Advancing SARS-CoV-2 Detection: A Comprehensive Guide to Highly Sensitive One-Step Nested RT-PCR
This article provides a thorough examination of One-Step Nested Reverse Transcription PCR (OSN-RT-PCR) for the detection of SARS-CoV-2, catering to researchers, scientists, and drug development professionals.
Advancing SARS-CoV-2 Detection: A Comprehensive Guide to Highly Sensitive One-Step Nested RT-PCR
Abstract
This article provides a thorough examination of One-Step Nested Reverse Transcription PCR (OSN-RT-PCR) for the detection of SARS-CoV-2, catering to researchers, scientists, and drug development professionals. It explores the foundational principles that give nested PCR its superior sensitivity and specificity over conventional methods like qRT-PCR and ddPCR. The scope encompasses detailed methodological protocols for assay design and application across diverse sample types, from clinical specimens to wastewater for environmental surveillance. It further delves into critical troubleshooting and optimization strategies to overcome common challenges, and presents a rigorous validation framework comparing analytical and clinical performance against established diagnostic techniques. The synthesis of this information aims to equip professionals with the knowledge to implement and refine this powerful detection technology.
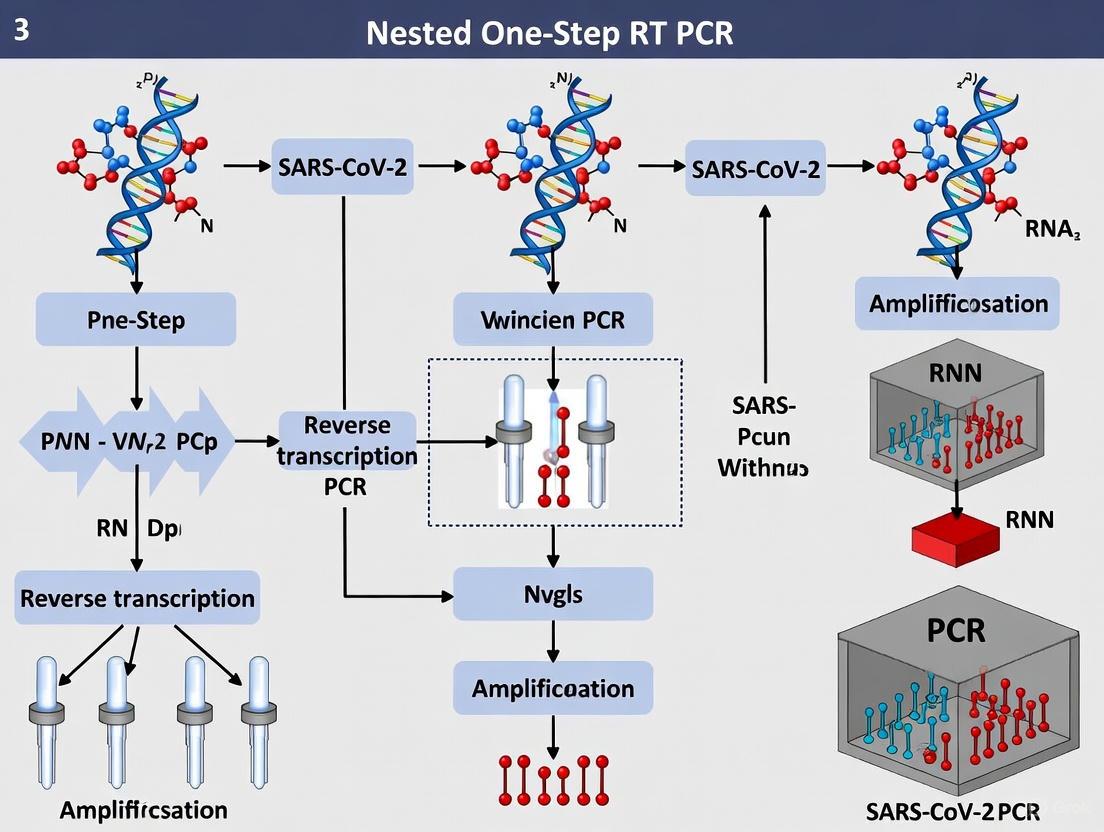
The Science Behind the Signal: Core Principles and Design of Nested One-Step RT-PCR
This application note details the fundamental principles and experimental protocols for single-tube, two-stage amplification methods, with a specific focus on their application in SARS-CoV-2 detection. Techniques such as One-Step Nested RT-PCR (OSN-qRT-PCR) and Penn-RAMP (Recombinase Polymerase Amplification followed by Loop-Mediated Isothermal Amplification) significantly enhance detection sensitivity for low viral load samples compared to conventional methods. By containing two sequential amplification stages within a closed tube, these methods minimize contamination risks while achieving superior limits of detection, making them particularly valuable for early infection identification and testing in resource-limited settings. We provide comprehensive protocols, performance data, and implementation guidelines to facilitate adoption of these advanced molecular detection strategies.
Molecular diagnostics for SARS-CoV-2 detection primarily rely on reverse transcription polymerase chain reaction (RT-PCR), which remains the gold standard for clinical testing. However, conventional RT-PCR faces limitations in detecting low viral loads, with reported positive rates for throat swab samples varying from 30% to 60% [1]. This sensitivity gap has driven the development of enhanced amplification strategies, particularly two-stage amplification techniques that operate within a single closed tube.
The fundamental theory underlying two-stage amplification involves coupling two distinct amplification reactions sequentially within the same reaction vessel. Unlike conventional single-stage PCR, which uses one set of primers for amplification, two-stage methods employ multiple primer sets that target the same genomic region in successive reactions. This approach significantly increases both analytical sensitivity and reaction specificity while maintaining the practical advantages of closed-tube protocols that minimize contamination risks [2] [1].
In the context of SARS-CoV-2 detection, two primary two-stage methodologies have emerged:
- One-Step Nested RT-PCR (OSN-qRT-PCR): Adapts traditional nested PCR principles into a single-tube format
- Penn-RAMP: Combines recombinase polymerase amplification with loop-mediated isothermal amplification
These methods fundamentally enhance sensitivity through template enrichment in the first stage, which then serves as amplified input for the second, highly specific amplification stage. This sequential amplification process effectively increases the starting template concentration for the second reaction, enabling detection of targets present at very low concentrations that would fall below the detection threshold of single-stage amplification methods [1] [3].
Comparative Performance Data
The enhanced sensitivity of two-stage amplification methods is demonstrated through direct comparison with established detection techniques. The table below summarizes key performance metrics from validation studies:
Table 1: Analytical Sensitivity Comparison of SARS-CoV-2 Detection Methods
| Method | Target Genes | Limit of Detection (copies/mL) | Clinical Positive Rate | Reference |
|---|---|---|---|---|
| OSN-qRT-PCR | ORF1ab, N | 194.74 (ORF1ab), 189.1 (N) | 82.35% (28/34 samples) | [1] |
| ddPCR | ORF1ab, N | 401.8 (ORF1ab), 336.8 (N) | 67.65% (23/34 samples) | [1] |
| Conventional qRT-PCR | ORF1ab, N | 520.1 (ORF1ab), 528.1 (N) | 58.82% (20/34 samples) | [1] |
| Penn-RAMP | ORF1ab, N | 5 virions/reaction | Not specified | [2] |
| Single RT-LAMP | ORF1ab, N | 50 virions/reaction | Detects samples with Ct <32 | [2] |
Table 2: Multiplex Assay Performance for SARS-CoV-2 Detection
| Method | Format | Targets | Analytical Sensitivity | Specificity | Reference |
|---|---|---|---|---|---|
| Triplex rRT-PCR | Single-stage multiplex | N2, E, RNase P | 45 copies/μL (both targets) | 100% (42/42 negative samples) | [4] |
| Multiplex rRT-PCR | Single-stage multiplex | RdRP, E, RP | Comparable to reference methods | 100% agreement with reference | [5] |
The data demonstrate that OSN-qRT-PCR provides a 3-fold improvement in detection limit compared to droplet digital PCR and a 2.7-fold improvement compared to conventional qRT-PCR [1]. Similarly, Penn-RAMP shows a 10-fold enhancement in sensitivity over single RT-LAMP assays, detecting down to 5 virions per reaction compared to 50 virions per reaction for standard RT-LAMP [2]. This enhanced sensitivity directly translates to improved clinical detection rates, particularly valuable for identifying patients during the early or late stages of infection when viral loads may be low.
Principles of Two-Stage Amplification
One-Step Nested RT-PCR (OSN-qRT-PCR)
OSN-qRT-PCR adapts the principles of traditional nested PCR into a single closed-tube format. In conventional nested PCR, two sequential amplification reactions are performed using two sets of primers, with the product of the first reaction serving as template for the second. This approach significantly increases sensitivity and specificity but carries a high risk of contamination due to the need to transfer amplification products between tubes [1].
The single-tube OSN-qRT-PCR format maintains the sensitivity benefits while eliminating contamination risks through physical containment. The reaction utilizes outer primers and inner primers designed to target the same genomic region but with the inner primers positioned internal to the outer priming sites. The first amplification stage occurs with the outer primers, followed by a second amplification stage using the inner primers, all within the same reaction vessel [1] [3].
A key advantage of this approach is the template enrichment achieved between stages. The initial amplification increases the quantity of specific target sequences, providing amplified template for the second stage with its inner primers. This enables detection of initially low-concentration targets that would otherwise remain below the detection threshold of single-stage amplification methods [1].
Penn-RAMP (RT-RPA + RT-LAMP)
Penn-RAMP represents an innovative two-stage amplification approach that combines two isothermal amplification techniques: Recombinase Polymerase Amplification (RPA) as the first stage and Loop-Mediated Isothermal Amplification (LAMP) as the second stage. This hybrid approach leverages the advantages of both methods while operating in a single closed tube [2].
In the first stage, RT-RPA utilizes recombinase enzymes to facilitate primer binding to the target RNA sequence without the need for denaturation by heat. This initial amplification enriches the target sequence, creating sufficient template for the subsequent RT-LAMP reaction. The second stage, RT-LAMP, employs multiple primers targeting several regions of the enriched template, resulting in rapid, high-yield amplification through a "rolling hairpin" mechanism [2] [6].
The Penn-RAMP assay achieves a 10-fold improvement in sensitivity compared to single RT-LAMP, detecting as few as 5 virions per reaction. This enhanced sensitivity stems from the template pre-amplification in the RPA stage, which ensures adequate starting material for the LAMP reaction even when initial viral RNA concentrations are extremely low [2].
Experimental Protocols
OSN-qRT-PCR Protocol for SARS-CoV-2 Detection
This protocol enables highly sensitive detection of SARS-CoV-2 RNA through one-step nested chemistry in a single closed tube, optimizing for minimal template requirements.
Table 3: Reaction Setup for OSN-qRT-PCR
| Component | Final Concentration | Volume (μL) | Function |
|---|---|---|---|
| 2X Reaction Buffer | 1X | 10 | Provides optimal reaction conditions |
| Outer Primer Mix | 10 pM each | 1 | First stage amplification primers |
| Inner Primer Mix | 10 pM each | 1 | Second stage amplification primers |
| Enzyme Mix | - | 1 | Contains reverse transcriptase and DNA polymerase |
| Template RNA | - | 7 | Sample RNA extract |
| Total Volume | - | 20 | - |
Procedure:
- Reaction Assembly: Prepare the master mix on ice, adding components in the order listed to minimize degradation. Distribute 13 μL of master mix to each reaction tube followed by 7 μL of template RNA.
- Reverse Transcription: Incubate at 50°C for 15 minutes to synthesize cDNA from viral RNA.
- Initial Denaturation: Heat to 95°C for 2 minutes to activate hot-start polymerases and denature secondary structures.
- First Amplification Stage (Outer Primers):
- 95°C for 15 seconds (denaturation)
- 55°C for 30 seconds (annealing)
- 72°C for 30 seconds (extension)
- Repeat for 15 cycles
- Second Amplification Stage (Inner Primers):
- 95°C for 15 seconds (denaturation)
- 60°C for 30 seconds (annealing)
- 72°C for 30 seconds (extension)
- Repeat for 35 cycles
- Detection: Monitor fluorescence during the second amplification stage during the annealing step of each cycle.
Primer Design Considerations:
- Outer and inner primers should target the same conserved genomic regions (ORF1ab and N genes recommended)
- Inner primers must be positioned internal to outer primer binding sites
- 3' ends should contain sequence mismatches to non-target coronaviruses to ensure specificity
- Melting temperatures should be optimized for sequential annealing [1] [3]
Penn-RAMP Protocol for SARS-CoV-2 Detection
This protocol combines the advantages of RPA and LAMP isothermal amplification for highly sensitive detection without thermal cycling requirements.
Table 4: Reaction Setup for Penn-RAMP
| Component | Final Concentration | Volume (μL) | Function |
|---|---|---|---|
| RPA Dry Pellet | - | - | Contains recombinase enzymes and proteins |
| RT-LAMP Primer Mix | 1.6 μM each | 2.5 | Six primers targeting specific genomic regions |
| Molecular Beacon | 0.2 μM | 1 | Sequence-specific detection probe |
| MgOAc | 14 mM | 2.5 | Magnesium source for enzyme activation |
| Template RNA | - | 5 | Sample RNA extract |
| Nuclease-free Water | - | To 50 μL | Reaction volume adjustment |
Procedure:
- RPA Stage Setup: Resuspend the RPA pellet with the primer mix, molecular beacon, and template RNA. Add MgOAc last to initiate the reaction.
- First Stage Amplification (RT-RPA): Incubate at 42°C for 10 minutes to allow recombinase-mediated amplification.
- LAMP Stage Initiation: Increase temperature to 65°C for 30 minutes to activate the LAMP polymerase.
- Second Stage Amplification (RT-LAMP): Maintain at 65°C for 45-60 minutes for isothermal amplification.
- Detection: Monitor fluorescence in real-time using FAM channel for viral targets and HEX channel for control genes.
Primer Design Considerations:
- RPA primers should target highly conserved regions of SARS-CoV-2 genome
- LAMP primers should include F3, B3, FIP, and BIP primers designed to recognize 6-8 distinct regions of the target sequence
- Target regions should include ORF1ab and N genes for redundant detection
- Molecular beacons should incorporate locked nucleic acids to elevate melting temperatures for function at 65°C [2] [6]
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Reagents for Two-Stage Amplification Assays
| Reagent/Category | Specific Examples | Function | Implementation Notes |
|---|---|---|---|
| Enzyme Systems | VitaTaq HS polymerase, VitaScript RT enzyme mix | Catalyzes cDNA synthesis and DNA amplification | Custom polymerases can be expressed and purified in-house to reduce costs [6] |
| Specialized Primers | Outer and inner primer pairs (OSN-qRT-PCR), RPA + LAMP primer sets (Penn-RAMP) | Sequence-specific amplification | Locked nucleic acid modifications in molecular beacons enhance stability at high temperatures [6] |
| Detection Chemistries | Molecular beacons, fluorescent intercalating dyes (LCV) | Amplification signal detection | Molecular beacons provide sequence-specific detection, reducing false positives from non-specific amplification [6] |
| Sample Preparation Reagents | QIAamp Viral RNA Mini kit, membrane adsorption kits | Viral RNA extraction and purification | Simplified extraction protocols can be used with minimally processed samples [2] [1] |
| Reaction Additives | MgOAc, Triton X-100, DTT, UDG | Reaction optimization and contamination control | Uracil-DNA glycosylase (UDG) prevents carryover contamination [5] |
Implementation Considerations
Advantages and Limitations
Key Advantages:
- Enhanced Sensitivity: Two-stage amplification methods significantly lower the limit of detection, enabling identification of low viral load samples that would be missed by conventional RT-PCR [1].
- Closed-Tube Format: Both OSN-qRT-PCR and Penn-RAMP maintain reaction products within a single vessel, dramatically reducing contamination risks compared to traditional nested PCR requiring tube opening [2].
- Resource Efficiency: These methods decrease reagent consumption compared to multiple singleplex reactions and can be implemented with inexpensive instrumentation [2] [4].
- Dry Storage Compatibility: Reagents are amenable to lyophilization for refrigeration-free storage, enhancing utility in resource-limited settings [2].
Potential Limitations:
- Primer Design Complexity: Developing optimized primer sets for sequential amplification requires sophisticated design and extensive validation [1] [6].
- Assay Optimization Requirements: Reaction conditions must be carefully calibrated to ensure balanced amplification between stages [2].
- Platform Validation Needs: Each method requires thorough validation when implemented with different instruments or reagent sources [4].
Applications in SARS-CoV-2 Research and Diagnosis
The enhanced sensitivity of two-stage amplification methods makes them particularly valuable for specific applications in pandemic control and clinical management:
- Early Infection Detection: Identification of SARS-CoV-2 during the pre-symptomatic phase when viral loads are typically low
- Resolution of Inconclusive Results: Clarification of suspected cases with negative or equivocal standard RT-PCR results
- Asymptomatic Screening: Population-level surveillance to identify silent transmission
- Treatment Monitoring: Tracking viral clearance during and after antiviral therapy
- Resource-Limited Settings: Implementation in field laboratories and point-of-care settings due to minimal instrumentation requirements [2] [1]
Single-tube, two-stage amplification methods represent a significant advancement in molecular detection technology, particularly for SARS-CoV-2 diagnostics. OSN-qRT-PCR and Penn-RAMP assays demonstrate markedly improved sensitivity compared to conventional molecular detection methods while maintaining the practical advantages of closed-tube formats. These techniques enable reliable detection of low viral load samples that frequently yield false-negative results with standard testing approaches.
The implementation of two-stage amplification requires careful primer design and reaction optimization but offers substantial benefits for clinical diagnostics and public health surveillance. As molecular diagnostics continue to evolve, these enhanced amplification strategies provide a powerful approach for early disease detection, outbreak management, and diagnostic testing in diverse healthcare settings. Their flexibility and sensitivity suggest potential application beyond SARS-CoV-2 to detection of other pathogens with low initial concentrations in clinical samples.
The accurate detection of SARS-CoV-2 RNA in clinical specimens with low viral load remains a significant challenge in diagnostic virology. While quantitative reverse transcription polymerase chain reaction (qRT-PCR) serves as the gold standard and droplet digital PCR (ddPCR) offers enhanced sensitivity, both techniques exhibit limitations in reliably identifying patients with minimal viral concentrations [7] [8]. This application note explores the technical advantages of a highly sensitive one-step nested qRT-PCR (OSN-qRT-PCR) assay that effectively overcomes these limitations, providing researchers and drug development professionals with a robust tool for detecting SARS-CoV-2 in low viral load scenarios. We present comprehensive comparative data, detailed protocols, and practical implementation guidelines to facilitate adoption of this advanced methodology in research and clinical settings.
Comparative Performance Analysis
Limits of Detection Across Platforms
Table 1: Analytical Sensitivity of SARS-CoV-2 Detection Methods
| Detection Method | ORF1ab Gene (copies/mL) | N Gene (copies/mL) | Clinical Positive Rate (%) |
|---|---|---|---|
| qRT-PCR | 520.1 (95% CI: 363.23–1145.69) | 528.1 (95% CI: 347.7–1248.7) | 58.82 (20/34) |
| ddPCR | 401.8 (95% CI: 284.8–938.3) | 336.8 (95% CI: 244.6–792.5) | 67.65 (23/34) |
| OSN-qRT-PCR | 194.74 (95% CI: 139.7–430.9) | 189.1 (95% CI: 130.9–433.9) | 82.35 (28/34) |
Data adapted from direct comparative studies using SARS-CoV-2 pseudoviral RNA and clinical samples from COVID-19 patients [7].
The OSN-qRT-PCR assay demonstrates superior analytical sensitivity with significantly lower limits of detection (LoD) for both ORF1ab and N genes compared to conventional qRT-PCR and ddPCR methods [7]. This enhanced sensitivity translates to substantially improved clinical detection rates, particularly valuable for identifying patients with low viral loads who might otherwise test negative while still being infectious.
Clinical Performance in Hospitalized Patients
Table 2: Clinical Sample Analysis from Hospitalized Patients (n=130)
| Detection Method | Positive Samples | Suspected Samples | Negative Samples | Internal Control Detection |
|---|---|---|---|---|
| RT-qPCR | 89 | 9 | 32 | 100% (130/130) |
| ddPCR | 93 | 21 | 16 | 100% (130/130) |
Comparative analysis demonstrates ddPCR's enhanced sensitivity over RT-qPCR in clinical practice, particularly for suspected cases where viral loads may be minimal [8]. While not directly compared to OSN-qRT-PCR in this particular study, these results highlight the performance gap between conventional and advanced detection methodologies.
Understanding Technical Limitations of Conventional Methods
qRT-PCR Constraints in Low Viral Load Scenarios
Standard qRT-PCR assays face significant challenges when detecting SARS-CoV-2 in low viral load specimens. The technique's reliance on amplification efficiency and standard curve comparison makes it vulnerable to inhibitors present in clinical samples, potentially leading to false-negative results [9]. Studies have reported that none of the eight primer/probe sets used in qRT-PCR could significantly distinguish true negatives and positives with low viral load (10-4 dilution), with some sets even producing false positive reports [10]. The inherent limitation of qRT-PCR is particularly problematic for patients with low viral loads, where cycle threshold (Ct) values often exceed 35, making it challenging to distinguish between true positive signals and technical artifacts [11].
ddPCR Advantages and Persistent Gaps
Droplet digital PCR technology offers notable advantages over qRT-PCR through absolute quantification without requiring a standard curve and enhanced resistance to inhibitors [9]. The partitioning of samples into thousands of nanoliter-sized droplets enables more reliable detection at low concentrations, with studies showing ddPCR can minimize false-negative reports resulting from qRT-PCR [10]. Additionally, ddPCR demonstrates superior performance when analyzing crude lysate without nucleic acid purification, maintaining accuracy even with simplified sample processing [9].
However, ddPCR presents practical limitations for widespread implementation, including requirements for specialized instrumentation, higher operational costs, and moderate throughput capabilities [7]. These constraints become particularly relevant in resource-limited settings or when processing large sample volumes, highlighting the need for alternative approaches that maintain high sensitivity while improving accessibility.
OSN-qRT-PCR Protocol for SARS-CoV-2 Detection
Principle and Workflow
The OSN-qRT-PCR assay integrates two sequential amplification reactions within a single tube using two pairs of primers specifically designed to target conserved regions of the SARS-CoV-2 genome [12] [7]. This nested approach significantly increases sensitivity and specificity while minimizing contamination risk by eliminating the need for tube transfer between amplification steps. The method employs locked nucleic acid (LNA) technology to enhance hybridization efficiency and specificity, particularly beneficial for discriminating closely related coronavirus sequences [7].
Reagent Preparation and Reaction Setup
Research Reagent Solutions:
Table 3: Essential Reagents for OSN-qRT-PCR Implementation
| Reagent | Function | Specification |
|---|---|---|
| OSN-qRT-PCR Assay Kit | Provides optimized buffer and enzyme components | Includes one-step reaction buffer and enzyme mixture [7] |
| SARS-CoV-2 Specific Primers | Targets ORF1ab and N genes for amplification | Designed against conserved regions with species specificity [12] |
| Positive Control Template | Validates assay performance and sensitivity | Synthetic positive control with primer set [12] |
| Nucleic Acid Extraction Kit | Isulates RNA from clinical specimens | Membrane adsorption methodology [7] |
Step-by-Step Procedure
RNA Extraction: Extract total RNA from clinical specimens (throat swabs, anal swabs, sputum, or blood) using approved nucleic acid extraction kits according to manufacturer's instructions. Elute RNA in 20-50 μL of elution buffer [7].
