNAs regulate gene expression through several mechanisms, with the outcome largely determined by the degree of complementarity between the miRNA and its target. Perfect or near-perfect complementarity typically leads to AGO2-mediated endonucleolytic cleavage and destruction of the target mRNA [5]. However, most animal miRNA-target interactions involve imperfect complementarity, particularly with central mismatches that prevent AGO2 cleavage activity [5]. In these cases, gene silencing occurs through translational repression coupled with mRNA destabilization via deadenylation and decapping [5].
The canonical targeting mechanism involves base pairing between the miRNA seed region and complementary sequences in the 3' UTR of target mRNAs [6]. However, functional miRNA binding sites have also been identified in 5' UTRs, coding sequences, and gene promoters, expanding the regulatory potential of miRNAs [5]. Under certain conditions, miRNA binding can even activate translation rather than repress it, demonstrating the context-dependent nature of miRNA-mediated regulation [5].
Table 1: Key Proteins in miRNA Biogenesis and Function
| Protein | Function | Localization |
|---|---|---|
| Drosha | RNase III enzyme that cleaves pri-miRNA to pre-miRNA | Nucleus |
| DGCR8 | DiGeorge syndrome critical region 8; cofactor for Drosha | Nucleus |
| Exportin-5 | Transports pre-miRNA from nucleus to cytoplasm | Nuclear membrane/Cytoplasm |
| Dicer | RNase III enzyme that cleaves pre-miRNA to mature miRNA duplex | Cytoplasm |
| Argonaute (AGO) | Core component of RISC; facilitates miRNA-guided target recognition | Cytoplasm |
| GW182 | Scaffolding protein that recruits effector complexes for silencing | Cytoplasm |
Figure 1: miRNA Biogenesis Pathway. The diagram illustrates the sequential nuclear and cytoplasmic processing steps from miRNA gene transcription to mature miRNA-mediated gene silencing.
Long Non-Coding RNAs (lncRNAs)
Definition and Genomic Origins
Long non-coding RNAs (lncRNAs) are broadly defined as RNA transcripts exceeding 200 nucleotides that lack significant protein-coding potential [2]. A more precise classification suggests lncRNAs should be considered as transcripts longer than 500 nucleotides, distinguishing them from other non-coding RNA classes [2]. These molecules display tremendous diversity in their genomic origins and structures. lncRNAs can be intergenic (lincRNAs), antisense, intronic, or sense-overlapping relative to protein-coding genes [2]. They are primarily transcribed by RNA Polymerase II and often undergo 5' capping, splicing, and polyadenylation, though notable exceptions exist [2]. The genomic organization of lncRNA genes is particularly complex, with many overlapping protein-coding genes or being located within intronic regions, creating challenges for functional annotation and genetic manipulation [2].
Structural Features and Functional Diversity
lncRNAs exhibit complex secondary and tertiary structures that are crucial for their function. They can form hairpins, stem-loops, and pseudoknots through base pairing, creating conserved short structural modules that mediate specific interactions [6]. For instance, SINEUP lncRNAs contain conserved modules that enhance translational efficiency, while TERRA lncRNAs interact with LSD1 through specific structural domains to promote R-loop formation and telomere maintenance via phase separation mechanisms [6]. The TubAR lncRNA exemplifies how specific secondary structures enable functional interactions, as it binds to α- and β-tubulin heterodimers to stabilize microtubules and support cerebellar myelination [6].
The functional repertoire of lncRNAs is equally diverse. They participate in transcriptional regulation by modulating chromatin accessibility and transcription factor activity [6] [3]. For example, LINC00673 can alter chromatin architecture in breast cancer cells, thereby influencing gene expression patterns [6]. lncRNAs also play important roles in epigenetic regulation by recruiting histone modification complexes or DNA methyltransferases to specific genomic loci [6]. Additionally, many lncRNAs function as competitive endogenous RNAs (ceRNAs) by sequestering miRNAs and preventing them from repressing their target mRNAs [1] [3]. NEAT1 represents a well-characterized example of this sponge function in HCC, where it regulates the miR-155/Tim-3 pathway in CD8+ T cells [3].
Table 2: lncRNA Functional Mechanisms and Examples
| Mechanism | Description | Example |
|---|---|---|
| Transcriptional Regulation | Modulate chromatin structure and transcription factor activity | LINC00673 in breast cancer [6] |
| Epigenetic Modification | Recruit histone/DNA modifying complexes to specific loci | Multiple lncRNAs in cancer [6] |
| miRNA Sponging | Sequester miRNAs to prevent target mRNA repression | NEAT1 in HCC [3] |
| Protein Scaffolding | Serve as platforms for assembling multi-protein complexes | TERRA in telomere maintenance [6] |
| Structural Role | Directly interact with cellular structures | TubAR in microtubule stabilization [6] |
Circular RNAs (circRNAs)
Biogenesis and Structural Characteristics
Circular RNAs (circRNAs) constitute a widespread class of covalently closed circular RNAs generated through a "back-splicing" mechanism where a downstream 5' splice site joins an upstream 3' splice site [8] [4]. This unique biogenesis creates circular molecules that lack free 5' and 3' ends, making them exceptionally resistant to exonuclease degradation and conferring greater stability than their linear counterparts [8] [4]. Based on their sequence composition, circRNAs are categorized into several types: exonic circRNAs (EciRNAs) derived solely from exons; circular intronic RNAs (ciRNAs) originating from introns; exonic-intronic circRNAs (EIciRNAs) containing both exonic and intronic sequences; and antisense or intergenic circRNAs transcribed from non-annotated genomic regions [4]. Approximately 80% of identified circRNAs are EciRNAs that predominantly localize to the cytoplasm, while ciRNAs and EIciRNAs are often nuclear [4].
Molecular Functions and Mechanisms
circRNAs employ diverse molecular mechanisms to regulate cellular processes:
miRNA Sponging: Many circRNAs function as competitive endogenous RNAs by containing multiple binding sites for specific miRNAs, effectively sequestering them and preventing their interaction with target mRNAs [8] [4]. For instance, circ_0056618 promotes angiogenesis in colorectal cancer by binding miR-206 and consequently upregulating CXCR4 and VEGFA expression [8].
Protein Interactions: circRNAs can bind to RNA-binding proteins (RBPs) to form ribonucleoprotein complexes that influence protein function, localization, or stability [8] [4]. This interaction can modulate various aspects of RNA metabolism, including splicing, stability, and translation.
Translation: Although traditionally classified as non-coding, some circRNAs have been shown to be translatable, producing unique peptides with biological functions [8]. This translation typically occurs through cap-independent mechanisms, often involving internal ribosome entry sites (IRES).
Gene Expression Regulation: Nuclear circRNAs can influence transcription by interacting with U1 small nuclear ribonucleoprotein (snRNP) or by modulating RNA Polymerase II activity [4]. EIciRNAs, for example, can enhance the expression of their parental genes through such mechanisms.
Figure 2: circRNA Functional Mechanisms. The diagram illustrates four primary functions of circRNAs: miRNA sponging, protein interactions, peptide translation, and transcription regulation.
ncRNA Crosstalk in the HCC Tumor Microenvironment
The Competitive Endogenous RNA (ceRNA) Hypothesis
The competitive endogenous RNA (ceRNA) hypothesis proposes a sophisticated regulatory network where different RNA species communicate through shared miRNA response elements (MREs) [1]. In this model, lncRNAs and circRNAs function as molecular "sponges" that compete for miRNA binding, thereby preventing these miRNAs from repressing their target mRNAs [1]. This ceRNA network creates an intricate layer of post-transcriptional regulation that fine-tunes gene expression dynamics. In HCC, this crosstalk is particularly relevant for regulating oncogenic pathways, immune responses, and cellular metabolism within the tumor microenvironment [1] [3].
ncRNA-Mediated Regulation of the HCC Immune Microenvironment
The HCC tumor microenvironment features a complex ecosystem where tumor cells interact with various immune cells, stromal components, and extracellular matrix [3]. ncRNAs play pivotal roles in shaping this microenvironment to either promote or suppress antitumor immunity. lncRNAs such as TUG1, LINC01116, CRNDE, and NEAT1 have been identified as key regulators of immune cell function in HCC [3]. For instance, NEAT1 and Tim-3 are significantly upregulated in peripheral blood mononuclear cells (PBMCs) of HCC patients, where NEAT1 promotes CD8+ T cell apoptosis and suppresses their cytolytic activity by regulating the miR-155/Tim-3 pathway [3]. Similarly, lnc-Tim3 directly binds to Tim-3 protein, preventing its interaction with Bat3 and consequently inhibiting downstream signaling in the Lck/NFAT1/AP-1 pathway, which contributes to T cell exhaustion [3].
CircRNAs also contribute significantly to immune regulation in HCC. Tumor-derived exosomes can deliver circRNAs to immune cells, influencing their function and promoting immune evasion [4]. For example, exosomal circ-0001068 from ovarian cancer cells enters T cells and upregulates PD-1 expression by sponging miR-28-5p, leading to T cell exhaustion [4]. Similarly, circRNA-002178 from lung adenocarcinoma can be transferred to CD8+ T cells via exosomes and upregulate PD-1 through miR-34a sponging [4]. Beyond T cells, circRNAs regulate other immune populations including natural killer cells and macrophages, further shaping the immunosuppressive HCC microenvironment [4].
Angiogenesis and Matrix Remodeling
ncRNAs play crucial roles in promoting tumor angiogenesis and extracellular matrix (ECM) remodeling in HCC. Multiple circRNAs regulate angiogenesis through the ceRNA network, with VEGF being a primary target [8]. For instance, circARF1 in glioblastoma stem cells upregulates ISL2 expression by sponging miR-342-3p, which in turn regulates VEGFA expression and promotes endothelial cell proliferation through the VEGFA-mediated ERK signaling pathway [8]. circRNAs also contribute to ECM remodeling by regulating the expression of collagen proteins (COL5A1, COL1A1) and other ECM components in various cancers, processes that are similarly relevant to HCC progression [8].
Table 3: ncRNA Dysregulation in HCC Tumor Microenvironment
| ncRNA | Class | Expression in HCC | Target/Mechanism | Functional Outcome |
|---|---|---|---|---|
| NEAT1 | lncRNA | Upregulated | miR-155/Tim-3 pathway | CD8+ T cell apoptosis, reduced cytolytic activity [3] |
| lnc-Tim3 | lncRNA | Upregulated | Binds Tim-3, disrupts Bat3 interaction | T cell exhaustion [3] |
| circ-0001068 | circRNA | Upregulated (exosomal) | miR-28-5p/PD-1 axis | T cell exhaustion [4] |
| circRNA-002178 | circRNA | Upregulated (exosomal) | miR-34a/PD-1 axis | CD8+ T cell exhaustion [4] |
| circARF1 | circRNA | Upregulated | miR-342-3p/ISL2/VEGFA | Angiogenesis promotion [8] |
Experimental Approaches and Research Reagents
Methodologies for ncRNA Research
Advanced technologies have been developed to identify, characterize, and functionally validate ncRNAs. High-throughput RNA sequencing, particularly with ribosomal RNA depletion protocols, enables comprehensive profiling of lncRNA and circRNA expression patterns [8] [4]. For circRNA identification, treatment with RNase R (which degrades linear RNAs but not circRNAs) followed by RNA sequencing provides a robust approach to enrich and detect circular transcripts [4]. Cross-linking and immunoprecipitation (CLIP) methods, particularly HITS-CLIP and PAR-CLIP, allow researchers to map the interactions between ncRNAs and RNA-binding proteins or between miRNAs and their targets [6]. Functional characterization typically involves loss-of-function approaches using RNA interference or CRISPR-based systems, and gain-of-function studies through plasmid-based overexpression or synthetic RNA delivery [3]. For circRNA-specific manipulation, algorithms that target the back-splicing junction are particularly effective [4].
Research Reagent Solutions
Table 4: Essential Research Reagents for ncRNA Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| RNase Inhibitors | RNaseOUT, SUPERase•In | Protect RNA during processing and analysis |
| Library Prep Kits | TruSeq Small RNA Library Prep Kit, SMARTer smRNA-Seq Kit | Sequencing library construction for different ncRNA classes |
| Enrichment Reagents | RNase R | Circular RNA enrichment by degrading linear RNAs |
| Detection Assays | qRT-PCR assays with divergent primers | circRNA-specific detection and quantification |
| Functional Tools | Locked Nucleic Acid (LNA) inhibitors, siRNA, shRNA, CRISPR-Cas9 systems | ncRNA knockdown and functional characterization |
| Delivery Systems | Lipid nanoparticles, viral vectors | Introduction of ncRNA mimics/inhibitors into cells |
| Exosome Isolation | Total Exosome Isolation Kits, ultracentrifugation protocols | Study of extracellular ncRNAs and their transfer mechanisms |
Concluding Perspectives
The intricate networks formed by miRNAs, lncRNAs, and circRNAs represent a critical regulatory layer in hepatocellular carcinoma biology, with particular significance for understanding and therapeutically targeting the tumor microenvironment. The ceRNA hypothesis provides a framework for understanding how these different ncRNA classes communicate to fine-tune gene expression patterns that drive HCC progression and immune evasion. Future research directions should focus on elucidating the specific molecular mechanisms by which individual ncRNAs function within the HCC TME, developing more sophisticated models to study ncRNA interactions, and translating this knowledge into novel diagnostic and therapeutic approaches. As technologies for ncRNA detection and manipulation continue to advance, targeting these molecules holds significant promise for improving outcomes in HCC and other cancers characterized by ncRNA dysregulation.
Hepatocellular carcinoma (HCC) represents a major global health challenge, ranking as the sixth most common cancer worldwide and the third leading cause of cancer-related deaths [9]. The tumor microenvironment (TME) has emerged as a critical determinant of HCC progression, therapeutic resistance, and patient outcomes. The HCC TME comprises a complex network of cellular components, including cancer-associated fibroblasts (CAFs), tumor-associated macrophages (TAMs), and infiltrating immune cells, alongside non-cellular factors such as extracellular matrix (ECM) proteins, cytokines, and angiogenic mediators [9]. These elements collectively promote immune evasion, stromal remodeling, and neovascularization, driving tumor aggressiveness [9]. Hypoxia, a pivotal characteristic of the HCC TME, is intimately linked to disease progression and unfavorable patient outcomes [10]. This in-depth technical guide examines the core components of the HCC TME and hypoxic niches within the broader context of non-coding RNA dysregulation, providing researchers and drug development professionals with current insights and methodologies for investigating this complex ecosystem.
Cellular Architecture of the HCC TME
The HCC TME features a highly organized cellular architecture where stromal and immune components interact dynamically with malignant hepatocytes. The table below summarizes the key cellular constituents, their origins, markers, and protumorigenic functions.
Table 1: Key Cellular Components of the HCC Tumor Microenvironment
| Cell Type | Origin | Key Markers | Major Protumorigenic Functions | Regulation by ncRNAs |
|---|---|---|---|---|
| Cancer-Associated Fibroblasts (CAFs) | Hepatic stellate cells (HSCs), portal fibroblasts, mesenchymal stem cells | α-SMA, FAP, COL1A1, COL1A2 [11] | ECM remodeling, secretion of growth factors (CXCL11, CCL5), recruitment of immunosuppressive cells (MDSCs, Tregs), promotion of angiogenesis via VEGF/PDGF [9] | miR-1228-3p delivered via exosomes promotes immune evasion [9] |
| Tumor-Associated Macrophages (TAMs) | Circulating monocytes, tissue-resident Kupffer cells | CD163, CD206, VEGF, ARG1 [11] | M2 polarization promotes immunosuppression via IL-4, IL-10, IL-13; angiogenesis via VEGF; tissue remodeling [12] [11] | Exosomal miR-3184-3p induces M2-like polarization [6] |
| Myeloid-Derived Suppressor Cells (MDSCs) | Immature myeloid cells | STAT3, NF-κB [11] | Expansion driven by GM-CSF, IL-6, VEGF; suppression of T cell function, promotion of Treg expansion [11] | Not specified in search results |
| Regulatory T Cells (Tregs) | CD4+ T cell differentiation | FOXP3, CD25, CTLA-4 [11] | Enforcement of immune tolerance via TGF-β and IL-2 signaling; recruitment via CCL22/CCL28 chemokines [11] | Lnc-Tim3 binding to Tim-3 modulates T cell activity [3] |
| CD8+ T Lymphocytes | Thymic development | PD-1, CTLA-4, TIM-3, LAG-3 [11] | Functional exhaustion characterized by upregulated inhibitory receptors and loss of effector cytokines (IFN-γ, TNF-α) [11] | NEAT1 regulates apoptosis and cytolytic activity via miR-155/Tim-3 pathway [3] |
| Natural Killer (NK) Cells | Hematopoietic stem cells | NKG2D, DNAM-1 [11] | Impaired cytotoxicity due to downregulation of activating receptors (NKG2D, DNAM-1) mediated by TGF-β and adenosine [11] | Not specified in search results |
CAFs are the predominant stromal population, accounting for 50-70% of TME cells [9]. Their activation primarily occurs through transdifferentiation of hepatic stellate cells (HSCs) stimulated by cytokines including TGF-β and PDGF [9]. Activated CAFs promote HCC metastasis through CCL5-mediated activation of the HIF1α/ZEB1 axis and directly enhance tumor proliferation via CXCL11 secretion [9]. The immune landscape within the HCC TME demonstrates significant heterogeneity, with high infiltration of MDSCs and Tregs associated with poor prognosis, while robust presence of activated cytotoxic T lymphocytes and NK cells correlates with better patient outcomes [12].
Hypoxic Niches in HCC
Hypoxia is a fundamental characteristic of the HCC TME, with oxygen tension (PaO2) decreasing from approximately 33 mmHg in normal liver tissue to as low as 6 mmHg in HCC tissues [10]. This hypoxic niche drives aggressive tumor behavior through multiple interconnected mechanisms.
Molecular Mediators of Hypoxia
The cellular response to hypoxia is primarily mediated by hypoxia-inducible factors (HIFs), particularly the HIF-1α subunit, which promotes tumor growth, metastasis, and therapy resistance [10]. Single-cell RNA sequencing analyses have identified distinct hypoxia subpopulations within HCC with significant overexpression of genes including MEG3, KLF6, and JUN [10]. Research has revealed that hypoxia induces epigenetic modifications such as m6A RNA demethylation, with HIF-1α binding to the promoter region of ALKBH5 (an m6A demethylase), thereby upregulating its expression and enhancing the stability of pro-tumorigenic transcripts like Galectin-1 [13].
Functional Consequences of Hypoxia
Hypoxia triggers multifaceted adaptations in the HCC TME:
- Angiogenesis: HIF-1α enhances angiogenesis through regulation of VEGF, driving the formation of abnormal tumor vasculature [10].
- Metabolic Reprogramming: Hypoxia induces metabolic changes that reduce ROS levels in TKI-treated HCC, contributing to drug resistance [10].
- Immunosuppression: Alterations in metabolite levels (glucose, lactate, adenosine) within the hypoxic TME collectively foster an immunosuppressive milieu that significantly hinders the efficacy of immune checkpoint inhibitors [10].
- Invasion and Metastasis: Hypoxic conditions promote epithelial-mesenchymal transition (EMT) and facilitate the formation of premetastatic niches (PMN) through exosome-mediated communication [10].
Diagram 1: Hypoxia signaling cascade in HCC. This diagram illustrates the central role of HIF-1α in mediating cellular responses to hypoxia, leading to angiogenesis, epigenetic modification, metastasis, and drug resistance. Created with DOT language.
Non-Coding RNA Dysregulation in the HCC TME
Non-coding RNAs (ncRNAs) have emerged as critical regulators of gene expression and cellular processes in the HCC TME, functioning as key intermediaries between hypoxic stress and tumor progression.
ncRNA Biogenesis and Classification
ncRNAs comprise several distinct classes:
MicroRNAs (miRNAs): Approximately 22 nucleotides long, single-stranded RNAs that regulate gene expression by binding to specific sequences in target mRNAs, leading to degradation, destabilization, or translational repression [6]. MiRNA biogenesis involves sequential processing from primary miRNA (pri-miRNA) to precursor miRNA (pre-miRNA) and finally to mature miRNA, which associates with Argonaute proteins to form the RNA-induced silencing complex (RISC) [6].
Long Non-coding RNAs (lncRNAs): RNA molecules exceeding 200 nucleotides that regulate gene expression through diverse mechanisms including transcriptional regulation, epigenetic modification, microRNA sponging, and splicing regulation [6] [3]. LncRNAs form complex secondary structures that enable specific molecular interactions.
Circular RNAs (circRNAs): A more recently characterized class of ncRNAs that form covalently closed continuous loops, often functioning as miRNA sponges or protein decoys [6].
Functional Roles of ncRNAs in TME Regulation
ncRNAs modulate the HCC TME through several key mechanisms:
Table 2: ncRNA-Mediated Regulation of the HCC Tumor Microenvironment
| ncRNA Class | Representative Molecules | Regulatory Targets/Mechanisms | Functional Outcomes in HCC |
|---|---|---|---|
| miRNAs | miR-1228-3p, miR-3184-3p, miR-155 | Target mRNA degradation/translational repression; delivered via exosomes [9] [6] | CAF-mediated immune evasion; macrophage polarization; T cell exhaustion |
| lncRNAs | NEAT1, lnc-Tim3, TUG1, LINC01116, CRNDE | miRNA sponging, chromatin remodeling, protein interactions [3] [14] | Regulation of T cell activity (via miR-155/Tim-3); modulation of autophagy; immune checkpoint regulation |
| circRNAs | circPS-MA1 | Activation of miR-637/Akt1/β-catenin axis [6] | Promotion of tumorigenesis, metastasis, and migration |
lncRNAs have been shown to regulate autophagy in HCC through integration into key signaling networks such as PI3K/AKT/mTOR, AMPK, and Beclin-1 pathways [14]. This regulatory function positions lncRNAs as critical modulators of the cellular stress response in the TME. The formation and function of lncRNAs involve transcription by RNA polymerase II, followed by processing including 5' capping, 3' polyadenylation, and splicing to generate mature transcripts that function in both nuclear and cytoplasmic compartments [3].
Experimental Methodologies for TME Investigation
Advanced technological approaches have enabled comprehensive dissection of the HCC TME at unprecedented resolution. The following experimental protocols represent cutting-edge methodologies for investigating hypoxic niches and ncRNA dysregulation.
Single-Cell RNA Sequencing (scRNA-seq) Workflow
scRNA-seq provides high-resolution analysis of cellular heterogeneity and gene expression patterns within the HCC TME [10].
Protocol: Single-Cell Transcriptomic Analysis of HCC TME
Sample Preparation: Obtain fresh HCC tissue samples (e.g., primary tumors, portal vein tumor thrombi, metastatic lymph nodes) and process immediately to preserve cell viability [10].
Single-Cell Suspension: Dissociate tissue using enzymatic digestion (collagenase/hyaluronidase mixtures) with gentle mechanical disruption. Filter through 40μm strainers to obtain single-cell suspensions.
Cell Viability Assessment: Evaluate viability using trypan blue exclusion or fluorescent viability dyes, maintaining >80% viability for optimal results.
Single-Cell Partitioning: Use microfluidic devices (10X Genomics Chromium system) to partition individual cells with barcoded beads.
Library Preparation: Perform reverse transcription, cDNA amplification, and library construction following manufacturer protocols. Incorporate unique molecular identifiers (UMIs) to account for amplification bias.
Sequencing: Conduct high-throughput sequencing on Illumina platforms (recommended depth: 50,000 reads/cell).
Bioinformatic Analysis:
- Quality control: Filter cells with mitochondrial content >20%, hemocyte content >3%, UMI counts 200-50,000, and gene counts 200-8,000 [10].
- Data normalization using Seurat package functions:
NormalizeData,FindVariableFeatures,ScaleData[10]. - Batch effect correction using Harmony algorithm.
- Dimensionality reduction with UMAP and t-SNE algorithms.
- Cell clustering using Louvain algorithm.
- Cell type annotation using marker panels:
- Neoplastic cells: CDH1, EPCAM, KRT18, KRT19
- Fibroblasts: SLRR1B, CD90, COL1A1, COL1A2
- Endothelial cells: CD31, CLDN2, VEGFR-1, RAMP2
- T-cells: CD3D/E/G, IMD7
- Myeloid cells: AMYLD5, SCARA2, CD16, CD68 [10]
Hypoxia Analysis: Identify hypoxic cell populations using specialized computational tools (e.g., CHPF software) that integrate scRNA-seq profiles with hypoxia-induced gene clusters [10].
Intercellular Communication: Analyze ligand-receptor interactions using CellChat package with
computeCommunProb,filterCommunication, andcomputeCommunProbPathwayfunctions [10].
Diagram 2: Single-cell RNA sequencing workflow for HCC TME analysis. Key steps include tissue processing, library preparation, sequencing, and bioinformatic analysis to characterize cellular heterogeneity and hypoxic niches. Created with DOT language.
Hypoxia-Related Prognostic Model Development
The construction of prognostic models based on hypoxia-related genes provides clinically relevant tools for outcome prediction [10].
Protocol: Development of Hypoxia Prognostic Signatures
Data Acquisition: Obtain transcriptomic data and clinical records from public databases (TCGA, ICGC). Convert expression data to TPM format followed by log2 transformation [10].
Hypoxia Cell Identification: Apply computational framework (CHPF software) to single-cell data to identify hypoxic cell populations and their characteristic gene expression patterns [10].
Differential Expression Analysis: Identify genes significantly overexpressed in hypoxic subpopulations (e.g., MEG3, KLF6, JUN) using FindAllMarkers function with thresholds: p-value <0.05, log2 fold change >0.25, expression proportion >0.1 [10].
Transcription Factor Analysis: Utilize SCENIC package with GRNboost2 software to construct gene regulatory networks and identify key transcription factors (e.g., NOP58, MED8) in hypoxic populations [10].
Prognostic Model Construction: Apply machine learning algorithms (LASSO Cox regression) to select most predictive features. Calculate risk scores based on gene expression weighted by regression coefficients.
Model Validation: Validate prognostic performance in independent datasets (e.g., LIRI-JP from ICGC) using survival analysis and receiver operating characteristic (ROC) curves [10].
ncRNA Functional Characterization
Elucidating the functional roles of specific ncRNAs in the HCC TME requires integrated experimental approaches.
Protocol: Functional Analysis of ncRNA in Hypoxic Niches
ncRNA Identification: Profile ncRNA expression patterns using small RNA-seq for miRNAs and total RNA-seq for lncRNAs/circRNAs from matched normoxic and hypoxic HCC regions.
Hypoxia Manipulation: Culture HCC cells in hypoxic chambers (1% O2) or with chemical hypoxia mimetics (CoCl2, DMOG) for specified durations (6-48 hours).
Loss/Gain-of-Function Studies:
- miRNA modulation: Transfect with miRNA mimics (gain-of-function) or inhibitors (loss-of-function)
- lncRNA/circRNA modulation: Use siRNA/shRNA-mediated knockdown or plasmid-based overexpression
- CRISPR/Cas9 systems for genomic editing of ncRNA loci
Phenotypic Assays:
- Proliferation: CCK-8, EdU incorporation assays
- Invasion: Transwell Matrigel invasion assays
- Angiogenesis: Endothelial tube formation assays using conditioned media
- Immune cell function: Coculture systems with peripheral blood mononuclear cells
Mechanistic Studies:
- miRNA target validation: Dual-luciferase reporter assays with wild-type and mutant 3'UTR constructs
- lncRNA-protein interactions: RNA immunoprecipitation (RIP), RNA pull-down assays
- lncRNA-miRNA sponging: Luciferase-based miRNA target reporters, AGO2-RIP
In Vivo Validation: Utilize orthotopic or subcutaneous xenograft models in immunodeficient mice. Implement ncRNA modulation via lentiviral transduction or nanoparticle-based delivery systems.
The Scientist's Toolkit: Essential Research Reagents
The table below summarizes key reagents and computational tools for investigating the HCC TME and hypoxic niches.
Table 3: Research Reagent Solutions for HCC TME Investigation
| Category | Reagent/Tool | Specific Application | Function/Utility |
|---|---|---|---|
| Computational Tools | Seurat Package (R) | scRNA-seq data analysis | Data normalization, dimensionality reduction, cell clustering, and visualization [10] |
| CHPF Software | Hypoxia cell identification | Predicts cellular hypoxia conditions by integrating scRNA-seq profiles with hypoxia-induced gene clusters [10] | |
| CellChat Package | Intercellular communication analysis | Infers and analyzes cell-cell communication networks from scRNA-seq data [10] | |
| SCENIC Package | Transcription factor analysis | Constructs gene regulatory networks from scRNA-seq data [10] | |
| Molecular Biology Reagents | Harmony Algorithm | Batch effect correction | Corrects for technical variations between different scRNA-seq batches [10] |
| Infercnv Package | Copy number variation analysis | Estimates CNV in tumor cells using endothelial cells as reference [6] | |
| Monocle2 Package | Cell trajectory analysis | Reconstructs cellular developmental trajectories from scRNA-seq data [10] | |
| Cell Culture Models | Hypoxic Chambers | Hypoxia modeling | Creates controlled low-oxygen environments (typically 1-5% O2) for in vitro studies [10] |
| Chemical Hypoxia Mimetics (CoCl2, DMOG) | HIF pathway stabilization | Stabilizes HIF-α subunits under normoxic conditions for hypoxia pathway studies [13] | |
| Therapeutic Agents | LNP-siRNA Formulations | ncRNA modulation in vivo | Enables efficient delivery of RNAi therapeutics to target specific ncRNAs in animal models [13] |
| 1H,2H,3H-pyrrolo[2,3-b]quinoline | 1H,2H,3H-pyrrolo[2,3-b]quinoline, CAS:40041-77-8, MF:C11H10N2, MW:170.215 | Chemical Reagent | Bench Chemicals |
| 2-methyl-1,2-thiazol-3-one;hydrate | 2-methyl-1,2-thiazol-3-one;hydrate|133.17 g/mol | 2-methyl-1,2-thiazol-3-one;hydrate (CAS 2089381-44-0) is a biocide preservative for research. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
The HCC tumor microenvironment represents a highly organized ecosystem where cellular components interact within hypoxic niches to drive tumor progression and therapeutic resistance. Non-coding RNAs serve as critical regulatory molecules in this ecosystem, mediating the cellular response to hypoxia and coordinating intercellular communication. Advanced methodologies including single-cell RNA sequencing, sophisticated computational algorithms, and functional genomic approaches provide powerful tools for dissecting this complexity. The integration of these technologies with mechanistic studies of ncRNA function offers promising avenues for identifying novel therapeutic targets and biomarkers. Future research should focus on validating specific ncRNA-autophagy axes, developing efficient ncRNA-targeting delivery systems, and exploring combination therapies that simultaneously target malignant cells and modulate the TME. Such integrated approaches hold significant potential for advancing precision medicine in HCC treatment.
Hepatocellular carcinoma (HCC) represents a major global health challenge characterized by a complex tumor microenvironment (TME) that plays a pivotal role in tumor progression and therapeutic response [3]. Within this ecosystem, non-coding RNAs (ncRNAs) have emerged as critical regulators of gene expression, influencing various biological processes despite not encoding proteins themselves [15] [6]. The TME comprises diverse cell types, including tumor cells, immune cells, fibroblasts, and endothelial cells, all interacting dynamically to influence tumor behavior [3]. Understanding how ncRNAs control gene expression within this microenvironment provides crucial insights into HCC pathogenesis and reveals potential therapeutic targets. This review explores the mechanisms through which different ncRNA classes—including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—orchestrate gene expression within the HCC TME, highlighting their roles as both regulators and effectors of tumor progression.
ncRNA Biogenesis and Functional Classes
MicroRNAs (miRNAs)
MiRNAs are approximately 22-nucleotide-long, single-stranded ncRNA molecules that regulate gene expression at the post-transcriptional level [6]. The biogenesis of miRNAs involves a meticulously controlled multi-step process: RNA polymerase II transcribes primary miRNAs (pri-miRNAs) containing imperfect hairpin structures from DNA [6]. In the nucleus, the Drosha-DGCR8 complex cleaves these hairpins to produce precursor miRNAs (pre-miRNAs) approximately 60-90 nucleotides long with distinctive 2-nucleotide 3' overhangs [6]. These pre-miRNAs are exported to the cytoplasm by XPO5 protein, where Dicer processes them into double-stranded RNA molecules of 19-22 nucleotides [6]. One strand (the guide strand) incorporates into the RNA-induced silencing complex (RISC), while the passenger strand is typically degraded [6]. The mature RISC complex uses the miRNA as a guide to recognize and bind target mRNAs through base pairing between its seed region (nucleotides 2-8) and specific sequences in the 3' untranslated region or coding region of target mRNAs, leading to mRNA degradation, destabilization, or translational repression [6].
Long Non-Coding RNAs (lncRNAs)
LncRNAs are RNA molecules exceeding 200 nucleotides in length that perform essential biological functions despite not coding for proteins [6]. The formation process of lncRNAs involves transcription from genomic DNA by RNA polymerase II, typically adjacent to or independently from protein-coding genes [3]. After transcription, lncRNAs undergo processing, including 5' capping, 3' polyadenylation, and splicing, to reach maturity [3]. Mature lncRNAs can function in both the nucleus and cytoplasm, regulating gene expression through interactions with DNA, RNA, or proteins [3]. Their structural complexity is evident in their ability to form secondary structures like hairpins, stem-loops, and pseudoknots via base pairing, which enhances their morphological diversity and contains conserved short modules crucial for specific functions [6]. For instance, SINEUP lncRNAs feature conserved short structural modules that boost translational enhancement [6].
Circular RNAs (circRNAs)
CircRNAs are produced by non-canonical splicing events that join a splice donor to an upstream splice acceptor, forming continuous closed loops [16]. RNA sequencing studies based on rRNA-depleted libraries have identified that approximately 85.82% of circRNAs originate from exonic regions, while 7.0% and 7.18% come from intergenic and intronic regions, respectively [16]. Notably, about 52.81% of genes produce more than two circRNA isoforms, indicating that alternative circularization extensively occurs in HCC and para-cancerous tissues [16]. These circRNAs can act as key regulators in cancer by regulating transcription or post-transcription of driver genes, often functioning as miRNA sponges or participating in other regulatory mechanisms [16].
Table 1: Major ncRNA Classes and Their Characteristics in HCC
| ncRNA Class | Size Range | Primary Functions | Key Features in HCC | Representative Examples |
|---|---|---|---|---|
| miRNA | ~22 nucleotides | mRNA degradation, translational repression | Frequently dysregulated by epigenetic mechanisms; can act as tumor suppressors or promoters | miR-122 (downregulated), miR-191 (upregulated) [15] |
| lncRNA | >200 nucleotides | Chromatin remodeling, transcriptional regulation, miRNA sponging | Often show copy number variations; regulate immune cell function in TME | NEAT1 (upregulated), FENDRR (downregulated) [15] [3] |
| circRNA | Variable | miRNA sponging, protein sequestration | Formed by back-splicing; highly stable structure; abundant in exosomes | cZRANB1 (upregulated), circTRIM33-12 (downregulated) [15] [16] |
Mechanisms of ncRNA Dysregulation in HCC
Genetic Alterations Driving ncRNA Dysregulation
Copy number variations (CNVs) represent one of the most common genetic alterations affecting ncRNA expression in HCC. Whole-genome sequencing data from 49 Chinese HCC patients revealed that lncRNAs are frequently amplified in HCC tumor tissues, with amplifications predominantly located on chromosomes 1q, 8q, 17q, and 20q [15]. Conversely, lncRNAs deleted in tumor tissues are mostly located on chromosomes 4q, 9q, 13q, and 16q [15]. TaqMan copy number assays of HCC tumors and normal liver tissues from 238 patients further confirmed that lncRNAs with copy number gain in >50% of HCC samples were consistently upregulated in tumor tissues [15]. Specific examples include the tumor suppressor lncRNA TSLNC8, located on chromosome 8p12, which is frequently deleted in HCC tissues [15], and FENDRR, which shows a pattern of decreased expression associated with CNV-driven dysregulation [15].
Epigenetic Modifications Regulating ncRNA Expression
Epigenetic mechanisms, particularly DNA methylation and histone modifications, play crucial roles in ncRNA dysregulation in HCC. DNA methylation of CpG islands within promoter regions can silence tumor suppressor miRNAs, while DNA hypomethylation can activate oncogenic miRNAs [15]. For instance, the CpG island of miR-1 is methylated in HCC cells (HepG2 and Hep3B) and tissues, with lower miR-1 expression in HCC tissues compared to normal liver tissues [15]. Treatment with the DNA hypomethylating agent 5-azacytidine restores miR-1 expression in HCC cells [15]. Conversely, hypomethylation of the CpG islands of miR-191 and miR-519d leads to their upregulated expression, enhancing epithelial-mesenchymal transition (EMT) in HCC [15].
Histone modifications also significantly contribute to ncRNA dysregulation. Enhancer of zeste homolog 2 (EZH2), an essential enzymatic unit of polycomb repressive complex 2 (PRC2), promotes H3K27me3, leading to the silencing of genes by interacting with miRNA promoters [15]. PRC2 mediates the downregulation of tumor suppressive miRNAs, including miR-101-1, miR-9, and miR-144/451a, by interacting with EZH2 in HCC [15]. Additionally, histone deacetylases (HDACs) contribute to ncRNA dysregulation, as demonstrated by HDAC9 and HDAC10 recruitment to the miR-223 promoter, where deacetylation contributes to miR-223 downregulation [15]. Similarly, HDAC3-mediated histone deacetylation regulates miR-195 expression [15].
Table 2: Epigenetic Regulation of ncRNAs in HCC
| Epigenetic Mechanism | Effect on ncRNAs | Regulatory Factors | Example ncRNAs | Functional Outcome |
|---|---|---|---|---|
| DNA Hypermethylation | Silencing of tumor suppressor ncRNAs | DNA methyltransferases | miR-1 [15] | Reduced expression; promotes tumor progression |
| DNA Hypomethylation | Activation of oncogenic ncRNAs | Demethylating agents | miR-191, miR-519d [15] | Increased expression; enhances EMT |
| H3K27me3 | Transcriptional repression | EZH2/PRC2 complex | miR-101-1, miR-9, miR-144/451a [15] | Silencing of tumor suppressors |
| Histone Deacetylation | Gene silencing | HDAC9, HDAC10, HDAC3 | miR-223, miR-195 [15] | Downregulation of tumor suppressive miRNAs |
| H3K27ac/H3K4me3 | Transcriptional activation | EP300, WDR5 | circSOD2 [15] | Enhanced expression; tumor promotion |
Functional Mechanisms of ncRNAs in the TME
Regulation of Immune Cell Function
Within the HCC TME, ncRNAs critically regulate the infiltration and function of various immune cells. The immune landscape of HCC features diverse immune cell populations, including T cells, natural killer (NK) cells, dendritic cells, and myeloid-derived suppressor cells (MDSCs), with the balance between these cell types determining anti-tumor immune effectiveness [3]. LncRNAs have emerged as important regulators of these immune cells, influencing both pro-tumor and anti-tumor activities [3].
