Beyond the Baseline: Strategies to Enhance PICADAR Sensitivity for Improved PCD Diagnosis
The Primary Ciliary Dyskinesia Rule (PICADAR) is a recommended predictive tool for estimating the likelihood of Primary Ciliary Dyskinesia (PCD), but recent evidence reveals critical limitations in its sensitivity, particularly...
Beyond the Baseline: Strategies to Enhance PICADAR Sensitivity for Improved PCD Diagnosis
Abstract
The Primary Ciliary Dyskinesia Rule (PICADAR) is a recommended predictive tool for estimating the likelihood of Primary Ciliary Dyskinesia (PCD), but recent evidence reveals critical limitations in its sensitivity, particularly in patients without laterality defects or hallmark ultrastructural ciliary defects. This article provides a comprehensive analysis for researchers and drug development professionals on the current performance landscape of PICADAR, explores methodological refinements and complementary tools like nasal nitric oxide (nNO), investigates strategies for optimizing its application in challenging patient subgroups, and validates its utility against other predictive instruments. By synthesizing foundational knowledge with emerging data, this review aims to guide the development of more robust, inclusive, and sensitive diagnostic pathways for this rare genetic disorder.
Deconstructing PICADAR: Current Performance and Established Limitations in PCD Prediction
What is the PICADAR score and what is its primary purpose?
The Primary Ciliary Dyskinesia Rule (PICADAR) is a clinical diagnostic prediction tool designed to identify patients who require specialized testing for Primary Ciliary Dyskinesia (PCD) [1]. PCD is a rare, genetically heterogeneous motile ciliopathy characterized by symptoms like neonatal respiratory distress, chronic wet cough, recurrent respiratory infections, and laterality defects [2]. As definitive PCD diagnostic tests are highly specialized and require experienced scientists, PICADAR serves as an initial, practical screening tool using readily obtainable patient history information to assess the likelihood of a PCD diagnosis before proceeding with complex confirmatory tests [1].
What are the core components and scoring system of the original PICADAR tool?
The original PICADAR tool, developed through a study of 641 consecutive referrals, applies to patients with a persistent wet cough and consists of seven predictive clinical parameters [1]. The tool assigns points for each feature present, and the total score indicates the probability of PCD. The table below details the core components and their assigned points.
| Predictive Parameter | Points Assigned |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms (at term) | 2 |
| Admission to a neonatal intensive care unit | 2 |
| Chronic rhinitis | 1 |
| Ear symptoms (chronic otitis media/effusions) | 1 |
| Situs inversus | 4 |
| Congenital cardiac defect | 2 |
Table: The seven predictive parameters of the PICADAR score and their point values [1].
How is the PICADAR score interpreted in clinical practice?
The total PICADAR score is calculated by summing the points for all parameters present in a patient. The score interpretation, based on the original validation study, is as follows:
| Total PICADAR Score | Interpretation / Probability of PCD |
|---|---|
| ≥ 5 points | High likelihood of PCD; recommends referral for diagnostic testing [1]. |
| < 5 points | Lower likelihood of PCD [1]. |
In the original study, a cut-off score of 5 points demonstrated a sensitivity of 0.90 and a specificity of 0.75 for predicting PCD. The area under the curve (AUC) for the internally and externally validated tool was 0.91 and 0.87, respectively [1].
What are the common challenges and limitations of using the PICADAR score?
Recent research has highlighted specific limitations of the PICADAR tool that users should be aware of during implementation.
- Initial Screening Question: The tool's initial question screens out patients without a daily wet cough. A 2025 study found that 7% (18/269) of genetically confirmed PCD individuals reported no daily wet cough and would have been ruled out from further testing by PICADAR [3] [4].
- Variable Sensitivity: The overall sensitivity of PICADAR was recently reported at 75% (202/269) [3] [4]. Its performance varies significantly across patient subgroups, as shown in the table below.
| Patient Subgroup | Reported Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| All Genetically Confirmed PCD (n=269) | 75% (202/269) | 7 (5 – 9) [3] [4] |
| Individuals with laterality defects | 95% | 10 (8 – 11) [3] [4] |
| Individuals with situs solitus (normal arrangement) | 61% | 6 (4 – 8) [3] [4] |
| Individuals with hallmark ultrastructural defects | 83% | Not Reported |
| Individuals without hallmark ultrastructural defects | 59% | Not Reported |
Table: Sensitivity of the PICADAR tool in different patient subgroups based on a 2025 study [3] [4].
These findings indicate that PICADAR has limited sensitivity, particularly in individuals without laterality defects (61%) or those without hallmark ultrastructural defects (59%) [3] [4]. Therefore, it should not be used as the sole factor to initiate a diagnostic work-up for PCD.
What is the recommended workflow for applying the PICADAR score in a diagnostic pathway?
The following diagram illustrates the logical workflow for applying the PICADAR score in a clinical setting, incorporating its limitations.
Diagram: Clinical Workflow for PICADAR Application
What are the essential research reagents and materials for PCD diagnostic testing?
For researchers conducting formal PCD diagnostics after a positive PICADAR screen, the following table lists key reagents and solutions used in the field.
| Research Reagent / Material | Function / Application in PCD Diagnostics |
|---|---|
| Nasal Nitric Oxide (nNO) Measurement Equipment | Measures nasal nitric oxide levels, which are typically very low in PCD patients; serves as a key screening test [2]. |
| High-Speed Videomicroscopy Analysis (HSVMA) System | Captures and analyzes ciliary beat frequency and pattern, a critical functional test for ciliary motility [2]. |
| Transmission Electron Microscopy (TEM) | Used for axonemal ultrastructure analysis to identify defects in dynein arms, nexin links, or microtubule organization [2]. |
| Immunofluorescent (IF) Staining Antibodies | Antibodies targeting specific ciliary proteins (e.g., DNAH5, GAS8) help identify the absence or mislocalization of proteins indicative of genetic defects [2]. |
| Genetic Testing Kits/Panels | Next-generation sequencing panels or whole-exome sequencing to identify pathogenic variants in over 50 known PCD-causing genes [2]. |
Table: Key Research Reagents and Materials for PCD Diagnostic Confirmation
FAQs: Understanding Sensitivity and Specificity in Diagnostic Research
Q1: What is the fundamental difference between sensitivity and specificity?
- Sensitivity (True Positive Rate) is the ability of a test to correctly identify individuals who have the disease. It is calculated as the number of true positives divided by the total number of individuals with the disease (true positives + false negatives) [5] [6]. A high-sensitivity test is excellent for "ruling out" a disease when the result is negative.
- Specificity (True Negative Rate) is the ability of a test to correctly identify individuals who do not have the disease. It is calculated as the number of true negatives divided by the total number of individuals without the disease (true negatives + false positives) [5] [6]. A high-specificity test is excellent for "ruling in" a disease when the result is positive.
Q2: Why is there often a trade-off between sensitivity and specificity?
Sensitivity and specificity are often inversely related [6] [7]. Adjusting the threshold for a positive test result to increase sensitivity (e.g., making it easier to test positive) will typically decrease specificity by increasing false positives. Conversely, raising the threshold to improve specificity will usually decrease sensitivity by increasing false negatives [5] [8]. This trade-off necessitates selecting a threshold that balances both metrics appropriately for the clinical or research context.
Q3: How can a predictive tool like PICADAR be used before advanced diagnostic testing?
The PICADAR tool is a clinical prediction rule that uses seven simple, clinically available parameters to estimate the probability of a patient having Primary Ciliary Dyskinesia (PCD) [1] [9]. It serves as a screening step to identify patients with a high pre-test probability who should be referred for complex, expensive confirmatory tests (like transmission electron microscopy or genetic testing). By using a tool with known sensitivity (0.90) and specificity (0.75), researchers and clinicians can streamline patient recruitment for studies and optimize resource use in specialized PCD centers [1].
Q4: What is the clinical significance of the Positive and Negative Predictive Values (PPV & NPV)?
While sensitivity and specificity are characteristics of the test itself, Predictive Values are highly dependent on disease prevalence in the population [6].
- Positive Predictive Value (PPV) is the probability that a subject with a positive test truly has the disease [10].
- Negative Predictive Value (NPV) is the probability that a subject with a negative test truly does not have the disease [10]. In a population where a disease is rare, even a test with high specificity can yield a low PPV, meaning many positive results will be false positives.
Troubleshooting Guides for Diagnostic Assay Development
Issue: Low Specificity (High False Positive Rate)
Potential Causes and Solutions:
- Cause 1: Non-specific binding or cross-reactivity in assay reagents.
- Solution: Optimize reagent concentrations and include blocking steps. Use more specific antibodies or probes.
- Cause 2: Contaminated samples or reagents.
- Solution: Implement strict sterile techniques and use fresh, quality-controlled reagents.
- Cause 3: Inadequate washing steps during the assay procedure.
- Solution: Increase the number or volume of washes and optimize wash buffer composition.
Issue: Low Sensitivity (High False Negative Rate)
Potential Causes and Solutions:
- Cause 1: Signal is below the detection limit of the instrument.
- Solution: Incorporate signal amplification methods or use a more sensitive detection system.
- Cause 2: Suboptimal sample collection or storage, leading to analyte degradation.
- Solution: Standardize sample handling protocols and ensure proper storage conditions.
- Cause 3: Inefficient capture or detection of the target analyte.
- Solution: Titrate and optimize all capture and detection reagents.
Issue: High Inter-Assay Variability
Potential Causes and Solutions:
- Cause 1: Inconsistent reagent preparation or lot-to-lot variability.
- Solution: Prepare large master batches of reagents, aliquot, and perform rigorous quality control on new lots.
- Cause 2: Environmental fluctuations (e.g., temperature, humidity).
- Solution: Perform assays in a controlled environment and standardize incubation times.
- Cause 3: Operator-to-operator differences in technique.
- Solution: Develop a detailed, step-by-step Standard Operating Procedure (SOP) and provide comprehensive training.
Experimental Protocols for Key Diagnostic Studies
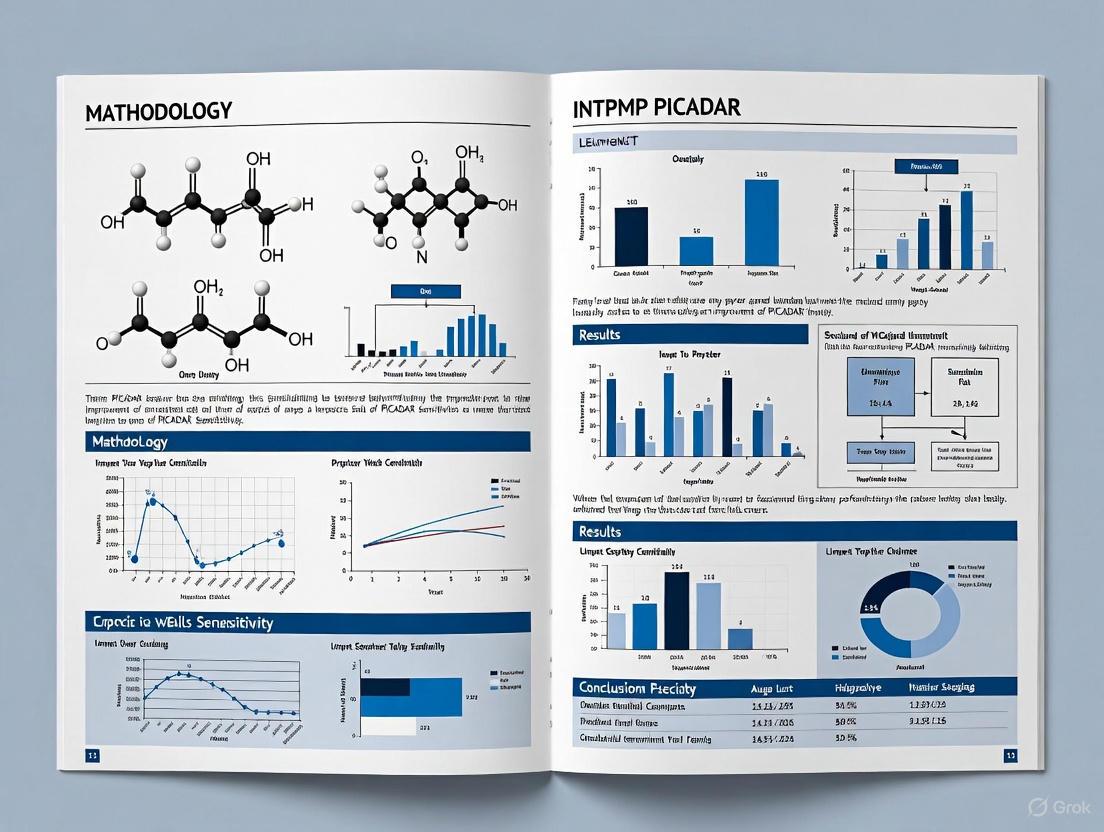
Protocol: Validating a Diagnostic Prediction Tool (Based on PICADAR Methodology)
Objective: To develop and validate a clinical prediction tool for identifying high-risk patients.
Methodology Summary from Foundational Study [9]:
- Study Population: Recruit consecutive patients referred for definitive diagnostic testing for the target condition (e.g., PCD).
- Data Collection: Collect information readily available from patient history prior to specialized testing using a standardized proforma.
- Diagnostic Outcome: Establish a definitive positive or negative diagnosis based on a pre-defined reference standard (e.g., a combination of hallmark ultrastructural defects and ciliary beat pattern analysis).
- Model Development:
- Compare characteristics of positive and negative referrals using appropriate statistical tests (t-test, Chi-squared).
- Use logistic regression analysis to identify significant predictors from the patient history data.
- Simplify the model by rounding regression coefficients to the nearest integer to create a practical scoring tool.
- Model Performance:
- Test the model's discrimination by plotting a Receiver Operating Characteristic (ROC) curve and calculating the Area Under the Curve (AUC).
- Determine the sensitivity and specificity at different score cut-offs.
- Assess calibration using the Hosmer-Lemeshow test.
- External Validation: Validate the scoring tool's performance in a separate, independent patient cohort from a different center.
Protocol: Conducting a Diagnostic Meta-Analysis
Objective: To systematically synthesize accuracy data (sensitivity, specificity) from multiple diagnostic studies.
Key Steps [11]:
- Literature Search: Perform a comprehensive search across multiple electronic databases with a pre-defined strategy.
- Study Selection: Apply inclusion and exclusion criteria to select relevant studies, typically involving a review of titles/abstracts followed by full-text assessment.
- Data Extraction: Extract data into standardized tables, including study baseline characteristics, true positives, false positives, false negatives, and true negatives.
- Quality Assessment: Evaluate the methodological quality of the included studies using tools like QUADAS-2.
- Statistical Synthesis and Meta-analysis:
- Pool estimates of sensitivity, specificity, positive likelihood ratio (LR+), and negative likelihood ratio (LR-).
- Create a hierarchical summary ROC (HSROC) curve to summarize the overall test performance and explore heterogeneity.
- Perform sub-group analyses to investigate sources of heterogeneity (e.g., by study quality, population characteristics).
- Assessment of Publication Bias: Use statistical or graphical methods (e.g., Deeks' funnel plot) to assess the potential for publication bias.
