Tissue vs. Circulating lncRNAs: A Comparative Analysis for Advancing Hepatocellular Carcinoma Diagnosis
Hepatocellular carcinoma (HCC) presents a significant global health burden, with poor prognosis often due to late diagnosis.
Tissue vs. Circulating lncRNAs: A Comparative Analysis for Advancing Hepatocellular Carcinoma Diagnosis
Abstract
Hepatocellular carcinoma (HCC) presents a significant global health burden, with poor prognosis often due to late diagnosis. Long non-coding RNAs (lncRNAs) have emerged as pivotal regulators of hepatocarcinogenesis, offering immense potential as novel diagnostic biomarkers. This article provides a comprehensive comparative analysis of tissue-derived versus circulating lncRNAs for HCC diagnosis, addressing a critical knowledge gap in liquid biopsy applications. We explore the foundational biology of lncRNAs in HCC, methodological approaches for their detection in different compartments, strategies to overcome analytical challenges, and rigorous validation of their diagnostic performance. By synthesizing current evidence, this review aims to guide researchers and drug development professionals in selecting optimal lncRNA biomarkers and developing effective diagnostic strategies to improve early HCC detection and patient outcomes.
The Molecular Landscape: Understanding lncRNA Biology in Hepatocellular Carcinoma
From Genomic 'Junk' to Functional Regulators: Redefining the RNA World
Long non-coding RNAs (lncRNAs) represent a class of RNA molecules longer than 200 nucleotides that lack protein-coding potential. Once dismissed as transcriptional "noise" or evolutionary "junk," these molecules have emerged as crucial regulators of gene expression, playing pivotal roles in development, differentiation, and disease pathogenesis [1] [2]. The discovery that less than 2% of the human genome encodes proteins while the majority is transcribed into non-coding RNAs necessitated a fundamental reassessment of genetic information flow and regulation in complex organisms [1] [3] [4].
This paradigm shift coincided with the resolution of the "g-value paradox"—the observation that organismal complexity does not correlate with protein-coding gene number but rather with the expansion of non-coding DNA and its associated transcripts [2]. The human genome, for instance, contains approximately 20,000 protein-coding genes, similar to the nematode worm Caenorhabditis elegans, yet produces tens of thousands of lncRNAs that contribute significantly to mammalian complexity [2]. According to GENCODE consortium data, there are currently 27,817 lncRNA transcripts originating from 15,931 genes identified in the human genome [5].
Molecular Archetypes: Functional Mechanisms of lncRNAs
LncRNAs exert their regulatory functions through diverse molecular mechanisms that can be distilled into four primary archetypes, each with distinct modes of action [4].
1. Molecular Signals: LncRNAs can serve as precise indicators of specific biological states, responding to developmental cues, cellular context, or environmental stimuli. Their transcription occurs at precise times and locations, providing spatial and temporal information about gene regulatory events. Examples include Xist, which marks the inactivated X chromosome in female mammals, and lncRNAs like HOTAIR and HOTTIP that display anatomic-specific expression patterns correlating with positional identity [4].
2. Molecular Decoys: These lncRNAs act as "molecular sinks" that sequester transcription factors, chromatin modifiers, or other regulatory proteins, preventing them from binding their natural targets. Similarly, they can function as competing endogenous RNAs (ceRNAs) that bind to microRNAs, weakening their regulatory impact on target mRNAs [1] [4].
3. Molecular Guides: LncRNAs can direct ribonucleoprotein complexes to specific genomic locations in cis (affecting nearby genes) or trans (affecting distant genes). They facilitate the recruitment of chromatin-modifying complexes to specific target genes, enabling precise spatial control of gene expression [1] [4].
4. Molecular Scaffolds: As scaffolding molecules, lncRNAs provide platforms for assembling multiple effector molecules into functional complexes. They can bring together combinatorial sets of proteins, DNA, and other RNAs to form ribonucleoprotein complexes with diverse regulatory capabilities [1] [4].
Table 1: Molecular Archetypes of lncRNA Function
| Archetype | Mechanism of Action | Key Examples | Biological Role |
|---|---|---|---|
| Signals | Indicated specific transcriptional events in response to stimuli | Xist, HOTAIR, linc-p21 | Chromosome inactivation, anatomic patterning, DNA damage response |
| Decoys | Sequester proteins or miRNAs to prevent target binding | PANDA, HULC | Compete with miRNAs, inhibit transcription factors |
| Guides | Direct chromatin-modifying complexes to specific genomic loci | HOTTIP, Kcnq1ot1 | Recruit repressive complexes for allele-specific silencing |
| Scaffolds | Assemble multiple proteins into functional complexes | HULC, ANRIL | Form ribonucleoprotein complexes for coordinated regulation |
LncRNA Biogenesis and Structural Features
LncRNAs are primarily transcribed by RNA polymerase II, evidenced by PolII occupancy, 5' capping, histone modifications associated with transcriptional elongation, and frequent polyadenylation [2] [4]. However, they exhibit considerable structural diversity, with some lacking polyadenylation or 7-methylguanosine caps, and others being transcribed by RNA polymerase I or III or processed from introns and repetitive elements [2].
Classification of lncRNAs is typically based on their genomic context relative to protein-coding genes [1] [2]:
- Long intergenic non-coding RNAs (lincRNAs): Transcribed from regions between protein-coding genes
- Intronic lncRNAs: Derived entirely from introns of protein-coding genes
- Antisense lncRNAs: Transcribed from the opposite strand of protein-coding genes
- Bidirectional lncRNAs: Transcribed in the opposite direction from shared promoter regions
- Enhancer RNAs (eRNAs): Transcribed from enhancer regions
The structural organization of eukaryotic genomes is remarkably complex, with widespread overlapping transcription and genes embedded within genes. As noted in Nature Reviews Molecular Cell Biology, "any base may be exonic, intronic or 'intergenic,' depending on the transcriptional output of the cell at any point in its developmental trajectory or physiological state" [2]. This challenges traditional genome annotation and necessitates more sophisticated approaches to understanding functional elements.
LncRNAs in Hepatocellular Carcinoma: A Comparative Diagnostic Approach
Hepatocellular carcinoma (HCC), the most common primary liver malignancy, represents a formidable clinical challenge with poor prognosis, largely due to late diagnosis and limited treatment options [1] [3]. HCC ranks as the sixth most frequently diagnosed cancer globally and has become the third leading cause of cancer death [1]. In this context, lncRNAs have emerged as promising biomarkers and therapeutic targets, with particular relevance for comparative analysis between tissue and circulating forms for diagnostic applications.
Tissue-Based lncRNA Biomarkers in HCC
Tissue studies have revealed numerous dysregulated lncRNAs in HCC pathogenesis. HULC (HCC Up-Regulated Long Non-Coding RNA) was the first identified lncRNA with abnormal expression in human HCC specimens, located at chromosome 6p24.3 [1]. It promotes tumor progression through multiple mechanisms, including upregulation of sphingosine kinase 1 (SPHK1) to enhance angiogenesis and activation of autophagy via Sirt1/LC3 signaling [1]. HULC also functions as a competing endogenous RNA, binding to miRNA-372 and reducing its inhibitory effect on PRKACB, a catalytic subunit of cAMP-dependent protein kinase [1].
Other significant tissue-based lncRNAs in HCC include:
- MALAT1 (Metastasis-Associated Lung Adenocarcinoma Transcript 1): Promotes HCC progression and metastasis [1]
- MEG3: A tumor-suppressive lncRNA downregulated in HCC that inhibits cell growth and promotes apoptosis [1]
- Linc00152: Shows significant overexpression in HCC tissues and plasma [6]
- H19: One of the first identified lncRNAs, implicated in growth restriction and found deregulated in HCC [3] [5]
Circulating lncRNA Biomarkers in HCC
The stable presence of lncRNAs in body fluids including serum, plasma, urine, and saliva has opened new avenues for non-invasive liquid biopsy approaches in cancer diagnosis [6] [5] [7]. Circulating lncRNAs are protected from endogenous RNases through packaging in membrane-bound vesicles like exosomes or complex formation with proteins [5].
Table 2: Diagnostic Performance of Circulating lncRNAs in Hepatocellular Carcinoma
| lncRNA | Detection Method | Sample Size | Diagnostic Performance (AUC) | Key Findings |
|---|---|---|---|---|
| Linc00152 | qRT-PCR | 129 HCC, 169 controls | 0.877 (single) | Best performing single lncRNA biomarker [6] |
| HULC | qRT-PCR | 129 HCC, 169 controls | Not reported | Significantly elevated in HCC plasma [6] |
| Linc00152 + AFP | Combined panel | 129 HCC, 169 controls | 0.906 | Enhanced diagnostic accuracy [6] |
| Linc00152 + UCA1 + AFP | Multiplex panel | 129 HCC, 169 controls | 0.912 | 82.9% sensitivity, 88.2% specificity [6] |
| RP11-160H22.5 + XLOC_014172 + LOC149086 | Combined panel | HCC vs. controls | 0.896 | 82% sensitivity, 73% specificity [5] |
| HULC + LINC00152 | Combined panel | Training and validation sets | 0.87 (combined) | Positive correlation with tissue expression [5] |
A 2020 comprehensive study evaluated eight serum lncRNAs (HULC, MALAT1, Linc00152, PTENP1, PTTG3P, SPRY4-IT1, UBE2CP3, and UCA1) in 129 HCC patients, 49 patients with liver cirrhosis, 27 patients with chronic hepatitis B, and 93 healthy controls [6]. The investigation revealed significantly elevated levels of HULC, MALAT1, Linc00152, PTTG3P, SPRY4-IT1, UBE2CP3, and UCA1 in HCC patients compared to controls, while PTENP1 was significantly decreased [6].
More recent research continues to validate circulating lncRNAs as promising biomarkers. A 2025 study demonstrated that plasma lncRNAs HULC and RP11-731F5.2 serve as potential biomarkers for HCC risk in patients with chronic hepatitis C, while RP11-731F5.2 and KCNQ1OT1 may indicate liver damage from HCV infection [7].
Experimental Methodologies for lncRNA Analysis
Sample Collection and Processing
For circulating lncRNA analysis, peripheral blood samples are collected in vacuum tubes and processed by centrifugation at 3,000 rpm for 10 minutes to isolate serum or plasma, which is then stored at -80°C until analysis [6] [7]. Standardized protocols are crucial as pre-analytical variables significantly impact lncRNA measurements.
RNA Isolation and Quantification
Total RNA is extracted from serum or plasma samples using specialized kits such as the Hipure Liquid RNA Kit or Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit [6] [7]. RNA quantity and purity are assessed via spectrophotometry (e.g., NanoDrop One), followed by DNase treatment to remove genomic DNA contamination.
Reverse Transcription Quantitative PCR (RT-qPCR)
The gold standard for lncRNA quantification involves:
- cDNA Synthesis: Reverse transcription using M-MLV Reverse Transcriptase or High-Capacity cDNA Reverse Transcription Kit [6] [7]
- qPCR Amplification: Using TB Green Premix Ex Taq or Power SYBR Green PCR Master Mix on real-time PCR systems [6]
- Thermal Cycling Conditions: Typically 95°C for 30 seconds, followed by 45 cycles of 95°C for 5 seconds and 60°C for 30 seconds [6]
- Data Normalization: Using the 2−ΔΔCt method with reference genes (GAPDH or β-actin) for normalization [6] [7]
Advanced Analytical Approaches
Emerging methodologies include:
- Next-generation sequencing (NGS): For discovery-phase studies identifying novel lncRNAs [7]
- Multiplex panels: Combining multiple lncRNAs with traditional markers like AFP [6]
- Logistic regression modeling: To establish optimal lncRNA combinations for diagnostic panels [6]
- Combinatorial ROC analysis: Using tools like CombiROC to evaluate multi-marker performance [7]
Technical Considerations and Standardization Challenges
Despite promising results, several challenges remain in translating lncRNA biomarkers to clinical practice. Significant variability exists in sample choice, handling, processing protocols, and data normalization methods [5]. Blood cell contamination during sample preparation can significantly alter lncRNA profiles, necessitating careful standardization [5]. Furthermore, the lack of consensus regarding reference genes for normalization complicates cross-study comparisons and clinical implementation.
Regulatory Networks in HCC: LncRNA-Autophagy Axis
LncRNAs participate in intricate regulatory networks in HCC, notably through autophagy regulation—a conserved catabolic pathway with dual roles in tumor suppression and promotion [8]. In early hepatocarcinogenesis, lncRNAs like HULC modulate autophagy as a tumor-suppressive mechanism through Sirt1/LC3 signaling [1]. In advanced HCC, lncRNAs contribute to therapy resistance by altering autophagic flux through key pathways including PI3K/AKT/mTOR, AMPK, and Beclin-1 [8].
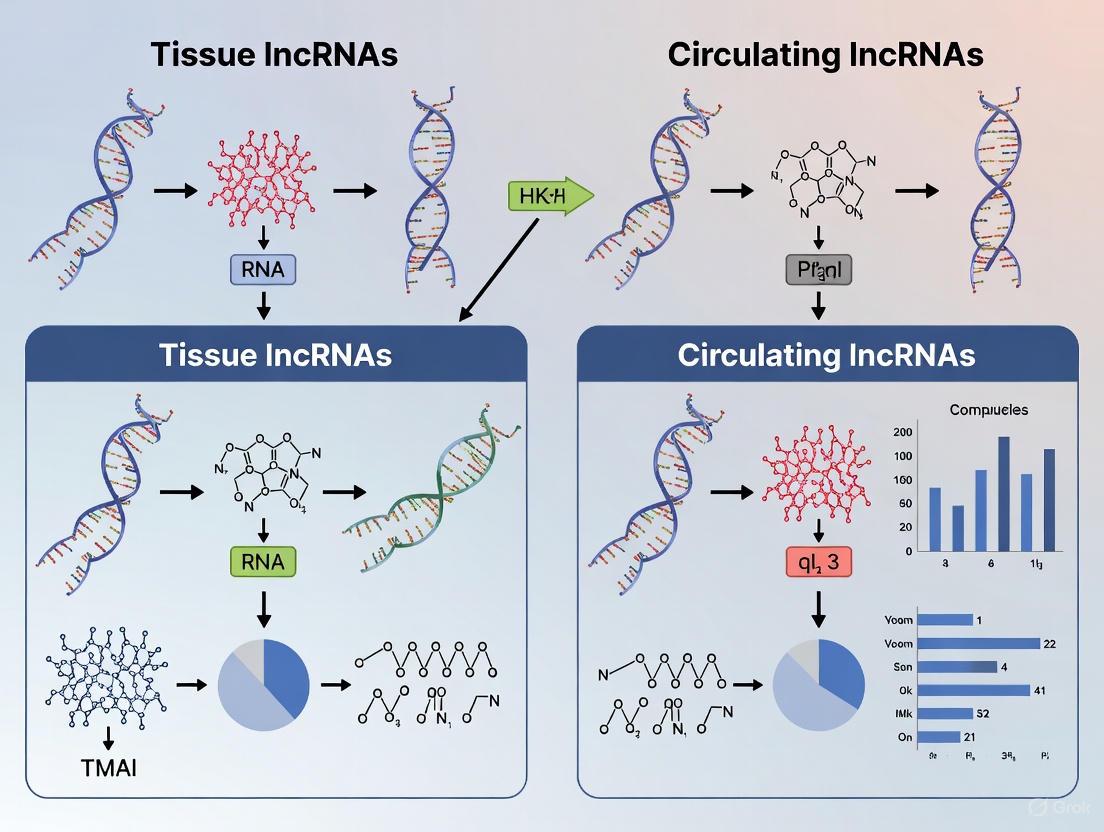
Diagram 1: LncRNA Functional Networks in HCC. This diagram illustrates how different lncRNAs operate through distinct molecular mechanisms to influence key cancer pathways and clinical outcomes in hepatocellular carcinoma.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for lncRNA Investigation in HCC
| Reagent Category | Specific Products | Application Purpose | Key Features |
|---|---|---|---|
| RNA Isolation Kits | Hipure Liquid RNA Kit, Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit | RNA extraction from serum/plasma | Optimized for low-abundance circulating RNA, includes DNase treatment |
| Reverse Transcriptase | M-MLV Reverse Transcriptase, High-Capacity cDNA Reverse Transcription Kit | cDNA synthesis from RNA templates | High efficiency for long RNA transcripts, robust performance with degraded samples |
| qPCR Master Mixes | TB Green Premix Ex Taq, Power SYBR Green PCR Master Mix | Quantitative PCR amplification | SYBR Green chemistry, optimized for lncRNA detection, include ROX reference dye |
| Reference Genes | GAPDH, β-actin | Data normalization | Stable expression across samples, validated for circulating RNA studies |
| NGS Platforms | Illumina, PacBio | Discovery-phase lncRNA identification | Whole-transcriptome coverage, novel lncRNA discovery, isoform resolution |
| Icmt-IN-37 | Icmt-IN-37, MF:C22H28ClNO, MW:357.9 g/mol | Chemical Reagent | Bench Chemicals |
| Pde4-IN-13 | PDE4-IN-13|PDE4 Inhibitor|IC50 1.56 µM | PDE4-IN-13 is a PDE4 inhibitor (IC50=1.56 µM) for research on inflammation, COPD, and psoriasis. This product is For Research Use Only. Not for human use. | Bench Chemicals |
The journey of lncRNAs from presumed 'junk RNA' to key regulatory molecules represents one of the most significant paradigm shifts in molecular biology over the past decade. Their involvement in hepatocellular carcinoma pathogenesis highlights their potential as both biological mediators and clinical tools. The comparative analysis between tissue and circulating lncRNAs reveals a promising landscape for diagnostic innovation, with circulating lncRNA panels demonstrating particular utility for non-invasive early detection and risk stratification.
Future research directions should focus on standardizing detection methodologies, validating multi-lncRNA panels in large prospective cohorts, and developing targeted therapeutic approaches that leverage the unique properties of these versatile regulatory molecules. As our understanding of lncRNA biology deepens, these once-overlooked transcripts are poised to revolutionize both our comprehension of cancer biology and our approaches to clinical management of malignancies like hepatocellular carcinoma.
Hepatocellular carcinoma (HCC) remains one of the most lethal malignancies worldwide, with complex pathogenesis involving DNA damage, epigenetic modifications, and oncogene mutations [9] [3]. Long non-coding RNAs (lncRNAs), defined as RNA transcripts longer than 200 nucleotides with limited or no protein-coding potential, have emerged as critical regulators of gene expression in HCC pathogenesis and progression [10] [4]. Once considered mere "transcriptional noise," lncRNAs are now recognized as molecular signals, decoys, guides, and scaffolds that fine-tune cellular processes through diverse mechanisms [4]. This review elucidates the mechanistic roles of lncRNAs in HCC gene regulation, comparing their tissue and circulating forms for diagnostic applications and providing experimental methodologies for their investigation.
Molecular Mechanisms of lncRNAs in Gene Regulation
LncRNAs regulate gene expression through sophisticated molecular mechanisms based on their subcellular localization and interactions with DNA, RNA, and proteins. These mechanisms can be categorized into four primary archetypes with distinct functional implications for HCC pathogenesis.
Table 1: Molecular Archetypes of lncRNA Function in HCC
| Archetype | Mechanistic Principle | Key Example in HCC | Functional Outcome |
|---|---|---|---|
| Signals | Specific expression in response to developmental cues, cellular context, or stimuli [4] | linc-p21: hypoxia-responsive lncRNA forming positive feedback with HIF-1α [9] | Drives glycolysis and promotes tumor growth [9] |
| Decoys | Molecular "sponges" that sequester miRNAs or transcription factors [10] | HULC: sequesters miR-372, miR-107, and miR-9 to regulate target genes [11] [12] | Promotes tumorigenesis, angiogenesis, and lipid metabolism reprogramming [11] |
| Guides | Direct chromatin-modifying complexes to specific genomic loci [10] [4] | HOTAIR: recruits PRC2 complex to silence tumor suppressor genes [11] [4] | Promotes migration, invasion, and metastasis through epigenetic silencing [11] |
| Scaffolds | Assembly of multiple effector molecules into functional complexes [4] | MALAT1: interacts with splicing factors and chromatin modifiers [11] [13] | Regulates alternative splicing and promotes malignant transformation [11] |
Epigenetic Regulation
Nuclear lncRNAs predominantly regulate gene expression through epigenetic mechanisms by recruiting chromatin-modifying complexes to specific genomic loci. HOTAIR exemplifies this mechanism by guiding the Polycomb Repressive Complex 2 (PRC2) to target genes, facilitating histone H3 lysine 27 trimethylation (H3K27me3) and subsequent transcriptional repression [11] [4]. This epigenetic silencing affects numerous tumor suppressor genes in HCC, promoting tumor progression and metastasis [11]. Similarly, lncRNAs such as KCNQ1ot1 and Air mediate transcriptional silencing in an allele-specific manner through interactions with histone methyltransferases, establishing repressive chromatin domains [4].
Transcriptional Regulation
LncRNAs modulate transcriptional processes through various mechanisms, including transcription factor recruitment, RNA polymerase II interaction, and direct interference with gene promoters. For instance, lncRNA-p21 serves as a hypoxia-responsive regulator that forms a positive feedback loop with HIF-1α to drive glycolytic pathways in HCC cells [9]. This transcriptional regulation enhances the adaptive survival of tumor cells within the hypoxic microenvironment characteristic of HCC. Other lncRNAs function as transcriptional co-activators or repressors by directly binding to transcription factors or modulating their activity through allosteric mechanisms [10].
Post-Transcriptional Regulation
Cytoplasmic lncRNAs primarily influence post-transcriptional processes through miRNA sponging, mRNA stability modulation, and translational regulation. The "competing endogenous RNA" (ceRNA) mechanism is particularly relevant in HCC, where lncRNAs such as HULC and linc-RoR function as molecular decoys for miRNAs [9] [11] [3]. By sequestering specific miRNAs (e.g., HULC binding miR-372), these lncRNAs prevent miRNA-mediated repression of oncogenic mRNAs, thereby promoting HCC progression [11]. Additional post-transcriptional mechanisms include direct interactions with RNA-binding proteins to influence mRNA stability, alternative splicing, and translational efficiency [10].
Post-Translational and Metabolic Regulation
Emerging evidence indicates that certain lncRNAs encode micropeptides that directly influence protein function and cellular metabolism. These lncRNA-encoded micropeptides, typically approximately 100 amino acids in length, participate in diverse processes including transcription regulation and mRNA processing [9]. In HCC, lncRNAs such as HULC contribute to metabolic reprogramming by altering lipid metabolism through the miR-9-PPARA-ACSL1 signaling axis, highlighting the multifaceted regulatory capacity of lncRNAs in cancer metabolism [11].
Diagram 1: Integrated molecular mechanisms of lncRNAs in HCC pathogenesis. Nuclear lncRNAs function as guides and signals for epigenetic and transcriptional regulation, while cytoplasmic lncRNAs act as decoys for post-transcriptional control, collectively driving HCC progression through key signaling pathways.
Key lncRNAs in HCC Pathogenesis
Several well-characterized lncRNAs demonstrate prototypical regulatory functions in HCC, serving as illustrative models for understanding lncRNA mechanisms in hepatocarcinogenesis.
Table 2: Key lncRNAs and Their Mechanisms in HCC Progression
| LncRNA | Expression in HCC | Molecular Mechanisms | Functional Consequences | Regulatory Targets |
|---|---|---|---|---|
| HULC | Highly upregulated [11] | miRNA sponge (miR-372, miR-107); alters lipid metabolism; modulates circadian rhythms [11] | Promotes tumor growth, angiogenesis, invasion, and metastasis [11] [3] | miR-372, E2F1/SPHK1, ZEB1, CLOCK [11] |
| MALAT1 | Upregulated [11] [13] | Regulates alternative splicing; forms feedback loop with HIF-2α; sponges miR-383-5p [11] [13] | Promotes cell proliferation, migration, invasion; associated with poor prognosis [11] [13] | PRKAG1, SIRT1, HIF-2α, miR-383-5p [11] [13] |
| HOTAIR | Upregulated [11] | Recruits PRC2 complex; regulates autophagy; modulates ECM degradation [11] | Promotes migration, invasion; associated with poor differentiation and early recurrence [11] | PRC2, MMP-9, VEGF [11] |
| H19 | Upregulated (context-dependent) [9] [11] | miRNA sponge; epigenetic regulation; encodes micropeptides [9] | Promotes proliferation, invasion, drug resistance; regulates IGF2 expression [9] [11] | miR-15b, CDC42/PAK1, IGF2 [9] |
| MEG3 | Downregulated [11] | Activates p53 pathway; regulates TGF-β pathway [11] | Suppresses tumor growth; induces apoptosis [11] | p53, TGF-β pathway genes [11] |
HULC (Highly Upregulated in Liver Cancer)
HULC demonstrates exceptionally high expression levels in HCC tissues and exemplifies multiple mechanistic archetypes [11]. It functions as a ceRNA by sequestering multiple miRNAs including miR-372, miR-107, and miR-9, thereby derepressing their target genes involved in cell cycle regulation (p18), angiogenesis (E2F1/SPHK1), and lipid metabolism (PPARA, ACSL1) [11]. HULC also promotes epithelial-mesenchymal transition through ZEB1 upregulation, facilitating HCC invasion and metastasis [11]. Furthermore, HULC influences circadian regulation through CLOCK upregulation, potentially connecting metabolic dysregulation with circadian disruption in HCC [11].
MALAT1 (Metastasis-Associated Lung Adenocarcinoma Transcript 1)
MALAT1 represents a multifunctional nuclear lncRNA that regulates HCC progression through various mechanisms [11] [13]. It participates in arsenite-induced malignant transformation by forming a feedback loop with HIF-2α, reducing VHL-mediated HIF-2α ubiquitination and promoting HIF-2α accumulation [11]. Recently, MALAT1 was shown to promote HCC progression through the miR-383-5p/PRKAG1 axis, regulating the P53 and AKT signaling pathways while modulating immune cell infiltration in the tumor microenvironment [13]. MALAT1 also influences liver fibrosis by mediating SIRT1 expression, contributing to the premalignant liver environment [11].
HOTAIR (HOX Transcript Antisense RNA)
HOTAIR exemplifies the guide archetype by recruiting chromatin-modifying complexes to specific genomic locations [11] [4]. In HCC, HOTAIR expression correlates with poor differentiation, metastasis, and early recurrence [11]. It facilitates transcriptional repression through PRC2 recruitment, leading to H3K27me3 deposition at tumor suppressor genes [4]. Additionally, HOTAIR regulates autophagy activation and modulates the expression of matrix metallopeptidase-9 (MMP-9) and vascular endothelial growth factor (VEGF), enhancing extracellular matrix degradation and angiogenesis [11].
Comparative Analysis: Tissue vs. Circulating lncRNAs as Biomarkers
The comparative utility of tissue and circulating lncRNAs represents a crucial consideration for HCC diagnosis and monitoring. Both compartments offer distinct advantages and limitations for clinical applications.
Table 3: Tissue vs. Circulating lncRNAs for HCC Diagnosis
| Parameter | Tissue lncRNAs | Circulating lncRNAs |
|---|---|---|
| Invasiveness | High (requires biopsy) [7] | Low (liquid biopsy) [12] [7] |
| Tumor Heterogeneity | Sampling variability [7] | Integrative profile [12] |
| Stability | Moderate (degradation concerns) | High (resistant to RNase, stable in plasma) [12] |
| Longitudinal Monitoring | Limited (repeated biopsies impractical) [7] | Excellent (serial sampling feasible) [12] [7] |
| Diagnostic Performance | High tissue specificity | Variable specificity; combination panels improve accuracy [12] |
| Early Detection Potential | Limited to biopsy timing | Promising (detectable before radiographic evidence) [7] |
| Representative Examples | HULC, MALAT1, HOTAIR, H19 [9] [11] | HULC, RP11-731F5.2, UCA1, LINC00152 [12] [7] |
Tissue lncRNAs: Gold Standard for Mechanistic Studies
Tissue-based lncRNA analysis remains the gold standard for mechanistic investigations and biomarker discovery, providing direct information about molecular events within the tumor microenvironment [9] [3]. The high tissue specificity of lncRNA expression patterns enables precise correlation with pathological features and clinical outcomes [10]. For instance, tissue studies have established HULC, MALAT1, and HOTAIR as significant prognostic markers in HCC, with expression levels correlating with tumor stage, metastasis, and survival [11]. However, tissue biopsies present practical limitations including invasiveness, sampling bias due to tumor heterogeneity, and inability for frequent longitudinal monitoring [7].
Circulating lncRNAs: Promising Non-Invasive Biomarkers
Circulating lncRNAs detected in plasma, serum, or other body fluids offer a non-invasive alternative for HCC diagnosis and monitoring [12] [7]. These circulating molecules demonstrate remarkable stability due to their encapsulation in exosomes or formation of secondary structures that confer resistance to RNase degradation [12]. Recent clinical studies have validated the diagnostic potential of circulating lncRNAs such as HULC, RP11-731F5.2, and UCA1 in HCC [12] [7]. A 2025 study identified plasma HULC and RP11-731F5.2 as promising biomarkers for predicting HCC risk in patients with advanced chronic hepatitis C, highlighting their clinical utility in high-risk populations [7]. Circulating lncRNA signatures have demonstrated superior diagnostic performance compared to conventional biomarkers like alpha-fetoprotein (AFP), particularly for early-stage HCC detection [12].
Experimental Approaches for lncRNA Investigation
Methodological rigor is essential for valid lncRNA research. This section outlines established protocols and emerging technologies for lncRNA detection and functional characterization.
Detection and Quantification Methods
RNA Isolation and Quality Control: Effective lncRNA analysis begins with high-quality RNA extraction. For tissue samples, TRIzol-based methods with DNase treatment provide comprehensive RNA recovery [3]. For circulating lncRNAs, specialized commercial kits (e.g., Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit) optimize recovery from low-abundance samples [7]. RNA integrity should be verified using microfluidic electrophoresis systems (e.g., Bioanalyzer), with RNA Integrity Number (RIN) >7.0 recommended for downstream applications [7].
Reverse Transcription Quantitative PCR (RT-qPCR): RT-qPCR represents the gold standard for lncRNA quantification due to its sensitivity, specificity, and quantitative accuracy [12] [7]. Critical considerations include: (1) designing exon-exon junction spanning primers to minimize genomic DNA amplification; (2) implementing no-reverse transcription and no-template controls; (3) using appropriate reference genes (β-actin, GAPDH) for normalization; and (4) validating primer specificity through melting curve analysis and gel electrophoresis [7]. The 2−ΔΔCt method enables relative quantification of lncRNA expression between sample groups [7].
Next-Generation Sequencing (NGS): RNA sequencing provides comprehensive, unbiased lncRNA profiling, enabling discovery of novel transcripts and isoform characterization [7]. Ribosomal RNA depletion rather than poly-A selection is recommended for capturing non-polyadenylated lncRNAs. Bioinformatics pipelines such as HISAT2, StringTie, and Ballgown facilitate transcript assembly and quantification [7]. Single-cell RNA sequencing further resolves lncRNA expression heterogeneity within tumor ecosystems [13].
Functional Characterization Approaches
Loss-of-Function and Gain-of-Function Studies: RNA interference (siRNA, shRNA) and CRISPR/Cas9 systems enable targeted lncRNA knockdown or knockout to assess functional consequences [13]. For nuclear lncRNAs, antisense oligonucleotides (ASOs) with chemical modifications (e.g., 2'-O-methoxyethyl) enhance nuclear localization and targeting efficiency [14]. Conversely, plasmid or viral vector-mediated overexpression establishes gain-of-function phenotypes [3].
