CRISPR-Cas9 Beta-Globin Mutation Correction: From Molecular Basis to Clinical Therapy in Sickle Cell Disease
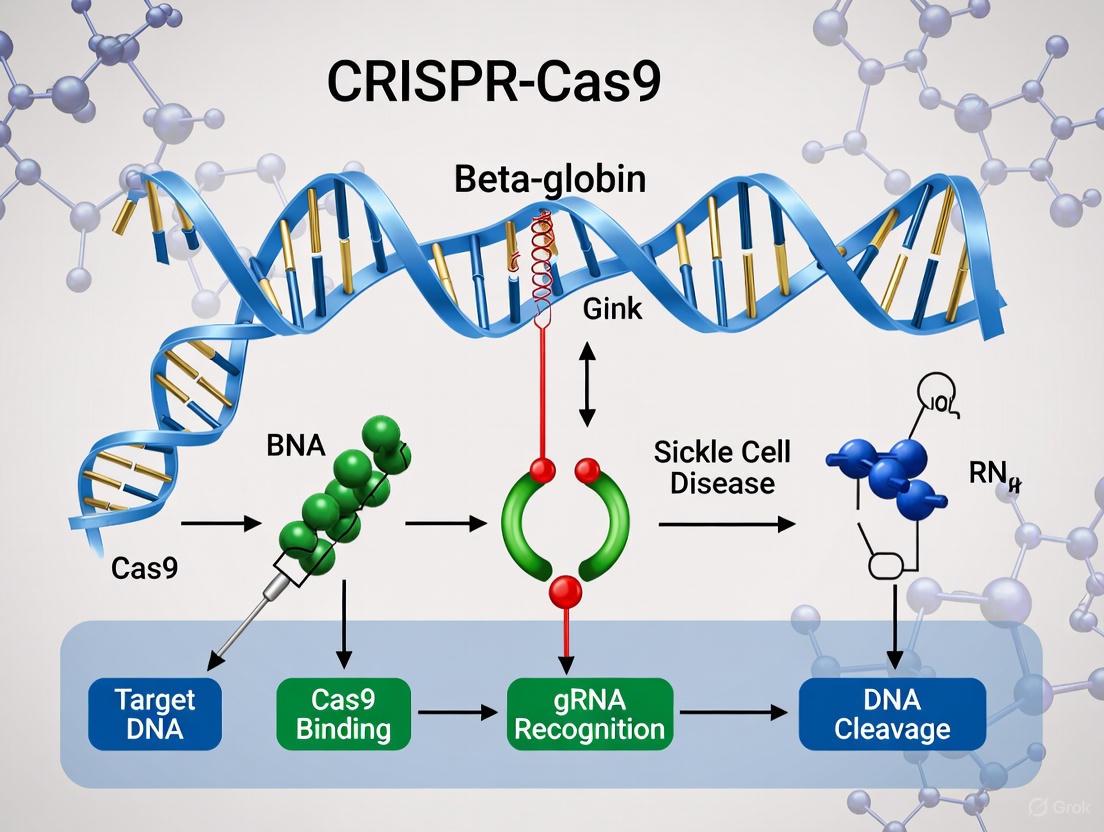
This comprehensive review synthesizes current advancements in CRISPR-based gene editing strategies for correcting the beta-globin mutation in sickle cell disease (SCD).
CRISPR-Cas9 Beta-Globin Mutation Correction: From Molecular Basis to Clinical Therapy in Sickle Cell Disease
Abstract
This comprehensive review synthesizes current advancements in CRISPR-based gene editing strategies for correcting the beta-globin mutation in sickle cell disease (SCD). Targeting researchers and drug development professionals, the article explores the molecular pathology of SCD, detailing various CRISPR methodologies including direct HBB correction, BCL11A targeting for fetal hemoglobin reactivation, and emerging base/prime editing approaches. It critically examines delivery challenges, safety considerations, and optimization strategies, while presenting clinical validation data from approved therapies like Casgevy. The analysis compares CRISPR approaches with conventional treatments and other gene therapy platforms, addressing technical hurdles, manufacturing scalability, and future directions for clinical translation of these transformative genetic medicines.
The Molecular Pathology of Sickle Cell Disease and CRISPR Therapeutic Rationale
The β-globin gene (HBB) encodes the beta-globin subunit of hemoglobin, the oxygen-carrying protein in red blood cells. Normal adult hemoglobin (HbA) is a tetramer consisting of two alpha-globin and two beta-globin chains, each associated with a heme group that binds oxygen [1]. Sickle cell disease (SCD) is a monogenetic disorder caused by a single nucleotide polymorphism (SNP) in the HBB gene. This A>T point mutation occurs in the sixth codon of the β-globin gene, resulting in the substitution of valine for glutamic acid at position 6 in the beta-globin chain (Glu6Val, E6V) [2] [1]. This specific genetic alteration leads to the production of an abnormal hemoglobin variant known as hemoglobin S (HbS).
The substitution of a hydrophilic amino acid (glutamic acid) with a hydrophobic one (valine) creates a hydrophobic interaction site on the surface of the beta-globin chain. Under deoxygenated conditions, these abnormal hemoglobin molecules polymerize into rigid, insoluble strands that deform red blood cells into the characteristic sickle shape [2]. These sickled cells exhibit decreased flexibility and increased adhesion to vascular endothelium, leading to microvascular occlusion, tissue ischemia, and both acute and chronic organ damage [2]. Additionally, sickled erythrocytes have a significantly shorter lifespan (10-20 days versus 120 days for normal red blood cells), resulting in chronic hemolytic anemia [2].
The clinical manifestations of SCD are primarily driven by these pathophysiological processes and include vaso-occlusive pain crises, acute chest syndrome, stroke, and progressive organ damage [2]. Interestingly, despite being a monogenic disorder, SCD exhibits considerable phenotypic heterogeneity influenced by genetic modifiers such as co-inheritance of alpha-thalassemia and polymorphisms in genes affecting fetal hemoglobin (HbF) production, including BCL11A and HBS1L-MYB [2].
Table 1: Genetic and Biochemical Basis of Sickle Cell Disease
| Aspect | Normal Physiology | Sickle Cell Pathophysiology |
|---|---|---|
| HBB Genotype | Two normal β-globin alleles | Homozygous Glu6Val (E6V) point mutation |
| Hemoglobin Type | Hemoglobin A (HbA) | Hemoglobin S (HbS) |
| Amino Acid Position 6 | Glutamic acid (hydrophilic) | Valine (hydrophobic) |
| Red Blood Cell Shape | Biconcave disc | Sickled crescent (when deoxygenated) |
| Primary Pathology | Normal oxygen transport | Hemoglobin polymerization, vaso-occlusion, hemolysis |
| Common Symptoms | None | Pain crises, anemia, infection risk, organ damage |
Current CRISPR-Based Therapeutic Strategies for HBB Mutation Correction
The precise understanding of the genetic defect in SCD has enabled the development of targeted gene correction strategies using CRISPR-Cas9 technology. Current approaches primarily focus on either directly correcting the pathogenic E6V point mutation or reactivating fetal hemoglobin (HbF) to compensate for the defective HbS. The direct gene correction strategy represents the most ideal curative approach as it addresses the fundamental genetic lesion while preserving physiologic regulation of gene expression [3].
Direct HBB Gene Correction
The direct correction approach utilizes high-fidelity Cas9 precomplexed with chemically modified guide RNAs to introduce a precise double-strand break near the E6V mutation in the HBB gene. This is followed by homology-directed repair (HDR) using a recombinant adeno-associated virus serotype 6 (rAAV6) vector delivering a donor DNA template with the correct nucleotide sequence [3]. This method has demonstrated up to 60% HBB allelic correction in clinical-scale manufacturing of patient-derived CD34+ hematopoietic stem and progenitor cells (HSPCs) [3]. Preclinical studies show long-term engraftment of these corrected cells in immunodeficient mice with multi-lineage correction frequencies of approximately 20% in hematopoietic organs, sufficient to reverse the sickling phenotype [3]. Toxicology studies have demonstrated no evidence of abnormal hematopoiesis, genotoxicity, or tumorigenicity from the engrafted gene-corrected cells, supporting the safety profile of this approach [3].
Fetal Hemoglobin Reactivation
An alternative strategy involves reactivating fetal hemoglobin through CRISPR-Cas9-mediated disruption of repressive regulatory elements. This approach targets the BCL11A gene enhancer or the LRF repressor binding sites in the γ-globin gene promoters [4] [5]. BCL11A is a master transcriptional regulator that suppresses γ-globin expression during development, and its disruption leads to sustained HbF production in adult red blood cells [5]. Similarly, targeting LRF binding sites in the γ-globin promoters has shown potent HbF synthesis in erythroid progeny derived from edited HSPCs [4]. This strategy has proven clinically successful, with the FDA approval of exagamglogene autotemcel (exa-cel), which utilizes CRISPR technology to inactivate BCL11A, for the treatment of SCD [6] [5].
Table 2: Comparison of CRISPR-Based Therapeutic Strategies for Sickle Cell Disease
| Parameter | Direct HBB Gene Correction | BCL11A Targeting (HbF Reactivation) | LRF Binding Site Disruption |
|---|---|---|---|
| Molecular Target | HBB gene E6V mutation | BCL11A erythroid enhancer | γ-globin promoter LRF binding sites |
| Therapeutic Goal | Restore normal β-globin | Increase γ-globin (HbF) | Increase γ-globin (HbF) |
| CRISPR Mechanism | Homology-directed repair | Non-homologous end joining | Non-homologous end joining |
| Donor Template Required | Yes (rAAV6) | No | No |
| Editing Efficiency | Up to 60% allelic correction [3] | High rate of indels at target site [5] | High frequency of disruption [4] |
| HbF Levels | Physiological HbA production | Significant HbF increase (>20%) | Potent HbF synthesis [4] |
| Clinical Status | Preclinical (Phase I/II planned) [3] | FDA approved (exa-cel) [6] | Preclinical/Clinical trials |
Experimental Protocols for HBB Gene Correction in Hematopoietic Stem Cells
The development of CRISPR-based therapies for SCD requires robust experimental protocols that can be translated to clinical applications. The following section details key methodologies for HBB gene correction in patient-derived hematopoietic stem and progenitor cells.
Isolation and Mobilization of CD34+ Hematopoietic Stem Cells
HSPCs are obtained from SCD patients via plerixafor mobilization rather than granulocyte colony-stimulating factor (G-CSF), which is contraindicated in SCD due to potential toxicity [3]. Plerixafor is a CXCR4 antagonist that induces rapid and reversible mobilization of CD34+ HSPCs into peripheral circulation [3]. CD34+ cells are then purified from leukapheresis products using immunomagnetic selection with clinical-grade CD34 MicroBeads and an AUTOMACS PRO system, achieving purities exceeding 90% [3] [7]. Cells are cultured in serum-free media supplemented with recombinant human cytokines (SCF, Fit3-L, TPO, IL-3) and small molecule enhancers (StemRegenin-1, UM171) to maintain stemness while promoting proliferation [3] [7].
CRISPR-Cas9 Delivery and HBB Gene Editing
The editing process utilizes ribonucleoprotein (RNP) complexes consisting of purified high-fidelity Cas9 protein complexed with synthetic, chemically modified single-guide RNAs (sgRNAs) targeting sequences near the E6V mutation [3] [4]. These RNP complexes are delivered to HSPCs via electroporation, providing efficient editing with reduced off-target effects compared to viral delivery methods. Following electroporation, cells are immediately transduced with rAAV6 donor vectors containing the homologous DNA template with the corrected HBB sequence and flanking homology arms of approximately 250 base pairs each [3]. The use of rAAV6 significantly enhances homology-directed repair efficiency in HSPCs. Edited cells are cultured for 48-72 hours before analysis of editing efficiency and transplantation.
Assessment of Editing Efficiency and Safety
Editing efficiency is quantified using droplet digital PCR (ddPCR) with allele-specific probes to distinguish between corrected and uncorrected HBB alleles [3]. Next-generation sequencing provides comprehensive analysis of on-target editing rates and potential off-target effects. In vitro erythroid differentiation is performed to assess functional correction by measuring HbS polymerization and sickling propensity under deoxygenated conditions [3] [4]. Safety assessments include karyotyping, whole-genome sequencing, and translocation assays to detect chromosomal abnormalities, with particular focus on known genomic fragile sites [4].
Preclinical Engraftment and Toxicology Studies
The functional potential of gene-corrected HSPCs is evaluated using immunodeficient mouse models (e.g., NGS mice) [3]. Cells are administered via intravenous or intra-femoral injection following sublethal irradiation. Engraftment is monitored over 16-24 weeks using flow cytometry to quantify human CD45+ cell chimerism and multi-lineage differentiation potential (myeloid, lymphoid, erythroid) [3]. Secondary transplantation assays evaluate long-term hematopoietic stem cell activity. Bone marrow is analyzed post-engraftment to assess persistence of gene correction and HbA production. Comprehensive toxicology studies examine potential genotoxicity, tumorigenicity, and abnormal hematopoiesis [3].
Figure 1: Experimental workflow for CRISPR-based HBB gene correction in sickle cell disease, showing key stages from hematopoietic stem cell collection to preclinical validation.
The Scientist's Toolkit: Essential Research Reagents and Solutions
The implementation of CRISPR-based gene correction protocols requires specialized reagents and tools optimized for working with hematopoietic stem cells. The following table details essential research solutions for HBB gene editing studies.
Table 3: Essential Research Reagents for HBB Gene Correction Studies
| Reagent/Category | Specific Examples | Function & Application |
|---|---|---|
| HSPC Mobilization | Plerixafor (Mozobil) | CXCR4 antagonist mobilizes CD34+ cells to peripheral blood for collection [3]. |
| Cell Separation | CD34 MicroBead Kit | Immunomagnetic selection of CD34+ hematopoietic stem/progenitor cells [7]. |
| Cell Culture Media | StemSpan Serum-Free Medium | Base medium for HSPC culture, maintains stemness while supporting proliferation [7]. |
| Cytokine Cocktail | SCF, Fit3-L, TPO, IL-3 | Essential growth factors for HSPC survival, expansion, and maintenance of multipotency [7]. |
| Small Molecule Enhancers | StemRegenin-1 (SR1), UM171 | Potent agonists that enhance HSPC expansion and self-renewal ex vivo [3] [7]. |
| CRISPR Enzyme | High-fidelity Cas9 (HiFi Cas9) | Engineered Cas9 variant with reduced off-target effects while maintaining high on-target activity [3]. |
| Guide RNA | Chemically modified sgRNAs | Synthetic single-guide RNAs with chemical modifications to enhance stability and editing efficiency [3] [4]. |
| Donor Template Vector | rAAV6 with HBB Donor | Recombinant AAV serotype 6 efficiently delivers homologous donor template for HDR in HSPCs [3]. |
| Delivery Method | Electroporation System | Non-viral delivery method for introducing RNP complexes into HSPCs (e.g., Neon, Amaxa) [3]. |
| Editing Assessment | ddPCR Assays | Ultra-sensitive quantification of HBB allelic correction frequency using allele-specific probes [3]. |
| Safety Assessment | Next-Generation Sequencing | Comprehensive analysis of on-target editing, off-target effects, and chromosomal rearrangements [4]. |
Clinical Translation and Regulatory Landscape
The transition from preclinical research to clinical application of CRISPR-based therapies for SCD has achieved significant milestones. Casgevy (exagamglogene autotemcel) became the first FDA-approved CRISPR-based medicine for SCD in late 2023, representing a landmark in the field [6] [8]. This therapy utilizes CRISPR-Cas9 to disrupt the BCL11A enhancer in patient-derived HSPCs, leading to sustained HbF production and inhibition of HbS polymerization [6]. Clinical trials have demonstrated that this approach can significantly reduce or eliminate vaso-occlusive crises in SCD patients [6].
Direct HBB gene correction strategies are advancing toward clinical trials, with foundational preclinical data supporting Investigational New Drug (IND) applications to the FDA [3]. Phase I/II trials will primarily evaluate safety, engraftment efficiency, and therapeutic efficacy of gene-corrected HSPCs. Current clinical-scale manufacturing protocols can process approximately 1-5×10^9 CD34+ cells with viability exceeding 80% post-editing [3].
The field is also exploring next-generation approaches including base editing and prime editing which offer potentially safer alternatives by minimizing DNA double-strand breaks [5]. Additionally, research continues into in vivo delivery systems that could eliminate the need for ex vivo manipulation of HSPCs, though this remains challenging for hematopoietic targets [6].
Figure 2: Logical pathway from genetic defect to clinical outcomes, showing how different CRISPR therapeutic strategies address the pathophysiology of sickle cell disease.
The successful clinical translation of CRISPR therapies requires addressing several challenges, including manufacturing scalability, cost reduction, and ensuring equitable access to these transformative treatments [6]. As of 2025, significant progress has been made in arranging reimbursement through state Medicaid programs and national health systems, though financial barriers remain substantial for these high-cost therapies [6]. The continued refinement of gene editing technologies promises to further enhance the safety, efficacy, and accessibility of curative approaches for sickle cell disease.
Sickle cell disease (SCD) is one of the most prevalent monogenic disorders worldwide, affecting millions of people globally [9] [10]. This hereditary hemoglobinopathy arises from a specific single nucleotide transversion point mutation in the β-globin gene (HBB) located on chromosome 11, which leads to the substitution of the sixth amino acid in the β-globin chain from glutamic acid to valine [9] [10] [11]. This single substitution results in the production of abnormal hemoglobin S (HbS), which undergoes polymerization under deoxygenated conditions, fundamentally altering red blood cell (RBC) physiology and triggering a complex pathophysiological cascade culminating in the vaso-occlusive crisis (VOC) that characterizes this debilitating disease [9] [11]. The understanding of this molecular pathway is particularly crucial in the current era of CRISPR-based gene editing approaches, which aim to correct the fundamental genetic defect underlying SCD.
The HbS Polymerization Cascade
The initial pathogenic event in SCD is the polymerization of deoxygenated HbS. The substitution of valine for glutamic acid establishes hydrophobic interactions between the valine of one HbS molecule and alanine, phenylalanine, and leucine residues of adjacent HbS molecules in the deoxygenated state [9]. This creates a hydrophobic patch that binds to the hydrophobic groove of a third HbS molecule, forming an HbS tetramer. The intermittent aggregation of these tetramers results in the formation of double-stranded polymer chains, which subsequently combine to form long helical fourteen-stranded insoluble fibers [9]. This polymerization process exhibits a characteristic delay time before the rapid phase of polymer formation, which is dependent on deoxy-HbS concentration and the transit time of RBCs through the microvasculature [12].
Table 1: Key Factors in HbS Polymerization
| Factor | Role in Polymerization | Therapeutic Implications |
|---|---|---|
| Deoxygenation | Promotes hydrophobic interactions enabling polymer formation | Oxygen therapy; Hyperbaric oxygen [13] |
| HbS Concentration | Higher concentrations decrease delay time and accelerate polymerization | Hydration therapy; Hemodilution [12] |
| Intracellular HbF Levels | Inhibits HbS polymerization by disrupting polymer contacts | Hydroxyurea; Genetic modulation of BCL11A [9] [14] |
| 2,3-DPG Levels | Decreases oxygen affinity, promoting deoxygenation and polymerization | Modulating erythrocyte metabolism [10] |
| Temperature | Affects polymerization kinetics | Avoiding hypothermia; Temperature control [9] |
| pH | Acidosis promotes polymerization | Managing metabolic acidosis [10] |
The polymerization of HbS transforms normally discoid, flexible RBCs into rigid, sickle-shaped cells with reduced deformability and shorter lifespan (10-20 days compared to 120 days for normal RBCs) [9]. These morphological changes are reversible initially with reoxygenation, but repeated sickling cycles cause irreversible membrane damage, leading to permanently sickled cells that are highly fragile and prone to hemolysis [10].
Pathophysiology of Vaso-Occlusion: A Multicellular Cascade
Vaso-occlusion in SCD represents a multistep, multicellular process involving complex interactions between sickled erythrocytes, leukocytes, platelets, and the vascular endothelium, rather than simply being a consequence of rigid sickle cells obstructing blood flow [12] [11]. The historical evolution of our understanding of VOC is summarized in Table 2.
Table 2: Evolution of Scientific Understanding of VOC
| Year | Scientific Observation | Contribution to VOC Understanding |
|---|---|---|
| 1910 | James Herrick's description of sickle-shaped RBCs | Original description of abnormal RBC morphology [12] |
| 1949 | Linus Pauling's demonstration of mutated hemoglobin | Identified SCD as a molecular disease of hemoglobin [12] |
| 1974 | Hofrichter and Eaton's "delay time" concept | Established kinetics of deoxy-HbS polymerization [12] |
| 1980 | Hebbel and Hoover's adhesion studies | Demonstrated increased propensity of SS-RBCs to adhere to endothelium [12] |
| 1989 | Kaul and Nagel's intravital studies | Showed SS reticulocytes initiate VOC by adhering to endothelium [12] |
| 2002 | Turhan and Frenette's leukocyte studies | Provided in vivo evidence for role of leukocytes in initiating VOC [12] |
| 2009 | Wallace and Linden's iNKT cell research | Identified role of iNKT cells in amplifying inflammation [12] |
The contemporary model of VOC pathogenesis involves several interconnected pathways:
Endothelial Activation and Adhesion
The vascular endothelium in SCD patients exists in a chronically activated state. Up to 50% of SCD patients experience endothelial dysfunction, primarily due to diminished nitric oxide (NO) bioavailability resulting from NO scavenging by cell-free plasma hemoglobin and L-arginine depletion by cell-free arginase released from hemolyzed RBCs [9]. This endothelial activation triggers increased expression of adhesion molecules including VCAM-1, ICAM-1, P-selectin, and E-selectin, which promote vascular occlusion and vasoconstriction [9] [12]. Activated platelets also contribute to this process through binding of platelet CD47 to endothelial thrombospondin, triggering exhibition of α2β3 on platelet surfaces that facilitates attachment to ICAM-4 on endothelial cells [9].
Hemolysis and Oxidative Stress
Intravascular hemolysis releases free hemoglobin and heme into the plasma, creating a pro-oxidant environment [10] [15]. Cell-free hemoglobin scavenges nitric oxide, while heme promotes neutrophil extracellular trap formation (NETosis) and activates inflammatory pathways through transcription factors such as BTB and CNC homologue (BACH) 1 and Spi-C [11]. Sickle erythrocytes exhibit increased NADPH oxidase activity and undergo HbS autoxidation at accelerated rates, generating excessive reactive oxygen species (ROS) including superoxide anion (O₂•⁻), hydrogen peroxide (H₂O₂), and hydroxyl radicals (•OH) [10] [15]. The antioxidant defense systems in SCD are compromised, with reduced levels of both enzymatic antioxidants (superoxide dismutase, catalase, glutathione peroxidase) and non-enzymatic antioxidants (glutathione, vitamin E, vitamin C), establishing a state of chronic oxidative stress [10].
Inflammation and Ischemia-Reperfusion Injury
SCD is characterized by a chronic inflammatory state with elevated baseline leukocyte counts and activated phenotypes of neutrophils, monocytes, and platelets [11]. Ischemia-reperfusion injury following microvascular occlusions promotes chronic inflammation through increased oxidant production and enhanced leukocyte adhesion to the endothelium [12] [11]. This inflammatory cascade is amplified by the activation of CD1d-restricted invariant natural killer T (iNKT) cells, which are more numerous and hyperresponsive to hypoxia/reoxygenation in SCD [12]. These cells secrete IFN-γ and chemokines that recruit additional lymphocytes to sites of inflammation, worsening tissue damage [12].
Pathophysiology of Vaso-Occlusive Crisis
Experimental Models and Methodologies
In Vitro Adhesion Assays
Early studies investigating VOC utilized in vitro adhesion assays to examine the adhesive interactions between sickle RBCs and endothelial cells. These experiments demonstrated that sickle RBCs, particularly low-density reticulocytes, exhibit increased adherence to vascular endothelium compared to normal RBCs [12]. Specific molecular interactions identified include α4β1 integrin on sickle RBCs binding directly to endothelial VCAM-1, and interactions between RBC LW (ICAM-4) and endothelial αvβ3 integrin [12]. These assays were instrumental in establishing the importance of RBC-endothelial adhesion in the initiation of VOC.
Animal Models of SCD
The development of transgenic murine models of SCD in the late 1990s represented a significant advancement in VOC research [12]. These models have enabled in vivo investigation of VOC pathophysiology using techniques such as intravital microscopy, which has visualized the preferential adhesion of sickle RBCs and leukocytes in postcapillary venules and the role of inflammatory stimuli in driving the vaso-occlusive cascade [12]. Studies in SCD mice have demonstrated diurnal variations in leukocyte recruitment, with higher densities of adherent leukocytes in venules at nighttime corresponding with more dramatic VOC phenotypes [12].
CRISPR/Cas9 Gene Editing Protocols
Recent advances in CRISPR/Cas9 gene editing have enabled precise correction of the SCD-causing E6V mutation in patient-derived hematopoietic stem cells (HSCs). The experimental workflow involves:
- HSC Collection: CD34+ hematopoietic stem and progenitor cells are collected from mobilized peripheral blood of SCD patients [16].
- Electroporation of RNP Complexes: Cells are electroporated with Cas9 ribonucleoproteins (RNPs) consisting of Cas9 complexed with chemically modified single-guide RNAs (sgRNAs) with 2'-O-methyl 3'phosphorothioate (MS) modifications at both termini to enhance stability and activity [16].
- rAAV6 Donor Delivery: Recombinant adeno-associated virus serotype 6 (rAAV6) vectors containing homology arms flanking the HBB target site are used to deliver homologous repair templates [16].
- Enrichment of Corrected Cells: At day 4 post-electroporation, successfully targeted cells are enriched based on high GFP expression (when using GFP-containing donors) through fluorescence-activated cell sorting (FACS) or magnetic bead selection, achieving populations with >90% targeted integration [16].
- Transplantation: Corrected HSCs are infused back into myeloablated recipients, where they engraft and reconstitute the hematopoietic system with RBCs capable of producing adult hemoglobin (HbA) [16].
This methodology has demonstrated efficient correction of the SCD mutation in multiple patient-derived HSC samples, with edited erythrocytes expressing normal β-globin mRNA and maintaining intact transcriptional regulation of edited HBB alleles [16].
CRISPR/Cas9 HSC Gene Editing Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for SCD Pathophysiology and Gene Editing Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Gene Editing Platforms | CRISPR/Cas9 RNPs, Base Editors (BEs), Prime Editors (PEs) | Precise correction of HBB E6V mutation; BCL11A targeting for HbF reactivation [14] [16] |
| Delivery Systems | rAAV6, Lipid Nanoparticles (LNPs), Electroporation | Efficient delivery of editing components to hematopoietic stem cells [14] [16] |
| Cell Culture Models | Patient-derived CD34+ HSPCs, Humanized SCD murine models | Preclinical testing of editing efficiency and safety; VOC pathophysiology studies [12] [16] |
| Adhesion Molecule Reagents | Anti-P-selectin aptamers, VCAM-1/ICAM-1 blocking antibodies | Investigating leukocyte-RBC-endothelial interactions in VOC [9] [12] |
| Oxidative Stress Assays | DCFDA, Lipid peroxidation kits, GSH/GSSG assays | Quantifying ROS production and antioxidant capacity in sickle erythrocytes [10] [15] |
| Analytical Tools | In-Out PCR, NGS off-target assays, HPLC for hemoglobin | Assessing targeted integration efficiency, safety profiles, and hemoglobin switching [16] |
Implications for CRISPR-Based Therapeutic Approaches
The detailed understanding of HbS polymerization and VOC pathophysiology has directly informed the development of CRISPR-based therapeutic strategies for SCD. Current approaches primarily focus on two strategic paradigms:
Direct Mutation Correction
The most straightforward approach involves precise correction of the E6V point mutation in the HBB gene using CRISPR/Cas9-mediated homology-directed repair. This strategy utilizes Cas9 ribonucleoproteins combined with rAAV6-delivered homologous donor templates to convert the sickle allele back to the normal β-globin sequence [16]. This approach has demonstrated allelic modification frequencies of approximately 19% in multiple HSPC donors, with the potential to restore normal hemoglobin production and prevent HbS polymerization entirely [16]. The development of enrichment protocols using FACS or magnetic beads to purify populations with >85% targeted integration has addressed the challenge of achieving therapeutic levels of corrected cells in vivo [16].
BCL11A Targeting for HbF Reactivation
An alternative strategy involves targeting the BCL11A gene, a transcriptional repressor of fetal hemoglobin (HbF). Reduction of BCL11A expression prevents HbS polymerization by increasing HbF expression, which incorporates into hemoglobin tetramers and disrupts the hydrophobic interactions necessary for HbS polymer formation [9] [14]. This approach has been successfully implemented in the FDA-approved therapy exagamglogene autotemcel (exa-cel), which has demonstrated robust and sustained improvements in quality of life for patients with severe SCD, with clinically meaningful improvements in physical, social, functional, and emotional well-being observed as early as six months post-treatment [17].