Data Presentation: Performance Metrics from Foundational Studies
| Parameter | Score Value | Performance Metric | Value (Derivation Cohort) | Value (Validation Cohort) |
|---|---|---|---|---|
| Full-term Gestation | 2 points | Sensitivity | 0.90 | - |
| Neonatal Chest Symptoms | 2 points | Specificity | 0.75 | - |
| Neonatal ICU Admission | 1 point | AUC | 0.91 | 0.87 |
| Chronic Rhinitis | 1 point | Cut-off Score | 5 points | - |
| Ear Symptoms | 1 point | Study Population | 641 patients | 187 patients |
| Situs Inversus | 2 points | PCD Prevalence | 12% | ~50% (selected) |
| Congenital Cardiac Defect | 2 points |
PICADAR: PrImary CiliARy DyskinesiA Rule; AUC: Area Under the ROC Curve
| Result | Has Disease | No Disease | Total | Metric | Calculation | Result |
|---|---|---|---|---|---|---|
| Positive | 369 (True Pos) | 58 (False Pos) | 427 | Sensitivity | 369 / (369 + 15) | 96.1% |
| Negative | 15 (False Neg) | 558 (True Neg) | 573 | Specificity | 558 / (558 + 58) | 90.6% |
| Total | 384 | 616 | 1000 | PPV | 369 / (369 + 58) | 86.4% |
| NPV | 558 / (558 + 15) | 97.4% |
Visualization of Workflows and Relationships
Diagnostic Prediction Tool Development Workflow
Sensitivity vs. Specificity Trade-off Relationship
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Diagnostic Test Evaluation
| Item / Reagent | Function in Research | Example from Foundational Studies |
|---|---|---|
| Standardized Clinical Proforma | Ensures uniform and systematic collection of patient history and clinical variables across all study participants. | Used in PICADAR study to collect data on neonatal symptoms, situs status, and chronic symptoms [9]. |
| Logistic Regression Model | A statistical method to identify which clinical variables are significant independent predictors of the disease outcome. | Used to develop the PICADAR score by weighting each of the 7 clinical parameters [1] [9]. |
| ROC Curve Analysis | A graphical plot that illustrates the diagnostic ability of a test by plotting sensitivity vs. (1-specificity) across all possible thresholds. | Used to evaluate PICADAR's discrimination (AUC=0.91) and select the optimal cut-off score of 5 points [1] [9]. |
| Reference Standard Test | The best available method for definitively confirming or excluding the disease, against which the new tool is validated. | For PCD, a combination of transmission electron microscopy (TEM) and high-speed video microscopy analysis (HSVMA) was used [9]. |
| External Validation Cohort | An independent set of data from a different location or time, used to test whether the tool performs well in a new population. | PICADAR was validated in a separate sample from the Royal Brompton Hospital, showing an AUC of 0.87 [9]. |
FAQs: Understanding PICADAR's Performance Gaps
What is the PICADAR score and what is its intended use? The PICADAR (PrImary CiliARy DyskinesiA Rule) score is a diagnostic prediction tool designed to help clinicians identify patients with a high probability of Primary Ciliary Dyskinesia (PCD) who should be referred for specialized diagnostic testing [9]. It utilizes seven readily available clinical parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care unit admission, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defect [9] [1]. In its initial validation, it demonstrated a sensitivity of 0.90 and a specificity of 0.75 at a recommended cut-off score of 5 points [9].
In which patient subgroups has PICADAR demonstrated notably low sensitivity? Recent evidence has identified two main subgroups where PICADAR's sensitivity is substantially reduced:
- Patients with situs solitus: PICADAR's sensitivity is significantly lower in PCD patients with situs solitus (the normal arrangement of thoracic and abdominal organs) compared to those with laterality defects like situs inversus [4] [3].
- Patients without hallmark ultrastructural defects: The tool also shows limited sensitivity in PCD patients who lack the hallmark defects in ciliary ultrastructure when examined by transmission electron microscopy (TEM) [4] [3].
What is the quantitative evidence for this performance gap? A 2025 study by Schramm et al. evaluated PICADAR in 269 individuals with genetically confirmed PCD. The findings on sensitivity are summarized in the table below [4] [3]:
| Subpopulation | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| Overall Cohort | 75% (202/269) | 7 (5 - 9) |
| With Laterality Defects | 95% | 10 (8 - 11) |
| With Situs Solitus | 61% | 6 (4 - 8) |
| With Hallmark Ultrastructural Defects | 83% | - |
| Without Hallmark Ultrastructural Defects | 59% | - |
Why does "situs solitus" create a sensitivity gap in PICADAR? The PICADAR scoring algorithm assigns points for the presence of situs inversus and congenital cardiac defects (often associated with heterotaxy) [9]. Patients with situs solitus, by definition, do not have situs inversus and are less likely to have major congenital heart defects [12] [13]. Therefore, they cannot accumulate these specific points, automatically lowering their total PICADAR score and reducing the probability of reaching the diagnostic threshold of 5 points [4]. This is a critical limitation, as studies show a significant portion of PCD patients, particularly in some populations like Japan, present with situs solitus [14].
Troubleshooting Guides & Experimental Protocols
Guide 1: Protocol for Validating Predictive Tool Performance in Subgroups
Objective: To critically evaluate the performance of a PCD predictive tool (e.g., PICADAR) across different patient subpopulations, specifically those with situs solitus and normal ciliary ultrastructure.
Materials and Reagents:
- Patient Cohort: A well-characterized cohort of patients with a confirmed or excluded PCD diagnosis.
- Clinical Data: A complete dataset for calculating the PICADAR score and other clinical variables.
- Genetic Confirmation: Results from genetic testing (e.g., next-generation sequencing panels for known PCD genes) to serve as a robust reference standard [4].
- Ultrastructural Data: Results from transmission electron microscopy (TEM) analysis of ciliary sections [4].
- Laterality Assessment: Imaging data (e.g., chest/abdominal radiograph, abdominal ultrasonography, CT scan) to definitively establish situs (solitus, inversus, or ambiguus) [13].
Methodology:
- Cohort Categorization: Divide the confirmed PCD-positive cohort into subgroups based on:
- Laterality: Situs solitus vs. situs inversus/heterotaxy.
- Ultrastructure: Presence or absence of hallmark TEM defects.
- Score Calculation: Calculate the PICADAR score for every patient in the cohort based on their clinical history [9].
- Sensitivity Analysis: For the entire cohort and for each pre-defined subgroup, calculate the sensitivity of the PICADAR tool. Sensitivity is defined as the number of genetically confirmed PCD patients with a PICADAR score ≥5, divided by the total number of genetically confirmed PCD patients in that group [4].
- Statistical Comparison: Compare the sensitivity and median PICADAR scores between subgroups (e.g., situs solitus vs. situs inversus) using appropriate statistical tests like the Mann-Whitney U test [4].
Guide 2: Strategy for Investigating Alternative Diagnostic Pathways
Objective: To establish a research workflow for identifying and validating new clinical parameters that could improve PCD detection in subgroups where PICADAR underperforms.
The following diagram illustrates a logical workflow for this investigative strategy:
Essential Research Reagent Solutions:
| Item | Function in Research Context |
|---|---|
| Genetic Sequencing Panel | To confirm PCD diagnosis and enable subgrouping by genotype, serving as a key reference standard [4]. |
| Transmission Electron Microscope | To analyze ciliary ultrastructure and categorize patients based on the presence or absence of hallmark defects [4]. |
| Nasal Nitric Oxide (nNO) Device | To provide an objective, non-invasive physiological measurement that is a validated screening tool for PCD [9]. |
| High-Speed Video Microscopy | To assess ciliary beat pattern and frequency, providing functional data on ciliary motion [9]. |
The following table details essential materials and their functions for research aimed at improving PCD diagnostics.
| Research Reagent / Material | Primary Function |
|---|---|
| Validated Clinical History Proforma | Standardized collection of patient data for accurate PICADAR calculation and discovery of new clinical features [9]. |
| Defined Genetic Reference Standard | A panel of known PCD-causing genes used to genetically confirm the diagnosis, which is crucial for validating new tools [4]. |
| Transmission Electron Microscopy (TEM) | Allows for the visualization and categorization of ciliary ultrastructural defects, a key parameter for patient stratification [4]. |
| Nasal Nitric Oxide (nNO) Measurement System | Provides an important objective biomarker; extremely low nNO levels are highly suggestive of PCD and useful for validation [9]. |
FAQs: Understanding the 'No Daily Wet Cough' Criterion in PICADAR
Q1: What is the PICADAR tool and what is its primary intended use? The PICADAR (PrImary CiliARy DyskinesiA Rule) tool is a clinical prediction rule developed to identify patients who should undergo specialized testing for Primary Ciliary Dyskinesia (PCD). It is designed to be a simple, evidence-based tool for general respiratory and ENT specialists to use in non-specialist settings before referring patients to specialized PCD diagnostic centers. Its purpose is to promote early diagnosis without overburdening specialized services with unnecessary referrals [1] [9].
Q2: Why does the PICADAR tool explicitly require "persistent wet cough" as a prerequisite? The tool was derived and validated specifically for patients presenting with a persistent wet cough. This symptom is a cornerstone of the classic PCD phenotype, as the disease is characterized by impaired mucociliary clearance leading to chronic, progressive respiratory symptoms. The research that developed PICADAR correlated readily available clinical information with diagnostic outcomes exclusively in a cohort of patients referred for testing who had this symptom. Therefore, its predictive accuracy of 0.90 sensitivity and 0.75 specificity is statistically validated only for this patient population [1] [9].
Q3: Which patient phenotypes are potentially excluded by the "no daily wet cough" criterion, and what is the risk? Strict adherence to this criterion creates a significant risk of diagnostic oversight in several key patient groups:
- Atypical PCD phenotypes: Not all genetically confirmed PCD cases present with the classic daily wet cough. Some genetic variants may have milder or atypical respiratory presentations.
- Infants and young children: The ability to manifest a productive, wet cough can be developmentally limited in very young children, even in the presence of significant lower airway infection and inflammation.
- Patients with dominant non-respiratory features: The tool may fail to identify patients whose primary manifestations are situs inversus, congenital cardiac defects, or severe neonatal respiratory distress at term, but who have a less prominent chronic cough [15]. European Respiratory Society (ERS) guidelines recommend testing for patients with several features, including situs anomalies and congenital cardiac defects, even without a documented wet cough [15].
Q4: How do current ERS guidelines address the limitations of single-criterion tools like PICADAR? The ERS guidelines take a more comprehensive approach. They recommend diagnostic testing for patients with several suggestive features, not solely a wet cough. These features include persistent wet cough, situs anomalies, congenital cardiac defects, persistent rhinitis, chronic middle ear disease, and a history of neonatal respiratory symptoms in term infants. The guidelines explicitly state that patients with normal situs but other suggestive symptoms should be referred, and they endorse the use of tools like PICADAR as part of a broader diagnostic work-up, not as a standalone gatekeeper [15].
Q5: What experimental approaches can researchers use to quantify the impact of this diagnostic oversight? Researchers can employ several methodologies to investigate this critical exclusion:
- Retrospective Cohort Analysis: Re-analyze data from PCD diagnostic centers to identify confirmed PCD patients who would have been missed by the PICADAR criterion alone. This can help quantify the false-negative rate attributable to the "no wet cough" rule.
- Prospective Validation in Broader Cohorts: Apply a modified PICADAR tool (with the wet cough prerequisite removed) to consecutive patients referred for testing due to clinical suspicion, and compare its sensitivity and specificity against the original tool.
- Genotype-Phenotype Correlation Studies: Systematically characterize the clinical presentation, including cough symptoms, across different genetic subtypes of PCD to identify genotypes associated with atypical or absent chronic cough.
Experimental Protocols for Evaluating and Improving PICADAR Sensitivity
Protocol 1: Retrospective Analysis of Missed PCD Diagnoses
Objective: To quantify the number and profile of confirmed PCD patients who did not present with a daily wet cough and would have been excluded from testing by the strict PICADAR criterion.
Methodology:
- Cohort Identification: Identify all patients with a definitive positive PCD diagnosis from a specialist center's database over a defined period.
- Data Extraction: Extract data for the seven PICADAR parameters (full-term gestation, neonatal chest symptoms, neonatal intensive care admittance, chronic rhinitis, ear symptoms, situs inversus, congenital cardiac defect) from patient records [9].
- Application of Criteria:
- Apply the official PICADAR rule, excluding any patient without a documented "persistent wet cough."
- Calculate the PICADAR score for the remaining cohort.
- Identify all patients with a confirmed PCD diagnosis who were excluded in the first step due to lack of wet cough.
- Phenotypic Characterization: Perform a detailed analysis of the clinical features of the excluded PCD patients to define the "atypical" phenotype.
Protocol 2: Prospective Validation of a Modified PICADAR Score
Objective: To develop and validate a modified version of PICADAR that does not require "persistent wet cough" as a mandatory prerequisite, thereby improving diagnostic sensitivity for atypical presentations.
Methodology:
- Study Population: Consecutive patients referred for PCD testing at multiple centers, regardless of their cough phenotype.
- Data Collection: Collect data on the seven original PICADAR parameters and the final diagnostic outcome (PCD positive/negative) [1] [9].
- Model Development:
- Use logistic regression analysis on the entire cohort, without pre-filtering for wet cough, to identify the most predictive clinical parameters.
- Develop a new scoring system (e.g., PICADAR-2) where "persistent wet cough" is one weighted parameter among others, not a gatekeeper.
- Performance Testing: Compare the sensitivity, specificity, and area under the curve (AUC) of the new PICADAR-2 model against the original PICADAR tool in the same cohort.
The following tables summarize key performance data from the original PICADAR validation study and related diagnostic criteria.
Table 1: Performance Metrics of the Original PICADAR Tool (Derivation Group) [1] [9]
| Parameter | Value | Description |
|---|---|---|
| Study Population | 641 patients | Consecutively referred for PCD testing |
| PCD Prevalence | 75 (12%) | Positive diagnoses in the cohort |
| PICADAR Cut-off | 5 points | Optimal score for referral |
| Sensitivity | 0.90 | Correctly identifies 90% of true PCD cases |
| Specificity | 0.75 | Correctly excludes 75% of non-PCD cases |
| Area Under Curve (AUC) | 0.91 (internal) | Indicator of very good diagnostic accuracy |
Table 2: PICADAR Scoring Parameters and Points [9]
| Clinical Parameter | Points |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Chronic ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 3 |
| Total Possible Score | 12 |
Table 3: ERS Guideline Recommendations for Referral (for comparison) [15]
| Recommendation | Strength of Recommendation |
|---|---|
| Test patients with several of the following: persistent wet cough, situs anomalies, congenital cardiac defects, persistent rhinitis, chronic middle ear disease, or neonatal respiratory symptoms in term infants. | Strong |
| Test patients with normal situs but other suggestive symptoms. | Strong |
| Test siblings of PCD patients, particularly if symptomatic. | Strong |
| Use combinations of symptoms and predictive tools (e.g., PICADAR) to identify patients. | Weak |
Diagnostic Pathway Visualization
The diagram below illustrates the standard PICADAR pathway and a proposed, more sensitive pathway for research validation.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Methods for PCD Diagnostic Research
| Item / Reagent | Function / Application in PCD Research |
|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | A chemiluminescence analyzer used as a key screening tool; nNO levels are characteristically very low in PCD patients. ERS guidelines recommend its use in the diagnostic work-up for patients aged >6 years [15]. |
| High-Speed Video Microscopy Analysis (HSVA) | Used to visualize and quantify ciliary beat frequency and, critically, ciliary beat pattern. Abnormal beat patterns are diagnostic for PCD. The ERS recommends it as part of the diagnostic work-up and advises repeating assessment after air-liquid interface (ALI) culture to improve accuracy [15]. |
| Transmission Electron Microscopy (TEM) | Allows for the examination of ciliary ultrastructure to identify hallmark defects (e.g., absent outer/inner dynein arms). It is a cornerstone of PCD diagnosis, though about 30% of patients may have normal ultrastructure [9] [15]. |
| Air-Liquid Interface (ALI) Culture | A cell culture technique that allows ciliated epithelium to differentiate and regenerate. Used to re-differentiate cilia after biopsy, helping to distinguish primary from secondary ciliary dyskinesia and improving the diagnostic accuracy of HSVA and TEM [9] [15]. |
| Genetic Testing Panels | Next-generation sequencing (NGS) panels for known PCD-causing genes are increasingly used for diagnosis and genotyping. In cases with strong clinical history but inconclusive other tests, genetic testing can provide a definitive diagnosis [15]. |
Refining the Toolbox: Methodological Enhancements and Integrated Diagnostic Approaches
Leveraging Nasal Nitric Oxide (nNO) as a Complementary Screening Metric
nNO Analyzers: Types and Technical Specifications
The selection of an appropriate analyzer is fundamental for reliable nasal Nitric Oxide (nNO) measurement. The following table compares the two primary types of analyzers.
