Single vs. Combined lncRNA Biomarkers in HCC: A Comprehensive Review of Diagnostic and Prognostic Efficacy
Hepatocellular carcinoma (HCC) is a global health challenge with high mortality, largely due to late diagnosis.
Single vs. Combined lncRNA Biomarkers in HCC: A Comprehensive Review of Diagnostic and Prognostic Efficacy
Abstract
Hepatocellular carcinoma (HCC) is a global health challenge with high mortality, largely due to late diagnosis. Long non-coding RNAs (lncRNAs) have emerged as promising biomarkers, offering new avenues for early detection and prognosis. This review synthesizes current evidence on the comparative efficacy of single versus combined lncRNA biomarkers in HCC. We explore the foundational biology of lncRNAs in hepatocarcinogenesis, evaluate methodological approaches for their detection in tissues and liquid biopsies, address challenges in clinical translation, and present a comparative analysis of their diagnostic and prognostic performance. Evidence indicates that while single lncRNAs like HULC, MALAT1, and UCA1 show promise, multi-lncRNA panels and combinations with traditional markers like AFP significantly enhance sensitivity, specificity, and prognostic stratification. This analysis provides researchers and drug development professionals with a critical resource for advancing lncRNA-based strategies toward clinical application in HCC management.
The Biological Landscape: Understanding lncRNA Roles in HCC Pathogenesis
The Clinical Challenge of Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) represents a major global health challenge as the most common form of primary liver cancer and a leading cause of cancer-related deaths worldwide [1] [2]. Despite advancements in therapeutic options, HCC prognosis remains poor, with a five-year survival rate of less than 20%, largely attributable to late-stage diagnosis when curative interventions are no longer feasible [3]. The disease typically arises in the context of chronic liver disease and cirrhosis, with key risk factors including chronic hepatitis B (HBV) and hepatitis C (HCV) infections, alcohol consumption, and metabolic dysfunction-associated steatotic liver disease (MASLD) [4] [2]. Current surveillance protocols for high-risk patients rely on abdominal ultrasound and serum alpha-fetoprotein (AFP) measurement, but both modalities present significant limitations in sensitivity and specificity, particularly in early-stage disease [3] [2] [5]. This diagnostic challenge has fueled extensive research into novel biomarkers that can enable earlier detection, more accurate prognosis, and better treatment selection.
Current Biomarker Landscape in HCC
The established biomarker landscape in HCC has long been dominated by alpha-fetoprotein (AFP), despite its well-documented limitations. AFP demonstrates inadequate sensitivity, as approximately one-third of HCC patients do not exhibit elevated levels, particularly in early-stage disease [2] [5]. Specificity is also suboptimal, as AFP elevations can occur in non-malignant chronic liver conditions including active hepatitis [5]. Additional biomarkers such as des-gamma-carboxyprothrombin (DCP) and glypican-3 (GPC3) have shown promise but still lack sufficient standalone performance for reliable early detection [6] [5].
To address these limitations, composite biomarker models have emerged. The GALAD score, which integrates gender, age, AFP, AFP-L3, and DCP, represents one of the most thoroughly validated integrative tools, demonstrating 82% sensitivity and 89% specificity for HCC detection, with an AUROC of 0.92 [2]. More recently, investigational models such as the HCC Early Detection Screening (HES) score and the aMAP score have shown potential for enhanced risk stratification and early detection [2]. These integrated approaches represent significant advances but still require broader validation and may not fully capture the molecular heterogeneity of HCC.
Table 1: Established and Emerging Biomarkers in HCC
| Biomarker Type | Examples | Performance Characteristics | Limitations |
|---|---|---|---|
| Traditional Serum Markers | AFP, DCP, GPC3 | AFP sensitivity ~50-60%; GALAD score: 82% sensitivity, 89% specificity [2] [5] | Limited sensitivity for early-stage HCC; false positives in benign liver disease [3] [5] |
| Imaging Modalities | Ultrasound, MRI, CT | Ultrasound is first-line but operator-dependent; MRI more accurate but costly [2] | Limited sensitivity in obese patients and severe steatosis; cost and accessibility barriers [2] |
| Molecular Panels | GALAD, HES score | GALAD: AUROC 0.92 for HCC detection [2] | Require further validation; limited adoption in clinical guidelines |
LncRNAs as Emerging Biomarkers in HCC
Long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers for HCC, representing a class of RNA transcripts longer than 200 nucleotides that lack protein-coding capacity [4]. These molecules play critical roles in regulating gene expression through various mechanisms, including epigenetic modification, transcriptional control, and post-transcriptional regulation [1] [4]. The relevance of lncRNAs in HCC stems from their extensive involvement in carcinogenic processes, where they function as either oncogenes or tumor suppressors to control malignant phenotypes including cell growth, proliferation, apoptosis, migration, and metastasis [1] [4].
LncRNAs offer several advantages as clinical biomarkers, including high tissue specificity, detectability in bodily fluids, and functional relevance to disease mechanisms [7] [4]. Their expression patterns are frequently altered in HCC tissues and circulation, making them accessible for liquid biopsy approaches [1] [8]. A 2017 meta-analysis of 40 studies encompassing 71 lncRNAs demonstrated that aberrant lncRNA expression significantly correlated with poor overall survival (pooled HR: 1.25) and recurrence-free survival (pooled HR: 1.66) in HCC patients [7].
Single vs. Combination LncRNA Biomarkers
Research has evolved from investigating individual lncRNAs to developing multi-lncRNA signatures that better capture HCC complexity. Single lncRNA biomarkers have demonstrated significant prognostic value in multiple studies. For instance, high expression of LINC00152 independently predicted shorter overall survival (HR: 2.524) [9], while elevated HOXC13-AS levels were associated with both reduced overall survival (HR: 2.894) and recurrence-free survival (HR: 3.201) [9]. Other single lncRNAs like LINC01146 and ELMO1-AS1 function as tumor suppressors, with their low expression predicting poorer outcomes [9].
Despite these promising results, combination lncRNA biomarkers generally demonstrate superior diagnostic and prognostic performance. A 2024 study developed a machine learning model integrating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters, achieving 100% sensitivity and 97% specificity for HCC diagnosis - significantly outperforming individual lncRNAs which showed sensitivity and specificity ranging from 60-83% and 53-67%, respectively [10]. Similarly, a 2025 study identified a plasma exosomal lncRNA-derived 6-gene risk signature (G6PD, KIF20A, NDRG1, ADH1C, RECQL4, MCM4) that effectively stratified HCC patients into molecular subtypes with distinct survival outcomes and treatment responses [8].
Table 2: Performance Comparison of Single vs. Combination LncRNA Biomarkers
| Biomarker Approach | Examples | Performance Metrics | Advantages |
|---|---|---|---|
| Single LncRNA | LINC00152 (HR: 2.524 for OS) [9] | Individual prognostic value | Simple measurement; clear biological interpretation |
| Single LncRNA | HOXC13-AS (HR: 2.894 for OS, 3.201 for RFS) [9] | Multivariate prognostic value | Independent prognostic factor |
| Single LncRNA | ELMO1-AS1 (HR: 0.518 for OS) [9] | Tumor suppressor activity | Counteracts oncogenic signals |
| Combination LncRNA | 4-lncRNA panel with machine learning [10] | 100% sensitivity, 97% specificity | Superior diagnostic accuracy; handles heterogeneity |
| Combination Signature | Exosomal lncRNA-derived 6-gene risk score [8] | Accurate prognostic stratification | Predicts treatment response; guides therapy |
Molecular Mechanisms of LncRNAs in HCC
LncRNAs contribute to hepatocellular carcinogenesis through diverse molecular mechanisms, which can be categorized into four primary functional patterns:
4.1 Signaling Molecules: Certain lncRNAs function as molecular signals in response to various stimuli. For example, the lncRNA MIR31HG responds to cellular stress and oncogenic signals, while H19 expression is induced by transforming growth factor-β (TGF-β) signaling to promote HCC progression [4].
4.2 Guides for Chromatin Modification: Many lncRNAs direct chromatin-modifying complexes to specific genomic locations. HOTAIR recruits polycomb repressive complex 2 (PRC2) to silence tumor suppressor genes, while DSCR8 facilitates transcriptional regulation through similar mechanisms [4].
4.3 Decoys for Transcription Factors or miRNAs: Numerous lncRNAs act as molecular decoys, sequestering transcription factors or microRNAs. Linc-RoR functions as a competitive endogenous RNA (ceRNA) that sponges tumor-suppressive miR-145, thereby activating downstream oncogenic pathways including p70S6K1, PDK1, and HIF-1α [4].
4.4 Scaffolds for Multi-protein Complexes: Some lncRNAs serve as structural platforms that assemble multiple protein components. NEAT1 facilitates the formation of nuclear paraspeckles and regulates gene expression through this scaffolding function [4].
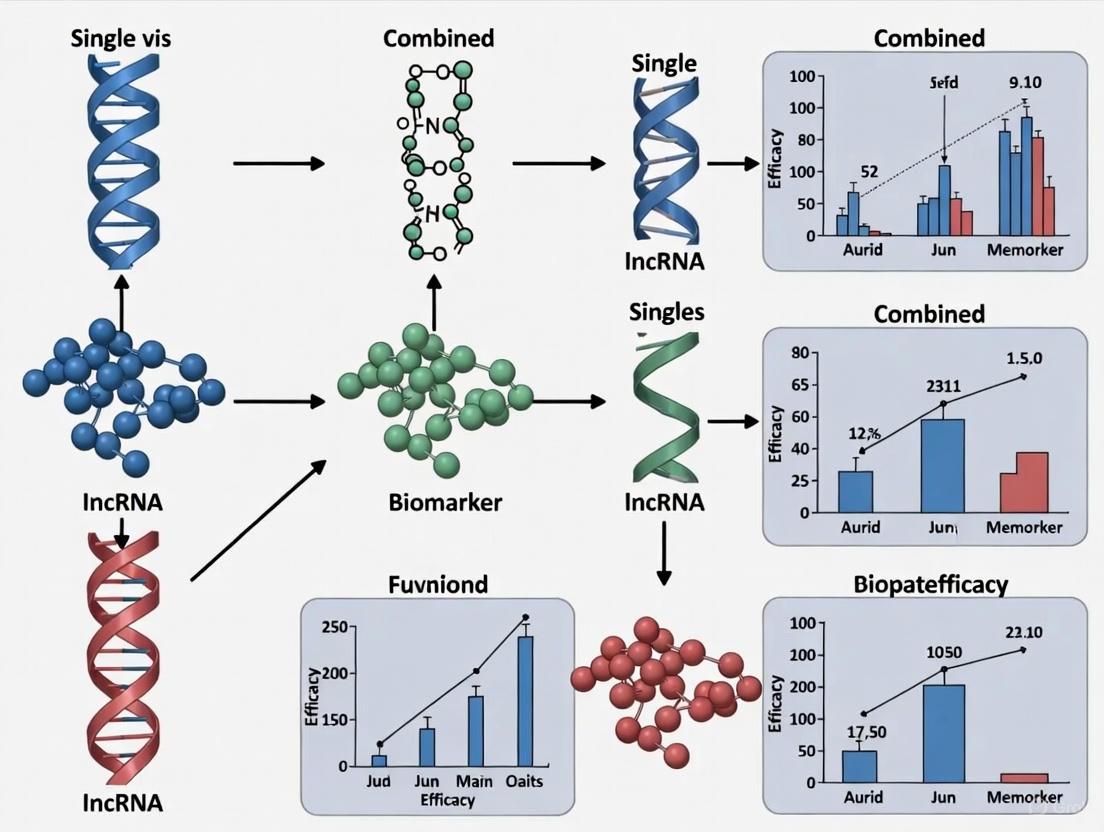
The diagram below illustrates these core mechanistic principles governing lncRNA functions in HCC:
Experimental Approaches for LncRNA Biomarker Validation
The development of robust lncRNA biomarkers requires rigorous experimental methodologies spanning discovery, validation, and clinical application phases. The following workflow outlines key experimental stages:
Sample Processing and Analysis
Standardized protocols are essential for reliable lncRNA biomarker development. The experimental workflow typically begins with sample collection from plasma, serum, or tissue specimens [8] [10]. RNA isolation is commonly performed using commercial kits such as the miRNeasy Mini Kit (QIAGEN), followed by cDNA synthesis using reverse transcription kits like RevertAid First Strand cDNA Synthesis Kit [10]. For quantification, quantitative real-time PCR (qRT-PCR) represents the gold standard, typically employing SYBR Green-based detection systems (e.g., PowerTrack SYBR Green Master Mix) with GAPDH or β-actin as reference genes for normalization [9] [10]. Data analysis generally utilizes the ΔΔCT method for relative quantification of lncRNA expression levels [10].
Advanced Analytical Approaches
Increasingly sophisticated computational methods are being applied to lncRNA biomarker research. Machine learning algorithms implemented in platforms like Python's Scikit-learn enable the integration of multiple lncRNAs with clinical parameters to develop predictive models with enhanced accuracy [8] [10]. For molecular subtyping, unsupervised consensus clustering of lncRNA-related genes can identify distinct HCC subtypes with different clinical outcomes and treatment responses [8]. Survival analysis using Cox proportional hazards models determines the prognostic significance of lncRNA biomarkers, while ROC curve analysis evaluates their diagnostic performance [7] [9] [10].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for LncRNA Biomarker Studies
| Category | Specific Product/Platform | Application in LncRNA Research |
|---|---|---|
| RNA Isolation | miRNeasy Mini Kit (QIAGEN) [10] | Total RNA extraction from plasma, serum, and tissues |
| cDNA Synthesis | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [10] | Reverse transcription of RNA to cDNA for qRT-PCR analysis |
| qRT-PCR Detection | PowerTrack SYBR Green Master Mix (Applied Biosystems) [10] | Quantitative measurement of lncRNA expression levels |
| Reference Genes | GAPDH, β-actin [9] [10] | Normalization of lncRNA expression data |
| Computational Tools | Python Scikit-learn [10] | Machine learning model development for biomarker integration |
| Bioinformatics | Competitive endogenous RNA (ceRNA) network analysis [8] | Construction of lncRNA-miRNA-mRNA regulatory networks |
| Validation Platforms | TIDE, oncoPredict algorithms [8] | Prediction of treatment response based on lncRNA signatures |
| Csnk2A-IN-1 | Csnk2A-IN-1, MF:C21H21N3O4, MW:379.4 g/mol | Chemical Reagent |
| Hdac6-IN-31 | Hdac6-IN-31, MF:C15H13FN4O2, MW:300.29 g/mol | Chemical Reagent |
The integration of lncRNA biomarkers into HCC research represents a paradigm shift in molecular diagnostics and personalized oncology. While single lncRNAs provide valuable biological insights and demonstrate independent prognostic value, combination approaches leveraging multiple lncRNAs integrated with clinical parameters and advanced computational methods show superior performance for HCC diagnosis, prognosis, and treatment prediction. The transition from single biomarkers to multi-analyte signatures reflects the molecular heterogeneity of HCC and enables more precise patient stratification. Future research directions should focus on validating these biomarkers in larger prospective cohorts, standardizing detection methodologies, and further elucidating the functional mechanisms through which lncRNAs drive hepatocarcinogenesis. As these efforts mature, lncRNA-based biomarkers hold significant promise for revolutionizing HCC management through earlier detection, more accurate prognosis, and personalized therapeutic strategies.
lncRNA Biogenesis and Functional Mechanisms in Gene Regulation
Long non-coding RNAs (lncRNAs) are defined as RNA transcripts longer than 200 nucleotides that lack protein-coding potential [11]. Once considered transcriptional "noise," lncRNAs are now recognized as critical regulators of gene expression, playing fundamental roles in cellular differentiation, development, and disease pathogenesis [12] [4]. In hepatocellular carcinoma (HCC), lncRNAs have emerged as crucial mediators of tumor initiation, progression, and metastasis through their ability to regulate oncogenes and tumor suppressor genes [13] [4]. The biogenesis of lncRNAs shares similarities with messenger RNAs (mRNAs), as most are transcribed by RNA polymerase II, and many undergo 5' capping, splicing, and polyadenylation [12] [14]. However, lncRNAs can also be processed through non-canonical mechanisms, including cleavage by ribonuclease P and circularization [12]. Their expression exhibits remarkable cell-type specificity and is frequently dysregulated in cancer, making them promising biomarkers and therapeutic targets [13] [12] [4].
Within the context of HCC research, a critical debate has emerged regarding the comparative efficacy of single lncRNA biomarkers versus multi-lncRNA signatures for prognosis prediction and clinical decision-making. This guide provides a comprehensive comparison of these approaches, supported by experimental data and methodological protocols, to inform researchers and drug development professionals in the field.
LncRNA Biogenesis, Localization, and Functional Classification
Genomic Origins and Processing Pathways
LncRNAs are classified based on their genomic context relative to protein-coding genes, which provides insight into their potential regulatory relationships [12] [14]. The major categories include:
- Intergenic lncRNAs: Transcribed from genomic regions between protein-coding genes [14]
- Intronic lncRNAs: Derived entirely from within introns of protein-coding genes [12]
- Antisense lncRNAs: Transcribed from the opposite strand of protein-coding genes [12] [14]
- Sense lncRNAs: Overlap with exons of protein-coding genes on the same strand [4]
- Enhancer RNAs: Transcribed from enhancer regions [14]
- Bidirectional lncRNAs: Transcribed in close proximity and opposite direction to protein-coding genes [12]
The subcellular localization of lncRNAs is a critical determinant of their function [15] [4]. Nuclear-enriched lncRNAs predominantly regulate chromatin organization, transcription, and RNA processing, while cytoplasmic lncRNAs primarily influence mRNA stability, translation, and post-translational modifications [15] [4]. Sequence elements including Alu repeats, specific secondary structures, and binding motifs for export factors govern this localization [15].
Molecular Mechanisms of Action
LncRNAs function through diverse molecular mechanisms, often characterized by five primary modes of action:
- Signals: LncRNAs whose expression indicates active signaling pathways or specific cellular states [12]
- Decoys: LncRNAs that "sponge" or sequester transcription factors, microRNAs, or regulatory proteins [12]
- Guides: LncRNAs that direct ribonucleoprotein complexes to specific genomic locations [12]
- Scaffolds: LncRNAs that serve as platforms for assembling multiple protein complexes [12]
- SINEUPs: LncRNAs that enhance translation of target mRNAs [12]
These functional mechanisms enable lncRNAs to regulate gene expression at epigenetic, transcriptional, and post-transcriptional levels, positioning them as master regulators of cellular homeostasis and pathogenesis [15] [12].
Diagram illustrating the biogenesis pathways and functional classification of long non-coding RNAs, highlighting key processing steps and mechanistic roles.
Comparative Analysis: Single vs. Combined LncRNA Biomarkers in HCC
Single LncRNA Biomarkers: Evidence and Limitations
Multiple studies have validated the independent prognostic value of individual lncRNAs in HCC tissues, as summarized in Table 1. These biomarkers demonstrate significant associations with overall survival (OS) and recurrence-free survival (RFS) in multivariate Cox regression analyses, accounting for conventional clinical factors [13].
Table 1: Validated Single LncRNA Biomarkers with Independent Prognostic Value in HCC
| LncRNA | Expression in Tumor | Hazard Ratio (HR) for OS | 95% CI | P-value | Cohort Size | Detection Method |
|---|---|---|---|---|---|---|
| LINC00152 | High | 2.524 | 1.661-4.015 | 0.001 | 63 | qRT-PCR |
| LINC00294 | High | 2.434 | 1.143-3.185 | 0.021 | 94 | ISH |
| LINC01094 | High | 2.091 | 1.447-3.021 | <0.001 | 365 | RNAseq |
| LINC01139 | High | 2.721 | 1.289-4.183 | 0.019 | 109 | qRT-PCR |
| LINC01146 | High | 0.38 | 0.16-0.92 | 0.033 | 85 | qRT-PCR |
| LINC01554 | Low | 2.507 | 1.153-2.832 | 0.017 | 167 | qRT-PCR |
| HOXC13-AS | High | 2.894 | 1.183-4.223 | 0.015 | 197 | qRT-PCR |
| LASP1-AS | Low | 3.539 | 2.698-6.030 | <0.0001 | 218 | qRT-PCR |
| ELF3-AS1 | High | 1.667 | 1.127-2.468 | 0.011 | 373 | RNAseq |
| ELMO1-AS1 | High | 0.430 | 0.225-0.824 | 0.011 | 112 | qRT-PCR |
| FOXP4-AS1 | High | 6.505 | 1.165-36.399 | 0.033 | 34 | qRT-PCR |
| GAS5-AS1 | High | 0.370 | 0.153-0.898 | 0.028 | 83 | qRT-PCR |
| HLA-F-AS1 | High | 2.290 | 1.191-4.403 | 0.013 | 100 | qRT-PCR |
The major advantage of single lncRNA biomarkers lies in their clinical practicality, as they can be rapidly measured using standardized techniques like qRT-PCR or RNA in situ hybridization, facilitating potential translation into diagnostic workflows [13]. However, significant limitations include biological redundancy, as HCC tumors frequently exhibit heterogeneous lncRNA expression patterns, and limited predictive power for complex phenotypes like therapeutic resistance [13] [16].
Combined LncRNA Signatures: Enhanced Prognostic Accuracy
Multi-lncRNA signatures address the limitations of single biomarkers by capturing the complexity of HCC biology through simultaneous assessment of multiple regulatory pathways. Recent studies have developed sophisticated risk models that significantly improve prognostic stratification and treatment response prediction [17] [18].
Table 2: Validated Multi-LncRNA Signatures for Prognostic Stratification in HCC
| Signature Type | Number of LncRNAs | Cohort Size | Risk Stratification | Clinical Applications | Validation Method |
|---|---|---|---|---|---|
| Amino Acid Metabolism-Related | 4 | 170 training, 170 validation | High-risk vs. Low-risk (HR: NA) | Immunotherapy response prediction, drug sensitivity | TCGA, GSVA, GSEA |
| Plasma Exosomal lncRNA-Derived | 6 mRNA signature from exosomal lncRNA network | 230 plasma exosomes, 831 HCC tissues | Three molecular subtypes (C1-C3) | Survival prediction, treatment stratification, immune microenvironment analysis | Random Survival Forest, TIDE algorithm |
| Competitive Endogenous RNA Network | 22 dysregulated exosomal lncRNAs | 112 HCC patients vs. 118 controls | Three subtypes with distinct survival | Molecular classification, therapeutic guidance | ceRNA network analysis, consensus clustering |
The plasma exosomal lncRNA-derived signature identified three molecular subtypes (C1-C3) with distinct clinical outcomes and microenvironment characteristics [18]. The C3 subtype exhibited the poorest overall survival, advanced tumor stage, immunosuppressive microenvironment (increased Treg infiltration, elevated PD-L1/CTLA4 expression), and hyperactivation of proliferation and metabolic pathways [18].
Comparative analysis of single versus combined lncRNA biomarker approaches highlighting advantages, limitations, and clinical applications in HCC management.
Experimental Protocols for LncRNA Biomarker Validation
Tissue-Based LncRNA Quantification Protocols
RNA Extraction and Quality Control
- Extract total RNA from fresh-frozen or FFPE HCC tissues using TRIzol reagent or commercial kits
- Determine RNA integrity number (RIN) using Bioanalyzer (minimum RIN ≥7.0 for sequencing)
- Verify absence of genomic DNA contamination via DNase I treatment and no-RT controls
Quantitative Reverse Transcription PCR (qRT-PCR)
- Synthesize cDNA using high-capacity reverse transcription kit with random hexamers
- Perform qPCR with SYBR Green or TaqMan chemistry using lncRNA-specific primers
- Normalize expression to reference genes (e.g., GAPDH, β-actin) using the 2^(-ΔΔCt) method
- Include no-template controls and inter-plate calibrators for technical validation
In Situ Hybridization (ISH) for Spatial Localization
- Design and validate locked nucleic acid (LNA) probes specific to target lncRNAs
- Deparaffinize tissue sections and perform antigen retrieval
- Hybridize with digoxigenin-labeled probes overnight at appropriate Tm
- Detect signals using anti-digoxigenin antibodies and colorimetric substrates
- Counterstain with hematoxylin and quantify using image analysis software
Liquid Biopsy and Exosomal LncRNA Analysis
Exosome Isolation and Characterization
- Isolate exosomes from plasma/serum using serial ultracentrifugation or commercial kits
- Validate exosome purity via transmission electron microscopy and nanoparticle tracking analysis
- Confirm presence of exosomal markers (CD63, CD81, TSG101) by western blotting
Exosomal RNA Extraction and Library Preparation
- Extract RNA using miRCURY RNA Isolation Kit with spike-in synthetic RNAs for normalization
- Assess RNA quality using Bioanalyzer Small RNA Assay
- Prepare sequencing libraries using SMARTer smRNA-Seq Kit for Illumina
- Alternatively, use targeted approaches like digital PCR for specific lncRNA quantification
Bioinformatic Analysis Pipeline
- Preprocess raw sequencing data with FastQC and Trimmomatic
- Align reads to reference genome using STAR aligner with lncRNA annotation from GENCODE
- Quantify lncRNA expression with featureCounts or StringTie
- Perform differential expression analysis using DESeq2 or edgeR
- Construct ceRNA networks using miRcode, miRTarBase, and TargetScan databases [18]
Table 3: Essential Research Tools for LncRNA Biomarker Discovery and Validation
| Category | Specific Tools/Reagents | Application | Key Features |
|---|---|---|---|
| Detection & Quantification | TRIzol Reagent, miRCURY RNA Isolation Kit, SYBR Green qPCR Master Mix, LNA ISH Probes | RNA extraction, quantification, and spatial localization | High sensitivity, lncRNA-specific detection, compatibility with multiple sample types |
| Sequencing & Analysis | SMARTer smRNA-Seq Kit, Illumina Sequencing Platforms, DESeq2, edgeR, CIRI, CIRCexplorer | Transcriptome profiling, differential expression, circular RNA detection | Comprehensive lncRNA coverage, accurate quantification, isoform resolution |
| Bioinformatic Databases | NONCODEV5, lnc2Function, exoRBase, miRcode, miRTarBase, TargetScan | lncRNA annotation, functional prediction, ceRNA network construction | Curated lncRNA collections, miRNA interaction prediction, tissue-specific expression |
| Functional Validation | LNATM GapmeRs, siRNA/shRNA constructs, Lipofectamine 3000, CCK-8 Assay Kit, Transwell Chambers | Loss-of-function studies, proliferation, migration, and invasion assays | Efficient lncRNA knockdown, phenotypic characterization, high-throughput compatibility |
| Data Integration & Modeling | ConsensusClusterPlus, randomForestSRC, Survival R package, TIDE algorithm, oncoPredict | Molecular subtyping, risk model development, therapy response prediction | Unsupervised clustering, survival analysis, immunotherapeutic response prediction |
The comprehensive analysis of lncRNA biomarkers in HCC reveals a clear evolutionary trajectory from single-marker approaches toward multi-parameter signatures that better reflect disease complexity. Single lncRNA biomarkers offer practical advantages for clinical implementation but face limitations in biological redundancy and predictive power for heterogeneous conditions like HCC [13]. In contrast, combined lncRNA signatures demonstrate superior prognostic accuracy and enable personalized treatment strategies by capturing the multifaceted nature of hepatocarcinogenesis [17] [18].
The emerging paradigm integrates multi-lncRNA signatures with clinicopathological variables, mutational profiles, and immune microenvironment data to construct comprehensive prognostic models [18]. These integrated approaches successfully stratify patients for targeted therapies, immunotherapies, and conventional treatments, ultimately advancing toward precision oncology in HCC management. Future research directions should focus on standardizing detection methodologies, validating signatures in prospective multicenter trials, and developing lncRNA-directed therapeutics that exploit the fundamental regulatory mechanisms elucidated in these studies.
Hepatocellular carcinoma (HCC) constitutes more than 90% of primary liver cancer cases and ranks as the third leading cause of cancer-related mortality worldwide [19] [13]. The pathogenesis of HCC involves complex biological processes, including DNA damage, epigenetic modifications, and oncogene mutations, often occurring against a background of chronic liver disease caused by risk factors such as hepatitis B and C viral infections, alcohol consumption, and non-alcoholic fatty liver disease [4]. Over the past decade, long non-coding RNAs (lncRNAs)—transcribed RNA molecules longer than 200 nucleotides with limited protein-coding potential—have emerged as crucial regulators of gene expression and central players in HCC pathogenesis [19] [4].
LncRNAs exert their functions through diverse mechanisms, including chromatin modification, transcriptional regulation, serving as microRNA sponges, and modulating protein activity [19]. They can be classified as either oncogenic or tumor-suppressive based on their roles in tumor development. Oncogenic lncRNAs, such as HULC, MALAT1, and HOTAIR, are frequently overexpressed in HCC and promote malignant phenotypes including cell proliferation, invasion, and metastasis. In contrast, tumor suppressor lncRNAs like GAS5 and LINC01146 are often downregulated, and their loss contributes to unchecked tumor growth [13] [10]. This comparative guide provides a systematic analysis of key lncRNAs in HCC, focusing on their molecular mechanisms, clinical relevance, and potential as diagnostic and prognostic biomarkers, with particular emphasis on the comparative efficacy of single versus combined lncRNA approaches in HCC research.
Comparative Analysis of Key Oncogenic and Tumor Suppressor lncRNAs
Table 1: Oncogenic lncRNAs in Hepatocellular Carcinoma
| lncRNA | Full Name | Expression in HCC | Molecular Mechanisms | Functional Consequences | Prognostic Value |
|---|---|---|---|---|---|
| HULC | Hepatocellular Carcinoma Up-Regulated Long Non-Coding RNA | Upregulated [20] | Functions as a miRNA sponge; modulates viral replication in HBV-related HCC [4] [21] | Promotes cell proliferation, inhibits apoptosis [19] | High expression correlated with poor survival [22] |
| MALAT1 | Metastasis Associated Lung Adenocarcinoma Transcript 1 | Upregulated [20] | Regulates alternative splicing; promotes aggressive tumor phenotypes [19] [10] | Enhances tumor invasion and metastasis [19] | Conflicting reports (both favorable & poor prognosis) [20] |
| HOTAIR | HOX Transcript Antisense RNA | Upregulated [23] | Recruits chromatin-modifying complexes; induces epigenetic silencing [23] | Promotes proliferation, metastasis; associated with poor survival [23] [10] | Poor overall and disease-free survival [10] |
| H19 | Imprinted Maternally Expressed Transcript | Upregulated [23] | Stimulates CDC42/PAK1 axis by down-regulating miRNA-15b [4] | Increases proliferation rate of HCC cells [4] | Associated with tumor expansion and metastasis [23] |
| LincRNA-UFC1 | Long Intergenic Non-Protein Coding RNA UFC1 | Upregulated [19] | Stabilizes β-catenin transcript in a HuR-dependent manner [19] | Promotes cell-cycle progression and proliferation [19] | Correlated with tumor size, cancer stage, and poor outcomes [19] |
Table 2: Tumor Suppressor lncRNAs in Hepatocellular Carcinoma
| lncRNA | Full Name | Expression in HCC | Molecular Mechanisms | Functional Consequences | Prognostic Value |
|---|---|---|---|---|---|
| GAS5 | Growth Arrest Specific 5 | Downregulated [10] | Triggers CHOP and caspase-9 signal pathways [10] | Inhibits proliferation, activates apoptosis [10] | High expression correlated with longer OS [13] |
| LINC01146 | Long Intergenic Non-Protein Coding RNA 1146 | Downregulated [13] | Mechanism not fully elucidated | Suppresses tumor growth [13] | High expression correlated with longer OS [13] |
| MIR31HG | MIR31 Host Gene | Downregulated [4] | Potential tumor suppressor mechanism under investigation | Inhibits tumor progression [4] | Potential therapeutic target [4] |
| LINC01554 | Long Intergenic Non-Protein Coding RNA 1554 | Downregulated [13] | Mechanism not fully elucidated | Suppresses tumor growth [13] | Low expression predicts shorter OS [13] |
| LncRNA-LET | Long Non-Coding RNA Low Expression in Tumor | Downregulated [19] | Regulated by hypoxia-induced histone deacetylase 3 | Prevents hypoxia-induced HCC cell invasion [19] | Down-regulated in HCC [19] |
Table 3: Clinically Validated Prognostic lncRNAs in HCC Tissues
| lncRNA | Patient Cohort Size | Detection Method | HR for Overall Survival | 95% CI | P-value |
|---|---|---|---|---|---|
| LINC00152 | 63 | qRT-PCR | 2.524 | 1.661-4.015 | 0.001 |
| LINC01139 | 109 | qRT-PCR | 2.721 | 1.289-4.183 | 0.019 |
| LINC01146 | 85 | qRT-PCR | 0.38 | 0.16-0.92 | 0.033 |
| HOXC13-AS | 197 | qRT-PCR | 2.894 | 1.183-4.223 | 0.015 |
| ELF3-AS1 | 373 | RNAseq | 1.667 | 1.127-2.468 | 0.011 |
| ELMO1-AS1 | 222 (training+validation) | qRT-PCR | 0.518 (training) | 0.277-0.968 | 0.039 |
Molecular Mechanisms and Signaling Pathways
LncRNAs regulate HCC pathogenesis through complex molecular interactions and signaling networks. The diagram below illustrates the key mechanistic roles of major oncogenic and tumor suppressor lncRNAs in HCC:
LncRNA-UFC1 exemplifies a novel mechanistic pathway in HCC pathogenesis. This cytosolic lncRNA promotes tumorigenesis by forming a complex with the RNA-binding protein HuR and β-catenin mRNA, facilitating their translocation from the nucleus to the cytoplasm. This interaction stabilizes the β-catenin transcript, increasing β-catenin protein levels and promoting nuclear translocation. Consequently, expression of β-catenin target genes such as c-myc and cyclin D1 is enhanced, driving cell-cycle progression and proliferation while inhibiting apoptosis [19].