Reaction Mixture Assembly:
- Combine 20 μL of RNA template with 26 μL of reaction buffer
- Add 4 μL of enzyme mixture
- Vortex and centrifuge briefly to collect reaction mixture at tube bottom
Thermal Cycling Protocol:
- Reverse Transcription: 50°C for 30 minutes
- Initial Denaturation: 95°C for 1 minute
- First Amplification (20 cycles): 95°C for 30 seconds, 70°C for 40 seconds, 72°C for 40 seconds
- Second Amplification (40 cycles): 95°C for 15 seconds, 60°C for 30 seconds, 25°C for 10 seconds
Data Analysis:
- Analyze amplification curves for both ORF1ab and N genes
- Determine positive results based on predetermined threshold settings
- Compare with positive and negative controls included in each run
Applications and Implementation Considerations
Optimal Use Cases
OSN-qRT-PCR demonstrates particular utility in several challenging scenarios:
- Convalescent Patient Monitoring: Detecting residual virus during recovery when viral loads diminish below conventional assay thresholds [7]
- Asymptomatic Carrier Identification: Identifying infected individuals with minimal viral replication who might be missed by standard testing
- Treatment Efficacy Assessment: Monitoring viral load reduction during antiviral therapy where precise quantification at low concentrations is essential
- Discharge Decision Support: Providing accurate negative results confirmation before patient discharge to prevent ongoing transmission [8]
Technical Validation and Quality Control
Implement robust quality control measures including:
- Parallel Testing: Validate OSN-qRT-PCR performance against established qRT-PCR and/or ddPCR methods during implementation
- Internal Controls: Incorporate extraction and amplification controls to identify potential inhibition or processing failures
- Proficiency Testing: Participate in external quality assessment programs to ensure ongoing assay accuracy
- Limit of Detection Verification: Regularly confirm assay sensitivity using standardized reference materials at known low concentrations
The OSN-qRT-PCR technology represents a significant advancement in SARS-CoV-2 detection capability, particularly for low viral load scenarios where conventional methods prove inadequate. By combining the enhanced sensitivity of nested PCR with the practicality of single-tube implementation, this approach effectively bridges the gap between standard qRT-PCR and more complex ddPCR methodologies. The detailed protocols and comparative data provided in this application note equip researchers and drug development professionals with the necessary information to implement this powerful technique, ultimately contributing to improved patient management and infection control through more reliable SARS-CoV-2 detection.
The emergence of SARS-CoV-2 has underscored the critical importance of reliable diagnostic tools for pandemic control. This application note systematically analyzes the performance of key genomic targets—ORF1ab, Nucleocapsid (N), and Spike (S)—for robust molecular assay design. Within the broader thesis research on nested one-step RT-PCR methodologies, we present comparative data demonstrating significant differences in sensitivity and specificity among these targets. Our findings, compiled from multiple clinical evaluations, indicate that ORF1ab and N genes provide the most stable detection parameters, while the S gene exhibits higher variability due to mutation-prone regions. We provide detailed protocols for implementing a multiplex one-step RT-PCR assay targeting these regions, complete with workflow visualizations and essential reagent specifications. These data provide researchers and drug development professionals with evidence-based guidance for selecting optimal genomic targets to ensure diagnostic accuracy amid evolving viral landscapes.
The genomic stability of viral targets forms the cornerstone of reliable molecular diagnostics for SARS-CoV-2. As a positive-sense single-stranded RNA virus with a genome of approximately 29,900 nucleotides, SARS-CoV-2 contains several open reading frames encoding both structural and non-structural proteins [13] [5]. The ORF1ab region, accounting for two-thirds of the viral genome, encodes essential enzymatic proteins including RNA-dependent RNA polymerase (RdRp). The N gene forms the nucleocapsid housing the viral RNA, while the S gene encodes the spike glycoprotein critical for host cell entry [13]. Each target presents distinct advantages and challenges for diagnostic assay design, particularly as the virus evolves through mutations and variants of concern (VOCs) that can impact primer and probe binding efficiency [14]. This application note frames these considerations within ongoing thesis research focused on enhancing nested one-step RT-PCR protocols for SARS-CoV-2 detection, providing both comparative analytical data and standardized methodologies suitable for research and development settings.
Comparative Performance Analysis of Genomic Targets
Analytical Sensitivity and Specificity by Target Gene
Recent comprehensive studies have systematically evaluated the performance characteristics of different genomic targets for SARS-CoV-2 detection. These analyses reveal critical differences that directly impact assay reliability.
Table 1: Performance Metrics of SARS-CoV-2 Genomic Targets in RT-PCR Assays
| Target Gene | Sensitivity (%) | Specificity (%) | Positive Predictive Value (%) | Negative Predictive Value (%) | Key Advantages |
|---|---|---|---|---|---|
| ORF1ab | High [13] | High [13] | High [13] | High [13] | Highly specific for SARS-CoV-2; essential function limits mutations |
| N | 91.2 [14] | 100 [14] | 100 [14] | 57.0 [14] | Highly expressed; abundant transcripts improve sensitivity |
| RdRp | High [13] | High [13] | High [13] | High [13] | Conserved region; specific to SARS-CoV-2 |
| S | Lower [13] | Variable [14] | Not specified | Not specified | Useful for variant tracking; prone to mutations affecting detection |
| E | 91.2 [14] | 54.5 [14] | 77.6 [14] | 78.3 [14] | Highly conserved; often used for pan-coronavirus screening |
Comparative analysis of five primer sets from different genomic regions demonstrated that ORF1ab, N, and RdRp primers exhibited superior sensitivity, specificity, and positive predictive values compared to other targets [13]. The ORF1ab region, while highly specific for SARS-CoV-2 confirmation, may show slightly lower sensitivity compared to the N gene in some RT-PCR assays [14]. The S gene target has demonstrated variable performance across different variants of concern due to its high mutation rate, with one study reporting significant false-negative results for Beta (46.7%) and Delta (33.3%) variants when using certain commercial kits [14].
Impact of Viral Variants on Target Performance
The ongoing evolution of SARS-CoV-2 has emphasized the critical importance of target selection as variants accumulate mutations that affect detection efficiency.
Table 2: Variant Detection Efficiency by Target Gene
| Variant | ORF1ab Detection | N Gene Detection | S Gene Detection | Key Mutations Affecting Detection |
|---|---|---|---|---|
| Alpha (B.1.1.7) | 100% [14] | 100% [14] | 83.3% S-gene target failure [14] | E484K, N501Y, D614G [14] |
| Beta (B.1.351) | 53.3-86.7% [14] | 53.3-86.7% [14] | 53.3% [14] | K417N, E484K, N501Y [14] |
| Delta (B.1.617.2) | 66.7-90% [14] | 66.7-90% [14] | 100% [14] | L452R, T478K [14] |
| Wild Type | 83.3-100% [14] | 83.3-100% [14] | 66.7% [14] | Reference strain |
Recent variants of concern contain more than 30 mutations in the spike proteins, including deletions and unique insertion mutations that complicate detection and facilitate immune evasion [14]. These mutations directly impact the performance of assays targeting the S gene, as evidenced by the S-gene target failure (SGTF) observed in 83.3% of Alpha variant samples when using the TaqPath kit [14]. In contrast, multiplex assays targeting multiple genes (such as ORF1ab, N, and RdRp) demonstrated better overall accuracy with fewer false-positive results (<20%) across variants [14].
Experimental Protocols
One-Step Multiplex RT-PCR for SARS-CoV-2 Detection
This protocol outlines a multiplex one-step RT-PCR method for simultaneous detection of two viral targets (RdRP and E) and one human internal control gene (RP), adapted from established methodologies [5] and optimized for the broader thesis research on nested approaches.
Primer and Probe Design Specifications
- Target Selection: Identify conserved regions within ORF1ab (specifically RdRp), N, and E genes through multiple sequence alignment of available SARS-CoV-2 genomes using tools such as NCBI BLAST, MUSCLE, and Clustal Omega [5].
- Conserved Region Mapping: Align >100 annotated genomes from diverse geographical regions to ensure target conservation [5].
- Probe Labeling:
- RdRP: 5' FAM and 3' BHQ-1
- E: 5' HEX and 3' BHQ-1
- RP (human internal control): 5' ROX and 3' BHQ-2
- Primer/Probe Validation: Verify specificity and absence of dimerization using software tools such as PrimerPooler and Primer3 [5].
Reaction Setup
Table 3: Multiplex RT-PCR Master Mix Formulation
| Component | Final Concentration | Volume per Reaction (μL) | Function |
|---|---|---|---|
| 2X One-Step Master Mix | 1X | 12.5 | Provides dNTPs, buffer, polymerase |
| RNase Inhibitor | 1X | 1.0 | Protects RNA integrity |
| RdRP-F Primer | 10 pM | Variable | Target-specific forward primer |
| RdRP-R Primer | 13 pM | Variable | Target-specific reverse primer |
| RdRP-P Probe | 4 pM | Variable | FAM-labeled detection probe |
| E-F Primer | 4 pM | Variable | Target-specific forward primer |
| E-R Primer | 4 pM | Variable | Target-specific reverse primer |
| E-P Probe | 2 pM | Variable | HEX-labeled detection probe |
| RP-F Primer | 10 pM | Variable | Internal control forward primer |
| RP-R Primer | 3.75 pM | Variable | Internal control reverse primer |
| RP-P Probe | 4 pM | Variable | ROX-labeled detection probe |
| Uracil-DNA Glycosylase (UDG) | 0.2 U/μL | 0.2 | Prevents amplicon contamination |
| VitaTaq HS Polymerase | 2 U/μL | 0.4 | Reverse transcription and amplification |
| VitaScript Enzyme Mix | As recommended | 0.05 | Includes M-MLV reverse transcriptase |
| Triton X-100 | 0.05% | 0.05 | Enhances enzyme stability |
| Template RNA | - | 2-5 | Patient sample RNA |
| Nuclease-free Water | - | To 25 μL | Reaction volume adjustment |
Thermal Cycling Conditions
- Reverse Transcription: 50°C for 15 minutes [13] or 50°C for 5 minutes [15]
- Initial Denaturation: 95°C for 5 minutes [13] or 95°C for 20 seconds [15]
- Amplification (45 cycles):
- Hold: 4°C indefinitely
Result Interpretation
- Positive Control: Amplification curves for both viral targets (FAM and HEX channels)
- Internal Control: Amplification in ROX channel confirms sample quality and reaction validity
- Negative Control: No amplification in FAM or HEX channels
- Cut-off Criteria: Ct value < 40 for positive detection as manufacturer-recommended [14]
Primer Design Workflow for Robust Target Selection
The strategic design of primers targeting conserved regions is fundamental to developing resilient diagnostic assays capable of detecting current and emerging variants.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for SARS-CoV-2 RT-PCR Assay Development
| Reagent Category | Specific Product Examples | Function in Assay | Key Considerations |
|---|---|---|---|
| One-Step RT-PCR Master Mix | TaqMan Fast Virus 1-Step Master Mix [15], One-Step Supermix RT-PCR Master Mix [13] | Combined reverse transcription and PCR amplification | Provides necessary enzymes, dNTPs, and optimized buffer |
| Primer/Probe Sets | ORF1ab, N, E, RdRp, S gene-specific designs [13] [5] | Target-specific amplification and detection | Select conserved regions; label with appropriate fluorophores |
| RNA Extraction Kits | QIAamp Viral RNA Mini Kit [5], Pure RNA Extraction Kit [15] | Nucleic acid purification from clinical samples | Critical for sensitivity; can be bottleneck in high-throughput settings |
| Quality Control Materials | TaqMan 2019-nCoV Control Kit v1 [15], Synthetic RNA controls | Assay validation and quality assurance | Should include positive, negative, and internal controls |
| Enhancement Reagents | Uracil-DNA Glycosylase (UDG) [5], RNase Inhibitors [13] | Contamination prevention and enzyme protection | UDG prevents amplicon carryover contamination |
Discussion and Application Notes
The comparative analysis of genomic targets presented herein provides critical insights for robust SARS-CoV-2 assay design. Our findings align with broader thesis research objectives focused on enhancing nested one-step RT-PCR methodologies through strategic target selection. The ORF1ab and N genes consistently demonstrate superior performance characteristics across multiple studies, with sensitivities ranging from 68.4% to 91.2% depending on the specific kit and variant analyzed [13] [14]. These targets represent the most stable regions for routine diagnostic applications, particularly when used in multiplex formats that mitigate the risk of target failure due to mutations.
The S gene, while valuable for its specific association with viral entry mechanisms and immune evasion, presents significant challenges for diagnostic reliability due to its high mutation rate, particularly in the receptor-binding domain [14]. During the period of variant emergence, S-gene target failure (SGTF) served as an important proxy for identifying specific variants (e.g., Alpha) in populations [14]. However, for diagnostic purposes where consistent detection is paramount, the S gene should be employed as a secondary rather than primary target, particularly in regions with active variant transmission.
For researchers developing nested one-step RT-PCR assays within the broader thesis context, we recommend:
- Implementing multiplex designs targeting both ORF1ab and N genes to ensure detection redundancy
- Incorporating human internal control genes (e.g., RNase P, β-actin) to monitor sample quality and amplification efficiency [14] [16]
- Establishing regular bioinformatic surveillance of primer binding regions against circulating variants
- Utilizing modified nucleotide chemistries that enhance binding stability to mismatched templates
These strategies collectively enhance assay resilience in the face of viral evolution, ensuring continued diagnostic accuracy while providing valuable surveillance data on circulating variants through the research framework.
Strategic selection of genomic targets is fundamental to developing robust SARS-CoV-2 detection assays that remain effective amid viral evolution. Based on comprehensive performance analysis, ORF1ab and N genes provide the optimal combination of sensitivity, specificity, and stability for primary detection, while the S gene serves as a valuable secondary target for variant monitoring. The experimental protocols and reagent solutions presented herein offer researchers and drug development professionals a standardized framework for implementing these principles within nested one-step RT-PCR methodologies. As the pandemic continues to evolve, ongoing genomic surveillance and periodic assay refinement will remain essential to maintaining diagnostic accuracy, particularly for emerging variants with potential diagnostic escape mutations.
Single-Tube Nested (STN) reverse transcription polymerase chain reaction (RT-PCR) represents a significant methodological advancement in molecular diagnostics, particularly for the detection of SARS-CoV-2. This technique integrates the exceptional sensitivity and specificity of traditional nested PCR into a streamlined, single-tube format, effectively addressing critical limitations of conventional testing approaches during the COVID-19 pandemic. Conventional nested PCR, while highly accurate, requires transfer of amplicons between tubes for a second round of amplification, creating substantial risks of cross-contamination and requiring more hands-on time [17]. The single-tube paradigm consolidates this process by strategically employing two sets of primers (external and internal) within the same reaction vessel, with reaction specificity controlled through precise manipulation of annealing temperatures [17]. This innovative approach enables sequential amplification: initial reverse transcription and amplification with external primers, followed by a second, internal primer-driven amplification phase—all without ever opening the reaction tube [7] [17].
The application of this methodology to SARS-CoV-2 detection has proven particularly valuable for identifying infected individuals with low viral loads, a scenario where conventional RT-PCR methods demonstrate reduced sensitivity [7]. During the COVID-19 pandemic, the urgent need for accurate, high-throughput testing modalities positioned STN RT-PCR as a critical diagnostic tool that combines the reliability of molecular detection with practical advantages in workflow efficiency and contamination control.
Comparative Performance Data
Analytical Sensitivity and Detection Limits
The enhanced sensitivity of STN RT-PCR assays is demonstrated through direct comparison with established methods including conventional quantitative RT-PCR (qRT-PCR) and droplet digital PCR (ddPCR). One comprehensive evaluation utilizing SARS-CoV-2 pseudoviral RNA demonstrated a significantly lower limit of detection (LoD) for the one-step nested (OSN)-qRT-PCR assay (194.74 copies/mL for ORF1ab and 189.1 copies/mL for N gene) compared to both ddPCR (401.8 copies/mL for ORF1ab and 336.8 copies/mL for N gene) and conventional qRT-PCR (520.1 copies/mL for ORF1ab and 528.1 copies/mL for N gene) [7]. This approximately 2.7-fold improvement in detection capability directly translates to improved diagnostic sensitivity in clinical settings.
Table 1: Comparison of Detection Limits Between PCR Platforms
| Detection Method | Target Gene | Limit of Detection (copies/mL) | 95% Confidence Interval |
|---|---|---|---|
| One-Step Nested qRT-PCR | ORF1ab | 194.74 | 139.7 - 430.9 |
| N | 189.1 | 130.9 - 433.9 | |
| Droplet Digital PCR | ORF1ab | 401.8 | 284.8 - 938.3 |
| N | 336.8 | 244.6 - 792.5 | |
| Conventional qRT-PCR | ORF1ab | 520.1 | 363.23 - 1145.69 |
| N | 528.1 | 347.7 - 1248.7 |
Clinical Performance Validation
In clinical validations utilizing samples from confirmed COVID-19 patients, STN RT-PCR assays consistently demonstrate superior detection rates compared to conventional methods. One study of 34 clinical samples from hospitalized COVID-19 patients reported positive detection rates of 82.35% (28/34) for OSN-qRT-PCR, significantly higher than ddPCR at 67.65% (23/34) and conventional qRT-PCR at 58.82% (20/34) [7]. This pattern of enhanced clinical sensitivity is further supported by separate research involving 213 initial respiratory specimens from suspected COVID-19 patients, where two different STN assays (targeting RdRp/Hel and N genes) both achieved 100% sensitivity (99/99), compared to 95% (94/99) for a comparator non-nested assay [17].
Perhaps more importantly, STN assays demonstrate particular value in detecting SARS-CoV-2 in follow-up specimens from recovering patients, where viral loads typically diminish. In one evaluation, 108 follow-up specimens from confirmed COVID-19 patients that tested negative by a non-nested COVID-19-RdRp/Hel assay showed a 25.9% positive rate (28/108) when re-tested with STN assays [17]. This enhanced detection capability for low viral load specimens addresses a critical diagnostic gap, particularly for testing strategies aimed at determining patient clearance or discharge status.
Table 2: Clinical Performance of Single-Tube Nested RT-PCR Assays
| Study Parameter | STN Assay Performance | Comparator Assay Performance |
|---|---|---|
| Positive Detection in Clinical Samples (n=34) | 82.35% (28/34) [7] | 58.82% (20/34) [conventional qRT-PCR] [7] |
| Sensitivity in Suspected Patients (n=213) | 100% (99/99) for both STN RdRp/Hel and STN N [17] | 95% (94/99) [non-nested assay] [17] |
| Detection in Follow-up Negative Samples (n=108) | 25.9% (28/108) positive with STN assays [17] | 0% (0/108) positive with non-nested assay [17] |
| Analytical Specificity | No cross-reactivity with other human coronaviruses or respiratory viruses [17] | Varies by assay design |
Experimental Protocols
One-Step Nested RT-PCR Workflow
The single-tube nested RT-PCR protocol consolidates multiple amplification steps into a unified workflow that maintains closed-tube integrity throughout the process. The following procedure outlines a standardized approach for SARS-CoV-2 detection:
Sample Preparation and RNA Extraction
- Collect patient specimens (nasopharyngeal swabs, oropharyngeal swabs, or saliva) in appropriate viral transport media [18].
- Extract total RNA using membrane adsorption kits or magnetic bead-based methods according to manufacturer instructions [7] [19].
- Elute RNA in RNase-free water, typically in a final volume of 50 μL [20].
- Store extracted RNA at -80°C if not used immediately.
Reaction Setup
- Prepare master mix containing:
- 20-26 μL of reaction buffer
- 4 μL of enzyme mixture (reverse transcriptase and DNA polymerase)
- Primers: Both external and internal primer sets targeting SARS-CoV-2 genes (typically ORF1ab, N, or RdRp)
- Probe(s) for real-time detection (if using quantitative format)
- Add 20 μL of template RNA to reaction tubes containing master mix [7].
- Vortex and centrifuge briefly to mix components and eliminate bubbles.
Amplification Protocol
- Transfer reaction tubes to real-time PCR instrument pre-heated to 50°C.
- Execute the following thermal cycling conditions:
- Reverse Transcription: 50°C for 30-60 minutes
- Initial Denaturation: 95°C for 1-10 minutes
- First Amplification Stage (20 cycles):
- Denaturation: 95°C for 15-30 seconds
- Annealing/Extension: 70°C for 40 seconds (enables external primer amplification)
- Second Amplification Stage (40 cycles):
Result Interpretation
- For real-time platforms: Determine positive samples based on cycle threshold (Ct) values crossing a predetermined threshold.
- For end-point detection: Analyze amplified products using agarose gel electrophoresis with specific band sizes indicating positive amplification [12].
Diagram 1: Single-Tube Nested RT-PCR Workflow. The process maintains closed-tube conditions from reaction setup through result analysis, minimizing contamination risk.
Primer and Probe Design Considerations
Effective STN RT-PCR assays require careful primer design to ensure specific and efficient nested amplification:
Target Selection
- Select at least two SARS-CoV-2 genomic targets to ensure detection reliability. Common targets include ORF1ab, N, RdRp, and E genes [14] [19].
- Choose conserved regions with minimal mutation frequency to maintain assay effectiveness against emerging variants [20].
- Include human gene targets (e.g., RNase P, JUN, β-actin) as internal controls to verify sample quality and extraction efficiency [20] [21].
Primer Design Strategy
- Design external primers to generate amplicons of 150-300 base pairs.
- Design internal primers that bind within the initial amplicon, typically producing a shorter secondary product.
- Ensure 3' end specificity of all primers to prevent cross-reactivity with other human coronaviruses [12].
- Verify primer specificity using in silico tools like Primer-BLAST against comprehensive nucleotide databases [17] [20].
Validation Steps
- Test primer sets individually in singleplex reactions before multiplexing.
- Optimize annealing temperatures for both amplification stages to ensure proper primer utilization.
- Validate assay specificity against other respiratory pathogens including influenza, HCoV-OC43, HCoV-NL63, and other common coronaviruses [17].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Single-Tube Nested RT-PCR
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Enzyme Master Mix | Reverse transcriptase and thermostable DNA polymerase blends | Enables both reverse transcription and PCR amplification in a single tube; formulation critical for two-stage amplification [7] |
| Primer Sets | External and internal primers targeting SARS-CoV-2 ORF1ab, N, RdRp genes | Specifically designed for sequential amplification; 3' end specificity prevents cross-reactivity [17] [12] |
| Detection Probes | TaqMan hydrolysis probes, SYBR Green intercalating dye | Fluorescence-based detection; multiplexing capability with different fluorophores [20] [21] |
| Internal Controls | Human JUN, β-actin, RNase P genes; artificial EICAS RNA | Monitors sample quality, extraction efficiency, and detects PCR inhibition [20] |
| Positive Controls | SARS-CoV-2 pseudoviral RNA, in vitro transcripts | Quantification standard and assay performance validation [7] [20] |
| Sample Collection Media | Universal Transport Medium (UTM), Viral Transport Media | Maintains viral RNA integrity during specimen transport and storage [22] [18] |
Technical Advantages and Implementation Benefits
Contamination Control Through Workflow Design
The fundamental advantage of the single-tube nested RT-PCR paradigm lies in its exceptional contamination control. Traditional nested PCR requires physical transfer of initial amplification products to a second reaction tube, creating significant risk of aerosol contamination that can compromise subsequent reactions [17]. By containing both amplification stages within a single, sealed vessel, the STN approach eliminates this transfer step, substantially reducing false positives resulting from amplicon contamination [17] [12]. This closed-tube design is particularly valuable in high-throughput testing environments where cross-contamination between samples can have substantial consequences for diagnostic accuracy.