T cell regulation represents a key mechanism through which lncRNAs modulate the immune microenvironment. Several oncogenic lncRNAs, including TUG1, LINC01116, CRNDE, MIAT, E2F1, LINC01132, and Lnc-Tim3, are overexpressed in HCC and influence T cell activity through various pathways [3]. For instance, NEAT1 and Tim-3 are significantly upregulated in the peripheral blood mononuclear cells (PBMCs) of HCC patients [3]. Downregulation of NEAT1 inhibits CD8+ T cell apoptosis and enhances their cytolytic activity against HCC cells by regulating the miR-155/Tim-3 pathway [3]. Similarly, Lnc-Tim3 specifically binds to Tim-3, preventing its interaction with Bat3 and thereby modulating downstream signaling in T cells [3].
Myeloid cell populations are also regulated by ncRNAs within the TME. Tumor-associated macrophages (TAMs) can be polarized toward M2-like immunosuppressive phenotypes under the influence of specific ncRNAs [6]. In gliomas, exosomes enriched with miR-3184-3p from cerebrospinal fluid not only boost glioma progression but also induce M2-like macrophage polarization, enhancing tumor aggression [6]. Although this specific example comes from glioma research, similar mechanisms likely operate in HCC, given the conserved nature of ncRNA-mediated regulation across different cancer types.
ceRNA Networks and miRNA Sponging
The competing endogenous RNA (ceRNA) hypothesis describes a mechanism through which different RNA species cross-regulate each other by competing for shared miRNA response elements. This network creates a complex regulatory system where lncRNAs, circRNAs, and mRNAs communicate through miRNA sponging [16]. In HCC, integrative analyses have uncovered specific ceRNA networks where circRNAs and lncRNAs function as miRNA sponges, regulating mRNA expression by competing for shared miRNAs [16]. For instance, cZRANB1, LINC00501, CTD-2008L17.2, and SLC7A11-AS1 may function as ceRNAs that regulate mRNAs by competing for shared miRNAs [16].
CircRNAs are particularly effective as miRNA sponges due to their stable circular structure and abundance of miRNA binding sites. The deregulation of specific circRNAs in HCC, such as the downregulation of circTRIM33-12, which serves as an independent risk factor for overall survival, highlights their importance in HCC pathogenesis [15]. Similarly, transcriptome sequencing has identified circRNA cZRANB1 as significantly upregulated not only in tumor tissues but also in blood exosomes of HCC patients compared with healthy donors, suggesting its potential as both a functional regulator and biomarker [16].
Regulation of Autophagy in the TME
The lncRNA-autophagy axis represents another crucial mechanism through which ncRNAs influence the HCC TME. Autophagy plays a paradoxical role in HCC, acting as a tumor suppressor during initiation but promoting survival and progression in advanced stages [14]. LncRNAs have emerged as critical regulators of autophagy, influencing tumorigenesis, metastasis, and therapy resistance through mechanisms such as miRNA sponging, chromatin remodeling, and protein interactions [14].
LncRNAs integrate into key signaling networks regulating autophagy, including the PI3K/AKT/mTOR, AMPK, and Beclin-1 pathways [14]. For instance, under nutrient deprivation conditions, AMPK activates ULK1 while inhibition of mTORC1 relieves its suppressive effect, resulting in ULK1 phosphorylating downstream autophagy-related proteins and initiating production of autophagic vesicles [14]. The PI3K complex, which includes VPS34 and Beclin-1, is essential for the nucleation of the phagophore—the initial membrane structure that gives rise to the autophagosome [14]. LncRNAs can modulate these pathways at multiple levels, thereby altering autophagic flux and associated molecular pathways that contribute to drug resistance, including resistance to first-line agents [14].
Experimental Approaches and Research Toolkit
Transcriptome Analysis Methodologies
Comprehensive transcriptome profiling utilizing next-generation sequencing (NGS) technologies has been instrumental in characterizing ncRNA dysregulation in HCC. The standard workflow for ncRNA detection and quantification involves parallel sequencing approaches for different ncRNA species [16]. For miRNA analysis, small RNA sequencing detects mature miRNAs annotated by miRBase and novel miRNAs identified by miRDeep2 [16]. For lncRNA and circRNA analysis, rRNA depletion-based total RNA sequencing enables the detection of both linear and circular transcripts, with circRNA prediction performed by tools such as CIRI2 [16].
Differential expression analysis typically involves quantifying ncRNAs at a count-based level and applying statistical tests to identify ncRNAs differentially expressed between HCC and para-cancerous tissues, using thresholds such as adjusted p-value <0.1 and fold-change >2 or <1/2 [16]. Validation in independent datasets is crucial, with studies reporting that approximately 65% of dysregulated lncRNAs, 76% of circRNAs, and 62% of miRNAs identified in discovery cohorts can be validated in independent patient cohorts [16].
Functional Validation Techniques
Functional characterization of ncRNAs requires a multi-faceted experimental approach. Gain-of-function and loss-of-function studies using techniques such as siRNA, shRNA, or CRISPR/Cas systems enable researchers to investigate the functional consequences of ncRNA modulation [14]. For instance, downregulation of NEAT1 has been shown to inhibit CD8+ T cell apoptosis and enhance their cytolytic activity against HCC cells, demonstrating its functional role in immune regulation [3].
Mechanistic insights often require additional techniques, including:
- RNA immunoprecipitation (RIP) and CLIP-seq to identify protein interaction partners
- Chromatin immunoprecipitation (ChIP) assays to study epigenetic regulation
- Luciferase reporter assays to validate direct miRNA-mRNA or miRNA-ncRNA interactions
- Fluorescent in situ hybridization (FISH) to determine subcellular localization
- Exosome isolation and characterization to study ncRNA secretion and intercellular communication
Table 3: Essential Research Reagents and Experimental Tools
| Research Tool Category | Specific Examples | Primary Application | Key Considerations |
|---|---|---|---|
| Sequencing Technologies | Small RNA sequencing, rRNA-depleted RNA sequencing | Comprehensive ncRNA profiling | Library preparation method affects ncRNA detection; validation required |
| Bioinformatics Tools | CIRI2 (circRNA prediction), miRDeep2 (miRNA prediction) | ncRNA identification and quantification | Multiple algorithms recommended for improved accuracy |
| Functional Modulation | siRNA, shRNA, CRISPR/Cas systems, ASOs | Gain/loss-of-function studies | Delivery efficiency and specificity crucial for interpretation |
| Interaction Studies | RIP, CLIP-seq, Luciferase reporter assays | Mechanistic validation | Controls essential for distinguishing direct vs. indirect effects |
| Localization Studies | FISH, Subcellular fractionation | Determining ncRNA localization | Critical for understanding mechanism of action |
| 3-Benzoylbenzenesulfonyl fluoride | 3-Benzoylbenzenesulfonyl Fluoride|Covalent Probe | Bench Chemicals | |
| 3-Hydroxy-2-isopropylbenzonitrile | 3-Hydroxy-2-isopropylbenzonitrile, CAS:1243279-74-4, MF:C10H11NO, MW:161.204 | Chemical Reagent | Bench Chemicals |
Concluding Remarks
The intricate mechanisms through which ncRNAs control gene expression in the HCC TME represent a rapidly advancing field with significant implications for both basic cancer biology and clinical translation. The dysregulation of ncRNAs through genetic and epigenetic mechanisms creates widespread effects on gene regulatory networks that ultimately shape the immunosuppressive TME characteristic of HCC. Understanding these mechanisms provides not only fundamental insights into HCC pathogenesis but also reveals novel therapeutic targets and biomarker opportunities.
The future of ncRNA research in HCC will likely focus on developing technologies to specifically target oncogenic ncRNAs while restoring tumor-suppressive ncRNAs, potentially through antisense oligonucleotides, small molecule inhibitors, or RNA-based therapeutics. Additionally, the exploration of exosomal ncRNAs as both therapeutic vehicles and diagnostic biomarkers represents a promising frontier. As our understanding of the complex ncRNA regulatory networks in the TME deepens, so too will our ability to develop effective ncRNA-based interventions for this devastating malignancy.
Hepatocellular carcinoma (HCC), the predominant form of primary liver cancer, represents a major global health challenge characterized by high mortality and limited therapeutic options for advanced disease [17] [3]. The tumor microenvironment (TME) of HCC plays a pivotal role in tumor progression and therapeutic resistance, with intratumoral hypoxia emerging as a critical hallmark [18] [19]. This hypoxic state originates from an imbalance between oxygen supply and consumption by rapidly proliferating tumor cells [19] [20]. In response to oxygen deprivation, cancer cells activate sophisticated genetic programs masterfully orchestrated by hypoxia-inducible factor-1 alpha (HIF-1α), the principal transcriptional regulator of cellular adaptation to hypoxia [18] [21].
HIF-1α exerts extensive influence over hypoxic gene expression and signaling networks, modulating processes including metabolism, angiogenesis, invasion, metastasis, and resistance to therapy [19] [22]. Meanwhile, advances in transcriptome analysis have revealed that non-coding RNAs (ncRNAs)—once considered transcriptional "noise"—occupy more than 95% of the human transcriptome and play critical regulatory roles in cancer pathogenesis [19] [20]. These ncRNAs, particularly microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), have emerged as crucial components in the hypoxic response of HCC tumors [18] [23].
This review comprehensively examines the intricate reciprocal regulation between HIF-1α and ncRNAs in HCC, focusing on their collective impact on tumorigenic processes, the potential of hypoxia-responsive ncRNAs as clinical biomarkers, and the therapeutic implications of targeting these regulatory networks in hepatocellular carcinoma.
Molecular Mechanisms of HIF-1α Regulation and Function
Oxygen-Dependent Regulation of HIF-1α Stability
Under normoxic conditions, HIF-1α undergoes rapid proteasomal degradation through an oxygen-sensitive mechanism [19] [22]. Prolyl hydroxylase domain enzymes (PHDs) utilize oxygen to hydroxylate conserved proline residues (Pro-402 and Pro-564) within the HIF-1α protein [19] [20]. This hydroxylation event enables the von Hippel Lindau (VHL) tumor suppressor protein to recognize HIF-1α as a substrate for ubiquitination, marking it for proteasomal destruction [19] [22]. Additionally, the transcriptional activity of HIF-1α is regulated by factor inhibiting HIF-1 (FIH-1), which hydroxylates an asparagine residue in the C-terminal transactivation domain, blocking its interaction with transcriptional coactivators CBP/p300 [19] [20].
In hypoxic conditions, oxygen deprivation halts the hydroxylation activities of both PHDs and FIH-1, leading to HIF-1α stabilization [19]. The stabilized HIF-1α protein translocates to the nucleus, dimerizes with HIF-1β, and recruits the CBP/p300 coactivator complex [19] [22]. This heterodimeric complex then binds to hypoxia-response elements (HREs) containing the core consensus sequence 5'-RCGTG-3' in the promoter regions of target genes, initiating a transcriptional program that facilitates cellular adaptation to hypoxia [19] [22].
HIF-1α-Mediated Transcriptional Programs in HCC
HIF-1α activation drives the expression of numerous genes implicated in key cancer hallmarks [18]. In HCC, this includes genes promoting angiogenesis (e.g., VEGF), metabolic reprogramming (e.g., glycolytic enzymes), invasion and metastasis (e.g., EMT transcription factors), and stemness maintenance [18] [19]. More than one thousand target genes have been reported to be regulated by HIF-1α to mediate hypoxic phenotypes, with hypoxia-responsive ncRNAs representing an especially noteworthy group [19] [20].
Figure 1: HIF-1α Regulation and Transcriptional Activation in Hypoxic HCC Microenvironment. Under normoxia, PHD enzymes hydroxylate HIF-1α, leading to VHL-mediated ubiquitination and proteasomal degradation. During hypoxia, HIF-1α stabilizes, translocates to the nucleus, dimerizes with HIF-1β, and binds to HREs to activate transcription of genes driving cancer hallmarks and hypoxia-responsive ncRNAs.
HIF-1α-Regulated Non-Coding RNAs in HCC
Classification and Mechanisms of Hypoxia-Responsive ncRNAs
Hypoxia-responsive ncRNAs (HRNs) can be categorized based on their regulatory relationships with HIF-1α [19]. In direct regulation, HIF-1α binds directly to HREs within the promoter regions of ncRNA genes to transactivate their expression [19] [20]. In indirect regulation, HIF-1α induces ncRNA expression through intermediate mechanisms, often involving epigenetic modifications mediated by histone deacetylases (HDACs) or other chromatin-modifying enzymes [19]. The major classes of HRNs in HCC include:
- MicroRNAs (miRNAs): Small ncRNAs (~22 nucleotides) that post-transcriptionally regulate gene expression by binding to target mRNAs, leading to translational repression or degradation [19] [6].
- Long non-coding RNAs (lncRNAs): Transcripts >200 nucleotides that regulate gene expression through chromatin modification, transcriptional, and post-transcriptional mechanisms [19] [3].
- Circular RNAs (circRNAs): Covalently closed circular molecules that function as miRNA sponges, protein decoys, or translational regulators [23] [22].
HIF-1α-Regulated microRNAs in HCC
miR-210: The Master HypoxamiR
Among hypoxia-responsive miRNAs, miR-210 stands out as the most consistently and strongly induced miRNA across multiple cancer types, including HCC [19] [20]. HIF-1α directly binds to HREs in the miR-210 promoter, driving its expression under hypoxic conditions [20]. In HCC, miR-210 promotes proliferation, inhibits apoptosis, and reduces radiosensitivity by targeting apoptosis-inducing factor mitochondria-associated 3 (AIFM3) [19]. It also enhances migration and invasion by regulating vacuole membrane protein 1 (VMP1) [19]. The table below summarizes key hypoxia-regulated miRNAs in HCC and their functional roles.
Table 1: HIF-1α-Regulated MicroRNAs in HCC and Their Functional Roles
| miRNA | Regulation by Hypoxia | Target Genes | Functional Outcomes in HCC | References |
|---|---|---|---|---|
| miR-210 | Upregulated | AIFM3, VMP1 | Promotes proliferation, inhibits apoptosis, enhances migration and invasion, reduces radiosensitivity | [19] |
| miR-21 | Upregulated | PTEN | Promotes colony formation, invasion, and migration | [19] |
| miR-382 | Upregulated | PTEN | Promotes proliferation, migration, and angiogenesis | [19] |
| miR-224 | Upregulated | RASSF8 | Promotes growth, migration, and invasion | [19] |
| miR-145 | Upregulated | N.A. | Promotes apoptosis | [19] |
Other Hypoxia-Regulated miRNAs
Beyond miR-210, numerous other miRNAs respond to hypoxic signaling in HCC. For instance, miR-21 is transcriptionally activated by HIF-1α and targets PTEN, thereby promoting colony formation, invasion, and migration in lung cancer models, with similar mechanisms likely operational in HCC [19]. miR-382 upregulation under hypoxia targets PTEN to promote proliferation, migration, and angiogenesis in gastric cancer, suggesting potential conserved functions in HCC [19]. The consistent targeting of tumor suppressors like PTEN by multiple hypoxia-induced miRNAs highlights the strategic importance of these regulatory networks in promoting HCC progression.
HIF-1α-Regulated Long Non-Coding RNAs in HCC
Oncogenic lncRNAs in the Hypoxic Niche
Several lncRNAs have been identified as critical mediators of HIF-1α-driven oncogenesis in HCC. The lncRNA HEIH (upregulated in hepatocellular carcinoma) demonstrates elevated expression in HCC tissues and functions as an oncogene [24]. HEIH primarily localizes to the cytoplasm but also accumulates in the nucleus, where it interacts with enhancer of Zeste homolog 2 (EZH2) to suppress cell cycle regulators including p15, p16, p21, and p57, facilitating cell cycle progression [24].
The lncRNA UCA1 has been shown to promote glycolysis, proliferation, and metastasis in HCC under hypoxic conditions by interacting with and stabilizing HIF-1α protein, creating a positive feedback loop that amplifies hypoxic responses [21]. Similarly, linc01132 and linc01116 are upregulated in HCC and contribute to immune evasion by modulating T cell activity within the TME [3].
Tumor-Suppressive lncRNAs Repressed by Hypoxia
Some lncRNAs function as tumor suppressors that are downregulated under hypoxic conditions. For example, MEG3 expression is reduced in HCC and associated with poor prognosis [21]. Restoration of MEG3 expression suppresses HIF-1α signaling and inhibits HCC growth, suggesting its potential as a therapeutic agent [21]. The dynamic balance between oncogenic and tumor-suppressive lncRNAs under hypoxia significantly influences HCC progression and therapeutic responses.
HIF-1α-Regulated Circular RNAs in HCC
While less characterized than miRNAs and lncRNAs, circRNAs are emerging as important players in the hypoxic HCC microenvironment. Several circRNAs are dysregulated in HCC and contribute to tumor progression through diverse mechanisms [23] [22]. For instance, circIPP2A2 is upregulated by the HIF-1α-induced writer protein METTL1, which catalyzes N7-methylguanosine (m7G) modification, promoting HCC progression [17]. Other circRNAs function as competitive endogenous RNAs (ceRNAs) that sequester miRNAs, preventing them from binding to their target mRNAs [23] [22].
Table 2: RNA Methylation Modifications in HCC and Their Hypoxia Connections
| Methylation Type | Writer Proteins | Eraser Proteins | Reader Proteins | Regulation by Hypoxia | Functional Impact in HCC |
|---|---|---|---|---|---|
| m6A | METTL3, METTL14, WTAP | FTO, ALKBH5 | IGF2BP1, YTHDF1 | HIF-1α influences expression of writers/erasers | METTL3 promotes HCC via inhibiting RDM1 transcription and promoting USP7 translation; METTL14 reduces HCC progression |
| m5C | NSUN2, NSUN5 | - | ALYREF, YBX1 | Potential indirect regulation | NSUN2 promotes HCC via increasing H19 stability; NSUN5 increases ZBED3 expression |
| m7G | METTL1, WDR4 | - | - | METTL1 upregulated by HIF-1α | METTL1 promotes HCC via increasing circIPP2A2 expression |
| m1A | TRM6/TRM61A | ALKBH3 | - | Potential indirect regulation | TRM6/TRM61A promotes HCC via promoting PPARδ translation |
Regulatory Feedback: ncRNAs Modulating HIF-1α Expression and Activity
The interplay between HIF-1α and ncRNAs extends beyond HIF-1α-mediated regulation to include extensive feedback mechanisms wherein ncRNAs modulate HIF-1α expression and activity at multiple levels.
Transcriptional and Post-Transcriptional Regulation of HIF-1α by ncRNAs
Several miRNAs directly target HIF-1α mRNA for degradation or translational repression. For example, miR-199a-5p has been shown to directly bind to the 3' untranslated region (3'UTR) of HIF-1α mRNA, reducing its stability and translation in cancer cells [22]. Similarly, miR-17-5p and miR-20a members of the miR-17-92 cluster, target HIF-1α mRNA, creating a negative feedback loop that fine-tunes hypoxic responses [22].
LncRNAs also participate in regulating HIF-1α expression. The lncRNA H19 is induced by hypoxia and promotes HIF-1α protein synthesis by acting as a competing endogenous RNA for miRNAs that target HIF-1α [21]. Conversely, the lncRNA MEG3 suppresses HIF-1α signaling by promoting its degradation or inhibiting its transcriptional activity [21].
Post-Translational Regulation of HIF-1α by ncRNAs
ncRNAs significantly influence HIF-1α protein stability and transcriptional activity through regulation of its modifying enzymes. Multiple miRNAs target the 3'UTRs of PHD enzymes, affecting their expression and consequently HIF-1α stability [22]. For instance, miR-31 directly targets PHD3, leading to enhanced HIF-1α stabilization under moderate hypoxia [22].
Additionally, epi-miRNAs—miRNAs that target epigenetic regulators—indirectly influence HIF-1α activity. miR-137 targets lysine-specific demethylase 1 (LSD1), an epigenetic modifier that stabilizes HIF-1α and facilitates expression of glycolytic genes such as hexokinase [23]. Through these multifaceted regulatory mechanisms, ncRNAs establish complex feedback loops that precisely calibrate the hypoxic response in HCC.
Functional Outcomes of HIF-1α-ncRNA Interplay in HCC Pathogenesis
Metabolic Reprogramming
The Warburg effect (aerobic glycolysis) represents a cornerstone of cancer metabolism that is profoundly influenced by HIF-1α-ncRNA interactions [23]. HIF-1α directly transactivates genes encoding glucose transporters and glycolytic enzymes, while ncRNAs provide additional layers of regulation. For example, miR-143 and miR-34a regulate key enzymes in glucose metabolism and the TCA cycle [23]. miR-122, frequently downregulated in HCC, suppresses glycolysis and lipid metabolism by targeting pyruvate kinase and fatty acid synthase (FASN) [23].
LncRNAs such as UCA1 enhance glycolytic flux by stabilizing HIF-1α and increasing its binding to promoters of glycolytic genes [21]. Circular RNAs contribute to metabolic reprogramming through their sponge functions; for instance, circPS-MA1 activates the miR-637/Akt1/β-catenin (cyclin D1) axis, promoting tumorigenesis and metabolism in triple-negative breast cancer, with similar mechanisms likely in HCC [6].
Immune Evasion and Modulation of the Tumor Microenvironment
The hypoxic HCC microenvironment shapes immune cell function and promotes immune evasion through HIF-1α-ncRNA networks [3] [24]. Myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs) accumulate in hypoxic regions, suppressing effector T cell function [3]. Multiple lncRNAs regulate this process; for example, NEAT1 and Tim-3 are significantly upregulated in peripheral blood mononuclear cells of HCC patients [3]. Downregulation of NEAT1 inhibits CD8+ T cell apoptosis and enhances their cytolytic activity against HCC cells by regulating the miR-155/Tim-3 pathway [3].
LncRNAs also modulate immune checkpoint expression. Lnc-Tim3 binds to Tim-3, preventing its interaction with Bat3 and thereby inhibiting downstream signaling in the Lck/NFAT1/AP-1 pathway, ultimately contributing to T cell exhaustion [3]. Similarly, HEIH influences PD-L1 expression and T cell function in the HCC microenvironment, promoting immune evasion [24].
Angiogenesis, Invasion, and Metastasis
HIF-1α is the master regulator of tumor angiogenesis, primarily through induction of VEGF expression [18] [19]. ncRNAs fine-tune this process through multiple mechanisms. For instance, miR-210 promotes angiogenesis by targeting FGFRL1, E2F3, VMP1, RAD52, and SDHD in lung cancer models [19]. miR-382 also promotes angiogenesis in gastric cancer through PTEN targeting [19].
Invasion and metastasis are enhanced through epithelial-mesenchymal transition (EMT), a process regulated by both HIF-1α and ncRNAs. In gastric cancer, miR-210 mediates HIF-1α-induced EMT by regulating homeobox A9 (HOXA9) expression [20]. Similarly, in prostate cancer, miR-210 promotes EMT, invasion, and migration by targeting TNIP1 and SOCS1 [19]. LncRNAs such as UCA1 and HEIH further contribute to metastatic progression by enhancing cell motility and invasion capabilities [21] [24].
Experimental Approaches for Studying HIF-1α-ncRNA Interactions
Methodologies for Investigating Hypoxia-ncRNA Networks
Figure 2: Experimental Workflow for Studying HIF-1α-ncRNA Interactions in HCC. The schematic outlines key methodological approaches from hypoxia induction to therapeutic testing.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for Studying HIF-1α-ncRNA Interactions in HCC
| Reagent Category | Specific Examples | Experimental Applications | Key Considerations |
|---|---|---|---|
| Hypoxia Inducers | Cobalt chloride (CoClâ‚‚), Deferoxamine (DFO), Hypoxia chambers (1% Oâ‚‚) | Mimicking tumor hypoxia in vitro | CoClâ‚‚ and DFO are chemical inducers; hypoxia chambers provide physiological oxygen levels |
| HIF-1α Modulators | PHD inhibitors (FG-4592), HIF-1α stabilizers, EZN-2968 (HIF-1α antagonist) | Manipulating HIF-1α activity | Specificity and off-target effects should be controlled |
| Gene Expression Analysis | RNA-seq kits, miRNA/qPCR arrays, Northern blot reagents | Profiling ncRNA expression under hypoxia | Normalization to appropriate housekeeping genes is critical |
| HIF-1α Binding Assays | ChIP-seq kits, HIF-1α antibodies, HRE luciferase reporters | Validating direct HIF-1α regulation of ncRNAs | Antibody specificity crucial for ChIP experiments |
| Functional Validation | CRISPR/Cas9 systems, siRNA/shRNAs, ASOs, ncRNA mimics/inhibitors | Loss/gain-of-function studies | Delivery efficiency and specificity must be optimized |
| Interaction Studies | RIP/qPCR kits, Biotin-labeled probe pulldown, Luciferase reporter vectors | Investigating ncRNA-protein interactions | Appropriate negative controls essential |
| HCC Models | HepG2, Huh7, PLC/PRF/5 cells, Patient-derived organoids, Mouse HCC models | In vitro and in vivo validation | Model selection should reflect specific research questions |
| 4-Methyl-4-chromanecarboxylic acid | 4-Methyl-4-chromanecarboxylic Acid | 4-Methyl-4-chromanecarboxylic acid is For Research Use Only. Not for human or veterinary use. Explore its applications in organic synthesis and pharmaceutical research. | Bench Chemicals |
| 2-acetylphenyl 4-methylbenzoate | 2-acetylphenyl 4-methylbenzoate, CAS:4010-26-8, MF:C16H14O3, MW:254.285 | Chemical Reagent | Bench Chemicals |
Clinical Implications and Therapeutic Perspectives
Diagnostic and Prognostic Biomarker Potential
The hypoxia-responsive ncRNA signature in HCC holds significant promise as a source of diagnostic and prognostic biomarkers [18] [19]. For instance, miR-210 expression correlates with HIF-1α levels and serves as an independent prognostic marker in breast cancer and clear cell renal cell cancer, with similar potential in HCC [19] [20]. High HEIH expression in serum and exosomes of HCC patients makes it a promising non-invasive diagnostic marker [24].
RNA methylation regulators also offer prognostic value in HCC. Elevated METTL3 expression is associated with unfavorable overall survival (OS) in HCC patients, while reduced METTL14 and ZC3H13 expression similarly correlates with poor prognosis [17]. These findings highlight the clinical potential of hypoxia-associated ncRNAs and their regulatory proteins as biomarkers for HCC management.
Therapeutic Targeting of HIF-1α-ncRNA Axes
Targeting HIF-1α-ncRNA networks presents innovative opportunities for HCC therapy. Several approaches show promise:
- Antisense oligonucleotides (ASOs) and RNAi technology: These can be designed to target oncogenic ncRNAs such as HEIH, UCA1, or NEAT1 [24]. ASOs complementary to specific lncRNAs can trigger their degradation or block functional interactions [24].
- CRISPR/Cas9 genome editing: This technology enables precise modification of ncRNA genes or their regulatory elements, offering potential for permanent disruption of oncogenic HIF-1α-ncRNA circuits [24].
- Small molecule inhibitors: Compounds that disrupt the interaction between lncRNAs and their protein partners, such as EZH2 inhibitors for HEIH targeting, represent another strategic approach [24].
- ncRNA mimics: Tumor-suppressive ncRNAs such as MEG3 or miR-199a-5p can be restored using synthetic mimics or expression vectors [21] [22].
Despite these promising approaches, challenges remain in delivery efficiency, tissue specificity, and potential toxicity, necessitating further development of targeted delivery systems such as lipid nanoparticles or ligand-conjugated formulations [6] [24].
Enhancing Response to Existing Therapies
Modulating HIF-1α-ncRNA axes may improve responses to conventional HCC therapies. For example, targeting HIF-1α-induced miR-210 could reverse radioresistance in HCC by restoring apoptosis sensitivity [19]. Similarly, combining immune checkpoint inhibitors with lncRNA-targeting approaches might overcome immunosuppression in the hypoxic TME [3] [24]. The lncRNA NEAT1 regulates T cell function through the miR-155/Tim-3 pathway, suggesting that NEAT1 inhibition could enhance checkpoint immunotherapy efficacy [3].
The intricate interplay between HIF-1α and ncRNAs represents a critical regulatory dimension in HCC pathogenesis, with hypoxia serving as a master regulator that coordinates multiple aspects of tumor biology through these networks. The reciprocal regulation between HIF-1α and ncRNAs—with HIF-1α driving ncRNA expression and ncRNAs fine-tuning HIF-1α activity—creates sophisticated feedback loops that amplify oncogenic signaling in the hypoxic TME.
Future research should focus on elucidating the complete landscape of hypoxia-responsive ncRNAs in HCC, particularly circular RNAs which remain relatively unexplored. The development of more sophisticated in vivo models that recapitulate the hypoxic HCC microenvironment will be essential for validating the therapeutic potential of targeting specific HIF-1α-ncRNA axes. Additionally, advancing delivery technologies for ncRNA-based therapeutics will be crucial for clinical translation.
As our understanding of the molecular intricacies between hypoxia and ncRNAs deepens, targeting these networks holds promise for innovative diagnostic strategies and therapeutic interventions in hepatocellular carcinoma, potentially overcoming the limitations of current treatment approaches and improving outcomes for patients with this devastating malignancy.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most prevalent cancer and the fourth leading cause of cancer-related mortality worldwide [25]. As the predominant form of primary liver cancer, HCC accounts for approximately 75-90% of all liver cancer cases, with its aggressive progression, unfavorable prognosis, and increasing incidence contributing to its substantial disease burden [26] [27]. The tumor microenvironment (TME) of HCC plays a pivotal role in tumor development, progression, and therapeutic resistance, with recent research highlighting exosomes as crucial mediators of intercellular communication within this niche [26] [25].
Exosomes are nanoscale (30-150 nm) membrane-bound vesicles secreted by nearly all cell types that facilitate intercellular communication by transferring bioactive molecules, including proteins, lipids, and nucleic acids [28] [25]. Among these molecules, non-coding RNAs (ncRNAs) have emerged as key regulatory elements in HCC pathogenesis. These exosomal ncRNAs include microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), which are selectively packaged and transferred between cells to modulate recipient cell behavior [28]. This review examines the multifaceted roles of exosomal ncRNAs in shaping the immunosuppressive HCC TME, with a focus on their mechanisms of action, experimental methodologies for their study, and their potential clinical applications.
Exosomal ncRNA Biogenesis and Functional Mechanisms
Biogenesis and Delivery
Exosome biogenesis begins with the formation of early endosomes through plasma membrane invagination, which mature into late endosomes or multivesicular bodies (MVBs) [28]. During this process, intraluminal vesicles (ILVs) are generated through inward budding of the endosomal membrane via both ESCRT (Endosomal Sorting Complexes Required for Transport)-dependent and ESCRT-independent mechanisms [28]. The ESCRT machinery, composed of four primary complexes (ESCRT-0, -I, -II, and -III) along with associated proteins including Hrs, Tsg101, and Alix, facilitates vesicle formation and cargo sorting [28]. ESCRT-independent pathways utilize ceramide-mediated trafficking and tetraspanin-enriched microdomains [28] [29].
The selective packaging of ncRNAs into exosomes involves RNA-binding proteins such as hnRNPA2B1 and YBX1, which recognize specific sequence motifs within ncRNAs [28]. Post-transcriptional modifications, including 3'-end uridylation, also influence ncRNA sorting into exosomes [28]. Once formed, ILVs are released as exosomes through MVB fusion with the plasma membrane, a process regulated by Rab GTPases (particularly Rab27a and Rab27b) and SNARE proteins [28].
Following release, exosomes execute their functions through receptor-ligand interactions on recipient cell membranes or via internalization through mechanisms including clathrin-mediated endocytosis, caveolin-dependent endocytosis, and direct membrane fusion [28] [27].
Functional Mechanisms of Exosomal ncRNAs
Upon internalization by recipient cells, exosomal ncRNAs exert their regulatory functions through diverse mechanisms depending on their structural classification:
Table 1: Functional Mechanisms of Different Exosomal ncRNA Types
| ncRNA Type | Size/Structure | Primary Functions | Examples in HCC |
|---|---|---|---|
| miRNAs | ~22 nucleotides; short single-stranded RNA | mRNA targeting leading to translational repression or degradation | miR-23a-3p downregulates PTEN in macrophages [30] |
| lncRNAs | >200 nucleotides; linear RNA | Chromatin modification, transcriptional regulation, miRNA sequestration | LncRNA HOTAIR induces epigenetic changes [28] |
| circRNAs | Closed-loop structure; covalently bonded | miRNA sponges, protein scaffolding, peptide encoding | circCCAR1 sponges miR-127-5p to promote immunotherapy resistance [30] |
MicroRNAs (miRNAs) primarily function by binding to complementary sequences on target mRNAs, leading to translational repression or direct degradation of the target transcripts [28]. For instance, HCC-derived exosomal miR-23a-3p downregulates PTEN expression in macrophages, activating the AKT pathway and promoting immunosuppression [30].
Long non-coding RNAs (lncRNAs) and circular RNAs (circRNAs) share several functional mechanisms: (1) chromatin modification through interactions with chromatin-modifying complexes; (2) transcriptional regulation by acting as co-activators or co-repressors; (3) mRNA processing through modulation of stability, splicing, or modification; (4) miRNA sequestration as competing endogenous RNAs (ceRNAs); (5) influence on post-translational protein modifications; and (6) functional peptide encoding in some cases [28].
The following diagram illustrates the biogenesis of exosomes and the functional mechanisms of their ncRNA cargo in recipient cells:
Exosomal ncRNAs in Shaping the Immunosuppressive HCC TME
Modulation of Adaptive Immunity
Exosomal ncRNAs play a critical role in suppressing adaptive immune responses in HCC through multiple mechanisms:
T Cell Dysfunction: HCC-derived exosomal circCCAR1 promotes CD8+ T cell dysfunction and mediates resistance to anti-PD-1 immunotherapy by sponging miR-127-5p and upregulating WTAP expression [30]. Similarly, endoplasmic reticulum stress in HCC cells promotes the release of exosomal miR-23a-3p, which downregulates PTEN in macrophages, activates the AKT pathway, increases PD-L1 expression, and ultimately leads to CD8+ T cell inhibition and apoptosis [30].
Regulatory T Cell Expansion: HCC-derived exosomes containing circGSE1 modulate the miR-324-5p/TGFBR1/Smad3 axis to promote regulatory T cell (Treg) expansion, further contributing to immune evasion [30]. This expansion enhances the immunosuppressive capacity of the TME by increasing the population of immune-inhibitory cells.
Innate Immune Cell Reprogramming
Macrophage Polarization: Tumor-associated macrophages (TAMs) are frequently polarized toward the M2 phenotype in HCC, promoting immunosuppression and tumor progression. HCC-derived exosomes enriched with miR-21-5p enhance transforming growth factor-β1 (TGF-β1) and interleukin-10 (IL-10) expression, thereby promoting M2 polarization [30]. Similarly, overexpression of miR-4669 in Hep3B cells induces the release of glyceraldehyde-3-phosphate dehydrogenase (GAPDH), which drives M2 polarization and contributes to immune suppression [30].
NK Cell Exhaustion: Natural killer (NK) cells are critical effectors of innate anti-tumor immunity. Exosomal circUHRF1, highly expressed in HCC tissues and plasma, promotes NK cell exhaustion by upregulating TIM-3 and downregulating miR-449c-5p, thereby reducing NK cell counts and impairing the secretion of IFN-γ and TNF-α [30]. Similarly, exosomal miR-17-5p suppresses NK cell cytotoxicity by downregulating RUNX1 and NKG2D expression [30].
The following diagram illustrates how HCC-derived exosomal ncRNAs coordinate immunosuppression in the tumor microenvironment:
Intercellular Communication Networks
Exosomal ncRNAs facilitate sophisticated communication networks between HCC cells and various stromal components in the TME. These ncRNAs can induce the activation of tumor cells and immunosuppressive immune cells including cancer-associated fibroblasts (CAFs), tumor-associated macrophages (TAMs), tumor-associated neutrophils (TANs), CD8+ T cells, regulatory T cells (Tregs), and regulatory B cells (Bregs) [26]. This cell-cell crosstalk triggered by exosomal ncRNAs promotes tumor proliferation and metastasis, angiogenesis, malignant phenotype transformation, and drug resistance [26].
Table 2: Exosomal ncRNAs Mediating Immunosuppression in HCC TME
| Exosomal ncRNA | Origin | Target Cell | Molecular Mechanism | Functional Outcome |
|---|---|---|---|---|
| circCCAR1 | HCC cells | CD8+ T cells | Sponges miR-127-5p, upregulates WTAP | T cell dysfunction, anti-PD-1 resistance [30] |
| miR-23a-3p | HCC cells (ER-stress) | Macrophages | Downregulates PTEN, activates AKT, upregulates PD-L1 | CD8+ T cell apoptosis [30] |
| circGSE1 | HCC cells | Tregs | Modulates miR-324-5p/TGFBR1/Smad3 axis | Treg expansion [30] |
| miR-21-5p | HCC cells | Macrophages | Enhances TGF-β1 and IL-10 expression | M2 polarization [30] |
| circUHRF1 | HCC cells | NK cells | Upregulates TIM-3, downregulates miR-449c-5p | NK cell exhaustion [30] |
| miR-17-5p | HCC cells | NK cells | Downregulates RUNX1 and NKG2D | Impaired NK cytotoxicity [30] |
Experimental Methodologies for Exosomal ncRNA Research
Exosome Isolation and Characterization
Standardized methodologies for exosome isolation and characterization are critical for reproducible research in this field. The following protocols represent current best practices:
Isolation Techniques: Size exclusion chromatography (SEC) is widely used for exosome isolation from conditioned cell culture media or patient samples [31]. For cell culture studies, media should first be centrifuged at 1500 × g for 10 minutes to remove cells and large particles, then concentrated using protein concentrators (100 K MWCO) before applying to SEC columns [31]. For patient samples (e.g., bone marrow aspirate supernatant or plasma), samples are centrifuged at 1500 × g for 10 minutes to remove large particles, then applied directly to SEC columns without concentration [31]. Following isolation, exosomes should be filtered through 0.2 µm filters and stored at -80°C [31].
Characterization Methods: Isolated exosomes should be characterized for size distribution and concentration using nanoparticle tracking analysis (e.g., NanoSight NS300) [31]. Additional characterization through transmission electron microscopy for morphological analysis and Western blotting for exosomal markers (e.g., tetraspanins CD81, CD63, CD9) is recommended to verify exosome identity and purity [31].
RNA Sequencing and Bioinformatics Analysis
Comprehensive RNA identification from exosomes requires specialized approaches due to the unique RNA composition in exosomes:
RNA Isolation and Library Preparation: RNA is isolated from exosomes using kits specifically designed for small RNA recovery (e.g., MagMAX mirVana Total RNA Isolation Kit) [31]. RNA concentration is determined using spectrophotometry (NanoDrop) and integrity assessed with bioanalyzer systems [31]. For library preparation, the isolated RNA is processed using small RNA-seq kits (e.g., NEXTFLEX Small RNA-Seq Kit v4) with procedures including 3' and 5' adapter ligation, reverse transcription, PCR amplification, and size selection [31].
Bioinformatics Analysis: Quality control of raw FASTQ files is assessed for each sample, followed by adapter trimming using tools like CUTADAPT with a quality cutoff of 20 [31]. For lncRNA analysis, alignment to reference genomes (e.g., GRCh38) is performed using STAR aligner, while miRNA data is aligned using Bowtie2 with appropriate seed parameters [31]. Differential expression analysis can be conducted using DESeq2 with adjusted p-value cutoffs of 0.01 based on the Benjamini-Hochberg algorithm to account for multiple testing [31].
