UHPLC-MS/MS Lipidomic Profiling in Diabetes and Hyperuricemia: Biomarker Discovery, Pathways, and Clinical Translation
The co-occurrence of diabetes mellitus (DM) and hyperuricemia (HUA) presents a significant clinical challenge, with growing evidence pointing to shared underlying disturbances in lipid metabolism.
UHPLC-MS/MS Lipidomic Profiling in Diabetes and Hyperuricemia: Biomarker Discovery, Pathways, and Clinical Translation
Abstract
The co-occurrence of diabetes mellitus (DM) and hyperuricemia (HUA) presents a significant clinical challenge, with growing evidence pointing to shared underlying disturbances in lipid metabolism. This article explores the application of Ultra-High-Performance Liquid Chromatography-Tandem Mass Spectrometry (UHPLC-MS/MS) for comprehensive lipidomic profiling to unravel the complex metabolic interplay in this comorbidity. We detail the foundational discoveries of specific lipid biomarkers and perturbed pathways, such as glycerophospholipid and glycerolipid metabolism. The discussion covers methodological best practices for UHPLC-MS/MS analysis, common troubleshooting scenarios, and the critical process of analytical and clinical validation. By integrating findings from recent studies, this review highlights the translational potential of lipidomics in developing diagnostic tools and personalized therapeutic strategies for patients with concurrent diabetes and hyperuricemia, ultimately aiming to improve risk prediction and clinical outcomes.
Unraveling the Lipid Landscape: Core Discoveries in Diabetes and Hyperuricemia
Clinical and Epidemiological Intersection
The comorbidity of Diabetes Mellitus (DM) and Hyperuricemia (HUA) represents a significant and growing challenge in metabolic medicine. Epidemiologically, these conditions are deeply intertwined. Hyperuricemia, defined as a serum uric acid (SUA) level exceeding 7.0 mg/dL in men or 6.0 mg/dL in women, ranks as the second most prevalent metabolic disorder after diabetes itself [1]. In China, the prevalence of HUA in the general population has been reported at 17.7% and can be as high as 21.24% among diabetic patients [2] [1]. This association is not merely coincidental but reflects shared pathophysiological underpinnings, as research indicates that for every 1 mg/dL increase in serum uric acid, the risk of developing diabetes increases by 17% [2].
The relationship between these conditions exhibits complex, sometimes paradoxical characteristics. A large-scale study from the Korean National Health and Nutrition Examination Survey found that hyperuricemia was associated with a decreased prevalence of diabetes mellitus in men (OR: 0.44) while simultaneously correlating with an increased prevalence of metabolic syndrome in both sexes [3]. This dual nature of uric acid—acting as both an antioxidant and a pro-oxidant depending on context—complicates the clinical picture and necessitates deeper investigation into the underlying mechanisms [4].
Table 1: Global Prevalence of Diabetes and Hyperuricemia
| Condition | Overall Prevalence | Prevalence in Diabetic Populations | Key Diagnostic Criteria |
|---|---|---|---|
| Diabetes Mellitus (DM) | 10.5% globally (536.6 million) [2] | - | Fasting blood glucose ≥7.0 mmol/L or random blood glucose >11.0 mmol/L [2] |
| Hyperuricemia (HUA) | 13.3%-17.7% in China [2] [5] | 21.24% in China [1] | SUA >420 μmol/L in men, >360 μmol/L in women [2] |
| DM-HUA Comorbidity | - | 20.70% in North America [1] | Co-occurrence of both conditions |
Lipidomic Alterations in Comorbid Diabetes-Hyperuricemia
Advanced lipidomic technologies, particularly UHPLC-MS/MS, have revealed profound disruptions in lipid metabolism in patients with combined diabetes and hyperuricemia. A 2025 study employing untargeted lipidomic analysis identified 1,361 lipid molecules across 30 subclasses in patient plasma, with 31 significantly altered lipid metabolites in the diabetes-hyperuricemia (DH) group compared to healthy controls [2]. The most prominent changes included significant upregulation of 13 triglycerides (TGs), 10 phosphatidylethanolamines (PEs), and 7 phosphatidylcholines (PCs), while one phosphatidylinositol (PI) was notably downregulated [2].
These alterations are not merely quantitative but represent fundamental shifts in lipid homeostasis. A separate multi-omics study on hyperuricemia patients confirmed 33 significantly upregulated lipid metabolites involved in five key metabolic pathways: arachidonic acid metabolism, glycerophospholipid metabolism, linoleic acid metabolism, glycosylphosphatidylinositol (GPI)-anchor biosynthesis, and alpha-linolenic acid metabolism [6]. The convergence of findings across studies highlights the centrality of glycerophospholipid and glycerolipid metabolism in this comorbidity.
Table 2: Key Altered Lipid Classes in Diabetes-Hyperuricemia Comorbidity
| Lipid Class | Change in DH Patients | Specific Examples | Biological Significance |
|---|---|---|---|
| Triglycerides (TGs) | Significant upregulation (13 TGs) [2] | TG(16:0/18:1/18:2) [2] | Energy storage, cardiovascular risk indicators |
| Phosphatidylethanolamines (PEs) | Significant upregulation (10 PEs) [2] | PE(18:0/20:4) [2] | Membrane structure, cell signaling |
| Phosphatidylcholines (PCs) | Significant upregulation (7 PCs) [2] | PC(36:1) [2] | Membrane integrity, lipoprotein assembly |
| Sphingomyelins (SMs) | Altered in T2DM with dyslipidemia [7] | SM(d18:1/24:0), SM(d18:1/16:1) [7] | Membrane microdomains, signaling pathways |
| Ceramides (Cer) | Altered in T2DM with dyslipidemia [7] | Cer(d18:1/24:0) [7] | Insulin resistance, apoptosis induction |
UHPLC-MS/MS Methodologies for Lipidomic Profiling
Sample Preparation and Extraction
The integrity of lipidomic analysis begins with meticulous sample preparation. In standard protocols, 100 μL of plasma is mixed with 200 μL of 4°C water and 240 μL of pre-cooled methanol before adding 800 μL of methyl tert-butyl ether (MTBE) for lipid extraction [2]. The mixture undergoes 20 minutes of sonication in a low-temperature water bath and 30 minutes of standing at room temperature, followed by centrifugation at 14,000 g for 15 minutes at 10°C [2]. The upper organic phase is collected and dried under nitrogen before being reconstituted for analysis. Quality control samples should be prepared by mixing equal volumes of all sample extracts and randomly inserted into the analysis sequence to ensure analytical consistency [2].
Chromatographic Separation
For chromatographic separation, the methodology typically employs a Waters ACQUITY UPLC BEH C18 column (2.1 mm × 100 mm, 1.7 μm particle size) maintained at 45°C [2] [6]. The mobile phase consists of: Mobile Phase A: 10 mM ammonium formate in acetonitrile-water solution, and Mobile Phase B: 10 mM ammonium formate in acetonitrile-isopropanol solution [2]. The gradient elution program generally starts at 30% mobile phase B (0-2 minutes), increases to 100% B (2-25 minutes), and is maintained before re-equilibration [6]. A constant flow rate of 300 μL/min with a 3 μL injection volume provides optimal separation conditions [6].
Mass Spectrometric Detection
The mass spectrometric analysis employs Q-Exactive series Orbitrap mass spectrometers or similar high-resolution instruments capable of accurate mass measurement [6] [8]. Typical source conditions include: heater temperature: 300°C, sheath gas flow rate: 45 arb, auxiliary gas flow rate: 15 arb, spray voltage: 3.0 kV (positive) or 2.5 kV (negative), and capillary temperature: 350°C [6]. Data acquisition involves full scans at a resolution of 70,000 at m/z 200 for MS1, with data-dependent MS2 scans at a resolution of 17,500 for top N precursors [6]. This configuration enables simultaneous identification and quantification of hundreds of lipid species across multiple classes.
Disrupted Metabolic Pathways and Signaling Mechanisms
The intersection of diabetes and hyperuricemia manifests in distinct metabolic pathway disruptions. Multivariate analyses reveal that glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) represent the most significantly perturbed pathways in diabetes-hyperuricemia patients [2]. These pathways are central to membrane integrity, signaling transduction, and energy homeostasis. The comparison of diabetes-hyperuricemia versus diabetes-alone groups identified 12 differential lipids also predominantly enriched in these same core pathways, underscoring their fundamental role in the pathophysiology of hyperuricemia complicating diabetes [2].
Beyond glycerophospholipid disruptions, research has highlighted the importance of sphingolipid metabolism, particularly in diabetes with dyslipidemia [7]. Specific ceramides and sphingomyelins—including Cer(d18:1/24:0), SM(d18:1/24:0), SM(d18:1/16:1), SM(d18:1/24:1), and SM(d18:2/24:1)—have been identified as crucial biomarkers strongly correlated with clinical parameters of glucose and lipid metabolism [7]. These sphingolipids participate in insulin resistance mechanisms through protein phosphatase inhibition and inflammatory pathway activation.
The immune-metabolic cross-talk in this comorbidity involves significant alterations in inflammatory mediators. Studies measuring immune factors in hyperuricemia patients found that IL-10, CPT1, IL-6, SEP1, TGF-β1, Glu, TNF-α, and LD were associated with glycerophospholipid metabolism disruptions [6]. Enzyme-linked immunosorbent assays (ELISA) confirmed significant differences in CPT1, TGF-β1, Glu, and LD between hyperuricemia patients and healthy controls across different ethnicities [6], highlighting the intricate connection between lipid metabolism and immune responses in this condition.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for UHPLC-MS/MS Lipidomics
| Reagent/Material | Specification | Function in Protocol |
|---|---|---|
| Chromatography Column | Waters ACQUITY UPLC BEH C18 (2.1 × 100 mm, 1.7 μm) [2] | Lipid separation by hydrophobicity |
| Extraction Solvent | Methyl tert-butyl ether (MTBE) [2] [6] | Lipid extraction from biological matrices |
| Mass Spectrometry Reference | Leucine-enkephalin [7] | Mass calibration and accuracy maintenance |
| Lipid Standards | LysoPC(18:0/0:0) and LysoPC(18:1/0:0) from Avanti Polar Lipids [7] | Quantification standardization and quality control |
| Mobile Phase Additive | 10 mM ammonium formate [2] [7] | Enhanced ionization efficiency in MS |
| Chromatography Solvents | MS-grade acetonitrile, methanol, isopropanol [7] | Mobile phase preparation for UHPLC separation |
| Data Processing Software | Compound Discoverer, LipidSearch, MS-DIAL [9] [8] | Lipid identification, quantification, and statistical analysis |
| Lipid Database | LIPID MAPS, LipidBlast [8] | Structural identification and annotation of lipid species |
| Phenethyl acetate | Phenethyl Acetate CAS 103-45-7 - Research Chemical | High-purity Phenethyl acetate for research. Study its role as an insect odorant receptor agonist and its applications. For Research Use Only. Not for human consumption. |
| Dimethylamine-SPDB | Dimethylamine-SPDB, CAS:1193111-73-7, MF:C15H19N3O4S2, MW:369.5 g/mol | Chemical Reagent |
Concluding Perspectives and Future Directions
The investigation of lipid metabolism in diabetes-hyperuricemia comorbidity through UHPLC-MS/MS lipidomics has revealed profound alterations in glycerophospholipid, glycerolipid, and sphingolipid pathways. These discoveries provide not only mechanistic insights but also potential biomarkers for early detection and risk stratification. The identified lipid species—particularly ceramides, sphingomyelins, and specific phospholipids—offer promising targets for therapeutic intervention and personalized treatment approaches.
Future research directions should prioritize the validation of these lipid biomarkers in independent, multi-center cohorts to establish standardized clinical applications. Additionally, the integration of lipidomics with other omics technologies—including genomics, proteomics, and metabolomics—will provide a more comprehensive understanding of the systemic metabolic disruptions in this comorbidity. As lipidomic methodologies continue to advance, particularly with the incorporation of artificial intelligence and machine learning for data analysis, the translation of these findings from research laboratories to clinical practice represents the next frontier in managing this complex metabolic comorbidity.
The comorbidity of diabetes mellitus (DM) and hyperuricemia (HUA) represents a significant clinical challenge, driven by intertwined pathophysiological mechanisms including insulin resistance, oxidative stress, and systemic metabolic dysregulation [10]. Lipidomics, a branch of metabolomics, has emerged as a powerful tool to characterize the specific lipid disturbances underlying this complex relationship. Advanced analytical techniques, particularly UHPLC-MS/MS, have enabled researchers to identify distinct lipidomic signatures associated with the progression from diabetes to diabetes with hyperuricemia (DH) [2]. This technical review synthesizes current evidence on the key lipid classes—triglycerides, glycerophospholipids, and sphingolipids—that are significantly altered in this comorbidity, providing a foundation for biomarker discovery and novel therapeutic strategies.
Key Lipid Classes and Their Alterations
Comprehensive lipidomic profiling reveals consistent and significant disturbances in three major lipid classes in patients with combined diabetes and hyperuricemia. The tables below summarize the specific lipid species and their directional changes.
Table 1: Triglyceride and Glycerophospholipid Species Altered in Diabetes with Hyperuricemia
| Lipid Class | Specific Species | Change in DH vs. Control | Biological Relevance |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) and 12 other TGs | Significantly Upregulated [2] | Marker of insulin resistance and central component of dyslipidemia. |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) and 9 other PEs | Significantly Upregulated [2] | Altered membrane permeability and fluidity. |
| Phosphatidylcholines (PCs) | PC(36:1) and 6 other PCs | Significantly Upregulated [2] | Disruption of cell membrane integrity and signaling. |
| Phosphatidylinositol (PI) | Not Specified | Significantly Downregulated [2] | Perturbation of intracellular signal transduction. |
| Lysophosphatidylcholine Plasmanyls | Multiple | Downregulated in HUA/Gout [11] | Potential anti-inflammatory role; reduction may promote inflammation. |
Table 2: Sphingolipid Species and Associated Enzymes in Metabolic Disease
| Sphingolipid Component | Specific Species / Enzyme | Change / Role in Diabetes/HUA | Functional Consequence |
|---|---|---|---|
| Ceramide | C24:0 Ceramide | Most abundant circulating species [12] | Promotes insulin resistance and apoptotic signaling. |
| Sphingomyelin | C16:0 Sphingomyelin | Most abundant sphingolipid in lipoproteins [12] | Alters membrane properties and lipoprotein function. |
| Sphingosine-1-Phosphate (S1P) | Various | Carried by HDL and albumin [12] | Generally promotes cell proliferation; balance with ceramide is crucial. |
| Serine Palmitoyltransferase (SPT) | SPTLC1, SPTLC2, SPTLC3 | Upregulated by inflammatory cytokines and fatty acids [13] | Rate-limiting enzyme in de novo synthesis; increased flux into sphingolipid pathway. |
Impacted Metabolic Pathways
Multivariate and enrichment analyses of lipidomic data consistently pinpoint specific metabolic pathways that are most significantly perturbed in the DH state.
Table 3: Significantly Perturbed Metabolic Pathways in Combined Diabetes and Hyperuricemia
| Metabolic Pathway | Impact Value (from MetaboAnalyst) | Key Lipid Classes Involved | Pathophysiological Significance |
|---|---|---|---|
| Glycerophospholipid Metabolism | 0.199 (Most significant) [2] | PCs, PEs, PIs, LPCs | Central to membrane biology, cell signaling, and inflammation. |
| Glycerolipid Metabolism | 0.014 [2] | Triglycerides, Diglycerides | Core pathway in energy storage and insulin resistance. |
| Arachidonic Acid Metabolism | Not Specified | PE(18:0/20:4) and other esters [14] | Generation of pro-inflammatory eicosanoids. |
| Sphingolipid Metabolism | Not Specified | Ceramide, Sphingomyelin, S1P [12] [13] | Regulation of insulin sensitivity, inflammation, and cell fate. |
Detailed Experimental Protocols
UHPLC-MS/MS Based Plasma Untargeted Lipidomics
The following protocol is adapted from the comprehensive methodology used in recent studies to identify lipid alterations in patient cohorts [2] [11].
Sample Collection and Pre-processing
- Blood Collection: Collect ~5 mL of fasting venous blood into sodium heparin or EDTA tubes.
- Plasma Separation: Centrifuge at 3,000 rpm (approximately 1,500-2,000 g) for 10 minutes at room temperature. Aliquot 0.2 mL of the upper plasma layer into 1.5 mL microcentrifuge tubes.
- Pooled QC: Create quality control (QC) samples by combining equal volumes of plasma from all experimental groups. Store all samples at -80°C.
- Lipid Extraction (Monophasic):
- Thaw plasma samples on ice.
- Pipette 100 μL of plasma into a 1.5 mL tube.
- Add 200 μL of ice-cold water and vortex.
- Add 240 μL of pre-cooled methanol and vortex.
- Add 800 μL of methyl tert-butyl ether (MTBE) and vortex vigorously.
- Sonicate for 20 minutes in a low-temperature water bath.
- Incubate for 30 minutes at room temperature.
- Centrifuge at 14,000 g for 15 minutes at 10°C.
- Transfer the upper organic phase to a new tube.
- Dry under a gentle stream of nitrogen gas.
- Reconstitute the dried lipid extract in 200 μL of 90% isopropanol/acetonitrile.
- Centrifuge at 14,000 g for 15 minutes at 10°C prior to MS analysis.
UHPLC-MS/MS Instrumentation and Conditions
- Chromatography:
- System: Ultra-High-Performance Liquid Chromatography (e.g., ExionLC, SCIEX or equivalent).
- Column: Waters ACQUITY UPLC BEH C18 column (2.1 mm × 100 mm, 1.7 μm) or a BEH C8 column for broader lipid coverage.
- Mobile Phase A: 10 mM ammonium formate in acetonitrile/water (e.g., 60:40, v/v).
- Mobile Phase B: 10 mM ammonium formate in acetonitrile/isopropanol (e.g., 10:90, v/v).
- Gradient: Typically from 30% B to 100% B over 20-25 minutes, followed by re-equilibration.
- Flow Rate: 0.3 mL/min.
- Column Temperature: 45°C.
- Injection Volume: 3 μL.
- Mass Spectrometry:
- System: Tandem Mass Spectrometer (e.g., QTRAP 6500+ or Q-Exactive Plus).
- Ionization: Electrospray Ionization (ESI), positive and negative ion modes.
- Source Parameters (Positive Mode): Sheath Gas Flow: 45 arb, Aux Gas Flow: 15 arb, Spray Voltage: 3.0 kV, Capillary Temperature: 350°C.
- Source Parameters (Negative Mode): Sheath Gas Flow: 45 arb, Aux Gas Flow: 15 arb, Spray Voltage: 2.5 kV, Capillary Temperature: 350°C.
- Scan Modes: Data-Dependent Acquisition (DDA) or Sequential Window Acquisition of All Theoretical Mass Spectra (SWATH) for untargeted analysis. MS1 full scan (e.g., m/z 200-1800) followed by MS2 scans of the top 10 most intense ions.
ELISA for Immune and Metabolic Biomarkers
To correlate lipidomic findings with inflammatory and metabolic status, key biomarkers can be quantified [14].
- Analytes: Tumor Necrosis Factor-α (TNF-α), Interleukin-6 (IL-6), Interleukin-10 (IL-10), Transforming Growth Factor-β1 (TGF-β1), Carnitine Palmitoyltransferase-1 (CPT1), Selenoprotein 1 (SEP1), Glucose (Glu), Lactic Acid (LD).
- Protocol:
- Coat ELISA plate with capture antibody.
- Block plates with a protein-based buffer (e.g., 1% BSA in PBS).
- Add standards and prediluted serum/plasma samples.
- Incubate, then wash to remove unbound material.
- Add detection antibody conjugated to an enzyme (e.g., Horseradish Peroxidase, HRP).
- Incubate and wash.
- Add enzyme substrate to develop color.
- Measure absorbance using a microplate reader (e.g., VersaMax).
- Calculate concentrations using a standard curve generated from known standards.
Pathway and Workflow Visualization
Sphingolipid Metabolism in Insulin Resistance
The following diagram illustrates the key pathways of sphingolipid metabolism and their involvement in promoting insulin resistance, a core defect in the diabetes-hyperuricemia comorbidity.
Diagram Title: Sphingolipid Metabolism in Insulin Resistance
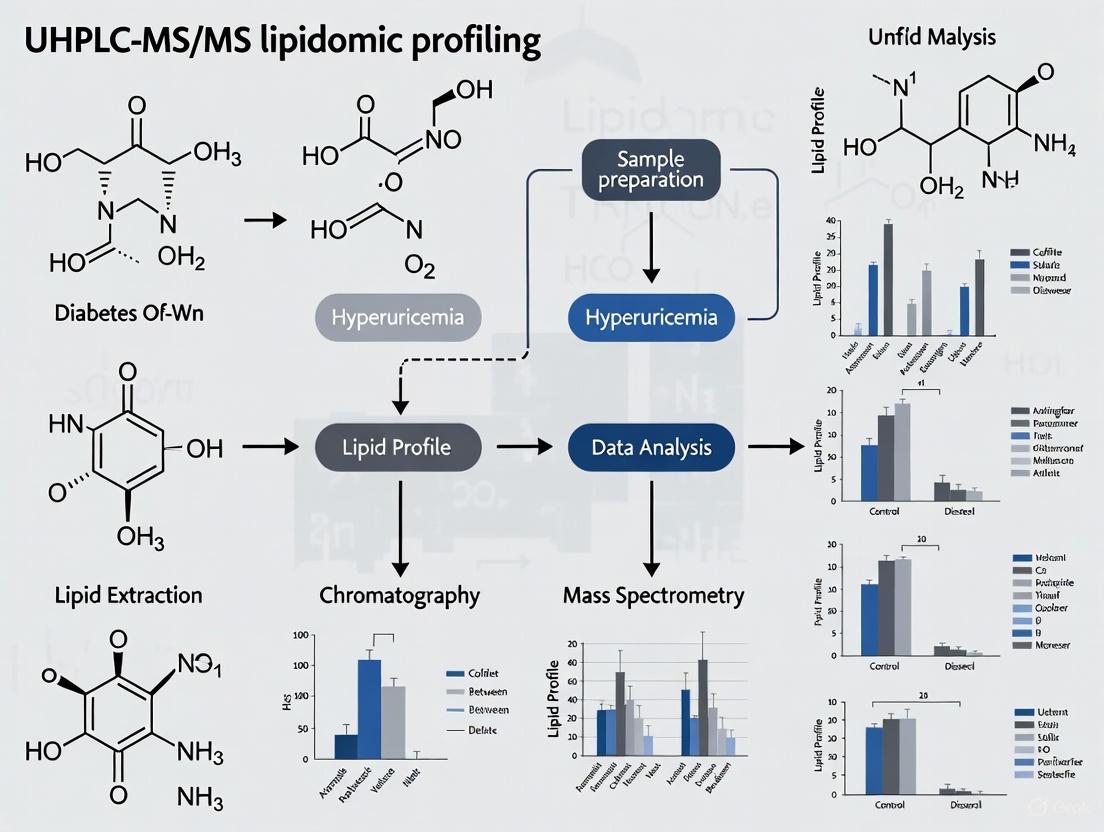
UHPLC-MS/MS Lipidomics Workflow
This diagram outlines the comprehensive workflow for a plasma untargeted lipidomics study, from sample collection to data analysis.
Diagram Title: UHPLC-MS/MS Lipidomics Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of the described protocols requires the following key reagents and instruments.
Table 4: Essential Research Reagents and Materials for Lipidomics Studies
| Category / Item | Specific Example / Specification | Critical Function in Workflow |
|---|---|---|
| Chromatography Column | Waters ACQUITY UPLC BEH C18 (2.1x100mm, 1.7µm) | High-resolution separation of complex lipid mixtures prior to MS detection. |
| Internal Standards | SPLASH LIPIDOMIX Mass Spec Standard; Deuterated Ceramide (d18:1-d7/15:0) | Correction for extraction efficiency and instrument variability; enables semi-quantitation. |
| Mass Spectrometer | QTRAP 6500+; Q-Exactive Plus | High-sensitivity detection and structural characterization of lipids via MS/MS. |
| Lipid Extraction Solvents | Methyl tert-butyl ether (MTBE), LC-MS Grade Isopropanol | Efficient, reproducible liquid-liquid extraction of a broad range of lipid classes from plasma. |
| Mobile Phase Additives | 10 mM Ammonium Formate, LC-MS Grade | Enhances ionization efficiency in ESI and helps control analyte adduct formation. |
| ELISA Kits | Commercial Kits for TNF-α, IL-6, CPT1, etc. | Multiplexed, specific quantification of protein biomarkers linked to lipid metabolic dysregulation. |
| Clocortolone | Clocortolone, CAS:4828-27-7, MF:C22H28ClFO4, MW:410.9 g/mol | Chemical Reagent |
| Thiol-PEG12-acid | Thiol-PEG12-acid, CAS:1032347-93-5; 2211174-73-9, MF:C27H54O14S, MW:634.78 | Chemical Reagent |
The application of advanced UHPLC-MS/MS lipidomics has definitively identified triglycerides, glycerophospholipids, and sphingolipids as the key lipid classes dysregulated in the complex interplay between diabetes and hyperuricemia. The consistent upregulation of specific TGs, PEs, and PCs, coupled with disturbances in glycerophospholipid and sphingolipid metabolism, provides a molecular rationale for the exacerbated insulin resistance and inflammatory state observed in comorbid patients. These findings not only illuminate the pathophysiological mechanisms but also establish a foundation for targeting these lipid pathways for future diagnostic and therapeutic innovations. The standardized protocols and tools outlined herein provide a roadmap for researchers to further validate and build upon these critical findings.
In the landscape of metabolic disease research, lipidomics has emerged as a powerful tool for elucidating the molecular mechanisms underlying disease pathophysiology. The dysregulation of glycerophospholipid and glycerolipid metabolism represents a critical metabolic axis in diabetes and its related complications, including hyperuricemia. These lipid classes are not only fundamental structural components of cellular membranes but also play dynamic roles in cellular signaling, energy storage, and metabolic homeostasis. Ultra-high performance liquid chromatography coupled with tandem mass spectrometry (UHPLC-MS/MS) has enabled researchers to characterize these alterations with unprecedented specificity and sensitivity, revealing complex lipid metabolic networks that are perturbed in disease states. This technical guide examines the core aspects of glycerophospholipid and glycerolipid dysregulation within the context of diabetes and hyperuricemia, providing researchers with comprehensive methodological frameworks, analytical approaches, and pathophysiological insights to advance investigation in this evolving field.
Lipidomic Alterations in Diabetes and Hyperuricemia
Clinical Lipidomic Profiling
Clinical studies utilizing UHPLC-MS/MS platforms have revealed consistent patterns of glycerophospholipid and glycerolipid dysregulation in patients with diabetes mellitus combined with hyperuricemia (DH). A recent investigation comparing DH patients, those with diabetes alone (DM), and healthy controls identified 1,361 lipid molecules across 30 subclasses, with multivariate analyses demonstrating significant separation among these groups [2].