Table 1: Comparison of nNO Measurement Analyzers [16]
| Feature | Chemiluminescence Analyzers | Electrochemical Analyzers |
|---|---|---|
| Accuracy & Data Display | + + + (High accuracy, real-time display for curve validation) | + (Limited data display, no real-time curve with some models) |
| Measurement Flexibility | + + + (Stable plateau identified without fixed minimum time) | + (Requires uninterrupted sampling for a fixed duration, e.g., ≥10s) |
| Validation & Cut-offs | + + + (Rigorously tested with validated cut-off values) | + (Limited published, validated cut-offs) |
| Ease of Use | + + (Requires rigorous operator training and expertise) | + + + (Simple to use) |
| Portability & Cost | + (Less portable, more expensive to purchase and maintain) | + + + (Small, portable, cost-effective) |
| Example Devices | CLD 88 sp, Sievers NOA 280i | NIOX VERO, NIOX MINO (discontinued), FeNO+ |
Essential Research Reagent Solutions
Table 2: Key Materials and Reagents for nNO Research
| Item | Function/Description | Examples & Notes |
|---|---|---|
| nNO Analyzer | Measures nitric oxide concentration in sampled nasal air. | See Table 1 for types and examples [16]. |
| Nasal Olive Probe | A soft probe inserted into the nostril to aspirate nasal air. | Must create a gentle seal; typically disposable or sterilizable. |
| Mouthpiece & Bacterial Filter | Used during exhalation maneuvers to protect the equipment and ensure hygiene. | Standard single-use components for respiratory testing. |
| Party Blower/Noisemaker | A resistance device to ensure velum closure during the "exhalation against resistance" manoeuvre. | A blow-out toy horn taped closed at the distal end [16]. |
| Saline Nasal Lavage | Used to clear nasal passages of excess mucus before testing. | Gentle saline solution; must be performed carefully to avoid mucosal injury [16]. |
Experimental Protocols & Methodologies
Protocol 1: Standard nNO Measurement via Exhalation Against Resistance
This is the recommended gold-standard method for cooperative patients [16].
Detailed Methodology:
- Patient Preparation: Confirm the patient has been free of acute viral infections or nose bleeds for 2-4 weeks. Ask the patient to blow their nose. Gently clear nasal passages with saline lavage if necessary [16].
- Equipment Setup: Connect a clean nasal olive probe to the sampling line of the nNO analyzer. Set up the mouthpiece with a resistor (creating 5-10 cm H₂O pressure) or a party blower noisemaker.
- Patient Maneuver:
- Instruct the patient to place the mouthpiece in their mouth and the nasal olive probe at the entrance of one nostril.
- The patient should take a deep inhalation.
- Then, the patient must exhale slowly and steadily against the resistance.
- Data Acquisition & Analysis:
- With Chemiluminescence Analyzer: Observe the real-time NO tracing. A valid plateau is reached when the nNO value remains stable for ≥3 seconds with a variation of ≤10% between the highest and lowest value. Manually select this plateau for the recorded value [16].
- With Electrochemical Analyzer: The device typically requires a slow oral exhalation for a set duration (e.g., ≥10 seconds). If the device software allows, visualize the curve post-measurement to manually select a plateau. Otherwise, accept the device's automated result [16].
- Repeats: The maneuver should be repeated twice in each nostril to assess intra- and inter-nostril repeatability.
Protocol 2: nNO Measurement in Young Children via Tidal Breathing
This is a feasible method for infants, young children (<5 years), and adults unable to perform velum-closing maneuvers [16].
Detailed Methodology:
- Patient Preparation: As per Protocol 1.
- Equipment Setup: As per Protocol 1, but no mouthpiece or resistor is used.
- Patient Maneuver: The nasal olive probe is held at the entrance of one nostril while the child breathes normally (tidal breathing) through their mouth. The velum remains open, which leads to dilution of nasal air with lower airway air and consequently lower measured nNO values.
- Data Acquisition: Sample the nasal air for a sufficient period to obtain a stable reading. The interpretation of results using this method must use age-specific reference values.
Protocol 3: Novel Electrochemical nNO Measurement during Laryngeal Mask Anesthesia (ECnNO LAMA)
This novel protocol enables nNO measurement in very young children using portable electrochemical devices, which normally require long, steady sampling times [17].
Detailed Methodology:
- Patient Preparation: This measurement is performed during scheduled bronchoscopy under general anesthesia. Standard pre-anesthetic protocols are followed.
- Equipment Setup: Place a laryngeal mask airway (LMA). Connect the electrochemical nNO analyzer's sampling line to the LMA.
- Patient Maneuver: During a brief breath-hold period (apnea) induced by the anesthesiologist, sample the air from the upper airways.
- Data Acquisition: The analyzer measures the nNO level during this apnea. The maneuver is repeated at least twice to assess repeatability. This method has shown substantial repeatability (ICC 0.974) in children under 5 years [17].
Diagnostic & Research Workflows
The following diagram illustrates the decision-making process for integrating nNO measurement into a PCD screening pathway, particularly for enhancing PICADAR.
Frequently Asked Questions (FAQs) & Troubleshooting
Q1: We obtained a very low nNO value, but the patient does not have a high PICADAR score. What could be the reason? A: A falsely low nNO reading can occur due to several factors unrelated to PCD. Before concluding, check for:
- Recent Illness: Acute viral infections can temporarily suppress nNO. Wait 2-4 weeks after full recovery before testing [16].
- Nasal Obstruction: Significant nasal polyps, congestion, or mucus can block NO diffusion. A saline lavage before testing may help; consider ENT evaluation for persistent obstruction [16].
- Technical Error: Ensure the sampling line is not kinked or obstructed. Check for air leaks around the nasal olive probe.
Q2: Our research involves preschool children. Which nNO measurement method is most feasible, and what are the caveats? A: For children under 5, the tidal breathing method is most feasible as it requires minimal cooperation [16]. The novel ECnNO LAMA technique also shows high repeatability in this age group when performed during anesthesia [17]. The major caveat is that tidal breathing values are inherently lower due to dilution from lower airway air, so you must use age-appropriate and method-specific reference values. Results cannot be directly compared to values obtained using velum-closure techniques.
Q3: How can nNO measurement specifically improve the sensitivity of the PICADAR score in a research setting? A: PICADAR is a clinical prediction tool, but it can miss patients with atypical presentations. nNO serves as an objective, continuous biomarker that can reclassify risk.
- A patient with a low PICADAR score but a consistently low nNO level should be flagged for further investigation, thereby improving sensitivity [18] [19].
- Conversely, a high PICADAR score with a normal nNO value may warrant a review before proceeding to more invasive diagnostics, potentially improving specificity. Research shows that combining a PICADAR score ≥2 with low nNO (<77 nL/min) provides a powerful screening combination [18].
Q4: Our electrochemical analyzer does not show a real-time curve. How can we ensure the quality of our measurements? A: This is a key limitation of some electrochemical devices. To ensure quality:
- Strict Adherence to Time: Ensure the patient maintains a steady exhalation for the entire device-specified duration (e.g., ≥10 seconds).
- Visual Feedback: Use a party blower noisemaker during the exhalation against resistance maneuver. The sound provides auditory feedback that the velum is closed and exhalation is steady.
- Repeat Measurements: Perform at least two technically satisfactory measurements per nostril. Good repeatability between measurements increases confidence in the result [16].
Q5: What are the critical environmental factors to control during nNO testing? A: Ambient nitric oxide levels can significantly affect results.
- Measure and Record: Always measure ambient NO levels in the testing room at the time of the procedure.
- High Ambient NO: If ambient NO is high (e.g., >20 ppb), this value must be subtracted from all patient measurements to avoid overestimation [16].
- Ventilation: Ensure the testing room is well-ventilated and not located near sources of high NO pollution (e.g., busy roads, certain laboratories).
The Role of Genetic and Ultrastructural Data in Informing Score Interpretation
Troubleshooting Guides and FAQs
This technical support resource addresses common challenges researchers face when interpreting PICADAR scores in primary ciliary dyskinesia (PCD) diagnostic workflows.
FAQ: Understanding PICADAR Performance Limitations
Q: Our research shows PICADAR sensitivity of only 75% in genetically confirmed PCD patients. Which patient subgroups are most likely to be missed?
A: Recent studies with genetically confirmed PCD cohorts reveal significant variability in PICADAR's performance across genetic and ultrastructural subgroups [4] [3]. The tool demonstrates particularly low sensitivity in:
- Patients with situs solitus (normal organ arrangement): 61% sensitivity [4] [3]
- Patients without hallmark ultrastructural defects: 59% sensitivity [4] [3]
- Patients reporting no daily wet cough: Approximately 7% of genetically confirmed PCD patients are automatically ruled out [4]
Q: What genetic and ultrastructural factors should we consider when interpreting low PICADAR scores?
A: Low PICADAR scores (<5 points) should be interpreted cautiously in patients with mutations known to cause subtle ciliary defects [20]. Key considerations include:
- DNAH11 mutations: Cause ODA defects with normal ultrastructure [20]
- HYDIN, RSPH9, RSPH4A mutations: Associated with central apparatus defects without laterality abnormalities [20]
- CCDC39, CCDC40 mutations: Cause IDA+MTD defects with more severe disease presentation [20]
Q: What experimental protocols can improve PICADAR sensitivity in research settings?
A: Supplement PICADAR with these methodological approaches:
- Structured clinical data collection using standardized proformas completed prior to diagnostic testing [9]
- Comprehensive genetic testing covering >50 known PCD-associated genes [20]
- Combined diagnostic techniques including nNO, HSVA, TEM, and genetic analysis [20]
Experimental Protocols for PICADAR Validation Studies
Protocol: Validating PICADAR in Specialized Populations
Objective: Assess PICADAR sensitivity in genetically confirmed PCD subgroups based on laterality and ultrastructural defects [4].
Methodology:
- Recruit consecutive patients with genetically confirmed PCD diagnosis
- Administer PICADAR questionnaire assessing seven predictive parameters [9]
- Calculate scores using established cutoff ≥5 points for positive prediction [4]
- Stratify analysis by:
Expected Outcomes: Median PICADAR scores of approximately 10 (IQR: 8-11) in patients with laterality defects versus 6 (IQR: 4-8) in those with situs solitus [4].
Data Presentation
Table 1: PICADAR Sensitivity Across Patient Subgroups
| Patient Subgroup | Sample Size | Sensitivity | Median PICADAR Score (IQR) | Statistical Significance |
|---|---|---|---|---|
| Overall PCD Population | 269 | 75% | 7 (5-9) | Reference |
| With Laterality Defects | Not specified | 95% | 10 (8-11) | p < 0.0001 |
| With Situs Solitus | Not specified | 61% | 6 (4-8) | p < 0.0001 |
| With Hallmark Ultrastructural Defects | Not specified | 83% | Not reported | p < 0.0001 |
| Without Hallmark Ultrastructural Defects | Not specified | 59% | Not reported | p < 0.0001 |
Data derived from Schramm et al. (2025) evaluation of 269 genetically confirmed PCD patients [4] [3].
Table 2: Genetic Mutations and Their Impact on PICADAR Scoring
| Genetic Mutation | Ultrastructural Defect | Laterality Defect Risk | Expected PICADAR Performance |
|---|---|---|---|
| DNAH5, DNAI1 | Outer Dynein Arm (ODA) Defect | Present (~50%) | Higher sensitivity |
| DNAH11 | ODA Defect (Normal TEM) | Present (~50%) | Variable |
| CCDC39, CCDC40 | IDA + Microtubule Disorganization | Reduced | Lower sensitivity |
| HYDIN, RSPH9, RSPH4A | Central Apparatus Defects | Absent | Lower sensitivity |
Genetic and ultrastructural relationships based on current PCD research [20].
Diagnostic Workflow Visualization
PICADAR Diagnostic with Genetic Overlay
The Scientist's Toolkit: Research Reagent Solutions
Essential Materials for PICADAR Validation Studies
| Research Reagent | Function in PICADAR Research | Application Notes |
|---|---|---|
| Standardized Clinical History Proforma | Ensures consistent data collection across research sites | Complete prior to diagnostic testing; captures 7 predictive parameters [9] |
| Genetic Testing Panels | Confirms PCD diagnosis through mutation identification | Should cover >50 known PCD-associated genes including DNAH5, DNAH11, CCDC39, CCDC40 [20] |
| Transmission Electron Microscopy (TEM) | Identifies hallmark ultrastructural defects | Differentiates ODA, IDA, MTD, and CP defects for patient stratification [20] |
| High-Speed Video Microscopy Analysis (HSVA) | Assesses ciliary beat pattern and function | Complements genetic and ultrastructural data [20] |
| Nasal Nitric Oxide (nNO) Measurement | Provides functional ciliary assessment | Low nNO supports PCD diagnosis but requires specialized equipment [9] |
Advanced Interpretation Guidelines
Protocol: Integrating Genetic Data with PICADAR Scoring
Objective: Enhance PICADAR interpretation through genetic correlation.
Methodology:
- Calculate PICADAR score using standard protocol [9]
- Perform comprehensive genetic testing
- Correlate specific genetic mutations with PICADAR parameters:
Interpretation: Low PICADAR scores in genetically confirmed cases most frequently occur in patients with situs solitus and central apparatus defects (HYDIN, RSPH9, RSPH4A mutations) [4] [20].
Table 3: PICADAR Parameter Weighting by Genetic Subtype
| PICADAR Parameter | DNAH5 Mutation (ODA Defect) | DNAH11 Mutation (Normal TEM) | CCDC39 Mutation (IDA+MTD) | HYDIN Mutation (CP Defect) |
|---|---|---|---|---|
| Situs Inversus | Strong predictor | Strong predictor | Reduced association | Typically absent |
| Congenital Cardiac Defect | Moderate predictor | Moderate predictor | Variable | Typically absent |
| Daily Wet Cough | Strong predictor | Strong predictor | Strong predictor | Strong predictor |
| Neonatal Respiratory Symptoms | Strong predictor | Moderate predictor | Strong predictor | Moderate predictor |
| Overall PICADAR Performance | High sensitivity | Moderate sensitivity | Variable sensitivity | Low sensitivity |
Theoretical weighting based on established genotype-phenotype correlations in PCD [20].
FAQs: PICADAR and Diagnostic Challenges
Q1: What is the PICADAR tool, and what is its intended use in PCD diagnosis? The PrImary Ciliary DyskinesiA Rule (PICADAR) is a predictive clinical tool designed to identify patients with a persistent wet cough who should be referred for definitive Primary Ciliary Dyskinesia (PCD) testing. It uses seven clinical parameters to generate a score that estimates the probability of a PCD diagnosis, helping to prioritize specialized testing [1].
Q2: What are the recognized limitations of the PICADAR tool? Recent research has highlighted significant limitations in PICADAR's sensitivity. A 2025 study found its overall sensitivity is 75%, meaning it misses about a quarter of genetically confirmed PCD cases. Performance is notably poorer in specific subgroups: sensitivity drops to 61% in individuals with normal organ placement (situs solitus) and to 59% in those without hallmark defects in ciliary ultrastructure [4].
Q3: How can genotype-phenotype correlations address PICADAR's limitations? PICADAR's reliance on a limited set of clinical features causes it to miss atypical presentations. Integrating genotype-phenotype correlations allows for a more nuanced risk stratification. For example, understanding that mutations in specific gene domains (like the T-Box domain in TBX4-associated diseases) are linked to more severe or earlier-onset phenotypes can help identify at-risk patients who would otherwise score low on PICADAR [21]. This facilitates a more personalized diagnostic approach.
Q4: What is a key difference between haploinsufficiency and dominant-negative pathogenic variants? In the context of genetic disorders like Marfan syndrome (caused by FBN1 variants), this distinction is critical. Haploinsufficiency (often from Premature Termination Codon variants) results from a reduced amount of the protein and is often associated with more severe aortic phenotypes. In contrast, dominant-negative (in-frame) variants produce an altered protein that disrupts the function of the normal protein from the healthy allele; these can be further stratified by their impact, such as cysteine content in fibrillin-1, which correlates with specific risks like ectopia lentis [22].
Q5: What are the essential components of a high-quality genotype-phenotype correlation study? A robust study requires:
- Comprehensive Genetic Data: Full gene sequencing and functional validation of variants (e.g., luciferase reporter assays to test for loss/gain-of-function) [21].
- Deep Phenotyping: Systematic, standardized collection of clinical data across all organ systems, not just the primary manifestations [22].
- Large, Unbiased Cohorts: Inclusion of consecutive patients and relatives, not just probands, to minimize referral bias and capture the full phenotypic spectrum [22].
Troubleshooting Guides
Guide 1: Resolving Low PICADAR Sensitivity in Patient Cohorts
Problem: The PICADAR tool fails to identify a significant number of true PCD cases, particularly those without classic symptoms like situs inversus.
Investigation & Solution:
- Step 1: Stratify by Laterality. Re-analyze your cohort based on situs (solitus vs. inversus). The diagnostic yield of PICADAR is significantly higher in patients with laterality defects (95% sensitivity) compared to those without (61%) [4].