Integrative Analysis: Weighted Gene Co-expression Network Analysis (WGCNA) using R packages can identify modules of highly correlated genes associated with specific traits [32]. This approach helps reconstruct co-expression networks and identify biologically meaningful modules associated with HCC progression [32].
Functional Validation Experiments
In Vitro Functional Assays: To validate the functional impact of identified exosomal ncRNAs, researchers employ various in vitro approaches including: (1) Transfection of mimic/inhibitor oligonucleotides to modulate ncRNA expression in donor cells; (2) Co-culture systems separating donor and recipient cells with transwell inserts to demonstrate exosome-mediated effects; (3) Flow cytometry analysis of immune cell markers and functional states; (4) Luciferase reporter assays to validate direct miRNA-mRNA interactions.
In Vivo Models: Animal models, particularly immunocompetent mouse models of HCC, are essential for validating the role of exosomal ncRNAs in shaping the TME and modulating immunotherapy responses. These models allow for assessment of tumor growth, metastasis, and immune cell infiltration in the context of ncRNA manipulation.
Table 3: Key Research Reagents and Resources for Exosomal ncRNA Studies
| Category | Specific Reagents/Resources | Application | Key Features |
|---|---|---|---|
| Cell Lines | Hep3B, Huh7, HepG2, PLC/PRF/5 | HCC modeling | Well-characterized HCC lines with varying etiologies |
| Culture Supplements | Exosome-depleted FBS | Cell culture | Prevents contamination with bovine exosomes |
| Isolation Kits | Size exclusion chromatography columns | Exosome isolation | Maintains exosome integrity and function |
| Characterization Instruments | NanoSight NS300 Nanoparticle Tracking Analyzer | Exosome characterization | Size distribution and concentration analysis |
| RNA Isolation Kits | MagMAX mirVana Total RNA Isolation Kit | RNA extraction from exosomes | Optimized for small RNA recovery |
| Sequencing Kits | NEXTFLEX Small RNA-Seq Kit v4 | Library preparation | Specifically designed for small RNA sequencing |
| Bioinformatics Tools | DESeq2, WGCNA, STAR, Bowtie2 | Data analysis | Differential expression, co-expression network analysis |
| Databases | exoRBase, circBank, Lncipedia | Data mining | Reference databases for exosomal RNA content |
Clinical Applications and Future Perspectives
Diagnostic and Prognostic Biomarkers
Exosomal ncRNAs show significant promise as non-invasive biomarkers for HCC diagnosis and prognosis. Serum exosomal long ncRNA FOXD2-AS1 has demonstrated promising diagnostic potential in colorectal cancer, achieving an area under the curve (AUC) of 0.736 across all patients and 0.758 specifically for early-stage cancer [29]. Similarly, exosomal lncRNA-GC1 has effectively distinguished gastric cancer patients from controls with AUCs exceeding 0.86, outperforming traditional markers including CEA and CA19-9 [29]. In HCC, exosomal circTMEM181 levels are associated with poor responses to anti-PD-1 therapy, highlighting their potential as predictive biomarkers [30].
Therapeutic Applications
The therapeutic potential of exosomal ncRNAs is being explored through multiple approaches:
Engineered Exosomes: Leveraging exosomes' inherent biocompatibility and targeting capabilities, engineered exosomes show promise as drug delivery vehicles [25]. These can be functionalized to deliver therapeutic payloads, including chemotherapeutic agents, siRNAs, and immunomodulatory molecules, specifically to tumor cells while minimizing off-target effects [30].
Targeting Oncogenic ncRNAs: Developing strategies to inhibit tumor-promoting exosomal ncRNAs or restore tumor-suppressive ncRNAs represents a promising therapeutic avenue. Approaches including antisense oligonucleotides, small molecule inhibitors, and CRISPR-based systems are under investigation to modulate exosomal ncRNA function in HCC [26] [30].
Current Challenges and Future Directions
Despite significant progress, several challenges remain in exosomal ncRNA research. Technical hurdles include standardization of exosome isolation techniques, characterization methods, and validation protocols across different laboratories [30]. Biological challenges encompass the heterogeneity of exosome populations and the complexity of ncRNA regulatory networks [26]. Future research should prioritize: (1) large-scale validation studies to confirm biomarker potential; (2) development of standardized protocols for clinical translation; (3) exploration of combination therapies targeting multiple ncRNA pathways; and (4) investigation of sex-specific differences in exosomal ncRNA regulation, as emerging evidence suggests sex-specific dysregulation of exosomal ncRNAs in other cancers [31].
In conclusion, exosomal ncRNAs represent crucial mediators of intercellular communication within the HCC TME, contributing significantly to immunosuppression and tumor progression. Understanding their precise mechanisms of action and developing strategies to target these molecules holds promise for improving HCC diagnosis, prognosis, and therapeutic outcomes.
From Mechanism to Therapy: Targeting ncRNA Networks for HCC Intervention
Hepatocellular carcinoma (HCC) represents a major global health challenge characterized by poor prognosis and high recurrence rates [33]. A core hallmark of HCC is metabolic reprogramming, an adaptive process where cancer cells alter their metabolic reactions to support rapid proliferation, survival, and metastasis [34] [35]. This reprogramming encompasses profound changes in glucose metabolism, lipid synthesis, and amino acid utilization, enabling cancer cells to thrive in the nutrient-poor and hypoxic conditions of the tumor microenvironment (TME) [34] [36]. The shifts in core metabolism are not merely consequences of cancer but are now recognized as fundamental drivers of hepatocarcinogenesis.
The discovery of non-coding RNAs (ncRNAs) has revolutionized our understanding of cancer regulation. Once considered "transcriptional noise," ncRNAs are now known to be critical regulators of gene expression [34] [33]. In the human genome, less than 2% of genes encode proteins; the vast majority are transcribed into ncRNAs [34] [24]. These molecules are broadly classified by size: small non-coding RNAs (sncRNAs, <200 nucleotides), including microRNAs (miRNAs), and long non-coding RNAs (lncRNAs, >200 nucleotides) [34] [6]. They exert regulatory control through diverse mechanisms, including epigenetic modification, chromatin remodeling, and post-transcriptional gene silencing [6] [36]. In HCC, specific ncRNAs are dysregulated and play pivotal roles as either oncogenic drivers or tumor suppressors, directly influencing the metabolic reprogramming that fuels tumor progression [34] [35] [37]. This whitepaper delves into the intricate mechanisms by which ncRNAs modulate key metabolic pathways in HCC, providing a technical guide for researchers and drug development professionals.
Core Metabolic Pathways and Regulatory ncRNAs in HCC
Glycolytic Reprogramming: The Warburg Effect
A cornerstone of cancer metabolism is the Warburg effect, where cancer cells preferentially metabolize glucose to lactate via glycolysis, even under oxygen-sufficient conditions (aerobic glycolysis) [35] [38] [36]. This switch from oxidative phosphorylation provides cancer cells with several advantages, including rapid ATP generation and the production of metabolic intermediates for biosynthesis [38]. ncRNAs finely tune this glycolytic switch by targeting key transporters and enzymes.
- Glucose Transporters (GLUTs): The first step in glycolysis is glucose uptake. ncRNAs regulate the expression of various GLUT isoforms. For instance, the tumor suppressor miR-1291 directly targets and inhibits GLUT1 in renal carcinoma cells, thereby reducing glucose uptake [35]. Conversely, the lncRNA PCGEM1 promotes GLUT1 expression in prostate cancer, while lncRNA-p21 is associated with HIF-1α-mediated upregulation of GLUT1 [37]. In bladder cancer, downregulation of miR-195-5p allows for the expression of GLUT3 [37].
- Glycolytic Enzymes: ncRNAs target rate-limiting enzymes throughout the glycolytic cascade. The tumor suppressor miR-143 decreases the glucose metabolic rate by inhibiting hexokinase 2 (HK2) expression [35]. Interestingly, the oncogenic miR-155 suppresses miR-143, leading to post-transcriptional upregulation of HK2 and enhanced glycolysis in breast cancer cells [35]. Pyruvate kinase M2 (PKM2), a critical regulator of the final step of glycolysis, is inhibited by miR-122 in breast cancer, promoting metastasis [35]. Furthermore, miR-375 ensures survival of gastric carcinoma cells by targeting pyruvate dehydrogenase kinase 1 (PDK1), a key enzyme that regulates the entry of pyruvate into the mitochondria [35].
Table 1: ncRNAs Regulating Glycolysis in HCC and Other Cancers
| Target Metabolic Process | Regulating ncRNA | Effect on Glycolysis | Molecular Target |
|---|---|---|---|
| Glucose Uptake | miR-1291 | Inhibitory | GLUT1 |
| Glucose Uptake | PCGEM1 (lncRNA) | Promotional | GLUT1 |
| Glucose Uptake | miR-195-5p | Inhibitory | GLUT3 |
| First Catalytic Step | miR-143 | Inhibitory | HK2 |
| First Catalytic Step | miR-155 | Promotional | Suppresses miR-143 |
| Final Catalytic Step | miR-122 | Inhibitory | PKM2 |
| Mitochondrial Entry | miR-375 | Promotional | PDK1 |
The diagram below illustrates how different classes of ncRNAs regulate key steps in the glycolytic pathway within the cancer cell.
Lipogenesis: Fueling Membrane Synthesis and Signaling
Cancer cells exhibit a marked increase in de novo lipid synthesis to support the production of membranes, signaling molecules, and energy storage [34] [36]. Key enzymes in the fatty acid synthesis pathway, such as ATP-citrate lyase (ACLY), acetyl-CoA carboxylase (ACC), and fatty acid synthase (FASN), are frequently upregulated in cancers, including HCC [36]. ncRNAs serve as critical modulators of this lipogenic switch.
- Sterol Regulatory Element-Binding Proteins (SREBPs): These are master transcription factors for lipid synthesis genes. The miR-33a/33b family has been accurately described as key regulators of lipid metabolism, primarily through their targeting of SREBP genes [35].
- Fatty Acid Metabolism Enzymes: Specific lncRNAs and miRNAs directly target enzymes involved in lipid synthesis and metabolism. For example, the HULC lncRNA (Highly Upregulated in Liver Cancer) is implicated in the reprogramming of lipid metabolism in HCC cells, although its precise molecular targets are still being elucidated [34]. The increased fatty acid synthesis under hypoxic conditions is also subject to ncRNA regulation, facilitating cancer cell adaptation to metabolic stress [36].
The reprogramming of lipid metabolism not only supports the structural and energy needs of cancer cells but also influences the TME. For instance, lipid synthesis in regulatory T cells (Tregs) within tumors relies on SREBPs, and targeting this pathway can potentiate antitumor immune responses [36].
Table 2: ncRNAs Regulating Lipogenesis and Autophagy in HCC
| Target Metabolic Process | Regulating ncRNA | Effect on Pathway | Molecular Target / Mechanism |
|---|---|---|---|
| Lipid Synthesis | miR-33a/33b | Inhibitory | SREBP transcription factors |
| Lipid Metabolism in HCC | HULC (lncRNA) | Promotional | Multiple enzymes (e.g., ACLY, ACC, FASN) |
| Autophagy Initiation | Multiple lncRNAs | Varies | PI3K/AKT/mTOR, AMPK pathways |
| Autophagy & Chemoresistance | Specific lncRNAs | Promotional | Modulate autophagic flux |
Autophagy: The Dual-Role Degradation Pathway
Autophagy is a conserved catabolic process that degrades damaged organelles and proteins to maintain cellular homeostasis and provide energy during stress. In cancer, autophagy plays a paradoxical, context-dependent role: it can act as a tumor suppressor in early stages by removing damaged components and preventing genomic instability, but it evolves into a tumor promoter in advanced cancers by enabling survival under metabolic duress and promoting therapy resistance [14].
LncRNAs have emerged as critical regulators of autophagy, influencing tumorigenesis, metastasis, and drug resistance through mechanisms such as miRNA sponging and interactions with key signaling proteins [14]. They integrate into core autophagy signaling networks:
- PI3K/AKT/mTOR Pathway: This is the primary negative regulator of autophagy. Numerous lncRNAs have been shown to modulate this pathway. For instance, the H19 lncRNA can drive glycolysis and tumor growth by forming a positive feedback loop with HIF-1α, a transcription factor that is also influenced by mTOR signaling [33].
- AMPK Pathway: As a central energy sensor and positive regulator of autophagy, the AMPK pathway is also a target of lncRNAs. LncRNAs can influence the activity of AMPK, thereby altering autophagic flux in response to energy stress [14].
- Beclin-1 Complex: The core autophagy initiation complex containing Beclin-1 and VPS34 is another regulatory node. Some lncRNAs can influence the formation or activity of this complex, directly impacting the nucleation of the autophagophore [14].
The modulation of autophagy by lncRNAs has direct therapeutic implications. In HCC, lncRNAs have been demonstrated to modulate resistance to first-line agents by altering autophagic flux and its associated molecular pathways [14]. Targeting these lncRNA-autophagy axes represents a promising frontier for overcoming chemoresistance.
The following diagram provides a simplified overview of the core autophagy machinery and its regulation by lncRNAs.
Experimental Protocols: Key Methodologies for Investigating ncRNA-Metabolism Axes
Studying the functional role of ncRNAs in metabolic reprogramming requires a multidisciplinary approach. Below is a detailed protocol for a core experiment investigating the impact of a specific lncRNA on glycolytic flux.
Protocol: Assessing Glycolytic Function Following LncRNA Knockdown
- Objective: To determine the functional consequences of a specific lncRNA (e.g., HULC) on glycolysis in HCC cell lines.
- Experimental Workflow:
- Cell Culture & Transfection: Maintain human HCC cell lines (e.g., HepG2, Huh-7) under standard conditions. Transfect cells with lncRNA-specific siRNAs or ASOs (Antisense Oligonucleotides) to achieve knockdown. Include a non-targeting siRNA (scramble) as a negative control.
- Validation of Knockdown: 48 hours post-transfection, harvest cells and extract total RNA. Perform qRT-PCR to quantify the knockdown efficiency of the target lncRNA.
- Functional Metabolic Assays: 72 hours post-transfection, perform the following assays using the transfected cells:
- Glucose Uptake Assay: Use a fluorescent 2-NBDG glucose analog. Measure cellular fluorescence by flow cytometry or fluorescence microscopy. Expected Outcome: Successful knockdown of an oncogenic lncRNA like HULC should result in decreased 2-NBDG uptake.
- Extracellular Acidification Rate (ECAR): Utilize a Seahorse XF Analyzer to measure real-time glycolytic flux. Key parameters to calculate include Glycolysis, Glycolytic Capacity, and Glycolytic Reserve. Expected Outcome: Knockdown of an oncogenic lncRNA should lead to a decreased ECAR, indicating reduced glycolysis.
- Lactate Production Assay: Collect cell culture media and measure lactate concentration using a colorimetric or fluorometric lactate assay kit. Normalize lactate levels to total cellular protein. Expected Outcome: Reduced lactate secretion upon lncRNA knockdown.
- Downstream Validation:
- Western Blotting: Analyze the protein levels of key glycolytic enzymes (e.g., HK2, PKM2, LDHA) and transporters (GLUT1) from cell lysates to confirm molecular changes.
- ATP Assay: Quantify intracellular ATP levels using a luminescent ATP assay kit to correlate glycolytic changes with energy production.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating ncRNA in Cancer Metabolism
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| LncRNA-specific siRNAs or ASOs | Selective knockdown of target lncRNA | Functional loss-of-function studies to assess metabolic impact of HULC or NEAT1 [14] [24]. |
| Seahorse XF Analyzer | Real-time measurement of metabolic rates (ECAR for glycolysis, OCR for OXPHOS) | Profiling glycolytic flux after ncRNA modulation [35]. |
| 2-NBDG | Fluorescent glucose analog for tracking glucose uptake | Quantifying changes in GLUT transporter activity via flow cytometry [37]. |
| qRT-PCR Assays | Quantification of ncRNA and mRNA expression levels | Validating knockdown efficiency and measuring target gene expression (e.g., HK2, SREBPs) [34] [35]. |
| CRISPR/Cas9 Systems | Genome editing for stable knockout or knock-in of ncRNA genes | Generating stable cell lines to study long-term metabolic effects of ncRNA dysregulation [14] [24]. |
| Colorimetric/Fluorometric Kits (e.g., for Lactate, ATP, Cholesterol) | Biochemical quantification of specific metabolites | Validating functional metabolic outputs predicted by transcriptomic or proteomic data [35] [36]. |
| 1-(5-Fluoropyrimidin-2-yl)indoline | 1-(5-Fluoropyrimidin-2-yl)indoline|CAS 2189498-59-5 | 1-(5-Fluoropyrimidin-2-yl)indoline (CAS 2189498-59-5) is a fluorinated heterocycle for anticancer and drug discovery research. For Research Use Only. Not for human or veterinary use. |
| 4-Amino-2-(methylthio)benzoic acid | 4-Amino-2-(methylthio)benzoic acid|CAS 1343844-11-0 | 4-Amino-2-(methylthio)benzoic acid (CAS 1343844-11-0) is a benzoic acid derivative for research use. This For Research Use Only product is not for human or veterinary use. |
The intricate interplay between ncRNA dysregulation and metabolic reprogramming in HCC represents a complex yet promising frontier in cancer research. As detailed in this whitepaper, specific miRNAs and lncRNAs exert precise control over the glycolytic, lipogenic, and autophagic pathways that power tumor progression. The growing understanding of these mechanisms opens up novel avenues for therapeutic intervention.
Future efforts should focus on translating this knowledge into clinical applications. This includes the development of ncRNA-based biomarkers for early diagnosis and prognosis, and the advancement of targeted therapies using ASOs, RNAi, or CRISPR/Cas9 technologies to specifically inhibit oncogenic ncRNAs or restore tumor-suppressive ncRNAs [14] [24]. A key challenge remains the efficient and specific delivery of these agents to tumor cells in vivo. Furthermore, given the complexity and redundancy of regulatory networks, combination therapies targeting multiple ncRNAs or co-targeting ncRNAs and key metabolic enzymes may yield superior efficacy. Integrating multi-omics data to build comprehensive models of the ncRNA-metabolism network will be crucial for identifying the most potent therapeutic nodes and advancing personalized medicine for HCC patients.
Hepatocellular carcinoma (HCC) represents a major global health challenge, characterized by a complex tumor microenvironment (TME) that plays a pivotal role in tumor progression and therapeutic response [39] [40]. The immune landscape of HCC is particularly critical, comprising various immune cell populations—including T cells, natural killer (NK) cells, dendritic cells, and myeloid-derived suppressor cells (MDSCs)—that dynamically interact to either promote anti-tumor immunity or facilitate tumor growth through immunosuppressive mechanisms [40] [3]. Long non-coding RNAs (lncRNAs), defined as RNA transcripts exceeding 200 nucleotides without protein-coding capacity, have emerged as master regulators of gene expression and cellular processes in cancer [33]. These molecules are now recognized as critical players in shaping the immune microenvironment of HCC by regulating immune cell functions, cytokine profiles, and checkpoint molecule expression [39] [40]. This review comprehensively examines the mechanistic roles of specific lncRNAs in modulating immune cell infiltration and checkpoint regulation within the HCC landscape, providing a technical resource for researchers and therapeutic developers.
LncRNA Regulation of Immune Cell Infiltration in HCC
LncRNAs profoundly influence the composition and functional state of immune cells within the HCC tumor microenvironment through diverse molecular mechanisms. Their impact varies significantly across different immune cell populations, as detailed below.
T Cell Regulation
T cells play a crucial role in the anti-tumor immune response of HCC, and lncRNAs regulate their function through multiple pathways. The lncRNA NEAT1 is significantly upregulated in peripheral blood mononuclear cells (PBMCs) of HCC patients and promotes CD8+ T cell apoptosis while suppressing their cytolytic activity. Mechanistically, NEAT1 functions as a competing endogenous RNA (ceRNA) that binds to and sequesters miR-155, leading to the upregulation of Tim-3, a critical exhaustion marker on T cells. Experimental evidence demonstrates that NEAT1 knockdown inhibits CD8+ T cell apoptosis and enhances their cytotoxicity against HCC cells, identifying it as a promising immunotherapeutic target [40] [3].
Lnc-Tim3 represents another crucial regulator of T cell exhaustion in HCC. This lncRNA specifically binds to the immune checkpoint protein Tim-3, preventing its interaction with the intracellular adaptor Bat3. This disruption inhibits downstream signaling through the Lck/NFAT1/AP-1 pathway while promoting Bat3 nuclear localization. Within the nucleus, Bat3 enhances the transcriptional activation of pro-apoptotic genes (including MDM2 and Bcl-2) through p300-dependent p53 and RelA pathways, ultimately driving T cell exhaustion [40] [3].
The lncRNA TUG1 is upregulated in HCC via METTL3-mediated m6A modification and contributes to immunosuppression through multiple mechanisms. Knockdown studies demonstrate that TUG1 suppression inhibits tumor growth and metastasis while simultaneously increasing infiltration of CD8+ T cells and M1 macrophages. TUG1 exerts its immunosuppressive effects partially through PD-L1 activation, highlighting its potential as a combination therapy target [40].
Table 1: LncRNAs Regulating T Cell Function in HCC
| LncRNA | Expression in HCC | Target/Mechanism | Functional Effect on T Cells |
|---|---|---|---|
| NEAT1 | Upregulated | Sponges miR-155, upregulates Tim-3 | Promotes CD8+ T cell apoptosis, suppresses cytotoxicity |
| Lnc-Tim3 | Upregulated | Binds Tim-3, inhibits Bat3 interaction | Drives T cell exhaustion, promotes apoptosis |
| TUG1 | Upregulated (m6A-dependent) | Activates PD-L1 signaling | Reduces CD8+ T cell infiltration, suppresses function |
| CRNDE | Upregulated | Multiple pathways | Promotes T cell dysfunction |
| MIAT | Upregulated | Multiple pathways | Promotes T cell dysfunction |
Macrophage Polarization
LncRNAs significantly influence macrophage polarization within the HCC microenvironment, primarily toward the pro-tumor M2 phenotype. LINC00543 is overexpressed in HCC and induces M2 polarization of macrophages, thereby contributing to tumorigenesis. It functions through the pre-miR-506-3p/FOXQ1 axis, establishing a pro-tumorigenic cross-talk between HCC cells and tumor-associated macrophages [41].
The lncRNA MIR155HG (host gene for miR-155) promotes proliferation, migration, and invasion in HCC cells while simultaneously modulating immune responses. It functions through the ANXA2/miR-650 pathway to alter macrophage activity within the TME, demonstrating how a single lncRNA can coordinately regulate both tumor-intrinsic properties and immune cell function [41].
RPPH1, transported via exosomes, promotes HCC cell migration, invasion, and epithelial-mesenchymal transition (EMT). It modulates macrophage function through TUBB3 interaction, facilitating metastasis and tumor growth through intercellular communication [41].
NK and Dendritic Cell Modulation
Beyond T cells and macrophages, lncRNAs regulate other critical immune populations. ELFN1-AS1 acts as an oncogene in HCC by suppressing natural killer (NK) cell function. It operates through the GDF15/NKG2D/GZMB pathway, impairing NK cell-mediated cytotoxicity and thus enabling immune evasion [41].
SNHG10, present in both nuclei and exosomes, contributes to immune evasion by modulating NK cell activity through the INHBC/TGF-β signaling axis. This pathway represents another mechanism by which HCC cells suppress innate anti-tumor immunity [41].
Table 2: LncRNAs Regulating Innate Immune Cells in HCC
| LncRNA | Expression | Target Immune Cell | Molecular Mechanism | Overall Effect |
|---|---|---|---|---|
| LINC00543 | Upregulated | Macrophages | pre-miR-506-3p/FOXQ1 axis | Induces M2 polarization |
| MIR155HG | Upregulated | Macrophages | ANXA2/miR-650 pathway | Promotes TME remodeling |
| RPPH1 | Upregulated (exosomal) | Macrophages | TUBB3 interaction | Promotes metastasis |
| ELFN1-AS1 | Upregulated | NK cells | GDF15/NKG2D/GZMB pathway | Suppresses NK cytotoxicity |
| SNHG10 | Upregulated | NK cells | INHBC/TGF-β signaling | Inhibits NK cell function |
| SATB2-AS1 | Downregulated | Dendritic cells | SATB2/CXCL9,10 regulation | Tumor suppressor |
LncRNA-Mediated Regulation of Immune Checkpoints
Immune checkpoint molecules represent critical regulators of anti-tumor immunity, and lncRNAs extensively modulate their expression and activity in HCC. This regulation occurs through both direct and indirect mechanisms, significantly impacting response to immunotherapy.
The lncRNA LINC00460 is upregulated in HCC and localizes to the cytoplasm, where it promotes tumor progression through multiple mechanisms. It functions as a ceRNA, sponging miR-186-3p to release its inhibition of MYC, leading to subsequent upregulation of CD47 and PD-L1. This dual checkpoint enhancement contributes significantly to immune evasion and is strongly associated with tumor metastasis and recurrence [41].
LINC01088, present in both nucleus and cytoplasm, facilitates immune evasion by regulating PD-L1 expression through the miR-548b-5p and miR-548c-5p/G3BP1/PD-L1 axis. This pathway enhances PD-L1-mediated suppression of CD8+ T cell function, highlighting how lncRNAs can fine-tune checkpoint expression through intricate RNA networks [41].
KCNQ1OT1, transported via exosomes, represents another important regulator of PD-L1 in HCC. It functions through the miR-30a-5p/USP22/PD-L1 pathway to promote tumor growth and EMT while simultaneously enhancing PD-L1-mediated immunosuppression. The exosomal nature of this lncRNA suggests potential roles in intercellular communication and regional modulation of the immune microenvironment [41].
SNHG29, localized to both nucleus and cytoplasm, modifies the tumor microenvironment through YAP/PD-L1 signaling. This connection links the Hippo signaling pathway to immune checkpoint regulation, demonstrating how lncRNAs can integrate developmental and immune signaling networks in HCC [41].
Table 3: LncRNAs Directly Regulating Immune Checkpoints in HCC
| LncRNA | Subcellular Localization | Target Checkpoint | Molecular Mechanism | Experimental Evidence |
|---|---|---|---|---|
| LINC00460 | Cytoplasm | CD47, PD-L1 | miR-186-3p/MYC axis | Promotes metastasis, angiogenesis |
| LINC01088 | Nucleus/Cytoplasm | PD-L1 | miR-548b-5p, miR-548c-5p/G3BP1 | Enhances tumor growth |
| PROX1-AS1 | Not specified | PD-L1 | PROX1-AS1/miR-520d/PD-L1 | Promotes viability, invasion |
| KCNQ1OT1 | Exosomes | PD-L1 | miR-30a-5p/USP22/PD-L1 | Promotes tumor growth, EMT |
| SNHG29 | Nucleus/Cytoplasm | PD-L1 | YAP/PD-L1 signaling | Modifies TME |
| CDR1AS | Not specified | PD-L1 | CDR1AS/CMTM4,6/PD-L1 | Promotes immune evasion |
Core Regulatory Circuitry and Network Biology
Advanced computational analyses have revealed that lncRNAs often function within complex regulatory networks rather than through simple linear pathways. The concept of ICP-related LncRNA-mediated Core Regulatory Circuitry Triplets (ICP-LncCRCTs) has emerged as a fundamental framework for understanding lncRNA functions in immune regulation [42].
These triplets consist of lncRNAs, immune-related genes, and immune checkpoint molecules that form coordinated regulatory units. Network-based analyses and Bayesian network inference have identified four major regulatory patterns: (1) lncRNA-mediated regulation of ICP by immune genes (LGI), (2) lncRNA-mediated direct regulation of ICP, further influencing immune genes (LIG), (3) coordinate regulation (COO), and (4) independent regulation (INDEP) [42].
Hub lncRNAs such as MIR155HG and ADAMTS9-AS2 play central roles in these regulatory networks. For example, the CXCL10-MIR155HG-ICOS triplet forms a cohesive regulatory unit that can better predict one-, three-, and five-year prognosis in melanoma compared to single molecules alone. When combined with tumor mutation burden (TMB), such ICP-LncCRCTs significantly improve prediction of ICI response in melanoma patients, highlighting their clinical potential [42].
Figure 1: Regulatory Patterns in ICP-LncRNA Core Circuitry. Four distinct patterns (LGI, LIG, COO, INDEP) describe how lncRNAs, immune genes, and immune checkpoints interact in regulatory networks.
Experimental Approaches and Methodologies
Identification of HCC-Associated lncRNAs
Comprehensive transcriptomic analysis represents the foundational approach for identifying dysregulated lncRNAs in HCC. The standard workflow begins with RNA extraction from paired tumor and adjacent non-tumor tissues, followed by RNA sequencing (RNA-Seq) or microarray analysis. Bioinformatic processing includes alignment to reference genomes, transcript assembly, and differential expression analysis using tools such as Cufflinks, DESeq2, or edgeR [43].
Validation of candidate lncRNAs typically employs quantitative reverse transcription PCR (qRT-PCR) on independent patient cohorts. For instance, in a recent study linking basement membrane and immune checkpoint-related lncRNAs, researchers developed a 10-lncRNA prognostic signature through univariable Cox regression followed by machine learning approaches (LASSO and SVM-RFE algorithms) applied to TCGA transcriptome data [43].
Functional Characterization of LncRNA Mechanisms
Loss-of-function experiments utilize siRNA or shRNA-mediated knockdown to assess lncRNA necessity. For example, in the characterization of LINC01224, researchers suppressed expression using specific siRNAs and observed inhibited migration of HCC cells in vitro, confirming its functional role in metastasis [43].
Gain-of-function approaches employ plasmid vectors or viral systems for lncRNA overexpression. This methodology helps establish sufficiency in driving specific phenotypes, such as immune checkpoint upregulation or macrophage polarization.
Mechanistic interrogation often involves RNA immunoprecipitation (RIP) to identify protein binding partners, chromatin isolation by RNA purification (ChIRP) to map genomic binding sites, and luciferase reporter assays to validate direct miRNA interactions. For instance, the interaction between NEAT1 and miR-155 was confirmed through RIP assays in CD8+ T cells from HCC patients [40] [3].
Assessing Immune Cell Interactions
Co-culture systems enable direct investigation of lncRNA-mediated cross-talk between HCC cells and immune cells. These typically involve:
- Establishing HCC cells with lncRNA modulation (knockdown/overexpression)
- Isolating primary immune cells (T cells, macrophages, NK cells) from peripheral blood
- Direct or indirect co-culture for specified durations
- Measuring functional outcomes (cytokine secretion, cytotoxicity, phagocytosis)
Exosome isolation and characterization utilize differential ultracentrifugation or commercial kits to isolate extracellular vesicles followed by nanoparticle tracking analysis and electron microscopy validation. Cargo transfer can be tracked using fluorescent labels or by measuring lncRNA levels in recipient immune cells via qRT-PCR [41].
Table 4: Research Reagent Solutions for LncRNA-Immune Function Studies
| Reagent/Category | Specific Examples | Experimental Function | Key Considerations |
|---|---|---|---|
| Knockdown Tools | siRNA, shRNA, ASO | LncRNA loss-of-function studies | Off-target effects, delivery efficiency |
| Expression Vectors | Plasmid, Lentivirus | LncRNA gain-of-function studies | Endogenous regulation, physiological expression levels |
| Co-culture Systems | Transwell, 3D spheroids | Cell-cell communication studies | Compartment separation, tissue context preservation |
| Exosome Isolation | Ultracentrifugation, Commercial kits | Extracellular vesicle studies | Purity, integrity preservation |
| Immune Cell Isolation | Magnetic sorting, FACS | Pure population studies | Activation state preservation, viability |
| Molecular Validation | qRT-PCR, Western, FACS | Mechanism confirmation | Antibody specificity, normalization controls |
Visualization of Key Signaling Pathways
The intricate relationships between lncRNAs and immune regulation in HCC can be visualized through several key pathways that highlight potential therapeutic targets.
Figure 2: LncRNA-Mediated Immune Regulation Pathways. Three major pathways (NEAT1/miR-155/Tim-3, Lnc-Tim3/Bat3, and LINC00460/miR-186/MYC) demonstrate how lncRNAs regulate immune cell function and checkpoint expression in HCC.
Concluding Perspectives and Future Directions
The comprehensive mapping of lncRNA functions in HCC immune regulation reveals a complex regulatory landscape with significant therapeutic implications. The accumulating evidence demonstrates that lncRNAs sit at the critical interface between tumor cells and the immune microenvironment, making them attractive targets for novel immunotherapeutic approaches.
Future research directions should prioritize several key areas:
- Therapeutic targeting development - Advancing delivery systems for lncRNA-targeting oligonucleotides, including nanoparticle-based approaches and tissue-specific delivery vehicles.
- Combination therapy strategies - Rational design of treatments combining lncRNA modulation with existing immunotherapies, particularly immune checkpoint inhibitors.
- Biomarker validation - Large-scale clinical validation of lncRNA signatures for predicting immunotherapy response and patient stratification.
- Single-cell resolution mapping - Application of single-cell sequencing technologies to delineate cell-type-specific lncRNA functions within the heterogeneous tumor microenvironment.
The integration of computational prediction with experimental validation will continue to accelerate the discovery of functional lncRNA-immune interactions. As our understanding of these complex regulatory networks deepens, lncRNA-based diagnostics and therapeutics hold promise for significantly improving outcomes in HCC patients by reshaping the immunosuppressive tumor landscape.
Hepatocellular carcinoma (HCC) is a major global health challenge, characterized by a complex tumor microenvironment (TME) that plays a pivotal role in tumor progression, immune evasion, and therapeutic resistance [3] [44]. The non-coding RNA (ncRNA) landscape within the HCC TME has emerged as a critical regulator of tumorigenesis, with dysregulation of various ncRNA species contributing significantly to disease pathogenesis [6] [45]. These ncRNAs, including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), constitute a sophisticated regulatory network that controls gene expression without encoding proteins [6]. Their stable nature, tissue specificity, and prevalence in bodily fluids make them promising targets for therapeutic intervention [45] [44].
The TME in HCC is a heterogeneous ecosystem comprising tumor cells, immune cells, fibroblasts, endothelial cells, and extracellular matrix components [3]. This microenvironment creates selective pressures that drive ncRNA dysregulation, which in turn modulates critical cancer hallmarks including sustained proliferation, evasion of immune surveillance, activation of invasion and metastasis, and resistance to cell death [6] [14]. The intricate interplay between different ncRNA species creates complex regulatory networks that can be exploited for therapeutic purposes. Understanding these networks is essential for developing effective ncRNA-targeted therapies that can reprogram the immunosuppressive TME and overcome current treatment limitations in HCC [3] [44].
ncRNA Replacement Therapy
Principles and Mechanisms
ncRNA replacement therapy involves restoring the function of tumor-suppressive ncRNAs that are downregulated in HCC. This strategy aims to reintroduce synthetic mimics of endogenous ncRNAs to re-establish their normal regulatory functions and counteract oncogenic pathways [45]. The approach is particularly relevant for miRNAs and lncRNAs that act as natural inhibitors of oncogenes or positive regulators of tumor suppressor pathways [46]. By delivering these synthetic ncRNAs to tumor cells, it is possible to restore lost regulatory functions and shift the balance from pro-tumorigenic to anti-tumorigenic signaling within the TME.
The therapeutic ncRNAs used in replacement strategies are designed to mimic the structure and function of their endogenous counterparts. For miRNA replacement, synthetic double-stranded RNA molecules are used, where the guide strand is identical to the mature miRNA sequence. These molecules are incorporated into the RNA-induced silencing complex (RISC) and direct it to target mRNAs for translational repression or degradation [6]. For lncRNA replacement, more complex synthetic RNAs are designed that recapitulate the functional domains of the endogenous lncRNA, enabling them to interact with binding partners and execute their regulatory roles [45].
Key Therapeutic Candidates and Targets
miR-122 Replacement: miR-122 is a liver-specific miRNA that is significantly downregulated in approximately 65% of HCC cases [45]. This miRNA serves as a key regulator of liver homeostasis and its loss contributes to hepatocarcinogenesis by promoting aberrant proliferation, modulating cell adhesion, and inducing a hepatoblastic signature [46]. Preclinical studies have demonstrated that restoring miR-122 expression using lipid nanoparticle-formulated mimics suppresses tumor growth by 55% in murine models and sensitizes HCC cells to chemotherapy [45]. The mechanism involves repression of oncogenic targets such as c-Myc and regulation of metabolic pathways specific to hepatocytes.
miR-26a Replacement: miR-26a is another frequently downregulated miRNA in HCC that functions as a potent tumor suppressor [46]. Its loss is associated with poor prognosis and reduced sensitivity to interferon therapy [46]. miR-26a replacement triggers cell cycle arrest in resting phases and modulates inflammatory responses through regulation of interleukin-6 signaling [46]. In vivo studies show that miR-26a delivery significantly reduces liver tumor development in animal models, highlighting its therapeutic potential [46].
LINC00152 Restoration: The lncRNA LINC00152 is downregulated in HCC and functions as a tumor suppressor [45]. Restoration of LINC00152 expression inhibits cell proliferation by recruiting histone deacetylase 1 (HDAC1) to repress c-Myc transcription [45]. Preclinical studies demonstrate that restoring LINC00152 reduces tumor growth by 40% in xenograft models, indicating its potential as a therapeutic agent [45].
Table 1: Key ncRNA Candidates for Replacement Therapy in HCC
| ncRNA | Expression in HCC | Primary Targets/Functions | Preclinical Efficacy |
|---|---|---|---|
| miR-122 | Downregulated (65% of cases) | Represses c-Myc, enhances chemosensitivity | 55% tumor growth suppression [45] |
| miR-26a | Downregulated | Modulates cell cycle, regulates IL-6 signaling | Reduces liver tumor development [46] |
| LINC00152 | Downregulated | Recruits HDAC1 to repress c-Myc | 40% tumor growth reduction [45] |
| miR-199a-3p | Downregulated | Inhibits MET and ERK signaling | Suppresses hyperactivation of oncogenic pathways [46] |
Experimental Protocol for ncRNA Replacement
Synthesis and Design of ncRNA Mimics:
- miRNA Mimics: Design double-stranded RNA molecules with perfect complementarity to the seed region of the endogenous miRNA. The guide strand should be identical to the mature miRNA sequence, while the passenger strand may include chemical modifications to enhance stability and promote RISC loading [6].
- lncRNA Replacement: Identify functional domains through structural analysis and design synthetic RNAs that recapitulate these domains. For LINC00152, focus on regions involved in HDAC1 recruitment and c-Myc repression [45].
Formulation and Delivery:
- Nanoparticle Formulation: Encapsulate ncRNA mimics in lipid nanoparticles (LNPs) optimized for hepatic delivery. LNPs should include ionizable lipids, phospholipids, cholesterol, and PEG-lipids in molar ratios of 50:10:38.5:1.5 [45].
- Surface Functionalization: Incorporate galactosylated lipids or peptide ligands for targeted delivery to hepatocytes and HCC cells [47].
In Vitro and In Vivo Validation:
- Cell Transfection: Transfect HCC cell lines (HepG2, Huh7, SMMC-7721) using LNP-formulated ncRNA mimics at concentrations of 10-50 nM. Use lipofectamine-based transfection for screening [48].
- Functional Assays: Assess proliferation (MTS assay), apoptosis (caspase-3 activity, Annexin V staining), and migration (transwell assay) at 24-72 hours post-transfection [49] [48].