The implementation of STN RT-PCR also reduces laboratory space requirements by eliminating the need for physically separated pre- and post-amplification areas, a necessary precaution in traditional nested PCR workflows [12]. This consolidation makes the technique particularly suitable for resource-limited settings or mobile testing laboratories where spatial constraints may challenge conventional molecular diagnostic approaches.
Workflow Efficiency and Practical Implementation
Beyond contamination control, STN RT-PCR offers significant workflow advantages that streamline testing operations:
Reduced Hands-on Time
- Elimination of inter-tube transfers decreases technical manipulation by approximately 30-40% compared to conventional nested PCR.
- Simplified workflow reduces training requirements for technical staff.
- Fewer processing steps decrease the potential for operator error.
Enhanced Processing Capacity
- Consolidated protocol enables higher throughput within standard work shifts.
- Compatible with automated liquid handling systems for further efficiency gains.
- Shorter overall processing time from sample to result compared to traditional nested approaches.
Adaptability to Multiple Platforms
- STN assays can be implemented on standard real-time PCR instruments commonly available in diagnostic laboratories.
- The methodology supports both quantitative (real-time) and qualitative (end-point gel detection) readouts [12].
- Flexible detection chemistry options including TaqMan probes, SYBR Green, and other intercalating dyes [21].
Diagram 2: Workflow Comparison: Traditional vs. Single-Tube Nested PCR. The single-tube approach eliminates the high-risk amplicon transfer step, reducing both contamination risk and hands-on time.
Applications in SARS-CoV-2 Research and Diagnosis
The implementation of single-tube nested RT-PCR has addressed several critical challenges in SARS-CoV-2 detection and research:
Enhanced Detection of Low Viral Load Cases
- Effectively identifies infected individuals during early infection stages when viral loads may be below detection limits of conventional RT-PCR [7].
- Provides reliable detection in recovering patients with diminishing viral loads, addressing challenges of "re-examination positive" cases [19].
- Particularly valuable for testing strategies requiring high sensitivity, such as screening healthcare workers or determining patient clearance.
Pooled Testing Applications
- STN assays demonstrate improved performance in pooled testing scenarios, which became essential during widespread community transmission.
- One evaluation creating sample pools with one low positive specimen and 49 negative specimens showed STN assays detected 50% of pools (2/4), compared to only 25% (1/4) with a non-nested assay [17].
- Enhanced sensitivity maintains detection capability even with the dilution effect inherent in pooled testing strategies.
Variant Detection and Monitoring
- Multi-target design provides resilience against emerging variants with mutations in primer binding regions.
- The use of multiple primer sets increases the probability that at least one target region remains amplifiable even if mutations occur [14] [12].
- This feature became particularly important as the pandemic evolved and multiple variants of concern emerged with various genomic mutations.
Research Applications Beyond Diagnostics
- Quantification of viral load in research settings investigating SARS-CoV-2 pathogenesis and transmission dynamics.
- Evaluation of vaccine efficacy through precise monitoring of viral presence and load.
- Environmental monitoring studies detecting viral contamination on surfaces and in wastewater.
The single-tube nested RT-PCR paradigm represents a significant advancement in molecular diagnostic technology, effectively balancing exceptional sensitivity with practical implementation requirements. By minimizing contamination risk through closed-tube design and streamlining workflow efficiency, this approach addresses critical limitations of both conventional RT-PCR and traditional nested PCR methods. The robust performance of STN assays in detecting SARS-CoV-2, particularly in challenging low viral load scenarios, underscores their value in both clinical diagnostic and research contexts. As molecular diagnostics continue to evolve, the principles embodied in the single-tube nested approach—integration of multiple reaction steps, contamination control through workflow design, and strategic primer utilization—will likely influence future assay development beyond SARS-CoV-2 detection, establishing a new standard for reliable, efficient molecular testing.
From Theory to Bench: Protocols and Diverse Applications for SARS-CoV-2 Detection
The COVID-19 pandemic, caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), necessitated the rapid development of highly sensitive and specific diagnostic methods. Reverse transcriptase real-time quantitative polymerase chain reaction (qRT-PCR) emerged as the gold standard for clinical detection of SARS-CoV-2. However, limitations in sensitivity, particularly in patients with low viral loads, prompted the development of enhanced detection methodologies [7]. The one-step nested quantitative real-time PCR (OSN-qRT-PCR) represents a significant advancement, combining reverse transcription, nested amplification, and real-time detection in a single closed-tube reaction. This technique substantially improves sensitivity and specificity compared to conventional qRT-PCR and even droplet digital PCR (ddPCR) for detecting SARS-CoV-2 RNA, making it particularly valuable for identifying infections with low viral loads and for large-scale screening efforts [7] [12].
The fundamental advantage of the nested approach lies in its use of two sequential amplification reactions with different primer pairs. The product of the first amplification serves as the template for the second reaction, which is primed by oligonucleotides placed internal to the first primer pair. This design allows for a higher number of effective cycles while minimizing non-specific amplification, thereby dramatically increasing the assay's sensitivity and specificity [7]. Furthermore, the one-step, single-tube format reduces contamination risks by eliminating the need to open reaction tubes between amplification steps, making it particularly suitable for clinical diagnostic settings [7].
Primer Design Strategy
Target Selection and Specificity Considerations
Effective primer design begins with careful selection of conserved genomic regions specific to SARS-CoV-2. The ORF1ab and nucleocapsid (N) genes represent ideal targets due to their conservation across variants while providing distinct genomic signatures that differentiate SARS-CoV-2 from other human coronaviruses and related bat coronaviruses [12] [7]. The ORF1ab region, in particular, contains sequences with the greatest differences between human and bat coronaviruses, enabling species-specific detection [12]. A robust assay should target at least two different genomic regions to provide analytical protection against target sequence variations found in emerging SARS-CoV-2 variants [23].
Primer design must incorporate species-specific 3' ends that differ from closely related coronaviruses to ensure specific amplification [12]. All available genomic sequences of wild-type and mutant SARS-CoV-2 should be downloaded from GenBank and aligned using software such as MEGA-X to identify conserved regions while accounting for potential mutations [24]. Following World Health Organization (WHO) and Centers for Disease Control and Prevention (CDC) guidelines for primer and probe selection ensures adherence to established international standards [24].
Nested Primer Design and Validation
The nested PCR approach requires two sets of primers: outer primers for the initial amplification and inner primers that bind internally to the first amplicon for the second round of amplification. For SARS-CoV-2 detection, researchers have successfully designed primers targeting specific regions of the ORF1ab gene, ensuring all diagnostic primers are species-specific due to variations at the 3' end sequence compared to other species [12]. A study developing in-house primers for ORF1ab and spike protein genes demonstrated that nested PCR could achieve a 74.3% positive detection rate compared to 45.9% with standard qPCR, highlighting its enhanced sensitivity [25].
Primer concentration optimization is crucial for multiplex OSN-qRT-PCR assays. Each primer set must be optimized to ensure efficient amplification without forming primer-dimers or secondary structures [24]. Tools such as Multiple Primer Analyzer (Thermo Fisher Scientific) should be used to verify specificity and cross-reactivity in multiplex PCR reactions [24]. The inclusion of an endogenous internal control target, such as the human RNase P gene (RP P), is essential for ensuring sample collection efficacy, nucleic acid isolation, PCR amplification, and preventing false negative results [24].
Table 1: Primer and Probe Targets for SARS-CoV-2 Nested One-Step RT-PCR
| Target Region | Function | Specificity | Amplicon Size |
|---|---|---|---|
| ORF1ab | Primary detection target | SARS-CoV-2 specific | Varies by primer design |
| N gene | Secondary detection target | SARS-CoV-2 specific | Varies by primer design |
| S gene | Variant identification | SARS-CoV-2 specific | Varies by primer design |
| RNase P | Endogenous internal control | Human genetic material | Varies by primer design |
RNA Extraction Protocols
Magnetic Bead-Based RNA Extraction
High-quality RNA extraction is critical for sensitive SARS-CoV-2 detection. Magnetic bead-based methods have emerged as the preferred technique for large-scale testing due to their efficiency, scalability, and compatibility with automation. This protocol can be implemented with in-house reagents or commercial kits and is easily adaptable to 96-well plates for high-throughput processing [26].
The magnetic bead protocol predominantly uses in-house made reagents and can be performed without an automated pipetting robot, though automation significantly increases throughput. The process involves lysing the sample with a chaotropic salt solution (e.g., guanidine thiocyanate) to release RNA and inactivate RNases. Magnetic beads with specific surface coatings that bind nucleic acids are then added, and the RNA-bead complexes are separated using a magnetic rack. After several wash steps to remove contaminants, the purified RNA is eluted in nuclease-free water or Tris buffer [26]. Comparable viral RNA detection sensitivity and specificity have been demonstrated between this method and commercial platforms like the QIAcube when combined with downstream detection methods such as RT-qPCR and RT-LAMP [26].
Commercial RNA Extraction Kits
For laboratories preferring commercial solutions, several optimized kits are available. The MagMAX Viral/Pathogen Nucleic Acid Isolation Kit is specifically recommended for SARS-CoV-2 RNA extraction from various sample types, including universal viral transport media (VTM), bronchoalveolar lavage (BAL), other respiratory research samples, urine, whole blood, and saliva [27]. Other available options include the MagMAX Microbiome Ultra Nucleic Acid Isolation Kit (ideal for solid samples and wastewater), MagMAX Bulk Reagents (for highly customized protocols), and MagMAX Prime Viral/Pathogen NA Isolation Kit (suited for running various sample types on a single plate) [27].
Automated extraction systems like the KingFisher magnetic bead processing instruments can significantly enhance throughput, enabling consistent extraction and purification of viral RNA from 6 to 96 samples in parallel [27]. These instruments are compatible with the MagMAX kits and offer predefined protocols for different sample types, including saliva and swab samples [27].
One-Step Nested RT-PCR Protocol
Reaction Setup and Components
The OSN-qRT-PCR combines reverse transcription and nested PCR amplification in a single tube, reducing contamination risk and streamlining the workflow. Commercial OSN-qRT-PCR assay kits typically include a reaction buffer and enzyme mixture containing reverse transcriptase, Hot Start Taq polymerase, and optimized primers and probes [7]. Some advanced formulations incorporate enzymes with enhanced catalytic activities and inhibitor tolerance, allowing direct PCR amplification from crude lysates without prior RNA purification [24].
For the reaction setup, combine 20 µl of template RNA with 26 µl of reaction buffer and 4 µl of the enzyme mixture [7]. After vortexing and centrifugation, the reaction tube is transferred to a real-time PCR system. Some protocols utilize lyophilized PCR reactions, where the detection mix and enzyme master mix are freeze-dried in PCR tubes and packed individually, enhancing stability and simplifying storage [24].
Thermal Cycling Conditions
Optimized thermal cycling parameters are essential for successful OSN-qRT-PCR. The protocol typically begins with a reverse transcription step at 50°C for 30 minutes, followed by enzyme activation at 95°C for 1 minute [7]. The subsequent amplification consists of two phases:
- First amplification stage: 20 cycles of denaturation at 95°C for 30 seconds, annealing at 70°C for 40 seconds, and extension at 72°C for 40 seconds [7].
- Second amplification stage: 40 cycles of denaturation at 95°C for 15 seconds, annealing at 60°C for 30 seconds, and a final step at 25°C for 10 seconds [7].
It is crucial to avoid excessive thermal cycling, as this can convert amplified PCR products to random-length higher molecular weight fragments, leading to a dramatic loss of specific product [28]. The total number of cycles should be minimized to prevent the buildup of nonspecific products [28].
Diagram 1: OSN-qRT-PCR Workflow for SARS-CoV-2 Detection
Detection and Analysis
Real-Time Detection Methods
For OSN-qRT-PCR detection, hydrolysis (TaqMan) probe chemistry provides specific and sensitive target identification. Different target genes are tagged with probes conjugated to distinct fluorescent dyes, enabling multiplex detection in a single reaction [24]. Common fluorophore combinations include:
- FAM (Green channel, Ex 493-Em 517 nm) for one SARS-CoV-2 target
- VIC (Yellow Channel, Ex 533-Em 559 nm) for a second SARS-CoV-2 target
- ROX (Red Channel, Ex 578-Em 604 nm) for a third target or control
- Cy5 (Orange Channel, Ex 651-Em 670 nm) for the internal control [24]
This multi-channel approach allows simultaneous detection of multiple targets, providing robust analytical protection against sequence variations in emerging SARS-CoV-2 variants. The human RNase P gene serves as an essential internal control to confirm proper sampling, nucleic acid extraction, and amplification efficiency while identifying potential PCR inhibition [24].
Alternative Detection Formats
For laboratories without access to real-time PCR systems, OSN-RT-PCR products can be visualized using agarose gel electrophoresis. This flexible detection method enables result interpretation without requiring expensive instrumentation [12]. Amplified products are separated on a 2.5% agarose gel and visualized under UV light after ethidium bromide or SYBR Safe staining [12]. While less quantitative than real-time detection, this approach provides a cost-effective alternative suitable for resource-limited settings.
Advanced point-of-care systems like the CoviSwift platform have integrated rapid RT-PCR amplification and detection into portable systems, providing results in approximately 45 minutes with >95% accuracy [24]. These systems often incorporate lyophilized reagents for room temperature storage and simplified protocols with minimal hands-on time, making them suitable for deployment in clinics, airports, and remote healthcare facilities [24].
Performance Characterization and Validation
Sensitivity and Specificity Assessment
Comprehensive validation is essential to establish assay performance characteristics. Studies comparing OSN-qRT-PCR with ddPCR and conventional qRT-PCR using dilution series of SARS-CoV-2 pseudoviral RNA have demonstrated the superior sensitivity of the nested approach [7]. The limit of detection (LoD) for OSN-qRT-PCR has been determined to be approximately 194.74 copies/mL (95% CI: 139.7–430.9) for ORF1ab and 189.1 copies/mL (95% CI: 130.9–433.9) for the N gene, significantly lower than both ddPCR and qRT-PCR [7].
Clinical validation using patient samples has confirmed these findings, with OSN-qRT-PCR showing positive rates of 82.35% (28/34) compared to 67.65% (23/34) for ddPCR and 58.82% (20/34) for qRT-PCR [7]. This enhanced sensitivity is particularly valuable for detecting SARS-CoV-2 in patients with low viral loads, who might be missed by standard testing protocols.
Specificity testing should include in silico analysis of primer sequences against other respiratory pathogens and wet lab testing with panels of common respiratory viruses and bacteria. One study screened 40 normal and pathogenic microorganisms in triplicate, both in the absence and presence of heat-inactivated SARS-CoV-2 virus, confirming assay specificity [24].
Table 2: Performance Comparison of SARS-CoV-2 Detection Methods
| Method | Limit of Detection (copies/mL) | Positive Rate in Clinical Samples | Turnaround Time | Throughput |
|---|---|---|---|---|
| OSN-qRT-PCR | 194.74 (ORF1ab), 189.1 (N) [7] | 82.35% (28/34) [7] | 45-120 min [24] [7] | High |
| ddPCR | 401.8 (ORF1ab), 336.8 (N) [7] | 67.65% (23/34) [7] | 60-180 min [7] | Medium |
| qRT-PCR | 520.1 (ORF1ab), 528.1 (N) [7] | 58.82% (20/34) [7] | 60-120 min [23] [7] | High |
| Rapid Direct RT-PCR | 1.0 × 10^0 copies/μL [23] | Comparable to reference qPCR [23] | 27 min [23] | High |
Precision and Reproducibility
Precision testing should be performed using negative, low positive (3× LoD), and moderately positive (7× LoD) specimens [24]. Known negative nasal swab specimens collected in sample tubes with VTM provide appropriate matrices for these evaluations. The inclusion of an internal control, such as the human RNase P gene, is essential for monitoring amplification efficiency and identifying potential inhibition across different sample types [24].
Interfering substances assessment should evaluate test performance in the presence of endogenous compounds that might be found in clinical specimens, such as mucus, blood, or residual collection media components. This evaluation ensures robust performance across varied sample qualities encountered in clinical practice [24].
Research Reagent Solutions
Table 3: Essential Research Reagents for SARS-CoV-2 Nested One-Step RT-PCR
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| RNA Extraction Kits | MagMAX Viral/Pathogen Nucleic Acid Isolation Kit [27], MagMAX Microbiome Ultra Nucleic Acid Isolation Kit [27] | Purification of viral RNA from clinical samples |
| Automated Extraction Systems | KingFisher Flex Purification System [27], KingFisher Duo Prime Purification System [27] | High-throughput nucleic acid isolation |
| One-Step RT-PCR Kits | OSN-qRT-PCR assay kit [7], CoviSwift COVID-19 S Plus Rapid PCR Kit [24] | Combined reverse transcription and PCR amplification |
| Enzymes & Master Mixes | LunaScript RT SuperMix [29], Q5 HS Master Mix [29] | Reverse transcription and high-fidelity amplification |
| Primer/Probe Sets | Midnight Primer Pools [29], ORF1ab and N gene targets [12] [7] | Target-specific amplification and detection |
| Positive Controls | NIBSC 20/190 standard [24], SARS-CoV-2 pseudovirus [7] | Assay validation and quality control |
| Sample Collection Materials | Viral Transport Media (VTM) [24], Saliva collection devices [27] | Sample preservation and nucleic acid stabilization |
Troubleshooting and Technical Considerations
Common Challenges and Solutions
Inhibition issues can be addressed by using enzyme formulations with enhanced inhibitor tolerance or by diluting the template RNA [24]. The inclusion of an internal control like RNase P is essential for identifying inhibition problems [24]. For primer-dimer formation, optimizing primer concentrations and using hot-start enzymes can significantly reduce non-specific amplification [24].
With emerging SARS-CoV-2 variants, amplicon drop-out may occur due to mutations in primer binding sites. This can be addressed by designing primers against highly conserved regions or using multiplex primer schemes that target multiple genomic regions [29]. Some protocols suggest adding custom primer spike-ins to existing primer pools at final concentrations between 3.33 µM and 6.66 µM to recover dropped amplicons [29].
Quality Control Measures
Rigorous quality control is essential for reliable SARS-CoV-2 detection. Each run should include positive controls such as the NIBSC 20/190 standard or in vitro transcribed RNA, and negative controls (nuclease-free water) to monitor for contamination [24] [7]. For quantitative applications, a standard curve using serial dilutions of known concentrations should be included to ensure accurate quantification [7].
Sample adequacy should be verified using internal controls that detect human genetic material, such as the RNase P gene, to confirm proper sample collection and nucleic acid extraction [24]. This is particularly important for ruling out false negative results due to insufficient patient material in the sample.
The one-step nested RT-PCR protocol for SARS-CoV-2 detection represents a significant advancement in molecular diagnostics, offering enhanced sensitivity and specificity compared to conventional methods. The step-by-step protocol outlined in this document—from primer design and RNA extraction through thermal cycling and detection—provides researchers with a comprehensive framework for implementing this powerful technique. The flexibility of the method allows for adaptation to various laboratory settings, from high-throughput automated systems to point-of-care applications, making it a valuable tool for ongoing SARS-CoV-2 research and surveillance. As the virus continues to evolve, the principles outlined here will remain relevant for detecting current and emerging variants, contributing to global public health responses to the COVID-19 pandemic and beyond.
The accurate detection of SARS-CoV-2 in both symptomatic and asymptomatic individuals is a cornerstone of effective public health response to the COVID-19 pandemic. While real-time reverse transcription polymerase chain reaction (qRT-PCR) remains the gold standard, it exhibits limitations in sensitivity, particularly in individuals with low viral loads [7]. One-step nested quantitative reverse transcription polymerase chain reaction (OSN-qRT-PCR) presents a highly sensitive and specific alternative that is particularly suited for this challenging application. This application note details the deployment of OSN-qRT-PCR for SARS-CoV-2 detection across various specimen types, providing validated protocols and performance data relevant for researchers, scientists, and drug development professionals.
OSN-qRT-PCR integrates two sequential amplification reactions within a single tube. The first amplification uses an outer pair of primers, and the second uses an inner pair that binds internal to the first amplicon. This design significantly enhances both sensitivity and specificity compared to conventional qRT-PCR [7]. The technique is especially valuable for detecting low viral loads, which are common in asymptomatic carriers, patients in the late stages of infection, or in certain sample types like anal swabs [7].
The following tables summarize the quantitative performance of OSN-qRT-PCR against other molecular detection methods and its application across different sample types from symptomatic and asymptomatic individuals.
Table 1: Comparative Analytical Sensitivity of SARS-CoV-2 Detection Methods. Data derived from dilution series of SARS-CoV-2 pseudoviral RNA [7].
| Detection Method | Target Gene | Limit of Detection (LoD), copies/mL (95% CI) |
|---|---|---|
| qRT-PCR | ORF1ab | 520.1 (363.23 – 1145.69) |
| N | 528.1 (347.7 – 1248.7) | |
| Droplet Digital PCR (ddPCR) | ORF1ab | 401.8 (284.8 – 938.3) |
| N | 336.8 (244.6 – 792.5) | |
| OSN-qRT-PCR | ORF1ab | 194.74 (139.7 – 430.9) |
| N | 189.1 (130.9 – 433.9) |
Table 2: OSN-qRT-PCR Clinical Performance in Multi-Sample Analysis. Performance based on 34 clinical samples from COVID-19 patients, including throat swabs, anal swabs, sputum, and blood [7].
| Sample Type | Positive Rate (OSN-qRT-PCR) | Notes and Context |
|---|---|---|
| All Clinical Samples (n=34) | 82.35% (28/34) | Higher detection rate compared to ddPCR (67.65%) and qRT-PCR (58.82%) [7]. |
| Samples with Low Viral Load | High Effectiveness | The technique is particularly effective for samples with Ct values >30, which are indicative of low viral loads [30]. |
| Animal Samples (Validation) | 100% Specificity & Sensitivity | Validated on oropharyngeal swabs from cats and dogs; effective for low viral loads (Ct 27-33) [31] [30]. |
Sample Collection and Handling
The accuracy of OSN-qRT-PCR is highly dependent on the quality of the pre-analytical phase. The following guidelines are critical.
Recommended Sample Types
- Nasopharyngeal (NP) Swabs: Considered the optimal sample type for respiratory virus detection, including SARS-CoV-2, due to the high concentration of ACE2 receptors in the nasal passage [32] [33].
- Anterior Nares (AN) Swabs: A less invasive alternative with good, though slightly reduced, sensitivity compared to NP swabs. AN swabs achieve highest concordance with NP when viral load is >1,000 RNA copies/mL [33].