- Step 2: Integrate Genetic Data. For patients with low PICADAR scores but high clinical suspicion, proceed directly to genetic testing. Genotype-phenotype knowledge can then reframe their clinical presentation.
- Step 3: Apply an Enhanced Protocol. Implement the diagnostic workflow below, which incorporates genetic information to supplement PICADAR.
Guide 2: Designing a Genotype-Phenotype Correlation Study
Problem: Inconsistent and non-reproducible correlations between genetic variants and clinical outcomes.
Investigation & Solution:
- Step 1: Standardize Variant Categorization. Do not rely solely on variant type (e.g., missense vs. nonsense). Perform functional assays to classify variants as Loss-of-Function (LoF) or Gain-of-Function (GoF), as these can have dramatically different clinical implications [21].
- Step 2: Implement Deep Phenotyping. Collect data across multiple organ systems using standardized protocols (e.g., specific echocardiography measurements, skeletal X-rays, slit-lamp examinations) [22]. This ensures consistent and comparable data.
- Step 3: Account for Modifying Factors. Acknowledge that age at diagnosis, environmental factors, and modifier genes can influence the phenotype. Use statistical methods like Kaplan-Meier survival curves to analyze time-to-event data (e.g., aortic dissection) [22].
The following workflow outlines a robust methodology for such a study.
Experimental Protocols
Protocol 1: Functional Validation of Genetic Variants Using a Luciferase Reporter Assay
Purpose: To determine whether a specific genetic variant results in Loss-of-Function (LoF) or Gain-of-Function (GoF) of the resulting protein [21].
Methodology:
- Plasmid Construction: Use site-directed mutagenesis to introduce the patient-specific variant into a wild-type cDNA sequence of the gene of interest (e.g., TBX4), cloned into an expression plasmid.
- Cell Transfection: Co-transfect cultured cells with:
- The experimental plasmid (wild-type, mutant, or empty vector control).
- A reporter plasmid containing a luciferase gene under the control of a promoter responsive to the target protein (e.g., a promoter with T-Box binding motifs).
- A control plasmid (e.g., Renilla luciferase) for normalization.
- Luciferase Assay: After 24-48 hours, lyse the cells and measure luminescence using a dual-luciferase reporter assay system.
- Data Analysis: Normalize the firefly luciferase activity to the Renilla control. Compare the transcriptional activity of the mutant protein to the wild-type protein.
- LoF Variant: Significantly reduced luciferase activity.
- GoF Variant: Significantly increased luciferase activity.
- Benign Variant: Activity similar to wild-type.
Protocol 2: Systematic Deep Phenotyping for Connective Tissue Disorders
Purpose: To comprehensively and consistently capture the multi-system clinical features of a genetic syndrome to enable robust genotype-phenotype correlations [22].
Methodology:
- Cardiovascular Evaluation:
- Perform transthoracic echocardiography.
- Measure aortic root diameters at the sinus of Valsalva and ascending aorta, standardized to body surface area (Z-scores).
- Document a history of aortic dissection or preventive surgery.
- Ophthalmologic Evaluation:
- Conduct a slit-lamp examination to detect ectopia lentis (lens dislocation).
- Record surgical history for lens replacement.
- Musculoskeletal Evaluation:
- Perform physical exam for features like pectus deformity, scoliosis, and arachnodactyly.
- Obtain spine and pelvis X-rays to quantify scoliosis and protrusio acetabuli.
- Data Integration: All findings are entered into a structured database during a multidisciplinary team meeting to confirm diagnoses and assign final phenotypes.
Data Presentation
Table 1: Performance Profile of the PICADAR Diagnostic Tool
This table summarizes the sensitivity of the PICADAR tool across different subpopulations as identified in a 2025 validation study [4].
| Patient Subgroup | PICADAR Sensitivity | Median PICADAR Score (IQR) | Key Implication |
|---|---|---|---|
| Overall Genetically Confirmed PCD | 75% (202/269) | 7 (5 - 9) | Misses 1 in 4 true PCD cases |
| With Laterality Defects (e.g., Situs Inversus) | 95% | 10 (8 - 11) | Functions well for classic presentation |
| With Situs Solitus (normal arrangement) | 61% | 6 (4 - 8) | Major limitation; high miss rate |
| With Hallmark Ciliary Defects | 83% | Data Not Provided | Moderate performance |
| Without Hallmark Ciliary Defects | 59% | Data Not Provided | Very high false-negative rate |
Table 2: Genotype-Phenotype Correlations inFBN1andTBX4Disorders
This table contrasts correlation patterns from two distinct genetic disorders, demonstrating generalizable principles [22] [21].
| Feature | FBN1 (Marfan Syndrome) | TBX4 (PAH & Lung Disease) |
|---|---|---|
| Key Correlated Genes | FBN1 | TBX4, BMPR2 |
| Variant Type & Effect | PTC/Haploinsufficiency: Severe aortic phenotype, higher scoliosis risk, shorter life expectancy. In-frame/Cysteine Loss: Higher risk of ectopia lentis. | LoF in T-Box/NLS domains: Early onset, severe lung disease. GoF variants: Later adult onset. |
| Associated Clinical Spectrum | Aortic dilation/dissection, ectopia lentis, scoliosis, dural ectasia. | Pulmonary arterial hypertension (PAH), developmental lung disease, skeletal features (SPS). |
| Impact on Survival | PTC variants associated with significantly shorter life expectancy. | T-Box domain mutations linked to shorter event-free survival. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Brief Explanation |
|---|---|
| Next-Generation Sequencing (NGS) Panels | For simultaneous screening of a curated set of genes associated with a disease phenotype (e.g., PCD or thoracic aortic aneurysms) [22]. |
| Dual-Luciferase Reporter Assay System | A functional assay kit to quantify the transcriptional activity of a protein of interest, crucial for classifying variants as LoF or GoF [21]. |
| Standardized Clinical Data Collection Forms | Structured protocols for deep phenotyping ensure consistent and comprehensive data capture across all patients in a cohort, which is vital for meaningful correlations [22]. |
| Kaplan-Meier Survival Analysis | A statistical method used to analyze "time-to-event" data (e.g., survival, aortic dissection), allowing for comparison of event risk between different genotype groups [22]. |
Frequently Asked Questions
Q1: What is the primary limitation of the current PICADAR tool identified by recent studies? Recent validation studies have demonstrated that PICADAR has significant sensitivity limitations, particularly missing PCD diagnoses in specific patient subgroups. The overall sensitivity was found to be 75% in a genetically confirmed PCD cohort, meaning it failed to identify 25% of actual PCD cases. Performance was substantially worse in patients without laterality defects (61% sensitivity) and those without hallmark ultrastructural defects (59% sensitivity). Additionally, the tool automatically excludes all patients without daily wet cough (approximately 7% of genuine PCD cases), creating a fundamental diagnostic gap [4] [3].
Q2: How does patient anatomy affect PICADAR's performance? PICADAR shows dramatically different performance based on the presence or absence of laterality defects (abnormal organ positioning). The sensitivity is 95% in patients with laterality defects but drops to only 61% in those with normal organ arrangement (situs solitus). This creates significant diagnostic inequality and missed diagnoses for a substantial portion of the PCD population [4].
Q3: What complementary diagnostic methods can improve PCD detection rates? Nasal nitric oxide (nNO) measurement has been shown to significantly enhance predictive power when combined with clinical scoring tools. One study found nNO improved the predictive capabilities of PICADAR and other clinical indices. High-speed video microscopy analysis (HSVMA) and transmission electron microscopy (TEM) remain essential confirmatory tests, though they require specialized equipment and expertise [19].
Q4: Are there alternative predictive tools to PICADAR for PCD diagnosis? Yes, researchers have developed other assessment tools including the Clinical Index (CI) and North America Criteria Defined Clinical Features (NA-CDCF). One comparative study found that CI may outperform PICADAR while having the advantage of not requiring assessment for laterality or congenital heart defects. These tools use different clinical parameters and scoring thresholds [19].
Quantitative Performance Analysis of PICADAR
Table 1: PICADAR Sensitivity Across Patient Subgroups
| Patient Subgroup | Sample Size | Sensitivity | Median Score | IQR |
|---|---|---|---|---|
| Overall PCD Population | 269 | 75% | 7 | 5-9 |
| With Laterality Defects | Information missing | 95% | 10 | 8-11 |
| With Situs Solitus (normal arrangement) | Information missing | 61% | 6 | 4-8 |
| With Hallmark Ultrastructural Defects | Information missing | 83% | Information missing | Information missing |
| Without Hallmark Ultrastructural Defects | Information missing | 59% | Information missing | Information missing |
Table 2: Comparison of PCD Predictive Tools
| Assessment Tool | Required Parameters | Key Advantages | Reported AUC | Study Population |
|---|---|---|---|---|
| PICADAR | 7 parameters including daily wet cough, situs abnormalities, gestational age | Previously validated, ERS recommended | 0.87 (external validation) | 641 patients [9] |
| Clinical Index (CI) | 7 symptoms from clinical history | Does not require assessment of laterality or cardiac defects | Larger than NA-CDCF (p=0.005) | 1401 patients [19] |
| NA-CDCF | 4 clinical criteria | Simpler parameter set | No significant difference from PICADAR | 1401 patients [19] |
Experimental Protocols & Methodologies
Protocol 1: Validating Predictive Tool Performance
Purpose: To evaluate the sensitivity and specificity of PCD predictive tools against genetically confirmed diagnoses.
Materials: Patient cohorts with confirmed PCD diagnosis, clinical history data, genetic confirmation results, statistical analysis software (SPSS, R, or equivalent).
Procedure:
- Recruit consecutive patients referred for PCD testing with definitive diagnostic outcomes
- Collect complete clinical history using standardized proforma prior to diagnostic testing
- Calculate PICADAR scores based on seven predictive parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care admittance, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defect
- Apply recommended cutoff score of ≥5 points to determine positive screening result
- Compare PICADAR results with definitive diagnostic outcome using receiver operating characteristic (ROC) curve analysis
- Perform subgroup analyses based on laterality defects and ultrastructural characteristics
- Calculate sensitivity, specificity, and area under the curve (AUC) metrics [9] [4]
Protocol 2: Comparative Analysis of Multiple Predictive Tools
Purpose: To directly compare the performance of CI, PICADAR, and NA-CDCF in the same patient population.
Materials: Patients with suspected PCD referred for diagnostic workup, structured medical documentation, nNO measurement equipment, HSVM equipment.
Procedure:
- Enroll patients with suspected PCD referred for high-speed video microscopy testing
- Extract relevant clinical signs and symptoms from structured medical documentation
- Calculate scores for all three predictive tools (CI, PICADAR, NA-CDCF) according to original publications
- Measure nasal nitric oxide (nNO) using electrochemical analyzer with tidal breathing technique or oral exhalation against resistance
- Perform HSVM via nasal brushing, analyzing ciliary beat frequency and movement pattern
- Conduct transmission electron microscopy (TEM) and genetic testing for definitive diagnosis
- Analyze predictive characteristics using ROC curves and compare AUC values [19]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PCD Diagnostic Research
| Item | Function/Application | Specifications/Protocols |
|---|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Non-invasive screening measure; low nNO values suggest PCD | Niox Mino or Niox Vero; aspiration at 5 mL·s⁻¹ via nasal olive probe [19] |
| High-Speed Video Microscopy (HSVMA) System | Analysis of ciliary beat frequency and pattern | Keyence Motion Analyzer Microscope VW-6000/5000; nasal brushing samples [19] |
| Transmission Electron Microscope (TEM) | Identification of ultrastructural ciliary defects | Processing of nasal brushings or endobronchial biopsies per international consensus guidelines [19] |
| Genetic Testing Panel | Identification of disease-causing mutations in PCD genes | Next-generation sequencing panel of ciliopathies (39 PCD genes); MLPA for DNAH5 and DNAI1 [19] |
| Clinical Data Collection Proforma | Standardized symptom assessment for tool validation | Structured form capturing neonatal history, respiratory symptoms, laterality defects, family history [9] |
Diagnostic Workflows and Scoring Systems
Diagram 1: PICADAR Diagnostic Workflow with Identified Gaps and Proposed Enhancements
Research Recommendations
Based on the current evidence, researchers should:
- Implement complementary screening approaches using both PICADAR and Clinical Index to maximize sensitivity across different patient phenotypes
- Prioritize nNO measurement as an objective screening measure that enhances predictive tool performance
- Develop population-specific scoring thresholds rather than relying on a universal cutoff score of ≥5
- Collect prospective validation data on proposed algorithmic refinements including weighted scoring systems and additional clinical variables
- Consider the impact of genetic heterogeneity on clinical presentation when refining predictive algorithms
The search for an optimal predictive algorithm continues, with current evidence suggesting that a multifaceted approach combining the best elements of existing tools with objective measures like nNO provides the most reliable screening strategy while awaiting further validation of refined scoring systems [19] [4] [3].
Navigating Diagnostic Challenges: Optimization Strategies for Complex PCD Cases
Optimizing PICADAR for Patients with Situs Solitus and Atypical Presentations
Technical Support Center
Frequently Asked Questions (FAQs)
Q1: What is the primary challenge when applying the PICADAR score to patients with situs solitus? The primary challenge is that the PICADAR tool includes "Laterality Defects," such as situs inversus, as a key diagnostic feature worth 2 points [20]. In patients with situs solitus (normal organ placement), this criterion is not met, reducing the maximum achievable score and potentially decreasing the tool's sensitivity for this patient subgroup. This can lead to missed or delayed diagnoses in individuals with atypical presentations [20].
Q2: Which clinical features in PICADAR are most frequently absent in atypical presentations? In atypical presentations, the features most often absent or less pronounced are:
- Laterality Defects: The absence of situs inversus is, by definition, a characteristic of situs solitus [20].
- Neonatal Respiratory Symptoms: While common, not all PCD neonates present with severe respiratory distress requiring prolonged support. Atypical cases might have milder, transient symptoms that are overlooked [20].
- Chronic Rhinitis: The persistent, non-seasonal nature of rhinitis may not be fully appreciated in infancy, leading to under-reporting [20].
Q3: How can genetic testing results be interpreted in the context of an optimized PICADAR score? Genetic testing can confirm PCD diagnosis by identifying mutations in over 50 known associated genes [20]. When optimizing PICADAR, genetic results can be used to validate the tool's predictions. For example, a patient with a low PICADAR score (lacking a laterality defect) but a confirmed pathogenic mutation in a PCD-associated gene (e.g., DNAH11) would represent a confirmed case of PCD with an atypical presentation, providing critical data for refining the scoring model [20].
Q4: What is the recommended workflow for diagnosing PCD when PICADAR sensitivity is low? Given the absence of a single gold-standard test, a multi-step diagnostic process is essential, especially when PICADAR sensitivity is low [20]. The following workflow integrates PICADAR with advanced diagnostic techniques:
Diagnostic Workflow for Low PICADAR Scores
Troubleshooting Guides
Issue: Inconclusive or borderline PICADAR score in a patient with situs solitus.
Potential Cause: The patient has PCD caused by a genetic mutation that does not cause situs inversus, such as those affecting the central pair of microtubules (e.g., RSPH4A, RSPH9, HYDIN) [20]. In these cases, the ciliary ultrastructure may appear normal, but function is impaired.
Solution:
- Proceed with Functional and Genetic Tests: As outlined in the workflow above, initiate testing with nNO and HSVA.
- Focus Genetic Panel: Prioritize genetic testing for genes associated with normal ultrastructure and central pair defects, which are less likely to cause laterality defects [20].
- Quantify Findings: Document the specific findings meticulously to contribute to research on refining PICADAR's weighting for situs solitus patients.
Issue: A patient has a high clinical suspicion for PCD but a low PICADAR score and negative initial genetic test.
Potential Cause: The genetic testing panel used may not have covered all known PCD-associated genes, or the patient may have mutations in a novel, not-yet-identified gene [20].
Solution:
- Re-evaluate Genetic Test Scope: Verify the comprehensiveness of the genetic panel used. Consider whole-exome or whole-genome sequencing.
- Utilize Immunofluorescence (IF): This modern method can detect the absence of specific ciliary proteins, which can be suggestive of a genetic defect even if the genetic variant is of unknown significance or not found [20].
- Refer to a Specialized Center: Collaborate with a research center focused on PCD to investigate the possibility of a novel gene mutation.