- In Vivo Administration: Administer LNP-formulated ncRNA mimics via tail vein injection to HCC mouse models (e.g., xenograft, DEN-induced) at doses of 1-5 mg/kg, twice weekly for 4 weeks [45].
- Efficacy Assessment: Monitor tumor volume by caliper measurements, perform immunohistochemistry for proliferation (Ki-67) and apoptosis (TUNEL) markers, and analyze gene expression in excised tumors [45].
Antisense Oligonucleotide (ASO) Therapeutics
Principles and Mechanisms
Antisense oligonucleotides are single-stranded DNA molecules typically 10-30 nucleotides in length that are designed to be complementary to specific target RNA sequences through Watson-Crick base pairing [50]. ASOs can modulate gene expression through several mechanisms, with the most common being RNase H-mediated degradation of the target RNA [50]. This enzyme recognizes DNA-RNA heteroduplexes and cleaves the RNA strand, leading to reduced levels of the target transcript. ASOs can also function by sterically blocking the translation machinery or splicing factors, modulating alternative splicing patterns, and sequestering miRNAs [50].
The effectiveness of ASO therapeutics depends heavily on chemical modifications that enhance stability, binding affinity, and pharmacokinetic properties. First-generation ASOs featured phosphorothioate backbone modifications, while second-generation ASOs incorporate 2'-O-methoxyethyl (2'-MOE) or 2'-O-methyl modifications that further improve nuclease resistance and binding affinity [50]. More recently, constrained ethyl (cEt) and phosphorodiamidate morpholino oligomer (PMO) modifications have been developed to optimize the therapeutic profile of ASOs [50].
Key Therapeutic Candidates and Targets
ASOs Targeting Oncogenic lncRNAs: The lncRNA HOTAIR is overexpressed in advanced HCC (75% in TNM III/IV vs. 25% in I/II stages) and promotes tumor progression through interaction with polycomb repressive complex 2 (PRC2), leading to epigenetic silencing of tumor suppressor genes [45]. ASOs targeting HOTAIR have demonstrated significant anti-tumor effects in preclinical models, inhibiting cell proliferation (IC50=20 nM) and inducing apoptosis (25% vs. 5% in controls) [45]. Similarly, ASOs targeting MALAT1, which is elevated in sorafenib-resistant HCC cells and functions as a miRNA sponge for miR-143, can reverse drug resistance and suppress tumor progression [45].
ASOs Targeting Protein-Coding Oncogenes: Midkine (MK) is overexpressed in HCC and promotes tumor survival by inhibiting caspase-dependent apoptosis and downregulating pro-apoptotic factors [49]. ASOs targeting MK (specifically ASODN5) induce apoptosis and increase chemosensitivity in HepG2 cells in a dose-dependent manner [49]. The mechanism involves reduced MK mRNA and protein levels, declined survivin and Bcl-2 expression, and increased caspase-3 activity [49]. This approach demonstrates the potential of ASOs to target non-coding and coding transcripts simultaneously for enhanced efficacy.
Metabolism-Targeting ASOs for NAFLD/NASH-HCC Spectrum: ASOs targeting key regulators of lipid metabolism show promise for treating metabolic liver diseases that predispose to HCC. ASOs against PNPLA3 (using 2'-4' constrained ethyl modification), Srebp-1c (phosphorothioate-modified), and Dgat2 (phosphorothioate with 2'-MOE) effectively inhibit lipid synthesis and can prevent progression from steatosis to HCC [50].
Table 2: Key ASO Candidates for HCC Therapy
| ASO Target | Target Type | Chemical Modifications | Mechanism of Action | Therapeutic Effects |
|---|---|---|---|---|
| HOTAIR | Oncogenic lncRNA | Not specified | RNase H-mediated degradation | 60% proliferation inhibition, 25% apoptosis [45] |
| Midkine (MK) | Protein-coding oncogene | Not specified | RNase H-mediated degradation | Increased apoptosis and chemosensitivity [49] |
| PNPLA3 | Lipid metabolism gene | 2'-4' constrained ethyl (cEt) | RNase H-mediated degradation | Inhibits lipid synthesis [50] |
| Srebp-1c | Lipid metabolism transcription factor | Phosphorothioate | RNase H-mediated degradation | Reduces hepatic steatosis [50] |
Experimental Protocol for ASO Therapeutics
ASO Design and Synthesis:
- Target Selection: Identify accessible target regions in the RNA secondary structure using computational tools (e.g., RNAfold, OligoWalk) [50].
- Sequence Design: Design 16-20 nucleotide ASOs with GC content of 40-60% to balance binding affinity and specificity. Avoid complementary sequences longer than 8 bases to prevent self-hybridization [50] [49].
- Chemical Modification: Incorporate phosphorothioate backbone modifications for nuclease resistance and 2'-O-methoxyethyl (2'-MOE) or 2'-4' constrained ethyl (cEt) modifications at wing positions for enhanced binding affinity [50].
In Vitro Screening:
- Cell Transfection: Transfect HCC cell lines with ASOs at concentrations of 50-400 nM using lipofectamine 2000. Include mismatch controls to assess sequence specificity [49].
- Dose-Response Analysis: Treat cells with ASO concentrations ranging from 10-500 nM for 48-72 hours and assess viability using MTS assay to determine IC50 values [49].
- Mechanistic Validation: Measure target mRNA and protein levels by RT-qPCR and Western blot, respectively. Assess apoptosis by caspase-3 activity and Annexin V staining [49].
In Vivo Evaluation:
- Formulation: Prepare ASOs in sterile PBS for subcutaneous administration or formulate with lipid nanoparticles for enhanced hepatic delivery [50].
- Dosing Regimen: Administer ASOs at 5-50 mg/kg, 2-3 times weekly for 4-6 weeks to HCC mouse models [50].
- Biodistribution and Efficacy: Quantify ASO accumulation in liver and tumor tissues by HPLC or hybridization-based assays. Monitor tumor growth and analyze gene expression in excised tissues [50].
Small Interfering RNA (siRNA) Technologies
Principles and Mechanisms
Small interfering RNAs are double-stranded RNA molecules typically 19-21 base pairs in length with 2-nucleotide 3' overhangs that mediate RNA interference (RNAi) - a conserved biological pathway for sequence-specific gene silencing [48]. The mechanism involves loading of the siRNA guide strand into the RNA-induced silencing complex (RISC), which then identifies complementary mRNA sequences and cleaves them between bases 10 and 11 relative to the 5' end of the siRNA guide strand [48]. This cleavage leads to degradation of the target mRNA and subsequent reduction in corresponding protein levels.
siRNA therapeutics offer several advantages for HCC treatment, including high specificity, potency, and the ability to target traditionally "undruggable" genes. However, effective delivery remains a significant challenge due to siRNA's susceptibility to degradation by nucleases, rapid renal clearance, and negative charge that impedes cellular uptake [47]. Advanced delivery systems, particularly lipid nanoparticles (LNPs) and GalNAc conjugates, have been developed to overcome these barriers and enable efficient siRNA delivery to hepatocytes and HCC cells [47].
Key Therapeutic Candidates and Targets
Multi-Target siRNA Strategies: HCC is a multigenic disease characterized by concurrent alterations in multiple oncogenic pathways. Multi-target siRNAs simultaneously inhibiting NET-1, EMS1, and VEGF genes have demonstrated superior efficacy compared to single-target approaches [48]. NET-1 (a tumor-related gene of the transmembrane 4 superfamily) promotes pathological grading and clinical progression; EMS1 (encoding cortactin) enhances cell motility and invasion; and VEGF drives angiogenesis [48]. The multi-target approach showed greater suppression of proliferation, migration, invasion, and angiogenesis, while inducing more pronounced apoptosis in HCC cells [48].
Oncogene-Targeting siRNAs: Single-target siRNAs against specific HCC-associated genes have shown promising results. siRNAs targeting circMET, an aberrantly expressed circRNA in HCC tumors, reduce tumor burden and increase CD8+ T cell infiltration through the miR-30-5p/Snail/DPP4 axis [44]. Combining DPP4 inhibitors with anti-PD1 immunotherapy enhances CD8+ T cell trafficking and improves response to immunotherapy [44]. Similarly, siRNAs against immune-related targets such as Lnc-Tim3 can specifically bind to Tim-3 and block its interaction with Bat3, inhibiting downstream Lck/NFAT1/AP-1 signaling and reducing CD8+ T cell exhaustion [44].
Immune-Modulating siRNAs: The complex immune microenvironment of HCC presents multiple opportunities for siRNA-mediated modulation. siRNAs targeting NEAT1, which is upregulated in peripheral blood mononuclear cells of HCC patients, can interfere with Tim-3 expression by binding to miR-155 [44]. Downregulation of NEAT1 inhibits CD8+ T cell apoptosis and enhances cytolytic activity against HCC cells, representing a promising approach to enhance immunotherapy efficacy [44].
Table 3: Key siRNA Candidates for HCC Therapy
| siRNA Target | Target Description | Delivery System | Therapeutic Effects |
|---|---|---|---|
| NET-1/EMS1/VEGF (multi-target) | Multiple oncogenes | Lipid nanoparticles | Superior suppression of proliferation, migration, invasion, and angiogenesis [48] |
| circMET | Oncogenic circRNA | Not specified | Reduces tumor burden, increases CD8+ T cell infiltration [44] |
| Lnc-Tim3 | Immune checkpoint regulator | Not specified | Reduces CD8+ T cell exhaustion [44] |
| NEAT1 | Oncogenic lncRNA | Not specified | Inhibits CD8+ T cell apoptosis, enhances cytolytic activity [44] |
Experimental Protocol for siRNA Technologies
siRNA Design and Synthesis:
- Target Site Selection: Identify potential target sites using algorithms that consider sequence specificity, secondary structure accessibility, and off-target potential. Favor sites with 30-50% GC content and avoid stretches of 4 or more identical nucleotides [48].
- siRNA Construction: Chemically synthesize 19 bp duplex RNAs with 2-nt 3' overhangs. For multi-target siRNAs, design long single-stranded RNAs (>21 nt) incorporating target sequences for multiple genes, produced by in vitro transcription with T7 RNA polymerase [48].
- Modification Strategy: Incorporate 2'-O-methyl modifications at specific positions to reduce immune activation and improve stability without compromising silencing activity.
Validation of Silencing Efficiency:
- Dual Luciferase Reporter Assay: Clone target sequences into siRNA validation vectors (e.g., siQuant). Co-transfect HEK293 cells with validation vectors and siRNAs using lipofectamine 2000. Measure firefly and renilla luciferase activities 24 hours post-transfection. Calculate normalized relative luciferase units to determine knockdown efficacy [48].
- RT-qPCR Analysis: Extract total RNA from transfected HCC cells using TRIzol reagent. Perform reverse transcription followed by quantitative PCR with gene-specific primers. Use GAPDH or β-actin as reference genes for normalization. Calculate fold-change using the 2^(-ΔΔCt) method [48].
- Western Blot Analysis: Confirm protein-level knockdown 48-72 hours post-transfection using specific antibodies against target proteins.
Functional Characterization:
- Proliferation Assays: Assess cell viability using MTS assay at 24, 48, and 72 hours post-transfection. Perform colony formation assays by staining with crystal violet after 10-14 days [48].
- Migration and Invasion Assays: Use transwell chambers with Matrigel coating for invasion assays and without coating for migration assays. Count cells that migrate through 8-μm pores after 24-48 hours [48].
- Apoptosis Analysis: Stain cells with Annexin V-FITC and propidium iodide 48 hours post-transfection and analyze by flow cytometry. Measure caspase-3/7 activity using luminescent substrates [48].
Visualization of Key Signaling Pathways and Experimental Workflows
ncRNA Therapeutic Mechanisms in HCC
Experimental Workflow for Therapeutic Development
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for ncRNA Therapeutic Development
| Reagent/Material | Function/Application | Key Specifications | Example Uses |
|---|---|---|---|
| Lipofectamine 2000 | In vitro transfection of nucleic acids | Cationic lipid formulation | Transfection of ASOs/siRNAs in HCC cell lines (HepG2, Huh7) [49] [48] |
| Lipid Nanoparticles (LNPs) | In vivo delivery of ncRNA therapeutics | Ionizable lipid:Phospholipid:Cholesterol:PEG-lipid (50:10:38.5:1.5) | Hepatic delivery of miRNA mimics and siRNAs [45] |
| T7 RNA Polymerase | In vitro transcription of siRNAs | High-yield RNA synthesis | Production of multi-target siRNAs [48] |
| Dual-Luciferase Reporter System | Validation of target engagement | Firefly and Renilla luciferase measurements | Confirmation of siRNA/ASO binding and efficacy [48] |
| GalNAc Conjugates | Hepatocyte-specific targeting | Triantennary N-acetylgalactosamine | Liver-directed delivery of ASOs and siRNAs [50] |
| MTS Assay Kit | Cell viability and proliferation assessment | Tetrazolium compound conversion | Measurement of anti-proliferative effects [49] [48] |
| Annexin V Apoptosis Kit | Apoptosis detection | FITC-labeled Annexin V and PI staining | Quantification of programmed cell death [49] [48] |
| Caspase-3 Activity Assay | Apoptosis pathway activation | Fluorogenic substrate cleavage | Measurement of caspase activation [49] |
| Decane-1,9-diol | Decane-1,9-diol, CAS:3208-05-7, MF:C10H22O2, MW:174.284 | Chemical Reagent | Bench Chemicals |
| (Acetylamino)(2-thienyl)acetic acid | (Acetylamino)(2-thienyl)acetic Acid|Research Chemical | (Acetylamino)(2-thienyl)acetic acid for research applications. This product is For Research Use Only and is not intended for diagnostic or therapeutic use. | Bench Chemicals |
The therapeutic targeting of ncRNA dysregulation in the HCC tumor microenvironment represents a promising frontier in precision oncology. The three major strategies - ncRNA replacement, antisense oligonucleotides, and siRNA technologies - offer complementary approaches to address the complexity of HCC pathogenesis. Each modality has distinct advantages: ncRNA replacement restores lost tumor suppressor functions, ASOs enable precise targeting of oncogenic transcripts, and siRNAs provide potent sequence-specific silencing with potential for multi-target approaches [50] [45] [48].
Future development in this field will likely focus on several key areas: (1) Advanced delivery systems with improved tumor specificity and reduced off-target effects; (2) Multi-target approaches that address the heterogeneous nature of HCC; (3) Rational combinations with existing therapies including immune checkpoint inhibitors; and (4) Personalized approaches based on individual ncRNA dysregulation patterns [47] [3] [44]. As these technologies mature, they hold significant potential to overcome current limitations in HCC treatment and improve outcomes for patients with this challenging malignancy.
The successful translation of ncRNA-targeted therapies will require continued optimization of chemical modifications, delivery vehicles, and target selection strategies. Furthermore, understanding the complex interactions within the HCC tumor microenvironment will be essential for developing therapies that can effectively reprogram the immunosuppressive landscape and overcome resistance mechanisms. With rapid advancements in RNA biology and delivery technologies, ncRNA-targeted therapies are poised to become increasingly important components of the HCC treatment arsenal.
The dysregulation of non-coding RNAs (ncRNAs), including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs), has been identified as a pivotal driver in the pathogenesis of hepatocellular carcinoma (HCC) [15]. These ncRNAs function as crucial epigenetic modifiers within the tumor microenvironment (TME), modulating tumor cell proliferation, invasion, migration, and immune cell infiltration [15] [51]. The therapeutic targeting of these dysregulated ncRNA networks holds immense promise for revolutionizing HCC treatment. However, the clinical translation of nucleic acid therapeutics—including siRNA, miRNA mimics/inhibitors, and CRISPR-based gene editors—is critically dependent on advanced delivery platforms that can overcome fundamental challenges such as nuclease degradation, poor cellular uptake, and off-target effects [52] [53]. This technical guide provides a comprehensive analysis of the leading liver-targeted delivery platforms, with a specific focus on their application in modulating the ncRNA landscape within the HCC TME.
The liver's unique vascular architecture, characterized by fenestrated sinusoidal endothelial cells, facilitates the passive accumulation of certain nanocarriers, while specific receptors highly expressed on hepatocytes enable active targeting strategies [54]. This combination of passive and active targeting mechanisms has positioned the liver at the forefront of nucleic acid therapeutics development. The following sections detail the core platforms—Lipid Nanoparticles (LNPs), GalNAc conjugates, and other non-viral vectors—that are expanding the possibilities for treating HCC by precisely intervening in ncRNA dysregulation.
Platform Fundamentals: Mechanisms, Components, and Workflows
Lipid Nanoparticles (LNPs)
Mechanism of Action: LNPs are the most clinically established non-viral delivery vehicles for RNA therapeutics. They are complex, multi-component systems that function by fully encapsulating their nucleic acid payload (e.g., siRNA, mRNA) within a lipid bilayer, protecting it from enzymatic degradation in the bloodstream [53]. Upon intravenous administration and passive accumulation in the liver, LNPs are internalized by hepatocytes via endocytosis. The key to their efficacy lies in the endosomal escape mechanism; ionizable lipids within the LNP structure become positively charged in the acidic environment of the endosome, facilitating destabilization and fusion with the endosomal membrane, thereby releasing the genetic payload into the cytoplasm [52] [53].
Standard Composition: A typical LNP formulation includes four key components, whose relative ratios can be optimized for specific applications [53]:
- Ionizable Cationic Lipid: Critical for endosomal escape (e.g., DLin-MC3-DMA).
- Phospholipid: Supports the lipid bilayer structure (e.g., DSPC).
- Cholesterol: Enhances membrane stability and integrity.
- PEGylated Lipid: Shields the particle surface, reduces opsonization, and modulates pharmacokinetics.
Figure 1: LNP Intracellular Delivery Mechanism. The process from systemic administration to cytoplasmic release of the therapeutic nucleic acid payload.
Experimental Workflow for LNP Development and Testing:
- Microfluidic Formulation: LNPs are typically assembled using microfluidic devices that mix an aqueous phase containing the nucleic acid payload with an ethanol phase containing the lipid mixture in a precise, rapid manner to form homogeneous particles.
- Physicochemical Characterization:
- Size and Polydispersity Index (PDI): Measured via Dynamic Light Scattering (DLS). Ideal LNP size for liver delivery is typically 70-120 nm.
- Zeta Potential: Measured via Laser Doppler Velocimetry.
- Encapsulation Efficiency: Quantified using a Ribogreen assay to determine the percentage of RNA successfully encapsulated within the particles.
- In Vitro Functional Testing:
- Cell Viability Assay: (e.g., MTT or CellTiter-Glo) to assess cytotoxicity in human hepatoma cell lines (e.g., HepG2, Huh-7).
- Gene Silencing/Expression Efficiency: Transfection with LNP-loaded siRNA or mRNA, followed by qPCR or Western Blot to measure target knockdown or protein expression.
- In Vivo Efficacy and Biodistribution:
- Animal Models: Typically performed in orthotopic or xenograft mouse models of HCC.
- Biodistribution: LNPs can be loaded with fluorescent dyes (e.g., DiR) or the RNA payload can be labeled to track organ accumulation using IVIS imaging. Quantitative PCR can also measure target engagement in excised tissues.
- Efficacy Endpoints: Tumor volume measurement (via caliper or imaging), analysis of ncRNA target levels in tumor tissue, and immunohistochemistry for proliferation (Ki-67) and apoptosis (TUNEL) markers.
GalNAc Conjugates
Mechanism of Action: N-Acetylgalactosamine (GalNAc) conjugates represent a paradigm of receptor-mediated, active targeting. This platform exploits the high-affinity interaction between GalNAc ligands and the asialoglycoprotein receptor (ASGPR), which is abundantly and almost exclusively expressed on the surface of hepatocytes [53]. The typical conjugate structure consists of a synthetic triantennary GalNAc ligand linked directly to the RNA therapeutic (e.g., siRNA) via a stable bridge. Upon subcutaneous administration, the conjugate enters the bloodstream, travels to the liver, and is rapidly internalized upon binding to ASGPR. The complex is trafficked to the endo-lysosomal system, where the acidic environment facilitates release of the RNA payload into the cytoplasm [52] [55].
Key Advantages: The primary strengths of the GalNAc platform are its exceptional simplicity, specificity, and proven clinical success. Its small size and synthetic nature avoid the toxicity and immunogenicity concerns associated with larger nanoparticles. The high specificity for hepatocytes minimizes off-target effects. This has led to multiple FDA-approved therapies, such as Givlaari and Oxlumo [55].
Standard Experimental Protocol for GalNAc-siRNA Conjugate Evaluation:
- Conjugate Synthesis: GalNAc-siRNA conjugates are synthesized via solid-phase phosphoramidite chemistry, incorporating the GalNAc ligand at the 3'-end of the sense strand during oligonucleotide synthesis.
- In Vitro Binding and Uptake:
- Surface Plasmon Resonance (SPR): Used to quantify binding affinity (KD) of the conjugate to recombinant ASGPR.
- Cellular Uptake Studies: Performed in ASGPR-expressing hepatoma cells using fluorescently labeled conjugates, with flow cytometry or confocal microscopy for analysis. Competition assays with free GalNAc confirm receptor-specificity.
- In Vivo Pharmacodynamics/Pharmacokinetics (PD/PK):
- Dosing: Conjugates are administered subcutaneously to mice with established HCC tumors.
- Target Engagement: qRT-PCR from liver and tumor homogenates is used to measure mRNA knockdown of the target gene.
- Biodistribution: Primarily assessed by quantifying siRNA levels in tissues (liver, tumor, kidney, etc.) using LC-MS/MS or hybridization ELISA, confirming preferential hepatic accumulation.
Emerging Non-Viral Vectors
While LNPs and GalNAc conjugates dominate the landscape, several emerging platforms offer unique capabilities for liver and HCC targeting.
Engineered Virus-Like Particles (eVLPs): eVLPs are non-infectious particles that mimic the structure of viruses but lack viral genetic material. They are engineered to package therapeutic cargo like ribonucleoproteins (RNPs) for CRISPR-based gene editing. Their key advantage for HCC therapy is the potential for cell-specific delivery and high editing efficiency with reduced off-target effects compared to viral vectors. A significant benefit is their inherent ability to be engineered to avoid liver tropism, making them suitable for targeting specific cell populations within the TME [53].
Polymer-Based Nanoparticles: Cationic polymers can condense nucleic acids into stable nanoparticles through electrostatic interactions. A modern approach, as exemplified by companies like Nanite Bio, involves high-throughput screening of large polymer libraries to discover novel, biodegradable polymers tailored for specific delivery applications. These systems can deliver both RNA and DNA, enabling more complex therapeutic strategies like gene insertion. They also offer improved stability, often at room temperature, circumventing cold-chain requirements [53].
Extracellular Vesicles (EVs): EVs are natural, lipid-bound vesicles secreted by cells, functioning as intercellular communication vehicles by transferring proteins, lipids, and nucleic acids. For therapeutic use, EVs can be isolated from stem cells and engineered to carry RNA payloads. They possess inherent homing capabilities to injured tissues and can be modified for tissue-specific targeting. In the context of HCC, their natural composition makes them low in immunogenicity and potentially powerful for delivering immune-modulating ncRNAs to specific cell types in the TME [53].
Quantitative Platform Comparison
The following tables provide a consolidated summary of the key characteristics, advantages, and challenges of the major delivery platforms, offering a direct comparison for researchers.
Table 1: Core Characteristics and Applications of Liver-Targeted Delivery Platforms
| Platform | Mechanism | Typical Payload | Administration Route | Key Clinical/Preclinical Example |
|---|---|---|---|---|
| LNP | Passive/active targeting, endosomal escape | siRNA, mRNA, CRISPR-Cas | Intravenous | Patisiran (Onpattro) for hATTR amyloidosis [55] |
| GalNAc Conjugate | ASGPR-mediated endocytosis | siRNA, miRNA antagonists/mimics | Subcutaneous | Givosiran (Givlaari) for Acute Hepatic Porphyria [55] |
| Polymeric NP | Electrostatic complexation, endosomal escape | DNA, RNA, CRISPR-Cas | Intravenous | High-throughput discovered polymers for gene insertion [53] |
| Engineered VLPs | Capsid-mediated cell entry | RNPs (for gene editing) | Intravenous | Tissue-specific editing with reduced off-target effects [53] |
| Extracellular Vesicles | Natural cell targeting and fusion | Proteins, ncRNAs, mRNAs | Intravenous | Stem cell-derived EVs for immunomodulation [53] |
Table 2: Performance and Practical Considerations for Platform Selection
| Platform | Targeting Specificity | Payload Capacity | Manufacturing Complexity | Key Advantages | Primary Challenges |
|---|---|---|---|---|---|
| LNP | Moderate (Liver-tropic) | High | Moderate | Proven clinical success; versatile payload capacity | Liver toxicity concerns; limited redosability [53] |
| GalNAc Conjugate | High (Hepatocyte-specific) | Low (Single siRNA) | Low | Simple, stable, high specificity; multiple FDA approvals | Limited to hepatocytes; restricted payload size [53] [55] |
| Polymeric NP | Tunable | High | Moderate | Room-temperature stability; delivers DNA & RNA | Less clinical precedent; potential immunogenicity [53] |
| Engineered VLPs | High (Engineerable) | Moderate | High | High editing efficiency; modular design | Cell-based manufacturing is complex [53] |
| Extracellular Vesicles | Innate/Engineerable | Moderate | High | Low immunogenicity; natural tropism | Scalable GMP manufacturing is challenging [53] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully developing and testing liver-targeted delivery systems requires a suite of specialized reagents and tools. The following table outlines core materials essential for research in this field.
Table 3: Essential Research Reagents and Materials for Liver-Targeted Delivery Research
| Reagent / Material | Function / Application | Example Product / Model |
|---|---|---|
| Ionizable Cationic Lipids | Core functional component of LNPs for RNA complexation and endosomal escape. | DLin-MC3-DMA, SM-102 |
| GalNAc Ligand (Triantennary) | Synthesized molecule for conjugation to siRNA, enabling ASGPR-mediated uptake. | Commercially available phosphoramidites for solid-phase synthesis. |
| Hepatocyte Cell Lines | In vitro models for testing uptake, toxicity, and efficacy in human liver cells. | HepG2, Huh-7, Hep3B, Primary Human Hepatocytes |
| ASGPR-Expressing Cells | Specific model for validating GalNAc-conjugate binding and internalization. | HepG2 cells, recombinant cell lines overexpressing ASGPR. |
| HCC Mouse Models | In vivo models for evaluating biodistribution, efficacy, and safety. | Diethylnitrosamine (DEN)-induced models, orthotopic/xenograft models (e.g., McA-RH7777). |
| Dynamic Light Scattering (DLS) Instrument | For characterizing the hydrodynamic diameter (size), and polydispersity (PDI) of nanoparticles. | Malvern Zetasizer Nano series |
| Ribogreen Assay Kit | Fluorescent quantification of RNA encapsulation efficiency within nanoparticles. | Quant-iT RiboGreen RNA Assay Kit (Thermo Fisher) |
| Microfluidic Mixer | For reproducible, scalable preparation of uniform LNPs and polymeric NPs. | NanoAssemblr (Precision NanoSystems) |
| 2-Propargyl-1-methyl-piperidine | 2-Propargyl-1-methyl-piperidine|C9H15N|Research Chemical | 2-Propargyl-1-methyl-piperidine (C9H15N) is a piperidine building block for pharmaceutical research. This product is For Research Use Only (RUO). Not for human use. |
| 4-(3-Aminopyridin-2-yl)benzoic acid | 4-(3-Aminopyridin-2-yl)benzoic Acid|CAS 886505-75-5 | 4-(3-Aminopyridin-2-yl)benzoic acid is a high-purity (≥98%) chemical building block for anticancer research. For Research Use Only. Not for human or veterinary use. |
The advancement of LNPs, GalNAc conjugates, and emerging non-viral vectors has created a powerful toolbox for translating ncRNA biology into tangible therapies for HCC. The future of this field lies in the strategic selection and continued optimization of these platforms. Key directions will include:
- Combination Therapies: Using these platforms to deliver ncRNAs that sensitize tumors to established chemotherapies or immunotherapies [15] [51].
- Targeting the TME: Developing vectors that can specifically deliver payloads to non-parenchymal cells within the TME, such as tumor-associated macrophages or cancer-associated fibroblasts, to disrupt the pro-tumorigenic niche [15] [54].
- Personalized Approaches: Leveraging the modular nature of these platforms to create therapies tailored to the unique ncRNA signature of an individual patient's tumor [52].
As the understanding of ncRNA dysregulation in HCC deepens, and as delivery technologies become increasingly sophisticated and targeted, the potential to develop transformative, mechanism-driven therapeutics that directly address the root of HCC pathogenesis is immense.
The complex immunosuppressive tumor microenvironment (TME) of hepatocellular carcinoma (HCC) significantly limits the efficacy of immune checkpoint inhibitors (ICIs), with response rates remaining below 20% as monotherapies. Non-coding RNAs (ncRNAs)—particularly long non-coding RNAs (lncRNAs) and circular RNAs (circRNAs)—have emerged as pivotal regulators of immune evasion mechanisms and promising therapeutic targets. This whitepaper examines the mechanistic basis, current experimental approaches, and clinical translation strategies for integrating ncRNA-targeting therapeutics with established immunotherapies. We detail how ncRNAs regulate key immunotherapy resistance pathways through immune checkpoint modulation, T-cell exhaustion, and myeloid cell reprogramming. Furthermore, we present innovative platforms employing artificial circRNAs as both miRNA sponges and immune modulator expression vehicles, alongside lncRNA-based prognostic signatures that may guide patient stratification. The integration of ncRNA therapeutics with existing immunomodulatory regimens represents a promising frontier for overcoming resistance mechanisms and improving outcomes in HCC.
Hepatocellular carcinoma exhibits remarkable heterogeneity and develops within a chronically inflamed, immunosuppressive liver environment. The HCC TME is characterized by dysfunctional cytotoxic CD8⺠T cells, enriched immunosuppressive populations (Tregs, MDSCs, M2-like TAMs), and upregulation of multiple immune checkpoints including PD-1, CTLA-4, LAG-3, and TIM-3 [56]. This immunologically "cold" phenotype limits the effectiveness of ICIs, which have revolutionized oncology but benefit only a minority of HCC patients [57].
Non-coding RNAs, once considered transcriptional "noise," are now recognized as master regulators of gene expression and cellular function. In HCC, dysregulated ncRNA networks contribute significantly to immune evasion and therapy resistance through several interconnected mechanisms:
- LncRNAs (>200 nucleotides) regulate gene expression via chromatin modification, transcriptional interference, miRNA sponging, and protein scaffolding [33].
- CircRNAs (covalently closed loops) function as efficient miRNA sponges, protein scaffolds, and occasionally translation templates, exhibiting enhanced stability compared to linear RNAs [58] [59].
- miRNAs (~22 nucleotides) post-transcriptionally regulate mRNA stability and translation, often targeting multiple components of immune signaling pathways [60].
The integration of ncRNA-targeting approaches with immunotherapies represents a promising strategy to reprogram the immunosuppressive HCC TME and overcome primary and acquired resistance mechanisms. This review examines the current state of this rapidly evolving field, with emphasis on mechanistic insights, experimental methodologies, and translational applications.
Core Mechanisms of ncRNA-Mediated Immunotherapy Resistance
Direct Immune Checkpoint Regulation
ncRNAs extensively regulate the expression of immune checkpoint molecules, directly influencing T-cell activation and anti-tumor immunity:
- PD-1/PD-L1 Axis: Multiple lncRNAs and circRNAs modulate this critical pathway. The lncRNA IFITM4P upregulates PD-L1 through dual mechanisms: cytoplasmic activation of NF-κB and nuclear recruitment of KDM5A to inhibit PTEN, thereby activating PI3K/AKT signaling [61]. Similarly, MALAT1 promotes PD-L1 expression by sponging miR-200 family members and potentially through EZH2 interaction and m6A-mediated stabilization [61]. CircRNAs also participate; CircKRT1 functions as a sponge for miR-495-3p, which normally downregulates PD-L1, thereby enhancing checkpoint expression [61].
- Novel Checkpoints: Beyond PD-1/PD-L1, ncRNAs regulate emerging checkpoints like TIM-3. The lncRNA NEAT1, significantly upregulated in peripheral blood mononuclear cells of HCC patients, promotes CD8⺠T cell apoptosis and inhibits their cytolytic activity by regulating the miR-155/Tim-3 pathway [3]. Another lncRNA, Lnc-Tim3, binds directly to Tim-3 and modulates its interaction with Bat3, thereby influencing downstream Lck/NFAT1/AP-1 signaling [3].
T Cell Dysfunction and Exhaustion
Continuous antigen exposure in the TME drives CD8⺠T cells toward an exhausted state (CD8Tex), characterized by reduced effector function and persistent expression of inhibitory receptors. ncRNAs are critically involved in this process. Single-cell RNA sequencing analyses have identified specific lncRNA signatures correlated with CD8Tex cells in HCC [62]. For instance, the lncRNA AL158166.1 demonstrates the strongest correlation with CD8⺠T cell exhaustion and poor prognosis, highlighting its potential as both a biomarker and therapeutic target [62]. Targeting these exhaustion-associated lncRNAs may rejuvenate anti-tumor T cell responses and enhance ICI efficacy.
Remodeling the Immunosuppressive Microenvironment
ncRNAs shape the broader immunosuppressive landscape by influencing the function of myeloid and stromal cells:
- Myeloid-Derived Suppressor Cells (MDSCs): MDSCs inhibit T cell activation by depleting L-arginine (via iNOS and ARG1), producing ROS/RNS, and expressing checkpoint ligands like PD-L1 and galectin-9 [56]. Specific lncRNAs regulate MDSC recruitment, expansion, and suppressive capacity within the HCC TME, though their identities are still being fully elucidated [3].
- Tumor-Associated Macrophages (TAMs): TAMs, particularly the M2-like phenotype, support tumor progression through angiogenesis, tissue remodeling, and immune suppression via IL-10, TGF-β, VEGF, and PD-L1 expression [56]. ncRNAs can influence macrophage polarization; for example, certain lncRNAs promote the M2 phenotype, further reinforcing an immunosuppressive milieu [3].
- Regulatory T Cells (Tregs): Tregs suppress effector T cells via cytokines (IL-10, TGF-β, IL-35), CTLA-4-mediated impairment of antigen presentation, IL-2 consumption (CD25), and generation of immunosuppressive adenosine (CD39/CD73) [56]. The circRNA hsacirc0069313 contributes to this axis by sponging miR-325-3p, leading to increased Foxp3 expression, a master regulator of Treg development and function [61].
Table 1: Key ncRNAs Regulating Immunotherapy Resistance in HCC
| ncRNA | Type | Molecular Mechanism | Functional Outcome in TME |
|---|---|---|---|
| NEAT1 [3] | lncRNA | Sponges miR-155, upregulating Tim-3 | Promotes CD8⺠T cell apoptosis, inhibits cytotoxicity |
| IFITM4P [61] | lncRNA | Activates NF-κB & PI3K/AKT via PTEN inhibition | Upregulates PD-L1 expression on tumor cells |
| MALAT1 [61] | lncRNA | Sponges miR-200 family; interacts with EZH2 | Upregulates PD-L1, promotes immune evasion |
| AL158166.1 [62] | lncRNA | Strongly correlated with CD8Tex gene signature | Drives T cell exhaustion, poor prognosis |
| CircKRT1 [61] | circRNA | Sponges miR-495-3p (a PD-L1 suppressor) | Upregulates PD-L1 expression |
| hsacirc0069313 [61] | circRNA | Sponges miR-325-3p, increasing Foxp3 | Promotes Treg differentiation and function |
The following diagram illustrates the multifaceted roles of ncRNAs in shaping an immunosuppressive tumor microenvironment in HCC.
Experimental Approaches for ncRNA Therapeutic Development
Artificial Circular RNA Engineering
CircRNAs offer unique advantages as therapeutic platforms due to their inherent stability from closed-loop structures, resisting exonuclease degradation. A pioneering study engineered a multifunctional artificial circRNA (circSC25-αPD1) to simultaneously target the oncogenic miRNA miR-25 and express a single-chain variable fragment (scFv) against PD-1 [58] [59].
Synthesis and Validation Workflow:
- Vector Construction: The circRNA vector was constructed using a plasmid containing self-splicing introns (e.g., permuted group I introns) to facilitate back-splicing and circularization. Key components included:
- miRNA Sponge Sites: Tandem repeats of complementary sequences to miR-25.
- Protein Expression Cassette: An internal ribosome entry site (IRES), notably optimized IRES from Coxsackievirus B3 (IRES-CVB3), followed by the coding sequence for anti-PD-1 scFv [59].
- In Vitro Transcription and Circularization: Linear RNA was transcribed from the plasmid, and a splicing reaction was performed to induce circularization. Successful circularization was confirmed via agarose gel electrophoresis (showing altered mobility) and Sanger sequencing across the junction site [59].
- Functional Validation:
- miRNA Sponging: qPCR demonstrated significant reduction in both miR-25-3p and miR-25-5p levels in HCC cells (Hepa1-6) transfected with circSC25-αPD1 [59].
- Protein Expression and Secretion: Western blotting confirmed efficient expression and extracellular secretion of the α-PD-1 scFv from transfected HEK-293T and Hepa1-6 cells [59].
- scFv Binding Efficacy: Flow cytometry analysis showed that the expressed scFv effectively bound to PD-1 on the surface of activated primary mouse T cells [59].
Table 2: Key Research Reagents for Engineering circRNA Therapeutics
| Reagent / Method | Function / Purpose | Example / Note |
|---|---|---|
| Self-Splicing Introns | Catalyze RNA circularization | Permuted group I introns (e.g., from T4 phage) [59] |
| Optimized IRES | Drives cap-independent translation | IRES-CVB3 (Coxsackievirus B3) for high protein yield [59] |
| miRNA Sponge Sequence | Binds and inhibits target miRNA | Tandem repeats fully complementary to mature miRNA [59] |
| scFv Coding Sequence | Encodes therapeutic antibody fragment | Derived from variable regions of anti-PD-1 mAb heavy/light chains [59] |
| In Vitro Transcription System | Produces linear RNA precursor | T7 or SP6 RNA polymerase-based kits [59] |
LncRNA Targeting and Prognostic Modeling
Beyond circRNAs, lncRNAs are investigated as targets and biomarkers. A common approach involves identifying lncRNAs correlated with specific immune cell states, like T cell exhaustion, and building prognostic models.
Protocol for Developing a CD8Tex-Associated LncRNA Signature [62]:
- Single-Cell Data Analysis:
- Dataset: Analyze single-cell RNA-seq data (e.g., GSE140228) to identify CD8⺠T cell exhaustion clusters.
- Differential Expression: Use Wilcoxon test to identify genes significantly upregulated in CD8Tex clusters compared to other CD8⺠T cells (log₂FC ≥ 1, FDR < 0.05).
- Bulk RNA-seq Correlation:
- Dataset: Utilize bulk transcriptome and clinical data from cohorts like TCGA-LIHC.
- LncRNA Identification: Perform Pearson correlation analysis to identify lncRNAs whose expression correlates with the CD8Tex gene signature (correlation coefficient > 0.4 and p < 0.001).
- Prognostic Model Construction:
- Univariate Cox Regression: Identify CD8Tex-related lncRNAs significantly associated with overall survival.
- LASSO Regression: Apply Least Absolute Shrinkage and Selection Operator (LASSO) regression to prevent overfitting and select the most robust lncRNAs for the model.