Table 1: Significantly Altered Lipid Species in Diabetes with Hyperuricemia
| Lipid Category | Lipid Subclass | Specific Lipid Species | Regulation Trend | Biological Relevance |
|---|---|---|---|---|
| Glycerophospholipids | Phosphatidylethanolamines (PE) | PE(18:0/20:4) | Upregulated | Membrane fluidity, signaling precursors |
| Phosphatidylcholines (PC) | PC(36:1) | Upregulated | Membrane integrity, choline metabolism | |
| Lysophosphatidylcholines (LysoPC) | Multiple species | Altered | Inflammatory modulation | |
| Phosphatidylinositol (PI) | Not specified | Downregulated | Insulin signaling, cellular trafficking | |
| Glycerolipids | Triglycerides (TG) | TG(16:0/18:1/18:2) | Upregulated | Energy storage, lipid accumulation |
| Diacylglycerols (DG) | Multiple species | Upregulated | Insulin resistance, signaling molecule |
The pathway analysis of these altered lipids revealed enrichment in six major metabolic pathways, with glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) identified as the most significantly perturbed in DH patients [2]. Notably, the comparison between DH and DM groups identified 12 differential lipids that were similarly enriched in these core pathways, underscoring their central role in the pathophysiology of hyperuricemia complicating diabetes.
Systemic Metabolic Implications
The dysregulation of glycerophospholipid and glycerolipid metabolism extends beyond diabetes with hyperuricemia to encompass various diabetic complications. In diabetic cardiomyopathy, increased fatty acid uptake and altered glycerophospholipid composition contribute to mitochondrial dysfunction, oxidative stress, and impaired cardiac function [15]. Similarly, lipidomic profiling of serum from patients with diabetic retinopathy has revealed distinctive glycerophospholipid and glycerolipid signatures that can distinguish between patients without retinopathy and those with non-proliferative diabetic retinopathy, offering potential diagnostic biomarkers [16].
The systemic nature of these lipid metabolic alterations is further evidenced by lipid traffic analysis studies in diabetic mouse models, which have shown that the spatial distribution of triglycerides (TGs), phosphatidylcholines (PCs), phosphatidylethanolamines (PEs), and phosphatidylinositols (PIs) is altered throughout the biological network, indicating fundamental changes in the systemic control of lipid metabolism [17].
UHPLC-MS/MS Methodologies for Lipidomic Analysis
Sample Preparation Protocols
Proper sample preparation is critical for reliable lipidomic profiling. For plasma/serum analysis, the following protocol has been successfully employed in diabetes hyperuricemia research:
- Sample Collection: Collect fasting blood samples (5 mL) in appropriate vacuum tubes and centrifuge at 3,000 rpm for 10 minutes at room temperature to separate plasma [2].
- Plasma Storage: Aliquot 0.2 mL of the upper plasma layer into 1.5 mL centrifuge tubes and store at -80°C until analysis [2].
- Lipid Extraction: Thaw samples on ice and vortex. For 100 μL of plasma, add 200 μL of 4°C water followed by 240 μL of pre-cooled methanol. After mixing, add 800 μL of methyl tert-butyl ether (MTBE) and sonicate in a low-temperature water bath for 20 minutes [2].
- Phase Separation: Allow the mixture to stand at room temperature for 30 minutes, then centrifuge at 14,000 g for 15 minutes at 10°C. Collect the upper organic phase and dry under a stream of nitrogen gas [2].
- Reconstitution: Reconstitute the dried lipid extract in 100 μL of isopropanol for UHPLC-MS/MS analysis [2].
For tissue-specific lipidomics, additional homogenization steps are required prior to lipid extraction. The MTBE extraction method has demonstrated excellent recovery across multiple lipid classes and is widely adopted in lipidomics research.
UHPLC-MS/MS Instrumental Configuration
Chromatographic Conditions:
- Column: Waters ACQUITY UPLC BEH C18 column (2.1 mm i.d. × 100 mm length, 1.7 μm particle size) [2] or Kinetex C18 (2.6 μm, 2.1 × 100 mm) [16]
- Mobile Phase A: 10 mM ammonium formate in acetonitrile/water [2]
- Mobile Phase B: 10 mM ammonium formate in acetonitrile/isopropanol [2]
- Gradient: Optimized linear gradients typically ranging from 60-90% mobile phase B over 15-25 minutes
- Temperature: Column compartment maintained at 45-55°C
- Injection Volume: 1-5 μL depending on sample concentration
Mass Spectrometry Parameters:
- Ionization: Electrospray ionization (ESI) in both positive and negative modes
- Ion Spray Voltage: +5,200 V (positive), -4,500 V (negative) [16]
- Ion Source Temperature: 350°C [16]
- Detection Mode: Multiple Reaction Monitoring (MRM) for targeted analysis; full scan for untargeted approaches
- Collision Energies: Optimized for specific lipid classes based on precursor and product ions
The experimental workflow for UHPLC-MS/MS lipidomic profiling in diabetes-hyperuricemia research encompasses sample collection, preparation, chromatographic separation, mass spectrometric detection, and data analysis, with specific methodology tailored to the biological question.
Data Processing and Statistical Analysis
Raw mass spectrometry data processing typically involves:
- Peak Detection and Alignment: Using platforms like SCIEX OS or open-source tools such as XCMS
- Lipid Identification: Based on retention time, precursor mass, and fragmentation patterns compared to standards
- Quantification: Using internal standards for semi-quantitative or absolute quantification
- Multivariate Statistical Analysis: Principal Component Analysis (PCA) and Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) to identify group separations
- Differential Analysis: Student's t-test and fold-change calculations to determine significantly altered lipids
- Pathway Analysis: Using platforms like MetaboAnalyst 5.0 to identify enriched metabolic pathways
Pathophysiological Mechanisms and Signaling Pathways
Glycerophospholipid Metabolism in Insulin Signaling
Glycerophospholipids, particularly phosphatidylinositols (PIs) and their phosphorylated derivatives, play fundamental roles in insulin signal transduction. In diabetic states, alterations in glycerophospholipid metabolism disrupt membrane fluidity, receptor function, and downstream signaling cascades. Research has demonstrated that specific PI species are significantly altered in diabetic models, with structural PIs (e.g., PI(36:1), PI(38:6)) showing distinct distribution patterns that may affect membrane physical properties and signaling functionality [17].
The interconnection between glycerophospholipid metabolism and insulin signaling involves multiple enzymes and lipid species that are dysregulated in diabetes, creating a pathological feedback loop that exacerbates insulin resistance.
Glycerolipid Dynamics and Lipid Droplet Pathology
Glycerolipids, particularly diacylglycerols (DGs) and triglycerides (TGs), are centrally implicated in the lipotoxicity that characterizes diabetes and its complications. DG accumulation has been identified as an early event in diabetic progression, with studies demonstrating its upregulation even during pre-symptomatic phases [18]. DGs activate protein kinase C (PKC) isoforms, which in turn phosphorylate insulin receptor substrates on inhibitory sites, blunting insulin signaling and promoting resistance [15].
In the context of hyperuricemia, uric acid has been shown to exacerbate glycerolipid dysregulation, promoting increased synthesis of TGs and altering the composition of lipid droplets (LDs) [19]. LDs are dynamic organelles that store neutral lipids, and their proper turnover is essential for maintaining lipid homeostasis. In diabetic states, LD dynamics become dysregulated, leading to ectopic lipid accumulation in non-adipose tissues such as the pancreas, liver, heart, and kidneys, contributing to cellular dysfunction and apoptosis [19].
Table 2: Lipid Droplet Dynamics in Diabetic Complications
| Tissue/Organ | LD Alteration | Functional Consequence | Molecular Mediators |
|---|---|---|---|
| Pancreatic β-cells | Increased LD accumulation | Impaired insulin secretion | PLIN2, PLIN5, ATGL |
| Liver | Excessive LD storage | Hepatic steatosis, insulin resistance | PNPLA3, CGI-58 |
| Heart | Cardiac lipid accumulation | Diabetic cardiomyopathy | CD36, PPARα |
| Kidney | Glomerular LD deposition | Diabetic nephropathy | ROS, ER stress |
| Retina | Altered retinal lipid metabolism | Diabetic retinopathy | DAG, PKC |
The interplay between glycerolipid metabolism and LD dynamics is regulated by numerous factors, including perilipin proteins (PLIN1-5), lipases (ATGL, HSL, MGL), and autophagy pathways. Therapeutic strategies that target LD dynamics are emerging as promising approaches for managing diabetes and its complications [19].
Advanced Research Applications
Spatial Lipidomics in Metabolic Research
Recent advances in mass spectrometry imaging (MSI) have enabled spatial resolution of lipid distributions within tissues, providing novel insights into region-specific lipid metabolic alterations in diabetes. Spatial-temporal lipidomics in mouse models of disease has revealed distinct lipidomic differences between various brain regions, with the thalamus exhibiting more significant lipid changes than the hippocampus in Alzheimer's disease models, highlighting the potential for similar approaches in diabetes research [18]. These techniques can be adapted to investigate pancreatic islets, liver lobules, and renal compartments in diabetes models, offering unprecedented resolution of metabolic zonation.
Biomarker Discovery and Validation
Lipidomic profiling has identified numerous potential biomarkers for early detection and monitoring of diabetes progression and complications. For diabetic retinopathy, a four-lipid combination diagnostic model (including TAG58:2-FA18:1) has demonstrated excellent predictive ability for distinguishing between patients without retinopathy and those with non-proliferative diabetic retinopathy [16]. Similarly, in newly diagnosed T2DM patients with dyslipidemia, ceramide (Cer(d18:1/24:0)) and sphingomyelin (SM(d18:1/24:0)) have emerged as promising biomarkers strongly correlated with clinical parameters [20].
The biomarker discovery and validation pipeline involves multiple stages from initial discovery to clinical implementation, with rigorous statistical evaluation at each step.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Lipidomic Studies in Diabetes-Hyperuricemia
| Category | Specific Reagents/Materials | Function/Application |
|---|---|---|
| Chromatography | Waters ACQUITY UPLC BEH C18 column | Lipid separation |
| Kinetex C18 column | Alternative separation column | |
| Ammonium formate | Mobile phase additive | |
| Acetonitrile, isopropanol, methanol | HPLC-grade solvents | |
| Sample Preparation | Methyl tert-butyl ether (MTBE) | Lipid extraction solvent |
| Internal standards: deuterated lipids | Quantification standardization | |
| Solid-phase extraction cartridges | Lipid cleanup and fractionation | |
| Mass Spectrometry | Reference standard lipid mixtures | Method development and calibration |
| Instrument calibration solutions | Mass accuracy maintenance | |
| Biological Reagents | CD36 antibodies | Fatty acid transporter studies |
| PPARα/γ agonists and antagonists | Pathway modulation | |
| Lipoprotein lipase inhibitors | Glycerolipid metabolism studies | |
| Data Analysis | LipidSearch Software | Lipid identification and quantification |
| MetaboAnalyst | Pathway analysis and visualization | |
| SIMCA-P | Multivariate statistical analysis | |
| Galanganone B | Galanganone B, MF:C34H40O6, MW:544.7 g/mol | Chemical Reagent |
| Anticancer agent 189 | Anticancer agent 189, MF:C42H56N4O10, MW:776.9 g/mol | Chemical Reagent |
The comprehensive characterization of glycerophospholipid and glycerolipid metabolism through UHPLC-MS/MS lipidomic profiling has fundamentally advanced our understanding of diabetes pathophysiology and its intersection with hyperuricemia. The intricate interplay between these lipid classes contributes significantly to insulin resistance, β-cell dysfunction, and the development of microvascular complications. The methodological frameworks outlined in this technical guide provide researchers with robust tools for investigating these metabolic pathways, while the identified lipid signatures and biomarkers offer potential targets for therapeutic intervention and early diagnosis. As lipidomic technologies continue to evolve, particularly with advancements in spatial resolution and single-cell analysis, our ability to decipher the complex metabolic networks underlying diabetes and hyperuricemia will undoubtedly expand, paving the way for more personalized and effective treatment strategies.
1. Introduction Lipidomic profiling via UHPLC-MS/MS is a cornerstone of modern metabolic disease research, providing a high-resolution snapshot of lipid dysregulation. In the context of diabetes and hyperuricemia, specific lipid species have emerged as critical biomarkers and potential mechanistic players. This guide details the analytical and biological significance of three key lipids: Triacylglycerol TG(16:0/18:1/18:2), Ceramide Cer(d18:1/24:0), and Sphingomyelin SM(d18:1/24:0), within this comorbid pathological framework.
2. Quantitative Lipid Biomarker Data in Diabetes-Hyperuricemia Dysregulated lipid levels are a hallmark of insulin resistance and hyperuricemia. The following table summarizes typical quantitative changes observed in patient serum/plasma studies.
Table 1: Quantitative Changes of Specific Lipid Biomarkers in Diabetes-Hyperuricemia Cohorts
| Lipid Biomarker | Full Name | Typical Change vs. Control | Approximate Fold-Change (Range) | Proposed Biological Implication |
|---|---|---|---|---|
| TG(16:0/18:1/18:2) | Triacylglycerol (Palmitic acid/Oleic acid/Linoleic acid) | ↑ Increased | 1.5 - 2.8 | Indicator of hepatic steatosis, impaired β-oxidation, and general lipotoxicity. |
| Cer(d18:1/24:0) | Ceramide (Sphingosine d18:1/Lignoceric acid) | ↓ Decreased | 0.4 - 0.7 | Loss of this longer-chain, less toxic ceramide may disrupt ceramide saturation balance, promoting insulin resistance. |
| SM(d18:1/24:0) | Sphingomyelin (Sphingosine d18:1/Lignoceric acid) | ↑ Increased | 1.3 - 2.0 | May reflect compensatory sphingomyelin synthesis or altered membrane microdomain composition in response to metabolic stress. |
3. Experimental Protocol: UHPLC-MS/MS Lipid Extraction and Profiling The following is a standardized protocol for lipidomic analysis from plasma/serum samples.
Materials:
- Biological Sample: Human plasma or serum (e.g., 10 µL aliquot).
- Extraction Solvent: Methyl tert-butyl ether (MTBE).
- Internal Standards: A mixture of stable isotope-labeled lipids (e.g., TG(16:0/18:1/18:2)-d5, Cer(d18:1/17:0), SM(d18:1/12:0)-d3).
- LC-MS Grade Solvents: Methanol, Water, Isopropanol, Acetonitrile, Ammonium Formate.
Procedure:
- Protein Precipitation & Lipid Extraction:
- To 10 µL of plasma in a glass vial, add 20 µL of internal standard mixture in methanol.
- Vortex for 10 seconds and incubate on ice for 10 minutes.
- Add 300 µL of MTBE and 100 µL of methanol.
- Sonicate for 15 minutes in an ice-cold water bath.
- Add 100 µL of LC-MS grade water to induce phase separation.
- Centrifuge at 14,000 x g for 15 minutes at 10°C.
- Collect the upper organic (MTBE) layer into a new vial.
- Evaporate the solvent to dryness under a gentle stream of nitrogen.
- Reconstitute the dried lipid extract in 100 µL of a 9:1 (v/v) isopropanol:acetonitrile mixture.
- UHPLC-MS/MS Analysis:
- Chromatography:
- Column: C8 or C18 reversed-phase column (e.g., 2.1 x 100 mm, 1.7 µm).
- Mobile Phase A: Acetonitrile/Water (60:40) with 10 mM Ammonium Formate.
- Mobile Phase B: Isopropanol/Acetonitrile (90:10) with 10 mM Ammonium Formate.
- Gradient: 30% B to 100% B over 15-20 minutes, hold at 100% B for 5 minutes.
- Flow Rate: 0.4 mL/min, Column Temp: 55°C.
- Mass Spectrometry:
- Ionization: Heated Electrospray Ionization (H-ESI) in positive and negative mode.
- Scan Mode: Data-Dependent Acquisition (DDA) or Parallel Reaction Monitoring (PRM).
- Source Parameters: Spray Voltage: 3.5 kV (pos), 2.8 kV (neg); Vaporizer Temp: 300°C; Sheath Gas: 40 arb; Aux Gas: 15 arb.
- Targeted MS/MS Transitions (for quantification):
- TG(16:0/18:1/18:2): [M+NH4]+ → 577.5 (18:2 fragment)
- Cer(d18:1/24:0): [M+H]+ → 264.3 (d18:1 sphingoid base)
- SM(d18:1/24:0): [M+H]+ → 184.1 (phosphocholine headgroup)
- Chromatography:
4. Visualizing Metabolic Pathways and Workflows
Sphingolipid Pathway in Metabolic Disease
UHPLC-MS/MS Lipidomics Workflow
5. The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for Lipid Biomarker Research
| Reagent / Material | Function / Application |
|---|---|
| Stable Isotope-Labeled Internal Standards (e.g., TG-d5, Cer-d7, SM-d9) | Critical for accurate quantification; corrects for matrix effects and recovery losses during sample preparation. |
| Methyl tert-butyl ether (MTBE) | Primary solvent for robust liquid-liquid extraction of a broad range of lipid classes. |
| C8 or C18 UHPLC Column (1.7-1.8 µm particle size) | Provides high-resolution separation of complex lipid mixtures prior to MS detection. |
| Ammonium Formate / Acetate | LC-MS compatible additive to mobile phases that promotes stable adduct formation (e.g., [M+NH4]+ for TGs). |
| Sphingolipid Pathway Inhibitors (e.g., Myriocin, Fumonisin B1) | Pharmacological tools to inhibit de novo ceramide synthesis (Myriocin) or ceramide synthase (Fumonisin B1) for functional studies. |
| Commercial Quality Control (QC) Plasma Pools | Used to monitor instrument performance and batch-to-batch reproducibility throughout a large analytical sequence. |
Linking Lipidomic Signatures to Pathophysiological Mechanisms and Disease Progression
Lipidomics, a specialized branch of metabolomics, has emerged as a powerful analytical approach for comprehensively profiling lipid species in biological systems. The lipidome encompasses a vast array of molecules that serve not only as structural components of cellular membranes but also as signaling mediators and energy reservoirs [21] [22]. Technological advances in ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) have enabled researchers to precisely characterize lipidomic signatures associated with various disease states, providing unprecedented insights into pathophysiological mechanisms [22] [23]. Within the context of diabetes mellitus and hyperuricemia research, lipidomic profiling offers exceptional potential for identifying novel biomarkers, elucidating metabolic disruptions, and monitoring disease progression [2] [24].
The integration of lipidomic data with clinical parameters facilitates a deeper understanding of how specific lipid classes contribute to disease pathogenesis. This technical guide explores the fundamental principles, methodologies, and applications of UHPLC-MS/MS-based lipidomics in characterizing lipid signatures in metabolic diseases, with particular emphasis on diabetes and hyperuricemia. By providing detailed experimental protocols, data interpretation frameworks, and visualization approaches, this resource aims to support researchers, scientists, and drug development professionals in advancing this rapidly evolving field.
Lipidomic Alterations in Diabetes and Hyperuricemia
Lipidomic Signatures in Diabetes Mellitus and Hyperuricemia
Comparative lipidomic analyses reveal distinct alterations in patients with diabetes mellitus (DM) and those with concomitant hyperuricemia (DH). A study investigating plasma untargeted lipidomics identified 1,361 lipid molecules across 30 subclasses, with multivariate analyses demonstrating significant separation trends among DH, DM, and normal glucose tolerance (NGT) groups [2]. This finding confirms distinct lipidomic profiles associated with these metabolic conditions.
Table 1: Significantly Altered Lipid Metabolites in Diabetes Mellitus with Hyperuricemia
| Lipid Category | Specific Lipid Molecules | Regulation Trend | Metabolic Pathway Association |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) and 12 other TGs | Significantly upregulated | Glycerolipid metabolism |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) and 9 other PEs | Significantly upregulated | Glycerophospholipid metabolism |
| Phosphatidylcholines (PCs) | PC(36:1) and 6 other PCs | Significantly upregulated | Glycerophospholipid metabolism |
| Phosphatidylinositol (PI) | Not specified | Downregulated | Glycerophospholipid metabolism |
The DH group exhibited 31 significantly altered lipid metabolites compared to NGT controls, with pronounced upregulation of 13 triglycerides (TGs), 10 phosphatidylethanolamines (PEs), and 7 phosphatidylcholines (PCs), while one phosphatidylinositol (PI) was downregulated [2]. Pathway enrichment analysis indicated these differential lipids predominantly affected glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014), highlighting these as the most significantly perturbed pathways in DH patients [2].
When comparing DH versus DM groups, researchers identified 12 differential lipids that were also predominantly enriched in these same core pathways, underscoring their central role in the pathophysiology of hyperuricemia complicating diabetes [2]. These findings suggest that hyperuricemia exacerbates lipid metabolic disturbances in diabetic patients, potentially accelerating disease progression and complication development.
Phenotype-Specific Lipidomic Patterns
Lipid metabolism displays phenotype-specific regulatory patterns across distinct clinical presentations. Research in pediatric populations has revealed that obesity is characterized by marked upregulation of triacylglycerols (TG), while hyperuricemia exhibits predominant downregulation of membrane lipids such as phosphatidylcholine (PC) and lysophosphatidylcholine (LPC), with phosphatidylinositol (PI) showing heterogeneous alterations [24]. The combined phenotype of obesity and hyperuricemia demonstrates more extensive disruptions across multiple metabolic pathways [24].
Correlation analyses have revealed consistent relationships between specific lipid classes and clinical parameters. TGs show an inverse relationship with glomerular filtration rate (GFR), ceramides (Cer) associate strongly with insulin metabolism, and LPC demonstrates a distinctive positive correlation with aspartate aminotransferase (AST) in hyperuricemia groups [24]. Carnitines (CAR) exhibit bidirectional associations with kidney function-related parameters, suggesting their potential as biomarkers for renal complications in metabolic diseases [24].
Experimental Workflows in Lipidomics Research
Sample Collection and Preparation
Proper sample collection and preparation are critical for reliable lipidomic profiling. For plasma samples, collection of fasting venous blood is recommended, followed by centrifugation at 3,000 rpm for 10 minutes at room temperature to separate plasma [2]. The resulting plasma should be aliquoted and stored at -80°C until analysis to preserve lipid stability [22].
Table 2: Key Research Reagent Solutions for Lipid Extraction and Analysis
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Methyl tert-butyl ether (MTBE) | Lipid extraction | Used in liquid-liquid extraction; 800μL added to 100μL plasma [2] |
| Methanol | Protein precipitation and lipid extraction | Pre-cooled; 240μL added to plasma sample [2] |
| Ammonium formate | Mobile phase additive | Enhances ionization; used at 10mM concentration in acetonitrile [2] |
| Internal standards | Quantification reference | Added prior to extraction to assess recovery and quantification accuracy [25] |
| Isopropanol | Solvent for lipid resuspension | Used at 90% with acetonitrile for sample reconstitution after drying [25] |
For lipid extraction, the MTBE/methanol method has demonstrated effectiveness. The protocol involves adding 200μL of 4°C water to 100μL of plasma, followed by 240μL of pre-cooled methanol and 800μL of MTBE [2]. After mixing, samples undergo sonication in a low-temperature water bath for 20 minutes and stand at room temperature for 30 minutes. Centrifugation at 14,000×g for 15 minutes at 10°C separates phases, with the upper organic phase collected and dried under nitrogen [2]. The dried lipids are then reconstituted in appropriate solvents for analysis.
UHPLC-MS/MS Analysis
Ultra-high performance liquid chromatography separation typically utilizes reversed-phase columns, such as Waters ACQUITY UPLC BEH C18 (2.1 mm × 100 mm, 1.7 μm particle size) [2]. The mobile phase commonly consists of acetonitrile-water mixtures with ammonium formate or formic acid as additives to enhance ionization [2] [25].
Mass spectrometry analysis employs both positive and negative ionization modes to comprehensively capture the lipidome. For Q-Exactive Plus instruments, positive ion spray voltage is typically set at 3.0 kV and negative ion spray voltage at 2.5 kV, with sheath gas flow of 45 arbitrary units and auxiliary gas flow of 15 arbitrary units [25]. The MS1 scanning range is generally set between 200-1800 m/z to cover most lipid species.
Data processing involves peak alignment, peak picking, and quantification using software such as Compound Discoverer, with subsequent matching against lipid databases including LIPID MAPS and LipidBlast for accurate qualitative and relative quantitative results [8].
Figure 1: Experimental Workflow for UHPLC-MS/MS Lipidomic Profiling
Analytical Techniques and Instrumentation
Mass Spectrometry Platforms
Various mass spectrometry platforms are available for lipidomic analyses, each with distinct advantages and limitations. The selection of an appropriate platform depends on research objectives, whether untargeted exploration or targeted quantification.
Table 3: Mass Spectrometry Platforms for Lipidomic Analysis
| Method | Advantages | Limitations | Applications |
|---|---|---|---|
| LC-QTOF/MS | High mass accuracy and resolution; suitable for untargeted analysis and identification of unknown compounds | Lower sensitivity than MRM mode scans; longer run times; high cost | Structural elucidation of novel lipid metabolites [22] |
| LC-Orbitrap | Enhanced separation of isotopic peaks with similar retention times; high mass resolution | Lower sensitivity than MRM mode scans; longer run times; high cost | Untargeted lipidomics with high resolution [22] |
| LC-Triple Quadrupole | Enhanced sensitivity and selectivity via MRM; optimal for targeted quantification | Lower resolution than QTOF or Orbitrap; less effective for unstable lipids | Targeted quantification of specific lipid classes [22] |
| Nano-ESI-MS | Small sample volume requirements; steady ionization environment; high signal intensities | Longer run times; narrow needles prone to clogging | Limited sample availability studies [22] |
| MALDI-TOF | Capable of generating 2D images depicting lipid localization in tissues | Low confidence in identifying lipid species without MS/MS | Spatial distribution studies in tissues [22] |
For comprehensive lipidomic profiling in diabetes and hyperuricemia research, LC-QTOF/MS and LC-Orbitrap platforms offer the necessary resolution and mass accuracy for untargeted analysis, enabling discovery of novel lipid biomarkers [22]. Conversely, for validation studies and targeted quantification of specific lipid panels, LC-Triple Quadrupole systems operating in multiple reaction monitoring (MRM) mode provide superior sensitivity and precision [22].
Data Processing and Statistical Analysis
Lipidomic datasets are inherently high-dimensional, requiring specialized statistical approaches for meaningful interpretation. Principal component analysis (PCA) and orthogonal partial least squares-discriminant analysis (OPLS-DA) are widely employed for visualizing group separations and identifying differentially abundant lipids [2]. These multivariate techniques help discern global lipidomic patterns among experimental groups while assessing data quality and outliers.
For feature selection in high-dimensional data, machine learning approaches such as least absolute shrinkage and selection operator (LASSO) regression have demonstrated utility in identifying the most informative lipid biomarkers [25] [8]. LASSO performs both feature selection and regularization simultaneously, enhancing model interpretability and predictive performance by selecting a subset of relevant lipids while constraining less relevant ones.
Pathway analysis tools such as MetaboAnalyst 5.0 enable researchers to identify enriched metabolic pathways from lists of differentially abundant lipids, providing biological context to lipidomic findings [2]. This platform facilitates the calculation of pathway impact values based on topological considerations, highlighting pathways most significantly perturbed in specific disease states.
Pathophysiological Mechanisms and Clinical Applications
Metabolic Pathways in Diabetes and Hyperuricemia
Lipidomic studies in diabetes and hyperuricemia have consistently identified glycerophospholipid and glycerolipid metabolism as central pathways disrupted in these conditions [2]. Glycerophospholipids, including phosphatidylcholines (PCs) and phosphatidylethanolamines (PEs), serve as crucial structural components of cellular membranes and play important roles in cellular signaling [21] [23]. Their disruption can impair membrane fluidity, receptor function, and signal transduction processes relevant to insulin resistance and inflammatory responses.
The observed upregulation of triglycerides (TGs) in diabetes with hyperuricemia reflects enhanced lipogenesis and altered energy storage patterns, potentially contributing to ectopic lipid accumulation and lipotoxicity mechanisms implicated in metabolic syndrome progression [2] [24]. These lipid alterations may promote insulin resistance through activation of inflammatory pathways and intracellular signaling cascades that interfere with insulin action.