Research Reagent Solutions
The following table details key materials and methods used in PCD diagnostic research, which are essential for experiments aimed at validating improvements to the PICADAR tool.
| Research Reagent / Method | Function in PCD Diagnostic Research |
|---|---|
| Extended Genetic Testing Panels | Identifies pathogenic mutations in over 50 known PCD-associated genes, crucial for confirming diagnosis in patients with atypical presentations and normal ultrastructure [20]. |
| High-Speed Video Microscopy Analysis (HSVA) | Allows for the direct visualization and analysis of ciliary beat pattern and frequency, identifying dynamic dysfunction that may not be evident from structure alone [20]. |
| Nasal Nitric Oxide (nNO) Measurement | Provides a non-invasive screening metric; low nNO levels are highly suggestive of PCD and can help triage patients for further testing [20]. |
| Transmission Electron Microscopy (TEM) | The historical gold standard for diagnosing PCD by revealing specific ultrastructural defects in the ciliary axoneme (e.g., absent dynein arms, microtubule disorganization) [20]. |
| Immunofluorescence (IF) Staining | A modern technique that uses antibodies to detect the presence or absence of specific ciliary proteins, providing functional insight into the consequences of genetic mutations [20]. |
| Model-Informed Drug Development (MIDD) | A quantitative framework that uses computational models to optimize drug development, which can be applied to create new therapies for PCD, such as gene corrections [23]. |
| Quantitative Systems Pharmacology (QSP) | An integrative modeling approach that can simulate disease mechanisms and patient responses, useful for predicting the efficacy of new treatments in different PCD genotypes [23]. |
Quantitative Data for PICADAR Optimization
The table below summarizes key quantitative data from the literature relevant to understanding the genetic basis of PCD and the potential limitations of the PICADAR score in specific genotypic subgroups.
Table 1: PCD Genetic Associations and Implications for PICADAR
| Ultrastructural Defect | Example Mutated Genes | Clinical/Diagnostic Notes | Relevance to PICADAR Optimization |
|---|---|---|---|
| Outer Dynein Arm (ODA) Defect | DNAH5, DNAI1 [20] | Often associated with a milder disease course [20]. | Commonly associated with situs inversus; absence in score reduces sensitivity for situs solitus patients with these mutations. |
| Microtubule Disorganization (MTD) + Inner Dynein Arm (IDA) Defect | CCDC39, CCDC40 [20] | Associated with more severe disease and poorer lung function [20]. | Strongly associated with situs inversus; their absence in a confirmed PCD case suggests a different genotype. |
| Central Pair (CP) Defect | RSPH9, RSPH4A, HYDIN [20] | Causes abnormal, swirling ciliary beating. Does not carry a risk of situs inversus [20]. | Critical for optimization: Patients with these genotypes will always have situs solitus and likely lower PICADAR scores. The score must be adjusted to be sensitive to these cases. |
| Normal Ultrastructure | DNAH11 [20] | Ciliary motility is impaired, but structure appears normal under TEM [20]. | Another key group for optimization, as these patients lack classic structural hallmarks and may have situs solitus, leading to under-assessment by PICADAR. |
Table 2: Diagnostic Test Characteristics for PCD
| Diagnostic Test | Typical Finding in PCD | Key Consideration for Atypical Cases |
|---|---|---|
| Nasal Nitric Oxide (nNO) | Very low levels [20] | A useful first-line screening tool, but requires patient cooperation, which can be difficult in young children. |
| High-Speed Video Microscopy (HSVA) | Abnormal ciliary beat pattern [20] | Can detect functional defects in cases with normal ultrastructure (e.g., DNAH11 mutations). |
| Transmission Electron Microscopy (TEM) | Specific axonemal defects (e.g., absent dynein arms) [20] | Will appear normal in approximately 30% of PCD cases (e.g., DNAH11, RSPH mutations), leading to false negatives if used alone [20]. |
| Genetic Testing | Bi-allelic pathogenic mutations in a PCD-associated gene [20] | The most comprehensive confirmatory test, especially as the number of known genes continues to grow beyond 50 [20]. |
Technical Support Center: FAQs & Troubleshooting Guides
This technical support resource provides troubleshooting guidance for researchers working on the diagnosis of Primary Ciliary Dyskinesia (PCD), with a specific focus on cases where ciliary ultrastructure appears normal. This content supports thesis research aimed at improving the sensitivity of the PICADAR (Primary Ciliary Dyskinesia Rule) clinical scoring tool.
Frequently Asked Questions (FAQs)
Q1: My transmission electron microscopy (TEM) results are normal, but the patient has a strong clinical PCD phenotype. What does this mean? It means your patient may fall into the approximately 30% of PCD cases where the disorder is present despite normal ciliary ultrastructure observable by standard TEM [24] [25]. This is a known diagnostic challenge. You should proceed with genetic testing or advanced imaging techniques like electron tomography, which can detect defects like the absence of DNAH11 that are invisible to conventional TEM [24].
Q2: What are the limitations of using TEM as the sole diagnostic tool in a research setting? Using TEM alone has a maximum diagnostic sensitivity of approximately 70% [25]. It requires proficient specimen collection, expensive infrastructure, and analytical expertise [25]. Furthermore, defects observed can sometimes be secondary (Class 2 defects) due to infection or inflammation, complicating interpretation without confirmatory tests [25].
Q3: What specific ultrastructural defects are considered confirmatory for PCD (Class 1 defects)? According to international consensus guidelines, confirmatory Class 1 defects, which must be present in more than 50% of transverse ciliary sections, include [25]:
- Absence or truncation of Outer Dynein Arms (ODA)
- Combined absence of Outer and Inner Dynein Arms (ODA+IDA)
- Microtubular disorganization with inner dynein arm loss
Q4: In a resource-limited setting where only TEM is available, how should I handle a case with inconclusive (Class 2) defects? A confirmatory diagnosis cannot be made with TEM alone in these cases. The international guidelines recommend using another PCD-testing modality to support the ultrastructural observations [25]. If this is not possible, a repeat brushing after treating any potential respiratory infection or inflammation may be considered, as some secondary defects are transient [25].
Troubleshooting Guide for Experimental Diagnostics
Issue: Inability to detect ultrastructural defects in genetically confirmed or clinically suspected PCD cases.
| Troubleshooting Step | Description & Action | Key Quantitative/Technical Data |
|---|---|---|
| 1. Validate Sample Quality | Ensure nasal brushings contain sufficient ciliated cells. Inadequate samples lead to false negatives. | One study noted that 83% (5 of 6) of cases requiring further testing had very few and sparsely ciliated cells [25]. |
| 2. Apply Advanced Tomography | Use electron tomography on existing araldite-embedded samples if standard TEM is normal [24]. | This 3D technique detected a >25% deficiency in proximal outer dynein arm volume in all patients with DNAH11 mutations (n=7), a defect missed by standard TEM [24]. |
| 3. Correlate with Genetic Findings | When TEM is normal, prioritize genetic analysis for known "normal ultrastructure" genes like DNAH11 [24]. | Up to 30% of PCD patients with bi-allelic mutations have normal ultrastructure [24] [25]. |
Experimental Protocols for Enhanced Diagnosis
The following protocols are designed to address the critical gap in diagnosing PCD with normal ultrastructure.
Protocol 1: Electron Tomography for 3D Ciliary Ultrastructure Analysis
This methodology is adapted from a study that successfully identified proximal outer dynein arm defects in patients with DNAH11 mutations [24].
1. Sample Preparation:
- Use existing nasal ciliary biopsies fixed and embedded in araldite resin, as prepared for standard TEM [24].
2. Data Acquisition - Tomogram Collection:
- Collect dual-axis tomograms from the embedded cilia samples using a transmission electron microscope equipped with tomography capabilities [24].
- Tilt the specimen through a range of angles (typically ±60°) to acquire a series of 2D images for 3D reconstruction.
3. 3D Modeling and Analysis:
- Software: Use specialized software such as IMOD and Chimera for 3D reconstruction and analysis [24].
- Focus Region: Specifically analyze the proximal region of the ciliary axoneme, as defects associated with DNAH11 are localized here [24].
- Quantitative Measurement: Calculate the volume of the outer dynein arms in the proximal region. A deficiency of more than 25% compared to healthy controls is considered indicative of a defect [24].
Protocol 2: Integrated Diagnostic Workflow for Resource-Limited Settings
For settings where advanced genetic testing or high-spec microscopy is unavailable, this protocol maximizes the utility of TEM and clinical data.
1. Clinical Pre-Screening:
- Calculate the patient's PICADAR score to assess the pre-test probability of PCD [25]. This helps prioritize cases for limited TEM resources.
2. Rigorous TEM Analysis & Reporting:
- Adhere to the international consensus guidelines for TEM reporting [25].
- Systematically analyze a minimum of 50 transverse ciliary sections.
- Categorize defects as Class 1 (confirmatory) or Class 2 (suggestive but inconclusive) [25].
3. Action Based on TEM Result:
- Class 1 Defect Found: Supports a confirmatory PCD diagnosis.
- Normal/Class 2 Result in High PICADAR Score: Strongly indicates a case of PCD with normal ultrastructure. The conclusion should be that another testing modality is required, and this limitation should be documented. Management can be initiated based on high clinical suspicion while seeking external confirmatory testing [25].
Visualizing Diagnostic Pathways & Strategies
Diagnostic Pathway for PCD with Normal Ultrastructure
Comparative Analysis of Diagnostic Techniques
The Scientist's Toolkit: Key Research Reagents & Materials
The following table details essential materials and their functions for conducting the experiments described in this guide.
| Item/Category | Function/Application in PCD Research | Specific Example / Technical Note |
|---|---|---|
| Nasal Brushing Brush | Collects ciliated epithelial cells from the inner turbinates for ultrastructural analysis. | Flexible nylon laparoscopy brush with twisted wire shaft (e.g., WS-1812XA3) [25]. |
| Electron Microscopy Fixative | Preserves ciliary ultrastructure immediately after sample collection. | 2.5% EM-grade glutaraldehyde in 0.1M sodium cacodylate buffer, osmotically adjusted with sucrose [25]. |
| 3D Reconstruction Software | Creates and analyzes 3D models of ciliary ultrastructure from tomographic data. | IMOD & Chimera software [24]. |
| Guidelines for TEM Reporting | Standardizes the analysis and classification of ciliary defects for consistent diagnosis. | International consensus guidelines for TEM-PCD diagnostic reporting [25]. |
| PICADAR Score Sheet | A clinical tool to rate the likelihood of PCD in children with chronic wet cough, helping to pre-select patients for further testing. | Scores based on term pregnancy, neonatal symptoms, situs inversus, cardiac defects, and chronic ear/nose symptoms [25]. |
FAQs: Addressing Common Research Challenges
1. Why is PICADAR sensitivity a concern in adult research populations? PICADAR's sensitivity is significantly lower in specific patient subgroups, which is problematic for adult populations where certain classic PCD symptoms may be less pronounced. Recent research demonstrates that while PICADAR shows an overall sensitivity of 75%, this figure drops to just 61% in patients with normal organ placement (situs solitus) and 59% in those without hallmark ultrastructural defects on transmission electron microscopy. Furthermore, the tool's initial question rules out PCD in the 7% of genetically confirmed patients who do not report a daily wet cough, creating an immediate diagnostic gap in adults who may have learned to manage or adapt to chronic symptoms [4].
2. What are the primary sources of data incompleteness in adult medical histories? Data incompleteness in adult medical records arises from several systemic issues [26] [27]:
- Memory Gaps and Geographic Mobility: Patients often forget treatments from years prior, especially routine visits. Moving between cities or states scatters medical records across multiple unconnected healthcare systems.
- Documentation Practices: In EHRs, a missing data field is frequently indistinguishable from a true negative value. A patient without a documented comorbidity may truly not have the condition, or it may simply never have been recorded.
- Multi-Provider Care and System Heterogeneity: Adults typically receive care from numerous specialists, urgent care centers, and hospital systems that do not share integrated electronic health records. Data is often stored in incompatible formats across different software platforms [28].
3. What analytical methods can help predict and manage incomplete data in research datasets? Researchers can conceptualize data incompleteness as a random variable and use statistical models to understand its patterns. Effective methods identified for predicting data incompleteness include [29]:
- Kolmogorov-Smirnov goodness of fit
- Mielke distribution
- Beta distributions
- Mixture density networks (a type of neural network)
These methods help identify which variables in a dataset are most likely to be incomplete, guiding mitigation strategies.
Troubleshooting Guides
Guide 1: Enhancing PICADAR Application in Adults with Incomplete Histories
Problem: Low diagnostic sensitivity when applying PICADAR to adult patients with fragmented or incomplete early life medical records.
Solution: Implement a multi-step data augmentation and scoring adjustment protocol.
Step 1: Proactive Medical Record Canvassing Go beyond standard record requests. One study found that 90% of comprehensive medical canvasses revealed additional records not discovered through initial requests [26]. Build a chronological medical timeline by canvassing:
- Birth and neonatal records (for data on full-term gestation, neonatal chest symptoms, and special care admittance).
- Pediatric primary care and school medical records.
- All known adult primary care and specialist providers.
Step 2: Differentiate "Missing" from "Negative" For data points that remain unobtainable after exhaustive canvassing, do not automatically assume a negative score. Instead, classify them as "Unknown" and use the scoring adjustment below.
Step 3: Apply a Modified Scoring Framework For patients with incomplete histories, treat missing PICADAR parameters not as absences (which default to a negative score) but as unknowns. Consider a lower threshold for referral to definitive testing (e.g., nNO, genetic testing) in adult patients with a strong clinical suspicion of PCD, even if their adjusted PICADAR score falls below the standard cutoff [4].
Guide 2: Handling Missing Data in Electronic Health Records for Research
Problem: Missing data in EHR-derived datasets introduces bias and reduces the validity of research conclusions.
Solution: Employ rigorous analytical techniques, primarily Multiple Imputation [27].
Step 1: Understand the Mechanism Identify why the data is missing. Is it missing completely at random (MCAR), at random (MAR), or not at random (MNAR)? This guides the choice of handling method.
Step 2: Utilize Multiple Imputation This is the preferred statistical method for addressing missing data. It creates several complete datasets by replacing missing values with plausible ones based on other available variables, analyzes each dataset separately, and then pools the results.
- Crucially, include powerful predictor variables in the imputation model, even if they are not primary variables of interest in your study. These should capture [27]:
- Overall health status: e.g., Charlson Comorbidity Index.
- Healthcare utilization: e.g., number of encounters, which provides more opportunities for documentation.
- Crucially, include powerful predictor variables in the imputation model, even if they are not primary variables of interest in your study. These should capture [27]:
Step 3: Consider Data Linkage Augment your EHR data by linking with other sources, such as national death indices, census data, or disease registries, to obtain less biased variables for imputation [27].
Experimental Protocols
Protocol 1: Comprehensive Medical History Canvassing
Objective: To reconstruct a complete patient medical history by identifying and retrieving records from all healthcare providers a patient has visited.
Methodology:
- Patient Interview: Conduct a structured interview using memory aids (e.g., life event timelines, maps of past residential locations).
- Provider Identification: Use database integration and advanced algorithms to identify potential sources of records that might be missed manually, including naming variations and past providers [26].
- Record Request: Systematically request records from all identified providers, including hospitals, primary care clinics, and specialist offices. Automated systems can ensure HIPAA compliance and streamline this process [26].
- Timeline Construction: Integrate all retrieved data into a standardized chronological timeline, noting all diagnoses, procedures, medications, and encounters.
Protocol 2: Diagnostic Testing for PCD in Complex Adult Cases
Objective: To achieve a definitive PCD diagnosis in adult patients where PICADAR and standard testing may be inconclusive.
Methodology (based on ERS guidelines and recent evidence) [30] [4]:
- Initial Assessment: Apply PICADAR with the acknowledgment of its sensitivity limitations.
- First-Line Test: Measure nasal nitric oxide (nNO). Consistently low nNO levels in a technically acceptable test strongly support a PCD diagnosis.
- Genetic Testing: Perform next-generation sequencing (NGS) of known PCD genes. This is critical as 15-20% of PCD cases have normal ciliary ultrastructure. Genetic testing can provide a diagnosis where other tests are ambiguous [30].
- Advanced Ciliary Functional Analysis: Use high-speed video microscopy analysis (HSVMA) in an expert center to identify characteristic ciliary beat patterns (e.g., immotile cilia, circular beating).
- Integrative Diagnosis: Combine all test results (clinical history, nNO, genetics, HSVMA) to assign a diagnostic certainty level per ERS guidelines, rather than relying on a single test.
