Validating lncRNA Prognostic Signatures in Hepatocellular Carcinoma: From Bench to Bedside
Hepatocellular carcinoma (HCC) remains a leading cause of cancer mortality worldwide, with a 5-year survival rate below 20% for advanced-stage patients.
Validating lncRNA Prognostic Signatures in Hepatocellular Carcinoma: From Bench to Bedside
Abstract
Hepatocellular carcinoma (HCC) remains a leading cause of cancer mortality worldwide, with a 5-year survival rate below 20% for advanced-stage patients. This comprehensive review explores the rapidly evolving field of long non-coding RNA (lncRNA) prognostic signatures for HCC, synthesizing evidence from multiple validation cohorts including TCGA and GEO databases. We examine the foundational biology establishing lncRNAs as key regulators in HCC pathogenesis, methodological frameworks for signature development using machine learning approaches like LASSO-Cox regression, optimization strategies addressing technical and biological challenges, and rigorous validation paradigms incorporating multi-omics data and functional studies. The analysis demonstrates that validated multi-lncRNA signatures—including models based on m6A modification, amino acid metabolism, and immune-related pathways—consistently outperform traditional clinical staging systems, with area under curve (AUC) values reaching 0.846 in some cohorts. These signatures not only predict survival but also inform immunotherapy response and potential therapeutic targeting, representing a paradigm shift in HCC prognostication and personalized treatment approaches.
The Biological Foundation: Understanding lncRNA Roles in HCC Pathogenesis
Clinical Context of Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) represents a major global health challenge, ranking as the sixth most common malignant tumor worldwide and the third leading cause of cancer-related deaths [1]. With over 900,000 new cases annually, HCC accounts for 75-90% of all primary liver cancers [2] [3] [4]. Despite advances in therapeutic options, the five-year survival rate for advanced HCC patients remains below 20%, largely due to late diagnosis and heterogeneous treatment responses [5]. Most concerning are the exceptionally high recurrence rates of 60-70% within five years post-resection, creating a critical management challenge [2].
The disease typically arises in the context of chronic liver diseases including hepatitis B or C infection, alcoholic liver disease, and metabolic dysfunction-associated steatotic liver disease [1] [3]. This complex etiology contributes to significant molecular heterogeneity, which profoundly impacts treatment efficacy and patient prognosis [6]. The insidious onset of HCC means a majority of patients present with advanced disease stages, precluding curative surgical intervention and substantially diminishing survival prospects [2] [1].
Table 1: Current Challenges in HCC Clinical Management
| Challenge Category | Specific Limitations | Clinical Impact |
|---|---|---|
| Diagnosis | Limited sensitivity of AFP for early-stage detection; inability of conventional imaging to identify micrometastatic disease [5] | Late-stage diagnosis in majority of patients |
| Prognostic Stratification | Inadequate accounting for molecular heterogeneity in current staging systems [6] | Inaccurate survival prediction and suboptimal treatment selection |
| Treatment Response | Low overall response rates (~20%) to immunotherapy; heterogeneous immune microenvironments [3] | Limited efficacy of systemic therapies |
| Recurrence Monitoring | High 5-year recurrence rates (60-70%) post-resection [2] | Poor long-term survival despite initial treatment success |
Limitations of Current Prognostic Systems
The Barcelona Clinic Liver Cancer (BCLC) classification system remains the global reference for HCC prognostication and treatment allocation, with the 2025 update preserving its direct linkage between stages and evidence-based first-option treatments [7]. However, this system faces significant limitations in addressing the profound molecular heterogeneity of HCC. The BCLC staging incorporates performance status, tumor burden, and liver function, but does not adequately account for biological variables that significantly influence outcomes [8].
Recognizing these limitations, the 2025 BCLC update has integrated the CUSE framework (Complexity, Uncertainty, Subjectivity, Emotion) to help multidisciplinary teams navigate evidence gaps and explicitly address uncertainty [7]. This framework turns "unavoidable doubt into a shared, iterative process" by defining therapeutic goals, grading options with evidence strength and gaps, aligning choices with comorbidities and patient values, and selecting plans with regular check-ins as new information emerges [7]. While this represents progress, it highlights the fundamental deficiency in objective molecular biomarkers to guide precision medicine approaches.
The European Association for the Study of the Liver (EASL) and ESMO guidelines emphasize standardized imaging using LI-RADS criteria and multiparametric CT or MRI for diagnosis and staging [8] [4]. However, the guidelines note that routine molecular analysis is not currently recommended for clinical decision-making, reflecting the translational gap between biomarker research and clinical application [8]. This gap is particularly problematic given that current biomarkers like alpha-fetoprotein (AFP) exhibit limited sensitivity for early-stage detection and response prediction [5].
The tumor immune microenvironment (TIME) introduces additional complexity, with immunosuppressive elements such as regulatory T cells (Tregs) and inactivated M0 macrophages contributing to treatment resistance [2]. Hypoxia and anoikis resistance further shape aggressive tumor phenotypes, yet these factors are not incorporated into conventional staging systems [2]. The evolving landscape of immunotherapy, while promising, has highlighted the critical need for biomarkers that can predict response to immune checkpoint inhibitors and combination regimens [3].
Emerging Prognostic Biomarkers and Signatures
LncRNA-Based Signatures
Long non-coding RNAs (lncRNAs) have emerged as powerful prognostic biomarkers in HCC due to their crucial roles in regulating tumor biology, including proliferation, metastasis, and therapeutic response [9]. These transcripts longer than 200 nucleotides function through diverse mechanisms: serving as signaling molecules that recruit transcription factors, guiding chromatin-modifying enzymes to specific genomic locations, sequestering transcription factors or microRNAs, and mediating the formation of multi-component complexes [9].
Table 2: Validated Single LncRNA Prognostic Biomarkers in HCC
| LncRNA | Expression in HCC | Hazard Ratio (HR) | 95% CI | P-value | Detection Method |
|---|---|---|---|---|---|
| LINC00152 | High | 2.524 | 1.661-4.015 | 0.001 | qRT-PCR [9] |
| LINC01554 | Low | 2.507 | 1.153-2.832 | 0.017 | qRT-PCR [9] |
| LINC01139 | High | 2.721 | 1.289-4.183 | 0.019 | qRT-PCR [9] |
| HOXC13-AS | High | 2.894 (OS), 3.201 (RFS) | 1.183-4.223 (OS), 1.372-4.653 (RFS) | 0.015 (OS), 0.004 (RFS) | qRT-PCR [9] |
| LASP1-AS | Low | 1.884 (training), 3.539 (validation) | 1.427-2.841 (training), 2.698-6.030 (validation) | <0.0001 | qRT-PCR [9] |
Multigene lncRNA signatures offer enhanced prognostic capability by capturing broader biological processes. A hypoxia- and anoikis-related nine-lncRNA signature effectively stratified HCC patients into distinct risk groups, with the high-risk group showing increased immunosuppressive elements (Tregs and inactivated M0 macrophages) and limited immunotherapy efficacy [2]. The signature included specifically downregulated lncRNAs (LINC01554, FIRRE, LINC01139, LINC01134, and NBAT1) that may influence apoptosis under hypoxia and anoikis conditions [2].
Plasma exosomal lncRNAs provide a promising liquid biopsy approach for non-invasive molecular stratification. A recent study integrating transcriptomic data from 230 plasma exosomes identified a 6-gene risk score (G6PD, KIF20A, NDRG1, ADH1C, RECQL4, MCM4) that demonstrated high prognostic accuracy [5]. This exosomal lncRNA-based framework classified HCC into three molecular subtypes (C1-C3), with the C3 subtype exhibiting the poorest overall survival, advanced grade and stage, and an immunosuppressive microenvironment characterized by increased Treg infiltration and elevated PD-L1/CTLA4 expression [5].
Other Molecular Signatures
Beyond lncRNAs, various molecular signatures have shown prognostic potential in HCC. A robust 8-gene signature (MCM10, CEP55, KIF18A, ORC6, KIF23, CDC45, CDT1, and PLK4) was identified through comprehensive transcriptomic analysis, with experimental validation confirming significant upregulation of MCM10, KIF18A, CDC45, and PLK4 in HCC tissues (p<0.05) [1]. These genes are primarily involved in cell cycle regulation and DNA replication, reflecting fundamental processes in hepatocarcinogenesis.
Integrating neutrophil extracellular traps (NETs) and immune-related genes has yielded another promising prognostic approach. A five-gene signature (HMOX1, MMP9, TNFRSF4, MMP12, and FLT3) demonstrated strong predictive ability, with enrichment analyses revealing pathways related to retinol metabolism and cytochrome P450 drug metabolism in different risk groups [6]. Immune infiltration analysis showed regulatory T cells positively correlated with MDSCs, both directly associated with the five prognostic genes [6].
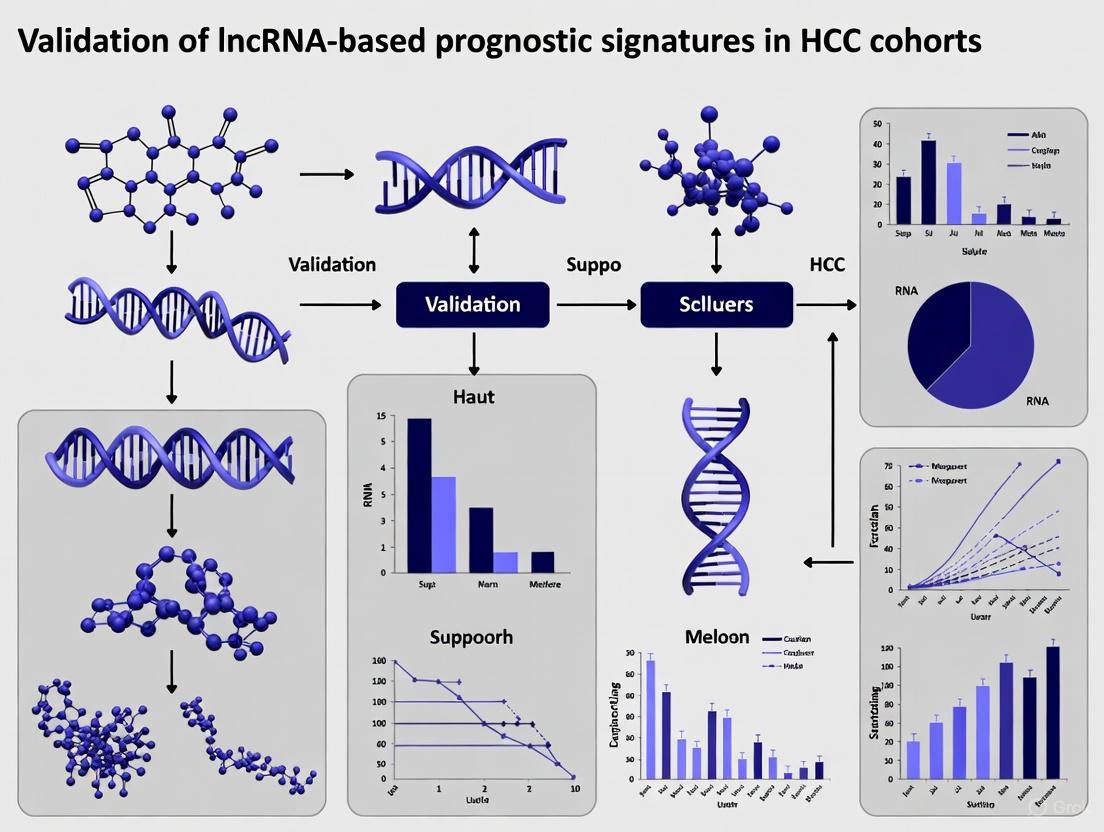
LncRNA Signature Development Workflow
Experimental Approaches and Methodologies
Computational Biology Methods
The development of lncRNA-based prognostic signatures relies on sophisticated computational approaches utilizing large-scale genomic datasets. Standard methodologies begin with RNA-seq data acquisition from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) [2] [1]. Data preprocessing includes transformation to transcripts per million (TPM) values, log2 conversion, and normalization to ensure comparability across datasets [2] [5].
Differential expression analysis is typically performed using the DESeq2 package with thresholds of p<0.05 and |log2 fold change| > 0.5-1.0 to identify significantly dysregulated lncRNAs [1] [6]. For molecular subtyping, unsupervised consensus clustering using the ConsensusClusterPlus package applies the Pearson distance metric, PAM clustering algorithm, 80% resampling ratio, and 1000 iterations to define robust molecular subtypes [2] [5].
Competitive endogenous RNA (ceRNA) network construction involves a multi-step process: miRNA binding sites of differentially expressed lncRNAs are predicted via the miRcode database, followed by integration of miRNA-mRNA relationships from miRTarBase, TargetScan, and miRDB databases [5]. The intersection of target genes of differentially expressed lncRNAs and upregulated mRNAs in HCC tissues defines exosome-related genes, with ternary regulatory networks visualized using Cytoscape [5].
Machine learning algorithms have become indispensable for prognostic model development. Recent studies systematically compare multiple algorithms including CoxBoost, stepwise Cox, LASSO, Ridge, elastic net, survival support vector machines, generalized boosted regression models, supervised principal components, partial least squares Cox, and random survival forests [1] [5]. These approaches employ 10-fold cross-validation frameworks, using the concordance index (C-index) to optimize hyperparameters and select the most predictive gene signatures.
Experimental Validation Techniques
While computational approaches identify candidate biomarkers, experimental validation remains essential for establishing biological and clinical relevance. Reverse transcription quantitative PCR (RT-qPCR) serves as the gold standard for validating expression patterns of identified lncRNAs and genes in independent patient cohorts and HCC cell lines [2] [1] [6].
Functional studies often employ in vitro models under controlled conditions to elucidate mechanisms. For hypoxia- and anoikis-related lncRNAs, human HCC cell lines like Li-7 are cultured under hypoxic conditions (1% O2) in ultra-low adsorption plates to simulate anchorage-independent growth [2]. Total RNA extraction using commercial kits (e.g., RNeasy Mini Kit) followed by cDNA synthesis and RT-qPCR with specifically designed primers enables quantification of lncRNA expression changes under these stress conditions [2].
Single-cell RNA sequencing provides unprecedented resolution for understanding cellular heterogeneity and validating cell-type-specific expression of prognostic genes. Analytical pipelines for scRNA-seq data include quality control, normalization, highly variable gene identification, dimensionality reduction, clustering, and cell type annotation [1]. This approach enables mapping of prognostic gene expression to specific cellular compartments within the tumor microenvironment.
Table 3: Essential Research Reagent Solutions for HCC Prognostic Biomarker Studies
| Research Tool Category | Specific Examples | Application in HCC Prognostic Research |
|---|---|---|
| RNA Extraction Kits | RNeasy Mini Kit [2] | High-quality RNA isolation from tissues/cells for transcriptomic studies |
| cDNA Synthesis Kits | PrimeScript RT Master Mix [2] | Preparation of cDNA templates for qPCR validation |
| qPCR Reagents | TB Green Premix [2] | Quantitative measurement of lncRNA and gene expression |
| Cell Culture Media | 1640 Medium with FBS [2] | Maintenance of HCC cell lines for functional studies |
| Bioinformatics Packages | DESeq2, ConsensusClusterPlus, CIBERSORT, ESTIMATE, glmnet [2] [1] [6] | Differential expression, clustering, immune infiltration, and machine learning analyses |
| Pathway Databases | GO, KEGG, HALLMARK [2] [1] | Functional enrichment analysis of prognostic signatures |
| Public Data Repositories | TCGA, GEO, ICGC, exoRBase [2] [1] [5] | Access to large-scale genomic and clinical data |
Signaling Pathways and Biological Mechanisms
LncRNAs influence HCC progression through regulation of critical signaling pathways and biological processes. Hypoxia- and anoikis-related lncRNAs converge on pathways controlling tumor stemness, immune suppression, and metastasis [2]. Hypoxia activates oncogenic pathways such as Wnt/β-catenin, enhancing invasion and migration while sustaining cancer stemness [2]. Simultaneously, hypoxia profoundly reshapes the tumor immune microenvironment by modulating immune cell infiltration and inducing immunosuppressive phenotypes [2].
Anoikis resistance enables epithelial-derived tumor cells to survive in suspension after detaching from the extracellular matrix, facilitating hematogenous dissemination [2]. In HCC, which arises from epithelial hepatocytes and exhibits strong vascularity, anoikis resistance significantly contributes to metastatic spread [2]. The integrated analysis of both hypoxia and anoikis mechanisms provides a more comprehensive understanding of tumor biology than either factor alone.
Plasma exosomal lncRNAs function within competitive endogenous RNA (ceRNA) networks that regulate oncogenic transcripts. These networks are significantly enriched in critical pathways including cell cycle regulation, TGF-β signaling, the p53 pathway, and ferroptosis [5]. The molecular subtypes defined by exosomal lncRNA profiles exhibit distinct pathway activations, with the poor-prognosis C3 subtype showing hyperactivation of proliferation pathways (MYC, E2F targets) and metabolic pathways (glycolysis, mTORC1) [5].
LncRNA Regulatory Mechanisms in HCC
The tumor immune microenvironment represents a critical mechanism through which prognostic signatures influence clinical outcomes. High-risk HCC subtypes consistently exhibit immunosuppressive characteristics including increased Treg infiltration, elevated expression of immune checkpoints (PD-L1, CTLA4), and higher TIDE scores predicting immunotherapy resistance [2] [5]. These features create a "cold" tumor microenvironment that limits effective anti-tumor immunity and diminishes response to immune checkpoint inhibitors [3].
Beyond the tumor microenvironment, prognostic genes identified in various signatures frequently participate in fundamental cellular processes driving hepatocarcinogenesis. The eight-gene signature (MCM10, CEP55, KIF18A, ORC6, KIF23, CDC45, CDT1, and PLK4) is enriched in cell cycle regulation and DNA replication functions [1]. Single-cell analysis reveals these prognostic genes are more highly expressed in the initial state of B cell differentiation and show the strongest interactions between B cells and macrophages in both HCC and control groups [1].
Clinical Translation and Therapeutic Implications
The ultimate goal of prognostic biomarker research is clinical translation to improve patient outcomes. LncRNA-based signatures show particular promise for guiding treatment selection across different HCC stages. For early-stage HCC, prognostic signatures could identify high-risk patients who might benefit from more aggressive adjuvant therapy despite current guidelines not recommending routine adjuvant treatment post-resection or ablation [8].
In advanced disease, risk stratification enables more personalized therapeutic approaches. Low-risk patients typically demonstrate superior responses to anti-PD-1 immunotherapy, while high-risk patients show increased sensitivity to DNA-damaging agents such as the Wee1 inhibitor MK-1775 and sorafenib [5]. Drug sensitivity analyses based on prognostic signatures can identify 74 drugs with differential sensitivity between risk groups, with compounds like axitinib showing lower sensitivity in high-risk patients, while ABT-888 demonstrates higher sensitivity in this group [6].
Molecular imaging represents an emerging approach for non-invasive assessment of tumor biology and treatment response. Techniques like positron emission tomography (PET) and magnetic resonance imaging (MRI) can visualize immune checkpoints, cell infiltration, and metabolic shifts, potentially enabling pretreatment stratification and early response monitoring [3]. These imaging modalities have demonstrated area under the curve (AUC) values >0.85 in predicting response to immunotherapy, though challenges remain including cirrhosis-induced imaging artifacts [3].
The integration of lncRNA signatures with current clinical decision-making frameworks like BCLC staging offers a path toward more personalized medicine. The CUSE framework incorporated in the 2025 BCLC update explicitly acknowledges the need to address complexity, uncertainty, subjectivity, and emotion in therapeutic decisions [7]. Molecular biomarkers could transform this process by providing objective data to define therapeutic goals, grade option strength, align choices with patient biology, and select personalized management plans with regular molecular monitoring.
Once dismissed as mere "transcriptional noise" or "junk DNA," long non-coding RNAs (lncRNAs) have undergone a dramatic re-evaluation over the past decades, emerging as crucial regulatory molecules in both normal physiology and disease states [10] [11] [12]. These RNA molecules, defined as transcripts longer than 200 nucleotides with limited or no protein-coding capacity, represent a major output of complex genomes [10]. The discovery that the number of protein-coding genes is similar in organisms with widely different developmental complexity (approximately 20,000 in both nematodes and humans) while non-coding DNA and RNA transcription increases with complexity forced a fundamental reassessment of genetic information flow [10]. This article examines the transformation of lncRNAs from biological curiosities to recognized key regulators, with a specific focus on their validation as prognostic signatures in hepatocellular carcinoma (HCC).
The early perception of lncRNAs as transcriptional artifacts stemmed from their generally low sequence conservation, low expression levels, and poor visibility in genetic screens [10]. However, foundational discoveries of specific functional lncRNAs such as H19 (first identified in mice in 1984), Xist (crucial for X-chromosome inactivation), and HOTAIR progressively challenged this dogma, revealing RNA molecules with specific regulatory roles in development, epigenetics, and cellular differentiation [10] [11] [12]. The first plant lncRNA, ENOD40, was isolated from nodule primordia in Medicago plants and found to be involved in symbiotic nodule organogenesis [11]. These pioneering examples paved the way for recognizing thousands of lncRNAs across diverse species, with current databases cataloging over 20,000 lncRNA genes in humans alone [12].
LncRNA Biogenesis, Classification, and Functional Mechanisms
Defining Characteristics and Biogenesis
LncRNAs share several similarities with messenger RNAs: they are predominantly transcribed by RNA polymerase II, can undergo 5' capping and 3' polyadenylation, and are frequently spliced [10] [11] [12]. However, they diverge from protein-coding transcripts in crucial aspects: they lack extensive open reading frames, exhibit lower sequence conservation, display more specific tissue expression patterns, and are often expressed at lower levels [12]. Some lncRNAs are transcribed by RNA polymerase I (such as ribosomal RNAs) or III (including 7SK, 7SL, and Alu RNAs), while others derive from processed introns or repetitive elements [10].
A significant proportion of lncRNAs undergo inefficient splicing compared to mRNAs, potentially due to differences in consensus sequences for splice sites or interactions with specific splicing factors [12]. While some lncRNAs are unstable, many are stabilized through polyadenylation or through secondary structures that protect them from degradation [12]. Their cellular localization—whether nuclear or cytoplasmic—profoundly influences their function and molecular partnerships [12].
Genomic Classification and Functional Mechanisms
LncRNAs are typically classified based on their genomic context relative to protein-coding genes [13]:
Table 1: LncRNA Classification by Genomic Context
| Classification | Genomic Position | Example |
|---|---|---|
| Intergenic (lincRNAs) | Located between protein-coding genes | HOTAIR, XIST |
| Intronic | Transcribed from introns of protein-coding genes | Various HCC-associated lncRNAs |
| Antisense | Transcribed from the opposite strand of protein-coding genes | HOTAIR, HOXC13-AS |
| Sense | Overlap with exons of protein-coding genes | Not specified in results |
| Enhancer RNAs (eRNAs) | Transcribed from enhancer regions | Implicated in chromatin looping |
| Promoter-associated | Transcribed from promoter regions | Involved in transcription initiation |
Functionally, lncRNAs operate through diverse molecular mechanisms that can be categorized into four primary modes of action [9]:
- Signaling molecules that respond to cellular stimuli
- Guiding molecules that direct ribonucleoprotein complexes to specific genomic locations
- Decoy molecules that sequester transcription factors or microRNAs
- Scaffolding molecules that assemble multiple-component complexes
Their functional roles are intimately linked to their subcellular localization—nuclear lncRNAs typically regulate transcription, chromatin organization, and RNA processing, while cytoplasmic lncRNAs often influence mRNA stability, translation, and post-translational modifications [13] [12].
Diagram 1: Diverse Functional Mechanisms of LncRNAs. LncRNAs exert their biological effects through distinct nuclear and cytoplasmic mechanisms depending on their subcellular localization.
LncRNAs in Hepatocellular Carcinoma: From Prognostic Signatures to Therapeutic Targets
The Clinical Challenge of Hepatocellular Carcinoma
Hepatocellular carcinoma represents a significant global health burden, ranking as the sixth most common cancer worldwide and the third leading cause of cancer-related mortality [14] [15] [9]. The disease is particularly challenging due to its frequent diagnosis at advanced stages and limited treatment options for late-stage patients [15] [16]. Chronic hepatitis B (HBV) and C (HCV) infections, alcohol consumption, non-alcoholic fatty liver disease, and aflatoxin B1 intake constitute major risk factors that promote HCC through induction of DNA damage, epigenetic alterations, and oncogenic mutations [13]. The poor 5-year survival rate of under 20% for advanced HCC patients underscores the urgent need for better early detection methods and novel therapeutic approaches [15].
In this context, lncRNAs have emerged as promising molecular tools for addressing these clinical challenges. Their high tissue specificity, detectability in bodily fluids, and critical roles in tumorigenic processes make them ideal candidates as diagnostic biomarkers, prognostic indicators, and therapeutic targets [13] [9] [16].
Validated LncRNA Prognostic Signatures in HCC
Multiple research groups have developed and validated lncRNA-based prognostic signatures for HCC using various methodological approaches. The table below summarizes key studies constructing multi-lncRNA prognostic models:
Table 2: Experimentally Validated LncRNA Prognostic Signatures in HCC
| Study Focus | LncRNAs in Signature | Validation Cohort | Performance (AUC) | Clinical Utility |
|---|---|---|---|---|
| Disulfidptosis-Related [14] | AC016717.2, AC124798.1, AL031985.3 | 369 TCGA patients (training n=185, validation n=184) | 1-year: 0.756, 3-year: 0.695, 5-year: 0.701 | Stratified patients into distinct risk groups with significant survival differences |
| Amino Acid Metabolism-Related [15] | 4-lncRNA signature (including AL590681.1) | 340 TCGA patients (170 training, 170 validation) | Not specified | High-risk patients showed lower OS; AL590681.1 functional role confirmed in HCC cell lines |
| Migrasome-Related [17] | LINC00839, MIR4435-2HG | 372 TCGA tumors + independent clinical cohort (n=100) | Consistent predictive value | MIR4435-2HG promotes malignant behaviors and immune evasion; model predicts immunotherapy response |
| Combination Biomarker [16] | LINC00152, LINC00853, UCA1, GAS5 | 52 HCC patients + 30 controls | Individual lncRNAs: 60-83% sensitivity, 53-67% specificity; ML model: 100% sensitivity, 97% specificity | Machine learning integration with conventional biomarkers enhanced diagnostic precision |
These studies consistently demonstrate that lncRNA signatures can effectively stratify HCC patients into distinct prognostic subgroups, potentially guiding personalized treatment approaches. The disulfidptosis-related model specifically highlighted that high-risk patients exhibited poorer overall survival, distinct immune function profiles, differential tumor mutational burden, and varied drug sensitivity [14]. Similarly, the amino acid metabolism-related signature revealed significant differences in immune cell infiltration and checkpoint expression between risk groups, with high-risk patients potentially benefiting more from anti-PD1 treatment [15].
Individual LncRNAs with Prognostic Value in HCC
Beyond multi-lncRNA signatures, numerous individual lncRNAs have demonstrated independent prognostic value in HCC through multivariate Cox regression analyses:
Table 3: Individual LncRNAs with Validated Prognostic Significance in HCC
| LncRNA | Expression in Tumor | Prognostic Impact | Study Details |
|---|---|---|---|
| LINC00152 | Upregulated | High expression → Shorter OS (HR: 2.524; 95% CI: 1.661-4.015; p=0.001) | 63 HCC patients, qRT-PCR detection [9] |
| LINC01146 | Downregulated | High expression → Longer OS (HR: 0.38; 95% CI: 0.16-0.92; p=0.033) | 85 HCC patients, qRT-PCR detection [9] |
| HOXC13-AS | Upregulated | High expression → Shorter OS (HR: 2.894) and RFS (HR: 3.201) | 197 HCC patients, qRT-PCR detection [9] |
| LASP1-AS | Downregulated | Low expression → Shorter OS and RFS (training: HR: 1.884; validation: HR: 3.539) | 423 HCC patients across two cohorts [9] |
| ELF3-AS1 | Upregulated | High expression → Shorter OS (HR: 1.667; 95% CI: 1.127-2.468; p=0.011) | 373 HCC patients, RNAseq detection [9] |
| GAS5 | Downregulated | Tumor suppressor role, activates CHOP and caspase-9 pathways | Induces apoptosis, inhibits proliferation [16] |
These individual lncRNAs contribute to HCC progression through diverse mechanisms. For instance, LINC00152 promotes cell proliferation through regulation of CCDN1 [16], while H19 stimulates the CDC42/PAK1 axis by down-regulating miRNA-15b expression [13]. The UCA1 lncRNA similarly promotes proliferation and inhibits apoptosis, though its exact mechanism in HCC is not completely understood [16].
Experimental Approaches and Methodologies
Standardized Workflow for LncRNA Signature Development
The development and validation of lncRNA prognostic signatures follows a relatively standardized workflow that integrates bioinformatic analyses with experimental validation:
Diagram 2: LncRNA Signature Development Workflow. The standardized approach for developing and validating lncRNA-based prognostic models in HCC.
Detailed Methodologies for Key Experimental Procedures
Signature Development and Statistical Analysis
The construction of lncRNA prognostic models typically employs sophisticated statistical approaches:
Data Acquisition and Preprocessing: Publicly available datasets (particularly TCGA-LIHC) provide transcriptomic data and corresponding clinical information. RNA sequencing data is normalized (typically to TPM - transcripts per million) and quality-controlled [14] [15] [17].