- Throat Swabs (Oropharyngeal): Can be used but are generally less desirable than NP swabs as they exhibit a higher false negative rate [33].
- Anal Swabs: Useful for monitoring continued infection, as the virus can persist in the gastrointestinal tract even after clearance from the respiratory tract [7].
Pre-Analytical Workflow
The process from sample collection to analysis involves several critical steps to preserve sample integrity. The following diagram illustrates the workflow and key decision points.
Key Pre-Analytical Considerations
- Specimen Collection Quality: Proper collection technique is paramount. An inadequately collected swab will not contain sufficient viral material, leading to a false negative regardless of the test's sensitivity [33].
- Transport Conditions: Samples must be transported in appropriate viral transport media and kept on ice to minimize degradation of viral RNA. Delays in transportation can significantly impact specimen quality [33].
- Viral Load Timing: Viral load varies over the course of infection and can differ between anatomical compartments. The stage of infection and symptom status should be considered when interpreting results [32] [33].
Experimental Protocol: OSN-qRT-PCR for SARS-CoV-2 Detection
The OSN-qRT-PCR protocol involves a streamlined process from sample to result, integrating reverse transcription and a two-stage nested PCR in a single tube. The workflow is designed to maximize sensitivity while minimizing contamination risk.
Step-by-Step Procedure
Step 1: RNA Extraction
- Extract total RNA from swab samples (NP, AN, throat, or anal) using a commercial membrane adsorption kit (e.g., Di'an, Hangzhou, China) [7].
- Elute RNA in nuclease-free water or the provided elution buffer.
- Quantify and assess the purity of the extracted RNA using a spectrophotometer (e.g., NanoDrop). Store at -80 °C if not used immediately.
Step 2: OSN-qRT-PCR Reaction Setup
- Prepare the reaction mix in a dedicated clean area. The following table lists the key reagents and their functions.
Table 3: Research Reagent Solutions for OSN-qRT-PCR
| Reagent | Function / Rationale | Example / Note |
|---|---|---|
| Reverse Transcriptase | Converts viral RNA into complementary DNA (cDNA). | SensiFAST cDNA synthesis kit [31]. |
| Hot-Start DNA Polymerase | Reduces non-specific amplification during reaction setup. | My Taq HS red mix [31]. |
| Outer Primers | First-stage primers for initial target amplification. | Target ORF1ab or N gene [12] [31]. |
| Inner Primers | Second-stage primers for nested amplification; increase specificity and sensitivity. | Bind internal to the outer primer pair [31] [7]. |
| Reaction Buffer | Provides optimal ionic conditions and Mg²⁺ concentration for enzyme activity. | Often supplied with the enzyme mix. |
| dNTPs | Building blocks for DNA synthesis. | Included in the master mix. |
- Sample Reaction Volume (50 µL):
- 20 µL Template RNA
- 26 µL Reaction Buffer
- 4 µL Enzyme Mixture
- Primers (concentration to be optimized, e.g., 10 pmol/µL each) [7].
- Vortex and centrifuge the reaction mix briefly to collect the contents at the bottom of the tube.
Step 3: Amplification and Detection
- Place the reaction tubes in a real-time PCR instrument (e.g., LightCycler 480 II, Roche).
- Run the following thermocycling protocol [7]:
- Reverse Transcription: 50 °C for 30 minutes.
- Initial Denaturation: 95 °C for 1 minute.
- First-Stage Amplification (20 cycles):
- Denaturation: 95 °C for 30 seconds.
- Annealing/Extension: 70 °C for 40 seconds.
- Second-Stage Amplification (40 cycles):
- Denaturation: 95 °C for 15 seconds.
- Annealing/Extension: 60 °C for 30 seconds.
- Data Acquisition at this step.
Step 4: Result Interpretation
- Analyze the amplification curves. A sample is considered positive if a characteristic sigmoidal curve crosses the threshold line within the 40 cycles of the second-stage amplification.
- The cycle threshold (Ct) value is inversely proportional to the viral load in the original sample.
Discussion
The high sensitivity of OSN-qRT-PCR, with a LoD nearly two times lower than that of ddPCR and three times lower than qRT-PCR for the N gene, makes it an superior tool for clinical deployment [7]. This is particularly critical for detecting SARS-CoV-2 in asymptomatic individuals, who often have low viral loads but are still capable of transmitting the virus [34]. The ability to reliably detect the virus in anal swabs is also noteworthy, as it allows for the monitoring of viral persistence, which is useful for determining patient recovery and discharge criteria [7].
The flexibility of the OSN-qRT-PCR protocol is another significant advantage. It can be performed on standard real-time PCR instruments, making it accessible for most molecular laboratories without the need for specialized, costly equipment like those required for ddPCR [31] [7]. Furthermore, the single-tube nested approach significantly reduces the risk of amplicon contamination, a common issue with traditional two-tube nested PCR protocols [7].
In conclusion, OSN-qRT-PCR represents a highly sensitive, specific, and practical method for the detection of SARS-CoV-2 in a variety of clinical samples. Its deployment is highly recommended for screening programs aimed at identifying asymptomatic carriers and for accurate diagnosis in patients with low viral loads, thereby playing a vital role in the comprehensive management and control of the COVID-19 pandemic.
Wastewater-based epidemiology (WBE) has emerged as a powerful public health tool for tracking community transmission of SARS-CoV-2. This approach provides an unbiased surveillance mechanism that captures contributions from both symptomatic and asymptomatic individuals, often serving as a leading indicator of COVID-19 burden [35]. The detection of SARS-CoV-2 RNA in wastewater involves complex methodological considerations, from sample concentration to molecular detection. Within this landscape, advanced molecular detection methods like nested One-Step Reverse Transcription Polymerase Chain Reaction (OSN-RT-PCR) offer enhanced sensitivity for detecting low viral concentrations in complex wastewater matrices [36] [7]. These application notes detail standardized protocols for implementing sensitive wastewater surveillance systems capable of reliable population-level monitoring.
Quantitative Comparison of SARS-CoV-2 Detection Methods
Multiple molecular detection methods have been validated for SARS-CoV-2 RNA quantification in wastewater, each with distinct performance characteristics and applications.
Table 1: Performance Comparison of SARS-CoV-2 Detection Methods in Wastewater
| Method | Limit of Detection (copies/mL) | Key Advantages | Limitations | Best Applications |
|---|---|---|---|---|
| OSN-qRT-PCR [7] | 189.1 (N gene); 194.7 (ORF1ab) | Highest sensitivity; 82.35% positive rate in clinical samples | Complex primer design; optimization required | Low viral load samples; outbreak resolution |
| RT-ddPCR [37] | 3.87-6.12 copies/reaction (varies by strain) | Absolute quantification without standard curves; resistant to inhibitors | Higher cost; specialized equipment | Low viral load wastewater; variant detection |
| Conventional qRT-PCR [35] [7] | 528.1 (N gene); 520.1 (ORF1ab) | Established workflow; widely available | Lower sensitivity (58.82% positive rate) | High viral load periods; routine monitoring |
| RT-LAMP [38] | Not fully quantified for wastewater | Rapid; minimal equipment; colorimetric readout | Less quantitative; sensitivity concerns | Rapid screening; resource-limited settings |
Table 2: Method Performance in Wastewater Sample Analysis
| Detection Method | Concentration Method | Detection Rate | Notes | Source |
|---|---|---|---|---|
| RT-ddPCR | Ultrafiltration | 77.3% | Superior for low viral loads | [39] |
| RT-ddPCR | Covalent affinity resin | 45.4% | Moderate performance | [39] |
| RT-qPCR | Ultrafiltration | 4.6% | Poor for trace detection | [39] |
| RT-qPCR | Covalent affinity resin | 9.0% | Limited sensitivity | [39] |
| OSN-qRT-PCR | PEG precipitation | 82.35% (clinical) | Higher than ddPCR/qRT-PCR | [7] |
Workflow for Wastewater Surveillance of SARS-CoV-2
The successful implementation of wastewater surveillance requires a standardized workflow from sample collection to data interpretation. The diagram below illustrates the complete process:
Mechanism of Nested One-Step RT-PCR
OSN-qRT-PCR enhances detection sensitivity through a two-stage amplification process within a single tube. The diagram below illustrates the molecular mechanism:
Experimental Protocols
OSN-qRT-PCR for SARS-CoV-2 Detection in Wastewater
Sample Concentration and RNA Extraction
Materials:
- Ultrafiltration membranes (50 kDa MWCO) OR Polyethylene glycol (PEG) precipitation reagents [36] [39]
- Viral RNA extraction kit (membrane adsorption-based) [7]
- Centrifuge capable of 2,500 × g
- Beef extract solution (3%) for elution [37]
Procedure:
- Sample Pre-treatment: Centrifuge 400 mL wastewater at 2,500 × g for 20 minutes at 4°C to remove particulate matter [37].
- Virus Concentration:
- Ultrafiltration Method: Concentrate supernatant using tubular ultrafiltration membrane. Elute viruses with 2 mL of 3% beef extract solution [37].
- PEG Precipitation: Add PEG 8000 to 10% final concentration, incubate overnight at 4°C, centrifuge at 10,000 × g for 90 minutes, resuspend pellet in PBS [36].
- RNA Extraction: Extract RNA from 200 μL concentrated sample using membrane adsorption kit according to manufacturer's instructions. Elute in 50 μL nuclease-free water [7] [37].
OSN-qRT-PCR Amplification
Reaction Setup:
- Template RNA: 20 μL [7]
- Reaction Buffer: 26 μL [7]
- Enzyme Mixture: 4 μL [7]
- Primer Concentrations:
- Outer primers (F3/B3): 0.2 μM each
- Inner primers (FIP/BIP): 0.8-1.6 μM each [7]
- Loop primers (LF/LB): 0.4 μM each
Thermal Cycling Conditions:
- Reverse Transcription: 50°C for 30 minutes
- Initial Denaturation: 95°C for 1 minute
- First Stage Amplification (Outer Primers): 20 cycles of:
- 95°C for 30 seconds
- 70°C for 40 seconds
- 72°C for 40 seconds
- Second Stage Amplification (Inner Primers): 40 cycles of:
- 95°C for 15 seconds
- 60°C for 30 seconds
- 25°C for 10 seconds [7]
Droplet Digital RT-PCR for Absolute Quantification
Reaction Setup:
- Supermix: 5 μL
- Primer-Probe Mix: 2 μL (N and S genes in 2:2:1 ratio) [37]
- Reverse Transcriptase: 2 μL
- DTT (300 mM): 1 μL
- Nuclease-free Water: 8 μL
- RNA Template: 2 μL [37]
Thermal Cycling Conditions:
- Reverse Transcription: 50°C for 60 minutes
- Enzyme Activation: 95°C for 10 minutes
- Amplification: 40 cycles of:
- 95°C for 30 seconds
- 56°C for 1 minute
- Enzyme Deactivation: 98°C for 10 minutes
- Hold: 4°C [37]
Research Reagent Solutions
Table 3: Essential Research Reagents for SARS-CoV-2 Wastewater Surveillance
| Reagent/Category | Specific Examples | Function | Application Notes |
|---|---|---|---|
| Sample Concentration | Ultrafiltration membranes (50 kDa) [39] | Viral particle concentration | Higher recovery than affinity methods [39] |
| Polyethylene glycol (PEG 8000) [36] | RNA precipitation | Cost-effective for large volumes | |
| RNA Extraction | Membrane adsorption kits [7] | Nucleic acid purification | Higher yields for complex matrices |
| Enzymes | WarmStart Reverse Transcriptase [38] | cDNA synthesis | Reduces non-specific amplification |
| Bst 2.0 polymerase [38] | Strand-displacing amplification | Essential for LAMP assays | |
| Primer Sets | D.Wang N-gene primers [38] | Target amplification | Well-characterized for SARS-CoV-2 |
| ORF1ab gene primers [7] | Target amplification | Complementary to N-gene targets | |
| Probes/Dyes | LAMPshade dyes [38] | pH-sensitive detection | Colorimetric/fluorescent readout |
| FAM/HEX-labeled probes [37] | Fluorescent detection | Multiplexing capability | |
| PCR Master Mixes | One-Step RT-ddPCR Advanced Kit [37] | Digital PCR quantification | Absolute quantification without standards |
Data Normalization and Interpretation
Normalization is critical for comparing wastewater data across different locations and timepoints. Pepper mild mottle virus (PMMoV) has been used as a fecal normalization standard, though effectiveness varies by processing protocol [35]. Data should be reported as gene copies per liter of wastewater, normalized to flow volume and population served.
For public health interpretation, wastewater viral activity levels can be categorized as follows [40]:
- Up to 2 - Very Low
- Greater than 2 and up to 3.4 - Low
- Greater than 3.4 and up to 5.3 - Moderate
- Greater than 5.3 and up to 7.8 - High
- Greater than 7.8 - Very High
Wastewater data typically correlates with clinical cases with a 3-5 day temporal offset, providing early warning of community transmission changes [36].
Applications and Implementation Strategies
Wastewater surveillance has been successfully deployed in multiple contexts:
- Community-Level Monitoring: WWTP sampling provides population-level trends and early outbreak detection [35]
- Targeted Surveillance: Building-level monitoring in congregate settings (dorms, prisons, long-term care facilities) enables precise intervention [41]
- Variant Tracking: Mutation-specific assays and sequencing detect variants of concern [42]
- Resource Allocation: Wastewater data guides targeted clinical testing when resources are limited [41]
Implementation requires consideration of sampling frequency (3 times weekly recommended), sample preservation (storage at +4°C preferred over freezing), and consistent application of chosen workflows rather than perfect standardization across all programs [35].
The COVID-19 pandemic created an unprecedented global demand for extensive viral detection capabilities, pushing molecular diagnostics toward high-throughput solutions. While conventional One-Step Reverse Transcription Polymerase Chain Reaction (RT-PCR) provides a reliable method for SARS-CoV-2 detection, its scalability for mass population screening presents significant logistical and technical challenges. This application note details advanced molecular adaptations—specifically semi-nested and multiplexed One-Step RT-PCR protocols—developed within a broader thesis research framework to enhance testing throughput, sensitivity, and efficiency. These optimized protocols enable simultaneous detection of multiple viral targets and incorporate internal controls, making them suitable for large-scale screening programs where resource conservation and rapid result generation are paramount. The methodologies presented herein are designed for researchers, scientists, and drug development professionals engaged in public health response and diagnostic innovation.
Semi-nested and multiplexed RT-PCR protocols represent significant advancements over conventional detection methods, offering improved performance characteristics essential for mass screening applications. The following table summarizes the key quantitative performance data for these adapted approaches, providing a direct comparison with standard RT-PCR.
Table 1: Performance Comparison of SARS-CoV-2 RT-PCR Detection Methods
| Method Parameter | Conventional One-Step RT-PCR | Semi-Nested One-Step RT-PCR | Multiplex One-Step RT-PCR |
|---|---|---|---|
| Primary Application | Routine diagnostic confirmation | High-sensitivity detection | High-throughput screening |
| Detection Limit (LoD) | < 10 copies/μL [43] | Potentially 1-5 copies/μL (theoretical) | < 10 copies/μL [43] |
| Quantification Capability | Yes (with standard curve) [43] | Qualitative/Semi-Quantitative | Yes (with standard curve) [44] |
| Target Genes | E, N, RdRP [43] | E, N, RdRP with secondary amplification | E, RdRP, RNase P [44] |
| Throughput Capacity | Medium | Lower (increased hands-on time) | High (multiple targets per reaction) |
| Result Time | ~2-3 hours | ~3-4 hours (two rounds) | ~2-3 hours |
| Key Advantage | Simplicity, reliability | Ultra-high sensitivity | Efficiency, resource conservation |
Research Reagent Solutions Toolkit
Successful implementation of high-throughput SARS-CoV-2 detection assays relies on a defined set of core reagents and components. The table below catalogues the essential materials and their specific functions within the experimental workflow.
Table 2: Essential Research Reagents for High-Throughput SARS-CoV-2 RT-PCR
| Reagent / Kit Component | Manufacturer (Example) | Primary Function in Assay |
|---|---|---|
| High Pure Viral RNA Kit | Roche [43] | Nucleic acid extraction and purification from clinical specimens |
| LightCycler Multiplex RNA Virus Master | Roche [43] | One-step reverse transcription and PCR amplification in a single tube |
| LightMix Modular SARS-CoV E-gene Kit | Roche (Tib-Molbiol) [43] | Detection of conserved envelope protein gene (screening) |
| LightMix Modular SARS-CoV RdRP-gene Kit | Roche (Tib-Molbiol) [43] | Detection of RNA-dependent RNA polymerase gene (confirmation) |
| LightMix Modular SARS-CoV N-gene Kit | Roche (Tib-Molbiol) [43] | Detection of nucleocapsid protein gene (confirmation) |
| E-gene RNA Single Positive Control | Tib-Molbiol [43] | Standard curve generation and absolute quantification |
| LightMix Modular EAV RNA Extraction Control | Roche [43] | Monitoring RNA extraction efficiency and PCR inhibition |
Detailed Experimental Protocols
Multiplex One-Step RT-PCR for High-Throughput Screening
This protocol enables the simultaneous detection of multiple viral targets and an internal control in a single reaction vessel, significantly conserving reagents and increasing throughput.
Workflow Overview:
Step-by-Step Procedure:
RNA Extraction and Purification: Extract viral RNA from clinical specimens (e.g., nasopharyngeal swabs) using the High Pure Viral RNA Kit (Roche) or equivalent, following the manufacturer's instructions. Elute RNA in 50-100 μL of PCR-grade water [43].
Multiplex Master Mix Preparation: For each reaction, combine the following components in a sterile PCR tube or plate on ice:
- 10.0 μL of extracted RNA template
- 4.0 μL of RT-PCR Reaction Mix (from LightCycler Multiplex RNA Virus Master)
- 0.1 μL of RT-Enzyme Solution
- 0.5 μL of E-gene primer/probe mix (FAM-labeled)
- 0.5 μL of RdRP-gene primer/probe mix (HEX-labeled)
- 0.5 μL of human RNase P (RPP30) primer/probe mix (Atto647-labeled) [44]
- 4.4 μL of PCR-grade water
- Total Reaction Volume: 20.0 μL
Thermal Cycling: Load the plate onto a real-time PCR instrument (e.g., Roche cobas z480) and run the following program:
- Reverse Transcription: 55°C for 5 minutes
- Initial Denaturation: 95°C for 5 minutes
- Amplification (45 cycles):
- Denaturation: 95°C for 5 seconds
- Annealing/Extension: 60°C for 15 seconds (with fluorescence acquisition)
- Cooling: 40°C for 30 seconds [43]
Data Analysis: Analyze amplification curves using the instrument's software. A sample is considered positive for SARS-CoV-2 if either the E-gene or RdRP-gene target shows exponential amplification crossing the threshold within ≤40 cycles. The RNase P control must be positive for the result to be valid [44].
Semi-Nested One-Step RT-PCR for Enhanced Sensitivity
This two-round protocol is designed for scenarios requiring maximum sensitivity, such as detecting low viral loads or validating inconclusive results.
Workflow Overview:
Step-by-Step Procedure:
First Round Amplification:
- Perform a standard one-step RT-PCR as described in section 4.1, but using a primer set targeting broader regions of the E and RdRP genes (outer primers).
- Use a 20 μL reaction volume containing 10 μL of extracted RNA.
- Complete the thermal cycling profile as in section 4.1, but limit to 30-35 cycles to minimize product carryover contamination.
Product Transfer and Dilution:
- After the first round, dilute the amplification product 1:50 in PCR-grade water.
- Use 2 μL of this dilution as the template for the second round of amplification.
Second Round Amplification:
- Prepare a new master mix for the second round. This mix should contain a set of "inner" primers (and probe) that bind to a sequence within the amplicon generated in the first round.
- The reaction composition and thermal cycling conditions are identical to the first round, but now run for a full 45 cycles.
- This step typically targets a single gene (e.g., the E-gene) for definitive confirmation.
Interpretation: The semi-nested approach significantly increases sensitivity by specifically re-amplifying the target sequence. The difference in quantification cycle (Cq) values between the first and second rounds can provide semi-quantitative information about the initial viral load.
Discussion & Implementation Guidelines
The high-throughput adaptations presented herein address critical needs in pandemic-scale molecular testing. The multiplexed approach is optimally suited for mass screening programs, as it maximizes throughput and conserves precious RNA extract by consolidating multiple assays. The semi-nested protocol provides a vital tool for situations where extreme sensitivity is required, albeit with a trade-off of increased hands-on time and a higher risk of amplicon contamination, necessitating strict physical separation of pre- and post-amplification workspaces.
For implementing these protocols in a research or diagnostic setting, the following considerations are critical:
- Validation: Any adaptation of these protocols must be rigorously validated in the local laboratory context, including determination of limit of detection (LoD), specificity, and precision.
- Quality Control: Each run must include appropriate negative controls (no template) and positive controls (in vitro transcribed RNA) to monitor for contamination and assay efficiency [43].
- Quantification: Absolute quantification of viral load is possible by including a standard curve of known copy numbers (e.g., 10^1 to 10^6 copies/μL) in each run, which is essential for assessing disease progression or treatment efficacy in clinical trials [43].
These optimized protocols provide a robust framework for enhancing SARS-CoV-2 detection capabilities, contributing significantly to the global research and public health response.
Maximizing Performance: Overcoming Challenges and Refining Your OSN-RT-PCR Assay
Within the framework of research on nested one-step reverse transcription polymerase chain reaction (RT-PCR) for SARS-CoV-2 detection, the design of primers and probes is a critical determinant of assay success. This diagnostic approach must reconcile two potentially competing objectives: high specificity to avoid cross-reactivity with related pathogens or host genetic material, and comprehensive variant coverage to ensure detection of evolving viral strains. The emergence of SARS-CoV-2 variants with numerous mutations, particularly in the spike protein, has highlighted the necessity for robust primer design strategies that maintain diagnostic efficacy amid viral evolution. This application note details evidence-based methodologies for designing primer and probe sets that achieve this balance, with particular emphasis on applications in nested one-step RT-PCR protocols.
Core Design Principles for Primers and Probes
Fundamental Parameters for Optimal Binding
The thermodynamic and compositional properties of primers and probes directly influence assay sensitivity and specificity. Adherence to established design parameters ensures efficient hybridization and amplification while minimizing non-specific binding events.
Table 1: Optimal Design Characteristics for Primers and Probes
| Parameter | Primers | Probes |
|---|---|---|
| Length | 18-24 nucleotides [45] | 15-30 nucleotides [45] |
| Melting Temperature (Tm) | 54°C or higher; 59°C optimal [45] [46] | 68-70°C [46] |
| GC Content | 40%-60% [45] [46] | 35%-60% [45] |
| GC Clamp | Max 3 G/C in last 5 bases at 3' end [45] | Avoid G at 5' end [45] |
| Amplicon Size | 50-120 nucleotides [46] | N/A |
The strategic placement of guanine (G) and cytosine (C) bases is crucial due to their three hydrogen bonds, which confer greater binding stability than the two bonds formed by adenine (A) and thymine (T) base pairs [45]. This principle underpins the recommendation for GC content between 40% and 60%. Furthermore, primers should avoid stretches of identical nucleotides (homopolymers), with no more than four consecutive Gs considered acceptable [46].