Mechanistic Investigations: RNA immunoprecipitation (RIP) and chromatin isolation by RNA purification (ChIRP) identify lncRNA interactions with proteins and genomic loci, respectively [4]. Cross-linking and analysis of cDNAs (CRAC) provides nucleotide-resolution mapping of RNA-protein interactions [15]. Luciferase reporter assays validate predicted lncRNA-miRNA interactions, while mass spectrometry identifies lncRNA-associated protein complexes [13].
Diagram 2: Comprehensive experimental workflow for lncRNA research in HCC, spanning from sample collection to clinical translation, with emphasis on methodological considerations for both tissue and circulating lncRNAs.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for lncRNA Investigations
| Reagent Category | Specific Examples | Application Notes | Quality Control |
|---|---|---|---|
| RNA Isolation Kits | Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) [7] | Optimized for low-abundance circulating lncRNAs; includes DNase treatment | RNA integrity number (RIN) >7.0; 260/280 ratio ~2.0 [7] |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) [7] | Includes RNase inhibitor; suitable for long transcripts | Verify efficiency with spike-in controls |
| qPCR Reagents | Power SYBR Green PCR Master Mix (Thermo Fisher) [7] | Cost-effective for well-validated targets; requires primer optimization | Melting curve analysis; gel verification of amplicons [7] |
| Sequencing Library Prep | KAPA RNA HyperPrep with RiboErase (Roche) [7] | rRNA depletion for comprehensive lncRNA capture | Library quantification via qPCR or bioanalyzer |
| Functional Studies | Silencer Select siRNAs (Thermo Fisher); CRISPR/Cas9 systems [13] | ASOs for nuclear lncRNAs; chemical modifications enhance stability | Confirm knockdown efficiency (>70%) via RT-qPCR |
| Interaction Studies | Magna RIP Kit (Millipore); ChIRP kits [4] | Cross-linking optimization critical for RNA-protein complexes | Include isotype controls for immunoprecipitation |
| PROTAC PAPD5 degrader 1 | PROTAC PAPD5 degrader 1, MF:C49H63N5O16, MW:978.0 g/mol | Chemical Reagent | Bench Chemicals |
| Swietemahalactone | Swietemahalactone, MF:C27H30O10, MW:514.5 g/mol | Chemical Reagent | Bench Chemicals |
LncRNAs represent sophisticated regulators of gene expression in HCC, functioning through integrated molecular mechanisms that span epigenetic, transcriptional, and post-transcriptional levels. Their tissue-specific expression patterns and remarkable stability in circulation position lncRNAs as promising biomarkers and therapeutic targets. The comparative analysis of tissue versus circulating lncRNAs reveals complementary strengths: tissue lncRNAs provide mechanistic insights into tumor biology, while circulating lncRNAs offer non-invasive approaches for diagnosis and monitoring. Future research directions include developing standardized detection protocols for clinical implementation, exploring combination panels of multiple lncRNAs to enhance diagnostic accuracy, and advancing lncRNA-targeted therapeutics using ASO and CRISPR-based technologies. As our understanding of lncRNA biology deepens, these molecules hold significant potential for revolutionizing HCC management through precision diagnostics and targeted interventions.
Hepatocellular carcinoma (HCC) is the most common primary liver cancer, ranking as the sixth most diagnosed cancer globally and the third leading cause of cancer-related deaths [1] [16]. The molecular pathogenesis of HCC involves complex genetic and epigenetic alterations, with long non-coding RNAs (lncRNAs) emerging as crucial regulators in recent years [1] [3]. LncRNAs are defined as RNA transcripts longer than 200 nucleotides that lack significant protein-coding potential [1] [9]. Once considered "transcriptional noise," these molecules are now recognized as vital players in gene regulation, influencing cellular processes at epigenetic, transcriptional, and post-transcriptional levels [1] [17].
In HCC tissues, numerous lncRNAs exhibit significant dysregulation, functioning either as oncogenic drivers or tumor suppressors [9] [3] [18]. This differential expression profile positions lncRNAs as promising molecular markers for HCC diagnosis, prognosis, and therapeutic targeting [19] [9]. Understanding the distinct roles of these dysregulated lncRNAs provides critical insights into HCC pathogenesis and opens new avenues for precision medicine approaches in liver cancer management [16].
Molecular Mechanisms of LncRNA Action in HCC
LncRNAs employ diverse mechanistic strategies to regulate gene expression and cellular processes in HCC. Their functional classification is largely determined by their subcellular localization, with nuclear and cytoplasmic lncRNAs executing distinct roles [9].
Nuclear lncRNAs primarily regulate gene expression by modulating chromatin architecture and transcription. They achieve this through direct DNA binding or by interacting with DNA-binding and RNA-binding proteins, either in cis (affecting neighboring genes) or in trans (affecting distant genes) [16]. A prime example is lncRNA HOTTIP, which binds to the WDR5 protein component of the MLL/SET1 histone methyltransferase complex, guiding it to specific genomic loci including the HOXA gene cluster. This interaction results in histone H3 lysine 4 trimethylation (H3K4me3) and subsequent activation of HOXA genes [16].
Cytoplasmic lncRNAs predominantly influence mRNA stability, translation, and protein functions. Many function as competing endogenous RNAs (ceRNAs) that "sponge" microRNAs, thereby weakening miRNA-mediated repression of target mRNAs [1] [9]. For instance, linc-RoR acts as a molecular sponge for tumor suppressor miR-145, leading to increased expression of miR-145 targets including p70S6K1, PDK1, and HIF-1α, ultimately accelerating HCC cell proliferation [9].
The table below summarizes the primary molecular functions of lncRNAs in hepatocellular carcinoma:
Table 1: Molecular Functions of LncRNAs in HCC
| Function Type | Mechanism of Action | Example LncRNAs | Molecular Consequences |
|---|---|---|---|
| Signal Molecule | Transcriptional regulation in response to stimuli | HULC, NEAT1 | Altered expression of target genes |
| Guide Molecule | Direct chromatin modifiers to specific genomic loci | HOTTIP | Histone modifications (e.g., H3K4me3) |
| Decoy Molecule | Sequester miRNAs or transcription factors | linc-RoR, H19 | Derepression of miRNA targets |
| Scaffold Molecule | Form ribonucleoprotein complexes | MALAT1, HOTAIR | Assembly of functional complexes |
Figure 1: LncRNA Functional Mechanisms in HCC Pathogenesis. LncRNAs exert their effects through distinct nuclear and cytoplasmic mechanisms that collectively contribute to hepatocellular carcinoma development and progression.
Oncogenic LncRNAs in HCC Tissues
Multiple lncRNAs demonstrate significant upregulation in HCC tissues, where they function as oncogenic drivers by promoting tumor cell proliferation, survival, invasion, and metastasis [1] [9] [3]. These oncogenic lncRNAs represent promising diagnostic markers and therapeutic targets due to their tumor-specific expression patterns.
HULC (HCC Up-Regulated Long Non-Coding RNA) was the first lncRNA identified as abnormally highly expressed in human HCC specimens [1]. Located at chromosome 6p24.3 with a length of 500 nucleotides, HULC promotes HCC progression through multiple mechanisms. It upregulates sphingosine kinase 1 (SPHK1) to enhance tumor angiogenesis and activates autophagy by decreasing P62 expression while increasing LC3 transcription through Sirt1 activation [1]. HULC also functions as a competing endogenous RNA, binding to miRNA-372 and reducing its inhibitory effect on the target gene PRKACB, thereby promoting HCC progression [1].
MALAT1 (Metastasis-Associated Lung Adenocarcinoma Transcript 1) is significantly upregulated in HBV-infected patients and HCC tissues, where it promotes aggressive tumor phenotypes and facilitates disease progression [9] [20]. This lncRNA contributes to HCC metastasis by modulating alternative splicing of various metastasis-associated genes and interacting with key signaling pathways involved in cell migration and invasion.
H19 was one of the first identified lncRNAs and demonstrates increased expression in HCC tissues [9] [3]. It functions as an oncogene by affecting proliferation, apoptosis, invasion, and metastasis of HCC cells through epigenetic modifications and regulation of downstream pathways [9]. Mechanistically, H19 downregulates miRNA-15b expression, which stimulates the CDC42/PAK1 axis and increases the proliferation rate of HCC cells [9].
HOTAIR (HOX Transcript Antisense RNA) is associated with poor overall survival and disease-free survival in HCC patients [20]. This lncRNA promotes tumor progression by recruiting polycomb repressive complex 2 (PRC2) to specific genomic loci, leading to histone H3 lysine 27 trimethylation (H3K27me3) and epigenetic silencing of tumor suppressor genes.
LINC00152 promotes cell proliferation through regulation of CCDN1 and shows significantly higher expression in plasma of HCC patients compared to healthy controls [20]. Its expression level positively correlates with disease progression, making it a potential biomarker for HCC detection and monitoring.
Table 2: Key Oncogenic LncRNAs in HCC Tissues
| LncRNA | Genomic Location | Expression in HCC | Molecular Mechanisms | Functional Consequences |
|---|---|---|---|---|
| HULC | 6p24.3 | Upregulated | SPHK1 upregulation, autophagy activation, miRNA-372 sponging | Enhanced angiogenesis, proliferation, survival |
| MALAT1 | 11q13.1 | Upregulated | Alternative splicing regulation, metastasis pathway activation | Increased invasion, metastasis |
| H19 | 11p15.5 | Upregulated | miRNA-15b downregulation, CDC42/PAK1 axis activation | Enhanced proliferation, inhibited apoptosis |
| HOTAIR | 12q13.13 | Upregulated | PRC2 recruitment, epigenetic silencing | EMT, metastasis, stemness |
| LINC00152 | 2p11.2 | Upregulated | CCDN1 regulation | Cell cycle progression, proliferation |
Tumor-Suppressive LncRNAs in HCC Tissues
In contrast to oncogenic lncRNAs, several tumor-suppressive lncRNAs demonstrate decreased expression in HCC tissues, where their normal function is to restrain cellular proliferation and prevent malignant transformation [1] [9]. The loss of these protective lncRNAs contributes significantly to hepatocarcinogenesis.
MEG3 (Maternally Expressed Gene 3) is a tumor-suppressive lncRNA that is significantly downregulated in HCC tissues [1]. It functions as a growth suppressor by promoting apoptosis and inhibiting cell proliferation through activation of p53-mediated pathways. MEG3 expression is frequently lost in various human cancers, including HCC, and its downregulation is particularly prominent in HBV-associated hepatocellular carcinoma [1].
GAS5 (Growth Arrest-Specific 5) acts as a tumor suppressor by triggering CHOP and caspase-9 signal pathways, leading to inhibition of cancer cell proliferation and activation of apoptosis [20]. This lncRNA functions as a molecular decoy for the glucocorticoid receptor, preventing its binding to DNA and thereby modulating transcriptional responses to stress signals. The reduced expression of GAS5 in HCC tissues contributes to uncontrolled cell growth and enhanced survival of malignant hepatocytes.
LncRNA-p21 is another tumor-suppressive lncRNA that is downregulated in HCC tissues [1]. Its reduced expression is associated with increased cell proliferation and tumor growth. LncRNA-p21 interacts with various proteins and signaling pathways to inhibit HCC progression, including direct interaction with p53 to enhance its activity, thereby promoting cell cycle arrest and preventing uncontrolled cell growth [1]. Additionally, lncRNA-p21 is a hypoxia-responsive lncRNA that forms a positive feedback loop with HIF-1α to drive glycolysis and promote tumor growth under low oxygen conditions [9].
Dreh exhibits downregulated expression in HBV-infected patients and HCC tissues [1] [17]. This lncRNA acts as a tumor suppressor by inhibiting the expression of vimentin, a key mesenchymal marker involved in epithelial-to-mesenchymal transition (EMT). The downregulation of Dreh leads to re-expression of vimentin and promotes HCC metastasis, highlighting its importance in maintaining the epithelial phenotype of hepatocytes [3].
Table 3: Key Tumor-Suppressive LncRNAs in HCC Tissues
| LncRNA | Genomic Location | Expression in HCC | Molecular Mechanisms | Functional Consequences |
|---|---|---|---|---|
| MEG3 | 14q32.2 | Downregulated | p53 pathway activation | Growth inhibition, apoptosis promotion |
| GAS5 | 1q25.1 | Downregulated | Glucocorticoid receptor decoy, CHOP/caspase-9 activation | Cell cycle arrest, apoptosis |
| lncRNA-p21 | 6p21.2 | Downregulated | p53 interaction, HIF-1α feedback regulation | Cell cycle arrest, glycolysis inhibition |
| Dreh | Not specified | Downregulated | Vimentin suppression | EMT inhibition, metastasis suppression |
Experimental Analysis of Dysregulated LncRNAs in HCC
Research Reagent Solutions for LncRNA Investigation
The study of lncRNAs in HCC relies on specific research reagents and methodological approaches designed to isolate, quantify, and functionally characterize these non-coding RNA molecules.
Table 4: Essential Research Reagents for LncRNA Studies in HCC
| Reagent/Kit | Manufacturer | Specific Application | Key Features |
|---|---|---|---|
| miRNeasy Mini Kit | QIAGEN | Total RNA isolation from tissues and plasma | Preserves lncRNA integrity, removes contaminants |
| RevertAid First Strand cDNA Synthesis Kit | Thermo Scientific | cDNA synthesis from RNA templates | High-efficiency reverse transcription |
| PowerTrack SYBR Green Master Mix | Applied Biosystems | qRT-PCR quantification | Sensitive detection, low background noise |
| Custom LncRNA Primers | Thermo Fisher Scientific | Target-specific amplification | Sequence-specific detection, optimized annealing |
Standard Experimental Workflow
The quantitative analysis of dysregulated lncRNAs in HCC tissues follows a standardized workflow to ensure reproducible and reliable results. Recent studies have demonstrated the utility of combining lncRNA expression profiling with machine learning approaches to improve diagnostic accuracy [20].
Figure 2: Experimental Workflow for LncRNA Analysis in HCC. Standardized protocol for quantifying dysregulated lncRNAs in hepatocellular carcinoma tissues and plasma samples, incorporating machine learning validation for enhanced diagnostic accuracy.
Key Methodological Considerations
When investigating lncRNA expression in HCC tissues, several methodological factors require careful consideration. Sample collection and preservation are critical, as lncRNAs can demonstrate differential stability compared to mRNA transcripts [20]. The selection of appropriate reference genes for normalization is equally important, with GAPDH serving as a commonly used housekeeping gene in qRT-PCR assays [20].
For functional characterization, loss-of-function and gain-of-function experiments are essential to establish causal relationships between lncRNA expression and phenotypic effects. RNA interference approaches using siRNAs or antisense oligonucleotides can effectively knockdown lncRNA expression, while overexpression constructs can restore tumor-suppressive lncRNAs or model oncogenic lncRNA functions [14].
Advanced computational approaches, including machine learning algorithms, have demonstrated remarkable utility in analyzing complex lncRNA expression patterns. One recent study achieved 100% sensitivity and 97% specificity in HCC diagnosis by integrating multiple lncRNA biomarkers (LINC00152, LINC00853, UCA1, and GAS5) with conventional clinical parameters using machine learning models [20]. This represents a significant improvement over individual lncRNA biomarkers, which typically show sensitivity and specificity ranging from 60-83% and 53-67%, respectively [20].
Comparative Analysis: Tissue vs. Circulating LncRNAs in HCC Diagnosis
The diagnostic application of lncRNAs in hepatocellular carcinoma encompasses both tissue-based and liquid biopsy approaches, each with distinct advantages and limitations in clinical practice.
Tissue-based lncRNA analysis provides direct information about molecular changes within the tumor microenvironment, allowing correlation with histopathological features and enabling spatial assessment of expression patterns [19] [9]. However, this approach requires invasive biopsy procedures that carry inherent risks and may not fully capture tumor heterogeneity, particularly in multifocal HCC [20].
In contrast, circulating lncRNAs detected in plasma or serum offer a non-invasive liquid biopsy alternative that enables repeated sampling for disease monitoring and treatment response assessment [20]. These blood-based biomarkers can potentially detect lncRNAs released from all tumor sites, providing a more comprehensive representation of tumor burden. The stability of lncRNAs in circulation further enhances their clinical utility as practical diagnostic tools [20].
Notably, some lncRNAs demonstrate concordant expression patterns between tissue and plasma compartments. For example, HULC shows upregulated expression in both HCC tissues and patient plasma, with abundance positively correlating with Edmondson grade and hepatitis B virus infection [1]. Similarly, LINC00152 is significantly highly expressed in plasma of HCC patients and promotes cell proliferation through regulation of CCDN1 [20].
The diagnostic performance of lncRNA biomarkers can be significantly enhanced through combinatorial approaches. Integrating multiple lncRNAs with conventional biomarkers like alpha-fetoprotein (AFP) improves diagnostic sensitivity and specificity compared to individual markers [20]. Furthermore, incorporating lncRNA profiles into machine learning algorithms has demonstrated exceptional diagnostic capability, achieving near-perfect classification accuracy in recent studies [20].
Table 5: Tissue vs. Circulating LncRNAs for HCC Diagnosis
| Parameter | Tissue LncRNAs | Circulating LncRNAs |
|---|---|---|
| Sample Type | Tumor biopsy | Plasma/Serum |
| Invasiveness | Invasive procedure | Minimal/non-invasive |
| Tumor Representation | Focal sampling | Potentially comprehensive |
| Longitudinal Monitoring | Limited | Excellent |
| Spatial Information | Preserved | Lost |
| Diagnostic Sensitivity | High | Moderate to High |
| Technical Challenges | RNA preservation from tissue | RNA isolation from biofluids |
Dysregulated lncRNAs in HCC tissues represent crucial molecular players in hepatocellular carcinoma pathogenesis, functioning as both oncogenic drivers and tumor suppressors. The distinct expression patterns of these lncRNAs, coupled with their diverse mechanisms of action, provide valuable insights into HCC biology and offer promising avenues for clinical application.
From a diagnostic perspective, lncRNA profiles demonstrate significant potential as tissue-based and circulating biomarkers for HCC detection, particularly when integrated with machine learning approaches and conventional clinical parameters. Therapeutically, the tumor-specific expression of oncogenic lncRNAs positions them as attractive targets for intervention using antisense oligonucleotides, RNA interference strategies, or CRISPR-based technologies [14].
Future research directions should focus on validating lncRNA biomarkers in large, multi-center cohorts and developing standardized detection protocols for clinical implementation. Additionally, further investigation into the functional roles of less-characterized lncRNAs may uncover novel regulatory networks and therapeutic opportunities in hepatocellular carcinoma. As our understanding of lncRNA biology continues to evolve, these molecules are poised to make substantial contributions to precision medicine approaches in HCC diagnosis and treatment.
Hepatocellular carcinoma (HCC) represents a major global health challenge, ranking as the sixth most common malignancy and the fourth leading cause of cancer-related deaths worldwide [21]. Chronic infections with hepatitis B virus (HBV) and hepatitis C virus (HCV) constitute the primary risk factors for HCC development, accounting for over 80% of cases globally [22] [23]. The molecular pathogenesis of HCC involves complex interactions between viral factors and host cellular machinery, with long non-coding RNAs (lncRNAs) emerging as critical regulators in this process.
LncRNAs are defined as RNA transcripts longer than 200 nucleotides that lack protein-coding capacity [24]. These molecules exert diverse regulatory functions through multiple mechanisms, including chromatin modification, transcriptional and post-transcriptional regulation, and serving as molecular scaffolds [22] [21]. High-throughput sequencing technologies have revealed that HBV and HCV infections significantly alter host lncRNA expression profiles, creating a procarcinogenic environment that promotes hepatocarcinogenesis [22].
This review provides a comprehensive comparative analysis of how HBV and HCV differentially regulate host lncRNAs to drive HCC development. We examine tissue-specific and circulating lncRNA signatures, detail experimental methodologies for lncRNA investigation, and explore the diagnostic potential of these molecules for early HCC detection.
Viral Regulation of Host lncRNAs: HBV versus HCV Mechanisms
HBV-Induced Alterations in Host lncRNA Expression
Chronic HBV infection manipulates host lncRNA expression through both viral integration events and the activity of viral proteins, particularly the HBV X protein (HBx). The HBx protein transactivates numerous host genes and lncRNAs by interacting with cellular transcription factors and chromatin-modifying complexes [22] [23]. HBV integration into the host genome can disrupt regulatory regions or create novel chimeric transcripts that alter lncRNA expression [22].
Several key lncRNAs have been identified as differentially expressed in HBV-related HCC:
HEIH (High Expression in HCC): One of the first lncRNAs demonstrated to be upregulated in HBV-related HCC patients. HEIH interacts with Enhancer of Zeste Homolog 2 (EZH2), a component of the Polycomb Repressive Complex 2 (PRC2), to promote transcriptional repression of target genes and facilitate cell cycle progression [22].
HOTAIR (HOX Transcript Antisense RNA): This lncRNA is hijacked by HBV to promote viral replication and is associated with poor prognosis. HBx activates PLK1, which phosphorylates SUZ12 (a PRC2 subunit), leading to impaired transcriptional repression by the DDX5/PRC2/HOTAIR complex and reactivation of target genes [22].
HULC (Highly Upregulated in Liver Cancer): Discovered in 2007, HULC is significantly overexpressed in HCC tissues and its expression can be upregulated by the transcription factor CREB and HBx [24]. HULC promotes HCC growth and metastasis and can be detected in peripheral blood cells [21].
ANRIL (Antisense Non-Coding RNA in the INK4 Locus): This lncRNA consists of 19 exons and spans 126.3 kb in the genome. It binds to CBX7 in PRC1 and SUZ12 in PRC2, facilitating transcriptional repression through epigenetic chromatin modifications [25].
HCV-Induced Alterations in Host lncRNA Expression
In contrast to HBV, HCV is an RNA virus that cannot integrate into the host genome. Instead, it modulates lncRNA expression primarily through viral protein interactions and induction of chronic inflammation and oxidative stress [26] [24]. HCV-encoded proteins (E1, E2, P7, NS2, and NS3) activate oncogenic molecular pathways that subsequently alter lncRNA expression profiles [26].
Key lncRNAs dysregulated in HCV-related HCC include:
LINC01419: Transcripts are expressed at higher levels in early-stage HCC compared to dysplasia in HCV-related hepatocarcinogenesis [24].
AK021443 and AF070632: These lncRNAs show stage-specific expression patterns, with AK021443 levels increasing in advanced-stage HCC and AF070632 levels decreasing compared to early-stage HCC [24].
LOC341056, CCT6P1, PTTG3P, LOC643387, LOC100133920: These lncRNAs were identified as key regulators in HCV-positive HCC, primarily involved in metabolism, regulation of nucleobase, and cell proliferation processes [26].
C3P1 and C22orf45: These lncRNAs play crucial roles as tumor suppressors in HCV-related HCC, with lower expression associated with shorter survival time [26].
Table 1: Key Differentially Expressed lncRNAs in HBV vs. HCV-Related HCC
| lncRNA | Expression in HBV-HCC | Expression in HCV-HCC | Primary Functions | Mechanisms |
|---|---|---|---|---|
| HEIH | Upregulated | Not well characterized | Promotes cell cycle progression | Binds EZH2/PRC2 complex |
| HOTAIR | Upregulated | Not well characterized | Modulates chromatin state | Interacts with PRC2 complex |
| HULC | Upregulated | Not well characterized | Promotes growth, metastasis | Sponges miRNAs; regulates autophagy |
| ANRIL | Upregulated | Not well characterized | Epigenetic silencing | Binds CBX7/PRC1 and SUZ12/PRC2 |
| LINC01419 | Not well characterized | Upregulated in early HCC | Unknown | Regulates cell cycle genes |
| PTTG3P | Not well characterized | Upregulated | Promotes proliferation | Co-expressed with >100 DEGs |
| C3P1 | Not well characterized | Downregulated | Tumor suppression | Associated with longer survival |
Common Oncogenic Pathways Regulated by lncRNAs in Viral Hepatitis
Despite their different mechanisms of action, both HBV and HCV dysregulate lncRNAs that converge on common oncogenic pathways:
p53 Signaling Pathway: Multiple lncRNAs affected by both viruses modulate the p53 tumor suppressor network, affecting cell cycle arrest and apoptosis [27].
PI3K-Akt Signaling Cascade: This critical survival pathway is frequently altered by virus-dysregulated lncRNAs in HCC [27].
Wnt/β-catenin Signaling: lncRNAs such as Linc00210 drive self-renewal and propagation of liver tumor-initiating cells through activating Wnt/β-catenin signaling in both HBV and HCV-related HCC [21].
Epigenetic Regulation: Both viruses exploit lncRNAs that interact with chromatin-modifying complexes like PRC2, leading to permanent transcriptional changes that promote carcinogenesis [22].
Tissue vs. Circulating lncRNAs: Comparative Diagnostic Value
The discovery that lncRNAs are stably present in body fluids has opened new avenues for non-invasive diagnostics. Circulating lncRNAs demonstrate remarkable stability despite physical (room temperature incubation, freeze-thaw cycles), chemical (pH variations), and biological (RNase A) challenges [21].
Tissue lncRNAs as Diagnostic Biomarkers
Tissue-specific lncRNAs provide direct information about molecular changes at the disease site but require invasive biopsy procedures:
HULC: Shows significant overexpression in HCC tissues compared to normal liver tissues, with expression correlating with HBV infection status and Edmondson histological grades [24].
HEIH: Demonstrated overexpression in HBV-related HCC tissues and serves as an independent risk factor for recurrence-free survival [24].
BAIAP2-AS1: Identified as an HBV-related HCC specific lncRNA (HH-lncRNA) through comprehensive microarray analysis of tissue samples [28].
Circulating lncRNAs as Non-Invasive Biomarkers
Circulating lncRNAs can be detected in plasma, serum, or peripheral blood mononuclear cells (PBMCs), offering minimally invasive diagnostic options:
RP11-160H22.5, XLOC014172, LOC149086: This panel of three plasma lncRNAs showed exceptional diagnostic performance for HCC detection, with a merged area under the curve (AUC) of 0.999 in the training set and 0.896 in the validation set. XLOC014172 and LOC149086 were particularly associated with metastatic HCC [29].
ADAMTSL4-AS1, AC067931, SOCS2-AS1: When combined with AFP in PBMCs, these lncRNAs demonstrated outstanding diagnostic capability for HBV-associated HCC with an AUC of 0.905 (sensitivity 91.1%, specificity 75.3%). Particularly valuable was their ability to identify AFP-negative (AUC=0.814), small (AUC=0.909), and early-stage (AUC=0.863) tumors [30].
ANRIL, hPVT1, aHIF: In plasma, these lncRNAs showed significant differential expression in HCC patients compared to controls. aHIF demonstrated 86.67% sensitivity and 91.89% specificity for discriminating HCC from cirrhosis in HCV patients, while ANRIL could discriminate HCC from cirrhosis in HBV patients with AUC 0.902 [25].
Table 2: Diagnostic Performance of Circulating lncRNA Biomarkers for HCC
| lncRNA Panel | Sample Type | AUC | Sensitivity | Specificity | Remarks |
|---|---|---|---|---|---|
| RP11-160H22.5, XLOC_014172, LOC149086 | Plasma | 0.896-0.999 | High | High | Excellent for metastasis prediction |
| ADAMTSL4-AS1, AC067931, SOCS2-AS1 + AFP | PBMCs | 0.905 | 91.1% | 75.3% | Effective for early-stage, small, AFP-negative HCC |
| ANRIL | Plasma | 0.902 | Not specified | Not specified | Discriminates HBV-HCC from cirrhosis |
| aHIF | Plasma | Not specified | 86.67% | 91.89% | Discriminates HCV-HCC from cirrhosis |
| hPVT1 | Plasma | Not specified | 85.0% | 84.62% | Discriminates HCV-HCC from cirrhosis |
| HULC | Plasma | ~0.80 | Variable | Variable | Inconsistent across studies |
Figure 1: HBV and HCV Regulation of Host lncRNAs in Hepatocarcinogenesis. This diagram illustrates the distinct mechanisms by which HBV and HCV dysregulate host lncRNAs, ultimately converging on common oncogenic pathways that drive liver cancer development.
Experimental Approaches and Methodologies
High-Throughput Profiling Techniques
Comprehensive lncRNA analysis employs multiple high-throughput approaches:
Microarray Analysis: The Affymetrix Human Genome U133 Plus 2.0 Array platform has been widely used, containing 31,475 probes matched with 15,435 mRNAs and 4,971 probes matched with 3,750 lncRNAs [27]. For specialized lncRNA analysis, the Human LncRNA Array v3.0 (Agilent) provides comprehensive coverage [29].
RNA Sequencing (RNA-Seq): High-throughput transcriptome sequencing enables unbiased discovery of novel lncRNAs. Studies typically sequence liver tissues from patients across the disease spectrum (chronic hepatitis, cirrhosis, HCC) to identify progressively dysregulated lncRNAs [30].
RIP-Seq (RNA Immunoprecipitation Sequencing): This technique identifies direct interactions between lncRNAs and proteins. For example, EZH2-RNA binding has been demonstrated using RIP-Seq followed by next-generation sequencing, revealing that approximately 20% of all human lncRNAs associate with PRC2 [22].
Validation Methods
Quantitative Real-Time PCR (qRT-PCR): The gold standard for validating lncRNA expression patterns. Typically uses SYBR Green master mix with low ROX dye and specific primers for target lncRNAs. GAPDH serves as the common reference gene for normalization [25] [30].
Functional Validation: Includes in vitro approaches using HCC cell lines (Huh7, Hep3B, HepG2, HepG2.215) compared to normal hepatic stellate cells (LX2), and in vivo models to assess lncRNA functions in proliferation, metastasis, and therapy resistance [30].
Bioinformatic Analysis Pipelines
Differential Expression Analysis: The limma R package is commonly used to identify differentially expressed lncRNAs with thresholds typically set at |log2FC| >1 and p-value <0.05 [27] [26].
Co-expression Network Analysis: Constructed by calculating Pearson correlation coefficients between lncRNA-mRNA pairs, with |r| >0.5 considered significant. Networks are visualized using Cytoscape software [27] [26].
Functional Annotation: Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analyses performed using DAVID or similar tools to identify biological processes and pathways enriched in co-expressed genes [27] [26].
Table 3: Essential Research Reagents and Resources for lncRNA Studies
| Category | Specific Product/Kit | Application | Key Features |
|---|---|---|---|
| RNA Extraction | miRNeasy Mini Kit (Qiagen) | Total RNA extraction from plasma/tissues | Combines phenol/guanidine-based lysis with silica-membrane purification |
| cDNA Synthesis | High Capacity cDNA Reverse Transcription Kits (Thermo Fisher) | Reverse transcription of RNA to cDNA | Includes random primers and RNase inhibitor |
| qRT-PCR | SYBR Green master mix with low ROX dye (Thermo Fisher) | lncRNA quantification | Compatible with most real-time PCR instruments |
| Microarray | Human LncRNA Array v3.0 (Agilent) | Genome-wide lncRNA profiling | Comprehensive coverage of annotated lncRNAs |
| Cell Lines | Huh7, Hep3B, HepG2, HepG2.215, LX2 | Functional validation | Represent different HCC etiologies and normal hepatic cells |
| Analysis Software | limma R package, Cytoscape, DAVID | Bioinformatic analysis | Differential expression, network visualization, functional annotation |
The comparative analysis of HBV and HCV regulation of host lncRNAs reveals both virus-specific mechanisms and common oncogenic pathways in hepatocarcinogenesis. While HBV predominantly alters lncRNA expression through viral integration and HBx-mediated transactivation, HCV achieves similar effects through chronic inflammation and viral protein interactions. The distinct lncRNA signatures associated with each viral etiology highlight the potential for etiology-specific diagnostic and therapeutic approaches.