- Risk Score Calculation: Generate a multivariate prognostic signature. For example:
Risk Score = Σ(Expression of LncRNA_i × Coefficient_i).
- Model Validation:
- Stratification: Divide patients into high-risk and low-risk groups based on the median risk score.
- Survival Analysis: Use Kaplan-Meier curves and log-rank tests to evaluate survival differences between groups.
- ROC Analysis: Assess the model's predictive accuracy using time-dependent receiver operating characteristic (ROC) curves.
This workflow identified the lncRNA AL158166.1 as a key factor correlated with T cell exhaustion and poor prognosis, nominating it for further functional validation and as a potential therapeutic target [62].
The following diagram summarizes the integrated experimental workflow from discovery to therapeutic development.
Clinical Translation and Biomarker Development
Circulating ncRNAs as Predictive Biomarkers
The low invasiveness of liquid biopsies makes circulating ncRNAs attractive for biomarker development. A post-hoc analysis of the phase II T1219 trial in advanced biliary tract cancer identified a three-miRNA signature (hsa-miR-16-5p, hsa-miR-93-5p, hsa-miR-126-3p) predictive of response to chemoimmunotherapy [60]. Patients with high baseline levels of these miRNAs had significantly longer progression-free survival (HR=0.44 for miR-16-5p) and overall survival (HR=0.34 for miR-16-5p) [60]. This underscores the potential of circulating ncRNA signatures to guide patient selection for immunotherapy-based regimens, a approach directly applicable to HCC.
LncRNA Signatures for Prognostic Stratification
Multivariate Cox regression analyses have identified numerous individual lncRNAs with independent prognostic value in HCC, as shown in the table below. Combining these into multi-lncRNA signatures can improve prognostic power and help stratify patients for more intensive or novel combination therapies.
Table 3: Selected LncRNAs with Independent Prognostic Significance in HCC
| LncRNA | Expression in Tumor | Hazard Ratio (HR) for OS | 95% CI | P-value | Clinical Implication |
|---|---|---|---|---|---|
| LINC00152 [63] | High | 2.524 | 1.661–4.015 | 0.001 | Shorter OS, potential oncogene |
| LINC01146 [63] | High | 0.38 | 0.16–0.92 | 0.033 | Longer OS, potential tumor suppressor |
| HOXC13-AS [63] | High | 2.894 | 1.183–4.223 | 0.015 | Shorter OS & RFS |
| LASP1-AS [63] | Low | 3.539 (Val. cohort) | 2.698–6.030 | <0.0001 | Shorter OS & RFS, tumor suppressor |
| ELF3-AS1 [63] | High | 1.667 | 1.127–2.468 | 0.011 | Shorter OS |
| ELMO1-AS1 [63] | High | 0.430 (Val. cohort) | 0.225–0.824 | 0.011 | Longer OS & RFS, tumor suppressor |
Key: OS: Overall Survival; RFS: Recurrence-Free Survival; CI: Confidence Interval; Val.: Validation.
Integrating ncRNA therapeutics with existing immunotherapies presents a multifaceted strategy to overcome resistance in HCC. Targeting oncogenic lncRNAs (e.g., NEAT1, MALAT1) or restoring tumor-suppressive ones, alongside using engineered circRNAs as multi-functional platforms, holds immense potential to reprogram the immunosuppressive TME and enhance ICI efficacy. The successful application of artificial circRNAs functioning as both miRNA sponges and immune modulator expression vectors in preclinical models marks a significant technical advance [58] [59].
Future progress depends on addressing key challenges: developing efficient and specific in vivo delivery systems (e.g., lipid nanoparticles, engineered viral vectors) for ncRNA therapeutics; deepening our understanding of ncRNA networks and their complex interactions within the HCC TME; and validating robust ncRNA biomarkers in prospective clinical trials to enable patient stratification. As these scientific and translational hurdles are cleared, ncRNA-based combination therapies are poised to become a powerful component of the next generation of precision immuno-oncology for HCC.
Navigating the Hurdles: Challenges and Optimization in ncRNA Therapeutic Development
The dysregulation of non-coding RNAs (ncRNAs) within the hepatocellular carcinoma (HCC) tumor microenvironment (TME) presents a promising frontier for therapeutic intervention. Long non-coding RNAs (lncRNAs), circular RNAs (circRNAs), and microRNAs (miRNAs) have been identified as critical regulators of tumorigenesis, immune evasion, and therapy resistance in HCC [6] [3] [14]. However, the clinical translation of therapeutics targeting these ncRNAs faces three fundamental delivery barriers: molecular stability, target specificity, and efficient cellular uptake. Native RNA molecules are highly susceptible to degradation by nucleases, exhibit poor intracellular uptake, and can trigger unintended immune responses [64] [65]. This technical guide examines current strategies to overcome these barriers, with a specific focus on applications within the complex HCC TME.
The HCC TME is characterized by a dense extracellular matrix, heterogeneous vasculature, and significant immune cell infiltration, creating substantial physical and biological barriers to effective drug delivery [3] [66]. Successfully navigating this environment requires sophisticated delivery solutions that protect therapeutic payloads, facilitate targeted accumulation in tumor tissue, and enable efficient intracellular delivery to both cancer and stromal cells. Advances in nanoparticle design, chemical modification, and biomimetic systems are providing new avenues to address these challenges, bringing ncRNA-based therapies closer to clinical reality for HCC patients.
Core Barrier 1: Molecular Stability of RNA Therapeutics
The inherent instability of RNA molecules constitutes the primary barrier to their therapeutic application. Unmodified RNA has a half-life of only a few minutes in the bloodstream due to rapid degradation by circulating nucleases [65]. This instability is particularly problematic in the context of HCC, where the therapeutic agent must remain intact long enough to traverse the circulation and reach the tumor site.
Chemical Modification Strategies
Chemical modifications to the RNA backbone and sugar moiety have proven highly effective in enhancing nuclease resistance and extending circulatory half-life. The most widely employed modifications are summarized in the table below.
Table 1: Key Chemical Modifications for Enhancing RNA Stability
| Modification Type | Chemical Structure | Primary Function | Example Applications |
|---|---|---|---|
| Phosphorothioate (PS) Backbone | Replacement of non-bridging oxygen with sulfur in phosphate backbone | Increased nuclease resistance, improved protein binding for tissue distribution | siRNA, ASO therapeutics |
| 2'-Sugar Modifications (-O-Me, -O-Et, -F) | Substitution of 2'-hydroxyl group | Dramatically reduced ribonuclease recognition and cleavage | siRNAs, miRNA mimetics/inhibitors |
| Locked Nucleic Acid (LNA) | 2'-O, 4'-C methylene bridge in ribose | Enhanced thermal stability, improved binding affinity, superior specificity | ASO gapmers, miRNA inhibitors |
| GalNAc Conjugation | Covalent linkage of triantennary N-acetylgalactosamine | Hepatocyte-specific targeting via asialoglycoprotein receptor (ASGPR) mediation | siRNA therapeutics for liver diseases |
These modifications function primarily by sterically hindering nuclease access to the RNA backbone and altering the electronic properties of the phosphate group, making it less susceptible to enzymatic cleavage [65]. When strategically incorporated, these modifications can increase the half-life of RNA therapeutics from minutes to several hours without significantly compromising biological activity.
Stability Considerations in the HCC Microenvironment
The unique conditions of the HCC TME present additional stability challenges. The presence of elevated ribonuclease activity in tumor tissue can degrade RNA molecules even after successful extravasation [65]. Furthermore, the hypoxic and acidic conditions characteristic of solid tumors can promote RNA degradation. Chemical modification strategies must therefore be optimized to withstand not only circulatory nucleases but also the specific enzymatic and chemical environment of the target tissue. For HCC applications, GalNAc conjugation represents a particularly valuable approach, leveraging the high expression of the asialoglycoprotein receptor on hepatocytes to facilitate liver-specific delivery while simultaneously enhancing molecular stability through carbohydrate conjugation [65].
Core Barrier 2: Delivery Specificity and Targeting
Achieving sufficient target tissue accumulation while minimizing off-target effects represents the second major challenge in ncRNA therapeutics for HCC. Passive targeting strategies exploit the enhanced permeability and retention (EPR) effect, wherein nanocarriers preferentially accumulate in tumor tissue due to leaky vasculature and impaired lymphatic drainage [66]. However, the EPR effect exhibits significant heterogeneity in HCC, necessitating more active targeting approaches.
Nanocarrier Systems for Targeted Delivery
Advanced nanocarrier systems have been engineered to provide both passive and active targeting capabilities. Lipid-based nanoparticles (LNPs), particularly those optimized for RNA delivery, represent the most clinically advanced platform [64] [65]. These systems protect RNA payloads from degradation, enhance circulation time, and can be modified with targeting ligands to improve HCC specificity. Other promising nanocarrier platforms include poly(lactic-co-glycolic acid) (PLGA) nanoparticles, which offer tunable release kinetics and excellent biocompatibility [66], and biomimetic systems utilizing cell membranes (e.g., platelet membranes) to evade immune clearance and enhance tumor homing [66].
Table 2: Nanocarrier Platforms for RNA Delivery to HCC TME
| Nanocarrier Type | Key Components | Targeting Mechanism | Advantages for HCC |
|---|---|---|---|
| Lipid Nanoparticles (LNPs) | Ionizable lipids, phospholipids, cholesterol, PEG-lipids | Passive (EPR); Active (with ligand conjugation) | Clinical validation, high RNA loading capacity, scalable production |
| Polymeric Nanoparticles | PLGA, chitosan, polyethyleneimine (PEI) | Passive (EPR); Surface-functionalization for active targeting | Tunable degradation rates, sustained release profiles |
| Biomimetic Systems | Platelet membranes, exosomes, lipoprotein mimics | Innate tropism of source cell/membrane | Immune evasion, natural tissue homing capabilities |
| Hybrid Systems | Iron oxide-PLGA composites [66] | Multimodal (magnetic + biological targeting) | Theranostic potential, enhanced targeting precision |
Microenvironment-Responsive Delivery Strategies
The distinct pathophysiological features of the HCC TME can be leveraged for targeted delivery. Stimuli-responsive nanocarriers designed to react to tumor-specific conditions such as acidic pH, elevated redox potential (glutathione), or overexpressed enzymes (matrix metalloproteinases) enable precise payload release within the tumor compartment [66]. For example, pH-sensitive LNPs undergo structural changes in the acidic HCC microenvironment, promoting RNA release specifically at the target site. Similarly, redox-sensitive nanoparticles utilizing disulfide bonds remain stable in circulation but degrade rapidly in the high intracellular glutathione concentrations of HCC cells, enabling intracellular payload release [66].
Core Barrier 3: Cellular Uptake and Intracellular Trafficking
The final delivery barrier involves crossing the cell membrane and navigating intracellular trafficking pathways to reach the target subcellular compartment. This process is particularly challenging for large, negatively charged RNA molecules.
Mechanisms of Cellular Internalization
The primary pathways for nanocarrier internalization in the HCC TME include clathrin-mediated endocytosis, caveolin-mediated endocytosis, and macropinocytosis [65] [67]. The specific pathway utilized significantly impacts subsequent intracellular trafficking and therapeutic efficacy. Recent research has identified specific membrane proteins that facilitate dsRNA uptake, including scavenger receptors (SRA, SRC) and lipoprotein receptors (LPR, LRP1-3), which form receptor complexes that mediate cellular internalization [67]. Understanding these natural RNA uptake mechanisms provides opportunities for biomimetic strategy design.
Endosomal Escape and Intracellular Fate
Following endocytosis, the majority of RNA therapeutics become trapped in endosomal compartments destined for lysosomal degradation. Facilitating endosomal escape represents perhaps the most critical bottleneck in RNA delivery. Several strategies have been developed to address this challenge:
- Ionizable LNPs: These lipids become positively charged in the acidic endosomal environment, interacting with anionic endosomal membranes to disrupt integrity and release payload into the cytoplasm [64] [65].
- Cell-Penetrating Peptides (CPPs): These short peptide sequences enhance cellular uptake and can promote endosomal escape through various mechanisms, including membrane pore formation or the "proton sponge" effect [65].
- V-ATPase Interference: Vacuolar-type H+-ATPase acidifies endosomes; interfering with this process can disrupt endosomal maturation and promote cargo release, as demonstrated in insect models [67].
The diagram below illustrates the complete journey of an RNA therapeutic from systemic administration to intracellular target engagement in an HCC cell, highlighting key barriers and overcoming strategies.
Experimental Protocols for Evaluating Delivery Efficiency
Rigorous assessment of delivery efficiency at each stage is essential for developing effective ncRNA therapeutics. Below are key methodological approaches for evaluating stability, specificity, and cellular uptake.
Stability Assessment Protocols
Serum Stability Assay:
- Procedure: Incubate modified and unmodified RNA in 50-90% fetal bovine serum (FBS) or human serum at 37°C. Aliquot samples at predetermined time points (0, 15, 30 min, 1, 2, 4, 8, 24 h).
- Analysis: Analyze integrity by denaturing urea-PAGE, capillary electrophoresis, or HPLC. Quantify intact RNA using densitometry or peak integration.
- Interpretation: Calculate half-life from degradation kinetics. Effective modifications should extend half-life from <30 min (unmodified) to >4-8 hours [65].
Tumor Homogenate Stability:
- Procedure: Prepare homogenates from fresh HCC tumor specimens or relevant cell lines. Incubate RNA constructs in homogenate and assess integrity as above.
- Significance: Provides more physiologically relevant stability data than serum alone, accounting for tissue-specific nucleases [65].
Cellular Uptake and Intracellular Trafficking Protocols
Flow Cytometry-Based Uptake Quantification:
- Reagent Preparation: Label RNA with fluorescent dyes (e.g., Cy5, FAM) using commercial labeling kits. Purify labeled RNA and incorporate into delivery systems.
- Cell Culture: Use relevant HCC cell lines (e.g., HepG2, Huh-7) cultured under standard conditions. Include primary hepatocytes or patient-derived organoids for more physiological relevance.
- Uptake Measurement: Incubate cells with fluorescent RNA formulations for 2-24 h. Wash extensively with PBS (pH 4.0) to remove surface-bound material. Detach cells, analyze by flow cytometry. Use inhibitors (e.g., chloroquine for endosomal escape) to probe mechanisms [65] [67].
Confocal Microscopy for Intracellular Localization:
- Cell Preparation: Plate cells on glass-bottom dishes. Treat with fluorescent RNA formulations.
- Staining: Counterstain cellular compartments with organelle-specific dyes (Lysotracker for lysosomes, ER-Tracker for endoplasmic reticulum).
- Imaging: Acquire z-stack images at appropriate intervals using confocal microscopy. Perform colocalization analysis with image processing software (e.g., ImageJ) to quantify distribution across compartments [67].
Mechanistic Uptake Studies:
- Inhibitor Screening: Pre-treat cells with pharmacological inhibitors of specific endocytic pathways (e.g., chlorpromazine for clathrin-mediated endocytosis, filipin for caveolae-mediated uptake, EIPA for macropinocytosis).
- Genetic Approaches: Use siRNA knockdown or CRISPR/Cas9 knockout of specific endocytic genes (e.g., SID-1 homologs, scavenger receptors) to confirm involvement in uptake [68] [67].
- Interpretation: Reduced uptake with specific inhibitors indicates pathway involvement, guiding delivery system optimization.
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of RNA delivery strategies requires specialized reagents and tools. The following table summarizes essential materials for studying ncRNA delivery in HCC models.
Table 3: Essential Research Reagents for RNA Delivery Studies
| Reagent Category | Specific Examples | Function/Application | Notes for HCC Research |
|---|---|---|---|
| Chemical Modification Reagents | 2'-F-UTP, 2'-O-Me ATP, LNA phosphoramidites, PS modification reagents | Enhance nuclease resistance, improve pharmacokinetics | Commercially available from Glen Research, Sigma-Aldrich, Thermo Fisher |
| Nanocarrier Components | Ionizable lipids (DLin-MC3-DMA), DSPC, cholesterol, DMG-PEG2000 | Formulate LNPs for RNA encapsulation and delivery | Pre-formulated LNP kits available for screening (e.g., Precision NanoSystems) |
| Targeting Ligands | GalNAc conjugates, RGD peptides, EGFR-targeting affibodies, transferrin | Enable receptor-mediated targeting to HCC cells/tumor vasculature | GalNAc essential for hepatocyte-specific targeting via ASGPR |
| Tracking & Detection | Cy5-labeled RNA, FAM-labeled RNA, Qdot nanocrystals, pHrodo dyes | Visualize and quantify cellular uptake, intracellular trafficking | pH-sensitive dyes valuable for monitoring endosomal escape |
| Endocytic Inhibitors | Chlorpromazine HCl, Filipin III, EIPA, Dynasore | Mechanistic studies of uptake pathways | Use dose-response to ensure specificity without cytotoxicity |
| HCC Model Systems | HepG2, Huh-7, PLC/PRF/5 cells, patient-derived organoids, PDX models | Biologically relevant screening platforms | Primary cells and 3D models better recapitulate TME complexity |
| Analysis Software | siRNA design algorithms (BLOCK-iT, IDT), ImageJ with colocalization plugins, FlowJo | Design, quantification, and data analysis | Critical for objective, reproducible quantification of delivery efficiency |
| 1-benzhydryl-3-(1H-indol-3-yl)urea | 1-benzhydryl-3-(1H-indol-3-yl)urea, CAS:899989-64-1, MF:C22H19N3O, MW:341.414 | Chemical Reagent | Bench Chemicals |
| 7-chloro-2-phenyl-4H-chromen-4-one | 7-chloro-2-phenyl-4H-chromen-4-one, CAS:1148-48-7, MF:C15H9ClO2, MW:256.69 | Chemical Reagent | Bench Chemicals |
Overcoming the triple barriers of stability, specificity, and cellular uptake is essential for realizing the therapeutic potential of ncRNA modulation in HCC. Integrated strategies combining chemical modifications, advanced nanocarriers, and targeting moieties show promising results in enhancing delivery efficiency. The continued development of HCC-specific delivery systems must account for the unique pathophysiological features of the liver TME, including its dense stromal structure, heterogeneous perfusion, and complex cellular composition.
Future advancements will likely emerge from several key areas: (1) Improved biomimetic systems that more effectively navigate biological barriers; (2) Smart nanocarriers responsive to multiple TME cues for precision release; (3) Computational approaches for optimizing RNA sequence design and nanoparticle formulation; and (4) Advanced disease models that better recapitulate human HCC heterogeneity for preclinical testing. As these technologies mature, they will enable more effective targeting of the ncRNA networks that drive HCC progression, ultimately improving therapeutic outcomes for this challenging malignancy.
Hepatocellular carcinoma (HCC) presents a complex therapeutic challenge, largely due to the dynamic and immunosuppressive nature of its tumor microenvironment (TME). Within this niche, non-coding RNAs (ncRNAs), including long non-coding RNAs (lncRNAs) and microRNAs (miRNAs), have emerged as master regulators of tumor initiation, progression, and immune evasion [6] [3]. The strategic targeting of these ncRNAs holds immense promise for a new class of therapeutics. However, the development of these precision tools, particularly those based on CRISPR-Cas systems and RNA-targeting technologies, is critically hampered by the dual challenges of off-target effects and unanticipated toxicity. Off-target effects can lead to genotoxicity, confounding experimental results and raising significant safety concerns for clinical translation [69] [70]. Furthermore, the biological differences between preclinical models and humans mean that toxicities observed in late-stage clinical trials or post-marketing surveillance often cannot be predicted by standard chemical-based assessments alone [71]. This whitepaper provides an in-depth technical guide to strategies that enhance the specificity of therapeutic and research interventions, with a specific focus on applications within the context of ncRNA dysregulation in the HCC TME. It outlines practical methodologies for experimental validation and introduces advanced computational frameworks for safety prediction, providing HCC researchers and drug development professionals with a comprehensive toolkit for developing safer, more effective targeted therapies.
Advanced Strategies for Minimizing Off-Target Effects
The journey toward precise genetic and epigenetic manipulation requires a multi-faceted approach to minimize unintended activity. The following strategies represent the forefront of ensuring specificity.
CRISPR-Cas System Engineering
The core component of CRISPR-based gene editing, the Cas nuclease, can be engineered for heightened fidelity. Moving beyond wild-type Cas9, several engineered variants have been developed.
- Rational Mutagenesis: This approach involves modifying specific amino acids in the Cas protein known to interact with the DNA backbone. By weakening these non-specific interactions, the engineered nuclease becomes more dependent on perfect complementarity for stable binding and cleavage. This strategy led to the creation of high-fidelity variants such as eSpCas9 and Cas9-HF1 [72].
- Random Mutagenesis with Directed Evolution: This method leverages the power of artificial evolution. Random mutations are introduced into the cas9 gene, and the resulting mutant libraries are screened in bacteria or yeast to isolate variants that maintain high on-target activity while exhibiting reduced off-target effects. Prominent examples developed through this approach include HiFi-Cas9, SNIPER-Cas9, and evoCas9 [72].
Table 1: Engineered High-Fidelity Cas9 Variants
| Variant Name | Development Approach | Key Feature |
|---|---|---|
| eSpCas9 | Rational Mutagenesis | Reduced non-specific DNA backbone interactions |
| Cas9-HF1 | Rational Mutagenesis | Mutated residues involved in DNA binding |
| HiFi-Cas9 | Directed Evolution | Optimized balance between on-target efficiency and specificity |
| evoCas9 | Directed Evolution | High-fidelity variant selected from a randomized library |
Alternative CRISPR Modalities
Beyond engineering the nuclease itself, altering the fundamental mechanism of DNA cleavage provides another powerful path to specificity.
- CRISPR Nickases: By mutating one of the two catalytic domains of Cas9 (HNH or RuvC), a nickase (nCas9) is created that can only cut a single DNA strand. To generate a double-strand break, two nickases with two distinct guide RNAs (sgRNAs) must bind opposite strands of the DNA target in close proximity and temporal overlap. This requirement for simultaneous nicking at a single locus dramatically reduces the probability of off-target double-strand breaks, as a single off-target nick is typically repaired without major consequences [72].
- Base and Prime Editing: These innovative technologies move beyond double-strand breaks. They use a catalytically impaired Cas nuclease fused to a deaminase enzyme to directly convert one base to another (Base Editing) or to more complex machinery that allows for precise small insertions or deletions (Prime Editing). Since they do not rely on generating double-strand breaks, they inherently avoid the associated genotoxic risks of traditional CRISPR-Cas nucleases [70].
Operational and Delivery Optimizations
How CRISPR components are delivered and their persistence within the cell are critical operational factors influencing off-target rates.
- Controlled Duration of Activity: The standard method of delivering CRISPR components as DNA plasmids can lead to their persistent expression over several days, significantly increasing the window for off-target activity. Switching to transient delivery formats, such as Cas9-gRNA ribonucleoprotein (RNP) complexes or mRNA, limits the active lifespan of the editing machinery to within 24-48 hours. This is often sufficient for efficient on-target editing while drastically reducing off-target effects [72].
- Improved gRNA Design: The design of the single-guide RNA is paramount. Utilizing modern computational tools that leverage deep learning can predict and minimize gRNA designs with high potential for off-target binding. These tools consider factors beyond simple seed sequence matching, including genomic context and epigenetic status, to select optimal guides [70].
Diagram 1: A multi-faceted strategy map for enhancing CRISPR-Cas specificity, covering nuclease engineering, delivery optimization, and alternative editing modalities.
Experimental Protocols for Off-Target Assessment
Rigorous, unbiased detection of off-target effects is a non-negotiable step in the development of any genome-editing therapeutic. The following methods represent the gold standard in the field.
Genome-Wide Sequencing-Based Methods
- CHANGE-seq: This is a high-throughput, in vitro method that comprehensively profiles the genome-wide activity of a CRISPR-Cas nuclease. It involves incubating the nuclease with fragmented genomic DNA, followed by a specialized library preparation and next-generation sequencing to map all potential cleavage sites. Its in vitro nature allows for scalable and unbiased screening [70].
- GUIDE-seq: An in cellulo method that identifies off-target sites by capturing double-strand breaks via the integration of a short, double-stranded oligodeoxynucleotide tag. The genomic DNA is then sequenced, and the tags allow for the precise mapping of both on-target and off-target cleavage events, providing a genome-wide profile of nuclease activity in a living cellular context [70].
- DISCOVER-Seq: This method leverages the cellular DNA repair machinery itself. It identifies off-target sites by mapping the binding of the MRE11 DNA repair protein to double-strand breaks in cells. As a key component of the repair process, MRE11 provides a natural, endogenous marker for CRISPR-induced breaks, offering a highly specific method for detecting off-target edits in vivo [70].
Table 2: Comparison of Key Off-Target Detection Methods
| Method | Principle | Context | Key Advantage |
|---|---|---|---|
| CHANGE-seq | In vitro cleavage of genomic DNA | In vitro | Unbiased, scalable, no cell culture required |
| GUIDE-seq | Tag integration at DSB sites | In cellulo | Genome-wide, sensitive detection in living cells |
| DISCOVER-Seq | MRE11 binding to DSB sites | In cellulo / In vivo | Uses endogenous repair factors; applicable in vivo |
| CIRCLE-seq | In vitro cleavage of circularized DNA | In vitro | Highly sensitive, can detect low-frequency events |
Protocol for GUIDE-seq
Objective: To identify genome-wide off-target sites of a CRISPR-Cas nuclease in a relevant cell line.
- Cell Transfection: Co-transfect your target cells (e.g., HepG2 for HCC studies) with (a) a plasmid expressing Cas9 (or a high-fidelity variant), (b) a plasmid expressing the sgRNA of interest, and (c) the GUIDE-seq double-stranded oligodeoxynucleotide (dsODN) tag using a high-efficiency method like nucleofection.
- Genomic DNA Extraction: Harvest cells 72 hours post-transfection. Extract high-molecular-weight genomic DNA using a standardized kit, ensuring minimal shearing.
- Library Preparation and Sequencing:
- Fragment the genomic DNA by sonication to an average size of 500 bp.
- Prepare sequencing libraries using adapters compatible with your sequencing platform.
- Perform a dsODN-specific enrichment step, typically via PCR, to selectively amplify fragments containing the integrated tag.
- Sequence the enriched library on a high-throughput sequencer (e.g., Illumina).
- Bioinformatic Analysis:
- Alignment: Map the sequenced reads to the reference human genome (e.g., hg38) using aligners like BWA or Bowtie2.
- Peak Calling: Use the GUIDE-seq computational pipeline (or other specialized tools) to identify genomic loci with a significant enrichment of dsODN-containing reads. These peaks represent potential off-target cleavage sites.
- Validation: The top candidate off-target sites must be validated using an independent method, such as targeted amplicon sequencing, to confirm editing efficiency at each locus.
AI-Driven Prediction of Toxicity and Human-Specific Risks
Overcoming the translational gap between preclinical models and human outcomes requires a new generation of predictive tools.
Incorporating Genotype-Phenotype Differences (GPD)
Traditional toxicity prediction models rely heavily on chemical structure, often failing to capture human-specific biology. A transformative approach involves using machine learning to incorporate Genotype-Phenotype Differences (GPD) between preclinical models (e.g., mice, cell lines) and humans [71]. This framework assesses discrepancies in three key biological contexts of a drug target:
- Gene Essentiality: Differences in whether a gene is critical for survival between models and humans.
- Tissue Specificity: Variations in gene expression profiles across tissues.
- Network Connectivity: Divergence in protein-protein interaction networks and pathway context.
A Random Forest model integrating GPD features with traditional chemical descriptors has been shown to significantly enhance the prediction of human drug toxicity (AUROC = 0.75 vs. baseline 0.50), particularly for neurotoxicity and cardiotoxicity, which are major causes of clinical failure [71].
AI and Deep Learning for Toxicity Endpoints
The expansion of large-scale toxicology databases has enabled the training of sophisticated AI models for early safety screening.
- Data Sources and Modeling: Public databases like Tox21 (12,000 compounds across 12 targets), ClinTox (drugs that failed vs. passed clinical trials), and DILIrank (drug-induced liver injury) serve as critical training data [73]. Models are trained using various algorithms, from Random Forest to advanced Graph Neural Networks (GNNs), which are particularly adept at learning from the inherent graph structure of molecules.
- Application in Virtual Screening: These models are integrated into early drug discovery pipelines to screen vast virtual compound libraries, filtering out those with predicted toxicity before they ever enter the wet lab. This creates a virtuous cycle where experimental results from downstream studies feed back to continuously improve the AI models [73].
Table 3: Selected Publicly Available Datasets for AI-Based Toxicity Prediction
| Dataset | Scope | Application |
|---|---|---|
| Tox21 | 8,249 compounds, 12 nuclear receptor & stress response assays | General toxicity, multi-task learning |
| ClinTox | Compounds that failed clinical trials due to toxicity vs. approved drugs | Clinical trial attrition risk |
| DILIrank | 475 drugs annotated for hepatotoxicity potential | Drug-induced liver injury prediction |
| hERG Central | >300,000 records on hERG channel inhibition | Cardiotoxicity risk prediction |
Targeting the HCC Tumor Microenvironment: Specificity and Toxicity Considerations
The strategies outlined above are paramount when developing therapies that target the intricate network of ncRNAs within the HCC TME.
The Role of lncRNAs in the HCC Immune Microenvironment
LncRNAs are critical regulators of the immunosuppressive HCC TME. For example:
- NEAT1 has been shown to promote CD8+ T cell apoptosis and suppress their cytolytic activity by regulating the miR-155/Tim-3 pathway. Targeting NEAT1 could thus enhance immunotherapy efficacy [3].
- Lnc-Tim3 can bind to the immune checkpoint protein Tim-3, modulating its function and contributing to T cell exhaustion, a key mechanism of immune evasion in HCC [3].
Strategies for Safe and Effective Targeting
Therapeutic intervention in this space must be highly specific to avoid disrupting tumor-suppressive ncRNAs or causing unintended immunotoxicity.
- CRISPR-Based lncRNA Modulation: Using high-fidelity Cas9 variants (e.g., HiFi-Cas9) or, more appropriately, CRISPR interference/activation (CRISPRi/a) systems that employ a catalytically dead Cas9 (dCas9) fused to repressive or activating domains can selectively modulate lncRNA expression without cutting DNA [14]. This is a safer approach for functional studies and potential therapeutics.
- Antisense Oligonucleotides (ASOs) and siRNAs: These nucleic acid-based drugs can be designed to specifically target and degrade oncogenic lncRNAs (e.g., TUG1, LINC01116) [14]. Chemical modifications (e.g., 2'-O-methyl, phosphorothioate backbones) enhance their stability and specificity, reducing the required dose and potential for off-target hybridization.
- Consideration of the Autophagy Axis: The lncRNA-autophagy network is a key signaling hub in HCC [14]. Targeting a specific lncRNA can have cascading effects on autophagic flux, which has a dual role in tumor suppression and promotion. Therefore, a deep understanding of this interaction is necessary to predict and mitigate potential on-target, mechanism-based toxicities.
Table 4: Essential Research Reagents for Specificity and Toxicity Analysis
| Reagent / Resource | Function | Example Use Case |
|---|---|---|
| High-Fidelity Cas9 (e.g., HiFi-Cas9) | Engineered nuclease with reduced off-target activity | Precise knockout of an oncogenic lncRNA in HCC cell lines. |
| GUIDE-seq dsODN Tag | Double-stranded tag for integration at DSBs | Genome-wide identification of off-target sites in an edited cell model. |
| CHANGE-seq Kit | In vitro kit for off-target profiling | Biophysical assessment of gRNA specificity before cellular experiments. |
| Anti-MRE11 Antibody | Immunoprecipitation of DNA repair complexes | Used in the DISCOVER-Seq method to map off-targets via endogenous repair. |
| Tox21 Dataset | Curated database of compound toxicity | Training or benchmarking an AI model for early toxicity prediction. |
| DILIrank Dataset | Annotated drug-induced liver injury data | Validating the hepatotoxicity risk of a novel small-molecule inhibitor. |
Diagram 2: A workflow for developing therapeutic strategies to target oncogenic lncRNAs in the HCC Tumor Microenvironment (TME), highlighting specific molecular tools and their functional impacts.
Drug resistance represents a pivotal challenge in the treatment of hepatocellular carcinoma (HCC), significantly limiting the efficacy of both chemotherapeutic agents and immunotherapies. Within the complex landscape of the HCC tumor microenvironment (TME), non-coding RNAs (ncRNAs) have emerged as critical regulators of resistance mechanisms. This technical review examines how the dysregulation of microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) drives resistance to conventional chemotherapy and emerging immunotherapies. We synthesize current understanding of ncRNA-mediated molecular pathways, provide detailed experimental methodologies for investigating these mechanisms, and visualize key signaling networks. Furthermore, we catalog essential research tools and reagents that enable the study of ncRNA functions, offering a comprehensive resource for researchers and drug development professionals working to overcome therapeutic resistance in HCC.
Hepatocellular carcinoma (HCC) ranks as the sixth most prevalent cancer and the fourth leading cause of cancer-related deaths globally, with its development often associated with chronic liver diseases including hepatitis B and C infections, cirrhosis, and metabolic disorders [74] [75]. Despite advancements in diagnostic technologies and treatment modalities, the prognosis for HCC patients remains poor, largely due to the development of drug resistance which leads to tumor recurrence and progression [75] [76].
The tumor microenvironment (TME) of HCC plays a crucial role in fostering therapeutic resistance through dynamic interactions between tumor cells, immune cells, fibroblasts, and endothelial cells [3] [77]. Within this complex milieu, non-coding RNAs (ncRNAs) have emerged as master regulators of gene expression and cellular function. Accounting for more than 90% of transcribed RNAs, ncRNAs do not encode proteins but exert profound influences on various biological processes, including cell proliferation, apoptosis, angiogenesis, and immune responses [78] [74].
This review focuses on three major classes of ncRNAs—microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—and their specific roles in mediating resistance to chemotherapy and immunotherapy in HCC. Understanding these mechanisms provides critical insights for developing novel strategies to overcome therapeutic resistance and improve patient outcomes.
ncRNA Dysregulation in the HCC Tumor Microenvironment
The HCC TME is characterized by significant heterogeneity and dynamic cellular interactions that promote tumor progression and therapeutic resistance. ncRNAs function as key regulatory molecules within this environment, influencing gene expression through diverse mechanisms including epigenetic modification, transcriptional regulation, and post-transcriptional control [74] [79].
miRNAs are approximately 22-nucleotide RNAs that regulate gene expression by binding to complementary sequences in target mRNAs, leading to translational repression or mRNA degradation [79]. Their biosynthesis involves multiple steps: RNA polymerase II transcribes primary miRNAs (pri-miRNAs) which are processed in the nucleus by the Drosha/DGCR8 complex to form precursor miRNAs (pre-miRNAs). After export to the cytoplasm via XPO5, Dicer cleaves pre-miRNAs into mature miRNAs that are incorporated into the RNA-induced silencing complex (RISC) to regulate target genes [79].
lncRNAs, exceeding 200 nucleotides in length, function through diverse mechanisms including chromatin modification, transcriptional regulation, and serving as molecular scaffolds [3]. They can form complex secondary structures that enable specific interactions with DNA, RNA, and proteins. For instance, SINEUP lncRNAs contain conserved structural modules that enhance translational efficiency, while TERRA lncRNAs interact with LSD1 to maintain telomere stability [79].
circRNAs form covalently closed continuous loops without 5' caps or 3' poly(A) tails, conferring exceptional stability [76]. They primarily function as miRNA sponges but can also regulate transcription and translate functional peptides. Their circular structure makes them resistant to exonuclease-mediated degradation, allowing persistent regulatory functions within the TME [76] [77].
The dysregulation of these ncRNAs in HCC is driven by various factors including genetic alterations, epigenetic modifications, and transcriptional misregulation. Once dysregulated, they profoundly influence multiple aspects of the TME, including immune cell infiltration, cytokine secretion, angiogenesis, and stromal activation, collectively contributing to the development of therapeutic resistance [3] [77] [79].
ncRNAs in Chemotherapy Resistance
Chemotherapy remains a cornerstone of systemic treatment for advanced HCC, but its efficacy is severely limited by both intrinsic and acquired drug resistance. ncRNAs mediate chemoresistance through diverse mechanisms, including regulation of drug efflux transporters, apoptosis pathways, autophagy, and DNA damage repair systems.
miRNAs and Multidrug Resistance
Multidrug resistance (MDR) presents a significant clinical challenge in HCC treatment, often involving enhanced efflux of chemotherapeutic agents through overexpression of ATP-binding cassette (ABC) transporters. miRNAs modulate these pathways through precise regulation of gene expression networks [78] [76].
Table 1: miRNAs Modulating Multidrug Resistance in HCC
| miRNA | Dysregulation | Target/Pathway | Chemotherapeutic Agents | Experimental Models |
|---|---|---|---|---|
| miR-122 | Downregulated | MDR-1, GST-pi, MRP, Bcl-w, cyclin B | Adriamycin, vincristine, cisplatin | HepG2 cells [78] |
| miR-223 | Downregulated | ABCB1 | Doxorubicin, paclitaxel | HCC cell lines [78] |
| miR-216b | Downregulated | HIF-2α-MALAT1-miR-216b axis | 5-FU, adriamycin, cisplatin | BEL-7402, SMMC-7721 cells [78] |
| miR-27a | Downregulated | FZD7/β-catenin pathway | 5-FU, adriamycin, mitomycin C | HepG2, Huh7 cells [78] |
| miR-21 | Upregulated | PTEN, PDCD4 | Interferon-α, 5-FU, cisplatin | HCC patient samples, cell lines [78] |
| miR-183 | Upregulated | IDH2/SOCS6-HIF-1α feedback loop | 5-FU | BEL-7402/5-FU cells [78] |
| miR-34a | Downregulated | LDHA, Bcl-2 | Radiotherapy, sorafenib | Hep3B, Huh7 cells [78] |
| miR-199a | Downregulated | ATG7, mTOR, c-Met | Cisplatin, doxorubicin | HepG2, Huh7 cells [78] |
| miR-491-3p | Downregulated | Sp3/ABCB1 axis | Doxorubicin, vinblastine | Huh7, Hep3B cells [78] |
| miR-137 | Downregulated | FBI-1 | Adriamycin | HepG2, BEL-7402 cells [78] |
The let-7 family demonstrates the complex roles miRNAs can play in chemoresistance. While most let-7 members function as tumor suppressors, with let-7g enhancing fluorouracil sensitivity by targeting HMGA2, let-7a is upregulated in certain HCC contexts and promotes resistance to interferon-γ, doxorubicin, and paclitaxel by targeting caspase-3 [78].
lncRNAs and circRNAs in Chemoresistance
lncRNAs contribute to chemoresistance through diverse mechanisms including miRNA sponging, regulation of epigenetic modifications, and modulation of key signaling pathways. For instance, the lncRNA H19 promotes stemness and sorafenib resistance in HCC organoids through upregulation of stemness-related and EMT-related genes including Myc, EGFR, TGFβ1, and E2F [75].
circRNAs function as competitive endogenous RNAs (ceRNAs) that sequester miRNAs, preventing them from binding to their target mRNAs. This sponge effect enables circRNAs to indirectly regulate gene expression networks involved in drug metabolism, cell survival, and DNA repair mechanisms [76] [77].