The path from the single nucleotide mutation in the β-globin gene to the devastating clinical manifestations of vaso-occlusive crisis in sickle cell disease involves a complex, multistep pathophysiology centered on HbS polymerization. This process initiates a cascade of events including erythrocyte sickling, chronic hemolysis, oxidative stress, endothelial activation, and persistent inflammation that culminates in episodic microvascular occlusion. The detailed elucidation of these mechanisms has been instrumental in guiding the development of novel CRISPR-based gene therapies that directly target the underlying genetic defect. As these innovative therapies progress through clinical trials and into clinical practice, they offer the promise of durable, potentially curative treatments for this debilitating monogenic disorder, transforming the lives of patients affected by sickle cell disease worldwide.
Sickle cell disease (SCD) management has long relied on a triad of therapeutic approaches: the pharmacologic agent hydroxyurea, chronic red blood cell transfusions, and hematopoietic stem cell transplantation (HSCT). While these interventions have improved patient survival and quality of life, they are characterized by significant limitations including variable efficacy, treatment-related toxicities, and accessibility challenges. This whitepaper provides a technical analysis of these foundational treatments, framing their shortcomings as the imperative driving current research into targeted genetic corrections, notably CRISPR-based therapies. Structured data on efficacy, implementation protocols, and mechanistic pathways are presented to equip researchers and drug development professionals with a consolidated reference on the pre-gene therapy landscape of SCD management.
Sickle cell disease is a monogenic autosomal recessive disorder caused by a point mutation in the β-globin gene (HBB), substituting valine for glutamic acid at position 6. This results in the production of hemoglobin S (HbS), which polymerizes under deoxygenated conditions, leading to erythrocyte sickling, hemolytic anemia, vaso-occlusion, and end-organ damage [18]. The clinical management of SCD has focused on mitigating these pathophysiological consequences. For decades, the therapeutic arsenal was confined to hydroxyurea, chronic transfusion regimens, and HSCT—each providing symptomatic relief or disease modification but falling short of a definitive, widely applicable cure. The limitations inherent in these conventional modalities have established a clear rationale for the development of therapies aimed directly at the underlying genetic defect.
Hydroxyurea: A Disease-Modifying Agent with Adherence Barriers
Mechanism of Action and Clinical Efficacy
Hydroxyurea, an oral, once-daily medication approved by the FDA in 1998, remains a first-line disease-modifying therapy. Its primary mechanism involves the cytotoxic inhibition of ribonucleotide reductase, leading to cellular stress that stimulates the production of fetal hemoglobin (HbF) [19]. Elevated HbF levels interfere with HbS polymerization, thereby reducing sickling of red blood cells. Clinically, this translates to fewer vaso-occlusive crises (VOCs) and acute chest syndrome (ACS) episodes, along with decreased need for blood transfusions [20].
Real-world, long-term studies confirm its sustained benefits. A 2024 analysis of 2,147 pediatric patients with severe SCD genotypes (HbSS/HbSβ⁰) demonstrated that hydroxyurea use was associated with 0.36 fewer emergency department visits and 0.84 fewer hospital days per patient-year compared to those not on the treatment [20]. The efficacy, however, is tightly linked to adherence; improvements in hemoglobin concentration are predominantly observed in patients with laboratory markers indicating consistent intake [20].
Documented Limitations and Barriers
Despite its efficacy, hydroxyurea is underutilized, with adherence being a central challenge. Barriers can be categorized within the framework of intentional and unintentional nonadherence, as identified in a large 2022 study [19].
Table 1: Barriers to Hydroxyurea Adherence and Utilization
| Barrier Category | Specific Barriers | Affected Population |
|---|---|---|
| Unintentional Nonadherence | Forgetting to take medication, competing life demands, challenges with pharmacy refills | Common across all age groups [19] |
| Intentional Nonadherence | Worry about long-term side effects (e.g., cancer risk, fertility impacts), aversion to medications, belief that "tried and it did not work" | Particularly prevalent in young adults and adults [19] |
| Provider-Level Barriers | Lack of familiarity with prescribing guidelines, hesitation to prescribe for non-HbSS/HbSβ⁰ genotypes despite indications | Contributes to under-prescription [19] |
| Formulation & Systemic Barriers | Lack of widely available liquid formulations for children, medication costs | Impacts accessibility, especially for pediatric populations [19] |
The perception of hydroxyurea's origin as a chemotherapy agent continues to fuel concerns about cancer risk and teratogenicity, despite studies showing long-term safety [19]. Furthermore, adults aged 26 and older are the demographic least likely to be on hydroxyurea therapy, highlighting a critical gap in lifelong care [19].
Experimental and Clinical Assessment Protocols
Protocol for Monitoring Hydroxyurea Efficacy in Clinical Trials:
- Baseline Assessment: Complete blood count (CBC) with differential, HbF percentage (by HPLC), renal and hepatic function panels.
- Dosing & Titration: Initiate therapy at 15-20 mg/kg once daily. Titrate every 8 weeks to maximum tolerated dose (MTD), typically capped at 35 mg/kg, targeting absolute neutrophil count (ANC) ≥ 2.0 x 10⁹/L [19].
- Efficacy Endpoints:
- Primary: Annual rate of VOCs requiring medical attention.
- Secondary: Change in HbF percentage from baseline, annual number of hospitalizations and ED visits, incidence of ACS, transfusion requirements.
- Adherence Monitoring: Use of pharmacy refill data, patient diaries, and laboratory markers such as mean corpuscular volume (MCV), which typically increases with consistent therapy.
Red Blood Cell Transfusion: Burden of Iron and Alloimmunization
Transfusion Modalities and Indications
Red blood cell transfusion is a cornerstone intervention for both acute complications and chronic management of SCD. It aims to improve oxygen-carrying capacity and dilute the proportion of HbS-containing red cells to prevent vaso-occlusion [21]. The three primary methodologies are:
- Simple Transfusion: Most widely available; involves infusion of RBC units without removal of patient blood. Carries a high risk of iron overload and hyperviscosity if hemoglobin is raised significantly above baseline [21].
- Manual Exchange Transfusion: Involves alternating phlebotomy and transfusion. Provides better control of HbS% and reduces iron accumulation compared to simple transfusion but is time-consuming and requires significant staff training [21].
- Automated Red Cell Exchange (RCE): Uses apheresis technology to simultaneously remove patient blood and replace it with donor RBCs. Offers the best control of HbS%, minimal iron loading, and allows for longer intervals between procedures. However, it requires specialized equipment, robust venous access, and is less widely available [21].
Table 2: Comparison of Transfusion Modalities in SCD
| Parameter | Simple Transfusion | Manual Exchange | Automated RCE |
|---|---|---|---|
| HbS% Control | Poor | Intermediate | Best |
| Iron Accumulation | High | Intermediate | Low |
| Time Consumption | Low | High | Intermediate |
| Specialist Equipment | Not required | Not required | Required |
| Venous Access | Peripheral | Peripheral/Central | Often Central |
| Availability | Widespread | Widespread | Limited |
Evidence for transfusion is strongest for primary and secondary stroke prevention, supported by randomized controlled trials [21]. Outside neurological indications, practice is guided by observational data and expert opinion, leading to significant variation. For instance, the proportion of patients transfused for recurrent pain across different centers varies from 16% to 54% [21].
Limitations and Global Burden
The chronicity of transfusion therapy introduces significant complications.
- Iron Overload: Each unit of transfused blood contains 200-250 mg of iron. Without iron chelation therapy, this leads to accumulation, causing endocrine dysfunction, cardiomyopathy, and liver cirrhosis. Patients on simple transfusion typically require chelation after approximately one year of regular therapy [21].
- Alloimmunization: The development of antibodies against foreign RBC antigens occurs in approximately 20-30% of patients with SCD. This complicates cross-matching, delays future transfusions, and can cause severe hemolytic reactions. It is often attributed to ethnic differences in antigen prevalence between predominantly Caucasian blood donors and African-American patients [22].
- Infection Risk: Despite improved screening, transmission of infections such as hepatitis B and C remains a concern, particularly in low- and middle-income countries (LMICs) where the blood supply may not meet WHO safety standards [22].
- Access and Logistics: In LMICs, access to safe, sustainable blood is a major barrier. Even in high-income nations, the burden of regular hospital visits for RCE or simple transfusion significantly impacts quality of life [22].
Standardized Transfusion Protocol
Protocol for Chronic Transfusion Therapy in SCD (Stroke Prevention):
- Pre-transfusion Testing: Extended RBC phenotyping (for C, E, K antigens) of the patient should be performed before the first transfusion to guide prophylactic antigen matching.
- Transfusion Goal: Maintain HbS% below a target threshold, typically 30-40%, to reduce stroke risk. The target hemoglobin should not exceed 10 g/dL to avoid hyperviscosity [21].
- Transfusion Interval: Typically every 3-4 weeks for simple transfusion; can be extended to 4-6 weeks for automated RCE.
- Adjunct Therapy:
- Iron Chelation: Initiate with deferasirox or deferoxamine when serum ferritin consistently exceeds 1000 ng/mL or after 1-2 years of chronic transfusion.
- Monitoring: Regularly monitor ferritin, liver function, and conduct echocardiography and T2* MRI for organ iron quantification.
Hematopoietic Stem Cell Transplantation: A Curative Yet High-Risk Option
Indications, Techniques, and Outcomes
Hematopoietic stem cell transplantation (HSCT) is currently the only widely available curative therapy for SCD. It involves replacing the patient's hematopoietic system with that of a healthy donor. The first successful transplant was performed in 1984 [23].
Indications: HSCT is generally reserved for patients with severe SCD manifestations, such as stroke, recurrent ACS, refractory VOC, or progressive organ damage. The availability of a fully matched sibling donor is a key requirement for optimal outcomes [23]. The procedure is most successful in children, with studies showing improved survival in those under 10 years of age [23].
Technique: The process involves a myeloablative conditioning regimen (e.g., busulfan/cyclophosphamide) to ablate the patient's bone marrow, followed by infusion of donor stem cells. Graft-versus-host disease (GVHD) prophylaxis is critical. Reduced-intensity conditioning regimens have been developed to reduce toxicity, particularly in older patients [23].
Efficacy: A decade-long follow-up from the DREPAGREFFE-1 trial demonstrated superior outcomes for children with SCD who received HSCT compared to those on standard care (chronic transfusion/hydroxyurea). Transplant recipients showed significantly better physical, school, and social functioning, improved cognitive performance, and a halt in the progression of silent cerebral infarcts [24]. A decision analysis model assigned the highest quality-of-life utility score to HSCT (0.85) compared to hydroxyurea (0.80) and chronic transfusion (0.71) [25].
Significant Limitations and Risks
The curative potential of HSCT is counterbalanced by substantial risks that limit its application.
- Graft-versus-Host Disease (GVHD): This occurs when donor immune cells attack the recipient's tissues. It can be acute (affecting skin, liver, gut) or chronic (a multi-system disorder), and can be fatal or cause significant long-term morbidity [23].
- Infertility: Myeloablative conditioning regimens commonly cause permanent infertility, a significant concern for patients and families. Fertility preservation procedures are recommended prior to transplant [24].
- Graft Rejection/Failure: The risk of the graft not "taking" or the disease recurring exists, particularly if adequate immunosuppression is not achieved.
- Donor Availability: Only about 15-20% of patients with SCD have a fully matched sibling donor, severely restricting eligibility [23].
- Treatment-Related Mortality: The procedure carries an estimated 5-10% risk of mortality from infections, organ toxicity, or GVHD [23].
- Long-Term Effects: Patients remain at risk for long-term complications from the conditioning regimen and chronic GVHD, requiring lifelong specialist follow-up.
HSCT Clinical Trial Methodology
Protocol for Myeloablative Allogeneic HSCT from a Matched Sibling Donor:
- Candidate Selection: Patients <16 years with severe SCD (e.g., stroke, recurrent ACS) and an HLA-matched sibling donor.
- Pre-transplant Preparation (Conditioning): Administer myeloablative regimen (e.g., Busulfan 14-16 mg/kg IV, Cyclophosphamide 200 mg/kg). GVHD prophylaxis with a calcineurin inhibitor (e.g., cyclosporine) and methotrexate.
- Stem Cell Source: Infuse bone marrow or umbilical cord blood-derived hematopoietic stem cells from the donor.
- Post-Transplant Monitoring:
- Engraftment: Monitor for neutrophil and platelet recovery.
- Chimerism: Assess donor-derived hematopoietic cells. A myeloid chimerism of ≥20% is sufficient for a clinical cure [23].
- Complications: Monitor for and manage infections, GVHD, and organ toxicity.
- Primary Efficacy Endpoint: Event-free survival (freedom from SCD-related events and transplant-related mortality).
The Scientist's Toolkit: Research Reagents for SCD Therapy Development
The transition from conventional treatments to gene-based cures relies on a specific toolkit of research reagents and model systems. The following table details key materials essential for preclinical research in HBB-targeted gene correction.
Table 3: Key Research Reagent Solutions for HBB Correction Studies
| Reagent / Material | Function in Research | Application Example |
|---|---|---|
| CD34+ Hematopoietic Stem/Progenitor Cells (HSPCs) | The target cell population for ex vivo gene editing; capable of reconstituting the entire hematopoietic system. | Sourced from mobilized peripheral blood, bone marrow, or umbilical cord blood of healthy donors or SCD patients for autologous therapy [18]. |
| CRISPR-Cas9 System (e.g., SpCas9) | Creates a precise double-strand break in the DNA at a targeted genomic locus to enable gene correction. | Used with a guide RNA (gRNA) targeting the HBB gene mutation site for knock-in correction or targeting the BCL11A erythroid enhancer for HbF induction [26]. |
| gRNA for HBB or BCL11A | Guides the Cas9 nuclease to the specific DNA sequence for cleavage. | HBB-gRNA directs correction of the Glu6Val mutation; BCL11A-gRNA disrupts the HbF repressor [26]. |
| AAV6 Donor Template | Serves as a viral vector to deliver the homologous donor DNA template for precise HDR-mediated correction. | Used to provide a correct HBB sequence for repairing the SCD mutation in CD34+ HSPCs after a CRISPR-induced cut [18]. |
| Base Editors / Prime Editors | Advanced genome editing tools that directly convert one base to another without causing a double-strand break, offering a safer alternative. | Used to convert the diseased HbS (GTG) codon into a non-pathogenic variant like HbG-Makassar (GCG) in human HSPCs [26]. |
| X-VIVO 15 or STEMSPAN Media | Serum-free cell culture media optimized for the expansion and maintenance of human HSPCs during ex vivo manipulation. | Used to culture CD34+ cells during the gene editing process [18]. |
| Cytokines (SCF, TPO, FLT3-L) | Recombinant growth factors that promote HSPC survival and proliferation during ex vivo culture. | Added to culture media to enhance cell viability and maintain stemness throughout the editing and transplantation workflow [18]. |
| NSG (NOD-scid-gamma) Mice | An immunodeficient mouse model that allows for the engraftment of human hematopoietic cells, enabling in vivo assessment of edited HSCs. | Used to transplant gene-edited human CD34+ cells to evaluate long-term engraftment, multi-lineage differentiation, and functional correction of the sickle phenotype [18]. |
The historical landscape of SCD treatment, defined by hydroxyurea, transfusions, and HSCT, is marked by a trade-off between efficacy and significant limitations. Hydroxyurea's potential is hampered by adherence barriers and perceptions of risk. Transfusions, while life-saving, introduce a cascade of complications like iron overload and alloimmunization, and their efficacy is highly dependent on the modality and consistent access. HSCT, though curative, is restricted by donor availability and associated with profound risks like GVHD and infertility.
These collective shortcomings underscore the clear and pressing need for therapies that address the root genetic cause of SCD without incurring the burdens of chronic care or the severe risks of allogeneic transplantation. The limitations of these conventional therapies form the foundational rationale for the development of autologous, targeted genetic interventions, such as CRISPR-Cas9-mediated gene correction, which aim to provide a durable, widespread, and safer curative solution.
β-hemoglobinopathies, primarily sickle cell disease (SCD) and β-thalassemia, are among the most common monogenic disorders worldwide, affecting millions and causing significant morbidity and mortality [27]. These conditions stem from mutations in the β-globin gene (HBB), which disrupt the structure or production of adult hemoglobin (HbA), leading to dysfunctional red blood cells [14] [28]. For SCD, a single nucleotide substitution (HBB: c.20A>T; p.Glu7Val) results in sickle hemoglobin (HbS) that polymerizes under deoxygenation, causing red blood cells to sickle and leading to vaso-occlusion, hemolysis, and end-organ damage [18]. In β-thalassemia, over 200 different HBB mutations can cause either absent (β⁰) or reduced (β⁺) β-globin synthesis, creating an imbalance in globin chain ratios, ineffective erythropoiesis, and chronic anemia [14] [27].
Current management strategies, including blood transfusions and iron chelation therapy, address symptoms but not the underlying genetic cause [14]. Allogeneic hematopoietic stem cell transplantation (HSCT) can be curative but is limited by donor availability and graft-versus-host disease risks [28]. The advent of CRISPR-based genome editing technologies has ushered in a new therapeutic paradigm focused on precise genetic correction to restore normal hemoglobin function [14] [28]. This whitepaper delineates the therapeutic goals and technical methodologies for genetic correction strategies within the broader context of CRISPR research for β-globin mutation correction.
Therapeutic Goals and Strategic Approaches
The primary therapeutic goal for genetic correction of β-hemoglobinopathies is to achieve durable production of functional non-pathogenic hemoglobin within erythrocytes, sufficient to ameliorate or eliminate disease pathophysiology. This overarching goal can be broken down into several key objectives and strategic approaches.
Table 1: Core Therapeutic Goals for Genetic Correction of β-Hemoglobinopathies
| Therapeutic Goal | Molecular/Physiological Outcome | Clinical Outcome |
|---|---|---|
| Eliminate HbS Polymerization | Reduce proportion of HbS tetramers below critical gelling threshold (<5-10%) [18] | Prevention of vaso-occlusive crises, hemolysis, and end-organ damage |
| Restore Hemoglobin Tetramer Stability | Ensure sufficient β-like globin chains to pair with α-globin chains, preventing α-globin precipitation [27] | Correction of anemia, reduction of ineffective erythropoiesis |
| Achieve Therapeutically Relevant Hemoglobin Levels | Attain total hemoglobin >9-10 g/dL or fetal hemoglobin (HbF) >30% in majority of circulating erythrocytes [27] | Transfusion independence, normalized quality of life [17] |
| Ensure Clonal Stability & Long-Term Engraftment | Maintain gene-corrected hematopoietic stem and progenitor cells (HSPCs) in bone marrow niche with multi-lineage differentiation potential [3] | Sustained, lifelong curative effect |
Three principal CRISPR-based strategic pathways have been developed to achieve these goals, each with distinct molecular mechanisms.
- Direct Mutation Correction: This strategy aims to precisely correct the specific pathogenic point mutation in the endogenous HBB gene. For SCD, this involves converting the single A>T nucleotide mutation back to the wild-type sequence, thereby restoring the production of normal adult hemoglobin (HbA) [3] [18]. This approach preserves the native regulatory control of the HBB locus.
- Fetal Hemoglobin (HbF) Reactivation: This indirect approach does not target the HBB gene itself. Instead, it disrupts repressors of the fetal γ-globin genes, such as BCL11A, or their binding sites in the globin locus [14] [28] [29]. This re-activates the production of HbF (α₂γ₂), which does not sickle and can effectively substitute for the defective adult hemoglobin, ameliorating the disease [27].
- Functional Gene Addition: This strategy uses lentiviral vectors to introduce a functional copy of the HBB gene (or an anti-sickling variant) into the HSPC genome, ensuring production of non-pathogenic hemoglobin [27]. This is not a gene editing approach per se but a gene therapy often discussed alongside editing strategies.
The following diagram illustrates the logical relationships and decision points between these core strategic pathways.
Quantitative Efficacy Benchmarks and Clinical Outcomes
The success of genetic correction strategies is quantified against specific biochemical and hematological benchmarks. Achieving these thresholds is strongly correlated with positive clinical outcomes, including transfusion independence in β-thalassemia and freedom from vaso-occlusive crises in SCD [17].
Table 2: Key Efficacy Benchmarks for Genetic Correction Strategies
| Parameter | Therapeutic Threshold | Reported Clinical Efficacy |
|---|---|---|
| HbF Reactivation (for SCD) | >30% HbF-containing erythrocytes (F-cells) [27] | Exa-cel therapy: Elimination of VOCs in 96.7% of SCD patients at 24 months [18] [17] |
| Donor Cell Chimerism | ≥20% donor myeloid chimerism in bone marrow [18] | Associated with reversal of sickle phenotype post-allogeneic HSCT |
| HBB Allelic Correction (Ex Vivo) | Up to 60% allelic correction achieved in clinical-scale manufacturing [3] | ~20% gene correction frequency post-engraftment in murine models [3] |
| Transfusion Independence (for TDT) | Total hemoglobin sustained >9 g/dL without transfusions [17] | Exa-cel therapy: 93.5% of TDT patients achieved transfusion independence for ≥12 months [17] |
| Patient-Reported Outcomes | Scores exceeding Minimal Clinically Important Difference (MCID) [17] | Exa-cel: Clinically meaningful improvements in quality of life, social, emotional, and sleep impacts [17] |
The clinical translation of these strategies has been highly successful. For the HbF reactivation strategy via BCL11A disruption, the approved therapy exagamglogene autotemcel (exa-cel, Casgevy) has demonstrated robust and sustained clinical benefits. As of a 2025 business update, approximately 115 patients had undergone cell collection for this treatment, with 29 patients having already received infusions [30]. Real-world application, as in the case of a 33-year-old with beta thalassemia major, demonstrates the therapeutic journey from lifelong monthly transfusions and iron chelation to the potential for a definitive cure [29].
Detailed Experimental Protocol for HBB Gene Correction
The following section provides a detailed methodology for an ex vivo CRISPR-based HBB gene correction protocol in hematopoietic stem and progenitor cells (HSPCs), as derived from foundational preclinical studies [3]. This protocol is representative of the processes used to develop clinically relevant genetic medicines.
The experimental workflow for ex vivo gene correction is complex and multi-staged, requiring precise execution at each step to ensure the yield of a therapeutically viable product. The entire process, from cell collection to infusion, can span several months.
Step-by-Step Protocol
Step 1: HSPC Mobilization and Collection
- Mobilization: Administer plerixafor (Mozobil), a CXCR4 antagonist, to mobilize CD34+ HSPCs from the bone marrow niche into peripheral blood. Plerixafor is preferred over G-CSF for SCD patients due to the risk of severe toxicity with G-CSF [3].
- Leukapheresis: Collect mobilized HSPCs via apheresis. Target cell dose should meet clinical-scale manufacturing requirements for a full human dose [3] [30].
Step 2: Cell Processing and Culture
- Isolation: Isulate CD34+ cells from the leukapheresis product using clinical-grade magnetic-activated cell sorting (MACS).
- Culture: Resuspend and culture CD34+ cells in serum-free medium supplemented with cytokines (e.g., SCF, TPO, FLT3-L) and the small molecule UM171, an agonist that has been shown to improve the protocol by supporting the maintenance and expansion of primitive hematopoietic stem cells during the ex vivo culture period [3].
Step 3: CRISPR Genome Editing
- Ribonucleoprotein (RNP) Complex Formation: Pre-complex a high-fidelity Cas9 protein with a chemically modified, single-guide RNA (sgRNA) targeting the specific genomic locus. Chemical modifications (e.g., 2'-O-methyl-3'phosphorothiate) on the sgRNA enhance stability and editing efficiency [3] [28].
- Donor Template Preparation: Prepare a recombinant adeno-associated virus serotype 6 (rAAV6) vector containing the homologous donor DNA template for the HBB gene. The donor template carries the intended correction (e.g., the wild-type sequence for SCD) flanked by homology arms.
- Co-Delivery: Deliver the Cas9 RNP complexes via electroporation into the cultured CD34+ HSPCs. Immediately following electroporation, transduce the cells with the rAAV6 donor template. This combination has been shown to achieve high frequencies of homology-directed repair (HDR) in long-term engrafting HSCs [3].
Step 4: Patient Conditioning
- Myeloablative Regimen: Administer a myeloablative conditioning regimen, typically with busulfan, to the patient. This is a critical step to create "space" in the bone marrow niche for the engraftment and expansion of the newly infused gene-corrected HSPCs [29].
Step 5: Product Infusion
- Final Formulation: The gene-corrected cell product (e.g., Drug Product-gcHBB-SCD) is washed, formulated in infusion medium, and released via quality control testing.
- Administration: Infuse the final cell product intravenously into the patient [3] [29].
Step 6: Engraftment and Monitoring
- Engraftment Period: Monitor the patient closely in the weeks following infusion for evidence of neutrophil and platelet engraftment, typically occurring within 2-4 weeks.
- Long-Term Follow-Up: Conduct weekly checkups for approximately six months to track blood counts and ensure the edited stem cells are producing healthy levels of all blood lineages. The definitive measure of success is transfusion independence for transfusion-dependent thalassemia or freedom from vaso-occlusive crises for SCD [29].
The Scientist's Toolkit: Essential Research Reagents
The execution of the aforementioned protocol relies on a suite of critical research reagents and materials. The following table details key components, their functions, and considerations for their use in developing genetic correction therapies for hemoglobinopathies.
Table 3: Essential Research Reagents for HBB Gene Correction Experiments
| Reagent/Material | Function | Key Features & Considerations |
|---|---|---|
| Plerixafor (Mozobil) | CXCR4 antagonist mobilizes HSPCs from bone marrow to peripheral blood for collection [3]. | Preferred over G-CSF for SCD patient mobilization due to safety profile [3]. |
| CD34 MicroBead Kit | Immunomagnetic selection and isolation of CD34+ HSPCs from heterogeneous leukapheresis product [3]. | Critical for obtaining a target cell population with >90% purity for editing [3]. |
| High-Fidelity Cas9 | Engineered CRISPR-associated nuclease with reduced off-target activity [3]. | Essential for enhancing the safety profile of the therapeutic edit. |
| Chemically Modified sgRNA | Single-guide RNA directs Cas9 to the specific target genomic locus (e.g., BCL11A erythroid enhancer or HBB locus) [3] [28]. | 2'-O-methyl-3'phosphorothiate modifications increase stability and editing efficiency [28]. |
| rAAV6 Serotype Vector | Delivery vehicle for the homologous donor DNA template to facilitate HDR-mediated gene correction [3]. | Demonstrates high efficiency of transduction in human HSPCs [3] [18]. |
| Electroporation System | Device for delivering Cas9 RNP complexes directly into the cytoplasm/nucleus of target HSPCs. | Enables transient, high-efficiency editing with low toxicity compared to viral delivery of editing components [28]. |
| UM171 Molecule | A small molecule agonist used in culture media to promote the maintenance and expansion of primitive hematopoietic stem cells ex vivo [3]. | Protocol optimization with UM171 can lead to higher in vivo retention of gene-corrected alleles [3]. |
| Lymphodepleting Agents (e.g., Busulfan) | Myeloablative chemotherapeutic agent used for patient conditioning to create bone marrow niche space [29]. | Critical for enabling successful engraftment of the infused gene-corrected HSPCs. |
The field of genetic correction for β-hemoglobinopathies has progressed from conceptual validation to clinical reality, as evidenced by the approval of CRISPR-based therapies like Casgevy [30]. The therapeutic goals are clearly defined: to restore normal hemoglobin function through direct mutation correction, fetal hemoglobin reactivation, or functional gene addition. Quantitative benchmarks, such as achieving HbF levels >30% or stable engraftment with ≥20% corrected cells, provide clear targets for therapeutic development.
Robust and detailed experimental protocols, leveraging reagents like plerixafor-mobilized CD34+ cells, high-fidelity Cas9 RNP, and rAAV6 donor templates, have enabled the transition from bench to bedside [3]. These foundational protocols continue to be refined, with next-generation research focusing on in vivo delivery of editing components to bypass the complex and costly ex vivo manufacturing process, and the development of targeted conditioning agents to reduce the toxicity of current regimens [30]. As the field advances, the ongoing challenge will be to broaden global access to these transformative therapies, particularly in regions with the highest prevalence of SCD and β-thalassemia [27].
CRISPR-Cas9 is an adaptive immune system found in prokaryotic organisms that has been repurposed for precise genome editing in eukaryotic cells [31]. The system consists of two key components: the Cas9 nuclease, which creates double-stranded breaks in DNA, and a guide RNA (gRNA), which directs Cas9 to specific genomic locations [31]. This technology has revolutionized genetic engineering, offering unprecedented precision in modifying DNA sequences. For therapeutic applications in monogenic disorders such as sickle cell disease (SCD), CRISPR-Cas9 enables researchers to target and correct the underlying genetic mutations responsible for pathogenesis [18] [26]. The fundamental mechanism involves a complex interplay between the gRNA's targeting capability and the Cas9 nuclease's DNA cleavage activity, which together facilitate precise genetic modifications through cellular repair processes.