Workflow Diagram
The following diagram illustrates a robust workflow for diagnosing PCD in adult populations while accounting for data gaps.
Research Reagent Solutions
Table: Essential Resources for PCD Diagnostic Research
| Research Reagent / Tool | Function / Application in PCD Research |
|---|---|
| PICADAR Score | A clinical prediction rule using seven patient history parameters to estimate the probability of PCD and determine referral for testing [9]. |
| Nasal Nitric Oxide (nNO) Analyzer | A chemiluminescence device used to measure nNO levels, which are characteristically very low in most PCD patients, serving as a key screening tool [30]. |
| Next-Generation Sequencing (NGS) Panels | Genetic test targeting over 30 known PCD-causative genes. Crucial for diagnosing the 15-20% of patients with normal ciliary ultrastructure [30] [4]. |
| High-Speed Video Microscopy (HSVMA) | Equipment to record and analyze ciliary beat frequency and pattern. Specific patterns are associated with genetic mutations and ultrastructural defects [30] [4]. |
| Transmission Electron Microscope (TEM) | Used to visualize the ultrastructure of respiratory cilia and identify hallmark defects (e.g., absent dynein arms) in approximately 80% of PCD cases [30]. |
| Multiple Imputation Software | Statistical software (e.g., R, Python with SciPy) and packages that implement multiple imputation methods to handle missing data in EHR-derived research datasets [29] [27]. |
| Clinical Data Warehouse (CDW) | An integrated data architecture that consolidates heterogeneous patient data from multiple hospital software platforms (EHR, labs, imaging) into a standardized format for research [28]. |
This technical support center is designed for researchers and scientists working to improve the sensitivity of the PICADAR (PrImary CiliAry DyskinesiA Rule) score, a predictive diagnostic tool for Primary Ciliary Dyskinesia (PCD). The guidance below addresses specific experimental challenges in defining and validating new risk thresholds to enhance triage accuracy in different patient populations.
Frequently Asked Questions (FAQs)
FAQ 1: What is the established PICADAR cut-off score, and why would it need adjustment?
The original PICADAR study established a cut-off score of 5 points for predicting PCD in children with persistent wet cough, yielding a sensitivity of 0.90 and specificity of 0.75 [1]. However, subsequent research has shown that this threshold may not be optimal for all patient groups. A study involving adults with bronchiectasis found that a modified PICADAR score using a cut-off of 2 points was more effective, achieving a sensitivity of 1.00 and specificity of 0.89 [18]. Adjusting the cut-off is therefore necessary when applying the tool to new populations (like adults) or when the clinical priority shifts towards maximizing case detection (sensitivity) over confirming diagnosis (specificity).
FAQ 2: My research involves adult populations. How should I modify the PICADAR parameters?
Your protocol should consider the modified parameters validated in adult bronchiectasis cohorts [18]. The core predictive components remain similar but are adapted for adult medical histories. The key is to ensure that data collection for parameters like "neonatal respiratory distress" is feasible and reliable in an adult population, where recall bias or missing neonatal records may be a factor. The modified score focuses on a set of clinical features including situs inversus, neonatal respiratory distress, congenital cardiac defect, chronic rhinosinusitis, and chronic ear and hearing symptoms [18].
FAQ 3: What is the role of Nasal Nitric Oxide (nNO) in validating a new PICADAR threshold?
nNO measurement is a crucial objective test to validate your new subjective PICADAR score. In a diagnostic workflow, a low nNO concentration is a highly specific indicator for PCD [18]. Researchers should use nNO as a key reference standard when performing Receiver Operating Characteristic (ROC) curve analysis to determine the new optimal PICADAR cut-off. In one study, an nNO level of 77 nL/min was identified as the best discriminative value for differentiating PCD from non-PCD bronchiectasis [18]. The concordance between a high PICADAR score and a low nNO value strengthens the evidence for a new threshold.
FAQ 4: How do I perform a robust statistical analysis to define a new cut-off score?
The standard methodology involves using ROC curve analysis [1] [18]. The following workflow outlines the core process.
FAQ 5: What are common pitfalls when developing a triage tool, and how can I avoid them?
A common pitfall is creating an overly complex flowchart that is difficult to implement and inaccessible [31]. For a triage tool, simplicity and clarity are paramount. Furthermore, ensure that the risk thresholds you define align with the clinical risk appetite—the degree of uncertainty or missed cases (false negatives) that is acceptable [32] [33]. A threshold that maximizes sensitivity might be chosen if the goal is to ensure no PCD cases are missed for further testing, even if it means more false positives.
Key Experimental Protocols
Protocol 1: ROC Curve Analysis for Threshold Optimization
This protocol details the steps for determining an optimal cut-off score for the PICADAR tool.
- Objective: To identify the PICADAR score that best discriminates between PCD and non-PCD patients in your specific cohort.
- Materials: Dataset of patients with calculated PICADAR scores and definitive diagnostic outcomes (PCD positive/negative).
- Methodology:
- Data Preparation: Arrange your data with each patient as a row. Required columns are: Patient ID, definitive diagnosis (PCD Yes/No), and the calculated PICADAR score (continuous value).
- Statistical Analysis: Use statistical software (e.g., R, SPSS, Python with scikit-learn) to generate an ROC curve.
- Threshold Selection: Analyze the ROC curve to find the score that maximizes both sensitivity and specificity. The Youden's J statistic (J = Sensitivity + Specificity - 1) is a common method to identify the optimal point.
- Performance Reporting: For the new cut-off, report the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) [1] [18].
- Troubleshooting:
- Low Area Under the Curve (AUC): If the AUC is below 0.8, the predictive power of the tool in your cohort may be weak. Re-evaluate the included parameters or the patient population.
- Conflicting Goals: If maximizing sensitivity drastically reduces specificity, you may need to define two thresholds: a low score for "high sensitivity" screening and a higher score for "high specificity" confirmation.
Protocol 2: Integrating nNO with PICADAR in a Diagnostic Pathway
This protocol describes how to combine the modified PICADAR score with nNO measurement in a sequential diagnostic algorithm.
- Objective: To create a efficient screening pathway that minimizes unnecessary expensive testing (like genetic analysis).
- Materials: Equipment for nNO measurement, trained personnel, patient data for PICADAR calculation.
- Methodology:
- Calculate the modified PICADAR score for all patients.
- For patients above the new risk threshold (e.g., ≥2 points), proceed to nNO measurement.
- Use the established nNO cut-off (e.g., <77 nL/min) to identify high-probability PCD cases [18].
- Refer only patients with both a high PICADAR score and low nNO for definitive genetic testing or ciliary electron microscopy.
The logical relationship of this pathway is shown below.
Data Presentation
Table 1: Comparison of Original and Modified PICADAR Score Performance
This table summarizes key quantitative data from foundational studies to inform your experimental benchmarks.
| Parameter | Original PICADAR (Children with Chronic Wet Cough) [1] | Modified PICADAR (Adults with Bronchiectasis) [18] |
|---|---|---|
| Study Population | Consecutive referrals for PCD testing | Adults with bronchiectasis |
| Optimal Cut-off Score | 5 points | 2 points |
| Sensitivity | 0.90 | 1.00 |
| Specificity | 0.75 | 0.89 |
| Area Under the Curve (AUC) | 0.91 (internal validation) | Not explicitly stated (ROC analysis used) |
| Key Predictive Parameters | Full-term gestation, neonatal chest symptoms, NICU admission, chronic rhinitis, ear symptoms, situs inversus, congenital cardiac defect | Situs inversus, neonatal respiratory distress, congenital cardiac defect, chronic rhinosinusitis, chronic ear/hearing symptoms |
Table 2: The Scientist's Toolkit: Essential Research Reagents & Materials
A list of key resources required for experiments in PICADAR sensitivity and PCD diagnostic research.
| Item | Function / Application | Example / Note |
|---|---|---|
| Patient Clinical Data | Retrospective or prospective collection of parameters for PICADAR score calculation and validation. | Ensure data includes the core parameters like situs inversus, neonatal symptoms, and chronic otorhinolaryngologic diseases [1] [18]. |
| Nasal Nitric Oxide (nNO) Analyzer | Objective physiological measurement used to validate the PICADAR score and as part of composite diagnostic pathways. | nNO levels are significantly lower in PCD patients (e.g., 25 nL/min vs. 227 nL/min in controls); a critical reference standard [18]. |
| Statistical Software | To perform ROC curve analysis, calculate sensitivity/specificity, and determine optimal cut-off scores. | Packages in R (pROC), SPSS, Stata, or Python (scikit-learn) are standard. |
| Genetic Testing Services / Electron Microscopy | The definitive "gold standard" tests to confirm PCD diagnosis in patients identified by the screening tool. | Used to establish the ground truth for your ROC analysis [18]. |
| High-Resolution CT (HRCT) Scanner | Confirms the presence and extent of bronchiectasis, which is a key clinical feature in the patient population. | Essential for characterizing the adult bronchiectasis cohort in validation studies [18]. |
Comparative Analysis and Validation: PICADAR in the Context of Evolving Diagnostic Standards
Frequently Asked Questions (FAQs)
1. Which predictive tool has the best overall performance? Based on a 2021 study comparing the tools in 1,401 patients, the Clinical Index (CI) demonstrated a potential to outperform both PICADAR and NA-CDCF. The Area Under the ROC Curve (AUC) for CI was statistically larger than that for NA-CDCF. While the AUC for CI was also larger than for PICADAR, this difference was not statistically significant [19] [34].
2. What is the most significant limitation of the PICADAR tool? The most significant limitation of PICADAR is its variable sensitivity, which is highly dependent on patient phenotype. A 2025 study found its overall sensitivity was 75%, but this dropped to 61% for patients with situs solitus (normal organ arrangement) and 59% for those without hallmark ultrastructural defects on transmission electron microscopy. Crucially, its initial question rules out PCD in patients without a daily wet cough, which excludes about 7% of genetically confirmed PCD patients [3] [4].
3. For which patients is the Clinical Index (CI) a particularly suitable tool? The CI is a highly feasible tool because, unlike PICADAR, it does not require the assessment of laterality defects or congenital heart defects to calculate a score. This makes it applicable to a broader patient population, including those where such information is not immediately available [19].
4. Can these predictive tools be used as a standalone diagnostic for PCD? No. These tools are predictive screening tools designed to identify high-risk patients who should be referred for definitive PCD testing. They are not a replacement for specialized diagnostic tests like nasal nitric oxide (nNO) measurement, genetic testing, or high-speed video microscopy [19] [20] [35].
5. How can the predictive power of these tools be improved? The 2021 study demonstrated that combining any of the three predictive tools with nasal nitric oxide (nNO) measurement significantly improved their predictive power for PCD [19] [34].
Troubleshooting Guides
Issue 1: Low PICADAR Score in a Patient with High Clinical Suspicion for PCD
Problem: A patient presents with strong clinical symptoms of PCD (e.g., chronic rhinitis, recurrent otitis), but scores below the PICADAR cutoff (≤5 points), suggesting a low probability of disease.
Solution:
- Action: Do not rule out PCD based on the low PICADAR score alone.
- Rationale: PICADAR has known limitations in sensitivity, especially in patients with situs solitus (61% sensitivity) or without hallmark ultrastructural defects (59% sensitivity) [3] [4].
- Next Steps:
- Use an alternative tool: Calculate the NA-CDCF or Clinical Index (CI) score. The CI may be particularly useful as it does not rely on laterality assessment [19].
- Proceed with objective testing: Refer the patient for definitive testing, such as nasal nitric oxide (nNO) measurement, which can improve the predictive power of any clinical tool [19] [34].
- Consider the phenotype: Be aware that patients with mutations in genes like DNAH11 or RSPH1 often have normal organ arrangement and may be missed by PICADAR [4] [20].
Issue 2: Applying a Predictive Tool to Adult Patients
Problem: Gathering accurate historical data for tools like PICADAR (e.g., gestational age, neonatal intensive care unit admission) is difficult for adult patients.
Solution:
- Action: Use the Clinical Index (CI) as a primary screening tool.
- Rationale: The seven items in the CI questionnaire focus on clinical symptoms that are easier to ascertain in a retrospective patient history, such as a history of pneumonia, multiple episodes of bronchitis, or chronic otitis [19].
- Alternative: If using PICADAR is mandatory, note that missing neonatal data will lower the score and reduce the tool's sensitivity. A low score in this context should be interpreted with caution, and further investigation may still be warranted [19].
Quantitative Data Comparison
Table 1: Direct Comparison of PCD Predictive Tools in a Cohort of 1,401 Suspected Patients [19]
| Tool | Full Name | Number of Items | Key Strengths | Key Limitations | Area Under the Curve (AUC) |
|---|---|---|---|---|---|
| Clinical Index (CI) | Clinical Index | 7 | Does not require assessment of laterality; high feasibility. | Less widely validated than PICADAR. | Largest AUC (larger than NA-CDCF, p=0.005) |
| PICADAR | Primary Ciliary Dyskinesia Rule | 7 (plus initial wet cough question) | Widely recognized and validated in chronic wet cough populations. | Cannot be scored in patients without chronic wet cough (6.1% of cohort); requires neonatal history. | AUC did not differ significantly from NA-CDCF (p=0.093) |
| NA-CDCF | North American Criteria Defined Clinical Features | 4 | Simple and quick to calculate. | Lower AUC than CI in head-to-head comparison. | Smaller AUC than CI (p=0.005) |
Table 2: Sensitivity Analysis of PICADAR in Genetically Confirmed PCD Patients (n=269) [3] [4]
| Patient Subgroup | Median PICADAR Score (IQR) | Sensitivity | Clinical Implication |
|---|---|---|---|
| All Genetically Confirmed PCD | 7 (5 – 9) | 75% | 1 in 4 PCD patients may be missed. |
| With Laterality Defects | 10 (8 – 11) | 95% | Tool works well for classic phenotypes. |
| With Situs Solitus (normal arrangement) | 6 (4 – 8) | 61% | High risk of false negatives in this group. |
| With Hallmark Ultrastructural Defects | Information missing | 83% | Better performance for clear structural abnormalities. |
| Without Hallmark Ultrastructural Defects | Information missing | 59% | Poor performance for normal ultrastructure genotypes. |
Experimental Protocols
Protocol 1: Validating a Predictive Tool in a Clinical Cohort
This methodology is based on the 2021 study that compared CI, PICADAR, and NA-CDCF [19].
1. Study Population Recruitment:
- Participants: Recruit patients referred to a tertiary center for suspected PCD. Inclusion criteria should mirror clinical practice (e.g., recurrent respiratory infections, bronchiectasis, laterality defects).
- Exclusion: Children under 1 year of age, as relevant clinical data for the questionnaires may be incomplete or lack predictive value.
2. Data Collection and Scoring:
- Clinical History: Collect a structured patient history conducted by a physician experienced in PCD. Record all signs and symptoms relevant to the CI, PICADAR, and NA-CDCF questionnaires.
- Tool Scoring: Calculate the scores for each of the three predictive tools based on their original published criteria [19] [36].
3. Definitive PCD Diagnosis (Reference Standard):
- Perform a multi-step diagnostic process according to international guidelines [19] [35]:
- Nasal Nitric Oxide (nNO): Measure nNO in patients older than 3 years using a standardized protocol.
- High-Speed Video Microscopy Analysis (HSVA): Analyze ciliary beat frequency and pattern via nasal brushing.
- Confirmatory Tests: Refer patients with high probability of PCD for transmission electron microscopy (TEM) and genetic testing via next-generation sequencing (NGS) of a PCD gene panel.
- Establish a definitive PCD diagnosis based on a clear ultrastructural defect or the presence of biallelic disease-causing mutations.
4. Data Analysis:
- Statistical Comparison: Use receiver operating characteristic (ROC) curves to calculate and compare the Area Under the Curve (AUC) for each predictive tool.
- Sensitivity/Specificity: Calculate the sensitivity and specificity at recommended score cutoffs (e.g., ≥5 for PICADAR).
- nNO Integration: Analyze how the addition of nNO measurement improves the predictive power of each tool.
Protocol 2: Assessing Tool Sensitivity Across Genotypes
This protocol is derived from the 2025 study highlighting PICADAR's limitations [3] [4].
1. Cohort Selection:
- Participants: Include only patients with a genetically confirmed PCD diagnosis to ensure an unambiguous reference standard.
2. Phenotypic and Genotypic Stratification:
- Data Grouping: Stratify the patient cohort into subgroups based on:
- Laterality: Situs inversus vs. situs solitus.