Multiple lncRNAs contribute to the Wnt/β-catenin signaling cascade, a pathway well-known for its involvement in cancer cell metabolism. HULC operates through a distinct mechanism by functioning as a competitive endogenous RNA (ceRNA) or "miRNA sponge," sequestering microRNAs and preventing them from binding to their target mRNAs. This mechanism effectively inactivates tumor-suppressive miRNAs, leading to increased expression of their oncogenic targets [19] [4]. Similarly, H19 stimulates the CDC42/PAK1 axis by down-regulating miRNA-15b expression, thereby increasing the proliferation rate of HCC cells [4].
Nuclear-enriched lncRNAs such as HOTAIR and MALAT1 primarily function through epigenetic mechanisms. HOTAIR recruits chromatin-modifying complexes to specific genomic locations, inducing epigenetic silencing of tumor suppressor genes [23]. MALAT1 regulates alternative splicing of various pre-mRNAs and promotes aggressive tumor phenotypes [19]. In contrast, tumor suppressor lncRNAs like GAS5 activate apoptosis through CHOP and caspase-9 signal pathways, thereby inhibiting HCC progression [10].
Diagnostic and Prognostic Applications
Single versus Combined lncRNA Biomarkers
The diagnostic and prognostic performance of lncRNAs varies significantly between single-marker approaches and multi-marker panels. Research demonstrates that combination approaches substantially enhance diagnostic accuracy and prognostic stratification in HCC.
Table 4: Diagnostic Performance of Single vs. Combined lncRNA Biomarkers
| Biomarker Approach | Sensitivity (%) | Specificity (%) | Clinical Utility | Study Details |
|---|---|---|---|---|
| LINC00152 (single) | 60-83 | 53-67 | Moderate individual diagnostic accuracy [10] | Plasma levels in HCC patients vs. controls [10] |
| GAS5 (single) | 60-83 | 53-67 | Moderate individual diagnostic accuracy [10] | Plasma levels in HCC patients vs. controls [10] |
| Four-lncRNA Panel | Information missing | Information missing | Superior to individual lncRNAs [10] | Combined LINC00152, LINC00853, UCA1, GAS5 [10] |
| Machine Learning Model | 100 | 97 | Excellent diagnostic performance [10] | Integration of lncRNAs with clinical laboratory parameters [10] |
| HULC + RP11-731F5.2 | Information missing | Information missing | HCC risk stratification in CHC patients [22] | Plasma biomarkers in chronic hepatitis C [22] |
A 2024 study investigating a four-lncRNA panel (LINC00152, LINC00853, UCA1, and GAS5) demonstrated that while individual lncRNAs exhibited moderate diagnostic accuracy with sensitivity and specificity ranging from 60-83% and 53-67% respectively, their combination significantly improved performance. Notably, integrating these lncRNAs with conventional laboratory parameters using a machine learning model achieved 100% sensitivity and 97% specificity, highlighting the superior efficacy of combinatorial approaches [10].
For prognostic applications, numerous studies have validated the independent prognostic significance of individual lncRNAs through multivariate Cox regression analysis. For instance, high pre-treatment expression of LINC00152 in tumor tissues independently predicted shorter overall survival (HR, 2.524; 95% CI, 1.661-4.015; P=0.001) in 63 HCC patients treated with curative surgical resection [13]. Similarly, high expression of HOXC13-AS was independently associated with shorter overall survival (HR, 2.894; 95% CI, 1.183-4.223; P=0.015) and recurrence-free survival (HR, 3.201; 95% CI, 1.372-4.653; P=0.004) in 197 HCC patients [13].
The prognostic value of lncRNAs extends beyond tumor tissue to circulating biomarkers. HULC has been detected in the blood of HCC patients, suggesting its potential as a non-invasive biomarker for disease diagnosis and monitoring [19] [22]. A study focusing on chronic hepatitis C patients found that plasma levels of HULC and RP11-731F5.2 could serve as potential biomarkers for HCC risk stratification, enabling early intervention in high-risk populations [22].
Emerging Risk Models and Clinical Applications
Recent research has explored the development of comprehensive risk models incorporating multiple lncRNAs for improved prognostic stratification. One study constructed a novel risk model based on four amino acid metabolism-related lncRNAs that effectively categorized HCC patients into distinct risk groups. Patients in the high-risk group had significantly lower overall survival rates and exhibited different immune infiltration patterns, with increased immunosuppressive cells and elevated expression of immune checkpoints including CD276, CTLA4, and TIGIT. Importantly, the high-risk group showed better responses to anti-PD1 immunotherapy, suggesting the model's utility in guiding treatment selection [17].
The experimental workflow for developing such comprehensive lncRNA signatures typically involves multiple stages, as illustrated below:
This comprehensive approach to lncRNA signature development enables robust prognostic stratification and therapeutic guidance, moving beyond the limitations of single-marker analysis.
Experimental Methodologies and Research Reagents
Standard Experimental Protocols for lncRNA Analysis
The analysis of lncRNAs in HCC research employs standardized molecular biology techniques with specific modifications for lncRNA detection and characterization:
RNA Isolation and Quality Control: Total RNA is typically isolated from fresh-frozen or preserved tissue samples and plasma/serum samples using commercial kits such as the Qiagen miRNeasy mini-kit or Norgen Biotek Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit [20] [22]. For liquid biopsies, larger plasma volumes (500 μL) are often processed to obtain sufficient RNA yield. RNA quality is confirmed using metrics such as RNA integrity number (RIN) ≥8 as measured by Agilent 2100 Bioanalyzer [20]. Treatment with Turbo DNase is performed to remove genomic DNA contamination [22].
cDNA Synthesis and Quantitative PCR: Reverse transcription is carried out using High-Capacity cDNA Reverse Transcription Kit or similar reagents [22]. Quantitative real-time PCR (qRT-PCR) is performed using SYBR Green or TaqMan chemistry with specific primers for target lncRNAs. The PCR conditions typically include initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 60-62°C for 1 minute [10] [22]. The housekeeping genes GAPDH and β-actin are commonly used for normalization [10] [22]. Each reaction is performed in triplicate with appropriate negative controls.
lncRNA Detection Techniques: Beyond qRT-PCR, various methods are employed for lncRNA detection and quantification:
- Microarray Analysis: Used for discovery-phase profiling of lncRNA expression patterns. Involves labeling with cyanine dyes and hybridization to whole human genome microarrays, followed by scanning and feature extraction [20].
- RNA Sequencing (RNAseq): Provides comprehensive transcriptome-wide analysis of lncRNA expression. Particularly valuable for identifying novel lncRNAs and isoform-specific expression [13].
- In Situ Hybridization (ISH): Enables spatial localization of lncRNAs within tissue sections, providing important information about subcellular distribution and cell-type-specific expression [13].
Functional Validation Experiments:
- In Vitro Studies: Include gene overexpression (using expression vectors) and knockdown approaches (using siRNA or shRNA) in HCC cell lines, followed by functional assays including CCK-8 assay for cell viability, colony formation assay for growth potential, migration and invasion assays [17].
- In Vivo Studies: Utilize xenograft models in immunodeficient mice (e.g., BALB/c nude mice) to assess tumor growth and metastasis [19].
Table 5: Key Research Reagent Solutions for lncRNA Studies in HCC
| Reagent/Resource Category | Specific Examples | Application Notes | Reference |
|---|---|---|---|
| RNA Isolation Kits | Qiagen miRNeasy mini-kit; Norgen Biotek Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit | For tissue and liquid biopsy samples respectively | [20] [22] |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit; RevertAid First Strand cDNA Synthesis Kit | Essential for cDNA synthesis from RNA templates | [22] [10] |
| qPCR Master Mixes | Power SYBR Green PCR Master Mix; PowerTrack SYBR Green Master Mix | Enable quantitative detection of lncRNAs | [22] [10] |
| Cell Culture Reagents | DMEM medium with 10% fetal bovine serum; Lipofectamine 3000 transfection reagent | For maintenance and genetic manipulation of HCC cell lines | [17] |
| Functional Assay Kits | CCK-8 assay kit; Colony formation assay reagents | For assessing cell viability and growth potential | [17] |
| HCC Cell Lines | THLE2, Hep-3B, Huh-1, Huh-7, HCCLM3 | Representative in vitro models for HCC studies | [17] |
| Public Databases | TCGA-LIHC; Molecular Signature Database (MSigDB) | Sources for transcriptomic data and gene sets | [17] |
The comprehensive analysis of oncogenic and tumor suppressor lncRNAs in HCC reveals a complex regulatory network with significant implications for cancer diagnosis, prognosis, and treatment. Key oncogenic lncRNAs including HULC, MALAT1, HOTAIR, H19, and LincRNA-UFC1 promote hepatocellular carcinoma through diverse mechanisms such as miRNA sponging, epigenetic regulation, and modulation of key signaling pathways like Wnt/β-catenin. Conversely, tumor suppressor lncRNAs such as GAS5, LINC01146, and LncRNA-LET inhibit tumor progression and are frequently downregulated in HCC.
The emerging paradigm in lncRNA research emphasizes the superiority of multi-marker panels over single lncRNA approaches for both diagnostic and prognostic applications. Machine learning integration of lncRNA signatures with conventional clinical parameters demonstrates remarkable accuracy in HCC diagnosis and risk stratification. Furthermore, lncRNA-based risk models show promise in predicting response to immunotherapy, potentially guiding treatment selection for advanced HCC.
Future research directions should focus on validating lncRNA signatures in larger, multi-center cohorts and standardizing detection methodologies for clinical translation. The development of lncRNA-targeted therapeutics, such as antisense oligonucleotides or small molecule inhibitors, represents an exciting frontier in precision oncology for hepatocellular carcinoma. As our understanding of lncRNA biology deepens, these non-coding molecules are poised to become integral components of comprehensive diagnostic, prognostic, and therapeutic strategies for HCC.
Hepatocellular carcinoma (HCC) remains one of the most lethal malignancies worldwide, ranking third in cancer-related mortality and posing a major global health concern [24] [4]. Despite advancements in treatment, the 5-year survival rate for HCC patients remains dismal, often below 20%, due to high recurrence rates, limited responsiveness to therapies, and frequent late-stage diagnosis [24] [25]. The pathogenesis of HCC involves complex biological processes including DNA damage, epigenetic modifications, and oncogene mutations that drive tumor initiation and progression [4]. Within this complex landscape, long non-coding RNAs (lncRNAs) have emerged as critical regulatory molecules that influence key pathways in HCC, including the PI3K/AKT/mTOR signaling axis, autophagic processes, and metabolic reprogramming [24] [26] [27]. This review examines the mechanistic roles of lncRNAs within these critical pathways and evaluates the comparative efficacy of single versus combined lncRNA biomarkers for advancing HCC diagnosis, prognosis, and therapeutic development.
LncRNAs in PI3K/AKT/mTOR Signaling
The PI3K/AKT/mTOR pathway represents a classic dysregulated signaling axis in HCC, profoundly influencing cell survival, proliferation, metabolism, and resistance to therapy [27]. This oncogenic pathway is regulated by numerous lncRNAs that show both oncogenic and tumor-suppressive functions in hepatocellular carcinoma.
Table 1: LncRNAs Regulating PI3K/AKT/mTOR Pathway in HCC
| LncRNA | Expression | Target/Mechanism | Biological Function | Clinical Relevance |
|---|---|---|---|---|
| HULC | Upregulated | miR-186/HMGA2; ERK/YB-1; Sirt1 [25] | Promotes tumorigenesis, progression, metastasis [25] | Diagnostic potential, chemotherapy resistance [25] |
| MALAT1 | Upregulated | miR-30a-5p; miR-195/EGFR; miR-143-3p/ZEB1 [25] | Promotes tumorigenesis, metastasis, chemotherapy resistance [25] | Predictor for recurrence [25] |
| NEAT1 | Upregulated | miR-139/TGF-β1; miR-485/STAT3; miR-101-3p/WEE1 [25] | Promotes tumor progression, metastasis [25] | Resistance to chemotherapy and radiotherapy [25] |
| PTTG3P | Upregulated | PTTG1/PI3K/AKT [25] | Promotes cell growth, metastasis [25] | Activates PI3K/AKT signaling [25] |
| CASC11 | Upregulated | PTEN and PI3K/AKT [25] | Promotes migration, invasion, EMT [25] | Activates PI3K/AKT signaling [25] |
| FOXD2-AS1 | Upregulated | DKK1 and Wnt/β-catenin [25] | Promotes tumor progression [25] | Activates Wnt/β-catenin signaling [25] |
| CASC2 | Downregulated | miR-24-3p; miR-367/FBXW7; miR-362-5p/NF-kB [25] | Inhibits tumor growth, migration, invasion [25] | Tumor suppressor [25] |
The mechanistic role of lncRNAs in PI3K/AKT/mTOR signaling involves sophisticated regulatory networks. Many lncRNAs function as competing endogenous RNAs (ceRNAs) that sequester microRNAs, preventing them from repressing target genes within the pathway [26] [27]. For instance, lncRNA HULC promotes HCC progression by acting as a miRNA sponge for miR-186, thereby upregulating HMGA2 expression and driving oncogenic signaling [25]. Similarly, lncRNA PTTG3P enhances HCC cell growth and metastasis by activating the PI3K/AKT pathway through interaction with PTTG1 [25]. The dysregulation of these lncRNAs has significant clinical implications, with many associated with clinicopathological features and clinical prognosis in HCC [27].
Figure 1: LncRNA Regulation of PI3K/AKT/mTOR Pathway in HCC. Oncogenic lncRNAs (yellow) promote pathway activation through miRNA sponging, while tumor suppressor lncRNAs (green) inhibit it. Pathway components (red) ultimately drive HCC progression (blue).
LncRNA-Autophagy Crosstalk in HCC
Autophagy plays a paradoxical, context-dependent role in hepatocellular carcinoma, acting as a tumor suppressor during early stages but promoting tumor survival and progression in advanced disease [24] [26]. This catabolic process is intricately regulated by lncRNAs that influence autophagic flux through multiple molecular mechanisms.
The molecular landscape of autophagy in HCC involves key steps including initiation, nucleation, elongation, maturation, and degradation, each controlled by specific protein complexes and regulatory molecules [24]. Two pivotal cellular energy sensors, mTOR and AMPK, tightly regulate autophagy initiation in response to environmental cues like nutrient availability and stress [24]. The PI3K complex, containing VPS34 and Beclin-1, is essential for phagophore nucleation, while the ATG8 system (including LC3 and GABARAP proteins) mediates elongation and closure of autophagosomal membranes [24].
Table 2: LncRNAs Modulating Autophagy in HCC
| LncRNA | Autophagy Role | Molecular Targets | Functional Outcome | Therapeutic Implications |
|---|---|---|---|---|
| Multiple Oncogenic lncRNAs | Promotes pro-tumor autophagy | miRNA sponging, chromatin remodeling, protein interactions [24] | Enhanced survival, therapy resistance [24] | Potential targets for combination therapies |
| HULC | Modulates drug resistance | Alters autophagic flux [24] | Promotes survival under treatment [24] | Target for overcoming chemoresistance |
| HOTAIR | Regulates energy metabolism | GLUT1/mTOR [25] | Supports nutrient utilization in TME [25] | Potential metabolic target |
| LncRNAs in Early HCC | Tumor suppressive via autophagy | Beclin1, ATG5, ATG7 [24] | Prevents genomic instability [24] | May require context-specific targeting |
LncRNAs regulate autophagy through diverse mechanisms including miRNA sponging, chromatin remodeling, and direct protein interactions [24]. They integrate into key autophagy signaling networks such as PI3K/AKT/mTOR, AMPK, and Beclin-1 pathways [24]. For instance, deficient macroautophagy in cancerous hepatocytes results in elevated oxidative stress and p62 accumulation, both playing critical roles in HCC development and malignant transformation [24]. The suppression of macroautophagy impairs lysosomal degradation of p62 and mutated proteins, leading to their accumulation and contributing to tumor progression [24].
The therapeutic implications of targeting the lncRNA-autophagy axis are significant. LncRNAs have been shown to modulate drug resistance, including resistance to first-line agents, by altering autophagic flux and associated molecular pathways [24]. Emerging strategies for targeting this axis include siRNAs, antisense oligonucleotides, and CRISPR/Cas systems that have shown promise in preclinical studies and may be adapted for HCC [24].
LncRNAs in Amino Acid Metabolic Reprogramming
While research on lncRNAs specifically regulating amino acid metabolism in HCC is still emerging, compelling evidence indicates their significant involvement in metabolic reprogramming, a hallmark of cancer. Tumor cells exhibit heightened demands for amino acids to support protein synthesis, nucleotide production, and energy metabolism, with lncRNAs serving as key regulators of these adaptive processes.
The regulatory mechanisms of lncRNAs in amino acid metabolism encompass multiple levels of control. LncRNAs can influence the expression of amino acid transporters, modulate the activity of metabolic enzymes, and regulate key signaling pathways that sense nutrient availability [24] [26]. For instance, under stressful conditions such as nutrient deprivation, tumor cells activate adaptive mechanisms including ER stress due to increased demand for protein biosynthesis [24]. The cellular response to these conditions determines whether pro-adaptive autophagy is induced or cell death mechanisms are activated [24].
The mTOR pathway, heavily influenced by lncRNAs as detailed in Section 2, serves as a central regulator of amino acid metabolism [24] [27]. mTORC1 is particularly sensitive to amino acid availability and coordinates cellular anabolic processes accordingly. LncRNAs that regulate mTOR signaling indirectly exert control over amino acid utilization, protein synthesis, and metabolic adaptation in HCC cells [24].
Furthermore, the interconnection between autophagy and amino acid metabolism creates a regulatory loop in which lncRNAs play integral roles. Autophagy recycles cellular components to generate free amino acids during nutrient deprivation, and lncRNAs modulating autophagy consequently influence amino acid pools and availability [24] [26]. This relationship highlights the complex networks through which lncRNAs coordinate metabolic adaptation in the challenging tumor microenvironment.
Single vs. Combined LncRNA Biomarkers: A Comparative Analysis
The development of reliable biomarkers represents a crucial frontier in improving HCC diagnosis and prognosis. Current evidence strongly supports the superior performance of combined lncRNA panels over single lncRNA biomarkers for clinical applications.
Table 3: Comparative Performance of Single vs. Combined LncRNA Biomarkers in HCC
| Biomarker Type | Examples | Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|
| Single lncRNA | LINC00152: HR 2.524 for OS [13] | Variable sensitivity/specificity [28] | Simpler analysis, lower cost | Limited robustness, context-dependent expression |
| LINC00294: HR 2.434 for OS [13] | ||||
| LINC01554: HR 2.507 for OS (low expression) [13] | ||||
| Combined Panels | 3-lncRNA signature (PTENP1, LSINCT-5, CUDR) [29] | Outperformed CEA and CA19-9 [29] | Higher specificity and sensitivity, robust classification | More complex analysis, validation challenges |
| 9-lncRNA hypoxia/anoikis model [30] | Stratified patients into distinct risk groups [30] | Incorporates biological pathways, prognostic value | Requires larger cohorts for development | |
| Combined with AFP | Linc00152 + AFP [29] | 82.9% sensitivity, 88.2% specificity [29] | Enhanced performance over single markers | Still requires validation in diverse populations |
The independent prognostic significance of individual lncRNAs has been demonstrated in multiple studies. For instance, Wang et al. revealed that high pre-treatment expression of LINC00152 in tumor tissues independently predicted shorter overall survival (HR 2.524) in HCC patients [13]. Similarly, Zhang et al. showed that high LINC00294 expression correlated with shorter OS (HR 2.434) [13], while Zheng et al. demonstrated that low LINC01554 expression predicted shorter OS (HR 2.507) [13]. These findings establish the fundamental prognostic value of individual lncRNAs in HCC.
However, combined lncRNA signatures demonstrate enhanced diagnostic and prognostic performance. A serum three-lncRNA signature consisting of PTENP1, LSINCT-5, and CUDR (UCA1) significantly outperformed conventional biomarkers CEA and CA19-9 in gastric cancer diagnostics [29]. Similarly, a nine-lncRNA prognostic model based on hypoxia- and anoikis-related lncRNAs effectively predicted overall survival in HCC patients, with high-risk groups showing increased immunosuppressive elements in the tumor microenvironment [30].
The integration of lncRNA biomarkers with traditional markers like AFP further enhances diagnostic performance. The combination of lncRNA Linc00152 with AFP demonstrated 82.9% sensitivity and 88.2% specificity in HCC diagnosis, superior to either marker alone [29]. This approach leverages the strengths of both established and novel biomarkers, potentially facilitating clinical translation while improving accuracy.
Experimental Methodologies and Research Toolkit
Robust experimental protocols are essential for investigating lncRNAs in HCC pathways and validating their clinical utility. Standardized methodologies have emerged across the field for lncRNA detection, functional characterization, and therapeutic targeting.
Core Methodologies for lncRNA Research
Detection and Quantification Methods:
- Quantitative Reverse-Transcription PCR (qRT-PCR): The gold standard for lncRNA quantification in tissue and blood specimens [13]. Provides high sensitivity for detecting expression changes in clinical samples.
- RNA Sequencing (RNAseq): Enables comprehensive profiling of lncRNA expression patterns [13] [30]. Essential for discovering novel lncRNAs and identifying expression signatures.
- In Situ Hybridization (ISH): Allows spatial localization of lncRNAs within tissues [13]. Critical for understanding tissue-specific expression patterns.
Functional Characterization Approaches:
- Gain/Loss-of-Function Studies: Utilizing siRNA, shRNA, or CRISPR/Cas systems to knockdown or knockout lncRNA expression [24] [26]. Assesses functional consequences on cellular phenotypes.
- Mechanistic Investigations: Employ RNA immunoprecipitation (RIP), chromatin isolation by RNA purification (ChIRP), and luciferase reporter assays to identify molecular interactions [26].
Bioinformatic Analyses:
- Differential Expression Analysis: Utilizing packages like limma with FDR threshold of 0.05 to identify significantly dysregulated lncRNAs [30].
- Survival Analysis: Using univariate Cox proportional hazard regression to evaluate prognostic significance [13] [30].
- Risk Model Construction: Applying LASSO Cox regression with 10-fold cross-validation to develop prognostic signatures [30].
Figure 2: Experimental Workflow for lncRNA Biomarker Development. Key steps include sample collection, lncRNA detection, bioinformatic analysis, functional validation, and model development.
Essential Research Reagent Solutions
Table 4: Essential Research Reagents for lncRNA Investigations in HCC
| Reagent Category | Specific Examples | Application Purpose | Technical Considerations |
|---|---|---|---|
| Detection Assays | qRT-PCR kits (TaqMan, SYBR Green) [13] | LncRNA quantification | Primers must span exon-exon junctions to avoid genomic DNA amplification |
| RNAseq library prep kits [13] [30] | Transcriptome-wide profiling | Ribosomal RNA depletion recommended for lncRNA enrichment | |
| Functional Tools | siRNA/shRNA constructs [24] | LncRNA knockdown | Multiple constructs recommended to control for off-target effects |
| CRISPR/Cas9 systems [24] | LncRNA knockout | sgRNA design critical for specific targeting | |
| Antisense oligonucleotides (ASOs) [24] | LncRNA inhibition | Chemical modifications enhance stability and delivery | |
| Cell Culture | HCC cell lines (Li-7, etc.) [30] | In vitro modeling | Authentication and mycoplasma testing essential |
| Hypoxia chambers (1% O2) [30] | Microenvironment modeling | Standardized oxygen control required for reproducibility | |
| Analysis Tools | LASSO Cox regression [30] | Prognostic model development | 10-fold cross-validation recommended for parameter selection |
| Tubulysin A intermediate-1 | Tubulysin A intermediate-1, MF:C31H52N4O7S, MW:624.8 g/mol | Chemical Reagent | Bench Chemicals |
| HCoV-OC43-IN-1 | HCoV-OC43-IN-1, MF:C23H22F6N4O2, MW:500.4 g/mol | Chemical Reagent | Bench Chemicals |
The investigation of lncRNAs in critical HCC pathways reveals an intricate regulatory network that profoundly influences tumor behavior through PI3K/AKT/mTOR signaling, autophagy, and metabolic reprogramming. The accumulated evidence demonstrates that combined lncRNA biomarkers significantly outperform single lncRNA approaches in diagnostic and prognostic accuracy, offering enhanced clinical utility for HCC management. Future research directions should focus on validating these findings in large, diverse patient cohorts, standardizing detection methodologies, and developing targeted therapeutic approaches that exploit the lncRNA-pathway interactions. As our understanding of these complex regulatory networks deepens, lncRNA-based biomarkers and therapies hold substantial promise for advancing precision medicine in hepatocellular carcinoma.
Long non-coding RNAs (lncRNAs) have emerged as pivotal regulators in hepatocellular carcinoma (HCC) pathogenesis, with significant implications for diagnosis and prognosis. This review comprehensively compares the efficacy of single versus combined lncRNA biomarkers in HCC research, demonstrating that multi-lncRNA signatures consistently outperform individual markers in prognostic accuracy and clinical utility. Through analysis of current experimental data and methodologies, we provide a structured evaluation of lncRNA biomarker performance, technical protocols, and emerging applications in clinical decision-making, offering researchers a validated framework for biomarker implementation in HCC management.
Hepatocellular carcinoma represents a significant global health challenge, ranking as the sixth most common malignancy worldwide and the third leading cause of cancer-related deaths [31]. The molecular complexity and heterogeneity of HCC have spurred extensive research into novel biomarkers for early detection, accurate prognosis, and personalized treatment strategies. Among these, long non-coding RNAs—transcripts longer than 200 nucleotides with limited or no protein-coding capacity—have emerged as promising candidates due to their tissue-specific expression, functional diversity, and presence in bodily fluids [32] [4].
LncRNAs regulate gene expression through multiple mechanisms: as signaling molecules recruiting transcription factors; as guides directing chromatin-modifying enzymes to specific genomic locations; as decoys sequestering transcription factors or microRNAs; and as scaffolds mediating the formation of multi-component complexes [13]. In HCC, dysregulated lncRNAs influence critical cancer hallmarks including proliferation, metastasis, angiogenesis, and drug resistance [31] [4]. More importantly, their detectable presence in both tissues and circulation positions them as ideal biomarkers for clinical application.
This review systematically evaluates the comparative efficacy of single versus combined lncRNA biomarkers within HCC research, providing structured experimental data, methodological protocols, and analytical frameworks to guide researchers and clinicians in leveraging these molecules for improved patient outcomes.
Molecular Mechanisms of lncRNAs in HCC Pathogenesis
LncRNAs exert their functional effects through diverse molecular mechanisms that impact HCC development and progression. Understanding these mechanisms provides crucial context for their utility as biomarkers.
Regulatory Paradigms and Functional Classes
The functional classification of lncRNAs is largely determined by their subcellular localization. Nuclear lncRNAs primarily regulate transcription and chromatin organization, while cytoplasmic lncRNAs influence mRNA stability, translation, and post-translational modifications [4]. Specifically in HCC, several regulatory paradigms have been established:
- Epigenetic Regulation: LncRNAs such as HOTAIR recruit chromatin-modifying complexes to specific genomic loci, enabling dynamic control of gene expression patterns [33] [4].
- Post-transcriptional Regulation: LncRNAs including NEAT1 function as competing endogenous RNAs (ceRNAs) by sequestering microRNAs, thereby preventing these miRNAs from binding to their target mRNAs [31] [4].
- Protein Scaffolding: LncRNAs serve as organizational platforms that bring multiple protein components into proximity, facilitating complex formation and signaling activation, as demonstrated by Linc-RoR in hypoxic HCC environments [4].
The diagram below illustrates the primary molecular mechanisms through which lncRNAs influence hepatocellular carcinoma development and progression:
Context-Specific lncRNA Functions in HCC Microenvironment
The functional impact of lncRNAs extends to specific aspects of the HCC tumor microenvironment. For instance, lnc-Tim3 directly binds to the immune checkpoint protein Tim-3 on CD8+ T cells, blocking interaction with Bat3 and inhibiting downstream signaling, thereby exacerbating T cell exhaustion and facilitating immune evasion [31]. Similarly, CircMET promotes immunosuppression through the miR-30-5p/Snail/DPP4 axis, reducing CD8+ T cell infiltration and potentially diminishing response to immunotherapy [31].
Metabolism-related lncRNAs also contribute significantly to HCC progression. In glucose-deprived conditions, linc-RoR acts as a miR-145 sponge, leading to upregulation of p70S6K1, PDK1, and HIF-1α, thereby enhancing glycolytic activity and supporting tumor cell survival under metabolic stress [4].
Comparative Analysis of Single vs. Combined lncRNA Biomarkers
Prognostic Performance of Individual lncRNA Biomarkers
Multiple individual lncRNAs demonstrate significant prognostic value in HCC, as validated through multivariate Cox regression analyses. The table below summarizes key single lncRNA biomarkers with independently verified prognostic significance:
Table 1: Single lncRNA Biomarkers with Independent Prognostic Value in HCC
| lncRNA | Expression in HCC | HR (95% CI) | P-value | Cohort Size | Endpoints | Detection Method |
|---|---|---|---|---|---|---|
| LINC00152 | Upregulated | 2.524 (1.661-4.015) | 0.001 | 63 | OS | qRT-PCR [13] |
| LINC00294 | Upregulated | 2.434 (1.143-3.185) | 0.021 | 94 | OS | ISH [13] |
| LINC01094 | Upregulated | 2.091 (1.447-3.021) | <0.001 | 365 | OS | RNAseq [13] |
| LINC01146 | Downregulated | 0.38 (0.16-0.92) | 0.033 | 85 | OS | qRT-PCR [13] |
| HOXC13-AS | Upregulated | 2.894 (1.183-4.223) | 0.015 | 197 | OS, RFS | qRT-PCR [13] |
| LASP1-AS | Downregulated | 3.539 (2.698-6.030) | <0.0001 | 423 | OS, RFS | qRT-PCR [13] |
| ELMO1-AS1 | Upregulated | 0.430 (0.225-0.824) | 0.011 | 222 | OS, RFS | qRT-PCR [13] |
| GAS5-AS1 | Upregulated | 0.370 (0.153-0.898) | 0.028 | 83 | OS | qRT-PCR [13] |
Individual lncRNAs demonstrate substantial prognostic value, with hazard ratios (HR) frequently exceeding 2.0 for upregulated markers or falling below 0.5 for tumor-suppressive lncRNAs. However, their individual performance characteristics vary considerably across different patient cohorts and detection platforms.