Identification of Relevant LncRNAs: Researchers typically identify lncRNAs of interest through correlation analysis with biologically relevant genes (e.g., disulfidptosis-related genes, amino acid metabolism genes, migrasome-related genes) using Pearson correlation with strict thresholds (|R| > 0.4-0.55, p < 0.001) [14] [15] [17].
Prognostic Model Construction: Univariate Cox regression analysis identifies lncRNAs significantly associated with overall survival. To prevent overfitting, LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression with k-fold cross-validation (typically 10-fold) is employed to select the most predictive lncRNAs. Finally, multivariate Cox regression assigns weights to each lncRNA to calculate a risk score: Risk Score = Σ(Coefficienti × Expressioni) [14] [15] [17].
Model Validation: The cohort is randomly split into training and validation sets. The model's predictive performance is assessed using Kaplan-Meier survival analysis (log-rank test) and time-dependent receiver operating characteristic (ROC) curve analysis. Increasingly, studies include external validation in independent patient cohorts [14] [15] [17].
Functional Validation Experiments
To establish biological relevance beyond statistical association, researchers employ various functional assays:
In Vitro Functional Studies: Following identification of key lncRNAs from signatures, researchers perform functional validation using HCC cell lines. This typically includes:
- Gene Knockdown: Using lncRNA-specific small interfering RNA (siRNA) or short hairpin RNA (shRNA) delivered via transfection reagents (e.g., Lipofectamine 3000) [15] [17].
- Proliferation Assays: Cell viability measured by CCK-8 assay or similar methods at various time points post-transfection [15].
- Colony Formation: Assessing long-term proliferative potential by staining and counting colonies after 14-day incubation [15].
- Migration/Invasion Assays: Transwell or wound-healing assays to evaluate metastatic potential [17].
- Gene Expression Analysis: Quantitative real-time PCR (qRT-PCR) to verify knockdown efficiency and measure downstream targets [15] [16] [17].
Molecular Mechanism Elucidation:
- Pathway Analysis: Gene set enrichment analysis (GSEA) identifies signaling pathways enriched in high-risk versus low-risk groups [14] [15].
- Immune Infiltration Analysis: Using algorithms like ESTIMATE or CIBERSORT to evaluate differences in tumor immune microenvironment between risk groups [14] [15] [17].
- Drug Sensitivity Prediction: Computational approaches (e.g., oncoPredict) assess potential differences in therapeutic response based on GDSC database [14].
Table 4: Essential Research Reagents and Resources for LncRNA Studies in HCC
| Reagent/Resource | Function/Application | Examples/Specifications |
|---|---|---|
| TCGA-LIHC Dataset | Primary source of transcriptomic and clinical data | 373 liver HCC tissues + 49 normal tissues; includes RNAseq data and clinical follow-up [14] |
| RNA Isolation Kits | Extraction of high-quality RNA from tissues/cells | miRNeasy Mini Kit (QIAGEN) - enables simultaneous isolation of miRNA and total RNA [16] |
| cDNA Synthesis Kits | Reverse transcription of RNA to cDNA | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [16] |
| qRT-PCR Systems | Quantification of lncRNA expression | PowerTrack SYBR Green Master Mix + ViiA 7 real-time PCR system (Applied Biosystems); GAPDH normalization [16] |
| siRNA/shRNA | Gene knockdown studies | LncRNA-specific sequences; Lipofectamine 3000 transfection reagent [15] |
| Cell Viability Assays | Assessment of proliferation | CCK-8 assay - measures metabolic activity as surrogate for cell number [15] |
| Immune Analysis Algorithms | Evaluation of tumor immune microenvironment | ESTIMATE, CIBERSORT, TIMER - computational deconvolution of immune cell populations [14] [15] |
| Drug Sensitivity Databases | Prediction of therapeutic response | GDSC (Genomics of Drug Sensitivity in Cancer) - correlates genomic features with drug response [14] |
Current Challenges and Future Perspectives
Despite significant progress, several challenges remain in translating lncRNA research into clinical practice. The functional characterization of most lncRNAs is still lacking, with only approximately 500-1,500 of the over 20,000 human lncRNA genes having been functionally characterized [12]. Additionally, the low conservation of many lncRNAs between species complicates the use of conventional animal models for functional studies [10]. Technical challenges include the inefficient splicing of many lncRNAs and their generally lower abundance compared to mRNAs [12].
Future research directions will likely focus on several key areas:
- Comprehensive Functional Characterization: Systematic efforts to assign biological functions to the thousands of uncharacterized lncRNAs.
- Therapeutic Targeting: Developing approaches to target oncogenic lncRNAs or replace tumor-suppressive lncRNAs, potentially through antisense oligonucleotides, small molecule inhibitors, or gene therapy approaches.
- Multi-omics Integration: Combining lncRNA data with genomic, epigenomic, and proteomic information to build more comprehensive models of HCC pathogenesis.
- Liquid Biopsy Applications: Optimizing detection of lncRNAs in circulating blood for non-invasive diagnosis and monitoring of HCC.
- Single-Cell Analyses: Resolving lncRNA expression and function at single-cell resolution to understand tumor heterogeneity.
The transformation of lncRNAs from "transcriptional noise" to key regulatory molecules represents one of the most significant paradigm shifts in molecular biology over the past decades. Their integration into prognostic signatures for HCC exemplifies how basic biological discoveries can translate into clinically relevant applications. As research methodologies continue to advance and our understanding of lncRNA biology deepens, these molecules are poised to become increasingly important in cancer diagnosis, prognosis, and treatment.
Hepatocellular carcinoma (HCC) ranks as the sixth most common cancer and the third leading cause of cancer-related deaths globally, characterized by its aggressive nature, frequent metastasis, and limited treatment options [18] [19]. The molecular pathogenesis of HCC involves complex genetic and epigenetic alterations, with long non-coding RNAs (lncRNAs) emerging as pivotal regulators in recent years [18] [13]. LncRNAs, defined as RNA transcripts longer than 200 nucleotides that lack protein-coding capacity, represent a rapidly growing class of functional RNA molecules that regulate gene expression at epigenetic, transcriptional, and post-transcriptional levels [13] [19]. This review provides a comprehensive mechanistic comparison of how specific lncRNAs drive HCC proliferation, invasion, and metastasis, framed within the context of validating lncRNA-based prognostic signatures in HCC cohorts. We synthesize experimental data and detailed methodologies to offer researchers, scientists, and drug development professionals a structured analysis of this dynamically evolving field.
Comparative Mechanisms of Key lncRNAs in HCC Progression
The table below summarizes the mechanisms and experimental evidence for critically important lncRNAs in HCC pathogenesis.
Table 1: Comparative Analysis of Key lncRNAs in HCC Progression
| LncRNA | Expression in HCC | Molecular Mechanism | Functional Outcome | Experimental Evidence |
|---|---|---|---|---|
| CR594175 | Upregulated from normal to primary HCC to metastasis [20] [21] | Acts as a molecular sponge for hsa-miR-142-3p, derepressing CTNNB1 (β-catenin) and activating Wnt signaling [20] [21] | Promotes cell proliferation, invasion in vitro and subcutaneous tumor growth in vivo [20] [21] | In vitro (HepG2 cells) and in vivo mouse models; lentiviral silencing; RT-qPCR, western blot [20] [21] |
| SOX2OT | Upregulated in metastatic HCC tissues and cell lines [22] | Sponges miR-122-5p to upregulate PKM2, enhancing aerobic glycolysis (Warburg effect) [22] | Increases metastatic potential, cell migration, and invasion [22] | Microarray, RT-qPCR in 105 HCC patient tissues; wound healing, Transwell assays in multiple cell lines (Huh-7, HCCLM3) [22] |
| MALAT1 | Upregulated in HCC cell lines and tissues [23] | Functions as a competing endogenous RNA (ceRNA) for miRNAs including miR-146b-5p and miR-195, activating TRAF6/Akt and EGFR pathways, respectively [23] | Enhances cell proliferation, migration, and invasion; associated with HCC recurrence [23] | siRNA silencing in vitro; correlation with patient recurrence post-liver transplantation [23] |
| HULC | Highly upregulated in liver cancer [23] | Acts as an endogenous sponge, sequestering miRNAs; epigenetic regulation [23] [19] | Promotes angiogenesis, cell proliferation, and metastasis [23] [19] | Identified via differential screening; extensive validation in clinical tissues [23] |
| H19 | Upregulated in HCC [13] | Downregulates miRNA-15b to activate the CDC42/PAK1 axis; interacts with HIF-1α to drive glycolysis [13] | Stimulates HCC cell proliferation and tumor growth [13] | Multiple mechanistic studies in cell lines and animal models [13] |
Detailed Experimental Protocols for Key Mechanistic Studies
Protocol for lncRNA-CR594175 Functional Validation
1. Lentivirus-Mediated Silencing:
- Vector Construction: A siRNA sequence (5′-GAATCCTCGGAGACAGCAG-3′) homologous to lncRNA-CR594175 was cloned into the pSIH1-H1-copGFP shRNA Vector using BamHI and EcoRI restriction sites. An invalid siRNA sequence served as a negative control (NC) [20] [21].
- Lentivirus Packaging: 293TN cells were co-transfected with the constructed pSIH1-shRNA-CR594175 vector or pSIH1-NC along with pPACK Packaging Plasmid Mix using Lipofectamine 2000. The viral supernatant was harvested 48 hours post-transfection, cleared by centrifugation, and filtered through a 0.45μm PVDF membrane [20] [21].
- Cell Infection: HepG2 cells in logarithmic growth phase were seeded into 6-well plates and infected with the viral solution at a multiplicity of infection (MOI) of 10. Infection efficiency was evaluated 72 hours post-infection via fluorescent marker analysis [20] [21].
2. In Vitro and In Vivo Functional Assays:
- Proliferation and Invasion Assays: Following lentiviral infection, HepG2 cell proliferation was assessed using MTT or CCK-8 assays. Cell invasion capability was measured via Transwell invasion chambers coated with Matrigel [20] [21].
- Subcutaneous Tumor Model: HepG2 cells stably expressing shRNA-CR594175 or control were subcutaneously injected into immunodeficient mice. Tumor volume was measured regularly, and tumors were harvested for further analysis after a set period, confirming that silencing inhibited subcutaneous tumor growth [20] [21].
3. Molecular Mechanism Elucidation:
- RT-qPCR and Western Blot: Total RNA and protein were extracted from tissues or cells. RT-qPCR measured lncRNA-CR594175 and hsa-miR142-3p levels. Western blot analyzed CTNNB1 and Wnt pathway-related proteins (E-cadherin, C-myc, CyclinD1, MMP-9) [20] [21].
- Luciferase Reporter Assay: A 127bp fragment of the CTNNB1 3'-UTR containing the hsa-miR-142-3p target site was cloned into a luciferase reporter vector. HepG2 cells were co-transfected with the reporter construct and miR-142-3p mimic or control, and luciferase activity was measured to confirm direct targeting [21].
Protocol for lncRNA-SOX2OT and Glycolysis Linkage
1. Correlation with Clinical Metastasis:
- Patient Imaging: 121 HCC patients underwent 18F-FDG PET scans. The maximum standardized uptake value (SUVmax) was calculated to evaluate glucose metabolism levels in tumors, with significantly higher SUVmax found in metastatic tissues [22].
- Microarray and RT-qPCR Validation: LncRNA expression profiles were analyzed in ten pairs of HCC samples with different metastatic outcomes using microarray. Differentially expressed lncRNAs were validated by RT-qPCR in a larger cohort of 105 paired HCC/non-tumor specimens [22].
2. In Vitro Metabolic and Metastatic Assays:
- Glycolytic Function Measurement: Five HCC cell lines (Hep3B, Huh-7, MHCC97-L, MHCC97-H, HCCLM3) and one normal liver cell line (WRL68) were assessed for glucose uptake, glycolysis rate, and lactate production to correlate with metastatic potential [22].
- Gain-and-Loss of Function: LncRNA-SOX2OT was stably overexpressed in low-metastatic potential cells (Huh-7) and knocked down in high-metastatic potential cells (HCCLM3). Wound-healing and Transwell migration/invasion assays were performed to assess metastatic capabilities [22].
- PKM2 Interaction: miR-122-5p was identified as a direct target of lncRNA-SOX2OT. Rescue experiments involving PKM2 inhibition or miR-122-5p restoration were conducted to confirm the lncRNA-SOX2OT/miR-122-5p/PKM2 axis in regulating Warburg effect and metastasis [22].
Visualization of Key Signaling Pathways
ceRNA Mechanism of lncRNA-CR594175 in Wnt Pathway Activation
Diagram 1: ceRNA Mechanism of lncRNA-CR594175. This diagram illustrates how highly expressed lncRNA-CR594175 acts as a molecular sponge for hsa-miR-142-3p, preventing it from negatively regulating CTNNB1. This derepression leads to Wnt pathway activation, promoting HCC proliferation and invasion [20] [21].
lncRNA-SOX2OT-Mediated Metabolic Reprogramming
Diagram 2: lncRNA-SOX2OT in Metabolic Reprogramming. This diagram shows how upregulated lncRNA-SOX2OT sequesters miR-122-5p, leading to increased PKM2 expression. This enhances aerobic glycolysis (Warburg effect), which in turn increases the metastatic potential of HCC cells [22].
Table 2: Key Research Reagents for lncRNA Mechanistic Studies in HCC
| Reagent/Resource | Function/Application | Specific Examples from Literature |
|---|---|---|
| Lentiviral Vectors | Delivery of shRNA for lncRNA silencing or cDNA for overexpression in vitro and in vivo | pSIH1-H1-copGFP shRNA Vector for CR594175 silencing [20] [21] |
| siRNA/shRNA Sequences | Sequence-specific knockdown of target lncRNAs | siRNA target sequence: 5′-GAATCCTCGGAGACAGCAG-3′ for lncRNA-CR594175 [20] [21] |
| Cell Lines | In vitro models for functional and mechanistic studies | HepG2, Huh-7, MHCC97-L, MHCC97-H, HCCLM3 with varying metastatic potential [20] [21] [22] |
| qRT-PCR Assays | Quantification of lncRNA, miRNA, and mRNA expression levels | Measurement of lncRNA-CR594175, hsa-miR-142-3p, and Wnt target genes [20] [21] [22] |
| Western Blot Reagents | Detection of protein expression and pathway activation | Analysis of CTNNB1, E-cadherin, C-myc, CyclinD1, MMP-9, PKM2 [20] [21] [22] |
| Luciferase Reporter Vectors | Validation of direct miRNA-mRNA or miRNA-lncRNA interactions | Cloning of CTNNB1 3'-UTR to verify miR-142-3p binding [21] |
| Transwell Assays | Measurement of cell invasion and migration capabilities | Matrigel-coated chambers to assess invasive potential after lncRNA modulation [20] [22] |
| Animal Models | In vivo validation of tumor growth and metastasis | Subcutaneous xenograft models in immunodeficient mice [20] [21] [22] |
The mechanistic insights into how lncRNAs drive HCC proliferation, invasion, and metastasis reveal a complex regulatory network centered on competing endogenous RNA (ceRNA) activities, metabolic reprogramming, and signaling pathway activation. The consistent experimental approaches across studies—employing lentiviral modulation, in vitro functional assays, and in vivo validation—provide a robust framework for future investigations. The growing body of evidence positions lncRNAs not only as promising prognostic biomarkers but also as potential therapeutic targets. As research progresses, integrating these molecular mechanisms with clinical validation in HCC cohorts will be essential for translating these findings into meaningful prognostic tools and targeted therapies for HCC patients.
Hepatocellular carcinoma (HCC) remains one of the most lethal malignancies worldwide, with its pathogenesis involving complex biological processes such as DNA damage, epigenetic modification, and oncogene mutation [13]. Over the past two decades, long non-coding RNAs (lncRNAs) have received increasing attention for their roles in the occurrence, metastasis, and progression of HCC [13]. These transcripts longer than 200 nucleotides lack protein-coding capacity but play critical roles as regulators of gene expression, affecting RNA transcription and mRNA stability [13]. The validation of lncRNA-based prognostic signatures in HCC cohorts represents a promising frontier for improving diagnosis, treatment stratification, and clinical outcomes. This review comprehensively compares four key oncogenic lncRNAs—H19, HOTAIR, HULC, and NEAT1—by examining their molecular mechanisms, clinical correlations, and experimental evidence, thereby providing researchers and drug development professionals with a structured analysis of their potential as biomarkers and therapeutic targets.
Comparative Analysis of Key Oncogenic lncRNAs
Table 1: Characteristics and Clinical Associations of Key Oncogenic lncRNAs in HCC
| lncRNA | Genomic Location | Expression in HCC | Key Functional Mechanisms | Clinical Correlations | Prognostic Value |
|---|---|---|---|---|---|
| H19 | 11p15.5 | Upregulated | Epigenetic modification, drug resistance, regulates proliferation/apoptosis via miR-675/PKM2 and AKT/GSK-3β/Cdc25A pathways [13] [24] | Associated with invasion and metastasis [24] | Poor survival, early recurrence |
| HOTAIR | 12q13.13 | Upregulated | Binds PRC2 and LSD1, regulates Wnt/β-catenin pathway, promotes EMT [13] [25] | Poor differentiation (P=0.002), metastasis (P=0.002), early recurrence (P=0.001) [25] | Shorter overall survival, independent prognostic factor |
| HULC | 6p24.3 | Upregulated | ceRNA for miR-372, activates CREB, promotes Warburg effect via LDHA/PKM2 phosphorylation [13] [26] | Advanced clinical stage, metastatic potential, HCV-positive status [26] | Poor prognosis, predicts metastasis post-resection |
| NEAT1 | 11q13.1 | Upregulated | Regulates proliferation, migration, and apoptosis through multiple mechanisms [13] | Associated with tumor progression [13] | Correlated with poor patient outcomes |
Table 2: Experimental Evidence from Functional Studies
| lncRNA | In Vitro Models | In Vivo Models | Key Functional Assays | Major Pathway Findings |
|---|---|---|---|---|
| H19 | Hep3B, HepG2 | Xenograft models | Knockdown reduces proliferation, invasion, and metastasis [24] | AKT/GSK-3β/Cdc25A signaling activation [24] |
| HOTAIR | HepG2 | Xenograft | shRNA knockdown suppresses proliferation (MTT) and invasion (Transwell) [25] | Regulates Wnt/β-catenin signaling; downregulation decreases Wnt and β-catenin [25] |
| HULC | Hep3B, HepG2 | Patient tissue analysis | qRT-PCR validation in clinical samples, rolling circle amplification detection [26] | Promotes glycolysis via LDHA/PKM2 phosphorylation; creates feedback loop with miR-372/CREB [26] |
| NEAT1 | Multiple HCC lines | Not specified in results | Proliferation, migration, and apoptosis assays [13] | Multiple oncogenic signaling pathways [13] |
Molecular Mechanisms and Signaling Pathways
The four lncRNAs drive hepatocarcinogenesis through distinct yet interconnected molecular mechanisms, functioning as crucial regulators of key signaling pathways in HCC progression.
H19 Oncogenic Networks
H19 exerts its oncogenic effects through several mechanistic axes. It functions as a competitive endogenous RNA (ceRNA) by sponging miR-675, which leads to the upregulation of Pyruvate Kinase M2 (PKM2) and subsequent acceleration of liver cancer stem cell proliferation [24]. Additionally, H19 inhibition has been shown to promote HCC invasion and metastasis through activation of the AKT/GSK-3β/Cdc25A signaling pathway [24]. H19 also regulates the CDC42/PAK1 axis by downregulating miRNA-15b expression, thereby increasing the proliferation rate of HCC cells [13].
HOTAIR-Mediated Epigenetic Regulation
HOTAIR promotes HCC progression primarily through epigenetic regulation and signaling pathway modulation. It interacts with Polycomb Repressive Complex 2 (PRC2) and lysine-specific histone demethylase 1A (LSD1), enabling genome-wide retargeting of chromatin remodeling complexes that silence multiple metastasis suppressor genes [25]. Functionally, HOTAIR depletion in HepG2 cells significantly suppresses cell proliferation and invasion in vitro and inhibits tumor growth in xenograft models [25]. Mechanistically, HOTAIR exerts its oncogenic effects partly through regulation of the Wnt/β-catenin signaling pathway, with studies showing that HOTAIR inhibition downregulates both Wnt and β-catenin expression [25].
HULC Metabolic Reprogramming
HULC drives hepatocellular carcinoma progression primarily through metabolic reprogramming and the establishment of autoregulatory loops. It promotes the Warburg effect (aerobic glycolysis) by directly binding to and increasing the phosphorylation of two key glycolytic enzymes—lactate dehydrogenase A (LDHA) and pyruvate kinase M2 (PKM2)—thereby enhancing glycolysis in HCC cell lines [26]. Furthermore, HULC participates in a positive feedback loop where it directly binds to and sequesters miR-372, leading to decreased miR-372 activity. This reduction in miR-372 activity alleviates its inhibitory effect on cAMP response element-binding protein (CREB) phosphorylation, consequently enhancing CREB-mediated transcription of HULC itself [26]. HULC also promotes autophagy through the miR-675/PKM2 axis, resulting in upregulation of Cyclin D1 and accelerated proliferation of liver cancer stem cells [26].
NEAT1 Functional Roles
While the specific molecular mechanisms of NEAT1 were less extensively detailed in the available search results, it has been identified as playing significant roles in regulating proliferation, migration, and apoptosis of HCC cells through various pathways [13]. Its oncogenic functions contribute substantially to HCC progression and patient outcomes.
Diagram Title: Oncogenic lncRNA Signaling Networks in HCC Progression
Research Methodologies and Experimental Approaches
Expression Analysis Protocols
RNA Extraction and qRT-PCR: Total RNA from frozen HCC and paired non-cancerous tissues or cell lines is extracted using commercial kits (e.g., Ultrapure RNA Kit) [25]. cDNA is synthesized by reverse transcribing total RNA using a HiFi-MMLV cDNA Kit [25]. Quantitative real-time PCR (qRT-PCR) is performed using systems like the ABI7500 with SYBR Green chemistry [25]. The expression of lncRNAs (H19, HOTAIR, HULC, NEAT1) is detected using specific primers, with β-actin serving as an internal control [25]. Expression levels are calculated using the 2−ΔΔCT method and normalized to the housekeeping gene [25].
Clinical Validation: Studies typically analyze dozens to hundreds of paired HCC and adjacent normal liver tissues obtained from patients who underwent partial liver resection [25] [27]. Tissue samples are immediately frozen in liquid nitrogen and stored at −80°C until use [25]. All samples are independently confirmed by pathologists, with comprehensive documentation of clinicopathological characteristics [25].
Functional Characterization Methods
Gene Knockdown Approaches: Lentivirus-mediated small hairpin RNA (shRNA) vectors are used for efficient and stable knockdown of target lncRNAs [25] [27]. For HOTAIR, specific sequences (e.g., 5′-UAACAAGACCAGAGAGCUGUU-3′) are designed and cloned into lentiviral vectors [25]. Transfection is performed using reagents such as HiPerFect [27]. Knockdown efficiency is validated via qRT-PCR [25] [27].
Phenotypic Assays:
- Cell Proliferation: MTT assays measure cell viability and proliferation rates after lncRNA knockdown [25] [27].
- Invasion and Migration: Transwell assays with Matrigel-coated chambers evaluate invasive capabilities [25].
- Colony Formation: Colony formation assays assess long-term proliferative capacity and clonogenic survival after lncRNA modulation [27].
- In Vivo Tumorigenesis: Xenograft models using immunodeficient mice subcutaneously injected with lncRNA-manipulated liver cancer cells monitor tumor growth rates and metastasis [25].
Mechanism Investigation Techniques
Pathway Analysis: Semi-quantitative RT-PCR detects expression level changes in signaling pathway molecules (e.g., Wnt/β-catenin) under conditions of lncRNA inhibition [25].
ceRNA Network Validation: Luciferase reporter assays, RNA immunoprecipitation (RIP), and pull-down assays validate direct interactions between lncRNAs and miRNAs or proteins [26].
Metabolic Studies: Seahorse extracellular flux analyzers and metabolic flux assays measure glycolysis and mitochondrial respiration changes following lncRNA manipulation [26].
Table 3: Essential Research Reagents and Resources
| Reagent/Resource | Specific Examples | Application | Key Considerations |
|---|---|---|---|
| Cell Lines | HepG2, Hep3B, Huh-7 | In vitro functional studies | Verify authenticity, mycoplasma-free status |
| qRT-PCR Reagents | Ultrapure RNA Kit, HiFi-MMLV cDNA Kit, SYBR Green Master Mix | Expression validation | Include proper controls, optimize primer efficiency |
| Lentiviral Vectors | shRNA constructs (e.g., HOTAIR: 5′-UAACAAGACCAGAGAGCUGUU-3′) | Stable gene knockdown | Monitor titer, include scramble controls |
| Functional Assay Kits | MTT assay, Transwell chambers with Matrigel, colony formation reagents | Phenotypic characterization | Standardize cell numbers, incubation times |
| Animal Models | Immunodeficient mice (e.g., BALB/c nude) | In vivo tumorigenesis | Follow IACUC protocols, adequate sample size |
The comprehensive analysis of H19, HOTAIR, HULC, and NEAT1 underscores their significant roles as oncogenic drivers in hepatocellular carcinoma. Each lncRNA contributes to HCC pathogenesis through distinct molecular mechanisms, ranging from epigenetic regulation (HOTAIR) and metabolic reprogramming (HULC) to complex ceRNA networks (H19, HULC) and proliferation control (NEAT1). Their consistent upregulation in HCC tissues and strong associations with clinicopathological features—particularly tumor differentiation, metastasis, and early recurrence—highlight their potential as robust prognostic biomarkers and therapeutic targets.
The validation of lncRNA-based prognostic signatures in HCC cohorts represents a critical step toward precision oncology applications. Future research should focus on standardizing detection methodologies, developing targeted delivery systems for lncRNA modulation, and validating multi-lncRNA signatures in prospective clinical trials. With continued investigation, these four oncogenic lncRNAs may form the foundation for novel diagnostic strategies and targeted therapies that ultimately improve outcomes for HCC patients.
The Rationale for Multi-lncRNA Signatures Over Single-Marker Approaches
In the pursuit of precision oncology, the discovery of reliable prognostic biomarkers has become a central focus of cancer research. Long non-coding RNAs (lncRNAs), once considered transcriptional "noise," have emerged as crucial regulators of gene expression and cellular functions, with growing evidence supporting their roles in tumorigenesis, metastasis, and treatment response [28]. Historically, cancer prognosis relied on single-marker approaches, but the complexity of cancer biology has driven a paradigm shift toward multi-gene signatures that better capture tumor heterogeneity. In hepatocellular carcinoma (HCC)—a cancer with high mortality and limited treatment options—this evolution is particularly relevant for improving patient stratification and therapeutic decision-making [29] [30].
The transition from single-marker to multi-marker approaches represents more than just quantitative increase in biomarkers; it reflects a fundamental recognition that cancer is driven by complex, interconnected molecular networks rather than isolated molecular alterations. This review comprehensively examines the theoretical foundations, empirical evidence, and practical advantages supporting multi-lncRNA signatures over single-marker approaches, with specific application to HCC prognosis validation.
Theoretical Foundations: Why Multi-lncRNA Signatures Outperform Single Markers
Biological Plausibility: Capturing Cancer Complexity
The superior performance of multi-lncRNA signatures is rooted in their ability to mirror the complex biological reality of cancer pathogenesis. Individual lncRNAs typically regulate specific aspects of cancer biology through discrete molecular mechanisms. For instance, the lncRNA HULC promotes tumor growth in HCC through multiple pathways, while LINC00152 is associated with shorter overall survival [28]. Similarly, LINC01146 and LINC01554 have been identified as protective markers associated with longer survival [28]. However, when used individually, each lncRNA captures only a fragment of the complex pathological process.
Multi-lncRNA signatures integrate complementary biological information by simultaneously accounting for multiple cancer hallmarks. A well-constructed signature can capture processes as diverse as immune evasion (through immune-related lncRNAs), sustained proliferation (via cell cycle-regulating lncRNAs), therapy resistance (through lncRNAs modulating drug efflux or DNA repair), and metastatic potential (via lncRNAs regulating epithelial-mesenchymal transition) [31] [28]. This comprehensive coverage of multiple cancer hallmarks provides a more holistic view of tumor behavior than any single marker can achieve.
Technical Advantages: Overcoming Analytical Limitations
Beyond biological considerations, multi-lncRNA signatures offer significant technical advantages. A critical innovation in this field is the development of relative expression ordering approaches that transform absolute expression values into relative rank relationships between lncRNA pairs. This method assigns a value of 1 when lncRNA A expression exceeds lncRNA B expression, and 0 for the opposite relationship [31]. This strategic approach effectively eliminates platform-specific technical variations and batch effects that often compromise single-marker analyses, as the relative ranking of genes within the same sample remains stable across different measurement platforms and normalization methods [31].
The robustness of multi-lncRNA signatures is further enhanced through statistical compensation mechanisms. When multiple markers are combined, measurement errors or biological variability in individual lncRNAs tend to average out, resulting in more stable prognostic estimates. This statistical resilience is particularly valuable in clinical settings where pre-analytical conditions and measurement techniques may vary.
Empirical Evidence: Performance Comparison in Hepatocellular Carcinoma
Direct Performance Comparisons in HCC Studies
Multiple studies have directly compared the prognostic performance of multi-lncRNA signatures against single lncRNA markers in hepatocellular carcinoma. The results consistently demonstrate the superiority of multi-marker approaches across various performance metrics.
