Beyond Situs Inversus: Advanced Strategies for Detecting Primary Ciliary Dyskinesia in Patients Without Laterality Defects
Primary Ciliary Dyskinesia (PCD) remains significantly underdiagnosed in patients who do not present with the classic hallmark of organ laterality defects.
Beyond Situs Inversus: Advanced Strategies for Detecting Primary Ciliary Dyskinesia in Patients Without Laterality Defects
Abstract
Primary Ciliary Dyskinesia (PCD) remains significantly underdiagnosed in patients who do not present with the classic hallmark of organ laterality defects. This creates a diagnostic blind spot, particularly for the estimated 50% of PCD patients with situs solitus. This article provides a comprehensive framework for researchers, scientists, and drug development professionals to bridge this diagnostic gap. We explore the foundational clinical phenotypes that should trigger suspicion, detail the evolving landscape of diagnostic methodologies—from nasal nitric oxide (nNO) to genetic panels and advanced imaging. The content further addresses critical troubleshooting in complex cases, optimizes referral pathways, and validates new technologies against established standards. By synthesizing current evidence and emerging innovations, this review aims to equip the biomedical community with the tools to enhance early detection, accelerate clinical trial enrollment, and pave the way for targeted therapeutic development for all PCD patients.
The Clinical Conundrum: Unmasking the PCD Phenotype Without Laterality Defects
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder of motile ciliary dysfunction that results in insufficient mucociliary clearance. The clinical presentation typically includes unexplained neonatal respiratory distress, chronic sino-oto-pulmonary congestion, and recurrent infections [1]. Nearly half of all patients with PCD have a laterality defect, such as situs inversus totalis (a complete mirror-image reversal of the thoracic and abdominal organs) or heterotaxy [2] [1]. This visible anatomical clue has historically served as a key indicator for clinicians to initiate a PCD diagnostic workup.
However, this reliance on laterality defects has created a significant epidemiological blind spot: patients who have PCD with situs solitus (normal organ arrangement) frequently remain undiagnosed or experience substantial diagnostic delays. This article examines the scale of this underdiagnosis, explores the underlying causes, and provides the scientific community with targeted troubleshooting guides and experimental protocols to enhance detection of PCD across all patient populations, particularly those without laterality defects.
Quantitative Analysis of the Diagnostic Gap
Epidemiological Data on Laterality Defects and PCD
Table 1: Epidemiology of Laterality Defects and Association with PCD
| Condition | Prevalence in Population | Prevalence of PCD within Condition | Key Clinical Associations |
|---|---|---|---|
| Situs Inversus Totalis | 1 in 6,500 - 1 in 25,000 births [2] [3] | 25% have Primary Ciliary Dyskinesia (PCD) [3] [4] | Kartagener Syndrome triad: situs inversus, chronic sinusitis, bronchiectasis [3] [5] |
| Heterotaxy (Situs Ambiguus) | ~1 in 10,000 births [2] [6] | Data insufficient but significantly increased risk [1] [6] | High prevalence (up to 100%) of complex congenital heart disease [6]. |
| Situs Solitus (Normal Anatomy) | >99.9% of population | Underdiagnosed; estimated PCD prevalence 1:10,000 - 1:25,000 [1] | Lacks the obvious anatomical red flag, leading to diagnostic oversight. |
Referral and Evaluation Rates: Revealing the Systemic Gap
A pivotal 2025 retrospective study provides the most compelling quantitative evidence of underdiagnosis. The research analyzed 369 patients with confirmed laterality defects, focusing on those who met the American Thoracic Society (ATS) criteria for PCD evaluation [1].
Table 2: PCD Evaluation Rates in Patients with Laterality Defects (2025 Study Data)
| Patient Cohort | Met ≥2 ATS PCD Criteria | Referred to Pulmonary Medicine | Actually Evaluated for PCD |
|---|---|---|---|
| All patients with laterality defects | 49% (n=180) | 41% | 16% |
| Patients meeting 2 criteria | 79 patients | 41% | 16% |
| Patients meeting all 4 criteria | 27 patients | 96% | 93% |
This data reveals a critical failure in the diagnostic pipeline: even when patients present with a known risk factor (a laterality defect) plus a second clinical symptom of PCD, the majority (84%) are not advanced to a definitive evaluation [1]. The study concluded that a "substantial number of pediatric patients meeting two PCD referral criteria are not referred to pediatric pulmonologists, and a larger number are not being evaluated for PCD" [1]. This demonstrates a systemic underestimation of PCD prevalence, particularly in the situs solitus population where the initial red flag of a laterality defect is absent.
FAQs: Troubleshooting PCD Diagnosis in Situs Solitus
Q1: What is the core clinical challenge in identifying PCD patients with situs solitus? A1: The primary challenge is the lack of a specific pathognomonic symptom. Clinical features like chronic cough and nasal congestion are highly common in childhood and overlap with more frequent conditions like recurrent viral infections, asthma, and allergic rhinitis [1]. Without the striking clue of situs inversus, clinicians often reasonably attribute symptoms to these more common ailments, leading to a low index of suspicion for PCD.
Q2: What are the key clinical criteria that should trigger a PCD evaluation in a patient with normal organ arrangement (situs solitus)? A2: Per the American Thoracic Society guidelines, the presence of any two of the following four criteria warrants a PCD evaluation [1]:
- Unexplained Neonatal Respiratory Distress: In a term infant, requiring oxygen or positive pressure for ≥24 hours.
- Persistent Daily Cough: Year-round, beginning before 6 months of age.
- Persistent Daily Nasal Congestion: Year-round, beginning before 6 months of age.
- An Organ Laterality Defect: Such as situs inversus or heterotaxy. (In situs solitus patients, this criterion is by definition absent, so two of the first three are required).
Q3: In a research setting, what is the recommended diagnostic workflow for confirming PCD? A3: A combination of diagnostic modalities is required for a definitive confirmation.
- Initial Screening: Measure Nasal Nitric Oxide (nNO). Chronically low nNO is a strong indicator of PCD [5].
- Genetic Analysis: Perform genetic testing for pathogenic variants in known PCD-associated genes. Given genetic heterogeneity, extended or whole-genome sequencing may be necessary.
- Ciliary Ultrastructure Analysis: If genetic results are inconclusive, proceed with Transmission Electron Microscopy (TEM) of a ciliary biopsy to assess dynein arm defects and other ultrastructural abnormalities [1] [5].
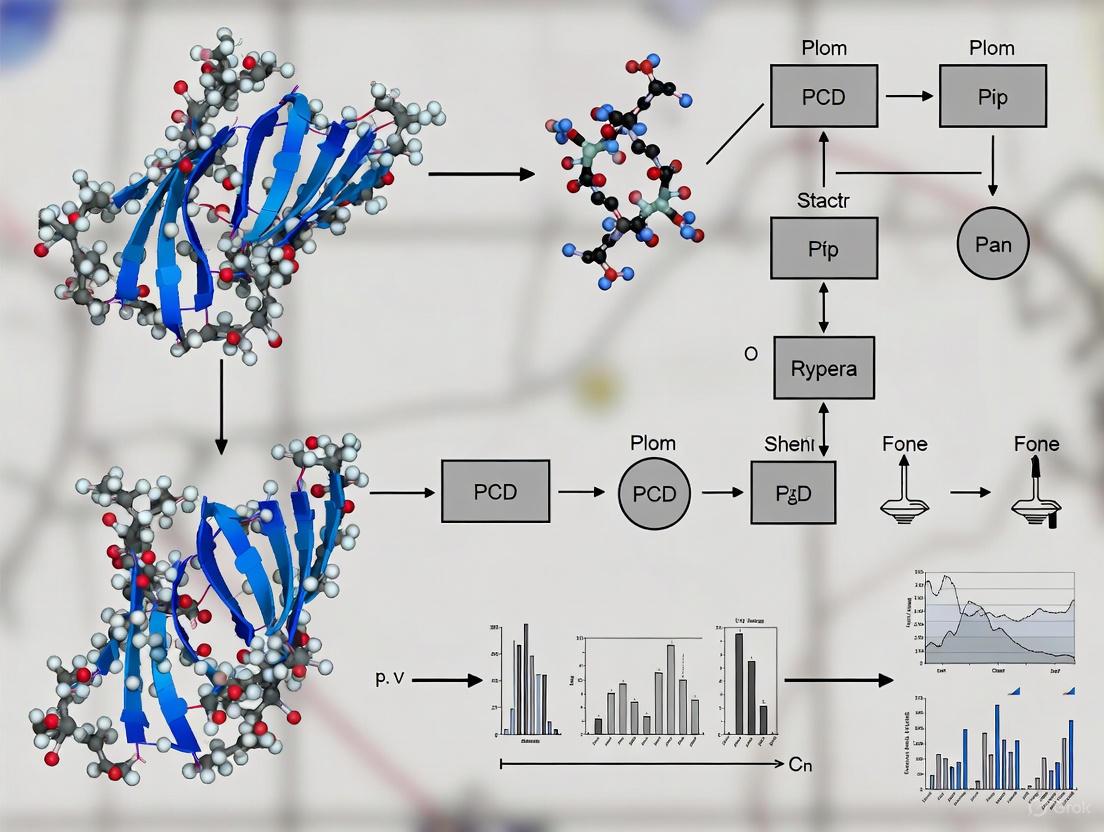
Diagram 1: Confirmatory PCD Diagnostic Workflow. This flowchart outlines the multi-modal approach required for a definitive PCD diagnosis, as per current guidelines.
Q4: Which genetic pathways and reagents are most critical for PCD research and diagnostics? A4: Over 100 genes have been linked to laterality defects, with a significant subset directly involved in PCD pathogenesis [2] [4]. Research focuses on genes affecting ciliary structure and function.
Table 3: Key Research Reagent Solutions for PCD Investigation
| Reagent / Assay Category | Specific Examples | Primary Function in PCD Research |
|---|---|---|
| Genetic Analysis Tools | Targeted NGS Panels (PCD-specific), Whole Exome/Genome Sequencing | Identification of pathogenic variants in genes like DNAH5, DNAI1, CCDC39, CCDC40, and other PCD-associated loci. |
| Antibodies for Protein Localization | Anti-DNAH5, Anti-DNALI1, Anti-GAS8 | Immunofluorescence staining to confirm protein expression and localization within ciliary axonemes. |
| Ciliary Functional Assays | High-Speed Video Microscopy Analysis Systems | Quantitative and qualitative assessment of ciliary beat frequency and pattern. |
| Ultrastructural Analysis | Transmission Electron Microscopy (TEM) Reagents | Visualization of ciliary cross-sections to identify defects in outer/inner dynein arms, nexin links, etc. |
Advanced Experimental Protocols
Protocol for a Prospective Study on Situs Solitus PCD Detection
Objective: To determine the prevalence of PCD in a cohort of children with situs solitus and persistent, otherwise unexplained respiratory symptoms.
Methodology:
- Recruitment: Enroll children aged 0-18 years with situs solitus and at least two of the three clinical ATS criteria (excluding laterality defect): unexplained neonatal respiratory distress, persistent daily cough, or persistent daily nasal congestion.
- Screening Phase:
- Perform nNO measurement on all participants.
- Exclude cystic fibrosis via sweat chloride test or genetic analysis.
- Confirmatory Phase:
- All participants with low nNO proceed to the confirmatory phase.
- Perform next-generation sequencing using a comprehensive PCD gene panel.
- For participants with inconclusive genetic results, obtain a nasal brush biopsy for TEM analysis of ciliary ultrastructure.
- Data Analysis:
- Calculate the point prevalence of confirmed PCD within the recruited cohort.
- Analyze the sensitivity and specificity of the ATS clinical criteria in the situs solitus population.
- Characterize the genetic and ultrastructural spectrum of PCD variants identified.
Diagram 2: Situs Solitus PCD Detection Study. This workflow details a proposed research protocol to actively identify and confirm PCD in the under-diagnosed situs solitus population.
The underdiagnosis of PCD in individuals with situs solitus represents a significant epidemiological gap and a failure in clinical translation. The quantitative evidence shows that even when clear clinical criteria are met, referral and evaluation rates remain unacceptably low. Overcoming this requires a paradigm shift from a suspicion based on rare anatomical clues to one driven by systematic screening for a constellation of common, persistent respiratory symptoms beginning in infancy. By employing the detailed troubleshooting guides, standardized diagnostic workflows, and targeted research protocols outlined herein, researchers and clinicians can collaborate to close this diagnostic gap, ensure timely interventions, and ultimately generate a more accurate understanding of the true prevalence and natural history of Primary Ciliary Dyskinesia.
Frequently Asked Questions (FAQs)
1. Why is "unexplained neonatal respiratory distress" in a term infant a red flag for PCD? Neonatal respiratory distress occurs in more than 80% of patients with Primary Ciliary Dyskinesia (PCD) and typically presents within the first 1-2 days of life [7]. In PCD, this distress is caused by impaired mucociliary clearance, leading to mucus impaction, atelectasis, and lobar collapse [7]. It is a significant indicator, especially in term infants without other risk factors (like surfactant deficiency common in prematurity) and when symptoms have a somewhat later onset, beginning 12-24 hours after birth [7]. Distinguishing it from other causes like transient tachypnea of the newborn (TTN) is crucial, as PCD is a chronic condition requiring long-term management.
2. What constitutes "chronic daily symptoms" in the context of PCD? The ATS clinical criteria emphasize early-onset, year-round symptoms that are present on a daily basis [7]. The core chronic daily symptoms of PCD are:
- A daily wet cough that is productive [7].
- Daily nasal congestion that begins early in life and persists year-round [7]. These symptoms are a direct result of stagnant purulent mucus in the respiratory system due to dysfunctional motile cilia [7].
3. How can we improve PCD detection in infants without laterality defects like situs inversus? Approximately half of PCD patients have situs inversus totalis, but a significant proportion do not [7]. Relying solely on the presence of situs inversus for suspicion of PCD leads to underdiagnosis. Key strategies include:
- Proactive Investigation: A PCD work-up should be initiated in any neonate with unexplained respiratory distress, persistent oxygen requirement, or consistent radiographic findings (like lobar atelectasis), even in the absence of laterality defects [7].
- Targeted Laterality Screening: Chest radiography (CXR) alone can miss situs ambiguus (SA). One study showed that using CXR with add-on targeted investigations (e.g., echocardiogram, abdominal ultrasound) significantly increased the detection of SA from 8% to 24% in a PCD cohort [8]. These defects can involve the cardiovascular system, intestines, or spleen [8].
- Genetic Testing: As over 45 genes are associated with PCD, genetic testing can confirm a diagnosis, especially in cases with normal ciliary ultrastructure on electron microscopy [7].
4. What is the typical diagnostic delay for PCD, and why does it happen? The diagnosis of PCD is often delayed to a mean age of 4.4–6 years [7]. This delay is attributed to:
- The transient nature of initial neonatal respiratory distress symptoms [7].
- Overlapping symptoms with more common respiratory diseases like cystic fibrosis, asthma, and protracted bacterial bronchitis [7].
- A low index of suspicion among clinicians, particularly if the classic sign of situs inversus is absent [7].
Troubleshooting Guide: Enhancing PCD Detection Without Overt Laterality Defects
| Challenge | Solution | Key Considerations |
|---|---|---|
| Atypical or Subtle Laterality | Employ targeted investigations beyond CXR [8]. | Order echocardiogram for heart defects, abdominal ultrasound for spleen/liver position, and consider splenic function tests [8]. |
| Overlap with Common Illnesses | Strictly apply ATS clinical criteria for chronic daily symptoms [7]. | Differentiate via the year-round, daily nature of wet cough and nasal congestion from infancy, unrelated to seasonal allergies or discrete infections [7]. |
| Non-Diagnostic Initial Tests | Utilize a multi-test diagnostic panel [7]. | Combine nasal nitric oxide (nNO) testing, genetic testing, high-speed video microscopy analysis (HSVA), and transmission electron microscopy (TEM), as no single test is 100% sensitive [7]. |
| Normal Ciliary Ultrastructure | Proceed with genetic testing for PCD [7]. | Approximately one-third of PCD-causing gene mutations do not result in obvious ultrastructural defects visible on TEM [7]. |
Quantitative Data on PCD Clinical Presentation
Table 1: Frequency of Key Clinical Features in PCD This table summarizes the prevalence of major symptoms to aid in clinical recognition and differential diagnosis [7].
| Clinical Feature | Prevalence in PCD |
|---|---|
| Neonatal Respiratory Distress | >80% |
| Year-Round Daily Wet Cough | Nearly 100% |
| Year-Round Daily Nasal Congestion | ~80% |
| Situs Inversus Totalis | ~50% |
| Situs Ambiguus (Heterotaxy) | ~12% |
| Chronic Otitis Media | Very Common |
| Male Infertility | Nearly 100% |
Table 2: Spectrum of Laterality Defects Identified with Targeted Imaging This data illustrates the improved detection of situs ambiguus (SA) when CXR is supplemented with other imaging modalities in 159 PCD patients [8].
| Situs Classification | CXR Alone | CXR + Targeted Investigations |
|---|---|---|
| Situs Solitus (SS) | 55% | 47% |
| Situs Inversus Totalis (SIT) | 37% | 29% |
| Situs Ambiguus (SA) | 8% | 24% |
Experimental Protocols for PCD Research
Protocol 1: Validating a Multi-Modal Diagnostic Workflow for Infants with Unexplained Respiratory Distress
- Patient Cohort: Recruit term neonates (>37 weeks gestation) presenting with respiratory distress of unknown etiology, particularly with onset after 12 hours of life and/or lobar atelectasis on chest imaging [7].
- Initial Screening:
- First-Line PCD Testing: Measure nasal nitric oxide (nNO); low nNO is a strong indicator of PCD [7].
- Confirmatory Testing:
- Genetic Analysis: Conduct next-generation sequencing using a targeted PCD gene panel (over 45 known genes) [7].
- Ciliary Functional and Structural Studies: Arrange for nasal brush biopsy to be analyzed by high-speed video microscopy analysis (HSVA) and transmission electron microscopy (TEM) at a specialist center [7].
- Data Correlation: Correlate genetic findings with clinical phenotype and ciliary function/structure results to establish a definitive diagnosis.
Protocol 2: Systematic Characterization of Laterality Defects in a PCD Population
- Study Population: Enroll patients with a confirmed or clinical diagnosis of PCD [8].
- Standardized Imaging:
- Chest Radiograph (CXR): Overread by a pediatric radiologist to assign initial situs (Solitus, Inversus, Ambiguus) [8].
- Echocardiogram: To identify congenital heart disease and vascular arrangement anomalies [8].