- Ultrastructural Group: As predicted by the genotype (e.g., outer dynein arm defects, inner dynein arm with microtubule disorganization, normal ultrastructure).
- Tool Application: Calculate the PICADAR score for every patient based on their retrospectively collected clinical data.
3. Sensitivity Calculation:
- Calculate the sensitivity of the tool for the overall cohort and for each pre-defined subgroup. Sensitivity is defined as the percentage of genetically confirmed PCD patients who score at or above the tool's recommended cutoff point.
Research Reagent Solutions
Table 3: Essential Materials for PCD Diagnostic Research
| Item / Technique | Function in PCD Research | Key Considerations |
|---|---|---|
| High-Speed Video Microscopy (HSVM) | To analyze ciliary beat frequency and pattern for functional assessment of cilia. | Requires specialized equipment and expert personnel for interpretation [19] [20]. |
| Transmission Electron Microscopy (TEM) | To visualize the ultrastructural defects of cilia (e.g., absent dynein arms). | Considered a definitive test, but some genetic forms have normal ultrastructure [19] [35]. |
| Next-Generation Sequencing (NGS) Gene Panels | To identify disease-causing mutations in over 50 known PCD-associated genes. | Essential for genetic confirmation, especially in cases with inconclusive other tests [19] [20]. |
| Nasal Nitric Oxide (nNO) Analyzer | To measure nasal NO levels, which are characteristically very low in most PCD patients. | A useful screening test; values improve the predictive power of clinical tools [19] [34]. |
Workflow and Relationship Visualizations
The development of the PrImary CiliARy DyskinesiA Rule (PICADAR) represents a significant advancement in identifying patients who require definitive testing for Primary Ciliary Dyskinesia (PCD), a rare genetic disorder characterized by abnormal ciliary function and chronic respiratory symptoms [9]. As a diagnostic predictive tool, PICADAR was designed to address the challenge posed by the non-specific nature of PCD symptoms and the highly specialized, expensive nature of confirmatory diagnostic tests [9]. The original derivation study, published in 2016, demonstrated promising performance with a sensitivity of 0.90 and specificity of 0.75 at a recommended cut-off score, with an Area Under the Curve (AUC) of 0.91 upon internal validation [9]. However, for a clinical prediction rule to achieve widespread adoption and trust within the scientific and clinical communities, it must demonstrate robust performance across diverse, independent international cohorts—a process known as external validation. This article establishes a technical support framework for researchers conducting such validations, providing troubleshooting guidance and methodological protocols to standardize this critical research and ultimately contribute to improving PICADAR's diagnostic sensitivity.
PICADAR Performance Metrics: A Comparative Analysis
The following tables summarize key performance metrics from the original derivation study and subsequent independent external validations, providing a benchmark for researchers.
Table 1: Performance Metrics of PICADAR from Validation Studies
| Study / Cohort | Sample Size (PCD+/Total) | Area Under Curve (AUC) | Sensitivity | Specificity | Recommended Cut-off |
|---|---|---|---|---|---|
| Original Derivation (UHS) [9] | 75 / 641 | 0.91 | 0.90 | 0.75 | 5 points |
| External Validation (RBH) [9] | 93 / 187 | 0.87 | Not Reported | Not Reported | Applied |
| Czech Republic Cohort (2021) [19] | 67 / 1401 | Comparable to original | Not Reported | Not Reported | Applied |
Table 2: PICADAR Scoring Criteria and Parameters [9]
| Predictive Parameter | Score |
|---|---|
| Full-term gestation (≥37 weeks) | 2 |
| Neonatal chest symptoms (at term) | 2 |
| Admission to Neonatal Intensive Care Unit (at term) | 1 |
| Chronic rhinitis (persisting >3 months) | 1 |
| Chronic ear symptoms (persisting >3 months) | 1 |
| Situs Inversus (confirmed by chest X-ray) | 2 |
| Congenital cardiac defect (confirmed by echocardiogram) | 2 |
| Total Possible Score | 11 |
The Researcher's Toolkit: Essential Reagents and Materials
Table 3: Key Research Reagent Solutions for PICADAR Validation
| Item / Reagent | Function / Application in Validation |
|---|---|
| Structured Data Collection Form | Standardizes the collection of the seven clinical parameters from patient histories across different study sites. |
| Reference Standard Diagnostic Tools | Confirms PCD diagnosis; includes High-Speed Video Microscopy (HSVM), Transmission Electron Microscopy (TEM), Genetic Testing, and Nasal Nitric Oxide (nNO) measurement [19]. |
| Nasal Nitric Oxide (nNO) Analyzer | Provides an objective, high-screening performance measure (e.g., Niox Mino/Vero) to use alongside PICADAR [19]. |
| Statistical Analysis Software (e.g., SPSS, R) | Used for performing Receiver Operating Characteristic (ROC) curve analysis and calculating AUC, sensitivity, and specificity [9]. |
Technical Support Center: Troubleshooting Common Validation Challenges
Frequently Asked Questions (FAQs)
1. In our cohort, PICADAR's sensitivity is significantly lower than the originally reported 0.90. What could be the cause?
This is a common finding in external validation. Potential causes and solutions include:
- Population Differences: Your cohort may have a different case mix, such as a higher proportion of patients without laterality defects (situs inversus) or with milder phenotypes. Solution: Conduct a subgroup analysis to identify which patient populations (e.g., those without situs inversus) are driving the lower sensitivity. This data is crucial for refining the tool [36].
- Spectrum Bias: The original study enrolled patients consecutively referred for testing, but your cohort might be skewed towards more or less severe cases. Solution: Clearly document the referral patterns and baseline characteristics of your cohort to contextualize your findings [9] [19].
- Misapplication of the Tool: Ensure PICADAR is only applied to patients with a persistent wet cough, as this was a prerequisite in the original study. Application to patients without this key symptom can impair performance [19].
2. How should we handle missing data for one or more of the seven PICADAR parameters?
- Best Practice: Aim for a complete case analysis where possible. In the original study, subjects with missing data were excluded on a case-wise basis [9].
- Advanced Technique: If missing data is substantial, consider using multiple imputation techniques to check for potential biases introduced by complete case analysis. The original developers used this method to confirm their model's accuracy [9].
3. Can PICADAR be used as a standalone tool to rule out PCD?
- Answer: No. PICADAR is a predictive rule to triage patients for specialized testing, not a diagnostic test itself. A score below the cut-off does not definitively exclude PCD. The European Respiratory Society guidelines recommend confirmation in a specialist centre using a combination of tests [9] [19]. It should be used as part of a multi-step diagnostic pathway.
4. How does PICADAR compare to other predictive tools like the Clinical Index (CI) or NA-CDCF?
- Evidence: A 2021 study found that while all tools (CI, PICADAR, NA-CDCF) effectively identified PCD patients, the CI may have certain practical advantages. Specifically, PICADAR could not be calculated for 6.1% of patients due to the absence of a chronic wet cough, whereas the CI does not have this prerequisite. Furthermore, combining any of these clinical tools with nNO measurement significantly improved predictive power [19].
Troubleshooting Guide for Experimental Protocols
This guide follows a logical, divide-and-conquer approach to diagnosing and resolving common methodological issues.
Scenario: Poor Specificity (High False Positive Rate) in Your Validation
You find that PICADAR identifies too many patients as high-risk who are later confirmed not to have PCD, overburdening specialist services.
Root Cause Analysis and Resolution Steps:
Verify the Cut-off Score:
- Action: Do not rely solely on the published cut-off of 5. Generate your own ROC curve and calculate the AUC. A high AUC (>0.8) with poor specificity at a cut-off of 5 suggests the optimal threshold for your population may be higher [9].
- Solution: Re-calibrate the cut-off score to improve specificity, even if it results in a slight reduction in sensitivity.
Enforce the "Persistent Wet Cough" Prerequisite:
- Action: Audit your patient cases. The PICADAR tool was explicitly developed for patients with a persistent wet cough. Including patients without this symptom can introduce noise and reduce specificity [9] [19].
- Solution: Ensure your inclusion criteria mirror the original study. Apply PICADAR only to eligible patients.
Objectively Verify Key Parameters:
- Action: Check how parameters like "situs inversus" and "congenital cardiac defect" were ascertained. Self-report or vague history is unreliable.
- Solution: As per the original protocol, "situs inversus" should be confirmed by imaging (e.g., chest X-ray or dextrocardia on ECG) and "congenital cardiac defect" by echocardiogram report [9]. This moves from subjective history to objective data.
Standardized Experimental Protocol for External Validation
To ensure consistency and comparability across research sites, adhere to the following detailed protocol.
Objective: To externally validate the PICADAR diagnostic prediction tool in an independent, consecutive cohort of patients referred for suspected PCD.
Workflow Overview:
Methodology:
Cohort Identification & Eligibility:
- Enroll consecutive patients referred to your center for PCD diagnostic testing.
- Inclusion Criteria: Patients with a persistent wet cough and clinical suspicion of PCD. Record age, gender, and ethnicity.
- Exclusion Criteria: Children under 1 year old, as relevant clinical history may be insufficient [19].
- Ethics Approval: Obtain informed consent and secure approval from the local ethics committee before study initiation [19].
Data Collection - PICADAR Parameters:
- Using a pre-piloted, structured form, collect the seven predictive parameters prior to definitive diagnostic testing [9].
- Key Definitions:
- Neonatal chest symptoms: Respiratory distress (e.g., tachypnea, grunting, supplemental oxygen requirement) in a full-term newborn.
- Chronic rhinitis/ear symptoms: Symptoms persisting for >3 months.
- Situs inversus & Cardiac defects: Must be confirmed by objective imaging (CXR, echocardiogram).
Reference Standard Testing:
- All patients must undergo a definitive reference standard test for PCD to determine their true disease status (PCD+ or PCD-).
- Follow international guidelines [19], using a combination of:
- Nasal Nitric Oxide (nNO): Measured with an electrochemical analyzer (e.g., Niox Mino/Vero) in patients older than 3 years. A low value (<30 nL·min⁻¹ or ~77 ppb) is suggestive of PCD [9] [19].
- High-Speed Video Microscopy (HSVM): Analyze ciliary beat frequency and pattern. Repeat after recovery from infection if secondary dyskinesia is suspected [19].
- Transmission Electron Microscopy (TEM): Identify hallmark ultrastructural defects [9] [19].
- Genetic Testing: Use next-generation sequencing panels for known PCD genes [19].
- A positive diagnosis is typically based on a characteristic clinical history plus at least two abnormal diagnostic tests (e.g., hallmark TEM defect + low nNO) [9].
Statistical Analysis & Performance Assessment:
- Calculate the PICADAR score (0-11) for each patient.
- Use the reference standard outcome as the gold standard to create a 2x2 contingency table.
- Perform ROC curve analysis to determine the AUC for PICADAR in your cohort.
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) at the published cut-off of 5 and other relevant thresholds. Use statistical software (e.g., SPSS, R) for these calculations [9].
Within the ongoing research aimed at improving the sensitivity of the PICADAR (PrImary CiliARy DyskinesiA Rule) predictive tool, a central tension exists between the competing values of diagnostic coverage and tool simplicity. PICADAR is a clinical prediction rule designed to identify patients who require specialized testing for Primary Ciliary Dyskinesia (PCD), a rare, genetically heterogeneous disorder caused by ciliary dysfunction [9] [20]. This technical support center addresses the key challenges researchers and clinicians face when employing PICADAR in diagnostic and research settings, providing targeted troubleshooting guides and FAQs to support its critical evaluation and refinement.
PICADAR at a Glance: Performance Data and Core Components
The diagnostic performance of PICADAR, as established in its original derivation and as revealed in recent validation studies, is summarized in the table below. This data is essential for benchmarking and understanding its limitations.
Table 1: Comparative Performance Metrics of the PICADAR Tool
| Study & Population | Reported Sensitivity | Reported Specificity | Area Under the Curve (AUC) | Key Limiting Factor Identified |
|---|---|---|---|---|
| Original Derivation Study (Behan et al., 2016) [9] | 0.90 | 0.75 | 0.91 (internal), 0.87 (external) | Original design target. |
| Recent Validation Study (Schramm et al., 2025) [3] [4] | 0.75 (Overall) | Not Reported | Not Reported | Overall sensitivity drop. |
| → Subgroup: With Laterality Defects (e.g., Situs Inversus) [3] [4] | 0.95 | Not Reported | Not Reported | High sensitivity maintained. |
| → Subgroup: With Situs Solitus (normal arrangement) [3] [4] | 0.61 | Not Reported | Not Reported | Severely reduced sensitivity. |
| → Subgroup: With Hallmark Ultrastructural Defects [3] [4] | 0.83 | Not Reported | Not Reported | Moderately high sensitivity. |
| → Subgroup: Without Hallmark Ultrastructural Defects [3] [4] | 0.59 | Not Reported | Not Reported | Severely reduced sensitivity. |
The PICADAR Logic and Workflow
The PICADAR tool operates on a specific logical pathway, starting with a key initial filter. The following diagram illustrates this workflow and the scoring process for patients who present with a persistent wet cough.
PICADAR Scoring Parameters: The seven predictive parameters, readily obtained from patient history, are [9]:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care unit admission
- Chronic rhinitis
- Chronic ear symptoms
- Situs inversus (a laterality defect where organs are mirrored)
- Congenital cardiac defect
Troubleshooting Guides
Guide 1: Addressing Low Sensitivity in Specific Patient Subgroups
Problem: The PICADAR tool fails to identify a significant number of true PCD cases, particularly in patients who do not present with classic "red flags" like situs inversus.
Background: Recent 2025 research has demonstrated that PICADAR's overall sensitivity is 75%, but it drops drastically to 61% in patients with situs solitus (normal organ arrangement) and 59% in patients without hallmark ciliary ultrastructural defects [3] [4]. This is because 7% of genetically confirmed PCD patients do not have a daily wet cough and are immediately ruled out by the tool's initial question [3].
Investigation Protocol:
- Confirm Patient Phenotype: Stratify your study cohort or patient by:
- Laterality: Situs solitus vs. situs inversus/heterotaxy.
- Genetic/Ultrastructural Status: Presence or absence of known hallmark defects (e.g., ODA/IDA defects) [20].
- Calculate Subgroup-Specific Sensitivity: Apply PICADAR to each subgroup separately. Compare the sensitivity values to the overall performance.
- Analyze False Negatives: Closely examine the clinical profiles of PCD-positive patients who scored below the PICADAR cut-off (<5 points). Identify which parameters (e.g., absence of neonatal symptoms, term gestation) are leading to the low score.
Solution:
- Do not use PICADAR in isolation. The 2025 study concludes that "PICADAR should not be the only factor to initiate diagnostic work-up for PCD" and should "be used with caution" [3] [4].
- Implement a multi-step diagnostic process as recommended by current guidelines [20]. PICADAR may serve as an initial trigger, but it must be followed by specialized tests (e.g., genetic testing, high-speed video microscopy, nasal nitric oxide measurement) in patients with a high clinical suspicion, even if their PICADAR score is low.
Guide 2: Resolving Tension Between Simplicity and Diagnostic Coverage
Problem: The tool's design prioritizes simplicity, using only easily available clinical data, but this inherent simplicity limits its ability to cover the full, complex spectrum of PCD.
Background: The value of "simplicity" in diagnostic tools is often assumed to guarantee accessibility and use in non-specialist settings [37]. However, this can be at odds with the biological complexity of diseases like PCD, which involves over 50 associated genes and diverse clinical presentations [20]. A tool that is too "simple" or "fluid" can be dangerous if it fails to accurately classify patients [37].
Investigation Protocol:
- Evaluate Workflow Integration: Assess if the simple, 7-question format integrates well into clinical workflow without increasing cognitive load [38].
- Test for "Fluidity": Determine if the tool's criteria are being interpreted consistently across different users and sites. Inconsistent interpretation can compromise the reliability of the score.
- Identify Gaps in "Coverage": Map the known genetic and ultrastructural variants of PCD against the parameters covered by PICADAR. This will visually highlight the phenotypic and genotypic groups that are poorly captured.
Solution:
- Develop complementary tools. Research efforts should focus on creating alternative or supplementary predictive tools for PCD subgroups with normal body composition (situs solitus) and normal ultrastructure [3].
- Adopt a human-centered design approach for new tools. This involves collaboration between developers, clinicians, and researchers to ensure new tools are usable, useful, and fit within clinical workflow without sacrificing necessary complexity [38]. The goal is a tool that is as simple as possible, but no simpler.