Table 1: Performance Comparison of Single vs. Multi-lncRNA Signatures in HCC
| Signature Type | Representative Markers | HR for Overall Survival | AUC (1-5 years) | Statistical Significance | Study |
|---|---|---|---|---|---|
| Single lncRNA | LINC00152 | 2.524 (1.661-4.015) | Not reported | P = 0.001 | [28] |
| Single lncRNA | LINC00294 | 2.434 (1.143-3.185) | Not reported | P = 0.021 | [28] |
| Single lncRNA | LINC01094 | 2.091 (1.447-3.021) | Not reported | P < 0.001 | [28] |
| 2-lncRNA signature | PRRT3-AS1, AL031985.3 | Not reported | 0.73-0.79 (1-3 year ROC) | Independent prognostic factor | [29] |
| 5-lncRNA signature | BOK-AS1, AC099850.3, AL365203.2, NRAV, AL049840.4 | 2.78-2.88 (high vs low risk) | 0.677-0.778 (3-year) | P < 0.001 | [30] |
The data reveal that while single lncRNAs show significant hazard ratios (typically 2-2.5), their predictive power as standalone markers is limited. In contrast, multi-lncRNA signatures demonstrate not only significant hazard ratios but also superior predictive accuracy as measured by time-dependent AUC values. The 5-lncRNA signature developed by [30] maintained AUC values above 0.67 for 3-year survival prediction across both training and validation cohorts, indicating robust discriminative ability that single markers rarely achieve.
Validation Robustness Across Platforms and Populations
Multi-lncRNA signatures have consistently demonstrated stronger validation performance across independent datasets—a critical metric for clinical applicability. For instance, a 5-lncRNA signature for HCC was successfully validated in both training and testing cohorts with highly consistent hazard ratios (2.88 and 2.78, respectively) and maintained significant predictive power for 1-, 3-, and 5-year overall survival [30]. Similarly, a breast cancer study incorporating 10 machine learning algorithms to develop a 9-lncRNA signature demonstrated superior predictive performance across 17 independent validation cohorts, outperforming 95 previously published models [32].
This cross-platform robustness stems from the inherent stability of combining multiple markers. While individual lncRNA measurements may fluctuate due to technical factors, the combined signature captures a stable biological signal that persists across different patient populations and measurement platforms. This validation robustness represents a significant advantage over single markers, which often fail to replicate their initial promising results in independent cohorts.
Methodological Framework: Constructing and Validating Multi-lncRNA Signatures
Standardized Workflow for Signature Development
The development of robust multi-lncRNA signatures follows a systematic workflow that integrates bioinformatics, statistical optimization, and experimental validation. The following diagram illustrates this standardized process:
This workflow typically begins with data acquisition from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO), which provide large-scale transcriptomic data with corresponding clinical information [33] [29] [30]. The subsequent differential expression analysis identifies lncRNAs significantly dysregulated in cancer tissues compared to normal controls, using thresholds such as |log2FC| > 1 and false discovery rate (FDR) < 0.05 [29].
For immune-related signatures, co-expression analysis with known immune genes further filters lncRNAs potentially involved in immune regulation, typically using correlation coefficients > 0.4-0.5 and p < 0.001 [29] [30]. The prognostic screening step applies univariate Cox regression to identify lncRNAs significantly associated with overall survival (p < 0.01) [29]. The most critical signature construction phase employs LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression with 10-fold cross-validation to select the optimal combination of lncRNAs while preventing overfitting [31] [33] [29].
Advanced Computational Approaches
Recent methodological advances have incorporated more sophisticated machine learning approaches to further enhance signature performance. One comprehensive study evaluated 101 combinations of 10 machine learning algorithms—including random survival forests, elastic net, CoxBoost, and survival SVMs—to identify optimal predictive models [32]. This multi-algorithm framework ensures that the final signature is robust and not dependent on the limitations of any single statistical method.
Another innovation involves the use of relative expression ordering of lncRNA pairs, which transforms continuous expression values into binary comparisons (0 or 1) based on which lncRNA in a pair is more highly expressed [31]. This approach eliminates the need for data normalization across platforms and reduces batch effects, significantly enhancing the clinical applicability of the resulting signatures.
Clinical Applications: Beyond Prognostic Prediction
Therapeutic Guidance and Treatment Selection
The true clinical value of multi-lncRNA signatures extends beyond mere prognosis to informing therapeutic decisions. Several studies have demonstrated that these signatures can predict response to specific treatments, including chemotherapy and immunotherapy. For example, a 9-lncRNA signature in breast cancer was shown to predict responses to paclitaxel chemotherapy, with low-risk patients potentially deriving greater benefit [32]. Similarly, in HCC, multi-lncRNA signatures have been correlated with immune cell infiltration patterns and expression of immune checkpoint molecules, suggesting potential utility in identifying patients most likely to respond to immunotherapy [30].
The relationship between lncRNA signatures and therapy response is biologically plausible, as lncRNAs regulate key drug resistance mechanisms. For instance, various lncRNAs have been identified to facilitate resistance to cisplatin, paclitaxel, 5FU, and other chemotherapeutic drugs through diverse mechanisms [31]. By capturing multiple resistance pathways simultaneously, multi-lncRNA signatures provide a more comprehensive assessment of therapeutic susceptibility than single markers.
Integration with Clinical Variables for Personalized Prediction
Multi-lncRNA signatures are frequently integrated with standard clinical parameters to create powerful predictive nomograms. These integrated tools provide personalized risk assessments that combine the molecular insights from lncRNAs with established clinical prognostic factors. For example, one HCC study combined a 2-lncRNA signature with clinicopathological features to develop a nomogram that showed satisfactory discrimination and consistency in predicting patient survival [29].
The development of such integrated models typically involves multivariate Cox regression analysis to confirm that the lncRNA signature provides prognostic information independent of clinical variables such as age, tumor stage, and histological grade [29] [30]. The resulting nomograms assign weighted points to each prognostic factor, enabling clinicians to calculate individual patient risk scores and tailor surveillance strategies and treatment intensities accordingly.
Technical Implementation: Research Reagent Solutions
The successful development and validation of multi-lncRNA signatures relies on a standardized set of research reagents and methodologies. The table below outlines essential resources for implementing these analyses.
Table 2: Essential Research Reagents and Resources for lncRNA Signature Development
| Category | Specific Resources | Application Purpose | Key Features |
|---|---|---|---|
| Data Resources | TCGA database (https://portal.gdc.cancer.gov/) | Primary data source for discovery | Standardized RNA-seq data, clinical annotations |
| GEO database (https://www.ncbi.nlm.nih.gov/geo/) | Independent validation | Multiple platforms, diverse populations | |
| ImmPort database | Immune-related gene annotations | 2,483 immune-related genes for co-expression analysis | |
| Computational Tools | R packages: limma, edgeR, glmnet, survival | Differential expression, LASSO regression, survival analysis | Statistical rigor, reproducibility |
| WGCNA (Weighted Gene Co-expression Network Analysis) | Identification of co-expression modules | Systems biology approach to network construction | |
| ssGSEA (single-sample GSEA) | Immune infiltration estimation | Quantification of tumor microenvironment composition | |
| Experimental Validation | qRT-PCR (TRIzol reagent, SYBR Green) | Confirmatory expression analysis | Gold standard for RNA quantification |
| RNA pull-down, ChIRP-MS | Protein interaction partner identification | Mapping lncRNA functional mechanisms | |
| LC-MS/MS platforms | Proteomic characterization | High-resolution identification of associated proteins |
These resources enable a comprehensive workflow from computational discovery to experimental validation. The computational tools facilitate the identification of candidate lncRNA signatures, while the experimental methods allow for confirmation of expression patterns and investigation of functional mechanisms. Importantly, the use of publicly available data resources enables independent validation—a critical step in verifying signature robustness.
The theoretical advantages and empirical evidence supporting multi-lncRNA signatures over single-marker approaches are compelling. By more accurately reflecting the biological complexity of cancer, providing robust prognostic stratification, and offering insights into therapeutic susceptibility, these multi-parameter signatures represent a significant advancement in cancer biomarker research. The standardized methodological frameworks and computational tools now available have matured to the point where clinical translation is increasingly feasible.
Future developments in this field will likely focus on several key areas. The integration of multi-omics data—combining lncRNA signatures with genomic, epigenomic, and proteomic information—will provide even more comprehensive molecular portraits of tumors. The application of advanced machine learning algorithms will further enhance predictive accuracy and biological interpretability. Most importantly, prospective clinical validation studies are needed to firmly establish the utility of these signatures in routine clinical practice, ultimately fulfilling their promise to guide personalized cancer therapy and improve patient outcomes.
Building Robust Prognostic Models: Methodological Frameworks and Signature Development
For researchers developing and validating lncRNA-based prognostic signatures in Hepatocellular Carcinoma (HCC), selecting appropriate genomic data repositories is a critical first step. The The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) represent two foundational resources that offer complementary data types and access methodologies. TCGA provides highly standardized, harmonized genomic data from controlled cancer studies, while GEO serves as a versatile repository for diverse functional genomics datasets submitted by researchers worldwide [34]. Understanding their distinct architectures, data acquisition protocols, and preprocessing requirements is essential for constructing robust prognostic models.
The research context for HCC biomarker discovery presents specific challenges that influence database selection. HCC exhibits substantial molecular heterogeneity influenced by etiology, making the availability of well-annotated clinical cohorts crucial for validation. Both repositories contain HCC-relevant datasets, including the TCGA-LIHC project and numerous GEO series investigating HBV/HCV-related hepatocarcinogenesis, immune microenvironment interactions, and therapeutic responses [35] [36]. This guide provides an objective comparison of TCGA and GEO functionalities to inform strategic data acquisition for lncRNA signature validation.
Database Comparison: Architecture and Data Access
Table 1: Core Architectural Differences Between TCGA and GEO Databases
| Feature | TCGA (via GDC) | GEO |
|---|---|---|
| Primary Focus | Curated cancer genomics projects | Community-submitted functional genomics |
| Data Model | Hierarchical, standardized metadata | Flexible, submitter-defined organization |
| Data Types | Genomic, transcriptomic, epigenomic, clinical | Array-based, high-throughput sequencing |
| Access Levels | Open and controlled (dbGaP authorization) | Primarily open access |
| Reference Genome | GRCh38 harmonized [34] | Submitter-dependent (often hg19/GRCh38) |
| Data Processing | Standardized pipelines (GDC Harmonization) [34] | Raw data + submitter-processed files |
| HCC Examples | TCGA-LIHC project | GSE251942, GSE269528 [35] [36] |
TCGA, accessed through the Genomic Data Commons (GDC), employs a highly structured data model with mandatory clinical annotations and consistent genomic processing. All sequencing data undergoes harmonization to GRCh38, ensuring cross-project comparability [34]. This standardization significantly reduces preprocessing burden but offers less flexibility in data types. The GDC requires dbGaP authorization for controlled access to potentially identifiable genomic data, with access decisions made by NIH Data Access Committees based on research compatibility with data use limitations [37].
GEO utilizes a more flexible submission model where individual researchers determine data organization and processing methods. Submitters must provide both raw data (e.g., FASTQ files) and processed data (e.g., count matrices), with metadata captured via spreadsheet templates [38]. This flexibility enables access to diverse experimental designs but increases variability in data quality and processing methods. GEO generally operates as an open-access resource, though submitters must comply with human subject guidelines when applicable [38].
Data Acquisition Protocols and Methodologies
TCGA Data Retrieval Workflow
The GDC provides multiple interfaces for data retrieval, each optimized for different use cases. The GDC Data Portal offers a web-based interface for querying and downloading small volumes of files, while the GDC Data Transfer Tool is recommended for large-scale downloads such as entire TCGA-LIHC datasets [34]. For programmatic access, the GDC API supports advanced queries using SQL-like syntax for precise dataset filtering.
A typical TCGA data acquisition protocol for lncRNA signature validation involves:
- Project Identification: Identify relevant cases using the TCGA-LIHC (Liver Hepatocellular Carcinoma) project
- Data Type Selection: Filter for transcriptomic profiling data (RNA-Seq)
- File Specification: Select BAM files for alignment-based analysis or FPKM/UQ-normalized counts for expression analysis
- Clinical Data Integration: Download corresponding clinical XML files for survival analysis and patient stratification
- Batch Effect Assessment: Examine technical batch variables using the GDC metadata
For controlled data access, researchers must first obtain dbGaP authorization through an NIH Data Access Committee, which reviews proposed research uses for consistency with data submission parameters [37].
GEO Data Retrieval and Submission Protocols
GEO data acquisition follows distinct pathways depending on whether researchers are downloading existing datasets or submitting new data:
Table 2: GEO Data Retrieval and Submission Methods
| Process | Primary Tools | Key Considerations |
|---|---|---|
| Dataset Download | GEO Accession Browser, SRA Toolkit | Supplemental files often contain processed data; Raw FASTQ via SRA |
| Data Submission | FTP transfer, metadata spreadsheet | Separate submissions per data type; Human data compliance required |
| Sequence Data | SRA Run Selector | Fastq preferred; BAM accepted but not preferred [38] |
| Metadata Requirements | GEO template spreadsheet | Detailed protocols, sample characteristics, data processing pipelines |
For HCC researchers validating lncRNA signatures, GEO datasets like GSE251942 (HBV-related HCC) provide valuable validation cohorts [35]. The acquisition protocol typically involves:
- Accession Search: Identify relevant datasets using GEO query tools
- Metadata Examination: Review experimental design and sample characteristics
- Processed Data Download: Obtain count matrices or normalized expression values
- Raw Data Access: Retrieve FASTQ files from SRA when reprocessing is necessary
- Clinical Data Integration: Merge expression data with available patient outcomes
For data submission to GEO – essential for publishing prognostic signature studies – researchers must prepare raw data files, processed data files, and complete metadata spreadsheets. The submission protocol requires FTP transfer to a personalized upload space followed by metadata file submission [38]. GEO specifically requires that processed data for sequencing studies have quantitative components (e.g., counts, FPKM, TPM) rather than alignment files (BAM/SAM), which are considered intermediary [38].
Experimental Design and Preprocessing Workflows
TCGA Data Preprocessing Framework
TCGA data undergoes standardized preprocessing through the GDC harmonization pipelines, which include:
- Alignment: RNA-Seq data aligned to GRCh38 using STAR
- Quantification: Gene-level counts derived from aligned reads
- Variant Calling: Somatic mutation identification using multiple callers
- Clinical Data Curation: Structured data extraction from original sources
For lncRNA analysis, researchers typically begin with raw count data, then apply quality control measures including library size assessment, gene filtering, and normalization. The GDC provides both raw counts and normalized expressions (FPKM, FPKM-UQ), though most prognostic signature studies utilize raw counts followed by appropriate normalization for differential expression analysis.
GEO Data Preprocessing Considerations
GEO data preprocessing requires customized approaches due to variability in submitted data. A generalized workflow includes:
- Format Conversion: Convert platform-specific formats to standardized count matrices
- Quality Assessment: Evaluate sequencing depth, gene detection rates, and sample outliers
- Batch Correction: Address technical artifacts using methods like ComBat when multiple batches are present
- Normalization: Apply appropriate normalization (e.g., TMM for RNA-seq, RMA for microarrays)
- lncRNA Annotation: Map probes or genes to comprehensive lncRNA databases
For example, in the HCC dataset GSE251942, the submitter provided both RSEM and STAR raw counts, allowing researchers to select their preferred quantification method [35]. This flexibility enables method consistency when comparing across datasets but requires careful documentation of preprocessing decisions.
GEO Data Preprocessing Workflow: This diagram outlines the key steps for preparing GEO data for lncRNA analysis, highlighting quality control and normalization stages.
Practical Applications in HCC lncRNA Research
Case Study: Integrating TCGA and GEO for Signature Validation
A robust protocol for validating lncRNA prognostic signatures in HCC involves:
- Discovery Phase: Utilize TCGA-LIHC as the primary cohort for initial signature identification through Cox regression and machine learning approaches
- Technical Validation: Confirm lncRNA measurements using orthogonal methods (e.g., RT-qPCR) in representative samples
- External Validation: Identify appropriate GEO HCC datasets matching inclusion criteria (etiology, stage distribution, treatment-naive)
- Clinical Utility Assessment: Evaluate signature performance in predicting survival, therapeutic response, or recurrence risk
For example, a researcher might develop an m6A-related lncRNA signature using TCGA-LIHC data, then validate it in GEO datasets such as GSE251942 (HBV-related HCC) [35] and GSE269528 (mouse model of HBV-induced HCC) [36]. This approach tests signature robustness across experimental systems and etiologies.
Experimental Reagent Solutions for Functional Validation
Table 3: Essential Research Reagents for lncRNA Functional Validation in HCC
| Reagent/Resource | Function | Example Application |
|---|---|---|
| A549/DDP Cell Line | Cisplatin-resistant LUAD model | Testing chemoresistance mechanisms [39] |
| TCGA RNA-seq Data | Discovery cohort for signature development | Identifying prognostic lncRNAs [40] |
| ssGSEA Algorithm | Immune infiltration quantification | Correlating lncRNAs with immune cells [40] |
| Illumina Platforms | High-throughput sequencing | Generating expression data (e.g., GPL18573) [35] |
| Feature Barcode Matrices | Single-cell RNA sequencing data | Characterizing cellular heterogeneity [38] |
| CIBERSORT/xCell | Immune cell deconvolution | Estimating immune contexture [40] |
Comparative Analysis and Strategic Recommendations
Performance Metrics for Database Evaluation
When assessing TCGA and GEO for HCC lncRNA research, several performance dimensions emerge:
- Data Standardization: TCGA provides superior standardization through harmonized processing, while GEO offers greater methodological diversity
- Clinical Annotation: TCGA includes comprehensive, structured clinical data; GEO clinical metadata varies substantially in depth and quality
- Sample Size: TCGA-LIHC provides ~370 cases; GEO offers numerous smaller datasets enabling meta-analysis
- Experimental Designs: GEO includes intervention studies, time series, and cross-species comparisons not available in TCGA
- Accessibility: GEO generally provides faster access to data; TCGA controlled access requires approval but offers richer clinical correlates
Strategic Implementation Framework
For researchers designing HCC lncRNA studies, the following strategic approach optimizes database utilization:
- Utilize TCGA for Discovery: Leverage TCGA-LIHC for initial signature identification due to standardized data and rich clinical annotation
- Employ GEO for Validation: Select GEO datasets with complementary etiologies and experimental designs to test signature generalizability
- Implement Cross-Platform Normalization: Develop robust normalization pipelines to address technical variability when integrating multiple datasets
- Document Preprocessing Decisions: Maintain detailed records of all filtering, normalization, and transformation steps for reproducibility
- Plan for Functional Follow-up: Identify model systems and reagents early to enable efficient transition from computational discovery to experimental validation
The integration of both resources creates a powerful framework for developing clinically relevant lncRNA signatures in HCC. While TCGA provides the foundational data for discovery, GEO offers the heterogeneous validation cohorts necessary to establish prognostic robustness across diverse patient populations and experimental conditions.
Hepatocellular carcinoma (HCC) represents a significant global health challenge, characterized by high mortality rates and limited therapeutic options for advanced disease. The heterogeneity of HCC contributes substantially to variable clinical outcomes, driving the need for reliable prognostic biomarkers that can guide clinical decision-making [41]. Long non-coding RNAs (lncRNAs), defined as RNA transcripts exceeding 200 nucleotides without protein-coding potential, have emerged as crucial regulators of oncogenic processes, including cell proliferation, invasion, metastasis, and treatment resistance [42] [28]. The development of lncRNA-based prognostic signatures through Cox regression methodologies provides a powerful approach for stratifying HCC patients based on survival probability, enabling more personalized management strategies. This review comprehensively examines the identification and validation of prognostic lncRNAs in HCC using univariate and multivariate Cox regression analyses, comparing various signatures and their clinical applicability.
Statistical Foundation: Cox Regression in Survival Analysis
Principles of Cox Proportional Hazards Model
The Cox proportional hazards model is a semi-parametric regression technique designed specifically for analyzing time-to-event data with censored observations, making it particularly suitable for cancer survival studies [43] [44]. The model evaluates the relationship between survival time and multiple predictor variables (covariates) simultaneously, allowing researchers to adjust for potential confounding factors when assessing the prognostic impact of individual variables.
The Cox model is mathematically expressed as:
[ h(t) = h0(t) \times \exp(b1x1 + b2x2 + \cdots + bpx_p) ]
Where:
- ( h(t) ) represents the hazard function at time ( t )
- ( h_0(t) ) denotes the baseline hazard function
- ( x1, x2, \ldots, x_p ) represent the predictor variables (covariates)
- ( b1, b2, \ldots, b_p ) are the regression coefficients measuring the impact of each covariate [43] [44]
The key output from Cox regression analysis is the hazard ratio (HR), calculated as ( \exp(b_i) ) for each covariate. A HR > 1 indicates increased hazard (worse prognosis) with higher values of the covariate, while HR < 1 suggests reduced hazard (better prognosis) [44].
Univariate and Multivariate Cox Regression
Univariate Cox regression assesses the relationship between each variable and survival outcome independently, without adjusting for other factors. This initial screening step identifies candidate prognostic markers with individual significance [30].
Multivariate Cox regression simultaneously incorporates multiple covariates to evaluate the independent prognostic value of each variable while controlling for potential confounders. This approach identifies factors that provide independent prognostic information beyond other clinical or molecular variables [43]. The application of both analytical steps is crucial for developing robust prognostic signatures, as univariate analysis alone may identify variables whose significance disappears when adjusted for other factors in multivariate analysis.
A critical assumption of the Cox model is proportional hazards, meaning the hazard ratio between any two groups should remain constant over time. Validation of this assumption is essential for ensuring model reliability [43] [44].
Experimental Workflows and Methodologies
Standardized Analytical Pipeline
The identification of prognostic lncRNAs typically follows a structured bioinformatics workflow, supplemented by experimental validation. The following diagram illustrates this standardized approach:
Data Acquisition and Preprocessing
Research groups typically acquire RNA sequencing data and corresponding clinical information from public repositories, primarily The Cancer Genome Atlas (TCGA) Liver Hepatocellular Carcinoma (LIHC) dataset [41] [45] [42]. Additional validation cohorts are often obtained from the International Cancer Genome Consortium (ICGC) and Gene Expression Omnibus (GEO) datasets [45] [42]. Data preprocessing includes:
- Quality Control: Exclusion of samples with low RNA quality or incomplete clinical data
- Normalization: Conversion of raw counts to transcripts per million (TPM) or fragments per kilobase million (FPKM) to enable cross-sample comparisons [41]
- Filtering: Removal of genes with low expression across most samples to reduce noise
- Annotation: Distinguishing lncRNAs from mRNAs using reference databases like GENCODE [41]
Differential Expression and Correlation Analyses
Differentially expressed lncRNAs (DElncRNAs) are identified by comparing tumor tissues with adjacent normal liver tissues using thresholds such as |log2 fold change| > 1 and adjusted p-value < 0.05 [41] [46]. For context-specific signatures, researchers often perform correlation analyses to identify lncRNAs associated with specific biological processes (e.g., disulfidptosis, costimulatory molecules) using Pearson correlation coefficients (typically |R| > 0.4, p < 0.001) [42] [30].
Prognostic Model Construction
The core analytical phase employs sequential Cox regression analyses:
Univariate Cox Regression: Initial screening to identify lncRNAs significantly associated with overall survival (OS), recurrence-free survival (RFS), or disease-free survival (DFS) [46] [30]
LASSO Cox Regression: Application of least absolute shrinkage and selection operator (LASSO) method to reduce overfitting and select the most relevant lncRNAs from univariately significant candidates [46] [42] [30]
Multivariate Cox Regression: Final model refinement to identify lncRNAs with independent prognostic value after adjusting for clinical covariates such as age, gender, tumor stage, and grade [41] [42]
The resulting risk score is calculated using the formula:
[ \text{Risk Score} = \sum (\text{Exp}{\text{lncRNA}i} \times \text{Coef}{\text{lncRNA}i}) ]
Where ( \text{Exp}{\text{lncRNA}i} ) represents the expression level of each lncRNA and ( \text{Coef}{\text{lncRNA}i} ) denotes its regression coefficient derived from multivariate Cox analysis [42] [30].
Model Validation and Evaluation
Prognostic signatures undergo rigorous validation using:
- Internal Validation: Random splitting of the primary cohort into training and testing sets [46] [30]
- External Validation: Application of the signature to independent patient cohorts from different institutions or databases [45] [42]
- Statistical Metrics: Time-dependent receiver operating characteristic (ROC) curves assessing 1-, 3-, and 5-year survival prediction accuracy [41] [30]
- Clinical Utility: Construction of nomograms integrating the lncRNA signature with clinical parameters for personalized prognosis prediction [41]
Functional Validation
Promising lncRNAs identified through computational analyses typically undergo experimental validation, including:
- In Vitro Assays: siRNA-mediated knockdown followed by functional assessments (CCK-8, colony formation, Transwell migration/invasion assays) to evaluate effects on proliferation, migration, and invasion [46] [42] [30]
- Molecular Techniques: Quantitative reverse transcription PCR (qRT-PCR) to verify expression patterns in cell lines and clinical specimens [42] [16]
- Mechanistic Studies: Investigation of regulatory networks, particularly competitive endogenous RNA (ceRNA) mechanisms where lncRNAs function as miRNA sponges [41]
Comparative Analysis of lncRNA Prognostic Signatures
Established lncRNA Signatures in HCC
Multiple research groups have developed and validated distinct lncRNA-based prognostic signatures for HCC, utilizing varied methodological approaches and biological rationales. The table below summarizes key signatures and their performance characteristics:
Table 1: Comparison of Prognostic lncRNA Signatures in Hepatocellular Carcinoma
| Signature Description | Component lncRNAs | Statistical Approach | Cohort Size | Performance (AUC) | Clinical Association |
|---|---|---|---|---|---|
| ceRNA Network-Based [41] | CRNDE, MYLK-AS1, CHEK1 | Differential network analysis + Multivariate Cox | 374 TCGA samples | 1-year: 0.7773-year: 0.7225-year: 0.630 | Independent prognostic factor; included in nomogram with pathological stage |
| 11-lncRNA Signature [46] | AC010547.1, AC010280.2, AC015712.7, GACAT3, AC079466.1, AC089983.1, AC051618.1, AL121721.1, LINC01747, LINC01517, AC008750.3 | Univariate Cox + LASSO + Multivariate Cox | 371 TCGA samples203 GEO samples | AUC: 0.846 | High-risk group showed poorer OS; GACAT3 promotes proliferation, invasion, migration |
| Costimulatory Molecule-Related [30] | BOK-AS1, AC099850.3, AL365203.2, NRAV, AL049840.4 | Correlation analysis + Univariate/LASSO/Multivariate Cox | 343 TCGA samples | Training: 1-year 0.778Testing: 1-year 0.735 | Risk score independent prognostic factor; associated with immune infiltration; AC099850.3 promotes proliferation |
| Disulfidptosis-Related [42] | 3-lncRNA signature (including TMCC1-AS1) | Pearson correlation + Univariate/LASSO/Multivariate Cox | 374 TCGA samples | Not specified | Associated with immune microenvironment; TMCC1-AS1 promotes proliferation, migration, invasion |
| Machine Learning Panel [16] | LINC00152, LINC00853, UCA1, GAS5 | Machine learning integration with clinical parameters | 52 HCC patients + 30 controls | Sensitivity: 100%Specificity: 97% | LINC00152/GAS5 ratio correlated with mortality risk |
Individual lncRNAs with Independent Prognostic Value
Beyond multi-lncRNA signatures, numerous individual lncRNAs demonstrate independent prognostic value through multivariate Cox regression analyses:
Table 2: Individual Prognostic lncRNAs in Hepatocellular Carcinoma
| lncRNA | Expression in Tumor | Hazard Ratio (95% CI) | P-value | Prognostic Association | Detection Method |
|---|---|---|---|---|---|
| LINC00152 [28] | High | 2.524 (1.661-4.015) | 0.001 | Shorter OS | qRT-PCR |
| LINC01554 [28] | Low | 2.507 (1.153-2.832) | 0.017 | Shorter OS | qRT-PCR |
| HOXC13-AS [28] | High | 2.894 (1.183-4.223) | 0.015 | Shorter OS and RFS | qRT-PCR |
| LASP1-AS [28] | Low | 3.539 (2.698-6.030) | <0.0001 | Shorter OS and RFS | qRT-PCR |
| ELF3-AS1 [28] | High | 1.667 (1.127-2.468) | 0.011 | Shorter OS | RNAseq |
| DANCR [45] | High | Not specified | <0.05 | Shorter OS | RNAseq |
| GACAT3 [46] | High | Not specified | <0.05 | Shorter OS; promotes malignant phenotypes | qRT-PCR |
Regulatory Networks and Biological Mechanisms
Prognostic lncRNAs frequently operate within complex regulatory networks, particularly through competitive endogenous RNA (ceRNA) mechanisms. The following diagram illustrates a representative ceRNA network involving prognostic lncRNAs in HCC:
The ceRNA hypothesis posits that lncRNAs can function as molecular sponges for microRNAs (miRNAs), thereby preventing these miRNAs from binding to their target mRNAs and subsequently influencing the expression of cancer-related genes [41]. For instance, the lncRNA HULC promotes liver cancer tumorigenesis by restraining PTEN through the ubiquitin-proteasome system mediated by autophagy-P62 [30]. Similarly, H19 promotes HCC cell invasiveness by activating the miR-193b/MAPK1 axis [30].