- Abdominal Ultrasound: To determine the position and morphology of the liver, spleen (e.g., polysplenia, asplenia), and stomach [8].
- Supplementary Investigations (as clinically indicated):
- Final Situs Classification: Compare the initial CXR classification with the final classification derived from the full suite of targeted investigations [8].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials for PCD Diagnostic Research
| Research Reagent / Tool | Function / Explanation |
|---|---|
| PCD Gene Panel (NGS) | Identifies pathogenic variants in over 45 known PCD-associated genes. Crucial for diagnosing patients with normal TEM or atypical presentations [7]. |
| High-Speed Video Microscopy Analysis (HSVA) | Visualizes and quantifies ciliary beat frequency and pattern. Can detect functional abnormalities even when ultrastructure appears normal [7]. |
| Transmission Electron Microscopy (TEM) | Assesses ciliary ultrastructure for classic defects (e.g., absent outer/inner dynein arms, microtubular disorganization) [7]. |
| Nasal Nitric Oxide (nNO) Device | Measures nNO levels, which are characteristically very low in most PCD patients, serving as a useful screening tool [7]. |
| Light Dosimeter | While used in EPP research in the search results, a analogous tool for quantifying ambient environmental exposures relevant to PCD symptoms is not standard but represents an area for methodological development. |
Visualizing the Diagnostic Pathway and Research Framework
The following diagram outlines a logical workflow for diagnosing PCD, with a specific focus on identifying cases without classic laterality defects.
Diagram 1: Diagnostic pathway for PCD, emphasizing key decision points.
This diagram illustrates the core research paradigm for improving PCD diagnosis, focusing on the critical role of neonatal respiratory distress and the challenge of cases without laterality defects.
Diagram 2: Research framework for enhancing PCD detection.
Diagnostic Troubleshooting Guide
Q1: A patient presents with a chronic wet cough and bronchiectasis. How can I differentiate between Primary Ciliary Dyskinesia (PCD), Cystic Fibrosis (CF), and Asthma in the absence of laterality defects?
A1: The absence of laterality defects, such as situs inversus, is a common diagnostic challenge, as this presentation occurs in approximately 50% of PCD cases [9]. Focus on the nature of symptoms, underlying pathophysiology, and specific diagnostic testing.
- Symptom Quality: A daily, year-round wet/productive cough that begins in the neonatal period is a hallmark of PCD and CF, whereas asthma typically features a dry, episodic cough that may be triggered by allergens, exercise, or viruses [9].
- Neonatal History: Unexplained respiratory distress in a full-term neonate is a key indicator for PCD, present in 80-90% of cases [9]. CF may also present in infancy, but often with meconium ileus or failure to thrive.
- Inflammatory Drivers: PCD and CF are primarily associated with neutrophilic inflammation due to impaired mucociliary clearance and chronic bacterial infection [10] [9]. Asthma, particularly the allergic (Th2-high) endotype, is characterized by eosinophilic inflammation [9] [11].
- Diagnostic Gold Standards:
- PCD: Genetic testing identifying biallelic pathogenic variants in a PCD-associated gene (e.g., DNAH5, DNAI1) or transmission electron microscopy revealing specific ciliary ultrastructural defects (e.g., absent outer dynein arms) [9].
- CF: An abnormal quantitative pilocarpine iontophoresis sweat chloride test (≥60 mmol/L) and/or genetic testing confirming biallelic pathogenic CFTR variants [12] [13].
- Asthma: Demonstration of variable expiratory airflow limitation via spirometry (e.g., significant bronchodilator reversibility or positive bronchoprovocation test) [9].
Q2: What are the key pathophysiological differences in mucociliary function between PCD and CF?
A2: While both diseases result in impaired mucociliary clearance, the fundamental mechanisms differ, as summarized below [9] [13].
Table 1: Pathophysiological Comparison of PCD and CF
| Feature | Primary Ciliary Dyskinesia (PCD) | Cystic Fibrosis (CF) |
|---|---|---|
| Primary Defect | Dysfunctional motile cilia structure/function | Defective ion transport due to CFTR protein malfunction |
| Ciliary Ultrastructure | Often abnormal (e.g., absent dynein arms, disrupted microtubules) | Typically normal |
| Mucus Composition | Primarily normal | Abnormally thick, dehydrated mucus due to defective chloride secretion and excess sodium absorption |
| Main Airway Consequence | Stagnant mucus due to ineffective ciliary beating | Physical obstruction by thick, adherent mucus plaques |
The following diagram illustrates the core pathophysiological pathways in PCD, CF, and Asthma.
Q3: What specific inflammatory biomarkers can help distinguish between these conditions?
A3: Biomarker profiles can provide critical evidence for differentiation, especially when clinical features overlap.
Table 2: Key Biomarkers for Differentiating PCD, CF, and Asthma
| Condition | Primary Inflammatory Biomarker | Other Relevant Biomarkers |
|---|---|---|
| PCD | Persistent Neutrophilia in sputum [9] | Nasal Nitric Oxide (nNO) is characteristically very low [9] |
| CF | Persistent Neutrophilia in sputum, often with chronic bacterial infection (e.g., P. aeruginosa, S. aureus) [10] | Elevated CRP during exacerbations; potential for allergic biomarkers if ABPA is present [12] |
| Asthma (Th2-high) | Elevated blood/sputum eosinophils [11] | Elevated Fractional Exhaled Nitric Oxide (FeNO); serum IgE (especially in allergic asthma) [11] |
Essential Experimental Protocols
Protocol for Genomic Characterization of Respiratory Pathogens
This protocol is adapted from a study characterizing bacterial isolates from pediatric CF patients, a methodology applicable to PCD research for understanding chronic infection profiles [10].
Objective: To identify and characterize bacterial sequence types (STs) and phenotypic adaptations, such as Small Colony Variants (SCVs), from respiratory specimens.
Materials & Reagents:
- Selective Culture Media: Mannitol-salt agar (Staphylococcus), Cetrimide agar (Pseudomonas), Endo medium (Gram-negative enterics), Columbia blood agar (non-selective growth and hemolysis).
- API 20E System (bioMérieux) or similar for biochemical identification.
- DNeasy UltraClean Microbial Kit (Qiagen) for genomic DNA extraction.
- KAPA Hyperplus Library Prep Kit (Roche) for WGS library construction.
- MiSeq Reagent Kit v3 (Illumina) for sequencing.
Methodology:
- Sample Collection & Culture: Inoculate respiratory specimens (sputum/BAL) onto selective and non-selective agars. Incubate for 24-72 hours at 37°C, with extended incubation at room temperature for up to 5 days to isolate slow-growing SCVs [10].
- Phenotypic Characterization: Identify SCVs by their characteristic small colony size (<1 mm), lack of pigment, absence of hemolysis, and "fried-egg" morphology. Perform antimicrobial susceptibility testing (AST) following EUCAST guidelines [10].
- Whole Genome Sequencing (WGS):
- Extract high-quality genomic DNA.
- Prepare sequencing libraries using the KAPA Hyperplus kit.
- Sequence on an Illumina MiSeq platform (2x300 bp chemistry).
- Bioinformatic Analysis:
- Use tools like
bbdukfor quality trimming and adapter removal. - Perform de novo assembly with
shovill. - Determine Sequence Types (STs) using
mlstfor Multi-Locus Sequence Typing. - Identify antimicrobial resistance (AMR) genes with
AMRFinderPlusandARIBA[10].
- Use tools like
Protocol for Symptom Phenotyping Using Machine Learning
This protocol uses k-means clustering to identify clinically meaningful symptom phenotypes, a technique demonstrated in CF and applicable to PCD for stratifying patient populations [14] [15].
Objective: To discover distinct symptom clustering patterns in patients at the onset of a pulmonary exacerbation.
Materials & Reagents:
- Clinical Data: Prospectively collected patient symptom data using a validated instrument (e.g., the CF Respiratory Symptom Diary - Chronic Respiratory Infection Symptom Score, CFRSD-CRISS).
- Software: R Studio with packages
NbClustand standard statistical libraries.
Methodology:
- Data Collection: Collect daily symptom scores (e.g., difficulty breathing, cough, sputum, wheezing) on a 0-4 scale for the first 21 days of an exacerbation.
- Clusterability Assessment:
- K-means Clustering: Apply the k-means algorithm to the Day 1 symptom data to assign patients to distinct clusters (e.g., Low-Symptom vs. High-Symptom phenotypes) [14] [15].
- Validation & Association: Use linear regression and multi-level growth models to test associations between cluster membership and clinical outcomes like hospitalization length and symptom resolution trajectory [14].
The workflow for this data-driven phenotyping approach is outlined below.
Research Reagent Solutions
Table 3: Essential Reagents for PCD and Chronic Infection Research
| Reagent / Kit | Primary Function | Application in PCD/CF Research |
|---|---|---|
| Selective Culture Media (e.g., Cetrimide agar) | Selective isolation of specific pathogens (e.g., Pseudomonas aeruginosa). | Profiling chronic respiratory infections and detecting polymicrobial cultures [10]. |
| API 20E System (bioMérieux) | Biochemical identification of Gram-negative bacteria. | Standardized phenotypic identification of Enterobacterales from patient samples [10]. |
| DNeasy UltraClean Microbial Kit (Qiagen) | High-quality genomic DNA extraction from bacterial cultures. | Preparation of DNA for Whole Genome Sequencing to determine STs and AMR genes [10]. |
| KAPA Hyperplus Library Prep Kit (Roche) | Preparation of Illumina-compatible sequencing libraries from DNA. | Essential step for WGS-based genotyping and phylogenetic analysis [10]. |
| CFRSD-CRISS Diary | Validated patient-reported outcome (PRO) instrument. | Quantifying respiratory symptom severity for machine learning-based phenotyping studies [14] [15]. |
Frequently Asked Questions (FAQs)
Q1: Why is Primary Ciliary Dyskinesia (PCD) particularly challenging to diagnose in patients with Congenital Heart Disease (CHD)? PCD diagnosis is often delayed or missed in CHD patients because the classic clinical hallmark, situs inversus (mirror-image organ arrangement), is not always present. In patients with CHD and heterotaxy (abnormal organ arrangement), respiratory symptoms can be incorrectly attributed solely to the cardiac defect or post-surgical complications, diverting attention from underlying ciliary dysfunction [16]. Furthermore, neonatal respiratory distress, a key symptom of PCD, is also common in neonates with complex CHD, creating a diagnostic overlap [5].
Q2: What are the key clinical red flags that should trigger PCD investigation in a patient with CHD? Clinicians should suspect PCD in CHD patients presenting with [16] [5]:
- Early-onset, recurrent respiratory issues: Including neonatal respiratory distress, recurrent otitis media, rhinosinusitis, and persistent wet cough.
- Laterality defects: Especially heterotaxy (which can include complex CHD and polysplenia or asplenia), not just classic situs inversus.
- Unexplained postoperative respiratory complications: Such as recurrent atelectasis that is difficult to resolve, particularly in a patient with known laterality defects.
Q3: What definitive diagnostic tests are recommended for confirming PCD in this patient population? A combination of tests is often necessary for a definitive diagnosis [16] [5]:
- Nasal Nitric Oxide (nNO) measurement: Typically low in PCD, useful as an initial screening tool.
- Genetic Testing: Identifying biallelic pathogenic variants in a known PCD-associated gene provides a definitive diagnosis.
- Transmission Electron Microscopy (TEM): Analysis of ciliary ultrastructure from a nasal or bronchial biopsy to identify specific defects (e.g., absent outer/inner dynein arms).
Q4: How can ciliary dysfunction impact the surgical and long-term outcomes for CHD patients? Evidence suggests that ciliary abnormalities may increase the risk of postoperative mortality and respiratory complications in patients with CHD [16]. Impaired mucociliary clearance leads to recurrent infections and atelectasis, which can complicate post-surgical recovery and contribute to progressive chronic heart failure [16].
Troubleshooting Guide: Navigating PCD Diagnosis in Complex CHD
This guide addresses common diagnostic challenges and offers evidence-based solutions for clinicians and researchers.
| Challenge | Symptom Overlap | Recommended Action & Experimental Protocol | Key Reagents & Techniques |
|---|---|---|---|
| Attributing respiratory symptoms solely to cardiac status | Atelectasis, wheezing, respiratory distress. | Action: Systematically investigate ciliary function in CHD patients with heterotaxy or recurrent respiratory issues, regardless of the primary cardiac diagnosis [16].Protocol: Implement a standardized screening protocol using nNO measurement followed by genetic testing or TEM confirmation [5]. | - nNO analyzer- PCD genetic testing panels (e.g., next-generation sequencing panels for >50 known PCD-related genes)- TEM fixatives (e.g., glutaraldehyde) |
| Distinguishing PCD from other ciliopathies with overlapping features | Heterotaxy, CHD, respiratory symptoms, developmental delay. | Action: Consider Joubert Syndrome and Related Disorders (JSRD), which affects primary cilia, and can co-present with motile cilia defects [16].Protocol: Perform brain MRI to identify the "molar tooth sign" characteristic of JSRD. For motile cilia, proceed with TEM and genetic testing for genes like OFD1 linked to both conditions [16]. | - MRI machine- Genetic analysis for OFD1 mutations- TEM |
| Managing poor postoperative respiratory outcomes | Recurrent atelectasis, difficult extubation, chronic pulmonary infections. | Action: In patients with confirmed or suspected ciliary dysfunction, employ aggressive perioperative pulmonary hygiene [16].Protocol: Implement rigorous chest physiotherapy, frequent suctioning, and consider early bronchoscopy to clear secretions. Maintain a high index of suspicion for PCD in this context [16]. | - Chest physiotherapy devices- Bronchoscope- Microbiological culture media for pathogen identification |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents and materials essential for conducting research into the mechanisms linking PCD and CHD.
| Research Reagent / Material | Function in Experimental Research |
|---|---|
| Anti-DNAH5 / DNAI1 Antibodies | Immunofluorescence staining to detect the presence and localization of key dynein arm proteins in ciliated cell cultures. Absence indicates specific ultrastructural defects [5]. |
| High-Speed Video Microscopy Analysis (HSVA) | To capture and analyze the ciliary beat pattern and frequency from fresh patient-derived ciliated epithelial cells. Dyskinetic or absent beating is diagnostic for PCD [5]. |
| PCD-Specific Genetic Panels (NGS) | Next-generation sequencing panels targeting all known PCD-causing genes to identify pathogenic variants and establish a genetic diagnosis, especially useful when TEM is inconclusive [5]. |
| Transmission Electron Microscope (TEM) | Visualization of the internal 9+2 microtubule structure of cilia to identify hallmark defects such as absent outer/inner dynein arms, which are common in PCD [16] [5]. |
Experimental Protocols for Key Diagnostics
Protocol 1: Transmission Electron Microscopy (TEM) for Ciliary Ultrastructure
- Sample Collection: Obtain nasal epithelial brush biopsies or bronchial samples.
- Fixation: Immediately place samples in primary fixative (e.g., 2.5% glutaraldehyde in cacodylate buffer) for a minimum of 24 hours at 4°C.
- Processing: Post-fix in 1% osmium tetroxide, dehydrate through a graded ethanol series, and embed in resin.
- Sectioning & Staining: Cut ultrathin sections (60-90 nm) and stain with uranyl acetate and lead citrate.
- Imaging & Analysis: Examine sections under TEM. Score for specific defects (e.g., outer dynein arm absence) by examining multiple cross-sections [16] [5].
Protocol 2: Nasal Nitric Oxide (nNO) Measurement as a Screening Tool
- Patient Preparation: The patient should be free from acute respiratory infections and not have eaten recently.
- Technique: Using a chemiluminescence analyzer, measure nNO while the patient exhales against resistance at a constant flow rate from a tidal breath held for 10-15 seconds (velum closure technique).
- Interpretation: nNO values persistently below a validated cutoff (e.g., 77 nL/min in children) are highly suggestive of PCD and warrant further investigation with TEM or genetic testing [5].
Diagnostic Pathways and Research Workflows
Diagram 1: Diagnostic Pathway for PCD in Patients with CHD. This flowchart outlines the sequential steps for investigating PCD in a patient with congenital heart disease, integrating screening and confirmatory tests. nNO: nasal Nitric Oxide; TEM: Transmission Electron Microscopy; JSRD: Joubert Syndrome and Related Disorders.
The Diagnostic Arsenal: From Standardized Screening to Cutting-Edge Confirmation
Nasal nitric oxide (nNO) measurement has emerged as a critical, non-invasive screening tool in the diagnostic pathway for Primary Ciliary Dyskinesia (PCD), a rare genetic disorder characterized by dysfunctional motile cilia. In the context of enhancing PCD detection, particularly for patients without classic laterality defects, nNO screening provides a valuable first-line investigation. The consistently low nNO levels observed in most PCD patients—approximately one-tenth of normal values—offer a reliable biochemical marker that can prompt further specialized testing, even when other clinical signs like situs inversus are absent [17]. This technical support center outlines standardized methodologies, troubleshooting guides, and analytical protocols to support researchers and clinicians in implementing robust nNO screening programs within their PCD diagnostic workflows.
Quantitative nNO Data in PCD and Respiratory Diseases
nNO measurement provides a key discriminatory value between PCD patients, healthy individuals, and those with other respiratory conditions. The table below summarizes quantitative findings from meta-analyses and clinical studies.
Table 1: Nasal Nitric Oxide (nNO) Levels Across Different Populations
| Population / Condition | Mean nNO Level (nL/min) | Standard Deviation | Sample Size (n) | Recommended Cut-off Value (nL/min) |
|---|---|---|---|---|
| Healthy Controls [18] | 265.0 | ± 118.9 | 338 | Not Applicable |
| PCD Patients [18] | 19.4 | ± 18.6 | 478 | < 77-100 [17] |
| Cystic Fibrosis Patients [18] | 133.5* | Not Specified | 415 | Not Applicable |
| PCD Patients (Tidal Breathing) [18] | Low (reduced discriminatory value) | Not Specified | Multiple Studies | Varies by technique |
| Symptomatic, Non-PCD (Winter) [19] | 123 (Median) | Not Specified | 434 | < 66 [19] |
| Symptomatic, Non-PCD (Summer) [19] | 167 (Median) | Not Specified | 434 | < 66 [19] |
*Calculated weighted mean difference for PCD vs. cystic fibrosis was 114.1 nL/min [18].
Core Methodologies and Experimental Protocols
Accurate nNO measurement requires strict adherence to standardized protocols. The following section details key experimental procedures.