Enhanced Predictive Accuracy with Multi-lncRNA Signatures
Combined lncRNA signatures consistently outperform individual biomarkers in prognostic accuracy and clinical utility across multiple studies. The table below compares representative multi-lncRNA signatures reported in recent literature:
Table 2: Combined lncRNA Signatures for HCC Prognostication
| lncRNA Signature | Number of lncRNAs | AUC (1-year) | AUC (3-year) | AUC (5-year) | Clinical Applications | Reference |
|---|---|---|---|---|---|---|
| Amino Acid Metabolism-Related | 4 | 0.79 | 0.75 | 0.72 | Prognosis, immunotherapy response prediction [17] | |
| Disulfidptosis-Related | 3 | 0.756 | 0.695 | 0.701 | Prognosis, drug sensitivity [34] | |
| Migrasome-Related (LINC00839, MIR4435-2HG) | 2 | 0.81 | 0.78 | 0.75 | Prognosis, immune microenvironment assessment [35] | |
| Plasma-based (LINC00152, LINC00853, UCA1, GAS5) | 4 | 1.00 (sensitivity) | 0.97 (specificity) | N/A | Early detection, machine learning integration [10] | |
| HEIH, MIAT, HOTAIR | 3 | N/A | N/A | N/A | Diagnostic signature, therapeutic targeting [33] |
The enhanced performance of multi-lncRNA signatures stems from their ability to capture the molecular heterogeneity of HCC and provide a more comprehensive representation of the disease biology than single biomarkers. For instance, the 4-lncRNA amino acid metabolism-related signature not only predicted prognosis but also identified patients with distinct immune microenvironment characteristics and differential responses to anti-PD1 immunotherapy [17].
Direct Performance Comparison: Individual vs. Combination Approaches
The comparative advantage of combination approaches becomes evident when examining studies that directly evaluate both individual and combined lncRNA biomarkers. In one analysis of plasma lncRNAs for HCC detection, individual markers (LINC00152, LINC00853, UCA1, and GAS5) demonstrated moderate diagnostic accuracy with sensitivity and specificity ranging from 60-83% and 53-67%, respectively [10]. However, when integrated within a machine learning model, the combination achieved 100% sensitivity and 97% specificity, significantly outperforming any single marker [10].
Similarly, in the disulfidptosis-related lncRNA study, the 3-lncRNA signature demonstrated time-dependent AUC values of 0.756, 0.695, and 0.701 for 1-, 3-, and 5-year survival, respectively—performance characteristics that exceeded those of individual lncRNAs in the same cohort [34]. This pattern of superior performance for combination approaches consistently emerges across studies employing diverse methodological frameworks.
Experimental Protocols and Methodological Considerations
Standardized Workflow for lncRNA Biomarker Validation
The translational pipeline for lncRNA biomarker development follows a structured workflow from discovery to clinical validation. The diagram below outlines the key stages in establishing and validating lncRNA biomarkers for HCC:
Essential Research Reagents and Methodological Specifications
Successful implementation of lncRNA biomarker studies requires standardized reagents and methodologies across laboratories. The table below details essential research solutions and their applications in lncRNA biomarker workflows:
Table 3: Essential Research Reagent Solutions for lncRNA Biomarker Studies
| Reagent/Category | Specific Examples | Application Purpose | Technical Considerations |
|---|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN), Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) | Isolation of high-quality RNA from tissues and biofluids | DNase treatment recommended to remove genomic DNA contamination [10] [22] |
| cDNA Synthesis Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific), High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | Reverse transcription of lncRNAs | Random hexamers or gene-specific primers; uniform reaction conditions essential [10] [22] |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems), Power SYBR Green PCR Master Mix (Thermo Fisher) | Quantitative detection of lncRNA expression | SYBR Green chemistry with melt curve analysis for specificity verification [10] [22] |
| Reference Genes | β-actin, GAPDH | Normalization of lncRNA expression data | Stability should be validated across sample types; multiple reference genes recommended [10] [22] |
| Bioinformatics Tools | CombiROC, TIDE, GDSC | Combinatorial analysis, immunotherapy response prediction, drug sensitivity | Web-based tools (CombiROC) enable optimal biomarker combination identification [22] |
Analytical Framework for Biomarker Performance Assessment
Rigorous statistical approaches are essential for evaluating lncRNA biomarker performance. The standard analytical sequence includes:
- Univariate Cox Regression: Initial screening of individual lncRNAs associated with clinical outcomes (typically P < 0.05) [17] [34]
- LASSO Cox Regression: Penalized regression method to select the most informative lncRNA combinations while preventing overfitting [17] [35] [34]
- Multivariate Cox Modeling: Construction of final risk score using the formula: Risk score = Σ(CoefficientlncRNAi × ExpressionlncRNAi) [35] [34]
- Stratification and Validation: Division of patients into high-risk and low-risk groups based on median risk score, followed by validation in independent cohorts [35] [34]
- Performance Metrics: Time-dependent receiver operating characteristic (ROC) analysis assessing sensitivity, specificity, and area under curve (AUC) at 1, 3, and 5 years [17] [34]
This structured analytical approach ensures robust biomarker development and facilitates direct comparison across different lncRNA signatures.
Clinical Translation and Practical Applications
Integration with Current Diagnostic and Prognostic Modalities
The clinical utility of lncRNA biomarkers is enhanced when integrated with established HCC assessment tools. For instance, combining lncRNA profiles with radiographic imaging (LI-RADS criteria) and standard serum markers (AFP) significantly improves early detection capabilities [10] [22]. Similarly, incorporating lncRNA signatures with clinical staging systems (BCLC, TNM) provides refined prognostic stratification beyond conventional clinicopathological parameters alone [13] [34].
The application of machine learning algorithms to integrate multi-lncRNA signatures with conventional biomarkers represents a particularly promising approach. One study demonstrated that a model combining four plasma lncRNAs with standard laboratory parameters achieved near-perfect discrimination between HCC patients and controls, substantially outperforming individual biomarkers [10].
Predictive Biomarkers for Therapy Selection
Beyond diagnosis and prognosis, lncRNA signatures show emerging utility as predictive biomarkers for treatment response. The amino acid metabolism-related lncRNA signature effectively stratified patients according to their likelihood of responding to anti-PD1 immunotherapy, with high-risk patients potentially deriving greater benefit from immune checkpoint inhibition [17]. Similarly, the migrasome-related lncRNA signature (LINC00839 and MIR4435-2HG) correlated with immunosuppressive microenvironment features, providing insights for patient selection for combination immunotherapy approaches [35].
Functional studies further support the therapeutic relevance of these biomarkers. Knockdown of MIR4435-2HG—a component of the migrasome-related signature—significantly reduced HCC cell proliferation, migration, epithelial-mesenchymal transition, and PD-L1 expression, confirming its role in both tumor progression and immune evasion mechanisms [35].
The comprehensive analysis presented herein demonstrates the clear advantage of multi-lncRNA signatures over individual biomarkers for HCC management. Combined lncRNA profiles consistently outperform single markers in prognostic accuracy, diagnostic precision, and clinical utility across diverse patient populations and methodological approaches.
Future developments in lncRNA biomarker research will likely focus on several key areas: standardization of detection methodologies across platforms, validation in large prospective clinical trials, integration with other molecular data types (genomic, proteomic), and development of point-of-care testing platforms for clinical implementation. Additionally, the functional characterization of lncRNAs included in prognostic signatures may reveal novel therapeutic targets, further expanding their clinical relevance beyond diagnostic applications.
As the field advances, lncRNA-based biomarkers hold exceptional promise for addressing critical challenges in HCC management, particularly through enabling earlier detection, personalizing therapeutic approaches, and improving prognostic precision in this clinically heterogeneous disease.
From Bench to Bedside: Detection Methods and Clinical Applications of lncRNA Biomarkers
Hepatocellular carcinoma (HCC) remains a major global health challenge, ranking third in mortality among all human cancers worldwide [13]. The discovery of independent prognostic biomarkers for early identification and timely treatment of HCC patients with poor prognosis is a critical goal for improving survival outcomes [13]. Long non-coding RNAs (lncRNAs) have emerged as one of the most investigated classes of non-coding RNAs, playing important roles in controlling HCC occurrence and development through regulation of oncogene and tumor suppressor gene expression [13]. The detection of these molecules in both tissue and blood specimens relies on three principal technological platforms: RT-qPCR, RNA sequencing, and in situ hybridization. This guide provides an objective comparison of these platforms' performance characteristics, experimental parameters, and applications within the evolving paradigm of single versus combined lncRNA biomarkers in HCC research.
Technological Platform Comparison
The selection of an appropriate detection platform is crucial for accurate lncRNA biomarker assessment. Each technology offers distinct advantages and limitations for research and potential clinical application.
Table 1: Performance Characteristics of lncRNA Detection Platforms
| Feature | RT-qPCR | RNA Sequencing | In Situ Hybridization |
|---|---|---|---|
| Sensitivity | High (detects low-abundance transcripts) [22] | High (broad dynamic range) [36] | Moderate (depends on probe design and abundance) [37] |
| Specificity | High (primers and probes) [22] | High (alignment to reference genome) [36] | High (sequence-specific probes) [37] |
| Throughput | Medium to High (multiplexing possible) | Very High (genome-wide) | Low (single marker per slide typically) |
| Quantification | Absolute or relative (precise) [22] | Absolute (digital counting) [36] | Semi-quantitative (based on signal intensity) [37] |
| Spatial Context | No (homogenized sample) | No (homogenized sample) | Yes (preserves tissue architecture) [37] |
| Primary Application | Targeted validation and quantification [22] | Discovery and transcriptome-wide profiling [36] | Localization within tissue morphology [37] |
| Sample Input | Low (nanograms of RNA) [22] | Moderate (tens to hundreds of ng) [36] | Tissue sections or cells [37] |
| Data Complexity | Low | High (requires bioinformatics) | Medium (requires pathology expertise) |
Table 2: Experimental and Practical Considerations
| Parameter | RT-qPCR | RNA Sequencing | In Situ Hybridization |
|---|---|---|---|
| Key Reagent Solutions | Sequence-specific primers, SYBR Green or TaqMan probes, reverse transcriptase [22] | Library prep kits, exome capture probes, sequencing flows cells [36] | Labeled antisense probes, hybridization buffers, detection enzymes [37] |
| Typified Protocol | RNA isolation, DNase treatment, cDNA synthesis, amplification with 40 cycles of 95°C/15s and 62°C/1min [22] | RNA/DNA isolation, library prep, hybridization & capture, sequencing on platforms like NovaSeq 6000 [36] | Cell fixation/permeabilization, incubation with biotinylated probe overnight, DAPI counterstaining [37] |
| Cost per Sample | Low | High | Medium |
| Turnaround Time | 1 day | Several days to weeks | 2-3 days |
| Tissue Compatibility | Fresh frozen, FFPE (with optimization) | Fresh frozen, FFPE (with optimization) [36] | FFPE, fresh frozen [37] |
| Blood/Plasma Compatibility | Yes (common for liquid biopsy) [22] | Yes (increasingly used) [38] | No (requires intact cells/tissue) |
Detailed Experimental Protocols
RT-qPCR for Circulating lncRNAs
The use of RT-qPCR for detecting lncRNAs in plasma, a form of liquid biopsy, involves specific steps to handle low-abundance targets [22]. Total RNA is isolated from 500 μL of plasma using specialized purification kits designed for circulating and exosomal RNA. Researchers treat RNA samples with Turbo DNase to eliminate genomic DNA contamination. Reverse transcription is performed using a High-Capacity cDNA Reverse Transcription Kit. The RT-qPCR itself is run using Power SYBR Green PCR Master Mix on a system like StepOne PlusTM with the following cycling conditions: initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 62°C for 1 minute [22]. The lncRNA expression level is calculated using the 2−ΔΔCt method with β-actin as an internal reference, and assay specificity is confirmed by dissociation melting curve analysis [22].
RNA Sequencing Workflow
The integrated RNA and DNA sequencing workflow provides a comprehensive molecular profile [36]. For nucleic acid isolation, the AllPrep DNA/RNA FFPE Kit or similar is used for formalin-fixed paraffin-embedded (FFPE) tumors. For library construction, 10–200 ng of input DNA or RNA is required. Library construction from FFPE tissue RNA is performed using exome capture kits (e.g., SureSelect XTHS2). Hybridization and capture use the SureSelect Human All Exon V7 + UTR exome probe for RNA. Sequencing is performed on a NovaSeq 6000, with stringent quality control at every stage, including Q30 > 90% and PF > 80% [36]. Bioinformatic processing includes alignment to the hg38 genome using STAR aligner, gene expression quantification with Kallisto, and variant calling from RNA-seq data using specialized tools like Pisces [36].
In Situ Hybridization Protocol
The ISH protocol preserves the spatial information of lncRNA expression within tissues [37]. Cells are seeded onto culture slides and allowed to adhere fully. They are then fixed, permeabilized, and blocked with a prehybridization solution. The cells are incubated overnight at 4°C with a biotinylated probe to enable specific binding. For subcellular localization, a key functional aspect of lncRNAs, nuclear and cytoplasmic fractions can be separated using a commercial extraction kit (e.g., Minute Cytoplasmic and Nuclear Extraction Kit), with U6 and GAPDH serving as internal controls for nuclear and cytoplasmic RNA, respectively [37]. Finally, the cell nuclei are stained with DAPI and imaged under a fluorescence microscope [37].
Research Reagent Solutions
Table 3: Essential Research Reagents and Kits
| Reagent/Kits | Function/Purpose | Example Uses |
|---|---|---|
| Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) [22] | Isolation of high-quality RNA from low-input, low-concentration biofluids. | Extraction of lncRNAs from patient plasma for liquid biopsy studies. |
| AllPrep DNA/RNA FFPE Kit (Qiagen) [36] | Co-isolation of genomic DNA and total RNA from a single FFPE tissue section. | Integrated DNA/RNA analysis from precious archival clinical samples. |
| SureSelect XTHS2 RNA Kit (Agilent) [36] | Preparation of strand-specific RNA-seq libraries from FFPE-derived RNA. | Target enrichment for transcriptome sequencing from challenging samples. |
| TruSeq Stranded mRNA Kit (Illumina) [36] | Preparation of sequencing libraries from poly-adenylated RNA. | Whole-transcriptome analysis for fusion detection and expression profiling. |
| Minute Cytoplasmic and Nuclear Extraction Kit (Invent) [37] | Rapid separation of cellular compartments to determine RNA localization. | Functional studies to determine if a lncRNA acts in the nucleus or cytoplasm. |
| Power SYBR Green PCR Master Mix (Thermo Fisher) [22] | Sensitive detection of amplified PCR products in real-time. | Quantitative measurement of specific lncRNA targets in validation experiments. |
Application in Single vs. Combined lncRNA Biomarker Research
The choice of detection platform is intrinsically linked to the strategic approach of investigating single versus combined lncRNA biomarkers.
For single lncRNA biomarkers, the research focus is on targeted, high-throughput validation. RT-qPCR is often the preferred tool due to its cost-effectiveness, simplicity, and quantitative precision. For example, studies have validated the independent prognostic value of single lncRNAs like LINC00152 (shorter OS: HR, 2.524) and LINC01146 (longer OS: HR, 0.38) in HCC tumor tissues using RT-qPCR [13]. ISH plays a complementary role by confirming the cellular origin and spatial distribution of these promising single markers within the tumor microenvironment, as demonstrated in the study of LINC00294 using in situ hybridization [13].
The paradigm is shifting toward combined biomarker panels to improve prognostic accuracy and overcome tumor heterogeneity. Here, RNA sequencing becomes the enabling technology. Its hypothesis-free, comprehensive nature allows for the discovery of multi-lncRNA signatures in a single assay [36]. This is crucial for developing clinically robust tools, as combinations of biomarkers can capture more of the molecular complexity of HCC. The analytical validation of integrated RNA-seq assays, which can detect gene expression, fusions, and sequence variants, is foundational for this approach [36].
Furthermore, the combination of different biomarker types is being explored. For instance, circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs) are promising blood-based biomarkers for detecting Minimal Residual Disease (MRD) in HCC, with sensitivities of 50–80% and specificities up to 94% [38]. A multi-omics approach that layers lncRNA data from RNA-seq with ctDNA mutations and protein biomarkers like AFP represents the cutting edge of HCC biomarker research.
Workflow Diagram for Platform Selection
The following diagram illustrates the decision-making workflow for selecting an appropriate detection platform based on research objectives and sample type.
The comparative analysis of RT-qPCR, RNA sequencing, and in situ hybridization reveals a complementary technological landscape for lncRNA detection in HCC research. RT-qPCR excels in cost-effective, sensitive, and high-throughput targeted validation, making it ideal for quantifying specific single or small-panel lncRNA biomarkers in blood and tissue. RNA sequencing provides a powerful discovery engine for identifying novel lncRNA signatures and enabling comprehensive multi-analyte approaches, which are fundamental for developing combined biomarker panels. In situ hybridization offers the unique advantage of morphological context, critical for understanding the tumor microenvironmental distribution of promising lncRNA markers.
The selection of the optimal platform is not a one-size-fits-all decision but must be strategically aligned with the research objective—whether it is discovery, validation, or localization—and the nature of the available sample. As the field progresses toward more complex, multi-analyte biomarker models for precise HCC prognosis and treatment stratification, the integration of data from these diverse technological platforms will be essential. The future of lncRNA biomarker research lies not in the supremacy of a single platform, but in their judicious combined application.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most prevalent cancer worldwide and the fourth most common cause of cancer-related mortality [10]. A critical factor contributing to its poor survival rate is that approximately 80% of cases are diagnosed at intermediate or advanced stages, missing the optimal window for curative treatments such as surgical resection [39]. The endemic prevalence of hepatitis B and C viruses further exacerbates the HCC burden in many regions, creating an urgent need for effective early detection methods [10] [21].
While alpha-fetoprotein (AFP) remains the most widely used serological biomarker in clinical practice, its sensitivity is significantly reduced in early-stage HCC detection, limiting diagnostic utility [39]. Conventional imaging modalities are similarly constrained by insufficient diagnostic accuracy. Against this backdrop, liquid biopsy has emerged as a promising minimally invasive approach for cancer diagnosis and monitoring. Among its various biomarkers, long non-coding RNAs (lncRNAs)—RNA molecules exceeding 200 nucleotides without protein-coding capacity—have recently gained attention for their critical regulatory functions in pivotal pathophysiological mechanisms, including cellular migration, angiogenesis, and tumorigenesis [39] [13]. LncRNAs are notably stable in circulation and can be detected in plasma and serum, making them ideal candidates for liquid biopsy applications [10].
This review examines the comparative efficacy of single versus combined lncRNA biomarkers in HCC research, focusing on their performance characteristics, methodological considerations, and clinical applicability.
Experimental Workflows for lncRNA Biomarker Studies
Sample Collection and Processing
The initial step in lncRNA biomarker research involves careful sample collection and processing. Studies typically obtain fasting venous blood samples from patients before treatment initiation. Blood for serum preparation is drawn into vacuum tubes containing inert separation gel and a procoagulant, while blood for plasma preparation uses anticoagulant tubes containing ethylenediaminetetraacetic acid (EDTA) [39]. The samples are centrifuged, and the separated serum/plasma is aliquoted and stored at -80°C for subsequent analyses, with the entire procedure completed within 2 hours of collection to preserve RNA integrity [39].
Extracellular Vesicle Isolation and Characterization
Since many circulating lncRNAs are encapsulated within extracellular vesicles (EVs) which protect them from degradation, EV isolation is a crucial step in the workflow. EVs are typically isolated from serum and plasma using size-exclusion chromatography and ultrafiltration methods [39]. After thawing, samples are pretreated with a 0.8 μm filter, then separated via a gel-permeation column, with PBS eluent collected and concentrated using a 100kD ultrafiltration tube [39].
Multiple validation techniques are employed to characterize the isolated EVs:
- Particle size distribution: Detected by nano-flow cytometry [39]
- Morphology assessment: Observed by transmission electron microscopy with uranyl acetate staining [39]
- Marker protein detection: Confirmed by Western blot for proteins such as TSG101, Alix, CD9, with Calnexin as a negative control [39]
RNA Extraction and Quantification
Total RNA is isolated from EVs or directly from plasma/serum using commercial purification kits. For EV-derived RNA, protocols typically involve adding specific buffers to the vesicle suspension, followed by vortexing and centrifugation [39]. The supernatant is combined with ethanol, loaded onto a purification column, and centrifuged multiple times with wash buffers before RNA elution [39].
Reverse transcription into complementary DNA (cDNA) is performed using standard kits, followed by quantitative real-time PCR (qRT-PCR) to measure lncRNA expression levels. Reactions are typically performed in triplicate using SYBR Green Master Mix on a real-time PCR system, with the housekeeping gene GAPDH used for normalization of expression data. The ΔΔCT method is employed for relative quantification and data analysis [10].
Validation and Statistical Analysis
Comprehensive statistical analyses are crucial for validating lncRNA biomarkers. Studies typically employ receiver operating characteristic (ROC) curve analysis to evaluate diagnostic accuracy, calculating area under the curve (AUC) values, sensitivity, and specificity for individual lncRNAs and combinations [10]. Machine learning approaches are increasingly utilized to integrate multiple lncRNAs with conventional laboratory parameters for improved diagnostic performance [10].
Figure 1: Experimental workflow for circulating lncRNA analysis in liquid biopsy, from sample collection to downstream applications.
Performance Comparison: Single vs. Combined lncRNA Biomarkers
Individual lncRNA Biomarkers and Their Diagnostic Performance
Multiple individual lncRNAs have demonstrated diagnostic and prognostic value in HCC research. The table below summarizes key lncRNAs investigated as single biomarkers and their performance characteristics:
Table 1: Performance characteristics of single lncRNA biomarkers in HCC
| lncRNA | Expression in HCC | Sample Type | Reported Sensitivity | Reported Specificity | Primary Functions |
|---|---|---|---|---|---|
| LINC00152 | Upregulated [10] | Plasma | 83% [10] | 67% [10] | Promotes cell proliferation through CCDN1 regulation [10] |
| UCA1 | Upregulated [10] | Plasma | 60% [10] | 53% [10] | Promotes proliferation and inhibits apoptosis [10] |
| GAS5 | Downregulated [10] | Plasma | 63% [10] | 60% [10] | Triggers CHOP and caspase-9 signal pathways, activating apoptosis [10] |
| LINC00853 | Upregulated [10] | Plasma | 67% [10] | 57% [10] | Not fully characterized [10] |
| LINC00152:GAS5 Ratio | Increased [10] | Plasma | N/A | N/A | Higher ratio correlated with increased mortality risk [10] |
Combined lncRNA Biomarkers and Their Enhanced Performance
Research consistently demonstrates that combinations of lncRNAs show superior diagnostic performance compared to individual markers. The integration of multiple lncRNAs into biomarker panels enhances sensitivity and specificity for HCC detection:
Table 2: Performance of combined lncRNA biomarkers and signature panels in HCC
| Biomarker Combination | Sample Type | Sensitivity | Specificity | Additional Notes |
|---|---|---|---|---|
| 4-lncRNA panel (LINC00152, LINC00853, UCA1, GAS5) with machine learning [10] | Plasma | 100% [10] | 97% [10] | Integration with conventional lab parameters; superior to individual markers [10] |
| 9-lncRNA signature (9LncSigAMI) [40] | Plasma | 93.88% [40] | 98% [40] | Originally developed for myocardial infarction; demonstrates potential for multi-disease application [40] |
| 3-disulfidptosis-related lncRNA signature [34] | Tissue | N/A | N/A | AUCs: 0.756 (1-year), 0.695 (3-year), 0.701 (5-year) for survival prediction [34] |
| Plasma exosomal lncRNA-related 6-gene signature [18] | Plasma exosomes | N/A | N/A | Random survival forest-derived; predicts immunotherapy response [18] |
| EV-derived lncRNA network [39] | Serum EVs | N/A | N/A | Identified 133 significantly differentially expressed lncRNAs in HCC; 10 core lncRNAs associated with progression [39] |
Prognostic Value of lncRNA Biomarkers
Beyond diagnostic applications, lncRNAs show significant promise as prognostic biomarkers in HCC. Multivariate Cox regression analyses have identified numerous lncRNAs as independent prognostic factors:
Table 3: Prognostic values of single lncRNA biomarkers in HCC tissues
| lncRNA | Hazard Ratio (HR) | 95% Confidence Interval | P-value | Prognostic Impact |
|---|---|---|---|---|
| LINC00152 [13] | 2.524 | 1.661-4.015 | 0.001 | Shorter overall survival |
| LINC00294 [13] | 2.434 | 1.143-3.185 | 0.021 | Shorter overall survival |
| LINC01094 [13] | 2.091 | 1.447-3.021 | <0.001 | Shorter overall survival |
| LINC01146 [13] | 0.38 | 0.16-0.92 | 0.033 | Longer overall survival |
| HOXC13-AS [13] | 2.894 | 1.183-4.223 | 0.015 | Shorter overall survival and recurrence-free survival |
| ELMO1-AS1 [13] | 0.518 (training) | 0.277-0.968 | 0.039 | Longer overall survival and recurrence-free survival |
| FOXP4-AS1 [13] | 2.712 (training) | 1.140-6.450 | 0.024 | Shorter overall survival and recurrence-free survival |
Molecular Mechanisms and Regulatory Networks
LncRNAs exert their functions through diverse molecular mechanisms, including serving as signaling molecules, guiding chromatin-modifying enzymes, functioning as decoy molecules to sequester transcription factors or microRNAs, and working as scaffolding molecules to mediate the formation of multi-component complexes [13]. In the context of HCC, lncRNAs participate in critical regulatory networks:
ceRNA Regulatory Networks
A particularly important mechanism involves the competitive endogenous RNA (ceRNA) network, where lncRNAs function as "molecular sponges" that sequester microRNAs, thereby derepressing their target mRNAs. For instance, upregulated exosomal lncRNAs in HCC form ceRNA networks regulating numerous genes significantly enriched in cell cycle regulation, TGF-β signaling, the p53 pathway, and ferroptosis [18].
Pathway Involvement
Functional enrichment analyses demonstrate that HCC-associated lncRNAs are involved in critical cancer-relevant processes including cell proliferation regulation, transmembrane ion transport, cytosol/plasma membrane localization, protein binding, and autophagy/MAPK pathways [39]. Protein-protein interaction (PPI) network analyses have identified hub genes such as NTRK2 and KCNJ10 within these lncRNA-mediated regulatory networks [39].
Figure 2: Molecular mechanisms of lncRNAs in HCC pathogenesis and their functional consequences.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 4: Essential research reagents and solutions for circulating lncRNA studies
| Category | Specific Product/Technology | Application Purpose | Key Features |
|---|---|---|---|
| EV Isolation | Size-exclusion chromatography (ES911 columns) [39] | EV isolation from serum/plasma | Preserves vesicle integrity; separates based on size |
| Ultrafiltration (100kD filters) [39] | Concentration of EV isolates | Retains EVs while removing contaminants | |
| Characterization | Transmission electron microscopy [39] | EV morphology assessment | Visual confirmation of vesicle structure |
| Nano-flow cytometry [39] | Particle size distribution | Quantitative analysis of EV size and concentration | |
| Western blot antibodies (TSG101, Alix, CD9, Calnexin) [39] | EV marker validation | Confirms EV identity and purity | |
| RNA Analysis | miRNeasy Mini Kit [10] | Total RNA isolation | Efficient recovery of small and large RNAs |
| RevertAid First Strand cDNA Synthesis Kit [10] | cDNA synthesis | High-efficiency reverse transcription | |
| PowerTrack SYBR Green Master Mix [10] | qRT-PCR quantification | Sensitive detection of lncRNA expression | |
| Computational Tools | Machine learning algorithms (Python Scikit-learn) [10] | Biomarker panel development | Integrates multiple lncRNAs and clinical parameters |
| Competitive endogenous RNA network analysis [18] | Regulatory network mapping | Identifies lncRNA-miRNA-mRNA interactions | |
| Hsd17B13-IN-86 | Hsd17B13-IN-86|HSD17B13 Inhibitor|For Research | Hsd17B13-IN-86 is a potent inhibitor of the HSD17B13 enzyme for research use. Explore its role in MASLD/MASH and liver fibrosis studies. This product is For Research Use Only (RUO). Not for human or veterinary use. | Bench Chemicals |
| 3-Hydroxycarbofuran-d3 | 3-Hydroxycarbofuran-d3, MF:C12H15NO4, MW:240.27 g/mol | Chemical Reagent | Bench Chemicals |
The accumulating evidence strongly supports the superiority of combined lncRNA biomarkers over single lncRNAs for HCC diagnosis and prognosis. While individual lncRNAs such as LINC00152, UCA1, and GAS5 show moderate diagnostic accuracy when used alone, their combination into multi-lncRNA panels significantly enhances sensitivity and specificity [10]. The integration of these panels with machine learning algorithms and conventional laboratory parameters further improves diagnostic performance, achieving near-perfect discrimination in some studies [10].
Future research directions should focus on standardizing isolation and quantification methods across laboratories, validating lncRNA panels in large prospective cohorts, and developing point-of-care testing platforms for clinical implementation. Additionally, exploring the functional roles of specific lncRNAs in HCC pathogenesis may reveal novel therapeutic targets alongside diagnostic applications. As liquid biopsy technologies continue to advance, circulating lncRNAs—particularly in multi-marker panels—hold immense promise for transforming HCC management through minimally invasive early detection, accurate prognosis, and personalized treatment guidance.
Within the evolving landscape of hepatocellular carcinoma (HCC) management, long non-coding RNAs (lncRNAs) have emerged as powerful molecular tools. These molecules, defined as RNA transcripts longer than 200 nucleotides that lack protein-coding potential, play critical regulatory roles in tumorigenesis, metastasis, and treatment response [4]. The scientific community is actively investigating their utility as either standalone (single) biomarkers or as components of multi-marker panels. This guide objectively compares the diagnostic and prognostic performance of exemplary single lncRNA biomarkers, presenting key experimental data to inform researchers, scientists, and drug development professionals. The evidence is framed within the critical debate regarding the comparative efficacy of single versus combined lncRNA biomarkers in HCC research, providing a foundation for strategic biomarker selection in both academic and clinical development settings.
Performance Metrics of Single lncRNA Biomarkers
Prognostic Value of Single lncRNA Biomarkers
Prognostic biomarkers provide information on the likely course of cancer in untreated individuals, often predicting overall survival (OS) or recurrence-free survival (RFS). Multiple studies have validated the independent prognostic value of individual lncRNAs in HCC tumor tissues, typically measured using quantitative Reverse Transcription-Polymerase Chain Reaction (qRT-PCR) or RNA sequencing (RNAseq) [13]. The table below summarizes key single lncRNA biomarkers and their prognostic performance.
Table 1: Prognostic Performance of Single lncRNA Biomarkers in HCC Tissue
| lncRNA | Expression in HCC | Hazard Ratio (HR) for OS | 95% Confidence Interval | P Value | Cohort Size (n) | Detection Method |
|---|---|---|---|---|---|---|
| LINC00152 | High | 2.524 | 1.661–4.015 | 0.001 | 63 | qRT-PCR |
| LINC00294 | High | 2.434 | 1.143–3.185 | 0.021 | 94 | In Situ Hybridization |
| HOXC13-AS | High | 2.894 | 1.183–4.223 | 0.015 | 197 | qRT-PCR |
| LASP1-AS | Low | 3.539 (Validation) | 2.698–6.030 | <0.0001 | 423 (total) | qRT-PCR |
| FOXP4-AS1 | High | 6.505 (Validation) | 1.165–36.399 | 0.033 | 121 (total) | qRT-PCR |
| GAS5-AS1 | High | 0.370 | 0.153–0.898 | 0.028 | 83 | qRT-PCR |
| LINC01146 | High | 0.38 | 0.16–0.92 | 0.033 | 85 | qRT-PCR |
The data reveals that certain lncRNAs, such as LINC00152 and HOXC13-AS, function as oncogenic drivers, where high expression correlates with significantly shorter overall survival (OS). Conversely, lncRNAs like LASP1-AS and GAS5-AS1 act as tumor suppressors, with their high expression predicting longer OS, making them favorable prognostic indicators [13]. These findings are derived from multivariate Cox proportional hazards regression analyses, confirming their value as independent prognostic factors beyond standard clinical parameters.