Figure 2: Pathophysiological Mechanisms Linking Lipid Alterations to Disease Progression
Biomarker Discovery and Clinical Translation
Lipidomic signatures show significant promise as biomarkers for disease diagnosis, prognosis, and therapeutic monitoring. In critical illness, phosphatidylethanolamines (PEs) have been identified as prognostic markers, with elevated levels associated with worse outcomes in both trauma and severe COVID-19 patients [26]. This suggests that certain lipidomic patterns may transcend specific disease etiologies, reflecting common pathophysiological pathways in systemic metabolic stress.
In schizophrenia research, a panel of three lipid biomarkers - PC(18:2e19:0), PE(53:7), and TG(16:2e19:0_20:5) - demonstrated capability to distinguish poor and good responders to antipsychotic treatment, achieving an AUC of 0.805 [25]. This highlights the potential of lipidomic profiling for predicting treatment response and guiding therapeutic decisions.
Similar approaches in diabetes and hyperuricemia research could yield biomarker panels for identifying patients at high risk for disease progression or complications, enabling targeted interventions and personalized treatment strategies. The distinct lipidomic signatures observed in patients with combined diabetes and hyperuricemia suggest potential for developing biomarkers that reflect the synergistic metabolic disturbances in this patient population [2] [24].
UHPLC-MS/MS-based lipidomic profiling provides a powerful approach for elucidating the complex relationships between lipid metabolism and disease pathophysiology in diabetes and hyperuricemia. The distinct lipid signatures associated with these conditions reflect underlying metabolic disruptions that contribute to disease progression and complications. Through standardized methodologies encompassing sample preparation, chromatographic separation, mass spectrometric analysis, and advanced data processing, researchers can obtain comprehensive lipidomic profiles that offer unique insights into disease mechanisms.
The integration of lipidomic data with clinical parameters and outcomes facilitates the discovery of novel biomarkers with diagnostic, prognostic, and therapeutic potential. As the field advances, standardization of analytical protocols and computational pipelines will enhance reproducibility and comparability across studies. Lipidomics holds particular promise for precision medicine approaches in metabolic diseases, potentially guiding targeted interventions based on individual lipidomic profiles to improve patient outcomes.
A Practical Guide to UHPLC-MS/MS Lipidomic Workflows for Metabolic Profiling
Lipidomics, a specialized branch of metabolomics, provides a comprehensive approach to analyzing the complete lipid profile within a biological system [27]. In the context of diabetes mellitus combined with hyperuricemia (DH), lipidomic profiling using ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) has revealed significant alterations in lipid metabolism pathways, specifically identifying 31 significantly altered lipid metabolites in DH patients compared to healthy controls [2]. These perturbations are primarily enriched in glycerophospholipid and glycerolipid metabolism pathways, offering crucial insights into the intertwined pathophysiological mechanisms of these metabolic disorders [2]. This technical guide details the essential workflow from sample collection to data acquisition for UHPLC-MS/MS-based lipidomic profiling, specifically framed within diabetes and hyperuricemia research.
Sample Collection and Preparation
Sample Collection Protocols
Proper sample collection and immediate processing are critical first steps in lipidomics, as lipids are prone to enzymatic and chemical degradation [28].
- Biological Matrices: Plasma/serum is commonly used. For DH studies, collect fasting blood samples [2].
- Collection Protocol: Draw 5 mL of fasting morning blood into appropriate collection tubes [2].
- Initial Processing: Centrifuge at 3,000 rpm for 10 minutes at room temperature to separate plasma [2].
- Aliquoting and Storage: Transfer 0.2 mL of the upper plasma layer into cryovials. Flash-freeze and store at -80°C to preserve lipid integrity [2] [28]. Avoid repeated freeze-thaw cycles.
For tissue samples, homogenization is essential to ensure equal lipid accessibility from all tissue regions. Methods include shear-force-based grinding (Potter-Elvehjem homogenizer) or crushing liquid-nitrogen-frozen tissue with a pestle and mortar [28].
Lipid Extraction Methodologies
Lipid extraction serves to reduce sample complexity by removing non-lipid compounds and enriching analytes of interest for improved signal-to-noise ratios [28].
Figure 1: MTBE-based Liquid-Liquid Extraction Workflow. Based on the protocol used in a diabetes with hyperuricemia lipidomic study [2].
The MTBE (methyl tert-butyl ether) method is widely used in lipidomics research [2] [28]. This method offers comparable efficiency to traditional chloroform-based protocols but with easier handling and enhanced safety [28]. The phase separation in MTBE extraction results in an upper organic phase containing lipids and a lower aqueous phase with salts and hydrophilic compounds, simplifying lipid recovery [28].
Alternative extraction methods include:
- Folch and Bligh & Dyer: Chloroform-based methods using ternary mixtures of chloroform, methanol, and water [28] [29].
- BUME method: A fully automated protocol using butanol/methanol sequentially added with heptane/ethyl acetate and acetic acid, suitable for high-throughput screening in 96-well plates [28].
- One-step protocols: Single-phase extractions using methanol, ethanol, 2-propanol, or acetonitrile followed by protein precipitation, offering higher efficiency for polar lipids but potentially increasing instrument contamination [28].
The Scientist's Toolkit: Essential Research Reagents
Table 1: Essential Reagents for UHPLC-MS/MS Lipidomics
| Reagent Category | Specific Examples | Function in Workflow |
|---|---|---|
| Extraction Solvents | Methyl tert-butyl ether (MTBE), Methanol, Chloroform, Butanol [2] [28] | Lipid solubilization and separation from non-lipid compounds during liquid-liquid extraction. |
| LC-MS Solvents | Acetonitrile, Isopropanol, Water (LC-MS grade) [2] [30] [31] | Mobile phase composition for UHPLC separation; minimizes background interference in MS detection. |
| Additives | Ammonium formate, Formic acid, Acetic acid [2] [32] [29] | Enhances ionization efficiency in the MS source and helps control chromatographic separation. |
| Internal Standards | Deuterated lipid standards (e.g., EquiSplash Lipidomix), 1,2,3-tripelargonoyl-glycerol [30] [33] | Normalization for extraction efficiency, instrument variability, and quantitative accuracy. |
| 8-pCPT-cGMP-AM | 8-pCPT-cGMP-AM, MF:C19H19ClN5O9PS, MW:559.9 g/mol | Chemical Reagent |
| TCO-PEG12-TFP ester | TCO-PEG12-TFP ester, MF:C42H67F4NO16, MW:918.0 g/mol | Chemical Reagent |
UHPLC-MS/MS Analysis: Instrumentation and Data Acquisition
Chromatographic Separation
Ultra-high performance liquid chromatography provides critical separation of complex lipid mixtures prior to mass spectrometry analysis, reducing ion suppression and enabling identification of isomeric lipids [30] [29].
- Column Technology: Use a Waters ACQUITY UPLC BEH C18 column (2.1 × 100 mm, 1.7 μm) or equivalent reversed-phase column [2] [29].
- Temperature Control: Maintain column at 50°C for enhanced elution of late-eluting lipids like triacylglycerols [29].
- Mobile Phase:
- Gradient Elution: Implement a multi-step gradient, for example: start at 65% A / 35% B, ramp to 80% B in 2 min, to 100% B in 7 min, and hold for 7 min [29].
- Flow Rate and Injection: 0.400 mL/min flow rate with 2.0 μL injection volume [29]. Total analysis time is approximately 12-16 minutes per sample.
Mass Spectrometric Detection
Mass spectrometry is the cornerstone of detection and identification in lipidomics due to its sensitivity, specificity, and dynamic range [32] [27].
- Ionization Source: Electrospray Ionization (ESI) is most common, capable of ionizing polar, thermally labile lipids [27]. Both positive and negative ionization modes are typically used, sometimes with polarity switching during a single run [32].
- Mass Analyzers: Quadrupole time-of-flight (Q-TOF) and Orbitrap instruments provide high resolution and mass accuracy, enabling precise lipid identification [27] [29]. Triple quadrupole (QqQ) systems offer high sensitivity for targeted analysis [31] [27].
- Data Acquisition Modes:
- Untargeted Lipidomics: Full scan mode at high resolution (e.g., m/z 300-1200) detects a broad range of lipids [27] [29].
- Data-Dependent Acquisition (DDA): Automatically selects abundant precursors for fragmentation, providing structural information [32].
- All Ion Fragmentation (AIF): Fragments all generated ions simultaneously at different collision energies, providing comprehensive structural data in a single run [32].
- Targeted Acquisition: For quantitative studies, use selected reaction monitoring (SRM) on QqQ instruments for highest sensitivity [31] [27].
Figure 2: UHPLC-MS/MS Data Acquisition Pathways. Multiple MS acquisition strategies can be employed depending on research goals [32] [27].
Data Processing, Analysis, and Application to Diabetes-Hyperuricemia
Data Processing and Lipid Identification
Processing raw UHPLC-MS/MS data requires specialized software for peak detection, alignment, and identification [29].
- Peak Processing: Use software like MZmine 2 for peak detection, alignment, integration, and normalization [29].
- Lipid Identification: Match accurate mass and retention time against internal spectral libraries [29]. Confirm identities using MS/MS fragmentation patterns compared to standards or database spectra [32].
- Quantification: Normalize using class-specific internal standards (e.g., deuterated lipids) [30] [29]. Response factors may be applied for absolute quantification.
Metabolic Pathway Analysis in Diabetes-Hyperuricemia
In DH research, multivariate statistical analyses like Principal Component Analysis (PCA) and Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) reveal separation trends among DH, DM, and healthy control groups [2]. Differential lipid molecules are subsequently analyzed for pathway enrichment.
Table 2: Key Lipid Alterations and Perturbed Pathways in Diabetes with Hyperuricemia
| Analytical Comparison | Significantly Altered Lipids | Perturbed Metabolic Pathways |
|---|---|---|
| DH vs. Healthy Controls | 13 Triglycerides (TGs) ↑10 Phosphatidylethanolamines (PEs) ↑7 Phosphatidylcholines (PCs) ↑1 Phosphatidylinositol (PI) ↓ [2] | Glycerophospholipid metabolism (Impact: 0.199)Glycerolipid metabolism (Impact: 0.014) [2] |
| DH vs. DM | 12 Differential Lipids identified [2] | Enriched in the same core pathways (Glycerophospholipid and Glycerolipid metabolism) [2] |
These findings underscore the central role of glycerophospholipid and glycerolipid metabolism disruptions in the pathophysiology of hyperuricemia complicating diabetes [2]. The identified lipid species and pathways serve as potential biomarkers for disease progression and therapeutic targets.
Method Validation and Quality Control
Rigorous validation and quality control are essential for generating reliable lipidomic data.
- Quality Control (QC) Samples: Prepare pooled QC samples from all study samples and inject regularly throughout the analytical sequence to monitor instrument stability [2].
- Method Validation: For targeted methods, validate linearity (typically over >4 orders of magnitude), accuracy, precision, and limits of quantitation (can reach femtomole levels on-column) [30].
- Standardization: Use standardized extraction protocols and internal standards to minimize technical variability [28].
This comprehensive workflow from sample collection through data acquisition provides a robust framework for conducting UHPLC-MS/MS lipidomic profiling in diabetes and hyperuricemia research, enabling the discovery of lipid biomarkers and mechanistic insights into these interconnected metabolic disorders.
Ultra-High-Performance Liquid Chromatography (UHPLC) has emerged as a cornerstone technique in modern lipidomics, particularly for the analysis of complex biological samples in disease research. Its superior speed, resolution, and sensitivity compared to traditional HPLC make it indispensable for unraveling the intricate lipid landscapes associated with metabolic diseases [34] [35]. This technical guide focuses on optimizing UHPLC conditions for separating complex lipid mixtures within the specific context of a broader thesis on UHPLC-MS/MS lipidomic profiling in diabetes mellitus (DM) and hyperuricemia (HUA) research. Lipid metabolism is profoundly disrupted in these conditions; disorders of lipid metabolism are a known risk factor for diabetes, and hyperuricemia can itself lead to lipid abnormalities [2] [14]. The intent of a quantitative bioanalytical method in this field is to provide a precise and accurate estimation of the concentration of target lipids in these complicated biological samples, which is essential for drug development, clinical analysis, and pharmacokinetic studies [34].
However, the inherent complexity of biological samples like plasma or serum presents significant challenges for UHPLC analysis. These samples are an intricate tapestry of proteins, lipids, carbohydrates, and other biomolecules, each with diverse physicochemical properties [34]. Two primary challenges are:
- Matrix Effects and Ion Suppression: During the ionization process in mass spectrometry, co-eluting biomolecules can interact with the analyte of interest, suppressing or enhancing its signal and leading to erroneous quantification. This is particularly problematic for low-concentration lipids and can mask their presence entirely. Phospholipids are especially known to cause significant ion suppression in electrospray ionization (ESI) [34].
- Analyte Diversity and Co-elution: Lipidomic samples harbor a vast array of molecules with diverse polarity, size, and charge. This diversity makes achieving optimal chromatographic separation a challenge, as lipids with similar properties may co-elute, resulting in overlapping peaks that hinder accurate identification and quantification [34].
Core UHPLC Optimization Parameters
Optimizing a UHPLC method for complex lipid mixtures requires meticulous attention to several key parameters to achieve efficient separation, minimize matrix effects, and improve overall sensitivity and accuracy.
Column Selection and Chemistry
The choice of chromatographic column is fundamental. UHPLC utilizes columns packed with sub-2 µm particles, which operate at very high pressures (up to 1000 bar or more) to provide dramatically reduced analysis times, enhanced resolution, and higher sensitivity compared to traditional HPLC [36] [35]. The typical peak widths generated are in the order of 1–2 seconds, which greatly improves chromatographic resolution and reduces the problem of ion suppression from co-eluting peaks [35]. For lipid separation, reversed-phase columns, particularly C18 chemistries, are most common.
Table 1: UHPLC Column and System Conditions for Lipidomics
| Parameter | Typical Specification for Lipidomics | Function and Impact |
|---|---|---|
| Column Chemistry | Waters ACQUITY UPLC BEH C18 [2] | Provides the stationary phase for analyte separation based on hydrophobicity. |
| Column Dimension | 2.1 mm i.d. × 100 mm length [2] | Standard format for UHPLC-MS/MS applications. |
| Particle Size | 1.7 µm [2] [35] | Smaller particles enable higher efficiency, resolution, and speed. |
| System Pressure | Operates at high pressure (up to 1000 bar+) [36] | Required to drive mobile phase through a column packed with sub-2 µm particles. |
| Column Temperature | 45°C [2] | Higher temperature can reduce mobile phase viscosity, improving efficiency. |
| Injection Volume | Lower than HPLC (e.g., 3 µL) [35] | Higher efficiency and sensitivity with minimal volume. |
Mobile Phase Composition and Gradient
The mobile phase composition and gradient profile are critical for eluting the wide range of lipids present in a sample. The mobile phase typically consists of a aqueous-based solvent (A) and an organic-rich solvent (B).
Table 2: Mobile Phase Components and Elution Protocols
| Component | Common Compositions | Role in Separation |
|---|---|---|
| Mobile Phase A | 10 mM ammonium formate in water [2] or ACN/H2O (60:40 v/v) with 10 mM ammonium formate [14] | Aqueous-based solvent for initial weak elution strength. Additives like ammonium formate improve ionization. |
| Mobile Phase B | 10 mM ammonium formate in acetonitrile:isopropanol (IPA) (e.g., 10:90) [2] or ACN:IPA (2:9 v/v) with 10 mM ammonium formate [14] | Organic-rich solvent for strong elution strength. IPA is effective at eluting more non-polar lipids. |
| Gradient Example | - 0-2 min: 30% B- 2-25 min: 30% B to 100% B- 25-35 min: 100% B (wash)- 35-35.1 min: 100% B to 30% B- 35.1-40 min: 30% B (re-equilibration) [2] [14] | A shallow or complex gradient is necessary to resolve the hundreds of lipid species with subtle differences in hydrophobicity. |
Sample Preparation
Effective sample preparation is critical for successful UHPLC-MS/MS analysis of lipids, as it removes proteins and other matrix interferences that can cause ion suppression and damage the instrument.
- Lipid Extraction: A common and robust method is a liquid-liquid extraction based on methyl tert-butyl ether (MTBE). A standard protocol involves:
- Vortexing 100 µL of plasma with 200 µL of water.
- Adding 240 µL of pre-cooled methanol, followed by 800 µL of MTBE.
- Sonicating in a low-temperature water bath for 20 minutes and standing at room temperature for 30 minutes.
- Centrifuging at 14,000 g for 15 minutes at 10°C.
- Collecting the upper organic phase and drying it under a stream of nitrogen.
- Reconstituting the dried lipids in 100 µL of isopropanol/acetonitrile (90:10) for analysis [2] [14].
- Protein Precipitation: While simple, protein precipitation using organic solvents like acetonitrile or methanol is often insufficient for lipidomics as it does not effectively remove phospholipids, which are a major source of matrix effects [34].
Experimental Protocols and Applications in Diabetes-Hyperuricemia Research
The following workflow and protocol details are derived from recent lipidomic studies investigating diabetes and hyperuricemia.
Diagram 1: Lipidomics workflow for diabetes-hyperuricemia research
Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for UHPLC-MS/MS Lipidomics
| Item | Function | Specific Example / Note |
|---|---|---|
| UHPLC System | High-pressure pump, autosampler, and column oven for precise separation. | Waters ACQUITY UPLC system or equivalent [2]. |
| Mass Spectrometer | High-resolution mass analyzer for accurate mass detection and structural characterization. | Q-Exactive Plus (Orbitrap) or other Q-TOF/Triple Quadrupole instruments [2] [35]. |
| Chromatography Column | The core component for separating lipid molecules. | Waters ACQUITY UPLC BEH C18 (1.7 µm, 2.1x100 mm) [2]. |
| Methyl tert-Butyl Ether (MTBE) | Primary solvent for liquid-liquid lipid extraction. | Effectively extracts a broad range of lipid classes [2] [14]. |
| HPLC-grade Solvents | Used for mobile phases and sample preparation to minimize background noise. | Acetonitrile, Isopropanol, Methanol, Water [2] [14]. |
| Ammonium Formate | Mobile phase additive to improve ionization efficiency and aid in adduct formation. | Typically used at 10 mM concentration [2] [14]. |
| Internal Standards | Correct for variability in sample prep, injection, and ionization. | Stable isotope-labeled lipid standards (SIL-IS) are ideal [34]. |
Key Findings and Differential Lipids
Application of the optimized UHPLC-MS/MS protocol in clinical research has revealed distinct lipid signatures associated with disease states. A study comparing patients with diabetes mellitus combined with hyperuricemia (DH), diabetes mellitus (DM) alone, and healthy controls (NGT) identified 1,361 lipid molecules across 30 subclasses [2]. Multivariate analyses confirmed distinct lipidomic profiles between these groups.
Table 4: Significantly Altered Lipid Metabolites in Diabetes-Hyperuricemia Research
| Lipid Class | Example Molecule(s) | Trend (DH vs NGT) | Biological Relevance |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) [2] | Significantly Upregulated | Associated with insulin resistance and core components of glycerolipid metabolism pathway [2]. |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) [2] | Significantly Upregulated | Key components of cell membranes; enriched in glycerophospholipid metabolism pathway [2]. |
| Phosphatidylcholines (PCs) | PC(36:1) [2] | Significantly Upregulated | Major membrane phospholipids; central to glycerophospholipid metabolism [2] [14]. |
| Phosphatidylinositol (PI) | Not Specified [2] | Downregulated | Involved in cell signaling; part of the disturbed glycerophospholipid metabolism network. |
Pathway analysis of these differential lipids using platforms like MetaboAnalyst 5.0 consistently identifies glycerophospholipid metabolism and glycerolipid metabolism as the most significantly perturbed pathways in patients with combined diabetes and hyperuricemia [2]. These findings are corroborated by other multiomics studies, which also found lipid metabolites involved in arachidonic acid metabolism and linoleic acid metabolism in hyperuricemia patients [14].
Diagram 2: Proposed lipid-immune pathway in diabetes-hyperuricemia
Furthermore, these lipid alterations are linked to changes in immune factors. Studies have shown that interleukin 6 (IL-6), carnitine palmitoyltransferase-1 (CPT1), glucose (Glu), and lactic acid (LD) are associated with the dysregulated glycerophospholipid metabolism pathway, suggesting a connection between lipid disorders and immune and metabolic shifts in patients with hyperuricemia [14].
Lipidomics, a specialized branch of metabolomics, has emerged as a powerful platform for comprehensively analyzing lipids in biological systems. This field is particularly relevant for understanding complex metabolic diseases such as diabetes mellitus (DM) and hyperuricemia, where dysregulated lipid metabolism plays a crucial pathophysiological role. The structural diversity of lipids—estimated to include hundreds of thousands of molecular species in biological systems—presents significant analytical challenges that conventional technologies cannot adequately address [37]. Recent advances in mass spectrometry, specifically the integration of high-resolution mass analyzers and tandem MS (MS/MS) capabilities, have revolutionized our ability to characterize lipidomes in unprecedented detail [38] [39]. These technological improvements have enabled researchers to move beyond simple lipid profiling to precise identification and quantification of individual molecular lipid species, even in complex biological samples.
The application of these advanced mass spectrometry techniques in studying diabetes combined with hyperuricemia (DH) has revealed specific lipid alterations that may serve as early biomarkers or therapeutic targets. A recent investigation utilizing UHPLC-MS/MS identified 1,361 lipid molecules across 30 subclasses in plasma samples, demonstrating the powerful resolving capacity of modern lipidomics platforms [2]. Such detailed molecular characterization provides critical insights into metabolic disturbances that underlie disease progression and comorbidity development. The convergence of high-resolution and tandem MS technologies has thus transformed lipidomics from a descriptive to a mechanistic science, enabling researchers to elucidate specific lipid pathways disrupted in metabolic disorders.
Technical Foundations of Lipid Identification
High-Resolution Mass Spectrometry
High-resolution mass spectrometry (HRMS) has fundamentally changed the strategy for lipidome characterization by enabling accurate mass measurements that distinguish isobaric species with minimal mass differences. The resolving power (R) of a mass spectrometer, calculated as the ratio of the ion peak mass to the peak width at half maximum height (FWHM), determines its ability to separate ions with similar mass-to-charge (m/z) ratios [39]. While unit mass resolution (the ability to distinguish peaks 1 Da apart) was once considered sufficient for lipidomics, modern Orbitrap and time-of-flight (TOF) instruments now routinely achieve resolutions of 60,000 to 100,000 or higher, allowing separation of lipid species differing in mass by only 0.0726 Da or less [39].
The exceptional value of HRMS in lipidomics lies in its capacity to differentiate isobaric lipids that share the same nominal mass but have different elemental compositions. For example, a phosphatidylcholine (PC) species (C44H85NO8P+) and a phosphatidylserine (PS) species (C42H75NO10P+) might both have a nominal mass of 786 Da, but their exact masses differ sufficiently to be resolved by HRMS [39]. This accurate mass measurement provides the elemental composition of lipid ions, delivering a critical first dimension of structural information without requiring fragmentation. Modern hybrid instruments combine high-resolution accurate mass (HRAM) detection with advanced fragmentation capabilities, providing a comprehensive solution for lipid identification and characterization [38] [30].
Tandem Mass Spectrometry (MS/MS)
Tandem mass spectrometry (MS/MS) adds a crucial dimension to lipid analysis by providing structural elucidation through controlled fragmentation of precursor ions. In MS/MS experiments, specific lipid molecular ions are isolated in the first stage of mass analysis, fragmented through collision-induced dissociation (CID) or higher-energy collisional dissociation (HCD), and the resulting product ions are analyzed in a second mass analysis stage [40]. These fragmentation patterns provide detailed structural information including head group composition, fatty acyl chain length, and double bond positions [40].
The diagnostic value of MS/MS spectra is particularly evident in distinguishing lipid isomers that share the same elemental composition but differ in their structural arrangements. For example, MS/MS can differentiate between plasmalogen phosphatidylethanolamines (PE-P) and diacyl phosphatidylethanolamines (PE) through characteristic fragmentation patterns that reveal the vinyl ether bond in plasmalogens [37]. Similarly, regioisomers of glycerolipids (e.g., sn-1 vs. sn-2 fatty acid positioning) and double bond positions in unsaturated fatty acyl chains can be determined through specific fragmentation signatures [40] [30]. This level of structural detail is essential for understanding the biological activity of lipid species in metabolic diseases like diabetes and hyperuricemia, where specific lipid molecular structures may have distinct pathophysiological roles.
Complementary Strengths of HRMS and MS/MS
The combination of high-resolution mass spectrometry and tandem MS creates a powerful synergistic platform for comprehensive lipidomics that leverages the unique strengths of both approaches. HRMS provides exceptional mass accuracy and resolution for determining elemental composition and distinguishing isobaric species, while MS/MS delivers structural specificity through characteristic fragmentation patterns [39]. This multi-dimensional approach is particularly valuable in complex biological samples where lipid diversity creates significant analytical challenges.
Table 1: Comparison of High-Resolution MS and Tandem MS Approaches in Lipidomics
| Analytical Feature | High-Resolution MS | Tandem MS (MS/MS) |
|---|---|---|
| Primary Information | Elemental composition | Structural fragments |
| Key Strength | Distinguishing isobaric species | Determining molecular structure |
| Typical Resolution | 60,000-100,000+ | Unit mass resolution often sufficient |
| Quantitation Capability | Excellent with proper standardization | Excellent with internal standards |
| Structural Specificity | Limited to formula assignment | High for class and chain composition |
| Throughput | High in full-scan mode | Lower due to sequential fragmentation |
This complementary relationship enables both untargeted lipid discovery (through HRMS) and targeted structural validation (through MS/MS) within a single analytical platform [38] [39]. For research on diabetes and hyperuricemia, this means that both expected and novel lipid perturbations can be detected and characterized in a single analysis, providing a comprehensive view of lipid metabolic disruptions associated with these conditions.
Integrated Analytical Workflows in Lipidomics Research
The power of modern lipidomics lies in the integration of complementary analytical techniques into structured workflows that maximize information recovery while maintaining analytical rigor. Two principal approaches—shotgun lipidomics and chromatography-coupled MS—each offer distinct advantages for different research applications.
Diagram 1: Integrated lipidomics workflow for metabolic disease research. The analytical approach selection (shotgun vs. LC-MS/MS) depends on research objectives, with shotgun favoring high-throughput and LC-MS/MS providing enhanced separation for complex samples.
Shotgun Lipidomics Approaches
Shotgun lipidomics employs the direct infusion of lipid extracts into the mass spectrometer without prior chromatographic separation [39]. This approach leverages the intrinsic chemical properties of different lipid classes to facilitate their identification and quantification through selective ionization and high-mass-resolution analysis. The primary advantage of shotgun methods is high throughput, as the elimination of chromatographic separation significantly reduces analysis time [39]. Additionally, the constant analyte composition during direct infusion enables extended signal averaging and the acquisition of multiple MS/MS spectra for comprehensive structural characterization.
The effectiveness of shotgun lipidomics is significantly enhanced by high-resolution mass analyzers, which can distinguish and quantify isobaric lipid species in total lipid extracts [39]. For example, the exact mass difference of 0.0726 Da between isobaric PC(36:1) and PS(36:2) species is readily resolved at a mass resolution of 100,000, allowing their independent quantification without MS/MS [39]. This capability streamlines lipidome characterization while maintaining analytical specificity. However, shotgun approaches can be limited by ion suppression effects in complex mixtures and may struggle with low-abundance lipid species [30]. The approach is therefore particularly well-suited for high-throughput screening applications where comprehensive lipid coverage is prioritized over absolute quantification of every molecular species.