Strategic Target Selection for Variant Coverage
For SARS-CoV-2 detection, target selection focuses on highly conserved genomic regions to maximize variant detection while ensuring specificity against closely related pathogens.
Table 2: SARS-CoV-2 Target Genes for Primer Design
| Target Gene | Conservation & Characteristics | Considerations |
|---|---|---|
| ORF1ab | Highly conserved among sarbecoviruses; contains RNA-dependent RNA polymerase (RdRp) [47] | Essential for viral replication; mutation rates require careful monitoring [47] |
| N (Nucleocapsid) | Highly conserved with abundant expression [47] [48] | Frequently used in diagnostic assays; offers multiple conserved regions [49] |
| E (Envelope) | Highly conserved among sarbecoviruses [47] | Smaller gene size may limit design options |
The VPrimer methodology addresses the challenge of viral evolution by systematically designing primers and probes that cover over 95% of variants while avoiding homology with host sequences and other viruses [50]. This approach utilizes comprehensive variant databases to identify conserved regions resilient to mutational changes, which is particularly valuable for RNA viruses characterized by high mutation rates [50].
Experimental Protocol: A Structured Workflow
In Silico Design and Validation
This protocol outlines a bioinformatics workflow for designing and validating primer-probe sets for SARS-CoV-2 detection, incorporating checks for specificity and variant coverage.
Step 1: Target Sequence Identification
- Identify conserved regions within target genes (ORF1ab, N) using multiple sequence alignments of SARS-CoV-2 variants and related coronaviruses [47].
- For variant discrimination, target regions containing characteristic single nucleotide polymorphisms (SNPs) or deletions specific to Variants of Concern (e.g., HV69-70 deletion in B.1.1.7) [49].
- Select a final target sequence of 100-200 nucleotides encompassing the desired primer binding sites.
Step 2: Specificity Verification via BLAST
- Perform nucleotide BLAST (blastn) against the "Human genomic + transcript" database to ensure no significant homology with human sequences [46].
- Conduct a second BLAST against the "nr" database to check for cross-reactivity with other microorganisms, particularly human coronaviruses (HCoV-229E, HCoV-NL63, HCoV-HKU1, HCoV-OC43, MERS-CoV, SARS-CoV) [47].
- Verify specificity against host species (e.g., feline genome) when designing assays for animal surveillance [48].
Step 3: Primer and Probe Design Using Primer3
- Input the target sequence into Primer3 (https://primer3.ut.ee/) [46].
- Set parameters according to Table 1: product size 50-120 bp, primer Tm 60-66°C, GC content 40-60% [46].
- Select "Pick hybridization probe" and set probe Tm to 68-70°C [46].
- Generate and evaluate multiple candidate sets based on compliance with design parameters.
Step 4: In Silico PCR Validation
- Utilize the UCSC Genome Browser's "In-Silico PCR" tool (https://genome.ucsc.edu/) to verify that primers amplify only the intended target region [46].
- Check for potential amplification of non-target genomic regions that could produce false-positive results.
Step 5: Variant Coverage Assessment
- Align primer and probe sequences against a comprehensive database of SARS-CoV-2 variants (e.g., GISAID) [50] [49].
- Calculate the percentage of variant sequences that perfectly match the primer-probe set, aiming for >95% coverage [50].
- For multiplex assays targeting specific variants, design primers that span characteristic mutations to ensure specific identification [49].
One-Step Nested RT-PCR Assay Protocol
This protocol describes the implementation of a one-step nested RT-PCR for SARS-CoV-2 detection, adapted from published methodologies [7] [51].
Reagent Preparation:
- Prepare reaction mix containing:
- 20 μL template RNA
- 26 μL reaction buffer
- 4 μL enzyme mixture (reverse transcriptase and DNA polymerase)
- Primers and probes at optimized concentrations (typically 200-400 nM each)
- For nested approaches, include both outer and inner primer sets in the same reaction [7] [51].
Thermal Cycling Conditions:
- Reverse Transcription: 50°C for 30 minutes [7]
- Initial Denaturation: 95°C for 1 minute [7]
- First Amplification Stage (20 cycles):
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 70°C for 40 seconds [7]
- Second Amplification Stage (40 cycles):
- Denaturation: 95°C for 15 seconds
- Annealing: 60°C for 30 seconds [7]
- Final Hold: 25°C for 10 seconds [7]
Detection and Analysis:
- Monitor fluorescence during the second amplification stage for real-time detection [7].
- For conventional nested PCR, analyze products by gel electrophoresis (2% agarose) following amplification [51] [48].
Performance Comparison and Validation
Sensitivity Across PCR Modalities
Rigorous validation is essential to establish assay performance characteristics. The following data compare the sensitivity of different PCR approaches for SARS-CoV-2 detection.
Table 3: Comparative Sensitivity of PCR Methods for SARS-CoV-2 Detection
| Method | Limit of Detection (copies/mL) | Positive Rate in Clinical Samples (n=34) | Reference |
|---|---|---|---|
| Traditional qRT-PCR | 520.1 (ORF1ab), 528.1 (N) | 58.82% (20/34) | [7] |
| Droplet Digital PCR (ddPCR) | 401.8 (ORF1ab), 336.8 (N) | 67.65% (23/34) | [7] |
| One-Step Nested qRT-PCR (OSN-qRT-PCR) | 194.74 (ORF1ab), 189.1 (N) | 82.35% (28/34) | [7] |
| Conventional Nested PCR | 0.015 ng/μL RNA | 100% in confirmed positive samples (45/45) | [48] |
The enhanced sensitivity of nested PCR formats, whether in real-time or conventional formats, makes them particularly valuable for detecting low viral loads in patient samples or environmental surveillance [7] [48]. The one-step nested approach offers the additional advantage of reduced contamination risk by containing the entire reaction within a single tube [7].
Specificity Testing
- Test primer-probe sets against panels of related pathogens to confirm specificity [48].
- For SARS-CoV-2, verify no cross-reactivity with other human coronaviruses (HCoV-229E, HCoV-NL63, HCoV-HKU1, HCoV-OC43, MERS-CoV, SARS-CoV) [47] [48].
- Include host genomic DNA to rule up non-specific amplification [48].
- For animal testing, validate against common pathogens that cause similar clinical symptoms (e.g., for feline testing: Feline herpesvirus, Feline calicivirus, Feline coronavirus) [48].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents for SARS-CoV-2 Primer and Probe Applications
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Nucleic Acid Extraction | ISOLATE II RNA Mini Kit [48] | RNA purification from swabs, BALF, tissue; critical for sample quality |
| Reverse Transcription | SensiFAST cDNA Synthesis Kit [48] | First-strand cDNA synthesis from viral RNA template |
| PCR Enzymes/Master Mixes | My Taq HS Red Mix [48]; SuperScript III RT/Platinum Taq High Fidelity Enzyme Mix [52] | Provides optimized buffer, dNTPs, and enzyme for efficient amplification |
| Real-Time PCR Reagents | Sansure OSN-qRT-PCR Assay Kit [7] | Pre-optimized mixtures for one-step nested quantitative detection |
| Positive Control | SARS-CoV-2 pseudovirus [7]; inactivated isolate SARS-CoV-2 USA/WA1/2020 [48] | Assay validation and run-to-run quality control |
| Primer/Probe Synthesis | Eurofins Genomics Oligo Synthesis [45] | Custom DNA oligonucleotides with optional modifications (e.g., FAM, MGB) |
Workflow Visualization
Diagram 1: Comprehensive workflow for bioinformatics design and validation of primers and probes for SARS-CoV-2 detection, emphasizing specificity checks and variant coverage assessment.
Diagram 2: One-step nested RT-PCR workflow for SARS-CoV-2 detection, illustrating the integrated two-stage amplification process within a single tube.
Effective primer and probe design for SARS-CoV-2 detection requires a multifaceted strategy that balances established thermodynamic principles with comprehensive variant coverage analysis. The nested one-step RT-PCR format provides enhanced sensitivity compared to conventional approaches, making it particularly valuable for detecting low viral loads. By implementing the bioinformatics workflows and experimental protocols outlined in this application note, researchers can develop robust detection assays that maintain performance across diverse SARS-CoV-2 variants while ensuring high specificity against related pathogens and host genetic material.
The accuracy of molecular diagnostics, particularly reverse transcription polymerase chain reaction (RT-PCR), is critically dependent on the purity of the sample nucleic acids. Complex matrices such as wastewater and sputum present significant challenges for SARS-CoV-2 detection because they contain numerous substances that can inhibit enzymatic reactions essential for RT-PCR. These inhibitors can co-purify with nucleic acids during extraction, leading to false-negative results and underestimation of viral load, which is especially problematic in public health surveillance and clinical diagnosis [53].
Wastewater contains a diverse range of PCR inhibitors, including humic acids, fulvic acids, polysaccharides, bile salts, metals ions, and lipids [53] [54]. The concentration and diversity of these inhibitors are influenced by factors such as population size, industrial and agricultural inputs, and climate [53]. Similarly, sputum contains inhibitors such as complex polysaccharides, proteins, and cellular debris that can interfere with molecular detection. The presence of these substances can inhibit reverse transcription, quench fluorescent signals, or interact directly with DNA polymerase, ultimately reducing amplification efficiency and detection sensitivity [53].
Effective inhibitor management is therefore essential for reliable SARS-CoV-2 detection, particularly when using highly sensitive methods like one-step nested RT-PCR (OSN-RT-PCR), which can be more susceptible to inhibition due to its multi-amplification design [7]. This application note provides detailed protocols and data for managing inhibitors in these complex matrices within the context of SARS-CoV-2 OSN-RT-PCR detection research.
Quantitative Comparison of Inhibitor Removal Techniques
The following table summarizes the key performance characteristics of various inhibitor management techniques applicable to complex matrices like wastewater and sputum.
Table 1: Comparison of Inhibitor Management Techniques for Complex Matrices
| Technique | Mechanism of Action | Target Matrices | Key Performance Findings | Considerations |
|---|---|---|---|---|
| Guanidinium Isothiocyanate (GIT) Extraction [55] | Denatures proteins and nucleases; separates RNA from inhibitors. | Sewage, latrine solids, stool [55]. | Increased enterovirus positive samples from 3/11 to 7/11; sensitive detection of 0.6-0.003 TCID50 for enteroviruses [55]. | Single-step purification; effective for diverse fecal wastes. |
| Polymeric Adsorbent (DAX-8) [54] | Binds and permanently removes humic acids via centrifugation. | Environmental water, wastewater [54]. | 5% DAX-8 increased MNV qPCR signals; effective permanent removal of humics [54]. | Potential virus adsorption needs evaluation; requires centrifugation. |
| PCR Additives: Bovine Serum Albumin (BSA) [53] | Binds to inhibitors in the reaction mix, reducing their interaction with enzymes. | Wastewater [53]. | BSA added to reaction mixture reduced inhibition and variability in SARS-CoV-2 RT-qPCR [53]. | Easy to implement; added directly to PCR master mix. |
| Sample Dilution [54] | Reduces concentration of inhibitors below an inhibitory threshold. | Complex environmental water, wastewater [54]. | Maximum MNV amplification achieved; optimal factor depends on inhibitor concentration [54]. | Simple but dilutes the target nucleic acid; may reduce sensitivity. |
| RT-qPCR Chemistry Selection [53] | Proprietary buffer components counteract inhibitors. | Wastewater [53]. | Fast Virus (FV) chemistry showed 40.5% reduction in mean inhibition & 57% reduction in variability vs. qScript [53]. | Chemistry-specific performance; requires validation. |
Detailed Experimental Protocols for Inhibitor Management
Protocol 1: DAX-8 Treatment for Wastewater Samples
DAX-8 is a non-soluble polymeric adsorbent highly effective at removing humic substances, a major class of PCR inhibitors in environmental waters [54].
- 1. Principle: Supelite DAX-8 resin binds to hydrophobic organic inhibitors like humic and fulvic acids. After a brief incubation, the resin with bound inhibitors is removed by centrifugation, leaving a purified supernatant for nucleic acid extraction [54].
- 2. Applications: This protocol is designed for concentrated wastewater samples, river water, and other environmental water samples prone to organic contamination.
- 3. Reagents and Equipment:
- Supelite DAX-8 resin (Sigma-Aldrich)
- Concentrated wastewater sample (e.g., post-PEG precipitation)
- Microcentrifuge tubes
- Benchtop centrifuge
- Vortex mixer
- 4. Step-by-Step Procedure:
- Resin Preparation: Ensure the DAX-8 resin is well-mixed.
- Sample Addition: Transfer 1 mL of the concentrated water sample to a microcentrifuge tube.
- Treatment: Add DAX-8 resin to the sample at a 5% (w/v) concentration (e.g., 50 mg per 1 mL sample).
- Incubation: Vortex the mixture thoroughly and incubate at room temperature for 15 minutes with continuous mixing (e.g., on a rotator).
- Separation: Centrifuge the sample at 8,000 rpm for 5 minutes at 4°C to pellet the resin and co-precipitated inhibitors.
- Recovery: Carefully transfer the clarified supernatant to a new tube, avoiding disturbance of the pellet.
- Downstream Processing: Proceed with nucleic acid extraction from the purified supernatant using your preferred kit.
- 5. Critical Notes:
- Virus Loss Control: A process control (e.g., murine norovirus) should be spiked into a separate aliquot to quantify potential target adsorption to the resin [54].
- The resin is not classified as a dangerous substance, but standard laboratory safety practices should be followed.
Protocol 2: Guanidinium Isothiocyanate (GIT) Extraction for Fecal-Rich Matrices
This method is effective for difficult matrices like sewage, latrine solids, and stool, where inhibitors are co-concentrated with viral particles [55].
- 1. Principle: GIT is a potent chaotropic agent that denatures proteins and nucleases, inactivates pathogens, and promotes the selective binding of RNA to silica membranes or its separation during phase separation, effectively removing many classes of PCR inhibitors [55].
- 2. Applications: Ideal for samples with high fecal content, including raw sewage, primary sludge, and clinical stool specimens.
- 3. Reagents and Equipment:
- Guanidinium isothiocyanate solution (e.g., 4M GIT, 0.1M Tris-HCl, pH 6.4)
- Nucleic acid extraction kit compatible with GIT
- Water bath or heating block
- Microcentrifuge
- 4. Step-by-Step Procedure:
- Lysis: Add an equal volume of GIT solution to the concentrated sample or viral pellet. Vortex vigorously for 15-30 seconds.
- Incubation: Incubate the mixture at 65-70°C for 10 minutes to ensure complete lysis and inhibitor dissociation.
- Purification:
- Option A (Silica Column): Add ethanol to the lysate and load onto the column. Proceed with wash steps as per the manufacturer's instructions.
- Option B (Phase Separation): Add phenol-chloroform-isoamyl alcohol, mix, and centrifuge. Transfer the aqueous phase containing RNA.
- Precipitation & Washing: Precipitate RNA with isopropanol, wash with 70% ethanol, and air-dry.
- Elution: Resuspend the purified RNA in nuclease-free water or elution buffer.
- 5. Critical Notes:
- This method was shown to enable detection of as few as 1-3 plaque-forming units of poliovirus in concentrated sewage [55].
- GIT is hazardous; perform all steps in a fume hood and wear appropriate personal protective equipment.
Protocol 3: Optimization of RT-qPCR Chemistry and Additives
The choice of master mix chemistry and additives can significantly mitigate residual inhibition without requiring additional sample pre-treatment steps [53].
- 1. Principle: Specific RT-qPCR chemistries contain enhancers and stabilizers that make the enzymatic reactions more resilient to inhibitors. Additives like BSA can further sequester residual inhibitors [53].
- 2. Applications: This is a "last-line" defense applicable to any complex matrix after nucleic acid extraction, or for routine analysis where inhibition is moderate.
- 3. Reagents and Equipment:
- Two or more commercial one-step RT-qPCR master mixes (e.g., based on "Fast Virus" and "qScript" chemistries)
- Molecular biology grade Bovine Serum Albumin (BSA)
- MgSO₄ (if required by the master mix)
- Real-time PCR instrument
- 4. Step-by-Step Procedure:
- Chemistry Comparison: Set up identical RT-qPCR reactions for the same extracted RNA samples using different master mixes. Follow the respective manufacturers' recommended primer/probe concentrations and cycling conditions.
- Additive Optimization: To the selected master mix, test the addition of:
- BSA at a final concentration of 0.1-0.5 µg/µL.
- MgSO₄ (if the master mix allows for supplementation) to enhance polymerase processivity.
- Inhibition Monitoring: Include an exogenous control RNA (EC RNA) in each reaction to quantify the degree of inhibition and inter-sample variability [53].
- 5. Critical Notes:
- A study found that Fast Virus-based chemistry with BSA and MgSO₄ reduced mean inhibition by 40.5% and inter-sample variability by 57% compared to qScript chemistry [53].
- Optimization of primer and probe concentrations is recommended when switching chemistries.
Workflow Integration for One-Step Nested RT-PCR
Integrating inhibitor management into the OSN-RT-PCR workflow is crucial for achieving the high sensitivity this method promises. The following diagram illustrates the logical pathway for processing complex samples.
Diagram 1: Integrated workflow for SARS-CoV-2 detection in complex matrices, highlighting the critical decision point for inhibitor removal method selection.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagent Solutions for Inhibitor Management in SARS-CoV-2 Research
| Reagent / Material | Function / Application | Specific Example / Note |
|---|---|---|
| Supelite DAX-8 | Polymeric adsorbent for removing humic acids from environmental water and wastewater concentrates. | Effective at 5% (w/v) concentration; requires validation for viral recovery [54]. |
| Guanidinium Isothiocyanate (GIT) | Chaotropic agent for lysis and inhibitor removal in fecal-rich matrices like sewage and stool. | Enables detection of low virus levels (1-3 PFU) in sewage; used in single-step extraction [55]. |
| Bovine Serum Albumin (BSA) | PCR additive that binds inhibitors, reducing their interference with polymerase activity. | Added directly to the RT-qPCR master mix at 0.1-0.5 µg/µL final concentration [53]. |
| Fast Virus-like RT-qPCR Master Mix | Optimized chemistry for sensitive detection in inhibitory matrices. | Shows reduced inhibition and variability compared to standard chemistries [53]. |
| PEG-6000 | Polymer for precipitating and concentrating viral particles from large volume samples. | Used in wastewater surveillance to enrich virions prior to nucleic acid extraction [54]. |
| Exogenous Control RNA | Non-target RNA sequence used to monitor and quantify RT-qPCR inhibition in each reaction. | Critical for data quality control; allows measurement of reverse transcription and amplification efficiency [53]. |
In the context of SARS-CoV-2 detection, optimizing the Limit of Detection (LoD) is paramount for identifying infected individuals and controlling disease spread. Nested One-Step RT-PCR represents a sophisticated molecular technique that combines reverse transcription and two rounds of amplification in a single tube, enhancing both sensitivity and specificity. This application note details systematic protocols for fine-tuning reaction components and cycling parameters to achieve optimal LoD, framed within broader thesis research on advanced SARS-CoV-2 diagnostics. The principles outlined are derived from established methodologies, including a one-step nested approach for SARS-CoV-2 that provides flexibility during reagent shortages [12] [3]. We provide a comprehensive guide for researchers seeking to maximize detection capabilities for low viral load samples, with all protocols validated in clinical and environmental settings.
Theoretical Foundations of LoD Optimization
The Limit of Detection represents the lowest concentration of target nucleic acid that can be reliably detected in a given assay. For SARS-CoV-2 diagnostics, improving LoD directly enhances early infection detection and monitoring capabilities in environmental samples. The fundamental principle underlying LoD optimization in nested One-Step RT-PCR involves enhancing the signal-to-noise ratio through strategic component manipulation and parameter refinement. This process requires a meticulous approach to each reaction component and thermal cycling parameter to maximize efficiency while minimizing non-specific amplification.
The one-step nested approach offers distinct advantages for LoD optimization. By incorporating two sets of primers in a single reaction, this method achieves a dual amplification effect, significantly enhancing sensitivity compared to conventional RT-PCR. The design employs outer primers that flank a region of DNA containing the amplicon of interest, while nested primers correspond to the precise internal region to be amplified [56]. This sequential priming strategy increases specificity by reducing the likelihood of amplifying non-target sequences, as any non-specific products generated by the outer primers are unlikely to be recognized by the second primer set. Research demonstrates that this method can achieve detection limits below 5 copies/reaction for SARS-CoV-2 when properly optimized [37].
Critical Reaction Components and Their Optimization
Core Reaction Components
Table 1: Essential Reaction Components for LoD Optimization in Nested One-Step RT-PCR
| Component | Optimal Concentration Range | Optimization Strategy | Impact on LoD |
|---|---|---|---|
| Primers (Outer & Nested) | 20-50 pmol per reaction [57] | Design with 40-60% GC content; avoid self-complementarity; ensure Tm within 5°C for all primers [57] | High: Specific binding reduces false negatives and improves low-copy detection |
| MgCl₂ Concentration | 1.5-4.0 mM [57] | Titrate in 0.5 mM increments; higher concentrations may help with GC-rich targets [58] | Critical: Affects enzyme processivity and primer annealing efficiency |
| dNTP Mix | 200 μM of each dNTP [57] | Use balanced concentrations; avoid excessive amounts that promote mispriming | Moderate: Sufficient pools ensure complete amplification of low-copy targets |
| DNA Polymerase | 0.5-2.5 units/50 μL reaction [57] | Use enzyme blends with reverse transcriptase and proofreading polymerase [59] | High: Enzyme processivity directly impacts amplification efficiency |
| Template RNA | 1-1000 ng [57] | Use high-purity RNA (A260/280 ~2.0); avoid repeated freeze-thaw cycles [60] | Fundamental: Input quality dictates maximum achievable sensitivity |
| Additives (DMSO, Betaine) | DMSO: 1-10%; Betaine: 0.5-2.5 M [57] | Incorporate for GC-rich targets (>65%); adjust annealing temperature accordingly [56] | Variable: Can dramatically improve amplification of difficult templates |
Advanced Optimization Strategies
Beyond basic component adjustment, several advanced strategies can further enhance LoD:
Hot-Start Technology: Employing hot-start DNA polymerases through antibody-based inhibition, affibodies, or chemical modification prevents non-specific amplification during reaction setup. This technology maintains enzyme inactivity at room temperature, only activating at high temperatures during initial denaturation. This approach significantly reduces primer-dimer formation and mispriming, which is particularly crucial in nested designs with multiple primer sets [56].
Enzyme Blending Systems: Combining highly processive enzymes with proofreading capabilities enhances performance for difficult targets. For instance, the OneTaq One-Step RT-PCR Kit blends ProtoScript II Reverse Transcriptase with reduced RNase H activity and increased thermostability with OneTaq Hot Start DNA Polymerase, enabling amplification of transcripts up to 9 kb while maintaining high sensitivity [59].
Multiplexing Considerations: When detecting multiple targets or incorporating internal controls, primer design becomes increasingly critical. All primers should have Tms within 5°C of each other, and amplicons should be of distinct sizes for clear resolution. Specialized multiplex PCR buffers with isostabilizing components can help maintain stable primer-template duplexes without extensive optimization [61] [56].