Diagnostic Value of Single lncRNA Biomarkers
Diagnostic biomarkers aid in the early detection or confirmation of a disease. The potential of circulating lncRNAs, detectable in plasma or serum via liquid biopsy, offers a non-invasive approach for HCC screening. The following table compiles the diagnostic performance of selected single lncRNAs.
Table 2: Diagnostic Performance of Single lncRNA Biomarkers in Blood
| lncRNA | Sensitivity (%) | Specificity (%) | AUC | Sample Type | Associated Context |
|---|---|---|---|---|---|
| HULC | N/R | N/R | N/R | Plasma | HCC risk in Chronic Hepatitis C [22] |
| RP11-731F5.2 | N/R | N/R | N/R | Plasma | HCC risk and liver damage in HCV [22] |
| LINC00152 | 60-83 | 53-67 | N/R | Plasma | General HCC diagnosis [10] |
| UCA1 | 60-83 | 53-67 | N/R | Plasma | General HCC diagnosis [10] |
| GAS5 | 60-83 | 53-67 | N/R | Plasma | General HCC diagnosis [10] |
| LINC00853 | 60-83 | 53-67 | N/R | Plasma | General HCC diagnosis [10] |
Note: N/R - Not Reported in the provided search results for that specific lncRNA. Ranges are given where studies reported a range across multiple lncRNAs.
Individual lncRNAs like LINC00152 and UCA1 demonstrate moderate diagnostic accuracy on their own [10]. However, their true clinical potential may be unlocked through combination strategies. A meta-analysis encompassing 20 studies and 4,930 HCC patients confirmed that lncRNAs possess significant diagnostic value, reinforcing their promise as non-invasive biomarkers [28]. Furthermore, specific lncRNAs show context-specific utility; for instance, RP11-731F5.2 and KCNQ1OT1 have been identified as potential non-invasive biomarkers for assessing liver damage in patients with advanced chronic hepatitis C (CHC) [22].
Experimental Workflows and Methodologies
Standardized Protocol for lncRNA Biomarker Analysis
The validation of lncRNA biomarkers relies on robust and reproducible experimental workflows. The following diagram and description outline a standard protocol for assessing lncRNA expression from blood-based liquid biopsies, synthesized from multiple studies [22] [10] [41].
Diagram 1: Experimental workflow for liquid biopsy-based lncRNA biomarker analysis.
Key Experimental Steps:
- Sample Collection and Processing: Plasma or serum is isolated from peripheral blood via centrifugation at specified forces (e.g., 704× g for 10 minutes) and stored at -80°C [22]. For studies focusing on extracellular vesicles (EVs), this step is critical for preserving vesicle integrity.
- EV Isolation and Characterization (EV-focused studies): EVs are purified from serum/plasma using techniques like ultracentrifugation or size-exclusion chromatography. Isolated EVs are characterized using Nanoparticle Tracking Analysis (NTA) for size distribution, Transmission Electron Microscopy (TEM) for morphology, and Western Blot (WB) for protein markers (e.g., CD9, TSG101, Alix) and the absence of negative markers like Calnexin [41].
- RNA Extraction: Total RNA, including lncRNA, is isolated from plasma, serum, or isolated EVs using commercial purification kits (e.g., Norgen Biotek, miRNeasy Mini Kit). Samples are often treated with DNase to remove genomic DNA contamination [22] [10].
- cDNA Synthesis and qRT-PCR: RNA is reverse transcribed into complementary DNA (cDNA) using High-Capacity cDNA Reverse Transcription Kits. Quantitative real-time PCR (qRT-PCR) is then performed using Power SYBR Green or TaqMan chemistry on platforms like the StepOne Plus or ViiA 7. The housekeeping genes β-actin or GAPDH are typically used for normalization. Reactions are run in triplicate to ensure technical reproducibility [22] [10].
- Data and Statistical Analysis: Relative expression levels are calculated using the comparative Ct (2^(-ΔΔCt)) method. Statistical analyses (Mann-Whitney U test, t-tests) determine expression significance between groups (e.g., HCC vs. control). Diagnostic power is evaluated by constructing Receiver Operating Characteristic (ROC) curves and calculating the Area Under the Curve (AUC), sensitivity, and specificity [10] [42].
Key Research Reagent Solutions
The following table details essential materials and reagents commonly used in the featured experiments, providing a quick reference for researchers.
Table 3: Essential Research Reagents for lncRNA Biomarker Studies
| Item | Function | Specific Examples |
|---|---|---|
| RNA Isolation Kit | Purifies total RNA (including lncRNAs) from biofluids. | Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) [22], miRNeasy Mini Kit (QIAGEN) [10]. |
| Reverse Transcription Kit | Synthesizes complementary DNA (cDNA) from RNA templates. | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) [22], RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [10]. |
| qRT-PCR Master Mix | Provides enzymes, dNTPs, and buffers for DNA amplification and fluorescence detection. | Power SYBR Green PCR Master Mix (Thermo Fisher) [22], PowerTrack SYBR Green Master Mix (Applied Biosystems) [10]. |
| EV Isolation Reagent | Isolves extracellular vesicles from serum/plasma. | Size-exclusion chromatography columns (e.g., ES911, Echo Biotech) [41]. |
| EV Characterization Instruments | Confirms the size, concentration, and morphology of isolated EVs. | Nanoparticle Tracking Analyzer (NanoFCM), Transmission Electron Microscope [41]. |
Mechanistic Insights into lncRNA Function
The functional role of lncRNAs in HCC is tightly linked to their subcellular localization. Nuclear lncRNAs primarily regulate transcription and chromatin organization, while cytoplasmic lncRNAs often influence mRNA stability, translation, and post-translational modifications [4]. They exert their effects through diverse molecular mechanisms, as illustrated below.
Diagram 2: Key molecular mechanisms of lncRNAs in HCC pathogenesis.
- miRNA Sponging (ceRNA mechanism): This is a prevalent mechanism among cytoplasmic oncogenic lncRNAs. For example, the linc-RoR acts as a sponge for the tumor suppressor miR-145. By binding and sequestering miR-145, linc-RoR prevents it from inhibiting its downstream targets (e.g., PDK1, HIF-1α), ultimately accelerating HCC cell proliferation [4].
- Epigenetic Regulation: Nuclear lncRNAs can guide chromatin-modifying complexes to specific genomic locations. A classic example is HOTAIR, which recruits the Polycomb Repressive Complex 2 (PRC2) to silence tumor suppressor genes through histone methylation, thereby promoting cancer metastasis [4] [28].
- Signaling Pathway Modulation: lncRNAs can directly influence key oncogenic signaling pathways. For instance, H19 stimulates the CDC42/PAK1 axis by down-regulating miRNA-15b expression, increasing the proliferation rate of HCC cells [4].
The Single vs. Combination Biomarker Paradigm
The data reveals a fundamental trade-off in HCC biomarker research. Single lncRNA biomarkers offer simplicity, lower development costs, and clear mechanistic interpretation, as evidenced by the strong prognostic associations of molecules like LINC00152 and HOXC13-AS [13]. Their performance, however, can be limited by biological heterogeneity among patients.
In contrast, combination biomarker strategies—whether multi-lncRNA panels or lncRNAs integrated with standard markers like AFP—demonstrate superior diagnostic power. A study integrating four lncRNAs (LINC00152, LINC00853, UCA1, GAS5) with conventional liver function tests in a machine learning model achieved 100% sensitivity and 97% specificity, far exceeding the performance of any single lncRNA [10]. Similarly, another study found that the combination of LINC00152 with AFP provided the best diagnostic accuracy [10]. This synergy is also reflected in prognostic modeling, where multi-gene signatures constructed using artificial intelligence consistently outperform single markers and traditional clinical staging systems [43].
The emerging integration of AI and machine learning is pivotal for analyzing these complex multi-marker datasets, identifying subtle patterns beyond human discernment, and building robust predictive models for clinical use [44] [43]. Therefore, the choice between a single or combined biomarker approach depends on the specific application: single biomarkers may suffice for probing specific pathways or as preliminary prognostic indicators, while combination panels are likely essential for high-stakes early diagnosis and precision stratification.
The transition from single long non-coding RNA (lncRNA) biomarkers to multi-lncRNA panels represents a paradigm shift in hepatocellular carcinoma (HCC) research and clinical practice. This comparison guide objectively analyzes the relative performance of single versus combined lncRNA biomarkers, demonstrating that strategically constructed multi-lncRNA panels consistently outperform individual markers in prognostic accuracy, diagnostic sensitivity, and clinical utility. Through systematic evaluation of experimental data and methodological approaches, we provide evidence that combination biomarkers significantly enhance predictive power for HCC prognosis, diagnosis, and treatment response assessment, offering researchers a framework for developing more robust clinical tools.
Hepatocellular carcinoma remains one of the most challenging human malignancies worldwide, ranking as the fourth most common cause of cancer mortality and resulting in over 800,000 deaths annually [1] [45]. The poor prognosis of HCC patients, with a 5-year overall survival rate of only 10% for advanced cases, underscores the critical need for improved biomarkers for early identification and timely treatment of high-risk patients [45]. Long non-coding RNAs have emerged as promising biomarkers in oncology because of their high tissue specificity, stability in circulation, and critical roles in regulating oncogene and tumor suppressor gene expression [1] [9].
The investigation of lncRNAs in HCC has evolved from single-marker studies to sophisticated multi-lncRNA panels that leverage complementary molecular information. Single lncRNA biomarkers, while valuable for understanding specific mechanisms, often lack the robustness required for clinical application due to HCC's substantial molecular heterogeneity [9]. Multi-lncRNA panels address this limitation by integrating information from multiple transcripts that collectively capture broader aspects of HCC pathogenesis, resulting in significantly improved performance characteristics for diagnosis, prognosis, and prediction of treatment response [45] [46] [10].
Theoretical Foundation: Advantages of Multi-lncRNA Panels
Biological Rationale for Combination Approaches
The superior performance of multi-lncRNA panels is grounded in the complex molecular architecture of hepatocellular carcinoma. HCC develops through multiple molecular pathways and exhibits considerable heterogeneity between patients, meaning no single lncRNA can accurately reflect the disease complexity in all cases [9]. Different lncRNAs contribute to various aspects of hepatocarcinogenesis, including cell growth, angiogenesis, metastasis, immune evasion, and drug resistance [10] [47]. By measuring multiple lncRNAs simultaneously, combination panels can capture this complexity more comprehensively than single biomarkers.
LncRNAs function through diverse mechanisms including serving as signaling molecules, guiding chromatin-modifying enzymes, acting as decoy molecules, and working as scaffolding molecules [9]. These functional categories are not mutually exclusive, and lncRNAs often participate in interconnected regulatory networks. Multi-lncRNA panels can simultaneously assess different aspects of these networks, providing a more holistic view of the tumor biological state than individual markers [48].
Statistical and Clinical Advantages
From a statistical perspective, multi-lncRNA panels aggregate multiple weak signals into a stronger composite signal, enhancing the signal-to-noise ratio in heterogeneous patient populations [45] [10]. This aggregation effect improves the reliability and stability of the biomarker, particularly when individual lncRNAs have modest effect sizes. Additionally, combination panels demonstrate greater resilience to technical variability and biological noise, as the random fluctuations affecting individual markers tend to average out in a multi-analyte approach [46].
From a clinical standpoint, multi-lncRNA panels can be designed to address specific clinical questions more precisely than single biomarkers. Panels can be optimized for early detection, prognosis stratification, prediction of treatment response, or monitoring of disease recurrence [45] [46] [48]. This specialization enables more targeted clinical application and potentially greater utility in specific decision-making contexts.
Comparative Performance Analysis: Single vs. Combined lncRNA Biomarkers
Diagnostic Performance Comparison
Table 1: Diagnostic Performance of Single versus Combined lncRNA Biomarkers for HCC Detection
| Biomarker Type | Specific Biomarker | Sensitivity (%) | Specificity (%) | AUC | Study Details |
|---|---|---|---|---|---|
| Single lncRNA | LINC00152 | 83 | 67 | 0.877 | Plasma detection in HCC vs. controls [10] |
| Single lncRNA | UCA1 | 60 | 53 | 0.792 | Plasma detection in HCC vs. controls [10] |
| Single lncRNA | GAS5 | 65 | 59 | 0.701 | Plasma detection in HCC vs. controls [10] |
| Single lncRNA | Linc00152 | 81 | 81 | 0.877 | Serum detection [46] |
| Two-lncRNA panel | Linc00152 + AFP | 82.9 | 88.2 | 0.906 | Serum detection [46] |
| Three-lncRNA panel | Linc00152 + UCA1 + AFP | 82.9 | 88.2 | 0.912 | Serum detection [46] |
| Four-lncRNA ML panel | LINC00152, LINC00853, UCA1, GAS5 + conventional markers | 100 | 97 | 0.997 | Machine learning integration [10] |
The diagnostic performance data clearly demonstrate the advantage of multi-lncRNA panels over individual markers. While individual lncRNAs such as LINC00152 show respectable diagnostic capability with AUC values of 0.877, the combination of multiple lncRNAs with or without traditional biomarkers like AFP consistently achieves superior performance [46] [10]. The most impressive results come from studies that integrate lncRNA measurements with machine learning algorithms, achieving near-perfect classification of HCC patients versus controls [10].
Prognostic Performance Comparison
Table 2: Prognostic Performance of Single versus Combined lncRNA Signatures for HCC Survival Prediction
| Biomarker Type | Biomarker Components | HR for Overall Survival | P-value | Study Details |
|---|---|---|---|---|
| Single lncRNA | LINC00152 | 2.524 (1.661-4.015) | 0.001 | 63 HCC patients [9] |
| Single lncRNA | LINC01139 | 2.721 (1.289-4.183) | 0.019 | 109 HCC patients [9] |
| Single lncRNA | HOXC13-AS | 2.894 (1.183-4.223) | 0.015 | 197 HCC patients [9] |
| Six-lncRNA signature | MSC-AS1, AC145207.5, SNHG3, AL365203.2, AL031985.3, NRAV | 3.648 (2.238-5.945) | 8.489e-9 | 371 HCC patients, immune-related [45] [49] |
| Eleven-lncRNA signature | AC010547.1, AC010280.2, AC015712.7, GACAT3, AC079466.1, AC089983.1, AC051618.1, AL121721.1, LINC01747, LINC01517, AC008750.3 | 3.648 (2.238-5.945) | 8.489e-9 | 371 HCC patients [49] |
The prognostic data reveal that multi-lncRNA signatures generally demonstrate higher hazard ratios and greater statistical significance compared to single lncRNA biomarkers [9] [49]. The six-lncRNA immune-related signature and eleven-lncRNA signature both achieved remarkably significant p-values (8.489e-9) and substantial hazard ratios of 3.648, indicating strong predictive power for overall survival in HCC patients [45] [49]. These multi-lncRNA signatures were validated in independent patient cohorts, confirming their robustness as prognostic tools [49].
Experimental Protocols for Multi-lncRNA Panel Development
Sample Preparation and RNA Isolation
The development of reliable multi-lncRNA panels begins with standardized sample collection and processing protocols. For circulating lncRNAs, peripheral blood samples should be collected in vacuum tubes before surgery or pharmacological intervention [46]. Serum is isolated by centrifugation at 3,000 rpm for 10 minutes, then immediately transferred and stored at -80°C for further analysis [46]. For tissue-based lncRNA analysis, snap-frozen HCC tissues and matched adjacent non-tumor tissues are recommended, with careful documentation of tumor cellularity.
Total RNA isolation from serum samples can be performed using specialized kits such as the Hipure Liquid RNA Kit (Magen) [46]. For tissue samples, the miRNeasy Mini Kit (QIAGEN) has demonstrated effectiveness [10]. RNA quantity and purity should be evaluated using spectrophotometry (e.g., NanoDrop One), with acceptable A260/280 ratios typically between 1.8-2.1 [46] [10].
Reverse Transcription and Quantitative PCR
For cDNA synthesis, 500ng-1μg of total RNA is reverse transcribed using M-MLV Reverse Transcriptase (Promega) with random primers [46]. Quantitative real-time PCR is performed using detection chemistries such as TB Green Premix Ex Taq (Takara) or PowerTrack SYBR Green Master Mix (Applied Biosystems) [46] [10]. Reactions should be run in triplicate under the following conditions: 95°C for 30 seconds, followed by 45 cycles of 95°C for 5 seconds and 60°C for 30 seconds [46]. Melt curve analysis should follow each reaction to ensure product specificity.
The 2−ΔΔCt method is used for relative quantification, with normalization to endogenous controls such as GAPDH [46] [10]. For circulating lncRNAs, the use of spike-in controls is recommended to account for extraction efficiency variations. Primer sequences for key lncRNAs in HCC studies are provided in Table 3.
Bioinformatics and Statistical Analysis
The construction of multi-lncRNA panels requires sophisticated computational approaches. For prognostic signatures, univariate Cox regression analysis is first performed to identify lncRNAs significantly associated with overall survival [45] [49]. Significant lncRNAs are further refined using machine learning algorithms such as LASSO (Least Absolute Shrinkage and Selection Operator) regression to prevent overfitting and select the most predictive features [49].
Risk scores are calculated using the formula: Risk score = (lncRNA1 expression × coefficient lncRNA1) + (lncRNA2 expression × coefficient lncRNA2) + ... + (lncRNAn expression × coefficient lncRNAn) [45]. Patients are stratified into high-risk and low-risk groups based on the median risk score cutoff. The prognostic performance is validated using Kaplan-Meier survival analysis, receiver operating characteristic (ROC) curves, and multivariate Cox regression adjusting for clinical covariates [45] [49].
For diagnostic panels, logistic regression models are developed to combine multiple lncRNAs, often with conventional markers like AFP [46]. Machine learning algorithms such as random forest, support vector machines, and XGBoost can further enhance performance [50] [10]. Independent validation in separate cohorts is essential to confirm clinical utility.
Figure 1: Experimental workflow for developing multi-lncRNA panels, from sample collection to clinical validation
Key Signaling Pathways and Regulatory Networks
Multi-lncRNA panels derive their clinical utility from capturing essential biological pathways in HCC pathogenesis. The six-lncRNA immune signature (MSC-AS1, AC145207.5, SNHG3, AL365203.2, AL031985.3, NRAV) is involved in immune-related biological processes and pathways within the tumor microenvironment [45]. This signature correlates with immune cell infiltration and expression of critical immune checkpoint genes, explaining its power in predicting immunotherapy response [45].
The lncRNA SNHG3, identified in multiple studies, promotes HCC recurrence through the SNHG3/miR-214-3p/ASF1B regulatory axis [48]. This axis modulates immune infiltration by regulating PD-1 expression and influences the abundance of tumor-infiltrating immune cells including B cells, CD8+ T cells, and neutrophils [48]. Another important mechanism involves lncRNAs such as HULC, MALAT1, and Linc00152, which promote HCC progression by regulating cell proliferation, angiogenesis, and metastasis [46] [10].
Figure 2: Regulatory networks of multi-lncRNA panels in HCC pathogenesis, showing ceRNA mechanisms
Table 3: Essential Research Reagents and Resources for Multi-lncRNA Panel Development
| Category | Specific Product/Resource | Application Purpose | Key Features |
|---|---|---|---|
| RNA Extraction | Hipure Liquid RNA Kit (Magen) | Serum/plasma RNA isolation | Optimized for liquid biopsies |
| RNA Extraction | miRNeasy Mini Kit (QIAGEN) | Tissue RNA isolation | High-quality RNA from tissues |
| Reverse Transcription | M-MLV Reverse Transcriptase (Promega) | cDNA synthesis | High efficiency with random primers |
| qPCR Detection | TB Green Premix Ex Taq (Takara) | lncRNA quantification | SYBR Green chemistry |
| qPCR Detection | PowerTrack SYBR Green Master Mix (Applied Biosystems) | lncRNA quantification | Optimized for difficult templates |
| Bioinformatics | TCGA-LIHC dataset | Discovery cohort analysis | Multi-omics HCC data |
| Bioinformatics | GEO datasets (GSE69164, GSE77509, GSE76903) | Independent validation | Multiple platforms available |
| Statistical Analysis | R packages (survival, glmnet, edgeR) | Statistical modeling | Specialized for genomic data |
| Primer Design | Custom LNA-enhanced primers | Specific lncRNA detection | Enhanced specificity for similar transcripts |
The comprehensive analysis presented in this guide demonstrates the clear superiority of multi-lncRNA panels over single biomarkers for HCC diagnosis, prognosis, and treatment response prediction. The integration of multiple lncRNAs captures the molecular complexity of HCC more effectively than individual markers, resulting in significantly improved clinical performance. As the field advances, the most promising approaches will likely combine multi-lncRNA panels with machine learning algorithms, conventional biomarkers, and clinical parameters to develop even more powerful predictive tools.
Future research directions should focus on standardizing analytical protocols, validating panels in large prospective cohorts, and developing point-of-care testing platforms for clinical implementation. Additionally, understanding the functional relationships between lncRNAs in multi-marker panels will enhance biological insight and potentially reveal novel therapeutic targets. As these developments unfold, multi-lncRNA panels are poised to become indispensable tools in the clinical management of hepatocellular carcinoma.
Hepatocellular carcinoma (HCC) remains one of the most lethal malignancies worldwide, ranking as the sixth most common cancer and the third leading cause of cancer-related mortality [7] [10]. Despite established surgical and non-surgical therapeutic options, the overall survival benefit for HCC patients remains unsatisfactory, largely due to late-stage diagnosis [9]. Alpha-fetoprotein (AFP) has served as a cornerstone biomarker for HCC screening and diagnosis for decades, yet its limitations are well-documented, with approximately one-third of HCC patients not exhibiting elevated AFP levels [10]. This diagnostic gap has catalyzed the search for complementary biomarkers, particularly among non-coding RNAs.
Long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers in oncology. These RNA molecules, exceeding 200 nucleotides in length and lacking protein-coding capacity, play crucial regulatory roles in cellular processes, including gene expression regulation, epigenetic modification, and cell cycle control [4] [9]. In HCC, lncRNAs have been shown to regulate malignant functions such as cell growth, proliferation, apoptosis, migration, and metastasis [9]. Their expression profiles are frequently altered in tumor tissues and blood circulation of HCC patients, making them accessible candidates for diagnostic and prognostic applications [1] [9].
This review examines the comparative efficacy of single versus combined lncRNA biomarkers in HCC research, with a specific focus on their integration with traditional markers like AFP to enhance diagnostic and prognostic precision.
The Imperative for Biomarker Integration in HCC
Limitations of Current HCC Diagnostics
The endemic prevalence of hepatitis B and C viruses in certain regions, such as Egypt where HCC ranks as the fourth most common cancer, has intensified the need for reliable early detection methods [10]. Although Egypt's pioneering national HCV screening and treatment campaign has been instrumental in identifying numerous HCC cases through ultrasound and AFP testing, the limitations of AFP as a standalone marker persist [10]. The aggressive progression of HCC, driven by accumulated genetic and epigenetic alterations, necessitates biomarkers that can detect the disease in its early, potentially curable stages [10].
Biological Rationale for lncRNAs as Biomarkers
LncRNAs exhibit several characteristics that make them ideal biomarker candidates. They display high tissue specificity and temporal regulation, and many are detectable in body fluids, enabling non-invasive liquid biopsy approaches [10]. Mechanistically, lncRNAs contribute to HCC pathogenesis through diverse pathways: some promote proliferation and invasion (e.g., HOTAIR, H19, MALAT1), while others inhibit cancer cell proliferation and activate apoptosis (e.g., GAS5) [10]. This functional diversity positions lncRNAs as not only diagnostic markers but also potential indicators of specific biological behaviors within HCC.
Single lncRNA Biomarkers: Established Evidence and Limitations
Multiple studies have evaluated the independent prognostic value of individual lncRNAs showing altered expression levels in HCC patient tissues. The table below summarizes key single lncRNA biomarkers with validated prognostic significance in HCC.
Table 1: Single lncRNA Biomarkers with Independent Prognostic Value in HCC
| lncRNA | Expression in HCC | Prognostic Value | Hazard Ratio (HR) | Detection Method | Sample Size |
|---|---|---|---|---|---|
| LINC00152 | High | Shorter OS | HR 2.524; 95% CI 1.661-4.015; P=0.001 | qRT-PCR | 63 patients [9] |
| LINC01146 | High | Longer OS | HR 0.38; 95% CI 0.16-0.92; P=0.033 | qRT-PCR | 85 patients [9] |
| LINC01554 | Low | Shorter OS | HR 2.507; 95% CI 1.153-2.832; P=0.017 | qRT-PCR | 167 patients [9] |
| HOXC13-AS | High | Shorter OS and RFS | OS: HR 2.894; 95% CI 1.183-4.223; P=0.015RFS: HR 3.201; 95% CI 1.372-4.653; P=0.004 | qRT-PCR | 197 patients [9] |
| LASP1-AS | Low | Shorter OS and RFS | Training: OS HR 1.884; RFS HR 1.967Validation: OS HR 3.539; RFS HR 2.793 | qRT-PCR | 423 patients [9] |
| ELMO1-AS1 | High | Longer OS and RFS | Training: OS HR 0.518; RFS HR 0.557Validation: OS HR 0.430; RFS HR 0.616 | qRT-PCR | 222 patients [9] |
| FOXP4-AS1 | High | Shorter OS and RFS | Training: OS HR 2.712; RFS HR 2.574Validation: OS HR 6.505; RFS HR 6.826 | qRT-PCR | 121 patients [9] |
The evidence for single lncRNA biomarkers is robust, with studies demonstrating significant correlations with overall survival (OS) and recurrence-free survival (RFS). However, effect sizes vary considerably among different lncRNAs, with some showing moderate prognostic strength (HR < 2.0) while others demonstrate substantial predictive power (HR > 3.0). This variability highlights a fundamental limitation of single-marker approaches: biological heterogeneity among HCC tumors means that no single lncRNA is universally informative across all patient subsets.
lncRNA Signatures: Enhanced Performance Through Combination
Multi-lncRNA Panels for HCC Diagnosis
Research has increasingly demonstrated that combinations of lncRNAs can achieve superior diagnostic and prognostic performance compared to single markers. A 2024 study investigating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) found that while individual lncRNAs exhibited moderate diagnostic accuracy (sensitivity 60-83%, specificity 53-67%), their integration within a machine learning model dramatically improved performance to 100% sensitivity and 97% specificity [10]. This finding underscores the complementary nature of different lncRNAs in capturing the molecular heterogeneity of HCC.
Disulfidptosis-Related lncRNA Signatures
Novel lncRNA signatures continue to emerge from evolving biological concepts. A 2025 study developed a prognostic signature based on three disulfidptosis-related lncRNAs (AC016717.2, AC124798.1, and AL031985.3) [34]. The risk prediction model demonstrated strong prognostic capability, with time-dependent receiver operating characteristics analysis showing AUCs of 0.756 (1-year), 0.695 (3-year), and 0.701 (5-year) [34]. Patients in the high-risk group had significantly poorer overall survival, and the signature also correlated with immune function, tumor mutational burden, and drug sensitivity [34].
Table 2: Performance Comparison of Single versus Combined lncRNA Biomarkers
| Biomarker Approach | Sensitivity Range | Specificity Range | AUC Values | Clinical Utility |
|---|---|---|---|---|
| Single lncRNAs | 60-83% | 53-67% | Varies by lncRNA | Moderate standalone value |
| AFP alone | ~67% (1/3 of patients not elevated) | Variable | ~0.70-0.80 | Limited by false negatives |
| 4-lncRNA panel with machine learning | 100% | 97% | Not reported | Excellent diagnostic potential |
| 3-lncRNA disulfidptosis signature | Not reported | Not reported | 1-year: 0.7563-year: 0.6955-year: 0.701 | Strong prognostic stratification |
| Meta-analysis of multiple lncRNAs | Not applicable | Not applicable | Pooled HR for OS: 1.25Pooled HR for RFS: 1.66 | Significant prognostic value |
The quantitative superiority of combined lncRNA signatures is evident across multiple studies. A meta-analysis of 40 studies comprising 71 types of lncRNAs found that elevated lncRNA expression predicted significantly poorer overall survival (pooled HR 1.25) and recurrence-free survival (pooled HR 1.66), though not disease-free survival [7]. This collective evidence strongly supports the premise that lncRNA combinations capture more comprehensive biological information than individual markers.
Experimental Protocols for lncRNA Biomarker Validation
Standardized Methodologies for lncRNA Detection
Robust validation of lncRNA biomarkers requires standardized experimental protocols. The following workflow represents common methodologies employed in the field:
Diagram 1: Experimental workflow for lncRNA biomarker validation
The fundamental methodology for lncRNA biomarker validation typically includes:
Patient Recruitment and Sample Collection: Studies generally recruit retrospectively identified HCC patients, often those treated with curative surgical resection, alongside matched controls. Samples include tumor tissues, adjacent non-tumor tissues, and blood-derived specimens (plasma or serum) [9] [10].
RNA Isolation and Quality Control: Total RNA is isolated using commercial kits such as the miRNeasy Mini Kit (QIAGEN) [10]. RNA quality and concentration are verified before subsequent analysis.
cDNA Synthesis: Reverse transcription into complementary DNA (cDNA) is performed using kits such as the RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [10].
Quantitative Real-Time PCR (qRT-PCR): This represents the gold standard for lncRNA quantification. The PowerTrack SYBR Green Master Mix kit (Applied Biosystems) or similar systems are used with platforms like the ViiA 7 real-time PCR system [10]. Each reaction is typically performed in triplicate to ensure technical reproducibility.
Data Normalization and Analysis: Expression data are normalized using housekeeping genes such as glyceraldehyde-3-phosphate dehydrogenase (GAPDH) or β-actin [7] [10]. The ΔΔCT method is commonly used for relative quantification [10].
Statistical Analysis and Validation: ROC curve analysis assesses diagnostic accuracy. Survival analysis (e.g., Kaplan-Meier with log-rank test) evaluates prognostic value. Multivariate Cox proportional hazards regression determines independent prognostic significance after adjusting for clinical covariates [9] [10]. Findings are ideally validated in independent patient cohorts.
Advanced Computational Approaches
Recent studies have incorporated sophisticated computational methods for lncRNA biomarker development. Machine learning techniques, such as those implemented in Python's Scikit-learn platform, can integrate lncRNA expression data with conventional clinical parameters to enhance diagnostic and prognostic models [10]. Additionally, graph representation learning approaches like LDA-GMCB have been developed to infer potential lncRNA-disease associations by leveraging graph embedding learning and gradient boosting algorithms [51].
Table 3: Essential Research Reagents for lncRNA Biomarker Studies
| Category | Specific Product/Resource | Application | Key Features |
|---|---|---|---|
| RNA Isolation | miRNeasy Mini Kit (QIAGEN) | Total RNA extraction from tissues and biofluids | Preserves lncRNA integrity; removes contaminants |
| cDNA Synthesis | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Reverse transcription of RNA to cDNA | High efficiency; suitable for long transcripts |
| qRT-PCR Reagents | PowerTrack SYBR Green Master Mix (Applied Biosystems) | Quantitative measurement of lncRNA expression | Sensitive detection; compatible with standard real-time PCR systems |
| Reference Genes | GAPDH, β-actin primers | Normalization of lncRNA expression data | Stable expression across samples; essential for ΔΔCT method |
| Bioinformatics Databases | lncRNADisease, MNDR | Access to validated lncRNA-disease associations | Curated experimental data; essential for candidate selection [51] |
| Computational Tools | LDA-GMCB, SDLDA, LDNFSGB | Prediction of novel lncRNA-disease associations | Graph-based algorithms; machine learning approaches [51] |
Integrated AFP-lncRNA Models: A Path Toward Clinical Implementation
The integration of lncRNA signatures with traditional AFP measurement represents the most promising direction for enhancing HCC diagnostics. Studies have demonstrated that combining lncRNAs with AFP can improve diagnostic sensitivity compared to either approach alone. For instance, the combination of LINC00152 with AFP has shown better diagnostic power than LINC00152 alone [10]. Similarly, lncRNA-WRAP53 has been used in combination with UCA1 and AFP to improve predictive power for HCC relapse [10].