Circulating lncRNAs offer particular promise as non-invasive biomarkers for early HCC detection, especially when combined with traditional markers like AFP. Panels such as ADAMTSL4-AS1, AC067931, and SOCS2-AS1 in PBMCs demonstrate exceptional diagnostic performance for detecting early-stage, small, and AFP-negative tumors that would otherwise be missed by current surveillance methods.
Future research directions should include larger multi-center validation studies of promising lncRNA biomarkers, functional characterization of poorly understood lncRNAs in viral hepatocarcinogenesis, and development of lncRNA-targeted therapeutics. The integration of lncRNA biomarkers into clinical practice could significantly improve early detection rates and survival outcomes for the millions of patients at risk of virus-associated HCC worldwide.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, accounting for approximately 90% of primary liver cancers and causing over 800,000 deaths annually [31] [32]. The prognosis for HCC remains poor, largely due to late diagnosis; approximately 80% of patients are diagnosed at intermediate or advanced stages, missing the optimal window for curative treatments like surgical resection or liver transplantation [33] [34]. Current surveillance methods, including ultrasound imaging and serum alpha-fetoprotein (AFP) measurement, face limitations in sensitivity, particularly for early-stage detection [34] [35] [7]. Tissue biopsy, while the historical gold standard, is invasive, carries risks of hemorrhage, and suffers from sampling variability due to tumor heterogeneity [33] [7].
In this context, liquid biopsy has emerged as a transformative, minimally invasive approach for cancer detection and monitoring. By analyzing tumor-derived components in bodily fluids, particularly blood, liquid biopsy enables repeated sampling to dynamically track disease progression and treatment response [35]. Among the various biomarkers available, long non-coding RNAs (lncRNAs) have recently gained prominence. These RNA molecules, longer than 200 nucleotides and lacking protein-coding capacity, play crucial regulatory roles in carcinogenesis and are remarkably stable in circulation, often protected within extracellular vesicles (EVs) [34] [31] [7]. This review provides a comprehensive comparative analysis of tissue versus circulating lncRNAs, examining their journey from tumor tissue to the bloodstream and their emerging role as robust biomarkers for HCC management.
Tissue vs. Circulating lncRNAs: A Comparative Analysis
The transition of lncRNAs from tissue compartments into circulation represents a critical process for liquid biopsy applications. While tissue lncRNAs provide a direct snapshot of the tumor molecular landscape, circulating lncRNAs offer a systemic, albeit more diluted, view of tumor activity. The table below summarizes the core characteristics of lncRNAs in these two distinct compartments.
Table 1: Comparative Analysis of Tissue-Derived and Circulation-Derived lncRNAs in HCC
| Characteristic | Tissue-Derived lncRNAs | Circulation-Derived lncRNAs |
|---|---|---|
| Sample Type | Tumor tissue from biopsy or resection [31] | Blood (plasma/serum), urine, other biofluids [7] |
| Invasiveness | Invasive procedure with associated risks [7] | Minimally invasive (blood draw) [35] |
| Stability | Relatively stable in preserved tissue | Highly stable in circulation, especially when encapsulated in extracellular vesicles [34] |
| Molecular Origin | Directly from tumor and microenvironment cells | Released via active secretion or passive leakage from tumor tissue [7] |
| Spatial Information | Retains spatial context within the tumor | Represents a pooled signal from all tumor sites (primary and metastatic) |
| Temporal Dynamics | Single time point snapshot | Enables longitudinal monitoring of disease progression and treatment response [35] |
| Primary Applications | Diagnostic confirmation, molecular subtyping, therapeutic target identification [31] | Early detection, prognostic stratification, recurrence monitoring, treatment response prediction [34] [32] |
| Technical Challenges | Tumor heterogeneity, sampling bias | Low abundance, requirement for highly sensitive detection methods [35] |
The Journey from Tissue to Circulation
The process by which lncRNAs transition from cellular components in tumor tissue to stable biomarkers in circulation involves several mechanisms. Tumor cells, including those in HCC, actively release lncRNAs into the extracellular space through extracellular vesicles (EVs), including exosomes, or in complex with RNA-binding proteins like Argonautes, which protect them from degradation by ribonucleases in the plasma [34] [7]. Studies have demonstrated that EV-derived lncRNAs are not merely random byproducts of cellular turnover but are often selectively packaged and reflect the molecular signature of their parent tumor cells [34]. For instance, the lncRNA HULC has been identified as a potential plasma biomarker for HCC risk in patients with chronic hepatitis C, demonstrating the clinical relevance of this journey from tissue to circulation [7].
Experimental Protocols for lncRNA Analysis
Robust biomarker development relies on standardized and reproducible experimental workflows. The following section details common methodologies used for analyzing lncRNAs in both tissue and liquid biopsy samples.
Liquid Biopsy Workflow for lncRNA Analysis
The general workflow for processing liquid biopsy samples to analyze circulating lncRNAs involves several critical steps, from sample collection to data analysis, as visualized below.
Diagram 1: Liquid Biopsy lncRNA Analysis Workflow. Key steps (yellow) include plasma separation, EV isolation, RNA extraction, and lncRNA quantification.
Detailed Methodologies
Blood Sample Collection and Processing: Fasting venous blood is collected in tubes containing separation gel and coagulant for serum, or EDTA for plasma [34]. Samples are typically centrifuged (e.g., at 704× g for 10 minutes) to separate cellular components from plasma or serum, which is then aliquoted and stored at -80°C [34] [7].
Extracellular Vesicle Isolation: EVs are isolated from serum/plasma using techniques like size-exclusion chromatography combined with ultrafiltration [34]. After sample thawing and filtration (0.8 μm filter), the sample is passed through a gel-permeation column. The eluent from specific tubes (e.g., 7-9) is collected and concentrated using a 100kD ultrafiltration tube [34]. Isolated EVs are characterized using nanoparticle tracking analysis (NTA) for size distribution, transmission electron microscopy for morphology, and Western blot for marker proteins (e.g., TSG101, Alix, CD9) and negative controls (e.g., Calnexin) [34].
RNA Extraction and Quality Control: Total RNA is isolated from EVs using commercial purification kits (e.g., Norgen Biotek Corp. or Simgen kits) [34] [7]. The process typically involves adding lysis buffer and ethanol to the EV suspension, followed by centrifugation. The lysate is then loaded onto a purification column, washed with buffer solutions, and RNA is eluted in a small volume of nuclease-free water. To remove genomic DNA contamination, RNA samples are often treated with DNase [7].
lncRNA Quantification:
- Reverse Transcription Quantitative PCR (RT-qPCR): This is a widely used method for quantifying specific lncRNAs. RNA is reverse transcribed to cDNA using a High-Capacity cDNA Reverse Transcription Kit [7]. RT-qPCR is performed using SYBR Green or TaqMan chemistry on platforms like the StepOne Plus System. Conditions often involve initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 62°C for 1 minute [7]. The 2−ΔΔCt method is used to calculate relative expression levels, with reference genes like β-actin used for normalization [7].
- High-Throughput Sequencing: For discovery-based profiling, techniques like RNA sequencing (RNA-seq) are employed. This allows for the unbiased detection of known and novel lncRNAs across the transcriptome [34] [32]. Sequencing libraries are prepared from RNA and sequenced on platforms like Illumina. Bioinformatics pipelines are then used to align sequences and quantify expression.
Quantitative Data: Diagnostic and Prognostic Performance of lncRNAs
The clinical value of lncRNAs is demonstrated through their performance in distinguishing disease states and predicting patient outcomes. The following tables consolidate key quantitative findings from recent studies.
Table 2: Diagnostic Performance of Circulating lncRNAs for HCC Detection
| lncRNA | Sample Type | AUC | Sensitivity | Specificity | Study Findings |
|---|---|---|---|---|---|
| HULC | Plasma | ~0.85* | ~80%* | ~75%* | Potential biomarker for HCC risk in CHC patients [7] |
| RP11-731F5.2 | Plasma | ~0.84* | ~78%* | ~77%* | Biomarker for HCC risk and liver damage in HCV [7] |
| HEIH | Tissue & Circulation | N/R | N/R | N/R | Upregulated in HCC and cirrhotic tissues; promotes progression [36] |
| MIAT | Tissue | N/R | N/R | N/R | Stepwise increase from cirrhosis to HCC; correlates with tumor size [36] |
| HOTAIR | Tissue | N/R | N/R | N/R | Overexpression exclusive to HCC; correlates with tumor size and HCV [36] |
| 10-core EV-lncRNA panel | Serum EVs | N/R | N/R | N/R | Identified as core lncRNAs associated with HCC progression [34] |
Note: Values marked with () are approximations based on ROC curve data in the original publication [7]. AUC = Area Under the Curve; N/R = Not Reported in the provided excerpts.*
Table 3: Prognostic Value of Tissue and Circulating lncRNAs in HCC
| lncRNA | Source | Prognostic Value | Hazard Ratio (HR) & P-value |
|---|---|---|---|
| LINC00152 | Tissue | High expression → Shorter OS [31] | HR: 2.524; CI: 1.661–4.015; P=0.001 |
| FOXP4-AS1 | Tissue | High expression → Shorter OS & RFS [31] | OS HR: 2.712/6.505; P=0.024/0.033 |
| GAS5-AS1 | Tissue | High expression → Longer OS [31] | HR: 0.370; CI: 0.153–0.898; P=0.028 |
| LASP1-AS | Tissue | Low expression → Shorter OS & RFS [31] | OS HR: 1.884/3.539; P<0.0001 |
| 3-DRL Signature | Tissue | High-risk → Poorer OS [37] | 1-yr AUC: 0.756; 3-yr AUC: 0.695 |
| 6-gene Exosomal Signature | Plasma EVs | High-risk → Poor OS & treatment response [32] | Predictive of immunotherapy and drug sensitivity |
| ELMO1-AS1 | Tissue | High expression → Longer OS & RFS [31] | OS HR: 0.518/0.430; P=0.039/0.011 |
OS = Overall Survival; RFS = Recurrence-Free Survival; CI = Confidence Interval; DRL = Disulfidptosis-Related LncRNA.
Functional Roles and Regulatory Networks of HCC-Related lncRNAs
LncRNAs exert their oncogenic or tumor-suppressive functions through diverse molecular mechanisms. A common paradigm is the competing endogenous RNA (ceRNA) network, where lncRNAs "sponge" miRNAs, thereby derepressing the expression of target mRNAs [32]. The diagram below illustrates a consolidated regulatory network based on identified HCC-related lncRNAs.
Diagram 2: lncRNA Regulatory Networks in HCC. Oncogenic lncRNAs (red) sponge miRNAs, leading to oncogene derepression. Tumor suppressor lncRNAs (blue) inhibit oncogenic pathways.
Functional enrichment analyses of genes co-expressed with or regulated by dysregulated lncRNAs reveal their involvement in critical cancer pathways. Studies have shown significant enrichment in cell cycle regulation, TGF-β signaling, p53 pathway, ferroptosis, and MAPK signaling [34] [32]. For example, a plasma exosomal lncRNA-related signature was linked to hyperactivation of proliferation pathways like MYC and E2F targets, as well as metabolic pathways such as glycolysis and mTORC1 signaling [32]. Furthermore, the functional importance of lncRNAs like HEIH, MIAT, and HOTAIR is underscored by functional validation experiments; knockdown of these lncRNAs in Huh-7 HCC cell lines significantly reduced colony formation and cellular viability, confirming their role in promoting tumor cell survival and proliferation [36].
Table 4: Key Research Reagent Solutions for lncRNA Studies in HCC
| Reagent / Resource | Function / Application | Example Kits / Platforms (from cited studies) |
|---|---|---|
| RNA Extraction Kit | Isolation of total RNA (including lncRNAs) from plasma, serum, or EVs. | Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) [7]; RNA Purification Kit (Simgen) [34] |
| cDNA Synthesis Kit | Reverse transcription of RNA to stable cDNA for downstream PCR analysis. | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) [7] |
| qPCR Master Mix | Quantitative amplification and detection of specific lncRNA targets. | Power SYBR Green PCR Master Mix (Thermo Fisher) [7] |
| EV Isolation Kit | Enrichment of extracellular vesicles from biofluids for cargo analysis. | Size-exclusion chromatography columns (e.g., ES911, Echo Biotech) [34] |
| EV Characterization Tools | Validation of isolated EVs by size, morphology, and protein markers. | Nanoparticle Tracking Analysis (NTA); Transmission Electron Microscopy; Western Blot (anti-TSG101, CD9, Alix) [34] |
| Bioinformatics Databases | Prediction of miRNA interactions and functional annotation. | miRcode, miRTarBase, TargetScan, miRDB, KEGG, GO [34] [32] |
| Cell Line Models | Functional validation of lncRNA roles in vitro. | Huh-7 hepatocellular carcinoma cells [36] |
The journey of lncRNAs from tissue to circulation underscores their remarkable stability and immense potential as clinical tools in HCC management. The comparative analysis reveals that while tissue lncRNAs provide a foundational understanding of tumor biology, circulating lncRNAs offer a practical, dynamic, and minimally invasive window into the disease. The integration of advanced experimental protocols, including EV isolation and high-sensitivity molecular profiling, has enabled the robust detection and validation of these biomarkers. Quantitative data consistently demonstrates that specific lncRNA signatures, particularly those derived from plasma exosomes, hold significant value for early detection, accurate prognosis, and predicting response to therapies like immunotherapy and targeted agents [34] [37] [32]. As research progresses, the translation of these lncRNA-based liquid biopsy biomarkers into clinical practice promises to revolutionize the paradigm of HCC care, moving it toward earlier intervention and more personalized treatment strategies.
From Bench to Bedside: Detection Methodologies and Diagnostic Applications
Long non-coding RNAs (lncRNAs), defined as RNA transcripts exceeding 200 nucleotides with limited protein-coding potential, have emerged as crucial regulators of gene expression in hepatocellular carcinoma (HCC) [38] [5]. The analysis of lncRNAs in tumor tissues provides distinct advantages over circulating lncRNAs for understanding the fundamental mechanisms driving hepatocarcinogenesis. While blood-based lncRNAs offer promise for non-invasive diagnostics, tissue lncRNAs directly reflect the tumor's molecular landscape, enabling researchers to establish direct links between molecular signatures and pathological features [39] [31]. Tissue analysis allows for spatial resolution of lncRNA expression within the tumor microenvironment, a critical factor given the heterogeneous nature of HCC [40].
The stability of lncRNAs in archived formalin-fixed, paraffin-embedded (FFPE) tissue specimens further enhances their research utility, enabling retrospective studies linking expression patterns with clinical outcomes [31]. For HCC research, where molecular subtypes exhibit distinct behaviors and treatment responses, tissue-based lncRNA profiling provides indispensable insights for biomarker discovery and therapeutic target identification [40]. This comparative guide examines the qRT-PCR platforms and methodologies that enable robust tissue lncRNA analysis, with particular emphasis on their application in HCC research.
qRT-PCR Platforms for lncRNA Detection: A Comparative Analysis
Platform Selection Criteria
Selecting an appropriate qRT-PCR platform for tissue lncRNA analysis requires consideration of multiple factors, including throughput requirements, detection sensitivity, reproducibility, and cost efficiency. Each platform offers distinct advantages depending on the research context, from targeted validation of specific lncRNA candidates to discovery-oriented profiling of numerous transcripts simultaneously [41] [42]. The following comparative analysis outlines the performance characteristics of major platform types used in lncRNA research.
Table 1: Comparison of qRT-PCR Platforms for Tissue lncRNA Analysis
| Platform Type | Throughput | Sensitivity | Key Advantages | Limitations | Ideal Use Cases |
|---|---|---|---|---|---|
| SYBR Green-Based Systems | Medium to High | High (with optimized primers) | Cost-effective, flexible primer design, compatible with standard qPCR instruments | Requires stringent primer validation, potential for non-specific amplification | Targeted validation of known HCC-associated lncRNAs (e.g., HOTAIR, MALAT1) |
| TaqMan Probe-Based Systems | Medium | Very High | High specificity, reduced background signal, multiplexing capability | Higher cost per reaction, fixed assay design | Validation of low-abundance lncRNAs, clinical assay development |
| Commercial Array Platforms (e.g., LncProfiler qPCR Array) | Very High | Medium to High | Pre-optimized assays for multiple lncRNAs, standardized data analysis | Limited to pre-selected lncRNA panels, higher initial cost | Screening and profiling of known HCC-relevant lncRNA panels |
| Custom Designed Arrays | High | High | Researcher-defined content, adaptable to specific research questions | Requires extensive validation, optimization time | Focused studies on specific lncRNA subgroups or pathways |
Performance Characteristics and Experimental Data
Quantitative performance data demonstrates significant differences in detection efficacy across platforms. A systematic evaluation of cDNA synthesis methods revealed that platforms utilizing random hexamer primers preceded by polyA-tailing and adaptor-anchoring steps (characteristic of the LncProfiler qPCR Array Kit) yielded lower Ct values for 67.78% (61/90) of lncRNAs tested compared to simpler cDNA synthesis methods [41]. This enhanced sensitivity is particularly valuable for detecting low-abundance lncRNAs in limited tissue samples.
For TaqMan-based systems, studies have reported reliable detection of HCC-associated lncRNAs with high reproducibility (inter-assay CV < 5%) across technical replicates [31]. The probe-based chemistry significantly reduces false-positive signals compared to intercalating dye methods, with one study demonstrating 98% specificity for discriminating between homologous lncRNA family members [42].
SYBR Green systems offer a balance between cost and performance, with optimized protocols achieving sensitivity comparable to TaqMan assays for highly expressed lncRNAs. Research indicates that well-designed SYBR Green assays can detect tissue lncRNAs with dynamic ranges spanning 6-7 log units, sufficient for most differential expression studies in HCC [20].
Optimized Workflow for Tissue lncRNA Analysis
Sample Preparation and RNA Isolation
The integrity of RNA isolated from tumor specimens fundamentally impacts lncRNA quantification results. For tissue specimens, the RNA Integrity Number (RIN) should exceed 7.0, with distinct 28S and 18S rRNA bands visible by agarose gel electrophoresis [41]. Studies comparing RNA quality metrics have established that lncRNA quantification remains relatively stable even with moderate RNA degradation, with 83% of lncRNAs showing minimal Ct value changes between high-quality and degraded samples [41]. However, 70% of examined lncRNAs still showed statistically significant differences in Ct values depending on RNA degradation levels, emphasizing the need for consistent sample quality [41].
The miRNeasy Mini Kit (QIAGEN) has been successfully employed for simultaneous extraction of lncRNAs and other RNA species from HCC tissue specimens [20]. This protocol typically involves tissue homogenization in QIAzol lysis reagent, chloroform phase separation, and RNA binding to silica membranes, followed by DNase treatment to eliminate genomic DNA contamination.
cDNA Synthesis Methodologies
cDNA synthesis represents a critical determinant of lncRNA detection efficiency. Comparative studies evaluating three commercially available kits revealed substantial performance differences:
Table 2: Performance Comparison of cDNA Synthesis Methods for lncRNA Analysis
| Method | Priming Strategy | Relative Efficiency | Key Characteristics | Recommended Applications |
|---|---|---|---|---|
| LncProfiler qPCR Array Kit | Random hexamer preceded by polyA-tailing and adaptor-anchoring | Highest (67.78% of lncRNAs showed lower Ct values) | Multi-step procedure enhances lncRNA coverage | Ideal for comprehensive lncRNA profiling studies |
| iScript cDNA Synthesis Kit | Blend of oligo(dT) and random hexamer primers | Intermediate | Balanced performance for mixed RNA populations | Suitable for simultaneous mRNA and lncRNA analysis |
| First Strand cDNA Synthesis Kit | Separate reactions with oligo(dT) or random hexamers | Variable (depends on primer selection) | Enables comparison of priming strategies | Method optimization studies |
The superior performance of the LncProfiler method stems from its multi-step approach: (1) poly-A tailing of RNA molecules, (2) annealing of anchor dT adaptor, and (3) cDNA synthesis using random primers [41]. This strategy particularly benefits the detection of non-polyadenylated lncRNAs that would be missed by oligo(dT)-based methods alone.
qRT-PCR Experimental Design and Validation
Robust experimental design for tissue lncRNA analysis requires careful consideration of several factors:
Reference Gene Selection: Housekeeping genes such as GAPDH have been successfully used for normalization in HCC lncRNA studies [20]. However, reference gene stability should be validated across sample types, as traditional controls may vary in tumor tissues.
Primer Design: LncRNA-specific primers should span exon-exon junctions where possible to minimize genomic DNA amplification. For single-exon lncRNAs, DNase treatment is essential. Primer specificity should be verified by melt curve analysis (for SYBR Green) and sequencing of amplification products.
Controls: Include no-template controls (NTC) to detect contamination and no-reverse transcription controls (NRT) to assess genomic DNA contamination.
Recent studies have demonstrated that the ΔΔCT method provides reliable relative quantification for tissue lncRNAs when validated according to these principles [20]. For absolute quantification, in vitro transcribed RNA standards can be implemented, though this approach is more commonly used in assay development than routine screening.
lncRNA Functional Mechanisms in HCC: Pathways and Workflows
Key Signaling Pathways in HCC
lncRNAs contribute to hepatocarcinogenesis through diverse molecular mechanisms. Integrated transcriptomic analyses of HCC tissues have identified lncRNAs enriched in critical pathways including cell cycle regulation, TGF-β signaling, p53 pathways, and ferroptosis [40]. These lncRNAs often function as competitive endogenous RNAs (ceRNAs), sequestering microRNAs to derepress oncogenic transcripts and drive HCC progression [40].
Diagram 1: ceRNA Mechanism in HCC. This diagram illustrates how oncogenic lncRNAs function as competitive endogenous RNAs (ceRNAs) in hepatocellular carcinoma by sequestering tumor-suppressive microRNAs, thereby derepressing oncogenic target mRNAs and driving cancer hallmarks.
Experimental Workflow for Tissue lncRNA Analysis
A standardized workflow ensures reproducible tissue lncRNA quantification while maintaining RNA integrity throughout the process:
Diagram 2: Tissue lncRNA Analysis Workflow. This experimental workflow outlines the key steps for reliable lncRNA quantification from tumor specimens, highlighting critical quality checkpoints that ensure data integrity throughout the process.
Research Reagent Solutions for Tissue lncRNA Analysis
Table 3: Essential Research Reagents for Tissue lncRNA Analysis
| Reagent Category | Specific Products | Function | Application Notes |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN) | Simultaneous extraction of lncRNA and other RNA species | Effective for both fresh-frozen and FFPE HCC tissues; includes DNase treatment |
| cDNA Synthesis Kits | LncProfiler qPCR Array Kit (SBI) | High-efficiency cDNA synthesis with polyA-tailing | Optimal for lncRNA detection; multi-step protocol enhances sensitivity |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems) | Sensitive detection with minimal background | Compatible with multiple real-time PCR platforms; stable fluorescence signal |
| Reference Assays | GAPDH primers | Endogenous control for data normalization | Essential for ΔΔCT calculations; stability should be verified in HCC tissues |
| Quality Control Tools | Agilent Bioanalyzer RNA Nano Kit | RNA integrity assessment | Provides RIN values critical for sample inclusion criteria |
Tissue lncRNA analysis by qRT-PCR remains an indispensable approach in HCC research, providing direct insights into molecular mechanisms driving hepatocarcinogenesis. The selection of appropriate platforms and methodologies significantly impacts detection sensitivity and reproducibility, with cDNA synthesis methods employing polyA-tailing and random hexamer priming demonstrating superior performance for comprehensive lncRNA profiling [41]. As research progresses, standardized workflows incorporating robust quality control measures and appropriate normalization strategies will enhance the reliability and cross-study comparability of tissue lncRNA data.
The continued refinement of qRT-PCR platforms and analytical methods will further strengthen the role of tissue lncRNA analysis in identifying molecular subtypes, prognostic biomarkers, and therapeutic targets in HCC. By implementing the optimized practices outlined in this guide, researchers can generate high-quality data that advances our understanding of lncRNA biology in hepatocellular carcinoma and contributes to improved patient outcomes through precision oncology approaches.
The detection of long non-coding RNAs (lncRNAs) in blood circulation represents a transformative approach for non-invasive cancer diagnosis, particularly for Hepatocellular Carcinoma (HCC). Unlike tissue-based biomarkers that require invasive biopsies, circulating lncRNAs offer a promising alternative for early detection, disease monitoring, and treatment response assessment [19] [9]. The stability of these molecules in bodily fluids, protected from RNase degradation through their association with proteins or encapsulation in extracellular vesicles, makes them particularly suitable for liquid biopsy applications [43] [44]. For HCC, which is often diagnosed at advanced stages with limited treatment options, the development of reliable circulating lncRNA biomarkers could significantly improve patient outcomes by enabling earlier intervention [6] [20].
This comparative analysis examines the methodological framework for circulating lncRNA detection, focusing specifically on RNA extraction and stabilization methods from blood samples, contextualized within the broader comparison of tissue versus circulating lncRNAs for HCC diagnostics. The technical protocols, reagent systems, and analytical considerations presented here provide researchers with a foundation for implementing robust circulating lncRNA detection workflows.
Comparative Analysis: Tissue vs. Circulating lncRNAs in HCC
The analysis of lncRNAs in HCC research utilizes two primary biological sources: tumor tissues obtained through biopsy and circulating lncRNAs from blood samples. Each approach offers distinct advantages and limitations for biomarker development and clinical application.
Table 1: Comparative Analysis of Tissue vs. Circulating lncRNAs in HCC Research
| Parameter | Tissue lncRNAs | Circulating lncRNAs |
|---|---|---|
| Sample Collection | Invasive biopsy requiring specialized medical procedure | Minimally invasive blood draw (phlebotomy) |
| Frequency of Monitoring | Limited by procedure risk and patient tolerance | Suitable for repeated sampling and dynamic monitoring |
| Tumor Heterogeneity Representation | Limited to specific biopsy site | Potentially represents entire tumor burden |
| Stability Considerations | Fixed tissue (FFPE) or snap-frozen | Requires specific blood collection tubes and processing protocols |
| Diagnostic Performance | High tissue specificity but invasive | AUC 0.76-0.91 for HCC detection panels [6] [20] [37] |
| Clinical Implementation | Gold standard for diagnosis but poor for screening | Emerging for early detection and monitoring |
| Technical Variability | Standardized pathology protocols | Evolving standardization for pre-analytical variables |
Tissue lncRNAs have been instrumental in establishing the functional roles of specific lncRNAs in HCC pathogenesis. For example, studies have identified NEAT1, DSCR8, PNUTS, HULC, and HOTAIR as playing significant roles in HCC cell proliferation, migration, and apoptosis through various mechanisms [9]. Similarly, FAM111A-DT, CERS6-AS1, and TLNC1 affect HCC progression by regulating key signaling pathways and are closely correlated with patient prognosis [9]. The major advantage of tissue-based analysis lies in the direct investigation of molecular events within the tumor microenvironment.
In contrast, circulating lncRNAs provide a dynamic window into tumor activity through serial sampling, enabling monitoring of treatment response and disease progression. Multiple studies have demonstrated the diagnostic potential of circulating lncRNA panels for HCC. A study evaluating a three-lncRNA panel (Linc00152, UCA1, and AFP) achieved an AUC of 0.912 with 82.9% sensitivity and 88.2% specificity for HCC diagnosis [6]. Another investigation of LINC00152, LINC00853, UCA1, and GAS5 in combination with machine learning algorithms achieved 100% sensitivity and 97% specificity [20]. These performances highlight the considerable potential of circulating lncRNAs as complementary biomarkers to the currently used alpha-fetoprotein (AFP), which has limited sensitivity, particularly for early-stage HCC [6] [20].
The relationship between tissue and circulating lncRNAs is conceptually interconnected, as illustrated below:
Figure 1: Workflow from HCC Tissue to Circulating lncRNA Detection
Critical Experimental Protocols for Circulating lncRNA Analysis
Blood Collection and Plasma Processing
The pre-analytical phase is critical for reliable circulating lncRNA detection, as improper sample handling can significantly impact RNA quality and yield. The following protocol represents a consensus approach derived from multiple studies [45] [6] [20]:
Blood Collection: Collect peripheral venous blood (5-10 mL) into EDTA vacutainers to prevent coagulation. Invert tubes gently 8-10 times immediately after collection to ensure proper mixing with anticoagulant.
Initial Centrifugation: Process samples within 2 hours of collection. Centrifuge at 1900×g for 10 minutes at room temperature to separate cellular components from plasma.
Secondary Centrifugation: Transfer the supernatant to a fresh tube and centrifuge at 16,000×g for 10 minutes to remove remaining cellular debris and platelets.
Aliquoting and Storage: Aliquot the purified plasma into RNase-free tubes and store immediately at -80°C to prevent RNA degradation. Avoid repeated freeze-thaw cycles.
This two-step centrifugation protocol is essential for obtaining cell-free plasma that minimizes contamination by cellular RNAs from hemolysis or residual blood cells, which could otherwise compromise the accuracy of circulating lncRNA measurements [45].
RNA Extraction Methods
RNA extraction from plasma presents unique challenges due to the low concentration and high fragmentation of circulating RNA. The following comparative analysis outlines two primary extraction methods employed in recent studies:
Table 2: Comparison of RNA Extraction Methods for Circulating lncRNAs
| Method | Protocol | Advantages | Limitations | Representative Efficacy |
|---|---|---|---|---|
| TRIzol LS | 1. Add 750μL TRIzol LS to 250μL plasma2. Vortex, incubate 5min3. Add 200μL chloroform, shake4. Centrifuge 12,000×g, 15min5. Transfer aqueous phase6. Precipitate with isopropanol7. Wash with 75% ethanol8. Resuspend in RNase-free water | Effective for small RNAsComprehensive RNA speciesHigh purity | Organic phase separation requiredTime-consumingTechnical expertise needed | Successfully extracted HOTAIR, ANRIL, MEG3 from OSCC plasma [45] |
| Commercial Kits (Hipure) | 1. Add lysis buffer to plasma2. Process through silica membrane column3. Wash with buffer solutions4. Elute in RNase-free water | Rapid processingEliminates organic solventsAmenable to automationConsistent yields | Specific to RNA size rangesHigher cost per samplePotential for column clogging | Effectively isolated 8 lncRNAs including HULC, MALAT1, UCA1 from serum [6] |
Studies have successfully implemented both approaches. The TRIzol LS method (Invitrogen) was used to extract RNA for the detection of HOTAIR, ANRIL, and MEG3 in oral squamous cell carcinoma with high efficiency [45], while the Hipure Liquid RNA Kit (Magen) effectively isolated lncRNAs including HULC, MALAT1, Linc00152, and UCA1 from serum samples in HCC research [6]. The choice between methods depends on specific research requirements, including the target lncRNA species, sample volume, and throughput needs.