Frequently Asked Questions (FAQs)
Q1: The original 2016 paper showed 90% sensitivity, but recent studies show 75%. Which one is correct, and why the discrepancy?
Both are likely correct for their respective study populations. The original 2016 study derived and validated the tool in a population referred for testing [9]. The 2025 study by Schramm et al. validated PICADAR in a cohort of genetically confirmed PCD patients, which includes the full spectrum of the disease, especially those with milder or atypical presentations (e.g., without laterality defects) that the original tool was not as effective in capturing [3] [4]. This highlights the importance of independent validation.
Q2: Our research focuses on a novel PCD gene not associated with situs inversus. Is PICADAR suitable for our study?
You should use PICADAR with great caution. The 2025 data shows a significant drop in sensitivity (to 61%) for patients with situs solitus [3]. Using PICADAR as a primary inclusion criterion for such a study could lead to a high rate of false negatives, omitting a large portion of your target population and biasing your results. Relying on genetic screening or other functional tests would be more appropriate.
Q3: How can we improve PICADAR's sensitivity without making it too complex for general clinicians to use?
This is the core challenge. Potential research directions include:
- Weighted Parameters: Investigating if certain parameters should be weighted more heavily, especially those more common in atypical PCD.
- New Predictive Variables: Exploring the addition of one or two other easily obtainable data points that are common in false-negative cases.
- Sequential Testing: Developing a two-stage rule where a low PICADAR score triggers a second, more specific (but still simple) set of questions or a readily available test like nasal nitric oxide.
Q4: What is the single most important takeaway for using PICADAR in a clinical research setting?
PICADAR is a useful initial screening tool but has major limitations. It performs excellently in "classic" PCD cases with laterality defects but misses a substantial number of patients with situs solitus. It should be a component of a diagnostic pathway, not the gatekeeper [3] [4] [20].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Materials for PCD Diagnostic Research
| Item | Function in Research | Relevance to PICADAR Validation |
|---|---|---|
| Genetic Testing Panels (For >50 known PCD genes) | Provides a definitive molecular diagnosis for PCD, serving as a key gold standard for validating diagnostic tools. [20] | Essential for confirming PCD status in study participants to calculate true sensitivity and specificity of PICADAR. |
| High-Speed Video Microscopy Analysis (HSVA) | Allows for the functional assessment of ciliary beat pattern and frequency. | Used as a key diagnostic test to correlate PICADAR scores with ciliary function. |
| Transmission Electron Microscopy (TEM) | Visualizes the ultrastructural defects in cilia (e.g., absent dynein arms). | Critical for stratifying PCD patients into subgroups (e.g., with/without hallmark defects) when analyzing PICADAR's performance. [3] [20] |
| Nasal Nitric Oxide (nNO) Measurement | A well-established screening test for PCD, as nNO is typically very low in patients. | Can be used alongside PICADAR in a multi-step diagnostic algorithm to improve overall accuracy. [9] [20] |
| Immunofluorescence (IF) Assays | Uses antibodies to detect the absence or mislocalization of specific ciliary proteins. | A modern technique that can provide a genetic diagnosis and help characterize variants, complementing TEM and genetics. [20] |
FAQs: PICADAR in Research and Clinical Practice
Q1: What is the PICADAR score and what is its primary purpose? The Primary Ciliary Ciliary DyskinesiA Rule (PICADAR) is a clinical prediction tool designed to help non-specialists identify patients with a high probability of Primary Ciliary Dyskinesia (PCD) who should be referred for definitive diagnostic testing [9] [1]. It was developed to address the challenge of PCD's non-specific symptoms and the highly specialized, expensive nature of confirmatory tests like genetic testing, transmission electron microscopy (TEM), and high-speed video microscopy analysis (HSVA) [9] [20].
Q2: What are the seven predictive parameters of the PICADAR tool? PICADAR is applied to patients with a persistent wet cough and assesses seven clinical parameters readily obtained from patient history [9] [1]:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care unit admittance
- Chronic rhinitis
- Ear symptoms (e.g., otitis media)
- Situs inversus
- Congenital cardiac defect
Q3: What was the original reported performance of PICADAR? In the original 2016 validation study, PICADAR demonstrated high accuracy [9] [1] [39]:
- Sensitivity: 0.90
- Specificity: 0.75
- Area Under the Curve (AUC): 0.91 (internal validation) and 0.87 (external validation) A score of ≥5 points was established as the cut-off, indicating a higher likelihood of PCD [9].
Q4: What are the key limitations of PICADAR identified by recent evidence? A 2025 study highlights significant limitations, revealing that PICADAR's sensitivity is not uniform across all PCD patient subgroups [3]. The tool has limited sensitivity in specific populations, which can lead to missed diagnoses if used as the sole screening factor.
Q5: How can a researcher troubleshoot low PICADAR sensitivity in their cohort? If your study population has a high proportion of PCD patients without laterality defects or with normal ciliary ultrastructure, PICADAR is likely to miss a substantial number of cases [3]. You should:
- Stratify your analysis based on the presence of laterality defects.
- Do not rely exclusively on PICADAR; consider it as part of a multi-tool framework that includes other clinical criteria or initial tests like nasal nitric oxide (nNO) measurement where available [20].
Table 1: Comparison of PICADAR Performance Metrics from Key Studies
| Study & Population | Sensitivity | Specificity | Area Under Curve (AUC) | Key Finding |
|---|---|---|---|---|
| Behan et al. (2016) - Original Derivation & Validation [9] [1] | 0.90 | 0.75 | 0.91 (internal)0.87 (external) | Validated as a simple, accurate prediction tool for general PCD referral. |
| Omran et al. (2025) - Genetically Confirmed PCD Cohort (n=269) [3] | 0.75 | Not Reported | Not Reported | Overall sensitivity is lower than originally reported. |
| Omran et al. (2025) - Subgroup with Situs Solitus (normal organ arrangement) [3] | 0.61 | Not Reported | Not Reported | Significantly reduced sensitivity in this large subgroup. |
| Omran et al. (2025) - Subgroup without Hallmark Ultrastructural Defects [3] | 0.59 | Not Reported | Not Reported | Significantly reduced sensitivity in this subgroup. |
| Omran et al. (2025) - Subgroup with Laterality Defects (e.g., situs inversus) [3] | 0.95 | Not Reported | Not Reported | High sensitivity, performs well in this classic phenotype. |
Table 2: PICADAR Scoring System and Probability of PCD [9] [39]
| Predictive Parameter | Points Assigned |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms | 1 |
| Neonatal intensive care unit admittance | 2 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 2 |
| Total Score Interpretation | Approximate Probability of PCD |
| ≥ 5 points | 11.1% |
| ≥ 10 points | > 90% |
Experimental Protocols
Protocol 1: Validating PICADAR in a Research Cohort
This protocol outlines the steps for evaluating the performance of the PICADAR tool within a specific patient population.
1. Objective: To determine the sensitivity, specificity, and predictive values of the PICADAR score in a cohort of patients referred for suspected PCD.
2. Materials: See "Research Reagent Solutions" below.
3. Methodology:
- Patient Recruitment: Consecutively enroll patients referred to a specialist center for PCD testing. The study should include all ages. Collect basic demographic data (age, sex, ethnicity) [9].
- Data Collection: Prior to definitive diagnostic testing, a clinician should conduct a clinical interview using a standardized proforma to collect data on the seven PICADAR parameters and other relevant clinical history [9].
- PICADAR Scoring: Calculate the PICADAR score for each patient. The tool is only applicable to patients with a persistent wet cough. Patients without a daily wet cough are considered screen-negative [3].
- Reference Standard (PCD Diagnosis): Establish a definitive diagnosis using a combination of advanced tests, as there is no single gold standard [20]. The European Respiratory Society guidelines recommend a combination of:
- Genetic Testing: Identify biallelic pathogenic mutations in a known PCD-associated gene [3] [20].
- Transmission Electron Microscopy (TEM): Identify hallmark ultrastructural defects in the ciliary axoneme (e.g., outer dynein arm defects) [9] [20].
- High-Speed Video Microscopy Analysis (HSVA): Identify characteristic abnormal ciliary beat patterns and frequency [9] [20].
- Nasal Nitric Oxide (nNO): Very low nNO is a strong indicator of PCD [9] [20].
- Data Analysis:
- Classify patients as PCD-positive or PCD-negative based on the reference standard.
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for the recommended PICADAR cut-off score (≥5).
- Perform subgroup analyses based on the presence of laterality defects and ciliary ultrastructure [3].
- Generate a Receiver Operating Characteristic (ROC) curve and calculate the Area Under the Curve (AUC) to assess overall discriminative ability [9].
Protocol 2: Evaluating PICADAR in a Multi-Tool Diagnostic Framework
1. Objective: To assess the incremental value of adding PICADAR to other screening tools like nasal nitric oxide (nNO) in a diagnostic algorithm for PCD.
2. Methodology:
- Study Design: A prospective cohort study of consecutive referrals.
- Interventions:
- All patients undergo the standard clinical history intake for PICADAR scoring.
- All patients undergo nNO measurement.
- All patients proceed to definitive testing (genetics, TEM, HSVA) as the reference standard.
- Data Analysis:
- Calculate the performance of PICADAR alone and nNO alone.
- Develop a diagnostic algorithm (e.g., proceed to definitive testing if either PICADAR ≥5 OR nNO is low) and calculate its sensitivity and specificity.
- Compare the performance of the combined algorithm against each tool in isolation.
Diagnostic Pathway & Sensitivity Analysis
Research Reagent Solutions
Table 3: Essential Materials and Reagents for PCD Diagnostic Research
| Item / Technique | Function / Role in PCD Diagnosis | Key Considerations |
|---|---|---|
| Genetic Testing Panels | Identifies pathogenic mutations in over 50 known PCD-associated genes (e.g., DNAH5, DNAI1, CCDC39, CCDC40) [20]. | Essential for a definitive diagnosis, especially in cases with normal ciliary ultrastructure. Critical for correlating genotype with PICADAR performance. |
| Transmission Electron Microscopy (TEM) | Visualizes the ultrastructure of ciliary axoneme to identify hallmark defects (e.g., absent outer dynein arms, microtubule disorganization) [9] [20]. | Considered a cornerstone diagnostic method. Required for subgroup analysis of PICADAR sensitivity based on ultrastructural phenotype [3]. |
| High-Speed Video Microscopy (HSVA) | Analyzes ciliary beat pattern and frequency to identify characteristic dyskinetic movements [9] [20]. | Requires experienced scientists for interpretation. Used in combination with other tests for a definitive diagnosis. |
| Nasal Nitric Oxide (nNO) Analyzer | Measures nasal NO levels; chronically low nNO is a highly sensitive and specific screening biomarker for PCD [9] [20]. | A valuable tool to use in conjunction with PICADAR in a multi-modal screening framework. |
| Cell Culture (Air-Liquid Interface) | Re-differentiates ciliated epithelium in vitro to rule out secondary ciliary dyskinesia caused by infection or inflammation [9]. | Used to confirm primary ciliary defects when initial tests are inconclusive. |
Conclusion
The PICADAR tool represents a significant step forward in systematizing the referral for PCD testing, yet its documented limitations necessitate a refined and nuanced application. Evidence confirms that its sensitivity is not uniform, being substantially lower in patients with situs solitus or without hallmark ultrastructural defects. Future directions must focus on developing integrated diagnostic algorithms that combine a potentially optimized PICADAR score with other tools like the Clinical Index and objective measures such as nasal nitric oxide. For researchers and drug developers, this underscores the importance of considering these patient subgroups in clinical trial design and the development of novel therapeutics. Ultimately, advancing PCD diagnostics will rely on a multifaceted strategy that enhances predictive tools, incorporates new genetic insights, and validates these approaches across diverse, real-world populations to ensure no patient is overlooked.
References
- 1. a diagnostic predictive tool for primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/26917608/]
- 2. Primary Ciliary Dyskinesia: A Clinical Review [https://www.mdpi.com/2073-4409/13/11/974]
- 3. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1691758/full]
- 4. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1]
- 5. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 6. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 7. 敏感性、特异性、灵敏度...检验人必须弄清楚的十大问题! [https://csmedlab.com/2022/09/02/%E6%95%8F%E6%84%9F%E6%80%A7%E3%80%81%E7%89%B9%E5%BC%82%E6%80%A7%E3%80%81%E7%81%B5%E6%95%8F%E5%BA%A6-%E6%A3%80%E9%AA%8C%E4%BA%BA%E5%BF%85%E9%A1%BB%E5%BC%84%E6%B8%85%E6%A5%9A%E7%9A%84%E5%8D%81/]
- 8. Specificity in Preclinical Drug Development Models [https://emulatebio.com/specificity-in-preclinical-drug-development-models-organ-chips/]
- 9. a diagnostic predictive tool for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819882/]
- 10. Sensitivity and Specificity Fundamentals [https://www.beckmancoulter.com/en/blog/diagnostics/sensitivity-and-specificity-fundamentals]
- 11. 写好诊断性meta分析的秘密(三) [https://www.xiahepublishing.com/2475-7543/MRP-2017-075]
- 12. Situs solitus [https://en.wikipedia.org/wiki/Situs_solitus]
- 13. Deciphering normal and anomalous viscero-atrial situs on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6818198/]
- 14. Analysis of the clinical features of Japanese patients with ... [https://www.sciencedirect.com/science/article/pii/S0385814621002248]
- 15. European Respiratory Society guidelines for the diagnosis of ... [https://publications.ersnet.org/content/erj/49/1/1601090]
- 16. Nasal nitric oxide measurement for the diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171850/]
- 17. Electrochemical nasal nitric oxide measurement during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598594/]
- 18. Thieme E-Journals - Pneumologie / Full Text [https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0043-111909?device=desktop]
- 19. Evaluation of a Clinical Index as a Predictive Tool for Primary Ciliary... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232329/]
- 20. Primary Ciliary Dyskinesia—Current Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525432/]
- 21. Understanding Genotype–Phenotype Correlations in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9757100/]
- 22. Clinical relevance of genotype–phenotype correlations ... [https://www.nature.com/articles/s41436-021-01132-x]
- 23. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 24. Primary ciliary dyskinesia with normal ultrastructure [https://pubmed.ncbi.nlm.nih.gov/29467202/]
- 25. Ultrastructure for the diagnosis of primary ciliary dyskinesia ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2023.1247638/full]
- 26. The Hidden Cost of Incomplete Medical Histories [https://isgvalue.com/the-hidden-cost-of-incomplete-medical-histories-why-comprehensive-record-canvassing-is-essential/]
- 27. Strategies for Handling Missing Data in Electronic Health ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4371484/]
- 28. Clinical data integration and processing challenges in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12461051/]
- 29. Analyzing the Data Completeness of Patients' Records ... [https://www.mdpi.com/2076-3417/12/21/10746]
- 30. Clinical care for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC9489029/]
- 31. Key Considerations for Flowchart Accessibility - MN.gov [https://mn.gov/mnit/about-mnit/accessibility/news/?id=38-436349]
- 32. What is Risk Threshold in Project Management? [https://projectriskcoach.com/what-is-risk-threshold-in-project-management/]
- 33. Role of Risk Thresholds in Risk Prioritization and Ranking [https://trustedinstitute.com/concept/pmi-rmp/risk-thresholds-triggers/risk-thresholds-in-risk-prioritization/]
- 34. Evaluation of a Clinical Index as a Predictive Tool for ... [https://pubmed.ncbi.nlm.nih.gov/34198708/]
- 35. Primary Ciliary Dyskinesia—Current Diagnostic and ... [https://www.mdpi.com/2077-0383/14/19/6808]
- 36. a diagnostic predictive tool for primary ciliary dyskinesia [https://www.semanticscholar.org/paper/PICADAR%3A-a-diagnostic-predictive-tool-for-primary-Behan-Dimitrov/6a07baf86d1b4853db031cd999d7c7f804482cea]
- 37. Valuing Simplicity: Developing a Good Point of Care ... [https://www.frontiersin.org/journals/sociology/articles/10.3389/fsoc.2020.00037/full]
- 38. Technology and Tools in the Diagnostic Process - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK338590/]
- 39. a diagnostic predictive tool for primary ciliary dyskinesia [https://www.academia.edu/55769744/PICADAR_a_diagnostic_predictive_tool_for_primary_ciliary_dyskinesia]