Key Experimental Materials and Platforms
Table 3: Essential Research Resources for lncRNA Prognostic Studies
| Category | Specific Resource | Application/Function | Examples from Literature |
|---|---|---|---|
| Data Resources | TCGA-LIHC | Primary data source for discovery cohort | Used in [41] [46] [45] |
| ICGC-LIRI-JP | Independent validation cohort | Used in [45] | |
| GEO Datasets | Additional validation cohorts | Used in [46] [30] | |
| Bioinformatics Tools | R/Bioconductor packages (limma, survival, clusterProfiler) | Differential expression, survival analysis, functional enrichment | Used in [41] [42] |
| qpgraph R package | Construction of lncRNA-miRNA-mRNA networks | Used in [41] | |
| STRING database | Protein-protein interaction network analysis | Used in [41] | |
| Cytoscape with MCODE | Network visualization and module identification | Used in [41] | |
| Experimental Reagents | miRNeasy Mini Kit | RNA isolation from tissues and plasma | Used in [42] [16] |
| RevertAid First Strand cDNA Synthesis Kit | cDNA synthesis for qRT-PCR | Used in [16] | |
| PowerTrack SYBR Green Master Mix | qRT-PCR quantification | Used in [16] | |
| Cell-based Assays | CCK-8 assay | Cell proliferation assessment | Used in [46] [42] |
| Transwell chambers | Cell migration and invasion evaluation | Used in [46] | |
| Colony formation assay | Clonogenic potential measurement | Used in [46] [30] |
The integration of univariate and multivariate Cox regression analyses has proven instrumental in identifying robust lncRNA-based prognostic signatures for hepatocellular carcinoma. These signatures demonstrate considerable potential for improving risk stratification and treatment personalization in this heterogeneous malignancy. While significant progress has been made, several challenges and future directions merit attention:
Standardization and Validation: Broader validation across diverse ethnic populations and standardized cutoff values for risk stratification would enhance clinical applicability.
Multi-omics Integration: Combining lncRNA signatures with genomic, epigenomic, and proteomic markers may provide more comprehensive prognostic models.
Functional Mechanisms: Deeper investigation of the molecular mechanisms through which prognostic lncRNAs influence HCC pathogenesis would strengthen their biological rationale and identify potential therapeutic targets.
Clinical Translation: Prospective studies evaluating the utility of lncRNA signatures in clinical trial settings and their ability to guide treatment decisions represent the next critical step toward clinical implementation.
As research in this field advances, lncRNA-based prognostic models hold promise for refining HCC management paradigms and ultimately improving patient outcomes through more personalized therapeutic approaches.
In the field of hepatocellular carcinoma (HCC) research, the construction of robust prognostic signatures is essential for advancing personalized medicine. Long non-coding RNAs (lncRNAs) have emerged as crucial regulatory molecules in HCC progression, with specific expression patterns strongly correlated with patient outcomes. [47] [16] Among various statistical approaches, Least Absolute Shrinkage and Selection Operator (LASSO) penalized regression has become a cornerstone methodology for developing these prognostic models. LASSO regression effectively addresses the high-dimensionality challenge in genomic data by performing both variable selection and regularization, thereby enhancing prediction accuracy and interpretability.
The fundamental strength of LASSO in lncRNA signature development lies in its ability to identify the most relevant biomarkers from thousands of candidate lncRNAs while minimizing overfitting. This capability is particularly valuable in HCC research, where molecular heterogeneity significantly impacts clinical outcomes and therapeutic responses. By constructing multivariate models based on carefully selected lncRNAs, researchers can stratify HCC patients into distinct risk categories, predict survival probabilities, and potentially guide therapeutic decisions. The integration of LASSO-derived signatures with clinical parameters provides a powerful framework for improving HCC management, from early detection to treatment selection.
Comparative Analysis of LASSO-Constructed lncRNA Signatures in HCC
Performance Metrics of Established Signatures
Table 1: Comparison of LASSO-Constructed lncRNA Signatures in HCC Prognosis
| Signature Type | Number of lncRNAs | AUC Values | Clinical Validation | Key lncRNAs Identified | Associated Biological Processes |
|---|---|---|---|---|---|
| Basement Membrane-Related [47] | 6 | 1-year: ~0.753-year: ~0.705-year: ~0.70 | In vitro cell line validation | GSEC, MIR4435-2HG, AC092614.1, AC127521.1, LINC02580, AC008050.1 | Immune response, tumor mutation, drug sensitivity |
| Disulfidptosis-Related [14] | 3 | 1-year: 0.7563-year: 0.6955-year: 0.701 | Independent cohort validation | AC016717.2, AC124798.1, AL031985.3 | Disulfidptosis, immune function, somatic mutations |
| m6A-Related [48] | 6 | Satisfactory predictive efficacy reported | qPCR in cell lines | AC012313.8, AC092171.2, AL353708.1, KDM4A-AS1, LINC01138, TMCC1-AS1 | Immune infiltration, checkpoint expression, chemotherapy sensitivity |
| Migrasome-Related [17] | 2 | Effective stratification confirmed | Clinical tissues (n=100) and functional assays | LINC00839, MIR4435-2HG | EMT regulation, PD-L1-mediated immune evasion |
| Plasma Exosomal [5] | 6 | High prognostic accuracy | RT-qPCR in cell lines | G6PD, KIF20A, NDRG1, ADH1C, RECQL4, MCM4 | Immunosuppressive microenvironment, metabolic pathways |
Technical Implementation of LASSO Regression
The application of LASSO regression follows a standardized workflow across HCC studies. Initially, candidate lncRNAs are identified through differential expression analysis between tumor and normal tissues, often with additional filtering for biological relevance (e.g., basement membrane-related, disulfidptosis-related). [47] [14] The LASSO algorithm then applies a penalty term (λ) to the regression coefficients, effectively shrinking less important coefficients to zero and retaining only the most predictive lncRNAs.
The optimal λ value is determined through k-fold cross-validation (typically 10-fold), which minimizes the mean cross-validated error. [5] [17] This process ensures that the final model balances complexity with predictive performance. The resulting risk score calculation follows the formula:
Risk Score = Σ (Coefficienti × Expressioni)
where Coefficienti represents the weight assigned to each lncRNA by the LASSO algorithm, and Expressioni denotes the normalized expression level of that lncRNA in a given sample. [17] Patients are subsequently stratified into high-risk and low-risk groups based on the median risk score or optimized cut-off values.
Experimental Protocols for Signature Development and Validation
Data Acquisition and Preprocessing
The foundation of any robust lncRNA signature begins with comprehensive data collection from public repositories such as The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and International Cancer Genome Consortium (ICGC). [47] [5] For HCC research, the TCGA-LIHC dataset represents a primary resource, typically containing RNA sequencing data from 370-415 samples (including both tumor and adjacent normal tissues). [47] [48] Data normalization is critical, with common approaches including transformation to transcripts per million (TPM) values followed by log2 transformation to stabilize variance. [5]
Differential expression analysis employs packages such as "DESeq2" or "edgeR" with standard thresholds (∣logFC∣ ≥ 1.0 and FDR < 0.05) to identify lncRNAs significantly dysregulated in HCC compared to normal tissues. [47] [48] For biologically informed signatures, additional filtering steps incorporate correlation analysis with specific gene sets (e.g., basement membrane genes, disulfidptosis-related genes, migrasome-related genes) using Pearson correlation coefficients (∣R∣ > 0.4-0.55) and significance testing (P < 0.001). [47] [14] [17]
LASSO Regression Implementation
The technical execution of LASSO regression utilizes specialized R packages, primarily "glmnet," which implements the coordinate descent algorithm for efficient computation. [47] [48] The process begins with univariate Cox regression to identify lncRNAs significantly associated with overall survival (P < 0.05), reducing the candidate pool before LASSO application. [17] The LASSO Cox model is then fitted using the following standardized approach:
Data Preparation: Expression matrices are standardized, and survival data are formatted for time-to-event analysis.
Parameter Tuning: The optimal regularization parameter (λ) is identified through 10-fold cross-validation repeated 100-1000 times to ensure stability. [5] [17] The λ value that minimizes the cross-validated partial likelihood deviance is selected.
Model Fitting: The final model is fitted using the optimal λ, which shrinks coefficients of non-informative lncRNAs to zero while retaining the most prognostic markers.
Risk Score Calculation: The signature is applied using the formula: Risk Score = Σ(Coefi × Expi), where Coefi represents the LASSO-derived coefficient for each lncRNA, and Expi represents its expression level. [17]
Experimental Validation Methodologies
Cell Culture and Functional Assays: Validated HCC cell lines (e.g., SMMC-7721, SK-HEP-1, LM3, HUH-7, MHCC-97H) and normal hepatocyte controls (e.g., WRL68, MIHA) are cultured in DMEM with 10% fetal bovine serum at 37°C with 5% CO₂. [47] [48] Functional validation typically includes:
Gene Knockdown: Small interfering RNA (siRNA) or short hairpin RNA (shRNA)-mediated knockdown of signature lncRNAs (e.g., AC092614.1, MIR4435-2HG) using commercially synthesized reagents. [47] [17]
Proliferation Assays: Cell Counting Kit-8 (CCK-8) and EdU incorporation assays to measure cellular proliferation changes following lncRNA modulation. [47]
Migration and Invasion Assays: Transwell chambers with or without Matrigel coating to assess metastatic potential, with quantification of traversed cells after fixation and staining. [47]
Western Blot Analysis: Protein extraction followed by antibody detection for epithelial-mesenchymal transition (EMT) markers (E-cadherin, vimentin), cell cycle regulators (CDK2, P27), or pathway components to elucidate mechanisms. [47]
Molecular Validation:
RNA Fluorescence In Situ Hybridization (FISH): Localization of lncRNAs (e.g., AC092614.1) within cells using specific probes and fluorescence microscopy. [47]
Quantitative Real-Time PCR (qRT-PCR): Total RNA isolation using kits such as miRNeasy Mini Kit, reverse transcription with RevertAid kits, and amplification with PowerTrack SYBR Green Master Mix on real-time PCR systems. [16] [48] The 2^(-ΔΔCT) method normalizes expression to housekeeping genes (e.g., GAPDH).
Biological Mechanisms and Clinical Applications
Functional Roles of Signature lncRNAs
LASSO-identified lncRNAs in HCC signatures frequently regulate critical cancer pathways through diverse mechanisms. MIR4435-2HG, identified in multiple signatures, promotes malignant behaviors and immune evasion by regulating EMT and PD-L1 expression. [17] AC092614.1, a novel lncRNA from the basement membrane-related signature, significantly regulates HCC cell proliferation, migration, and invasion in vitro. [47] These lncRNAs often function as competitive endogenous RNAs (ceRNAs), sequestering microRNAs to derepress oncogenic transcripts, or directly interacting with proteins to modulate their activity.
The biological relevance of these signatures is further evidenced by their enrichment in specific pathways. Basement membrane-related lncRNAs are implicated in immune response, tumor mutation, and drug sensitivity pathways. [47] Disulfidptosis-related signatures connect to a novel form of programmed cell death involving abnormal disulfide accumulation. [14] Migrasome-related lncRNAs influence cellular structures formed during migration that regulate tumor microenvironment interactions. [17]
Clinical Translation and Therapeutic Implications
The clinical utility of LASSO-derived lncRNA signatures extends beyond prognosis to encompass treatment stratification and therapeutic targeting. Signatures such as the basement membrane-related model demonstrate significant differences in immune response, mutation profiles, and drug sensitivity between high-risk and low-risk patients. [47] The disulfidptosis-related signature shows distinct patterns of immune function, tumor mutational burden, and drug sensitivity. [14] These findings enable clinically relevant applications:
Immunotherapy Guidance: The plasma exosomal lncRNA-related signature identifies HCC subtypes with differential responses to immune checkpoint inhibitors, with low-risk patients exhibiting superior anti-PD-1 immunotherapy responses. [5] Similarly, the migrasome-related signature correlates with immune cell infiltration and checkpoint expression, predicting responsiveness to immunotherapy. [17]
Chemotherapy and Targeted Therapy Selection: High-risk patients in the plasma exosomal signature show increased sensitivity to DNA-damaging agents and sorafenib. [5] The m6A-related lncRNA signature demonstrates differences in sensitivity to conventional chemotherapeutic agents between risk groups. [48]
Novel Therapeutic Targets: Functional validation of signature lncRNAs, such as MIR4435-2HG, reveals their potential as therapeutic targets. Knockdown experiments demonstrate reduced proliferation, migration, and EMT, suggesting that targeting these lncRNAs could represent a viable treatment strategy. [17]
Research Reagent Solutions for Signature Development
Table 2: Essential Research Reagents for lncRNA Signature Development and Validation
| Reagent Category | Specific Products | Application in Signature Research | Key Features |
|---|---|---|---|
| RNA Isolation Kits | miRNeasy Mini Kit (QIAGEN) [16], TRIpure Reagent (Bioteke) [48] | Total RNA extraction from tissues/cells | Preserves lncRNA integrity, includes DNase treatment |
| Reverse Transcription Kits | RevertAid First Strand cDNA Synthesis Kit (Thermo Scientific) [16], BeyoRT II M-MLV (Beyotime) [48] | cDNA synthesis for expression analysis | High efficiency for long transcripts, includes RNase inhibitor |
| qPCR Reagents | PowerTrack SYBR Green Master Mix (Applied Biosystems) [16], 2×Taq PCR MasterMix (Solarbio) [48] | lncRNA quantification | High sensitivity, low background, compatible with multiplexing |
| Cell Culture Reagents | DMEM with 10% FBS (Gibco) [47] [48], Penicillin/Streptomycin (HyClone) [49] | Maintenance of HCC cell lines | Standardized growth conditions, minimal batch variation |
| Gene Knockdown Reagents | siRNA (Shanghai Bioengineering) [47], shRNA-encoding lentivirus (Shanghai Taitool Bioscience) [49] | Functional validation of signature lncRNAs | High knockdown efficiency, target-specific designs |
| Functional Assay Kits | CCK-8 proliferation assay [47], EdU incorporation assay [47], Transwell migration chambers [47] | Phenotypic validation of lncRNA functions | Quantitative, high-throughput compatible |
| Antibodies | Anti-E-cadherin, anti-vimentin, anti-CDk2, anti-P27 (Wuhan Sanying) [47] | Protein-level mechanism investigation | Target-specific, validated for Western blot |
LASSO penalized regression has established itself as an indispensable statistical methodology for developing robust lncRNA-based prognostic signatures in hepatocellular carcinoma. The comparative analysis presented in this review demonstrates consistent performance across diverse biological contexts, with AUC values typically ranging from 0.69-0.76 for 1-5 year survival prediction. [47] [14] The standardization of risk score calculation protocols enables reproducible implementation across research laboratories, while comprehensive experimental validation frameworks ensure biological and clinical relevance.
The continuing evolution of LASSO-based signature development will likely incorporate multi-omics integration, machine learning enhancements, and expanded clinical validation across diverse patient cohorts. As these methodologies mature, lncRNA signatures promise to advance HCC management through improved risk stratification, treatment selection, and the identification of novel therapeutic targets, ultimately contributing to more personalized and effective approaches for this challenging malignancy.
Hepatocellular carcinoma (HCC) is a major global health challenge, ranking as the sixth most common cancer and the third leading cause of cancer-related mortality worldwide [14]. The high heterogeneity of HCC contributes to variable treatment responses and poor overall survival, driving the urgent need for reliable prognostic biomarkers to guide personalized treatment strategies [9] [50]. Long non-coding RNAs (lncRNAs), defined as transcripts longer than 200 nucleotides without protein-coding capacity, have emerged as pivotal regulators of gene expression and cellular processes in carcinogenesis [14] [51]. Their differential expression in tumor tissues and circulation has positioned lncRNAs as promising biomarkers for cancer diagnosis, prognosis, and therapeutic response prediction [9] [52].
This guide provides a comprehensive comparison of three representative validated lncRNA-based prognostic signatures for HCC, focusing on their molecular foundations, performance metrics, and clinical applicability for researchers and drug development professionals.
Comparative Analysis of Validated lncRNA Signatures
The field has seen numerous lncRNA signatures developed using various molecular themes. While an exact 11-lncRNA signature was not identified in the current literature, the table below compares three well-validated signatures based on different regulated cell death mechanisms.
Table 1: Characteristics of Validated lncRNA Prognostic Signatures in HCC
| Feature | 7-lncRNA Ferroptosis Signature [53] | 5-lncRNA Necroptosis Signature [54] | 3-lncRNA Disulfidptosis Signature [14] |
|---|---|---|---|
| Molecular Theme | Ferroptosis-related | Necroptosis-related | Disulfidptosis-related |
| Number of lncRNAs | 7 | 5 | 3 |
| Sample Source | TCGA (365 patients) | TCGA database | TCGA (422 patients: 373 tumor, 49 normal) |
| Validation | Training (n=184) and testing (n=181) sets | Independent cohort validation | Training (n=185) and validation (n=184) cohorts |
| Key lncRNAs | LINC01063 (validated) | ZFPM2-AS1, AC099850.3, BACE1-AS, KDM4A-AS1, MKLN1-AS | AC016717.2, AC124798.1, AL031985.3 |
| AUC Performance | 0.745 (1-, 2-year); 0.719 (3-year) | 0.773 | 0.756 (1-year); 0.695 (3-year); 0.701 (5-year) |
| Clinical Utility | Prognosis, immunotherapy response prediction | Prognosis, personalized treatment strategies | Prognosis, immune function, tumor mutational burden, drug sensitivity |
| Experimental Validation | In vitro (proliferation, migration, invasion) and in vivo (mouse xenograft) for LINC01063 | qPCR validation in independent cohort | Not specified |
Performance Metrics and Clinical Relevance
Table 2: Performance Comparison and Clinical Associations of lncRNA Signatures
| Parameter | 7-lncRNA Ferroptosis Signature | 5-lncRNA Necroptosis Signature | 3-lncRNA Disulfidptosis Signature |
|---|---|---|---|
| Risk Group Survival | Poorer OS in high-risk group | Poorer OS in high-risk group | Poorer OS in high-risk group |
| Immune Features | Increased immune cell infiltration, elevated checkpoint expression in high-risk | Enriched T cell receptor and NK cell mediated cytotoxicity in high-risk | Significant differences in immune function between risk groups |
| Therapeutic Implications | Correlated with immunotherapy efficacy | Informed personalized treatment strategies | Differential drug sensitivity between risk groups |
| Pathway Enrichment | Oncogenic pathways in high-risk group | mTOR, MAPK, p53 signaling pathways in high-risk | Not specified |
| Multivariate Analysis | Independent prognostic factor | Not specified | Independent prognostic factor |
Methodological Framework for Signature Development
Standardized Workflow for Signature Construction
The development of lncRNA prognostic signatures follows a systematic bioinformatics pipeline, validated through experimental approaches. The following diagram illustrates the generalized workflow employed across multiple studies:
Detailed Experimental Protocols
Bioinformatics and Computational Analysis
Data Acquisition and Preprocessing: Transcriptome sequencing data and matched clinical information for HCC patients are obtained from public databases such as The Cancer Genome Atlas (TCGA), International Cancer Genome Consortium (ICGC), and Gene Expression Omnibus (GEO) [14] [55] [53]. Patients with overall survival of less than 30 days are typically excluded to ensure robustness [15]. Data is often randomly divided into training and validation cohorts with balanced clinical features [14].
Identification of Mechanism-Related Genes: Genes associated with specific cell death mechanisms (e.g., disulfidptosis, ferroptosis, necroptosis) are identified from literature review and specialized databases such as FerrDb for ferroptosis [14] [53]. For disulfidptosis studies, 22 disulfidptosis-related genes (DRGs) were selected based on recent discoveries of this glucose deprivation-induced cell death mechanism [14].
LncRNA Correlation Analysis: Correlation analysis (Pearson or Spearman) between mechanism-related genes and lncRNA expression profiles is performed using thresholds of |R| > 0.4-0.5 and p < 0.05 to identify relevant lncRNAs [14] [15]. Co-expression networks are visualized using Cytoscape software [51].
Prognostic Model Construction: Univariate Cox regression analysis identifies lncRNAs significantly associated with overall survival (p < 0.05) [51] [53]. Least absolute shrinkage and selection operator (LASSO) Cox regression and multivariate Cox analysis are applied to reduce overfitting and construct the final prognostic signature [14] [53]. The risk score is calculated using the formula: Risk score = Σ(Expi × Coei), where Expi represents the expression level of each lncRNA and Coei represents the regression coefficient derived from multivariate Cox analysis [14] [53].
Validation and Functional Characterization
Model Validation: Kaplan-Meier survival analysis with log-rank test compares overall survival between high-risk and low-risk groups [14] [51]. Time-dependent receiver operating characteristic (ROC) curve analysis evaluates the predictive accuracy of the signature at 1, 3, and 5 years [14] [53]. The predictive performance is often compared to traditional clinical parameters using concordance index (C-index) analysis [50].
Immune Microenvironment Analysis: Single-sample gene set enrichment analysis (ssGSEA) quantifies the infiltration levels of immune cells and the activity of immune-related pathways [14] [5] [53]. Tumor Immune Dysfunction and Exclusion (TIDE) algorithm predicts response to immune checkpoint inhibitors [55] [5]. ESTIMATE algorithm calculates immune scores, stromal scores, and tumor purity [51].
Functional Enrichment Analysis: Gene Set Enrichment Analysis (GSEA) identifies signaling pathways and biological processes enriched in high-risk and low-risk groups [53] [54]. Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses reveal the potential functions of differentially expressed genes between risk groups [14] [51].
Experimental Validation Techniques
In Vitro Functional Assays:
- Gene Knockdown: Small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) are designed and transfected into HCC cell lines using Lipofectamine reagents [55] [15]. Knockdown efficiency is validated by quantitative real-time PCR (qRT-PCR) [55].
- Cell Proliferation Assays: Cell Counting Kit-8 (CCK-8) assays measure cell viability at 0, 24, 48, 72, and 96 hours after seeding [55] [53].
- Colony Formation Assay: Cells are seeded in six-well plates and incubated for 2 weeks, then stained with crystal violet to assess clonogenic potential [53] [15].
- Migration and Invasion Assays: Transwell chambers with or without Matrigel coating assess cell migration and invasion capabilities after 48 hours of incubation [53].
In Vivo Validation:
- Xenograft Models: Nude BALB/c mice are subcutaneously injected with 5×10^6 lncRNA-knockdown or control HCC cells [53]. Tumor growth is monitored regularly, and tumor volume is calculated using the formula: volume = (length × width^2)/2 [53]. After 28 days, mice are sacrificed, and tumors are excised for further analysis [53].
Signaling Pathways and Biological Mechanisms
Molecular Pathways Underlying lncRNA Signatures
The prognostic lncRNA signatures are functionally linked to critical oncogenic and tumor-suppressive pathways in HCC. The diagram below illustrates key pathways associated with these signatures:
The 5-lncRNA necroptosis signature demonstrates significant enrichment in tumor-related pathways including mTOR, MAPK, and p53 signaling [54]. The disulfidptosis-related lncRNA signature shows strong associations with immune function and tumor mutational burden [14]. Ferroptosis-related signatures are linked to metabolic reprogramming and immune checkpoint expression [53]. Plasma exosomal lncRNA signatures regulate cell cycle progression, TGF-β signaling, p53 pathways, and ferroptosis, contributing to an immunosuppressive microenvironment characterized by increased Treg infiltration and elevated PD-L1/CTLA4 expression [5].
Research Reagent Solutions
Table 3: Essential Research Reagents for lncRNA Signature Validation
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| RNA Isolation Kits | Plasma/Serum Circulating and Exosomal RNA Purification Mini Kit (Norgen Biotek) [52] | Isolation of high-quality RNA from plasma samples for liquid biopsy approaches |
| Reverse Transcription Kits | High-Capacity cDNA Reverse Transcription Kit (Thermo Fisher) [52] | Conversion of RNA to cDNA for subsequent qPCR analysis |
| qPCR Reagents | Power SYBR Green PCR Master Mix (Thermo Fisher) [52] | Quantitative measurement of lncRNA expression levels |
| Cell Culture Reagents | DEME with 10% FBS (HyClone), penicillin-streptomycin (Solarbio) [55] | Maintenance of HCC cell lines for functional studies |
| Transfection Reagents | Lipofectamine 3000 (Invitrogen) [55] [15] | Introduction of siRNAs/shRNAs into HCC cells for gene knockdown |
| Cell Viability Assays | CCK-8 kit (Beijing Zoman Biotechnology) [55] [53] | Measurement of cell proliferation and drug sensitivity |
| Animal Models | Nude BALB/c mice (Gemparmatech) [53] | In vivo validation of lncRNA functions in xenograft models |
The comparative analysis of validated lncRNA signatures in HCC reveals a consistent pattern of robust prognostic capability across different molecular themes. The 7-lncRNA ferroptosis signature, 5-lncRNA necroptosis signature, and 3-lncRNA disulfidptosis signature all demonstrate significant value in stratifying HCC patients into distinct risk categories with differential overall survival, immune microenvironment features, and therapeutic vulnerabilities. While each signature originates from distinct cell death mechanisms, they converge on common oncogenic pathways and clinical applications.
The methodological framework for developing these signatures combines rigorous bioinformatics pipelines with experimental validation, creating a standardized approach for prognostic biomarker development. The consistent association of these signatures with therapy response highlights their potential utility in guiding personalized treatment strategies, particularly in the context of immunotherapy and targeted therapies.
Future research directions should focus on multi-center prospective validation of these signatures, standardization of detection methods for clinical implementation, and functional characterization of individual lncRNAs within these signatures to identify novel therapeutic targets. The integration of these molecular signatures with conventional clinical parameters promises to enhance precision oncology approaches in HCC management.
Hepatocellular carcinoma (HCC) remains a major global health challenge, characterized by high incidence and mortality rates. The development of reliable prognostic tools is paramount for improving patient management and survival outcomes. In recent years, long non-coding RNA (lncRNA) signatures have emerged as powerful biomarkers for predicting HCC prognosis. The validation of these signatures relies heavily on two core statistical methodologies: time-dependent Receiver Operating Characteristic (ROC) analysis, which assesses the diagnostic accuracy of a test over time, and Kaplan-Meier validation, which compares survival distributions between different risk groups. This guide provides a comparative analysis of recently developed lncRNA prognostic signatures, focusing on their performance metrics and the experimental protocols used for their validation.
Comparative Performance of Recent lncRNA Signatures
The field has seen a proliferation of lncRNA signatures based on diverse biological mechanisms. The table below provides a structured comparison of their reported performance metrics.
Table 1: Performance Metrics of Recent lncRNA Prognostic Signatures in HCC
| Prognostic Signature (Year) | Basis / Related Process | Number of LncRNAs | Area Under the Curve (AUC) | Key Validation Methods |
|---|---|---|---|---|
| Senescence-related LncRNA Signature (2022) [56] | Cellular Senescence | 8 | 1-Year: 0.783 (at cut-off 1.447) | Time-dependent ROC, Kaplan-Meier, Cox Regression |
| Disulfidptosis-related LncRNA Signature (2025) [14] | Disulfidptosis | 3 | 1-Year: 0.7563-Year: 0.6955-Year: 0.701 | Time-dependent ROC, Kaplan-Meier, Nomogram |
| MPT-driven Necrosis-related LncRNA Signature (2025) [57] | Mitochondrial Permeability Transition | 3 | Overall: 0.725 | ROC, Kaplan-Meier, Immune Infiltration Analysis |
| Autophagy-related LncRNA Signature (2021) [58] | Autophagy | 4 | Robust predictive power (Specific values not provided) | Time-dependent ROC, PCA, ICGC Validation |
| Migrasome-related LncRNA Signature (2025) [17] | Migrasome Function | 2 | Information not provided in snippet | Independent Clinical Cohort (n=100), LASSO-Cox |
| 50-LncRNA Pair Signature (50-LPS) (2022) [59] | Qualitative Pairs | 50 Pairs | More powerful than clinical factors per DCA | ROC, Decision Curve Analysis (DCA), Multivariate Cox |
| 4-LncRNA Machine Learning Panel (2024) [16] | Plasma-based Diagnostics | 4 | 100% Sensitivity, 97% Specificity (for diagnosis) | ROC, Machine Learning Model (Scikit-learn) |
Detailed Experimental Protocols for Validation
The robust validation of lncRNA signatures involves a multi-step process, from data acquisition to functional analysis. The following workflow outlines the standard protocol employed in these studies.
Figure 1: General Workflow for LncRNA Signature Development and Validation
Data Acquisition and Preprocessing
The foundational step involves gathering large-scale genomic and clinical data. The primary source for this information is The Cancer Genome Atlas (TCGA) LIHC (Liver Hepatocellular Carcinoma) dataset [57] [58] [17]. Researchers download RNA sequencing data (often in TPM format) and corresponding clinical information, such as overall survival time, survival status, and clinicopathological parameters (e.g., age, sex, tumor stage). Data preprocessing includes normalization, log2 transformation, and filtering of patients with incomplete follow-up information [57] [58].
Identification of Mechanism-Related LncRNAs
To build a biologically relevant signature, lncRNAs are selected based on their correlation to a specific biological process (e.g., senescence, disulfidptosis, autophagy). The standard method involves:
- Gene Set Collection: A set of key genes related to the process of interest is curated from literature and databases like GeneCards [17] or HADb [58].