Core Mechanism: gRNA Design and Cas9 Nuclease Function
Guide RNA (gRNA) Design Principles
The guide RNA is a synthetic fusion molecule that combines the functions of CRISPR RNA (crRNA) and trans-activating crRNA (tracrRNA) into a single-guide RNA (sgRNA) [31]. This ~100 nucleotide RNA molecule contains a 20-nucleotide spacer sequence at its 5' end that is complementary to the target DNA site, and a scaffold sequence at its 3' end that facilitates binding to the Cas9 nuclease. Effective gRNA design requires careful selection of the spacer sequence to ensure specificity and efficiency. The target site must be adjacent to a Protospacer Adjacent Motif (PAM) with the sequence 5'-NGG-3' for the commonly used Streptococcus pyogenes Cas9 [31]. The PAM sequence is essential for Cas9 recognition but is not part of the gRNA targeting sequence. gRNAs are typically designed to target sites as close as possible to the pathogenic mutation to maximize correction efficiency while minimizing off-target effects. For sickle cell disease research, gRNAs can be designed to target either the mutated β-globin gene (HBB) itself or regulatory genes such as BCL11A that control fetal hemoglobin expression [18] [26].
Cas9 Nuclease Mechanism
The Cas9 nuclease is a multi-domain enzyme that creates double-stranded breaks in DNA through its two distinct nuclease domains: HNH and RuvC [31]. The HNH domain cleaves the DNA strand complementary to the gRNA spacer sequence, while the RuvC domain cleaves the non-complementary strand. Upon gRNA binding to the target DNA sequence, Cas9 undergoes a conformational change that activates its nuclease activity, resulting in a blunt-ended double-strand break approximately 3-4 nucleotides upstream of the PAM site. This break then triggers the cell's innate DNA repair mechanisms, primarily non-homologous end joining (NHEJ) or homology-directed repair (HDR) [26]. NHEJ is an error-prone process that often results in small insertions or deletions (indels) that can disrupt gene function, while HDR uses a donor DNA template to enable precise genetic corrections—the preferred pathway for therapeutic correction of the sickle cell mutation [18].
Figure 1: CRISPR-Cas9 Mechanism and DNA Repair Pathways. The gRNA:Cas9 complex binds target DNA adjacent to a PAM sequence, creating double-strand breaks repaired via NHEJ or HDR pathways.
Quantitative Parameters for gRNA Selection
Table 1: Key Parameters for Optimal gRNA Design
| Parameter | Optimal Value/Range | Functional Significance |
|---|---|---|
| gRNA Length | 20 nucleotides | Balances specificity and efficiency |
| GC Content | 40-60% | Prevents secondary structures; improves stability |
| PAM Sequence | 5'-NGG-3' | Essential for Cas9 recognition and binding |
| Off-Target Score | >90 (prediction tools) | Minimizes unintended genomic edits |
| On-Target Score | >50 (prediction tools) | Maximizes editing efficiency at intended target |
Therapeutic Application in Sickle Cell Disease
Sickle cell disease is caused by an A>T point mutation at codon 6 of the β-globin gene (HBB: c.20A>T), resulting in the substitution of valine for glutamic acid (p.Glu7Val) and the production of pathological hemoglobin S (HbS) [18]. This single nucleotide polymorphism leads to hemoglobin polymerization under deoxygenated conditions, causing red blood cells to assume a sickled shape, chronic hemolytic anemia, vaso-occlusive crises, and multi-organ damage [32]. CRISPR-Cas9 therapy offers two primary strategic approaches for treating SCD: direct correction of the HBB mutation or indirect therapeutic approaches through manipulation of hemoglobin switching regulators.
Direct Correction Strategy
The direct correction approach involves designing gRNAs that target sequences immediately adjacent to the sickle cell mutation in the HBB gene, enabling precise correction through HDR using a donor DNA template containing the wild-type sequence [18]. This strategy requires the co-delivery of Cas9, gRNA, and a donor template into hematopoietic stem and progenitor cells (HSPCs). The donor template typically contains the correct nucleotide (A instead of T) along with homologous arms ranging from 400-800 bp to facilitate efficient HDR. This method achieves permanent genetic correction at the endogenous HBB locus, restoring normal β-globin expression and function. Research has demonstrated successful correction of the sickle mutation in human HSPCs using this approach, with corrected cells demonstrating reduced sickling and improved survival [18]. However, the efficiency of HDR remains a challenge, as it competes with the more prevalent NHEJ pathway, which can introduce unintended mutations at the target site.
Indirect Therapeutic Approaches
Indirect approaches target regulatory genes rather than the mutated HBB gene itself. The most advanced strategy involves disrupting the BCL11A gene, which encodes a transcriptional repressor of fetal hemoglobin (HbF) [26]. Naturally occurring mutations in the BCL11A enhancer are associated with hereditary persistence of fetal hemoglobin and ameliorated SCD symptoms. CRISPR-Cas9 can be used to disrupt the BCL11A gene or its enhancer in HSPCs, thereby reducing BCL11A expression and allowing for persistent HbF production in adult red blood cells. HbF contains gamma-globin chains that do not polymerize with HbS and effectively interfere with HbS polymerization, preventing sickling of red blood cells [26]. This approach has led to the development of Casgevy (exagamglogene autotemcel), the first FDA-approved CRISPR-based therapy for SCD, which has demonstrated clinical efficacy in multiple patients [26].
Figure 2: CRISPR-Cas9 Therapeutic Strategies for Sickle Cell Disease. Two main approaches either correct the HBB mutation directly or disrupt BCL11A to induce fetal hemoglobin production.
Quantitative Therapeutic Thresholds
Table 2: Therapeutic Efficacy Parameters for SCD Gene Editing
| Parameter | Therapeutic Threshold | Clinical Significance |
|---|---|---|
| HDR Efficiency | >20% | Minimum for phenotypic correction |
| Donor Myeloid Chimerism | ≥20% | Correlates with 100% donor RBCs in peripheral blood |
| HbF Levels | >20% | Sufficient to inhibit HbS polymerization |
| Vector Copy Number (VCN) | <5 | Safety threshold for lentiviral approaches |
| Engraftment Efficiency | >80% | For sustained therapeutic effect |
Experimental Workflow for SCD Gene Correction
Hematopoietic Stem Cell Collection and Preparation
The therapeutic workflow begins with the collection of hematopoietic stem and progenitor cells (HSPCs) from the patient. CD34+ cells can be isolated from bone marrow harvest or through mobilization into peripheral blood using plerixafor, a CXCR4 antagonist [32]. Granulocyte colony-stimulating factor (G-CSF) is typically avoided in SCD patients due to the risk of vaso-occlusive crises. The collected CD34+ cells are then cultured in cytokine-rich media (SCF, TPO, FLT3-L) to maintain stemness while promoting cell cycle progression, which is essential for efficient CRISPR editing as HDR primarily occurs in cycling cells [32].
CRISPR-Cas9 Delivery and Electroporation
For clinical applications, CRISPR-Cas9 components are typically delivered to HSPCs via electroporation of ribonucleoprotein (RNP) complexes [18]. These complexes consist of purified Cas9 protein pre-assembled with synthetic gRNA, which enables rapid genome editing while minimizing off-target effects associated with prolonged Cas9 expression. The RNP delivery method results in rapid clearance of CRISPR components, reducing immunogenicity and potential off-target activity. For HDR-based approaches, a single-stranded oligodeoxynucleotide (ssODN) or adeno-associated virus (AAV) donor template is co-electroporated with the RNP complex. Optimization of electroporation parameters is critical for maintaining high cell viability while achieving efficient editing.
Transplantation and Engraftment
Following CRISPR editing, cells are infused back into the patient after myeloablative conditioning with busulfan to create niche space in the bone marrow [32]. Busulfan conditioning is essential for efficient engraftment of the modified HSPCs. Patients require close monitoring for engraftment signs, typically evidenced by neutrophil and platelet count recovery within 2-4 weeks post-transplantation. The establishment of ≥20% donor myeloid chimerism has been shown to correlate with 100% donor-derived red blood cells in peripheral blood due to the selective survival advantage of corrected RBCs over sickle RBCs [32].
Figure 3: Experimental Workflow for SCD Gene Therapy. Key steps from HSPC collection to transplantation and therapeutic outcome assessment.
Research Reagent Solutions for SCD Gene Editing
Table 3: Essential Reagents for CRISPR-Based Sickle Cell Disease Research
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| Nuclease Systems | SpCas9, Cas12a (Cpf1), MAD7 | DNA cleavage with varying PAM requirements |
| gRNA Design Tools | ICE (Inference of CRISPR Edits), CRISPick | Design and analysis of gRNA efficiency and specificity |
| Delivery Methods | Electroporation systems, AAV6 serotype | Introduction of CRISPR components into HSPCs |
| HDR Donor Templates | ssODNs, AAV donor vectors, dsDNA templates | Precise correction of sickle mutation |
| Cell Culture Media | StemSpan, cytokines (SCF, TPO, FLT3-L) | Maintenance and expansion of HSPCs |
| Analysis Tools | Sanger sequencing, NGS, ICE analysis, MAGeCK | Assessment of editing efficiency and specificity |
Analytical Methods for CRISPR Editing Assessment
Editing Efficiency Quantification
The Inference of CRISPR Edits (ICE) tool enables robust analysis of CRISPR editing efficiency from Sanger sequencing data, providing NGS-quality analysis at significantly reduced cost [33]. ICE analyzes sequencing chromatograms from edited samples by deconvoluting the complex traces resulting from heterogeneous editing outcomes. The algorithm calculates indel percentages, knockout scores (proportion of cells with frameshift or 21+ bp indels), and knock-in scores (proportion of sequences with desired knock-in edit) [33]. For HDR-based approaches, digital droplet PCR (ddPCR) or next-generation sequencing (NGS) is employed to precisely quantify correction rates at the target locus.
Off-Target Analysis
Comprehensive off-target analysis is essential for therapeutic applications. In silico prediction tools identify potential off-target sites based on sequence similarity to the gRNA spacer. Empirically, genome-wide methods such as GUIDE-seq or CIRCLE-seq can detect actual off-target cleavage events [18]. For clinical applications, targeted deep sequencing of predicted off-target sites is performed to ensure the safety of the edited cell product.
Functional Validation
Functional assessment of edited cells includes in vitro differentiation of HSPCs into erythroid lineages followed by analysis of hemoglobin expression via HPLC and measurement of sickling propensity under low-oxygen conditions [18]. For preclinical validation, edited HSPCs are transplanted into immunodeficient mice to assess long-term engraftment potential and lineage differentiation in vivo.
The CRISPR-Cas9 system represents a transformative technology for the treatment of sickle cell disease through precise genome editing of hematopoietic stem cells. The dual strategies of direct HBB mutation correction and BCL11A-targeted fetal hemoglobin induction offer promising therapeutic avenues, with the latter already achieving clinical validation and regulatory approval. Continued optimization of gRNA design, delivery methods, and editing efficiency will further enhance the safety and efficacy of these approaches. As the field advances, CRISPR-based therapies hold the potential to provide durable, one-time treatments for sickle cell disease and other monogenic disorders, moving from innovative research concepts to established clinical modalities.
CRISPR Editing Strategies for Beta-Globin Correction: Technical Approaches and Workflows
Sickle cell disease (SCD) is a monogenic autosomal recessive disorder and one of the most prevalent severe monogenic diseases worldwide, affecting approximately 500,000 neonates globally each year [18]. The molecular pathogenesis of SCD stems from a single-nucleotide transversion in the β-globin gene (HBB), where an adenine-to-thymine substitution results in the replacement of glutamic acid with valine at codon 6 (HBB: c.20A>T; p.Glu7Val) [18]. This specific point mutation leads to the production of sickle hemoglobin (HbS), which polymerizes under deoxygenated conditions, distorting red blood cells into a characteristic sickle shape [18]. The abnormal erythrocytes trigger downstream pathological events including vaso-occlusion, hemolytic anemia, ischemic damage to organs and tissues, and significantly reduced lifespan—averaging 42 years for females and 38 years for males in the United States [18].
Direct correction of the SCD point mutation via Homology-Directed Repair (HDR) represents a paradigm shift in therapeutic strategies, moving beyond symptomatic management toward a curative genetic intervention. Unlike approaches that introduce exogenous genes or modulate related pathways, HDR-based correction aims to precisely revert the pathogenic mutation to the wild-type sequence at the endogenous HBB locus, thereby restoring normal β-globin production and hemoglobin function while maintaining native regulatory control [27]. This technical guide examines the current methodologies, challenges, and applications of HDR-mediated HBB gene correction within the broader context of CRISPR research for SCD.
Fundamental Principles of HDR-Mediated Gene Correction
Homology-Directed Repair is a precise DNA repair pathway that becomes active primarily in the S and G2 phases of the cell cycle, utilizing homologous DNA sequences as templates to faithfully repair double-strand breaks (DSBs) [34]. In the context of gene editing for SCD, this natural cellular mechanism is co-opted by introducing a site-specific DSB near the pathogenic mutation using programmable nucleases alongside a donor template containing the correct HBB sequence with homologous arms.
The competitive relationship between HDR and error-prone non-homologous end joining (NHEJ) presents a significant challenge for therapeutic applications. NHEJ frequently dominates DSB repair in hematopoietic stem cells (HSCs), particularly in quiescent populations, often resulting in insertions or deletions (indels) that disrupt the HBB gene rather than correcting it [34] [35]. This competition underscores the importance of optimizing experimental conditions to favor HDR outcomes, including cell cycle synchronization, delivery methods, and the design of editing reagents.
The fundamental workflow for HDR-based HBB correction involves several critical steps: (1) isolation of hematopoietic stem and progenitor cells (HSPCs) from a patient; (2) introduction of sequence-specific nucleases to create a DSB near the E6V mutation; (3) co-delivery of a donor template with the correct HBB sequence; (4) ex vivo culture to allow for repair and expansion; and (5) reinfusion of corrected cells following conditioning [18] [27]. Successful engraftment of these corrected HSCs can then theoretically restore normal erythropoiesis, with even partial chimerism demonstrating therapeutic potential—studies suggest that as little as 20% donor myeloid chimerism may be sufficient to reverse the sickle phenotype [18].
Donor Template Design and Delivery Strategies
Donor Template Variants and Design Considerations
The design of the donor template is a critical determinant of HDR efficiency and safety. Currently, two primary template types dominate HBB correction strategies: viral-based templates (particularly recombinant adeno-associated virus serotype 6, rAAV6) and synthetic single-stranded oligodeoxynucleotides (ssODNs) [34] [35].
Table 1: Comparison of Donor Template Platforms for HBB Gene Correction
| Template Type | Size Capacity | HDR Efficiency (In Vitro) | Engraftment Persistence (In Vivo) | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| rAAV6 | ~4.7 kb | High (34% reported with optimized cassettes) [36] | Reduced long-term persistence in some studies [34] | High transduction efficiency in HSPCs, large cargo capacity | Potential immune responses, production complexity |
| ssODN | <200 bp | Moderate | Superior long-term persistence in engrafting HSCs [34] | Simple design, cost-effective, minimal immunogenicity | Limited homology arm length, lower HDR efficiency for large edits |
| Adenovirus 5/35 | ~36 kb | Variable | Limited data available | Very large cargo capacity | Increased cytotoxicity, complex production |
| IDLV | ~8 kb | Moderate | Limited data available | Non-integrating, extended template persistence | Lower HDR efficiency compared to AAV6 |
Recent innovations in donor template design have focused on overcoming the challenge of sequence homology, which can lead to unpredictable recombination events. Wienert and colleagues developed a novel HBB gene replacement strategy utilizing a diverged HBB coding sequence with heterologous introns (specifically truncated γ-globin introns) to avoid homologous recombination while maintaining physiological β-globin expression levels [36]. This approach achieved 34% HDR efficiency in HSPCs and successfully rescued β-globin expression in SCD models, demonstrating the importance of strategic template engineering [36].
Nuclease Platforms for HBB-Targeted DSB Induction
The induction of a clean DSB at the target locus is prerequisite for HDR. Multiple nuclease platforms have been employed for HBB correction, each with distinct characteristics:
CRISPR-Cas9: The most widely used system utilizes a guide RNA (typically sgRNA-g1 or sgRNA-g6 targeting exon 1 of HBB) complexed with Cas9 nuclease, delivered as ribonucleoprotein (RNP) complexes to minimize oncogenic risks and off-target effects [34]. HiFi Cas9 variants are increasingly employed to enhance specificity [36].
Zinc Finger Nucleases (ZFNs): The first targetable genome-editing nucleases, ZFNs link zinc-finger DNA-binding domains with the FokI nuclease domain. While demonstrating efficacy in HBB correction, they present greater design challenges compared to CRISPR systems [18] [35].
Transcription Activator-Like Effector Nucleases (TALENs): Although successfully used to edit the sickle mutation in cell lines and iPSCs, evidence of TALEN efficacy in primary HSPCs for HBB targeting remains limited [35].
Table 2: Nuclease Performance Metrics in HBB Gene Correction
| Nuclease System | Delivery Method | On-Target Efficiency | Key Advantages | Clinical Translation Status |
|---|---|---|---|---|
| CRISPR-Cas9 RNP | Electroporation | 35-86% (varies by system and cell source) [34] | Easy programmability, high efficiency | FDA-approved (CASGEVY) for BCL11A targeting; HDR correction in trials |
| ZFN mRNA | Electroporation | Comparable to CRISPR-Cas9 in some studies [35] | Smaller size, longer clinical history | Earlier clinical experience but less current use |
| TALEN | mRNA electroporation | Limited data in HSPCs | High specificity | Primarily research-based for HBB correction |
Experimental Protocols for HBB HDR Correction
HDR-Mediated Correction in CD34+ HSPCs
The following protocol outlines a standardized approach for HDR-mediated correction of the SCD mutation in human CD34+ hematopoietic stem and progenitor cells, synthesizing methodologies from multiple recent studies [34] [36] [35].
Step 1: HSPC Isolation and Culture
- Isolate CD34+ cells from mobilized peripheral blood, bone marrow, or cord blood using immunomagnetic selection.
- Culture cells in serum-free medium supplemented with SCF, FMS-related tyrosine kinase 3 ligand (Flt-3L), and thrombopoietin (TPO) at 37°C and 5% CO₂ for 24-48 hours prior to editing.
- Optimal cell density: 1-2×10⁶ cells/mL.
Step 2: RNP Complex Formation and Donor Template Preparation
- For CRISPR-Cas9: Complex HiFi Cas9 protein with sgRNA targeting the HBB locus (e.g., sgRNA-g1: 5'-GTAACGGCAGACTTCTCCTC-3') at a molar ratio of 1:2.5 (Cas9:sgRNA) in R buffer. Incubate at room temperature for 10-20 minutes to form RNP complexes.
- Prepare donor template: For AAV6 delivery, titers of 1×10⁵ - 4×10⁴ vector genomes per cell are typically used. For ssODN donors, use 1-4 µM final concentration.
Step 3: Electroporation and Template Delivery
- Use Lonza 4D-Nucleofector system with P3 Primary Cell solution or comparable electroporation system.
- Program: Code DZ-100 or EN-138 for human CD34+ cells.
- Combine 1×10⁵ - 1×10⁶ cells with pre-formed RNP complexes in a single reaction.
- Immediately following electroporation, add AAV6 donor vectors to culture medium if using viral delivery.
- Plate cells in recovery medium with cytokines at 37°C.
Step 4: Post-Editing Culture and Analysis
- Culture cells for 48-72 hours in cytokine-supplemented medium before transplantation or functional analysis.
- Assess editing efficiency: Perform droplet digital PCR (ddPCR) using allele-specific probes or amplicon next-generation sequencing (NGS) to quantify HDR and NHEJ frequencies at the HBB locus.
- Evaluate cytotoxicity: Measure viability via trypan blue exclusion and Annexin V staining, and assess differentiation potential via colony-forming unit (CFU) assays.
In Vivo Functional Validation in SCD Models
Robust in vivo validation is essential to establish the therapeutic potential of HDR-corrected HSPCs. The Townes-SCD mouse model (which expresses human α- and βS-globin genes) provides a relevant system for functional assessment [37].
Transplantation Protocol:
- Condition recipient Townes-SCD mice with 9.5 Gy radiation (split dose) to clear endogenous hematopoiesis. Provide supportive care including blood transfusions to mitigate radiation toxicity.
- Transplant 1×10⁶ - 2×10⁶ gene-corrected CD34+ cells via tail vein injection.
- Monitor engraftment weekly for 12-20 weeks via peripheral blood collection and flow cytometry for human CD45+ cells.
- Assess functional correction: Measure hemoglobin A (HbA) production by HPLC, evaluate RBC sickling propensity under hypoxic conditions, and monitor reticulocyte counts and RBC half-life as indicators of improved erythropoiesis.
Key Validation Endpoints:
- Molecular: HDR allele frequency in bone marrow-derived myeloid and lymphoid cells.
- Hematological: Proportion of HbA-positive erythrocytes, reduction in sickle cells.
- Physiological: Improved RBC survival, decreased reticulocytosis, resolution of anemia.
Quantitative Assessment of Editing Outcomes
The therapeutic potential of HDR-based strategies must be evaluated through multiple quantitative metrics, including correction efficiency, safety parameters, and functional outcomes.
Table 3: HDR Correction Efficiencies Across Experimental Systems
| Cell Type / Model | Nuclease System | Donor Template | HDR Efficiency (In Vitro) | In Vivo Engraftment/Correction | Reference |
|---|---|---|---|---|---|
| Human CD34+ mPBSCs | CRISPR-Cas9 RNP | rAAV6 | Up to 34% [36] | Significant reduction in engrafted cells [34] | [34] [36] |
| Human CD34+ mPBSCs | CRISPR-Cas9 RNP | ssODN | Lower than AAV6 in vitro [34] | ~6-fold higher persistence vs. AAV6 [34] | [34] |
| Townes-SCD Mouse HSCs | CRISPR-Cas9 RNP | AAV6 | ~25% (Rosa26 target) [37] | Stable HbA production (>20 weeks), correlation with chimerism [37] | [37] |
| β039-Thalassemia ErPCs | CRISPR-Cas9 | ssODN | Demonstrated at genomic, transcriptomic, protein levels [38] | Not assessed | [38] |
Critical to clinical translation is the relationship between HDR efficiency and therapeutic efficacy. Studies indicate that maintaining donor myeloid chimerism above approximately 20% in the bone marrow may be sufficient to reverse the sickle phenotype [18]. Importantly, even low levels of HDR-corrected HSCs can yield substantial therapeutic benefits—in Townes-SCD mice, low levels of chimerism resulted in robust hemoglobin A production and significant improvement in RBC parameters [37].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for HDR-Based HBB Correction Research
| Reagent Category | Specific Examples | Function/Application | Considerations for Use |
|---|---|---|---|
| Nucleases | HiFi Cas9 protein, ZFN mRNA | Induction of site-specific DSBs at HBB locus | RNP delivery reduces off-target effects and cytotoxicity |
| Guide RNAs | sgRNA-g1 (targeting HBB exon 1) | Targets nuclease activity to specific genomic locus | Verify specificity using predictive algorithms (CCTOP) |
| Donor Templates | rAAV6-HBBdiv-HBG2i, ssODN with ~100 nt homology arms | Provides correct template for HDR repair | AAV6 offers higher HDR; ssODN shows better engraftment persistence |
| Cell Culture Reagents | StemSpan SFEM, cytokine cocktails (SCF, TPO, Flt-3L) | Supports HSPC maintenance and expansion | Critical for preserving stemness during ex vivo culture |
| Delivery Systems | Lonza 4D-Nucleofector, Neon Transfection System | Introduces editing reagents into HSPCs | Optimization required for specific cell sources |
| Analysis Tools | ddPCR (allele-specific), Amplicon NGS, HPLC for hemoglobin | Quantifies editing efficiency and functional outcomes | Multiplexed approaches recommended for comprehensive assessment |
Current Challenges and Future Directions
Despite significant progress, HDR-based HBB correction faces several technical hurdles. The inherently low efficiency of HDR in primitive HSCs remains a primary challenge, compounded by the competitive dominance of NHEJ repair pathways [34] [35]. Additionally, cytotoxicity associated with electroporation and nuclease activity can impair engraftment potential, while the potential for off-target editing necessitates comprehensive genomic safety assessments [35] [39].
Future directions focus on enhancing HDR efficiency through small molecule inhibitors of NHEJ components or cell cycle synchronization agents, developing novel delivery systems to reduce cytotoxicity, and optimizing donor designs for improved recombination rates [18] [36]. The emergence of precision editing technologies like base editing and prime editing offer promising alternatives that circumvent some limitations of HDR-based approaches [39]. Base editors can directly convert the pathogenic E6V mutation without requiring DSBs, while prime editors offer greater versatility for installing various sequence changes [39]. However, these technologies currently face their own limitations in efficiency and delivery.
The recent FDA approval of CASGEVY, a CRISPR-based therapy that targets BCL11A to reactivate fetal hemoglobin, validates the broader gene editing approach for SCD while highlighting that multiple strategic paths can yield therapeutic benefits [26]. As HDR-based correction technologies continue to mature, they offer the potential for a more precise physiological solution—restoring native adult hemoglobin regulation while addressing the fundamental genetic cause of sickle cell disease.
Diagram 1: HBB Gene Correction via HDR Workflow. The process begins with isolation of hematopoietic stem and progenitor cells (HSPCs) from a sickle cell disease (SCD) patient, followed by simultaneous delivery of nuclease and donor template. After double-strand break (DSB) induction and homology-directed repair (HDR), corrected cells undergo validation and autologous transplantation, ultimately producing therapeutic hemoglobin A (HbA).
Diagram 2: Donor Template Design Strategies. Key design elements for AAV6 and ssODN donor templates include heterologous introns and diverged coding sequences to maintain physiological expression while avoiding homologous recombination. AAV6 offers larger capacity and higher HDR efficiency, while ssODNs demonstrate superior in vivo persistence.
Sickle cell disease (SCD) is a monogenic autosomal recessive disorder caused by a point mutation in the β-globin gene (HBB), leading to the production of abnormal sickle hemoglobin (HbS) and a spectrum of severe clinical complications [18] [26]. While allogeneic hematopoietic stem cell transplantation offers a cure, its applicability is limited by donor availability and graft-versus-host disease [40]. Direct correction of the HBB mutation via homology-directed repair (HDR) represents a definitive therapeutic strategy [18] [16]. However, this approach faces technical challenges, including achieving robust HDR efficiency in long-term repopulating hematopoietic stem cells (HSCs) [18] [16].
An alternative, indirect strategy has emerged: reactivating fetal hemoglobin (HbF, α2γ2). HbF does not polymerize with HbS and can effectively displace the mutant β-globin chain in hemoglobin tetramers, thereby inhibiting the root pathophysiology of SCD [41]. In healthy development, a switch from fetal (γ-globin) to adult (β-globin) hemoglobin occurs postnatally, coordinated by transcriptional repressors, including BCL11A [42] [43]. This review details the rationale, molecular mechanisms, and technical protocols for disrupting the BCL11A gene as a therapeutic modality to induce HbF for treating SCD, contextualized within the broader goal of HBB mutation correction.
BCL11A as a Master Regulator of Fetal Hemoglobin
Molecular Biology of BCL11A
BCL11A is a zinc-finger transcription factor predominantly expressed in brain and hematopoietic tissues [42]. It functions primarily as a transcriptional repressor [42]. The gene encodes multiple isoforms, with the XL and L isoforms being critical in adult human erythroid cells [43]. Structurally, the BCL11A-XL isoform contains six C2H2-type zinc-finger (ZF) domains organized into two tandem arrays: a low-affinity ZF2-3 array and a high-affinity ZF4-6 array, separated by a ~300-amino-acid linker [43]. This linker enables the protein to bind clustered short DNA sequence motifs across a broader genomic span, enhancing its repressive function [43].
Mechanism of HbF Silencing
BCL11A directly suppresses the expression of the fetal γ-globin genes (HBG1 and HBG2). It binds to specific recognition motifs within the γ-globin gene promoters, particularly at approximately -115 nucleotides upstream of the transcription start site [40]. Crystallographic studies reveal that DNA sequence recognition is mediated by key residues, including Asn756 (ZF4), Lys784, and Arg787 (ZF5) [43]. Disruption of this binding site, as seen in hereditary persistence of fetal hemoglobin (HPFH) mutations, prevents repression and leads to continued HbF expression in adulthood [40] [42]. BCL11A expression is itself regulated by complex mechanisms, including microRNAs (e.g., let-7 family, miR-210, miR-486-3p) and transcription factors like KLF1 [42].
The following diagram illustrates the core therapeutic strategy of BCL11A disruption for HbF reactivation.
Clinical and Preclinical Validation
FDA Approval and Clinical Trial Data
The most significant validation of this approach is the 2023 FDA approval of Casgevy (exagamglogene autotemcel), the first CRISPR-Cas9-based therapy for SCD [44]. Casgevy utilizes an ex vivo strategy where a patient's own CD34+ hematopoietic stem and progenitor cells (HSPCs) are edited to disrupt the BCL11A gene, subsequently reducing BCL11A protein levels and reactivating HbF synthesis [26] [44].
Pivotal clinical trial data demonstrates its efficacy and safety [44]:
- Efficacy: In the ongoing trial, 44 patients with SCD were treated. Of the 31 patients with sufficient follow-up, 29 (93.5%) achieved freedom from severe vaso-occlusive crises (VOCs) for at least 12 consecutive months.
- Safety: All treated patients achieved successful engraftment with no graft failure or rejection. Common side effects were consistent with myeloablative conditioning and included low platelet/white blood cell counts, mouth sores, nausea, and febrile neutropenia.