Protocol 1: nNO Measurement with Breath-Hold Maneuver
The breath-hold technique with velum closure is the gold-standard method for cooperative patients, typically those over 5 years of age [20] [17].
Primary Workflow Diagram
Materials and Equipment:
- Chemiluminescence or electrochemical NO analyzer [20]
- Nasal catheter or olive with airtight foam sleeve
- Calibration gases (NO standard, zero air)
- Disposable mouthpieces (if applicable)
Procedure:
- Patient Preparation: Ensure the patient is seated comfortably. Exclude individuals with acute upper respiratory infections (within 2-4 weeks) or active nosebleeds, as these can cause falsely low nNO [20].
- Equipment Calibration: Calibrate the NO analyzer according to the manufacturer's instructions using certified calibration gases before the first test of the day.
- Maneuver Execution: Insert the nasal olive into one nostril, ensuring an airtight seal. Instruct the patient to exhale fully, then inhale deeply to total lung capacity through the mouth. The patient must then hold their breath while keeping the velum (soft palate) closed to prevent contamination from lung air, which has lower NO concentrations [18] [17].
- Sampling: Aspirate air from the nasal cavity at a constant flow rate. Common flow rates are between 0.3 to 5 mL/s, though 3 mL/s is frequently used. The nNO output (nL/min) should be recorded once a stable plateau is observed [18] [20].
- Repeat: Perform at least two technically acceptable measurements per nostril. The results are typically reported as the mean value.
Protocol 2: nNO Measurement During Tidal Breathing
For young children (<5 years) or individuals unable to perform the breath-hold maneuver, tidal breathing is an acceptable alternative, though with reduced discriminatory power [18] [20].
Procedure:
- Setup: Position the patient and insert the nasal olive as described in Protocol 1.
- Sampling: During quiet, tidal breathing through the mouth, aspirate nasal air at a controlled flow rate. The patient should breathe normally with the mouth slightly open, which helps close the velum passively.
- Recording: Record the nNO output once a stable reading is achieved. Note that values obtained via tidal breathing are generally lower than those from breath-hold and have a different, typically lower, diagnostic cut-off point [18].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 2: Key Materials and Equipment for nNO Measurement
| Item | Function/Description | Examples & Notes |
|---|---|---|
| Chemiluminescence Analyzer | Gold-standard device; measures NO via reaction with ozone producing light [20] [21]. | Highly accurate and reliable for real-time measurement; less portable and more expensive [20]. |
| Electrochemical Analyzer | Portable device; measures NO via electrical current produced in a chemical reaction [20]. | Increasingly used; more portable and cost-effective; performance validation is crucial [20]. |
| Nasal Olives/Probes | Creates an airtight seal in the nostril to prevent ambient air dilution. | Disposable or reusable olives with different sizes are needed for various patient ages. |
| Calibration Gases | Essential for daily calibration to ensure measurement accuracy. | Requires a known concentration of NO in an inert gas (e.g., nitrogen) and a zero gas [21]. |
| Nose Clip | May be used during tidal breathing to ensure nasal-only breathing. | Simple physical barrier. |
Troubleshooting Guides & FAQs
This section addresses common technical and interpretative challenges encountered during nNO testing.
FAQ 1: What are the most common causes of falsely low nNO readings, and how can they be mitigated?
Falsely low nNO is a significant concern as it can lead to unnecessary further testing. The main causes and solutions are:
- Acute Viral Infections: Upper respiratory infections can transiently lower nNO. Solution: Postpone testing until at least 2-4 weeks after full symptom resolution [20].
- Seasonal Variability: nNO levels are statistically significantly lower in winter compared to summer in subjects without PCD. Solution: If an unexpectedly low nNO is found in winter in a symptomatic patient, consider repeating the test in the summer before proceeding to invasive diagnostics [19].
- Technical Errors: Inadequate velum closure during breath-hold contaminates the sample with low-NO lung air. Solution: Properly train the patient on the maneuver. Use visual or verbal cues to ensure breath-holding with a closed glottis.
- Nasal Polyps or Obstruction: Significant blockage can impede airflow. Solution: Perform a brief visual inspection of the nares before testing.
FAQ 2: How do we account for nNO variability in children versus adults?
Cooperation is the primary differentiator.
- Children >5 years: Can often perform the breath-hold maneuver. Use the same protocol as for adults for the most discriminatory result [17].
- Young Children (<5 years) / Uncooperative: The tidal breathing method must be employed. Critical Note: The reference ranges and diagnostic cut-offs for tidal breathing are distinct from and lower than those for the breath-hold technique. Laboratories must establish or use validated reference values for their specific tidal breathing protocol [18] [20].
FAQ 3: Our research involves PCD patients without laterality defects. Is nNO still a reliable marker?
Yes. Low nNO is a consequence of the underlying ciliary dysfunction in the nasal epithelium, which is independent of organ placement. The genetic defects causing PCD affect motile cilia throughout the body. Therefore, nNO is consistently low in most forms of PCD, regardless of whether the patient has situs solitus (normal arrangement), situs inversus, or situs ambiguus [8] [17]. This makes it a powerful tool for identifying PCD in the entire patient spectrum.
FAQ 4: When should we use a portable electrochemical analyzer versus a stationary chemiluminescence analyzer?
- Chemiluminescence Analyzers: are ideal for a central lab or clinic setting. They are considered the most accurate and reliable for real-time measurement and have been validated in multicentre studies. Use these for definitive diagnostic testing [20].
- Electrochemical Analyzers: are best for field studies, satellite clinics, or situations where portability is paramount. They are more affordable but require rigorous validation against chemiluminescence standards to ensure data reliability [18] [20].
Advanced Analytical Considerations
Impact of Seasonal Variability on Research Protocols
The observed seasonal fluctuation in nNO has direct implications for study design and data interpretation.
Seasonal Impact Diagram
Research Recommendation: For longitudinal studies or when screening symptomatic cohorts, the season of testing should be recorded as a key variable. A low nNO measurement obtained in winter should be interpreted with caution and, where possible, confirmed with a repeat test in the summer to minimize false positives [19].
Integration with the Broader PCD Diagnostic Pathway
nNO is a screening tool, not a standalone diagnostic. The following workflow integrates nNO into a comprehensive diagnostic strategy for PCD, particularly in cases without laterality defects.
Comprehensive Diagnostic Pathway
This integrated approach ensures that nNO's high sensitivity is leveraged to identify at-risk individuals, who then undergo definitive testing, thus streamlining the diagnostic journey and reducing delays.
### Frequently Asked Questions (FAQs) and Troubleshooting
Q1: Our genetic testing results show a high number of Variants of Uncertain Significance (VUS). Is this common, and what factors contribute to it?
A: Yes, a high VUS rate is a well-documented challenge in modern genetic testing. The frequency of VUS findings is not uniform and can vary significantly based on the clinical context and the patient population being tested [22].
Key factors influencing VUS rates include:
- Patient Ancestry: Individuals from populations underrepresented in genomic databases (e.g., Middle Eastern, Asian, Hispanic) have a higher probability of receiving a VUS result [23] [22]. One study found a 3-fold variation in VUS rates based on self-reported race [22].
- Test Indication: The primary reason for genetic testing can lead to over a 14-fold difference in the number of VUS reported relative to pathogenic variants [22].
- Gene Panels: The evolution from single-gene testing (e.g., BRCA1/2 only) to large multigene panels has broadened the scope of testing, inevitably increasing the detection of rare variants with limited available evidence [23].
Q2: What are the practical steps for reclassifying a VUS?
A: Reclassification is a systematic process that relies on gathering additional evidence. The following methodology, adapted from published studies, provides a robust framework [23]:
- Evidence Review: Compile population frequency data from databases like gnomAD. A very high allele frequency is inconsistent with a highly penetrant disease.
- Computational Prediction: Utilize in-silico predictors (e.g., SIFT, PolyPhen-2) to assess the variant's potential impact on protein function.
- Segregation Analysis: Test family members to see if the variant co-segregates with the disease phenotype.
- Functional Studies: Generate experimental data on the variant's effect, though this is often not feasible in a clinical setting.
- Literature and Database Mining: Search for new peer-reviewed evidence or updated classifications in ClinVar.
- Expert Consensus: Apply established guidelines, such as the ACMG/AMP 2015 criteria or the ClinGen ENIGMA methodology for specific genes, to assign a new pathogenicity class [23].
Q3: We are experiencing issues with SNP genotyping assays, such as failed amplification or multiple clusters in the data. What could be the cause?
A: Several technical issues can lead to these problems [24]:
- Failed Amplification: This can result from inaccurately quantitated DNA, degraded DNA, inhibitors in the sample, or an error in the reaction setup. If you are designing a custom assay, an incorrect input sequence can also cause failure.
- Multiple or Trailing Clusters: This is often due to a hidden SNP under the probe or primer binding site. You can search dbSNP for other polymorphisms in the region. Alternatively, the region might be within a copy number variation. Trailing clusters can also be caused by significant variation in the quality or concentration of the gDNA samples across your study [24].
Q4: How can we ensure our genetic tests are discoverable and transparent to the clinical and research community?
A: The NIH's Genetic Testing Registry (GTR) is a centralized, publicly available database for this purpose [25]. Test providers, including both U.S. and international clinical and research laboratories, can voluntarily submit detailed information about their tests. This includes the test's purpose, methodology, analytical validity, and evidence of clinical validity. Registering your test in the GTR provides a unique accession number, enhancing transparency and allowing for uniform referencing in publications and health records [25].
Q5: A significant number of our patients with laterality defects are not being evaluated for Primary Ciliary Dyskinesia (PCD), despite meeting clinical criteria. How can we improve this?
A: This is a recognized issue. A recent study found that while 96% of patients meeting all four PCD criteria were referred to a pulmonologist, only 41% of those meeting the minimum of two criteria were referred [1]. Improving detection requires:
- Education: Increase awareness among pediatricians and specialists about the PCD clinical criteria: laterality defect, chronic daily cough, year-round nasal congestion starting in infancy, and unexplained neonatal respiratory distress syndrome (NRDS) in a term infant [1] [26].
- Lower Referral Threshold: Have a heightened suspicion for PCD even when other diagnoses, like congenital heart disease (which is common in patients with laterality defects), are present and could explain respiratory symptoms [1].
- Utilize Available Diagnostics: Increase the use of screening tools like nasal nitric oxide (nNO) measurement and commercially available genetic panels, which have made definitive diagnosis more accessible outside of highly specialized centers [26].
Q6: How significant is the problem of outdated variant classifications in clinical care?
A: This is a critical systems-level challenge. Research using an EHR-linked database found that at least 1.6% of variant classifications used in the EHR for clinical care are outdated based on current ClinVar data [22]. The same study identified 26 specific instances where a testing lab had updated a variant's classification in ClinVar, but this reclassification was never communicated to the patient, meaning clinical decisions were being made using obsolete information [22]. This highlights a major bottleneck in the dissemination of knowledge between databases, testing labs, and providers.
### Key Quantitative Data on VUS and PCD Detection
Table 1: VUS Reclassification Outcomes in a Middle Eastern HBOC Cohort [23]
| Metric | Value |
|---|---|
| Total VUS detected before reclassification | 160 |
| VUS successfully reclassified | 52 (32.5%) |
| VUS upgraded to Pathogenic/Likely Pathogenic | 4 (2.5% of total VUS) |
| Median number of total VUS per patient | 4 |
| Non-informative (VUS) result rate in cohort | 40% |
Table 2: Referral and Evaluation Patterns for PCD in Patients with Laterality Defects [1]
| Patient Group | Referral to Pulmonary | Evaluation for PCD |
|---|---|---|
| All patients meeting ≥2 PCD criteria (n=79) | 41% | 16% |
| Patients meeting all 4 PCD criteria (n=27) | 96% | 93% |
| Patients with only 1 criterion (laterality defect, n=189) | Not reported | Not reported |
### Experimental Protocols
Protocol 1: Variant Reclassification Workflow
This protocol is adapted from the retrospective reclassification study performed on a Hereditary Breast and Ovarian Cancer (HBOC) cohort [23].
- Variant Collection: Compile all germline variants initially classified as VUS (Class 3) from clinical genetic test reports.
- Independent Review: Two independent assessors (e.g., a certified laboratory geneticist and an experienced laboratory scientist) review each variant.
- Evidence Gathering: For each variant, reviewers systematically gather and evaluate the following:
- Population Frequency: Query the Genome Aggregation Database (gnomAD) for allele frequency.
- In-silico Analysis: Run the variant through computational predictors like SIFT, PolyPhen-2, and the Variant Effect Predictor (VEP).
- Literature and Database Review: Search for functional, clinical, or segregation data in published literature and the ClinVar database.
- Apply Classification Guidelines: Score the assembled evidence using the latest ACMG/AMP 2015 criteria. For genes like BRCA1 and BRCA2, the more specific ClinGen ENIGMA methodology should be applied.
- Consensus Meeting: Reviewers meet to discuss their independent classifications, resolve any discrepancies, and assign a final pathogenicity class (1-5) for each variant.
Protocol 2: Assessing PCD Referral Patterns
This protocol is based on a retrospective chart review study investigating PCD detection [1].
- Cohort Identification: Use the Electronic Medical Record (EMR) system to identify all pediatric patients (e.g., ≤18 years) over a defined period (e.g., 12 years) with diagnoses indicating a laterality defect (e.g., heterotaxy, dextrocardia, situs inversus).
- Apply Inclusion/Exclusion Criteria:
- Inclusion: Patients with at least one laterality defect.
- Exclusion: Patients without laterality defects, those with unavailable symptom data, and those deceased at or before 2 years of age.
- Data Abstraction: For each included patient, manually review the chart to record:
- Presence or absence of the four PCD clinical criteria (laterality defect, chronic daily cough, year-round nasal congestion starting in infancy, unexplained NRDS requiring >24h of oxygen/positive pressure).
- Documentation of referral to pediatric pulmonology or genetics.
- Documentation of any evaluation for PCD (e.g., nNO, genetic testing, TEM).
- Demographics (sex, race, ethnicity, insurance type).
- Statistical Analysis: Analyze data to determine referral and evaluation rates. Use Chi-square tests and logistic regression to examine the impact of the number of PCD criteria and patient demographics on referral rates.
### Visual Workflows
### The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Genetic Testing and Variant Interpretation
| Item | Function |
|---|---|
| Genome Aggregation Database (gnomAD) | Public repository of population allele frequencies critical for assessing if a variant is too common to be causative for a rare disease [23]. |
| ClinVar | Public archive of reports on the relationships between human variants and phenotypes, with supporting evidence; essential for comparing your variant classification with the community [23] [22]. |
| ACMG/AMP Classification Guidelines | The standardized framework for interpreting sequence variants, providing criteria to classify variants as Pathogenic, Likely Pathogenic, VUS, Likely Benign, or Benign [23]. |
| Genetic Testing Registry (GTR) | A centralized NIH database for test providers to voluntarily submit information about their genetic tests, improving transparency and discoverability for clinicians and researchers [25]. |
| Variant Effect Predictor (VEP) | A powerful tool that determines the effect of your variants (e.g., missense, synonymous) on genes, transcripts, and protein sequence, as well as regulatory regions [23]. |
| TaqMan Genotyper Software | An example of specialized software for analyzing and automating calls in SNP genotyping experiments, which can have improved clustering algorithms over standard instrument software [24]. |
The Evolving Role of Transmission Electron Microscopy (TEM) in a Genetic-First Diagnostic World
Primary Ciliary Dyskinesia (PCD) is a rare genetic disorder affecting approximately 1 in 20,000 individuals, characterized by dysfunction of motile cilia leading to chronic respiratory infections, bronchiectasis, and laterality defects in approximately 50% of cases [27]. In the current diagnostic landscape, genetic testing has emerged as a powerful first-line tool, with approximately 50 known causative genes identified [27]. Despite this genetic-focused approach, Transmission Electron Microscopy (TEM) maintains a crucial role in the diagnostic algorithm, particularly for confirming diagnosis in cases of variant of uncertain significance or novel genetic findings.
This technical support center addresses the practical challenges researchers face when integrating TEM with genetic testing, providing troubleshooting guidance to enhance diagnostic accuracy. The continued evolution of TEM protocols and international standardization efforts ensures its place as an indispensable component of comprehensive PCD diagnosis, enabling researchers to confirm ultrastructural defects that correlate with genetic variants and clinical presentations.
Diagnostic Frameworks: Integrating TEM with Genetic Testing
Current Diagnostic Criteria and Classifications
Modern PCD diagnosis utilizes a multifaceted approach, with TEM providing critical evidence for definitive diagnosis. According to recent guidelines, a definitive PCD diagnosis requires exclusion of cystic fibrosis and primary immunodeficiency, at least one characteristic clinical feature, and a positive result from specific confirmatory tests [27].
Table 1: Diagnostic Categories for PCD Confirmation
| Diagnostic Category | Clinical Features Required | Laboratory Evidence Required | Genetic Correlation |
|---|---|---|---|
| Definite PCD | At least one of six defined clinical features | • Class 1 defect on TEM OR • Pathogenic/likely pathogenic variants in PCD-related gene OR • Impairment of ciliary motility repairable by gene correction in iPS cells | Genetic testing can confirm but is not always required if TEM shows definitive defect |
| Probable PCD | Clinical features suggestive of PCD | Class 2 defect on TEM OR borderline/low nNO with supportive clinical picture | May have variants of uncertain significance |
| Possible PCD | Incomplete or atypical clinical presentation | Equivocal or conflicting laboratory findings | May lack genetic confirmation |
The international BEAT PCD TEM Criteria provide standardized classification for ultrastructural defects, defining Class 1 defects as diagnostic for PCD and Class 2 defects as indicative of PCD when combined with other supporting evidence [28]. This classification system has been validated across 18 diagnostic centers in 14 countries, enabling consistent reporting and interpretation of TEM findings globally.
TEM Defect Classification in the Genetic Era
Table 2: TEM Ultrastructural Defects in PCD Diagnosis
| Defect Category | Specific Defects | Diagnostic Significance | Common Genetic Associations |
|---|---|---|---|
| Class 1 (Diagnostic) | • Outer dynein arm defects • Combined outer and inner dynein arm defects • Microtubular disorganization with central pair defects • Absent inner dynein arms with microtubular disorganization | Definitive for PCD | Strong correlation with multiple known PCD genes including DNAH5, DNAI1, CCDC39, CCDC40 |
| Class 2 (Supportive) | • Isolated inner dynein arm defects • Central apparatus defects • Miscellaneous defects including radial spoke defects | Require additional supportive evidence for diagnosis | Variable genetic associations, some genes not yet identified |
| Normal Ultrastructure | Normal ciliary axonemal structure | Does not exclude PCD (up to 30% of cases) | May indicate genetic defects affecting ciliary function without structural defects |
The integration of TEM with genetic testing creates a powerful diagnostic synergy. While genetic testing can identify pathogenic variants, TEM provides functional validation of the structural impact of these variants, particularly important for novel gene discoveries or variants of uncertain significance.