Liquid Chromatography-Mass Spectrometry Approaches
Liquid chromatography coupled to mass spectrometry (LC-MS) introduces an additional separation dimension that alleviates many limitations of shotgun approaches. Ultrahigh performance liquid chromatography (UHPLC) employing sub-2µm particle columns provides exceptional chromatographic resolution, separating lipids by both acyl chain length and degree of unsaturation prior to mass analysis [2] [30]. This separation reduces ion suppression effects and increases analytical sensitivity, particularly for low-abundance lipid species [30]. Additionally, the temporal separation of isobaric and isomeric species ensures that MS/MS spectra originate from single lipid precursors, simplifying data interpretation and improving identification confidence [30].
A representative UHPLC-MS method for lipidomics utilizes reversed-phase C18 columns with a binary mobile phase gradient ranging from aqueous to organic solvents [2] [37]. Typical analysis times of 10-20 minutes provide sufficient chromatographic resolution while maintaining practical throughput for large sample sets [37]. The coupling of UHPLC with high-resolution tandem mass spectrometry creates a particularly powerful platform for global lipidomic profiling, enabling the identification and quantification of hundreds to thousands of lipid species across multiple classes in a single analysis [2] [30]. This comprehensive approach has been successfully applied to investigate lipid disturbances in diabetes with hyperuricemia, revealing specific alterations in glycerophospholipid and glycerolipid metabolism pathways [2].
Experimental Protocols for Lipidomics in Diabetes-Hyperuricemia Research
Sample Preparation Methodology
Robust sample preparation is fundamental to successful lipidomics studies. A standardized protocol derived from recent diabetes-hyperuricemia research ensures reproducible lipid extraction and recovery [2]:
Sample Collection: Collect 5 mL of fasting morning blood in appropriate anticoagulant tubes. Centrifuge at 3,000 rpm for 10 minutes at room temperature to separate plasma. Aliquot 0.2 mL of the upper plasma layer into 1.5 mL centrifuge tubes and store at -80°C until analysis.
Lipid Extraction: Thaw samples on ice and vortex thoroughly. Transfer 100 µL of plasma to a 1.5 mL centrifuge tube. Add 200 µL of 4°C water followed by 240 µL of pre-cooled methanol and mix thoroughly. Add 800 µL of methyl tert-butyl ether (MTBE), sonicate in a low-temperature water bath for 20 minutes, and let stand at room temperature for 30 minutes. Centrifuge at 14,000 g for 15 minutes at 10°C. Collect the upper organic phase and dry under a nitrogen stream [2].
Quality Control: Prepare pooled quality control (QC) samples by combining equal aliquots from all samples. Insert QC samples randomly throughout the analysis sequence to monitor instrument performance and data quality.
UHPLC-MS/MS Analysis Conditions
The analytical separation and detection parameters are critical for comprehensive lipidome characterization [2] [37]:
Chromatographic Conditions:
- Column: Waters ACQUITY UPLC BEH C18 (2.1 × 100 mm, 1.7 µm)
- Mobile Phase A: 10 mM ammonium formate in water
- Mobile Phase B: 10 mM ammonium formate in acetonitrile-isopropanol solution
- Gradient Program: Initiate at 35% B, increase to 80% B in 2 minutes, 100% B in 7 minutes, hold for 7 minutes
- Flow Rate: 0.400 mL/min
- Column Temperature: 50°C
- Injection Volume: 2.0 µL
Mass Spectrometry Conditions:
- Ionization: Electrospray ionization (ESI) in positive and negative modes
- Mass Analyzer: Quadrupole-time-of-flight (Q-TOF) or Orbitrap-based instrument
- Mass Resolution: ≥60,000 for high-resolution applications
- Mass Range: m/z 300-1200
- Data Acquisition: Full MS scans combined with data-dependent MS/MS (dd-MS²) for top N precursors
Data Processing and Lipid Identification
Raw data processing converts instrumental data into biologically meaningful lipid identifications [2] [37]:
- Chromatographic Processing: Perform peak detection, alignment, and integration using specialized software (e.g., MZmine, XCMS, or vendor-specific packages).
- Lipid Identification: Match accurate mass (typically <5 ppm error) and retention time against authentic standards when available. Confirm identifications through MS/MS spectral matching to reference libraries or theoretical fragmentation patterns.
- Quantitation: Normalize lipid peak areas using internal standards (e.g., deuterated or odd-chain lipid species) to account for extraction and ionization variability.
- Statistical Analysis: Apply multivariate statistics (PCA, OPLS-DA) to identify differentially abundant lipids. Perform pathway analysis (e.g., MetaboAnalyst) to determine affected metabolic pathways.
Lipidomic Findings in Diabetes with Hyperuricemia
Application of the above methodologies to diabetes with hyperuricemia (DH) research has revealed specific lipid disturbances that provide mechanistic insights into this metabolic comorbidity. A recent UHPLC-MS/MS study comparing DH patients with diabetic controls and healthy subjects identified 31 significantly altered lipid metabolites in the DH group [2]. These differential lipids were predominantly upregulated and included specific molecular species of triglycerides (TGs), phosphatidylethanolamines (PEs), and phosphatidylcholines (PCs) [2].
Table 2: Significantly Altered Lipid Classes in Diabetes with Hyperuricemia
| Lipid Class | Representative Molecules | Change in DH | Biological Relevance |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) | Significantly upregulated | Energy storage, insulin resistance association |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) | Significantly upregulated | Membrane fluidity, signaling precursors |
| Phosphatidylcholines (PCs) | PC(36:1) | Significantly upregulated | Membrane structure, lipoprotein assembly |
| Phosphatidylinositols (PIs) | Not specified | Downregulated | Signaling precursors, insulin signaling |
Pathway analysis of these altered lipids revealed enrichment in several key metabolic pathways, with glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) identified as the most significantly perturbed in DH patients [2]. These pathway disturbances highlight the interconnected nature of lipid metabolic networks in complex metabolic diseases and suggest potential points for therapeutic intervention.
Diagram 2: Perturbed lipid metabolism pathways in diabetes with hyperuricemia. Upregulated lipid classes in DH are highlighted in green, while downregulated PIs are shown in red. The pathway illustrates key branch points in glycerophospholipid and glycerolipid metabolism that are disrupted in the comorbidity.
The comparison between DH and DM-only groups further identified 12 differential lipids that were similarly enriched in these core pathways, underscoring their central role in the pathophysiology of hyperuricemia complicating diabetes [2]. These specific lipid alterations may serve as potential biomarkers for identifying diabetic patients at risk for developing hyperuricemia or for monitoring disease progression and therapeutic responses.
Table 3: Key Research Reagent Solutions for Lipidomics Studies
| Resource Category | Specific Examples | Function/Application |
|---|---|---|
| Chromatography Columns | Waters ACQUITY UPLC BEH C18 (2.1 × 100 mm, 1.7 µm) | Reversed-phase separation of lipid molecular species by hydrophobicity |
| Mass Spectrometry Systems | Q-TOF Premier (Waters), LTQ-Orbitrap (Thermo Fisher) | High-resolution mass analysis and tandem MS fragmentation |
| Internal Standards | LIPID MAPS quantitative lipid standards, deuterated analogs (e.g., PC(16:1/16:1-D6)) | Quantitation normalization, quality control, and method validation |
| Extraction Solvents | Methyl tert-butyl ether (MTBE), chloroform:methanol (2:1) | Efficient lipid extraction from biological matrices with minimal degradation |
| Data Processing Software | MZmine 2, MS DIAL, Lipostar | Peak detection, alignment, identification, and quantitation |
| Lipid Database Resources | LIPID MAPS, CFM-ID, MetaboAnalyst | Lipid structure identification, pathway analysis, and functional interpretation |
The integration of high-resolution mass spectrometry with tandem MS capabilities has transformed lipidomics into a powerful platform for investigating complex metabolic diseases such as diabetes with hyperuricemia. The exceptional mass accuracy and resolution of modern instruments enable discrimination of isobaric lipid species, while MS/MS provides structural confirmation and detailed molecular characterization. When coupled with robust chromatographic separation and standardized sample preparation, these techniques can comprehensively characterize hundreds to thousands of lipid species across multiple classes in a single analysis.
Application of these advanced lipidomics technologies to diabetes with hyperuricemia research has revealed specific alterations in glycerophospholipid and glycerolipid metabolism pathways, with particular upregulation of triglyceride, phosphatidylethanolamine, and phosphatidylcholine species. These lipid disturbances provide mechanistic insights into the metabolic interactions between diabetes and hyperuricemia and may yield biomarkers for early detection, risk stratification, or therapeutic monitoring. As lipidomics technologies continue to evolve toward greater sensitivity, resolution, and throughput, their application to metabolic disease research promises to uncover increasingly detailed understanding of lipid-mediated pathophysiological processes, potentially leading to improved diagnostic and therapeutic approaches for these increasingly prevalent conditions.
Ultra-High-Performance Liquid Chromatography-Tandem Mass Spectrometry (UHPLC-MS/MS) has become an indispensable tool for untargeted lipidomics, enabling the identification and quantification of thousands of lipid molecules from biological samples [41]. This capability is crucial for investigating complex metabolic disorders such as Diabetes Mellitus (DM) and Diabetes Mellitus combined with Hyperuricemia (DH). In such research, the robust processing of raw mass spectrometry data is not merely a preliminary step but the foundation upon which valid biological insights are built. The initial data, comprising thousands of mass-to-charge (m/z) and retention time (RT) pairs, are vast and complex [41]. Without sophisticated processing strategies—including peak alignment to correct for analytical drift, normalization to account for technical variance, and multivariate statistical analysis to discern meaningful patterns—researchers cannot reliably identify the lipid metabolic signatures that distinguish diseased states from healthy controls. For instance, a study investigating DH identified 1,361 lipid molecules across 30 subclasses, and the application of Principal Component Analysis (PCA) and Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA) was critical in confirming distinct lipidomic profiles among the DH, DM, and healthy control groups [2]. This technical guide details the core data processing strategies required to transform raw UHPLC-MS/MS data into biologically significant findings within the context of diabetes and hyperuricemia research.
Experimental Workflow in UHPLC-MS/MS Lipidomics
A typical lipidomics study involves a multi-stage process, from sample preparation to biological interpretation. The data processing steps of peak alignment, normalization, and multivariate analysis are central to extracting meaningful results from the raw data acquired by the mass spectrometer. The following diagram illustrates the complete experimental workflow, highlighting the critical stages of data processing.
Peak Alignment
Objective: To correct for minor, unavoidable fluctuations in retention time (RT) and m/z values across multiple sample runs, ensuring that the same lipid species is correctly aligned and compared across all samples in the dataset [41].
Detailed Methodology: The process begins after raw data files have been converted from proprietary formats to an open format like mzXML using tools such as ProteoWizard [41].
- Peak Detection: The first step is to identify all the chromatographic peaks in each sample's data file. Software like the XCMS Bioconductor package in R scans the data for regions with elevated ion counts relative to the baseline, defining each peak by its m/z, RT, and intensity [41].
- Correspondence Analysis: After individual peaks are identified, the algorithm performs "correspondence analysis," which groups peaks with similar m/z and RT across different samples. This step is crucial for matching the same lipid species measured in different runs [41].
- Retention Time Correction: To improve the accuracy of the correspondence, advanced algorithms can adjust the retention time of peaks across samples to a common reference. This corrects for drifts caused by changes in column performance or mobile phase composition over the course of a long analytical sequence. The Bioconductor package IPO can be used to optimize the parameters for this alignment process [41].
Considerations for Diabetes/Hyperuricemia Research:
- Batch Effects: Large-scale studies are often run in multiple batches. It is critical to distribute samples from different groups (e.g., DH, DM, Control) across batches and to include quality control (QC) samples in each batch to monitor and correct for technical variation [41].
- Folder Structure: The organization of raw data files in folders can influence how XCMS groups samples. Files from similar groups or technical replicates should be placed in subfolders to guide the alignment algorithm [41].
Normalization
Objective: To remove non-biological, technical variances from the data (e.g., variations in sample injection volume, instrument sensitivity, or sample preparation efficiency), thereby ensuring that the differences in lipid abundance reflect true biological variation.
Detailed Methodology:
- Internal Standard (IS) Normalization: This is the most critical and preferred method in lipidomics.
- Procedure: A known amount of one or more isotope-labeled internal standards (IS), representing different lipid classes, is added to each sample at the very beginning of the extraction process [41].
- Calculation: The abundance of each endogenous lipid feature is divided by the abundance of a relevant internal standard. For example, a phosphatidylcholine (PC) lipid would be normalized to an isotope-labeled PC standard. This corrects for losses during sample preparation and ionization suppression/enhancement during MS analysis.
- Quality Control (QC) Sample-Based Normalization: A pooled QC sample, created by combining a small aliquot of every sample in the study, is analyzed repeatedly throughout the analytical sequence.
- Procedure: The data from the QC injections is used to monitor instrument stability. Signal drift can be modeled and corrected for each lipid feature across the run order.
- Data Cleaning and Filtering: Post-normalization, the data is cleaned by removing lipid features with high variance in the QC samples (typically >20-30%) and those with a high prevalence in blank samples, indicating potential contamination [41].
Application in Metabolic Research: In the DH/DM study, the use of internal standards and QC samples was integral to the protocol, allowing for the reliable identification of 31 significantly altered lipid metabolites in the DH group compared to controls [2].
Multivariate Statistical Analysis (PCA & OPLS-DA)
Objective: To provide a high-level, unsupervised (PCA) and supervised (OPLS-DA) overview of the data, identify global patterns, and pinpoint the specific lipid features most responsible for the differences between predefined groups (e.g., DH vs. DM).
Detailed Methodology:
- Principal Component Analysis (PCA):
- An Unsupervised Method: PCA is used to explore the data without using prior knowledge of group membership.
- Procedure: PCA reduces the dimensionality of the dataset by creating new, uncorrelated variables called Principal Components (PCs). The first PC (PC1) explains the largest possible variance in the data, the second PC (PC2) explains the next largest, and so on.
- Output: The results are visualized in a scores plot, which shows the natural clustering or separation of samples, and a loadings plot, which identifies which lipid variables contribute most to the separation seen in the scores plot. The DH/DM study used PCA to observe the overall distribution trend between groups [2].
- Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA):
- A Supervised Method: OPLS-DA uses the known class labels to maximize the separation between predefined groups.
- Procedure: The model separates the systematic variance in the data into two parts: (1) the predictive variance, which is correlated to the class labels (e.g., Disease vs. Control), and (2) the orthogonal variance, which is uncorrelated to the class labels (e.g., batch effects, age). This separation simplifies interpretation.
- Model Validation: To avoid overfitting, the model must be rigorously validated. This is typically done using a permutation test (e.g., randomly permuting class labels hundreds of times to ensure the original model is significantly better than chance) and by using cross-validation to calculate metrics like R²Y and Q². The DH/DM study employed OPLS-DA to confirm distinct lipidomic profiles and pinpoint differential lipids [2].
The relationship between the data, the models, and their validation is summarized below.
The Scientist's Toolkit: Essential Reagents and Materials
The following table catalogues the key reagents, software, and analytical tools essential for executing a UHPLC-MS/MS based lipidomics study in the context of diabetes research.
Table 1: Key Research Reagent Solutions for UHPLC-MS/MS Lipidomics
| Item Name | Function/Brief Explanation | Relevant Context in Diabetes/Hyperuricemia Research |
|---|---|---|
| Isotope-Labeled Internal Standards | Added to each sample prior to extraction to correct for technical variability during normalization [41]. | Enables accurate quantification of lipid species like TGs, PCs, and PEs, which are often dysregulated in diabetes and hyperuricemia [2]. |
| Methyl tert-butyl ether (MTBE) | A common organic solvent used in lipid extraction protocols to efficiently separate lipids from proteins and other aqueous components [2]. | Used in the sample preparation for the DH/DM study to extract a wide range of lipid classes from plasma [2]. |
| UHPLC System with BEH C18 Column | Provides high-resolution chromatographic separation of complex lipid mixtures prior to mass spectrometry analysis [2] [41]. | The DH/DM study utilized a Waters ACQUITY UPLC BEH C18 column (2.1 mm x 100 mm, 1.7 µm) for separation [2]. |
| QC Pooled Sample | A quality control sample created by pooling a small aliquot of every sample; analyzed repeatedly to monitor instrument stability and for data correction [41]. | Critical for large batch studies to ensure data quality and correct for signal drift over time, a necessity for reliable biomarker discovery. |
| XCMS Software (R/Bioconductor) | A widely used open-source package for peak detection, alignment, and statistical analysis of mass spectrometry data [41]. | Provides the computational framework for implementing the core data processing strategies outlined in this guide. |
| MetaboAnalyst 5.0 Platform | A web-based tool for comprehensive metabolomic data analysis, including pathway analysis and biomarker profiling. | Used in the DH/DM study to analyze and identify significantly perturbed lipid metabolic pathways, such as glycerophospholipid metabolism [2]. |
| BC21 | BC21, MF:C32H40Cl2Cu2N2O2+, MW:682.7 g/mol | Chemical Reagent |
| Jqad1 | Jqad1, MF:C48H52F4N6O9, MW:933.0 g/mol | Chemical Reagent |
The path from raw UHPLC-MS/MS data to biologically actionable insights in diabetes and hyperuricemia research is paved with meticulous data processing. The sequential application of robust peak alignment, careful normalization using internal standards, and insightful multivariate statistical analysis with PCA and OPLS-DA is non-negotiable. These strategies, when executed correctly, transform an overwhelming dataset into a clear story, revealing the specific lipid molecules and perturbed metabolic pathways—such as glycerophospholipid and glycerolipid metabolism—that underpin complex metabolic diseases [2]. As lipidomics continues to evolve, these core data processing strategies remain the bedrock of rigorous, reproducible, and impactful scientific discovery.
Pathway analysis is a cornerstone of systems biology, providing a powerful means to interpret complex high-throughput biological data by identifying relevant groups of related genes or metabolites that are altered in experimental conditions compared to controls [42]. In the context of UHPLC-MS/MS lipidomic profiling for research on diabetes mellitus (DM) combined with hyperuricemia (HUA), this approach moves beyond a simple list of dysregulated lipids to reveal the underlying metabolic pathways and biological processes that are perturbed, thereby generating actionable hypotheses [2] [42]. This technical guide outlines the methodology and application of pathway analysis, with a specific focus on using tools like MetaboAnalyst, for researchers and scientists in the field of metabolic disease drug development.
Theoretical Foundations of Pathway Analysis
The Core Concept
The fundamental principle of pathway analysis is the recognition that complex biological phenotypes are rarely the product of a single molecule but rather emerge from the interactions of multiple biomolecules within functional pathways [42]. Pathway analysis methods couple existing biological knowledge from curated databases with statistical testing and computational algorithms to overcome the challenge of interpreting overwhelmingly large lists of significant but isolated molecules [42].
Key Methodological Classes
Several methodological approaches exist for pathway analysis [42]:
- Over-Representation Analysis (ORA): This traditional method tests whether a specific pathway or functional group is over-represented in a list of statistically significant molecules (e.g., lipids), compared to what would be expected by chance.
- Functional Class Scoring (FCS): FCS methods consider the subtle, coordinated changes in a group of related molecules, which may not all pass individual significance thresholds but together indicate a pathway perturbation.
- Pathway Topology-based Methods: These more advanced approaches incorporate information about the structure and interactions within a pathway (e.g., position of a molecule in a network, interaction strength) to yield more biologically nuanced results.
Practical Application in Lipidomics: A Workflow from Data to Biological Insight
The following workflow, generated using the specified DOT language and color palette, illustrates the pathway analysis process for a UHPLC-MS/MS lipidomics study.
Diagram 1: The pathway analysis workflow for lipidomics data.
Input Data Preparation
The pathway analysis workflow begins with the results from a UHPLC-MS/MS experiment. After raw data is processed (peak picking, alignment, normalization), statistical analysis (e.g., t-tests, fold-change calculation) is performed to generate a list of lipid molecules that are significantly altered between experimental groups [2] [43]. For input into MetaboAnalyst, this typically requires a compound list with unique identifiers (e.g., Lipid Maps ID, HMDB ID) and associated quantitative measures of change and statistical significance [2].
Execution in MetaboAnalyst
MetaboAnalyst is a comprehensive web-based platform specifically designed for metabolomics data analysis [2] [43]. Its pathway analysis module performs the following key steps [2]:
- Identifier Mapping: The user-provided list of lipid identifiers is mapped to biological pathways within knowledge bases like the Kyoto Encyclopedia of Genes and Genomes (KEGG).
- Pathway Enrichment Analysis: The tool calculates whether any pathways contain a statistically significant number of altered lipids. This is often evaluated using a p-value from an enrichment test (e.g., Fisher's exact test) and an impact value derived from pathway topology.
- Visualization and Output: Results are presented as interactive tables and plots, most notably the pathway overview, which graphically displays the pathways and highlights the matched compounds.
Case Study: Pathway Analysis in Diabetes and Hyperuricemia Research
To ground this methodology in a concrete example, we can examine its application in a study investigating the lipidomic profiles of patients with diabetes mellitus combined with hyperuricemia (DH) [2].
Experimental Protocol
- Study Population: The study employed a case-control design with 17 patients each in the DH, DM-only, and normal glucose tolerance (NGT) groups, matched for age and sex [2].
- Sample Preparation: Fasting plasma samples were collected. Lipids were extracted using a liquid-liquid extraction method with methyl tert-butyl ether (MTBE) and methanol after protein precipitation. The extracted lipids were reconstituted in isopropanol for analysis [2].
- UHPLC-MS/MS Analysis: Lipid separation was achieved on a Waters ACQUITY UPLC BEH C18 column using a gradient mobile phase. Untargeted lipidomic analysis was performed using tandem mass spectrometry [2].
- Data Processing and Pathway Analysis: Differential lipids were identified using multivariate statistics (OPLS-DA), and pathway analysis was conducted using the MetaboAnalyst 5.0 platform [2].
Key Findings and Interpretation
The pathway analysis revealed critical insights into the metabolic disturbances in DH. The following table summarizes the quantitative findings of differential lipids and enriched pathways from the study [2].
Table 1: Summary of Lipidomic and Pathway Analysis Findings in DH vs. NGT [2]
| Analysis Category | Specific Finding | Quantity | Examples |
|---|---|---|---|
| Total Identified Lipids | 30 subclasses | 1,361 molecules | --- |
| Differential Lipids | Significantly altered in DH vs. NGT | 31 metabolites | TG(16:0/18:1/18:2), PE(18:0/20:4), PC(36:1) |
| Â Upregulated Triglycerides (TGs) | 13 | ||
| Â Upregulated Phosphatidylethanolamines (PEs) | 10 | ||
| Â Upregulated Phosphatidylcholines (PCs) | 7 | ||
| Â Downregulated Phosphatidylinositol (PI) | 1 | ||
| Enriched Pathways | Glycerophospholipid metabolism | Impact: 0.199 | |
| Glycerolipid metabolism | Impact: 0.014 |
The identification of glycerophospholipid and glycerolipid metabolism as the most perturbed pathways provides a mechanistic understanding of the lipid disorder in DH. These pathways are central to membrane integrity, energy storage, and signaling, and their disruption aligns with the known pathophysiology of both diabetes and hyperuricemia [2]. A separate study on hyperuricemia with hyperlipidaemia also found perturbations in pathways like linoleic acid metabolism and glycine, serine, and threonine metabolism, suggesting interconnected metabolic axes [43].
The relationships between these key findings and their potential biological consequences are visualized in the following diagram.
Diagram 2: The relationship between metabolic disturbances and biological outcomes.
The Scientist's Toolkit: Essential Reagents and Materials
Successfully executing a lipidomics study with pathway analysis requires a suite of specialized reagents and tools. The following table details essential items and their functions based on the protocols cited [2] [43] [9].
Table 2: Key Research Reagent Solutions for UHPLC-MS/MS Lipidomics and Pathway Analysis
| Category | Item | Function / Application |
|---|---|---|
| Sample Collection & Prep | EDTA or Heparin tubes (for plasma) | Collection of fasting blood samples while preventing coagulation [2]. |
| Methyl tert-butyl ether (MTBE), Methanol, Acetonitrile, Isopropanol | Organic solvents for liquid-liquid extraction of lipids from biological matrices [2] [43]. | |
| Ammonium formate | Mobile phase additive in UHPLC to improve ionization efficiency and peak shape [2]. | |
| Chromatography | UHPLC system (e.g., Thermo Vanquish, Waters ACQUITY) | High-pressure separation of complex lipid extracts prior to mass spectrometry [2] [43]. |
| C18 reversed-phase column (e.g., Waters BEH C18) | The standard workhorse column for separating a wide range of lipid species by hydrophobicity [2]. | |
| Mass Spectrometry | High-resolution mass spectrometer (e.g., Orbitrap) | Accurate mass measurement for lipid identification and quantification in untargeted analysis [2] [43] [9]. |
| Data Analysis | MetaboAnalyst 5.0 platform | Web-based tool for statistical and pathway analysis of metabolomics/lipidomics data [2] [43]. |
| Human Metabolome Database (HMDB), KEGG, LIPID MAPS | Reference databases for lipid identification, pathway mapping, and functional annotation [43] [9]. | |
| Sucrose, monolaurate | Sucrose, monolaurate, MF:C24H46O13, MW:542.6 g/mol | Chemical Reagent |
| Reactive Blue 19 | Reactive Blue 19, CAS:110540-35-7, MF:C22H16N2Na2O11S3, MW:626.5 g/mol | Chemical Reagent |
Pathway analysis, implemented through platforms like MetaboAnalyst, is an indispensable method for translating raw UHPLC-MS/MS lipidomic data into biologically meaningful insight. By applying this methodology to the study of complex metabolic diseases like diabetes with hyperuricemia, researchers can move from observing a list of dysregulated lipids to understanding the specific metabolic pathways that are compromised. This systems biology approach not only elucidates disease mechanisms but also pinpoints potential biomarkers and therapeutic targets, thereby directly supporting drug development and personalized medicine initiatives.
Overcoming Analytical Hurdles: Troubleshooting and Optimizing Lipidomic Data
In the meticulous world of clinical research, particularly for high-resolution techniques like UHPLC-MS/MS-based lipidomic profiling, the integrity of final data is inextricably linked to the very first steps of sample handling. Pre-analytical variability encompasses all processes from patient preparation and sample collection to processing and storage, prior to the analytical measurement itself. Within the specific context of diabetes mellitus (DM) and hyperuricemia (DH) research, where subtle lipidomic signatures are sought for mechanistic insights and biomarker discovery, controlling this phase is not merely good practice—it is a scientific imperative. Studies consistently demonstrate that the pre-analytical phase is the most prolific source of error in laboratory medicine, accounting for up to 75% of all mistakes [44]. Another recent review corroborates this, noting that pre-analytical errors contribute to around 60-70% of laboratory errors [45]. For lipidomics, which aims to provide a comprehensive and quantitative profile of hundreds of lipid species in a biological system, factors such as hemolysis, improper fasting, or suboptimal storage can introduce profound artifacts, obscuring true biological signals and leading to irreproducible results [2] [46]. This guide provides a detailed framework for standardizing sample collection and preparation, specifically tailored for researchers investigating the lipidomic interplay between diabetes and hyperuricemia.