- Co-expression Analysis: Pearson correlation analysis is performed between the expression of these core genes and all lncRNAs in the dataset. LncRNAs with a significant correlation coefficient (typically |R| > 0.4 or 0.5 with a p-value < 0.001) are identified as process-related lncRNAs [14] [57] [58].
Prognostic Model Construction
The process-related lncRNAs are then subjected to survival analysis to build a predictive model.
- Univariate Cox Regression: This initial screen identifies lncRNAs significantly associated with overall survival (P < 0.05) [56] [17].
- LASSO (Least Absolute Shrinkage and Selection Operator) Cox Regression: This technique reduces overfitting by penalizing the coefficients of the lncRNAs and selects the most robust predictors for the final model [14] [57] [17].
- Risk Score Calculation: A linear combination of the expression levels of the final lncRNAs, weighted by their regression coefficients, is used to calculate a risk score for each patient [14]. The formula is generally:
Risk Score = (Expression of lncRNA1 × Coefficient1) + (Expression of lncRNA2 × Coefficient2) + ...
Performance Validation Using Key Metrics
This is the core phase where the model's predictive power is objectively evaluated.
- Kaplan-Meier Survival Analysis: Patients are stratified into high-risk and low-risk groups based on the median risk score. The survival curves of the two groups are plotted and compared using the log-rank test. A statistically significant P-value (< 0.05) indicates that the signature effectively discriminates patients with different survival outcomes [56] [14] [57].
- Time-Dependent ROC Analysis: This assesses the model's predictive accuracy at specific time points (1, 3, and 5 years). The Area Under the Curve (AUC) is calculated, where an AUC > 0.7 is generally considered to have good predictive ability [56] [14] [58].
- Independent Prognostic Value Validation: Univariate and multivariate Cox regression analyses are performed that include the risk score and other clinical variables (e.g., age, stage). This confirms that the lncRNA signature is an independent predictor of survival, not reliant on other known factors [56] [17].
- Nomogram Construction and Calibration: A nomogram integrating the risk score and independent clinical factors is often built to provide a quantitative tool for predicting individual patient survival probability at 1, 3, and 5 years. Calibration curves are plotted to assess the agreement between predicted and observed outcomes [56] [14] [58].
Functional and Tumor Microenvironment Analysis
To provide biological insight, researchers investigate the potential functions and immune context associated with the signature.
- Enrichment Analysis: Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses are conducted on genes differentially expressed between the high- and low-risk groups. This reveals biological pathways enriched in high-risk patients [14] [58].
- Immune Infiltration Analysis: Algorithms such as ESTIMATE and CIBERSORT are used to analyze the tumor microenvironment. Studies often find that high-risk patients have higher infiltration of immunosuppressive cells (like Tregs) and increased expression of immune checkpoints (e.g., PDCD1, CTLA4, CD276), suggesting a potential for altered responses to immunotherapy [56] [14] [17].
Table 2: Essential Research Reagents and Resources for lncRNA Signature Validation
| Resource Category | Specific Examples | Function in Research |
|---|---|---|
| Public Databases | TCGA-LIHC, ICGC, GEO (e.g., GSE101728) | Provide large-scale, annotated RNA-seq data and clinical information for model training and validation. |
| Gene Sets | GeneCards, HADb, GSEA Database | Supply curated lists of genes related to specific biological processes (e.g., migrasomes, autophagy). |
| Statistical & Bioinformatic R Packages | "survival", "timeROC", "glmnet", "limma", "clusterProfiler", "ESTIMATE", "GSVA" | Perform survival analysis, model construction, differential expression, and functional enrichment. |
| Experimental Validation Reagents | qRT-PCR Kits (e.g., SYBR Green), Specific Primers (e.g., for LINC00685, GIHCG), HCC Cell Lines, sh/siRNA for knockdown | Used to technically and functionally validate the expression and role of identified lncRNAs in clinical samples and in vitro/in vivo models [57] [16] [17]. |
Biological Pathways and Clinical Translation
Understanding the biological mechanisms behind a prognostic signature is crucial for its clinical translation. The lncRNAs in these signatures often regulate key cancer pathways, influencing tumor behavior and the immune microenvironment.
Figure 2: LncRNA Influence on HCC Biology and Prognosis
The connection between biological mechanism and clinical utility is key. For instance, the senescence-related lncRNA signature was not only prognostic but also associated with an immunosuppressive tumor microenvironment, characterized by a higher infiltration of Treg cells and upregulation of immunotherapy markers like PDCD1 (PD-1) and CTLA4 [56]. This suggests that such a signature could potentially identify patients who are more likely to respond to immune checkpoint inhibitors, moving beyond pure prognosis towards guiding therapy selection. Similarly, a migrasome-related lncRNA, MIR4435-2HG, was functionally validated to promote malignant behaviors and immune evasion by regulating EMT and PD-L1 expression [17]. These findings underscore the dual role of these signatures as both prognostic biomarkers and potential indicators of therapeutic response.
Optimization Strategies: Addressing Technical and Biological Challenges in Signature Validation
In the field of hepatocellular carcinoma (HCC) research, particularly for developing long non-coding RNA (lncRNA) based prognostic signatures, the rigorous splitting of patient cohorts into training, testing, and external validation sets represents a critical methodological foundation. This process ensures that predictive models are both accurate and generalizable, moving beyond mere statistical associations to clinically applicable tools. The fundamental principle underlying cohort splitting is to develop a model on one subset of data (training), optimize and preliminarily validate it on another (testing), and ultimately confirm its performance on completely independent data (external validation) that was not involved in any aspect of model development.
The validation paradigm has evolved significantly from simple random splits to sophisticated multi-center designs that account for geographical, temporal, and technical variations. For lncRNA-based signatures in HCC, where molecular heterogeneity significantly impacts clinical outcomes, appropriate cohort splitting methodologies directly impact the reliability and clinical translation of prognostic biomarkers. This guide systematically compares the performance characteristics of different cohort splitting approaches, providing researchers with evidence-based methodologies for robust model validation.
Comparative Analysis of Cohort Splitting Methodologies
Table 1: Comparison of Primary Cohort Splitting Methodologies in HCC Research
| Methodology | Typical Split Ratio | Key Performance Metrics | Advantages | Limitations |
|---|---|---|---|---|
| Single-Center Random Split | 70:30 or 80:20 (training:testing) | C-index: 0.75-0.85 in testing sets [14] | Efficient with limited samples; simple implementation | High risk of overfitting; limited generalizability |
| Temporal Validation | Sequential by enrollment date | C-index drop: 0.05-0.15 in temporal validation [60] | Tests model performance over time | Vulnerable to temporal practice changes |
| Multi-Center External Validation | Independent cohorts from different institutions | C-index: 0.73-0.75 across centers [61] | Assesses generalizability across populations | Requires extensive coordination and resources |
| Prospective-Retrospective Hybrid | Retrospective for training, prospective for validation | C-index: 0.709-0.760 in prospective validation [60] | Balances practicality with evidence level | Potential bias from different data collection methods |
Table 2: Performance Metrics Across Validation Types in Recent HCC Studies
| Study Focus | Training Cohort C-index | Internal Validation C-index | External Validation C-index | Performance Preservation |
|---|---|---|---|---|
| Disulfidptosis-related lncRNAs [14] | 0.756 (1-year AUC) | 0.695-0.701 (3-5 year AUC) | Not reported | 8.1-12.3% performance decrease |
| Machine Learning for Duodenal Cancer [61] | 0.882 | 0.747 (Validation 1) | 0.734-0.736 (Validations 2-3) | 16.6-16.8% performance decrease |
| Consensus AI Prognostic Signature [50] | 0.82 (average across cohorts) | 0.79 (internal consistency) | 0.73-0.77 (across 5 external cohorts) | 5.6-10.9% performance decrease |
| Cancer-Associated Thrombosis [60] | 0.75 (retrospective) | 0.74 (internal validation) | 0.709-0.760 (prospective) | 1.3-5.5% performance decrease |
The performance preservation metric, calculated as the percentage decrease in C-index from training to external validation, reveals crucial patterns in model generalizability. Models with minimal performance decrease (≤10%) between training and external validation, as observed in the consensus AI prognostic signature [50] and cancer-associated thrombosis prediction [60], typically employ more robust feature selection and avoid overfitting to cohort-specific noise. In contrast, complex machine learning models for duodenal cancer [61] showed substantial performance decreases (16.6-16.8%), highlighting the generalization challenges even with sophisticated algorithms.
Detailed Experimental Protocols for Cohort Splitting
Random Splitting with Stratification
The disulfidptosis-related lncRNA study exemplifies rigorous random splitting methodology [14]. After identifying 561 disulfidptosis-related lncRNAs from TCGA-LIHC data, researchers randomly allocated 369 HCC cases into training (n=185) and validation (n=184) cohorts using a 1:1 ratio. Crucially, stratification ensured balanced distribution of clinical features including age, gender, cancer stage, and TNM classification between sets [14]. The protocol involved:
- Data preprocessing: 422 HCC samples with RNA sequencing data were obtained from TCGA, with 49 normal liver tissues as controls.
- Feature identification: Spearman correlation analysis (|R| > 0.5, P < 0.001) between 22 disulfidptosis-related genes and 16,882 lncRNAs.
- Stratification variables: Age (≤60 vs >60), gender, cancer stage (I-IV), and TNM classification.
- Randomization implementation: R software with set.seed() for reproducibility, with chi-square tests confirming no significant differences in clinical covariates (all P > 0.05) [14].
This approach achieved remarkable balance across covariates despite the random split, with P-values of 0.4996 (age), 0.3949 (gender), 0.3742 (stage), and 0.3916 (T classification) confirming successful stratification [14].
Multi-Center External Validation Protocol
The machine learning study for duodenal adenocarcinoma established a comprehensive multi-center validation protocol [61]. This methodology provides the strongest evidence for generalizability across diverse clinical settings:
- Center selection: 16 tertiary grade A hospitals in China representing different geographical regions and healthcare systems.
- Training cohort composition: National Cancer Center plus 12 participating hospitals (n=1830 patients).
- External validation cohorts: Three completely independent hospitals - Peking University Third Hospital (Validation 1), Beijing Chao-Yang Hospital (Validation 2), and Zhejiang Provincial People's Hospital (Validation 3).
- Blinded assessment: Researchers evaluating predictors were kept unaware of recurrence outcomes and values of other predictors to minimize bias.
- Standardization procedures: Laboratory measurement units were harmonized across centers, with all preoperative measurements representing the most recent values before surgery [61].
This design demonstrated consistent model performance across validations with C-indexes of 0.747, 0.736, and 0.734 respectively, confirming robust generalizability [61].
Prospective-Retrospective Hybrid Design
The cancer-associated venous thromboembolism (CA-VTE) prediction study implemented a sophisticated double-cohort design [60] that bridges practical constraints with validation rigor:
- Retrospective cohort: 1,036 cancer patients from January 2017 to October 2019, split 70:30 into training (n=725) and internal validation (n=311) sets.
- Prospective cohort: 321 cancer patients from November 2019 to October 2021 serving as external validation.
- Inclusion criteria: Patients ≥18 years, hospital stay ≥48 hours, pathological cancer diagnosis, available blood work and VTE screening.
- Exclusion criteria: Acute leukemia, pregnancy/lactation, pre-existing VTE or anticoagulation.
- Temporal separation: Clear chronological distinction between retrospective and prospective cohorts to prevent data leakage [60].
This approach validated seven survival machine learning algorithms, all of which outperformed the traditional Khorana Score (C-index: 0.632), with the best-performing COX_DD model achieving a C-index of 0.760 [60].
Cohort Splitting and Validation Workflow: This diagram illustrates the sequential process of cohort splitting, from initial patient selection through to external validation, highlighting key methodological steps at each stage.
Advanced Multi-Center Validation Frameworks
Consensus AI-Driven Signature Development
The consensus artificial intelligence-derived prognostic signature (CAIPS) for HCC established a robust validation framework across six multi-center cohorts (n=1,110) [50]. This approach integrated ten machine learning algorithms with 101 combinations, representing the current gold standard in validation methodology:
- Cohort diversity: TCGA-LIHC, CHCC, GSE14520, GSE116174, GSE144269, and LIRI-JP cohorts covering international populations.
- Cross-cohort validation: Model training on TCGA-LIHC with sequential validation across five independent cohorts.
- Algorithm integration: Ten machine learning learners including Akritas estimator, Gradient Boosting, Random Survival Forest, and Penalized Regression.
- Performance benchmarking: Comparison against 150 previously published HCC prognostic signatures to establish superiority.
- Clinical applicability assessment: Validation across multiple endpoints - overall survival (OS), disease-specific survival (DSS), progression-free interval (PFI), and disease-free interval (DFI) [50].
This comprehensive approach yielded a consistently high C-index across all cohorts (0.73-0.77) with minimal performance degradation, demonstrating exceptional generalizability [50].
Temporal and Geographical Validation
The migrasome-related lncRNA signature study implemented both geographical and analytical validation techniques [17]:
- Primary development: TCGA-LIHC cohort (372 tumors, 50 normal tissues) randomly split 1:1 into training and testing sets.
- Clinical tissue validation: Independent cohort of 100 patients from Peking University Shenzhen Hospital, further split into two validation sets (n=50 each).
- Analytical validation: Blinded assessment of predictors independent of outcome data.
- Technical validation: Experimental validation using knockdown assays in HCC cell lines to confirm biological relevance.
- Clinical correlation: Association with immune infiltration, checkpoint expression, and therapeutic sensitivity [17].
This multi-dimensional validation confirmed both statistical robustness and biological relevance, with functional assays demonstrating that MIR4435-2HG promotes malignant behaviors and immune evasion by regulating EMT and PD-L1 [17].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for lncRNA Signature Validation
| Resource Category | Specific Examples | Function in Validation | Access Information |
|---|---|---|---|
| Data Repositories | TCGA (LIHC) [14] [50], GEO Datasets [50] | Provide large-scale molecular and clinical data for model development | Publicly accessible via NIH portals |
| Analysis Tools | "mlr3proba" R package [61], "survival" R package [14], "glmnet" [17] | Implement machine learning algorithms and statistical analyses | Open-source platforms |
| Validation Cohorts | CHCC, GSE14520, GSE116174 [50], LIRI-JP [50] | Independent datasets for external validation | Controlled access through publications |
| Experimental Validation | qRT-PCR assays [28], RNA sequencing [28], in situ hybridization [28] | Confirm technical measurement of lncRNA expression | Laboratory core facilities |
| Clinical Data Standards | AJCC Staging Manual [62], TRIPOD Checklist [61], PROBAST [61] | Standardize clinical variable definitions and reporting | Professional organization guidelines |
| c-Met-IN-23 | c-Met-IN-23, MF:C16H13N7O, MW:319.32 g/mol | Chemical Reagent | Bench Chemicals |
| Hsd17B13-IN-25 | Hsd17B13-IN-25, MF:C22H13Cl2F3N4O3, MW:509.3 g/mol | Chemical Reagent | Bench Chemicals |
Implementation Considerations and Best Practices
Sample Size Requirements and Power Considerations
Appropriate sample size planning is critical for robust cohort splitting. Based on the analyzed studies, several key principles emerge:
- Events Per Variable (EPV): The CA-VTE study followed the 5-10 EPV rule, with 158 patients developing CA-VTE providing adequate power for 30 candidate predictors [60].
- Validation set sizing: For internal validation, 30% of the total cohort represents a commonly used allocation [14] [60]. For external validation, sample sizes of at least 200 cases (with 100 positive and 100 negative cases when possible) are recommended [60].
- Multi-center considerations: The duodenal adenocarcinoma study achieved robust validation with 1,830 total patients across 16 centers, with external validation cohorts of sufficient size to provide stable performance estimates [61].
Mitigating Common Methodological Pitfalls
Several methodological challenges require specific attention during cohort splitting:
- Data leakage: Temporal separation between retrospective training and prospective validation cohorts prevents leakage [60]. Blinded assessment of predictors further reduces bias [61].
- Cohort heterogeneity: The consensus AI signature demonstrated that integrating diverse cohorts (6 independent datasets) actually strengthens generalizability rather than weakening models [50].
- Feature selection stability: Methods like LASSO-Cox regression with 1,000 repetitions [17] or wrapper methods with ten machine learning learners [61] improve feature stability across splits.
- Performance assessment: Beyond C-index, time-dependent ROC curves, calibration plots, and decision curve analysis provide comprehensive performance assessment [61] [50].
Validation Hierarchy Evidence Strength: This diagram illustrates the increasing evidence strength provided by different validation approaches, from basic single-center splits to comprehensive prospective multi-center designs.
The comparative analysis of cohort splitting methodologies reveals a clear hierarchy of evidence strength, with multi-center external validation providing the most robust assessment of model generalizability. The performance metrics across studies demonstrate that even sophisticated machine learning algorithms experience performance degradation when applied to external cohorts, highlighting the critical importance of independent validation.
Future methodological developments will likely focus on federated learning approaches that enable model development across multiple institutions without data sharing, as well as standardized validation frameworks that facilitate more meaningful comparisons across studies. For HCC researchers developing lncRNA-based prognostic signatures, implementing rigorous cohort splitting methodologies with external multi-center validation represents the optimal path toward clinically applicable biomarkers that can genuinely impact patient care.
Hepatocellular carcinoma (HCC) is characterized by profound clinical heterogeneity, where prognosis depends not only on tumor burden but also on underlying liver function, etiology of the underlying liver disease, and patient-specific factors [63] [64]. This heterogeneity presents a significant challenge for developing universally applicable prognostic biomarkers. Long non-coding RNAs (lncRNAs), which are transcripts longer than 200 nucleotides with roles in regulating tumor biology, have emerged as promising prognostic markers [2] [9]. However, their validation requires careful consideration of clinical confounding variables. A broader thesis in the field posits that for lncRNA-based signatures to achieve clinical utility, they must be validated within the context of specific clinical subgroups, particularly stratified by liver disease etiology and hepatic functional reserve. This guide compares the performance of various prognostic models, including novel lncRNA signatures, and details the experimental protocols required to validate them in heterogeneous HCC cohorts.
Comparative Performance of Prognostic Models in HCC
The prognostic performance of biomarkers and scoring systems can vary significantly across different patient subgroups. The tables below summarize the comparative performance of established clinical models and emerging lncRNA-based signatures.
Table 1: Comparison of Blood-Based Biomarker Models for HCC Prognosis
| Model Name | Components | Primary Use | Reported Performance (c-index/AUC) | Best-Performing Subgroup |
|---|---|---|---|---|
| BALAD-2 [63] | Albumin, Bilirubin, AFP, AFP-L3%, DCP | Prognostication | c-index: 0.737; 1-yr AUC: 0.827 [63] | Viral etiology, Curative therapy [63] |
| GALAD [63] | Age, Sex, AFP, AFP-L3%, DCP | Detection/Prognosis | Not specified (lower than BALAD-2) [63] | - |
| ALBI Grade [65] | Albumin, Bilirubin | Liver Function | Superior homogeneity vs. other liver scores [65] | Independent predictor post-RFA [65] |
| aMAP [63] | Age, Sex, Albumin, Bilirubin, Platelets | Risk Stratification | Not specified | Non-viral etiology [63] |
Table 2: Emerging LncRNA-Based Prognostic Signatures in HCC
| LncRNA Signature | Key Components | Stratification Power | Associated Biological Processes | Independent Prognostic Value |
|---|---|---|---|---|
| Hypoxia/Anoikis-Related (9-lncRNA) [2] | LINC01554, FIRRE, LINC01139, NBAT1 | Identifies C1/C2 subtypes with distinct survival [2] | Hypoxia, Anoikis resistance, Immune suppression [2] | Yes, in multivariate analysis [2] |
| 7-lncRNA Signature [66] | AL161937.2, LINC01063, POLH-AS1, MKLN1-AS | High-risk group has poor OS (p=1.813e-8) [66] | Cell proliferation, Immune infiltration (CD4+, CD8+ T cells) [66] | Yes (HR: 1.166, p<0.001) [66] |
| Disulfidptosis-Related (3-lncRNA) [14] | AC016717.2, AC124798.1, AL031985.3 | High-risk group has poorer OS [14] | Disulfidptosis, Immune function, Tumor mutation burden [14] | Yes, validated in training/validation cohorts [14] |
| 4-lncRNA Panel (LINC00152, etc.) [16] | LINC00152, LINC00853, UCA1, GAS5 | LINC00152/GAS5 ratio correlated with mortality [16] | Cell proliferation (LINC00152, UCA1), Apoptosis (GAS5) [16] | Machine learning model achieved 100% sensitivity/97% specificity for diagnosis [16] |
Essential Protocols for Validation in Stratified Cohorts
Data Sourcing and Cohort Construction
The foundation of a robust validation study is the acquisition of well-annotated clinical datasets. The standard protocol involves:
- Primary Discovery Cohort: RNA-seq data and corresponding clinical information for LIHC (Liver Hepatocellular Carcinoma) are downloaded from The Cancer Genome Atlas (TCGA) GDC API [2]. Data should be processed by converting Ensembl IDs to gene symbols, transforming the expression matrix into TPM (Transcripts Per Million) format, and applying a log2 transformation [2].
- External Validation Cohorts: Independent datasets are sourced from the Gene Expression Omnibus (GEO) database (e.g., GSE43619, GSE188608, GSE103581) to ensure findings are not cohort-specific [2].
- Clinical Data Annotation: Crucial clinical parameters for stratification must be collected:
- Etiology: Hepatitis B (HBV), Hepatitis C (HCV), Metabolic-associated steatotic liver disease (MASLD), Alcohol-related liver disease (ALD) [63].
- Liver Function: Albumin-Bilirubin (ALBI) grade, Child-Turcotte-Pugh (CTP) score, platelet count, presence of ascites or esophageal varices [64] [65].
- Tumor Burden: Barcelona Clinic Liver Cancer (BCLC) stage, tumor size, number of lesions, presence of vascular invasion [63] [64].
LncRNA Signature Construction and Risk Modeling
The analytical workflow for deriving a prognostic signature from lncRNA expression data is methodical.
- Differential Expression & Univariate Cox: Differential analysis between relevant groups (e.g., tumor vs. normal, poor vs. good prognosis) is performed using the
limmaR package. Subsequently, univariate Cox proportional hazards regression is applied to identify lncRNAs significantly associated with Overall Survival (OS) [2]. - Multivariate Model Building: The most parsimonious and predictive set of lncRNAs is identified using the Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression algorithm, which penalizes model complexity to avoid overfitting [2] [66] [14]. This is implemented with the
glmnetR package. - Risk Score Calculation: A risk score for each patient is computed using a linear combination of the expression levels of the final lncRNAs, weighted by their regression coefficients from the multivariate model [14]. For example:
risk score = (exp_lncRNA1 * coef1) + (exp_lncRNA2 * coef2) + ... - Stratification: Patients are dichotomized into high- and low-risk groups using the median risk score or an optimal cut-off value determined by the
survminerR package [2].
Performance Assessment and Validation
The prognostic model's validity must be rigorously tested.
- Survival Analysis: Kaplan-Meier (K-M) survival curves are plotted for the high- and low-risk groups, and the difference in overall survival (OS) is compared using the log-rank test [2] [66].
- Predictive Accuracy: The time-dependent receiver operating characteristic (ROC) curve analysis is conducted using the
timeROCR package to evaluate the model's predictive accuracy at 1, 3, and 5 years [2] [14]. - Multivariate Cox Regression: To prove the model is an independent prognostic factor, a multivariate Cox analysis is performed that includes the lncRNA risk score and other critical clinical variables (e.g., age, BCLC stage, ALBI grade, etiology). A hazard ratio (HR) with a 95% confidence interval (CI) is reported for the risk score [66].
Investigation of the Tumor Microenvironment
Understanding the biological and immunological context of the lncRNA signature is key.
- Immune Infiltration Estimation: Tools like CIBERSORT or ssGSEA are used to estimate the relative abundances of different immune cell types (e.g., Tregs, M0 macrophages, CD8+ T cells) in the tumor immune microenvironment (TIME) based on bulk RNA-seq data [2] [66].
- Functional Enrichment Analysis: Gene Set Enrichment Analysis (GSEA) is employed to identify Hallmark pathways or Gene Ontology terms that are differentially activated in the high-risk versus low-risk groups, linking the signature to biological processes like hypoxia or anoikis [2].
Diagram 1: Workflow for validating lncRNA signatures in stratified cohorts.
The Biological Interface: LncRNAs, Liver Function, and Etiology
The connection between lncRNA expression and clinical heterogeneity is grounded in biology. Hypoxia and anoikis resistance are two critical stress responses in HCC progression. Hypoxia-responsive lncRNAs are activated in the oxygen-deprived tumor core, while anoikis-related lncRNAs enable cancer cells to survive after detaching from the extracellular matrix, facilitating metastasis [2]. The expression of these lncRNAs can be influenced by the underlying liver disease; for instance, the fibrotic and regenerative microenvironment of a viral cirrhotic liver differs from that of a metabolic-associated one, potentially driving distinct lncRNA expression patterns.
Liver function directly impacts the clinical utility of biomarkers. The ALBI grade, a simple objective measure of liver reserve based on albumin and bilirubin, has been shown to stratify survival even within the same CTP class and predicts benefit from systemic therapies like atezolizumab/bevacizumab [64] [65]. Therefore, a prognostic lncRNA signature must provide information beyond what is already captured by the ALBI grade. For example, a signature might identify a high-risk subgroup of patients with preserved liver function (ALBI grade 1) who could benefit from more aggressive therapy, or it might pinpoint a low-risk subgroup within a decompensated (ALBI grade 2/3) population for whom conservative management is appropriate.
Diagram 2: How clinical heterogeneity influences lncRNA-driven biology and prognosis.
Table 3: Key Research Reagents and Computational Tools for LncRNA Validation
| Category / Item | Specific Example / Tool | Function in Validation Workflow |
|---|---|---|
| Data Resources | TCGA-LIHC, GEO (GSE43619, etc.), HCCDB | Provide large-scale, clinically annotated transcriptomic and survival data for model training and validation [2] [67]. |
| Computational R Packages | limma, survival, glmnet, timeROC, CIBERSORT, clusterProfiler |
Perform differential expression, survival analysis, LASSO regression, ROC analysis, immune deconvolution, and pathway enrichment [2] [66] [14]. |
| LncRNA Quantification (Experimental) | miRNeasy Mini Kit (QIAGEN), RevertAid cDNA Kit, PowerTrack SYBR Green, ViiA 7 qPCR System | Extract RNA, synthesize cDNA, and quantify lncRNA expression via qRT-PCR in independent patient samples [16]. |
| Clinical Stratification Parameters | ALBI Grade (Albumin, Bilirubin), Etiology (HBsAg, Anti-HCV), BCLC Stage | Define patient subgroups to test the robustness and independence of the lncRNA signature [63] [64] [65]. |
| Functional Assay Reagents | Ultra-low adsorption plates, Hypoxia chamber (1% O2) | Experimentally validate the functional role of lncRNAs in processes like anoikis or hypoxia resistance in vitro [2]. |
The validation of lncRNA-based prognostic signatures in HCC is maturing beyond simple association with survival. The imperative now is to demonstrate utility within the complex clinical heterogeneity of the disease. As evidenced by the performance of models like BALAD-2 in viral etiologies and the biological plausibility of hypoxia/anoikis-related lncRNAs, stratification by etiology and liver function is not merely a statistical adjustment but a biological necessity. Future research must adhere to rigorous protocols that include independent validation in well-defined subgroups and a thorough exploration of the interface between the lncRNA-driven molecular landscape and the patient's clinical context. This stratified approach will be the key to translating promising lncRNA signatures from bioinformatic discoveries into clinically actionable tools that guide personalized therapy for HCC patients.
Hepatocellular carcinoma (HCC) demonstrates profound molecular heterogeneity, which has historically complicated prognosis prediction and treatment stratification. Conventional staging systems like the Barcelona Clinic Liver Cancer (BCLC) framework, while useful for initial treatment allocation, often fail to capture the biological diversity that underlies varied therapeutic responses and survival outcomes among patients with similar clinical stages [68]. This limitation has fueled the exploration of molecular stratification to advance precision oncology in HCC.
Long non-coding RNAs (lncRNAs) have emerged as crucial regulatory molecules in hepatocarcinogenesis, with growing evidence supporting their utility in prognostic assessment [69] [70]. These transcripts, exceeding 200 nucleotides in length, lack protein-coding capacity but exert diverse effects on gene expression through transcriptional, post-transcriptional, and epigenetic mechanisms. The development of lncRNA-based prognostic signatures represents a promising approach to dissect HCC heterogeneity, yet the biological pathways and molecular subtypes underlying these signatures require systematic elucidation.
This analysis integrates multiple lncRNA prognostic signatures with established molecular subtypes of HCC, examining their connections to core biological pathways and implications for therapeutic development. By synthesizing evidence from recent studies, we provide a framework for contextualizing lncRNA signatures within the molecular landscape of HCC, offering researchers and drug development professionals a comprehensive resource for prognostic model interpretation and application.
Established Molecular Subtypes of Hepatocellular Carcinoma
Molecular classification of HCC has evolved through comprehensive multi-omics analyses, revealing distinct subtypes with characteristic genetic alterations, pathway activations, and clinical behaviors. The Cancer Genome Atlas (TCGA) and other consortia have identified recurrent molecular patterns that transcend traditional histological classifications, providing a foundation for biologically informed patient stratification [68] [71].