Technical Support Center: TEM Troubleshooting and Methodologies
Frequently Asked Questions: TEM in PCD Diagnosis
Q1: What constitutes an adequate ciliary sample for TEM analysis, and how can I avoid common sampling errors? A: An adequate diagnostic sample requires properly oriented ciliary cross-sections from at least 60-70 different cilia. Common issues include tangential sectioning (producing longitudinal views), excessive mucus contamination, and processing artifacts. To ensure proper orientation, look for the classic "9+2" microtubule arrangement in circular profiles. Samples with predominantly oblique or longitudinal sections should be considered inadequate for diagnosis and require re-biopsy [28].
Q2: How does the BEAT PCD TEM Criteria system distinguish between Class 1 and Class 2 defects? A: The internationally validated BEAT PCD TEM Criteria defines Class 1 defects as those with definitive diagnostic value, including outer dynein arm absence, combined outer and inner dynein arm defects, and specific microtubular disorganization patterns. Class 2 defects have more variable diagnostic significance and require correlation with other tests such as genetic analysis or nasal nitric oxide measurement. Isolated inner dynein arm defects fall into this category, as they can be more challenging to identify consistently and may have partial presentations [28].
Q3: What are the most common artifacts that can mimic PCD ultrastructural defects, and how can I distinguish them? A: Common artifacts include secondary ciliary dyskinesia from infection or inflammation, processing-induced microtubule disorganization, and oblique sectioning that creates false appearance of defects. Key distinguishing factors: primary ciliary defects affect virtually all cilia consistently, while secondary defects show patchy involvement and are often reversible with clinical improvement. Always correlate TEM findings with clinical presentation and consider repeat sampling after treating active infection [28].
Q4: In a genetic-first diagnostic approach, when is TEM analysis still indicated? A: TEM remains crucial in these scenarios: (1) when genetic testing identifies variants of uncertain significance; (2) when no pathogenic variants are identified despite strong clinical suspicion (covering the 20-30% of cases where genetic testing is negative); (3) for functional validation of novel gene variants; and (4) when establishing new PCD diagnostic programs and validating genetic testing panels [27] [28].
Q5: What technical factors most significantly impact TEM image quality for ciliary analysis? A: Critical factors include: proper fixation (fresh glutaraldehyde fixation within 2 hours of biopsy), avoidance of freezing artifacts, appropriate staining protocols, correction of contrast transfer function, and precise defocus determination. Sample preparation must maintain ciliary orientation and ultrastructural integrity throughout processing [29].
Advanced Troubleshooting Guide
Issue: Inconsistent Identification of Inner Dynein Arm Defects Solution: Implement high-contrast staining protocols and ensure optimal section thickness (70-90 nm). Use standardized imaging protocols with multiple independent reviewers. Consider that some genetic forms of PCD (e.g., CCDC39-related) show complete axonemal disorganization rather than isolated inner dynein arm defects [28].
Issue: Discrepancy Between Genetic Findings and TEM Ultrastructure Solution: This may occur in 10-15% of cases. Consider these possibilities: (1) genetic variants affecting ciliary function without structural defects (e.g., GAS8-related PCD); (2) technical limitations in TEM sensitivity; or (3) secondary ciliary modifications. Utilize complementary functional tests like high-speed videomicroscopy or ciliary waveform analysis [27].
Issue: Poor Sample Preservation Affecting Diagnostic Interpretation Solution: Optimize the biopsy-to-fixation time, using immediate immersion in glutaraldehyde-based fixatives. For difficult cases, consider protocol modifications from large-sample TEM studies that have addressed preservation challenges in centimeter-scale samples, including extended osmium tetroxide incubation with temperature control and modified washing steps to prevent microbreakages [30].
Research Reagent Solutions for TEM Analysis
Table 3: Essential Reagents for PCD TEM Diagnostics
| Reagent/Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| Primary Fixatives | Glutaraldehyde (2.5-3%), Paraformaldehyde | Tissue preservation and ultrastructural maintenance | Critical for biopsy-to-fixation time (<2 hours); buffer with cacodylate or phosphate |
| Secondary Fixatives | Osmium tetroxide (1-2%) | Lipid membrane stabilization and electron density | Requires careful handling; temperature control vital for large samples [30] |
| Staining Agents | Uranyl acetate, Lead citrate | Heavy metal contrast enhancement for membrane visualization | Can be applied en bloc or section staining; protocols exist for large samples [30] |
| Embedding Media | Epon, Spurr's epoxy resin | Tissue support for ultrathin sectioning | Infiltration protocols must be adjusted for sample size; viscosity critical [30] |
| Specialty Reagents | Thiocarbohydrazide (TCH), Pyrogallol (Pg) | Enhanced conductive staining for large samples | Pyrogallol can replace TCH to reduce sample breakage in large specimens [30] |
Experimental Protocols and Workflows
Integrated PCD Diagnostic Protocol
Figure 1: Contemporary PCD Diagnostic Workflow Integrating Genetic and TEM Approaches
Detailed TEM Sample Preparation Protocol
For optimal ciliary ultrastructure preservation, follow this standardized protocol derived from current best practices:
Sample Collection and Primary Fixation
- Obtain nasal brush biopsy or bronchial biopsy using appropriate clinical techniques
- Immediately immerse sample in cold (4°C) 2.5% glutaraldehyde in 0.1M cacodylate buffer (pH 7.4)
- Fix for minimum 2 hours at 4°C, with gentle agitation if possible
- Wash 3× in cacodylate buffer (10 minutes each)
Secondary Fixation and Staining
- Post-fix in 1% osmium tetroxide in cacodylate buffer for 90 minutes at 4°C
- For larger tissue samples, extend osmium incubation to 3-6 days with temperature control to prevent peripheral ultrastructural disintegration [30]
- Rinse thoroughly with buffer (3×10 minutes)
- For en bloc staining, incubate with 1% uranyl acetate for 60 minutes
Dehydration and Embedding
- Dehydrate through graded ethanol series (50%, 70%, 90%, 100% ×3), 10 minutes each step
- Transition through propylene oxide (2×10 minutes)
- Infiltrate with epoxy resin mixtures (1:2, 1:1, 2:1 resin:propylene oxide) for 2 hours each step
- For samples >2mm, add 95% resin in 5% acetone step to decrease viscosity and extend incubation times [30]
- Transfer to pure resin for overnight infiltration
- Embed in fresh resin and polymerize at 60°C for 48 hours
Sectioning and Imaging
- Prepare semi-thin sections (0.5-1μm) and stain with toluidine blue for orientation
- Cut ultrathin sections (70-90nm) using diamond knife
- Collect sections on coated grids
- Stain with uranyl acetate and lead citrate
- Image at 80-100kV using calibrated TEM
Advanced Large-Sample TEM Protocol for Research Applications
For connectomics research or large tissue samples, modified protocols enable homogeneous staining of samples up to centimeter scale:
Figure 2: Advanced Large-Sample TEM Staining Workflow
Key modifications for large samples include:
- Extended initial osmium tetroxide incubation (3-6 days) with temperature control at 4°C to prevent peripheral ultrastructural disintegration while ensuring central penetration [30]
- Replacement of thiocarbohydrazide with pyrogallol to reduce sample breakage
- Additional osmium tetroxide step after ferrocyanide reduction to enhance sample stability during aqueous incubations
- Cold resin infiltration (4°C) with extended times and inclusion of 95% resin in 5% acetone to maintain low viscosity and ensure complete infiltration [30]
Emerging Technologies and Future Directions
Machine Learning in PCD Diagnosis
Recent research demonstrates the feasibility of machine learning (ML) approaches to identify patients with possible PCD, even in the absence of specific ICD codes. One study utilized random forest models trained on claims data, showing promising performance with sensitivity of 0.75-0.94 and positive predictive value of 0.45-0.73 [31]. This approach classified 7,705 patients as PCD-positive from a cohort of 1.32 million pediatric patients, consistent with estimated PCD prevalence of 1:7,554 [31].
These ML models utilize diagnostic, procedural, and pharmaceutical codes associated with PCD clinical features, creating scalable screening methods that could reduce diagnostic delays. Future integration of TEM findings with ML algorithms may further enhance predictive accuracy, creating decision support tools that prioritize patients for specialized testing.
Technical Innovations in TEM Methodology
Advanced staining protocols now enable high-contrast en bloc staining of large tissue samples, overcoming previous limitations in sample size. These developments address critical challenges including staining inhomogeneity, sample instability, and incomplete resin infiltration that previously limited large-volume connectomic analyses [30].
Innovations such as the incorporation of contrast transfer function (CTF) correction have revolutionized TEM image quality, ensuring accurate representation of biological structures at high resolution. Precise defocus determination and CTF correction are now recognized as essential for valid structural interpretation, preventing distortion of morphological details [29].
In the evolving genetic-first diagnostic landscape, TEM maintains its essential role in the PCD diagnostic algorithm. The synergy between genetic testing and TEM ultrastructural analysis creates a powerful diagnostic combination, particularly for cases with variants of uncertain significance or novel genetic findings. By implementing the standardized protocols, troubleshooting guides, and reagent solutions outlined in this technical support center, researchers can enhance diagnostic accuracy and continue to advance our understanding of PCD pathogenesis and phenotypic expression.
The future of PCD diagnosis lies not in choosing between genetic or TEM approaches, but in their intelligent integration, supported by emerging technologies including machine learning and advanced imaging modalities. This comprehensive approach will ultimately reduce diagnostic delays and improve outcomes for patients with this complex genetic disorder.
Troubleshooting Guides
Guide 1: Troubleshooting Inconsistent Laterality Classifications
Problem: Initial chest X-ray (CXR) suggests situs solitus (normal organ arrangement) or situs inversus totalis (mirror-image arrangement), but you suspect a more complex situs ambiguus (heterotaxy) is present [8].
- 1. Identify the Problem: Standard CXR is insufficient to rule out subtle laterality defects. A study found that using CXR alone classified only 8% of a PCD cohort as having situs ambiguus (SA). When add-on targeted investigations were used, the prevalence of SA increased threefold to 24% [8].
- 2. List Possible Explanations:
- Cardiovascular Defects: Simple or complex congenital heart defects not visible on CXR [32] [8].
- Abdominal Situs Defects: Midline liver, intestinal malrotation, or abnormal spleen location/function [32] [6].
- Vascular Defects: Interrupted inferior vena cava, anomalous pulmonary venous return, or a right-sided aortic arch [32].
- 3. Collect the Data: Implement a standardized imaging protocol beyond CXR.
- Echocardiogram (ECHO): Essential for identifying atrial isomerism, septal defects, and transposition of the great arteries [8] [6].
- Abdominal Ultrasound (AUS): Screens for midline liver, polysplenia, asplenia, and abdominal vessel arrangement [8] [6].
- Chest CT Scan: Provides detailed bronchial anatomy (e.g., bronchial isomerism) and vascular anatomy. It is the preferred examination for definitive diagnosis [8] [6].
- 4. Eliminate Explanations: Correlate findings from all imaging modalities. A patient with a normal heart on ECHO but with a midline liver on AUS and bilateral bilobed lungs on CT would be classified as SA with left isomerism [6].
- 5. Check with Experimentation: For confirmed SA cases with respiratory symptoms, proceed with PCD-specific diagnostics (nasal nitric oxide testing, genetic sequencing) to investigate the underlying ciliopathy [32].
- 6. Identify the Cause: The inconsistent classification is resolved by using a multi-modality imaging approach, leading to an accurate situs ambiguus diagnosis and guiding further management [8].
Guide 2: Troubleshooting Missed Cardiovascular Defects in PCD Research
Problem: A research subject with confirmed PCD and situs solitus has no documented cardiac workup, potentially missing critical phenotype data.
- 1. Identify the Problem: Laterality defects exist on a spectrum. Isolated cardiovascular defects can be the only manifestation of heterotaxy in a PCD population, occurring in approximately 2.3% of patients [32]. Relying solely on the absence of situs inversus can miss these defects.
- 2. List Possible Explanations:
- 3. Collect the Data:
- 4. Eliminate Explanations: A normal ECHO rules out the most common simple cardiac malformations. In a research context, this subject could then be confidently classified as PCD with situs solitus and no cardiac involvement.
- 5. Check with Experimentation: Integrate ECHO into the standard baseline assessment for all PCD research subjects, regardless of their initial situs classification.
- 6. Identify the Cause: The protocol for phenotyping in PCD research was inadequate. Implementing routine echocardiography ensures comprehensive detection of laterality defects, enriching the research data [32] [8].
Frequently Asked Questions (FAQs)
Q1: Why is it critical to look for laterality defects beyond situs inversus totalis in PCD research?
The presence of any laterality defect is a major diagnostic criterion for PCD. Focusing only on the classic situs inversus totalis (which occurs in about 41% of PCD cases) misses the 12% or more of patients who have situs ambiguus [32] [8]. These patients have a 200-fold increased risk of congenital heart disease compared to the general population, which significantly impacts their clinical management and is a crucial variable in research studies aiming to fully characterize the PCD phenotype [6].
Q2: What is the minimum set of imaging investigations recommended to comprehensively assess organ laterality in a PCD cohort?
While CXR is a common first step, evidence shows it is inadequate alone [8]. A robust imaging protocol should include:
- Echocardiogram (ECHO): To rule out complex and simple congenital heart disease [32] [8].
- Abdominal Ultrasound (AUS): To determine spleen status (asplenia/polysplenia) and liver position [8] [6].
- Chest CT Scan: To evaluate bronchial anatomy (e.g., bilateral eparterial bronchi in right isomerism) and vascular structures [6].
Q3: How do we classify a patient with isolated intestinal malrotation or an isolated right aortic arch?
In the context of PCD research, these isolated defects are considered part of the situs ambiguus spectrum. Studies classify such findings as "SA without cardiac malformation" or an "isolated possible laterality defect" [32]. For consistency, adopt a predefined classification system, such as one based on Botto et al., which accounts for these solitary lesions [32].
Q4: What are the common pitfalls in image interpretation for laterality defects?
The primary pitfall is a lack of systematic review. Key structures must be actively assessed [6]:
- Atrial morphology: Determine if there is right or left isomerism.
- Bronchial anatomy: The length and branching pattern of the main bronchi are key indicators of atrial situs.
- Abdominal great vessels: Note the position of the aorta and inferior vena cava relative to the spine.
- Spleen status: Confirm the presence, number, and location of the spleen.
Table 1: Prevalence of Laterality Defects in Classic PCD (Prospective Study, n=305) [32]
| Situs Classification | Prevalence in PCD (%) | Key Characteristics |
|---|---|---|
| Situs Solitus (SS) | 46.9% | Normal organ arrangement. |
| Situs Inversus Totalis (SI) | 41.0% | Complete mirror-image organ arrangement. |
| Situs Ambiguus (SA) | 12.1% | Spectrum of organ laterality defects. |
| SA Subgroup: Complex Cardiac Defects | 2.6% | Heterotaxy with severe cardiac malformations. |
| SA Subgroup: Simple Cardiac Defects | 2.3% | e.g., ASD, VSD, dextrocardia. |
| SA Subgroup: No Cardiac Defects | 4.6% | Vascular, abdominal, or pulmonary defects only. |
| SA Subgroup: Isolated Laterality Defect | 2.6% | A single defect, e.g., intestinal malrotation. |
Table 2: Detection of Situs Ambiguus: CXR Alone vs. Targeted Imaging (Retrospective Study, n=159) [8]
| Imaging Method | Situs Solitus (%) | Situs Inversus Totalis (%) | Situs Ambiguus (%) |
|---|---|---|---|
| Chest X-Ray (CXR) Alone | 88 (55%) | 59 (37%) | 12 (8%) |
| CXR + Targeted Investigations | 75 (47%) | 46 (29%) | 38 (24%) |
| Common SA Defects Found | --- | --- | Cardiovascular (13%), Splenic (10%), Intestinal (6%) |
Experimental Protocols & Workflows
Standardized Laterality Assessment Workflow
Diagnostic Troubleshooting Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Laterality Defect Research in PCD
| Item / Reagent | Function / Application | Example / Note |
|---|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Diagnostic screening for PCD. Low nNO is a hallmark feature. | CLD 88 series, NIOX Flex. nNO <77 nL/min (velum closure) is indicative of PCD [32]. |
| Transmission Electron Microscope (TEM) | Identifies hallmark ciliary ultrastructural defects (ODA, IDA, CA). | e.g., Zeiss EM900. Used for definitive PCD diagnosis in a research context [32]. |
| Genetic Sequencing Panels | Identifies biallelic mutations in known PCD-causing genes. | Genes include DNAH5, DNAI1 (ODA defects); CCDC39, CCDC40 (IDA/CA defects); DNAH11 (normal ultrastructure) [32]. |
| Echocardiography System | Gold standard for non-invasive identification of associated congenital heart defects. | Critical for detecting defects like AVSD, TGA, and atrial isomerism in situs ambiguus cases [8] [6]. |
| Computed Tomography (CT) Scanner | Provides definitive anatomic detail for thoracic and abdominal situs determination. | Used to confirm bronchial anatomy, liver/stomach position, and great vessel arrangement [6]. |
Overcoming Diagnostic Hurdles: Optimizing Pathways and Interpreting Ambiguous Results
For researchers and drug development professionals working to enhance PCD (Primary Ciliary Dyskinesia) detection, particularly in cases without laterality defects such as situs inversus, a significant and often overlooked roadblock exists: the low engagement of pulmonary subspecialists in the patient referral process. This disengagement directly impacts research cohorts by limiting patient accrual and creating selection biases that can skew study results. The challenge is particularly acute for PCD, a rare, genetically heterogeneous disease affecting approximately 1 in 10,000 people, where dysfunction of motile cilia leads to progressive sino-pulmonary disease [17] [33]. A substantial proportion of patients—estimated at 6–12%—present with laterality defects other than situs inversus, such as heterotaxy, which can include complex congenital heart disease [33]. Identifying patients without these obvious anatomical clues requires a high index of suspicion and reliable access to specialized diagnostic pathways. This article establishes a technical support framework to analyze and troubleshoot the specific barriers that prevent pulmonary subspecialists from consistently referring patients into these critical research streams.