Understanding the sources and magnitudes of pre-analytical variability is the first step toward its mitigation. Errors during this phase can compromise data quality, leading to inaccurate conclusions and failed biomarker validation.
The following table summarizes the primary categories of pre-analytical errors and their frequency, highlighting the areas requiring maximum vigilance [45].
Table 1: Common Sources and Distributions of Pre-analytical Errors
| Category of Pre-analytical Error | Specific Examples | Reported Frequency |
|---|---|---|
| Poor Blood Sample Quality | Hemolysis, lipemia, icterus, clotting | 80-90% of pre-analytical errors |
| Incorrect Sample Volume | Insufficient or overfilled collection tubes | 10-20% |
| Use of Wrong Container | Incorrect anticoagulant or preservative | 5-15% |
| Clotted Samples | Inadequate mixing of anticoagulant tubes | 5-10% |
| Patient Misidentification | Wrong labels, failure to use two identifiers | ~16% of phlebotomy process errors |
| Improper Tube Labeling | Missing information, legibility issues | ~56% of phlebotomy process errors |
Key Variables Affecting Lipidomic Analysis
For lipidomic studies in metabolic diseases, specific pre-analytical factors are of critical importance:
- Patient Preparation: Diet is a major source of variability. Food ingestion significantly alters lipid levels; an overnight fast of 10-14 hours is optimal for minimizing variations in analytes like triglycerides and glucose [44]. Caffeine, alcohol, and smoking must also be controlled as they can markedly increase the metabolic rate of triglyceride-rich lipoproteins [45]. Furthermore, a patient's posture and physical activity level can impact results. A change from lying to standing can cause a 9% elevation in serum concentrations of proteins or protein-bound constituents due to a shift in blood volume [44].
- Sample Collection: Prolonged tourniquet application (over one minute) can cause hemoconcentration, increasing the concentration of non-filterable elements like proteins and lipids [47]. The order of draw is critical to avoid cross-contamination between tubes, and gentle inversion of anticoagulant tubes (5-10 times) is necessary to prevent clot formation or hemolysis [47].
- Sample Processing and Storage: The timing of sample processing is crucial. Delays in the separation of plasma or serum from cells can lead to glycolysis, evaporation, and the release of intracellular constituents. For lipidomic stability, immediate centrifugation and subsequent storage at -80°C is the gold standard, as demonstrated in studies of diabetic and hyperuricemic patients [2] [46]. Freeze-thaw cycles must be minimized as they can degrade labile lipid species.
The relationship between these variables and their impact on the research workflow can be visualized as follows:
Standardized Protocols for Lipidomics in DM/DH Research
To ensure the generation of high-fidelity lipidomic data, laboratories must implement and rigorously adhere to detailed Standard Operating Procedures (SOPs). The following protocols are synthesized from current research practices in the field [2] [46].
Patient Preparation and Blood Collection Protocol
- Patient Instruction: Participants should be instructed to fast for 12 hours overnight (water is permitted) and abstain from alcohol, strenuous exercise, and smoking for at least 24 hours prior to blood collection. Consumption of chewing gum should be prohibited [45].
- Timing: Fasting morning blood samples should be collected to minimize circadian variation. The actual time of draw must be meticulously documented [44].
- Patient Positioning: The patient should be seated for at least 5 minutes prior to phlebotomy. Prolonged bed rest in hospitalized patients can also dramatically affect results [44].
- Phlebotomy Technique:
- Apply a tourniquet for less than one minute. Probing or massaging the site should be avoided.
- Perform venipuncture and collect blood into the appropriate vacuum tubes. For lipidomics, tubes containing EDTA (purple top) or heparin (green top) are typically used for plasma separation.
- Release the tourniquet as soon as blood flow is established.
- Gently invert tubes with additives 5-10 times to ensure proper mixing without inducing hemolysis [47].
Sample Processing and Storage Protocol for Plasma Lipidomics
The workflow for processing blood samples into analysis-ready plasma extracts must be optimized for lipid stability and reproducibility.
Table 2: Key Reagents and Materials for Lipidomic Sample Preparation
| Research Reagent / Material | Function / Explanation | Example from Literature |
|---|---|---|
| EDTA or Heparin Tubes | Anticoagulant for plasma separation; prevents clotting. | Standard for plasma collection in lipidomic studies [2] [46]. |
| Methyl tert-butyl ether (MTBE) | Organic solvent for liquid-liquid extraction; efficiently partitions lipids from aqueous phase. | Used in the MTBE-based extraction method for human plasma [2]. |
| Methanol (MeOH) & Isopropanol (IPA) | Polar solvents used to denature proteins and facilitate lipid extraction. | Used in combination with MTBE in a 1:2 (sample:MTBE) ratio [2]. |
| SPLASH LIPIDOMIX Standard | A stable isotope-labeled internal standard mixture for semi-quantification of multiple lipid classes. | Added to plasma prior to extraction to correct for technical variability [46]. |
| Ammonium Formate | A volatile salt used in LC-MS mobile phases to improve ionization efficiency. | Used in acetonitrile and isopropanol solutions for UHPLC separation [2]. |
| C18 UHPLC Column | Reversed-phase chromatography column for separating individual lipid species by hydrophobicity. | Waters ACQUITY UPLC BEH C18 column (1.7 µm particle size) [2]. |
The following diagram outlines the critical steps for processing plasma samples from collection to mass spectrometry injection, based on established methodologies [2].
Detailed Lipid Extraction Protocol (based on [2]):
- Aliquoting: Transfer 100 µL of plasma into a 1.5 mL microcentrifuge tube.
- Protein Precipitation & Extraction:
- Add 200 µL of ice-cold water and vortex.
- Add 240 µL of pre-cooled methanol and vortex to precipitate proteins.
- Add 800 µL of MTBE, vortex vigorously, and sonicate in a low-temperature water bath for 20 minutes.
- Allow the mixture to stand at room temperature for 30 minutes to facilitate phase separation.
- Phase Separation: Centrifuge at 14,000 g for 15 minutes at 10°C. The upper organic phase (MTBE), which contains the extracted lipids, will be clearly separated from the lower aqueous phase.
- Collection and Concentration: Carefully collect the upper organic phase without disturbing the interface. Transfer it to a new tube and evaporate to dryness under a gentle stream of nitrogen gas.
- Reconstitution: Reconstitute the dried lipid extract in 100 µL of isopropanol, vortex thoroughly, and transfer to an LC-MS vial for analysis.
Quality Control and Monitoring in the Pre-analytical Phase
Robust quality control (QC) mechanisms are essential for detecting pre-analytical errors and ensuring long-term data consistency.
- Automated Sample Quality Assessment: Modern clinical chemistry analyzers can determine serum indices, which are spectrophotometric estimates of hemoglobin (hemolysis index), bilirubin (icterus index), and lipids (lipemia index). These indices provide an objective measure of sample quality and can be used to flag samples that may yield unreliable results [44].
- Utilization of Quality Indicators (QIs): Laboratories should adopt standardized QIs to monitor the pre-analytical phase proactively. Examples recommended by the International Federation for Clinical Chemistry and Laboratory Medicine (IFCC) include monitoring the rate of samples lost or not received, mislabeled samples, and samples collected in the wrong container [44].
- Application in Lipidomic Workflows: For targeted and untargeted lipidomics, the use of pooled quality control samples (prepared from an aliquot of all samples in the study) is critical. These QC samples are injected at regular intervals throughout the analytical sequence to monitor instrument stability, evaluate reproducibility, and correct for signal drift [2].
In the pursuit of discovering robust lipidomic biomarkers and understanding the metabolic crosstalk in complex conditions like diabetes and hyperuricemia, standardizing the pre-analytical phase is not a secondary concern but a foundational requirement. The high sensitivity of UHPLC-MS/MS is a double-edged sword: it can detect subtle, biologically significant lipid alterations, but it is equally susceptible to pre-analytical artifacts. By implementing the rigorous protocols outlined in this guide—from controlled patient preparation and meticulous phlebotomy to standardized, cold-processed lipid extraction—research teams can significantly reduce unwanted variability. This commitment to pre-analytical rigor is the bedrock upon which reliable, reproducible, and meaningful lipidomic data is built, ultimately accelerating the translation of research findings into clinical insights.
Lipidomics, the large-scale study of cellular lipids, has become an indispensable tool for understanding the metabolic dysregulation underlying diseases such as diabetes mellitus combined with hyperuricemia (DH). The comprehensive characterization of lipid species is crucial for identifying biomarkers and understanding pathological mechanisms [2]. However, two significant analytical challenges persist: the separation of lipid isomers and the confident identification of low-abundance species. These challenges are particularly relevant in DH research, where subtle alterations in lipid metabolism may hold key diagnostic and therapeutic insights.
The structural diversity of lipids is immense, with cells expressing hundreds of enzymes that synthesize tens of thousands of different lipids [48]. This diversity leads to numerous isobaric and isomeric compounds in biological samples. Isomers may differ due to subclasses having the same chemical composition, varied acyl chain connectivities (sn-1, sn-2, or sn-3), distinct double bond positions and orientations (cis or trans), and different functional group stereochemistry (R versus S) [48]. Fully understanding the roles of lipids in biological processes therefore requires separating and evaluating how these isomers change in disease states [48].
Simultaneously, the detection and identification of low-abundance lipid species remains analytically challenging. These minor species, while difficult to detect against the background of more abundant lipids, may play significant roles in physiological and pathological processes [49]. In diabetes and hyperuricemia research, where lipid abnormalities are known to coexist [2], overcoming these analytical challenges is paramount for advancing our understanding of disease mechanisms.
Advanced Separation Techniques for Lipid Isomers
Ion Mobility Spectrometry and Its Variants
Ion mobility spectrometry (IMS) has emerged as a powerful technology for lipid class and isomer separations, with several variants offering complementary approaches:
Field Asymmetric Waveform IMS (FAIMS), also known as differential ion mobility spectrometry (DMS), distinguishes ions based on their mobility differences at high and low electric fields. FAIMS can baseline separate lipids from different classes and subclasses in less than one second and has demonstrated the ability to characterize different lipid classes into specific 'trend lines' groupings [48]. In the analysis of glycerophospholipids, lysophosphatidylcholine (LPC) separates first followed by phosphatidylcholine (PC), phosphatidic acid (PA), phosphatidylethanolamine (PE), phosphatidylglycerol (PG), and phosphatidylserine (PS) [48].
Drift Tube IMS (DTIMS) and Traveling Wave IMS (TWIMS) separate ions based on their mobility differences as they move through a buffer gas. DTIMS with a 4 Torr pressure and 1 m long IMS drift region has been shown to separate lipid isomers including sn-1/sn-2 positional isomers, cis/trans double bond orientation isomers, and stereochemical isomers (R versus S) [48]. Research has revealed that when the smaller fatty acyl chain is in the sn-1 position, the lipid has a smaller structure, and cis double bonds form smaller structures than trans double bonds [48].
Trapped Ion Mobility Spectrometry (TIMS) represents a recent advancement where ions entering the TIMS analyzer are positioned in an electrical field by the drag of a gas flow. By gradually lowering the electrical force, ions elute from the TIMS device according to their ion mobility [50]. When coupled with the parallel accumulation serial fragmentation (PASEF) scan mode, TIMS enables high-speed analysis and efficient ion usage [50].
Table 1: Comparison of Ion Mobility Techniques for Lipid Isomer Separation
| Technique | Separation Principle | Separation Capabilities | Analysis Speed |
|---|---|---|---|
| FAIMS/DMS | Mobility differences at high/low electric fields | Lipid classes and subclasses | < 1 second |
| DTIMS | Uniform electric field | sn-1/sn-2 isomers, cis/trans, stereoisomers | Seconds |
| TWIMS | Dynamic travelling voltage wave | sn-1/sn-2 isomers, cis/trans, stereoisomers | Seconds |
| TIMS | Electrical field with gas flow drag | cis/trans isomers with high resolution | Seconds |
Chromatographic Approaches
While IMS techniques provide powerful gas-phase separation, liquid chromatography remains fundamental to lipidomic workflows:
Reversed-Phase LC (RPLC) separates lipids mainly based on their fatty acyl composition, with lysolipids (containing one fatty acyl group) eluting before triacylglycerides (with three fatty acyl chains) [48]. This technique is particularly effective for separating lipid species within the same class based on their acyl chain length and degree of unsaturation.
Normal-Phase LC (NPLC) separates lipids based on their head groups or lipid classes, providing complementary separation to reversed-phase methods [48]. This approach is valuable for class-based lipid profiling.
Hydrophilic Interaction Liquid Chromatography (HILIC) has shown promising results for lipid separations, particularly for lysophospholipid regioisomers [48]. The combination of different chromatographic modes can provide comprehensive lipid coverage.
Supercritical Fluid Chromatography (SFC) has recently been explored as a higher throughput method for lipidomic class separations, as its separations are inherently faster than traditional LC and generally involve minimal solvent consumption through the use of COâ‚‚ as a mobile phase [48].
Four-Dimensional Lipidomics
The integration of multiple separation dimensions has led to the emergence of four-dimensional (4D) lipidomics, which combines retention time, collision cross section (CCS), mass-to-charge ratio (m/z), and MS/MS spectra [50]. This approach enables the implementation of stringent criteria for lipid annotation, significantly reducing false discovery rates that can approach 50% in conventional workflows [50].
In 4D lipidomics utilizing LC-TIMS-MS with PASEF, researchers have achieved highly reproducible profiling with median variability of 0.58 ppm for mass accuracy, median CV of 0.19% for retention time, and 0.11% for CCS values [50]. This high inter-day reproducibility allows for the implementation of stringent variability criteria for RT-based lipid annotation and curation, substantially reducing false-positive structural assignments [50].
Strategies for Low-Abundance Lipid Detection
High-Resolution Mass Spectrometry
The detection of low-abundance lipids in complex biological matrices requires instruments with high sensitivity and resolution:
Fourier Transform Ion Cyclotron Resonance (FT-ICR) and Orbitrap mass analyzers provide the high molecular specificity needed to resolve near-isobaric lipid species in a narrow mass range [49] [51]. The high mass resolution and accuracy of these instruments allow for the determination of molecular formulas by exact mass measurements, which is crucial for identifying low-abundant species against a complex background [49].
The exceptional sensitivity and mass accuracy of these techniques enable the detection of lipid species present at low concentrations that may nonetheless be biologically significant. For example, in studies of human breast cancer xenografts, high-resolution MALDI-FTICR MS imaging has enabled the localization and identification of specific low-abundant phospholipids in different tumor microenvironments, revealing their association with distinct biological processes such as proliferation, hypoxia, and inflammation [49].
Spatial Localization Techniques
Matrix-Assisted Laser Desorption/Ionization Mass Spectrometry Imaging (MALDI MSI) has emerged as a powerful application for lipid research, enabling the in situ identification and localization of lipids directly on tissue sections without the requirement of specific probes or staining [49]. This technique preserves spatial information that is lost in extraction-based methods.
When combined with liquid chromatography-electrospray ionization mass spectrometry (LC-ESI-MS) after extraction from regions of interest defined by MALDI imaging, researchers can confirm the identity of low-abundant lipids localized to specific tissue compartments [49]. This combined approach has been successfully applied to characterize the heterogeneous distribution of low-abundant lipid species in complex histological samples, revealing their biological significance in different tissue microenvironments [49].
Enrichment and Targeted Approaches
While not explicitly detailed in the search results, the literature suggests that enrichment strategies and targeted mass spectrometry approaches are essential for comprehensive analysis of low-abundance lipids. These typically include:
- Selective sample preparation techniques that enrich for specific lipid classes
- Chemical derivatization to enhance ionization efficiency of low-abundance species
- Multiple reaction monitoring (MRM) and other targeted MS methods that increase sensitivity for specific lipids of interest
Experimental Protocols for Comprehensive Lipid Identification
Sample Preparation for Lipidomics
Robust sample preparation is critical for reliable lipid identification. For plasma lipid analysis in diabetes and hyperuricemia research, the following protocol has been employed:
Plasma Collection and Processing: Collect 5 mL of fasting morning blood and centrifuge at 3,000 rpm for 10 minutes at room temperature. Aliquot 0.2 mL of the upper plasma layer into 1.5 mL centrifuge tubes, with quality control samples prepared by mixing equal groups of samples [2].
Lipid Extraction: Adapting the MTBE-based extraction method: Take 100 μL of plasma into a 1.5 mL centrifuge tube, add 200 μL of 4°C water followed by 240 μL of pre-cooled methanol after mixing. Add 800 μL of methyl tert-butyl ether (MTBE), sonicate for 20 minutes in a low-temperature water bath, and let stand at room temperature for 30 minutes. Centrifuge at 14,000 g for 15 minutes at 10°C, collect the upper organic phase, and dry under nitrogen [2].
High-Throughput Automated Extraction: For clinical applications, automated lipid extraction on a robotic platform significantly improves throughput and reproducibility. Optimization of robotic handling station parameters—including pipetting volume, depth, and speed of pipette immersion in the organic phase—enables maximal removal of organic solvent without contamination with the polar phase [50]. This approach reduces processing time to 3 hours per 96-well plate and demonstrates CV values for normalized lipid peak areas below 10% for most lipids [50].
Instrumental Analysis Conditions
Chromatographic Conditions: Employ a Waters ACQUITY UPLC BEH C18 column (2.1 mm i.d. × 100 mm length, 1.7 μm particle size). Use a mobile phase consisting of A: 10 mM ammonium formate acetonitrile solution in water and B: 10 mM ammonium formate acetonitrile isopropanol solution [2]. Microflow UHPLC/ESI-TIMS-MS provides high ionization efficiency with reduced adduct formation in both ionization modes and efficient chromatographic resolution within 20 minutes [50].
MS Data Acquisition: For comprehensive lipid coverage, employ data-dependent acquisition (DDA) or data-independent acquisition (DIA) methods. When using TIMS-PASEF, leverage the parallel accumulation serial fragmentation mode to enhance the signal-to-noise ratio and enable simultaneous fragmentation of multiple precursors in a single scan [50].
Data Processing and Lipid Identification
4D Feature Annotation: Confident lipid annotation requires matching multiple data quality indicators against reference libraries. Implement stringent parameters for retention time, accurate mass, CCS, isotopic pattern, and MS/MS spectral matching [50]. The low variability of CCS values (average CV less than 0.18%) permits inclusion of CCS deviation as an additional data attribute for confident automatic annotation [50].
Statistical Analysis and Validation: Employ appropriate statistical methods including t-tests for comparing two groups, ANOVA for multiple groups, and multivariate techniques such as Principal Component Analysis (PCA) and Orthogonal Partial Least Squares Discriminant Analysis (OPLS-DA) [2] [52]. For validation, cross-reference findings with existing literature and databases such as PubMed, HMDB (Human Metabolome Database), and LipidMaps [52].
Table 2: Key Research Reagent Solutions for Lipidomics
| Reagent/Resource | Function | Application Note |
|---|---|---|
| MTBE (Methyl tert-butyl ether) | Lipid extraction solvent | Forms upper non-polar phase; advantageous for automated platforms |
| Ammonium formate | Mobile phase additive | Enhances ionization in positive and negative modes |
| 1,5-DAN matrix | MALDI matrix | Provides rich lipid signatures without analyte delocalization |
| Lipid internal standards | Quantification reference | Enables reproducible quantification using level-3 internal standards |
| CCS libraries | Lipid identification | Provides collision cross section values for confident annotation |
Application to Diabetes and Hyperuricemia Research
In the context of diabetes mellitus combined with hyperuricemia (DH), advanced lipid identification techniques have revealed significant alterations in lipid metabolism. Using UHPLC-MS/MS-based untargeted lipidomic analysis, researchers have identified 1,361 lipid molecules across 30 subclasses in plasma samples from DH patients [2].
Multivariate analyses revealed a significant separation trend among the DH, diabetes mellitus (DM), and normal glucose tolerance (NGT) groups, confirming distinct lipidomic profiles [2]. Specifically, 31 significantly altered lipid metabolites were pinpointed in the DH group compared to NGT controls. Among the most relevant individual metabolites, 13 triglycerides (TGs), 10 phosphatidylethanolamines (PEs), and 7 phosphatidylcholines (PCs) were significantly upregulated, while one phosphatidylinositol (PI) was downregulated [2].
Pathway analysis of these altered metabolites revealed their enrichment in six major metabolic pathways, with glycerophospholipid metabolism (impact value of 0.199) and glycerolipid metabolism (impact value of 0.014) identified as the most significantly perturbed pathways in DH patients [2]. Furthermore, comparison of DH versus DM groups identified 12 differential lipids, which were also predominantly enriched in these same core pathways, underscoring their central role in the pathophysiology of hyperuricemia complicating diabetes [2].
These findings demonstrate how advanced lipid identification techniques can uncover specific metabolic disruptions in complex diseases, providing insights into potential biomarkers and therapeutic targets.
Workflow and Pathway Diagrams
Diagram 1: Comprehensive Lipidomics Workflow. This diagram illustrates the integrated approach for advanced lipid identification, from sample preparation to biological interpretation.
Diagram 2: Perturbed Lipid Pathways in Diabetes-Hyperuricemia. This diagram highlights the glycerophospholipid and glycerolipid metabolism pathways significantly altered in DH, with key upregulated lipids colored red.
In UHPLC-MS/MS-based lipidomic profiling, particularly for complex metabolic diseases like diabetes mellitus combined with hyperuricemia (DH), ensuring data integrity is paramount. The intricate lipid perturbations characteristic of these conditions demand rigorous analytical workflows to generate reliable, reproducible, and biologically meaningful data. This technical guide details the foundational role of quality control (QC) samples and internal standards in maintaining analytical precision and accuracy throughout the lipidomic pipeline. We outline standardized protocols for their implementation, present quantitative performance data from validation studies, and frame these practices within the specific context of DH research, providing a robust framework for researchers and drug development professionals.
Lipidomics, a branch of metabolomics, has become an indispensable tool for characterizing the specific lipid perturbations that precede and accompany complex metabolic diseases [2]. In the study of diabetes mellitus (DM) and its comorbidity with hyperuricemia (HU), lipidomic profiling via ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) can reveal distinct lipidomic signatures and illuminate altered metabolic pathways [2]. However, the analytical process—from sample preparation to data acquisition—is susceptible to numerous sources of variation, including instrument drift, matrix effects, and batch-to-batch inconsistencies.
The integration of a rigorous quality control system is therefore not optional but essential. It ensures that the observed biological variation truly reflects the pathophysiology of the disease and is not an artifact of the analytical process. This whitepaper examines the critical function of QC samples and internal standards, providing a detailed technical roadmap for their application in UHPLC-MS/MS lipidomic studies, with a specific focus on diabetes and hyperuricemia research.
The Pillars of Analytical Quality Control
Quality Control (QC) Samples
QC samples are used to monitor the stability and performance of the analytical system over the entire sequence of a study.
- Pooled QC (PQC) Samples: A PQC is created by combining equal aliquots from all individual study samples, resulting in a composite matrix that mirrors the average composition of the entire sample set [2] [53]. In a study comparing DH, DM, and normal glucose tolerance (NGT) groups, PQC samples are injected at regular intervals (e.g., every 5-10 samples) throughout the analytical run [2]. This allows for the monitoring of instrumental sensitivity, retention time stability, and mass accuracy, and facilitates the correction of signal drift during data pre-processing.
- Surrogate QC (sQC) and Long-Term Reference (LTR): Commercial quality control plasma can serve as a surrogate QC (sQC), providing a consistent reference material across multiple analytical batches or even different laboratories [53]. When maintained as a long-term reference (LTR), it enables performance tracking and data comparability over extended periods.
Internal Standards (IS)
Internal standards are isotopically labeled analogs of the target analytes (lipids) that are added to each sample at a known concentration before the extraction process. They are critical for correcting for losses during sample preparation, variability in ionization efficiency, and matrix effects [30].
- Stable-Isotope Labeled Lipids: Commonly used IS include deuterated (d5) triglycerides (TG), diglycerides (DG), ceramides, and various phospholipid classes [30]. The selection should cover the broad range of lipid classes being investigated. For instance, a DH lipidomic study would require IS for triglycerides, phosphatidylethanolamines (PEs), and phosphatidylcholines (PCs), given their reported upregulation in this condition [2].
- Method Validation: The use of IS is integral to method validation. A validated UHPLC-MS/MS lipidomics method should demonstrate a linearity range of over four orders of magnitude, high accuracy and precision, and limits of quantitation in the femtomole range on-column [30].
Experimental Protocols for QC in Lipidomics
Sample Preparation and QC Integration
The following protocol, adapted from DH research, details the integration of QC measures from the outset [2].
- Sample Collection: Collect fasting blood samples (e.g., 5 mL) and centrifuge at 3,000 rpm for 10 minutes at room temperature to isolate plasma.
- Aliquot and Pool: Aliquot the upper plasma layer (e.g., 0.2 mL) into individual vials. To create the PQC, combine equal volumes (e.g., 10 µL) from every individual study sample into a separate vial.
- Lipid Extraction: Perform a liquid-liquid extraction. For example:
- To 100 µL of plasma, add 200 µL of cold water and 240 µL of pre-cooled methanol.
- Add 800 µL of methyl tert-butyl ether (MTBE), vortex, and sonicate in a low-temperature water bath for 20 minutes.
- Let the mixture stand at room temperature for 30 minutes.
- Centrifuge at 14,000 g at 10°C for 15 minutes.
- Collect the upper organic phase and dry under a gentle nitrogen stream [2].
- Add Internal Standards: A critical step. Reconstitute the dried lipid extracts with 100 µL of isopropanol containing a predefined cocktail of internal standards (e.g., d5-TG, d5-DG, ceramide/sphingoid internal standard mixture) [2] [30].
- Instrumental Analysis: Inject samples onto the UHPLC-MS/MS system. The injection sequence should be randomized to avoid bias. The PQC sample is injected at the beginning of the run to "condition" the system, and then repeatedly after every 4-8 experimental samples.
UHPLC-MS/MS Conditions for Lipidomics
Robust chromatographic separation is key to resolving the complex lipidome and minimizing ion suppression.
- Chromatography: Utilize a reversed-phase column (e.g., Waters ACQUITY UHPLC BEH C18, 2.1 mm x 100 mm, 1.7 µm) [2] [30]. The mobile phase typically consists of (A) 10 mM ammonium formate in water and (B) 10 mM ammonium formate in acetonitrile:isopropanol. A gradient elution is used to separate lipids by acyl chain length and unsaturation [2].
- Mass Spectrometry: Operate the mass spectrometer in both positive and negative ionization modes. Data-dependent acquisition (DDA) or multiple reaction monitoring (MRM) can be employed. High-resolution mass analyzers like Orbitraps are preferred for their ability to deliver elemental composition with high mass accuracy [30].
The workflow below summarizes the integrated QC process.
Quantitative Data and Performance Metrics
The implementation of a rigorous QC framework enables the measurement of key analytical performance parameters. The table below summarizes typical validation data for a quantitative UHPLC-MS/MS lipidomics method.
Table 1: Performance Metrics from a Validated Quantitative UHPLC-MS/MS Lipidomics Method [30]
| Performance Parameter | Result / Value | Context and Implication |
|---|---|---|
| Linearity Range | > 4 orders of magnitude | Allows for accurate quantification of lipids across a wide concentration range, from very low to high abundance. |
| Limit of Quantitation (LOQ) | A few femtomoles (fmol) on-column | Enables detection of low-abundance but biologically significant lipid species. |
| Accuracy & Precision | Good at biologically relevant levels | Ensures data is both correct (accuracy) and reproducible (precision), which is critical for identifying true biomarkers. |
The effectiveness of the QC system during an analytical run can be visualized by monitoring the signal from the internal standards and PQC samples. Stable retention times and consistent peak intensities across the PQC injections indicate a well-controlled system.