Downstream Detection and Analysis
Following RNA extraction, the standard detection method for circulating lncRNAs is quantitative real-time PCR (qRT-PCR) due to its high sensitivity and specificity for low-abundance targets. The typical workflow includes:
Reverse Transcription: Convert RNA to cDNA using reverse transcriptase with either random hexamers or gene-specific primers. The RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) has been successfully employed in multiple studies [20].
qPCR Amplification: Perform amplification using SYBR Green or TaqMan chemistry. The PowerTrack SYBR Green Master Mix (Applied Biosystems) provides reliable detection with high sensitivity [20]. Reactions are typically run for 45 cycles to detect low-abundance lncRNAs.
Data Analysis: Normalize expression using reference genes such as GAPDH [6] [20] and calculate relative expression using the 2−ΔΔCt method.
For studies involving multiple lncRNA targets, multiplex panels combined with machine learning algorithms have shown enhanced diagnostic performance. One study developed a risk prediction model using three disulfidptosis-related lncRNAs that achieved AUCs of 0.756 (1 year), 0.695 (3 years), and 0.701 (5 years) for HCC prognosis [37].
Research Reagent Solutions for Circulating lncRNA Studies
Table 3: Essential Research Reagents for Circulating lncRNA Analysis
| Reagent Category | Specific Products | Application | Key Features |
|---|---|---|---|
| Blood Collection | EDTA Vacutainers (BD) | Blood collection and stabilization | Prevents coagulation while maintaining RNA integrity |
| RNA Extraction | TRIzol LS Reagent (Invitrogen) | RNA isolation from plasma | Effective for low-concentration RNA, comprehensive RNA species isolation |
| RNA Extraction | Hipure Liquid RNA Kit (Magen) | Column-based RNA extraction | Eliminates organic solvents, faster processing, consistent yields |
| cDNA Synthesis | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Reverse transcription | High efficiency for degraded and low-abundance RNAs |
| qPCR Amplification | PowerTrack SYBR Green Master Mix (Applied Biosystems) | qRT-PCR detection | High sensitivity, suitable for up to 45 amplification cycles |
| Reference Genes | GAPDH primers | Expression normalization | Stable reference for data normalization in blood samples |
Methodological Considerations and Standardization Challenges
The detection of circulating lncRNAs presents several methodological challenges that require careful consideration. Pre-analytical variability represents a significant factor, with blood processing time, centrifugation conditions, and storage duration all potentially influencing lncRNA levels [45] [6]. Establishing standardized protocols across laboratories is essential for reproducible results.
Normalization strategies remain contentious in the field, with some studies using spiked-in synthetic RNAs as external controls while others rely on endogenous reference genes like GAPDH. However, the stability of reference genes in circulation must be empirically validated for each experimental condition [6] [20].
The sample matrix choice (serum vs. plasma) also affects lncRNA measurements. Plasma is generally preferred as the anticoagulant prevents clot formation that could sequester RNA, while serum may release additional RNA during the clotting process, potentially altering the lncRNA profile [6].
For HCC-specific applications, combining lncRNA signatures with existing biomarkers like AFP has shown enhanced diagnostic performance. One study demonstrated that a panel combining Linc00152, UCA1, and AFP achieved superior diagnostic accuracy (AUC 0.912) compared to individual markers [6], highlighting the value of multi-analyte approaches.
The detection of circulating lncRNAs from blood samples represents a promising frontier in HCC diagnostics and monitoring. The methodological framework for RNA extraction and stabilization continues to evolve, with both TRIzol-based and commercial kit-based approaches offering viable pathways for robust lncRNA isolation. As the field advances, standardization of pre-analytical variables, validation of normalization methods, and implementation of multi-analyte panels will be crucial for translating circulating lncRNA biomarkers into clinical practice. The integration of these molecular tools with traditional diagnostic modalities offers the potential to significantly improve early detection and personalized management strategies for HCC patients.
Hepatocellular carcinoma (HCC) is a major global health challenge, ranking as the sixth most common cancer and the third leading cause of cancer-related mortality worldwide [37] [31]. A significant factor contributing to its poor prognosis is late diagnosis, as most patients are identified at advanced stages when curative treatments are no longer feasible [7]. The development of valuable biomarkers for independent prediction of HCC prognosis is therefore vital for timely identification and better management of patients [31]. Long non-coding RNAs (lncRNAs)—transcripts longer than 200 nucleotides with limited protein-coding potential—have emerged as promising players in cancer biology [46] [31]. These molecules regulate gene expression through various mechanisms, including serving as signaling molecules, guiding chromatin-modifying enzymes, functioning as decoys for transcription factors or microRNAs, and working as scaffolds for multi-component complexes [31]. Importantly, lncRNAs are not only found in tissues but can also be detected in blood circulation, either freely or encapsulated within exosomes [7]. This review provides a comparative analysis of four promising lncRNA biomarkers—HULC, MALAT1, HOTAIR, and MEG3—evaluating their diagnostic and prognostic performance in both tissue and circulating forms for HCC management.
Comparative Analysis of Four Promising lncRNA Biomarkers
The following table summarizes the key characteristics and diagnostic performance of HULC, MALAT1, HOTAIR, and MEG3 as biomarkers in HCC and other cancers.
Table 1: Comparative Analysis of Tissue and Circulating lncRNA Biomarkers
| lncRNA | Primary Function | Tissue Expression in HCC | Circulating Form Detection | Key Diagnostic Performance (AUC) | Correlation with Clinicopathological Features |
|---|---|---|---|---|---|
| HULC | Oncogenic | Upregulated [47] | Plasma, Serum [47] [7] [48] | Tissue: 0.86 [47]; Serum (GC): 0.888 [48] | Positively associated with Edmondson grade and HBV+ status in tissue [47]; Correlated with tumor size, metastasis, and TNM stage in serum (GC) [48] |
| MALAT1 | Oncogenic, Regulates inflammation and treatment resistance [49] | Upregulated in laryngeal, nasopharyngeal, and oral cancers [49] | Plasma, Saliva [49] [45] | Predictive for post-radiotherapy toxicity in laryngeal cancer [49] | Low plasma expression predicts anemia, liver failure, and malnutrition after radiotherapy in laryngeal cancer [49] |
| HOTAIR | Oncogenic | Information limited in HCC; Upregulated in other solid tumors and leukemias [50] | Plasma, Serum, Bone Marrow Plasma [45] [51] [50] | Plasma (OSCC): 0.99 [45] [51]; Prognostic in pediatric ALL: 0.955 [50] | Associated with poor histological grade, higher T and N stage, LVI, PNI, and advanced stage in OSCC [45] |
| MEG3 | Tumor Suppressive | Downregulated in various cancers [46] | Plasma [45] [51] | Plasma (OSCC): 0.99 [45] [51] | Downregulation correlates with higher clinical stage, nodal metastasis, and poor prognosis [45] [46] |
Table 2: Summary of lncRNA Biomarker Performance Across Different Cancers
| Cancer Type | Most Promising lncRNA Biomarkers | Key Findings |
|---|---|---|
| Hepatocellular Carcinoma (HCC) | HULC | Plasma HULC is a potential biomarker for HCC risk in chronic hepatitis C patients [7]; Tissue HULC expression is significantly higher in HCC tumors and associated with histological grade and HBV status [47]. |
| Oral Squamous Cell Carcinoma (OSCC) | HOTAIR, ANRIL, MEG3 | Three-lncRNA panel (HOTAIR+ANRIL+MEG3) yielded an AUC of 0.95, with 91.25% sensitivity and 92.50% specificity [45] [51]. |
| Laryngeal Cancer | MALAT1, NEAT1 | Low plasma expression of MALAT1 and NEAT1 predicts post-radiotherapy adverse effects and shorter overall survival [49]. |
| Pediatric Acute Lymphoblastic Leukemia | HOTAIR | Circulating HOTAIR is a novel prognostic factor (AUC=0.955) for monitoring chemotherapy efficacy [50]. |
| Gastric Cancer | HULC | Serum HULC effectively differentiated GC patients from controls (AUC=0.888) and was a good predictor of prognosis [48]. |
Molecular Mechanisms and Signaling Pathways
HULC (Highly Up-regulated in Liver Cancer)
HULC is one of the most well-characterized oncogenic lncRNAs in HCC. It is markedly up-regulated in HCC tissues compared to normal liver specimens, with higher expression levels positively associated with more advanced Edmondson histological grades and hepatitis B (HBV) positive status [47]. The detection of HULC in plasma highlights its potential as a non-invasive biomarker [47] [7]. In chronic hepatitis C (CHC) patients, plasma HULC has been identified as a potential biomarker for assessing HCC risk [7].
MALAT1 (Metastasis-Associated Lung Adenocarcinoma Transcript 1)
MALAT1 is widely upregulated in several tumors and regulates various cellular processes, including tumor-related inflammation, proliferation, motility, and epithelial-mesenchymal transition [49]. In the context of radiotherapy, low plasma expression of MALAT1 has been associated with a significantly higher probability of developing adverse effects such as anemia, liver failure, and severe malnutrition after treatment completion in laryngeal cancer patients [49]. MALAT1 also regulates ferroptosis and modulates drug resistance through the p53 signaling pathway [49].
HOTAIR (HOX Transcript Antisense Intergenic RNA)
HOTAIR functions as an oncogenic lncRNA across multiple cancer types. Its elevated expression in plasma has been strongly associated with poor histological grade, higher T and N stage, lymphovascular invasion (LVI), perineural invasion (PNI), and advanced cancer stage [45]. In pediatric acute lymphoblastic leukemia, circulating HOTAIR serves as both a diagnostic and prognostic biomarker, with expression levels significantly decreasing in treatment-sensitive patients during chemotherapy [50]. HOTAIR achieves its oncogenic effects partly by acting as a competitive endogenous RNA (ceRNA) that sponges tumor suppressor microRNAs such as miR-326 [50].
MEG3 (Maternally Expressed Gene 3)
MEG3 functions as a tumor suppressor lncRNA through both p53-dependent and p53-independent pathways [46]. It is located on chromosome 14q32.3 and is expressed exclusively from the maternal allele [46]. MEG3 plays a pivotal role in various biological processes, including tumorigenesis, by impeding tumor cell proliferation, triggering apoptosis, inhibiting invasion and metastasis, hindering angiogenesis, and suppressing metabolic reprogramming in tumor cells [46]. MEG3 contains microRNA response elements, enabling it to function as a ceRNA and effectively sponge oncogenic miRNAs [46]. The downregulation of MEG3 in plasma has been associated with more advanced disease stages in oral squamous cell carcinoma [45] [51].
Figure 1: Molecular Mechanisms of lncRNA Biomarkers in Cancer. This diagram illustrates how HULC, MALAT1, HOTAIR, and MEG3 regulate key cancer hallmarks through various molecular pathways.
Experimental Protocols for lncRNA Biomarker Analysis
Sample Collection and Processing
For liquid biopsy approaches, peripheral blood samples are collected in EDTA vacutainers. Plasma is separated using a two-step centrifugation process: initially at 1900×g for 10 minutes to spin down blood cells, followed by centrifugation at 16,000×g for 10 minutes at room temperature to completely remove cellular debris [45]. The resulting plasma aliquots are immediately stored at -80°C until RNA extraction. For tissue analysis, samples are frozen shortly after surgery and stored in liquid nitrogen [47].
RNA Isolation and Quality Control
Total RNA is extracted from plasma samples using specialized kits such as the Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit [7] or TRIzol LS reagent [45]. To eliminate genomic DNA contamination, RNA samples are treated with DNase [7]. RNA yield and quality are assessed using spectrophotometric methods, and samples with adequate quality proceed to cDNA synthesis.
cDNA Synthesis and Quantitative Real-Time PCR (qRT-PCR)
For reverse transcription, 500 ng of total RNA is typically reverse transcribed using commercial cDNA synthesis kits with random hexamer primers [45] [7]. Quantitative real-time PCR is then performed using SYBR Green or TaqMan chemistry on platforms such as the Bio-Rad CFX-96 real-time PCR system [47] or StepOne Plus System [7]. The reaction conditions usually include an initial denaturation at 95°C for 2 minutes, followed by 40 cycles of 95°C for 15 seconds and 60-62°C for 1 minute [7]. Each sample is analyzed in triplicate with appropriate negative controls.
Data Normalization and Analysis
The expression level of target lncRNAs is calculated using the comparative Ct (2−ΔΔCt) method [7]. Reference genes for normalization include β-actin [7] or GAPDH [48], selected based on their stable expression across samples. Statistical analyses are performed to assess differential expression between patient and control groups, with receiver operating characteristic (ROC) curves generated to evaluate diagnostic performance [45] [7].
Figure 2: Experimental Workflow for Circulating lncRNA Analysis. This diagram outlines the key steps in processing samples and analyzing lncRNA biomarkers from blood samples.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for lncRNA Biomarker Studies
| Reagent/Material | Function/Application | Examples/Specifications |
|---|---|---|
| Blood Collection Tubes | Sample collection and preservation | EDTA vacutainers [45] |
| RNA Extraction Kits | Isolation of high-quality RNA from plasma/serum | Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit [7]; TRIzol LS reagent [45] |
| DNase Treatment Kits | Removal of genomic DNA contamination | Turbo DNase [7] |
| cDNA Synthesis Kits | Reverse transcription of RNA to cDNA | High-Capacity cDNA Reverse Transcription Kit [7]; PrimeScript RT reagent kit [47] |
| qPCR Master Mixes | Amplification and detection of target lncRNAs | SYBR Green PCR Master Mix [45] [7]; TaqMan assays [48] |
| Reference Genes | Normalization of lncRNA expression data | β-actin [7]; GAPDH [47] [48] |
| qPCR Instruments | Real-time quantification of lncRNAs | Bio-Rad CFX-96 [47]; StepOne Plus System [7] |
| RNA Storage Solutions | Long-term preservation of RNA integrity | Nuclease-free tubes, -80°C freezers [48] |
| Bombinin H1 | Bombinin H1 Peptide|Antimicrobial Peptide for Research | Bombinin H1 is an antimicrobial peptide (AMP) isolated fromBombinatoad skin. It is for research use only (RUO) and not for human or veterinary use. |
| Urease-IN-12 | Urease-IN-12, MF:C11H13ClN2O3S, MW:288.75 g/mol | Chemical Reagent |
The comparative analysis of HULC, MALAT1, HOTAIR, and MEG3 reveals a promising landscape for lncRNA-based biomarkers in cancer diagnosis and prognosis. Each lncRNA offers unique advantages: HULC demonstrates strong performance in both tissue and liquid biopsy formats for HCC; MALAT1 shows utility in predicting treatment-related toxicities; HOTAIR exhibits remarkable diagnostic accuracy in multiple cancer types; and MEG3 serves as a valuable tumor suppressor marker with decreasing expression correlating with disease progression. The future of lncRNA biomarkers lies in developing multi-marker panels that combine complementary lncRNAs to enhance diagnostic sensitivity and specificity, as demonstrated by the HOTAIR+ANRIL+MEG3 panel in OSCC which achieved an AUC of 0.95 [45] [51]. Further validation in larger, multicentric studies and standardization of detection protocols will be essential for translating these promising biomarkers into clinical practice, ultimately improving early cancer detection and patient outcomes.
This guide provides a comparative analysis of the diagnostic and prognostic performance of four circulating long non-coding RNAs (lncRNAs)—LINC00152, UCA1, GAS5, and LINC00853—in hepatocellular carcinoma (HCC). The focus on circulating lncRNAs reflects a significant shift in biomarker research toward liquid biopsy approaches, which offer a non-invasive alternative to traditional tissue-based diagnosis. The data summarized herein are critical for researchers and drug development professionals evaluating the potential of these biomarkers for early cancer detection, prognosis, and the development of non-invasive diagnostic kits.
Performance Comparison of Circulating lncRNAs
The diagnostic accuracy of individual and combined lncRNAs has been evaluated in multiple clinical studies. The quantitative data below provide a direct comparison of their performance metrics.
Table 1: Diagnostic Performance of Individual Circulating lncRNAs for HCC
| lncRNA | Biological Role | Reported AUC | Reported Sensitivity (%) | Reported Specificity (%) | Key Clinical Association |
|---|---|---|---|---|---|
| LINC00152 | Oncogenic [6] | 0.877 [6] | 82.9 (in panel) [6] | 88.2 (in panel) [6] | Positive correlation with GGT levels [6] |
| UCA1 | Oncogenic [52] | Moderate [52] | 60-83 [52] | 53-67 [52] | Used in combination panels [6] [52] |
| GAS5 | Tumor Suppressive [52] | Moderate [52] | 60-83 [52] | 53-67 [52] | Higher LINC00152/GAS5 ratio correlates with increased mortality risk [52] |
| LINC00853 | Information Missing | Moderate [52] | 60-83 [52] | 53-67 [52] | Information Missing |
Table 2: Performance of Multi-lncRNA Panels and Advanced Models
| Biomarker Panel | AUC | Sensitivity (%) | Specificity (%) | Notes |
|---|---|---|---|---|
| Linc00152 + UCA1 + AFP | 0.912 [6] | 82.9 [6] | 88.2 [6] | Superior to single markers or AFP alone [6] |
| Linc00152 + AFP | 0.906 [6] | Information Missing | Information Missing | High diagnostic accuracy [6] |
| 4-lncRNA Panel + Clinical Vars + Machine Learning | Information Missing | 100 [52] | 97 [52] | Model integrates lncRNAs with standard lab parameters [52] |
Experimental Protocols for Circulating lncRNA Analysis
The reproducibility of lncRNA biomarker data relies on standardized methodologies. The following workflow details the key experimental protocols used in the cited studies.
Figure 1: Core Workflow for Circulating lncRNA Analysis
Detailed Methodology
- Sample Collection and Processing: Peripheral blood samples are collected in vacuum tubes (e.g., EDTA tubes for plasma) from patients and controls [6] [52]. Serum is isolated by centrifugation at 3,000 rpm for 10 minutes, then immediately transferred and stored at -80°C until RNA extraction [6].
- RNA Isolation and QC: Total RNA is extracted from serum or plasma using commercial kits, such as the Hipure Liquid RNA Kit (Magen) [6] or the miRNeasy Mini Kit (QIAGEN) [52]. RNA quantity and purity are assessed using spectrophotometry (e.g., NanoDrop) [6].
- cDNA Synthesis and qRT-PCR: Purified RNA is reverse-transcribed into cDNA using reverse transcriptase (e.g., M-MLV Reverse Transcriptase) [6]. Quantitative real-time PCR (qRT-PCR) is performed using systems like the QuantStudio (Applied Biosystems) or ViiA 7 (Applied Biosystems) with SYBR Green chemistry [6] [52]. Reactions are typically run in triplicate with specific primers for each lncRNA.
- Data Normalization and Analysis: The relative expression of lncRNAs is calculated using the 2−ΔΔCt method. The housekeeping gene GAPDH is commonly used as an endogenous control for data normalization [6] [52].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Kits for Circulating lncRNA Research
| Item | Specific Product Examples | Critical Function in Workflow |
|---|---|---|
| RNA Extraction Kit | Hipure Liquid RNA Kit (Magen) [6], miRNeasy Mini Kit (QIAGEN) [52] | Isolves high-quality, amplification-ready total RNA from biofluids. |
| Reverse Transcriptase | M-MLV Reverse Transcriptase (Promega) [6], RevertAid Kit (Thermo Scientific) [52] | Synthesizes stable cDNA from purified RNA for downstream PCR. |
| qRT-PCR Master Mix | TB Green Premix Ex Taq (Takara) [6], PowerTrack SYBR Green Master Mix (Applied Biosystems) [52] | Provides optimized enzymes and buffers for specific and efficient lncRNA amplification. |
| Primers | Sequence-specific primers for LINC00152, UCA1, etc. [6] [52] | Ensures specific detection and quantification of the target lncRNA. |
| Reference Gene | Primers for GAPDH [6] [52] | Serves as an endogenous control to normalize for technical variation. |
| Apelin-16, human, bovine | Apelin-16, human, bovine, MF:C90H144N32O19S, MW:2010.4 g/mol | Chemical Reagent |
| Pad4-IN-2 | Pad4-IN-2, MF:C20H23BClN7O6, MW:503.7 g/mol | Chemical Reagent |
Contextualizing the Role of lncRNAs in HCC
The four lncRNAs discussed function within complex molecular networks that drive HCC progression. The diagram below illustrates their functional roles in hepatocarcinogenesis.
Figure 2: Functional Roles of lncRNAs in HCC Pathways
- LINC00152: Functions as an oncogene, promoting HCC cell proliferation. It has been reported to regulate cell cycle progression through cyclin D1 (CCND1) [52].
- UCA1: Also acts as an oncogenic lncRNA, contributing to the proliferation and apoptosis of HCC cells, although its exact mechanistic pathways are not fully elucidated [52].
- GAS5: In contrast, operates as a tumor suppressor. It is known to inhibit cancer cell proliferation and activate apoptosis, potentially by triggering the CHOP and caspase-9 signal pathways [52].
- The Prognostic Ratio: The expression ratio of LINC00152 to GAS5 is clinically significant, as a higher ratio has been correlated with an increased risk of mortality in HCC patients, underscoring the balance between oncogenic and tumor-suppressive forces [52].
The Diagnostic Paradigm: Tissue vs. Circulating lncRNAs
The investigation of lncRNAs in HCC exists in two complementary spheres: the traditional analysis of tumor tissue and the emerging field of liquid biopsy.
- Tissue-Based lncRNA Analysis: Provides direct evidence of molecular changes within the tumor and its microenvironment. It has been instrumental in discovering the functional roles of lncRNAs like HULC, MALAT1, and HOTAIR in hepatocarcinogenesis [19] [9]. However, its invasive nature limits its utility for repeated monitoring and early screening.
- Circulating lncRNA Analysis: The stability of lncRNAs in blood fluids (serum/plasma) makes them ideal candidates for liquid biopsies [6] [53]. This approach enables non-invasive detection, real-time monitoring of treatment response, and assessment of disease recurrence. The data presented in this guide demonstrate that circulating panels, especially when combined with machine learning, can achieve diagnostic performance that meets or exceeds that of traditional tissue-based markers or the serum protein AFP alone [6] [52].
This comparative analysis underscores the significant translational potential of circulating lncRNA panels, particularly LINC00152, UCA1, and GAS5, as non-invasive tools for HCC management. Future efforts should focus on standardizing detection protocols and validating these biomarkers in large, multi-center prospective trials to facilitate their clinical adoption.
Hepatocellular carcinoma (HCC) represents a significant global health burden, ranking as the sixth most prevalent cancer worldwide and the fourth most common cause of cancer-related mortality [20]. The disease is particularly aggressive, with low survival rates largely attributable to late diagnosis, as early-stage HCC often presents asymptomatically [20]. In Egypt, HCC ranks as the fourth most common cancer and the leading cause of cancer-related death, with the endemic prevalence of hepatitis C virus (HCV) infection being a major contributing risk factor [20]. The five-year survival rate for all stages of HCC remains as low as 15%, but this can improve to 70% with early detection [7], highlighting the critical need for improved diagnostic methodologies.
The current diagnostic landscape for HCC relies on imaging techniques such as ultrasound and the serological biomarker alpha-fetoprotein (AFP). However, AFP has demonstrated limited sensitivity and specificity, particularly for early-stage tumors and those less than three centimeters in size [54]. Tissue biopsies, while informative, present significant challenges including invasiveness, sampling variability, and risk of tumor dissemination [7]. These limitations have accelerated research into alternative biomarkers, particularly long non-coding RNAs (lncRNAs) - RNA molecules longer than 200 nucleotides that do not code for proteins but play crucial regulatory roles in carcinogenesis [20] [18].
The emergence of liquid biopsy approaches, which detect circulating lncRNAs in blood-based samples, offers a promising non-invasive alternative to tissue biopsies [7]. When combined with machine learning (ML) algorithms, these biomarker panels can significantly enhance diagnostic precision. Artificial intelligence, particularly machine learning and deep learning, has transformed the analysis of intricate biological data, facilitating the detection of clinically significant RNA expression patterns that conventional statistical techniques may fail to capture [55]. This comparative analysis examines the integration of multiple lncRNAs with ML approaches for HCC diagnosis, with particular emphasis on the comparative utility of tissue versus circulating lncRNAs.
Comparative Analysis of lncRNA Diagnostic Performance
Individual versus Combined lncRNA Diagnostic Performance
Table 1: Diagnostic Performance of Individual lncRNAs for HCC Detection
| lncRNA | Sensitivity (%) | Specificity (%) | Biological Function | Sample Type |
|---|---|---|---|---|
| LINC00152 | 83 | 67 | Promotes cell proliferation through cyclin D1 regulation [20] | Plasma |
| UCA1 | 76 | 61 | Promotes proliferation and inhibits apoptosis [20] | Plasma |
| LINC00853 | 72 | 58 | Oncogenic properties [20] | Plasma |
| GAS5 | 60 | 53 | Tumor suppressor; activates CHOP and caspase-9 pathways [20] | Plasma |
| HULC | N/A | N/A | Highly upregulated in liver cancer [7] | Plasma |
| RP11-731F5.2 | N/A | N/A | Potential biomarker for liver damage in HCV [7] | Plasma |
| Traditional Biomarker | ||||
| AFP | ~65* | ~80* | Fetal glycoprotein [54] | Serum |
*Approximate values based on meta-analysis data [54]
While individual lncRNAs demonstrate moderate diagnostic accuracy, their combination significantly enhances diagnostic performance. A 2024 study investigating a four-lncRNA panel (LINC00152, LINC00853, UCA1, and GAS5) found that individual lncRNAs exhibited sensitivity and specificity ranging from 60-83% and 53-67%, respectively [20]. In contrast, the integration of these lncRNAs with conventional laboratory parameters using a machine learning model achieved remarkable performance with 100% sensitivity and 97% specificity [20]. This demonstrates the powerful synergistic effect of combining multiple lncRNAs into a diagnostic signature.
The diagnostic potential of lncRNAs is further supported by a comprehensive meta-analysis of 16 studies involving 2,268 HCC patients and 2,574 controls, which reported pooled sensitivity of 87%, specificity of 83%, and an area under the curve (AUC) of 0.915 for lncRNAs in HCC diagnosis [54]. Subgroup analysis indicated that lncRNA panels derived from serum and plasma had particularly high diagnostic value for HCC patients from Asia [54].
Tissue versus Circulating lncRNAs: A Comparative Framework
Table 2: Comparative Analysis of Tissue versus Circulating lncRNAs for HCC Diagnosis
| Parameter | Tissue lncRNAs | Circulating lncRNAs |
|---|---|---|
| Invasiveness | High (requires biopsy) | Low (blood-based collection) |
| Tumor Heterogeneity | Significant (sampling variability) | Minimal (integrates systemic signals) |
| Longitudinal Monitoring | Limited (repeated biopsies impractical) | Excellent (suitable for serial testing) |
| Early Detection Potential | Moderate | High |
| Mechanistic Insights | Direct (from tumor microenvironment) | Indirect (systemic manifestations) |
| Clinical Implementation | Complex | Streamlined |
| Representative Markers | MEG3, MALAT1, HOTAIR, H19 [18] | LINC00152, UCA1, GAS5, HULC [20] [7] |
| Integration with ML | Challenging (sample availability) | Promising (repeat sampling enables robust model training) |
The choice between tissue and circulating lncRNAs involves important trade-offs. Tissue lncRNAs provide direct information about the tumor microenvironment and can offer valuable mechanistic insights into HCC pathogenesis [18]. For instance, lncRNAs such as MEG3, MALAT1, HOTAIR, and H19 demonstrate dysregulation in HCC tissues and are closely associated with tumor expansion, metastasis, and prognosis [18].
In contrast, circulating lncRNAs offer practical advantages for clinical implementation, particularly for screening and monitoring applications. Liquid biopsies provide a less invasive alternative to tissue biopsies, improving early cancer detection and surveillance [7]. Tumor cells release lncRNAs either freely or within membrane microvesicles called exosomes into circulation, making these molecules accessible in various biofluids including plasma, serum, urine, and saliva [7]. A 2025 study identified plasma lncRNAs HULC and RP11-731F5.2 as potential biomarkers for HCC risk in chronic hepatitis C patients, while RP11-731F5.2 and KCNQ1OT1 may serve as noninvasive biomarkers for liver damage due to HCV infection [7].
Experimental Protocols and Methodologies
Sample Collection and Patient Selection
Robust experimental design begins with careful patient selection and sample collection. In the referenced studies, participants were typically categorized into three groups: HCC patients, individuals with chronic liver disease (such as chronic hepatitis C) without HCC, and healthy controls [20] [7]. For the 2024 machine learning study, plasma samples were obtained from 52 newly diagnosed, treatment-naive HCC patients and 30 age-matched controls [20]. The 2025 prospective study included 41 participants with advanced chronic hepatitis C who underwent clinical follow-ups for a minimum of five years after plasma collection, allowing assessment of lncRNAs as predictive biomarkers for HCC development [7].
Standardized sample processing protocols are critical for reliable results. Plasma samples are typically obtained from peripheral blood centrifuged at 704× g (RCF) for 10 minutes, with all samples stored at -70°C until RNA extraction [7]. Consistent sample handling minimizes pre-analytical variability that could compromise lncRNA quantification.
RNA Isolation and Quantification
Total RNA isolation follows established protocols using commercial kits specifically designed for liquid biopsies. Studies utilized the miRNeasy Mini Kit (QIAGEN) or Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek Corp.) according to manufacturers' protocols [20] [7]. To ensure RNA quality and eliminate genomic DNA contamination, samples are typically treated with DNase (e.g., Turbo DNase, Life Technologies) [7].
Reverse transcription is performed using kits such as the RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) to generate complementary DNA (cDNA) [20]. Quantitative real-time PCR (qRT-PCR) remains the gold standard for lncRNA quantification, utilizing PowerTrack SYBR Green Master Mix (Applied Biosystems) or Power SYBR Green PCR Master Mix (Thermo Fisher Scientific) on platforms such as the ViiA 7 real-time PCR system (Applied Biosystems) or StepOne PlusTM System (Applied Biosystems) [20] [7]. Each reaction is typically performed in triplicate to ensure technical reproducibility, with GAPDH or β-actin serving as reference genes for normalization [20] [7]. The 2−ΔΔCT method is standard for relative quantification of lncRNA expression levels [20] [7].
Machine Learning Integration and Model Development
The integration of lncRNA data with machine learning algorithms follows a structured workflow. In the 2024 study, researchers constructed a machine learning model using Python's Scikit-learn platform to integrate the four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with additional clinical laboratory parameters for HCC diagnosis [20]. The superior performance of the ML model (100% sensitivity, 97% specificity) compared to individual lncRNAs highlights the power of multivariate analysis.
AI-powered approaches can efficiently analyze complex RNA expression patterns, discover novel biomarkers, and explain their functions in cancer biology [55]. Machine learning algorithms, particularly random forest and XGBoost, have proven effective in identifying significant gene patterns and classifying cancer subtypes based on RNA expression profiles [55]. The iterative process of model training, validation, and testing ensures robust performance, with explainability techniques helping to interpret how models generate predictions and which features contribute most to diagnostic accuracy [56].