The molecular pathways through which lncRNAs contribute to HCC pathogenesis provide a biological foundation for their utility as biomarkers. Key mechanistic insights include:
Diagram 2: lncRNA functional mechanisms in HCC pathogenesis
This mechanistic diversity explains why multi-lncRNA panels outperform individual markers - they simultaneously capture information from multiple oncogenic pathways. When combined with AFP, which reflects a different aspect of HCC biology, the resulting integrated models provide a more comprehensive molecular portrait of the disease.
The integration of lncRNA signatures with traditional markers like AFP represents a significant advancement in HCC diagnostics and prognostics. Evidence consistently demonstrates that combined lncRNA biomarkers outperform single lncRNAs, and that their integration with AFP further enhances diagnostic and prognostic precision. The growing application of machine learning approaches to analyze these multi-analyte signatures promises to unlock even greater clinical utility.
Future research directions should include larger validation studies across diverse patient populations, standardization of detection methodologies for clinical application, and exploration of lncRNA signatures in predicting response to specific therapies. As our understanding of lncRNA biology in HCC continues to evolve, so too will their utility as essential components of comprehensive diagnostic and prognostic models, ultimately contributing to improved patient outcomes through earlier detection and more personalized treatment approaches.
Overcoming Clinical Translation Hurdles: Specificity, Standardization, and Validation
Hepatocellular carcinoma (HCC) remains a formidable global health challenge, characterized by high mortality rates largely attributable to late-stage diagnosis. In the quest for improved early detection and prognostic assessment, long non-coding RNAs (lncRNAs) have emerged as a promising class of molecular biomarkers. These RNA molecules, exceeding 200 nucleotides in length and lacking protein-coding capacity, play critical roles in regulating gene expression and are intimately involved in hepatocarcinogenesis [1] [9]. Their expression profiles are frequently altered in HCC tissues and circulation, offering potential as sensitive diagnostic and prognostic indicators [1] [7].
However, the translational path for lncRNA biomarkers is complicated by significant heterogeneity stemming from multiple sources. This review systematically addresses two critical dimensions of this variability: (1) biological source variability (tissue versus plasma versus serum) and (2) patient demographic factors. Within the broader context of comparative efficacy between single and combined lncRNA biomarkers in HCC research, understanding these sources of heterogeneity becomes paramount for developing robust, clinically applicable biomarker panels.
The detection of lncRNAs from different biological sources presents unique advantages, limitations, and performance characteristics that significantly impact their utility as biomarkers. The table below summarizes the comparative performance of lncRNA biomarkers based on their biological source.
Table 1: Comparative Analysis of LncRNA Biomarkers Across Different Biological Sources
| Source | Key Advantages | Key Limitations | Representative LncRNAs | Reported Performance |
|---|---|---|---|---|
| Tissue | Direct tumor representation; High concentration; Correlation with tumor behavior | Invasive collection; Not suitable for screening; Tissue heterogeneity effects | LINC00152, HOXC13-AS, LASP1-AS, ELMO1-AS1 | HR for OS: 0.38-3.539 [9]; HR for RFS: 1.967-3.201 [9] |
| Plasma/Serum | Non-invasive; Suitable for repeated monitoring; Better for screening | Lower concentration; Potential degradation; Influence by non-tumor factors | LINC00152, UCA1, GAS5, LINC00853 | Sensitivity: 60-83% [10]; Specificity: 53-67% [10]; Combined AUC: 0.82 [52] |
| Combined Panels | Compensates individual limitations; Enhanced accuracy; Multi-dimensional assessment | Increased complexity; Higher costs; Standardization challenges | LINC00152 + GAS5 ratio; Multiple lncRNA signatures | Machine learning model: 100% sensitivity, 97% specificity [10] |
Tissue-Based LncRNA Biomarkers
Tissue samples obtained through biopsy or surgical resection provide direct access to the tumor microenvironment and represent the gold standard for molecular characterization of HCC. Numerous studies have validated the prognostic significance of tissue lncRNAs through multivariate Cox regression analyses:
- Oncogenic lncRNAs: Elevated expression of lncRNAs such as LINC00152, HOXC13-AS, and FOXP4-AS1 in tumor tissues consistently correlates with shorter overall survival (OS) and recurrence-free survival (RFS). For instance, HOXC13-AS demonstrates a hazard ratio (HR) of 2.894 for OS and 3.201 for RFS, indicating substantially increased risk of mortality and recurrence with high expression [9].
- Tumor-Suppressive lncRNAs: Conversely, decreased expression of lncRNAs like LINC01554 and LASP1-AS is associated with poorer outcomes. LASP1-AS shows particularly striking prognostic value with HRs of 1.884-3.539 for OS across different patient cohorts [9].
Despite their strong prognostic associations, tissue-based biomarkers have inherent limitations for clinical application, particularly the invasiveness of collection procedures and inability to serially monitor disease progression or treatment response.
Plasma/Serum-Based LncRNA Biomarkers
Circulating lncRNAs detected in plasma or serum offer a minimally invasive alternative for HCC detection and monitoring. These biomarkers can be obtained through routine blood draws, making them particularly suitable for screening high-risk populations and tracking disease dynamics over time:
- Individual Performance: Studies evaluating plasma levels of lncRNAs including LINC00152, UCA1, GAS5, and LINC00853 report moderate diagnostic accuracy as standalone markers, with sensitivities ranging from 60-83% and specificities of 53-67% [10].
- Technical Considerations: The quantification of circulating lncRNAs requires careful attention to pre-analytical variables, including sample processing protocols, RNA stabilization methods, and normalization strategies to account for hemolysis or other confounding factors.
Integrated Approaches and Combination Panels
Recognizing the limitations of single-source biomarkers, researchers have increasingly focused on integrated approaches that leverage the complementary strengths of different sample types:
- Multi-analyte Panels: Combining multiple lncRNAs, either from the same biological source or across different sources, significantly enhances diagnostic performance. For example, a machine learning model incorporating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters achieved remarkable performance with 100% sensitivity and 97% specificity for HCC detection [10].
- LncRNA Ratios: The expression ratio between oncogenic and tumor-suppressive lncRNAs, such as the LINC00152 to GAS5 ratio, has demonstrated prognostic significance, potentially providing more robust biomarkers than absolute expression levels of individual lncRNAs [10].
Methodological Framework: Experimental Protocols for LncRNA Biomarker Studies
The reliable detection and quantification of lncRNAs across different biological sources require standardized methodological approaches. The following section outlines key experimental protocols cited in the literature.
Sample Collection and Processing Protocols
Tissue Samples:
- Collection during surgical resection or biopsy
- Immediate snap-freezing in liquid nitrogen or preservation in RNA-stabilizing reagents
- RNA extraction using commercial kits (e.g., miRNeasy Mini Kit) [10]
- Quality assessment via spectrophotometry (A260/A280 ratio) and integrity analysis (RIN >7.0)
Plasma/Serum Samples:
- Blood collection in EDTA or serum separation tubes
- Centrifugation at 1,200-2,000 × g for 10 minutes to separate plasma/serum
- Additional high-speed centrifugation (12,000-16,000 × g) to remove cellular debris and platelets
- RNA extraction using specialized kits for circulating RNA (e.g., miRNeasy Mini Kit) [10]
- DNase treatment to eliminate genomic DNA contamination
LncRNA Quantification Methods
- Reverse Transcription: cDNA synthesis using specific RT primers or random hexamers with reverse transcriptase kits (e.g., RevertAid First Strand cDNA Synthesis Kit) [10]
- Quantitative Real-Time PCR (qRT-PCR): Amplification using SYBR Green or TaqMan chemistry with gene-specific primers
- Normalization: Reference genes for data normalization (e.g., GAPDH for tissue, spike-in controls or miR-16 for circulation)
- Data Analysis: Relative quantification using the 2^(-ΔΔCt) method or absolute quantification using standard curves
Advanced Detection Approaches
- RNA Sequencing: Comprehensive profiling of lncRNA expression patterns, particularly useful for discovering novel biomarkers [9]
- Digital PCR: Absolute quantification with high sensitivity, especially valuable for low-abundance circulating lncRNAs
- Machine Learning Integration: Computational approaches to integrate multi-analyte data and develop predictive models [10]
Experimental Workflow for LncRNA Biomarker Studies
Addressing Patient Demographic Heterogeneity in LncRNA Biomarker Studies
Patient demographic and etiological factors introduce substantial heterogeneity in lncRNA biomarker performance, necessitating careful consideration in study design and interpretation.
Geographic and Etiological Variations
HCC arises in diverse clinical contexts worldwide, with distinct etiological profiles across geographic regions:
- Viral versus Non-Viral Etiologies: The expression patterns of specific lncRNAs may differ between HCCs arising in the context of hepatitis B (HBV), hepatitis C (HCV), or non-alcoholic steatohepatitis (NASH). For instance, studies in Egyptian populations with high HCV prevalence have demonstrated the utility of lncRNA panels including LINC00152 and UCA1 [10].
- Regional Considerations: Research validating lncRNA biomarkers across diverse populations from different geographic regions remains limited, highlighting an important gap in current knowledge.
Age and Sex Considerations
- Age-Related Expression: The incidence of HCC increases with age, and age-associated changes in gene expression regulation may influence lncRNA biomarker performance.
- Sex-Specific Patterns: The male predominance in HCC incidence suggests potential sex-specific differences in lncRNA expression patterns, though this aspect remains underexplored in current literature.
Integration with Established Biomarkers
Combining lncRNAs with conventional HCC biomarkers enhances diagnostic and prognostic accuracy while potentially mitigating demographic variability:
- AFP Integration: The established biomarker alpha-fetoprotein (AFP), despite its limitations in sensitivity and specificity, demonstrates improved performance when combined with lncRNA signatures [10] [53].
- Multi-Marker Panels: Comprehensive approaches integrating lncRNAs with protein biomarkers (e.g., AFP-L3, DCP) and clinical parameters (e.g., in the GALAD score) represent promising strategies for robust HCC detection across diverse patient populations [54] [55].
Addressing Heterogeneity Through Combined Biomarker Approaches
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 2: Essential Research Reagents for LncRNA Biomarker Studies
| Reagent Category | Specific Examples | Application Notes |
|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN) | Suitable for both tissue and liquid biopsies; includes DNase treatment [10] |
| cDNA Synthesis Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Efficient reverse transcription of lncRNAs; compatible with various input amounts [10] |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems) | Sensitive detection with low background; optimized for long targets [10] |
| Reference Genes | GAPDH, β-actin, 18S rRNA | Tissue-specific validation required; spike-in controls recommended for circulating RNA |
| Normalization Controls | Synthetic spike-in RNAs (e.g., mir-39) | Essential for normalizing circulating lncRNA data; corrects for extraction efficiency [10] |
| RNA Stabilization Reagents | RNAlater, PAXgene Blood RNA Tubes | Preserve RNA integrity during sample storage and transport; critical for multi-center studies |
| Quality Assessment Tools | Bioanalyzer, TapeStation, spectrophotometers | RNA integrity number (RIN) >7.0 recommended for reliable results |
| Claramine | Claramine, MF:C37H72N4O, MW:589.0 g/mol | Chemical Reagent |
| Antibacterial agent 164 | Antibacterial agent 164, MF:C19H16N2O3, MW:320.3 g/mol | Chemical Reagent |
The development of lncRNA-based biomarkers for HCC must contend with substantial heterogeneity arising from biological source variability and patient demographic factors. Tissue-based lncRNAs provide valuable prognostic information with direct relevance to tumor biology but have limitations for serial monitoring and screening applications. Circulating lncRNAs offer non-invasive alternatives but may be influenced by various non-tumor factors and exhibit more variable performance as individual markers.
The path forward lies in the strategic integration of multiple biomarkers across different biological sources, combined with clinical parameters through sophisticated computational approaches. Future research must prioritize the validation of lncRNA biomarkers across diverse patient populations with varying etiologies and demographic characteristics. Standardization of pre-analytical and analytical protocols will be essential to enable comparison across studies and facilitate clinical translation. As our understanding of lncRNA biology in HCC continues to evolve, these molecular signatures hold tremendous promise for advancing personalized approaches to HCC detection, prognosis, and treatment selection.
In the pursuit of reliable hepatocellular carcinoma (HCC) biomarkers, long non-coding RNAs (lncRNAs) have emerged as promising candidates for both single and combination prognostic signatures [1] [9]. However, the technical challenges of maintaining RNA stability, ensuring efficient extraction, and implementing proper data normalization significantly impact the validity and reproducibility of research findings. The integrity of RNA specimens directly influences the accurate quantification of transcript levels, which is paramount when comparing the efficacy of single lncRNA biomarkers against multi-lncRNA signatures.
Altered expression levels of numerous lncRNAs are frequently observed in HCC tissues and blood circulation, and they have demonstrated independent prognostic value in predicting patient survival [9]. For instance, studies have validated multiple individual lncRNAs as prognostic biomarkers, with hazard ratios (HR) for overall survival ranging from 2.091 for LINC01094 to 3.539 for LASP1-AS in validation cohorts [9]. The technical precision required to detect these meaningful biological signals demands rigorous attention to pre-analytical variables, particularly those affecting RNA integrity.
RNA Extraction Efficiency: Methodological Comparisons for lncRNA Recovery
The efficiency of RNA extraction methodologies varies considerably, directly impacting the yield and quality of recovered lncRNAs. Different extraction techniques demonstrate distinct performance characteristics in preserving both large and small RNA species, which is crucial for comprehensive transcriptome analyses in HCC research.
Comparative Performance of RNA Extraction Methods
A systematic comparison of three RNA extraction methods revealed significant differences in their ability to recover high-quality RNA suitable for next-generation sequencing applications [56]:
Table 1: Performance Comparison of RNA Extraction Methods
| Extraction Method | Average Yield | RNA Integrity Number (RIN) | sRNA Recovery | gDNA Contamination |
|---|---|---|---|---|
| Phenol-free kit | Highest | 9.85 ± 0.3 | Good | Minimal after DNase I |
| RNeasy Mini kit | Moderate | Good | Trace amounts | Present |
| TRI Reagent | Lowest | - | Enriched | Present |
The Phenol-free total RNA purification kit coupled with DNase I treatment yielded the highest quality RNAs with the best integrity scores and effective recovery of both high and low molecular weight transcripts [56]. This balanced recovery is particularly important for lncRNA studies, as it ensures adequate representation of both the large lncRNAs and smaller regulatory RNAs that might interact in HCC pathways.
Experimental Protocol for Optimal RNA Extraction
The following detailed protocol has been validated for efficient RNA extraction from bacterial samples, with principles applicable to HCC tissue samples [56]:
Cell Preparation: Harvest 1 × 10^9 cells by centrifugation at 10,000 × g for 10 minutes at 4°C. Discard supernatant and keep pellet on ice for immediate processing.
Cell Lysis: Use the proprietary lysis buffer provided in the Phenol-free total RNA purification kit. Thoroughly homogenize the cell pellet to ensure complete lysis.
RNA Binding and Washing: Transfer the lysate to the spin column provided in the kit. Centrifuge at 12,000 × g for 1 minute. Wash the membrane with the provided wash buffers according to manufacturer's specifications.
DNase I Treatment (Critical Step):
- Prepare DNase I reaction mixture: 10 U DNase I, 1× DNase I buffer, 80 U recombinant RNasin ribonuclease inhibitor.
- Apply directly to the membrane and incubate at 37°C for 1 hour.
- This step is essential for removing contaminating genomic DNA that could interfere with subsequent analyses.
RNA Elution: Elute RNA with nuclease-free water. Pre-heating elution buffer to 65°C may improve yield.
Quality Assessment:
- Determine RNA concentration and integrity using Agilent 2100 Bioanalyzer with RNA Nano 6000 LabChip kit.
- Verify absence of genomic DNA contamination by PCR using species-specific primers (e.g., 16S rDNA primers for bacterial samples).
- Repeat DNase I treatment if genomic DNA contamination is detected.
This protocol, when applied to Pseudomonas aeruginosa, enabled excellent sequencing coverage across RNA size ranges, detecting 5435 coding genes, 452 sRNAs, and 7 potential novel intergenic sRNAs in a single sequencing run [56].
Diagram 1: RNA Extraction Workflow and Quality Impact on lncRNA Research
RNA Stability: Preserving lncRNA Integrity for HCC Biomarker Discovery
RNA stability presents a formidable challenge in HCC research due to the rapid degradation of RNA transcripts by ubiquitous RNases. The integrity of lncRNAs is particularly crucial as their expression levels serve as direct readouts for biomarker potential in prognostic models.
Strategic Approaches to Maintain RNA Stability
Several critical strategies must be implemented throughout the experimental workflow to preserve RNA integrity:
RNase Inhibition: The use of RNase inhibitors is essential during RNA extraction and subsequent handling. In the optimized protocol, 80 U of recombinant RNasin ribonuclease inhibitor was incorporated during the DNase I treatment step to prevent RNA degradation [56].
Temperature Control: Immediate processing of samples after collection and maintaining cold chain conditions (4°C during centrifugation, -80°C for storage) is crucial. Flash-freezing in liquid nitrogen is recommended for tissue specimens.
Rapid Stabilization: For clinical samples, the use of RNA stabilization reagents (such as RNAprotect Bacteria Reagent) immediately after collection preserves the in vivo RNA expression profile and prevents degradation.
The half-life of lncRNAs can vary significantly based on their secondary structure and cellular context, making standardized stabilization protocols essential for comparative analyses between single and combined lncRNA biomarker panels [9].
Data Normalization: Ensuring Reliable lncRNA Quantification in HCC Studies
Proper data normalization is fundamental for accurate comparison of lncRNA expression levels across HCC patient samples. The technical variability introduced during RNA extraction and analysis must be accounted for to draw valid biological conclusions about biomarker efficacy.
Normalization Strategies for Transcriptomic Data
Multiple normalization approaches can be employed depending on the analytical platform:
Reference Gene Normalization: Using stably expressed housekeeping genes (e.g., GAPDH, ACTB) as internal controls for qRT-PCR experiments. This approach requires preliminary validation of reference gene stability in the specific experimental system.
Global Mean Normalization: For sequencing-based approaches, normalizing to the global mean of expressed transcripts can account for technical variations in library preparation and sequencing depth.
Upper Quartile Normalization: This method scales counts based on the upper quartile of expressed genes, reducing the impact of highly variable low-abundance transcripts.
In machine learning approaches for HCC prediction, data normalization has been shown to significantly improve model performance, with accuracy improvements of up to 97.33% for Naive Bayes classifiers after proper normalization and feature reduction [57].
Impact on lncRNA Biomarker Validation
The choice of normalization strategy directly impacts the prognostic value derived from lncRNA biomarkers. For instance, in studies validating single lncRNA biomarkers, normalized expression levels of LINC01146 showed an independent association with longer overall survival (HR, 0.38; 95% CI, 0.16-0.92; P = 0.033), while LINC01139 high expression predicted shorter survival (HR, 2.721; 95% CI, 1.289-4.183; P = 0.019) [9]. These hazard ratios, central to biomarker validation, are highly dependent on the accuracy of the normalized expression measurements.
Diagram 2: Data Normalization Impact on lncRNA Biomarker Validation
Table 2: Essential Research Reagents for RNA-Based HCC Biomarker Studies
| Reagent/Resource | Specific Function | Application in lncRNA Research |
|---|---|---|
| Phenol-free RNA purification kit | Total RNA isolation with high integrity | Optimal recovery of full-length lncRNAs |
| DNase I (RNase-free) | Genomic DNA elimination | Prevents false positives in qRT-PCR and sequencing |
| Recombinant RNasin inhibitor | Protection against RNase degradation | Maintains lncRNA integrity during processing |
| RNAprotect Tissue Reagent | RNA stabilization at collection | Preserves in vivo lncRNA expression profiles |
| Agilent Bioanalyzer RNA chips | RNA integrity quantification | Quality control for reliable lncRNA detection |
| Reference genes (GAPDH, ACTB) | qRT-PCR normalization | Enables accurate lncRNA quantification |
| lncRNA-specific primers | Target amplification | Precise detection of individual lncRNA biomarkers |
Comparative Efficacy: Technical Considerations for Single vs. Combined lncRNA Biomarkers
The technical challenges of RNA stability, extraction efficiency, and data normalization manifest differently when working with single lncRNA biomarkers compared to multi-lncRNA signatures.
Single lncRNA Biomarker Requirements
For individual lncRNAs, the technical requirements include:
- Highly specific detection methods such as qRT-PCR with validated primer sets
- Stringent normalization to account for sample-to-sample variation
- Optimized extraction to ensure consistent recovery of the specific lncRNA
Examples of successfully validated single lncRNA biomarkers include LINC01554, where low pre-treatment expression independently predicted shorter overall survival (HR, 2.507; 95% CI, 1.153-2.832; P = 0.017), and HOXC13-AS, where high expression predicted shorter overall survival (HR, 2.894; 95% CI, 1.183-4.223; P = 0.015) and recurrence-free survival (HR, 3.201; 95% CI, 1.372-4.653; P = 0.004) [9].
Multi-lncRNA Signature Considerations
For combination lncRNA biomarkers, additional technical factors must be addressed:
- Balanced extraction efficiency across multiple lncRNA species with varying lengths and structures
- Comprehensive normalization strategies that account for coordinated expression patterns
- Reduced technical variance to enable detection of subtle but biologically relevant expression changes across multiple targets
The computational approaches for analyzing multi-lncRNA signatures benefit from advanced normalization techniques, with studies demonstrating that feature reduction methods can improve machine learning algorithm accuracy for HCC prediction from below 70.6% to over 96% for multiple algorithms including Decision Trees, Neural Networks, and SVM [57].
The technical challenges of RNA stability, extraction efficiency, and data normalization represent critical factors in the validation of both single and combined lncRNA biomarkers for hepatocellular carcinoma. The selection of appropriate RNA extraction methodologies, particularly phenol-free systems with rigorous DNase treatment, provides the foundation for reliable lncRNA recovery. Coupled with stringent RNA stabilization protocols and sophisticated data normalization approaches, these technical considerations enable researchers to accurately discern the comparative efficacy of individual lncRNAs versus multi-lncRNA signatures as prognostic indicators in HCC. As the field advances toward clinical implementation of these biomarkers, standardized technical protocols will be essential for translating laboratory findings into clinically actionable diagnostic and prognostic tools.
The transition of long non-coding RNAs (lncRNAs) from research discoveries to clinically applicable biomarkers for hepatocellular carcinoma (HCC) confronts two fundamental analytical challenges: establishing standardized cut-off values for risk stratification and implementing robust protocols to mitigate batch effects across multi-center studies. These technical roadblocks substantially impact the comparative efficacy of single versus combined lncRNA biomarkers, influencing their reliability in prognostic prediction and therapeutic decision-making. While combined lncRNA signatures demonstrate enhanced prognostic accuracy through complementary pathways—such as the RAB30-DT/SRPK1 axis regulating alternative splicing and the NEAT1/miR-155 pathway modulating CD8+ T cell function—their clinical translation depends on resolving these analytical variabilities [58] [59]. This guide systematically compares experimental approaches to these challenges, providing objective performance data and methodological frameworks essential for robust biomarker implementation.
Establishing Cut-off Values: Methodologies and Comparative Performance
Technical Approaches for Cut-off Determination
Cut-off values transform continuous lncRNA expression data into clinically actionable binary classifications (high-risk vs. low-risk). The methodologies employed directly impact prognostic accuracy and clinical applicability, with significant differences observed between single and multi-marker approaches.
- Statistical Distribution-Based Methods: Single lncRNA biomarkers frequently utilize median expression values (e.g., LINC00152, LINC00294) or percentile-based stratification (e.g., top vs. bottom quartile) as objective, data-driven cut-offs. This approach demonstrates utility in homogeneous patient cohorts but shows reduced transferability across diverse populations [13] [43].
- Outcome-Oriented Optimization: Maximally Selected Rank Statistics identify cut-offs that optimally separate survival outcomes, as applied in studies of LINC01146 and ELMO1-AS1. This method directly links expression thresholds to clinical endpoints but risks overfitting to specific cohorts without independent validation [13].
- Machine Learning-Derived Thresholds: Multi-marker signatures increasingly employ algorithm-generated continuous risk scores with thresholds determined by unsupervised clustering (K-means) or supervised methods. The Consensus Artificial Intelligence-derived Prognostic Signature (CAIPS) exemplifies this approach, leveraging ten machine learning algorithms to establish stable cut-offs across six multi-center cohorts (n=1,110) [43].
Table 1: Comparative Performance of Cut-off Establishment Methods in HCC lncRNA Studies
| Method Category | Specific Technique | Representative Biomarker | Cohort Size | Prognostic Performance (HR Range) | Key Advantages | Major Limitations |
|---|---|---|---|---|---|---|
| Distribution-Based | Median Split | LINC00152, LINC00294 | 63-94 patients | HR: 2.434-2.524 [13] | Computational simplicity, objectivity | Population-dependent, may not optimize prognostic separation |
| Outcome-Oriented | Maximally Selected Rank Statistics | LINC01146, ELMO1-AS1 | 85-222 patients | HR: 0.38-0.518 [13] | Direct clinical relevance, optimized separation | Overfitting risk, reduced cross-cohort stability |
| Machine Learning | Risk Score Clustering | CAIPS (7-gene) | 1,110 patients | Highest C-index vs. 150 existing models [43] | Multi-dimensional integration, enhanced stability | Computational complexity, requires large sample sizes |
Experimental Protocols for Cut-off Validation
Robust establishment of lncRNA cut-off values requires a multi-stage validation protocol:
- Discovery Phase: In initial cohort analysis, apply Receiver Operating Characteristic (ROC) curve analysis against clinical endpoints (overall survival, recurrence-free survival) to identify candidate thresholds maximizing sensitivity and specificity. For continuous risk scores, use time-dependent ROC analysis to evaluate predictive accuracy at specific clinical timepoints (1-, 3-, 5-year survival) [43] [60].
- Validation Phase: Confirm established cut-offs in temporally or geographically distinct validation cohorts using identical quantification methodologies. The study by Yin et al. exemplifies this approach, validating LASP1-AS cut-offs in 218 independent patients after initial establishment in 205 patients [13].
- Clinical Utility Assessment: Evaluate stratification performance through Kaplan-Meier survival analysis with log-rank testing and multivariate Cox regression to confirm independent prognostic value after adjusting for clinical covariates (age, stage, etiology) [13] [43].
The following workflow diagram illustrates the standardized protocol for establishing and validating cut-off values in lncRNA biomarker studies:
Overcoming Batch Effects: Strategies for Multi-Center Consistency
Batch effects introduce non-biological variation arising from differences in sample processing, reagent lots, instrumentation, and personnel across collection sites or processing dates. In lncRNA studies, these effects particularly impact:
- RNA extraction efficiency (column-based vs. liquid-phase separation)
- Reverse transcription efficiency (enzyme selection, priming methods)
- Amplification bias (qPCR efficiency, primer lot variability)
- Platform-specific detection (RNA-seq library prep, sequencing depth) [43] [22]
The CAIPS multi-center study demonstrated that uncontrolled batch effects can reduce prognostic accuracy by up to 40% compared to batch-corrected models, emphasizing the critical need for standardization [43].
Comparative Batch Effect Correction Strategies
Table 2: Experimental Approaches for Batch Effect Mitigation in Multi-Center lncRNA Studies
| Correction Strategy | Implementation Method | Suitable Study Designs | Performance Evidence | Technical Requirements |
|---|---|---|---|---|
| Pre-analytical Standardization | Standardized RNA extraction, unified platforms, reference materials | Prospective multi-center studies | 30% improvement in inter-site correlation [22] | Centralized protocol development, training programs |
| Reference Sample Integration | Inter-laboratory reference standards, spike-in controls | Cross-platform comparisons, longitudinal studies | 25% reduction in technical CV [43] | Access to synthetic lncRNAs or stable reference materials |
| Bioinformatic Correction | ComBat, Harmony algorithm, RUV normalization | Retrospective analyses, data integration | C-index improvement from 0.65 to 0.82 in integrated cohorts [43] [60] | Computational expertise, raw data availability |
| Sample Randomization | Balancing experimental batches across clinical groups | Single-center studies with large sample sizes | Prevents confounding but doesn't eliminate variability | Careful experimental planning, sufficient sample numbers |
Experimental Protocols for Batch Effect Management
Pre-analytical Phase Control:
- Implement identical RNA stabilization methods (e.g., PAXgene tubes) across collection sites
- Utilize single-lot reagent purchases for multi-center studies or validate cross-lot consistency
- Establish RNA quality thresholds (RIN >7.0 for RNA-seq, DV200 >30% for FFPE samples) [22]
Reference Material Integration:
- Incorporate external RNA controls (e.g., Synthetic lncRNA spike-ins) at RNA extraction stage
- Include inter-plate calibrators across all processing batches
- Use pooled reference samples representing all experimental groups [43]
Bioinformatic Normalization:
The following diagram illustrates the comprehensive strategy for managing batch effects throughout the experimental workflow:
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for lncRNA Biomarker Studies
| Reagent/Platform Category | Specific Examples | Primary Function | Performance Considerations | Compatibility with Correction Methods |
|---|---|---|---|---|
| RNA Stabilization Reagents | PAXgene Blood RNA tubes, RNAlater | Preserve RNA integrity during storage/transport | Critical for circulating lncRNA studies; reduces hemolysis effects [22] | Enables multi-center standardization |
| Nucleic Acid Extraction Kits | Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) | Isolation of circulating lncRNAs from biofluids | Determines yield and purity; impacts downstream efficiency [22] | Kit lot consistency essential for batch effect control |
| Reverse Transcription Systems | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | cDNA synthesis with minimal bias | Enzyme choice affects lncRNA detection efficiency | Enables spike-in control incorporation |
| qPCR Detection Platforms | Power SYBR Green PCR Master Mix, TaqMan assays | lncRNA quantification | SYBR Green requires optimization of primer specificity | Multi-plate calibration reduces inter-run variability |
| Reference Materials | Synthetic lncRNA spike-ins, External RNA Controls Consortium (ERCC) standards | Batch effect monitoring and normalization | Must be added pre-extraction for accurate normalization | Enables bioinformatic correction validation |
| Bioinformatic Tools | Harmony, ComBat, sva, limma packages | Computational batch effect correction | Harmony excels for single-cell data; ComBat for bulk RNA-seq | Requires raw data access for optimal implementation |
| Exatecan intermediate 8 | Exatecan intermediate 8, MF:C30H34FN3O9S, MW:631.7 g/mol | Chemical Reagent | Bench Chemicals |
Overcoming the dual challenges of cut-off establishment and batch effect mitigation requires methodical implementation of standardized protocols across the biomarker development pipeline. The experimental data presented demonstrates that multi-marker signatures incorporating bioinformatic correction strategies consistently outperform single lncRNA biomarkers in multi-center applications, with the CAIPS model maintaining superior prognostic accuracy (C-index >0.7) across six independent cohorts [43]. Future directions should prioritize reference material development specifically for lncRNA quantification and machine learning frameworks that simultaneously optimize cut-offs while correcting for technical variability. Through rigorous attention to these analytical fundamentals, the promising efficacy of lncRNA biomarkers—particularly combination signatures—can be reliably translated into clinically applicable tools for HCC management.
Hepatocellular carcinoma (HCC) typically arises from a background of chronic liver disease, most often in patients with hepatitis B (HBV), hepatitis C (HCV), or cirrhosis from various etiologies [61] [62]. This pathogenic continuum presents a significant diagnostic challenge: accurately distinguishing early-stage HCC from benign chronic liver conditions. While cirrhosis is a well-established prerequisite for most HCC cases, emerging evidence indicates that a substantial proportion (approximately 28%) of HCCs develop in non-cirrhotic livers, particularly those associated with HBV, underscoring the need for highly specific biomarkers beyond conventional indicators of liver dysfunction [61].