Cycling Parameter Optimization
Thermal cycling parameters directly influence reaction efficiency and must be systematically optimized for each primer-template system. The following parameters represent the most critical factors affecting LoD.
Table 2: Thermal Cycling Parameters for LoD Optimization
| Parameter | Standard Conditions | Optimization Approaches | Effect on LoD |
|---|---|---|---|
| Initial Denaturation | 94-98°C for 1-3 min [58] | Increase to 98°C for GC-rich templates; extend time to 5 min for complex genomic DNA [58] | High: Complete template denaturation is essential for efficient priming |
| Denaturation | 94-98°C for 15s-2 min [58] | Increase temperature to 98°C for difficult templates; shorten time for fast cycling [56] | Moderate: Affects template accessibility in each cycle |
| Annealing Temperature | Primer Tm - (3-5°C) [58] | Use gradient PCR; increase temperature incrementally to reduce nonspecific products [62] | Critical: Single most important parameter for specificity |
| Annealing Time | 0.5-2 min [58] | Generally sufficient at 30-60s; can be reduced in fast cycling protocols [56] | Low-Moderate: Sufficient time for specific hybridization |
| Extension Temperature | 70-75°C [58] | Match to polymerase optimum; combine with annealing in two-step PCR [58] | Moderate: Affects polymerase processivity and fidelity |
| Extension Time | 1-2 min/kb [58] | Increase for long amplicons (>3 kb); decrease with highly processive enzymes [61] | High: Inadequate time results in incomplete products |
| Cycle Number | 25-40 cycles [58] | Increase to 40-45 for low-copy targets (<10 copies); avoid >45 cycles to prevent nonspecific amplification [58] | High: Directly impacts signal strength for low-abundance targets |
| Final Extension | 72°C for 5-15 min [58] | Extend to 30 min for complete product formation and A-tailing for cloning [58] | Low-Moderate: Ensures complete product formation |
Advanced Cycling Strategies
Touchdown PCR: This approach begins with an annealing temperature 3-5°C above the calculated Tm of the primers, then gradually decreases the temperature by 1°C per cycle until the optimal annealing temperature is reached. This method preferentially enriches specific targets during early cycles when temperature stringency is high, effectively reducing nonspecific amplification and improving LoD for difficult samples [56].
Two-Step PCR: When the annealing temperature of primers is within 3°C of the extension temperature, combining these steps into a single incubation reduces total cycle time and may improve efficiency. This approach is particularly effective with highly processive DNA polymerases that maintain activity across broader temperature ranges [58].
Fast Cycling Modifications: Utilizing highly processive enzymes enables significant reduction of extension times - as short as 30 seconds per kb compared to 1-2 minutes per kb for conventional polymerases. This approach not only speeds up the reaction but can also improve product yield by reducing enzyme exposure to denaturing temperatures [61] [56].
Experimental Protocol for LoD Optimization
Primer Design and Validation
Target Selection: Identify unique genomic regions with maximal sequence differences from related viruses. For SARS-CoV-2, the ORF1ab gene has shown high specificity with significant differences from bat coronaviruses [12] [3].
Primer Design Criteria:
- Design outer primers to flank the target region (amplicon size: 200-500 bp)
- Design nested primers to bind internally (amplicon size: 100-300 bp)
- Primer length: 15-30 nucleotides [57]
- GC content: 40-60% [57]
- Avoid 3' end complementarity to prevent primer-dimer formation [57]
- Tm difference between all primers: ≤5°C [57]
Specificity Validation:
- Use BLAST analysis against SARS-CoV-2 sequence database
- Check for cross-reactivity with human genome and common respiratory pathogens
- Validate with positive and negative control samples
Reaction Setup and Optimization
Materials:
- One-Step RT-PCR kit (e.g., SuperScript IV UniPrime, OneTaq One-Step) [61] [59]
- RNA template (SARS-CoV-2 positive control)
- Primers (outer and nested sets)
- Nuclease-free water
- Thermal cycler with gradient capability
Basic Reaction Setup (50 μL reaction) [57]:
- 5 μL 10X One-Step Reaction Buffer
- 1 μL dNTP Mix (10 mM each)
- 1 μL Outer Forward Primer (20 μM)
- 1 μL Outer Reverse Primer (20 μM)
- 1 μL Nested Forward Primer (20 μM)
- 1 μL Nested Reverse Primer (20 μM)
- 2 μL One-Step Enzyme Mix
- 5 μL RNA Template (1-1000 ng)
- 33 μL Nuclease-Free Water
Annealing Temperature Optimization:
- Set up identical reactions as above
- Use thermal cycler with gradient capability across annealing temperatures (e.g., 50-65°C)
- Analyze products by agarose gel electrophoresis for specific amplification
- Select temperature yielding strongest specific signal with minimal background
Mg²⁺ Concentration Optimization:
- Prepare reactions with MgCl₂ concentrations from 1.0-4.0 mM in 0.5 mM increments
- Use optimal annealing temperature determined above
- Compare amplification efficiency and specificity
- Select concentration with optimal performance
LoD Determination Protocol
Standard Curve Preparation:
- Use quantified SARS-CoV-2 RNA standard (e.g., from cultured virus)
- Prepare 10-fold serial dilutions from 10⁶ to 10⁰ copies/μL
- Include at least 5 replicates per dilution
Amplification:
- Run all dilutions with optimized protocol
- Include no-template controls (NTC) for contamination monitoring
- Use standardized positive controls for process validation
Data Analysis:
- For real-time detection: Determine the dilution where 95% of replicates test positive [37]
- For end-point detection: Use agarose gel electrophoresis to visualize the lowest dilution with detectable bands
- Calculate copy number using the formula: Copies/μL = (Concentration (g/μL) / (Transcript Length × 660)) × 6.022 × 10²³
Validation:
- Test against clinical samples with known viral load
- Compare with reference method (e.g., RT-qPCR) [60]
- Assess inter-assay and intra-assay variability
Research Reagent Solutions
Table 3: Essential Research Reagents for Nested One-Step RT-PCR
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| One-Step RT-PCR Kits | SuperScript IV UniPrime One-Step RT-PCR System [61] | Combined RT and PCR with universal annealing temperature (60°C); resistant to inhibitors; suitable for multiplexing |
| One-Step RT-PCR Kits | OneTaq One-Step RT-PCR Kit [59] | Blends ProtoScript II Reverse Transcriptase with OneTaq Hot Start DNA Polymerase; amplifies targets up to 9 kb; direct gel loading capability |
| Hot-Start DNA Polymerases | Platinum II Taq Hot-Start DNA Polymerase [56] | Antibody-mediated hot-start; enables room-temperature setup; high processivity for fast cycling |
| Reverse Transcriptases | ProtoScript II Reverse Transcriptase [59] | Reduced RNase H activity; increased thermostability; optimal for GC-rich templates and long transcripts |
| RNA Extraction Kits | RNeasy Mini Kit [37] | High-purity RNA extraction; minimal inhibitor carryover; compatible with various sample types |
| Inhibitor-Resistant Enzymes | Platinum SuperFi II DNA Polymerase [61] | Maintains activity in presence of PCR inhibitors; high fidelity; suitable for direct amplification |
| Quantitative Reference Materials | SARS-CoV-2 Pseudovirus Quantification Reference [37] | Absolute quantification standard; enables copy number determination; validation of LoD claims |
Workflow and Optimization Pathways
The following diagram illustrates the complete workflow for LoD optimization of nested One-Step RT-PCR, incorporating both reaction component and cycling parameter refinement:
Nested One-Step RT-PCR LoD Optimization Workflow
Systematic optimization of both reaction components and cycling parameters is essential for achieving the lowest possible Limit of Detection in nested One-Step RT-PCR for SARS-CoV-2 detection. The protocols outlined provide a comprehensive framework for researchers to enhance assay sensitivity while maintaining specificity. Through iterative refinement of primer design, Mg²⁺ concentration, enzyme selection, annealing temperature, and cycling conditions, detection limits below 5 copies/reaction are achievable. These optimized protocols support critical applications in early infection detection, wastewater surveillance, and clinical diagnostics where maximum sensitivity is required. The nested one-step approach offers particular advantages during reagent shortages or when processing samples with low viral loads, making it a valuable methodology in ongoing pandemic response and future infectious disease surveillance.
The relentless evolution of SARS-CoV-2 has resulted in successive Variants of Concern (VOCs) characterized by mutations that can alter viral transmissibility, disease severity, and crucially, detection by molecular diagnostics [63] [64]. For assays based on specific genetic sequences, such as the highly sensitive one-step nested reverse transcription polymerase chain reaction (OSN-RT-PCR), these mutations pose a significant threat to diagnostic efficacy. A study evaluating commercial RT-PCR kits found that their sensitivity varied considerably against different VOCs, with some kits failing to detect up to 46.7% of Beta variant samples and 36.7% of Delta variant samples [14]. This underscores the critical need for proactive strategies to ensure diagnostic assays remain effective.
This application note details a comprehensive bioinformatic workflow integrated with experimental validation protocols to monitor circulating SARS-CoV-2 variants, assess their impact on OSN-RT-PCR assay performance, and guide timely primer/probe redesign to maintain the highest diagnostic sensitivity and specificity.
Bioinformatic Strategy for VOC Surveillance and Primer Assessment
A robust bioinformatic pipeline is fundamental for tracking viral evolution and its implications for diagnostic assays. The following workflow outlines the key steps from genomic data acquisition to functional analysis.
The diagram below illustrates the core bioinformatic workflow for maintaining assay efficacy:
Data Acquisition and Variant Monitoring
Continuous monitoring of publicly available genomic databases is the first critical step. The National Center for Biotechnology Information (NCBI) and the Global Initiative on Sharing All Influenza Data (GISAID) are primary repositories for SARS-CoV-2 genomic sequences [65] [63]. The Centers for Disease Control and Prevention (CDC) uses genomic surveillance to track variant proportions, providing empiric estimates based on observed data and Nowcast estimates to project trends for the most recent periods [63]. This surveillance identifies variants with mutations in the spike protein and other genomic regions that could impact viral behavior and diagnostic accuracy.
In Silico Primer and Probe Evaluation
Once VOC sequences are obtained, multiple sequence alignment tools (e.g., MEGA, Clustal Omega) are used to compare them against the assay's primer and probe sequences. This analysis identifies mutations within the binding regions that could hinder hybridization. The Pango lineage nomenclature system is used to track the transmission and spread of variants, providing a standardized framework for classification [63].
Bioinformatic tools such as MFEprimer can then be employed to evaluate the thermodynamic stability of the primer-template duplex [3]. Key parameters to assess include:
- Binding Affinity (ΔG): A significant reduction in binding energy suggests weaker hybridization.
- Melting Temperature (Tm): Shifts in Tm can indicate reduced binding efficiency.
- Mismatch Tolerance: The position and type of mismatch (e.g., G-T vs. A-C) determine its severity.
Table 1: Key Mutations in SARS-CoV-2 VOCs and Their Potential Impact on Diagnostic Assays
| Variant (Pango Lineage) | Signature Spike Protein Mutations | Potential Diagnostic Impact |
|---|---|---|
| Alpha (B.1.1.7) | N501Y, D614G, P681H, ∆69-70 | S-gene target failure (SGTF) in some assays [64] [66] |
| Beta (B.1.351) | K417N, E484K, N501Y, D614G | Potential false negatives in kits targeting the E and RdRp genes [14] |
| Delta (B.1.617.2) | L452R, T478K, D614G, P681R | Reduced sensitivity (up to 33.3% false negatives in some kits) [14] |
| Omicron (B.1.1.529) | Extensive mutations including K417N, N501Y, D614G, ∆69-70, P681H | Altered antigenicity; potential for SGTF and primer/probe binding issues [65] [64] |
Experimental Protocol for Validating Assay Performance Against VOCs
Bioinformatic predictions must be confirmed experimentally. The following protocol outlines the validation of an OSN-RT-PCR assay against current VOCs.
Sample and Reagent Preparation
- Viral RNA Sources: Obtain certified RNA from SARS-CoV-2 pseudoviruses engineered to contain the full sequences of target VOCs (Alpha, Beta, Delta, Omicron, etc.) [1] [67]. Alternatively, use residual clinical specimens from patients infected with specific VOCs, as confirmed by whole-genome sequencing [64].
- RNA Extraction: Extract total RNA using membrane adsorption kits (e.g., Di'an, Hangzhou). Elute RNA in nuclease-free water or the buffer provided in the kit [1].
- Assay Components: Prepare the OSN-RT-PCR master mix. The OSN-RT-PCR method typically uses an outer and an inner set of primers in a single tube to amplify a specific region, such as the ORF1ab gene, enhancing sensitivity and specificity [1] [3].
One-Step Nested RT-PCR Assay Procedure
- Reaction Setup: In a single tube, combine the following:
- 5-10 µL of extracted RNA template.
- 12.5 µL of 2X RT-PCR buffer.
- 1 µL of each primer (outer forward, outer reverse, inner forward, inner reverse) at a concentration of 10 µM.
- 0.5 µL of probe (e.g., FAM-labeled) at 10 µM.
- 1 µL of reverse transcriptase enzyme.
- Nuclease-free water to a final volume of 25 µL.
- Thermal Cycling: Run the reaction on a real-time PCR instrument using the following optimized cycling conditions [1] [3]:
- Reverse Transcription: 50°C for 60 minutes.
- Initial Denaturation: 95°C for 10 minutes.
- First-Stage Amplification (Outer Primers): 20 cycles of:
- 95°C for 30 seconds
- 56-60°C for 1 minute
- Second-Stage Amplification (Inner Primers): 40 cycles of:
- 95°C for 15 seconds
- 56-60°C for 30 seconds (with fluorescence acquisition)
Data Analysis and Interpretation
- Cycle Threshold (Ct) Analysis: Record the Ct values for each VOC sample and compare them to the wild-type or a reference strain. A significant and consistent increase in Ct value (e.g., > 3 cycles) for a specific variant indicates reduced assay efficiency [14].
- Limit of Detection (LoD) Determination: Perform a dilution series of pseudoviral RNA for each VOC. The LoD is the lowest concentration at which 95% of the replicates are detected. Compare the LoD across variants to identify any loss of sensitivity [1].
- Specificity Assessment: Ensure the assay does not cross-react with other human coronaviruses or respiratory pathogens.
Table 2: Performance Comparison of SARS-CoV-2 Detection Methods Against VOCs
| Method | Principle | Key Advantage | Reported Sensitivity vs. VOCs | Limitation |
|---|---|---|---|---|
| Conventional qRT-PCR | One-step reverse transcription and real-time PCR | Widely available, high throughput | Variable; 58.82% positive rate in one clinical study [1] | Susceptible to primer/probe mismatches leading to false negatives [14] |
| OSN-qRT-PCR | Single-tube nested PCR with two sequential amplifications | High sensitivity (82.35% positive rate); better for low viral loads [1] | Superior sensitivity for low viral load samples; less impacted by minor mismatches due to dual amplification [1] | Requires careful primer design to avoid primer-dimer formation |
| RT-PCR Genotyping | PCR assays targeting specific VOC mutations | Rapid, high-throughput screening for known VOCs; median 3 days to result [64] [66] | High accuracy for defined variants (e.g., sensitivity: 0.98 for Delta; PPV: 1.00) [66] | Only detects pre-defined mutations; cannot identify novel variants |
| Digital PCR (ddPCR) | Absolute quantification via sample partitioning | High precision and resistance to PCR inhibitors | Good sensitivity (67.65% positive rate), but lower than OSN-qRT-PCR [1] | High cost, specialized equipment, moderate throughput [1] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Kits for OSN-RT-PCR Validation
| Reagent/Kits | Function | Example Use Case |
|---|---|---|
| SARS-CoV-2 Pseudovirus RNA (VOCs) | Provides a safe and consistent source of viral RNA for assay validation | Used as a quantitative standard for determining LoD and assessing PCR efficiency against specific variants [1] [67] |
| Nucleic Acid Extraction Kits | Isolates and purifies viral RNA from complex clinical matrices | Membrane adsorption kits (e.g., Di'an) are used to prepare RNA from nasopharyngeal swabs and other specimens [1] |
| One-Step Nested RT-PCR Master Mix | Contains reverse transcriptase, DNA polymerase, and optimized buffers for the nested reaction | The core component for performing the OSN-RT-PCR assay, enabling sensitive detection of target genes (ORF1ab, N) [1] [3] |
| VOC-Specific Genotyping Kits | Detects specific spike protein mutations (e.g., N501Y, L452R, K417N) | Used to rapidly screen and confirm the presence of specific VOCs in clinical samples as part of the validation process [64] |
| MFEprimer Software | Bioinformatics tool for checking primer specificity and predicting secondary structures | Used during the primer redesign phase to select optimal primer sequences with minimal off-target binding and stable thermodynamics [3] |
Implementation and Workflow Integration
To maintain diagnostic integrity, a continuous cycle of surveillance, assessment, and validation is required. The diagram below outlines the integrated workflow from detection to action:
This integrated approach ensures that OSN-RT-PCR assays remain a powerful tool for SARS-CoV-2 detection. By combining bioinformatic vigilance with rigorous experimental validation, diagnostic assays can be rapidly adapted to address the challenges posed by viral evolution, thereby ensuring continued reliable performance in clinical and public health settings.
Proof of Excellence: Analytical Validation and Benchmarking Against Gold Standards
Within the broader research on nested One-Step RT-PCR for SARS-CoV-2 detection, a critical objective is to rigorously evaluate its analytical performance against established benchmark technologies. Quantitative real-time polymerase chain reaction (qRT-PCR) has been the standard method for clinical diagnosis of COVID-19, while droplet digital PCR (ddPCR) is recognized for its superior precision and sensitivity in nucleic acid quantification. This application note provides a detailed, evidence-based comparison of the sensitivity and specificity of a highly sensitive One-Step Nested qRT-PCR (OSN-qRT-PCR) assay against both qRT-PCR and ddPCR, using standardized samples and clinical specimens. The data confirms that OSN-qRT-PCR presents a formidable alternative, particularly for detecting low viral loads, combining the high sensitivity of digital PCR with the practicality of conventional real-time PCR.
Performance Comparison of Detection Methods
Limit of Detection (LoD) and Clinical Sensitivity
A direct comparison of the LoD and clinical performance reveals a clear hierarchy in sensitivity between the three methods. The following table summarizes key quantitative findings from a controlled study using pseudoviral RNA and clinical samples from COVID-19 patients [7].
Table 1: Analytical and Clinical Sensitivity of SARS-CoV-2 Detection Methods
| Detection Method | LoD for ORF1ab (copies/mL) | LoD for N Gene (copies/mL) | Positive Rate in Clinical Samples (n=34) |
|---|---|---|---|
| qRT-PCR | 520.1 (95% CI: 363.23–1145.69) | 528.1 (95% CI: 347.7–1248.7) | 58.82% (20/34) |
| ddPCR | 401.8 (95% CI: 284.8–938.3) | 336.8 (95% CI: 244.6–792.5) | 67.65% (23/34) |
| OSN-qRT-PCR | 194.74 (95% CI: 139.7–430.9) | 189.1 (95% CI: 130.9–433.9) | 82.35% (28/34) |
As shown in Table 1, OSN-qRT-PCR demonstrates a lower LoD for both the ORF1ab and N gene targets compared to qRT-PCR and ddPCR, indicating higher analytical sensitivity. This translates directly to superior clinical performance, with OSN-qRT-PCR detecting over 23% more positive cases in clinical samples than standard qRT-PCR [7]. Another study corroborates that ddPCR outperforms qRT-PCR in sensitivity, particularly for low-viral-load specimens, by minimizing false-negative results [10]. However, the OSN-qRT-PCR method achieves this even more effectively.
Specificity and Robustness
Specificity is paramount for accurate diagnosis. The OSN-qRT-PCR assay was designed with primers targeting a specific region in the ORF1ab gene that has the greatest differences between human coronaviruses and bat coronaviruses, ensuring species specificity [12] [3]. Furthermore, the nested approach, which uses two pairs of primers in a single tube, inherently increases specificity by requiring successful amplification with two distinct primer sets.
A significant challenge for all PCR-based methods is the virus's rapid mutation rate. Mutations in the primer-probe binding regions can significantly reduce detection sensitivity for both qRT-PCR and ddPCR [68]. The design of OSN-qRT-PCR, which employs four diagnostic primers, offers a built-in advantage: if a mutation occurs in one of the key amplification nucleotides, at least one other primer pair can still amplify the target, thereby enhancing the assay's robustness against emerging variants [12].
Experimental Protocols
Protocol 1: One-Step Nested qRT-PCR (OSN-qRT-PCR)
This protocol is adapted from the highly sensitive method validated by Liu et al. (2020) for the detection of SARS-CoV-2 [7].
Principle: The assay combines reverse transcription, first-round PCR, and second-round nested PCR in a single closed tube. This design minimizes contamination risk and improves sensitivity by performing a second amplification with internal primers.
Workflow Diagram:
Reagents:
- OSN-qRT-PCR Assay Kit (e.g., Sansure)
- Template RNA (20 µL per reaction)
- Nuclease-free water
Procedure:
- Reaction Setup: Prepare a master mix on ice containing 26 µL of reaction buffer and 4 µL of the enzyme mixture per reaction. Aliquot 30 µL of the master mix into each PCR tube or plate well.
- Add Template: Add 20 µL of extracted RNA template to each reaction, bringing the total volume to 50 µL. Vortex and centrifuge briefly to mix and collect the contents.
- Amplification: Place the reaction tube in a real-time PCR instrument (e.g., LightCycler 480 II, Roche). Run the following thermal cycling protocol [7]:
- Reverse Transcription: 50°C for 30 minutes.
- Initial Denaturation: 95°C for 1 minute.
- First-Stage Amplification (20 cycles):
- Denature: 95°C for 30 seconds.
- Anneal/Extend: 70°C for 40 seconds.
- Second-Stage Nested Amplification (40 cycles):
- Denature: 95°C for 15 seconds.
- Anneal/Extend: 60°C for 30 seconds.
- Data Acquisition: 25°C for 10 seconds (acquire fluorescence at this step).
- Analysis: Analyze the amplification curves. A sample is considered positive if it produces a characteristic sigmoidal curve that crosses the threshold line within the 40 cycles of the second-stage amplification.
Protocol 2: Droplet Digital PCR (ddPCR)
This protocol is based on the methods used in comparative studies for SARS-CoV-2 detection [10] [7].
Principle: The reaction mixture is partitioned into thousands of nanoliter-sized droplets. PCR amplification occurs within each droplet, and after cycling, the droplets are analyzed individually to count the number of positive (fluorescent) and negative (non-fluorescent) reactions for absolute quantification.
Workflow Diagram:
Reagents:
- ddPCR Supermix for Probes (no dUTP) (Bio-Rad)
- Reverse Transcriptase
- 300 mM DTT
- SARS-CoV-2 primer-probe reaction solution (targeting ORF1ab and N)
- Template RNA (7 µL per reaction)
- Droplet Generation Oil
Procedure:
- Reaction Setup: On ice, prepare a master mix for the desired number of reactions. Per reaction, combine:
- 5 µL of ddPCR Supermix
- 2 µL of Reverse Transcriptase
- 1 µL of 300 mM DTT
- 5 µL of SARS-CoV-2 primer-probe solution
- 7 µL of RNA template
- Total Volume: 20 µL
- Droplet Generation: Load 20 µL of the reaction mix and 70 µL of droplet generation oil into a DG8 cartridge. Place the cartridge in the QX200 Droplet Generator to create nanoliter-sized droplets.