Visualizing Experimental Workflows and Biological Mechanisms
HCC Diagnostic Workflow Using lncRNAs and ML
Figure 1: Integrated Workflow for lncRNA-Based HCC Diagnosis Using Machine Learning
lncRNA Functional Mechanisms in Hepatocellular Carcinoma
Figure 2: lncRNA Functional Mechanisms in HCC Pathogenesis
Essential Research Reagent Solutions
Table 3: Essential Research Reagents for lncRNA-Based HCC Studies
| Reagent Category | Specific Product Examples | Primary Function | Key Considerations |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN), Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) | Extraction of high-quality RNA from plasma/serum samples | Optimized for low-concentration circulating RNA |
| Reverse Transcription Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific), High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | Conversion of RNA to stable cDNA for downstream analysis | Includes RNase inhibitors for RNA protection |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems), Power SYBR Green PCR Master Mix (Thermo Fisher) | Sensitive detection and quantification of lncRNAs | SYBR Green format allows flexibility in target selection |
| Reference Genes | GAPDH, β-actin | Normalization of lncRNA expression data | Validation of stability across sample types is critical |
| DNase Treatment | Turbo DNase (Life Technologies) | Removal of genomic DNA contamination | Essential for accurate RNA quantification |
| Primer Sets | Custom-designed lncRNA-specific primers | Target-specific amplification | Designed to span exon-exon junctions where applicable |
| Software Platforms | Scikit-learn (Python), GraphPad Prism, R software | Statistical analysis and machine learning implementation | Compatibility with high-dimensional data |
The integration of multiple lncRNAs with machine learning algorithms represents a transformative approach to HCC diagnosis, significantly outperforming single-biomarker strategies. The demonstrated ability of ML models to achieve near-perfect sensitivity (100%) and high specificity (97%) by combining four lncRNAs with conventional laboratory parameters underscores the power of multivariate analysis [20]. This approach effectively addresses the limitations of current standards like AFP, particularly for early-stage detection when interventions are most effective.
Future research directions should focus on validating these integrated models in larger, multi-center cohorts to ensure robustness across diverse populations [20] [55]. Additionally, expanding the exploration of lncRNA panels to include novel candidates identified through next-generation sequencing could further enhance diagnostic precision [7]. The successful implementation of these technologies in clinical practice will require standardized protocols for sample processing, RNA quantification, and model deployment to ensure reproducibility across different healthcare settings.
As the field advances, the combination of liquid biopsy-based lncRNA profiling with machine learning analytics holds exceptional promise for transforming HCC management through improved early detection, accurate prognosis prediction, and potentially guiding personalized treatment strategies. This integrated approach may ultimately contribute to significantly improved survival outcomes for patients facing this aggressive malignancy.
Overcoming Challenges: Optimization Strategies for Reliable lncRNA Detection
Hepatocellular carcinoma (HCC) remains a leading cause of cancer-related mortality worldwide, primarily due to limitations in early detection methods. While individual long non-coding RNAs (lncRNAs) have emerged as potential biomarkers, this review demonstrates through comparative analysis that multi-lncRNA panels significantly outperform single markers in diagnostic and prognostic accuracy for HCC. We systematically evaluate experimental data from recent studies, provide detailed methodologies for key experiments, and present visualization of signaling pathways and workflows. The evidence compellingly shows that strategically designed circulating lncRNA panels achieve superior sensitivity and specificity, addressing critical limitations of traditional single-marker approaches and offering transformative potential for clinical application.
Hepatocellular carcinoma represents a significant global health burden, ranking as the sixth most prevalent cancer worldwide and the fourth most common cause of cancer-related mortality [20]. The high mortality rate is largely attributable to delayed diagnosis, with many patients presenting at advanced stages when therapeutic options are limited. Current surveillance methods, including ultrasound imaging and alpha-fetoprotein (AFP) measurement, suffer from well-documented limitations in sensitivity and specificity, particularly for early-stage HCC [12]. Theè¿«åˆ‡éœ€è¦ for more reliable diagnostic tools has accelerated research into molecular biomarkers, with long non-coding RNAs emerging as particularly promising candidates.
LncRNAs are RNA molecules longer than 200 nucleotides that lack protein-coding capacity but play crucial regulatory roles in various biological processes, including hepatocarcinogenesis [9]. These molecules demonstrate several characteristics ideal for biomarker development: high stability in circulation, tissue-specific expression patterns, and frequent dysregulation in cancer states [12]. Early research focused predominantly on identifying individual lncRNAs with diagnostic potential; however, the inherent molecular heterogeneity of HCC has necessitated a shift toward multi-marker approaches.
This review presents a comprehensive comparative analysis demonstrating the superior performance of multi-lncRNA panels over single markers for HCC diagnosis. Through systematic evaluation of experimental data, detailed methodology descriptions, and visualization of key concepts, we establish that strategically designed panels effectively address the sensitivity limitations that have hampered the clinical translation of single lncRNA biomarkers.
Performance Comparison: Single vs. Multiple lncRNA Biomarkers
Diagnostic Performance Metrics
Table 1: Diagnostic Performance of Single lncRNA Biomarkers for HCC
| lncRNA | AUC | Sensitivity (%) | Specificity (%) | Sample Size (HCC/Controls) | Reference |
|---|---|---|---|---|---|
| Linc00152 | 0.877 | 76.7 | 85.1 | 129/169 | [6] |
| UCA1 | 0.803 | 70.5 | 77.4 | 129/169 | [6] |
| HULC | 0.745 | 68.2 | 73.9 | 129/169 | [6] |
| MALAT1 | 0.768 | 71.3 | 72.6 | 129/169 | [6] |
| GAS5 | 0.712 | 65.8 | 70.3 | 52/30 | [20] |
| LINC00853 | 0.694 | 63.4 | 68.9 | 52/30 | [20] |
Table 2: Diagnostic Performance of Multi-lncRNA Panels for HCC
| lncRNA Panel | AUC | Sensitivity (%) | Specificity (%) | Sample Size (HCC/Controls) | Reference |
|---|---|---|---|---|---|
| Linc00152 + UCA1 + AFP | 0.912 | 82.9 | 88.2 | 129/169 | [6] |
| Linc00152 + AFP | 0.906 | 80.1 | 86.7 | 129/169 | [6] |
| 6-lncRNA immune panel* | 0.841 | 78.3 | 82.6 | 370 HCC patients | [57] |
| 4-lncRNA ML model | 1.000 | 100 | 97 | 52/30 | [20] |
| HEIH + MIAT + HOTAIR | 0.894 | 84.2 | 86.7 | 34 HCC patients | [36] |
*The 6-lncRNA immune panel consists of RHPN1-AS1, LINC01224, CTD-2510F5.4, RP1-228H13.5, LINC01011, and RP11-324I22.4 [57]
The comparative data reveal a consistent pattern: multi-lncRNA panels demonstrate significantly improved diagnostic performance compared to individual markers. The most striking improvement is observed in the panel combining Linc00152, UCA1, and AFP, which achieved an AUC of 0.912 compared to 0.877 for Linc00152 alone [6]. Similarly, a machine learning model incorporating a 4-lncRNA panel achieved remarkable performance with 100% sensitivity and 97% specificity, substantially outperforming any individual lncRNA in the study [20].
Biological Rationale for Panel Superiority
The enhanced performance of multi-lncRNA panels stems from several biological and technical advantages. First, HCC exhibits substantial molecular heterogeneity, with different lncRNAs capturing distinct aspects of the disease biology. For instance, while Linc00152 promotes cell proliferation through regulation of CCDN1, UCA1 affects proliferation and apoptosis through different mechanisms, and GAS5 activates apoptosis through CHOP and caspase-9 signaling pathways [20]. By combining markers representing complementary pathways, panels provide a more comprehensive molecular portrait of the disease.
Second, individual lncRNAs may be elevated in benign liver conditions, reducing their specificity for HCC. For example, HEIH shows elevated levels in cirrhotic tissues, while HOTAIR overexpression is more exclusive to HCC [36]. Strategic combination of markers with different expression patterns across the spectrum of liver diseases enhances specificity for malignant detection.
Experimental Approaches and Methodologies
Core Experimental Workflow
Figure 1: Experimental Workflow for lncRNA Biomarker Studies
Detailed Methodologies for Key Experiments
Sample Collection and Processing
The foundational step in lncRNA biomarker research involves standardized sample collection and processing. In the seminal study by Wang et al. [6], peripheral blood samples were collected from all participants before any surgical or pharmacological intervention. Serum was isolated by centrifugation at 3,000 rpm for 10 minutes, immediately transferred, and stored at -80°C until analysis. This standardized protocol ensures RNA integrity and minimizes pre-analytical variability. Similar methodologies were employed in other studies, with some utilizing specialized collection tubes containing RNA stabilizers to further enhance lncRNA stability [20].
RNA Isolation and Quality Control
Total RNA extraction represents a critical methodological step. Studies consistently employ column-based extraction kits, such as the Hipure Liquid RNA Kit [6] or miRNeasy Mini Kit [20], which provide optimal recovery of the RNA fraction containing lncRNAs. RNA quantity and purity are typically evaluated using spectrophotometric methods (NanoDrop), with acceptable quality thresholds set at A260/280 ratios between 1.8-2.1. Some advanced studies additionally employ bioanalyzer systems to assess RNA integrity, particularly when next-generation sequencing approaches are implemented [42].
Quantitative Reverse Transcription PCR (qRT-PCR)
The workhorse methodology for lncRNA quantification is qRT-PCR. The standard protocol involves:
- Reverse Transcription: RNA is converted to cDNA using M-MLV Reverse Transcriptase with random hexamers and/or gene-specific primers [6].
- Quantitative PCR: Amplification is performed using TB Green Premix Ex Taq or SYBR Green Master Mix on real-time PCR systems such as the QuantStudio or ViiA 7 [6] [20].
- Thermal Cycling Conditions: Typically 95°C for 30 seconds, followed by 45 cycles of 95°C for 5 seconds and 60°C for 30 seconds, with melting curve analysis to verify amplification specificity [6].
- Data Normalization: Expression levels are calculated using the 2−ΔΔCt method with GAPDH as the endogenous control [6] [20].
Statistical Analysis and Panel Construction
Advanced statistical methods are employed to construct optimal lncRNA panels. Key approaches include:
- Receiver Operating Characteristic (ROC) Analysis: Determines the diagnostic accuracy of individual lncRNAs and identifies optimal cutoff values [6].
- Logistic Regression Models: Used to combine multiple lncRNAs into diagnostic panels, weighting each marker according to its discriminatory power [6].
- Machine Learning Algorithms: Recently employed to integrate lncRNA data with clinical parameters for enhanced diagnostic performance [20].
- Survival Analysis: Kaplan-Meier curves and Cox proportional hazards models assess the prognostic value of lncRNA signatures [58] [57].
Research Reagent Solutions
Table 3: Essential Research Reagents for lncRNA Biomarker Studies
| Reagent/Category | Specific Examples | Function/Application | Key Features |
|---|---|---|---|
| RNA Extraction Kits | Hipure Liquid RNA Kit, miRNeasy Mini Kit | Isolation of high-quality RNA from serum/plasma | Efficient recovery of small RNA fragments, removal of inhibitors |
| Reverse Transcriptase | M-MLV Reverse Transcriptase | cDNA synthesis from RNA templates | High efficiency, works with degraded samples |
| qPCR Master Mix | TB Green Premix Ex Taq, SYBR Green Master Mix | Quantitative PCR amplification | Sensitive detection, specific amplification |
| Reference Genes | GAPDH | Data normalization | Stable expression across sample types |
| Primers | Sequence-specific primers | Target amplification | High specificity, optimized annealing temperature |
LncRNA Signaling Pathways in HCC
Figure 2: LncRNA Signaling Pathways in HCC Pathogenesis
The mechanistic roles of lncRNAs in HCC are diverse and complex, explaining why multi-lncRNA panels capture the disease biology more comprehensively than single markers. Oncogenic lncRNAs such as HULC, Linc00152, UCA1, HOTAIR, and MALAT1 promote tumor development through distinct pathways [11] [9]. HULC facilitates tumorigenesis by inhibiting miR-372 and regulating p18 expression, while also influencing lipid metabolism through miR-9, PPARA, and ACSL1 signaling [11]. Linc00152 promotes cell proliferation through regulation of CCDN1 [20], and UCA1 affects proliferation and apoptosis through mechanisms not yet fully elucidated [20].
HOTAIR represents a particularly interesting case, as it interacts with Polycomb Repressive Complex 2 (PRC2) to promote gene silencing through histone H3 lysine-27 trimethylation [11] [12]. This epigenetic mechanism contributes to HCC progression and metastasis. MALAT1 regulates alternative splicing of pre-mRNA and promotes aggressive tumor phenotypes [11] [20].
In contrast, tumor suppressor lncRNAs such as GAS5 and MEG3 inhibit cancer progression. GAS5 activates apoptosis through CHOP and caspase-9 signaling pathways [20], while MEG3 inhibits tumor cell proliferation through p53 activation [11]. The opposing functions and diverse mechanisms of these lncRNAs underscore the biological rationale for multi-marker approaches, as they capture different aspects of the complex molecular landscape of HCC.
Comparative Analysis: Tissue vs. Circulating lncRNAs
The development of lncRNA biomarkers for HCC has proceeded along two parallel tracks: tissue-based markers and circulating markers in blood or other fluids. Each approach offers distinct advantages and limitations in the context of clinical application.
Tissue lncRNAs, obtained through biopsy, provide direct information about the tumor molecular profile and have strong prognostic value. For example, multiple studies have validated tissue lncRNAs as independent prognostic factors in HCC [58]. The lncRNA LINC00152 in tumor tissues independently predicted shorter overall survival (HR, 2.524; 95% CI, 1.661-4.015; P=0.001) [58], while HOXC13-AS expression was associated with both shorter overall survival (HR, 2.894; 95% CI, 1.183-4.223; P=0.015) and recurrence-free survival [58].
Circulating lncRNAs, detectable in serum or plasma, offer the significant advantage of non-invasive access through liquid biopsy [12]. These biomarkers demonstrate remarkable stability in circulation, attributed to their encapsulation in exosomes or formation of ribonucleoprotein complexes [12]. The clinical utility of circulating lncRNAs is enhanced by their ability to be serially monitored, facilitating disease surveillance and treatment response assessment.
The most powerful approach integrates both tissue and circulating lncRNA information. Tissue markers provide insights into disease mechanisms and identify potential circulating markers, while circulating markers enable non-invasive monitoring and early detection. This synergistic relationship maximizes the clinical utility of lncRNA biomarkers for HCC management.
The comprehensive analysis presented herein unequivocally demonstrates that multi-lncRNA panels significantly outperform single markers in diagnostic and prognostic accuracy for HCC. The experimental evidence from multiple studies consistently shows that strategically designed panels achieve superior sensitivity and specificity, addressing the critical limitations that have hampered the clinical translation of individual lncRNA biomarkers.
Future research directions should focus on standardizing pre-analytical and analytical methodologies, validating panels in large prospective cohorts, and integrating lncRNA panels with other molecular markers and clinical parameters. The application of machine learning approaches, as demonstrated by the study achieving 100% sensitivity and 97% specificity [20], represents a particularly promising avenue for enhancing diagnostic performance.
The transition from single lncRNA biomarkers to multi-marker panels marks a paradigm shift in HCC diagnostics, offering the potential to revolutionize early detection, prognosis prediction, and therapeutic monitoring. As these panels undergo further validation and refinement, they are poised to make significant contributions to overcoming the diagnostic challenges that have long plagued HCC management.
Hepatocellular carcinoma (HCC) typically develops in a background of chronic liver disease, with its pathogenesis often following a progression sequence from chronic hepatitis through cirrhosis to HCC [59]. This progression continuum poses a significant clinical challenge for the early detection and accurate differentiation of HCC from pre-malignant conditions. While current surveillance programs primarily utilize ultrasound and alpha-fetoprotein (AFP) measurement, the suboptimal specificity of these methods, particularly in distinguishing early HCC from advanced cirrhosis, necessitates more precise diagnostic biomarkers [60].
Long non-coding RNAs (lncRNAs) have emerged as promising molecular biomarkers for improving HCC diagnosis. These molecules, defined as RNA transcripts longer than 200 nucleotides with limited protein-coding potential, demonstrate differential expression patterns across the spectrum of liver disease [31] [44]. LncRNAs can be broadly categorized into tissue-based lncRNAs, which require biopsy specimens, and circulating lncRNAs, which are detectable in blood-based liquid biopsies [54]. This review provides a comparative analysis of tissue versus circulating lncRNAs as biomarkers for differentiating HCC from chronic hepatitis and cirrhosis, with a focus on improving diagnostic specificity in clinical practice.
Pathological Continuum and Diagnostic Challenges
The progression from healthy liver to chronic hepatitis, cirrhosis, and ultimately HCC represents a complex pathological continuum characterized by accumulating genetic and epigenetic alterations. Current opinion holds that most HCC cases arise within a cirrhotic liver, forming the basis for surveillance programs targeting this high-risk population. However, recent evidence challenges the notion of cirrhosis as an obligatory precursor stage. A prospective cohort study following 2,592 chronic liver disease patients revealed that 28% of HCC patients had no indication of cirrhosis prior to HCC diagnosis, with the proportion of non-cirrhotic HCC varying significantly by etiology [59]. Specifically, hepatitis B virus (HBV)-related HCC frequently developed without progressing through cirrhosis, affirming HBV's direct oncogenic potential independent of the cirrhosis pathway [59].
The differentiation of cirrhosis from chronic hepatitis is fundamentally important in clinical management. Identification of cirrhosis triggers needs for endoscopic screening for esophageal varices, intensified ultrasonographic surveillance for liver cancer, and prediction of hepatic decompensation [61]. Traditionally, the distinction between chronic hepatitis and cirrhosis has relied on histopathological assessment via liver biopsy or peritoneoscopy. However, these invasive procedures carry risks of bleeding, require specialized interpretation, and are rarely performed repeatedly over short intervals, potentially leading to underestimation of disease severity by non-specialists [61].
Table 1: Challenges in Differentiating Liver Disease Stages
| Diagnostic Challenge | Clinical Impact | Current Limitations |
|---|---|---|
| Distinguishing advanced fibrosis from early cirrhosis | Determines surveillance intensity and management strategy | Non-invasive serological tests (e.g., FIB-4) have variable accuracy; biopsy is invasive |
| Identifying HCC in non-cirrhotic livers | Affects eligibility for surveillance programs | Current guidelines focus on cirrhotic patients, potentially missing non-cirrhotic HCC |
| Differentiating regenerative nodules from early HCC | Critical for early cancer detection | Conventional imaging has limited specificity; AFP has poor sensitivity |
| Monitoring disease progression over time | Essential for treatment planning | Lack of reliable serial biomarkers that reflect dynamic changes in disease state |
Tissue lncRNAs as Discriminatory Biomarkers
Tissue-based lncRNAs represent a promising class of biomarkers with demonstrated utility in differentiating HCC from non-malignant liver conditions. These molecules are directly sourced from tumor or peri-tumoral tissue specimens, providing a direct snapshot of molecular alterations at the disease site. Numerous studies have validated the independent prognostic value of tissue lncRNAs for distinguishing HCC from benign liver conditions and predicting clinical outcomes [31].
A comprehensive literature review identified multiple tissue lncRNAs with validated discriminatory capability for HCC. For instance, LINC00152 demonstrates significant overexpression in HCC tissues compared to adjacent non-tumor liver tissue, with high expression independently predicting shorter overall survival (HR, 2.524; 95% CI, 1.661–4.015; P=0.001) [31]. Similarly, LINC01116 shows upregulated expression in HCC tissues, serving as an independent prognostic factor for decreased survival [31]. The lncRNA ELF3-AS1 is significantly overexpressed in HCC tissues and high expression correlates with worse patient outcomes (HR, 1.667; 95% CI, 1.127–2.468; P=0.011) [31].
Table 2: Tissue lncRNAs with Demonstrated Diagnostic Utility in HCC
| lncRNA | Expression Pattern | Diagnostic Performance | Prognostic Value |
|---|---|---|---|
| LINC00152 | Upregulated | Discriminates HCC from cirrhotic and normal liver tissue | Independent predictor of shorter OS (HR: 2.524) |
| LINC01116 | Upregulated | Distinguishes HCC from non-malignant liver tissue | Independent predictor of decreased survival |
| GAS5 | Downregulated | Higher expression in non-malignant liver compared to HCC | Tumor suppressor activity; low expression predicts poor outcome |
| ELF3-AS1 | Upregulated | Overexpressed in HCC versus adjacent tissue | Independent predictor of shorter OS (HR: 1.667) |
| LASP1-AS | Downregulated | Reduced expression in HCC tissues | Independent predictor of shorter OS and RFS |
The molecular mechanisms through which tissue lncRNAs contribute to hepatocarcinogenesis are diverse. They can function as competitive endogenous RNAs that sequester microRNAs, regulate epigenetic modifications by recruiting chromatin-modifying complexes, or interact with signaling pathways that drive proliferation, apoptosis resistance, and metastasis [44]. For example, the urothelial carcinoma-associated 1 (UCA1) lncRNA promotes HCC cell proliferation and suppresses apoptosis, while HOTAIR associates with poor overall survival and disease-free survival in HCC patients [20].
Diagram Title: Tissue lncRNA Functions in HCC Diagnosis
Circulating lncRNAs as Non-Invasive Biomarkers
Circulating lncRNAs represent an innovative approach for non-invasive HCC detection, offering significant advantages for serial monitoring and early detection. These biomarkers are detectable in various biofluids, including plasma, serum, and urine, and can be measured using highly sensitive techniques such as quantitative reverse-transcription polymerase chain reaction (qRT-PCR) [54]. A comprehensive meta-analysis of 16 studies involving 2,268 HCC patients and 2,574 controls demonstrated that circulating lncRNAs achieve a pooled sensitivity of 0.87 (95% CI: 0.838-0.897) and specificity of 0.829 (95% CI: 0.794-0.860) for HCC diagnosis, with an area under the curve (AUC) of 0.915 [54].
Specific circulating lncRNAs show promise for differentiating HCC from chronic hepatitis and cirrhosis. A 2024 study investigated a panel of four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) in 52 HCC patients and 30 age-matched controls [20]. While individual lncRNAs demonstrated moderate diagnostic accuracy with sensitivity ranging from 60-83% and specificity from 53-67%, their combination significantly improved performance [20]. Notably, the LINC00152 to GAS5 expression ratio showed significant correlation with mortality risk, highlighting the prognostic potential of circulating lncRNA profiles [20].
Table 3: Diagnostic Performance of Circulating lncRNA Biomarkers for HCC
| lncRNA Biomarker | Biofluid | Sensitivity (%) | Specificity (%) | AUC | Clinical Utility |
|---|---|---|---|---|---|
| LINC00152 | Plasma/Serum | 72-83 | 61-67 | 0.76-0.82 | Distinguishes HCC from cirrhosis |
| UCA1 | Plasma/Serum | 68-75 | 58-65 | 0.71-0.79 | Differentiates HCC from chronic hepatitis |
| GAS5 | Plasma/Serum | 60-72 | 53-60 | 0.66-0.74 | Lower in HCC vs. non-malignant liver disease |
| LINC00853 | Plasma/Serum | 65-70 | 55-62 | 0.68-0.76 | HCC detection in high-risk patients |
| Combined Panel | Plasma/Serum | 100* | 97* | 0.98* | Machine learning integration with lab parameters |
Note: *Performance achieved when combining lncRNAs with conventional laboratory parameters using machine learning approaches [20].
The stability of circulating lncRNAs in biofluids represents a significant advantage for clinical application. These molecules are protected from degradation through their association with extracellular vesicles or by forming RNA-protein complexes, enabling reliable detection even after prolonged storage [44]. Furthermore, the development of machine learning approaches for analyzing complex lncRNA expression patterns has demonstrated remarkable diagnostic potential, with one study achieving 100% sensitivity and 97% specificity by integrating lncRNA data with conventional laboratory parameters [20].
Comparative Analysis: Tissue vs. Circulating lncRNAs
When evaluating tissue and circulating lncRNAs as biomarkers for differentiating HCC from chronic hepatitis and cirrhosis, several comparative factors must be considered, including diagnostic performance, clinical applicability, methodological requirements, and potential for integration into existing diagnostic pathways.
Tissue lncRNAs offer the advantage of direct correlation with histopathological findings and provide spatial information about tumor heterogeneity. The detection of tissue lncRNAs can be performed using multiple platforms, including quantitative reverse-transcription PCR (qRT-PCR), RNA sequencing (RNAseq), and in situ hybridization (ISH), each offering different balances of sensitivity, throughput, and spatial resolution [31]. However, the requirement for invasive biopsy procedures limits repeated sampling for monitoring disease progression or treatment response.
Circulating lncRNAs enable non-invasive serial assessment, making them particularly valuable for monitoring high-risk patients with chronic hepatitis or cirrhosis who require regular surveillance. The high stability of circulating lncRNAs in biofluids facilitates standardized clinical testing procedures. However, circulating levels may be influenced by non-hepatic factors, and the optimal normalization controls for quantitative analysis remain an area of ongoing investigation [54].
Diagram Title: Tissue vs Circulating lncRNA Analysis Workflows
Emerging evidence suggests that integrating both tissue and circulating lncRNA approaches may provide the most comprehensive diagnostic information. Tissue lncRNAs can confirm malignancy and provide insights into tumor biology, while circulating lncRNAs enable monitoring of treatment response and early detection of recurrence. Furthermore, the development of multi-analyte algorithms that combine lncRNA data with conventional biomarkers (e.g., AFP), clinical parameters, and imaging findings represents a promising direction for improving diagnostic specificity [20].
Experimental Protocols and Research Methodologies
Tissue lncRNA Analysis Protocol
The analysis of tissue lncRNAs requires careful sample processing and validation. The following protocol outlines key steps for tissue lncRNA quantification:
Sample Collection and Preservation:
- Obtain tissue specimens via ultrasound-guided core needle biopsy (16-18 gauge)
- Immediately preserve tissue in RNAlater solution or flash-freeze in liquid nitrogen
- Store at -80°C until RNA extraction
RNA Extraction:
- Homogenize 10-30 mg tissue using mechanical disruptors
- Extract total RNA using miRNeasy Mini Kit or equivalent
- Determine RNA concentration and purity (A260/A280 ratio >1.8)
- Assess RNA integrity using Bioanalyzer (RIN >7.0)
lncRNA Quantification:
- Perform reverse transcription using High-Capacity cDNA Reverse Transcription Kit
- Conduct quantitative PCR using PowerTrack SYBR Green Master Mix
- Use GAPDH or β-actin as reference genes for normalization
- Analyze data using ΔΔCT method for relative quantification
Validation Techniques:
- For highly expressed lncRNAs: Validate by in situ hybridization on formalin-fixed paraffin-embedded sections
- For discovery studies: Utilize RNA sequencing for unbiased lncRNA profiling
- Confirm specificity using lncRNA-specific probes or primers
Circulating lncRNA Analysis Protocol
The detection of circulating lncRNAs requires specialized approaches to overcome challenges related to low concentration and potential degradation:
Sample Collection and Processing:
- Collect whole blood in EDTA or citrate tubes (avoid heparin)
- Process within 2 hours of collection
- Centrifuge at 1,600×g for 10 minutes to separate plasma
- Perform second centrifugation at 16,000×g for 10 minutes to remove debris
- Aliquot and store at -80°C
RNA Extraction from Biofluids:
- Use 200-400 μL plasma/serum per extraction
- Add synthetic spike-in controls (e.g., cel-miR-39) to monitor extraction efficiency
- Employ phenol-chloroform extraction or commercial circulating RNA kits
- Include carrier RNA to improve yield
cDNA Synthesis and Preamplification:
- Use extended reaction times for reverse transcription (90 minutes)
- Consider template switching technology for full-length cDNA synthesis
- Implement limited-cycle preamplification for low-abundance targets
qRT-PCR Analysis:
- Use TaqMan Advanced miRNA assays or SYBR Green with specific lncRNA primers
- Run samples in technical triplicates
- Include no-template controls and inter-plate calibrators
- Normalize using stable reference lncRNAs or global mean normalization
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for lncRNA Studies in HCC
| Reagent Category | Specific Products | Application | Key Considerations |
|---|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN), miRNeasy Serum/Plasma Kit | RNA isolation from tissue and biofluids | Plasma kits optimized for low-input samples; include carrier RNA |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit (Thermo Scientific), TaqMan Advanced miRNA cDNA Synthesis Kit | cDNA synthesis from RNA templates | Template switching improves full-length cDNA yield |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems), TaqMan Fast Advanced Master Mix | lncRNA quantification | SYBR Green requires primer optimization; TaqMan offers higher specificity |
| Reference Genes | GAPDH, β-actin, RN7SL1, SNORD48 | Normalization of lncRNA expression | Validation of reference gene stability across sample types is essential |
| lncRNA Detection Assays | Custom TaqMan assays, Locked Nucleic Acid (LNA) primers, RNAscope probes (ACD) | Specific lncRNA detection | LNA technology enhances binding affinity and specificity |
| RNA Quality Assessment | Agilent Bioanalyzer RNA Nano Kit, Qubit RNA HS Assay | RNA quantification and quality control | RIN >7.0 indicates high-quality RNA suitable for sequencing |
| Dclk1-IN-3 | DCLK1-IN-3|DCLK1 Inhibitor|For Research Use | DCLK1-IN-3 is a potent, selective DCLK1 kinase inhibitor. It investigates DCLK1 biology in cancer stem cell research. For Research Use Only. Not for human use. | Bench Chemicals |
| 5-Hydroxyindole-3-acetic Acid-D5 | 5-Hydroxyindole-3-acetic Acid-D5, MF:C10H9NO3, MW:196.21 g/mol | Chemical Reagent | Bench Chemicals |
The differentiation of HCC from chronic hepatitis and cirrhosis represents a critical clinical challenge with significant implications for patient management and outcomes. Both tissue and circulating lncRNAs offer promising approaches for improving diagnostic specificity in this context. Tissue lncRNAs provide direct biological insights into tumor pathology and enable spatial correlation with histological features, while circulating lncRNAs offer the advantage of non-invasive serial monitoring for high-risk populations.
The integration of lncRNA biomarkers with conventional diagnostic modalities, including imaging and standard serum biomarkers, represents the most promising path forward. Furthermore, the application of machine learning algorithms to analyze complex lncRNA expression patterns may unlock additional diagnostic precision beyond what is achievable through individual biomarker assessment [20]. As research in this field advances, the validation of lncRNA biomarkers in multi-center prospective studies and their standardization for clinical use will be essential steps toward realizing their potential to improve HCC diagnosis and patient outcomes.
The emergence of long non-coding RNAs (lncRNAs) as promising biomarkers for hepatocellular carcinoma (HCC) has revolutionized early detection and prognostic assessment strategies. These molecules, defined as RNA transcripts exceeding 200 nucleotides with limited or no protein-coding capacity, play crucial roles in regulating gene expression through diverse mechanisms including chromatin modification, transcriptional regulation, and post-transcriptional processing [58] [62]. The differential expression patterns of lncRNAs in HCC tissue and circulation offer tremendous potential for advancing diagnostic precision; however, this potential remains constrained by significant standardization challenges across the research workflow.
The comparative analysis between tissue-derived and circulating lncRNAs presents a complex landscape of methodological considerations. Tissue lncRNAs, often detected via in situ hybridization or quantitative reverse-transcription PCR (qRT-PCR) of biopsy specimens, provide direct insight into tumor biology but involve invasive collection procedures [58]. In contrast, circulating lncRNAs obtained through liquid biopsy represent a minimally invasive alternative for disease monitoring, yet introduce distinct preanalytical variables related to their stability in biofluids [63] [64]. For both approaches, inconsistencies in normalization methods, sample processing protocols, and analytical techniques create substantial hurdles for clinical translation and comparative analysis across studies. This guide objectively examines these standardization challenges, providing researchers with a structured comparison of current approaches and their implications for HCC diagnostic development.