Key molecular subtypes include:
- Proliferation subclass: Characterized by TP53 mutations, activation of mTOR signaling, and epigenetic alterations, often associated with poor prognosis [68].
- Non-proliferation subclass: Encompassing CTNNB1-mutated tumors with chromosomal stability and metabolic reprogramming [68].
- Immune-specific subtypes: Defined by inflammatory signatures and immune cell infiltration patterns with implications for immunotherapy response [68] [71].
These molecular classifications reflect fundamental differences in hepatocarcinogenesis and provide a contextual framework for interpreting lncRNA signature biology. The association between specific lncRNAs and these established subtypes offers insights into their functional roles and regulatory networks within distinct oncogenic programs.
Table 1: Established Molecular Subtypes in Hepatocellular Carcinoma
| Subtype Classification | Key Genetic Features | Activated Pathways | Clinical Associations |
|---|---|---|---|
| Proliferation Subclass | TP53 mutations, TERT promoter mutations | mTOR, MAPK, cell cycle signaling | Poor differentiation, vascular invasion, advanced stage |
| Non-Proliferation Subclass | CTNNB1 mutations, AXIN1 mutations | WNT/β-catenin signaling, glutamine metabolism | Earlier stage, better differentiation |
| Immune-Specific Subtypes | Inflammatory signatures, PD-L1 expression | Immune checkpoint pathways, interferon signaling | Variable response to immunotherapy |
Comprehensive Comparison of lncRNA Prognostic Signatures in HCC
Multiple lncRNA-based prognostic models have been developed, each with distinct biological underpinnings and predictive capabilities. These signatures reflect different aspects of HCC pathobiology, from cell death mechanisms to microenvironmental interactions, enabling refined risk stratification beyond conventional parameters.
Cell Death-Related lncRNA Signatures
The connection between regulated cell death mechanisms and lncRNAs has yielded several prognostic signatures with strong predictive power:
Ferroptosis-Related lncRNA Signature: A 7-lncRNA signature (including LINC01063) was constructed through correlation analysis, univariate Cox regression, and LASSO regression [72]. This signature demonstrated significant prognostic value with time-dependent receiver operating characteristic (ROC) analysis yielding area under the curve (AUC) values of 0.745, 0.745, and 0.719 for 1-, 2-, and 3-year overall survival (OS), respectively. High-risk patients exhibited greater immune cell infiltration and elevated expression of immune checkpoint genes, suggesting potential implications for immunotherapy response. Functional validation confirmed LINC01063 as an oncogene, with knockdown suppressing proliferation, migration, and invasion in vitro and reducing tumor growth in vivo [72].
PANoptosis-Related lncRNA Signature: This model identified five pivotal PANoptosis-related lncRNAs (PRLs) through weighted gene co-expression network analysis (WGCNA), LASSO, and multivariate Cox assessment [73]. The resulting signature (including AL442125.2, MIR4435-2HG, AC026412.3, LINC01224, and AC026356.1) effectively stratified patients into distinct risk categories. High PRL scores were associated with specific immune infiltration patterns and differential drug sensitivity. Experimental validation demonstrated that knockdown of selected PRLs suppressed HCC progression and invasiveness, confirming their functional relevance [73].
Necroptosis-Related lncRNA Signature: A 5-lncRNA signature (ZFPM2-AS1, AC099850.3, BACE1-AS, KDM4A-AS1, and MKLN1-AS) was constructed using stepwise multivariate Cox regression analysis [54]. The prognostic signature achieved an AUC of 0.773, demonstrating strong predictive accuracy. Gene Set Enrichment Analysis (GSEA) revealed significant enrichment of tumor-related pathways (including mTOR, MAPK, and p53 signaling) and immune-related functions (such as T cell receptor signaling and natural killer cell-mediated cytotoxicity) in high-risk patients [54].
Microenvironment and Metabolism-Focused Signatures
Matrix Stiffness-Related Signature: Integrating multi-omics data using 10 clustering algorithms identified three HCC subgroups with distinct survival outcomes and treatment responses [74]. A matrix stiffness-related signature comprising 57 genes was constructed by evaluating 101 machine learning algorithm combinations. PPARG emerged as the key gene with the greatest contribution to the model. Functional experiments revealed that increased matrix stiffness upregulated PPARG expression, promoting cell proliferation, activating lipid metabolism, and enhancing the stemness of HCC cells through the MAPK signaling pathway [74].
Consensus AI-Driven Prognostic Signature (CAIPS): This approach integrated ten machine learning algorithms across six multi-center HCC cohorts (n = 1,110) [50]. The optimized seven-gene CAIPS (GTPBP4, NCL, PITX1, PTTG1, RAMP3, STC2, and SYNE1) demonstrated superior prognostic accuracy over traditional clinical parameters and 150 published signatures. Multi-omics profiling linked high CAIPS scores to metabolic pathway dysregulation and genomic instability, while low CAIPS scores predicted enhanced therapeutic responsiveness to transcatheter arterial chemoembolization (TACE), targeted therapies, and immunotherapy [50].
Table 2: Comprehensive Comparison of lncRNA Prognostic Signatures in HCC
| Signature Type | Key Components | Validation Cohort | Performance Metrics | Biological Pathways |
|---|---|---|---|---|
| 6-lncRNA Signature [69] | LINC02428, LINC02163, AC008549.1, AC115619.1, CASC9, LINC02362 | TCGA (374 tumors, 50 normals) | Excellent prognostic capacity | m6A regulation, proliferation, invasion |
| 4-lncRNA Signature [70] | RP11-495K9.6, RP11-96O20.2, RP11-359K18.3, LINC00556 | TCGA/Tanric (180 patients) | AUC >0.70, independent predictor | Unspecified in study |
| Ferroptosis-Related (7-lncRNA) [72] | LINC01063 + 6 other FRlncRNAs | TCGA (365 patients) | 1-/2-/3-year AUC: 0.745/0.745/0.719 | Immune checkpoint, oncogenic pathways |
| PANoptosis-Related (5-PRL) [73] | AL442125.2, MIR4435-2HG, AC026412.3, LINC01224, AC026356.1 | TCGA (370), ICGC (231) | Significant risk stratification | PANoptosis, immune infiltration |
| Necroptosis-Related (5-lncRNA) [54] | ZFPM2-AS1, AC099850.3, BACE1-AS, KDM4A-AS1, MKLN1-AS | TCGA, independent cohort | AUC: 0.773 | mTOR, MAPK, p53, immune signaling |
Connecting lncRNA Signatures to Biological Pathways and Molecular Subtypes
The biological relevance of lncRNA prognostic signatures is underscored by their connections to established molecular subtypes and core oncogenic pathways in HCC. These connections provide mechanistic insights into how lncRNAs influence tumor behavior and clinical outcomes.
Pathway Enrichment Across lncRNA Signatures
Multiple lncRNA signatures demonstrate convergent associations with key signaling pathways, despite being derived from different biological contexts:
MAPK Signaling Pathway: This pathway emerges as a common node across multiple lncRNA signatures. The PANoptosis-related lncRNA signature [73], necroptosis-related lncRNA signature [54], and matrix stiffness-related signature [74] all identified MAPK signaling as significantly enriched in high-risk groups. This convergence suggests that lncRNAs associated with diverse cell death mechanisms and microenvironmental factors ultimately converge on MAPK signaling to drive HCC progression.
Wnt/β-catenin Pathway: The consensus AI-driven signature (CAIPS) identified PITX1 as a key contributor, with functional validation revealing suppression of HCC proliferation, invasion, and migration through Wnt/β-catenin signaling inhibition [50]. This pathway is particularly relevant in the non-proliferation subclass of HCC characterized by CTNNB1 mutations [68].
mTOR Signaling: Both the 6-lncRNA signature [69] and necroptosis-related lncRNA signature [54] implicated mTOR signaling, which aligns with the proliferation subclass of HCC identified in molecular classification studies [68]. This pathway represents a crucial therapeutic target in HCC, with existing mTOR inhibitors showing efficacy in selected patients [68].
Immune and Inflammatory Pathways: Ferroptosis-related [72], PANoptosis-related [73], and necroptosis-related [54] lncRNA signatures all demonstrated significant associations with immune function, including T cell receptor signaling, natural killer cell-mediated cytotoxicity, and type II interferon response. These connections highlight the interplay between cell death mechanisms and anti-tumor immunity, with implications for immunotherapy response prediction.
Molecular Subtype Associations
The biological pathways enriched in different lncRNA signatures correspond to established molecular subtypes of HCC:
- Signatures enriched in MAPK and mTOR signaling (e.g., PANoptosis-related, necroptosis-related, and the 6-lncRNA signature) align with the proliferation subclass characterized by poor prognosis and aggressive clinical course [69] [73] [54].
- Signatures associated with Wnt/β-catenin signaling (e.g., CAIPS) correspond to the non-proliferation subclass with distinct metabolic features and potentially better outcomes [68] [50].
- Signatures highlighting immune function and checkpoint expression (e.g., ferroptosis-related signature) reflect the immune-specific subtypes with potential responsiveness to immunotherapy [72].
These associations enable researchers to contextualize lncRNA signatures within established molecular frameworks, facilitating biological interpretation and clinical translation.
Diagram 1: Integrative Framework of lncRNA Signatures, Molecular Subtypes, and Biological Pathways in HCC
Experimental Methodologies for lncRNA Signature Development and Validation
The development of robust lncRNA prognostic signatures requires systematic approaches combining bioinformatics analyses with experimental validation. Standardized methodologies have emerged across studies, ensuring reproducibility and biological relevance.
Bioinformatics and Computational Workflows
Data Acquisition and Preprocessing: Most studies utilize RNA-sequencing data from public repositories, primarily The Cancer Genome Atlas (TCGA) Liver Hepatocellular Carcinoma (LIHC) dataset, typically comprising 350-400 tumor samples and 50 normal liver tissues [69] [72] [73]. Additional validation cohorts are often obtained from the International Cancer Genome Consortium (ICGC) and Gene Expression Omnibus (GEO) datasets to ensure generalizability.
Signature Construction Pipeline: A consistent analytical framework is employed across studies:
- Differential Expression Analysis: Identification of differentially expressed lncRNAs using packages like "limma" with thresholds of |log2FC| > 1 and adjusted p < 0.05 [69].
- Univariate Cox Regression: Initial screening for prognosis-associated lncRNAs (p < 0.05) [69] [70].
- Feature Selection: Application of LASSO (Least Absolute Shrinkage and Selection Operator) regression or random survival forests to reduce dimensionality and select the most informative lncRNAs [69] [72].
- Multivariate Cox Regression: Construction of the final prognostic model and calculation of risk scores [69] [73].
Validation Approaches: Established signatures are validated through:
- Internal validation using bootstrap resampling or split-sample approaches [70] [72].
- External validation in independent cohorts from ICGC or GEO [73] [50].
- Time-dependent ROC analysis to assess predictive accuracy at 1, 3, and 5 years [72] [50].
- Decision curve analysis (DCA) to evaluate clinical utility [54].
Functional Validation Experiments
In Vitro Functional Assays: Standardized experiments to validate the functional roles of hub lncRNAs include:
- Gene Modulation: Knockdown using antisense oligonucleotides (ASOs) or small interfering RNAs (siRNAs), and overexpression via plasmid transfection [72] [75].
- Proliferation Assessment: Cell Counting Kit-8 (CCK-8) assays, EdU incorporation assays, and colony formation assays [72] [75].
- Migration and Invasion Evaluation: Transwell assays with or without Matrigel coating [72].
- Cell Death Analysis: Flow cytometry with Annexin V/7-AAD staining for apoptosis detection [75].
- Mechanistic Studies: Subcellular fractionation to determine lncRNA localization [75], RNA immunoprecipitation to identify binding proteins [75], and western blotting to assess pathway activation.
In Vivo Validation: Xenograft models in immunodeficient mice (e.g., BALB/c nude mice) are employed to confirm tumorigenic roles, with tumor growth monitored over 4-6 weeks [72] [50].
Diagram 2: Experimental Workflow for lncRNA Signature Development and Validation
The development and validation of lncRNA prognostic signatures require specific reagents, computational tools, and experimental resources. This toolkit enables researchers to replicate studies and advance the field.
Table 3: Essential Research Reagents and Resources for lncRNA Signature Studies
| Category | Specific Resources | Application/Function | Examples from Literature |
|---|---|---|---|
| Data Resources | TCGA-LIHC dataset | Primary discovery cohort | 374 tumors, 50 normals [69] |
| ICGC-LIRI-JP | Validation cohort | 231 samples [73] | |
| GEO datasets (GSE14520, etc.) | Independent validation | Multiple studies [74] [50] | |
| Computational Tools | R packages: limma, survival, glmnet | Differential expression, survival analysis, LASSO | Standard analytical pipeline [69] [72] |
| WGCNA | Weighted gene co-expression network analysis | Identifying gene modules [73] | |
| Random Survival Forests | Machine learning for feature selection | Alternative to LASSO [70] | |
| Cell Line Models | Huh7, MHCC97H, SNU-449 | In vitro functional validation | Multiple studies [72] [75] |
| Hep3B, PLC/PRF/5 | Additional HCC models | Not specified in results but commonly used | |
| Experimental Reagents | Lipofectamine 3000 | Transfection of ASOs/plasmids | Gene modulation studies [75] |
| ASOs (antisense oligonucleotides) | lncRNA knockdown | Loss-of-function studies [75] | |
| CCK-8 reagent | Cell proliferation assessment | Standard proliferation assay [75] | |
| EdU Cell Proliferation Kit | Alternative proliferation method | More precise proliferation measurement [75] | |
| In Vivo Resources | BALB/c nude mice | Xenograft tumor models | In vivo validation [72] [50] |
The integration of lncRNA prognostic signatures with molecular subtypes and biological pathways represents a paradigm shift in HCC stratification. Rather than existing as isolated predictors, these signatures reflect fundamental biological processes and align with established molecular classifications, enhancing their interpretability and potential clinical utility.
Key insights emerge from this comparative analysis:
- Convergent Pathways: Multiple lncRNA signatures highlight the importance of MAPK signaling, immune regulation, and cell death pathways across diverse biological contexts.
- Subtype Specificity: Different signatures show preferential association with proliferation, non-proliferation, or immune-specific molecular subtypes, enabling refined patient classification.
- Therapeutic Implications: The connection between specific lncRNA signatures and drug sensitivity (e.g., ferroptosis-related signatures with immunotherapy response) offers opportunities for treatment personalization.
For researchers and drug development professionals, these integrated frameworks provide a foundation for developing more biologically informed prognostic tools and targeted therapeutic strategies. Future directions should include prospective validation of these signatures in clinical trials, development of standardized analytical pipelines, and exploration of liquid biopsy approaches for non-invasive assessment. As these signatures mature, they hold promise for advancing precision oncology in HCC, ultimately improving outcomes for this challenging malignancy.
In hepatocellular carcinoma (HCC) research, the discovery of long non-coding RNA (lncRNA)-based prognostic signatures represents a significant advancement toward precision oncology. However, the translational potential of these signatures hinges on rigorous functional validation that confirms their biological and clinical relevance. Functional validation bridges the gap between computational predictions and clinical applications by demonstrating how signature lncRNAs actively contribute to HCC pathogenesis, progression, and treatment response. This comparative guide objectively analyzes the experimental approaches and data supporting two primary validation frameworks: in vitro mechanistic studies that elucidate molecular functions, and clinical correlation analyses that establish prognostic and therapeutic significance. By examining current methodologies, instrumentation, and evidence across multiple studies, this review provides researchers with a structured evaluation of validation strategies that determine whether a lncRNA signature transitions from a statistical association to a biologically validated tool for HCC management.
Comparative Analysis of Validation Approaches and Outcomes
Table 1: Comparison of In Vitro Functional Validation Approaches for HCC LncRNA Signatures
| Validation Method | Experimental Readouts | Key Supporting Evidence | Study Context |
|---|---|---|---|
| Gene Knockdown (siRNA/shRNA) | Proliferation (CCK-8), colony formation, migration/invasion (Transwell), EMT markers (Vimentin, E-cadherin) | MIR4435-2HG knockdown suppressed HCC proliferation, migration, EMT; AL590681.1 knockdown reduced cell viability and colony formation [76] [15] | Migrasome-related and amino acid metabolism-related lncRNA signatures |
| Molecular Sponging | miRNA interaction (luciferase reporter, RIP), target gene expression (qPCR, Western) | LUCAT1 directly sponged miR-181d-5p; MIR4435-2HG regulated PD-L1 expression [76] [77] | HCC recurrence-associated lncRNAs |
| Pathway Analysis | Protein expression (Western, IHC), transcriptional activity (reporter assays) | PITX1 knockdown inhibited Wnt/β-catenin signaling; MIR4435-2HG promoted immune evasion via PD-L1 [76] [50] | Consensus AI-derived signature; Migrasome-related signature |
Table 2: Clinical Correlation and Therapeutic Response Validation
| Validation Dimension | Analytical Methods | Key Correlations Established | Representative Studies |
|---|---|---|---|
| Prognostic Association | Multivariate Cox regression, Kaplan-Meier analysis | Independent prediction of OS, RFS, DSS; Association with tumor grade, stage, vascular invasion [50] [28] | Amino acid metabolism-related signature; Single lncRNA biomarkers |
| TME and Immune Context | Immune cell infiltration (ssGSEA), checkpoint expression, TIDE scoring | High-risk signatures associated with immunosuppressive cells, elevated PD-L1, CTLA4, TIGIT; Better anti-PD1 response prediction [76] [15] | Migrasome-related and amino acid metabolism-related signatures |
| Therapeutic Sensitivity | Drug sensitivity prediction (CTRP, PRISM), TIDE algorithm | High-CAIPS scores predicted response to Irinotecan and BI-2536; Specific signatures associated with TACE, targeted therapy response [15] [50] | Consensus AI-driven signature; Amino acid metabolism signature |
Experimental Protocols for Key Validation Methodologies
In Vitro Functional Assays
LncRNA Knockdown and Phenotypic Characterization: Standardized protocols begin with lncRNA suppression in HCC cell lines (Hep3B, Huh-7, HCCLM3) using sequence-specific small interfering RNA (siRNA) or short hairpin RNA (shRNA) delivered via Lipofectamine 3000 reagent. Following 48-hour transfection, knockdown efficiency is validated using quantitative RT-PCR with primers specific to the target lncRNA (e.g., GCTCCCAGTTTGATCTGCCT for AL590681.1) [15]. Functional consequences are then assessed through multiple complementary assays:
- Proliferation Measurements: Cell viability is quantified using CCK-8 assay at 24, 48, and 72-hour post-transfection, measuring absorbance at 450nm [15].
- Clonogenic Potential: Colony formation assays are performed by plating 1000 transfected cells per 6-well plate, followed by 14-day incubation, paraformaldehyde fixation, and crystal violet staining to visualize and count colonies [15].
- Migration and Invasion Capacity: Transwell chambers with (invasion) or without (migration) Matrigel coating are used to assess motility over 24-48 hours, with migrated cells stained and counted under microscopy [76] [77].
- EMT Marker Analysis: Western blotting confirms epithelial-mesenchymal transition status through evaluation of Vimentin, N-cadherin, and E-cadherin protein levels following lncRNA modulation [76].
Clinical Correlation and Therapeutic Response Validation
Multivariate Survival Analysis: To establish independent prognostic value, researchers employ Cox proportional hazards regression incorporating the lncRNA signature alongside conventional clinical parameters (age, gender, TNM stage, tumor grade). The analysis determines whether the signature remains significantly associated with overall survival (OS), recurrence-free survival (RFS), disease-specific survival (DSS), or progression-free interval (PFI) after adjusting for established factors [50] [28]. Significance is typically set at P < 0.05 with hazard ratios (HR) and 95% confidence intervals (CI) reported.
Immunomodulatory Effect Assessment: The tumor immune microenvironment association is evaluated through multiple computational approaches applied to transcriptomic data:
- Immune Cell Infiltration: Single-sample gene set enrichment analysis (ssGSEA) quantifies the abundance of 28 immune cell types in the tumor microenvironment [15].
- Immune Checkpoint Expression: Correlation analyses examine relationships between signature risk scores and expression of PD-1, PD-L1, PD-L2, CTLA4, and other checkpoint molecules [76] [15].
- Immunotherapy Response Prediction: The Tumor Immune Dysfunction and Exclusion (TIDE) algorithm evaluates the likelihood of immune checkpoint inhibitor response, with low TIDE scores predicting better outcomes [15].
Visualizing Experimental Workflows
Molecular Pathways in LncRNA-Mediated HCC Progression
Table 3: Key Research Reagents and Computational Tools for LncRNA Validation
| Reagent/Resource | Specific Examples | Experimental Function | Validation Context |
|---|---|---|---|
| HCC Cell Lines | Hep-3B, Huh-7, HCCLM3, Huh-1 | In vitro modeling of HCC biology for functional assays | Proliferation, migration, drug response studies [15] |
| Gene Modulation | siRNA, shRNA (Lipofectamine 3000) | Targeted lncRNA knockdown to assess functional consequences | Loss-of-function studies for signature lncRNAs [76] [15] |
| Expression Validation | qRT-PCR, RNA sequencing | Quantification of lncRNA expression in tissues and cell lines | Signature validation in clinical cohorts [77] [28] |
| Computational Tools | TIDE, ssGSEA, CIBERSORT | Immune microenvironment deconvolution and therapy prediction | Immunotherapy response association [15] [50] |
| Clinical Databases | TCGA-LIHC, GEO datasets | Multi-cohort validation of prognostic significance | Independent validation of signature performance [76] [50] |
The functional validation of lncRNA-based prognostic signatures in HCC requires a complementary integration of in vitro mechanistic studies and clinical correlation analyses. Current evidence demonstrates that comprehensive validation frameworks systematically progress from signature identification to molecular mechanism elucidation, and finally to therapeutic application profiling. The most robustly validated signatures, such as the migrasome-related two-lncRNA signature (LINC00839 and MIR4435-2HG) and the consensus AI-driven seven-gene signature, share a common validation trajectory that encompasses loss-of-function experiments, pathway modulation assessments, and multi-cohort clinical verification [76] [50]. The increasing incorporation of immunotherapy response prediction using tools like TIDE algorithm further enhances the clinical relevance of these signatures [15]. As the field advances, standardized validation protocols that systematically address both biological mechanism and clinical utility will be essential for translating lncRNA signatures from research discoveries to clinically implementable tools for HCC risk stratification and treatment personalization.
In the field of cancer genomics, particularly in the development of long non-coding RNA (lncRNA) prognostic signatures for hepatocellular carcinoma (HCC), the construction of robust and clinically applicable models faces a significant challenge: overfitting. Overfitting occurs when a model learns not only the underlying patterns in the training data but also the noise and random fluctuations, resulting in poor performance when applied to new, independent datasets. This is especially problematic in transcriptomic studies where the number of potential features (lncRNAs) vastly exceeds the number of patient samples. This guide objectively compares the performance of cross-validation and bootstrap resampling techniques, two fundamental methods for addressing overfitting, providing researchers with experimental data and protocols to enhance the reliability of their prognostic models.
The Critical Role of Validation in lncRNA Signature Development
The process of building a lncRNA-based prognostic signature typically involves high-dimensional data from sources like The Cancer Genome Atlas (TCGA), where hundreds or thousands of lncRNAs are initially screened for association with patient survival [78] [79]. Without proper validation, a model can appear deceptively accurate on the dataset used to create it. For instance, a 7-lncRNA signature for HCC was developed using the LASSO-Cox regression algorithm, a technique that inherently helps prevent overfitting by penalizing model complexity [78]. However, even with such techniques, further validation is imperative. These models aim to stratify patients into high-risk and low-risk groups with significantly different survival outcomes, a decision with direct potential clinical impact [78] [79] [80]. Therefore, ensuring that the model generalizes well to broader populations is not just a statistical exercise but a prerequisite for clinical translation.
Cross-Validation: Methodology and Experimental Evidence
Protocol and Workflow
Cross-validation is a cornerstone technique for estimating how a model will perform in practice. The most common form is k-fold cross-validation, and its application in lncRNA signature development follows a standardized workflow:
- Data Partitioning: The entire dataset is randomly split into
kroughly equal-sized folds or subsets. A common strategy is to use a function likecreateDataPartitionfrom the Rcaretpackage to ensure the distribution of key labels (e.g., survival status) is consistent across folds [78]. - Iterative Training and Validation: The model is trained
ktimes. In each iteration,k-1folds are used as the training set, and the remaining single fold is used as the validation set. - Performance Aggregation: The performance metric (e.g., AUC, C-index) from each of the
kiterations is averaged to produce a single, more robust estimate. Ten-fold cross-validation is a frequently used standard [81] [82].
Table 1: Key Parameters for k-Fold Cross-Validation in cited Studies
| Study Context | Value of k | Number of Iterations | Primary Performance Metric |
|---|---|---|---|
| Urine Biomarker Panel for HCC Screening [81] | 10 | 1,000 | Sensitivity, Specificity, AUC |
| HBV-related cACLD Machine Learning Model [82] | 10 | Not Specified | AUC, Accuracy, Sensitivity |
| LASSO-Cox Regression for lncRNA Signature [80] | 10 | 1,000 | Model Coefficients |
Supporting Data and Comparative Performance
Cross-validation provides a critical check on model performance before external validation. In a study comparing statistical methods for an HCC screening test, models were evaluated through repeated 10-fold cross-validation (1,000 iterations). This rigorous process assessed not only accuracy but also the robustness (low variability) of the models [81]. The study demonstrated that models like Random Forest (RF) and a novel Two-Step (TS) model showed higher sensitivity and specificity than traditional logistic regression, with cross-validation ensuring these claims were not due to overfitting [81].
Another study developed a prognostic model for intermediate-stage HCC patients treated with TACE. The model's discriminatory ability was quantified by the C-statistic (equivalent to AUC), which was calculated through cross-validation, yielding a value of 0.66. This provided evidence that the model's performance was reliable and superior to an existing subclassification system (C-statistic 0.60) [83] [84].
Diagram 1: k-Fold Cross-Validation Workflow. This diagram illustrates the iterative process of partitioning data into k folds, training and validating the model k times, and aggregating the results.
Bootstrap Resampling: Methodology and Experimental Evidence
Protocol and Workflow
Bootstrap resampling is a powerful technique for assessing the stability and uncertainty of model predictions. Instead of partitioning data into folds, it creates multiple new datasets by random sampling with replacement from the original dataset.
- Resampling: From a dataset of size
N, a bootstrap sample is created by randomly selectingNobservations, one at a time, with replacement. This means some observations may be selected multiple times, while others may not be selected at all. The unsampled observations form the "out-of-bag" (OOB) sample. - Model Building and Validation: A model is built on the bootstrap sample and can be validated on the OOB sample.
- Repetition and Averaging: This process is repeated many times (e.g., 1,000 times). The results across all bootstrap samples are averaged to estimate the model's performance and the stability of its parameters [83] [84].
Supporting Data and Comparative Performance
Bootstrap resampling is extensively used for internal validation of prognostic models. In the development of a cuproptosis-related lncRNA model for HBV-HCC, the researchers used the R boot package to perform bootstrap resampling with replacement as a method for the internal validation of their prognostic model [80]. This approach helped confirm that their 3-lncRNA signature was robust.
Similarly, in the TACE prognosis study, bootstrap resampling (1,000 data re-samplings) was used specifically to assess the model's discriminatory ability (C-statistic) and for model selection [84]. The resampling demonstrated that the model maintained sufficient discriminant power, with an average C-statistic of 0.66 (95% CI: 0.65-0.68) [83] [84]. This narrow confidence interval, derived from bootstrapping, provides strong evidence for the model's stability.
Table 2: Application of Bootstrap Resampling in cited Studies
| Study Context | Number of Resamples | Primary Purpose | Outcome |
|---|---|---|---|
| Prognosis after cTACE [83] [84] | 1,000 | Assess discriminatory ability & model selection | C-statistic: 0.66 (95% CI 0.65-0.68) |
| Cuproptosis-related lncRNA Signature [80] | Not Specified | Internal validation of the risk model | Validation of a 3-lncRNA signature |
| Machine Learning for HCC Risk [82] | Implied in feature selection | Feature selection stability | Identified 5 key predictors (e.g., LSM, age) |
Diagram 2: Bootstrap Resampling Process. This diagram shows the creation of multiple bootstrap samples by sampling with replacement, used to build and validate models to assess performance and parameter stability.
Direct Comparison and Guidelines for Use
While both techniques aim to improve model generalizability, they have different strengths and can be used complementarily.
Table 3: Cross-Validation vs. Bootstrap Resampling
| Feature | Cross-Validation | Bootstrap Resampling |
|---|---|---|
| Primary Strength | Less biased estimate of model performance on unseen data. | Excellent for estimating the stability and variance of model parameters and performance. |
| Data Usage | Efficient as every observation is used for both training and validation exactly once. | Some observations are used multiple times, others not at all in a given sample. |
| Common Application | Model Evaluation & Selection: Comparing different models or algorithms to choose the best performer. | Internal Validation & Stability Assessment: Validating a final model and understanding the confidence of its predictions. |
| Output | A robust estimate of a performance metric (e.g., mean AUC). | A distribution of a performance metric or model parameter, allowing for confidence interval calculation. |
| Typical Setup | 5- or 10-fold is standard. | 1,000+ resamples are common for stable estimates. |
The choice between them often depends on the research goal. Cross-validation is often preferred for model selection and tuning during the development phase. For instance, when using LASSO regression, 10-fold cross-validation is the standard method for selecting the optimal penalization parameter (λ) [80] [82]. Conversely, bootstrap resampling is highly effective for the internal validation of a final chosen model and for quantifying the confidence in its predictions, as seen in the prognostic models for HCC [83] [80] [84]. For the most rigorous validation, a combination of both is recommended—using cross-validation for model selection and bootstrap to assess the final model's stability.