The following diagram illustrates the logical relationship between different QC materials and their primary functions in ensuring data quality.
The Scientist's Toolkit: Essential Research Reagents and Materials
A successful lipidomics study relies on a suite of high-purity reagents and standardized materials. The following table details key components used in the featured DH lipidomic research.
Table 2: Essential Research Reagents and Materials for UHPLC-MS/MS Lipidomics [2] [30]
| Item | Function / Application | Specific Examples |
|---|---|---|
| Internal Standard Mixtures | Correct for variability in sample prep and analysis; enable absolute quantification. | d5-TG internal standard mixture; d5-DG internal standard mixture; ceramide/sphingoid internal standard mixture [30]. |
| Lipid Extraction Solvents | Liquid-liquid extraction of a broad range of lipid classes from biological matrices. | Methyl tert-butyl ether (MTBE), chloroform, methanol, isopropanol (all Chromasolv or LC/MS grade) [2] [30]. |
| UHPLC Mobile Phase Additives | Promote efficient ionization and aid in chromatographic separation. | Ammonium formate (LC/MS grade), formic acid [2]. |
| Chromatography Columns | High-resolution separation of complex lipid mixtures. | Reversed-phase columns (e.g., Waters ACQUITY UHPLC BEH C18, 1.7 µm) [2] [54]. |
| Standard Reference Materials | Method development, calibration, and identification of lipid species. | LIPID MAPS quantitative lipid standards for various phospholipid classes (PC, PE, PS, PI, PG) and glycerolipids [30]. |
| Plga-peg-NH2 | Plga-peg-NH2, MF:C9H17NO6, MW:235.23 g/mol | Chemical Reagent |
In the pursuit of elucidating the lipidomic underpinnings of diabetes mellitus and hyperuricemia, data quality is the foundation upon which valid biological insights are built. The consistent and meticulous application of QC samples and internal standards throughout the analytical workflow is non-negotiable. These practices mitigate analytical variance, ensure system stability, and provide the necessary benchmarks for data correction and validation. By adhering to the detailed protocols and principles outlined in this guide, researchers can generate lipidomic data of the highest integrity, thereby confidently identifying novel biomarkers and perturbed pathways that drive these interconnected metabolic diseases.
Reproducibility is a cornerstone of scientific research, yet it remains a significant challenge in the niche field of UHPLC-MS/MS lipidomic profiling for complex metabolic diseases such as diabetes mellitus (DM) and hyperuricemia (HUA). The intricate nature of lipid molecules, combined with technical variations in analytical platforms and a lack of standardized protocols, often leads to inconsistencies that hinder the validation of biomarkers and the translation of research findings into clinical applications. This whitepaper details the primary sources of variability in lipidomics workflows and provides a structured framework for inter-laboratory standardization, with a specific focus on research involving diabetes and hyperuricemia.
The journey from sample collection to data analysis is fraught with potential pitfalls that can compromise reproducibility. The table below summarizes the core challenges and their impacts on lipidomic studies.
Table 1: Key Sources of Variability in UHPLC-MS/MS Lipidomics and Their Impacts
| Stage | Source of Variability | Impact on Reproducibility |
|---|---|---|
| Sample Preparation | Lipid extraction efficiency (e.g., MTBE vs. chloroform-based methods), sample storage conditions, freeze-thaw cycles | Alters absolute concentrations of lipid species, especially oxidizable polyunsaturated fatty acids and lysophospholipids [2] [55]. |
| Chromatography | Column chemistry (C18, C8), mobile phase composition, gradient profile, and temperature | Changes retention times and separation of critical isomeric lipids (e.g., C18:1 vs. C18:2), leading to misidentification [2] [20]. |
| Mass Spectrometry | Ionization efficiency (ESI, APCI), instrument calibration, mass resolution, and collision energy | Causes significant differences in signal response for different lipid classes, affecting quantitative accuracy across platforms [55] [56]. |
| Data Processing | Peak picking algorithms, alignment parameters, and database matching for lipid identification | Introduces inconsistencies in the final lipid count and relative abundances between software solutions [46] [57]. |
Standardized Experimental Protocols for Key Applications
To ensure consistency across studies, particularly in diabetes and hyperuricemia research, adherence to detailed methodological protocols is paramount. The following section outlines standardized procedures based on current literature.
Protocol: Plasma Lipidomic Profiling for Diabetes and Hyperuricemia
This protocol is adapted from a study investigating lipid alterations in patients with diabetes mellitus combined with hyperuricemia (DH) [2].
- Sample Collection and Pre-processing: Collect fasting venous blood (e.g., 5 mL) into EDTA tubes. Centrifuge at 3,000 rpm for 10 minutes at room temperature to isolate plasma. Aliquot 0.2 mL of plasma into cryovials and store immediately at -80°C. Before analysis, thaw samples on ice and prepare a pooled quality control (QC) sample by combining equal volumes from all samples to be used for monitoring instrument performance [2] [57].
- Lipid Extraction: Employ a modified methyl tert-butyl ether (MTBE) protocol. Briefly, vortex 100 μL of plasma with 200 μL of cold water. Add 240 μL of pre-cooled methanol and 800 μL of MTBE. Sonicate the mixture in a low-temperature water bath for 20 minutes and allow it to stand at room temperature for 30 minutes. Centrifuge at 14,000 g at 10°C for 15 minutes. Collect the upper organic phase and dry it under a gentle stream of nitrogen. Reconstitute the dried lipids in a suitable solvent, such as 100 μL of isopropanol, for LC-MS analysis [2] [57].
- UHPLC Conditions:
- Column: Waters ACQUITY UPLC BEH C18 (2.1 mm × 100 mm, 1.7 μm particle size).
- Mobile Phase: A: 10 mM ammonium formate in acetonitrile/water; B: 10 mM ammonium formate in acetonitrile/isopropanol.
- Gradient: Utilize a linear gradient optimized for comprehensive lipid separation, typically from 30% B to 100% B over 15-20 minutes.
- Temperature: Maintain column oven at 45-55°C.
- Injection Volume: 2-5 μL [2] [20].
- MS/MS Conditions: Operate the mass spectrometer in both positive and negative electrospray ionization (ESI) modes with data-dependent acquisition (DDA) or multiple reaction monitoring (MRM) for targeted analysis. Key parameters include a gas temperature of 300°C, a drying gas flow rate of 10 L/min, a nebulizer pressure of 45 psi, and a fragmentor voltage optimized for different lipid classes [2] [55].
The following workflow diagram visualizes this standardized protocol.
Protocol: Quality Control and Validation
Implementing rigorous QC is non-negotiable for inter-laboratory standardization.
- Internal Standards: Spike samples with a standardized mixture of deuterated or odd-chain lipid internal standards (e.g., SPLASH LIPIDOMIX) prior to extraction to correct for variations in recovery and ionization efficiency [46] [55].
- Quality Control Samples: Analyze pooled QC samples repeatedly throughout the acquisition batch—at the beginning for system conditioning, after every 10 experimental samples, and at the end. This monitors instrument stability, retention time drift, and signal intensity [57].
- Data Quality Metrics: Establish acceptance criteria for the QC data. Common metrics include a relative standard deviation (RSD) of < 30% for the peak areas of the majority of lipids detected in the QC samples, indicating satisfactory analytical precision [56].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful and reproducible lipidomics relies on a core set of high-quality reagents and materials.
Table 2: Essential Research Reagent Solutions for UHPLC-MS/MS Lipidomics
| Category | Item | Function and Importance |
|---|---|---|
| Sample Prep | MTBE (Methyl tert-butyl ether) | Primary solvent for lipid extraction; provides high recovery of diverse lipid classes [2]. |
| Deuterated Internal Standards (e.g., SPLASH LIPIDOMIX) | Enables precise quantification by accounting for losses during preparation and matrix effects during ionization [46] [55]. | |
| Chromatography | UHPLC Column (e.g., C18, 1.7μm) | Provides high-resolution separation of complex lipid mixtures, critical for isolating isomers [2] [20]. |
| LC-MS Grade Solvents (Acetonitrile, Isopropanol) | Minimizes background noise and ion suppression, ensuring high signal-to-noise ratios [46]. | |
| Calibration & QC | Standard Reference Material (e.g., NIST SRM 1950) | A standardized human plasma material used for inter-laboratory method validation and benchmarking [46]. |
| Ceramide (d18:1-d7/15:0) | A specific internal standard for quantifying sphingolipids, a class often dysregulated in diabetes [46] [20]. |
Case Study: Lipidomic Profiling in Diabetes and Hyperuricemia
Applying standardized methods to the study of diabetes and hyperuricemia has revealed specific, reproducible lipid signatures.
- Key Lipid Alterations: A study comparing diabetic patients with hyperuricemia (DH) to healthy controls (NGT) identified 31 significantly altered lipid metabolites. These included 13 triglycerides (TGs), 10 phosphatidylethanolamines (PEs), and 7 phosphatidylcholines (PCs) that were significantly upregulated, while one phosphatidylinositol (PI) was downregulated [2]. Another large-scale study in a Chinese population confirmed diacylglycerols (DAGs) and specific TGs as the most significant lipid signatures positively associated with HUA risk, while lysophosphatidylcholine (LPC (20:2)) was inversely associated [57].
- Perturbed Metabolic Pathways: Multivariate and enrichment analyses consistently point to the same core pathways being disrupted. Glycerophospholipid metabolism and glycerolipid metabolism have been identified as the most significantly perturbed pathways in patients with combined diabetes and hyperuricemia [2]. These findings are corroborated by other studies highlighting sphingolipid and glycerophospholipid metabolism in diabetic dyslipidemia [20] and by research showing profound changes in glycerophospholipids in young hyperuricemia and gout patients [46].
The diagram below synthesizes these findings into a proposed mechanistic pathway linking lipid dysregulation to disease pathology.
A Framework for Inter-laboratory Standardization
To overcome reproducibility challenges, the field must adopt a unified set of practices. The following table outlines actionable recommendations.
Table 3: Framework for Enhancing Reproducibility and Standardization in Lipidomics
| Area | Standardization Action | Expected Outcome |
|---|---|---|
| Pre-analytical | Adopt a universal standard operating procedure (SOP) for blood collection, plasma separation, and storage at -80°C with limited freeze-thaw cycles. | Minimized pre-analytical bias and degradation of labile lipids. |
| Analytical | Use a common set of internal standards and reference materials (e.g., NIST SRM 1950) across labs. Harmonize key UHPLC-MS/MS parameters within feasible limits. | Improved inter-laboratory quantitative accuracy and comparability of data. |
| Data Processing | Implement standardized data processing workflows with agreed-upon parameters for peak picking, alignment, and identification. | Reduced variability introduced by software and algorithms. |
| Reporting | Adhere to the guidelines set by the Lipidomic Standards Initiative for reporting metadata, methodologies, and results. | Enhanced transparency, allowing for critical evaluation and replication of studies [56]. |
In the evolving landscape of biomedical research, lipidomics has emerged as a critical discipline for understanding metabolic pathways and their disruption in disease states. The comprehensive analysis of lipids in biological systems provides unique insights into cellular functions, signaling cascades, and homeostatic balance [58]. When investigating complex conditions such as diabetes mellitus (DM) and diabetes mellitus combined with hyperuricemia (DH), lipidomic profiling using advanced techniques like ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) reveals profound alterations in lipid metabolism that underlie disease pathophysiology [2]. However, the true power of lipidomics is unlocked only when these molecular profiles are systematically integrated with clinical phenotypes and genomic data, creating a multidimensional understanding of disease mechanisms that no single data type can provide independently.
The challenge of data integration lies in the technical and computational complexities of harmonizing disparate data types—each with distinct scales, structures, and biological interpretations. Lipidomic data itself presents unique annotation challenges due to the tremendous structural diversity of lipid species, requiring sophisticated analytical and bioinformatic approaches for reliable identification [58]. This technical guide provides a comprehensive framework for optimizing the integration of lipidomic profiles with clinical and genomic data, with specific application to UHPLC-MS/MS-based diabetes and hyperuricemia research. Through structured methodologies, visualization strategies, and practical tools, we aim to equip researchers with the necessary approaches to advance systems-level understanding of metabolic diseases.
Lipidomic Profiling Foundations: Analytical Methods and Experimental Design
UHPLC-MS/MS Methodologies for Comprehensive Lipidomics
The foundation of any successful integration begins with robust, high-quality lipidomic data. UHPLC-MS/MS has become the gold standard for lipidomic analysis due to its superior separation capability, sensitivity, and structural elucidation power [58]. The technical workflow begins with sample preparation—a critical step that significantly impacts data quality. For plasma samples, as used in diabetes-hyperuricemia studies, the recommended protocol involves protein precipitation and lipid extraction using methyl tert-butyl ether (MTBE) [2]. Specifically, 100μL of plasma is mixed with 200μL of ice-cold water, followed by addition of 240μL of pre-cooled methanol and 800μL of MTBE. After sonication in a low-temperature water bath and centrifugation at 14,000g for 15 minutes at 10°C, the upper organic phase containing lipids is collected and dried under nitrogen [2].
Chromatographic separation is typically performed using a Waters ACQUITY UPLC BEH C18 column (2.1 × 100 mm, 1.7μm particle size) with a mobile phase consisting of: (A) 10mM ammonium formate in acetonitrile-water solution and (B) 10mM ammonium formate in acetonitrile-isopropanol solution [2]. This setup provides excellent resolution of diverse lipid classes, including phospholipids, sphingolipids, glycerolipids, and sterol lipids. For mass spectrometric detection, both positive and negative ion modes are essential for comprehensive coverage. Negative ion mode is particularly valuable for identifying fatty acyl chains of phospholipids and determining their sn1/sn2 positions on the glycerol moiety based on relative carboxylate ion intensities [58].
Table 1: Key Lipid Classes and Their Pathophysiological Significance in Diabetes and Hyperuricemia
| Lipid Class | Subclasses | Biological Functions | Relevance to DM/DH |
|---|---|---|---|
| Glycerophospholipids | Phosphatidylcholine (PC), Phosphatidylethanolamine (PE), Phosphatidylinositol (PI), Phosphatidylserine (PS) | Membrane structure, cell signaling, inflammatory mediator precursor | PC and PE significantly upregulated in DH; involved in inflammatory responses [2] |
| Sphingolipids | Ceramides (Cer), Sphingomyelins | Apoptosis regulation, inflammation, insulin resistance | Ceramides mediate apoptosis via caspase-3 and inflammation through IL-1β/IL-6 release [58] |
| Glycerolipids | Triglycerides (TG), Diglycerides (DAG) | Energy storage, signaling molecules | 13 TGs including TG(16:0/18:1/18:2) significantly upregulated in DH [2] |
| Fatty Acids | Arachidonic acid, other polyunsaturated fatty acids | Eicosanoid precursor, inflammatory signaling | Pro-inflammatory fatty acids originating from phospholipid cleavage [58] |
Lipid Annotation and Validation Strategies
Reliable lipid identification requires multiple analytical features: retention time (tR), accurate precursor ion m/z value, isotopic ratio, and MS/MS data comparison with reference compounds [58]. Molecular networking has emerged as a powerful computational strategy for organizing and visualizing hundreds of lipid molecules based on MS/MS spectral similarities, operating on the principle that structurally related molecules display similar product ion spectra [58]. Platforms such as GNPS (Global Natural Products Social Molecular Networking) enable the generation of molecular networks that cluster lipids by structural similarity, facilitating the annotation of unknown species based on their proximity to known standards in the network.
For phospholipid annotation in negative ion mode, six diagnostic product ions are typically monitored: the deprotonated demethylated phosphocholine ion (for PC), carboxylate ions for both fatty acyl chains, and demethylated lysophosphatidylcholine ions corresponding to the loss of each fatty acyl chain [58]. Optimal collision energies must be determined experimentally—for PC species, a ramp between 20-40eV proves suitable for obtaining diagnostic ions with sufficient sensitivity and mass accuracy (Δ < 10ppm) [58]. Annotation is further reinforced by comparing experimental retention times with predicted values based on lipid structural properties, providing an additional orthogonal identification parameter that helps discriminate isobaric compounds [58].
Multi-Omics Integration Framework: Technical Approaches and Computational Strategies
Data Preprocessing and Quality Assessment
Prior to integration, each data type requires specialized preprocessing and rigorous quality control. Lipidomic data processing involves peak detection, alignment, and normalization using software such as MZmine 2, followed by missing value imputation appropriate for mass spectrometry data [58]. Batch effects must be carefully addressed through randomized sample running orders and statistical correction methods. Quality control samples—including pooled samples from all groups and technical replicates—should be interspersed throughout the analytical sequence to monitor instrument performance and reproducibility [2].
Clinical data harmonization involves standardizing measurement units, handling missing values through appropriate imputation methods, and normalizing continuous variables to account for different scales. Genomic data, whether from microarray or sequencing platforms, requires standard preprocessing including background correction, normalization, and probe summarization for gene expression data, or quality control, alignment, and variant calling for genomic sequencing data. The creation of a unified data matrix for integration requires careful matching of sample identifiers across all three domains and addressing any sample mismatches or technical artifacts.
Statistical Integration and Pathway Analysis
Multivariate statistical methods provide powerful approaches for integrating lipidomic, clinical, and genomic data. Principal component analysis (PCA) and orthogonal partial least squares-discriminant analysis (OPLS-DA) effectively visualize separation trends between experimental groups and identify variables driving these separations [2]. These methods can be extended through multiblock approaches that simultaneously model relationships across different data types while preserving their unique structures.
Differential analysis should be performed within each data type before integration. For lipidomic data, Student's t-test and fold change calculations identify significantly altered lipid species between groups, with false discovery rate correction for multiple testing [2]. In DH research, this approach identified 31 significantly altered lipid metabolites compared to normal glucose tolerance controls, including 13 triglycerides, 10 phosphatidylethanolamines, and 7 phosphatidylcholines that were significantly upregulated, and one downregulated phosphatidylinositol [2]. These differential lipids can then be mapped to metabolic pathways using platforms such as MetaboAnalyst 5.0, which in DH research revealed enrichment in glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) as the most significantly perturbed pathways [2].
Diagram 1: Multi-Omics Data Integration Workflow for Lipidomic, Clinical, and Genomic Data
Correlation-Based Integration Networks
Correlation network analysis provides a powerful framework for identifying interconnected molecular features across data types. By calculating pairwise correlations between significantly altered lipids, clinical parameters (such as fasting glucose, HbA1c, and uric acid levels), and gene expression values, researchers can construct multi-omics networks that reveal systems-level relationships. These networks can be visualized using cytoscape or similar tools, with nodes representing lipid species, clinical traits, or genes, and edges representing significant correlations.
In the context of diabetes and hyperuricemia, such networks might reveal, for example, that specific triglyceride species correlate strongly with uric acid levels and expression of genes involved in purine metabolism, suggesting novel mechanistic connections between lipid and purine metabolic pathways. Similarly, phosphatidylcholine species that correlate with insulin resistance markers and inflammatory gene expression could highlight specific molecular links between lipid metabolism and inflammatory processes in diabetes complications.
Experimental Protocols for Validation Studies
Targeted Lipidomic Validation
Following untargeted discovery and integration analyses, putative biomarkers require validation using targeted methods. Liquid chromatography with multiple reaction monitoring (LC-MRM) provides the gold standard for sensitive, specific, and quantitative validation of lipid species of interest. The protocol involves:
- Selection of target lipids based on integration analysis results and commercial standard availability
- Optimization of MRM transitions for each lipid using pure standards, determining optimal collision energies for precursor→product ion transitions
- Preparation of calibration curves using stable isotope-labeled internal standards for absolute quantification
- Analysis of patient samples using validated MRM methods with quality controls
- Data processing using vendor software or open-source alternatives like Skyline
This approach was applied in DH research to validate alterations in key lipid classes including triglycerides, phosphatidylethanolamines, and phosphatidylcholines that were identified through untargeted screening [2].
Functional Validation in Cellular Models
To establish causal relationships between lipid alterations and disease phenotypes, functional validation in relevant cellular models is essential. For diabetes-hyperuricemia research, appropriate models might include hepatic cell lines (HepG2), adipocytes, or renal tubular cells exposed to high glucose and uric acid conditions. The experimental workflow includes:
- Lipid supplementation or inhibition: Treating cells with specific lipid species identified in human studies (e.g., ceramides, oxidized phospholipids) or inhibitors of lipid metabolism enzymes
- Phenotypic assessment: Measuring insulin signaling (via phospho-Akt Western blot), inflammatory responses (IL-1β, IL-6 secretion), and metabolic flux
- Gene expression analysis: qPCR or RNA-seq of relevant metabolic genes
- Pathway manipulation: siRNA knockdown or CRISPR inhibition of genes identified through integration analysis
For example, in studies of dry eye disease—another condition involving lipid disruption—human corneal epithelial cells exposed to hyperosmolarity demonstrated changes in 54 lipid species, several involved in inflammatory responses [58]. Similar approaches can be applied to DH research, with exposure of relevant cell types to high glucose and uric acid conditions to recapitulate the lipid alterations observed in patient samples.
Table 2: Essential Research Reagents and Computational Tools for Integrated Lipidomics
| Category | Item/Platform | Specification/Application | Functional Role |
|---|---|---|---|
| Chromatography | Waters ACQUITY UPLC BEH C18 Column | 2.1 × 100 mm, 1.7μm particle size | High-resolution separation of complex lipid mixtures [2] |
| Lipid Standards | SPLASH LIPIDOMIX Mass Spec Standard | Deuterated lipids across multiple classes | Internal standards for retention time alignment and quantification |
| Extraction Solvents | Methyl tert-butyl ether (MTBE) | HPLC grade | Lipid extraction from plasma/tissues with high recovery of diverse lipid classes [2] |
| Mobile Phase Additives | Ammonium formate | 10mM in acetonitrile-water or acetonitrile-isopropanol | Enhanced ionization efficiency and adduct formation in MS analysis [2] |
| Data Processing | MZmine 2 | Open-source platform | Peak detection, alignment, and normalization of LC-MS data [58] |
| Molecular Networking | GNPS (Global Natural Products Social Molecular Networking) | Web-based platform | Organization and annotation of lipid species based on MS/MS spectral similarity [58] |
| Pathway Analysis | MetaboAnalyst 5.0 | Web-based platform | Enrichment analysis and pathway mapping of altered lipids [2] |
| Multi-Omics Integration | MixOmics | R/Bioconductor package | Multivariate integration of lipidomic, clinical, and genomic datasets |
Biological Pathways and Visualization of Integrated Findings
The integration of lipidomic, clinical, and genomic data ultimately serves to elucidate the complex biological pathways disrupted in disease states. In diabetes with hyperuricemia, research has identified glycerophospholipid metabolism and glycerolipid metabolism as central disrupted pathways [2]. These pathways intersect with inflammatory processes and cell death signaling, creating a network of molecular interactions that drive disease progression.
Ceramides, a sphingolipid subclass identified as significant in lipidomic studies, mediate apoptosis through caspase-3 dependent mechanisms and inflammation through cytokine release (IL-1β, IL-6) [58]. Similarly, arachidonic acid—often cleaved from phospholipids—serves as a pro-inflammatory fatty acid precursor to eicosanoids [58]. These molecular connections illustrate how lipid alterations identified through lipidomic profiling can directly link to clinical manifestations of disease through defined biological mechanisms.
Diagram 2: Integrated Pathway Mapping of Lipid Alterations in Diabetes-Hyperuricemia
The integration of lipidomic data with clinical and genomic information represents a powerful paradigm for advancing our understanding of complex metabolic diseases such as diabetes with hyperuricemia. The strategies outlined in this technical guide—from robust UHPLC-MS/MS lipidomic profiling to sophisticated computational integration methods—provide a roadmap for researchers to uncover novel mechanistic insights and potential therapeutic targets. As the field advances, several emerging technologies promise to further enhance integration capabilities, including single-cell lipidomics, spatial lipidomics, and artificial intelligence approaches for pattern recognition in multi-omics datasets. By systematically applying these integration strategies, the research community can accelerate the translation of lipidomic discoveries into clinical applications for improved diagnosis, risk stratification, and treatment of metabolic diseases.
From Discovery to Clinic: Validating and Contextualizing Lipid Biomarkers
Analytical validation forms the cornerstone of any rigorous lipidomics study, ensuring that the data generated are reliable, reproducible, and fit for their intended purpose [59]. In the context of research on diabetes mellitus combined with hyperuricemia (DH), a complex metabolic disorder, the application of ultra-high-performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) for untargeted lipidomic profiling demands stringent validation to accurately capture the subtle lipid alterations associated with the disease [2]. The intricate lipidomic changes observed in DH, including significant upregulation of specific triglycerides (TGs), phosphatidylethanolamines (PEs), and phosphatidylcholines (PCs), as well as perturbations in glycerophospholipid and glycerolipid metabolism pathways, underscore the necessity for highly sensitive and specific analytical methods [2]. This guide details the core principles and practical protocols for validating UHPLC-MS/MS methods within the specific framework of DH lipidomic research, providing a technical roadmap for scientists and drug development professionals.
Core Validation Parameters in Lipidomics
A comprehensive analytical validation for UHPLC-MS/MS lipidomics must evaluate a suite of performance criteria. These parameters collectively guarantee that the method can consistently detect and quantify lipid species with accuracy and precision amidst the complex biological matrix of plasma or serum samples from diabetic and hyperuricemic patients [59]. The validation should move beyond simple standard mixtures and be performed using representative sample matrices, such as pooled patient plasma, to accurately assess matrix effects [59].
Table 1: Key Analytical Validation Parameters for UHPLC-MS/MS Lipidomics.
| Validation Parameter | Definition | Target Acceptance Criteria | Assessment Method |
|---|---|---|---|
| Reproducibility | The precision of the method under varied conditions, including within-batch (intra-day) and between-batch (inter-day) analysis [59]. | Coefficient of variation (CV) < 15% for most lipids; <20% for lipids near LLOQ. | Repeated analysis of quality control (QC) samples (e.g., pooled plasma) over multiple days and batches. |
| Accuracy | The closeness of agreement between the measured value and a known reference value [59]. | Bias within ±15% of the true value. | Analysis of certified reference materials (e.g., NIST SRM 1950 [60]) or spiked recovery experiments in the biological matrix. |
| Sensitivity | The ability of the method to detect and quantify low-abundance lipids. | Limit of Detection (LOD): Signal-to-Noise (S/N) ≥ 3. Lower Limit of Quantification (LLOQ): CV <20%, accuracy 80-120% [61]. | Serial dilution of a standard or sample to determine the lowest concentration meeting criteria. |
| Specificity | The ability to unequivocally assess the analyte in the presence of other components, such as isomers or matrix interferences [61]. | No significant interference at the retention time and mass transition of the target lipid. | Analysis of blank matrix samples and examination of chromatographic separation. |
| Linear Dynamic Range | The concentration range over which the instrumental response is linearly proportional to the analyte concentration [59]. | A coefficient of determination (R²) > 0.99. | Calibration curves with a minimum of 5-6 concentration levels. |
| Carry-Over | The presence of a measurable signal from a previous sample in the analysis of a subsequent blank sample [59]. | Peak area in blank < 20% of LLOQ. | Injection of a blank solvent or matrix sample immediately after a high-concentration sample. |
| Sample Stability | The integrity of lipids during sample collection, storage, and preparation [59]. | Concentration change < 15% from baseline. | Analysis of QC samples after short-term (bench-top) and long-term (freezer) storage, and through freeze-thaw cycles. |
Experimental Workflow for a Validated DH Lipidomics Study
A robust lipidomics workflow encompasses all steps from sample collection to data interpretation, with validation integrated throughout. The following diagram and protocol outline a typical validated approach for a DH study.