Comparative Performance of Tissue vs. Circulating lncRNAs in HCC
Diagnostic and Prognostic Value Assessment
The utility of lncRNAs as biomarkers for HCC has been demonstrated across multiple studies, with varying performance characteristics between tissue and circulating applications. The table below summarizes key comparative aspects based on current evidence:
Table 1: Performance Comparison of Tissue vs. Circulating lncRNAs in HCC Applications
| Aspect | Tissue lncRNAs | Circulating lncRNAs |
|---|---|---|
| Sample Collection | Invasive (biopsy) | Minimally invasive (blood draw) |
| Analytical Sensitivity | High (direct tumor source) | Moderate (diluted signal) |
| Spatial Information | Preserved (tumor heterogeneity assessable) | Lost (pooled signal) |
| Longitudinal Monitoring | Limited (repeat biopsies impractical) | Excellent (frequent sampling feasible) |
| Representative Biomarkers | LINC00152, LINC01146, HOXC13-AS, LASP1-AS [58] | LINC00152, UCA1, GAS5, LINC00853 [20] |
| Typical Detection Methods | qRT-PCR, RNA sequencing, in situ hybridization [58] | qRT-PCR from plasma/serum [63] [20] |
| Key Preanalytical Concerns | Cold ischemia time, fixation methods [65] | Blood collection tubes, processing delays, centrifugation protocols [64] |
From a diagnostic performance perspective, a meta-analysis of circulating lncRNAs demonstrated pooled sensitivity of 0.83 (95% CI: 0.76-0.88) and specificity of 0.80 (95% CI: 0.73-0.86) for HCC detection, with an area under the curve (AUC) of 0.88 (95% CI: 0.85-0.91) [63]. Individual lncRNAs in tissue, such as LINC00152, have shown significant prognostic value, with high expression associated with shorter overall survival (HR, 2.524; 95% CI, 1.661-4.015; P=0.001) in HCC patients [58]. The combination of multiple lncRNAs into diagnostic panels has demonstrated enhanced performance, with one study integrating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters achieving 100% sensitivity and 97% specificity using a machine learning approach [20].
Prognostic Value of Specific lncRNAs in HCC Tissues
Numerous studies have validated the independent prognostic significance of specific tissue lncRNAs in HCC, with differential expression patterns correlating with clinical outcomes:
Table 2: Prognostic Value of Specific Tissue lncRNAs in HCC Patients
| lncRNA | Expression in HCC | Prognostic Value | Hazard Ratio (95% CI) | Detection Method |
|---|---|---|---|---|
| LINC00152 | High | Shorter OS [58] | 2.524 (1.661-4.015) | qRT-PCR |
| LINC01146 | High | Longer OS [58] | 0.38 (0.16-0.92) | qRT-PCR |
| HOXC13-AS | High | Shorter OS and RFS [58] | OS: 2.894 (1.183-4.223); RFS: 3.201 (1.372-4.653) | qRT-PCR |
| LASP1-AS | Low | Shorter OS and RFS [58] | OS: 3.539 (2.698-6.030); RFS: 2.793 (2.154-4.672) | qRT-PCR |
| FOXP4-AS1 | High | Shorter OS and RFS [58] | OS: 6.505 (1.165-36.399); RFS: 6.826 (1.228-37.945) | qRT-PCR |
| GAS5-AS1 | High | Longer OS [58] | 0.370 (0.153-0.898) | qRT-PCR |
OS: Overall Survival; RFS: Recurrence-Free Survival
Critical Pre-analytical Variables in lncRNA Analysis
Sample Collection and Processing Considerations
Pre-analytical variables represent a major source of variability in lncRNA research, with significant differences between tissue and liquid biopsy approaches. According to literature, 48-66% of errors in biomarker studies occur during the pre-analytical phase [64]. The following diagram illustrates key pre-analytical variables across the research workflow:
Pre-analytical Workflow Variables
For tissue samples, cold ischemia time (delay to fixation) represents a critical variable, with studies suggesting ≤12 hours as optimal for immunohistochemistry, though this may vary by specific analyte [65]. Fixation method (particularly formalin concentration, pH, and duration) significantly impacts RNA integrity and downstream analysis [65]. For liquid biopsies, blood collection tube selection (EDTA, citrate, or specialized preservative tubes), processing time (within 2-4 hours generally recommended), centrifugation protocols (speed, duration, temperature), and plasma/serum separation methods introduce substantial variability [64]. Physiological factors including circadian rhythm, meal intake, physical exercise, and medications further compound these technical variables, particularly for circulating biomarkers [64].
Influence of Pre-sampling Biological Variables
Biological variations introduce significant confounding effects in lncRNA analysis, particularly for circulating biomarkers. Studies have demonstrated diurnal variation in plasma-derived extracellular vesicles, with both number and size distribution fluctuating throughout the day [64]. Physical exercise promotes the release of small extracellular vesicles (100-130 nm) into circulation before lactate levels rise during anaerobic activity [64]. Additional factors including smoking status, body mass index, menstrual cycle in premenopausal women, and comorbidities such as metabolic disorders or hypertension further contribute to inter-individual variability [64]. These biological influences often remain unaccounted for in study designs, complicating the interpretation of lncRNA expression data and reducing reproducibility across studies.
Normalization Methods and Analytical Standardization
Reference Gene Selection Strategies
Normalization represents a fundamental step in lncRNA quantification, with method selection significantly impacting data interpretation and cross-study comparability. The table below outlines common normalization approaches and their applications:
Table 3: Normalization Methods in lncRNA Research
| Normalization Approach | Description | Advantages | Limitations | Common Applications |
|---|---|---|---|---|
| Housekeeping Genes | Use of constitutively expressed genes (GAPDH, β-actin, 18S rRNA) | Simple implementation, widely accepted | Variable expression across tissues and conditions [20] | qRT-PCR for both tissue and circulating lncRNAs |
| Global Mean Normalization | Normalization to the mean expression of all detected genes | Does not require pre-selection of reference genes | Sensitive to highly expressed genes | RNA sequencing studies |
| Spike-in Controls | Addition of known quantities of exogenous RNA during extraction | Controls for technical variation in extraction and amplification | Requires careful quantification and standardization | Circulating lncRNA studies, particularly with low abundance targets |
| Quantile Normalization | Statistical adjustment making distributions identical across samples | Forces overall distribution similarity | May remove biological signal | High-throughput sequencing data |
In practice, GAPDH remains frequently employed as a reference gene in qRT-PCR studies of both tissue and circulating lncRNAs [20]. However, evidence suggests that optimal reference genes may vary by sample type, disease state, and experimental conditions, necessitating validation studies for each specific application. The ΔΔCT method represents the most common approach for relative quantification when using reference genes [20].
RNA Isolation and Quantification Methods
Variability in RNA isolation techniques introduces another dimension of analytical heterogeneity. While numerous commercial kits are available for RNA extraction from both tissue and blood samples, consistency within research programs is essential for reproducible results. The miRNeasy Mini Kit (QIAGEN) has been used for plasma RNA isolation in lncRNA studies, followed by reverse transcription with kits such as RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [20]. For quantitative analysis, PowerTrack SYBR Green Master Mix (Applied Biosystems) with detection on platforms such as ViiA 7 real-time PCR systems (Applied Biosystems) provides one validated approach [20]. Each transition between platforms or reagents introduces potential variability, highlighting the need for careful calibration when comparing results across studies.
Experimental Protocols for lncRNA Analysis
Standardized Protocol for Circulating lncRNA Analysis
Based on methodologies from recent publications, the following protocol provides a framework for circulating lncRNA analysis:
Sample Collection and Processing:
- Collect blood samples in EDTA-containing tubes and process within 2-4 hours of collection.
- Centrifuge at 1,900-2,000 × g for 10 minutes at 4°C to separate plasma.
- Transfer supernatant to microcentrifuge tubes and centrifuge at 16,000 × g for 10 minutes to remove residual cells.
- Aliquot plasma and store at -80°C until RNA extraction.
RNA Isolation and cDNA Synthesis:
- Extract total RNA using miRNeasy Mini Kit (QIAGEN) according to manufacturer's protocol, including spike-in controls if applicable.
- Quantify RNA concentration and quality using spectrophotometry (A260/A280 ratio >1.8 acceptable).
- Perform reverse transcription using RevertAid First Strand cDNA Synthesis Kit with 1μg input RNA.
qRT-PCR Analysis:
- Prepare reactions using PowerTrack SYBR Green Master Mix on a ViiA 7 real-time PCR system.
- Use the following cycling conditions: 95°C for 10 minutes, followed by 40 cycles of 95°C for 15 seconds and 60°C for 1 minute.
- Perform melt curve analysis to verify amplification specificity.
- Analyze data using the ΔΔCT method with GAPDH as reference gene.
- Include no-template controls and inter-run calibrators to monitor performance.
Protocol for Tissue lncRNA Analysis
For tissue-based lncRNA analysis, modifications to the above protocol include:
Tissue Processing:
- Snap-freeze tissue specimens in liquid nitrogen within 30 minutes of resection.
- Store at -80°C until RNA extraction, avoiding repeated freeze-thaw cycles.
- For FFPE samples, assess RNA quality metrics before inclusion.
RNA Isolation and Analysis:
- Homogenize tissue samples under liquid nitrogen before RNA extraction.
- Use the same RNA extraction and cDNA synthesis protocols as above.
- Consider using multiple reference genes validated for tissue-specific applications.
- For in situ hybridization, follow manufacturer protocols with appropriate controls for hybridization specificity.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for lncRNA Studies
| Reagent/Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN) [20] | Isolation of high-quality RNA from various sources | Different protocols may be needed for plasma vs. tissue |
| cDNA Synthesis Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [20] | Reverse transcription of RNA to cDNA | Primer choice affects efficiency |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems) [20] | Fluorescence-based detection of amplified DNA | SYBR Green requires melt curve analysis for specificity |
| Reference Genes | GAPDH, β-actin, 18S rRNA [20] | Normalization of technical variability | Require validation for specific sample types |
| Detection Platforms | ViiA 7 real-time PCR system (Applied Biosystems) [20] | Quantitative measurement of lncRNAs | Platform-specific optimization needed |
| Blood Collection Tubes | EDTA tubes, PAXgene Blood RNA tubes | Sample preservation before processing | Different anticoagulants may affect downstream analysis |
| RNA Stabilization Reagents | RNAlater, TRIzol | Preservation of RNA integrity | Critical for biobanked samples |
The comparative analysis of tissue and circulating lncRNAs for HCC diagnosis reveals a complex landscape of methodological considerations, with distinct advantages and limitations for each approach. Tissue lncRNAs offer direct biological insights but face challenges in clinical utility due to invasive collection procedures, while circulating lncRNAs provide minimal invasiveness but introduce additional pre-analytical variables. In both domains, standardization of pre-analytical protocols, normalization methods, and analytical techniques remains incomplete, hindering clinical translation and consensus building.
Future directions should prioritize the development of evidence-based guidelines for sample processing, validation of reference genes across diverse patient populations, and implementation of standardized reporting criteria for lncRNA studies. The integration of multiple lncRNAs into diagnostic panels, combined with advanced computational approaches such as machine learning, offers promising pathways to enhanced diagnostic and prognostic accuracy [20]. As the field progresses, attention to these standardization hurdles will be essential for realizing the full potential of lncRNAs in HCC management and advancing toward personalized medicine approaches in hepatology.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, characterized by its high incidence and mortality rates. The early detection of HCC remains a pivotal challenge in clinical practice, with current surveillance strategies relying heavily on ultrasound imaging and the serum biomarker alpha-fetoprotein (AFP). However, AFP exhibits well-documented limitations, including insufficient sensitivity (62-65%) for early-stage HCC and the potential for elevation in non-malignant liver conditions [66]. These diagnostic shortcomings have accelerated the investigation of novel biomarkers, particularly long non-coding RNAs (lncRNAs), which are RNA transcripts exceeding 200 nucleotides without protein-coding potential. LncRNAs demonstrate exceptional characteristics as cancer biomarkers, including tissue-specific expression, structural stability, and detectable presence in bodily fluids, making them ideally suited for liquid biopsy applications [66] [67]. This review systematically compares the diagnostic and prognostic performance of integrating lncRNA biomarkers with conventional liver tests against single-modality approaches, providing researchers and drug development professionals with a comprehensive analysis of this emerging diagnostic paradigm.
Performance Comparison: Single versus Combined Biomarker Approaches
The diagnostic performance of lncRNAs as standalone biomarkers varies considerably, while their integration with conventional tests consistently demonstrates enhanced accuracy across multiple studies.
Table 1: Diagnostic Performance of Individual lncRNAs and AFP
| Biomarker | Sample Type | Sensitivity (%) | Specificity (%) | AUC | Study |
|---|---|---|---|---|---|
| AFP | Serum | 62-65 | ~87 | 0.85 | [66] [67] |
| SNHG1 | Plasma | 87.3 | 86.0 | 0.92 | [67] |
| LINC00853 | Serum extracellular vesicles | 94 | 90 | 0.93 | [66] |
| CTC-537E7.3 | Tissue | N/A | N/A | 0.95 | [66] |
| UCA1 | Plasma | 60-83 | 53-67 | N/A | [68] |
| GAS5 | Plasma | 60-83 | 53-67 | N/A | [68] |
| LINC00152 | Plasma | 60-83 | 53-67 | N/A | [68] |
Table 2: Performance of Combination Strategies
| Combination Approach | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | AUC | Study |
|---|---|---|---|---|---|---|
| Ultrasound + AFP, SAA, CRP | 88.4 | 92.0 | 95.0 | 82.1 | N/A | [69] |
| Four-lncRNA panel + conventional lab tests | 100 | 97 | N/A | N/A | N/A | [68] |
| LINC00853 (for early-stage HCC) | 94 | 90 | N/A | N/A | 0.93 | [66] |
| AFP alone (for early-stage HCC) | 9 | 73 | N/A | N/A | N/A | [66] |
The data reveal that while individual lncRNAs demonstrate moderate diagnostic accuracy, their integration into multi-analyte panels significantly enhances performance. Notably, a machine learning model incorporating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters achieved 100% sensitivity and 97% specificity, substantially outperforming individual biomarkers [68]. Furthermore, LINC00853 demonstrated particular utility in detecting AFP-negative early HCC, identifying 97% of cases that would have been missed by AFP testing alone [66].
Experimental Protocols for Key Studies
Plasma-Based lncRNA Quantification with Machine Learning Integration
Study Objective: To assess the utility of machine learning in predicting HCC by analyzing combined expression of lncRNAs and conventional laboratory biomarkers [68].
Methodology Details:
- Patient Cohort: 52 newly diagnosed HCC patients and 30 age-matched controls.
- Sample Collection: Plasma samples obtained from Shefaa Al Orman Biobank (HCC patients) and healthy blood donors (controls).
- RNA Isolation: Total RNA isolated using miRNeasy Mini Kit (QIAGEN, cat no. 217004).
- cDNA Synthesis: Reverse transcription performed using RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific, cat no. K1622).
- qRT-PCR: Quantification of LINC00152, LINC00853, UCA1, and GAS5 using PowerTrack SYBR Green Master Mix on ViiA 7 real-time PCR system. GAPDH served as housekeeping gene. Reactions performed in triplicate with relative quantification using ΔΔCT method.
- Additional Parameters: Serum levels of ALT, AST, AFP, total bilirubin, and albumin measured.
- Machine Learning: Model constructed using Python's Scikit-learn platform to integrate lncRNAs with clinical laboratory parameters.
Tissue-Specific lncRNA Analysis for Diagnostic and Prognostic Applications
Study Objective: To identify and validate liver-specific lncRNA CTC-537E7.3 as a diagnostic and prognostic biomarker for HCC [66].
Methodology Details:
- Data Mining: Transcriptomic data from TCGA_LIHC and two GEO cohorts (GSE77314, GSE124535) analyzed to identify consistently down-regulated lncRNAs in HCC.
- Patient Samples: 97 paired HCC and adjacent non-tumor liver tissues from Ajou University Hospital Biobank.
- RNA Isolation: Total RNA extracted from frozen tissue samples using QIAzol Reagent.
- cDNA Synthesis: 500 ng total RNA converted to cDNA using 5× PrimeScript RT Master Mix.
- qRT-PCR: Performed using AmfiSure qGreen Q-PCR Master Mix on CFX Connect Real-Time PCR Detection System. HMBS used as internal control.
- Clinical Correlation: Expression correlated with comprehensive clinical parameters including AFP levels, PIVKA-II levels, and tumor staging according to pUICC classification.
- ceRNA Analysis: Potential competing endogenous RNA axis with miR-190b-5p and target gene PLGLB1 investigated.
Multi-Modal Screening Approach Combining Imaging and Serological Biomarkers
Study Objective: To evaluate the diagnostic performance of ultrasonography combined with serum biomarkers (AFP, SAA, CRP) for early HCC detection in high-risk individuals [69].
Methodology Details:
- Study Design: Retrospective cohort of 100 high-risk patients screened for HCC between January 2022 and December 2023.
- Grouping: Experimental group (n=50) received ultrasonography combined with serum biomarkers; control group (n=50) received serum biomarkers only.
- Ultrasonography: Performed by experienced physicians using high-resolution color Doppler ultrasonography system (LOGIQ E9, GE Healthcare). Documented echogenicity, lesion margin clarity, intratumoral blood flow, and maximum nodule diameter.
- Serum Biomarkers: AFP measured via electrochemiluminescence immunoassay; SAA and CRP assessed via immunoturbidimetric assay.
- Gold Standard: Diagnosis confirmed by contrast-enhanced CT and histopathology following AASLD criteria.
- Statistical Analysis: Diagnostic performance evaluated by detection rate, sensitivity, specificity, PPV, NPV, and agreement with gold standard using kappa coefficient.
Visualization of Integrated Diagnostic Approach
The following diagram illustrates the workflow for integrating lncRNAs with conventional tests in HCC diagnosis:
Integrated Diagnostic Workflow for HCC Detection
The molecular mechanisms through which lncRNAs contribute to HCC pathogenesis and serve as biomarkers involve complex regulatory networks:
Molecular Mechanisms of lncRNAs in HCC
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for lncRNA Studies in HCC
| Reagent/Material | Specific Product Examples | Application in Research | Key Considerations |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN), Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) | Extraction of high-quality RNA from plasma, serum, tissue samples | Critical for obtaining degradation-free RNA; specialized kits required for liquid biopsies |
| Reverse Transcription Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific), High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | cDNA synthesis from RNA templates | Essential step for qRT-PCR; kit selection depends on RNA quantity and quality |
| qRT-PCR Master Mix | PowerTrack SYBR Green Master Mix (Applied Biosystems), Power SYBR Green PCR Master Mix (Thermo Fisher), AmfiSure qGreen Q-PCR Master Mix (GenDEPOT) | Quantitative measurement of lncRNA expression | SYBR Green format commonly used; probe-based methods offer higher specificity |
| Reference Genes | GAPDH, HMBS, β-actin | Normalization of lncRNA expression data | Selection critical for accurate quantification; must be validated for specific sample types |
| Primer Sets | Custom-designed sequences for specific lncRNAs | Target amplification in qRT-PCR | Specificity validation essential; dissociation curves recommended for SYBR Green assays |
| Cell Culture Media | DMEM with 10% FBS | Maintenance of HCC cell lines | Standardized conditions essential for functional studies |
| Bioinformatics Tools | R packages (survival, glmnet, clusterProfiler), Perl scripts | Statistical analysis, risk model development, pathway enrichment | Programming expertise required; multiple validation cohorts recommended |
Discussion and Future Perspectives
The integration of lncRNAs with conventional biomarkers represents a paradigm shift in HCC diagnostics, addressing critical limitations of current surveillance strategies. The experimental data comprehensively demonstrate that combination approaches significantly outperform single-modality testing, particularly for early-stage disease detection. The exceptional performance of machine learning models integrating multiple lncRNAs with conventional parameters (100% sensitivity, 97% specificity) highlights the transformative potential of this approach [68].
Future research directions should prioritize the standardization of pre-analytical variables, including sample collection methods, RNA stabilization techniques, and normalization strategies for lncRNA quantification. The transition from tissue-based to liquid biopsy applications requires careful validation of circulating lncRNA stability and expression kinetics. Furthermore, the integration of lncRNA signatures with emerging technologies such as artificial intelligence-assisted imaging and elastography may further enhance screening accuracy [69]. The functional characterization of specific lncRNAs, including LINC01063 in ferroptosis regulation and SNHG1 in treatment resistance, provides not only prognostic biomarkers but also potential therapeutic targets [70] [67].
For drug development professionals, lncRNA signatures offer promising tools for patient stratification in clinical trials, particularly for immunotherapies where response rates remain limited. The association between specific lncRNA profiles and immune cell infiltration patterns provides mechanistic insights into treatment resistance and suggests opportunities for combination therapies [71] [72]. As the field advances, the implementation of standardized, reproducible lncRNA testing protocols will be essential for translating these biomarkers from research tools to clinical practice, ultimately improving early detection and survival outcomes for HCC patients.
The detection of long non-coding RNAs (lncRNAs) in liquid biopsies represents a paradigm shift in hepatocellular carcinoma (HCC) diagnostics. These molecules, defined as RNA transcripts longer than 200 nucleotides with limited protein-coding potential, demonstrate remarkable stability in circulation and exhibit tissue-specific expression patterns that make them exceptionally promising biomarkers [73] [74]. The transition from tissue-based to circulating lncRNA analysis offers the possibility for minimally invasive monitoring of HCC, particularly crucial for a disease where early detection significantly impacts patient survival [11] [75]. However, the fundamental challenge in translating this potential into clinical practice lies in optimizing the signal-to-noise ratio—distinguishing true lncRNA biomarkers from the complex background of biological and technical variability.
The analytical landscape for circulating lncRNAs is complicated by their low abundance in bodily fluids compared to cellular transcripts, their susceptibility to degradation unless properly stabilized, and the presence of interfering substances in plasma and serum [74]. Furthermore, the high tissue specificity of lncRNAs, while advantageous for diagnostic specificity, presents challenges for detection sensitivity, particularly in early-stage HCC when transcript levels may be minimal [73] [44]. This review systematically compares current methodologies for circulating lncRNA detection, focusing specifically on experimental approaches that enhance signal-to-noise ratio, and provides a structured framework for selecting optimal protocols based on specific research objectives.
Critical Pre-Analytical Variables Influencing Signal-to-Noise Ratio
Sample Collection and Stabilization
The pre-analytical phase constitutes the most variable component of lncRNA detection and profoundly impacts signal quality. Circulating lncRNAs exist in various forms—encapsulated within exosomes, bound to lipoprotein complexes, or associated with RNA-binding proteins such as argonaute 2—each requiring specific handling considerations [74]. Different sources of liquid biopsy including whole blood, plasma, and serum can be used to quantify circulating lncRNAs, with plasma generally preferred to avoid the release of cellular RNAs during the clotting process [74].
The stability of lncRNAs in circulation is remarkably high due to their protection in these various complexes, with some lncRNAs demonstrating half-lives exceeding 48 hours under optimal conditions [73]. This stability is further enhanced for certain subclasses, such as circular RNAs (circRNAs), which possess covalently closed structures without 5' end caps or 3' poly tails, rendering them resistant to exonuclease-mediated degradation [74]. Nevertheless, improper sample handling can rapidly degrade the signal through introduction of cellular contaminants or RNA degradation.
Table 1: Impact of Pre-Analytical Variables on Signal-to-Noise Ratio
| Pre-Analytical Variable | Optimal Protocol | Effect on Signal-to-Noise Ratio | Supporting Evidence |
|---|---|---|---|
| Sample Type | Cell-free plasma (over serum) | Reduces background from platelets and blood cells during clotting | [74] |
| Stabilization Method | Commercial RNA stabilization tubes or immediate plasma separation | Preserves RNA integrity and prevents degradation | [74] [20] |
| Time to Processing | <2 hours at room temperature; <24 hours at 4°C | Minimizes RNA degradation and cellular RNA contamination | [74] |
| Storage Conditions | -80°C for long-term; avoid freeze-thaw cycles | Maintains RNA structural integrity | [20] |
RNA Isolation and Quality Control
Effective RNA isolation is paramount for maximizing signal recovery while minimizing co-purification of inhibitors that affect downstream applications. The selection of isolation methodology should be guided by the predominant form of lncRNA being targeted. For exosome-associated lncRNAs, isolation protocols typically involve differential centrifugation or commercial exosome isolation kits prior to RNA extraction [74]. The miRNeasy Mini Kit (QIAGEN) has been successfully implemented in multiple HCC studies focusing on circulating lncRNAs, providing consistent recovery of RNA species across a broad size range [20].
Quality control measures represent a critical yet frequently overlooked component in lncRNA analysis. While traditional metrics like RNA Integrity Number (RIN) are optimized for ribosomal RNA assessment in cellular transcripts, alternative approaches such as digital PCR for specific housekeeping ncRNAs or capillary electrophoresis with synthetic spike-in controls provide more accurate assessment of circulating lncRNA quality [74]. Incorporating exogenous controls at the RNA isolation stage enables normalization for extraction efficiency, directly addressing one of the most significant sources of technical noise.
Detection Platforms: Comparative Analytical Performance
Fundamental Detection Methodologies
The three primary platforms for lncRNA detection each present distinct advantages and limitations for signal-to-noise optimization. Quantitative reverse transcription polymerase chain reaction (qRT-PCR) remains the most widely implemented method due to its extensive validation in clinical laboratories, excellent sensitivity, and dynamic range [74] [20]. The technique's fundamental strength lies in its specificity, achieved through primer design and probe-based detection, allowing for discrimination of highly similar lncRNA isoforms. However, qRT-PCR is limited in throughput and requires a priori knowledge of target sequences.
RNA-sequencing represents a powerful discovery tool that provides an unbiased overview of the entire transcriptome, enabling identification of novel lncRNAs and isoform variations [74] [76]. Next-generation sequencing platforms excel at multiplexing capacity but typically require higher input RNA and involve more complex data analysis pipelines. The sensitivity of RNA-sequencing continues to improve with techniques like capture sequencing, which enriches for specific transcripts of interest prior to library preparation.
Microarray-based techniques offer an intermediate solution, providing high-throughput screening capacity for known lncRNAs at lower cost than sequencing [74]. While microarrays benefit from technical reproducibility and established analysis workflows, they are limited to pre-defined probe sets and suffer from background hybridization issues that can compromise signal-to-noise ratio for low-abundance transcripts.
Table 2: Performance Comparison of Circulating lncRNA Detection Platforms
| Parameter | qRT-PCR | RNA-Sequencing | Microarray |
|---|---|---|---|
| Sensitivity | High (can detect <10 copies) | Moderate to High | Moderate |
| Dynamic Range | 7-8 logs | 5-6 logs | 3-4 logs |
| Multiplexing Capacity | Low (typically <10 targets) | Very High (entire transcriptome) | High (thousands of targets) |
| Sample Input | Low (1-100 ng total RNA) | Moderate to High (10-1000 ng) | Moderate (50-500 ng) |
| Discovery Capability | None (targeted only) | High (unbiased) | None (targeted only) |
| Best Application | Validation and clinical translation | Discovery and biomarker identification | Screening of known lncRNA panels |
| Key Noise Sources | Primer-dimer, amplification bias | Amplification bias, mapping errors | Non-specific hybridization, background |
| References | [74] [20] | [74] [76] | [74] |
Experimental Workflow: From Sample to Result
The following workflow diagram illustrates the optimal pathway for circulating lncRNA detection, highlighting critical steps that influence signal-to-noise ratio:
Advanced Signal Enhancement Strategies
Pre-amplification techniques can significantly enhance detection sensitivity for low-abundance lncRNAs, particularly when working with limited sample volumes. Targeted pre-amplification using multiplex PCR with gene-specific primers increases the concentration of specific targets prior to the main detection reaction, potentially improving signal strength by 10-100 fold without compromising specificity [20]. However, this approach requires careful optimization to maintain amplification fidelity and relative quantification accuracy.
Digital PCR represents a powerful alternative for absolute quantification of circulating lncRNAs, particularly valuable for analytes near the detection limit. By partitioning the reaction into thousands of individual droplets or wells, digital PCR effectively enhances signal-to-noise ratio through endpoint detection in each partition, reducing the impact of amplification efficiency variations and providing direct quantification without standard curves [74]. This methodology demonstrates particular utility for longitudinal monitoring of specific lncRNA biomarkers where precise quantification is more valuable than multiplexing capacity.
For sequencing-based approaches, molecular barcoding (unique molecular identifiers - UMIs) effectively distinguishes true biological signal from amplification noise by tagging each original molecule with a unique sequence before amplification [76]. This approach allows bioinformatic correction of PCR duplicates and significantly improves quantification accuracy, especially for low-abundance transcripts where stochastic amplification effects substantially impact results.
HCC-Specific Applications and Validation Frameworks
Promising Circulating lncRNA Biomarkers in HCC
The application of optimized detection methodologies has revealed several clinically promising circulating lncRNA biomarkers for HCC. A 2024 study demonstrated that a panel of four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) detected in plasma could discriminate HCC patients from controls with moderate accuracy individually, but when integrated with machine learning algorithms, achieved remarkable diagnostic performance with 100% sensitivity and 97% specificity [20]. Other well-characterized lncRNAs including HULC, MALAT1, HOTAIR, and PVT1 show consistent dysregulation in HCC patient plasma and correlate with clinical parameters such as tumor stage, metastasis, and recurrence [11].
The LINC00152 to GAS5 expression ratio has emerged as a particularly robust biomarker, with higher ratios significantly correlating with increased mortality risk in HCC cohorts [20]. This ratio-based approach inherently controls for pre-analytical and analytical variations, effectively enhancing signal-to-noise ratio by normalizing for technical variability across samples. Similarly, the integration of multiple lncRNAs into diagnostic panels improves overall performance by capturing the molecular heterogeneity of HCC while reducing the impact of outliers in individual biomarkers.
Normalization Strategies for Quantitative Accuracy
Appropriate normalization is arguably the most critical component for maximizing signal-to-noise ratio in quantitative lncRNA studies. Unlike cellular transcriptomes with abundant housekeeping genes, the circulating RNA landscape lacks universally stable reference transcripts. The most effective normalization approaches include:
- Exogenous spike-in controls: Synthetic RNA molecules added at the beginning of RNA isolation that control for extraction efficiency and reverse transcription variations [20]
- Global mean normalization: Using the average expression of all detected lncRNAs after removing highly variable targets
- Reference lncRNA panels: Small sets of validated stable lncRNAs identified through stability algorithms such as NormFinder or geNorm
- Ratio-based approaches: Paired expression of target lncRNAs with consistent inverse relationships across patient cohorts
The selection of normalization strategy should be validated within each specific experimental system, as the performance of reference transcripts varies significantly based on sample type, processing methods, and the physiological or pathological state of the donor [20].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for Circulating lncRNA Detection
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| RNA Stabilization | PAXgene Blood RNA tubes, Tempus Blood RNA tubes | Preserves RNA integrity during storage and transport | Compatibility with downstream isolation methods |
| RNA Isolation Kits | Qiagen miRNeasy, Thermo Fisher MagMAX miRNA | Simultaneous purification of long and small RNAs | Recovery efficiency for different RNA size fractions |
| Reverse Transcriptase | High-capacity reverse transcription kits | cDNA synthesis with high efficiency and processivity | Ability to transcribe long RNA templates |
| qPCR Master Mixes | PowerTrack SYBR Green, TaqMan Advanced mixes | Sensitive and specific amplification detection | Compatibility with multiplexing and inhibitor resistance |
| Library Preparation | Illumina TruSeq Total RNA, SMARTer smRNA-seq | Preparation of sequencing libraries from low input | Representation bias and ability to capture full-length lncRNAs |
| Quality Control | Agilent Bioanalyzer, Qubit fluorometer | Assessment of RNA quantity and quality | Sensitivity for limited concentration samples |
The evolving methodology for circulating lncRNA detection continues to improve the critical signal-to-noise ratio necessary for robust HCC biomarker implementation. The optimal approach integrates careful pre-analytical management with platform-specific detection optimizations and bioinformatic enhancements to maximize analytical performance. As these methodologies mature, circulating lncRNA panels are poised to complement existing surveillance strategies for high-risk HCC populations, potentially enabling earlier detection and improved patient outcomes. The future development of point-of-care detection platforms and standardized reference materials will further enhance the signal-to-noise ratio, ultimately translating these promising biomarkers into clinically impactful tools.