Long non-coding RNAs (lncRNAs), defined as RNA transcripts longer than 200 nucleotides with limited protein-coding potential, have emerged as promising molecular biomarkers in oncology [13] [4]. Their high tissue specificity, stability in circulating biofluids, and central roles in regulating carcinogenic processes make them particularly attractive for addressing this diagnostic challenge [39] [22]. This review evaluates the comparative efficacy of single versus combined lncRNA biomarkers in optimizing diagnostic specificity for distinguishing HCC from chronic hepatitis and cirrhosis, providing researchers and drug development professionals with a critical analysis of current methodologies and emerging signatures.
The Diagnostic Challenge: HCC in the Context of Chronic Liver Disease
The progression from healthy liver to chronic hepatitis, cirrhosis, and ultimately hepatocellular carcinoma involves complex molecular alterations that create a difficult diagnostic landscape. Cirrhosis, characterized by progressive liver fibrosis and scarring, remains the most significant risk factor for HCC, with annual incidence rates of 1-8% among affected individuals [63] [62]. However, recent analyses of prospectively accrued cohorts challenge the notion of cirrhosis as an obligatory precursor stage, revealing that 28% of HCC patients showed no indication of cirrhosis prior to cancer diagnosis [61]. The etiology of underlying liver disease significantly influences HCC risk, with HCV-cirrhosis demonstrating higher HCC incidence compared to cirrhosis related to alcoholic liver disease (ALD) or non-alcoholic fatty liver disease (NAFLD) [63].
Conventional surveillance methods, including abdominal ultrasound and serum alpha-fetoprotein (AFP) measurement, face limitations in sensitivity and specificity, particularly for early-stage HCC detection [39] [22]. Ultrasound examination is operator-dependent and less sensitive in obese patients or those with nodular livers, while AFP demonstrates suboptimal sensitivity and specificity, especially for early-stage tumors [22]. Tissue biopsy, while definitive, carries risks of hemorrhage, tumor seeding, and sampling error due to tumor heterogeneity [22]. These limitations highlight the urgent need for more reliable, non-invasive molecular biomarkers that can detect HCC at its earliest, most treatable stages, particularly in high-risk populations with chronic liver disease.
Table 1: Current Limitations in HCC Diagnosis
| Diagnostic Method | Key Limitations | Impact on Clinical Management |
|---|---|---|
| Abdominal Ultrasound | Operator-dependent; Reduced sensitivity in obese patients/nodular livers; Limited detection of early lesions | Delayed diagnosis of early-stage HCC |
| Alpha-fetoprotein (AFP) | Suboptimal sensitivity (particularly in early HCC); False positives in active hepatitis | Limited utility for population screening |
| Liver Biopsy | Invasive procedure with risk of hemorrhage (1-5%); Tumor seeding along needle track (~2.5%); Sampling variability | Restricted to indeterminate cases; Not suitable for serial monitoring |
LncRNAs: Mechanisms and Methodologies
Biological Functions of LncRNAs in Hepatocarcinogenesis
LncRNAs exert their regulatory functions through diverse molecular mechanisms, functioning as critical modulators of gene expression at epigenetic, transcriptional, and post-transcriptional levels [13] [4]. They can act as signaling molecules recruiting transcription factors in response to cellular stimuli; guiding molecules directing chromatin-modifying enzymes to specific genomic locations; decoy molecules sequestering transcription factors or microRNAs from their targets; and scaffolding molecules mediating the formation of multi-component complexes [13]. Their functional roles are largely determined by subcellular localization—nuclear lncRNAs predominantly regulate RNA transcription and chromatin organization, while cytoplasmic lncRNAs influence mRNA stability, translation, and protein functions [4].
In HCC, specific lncRNAs drive tumorigenesis through defined molecular pathways. For instance, lncRNA H19 stimulates the CDC42/PAK1 axis by downregulating miRNA-15b expression, accelerating HCC cell proliferation [4]. The hypoxia-responsive lncRNA-p21 forms a positive feedback loop with HIF-1α to drive glycolysis and promote tumor growth [4]. Linc-RoR functions as a molecular sponge for tumor suppressor miR-145 during hypoxic conditions, enabling cancer cell self-renewal through upregulation of miR-145 downstream targets p70S6K1, PDK1, and HIF-1α [4]. These defined mechanistic roles make lncRNAs not only promising biomarkers but also potential therapeutic targets.
Experimental Workflows for LncRNA Biomarker Validation
Robust validation of lncRNA biomarkers requires standardized methodologies across sample collection, processing, and analytical phases. The typical workflow begins with sample acquisition from either tissue or liquid biopsy sources. For blood-based lncRNA detection, fasting venous blood is collected in EDTA-containing vacuum tubes for plasma preparation or tubes with inert separation gel and procoagulant for serum preparation [39]. Samples should be centrifuged promptly (within 2 hours of collection), with separated serum/plasma aliquoted and stored at -80°C until analysis.
Extracellular vesicle (EV) isolation represents a crucial step for analyzing circulating lncRNAs, as EVs protect their RNA cargo from degradation. The size-exclusion chromatography and ultrafiltration method provides high-quality EV preparations: after thawing, samples are pretreated with a 0.8μm filter, then separated via a gel-permeation column (e.g., ES911, Echo Biotech), with PBS eluent collected and concentrated using a 100kD ultrafiltration tube [39]. EV characterization should include nanoparticle tracking analysis for particle size distribution, transmission electron microscopy for morphological assessment, and Western blot analysis for marker proteins (TSG101, Alix, CD9) with Calnexin as a negative control [39].
RNA extraction from EVs or tissues employs commercial kits optimized for different sample types. For plasma EV RNA isolation, the Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek Corp.) effectively processes 500μL starting material, with subsequent DNase treatment (Turbo DNase, Life Technologies) to remove genomic DNA contamination [22]. Reverse transcription utilizes the High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher Scientific), followed by quantitative PCR with Power SYBR Green PCR Master Mix (Thermo Fisher Scientific) on platforms such as the StepOne Plus System (Applied Biosystems) [22]. PCR conditions typically include initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 62°C for 1 minute, with specificity confirmed through dissociation melting curves and polyacrylamide gel electrophoresis [22].
Single LncRNA Biomarkers: Diagnostic and Prognostic Performance
Numerous individual lncRNAs demonstrate altered expression in HCC tissues and circulation, showing promise as discriminatory biomarkers. Well-characterized examples include HULC, which is significantly upregulated in plasma from chronic hepatitis C patients who develop HCC compared to those who do not [22]. Similarly, lncRNA RP11-731F5.2 shows differential expression in CHC patients with and without HCC progression, suggesting utility in risk stratification [22]. The diagnostic potential of single lncRNAs extends beyond mere presence/absence discrimination to correlation with clinical parameters. For instance, MIAT and HOTAIR levels positively correlate with tumor size ≥5 cm and HCV-positive status, providing quantitative relationships with disease severity [33].
The prognostic value of single lncRNA biomarkers is substantiated by multivariate Cox proportional hazards regression analyses across multiple studies. Investigations in retrospectively recruited HCC patient cohorts reveal independent prognostic significance for various lncRNAs. For example, elevated LINC00152 expression independently predicts shorter overall survival (HR, 2.524; 95% CI, 1.661-4.015; P=0.001) [13]. Similarly, high LINC00294 levels correlate with reduced survival (HR, 2.434; 95% CI, 1.143-3.185; P=0.021) [13]. Conversely, some lncRNAs like LINC01146 demonstrate tumor-suppressive properties, with high expression independently associated with longer overall survival (HR, 0.38; 95% CI, 0.16-0.92; P=0.033) [13].
Table 2: Single LncRNA Biomarkers with Prognostic Significance in HCC
| LncRNA | Expression in HCC | Hazard Ratio (95% CI) | P-value | Clinical Significance |
|---|---|---|---|---|
| LINC00152 | Upregulated | 2.524 (1.661-4.015) | 0.001 | Independent predictor of shorter OS [13] |
| LINC00294 | Upregulated | 2.434 (1.143-3.185) | 0.021 | Independently correlated with shorter OS [13] |
| LINC01146 | Downregulated | 0.38 (0.16-0.92) | 0.033 | Independent association with longer OS [13] |
| HOXC13-AS | Upregulated | OS: 2.894 (1.183-4.223)RFS: 3.201 (1.372-4.653) | 0.0150.004 | Independent association with shorter OS and RFS [13] |
| LASP1-AS | Downregulated | Training: 1.884 (1.427-2.841)Validation: 3.539 (2.698-6.030) | <0.0001<0.0001 | Independent predictor of shorter OS in training and validation cohorts [13] |
Beyond diagnostic applications, functional studies establish the therapeutic relevance of specific lncRNAs. Efficient knockdown of oncogenic lncRNAs HEIH, MIAT, and HOTAIR significantly reduces colony formation and cellular viability in Huh-7 HCC cells, confirming their functional roles in maintaining malignant phenotypes [33]. This dual utility as both biomarker and therapeutic target enhances the clinical value of individual lncRNAs in HCC management.
Combined LncRNA Signatures: Enhanced Specificity and Clinical Utility
While individual lncRNAs show promise, combined biomarker signatures significantly enhance diagnostic specificity for distinguishing HCC from benign liver conditions. Multi-lncRNA panels address tumor heterogeneity and compensate for variations in individual marker expression, providing more robust classification accuracy. A notable three-lncRNA signature comprising MIAT, HEIH, and HOTAIR demonstrates superior discriminatory power, with each component contributing unique diagnostic information: HEIH shows elevated levels in both cirrhotic and HCC tissues, MIAT displays a stepwise increase from cirrhosis to HCC, while HOTAIR overexpression is exclusive to HCC tissue [33].
High-throughput transcriptomic approaches facilitate identification of complex lncRNA signatures specifically tailored for distinguishing disease stages. Systematic RNA sequencing of serum extracellular vesicles across the liver disease spectrum (chronic hepatitis B, cirrhosis, hepatic adenoma, and HCC) identified 133 significantly differentially expressed lncRNAs in the HCC group [39]. Through multi-step screening and time-series analysis, researchers distilled these to 10 core lncRNAs specifically associated with HCC progression, which were incorporated into a regulatory network comprising 62 nodes and 68 edges [39]. This systems biology approach captures the complexity of lncRNA interactions in hepatocarcinogenesis, moving beyond single-marker paradigms.
The diagnostic performance of combined lncRNA signatures frequently surpasses conventional biomarkers. For instance, the combination of plasma lncRNAs HULC and RP11-731F5.2 demonstrates enhanced predictive value for HCC risk stratification in chronic hepatitis C patients compared to either marker alone [22]. Similarly, lncRNA pairs such as RP11-731F5.2 and KCNQ1OT1 may serve as complementary biomarkers for liver damage due to HCV infection, offering noninvasive monitoring tools for disease progression [22]. These multi-analyte approaches align with the recognition that HCC development involves coordinated alterations in multiple regulatory pathways rather than isolated molecular events.
Table 3: Combined LncRNA Signatures for HCC Detection
| LncRNA Signature | Components | Diagnostic Utility | Sample Source | Key Findings |
|---|---|---|---|---|
| Three-LncRNA Signature | MIAT, HEIH, HOTAIR | Distinguishes HCC from cirrhosis and normal liver | Liver tissue | MIAT: Stepwise increase from cirrhosis to HCCHOTAIR: Exclusive to HCCHEIH: Elevated in cirrhosis and HCC [33] |
| EV-derived 10-LncRNA Panel | 10 core lncRNAs | Tracks progression from hepatitis to HCC | Serum extracellular vesicles | Identified through high-throughput sequencing; Incorporated into regulatory network (62 nodes, 68 edges) [39] |
| Plasma Risk Stratification Panel | HULC, RP11-731F5.2 | HCC risk assessment in CHC patients | Plasma | Complementary performance for identifying CHC patients who will develop HCC [22] |
| Liver Damage Monitoring Panel | RP11-731F5.2, KCNQ1OT1 | Monitoring liver damage in HCV infection | Plasma | Potential noninvasive biomarkers for liver damage due to HCV [22] |
Comparative Analysis: Single vs. Combined LncRNA Biomarkers
The strategic selection between single and combined lncRNA biomarkers depends on specific clinical applications, weighing advantages and limitations of each approach. Single lncRNA biomarkers offer practical advantages in clinical translation, including simpler analytical validation, reduced development costs, and more straightforward regulatory approval pathways. Their implementation in routine clinical practice requires less complex instrumentation and interpretation algorithms. However, they face limitations in addressing the substantial molecular heterogeneity of HCC, with variable expression across etiologies (HBV-, HCV-, or NAFLD-related HCC) and tumor stages [63].
Combined lncRNA signatures demonstrate superior diagnostic performance metrics, particularly in specificity and positive predictive value. By integrating multiple markers with complementary expression patterns, these panels better capture the molecular diversity of HCC and show increased robustness against technical and biological variations. The statistical advantage of multi-analyte panels is evident in receiver operating characteristic (ROC) analyses, where combinations frequently achieve area under the curve (AUC) values exceeding those of individual markers [39] [22]. However, these enhancements come with practical challenges, including more complex analytical procedures, requirement for multivariate statistical models, and increased regulatory hurdles for clinical implementation.
The optimal application of each approach varies by clinical context. Single lncRNAs may suffice for monitoring treatment response or recurrence risk in established HCC cases, where baseline expression levels are known. In contrast, combined signatures prove more valuable for initial diagnosis and distinguishing HCC from benign liver conditions, where maximizing diagnostic specificity is paramount. For comprehensive HCC management, a tiered approach may be optimal: using combined signatures for initial screening and risk stratification, followed by specific individual lncRNAs for monitoring disease progression or treatment response.
Essential Research Reagents and Methodologies
Standardized research methodologies and high-quality reagents are fundamental to generating reproducible lncRNA biomarker data. Key experimental components include sample collection systems such as vacuum tubes containing inert separation gel and procoagulant for serum preparation or EDTA-containing tubes for plasma preparation (SEKISUI MEDICAL TECHNOLOGY LTD) [39]. For EV isolation, size-exclusion chromatography columns (ES911, Echo Biotech) combined with 100kD ultrafiltration tubes enable high-purity extracellular vesicle recovery [39].
RNA isolation represents a critical step, with specialized kits like the Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek Corp.) optimized for challenging biofluid samples [22]. DNase treatment reagents (Turbo DNase, Life Technologies) ensure removal of contaminating genomic DNA, while reverse transcription kits (High-Capacity cDNA Reverse Transcription Kit, Thermo Fisher Scientific) and qPCR master mixes (Power SYBR Green PCR Master Mix, Thermo Fisher Scientific) maintain analytical sensitivity and specificity [22].
Validation methodologies extend beyond expression profiling to functional characterization. For in vitro functional studies, siRNA transfection reagents (HiPerFect, Qiagen) enable efficient lncRNA knockdown in hepatoma cell lines (e.g., Huh-7), with subsequent phenotypic assessments using MTT assays for cell viability and colony formation assays for proliferative capacity [33]. Analytical instrumentation spans nanoparticle tracking analyzers (Flow NanoAnalyzer, NanoFCM Inc.) for EV characterization, transmission electron microscopes (H-7650, Hitachi) for morphological analysis, and qPCR systems (StepOne Plus, Applied Biosystems) for expression quantification [39] [22].
Table 4: Essential Research Reagents for LncRNA Biomarker Studies
| Category | Specific Reagents/Instruments | Application | Key Features |
|---|---|---|---|
| Sample Collection | Vacuum tubes with separation gel (serum); EDTA tubes (plasma) | Blood sample acquisition | Preserves RNA integrity; Minimizes hemolysis |
| EV Isolation | Size-exclusion chromatography columns (ES911, Echo Biotech); 100kD ultrafiltration tubes | Extracellular vesicle isolation | Maintains vesicle integrity; High purity recovery |
| RNA Extraction | Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) | RNA isolation from biofluids | Optimized for low-concentration circulating RNA |
| Molecular Analysis | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher); Power SYBR Green PCR Master Mix (Thermo Fisher) | lncRNA expression quantification | High sensitivity; Wide dynamic range |
| Functional Validation | HiPerFect Transfection Reagent (Qiagen); Huh-7 cell line | lncRNA knockdown studies | Efficient siRNA delivery; Relevant HCC model |
The strategic implementation of lncRNA biomarkers represents a paradigm shift in distinguishing hepatocellular carcinoma from chronic hepatitis and cirrhosis. While individual lncRNAs provide valuable diagnostic and prognostic information, combined multi-lncRNA signatures demonstrate superior specificity for differentiating HCC from benign liver conditions. The evolving understanding of lncRNA regulatory networks in hepatocarcinogenesis, particularly their roles in modulating immune responses, autophagy, and key signaling pathways, continues to reveal new biomarker opportunities.
Future directions in lncRNA-based HCC diagnostics should focus on validating these biomarkers in large, multi-center prospective cohorts, with particular attention to standardized pre-analytical procedures and analytical thresholds. Integration of lncRNA signatures with existing clinical parameters and conventional biomarkers may further enhance diagnostic accuracy. For research and drug development applications, combined lncRNA panels offer the most promising approach for early detection and risk stratification, while single lncRNAs retain utility for monitoring disease progression and treatment response. As lncRNA research advances, these molecular tools hold immense potential to improve HCC detection and patient outcomes through precision diagnostics.
The investigation of long non-coding RNAs (lncRNAs) as biomarkers for hepatocellular carcinoma (HCC) represents a rapidly advancing frontier in molecular oncology. As research progresses from single-center discovery studies to multi-center validation, the field faces a critical challenge: transitioning from promising but isolated findings to clinically applicable, reproducible diagnostic tools. The comparative efficacy of single lncRNA biomarkers versus multi-lncRNA panels remains a central question in this maturation process, with significant implications for early detection, prognostic stratification, and therapeutic guidance in HCC management.
Current evidence suggests that while individual lncRNAs show moderate diagnostic accuracy, their combination into integrated panels significantly enhances performance characteristics. For instance, individual lncRNAs typically demonstrate sensitivity and specificity ranging from 60-83% and 53-67%, respectively, whereas machine learning models integrating multiple lncRNAs with conventional biomarkers can achieve remarkable performance improvements up to 100% sensitivity and 97% specificity [10]. This stark contrast underscores the necessity for standardized protocols that can ensure the reproducibility of these findings across diverse patient populations and research institutions.
This guide systematically compares the performance of single and combined lncRNA biomarkers through the lens of multi-center validation, providing a structured framework for experimental design, methodology, and data analysis to advance the field toward clinically implementable standards.
Comparative Performance of Single vs. Combined lncRNA Biomarkers
Quantitative Performance Metrics
Table 1: Diagnostic Performance of Single lncRNA Biomarkers for HCC
| lncRNA | Sensitivity (%) | Specificity (%) | AUC | Sample Size (HCC/Control) | Reference |
|---|---|---|---|---|---|
| LINC00152 | 83 | 67 | 0.79 | 52/30 | [10] |
| LINC00853 | 60 | 53 | 0.62 | 52/30 | [10] |
| UCA1 | 75 | 60 | 0.71 | 52/30 | [10] |
| GAS5 | 65 | 58 | 0.66 | 52/30 | [10] |
| HOTAIR | 81 | 76 | 0.84 | 60/60 | [64] |
| MALAT1 | 85 | 72 | 0.86 | 60/60 | [64] |
| HOST2 | 78 | 70 | 0.81 | 60/60 | [64] |
| HOXA-AS2 | 80 | 69 | 0.82 | 60/60 | [64] |
Table 2: Performance of Combined lncRNA Biomarkers and Integrated Models
| Biomarker Combination | Sensitivity (%) | Specificity (%) | AUC | Sample Size (HCC/Control) | Reference |
|---|---|---|---|---|---|
| 4-lncRNA Panel + Machine Learning | 100 | 97 | 0.99 | 52/30 | [10] |
| MALAT1 + AFP | 92 | 85 | 0.94 | 60/60 | [64] |
| HOTAIR + AFP | 90 | 83 | 0.92 | 60/60 | [64] |
| 6-gene Risk Score (Exosomal lncRNA-derived) | 89 | 91 | 0.95 | 230 plasma exosomes | [18] |
| AAM-related lncRNA Risk Model (4 lncRNAs) | 87 | 85 | 0.91 | 170 training/170 validation | [17] |
The quantitative comparison reveals a consistent pattern: while individual lncRNAs demonstrate moderate diagnostic utility, their integration into multi-marker panels substantially enhances discriminatory power. The most pronounced improvement emerges when lncRNA combinations are processed through machine learning algorithms, achieving near-perfect classification in controlled studies [10]. This performance enhancement stems from the ability of combined panels to capture the molecular heterogeneity of HCC, which single biomarkers cannot adequately represent.
Prognostic and Therapeutic Stratification Value
Beyond diagnostic applications, lncRNA biomarkers show increasing utility in prognostic stratification and treatment response prediction. A plasma exosomal lncRNA-derived 6-gene risk score (G6PD, KIF20A, NDRG1, ADH1C, RECQL4, MCM4) successfully categorized HCC patients into distinct molecular subtypes with differential survival outcomes and treatment sensitivities [18]. Similarly, amino acid metabolism-related lncRNA signatures can stratify patients according to immune microenvironment characteristics and predicted response to immunotherapy [17].
Table 3: Prognostic Stratification Capabilities of lncRNA Signatures
| lncRNA Signature | Stratification Power | Clinical Applications | Validation Cohort |
|---|---|---|---|
| AAM-related 4-lncRNA Risk Model | High-risk group had significantly lower OS | Predicts immunotherapy response; high-risk group shows better response to anti-PD1 | 170 training/170 validation |
| Exosomal lncRNA-derived Molecular Subtyping | Three subtypes (C1-C3) with distinct survival | C3 subtype: poorest OS, immunosuppressive microenvironment | 831 HCC tissues |
| LINC00152 to GAS5 Expression Ratio | Correlates with mortality risk | Prognostic stratification | 52 HCC patients |
Standardized Experimental Protocols for lncRNA Biomarker Validation
Sample Collection and RNA Isolation
Patient Selection and Ethical Considerations Multi-center validation studies should establish consistent eligibility criteria across participating sites. Standardized protocols should include: (1) adult patients (≥18 years) with HCC diagnosed according to LI-RADS imaging criteria or histopathological examination; (2) treatment-naive individuals before sample collection; (3) age- and gender-matched controls without history of liver disease, cancer, or chronic inflammatory disorders [10]. Exclusion criteria must encompass patients on immunosuppressive drugs, those with non-HCC liver tumors, or other past/concurrent malignancies. The study protocol requires approval by institutional review boards at each participating site, with written informed consent obtained from all participants [10] [64].
Sample Collection and Processing Plasma samples should be collected following standardized protocols. For HCC patients, samples can be retrieved from institutional biobanks, while control samples require collection following identical standard operating procedures. All samples must be processed uniformly: (1) collection in EDTA tubes; (2) centrifugation at 2,000-3,000 × g for 10 minutes to separate plasma; (3) aliquoting and storage at -80°C until RNA extraction [10] [18].
RNA Isolation Protocol Total RNA isolation should utilize commercial kits such as the miRNeasy Mini Kit (QIAGEN, cat no. 217004) according to manufacturer's protocol [10]. The isolation procedure should include: (1) sample homogenization; (2) RNA separation through phase separation; (3) RNA precipitation with ethanol; (4) washing steps; (5) elution in RNase-free water. RNA quality and quantity should be assessed using spectrophotometry (A260/A280 ratio >1.8) or automated electrophoresis systems. Consistent RNA quality thresholds (e.g., RNA integrity number >7) should be established across centers.
cDNA Synthesis and Quantitative Real-Time PCR
Reverse Transcription The cDNA synthesis should employ the RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, cat no. K1622) or equivalent standardized across centers [10]. The reaction mixture typically includes: (1) total RNA template (100ng-1μg); (2) random hexamer or gene-specific primers; (3) reaction buffer; (4) RNase inhibitor; (5) reverse transcriptase enzyme. The thermal cycler conditions should be standardized: 25°C for 5 minutes (annealing), 42°C for 60 minutes (elongation), and 70°C for 5 minutes (enzyme inactivation).
qRT-PCR Analysis Quantitative real-time PCR should be performed using the PowerTrack SYBR Green Master Mix kit (Applied Biosystems, cat no. A46012) on a ViiA 7 real-time PCR system (Applied Biosystems) or equivalent instruments calibrated across centers [10]. Each reaction should be performed in triplicate with a reaction volume of 10-20μL containing: (1) cDNA template; (2) forward and reverse primers (sequences provided in Table 4); (3) SYBR Green Master Mix; (4) nuclease-free water. The thermal cycling conditions should be standardized: 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 60°C for 1 minute. The housekeeping gene GAPDH should be used for normalization, with the ΔΔCT method employed for relative quantification [10].
Table 4: Primer Sequences for Key lncRNAs in HCC Biomarker Studies
| lncRNA | Forward Primer (5'-3') | Reverse Primer (5'-3') | Amplicon Size (bp) |
|---|---|---|---|
| LINC00152 | Custom sequence per study | Custom sequence per study | Varies |
| LINC00853 | Custom sequence per study | Custom sequence per study | Varies |
| UCA1 | Custom sequence per study | Custom sequence per study | Varies |
| GAS5 | Custom sequence per study | Custom sequence per study | Varies |
| HOTAIR | Custom sequence per study | Custom sequence per study | Varies |
| MALAT1 | Custom sequence per study | Custom sequence per study | Varies |
Note: Specific primer sequences should be standardized across participating centers and validated for efficiency. Primer sequences for commonly investigated lncRNAs are available in publications such as [10].
Data Integration and Computational Analysis
Machine Learning Frameworks For integrated biomarker panels, machine learning analysis should be conducted using Python's Scikit-learn platform or equivalent computational environments [10]. The analysis pipeline should include: (1) data normalization and preprocessing; (2) feature selection using univariate Cox analysis, LASSO, and multivariate Cox analysis; (3) model construction with multiple algorithms (CoxBoost, stepwise Cox, Lasso, Ridge, elastic net, survival-SVMs, GBMs, SuperPC, plsRcox, and random survival forest); (4) 10-fold cross-validation for model optimization; (5) performance evaluation using concordance index (C-index) as the primary metric [18].
ceRNA Network Construction For functional characterization of lncRNA biomarkers, competitive endogenous RNA (ceRNA) networks should be constructed through a multi-database integration strategy: (1) prediction of miRNA binding sites of differentially expressed lncRNAs via miRcode database; (2) integration of miRNA-mRNA relationships from miRTarBase, TargetScan, and miRDB databases; (3) intersection of target genes of differentially expressed lncRNAs and upregulated mRNAs in HCC tissues; (4) network visualization using Cytoscape 3.9.1 [18].
Visualization of Experimental Workflows and Biological Mechanisms
Multi-Center lncRNA Validation Workflow
Diagram 1: Standardized multi-center workflow for lncRNA biomarker validation, encompassing protocol harmonization, experimental procedures, computational analysis, and cross-site performance verification.
lncRNA Functional Mechanisms in HCC
Diagram 2: Molecular mechanisms of lncRNAs in HCC pathogenesis, illustrating how oncogenic and tumor suppressor lncRNAs influence hepatocellular carcinoma progression through diverse regulatory pathways.
Essential Research Reagent Solutions
Table 5: Key Research Reagents for lncRNA Biomarker Studies
| Reagent Category | Specific Product Examples | Application in lncRNA Research | Performance Considerations |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN) | Total RNA extraction including small RNAs | Ensures high-quality RNA with RIN >7; compatible with plasma samples |
| cDNA Synthesis Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Reverse transcription for lncRNA analysis | High efficiency for long transcripts; minimal primer-dimer formation |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems) | Quantitative detection of lncRNAs | High sensitivity, specific amplification, low background noise |
| Reference Genes | GAPDH, β-actin | Normalization of lncRNA expression | Stable expression across samples; validated for tissue/plasma |
| lncRNA-Specific Primers | Custom-designed sequences | Target-specific amplification | Validation of specificity and efficiency required; minimal secondary structure |
Discussion: Toward Clinically Implementable lncRNA Biomarkers
The pathway to standardization in lncRNA biomarker research requires meticulous attention to methodological harmonization across multiple centers. The experimental protocols and comparative data presented herein provide a framework for achieving the reproducibility necessary for clinical translation. Key considerations for successful multi-center validation include:
Pre-analytical Variables: Standardization of sample collection, processing, and storage conditions is paramount, as variations in these pre-analytical factors can significantly impact lncRNA stability and quantification accuracy. The implementation of standardized blood collection tubes, uniform centrifugation protocols, and consistent RNA extraction methods across participating centers minimizes technical variability.
Analytical Validation: Rigorous assessment of assay performance characteristics—including sensitivity, specificity, precision, and linearity—must be conducted at each participating site using shared reference materials. The establishment of inter-laboratory quality control programs ensures consistent performance across centers.
Bioinformatic Harmonization: Computational analysis pipelines must be standardized to enable direct comparison of results across institutions. This includes consistent normalization strategies, uniform quality control thresholds, and shared reference databases for annotation.
The emerging consensus from current literature strongly supports the superiority of combined lncRNA panels over single biomarkers for HCC detection and prognostication. However, this enhanced performance comes with increased complexity in validation and implementation. Future efforts should focus on streamlining these multi-marker panels into clinically practical formats while maintaining their discriminatory power. As the field advances, the establishment of standardized protocols for multi-center validation will be the critical pathway from research discovery to clinical utility in hepatocellular carcinoma management.
Head-to-Head Comparison: Evaluating Diagnostic Accuracy and Prognostic Value
Hepatocellular carcinoma (HCC) constitutes over 75% of primary liver cancer cases worldwide and ranks as the third leading cause of cancer-related mortality [9] [4]. The insidious onset of HCC, coupled with limited early diagnostic options, results in over 80% of patients being diagnosed at advanced stages, contributing to a dismal 5-year survival rate of less than 20% [17] [28]. Alpha-fetoprotein (AFP), the current standard serological biomarker, demonstrates insufficient sensitivity and specificity, particularly for early-stage detection [65] [10].
Long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers for HCC diagnosis and prognosis. These transcripts longer than 200 nucleotides regulate gene expression through diverse mechanisms including epigenetic modification, transcriptional control, and post-transcriptional processing [4] [22]. Their differential expression in tumor tissues and stable detection in circulating blood make them ideal candidates for non-invasive liquid biopsies [22] [10].
This analysis synthesizes evidence from multiple meta-analyses and recent studies to evaluate the comparative efficacy of single versus combined lncRNA biomarkers for HCC detection, providing researchers with quantitative diagnostic performance metrics and methodological frameworks for clinical validation.
Pooled Diagnostic Performance of lncRNAs
Comprehensive meta-analyses have established that lncRNAs demonstrate moderate to high diagnostic accuracy for HCC. A 2017 meta-analysis of 19 studies involving 1,454 HCC patients and 1,300 controls revealed a pooled sensitivity of 0.83 (95% CI: 0.76–0.88) and specificity of 0.80 (95% CI: 0.73–0.86) [65]. The area under the summary receiver operating characteristic (sROC) curve was 0.88 (95% CI: 0.85–0.91), indicating substantial discriminatory power [65].
A more recent 2021 meta-analysis incorporating 20 studies with 4,930 HCC patients and 4,614 controls confirmed these findings, reporting similar pooled sensitivity and specificity estimates [28]. The diagnostic odds ratio (DOR), which represents the ratio of the odds of positivity in diseased persons relative to the odds of positivity in non-diseased persons, was 20 (95% CI: 11–34) in the 2017 analysis, further supporting the diagnostic capability of lncRNAs for HCC [65].