Detailed Experimental Protocol
1. Sample Collection and Pre-processing:
- Collection: Collect fasting blood samples from enrolled subjects (e.g., DH patients, diabetes mellitus (DM) patients, and healthy controls (NGT)) into appropriate anticoagulant tubes [2].
- Processing: Centrifuge blood samples at 3,000 rpm for 10 minutes at room temperature to isolate plasma. Aliquot the supernatant (e.g., 0.2 mL) into sterile tubes.
- Storage: Immediately store aliquots at -80°C to preserve lipid stability until analysis [2] [61].
2. Lipid Extraction:
- Method: Employ a robust liquid-liquid extraction (LLE) method, such as a modified Folch or Bligh and Dyer protocol, considered the "gold standard" for lipidomics [61].
- Procedure: Thaw plasma samples on ice. Aliquot 100 µL of plasma into a glass vial. Add a pre-cooled mixture of chloroform and methanol (e.g., 2:1 v/v) to precipitate proteins and extract lipids. Vortex and sonicate the mixture. Add water or buffer to induce phase separation. Centrifuge and collect the lower organic phase containing the lipids [2] [61].
- Quality Control: Prepare pooled quality control (QC) samples by combining equal volumes of all study samples. These QCs are used to monitor instrument performance and validate reproducibility throughout the analytical run.
3. Chemical Derivatization (Optional for Enhanced Sensitivity):
- Reagent: Use benzoyl chloride for targeted analysis of lipid classes that lack characteristic MRM transitions and have poor sensitivity in conventional methods, such as monoacylglycerols (MG), diacylglycerols (DG), sphingoid bases (SPB), and free sterols (ST) [60].
- Protocol: Redissolve the dried lipid extract in a pyridine/acetonitrile mixture. Add benzoyl chloride in acetonitrile and react for 60 minutes at ambient temperature with slow stirring. Terminate the reaction and remove excess reagent using a modified Folch extraction with ammonium carbonate [60].
4. UHPLC-MS/MS Analysis:
- Chromatography:
- Column: Use a reversed-phase column, such as a Waters ACQUITY UPLC BEH C18 (e.g., 2.1 mm x 100 mm, 1.7 µm) [2] [60].
- Mobile Phase: Employ a binary gradient. Mobile phase A is often 10 mM ammonium formate in acetonitrile/water, and phase B is 10 mM ammonium formate in acetonitrile/isopropanol [2].
- Gradient: Implement a linear gradient elution from a high percentage of A to a high percentage of B over 10-30 minutes to separate diverse lipid classes based on hydrophobicity.
- Temperature: Maintain column temperature at 55°C [60].
- Mass Spectrometry:
- Ionization: Utilize electrospray ionization (ESI) in both positive and negative modes to cover the broad range of lipid polarities.
- Scanning: For untargeted profiling, use data-dependent acquisition (DDA) or data-independent acquisition (DIA). For targeted validation and quantification, use multiple reaction monitoring (MRM) for its high sensitivity and specificity [60] [61].
- Parameters: Optimize source parameters (gas flows, temperature) and collision energies for specific lipid classes.
5. Data Processing and Validation:
- Processing: Use specialized software (e.g., LipidSearch, MarkerView) for peak picking, alignment, and lipid identification against databases (e.g., LIPID MAPS). For targeted methods, use the internal standard for peak area ratio calculation for quantification [61].
- Validation: Integrate the validation parameters from Table 1 throughout the process. Analyze QC samples intermittently to assess reproducibility and accuracy. Process and statistically analyze the validated data to identify significantly altered lipids and pathways, such as glycerophospholipid metabolism, in DH patients [2] [59].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful execution of a validated lipidomics study requires carefully selected reagents and materials.
Table 2: Key Research Reagent Solutions for UHPLC-MS/MS Lipidomics.
| Item | Function/Application | Specific Example/Note |
|---|---|---|
| Internal Standards (IS) | Correct for variability in extraction, ionization, and analysis; enable quantification [60]. | Deuterated or odd-chain lipid standards (e.g., PC(15:0/18:1-d7), SM(d18:1/12:0)), added at the beginning of sample preparation. |
| Certified Reference Material | Assess method accuracy and enable cross-laboratory comparison [60]. | NIST SRM 1950 - Metabolites in Human Plasma. |
| LC-MS Grade Solvents | Minimize background noise and ion suppression, ensuring high sensitivity and reproducibility. | Chloroform, Methanol, Acetonitrile, 2-Propanol, Water. |
| Derivatization Reagents | Enhance chromatographic retention and MS sensitivity for poorly ionizing lipid classes [60]. | Benzoyl Chloride (for MG, DG, SPB, ST). |
| Solid Phase Extraction (SPE) Cartridges | Fractionate complex lipid extracts or clean up samples to reduce matrix effects. | Aminopropyl (NH2) or C18 cartridges. |
| Quality Control (QC) Material | Monitor system stability, data quality, and reproducibility throughout the analytical sequence [59]. | Pooled plasma from all study samples. |
| UHPLC Column | High-efficiency separation of complex lipid mixtures. | Reversed-Phase C18 column (e.g., 1.7 µm particle size, 2.1 x 100 mm). |
The path to discovering robust lipid biomarkers and understanding the metabolic pathophysiology of diabetes mellitus with hyperuricemia is paved with analytically sound data. A rigorous validation framework assessing reproducibility, sensitivity, and specificity is not an optional supplement but a fundamental requirement. By adhering to the detailed parameters, workflows, and reagent standards outlined in this guide, researchers can generate lipidomic profiles for DH with the high degree of confidence needed for meaningful biological interpretation and future translational application.
Ultra-high-performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) based lipidomics has emerged as a powerful phenotyping tool that offers unprecedented insights into metabolic health and disease pathophysiology. Within the specific research domain of diabetes mellitus (DM) and hyperuricemia (HUA), lipidomic signatures are transitioning from mere observational findings to clinically validated biomarkers for disease subtyping, prognosis, and understanding underlying mechanisms. This technical guide details the core principles and methodologies for robustly correlating lipidomic profiles with clinical parameters, focusing on validating their biological and clinical significance for researchers and drug development professionals. The intricate interplay between lipid metabolism, glucose homeostasis, and uric acid regulation provides a compelling rationale for using lipid signatures to decipher the shared pathophysiology of these common metabolic disorders.
Lipidomic Signatures in Diabetes and Hyperuricemia
Comprehensive lipidomic profiling consistently reveals specific alterations in the plasma lipidome of patients with diabetes, hyperuricemia, and their co-occurrence. The table below summarizes key validated lipid signatures associated with these conditions.
Table 1: Clinically Validated Lipid Signatures in Diabetes and Hyperuricemia
| Disease Context | Lipid Class | Specific Lipid Metabolites | Direction of Change | Associated Clinical Parameters & Correlations |
|---|---|---|---|---|
| DM with HUA (DH) | Triglycerides (TGs) | TG(16:0/18:1/18:2) and 12 other TGs [2] | ↑ Upregulated | Positively correlated with HUA risk; associated with de novo lipogenesis fatty acids (e.g., 16:1n-7) [57] |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) and 9 other PEs [2] | ↑ Upregulated | Enriched in persistent critical illness; prognostic for worse outcomes [26] | |
| Phosphatidylcholines (PCs) | PC(36:1) and 6 other PCs [2] | ↑ Upregulated | ||
| Hyperuricemia (HUA) | Diacylglycerols (DAGs) | DAG(16:0/22:5), DAG(16:0/22:6), DAG(18:1/20:5), DAG(18:1/22:6) [57] | ↑ Upregulated | Positively associated with plasma uric acid levels and HUA risk [57] |
| Lysophosphatidylcholine (LPC) | LPC(20:2) [57] | ↓ Downregulated | Inversely associated with HUA risk [57] | |
| T2DM with Dyslipidemia | Sphingomyelins (SMs) & Ceramides (Cer) | SM(d18:1/24:0), SM(d18:1/16:1), Cer(d18:1/24:0) [7] | Significantly Altered | Strong correlation with clinical glucose and lipid metabolism markers (HbA1c, FPG, TG); potential for enhanced risk prediction [7] |
These signatures are not isolated findings; network analyses often show co-regulation, such as a positive association between modules containing TGs, PCs, and DAGs with HUA risk [57]. Furthermore, these lipidomic associations can be influenced by mediating factors. For instance, the association between specific lipids and HUA is partially mediated (5-14%) by retinol-binding protein 4 (RBP4), an adipokine linked to dyslipidemia and insulin resistance [57].
Experimental Protocols for Validation
Robust clinical validation of lipid signatures requires standardized, high-throughput protocols that ensure data reproducibility and biological relevance.
Sample Collection and Pre-processing
The foundation of reliable lipidomics data is careful sample handling. A typical protocol is as follows [2] [62]:
- Collection: Collect fasting venous blood (e.g., 5 mL) into tubes containing anticoagulants like EDTA.
- Plasma Separation: Centrifuge at 3,000 rpm for 10-15 minutes at 4°C to separate plasma.
- Aliquoting and Storage: Aliquot the supernatant (plasma) into cryovials and immediately store at -80°C.
- Lipid Extraction (MTBE method):
- Thaw plasma samples on ice.
- Aliquot 100 μL of plasma into a new tube.
- Add 200 μL of cold methanol and 800 μL of methyl tert-butyl ether (MTBE).
- Sonicate in a low-temperature water bath for 20 minutes and incubate at room temperature for 30 minutes.
- Centrifuge at 14,000 g for 15 minutes at 10°C.
- Collect the upper organic phase and dry under a gentle nitrogen stream.
- Reconstitute the dried lipids in a suitable solvent (e.g., 100 μL isopropanol) for MS analysis.
- Quality Control (QC): Create a pooled QC sample by combining equal volumes from all samples. QC samples are injected at regular intervals throughout the analytical sequence to monitor instrument stability and data quality [7].
UHPLC-MS/MS Analysis Conditions
The core analytical method utilizes UHPLC coupled with tandem mass spectrometry.
Table 2: Standard UHPLC-MS/MS Conditions for Lipidomics
| Component | Specifications | Typical Conditions |
|---|---|---|
| Chromatography | Column: | Waters ACQUITY UPLC BEH C18 (2.1 x 100 mm, 1.7 μm) [2] or equivalent (e.g., Phenomenex Kinetex C18) [62]. |
| Mobile Phase A: | 10 mM ammonium formate in acetonitrile/water (e.g., 60:40, v/v) [2] [62]. | |
| Mobile Phase B: | 10 mM ammonium formate in isopropanol/acetonitrile (e.g., 90:10, v/v) [2] [62]. | |
| Gradient: | Nonlinear gradient from 40% B to 100% B over 10-18 minutes [2] [62]. | |
| Temperature: | 55°C [62]. | |
| Flow Rate: | 0.30 mL/min [62]. | |
| Injection Volume: | 2 μL [62]. | |
| Mass Spectrometry | Instrument Platform: | Triple-quadrupole (QTRAP) or high-resolution (e.g., timsTOF) mass spectrometers [63] [62]. |
| Ionization Mode: | Electrospray Ionization (ESI), positive and/or negative mode. | |
| Scan Mode: | Data-Dependent Acquisition (DDA) or Multiple Reaction Monitoring (MRM) for quantification. | |
| Mass Range: | m/z 100 - 1350 [62]. |
Data Processing and Statistical Analysis
The raw data processing pipeline involves:
- Lipid Annotation: Using specialized software (e.g., Lipid4DAnalyzer, Analyst) for peak picking, alignment, and identification based on m/z and fragmentation patterns [62].
- Data Pre-processing: Filtering features, imputing missing values (e.g., K-Nearest Neighbors method), and normalizing data using QC samples (e.g., RSD < 30% in QCs is acceptable) [7] [62].
- Multivariate Statistics:
- Principal Component Analysis (PCA): For unsupervised overview of data and detecting outliers.
- Orthogonal Partial Least Squares-Discriminant Analysis (OPLS-DA): For supervised identification of lipids most responsible for separating pre-defined groups (e.g., DH vs. healthy controls). Model validity is checked with permutation testing [2] [7].
- Differential Analysis: Univariate tests (Student's t-test) combined with fold-change (FC) analysis to pinpoint significantly altered lipids [2].
- Pathway Analysis: Using platforms like MetaboAnalyst 5.0 to identify enriched metabolic pathways (e.g., glycerophospholipid metabolism) based on the differential lipids [2].
Metabolic Pathway Mapping and Visualization
Integrating lipid signatures into known biochemical pathways is crucial for mechanistic insight. Studies on diabetes with hyperuricemia consistently identify glycerophospholipid metabolism and glycerolipid metabolism as the most significantly perturbed pathways [2] [7].
The following diagram illustrates the interconnected nature of these pathways and the points where validated lipid signatures are dysregulated.
Figure 1: Key Perturbed Lipid Pathways. This flow diagram synthesizes findings from multiple studies [2] [57], showing the cascade from glycerol-3-phosphate to key lipid classes. Lipid species significantly upregulated in Diabetes-Hyperuricemia (DH) or Hyperuricemia (HUA) are highlighted in red, while a downregulated species is highlighted in green. The diagram illustrates that disturbances are concentrated in the branches leading to Triglycerides (TAG), Diacylglycerols (DAG), and Phosphatidylethanolamines (PE).
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful execution of a clinical lipidomics study requires a suite of reliable, high-quality reagents and materials.
Table 3: Essential Research Reagent Solutions for UHPLC-MS/MS Lipidomics
| Category | Item | Critical Function & Rationale |
|---|---|---|
| Chromatography | UHPLC BEH C18 Column (1.7 μm) | High-resolution separation of complex lipid mixtures prior to MS detection [2]. |
| MS-Grade Solvents (Acetonitrile, Methanol, Isopropanol) | High-purity solvents prevent ion suppression and background noise, ensuring sensitivity and reproducibility [7]. | |
| Ammonium Formate | Mobile phase additive that promotes consistent ionization efficiency of lipids [2] [62]. | |
| Sample Prep | Methyl tert-butyl ether (MTBE) | Primary solvent for robust lipid extraction from plasma via the MTBE method [2]. |
| Deuterated Lipid Internal Standards (e.g., d7-PC, d5-TG) | Critical for accurate quantification; correct for extraction efficiency and MS variability [63] [64]. | |
| Quality Control | National Institute of Standards and Technology (NIST) Plasma | Reference material analyzed intermittently to monitor batch-to-batch reproducibility and ensure data quality across large studies [64]. |
| Data Acquisition | Commercially Available Lipid Standard Mixtures | Used for constructing calibration curves and validating lipid identification based on retention time and fragmentation [7]. |
The clinical validation of lipid signatures is a multi-step process that bridges from analytical chemistry to clinical pathophysiology. By employing rigorous UHPLC-MS/MS protocols, robust statistical frameworks, and pathway-based integration, researchers can transform lipidomic data into actionable insights. In the context of diabetes and hyperuricemia, the consistent identification of specific lipid subclasses (TGs, DAGs, PEs) and their associated metabolic pathways provides a solid foundation for developing these signatures into tools for patient stratification, prognostic assessment, and targeted drug development. The high individuality and sex specificity of the circulatory lipidome further underscore its potential for next-generation personalized metabolic health monitoring [64].
Lipidomics, a specialized branch of metabolomics, provides a comprehensive platform for identifying and quantifying the entire lipid pool within a biological system. The application of advanced analytical technologies, particularly ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS), has enabled the detailed characterization of lipid profiles associated with metabolic diseases [65]. This technical guide synthesizes current lipidomic research to delineate the distinct lipid disturbances in Diabetes Mellitus (DM), Hyperuricemia (HUA), and their co-occurrence (DH), framing these findings within the context of UHPLC-MS/MS methodologies for a research-focused audience.
Lipidomic Alterations Across Disease States
Comparative lipidomic analyses reveal distinct and overlapping lipid signatures in DM, HUA, and DH. The following table synthesizes key lipid alterations identified in recent studies.
Table 1: Significantly Altered Lipid Classes and Species in Diabetes, Hyperuricemia, and their Combination
| Lipid Class / Species | Diabetes Mellitus (DM) | Hyperuricemia (HUA) | Diabetes with HUA (DH) | Citations |
|---|---|---|---|---|
| Triglycerides (TGs) | Upregulated | Upregulated (e.g., TAG(53:0)) | Significantly upregulated (13 TGs, e.g., TG(16:0/18:1/18:2)) | [2] [66] |
| Diacylglycerols (DAGs) | Associated with T2DM | Upregulated (e.g., DAG(16:0/22:5), DAG(16:0/22:6)) | Information not specified | [66] [67] |
| Phosphatidylcholines (PCs) | Alterations reported | Upregulated (e.g., PC(16:0/20:5)) | Significantly upregulated (7 PCs, e.g., PC(36:1)) | [2] [66] [7] |
| Phosphatidylethanolamines (PEs) | Alterations reported | Information not specified | Significantly upregulated (10 PEs, e.g., PE(18:0/20:4)) | [2] |
| Lysophosphatidylcholines (LPCs) | Information not specified | Downregulated (e.g., LPC(20:2)) | Information not specified | [66] |
| Sphingomyelins (SMs) | Alterations reported (e.g., SM(d18:1/24:0)) | Information not specified | Information not specified | [7] |
| Ceramides (Cers) | Alterations reported (e.g., Cer(d18:1/24:0)) | Information not specified | Information not specified | [7] |
Core Perturbed Metabolic Pathways
Pathway enrichment analysis of differential lipids consistently implicates several key metabolic pathways across the disease states. The following table ranks these pathways based on their reported significance.
Table 2: Enriched Metabolic Pathways in Diabetes, Hyperuricemia, and their Combination
| Metabolic Pathway | Reported Impact in DH | Association with HUA | Association with DM | Citations |
|---|---|---|---|---|
| Glycerophospholipid Metabolism | Most significantly perturbed (Impact value: 0.199) | Strongly associated | Strongly associated | [2] [14] [68] |
| Glycerolipid Metabolism | Significantly perturbed (Impact value: 0.014) | Strongly associated (via TGs, DAGs) | Strongly associated | [2] [66] [67] |
| Sphingolipid Metabolism | Information not specified | Associated | Strongly associated | [68] [7] |
| Arachidonic Acid Metabolism | Information not specified | Associated | Information not specified | [14] [68] |
| Linoleic Acid Metabolism | Information not specified | Associated | Information not specified | [14] [68] |
The interconnection of these pathways and their relationship to disease pathophysiology can be visualized as follows:
Detailed Experimental Protocols for UHPLC-MS/MS Lipidomics
Sample Collection and Preparation
Robust sample preparation is critical for reliable lipidomic profiling. The following protocol is synthesized from multiple studies:
Sample Collection: Collect fasting venous blood into tubes containing anticoagulants (e.g., EDTA). Centrifuge at 3,000 rpm for 10-15 minutes at 4°C to isolate plasma or serum [2] [66]. Aliquot and store immediately at -80°C.
Lipid Extraction (MTBE Method):
- Thaw samples on ice and vortex.
- Aliquot 100 μL of plasma into a 1.5 mL microcentrifuge tube.
- Add 200 μL of 4°C HPLC-grade water and vortex.
- Add 240 μL of pre-cooled methanol and vortex thoroughly.
- Add 800 μL of methyl tert-butyl ether (MTBE), vortex, and sonicate in a low-temperature water bath for 20 minutes.
- Incubate at room temperature for 30 minutes.
- Centrifuge at 14,000 g for 15 minutes at 10°C to achieve phase separation.
- Collect the upper organic phase and dry under a gentle nitrogen stream.
- Reconstitute the dried lipids in 100-200 μL of 90% isopropanol/acetonitrile for MS analysis [2] [14].
Quality Control: Prepare pooled quality control (QC) samples by combining equal volumes of all study samples. Insert QC samples randomly throughout the analytical sequence to monitor instrument stability and data reproducibility [2] [7].
UHPLC-MS/MS Instrumental Analysis
The core analytical workflow for lipid separation and detection is outlined below:
Chromatographic Conditions:
- Column: Waters ACQUITY UPLC BEH C18 column (2.1 mm × 100 mm, 1.7 μm particle size) or equivalent [2] [7].
- Mobile Phase:
- Gradient: Non-linear gradient from 30% B to 100% B over 25 minutes [14].
- Flow Rate: 0.3-0.4 mL/min [14] [68].
- Column Temperature: 45-55°C [14] [68].
- Injection Volume: 2-5 μL [68].
Mass Spectrometric Conditions:
- Ionization: Electrospray ionization (ESI) in both positive and negative ion modes [14] [68].
- Spray Voltage: 3.0 kV (positive mode), 2.5 kV (negative mode) [14].
- Source Temperature: 300-350°C [14].
- Scan Range: m/z 200-1800 [14].
- Data Acquisition: Data-dependent acquisition (DDA) or data-independent acquisition (DIA) modes, collecting both MS1 and MS/MS spectra for lipid identification [14].
Data Processing and Statistical Analysis
- Peak Processing: Use specialized software (e.g., LipidSearch, Progenesis QI, ADViSELipidomics) for peak picking, alignment, and normalization [65] [68].
- Lipid Identification: Annotate lipids based on accurate mass, retention time, and MS/MS fragmentation patterns, referencing databases such as LIPID MAPS [65].
- Multivariate Statistics:
- Differential Analysis: Apply univariate tests (e.g., Student's t-test) with correction for multiple testing (e.g., False Discovery Rate) and fold-change analysis to identify significantly altered lipids [2] [7].
- Pathway Analysis: Utilize platforms like MetaboAnalyst 5.0 to identify enriched metabolic pathways from the list of differential lipids [2].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Reagents and Materials for UHPLC-MS/MS Lipidomics
| Item | Function / Application | Examples / Specifications |
|---|---|---|
| UHPLC System | High-resolution chromatographic separation of complex lipid mixtures | Waters ACQUITY UPLC, Shimadzu Nexera systems |
| Mass Spectrometer | Accurate mass detection and structural characterization | Q-TOF, Orbitrap, QqQ instruments (e.g., SCIEX 5500 QTRAP) |
| C18 Chromatography Column | Reverse-phase separation of lipid species | Waters ACQUITY UPLC BEH C18 (1.7 μm) |
| MS-Grade Solvents | Mobile phase preparation and sample reconstitution | Methanol, Acetonitrile, Isopropanol, Water |
| Lipid Extraction Solvents | Liquid-liquid extraction of lipids from biological matrices | Methyl tert-butyl ether (MTBE), Chloroform, Methanol |
| Internal Standards | Normalization for quantification and monitoring of extraction efficiency | Deuterated or odd-chain lipid standards for multiple classes |
| Ammonium Formate / Acetate | Mobile phase additive to promote ionization efficiency | 10 mM concentration in mobile phases |
| Data Processing Software | Lipid identification, quantification, and statistical analysis | LipidSearch, Progenesis QI, ADViSELipidomics, LIQUID |
UHPLC-MS/MS-based lipidomics has unveiled distinct and overlapping perturbations in the lipidomes of diabetes, hyperuricemia, and their combination. The consistent upregulation of specific triglycerides, glycerophospholipids, and diacylglycerols, along with the central disruption of glycerophospholipid and glycerolipid metabolism pathways, provides a mechanistic link between these comorbid conditions. The standardized protocols and resource toolkit outlined in this guide provide a foundation for advancing research in this field, with the potential to identify novel biomarkers and therapeutic targets for these interconnected metabolic disorders.
The integration of machine learning (ML) with high-throughput omics technologies is revolutionizing biomarker discovery, moving the field beyond single-molecule identification towards robust, multi-feature panels. For researchers in areas such as UHPLC-MS/MS lipidomic profiling of complex conditions like diabetes mellitus combined with hyperuricemia (DH), rigorous validation of these panels is not merely a final step but a fundamental component of the discovery pipeline [2] [9]. Techniques like Least Absolute Shrinkage and Selection Operator (LASSO) and Random Forest provide powerful frameworks for feature selection, while Receiver Operating Characteristic (ROC) analysis offers a critical means of evaluating diagnostic performance. This technical guide details advanced methodologies for developing and validating biomarker panels, with a specific focus on applications within lipidomics and metabolic disease research, providing a solid foundation for a thesis investigating the lipidomic signatures of diabetes and hyperuricemia.
Core Machine Learning Techniques for Biomarker Validation
LASSO Regression for Sparse Biomarker Selection
LASSO (Least Absolute Shrinkage and Selection Operator) regression is a paramount technique for developing parsimonious biomarker panels from high-dimensional omics data. Its primary function is feature selection by applying an L1-penalty that shrinks the coefficients of irrelevant features to exactly zero, thus yielding a sparse, interpretable model [69] [70].
A key advancement in this area is the SMAGS-LASSO framework, which modifies the traditional objective function to maximize sensitivity at a given specificity (SP). This is crucial for clinical applications like early cancer detection or screening for disease complications, where missing a positive case (low sensitivity) has severe consequences [69]. The objective function is formulated as:
$$ \max{\beta, \beta0} \frac{\sum{i=1}^{n} \hat{y}i \cdot yi}{\sum{i=1}^{n} yi} - \lambda \|\beta\|1, \quad \text{Subject to} \quad \frac{\mathbf{1 - y}^T (\mathbf{1} - \mathbf{\hat{y}})}{\mathbf{1 - y}^T (\mathbf{1} - \mathbf{y})} \geq SP $$
Here, $\hat{y}i = I(\sigma(xi^T \beta + \beta_0) > \theta)$ is the predicted class, and $\theta$ is a threshold adaptively determined to control the specificity level [69]. The optimization employs a multi-pronged strategy, initializing coefficients with standard logistic regression and then applying multiple algorithms (Nelder-Mead, BFGS, CG, L-BFGS-B) in parallel, finally selecting the solution with the highest sensitivity [69].
For standard LASSO, the regularization parameter $\lambda$ is typically chosen via k-fold cross-validation (e.g., k=5) to minimize classification error. In contrast, SMAGS-LASSO's cross-validation is designed to select the $\lambda$ that minimizes sensitivity mean squared error (MSE), ensuring the model maintains high sensitivity under the specificity constraint [69].
Random Forest for Non-Linear Pattern Recognition
Random Forest is an ensemble learning method that operates by constructing a multitude of decision trees at training time. It is particularly effective for biomarker discovery due to its ability to handle non-linear relationships and complex interactions between features without strong assumptions about the underlying data distribution [71] [72].
The algorithm's robustness stems from two key mechanisms: bagging (bootstrap aggregating), which reduces variance and mitigates overfitting, and feature randomness, which ensures that each tree is de-correlated from the others [71]. A critical output is the variable importance measure, which quantifies the contribution of each feature (biomarker) to the model's predictive accuracy. Features with higher importance scores are strong candidates for the final biomarker panel [72] [70].
In practice, as demonstrated in a study on primary myelofibrosis, LASSO and Random Forest can be integrated. The Random Forest algorithm is used to rank genes by their importance score, and those exceeding a predefined threshold (e.g., score > 2) are retained. The intersection of these genes with those selected by LASSO provides a robust set of hub biomarkers, balancing both linear and non-linear model strengths [72].
Evaluation Metrics and ROC Analysis
Once a biomarker panel is selected, its diagnostic performance must be rigorously evaluated. The Receiver Operating Characteristic (ROC) curve is a fundamental tool for this purpose, plotting the True Positive Rate (Sensitivity) against the False Positive Rate (1 - Specificity) across all possible classification thresholds [69] [72].