Comparative Preclinical Studies
Recent preclinical research has further refined this approach. A 2025 study directly compared disrupting the BCL11A binding site to disrupting the binding site of another repressor, ZBTB7A/LRF, in HSPCs from healthy donors and β⁰-thalassemia/HbE patients [40].
Table 1: Comparative Editing Efficiencies and HbF Induction in Preclinical Models [40]
| Cell Source | Target Site | Editing Efficiency (Indel %) | HbF Induction | Common Indel |
|---|---|---|---|---|
| Healthy Donor HSPCs | BCL11A (-115) | 75 - 92% | 26.2 ± 1.4% | 13-bp deletion |
| ZBTB7A/LRF (-197) | 57 - 60% | 27.9 ± 1.5% | 6-bp deletion | |
| β⁰-thalassemia/HbE HSPCs | BCL11A (-115) | ~88.5% | 62.7 ± 0.9% | 13-bp deletion |
| ZBTB7A/LRF (-197) | ~68.2% | 64.0 ± 1.6% | 6-bp deletion |
This study confirmed that disrupting the BCL11A binding site is a highly effective strategy, resulting in HbF levels sufficient to ameliorate the disease pathophysiology. Notably, editing efficiency for the BCL11A site was generally higher than for the ZBTB7A/LRF site [40]. Furthermore, the study reported an absence of detectable off-target effects in BCL11A-edited cells, a critical safety consideration [40].
Experimental Protocols for BCL11A Disruption
This section provides a detailed methodology for BCL11A gene disruption in human HSPCs using CRISPR-Cas9 ribonucleoproteins (RNPs), a method successfully employed in clinical and preclinical studies [40] [16].
Detailed Step-by-Step Workflow
The experimental workflow for ex vivo gene therapy is complex and requires strict adherence to Good Manufacturing Practices (GMP). The following diagram outlines the key stages from cell collection to transplantation.
1. Isolation of Human CD34+ HSPCs:
- Source: Collect HSPCs from a patient's mobilized peripheral blood (using G-CSF) or bone marrow aspirate [44].
- Processing: Isolate CD34+ cells using clinical-grade immunomagnetic bead separation (e.g., CliniMACS system). Cryopreserve cells if not used immediately.
2. Preparation of CRISPR-Cas9 RNP Complex:
- sgRNA Design: Use a chemically synthesized, chemically modified sgRNA (e.g., with 2'-O-methyl 3'-phosphorothioate modifications at both termini) targeting the BCL11A binding site in the HBG promoter (e.g., -115 position) or a BCL11A enhancer region [40] [16]. Example sg-BCL11A sequence (from [40]).
- RNP Complex Formation: Complex high-purity, GMP-grade S. pyogenes Cas9 protein with the sgRNA at a molar ratio of 1:2 (e.g., 60 µg Cas9: 100 µg sgRNA) in an appropriate buffer. Incubate at room temperature for 10-20 minutes to form the RNP complex prior to electroporation [16].
3. Electroporation and Editing:
- Cell Preparation: Thaw and pre-stimulate CD34+ HSPCs in serum-free medium (e.g., StemSpan) supplemented with cytokines (SCF, TPO, FLT3-L) for 24-48 hours.
- Electroporation: Use a clinical-grade electroporator (e.g., Lonza 4D-Nucleofector). Resuspend 1x10^6 cells in 100 µL of electroporation buffer, mix with the pre-formed RNP complex (e.g., 4 µM final concentration), and electroporate using a validated program (e.g., EO-100 pulse code) [40] [16].
- Post-Electroporation Recovery: Immediately transfer cells to pre-warmed culture medium and incubate at 37°C, 5% CO₂.
4. Analysis of Editing Efficiency:
- Genomic DNA Extraction: Harvest cells 48-72 hours post-electroporation.
- Next-Generation Sequencing (NGS): Amplify the targeted genomic region by PCR and perform deep sequencing to quantify indel frequencies and characterize the spectrum of mutations (e.g., 13-bp deletion being most common for BCL11A site editing) [40].
5. Functional Validation: Erythroid Differentiation and HbF Analysis:
- In Vitro Erythroid Differentiation: Culture edited CD34+ cells for up to 21 days in a multi-phase erythroid differentiation medium containing stepwise changes in cytokine combinations (SCF, EPO, IL-3, etc.) to drive maturation into enucleated erythrocytes [40].
- HbF Quantification:
- HPLC: Use Cation-Exchange High-Performance Liquid Chromatography (HPLC) to quantify the percentage of HbF in lysates from differentiated erythroid cells. This provides a direct biochemical measurement [40].
- Flow Cytometry: Intracellularly stain for HbF protein (using fluorescently labeled anti-HbF antibodies) in differentiated cells to determine the proportion of F-cells (HbF-positive cells) [40].
- qRT-PCR: Isolve RNA and perform quantitative reverse transcription PCR (qRT-PCR) to measure γ-globin (HBG) mRNA expression levels, normalized to housekeeping genes [40].
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues critical reagents and their functions for implementing BCL11A disruption experiments.
Table 2: Essential Research Reagents for BCL11A Disruption Studies
| Reagent / Tool | Function / Purpose | Example & Notes |
|---|---|---|
| CRISPR-Cas9 RNP | Induces site-specific DNA double-strand break. RNP delivery minimizes off-target effects and reduces cytotoxicity [40] [16]. | Chemically modified sgRNA (e.g., MS sgRNA) complexed with recombinant Cas9 protein. |
| CD34+ HSPCs | Target cell for ex vivo editing; capable of reconstituting the entire hematopoietic system [16]. | Sourced from mobilized peripheral blood, bone marrow, or cord blood. |
| Electroporation System | Enables efficient delivery of RNP complexes into hard-to-transfect primary HSPCs [16]. | Lonza 4D-Nucleofector System. |
| Erythroid Differentiation Media | Supports in vitro maturation of HSPCs into erythroid lineage, allowing functional assessment of HbF induction [40]. | Multi-phase media with SCF, EPO, LDL, and steroids. |
| AAV6 Homology Donor (for HDR) | Provides a homologous DNA template for precise gene correction via HDR. AAV6 serotype shows high tropism for HSPCs [16]. | Used in strategies for direct HBB correction, not typically for BCL11A knockout. |
| HPLC System | Gold-standard method for quantifying different hemoglobin types (HbA, HbS, HbF) in erythroid cell lysates [40]. | Cation-exchange HPLC. |
| NGS Platform | High-throughput analysis of editing efficiency (indel %), allelic diversity, and off-target profiling [40]. | Illumina MiSeq/NextSeq. |
Disruption of the BCL11A gene represents a paradigm-shifting, indirect therapeutic approach for sickle cell disease. By reactivating fetal hemoglobin, this strategy effectively bypasses the toxic gain-of-function caused by the HBB mutation. The rigorous preclinical validation and subsequent FDA approval of Casgevy underscore the therapeutic viability of this mechanism. While the field continues to advance direct correction strategies for the HBB mutation, BCL11A disruption has proven to be a powerful and clinically successful application of CRISPR/Cas9 technology, offering a one-time, potentially curative treatment for patients with SCD.
Sickle cell disease (SCD) is a monogenic disorder caused by an A-to-T point mutation in the β-globin gene (HBB), which leads to the production of sickle hemoglobin (HbS) and subsequent red blood cell sickling, hemolytic anemia, vaso-occlusive episodes, and multi-organ damage [32] [45]. Ex vivo hematopoietic stem cell (HSC) gene therapy represents a transformative one-time curative approach that involves harvesting a patient's own HSCs, genetically modifying them outside the body to correct the underlying genetic defect, and reinfusing them back into the patient following conditioning chemotherapy [32]. This autologous approach avoids the immunogenic complications of allogeneic transplantation while enabling permanent correction at the DNA level, with modified HSCs capable of self-renewal and lifelong production of healthy erythrocytes [32]. This technical guide details the core protocols for ex vivo HSC gene editing using CRISPR-Cas9 systems, with specific application to SCD therapy development.
HSC Harvesting and Source Cell Preparation
HSC Mobilization and Collection
The initial critical step involves obtaining sufficient quantities of hematopoietic stem and progenitor cells (HSPCs) from the patient. For SCD patients, special considerations must be made due to their unique pathophysiology.
- Collection Sources: HSCs can be harvested directly from bone marrow (BM) under general anesthesia or from mobilized peripheral blood [32].
- Mobilization Agents: Granulocyte colony-stimulating factor (G-CSF) is contraindicated in SCD due to the risk of severe vaso-occlusive episodes and even death. Instead, plerixafor, a CXCR4 antagonist, is used to mobilize CD34+ HSCs from bone marrow to peripheral blood for collection via apheresis [32].
- Purity Challenges: SCD patients exhibit stress-induced erythropoiesis which expands CD34+CD235a+ erythroid progenitors in the bone marrow, potentially reducing HSC purity within the CD34+ population and impacting lentiviral transduction efficiency [32]. Multiple collection rounds may be necessary to obtain adequate CD34+ cells for therapy.
HSC Selection and Enrichment
Following collection, CD34+ cell selection is performed to enrich the HSC concentration for genetic modification. Immunomagnetic selection for CD34+ cells is standard, with further enrichment possible using phenotypic markers to target primitive HSCs. Studies demonstrate that isolating CD34+CD90+CD45RA– cells enriches for long-term repopulating HSCs, allowing for a 10-fold reduction in the number of cells required for transplantation while maintaining durable engraftment [46].
Table 1: Key Cell Populations in HSC Harvesting for SCD Gene Therapy
| Cell Population | Phenotypic Markers | Functional Significance | Considerations for SCD |
|---|---|---|---|
| Bulk HSC/HSPCs | CD34+ | Contains hematopoietic stem and progenitor cells | Standard collection target; may contain excess erythroid progenitors |
| Primitive HSCs | CD34+CD90+CD45RA– | Enriched for long-term engrafting stem cells | Enables dose reduction; improves editing efficiency in true HSCs |
| Erythroid Progenitors | CD34+CD235a+ | Committed erythroid lineage cells | Expanded in SCD BM; can reduce HSC purity and transduction efficiency |
Ex Vivo Genetic Modification Strategies
CRISPR-Cas9 Genome Editing Approaches
Ex vivo CRISPR-Cas9 editing enables precise genetic modification of HSCs to address the underlying pathology of SCD. The primary strategies include gene knockout to reactivate fetal hemoglobin and direct gene correction of the HBB mutation.
Gene Knockout for HbF Reactivation: The FDA-approved therapy Casgevy (exagamglogene autotemcel) utilizes this approach. CRISPR-Cas9 ribonucleoproteins (RNPs) are delivered to CD34+ cells to disrupt a BCL11A erythroid enhancer region, a key repressor of fetal hemoglobin (HbF) [26] [47]. This disruption recapitulates natural hereditary persistence of fetal hemoglobin (HPFH) mutations, leading to sustained HbF production which interferes with HbS polymerization and prevents sickling [46] [26]. Editing efficiencies of 70-80% in the infusion product have been reported, with the 13-nucleotide HPFH deletion being a predominant outcome [46].
Direct Gene Correction: An alternative strategy uses homology-directed repair (HDR) to correct the pathogenic HBB mutation (HBB:c.20A>T) at the endogenous locus. A CRISPR-Cas9-induced double-strand break is repaired using a donor DNA template containing the correct sequence, restoring normal adult hemoglobin production [26]. While precise, this approach faces challenges with lower efficiency compared to non-homologous end joining (NHEJ)-based knockouts.
Editing Workflow and Optimization
The technical workflow for HSC modification requires careful optimization to maximize editing efficiency while preserving stem cell viability and function.
Delivery Method: Electroporation is the standard method for delivering CRISPR-Cas9 as RNP complexes into CD34+ HSCs. This method provides rapid intracellular delivery with transient nuclease presence, reducing off-target risks [46].
Editing Conditions: Optimal conditions differ between species and cell sources. For non-human primate CD34+ cells, a 1:10 molar ratio of Cas9 protein to chemically modified guide RNA achieved ~75% editing efficiency, whereas human cells required different ratios [46]. A typical protocol involves pre-stimulation of CD34+ cells in cytokine media (SCF, TPO, FLT3L) for 24-48 hours, followed by RNP electroporation and recovery in culture medium [46].
Preserving Stemness: Editing can activate p53-mediated DNA damage response, potentially compromising HSC function. Transient p53 upregulation and increased apoptosis peaks 24-48 hours post-electroporation [46]. Colony-forming unit (CFU) assays should confirm that editing does not impair the multilineage differentiation potential of HSCs [46].
Figure 1: Experimental workflow for ex vivo CRISPR editing of hematopoietic stem cells
Conditioning and Reinfusion of Edited HSCs
Pre-transplant Conditioning
Successful engraftment of gene-edited HSCs requires creation of space in the bone marrow niche through myeloablative conditioning, typically with busulfan [32]. This alkylating agent eliminates native HSCs, preventing competition with edited cells while enabling durable engraftment. Unlike allogeneic transplantation, lymphocyte suppression is unnecessary in autologous settings, reducing regimen intensity [32]. Reduced-intensity conditioning has been explored but may result in lower vector copy numbers and therapeutic hemoglobin levels due to mixed chimerism [32].
Engraftment and Persistence Monitoring
Following reinfusion, patients are monitored for hematopoietic recovery and persistence of edited cells. Meta-analyses of preclinical studies reveal that CRISPR-Cas9 edited HSCs initially engraft similarly to unedited cells but may demonstrate reduced persistence at later timepoints and in secondary transplants [48]. In non-human primate models, edited cells maintained up to 30% engraftment for over one year, with corresponding HbF reactivation evidenced by up to 18% HbF-expressing erythrocytes in peripheral blood [46]. Clinical monitoring includes tracking:
- Hematological Recovery: Neutrophil and platelet reconstitution
- Editing Persistence: Vector copy number (VCN) assessment in peripheral blood and bone marrow
- Therapeutic Efficacy: HbF levels, percentage of F-cells, and resolution of SCD symptoms
Table 2: Quantitative Outcomes of Ex Vivo HSC Editing in Preclinical and Clinical Studies
| Study Model | Editing Target | Editing Efficiency | Engraftment/Persistence | Functional Outcome |
|---|---|---|---|---|
| NHP autologous transplant [46] | HBG promoter (BCL11A binding site) | 70-75% in infusion product | Up to 30% for >1 year; ~25% in PB at 1 year | Up to 18% HbF+ erythrocytes |
| NHP with CD34+CD90+CD45RA– cells [46] | HBG promoter | Comparable to bulk CD34+ | Durable multilineage engraftment with 10-fold fewer cells | Stable HbF reactivation |
| Clinical trial (Casgevy) [26] | BCL11A enhancer | High efficiency in clinical product | Sustained engraftment observed | Elimination of VOEs; transfusion independence |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for Ex Vivo HSC Editing
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| HSC Mobilization | Plerixafor (CXCR4 antagonist) | Mobilizes CD34+ HSCs to peripheral blood for collection; essential for SCD patients [32] |
| Cell Separation | Anti-CD34 magnetic beads | Immunomagnetic selection and enrichment of target HSC population from heterogeneous collection |
| Cell Culture | StemSpan media; SCF, TPO, FLT3L | Pre-stimulation cytokine cocktail to promote cell cycling and enhance editing efficiency [46] |
| CRISPR Delivery | Cas9 protein, synthetic sgRNA | Formation of ribonucleoprotein (RNP) complexes for electroporation; reduces off-target risks [46] |
| Editing Assessment | Next-generation sequencing, T7E1 assay | Quantification of editing efficiency and characterization of indel patterns [46] |
| Functional Validation | Colony-forming unit (CFU) assays | Confirmation of multipotent differentiation potential post-editing [46] |
Ex vivo HSC editing protocols represent a groundbreaking therapeutic modality for sickle cell disease, transitioning from research concept to clinical reality with the recent approval of Casgevy. The intricate workflow—from patient-specific HSC collection with plerixafor mobilization through precision CRISPR editing to conditioned reinfusion—demands rigorous optimization and quality control at each stage. Current research focuses on enhancing the efficiency and safety of these protocols, particularly through improved HSC targeting, reduced conditioning toxicity, and innovative approaches to ensure durable persistence of edited cells. As these technologies evolve, ex vivo HSC editing promises to expand its therapeutic reach beyond hemoglobinopathies to address a growing spectrum of genetic disorders.
The emergence of precision genome editing technologies represents a paradigm shift in genetic engineering, moving beyond traditional nuclease-based approaches that rely on double-strand breaks (DSBs) and error-prone repair mechanisms. Base editing and prime editing constitute a new generation of tools that enable precise nucleotide conversion without creating DSBs, thereby minimizing unintended mutations and enhancing safety profiles [49]. These technologies hold particular promise for therapeutic applications where precision is paramount, such as correcting the single-point mutation responsible for sickle cell disease (SCD) [50] [51].
Sickle cell disease, caused by an A•T-to-T•A transversion in the β-globin gene (HBB), represents an ideal target for precision editing approaches [51]. While conventional CRISPR-Cas9 systems have shown therapeutic potential, they generate DSBs that can lead to uncontrolled insertion/deletion (indel) mutations, p53 activation, and chromosomal abnormalities [49] [50]. Base editors and prime editors overcome these limitations by offering more precise genetic modifications, making them particularly suitable for therapeutic correction of the SCD mutation and other monogenic disorders [49] [50] [51].
Technical Foundations of Base Editing
Molecular Mechanism
Base editing utilizes a catalytically impaired Cas9 protein (nCas9) fused to a nucleobase deaminase enzyme, enabling direct chemical conversion of one DNA base pair to another without generating DSBs [49] [52]. Cytosine base editors (CBEs) convert cytosine (C) to thymine (T) through deamination of cytidine to uridine, while adenine base editors (ABEs) convert adenine (A) to guanine (G) through deamination of adenosine to inosine [49] [52]. The editing window is typically restricted to a narrow range of four to five nucleotides within the protospacer adjacent motif (PAM) region, which enhances precision but limits targeting scope [49].
Therapeutic Application for Sickle Cell Disease
For SCD treatment, base editing has been employed to disrupt the BCL11A binding site or create novel transcription factor binding sites to reactivate fetal hemoglobin (HbF) expression [50]. This approach leverages the natural protective effect of HbF against sickling, offering a potential "one-size-fits-all" treatment for SCD and β-thalassemia [50]. In comparative studies, base editing demonstrated 2- to 4-fold greater HbF induction than Cas9 nuclease approaches, with more uniform outcomes across cell populations and reduced genotoxic risks [50].
Technical Foundations of Prime Editing
Molecular Architecture and Mechanism
Prime editing represents a more versatile "search-and-replace" genome editing technology that directly writes new genetic information into a specified DNA site [49] [52]. The system consists of two primary components: (1) a prime editor protein comprising a Cas9 nickase (H840A) fused to an engineered reverse transcriptase (RT), and (2) a specialized prime editing guide RNA (pegRNA) that both specifies the target site and encodes the desired edit [49] [52].
The editing process occurs through a coordinated series of molecular events:
- Target Recognition and Binding: The pegRNA directs the prime editor complex to the target DNA sequence through standard Cas9 complementarity [52].
- DNA Strand Nicking: The Cas9 nickase cleaves the non-target DNA strand, exposing a 3'-hydroxyl group [49] [52].
- Reverse Transcription: The exposed 3'-OH serves as a primer for reverse transcription using the pegRNA's template region [49] [52].
- Flap Resolution and Integration: Cellular repair mechanisms resolve the resulting DNA flap structure, incorporating the newly synthesized edited strand into the genome [49].
Table 1: Evolution of Prime Editor Systems
| Editor Version | Key Components | Editing Efficiency | Notable Features |
|---|---|---|---|
| PE1 | Nickase Cas9 (H840A) + M-MLV RT | ~10-20% in HEK293T | Initial proof-of-concept system |
| PE2 | Optimized RT + enhanced pegRNA design | ~20-40% in HEK293T | Improved reverse transcriptase engineering |
| PE3 | PE2 + additional sgRNA for non-edited strand nicking | ~30-50% in HEK293T | Dual nicking strategy enhances efficiency |
| PEmax | Optimized Cas9/NLS + codon usage | 1.3-3.5× improvement over PE2 | Enhanced editing across multiple loci |
| PE4/PE5 | PEmax + dominant-negative MLH1 | Variable by cell type | MMR inhibition to reduce editing rejection |
pegRNA Design and Optimization
The pegRNA represents a critical innovation in prime editing, incorporating four distinct functional elements: (1) the spacer sequence that identifies the target DNA site (~20 nucleotides), (2) the scaffold sequence that binds Cas9 nickase, (3) the reverse transcription template (RTT) containing the desired edit (25-40 nucleotides), and (4) the primer binding site (PBS) that anchors reverse transcription initiation (10-15 nucleotides) [52]. The complete pegRNA typically ranges from 120-145 nucleotides, with recent advances incorporating engineered pegRNAs (epegRNAs) that include 3' structural motifs to protect against exonuclease degradation [51].
Comparative Analysis of Editing Platforms
Quantitative Performance Metrics
Table 2: Performance Comparison of Genome Editing Platforms for Sickle Cell Disease Correction
| Editing Platform | Editing Efficiency in HSPCs | Key Edit Type | DSB Formation | Indel Formation | Therapeutic Outcome |
|---|---|---|---|---|---|
| CRISPR-Cas9 Nuclease | Variable (depends on HDR efficiency) | NHEJ/HDR-dependent | Yes | High (uncontrolled mixtures) | HbF induction via BCL11A disruption |
| Adenine Base Editing | 2-4× higher HbF vs. Cas9 | A•T to G•C conversion | No | Low | HbF induction via novel TF binding sites |
| Prime Editing | 15-41% correction in SCD HSPCs | All 12 possible base-to-base conversions | No | Minimal | Direct reversion of HBBS to HBBA |
Therapeutic Specificity and Safety Profiles
Prime editing demonstrates a superior safety profile for SCD correction, with minimal off-target effects observed at over 100 experimentally nominated candidate sites in genome-wide analyses [51]. In contrast, base editors can exhibit off-target RNA and DNA editing due to deaminase activity, while conventional Cas9 nucleases generate unpredictable indel mixtures [49] [50]. Prime editing's ability to correct the SCD mutation without DSBs or donor DNA templates eliminates risks associated with p53 activation, chromosomal rearrangements, and AAV vector integration [51].
Experimental Implementation for Sickle Cell Disease
Prime Editing Workflow for SCD Correction
The following diagram illustrates the complete experimental workflow for correcting the SCD mutation using prime editing in hematopoietic stem and progenitor cells (HSPCs):
Research Reagent Solutions
Table 3: Essential Research Reagents for Prime Editing in Sickle Cell Disease Models
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Prime Editor Proteins | PEmax, PE2, PE3 | Catalytic core for editing | PEmax shows 1.3-3.5× higher efficiency in HSPCs |
| pegRNA Design Tools | pegLIT algorithm | Optimize linker and RTT design | Critical for editing efficiency; visual inspection less effective |
| Delivery Systems | RNA electroporation | Component delivery to HSPCs | Clinical compatibility; avoids viral vector limitations |
| HSPC Culture Media | Serum-free expansion media | Maintain stemness during editing | Preserves engraftment potential post-editing |
| Assessment Assays | CIRCLE-seq, HbA HPLC | Off-target profiling and functional validation | Essential for safety and efficacy evaluation |
Protocol for SCD Mutation Correction in HSPCs
The following protocol details the optimal methodology for correcting the SCD mutation using prime editing, based on successful implementation in preclinical studies [51]:
HSPC Isolation and Culture: Isolate CD34+ hematopoietic stem and progenitor cells from SCD patient peripheral blood or bone marrow using clinical-grade magnetic-activated cell sorting. Maintain cells in serum-free expansion media supplemented with SCF, TPO, and FLT3-L at 37°C with 5% CO₂.
pegRNA Design and Synthesis: Design pegRNA targeting the HBB sickle mutation (chr11:5,248,233 in GRCh38) with the following specifications:
- Spacer sequence: 20-nt complementary to HBB target site
- Reverse transcription template: Encodes the A•T-to-T•A correction with 5-nt flanking homology
- Primer binding site: 13-nt length for optimal reverse transcription initiation
- Utilize epegRNA architecture with 3' structural motif to enhance stability
Component Delivery via Electroporation: Electroporate 1×10⁵ HSPCs with the following RNA components:
- 10 μg PEmax mRNA
- 5 μg synthetic epegRNA
- 5 μg nicking sgRNA (for PE3 system)
- Use optimized electroporation parameters: 500V, 5ms pulse for human HSPCs
Transplantation and Engraftment Assessment: Transplant edited HSPCs into immunodeficient NSG mice via tail vein injection (1×10⁵ cells/mouse). Monitor engraftment weekly via peripheral blood sampling for 17 weeks to assess long-term stability of editing.
Functional Validation: Isolate human erythroblasts and reticulocytes from mouse bone marrow at 17 weeks post-transplantation. Assess:
- HbA expression via HPLC (therapeutic threshold: >20% correction)
- Hypoxia-induced sickling propensity (measure reduction from ~67% to ~37%)
- Off-target editing profiling via CIRCLE-seq at >100 nominated sites
Current Challenges and Future Directions
Despite promising results, several technical challenges remain for clinical translation of prime editing for SCD. Delivery efficiency is hampered by the large size of pegRNAs and the need for co-delivery of multiple components [52]. Cellular mismatch repair systems can reverse prime edits, though inhibition strategies using dominant-negative MLH1 (PE4/PE5 systems) show variable efficacy across cell types [51]. Potential immune responses against bacterial-derived Cas9 components must also be addressed through engineered variants with reduced immunogenicity [52].
Future innovations focus on optimizing all components of the prime editing system. Enhanced reverse transcriptase engineering aims to improve processivity and fidelity, while novel Cas9 variants with altered PAM specificities will expand the targeting scope [49] [52]. Advanced delivery systems, including lipid nanoparticles specifically engineered for pegRNA delivery, show promise for in vivo therapeutic applications that could eventually bypass the need for ex vivo HSPC manipulation [52].
Base editing and prime editing represent significant advancements in precision genome editing, offering versatile solutions for therapeutic correction of the SCD mutation. Prime editing particularly stands out for its ability to directly revert the pathogenic HBBS allele to wild-type HBBA without DSBs or donor DNA templates, achieving correction rates of 15-41% in patient-derived HSPCs with minimal off-target effects [51]. As these technologies continue to evolve, they hold tremendous promise for developing safe, effective, and durable therapies for sickle cell disease and other monogenic disorders. The ongoing optimization of editing efficiency, delivery methods, and safety profiles will be crucial for successful clinical translation in the coming years.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated protein 9 (Cas9) system has emerged as the most effective, efficient, and precise genome-editing technology currently available [53]. For sickle cell disease (SCD), a monogenic disorder caused by an A-to-T point mutation in the β-globin gene (HBB), CRISPR-Cas9 represents a promising therapeutic approach to correct the underlying genetic defect [18] [54]. The system consists of two fundamental components: a guide RNA (gRNA) that directs the complex to a specific DNA sequence, and the Cas9 nuclease that creates a double-stranded break at the targeted location [53] [55].
A paramount challenge in therapeutic CRISPR application is the safe and efficient delivery of these components into target cells [53] [55]. The choice of delivery system critically influences the safety profile, editing efficiency, and therapeutic potential of CRISPR-based treatments for SCD. Delivery strategies are broadly categorized into viral vectors, non-viral nanoparticles (notably Lipid Nanoparticles, LNPs), and physical methods such as electroporation [56]. For SCD, therapies can be administered either ex vivo, where patient-derived hematopoietic stem and progenitor cells (HSPCs) are edited outside the body and then reinfused, or in vivo, where the editing machinery is delivered directly into the patient's body [6] [26].
The delivery of CRISPR-Cas9 requires transporting the functional payload—which can be in the form of DNA, mRNA, or preassembled ribonucleoprotein (RNP)—to the nucleus of target cells [56]. The table below summarizes the core characteristics of the primary delivery platforms used in SCD research.
Table 1: Comparison of Key CRISPR-Cas9 Delivery Systems for SCD Therapy
| Delivery System | Mechanism of Action | Primary Cargo Format | Editing Paradigm | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | Viral transduction; delivers genetic material for Cas9 and gRNA expression [53]. | DNA | Primarily in vivo [53]. | Low immunogenicity/profile; proven clinical success; natural tropisms for specific tissues [53] [57]. | Severely limited cargo capacity (<5 kb); potential for long-term persistence and off-target editing; pre-existing immunity in many patients [53] [56]. |
| Lentivirus (LV) | Viral transduction; integrates into host genome to provide stable expression [56]. | DNA | Ex vivo [26]. | High efficiency for cell engineering; large cargo capacity; stable, long-term expression [56]. | Permanent integration raises insertional mutagenesis concerns; safety implications of HIV backbone [56]. |
| Lipid Nanoparticles (LNPs) | Synthetic particles that encapsulate and protect cargo, fusing with cell membranes for delivery [58]. | mRNA or RNP | In vivo or ex vivo [6] [58]. | Transient activity reduces off-target risks; suitable for re-dosing [6]; high efficiency for liver-targeted delivery [6] [58]. | Can trigger infusion-related reactions; largely limited to hepatic targets with current formulations; endosomal escape can be inefficient [6] [58]. |
| Electroporation | Physical method using electrical pulses to create transient pores in the cell membrane [26]. | RNP (preferred) or mRNA | Ex vivo [26]. | High efficiency in hard-to-transfect cells like HSPCs; RNP delivery is rapid and minimizes off-target effects [26]. | Specialized equipment required; can cause significant cell death and stress; not suitable for in vivo delivery [26]. |
Delivery System Architectures and Workflows
The functional workflow of a CRISPR-Cas9 experiment, from design to analysis, involves a sequence of critical steps common across delivery methods. The following diagram outlines this generalized workflow, highlighting key decision points.