Diagnosing the Problem: A Barrier Analysis for Research Operations
Understanding the barriers to referral is the first step in developing effective countermeasures for your research operations. The following table synthesizes qualitative findings from healthcare studies, translating them into a research context to diagnose the core issues [34] [35].
Table 1: Analysis of Referral Barriers and Research Implications
| Barrier Category | Specific Barrier | Impact on PCD Research | Supporting Evidence |
|---|---|---|---|
| Knowledge & Awareness | Limited awareness of available PCD research studies/registries. | Missed opportunities to enroll eligible patients into cohorts. | Hospitalists and ED physicians reported low awareness of available programs/resources [34]. |
| Unfamiliarity with PCD phenotypes, especially without laterality defects. | Failure to identify potential PCD cases, leading to under-diagnosis and exclusion from research. | PCD diagnosis is often delayed due to symptom overlap with other disorders [17]. | |
| Process & Resources | Lack of clear referral pathways from clinical to research settings. | Cumbersome processes deter time-constrained subspecialists. | HCPs suggested "clear guidelines" and a "pathway to directly refer" as needed improvements [34]. |
| Inadequate diagnostic resources (e.g., nasal NO, TEM, genetic testing). | Inability to confirm PCD diagnosis, a common prerequisite for research enrollment. | Diagnosis is complex and requires a multi-test approach; access to modern facilities is unequal [33]. | |
| Perceptual & Structural | Perception of research as an extra burden with low relative advantage. | Low motivation to engage in activities perceived as outside core clinical duties. | While HCPs saw the benefit of interventions, this was offset by other systemic barriers [34]. |
| Organizational and governmental context (e.g., funding, priorities). | Lack of institutional support for research activities, including protected time for referrals. | Barriers exist at personal, familial, social, financial, organizational, and governmental levels [35]. |
Troubleshooting Guides & FAQs for Research Teams
This section provides actionable, step-by-step protocols to address the identified barriers and strengthen the referral pipeline for your studies.
Troubleshooting Guide: Building a Robust Referral Pathway
Problem: A low rate of referrals from pulmonary subspecialists is slowing patient accrual for a PCD natural history study.
Solution: Implement a systematic troubleshooting protocol to identify and resolve the root cause.
Table 2: Troubleshooting Guide for Low Referral Rates
| Step | Action Item | Expected Outcome | Tools/Resources |
|---|---|---|---|
| 1. Diagnose | Survey referring physicians to gauge awareness of your study and perceived barriers. | Data-driven identification of the primary barrier (e.g., awareness, process, perception). | Custom survey based on barriers in Table 1. |
| 2. Address Awareness | If awareness is low, deploy a multi-channel communication strategy. | Increased visibility of the research study and its eligibility criteria among subspecialists. | - Educational seminars on PCD phenotypes.- Laminated quick-reference guides for clinical areas.- Regular updates in institutional newsletters. |
| 3. Streamline Process | If the process is a barrier, simplify the referral mechanism. | A referral process that takes less than 2 minutes to initiate. | - Single-page referral form with checkboxes.- Dedicated research coordinator contact info.- Integration with electronic health records (EHR) if possible. |
| 4. Provide Feedback | Close the loop by acknowledging every referral and updating referrers on patient status. | Reinforced behavior, making referrers feel valued and part of the research team. | - Personalized thank-you email.- Periodic summaries of aggregate study progress. |
| 5. Monitor & Adapt | Track referral sources over time and be prepared to iterate. | A sustainable and effective referral pipeline that supports long-term research goals. | Simple tracking database (e.g., REDCap, Excel). |
Frequently Asked Questions (FAQs)
Q1: A clinician asks, "Why should I refer my PCD patients to a research registry? What's the immediate benefit to my patient or my practice?"
- A: Emphasize the value. Explain that participation in registries like those developed by the BEAT-PCD Clinical Research Collaboration contributes to a larger evidence base, which ultimately leads to better-defined disease phenotypes, standardized care guidelines, and future access to clinical trials [33]. For the practice, it provides structured follow-up data and connects them to an international network of experts.
Q2: "My patient doesn't have situs inversus. Could they still have PCD and be eligible for your study on enhanced detection?"
- A: Absolutely. Approximately half of PCD patients do not have situs inversus. A significant minority (6-12%) have other laterality defects (heterotaxy), and the rest have situs solitus (normal organ arrangement) [17] [33]. Key clinical symptoms that should trigger suspicion include neonatal respiratory distress in term infants, chronic wet cough year-round that begins in infancy, and chronic rhinosinusitis or otitis media [17].
Q3: "What is the minimum diagnostic evidence I need to refer a patient for a PCD research study?"
- A: Requirements vary by study, but generally, suspicion can be based on clinical phenotype. However, for genetic studies, a definitive diagnosis is often required. The current diagnostic workflow is multi-test, as there is no single stand-alone test. The following diagram outlines the standard diagnostic pathway and where research referrals can be integrated.
Q4: "We don't have access to nasal nitric oxide testing or electron microscopy. How can we participate in PCD research?"
- A: This is a common challenge. International networks like BEAT-PCD aim to support centers with limited diagnostic resources [33]. You can:
- Collect Clinical Data: Systematically document the clinical phenotype using standardized forms like FOLLOW-PCD.
- Refer for Testing: Establish a collaboration with a reference diagnostic center for sending samples (e.g., nasal brushings for genetic analysis).
- Utilize Genetic Testing: As genetic panels become more accessible, they can be a powerful first-line diagnostic tool, especially when combined with strong clinical evidence.
The Scientist's Toolkit: Key Research Reagents & Materials
For research focused on improving PCD detection, a core set of reagents and methodologies is essential. The following table details key solutions used in the field.
Table 3: Essential Research Reagents and Materials for PCD Detection Studies
| Item Name | Function/Application in PCD Research | Key Considerations |
|---|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Non-invasive screening tool; measures very low nNO levels characteristic of PCD (approx. 10-15% of normal) [17]. | Critical for patient recruitment and stratification. No FDA-approved device is currently available in the US, though used clinically in Europe. |
| Transmission Electron Microscope (TEM) | Visualizes ciliary ultrastructure to identify defects in dynein arms, radial spokes, or microtubule organization [17]. | Requires specialized expertise and standardized protocols. May miss cases with normal ultrastructure but genetic defects (e.g., DNAH11). |
| PCD Genetic Sequencing Panel | Definitive diagnosis by identifying biallelic pathogenic mutations in one of over 50 known PCD-related genes [17] [33]. | Handles genetic heterogeneity. Essential for correlating genotype with phenotype, especially in patients without laterality defects. |
| High-Speed Video Microscopy System | Analyzes ciliary beat frequency and pattern to detect dyskinesia that may not be evident structurally [17]. | A specialized technique that can differentiate between specific beat patterns associated with different ultrastructural defects. |
| Standardized Clinical Data Forms (e.g., FOLLOW-PCD) | Collects uniform clinical, diagnostic, and patient-reported outcome data across research sites for robust cohort studies [33]. | Promotes data comparability and is vital for large, multi-center studies and registries. |
Experimental Protocol: Standardized nNO Measurement for Research Cohorts
Accurate and consistent measurement of nasal nitric oxide is a cornerstone of PCD screening in research. The following protocol is adapted from current methodologies to ensure reliable, reproducible data.
Objective: To obtain a quantifiable nasal nitric oxide (nNO) measurement from a research participant for the purpose of PCD screening.
Background: nNO is severely reduced in PCD patients due to unknown mechanisms, making it a highly sensitive screening tool. The measurement is expressed as nL/min (nanoliters per minute) to standardize for flow rate [17].
Materials:
- Chemiluminescence nNO analyzer
- Nasal olive or catheter with foam sleeve
- Nose clips
- Calibration gases
- Data recording forms
Step-by-Step Methodology:
- Participant Preparation: The participant should refrain from smoking, drinking alcohol, or eating for at least one hour prior to testing. They should also be free of acute upper respiratory infections.
- Equipment Calibration: Calibrate the nNO analyzer according to the manufacturer's specifications using certified calibration gases before each testing session.
- Participant Positioning: Seat the participant comfortably. Explain the procedure, emphasizing the need for velum closure (soft palate closure) to prevent contamination from lung air.
- Velum Closure Training: Instruct the participant to practice breathing gently through their mouth while keeping their lips sealed. Alternatively, they can perform a slow vital capacity maneuver against resistance.
- Measurement:
- Gently insert the nasal olive into one nostril, ensuring a tight seal.
- Instruct the participant to perform the velum closure maneuver.
- Aspirate air from the nasal cavity at a constant, recommended flow rate (typically 0.3-0.5 L/min) for 30-45 seconds or until a stable plateau of nNO concentration is observed.
- Record the plateau nNO concentration in parts per billion (ppb) and the flow rate.
- Calculation: Calculate nNO output: nNO (nL/min) = [NO] (ppb) × Flow Rate (L/min). Most modern analyzers perform this calculation automatically.
- Replication: Repeat the measurement at least twice in each nostril to ensure reproducibility. Average the results for the final value.
Interpretation of Results:
- nNO values consistently below 100 nL/min are highly suggestive of PCD and warrant further confirmatory testing [17].
- Note that low nNO can occasionally occur in other conditions like cystic fibrosis or severe sinus disease, so it should be interpreted within the full clinical and research context.
Strategies for Optimizing nNO Testing in Young and Uncooperative Patients
Frequently Asked Questions (FAQs) on nNO Testing Challenges
Q1: Why is measuring nasal nitric oxide (nNO) challenging in young children, and what are the clinical consequences? nNO measurement in young children is challenging primarily due to their inability to perform the coordinated breath-hold maneuver required for standard testing protocols. This can lead to falsely low nNO readings that overlap with levels seen in Primary Ciliary Dyskinesia (PCD). A comparative study found that while PCD patients had consistently low nNO levels (29.7 ± 5.7 ppb), uncooperative healthy children could also present with similarly low values (e.g., 128.1 ± 16.2 ppb in children ≤6 months), creating a diagnostic challenge [36]. Failure to optimize testing for this population can result in misdiagnosis or delayed diagnosis of PCD, particularly in patients who do not have the classic laterality defect, situs inversus totalis [37].
Q2: What are the key technical differences between testing cooperative versus uncooperative patients? The key technical difference lies in the breathing maneuver required. The gold standard for cooperative patients is a breath-hold maneuver with velum closure, which yields higher nNO values (e.g., 687.7 ± 96.9 ppb in healthy cooperative children) [36]. For uncooperative young children, an alternative is tidal breathing—breathing quietly without a breath-hold. However, this method typically produces lower nNO values (e.g., 335.9 ± 57.9 ppb in the same children) and has a wider range of normal values, which must be considered when interpreting results [36].
Q3: A patient's initial nNO value was low, suggesting PCD. What is the recommended next step? A single low nNO measurement in a young, uncooperative child should not be considered diagnostic for PCD. The recommended strategy is to schedule a repeat evaluation after a time interval. Research shows that in 24 uncooperative healthy children with initial nNO values ≤200 ppb, levels significantly increased from 104.7 ± 10.5 ppb to 169.9 ± 19.6 ppb when re-tested at least six months later [36]. Repeated measurements are often necessary to distinguish true PCD from transiently low values due to poor cooperation or young age.
Q4: Beyond cooperation, what other factors can affect nNO levels and should be controlled for during testing? It is critical to perform nNO testing when the patient is in a period of clinical stability. Acute respiratory illnesses can significantly alter nNO values, potentially leading to false positives or negatives [38]. Testing should be postponed if the patient has had a recent upper respiratory tract infection. Furthermore, the proper functioning of motile cilia in the respiratory tract is essential for normal nNO production, and acute infections can cause secondary, transient ciliary dysfunction [38].
Troubleshooting Guides for Common nNO Testing Scenarios
Scenario 1: The Uncooperative Preschooler
- Presenting Issue: Patient (age 2-5 years) is unable or unwilling to perform a breath-hold maneuver.
- Step-by-Step Resolution:
- Switch to Tidal Breathing Protocol: Use the tidal breathing method with a soft, well-sealed nose olive.
- Engage the Child: Use child-friendly techniques—demonstrate the process on a parent or a toy, use colorful visuals, or allow the child to handle the equipment (with supervision).
- Ensure a Leak-Free Seal: Check that the nasal olive fits snugly. A small leak can lead to a falsely low reading.
- Record Multiple Measurements: Take several recordings over a short period to ensure consistency and obtain a reliable average value.
- Interpret with Age-Specific Norms: Compare the result against established reference values for tidal breathing in the specific age group, not against breath-hold norms [36].
- Plan for Follow-up: If the value is low, schedule a repeat test in 6-12 months to monitor for the expected age-related increase in nNO, rather than concluding a PCD diagnosis immediately [36].
Scenario 2: Inconclusive Low nNO Without Laterality Defects
- Presenting Issue: A patient with a strong clinical phenotype of PCD (e.g., year-round wet cough, neonatal respiratory distress) has persistently low nNO but no laterality defects (situs solitus), making diagnosis less straightforward.
- Step-by-Step Resolution:
- Verify Testing Conditions: Confirm the test was performed during a clinically stable period, free from active infection [38].
- Repeat the nNO Test: A second or third low nNO measurement strengthens the suspicion of PCD.
- Proceed to Advanced Diagnostics: Recognize that nNO is a screening tool. A low value should trigger a referral for definitive PCD testing, which is a multi-modal approach [38]:
- Genetic Testing: Identify biallelic pathogenic mutations in a known PCD-associated gene.
- Transmission Electron Microscopy (TEM): Analyze ciliary ultrastructure from a nasal brush biopsy for hallmark defects (e.g., absent outer/inner dynein arms).
- Consider Phenotypic nuances: Be aware that patients with PCD and situs solitus (no laterality defects) are common, representing about 47% of one classic PCD cohort [37]. The absence of laterality defects does not rule out PCD.
The following table consolidates key nNO values from research to aid in the interpretation of results across different patient groups and testing methods.
Table 1: Nasal Nitric Oxide (nNO) Levels in Various Patient Groups and Testing Conditions
| Patient Group / Condition | Testing Method | Typical nNO Value (ppb) | Key Context for Interpretation |
|---|---|---|---|
| PCD Patients | Not specified (presumed breath-hold) | 29.7 ± 5.7 [36] | Consistently low, typically <100 ppb. A strong positive indicator for PCD. |
| Healthy Cooperative Children | Breath-hold maneuver | 650 ± 60.6 [36] | Represents the "normal" target for cooperative patients using the standard method. |
| Healthy Uncooperative Children (>6 mos) | Tidal breathing | 309.1 ± 45.9 [36] | Normal range for tidal breathing is lower than breath-hold. Values can overlap with PCD. |
| Healthy Uncooperative Children (≤6 mos) | Tidal breathing | 128.1 ± 16.2 [36] | Normal values can be very low in infancy. Repeat testing is essential. |
| PCD with Situs Ambiguus (SA) | Not specified | Median: 12 nL/min [37] | Confirms that low nNO is a robust marker for PCD, even in patients with complex laterality defects. |
Table 2: Key Reagents and Materials for nNO Research and Diagnostic Testing
| Research Reagent / Material | Function in nNO Testing and PCD Diagnostics |
|---|---|
| Chemiluminescence Nitric Oxide Analyzer | The core analytical instrument that accurately measures the concentration of NO in nasal air samples. |
| Nasal Olive or Nasal Probe | A soft, disposable attachment that creates a leak-free seal in the nostril for direct sampling of nasal air. |
| Biofeedback Software/Visual Aids | Tools to help coach cooperative patients on maintaining the proper breath-hold technique during testing. |
| Cell Culture Media & Supplies | Used for cultivating ciliated epithelial cells from nasal brush biopsies for functional tests like High-Speed Video Microscopy Analysis (HSVA). |
| Electron Microscopy Fixatives | Chemicals (e.g., glutaraldehyde) for immediate fixation of nasal brush biopsy samples to preserve ciliary ultrastructure for TEM analysis. |
Experimental Protocol: nNO Measurement via Tidal Breathing
Objective: To obtain a reliable nasal nitric oxide measurement from a young or uncooperative patient who cannot perform a breath-hold maneuver.
Materials:
- Chemiluminescence NO analyzer (calibrated according to manufacturer specifications)
- Appropriate-sized nasal olives to ensure a tight seal
- Disposable tubing
- Data recording software or system
Step-by-Step Methodology:
- Patient Preparation: Seat the patient comfortably. Explain the procedure to the parent and, in age-appropriate terms, to the child. Ensure the patient has been free of acute respiratory symptoms for at least 2-4 weeks.
- Equipment Setup: Connect a new, clean nasal olive to the sampling tube. Select the "tidal breathing" protocol on the analyzer if available.
- Olive Placement: Gently insert the nasal olive into one nostril, ensuring a soft but complete seal. The other nostril remains open and unobstructed.
- Initiate Measurement: Instruct the patient to breathe normally through their mouth while keeping their lips closed. Visually monitor the pressure trace on the analyzer to ensure stable, leak-free sampling.
- Data Recording: Record the nNO concentration once a stable plateau is observed, typically over a 30-45 second period. Repeat the measurement in the same nostril or the contralateral nostril to obtain a minimum of two reproducible plateau values.
- Data Analysis: Calculate the mean of the stable plateau values. Interpret this value against published normative data for the tidal breathing method in the patient's age group [36].
Diagnostic Workflow and Pathway Diagrams
The following diagram illustrates the integrated diagnostic pathway for identifying PCD, emphasizing the role of nNO testing within a broader multimodal strategy, especially for patients without laterality defects.
Diagram 1: Integrated Diagnostic Pathway for PCD Using nNO. This workflow highlights the critical steps for using nNO testing, including the need for repeat testing in young children and the subsequent use of advanced diagnostic modalities to confirm a PCD diagnosis.
Troubleshooting Genetic Test Interpretation
Genetic testing is a powerful tool for diagnosing Primary Ciliary Dyskinesia (PCD), yet the interpretation of results is fraught with challenges that can lead to misdiagnosis and improper patient management.
Frequently Asked Questions (FAQs) on Genetic Results
What constitutes an inconclusive genetic result? The most common inconclusive result is a Variant of Unknown Significance (VUS), where a genetic change is identified but its link to disease is unclear. Other challenges include interpreting missense variants and distinguishing between pathogenic changes and benign population polymorphisms [39].
Why is there such a high rate of misinterpretation? A survey of genetics professionals found that 83% were aware of at least one case of genetic test misinterpretation. Contributing factors include unclear report wording, lack of genetic counseling, and suboptimal communication among healthcare providers, many of whom may not have formal training in genetics [39].