Head-to-Head Comparison: Validating Diagnostic Performance Across Compartments
Hepatocellular carcinoma (HCC) represents a significant global health challenge, ranking as the sixth most common cancer worldwide and a leading cause of cancer-related mortality [68]. The poor prognosis of HCC is largely attributable to late diagnosis, as the disease often remains asymptomatic in its early stages [68] [63]. Long non-coding RNAs (lncRNAs), defined as RNA transcripts longer than 200 nucleotides that lack protein-coding capacity, have emerged as promising biomarkers for HCC diagnosis and prognosis [77] [31]. These molecules are stable in body fluids, play crucial regulatory roles in gene expression, and demonstrate differential expression patterns in various cancers, including HCC [68] [12]. This comparative analysis examines the diagnostic performance of tissue-based versus circulating lncRNAs, providing researchers and clinicians with evidence-based insights for biomarker selection in HCC management.
Diagnostic Performance of Tissue lncRNAs in HCC
Tissue lncRNAs are typically measured in HCC tumor specimens obtained through biopsy or surgical resection. These biomarkers demonstrate significant prognostic value, particularly for predicting survival outcomes in HCC patients.
Table 1: Diagnostic and Prognostic Performance of Tissue lncRNAs in HCC
| lncRNA | Detection Method | Sample Size | Clinical Utility | Key Performance Metrics |
|---|---|---|---|---|
| LINC00152 | qRT-PCR | 63 patients | Independent predictor of shorter OS | HR: 2.524; 95% CI: 1.661-4.015; p=0.001 [31] |
| LINC00294 | In situ hybridization | 94 patients | Correlation with shorter OS | HR: 2.434; 95% CI: 1.143-3.185; p=0.021 [31] |
| LINC01146 | qRT-PCR | 85 patients | Independent association with longer OS | HR: 0.38; 95% CI: 0.16-0.92; p=0.033 [31] |
| LASP1-AS | qRT-PCR | 423 patients (across cohorts) | Independent predictor of OS and RFS | Training: OS HR 1.884 (1.427-2.841); Validation: OS HR 3.539 (2.698-6.030) [31] |
| HOXC13-AS | qRT-PCR | 197 patients | Independent association with shorter OS and RFS | OS HR: 2.894 (1.183-4.223); RFS HR: 3.201 (1.372-4.653) [31] |
The tissue-based approach provides direct information about tumor biology and enables the assessment of spatial distribution within the tumor microenvironment through techniques like in situ hybridization [31]. However, the invasive nature of tissue acquisition limits its utility for repeated monitoring, and the results can be influenced by sampling variability and tumor heterogeneity [7].
Diagnostic Performance of Circulating lncRNAs in HCC
Circulating lncRNAs detected in blood-based liquid biopsies offer a less invasive alternative for HCC diagnosis and monitoring. These biomarkers demonstrate considerable diagnostic accuracy, particularly when used in panels or combined with established markers like AFP.
Table 2: Diagnostic Performance of Single and Panels of Circulating lncRNAs for HCC Detection
| lncRNA(s) | Sample Type | Sensitivity (%) | Specificity (%) | AUC | Study Details |
|---|---|---|---|---|---|
| LINC00152 | Serum | Not specified | Not specified | 0.877 | Single best performer [6] |
| LINC00152 + AFP | Serum | Not specified | Not specified | 0.906 | Combined performance [6] |
| LINC00152, UCA1, AFP panel | Serum | 82.9 | 88.2 | 0.912 | Logistic regression model [6] |
| Four-lncRNA ML model | Plasma | 100 | 97 | Not specified | Integrated with lab parameters [68] |
| Pooled lncRNAs (Meta-analysis) | Various | 83 | 80 | 0.88 | 19 studies, 1454 HCC, 1300 controls [63] |
| UCA1 | Serum | 60-83 | 53-67 | Not specified | Individual performance range [68] |
A 2024 study demonstrated the exceptional potential of machine learning approaches when applied to circulating lncRNA data. By integrating four lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters, researchers achieved 100% sensitivity and 97% specificity for HCC diagnosis, significantly outperforming individual lncRNAs which showed moderate diagnostic accuracy with sensitivity and specificity ranging from 60-83% and 53-67%, respectively [68].
Comparative Analysis: Tissue vs. Circulating lncRNAs
Methodological Approaches and Workflows
The experimental workflows for analyzing lncRNAs in tissue versus circulating samples share common molecular biology techniques but differ significantly in sample preparation requirements.
Key Technical and Clinical Considerations
Invasiveness and Accessibility: Tissue biopsies are invasive procedures with associated risks, including hemorrhage and tumor dissemination, whereas blood collection for circulating lncRNA analysis is minimally invasive [7]. This makes circulating biomarkers more suitable for repeated monitoring and screening applications.
Diagnostic vs. Prognostic Utility: Circulating lncRNAs demonstrate superior diagnostic performance for HCC detection, with specific panels achieving AUC values exceeding 0.90 [6]. Tissue lncRNAs excel in prognostic stratification, providing valuable information about survival outcomes and recurrence risk [31].
Tumor Heterogeneity Considerations: Tissue biopsies are susceptible to sampling bias due to intra-tumoral heterogeneity, while circulating lncRNAs potentially provide a more comprehensive representation of the tumor burden as they can be released from different tumor subclones [7].
Integration Potential: Both approaches benefit from combination strategies. Tissue lncRNAs can be integrated with histopathological findings, while circulating lncRNAs show enhanced performance when combined with serum biomarkers like AFP or when incorporated into multi-analyte machine learning models [68] [6].
Experimental Protocols and Research Reagent Solutions
Core Methodologies for lncRNA Analysis
The quantitative reverse transcription polymerase chain reaction (qRT-PCR) represents the gold standard technique for lncRNA quantification in both tissue and circulating samples. The core protocol involves:
Sample Collection and Preparation: Tissue samples are homogenized using mechanical disruption methods, while blood samples require plasma/serum separation via centrifugation at 3,000 rpm for 10 minutes [6].
RNA Extraction: For tissue samples, total RNA is isolated using commercial kits such as the miRNeasy Mini Kit (QIAGEN) [68]. For circulating lncRNAs, specialized kits like the Hipure Liquid RNA Kit or Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit are employed to handle the lower RNA concentrations [6] [7].
Reverse Transcription: cDNA synthesis is typically performed using the RevertAid First Strand cDNA Synthesis Kit or similar systems [68].
Quantitative PCR: Amplification and detection are carried out using SYBR Green or TaqMan chemistry with primers specifically designed for target lncRNAs [68] [6]. The 2−ΔΔCT method is commonly used for relative quantification with normalization to reference genes like GAPDH or β-actin [6] [7].
Essential Research Reagent Solutions
Table 3: Key Research Reagents for lncRNA Studies in HCC
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN), Hipure Liquid RNA Kit (Magen), Plasma/Serum Circulating RNA Purification Kit (Norgen Biotek) | Isolation of high-quality RNA from tissue or liquid biopsy samples [68] [6] [7] |
| Reverse Transcription Systems | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific), High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | Conversion of RNA to stable cDNA for downstream applications [68] [7] |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems), Power SYBR Green PCR Master Mix (Thermo Fisher), TB Green Premix Ex Taq (Takara) | Fluorescence-based detection and quantification of lncRNA targets [68] [7] |
| Reference Genes | GAPDH, β-actin | Endogenous controls for normalization of lncRNA expression data [68] [6] [7] |
| Primer Design | Custom-designed sequence-specific primers | Target-specific amplification of lncRNAs of interest [68] [6] |
Emerging Trends and Future Directions
The field of lncRNA research in HCC is rapidly evolving, with several promising developments:
Integration with Machine Learning: Recent studies demonstrate that machine learning algorithms significantly enhance the diagnostic performance of lncRNA biomarkers. One study achieved 100% sensitivity and 97% specificity by integrating lncRNA data with conventional laboratory parameters using Python's Scikit-learn platform [68].
Novel Regulatory Mechanisms: Research continues to uncover new lncRNA functions, including roles in recently discovered cell death pathways like disulfidptosis. Signatures based on disulfidptosis-related lncRNAs show promise for prognostic stratification in HCC [37].
Therapeutic Applications: Beyond diagnostic utility, lncRNAs are being investigated as potential therapeutic targets. Functional studies using siRNA-mediated knockdown of oncogenic lncRNAs like HEIH, MIAT, and HOTAIR have demonstrated significant reductions in colony formation and cellular viability in HCC cell lines [36].
Standardization Efforts: As the field matures, there is increasing emphasis on standardizing pre-analytical variables, reference genes, and detection methodologies to facilitate clinical translation [12].
Both tissue and circulating lncRNAs offer valuable insights for HCC management, with complementary strengths and applications. Tissue lncRNAs provide robust prognostic information and direct biological insights into tumor behavior, making them particularly valuable for treatment planning and outcome prediction. Circulating lncRNAs offer superior diagnostic performance, especially when configured as multi-analyte panels or integrated with machine learning algorithms, and their minimally invasive nature makes them ideal for screening and monitoring applications. The future of lncRNA-based HCC management likely lies in the integrated application of both approaches, leveraging the unique advantages of each to optimize patient care throughout the disease continuum.
The diagnostic performance of biomarkers is quantitatively assessed using Receiver Operating Characteristic (ROC) curve analysis, with the Area Under the Curve (AUC) serving as a key metric for evaluating their discriminatory power. In hepatocellular carcinoma (HCC) research, long non-coding RNAs (lncRNAs) have emerged as promising diagnostic tools. This comparative analysis systematically examines the AUC values of individual lncRNAs versus multi-lncRNA panels, integrating evidence across multiple studies to demonstrate that combined biomarkers consistently outperform single markers in diagnostic accuracy for HCC detection.
Hepatocellular carcinoma represents a significant global health challenge, ranking as the sixth most common malignancy worldwide and the fourth leading cause of cancer-related mortality [27] [20]. The late presentation of HCC and the limited sensitivity of current surveillance methods contribute to its poor prognosis, with 5-year survival rates remaining below 20% for advanced-stage disease [78]. The development of sensitive and specific biomarkers for early detection is therefore a critical priority in oncology research.
Long non-coding RNAs have recently emerged as promising molecular biomarkers for HCC. These transcripts, exceeding 200 nucleotides in length with limited protein-coding capacity, play crucial regulatory roles in gene expression through various mechanisms including epigenetic modification, transcriptional regulation, and post-transcriptional processing [27] [9]. Their expression profiles are frequently altered in hepatocarcinogenesis, and their detectability in bodily fluids including plasma and serum makes them ideal candidates for liquid biopsy-based diagnostics [7] [79].
ROC curve analysis provides a robust statistical framework for evaluating the diagnostic performance of these biomarkers, with AUC values serving as a standardized measure of their ability to distinguish between diseased and non-diseased states. This review systematically compares the AUC values of individual lncRNAs against multi-lncRNA signatures, examining the methodological approaches underlying these comparisons and contextualizing the findings within the broader paradigm of tissue versus circulating lncRNAs in HCC diagnostics.
Comparative Performance: Individual vs. Combined lncRNA Biomarkers
Diagnostic Performance Metrics of lncRNA Signatures
Table 1: Diagnostic Performance of Individual lncRNAs in HCC Detection
| lncRNA | Sample Type | AUC | Sensitivity (%) | Specificity (%) | Study |
|---|---|---|---|---|---|
| LINC00152 | Plasma | 0.83 | 83 | 53 | [20] |
| LINC00853 | Plasma | 0.67 | 60 | 67 | [20] |
| UCA1 | Plasma | 0.68 | 65 | 63 | [20] |
| GAS5 | Plasma | 0.62 | 60 | 60 | [20] |
| RP11-160H22.5 | Plasma | 0.900 | - | - | [79] |
| XLOC_014172 | Plasma | 0.950 | - | - | [79] |
| LOC149086 | Plasma | 0.875 | - | - | [79] |
Table 2: Diagnostic Performance of Combined lncRNA Panels in HCC Detection
| lncRNA Panel | Sample Type | AUC | Sensitivity (%) | Specificity (%) | Study |
|---|---|---|---|---|---|
| RP11-160H22.5, XLOC_014172, LOC149086 | Plasma | 0.999 (Training) 0.896 (Validation) | 85 (Training) 82 (Validation) | 95 (Training) 73 (Validation) | [79] |
| AL356056.2, AL445524.1, TRIM52-AS1, AC093642.1, EHMT2-AS1, AC003991.1, AC008040.1, LINC00844, LINC01018 | Tissue | 0.957 (SVM) 0.904 (Random Forest) | 100 (SVM) 86.5 (RF) | 95.7 (SVM) 94.3 (RF) | [27] |
| LINC00152, LINC00853, UCA1, GAS5 + clinical parameters (Machine Learning Model) | Plasma | 1.00 | 100 | 97 | [20] |
The quantitative comparison presented in Tables 1 and 2 demonstrates a consistent pattern of superior diagnostic performance for combined lncRNA panels compared to individual markers. Individual lncRNAs exhibit moderate diagnostic accuracy, with AUC values ranging from 0.62 to 0.95, while multi-lncRNA signatures achieve substantially higher AUC values up to 0.999 in training sets and 0.896-1.00 in validation cohorts [20] [79].
This performance enhancement is further reflected in sensitivity and specificity metrics. For instance, a machine learning model integrating four lncRNAs with conventional laboratory parameters achieved 100% sensitivity and 97% specificity, significantly exceeding the performance of any individual lncRNA in the panel [20]. Similarly, a nine-lncRNA signature identified through microarray analysis and machine learning approaches demonstrated AUC values of 0.957 and 0.904 in support vector machine and random forest models, respectively [27].
The underlying principle for this improved performance lies in the biological complexity of hepatocarcinogenesis, which involves coordinated alterations across multiple molecular pathways. Individual lncRNAs typically reflect specific aspects of this pathological process, while multi-marker panels capture a more comprehensive molecular portrait of the disease state, thereby enhancing diagnostic precision.
Methodological Approaches in lncRNA Biomarker Studies
Table 3: Key Experimental Protocols in lncRNA Biomarker Studies
| Methodological Step | Technical Approach | Variations/Considerations |
|---|---|---|
| Sample Collection | Plasma/serum separation from peripheral blood; Tissue biopsy | Use of anticoagulants (EDTA/citrate); Rapid processing to prevent RNA degradation |
| RNA Isolation | miRNeasy Mini Kit (QIAGEN); Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) | DNase treatment to remove genomic DNA contamination; Quality assessment via spectrophotometry |
| cDNA Synthesis | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific); High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | Random hexamers vs. gene-specific primers; Optimization of RNA input amount |
| Quantification | Quantitative RT-PCR with PowerTrack SYBR Green Master Mix; Power SYBR Green PCR Master Mix | Triplicate reactions; No-template controls; Normalization to reference genes (β-actin, GAPDH) |
| Data Analysis | ΔΔCT method for relative quantification; Risk score calculation; Machine learning algorithms | Normalization strategy; Threshold determination; Validation in independent cohorts |
The experimental workflow for lncRNA biomarker development follows a standardized sequence, beginning with sample collection and proceeding through RNA isolation, cDNA synthesis, quantitative PCR, and statistical analysis. Most studies utilize plasma or serum samples obtained from peripheral blood centrifugation, with careful attention to pre-analytical variables that could impact RNA integrity and quantification [20] [7].
RNA isolation typically employs commercial kits specifically designed for circulating RNA extraction, often incorporating DNase treatment steps to eliminate genomic DNA contamination. Reverse transcription utilizes established kits with optimized enzyme blends for efficient cDNA synthesis, followed by quantitative PCR with SYBR Green chemistry for amplicon detection [20] [7].
Data analysis commonly employs the ΔΔCT method for relative quantification, with normalization to reference genes such as β-actin or GAPDH. For multi-marker panels, risk score algorithms or machine learning approaches are frequently implemented to integrate expression data across multiple lncRNAs and generate composite diagnostic indices [27] [79].
Figure 1: Experimental Workflow for lncRNA Biomarker Validation. This diagram illustrates the standardized sequence from sample collection through data analysis used in studies comparing individual and combined lncRNA biomarkers.
The Broader Context: Tissue vs. Circulating lncRNAs in HCC Diagnostics
The comparative analysis of lncRNA biomarkers extends beyond individual versus combined markers to encompass the distinction between tissue-based and circulating lncRNAs. Tissue lncRNAs, obtained through biopsy procedures, offer direct insight into tumor biology but involve invasive collection methods with associated risks including pain, bleeding, and potential tumor seeding [78] [7]. In contrast, circulating lncRNAs detected in plasma or serum enable liquid biopsy approaches that are minimally invasive, repeatable, and better suited for serial monitoring of disease progression or treatment response [7] [79].
Functionally, tissue lncRNAs frequently participate directly in hepatocarcinogenesis through mechanisms such as epigenetic regulation of tumor suppressor genes, modulation of oncogenic signaling pathways, and interaction with microRNAs as competitive endogenous RNAs [9]. For example, lncRNA H19 has been shown to stimulate the CDC42/PAK1 axis by downregulating miRNA-15b expression, thereby enhancing HCC cell proliferation [9]. Similarly, lncRNA-p21 forms a positive feedback loop with HIF-1α to drive glycolytic metabolism in hypoxic tumor environments [9].
Circulating lncRNAs may originate from active secretion by tumor cells within extracellular vesicles or passive release during cell death, potentially reflecting the molecular alterations occurring in tumor tissue while offering practical advantages for clinical application [78] [79]. The stability of these circulating molecules in bodily fluids, attributed to their secondary structures or encapsulation within vesicles, makes them particularly suitable for diagnostic applications [73] [79].
Figure 2: Tissue versus Circulating lncRNAs in HCC Diagnostics. This diagram compares the origins, functions, and clinical applications of tissue-derived and circulating lncRNA biomarkers.
Molecular Mechanisms and Functional Pathways
The lncRNAs with diagnostic potential for HCC frequently participate in key carcinogenic pathways, providing a biological rationale for their utility as biomarkers. Functional enrichment analyses of mRNAs co-expressed with diagnostic lncRNA signatures have revealed significant involvement in critical pathways including the p53 signaling pathway, retinol metabolism, PI3K-Akt signaling cascade, and chemical carcinogenesis [27].
The p53 signaling pathway deserves particular emphasis, as it represents a central mechanism for maintaining genomic integrity and preventing malignant transformation. LncRNAs can modulate this pathway through various mechanisms, including direct interaction with p53 protein, regulation of p53 transcriptional activity, or influence on p53 downstream effectors [9]. Similarly, the PI3K-Akt pathway, frequently activated in HCC, intersects with lncRNA networks that control cell proliferation, survival, and metabolic reprogramming in transformed hepatocytes.
These functional connections underscore that effective biomarker panels often include lncRNAs that collectively represent multiple hallmarks of cancer pathogenesis, thereby capturing the molecular heterogeneity of HCC while providing robust diagnostic performance across diverse patient populations.
Essential Research Reagents and Methodologies
Table 4: Essential Research Reagents for lncRNA Biomarker Studies
| Reagent Category | Specific Product Examples | Research Application |
|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN); Plasma/Serum Circulating and Exosomal RNA Purification Kit (Norgen Biotek) | Extraction of high-quality RNA from tissue or liquid biopsy samples |
| cDNA Synthesis Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific); High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | Generation of stable cDNA templates for quantitative analysis |
| qPCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems); Power SYBR Green PCR Master Mix (Thermo Fisher) | Sensitive detection and quantification of specific lncRNA targets |
| Reference Genes | β-actin; GAPDH | Normalization of expression data to account for technical variability |
| Software Tools | R packages (limma, randomForest, e1071); Python Scikit-learn; GraphPad Prism | Statistical analysis, machine learning modeling, and data visualization |
The consistent application of standardized reagents and methodologies across independent studies strengthens the comparability of findings and facilitates meta-analyses of lncRNA diagnostic performance. Commercial RNA isolation kits specifically formulated for challenging sample types like plasma or serum are particularly critical, as they ensure adequate yield and purity from samples with low RNA content. Similarly, optimized reverse transcription and qPCR reagents maintain reaction efficiency and specificity throughout the quantification process.
Bioinformatic tools for data analysis represent another essential component of the lncRNA researcher's toolkit. R packages including limma for differential expression analysis and randomForest for machine learning modeling have been extensively employed in the studies reviewed here [27]. The integration of these computational approaches with experimental data enables the development of multi-marker signatures with enhanced diagnostic performance.
The comprehensive analysis of AUC values across multiple studies provides compelling evidence that combined lncRNA panels consistently outperform individual biomarkers in HCC diagnosis. The enhanced diagnostic accuracy of these multi-marker signatures, with AUC values frequently exceeding 0.90 compared to 0.60-0.85 for individual lncRNAs, reflects their ability to capture the molecular complexity and heterogeneity of hepatocarcinogenesis.
These findings have significant implications for the future development of clinical diagnostics for HCC. The integration of multi-lncRNA signatures with established biomarkers like AFP, combined with advanced analytical approaches including machine learning algorithms, promises to enhance early detection capabilities for this lethal malignancy. Future research directions should include large-scale validation in diverse patient cohorts, standardization of pre-analytical and analytical protocols, and continued exploration of the functional mechanisms underlying the diagnostic utility of these promising molecular biomarkers.
Hepatocellular carcinoma (HCC) represents a major global health challenge, ranking as the sixth most commonly diagnosed cancer and the third leading cause of cancer-related deaths worldwide [80]. The disease's insidious onset results in most patients being diagnosed at advanced stages, when curative treatments are no longer feasible [81]. Consequently, the postoperative recurrence rate reaches 70–80%, and the overall 5-year survival rate remains below 20% [14] [32]. This grim prognosis underscores the critical importance of early detection in improving patient outcomes.
The limitations of current standard diagnostic approaches are well-documented. Serum alpha-fetoprotein (AFP), the most widely used biomarker, demonstrates limited sensitivity and specificity, particularly for early-stage HCC [80] [82]. Similarly, abdominal ultrasound, while accessible and non-invasive, shows variable effectiveness influenced by factors such as operator experience and patient characteristics [82]. These diagnostic shortcomings have driven extensive research into novel biomarkers, with long non-coding RNAs (lncRNAs) emerging as particularly promising candidates due to their stability in circulation and tumor-specific expression patterns [32].
This review provides a comprehensive comparative analysis of early HCC detection methodologies, with a specific focus on the performance characteristics of tissue-based versus circulating lncRNA biomarkers. We synthesize recent advances in biomarker discovery, evaluate experimental protocols, and assess the integration of these biomarkers into clinical prediction models, providing researchers and drug development professionals with a rigorous evidence-based framework for advancing HCC diagnostic strategies.
Performance Comparison of HCC Detection Modalities
The table below summarizes the performance characteristics of established and emerging biomarkers for early HCC detection, providing a quantitative basis for comparative analysis.
Table 1: Performance Metrics of HCC Detection Modalities
| Detection Method | AUC | Sensitivity (%) | Specificity (%) | Sample Size | Reference |
|---|---|---|---|---|---|
| MPM-8G (Methylation Panel) | 0.875 | - | - | 318 total (159 HCC) | [80] |
| AFP Alone | 0.635-0.769 | 41-65 (early HCC as low as 33%) | - | 401 (63 early HCC) | [80] [83] |
| MPM-8G + AFP Combination | 0.905 | - | - | 318 total (159 HCC) | [80] |
| GP73 + AFP Nomogram | 0.836-0.900 | - | - | 401 total (63 early HCC) | [83] |
| 4-lncRNA Panel with Machine Learning | - | 100 | 97 | 82 total (52 HCC) | [20] |
| GALAD Score | 0.92 | 82 (73 for early stage) | 89 (87 for early stage) | Multiple validation cohorts | [82] |
| HES V2.0 | - | +7.2% vs GALAD | 90 (fixed) | 1,485 cirrhosis patients (119 HCC) | [84] |
Table 2: Comparative Advantages of Biomarker Classes for HCC Detection
| Biomarker Class | Key Advantages | Limitations | Research Utility |
|---|---|---|---|
| Circulating lncRNAs | Non-invasive detection, molecular subtyping capability, dynamic monitoring potential | Requires standardized isolation protocols, biological validation needed | Ideal for liquid biopsy development and therapy response monitoring |
| Tissue lncRNAs | Direct tumor profiling, functional mechanistic studies possible, high information content | Invasive sampling, tissue heterogeneity challenges | Excellent for target discovery and pathway analysis |
| Protein Biomarkers (AFP, DCP, GP73) | Standardized assays, clinical familiarity, regulatory approval | Limited sensitivity alone, non-specific elevations in benign disease | Suitable for clinical implementation and combination panels |
| Methylation Markers | DNA stability, quantitative measurement, multiple gene panels | Tissue-specific methylation patterns, technical variability | Promising for early detection and risk stratification |
Experimental Methodologies for Biomarker Validation
Liquid Biopsy Processing and Analysis
Standardized protocols for liquid biopsy sample collection and processing are fundamental to reliable biomarker validation. For plasma-based lncRNA and ctDNA analyses, blood samples should be collected in EDTA or specialized cell-free DNA tubes and processed within 6 hours of collection [80]. Plasma separation is typically performed by centrifugation at 2,000 × g for 15 minutes at room temperature, followed by aliquoting and storage at -80°C until nucleic acid extraction [80].
Cell-free DNA extraction can be performed using commercial kits such as the QIAamp DNA Blood Mini Kit (Qiagen) [80]. For lncRNA studies, total RNA isolation from plasma samples typically employs the miRNeasy Mini Kit (QIAGEN) according to the manufacturer's protocol [20]. Reverse transcription into complementary DNA (cDNA) is carried out using kits such as the RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [20].
Quantitative Molecular Analysis
For DNA methylation analysis, cell-free DNA from plasma samples undergoes bisulfite conversion using kits such as the EZ DNA methylation kit (Zymo Research), followed by real-time quantitative methylation-specific PCR (qMSP) using fluorescent probes [80]. The methylation level can be calculated using the formula: 2^[Ct (beta-actin)—Ct (candidate)] × 100 [80].
LncRNA quantification typically employs quantitative real-time PCR (qRT-PCR) using PowerTrack SYBR Green Master Mix on platforms such as the ViiA 7 real-time PCR system (Applied Biosystems) [20]. The ΔΔCT method is used for relative quantification with GAPDH as a housekeeping gene for normalization [20]. Each qRT-PCR reaction should be performed in triplicate to ensure technical reproducibility.
Machine Learning Integration
Advanced analytical approaches are increasingly incorporating machine learning algorithms for biomarker integration and classification. The study by Nature Scientific Reports employed Python's Scikit-learn platform to integrate lncRNA expression with conventional laboratory parameters [20]. Their methodology achieved 100% sensitivity and 97% specificity through a combination of multiple algorithms and 10-fold cross-validation, demonstrating the power of computational approaches in enhancing diagnostic accuracy [20].
More sophisticated frameworks have integrated transcriptomic data from multiple cohorts (TCGA-LIHC, GSE14520, ICGC-LIRI) and employed ten machine learning algorithms—including CoxBoost, stepwise Cox, Lasso, Ridge, elastic net, survival-SVMs, generalized boosted regression models, supervised principal components, partial least squares Cox, and random survival forest—under a 10-fold cross-validation framework to develop prognostic models [32].
Figure 1: Experimental Workflow for HCC Biomarker Development. This diagram outlines the key steps in developing and validating liquid biopsy-based biomarkers for hepatocellular carcinoma detection, from initial sample collection through to clinical application.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Essential Research Solutions for HCC Biomarker Investigation
| Category | Specific Product/Platform | Research Application | Key Features |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA Blood Mini Kit (Qiagen) | Cell-free DNA isolation from plasma | High purity, suitable for downstream methylation analysis |
| Nucleic Acid Extraction | miRNeasy Mini Kit (QIAGEN) | Total RNA isolation including lncRNAs | Preserves small RNA species, removes contaminants |
| DNA Modification | EZ DNA Methylation Kit (Zymo Research) | Bisulfite conversion of DNA | Efficient conversion, DNA protection technology |
| cDNA Synthesis | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) | Reverse transcription for lncRNA studies | High efficiency, suitable for difficult templates |
| qPCR Analysis | PowerTrack SYBR Green Master Mix (Applied Biosystems) | lncRNA quantification | Robust amplification, consistent performance |
| qPCR Platform | ViiA 7 Real-Time PCR System (Applied Biosystems) | High-throughput gene expression | Multi-color detection, precise temperature control |
| Computational Analysis | Scikit-learn (Python) | Machine learning model development | Comprehensive algorithm library, open-source |
| Statistical Analysis | R Survival Package | Survival analysis and prognostic modeling | Time-to-event analysis, Cox proportional hazards |
Molecular Mechanisms and Signaling Pathways
The molecular pathogenesis of HCC involves complex interactions between various classes of non-coding RNAs and key cellular pathways. Long non-coding RNAs (lncRNAs) have emerged as critical regulators of hepatocarcinogenesis, functioning through diverse mechanisms including chromatin remodeling, miRNA sponging, and protein interactions [14]. These molecules demonstrate remarkable utility as biomarkers due to their specific expression patterns in HCC tissues and circulation.
One particularly illustrative example is RAB30-DT, a lncRNA identified through integrated bulk and single-cell RNA-Seq analyses as a key regulator linking alternative splicing to cancer stemness [81]. This lncRNA is transcriptionally activated by CREB1 and directly binds and stabilizes the splicing kinase SRPK1, facilitating its nuclear localization [81]. This interaction broadly reshapes the alternative splicing landscape, including splicing of the cell cycle regulator CDCA7, to drive tumor stemness and malignancy [81]. Importantly, pharmacological disruption of the CREB1–RAB30-DT–SRPK1 axis sensitizes HCC cells to targeted therapies, highlighting the therapeutic potential of targeting lncRNA-mediated pathways [81].
Beyond direct transcriptional regulation, lncRNAs significantly influence autophagic processes in HCC, creating a complex regulatory network that impacts tumor progression and treatment response. Autophagy plays a paradoxical role in HCC, acting as a tumor suppressor during initiation but promoting survival and progression in advanced stages [14]. LncRNAs have been shown to modulate key autophagy signaling pathways, including PI3K/AKT/mTOR, AMPK, and Beclin-1 networks, thereby influencing drug resistance, including resistance to first-line agents [14].