Table 2: Experimental Models for Studying ncRNA-Mediated Chemoresistance
| Experimental Approach | Key Methodologies | Application in HCC Resistance Research |
|---|---|---|
| In vitro models | Stable cell line generation, miRNA mimics/inhibitors, siRNA/shRNA knockdown, luciferase reporter assays | Functional validation of ncRNA targets, drug sensitivity assays [78] [76] |
| Ex vivo models | Patient-derived organoids, 3D culture systems | Study of stemness-related resistance, tumor heterogeneity [75] |
| In vivo models | Xenograft models, patient-derived xenografts (PDX), genetically engineered mouse models | Evaluation of therapeutic efficacy, biodistribution studies [78] [75] |
| Omics technologies | RNA sequencing, single-cell RNA-seq, ATAC-seq, proteomics | Identification of dysregulated ncRNAs, pathway analysis [17] |
| Molecular techniques | RIP-seq, CLIP-seq, ChIRP-seq, RNA-FISH | Investigation of ncRNA-protein/DNA interactions [79] |
Diagram 1: ncRNA-Mediated Chemotherapy Resistance Pathways. This diagram illustrates how different classes of ncRNAs regulate multiple mechanisms that contribute to chemotherapy resistance in HCC.
ncRNAs in Immunotherapy Resistance
Immunotherapy, particularly immune checkpoint inhibitors (ICIs), has revolutionized cancer treatment, but response rates in HCC remain limited to 15-20% of patients [75]. ncRNAs play pivotal roles in shaping the immunosuppressive TME and driving resistance through multiple mechanisms.
Regulation of Immune Checkpoints
lncRNAs directly modulate the expression of critical immune checkpoint molecules. For instance, lncRNA NEAT1 is significantly upregulated in peripheral blood mononuclear cells (PBMCs) of HCC patients and promotes CD8+ T cell apoptosis while reducing cytolytic activity through regulation of the miR-155/Tim-3 pathway [3]. Downregulation of NEAT1 enhances CD8+ T cell function and represents a promising strategy to overcome immunotherapy resistance.
The lnc-Tim3 directly binds to Tim-3, preventing its interaction with Bat3 and thereby inhibiting downstream signaling in the Lck/NFAT1/AP-1 pathway, ultimately contributing to T cell exhaustion and impaired anti-tumor immunity [3]. Similarly, multiple lncRNAs have been identified that regulate PD-L1 expression through various mechanisms including epigenetic modification, transcriptional regulation, and post-transcriptional stabilization [3] [77].
Modulation of Immune Cell Infiltration and Function
ncRNAs profoundly influence the composition and functional state of immune cells within the TME. They regulate the recruitment, differentiation, and activity of various immune cell populations including T cells, natural killer (NK) cells, myeloid-derived suppressor cells (MDSCs), and tumor-associated macrophages (TAMs) [3] [77].
Table 3: ncRNAs Mediating Immunotherapy Resistance in HCC
| ncRNA | Type | Molecular Target/Pathway | Effect on Immune Microenvironment | Therapeutic Implications |
|---|---|---|---|---|
| NEAT1 | lncRNA | miR-155/Tim-3 pathway | Promotes CD8+ T cell apoptosis, reduces cytolytic activity | Potential target to enhance CD8+ T cell function [3] |
| lnc-Tim3 | lncRNA | Tim-3/Bat3 interaction | Induces T cell exhaustion, inhibits Lck/NFAT1/AP-1 signaling | Target for reversing T cell exhaustion [3] |
| miR-449c | miRNA | CXCR2 signaling in myeloid cells | Enhances immunosuppressive cell activity | Modulation may reduce immunosuppression [77] |
| MALAT1 | lncRNA | Multiple immune checkpoints | Promotes immunosuppressive microenvironment | Combined targeting with ICIs [3] |
| miR-221 | miRNA | DDIT4/mTOR pathway, PTEN, TIMP3 | Enhances proliferation, inhibits apoptosis | OncomiR with therapeutic targeting potential [74] |
| miR-122 | miRNA | Multiple immune regulators | Attenuates HCC progression, modulates immune response | TS-miR with supplementation potential [74] |
| miR-29 | miRNA | IGF2BP1, VEGFA, BCL2 | Contrasts HCC progression, inhibits angiogenesis | TS-miR with therapeutic potential [74] |
miRNAs function as crucial regulators of immunosuppressive cells in the TME. miR-449c upregulation in myeloid progenitor cells enhances the activity of immunosuppressive cells through CXCR2 signaling, fostering an environment conducive to immune evasion and resistance to ICIs [77]. Conversely, tumor suppressor miRNAs like miR-122 and miR-29 can attenuate HCC progression and modulate immune responses, suggesting their potential as therapeutic agents to sensitize tumors to immunotherapy [74].
Experimental Approaches for Studying Immunotherapy Resistance
Investigating ncRNA functions in immunotherapy resistance requires specialized experimental approaches that capture the complexity of immune-tumor interactions. Co-culture systems combining immune cells with HCC cells enable study of cell-cell communication and ncRNA transfer via exosomes. Syngeneic mouse models that retain intact immune systems are essential for evaluating ncRNA targeting strategies in immunocompetent environments. Advanced techniques like single-cell RNA sequencing of patient samples before and during ICI treatment can identify ncRNA signatures associated with response or resistance [3] [77].
Diagram 2: ncRNA-Mediated Immunotherapy Resistance Mechanisms. This diagram illustrates how different classes of ncRNAs regulate immune checkpoints, immune cell function, and cytokine signaling to promote an immunosuppressive microenvironment and resistance to immunotherapy.
The Scientist's Toolkit: Research Reagent Solutions
Investigating ncRNA functions in drug resistance requires specialized reagents and experimental tools. The following table catalogues essential research solutions for studying ncRNA-mediated resistance mechanisms in HCC.
Table 4: Essential Research Reagents for Investigating ncRNA in Drug Resistance
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| ncRNA Modulation | miRNA mimics/inhibitors, siRNA/shRNA, CRISPR-Cas9 systems, ASOs | Functional validation of specific ncRNAs, target identification | Delivery efficiency, off-target effects, duration of effect [78] [76] |
| Detection & Quantification | qRT-PCR primers, RNA-FISH probes, Northern blot reagents | Expression analysis, spatial localization, isoform detection | Sensitivity, specificity, multiplexing capability [76] [79] |
| Interaction Studies | Biotin-labeled probes, antibody for RIP, ChIRP reagents | Identification of ncRNA-protein/DNA interactions, mechanistic studies | Cross-linking efficiency, background noise, validation requirements [79] |
| Delivery Systems | Lipid nanoparticles, viral vectors (lentivirus, AAV), exosome isolation kits | Therapeutic application studies, in vivo functional validation | Cell/tissue specificity, immunogenicity, loading efficiency [76] [79] |
| Cell Culture Models | Patient-derived organoids, 3D culture systems, co-culture kits | Study of tumor heterogeneity, TME interactions, drug screening | Physiological relevance, reproducibility, cost [75] |
| Animal Models | PDX models, genetically engineered mice, syngeneic models | Preclinical validation, biodistribution studies, toxicity assessment | Human-mouse differences, engraftment success, cost and timeline [78] [75] |
| Omics Technologies | RNA-seq kits, single-cell sequencing platforms, arrays | Discovery phase, biomarker identification, pathway analysis | Data complexity, computational requirements, integration challenges [17] |
The critical roles of ncRNAs in mediating drug resistance in HCC represent both a challenge and an opportunity. As master regulators of gene expression networks, ncRNAs influence virtually every aspect of therapy resistance, from drug efflux and cell survival pathways to immune evasion mechanisms. The growing understanding of these functions opens new avenues for overcoming therapeutic resistance.
Future research directions should focus on several key areas: First, comprehensive mapping of ncRNA interaction networks in specific HCC etiologies and molecular subtypes will enable more precise targeting strategies. Second, developing advanced delivery systems that can specifically target ncRNAs in tumor cells while sparing normal tissues remains a critical challenge. Nanoparticles, exosomes, and virus-like particles show promise for achieving tissue-specific delivery. Third, exploring combination therapies that target multiple ncRNAs or ncRNAs with conventional therapies may yield synergistic effects and prevent compensatory resistance mechanisms.
The clinical translation of ncRNA-based therapeutics faces several hurdles, including stability issues, delivery efficiency, and potential off-target effects. However, ongoing advances in chemical modification strategies and delivery platforms are steadily addressing these challenges. As our understanding of ncRNA biology in the HCC TME continues to deepen, ncRNA-based diagnostics and therapeutics are poised to become powerful tools for overcoming drug resistance and improving outcomes for HCC patients.
The integration of ncRNA biomarkers into clinical practice could enable better patient stratification and treatment selection, while ncRNA-targeting therapies may help reverse established resistance or prevent its development. With continued research innovation, targeting ncRNAs represents a promising strategy for addressing the critical challenge of therapy resistance in HCC.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, characterized by molecular heterogeneity, poor prognosis, and limited therapeutic options [80]. The translational pathway from preclinical discovery to clinical application faces unique challenges in HCC due to limited accessibility to human tumor samples, lack of homogeneous oncogenic driver mutations, and insufficient experimental models that accurately recapitulate the human disease [81]. Within this complex landscape, non-coding RNA dysregulation has emerged as a critical regulatory layer in HCC pathogenesis, offering promising avenues for biomarker discovery and therapeutic intervention [33]. This technical guide examines the model systems and validation frameworks essential for bridging the gap between preclinical findings and clinical applications in HCC research, with particular emphasis on the tumor microenvironment and non-coding RNA biology.
The complexity of HCC arises from its diverse etiologies, including chronic hepatitis B and C infections, cirrhosis, metabolic disorders, and environmental carcinogen exposure [80]. This etiological diversity is reflected in substantial molecular heterogeneity, with recurrent alterations in genes including TERT promoter, TP53, CTNNB1, and ARID1A, as well as dysregulation of key signaling pathways such as Wnt/β-catenin, PI3K/AKT, and Hippo [80]. Within this molecular landscape, long non-coding RNAs (lncRNAs) have emerged as important regulators of gene expression, affecting RNA transcription, mRNA stability, and protein functions [33].
Experimental Model Systems for HCC Research
In Vitro Model Systems
Two-Dimensional (2D) Cell Cultures: Traditional 2D monolayer cultures provide a simplified system for initial mechanistic studies but lack the physiological complexity of the tumor microenvironment [80]. These models are suitable for high-throughput screening and foundational investigations into lncRNA function and regulation.
Three-Dimensional (3D) Model Systems: Advanced in vitro models including tumor spheroids, organoids, and organ-on-a-chip platforms better recapitulate the spatial architecture, cell-cell interactions, and gradient conditions found in vivo [80]. These systems preserve the tumor microenvironment characteristics essential for studying lncRNA-mediated mechanisms in HCC progression and therapy resistance.
Table 1: Comparison of In Vitro Model Systems for HCC Research
| Model Type | Key Characteristics | Applications in ncRNA Research | Limitations |
|---|---|---|---|
| 2D Monolayers | Simplified system, high reproducibility, suitable for high-throughput screening | Initial functional validation of ncRNAs, gain/loss-of-function studies, mechanistic investigations | Lack TME context, poor clinical predictive value |
| 3D Spheroids | Multicellular aggregates, recapitulate some TME features, gradient conditions | Studying ncRNA roles in cell-cell interactions, hypoxia response, drug penetration | Limited complexity, variable size and organization |
| Organoids | Patient-derived, retain genetic heterogeneity, include multiple cell types | Personalized ncRNA biomarker validation, drug response studies, precision medicine applications | technically challenging, costly, variable success rates |
| Organ-on-a-Chip | Microfluidic systems, dynamic flow conditions, precise microenvironment control | Investigating ncRNA-mediated endothelial interactions, metastasis, nutrient signaling | Complex operation, specialized equipment required |
In Vivo Model Systems
Mouse Models: Genetically engineered mouse models (GEMMs) and patient-derived xenografts (PDXs) provide invaluable platforms for studying HCC pathogenesis and therapeutic response in a physiological context [80]. These systems enable investigation of lncRNA function within intact tumor-stroma interactions and immune responses.
Limitations of Conventional Models: Traditional models often fail to fully recapitulate the human immune microenvironment and the chronic liver disease background typical of human HCC [81]. This limitation is particularly relevant for immunotherapy studies and investigation of immune-related lncRNAs.
Emerging Model Systems
Patient-Derived Models: Bioengineered preclinical models that preserve in vivo tumor characteristics show great promise for circumventing tumor heterogeneity and overcoming drug resistance [82]. These include patient-derived organoids and xenografts that maintain the genetic and phenotypic features of original tumors.
Humanized Mouse Models: Immunodeficient mice engrafted with human immune cells provide a more physiologically relevant system for studying immunotherapy and immune-related lncRNAs in HCC [81].
Methodological Framework for ncRNA Research in HCC
Discovery Approaches for Dysregulated ncRNAs
RNA Sequencing (RNA-Seq): High-throughput transcriptome sequencing enables comprehensive profiling of lncRNA expression in HCC tissues compared to normal adjacent tissue [83]. Bulk RNA-Seq provides quantitative expression data, while single-cell RNA-Seq offers resolution at the cellular level, revealing cell type-specific lncRNA expression patterns within the tumor microenvironment.
Experimental Protocol: RNA-Seq for ncRNA Discovery
- Sample Preparation: Isolate total RNA from matched tumor and normal adjacent tissues (minimum 70% tumor content recommended) using column-based purification methods [84].
- RNA Quality Control: Assess RNA integrity using Bioanalyzer (RIN >7.0 required), quantify using spectrophotometric methods [84].
- Library Preparation: Use ribosomal RNA depletion rather than poly-A selection to retain non-polyadenylated lncRNAs. Employ strand-specific protocols to accurately determine transcription direction.
- Sequencing: Perform paired-end sequencing (≥75bp) with sufficient depth (typically 50-100 million reads per sample) to detect low-abundance lncRNAs.
- Bioinformatic Analysis: Align reads to reference genome using splice-aware aligners. Reconstruct transcripts and quantify expression. For lncRNA identification, utilize annotation databases (GENCODE, LNCIpedia) and coding potential calculators (CPC, PhyloCSF).
Microarray Analysis: Although largely superseded by RNA-Seq, microarray platforms with customized lncRNA content provide a cost-effective alternative for targeted transcriptome profiling [83] [84].
Validation Methodologies
RT-qPCR Validation: Technical and biological validation of candidate lncRNAs using quantitative reverse transcription PCR remains the gold standard [84].
Experimental Protocol: RT-qPCR for lncRNA Validation
- RNA Extraction: Use column-based methods with DNase treatment to eliminate genomic DNA contamination.
- Reverse Transcription: Employ gene-specific primers or random hexamers. Include controls without reverse transcriptase to assess DNA contamination.
- qPCR Amplification: Design primers spanning exon-exon junctions where possible. Use SYBR Green or probe-based detection. Include multiple reference genes (TBP, GAPDH, β-actin) for normalization [84].
- Data Analysis: Calculate expression using the 2−ΔΔCt method. Perform statistical analysis using appropriate tests (paired t-test for matched samples).
Functional Validation Approaches:
- Gain-of-Function: cDNA overexpression, viral transduction, inducible expression systems
- Loss-of-Function: siRNA, shRNA, CRISPRi, ASO-mediated knockdown
- Mechanistic Studies: RNA immunoprecipitation (RIP), chromatin isolation by RNA purification (ChIRP), luciferase reporter assays
Integration with Multi-Omics Data
Advanced computational approaches integrating lncRNA expression with genomic, epigenomic, and proteomic data provide insights into regulatory networks and functional mechanisms [85]. Weighted Gene Co-expression Network Analysis (WGCNA) identifies modules of co-expressed genes associated with clinical phenotypes, while pathway enrichment analysis reveals biological processes influenced by dysregulated lncRNAs [85].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for HCC ncRNA Studies
| Reagent/Category | Specific Examples | Application Function | Technical Notes |
|---|---|---|---|
| RNA Isolation Kits | Direct-zol RNA MiniPrep, miRNeasy | High-quality total RNA extraction with preservation of small and long ncRNAs | Include DNase treatment step; assess RIN >7.0 |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription, PrimeScript RT | cDNA synthesis with high efficiency for subsequent qPCR validation | Use random hexamers for comprehensive ncRNA coverage |
| qPCR Reagents | SYBR Green Master Mix, TaqMan assays | Quantitative measurement of ncRNA expression levels | Design primers spanning exon junctions; validate specificity |
| Library Prep Kits | TruSeq Stranded Total RNA, SMARTer Stranded RNA-Seq | Preparation of sequencing libraries for transcriptome analysis | Use ribosomal depletion for comprehensive ncRNA capture |
| Cell Culture Media | DMEM/F-12, specialized organoid media | Maintenance of HCC cell lines and patient-derived models | Optimize for specific model systems; include essential supplements |
| Transfection Reagents | Lipofectamine RNAiMAX, DharmaFECT | Delivery of siRNAs, ASOs for functional studies | Optimize ratio for specific cell models; include proper controls |
| Immunoassay Reagents | ELISA kits, flow cytometry antibodies | Analysis of protein biomarkers, immune cell profiling | Validate for specific applications; use isotype controls |
Signaling Pathways and Workflow Visualization
Diagram 1: Integrated Workflow for HCC ncRNA Research Translation
Diagram 2: LncRNA Regulatory Networks in HCC Signaling Pathways
Therapeutic Targeting and Clinical Translation
Targeting Oncogenic lncRNAs
Multiple strategies have emerged for therapeutic targeting of dysregulated lncRNAs in HCC:
Antisense Oligonucleotides (ASOs): Chemically modified single-stranded DNA analogs that trigger RNase H-mediated degradation of complementary RNA transcripts [14]. ASOs can be designed to target oncogenic lncRNAs such as NEAT1, HULC, and HOTAIR, which play critical roles in HCC progression [33].
RNA Interference Approaches: Small interfering RNAs (siRNAs) and short hairpin RNAs (shRNAs) enable sequence-specific silencing of target lncRNAs. Lipid nanoparticles and viral vectors facilitate efficient delivery to tumor cells [14].
CRISPR-Based Technologies: CRISPR/Cas9 systems can delete genomic loci encoding oncogenic lncRNAs, while CRISPR interference (CRISPRi) enables transcriptional repression without DNA cleavage [14].
Biomarker Development and Clinical Application
LncRNAs show considerable promise as diagnostic, prognostic, and predictive biomarkers in HCC:
Diagnostic Biomarkers: Differential expression of lncRNAs such as AL355075.4, AC012076.1, and AC136475.8 between tumor and normal tissue enables non-invasive detection of HCC [86]. Panels combining multiple lncRNAs can achieve high diagnostic accuracy (AUC 0.919 in some studies) [86].
Prognostic Models: Integration of multiple immune-related lncRNAs into prognostic signatures enables risk stratification and outcome prediction [85]. Cox regression models incorporating lncRNAs such as HHLA3, LINC01232, and MSC-AS1 have demonstrated significant predictive value for patient survival [85].
Therapy Response Prediction: LncRNA expression patterns may predict response to targeted therapies and immunotherapy. For instance, NEAT1 expression correlates with Tim-3 levels and CD8+ T cell function, potentially influencing immunotherapy outcomes [3].
Integration with Current Treatment Paradigms
The development of lncRNA-targeted approaches must consider their integration with established HCC treatments:
Combination with Targeted Therapies: LncRNA-targeting strategies may enhance response to tyrosine kinase inhibitors (sorafenib, lenvatinib, regorafenib) by overcoming resistance mechanisms [82]. For example, targeting lncRNAs involved in FGF signaling may augment response to VEGFR inhibitors [82].
Immunotherapy Combinations: Given the role of lncRNAs in regulating immune checkpoint molecules and tumor immunogenicity, combining lncRNA-targeting approaches with immune checkpoint inhibitors may yield synergistic effects [3] [81].
The translation of preclinical findings in HCC lncRNA research to clinical applications requires rigorous validation across model systems and careful consideration of therapeutic windows and delivery strategies. Future efforts should focus on standardizing methodologies, improving model systems to better recapitulate the human tumor microenvironment, and developing efficient delivery platforms for lncRNA-targeting therapeutics. As our understanding of lncRNA biology in HCC continues to evolve, these molecules hold substantial promise as biomarkers for patient stratification and as targets for novel therapeutic interventions that address the significant unmet needs in HCC management.
The successful translation of lncRNA research from preclinical models to clinical application will require interdisciplinary collaboration between molecular biologists, computational scientists, clinical researchers, and drug development experts. By leveraging advanced model systems, robust validation methodologies, and innovative therapeutic platforms, the field is poised to harness the potential of ncRNA biology to improve outcomes for HCC patients.
Hepatocellular carcinoma (HCC) is the third leading cause of cancer-related mortality worldwide, posing a significant and growing public health burden [87]. The tumor microenvironment (TME) of HCC exhibits extreme heterogeneity, characterized by complex interactions between malignant hepatocytes, immune cells, stromal cells, and abundant non-coding RNA (ncRNA) networks that collectively drive tumor progression [15]. Non-coding RNAs—including microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—have emerged as pivotal regulators of gene expression in cancer biology, modulating critical processes such as cell proliferation, death, metastasis, and therapy resistance [88].
The dysregulation of ncRNA expression in HCC arises through multiple mechanisms, including copy number variations, histone modifications, and DNA methylation changes [15]. For instance, lncRNAs are frequently amplified in HCC tumor tissues, particularly on chromosomes 1q, 8q, 17q, and 20q, while deletions often occur on chromosomes 4q, 9q, 13q, and 16q [15]. Histone modifications mediated by enzymes such as EZH2 (which promotes H3K27me3) lead to silencing of tumor-suppressive miRNAs including miR-101-1, miR-9, and miR-144/451a [15]. Similarly, DNA hypermethylation silences tumor suppressor miRNAs, while hypomethylation activates oncogenic miRNAs [15].
Therapeutic targeting of dysregulated ncRNAs in HCC represents a promising frontier, but faces substantial pharmacokinetic challenges. Naked RNA molecules exhibit poor stability, rapid clearance, and limited target selectivity, necessitating sophisticated chemical modifications and formulation strategies to achieve therapeutic efficacy [89]. This technical guide comprehensively addresses these challenges, providing researchers with experimental frameworks for optimizing ncRNA-based therapeutics for HCC treatment.
Chemical Modification Strategies for ncRNA Therapeutics
Chemical modifications to ncRNA backbones, sugars, and bases significantly enhance metabolic stability, binding affinity, and pharmacokinetic profiles while reducing immunogenicity.
Sugar and Backbone Modifications
Table 1: Common Chemical Modifications for Improved ncRNA Stability and Pharmacokinetics
| Modification Type | Chemical Structure | Key Benefits | Potential Limitations | HCC Application Examples |
|---|---|---|---|---|
| 2'-O-Methyl (2'-O-Me) | 2'-O-methyl group on ribose | Enhanced nuclease resistance, reduced immunogenicity, improved binding affinity | Possible reduced silencing efficacy | miRNA mimics/anti-miRs for HCC [90] |
| 2'-Fluoro (2'-F) | 2'-fluoro substitution | Superior metabolic stability to 2'-O-Me, maintained A-form helix | Potential for off-target effects | circRNA stabilization in HCC models [15] |
| Phosphorothioate (PS) | Sulfur substitution for non-bridging oxygen | Increased protein binding, prolonged circulation half-life | Dose-dependent toxicity observed | LNAs for targeting lncRNAs in HCC [90] |
| Locked Nucleic Acid (LNA) | 2'-O,4'-C-methylene bridge | Extremely high binding affinity, excellent mismatch discrimination | Hepatotoxicity at high doses | Gapmer designs for HCC-specific ncRNAs [90] |
| 2'-O-Methoxyethyl (2'-MOE) | 2'-O-methoxyethyl extension | Enhanced nuclease resistance, favorable pharmacokinetics | Synthetic complexity | Clinical-stage oligonucleotides [90] |
Mechanism-Based Modification Strategies
The diversity of post-transcriptional RNA modifications—including splicing, polyadenylation, methylation, and editing—generates numerous mature RNA forms with distinct functional implications in HCC [90]. Adenosine-to-inosine (A-to-I) editing in mRNA involves site-specific nucleotide substitution in pre-mRNA before splicing, mediated by ADAR enzymes. In HCC, aberrant expression of ADAR1 or ADAR2 editing enzymes is strongly associated with cancer development, making them attractive therapeutic targets [90].
Chemical modification approaches must be tailored to specific ncRNA categories:
miRNA therapeutics: Utilize antagoniRs (inhibitors) or miRNA mimics with 2'-O-Me, 2'-F, or LNA modifications, particularly at seed region positions [88]. For example, miR-221/222 is overexpressed in approximately 70% of HCCs and can be targeted with LNA-modified anti-miRs [88].
lncRNA targeting: Apply gapmer technology with LNA or 2'-MOE modifications to degrade oncogenic lncRNAs such as MCM3AP-AS1, which is highly expressed in HCC and associated with large tumor size and shorter survival [15].
circRNA approaches: Employ ASO strategies with extensive phosphorothioate linkages to counter circRNA dysregulation, such as circTRIM33-12, which is downregulated in HCC tissues and serves as an independent risk factor for overall survival [15].
Diagram Title: ncRNA Dysregulation Cascade in HCC TME
Formulation Strategies for Enhanced ncRNA Delivery
Biomaterial-Based Delivery Systems
Stimuli-responsive biomaterials represent a promising frontier for ncRNA delivery in HCC, enabling precise spatiotemporal control of drug release while enhancing therapeutic efficacy and reducing side effects [89]. These advanced materials can be engineered to respond to specific endogenous cues (e.g., pH, enzymes, redox conditions) and exogenous stimuli (e.g., light, magnetic fields) within the HCC TME.
Table 2: Formulation Strategies for ncRNA Delivery in HCC
| Formulation Platform | Responsive Mechanism | Key Components | Advantages for HCC | Experimental Evidence |
|---|---|---|---|---|
| pH-sensitive nanoparticles | Low TME pH trigger | Poly(β-amino ester), PLGA-PEG | Selective release in acidic TME | Improved tumor accumulation in HCC models [89] |
| Enzyme-responsive hydrogels | MMP-2/9 cleavage | MMP-sensitive peptide crosslinkers | Degradation in MMP-rich TME | Sustained release profiles demonstrated [89] [91] |
| Redox-responsive carriers | GSH-triggered disulfide cleavage | Disulfide-containing polymers | Enhanced intracellular release | Improved endosomal escape in hepatoma cells [89] |
| Magnetic field-guided systems | External magnetic targeting | SPIONs, magnetic liposomes | Active tumor targeting | Enhanced localization in preclinical HCC [89] |
| Apoferritin nanocages | TFR1 receptor targeting | Recombinant apoferritin | Natural tropism for hepatocytes | Effective TAM reprogramming in HCC [91] |
TME-Targeted Formulation Design
The HCC TME exhibits distinctive features that can be leveraged for targeted delivery, including:
Acidic pH: The HCC TME typically maintains a pH of 6.5-6.9 compared to 7.4 in normal tissue, enabling pH-responsive release from systems containing ionizable groups (e.g., poly(β-amino ester)s, sulfonamide derivatives) [89].
Overexpressed enzymes: Matrix metalloproteinases (MMPs), particularly MMP-2 and MMP-9, are highly active in HCC invasion and metastasis. Enzyme-responsive systems incorporating MMP-cleavable peptides (e.g., PVGLIG) enable TME-specific activation [89].
Elevated glutathione (GSH): Intracellular GSH concentrations in HCC cells (2-10 mM) are significantly higher than extracellular levels (2-20 μM), facilitating redox-responsive disulfide bond cleavage for intracellular payload release [89].
Specific receptor overexpression: Transferrin receptor 1 (TFR1) is overexpressed in HCC cells, enabling targeting with apoferritin-based systems. Similarly, asialoglycoprotein receptor (ASGPR) expression permits galactose-mediated hepatocyte targeting [91].
Experimental Protocols for Pharmacokinetic Optimization
Protocol: Evaluating Chemical Modification Stability in HCC Models
Objective: Assess metabolic stability of chemically modified ncRNA constructs in HCC-relevant biological environments.
Materials:
- Chemically modified ncRNAs (LNA, 2'-MOE, PS backbones)
- Human hepatocellular carcinoma cell lines (HepG2, Huh7, PLC/PRF/5)
- Human plasma and liver S9 fractions
- Denaturing polyacrylamide gel electrophoresis (PAGE) system
- Quantitative RT-PCR reagents
- Nuclease-free water and buffers
Methodology:
- Incubation conditions: Prepare 5 μM solutions of modified ncRNAs in:
- 50% human plasma (v/v) in PBS, pH 7.4
- Liver S9 fractions (1 mg/mL protein) with NADPH regeneration system
- Complete cell culture media with 10% FBS
- HCC cell lysates (1 mg/mL total protein)
Time-course sampling: Aliquot samples at 0, 0.5, 1, 2, 4, 8, 12, and 24 hours. Terminate reactions with 2 volumes of phenol:chloroform:isoamyl alcohol (25:24:1).
Analysis:
- Extract RNA and analyze by denaturing PAGE (15% gel) with ethidium bromide staining
- Quantify intact ncRNA using densitometry or qRT-PCR
- Calculate half-life (t½) using one-phase exponential decay nonlinear regression
HCC-specific validation: Transfer modified ncRNAs to HCC cell lines and measure intracellular persistence over 72 hours using qRT-PCR with modification-specific primers.
Expected Outcomes: LNA and 2'-MOE modifications typically extend ncRNA half-life from <2 hours (unmodified) to >24 hours in plasma and >48 hours intracellularly in HCC models [90].
Protocol: Formulation Efficacy Testing in 3D HCC Spheroids
Objective: Evaluate TME penetration and efficacy of formulated ncRNA therapeutics in physiologically relevant 3D HCC models.
Materials:
- Huh7 or HepG2 cells for spheroid formation
- Ultra-low attachment 96-well plates
- Fluorescently labeled ncRNAs (Cy5 or FAM labels)
- Confocal microscopy system with z-stack capability
- RNA extraction and qPCR equipment
- Apoptosis/cell viability assay kits
Methodology:
- Spheroid generation:
- Seed 1000 cells/well in ultra-low attachment plates
- Centrifuge at 300×g for 10 minutes to enhance cell contact
- Culture for 96 hours until compact spheroids form (200-300 μm diameter)
Treatment application:
- Apply fluorescent ncRNA formulations at 100 nM concentration
- Include unformulated ncRNAs as control
- Incubate for 24, 48, and 72 hours
Analysis:
- Penetration assessment: Fix spheroids in 4% PFA, image using confocal microscopy with z-stacking (10 μm intervals). Quantify fluorescence intensity from periphery to core using ImageJ.
- Gene expression: Extract total RNA, perform qPCR for target genes (e.g., downregulation of oncogenes after tumor suppressor miRNA delivery).
- Functional effects: Measure spheroid growth inhibition, apoptosis (caspase-3/7 activation), and viability (Alamar Blue assay).
Interpretation: Effective formulations should demonstrate >50% penetration into spheroid core, significant target modulation (>70% knockdown), and ICâ‚…â‚€ values at least 2-fold lower than unformulated controls in HCC spheroids [89].
Diagram Title: ncRNA Therapeutic Optimization Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for ncRNA Therapeutic Development in HCC
| Reagent/Category | Specific Examples | Function in Development | HCC-Specific Considerations |
|---|---|---|---|
| Chemical Modification Reagents | LNA phosphoramidites, 2'-O-Me RNA monomers, PS reagents | Introduce nuclease-resistant modifications during synthesis | Optimize for hepatocyte uptake and HCC intracellular environment |
| Delivery Materials | Ionizable lipids (DLin-MC3-DMA), PEG-lipids, chitosan, PLGA | Formulate ncRNAs into nanoparticles | Incorporate HCC-targeting ligands (galactose, lactosamine) |
| Characterization Kits | Zeta potential analyzers, DLS instruments, RiboGreen assay | Determine particle size, PDI, encapsulation efficiency | Validate in HCC-relevant media (high protein, bile salts) |
| In Vitro Models | HepG2, Huh7, PLC/PRF/5 cells, 3D spheroid kits, co-culture systems | Evaluate efficacy, uptake, and safety | Include models with different HCC etiologies (HBV, HCV, MASH) |
| Analytical Tools | HPLC/UPLC with ion-pairing, LC-MS/MS, PAGE, qRT-PCR | Quantity intact ncRNA, metabolites, and target engagement | Develop HCC biomarker-coupled assays (AFP, GPC3, DCP) |
| In Vivo Models | Orthotopic HCC models, PDX models, immunocompetent mice | Assess biodistribution, efficacy, and toxicity | Consider liver-specific promoter systems (Albumin, AAT) |
The optimization of ncRNA therapeutics for HCC requires systematic integration of chemical modifications and advanced formulation technologies. The synergistic combination of stabilizing chemical modifications (LNA, 2'-MOE, phosphorothioate) with TME-responsive delivery systems (pH-sensitive, enzyme-cleavable, redox-responsive) creates a powerful approach to overcome the substantial pharmacokinetic challenges in HCC treatment.
Future directions should focus on developing multi-stimuli responsive systems that sequentially respond to different TME cues, incorporating real-time imaging capabilities for therapeutic monitoring, and creating personalized formulation approaches based on individual HCC molecular subtypes. As our understanding of ncRNA dysregulation in HCC deepens, particularly regarding the roles of specific miRNAs, lncRNAs, and circRNAs in therapy resistance and immune evasion, the strategic application of these chemical and formulation principles will be essential for translating ncRNA therapeutics from research tools to clinical reality.
The experimental frameworks provided in this guide offer comprehensive methodologies for researchers to systematically optimize ncRNA therapeutics, with the ultimate goal of developing effective, targeted interventions that improve outcomes for HCC patients facing this challenging malignancy.
Clinical Translation and Biomarker Potential: Validating ncRNAs for HCC Prognosis and Treatment Stratification
Hepatocellular carcinoma (HCC) represents a major global health challenge, ranking as the third leading cause of cancer-related mortality worldwide [92]. The prognosis for HCC patients remains poor, with a 5-year overall survival rate of less than 12%, largely due to late diagnosis and the limitations of current surveillance methods [92]. The early detection of HCC is crucial as therapeutic options are significantly more effective in initial disease stages [93]. Traditional diagnostic approaches, including ultrasound examination with sensitivity ranging from 51% to 87% and alpha-fetoprotein (AFP) testing with sensitivity of only 20% to 65%, lack sufficient accuracy for reliable early detection [93] [92]. Approximately 40% of small HCCs do not secrete AFP at all, further limiting its diagnostic utility [92].
In this context, liquid biopsy has emerged as a promising minimally invasive approach for early HCC detection and monitoring [92]. Unlike tissue biopsy, which carries risks of pain, bleeding, and sampling bias, liquid biopsy allows for multiple tests and real-time monitoring of HCC evolution [92]. Among the most promising candidates in liquid biopsy are non-coding RNAs (ncRNAs), which include microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs) [93]. These molecules regulate gene expression through various mechanisms and demonstrate altered expression patterns in HCC that reflect disease status [92]. Their stability in bodily fluids and disease-specific expression patterns render them highly promising as diagnostic and prognostic biomarkers for HCC [94].
ncRNA Biogenesis and Functional Mechanisms in HCC
Non-coding RNAs constitute a diverse class of RNA molecules that do not encode proteins but exert crucial regulatory functions in HCC pathogenesis and progression. The three primary classes—miRNAs, lncRNAs, and circRNAs—differ in their biogenesis and mechanisms of action.
MicroRNAs (miRNAs) are single-stranded RNAs of 19-25 nucleotides that regulate protein expression through mRNA degradation and translational inhibition by binding to the 3'-untranslated region of target mRNAs [93]. They can function as either tumor suppressors or oncogenes, with aberrant expression linked to carcinogenesis processes including tumor angiogenesis, cell proliferation, invasion, and metastasis [93].
Long non-coding RNAs (lncRNAs) exceed 200 nucleotides in length and typically do not code for proteins [93]. They regulate gene expression through various mechanisms, including acting as miRNA sponges or competing endogenous RNAs (ceRNAs) [93]. Their dysregulation affects carcinogenic processes including cell differentiation and proliferation by altering gene expression [93]. In the immune microenvironment of HCC, lncRNAs are transcribed by RNA polymerase II and undergo processing including 5' capping, 3' polyadenylation, and splicing to become mature functional molecules [3].
Circular RNAs (circRNAs) are endogenous circular ncRNAs with covalently closed linked ends produced by the backsplicing of exons and/or introns on precursor mRNAs [93]. Unlike linear RNAs, circRNAs are resistant to RNase because they lack a 5' cap and 3' polyadenylated tail, enhancing their stability in bodily fluids [93]. Similar to lncRNAs, they can function as miRNA sponges or ceRNAs at both transcriptional and posttranscriptional levels [93].
Diagram 1: Biogenesis pathways and functional mechanisms of different ncRNA classes in HCC.
Exosomal ncRNAs as Diagnostic Biomarkers in HCC
Exosomes are nanoscale vesicles (30-100 nm) secreted by most cell types and detectable in body fluids such as serum, urine, and ascitic fluid [93]. These cup-shaped or double concave disc-shaped vesicles play crucial roles in cell-to-cell communication by transferring genetic information between donor and recipient cells [93]. Exosomes contain cell-specific mRNAs, ncRNAs, and proteins that are stabilized in circulation due to protective functions against RNase degradation [93]. The discovery that exosomal ncRNAs can reflect the molecular characteristics of their cell of origin has positioned them as promising diagnostic tools for HCC.
Table 1: Exosomal ncRNAs as Diagnostic Biomarkers in HCC
| ncRNA Type | Specific ncRNA | Change in HCC | Biological Source | Target Genes/Pathways | Diagnostic Significance |
|---|---|---|---|---|---|
| miRNA | miRNA-21 | Upregulated | Serum | NA | Potential biomarker for HCC diagnosis [93] |
| miRNA | miRNA-10b-5p | Upregulated | Serum | NA | Potential diagnostic biomarker for early-stage HCC [93] |
| miRNA | miRNA-148a | Downregulated | Plasma | NA | Novel noninvasive biomarker for diagnosis of HCC [93] |
| miRNA | miRNA-155-5p | Upregulated | Serum | PTEN | Novel target for HCC diagnosis and therapy [93] |
| lncRNA | lncRNA-HEIH | Upregulated | Serum | NA | Distinguishable marker of HCC from chronic hepatitis C or liver cirrhosis [93] |
| lncRNA | lncRNA-HULC | Upregulated | Plasma | HULC/miRNA-2052/MET | Diagnostic and prognostic maker in HCC [93] |
| lncRNA | linc00152 | Upregulated | Serum | EpCAM | Diagnostic markers in HCC [93] |
| lncRNA | lncRNA-UCA1 | Upregulated | Serum | miRNA-216b, FGFR1/ERK | Diagnostic/therapeutic marker in HCC [93] |
| lncRNA | lncRNA-MALAT1 | Upregulated | Serum | miRNA-204/SIRT, miRNA-200a | Diagnostic marker in HCC [93] |
The diagnostic potential of exosomal ncRNAs is particularly valuable for distinguishing HCC from other liver conditions. For instance, the combination of exosomal miRNA-122, miRNA-148a, and miRNA-1246 can distinguish HCC from liver cirrhosis (LC) and normal controls (NC), especially when combined with AFP testing [93]. Similarly, panels including miRNA-18a, miRNA-221, miRNA-222, and miRNA-224 show upregulated expression in HCC compared to chronic hepatitis B (CHB) or LC, while miRNA-101, miRNA-106b, miRNA-122, and miRNA-195 demonstrate downregulation [93].