- Transfer: Carefully transfer the generated droplets (approximately 40 µL) to a 96-well PCR plate. Seal the plate with a foil heat seal.
- Amplification: Place the sealed plate in a thermal cycler (e.g., C1000 Touch, Bio-Rad). Run the following protocol [7]:
- Reverse Transcription: 50°C for 60 minutes.
- Enzyme Activation: 95°C for 10 minutes.
- Amplification (40 cycles):
- Denature: 95°C for 30 seconds.
- Anneal/Extend: 56°C for 1 minute.
- Enzyme Deactivation: 98°C for 10 minutes.
- Hold: 4°C forever.
- Droplet Reading: Place the plate in the QX200 Droplet Reader. The instrument will count the number of positive and negative droplets for the FAM (ORF1ab) and HEX (N) channels.
- Analysis: Use the manufacturer's software to apply a fluorescence amplitude threshold and calculate the concentration (copies/µL) of the target based on Poisson statistics.
Analysis of Mutations in Primer-Probe Regions
Principle: Viral mutations can affect primer/probe binding, leading to reduced sensitivity. This protocol involves monitoring known variant sequences and evaluating their impact on established assays [68].
Workflow Diagram:
Procedure:
- Sequencing and Identification: Perform whole genome sequencing of circulating SARS-CoV-2 variants in your region. Analyze the sequences to identify Single Nucleotide Variants (SNVs) located within the binding regions of commonly used primer-probe sets (e.g., CDC-N1, Charité-E).
- In Silico Analysis: Use alignment software to assess the impact of identified SNVs on the thermodynamic stability of primer-probe binding. Mismatches, especially near the 3' end of primers, are likely to impair amplification efficiency.
- Experimental Validation: Test the effect of mutations by performing qRT-PCR and ddPCR on synthetic controls or patient samples harboring the specific SNVs. Compare the Ct values and copy number quantification to wild-type controls.
- Assay Refinement: If a significant drop in sensitivity is confirmed, design and validate new primer-probe sets that are complementary to the mutated sequences, thereby restoring detection accuracy [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for SARS-CoV-2 PCR Detection Assays
| Reagent / Kit | Function / Description | Example Use Case |
|---|---|---|
| Nucleic Acid Extraction Kit | Purifies RNA from clinical samples (swabs, sputum). Essential for sample prep. | Used in all protocols (OSN-qRT-PCR, ddPCR, qRT-PCR) to obtain template RNA [7]. |
| OSN-qRT-PCR Assay Kit | Contains optimized buffers, enzymes, and primers for one-step nested detection. | Specific to the high-sensitivity OSN-qRT-PCR protocol [7]. |
| ddPCR Supermix for Probes | A reaction mix for probe-based digital PCR, optimized for droplet formation. | Forms the core of the ddPCR reaction mixture [7]. |
| SARS-CoV-2 Primer-Probe Sets | Specific oligonucleotides targeting conserved regions (e.g., ORF1ab, N, E). | Critical for assay specificity. Must be monitored for mismatches due to mutations [10] [68]. |
| Droplet Generation Oil & Cartridges | Consumables for partitioning the ddPCR reaction into nanoliter droplets. | Required for the droplet generation step in the QX200 system [7]. |
| SARS-CoV-2 RNA Transcript Standards | Synthetic RNA of known concentration used as a quantitative standard. | Essential for determining the Limit of Detection (LoD) and assay validation [69]. |
The accurate identification of individuals infected with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) remains a cornerstone of effective public health response to the COVID-19 pandemic. While reverse transcriptase real-time quantitative polymerase chain reaction (qRT-PCR) has been widely adopted as the gold standard for clinical detection, its reported positive rates for throat swab samples vary considerably, often falling between 30% and 60% [70]. This limitation in sensitivity can lead to false-negative results, particularly in patients with low viral loads, complicating clinical management and outbreak control efforts. Consequently, there is a pressing need for more sensitive detection methodologies. This application note evaluates the clinical performance of a highly sensitive one-step nested qRT-PCR (OSN-qRT-PCR) assay for SARS-CoV-2 detection, comparing its positive detection rates against those of qRT-PCR and droplet digital PCR (ddPCR) in confirmed patient cohorts. The data presented herein provide researchers and clinical laboratory professionals with robust evidence for implementing superior detection strategies in both diagnostic and research settings.
Results
Comparative Analytical Sensitivity of PCR Platforms
The limit of detection (LoD) is a fundamental parameter for evaluating the analytical sensitivity of any molecular assay. We determined the LoD for three PCR platforms—qRT-PCR, ddPCR, and OSN-qRT-PCR—using a dilution series of SARS-CoV-2 pseudoviral RNA. The results, quantified for both the ORF1ab and N genes, demonstrate a clear hierarchy in sensitivity.
Table 1: Comparison of Detection Limits for SARS-CoV-2 PCR Assays
| PCR Platform | Target Gene | Limit of Detection (copies/mL) with 95% CI |
|---|---|---|
| qRT-PCR | ORF1ab | 520.1 (363.23 - 1145.69) |
| N | 528.1 (347.7 - 1248.7) | |
| ddPCR | ORF1ab | 401.8 (284.8 - 938.3) |
| N | 336.8 (244.6 - 792.5) | |
| OSN-qRT-PCR | ORF1ab | 194.74 (139.7 - 430.9) |
| N | 189.1 (130.9 - 433.9) |
As summarized in Table 1, the OSN-qRT-PCR assay demonstrated a superior analytical sensitivity, with LoDs approximately 2.7 times lower than those of qRT-PCR and 2.0 times lower than those of ddPCR for the ORF1ab gene [70]. This enhanced sensitivity is attributable to the nested primer design, which employs two sequential amplification reactions in a single tube, thereby increasing the specificity and yield of the target amplicon.
Clinical Performance in Confirmed Patient Cohorts
The clinical sensitivity of each platform was validated using a cohort of 34 clinical specimens from hospitalized patients with confirmed COVID-19. The samples comprised various types, including throat swabs, anal swabs, sputum, and blood, reflecting real-world diagnostic scenarios.
Table 2: Positive Detection Rates in Clinical Samples (n=34)
| PCR Platform | Positive Cases | Positive Rate (%) |
|---|---|---|
| qRT-PCR | 20 | 58.82 |
| ddPCR | 23 | 67.65 |
| OSN-qRT-PCR | 28 | 82.35 |
The clinical performance data (Table 2) reveal that OSN-qRT-PCR achieved a significantly higher positive detection rate (82.35%) compared to both ddPCR (67.65%) and qRT-PCR (58.82%) [70]. This translates to OSN-qRT-PCR identifying 8 more positive patients than standard qRT-PCR within this cohort, underscoring its potential to substantially reduce false-negative results. The superior performance of ddPCR over qRT-PCR is consistent with its known advantages for absolute quantification and resilience to PCR inhibitors, yet it was still outperformed by the nested approach.
Experimental Protocols
Workflow for One-Step Nested qRT-PCR (OSN-qRT-PCR)
The following protocol details the optimized OSN-qRT-PCR assay for the detection of SARS-CoV-2.
Principle: OSN-qRT-PCR integrates two consecutive amplification rounds within a single, sealed tube. The first amplification uses an outer primer pair, and the product from this reaction serves as the template for the second amplification, which is primed by oligonucleotides placed internal to the first pair. This design enhances both sensitivity and specificity while minimizing the risk of amplicon contamination [70] [12].
Reagent Setup:
- Template RNA: 20 µL of extracted total RNA.
- OSN-qRT-PCR Master Mix: 26 µL of reaction buffer.
- Enzyme Mixture: 4 µL.
- Total Reaction Volume: 50 µL.
Procedure:
- Assembly: Combine the reaction buffer, enzyme mixture, and template RNA in a PCR tube. Vortex and centrifuge briefly to ensure mixing.
- Reverse Transcription and First PCR Round:
- Place the tube in a real-time PCR instrument, such as the LightCycler 480 II (Roche).
- Incubate at 50°C for 30 minutes (reverse transcription).
- Incubate at 95°C for 1 minute (initial denaturation).
- Perform 20 cycles of:
- 95°C for 30 seconds (denaturation)
- 70°C for 40 seconds (annealing of outer primers)
- 72°C for 40 seconds (extension)
- Second Nested PCR Round:
- Perform 40 cycles of:
- 95°C for 15 seconds (denaturation)
- 60°C for 30 seconds (annealing of inner primers)
- 25°C for a minimal hold time [70].
- Perform 40 cycles of:
- Analysis: Fluorescence is collected during the annealing or extension step of the second round of amplification. The cycle threshold (Ct) values are determined by the instrument's software.
Reference Protocols for Comparative Platforms
For context, abbreviated protocols for the comparator platforms are provided below.
Droplet Digital RT-PCR (RT-ddPCR)
- Reaction Setup: Combine 5 µL of ddPCR Supermix, 2 µL of reverse transcriptase, 1 µL of 300 mM DTT, 5 µL of SARS-CoV-2 primer-probe reaction solution, and 7 µL of RNA template [70] [37].
- Droplet Generation: Load 20 µL of the reaction mix into a droplet generator (e.g., QX200, Bio-Rad) to partition the sample into thousands of nanoliter-sized droplets [70].
- Thermal Cycling: Perform amplification on a thermal cycler with the following protocol: 50°C for 60 min (RT); 95°C for 10 min; 40 cycles of 95°C for 30 s and 56°C for 1 min; 98°C for 10 min; and a 4°C hold [70] [37].
- Reading and Analysis: Transfer the cycled plate to a droplet reader. The fraction of positive droplets for targets (e.g., FAM for ORF1ab, HEX for N) is counted, and the absolute copy number is calculated using Poisson statistics [70] [37].
Conventional qRT-PCR
- Procedure: Follow the manufacturer's instructions for commercial qRT-PCR kits. Typically, this involves a one-step protocol combining reverse transcription (e.g., 50°C for 15-30 min) and PCR amplification (40-45 cycles of 95°C for 10-15 s and 55-60°C for 30-60 s) with continuous fluorescence monitoring [70].
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for OSN-qRT-PCR
| Item | Function and Description |
|---|---|
| OSN-qRT-PCR Assay Kit | Provides optimized buffer, enzyme mix, and primers for the one-step nested reaction. The kit typically contains a specialized reverse transcriptase and a hot-start DNA polymerase for robust and specific amplification [70]. |
| SARS-CoV-2 Primers (Outer & Inner) | Species-specific primers targeting conserved regions of the SARS-CoV-2 genome, such as ORF1ab and N. The nested design ensures high specificity and sensitivity, potentially offering redundancy if mutations occur in one primer binding site [70] [12]. |
| Nucleic Acid Extraction Kit | For purifying total RNA from clinical specimens (e.g., swabs, sputum). Membrane adsorption-based kits are commonly used to obtain high-quality, PCR-inhibitor-free RNA [70]. |
| Positive Control Template | SARS-CoV-2 pseudoviral RNA or synthetic RNA transcripts of known concentration. Essential for validating assay performance, determining the LoD, and ensuring day-to-day run quality [70]. |
| Real-Time PCR System | Instrument capable of precise thermal cycling and fluorescence detection (e.g., LightCycler 480 II, Roche). Required for real-time monitoring of the nested amplification [70]. |
Discussion
The data presented in this application note firmly establish the OSN-qRT-PCR assay as a superior method for detecting SARS-CoV-2 in clinical samples. Its significantly higher positive detection rate of 82.35% in a confirmed patient cohort, compared to 58.82% for qRT-PCR, demonstrates a critical advantage in clinical sensitivity [70]. This is particularly relevant for patient management and public health, as it can drastically reduce the number of false-negative results, enabling more effective isolation and treatment strategies.
The enhanced performance of OSN-qRT-PCR stems from its fundamental design. The two-stage amplification process, utilizing two pairs of primers, significantly increases the amount of specific amplicon while reducing non-specific amplification and the impact of PCR inhibitors present in clinical samples [70] [12]. While ddPCR also offers high sensitivity and absolute quantification without a standard curve, its requirement for specialized instrumentation and reagents, higher running costs, and moderate throughput can be limiting for routine clinical use [70]. OSN-qRT-PCR, in contrast, achieves higher sensitivity while maintaining compatibility with standard real-time PCR instruments, offering a compelling balance of performance, practicality, and cost-effectiveness.
In conclusion, for researchers and drug development professionals focused on maximizing detection capability for SARS-CoV-2, especially in samples with low viral loads, OSN-qRT-PCR represents a highly sensitive and specific alternative to both qRT-PCR and ddPCR. Its implementation can greatly enhance the accuracy of clinical diagnostics, epidemiological studies, and therapeutic monitoring.
Accurate detection of SARS-CoV-2 is fundamental to controlling infection and understanding disease dynamics. This application note explores the critical correlation between viral load and detection sensitivity across different molecular methods, with a specific focus on the enhanced performance of one-step nested reverse transcription quantitative polymerase chain reaction (OSN-qRT-PCR) within the broader context of SARS-CoV-2 research. As viral load fluctuates throughout the infection cycle, selecting an appropriately sensitive detection method becomes paramount for reliable diagnosis, particularly during phases of low viral shedding. We present structured quantitative data, detailed protocols, and analytical tools to guide researchers in implementing these advanced detection strategies for both clinical and research applications.
Data Analysis: Comparative Assay Performance and Viral Load Correlation
Quantitative Comparison of SARS-CoV-2 Detection Assays
The limit of detection (LoD) is a crucial parameter for evaluating the performance of any diagnostic assay, particularly for identifying patients with low viral loads. The following table summarizes the comparative analytical sensitivity of three primary PCR-based methods for SARS-CoV-2 detection, as established using pseudoviral RNA dilution series [1] [7].
Table 1: Comparative Limits of Detection for SARS-CoV-2 Assays
| Detection Method | LoD for ORF1ab (copies/mL) | LoD for N Gene (copies/mL) | Key Characteristics |
|---|---|---|---|
| qRT-PCR | 520.1 (95% CI: 363.23–1145.69) | 528.1 (95% CI: 347.7–1248.7) | Considered the gold standard; widely available. |
| Droplet Digital PCR (ddPCR) | 401.8 (95% CI: 284.8–938.3) | 336.8 (95% CI: 244.6–792.5) | Absolute quantification without a standard curve; high sensitivity. |
| OSN-qRT-PCR | 194.74 (95% CI: 139.7–430.9) | 189.1 (95% CI: 130.9–433.9) | Highest sensitivity; superior for low viral load detection. |
This data demonstrates that OSN-qRT-PCR achieves an approximately 2.7-fold lower LoD (i.e., higher sensitivity) for both the ORF1ab and N genes compared to standard qRT-PCR, making it particularly suitable for detecting low-level infections [1] [7].
Clinical validation studies further corroborate this analytical superiority. In a study of 34 clinical samples from COVID-19 patients, OSN-qRT-PCR detected 28 positives (82.35%), outperforming both ddPCR (23 positives, 67.65%) and standard qRT-PCR (20 positives, 58.82%) [1] [7].
Cycle Threshold (Ct) as a Surrogate for Viral Load and Its Applications
The Cycle Threshold (Ct) value from qRT-PCR assays serves as an inverse correlate of viral load, with lower Ct values indicating higher viral RNA concentration in the sample. This relationship has significant implications for epidemic tracking and transmission risk assessment.
Table 2: Correlation of Ct Values with Epidemiological and Contamination Metrics
| Metric | Correlation with Ct Value (Gene Target) | Statistical Significance | Public Health Implication |
|---|---|---|---|
| Current Month Positivity Rate | Strong inverse correlation (ORF1ab: r = -0.692; N: r = -0.629) | P = 0.004 (ORF1ab); P = 0.012 (N) | Lower median Ct values (higher viral loads) in a population predict higher current case rates. |
| Following Month Positivity Rate | Extreme inverse correlation (ORF1ab: r = -0.801); Strong inverse correlation (N: r = -0.620) | P = 0.001 (ORF1ab); P = 0.018 (N) | Ct value distribution can serve as a leading indicator for forecasting epidemic trends. |
| Surface Contamination Risk | Ct < 29.09 (ORF1ab) = 11.25x higher odds; Ct < 28.03 (N) = 10.48x higher odds | P < 0.001 | Patient Ct values are effective predictors of environmental contamination risk, informing infection control protocols. |
Data from a study analyzing inbound overseas travelers showed that lower median Ct values were strongly to extremely inversely correlated with the positivity rate not only in the current month but also in the subsequent month, highlighting its predictive value for epidemic dynamics [71]. Furthermore, specific Ct value cut-offs were identified for monitoring surface contamination. Patients with an ORF1ab Ct value below 29.09 were 11.25 times more likely to contaminate their environment, while an N gene Ct below 28.03 increased the odds by 10.48 times [71].
The temporal dynamics of Ct values relative to symptom onset for SARS-CoV-2 generally mirror patterns seen with other respiratory viruses. Ct values are typically in the 25-30 range at symptom onset, decrease (indicating higher viral load) over the next 1-3 days, and then progressively increase, often rising above 30 after one week for most viruses [72].
Experimental Protocols
Detailed OSN-qRT-PCR Workflow for SARS-CoV-2 Detection
The following protocol is adapted from the validated OSN-qRT-PCR method described in the search results, which uses a single-tube, two-step amplification process to enhance sensitivity and specificity [1] [7].
Protocol: OSN-qRT-PCR for SARS-CoV-2
Principle: This assay combines reverse transcription and two consecutive PCR amplifications in a single tube. The first PCR uses an outer primer pair, and the second PCR uses an inner primer pair that binds internally to the first amplicon. This nested approach significantly increases specificity and sensitivity compared to standard qRT-PCR.
Key Reagents and Equipment [1] [7]:
- OSN-qRT-PCR Assay Kit (e.g., from Sansure Biotech)
- RNA Template (extracted from clinical samples)
- Real-Time PCR System (e.g., LightCycler 480 II, Roche)
- Microcentrifuge Tubes and Pipettes
Procedure:
- Reaction Mix Preparation: In a sterile PCR tube, combine the following components on ice:
- 26 µL of OSN Reaction Buffer
- 4 µL of Enzyme Mixture (containing reverse transcriptase, and inner/outer primers)
- 20 µL of extracted RNA template
- Total Reaction Volume: 50 µL.
- Mix and Centrifuge: Gently vortex the reaction tube for 5-10 seconds, then briefly centrifuge to collect the contents at the bottom of the tube.
- Amplification: Place the tube in the real-time PCR instrument and run the following thermal cycling protocol:
- Reverse Transcription: 50°C for 30 minutes.
- Initial Denaturation: 95°C for 1 minute.
- First-Stage PCR (20 cycles):
- Denaturation: 95°C for 30 seconds
- Annealing/Extension: 70°C for 40 seconds
- Second-Stage PCR (40 cycles):
- Denaturation: 95°C for 15 seconds
- Annealing/Extension: 60°C for 30 seconds
- Data acquisition is performed at this step.
- Result Interpretation: Analyze the amplification curves. A sample is considered positive if a characteristic sigmoidal curve crosses the threshold line within the 40 cycles of the second-stage PCR. The Ct value is recorded for relative quantification.
Droplet Digital PCR (ddPCR) Protocol for Absolute Quantification
For absolute quantification of viral load without a standard curve, ddPCR offers a highly sensitive alternative. This protocol is based on the QX200 Droplet Digital PCR System [1] [37].
Protocol: RT-ddPCR for SARS-CoV-2 Absolute Quantification
Principle: The reaction mixture is partitioned into thousands of nanoliter-sized droplets. PCR amplification occurs in each droplet independently, and the fraction of positive droplets is counted to absolutely quantify the target nucleic acid using Poisson statistics.
Key Reagents and Equipment [1] [37]:
- QX200 Droplet Digital PCR System (Bio-Rad), including droplet generator and reader.
- ddPCR Supermix (e.g., One-Step RT-ddPCR Advanced Kit for Probes, Bio-Rad).
- SARS-CoV-2 Primer/Probe Sets (FAM-labeled for ORF1ab, HEX-labeled for N gene).
- RNA Template.
Procedure:
- Reaction Mix Preparation: Prepare the following mix on ice (for one reaction):
- 5 µL of ddPCR Supermix
- 2 µL of Reverse Transcriptase
- 1 µL of 300 mM DTT
- 5 µL of SARS-CoV-2 Primer-Probe Reaction Solution
- 7 µL of RNA Template
- Total Volume: 20 µL.
- Droplet Generation: Transfer the 20 µL reaction mix to the droplet generator. Following the manufacturer's instructions, generate droplets. The output will be approximately 40 µL of droplet emulsion.
- PCR Amplification: Carefully transfer the droplet emulsion to a 96-well PCR plate. Seal the plate and place it in a thermal cycler. Run the following protocol:
- Reverse Transcription: 50°C for 60 minutes.
- Enzyme Activation/Denaturation: 95°C for 10 minutes.
- Amplification (40 cycles): 95°C for 30 seconds, then 56°C for 1 minute.
- Enzyme Deactivation: 98°C for 10 minutes.
- Hold: 4°C.
- (Note: Ramp rate should be 2°C/second for all steps).
- Droplet Reading and Analysis: Place the plate in the QX200 droplet reader. The reader will count the number of positive and negative droplets for each fluorescent channel (FAM and HEX). The copy number concentration (copies/µL) in the original reaction is calculated automatically by the instrument's software using Poisson distribution analysis.
The Scientist's Toolkit: Key Research Reagent Solutions
Successful implementation of sensitive SARS-CoV-2 detection assays relies on a core set of validated reagents and instruments.
Table 3: Essential Reagents and Tools for SARS-CoV-2 Nucleic Acid Detection
| Item | Function/Description | Example Use Case |
|---|---|---|
| Nucleic Acid Extraction Kit | Purifies viral RNA from clinical matrices (swabs, sputum). | Membrane adsorption kits (e.g., Di'an) for consistent yield [1]. |
| OSN-qRT-PCR Master Mix | Contains optimized buffers, enzymes, and nested primers for a single-tube reaction. | Sansure Biotech kit for high-sensitivity detection of ORF1ab and N genes [1] [7]. |
| ddPCR Supermix for Probes | Reagent for partitioning and amplifying target nucleic acids in droplets. | Bio-Rad One-Step RT-ddPCR Advanced Kit for absolute viral load quantification [1] [37]. |
| SARS-CoV-2 Pseudovirus | Non-replicating viral particle containing target RNA sequences; used as a positive control and for LoD studies. | Quantification of ORF1ab and N genes from lentiviral backbone [1] [7]. |
| Real-Time PCR Cycler | Instrument for thermal cycling and fluorescence detection in qPCR. | LightCycler 480 II (Roche) for running OSN-qRT-PCR protocols [7]. |
| Droplet Digital PCR System | Instrument suite for generating, amplifying, and reading droplets. | QX200 System (Bio-Rad) for absolute quantification of viral RNA [1] [37]. |
Visualizing Detection Dynamics and Viral Load
The relationship between the infection cycle, viral load, and the capability of different detection methods is complex. The following diagram synthesizes these dynamics to provide a clear conceptual framework.