What are the clinical consequences of misinterpretation? Incorrect interpretation can trigger a cascade of negative outcomes, including unnecessary follow-up tests, improperly altered clinical management, incorrect diagnoses, increased psychosocial stress for patients and families, and the misuse of healthcare dollars [39].
How can our team minimize interpretation errors? Adhere to the standardized five-tier terminology system recommended by the American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology (AMP). All clinical genetic testing should be performed in a CLIA-approved laboratory and interpreted by a board-certified clinical molecular geneticist or equivalent [40].
What genes are most critical to analyze for PCD? Focus on genes known to cause PCD with and without laterality defects. Note that mutations in genes encoding for central pair microtubules and radial spokes (e.g., RSPH4A, RSPH9, RSPH1) typically cause PCD without laterality defects, as embryonic nodal cilia have a 9+0 ultrastructure lacking these components [41].
| Classification Tier | Definition | Implied Action for Clinical Management |
|---|---|---|
| Pathogenic (P) | >90% certainty of being disease-causing | Can be used for diagnostic and therapeutic decisions. |
| Likely Pathogenic (LP) | >90% certainty of being disease-causing | Can be used for diagnostic and therapeutic decisions. |
| Uncertain Significance (VUS) | Not classifiable as pathogenic or benign | Should not be used for clinical decision-making; requires further evidence. |
| Likely Benign (LB) | >90% certainty of being benign | Generally not reported. |
| Benign (B) | No clinical significance for the disorder | Generally not reported. |
Workflow for Classifying Genetic Variants
The following diagram outlines the standardized process for interpreting sequence variants, as per joint consensus recommendations.
Troubleshooting Transmission Electron Microscopy (TEM) in PCD
TEM analysis of ciliary ultrastructure is a cornerstone of PCD diagnosis. However, technical artifacts can obscure results and lead to false negatives or incorrect characterization of defects.
Frequently Asked Questions (FAQs) on TEM Findings
What are the most common TEM artifacts that hinder analysis? Scientists report several common, troublesome artifacts:
- Crystalline Ice Contaminants (in cryo-TEM)
- Stain Crystal Clusters (in negative stain TEM)
- Carbon Film Artifacts
- Sample Drift
- Grid Imperfections [42]
How can I distinguish true ciliary defects from ice contamination? Crystalline ice appears as dense, variably-sized contaminants embedded in the vitreous ice. It is more electron-dense than the ice layer and embedded particles. While minor contamination can be tolerated, excessive ice crystals can obscure or mimic particles, interfering with sizing, morphology analysis, and interpretation. Preparing grids in a dehumidified environment and optimizing vitrification parameters can mitigate this issue [42].
Our negative stain images have an uneven background with crystal clusters. What is the cause? Clusters of stain crystals are often due to an interaction between the sample buffer and the heavy metal stain (e.g., uranyl acetate). This can usually be resolved by making a new grid or preparing a fresh stain solution [42].
Is there a standardized method for quantifying organelle morphology from TEM images? Yes, using open-source software like ImageJ (Fiji) provides a standardized approach. Key measurable features include:
- Length & Width: Calculated using the Pythagorean theorem on pixel coordinates.
- Area & Perimeter: Measured for defined shapes (circles, rectangles).
- Circularity Index: A unitless value (Ci = 4π*Area/Perimeter²) where 1.0 indicates a perfect circle [43].
| Artifact | Description & Impact | Troubleshooting Solution |
|---|---|---|
| Crystalline Ice | Dense, crystalline forms in vitreous ice; obscures particles and compromises image quality. | Use freshly dispensed liquid nitrogen; work in a dehumidified environment; optimize blotting time and vitrification parameters. |
| Stain Crystal Clusters | Electron-dense crystals creating an uneven background in negative stain TEM. | Prepare a fresh stain solution; make a new grid; check for sample buffer compatibility with the stain. |
| Carbon Artifacts | Defects (e.g., wrinkles, tears) in the thin carbon support film; can be mistaken for biological structures. | Use a new batch of carbon-coated grids; carefully check the carbon layer integrity during grid preparation. |
| Drift | Blurred images caused by sample movement during exposure. | Ensure the grid is securely mounted; check for environmental vibrations; assess ice/grid stability. |
| Grid Imperfections | Flaws from the manufacturing process (e.g., irregular holes). | Select grids from a reliable supplier; screen multiple grid squares for optimal regions. |
Workflow for Systematic TEM Image Analysis
This workflow, based on established protocols, ensures accurate and reproducible quantification of organelles like mitochondria and endoplasmic reticulum from TEM images [43].
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Material | Function / Application | Key Considerations |
|---|---|---|
| Nasal Nitric Oxide (nNO) Measurement | A key screening tool for PCD; nNO levels are extremely low in most PCD patients [37]. | Must be performed with age-appropriate protocols. Low nNO is sensitive but not specific for PCD. |
| Heavy Metal Stains (e.g., Uranyl Formate) | Provides electron-dense background in negative stain TEM for high-contrast visualization of particles like viruses and protein complexes [42]. | Prepare fresh solutions; crystals can form and obscure particles if the stain is old or interacts with sample buffer. |
| Liquid Ethane / Cryogen | Used for rapid freezing of aqueous samples to form non-crystalline, vitreous ice for cryo-TEM, preserving native particle structure [42]. | High cooling rates are critical to prevent destructive ice crystal formation. |
| PureLink Genomic DNA Mini Kit | For isolation of high-quality chromosomal DNA from bacterial or human cells, used as a template for subsequent PCR amplification of target genes [44]. | Follow manufacturer's protocol for consistent yield and purity; critical step for downstream genetic analyses. |
| BD Matrigel | A basement membrane matrix used to coat culture dishes for plating and differentiating sensitive cells, such as satellite cells used in metabolic studies [43]. | Provides a biologically relevant substrate that promotes cell adhesion, differentiation, and maintenance of specialized functions. |
| ImageJ / Fiji Software | Open-source image analysis platform for quantifying morphological features (length, area, circularity) from TEM and other microscopy images [43]. | Enables standardized, reproducible measurements. The analysis should be performed by a blinded team to reduce subjective bias. |
Integrating Findings in PCD Without Classic Laterality Defects
Enhancing PCD detection in patients without situs inversus totalis (SI) requires a multifaceted approach, as a significant proportion of cases present with situs ambiguus (SA) or situs solitus (SS).
Quantitative Data on Laterality Defects in PCD
The table below summarizes the prevalence of different situs states from two key studies, highlighting that laterality defects are a spectrum and SA is more common than once thought.
| Situs Classification | Prevalence in Classic PCD (Shapiro et al.) [37] | Prevalence in PCD (Wong et al.) [8] | Key Associated Features |
|---|---|---|---|
| Situs Solitus (SS) | 46.9% (143/305) | 47% (75/159) | Normal organ arrangement. PCD diagnosis can be missed without respiratory symptoms. |
| Situs Inversus Totalis (SI) | 41.0% (125/305) | 29% (46/159) | Mirror-image organ arrangement. Classic Kartagener's Syndrome triad. |
| Situs Ambiguus (SA) | 12.1% (37/305) | 24% (38/159) | Includes heterotaxy. High risk of congenital heart disease (200x general population) and other defects [8]. |
Diagnostic Pathway for PCD with Atypical Laterality
A proactive diagnostic approach is essential for identifying PCD in cases with subtle or no laterality defects.
Developing Institutional Algorithms to Streamline Triage and Multidisciplinary Evaluation
Frequently Asked Questions (FAQs)
Q1: What are the key clinical features that should trigger a PCD evaluation in a patient without a laterality defect? The American Thoracic Society (ATS) algorithm recommends evaluation for PCD if a patient exhibits at least two of the following four key clinical features:
- Unexplained neonatal respiratory distress syndrome (NRDS) in a term infant, requiring oxygen or positive pressure for at least 24 hours.
- Year-round daily cough beginning before 6 months of age.
- Year-round daily nasal congestion beginning before 6 months of age.
- An organ laterality defect (e.g., situs inversus totalis, heterotaxy) [1] [5].
For patients without a laterality defect, the presence of any two of the first three criteria warrants a referral for evaluation. A chronic wet cough and a history of recurrent otitis media are also strong indicators [5].
Q2: A significant number of eligible patients are not being referred for PCD evaluation. What are the common pitfalls and how can they be avoided? A common pitfall is attributing respiratory symptoms solely to a coexisting condition, such as congenital heart disease (CHD), which is frequently present in patients with laterality defects. This often leads to a missed diagnosis of PCD [1]. To avoid this:
- Maintain a High Index of Suspicion: Adhere strictly to the ATS criteria. The presence of another explanatory diagnosis (like CHD) should not automatically rule out a concurrent PCD evaluation, especially if multiple criteria are met [1].
- Document Symptom Chronicity: Ensure that symptoms like cough and nasal congestion are documented as "daily" and "year-round" in the patient's record, as this is a specific requirement of the evaluation criteria [1].
- Implement an Institutional Referral Algorithm: Use a standardized triage and referral pathway to ensure that all patients who meet the minimum criteria are automatically flagged for pulmonary and genetics specialist review [1].
Q3: What is the role of nasal nitric oxide (nNO) testing in the diagnostic workflow? Nasal nitric oxide (nNO) is a valuable, non-invasive screening tool for PCD. It is typically used as a first-line test at specialty centers. Low nNO levels are highly suggestive of PCD and should be followed by confirmatory genetic testing. It is important to note that some genetic variants may present with normal nNO levels, so a normal test does not completely rule out PCD [5].
Q4: What is the recommended sequence of diagnostic tests once a patient is referred? The following standardized diagnostic pathway is recommended [1] [5]:
- Initial Screening: Perform nNO testing at a specialty center, if available.
- Genetic Testing: If nNO is low or unavailable, proceed with genetic testing for pathogenic variants in known PCD-associated genes.
- Confirmatory Testing: If genetic test results are inconclusive or normal but clinical suspicion remains high, transmission electron microscopy (TEM) of ciliary ultrastructure should be performed. Cystic fibrosis (CF) must be excluded as part of the differential diagnosis.
Troubleshooting Guides
Issue 1: Inconclusive Genetic Test Results
Problem: A patient has strong clinical features of PCD, but genetic testing returns variants of uncertain significance (VUS) or is inconclusive.
Solution:
- Proceed to TEM: Transmission Electron Microscopy remains the gold standard for identifying classic ciliary ultrastructural defects (e.g., outer dynein arm defects). This can provide definitive confirmatory evidence [1] [5].
- Expanded Genetic Analysis: Consider re-analysis with an expanded or updated PCD gene panel, as new genes continue to be discovered. Seek collaboration with specialized research or diagnostic centers for further interpretation of VUS [1].
- Functional Assays: In research settings, ciliary beat frequency and pattern analysis can provide functional data to support the diagnosis, though these are highly specialized tests [5].
Issue 2: Differentiating PCD from Other Causes of Chronic Respiratory Symptoms
Problem: Symptoms like chronic cough and nasal congestion overlap with common conditions like asthma, allergic rhinitis, and recurrent viral infections.
Solution:
- Focus on Onset and Pattern: PCD symptoms are typically daily and begin in infancy (before 6 months of age). This pattern is distinct from the intermittent or seasonal nature of allergies and common infections [1].
- Look for "Red Flag" Comorbidities: A history of recurrent otitis media with effusion, chronic rhinosinusitis, or bronchiectasis in a child increases the probability of PCD [5].
- Utilize Diagnostic Triangulation: Rely on a combination of tests rather than a single data point. The concordance of low nNO, a pathogenic genetic variant, and a compatible clinical phenotype provides a definitive diagnosis.
Evidence and Data Foundation
The development of an effective algorithm is grounded in data that reveals current gaps in clinical practice. The table below summarizes key quantitative findings from a recent study on PCD referral patterns.
Table 1: Rates of Referral and Evaluation for PCD in Patients with Laterality Defects
| Number of PCD Criteria Met | Percentage Referred to Pulmonary | Percentage Referred to Genetics | Percentage Evaluated for PCD |
|---|---|---|---|
| 2 or more criteria | 41% | 18% | 16% |
| All 4 criteria | 96% | 85% | 93% |
Source: Retrospective chart review of 369 patients with laterality defects at a pediatric academic center [1].
This data highlights a significant gap: while patients meeting all four criteria are highly likely to be evaluated, nearly 60% of those meeting the minimum of two criteria are not referred to a pulmonologist, leading to substantial underdiagnosis [1].
Experimental Protocols
Protocol 1: Implementing a Triage Algorithm for PCD Suspect Identification
Objective: To systematically identify patients within a healthcare system who meet the criteria for PCD evaluation and ensure appropriate referral.
Methodology:
- Electronic Medical Record (EMR) Flagging: Configure the EMR system to flag pediatric patients with one or more of the following diagnostic codes: heterotaxy, dextrocardia, isomerism, or situs inversus [1].
- Structured Data Extraction: For flagged patients, create a structured data dashboard or report that extracts and displays:
- Documented history of NRDS requiring >24 hours of respiratory support.
- Problem list entries of "chronic daily cough" or "chronic daily nasal congestion."
- Age of onset for respiratory symptoms (to confirm onset in infancy).
- Triage Categorization: Apply a standardized triage color system to categorize urgency and required actions based on the number of criteria met [45] [46].
- Red (Immediate): Meets 3-4 criteria → Automatic referral to Pulmonary and Genetics.
- Yellow (Delayed): Meets 2 criteria → Automatic referral to Pulmonary.
- Green (Minor/Monitor): Meets only 1 criterion → Document for future monitoring if new symptoms arise.
- Multidisciplinary Notification: The algorithm should automatically notify the respective clinical teams (Pulmonary, Genetics) and trigger a referral order for patients in the Red and Yellow categories.
Protocol 2: Standardized Diagnostic Workflow for PCD Confirmation
Objective: To provide a clear, step-by-step protocol for confirming a PCD diagnosis after a patient is referred.
Methodology:
- Exclusion of Cystic Fibrosis: Perform a sweat chloride test and/or CFTR genetic testing to rule out cystic fibrosis [1].
- Nasal Nitric Oxide (nNO) Measurement: Schedule nNO testing at a specialty center. Consistently low nNO measurements on repeated attempts are highly suggestive of PCD [5].
- Genetic Testing: Order a next-generation sequencing panel for all known PCD-associated genes. A positive finding of biallelic pathogenic variants confirms the diagnosis [1] [5].
- Transmission Electron Microscopy (TEM): If genetic testing is non-diagnostic, proceed with a nasal brush biopsy to obtain ciliated epithelium for TEM analysis to assess for ultrastructural defects [1] [5].
Workflow Visualization
The following diagram illustrates the logical pathway for triaging patients and the subsequent multidisciplinary diagnostic evaluation.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and assays essential for the research and diagnostic evaluation of PCD.
Table 2: Essential Reagents and Materials for PCD Research and Diagnostics
| Item Name | Function/Brief Explanation |
|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | A non-invasive device to measure nasal NO concentration. Consistently low nNO levels are a key screening biomarker for PCD due to impaired production in the nasal epithelium [5]. |
| PCD Gene Panel (NGS) | A next-generation sequencing panel targeting all known PCD-associated genes. This is a core diagnostic tool for identifying pathogenic genetic variants responsible for the disease [1] [5]. |
| Transmission Electron Microscope (TEM) | Used to visualize the ultrastructure of cilia obtained from nasal brush biopsies. Identifies classic defects such as the absence of outer or inner dynein arms, which are pathognomonic for many forms of PCD [1] [5]. |
| Cell Culture Media for Ciliated Epithelium | Specialized media used to grow and differentiate human airway epithelial cells at an air-liquid interface (ALI). This creates a model for studying ciliary function and beat frequency in vitro [5]. |
Benchmarking Progress: Validating New Technologies and Comparative Diagnostic Accuracy
The following tables summarize the key performance metrics for nasal Nitric Oxide (nNO), genetic testing, and transmission electron microscopy (TEM) in the diagnosis of Primary Ciliary Dyskinesia (PCD), based on current literature and clinical guidelines.
Table 1: Overall Sensitivity, Specificity, and Key Characteristics of PCD Diagnostic Tests
| Test Modality | Reported Sensitivity | Reported Specificity | Key Strengths | Major Limitations |
|---|---|---|---|---|
| Nasal Nitric Oxide (nNO) | 96.3% [47] | 96.4% [47] | Non-invasive; useful screening tool [47]. | Not a standalone test; low in other conditions like cystic fibrosis; requires specialized equipment [48] [47]. |
| Genetic Testing | ~70% (for known genes) [47] | High (for identified pathogenic variants) [47] | Provides definitive molecular diagnosis; implications for management [48]. | Locus heterogeneity; ~30% of patients have no identified genetic cause; VUS challenges [48] [47]. |
| Transmission Electron Microscopy (TEM) | ~70% (estimates vary) [47] | High (for classic ultrastructural defects) [47] | Identifies classic ultrastructural defects (e.g., ODA, IDA) [8]. | ~30% of PCD patients have normal ultrastructure; sample processing and interpretation challenges [47]. |
Table 2: Real-World Performance and Clinical Utility Data
| Performance Aspect | nNO Findings | Genetic Testing Findings |
|---|---|---|
| Impact on Diagnostic Workflow | 75% of patients with a single nNO value above cutoff avoided further confirmatory testing [47]. | The positivity rate was 50% when performed after a positive nNO screen, versus 8% when used as a first-line test [47]. |
| Result Interpretation | 91% of patients with a single above-cutoff nNO value were determined to have PCD "unlikely" without additional testing [47]. | A confirmed genetic diagnosis is possible when two pathogenic/likely pathogenic variants are found in a PCD-associated gene [8]. |
| Challenging Scenarios | Patients with repeatedly low nNO but negative confirmatory tests may still be managed as having PCD [47]. | Genetic diagnosis is confounded by variants of uncertain significance (VUS), requiring correlation with other tests [48]. |
Experimental Protocols for Key Diagnostic Tests
FAQ: What is the standardized protocol for nNO measurement?
Answer: The American Thoracic Society (ATS) and European Respiratory Society (ERS) recommend specific technical standards for nNO measurement [48] [47].
- Methodology: The preferred method for cooperative patients (typically ≥5 years old) is measurement during velum closure with a chemiluminescence device and resistor technique. For younger patients (2-5 years) unable to perform this maneuver, measurement during tidal breathing can be used, though with lower accuracy and more variability [48].
- Diagnostic Cut-off: When using the resistor technique in children ≥5 years old, a value of ≤77 nL/min is a commonly used diagnostic cutoff [47].
- Critical Considerations:
FAQ: What are the standard methodologies for genetic testing and TEM analysis in PCD?