Exosomal lncRNAs also show remarkable diagnostic potential. lncRNA-HEIH is significantly upregulated in HCC serum compared to chronic hepatitis C and liver cirrhosis patients [93]. Other lncRNAs such as linc00152, linc00853, and lncRNA-00161 demonstrate significant upregulation in HCC patients compared to controls [93]. The combination of multiple exosomal ncRNAs often enhances diagnostic sensitivity and specificity compared to single markers, suggesting future diagnostic approaches may rely on signature panels rather than individual molecules.
ncRNAs as Prognostic Biomarkers and Therapeutic Targets
Beyond diagnosis, ncRNAs show significant promise as prognostic indicators in HCC, with expression levels often correlating with disease progression, treatment response, and survival outcomes. The regulatory functions of ncRNAs in key cancer hallmarks position them as valuable markers for predicting disease course and therapeutic efficacy.
In the context of the tumor microenvironment (TME), hypoxia is a critical factor influencing HCC progression [95]. Hypoxia-inducible factor-1α (HIF-1α) serves as a master regulator of cellular response to low oxygen conditions, and numerous ncRNAs are involved in modulating this pathway [95]. These hypoxia-responsive ncRNAs (HRNs) can be categorized based on their interactions with the HIF-1α complex, including those participating in HIF-1α-mediated direct regulation and those involved in indirect regulation [95].
Table 2: Functional Roles of ncRNAs in HCC Progression and Prognosis
| Functional Role | ncRNA Type | Specific ncRNA | Molecular Targets/Pathways | Prognostic Significance |
|---|---|---|---|---|
| EMT and Metastasis | lncRNA | TUG1, LINC01116, CRNDE | Various miRNAs and signaling pathways | Promotes tumor progression [3] |
| Immune Evasion | lncRNA | NEAT1 | miR-155/Tim-3 pathway | Inhibition enhances CD8+ T cell activity against HCC [3] |
| Angiogenesis | HIF-1α regulated ncRNAs | Multiple | IL-8/NF-κB axis, TM4SF1-AS1/TM4SF1 | Promotes migration and invasion [95] |
| Proliferation | HIF-1α regulated ncRNAs | Multiple | KDM4A-AS1/KPNA2/AKT pathway | Promotes tumor proliferation [95] |
| Lipid Metabolism | HIF-1α regulated ncRNAs | Multiple | FABP5/HIF-1α axis | Promotes lipid accumulation and cell proliferation [95] |
| Drug Resistance | HIF-1α regulated ncRNAs | Multiple | PFKFB3/HIF-1α feedback loop | Contributes to therapy resistance [95] |
The prognostic significance of ncRNAs extends to their roles in modulating the immune microenvironment of HCC. For instance, lncRNA NEAT1 is significantly upregulated in peripheral blood mononuclear cells (PBMCs) of HCC patients [3]. Downregulation of NEAT1 inhibits apoptosis of CD8+ T cells and enhances their cytolytic activity against HCC cells through regulation of the miR-155/Tim-3 pathway [3]. This mechanism highlights the potential of targeting specific lncRNAs to improve immunotherapy outcomes in HCC.
LncRNAs also regulate immune checkpoint molecules that are critical for immunotherapy response. Several lncRNAs have been identified as regulators of PD1, PD-L1, and CTLA-4 expression, potentially influencing the efficacy of immune checkpoint inhibitors in HCC treatment [3]. The expression of these lncRNAs may serve as predictive biomarkers for immunotherapy response, allowing for more personalized treatment approaches.
The Researcher's Toolkit: Experimental Approaches for ncRNA Biomarker Validation
Sample Collection and Processing Protocols
The validation of ncRNAs as biomarkers requires standardized protocols for sample collection, processing, and analysis. For serum or plasma isolation, blood samples should be collected in EDTA tubes and processed within 2 hours of collection [93]. Centrifugation protocols typically involve an initial low-speed spin (1,500-2,000 × g for 10 minutes at 4°C) to remove cells and debris, followed by a high-speed centrifugation (10,000-20,000 × g for 30 minutes at 4°C) to obtain platelet-poor plasma or serum [93]. Samples should be aliquoted and stored at -80°C until exosome isolation to prevent repeated freeze-thaw cycles.
Exosome Isolation and Characterization
Multiple methods exist for exosome isolation, each with advantages and limitations:
Ultracentrifugation: Considered the gold standard, this method involves sequential centrifugation steps culminating in high-speed spins (100,000-120,000 × g) to pellet exosomes [93]. While providing high purity, it requires specialized equipment and may cause exosome aggregation.
Precipitation-based Kits: Commercial kits utilizing polymer-based precipitation offer convenient alternatives with reasonable recovery rates, though they may co-precipitate contaminants [93].
Size-exclusion Chromatography: This method separates exosomes based on size, preserving vesicle integrity and functionality while providing good purity [93].
Immunoaffinity Capture: Using antibodies against exosomal surface markers (CD63, CD81, CD9), this approach offers high specificity but may select for specific exosome subpopulations [93].
Following isolation, exosomes should be characterized by transmission electron microscopy for morphology, nanoparticle tracking analysis for size distribution, and western blotting for exosomal markers (CD63, CD81, CD9) to confirm isolation quality [93].
ncRNA Extraction and Quantification
Total RNA from exosomes can be extracted using commercial kits specifically optimized for small RNAs. Quality control should include assessment of RNA integrity and quantification. For ncRNA expression analysis, several approaches are commonly employed:
Reverse Transcription Quantitative PCR (RT-qPCR): The most accessible method for targeted analysis of specific ncRNAs. Stem-loop primers are often used for miRNA detection to enhance specificity [93].
Next-generation Sequencing (NGS): Provides comprehensive profiling of all ncRNA species without prior target selection, enabling discovery of novel biomarkers [93]. Both small RNA-seq and total RNA-seq approaches can be applied depending on the ncRNA classes of interest.
Microarrays: Offer a cost-effective alternative for profiling known ncRNAs, though with less dynamic range and sensitivity compared to NGS [93].
Table 3: Essential Research Reagents and Resources for ncRNA Biomarker Studies
| Reagent/Resource Category | Specific Examples | Application Notes |
|---|---|---|
| Exosome Isolation Kits | Total Exosome Isolation Kits, ExoQuick | Polymer-based precipitation for serum/plasma exosome isolation [93] |
| RNA Extraction Kits | miRCURY RNA Isolation Kits, miRNeasy | Optimized for small RNA retention including miRNAs [93] |
| Reverse Transcription Reagents | TaqMan MicroRNA Reverse Transcription Kit, miScript II RT Kit | Include stem-loop primers for specific miRNA detection [93] |
| qPCR Detection Systems | TaqMan assays, SYBR Green-based detection | Provide high sensitivity for low-abundance ncRNAs [93] |
| Sequencing Platforms | Illumina NextSeq, NovaSeq | Enable comprehensive ncRNA profiling [93] |
| Validation Antibodies | Anti-CD63, Anti-CD81, Anti-CD9 | Confirm exosomal identity after isolation [93] |
| Reference Genes | miR-16-5p, miR-92a-3p, U6 snRNA | Commonly used for normalization in ncRNA studies [93] |
Diagram 2: Experimental workflow for exosomal ncRNA biomarker discovery and validation.
The field of ncRNAs as diagnostic and prognostic biomarkers in HCC has progressed remarkably, with numerous candidates showing promising clinical utility. From serum to exosomal signatures, these molecules offer unprecedented opportunities for early detection, risk stratification, and treatment monitoring. The stability of ncRNAs in circulation, particularly when protected within exosomes, enhances their practical applicability as liquid biopsy biomarkers.
Future developments in this field will likely focus on several key areas. First, the validation of multi-ncRNA panels rather than single markers may provide enhanced sensitivity and specificity for HCC detection and classification. Second, standardized protocols for exosome isolation and ncRNA quantification need to be established across laboratories to ensure reproducible results. Third, the integration of ncRNA biomarkers with other molecular markers (CTCs, cfDNA) and imaging modalities may enable comprehensive patient profiling for personalized treatment approaches.
From a therapeutic perspective, the regulatory roles of ncRNAs in key cancer pathways and the immune microenvironment position them as attractive therapeutic targets. RNA-based therapeutics, including antisense oligonucleotides and small interfering RNAs, offer potential strategies for modulating ncRNA expression in HCC. As research continues to unravel the complex networks of ncRNA interactions in HCC pathogenesis, the translation of these findings into clinical practice holds significant promise for improving patient outcomes in this challenging malignancy.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the third leading cause of cancer-related deaths worldwide [96] [97]. The tumor microenvironment (TME) plays a crucial role in hepatocarcinogenesis, progression, immune escape, and therapeutic resistance [98]. Within the TME, long non-coding RNAs (lncRNAs)—transcripts longer than 200 nucleotides with limited protein-coding potential—have emerged as master regulators of gene expression through transcriptional, post-transcriptional, and epigenetic mechanisms [99] [100].
The dysregulation of lncRNAs is increasingly recognized as a critical factor in HCC pathogenesis. Proliferating tumor cells alter their amino acid metabolism to meet the demands of new protein synthesis, and lncRNAs have been found to regulate these metabolic pathways, affecting the expression of amino acid transporters and metabolic enzymes [99]. This review explores the cutting-edge research on TME-related lncRNA signatures as prognostic tools and risk stratification models in HCC, framing this discussion within the broader context of non-coding RNA dysregulation in HCC tumor microenvironment research.
TME-Related lncRNA Signatures for Prognostic Stratification
Established Risk Models and Their Clinical Value
Recent studies have successfully developed multiple risk models based on TME-related lncRNAs that effectively stratify HCC patients into distinct prognostic groups. These models leverage computational algorithms to analyze transcriptomic data and identify lncRNA signatures with significant prognostic value.
Table 1: Established TME-Related lncRNA Risk Models in HCC
| Study Model | Number of lncRNAs | Risk Stratification | Clinical Application | Reference |
|---|---|---|---|---|
| TME-Related Signature | 6 lncRNAs | High-risk vs. low-risk groups | Prognostic prediction and immunotherapy response | [98] |
| AAM-Related Signature | 4 lncRNAs | High-risk vs. low-risk groups | Prognostic prediction and immunotherapy response | [99] |
| Six-lncRNA TME Signature | 6 lncRNAs | High-risk vs. low-risk groups | Independent prognostic biomarker | [98] |
The ESTIMATE (Estimation of Stromal and Immune Cells in Malignant Tumor Tissues Using Expression Data) algorithm has been instrumental in quantifying stromal and immune components within the HCC TME [98]. Studies utilizing this approach have revealed that stromal, immune, and ESTIMATE scores significantly correlate with patient survival, with higher scores associated with better prognosis [98]. One particularly robust model identified six TME-related lncRNAs that effectively stratified patients into high-risk and low-risk groups with significantly different overall survival outcomes [98].
Another innovative approach focused on amino acid metabolism (AAM)-related lncRNAs, constructing a risk model based on 24 lncRNAs associated with AAM, ultimately identifying a 4-lncRNA signature for prognostic stratification [99]. Patients in the high-risk group demonstrated significantly lower overall survival rates compared to low-risk patients, highlighting the clinical utility of this approach [99].
Quantitative Survival Analysis of lncRNA Risk Models
The prognostic value of TME-related lncRNA signatures is substantiated by robust quantitative survival data across multiple studies.
Table 2: Survival Analysis of HCC Patients Stratified by lncRNA Risk Models
| Risk Model | High-Risk Group Survival | Low-Risk Group Survival | Hazard Ratio (HR) | Statistical Significance | |
|---|---|---|---|---|---|
| Six-lncRNA TME Signature | Poor prognosis | Better prognosis | Not specified | p < 0.001 | [98] |
| AAM-Related lncRNA Model | Lower OS rate | Higher OS rate | Not specified | p < 0.05 | [99] |
| Overall lncRNA Expression (Meta-analysis) | Poor OS | Better OS | 1.25 (95% CI: 1.03-1.52) | p = 0.03 | [101] |
| Recurrence-Free Survival (Meta-analysis) | Poor RFS | Better RFS | 1.66 (95% CI: 1.26-2.17) | Significant | [101] |
A comprehensive meta-analysis of 40 studies further validated the prognostic significance of lncRNAs in HCC, demonstrating that elevated levels of oncogenic lncRNAs were associated with a 1.25-fold increased risk of poor overall survival and a 1.66-fold increased risk of poor recurrence-free survival [101]. Interestingly, this analysis found no significant association between lncRNA expression and disease-free survival (pooled HR: 1.04; 95% CI: 0.52-2.07; p = 0.91) [101].
Experimental Methodologies for TME-Related lncRNA Profiling
Data Acquisition and Processing
The standard workflow for developing TME-related lncRNA signatures begins with comprehensive data acquisition and processing:
Data Collection: Transcriptome expression data and corresponding clinical information for HCC patients are acquired from public databases such as The Cancer Genome Atlas (TCGA-LIHC) [99] [98]. Sample sizes typically range from 374 tumor samples with 50 normal samples to larger cohorts depending on the study [98].
lncRNA Annotation: Genes are annotated and classified as lncRNAs (14,142) and protein-coding genes (19,659) according to the ENSEMBL database [98]. Low-expression lncRNAs (average expression < 0.1) are typically filtered out, retaining approximately 3,848 lncRNAs for subsequent analysis [98].
TME Scoring: The ESTIMATE algorithm is applied to calculate stromal, immune, and ESTIMATE scores for each HCC sample, representing the relative abundance of stromal and immune cells in the TME [98].
Cohort Assignment: Patients are randomly assigned to training and validation cohorts, typically in a 1:1 ratio [99] or 7:3 ratio [98], to ensure robust model development and validation.
Identification of TME-Related lncRNAs and Model Construction
The core process of signature development involves multiple analytical steps:
Differential Expression Analysis: Differentially expressed lncRNAs (DElncRNAs) are identified based on their correlation with stromal and immune scores using Pearson correlation analysis (|Pearson R| > 0.4 and p < 0.05) [99] [98].
Prognostic lncRNA Screening: Univariate Cox regression analysis is performed to identify DElncRNAs significantly associated with overall survival (p < 0.05) [99].
Signature Construction: Least absolute shrinkage and selection operator (LASSO) Cox regression analysis is applied to prevent overfitting and select the most prognostic lncRNAs [99] [98]. Multivariate Cox regression analysis is then used to construct the final risk model and calculate risk scores for each patient.
Risk Stratification: Patients are divided into high-risk and low-risk groups based on the median risk score [99].
Model Validation: The prognostic value of the risk model is validated using Kaplan-Meier survival analysis and time-dependent receiver operating characteristic (ROC) curve analysis in both training and validation datasets [99] [98].
The following diagram illustrates the complete workflow for developing and validating a TME-related lncRNA signature:
Molecular Mechanisms of TME-Related lncRNAs in HCC
Mechanisms of lncRNA Dysregulation
The aberrant expression of lncRNAs in HCC can arise through multiple molecular mechanisms:
Copy Number Variations (CNVs): CNVs are the most common DNA variations in cancer cells and frequently affect noncoding protein regions. Whole-genome sequencing of HCC patients has revealed that lncRNAs are often amplified in tumor tissues (particularly on chromosomes 1q, 8q, 17q, and 20q) or deleted (mostly on chromosomes 4q, 9q, 13q, and 16q) [15]. For instance, the lncRNA TSLNC8, located on chromosome 8p12, functions as a tumor suppressor and is frequently deleted in HCC tissues [15].
Epigenetic Modifications:
- Histone Modification: Dysregulation of ncRNAs is commonly mediated by various types of histone modifications, including histone acetylation, deacetylation, H3K27ac, and H3K27me3 [15]. Enhancer of zeste homolog 2 (EZH2), the sole histone methyltransferase promoting H3K27me3, silences tumor suppressive miRNAs (including miR-101-1, miR-9, and miR144/451a) by interacting with their promoters [15].
- DNA Methylation: DNA methylation of CpG islands within promoter regions can silence tumor suppressor genes. Multiple miRNAs with tumor suppressor characteristics have been found to be silenced by promoter DNA hypermethylation in HCC, while some tumor-promoting miRNAs are upregulated by promoter DNA hypomethylation [15].
m6A RNA Methylation: N6-methyladenosine (m6A) modifications play critical roles in regulating lncRNA stability and function. For example, METTL3 increases m6A modification and stability of the lncRNA RNF144A-AS1 in an IGF2BP1-dependent manner, promoting HCC progression [102].
Functional Mechanisms in HCC Pathogenesis
TME-related lncRNAs contribute to HCC pathogenesis through diverse molecular mechanisms:
Regulation of Immune Checkpoints: LncRNAs can modulate the expression of immune checkpoint molecules. The high-risk group defined by AAM-related lncRNAs showed increased expression of immunosuppressive checkpoints including CD276, CTLA4, and TIGIT [99].
Metabolic Reprogramming: LncRNAs regulate amino acid metabolism in HCC cells by affecting the expression of amino acid transporters and metabolic enzymes, thereby supporting tumor growth and survival under nutrient stress [99].
ceRNA Networks: Many lncRNAs function as competing endogenous RNAs (ceRNAs) or "miRNA sponges." For instance, lncRNA RNF144A-AS1 promotes HCC malignant phenotypes by sequestering miR-1301-3p, thereby preventing miR-1301-3p-mediated degradation of its target RNF38 [102].
Transcriptional and Epigenetic Regulation: Nuclear lncRNAs can recruit chromatin-modifying complexes to specific genomic loci. For example, the lncRNA ANRIL promotes HCC cell proliferation by recruiting polycomb repressive complex 2 (PRC2) to the promoter region of KLF2, resulting in H3K27 trimethylation and KLF2 silencing [100].
The following diagram summarizes these key molecular mechanisms:
Table 3: Key Research Reagents and Resources for TME-Related lncRNA Studies
| Reagent/Resource | Specific Example | Application/Function | Reference |
|---|---|---|---|
| Cell Lines | THLE2, Hep-3B, Huh-1, Huh-7, HCCLM3 | In vitro models for functional validation of lncRNAs | [99] |
| Transfection Reagent | Lipofectamine 3000 | Delivery of nucleic acids (siRNA, plasmids) into cells | [99] |
| Gene Silencing | AL590681.1-specific shRNA | Knockdown of specific lncRNAs for functional studies | [99] |
| Cell Viability Assay | CCK-8 kit | Measurement of cell proliferation and viability | [99] [102] |
| Clonogenic Assay | Colony formation assay | Assessment of single-cell growth potential and proliferation | [99] |
| Migration/Invasion Assays | Transwell and scratch assays | Evaluation of cell migratory and invasive capabilities | [102] |
| RNA Detection | Quantitative RT-PCR (qRT-PCR) | Measurement of lncRNA expression levels | [99] [102] [103] |
| Fluorescence In Situ Hybridization | FISH assay with specific probes | Spatial localization of lncRNAs in tissues and cells | [102] |
| Protein Analysis | Western blot | Detection of protein expression and signaling pathways | [102] |
| Database | TCGA-LIHC | Source of transcriptomic and clinical data | [99] [98] |
| Computational Tool | ESTIMATE algorithm | Calculation of stromal and immune scores in TME | [98] |
Clinical Applications and Therapeutic Implications
Predicting Immunotherapy Response
TME-related lncRNA signatures show significant promise as predictors of response to immune checkpoint inhibitors (ICIs) in HCC. Studies have demonstrated that high-risk patients, as defined by AAM-related lncRNA signatures, exhibit more immunosuppressive immune cell infiltration and increased expression of immune checkpoints including CD276, CTLA4, and TIGIT [99]. Importantly, these patients may derive greater benefit from anti-PD1 therapy compared to low-risk patients [99].
The TIDE (Tumor Immune Dysfunction and Exclusion) framework, a computational method designed to predict cancer patients' responses to immune checkpoint inhibitors, has been successfully applied to evaluate the predictive value of lncRNA signatures [99]. This approach has revealed significant correlations between specific lncRNA risk scores and expression of established immune checkpoints such as PD-1, PD-L1, PD-L2, and CTLA4 [99] [98].
Integration with Machine Learning Approaches
Advanced computational methods are enhancing the diagnostic and prognostic potential of lncRNA-based biomarkers. A recent study integrated four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters using machine learning algorithms, achieving 100% sensitivity and 97% specificity in HCC diagnosis—significantly outperforming individual lncRNAs or standard biomarkers like AFP [103]. Furthermore, the LINC00152 to GAS5 expression ratio significantly correlated with mortality risk, highlighting the prognostic value of lncRNA combinations [103].
TME-related lncRNA signatures represent powerful tools for risk stratification and prognostic prediction in HCC. The integration of these molecular signatures with clinical parameters and advanced computational approaches offers a promising path toward personalized management of HCC patients. Future research should focus on validating these signatures in prospective clinical trials and exploring their utility in guiding therapeutic decisions, particularly in the context of immunotherapy. As our understanding of the complex regulatory networks involving lncRNAs in the TME continues to expand, so too will opportunities for developing novel diagnostic, prognostic, and therapeutic strategies for this lethal malignancy.
Hepatocellular carcinoma (HCC) represents a major global health challenge, characterized by a complex tumor microenvironment (TME) and limited response rates to immune checkpoint inhibitor (ICI) therapies. The discovery of robust predictive biomarkers is crucial for identifying patients who will benefit from immunotherapy. Non-coding RNAs (ncRNAs), particularly long non-coding RNAs (lncRNAs) and microRNAs (miRNAs), have emerged as critical regulators of the immune landscape in HCC, influencing immune cell function, checkpoint expression, and therapeutic resistance [3] [24]. These molecules offer unprecedented potential as predictive biomarkers for immunotherapeutic outcomes and as targets for novel combination strategies. This technical review synthesizes current evidence on ncRNA profiling as a tool for predicting ICI response in HCC, providing detailed methodologies for researchers and clinicians working at the intersection of cancer genomics and immuno-oncology.
Core ncRNA Classes and Their Mechanisms in Immune Regulation
Long Non-Coding RNAs (lncRNAs)
LncRNAs are transcripts longer than 200 nucleotides that regulate gene expression through diverse mechanisms, including chromatin remodeling, transcriptional interference, and post-transcriptional processing [24]. In the context of HCC immunotherapy, lncRNAs function as master regulators of the tumor immune microenvironment through several key mechanisms:
- Immune Checkpoint Regulation: LncRNAs such as HEIH directly modulate the expression of immune checkpoint molecules like PD-1, PD-L1, and CTLA-4, enabling tumor immune evasion [24].
- Immune Cell Differentiation and Recruitment: LncRNAs influence the differentiation, recruitment, and function of various immune cells, including T cells, natural killer (NK) cells, tumor-associated macrophages (TAMs), and myeloid-derived suppressor cells (MDSCs) [3].
- Cytokine and Chemokine Signaling: These molecules shape the immunosuppressive TME by regulating the production of cytokines and chemokines that determine immune cell trafficking and activation states [3].
Table 1: Key lncRNAs Implicated in HCC Immunotherapy Response
| LncRNA | Expression in HCC | Mechanism of Action | Impact on ICI Response |
|---|---|---|---|
| HEIH | Upregulated | Binds EZH2; suppresses CD8+ T cell function; upregulates PD-L1 | Predictive of resistance [24] |
| AL590681.1 | Upregulated | Enhances HCC cell activity; modulates amino acid metabolism | High expression correlates with poor survival [99] |
| MIR4435-2HG | Upregulated | Promotes EMT; upregulates PD-L1 expression | Associated with immune evasion [104] |
| LINC00839 | Upregulated | Migrasome-related; modulates immune infiltration | High risk score predicts poor outcome [104] |
| NEAT1 | Upregulated | Regulates miR-155/Tim-3 pathway in CD8+ T cells | Modulates T cell cytolytic activity [3] |
MicroRNAs (miRNAs)
MiRNAs are small non-coding RNAs (~22 nucleotides) that typically function by binding to target messenger RNAs (mRNAs), leading to their degradation or translational repression [105]. In HCC immunotherapy:
- Checkpoint Pathway Regulation: Specific miRNAs directly target immune checkpoint components, with miR-197 shown to regulate the PD-L1 axis in multiple cancers [105].
- Immune Cell Function: MiRNAs modulate T cell exhaustion, functional suppression, and regulatory T cell (Treg) promotion within the TME [105].
- Circulating Biomarkers: Plasma miRNAs such as hsa-miR-16-5p, hsa-miR-93-5p, and hsa-miR-126-3p demonstrate predictive value for chemoimmunotherapy response in biliary tract cancers, with potential applicability to HCC [60].
Methodological Framework for ncRNA Biomarker Discovery
Transcriptomic Data Acquisition and Preprocessing
The standard workflow begins with acquiring high-quality RNA-seq data and corresponding clinical information from large-scale databases such as The Cancer Genome Atlas (TCGA-LIHC) and Gene Expression Omnibus (GEO) [99] [104]. Key preprocessing steps include:
- Data Normalization: Conversion of raw counts to transcripts per million (TPM) followed by log2 transformation to ensure comparability across samples [104].
- Quality Control: Removal of patients with overall survival of less than 30 days to ensure robustness in survival analyses [99].
- LncRNA Identification: Extraction of lncRNA expression profiles from transcriptomic data using genomic annotation files (e.g., GENCODE) to distinguish from protein-coding transcripts.
Identification of Therapy-Relevant ncRNA Signatures
The identification of prognostic ncRNA signatures involves multiple computational biology approaches:
- Correlation Analysis: Pearson correlation analysis between genes of interest (e.g., amino acid metabolism genes, migrasome-related genes) and lncRNA expression levels, with thresholds typically set at |correlation coefficient| >0.4 and p < 0.05 [99] [104].
- Survival Analysis: Univariate Cox regression to identify ncRNAs significantly associated with overall survival (p < 0.05) [99] [104].
- Feature Selection: LASSO Cox regression analysis with 10-fold cross-validation to select the most prognostic ncRNAs while preventing overfitting [99] [104].
- Risk Model Construction: Development of a multivariate Cox proportional hazards model using selected ncRNAs, with risk scores calculated using the formula:
Validation and Functional Characterization
Robust biomarker development requires rigorous validation and functional assessment:
- Cohort Validation: Internal validation through random splitting of datasets into training and testing cohorts (typically 1:1 ratio), followed by external validation using independent patient cohorts [104] [106].
- Survival Statistics: Kaplan-Meier analysis with log-rank test to compare survival between high-risk and low-risk groups, complemented by time-dependent receiver operating characteristic (ROC) curve analysis to evaluate predictive accuracy [99] [104].
- Immune Correlates: Analysis of tumor immune microenvironment using CIBERSORT or single-sample gene set enrichment analysis (ssGSEA) to quantify immune cell infiltration [99] [104].
- Therapy Response Prediction: Application of the Tumor Immune Dysfunction and Exclusion (TIDE) algorithm and subclass mapping (SubMap) to predict ICI response based on ncRNA signatures [99] [104].
Diagram 1: Experimental workflow for ncRNA biomarker discovery in HCC immunotherapy.
Established ncRNA Signatures and Their Predictive Value
Amino Acid Metabolism-Related lncRNA Signature
A recent study constructed a risk model based on amino acid metabolism (AAM)-related lncRNAs that effectively stratifies HCC patients for immunotherapeutic outcomes [99]. The methodology included:
- Signature Identification: Univariate Cox, LASSO, and multivariate Cox analyses identified 4 prognostic AAM-related lncRNAs from an initial 24 candidates associated with overall survival.
- Risk Stratification: Patients in the high-risk group demonstrated significantly lower overall survival rates compared to low-risk patients (p < 0.001).
- Immune Profiling: The high-risk group exhibited increased infiltration of immunosuppressive cells and elevated expression of immune checkpoints CD276, CTLA4, and TIGIT.
- Therapeutic Implications: Despite the immunosuppressive profile, high-risk patients showed better survival prospects with anti-PD1 treatment, suggesting potential for patient selection.
- Functional Validation: The key gene AL590681.1 was overexpressed in various HCC cell lines and demonstrated enhancement of HCC cell activity in functional assays.
Migrasome-Related lncRNA Signature
Another innovative approach identified migrasome-related lncRNAs (MRlncRNAs) as potent predictors of immunotherapy response [104]:
- Signature Development: A robust 2-lncRNA signature (LINC00839 and MIR4435-2HG) was constructed using LASSO-Cox regression from TCGA data.
- Prognostic Value: The signature effectively stratified HCC patients by prognosis and immunotherapy responsiveness, validated in an independent cohort (n = 100).
- Mechanistic Insights: High-risk patients exhibited elevated immunosuppressive cell infiltration and immune checkpoint expression.
- Functional Evidence: Knockdown of MIR4435-2HG in HCC cells impaired malignant behaviors and immune evasion by regulating epithelial-mesenchymal transition (EMT) and PD-L1 expression.
Table 2: Quantitative Performance of Established ncRNA Signatures in Predicting HCC Immunotherapy Response
| Signature Type | Key Components | Cohort Size | Predictive Performance | Clinical Correlates |
|---|---|---|---|---|
| AAM-Related lncRNAs [99] | 4-lncRNA signature | Training: 170Validation: 170 | ROC AUC: 0.75-0.80High-risk: worse OS (p<0.001) | Increased CD276, CTLA4, TIGITBetter anti-PD1 response |
| Migrasome-Related lncRNAs [104] | LINC00839, MIR4435-2HG | Primary: 372Validation: 100 | Effective risk stratificationHigh-risk: immunosuppressive TME | Promotes EMT, PD-L1 expressionEnriched in cancer-associated fibroblasts |
| Circulating miRNAs [60] | hsa-miR-16-5p, hsa-miR-93-5p, hsa-miR-126-3p | 46 patients | AUC = 0.81 for response prediction | High miR-16-5p: longer PFS (HR=0.44) and OS (HR=0.34) |
| Hypoxia/Anoikis-Related lncRNAs [107] | 9-lncRNA signature | TCGA: 365External validation | Effective risk stratificationHigh-risk: immunosuppressive profile | Increased Tregs, M0 macrophagesLimited immunotherapy efficacy |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for ncRNA Biomarker Discovery
| Reagent/Platform | Specific Examples | Application in ncRNA Research | Technical Considerations |
|---|---|---|---|
| Transcriptomic Databases | TCGA-LIHC, GEO (GSE43619, GSE188608) | Source of RNA-seq data and clinical correlations | Ensure consistent preprocessing (TPM, log2) and batch effect correction |
| Bioinformatics Tools | CIBERSORT, ESTIMATE, ssGSEA | Immune cell infiltration quantification | Platform-specific normalization critical for comparability |
| Therapy Response Predictors | TIDE algorithm, SubMap analysis | ICI response prediction based on gene expression | Requires appropriate reference datasets for accurate prediction |
| ncRNA Functional Validation | siRNA/shRNA (e.g., Lipofectamine 3000) | Knockdown of target lncRNAs (e.g., AL590681.1, MIR4435-2HG) | Optimization of transfection efficiency critical for HCC cell lines |
| Cell Culture Models | HCC cell lines (Hep-3B, Huh-7, HCCLM3) | Functional assays for proliferation, migration, invasion | Include appropriate controls (e.g., THLE2 normal liver cells) |
| Molecular Assays | RT-qPCR, Western immunoblotting, nanoparticle tracking analysis | Validation of ncRNA expression and functional effects | Primer design critical for specific lncRNA detection |
| Pathway Analysis | GO, KEGG, GSEA enrichment analysis | Elucidation of biological processes and pathways | Use updated gene sets and appropriate FDR correction |
ncRNA-Mediated Immunosuppressive Mechanisms in HCC
The predictive value of ncRNA signatures stems from their fundamental roles in shaping the immunosuppressive HCC microenvironment. Key mechanisms include:
Direct Immune Checkpoint Regulation
LncRNAs directly regulate the expression of critical immune checkpoint molecules:
- HEIH: This well-characterized oncogenic lncRNA is upregulated in HCC and promotes immune evasion through multiple pathways, including enhancement of PD-L1 expression and suppression of CD8+ T cell function [24].
- MIR4435-2HG: Functional assays demonstrate that this migrasome-related lncRNA promotes immune evasion by regulating PD-L1 expression, providing a direct link between migrasome formation and immune checkpoint regulation [104].
T Cell Function Modulation
ncRNAs significantly influence T cell activity and differentiation in the HCC TME:
- NEAT1: Regulation of the miR-155/Tim-3 pathway in CD8+ T cells, where NEAT1 downregulation inhibits CD8+ T cell apoptosis and enhances cytolytic activity against HCC cells [3].
- Lnc-Tim3: Binds to Tim-3 and prevents interaction with Bat3, inhibiting downstream signaling in the Lck/NFAT1/AP-1 pathway and contributing to T cell exhaustion [3].
Metabolic Reprogramming of the TME
ncRNAs mediate metabolic alterations that support immunosuppression:
- AAM-Related lncRNAs: Amino acid metabolism plays a crucial role in HCC progression, with specific lncRNAs regulating metabolic pathways that influence mTOR signaling and T cell function [99].
- Hypoxia-Related lncRNAs: The hypoxic TME characteristic of HCC drives the expression of lncRNAs that promote angiogenesis, metabolic adaptation, and immune evasion through HIF-1α stabilization and downstream signaling [107].
Diagram 2: ncRNA-mediated mechanisms of immunotherapy resistance in HCC.
The integration of ncRNA profiling into predictive models for HCC immunotherapy represents a paradigm shift in precision oncology. The established signatures discussed in this review—including amino acid metabolism-related lncRNAs, migrasome-related lncRNAs, and circulating miRNAs—demonstrate robust performance in stratifying patients based on their likelihood of responding to ICI therapy. The methodological framework outlined provides a standardized approach for biomarker discovery and validation, essential for translating these findings into clinical practice.
Future research directions should focus on the development of multi-analyte signatures that integrate ncRNA profiles with traditional biomarkers such as PD-L1 expression, tumor mutational burden, and radiological features. Additionally, the therapeutic targeting of oncogenic ncRNAs using antisense oligonucleotides, RNA interference, or CRISPR/Cas9 systems represents a promising strategy to overcome resistance and enhance the efficacy of existing immunotherapies. As our understanding of ncRNA biology in the HCC TME deepens, these molecules will undoubtedly play an increasingly central role in guiding immunotherapeutic strategies and improving patient outcomes.
The dysregulation of non-coding RNAs (ncRNAs) within the hepatocellular carcinoma (HCC) tumor microenvironment (TME) presents a complex landscape of therapeutic opportunities and challenges. This review provides a comparative analysis of the three principal ncRNA classes—microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—evaluating their respective strengths and limitations as therapeutic targets. We examine their biogenesis, regulatory mechanisms, stability, and delivery considerations within the context of HCC pathogenesis. Furthermore, we detail essential experimental methodologies for investigating ncRNA function and therapeutic potential, supported by visualization of key pathways and a comprehensive toolkit for researchers. The integration of ncRNA-targeting strategies, particularly using nanomedicine approaches, holds significant promise for advancing precision oncology in HCC treatment.
In the complex molecular ecology of the hepatocellular carcinoma (HCC) tumor microenvironment (TME), non-coding RNAs (ncRNAs) have emerged as master regulators of cancer progression, immune evasion, and therapeutic response. Once dismissed as "junk DNA," ncRNAs are now recognized as crucial players in gene regulation, cellular development, and disease progression [108]. The dysregulation of specific ncRNA classes creates distinct molecular vulnerabilities that can be exploited for therapeutic intervention. In HCC, as in other cancers, the major ncRNA classes—microRNAs (miRNAs), long non-coding RNAs (lncRNAs), and circular RNAs (circRNAs)—exhibit unique characteristics that define their potential as therapeutic targets [15] [109]. Understanding their comparative strengths and limitations is essential for developing effective ncRNA-based therapeutics that can navigate the challenges of the HCC TME, including immune cell infiltration, epithelial-mesenchymal transition (EMT), angiogenesis, and drug resistance [44] [110]. This analysis examines these ncRNA classes through multiple lenses: their molecular mechanisms, therapeutic malleability, delivery requirements, and integration within the broader context of HCC pathogenesis.
ncRNA Classes: Molecular Mechanisms and Functional Roles in HCC
MicroRNAs (miRNAs): Master Post-Transcriptional Regulators
Biogenesis and Mechanism: miRNA biogenesis begins with RNA polymerase II/III transcription in the nucleus, producing primary miRNAs (pri-miRNAs) that are processed by the Drosha-DGCR8 complex into precursor miRNAs (pre-miRNAs) of approximately 70 nucleotides [109]. These pre-miRNAs are exported to the cytoplasm via Exportin-5, where Dicer cleavage generates mature miRNA duplexes of 21-25 nucleotides. One strand of this duplex is loaded into the RNA-induced silencing complex (RISC), where the Argonaute (AGO2) protein facilitates guide strand binding to complementary messenger RNA (mRNA) targets, primarily at the 3'-untranslated region (3'-UTR) [109]. This interaction leads to either translational repression or degradation of the target mRNA, depending on the degree of complementarity [108].
Therapeutic Strengths: miRNAs present exceptional therapeutic advantages due to their ability to simultaneously regulate multiple genes within a pathway. A single miRNA can target hundreds of mRNAs, making them powerful tools for modulating complex disease processes like carcinogenesis [109]. Their small size (approximately 22 nucleotides) facilitates chemical synthesis and modification for enhanced stability. Furthermore, their well-characterized mechanism of action through the RISC pathway provides a predictable framework for therapeutic design.
Key Limitations: The pleiotropic nature of miRNAs constitutes a significant therapeutic challenge, as off-target effects can lead to unintended consequences [65]. Additionally, miRNAs exhibit functional duality—the same miRNA can act as either an oncogene or tumor suppressor depending on cellular context. For instance, miR-122 functions as a tumor suppressor in HCC, with decreased expression associated with increased invasiveness and metastasis, while miR-221 acts as an oncomiR with elevated expression in HCC tissues [110].
Long Non-Coding RNAs (lncRNAs): Complex Architectural Regulators
Biogenesis and Mechanism: lncRNAs are defined as transcripts longer than 200 nucleotides that lack significant protein-coding potential. They are transcribed by RNA polymerase II and often undergo splicing and polyadenylation similar to mRNAs [109]. Their mechanisms of action are remarkably diverse, functioning as signals, decoys, guides, or scaffolds in regulatory processes ranging from epigenetic modifications to protein stabilization [44]. In the HCC TME, lncRNAs such as NEAT1 and Lnc-Tim3 play crucial roles in regulating immune cell function—NEAT1 modulates Tim-3 expression by binding miR-155, thereby influencing CD8+ T-cell exhaustion, while Lnc-Tim3 directly binds to Tim-3, disrupting its interaction with Bat3 and promoting T-cell exhaustion [44].
Therapeutic Strengths: The complex structural domains of lncRNAs provide multiple targeting opportunities for therapeutic intervention. Their high specificity—both tissue-specific and context-specific—offers potential for highly targeted therapies with reduced off-target effects [44]. Some lncRNAs, such as TSLNC8, function as tumor suppressors that are frequently deleted in HCC, suggesting potential replacement therapy strategies [15].
Key Limitations: The large size of lncRNAs (often >1kb) presents significant challenges for synthetic production and delivery [44]. Their structural complexity and numerous isoforms further complicate therapeutic targeting. Additionally, the functions of many lncRNAs remain poorly characterized, creating substantial knowledge gaps for therapeutic development.