The COVID-19 pandemic underscored the critical need for diagnostic methods that are not only sensitive and specific but also robust and reproducible across different laboratory settings. While real-time reverse transcriptase quantitative polymerase chain reaction (qRT-PCR) remains the gold standard for SARS-CoV-2 detection, its technical limitations in detecting low viral loads have prompted the development of more advanced techniques [7]. Nested one-step RT-PCR represents a significant methodological evolution, combining the principle of nested PCR—with its superior sensitivity and specificity—with the streamlined workflow of a single-tube reaction [7] [73]. This application note systematically evaluates the robustness and reproducibility of nested one-step RT-PCR for SARS-CoV-2 detection within the context of multi-center and inter-laboratory studies, providing validated protocols and performance metrics essential for researchers and drug development professionals.
Performance Comparison of SARS-CoV-2 Detection Methods
Analytical Sensitivity and Clinical Performance
The enhanced sensitivity of nested one-step RT-PCR is demonstrated through direct comparison with established methods across multiple studies.
Table 1: Comparative Analytical Sensitivity of SARS-CoV-2 Detection Methods
| Method | Target Gene | Limit of Detection (copies/mL) | 95% Confidence Interval | Reference |
|---|---|---|---|---|
| One-Step Nested qRT-PCR (OSN-qRT-PCR) | ORF1ab | 194.74 | 139.7 - 430.9 | [7] |
| N | 189.1 | 130.9 - 433.9 | [7] | |
| Droplet Digital PCR (ddPCR) | ORF1ab | 401.8 | 284.8 - 938.3 | [7] |
| N | 336.8 | 244.6 - 792.5 | [7] | |
| Conventional qRT-PCR | ORF1ab | 520.1 | 363.23 - 1145.69 | [7] |
| N | 528.1 | 347.7 - 1248.7 | [7] | |
| Conventional Nested PCR | N | 0.015 ng/μL (RNA concentration) | N/A | [74] |
Table 2: Clinical Performance in Patient Samples
| Method | Positive Detection Rate | Number of Positive Samples/Total | Population | Reference |
|---|---|---|---|---|
| One-Step Nested qRT-PCR | 82.35% | 28/34 | COVID-19 Patients | [7] |
| Droplet Digital PCR (ddPCR) | 67.65% | 23/34 | COVID-19 Patients | [7] |
| Conventional qRT-PCR | 58.82% | 20/34 | COVID-19 Patients | [7] |
| Conventional Nested PCR | 100% (Sensitivity & Specificity) | 45/45 positive; 45/45 negative | Human & Cat Samples | [74] |
The data demonstrates that OSN-qRT-PCR offers a lower limit of detection (LoD) than both ddPCR and qRT-PCR, making it particularly suitable for identifying patients with low viral loads [7]. The clinical superiority is further evidenced by its significantly higher positive detection rate in samples from confirmed COVID-19 patients [7]. The high sensitivity and specificity of conventional nested PCR formats have also been independently validated in both human and animal populations [74] [30].
Robustness Across Sample Types and Viral Loads
The reliability of a diagnostic method is tested by its performance across diverse sample types and a broad range of viral loads. Nested PCR has proven effective in detecting SARS-CoV-2 in various human sample types, including throat swabs, anal swabs, sputum, and blood [7]. Its particular value extends to animal surveillance, where it has successfully identified the virus in oropharyngeal swabs from dogs and cats with low viral loads (Ct values 27-33), a challenge for some standard qRT-PCR assays [30]. This ability to consistently detect the virus in different matrices and at low concentrations is a key indicator of methodological robustness, crucial for large-scale screening and surveillance studies [30].
Experimental Protocols for Multi-Center Validation
One-Step Nested qRT-PCR Protocol
The following protocol is adapted from a validated one-step nested qRT-PCR assay for SARS-CoV-2, targeting the ORF1ab and N genes [7].
Workflow Overview:
Detailed Reagents and Procedure:
Reaction Mix Preparation: In a single tube, combine the following components to a final volume of 50 μL:
- 20 μL of template RNA
- 26 μL of reaction buffer
- 4 μL of enzyme mixture (including reverse transcriptase and thermostable DNA polymerase)
- Primers and probes for the first (external) and second (internal) primer sets. The exact sequences and concentrations should be optimized and fixed for inter-laboratory studies. The WHO-recommended primers (e.g., BNIoutS/BNIoutAs for the first round and BNIinS/BNIinAs for the nested round) can be used as a reference [75].
Thermal Cycling Conditions: Run the reaction on a real-time PCR instrument (e.g., LightCycler 480 II) using the following profile:
- Reverse Transcription: 50°C for 30 minutes.
- Initial Denaturation: 95°C for 1 minute.
- First-Stage Amplification (20 cycles):
- Denaturation: 95°C for 30 seconds.
- Annealing/Extension: 70°C for 40 seconds.
- Second-Stage (Nested) Amplification (40 cycles):
- Denaturation: 95°C for 15 seconds.
- Annealing/Extension: 60°C for 30 seconds (with fluorescence acquisition).
- Final Step: 25°C for 10 seconds [7].
Critical Considerations for Reproducibility:
- Template Switching: The one-step nested protocol is designed to occur in a single tube, where the internal primers take over amplification upon exhaustion of the external primers, minimizing the risk of contamination [7] [73].
- Cycle Number Optimization: The number of cycles in the first-stage amplification (typically 20-25 cycles) must be carefully controlled to remain within the linear amplification range, ensuring accurate quantification in the second stage [75].
- Positive and Negative Controls: Each run must include a negative control (nuclease-free water) and a positive control (SARS-CoV-2 RNA of known concentration) to monitor for contamination and assay performance.
Conventional Two-Step Nested RT-PCR Protocol
For laboratories without access to advanced real-time systems, a conventional nested RT-PCR offers a highly sensitive and cost-effective alternative, particularly for end-point detection [74] [30].
Workflow Overview:
Detailed Reagents and Procedure:
Reverse Transcription (First Step):
- Combine 7 μL RNA, 4 μL TransAmp buffer, 1 μL reverse transcriptase enzyme, and 8 μL DEPC-treated water.
- Incubate at 25°C for 10 min, 42°C for 15 min, and 80°C for 5 min [74].
First Round of PCR:
- Reaction Mix: 12.5 μL 2x My Taq HS Red Mix, 1 μL each of external forward and reverse primers (10 pmol/μL), 4 μL cDNA, and 6.5 μL PCR-grade water.
- Thermal Cycling: Initial denaturation at 95°C for 1 min; followed by 35-40 cycles of 95°C for 15 s, 49-55°C for 15 s, 72°C for 15 s; final extension at 72°C for 1 min [74] [30].
Second Round (Nested) PCR:
- Reaction Mix: 12.5 μL 2x My Taq HS Red Mix, 1 μL each of internal forward and reverse primers (10 pmol/μL), 0.5-1 μL of the first-round PCR product, and 10 μL PCR-grade water.
- Thermal Cycling: Use a similar profile to the first round, but with an internal annealing temperature (e.g., 51-56°C) [74] [30].
Detection: Analyze 5-10 μL of the final PCR product by agarose gel electrophoresis (e.g., 2% agarose). A clear band of the expected size (e.g., 633 bp for the N gene target in one assay) indicates a positive result [74].
Critical Considerations for Reproducibility:
- Amplicon Size Design: The nested amplicon should be designed to be smaller than and fully contained within the first-round amplicon.
- Contamination Control: Physical separation of pre- and post-PCR areas, use of dedicated equipment and aerosol-resistant filter tips are mandatory to prevent false positives from amplicon carryover [75].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Nested One-Step RT-PCR
| Reagent/Category | Specific Example(s) | Function & Importance for Reproducibility |
|---|---|---|
| Nucleic Acid Extraction Kits | ISOLATE II RNA Mini Kit; QIAamp viral RNA mini kit; Membrane adsorption kits (Di'an) | Consistent yield and purity of template RNA are foundational. Automated systems or validated manual kits reduce inter-lab variability [7] [74] [76]. |
| One-Step Nested RT-PCR Master Mix | Sansure Biotech OSN-qRT-PCR assay kit | Optimized proprietary mix containing reverse transcriptase, DNA polymerase, and salts. Using a common, validated master mix across centers is critical for reproducibility [7]. |
| Primer & Probe Sets | Targets: ORF1ab, N gene; WHO-recommended primers (BNIoutS/BNIoutAs, BNIinS/BNIinAs) | Primers must be highly specific and validated against circulating variants. Aliquot and use at a standardized concentration in all studies [7] [75]. |
| Positive Control RNA | SARS-CoV-2 pseudoviral RNA; Inactivated isolate (e.g., USA-WA1/2020) | Essential for calibrating instruments, determining LoD, and monitoring inter-assay performance. Should be a quantified standard traceable to an international standard [7] [74]. |
| Thermal Cyclers | LightCycler 480 II (Roche); QB96 (Quanta Biotech) | Instrument-specific thermal performance can affect efficiency. Calibration and using the same model/software version across sites enhances data uniformity [7] [74]. |
The rigorous assessment of nested one-step RT-PCR confirms its exceptional robustness, reproducibility, and high sensitivity for detecting SARS-CoV-2. These attributes make it an indispensable tool not only for clinical diagnostics of low viral load infections but also for large-scale epidemiological studies and animal surveillance programs where cost and sensitivity are paramount [7] [30]. The standardized protocols and reagent specifications outlined in this application note provide a clear framework for implementing this powerful technique in multi-center research, ensuring the generation of reliable, high-quality, and comparable data across the scientific community.
Conclusion
One-Step Nested RT-PCR establishes itself as a superior molecular tool for SARS-CoV-2 detection, particularly where sensitivity is paramount. Evidence consistently demonstrates its enhanced performance over conventional qRT-PCR and even ddPCR, especially in clinical and environmental samples with low viral loads. The methodology's robustness, cost-effectiveness, and adaptability for high-throughput screening make it an invaluable asset for clinical diagnostics, public health surveillance, and drug development research. Future directions should focus on the development of standardized, commercially available kits, further automation to increase accessibility, and the continuous adaptation of primer sets to ensure detection fidelity in the face of ongoing SARS-CoV-2 evolution. Its application is also poised to extend beyond COVID-19, serving as a blueprint for detecting other emerging pathogens with high sensitivity and speed.
References
- 1. Analysis and validation of a highly sensitive - one ... step nested [https://pmc.ncbi.nlm.nih.gov/articles/PMC7768088/]
- 2. - and Single - Two , Closed- Stage , Point-of-Care, Molecular... Tube [https://pubmed.ncbi.nlm.nih.gov/34541844/]
- 3. (PDF) One - step - nested for COVID-19 detection: A flexible... RT PCR [https://www.academia.edu/61873313/One_step_nested_RT_PCR_for_COVID_19_detection_A_flexible_locally_developed_test_for_SARS_CoV2_nucleic_acid_detection]
- 4. Triplex Real-Time RT-PCR for Severe Acute Respiratory Syndrome Coronavirus 2 - Volume 26, Number 7—July 2020 - Emerging Infectious Diseases journal - CDC [https://wwwnc.cdc.gov/eid/article/26/7/20-1285_article]
- 5. Development of multiplex real-time RT-PCR assay for the detection of SARS-CoV-2 | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0250942]
- 6. of Detection - SARS - CoV RNA using RT-LAMP and molecular beacons 2 [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-021-02387-y]
- 7. Analysis and validation of a highly sensitive one-step nested... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-020-01467-y]
- 8. Comparison of reverse-transcription qPCR and droplet digital PCR for the detection of SARS-CoV-2 in clinical specimens of hospitalized patients - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8933867/]
- 9. Digital droplet PCR accurately quantifies SARS-CoV-2 viral load from crude lysate without nucleic acid purification | Scientific Reports [https://www.nature.com/articles/s41598-020-80715-1]
- 10. Analytical comparisons of SARS-COV-2 detection by qRT - PCR and... [https://pubmed.ncbi.nlm.nih.gov/32448084/]
- 11. Frontiers | Evaluation of droplet digital qRT-PCR (dd qRT-PCR) for quantification of SARS CoV-2 RNA in stool and urine specimens of COVID-19 patients [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2023.1148688/full]
- 12. - One - step for COVID-19 nested : A flexible, locally... RT PCR detection [https://pubmed.ncbi.nlm.nih.gov/32794453/]
- 13. Comparison five primer sets from different genome of... region [https://pmc.ncbi.nlm.nih.gov/articles/PMC7340604/]
- 14. Evaluation of RT-PCR assays for detection of SARS-CoV-2 variants of concern | Scientific Reports [https://www.nature.com/articles/s41598-023-28275-y]
- 15. The Comparative Analysis of Two RT-qPCR Kits for Detecting SARS-CoV-2 Reveals a Higher Risk of False-Negative Diagnosis in Samples with High Quantification Cycles for Viral and Internal Genes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9259548/]
- 16. Rapid detection of SARS-CoV-2 RNA using a one -step fast multiplex... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-10296-1]
- 17. Development and Evaluation of Novel and Highly Sensitive Single-Tube Nested Real-Time RT-PCR Assays for SARS-CoV-2 Detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7461039/]
- 18. Diagnosis of SARS-CoV-2 by RT-PCR Using Different Sample Sources: Review of the Literature - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7459180/]
- 19. Sensitivity evaluation of 2019 novel coronavirus (SARS-CoV-2) RT-PCR detection kits and strategy to reduce false negative - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7673793/]
- 20. -ID, a MIQE-compliant sub-20-min 5-plex CoV - 2 assay... RT PCR [https://www.nature.com/articles/s41598-020-79233-x?error=cookies_not_supported&code=fab577fb-9397-4802-b526-42c2f2f6d42a]
- 21. Development and validation of cost-effective one-step multiplex... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9019801/]
- 22. A multicenter study to assess the performance of the point-of-care RT-PCR Cobas SARS-CoV-2 & Influenza A/B nucleic acid test for use on the Cobas Liat system in comparison with centralized assays across healthcare facilities in the United States - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345166/]
- 23. Rapid thermal cycling approach for the detection of SARS-CoV-2 [https://www.news-medical.net/news/20211115/Rapid-thermal-cycling-approach-for-the-detection-of-SARS-CoV-2.aspx]
- 24. ‘CoviSwiftTM’: A point-of-care RT-PCR device for SARS-CoV-2 and its variant detection - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10023201/]
- 25. Development of an in-house primer design: Nested polymerase chain reaction for coronavirus disease 2019 detection based on open reading frame 1a/b and spike [https://onehealthjournal.org/Vol.10/No.2/3.php]
- 26. - SARS - CoV Using Magnetic Beads for Rapid... 2 RNA Extraction [https://pubmed.ncbi.nlm.nih.gov/32784757/]
- 27. Viral RNA Kits for Extraction - SARS - CoV 2 Research [https://www.thermofisher.com/ng/en/home/life-science/dna-rna-purification-analysis/automated-purification-extraction/sars-cov-2-nucleic-acid-extraction.html]
- 28. EXCESSIVE THERMAL CYCLING CONVERTS AMPLIFIED PCR PRODUCTS TO RANDOM-LENGTH HIGHER MOLECULAR WEIGHT FRAGMENTS | Science Inventory | US EPA [https://cfpub.epa.gov/si/si_public_record_Report.cfm?LAB=NHEERL&dirEntryID=36809]
- 29. - SARS - CoV virus PCR tiling and sequencing from 2 using... RNA [https://nanoporetech.com/document/pcr-tiling-of-sars-cov-2-virus-rbk114-and-midnight-rt]
- 30. Nested PCR effective to detect low viral loads of SARS-CoV-2 in animal samples - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0167587724001892]
- 31. Development of Nested PCR for SARS-CoV-2 Detection and Its Application for Diagnosis of Active Infection in Cats - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9231004/]
- 32. A review of nasopharyngeal swab and saliva tests for SARS‐CoV‐2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8242677/]
- 33. Comparison of SARS-CoV-2 Specimen Types: Nasal Swabs, Nasopharyngeal ... [https://health.ucdavis.edu/blog/lab-best-practice/comparison-of-sars-cov-2-specimen-types-nasal-swabs-nasopharyngeal-swabs-and-beyond/2021/09]
- 34. International Journal of Molecular Medicine [https://www.spandidos-publications.com/10.3892/ijmm.2021.4933]
- 35. Frontiers | Consistent trends from different methods for monitoring... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1547831/full]
- 36. Comparison of ordinary reverse transcription real-time polymerase ... [https://pubmed.ncbi.nlm.nih.gov/37553492/]
- 37. Frontiers | Droplet digital RT - PCR method for SARS - CoV - 2 variants... [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1635733/full]
- 38. Direct detection of SARS-CoV-2 RNA using high-contrast pH-sensitive dyes - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8730524/]
- 39. Validation of methods for enriching and detecting - SARS - CoV RNA... 2 [https://link.springer.com/article/10.1007/s10311-025-01843-6]
- 40. COVID-19 Wastewater Data – National Trends | NWSS | CDC [https://www.cdc.gov/nwss/rv/COVID19-national-data.html]
- 41. Integrating wastewater analysis and targeted clinical testing for early... [https://pubs.rsc.org/en/content/articlelanding/2025/ew/d4ew00654b]
- 42. for public health: timely, sensitive, and reliable... Wastewater [https://pubs.rsc.org/EN/content/articlelanding/2025/ew/d4ew00845f]
- 43. Establishment of a quantitative RT - PCR detection of SARS - CoV - 2 virus [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-021-00608-5]
- 44. Detection and Quantification of SARS - CoV - 2 by Real-Time RT - PCR ... [https://pubmed.ncbi.nlm.nih.gov/35554902/]
- 45. guide - 5 tips for best PCR results Primer design [https://the-dna-universe.com/2022/09/05/primer-design-guide-the-top-5-factors-to-consider-for-optimum-performance/]
- 46. PCR Primer or Primer + Probe design [https://www.biostars.org/p/9473967/]
- 47. for quantitative real-time PCR for the emerging... Primer design [https://www.thno.org/v10p7150.htm]
- 48. Development of Nested PCR for SARS-CoV-2 Detection and Its Application for Diagnosis of Active Infection in Cats [https://www.mdpi.com/2306-7381/9/6/272]
- 49. to detect SARS-CoV-2 Primer | Kilobaser design Variants [https://kilobaser.com/post/primer-design-for-sars-cov-2-variants]
- 50. VPrimer: A Method of Designing and Updating Primer ... and Probe [https://pubmed.ncbi.nlm.nih.gov/34951850/]
- 51. One-step nested RT-PCR for COVID-19 detection: A flexible, locally developed test for SARS-CoV2 nucleic acid detection | The Journal of Infection in Developing Countries [https://jidc.org/index.php/journal/article/view/32794453]
- 52. Comparison of a one-step real-time RT-PCR and a nested real-time RT-PCR for a genogroup II norovirus reveals differences in sensitivity depending upon assay design and visualization | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0248581]
- 53. The Inhibition and Variability of Two Different RT-qPCR Assays Used for Quantifying SARS-CoV-2 RNA in Wastewater | Food and Environmental Virology [https://link.springer.com/article/10.1007/s12560-022-09542-z]
- 54. Assessment of PCR Inhibitor Removal Methods to Monitor Viruses in Environmental Water Samples: DAX-8 Outperforms Competitors | Water, Air, & Soil Pollution [https://link.springer.com/article/10.1007/s11270-023-06821-8]
- 55. Methods to remove inhibitors in sewage and other fecal wastes for enterovirus detection by the polymerase chain reaction - PubMed [https://pubmed.ncbi.nlm.nih.gov/7559857/]
- 56. PCR Methods - Top Ten Strategies | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-methods.html]
- 57. : Basic Protocol Plus Troubleshooting... Polymerase Chain Reaction [https://www.jove.com/t/3998/polymerase-chain-reaction-basic-protocol-plus-troubleshooting]
- 58. PCR Cycling Parameters—Six Key Considerations for Success | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-cycling-considerations.html]
- 59. OneTaq One - Step - RT Kit - New England Biolabs GmbH PCR [https://www.neb-online.de/en/pcr-and-dna-amplification/reverse-transcription-cdna-synthesis/onetaq-one-step/]
- 60. Evaluation and comparison of one - step real-time PCR and one - step ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-024-09574-9]
- 61. - One - Step Systems | Thermo Fisher Scientific - RU RT PCR [https://www.thermofisher.com/ru/ru/home/life-science/pcr/reverse-transcription/superscript-iv-one-step-rt-pcr-system.html]
- 62. Stepwise Optimization of Real-Time RT-PCR Analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/36995635/]
- 63. Variants and Genomic Surveillance | COVID-19 | CDC [https://www.cdc.gov/covid/php/variants/variants-and-genomic-surveillance.html]
- 64. Tracking SARS-CoV-2 variants through pandemic waves using RT-PCR testing in low-resource settings - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10234525/]
- 65. Characteristic analysis of Omicron-included SARS - CoV - 2 ... variants of [https://pubmed.ncbi.nlm.nih.gov/35434714/]
- 66. RT-PCR genotyping assays to identify SARS-CoV-2 variants in England in 2021: a design and retrospective evaluation study - UK Health Security Agency [https://researchportal.ukhsa.gov.uk/en/publications/rt-pcr-genotyping-assays-to-identify-sars-cov-2-variants-in-engla]
- 67. Molecular insights into receptor binding of... | Nature Communications [https://www.nature.com/articles/s41467-021-26401-w?error=cookies_not_supported&code=73d2f41a-966e-420c-8f79-23812ba4c705]
- 68. Sensitivity analysis of RT-qPCR and RT-ddPCR for SARS-CoV-2 detection with mutations on N1 and E primer-probe region - PubMed [https://pubmed.ncbi.nlm.nih.gov/38916349/]
- 69. Analytical sensitivity and efficiency comparisons of SARS-COV-2 qRT-PCR primer-probe sets | medRxiv [https://www.medrxiv.org/content/10.1101/2020.03.30.20048108v3]
- 70. Analysis and validation of a highly sensitive one - step ... nested [https://link.springer.com/article/10.1186/s12985-020-01467-y]
- 71. Evaluation of the cycle threshold values of RT-PCR for SARS-CoV-2 in COVID-19 patients in predicting epidemic dynamics and monitoring surface contamination - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9671601/]
- 72. Cycle threshold dynamics of non–severe acute respiratory coronavirus virus 2 (SARS-CoV-2) respiratory viruses | Infection Control & Hospital Epidemiology | Cambridge Core [https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiology/article/abs/cycle-threshold-dynamics-of-nonsevere-acute-respiratory-coronavirus-virus-2-sarscov2-respiratory-viruses/A078FE22A5801B63A8BF43F116691E3B]
- 73. Sensitive and quantitative detection of pathogens by real-time nested PCR - National Health Research Institutes [https://www.freepatentsonline.com/y2005/0233314.html]
- 74. Veterinary Sciences | Free Full-Text | Development of Nested PCR for SARS-CoV-2 Detection and Its Application for Diagnosis of Active Infection in Cats [https://www.mdpi.com/2306-7381/9/6/272/htm]
- 75. Sensitive and Quantitative Detection of Severe Acute Respiratory Syndrome Coronavirus Infection by Real-Time Nested Polymerase Chain Reaction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7107825/]
- 76. 2.1. Analysis for the detection and confirmation of COVID 19 [https://bio-protocol.org/exchange/minidetail?id=9403912&type=30]