Ex Vivo Editing Workflow for SCD
The ex vivo approach is the basis for the first FDA-approved CRISPR therapy for SCD, Casgevy [26]. This multi-step process involves isolating a patient's own cells, editing them outside the body, and then returning them.
Table 2: Key Research Reagents for Ex Vivo SCD Gene Editing
| Research Reagent / Material | Function in the Protocol |
|---|---|
| CD34+ HSPCs | The target cell population, harboring the sickle cell mutation. These are therapeutically relevant cells capable of reconstituting the entire blood system [18] [26]. |
| CRISPR RNP Complex | The active editing machinery. Comprising the purified Cas9 protein and synthetic sgRNA, it offers immediate activity and rapid degradation, which enhances precision and reduces off-target effects [56] [26]. |
| Electroporation System | Specialized instrumentation (e.g., Lonza 4D-Nucleofector) that uses electrical pulses to transiently permeabilize cell membranes, allowing the RNP complex to enter the CD34+ cells efficiently [26]. |
| Stem Cell Culture Media | A precisely formulated medium (e.g., StemSpan) containing cytokines (SCF, TPO, FLT3-L) that maintains the viability and stemness of HSPCs during the ex vivo manipulation process [18]. |
| Donor DNA Template | A synthetic DNA molecule containing the correct HBB sequence, used to guide the cell's Homology-Directed Repair (HDR) machinery to precisely correct the mutation [18] [26]. |
In Vivo Delivery Workflow for SCD
In vivo delivery aims to administer the CRISPR therapeutic directly to the patient, offering a less invasive alternative. The success of this approach hinges on the delivery vehicle reaching the target tissue—most often the liver or hematopoietic stem cells in the bone marrow.
Experimental Protocols for SCD Research
Ex Vivo HSC Editing via Electroporation of RNP
This protocol is adapted from methods used in clinical trials for SCD, including the development of Casgevy, which involves knocking out the BCL11A gene to reactivate fetal hemoglobin [26].
- CD34+ HSPC Mobilization and Collection: Mobilize HSPCs from the patient's bone marrow into the peripheral blood using granulocyte colony-stimulating factor (G-CSF). Collect the cells via leukapheresis [26].
- Cell Isolation and Purity: Isulate CD34+ cells from the apheresis product using clinical-grade immunomagnetic beads. Confirm cell viability and purity via flow cytometry. Maintain cells in serum-free medium supplemented with stem cell cytokines (SCF, TPO, FLT3-Ligand) [18].
- RNP Complex Formation: Combine 100 µg of high-fidelity Cas9 protein with a 1.2x molar ratio of synthetic sgRNA (targeting the BCL11A erythroid enhancer or the HBB gene locus) in a sterile buffer. Incubate at room temperature for 10-20 minutes to allow RNP complex assembly [26].
- Electroporation: Resuspend 1x10^5 CD34+ cells in 100 µL of electroporation buffer. Mix with the pre-formed RNP complex and transfer to an electroporation cuvette. Electroporate using a designated program (e.g., for human CD34+ cells on a Lonza 4D-Nucleofector). Immediately after pulsing, add pre-warmed culture medium to the cells [26].
- Post-Electroporation Culture and Analysis: Culture the edited cells in cytokine-enriched medium for 48-72 hours. Analyze editing efficiency using targeted next-generation sequencing (NGS) to quantify Indel formation at the BCL11A locus or HDR-mediated correction at the HBB locus. Perform flow cytometry to assess fetal hemoglobin (HbF) expression in erythroid cells derived from edited progenitors after in vitro differentiation [18] [26].
- Transplantation: Prior to reinfusion, the patient undergoes myeloablative conditioning (e.g., with busulfan) to clear the bone marrow niche. The edited CD34+ cells are then infused back into the patient [26].
In Vivo Editing via LNP Delivery of mRNA
This protocol is based on recent clinical advances, such as the use of LNPs to deliver CRISPR components systemically for the treatment of hereditary transthyretin amyloidosis (hATTR), demonstrating the potential for in vivo application to other genetic diseases [6].
- LNP Formulation: Prepare ionizable cationic lipids, phospholipids, cholesterol, and PEG-lipid in an ethanol phase. Prepare the aqueous phase containing the CRISPR payload—either Cas9 mRNA and sgRNA, or a single mRNA encoding both Cas9 and the sgRNA. Use a microfluidic mixer to combine the two phases rapidly, forming LNPs that encapsulate the nucleic acids. Dialyze the LNP formulation against a buffer to remove ethanol and calibrate the final concentration [58].
- Quality Control: Characterize the LNP preparation by measuring particle size and polydispersity index (PDI) via dynamic light scattering. Determine encapsulation efficiency using a Ribogreen assay. Confirm sterility through standard microbiological tests [58].
- In Vivo Administration: Administer the LNP formulation to the animal model or human patient via intravenous infusion. Clinical trials have used doses in the range of 0.1-1.0 mg of mRNA per kg of body weight, infused over several hours to mitigate infusion-related reactions [6].
- Efficacy and Safety Monitoring: Collect blood and tissue samples at regular intervals post-administration. For SCD-relevant targets, quantify the reduction of the disease-related protein (e.g., serum TTR for hATTR) or the level of target gene editing in circulating cells via NGS. Monitor for potential immune responses and liver enzymes (ALT, AST) to assess toxicity [6].
Emerging Technologies and Future Directions
The field of CRISPR delivery is rapidly evolving. Several emerging technologies and strategic shifts are poised to enhance the safety, efficacy, and applicability of SCD therapies.
- Advanced LNP Formulations: Research is focused on developing Selective Organ Targeting (SORT) LNPs. By incorporating additional SORT molecules, these LNPs can be engineered to shift their tropism from the liver to other tissues, such as the bone marrow, which is critical for directly targeting HSCs in vivo [58] [56].
- Virus-Like Particles (VLPs): VLPs are engineered particles that consist of an empty viral capsid but lack the viral genome. This platform offers the cell-targeting ability of viral vectors without the risks of genomic integration. VLPs deliver CRISPR components transiently, reducing the potential for long-term off-target effects, and are being explored for delivering base editors and prime editors [56].
- AI-Powered Experimental Design: Tools like CRISPR-GPT, an AI large language model trained on over a decade of CRISPR experimental data, are now assisting researchers in designing gRNAs, predicting off-target effects, and troubleshooting experimental designs. This AI copilot can significantly accelerate the preclinical development timeline for novel therapies [59].
- In Vivo Reprogramming for Rare Diseases: A landmark case in 2025 demonstrated the first personalized in vivo CRISPR treatment for an infant with a rare genetic disease (CPS1 deficiency). The therapy was developed and delivered via LNP in just six months, establishing a regulatory precedent for "on-demand" gene editing platforms that could be adapted for SCD variants [6].
- Redosing Potential of LNP Therapies: Unlike viral vectors, which often trigger strong immune responses that prevent re-administration, LNP-based CRISPR therapies have shown potential for redosing. In clinical trials for hATTR, participants safely received a second, higher dose of the LNP-CRISPR therapy, and the personalized therapy for infant KJ involved three separate doses, each providing additional therapeutic benefit [6].
The translation of CRISPR-based genetic correction for sickle cell disease from a laboratory concept to an approved medicine represents a triumph of modern biotechnology. The strategic selection and continuous refinement of delivery systems—viral vectors, LNPs, and electroporation—have been instrumental in this success. Each platform offers a distinct set of advantages tailored to specific therapeutic contexts, from the ex vivo engineering of HSCs using electroporation to the emerging potential of in vivo reprogramming via LNPs. As research progresses, innovations in vector engineering, such as targeted LNPs and safer viral constructs, combined with AI-driven design tools, promise to further enhance the precision, safety, and accessibility of these transformative therapies, ultimately broadening their impact for patients suffering from sickle cell disease and other genetic disorders.
The approval of CASGEVY (exagamglogene autotemcel) by the U.S. Food and Drug Administration represents a watershed moment in translational medicine, marking the first clinical application of CRISPR/Cas9 genome editing technology [44]. This autologous cell-based gene therapy is indicated for patients aged 12 years and older with severe sickle cell disease (SCD) or transfusion-dependent beta thalassemia (TDT), addressing a significant unmet need for curative treatments for these inherited hemoglobinopathies [44]. The development pathway for Casgevy exemplifies a successful transition from preclinical target identification through clinical validation to regulatory approval, establishing a blueprint for future genome-editing therapeutics. This review delineates the comprehensive translational journey of Casgevy, with particular emphasis on its context within broader CRISPR-based research aimed at correcting the sickle cell disease beta-globin mutation.
Molecular Pathogenesis and Therapeutic Rationale
Sickle Cell Disease Pathophysiology
Sickle cell disease is an inherited hemoglobinopathy caused by a single nucleotide substitution (A>T) in the β-globin gene (HBB) on chromosome 11, resulting in a missense mutation (Glu6Val) that produces abnormal sickle hemoglobin (HbS) [60]. Under deoxygenated conditions, HbS polymerizes, causing red blood cells to adopt a characteristic sickle shape that leads to recurrent vaso-occlusive crises (VOCs), chronic hemolytic anemia, progressive multiorgan damage, and early mortality [44] [60]. The clinical hallmark of SCD is the vaso-occlusive crisis, a painful event requiring medical intervention that significantly diminishes patient quality of life [61].
The Fetal Hemoglobin Reactivation Strategy
A key physiological observation informed Casgevy's therapeutic strategy: individuals with SCD who co-inherit genetic mutations causing hereditary persistence of fetal hemoglobin (HPFH) experience markedly milder disease [60]. Fetal hemoglobin (HbF, α₂γ₂), which is naturally expressed during fetal development but declines postnatally, does not incorporate the mutated β-globin chain and effectively inhibits HbS polymerization [62]. The developmental switch from γ-globin (HbF) to β-globin (adult hemoglobin) expression is primarily governed by the transcriptional repressor BCL11A, which silences the HBG1 and HBG2 genes encoding γ-globin [62] [60]. Casgevy's mechanism involves disrupting the BCL11A gene in hematopoietic stem cells to reactivate HbF production, thereby compensating for the defective adult hemoglobin in SCD patients [62].
Table 1: Key Molecular Targets in Sickle Cell Disease Gene Therapy
| Target | Biological Function | Therapeutic Approach | Outcome |
|---|---|---|---|
| BCL11A Gene | Transcriptional repressor of fetal hemoglobin (HbF) | CRISPR/Cas9 editing of erythroid-specific enhancer [62] | Silencing of BCL11A in erythroid lineage [62] |
| HbF (γ-globin) | Fetal hemoglobin form that resists polymerization | Reactivation via BCL11A disruption [44] | Increased HbF levels, reduced sickling [61] |
| BCL11A Enhancer | Regulatory element controlling BCL11A expression | Precise double-strand break by CRISPR/Cas9 [62] | Disruption of 3D chromatin structure, gene silencing [62] |
Preclinical Development and Mechanism Elucidation
Target Validation and CRISPR Tool Selection
Preclinical studies established BCL11A as a promising therapeutic target through genetic association studies and conditional knockout mouse models demonstrating that BCL11A deficiency robustly induces HbF without catastrophic consequences for erythropoiesis [62]. The CRISPR/Cas9 system was selected as the preferred genome editing platform due to its high efficiency, precision, and relatively simpler design compared to earlier technologies like zinc finger nucleases (ZFNs) and transcription activator-like effector nucleases (TALENs) [14] [63].
Casgevy employs a non-viral, ex vivo CRISPR/Cas9 editing approach where patient-derived CD34+ hematopoietic stem and progenitor cells (HSPCs) are genetically modified to disrupt an erythroid-specific enhancer region of the BCL11A gene [64]. This strategy enables erythroid-specific knockdown of BCL11A while preserving its expression in non-erythroid cells where it serves important functions in B-lymphopoiesis and neurodevelopment [62].
Elucidation of the Three-Dimensional Genome Mechanism
Recent research has illuminated the precise molecular mechanism through which Casgevy achieves BCL11A silencing. The targeted enhancer region forms a specific three-dimensional "chromatin rosette" structure that maintains high-level BCL11A expression in red blood cell precursors by facilitating contacts between critical regulatory elements [62]. The CRISPR/Cas9-induced double-strand break disrupts this chromatin architecture, allowing repressive proteins to access the locus and permanently silence BCL11A expression [62]. Furthermore, investigators discovered that this enhancer produces a specific enhancer RNA (eRNA) that is essential for maintaining the chromatin structure, revealing a potential alternative target for therapeutic intervention using antisense oligonucleotides [62].
Diagram 1: BCL11A Targeting Mechanism - This diagram illustrates how Casgevy disrupts the normal three-dimensional chromatin structure of the BCL11A gene, leading to its silencing and subsequent reactivation of fetal hemoglobin (HbF).
Clinical Trial Program and Outcomes
Clinical Trial Design
The clinical development program for Casgevy consisted of multiple open-label trials designed to evaluate safety and efficacy in patients with severe SCD or TDT. The pivotal trials included:
- CLIMB-121: Phase 1/2/3 trial for SCD patients ages 12-35 with recurrent VOCs (≥2 severe VOCs annually) [64] [61]
- CLIMB-111: Phase 1/2/3 trial for TDT patients requiring regular transfusions [64]
- CLIMB-131: Long-term follow-up study designed to monitor patients for up to 15 years post-treatment [64]
All trials employed an autologous hematopoietic stem cell transplantation approach wherein patients underwent myeloablative conditioning with busulfan followed by infusion of CRISPR-edited CD34+ cells [44] [61]. The primary efficacy endpoints differed between indications: freedom from severe VOCs for at least 12 consecutive months for SCD, and transfusion independence for at least 12 consecutive months with weighted average hemoglobin ≥9 g/dL for TDT [44] [64].
Efficacy Outcomes
Clinical trials demonstrated remarkable efficacy for Casgevy in both SCD and TDT populations. In the interim analysis of the SCD trial, 29 of 31 evaluable patients (93.5%) achieved freedom from severe VOCs for at least 12 consecutive months during the 24-month follow-up period [44]. All evaluable patients (30/30) were free from hospitalizations for severe VOCs for the same duration [61]. Updated data presented in 2025 with longer follow-up (mean 39.4 months, extending beyond 5.5 years) showed that 43 of 45 evaluable patients (95.6%) maintained VOC-free status for at least 12 consecutive months, with a mean VOC-free duration of 35.0 months [64].
For TDT patients, the results were equally impressive, with 54 of 55 evaluable patients (98.2%) achieving transfusion independence for at least 12 consecutive months, with a mean duration of 40.5 months [64]. Furthermore, 69.6% of treated TDT patients (39/56) were able to discontinue iron removal therapy for more than 6 months following Casgevy infusion, demonstrating correction of ineffective erythropoiesis and iron overload [64].
Table 2: Casgevy Clinical Efficacy Outcomes (2025 Updated Analysis)
| Parameter | Sickle Cell Disease (SCD) | Transfusion-Dependent Beta Thalassemia (TDT) |
|---|---|---|
| Primary Endpoint | Freedom from severe VOCs for ≥12 consecutive months [64] | Transfusion independence for ≥12 consecutive months with Hb ≥9 g/dL [64] |
| Evaluable Patients | n=45 | n=55 |
| Responders | 43/45 (95.6%) | 54/55 (98.2%) |
| Mean Response Duration | 35.0 months (range 14.4-66.2) [64] | 40.5 months (range 13.6-70.8) [64] |
| Key Secondary Endpoint | Freedom from hospitalization for severe VOCs: 45/45 (100%) [64] | Discontinuation of iron chelation: 39/56 (69.6%) [64] |
| Longest Follow-up | >5.5 years [64] | >6 years [64] |
Safety Profile
The safety profile of Casgevy was generally consistent with the effects of myeloablative conditioning with busulfan and autologous hematopoietic stem cell transplantation [64]. The most common adverse effects included:
- Low levels of platelets and white blood cells [44]
- Mouth sores (stomatitis) [44]
- Nausea, musculoskeletal pain, abdominal pain [44]
- Febrile neutropenia [44]
These cytopenias represent expected consequences of myeloablative conditioning and were managed with standard supportive care until hematopoietic recovery occurred [61]. No graft-versus-host disease was observed, which represents a significant safety advantage over allogeneic transplantation [60]. Patients continued to demonstrate stable levels of fetal hemoglobin and allelic editing throughout the follow-up period, indicating durable engraftment and persistence of the therapeutic effect [64].
Manufacturing and Regulatory Pathway
Cell Processing and Therapeutic Manufacturing
Casgevy manufacturing follows a complex, multi-step process that requires approximately six months from cell collection to final product delivery [61]:
- Stem Cell Mobilization and Collection: Patients receive mobilization medicine to move hematopoietic stem cells from bone marrow to peripheral blood, followed by apheresis collection [61]
- CRISPR Genome Editing: Collected CD34+ HSPCs are edited ex vivo using CRISPR/Cas9 to target the BCL11A erythroid-specific enhancer [64]
- Myeloablative Conditioning: Patients receive busulfan conditioning to clear bone marrow space for engraftment of edited cells [44]
- Product Infusion: Edited cells are administered via intravenous infusion [61]
- Engraftment and Recovery: Patients require 4-6 weeks of hospitalization for monitoring and supportive care until hematological recovery [61]
A critical step in the process is the collection and cryopreservation of "rescue cells" - a portion of the patient's unmodified hematopoietic stem cells that can be reinfused if the edited cells fail to engraft or if manufacturing fails [61].
Regulatory Review and Approval
The Casgevy development program received multiple regulatory designations that accelerated its clinical development and review:
- Priority Review: Expedited review timeline for products offering significant advantages [44]
- Orphan Drug Designation: Incentives for drugs treating rare diseases [44]
- Fast Track Designation: Facilitated development and expedited review [44]
- Regenerative Medicine Advanced Therapy (RMAT) Designation: Accelerated development of regenerative medicine products [44]
These designations reflected the transformative potential of Casgevy for serious conditions with limited treatment options. The FDA approval in December 2023 was based on the robust efficacy and manageable safety profile demonstrated in the clinical trials [44].
Diagram 2: Clinical Translation Pathway - This diagram outlines the key stages in Casgevy's development from preclinical research through manufacturing, clinical trials, and regulatory approval.
Technical and Implementation Considerations
The Scientist's Toolkit: Essential Research Reagents
The development and manufacturing of CRISPR-based therapeutics like Casgevy require specialized reagents and materials that adhere to stringent quality standards:
Table 3: Essential Research Reagents for CRISPR Therapy Development
| Reagent/Material | Function | Considerations |
|---|---|---|
| GMP-grade gRNA [63] | Guides Cas9 to specific genomic target (BCL11A enhancer) | Must be true GMP-grade, not "GMP-like"; critical for consistency [63] |
| GMP-grade Cas9 Nuclease [63] | Creates precise double-strand DNA breaks | High purity and activity essential for editing efficiency [63] |
| Mobilization Agents | Moves stem cells from bone marrow to peripheral blood | Required for stem cell collection via apheresis [61] |
| Myeloablative Conditioning Agents | Clears bone marrow space for engrafted cells | Busulfan used in Casgevy trials [44] |
| Cryopreservation Media | Preserves cells during manufacturing and storage | Maintains cell viability throughout process [61] |
Implementation Challenges and Solutions
The translation of Casgevy from bench to bedside has faced several significant challenges:
Manufacturing Complexity: The multi-month, patient-specific manufacturing process requires sophisticated facilities and rigorous quality control [61] [63]. Solution: Closed-system automated processing and standardized protocols.
Toxic Conditioning Regimen: The myeloablative conditioning carries significant toxicity [60]. Solution: Ongoing research into reduced-intensity conditioning regimens.
Healthcare Infrastructure Requirements: Treatment requires specialized academic medical centers with stem cell transplantation expertise [60]. Solution: Establishment of certified treatment centers and specialized training programs.
Economic Considerations: The high cost of therapy presents accessibility challenges [6]. Solution: Outcomes-based reimbursement agreements and innovative payment models developed by the manufacturer [64].
The successful clinical translation of Casgevy from preclinical models to FDA-approved therapy represents a paradigm shift in the treatment of genetic disorders. By demonstrating that precise genome editing can produce durable clinical benefits with an acceptable safety profile, Casgevy has established a new therapeutic modality with applications extending far beyond hemoglobinopathies. The continued follow-up of treated patients beyond six years provides increasing confidence in the long-term durability of the treatment effect [64].
Future directions in the field include the development of in vivo genome editing approaches that could eliminate the need for complex ex vivo manufacturing and myeloablative conditioning [6], next-generation editing technologies such as base and prime editing that offer potentially greater precision [14], and alternative targeting strategies such as antisense oligonucleotides against BCL11A enhancer RNA that might offer more accessible treatment options [62]. As the field advances, Casgevy will stand as a landmark achievement that paved the way for a new generation of genomic medicines.
Overcoming Technical Hurdles: Optimization Strategies for Enhanced Efficiency and Safety
The promise of CRISPR-Cas9 technology for curing genetic disorders like sickle cell disease (SCD) is undeniable, with the first therapies already receiving regulatory approval. However, the transition from laboratory research to widespread clinical application hinges on solving one fundamental challenge: the safe, efficient, and targeted delivery of CRISPR components to therapeutically relevant cells in vivo. For SCD, caused by an A-to-T point mutation in the β-globin gene (HBB), the ultimate therapeutic goal is to correct this mutation in hematopoietic stem cells (HSCs) [18]. The delivery system must navigate multiple biological barriers, protect its cargo from degradation, achieve specific cellular uptake, and facilitate nuclear entry—all while minimizing off-target effects and immune reactions [65] [66]. This technical guide examines the current landscape of delivery platforms, focusing on strategies for organ-specific targeting and enhanced cellular uptake critical for translating HBB correction strategies from bench to bedside.
Cargo Options: Balancing Efficiency, Specificity, and Safety
The choice of CRISPR cargo format significantly influences editing efficiency, specificity, and potential immunogenicity. Researchers primarily work with three deliverable forms, each with distinct advantages and limitations [65] [67].
Table 1: Comparison of CRISPR-Cas9 Delivery Cargo Formats
| Cargo Type | Components | Key Advantages | Major Limitations | Best Applications |
|---|---|---|---|---|
| Plasmid DNA (pDNA) | DNA plasmid encoding Cas9 and sgRNA [65] | Economical, high stability, easy to produce [65] | Large size, low nuclear entry efficiency, prolonged expression increasing off-target risk [65] [67] | In vitro research where cost is a primary factor |
| Messenger RNA (mRNA) | Cas9 mRNA + separate sgRNA molecule [65] | Transient expression, reduced off-target risk compared to pDNA, faster action than pDNA [65] [67] | Lower stability, potential for premature sgRNA degradation, requires simultaneous delivery of two components [65] | In vivo applications where transient activity is desirable |
| Ribonucleoprotein (RNP) | Pre-complexed Cas9 protein and sgRNA [65] [67] | Immediate activity, highest editing efficiency, lowest off-target effects, minimal immunogenicity concern [67] [68] | Most challenging to deliver in vivo due to large size and stability during formulation [68] | Clinical applications prioritizing safety and precision; ex vivo editing (e.g., CASGEVY) [67] |
For SCD therapy, the RNP complex is often the preferred cargo, particularly for ex vivo approaches like the FDA-approved CASGEVY therapy, where patient HSCs are edited outside the body before reinfusion [67] [26]. The immediate activity of RNPs shortens the time window for unintended edits, and their rapid degradation limits off-target effects [67]. However, achieving efficient in vivo delivery of large RNP complexes remains a significant technical hurdle, driving the development of advanced nanoparticle systems [68].
Delivery Vehicles: Navigating the Biological Landscape
Delivery vehicles are engineered to protect CRISPR cargo and facilitate its journey into target cells. They are broadly categorized into viral, non-viral, and physical methods.
Viral Vectors
Viral vectors are engineered viruses that exploit natural viral infection pathways for high-efficiency gene delivery.
Table 2: Viral Delivery Systems for CRISPR-Cas9
| Vector Type | Payload Capacity | Integration into Genome | Key Advantages | Major Limitations |
|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | ~4.7 kb [56] [66] | No [56] | Low immunogenicity, mild immune response, high tissue tropism variety [56] | Limited payload capacity (too small for full SpCas9 + sgRNA + donor template), potential for pre-existing immunity [56] [66] |
| Lentivirus (LV) | ~8 kb [56] | Yes [56] | High transduction efficiency, can infect dividing and non-dividing cells, large cargo capacity [56] | Insertional mutagenesis risk, safety concerns due to HIV backbone [56] |
| Adenovirus (AdV) | ~36 kb [56] | No [56] | Very large cargo capacity, high transduction efficiency [56] | Strong immune response, potential toxicity [56] |
AAVs are the most prominent viral vector for in vivo gene therapy due to their favorable safety profile. However, their limited payload capacity is a critical constraint for CRISPR systems. Strategies to overcome this include using two separate AAVs or employing smaller Cas9 orthologs (e.g., Cas12a) [56].
Non-Viral Nanocarriers
Non-viral nanocarriers have gained prominence for their improved safety profile, reduced immunogenicity, and greater payload flexibility compared to viral vectors.
- Lipid Nanoparticles (LNPs): LNPs are the most clinically advanced non-viral platform, proven successful in mRNA-based COVID-19 vaccines and CRISPR therapies [67]. They are synthetic particles comprising ionizable lipids, phospholipids, cholesterol, and PEG-lipids [68]. The ionizable lipids are crucial for endosomal escape, a major barrier to intracellular delivery. Recent advances include Selective Organ Targeting (SORT) LNPs, where the addition of supplemental lipids (e.g., permanently cationic lipids) enables precise redirection of LNPs to specific organs like the lungs, liver, and spleen following intravenous administration [56] [68]. LNPs naturally accumulate in the liver, making them ideal for targeting hepatocytes for diseases like hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) [6].
- Other Non-Viral Platforms:
- Extracellular Vesicles (EVs): Natural, cell-derived lipid vesicles with inherent biocompatibility and potential for homing to specific tissues. However, challenges in production scalability and cargo loading heterogeneity remain [56].
- Polymer-Based Nanoparticles: Cationic polymers form polyplexes with nucleic acids or proteins via electrostatic interactions, but can suffer from toxicity and lower efficiency compared to LNPs [56].
- Gold Nanoparticles (AuNPs): Inorganic particles that can be conjugated with CRISPR components, often used with physical methods like electroporation [67].
Physical Delivery Methods
Physical methods use external forces to transiently disrupt the cell membrane, allowing direct cargo passage.
- Electroporation: Applying electrical pulses to cells in suspension creates temporary pores in the cell membrane. This is the gold standard for ex vivo CRISPR delivery, as used in the CASGEVY therapy for SCD, where patient HSCs are electroporated with RNP complexes targeting the BCL11A enhancer [67] [26].
- Microinjection: A glass micropipette is used to inject CRISPR components directly into a single cell, commonly used for genetic engineering of animal embryos and in vitro fertilized zygotes [66].
Organ-Specific Targeting Strategies
Moving from broad systemic distribution to precise organ-specific delivery is a primary focus of next-generation delivery systems.
Liver-Targeted Delivery
The liver is a naturally accessible organ for nanocarriers due to sinusoidal fenestrations and resident phagocytic Kupffer cells. Lipid Nanoparticles (LNPs) show a natural tropism for the liver following intravenous administration, making them an ideal platform for hepatic gene editing [6]. This has been successfully leveraged in clinical trials for hATTR and HAE, where LNPs deliver CRISPR components to hepatocytes to disrupt disease-driving genes [6]. The high protein production capacity of the liver means that editing a relatively small percentage of hepatocytes can yield a significant therapeutic effect.
Lung-Targeted Delivery
Engineering LNPs for lung targeting requires specific formulation adjustments. Research has demonstrated that incorporating permanently cationic lipids (e.g., DOTAP) into standard LNP formulations can redirect them to the lung endothelium and epithelium following intravenous injection [68]. This approach has enabled multiplexed gene editing in mouse lungs, showcasing its potential for treating genetic respiratory diseases like cystic fibrosis.
Hematopoietic Stem Cell (HSC) Targeting for Sickle Cell Disease
For SCD, the therapeutic target is the population of HSCs residing in the bone marrow. The clinically approved therapy CASGEVY uses an ex vivo approach: HSCs are harvested from the patient, edited outside the body using electroporation to deliver RNP complexes, and then reinfused back into the patient [26]. While effective, this process is complex and costly. The development of in vivo delivery systems that can directly target HSCs within the bone marrow represents a major frontier in SCD therapy. While still preclinical, strategies involving direct bone marrow injection or systemically administered nanoparticles with specific bone marrow homing properties are under active investigation.
Detailed Experimental Protocol: LNP-Mediated RNP Delivery for In Vivo Editing
The following protocol details a methodology for the systemic delivery of Cas9 RNP complexes via engineered LNPs to achieve tissue-specific genome editing in vivo, based on a successfully published approach [68].