Answer: Both tests require specialized expertise and have specific procedural standards.
- Genetic Testing Protocol:
- Test Selection: Use an extended genetic testing panel that covers all known PCD-associated genes (over 50 genes are currently known) [47].
- Analysis: Sequence analysis is performed to identify pathogenic or likely pathogenic variants.
- Interpretation: A confirmed genetic diagnosis is typically made when biallelic pathogenic variants (two pathogenic/likely pathogenic variants) are identified in a PCD-associated gene [8]. The presence of variants of uncertain significance (VUS) requires correlation with other test results, such as immunofluorescence (IF) [48].
- Transmission Electron Microscopy (TEM) Protocol:
- Sample Collection: A ciliary biopsy is obtained from the nasal epithelium.
- Processing: The sample is processed and sectioned for ultrastructural analysis under the electron microscope.
- Analysis: The ciliary ultrastructure is examined for definitive defects, such as the absence of outer dynein arms (ODA), combined absence of inner and outer dynein arms (ODA/IDA), or inner dynein arm defects with microtubular disorganization (IDA/MTD) [8].
- Critical Consideration: Samples must be collected when the patient is at baseline health, as acute infection can cause secondary, temporary ultrastructural changes that mimic PCD [47].
Diagnostic Pathways and Workflows
The following diagram illustrates the logical workflow for diagnosing PCD, integrating multiple tests as recommended by international guidelines.
Diagram 1: Integrated Diagnostic Workflow for PCD. This flowchart outlines the multi-test algorithm recommended by guidelines, emphasizing that no single test is sufficient to rule in or rule out PCD [48] [47].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for PCD Diagnostic Research
| Item/Category | Function in PCD Diagnostics | Specific Examples / Notes |
|---|---|---|
| Chemiluminescence Analyzer | Measures nasal nitric oxide (nNO) levels with high accuracy. | Required for standardized nNO measurement per ATS/ERS guidelines; uses resistor technique for velum closure [48] [47]. |
| Antibody Panels for Immunofluorescence (IF) | Detects absence or mislocalization of ciliary proteins. | Used as an adjunct test; accuracy depends on antibody panel quality and breadth; batch-to-battery variability is a concern [48]. |
| Extended Genetic Panels | Identifies pathogenic variants in PCD-associated genes. | Should include all known genes (>50); crucial for confirming diagnosis and guiding management [48] [47]. |
| High-Speed Video Microscopy (HSVM) | Analyzes ciliary beat frequency and pattern. | Requires post-cell culture analysis for higher specificity; should be performed in expert centers with high sample throughput [48]. |
| Electron Microscope & Processing Reagents | Visualizes ciliary ultrastructure for defects (e.g., ODA, IDA). | Used for TEM analysis; sample integrity is critical to avoid artifacts from inflammation [47] [8]. |
Validating Novel Biomarkers and High-Throughput Sequencing Approaches for PCD
Frequently Asked Questions (FAQs) on PCD Diagnostics and Sequencing
Q1: What are the key diagnostic challenges for PCD, especially in cases without laterality defects? A major challenge is that no single test is sufficient for a definitive diagnosis. A combination of tests is required, as each has limitations in sensitivity and specificity [49] [50]. For patients without situs inversus (approximately 50% of PCD cases), clinical suspicion is often lower, leading to significant diagnostic delays [51] [49]. Furthermore, up to 30% of patients with PCD have normal ciliary ultrastructure when examined by transmission electron microscopy (TEM), making diagnosis reliant on other modalities like genetic testing or immunofluorescence [51] [50].
Q2: Which high-throughput sequencing approach is preferred for PCD biomarker discovery: bulk RNA-Seq or single-cell RNA-Seq? Both approaches have complementary strengths. Bulk RNA-Seq is excellent for identifying overall gene expression differences between patient and control groups and is a robust starting point for biomarker discovery [52] [53]. Single-cell RNA-Seq (scRNA-seq) is powerful for deconvoluting cellular heterogeneity and identifying which specific cell types express your biomarkers of interest, providing deeper insights into disease mechanisms [54]. The choice depends on your research goal: bulk RNA-Seq for a broad transcriptional profile, and scRNA-seq to pinpoint cellular sources of dysregulation.
Q3: What is the minimum number of biological replicates required for a robust RNA-Seq experiment in PCD research? For RNA-Seq experiments, a minimum of 3 biological replicates per condition is required, but 4 is considered the optimal minimum to ensure statistical power and reliability [55]. Biological replicates (samples from different individuals) are strongly recommended over technical replicates (repeated measurements from the same sample) to account for natural biological variation [55].
Q4: How can I validate biomarkers identified from sequencing data? A multi-step validation strategy is considered best practice. This typically involves:
- Cross-dataset Validation: Confirming that the biomarkers are consistently dysregulated in an independent, publicly available cohort [53].
- Experimental Validation: Using reverse transcription-quantitative polymerase chain reaction (RT-qPCR) on a new set of patient and control samples to verify mRNA expression levels [53]. This is a gold-standard method for confirming sequencing findings.
- Functional Validation: Employing techniques like gene set enrichment analysis (GSEA) to determine if your biomarkers are involved in biologically relevant pathways, such as ciliary assembly or function [52] [54].
Troubleshooting Guides for Common Experimental Issues
Low Nasal Nitric Oxide (nNO) Measurement Quality
Problem: Inconsistent or unreliable nNO readings, which is a common screening test for PCD [49].
| Symptom | Possible Cause | Solution |
|---|---|---|
| Unstable nNO reading | Velum not closed, contaminating the sample with lower airway gas. | Ensure the patient exhales against resistance (e.g., against a pressure of 10 cm H₂O) to close the velum during aspiration [49]. |
| Low nNO in a non-PCD patient | Recent nasal inflammation or infection. | Postpone testing until after acute symptoms resolve. A normal nNO measurement effectively rules out PCD in most cases [49]. |
| nNO value is borderline | Lack of age-specific reference values or use of a portable analyzer. | Use a chemiluminescence analyzer if possible, and compare to reference values generated by your own center. A value below 77 nL·min⁻¹ is highly suggestive of PCD in children and adults [49]. |
RNA-Seq Batch Effects and Quality Control
Problem: Unwanted technical variation in RNA-Seq data that can obscure true biological signals.
| Symptom | Possible Cause | Solution |
|---|---|---|
| Samples cluster by processing date in PCA plot. | RNA extractions or library preparations performed at different times. | Process all RNA extractions simultaneously. If batched processing is unavoidable, ensure each batch contains replicates from all experimental conditions to allow for bioinformatic correction [55]. |
| Poor sequencing library quality. | Degraded RNA or incorrect library preparation method. | Check RNA Integrity Number (RIN); it should be >8 for mRNA-seq. Use total RNA library prep if RNA is degraded or if studying non-coding RNA [55]. |
| Insufficient sequencing depth. | Low number of sequenced reads per sample. | Aim for 10-20 million paired-end reads for mRNA-seq studies focused on coding genes [55]. |
Biomarker Validation Failure
Problem: Biomarkers identified in a discovery cohort fail to validate in a second dataset or via RT-qPCR.
| Symptom | Possible Cause | Solution |
|---|---|---|
| Biomarker is not significant in the validation cohort. | Overfitting in the initial discovery analysis or cohort-specific biases. | Use machine learning feature selection methods like SVM-RFE or LASSO regression in the discovery phase to identify robust biomarkers [52] [53]. Ensure validation cohorts are well-matched and of sufficient size. |
| RT-qPCR results do not match sequencing fold-change. | PCR primer inefficiency or sample degradation. | Design and validate high-efficiency primers. Use the same RNA aliquot for both sequencing and RT-qPCR to avoid sample quality discrepancies [53]. |
| Biomarker shows high variability. | Underlying biological heterogeneity in PCD. | Increase sample size. Stratify patients based on genetic mutation or clinical phenotype (e.g., with/without neonatal respiratory distress) to identify subgroup-specific biomarkers [51] [49]. |
Detailed Experimental Protocols
Protocol: Bulk RNA-Seq for PCD Biomarker Discovery from Blood
This protocol is adapted from methodologies used in recent studies on programmed cell death, which can be applied to PCD research [52] [54] [53].
1. Sample Collection and RNA Extraction:
- Collect peripheral blood mononuclear cells (PBMCs) from confirmed PCD patients and matched healthy controls. Informed consent and ethical approval are mandatory.
- Extract total RNA using a standardized method like TRIzol reagent. Quantify RNA concentration and purity using a spectrophotometer (e.g., NanoDrop). Assess RNA integrity with a Bioanalyzer; a RIN > 8.0 is recommended.
2. Library Preparation and Sequencing:
- Use 1 µg of total RNA for library preparation. Isolate mRNA using poly-A selection beads.
- Synthesize double-stranded cDNA using random hexamer primers and a SuperScript double-stranded cDNA synthesis kit.
- Perform end-repair, phosphorylation, and adapter ligation on the synthesized cDNA. Size-select for fragments of ~300 bp.
- Amplify the library with PCR for 15 cycles.
- Sequence the libraries on an Illumina platform (e.g., NovaSeq X Plus) to a depth of 25-60 million paired-end 150 bp reads to ensure adequate coverage [55].
3. Data Analysis:
- Quality Control: Use FASTQC for initial read quality assessment. Trim adapters and low-quality bases with tools like NGS QC Toolkit.
- Alignment: Map clean reads to the human reference genome (e.g., GRCh38) using HISAT2.
- Quantification: Assemble transcripts and calculate gene-level counts (e.g., TPM) using StringTie.
- Differential Expression: Identify Differentially Expressed Genes (DEGs) using R package
DESeq2orlimma, with thresholds of |log2FC| > 0.5 and adjusted p-value < 0.05 [53].
Protocol: Cross-Modal Validation of PCD Biomarkers
This protocol outlines steps to move from a genetic signature to a clinically usable biomarker [53].
1. Computational Validation with Public Data:
- Identify Candidate Genes: Perform differential expression analysis on your discovery RNA-Seq dataset (e.g., PCD vs. control) to obtain a list of candidate genes.
- Functional Enrichment: Conduct Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis using the
clusterProfilerR package to ensure genes are involved in relevant biological processes (e.g., ciliary assembly, axonemal structure). - Independent Cohort Validation: Test the expression signature of your candidate biomarkers in an independent, publicly available dataset (if available) to confirm generalizability.
2. Experimental Validation with RT-qPCR:
- Primer Design: Design and validate high-efficiency primers for your candidate genes and reference genes (e.g., GAPDH, ACTB).
- Reverse Transcription: Convert 1 µg of total RNA from a new set of PCD and control samples into cDNA.
- qPCR Reaction: Perform qPCR reactions in triplicate for each sample-primer pair. Use a standard 2-step amplification protocol.
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method. Perform statistical analysis (e.g., t-test) to confirm significant dysregulation of your biomarkers in the PCD cohort.
Key Signaling Pathways and Experimental Workflows
PCD Diagnostic Pathway for Patients Without Laterality Defects
This diagram outlines the integrated diagnostic workflow recommended for patients with suspected PCD but no situs inversus, emphasizing the need for multiple confirmatory tests [49] [50].
High-Throughput Biomarker Discovery & Validation Workflow
This diagram illustrates the multi-stage process from initial high-throughput sequencing to final biomarker validation, integrating computational and experimental biology techniques [52] [54] [53].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for PCD Biomarker Research
| Item | Function/Description | Example/Note |
|---|---|---|
| TRIzol Reagent | A ready-to-use monophasic solution for the isolation of high-quality total RNA from cells and tissues. Prevents RNA degradation during isolation [54] [53]. | Standard for RNA extraction prior to sequencing or RT-qPCR. |
| Poly-A Selection Beads | Magnetic beads that bind the poly-A tails of messenger RNA (mRNA) to enrich for coding transcripts during RNA-Seq library prep [55]. | Used to isolate mRNA from total RNA. Critical for mRNA-seq protocols. |
| SuperScript ds-cDNA Synthesis Kit | A set of reagents for the efficient synthesis of double-stranded cDNA from RNA templates, which is required for Illumina sequencing library construction [54]. | |
| Illumina NovaSeq X Plus | A high-throughput sequencing platform capable of generating massive amounts of data, suitable for whole transcriptome sequencing of large cohorts [54]. | Recommended sequencing depth: 25-60M PE reads for total RNA-seq [55]. |
| SYBR Green qPCR Master Mix | A ready-to-use mix containing all components (except primers and template) for quantitative real-time PCR, used for biomarker validation [53]. | Enables sensitive and specific detection of amplified DNA. |
| CIBERSORT/ssGSEA Software | Bioinformatic tools used to estimate the abundance of immune cell types in a mixed population from bulk RNA-Seq data [52] [54]. | Helps characterize the immune microenvironment in PCD samples. |
| STRING Database | A database of known and predicted protein-protein interactions (PPIs), used to build functional networks around candidate biomarker genes [53]. | Essential for understanding the functional context of discovered biomarkers. |
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Our model for identifying PCD without laterality defects shows good accuracy on historical data but performance drops significantly in current clinical use. What is the cause and solution?
A: This is a classic sign of model drift, where the relationship between the input data and the target variable changes over time. In clinical environments, this can be caused by changes in medical practices, technologies, or patient populations [56].
- Troubleshooting Steps:
- Implement a Temporal Validation Framework: Use a diagnostic framework to systematically evaluate model performance over time. Split your data by time (e.g., train on 2015-2019 data and validate on 2020-2022 data) to assess temporal consistency [56].
- Characterize Temporal Evolution: Analyze how patient outcomes (labels) and characteristics (features) have evolved. For instance, the introduction of new diagnostic codes or changes in PCD diagnostic criteria can create drift [56].
- Explore Data Quantity-Recency Trade-offs: Test if models trained on smaller, more recent datasets outperform those trained on larger, older datasets. Retrain your model using a "sliding window" of the most recent, relevant data [56].
- Preventive Strategy: Integrate continuous monitoring of model performance and data distributions into your deployment pipeline, with plans for periodic retraining.
Q2: We are struggling to get clinicians to refer patients for PCD evaluation, even when they meet multiple diagnostic criteria. How can we improve this workflow?
A: This is primarily a workflow and awareness challenge. Research shows that for patients with laterality defects who meet only two PCD criteria, referral rates to pulmonary specialists can be as low as 41% [1]. The presence of a competing diagnosis like Congenital Heart Disease (CHD) is often the reason for non-referral [1].
- Troubleshooting Steps:
- Conduct a Bottleneck-Focused Analysis: Map the clinician's decision-making process to identify the specific point where the referral stops. Is it a lack of knowledge, a cumbersome referral process, or diagnostic overshadowing? [57].
- Implement a Value-Added Analysis: Show clinicians that adding a PCD referral to their workflow, while taking extra time, provides high value by preventing long-term lung damage in patients [57].
- Simplify the Referral Pathway: Integrate automated prompts into the Electronic Medical Record (EMR) when a patient meets a minimum number of PCD evaluation criteria (e.g., two or more), such as chronic daily cough and neonatal respiratory distress [1].
- Preventive Strategy: Develop ongoing education for pediatricians and specialists on the PCD evaluation criteria, emphasizing the need for a high index of suspicion even when other explanatory diagnoses are present [1].
Q3: Our voice biomarker model for PCD detection performs well in the lab but fails to generalize across diverse patient demographics. How can we improve its robustness?
A: This is a common issue of data scarcity and lack of diversity in training data, leading to poor model generalizability [58].
- Troubleshooting Steps:
- Enhance Data Collection: Prioritize the creation of larger, high-quality, and diverse medical voice datasets that include variations in age, ethnicity, accent, and background noise [58].
- Employ Advanced Feature Engineering: Move beyond basic acoustic features (e.g., jitter, shimmer). Leverage proprietary, musicologically-informed AI (Musicology AI) that can capture more complex, clinically relevant patterns in voice data that are consistent across demographics [58].
- Strengthen Clinical Partnerships: Collaborate with multiple clinical centers to access a broader patient population and ensure your data reflects real-world variability [58].
- Preventive Strategy: From the project's inception, plan for multi-site data collection and use rigorous, scalable clinical validation methods that test the model across different subgroups [58].
Q4: The AI diagnostic tool we deployed is computationally expensive and cannot handle the growing patient load at our clinic. How can we improve its scalability?
A: This indicates a need for a formal AI Model Evaluation for Scalability [59].
- Troubleshooting Steps:
- Evaluate Key Scalability Metrics: Move beyond accuracy and measure latency (response time), throughput (number of processed samples per second), and resource utilization (CPU/GPU memory) under increasing load [59].
- Simulate Real-World Conditions: Use load-testing tools to simulate the model's performance with a higher volume of concurrent users or larger datasets than currently experienced [59].
- Optimize and Iterate: Identify computational bottlenecks. Consider using more efficient model architectures, optimizing code, or leveraging scalable cloud infrastructure and containerization tools like Kubernetes [59].
- Preventive Strategy: Select frameworks with built-in scalability features (e.g., TensorFlow Extended, Apache Spark) and adopt a continuous evaluation approach to monitor performance as usage grows [59].
Key Diagnostic Criteria and Referral Rates for PCD
The American Thoracic Society (ATS) criteria for PCD evaluation provide a foundation for identifying patients, including those without classic laterality defects. The following table summarizes referral patterns based on how many criteria a patient meets, highlighting the diagnostic gap.
Table 1: PCD Evaluation Criteria and Observed Referral Rates in Patients with Laterality Defects [1]
| Number of PCD Criteria Met | Example Criteria Combination | Referral Rate to Pulmonary Medicine | Rate of PCD Evaluation Completion |
|---|---|---|---|
| 2 Criteria | Laterality defect + chronic daily cough | 41% | 16% |
| 4 Criteria | Laterality defect + chronic daily cough + chronic nasal congestion + unexplained NRDS | 96% | 93% |
Abbreviations: NRDS, Neonatal Respiratory Distress Syndrome; PCD, Primary Ciliary Dyskinesia.
Experimental Protocols for Model Validation
Protocol 1: Temporal Validation Framework for Clinical ML Models
This protocol is designed to diagnose and address model drift, ensuring that diagnostic models remain accurate over time [56].
Methodology:
- Cohort Construction: Extract patient data from the EHR using a specific index date (e.g., date of first clinical suspicion of PCD). Define the feature set using data from a standardized period (e.g., 180 days) before the index date.
- Data Partitioning for Temporal Validation: Instead of random splitting, partition data by time.
- Training Set: Data from years 2010-2018.
- Internal Validation Set: A random 10% sample from the 2010-2018 period.
- Prospective Test Set: Data from years 2019-2022.