Table 1: Pooled Diagnostic Accuracy of lncRNAs from Meta-Analyses
| Meta-Analysis Year | Number of Studies | Patients/Controls | Sensitivity (95% CI) | Specificity (95% CI) | sAUC (95% CI) | DOR (95% CI) |
|---|---|---|---|---|---|---|
| 2017 [65] | 19 | 1,454/1,300 | 0.83 (0.76–0.88) | 0.80 (0.73–0.86) | 0.88 (0.85–0.91) | 20 (11–34) |
| 2021 [28] | 20 | 4,930/4,614 | Comparable results | Comparable results | - | - |
Single lncRNA Biomarkers
Individual lncRNAs demonstrate variable but generally moderate diagnostic performance. A 2024 investigation evaluating four specific lncRNAs reported the following individual diagnostic accuracies [10]:
Table 2: Diagnostic Performance of Single lncRNA Biomarkers
| lncRNA | Sensitivity | Specificity | Clinical Significance |
|---|---|---|---|
| LINC00152 | 83% | 67% | Oncogenic, promotes cell proliferation via CCDN1 regulation [10] |
| UCA1 | 77% | 53% | Promotes proliferation and apoptosis resistance [10] |
| LINC00853 | 60% | 67% | Investigated as potential diagnostic marker [10] |
| GAS5 | 63% | 67% | Tumor suppressor, activates CHOP and caspase-9 pathways [10] |
Other notable single lncRNAs with diagnostic potential include HULC, HOTAIR, and MIAT. A study in Egyptian patients with non-metastatic HCC found significant upregulation of HEIH, MIAT, and HOTAIR in HCC tissues compared to adjacent non-tumorous and cirrhotic tissues [33]. Functional analyses demonstrated that knockdown of these lncRNAs significantly reduced colony formation and cellular viability in Huh-7 cells, confirming their oncogenic roles [33].
Combined lncRNA Biomarkers
Evidence consistently demonstrates that biomarker panels combining multiple lncRNAs outperform single lncRNAs in diagnostic accuracy:
- A 2024 study developed a machine learning model integrating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters, achieving 100% sensitivity and 97% specificity for HCC diagnosis, substantially superior to any individual lncRNA [10].
- Another 2024 study constructed a risk model based on four amino acid metabolism-related lncRNAs that effectively stratified HCC patients into high-risk and low-risk groups with distinct overall survival outcomes [17].
- Research on Egyptian HCC patients revealed that a combination of MIAT and HOTAIR levels correlated with tumor size ≥5 cm and HCV-positive status, suggesting their combined utility in identifying aggressive disease subtypes [33].
- A study focusing on HCC risk in chronic hepatitis C patients identified plasma lncRNAs HULC and RP11-731F5.2 as potential biomarkers for HCC risk assessment, while RP11-731F5.2 and KCNQ1OT1 showed promise as noninvasive biomarkers for liver damage due to HCV infection [22].
Table 3: Diagnostic Performance of Combined lncRNA Biomarkers
| Combination Approach | Sensitivity | Specificity | Clinical Application |
|---|---|---|---|
| ML model with 4 lncRNAs + conventional markers [10] | 100% | 97% | HCC diagnosis |
| Amino acid metabolism-related 4-lncRNA signature [17] | - | - | Prognostic stratification |
| MIAT + HOTAIR [33] | - | - | Identification of aggressive tumors |
| HULC + RP11-731F5.2 [22] | - | - | HCC risk assessment in CHC patients |
Experimental Methodologies for lncRNA Biomarker Validation
Sample Collection and Preparation
Standardized protocols for sample collection and processing are critical for reliable lncRNA quantification. For liquid biopsies, peripheral blood samples should be collected in EDTA-containing tubes and processed within 2 hours of collection [22] [10]. Plasma separation involves centrifugation at 704-800 × g (RCF) for 10 minutes at 4°C, followed by aliquoting and storage at -70°C until RNA extraction [22] [10]. For tissue analyses, surgically resected HCC and adjacent non-tumorous tissues should be snap-frozen in liquid nitrogen and stored at -80°C [33].
RNA Extraction and Quality Control
Total RNA extraction from plasma requires specialized kits designed for low-abundance nucleic acids, such as the Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit [22] or miRNeasy Mini Kit [10]. The extraction protocol typically includes:
- Sample lysis with denaturing reagents containing guanidine thiocyanate
- Acid-phenol:chloroform extraction
- RNA precipitation with ethanol
- RNA washing and elution in nuclease-free water [22] [10]
DNA contamination is eliminated through DNase treatment using reagents such as Turbo DNase [22]. RNA quality and concentration should be assessed using spectrophotometry (A260/A280 ratio >1.8) or automated electrophoresis systems.
Reverse Transcription Quantitative PCR (RT-qPCR)
RT-qPCR represents the gold standard for lncRNA quantification due to its sensitivity, specificity, and quantitative capabilities. The standard workflow includes:
Diagram 1: RT-qPCR Workflow for lncRNA Quantification. The process involves reverse transcription of RNA to cDNA, followed by quantitative PCR with SYBR Green chemistry, and data analysis using the ΔΔCt method. Critical parameters include specific primer design, appropriate controls, and technical replicates.
Reverse transcription is performed using High-Capacity cDNA Reverse Transcription Kit with 100-500 ng total RNA input [22]. qPCR reactions utilize SYBR Green Master Mix with standardized cycling conditions: initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 60-62°C for 1 minute [22] [10]. Primer sequences must be validated for specificity through melting curve analysis and gel electrophoresis [22].
Data Normalization and Analysis
Proper normalization is critical for accurate lncRNA quantification. Reference genes for plasma lncRNA normalization include β-actin [22] or GAPDH [10]. The comparative ΔΔCt method is used for relative quantification, with results expressed as fold-change relative to control groups [22] [10]. For diagnostic accuracy assessment, receiver operating characteristic (ROC) curves are generated, and area under the curve (AUC) values calculated to determine optimal cutoff values that maximize both sensitivity and specificity [10].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for lncRNA Biomarker Studies
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit, Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit | Isolation of high-quality RNA from plasma/tissue | Select kits specifically validated for circulating RNA |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit, RevertAid First Strand cDNA Synthesis Kit | cDNA synthesis from RNA templates | Include genomic DNA removal steps |
| qPCR Master Mixes | Power SYBR Green PCR Master Mix, PowerTrack SYBR Green Master Mix | Fluorescent detection of amplified products | Optimize for specific primer sets |
| Reference Genes | β-actin, GAPDH | Normalization of lncRNA expression levels | Validate stability in specific sample matrices |
| Primers | LINC00152, UCA1, GAS5, HULC, HOTAIR-specific sequences | Target amplification | Design to span exon-exon junctions where applicable |
The accumulating meta-analysis evidence firmly establishes that lncRNAs offer substantial diagnostic value for hepatocellular carcinoma, with pooled sensitivity and specificity estimates of approximately 83% and 80%, respectively. While individual lncRNAs demonstrate moderate diagnostic performance, combination approaches integrating multiple lncRNAs with conventional biomarkers significantly enhance diagnostic accuracy, with some studies reporting near-perfect sensitivity and specificity when implemented within machine learning frameworks.
The superior performance of combined lncRNA panels stems from their ability to capture the molecular heterogeneity of HCC and compensate for individual biomarker limitations. As research progresses toward standardized methodologies and validated biomarker panels, lncRNA-based diagnostics hold immense promise for revolutionizing early HCC detection, risk stratification, and precision monitoring—ultimately addressing critical unmet needs in hepatocellular carcinoma management.
Hepatocellular carcinoma (HCC) continues to pose a significant global health challenge, characterized by high mortality rates often due to late-stage diagnosis. The exploration of long non-coding RNAs (lncRNAs) as biomarkers has emerged as a promising avenue for improving early detection and prognostic assessment. Within this field, a central question has developed regarding the comparative efficacy of single lncRNA biomarkers versus multi-lncRNA signature panels. This analysis directly addresses this question by synthesizing available experimental data to objectively compare the diagnostic and prognostic performance, as measured by the Area Under the Curve (AUC), of single versus combined lncRNA approaches. The evidence consistently demonstrates that multi-lncRNA signatures significantly enhance predictive accuracy for HCC, offering researchers and clinicians a more powerful tool for patient management [46] [66] [10].
Performance Metrics: Single vs. Combination LncRNA Signatures
The comparative diagnostic and prognostic performance of single and multi-lncRNA signatures has been quantitatively assessed across multiple studies, with the Area Under the Receiver Operating Characteristic Curve (AUC) serving as a key metric.
Diagnostic Performance for HCC Detection
Data from independent research groups consistently show that combining multiple lncRNAs, often with the traditional biomarker AFP, yields superior diagnostic power compared to any single lncRNA.
Table 1: Diagnostic AUC of Single vs. Combined LncRNAs for HCC Detection
| Biomarker Type | Specific Biomarker(s) | AUC Value | Key Context / Cohort | Reference |
|---|---|---|---|---|
| Single lncRNA | LINC00152 | 0.877 | Best-performing single lncRNA in a 8-lncRNA screen | [46] |
| Single lncRNA | UCA1 | 0.783 | Part of an 8-lncRNA screen for HCC diagnosis | [46] |
| Two-lncRNA Panel | LINC00152 + UCA1 | 0.892 | Combined two-lncRNA panel for diagnosis | [46] |
| lncRNA + AFP | LINC00152 + AFP | 0.906 | Combination of best single lncRNA with standard biomarker | [46] |
| Multi-lncRNA Panel | LINC00152 + UCA1 + AFP | 0.912 | Highest diagnostic accuracy from a triple-panel | [46] |
| Machine Learning Panel | 4 lncRNAs + Lab Parameters | ~1.00 | Integration with ML model; sensitivity 100%, specificity 97% | [10] |
A 2020 study systematically evaluating eight serum lncRNAs found that while LINC00152 was the best single performer (AUC=0.877), its combination with AFP improved the AUC to 0.906. The most accurate diagnostic tool was a triple-panel of LINC00152, UCA1, and AFP, which achieved an AUC of 0.912, providing 82.9% sensitivity and 88.2% specificity [46]. A more recent study from 2024 further underscored the power of integration, demonstrating that a machine learning model incorporating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) along with standard laboratory parameters could achieve near-perfect diagnostic accuracy (100% sensitivity, 97% specificity) [10].
Prognostic Performance for Survival Prediction
Beyond diagnosis, lncRNA signatures are critical for predicting patient outcomes, such as Overall Survival (OS). Multi-lncRNA prognostic models consistently show higher time-dependent AUC values compared to single clinical variables or smaller signatures.
Table 2: Prognostic Performance of Multi-lncRNA Signatures for HCC Survival
| Signature Type / Name | Number of LncRNAs | Prognostic AUC (1-/3-/5-year) | Clinical Utility | Reference |
|---|---|---|---|---|
| Disulfidptosis-Related | 3 | 0.756 / 0.695 / 0.701 | Predicts OS, immune function, and drug sensitivity | [34] |
| Autophagy-Related | 7 | 0.786 (OS) | Superior to AFP (0.575), AJCC stage (0.631) | [67] |
| Amino Acid Metabolism-Related | 4 | N/A | Independent prognostic factor; predicts immunotherapy response | [68] |
| Basement Membrane-Related | 6 | N/A | Predicts OS; high-risk score linked to worse prognosis | [69] |
| General Prognostic (TCGA) | 6 | N/A | Excellent prognostic capacity for OS in HCC patients | [66] |
For instance, a disulfidptosis-related lncRNA signature comprising three lncRNAs demonstrated robust prognostic accuracy for 1-, 3-, and 5-year overall survival [34]. Similarly, a 7-lncRNA autophagy-related signature significantly outperformed traditional clinical indicators like AFP level, AJCC stage, and Child-Pugh grade in predicting survival [67]. These complex signatures not only predict survival but also provide insights into tumor biology and potential therapeutic vulnerabilities, such as immune infiltration and drug sensitivity [34] [68].
Experimental Workflows and Methodologies
The development and validation of single and multi-lncRNA biomarkers follow a structured experimental pipeline, from sample collection to final validation. The workflow below illustrates the general process for establishing a multi-lncRNA signature.
General Workflow for Developing a Multi-lncRNA Signature
Core Experimental Protocol for Circulating lncRNAs
The following detailed methodology is adapted from studies that established high-performing lncRNA panels [46] [10].
- Cohort Recruitment and Sample Collection: Participants are recruited into well-defined groups (e.g., HCC patients, patients with benign liver diseases like cirrhosis or chronic hepatitis, and healthy controls). Peripheral blood is collected in vacuum tubes. Serum or plasma is isolated by centrifugation (e.g., 3,000 rpm for 10 minutes), aliquoted, and immediately stored at -80°C until RNA extraction [46] [22].
- RNA Isolation: Total RNA is extracted from serum or plasma samples using specialized commercial kits (e.g., Hipure Liquid RNA Kit, miRNeasy Mini Kit, or Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit). The quantity and purity of the extracted RNA are assessed using a spectrophotometer [46] [10].
- Reverse Transcription and Quantitative Real-Time PCR (qRT-PCR):
- cDNA Synthesis: Purified RNA is reverse transcribed into complementary DNA (cDNA) using a reverse transcriptase kit (e.g., M-MLV Reverse Transcriptase or RevertAid First Strand cDNA Synthesis Kit) [46] [10].
- qRT-PCR Amplification: The expression levels of target lncRNAs are quantified by qRT-PCR using a detection system (e.g., SYBR Green Master Mix on a QuantStudio or ViiA 7 system). Reactions are typically run in triplicate under the following conditions: 95°C for 30 seconds, followed by 45 cycles of 95°C for 5 seconds and 60°C for 30 seconds [46] [10].
- Data Normalization: The relative expression of each lncRNA is calculated using the 2^(-ΔΔCt) method, with normalizing to a stable internal control gene such as GAPDH or β-actin [46] [22] [10].
- Statistical Analysis and Model Building:
- Differential Expression: Non-parametric tests (e.g., Mann-Whitney U test) are used to compare lncRNA levels between groups.
- ROC Analysis: The diagnostic performance of individual lncRNAs is evaluated by generating Receiver Operating Characteristic (ROC) curves and calculating the Area Under the Curve (AUC).
- Logistic Regression & Machine Learning: To build a multi-lncRNA panel, a logistic regression model or machine learning algorithm is employed. This model assigns optimal weights to each lncRNA to create a combined score that maximizes diagnostic or prognostic power [46] [10].
- Survival Analysis: For prognostic studies, Kaplan-Meier survival analysis and Cox proportional hazards regression models are used to assess the association between lncRNA expression levels (or a risk score) and patient overall survival or recurrence-free survival [13] [66].
Pathway and Functional Relationship Diagrams
Multi-lncRNA signatures are powerful because they capture the regulation of multiple oncogenic pathways. The diagram below illustrates how a hypothetical 3-lncRNA signature might co-regulate key cellular processes driving HCC.
Multi-lncRNA Signature Regulates Key Pathways
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and kits commonly used in the cited studies for lncRNA biomarker research, providing a practical resource for experimental design.
Table 3: Essential Reagents and Kits for lncRNA Biomarker Research
| Reagent / Kit Name | Function / Application | Specific Example (from search results) |
|---|---|---|
| Plasma/Serum RNA Kit | Isolation of circulating RNA from blood samples. | Hipure Liquid RNA Kit (Magen) [46]; Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) [22]. |
| miRNA/RNA Mini Kit | General-purpose RNA isolation from various samples. | miRNeasy Mini Kit (QIAGEN) [10]. |
| Reverse Transcriptase | Synthesis of cDNA from purified RNA template. | M-MLV Reverse Transcriptase (Promega) [46]; RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [10]. |
| SYBR Green Master Mix | Fluorescent detection for qRT-PCR amplification. | TB Green Premix Ex Taq (Takara) [46]; PowerTrack SYBR Green Master Mix (Applied Biosystems) [10]. |
| qRT-PCR System | Instrument platform for quantitative gene expression. | QuantStudio System (Applied Biosystems) [46]; ViiA 7 Real-Time PCR System (Applied Biosystems) [10]; StepOne Plus System (Applied Biosystems) [22]. |
| NanoDrop Spectrophotometer | Rapid assessment of RNA concentration and purity. | NanoDrop One (Thermo Scientific) [46]. |
The collective evidence from recent studies provides a definitive answer to the question of comparative efficacy. While single lncRNAs like LINC00152 can serve as good biomarkers (AUC ~0.88), the integration of multiple lncRNAs into a single signature consistently yields superior diagnostic and prognostic performance (AUC >0.90). The synergistic effect of multi-lncRNA panels enhances accuracy, robustness, and clinical utility by capturing the complexity and heterogeneity of hepatocellular carcinoma. Future research directions should focus on the standardization of these panels and the integration of machine learning models to further unlock their potential in personalized oncology.
Hepatocellular carcinoma (HCC) is a highly aggressive malignancy and a leading cause of cancer-related mortality worldwide [70]. A significant challenge in managing HCC is that most patients are diagnosed at advanced stages due to the lack of early symptoms, resulting in poor prognosis [70] [71]. The current standard for HCC surveillance in at-risk populations involves ultrasound imaging and measurement of serum alpha-fetoprotein (AFP), but both methods have limitations [71]. Ultrasound lacks specificity and sensitivity, while AFP exhibits limited diagnostic performance, particularly for early-stage HCC, with sensitivities ranging from 68% to 79.4% depending on the cutoff used [70] [71] [72]. This diagnostic gap has spurred research into novel biomarkers, particularly long non-coding RNAs (lncRNAs), which have emerged as promising candidates due to their stable presence in body fluids and involvement in hepatocarcinogenesis [70] [1]. This case study examines the experimental validation and diagnostic performance of a specific multi-analyte approach—the combination of lncRNA PTTG3P, mRNA PTTG1, and AFP—demonstrating the superior power of combined biomarkers over single-analyte tests in HCC detection.
The Biological Foundation: PTTG3P and PTTG1 in Hepatocarcinogenesis
Molecular Characteristics and Oncogenic Functions
LncRNA PTTG3P is a processed pseudogene located at chromosome 8q13.1 that has been demonstrated to participate in the development of various cancers, including HCC [70]. Previous research has established that lncRNA PTTG3P functions as an oncogene in HCC by elevating mRNA PTTG1 and activating the PI3K/AKT signaling pathway, thereby promoting tumor growth and metastasis [70]. The PTTG3P/PTTG1 axis represents a functionally interconnected pathway where the lncRNA directly influences the expression of its protein-coding counterpart, creating an amplification loop that drives carcinogenesis.
Table 1: Biological Characteristics of PTTG3P and PTTG1
| Biomarker | Type | Chromosomal Location | Primary Function in HCC | Regulatory Mechanism |
|---|---|---|---|---|
| PTTG3P | Long non-coding RNA | 8q13.1 | Oncogene | Activates PI3K/AKT signaling pathway |
| PTTG1 | mRNA | - | Promotes tumor growth and metastasis | Molecular target of PTTG3P |
Signaling Pathway Schematic
The following diagram illustrates the molecular mechanism through which the PTTG3P/PTTG1 axis promotes hepatocellular carcinoma development:
Experimental Validation: Methodology and Workflow
Study Population and Sample Collection
The foundational study validating the PTTG3P/PTTG1/AFP panel enrolled 373 participants across multiple clinical groups [70] [73]. The cohort composition is detailed in the table below.
Table 2: Study Population Demographics
| Participant Group | Number of Subjects | Key Characteristics |
|---|---|---|
| HCC Patients | 73 | Diagnosed by histological examination; treatment-naïve |
| Chronic Hepatitis B (CHB) | 100 | Diagnosed per EASL Clinical Practice Guidelines |
| Liver Cirrhosis (LC) | 100 | Diagnosed per AASLD Practice Guidelines |
| Healthy Controls (HCs) | 100 | Recruited during routine medical examinations |
Peripheral blood samples were collected in vacuum tubes from all participants prior to any surgical or pharmacological intervention [70]. For 36 HCC patients, paired preoperative and postoperative plasma samples were obtained, with postoperative samples collected 10 days after surgery [70]. All serum samples were stored at -80°C until analysis to preserve RNA integrity [70].
RNA Isolation and Quantitative Analysis
The experimental workflow for biomarker quantification followed a standardized protocol to ensure reproducibility and accuracy [70]:
- RNA Extraction: Serum RNA was isolated using a HiPure Liquid RNA Kit, with contaminating DNA removed using a DNase On Column Kit [70].
- Quality Control: RNA quantity and purity were verified using a NanoDrop 2000c Spectrophotometer to ensure sample quality [70].
- cDNA Synthesis: Reverse transcription was performed using Evo M-MLV RT Premix for qPCR according to manufacturer's protocol [70].
- Quantitative PCR: Expression levels were assessed by qPCR using SYBR Green Premix Pro Taq HS qPCR Kit on an LC480 Real Time PCR system [70]. The reaction conditions consisted of an initial denaturation at 95°C for 30 seconds, followed by 40 cycles of 95°C for 5 seconds and 60°C for 30 seconds [70].
- Normalization: U6 and β-actin were used as internal controls for data normalization, with quantification performed using the 2−ΔΔCq method [70].
Primer Sequences
The specific primer sequences used for amplification of each target are documented in the table below.
Table 3: Primer Sequences for RT-qPCR Analysis
| Gene Symbol | Primer Sequences (5'→3') |
|---|---|
| U6 | Sense: CTCGCTTCGGCAGCACA Antisense: AACGCTTCACGAATTTGCGT |
| PTTG3P | Sense: GGGGTCTGGACCTTCAATCAA Antisense: GCTTTAGGTAAGGATGTGGGA |
| PTTG1 | Sense: ACCCGTGTGGTTGCTAAGG Antisense: ACGTGGTGTTGAAACTTGAGAT |
| β-actin | Sense: TGGCACCCAGCACAATGAA Antisense: CTAAGTCATAGTCCGCCTAGAA |
Analytical Measurements
Liver function indicators—including GGT, AST, ALT, ALP, total protein, albumin, total bilirubin, and direct bilirubin—were detected on a Roche Cobas 8000 c702 chemistry analyzer [70]. Serum AFP was measured using the Roche Cobas 8000 e602 electrochemiluminescence immunoanalyzer [70]. These standardized clinical chemistry platforms ensured consistent and comparable results across all samples.
Diagnostic Performance: Comparative Analysis
Expression Patterns and Clinical Correlations
The experimental results revealed that expression levels of both lncRNA PTTG3P and mRNA PTTG1 were significantly elevated in the serum of HCC patients compared to healthy controls [70]. Importantly, these biomarkers were also increased in patients with chronic hepatitis B, suggesting a potential role in the progression from chronic liver disease to HCC [70]. A particularly significant finding was that postoperative levels of both lncRNA PTTG3P and mRNA PTTG1 were significantly lower than preoperative concentrations in the 36 paired HCC patients, indicating their potential utility for monitoring treatment response [70]. Statistical analysis using Spearman's correlation coefficient demonstrated that serum lncRNA PTTG3P was specifically correlated with aspartate transaminase (AST), linking its expression to liver damage [70].
Diagnostic Accuracy of Individual and Combined Biomarkers
Receiver operating characteristic (ROC) curve analysis was performed to evaluate the diagnostic performance of each biomarker individually and in combination [70]. The area under curve (AUC) values provide a comprehensive metric of diagnostic accuracy.
Table 4: Diagnostic Performance of Individual and Combined Biomarkers for HCC Detection
| Biomarker or Panel | AUC Value | Sensitivity (%) | Specificity (%) |
|---|---|---|---|
| PTTG3P alone | 0.636 | - | - |
| PTTG1 alone | 0.634 | - | - |
| AFP alone | - | 68.0* | - |
| PTTG3P + PTTG1 + AFP | - | - | - |
| PTTG3P + PTTG1 + AFP + ALT + AST + GGT + ALP | 0.959 | 90.4 | 98.0 |
| 5-miRNA Panel + AFP [71] | 0.924 | - | - |
| GALAD Score [72] | - | 91.0 | 85.0 |
*Sensitivity for AFP alone from independent study [72]
The most striking finding was that the combination of PTTG3P, PTTG1, AFP, and standard liver function tests (ALT, AST, GGT, ALP) achieved exceptional diagnostic performance with an AUC of 0.959, sensitivity of 90.4%, and specificity of 98.0% [70]. This represents a substantial improvement over any individual biomarker and demonstrates the powerful synergistic effect of multi-analyte approaches.
Comparative Diagnostic Performance Visualization
The following diagram illustrates the progressive improvement in diagnostic accuracy achieved by combining multiple biomarkers, culminating in the superior performance of the comprehensive panel:
Comparative Context with Alternative Multi-Analyte Approaches
The diagnostic superiority of combined biomarker approaches is further evidenced by other multi-analyte panels developed for HCC detection. The GALAD score, which incorporates gender, age, AFP-L3, total AFP, and des-carboxy-prothrombin (DCP), has demonstrated sensitivities of 86-91% with specificities of 85-97% in validation studies [72]. Similarly, a recently developed 5-miRNA panel (miR-361-5p, miR-130a-3p, miR-27a-3p, miR-30d-5p, miR-193a-5p) combined with AFP achieved an AUC of 0.924, significantly outperforming AFP alone (AUC: 0.794) [71]. These independent validations reinforce the fundamental principle that multi-analyte approaches consistently surpass single-marker tests in HCC diagnostics.
Table 5: Comparison of Multi-Analyte Biomarker Panels for HCC Detection
| Panel | Components | Performance | Advantages |
|---|---|---|---|
| PTTG3P/PTTG1/AFP Panel | lncRNA PTTG3P, mRNA PTTG1, AFP, liver function tests | AUC: 0.959Sensitivity: 90.4%Specificity: 98.0% | Functional biomarker relationship; includes routine liver tests |
| GALAD Score [72] | Gender, Age, AFP-L3, AFP, DCP | Sensitivity: 91%Specificity: 85% | Extensively validated; includes demographic risk factors |
| 5-miRNA Panel [71] | miR-361-5p, miR-130a-3p, miR-27a-3p, miR-30d-5p, miR-193a-5p, AFP | AUC: 0.924 | Superior to AFP alone; effective for early-stage detection |
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 6: Key Research Reagents and Instrumentation for lncRNA Biomarker Studies
| Reagent/Instrument | Specific Product | Application/Function |
|---|---|---|
| RNA Extraction Kit | HiPure Liquid RNA Kit | Serum RNA isolation |
| DNA Removal Kit | DNase On Column Kit B | Genomic DNA elimination |
| Reverse Transcription Kit | Evo M-MVL RT Premix for qPCR | cDNA synthesis from RNA templates |
| qPCR Master Mix | SYBR Green Premix Pro Taq HS qPCR Kit | Fluorescence-based quantification of amplified DNA |
| qPCR Instrument | LC480 Real Time PCR System | High-throughput quantitative PCR analysis |
| Spectrophotometer | NanoDrop 2000c | RNA quantification and quality assessment |
| Clinical Chemistry Analyzer | Roche Cobas 8000 c702 | Automated measurement of liver function tests |
| Immunoassay Analyzer | Roche Cobas 8000 e602 | Precise quantification of AFP and other protein biomarkers |
This case study demonstrates that the PTTG3P/PTTG1/AFP panel represents a significant advancement in HCC diagnostics, with experimentally validated performance metrics that substantially exceed conventional single-analyte approaches. The comprehensive multi-analyte panel combining PTTG3P, PTTG1, AFP, and standard liver function tests achieved exceptional diagnostic accuracy (AUC: 0.959), highlighting the transformative potential of integrated biomarker strategies [70]. These findings strongly support the broader thesis that combined lncRNA-based biomarkers offer superior diagnostic efficacy compared to single-marker tests in HCC. The functional relationship between PTTG3P and PTTG1 within a defined oncogenic pathway provides biological plausibility for their coordinated use as biomarkers. Future research directions should include validation in larger, multi-center cohorts; standardization of pre-analytical and analytical procedures; and exploration of these biomarkers for monitoring treatment response and predicting recurrence in HCC patients undergoing therapy.
The development of accurate prognostic biomarkers is critical for managing hepatocellular carcinoma (HCC), which continues to exhibit high mortality rates despite therapeutic advances. Long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers due to their specific expression patterns in cancer tissues and circulation. This review systematically compares the prognostic efficacy of single lncRNA biomarkers against multi-lncRNA signatures in predicting overall survival (OS) and recurrence-free survival (RFS) in HCC patients. Current evidence demonstrates that while certain individual lncRNAs show significant prognostic value, combined lncRNA signatures consistently outperform single markers in predictive accuracy, stability, and clinical applicability. Through direct comparison of quantitative hazard ratios, area under curve values, and multivariate analysis results, we provide a comprehensive assessment of the comparative efficacy of these approaches, offering evidence-based guidance for researchers and clinicians in prognostic stratification strategies.
Hepatocellular carcinoma represents a significant global health challenge, ranking as the third leading cause of cancer-related mortality worldwide [7]. Despite improvements in diagnostic techniques and therapeutic options, the 5-year survival rate for advanced HCC remains disappointingly low, primarily due to frequent recurrence and metastasis [4]. The complex molecular heterogeneity of HCC has complicated the development of accurate prognostic tools, creating an urgent need for biomarkers that can reliably stratify patients based on their recurrence risk and survival probability [9].
Long non-coding RNAs have recently emerged as crucial regulators of carcinogenesis and cancer progression, with demonstrated roles in controlling oncogene and tumor suppressor gene expression [9]. These transcripts, exceeding 200 nucleotides in length without protein-coding capacity, participate in diverse cellular processes through various mechanisms including epigenetic regulation, transcriptional control, and post-transcriptional modifications [4]. The discovery that lncRNAs exhibit tissue-specific expression patterns and remarkable stability in body fluids has positioned them as attractive candidates for cancer biomarker development [22].
Two predominant approaches have emerged in lncRNA-based prognostic assessment: single-marker analysis and multi-marker signatures. Single lncRNA biomarkers offer simplicity and potentially lower implementation costs, while combined lncRNA signatures may provide enhanced predictive power through the integration of multiple molecular pathways. This review systematically evaluates the comparative efficacy of these approaches, examining their respective strengths and limitations in predicting OS and RFS in HCC patients.
Single lncRNA Biomarkers: Established Prognostic Indicators
Numerous individual lncRNAs have demonstrated significant prognostic value for HCC outcomes, with their expression levels independently correlating with survival in multivariate analyses. The prognostic impact of these single lncRNAs is typically categorized based on their association with either favorable or unfavorable clinical outcomes.
Table 1: Single lncRNA Biomarkers with Prognostic Significance in HCC
| LncRNA Name | Expression in HCC | Survival Endpoint | Hazard Ratio (HR) | 95% Confidence Interval | P-value |
|---|---|---|---|---|---|
| LINC00152 | High | OS | 2.524 | 1.661-4.015 | 0.001 |
| LINC00294 | High | OS | 2.434 | 1.143-3.185 | 0.021 |
| HOXC13-AS | High | OS | 2.894 | 1.183-4.223 | 0.015 |
| HOXC13-AS | High | RFS | 3.201 | 1.372-4.653 | 0.004 |
| LASP1-AS | Low | OS | 3.539 | 2.698-6.030 | <0.0001 |
| LASP1-AS | Low | RFS | 2.793 | 2.154-4.672 | <0.0001 |
| ELMO1-AS1 | High | OS | 0.430 | 0.225-0.824 | 0.011 |
| GAS5-AS1 | High | OS | 0.370 | 0.153-0.898 | 0.028 |
Mechanistically, oncogenic lncRNAs such as LINC00152 and HOXC13-AS promote tumor progression through various pathways, including cell proliferation, invasion, and metastasis [9]. In contrast, tumor-suppressive lncRNAs like LASP1-AS and ELMO1-AS1 are frequently downregulated in HCC, with their decreased expression associated with worse patient outcomes [9]. The meta-analysis by Wang et al. consolidated evidence from 40 studies, demonstrating that elevated expression of detrimental lncRNAs was associated with a 1.25-fold increased risk of poor OS and a 1.66-fold increased risk of poor RFS [7].
From a clinical perspective, single lncRNA biomarkers offer relative simplicity in assay development and implementation. Their detection via quantitative real-time PCR (qRT-PCR) provides a technically straightforward approach applicable to both tissue samples and liquid biopsies [22]. However, the inherent molecular complexity of HCC and the limited explanatory power of individual molecules represent significant limitations of this approach.