Materials and Reagents
Table 3: Key Research Reagents for LNP-RNP Formulation
| Reagent / Material | Function / Purpose | Example / Notes |
|---|---|---|
| Cas9 Nuclease | Endonuclease that creates DSB at target DNA sequence | Recombinantly purified, preferably with NLS tags |
| sgRNA | Synthetic RNA guiding Cas9 to specific genomic locus | Target-specific (e.g., for BCL11A enhancer in SCD) |
| Ionizable Cationic Lipid | Core LNP component for cargo encapsulation and endosomal escape | e.g., 5A2-SC8 [68] |
| Permanently Cationic Lipid | Enhances RNP encapsulation at neutral pH; directs organ tropism | e.g., DOTAP (10-20 mol% of total lipid) [68] |
| Helper Lipids (DOPE, Cholesterol) | Stabilize LNP structure and promote membrane fusion | DOPE and Cholesterol are standard components |
| PEG-Lipid | Provides LNP surface stability and reduces non-specific uptake | e.g., DMG-PEG 2000 [68] |
| Microfluidic Device | Enables precise, reproducible mixing of lipid and aqueous phases | e.g., NanoAssemblr Ignite |
Step-by-Step Methodology
- RNP Complex Preparation: Complex purified Cas9 protein with synthetic sgRNA at a molar ratio of 1:3 (Cas9:sgRNA) in phosphate-buffered saline (PBS). Incubate at room temperature for 10-15 minutes to allow for complete RNP complex formation [68].
- Lipid Mixture Preparation: Prepare an ethanol solution containing the lipid blend. A sample formulation is 5A2-SC8/DOPE/Cholesterol/DMG-PEG2000/DOTAP at a molar ratio of 15/15/30/3/7. The inclusion of 10-20 mol% DOTAP is critical for efficient RNP encapsulation under neutral pH conditions [68].
- LNP Formulation via Microfluidics: Use a microfluidic device to rapidly mix the lipid solution (in ethanol) with the aqueous RNP solution (in PBS) at a controlled flow rate and ratio (typically 1:3 organic-to-aqueous ratio). This process drives nanoscale self-assembly, resulting in monodisperse LNPs encapsulating the RNP cargo.
- Buffer Exchange and Purification: Dialyze the freshly formulated LNP suspension against a large volume of PBS (pH 7.4) for several hours at 4°C to remove residual ethanol and concentrate if necessary. Sterile-filter the final LNP product using a 0.22 µm filter.
- Characterization and Quality Control:
- Size and Dispersity: Measure the hydrodynamic diameter and polydispersity index (PDI) via Dynamic Light Scattering (DLS). Target a size of <200 nm with PDI <0.2.
- Encapsulation Efficiency: Quantify the percentage of RNP cargo successfully encapsulated within the LNPs using a Ribogreen assay or similar method.
- In Vitro Potency Validation: Transfect a reporter cell line (e.g., HeLa-GFP) and measure editing efficiency (e.g., % GFP knockout) via flow cytometry or T7 Endonuclease I assay before proceeding to in vivo studies [68].
- In Vivo Administration and Analysis: Administer the LNP-RNP formulation to animal models (e.g., mice) via low-dose intravenous injection. After 3-7 days, harvest target organs (e.g., liver, lung).
- Editing Efficiency Analysis: Isolate genomic DNA from tissues and assess indel formation at the target locus using next-generation sequencing (NGS) of PCR amplicons.
- Protein-Level Analysis: For knockouts, measure reduction in target protein levels (e.g., via Western blot or ELISA). For corrections, assess functional protein restoration via appropriate assays.
The trajectory of CRISPR-based therapeutics for sickle cell disease and other genetic disorders is inextricably linked to advances in delivery technology. While significant progress has been made, evidenced by approved ex vivo therapies, the development of safe and effective in vivo delivery systems remains the field's paramount challenge. The future lies in designing next-generation smart nanoparticles that combine enhanced tissue specificity, high editing efficiency, and minimized immunogenicity. The continued refinement of organ-specific LNPs, along with emerging technologies such as virus-like particles (VLPs) and advanced base editors deliverable by these platforms, will be crucial for unlocking the full potential of CRISPR as a universal therapeutic modality.
The advent of CRISPR-based gene editing has opened a revolutionary path toward curing genetic disorders, with sickle cell disease (SCD) standing at the forefront of this breakthrough. SCD is caused by a single nucleotide mutation in the beta-globin (HBB) gene, leading to the production of defective hemoglobin S (HbS). The recent approval of Casgevy (exa-cel), a CRISPR-based therapy, marks a pivotal milestone. This therapy successfully ameliorates SCD by reactivating fetal hemoglobin, thereby compensating for the defective HbS [69]. However, a significant challenge in the clinical development of such therapies is CRISPR off-target editing—the non-specific activity of the Cas nuclease at unintended sites in the genome [69]. These off-target effects can confound experimental results, delay clinical pipelines, and pose critical safety risks to patients, including the potential for oncogenic mutations [69] [70]. This guide provides an in-depth technical overview of strategies to minimize these risks, specifically within the context of SCD HBB correction, focusing on gRNA optimization and the use of high-fidelity Cas9 variants.
Understanding CRISPR Off-Target Effects in Therapeutic Contexts
In the context of developing a cure for SCD, the risk profile of off-target effects is particularly high. When CRISPR components are delivered to a patient's hematopoietic stem and progenitor cells (HSPCs), any off-target edit could have long-term consequences.
- Mechanism of Off-Target Activity: The wild-type Cas9 nuclease from Streptococcus pyogenes (SpCas9) possesses a notable tolerance for mismatches between the guide RNA (gRNA) and the target DNA sequence. It can tolerate between three and five base pair mismatches, potentially creating double-stranded breaks at multiple genomic sites that bear similarity to the intended
HBBtarget and possess the correct Protospacer Adjacent Motif (PAM) sequence [69]. - Consequences in SCD Therapy: The risk level is elevated for in vivo therapies but is somewhat mitigated for SCD treatments like Casgevy, which utilize an ex vivo approach. In ex vivo editing, patient HSPCs are edited outside the body, allowing for the selection and validation of correctly edited cells before autologous transplantation [69] [71]. Nonetheless, the FDA has emphasized the need for thorough off-target characterization, noting that individuals with rare genetic variants may be at higher risk [69]. An off-target edit within a proto-oncogene or tumor suppressor gene in a repopulating HSC could theoretically lead to clonal expansion and malignancy, underscoring the need for stringent safety measures [69].
gRNA Optimization Strategies for Enhanced Specificity
The design of the single guide RNA (sgRNA) is the first and most critical factor in determining editing specificity. Meticulous gRNA design can drastically reduce the potential for off-target binding.
1In SilicogRNA Design and Selection
The initial step involves using computational tools to select a gRNA with maximal on-target and minimal off-target potential.
- Guide Design Software: Tools like CRISPOR are indispensable for the design process [69]. They analyze potential gRNA sequences against the reference genome to predict on-target efficiency and identify sites with significant homology that could serve as off-target loci.
- Selection Criteria: These tools typically provide a ranking or score for each potential gRNA. A high-ranking guide is characterized by a high predicted on-target activity and a low risk of off-target editing. Researchers often select several top-ranked guides for empirical testing, as the top in silico candidate may not always perform best in biological systems [69].
Chemical and Structural gRNA Modifications
Beyond sequence selection, synthetic gRNAs can be chemically modified to enhance their stability and specificity.
- Common Modifications: The addition of 2'-O-methyl analogs (2'-O-Me) and 3' phosphorothioate bonds (PS) to the gRNA backbone is a common strategy. These modifications improve nuclease resistance, reduce off-target editing, and can increase on-target efficiency [69].
- Guide Length Optimization: Truncating the gRNA length to 17-18 nucleotides (from the standard 20) has been shown to reduce off-target activity by tolerating fewer mismatches, though this must be balanced against potential reductions in on-target efficiency [69].
GC Content and Specificity
The GC content of the gRNA spacer sequence also influences specificity. A higher GC content stabilizes the DNA:RNA duplex when the guide binds to its intended target, which promotes on-target editing and reduces off-target binding [69].
The diagram below illustrates the multi-faceted workflow for designing and validating a high-specificity gRNA for HBB correction.
High-Fidelity Cas9 Variants for Reduced Off-Target Cleavage
While gRNA optimization targets the source of specificity, protein engineering of the Cas9 nuclease itself has yielded "high-fidelity" variants with dramatically reduced off-target activity.
Mechanism and Trade-offs
These high-fidelity variants, such as SpCas9-HF1 and HiFi Cas9, are engineered through point mutations (e.g., N497A, R661A, Q695A, Q926A) that disrupt the nuclease's non-specific interactions with the DNA phosphate backbone. This makes the enzyme more dependent on perfect complementarity between the gRNA and target DNA for cleavage [72]. A critical consideration is that these high-fidelity variants can sometimes come with a trade-off of reduced on-target editing efficiency [69]. Therefore, empirical testing is essential to identify a variant that maintains therapeutic levels of on-target activity while maximizing specificity.
Quantitative Performance of High-Fidelity Cas9
Evidence from various studies demonstrates the clear benefit of using high-fidelity variants. The table below summarizes a direct comparison between wild-type and a high-fidelity Cas9 in a relevant model system.
Table 1: Quantitative Comparison of Wild-Type vs. High-Fidelity Cas9 Performance
| Cas9 Nuclease | Target | Editing Efficiency | Key Finding | Source |
|---|---|---|---|---|
| Wildtype SpCas9 | Chicken provirus (EAV-HP) | 29% provirus deletion | Served as a baseline for efficiency | [72] |
| High-Fidelity Cas9 variant | Chicken provirus (EAV-HP) | 69% provirus deletion | ~2.4-fold increase in successful large deletion compared to wildtype | [72] |
| HiFi Cas9 | Human HSPCs (Clinical relevant) | High on-target, reduced off-target | Demonstrated utility in therapeutic editing of stem cells | [37] |
This data confirms that high-fidelity variants can not only reduce off-target effects but also, in some contexts, significantly enhance the desired on-target outcome, making them highly suitable for clinical applications [72].
Experimental Protocols for Off-Target Assessment
After performing CRISPR editing, rigorous detection and quantification of off-target effects are mandatory. No single method is perfect, and a combination of approaches is often employed.
Detection and Analysis Methods
- Candidate Site Sequencing: This method involves sequencing the genomic loci identified as potential off-target sites during the in silico prediction phase. It is cost-effective but limited by the completeness of the prediction algorithm [69].
- Targeted Sequencing Methods: These are more comprehensive, empirical methods that identify off-target sites directly from the edited sample.
- Whole Genome Sequencing (WGS): WGS is the most unbiased and comprehensive method, capable of detecting off-target edits and chromosomal aberrations across the entire genome. However, it is cost-prohibitive for routine screening and requires sophisticated bioinformatic analysis [69].
Quantitative Analysis of Editing Outcomes
For the quantitative analysis of both on-target and known off-target edits, several robust methods exist.
- qEva-CRISPR: This is a quantitative, ligation-based (MLPA) method that allows for parallel, multiplex analysis of a target site and its predicted off-targets. Its key advantage is the ability to detect all mutation types, including point mutations and large deletions, with high sensitivity. It is also suitable for analyzing "difficult" genomic regions, such as those with high GC content or repeats [73].
- Digital PCR (dPCR): As demonstrated in the chicken provirus study, dPCR provides absolute quantification of editing efficiencies. It is highly sensitive and allows for the precise measurement of the ratio between modified and unmodified alleles in a heterogeneous cell population [72].
- Inference of CRISPR Edits (ICE): A widely cited, accessible tool from Synthego, ICE uses Sanger sequencing data to provide quantitative analysis of editing efficiency and indel profiles. While excellent for analyzing on-target efficiency and characterizing the spectrum of indels, it is not a discovery tool for novel off-target sites [33].
Table 2: Key Methods for Detecting and Analyzing CRISPR Edits
| Method | Principle | Key Advantage | Key Limitation | Best Used For |
|---|---|---|---|---|
| qEva-CRISPR [73] | Multiplex Ligation-dependent Probe Amplification (MLPA) | Quantifies all mutation types; works in difficult genomic regions. | Requires prior knowledge of target/off-target loci. | Quantitative, multiplex analysis of known sites. |
| Digital PCR [72] | Partitioning and absolute quantification of DNA molecules | High sensitivity; absolute quantification without standards. | Low throughput; requires specific assay design. | Validating and precisely quantifying edits at specific loci. |
| ICE [33] | Decomposition of Sanger sequencing traces | Low cost; user-friendly; provides indel spectrum. | Not for off-target discovery; relies on Sanger quality. | Rapid, cost-effective assessment of on-target efficiency. |
| GUIDE-seq [69] | Empirical capture of DSBs in cells | Unbiased identification of off-target sites within cells. | Requires specialized library prep and sequencing. | Comprehensive off-target discovery in relevant cell types. |
| Whole Genome Sequencing [69] | Sequencing of the entire genome | Most comprehensive; detects structural variations. | Very high cost and complex data analysis. | Final, thorough safety assessment of clinical candidates. |
The following diagram outlines a recommended workflow for profiling off-target effects, from prediction to validation, integrating the methods described above.
The Scientist's Toolkit: Essential Reagents for SCD Gene Correction
The successful implementation of the strategies outlined above relies on a suite of key reagents and tools. The following table details essential components for a typical SCD HBB correction workflow.
Table 3: Research Reagent Solutions for HBB Gene Correction in SCD
| Reagent / Tool | Function | Example Use Case |
|---|---|---|
| High-Fidelity Cas9 Nuclease | Engineered nuclease with reduced off-target activity. | HiFi Cas9 protein for RNP delivery to patient HSPCs to correct the HBB locus safely [37] [72]. |
| Chemically Modified sgRNA | Synthetic guide RNA with enhanced stability and specificity. | 2'-O-Me/PS-modified sgRNA targeting the HBB mutation or BCL11A enhancer for Casgevy-like approach [69]. |
| CRISPOR | Bioinformatics tool for gRNA design and off-target prediction. | Identifying optimal sgRNAs with high on-target scores for HBB and low predicted off-target sites in the human genome [69]. |
| AAV6 Serotype | Highly efficient delivery vector for homologous repair templates. | Delivering a donor template with the correct HBB sequence to patient HSPCs for homology-directed repair (HDR) [37]. |
| ICE Analysis Tool | Software for analyzing CRISPR editing efficiency from Sanger data. | Rapid, cost-effective initial assessment of on-target indel rates in HBB-edited HSPC populations [33]. |
| qEva-CRISPR Assay | Quantitative, multiplex assay for target and off-target validation. | Simultaneously measuring correction at the HBB locus and mutation rates at top predicted off-target sites [73]. |
The path to a safe and durable CRISPR-based cure for sickle cell disease hinges on the precise targeting of the HBB locus. Minimizing off-target effects is not a single-step solution but a multi-layered strategy combining bioinformatically optimized gRNAs, high-fidelity Cas9 variants, and rigorous empirical validation using sensitive detection methods. As the field progresses, the adoption of these combined best practices will be paramount for ensuring the safety and efficacy of not only SCD therapies but the entire next generation of CRISPR-based genetic medicines.
Precise CRISPR-Cas9 genome editing via Homology-Directed Repair (HDR) is a powerful strategy for correcting the sickle cell disease (SCD) beta-globin mutation. The single nucleotide substitution (E6V A>T) in the HBB gene causes this monogenic disorder, making it an ideal candidate for HDR-based correction [74] [26] [27]. However, the inherent inefficiency of HDR compared to the error-prone non-homologous end joining (NHEJ) pathway presents a major technical challenge [75]. This whitepaper examines two pivotal strategies for enhancing HDR efficiency—cell cycle synchronization and small molecule enhancers—within the context of SCD research, providing technical guidance and experimental protocols for researchers and therapeutic developers.
Biological Foundations of HDR and Rationale for Enhancement
The DNA Repair Pathway Competition
After CRISPR-Cas9 induces a double-strand break (DSB), cellular repair machinery can utilize two principal pathways: the precise HDR pathway or the error-prone NHEJ pathway [76] [75]. NHEJ is active throughout the cell cycle and represents the dominant pathway in mammalian cells, often resulting in insertions or deletions (indels) [75]. HDR, in contrast, is restricted to the late S and G2 phases of the cell cycle when a sister chromatid template is available [74] [75]. This cell cycle dependence fundamentally limits HDR efficiency and forms the rationale for synchronization strategies.
HDR Pathway Mechanics and Enhancement Targets
The following diagram illustrates the key cellular decision points between NHEJ and HDR pathways, along with strategic intervention opportunities for enhancing HDR efficiency.
Quantitative Analysis of HDR Enhancement Strategies
Performance Comparison of Small Molecule Enhancers
Research utilizing the BEL-A erythroid cell line for SCD modeling systematically evaluated several small molecule HDR enhancers, yielding the following comparative data [74] [77]:
Table 1: Efficacy Profile of Small Molecule HDR Enhancers in Erythroid Cells
| Small Molecule | Target | Optimal Concentration | HDR Increase | Cell Viability | Key Considerations |
|---|---|---|---|---|---|
| Nedisertib | DNA-PKcs inhibitor | 0.25 µM | +24% (vs. control) | 74% | Best compromise of efficiency and viability |
| NU7441 | DNA-PKcs inhibitor | Not specified | +11% (vs. control) | Moderate | Second most effective molecule tested |
| Alt-R HDR Enhancer | Proprietary protein | Not specified | No significant increase | Reduced | Negative impact on cell viability |
| SCR-7 | DNA Ligase IV inhibitor | Not specified | No significant increase | Not significantly affected | Ineffective in this system |
Cell Cycle Synchronization Outcomes
The same study investigated cell cycle synchronization using nocodazole, which arrests cells in G2/M phase by inhibiting microtubule polymerization [74] [77]. Despite a solid theoretical foundation, the experimental results were unfavorable:
- Protocol: Cells treated with nocodazole for 18 hours prior to transfection, with release either immediately or 6 hours post-transfection.
- Efficiency Outcome: No boost in HDR efficiency beyond what was achieved with Nedisertib or NU7441 alone.
- Viability Impact: Marked reduction in cell viability was observed.
- Conclusion: While HDR is confined to late S and G2 phases [74], practical implementation of synchronization did not provide a net benefit for HDR in this erythroid model.
Advanced HDR Enhancement Techniques and Safety Considerations
DNA Template Engineering Strategies
Recent investigations reveal that modifying the DNA donor template itself can dramatically enhance HDR efficiency [78]:
Table 2: DNA Template Modification Strategies for Enhanced HDR
| Strategy | Mechanism | Reported Efficacy | Notes |
|---|---|---|---|
| Template Denaturation | Using heat-denatured ssDNA instead of dsDNA | 4-fold increase in correctly targeted animals | Reduces unwanted template concatemerization |
| 5'-Biotin Modification | Enhances donor recruitment to Cas9 complex | Up to 8-fold increase in single-copy integration | Potential for reduced multimerization |
| 5'-C3 Spacer | 5'-end modification with propyl group | Up to 20-fold increase in correctly edited mice | Effective regardless of donor strandness |
| RAD52 Supplementation | Promotes ssDNA integration in HDR | 4-fold increase in ssDNA integration | Higher rate of template multiplication |
Critical Safety Considerations for Clinical Translation
While strategies to enhance HDR are technologically promising, significant safety considerations must be addressed for therapeutic applications, particularly for SCD [76]:
- Structural Variations: The use of DNA-PKcs inhibitors (including Nedisertib) has been associated with increased frequencies of large, on-target chromosomal deletions and chromosomal translocations [76].
- Analysis Limitations: Traditional short-read sequencing often fails to detect these large aberrations, potentially leading to overestimation of HDR efficiency and underestimation of genotoxic risk [76].
- Risk-Benefit Assessment: The genotoxic potential of HDR-enhancing strategies must be carefully weighed against the therapeutic benefit, particularly for ex vivo editing of hematopoietic stem cells for SCD therapy [76].
Integrated Experimental Protocol for SCD Mutation Correction
Workflow for HDR-Mediated Beta-Globin Correction
The following diagram outlines a comprehensive experimental workflow for correcting the SCD E6V A>T mutation in erythroid cells, incorporating optimal HDR enhancement strategies.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Core Research Reagents for HDR Enhancement in SCD Models
| Reagent / Solution | Specification | Function in Workflow |
|---|---|---|
| RNP Complex | Cas9 protein + sgRNA at 1:2.5 ratio | CRISPR cleavage complex; RNP format reduces off-target effects |
| ssODN Donor Template | 127-nt with asymmetric homology arms | HDR template for E6V A>T correction; ssDNA reduces cytotoxicity |
| Nedisertib (M3814) | DNA-PKcs inhibitor, 0.25 µM working concentration | Shifts repair balance toward HDR by suppressing NHEJ pathway |
| Nucleofector System | Amaxa 4D-Nucleofector with DZ-100 program | High-efficiency delivery of RNP complexes to hard-to-transfect cells |
| BEL-A Cell Line | Immortalized human erythroid line | Disease modeling; recapitulates normal erythroid differentiation |
| Hypoxia Chamber | Controlled oxygen environment | Phenotypic validation of sickling behavior in corrected cells |
The strategic enhancement of HDR efficiency is paramount for advancing CRISPR-based correction of the SCD beta-globin mutation. Small molecule inhibitors of DNA-PKcs, particularly Nedisertib at optimized concentrations (0.25 µM), currently represent the most effective and practical approach, achieving up to 73% editing efficiency in erythroid cell lines [74] [77]. While theoretically sound, cell cycle synchronization has not demonstrated net experimental benefits in these systems due to viability costs.
Emerging strategies focusing on DNA template engineering—including 5'-modifications and RAD52 supplementation—show remarkable promise, with some reports of up to 20-fold improvements in HDR efficiency [78]. However, comprehensive safety assessments using long-read sequencing and structural variation detection methods must accompany these efficiency gains, particularly given the concerning association between DNA-PKcs inhibition and chromosomal rearrangements [76].
For SCD therapeutic development, the optimal path forward likely combines RNP delivery, optimized ssDNA donor design, and carefully titrated small molecule enhancers, with rigorous safety profiling to ensure the therapeutic benefit outweighs potential genotoxic risk. As the field progresses, continued refinement of these approaches will be essential for developing accessible and safe CRISPR-based therapies for sickle cell disease.
Sickle cell disease (SCD) is a monogenic blood disorder caused by a single-nucleotide point mutation in the β-globin gene (HBB), where an adenine-to-thymine substitution results in the production of abnormal sickle hemoglobin (HbS) [60]. This molecular defect triggers a pathophysiological cascade characterized by hemoglobin polymerization under hypoxic conditions, leading to rigid, sickle-shaped erythrocytes that cause vaso-occlusion, chronic hemolysis, and progressive multiorgan damage [18]. While the recent approval of Casgevy (exa-cel), a CRISPR-Cas9-based therapy, represents a landmark achievement, this approach relies on the creation of DNA double-strand breaks (DSBs) to disrupt the BCL11A erythroid enhancer and induce fetal hemoglobin (HbF) [6] [60]. Although clinically effective, DSB-dependent editing carries inherent genotoxic risks, including unwanted insertions/deletions (indels), chromosomal rearrangements, and p53-mediated cellular stress responses [49] [79].
The limitations of DSB-based editing have accelerated the development of precision genome editing tools that operate without creating double-strand breaks. Base editors (BEs) and prime editors (PEs) represent novel "search-and-replace" technologies that enable precise nucleotide conversions and small insertions/deletions while largely avoiding the genotoxic consequences of conventional CRISPR-Cas9 systems [49] [80]. For SCD therapy, these platforms offer two fundamental strategies: direct correction of the causative Glu6Val point mutation in HBB, or induction of protective fetal hemoglobin through precise manipulation of regulatory elements [18] [60]. This technical guide examines the mechanisms, comparative genotoxicity profiles, and experimental implementation of these DSB-independent editing platforms within the context of SCD therapeutic development.
Molecular Mechanisms of DSB-Independent Editing
Base Editing Architecture and Function
Base editors are fusion proteins that typically combine a catalytically impaired Cas9 nickase (nCas9) with a nucleotide deaminase enzyme, enabling direct chemical conversion of one DNA base to another without double-strand breaks [79] [81]. These systems achieve single-nucleotide precision through a multi-component architecture:
- Catalytic Core: nCas9 (H840A) creates a single-strand nick in the non-target DNA strand, biasing cellular repair toward the edited strand [49].
- Deaminase Domain: Cytidine deaminase (for CBEs) or engineered adenosine deaminase (for ABEs) catalyzes the conversion of cytidine-to-thymine (C•G to T•A) or adenine-to-guanine (A•T to G•C), respectively [79].
- Accessory Components: Uracil glycosylase inhibitor (UGI) domains in CBEs prevent excision of the edited base uracil by base excision repair (BER) pathways, enhancing editing efficiency [79].
The editing process begins with the base editor complex binding to the target DNA sequence guided by a single guide RNA (sgRNA). The nCas9 domain positions the deaminase enzyme within a narrow "editing window" (typically 4-5 nucleotides) of the protospacer adjacent motif (PAM), where it acts on the single-stranded DNA bubble created by Cas9 binding [49]. For SCD therapeutic applications, the primary strategy involves using adenine base editors (ABEs) to directly correct the pathogenic A•T to G•C mutation in codon 6 of the HBB gene, restoring normal glutamic acid residue and functional adult hemoglobin production [18].
Prime Editing: A Versatile Search-and-Replace Platform
Prime editing represents a more recent advancement that overcomes key limitations of base editing, including the inability to perform all possible base-to-base conversions and the risk of bystander editing within the editing window [49]. The prime editing system consists of two primary components:
- Editor Protein: A fusion of nCas9 (H840A) with an engineered reverse transcriptase (RT) domain [49].
- Specialized Guide RNA: A prime editing guide RNA (pegRNA) that both specifies the target site and encodes the desired edit within its extension segment [49].
The prime editing mechanism involves a coordinated multi-step process. First, the nCas9 domain nicks the target DNA strand, exposing a 3'-hydroxyl group that serves as a primer for reverse transcription. The RT then uses the pegRNA's extension template to synthesize a DNA flap containing the desired edit. Cellular repair mechanisms subsequently resolve the resulting heteroduplex structure, preferentially incorporating the edited strand into the genome [49]. This elegant mechanism enables precise correction of the SCD point mutation while minimizing unintended genetic alterations, making it particularly suitable for therapeutic applications where precision is paramount.
Table 1: Comparison of Genome Editing Platforms for Sickle Cell Disease
| Editing Platform | Editing Mechanism | SCD Application | Key Advantages | Primary Limitations |
|---|---|---|---|---|
| CRISPR-Cas9 Nuclease | Creates DSBs, relies on endogenous repair | BCL11A enhancer disruption to induce HbF [60] | High efficiency, clinically validated | DSB-associated genotoxicity, unpredictable indels [79] |
| Cytidine Base Editor (CBE) | Converts C•G to T•A without DSBs | Limited application for direct HBB correction | Avoids DSBs, high efficiency for specific conversions | Off-target editing, bystander mutations [79] |
| Adenine Base Editor (ABE) | Converts A•T to G•C without DSBs | Direct correction of HBB Glu6Val mutation [18] | Direct mutation correction, no DSBs | Cannot create all edit types, size constraints [49] |
| Prime Editor (PE) | Reverse transcription of edited sequence using pegRNA | Direct correction of HBB Glu6Val mutation [18] | All possible base-to-base changes, minimal byproducts | Lower efficiency, complex pegRNA design [49] |
Diagram 1: Comparative mechanisms of DSB-dependent and independent editing platforms. Base and prime editors bypass double-strand breaks, reducing genotoxic outcomes.
Genotoxicity Profiles: Comparative Analysis of Editing Platforms
DSB-Associated Genotoxicity in CRISPR-Cas9 Editing
Conventional CRISPR-Cas9 nucleases introduce deliberate double-strand breaks at target genomic loci, activating competing DNA repair pathways that determine editing outcomes [82]. The error-prone non-homologous end joining (NHEJ) pathway frequently generates insertions and deletions (indels) at the break site, while microhomology-mediated end joining (MMEJ) produces larger, predictable deletions [82]. In the context of SCD therapy targeting the BCL11A enhancer, these unpredictable mutations can successfully disrupt the HbF repressor, but at the cost of potential genomic instability [79].
Comprehensive studies in human hematopoietic stem and progenitor cells (HSPCs) have demonstrated that Cas9-induced DSBs trigger p53-dependent DNA damage responses, leading to cell cycle arrest, apoptosis, and reduced engraftment potential in xenotransplantation models [79]. Perhaps more concerning are observations that DSB repair can generate large deletions, chromosomal translocations, and complex rearrangements extending far beyond the target site, presenting significant safety concerns for therapeutic applications [79] [83]. These genotoxic effects are particularly problematic in long-term repopulating HSCs, where cumulative DNA damage could potentially contribute to malignant transformation.
Genotoxicity of Base Editing Systems
While base editors theoretically avoid DSB formation, recent comprehensive analyses reveal a more nuanced genotoxicity profile. In HSPCs edited with cytidine base editors (BE4max) targeting the B2M locus, approximately one-third of edited alleles contained indels rather than the intended base transitions, with the frequency influenced by cellular base excision repair activity [79]. These unintended indels predominantly occurred between the nCas9 nick site and the base editing window, suggesting a mechanism where concurrent nicking and base excision repair activities create de facto double-strand breaks [79] [81].