Table 4: Key Reagent Solutions for lncRNA Prognostic Signature Development
| Reagent / Resource | Function / Application | Example Use in Context |
|---|---|---|
| TCGA-LIHC Dataset | Provides comprehensive transcriptomic (RNA-seq) and clinical data for HCC patients. | Primary data source for identifying differentially expressed lncRNAs and survival analysis [78] [79]. |
| R Statistical Software | Open-source environment for statistical computing and graphics. | Platform for all data analysis, including implementation of cross-validation and bootstrap resampling [78] [85]. |
R glmnet Package |
Fits LASSO and Elastic-Net regularized regression models. | Key for building parsimonious prognostic signatures by selecting the most relevant lncRNAs from a large pool [78] [80]. |
R caret Package |
Streamlines the process for creating predictive models. | Used for data partitioning (e.g., createDataPartition) and training control in cross-validation [78]. |
R boot Package |
Provides facilities for bootstrapping and related resampling methods. | Used for performing bootstrap resampling for internal model validation [80]. |
R survival Package |
Core package for survival analysis. | Used for Kaplan-Meier curves, log-rank tests, and Cox proportional hazards regression [78] [85]. |
| CIBERSORT/quanTIseq | Computational tools for deconvoluting immune cell fractions from bulk RNA-seq data. | Used to explore the correlation between the lncRNA signature and the tumor immune microenvironment [78] [85]. |
| Cell Culture & siRNA | Experimental Validation: In vitro models for functional studies. | Used to knock down lncRNAs (e.g., MKLN1-AS) to confirm their role in HCC cell proliferation [78] [80]. |
In the pursuit of clinically relevant lncRNA-based prognostic signatures for HCC, cross-validation and bootstrap resampling are not optional but essential. Cross-validation provides a robust framework for model selection and performance estimation, while bootstrap resampling offers deep insights into model stability and reliability. The experimental data and protocols outlined in this guide demonstrate that these techniques, when applied rigorously, can significantly improve the transparency and credibility of research findings. As the field moves towards more complex models, including those built with machine learning [81] [82], the disciplined application of these validation strategies will be the cornerstone of generating prognostic tools that truly benefit patients.
Rigorous Validation and Clinical Translation: From Signatures to Applications
In the field of hepatocellular carcinoma (HCC) research, the development of long non-coding RNA (lncRNA) based prognostic signatures has emerged as a pivotal strategy for risk stratification and treatment personalization [9]. The translation of these molecular signatures from research discoveries to clinically applicable tools hinges on the rigor of their statistical validation. This guide objectively compares the performance of different validation methodologies—specifically the use of internal versus external validation cohorts—employed in recent HCC lncRNA studies. The paradigm has shifted from simple single-cohort analyses to complex multi-tiered validation frameworks that incorporate machine learning, multi-omics integration, and functional experimental confirmation [86] [73]. By examining experimental protocols and performance metrics across recent studies, this guide provides researchers with a standardized framework for evaluating and implementing robust validation strategies in HCC biomarker development.
Comparative Analysis of Validation Cohort Methodologies
Table 1: Overview of Validation Cohort Designs in Recent HCC lncRNA Studies
| Study Focus | Internal Validation Approach | External Validation Source | Cohort Splitting Ratio | Key Performance Metrics |
|---|---|---|---|---|
| PANoptosis-related lncRNAs [73] | Training/Test split (TCGA) | ICGC database (n=231) | 70:30 | C-index: 0.681; 1-,3-,5-year AUCs |
| Plasma Exosomal lncRNAs [86] | 10-fold cross-validation | ICGC/GSE14520 | Not specified | C-index; AUC for risk stratification |
| Disulfidptosis-related lncRNAs [14] | Training/Validation (TCGA) | None | 50:50 | 1-year AUC: 0.756; 3-year: 0.695 |
| Four-DRL Signature [87] | Multivariate Cox with LASSO | Clinical sample validation | Not specified | 1-year AUC: 0.750; 3-year: 0.709 |
| Migrasome-related lncRNAs [17] | Training/Testing split | Independent clinical cohort (n=100) | 50:50 | Time-dependent ROC analysis |
Table 2: Performance Metrics Comparison Across Validation Types
| Validation Type | Average 1-Year AUC | Average 3-Year AUC | Statistical Power Assessment | Clinical Translational Potential |
|---|---|---|---|---|
| Internal Validation Only | 0.72-0.76 | 0.69-0.71 | Limited | Moderate |
| Internal + Database External | 0.75-0.81 | 0.70-0.78 | Moderate | High |
| Internal + Clinical External | 0.76-0.83 | 0.72-0.80 | Strong | Very High |
| Multi-Cohort External | 0.78-0.85 | 0.75-0.82 | Very Strong | Highest |
Experimental Protocols for Cohort Validation
Internal Validation Methodologies
Data Preprocessing and Quality Control
The foundational step across all studies involves rigorous data preprocessing from publicly available databases such as The Cancer Genome Atlas (TCGA-LIHC). The standard protocol includes RNA-seq data normalization using TMM (Trimmed Mean of M-values) method in edgeR, filtering of low-expression genes (Counts Per Million >1 in at least 50% of samples), and log2(CPM+1) transformation [87]. Principal component analysis (PCA) is routinely performed to identify and address batch effects. For studies incorporating machine learning approaches, the data preprocessing pipeline expands to include missing data imputation, feature scaling, and dimensionality reduction prior to model training [86].
Cohort Partitioning Strategies
Random partitioning of the primary cohort into training and testing subsets represents the most common internal validation approach. The partitioning ratios vary significantly across studies, with 70:30 and 50:50 being the most prevalent [73] [14]. The 70:30 ratio provides more data for model development while maintaining adequate testing samples, whereas the 50:50 approach offers balanced sets for both training and validation. For smaller cohorts (<200 samples), repeated k-fold cross-validation (typically 10-fold) is preferred to maximize data utilization and obtain more stable performance estimates [86]. The survival package in R serves as the primary tool for conducting survival analyses and calculating hazard ratios with 95% confidence intervals.
External Validation Frameworks
Independent Database Validation
The use of independent genomic databases represents the most accessible form of external validation. The standard protocol involves applying the established risk model to completely independent datasets such as the International Cancer Genome Consortium (ICGC-LIRI) or Gene Expression Omnibus (GSE14520) cohorts [86] [73]. This approach validates the generalizability of the signature across different populations and sequencing platforms. The validation process includes recalculating risk scores using the original model coefficients, stratifying patients into high- and low-risk groups based on the predetermined cutoff, and assessing prognostic performance through Kaplan-Meier survival analysis and time-dependent receiver operating characteristic (ROC) curves.
Prospective Clinical Cohort Validation
The most rigorous validation involves prospective collection of clinical samples. The protocol described in migrasome-related lncRNA research involves collecting 100 independent HCC tissue samples with complete clinical follow-up [17]. This cohort is typically further divided into multiple validation sets (e.g., 50:50 split) to assess consistency. The experimental workflow includes RNA extraction, quantitative reverse transcription PCR (qRT-PCR) analysis of the signature lncRNAs, and application of the predefined risk score formula. This approach not only validates the molecular signature but also confirms its practical applicability in a clinical setting, addressing pre-analytical variables and assay performance.
Machine Learning Integration in Validation
Advanced studies have incorporated multiple machine learning algorithms to enhance validation robustness. The methodology involves systematically comparing ten algorithms including CoxBoost, stepwise Cox, LASSO, Ridge, elastic net, survival-SVMs, generalized boosted regression models, supervised principal components, partial least squares Cox, and random survival forests [86]. These algorithms are evaluated under a 10-fold cross-validation framework, with the concordance index (C-index) serving as the primary metric for model selection. The optimal model is then validated across external cohorts to ensure algorithmic stability and predictive performance independent of the training data characteristics.
Visualization of Validation Workflows
Statistical Validation Workflow in HCC lncRNA Studies
Table 3: Essential Research Reagents and Computational Tools for Validation Studies
| Category | Specific Tools/Reagents | Function in Validation | Example Implementation |
|---|---|---|---|
| Bioinformatics Tools | edgeR, DESeq2, limma | Data normalization and differential expression | TMM normalization in disulfidptosis studies [87] |
| Statistical Packages | survival, survminer, timeROC (R) | Survival analysis and ROC curve generation | Kaplan-Meier plots and AUC calculation [14] |
| Machine Learning Libraries | glmnet, randomForestSRC, caret | Predictive model building and validation | 10-algorithm comparison framework [86] |
| Experimental Validation | qRT-PCR reagents, cell lines (Huh7, MIHA) | Technical verification of lncRNA expression | AC026412.3 functional validation [87] |
| Data Resources | TCGA-LIHC, ICGC, GEO, exoRBase | Primary and external validation cohorts | Multi-database integration (n=831 samples) [86] |
The comparative analysis of validation paradigms in HCC lncRNA research reveals a clear hierarchy of methodological rigor. Internal validation through cohort partitioning provides the foundational evidence for prognostic performance, while external validation against independent databases establishes generalizability across platforms and populations. The most compelling evidence emerges from studies that incorporate prospective clinical cohorts and functional experimental validation, as demonstrated in the migrasome-related lncRNA study [17] and the disulfidptosis-related lncRNA research [87]. The integration of multiple machine learning algorithms represents an emerging best practice that enhances model robustness and minimizes algorithmic bias. For researchers developing lncRNA-based prognostic signatures, implementing a comprehensive validation framework that spans internal, external, and clinical verification is essential for translating molecular discoveries into clinically applicable tools. Future standards should emphasize prospective multi-center validation cohorts and standardized performance reporting to facilitate cross-study comparison and clinical adoption.
Hepatocellular carcinoma (HCC) presents a significant global health challenge, characterized by high molecular heterogeneity and variable patient outcomes. Traditional prognostic assessment relying on clinicopathological staging systems such as the Tumor-Node-Metastasis (TNM) classification and Barcelona Clinic Liver Cancer (BCLC) staging has demonstrated limitations in accuracy and fails to fully capture the underlying molecular drivers of tumor behavior [88]. In recent years, long non-coding RNA (lncRNA) signatures have emerged as powerful molecular prognostic tools. This guide provides an objective comparison of the performance between novel lncRNA-based prognostic signatures and conventional staging systems, offering experimental validation data and methodological insights for researchers and drug development professionals.
Performance Comparison: Quantitative Data Analysis
Multiple independent studies conducted in 2025 have systematically compared the prognostic performance of lncRNA signatures against conventional staging systems. The quantitative data below demonstrate the superior predictive accuracy of lncRNA-based approaches.
Table 1: Comparative Performance of lncRNA Signatures vs. Conventional Staging
| Prognostic Model | Study Cohort | Predictive Accuracy (C-index/AUC) | Comparison to Conventional Staging | Reference |
|---|---|---|---|---|
| 4-DRL disulfidptosis signature | TCGA-LIHC (n=365) | 1-year AUC: 0.7503-year AUC: 0.7095-year AUC: 0.720C-index: 0.681 | Outperformed BCLC, CLIP, TNM staging systems | [88] |
| Consensus AI-driven Prognostic Signature (CAIPS) | Multi-center (n=1110) | Highest C-index across 6 cohorts | Surpassed traditional clinical parameters and 150 published signatures | [50] |
| 7-lncRNA risk model | TCGA-LIHC | AUC: 0.827 (training)0.757 (all patients) | Predictive accuracy superior to TNM stage | [66] |
| Plasma exosomal lncRNA 6-gene risk score | Multi-cohort (n=831) | High prognostic accuracy demonstrated | Provided molecular stratification beyond conventional staging | [5] [89] |
| PANoptosis-related lncRNA (PRL) score | TCGA+ICGC validation | Significant prognostic stratification (p<1.813×10â»â¸) | Independent prognostic value beyond clinical parameters | [73] |
Table 2: Clinical Utility and Therapeutic Prediction Capabilities
| Model Type | Therapeutic Response Prediction | Immune Microenvironment Insights | Experimental Validation | |
|---|---|---|---|---|
| Disulfidptosis-related lncRNAs | Identified sensitivity to 5 agents (Osimertinib, Paclitaxel, etc.); High TIDE scores predict immunotherapy non-response | Elevated M0 macrophage infiltration; Immunosuppressive microenvironment | AC026412.3 knockdown suppressed proliferation, invasion, migration in vitro and in vivo | [88] |
| Plasma exosomal lncRNA signature | Low-risk: superior anti-PD-1 responseHigh-risk: sensitivity to DNA-damaging agents, sorafenib | C3 subtype showed Treg infiltration, elevated PD-L1/CTLA4, highest TIDE score | Six-gene signature validated in HCC cell lines | [5] [89] |
| Consensus AI-derived signature | Low-score: enhanced response to TACE, targeted therapies, immunotherapy | Linked to metabolic pathway dysregulation and genomic instability | PITX1 knockdown suppressed HCC proliferation via Wnt/β-catenin inhibition | [50] |
| PANoptosis-related lncRNAs | Drug sensitivity prediction via GDSC database | Immune infiltration analysis via ssGSEA | PRL knockdown suppressed HCC progression and invasiveness | [73] |
Methodological Approaches: Experimental Protocols
Signature Development and Validation Workflow
The construction of robust lncRNA prognostic signatures follows a systematic multi-step process that integrates high-throughput transcriptomic data with advanced computational approaches:
Data Acquisition and Preprocessing: Transcriptomic data are obtained from public databases such as The Cancer Genome Atlas (TCGA-LIHC), Gene Expression Omnibus (GEO), and International Cancer Genome Consortium (ICGC). RNA-seq data undergo quality control, normalization (e.g., log2(CPM+1) transformation), and batch effect correction [88].
Identification of Prognostic lncRNAs: Differential expression analysis identifies lncRNAs significantly dysregulated in HCC versus normal tissues. Weighted Gene Co-expression Network Analysis (WGCNA) and correlation analyses pinpoint functional lncRNA modules associated with clinical traits or specific biological processes (e.g., PANoptosis, disulfidptosis) [73] [90].
Feature Selection and Model Construction: Machine learning algorithms systematically evaluate candidate lncRNAs. The 2025 multi-center study by Yang et al. integrated ten machine learning algorithms (101 method combinations), identifying StepCox[both] combined with Generalized Boosted Regression Models (GBM) as optimal for constructing a consensus artificial intelligence-derived prognostic signature (CAIPS) [50]. Alternative approaches employ LASSO-Cox regression to prevent overfitting [66] [88].
Validation and Performance Assessment: Models are validated internally via cross-validation and externally using independent cohorts. Time-dependent receiver operating characteristic (ROC) analysis evaluates predictive accuracy at 1, 3, and 5 years. Concordance indices (C-index) and hazard ratios from multivariate Cox regression establish independent prognostic value [88].
Clinical Translation: Nomograms integrate lncRNA risk scores with conventional clinical parameters (TNM stage, Child-Pugh grade) to enhance prognostic precision [66] [90].
Figure 1: Workflow for lncRNA Prognostic Signature Development and Validation
Functional Validation Protocols
Rigorous experimental validation confirms the biological relevance and functional roles of signature lncRNAs:
In Vitro Functional Assays:
- Gene Expression Validation: RT-qPCR confirms dysregulation of identified lncRNAs in HCC cell lines (e.g., Huh7) compared to normal hepatocytes [5] [73].
- Phenotypic Functional Tests: Knockdown approaches (siRNA/shRNA) assess the impact of candidate lncRNAs on malignant phenotypes. For example, AC026412.3 suppression significantly inhibited HCC cell proliferation, invasion, and migration in vitro [88]. Similarly, MKLN1-AS suppression reduced cell proliferation in CCK8 assays [66].
In Vivo Validation:
- Xenograft Tumor Models: Orthotopic implantation models demonstrate the necessity of lncRNAs for primary tumor growth and metastasis. AC026412.3 was essential for pulmonary metastasis and epithelial-mesenchymal transition activation in vivo [88].
- Angiogenesis Assessment: Chorioallantoic membrane assays evaluate the impact of lncRNAs on tumor angiogenesis [88].
Mechanistic Investigations:
- Pathway Analysis: Western blot analysis and luciferase reporter assays elucidate signaling pathways. PITX1 knockdown was mechanistically attributed to Wnt/β-catenin signaling inhibition [50].
- Immune Microenvironment Characterization: CIBERSORT algorithm and gene set enrichment analysis (GSEA) evaluate immune cell infiltration and pathway activity [5] [90].
Key Signaling Pathways and Biological Mechanisms
lncRNA signatures capture critical biological processes beyond the resolution of conventional staging:
Figure 2: Biological Mechanisms Captured by lncRNA Prognostic Signatures
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for lncRNA Signature Validation
| Reagent/Resource | Primary Application | Specific Function | Example Implementation |
|---|---|---|---|
| TCGA-LIHC Dataset | Bioinformatics Analysis | Provides transcriptomic and clinical data for model development | Primary cohort for signature discovery [66] [88] |
| ICGC-LIRI-JP Cohort | Independent Validation | External validation cohort for model generalization | Validation of disulfidptosis-related lncRNA signature [88] |
| Huh7 Cell Line | In Vitro Experiments | Human HCC cell model for functional studies | Validation of AC026412.3 oncogenic functions [88] |
| CIBERSORT Algorithm | Immune Microenvironment Analysis | Deconvolutes immune cell infiltration from transcriptomic data | Identified M0 macrophage enrichment in high-risk groups [5] [90] |
| TIDE Platform | Immunotherapy Response Prediction | Computational framework for assessing immune evasion potential | Predicted anti-PD-1 response in plasma exosomal lncRNA study [5] |
| oncoPredict R Package | Drug Sensitivity Screening | Predicts chemotherapeutic response from genomic data | Identified sensitivity to Wee1 inhibitor MK-1775 in high-risk patients [5] |
| GDSC Database | Pharmacogenomic Profiling | Database linking genomic features to drug sensitivity | Screening for candidate therapeutics (e.g., Irinotecan, BI-2536) [50] [73] |
| Noxa B BH3 | Noxa B BH3, MF:C95H164N30O31S, MW:2254.6 g/mol | Chemical Reagent | Bench Chemicals |
The comprehensive evidence from recent 2025 studies demonstrates that lncRNA-based prognostic signatures consistently outperform conventional staging systems in HCC prognosis. These molecular tools provide superior predictive accuracy, with disulfidptosis-related signatures achieving C-indices of 0.681 and AUC values up to 0.750 at 1-year survival prediction [88]. Beyond prognostic stratification, lncRNA signatures offer unprecedented insights into tumor biology, capturing dysregulation in programmed cell death pathways, immune microenvironment composition, and metabolic pathways. Critically, they enable prediction of therapeutic responses to immunotherapy, targeted agents, and chemotherapy, guiding personalized treatment decisions. While conventional staging remains valuable for initial assessment, the integration of lncRNA signatures represents a paradigm shift toward molecular-driven precision oncology in HCC management. Future directions should focus on standardizing analytical protocols and translating these biomarkers into clinical practice through prospective trials.
Within the broader thesis on validating long non-coding RNA (lncRNA)-based prognostic signatures in hepatocellular carcinoma (HCC) cohorts, multivariate Cox regression analysis emerges as an indispensable statistical tool. This method enables researchers to determine whether a newly discovered lncRNA signature provides prognostic information independent of established clinical factors such as tumor stage, grade, and patient age [91] [92]. The integration of molecular biomarkers with traditional clinicopathological features represents a paradigm shift in prognostic model development, moving beyond staging systems that rely solely on clinical and morphological characteristics [92]. As the field advances toward personalized medicine, the rigorous validation of lncRNA signatures through multivariate Cox regression becomes crucial for establishing their clinical utility in HCC risk stratification and treatment decision-making.
Experimental Protocols for Signature Development and Validation
Data Acquisition and Preprocessing
The foundational step in constructing lncRNA-based prognostic signatures involves the acquisition of high-quality, comprehensive datasets. Researchers typically obtain RNA sequencing data and corresponding clinical information from large-scale repositories such as The Cancer Genome Atlas (TCGA) Liver Hepatocellular Carcinoma (LIHC) dataset [91] [92] [14]. For example, one study utilized 374 HCC samples from TCGA, while another analyzed 377 HCC samples alongside 50 adjacent non-tumor tissues [91] [30]. The preprocessing pipeline includes quality control measures, normalization of raw read counts (often using FPKM or TPM methods), and annotation of lncRNAs using reference databases like GENCODE [91]. Clinical data must be carefully curated, with particular attention to overall survival (OS) and relapse-free survival (RFS) endpoints, along with standard clinicopathological variables including tumor stage, grade, and patient demographics.
Identification of Prognostic LncRNA Candidates
The process of identifying lncRNAs with potential prognostic value typically involves a multi-step analytical approach:
Differential Expression Analysis: Researchers compare lncRNA expression profiles between tumor and adjacent normal tissues using statistical packages such as "edgeR" and "limma" in R [91]. Standard thresholds (e.g., |log2FC| > 0.5 or 1.0 with adjusted p-value < 0.05) identify significantly dysregulated lncRNAs in HCC.
Univariate Cox Regression Screening: Each differentially expressed lncRNA undergoes initial screening for association with survival outcomes using univariate Cox proportional hazards models [92] [14]. LncRNAs demonstrating significant association (typically p < 0.05 or more stringent thresholds) advance to subsequent modeling phases.
Incorporation of Biological Context: Some studies further refine candidate lncRNAs by focusing on those associated with specific biological processes, such as T-cell exclusion in the tumor microenvironment [91], costimulatory molecules [30], or novel cell death mechanisms like disulfidptosis [14].
Signature Construction via LASSO and Multivariate Cox Regression
The core analytical workflow for developing a refined prognostic signature integrates machine learning techniques with survival analysis:
Dataset Partitioning: The complete cohort is randomly divided into training and validation sets, typically at a 1:1 ratio, using R packages like "caret" to ensure balanced distribution of clinical characteristics [91] [14].
LASSO (Least Absolute Shrinkage and Selection Operator) Regression: This regularization technique addresses overfitting by penalizing the magnitude of coefficients and effectively selecting the most predictive lncRNAs from the candidate pool [91] [92]. The process involves 10-20 fold cross-validation to determine the optimal penalty parameter (lambda) that minimizes prediction error.
Multivariate Cox Regression Modeling: The lncRNAs retained from LASSO regression enter a multivariate Cox proportional hazards model alongside key clinicopathological variables [91] [92] [30]. This critical step determines whether each lncRNA retains independent prognostic value after adjusting for established clinical factors. The final output includes regression coefficients for each lncRNA in the signature.
Risk Score Calculation: A personalized risk score is computed for each patient using the formula: Risk score = Σ(Expressioni × Coefficienti), where Expressioni represents the normalized expression level of each lncRNA in the signature, and Coefficienti is its corresponding weight derived from the multivariate Cox model [91] [14].
Model Validation and Performance Assessment
Rigorous validation protocols ensure the reliability and generalizability of the prognostic signature:
Survival Analysis: Patients are stratified into high-risk and low-risk groups based on the median risk score or optimal cut-off value. Kaplan-Meier curves with log-rank tests compare survival distributions between these groups in both training and validation cohorts [92] [14] [30].
Time-Dependent ROC Analysis: Receiver operating characteristic (ROC) curves at 1, 3, and 5 years evaluate the predictive accuracy of the signature, with the area under the curve (AUC) providing a quantitative measure of performance [92] [14].
Comparison with Established Staging Systems: Researchers assess whether the lncRNA signature provides incremental prognostic value beyond conventional staging systems (e.g., BCLC, TNM) through statistical measures such as Harrell's concordance index (C-index) [93] [92].
Clinical Utility Assessment: Decision curve analysis and calibration plots evaluate the potential clinical net benefit of using the signature for risk stratification [94].
The following diagram illustrates the comprehensive experimental workflow for developing and validating lncRNA-based prognostic signatures using multivariate Cox regression analysis:
Comparative Performance of LncRNA-Based Prognostic Signatures
Established LncRNA Signatures in HCC
Multiple lncRNA-based prognostic signatures have been developed and validated through multivariate Cox regression analysis, demonstrating variable predictive performance across studies. The table below summarizes key signatures reported in recent literature:
Table 1: Comparison of LncRNA-Based Prognostic Signatures in HCC
| Signature Name/Description | Number of LncRNAs | Validation Cohort | Key Clinicopathological Features Adjusted | Performance Metrics (AUC) | Independent Prognostic Value |
|---|---|---|---|---|---|
| 11LNCPS (TCE-associated) [91] | 11 | TCGA (n=373, 1:1 split) | Age, gender, stage, T cell exclusion | Not specified | Yes (p<0.05) |
| OS Classifier [92] | 8 | TCGA (n=369) | TNM stage, grade | 1-year: 0.778, 3-year: 0.677, 5-year: 0.712 (training) | Yes (p<0.001) |
| RFS Classifier [92] | 6 | TCGA (n=369) | TNM stage, grade | Not specified for RFS | Yes (p<0.001) |
| Disulfidptosis-Related Signature [14] | 3 | TCGA (n=369, 1:1 split) | Age, gender, stage, TNM | 1-year: 0.756, 3-year: 0.695, 5-year: 0.701 | Yes (p<0.01) |
| Costimulatory Molecule-Related Signature [30] | 5 | TCGA (n=343, 1:1 split) | Age, gender, stage | 1-year: 0.778, 3-year: 0.677, 5-year: 0.712 (training) | Yes (p<0.001) |
Comparison with Traditional Biomarker Models
Traditional biomarker-based prognostic models for HCC have primarily relied on serum proteins, with recent composite models incorporating multiple biomarkers. The BALAD-2 model, which integrates bilirubin, albumin, AFP-L3%, AFP, and des-gamma-carboxy prothrombin (DCP), has demonstrated robust performance in recent comparative studies [93]. When evaluated in a biobank-based cohort of 186 HCC patients, BALAD-2 achieved a C-index of 0.737 and the highest AUC values at 1 year (0.827), 2 years (0.846), 3 years (0.781), and 5 years (0.716), outperforming other biomarker models including GALAD, ASAP, and aMAP [93]. This model maintained superior discrimination across patient subgroups, particularly among those receiving curative therapy and those with viral etiologies.
Integration of LncRNA Signatures with Clinicopathological Features
Multivariate Cox regression analyses consistently demonstrate that lncRNA-based signatures retain independent prognostic value after adjusting for established clinicopathological variables. Key findings include:
- The 11-lncRNA prognostic signature (11LNCPS) remained significantly associated with overall survival after adjusting for T cell exclusion levels and immune cell infiltration patterns [91].
- A 5-lncRNA costimulatory molecule-related signature maintained independent prognostic value in both training (HR=2.88, 95% CI: 1.65-5.05) and validation cohorts (HR=2.78, 95% CI: 1.62-4.79) after adjusting for standard clinical parameters [30].
- A disulfidptosis-related 3-lncRNA signature significantly predicted overall survival in multivariate analysis that included age, gender, and TNM stage [14].
Table 2: Multivariate Cox Regression Analyses of Selected LncRNA Signatures
| Signature | Clinical Covariates Included | Hazard Ratio (High vs. Low Risk) | 95% Confidence Interval | P-value |
|---|---|---|---|---|
| 11LNCPS [91] | Age, gender, stage, TCE status | Not specified | Not specified | <0.05 |
| 5-lncRNA Costimulatory Signature [30] | Age, gender, stage | 2.88 (training) | 1.65-5.05 | <0.001 |
| 5-lncRNA Costimulatory Signature [30] | Age, gender, stage | 2.78 (validation) | 1.62-4.79 | <0.001 |
| 3-lncRNA Disulfidptosis Signature [14] | Age, gender, stage, TNM | Not specified | Not specified | <0.01 |
Table 3: Key Research Reagents and Computational Tools for LncRNA Prognostic Model Development
| Resource Category | Specific Tools/Databases | Application in Prognostic Model Development |
|---|---|---|
| Data Sources | TCGA-LIHC dataset [91] [92] [14] | Primary source of RNA-seq data and clinical annotations for HCC |
| GEO datasets (e.g., GSE146115) [91] | Supplementary data for validation and single-cell analyses | |
| Computational Tools | R packages: "edgeR", "limma" [91] | Differential expression analysis |
| R packages: "survival", "glmnet" [91] [92] | LASSO and Cox regression analysis | |
| R package: "survivalROC" [14] | Time-dependent ROC analysis | |
| R package: "rms" [91] [14] | Nomogram construction and calibration plots | |
| TIDE algorithm [91] | Assessment of T-cell exclusion and dysfunction | |
| Experimental Validation | Plasma/Serum RNA Purification Kits [52] | RNA isolation from liquid biopsies |
| RT-qPCR reagents and systems [52] | Validation of lncRNA expression patterns | |
| Cell culture models and functional assay reagents [30] | In vitro validation of lncRNA biological functions |
Multivariate Cox regression analysis serves as the statistical cornerstone for validating the independent prognostic value of lncRNA signatures in HCC. The growing body of evidence demonstrates that rigorously developed lncRNA-based models consistently predict patient survival outcomes after adjusting for established clinicopathological features. While traditional serum biomarker models like BALAD-2 show impressive performance, lncRNA signatures offer complementary molecular insights into tumor biology and microenvironment interactions. The integration of these molecular signatures with conventional clinical staging systems represents the most promising path toward refined HCC prognostication. Future research directions should include external validation in prospective cohorts, standardization of analytical pipelines, and development of clinically implementable platforms for lncRNA quantification in routine practice.