Circular RNAs (circRNAs): Stable Regulatory Sponges
Biogenesis and Mechanism: circRNAs are generated through a unique back-splicing mechanism where a downstream 5' splice site joins with an upstream 3' splice site, forming a covalently closed loop structure without 5' caps or 3' poly(A) tails [111]. This circular configuration confers exceptional resistance to exonucleases, resulting in significantly extended half-lives compared to linear RNAs. circRNAs function primarily as miRNA "sponges" that sequester miRNAs and prevent their interaction with target mRNAs [111] [44]. In HCC, circMET drives tumor progression through the miR-30-5p/Snail/DPP4 axis, impairing CD8+ T-cell infiltration and contributing to an immunosuppressive TME [44].
Therapeutic Strengths: The outstanding molecular stability of circRNAs—with half-lives exceeding 48 hours compared to approximately 10 hours for linear mRNAs—makes them exceptionally attractive therapeutic modalities [111]. Their closed-loop structure eliminates the need for 5'-capping and 3'-polyadenylation in synthetic production. Recent advances have demonstrated that engineered circRNAs can possess protein-coding capability, expanding their therapeutic potential [111].
Key Limitations: Production of circRNAs through in vitro transcription remains technically challenging, with potential for linear RNA contaminants. Their large size also presents delivery difficulties similar to those of lncRNAs. Furthermore, the sponge function of circRNAs can have unpredictable network effects due to simultaneous regulation of multiple miRNA targets.
Table 1: Comparative Analysis of ncRNA Classes as Therapeutic Targets
| Parameter | miRNAs | lncRNAs | circRNAs |
|---|---|---|---|
| Size | Small (~22 nt) | Large (>200 nt) | Variable (often large) |
| Stability | Moderate | Moderate | Very high |
| Synthetic Production | Straightforward | Challenging | Technically complex |
| Delivery Ease | High | Low | Low |
| Specificity | Low (pleiotropic) | High | Moderate |
| Therapeutic Versatility | miRNA mimics, antagomirs, sponges | ASOs, CRISPR-based, small molecules | Sponges, protein coding |
| Clinical Stage | Multiple in trials | Early preclinical | Early preclinical |
| Key Challenge | Off-target effects | Delivery, limited functional data | Production complexity |
Experimental Methodologies for ncRNA Investigation in HCC
Expression Profiling and Functional Validation
Comprehensive investigation of ncRNAs in the HCC TME requires integrated methodological approaches that address both expression dynamics and functional significance. The following protocols represent established standards in the field:
Expression Profiling Protocol:
- Sample Collection: Obtain paired HCC and adjacent non-tumor liver tissues, preferably with detailed clinical annotation including etiology (NAFLD, HBV, HCV), tumor stage, and treatment history [15].
- RNA Extraction: Use mirVana miRNA Isolation Kit (Thermo Fisher) for simultaneous isolation of small and large RNAs. Assess RNA integrity using Agilent Bioanalyzer (RIN >7.0 required) [109].
- Library Preparation and Sequencing:
- For miRNAs: Employ NEBNext Small RNA Library Prep Set following manufacturer's instructions.
- For lncRNAs/circRNAs: Use Ribo-zero Gold Kit (Illumina) to deplete ribosomal RNA followed by NEBNext Ultra II Directional RNA Library Prep [44].
- Bioinformatic Analysis:
- Process raw data through FastQC for quality control.
- Align reads to reference genome (GRCh38) using STAR aligner.
- Identify differentially expressed ncRNAs using DESeq2 (FDR <0.05, log2FC >1).
- Predict targets: miRDB for miRNAs, CRISPRi for lncRNAs, circInteractome for circRNAs.
- Validation: Confirm findings by qRT-PCR using TaqMan assays with U6 (miRNAs) or GAPDH (lncRNAs/circRNAs) as endogenous controls [15].
Functional Validation Workflow:
- Gain-of-Function: Transfect ncRNA mimics (miRNAs) or expression vectors (lncRNAs/circRNAs) using Lipofectamine 3000 into HCC cell lines (HepG2, Huh7).
- Loss-of-Function: Introduce antagomirs (miRNAs) or siRNA/shRNA (lncRNAs/circRNAs) using appropriate transfection reagents.
- Phenotypic Assays:
- Conduct MTT and colony formation assays at 24h, 48h, and 72h post-transfection to assess proliferation.
- Perform Transwell migration and invasion assays with Matrigel-coated membranes.
- Analyze apoptosis using Annexin V-FITC/PI staining with flow cytometry.
- In Vivo Validation: Establish subcutaneous or orthotopic HCC models in immunocompromised (nu/nu) or humanized mice, administering ncRNA modulators via hydrodynamic injection or nanoparticle delivery [44].
Pathway Analysis and Mechanism Elucidation
Understanding ncRNA mechanisms within the HCC TME requires sophisticated molecular techniques to map interaction networks and functional consequences:
Mechanistic Investigation Protocol:
- Target Identification:
- For miRNAs: Perform Ago2-CLIP followed by high-throughput sequencing to identify direct mRNA targets.
- For lncRNAs: Conduct CHIRP or ChIRP-MS to identify interacting DNA and protein partners.
- For circRNAs: Implement RNA pulldown with biotinylated probes followed by mass spectrometry.
- Pathway Analysis:
- Use KEGG and Gene Ontology enrichment analyses of identified targets.
- Validate key pathways (e.g., PI3K/AKT, Wnt/β-catenin, immune checkpoints) through Western blotting and immunofluorescence.
- TME Interaction Studies:
- Establish coculture systems with HCC cells and immune cells (CD8+ T cells, macrophages).
- Analyze cytokine profiles using Luminex arrays.
- Evaluate immune cell function through cytotoxicity assays (CD8+ T cells) and phagocytosis assays (macrophages) [44].
The following diagram illustrates the core experimental workflow for ncRNA functional analysis in HCC:
Therapeutic Targeting Strategies and Delivery Considerations
ncRNA-Targeted Therapeutic Approaches
The development of ncRNA-based therapeutics for HCC has generated diverse strategic approaches, each with distinct molecular mechanisms and implementation considerations:
miRNA-Targeted Therapies:
- miRNA Mimics: Synthetic double-stranded RNA molecules designed to replace downregulated tumor-suppressor miRNAs (e.g., miR-122, miR-34a) in HCC [110]. These molecules are processed similarly to endogenous miRNAs and incorporated into RISC to restore lost regulatory functions. Chemical modifications (2'-O-methyl, 2'-fluoro) enhance stability and reduce immunogenicity.
- Antagomirs (Anti-miRs): Single-stranded oligonucleotides with complete complementarity to oncogenic miRNAs (e.g., miR-221, miR-21), often incorporating locked nucleic acid (LNA) modifications for increased binding affinity and nuclease resistance [65]. These molecules sterically block miRNA function or trigger degradation through RNase H recruitment.
- miRNA Sponges: Ectopically expressed transcripts containing multiple tandem binding sites for a miRNA family, competitively inhibiting miRNA activity across entire functional families [108].
lncRNA-Targeted Approaches:
- Antisense Oligonucleotides (ASOs): Gapmer designs incorporating LNA modifications enable RNase H1-mediated degradation of oncogenic lncRNAs (e.g., HOTAIR, MALAT1) [112]. Recent advances include cEt bicyclic nucleic acids with improved potency and tissue retention.
- Small Molecule Inhibitors: High-throughput screening approaches identify chemical compounds that disrupt lncRNA structure or protein interactions. For example, compounds targeting the interaction between lncRNA MYU and hnRNP-K show promise in preclinical HCC models [44].
- CRISPR-Based Interventions: CRISPRi (interference) systems utilizing catalytically dead Cas9 (dCas9) fused to transcriptional repressors (KRAB) enable precise epigenetic silencing of oncogenic lncRNA loci without DNA damage [113].
circRNA-Specific Strategies:
- RNAi-Mediated Knockdown: siRNAs targeting back-splice junction sequences enable specific circRNA inhibition without affecting linear counterparts [111].
- Therapeutic circRNA Expression: Engineered circRNAs incorporating internal ribosome entry sites (IRES) enable sustained therapeutic protein expression, leveraging circRNA's exceptional stability for long-term transgene expression in HCC models [111].
Table 2: Therapeutic Approaches by ncRNA Class
| Therapeutic Approach | Mechanism | Example Targets | Development Status |
|---|---|---|---|
| miRNA Mimics | Restore tumor-suppressor function | miR-34a, miR-122 | Phase I trials |
| Antagomirs | Inhibit oncomiR function | miR-221, miR-21 | Preclinical/Phase I |
| LNA Gapmers | RNase H-mediated degradation of lncRNAs | HOTAIR, MALAT1 | Preclinical development |
| CRISPRi | Epigenetic silencing | PVT1, NEAT1 | Preclinical optimization |
| circRNA Expression | Stable protein production | Immunomodulators | Early preclinical |
| Small Molecules | Disrupt RNA-protein interactions | MYU-hnRNP-K | Screening phase |
Nanomedicine Delivery Solutions
Effective delivery of ncRNA therapeutics to the HCC TME requires sophisticated nanocarrier systems that overcome biological barriers while ensuring precise cellular targeting:
Lipid-Based Systems:
- Lipid Nanoparticles (LNPs): The most clinically advanced delivery platform, comprising ionizable lipids, phospholipids, cholesterol, and PEG-lipids that self-assemble into nanoparticles capable of encapsulating nucleic acids and facilitating endosomal escape [108] [65]. Recent HCC-targeted formulations incorporate galactose derivatives for asialoglycoprotein receptor (ASGPR)-mediated hepatocyte-specific delivery.
- Lipid-Derived Nanocarriers: Stable nucleic acid lipid particles (SNALPs) with optimized ionizable lipid compositions (DLin-MC3-DMA) demonstrate enhanced potency and tolerability in HCC models, enabling efficient siRNA/miRNA delivery at reduced doses [65].
Polymer-Based Systems:
- Polyethylenimine (PEI) Derivatives: Cationic polymers that complex nucleic acids through electrostatic interactions, with linear PEI (25 kDa) representing the gold standard for in vitro transfection despite cytotoxicity concerns [108].
- Biodegradable Polymeric NPs: Poly(lactic-co-glycolic acid) (PLGA) nanoparticles provide sustained release kinetics and excellent biocompatibility, with surface functionalization enabling active targeting of HCC cells [108].
Inorganic and Hybrid Systems:
- Porous Silicon Nanoparticles: Biodegradable multistage delivery systems that protect nucleic acids from degradation and provide tunable release kinetics, with demonstrated efficacy in orthotopic HCC models [65].
- Gold Nanoparticle Conjugates: Spherical nucleic acid (SNA) constructs with dense oligonucleotide surface functionalization show enhanced cellular uptake and endosomal escape without transfection reagents [108].
Cell-Derived Systems:
- Exosome-Based Delivery: Native or engineered exosomes harness natural intercellular communication pathways for efficient ncRNA delivery, with demonstrated tropism for HCC cells through inherent homing properties [65].
The following diagram illustrates the major nanocarrier systems for ncRNA delivery in HCC therapeutics:
The Scientist's Toolkit: Essential Research Reagents
Successful investigation of ncRNA therapeutics for HCC requires carefully selected research tools and methodologies. The following table details essential reagents and their applications in ncRNA research:
Table 3: Research Reagent Solutions for ncRNA Investigation in HCC
| Reagent Category | Specific Products | Application in ncRNA Research | Key Considerations |
|---|---|---|---|
| RNA Isolation | miRVana miRNA Isolation Kit (Thermo Fisher), miRNeasy Mini Kit (Qiagen) | Simultaneous purification of small and large RNAs from HCC tissues and cell lines | Assess RNA integrity number (RIN) for sequencing applications |
| qRT-PCR Assays | TaqMan MicroRNA Assays, SYBR Green-based detection | Validation of sequencing results, expression profiling across patient cohorts | Use appropriate endogenous controls (U6, RNU44 for miRNAs; GAPDH for lncRNAs/circRNAs) |
| Sequencing Kits | NEBNext Small RNA Library Prep, SMARTer smRNA-Seq Kit (Takara Bio) | Library preparation for miRNA sequencing | Optimize for input amount, incorporate unique molecular identifiers (UMIs) |
| Transfection Reagents | Lipofectamine RNAiMAX, DharmaFECT (Horizon Discovery), INTERFERin (Polyplus) | Introduction of miRNA mimics/inhibitors, siRNAs targeting lncRNAs/circRNAs | Optimize reagent:RNA ratio for each HCC cell line; assess cytotoxicity |
| Functional Assays | MTT Cell Proliferation Kit, Transwell Chambers, Annexin V-FITC Apoptosis Kit | Assessment of phenotypic effects following ncRNA modulation | Include appropriate controls (scrambled RNAs, empty vectors) |
| In Vivo Delivery | Invivofectamine 3.0 (Thermo Fisher), JetPEI-Hepatocyte (Polyplus) | Preclinical testing in mouse HCC models (subcutaneous, orthotopic) | Consider hydrodynamic injection for high-efficiency hepatocyte delivery |
| Nanoparticle Formulation | GenVoy-ILM Precision Particle Kit (Precision NanoSystems) | LNP formulation for therapeutic ncRNA delivery | Characterize particle size, PDI, encapsulation efficiency |
The comparative analysis of ncRNA classes reveals a complex therapeutic landscape with complementary strengths and limitations. miRNAs offer immediate therapeutic potential with relatively straightforward delivery but face challenges with specificity and pleiotropic effects. lncRNAs provide exceptional targeting specificity but present substantial delivery hurdles due to their size and structural complexity. circRNAs offer unprecedented stability but require further technical development in production methodologies. The future of ncRNA therapeutics in HCC will likely involve integrated approaches that target multiple ncRNA classes simultaneously, address the unique challenges of the immunosuppressive HCC TME, and leverage advances in nanomedicine for targeted delivery. As our understanding of ncRNA dysregulation in HCC deepens, these RNA-based approaches hold exceptional promise for personalized medicine strategies that can be rapidly adapted to individual patient profiles and evolving tumor dynamics.
The dysregulation of non-coding RNAs (ncRNAs) within the hepatocellular carcinoma (HCC) tumor microenvironment (TME) presents a complex landscape that demands rigorous validation techniques. This technical guide details established and emerging methodologies for validating ncRNA findings, integrating multi-omics data, and translating discoveries into clinically applicable assays. We provide a comprehensive framework encompassing high-throughput sequencing verification, computational integration strategies, and clinical performance evaluation, specifically contextualized for HCC research and drug development. Structured protocols, comparative tables, and visual workflows are included to equip researchers with practical tools for advancing ncRNA-based biomarkers and therapeutic targets.
Hepatocellular carcinoma (HCC) is characterized by a complex TME where ncRNAs—including long non-coding RNAs (lncRNAs), microRNAs (miRNAs), and circular RNAs (circRNAs)—play critical regulatory roles in immune evasion, tumor progression, and therapy resistance [6] [3]. For instance, specific lncRNAs such as NEAT1 and LINC01116 have been implicated in modulating T-cell function and promoting an immunosuppressive environment in HCC [3]. The transition from observational ncRNA discoveries to mechanistic insights and clinical applications hinges on robust validation frameworks that ensure findings are reproducible, biologically relevant, and clinically actionable.
High-throughput technologies generate vast datasets, but their clinical translation is often hampered by technical artifacts, biological heterogeneity, and analytical challenges. This guide addresses these hurdles by systematically outlining validation techniques across the research continuum—from initial sequencing data confirmation through multi-omics integration to final clinical assay development—with a specific focus on overcoming the unique challenges presented by the HCC TME.
High-Throughput Sequencing Validation
Orthogonal Verification of NGS Findings
Next-generation sequencing (NGS) has revolutionized ncRNA discovery, but its inherent limitations necessitate orthogonal validation to confirm findings, especially when working with clinical samples.
Sanger Sequencing remains a widely used method for validating single-nucleotide variants or small indels in ncRNAs identified through NGS. While often considered a gold standard, it is not without pitfalls. Key considerations include:
- Primer Design: Design primers flanking the region of interest, ensuring they do not overlap with known single-nucleotide polymorphisms (SNPs) that could cause allelic dropout [114]. Use tools like Primer-BLAST to check specificity.
- Amplification and Sequencing: Perform PCR amplification followed by capillary electrophoresis. A typical reaction uses 50 ng/μl genomic DNA, FastStart Taq DNA Polymerase, and BigDye Terminator chemistry [114].
- Limitations: Sanger sequencing can suffer from allelic dropout (ADO) due to polymorphisms in primer-binding sites, potentially leading to false negatives. Studies show that when NGS data meets high-quality thresholds (phred score ≥30, coverage depth >30×), discrepancies with Sanger sequencing often originate from Sanger artifacts rather than NGS errors [114].
High-Throughput Genotyping Assays provide scalable validation for CRISPR-edited cell lines or population studies. The genoTYPER-NEXT platform exemplifies a NGS-based approach suitable for validating ncRNA edits in high-throughput formats [115]:
- Sample Preparation: Submit CRISPR-edited cells in 96- or 384-well plates.
- Cell Lysis and Targeted Amplification: Lyse cells and perform PCR with barcoded primers targeting the edited ncRNA region.
- Pooled Sequencing: Pool amplicons and sequence on an Illumina platform.
- Data Analysis: Utilize interactive browsers to visualize indel frequencies, allele-specific expression, and frameshift consequences [115].
This method offers high sensitivity (detection of <1% allele frequency), eliminates the need for pre-screening or TA cloning, and enables the processing of thousands of samples simultaneously, making it ideal for large-scale functional validation of ncRNA candidates [115].
Table 1: Comparison of NGS Validation Techniques
| Technique | Throughput | Key Applications | Sensitivity | Limitations |
|---|---|---|---|---|
| Sanger Sequencing | Low | Validation of single variants; confirmation of small indels | ~15-20% allele frequency | Low throughput; prone to allelic dropout [114] |
| genoTYPER-NEXT | High (10,000 samples/run) | CRISPR validation; large-scale screening of ncRNA edits | <1% allele frequency | Requires NGS infrastructure; data analysis complexity [115] |
| Digital PCR | Medium | Absolute quantification of ncRNA expression; rare variant detection | <0.1% allele frequency | Limited multiplexing capability; higher cost per sample |
Analytical Validation for ncRNA Biomarkers
Before clinical application, ncRNA assays must undergo rigorous analytical validation to establish performance characteristics:
- Specificity and Sensitivity: Demonstrate the assay accurately detects the target ncRNA without cross-reacting with similar sequences. For miRNA, this includes distinguishing between family members with seed sequence homology.
- Reproducibility and Precision: Determine intra- and inter-assay coefficients of variation through repeated measurements across different days, operators, and instruments [116].
- Dynamic Range and Linearity: Establish the quantitative range over which the assay provides accurate measurements, typically through serial dilutions of synthetic RNA standards.
- Limit of Detection (LoD) and Quantification (LoQ): Determine the lowest concentration of the ncRNA that can be reliably detected and quantified, crucial for detecting low-abundance ncRNAs in liquid biopsies [116].
Multi-Omics Integration Strategies
The integration of multiple omics layers is essential for understanding the mechanistic role of ncRNAs within the HCC TME and for moving beyond correlation to causation.
Computational Integration Frameworks
Multi-omics integration strategies can be categorized based on data availability and the biological questions being addressed. The key challenge lies in reconciling data of different scales, noise ratios, and biological meanings—for instance, the imperfect correlation between chromatin accessibility and transcript levels, or between mRNA abundance and protein expression [117].
Table 2: Multi-Omics Integration Tools and Their Applications in HCC ncRNA Research
| Tool | Methodology | Integration Capacity | Best Suited for HCC ncRNA Studies |
|---|---|---|---|
| MOFA+ [117] | Factor analysis | mRNA, DNA methylation, chromatin accessibility, protein | Identifying latent factors driving lncRNA expression and immune cell infiltration in TME |
| Seurat v4/v5 [117] | Weighted nearest neighbor; Bridge integration | mRNA, chromatin accessibility, protein, spatial coordinates | Mapping ncRNA expression to specific cell subtypes in HCC spatial transcriptomics data |
| GLUE [117] | Graph-linked unified embedding | Chromatin accessibility, DNA methylation, mRNA | Integrating unmatched omics data to infer lncRNA regulatory networks |
| MultiVI [117] | Probabilistic modeling | mRNA, chromatin accessibility | Mosaic integration of scRNA-seq and scATAC-seq to link enhancer activity to ncRNA expression |
| LIGER [117] | Integrative non-negative matrix factorization | mRNA, DNA methylation | Identifying conserved and context-specific ncRNA programs across multiple HCC patient cohorts |
Practical Integration Workflow for HCC ncRNA Studies
A typical integration workflow for investigating ncRNAs in the HCC TME involves:
Data Acquisition and Preprocessing: Source multi-omics data from repositories like The Cancer Genome Atlas (TCGA), International Cancer Genomics Consortium (ICGC), or in-house generated datasets [118]. Preprocess each omics layer individually (quality control, normalization, batch correction).
Matched Integration (Vertical Integration): For data profiled from the same cells (e.g., scRNA-seq + scATAC-seq), use tools like Seurat v4 or MOFA+.
This approach allows the identification of cell populations defined by both their transcriptome (including lncRNAs) and epigenome, revealing how chromatin accessibility in immune cells correlates with lncRNA expression in the HCC TME [117].
Unmatched Integration (Diagonal Integration): For data from different cells or studies, tools like GLUE or BindSC use manifold alignment or canonical correlation analysis to infer shared biological states [117]. This is particularly useful for integrating public HCC transcriptomic data (including ncRNA expression) with in-house proteomic or metabolomic data.
Biological Interpretation: Extract and interpret the factors from MOFA+ or the shared embeddings from GLUE to identify:
- ncRNAs associated with specific immune cell states (e.g., T-cell exhaustion, M2 macrophage polarization).
- Regulatory networks linking transcription factor activity, chromatin accessibility, and ncRNA expression.
- Multi-omics subtypes of HCC with distinct prognostic implications and ncRNA dependencies.
Clinical Assay Development and Performance Evaluation
Translating research findings on ncRNAs into clinically applicable diagnostic tests requires careful consideration of regulatory standards and performance metrics.
Design Considerations for Clinical Assays
When developing molecular diagnostic tests for ncRNAs in HCC, several factors must be addressed:
- Intended Use: Clearly define the test's purpose—whether for risk stratification, early detection, prognosis, or prediction of therapy response (e.g., to immunotherapies) [116]. This determines the required performance characteristics.
- Sample Type: Choose appropriate specimen types (e.g., formalin-fixed paraffin-embedded tissue, plasma, serum) and validate the stability of ncRNAs in these matrices.
- Platform Selection: Select technologies that meet clinical laboratory requirements for robustness, throughput, and cost-effectiveness. Options include RT-digital PCR, targeted NGS panels, or hybridization-based assays.
Statistical Framework for Performance Evaluation
The clinical performance of a molecular diagnostic test is typically evaluated using several key metrics, ideally with a dichotomous outcome (positive/negative) [116]:
- Sensitivity and Specificity: Calculate with 95% confidence intervals against an appropriate reference standard.
- Positive and Negative Predictive Values: These are prevalence-dependent and crucial for understanding clinical utility.
- Area Under the Curve (AUC): For continuous tests, report the AUC of the Receiver Operating Characteristic curve.
- Reproducibility: Assess inter-laboratory and inter-operator variability.
It is critical to avoid common biases in test evaluation. Spectrum bias occurs when the patient population used for validation does not represent the intended-use population. Verification bias happens when only a subset of patients receives the reference standard test. Review bias can occur when the interpretation of the index test or reference standard is not blinded [116].
Table 3: Key Considerations for Clinical Assay Validation of ncRNA Biomarkers in HCC
| Parameter | Requirements | Example for HCC ncRNA Liquid Biopsy Assay |
|---|---|---|
| Analytical Sensitivity | Limit of Detection (LoD) established with dilution series | LoD of 5 copies/mL for plasma lncRNA HULC |
| Analytical Specificity | Demonstrate no cross-reactivity with homologous sequences | No amplification of similar lncRNAs (e.g., MALAT1) |
| Precision | ≤15% CV for intra-assay; ≤20% CV for inter-assay | CV of 12% for repeated measures of miR-122 across 10 runs |
| Reportable Range | Defined linear range of quantification | 10-10^6 copies/reaction for circRNA_100338 |
| Reference Range | Established from healthy and disease controls | 95th percentile of lncRNA UCA1 in healthy donors: <50 copies/mL |
| Clinical Cutoff | Optimized for intended use (screening vs. monitoring) | Optimized for 90% sensitivity in early HCC detection |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Key Research Reagent Solutions for HCC ncRNA Validation Studies
| Reagent/Platform | Function | Example Applications in HCC ncRNA Research |
|---|---|---|
| Illumina MiSeq [114] | Targeted NGS platform | High-throughput validation of ncRNA sequencing findings; CRISPR validation |
| genoTYPER-NEXT [115] | NGS-based genotyping service | Scalable validation of ncRNA edits in CRISPR-engineered cell lines |
| SureSelect/HaloPlex [114] | Target enrichment systems | Custom panels for capturing ncRNAs and their regulatory regions |
| Seurat v4/v5 [117] | Single-cell multi-omics analysis | Integration of scRNA-seq and scATAC-seq to map ncRNA regulation in HCC TME |
| MOFA+ [117] | Multi-omics factor analysis | Deconvolution of latent factors driving ncRNA dysregulation in HCC progression |
| GLUE [117] | Graph-linked unified embedding | Integration of unmatched omics data to infer ncRNA regulatory networks |
| Anti-PD-1/PD-L1 [3] | Immune checkpoint inhibitors | Functional validation of lncRNAs modulating immunotherapy response |
The path from initial discovery of dysregulated ncRNAs in the HCC TME to clinically applicable biomarkers and therapeutic targets requires a rigorous, multi-stage validation pipeline. This guide has outlined a comprehensive framework encompassing orthogonal verification of NGS findings, sophisticated multi-omics integration strategies, and stringent clinical assay evaluation. By adopting these standardized validation techniques and leveraging the featured research tools, scientists can enhance the reproducibility, biological relevance, and clinical translatability of their findings, ultimately accelerating the development of ncRNA-based diagnostics and therapeutics for hepatocellular carcinoma.
Conclusion
The dysregulation of ncRNAs is a cornerstone of Hepatocellular Carcinoma pathogenesis, profoundly influencing the tumor microenvironment by driving metabolic reprogramming, immune suppression, and therapy resistance. This review has synthesized evidence across four key areas: foundational mechanisms, therapeutic applications, developmental challenges, and clinical validation. The future of HCC management lies in leveraging this knowledge to develop sophisticated ncRNA-based therapeutics and biomarkers. Promising directions include creating multi-targeted delivery systems, integrating ncRNA strategies with conventional therapies to overcome resistance, and employing multi-omics approaches to build personalized diagnostic and prognostic models. Successfully translating these insights from bench to bedside holds the potential to significantly improve outcomes for HCC patients.
References
- 1. Functional Interactions Between lncRNAs/circRNAs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8858953/]
- 2. Long non-coding RNAs: definitions, functions, challenges ... [https://www.nature.com/articles/s41580-022-00566-8]
- 3. Long non-coding rnas as key modulators of the immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1523190/full]
- 4. Regulation of the tumor immune microenvironment by ... [https://www.nature.com/articles/s41419-023-05647-w]
- 5. Overview of MicroRNA Biogenesis, Mechanisms of Actions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6085463/]
- 6. Unraveling the advances of non-coding RNAs on the tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12131439/]
- 7. miRNA Biogenesis | Thermo Fisher Scientific - ET [https://www.thermofisher.com/et/en/home/life-science/epigenetics-noncoding-rna-research/epigenetics-learning-center/mirna/mirna-biogenesis.html]
- 8. Roles of circRNAs in regulating the tumor microenvironment [https://pmc.ncbi.nlm.nih.gov/articles/PMC10567871/]
- 9. The tumor microenvironment in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150456/]
- 10. Deciphering hypoxia's role in hepatocellular carcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12297087/]
- 11. Review Interactions in hepatic tumor microenvironment [https://www.sciencedirect.com/science/article/abs/pii/S0344033825002675]
- 12. Immune microenvironment in hepatocellular carcinoma [https://www.nature.com/articles/s41423-025-01308-4]
- 13. Hypoxia-induced m6A demethylation promotes ... [https://www.sciencedirect.com/science/article/pii/S2352304225003496]
- 14. Long non-coding RNAs and autophagy: dual drivers of ... [https://www.nature.com/articles/s41420-025-02667-7]
- 15. The Mechanism Underlying the ncRNA Dysregulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8904560/]
- 16. Transcriptome sequencing of hepatocellular carcinoma ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2022.927524/full]
- 17. RNA methylation in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12486860/]
- 18. The interplay between HIF - 1 and α RNAs in cancer noncoding [https://pubmed.ncbi.nlm.nih.gov/32014012/]
- 19. The interplay between HIF-1α and noncoding RNAs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6998277/]
- 20. The interplay between HIF - 1 and α RNAs in cancer noncoding [https://link.springer.com/article/10.1186/S13046-020-1535-Y]
- 21. Interplay of long non-coding RNAs and HIF-1α [https://www.sciencedirect.com/science/article/pii/S0304383520305991]
- 22. Interactions Between Non-Coding RNAs and HIF-1alpha in ... [https://www.mdpi.com/2218-273X/15/4/510]
- 23. Non-coding RNAs at the intersection of epigenetics and ... [https://www.frontiersin.org/journals/epigenetics-and-epigenomics/articles/10.3389/freae.2025.1699969/full]
- 24. Long non-coding RNAs as immune landscape regulators ... [https://www.sciencedirect.com/science/article/abs/pii/S104084282500280X]
- 25. Frontiers | Multidimensional insights into exosomes in hepatocellular ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1628573/full]
- 26. : Multifunctional contributors to the... Exosomal ncRNAs [https://pubmed.ncbi.nlm.nih.gov/38460375/]
- 27. Insights about exosomal circular RNAs as novel ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11496148/]
- 28. Immune cell-derived exosomal non-coding RNAs in tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12062983/]
- 29. Exosomal ncRNAs in liquid biopsy: a new paradigm for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1615433/full]
- 30. The role and potential mechanisms of exosomes in the progression of... [https://link.springer.com/article/10.1007/s44178-025-00171-7]
- 31. Sex-specific dysregulation of exosomal non-coding RNAs ... [https://www.nature.com/articles/s41408-025-01362-1]
- 32. Integrative analysis of exosomal ncRNAs and their regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11992429/]
- 33. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 34. The role and mechanism of noncoding RNAs in regulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9325518/]
- 35. The role of noncoding RNAs in metabolic reprogramming of ... [https://cmbl.biomedcentral.com/articles/10.1186/s11658-023-00447-8]
- 36. Metabolic reprogramming and epigenetic modifications in ... [https://www.nature.com/articles/s12276-023-01020-1]
- 37. Insights into the Regulatory Role of Non-coding RNAs in ... [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2016.00342/full]
- 38. Metabolic Reprogramming in Melanoma: An Epigenetic ... [https://www.mdpi.com/1424-8247/18/6/853]
- 39. Long non-coding rnas as key modulators of the immune ... [https://pubmed.ncbi.nlm.nih.gov/40352941/]
- 40. Long non-coding rnas as key modulators of the immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12061944/]
- 41. Functions and mechanisms of lncRNAs in immune escape ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180200/]
- 42. The landscape of immune checkpoint-related long non- ... [https://www.nature.com/articles/s42003-024-06004-z]
- 43. Comprehensive analysis of basement membrane and ... [https://www.sciencedirect.com/science/article/pii/S2405844023076703]
- 44. Non-coding RNAs in hepatocellular carcinoma: Insights ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.985815/full]
- 45. Non-coding RNAs in Hepatocellular Carcinoma [https://www.genesispub.org/non-coding-rnas-in-hepatocellular-carcinoma]
- 46. Non-Coding RNAs as Therapeutic Targets in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3916140/]
- 47. Recent advances in optimizing siRNA delivery to ... [https://pubmed.ncbi.nlm.nih.gov/40126051/]
- 48. Multi-target siRNA: Therapeutic Strategy for Hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4934040/]
- 49. Antisense oligonucleotides targeting midkine induced ... [https://www.nature.com/articles/aps2006218]
- 50. Antisense oligonucleotide is a promising intervention for liver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9780395/]
- 51. Deciphering the nexus between long non-coding RNAs ... [https://www.nature.com/articles/s41420-024-02200-2]
- 52. Nucleic acid therapeutics for liver diseases: A decade ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12496246/]
- 53. Beyond LNPs 4 Non-Viral Delivery Vehicles Expanding ... [https://www.advancingrna.com/doc/beyond-lnps-non-viral-delivery-vehicles-expanding-the-possibilities-of-mrna-therapeutics-0001]
- 54. Liver-specific drug delivery platforms - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC9521517/]
- 55. The State and Future of Viral, Nonviral Vectors for Gene ... [https://www.ajmc.com/view/the-state-and-future-of-viral-non-viral-vectors-for-gene-therapy]
- 56. Combination immunotherapy in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465164/]
- 57. Hepatocellular carcinoma: signaling pathways and ... [https://www.nature.com/articles/s41392-024-02075-w]
- 58. Utilization of artificial circular RNAs as miRNA sponges ... [https://pubmed.ncbi.nlm.nih.gov/40568595/]
- 59. Utilization of artificial circular RNAs as miRNA sponges ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1609165/full]
- 60. Circulating miRNAs as potentially predictive biomarkers for ... [https://www.nature.com/articles/s41698-025-01099-x]
- 61. The role and targeting strategies of non-coding RNAs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597961/]
- 62. CD8 T cell exhaustion-associated LncRNA signature reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508406/]
- 63. Long non-coding RNA-based single and combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405140/]
- 64. Advances in RNA-based cancer therapeutics: pre-clinical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512572/]
- 65. RNA Therapeutics: Delivery Problems and Solutions—A Review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12567017/]
- 66. Advances in Nano-Drug Delivery for Tumor ... [https://www.mdpi.com/1999-4923/17/7/942]
- 67. Molecular mechanisms of dsRNA uptake and intracellular ... [https://pubmed.ncbi.nlm.nih.gov/41177182/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1rE397IRBYU1-pjfvDdvo9knO2Yg65lpHsr4I4xr_6SQOWToB1&fc=None&ff=20251104051646&v=2.18.0.post22+67771e2]
- 68. New Study Reveals How RNA Travels Between Cells to ... [https://cmns.umd.edu/news-events/news/new-study-reveals-how-rna-travels-between-cells-control-genes-across-generations]
- 69. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 70. Measurement and clinical interpretation of CRISPR off- ... [https://www.nature.com/articles/s41588-025-02428-3]
- 71. Drug toxicity prediction based on genotype-phenotype ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12597050/]
- 72. Strategies to Avoid and Reduce Off-Target Effects [https://crisprmedicinenews.com/news/strategies-to-avoid-and-reduce-off-target-effects/]
- 73. Recent advances in AI-based toxicity prediction for drug ... [https://www.frontiersin.org/journals/chemistry/articles/10.3389/fchem.2025.1632046/full]
- 74. Role of Non-Coding RNAs in Hepatocellular Carcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10647270/]
- 75. Mechanisms of drug resistance in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12117952/]
- 76. The interplay between noncoding RNAs and drug resistance ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-023-04238-9]
- 77. Noncoding RNAs as an emerging resistance mechanism to ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1268745/full]
- 78. Non-coding RNA in drug resistance of hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6177555/]
- 79. Unraveling the advances of non-coding RNAs on the tumor ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06629-6]
- 80. Experimental Models of Hepatocellular Carcinoma—A Preclinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8344976/]
- 81. research on drug development and biomarker discovery... Translational [https://jbiomedsci.biomedcentral.com/articles/10.1186/s12929-024-01011-y]
- 82. Frontiers | Personalized treatment for hepatocellular carcinoma in the... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1150151/full]
- 83. Discovery and Validation of Clinically Relevant Long Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405614/]
- 84. Long non-coding RNA dysregulation is a frequent event in ... [https://www.nature.com/articles/s41416-020-0742-9]
- 85. Potential role of immune-related LncRNAs in prognosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399479/]
- 86. RNA high-throughput sequencing and clinical outcome ... [https://www.sciencedirect.com/science/article/pii/S2950588725000795]
- 87. Applying the multiphase optimisation strategy to develop ... [https://pubmed.ncbi.nlm.nih.gov/41248332/]
- 88. Exploring non-coding RNA mechanisms in hepatocellular ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1400744/full]
- 89. Responsive biomaterials for therapeutic strategies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405289/]
- 90. The roles and mechanisms of coding and noncoding RNA ... [https://www.nature.com/articles/s12276-024-01307-x]
- 91. Self-healing hydrogel loaded with M2pep-modified ... [https://www.sciencedirect.com/science/article/pii/S2590156725000994]
- 92. Non-Coding RNAs as Potential Diagnostic/Prognostic ... [https://www.mdpi.com/1422-0067/25/22/12235]
- 93. Clinical significance of exosomal noncoding RNAs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11812098/]
- 94. Non-coding RNAs as key regulators in hepatitis B virus- ... [https://pubmed.ncbi.nlm.nih.gov/40625740/]
- 95. The role of noncoding RNAs in the tumor microenvironment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10686793/]
- 96. Hepatocellular Carcinoma Risk Stratification for Cirrhosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422879/]
- 97. Hepatocellular carcinoma risk stratification to identify ... [https://link.springer.com/article/10.1007/s00330-025-12060-8]
- 98. Identification of Novel Tumor Microenvironment-Related ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.781307/full]
- 99. Amino acid metabolism-related LncRNAs as prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12545943/]
- 100. Dysregulated long noncoding RNAs (lncRNAs) in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-017-0734-4]
- 101. lncRNAs as prognostic molecular biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5601763/]
- 102. m6A methylation-mediated lncRNA RNF144A-AS1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12306006/]
- 103. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 104. A migrasome-related lncRNA signature predicts prognosis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581122/full]
- 105. The role and targeting strategies of non-coding RNAs in ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1642417/full]
- 106. Extracellular vesicle-derived lncRNA-GC1 serves as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12392478/]
- 107. Hypoxia- and Anoikis-Related lncRNA Signature Defines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533731/]
- 108. Role of non-coding RNA through nanomedicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579740/]
- 109. Non-coding RNAs: emerging biomarkers and therapeutic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1534862/full]
- 110. Role of Non-Coding RNAs in Hepatocellular Carcinoma ... [https://www.mdpi.com/2072-6694/15/21/5178]
- 111. The potential and challenges of circular RNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12423345/]
- 112. Advancements in clinical RNA therapeutics: Present ... [https://www.sciencedirect.com/science/article/pii/S2666379124002477]
- 113. Advances in RNA therapeutics: Classes, innovations and ... [https://www.sciencedirect.com/science/article/pii/S3050632825000162]
- 114. Sanger Validation of High-Throughput Sequencing in ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.592588/full]
- 115. High-Throughput Genotyping | CRISPR Validation [https://www.genewiz.com/public/services/next-generation-sequencing/high-throughput-genotyping]
- 116. Clinical Performance Evaluation of Molecular Diagnostic ... [https://pubmed.ncbi.nlm.nih.gov/27639547/]
- 117. A Guide to Multi-omics Integration Strategies [https://frontlinegenomics.com/a-guide-to-multi-omics-integration-strategies/]
- 118. Multi-omics Data Integration, Interpretation, and Its Application [https://pmc.ncbi.nlm.nih.gov/articles/PMC7003173/]