Comparative transcriptomic analyses further revealed that cytidine base editors trigger detrimental innate immune responses and p53 pathway activation, though at reduced magnitude compared to Cas9 nucleases [79] [81]. These cellular stressors reduced editing efficiency and negatively impacted hematopoietic repopulation capacity in transplanted mice. Additionally, genome-wide sequencing of base-edited HSPCs demonstrated an increased load and altered spectrum of single-nucleotide variants across the genome, suggesting potential gRNA-independent mutagenic effects of constitutively active deaminase domains [79].
Genotoxicity of Prime Editing Systems
Prime editors generally demonstrate superior genotoxicity profiles compared to both Cas9 nucleases and base editors. In HSPCs, PE2 and PE3 systems produce significantly fewer indels and genomic alterations at both on-target and off-target sites [79]. The reduced genotoxicity stems from the avoidance of both DSBs and the provocative deaminase activity that characterizes base editors.
However, prime editing is not completely free of genotoxic concerns. At high expression levels, the reverse transcriptase component can cause low-frequency DNA damage and activate p53 signaling, albeit to a lesser extent than base editors [79] [81]. Additionally, imperfect resolution of the edited DNA flaps can generate low-abundance indels, though these occur at substantially reduced rates compared to DSB-dependent editing [49] [79].
Table 2: Quantitative Genotoxicity Comparison in Human Hematopoietic Stem Cells
| Genotoxicity Metric | CRISPR-Cas9 | Cytidine Base Editor | Adenine Base Editor | Prime Editor |
|---|---|---|---|---|
| Indel Frequency at Target Site | 60-80% [79] | 20-35% [79] | 5-15% [79] | 1-5% [79] |
| p53 Pathway Activation | High [79] | Moderate [79] | Low [79] | Low [79] |
| Large Deletions/Translocations | Present [79] | Rare [79] | Very Rare [79] | Extremely Rare [79] |
| Innate Immune Activation | Moderate [81] | High [81] | Moderate [81] | Low [79] |
| Genome-Wide Mutational Burden | Unchanged [79] | Increased SNVs [79] | Mild Increase [79] | Unchanged [79] |
| HSPC Engraftment Efficiency | Reduced [79] | Moderately Reduced [79] | Mildly Reduced [79] | Near Normal [79] |
Experimental Optimization for SCD Therapeutic Development
Delivery and Workflow Considerations
Successful therapeutic editing for SCD requires optimized delivery systems and workflows tailored to hematopoietic stem cells. The following experimental protocol has demonstrated efficacy in preclinical SCD models:
HSPC Isolation and Culture: Isolate CD34+ hematopoietic stem/progenitor cells from mobilized peripheral blood, bone marrow, or cord blood. Maintain cells in serum-free expansion media supplemented with SCF, TPO, and FMS-like tyrosine kinase 3 ligand (Flt3L) [79] [71].
Editor Delivery: Deliver base or prime editor as ribonucleoprotein (RNP) complexes via electroporation. For in vivo delivery, utilize lipid nanoparticles (LNPs) optimized for hematopoietic tissue targeting [6] [83].
Editing Validation: Assess editing efficiency 72 hours post-delivery using next-generation sequencing of the HBB target locus. For SCD-specific correction, monitor the Glu6Val mutation frequency and detect the restoration of wild-type glutamic acid codon [18].
Functional Validation: Differentiate edited HSPCs in vitro into erythroid lineages and assess hemoglobin patterns via HPLC, specifically monitoring correction of HbS to HbA and reduced sickle cell formation under hypoxic conditions [18] [60].
Diagram 2: Experimental workflow for base and prime editing in sickle cell disease therapeutic development.
Mitigation Strategies for Residual Genotoxicity
Despite the improved safety profiles of DSB-independent editors, several strategies can further minimize residual genotoxicity:
Editor Expression Optimization: Use self-inactivating mRNA systems with optimized 5' caps and 3' poly(A) tails to limit editor persistence and reduce off-target activity [79] [81].
pegRNA Engineering: Implement engineered pegRNAs (epegRNAs) with structural motifs that enhance stability and editing efficiency, allowing lower editor doses [49].
MMR Inhibition: Co-express dominant-negative MLH1 (MLH1dn) to temporarily suppress mismatch repair, increasing prime editing efficiency 2-3 fold while reducing template-independent mutations [49].
Dose Titration: Determine the minimum effective editor dose through careful titration, as reducing BE4max concentration 4-fold decreased indels from >30% to <5% while maintaining therapeutic editing levels [79].
The Scientist's Toolkit: Essential Reagents for DSB-Independent Editing
Table 3: Research Reagent Solutions for Base and Prime Editing Applications
| Reagent Category | Specific Examples | Function and Application | Considerations for SCD Therapy |
|---|---|---|---|
| Base Editor Systems | BE4max (CBE), ABE8.20-m (ABE) [79] | Direct point mutation correction; BE4max for C•G to T•A, ABE8 for A•T to G•C conversions | ABE8.20-m enables direct correction of HBB Glu6Val mutation [18] |
| Prime Editor Systems | PE2, PE3, PE5, PE6 variants [49] | Versatile editing without DSBs; PE2 for foundational editing, PE3 with additional nicking sgRNA for enhanced efficiency | PE6 variants with compact RT show improved efficiency in HSPCs [49] |
| Delivery Vehicles | Lipid nanoparticles (LNPs), Electroporation systems, Virus-like particles (VLPs) [6] [83] | LNP for in vivo delivery; electroporation for ex vivo RNP delivery; VLPs for protein delivery to difficult cells | LNPs enable in vivo editing without stem cell mobilization [6] |
| Guide RNA Formats | pegRNA, epegRNA, sgRNA [49] | pegRNA for prime editing; epegRNA with stability motifs; sgRNA for base editing | epegRNAs reduce degradation and improve editing efficiency in HSPCs [49] |
| HSPC Culture Supplements | SCF, TPO, Flt3L, SR1 [79] [71] | Maintain stemness during ex vivo culture; enhance engraftment potential; improve editing efficiency in primitive cells | Culture duration (1 vs 3 days) impacts editing efficiency and stem cell function [79] |
| Genotoxicity Assays | NGS for on-target/off-target, γH2AX staining, p53 pathway analysis, RNA-seq [79] | Comprehensive safety profiling; detect DSBs and cellular stress responses; identify genome-wide mutations | Essential for preclinical safety assessment of SCD therapeutics [79] [81] |
Base and prime editing technologies represent significant advances in the quest for precise, safe genetic correction of the sickle cell disease mutation. While not completely free of genotoxic concerns, these DSB-independent platforms offer substantially improved safety profiles compared to conventional CRISPR-Cas9 nucleases [79] [81]. The residual genotoxicity observed with base editors, particularly cytidine base editors, underscores the importance of continued optimization and thorough safety assessment in therapeutically relevant cells like HSPCs [79].
For SCD therapeutic development, both platforms present compelling opportunities. Adenine base editors enable direct correction of the pathogenic HBB mutation with high efficiency, while prime editors offer unparalleled versatility for precise genetic surgery [18]. As these technologies continue to evolve—with improvements in editor efficiency, delivery systems, and safety profiling—they hold tremendous promise for delivering safe, effective, and accessible therapies for sickle cell disease patients worldwide [80] [60]. The ongoing clinical evaluation of these platforms will ultimately determine their therapeutic potential and position in the expanding arsenal of genetic medicines for monogenic blood disorders.
The advent of CRISPR-based therapies for sickle cell disease (SCD) represents a paradigm shift in precision medicine, with the first approved treatment, CASGEVY (exagamglogene autotemcel), demonstrating remarkable clinical success [6] [84]. However, translating these scientific breakthroughs into commercially viable and widely accessible treatments requires overcoming formidable manufacturing scalability challenges. The complex, multi-step process of clinical-grade production for autologous CRISPR therapies presents unique obstacles in process optimization, quality control, and supply chain management that must be addressed to meet global patient demand.
SCD affects millions globally, with approximately 100,000 individuals in the United States and over 300,000 annual births worldwide affected by this monogenic disorder [85] [84]. The therapeutic approach for CRISPR-based SCD treatments involves precise genetic modification of a patient's own hematopoietic stem cells (HSCs) to correct the underlying β-globin mutation or reactivate fetal hemoglobin production. This autologous ex vivo manufacturing paradigm creates significant scalability constraints that this technical guide will address through optimized protocols, standardized metrics, and innovative manufacturing approaches.
Current Clinical Landscape and Manufacturing Framework
Approved Therapies and Manufacturing Workflows
The CRISPR therapeutic landscape for SCD has matured rapidly, with CASGEVY receiving FDA approval in December 2023 based on demonstrated efficacy in clinical trials where 93.5% of patients (29 of 31) achieved freedom from severe vaso-occlusive crises for at least 12 consecutive months during the 24-month follow-up period [84]. This therapy utilizes a precise CRISPR-Cas9-mediated disruption of the BCL11A erythroid enhancer to reactivate fetal hemoglobin production, achieving editing frequencies of 85.8±14.7% in CD34+ cells from persons with sickle cell disease [84].
The manufacturing workflow for autologous CRISPR therapies follows a defined sequence: (1) HSC collection via apheresis, (2) cell processing and activation, (3) CRISPR system delivery via electroporation, (4) expansion of edited cells, (5) quality control and release testing, and (6) reinfusion into the patient following myeloablative conditioning [84] [67]. Each stage presents distinct scalability challenges that must be optimized for clinical-grade production.
Table 1: Key Manufacturing Metrics for CRISPR-Based SCD Therapies
| Manufacturing Parameter | CASGEVY (exa-cel) | LentiGlobin (lovo-cel) | Optimization Target |
|---|---|---|---|
| Editing Efficiency | 85.8±14.7% indels in BCL11A enhancer [84] | 1.0-1.2 vector copies per cell [84] | >90% consistency |
| Cell Viability Post-Electroporation | High (specific data not provided) | High (specific data not provided) | >80% recovery |
| Manufacturing Timeline | Approximately 6-8 weeks | Approximately 6-8 weeks | <4 weeks |
| Dose | Targeted CD34+ cell count: >2×10^6 cells/kg | Targeted CD34+ cell count: >2×10^6 cells/kg | Consistent engraftment |
| Vector/RNP Delivery Efficiency | Up to 90% in HSPCs [67] | Not applicable | >95% consistency |
CRISPR Delivery System Optimization
Efficient delivery of CRISPR components into target HSCs remains a critical bottleneck in manufacturing scalability. The choice of delivery vehicle significantly impacts editing efficiency, cell viability, and ultimately therapeutic efficacy. Current approaches include physical methods (electroporation), viral vectors, and non-viral nanoparticles, each with distinct advantages and limitations for scale-up.
Table 2: CRISPR Delivery Systems for Clinical-Scale Manufacturing
| Delivery Method | Editing Efficiency | Scalability Considerations | Clinical Applications |
|---|---|---|---|
| Electroporation (RNP) | Up to 90% indels in HSPCs [67] | Closed-system automation available; requires optimization of voltage parameters | CASGEVY for SCD [67] |
| Lentiviral Vectors | 1.0-1.2 copies per cell [84] | Complex GMP manufacturing; insertional mutagenesis concerns | LentiGlobin for SCD [84] |
| Lipid Nanoparticles (LNPs) | Efficient in hepatocytes (in vivo) [6] | Scalable for in vivo use; limited data for ex vivo HSC editing | Intellia's hATTR program [6] |
| AAV Vectors | High efficiency in some targets | Immunogenicity concerns; scalable production challenges | Preclinical studies [18] |
Electroporation of ribonucleoprotein (RNP) complexes has emerged as the preferred method for clinical-scale manufacturing due to precise temporal control, reduced off-target effects, and avoidance of genomic integration [67]. However, optimization of electroporation parameters (voltage, pulse length, cell density) and RNP formulation is essential for maintaining high cell viability while achieving efficient editing. Recent advances include the development of proprietary electroporation systems that improve viability of sensitive HSCs post-editing.
Diagram 1: CRISPR Manufacturing Workflow for SCD Therapies
Process Optimization Strategies for Scale-Up
Closed-System Automation and Bioprocess Integration
Transitioning from manual, open-process operations to closed, automated systems represents the most significant opportunity for enhancing manufacturing scalability. Current clinical-scale production of CRISPR therapies relies heavily on labor-intensive processes in Grade A cleanrooms with limited batch size capacity. Implementing integrated closed-system bioreactors with automated monitoring and control systems can dramatically increase throughput while reducing contamination risk and operator-dependent variability.
Advanced bioreactor systems with perfusion capabilities enable continuous medium exchange during the critical post-electroporation expansion phase, maintaining optimal nutrient concentrations and removing waste products that can impair cell growth. Process analytical technologies (PAT) incorporating real-time monitoring of critical quality attributes (CQAs) such as glucose consumption, lactate production, and oxygen uptake rates allow for dynamic process control and early detection of batch failures. Integration of these technologies has demonstrated potential to reduce manufacturing timelines by 30-40% while improving process consistency [67].
CRISPR Reagent Manufacturing and Standardization
The quality and consistency of CRISPR components directly impact editing efficiency and product safety. Clinical-grade production requires GMP-compliant manufacturing of Cas9 nuclease (as protein or mRNA) and guide RNA with stringent specifications for purity, potency, and endotoxin levels. Process optimization includes:
Cas9 Protein Production: Development of high-yield microbial expression systems with purification processes that minimize protein aggregation, which can reduce editing efficiency and compromise delivery [67]. Advanced chromatography methods can achieve >95% purity with residual host cell DNA <10 pg/mg and endotoxin levels <1 EU/mg.
Guide RNA Synthesis: Implementation of novel chemistry for large-scale gRNA synthesis with modified nucleotides to enhance stability and reduce immunogenicity. Process optimization focuses on improving coupling efficiency and reducing deletion sequences that can impair editing specificity.
RNP Complex Formation: Standardization of RNP assembly conditions (stoichiometry, buffer composition, incubation parameters) to ensure complete complex formation and stability during storage and processing.
Table 3: Critical Quality Attributes for CRISPR Reagents
| Reagent | Critical Quality Attributes | Analytical Methods | Target Specifications |
|---|---|---|---|
| Cas9 Protein | Purity, aggregation state, enzymatic activity, endotoxin, sterility | SEC-HPLC, SDS-PAGE, in vitro cleavage assay, LAL test, microbiological testing | >95% purity, <5% aggregates, >90% activity, <1 EU/mg |
| Guide RNA | Identity, purity, integrity, modification efficiency, endotoxin | LC-MS, IP-HPLC, denaturing PAGE, ELISA | >90% purity, >85% full-length, >95% modification |
| RNP Complex | Complex formation efficiency, size distribution, stability | Native PAGE, DLS, EMSA, HPLC | >95% complex formation, monodisperse distribution |
Analytical Development and Quality Control
Comprehensive characterization of CRISPR-edited cell products requires robust analytical methods to assess critical quality attributes including editing efficiency, on-target specificity, cell viability, potency, and safety. Method validation and standardization across manufacturing sites is essential for ensuring product consistency during scale-up.
Editing Efficiency Assessment: Digital PCR and next-generation sequencing methods validated for precision (RSD <15%) and accuracy (85-115% of reference value) to quantify on-target modification rates at the BCL11A enhancer or HBB gene locus.
Off-Target Analysis: Orthogonal approaches including GUIDE-seq, CIRCLE-seq, and in silico prediction tools to profile potential off-target sites, with follow-up confirmation by targeted NGS in clinical batches.
Potency Assays: In vitro erythroid differentiation assays measuring HbF expression and percentage of F-cells, correlated with clinical efficacy. Validation of assay linearity, range, and intermediate precision to ensure reliable potency determination.
Safety Testing: Sterility, mycoplasma, endotoxin, and adventitious virus testing per pharmacopeial methods, plus specific assays for replication-competent lentivirus (for vector-based approaches) and karyotypic analysis to detect chromosomal abnormalities.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagent Solutions for CRISPR Manufacturing Optimization
| Reagent/Category | Function in Manufacturing Process | Application Example |
|---|---|---|
| GMP-grade Cas9 Nuclease | CRISPR system enzyme component for precise DNA cleavage | BCL11A enhancer editing in HSCs for HbF reactivation [84] |
| Clinical-grade sgRNA | Target-specific guide RNA directing Cas9 to genomic locus | HBG1/HBG2 promoter targeting in SCD therapies [84] |
| Electroporation Enhancers | Improve delivery efficiency while maintaining cell viability | Small molecules that transiently permeabilize cell membranes [67] |
| Stem Cell Media Formulations | Support HSC expansion while maintaining pluripotency | Serum-free, xeno-free media with optimized cytokine cocktails |
| Cell Separation Matrices | Isolation of CD34+ cells from apheresis products | Clinical-grade antibodies for magnetic bead separation |
| Cryopreservation Solutions | Maintain cell viability and potency during frozen storage | DMSO-based formulations with optimized cooling rate protocols |
Technical Protocols for Process Optimization
High-Efficiency Electroporation of Hematopoietic Stem Cells
This optimized protocol for CRISPR RNP delivery into CD34+ HSCs achieves >80% editing efficiency while maintaining high cell viability and multipotent differentiation capacity.
Materials:
- GMP-grade CD34+ cells (≥90% purity)
- CRISPR RNP complex (Cas9:sgRNA molar ratio 1:2.5)
- Electroporation buffer (commercial formulation)
- Electroporation device with specialized HSC program
- Recovery medium with Rho-associated kinase (ROCK) inhibitor
Procedure:
- Cell Preparation: Harvest and wash CD34+ cells, resuspend in electroporation buffer at 1×10^8 cells/mL. Maintain cells at 2-8°C during preparation.
- RNP Complex Formation: Incubate Cas9 protein with sgRNA at room temperature for 10 minutes to form RNP complexes.
- Electroporation: Mix cell suspension with RNP complexes (final concentration 10-20 μM), transfer to electroporation cuvette, and pulse using optimized parameters (typically 1500V, 10ms pulse length, 3 pulses).
- Post-Electroporation Recovery: Immediately transfer cells to pre-warmed recovery medium containing ROCK inhibitor, incubate at 37°C for 30-60 minutes.
- Cell Expansion: Wash cells and transfer to expansion medium with cytokine cocktail (SCF, TPO, FLT3-L). Culture for 48-72 hours before quality assessment.
Critical Parameters:
- Cell density: 1×10^8 cells/mL optimal for most systems
- RNP concentration: Titrate between 5-20 μM for optimal efficiency/viability balance
- Post-electroporation recovery: Essential for reducing apoptosis; ROCK inhibitor concentration typically 10-20 μM
Process Monitoring and Quality Control Testing
Implementing rigorous in-process controls throughout manufacturing is essential for detecting deviations early and ensuring batch consistency.
Key Analytical Timepoints:
- Post-Apheresis: Cell count, viability, CD34+ percentage, sterility
- Post-Electroporation: Editing efficiency (digital PCR), viability, cell recovery
- Pre-Release: Comprehensive panel including potency, sterility, mycoplasma, endotoxin, identity, and purity
Process Monitoring:
- Metabolic Parameters: Glucose consumption rate, lactate production, dissolved oxygen
- Growth Kinetics: Population doublings, expansion factor, viability trend
- Genetic Stability: Karyotyping at pre-release stage for master cell banks
Scaling Challenges and Future Directions
Despite significant advances, manufacturing scalability for CRISPR-based SCD therapies faces several persistent challenges. The autologous nature of these treatments creates inherent limitations in batch size and requires patient-specific production, resulting in high costs currently exceeding $1 million per treatment [6] [84]. Additionally, the complex supply chain involving apheresis centers, manufacturing facilities, and treatment centers creates logistical hurdles that must be addressed through distributed manufacturing models.
Future process optimization will focus on three key areas: (1) reducing manufacturing timelines through accelerated expansion protocols and reduced hold times, (2) increasing automation to reduce labor requirements and improve consistency, and (3) developing allogeneic approaches that would enable large-batch production of off-the-shelf CRISPR-edited cell therapies. Emerging technologies like point-of-care manufacturing systems and advanced analytics for real-time release testing show promise for addressing current scalability constraints.
Diagram 2: Scaling Trajectory for CRISPR Manufacturing
The ongoing development of in vivo CRISPR delivery approaches using lipid nanoparticles (LNPs) or viral vectors could potentially bypass many current manufacturing challenges by eliminating the need for ex vivo cell processing [6]. However, these approaches present their own scale-up challenges related to vector production and targeted delivery efficiency. As the field advances, harmonization of regulatory standards and development of platform manufacturing processes will be essential for achieving the scalability needed to address the global burden of sickle cell disease.
Conditioning regimens represent a critical determinant of success in hematopoietic stem cell (HSC) transplantation for sickle cell disease (SCD). These regimens, designed to create space in the bone marrow niche and eliminate disease-causing cells, must strike a delicate balance between sufficient myeloablation to enable engraftment of genetically corrected cells and minimal toxicity to ensure patient safety [32]. Within the context of novel CRISPR/Cas9-based therapies for β-globin mutation correction, optimizing these regimens becomes paramount to achieving durable clinical outcomes while mitigating treatment-related risks. The recent approval of the first CRISPR-based gene therapy for SCD, Casgevy, which utilizes myeloablative conditioning with busulfan, underscores the clinical relevance of regimen optimization [44]. This technical guide examines current conditioning approaches, emerging safety data, and innovative strategies aimed at refining the risk-benefit profile for SCD patients undergoing autologous HSC transplantation with gene-corrected cells.
Current Conditioning Landscape in SCD Gene Therapy
Myeloablative Conditioning: Standard Approaches and Clinical Evidence
Myeloablative conditioning with alkylating agents remains the foundation for autologous HSC gene therapy protocols. The primary objective is to sufficiently clear the bone marrow niche to allow engraftment of genetically modified CD34+ hematopoietic stem and progenitor cells (HSPCs) [32]. Busulfan stands as the most extensively validated conditioning agent in this setting, with demonstrated efficacy in supporting engraftment of gene-corrected HSCs.
Table 1: Current Conditioning Agents in SCD Gene Therapy Trials
| Agent | Mechanism of Action | Dosing Strategy | Clinical Efficacy | Key Toxicities |
|---|---|---|---|---|
| Busulfan | DNA alkylation, myeloablation | Weight-based or targeted (AUC 65-75 ng·h/mL) [86] | 100% engraftment in busulfan-conditioned patients (n=25) [86] | Mucositis, hepatic VOD, infertility, secondary malignancies |
| Treosulfan | Bifunctional alkylating agent | 3 × 14 g/m² [86] | 33% graft failure rate (2/6 patients) [86] | Similar to busulfan but potentially less toxic |
| Plerixafor | CXCR4 antagonist, HSC mobilization | Single agent for HSPC collection [32] [3] | Safe mobilization in SCD patients [87] | Minimal toxicity, contraindicated for G-CSF |
The functional consequence of effective conditioning is demonstrated through robust engraftment metrics. In the Casgevy trial, all treated patients achieved successful engraftment with no graft failure or rejection [44]. Similarly, a comparative study of 31 SCD patients undergoing allogeneic transplantation demonstrated superior outcomes with busulfan-based conditioning (0% graft failure in 25 patients) compared to treosulfan-based regimens (33% graft failure in 6 patients) [86].
Efficacy Endpoints and Engraftment Metrics
Conditioning efficacy is quantified through specific hematopoietic recovery parameters and engraftment durability. Neutrophil engraftment typically occurs within 14-19 days post-transplantation, while platelet recovery may extend to 19-63 days depending on the conditioning intensity and product characteristics [87]. The critical threshold for therapeutic success appears to be approximately 20% donor myeloid chimerism, which translates to nearly 100% healthy red blood cell circulation due to the selective survival advantage of non-sickling erythrocytes [32].
Molecular outcomes following conditioning include vector copy number (VCN) stability in lentiviral-based approaches and allelic correction frequencies in CRISPR-based strategies. Studies report VCNs of 0.9±0.2 in drug products with variable retention post-transplantation (1.2 to 5.5-fold decreases observed in clinical trials) [87]. For CRISPR-corrected HBB alleles, preclinical models demonstrated up to 60% correction in clinical-scale manufacturing with approximately 20% multilineage correction following engraftment [3].
Safety Considerations and Toxicity Profiles
Regimen-Related Toxicities and Risk Mitigation
The intensified inflammatory state and organ damage characteristic of SCD renders patients particularly vulnerable to conditioning-related toxicities. Myeloablative busulfan conditioning carries significant risks, including infections, mucosal damage, hepatic veno-occlusive disease (VOD), infertility, and secondary malignancies [32]. These toxicities necessitate comprehensive supportive care strategies during the peri-transplant period.
Table 2: Adverse Events Associated with Conditioning Regimens in SCD Patients
| Toxicity Category | Specific Adverse Events | Preventive/Mitigation Strategies | Clinical Incidence |
|---|---|---|---|
| Hematologic | Febrile neutropenia, thrombocytopenia | Prophylactic antibiotics, transfusion support | Nearly universal during aplasia period |
| Gastrointestinal | Mucositis, nausea, vomiting | Aggressive hydration, mucosal cryotherapy, antiemetics | Common (Casgevy trial: mouth sores) [44] |
| Hepatic | Veno-occlusive disease | Busulfan dose adjustment, ursodiol, defibrotide prophylaxis | <5% with targeted busulfan [86] |
| Long-term | Infertility, secondary malignancies | Fertility preservation, long-term monitoring | Requires ongoing evaluation [32] |
Clinical data from the Lyfgenia trial highlighted hematologic malignancies as a significant concern, warranting a black box warning in its labeling [44]. This finding underscores the importance of lifelong monitoring for patients receiving gene therapies with integrating vectors or following genotoxic conditioning.
Patient-Specific Factors Influencing Toxicity
Recent investigations reveal that intrinsic patient factors significantly modulate conditioning toxicity and engraftment efficacy. Single-cell transcriptome analyses of HSPCs from SCD patients demonstrate an exacerbated inflammatory signature mediated through IL-1, TNF-α, and interferon signaling pathways [87]. This inflammatory state correlates with lineage bias and impaired engraftment potential, potentially explaining the variable efficacy observed in clinical trials despite similar vector copy numbers in drug products.
The underlying SCD pathophysiology further complicates conditioning safety. Chronic hemolysis, iron overload, and end-organ damage (particularly renal and hepatic impairment) may alter drug metabolism and increase susceptibility to regimen-related toxicities [87]. These findings highlight the need for patient-specific conditioning strategies that account for inflammatory status and disease-related comorbidities.
Emerging Strategies for Reduced-Toxicity Conditioning
Reduced-Intensity and Targeted Conditioning Approaches
Novel conditioning strategies aim to maintain efficacy while improving safety profiles through reduced-intensity approaches and targeted drug delivery systems. Reduced-intensity conditioning (RIC) protocols utilizing lower busulfan doses have demonstrated feasibility, though with potentially compromised engraftment levels and therapeutic protein expression [32]. The optimal RIC regimen would sufficiently immunosuppress the host to allow donor cell engraftment while minimizing damage to non-hematopoietic tissues.
Antibody-based conditioning represents a promising targeted approach under investigation. These regimens employ monoclonal antibodies or antibody-drug conjugates that specifically target HSC surface markers (e.g., CD117, CD45), enabling efficient niche clearance without the broad cytotoxic effects of conventional chemotherapy [32]. Early-phase clinical trials are evaluating the efficacy of these targeted approaches in creating space for genetically modified HSCs while substantially reducing off-target toxicity.
In Vivo Gene Editing and Minimally Invasive Conditioning
The development of in vivo gene editing approaches could potentially circumvent the need for intensive conditioning regimens altogether. While still in preclinical stages, these strategies envision direct administration of genome editing reagents to patients, eliminating ex vivo HSC manipulation and associated toxicities [32] [27]. Successful implementation would represent a paradigm shift in SCD gene therapy, dramatically simplifying treatment and expanding accessibility.
Current research focuses on optimizing delivery vehicles for in vivo approaches, including viral vectors and lipid nanoparticles capable of targeting HSCs with high specificity. The minimal effective conditioning requirements for these approaches remain an active area of investigation, with potential for substantially reduced intensity compared to current standards.
Experimental Protocols and Methodologies
Preclinical Conditioning and Transplantation Model
The following protocol outlines the conditioning and transplantation approach used in the Townes-SCD mouse model to evaluate HBB gene correction, providing a template for preclinical conditioning optimization studies [37]:
Materials:
- Busulfan (or alternative conditioning agent)
- Irradiation equipment (for murine models)
- Supportive care medications (analgesics, antibiotics)
- Transfusion support products
Methodology:
- Pre-conditioning stabilization: Implement partial exchange transfusions to reduce HbS levels to approximately 30-35% in the week preceding conditioning [86].
- Conditioning administration: Administer myeloablative busulfan via weight-based dosing or targeted dosing to achieve AUC of 65-75 ng·h/mL over 3-4 days [86]. For murine models, utilize 9.5 Gy radiation with supportive blood transfusions to mitigate radiation toxicity [37].
- Cell transplantation: Infuse CRISPR-corrected CD34+ HSPCs at a dose of 5.97-8.1 × 10^6 cells/kg [87] via intravenous injection.