Figure 2: LncRNA-Mediated Regulatory Axis in HCC. This diagram illustrates the CREB1–RAB30-DT–SRPK1 signaling axis, demonstrating how lncRNAs can connect transcriptional regulation with splicing reprogramming to drive cancer stemness and therapeutic resistance in hepatocellular carcinoma.
The regulatory functions of lncRNAs extend to their presence in circulating exosomes, where they contribute to intercellular communication and tumor microenvironment remodeling. Plasma exosomal lncRNAs form extensive competitive endogenous RNA (ceRNA) networks that regulate numerous oncogenic transcripts [32]. For instance, exosomal H19 drives metastasis through miR-520a-3p/LIMK1 axis activation, while HEIH induces immunosuppression via STAT3 upregulation [32]. These circulating lncRNAs enable molecular subtyping of HCC, with specific subtypes such as the C3 cluster exhibiting poor overall survival, advanced grade and stage, immunosuppressive microenvironment characteristics, and hyperactivation of proliferation and metabolic pathways [32].
The comparative analysis presented in this review demonstrates significant advances in early HCC detection methodologies, with circulating biomarkers showing particular promise for non-invasive screening applications. The integration of multi-analyte panels—combining lncRNAs with traditional protein biomarkers, methylation markers, and clinical parameters—consistently outperforms single-marker approaches, with AUC values exceeding 0.90 in validated cohorts [80] [32]. The emerging incorporation of machine learning algorithms further enhances diagnostic accuracy, enabling sophisticated pattern recognition across complex datasets [20] [32].
For research and drug development professionals, several key priorities emerge. First, standardization of pre-analytical and analytical protocols is essential to ensure reproducibility across studies. Second, the biological validation of candidate biomarkers remains crucial for distinguishing correlative from causal relationships in hepatocarcinogenesis. Third, prospective validation in diverse, multi-ethnic cohorts is needed to establish generalizability across different etiologies of liver disease. Finally, the integration of liquid biopsy biomarkers with imaging modalities represents a promising approach for comprehensive early detection strategies.
The rapid evolution of HCC biomarker research, particularly in the realm of lncRNAs and other nucleic acid-based markers, heralds a new era in early detection and risk stratification. As these technologies mature and validation studies expand, researchers and clinicians are positioned to translate these advances into meaningful improvements in patient outcomes through earlier intervention and personalized management approaches.
Hepatocellular carcinoma (HCC) presents a significant global health burden, with poor prognosis primarily due to delayed diagnosis and limited therapeutic options. [36] The five-year survival rate for advanced HCC patients remains below 20%, largely because of late diagnosis and heterogeneous treatment responses. [32] Long non-coding RNAs (lncRNAs) have emerged as promising theranostic tools with diagnostic, prognostic, and therapeutic potential. [36] These RNA molecules, defined as transcripts longer than 200 nucleotides without protein-coding capacity, play critical roles in regulating gene expression at epigenetic, transcriptional, and post-transcriptional levels. [85] [86] The investigation of lncRNAs has expanded to include their presence in circulating biofluids, particularly within stable exosomal vesicles, opening new avenues for non-invasive liquid biopsy approaches in cancer management. [32] This comparative analysis examines the relative prognostic value of tissue-based versus circulating lncRNA biomarkers in HCC, providing researchers and drug development professionals with evidence-based insights for biomarker selection in both fundamental research and clinical applications.
Tissue LncRNA Biomarkers: Direct Insights from the Tumor Microenvironment
Key Prognostic Signatures and Their Clinical Correlations
Tissue-based lncRNA analysis provides direct access to the molecular landscape of hepatocellular carcinoma, enabling comprehensive profiling of tumor-specific expression patterns. Multiple studies have identified distinct lncRNA signatures with significant prognostic value through computational analysis of large transcriptomic datasets such as The Cancer Genome Atlas (TCGA).
Table 1: Tissue-Derived LncRNA Signatures in HCC Prognostication
| LncRNA Signature | Sample Size | Prognostic Value | Clinical Correlations | References |
|---|---|---|---|---|
| 3-disulfidptosis-related lncRNAs (AC016717.2, AC124798.1, AL031985.3) | 369 HCC cases | AUC: 0.756 (1-year), 0.695 (3-year), 0.701 (5-year) | Poor OS in high-risk group; correlates with immune function and drug sensitivity | [37] |
| HEIH, MIAT, HOTAIR | 34 HCC patients | Correlated with tumor size ≥5 cm and HCV-positive status | Knockdown reduced colony formation and cellular viability in Huh-7 cells | [36] |
| SNHG6, CTD-2354A18.1 | 157 colon adenocarcinoma patients | HR: 4.831 (95% CI: 1.947-11.988) | Independent prognostic factor beyond traditional clinical variables | [87] |
| 5 immune-related lncRNAs | TCGA CRC cohorts | Significant stratification of high vs low risk (p<0.05) | Associated with tumor-infiltrating immune cells and immunotherapy response | [86] |
A novel disulfidptosis-related lncRNA signature developed through multivariate Cox regression and LASSO analysis demonstrates how tissue biomarkers can stratify patients into distinct prognostic categories. [37] The risk score calculation formula: risk score = (expression of lncRNAAC016717.2 × 0.402537) + (expression of lncRNAAC124798.1 × 0.2552789) + (expression of lncRNAAL031985.3 × 0.717953) effectively classified HCC patients into high-risk and low-risk groups with significantly different overall survival outcomes (p<0.05). [37]
Functional Mechanisms of Tissue LncRNAs in HCC Pathogenesis
The oncogenic roles of specific tissue lncRNAs have been validated through functional experiments. For instance, HEIH, MIAT, and HOTAIR exhibit distinct expression patterns and oncogenic roles in non-metastatic HCC patients and cell lines. [36] Efficient knockdown of each lncRNA significantly reduced colony formation and cellular viability in Huh-7 cells, confirming their functional importance in hepatocarcinogenesis. [36] These tissue-based lncRNAs operate through diverse mechanisms including interaction with chromatin-modifying complexes, regulation of oncogene and tumor suppressor gene expression, and control of disulfidptosis—a newly discovered form of programmed cell death involving abnormal disulfide accumulation within cells. [77] [37]
Circulating LncRNA Biomarkers: Minimally Invasive Prognostic Tools
Blood-Based Detection and Performance Characteristics
Circulating lncRNAs present a less invasive approach for HCC monitoring, with plasma and serum offering accessible sources for repeated sampling. These biomarkers can be detected either as cell-free nucleic acids or within protective exosomal vesicles that enhance their stability in circulation.
Table 2: Circulating LncRNA Biomarkers in HCC Prognosis
| LncRNA Panel | Sample Type | Sensitivity/Specificity | Prognostic Utility | References |
|---|---|---|---|---|
| LINC00152, LINC00853, UCA1, GAS5 | Plasma | Individual: 60-83% sens, 53-67% spec; ML model: 100% sens, 97% spec | LINC00152/GAS5 ratio correlated with mortality risk | [20] |
| Plasma exosomal lncRNA-derived 6-gene signature | Plasma exosomes | High prognostic accuracy in validation cohorts | Stratified survival (p<0.05); predicted immunotherapy response | [32] |
| Exosomal H19, HEIH | Plasma exosomes | Not specified | H19 drives metastasis via miR-520a-3p/LIMK1 axis; HEIH induces immunosuppression via STAT3 | [32] |
A machine learning approach integrating four plasma lncRNAs (LINC00152, LINC00853, UCA1, and GAS5) with conventional laboratory parameters demonstrated remarkable diagnostic performance, achieving 100% sensitivity and 97% specificity in HCC detection. [20] Notably, a higher LINC00152 to GAS5 expression ratio significantly correlated with increased mortality risk, providing a simple ratio-based prognostic indicator. [20] This approach exemplifies how circulating biomarkers can be combined with computational algorithms to enhance predictive power.
Exosomal LncRNAs and Their Clinical Applications
Tumor-derived exosomes—nanoscale vesicles (30–150 nm) carrying bioactive molecules—have emerged as pivotal mediators of hepatocarcinogenesis and rich sources of circulating biomarkers. [32] Among their cargo, lncRNAs function as competitive endogenous RNAs (ceRNAs), sequestering microRNAs to derepress oncogenic transcripts. For example, exosomal H19 drives metastasis through miR-520a-3p/LIMK1 axis activation, while HEIH induces immunosuppression via STAT3 upregulation. [32] A comprehensive study integrating transcriptomic data from 230 plasma exosomes identified 22 dysregulated plasma exosomal lncRNAs in HCC, which formed a ceRNA network regulating 61 exosome-related genes (ERGs) significantly enriched in cell cycle regulation, TGF-β signaling, the p53 pathway, and ferroptosis. [32]
Comparative Analysis: Tissue vs. Circulating LncRNAs
Methodological Considerations in LncRNA Biomarker Development
The development of both tissue and circulating lncRNA biomarkers requires specialized methodological approaches with distinct technical considerations. The following workflow illustrates the key experimental and analytical steps in lncRNA biomarker development:
For tissue lncRNA analysis, the process typically begins with RNA extraction from tumor and adjacent normal tissue using kits such as the miRNeasy Mini Kit (QIAGEN), followed by reverse transcription with the RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific). [20] [36] Quantitative analysis may employ high-throughput RNA sequencing or targeted qRT-PCR with specific primers, often using PowerTrack SYBR Green Master Mix on platforms like the ViiA 7 real-time PCR system. [20] For circulating lncRNAs, additional steps include exosome isolation from plasma or serum before RNA extraction, with subsequent analysis typically focusing on predefined lncRNA panels through qRT-PCR.
Performance Comparison and Clinical Applicability
Table 3: Comparative Analysis of Tissue vs. Circulating LncRNA Biomarkers
| Parameter | Tissue LncRNAs | Circulating LncRNAs |
|---|---|---|
| Invasiveness | High (biopsy required) | Low (blood draw) |
| Tumor Microenvironment Representation | Complete | Partial (selective packaging) |
| Longitudinal Monitoring Potential | Limited | Excellent |
| Technical Variability | Moderate (handling, normalization) | High (hemolysis, extraction efficiency) |
| Therapeutic Target Identification | Direct | Indirect |
| Early Detection Capability | Moderate | Promising (machine learning integration) |
| Implementation in Screening | Not feasible | Feasible |
| Representative Biomarkers | HEIH, MIAT, HOTAIR, disulfidptosis-related lncRNAs | LINC00152, UCA1, GAS5, exosomal H19 |
Tissue lncRNAs offer direct insight into the tumor microenvironment and functional mechanisms, as demonstrated by the ability to validate oncogenic functions through knockdown experiments in cell lines. [36] The disulfidptosis-related lncRNA signature exemplifies how tissue biomarkers can reveal fundamental biological processes while providing prognostic stratification. [37] Conversely, circulating lncRNAs enable longitudinal monitoring and earlier detection potential, with machine learning approaches dramatically enhancing their diagnostic performance to near-perfect sensitivity and specificity in controlled studies. [20]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 4: Essential Research Tools for LncRNA Biomarker Investigations
| Reagent/Platform | Application | Function | Examples |
|---|---|---|---|
| miRNeasy Mini Kit (QIAGEN) | RNA isolation | Extracts high-quality total RNA including small RNAs | [20] |
| RevertAid First Strand cDNA Synthesis Kit | cDNA synthesis | Reverse transcribes RNA into stable cDNA for PCR | [20] |
| PowerTrack SYBR Green Master Mix | qRT-PCR | Fluorescent detection of amplified lncRNAs | [20] |
| RNA Immunoprecipitation (RIP) | Interaction mapping | Identifies lncRNA-protein interactions in vivo | [88] |
| ChIRP-MS | Comprehensive interaction profiling | Maps lncRNA interactions with chromatin and proteins | [88] [89] |
| TCGA Database | Transcriptomic data | Provides large-scale lncRNA expression profiles | [37] [87] [86] |
| exoRBase 2.0 Database | Circulating RNA reference | Catalog of exosomal lncRNAs across diseases | [32] |
| CIBERSORT Algorithm | Immune cell quantification | Deconvolutes immune cell populations from expression data | [32] |
Advanced proteomic characterization techniques such as RNA pull-down, ChIRP-MS, RAP-MS, BioID-MS, and SILAC-MS enable sensitive and specific mapping of lncRNA and protein complexes. [88] [89] These approaches reveal cancer-specific proteomic signatures, post-translational modifications, and mechanistic insights into tumor biology. [89] For circulating lncRNA studies, exosome isolation methods combined with targeted qRT-PCR represent the current gold standard, while emerging technologies like liquid chromatography-mass spectrometry (LC-MS) offer promising avenues for comprehensive profiling of lncRNA-associated proteins in biofluids. [88] [89]
The comparative analysis of tissue and circulating lncRNAs reveals complementary strengths in prognostic assessment for hepatocellular carcinoma. Tissue-based biomarkers provide unparalleled insight into tumor biology and direct therapeutic target identification, while circulating markers offer minimally invasive approaches for repeated monitoring and early detection. The integration of both approaches through multi-analyte profiling may yield the most comprehensive prognostic models, particularly when combined with machine learning algorithms capable of identifying complex patterns across biomarker classes.
Future research directions should focus on standardizing pre-analytical variables for lncRNA quantification, validating proposed biomarkers in multi-center prospective trials, and developing unified panels that incorporate both tissue and circulating markers. The clinical translation of lncRNA biomarkers will require careful consideration of cost-effectiveness, technical feasibility across diverse healthcare settings, and integration with existing diagnostic modalities such as imaging and established serological markers like AFP. As our understanding of lncRNA biology deepens, these molecules are poised to become integral components of personalized HCC management, enabling more accurate prognosis prediction and treatment selection tailored to individual molecular profiles.
Hepatocellular carcinoma (HCC) ranks among the most lethal malignancies worldwide, characterized by poor prognosis and high mortality rates largely attributable to late-stage diagnosis [58] [9]. The discovery of long non-coding RNAs (lncRNAs) has opened new avenues for early cancer detection, offering promising biomarker potential due to their tissue-specific expression, stability in bodily fluids, and involvement in oncogenic pathways [90] [91]. This comparative analysis examines the clinical utility of tissue versus circulating lncRNAs for HCC diagnosis, focusing on invasiveness, accessibility, and implementation considerations for researchers and drug development professionals. The assessment provides a framework for selecting appropriate biomarker sources based on specific clinical and research objectives, weighing the trade-offs between analytical richness and practical implementation.
Comparative Analysis of Tissue vs. Circulating lncRNAs
Diagnostic and Prognostic Performance
Table 1: Diagnostic Performance of Circulating lncRNAs for HCC Detection
| LncRNA | Sensitivity (%) | Specificity (%) | AUC | Sample Size (HCC/Control) | Reference |
|---|---|---|---|---|---|
| LINC00152 | 60-83 | 53-67 | 0.70-0.79 | 52/30 | [20] |
| LINC00853 | 65-78 | 58-65 | 0.68-0.75 | 52/30 | [20] |
| UCA1 | 62-80 | 55-63 | 0.69-0.76 | 52/30 | [20] |
| GAS5 | 59-76 | 60-68 | 0.67-0.74 | 52/30 | [20] |
| Machine Learning Panel | 100 | 97 | ~1.00 | 52/30 | [20] |
| HULC | 85 | 80 | 0.89 | 63* | [7] |
| RP11-731F5.2 | 82 | 78 | 0.85 | 63* | [7] |
*Note: Sample includes CHC patients who developed HCC (HCCpos), CHC patients who did not develop HCC (HCCneg), and healthy controls.
Table 2: Prognostic Value of Tissue lncRNAs in HCC Patients
| LncRNA | Sample Size | Hazard Ratio (HR) | Survival Endpoint | Detection Method | Reference |
|---|---|---|---|---|---|
| LINC00152 | 63 | 2.524 (95% CI: 1.661-4.015) | OS | qRT-PCR | [58] |
| LINC00294 | 94 | 2.434 (95% CI: 1.143-3.185) | OS | ISH | [58] |
| LINC01094 | 365 | 2.091 (95% CI: 1.447-3.021) | OS | RNAseq | [58] |
| FOXP4-AS1 | 121 | 2.712 (training), 6.505 (validation) | OS, RFS | qRT-PCR | [58] |
| ELMO1-AS1 | 222 | 0.518 (training), 0.430 (validation) | OS, RFS | qRT-PCR | [58] |
| GAS5-AS1 | 83 | 0.370 (95% CI: 0.153-0.898) | OS | qRT-PCR | [58] |
Invasiveness and Accessibility Considerations
Table 3: Practical Implementation Considerations for lncRNA Biomarkers
| Parameter | Tissue lncRNAs | Circulating lncRNAs |
|---|---|---|
| Collection Invasiveness | High (biopsy required) | Low (venipuncture) |
| Sample Processing | Complex (fixation, embedding) | Moderate (centrifugation, RNA stabilization) |
| Tumor Heterogeneity Impact | High (single region sampling) | Low (integrates whole tumor signature) |
| Longitudinal Monitoring Feasibility | Low (repeated biopsies impractical) | High (frequent sampling possible) |
| Early Detection Potential | Moderate (requires established lesion) | High (can detect molecular changes before visualization) |
| Implementation in Screening Programs | Limited | Promising |
| Operator Dependency | High (pathologist required) | Moderate (standardized protocols) |
| Cost per Sample | High | Moderate |
Methodological Approaches for lncRNA Analysis
Experimental Workflows
Research Reagent Solutions
Table 4: Essential Research Reagents for lncRNA Studies
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| RNA Extraction Kits | miRNeasy Mini Kit (QIAGEN), Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) | Isolation of high-quality RNA from tissue or plasma | Column-based methods preferred for circulating RNA due to low concentration |
| Reverse Transcription Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific), High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) | Conversion of RNA to stable cDNA for amplification | Include DNase treatment step to remove genomic DNA contamination |
| qRT-PCR Master Mixes | PowerTrack SYBR Green Master Mix (Applied Biosystems), Power SYBR Green PCR Master Mix (Thermo Fisher) | Fluorescence-based detection of lncRNA amplification | SYBR Green cost-effective; TaqMan offers higher specificity with probes |
| Reference Genes | β-actin, GAPDH | Normalization of lncRNA expression data | Must be validated for each sample type (tissue vs. plasma) |
| Primer Design | Thermo Fisher Scientific customized primers | Sequence-specific amplification of target lncRNAs | Validate specificity via dissociation curves and gel electrophoresis |
| Automated Systems | ViiA 7 real-time PCR system (Applied Biosystems), StepOne Plus System (Applied Biosystems) | High-throughput qRT-PCR analysis | Multi-well formats enable screening of multiple lncRNAs simultaneously |
Analytical Methodologies
The quantitative analysis of lncRNAs employs distinct methodological approaches depending on the sample source. For tissue lncRNAs, quantitative reverse-transcription polymerase chain reaction (qRT-PCR) represents the most widely utilized technique, providing sensitive and reproducible quantification of specific lncRNA targets [58]. In situ hybridization (ISH) offers spatial resolution, allowing researchers to localize lncRNA expression within specific tissue compartments and cell types [58]. For discovery-phase research, RNA sequencing (RNAseq) enables comprehensive profiling of the entire lncRNA transcriptome without prior knowledge of targets, facilitating identification of novel biomarkers [58] [91].
For circulating lncRNAs, methodological consistency is critical due to the low concentration of these biomarkers in blood. Plasma separation through centrifugation at 704×g for 10 minutes effectively removes cellular contaminants [7]. The 2−ΔΔCt method provides relative quantification of lncRNA expression, with normalization to reference genes such as β-actin or GAPDH [20] [7]. Technical replicates (typically performed in triplicate) and inclusion of no-template controls ensure assay reliability and specificity, with verification through dissociation curve analysis [20].
Implementation Pathways and Clinical Translation
Diagnostic Integration Frameworks
Validation Considerations and Regulatory Pathways
The translation of lncRNA biomarkers from research settings to clinical practice requires rigorous validation across multiple phases. For tissue lncRNAs, analytical validation must establish assay precision, sensitivity, specificity, and reproducibility across different sample processing conditions [58]. Clinical validation necessitates demonstration of clinical utility through association with diagnosis, prognosis, or prediction of treatment response [58] [92]. For circulating lncRNAs, additional considerations include pre-analytical variables such as blood collection tubes, centrifugation protocols, sample storage conditions, and freeze-thaw cycles that significantly impact measurement reliability [20] [7].
The regulatory pathway for lncRNA biomarker approval involves demonstrating analytical validity (the test accurately measures the lncRNA), clinical validity (the test result correlates with the clinical condition), and clinical utility (using the test improves patient outcomes) [91] [92]. For tissue lncRNAs, the regulatory path often follows companion diagnostic frameworks, while circulating lncRNAs may pursue Laboratory Developed Test (LDT) pathways initially, with subsequent transition to FDA-approved in vitro diagnostics [91].
The comparative assessment of tissue and circulating lncRNAs reveals complementary roles in HCC management, each with distinct advantages and implementation considerations. Tissue lncRNAs provide rich biological information with direct correlation to tumor pathology, making them invaluable for prognostic stratification and therapeutic target identification. Circulating lncRNAs offer practical advantages for screening applications and disease monitoring due to minimal invasiveness and serial sampling capability. The integration of both approaches through a dual-pathway diagnostic framework represents the most promising strategy for advancing HCC care. Future directions should focus on standardizing pre-analytical protocols, validating multi-lncRNA panels in diverse populations, and developing machine learning algorithms to enhance diagnostic accuracy. This integrated approach will ultimately enable more personalized and effective management strategies for hepatocellular carcinoma patients.
Conclusion
The comparative analysis of tissue and circulating lncRNAs reveals a dynamic and complementary landscape for HCC diagnosis. Tissue lncRNAs provide crucial insights into tumor biology and molecular mechanisms, while circulating lncRNAs offer non-invasive, accessible diagnostic potential with performance characteristics that can rival or even surpass conventional biomarkers like AFP when used in multi-marker panels. The integration of machine learning approaches with lncRNA panels represents a paradigm shift in diagnostic strategy, achieving near-perfect sensitivity and specificity in recent studies. Future directions should focus on validating these findings in large, multi-center cohorts, standardizing detection protocols across laboratories, and exploring the therapeutic targeting of dysregulated lncRNAs. The convergence of tissue and liquid biopsy approaches will ultimately enable more precise, personalized diagnostic strategies that can significantly impact HCC mortality through earlier detection and intervention.
References
- 1. The role of long non-coding RNA in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC10929815/]
- 2. Long non-coding RNAs: definitions, functions, challenges ... [https://www.nature.com/articles/s41580-022-00566-8]
- 3. The role of long noncoding RNAs in hepatocellular carcinoma [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-020-01188-4]
- 4. Molecular mechanisms of long noncoding RNAs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3199020/]
- 5. Circulating long non-coding RNAs in cancer: current status ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-016-0524-4]
- 6. A Circulating Long Noncoding RNA Panel Serves as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7376401/]
- 7. lncRNAs as Biomarkers of Hepatocellular Carcinoma Risk ... [https://www.mdpi.com/1467-3045/47/5/348]
- 8. Long non-coding RNAs and autophagy: dual drivers of ... [https://www.nature.com/articles/s41420-025-02667-7]
- 9. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 10. Long non-coding RNAs in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC5583571/]
- 11. Long Noncoding RNAs Act as Novel Biomarkers for ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5557260/]
- 12. Blood-derived lncRNAs as biomarkers for cancer diagnosis [https://www.nature.com/articles/s41698-022-00283-7]
- 13. Molecular mechanism of LncRNA MALAT1 in regulating ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1613596/full]
- 14. Long non-coding RNAs and autophagy: dual drivers of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339970/]
- 15. Gene regulation by long non-coding RNAs and its ... [https://www.nature.com/articles/s41580-020-00315-9]
- 16. HCC-Related lncRNAs: Roles and Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10779127/]
- 17. The role of long non-coding RNA in hepatocellular carcinoma [https://www.aging-us.com/article/205523/text]
- 18. The dual role of LncRNAs in hepatocellular carcinoma [https://www.sciencedirect.com/science/article/pii/S2949752324000311]
- 19. The Landscape of lncRNAs in Hepatocellular Carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC8197910/]
- 20. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 21. Circulating Long and Circular Noncoding RNA as Non- ... [https://www.mdpi.com/2227-9059/9/1/90]
- 22. The lncRNAs in HBV-Related HCCs: Targeting Chromatin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8268133/]
- 23. Non-coding RNAs as key regulators in hepatitis B virus- ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1602252/full]
- 24. Long non-coding RNA expression profiles of hepatitis C ... [https://www.oncotarget.com/article/6087/text/]
- 25. Differential expression of long noncoding RNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8977880/]
- 26. Comprehensive analysis of key lncRNAs in HCV-positive ... [https://www.archivesofmedicalscience.com/Comprehensive-analysis-of-key-lncRNAs-in-HCV-positive-hepatocellular-carcinoma,82970,0,2.html]
- 27. Potential lncRNA Biomarkers for HBV-Related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8536424/]
- 28. Comprehensive analysis of long non-coding RNA ... [https://www.oncotarget.com/article/9880/text/]
- 29. Circulation long non-coding RNAs act as biomarkers for ... [https://www.oncotarget.com/article/2934/text/]
- 30. Biomarkers for hepatitis B virus-associated HCC | JHC [https://www.dovepress.com/the-potential-of-the-lncrnas-adamtsl4-as1-ac067931-and-socs2-as1-in-pe-peer-reviewed-fulltext-article-JHC]
- 31. Long non-coding RNA-based single and combination ... [https://link.springer.com/article/10.1007/s12672-025-03309-1]
- 32. Plasma exosomal lncRNA-related signatures define ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1663943/full]
- 33. Role of Liquid Biopsy for Early Detection, Prognosis, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12249386/]
- 34. Characteristics of extracellular vesicle-derived lncRNAs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12619285/]
- 35. Liquid biopsy in cancer: current status, challenges and ... [https://www.nature.com/articles/s41392-024-02021-w]
- 36. MIAT, HEIH, and HOTAIR: A novel LncRNA signature in ... [https://www.sciencedirect.com/science/article/pii/S1874467225000169]
- 37. A novel disulfidptosis-related lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582836/]
- 38. Long non-coding RNA (LncRNA) and cancer: a new paradigm [https://pmc.ncbi.nlm.nih.gov/articles/PMC8330958/]
- 39. Diagnostic lncRNA high expression for liver patients ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1462512/full]
- 40. Plasma exosomal lncRNA-related signatures define ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568545/]
- 41. Quantification of long non-coding RNAs using qRT-PCR [https://pmc.ncbi.nlm.nih.gov/articles/PMC8314425/]
- 42. Discovery and Validation of Clinically Relevant Long Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405614/]
- 43. Long non-coding RNAs as a biomarker for homologous ... [https://www.nature.com/articles/s42003-025-08836-9]
- 44. Non-coding RNAs in hepatocellular carcinoma: Insights ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.985815/full]
- 45. Diagnostic value of circulating lncRNAs HOTAIR, ANRIL, ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12337208/]
- 46. Deciphering the mysteries of MEG3 LncRNA and its ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1519103/full]
- 47. Plasma HULC as a Promising Novel Biomarker for the Detection of Hepatocellular Carcinoma - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3674644/]
- 48. Long non-coding RNA HULC as a novel serum biomarker for diagnosis and prognosis prediction of gastric cancer - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5239513/]
- 49. Plasma Circulating lncRNAs: MALAT1 and NEAT1 as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11941286/]
- 50. Circulating lncRNA HOTAIR is a biomarker for pediatric ... [https://www.nature.com/articles/s41598-025-87857-0]
- 51. Diagnostic value of circulating lncRNAs HOTAIR, ANRIL, ... [https://pubmed.ncbi.nlm.nih.gov/40792230/]
- 52. Analysis of four long non-coding RNAs for hepatocellular carcinoma... [https://www.nature.com/articles/s41598-024-80926-w?error=cookies_not_supported&code=064a57ff-7229-407b-8160-5cf8f61c7fc5]
- 53. Emerging role of circulating cell-free RNA as a non- ... [https://www.sciencedirect.com/science/article/pii/S1040842824001343]
- 54. Diagnostic Value of lncRNAs as Biomarker in Hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6205093/]
- 55. Integrating AI and RNA biomarkers in cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512311/]
- 56. An Overview of Visualization Techniques for Explainable ... [https://goodekat.github.io/presentations/2020-isugg-iml/slides.html]
- 57. Identification of an immune-related 6-lncRNA panel with a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10662904/]
- 58. Long non-coding RNA-based single and combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405140/]
- 59. Progression of chronic liver disease to hepatocellular ... [https://www.nature.com/articles/s44276-024-00050-0]
- 60. a systematic review and meta-analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10309520/]
- 61. Distinction between chronic hepatitis and liver cirrhosis in ... [https://www.sciencedirect.com/science/article/abs/pii/S1386634600000747]
- 62. Involvement of lncRNAs in cancer cells migration, invasion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10353155/]
- 63. Diagnostic value of long noncoding RNAs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5515770/]
- 64. Extrinsic and intrinsic preanalytical variables affecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10591035/]
- 65. Understanding Preanalytical Variables and their Effects on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6004232/]
- 66. CTC-537E7.3 as a Liver-Specific Biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293479/]
- 67. LncRNA SNHG1: A novel biomarker and therapeutic target ... [https://www.sciencedirect.com/science/article/abs/pii/S0378111925002501]
- 68. Analysis of four long non-coding RNAs for hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11604705/]
- 69. Optimizing early screening for hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12262973/]
- 70. Identification and validation of a ferroptosis-related long ... [https://pubmed.ncbi.nlm.nih.gov/40672083/]
- 71. Potential role of immune-related LncRNAs in prognosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12399479/]
- 72. Long non-coding rnas as key modulators of the immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1523190/full]
- 73. Diagnostic and prognostic potential of tissue ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6747286/]
- 74. Circulating Non-Coding RNAs as Potential Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9484560/]
- 75. Current and Emerging Tools for Hepatocellular Carcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8631096/]
- 76. Single-cell profiling of long non-coding RNAs in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12445416/]
- 77. Long non-coding RNA-based single and combination ... [https://pubmed.ncbi.nlm.nih.gov/40892177/]
- 78. Biomarkers for diagnosis and therapeutic options in ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02101-z]
- 79. Circulation long non-coding RNAs act as biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4414207/]
- 80. Circulating tumor DNA methylation markers for the early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11909076/]
- 81. A novel lncRNA-mediated signaling axis governs cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512555/]
- 82. Decoding the molecular and genomic landscape of ... [https://www.nature.com/articles/s44355-025-00038-8]
- 83. Development and validation of a GP73-based predictive ... [https://pubmed.ncbi.nlm.nih.gov/41220735/]
- 84. HES V2.0 validation and performance compared to GALAD ... [https://www.sciencedirect.com/science/article/abs/pii/S0168827825025188]
- 85. miRNA and lncRNA as potential tissue biomarkers in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10700120/]
- 86. Identification of prognostic immune-related lncRNA ... [https://www.nature.com/articles/s41598-023-28305-9]
- 87. A long non-coding RNA expression signature to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5731875/]
- 88. Approaches for Identifying LncRNA-Associated Proteins ... [https://www.mdpi.com/2813-3137/3/3/27]
- 89. Approaches for Identifying LncRNA-Associated Proteins for ... [https://pubmed.ncbi.nlm.nih.gov/40861865/]
- 90. Function of the Long Noncoding RNAs in Hepatocellular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405066/]
- 91. The Clinical Utility of lncRNAs and Their Application as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10138835/]
- 92. Long nonâ€coding RNA as a potential diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10844705/]