The Area Under the ROC Curve (AUC) summarizes the overall performance, where an AUC of 1 represents a perfect test and 0.5 represents a worthless test. For clinical applications, the partial AUC in a specific, clinically relevant region of high specificity (e.g., 90-100%) can be more informative than the full AUC [69].
Table 1: Key Metrics for Biomarker Panel Evaluation
| Metric | Formula | Interpretation |
|---|---|---|
| Sensitivity | $\frac{TP}{TP+FN}$ | Ability to correctly identify positive cases |
| Specificity | $\frac{TN}{TN+FP}$ | Ability to correctly identify negative cases |
| Area Under Curve (AUC) | Area under ROC curve | Overall diagnostic performance |
| Biomarker Probability Score | Normalized summative rank from ML models [73] | Ranks potential biomarkers for further validation |
The Biomarker Probability Score (BPS), a normalized summative rank from multiple ML models, has been proposed as a useful metric for prioritizing biomarkers for further validation [73].
Experimental Protocols and Workflows
Integrated ML-Workflow for Biomarker Panel Discovery
The following diagram illustrates a generalized, robust workflow for biomarker panel discovery and validation, integrating LASSO and Random Forest.
Protocol: Biomarker Panel Validation using LASSO and Random Forest
Objective: To identify and validate a minimal biomarker panel from high-dimensional lipidomic data for distinguishing patients with diabetes mellitus and hyperuricemia (DH) from healthy controls (NGT) and diabetic patients (DM) [2].
Step 1: Data Preparation and Preprocessing
- Acquire lipidomic data via UHPLC-MS/MS, ensuring quality control (e.g., using pooled quality control samples) [2] [9].
- Perform peak alignment, normalization, and log-transformation to stabilize variance.
- Split the dataset into a training set (e.g., 80%) for model development and a hold-out test set (e.g., 20%) for final validation. Use stratified splitting to maintain class distribution.
Step 2: Application of LASSO Regression
- On the training set, fit a LASSO logistic regression model using the
glmnetpackage in R [72] [70]. - Perform 10-fold cross-validation (
cv.glmnet) with alpha set to 1 to determine the optimal $\lambda$ value ($\lambda_{1se}$) that minimizes the binomial deviance [72]. - Extract the non-zero coefficients at $\lambda_{1se}$ to obtain the first candidate list of biomarkers.
Step 3: Application of Random Forest
- On the same training set, train a Random Forest model using the
randomForestpackage in R. - Set a sufficient number of trees (
ntree=1000) and tune themtryparameter. - Calculate the Mean Decrease Gini or Mean Decrease Accuracy as the variable importance measure.
- Retain features with an importance score exceeding a predefined threshold (e.g., above the median or a specific value from the literature) [72] for the second candidate list.
Step 4: Hub Biomarker Identification
- Take the intersection of biomarkers selected by both LASSO and Random Forest. This combined list of "hub biomarkers" leverages the strengths of both methods [72].
- Alternatively, if the intersection is too small, create a union set and use domain knowledge (e.g., biological plausibility from pathway analysis [2]) for final selection.
Step 5: Model Building and ROC Analysis
- Build a final, simpler classifier (e.g., logistic regression) using only the selected hub biomarkers on the training set.
- Predict on the held-out test set and generate the ROC curve using the
pROCpackage in R [72]. - Report the AUC, sensitivity, and specificity at the optimal cutoff (e.g., Youden's index) [74].
- For clinical utility, report sensitivity at a fixed, high specificity (e.g., 95% or 98.5%) as required by the screening context [69].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Platforms for Biomarker Validation
| Category/Item | Specific Example / Kit | Function in Workflow |
|---|---|---|
| Chromatography System | Waters ACQUITY UHPLC System | High-resolution separation of complex lipid samples prior to MS analysis [2]. |
| Mass Spectrometer | Tandem Quadrupole Mass Spectrometer (MS/MS) | Precise identification and quantification of lipid molecular species [2] [9]. |
| Chromatography Column | Waters ACQUITY UHPLC BEH C18 Column (2.1x100mm, 1.7µm) | Stationary phase for retaining and separating lipid molecules based on hydrophobicity [2]. |
| Lipid Extraction Solvent | Methyl-tert-butyl ether (MTBE) / Methanol | Liquid-liquid extraction of a broad range of lipids from plasma or tissue samples [2]. |
| Statistical Software | R Statistical Software (v4.3.3+) | Platform for data preprocessing, statistical analysis, and machine learning modeling [70]. |
| R Packages - ML | glmnet, randomForest, Boruta |
Implementation of LASSO, Random Forest, and other feature selection algorithms [72] [70]. |
| R Packages - Validation | pROC, caret |
Generation of ROC curves, calculation of AUC, and general model training functions [72]. |
Signaling Pathways and Logical Workflows in Biomarker Discovery
From Lipidomic Data to Clinical Insight
The final diagram maps the logical flow from raw data generation through to clinical insight, highlighting the central role of machine learning validation in the context of diabetes and hyperuricemia research.
The rigorous application of machine learning validation techniques, particularly LASSO and Random Forest, combined with robust ROC analysis, is indispensable for transforming high-dimensional UHPLC-MS/MS lipidomic data into clinically actionable biomarker panels. The structured workflows and protocols detailed in this guide provide a roadmap for researchers to navigate the complexities of feature selection, model validation, and performance evaluation. By adhering to these advanced technical standards, the discovery of lipidomic biomarkers for complex metabolic diseases like diabetes and hyperuricemia can be accelerated, paving the way for improved diagnostic precision and personalized therapeutic strategies.
The complexity of metabolic diseases such as diabetes mellitus and hyperuricemia demands research approaches that transcend the limitations of single-study designs. Multi-cohort and cross-population studies have emerged as powerful methodologies that strengthen the evidence base for clinical translation by validating findings across diverse populations, increasing statistical power, and enhancing the generalizability of results. The integration of advanced omics technologies, particularly ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) lipidomic profiling, with multi-cohort frameworks represents a cutting-edge approach to unraveling the intricate metabolic disruptions underlying complex conditions like diabetes with hyperuricemia comorbidity.
The global burden of metabolic diseases underscores the urgency of this research. Diabetes mellitus affects approximately 10.5% of the global adult population (536.6 million individuals), with prevalence continuing to rise [2]. Hyperuricemia, originally more common in Western nations, has become increasingly prevalent in Eastern countries, with a recent cross-sectional study in mainland China reporting a 17.7% prevalence rate [2]. The coexistence of these conditions presents particular clinical challenges, as hyperuricemia occurs more frequently in diabetic populations and elevates the risk of diabetic complications including nephropathy, adverse cardiac events, and peripheral vascular disease [2].
Theoretical Foundations of Multi-Cohort Research
Conceptual Framework and Definitions
Multi-cohort studies involve the integration and harmonization of data from multiple independent cohort studies to investigate scientific questions beyond the scope of a single institution. These initiatives can be categorized into two primary approaches: (1) prospective collaborative consortia that establish unified protocols from inception, and (2) retrospective harmonization projects that integrate existing cohorts with varied original designs [75] [76].
The fundamental value proposition of multi-cohort research lies in its ability to overcome the limitations inherent in individual studies, including limited sample sizes, restricted demographic diversity, and cohort-specific biases. By combining data across studies, researchers can achieve sufficient statistical power for robust analyses, particularly for investigating rare conditions, subgroup effects, or complex interactions [75] [77].
Advantages and Methodological Strengths
The primary advantages of multi-cohort approaches include:
- Enhanced Statistical Power: Larger sample sizes enable detection of smaller effect sizes and provide greater precision in estimating associations [76].
- Improved Generalizability: Validation across heterogeneous populations increases confidence that findings are not cohort-specific artifacts [78] [79].
- Accelerated Discovery: Efficient reuse of existing data and samples accelerates research progress and maximizes resource utilization [75].
- Stratification Capabilities: Sufficient sample sizes allow examination of subgroups based on sex, ethnicity, comorbidities, or other relevant characteristics [78].
The SYNCHROS (SYNergies for Cohorts in Health: integrating the ROle of all Stakeholders) project, a 3-year initiative funded by the Horizon 2020 Program, successfully mapped 1000 multi-cohort projects across 11 countries, demonstrating the growing recognition of this approach's value in personalized medicine [75].
Methodological Considerations for Multi-Cohort Studies
Cohort Harmonization and Data Integration
The process of harmonizing data across multiple cohorts presents significant technical and methodological challenges. Different cohorts typically employ varied data structures, terminologies, measurement tools, and data collection protocols, creating obstacles for integrated analysis. The methodology proposed by [77] provides a framework for semi-automatic harmonization of large amounts of medical concepts across clinical studies, inspired by the OHDSI Common Data Model. This approach involves:
- Metadata Analysis: Comprehensive documentation of source data structures and semantics.
- Concept Mapping: Establishing equivalence between different coding systems and measurement approaches.
- Data Transformation: Converting source data into a common standardized format.
- Quality Validation: Ensuring accuracy and completeness of the harmonization process.
This methodology has been successfully applied in Alzheimer's Disease research, harmonizing 6,669 subjects and 172 clinical concepts across multiple international cohorts [77].
Cross-Study Normalization and Batch Effect Correction
In lipidomic studies, technical variation between cohorts introduced by different instrumentation, laboratory protocols, or sample handling procedures can create batch effects that obscure biological signals. Cross-study normalization approaches are essential to address these technical artifacts. Research has demonstrated that appropriate normalization can enhance predictive performance in multi-cohort analyses, though benefits may vary across studies, indicating that normalization strategies should be tailored to cohort-specific characteristics [78].
Ethical, Legal, and Governance Frameworks
Multi-cohort research introduces complex ethical and legal considerations, particularly regarding data privacy, informed consent, and data governance. Each cohort typically has established policies, governance structures, and data sharing agreements that must be respected [75]. The process often requires approval from multiple ethics committees and scientific boards, a process that can be time-consuming. The PGX-link project, a Swiss multi-cohort initiative, required a one-year preparation phase solely to navigate these administrative requirements before research activities could commence [75].
Table 1: Key Challenges in Multi-Cohort Studies and Potential Mitigation Strategies
| Challenge Category | Specific Challenges | Potential Mitigation Strategies |
|---|---|---|
| Data Harmonization | Different data structures, terminologies, measurement tools | Common Data Models (e.g., OHDSI CDM), semantic mapping tools |
| Technical Variation | Batch effects, different analytical platforms | Cross-study normalization, reference standards, quality control samples |
| Governance | Diverse ethics requirements, data sharing agreements | Early engagement with cohort governance bodies, standardized material transfer agreements |
| Statistical Methods | Heterogeneity across cohorts, varying follow-up durations | Appropriate mixed-effects models, sensitivity analyses, stratification approaches |
UHPLC-MS/MS Lipidomic Profiling in Multi-Cohort Diabetes and Hyperuricemia Research
Analytical Methodology for Lipidomic Profiling
UHPLC-MS/MS has emerged as the gold standard for comprehensive lipidomic analysis in metabolic disease research due to its high sensitivity, resolution, and capacity to characterize hundreds of lipid species simultaneously. The technical workflow typically involves:
Sample Preparation:
- Plasma or serum collection after fasting [2] [43]
- Protein precipitation using pre-cooled methanol [2]
- Lipid extraction with methyl tert-butyl ether (MTBE) or methanol/acetonitrile/water mixtures [2] [43]
- Low-temperature sonication and centrifugation [2]
- Nitrogen drying of organic phase and reconstitution in isopropanol [2]
Chromatographic Conditions:
- Column: Waters ACQUITY UPLC BEH C18 (2.1 mm × 100 mm, 1.7 μm particle size) [2]
- Mobile Phase: A: 10 mM ammonium formate in acetonitrile/water; B: 10 mM ammonium formate in acetonitrile/isopropanol [2]
- Gradient elution with precise temperature control
Mass Spectrometric Analysis:
- Instrumentation: Thermo Exactive Plus Orbitrap mass spectrometer [43]
- Ionization Mode: Positive and/or negative electrospray ionization
- Mass Resolution: High-resolution accurate mass measurement
- Data Acquisition: Data-dependent MS/MS fragmentation for structural characterization
Quality Control:
- Implementation of pooled quality control samples throughout analytical sequence [2] [43]
- Monitoring of retention time stability and mass accuracy
- Calculation of coefficients of variation for quality control samples (<15% acceptable) [43]
Diagram 1: Experimental workflow for UHPLC-MS/MS lipidomic profiling
Multi-Cohort Lipidomic Findings in Diabetes and Hyperuricemia
Recent multi-cohort lipidomic studies have revealed profound disruptions in lipid metabolism in patients with diabetes and hyperuricemia. A study comparing patients with diabetes mellitus (DM), diabetes mellitus combined with hyperuricemia (DH), and healthy controls (NGT) identified 1,361 lipid molecules across 30 subclasses, with multivariate analyses revealing significant separation trends among the groups [2].
Table 2: Significantly Altered Lipid Classes in Diabetes with Hyperuricemia
| Lipid Class | Direction of Change | Specific Examples | Proposed Biological Significance |
|---|---|---|---|
| Triglycerides (TGs) | Significantly upregulated | TG(16:0/18:1/18:2) | Energy storage, lipid accumulation, insulin resistance |
| Phosphatidylethanolamines (PEs) | Significantly upregulated | PE(18:0/20:4) | Membrane fluidity, signaling precursors |
| Phosphatidylcholines (PCs) | Significantly upregulated | PC(36:1) | Membrane composition, cholesterol metabolism |
| Phosphatidylinositols (PIs) | Downregulated | Not specified | Cell signaling, insulin signaling pathway |
The most significantly perturbed metabolic pathways identified in patients with combined diabetes and hyperuricemia include glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) [2]. These pathway disturbances highlight the interconnected nature of lipid and purine metabolism in these conditions.
Comparison of lipid profiles between asymptomatic hyperuricemic and gout patients has revealed additional nuances in lipid disruptions. A study identifying 116 differential metabolites between these groups found that a biomarker panel containing TAG(18:1-20:0-22:1) and TAG(14:0-16:0-16:1) could differentiate between hyperuricemia and gout with high accuracy (AUC: 0.8288) [80].
Diagram 2: Key metabolic pathway disruptions in diabetes with hyperuricemia
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of multi-cohort UHPLC-MS/MS lipidomic studies requires carefully selected reagents and materials to ensure reproducibility and data quality across sites.
Table 3: Essential Research Reagents for Multi-Cohort Lipidomic Studies
| Reagent/Material | Specification | Function in Workflow | Quality Considerations |
|---|---|---|---|
| Chromatography Column | Waters ACQUITY UPLC BEH C18 (2.1×100mm, 1.7μm) | Lipid separation | Column batch consistency, lifetime monitoring |
| Mobile Phase Additive | 10 mM ammonium formate | MS compatibility, adduct formation | High purity, fresh preparation |
| Lipid Extraction Solvent | Methyl tert-butyl ether (MTBE) or methanol/acetonitrile/water (5:3:2) | Lipid extraction from biological matrix | HPLC grade, antioxidant stabilization |
| Quality Control Material | Sigma human serum matrix | Inter-batch normalization | Consistent source, stability monitoring |
| Internal Standards | Stable isotope-labeled lipid standards | Quantitation accuracy | Coverage of multiple lipid classes |
| Sample Collection Tubes | EDTA or heparin plasma tubes | Pre-analytical standardization | Lot consistency, polymer contamination screening |
Machine Learning and Predictive Modeling in Multi-Cohort Studies
The integration of machine learning with multi-cohort data offers powerful approaches for risk prediction and biomarker discovery. Multi-cohort machine learning models have demonstrated advantages over single-cohort models in terms of performance stability and robustness, despite the more challenging nature of prediction tasks across heterogeneous populations [78].
In Parkinson's disease research, multi-cohort models for predicting cognitive impairment showed comparable performance to single-cohort models while providing more stable performance statistics across cross-validation cycles [78]. This improved stability reduces cohort-specific biases and increases clinical prediction reliability, essential qualities for translational applications.
For diabetes risk prediction, a multicohort study developed a novel diabetes index using logistic regression that achieved exceptional performance (AUROC: 0.93-0.94) [81]. The model incorporated 16-18 variables including glycosuria (showing the highest odds ratio in men) and high triglyceride levels (highest odds ratio in women), highlighting sex-specific risk factors [81]. External validation in a prospective cohort demonstrated the model's ability to stratify patients into risk groups with significantly different cumulative incidence of diabetes [81].
Explainable Artificial Intelligence (XAI) methods such as SHapley Additive exPlanations (SHAP) value plots enable interpretation of complex machine learning models and identification of consistent predictors across cohorts [78]. This transparency is crucial for clinical translation and biological insight generation.
Multi-cohort and cross-population studies represent a paradigm shift in metabolic disease research, enabling robust validation of findings and enhancing the translational potential of discoveries. The integration of UHPLC-MS/MS lipidomic profiling with multi-cohort frameworks has revealed specific lipid disturbances and metabolic pathway alterations in diabetes with hyperuricemia, providing insights into the underlying pathophysiology and potential biomarkers for risk stratification.
Future directions in this field include the development of standardized harmonization protocols specifically for lipidomic data, implementation of federated learning approaches that enable analysis without centralizing sensitive data, and increased inclusion of diverse populations to ensure equity in biomarker discovery and clinical translation. As these methodologies continue to mature, multi-cohort lipidomic studies will play an increasingly central role in precision medicine approaches to metabolic disease prevention, diagnosis, and treatment.
Conclusion
UHPLC-MS/MS-based lipidomics has unequivocally illuminated the profound lipid metabolic disruptions characteristic of the diabetes-hyperuricemia comorbidity, identifying specific biomarkers and highlighting glycerophospholipid and glycerolipid metabolism as central perturbed pathways. The integration of robust methodological workflows with advanced data analysis and validation frameworks is paramount for translating these discoveries from research benches to clinical settings. Future efforts must focus on large-scale, multi-center validation studies, the standardization of analytical protocols to ensure reproducibility, and the development of regulatory-approved diagnostic panels. The synergy of lipidomics with other omics technologies and artificial intelligence holds immense promise for pioneering personalized risk assessment, early diagnosis, and novel therapeutic interventions, ultimately reshaping the management of complex metabolic syndromes.
References
- 1. The link between hyperuricemia and diabetes: insights from a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11842261/]
- 2. UHPLC-MS/MS-based plasma untargeted lipidomic ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1656458/full]
- 3. Hyperuricemia is Associated With an Increased Prevalence ... [https://www.jrd.or.kr/journal/view.html?doi=10.4078/jrd.2020.27.4.247]
- 4. Hyperuricemia and its related diseases: mechanisms and ... [https://www.nature.com/articles/s41392-024-01916-y]
- 5. Correlation between remnant cholesterol and hyperuricemia ... [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-024-02148-3]
- 6. The effect of lipid metabolism disorder on patients with ... [https://www.nature.com/articles/s41598-023-45564-8]
- 7. based on Lipidomics /Q-TOF- UHPLC to characterize lipid... MS [https://pmc.ncbi.nlm.nih.gov/articles/PMC10884851/]
- 8. Research on Lipidomic Profiling and Biomarker ... [https://www.mdpi.com/2227-9059/12/12/2827]
- 9. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/pii/S0009898125005777?dgcid=rss_sd_all]
- 10. Revisiting the metabolic crosstalk between type 2 diabetes ... [https://www.sciencedirect.com/science/article/abs/pii/S0925443925004521]
- 11. Alterations in lipidome profiles distinguish early-onset ... [https://arthritis-research.biomedcentral.com/articles/10.1186/s13075-023-03204-6]
- 12. Circulating Sphingolipids in Insulin Resistance, Diabetes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10531201/]
- 13. Sphingolipids in Obesity, Type 2 Diabetes, and Metabolic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4091661/]
- 14. The effect of lipid metabolism disorder on patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10598229/]
- 15. Molecular mechanisms of metabolic dysregulation in ... [https://www.frontiersin.org/journals/cardiovascular-medicine/articles/10.3389/fcvm.2024.1375400/full]
- 16. Clinical serum lipidomic profiling revealed potential lipid ... [https://www.nature.com/articles/s41598-024-66157-z]
- 17. Lipid metabolism is dysregulated in a mouse model of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9156495/]
- 18. Spatial-temporal lipidomics reveals dysregulated lipid ... [https://pubmed.ncbi.nlm.nih.gov/40865635/]
- 19. Lipid droplet dynamics in type 2 diabetes and its complications [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-025-02747-8]
- 20. Lipidomics based on UHPLC/Q-TOF-MS to characterize ... [https://www.sciencedirect.com/science/article/pii/S2405844024023570]
- 21. Exploring the Lipidome: Current Lipid Extraction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7345237/]
- 22. Lipidomics in Understanding Pathophysiology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9030008/]
- 23. A Critical Overview of HPLC-MS-Based Lipidomics in ... [https://www.mdpi.com/2304-8158/12/17/3177]
- 24. Profiling Reveals Phenotype-Specific Metabolic Signatures... Lipidomic [https://pubmed.ncbi.nlm.nih.gov/41126449/]
- 25. Identifying serum lipidomic signatures related to prognosis in ... [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-025-06802-7]
- 26. Lipidomic signatures align with inflammatory patterns and ... [https://www.nature.com/articles/s41467-022-34420-4]
- 27. Mass Spectrometry in Analytical Lipidomics [https://www.chromatographyonline.com/view/mass-spectrometry-analytical-lipidomics]
- 28. Lipidomics from sample preparation to data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC7118050/]
- 29. Ultrahigh-Performance Liquid Chromatography–Mass ... [https://www.spectroscopyonline.com/view/ultrahigh-performance-liquid-chromatography-mass-spectrometry-lipidomics]
- 30. Lipidomics by ultrahigh performance liquid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6013032/]
- 31. A targeted UHPLC-MS/MS method to monitor lipidomic ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708523001425]
- 32. Versatile lipid profiling by liquid chromatography–high ... [https://www.sciencedirect.com/science/article/abs/pii/S0003267013010544]
- 33. Microwave-Assisted Extraction/UHPLC-Q-Orbitrap-MS-Based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11012187/]
- 34. Optimizing Ultra-High-Performance Liquid Chromatography (UHPLC) Methods for Rapid Analysis of Complex Biological Samples | IntechOpen [https://www.intechopen.com/chapters/1188571]
- 35. Ultra High Performance Liquid Chromatography - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/immunology-and-microbiology/ultra-high-performance-liquid-chromatography]
- 36. Principles and Applications of High-Performance Liquid Chromatography (HPLC): A Review – Biomedical and Pharmacology Journal [https://biomedpharmajournal.org/vol18no2/principles-and-applications-of-high-performance-liquid-chromatography-hplc-a-review/]
- 37. Ultrahigh-Performance Liquid Chromatography–Mass ... [https://www.chromatographyonline.com/view/ultrahigh-performance-liquid-chromatography-mass-spectrometry-lipidomics-2]
- 38. HIGH RESOLUTION MASS SPECTROMETRY IN ... [https://pubmed.ncbi.nlm.nih.gov/32233039/]
- 39. Shotgun Lipidomics on High Resolution Mass Spectrometers [https://pmc.ncbi.nlm.nih.gov/articles/PMC3181034/]
- 40. Tandem Mass Spectrometry in Untargeted Lipidomics [https://pubmed.ncbi.nlm.nih.gov/39596146/]
- 41. The Hitchhiker's Guide to Untargeted Lipidomics Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8624948/]
- 42. Pathway Analysis: State of the Art - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4681784/]
- 43. Metabolic pathway analysis of hyperuricaemia patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9805114/]
- 44. Pre-Analytical Variation | myadlm.org [https://myadlm.org/cln/articles/2016/july/preanalytical-variation-the-leading-cause-of-error-in-laboratory-medicine]
- 45. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 46. Alterations in lipidome profiles distinguish early-onset ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10693150/]
- 47. Preanalytical, analytical, and postanalytical variables [https://webpath.med.utah.edu/EXAM/LabMedCurric/LabMed01_04.html]
- 48. Recent Advances in Lipid Separations and Structural ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5828972/]
- 49. Towards Lipidomics of Low-Abundant Species for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3876128/]
- 50. Four-dimensional trapped ion mobility spectrometry ... [https://www.nature.com/articles/s41467-023-36520-1]
- 51. An analytical evaluation of tools for lipid isomer ... [https://www.sciencedirect.com/science/article/abs/pii/S1387380624000794]
- 52. How to Interpret Lipidomics Data: A Step-by-Step Guide [https://lipidomics.creative-proteomics.com/resource/how-to-interpret-lipidomics-data-a-step-by-step-guide.htm]
- 53. Analytical quality control in targeted lipidomics [https://www.sciencedirect.com/science/article/pii/S0003267025006191]
- 54. Improved Performance of UHPLC–MS Hyphenated Systems [https://www.chromatographyonline.com/view/improved-performance-of-uhplc-ms-hyphenated-systems]
- 55. Unveiling Lipidomics Quantitative Analysis: What, Why, ... [https://dmpkservice.wuxiapptec.com/articles/479-unveiling-lipidomics-quantitative-analysis-what-why-and-how/]
- 56. Quantitative Lipid Analysis of Extracellular Vesicle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11911390/]
- 57. Associations of Plasma Lipidomic Profiles with Uric Acid ... [https://link.springer.com/article/10.1007/s43657-024-00157-x]
- 58. Lipid Annotation by Combination of UHPLC-HRMS (MS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7345884/]
- 59. Method Validation – lipidomicstandards.org [https://lipidomicstandards.org/method-validation/]
- 60. Benzoyl chloride derivatization improves selectivity and ... [https://link.springer.com/article/10.1007/s00216-025-06151-0]
- 61. Recent Analytical Methodologies in Lipid Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10889185/]
- 62. Plasma lipidomic signatures reveal age-associated ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1659425/full]
- 63. Dynamic lipidome alterations associated with human ... [https://www.nature.com/articles/s42255-023-00880-1]
- 64. Clinical lipidomics reveals high individuality and sex ... [https://www.sciencedirect.com/science/article/pii/S0022227525000409]
- 65. ADViSELipidomics: a workflow for analyzing lipidomics data [https://pmc.ncbi.nlm.nih.gov/articles/PMC9750127/]
- 66. Associations of Plasma Lipidomic Profiles with Uric Acid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11584823/]
- 67. Lipidomics and metabolomics investigation into the effect of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11416290/]
- 68. High-Throughput Untargeted Serum Metabolomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8216829/]
- 69. SMAGS-LASSO: A Novel Feature Selection Method for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570486/]
- 70. Identification of optimal biomarkers associated with distant ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-14664-1]
- 71. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 72. Machine learning identifies inflammation-related diagnostic ... [https://www.nature.com/articles/s41598-025-24756-4]
- 73. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 74. Development and validation of machine learning models ... [https://www.sciencedirect.com/science/article/pii/S2589537025000744]
- 75. Collaborative Challenges of Multi-Cohort Projects in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9562084/]
- 76. Cohort profile: The MULTI sTUdy Diabetes rEsearch ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5942412/]
- 77. A methodology for cohort harmonisation in multicentre ... [https://www.sciencedirect.com/science/article/pii/S2352914821002343]
- 78. Multi-cohort machine learning identifies predictors of ... [https://www.nature.com/articles/s41746-025-01862-1]
- 79. Development and multi-cohort validation of a clinical score for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0218933]
- 80. Serum lipidomics reveals distinct metabolic profiles for ... [https://pubmed.ncbi.nlm.nih.gov/34599805/]
- 81. Development and validation of a new diabetes index for ... [https://www.nature.com/articles/s41598-021-95341-8]