Functional enrichment analysis is a cornerstone for interpreting high-throughput genomic data, enabling researchers to transition from lists of differentially expressed genes to understanding underlying biological processes [95] [96]. Within the specific research context of validating long non-coding RNA (lncRNA)-based prognostic signatures in Hepatocellular Carcinoma (HCC), selecting the appropriate enrichment methodology is crucial for uncovering the biological mechanisms driven by these signatures and their connection to the tumor immune microenvironment [97] [17] [90].
This guide objectively compares the performance of Gene Set Enrichment Analysis (GSEA) against other common alternatives, namely Over-Representation Analysis (ORA) and topology-based pathway analysis. We focus on their application in HCC research, particularly for studies investigating immune-related lncRNA signatures and their correlation with immune infiltration patterns. Supporting experimental data from recent HCC studies is provided to illustrate key performance differences.
Methodological Comparison: GSEA vs. ORA vs. Topology-Based Analysis
Understanding the fundamental differences between these approaches is the first step in selecting the right tool.
Core Principles and Definitions
- Gene Set Enrichment Analysis (GSEA): A functional class scoring method that uses a ranked list of all genes from an expression dataset to determine whether predefined gene sets are enriched at the top or bottom of the list. It does not require a predefined significance cutoff for individual genes [95] [96] [98].
- Over-Representation Analysis (ORA): Tests whether genes from a predefined gene set are disproportionately represented (over-represented) in a list of differentially expressed genes (DEGs) compared to what would be expected by chance. It relies on a prior cutoff to define DEGs [95] [98].
- Topology-Based (TB) Pathway Analysis: Goes beyond treating pathways as simple gene lists by incorporating known pathway structures, including the type, direction, and position of interactions between genes. Methods like Impact Analysis and SPIA fall into this category [98].
Key Performance Differentiators in HCC Research
The table below summarizes the critical differences between these methods, highlighting their implications for research on lncRNA signatures in HCC.
Table 1: Performance Comparison of Functional Enrichment Methods in HCC Research
| Feature | GSEA | ORA | Topology-Based Analysis |
|---|---|---|---|
| Input Data | All genes, ranked by expression change [95] [96] | A list of differentially expressed genes (DEGs) [95] [98] | Gene expression data with pathway topology [98] |
| Handling of Subtle Changes | Excellent. Detects coordinated, subtle shifts in expression across a gene set [95] [96] | Poor. Only considers genes passing a strict cutoff, missing subtle effects [98] | Varies. Can be sensitive if the topology amplifies subtle changes [98] |
| Use of Expression Data | Uses the full ranked list; calculates an Enrichment Score (ES) and Normalized ES (NES) [95] | Uses only a binary (yes/no) classification of genes as DEGs [98] | Uses expression changes in the context of pathway structure [98] |
| Biological Insight | Identifies pathways activated (positive NES) or suppressed (negative NES) as a whole [95] | Identifies pathways that are over-represented in the DEG list [95] | Predicts pathway perturbation and signal propagation [98] |
| Ideal Use Case in HCC | Identifying global pathway dysregulation from full transcriptomic data [97] [99] | Quick analysis when a clear, high-confidence DEG list is available [95] | Understanding mechanism and downstream effects of dysregulation [98] |
Experimental Protocols and Applications in HCC
The following section outlines standard protocols for these methods, illustrated with examples from recent HCC studies on lncRNA prognostic signatures.
Standard GSEA Protocol
A typical GSEA workflow involves the following steps, which have been applied in recent HCC transcriptomic studies [97] [99]:
- Gene Ranking: All genes from the RNA-seq or microarray dataset are ranked based on their differential expression between conditions (e.g., high-risk vs. low-risk HCC patient groups). The ranking metric is often the signal-to-noise ratio or -log10(p-value) multiplied by the sign of the fold change [95].
- Enrichment Score Calculation: For each gene set (e.g., from MSigDB), GSEA walks down the ranked list, increasing a running enrichment score when a gene in the set is encountered and decreasing it when it is not. The Enrichment Score (ES) is the maximum deviation from zero encountered [95].
- Significance Assessment: The ES is normalized for gene set size to produce the Normalized Enrichment Score (NES). A p-value is calculated by comparing the observed ES to a null distribution generated by permuting the gene labels [95].
- Interpretation: A high positive NES indicates the gene set is enriched at the top of the list (associated with the first phenotype), while a high negative NES indicates enrichment at the bottom (associated with the second phenotype) [95].
Table 2: Key Research Reagent Solutions for Functional Enrichment Analysis
| Reagent / Resource | Function / Description | Example in HCC Research |
|---|---|---|
| MSigDB (Molecular Signatures Database) | A curated collection of annotated gene sets for GSEA and ORA [98]. | Used to investigate enrichment in Hallmark pathways, immunologic signatures, and oncogenic signatures [97]. |
| fGSEA R package | A fast implementation for pre-ranked GSEA, significantly reducing computation time [100]. | Ideal for rapid iterative analysis during model development of lncRNA signatures. |
| clusterProfiler R package | A versatile tool for performing and visualizing ORA and GSEA, integrating GO and KEGG databases [86] [90]. | Commonly used for functional annotation of DEGs derived from HCC prognostic models [90]. |
| CIBERSORT / ssGSEA | Algorithms for estimating immune cell infiltration from bulk transcriptome data [97] [90]. | Used to correlate lncRNA signature risk scores with levels of specific immune cells (e.g., T cells, macrophages) [97] [17]. |
| EnrichmentMap (Cytoscape App) | A network-based visualization tool for GSEA results, clustering related pathways [100]. | Helps visualize and interpret complex enrichment results, such as clusters of immune-related pathways. |
Supporting Data from HCC Studies
Recent studies validating lncRNA-based prognostic models in HCC consistently utilize GSEA to provide a deeper biological context for their findings.
- Immune and Metabolic Pathways: A study on a migrasome-related lncRNA signature used GSEA to demonstrate that high-risk HCC patients were significantly enriched in immune-related pathways (e.g., inflammatory response) and metabolic pathways, providing a mechanistic link to aggressive tumor behavior [17].
- Pathway-Level Validation: Research into a plasma exosomal lncRNA signature applied GSEA to validate the hyperactivation of specific biological processes in the high-risk subgroup, including glycolysis, E2F targets, and mTORC1 signaling [86].
- Single-Cell Validation: In the context of microvascular invasion (MVI), GSEA was applied to genes derived from single-cell RNA-sequencing. This analysis revealed significant enrichment in pathways critical to HCC progression, such as DNA replication, cell cycle regulation, and immune-related pathways [99].
Visualizing Analytical Workflows and Pathway Relationships
The following diagrams, generated using Graphviz DOT language, illustrate the core analytical workflows and logical relationships in functional enrichment analysis.
GSEA Workflow for HCC lncRNA Signatures
Pathway Enrichment Analysis Comparison
The choice between GSEA, ORA, and topology-based methods is not one of absolute superiority but of strategic application. For research focused on validating lncRNA-based prognostic signatures in HCC, GSEA offers a powerful advantage by capturing subtle, coordinated changes in biological pathways that are often central to cancer progression and immune evasion. Its ability to utilize a full ranked gene list makes it exceptionally suited for identifying pathway-level dysregulation that may be missed by ORA's strict cutoff approach. Topology-based methods provide the deepest layer of mechanistic insight. The consistent use of GSEA in recent, high-quality HCC studies [97] [86] [17] underscores its value as a critical tool for bridging the gap between a prognostic signature and its functional biological implications, particularly in the complex landscape of tumor immunology.
Hepatocellular carcinoma (HCC) represents a major global health challenge, ranking as the third leading cause of cancer-related deaths worldwide [3]. The treatment paradigm for advanced HCC has undergone a significant transformation with the introduction of immune checkpoint inhibitors (ICIs), which have demonstrated remarkable outcomes in subsets of patients [101] [102]. However, response rates to single-agent ICIs remain around 15-20%, highlighting the critical need for reliable predictive biomarkers [103] [102]. The complex heterogeneity of HCC's tumor immune microenvironment (TIME) necessitates sophisticated tools for patient stratification [3].
Long non-coding RNAs (lncRNAs), defined as RNA transcripts exceeding 200 nucleotides with limited protein-coding potential, have emerged as promising biomarker candidates [70]. They play critical regulatory roles in various biological processes, including immune response modulation, cell proliferation, and apoptosis [91] [73]. Their expression patterns are frequently dysregulated in HCC and can be quantitatively measured, making them suitable for developing multi-gene prognostic signatures [70] [46]. This review comprehensively compares established lncRNA-based prognostic signatures, evaluates their clinical utility for predicting immunotherapy response, and identifies therapeutic vulnerabilities in HCC.
Comparative Analysis of Established lncRNA Signatures
Researchers have employed various bioinformatics approaches and machine learning algorithms to identify and validate lncRNA signatures with prognostic value in HCC. The table below summarizes key multi-lncRNA signatures and their clinical performance characteristics.
Table 1: Comparison of Established lncRNA Prognostic Signatures in HCC
| Signature Name | Components (lncRNAs) | Development Cohort | Performance (AUC) | Clinical Utility |
|---|---|---|---|---|
| Four-lncRNA Signature [70] | RP11-495K9.6, RP11-96O20.2, RP11-359K18.3, LINC00556 | 180 HCC (TCGA/TANRIC) | >0.70 (Training) | Prognostic stratification; Independent of TNM stage |
| 11-lncRNA Prognostic Signature (11LNCPS) [91] | LINC01134, AC116025.2, +9 others | 374 HCC (TCGA) | 0.846 (Model) | Predicts immune cell infiltration (CD8+ T cells, DCs); Correlates with T-cell exclusion |
| Five-lncRNA PANoptosis Signature [73] | AL442125.2, MIR4435-2HG, AC026412.3, LINC01224, AC026356.1 | 370 HCC (TCGA), 231 (ICGC) | Not Specified | Links cell death mechanisms (PANoptosis) to prognosis and immune infiltration |
| Costimulatory Molecule-related Signature [30] | BOK-AS1, AC099850.3, AL365203.2, NRAV, AL049840.4 | 343 HCC (TCGA) | 1-year: 0.778, 3-year: 0.677, 5-year: 0.712 (Training) | Based on costimulatory molecules; AC099850.3 promotes HCC cell proliferation |
The performance of these signatures is frequently validated in independent test cohorts and sometimes external datasets like the International Cancer Genome Consortium (ICGC), confirming their robustness [73]. Notably, the 11LNCPS signature demonstrates superior predictive accuracy with an Area Under the Curve (AUC) of 0.846, outperforming several earlier models [91]. These signatures consistently categorize patients into high-risk and low-risk groups with significantly different overall survival (OS) outcomes. For instance, the four-lncRNA signature showed a median survival of 1.81 years for high-risk patients versus 8.56 years for low-risk patients in the training set [70].
Methodological Framework for Signature Development
The construction of a reliable lncRNA prognostic signature follows a structured analytical workflow. The following diagram illustrates the key steps from data acquisition to final model validation.
Key Analytical Techniques
Data Acquisition and Processing: The process typically begins with acquiring lncRNA expression data and corresponding clinical information from public repositories such as The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), or ICGC [70] [91] [73]. Data preprocessing involves normalization (e.g., converting raw counts to FPKM fragments per kilobase of transcript per million) and quality control, often removing patients with incomplete survival data [73] [30].
Identification of Prognostic LncRNAs: Differentially expressed lncRNAs between tumor and adjacent normal tissues are identified. Subsequently, univariate Cox regression analysis is performed to select lncRNAs significantly associated with overall survival (OS) [70] [91]. Many studies incorporate an additional filtering layer based on a biological theme, such as association with T-cell exclusion (TCE), PANoptosis, or co-expression with costimulatory molecules [91] [73] [30].
Signature Construction and Validation: The least absolute shrinkage and selection operator (LASSO) Cox regression is a widely used machine learning method to prevent overfitting and select the most predictive lncRNAs from the candidate pool [91] [73] [30]. A multivariate Cox proportional hazards model is then built to assign a coefficient (weight) to each selected lncRNA, forming a risk score formula:
Risk score = Σ(Coefficient_i × Expression_i)[91]. The model's performance is rigorously evaluated using time-dependent Receiver Operating Characteristic (ROC) curves, Kaplan-Meier survival analysis with log-rank tests, and concordance index (C-index) calculation, and validated in an independent test cohort [70] [91] [30].
Predicting Immunotherapy Response and Immune Landscape
A primary clinical application of lncRNA signatures is their ability to predict responses to immunotherapy and characterize the tumor immune microenvironment. These signatures provide insights beyond traditional biomarkers like PD-L1 expression, which has limited predictive utility in HCC [103].
Table 2: LncRNA Signatures and Association with Tumor Immune Microenvironment
| Signature | Immune Cell Correlations | Immunotherapy Prediction Value | Underlying Mechanisms |
|---|---|---|---|
| 11LNCPS [91] | ↓ CD8+ T cells, ↓ Dendritic Cells, ↓ Th1/Th2 cells | High-score patients transcriptomically similar to PDL1 inhibitor responders | Promotes T-cell exclusion (TCE); Alters chemokine/cytokine networks |
| PANoptosis Signature [73] | Correlated with specific immune infiltration patterns | Informs on chemotherapy and PD-1/PD-L1 treatment response | Regulates inflammatory programmed cell death (PANoptosis) |
| Costimulatory Signature [30] | Significant differences in immune infiltration levels | Provides insight for immunotherapeutic strategies | Based on direct link to B7-CD28/TNF costimulatory pathways |
The 11LNCPS signature is particularly notable for its direct link to immunosuppression. Patients with high 11LNCPS scores exhibit significant T-cell exclusion, characterized by reduced infiltration of cytotoxic CD8+ T cells and dendritic cells into the tumor bed, effectively creating an "immune-cold" phenotype [91]. This is mechanistically supported by single-cell RNA sequencing analysis, which suggests that lncRNAs like LINC01134 and AC116025.2 disrupt communication between HCC cells and CD8+ T cells by affecting chemokine, cytokine, and immune checkpoint ligand-receptor interactions [91]. Consequently, these signatures can identify patients who are less likely to benefit from ICIs monotherapy and may require combination strategies to overcome immune resistance.
Therapeutic Vulnerabilities and Research Toolkit
Beyond prognostication, lncRNA signatures unveil potential therapeutic vulnerabilities. Functional experiments on specific lncRNAs within these signatures confirm their oncogenic roles. For example, silencing GACAT3 (from an 11-lncRNA signature) significantly suppressed HCC cell proliferation, invasion, and migration in vitro [46]. Similarly, knockdown of AC099850.3 (from a costimulatory-related signature) strongly impaired HCC cell proliferation, identifying it as a potential therapeutic target [30].
The following table lists essential reagents and resources for researchers aiming to explore lncRNA biology and therapeutic potential in HCC.
Table 3: Research Reagent Solutions for LncRNA Investigation in HCC
| Reagent/Resource | Function/Application | Examples from Literature |
|---|---|---|
| Public Genomic Databases | Source for lncRNA expression data and clinical correlations | TCGA (The Cancer Genome Atlas), ICGC, GEO (Gene Expression Omnibus) [70] [91] [73] |
| Bioinformatics Software (R Packages) | Statistical analysis, model building, and visualization | "edgeR", "limma" (differential expression); "survival", "glmnet" (Cox/LASSO); "pROC", "survivalROC" (validation) [91] [73] |
| siRNAs/shRNAs | Gene knockdown to assess lncRNA function in vitro | Used for silencing GACAT3, AC099850.3 to confirm roles in proliferation/invasion [46] [30] |
| Cell Proliferation & Invasion Assays | Functional validation of lncRNA effects on malignancy | CCK-8, colony formation, Transwell invasion/migration assays [46] [30] |
| Pathway Analysis Tools | Uncover biological processes and signaling pathways affected | GSEA (Gene Set Enrichment Analysis), KEGG, GO (Gene Ontology) enrichment [70] [91] [73] |
Integrated Pathway of LncRNA-Mediated Immunosuppression
The mechanistic role of prognostic lncRNAs in shaping an immunosuppressive tumor microenvironment and promoting therapy resistance can be visualized through a unified signaling pathway. The following diagram synthesizes findings from multiple studies to illustrate this process.
This integrated pathway shows how dysregulated lncRNAs drive immunosuppression through multiple interconnected mechanisms: altering chemokine networks to impair T-cell recruitment, disrupting costimulatory signals needed for T-cell activation, and promoting inflammatory cell death pathways that shape a hostile microenvironment [91] [73] [30]. The resultant "cold" tumor phenotype, characterized by T-cell exclusion, directly contributes to reduced efficacy of ICIs [91].
LncRNA-based prognostic signatures represent a powerful and refined tool for risk stratification in HCC. Their ability to predict immunotherapy response and reveal therapeutic vulnerabilities positions them at the forefront of precision oncology. The integration of these molecular signatures with established clinical variables and emerging modalities like radiomics holds promise for developing more accurate predictive models [3] [104]. Future efforts should focus on the standardization of analytical protocols, technical validation of signatures in prospective clinical trials, and the functional characterization of individual lncRNAs to unlock their potential as novel therapeutic targets. The ongoing translation of these biomarkers from bioinformatics discoveries to clinical applications will be crucial for improving outcomes for HCC patients in the immunotherapy era.
Conclusion
The validation of lncRNA-based prognostic signatures represents a transformative approach in HCC management, addressing critical limitations of conventional staging systems. Synthesizing evidence across multiple studies reveals that rigorously validated multi-lncRNA models consistently demonstrate superior prognostic accuracy, with AUC values frequently exceeding 0.75-0.85 for predicting overall and recurrence-free survival. The integration of these signatures with specific biological pathways—including m6A modification, amino acid metabolism, and costimulatory molecule networks—provides not only prognostic value but also mechanistic insights into HCC pathogenesis. Future directions should focus on standardizing analytical pipelines, validating signatures in prospective multicenter trials, and developing lncRNA-targeted therapeutics. The functional validation of signature components like GACAT3 and AC099850.3, which demonstrate direct roles in HCC cell proliferation and invasion, underscores the dual utility of these signatures as both prognostic tools and sources of therapeutic targets. As the field advances, lncRNA signatures are poised to become integral components of precision oncology for HCC, enabling risk-adapted treatment strategies and ultimately improving patient outcomes.
References
- 1. Clinical potential and experimental validation of prognostic ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1541252/full]
- 2. Hypoxia- and Anoikis-Related lncRNA Signature Defines ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533731/]
- 3. Advances and challenges in immunotherapy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521690/]
- 4. New ESMO Clinical Guidelines for the diagnosis and ... [https://www.clinicbarcelona.org/en/news/new-esmo-clinical-guidelines-for-the-diagnosis-and-treatment-of-hepatocellular-carcinoma]
- 5. Plasma exosomal lncRNA-related signatures define ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1663943/full]
- 6. A reliable prognostic model for hepatocellular carcinoma ... [https://www.nature.com/articles/s41598-025-01335-1]
- 7. BCLC strategy for prognosis prediction and treatment ... [https://www.sciencedirect.com/science/article/abs/pii/S0168827825025711]
- 8. EASL 2025: Update to Guidance on the Management of ... [https://reference.medscape.com/cc1/p10/easl-2025-update-guidance-management-hepatocellular-2025a100082k]
- 9. Long non-coding RNA-based single and combination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12405140/]
- 10. Long non-coding RNAs: definitions, functions, challenges ... [https://www.nature.com/articles/s41580-022-00566-8]
- 11. Long Non-Coding RNAs, the Dark Matter - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC7795044/]
- 12. Localization is the key to action: regulatory peculiarities of ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2024.1478352/full]
- 13. Long non-coding RNA in hepatocellular carcinoma [https://link.springer.com/article/10.1007/s13402-025-01119-9]
- 14. A novel disulfidptosis-related lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12582836/]
- 15. Amino acid metabolism-related LncRNAs as prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12545943/]
- 16. Analysis of four long non-coding RNAs for hepatocellular ... [https://www.nature.com/articles/s41598-024-80926-w]
- 17. A migrasome-related lncRNA signature predicts prognosis ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581122/full]
- 18. HCC-Related lncRNAs: Roles and Mechanisms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10779127/]
- 19. The role of long non-coding RNA in hepatocellular carcinoma [https://www.aging-us.com/article/205523/text]
- 20. A study of the mechanism of lncRNA -CR594175 in regulating... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7510120/]
- 21. A study of the mechanism of lncRNA-CR594175 in regulating ... [https://infectagentscancer.biomedcentral.com/articles/10.1186/s13027-020-00321-8]
- 22. lncRNA-SOX2OT promotes hepatocellular carcinoma ... [https://www.nature.com/articles/s41389-020-0242-z]
- 23. lncRNA involvement in hepatocellular carcinoma metastasis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6295623/]
- 24. Emerging role of long noncoding RNAs in recurrent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8610931/]
- 25. Long non-coding RNA HOTAIR is a marker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4774541/]
- 26. Roles of long non-coding RNA HULC in human digestive ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1642425/full]
- 27. MIAT, HEIH, and HOTAIR: A novel LncRNA signature in ... [https://www.sciencedirect.com/science/article/pii/S1874467225000169]
- 28. Long non-coding RNA-based single and combination ... [https://link.springer.com/article/10.1007/s12672-025-03309-1]
- 29. Development and Validation of an Immune-Related ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.01037/full]
- 30. Identification of a novel prognostic signature for HCC and ... [https://www.nature.com/articles/s41598-022-13792-z]
- 31. A new marker constructed from immune-related lncRNA pairs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10433616/]
- 32. Machine learning combined with multi-omics to identify ... [https://www.nature.com/articles/s41598-025-10186-9]
- 33. Identification and Validation of a Prognostic lncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7298074/]
- 34. GDC FAQs - NCI Genomic Data Commons [https://gdc.cancer.gov/about-gdc/gdc-faqs]
- 35. GSE251942 - GEO Accession viewer - NIH [https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE251942]
- 36. GSE269528 [https://www.ncbi.xyz/geo/query/acc.cgi?acc=GSE269528]
- 37. Data Access Policies - NCI Genomic Data Commons [http://gdc.cancer.gov/access-data/data-access-policies]
- 38. Submitting high-throughput sequence data to GEO - NCBI - NIH [https://www.ncbi.nlm.nih.gov/geo/info/seq.html]
- 39. Development of a Prognostic m6A-Related lncRNA ... [https://pubmed.ncbi.nlm.nih.gov/41048653/]
- 40. Identification and Validation of Immune-Related LncRNA ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.681277/full]
- 41. Construction of a diseaseâ€specific lncRNA â€miRNAâ€mRNA regulatory... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7774738/]
- 42. Integrating bioinformatics and experimental validation to unveil... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-023-03208-x]
- 43. Survival Analysis Part II: Multivariate data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2394368/]
- 44. Cox Proportional-Hazards Model - Easy Guides - Wiki [https://www.sthda.com/english/wiki/cox-proportional-hazards-model]
- 45. Expression levels of lncRNAs are prognostic for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7269992/]
- 46. Identification and Validation of a Prognostic lncRNA ... [https://pubmed.ncbi.nlm.nih.gov/32587825/]
- 47. Identification and Validation of Basement Membrane ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12144066/]
- 48. Prognostic Signature of Hepatocellular Carcinoma and ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.691372/full]
- 49. Identification of a LncRNA based CeRNA network ... [https://www.nature.com/articles/s41598-025-05105-x]
- 50. a multi-center and large-scale study | npj Precision Oncology [https://www.nature.com/articles/s41698-025-01010-8]
- 51. Development and Validation of a Prognostic Signature ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2021.762570/full]
- 52. lncRNAs as Biomarkers of Hepatocellular Carcinoma Risk ... [https://www.mdpi.com/1467-3045/47/5/348]
- 53. Identification and validation of a ferroptosis-related long non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261030/]
- 54. Identification and validation of a five-necroptosis-related ... [https://www.sciencedirect.com/science/article/pii/S2405844024134342]
- 55. Integrating bioinformatics and experimental validation to ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1614702/full]
- 56. The development and validation of a novel senescence-related long-chain non-coding RNA (lncRNA) signature that predicts prognosis and the tumor microenvironment of patients with hepatocellular carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/35965795/]
- 57. The construction and evaluation of a prognostic risk score ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336248/]
- 58. Development and Validation of a Prognostic Signature Associated With Tumor Microenvironment Based on Autophagy-Related lncRNA Analysis in Hepatocellular Carcinoma - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8712323/]
- 59. A novel qualitative signature based on lncRNA pairs for prognosis prediction in hepatocellular carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/35193591/]
- 60. Development, validation, and clinical utility of risk prediction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12032184/]
- 61. Development and external validation of a machine learning ... [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-025-03912-7]
- 62. Cancer treatment and survivorship statistics, 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12223361/]
- 63. BALAD-2 Emerges as the Most Accurate Prognostic Model ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12610203/]
- 64. Proper assessment and prognostication of patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10919536/]
- 65. Prognostic Performance of Ten Liver Function Models in ... [https://www.nature.com/articles/s41598-018-19251-y]
- 66. Assessment of prognostic role of a novel 7-lncRNA ... [https://www.sciencedirect.com/science/article/pii/S2405844023057018]
- 67. Intra-tumor heterogeneity and prognostic risk signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9638959/]
- 68. Molecular subtyping of hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC7743018/]
- 69. Identification of a novel lncRNA prognostic signature and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10442647/]
- 70. A fourâ€long noncoding RNA signature predicts survival of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7521318/]
- 71. Decoding the molecular and genomic landscape of ... [https://www.nature.com/articles/s44355-025-00038-8]
- 72. Identification and validation of a ferroptosis-related long ... [https://pubmed.ncbi.nlm.nih.gov/40672083/]
- 73. Identification and validation of PANoptosis-related ... [https://www.nature.com/articles/s41598-025-90498-y]
- 74. Identification of matrix stiffness-related molecular subtypes in ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06733-7]
- 75. The LncRNA lnc-POTEM-4:14 promotes HCC progression ... [https://www.nature.com/articles/s41598-025-92614-4]
- 76. A migrasome-related lncRNA signature predicts prognosis ... [https://pubmed.ncbi.nlm.nih.gov/40843374/]
- 77. LncRNAs as novel players in hepatocellular carcinoma ... [https://www.oncotarget.com/article/26202/text/]
- 78. Assessment of prognostic role of a novel 7-lncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10382640/]
- 79. Prognosis-Predictive Signature and Nomogram Based on ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2020.608668/full]
- 80. A New Cuproptosis-Related lncRNAs Model for Predicting the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11645962/]
- 81. Development and Evaluation of Novel Statistical Methods ... [https://www.nature.com/articles/s41598-018-21922-9]
- 82. Machine learning-based hepatocellular carcinoma risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504168/]
- 83. A New Prediction Model for Prognosis of Patients ... [https://pubmed.ncbi.nlm.nih.gov/31777583/]
- 84. A new prediction model for prognosis of patients with ... [https://www.jcancer.org/v10p6535.htm]
- 85. Identification and evaluation of a six-lncRNA prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11147969/]
- 86. Plasma exosomal lncRNA-related signatures define ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12568545/]
- 87. a prognostic disulfidptosis-related LncRNAs model perspective [https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-025-04174-6]
- 88. Elucidating the role of AC026412.3 in hepatocellular carcinoma [https://pmc.ncbi.nlm.nih.gov/articles/PMC12341353/]
- 89. Plasma exosomal lncRNA-related signatures define ... [https://pubmed.ncbi.nlm.nih.gov/41169384/]
- 90. Potential role of immune-related LncRNAs in prognosis ... [https://link.springer.com/article/10.1007/s12672-025-03497-w]
- 91. Establishment of a lncRNA-Based Prognostic Gene ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.880288/full]
- 92. Identification of prognostic long non-coding RNA signature ... [https://www.aging-us.com/article/203322/text]
- 93. BALAD-2 Emerges as the Most Accurate Prognostic Model ... [https://pubmed.ncbi.nlm.nih.gov/41228250/]
- 94. Comparison of machine learning and Cox regression ... [https://www.sciencedirect.com/science/article/pii/S2589845025000570]
- 95. GSEA vs ORA: Two key pathway analysis approach... [https://pluto.bio/resources/Learning%20Series/gsea-vs-ora-two-key-pathway-analysis-approaches-for-next-gen-sequencing-data]
- 96. GO vs KEGG vs GSEA: How to Choose the Right ... [https://www.metwarebio.com/go-vs-kegg-vs-gsea-enrichment-analysis/]
- 97. CD8 T cell exhaustion-associated LncRNA signature reveals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12508406/]
- 98. Pathway Analysis vs Gene Set Analysis [https://advaitabio.com/science/pathway-analysis-vs-gene-set-analysis/]
- 99. Development of a MVI associated HCC prognostic model ... [https://www.nature.com/articles/s41598-025-91475-1]
- 100. Gene-set enrichment analysis and visualization on the web ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12373637/]
- 101. Hepatocellular carcinoma: signaling pathways and ... [https://www.nature.com/articles/s41392-024-02075-w]
- 102. Immunotherapy for hepatocellular carcinoma: Current status ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9950866/]
- 103. Predictive Biomarkers for Immune-Checkpoint Inhibitor ... [https://pubmed.ncbi.nlm.nih.gov/37108802/]
- 104. The evolving landscape of biomarkers for systemic therapy in ... [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-025-00774-2]