Combined lncRNA Signatures: Enhanced Predictive Power
Multi-lncRNA signatures integrate information from several lncRNAs into a single prognostic model, typically using computational approaches to weight each component based on its relative contribution to risk prediction. These signatures demonstrate consistently superior performance compared to individual markers, reflecting the biological complexity of HCC progression.
Table 2: Combined lncRNA Signatures for HCC Prognosis
| LncRNA Signature | Number of lncRNAs | Survival Endpoint | AUC Value | Median Survival (High vs Low Risk) | P-value |
|---|---|---|---|---|---|
| Four-lncRNA (TCGA) | 4 | OS | >0.70 | 1.81 vs 8.56 years | <0.001 |
| RP11-495K9.6 based | 4 | OS | >0.70 | 1.95 vs 5.80 years | 0.007 |
| Machine Learning Panel | 4 | Diagnostic | 0.97 (Sens:100%, Spec:97%) | N/A | N/A |
| Seven-lncRNA (Breast CA) | 7 | OS | 0.780 (5-year) | Significant difference | <0.05 |
The four-lncRNA signature comprising RP11-495K9.6, RP11-96O20.2, RP11-359K18.3, and LINC00556 demonstrated remarkable prognostic efficacy in TCGA datasets, effectively stratifying patients into distinct risk groups with significantly different survival outcomes [74]. The high-risk group identified by this signature had a median survival of only 1.81 years compared to 8.56 years for the low-risk group in the training cohort, with consistent results in validation cohorts [74].
Advanced computational approaches further enhance the utility of combined lncRNA signatures. A machine learning model incorporating LINC00152, LINC00853, UCA1, and GAS5 expression achieved remarkable diagnostic performance with 100% sensitivity and 97% specificity for HCC detection, significantly outperforming individual lncRNAs which showed moderate accuracy (sensitivity: 60-83%, specificity: 53-67%) [10]. This highlights how integrated computational analysis can extract synergistic prognostic information from multiple lncRNAs.
The development of immune-related lncRNA signatures represents another advancement, connecting lncRNA expression patterns with tumor immune microenvironment characteristics. Studies in lung adenocarcinoma have established eight-lncRNA prognostic signatures that not only predict survival but also correlate with immune cell infiltration patterns, offering insights into potential immunotherapy responsiveness [75]. Similar approaches in colorectal cancer have yielded five-lncRNA signatures that accurately stratify patients while providing information about immune status and potential response to immunotherapy [76].
Direct Comparison: Single versus Combined lncRNA Approaches
When directly comparing the prognostic performance of single versus combined lncRNA biomarkers, several key differentials emerge that have significant implications for clinical translation and research applications.
Predictive Accuracy and Stability
Combined lncRNA signatures consistently demonstrate superior predictive accuracy compared to individual markers. The area under the curve (AUC) values for multi-lncRNA signatures frequently exceed 0.70, reaching up to 0.780 for 5-year survival prediction in some models [74] [77]. In contrast, individual lncRNAs typically show more modest effect sizes, with hazard ratios generally ranging from 1.5 to 3.5 for overall survival [9]. This enhanced performance likely reflects the ability of combined signatures to capture the complexity of HCC pathogenesis by integrating information from multiple molecular pathways simultaneously.
Furthermore, combined signatures exhibit greater stability across different patient populations and datasets. The four-lncRNA signature validated in TCGA datasets maintained its prognostic significance across training, testing, and complete cohorts, demonstrating robust generalizability [74]. Single lncRNAs, while statistically significant in specific populations, may show variable performance across different ethnic groups or etiological subtypes of HCC due to their more limited biological scope.
Biological Comprehensiveness
The biological rationale supporting combined signatures is inherently more comprehensive than that of single markers. HCC progression involves coordinated dysregulation across multiple cellular processes, including proliferation, apoptosis, invasion, and immune evasion. While individual lncRNAs typically regulate specific pathways, combined signatures can simultaneously capture information about multiple cancer hallmarks.
For instance, the seven-lncRNA signature identified for breast cancer prognosis was found to participate in multiple pathways related to tumorigenesis through enrichment analysis of co-expressed protein-coding genes [77]. Similarly, immune-related lncRNA signatures connect prognostic prediction with specific immune cell infiltration patterns and potential immunotherapy responsiveness, providing clinically actionable insights beyond simple risk stratification [75] [76].
Technical Implementation Considerations
Despite their superior performance, combined lncRNA signatures present greater technical challenges for clinical implementation. The requirement to accurately measure multiple RNA species simultaneously demands more complex assay validation and quality control procedures. The computational algorithms needed to integrate these measurements into risk scores also represent a barrier to routine clinical use.
Single lncRNA biomarkers, with their more straightforward measurement and interpretation, may offer practical advantages in resource-limited settings or as rapid screening tools. The development of standardized detection kits for individual lncRNAs like HULC or RP11-731F5.2 could facilitate their translation into clinical practice [22].
Diagram: Comparative mechanistic pathways of single versus combined lncRNA biomarkers in HCC prognosis
Experimental Approaches and Methodologies
Sample Processing and RNA Isolation
Robust lncRNA analysis begins with appropriate sample collection and processing. Plasma samples are typically obtained from peripheral blood centrifuged at 704× g (RCF) for 10 minutes to separate cellular components, followed by storage at -70°C until RNA extraction [22]. For tissue-based analyses, surgically resected HCC specimens and adjacent non-tumor tissues are immediately preserved in RNA-stabilizing solutions.
Total RNA isolation from plasma typically employs specialized kits such as the Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit, with subsequent DNase treatment to eliminate genomic DNA contamination [22]. For tissue samples, the miRNeasy Mini Kit provides effective RNA extraction, ensuring high-quality RNA suitable for downstream applications [10].
LncRNA Quantification Methods
Quantitative real-time PCR (qRT-PCR) represents the gold standard for lncRNA quantification in both research and clinical settings. The process begins with reverse transcription using High-Capacity cDNA Reverse Transcription Kits, followed by amplification with Power SYBR Green PCR Master Mix on platforms such as the StepOne Plus System or ViiA 7 real-time PCR system [10] [22].
Primer design specificity is crucial for accurate lncRNA measurement, with amplification conditions typically including initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 62°C for 1 minute [22]. The comparative Ct (ΔΔCt) method normalizes lncRNA expression against reference genes such as GAPDH or β-actin, with all reactions performed in technical triplicates to ensure reproducibility [10].
Signature Development and Validation
The development of multi-lncRNA signatures follows rigorous statistical workflows. For the four-lncRNA signature identified from TCGA data, researchers initially selected lncRNAs with coefficient of variance >0.1, followed by univariate Cox regression to identify survival-associated transcripts [74]. The random survival forests-variable hunting algorithm further refined the candidate list, with final signature selection based on optimal AUC values (>0.7) and significant log-rank P-values in Kaplan-Meier analysis [74].
Validation occurs through multiple phases, beginning with training cohorts (typically 50-70% of samples) followed by testing in independent validation sets. For the seven-lncRNA signature in breast cancer, researchers employed 3-fold cross-validation, dividing 913 patients into training (n=608) and testing (n=305) datasets to ensure robust performance assessment [77].
Diagram: Experimental workflow for lncRNA biomarker development
Table 3: Essential Research Reagents for lncRNA Prognostic Studies
| Reagent/Resource | Specific Example | Application Purpose | Technical Notes |
|---|---|---|---|
| RNA Isolation Kit | miRNeasy Mini Kit (QIAGEN) | Total RNA extraction from tissues | Maintain RNA integrity for accurate quantification |
| Plasma RNA Kit | Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) | Cell-free RNA isolation from blood | Specialized for low-concentration circulating RNA |
| Reverse Transcription Kit | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | cDNA synthesis from RNA templates | Essential for downstream qRT-PCR applications |
| qRT-PCR Master Mix | Power SYBR Green PCR Master Mix (Thermo Fisher) | Amplification and detection of lncRNAs | Enables quantitative measurement of expression |
| Reference Genes | GAPDH, β-actin | Expression normalization | Critical for accurate ΔΔCt calculations |
| Bioinformatics Tool | Random Survival Forests Algorithm | Signature development from expression data | Identifies optimal lncRNA combinations |
| Validation Software | R package "survivalROC" | Prognostic model performance assessment | Calculates time-dependent ROC curves |
The comprehensive comparison between single and combined lncRNA biomarkers for HCC prognosis reveals a consistent pattern of superior performance for multi-marker signatures across multiple metrics. While individual lncRNAs such as LINC00152, HOXC13-AS, and LASP1-AS provide valuable prognostic information with practical advantages in implementation simplicity, their predictive power remains limited compared to integrated signatures.
The emerging paradigm of immune-related lncRNA signatures represents a particularly promising direction, connecting prognostic stratification with potential therapeutic implications. The eight-lncRNA signature in lung adenocarcinoma and five-lncRNA signature in colorectal cancer not only predict survival but also provide insights into tumor immune microenvironment characteristics, potentially guiding immunotherapy decisions [75] [76].
Future developments will likely focus on standardizing detection methodologies, validating signatures across diverse populations, and integrating lncRNA biomarkers with existing clinical parameters such as TNM staging and AFP levels. The incorporation of machine learning approaches, as demonstrated by the 100% sensitivity and 97% specificity achieved in HCC diagnosis, will further enhance the clinical utility of lncRNA-based prognostic tools [10].
As lncRNA research continues to evolve, the optimal approach to prognostic stratification may involve a tiered system combining rapidly assessable single lncRNAs for initial screening followed by comprehensive multi-lncRNA signatures for refined risk assessment and therapeutic guidance. This integrated strategy promises to advance personalized medicine in HCC, ultimately improving patient outcomes through more accurate prognosis and tailored treatment approaches.
Long non-coding RNAs (lncRNAs), defined as RNA transcripts exceeding 200 nucleotides with limited protein-coding potential, have emerged as critical regulators of gene expression through diverse mechanisms including chromatin modification, transcriptional regulation, and post-transcriptional processing [78]. Their expression exhibits remarkable tissue specificity and they play essential roles in carcinogenesis, tumor progression, and therapy response through interactions with DNA, RNA, and proteins [50] [78]. The discovery that lncRNAs are stably present in body fluids such as blood serum and plasma, often protected within exosomes or by RNA-binding proteins, has positioned them as promising non-invasive biomarkers [50] [79].
lncRNA signatures—panels of multiple lncRNAs analyzed in combination—represent a transformative approach in cancer theranostics. Unlike single biomarkers, these multi-lncRNA signatures capture the complexity of tumor biology and heterogeneity, providing superior prognostic and predictive capability [1] [9]. Within the specific context of hepatocellular carcinoma (HCC), the comparative efficacy of single versus combined lncRNA biomarkers represents a critical frontier in precision oncology, with growing evidence suggesting that combination signatures offer enhanced stratification power for predicting responses to emerging immunotherapies and targeted therapies.
Single versus Combination lncRNA Biomarkers: Comparative Efficacy in HCC
HCC demonstrates the evolving paradigm from single lncRNA biomarkers toward multi-lncRNA signatures. Numerous individual lncRNAs have established independent prognostic value in HCC, as validated through multivariate Cox regression analyses [9]. For instance, elevated pre-treatment levels of LINC00152 independently predicted shorter overall survival (HR, 2.524; 95% CI, 1.661–4.015; P=0.001), while high LINC01146 expression was associated with longer survival (HR, 0.38; 95% CI, 0.16–0.92; P=0.033) [9]. Similarly, HOXC13-AS significantly predicted both overall survival (HR, 2.894; 95% CI, 1.183–4.223; P=0.015) and recurrence-free survival (HR, 3.201; 95% CI, 1.372–4.653; P=0.004) [9].
Despite these validated single biomarkers, combination lncRNA signatures demonstrate superior prognostic and predictive performance by capturing broader biological networks and overcoming tumor heterogeneity. Multi-lncRNA classifiers can simultaneously evaluate multiple oncogenic pathways, immune evasion mechanisms, and drug resistance pathways, providing a more comprehensive assessment of tumor behavior [1]. The statistical advantage of combination signatures lies in their ability to mitigate the limitations of any single biomarker, including spatial heterogeneity and dynamic expression changes during treatment.
Table 1: Comparative Analysis of Single versus Combination lncRNA Biomarkers in HCC
| Feature | Single lncRNA Biomarkers | Combination lncRNA Signatures |
|---|---|---|
| Statistical Power | Moderate effect sizes (HR typically 2-3) | Enhanced predictive accuracy through combined risk scores |
| Biological Coverage | Limited to specific pathways or mechanisms | Captures multiple oncogenic processes simultaneously |
| Technical Robustness | Vulnerable to tumor heterogeneity | Reduces impact of spatial heterogeneity through multi-analyte assessment |
| Clinical Validation | Multiple individually validated markers (LINC00152, HOXC13-AS, LASP1-AS) | Emerging evidence for superior stratification in HCC cohorts |
| Therapeutic Prediction | Limited to general prognosis | Potential for predicting specific therapy responses (immunotherapy, targeted agents) |
Pan-Cancer Applications of lncRNA Signatures in Therapy Prediction
Predicting Immunotherapy Response
lncRNA signatures demonstrate remarkable utility in predicting response to immune checkpoint inhibitors across multiple cancer types. In non-small cell lung cancer (NSCLC), immune-related lncRNA signatures have identified three distinct tumor microenvironment subtypes: immune-inflamed (enriched with B/T cells and HLA expression), immune-escape (interferon-driven MHC upregulation), and immune-desert (minimal immune infiltration) [80]. These subtypes show significant differences in predicted immunotherapy sensitivity, with the immune-inflamed subtype demonstrating superior response [80].
In lung adenocarcinoma (LUAD), a novel 4-cuproptosis-related lncRNA signature (AC026355.2, AP000695.1, ARHGEF26-AS1, and AP005137.2) effectively stratifies patients by survival outcomes and immunotherapy response [81] [82]. This signature, derived from correlation analysis with 19 cuproptosis-related genes, functions as an independent prognostic factor and distinguishes patients with differential responses to immune checkpoint blockade [81]. Similarly, in gastric cancer, a 5-lncRNA signature (AC010333.1, LINC01579, AP000695.2, LINC00922, and AL121772.1) developed through ceRNA network analysis predicts prognosis and immunotherapy response, with elevated VCAN expression correlated with reduced anti-PD-1 response [83].
Predicting Targeted Therapy Response
lncRNA signatures show increasing promise in predicting response to molecularly targeted agents. In HER2+ metastatic breast cancer, a serum-based 4-lncRNA signature (LINP1, EGOT, BREA2, and LINC01503) accurately predicts treatment response to ado-trastuzumab emtansine (T-DM1) [79]. Developed through microarray profiling and validated using qRT-PCR across multiple cohorts, this signature classifies patients into high-risk and low-risk groups with significantly different progression-free survival outcomes [79]. The signature's validation in serum represents a significant advance for non-invasive treatment monitoring.
In high-grade serous ovarian cancer, a 29-lncRNA signature demonstrates predictive value for homologous recombination deficiency (HRD) and PARP inhibitor sensitivity [50]. Among these, ENSG00000272172.1 shows significant upregulation in HRD-positive tumors and is detectable in both formalin-fixed tissue and plasma, supporting its use as a minimally invasive biomarker [50]. Functional analyses reveal this lncRNA contributes to genome stability by modulating replication dynamics, providing mechanistic insight into its predictive capacity [50].
Table 2: Pan-Cancer Applications of Predictive lncRNA Signatures
| Cancer Type | lncRNA Signature | Therapy Type | Predictive Performance |
|---|---|---|---|
| Lung Adenocarcinoma | 4-cuproptosis-related lncRNAs (AC026355.2, AP000695.1, ARHGEF26-AS1, AP005137.2) | Immunotherapy | Effectively discriminates immunotherapy responders; independent prognostic factor (P<0.001) |
| HER2+ Breast Cancer | 4-lncRNA serum signature (LINP1, EGOT, BREA2, LINC01503) | T-DM1 (targeted) | Accurately classifies high/low risk groups (P<0.01); validated in multiple cohorts |
| Ovarian Cancer | 29-lncRNA panel (including ENSG00000272172.1) | PARP inhibitors | Predicts HRD status and PARP inhibitor sensitivity; detectable in plasma |
| Gastric Cancer | 5-lncRNA ceRNA signature (AC010333.1, LINC01579, AP000695.2, LINC00922, AL121772.1) | Immunotherapy (anti-PD-1) | Correlates with immunotherapy response; elevated VCAN associated with resistance |
| NSCLC | Immune-related lncRNA clusters | Immunotherapy | Identifies three TME subtypes with differential immunotherapy sensitivity |
Experimental Workflows and Methodological Frameworks
Signature Development and Validation Pipeline
The development of predictive lncRNA signatures follows a systematic workflow encompassing discovery, validation, and functional characterization. Initial discovery typically begins with transcriptomic data from sources like The Cancer Genome Atlas (TCGA), with lncRNAs identified through correlation analysis with known therapeutic response genes (e.g., cuproptosis genes for LUAD) [81] [82]. Feature selection employs multivariate statistical approaches including univariate Cox regression followed by LASSO and multivariate Cox regression to identify the most predictive lncRNA combinations [81] [83] [79].
Signature validation utilizes independent patient cohorts, with Kaplan-Meier survival analysis, principal component analysis, and functional enrichment analysis confirming prognostic and predictive utility [81] [82]. For clinical translation, nomograms integrating the lncRNA signature with standard clinicopathological features are developed to enhance predictive accuracy [81]. Finally, experimental validation through reverse transcription-quantitative PCR in patient tissues or cell lines confirms differential expression of signature lncRNAs [81] [83].
Methodological Details for Key Studies
The development of the 4-cuproptosis-related lncRNA signature in LUAD exemplifies rigorous methodology [81] [82]. Researchers extracted gene expression data of 16,876 lncRNAs and 19 cuproptosis-related genes from TCGA-LUAD. Cuproptosis-related lncRNAs were identified through Pearson correlation analysis (|R|>0.3, P<0.001), yielding 3,385 candidates. After random partitioning of patients into training (70%) and test (30%) cohorts, univariate Cox regression identified prognostic lncRNAs, followed by LASSO-Cox regression to reduce overfitting and multivariate Cox regression to establish the final 4-lncRNA signature [82]. The risk score was calculated as: Risk score = Σ(coefficientlncRNA × expressionlncRNA) for all four lncRNAs.
For the serum 4-lncRNA signature predicting T-DM1 response in HER2+ breast cancer, researchers performed lncRNA microarray profiling on serum samples from sensitive versus resistant patients, identifying 23 differentially expressed lncRNAs [79]. After qRT-PCR validation, machine learning approaches including LASSO Cox regression with 200 bootstrap replicates selected the final 4-lncRNA panel. The risk score was calculated as: (0.574 × LINP1) + (0.29 × EGOT) + (-0.42 × BREA2) + (-0.64 × LINC01503), with an optimal cutoff of 0.17 distinguishing high-risk and low-risk patients [79].
Signaling Pathways and Biological Mechanisms
lncRNA signatures exert their predictive power through regulation of critical cancer pathways. The ceRNA (competing endogenous RNA) network represents a fundamental mechanism, where lncRNAs function as molecular sponges for miRNAs, thereby modulating the expression of miRNA target genes [83] [78]. In gastric cancer, AP000695.2 promotes tumor growth through a ceRNA mechanism by sequestering miR-144-3p and miR-7-5p, thereby increasing expression of oncogenic genes including CDH11, COL5A2, COL12A1, and VCAN [83]. This network directly influences immunotherapy response, with elevated VCAN expression correlating with reduced anti-PD-1 efficacy [83].
Cuproptosis-related lncRNAs in LUAD connect copper metabolism to immune regulation and therapy response [81] [82]. Cuproptosis itself represents a novel form of copper-dependent cell death driven by mitochondrial copper accumulation and proteotoxic stress. lncRNAs associated with this process likely modulate key cuproptosis regulators including FDX1, DLAT, and other TCA cycle components, ultimately influencing cellular sensitivity to copper-induced death and corresponding immune activation [82].
RNA modification (RM)-related lncRNAs represent another mechanism, with 12 different RNA modifications (m5C, m6A, m7G, etc.) linked to lncRNA function in NSCLC [84]. These modifications influence RNA metabolism, stability, and translation, creating an additional layer of regulation that lncRNAs exploit to control cancer-relevant pathways. RM-related lncRNA clusters show distinct mutation patterns (e.g., TP53, TTN), immune cell infiltration, and immune checkpoint gene expression, ultimately influencing therapeutic susceptibility [84].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Reagents and Platforms for lncRNA Signature Development
| Reagent/Platform | Function | Application Example |
|---|---|---|
| TCGA Database | Source of RNA-seq data and clinical annotations | Pan-cancer lncRNA identification and correlation with clinical outcomes [81] [84] [82] |
| LASSO-Cox Regression | Statistical method for feature selection and overfitting reduction | Identification of most predictive lncRNAs from thousands of candidates [81] [79] |
| WGCNA | Weighted gene co-expression network analysis | Identification of lncRNA modules correlated with biological traits [84] [83] |
| CIBERSORT/XCELL | Computational deconvolution of immune cell populations | Assessment of immune infiltration in TME subtypes [84] [83] |
| qRT-PCR | Experimental validation of lncRNA expression | Confirmation of differential expression in patient tissues/sera [81] [83] [79] |
| GDSC Database | Drug sensitivity and compound screening resource | Identification of candidate therapeutic agents targeting high-risk groups [82] |
| TIDE Algorithm | Computational framework for immunotherapy response prediction | Evaluation of lncRNA signature association with immunotherapy outcome [82] |
lncRNA signatures represent a transformative approach in cancer theranostics, offering superior prognostic and predictive capability compared to single biomarkers. The development of these multi-analyte signatures has been accelerated by integrated bioinformatics pipelines, machine learning approaches, and validation across independent cohorts. In HCC, the transition from single lncRNA biomarkers to combination signatures mirrors the broader evolution in cancer biomarker development, addressing tumor heterogeneity and capturing complex biological networks.
Future developments will likely focus on standardizing analytical frameworks, validating signatures in prospective clinical trials, and integrating lncRNA signatures with existing biomarkers such as PD-L1 expression and tumor mutational burden. The successful development of serum-based lncRNA signatures [79] highlights the potential for non-invasive "liquid biopsy" applications, enabling dynamic monitoring of treatment response. As functional characterization of predictive lncRNAs advances, these signatures may not only predict treatment response but also reveal novel therapeutic targets, ultimately advancing personalized cancer therapy.
Conclusion
The evidence overwhelmingly demonstrates that combined lncRNA biomarker strategies significantly outperform single lncRNA assays in both diagnostic accuracy and prognostic prediction for HCC. Panels that integrate multiple lncRNAs or combine lncRNAs with traditional markers like AFP achieve superior sensitivity and specificity, with some combinations reaching AUC values exceeding 0.95. This enhanced performance is critical for early detection, patient risk stratification, and guiding personalized treatment decisions. Future research must focus on standardizing detection protocols, validating panels in large, multi-center prospective cohorts, and integrating lncRNA biomarkers with other omics data and imaging features. The ultimate goal is the development of clinically robust, non-invasive liquid biopsy tests that can be seamlessly incorporated into HCC surveillance programs for high-risk populations, ultimately improving patient survival through earlier and more precise intervention.
References
- 1. Long non-coding RNA-based single and combination ... [https://pubmed.ncbi.nlm.nih.gov/40892177/]
- 2. Decoding the molecular and genomic landscape of ... [https://www.nature.com/articles/s44355-025-00038-8]
- 3. New insights into biomarkers and risk stratification to predict ... [https://pubmed.ncbi.nlm.nih.gov/40269686/]
- 4. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 5. Biomarker discovery in hepatocellular carcinoma (HCC) for ... [https://www.sciencedirect.com/science/article/abs/pii/S1359610124000674]
- 6. Biomarker discovery in hepatocellular carcinoma (HCC) for ... [https://pubmed.ncbi.nlm.nih.gov/39191624/]
- 7. lncRNAs as prognostic molecular biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5601763/]
- 8. Plasma exosomal lncRNA-related signatures define ... [https://pubmed.ncbi.nlm.nih.gov/41169384/]
- 9. Long non-coding RNA-based single and combination ... [https://link.springer.com/article/10.1007/s12672-025-03309-1]
- 10. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 11. Long non-coding RNAs: definitions, functions, challenges ... [https://www.nature.com/articles/s41580-022-00566-8]
- 12. Long non-coding RNAs: Biogenesis, functions, and clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8637188/]
- 13. Long non-coding RNA-based single and combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405140/]
- 14. Biogenesis and transcriptional regulation of long non-coding ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5140008/]
- 15. Gene regulation by long non-coding RNAs and its ... [https://www.nature.com/articles/s41580-020-00315-9]
- 16. Biomarkers for diagnosis and therapeutic options in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02101-z]
- 17. Amino acid metabolism-related LncRNAs as prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12545943/]
- 18. Plasma exosomal lncRNA-related signatures define ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1663943/full]
- 19. Long Noncoding RNAs and Hepatocellular Carcinoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8985762/]
- 20. Prognostic Value of Long Non-Coding RNA HULC and ... [https://www.nature.com/articles/s41598-017-16260-1]
- 21. Current progress and role of lncRNAs in HBV infection ... [https://www.sciencedirect.com/science/article/pii/S2352304225003678]
- 22. lncRNAs as Biomarkers of Hepatocellular Carcinoma Risk ... [https://www.mdpi.com/1467-3045/47/5/348]
- 23. The dual role of LncRNAs in hepatocellular carcinoma [https://www.sciencedirect.com/science/article/pii/S2949752324000311]
- 24. Long non-coding RNAs and autophagy: dual drivers of ... [https://www.nature.com/articles/s41420-025-02667-7]
- 25. Long Non-Coding RNAs: Potential Biomarkers and Targets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7757045/]
- 26. Targeting Autophagy Using Long Non-Coding RNAs (LncRNAs) [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000689/]
- 27. PI3K/AKT/mTOR pathway-related long non-coding RNAs [https://pubmed.ncbi.nlm.nih.gov/32916254/]
- 28. Long noncoding RNAs as biomarkers for the diagnosis of ... [https://www.sciencedirect.com/science/article/abs/pii/S0344033821002077]
- 29. Blood-derived lncRNAs as biomarkers for cancer diagnosis [https://www.nature.com/articles/s41698-022-00283-7]
- 30. Hypoxia- and Anoikis-Related lncRNA Signature Defines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533731/]
- 31. Non-coding RNAs in hepatocellular carcinoma: Insights ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.985815/full]
- 32. Unveiling the Role of LncRNAs in Tumorigenesis [https://www.sciencedirect.com/science/article/pii/S305078712500085X]
- 33. MIAT, HEIH, and HOTAIR: A novel LncRNA signature in ... [https://www.sciencedirect.com/science/article/pii/S1874467225000169]
- 34. A novel disulfidptosis-related lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582836/]
- 35. A migrasome-related lncRNA signature predicts prognosis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581122/full]
- 36. Clinical and analytical validation of a combined RNA ... [https://www.nature.com/articles/s43856-025-00934-3]
- 37. The LncRNA lnc-POTEM-4:14 promotes HCC progression ... [https://www.nature.com/articles/s41598-025-92614-4]
- 38. Circulating blood biomarkers for minimal residual disease ... [https://www.sciencedirect.com/science/article/pii/S0305737225000301]
- 39. Characteristics of extracellular vesicle-derived lncRNAs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619285/]
- 40. Identification of long non-coding RNAs biomarkers for early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5341997/]
- 41. Characteristics of extracellular vesicle-derived lncRNAs ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-15237-y]
- 42. Diagnostic lncRNA high expression for liver patients ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1462512/full]
- 43. a multi-center and large-scale study | npj Precision Oncology [https://www.nature.com/articles/s41698-025-01010-8]
- 44. Integrating AI and RNA biomarkers in cancer: advances in ... [https://biosignaling.biomedcentral.com/articles/10.1186/s12964-025-02434-2]
- 45. Construction of an Immune-Related Six-lncRNA Signature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8283691/]
- 46. A Circulating Long Noncoding RNA Panel Serves as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7376401/]
- 47. Non-coding RNAs: emerging biomarkers and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11931079/]
- 48. Construction of Novel lncRNA–miRNA–mRNA Network ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.626663/full]
- 49. Identification and Validation of a Prognostic lncRNA ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2020.00780/full]
- 50. Long non-coding RNAs as a biomarker for homologous ... [https://www.nature.com/articles/s42003-025-08836-9]
- 51. Decoding potential lncRNA and disease associations ... [https://www.nature.com/articles/s41598-025-16177-0]
- 52. Long Noncoding RNA Serve as a Potential Predictive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7238389/]
- 53. Evaluation of Individual and Combined Applications ... [https://www.mdpi.com/1422-0067/14/12/23559]
- 54. Updating the Clinical Application of Blood Biomarkers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10001986/]
- 55. Serum Biomarkers for the Prediction of Hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8038187/]
- 56. of small and large RNAs in bacteria for excellent... Efficient extraction [https://bmcresnotes.biomedcentral.com/articles/10.1186/s13104-015-1726-3]
- 57. Feature reduction for hepatocellular carcinoma prediction ... [https://journalofbigdata.springeropen.com/articles/10.1186/s40537-024-00944-3]
- 58. A novel lncRNA-mediated signaling axis governs cancer ... [https://jeccr.biomedcentral.com/articles/10.1186/s13046-025-03546-w]
- 59. Long non-coding rnas as key modulators of the immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1523190/full]
- 60. single-cell analysis and identification of prognostic biomarkers [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605361/]
- 61. Progression of chronic liver disease to hepatocellular ... [https://www.nature.com/articles/s44276-024-00050-0]
- 62. Hepatocellular carcinoma (HCC) - Symptoms and causes [https://www.mayoclinic.org/diseases-conditions/hepatocellular-carcinoma/symptoms-causes/syc-20589101]
- 63. Differences in hepatocellular carcinoma risk, predictors and ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0204412]
- 64. Detection and validity of long non-coding RNAs HOST2, ... [https://www.sciencedirect.com/science/article/abs/pii/S2773044124000937]
- 65. Diagnostic value of long noncoding RNAs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5515770/]
- 66. Identification of a novel lncRNA prognostic signature and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10442647/]
- 67. The prognostic value of an autophagy-related lncRNA ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-021-04123-6]
- 68. Amino acid metabolism-related LncRNAs as prognostic ... [https://link.springer.com/article/10.1007/s12672-025-03789-1]
- 69. Basement membrane-related lncRNA signature for the ... [https://www.sciencedirect.com/science/article/pii/S2405844024064703]
- 70. The combination of serum lncRNA PTTG3P and mRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11632297/]
- 71. Establishing a miRNA panel for hepatocellular carcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12275877/]
- 72. Hepatocellular Carcinoma Risk Panel with GALAD Score [https://news.mayocliniclabs.com/2023/07/24/hepatocellular-carcinoma-risk-panel-with-galad-score/]
- 73. Molecular Medicine Reports [https://www.spandidos-publications.com/10.3892/mmr.2024.13409/abstract]
- 74. A fourâ€long noncoding RNA signature predicts survival of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7521318/]
- 75. Identification and Validation of Immune-Related LncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8301374/]
- 76. Identification of prognostic immune-related lncRNA ... [https://www.nature.com/articles/s41598-023-28305-9]
- 77. A seven-lncRNA signature for predicting prognosis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8797290/]
- 78. Non-coding RNAs: emerging biomarkers and therapeutic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1534862/full]
- 79. A long noncoding RNA-based serum signature predicts ... [https://www.nature.com/articles/s41420-025-02701-8]
- 80. Immune-Related lncRNA Signatures Define Tumor ... [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.21203/rs.3.rs-7575439/v1]
- 81. A 4-cuproptosis-related lncRNA theragnostic signature ... [https://pubmed.ncbi.nlm.nih.gov/41220401/]
- 82. Molecular and Clinical Oncology [https://www.spandidos-publications.com/10.3892/mco.2025.2912?text=fulltext]
- 83. Identification of a LncRNA based CeRNA network ... [https://www.nature.com/articles/s41598-025-05105-x]
- 84. Enhanced multi-omics analysis reveals a lncRNA signature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521086/]