- Model Training and Evaluation: Train multiple models (e.g., LASSO, XGBoost) on the training set. Evaluate performance on both the internal and prospective test sets. A significant performance drop on the prospective set indicates temporal drift.
- Analysis of Drift:
- Label Shift: Analyze the temporal evolution of the target variable (e.g., proportion of patients diagnosed with PCD over the years).
- Feature Shift: Track the statistical properties of key input features over time.
- Quantity-Recency Trade-off: Experiment with training models on sliding windows of data (e.g., 2015-2018 vs. 2010-2018) to determine the optimal balance between data volume and relevance.
Protocol 2: Workflow Efficiency Analysis for Diagnostic Referrals
This protocol uses business process analysis to identify and fix inefficiencies in the patient referral pathway for PCD evaluation [57].
Methodology:
- Identify the Workflow: Define the scope as "the process from a patient presenting with symptoms to a referral for PCD evaluation being initiated."
- Map the Current Workflow:
- Create a detailed flowchart or swimlane diagram that visually tracks every step, decision point, and handoff between departments.
- Conduct time-based analysis by measuring the cycle time for each step and identifying stages with long wait times.
- Gather Data and Insights:
- Quantitative: Collect metrics like cycle time, referral rate (see Table 1), and error rate (e.g., referrals sent to the wrong department).
- Qualitative: Interview clinicians to understand their frustrations and the reasons for non-referral (e.g., "CHD explains all symptoms").
- Identify Areas for Improvement:
- Use bottleneck analysis to find the step that most slows down the entire process (e.g., getting attending physician approval).
- Use value-added analysis to tag steps as "value-added" (e.g., patient examination) or "non-value-added" (e.g., duplicate data entry).
- Propose and Implement Improvements:
Visualization of Workflows and System Architecture
Diagnostic Model Implementation Workflow
Health xAI Implementation Framework Architecture
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Tools and Frameworks for Implementing Scalable Diagnostic Models
| Item Name | Specification / Version | Primary Function in Research |
|---|---|---|
| Electronic Health Record (EMR) Data | Epic, Cerner, etc. | Provides real-world, longitudinal patient data for model training and validation. Essential for defining cohorts (e.g., patients with chronic cough) and extracting clinical features [1] [56]. |
| Temporal Validation Framework | Model-agnostic diagnostic framework [56] | A systematic method to evaluate ML model performance over time, diagnose model drift, and determine the optimal trade-off between data quantity and recency. |
| Health xAI Implementation Framework | Integrated Bandit Learning & Privacy [60] | A comprehensive framework for deploying multiple AI models in healthcare. It combines privacy preservation, model selection via reinforcement learning, and explainable AI for clinical interpretability [60]. |
| Workflow Analysis Tools | Process Mapping, Bottleneck Analysis [57] | A set of methodologies (e.g., time-based, bottleneck-focused analysis) to identify and eliminate inefficiencies in clinical and diagnostic pathways. |
| Voice Biomarker Analysis Platform | Musicology AI, openSMILE [58] | Software for extracting and analyzing acoustic features (jitter, shimmer, MFCC) or more complex, musicologically-informed patterns from voice recordings to develop non-invasive diagnostic biomarkers. |
| Scalable ML Infrastructure | TensorFlow Extended (TFX), Kubernetes, Apache Spark [59] | Software platforms and tools that enable the deployment, management, and scaling of AI models in production environments, ensuring they can handle large datasets and user loads. |
► FAQ: Navigating PCD Diagnosis Without Laterality Defects
What is the primary diagnostic challenge in PCD patients with normal organ arrangement (situs solitus)?
The main challenge is the significantly lower sensitivity of common screening tools. The PICADAR clinical scoring tool, for instance, has a sensitivity of only 61% in patients with situs solitus, compared to 95% in those with laterality defects [61]. Furthermore, the clinical presentation can be more subtle, lacking the clear red flag of situs inversus, which often leads to these cases being overlooked or diagnosed late [61] [62].
Which diagnostic tests are recommended by international consortia, and what are their key limitations?
International guidelines from the European Respiratory Society (ERS) and American Thoracic Society (ATS) strongly recommend a multi-test approach, as no single test is sufficient to confirm or exclude PCD [48] [63]. The following table summarizes the recommended tests and their critical limitations.
| Diagnostic Test | Recommendation Strength & Certainty | Key Limitations & Requirements |
|---|---|---|
| Nasal Nitric Oxide (nNO) | Strong (Moderate certainty for velum closure) [48] | Not a standalone test. Normal result does not exclude PCD. Lower accuracy in tidal breathing (often used in young children) [48] [63]. |
| Immunofluorescence (IF) | Strong (High certainty) [48] | Not a standalone test. Accuracy depends on antibody panel quality and laboratory expertise. Batch-to-batch antibody variability is common [48] [63]. |
| High-Speed Video Microscopy (HSVM) | Strong (Very low certainty) [48] | Not a standalone test. Should be performed post-culture. Requires a high sample throughput to maintain expertise; best done in specialist centres [48] [63]. |
| Genetic Testing | Encouraged as a reference test [48] | - |
| Transmission Electron Microscopy (TEM) | A reference test [48] | Cannot detect all forms of PCD (e.g., those with normal ultrastructure) [61]. |
How can we improve the detection of PCD cases with normal ciliary ultrastructure?
Cases with normal ultrastructure (e.g., associated with pathogenic variants in genes like DNAH11 or HYDIN) are a key diagnostic pitfall. A combination of the following methods is crucial:
- HSVM is particularly valuable here, as it can directly visualize ciliary dyskinesia even when ultrastructure appears normal [63].
- Immunofluorescence can show absent localisation of specific proteins (e.g., SPEF2 in HYDIN-related PCD), providing critical evidence for a diagnosis, especially when genetic results are uncertain [63].
- Genetic Testing is essential. Pursuing a genetic diagnosis is strongly encouraged for its implications on management and eligibility for future therapies [63] [50].
What are the essential clinical symptoms that should trigger a PCD diagnostic workup?
Key clinical features, especially in children, include [62]:
- Neonatal respiratory distress in a full-term infant requiring supplemental oxygen or ventilation for ≥24 hours.
- Year-round, daily wet cough that begins in the first 6 months of life.
- Year-round, daily nasal congestion that begins in the first 6 months of life.
- Any organ laterality defect (situs inversus totalis or situs ambiguus). The presence of any two of the first three symptoms, or any one symptom combined with a laterality defect, should prompt referral for diagnostic testing [62].
► The Scientist's Toolkit: Research Reagent Solutions for PCD Diagnostics
The following table details key materials and technologies used in advanced PCD diagnostic workflows.
| Research Reagent / Technology | Function in PCD Diagnostics |
|---|---|
| Antibody Panels for Immunofluorescence | Used to detect the absence or mislocalisation of specific ciliary proteins (e.g., dynein arms, radial spokes). A broad panel (≥10 antibodies) is recommended for higher accuracy [48]. |
| Cell Culture Media for Ciliogenesis | Supports the regrowth of cilia on biopsied epithelial cells after dedifferentiation in culture. This is a critical step for post-culture HSVM and TEM, improving diagnostic specificity [48]. |
| Next-Generation Sequencing (NGS) Panels | Target enrichment for known PCD-associated genes. Whole-exome or whole-genome sequencing is used to discover novel disease-causing variants [64] [65]. |
| Machine Learning Algorithms | Analyze complex datasets (e.g., health claims data, clinical features) to identify patients with a high probability of PCD for targeted screening, helping to reduce diagnostic delays [31]. |
► Experimental Protocol: Integrated Diagnostic Pathway for PCD
Workflow Diagram
The following diagram illustrates the multi-test diagnostic pathway for PCD, emphasizing the process for challenging cases without laterality defects.
Detailed Methodology
Patient Identification & Clinical Assessment:
- Purpose: To identify patients with a high pre-test probability of PCD.
- Procedure: Systematically assess for key clinical features: neonatal respiratory distress in term infants, year-round wet cough/nasal congestion starting before 6 months of age, and laterality defects [62]. Use of the PICADAR tool should be done with caution, recognizing its low sensitivity (61%) in situs solitus patients [61].
Initial Screening with Nasal Nitric Oxide (nNO):
- Purpose: A non-invasive, high-sensitivity screening test.
- Procedure: Measure nNO production rate following ATS/ERS technical standards [48]. Velum closure techniques are preferred for accuracy. Tidal breathing is an alternative for young children (2-5 years) but has greater variability.
- Troubleshooting: A normal nNO level does not rule out PCD. If clinical suspicion remains high, proceed with further testing [48] [63].
Reference and Specialist Tests:
- Purpose: To provide functional and structural evidence of ciliary dysfunction.
- Procedure:
- Nasal Brush Biopsy: Obtain ciliated epithelial cells from the inferior nasal turbinate.
- High-Speed Video Microscopy (HSVM): Analyze ciliary beat pattern and frequency. Perform analysis post-cell culture to correct for secondary dyskinesia, whenever possible [48].
- Transmission Electron Microscopy (TEM): Examine ciliary ultrastructure for hallmark defects (e.g., absent outer/inner dynein arms).
- Immunofluorescence (IF): Use a panel of validated antibodies to assess protein localization within the ciliary axoneme [48].
- Troubleshooting: These tests require specialist centers with high throughput to maintain expertise. Inconclusive results from one test should be supplemented with others [48] [63].
Genetic Testing & Advanced Analysis:
- Purpose: To identify bi-allelic (or hemizygous/mono-allelic) pathogenic variants in one of the over 50 known PCD-associated genes, providing a definitive diagnosis.
- Procedure: Use next-generation sequencing (NGS), such as targeted PCD gene panels or whole-exome sequencing [64]. Variants should be interpreted according to ACMG/AMP guidelines [61].
- Troubleshooting: In cases of variants of uncertain significance (VUS), results from IF or HSVM can provide functional evidence to support pathogenicity [48] [63]. A negative genetic test does not exclude PCD, as not all causative genes are known.
► Quantitative Data: Performance of Diagnostic Tools
Sensitivity of the PICADAR Tool in Genetically Confirmed PCD (n=269)
This table summarizes the performance of the PICADAR clinical score, highlighting its limitations in key subgroups [61].
| Patient Subgroup | Median PICADAR Score (IQR) | Sensitivity |
|---|---|---|
| Overall Cohort | 7 (5 – 9) | 75% (202/269) |
| With Laterality Defects | 10 (8 – 11) | 95% |
| With Situs Solitus (normal arrangement) | 6 (4 – 8) | 61% |
| With Hallmark Ultrastructural Defects | Information not available in source | 83% |
| Without Hallmark Ultrastructural Defects | Information not available in source | 59% |
Conclusion
Enhancing the detection of Primary Ciliary Dyskinesia in patients without laterality defects is an achievable and critical goal for improving patient outcomes and advancing research. A multi-pronged strategy is essential, combining heightened clinical awareness of key neonatal and chronic symptoms with the systematic application of available diagnostic tools. The journey forward requires a concerted effort to dismantle referral barriers, optimize and validate integrated diagnostic algorithms, and embrace emerging genetic and biomarker technologies. For researchers and drug developers, success in this area is paramount. Improving diagnostic accuracy directly fuels the ability to identify and enroll well-characterized patient cohorts into clinical trials, which is the foundation for developing the first disease-modifying therapies for PCD. Future efforts must focus on the translation of these advanced diagnostic frameworks into global, accessible standards of care, ultimately ensuring that no PCD patient, regardless of their situs status, remains undiagnosed.
References
- 1. Referral Rates and Diagnostic Evaluation for Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12139576/]
- 2. Situs Inversus Totalis: A Clinical Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8901252/]
- 3. Situs inversus [https://en.wikipedia.org/wiki/Situs_inversus]
- 4. Situs Inversus: Causes & Outlook [https://my.clevelandclinic.org/health/diseases/23486-situs-inversus]
- 5. Primary ciliary dyskinesia: A review [https://www.sciencedirect.com/science/article/pii/S2950008725000420]
- 6. Situs Inversus Imaging: Practice Essentials, Radiography, ... [https://emedicine.medscape.com/article/413679-overview]
- 7. Respiratory Distress in the Newborn with Primary Ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7922088/]
- 8. Investigating laterality defects in primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC9186022/]
- 9. as a Comorbidity in Primary Ciliary Dyskinesia... | IntechOpen Asthma [https://www.intechopen.com/online-first/1223303]
- 10. Genomic and phenotypic characterization of respiratory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12587554/]
- 11. Biologics and Biomarkers in 2025: Evolving Strategies for ... [https://www.hcplive.com/view/biologics-and-biomarkers-in-2025-evolving-strategies-for-asthma-and-copd]
- 12. in Asthma : Definitions and Implications of This... Cystic Fibrosis [https://pubmed.ncbi.nlm.nih.gov/33560464/]
- 13. Cystic fibrosis and primary ciliary dyskinesia [https://www.sciencedirect.com/science/article/pii/S0954611123000574]
- 14. Symptom Phenotyping in People with Cystic Fibrosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11624099/]
- 15. Symptom phenotyping in people with cystic fibrosis during ... [https://www.sciencedirect.com/science/article/abs/pii/S1569199324000778]
- 16. Challenges in postoperative management of a patient with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550884/]
- 17. Primary ciliary dyskinesia: improving the diagnostic approach [https://pmc.ncbi.nlm.nih.gov/articles/PMC3665363/]
- 18. Nasal nitric oxide screening for primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/25323224/]
- 19. Impact of Seasonal Variability in Nasal Nitric Oxide ... [https://pubmed.ncbi.nlm.nih.gov/41022559/]
- 20. Nasal nitric oxide measurement for the diagnosis of ... [https://pubmed.ncbi.nlm.nih.gov/40529313/]
- 21. Nitric oxide detection methods in vitro and in vivo - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7802420/]
- 22. Systematic gaps in reporting variants of uncertain ... [https://www.sciencedirect.com/science/article/pii/S1098360025001480]
- 23. The Frequency and Reclassification of Variants Uncertain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577467/]
- 24. SNP Genotyping Support—Troubleshooting [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/real-time-digital-PCR-applications-support-center/snp-genotyping-support/snp-genotyping-support-troubleshooting.html]
- 25. Frequently Asked Questions (FAQ) for the NIH Genetic Testing ... [https://www.ncbi.nlm.nih.gov/gtr/docs/faq]
- 26. CHEST Pulmonary Reviews Primary Ciliary Dyskinesia [https://www.sciencedirect.com/science/article/pii/S2949789223000041]
- 27. Practical guide for the diagnosis and management of ... [https://www.sciencedirect.com/science/article/pii/S0385814624000166]
- 28. International consensus guideline for reporting ... [https://pubmed.ncbi.nlm.nih.gov/32060067/]
- 29. Critical importance of the correction of contrast transfer ... [https://jast-journal.springeropen.com/articles/10.1186/2093-3371-4-14]
- 30. High-contrast en bloc staining of mouse whole-brain and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10250191/]
- 31. Feasibility of machine learning analysis for the identification of ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-03966-z]
- 32. Laterality Defects Other Than Situs Inversus Totalis in Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4219335/]
- 33. The BEAT-PCD (Better Experimental Approaches to Treat ... [https://publications.ersnet.org/content/erj/57/2/2004601]
- 34. Assessing the Barriers and Facilitators to Pulmonary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11141829/]
- 35. Exploring the barriers to pulmonary rehabilitation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8369747/]
- 36. Nasal nitric oxide for early diagnosis of primary ciliary ... [https://pubmed.ncbi.nlm.nih.gov/18187313/]
- 37. Laterality Defects Other Than Situs Inversus Totalis in ... [https://www.sciencedirect.com/science/article/abs/pii/S0012369215523854]
- 38. The Challenges of Diagnosing Primary Ciliary Dyskinesia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3209576/]
- 39. Pitfalls and challenges in genetic test interpretation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8489659/]
- 40. Standards and guidelines for the interpretation of ... [https://www.nature.com/articles/gim201530]
- 41. Spectrum of Genetic Variants in a Cohort of 37 Laterality ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.861236/full]
- 42. A Guide to Understanding & Overcoming TEM Imaging ... [https://www.nanoimagingservices.com/about/blog/a-guide-to-understanding-overcoming-tem-imaging-challenges]
- 43. A Universal Approach to Analyzing Transmission Electron ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8465115/]
- 44. Exploring the TEM β-Lactamase in E. coli From Urinary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12519961/]
- 45. START Adult Triage Algorithm: Text Version [https://remm.hhs.gov/startalgotext.htm]
- 46. Triage Color System [https://www.process.st/templates/triage-color-system/]
- 47. The Utility of Nasal Nitric Oxide in the Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11058016/]
- 48. Diagnosis of Primary Ciliary Dyskinesia [https://www.guidelinecentral.com/guideline/7172/]
- 49. Diagnosis of primary ciliary dyskinesia: potential options for ... [https://publications.ersnet.org/content/errev/26/143/160058]
- 50. European Respiratory Society and American Thoracic ... [https://pubmed.ncbi.nlm.nih.gov/41005984/]
- 51. Primary Ciliary Dyskinesia. Recent Advances in Diagnostics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3826280/]
- 52. insights from PCD gene expression and machine learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003219/]
- 53. Identification and experimental validation of biomarkers ... [https://www.nature.com/articles/s41598-025-17606-w]
- 54. Comprehensive analysis of the role of diverse programmed ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1685533/full]
- 55. Experimental Design: Best Practices - Bioinformatics [https://bioinformatics.ccr.cancer.gov/ccbr/project-support/experimental-design-best-practices/]
- 56. Diagnostic framework to validate clinical machine learning ... [https://www.nature.com/articles/s43856-025-00965-w]
- 57. Workflow Efficiency Analysis: A Practical Guide [https://www.getclockwise.com/blog/workflow-efficiency-analysis-steps-tools-business-processes]
- 58. Bridging AI innovation and healthcare: scalable clinical ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1575753/full]
- 59. AI Model Evaluation For Scalability [https://www.meegle.com/en_us/topics/ai-model-evaluation/ai-model-evaluation-for-scalability]
- 60. Implementation framework for AI deployment at scale in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083986/]
- 61. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1.full-text]
- 62. Primary ciliary dyskinesia - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12316531/]
- 63. ERS and ATS unite for universal PCD diagnosis guideline [https://thelimbic.com/respiratory/ers-and-ats-unite-for-universal-pcd-diagnosis-guideline/]
- 64. Genotypic and Phenotypic Characterization of Axonal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12385308/]
- 65. Advancing Discoveries in Charcot-Marie-Tooth Disease [https://inc.rarediseasesnetwork.org/news/consortium-spotlight-advancing-discoveries-charcot-marie-tooth-disease]