- Engraftment monitoring: Track neutrophil recovery (expected by day 14-19) and platelet recovery (expected by day 19-63) [87].
- Efficacy assessment: Quantify donor chimerism (>20% target), vector copy number stability, and hemoglobin A production at regular intervals post-transplantation.
Clinical Conditioning Optimization Trial Design
For clinical investigators designing conditioning optimization trials, the following elements should be incorporated:
- Primary endpoints: Event-free survival (freedom from graft failure and severe regimen-related toxicity) [86].
- Secondary endpoints: Time to hematopoietic recovery, levels of donor chimerism, therapeutic hemoglobin expression, and incidence of graft-versus-host disease in allogeneic settings.
- Safety monitoring: Comprehensive assessment of organ-specific toxicities, infectious complications, and long-term sequelae including fertility preservation and malignancy risk.
- Correlative studies: Evaluation of inflammatory biomarkers, HSC lineage bias, and pharmacogenomic factors influencing conditioning agent metabolism.
Diagram Title: Conditioning Optimization Feedback Loop
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Research Reagents for Conditioning Regimen Studies
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Conditioning Agents | Busulfan, Treosulfan, Fludarabine | Myeloablation efficacy studies | Pharmacokinetic monitoring essential for busulfan [86] |
| HSC Mobilization Agents | Plerixafor (CXCR4 antagonist) | HSPC collection for ex vivo manipulation | Safe in SCD vs. G-CSF contraindication [32] [3] |
| Immunosuppressants | Sirolimus, Tacrolimus, PTCy | GVHD prevention in allogeneic settings | Sirolimus promotes mixed chimerism [32] |
| Supportive Care Agents | Acyclovir, Levetiracetam | Infection/prophylaxis management | Standardized protocols reduce variability [86] |
| Analytical Tools | ddPCR, NGS, Flow Cytometry | Engraftment and chimerism quantification | Single-cell RNAseq reveals inflammatory signatures [87] |
Conditioning regimen optimization represents a dynamic frontier in the advancement of CRISPR-based therapies for sickle cell disease. The current standard of myeloablative busulfan conditioning effectively supports engraftment of gene-corrected HSCs but carries significant toxicity risks that may be exacerbated by the underlying inflammatory state of SCD patients. Emerging strategies employing reduced-intensity approaches, antibody-based conditioning, and in vivo gene editing platforms promise to redefine the therapeutic landscape by improving safety profiles while maintaining efficacy. Future success will depend on continued refinement of patient-specific conditioning intensities based on individualized risk assessments and comprehensive biomarker evaluation. As the field progresses, optimized conditioning regimens will be essential for maximizing the therapeutic potential of gene correction strategies while ensuring favorable risk-benefit profiles for all SCD patients.
Clinical Validation and Comparative Analysis of CRISPR Therapies in SCD Treatment
Casgevy (exagamglogene autotemcel) represents a landmark advancement in the treatment of hemoglobinopathies, being the first FDA-approved therapy utilizing CRISPR/Cas9 genome editing technology [44]. This autologous cell-based gene therapy is approved for patients aged 12 years and older with sickle cell disease (SCD) who experience recurrent vaso-occlusive crises (VOCs) or for those with transfusion-dependent beta thalassemia (TDT) [61] [88] [44]. The therapeutic approach involves precise genome editing of the patient's own hematopoietic stem cells to disrupt the BCL11A gene, a key transcriptional repressor of fetal hemoglobin (HbF) [89]. By reactivating HbF production, Casgevy addresses the fundamental pathophysiology of both diseases—reducing sickling of red blood cells in SCD and ameliorating chronic anemia in TDT [89]. This in-depth technical review examines the comprehensive clinical trial data, mechanistic insights, and long-term outcomes supporting Casgevy's therapeutic profile, providing researchers and drug development professionals with a detailed analysis of this transformative CRISPR-based intervention.
Clinical Trial Design and Participant Demographics
Clinical Trial Program Structure
The clinical development program for Casgevy consists of three ongoing Phase 1/2/3 open-label trials: CLIMB-111 (NCT03655678) for TDT, CLIMB-121 (NCT03745287) for SCD, and CLIMB-131 (NCT04208529) for long-term follow-up [89] [90]. These single-arm, multi-center studies were designed to evaluate the safety and efficacy of a single dose of Casgevy in patients aged 12-35 years [61] [89] [88]. The trials are open-label, meaning all participants and investigators knew the treatment being administered, with no placebo control group [61] [88]. The primary efficacy outcomes were measured at 12 months, but the studies continue to collect data, with CLIMB-131 designed to follow patients for up to 15 years after infusion to assess long-term safety and durability [89].
Participant Characteristics and Eligibility Criteria
The trials enrolled carefully selected patient populations with significant disease burden. For the sickle cell disease trial, participants had a history of at least two severe VOCs per year in the two years preceding the study [61]. Severe VOCs were protocol-defined as pain events requiring medical facility visits and parenteral pain medication or red blood cell transfusions, acute chest syndrome, priapism, or splenic sequestration [61]. For the beta thalassemia trial, participants had transfusion-dependent beta thalassemia requiring regular blood transfusions [88]. As of recent data cuts, 44 patients with SCD and 52 patients with TDT have received Casgevy across the trials [61] [88]. The demographic profile spans adolescents and young adults, with efficacy evaluated in subsets who had sufficient follow-up time (31 SCD patients and 35 TDT patients at initial analysis) [61] [88].
Table 1: Clinical Trial Participant Demographics and Baseline Characteristics
| Characteristic | Sickle Cell Disease Trial | Beta Thalassemia Trial |
|---|---|---|
| Total Treated | 44 patients | 52 patients |
| Evaluable for Efficacy | 31 patients (at initial analysis) | 35 patients (at initial analysis) |
| Age Range | 12-35 years | 12-35 years |
| Key Inclusion Criteria | ≥2 severe VOCs/year for 2 years prior to study | Transfusion-dependent beta thalassemia |
| Baseline Disease Severity | High VOC frequency: median of 3.5-4.0 severe VOCs annually [91] | Regular transfusion requirements pre-treatment |
Comprehensive Efficacy Outcomes
Sickle Cell Disease: VOC Reduction and Hospitalization Freedom
Casgevy demonstrated remarkable efficacy in eliminating severe vaso-occlusive crises in patients with sickle cell disease. In the primary efficacy analysis, 93.5% (29 out of 31) of evaluable patients achieved freedom from severe VOCs for at least 12 consecutive months after receiving Casgevy [61] [91]. Importantly, 100% (30 out of 30) of evaluable patients were free from hospitalizations for severe VOCs for the same duration [61]. Updated interim analyses from February 2025 with 46 patients show consistent results, with 93% (39 out of 42) of evaluable patients maintaining freedom from VOCs for at least 12 consecutive months [89]. The durability of response is particularly noteworthy, with the mean duration of VOC-free period extending to 30.9 months, and a maximum of 59.6 months in long-term follow-up [89]. Even the small subset of evaluable patients who did not achieve the full 12-month VOC-free endpoint still derived substantial clinical benefit, demonstrating reductions in hospitalization rates for VOCs by 71-100% [89].
Beta Thalassemia: Transfusion Independence
In patients with transfusion-dependent beta thalassemia, Casgevy achieved similarly impressive results, with 91.4% (32 out of 35) of evaluable patients no longer requiring transfusions for at least 12 consecutive months after treatment [88]. The median duration of transfusion independence was 20.8 months in initial analyses [88], with more recent data showing a mean duration of 34.5 months and a maximum of 64.1 months in long-term follow-up [89]. Among the 54 evaluable patients in updated analyses, 98% achieved transfusion independence for at least 12 consecutive months with a weighted average hemoglobin of at least 9 g/dL [89]. The single evaluable patient who had not yet achieved this endpoint still demonstrated meaningful clinical improvement, remaining transfusion-free for 8.2 months [89].
Hematological and Biochemical Parameters
Beyond the primary clinical endpoints, Casgevy treatment resulted in significant improvements in key laboratory parameters. Patients exhibited substantial and sustained increases in fetal hemoglobin (HbF) levels, with corresponding elevations in total hemoglobin [61] [88]. The elevated HbF facilitates oxygen delivery and prevents sickling of red blood cells in SCD, while in TDT, it compensates for the deficient adult hemoglobin production [89]. These biochemical improvements correlate with the observed clinical benefits and demonstrate the mechanistic efficacy of BCL11A gene editing.
Table 2: Summary of Primary Efficacy Outcomes from Clinical Trials
| Efficacy Parameter | Sickle Cell Disease Results | Beta Thalassemia Results |
|---|---|---|
| Primary Endpoint | Freedom from severe VOCs for ≥12 months | Transfusion independence for ≥12 months |
| Efficacy Rate (Initial) | 93.5% (29/31 patients) [61] [91] | 91.4% (32/35 patients) [88] |
| Efficacy Rate (Updated) | 93% (39/42 patients) [89] | 98% (53/54 patients) [89] |
| Duration of Response (Mean) | 30.9 months [89] | 34.5 months [89] |
| Maximum Observed Duration | 59.6 months [89] | 64.1 months [89] |
| Hospitalization Freedom | 100% free from VOC hospitalizations for ≥12 months [61] | Not applicable |
Safety Profile and Adverse Event Management
Adverse Event Spectrum and Incidence
The safety profile of Casgevy is consistent with that expected from myeloablative conditioning with busulfan and autologous hematopoietic stem cell transplant (HSCT) [89] [92]. In the SCD trial, serious adverse reactions occurred in 45% of patients after myeloablative conditioning and Casgevy infusion [92]. The most common serious adverse reactions (occurring in ≥2 patients) included cholelithiasis, pneumonia, abdominal pain, constipation, pyrexia, upper abdominal pain, non-cardiac chest pain, oropharyngeal pain, pain, and sepsis [92]. One patient (2%) died due to COVID-19 infection and subsequent respiratory failure, which was assessed as unrelated to Casgevy [92]. Updated safety data from February 2025 show consistent findings, with serious adverse events observed in 47.8% of patients [92].
Hematological Recovery and Engraftment
A critical phase following Casgevy treatment involves the period of cytopenia before successful engraftment. Patients experience low levels of platelets and white blood cells until the edited cells engraft in the bone marrow [61] [92]. Neutrophil engraftment occurred at a median of 27 days (range: 15-40 days), while platelet engraftment occurred at a median of 35 days (range: 23-126 days) [92]. All patients achieved successful engraftment with no cases of graft failure, graft rejection, or graft-versus-host disease reported [92]. No patients required backup CD34+ cells, indicating robust engraftment of the edited cells [92].
Management of Treatment-Emergent Adverse Events
Clinical management during the treatment period focuses on monitoring and supporting patients through the cytopenic phase. Healthcare providers regularly test blood counts to monitor platelet and white blood cell levels [61]. Patients are instructed to report symptoms suggestive of low platelet levels (severe headache, abnormal bruising, prolonged bleeding, bleeding without injury) or low white blood cell levels (fever, chills, infections) [61]. Additional common side effects include mucositis, nausea, vomiting, and febrile neutropenia, which are managed with standard supportive care measures [92].
Table 3: Grade 3 or 4 Adverse Reactions in ≥10% of SCD Patients (N=44)
| Adverse Reaction | Frequency n (%) |
|---|---|
| Mucositis | 41 (93%) |
| Febrile Neutropenia | 40 (91%) |
| Neutropenia | 6 (14%) |
| Decreased Appetite | 9 (20%) |
| Pruritus | 7 (16%) |
| Pain | 5 (11%) |
| Headache | 5 (11%) |
Source: Casgevy Prescribing Information [92]
Experimental Protocols and Methodologies
CASGEVY Manufacturing and Treatment Process
The Casgevy treatment protocol involves a multi-step manufacturing process conducted at specialized facilities [61]. The workflow can be visualized as follows:
CRISPR Editing Mechanism and Molecular Validation
The core technology underlying Casgevy involves precise CRISPR/Cas9-mediated editing of the BCL11A gene in hematopoietic stem cells [89]. The experimental methodology for gene editing validation includes:
- Guide RNA Design: Selection of specific gRNA sequences targeting the erythroid-specific enhancer region of the BCL11A gene to disrupt its expression specifically in red blood cell lineage [89]
- Electroporation Protocol: Optimization of delivery parameters for introducing CRISPR/Cas9 ribonucleoprotein complexes into CD34+ hematopoietic stem and progenitor cells [89]
- Clonogenic assays: Assessment of hematopoietic progenitor cell function and differentiation potential post-editing
- Off-target analysis: Comprehensive genomic assessment using GUIDE-seq or similar methods to identify and validate editing specificity [93]
- Engraftment validation: Xenotransplant models to evaluate long-term repopulation capacity of edited cells and lineage distribution
Quality Control and Release Testing
Rigorous quality control measures are implemented throughout the manufacturing process, including:
- Viability and potency assays of the final cell product
- Microbiological testing for sterility
- Vector copy number analysis (for lentiviral components if used)
- Determination of editing efficiency at the BCL11A target site
- Cell dose quantification to ensure adequate CD34+ cell count for transplantation
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for CRISPR-Based Hematopoietic Stem Cell Research
| Reagent/Category | Function in Experimental Workflow | Specific Application Examples |
|---|---|---|
| CRISPR/Cas9 System | Site-specific DNA cleavage for gene editing | BCL11A enhancer disruption [89] |
| Base Editors (ABE/CBE) | Precise single-nucleotide conversions without double-strand breaks | Direct correction of HBB mutations [93] |
| Lentiviral Vectors | Delivery of editing components or therapeutic transgenes | Alternative gene therapy approaches [44] |
| Lipid Nanoparticles (LNPs) | Non-viral delivery of editing components | In vivo delivery for liver-targeted editing [6] |
| CD34+ Selection Kits | Isolation of hematopoietic stem cells | Patient cell processing for ex vivo editing |
| Myeloablative Agents (Busulfan) | Bone marrow conditioning | Create niche for engrafted cells [92] |
| Cytokine Cocktails | Stem cell mobilization and expansion | Enhance stem cell collection and culture |
Long-Term Patient Outcomes and Durability
Sustained Efficacy and Hemoglobin Stability
Long-term follow-up data from the CLIMB-131 trial demonstrate remarkable durability of treatment response. For SCD patients, the clinical benefits persist with a mean VOC-free duration of 30.9 months and maximum observed duration of 59.6 months [89]. Similarly, TDT patients maintain transfusion independence for a mean of 34.5 months, with some patients reaching 64.1 months without transfusions [89]. These data indicate that the therapeutic effect of a single Casgevy treatment is sustained over multiple years. Patients continue to demonstrate stable levels of fetal hemoglobin and allelic editing across all ages and genotypes in the trials, confirming the permanent nature of the genetic modification and its functional consequences [89].
Quality of Life and Functional Outcomes
Beyond the primary hematological and clinical endpoints, patients treated with Casgevy report sustained and clinically meaningful improvements in quality of life metrics [89]. Comprehensive assessments measuring physical, emotional, social/family, and functional well-being show significant enhancements following treatment [89]. These improvements reflect the substantial reduction in disease-related complications and hospitalizations, allowing patients to experience better overall health status and daily functioning.
Safety and Monitoring in Long-Term Follow-Up
The long-term safety profile of Casgevy continues to be consistent with myeloablative conditioning and autologous hematopoietic stem cell transplant, with no new safety signals emerging in extended follow-up [89] [90]. Patients will be monitored for up to 15 years after treatment to comprehensively assess long-term risks and benefits [89]. Critical monitoring parameters include complete blood counts, hemoglobin electrophoresis, vector integration sites (if applicable), and screening for any late-effects of genome editing.
Casgevy represents a paradigm shift in the treatment of sickle cell disease and transfusion-dependent beta thalassemia, demonstrating that a single course of CRISPR/Cas9-mediated gene editing can produce durable clinical benefits with a manageable safety profile. The robust clinical trial data show consistent and sustained efficacy across patient populations, with over 90% of evaluable patients achieving the primary endpoints of VOC freedom or transfusion independence. The safety profile, while significant, is consistent with the known risks of myeloablative conditioning and autologous HSCT. As research progresses, future developments will likely focus on optimizing manufacturing processes, expanding patient eligibility, and potentially combining Casgevy with other innovative approaches. The success of Casgevy validates CRISPR-based genome editing as a therapeutic modality and paves the way for applications to other genetic disorders.
Sickle Cell Disease (SCD) is a monogenic disorder caused by a point mutation in the β-globin gene (HBB), which leads to the production of abnormal sickle hemoglobin (HbS) [60] [27]. This results in chronic hemolytic anemia, vaso-occlusive crises, and progressive multi-organ damage [18]. The recent approval of both CRISPR-based (Casgevy) and lentiviral vector-based (Lyfgenia) gene therapies represents a paradigm shift in the treatment landscape, offering potential cures through autologous hematopoietic stem cell (HSC) transplantation [27]. This analysis provides a technical comparison of these two groundbreaking approaches, focusing on their molecular mechanisms, efficacy, safety, and practical implementation for researchers and drug development professionals.
Molecular Mechanisms and Therapeutic Targets
The two therapies employ fundamentally distinct strategies to counteract the pathological effects of HbS.
CRISPR-Based Therapy (Casgevy): HbF Reactivation This approach indirectly addresses the SCD mutation by reactivating the production of fetal hemoglobin (HbF). HbF (α2γ2) does not incorporate the defective βS-globin chain and can effectively prevent HbS polymerization [60] [27]. Casgevy utilizes CRISPR-Cas9 to create a double-strand break in the gene encoding BCL11A, a key transcriptional repressor of the γ-globin genes (HBG1 and HBG2) [26]. The break is repaired via non-homologous end joining (NHEJ), leading to gene knockout. This disruption de-represses γ-globin expression, leading to sustained production of HbF in red blood cells, which dilutes HbS and inhibits its polymerization [60] [26].
Lentiviral Vector Therapy (Lyfgenia): Anti-Sickling Globin Addition Lyfgenia employs a direct gene addition strategy. It uses a lentiviral vector to introduce a functional, modified β-globin gene into the patient's HSCs [60] [27]. The transgene, β^A-T87Q-globin, encodes an anti-sickling hemoglobin variant (HbA^T87Q) containing three specific amino acid substitutions (G16D, E22A, T87Q) that prevent HbS polymerization under hypoxic conditions [94] [60]. This therapeutic globin is driven by a lentiviral vector that incorporates elements of the β-globin locus control region (LCR) to ensure high-level, erythroid-specific expression [27]. The modified HSCs then produce red blood cells containing the anti-sickling HbA^T87Q.
The following diagram illustrates the core mechanistic differences between these two strategies.
Comparative Efficacy and Safety Data
Preclinical and clinical data reveal distinct efficacy and safety profiles for each modality. A direct comparison of key parameters is summarized in the table below.
Table 1: Quantitative Comparison of CRISPR and Lentiviral Therapies for SCD
| Parameter | CRISPR-based (Casgevy) | Lentiviral (Lyfgenia) | References |
|---|---|---|---|
| Therapeutic Molecule | Fetal Hemoglobin (HbF) | Anti-sickling β-globin (HbA^T87Q) | [60] [27] |
| Therapeutic Globin Level | ~62% γ-globin (in mouse model) | ~38% β^A-T87Q-globin (in mouse model) | [95] |
| Reduction in RBC Sickling | ~30% (in mouse model) | ~50% (in mouse model) | [95] |
| Integration Pattern | Targeted gene knockout (NHEJ) | Semi-random genomic integration | [96] [94] |
| Primary Safety Concerns | Off-target editing, chromosomal rearrangements | Insertional mutagenesis, globin chain imbalance, theoretical risk of myeloid malignancy | [96] [94] [60] |
| Vector Copy Number (VCN) | Not applicable (non-viral editing) | ~2.0 copies/diploid genome (target range) | [95] |
| Clinical VOC Resolution | Near-complete resolution demonstrated | Near-complete resolution demonstrated | [60] |
3.1 Efficacy Outcomes Both therapies have demonstrated profound clinical benefits, including a near-complete resolution of vaso-occlusive crises (VOCs) in clinical trial participants [60]. In a comparative mouse model study, the CRISPR approach targeting BCL11A resulted in 62% γ-globin production and a 30% reduction in sickling. In contrast, the lentiviral approach (using the BB305 vector, the basis for Lyfgenia) achieved 38% β^A-T87Q-globin production and a 50% reduction in sickling [95]. This suggests that while both are effective, the mechanisms lead to different levels of corrective globins and phenotypic rescue.
3.2 Safety Profiles The safety profiles are dictated by the underlying technology.
- CRISPR (Casgevy): The primary concerns are off-target effects, where unintended genomic loci could be edited, and the potential for on-target chromosomal rearrangements (e.g., large deletions, translocations) at the BCL11A cut site [96]. Advanced specificity analyses, such as rhAmpSeq across 82 predicted off-target sites, have found no evidence of indels in pre-clinical studies, highlighting the importance of thorough off-target screening [96].
- Lentiviral (Lyfgenia): The main risk is insertional mutagenesis, where the semi-random integration of the lentiviral vector could disrupt a tumor suppressor gene or activate an oncogene, potentially leading to clonal expansion and malignancy [94] [60]. While current self-inactivating (SIN) lentiviral vectors have a improved safety profile, cases of aberrant vector-gene fusion transcripts and clonal expansions have been reported in other lentiviral therapies [96] [60]. Additionally, globin chain imbalance remains a theoretical risk if the expression of the therapeutic β-globin is insufficient to pair with endogenous α-globin chains [60].
Experimental and Manufacturing Workflows
The ex vivo manufacturing processes for both therapies share initial and final steps but differ critically in the genetic modification phase.
Table 2: Comparative Experimental Protocols for SCD Gene Therapies
| Process Step | CRISPR-based (Casgevy) | Lentiviral (Lyfgenia) |
|---|---|---|
| 1. HSPC Mobilization & Collection | Apheresis of CD34+ HSCs after G-CSF (± Plerixafor) mobilization. | Identical process. |
| 2. Pre-stimulation | Culture in StemSpanII or X-Vivo 10 medium with SCF, Flt3-L, TPO for 48 hours. | Culture in X-Vivo 10 medium with SCF, Flt3-L, TPO for 48 hours. |
| 3. Genetic Modification | Electroporation of CRISPR-Cas9 Ribonucleoprotein (RNP) complex. Co-delivery of i53 mRNA to transiently inhibit p53 and improve HSC viability may be used [96]. | Lentiviral Transduction with clinical-grade LV vector. Use of enhancers (e.g., LentiBoost, dmPGE2) to improve transduction efficiency [96] [94]. |
| 4. Donor Template | Not applicable for BCL11A knockout strategy. (For HDR-based correction, an AAV6 or ssDNA donor would be used). | The lentiviral vector itself acts as the donor. |
| 5. Expansion & Quality Control | Assessment of viability, indels (via TIDE or NGS), and off-target analysis. | Assessment of viability, Vector Copy Number (VCN) via qPCR/ddPCR, and transduction efficiency. |
| 6. Patient Conditioning | Myeloablative busulfan conditioning. | Myeloablative busulfan conditioning. |
| 7. Re-infusion | Intravenous infusion of genetically modified autologous CD34+ cells. | Intravenous infusion of genetically modified autologous CD34+ cells. |
The following workflow provides a visual overview of the parallel processes.
The Scientist's Toolkit: Essential Research Reagents
Developing and optimizing these therapies requires a suite of specialized reagents and tools.
Table 3: Key Research Reagent Solutions for SCD Gene Therapy Development
| Reagent / Tool | Function | Application in SCD Research |
|---|---|---|
| CRISPR-Cas9 RNP | Pre-assembled complex of Cas9 protein and synthetic guide RNA (sgRNA). Enables immediate activity upon delivery, reducing off-target effects. | Used for knocking out BCL11A or, with a donor template, for precise HBB correction [26] [97]. |
| Lentiviral Vector (SIN) | Delivery vehicle for stable integration of transgenes into the host genome. Self-Inactivating (SIN) design improves safety. | Used to deliver the anti-sickling β^A-T87Q-globin gene (Lyfgenia) or shRNAs against BCL11A [94] [27]. |
| rAAV6 Donor Template | Recombinant Adeno-Associated Virus serotype 6. Highly efficient at delivering donor DNA for HDR in HSCs. | Used in CRISPR strategies requiring precise gene correction (e.g., converting HbS to HbA) [96]. |
| Lentiviral Transduction Enhancers | Small molecules (e.g., LentiBoost, 16,16-dimethyl PGE2) that increase transduction efficiency of HSCs. | Critical for achieving high VCN in a large proportion of CD34+ cells with lower vector doses [96] [94]. |
| HSPC Culture Media | Serum-free media (e.g., StemSpan II, X-Vivo 10) optimized for pre-stimulation and maintenance of HSCs. | Supports cell viability and proliferation during the ex vivo culture and genetic modification steps [96]. |
| Electroporation System | Device for delivering electrical pulses to create transient pores in cell membranes, allowing RNP entry. | Standard method for non-viral delivery of CRISPR RNP into sensitive CD34+ HSCs [97]. |
The advent of both CRISPR-based and lentiviral gene therapies marks a new era for SCD treatment. The choice between these modalities involves a careful trade-off:
- Casgevy (CRISPR) offers a highly precise, non-viral mechanism with a potentially favorable long-term genotoxicity profile due to the absence of random vector integration. However, it requires vigilant monitoring for off-target effects [96] [97].
- Lyfgenia (Lentiviral) delivers a proven, potent anti-sickling globin via a well-characterized delivery platform but carries the inherent, albeit mitigated, risk of insertional mutagenesis and requires careful monitoring of VCN [94] [60].
Future research will focus on enhancing the safety and efficacy of both platforms. For CRISPR, this includes developing high-fidelity Cas variants and novel delivery methods like lipid nanoparticles (LNPs) for in vivo editing, which could eliminate the need for complex ex vivo manufacturing [6] [97]. For lentiviral therapies, further refinements to vector design to direct integration to safe genomic harbors are underway. The ultimate goal is to simplify these therapies, reduce their cost, and improve global accessibility, particularly in regions with a high prevalence of SCD. The continued evolution of both strategies will be instrumental in achieving this objective.
Sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TDT) are monogenic hemoglobinopathies representing a significant global health burden. For SCD, a single point mutation in the β-globin gene (HBB) leads to the production of sickle hemoglobin (HbS), which polymerizes under deoxygenation, causing red blood cells to distort into a sickle shape. This results in chronic hemolytic anemia, vaso-occlusive crises (VOCs), and progressive multi-organ damage [27]. TDT results from mutations that cause absent or significantly reduced β-globin chain synthesis, leading to severe anemia requiring lifelong red blood cell transfusions [64]. The therapeutic goal of novel CRISPR-based gene therapies is to address the root genetic cause, with efficacy measured through key clinical and laboratory metrics: elevation of fetal hemoglobin (HbF), reduction in VOC frequency, and achievement of transfusion independence. This whitepaper examines these critical efficacy endpoints within the context of CRISPR-Cas9 mediated beta-globin mutation correction.
Core Therapeutic Efficacy Metrics
Fetal Hemoglobin (HbF) Levels
HbF (α2γ2) is the dominant form of hemoglobin during fetal development but is largely replaced by adult hemoglobin (HbA, α2β2) after birth. Elevated HbF levels are a well-established modifier of disease severity in both SCD and TDT. In SCD, HbF interferes with the polymerization of HbS, while in TDT, γ-globin chains pair with excess α-globin chains to form functional HbF, ameliorating the α-globin chain imbalance and ineffective erythropoiesis [27]. Consequently, increasing HbF expression to a therapeutic threshold of approximately 30% is a primary objective of many gene therapies [27].
Table 1: HbF Elevation Across Therapeutic Modalities
| Therapeutic Modality | Mechanism of Action | Average HbF Increase | Key Supporting Evidence |
|---|---|---|---|
| Hydroxyurea (Pharmacologic) [98] | Cytostatic agent inducing "stress erythropoiesis"; exact mechanism of HbF induction not fully understood. | ~18% (with 20 mg/kg/day dose) | Meta-analysis of 45 articles (2003-2023). |
| CASGEVY (exa-cel) - CRISPR [64] [89] | Ex vivo knockout of BCL11A enhancer in HSPCs to disrupt HbF repression. | Stable, high levels sustained for >5.5 years (SCD) and >6 years (TDT). | Long-term follow-up data from CLIMB trials; stable allelic editing. |
| LRF Repressor Disruption (CRISPR) [4] | Ex vivo disruption of LRF binding sites in the γ-globin promoters in HSPCs. | Potent HbF synthesis in erythroid progeny. | Preclinical study in healthy donor and patient-derived HSPCs. |
| HBB Gene Correction (CRISPR) [3] | Ex vivo precision correction of the E6V point mutation in the HBB gene in HSPCs. | Data focused on engraftment and safety; goal is restored HbA production. | Preclinical study demonstrating up to 60% allelic correction in manufacturing. |
Reduction in Vaso-Occlusive Crises (VOCs)
VOCs are the acute, painful hallmark of SCD, occurring when sickled red blood cells obstruct blood flow. A reduction in VOC frequency is a direct measure of clinical improvement and a primary efficacy endpoint in SCD clinical trials.
Table 2: VOC Reduction in Sickle Cell Disease Therapies
| Therapy | Study / Context | VOC Reduction Outcome | Follow-up Duration |
|---|---|---|---|
| Hydroxyurea [99] | Systematic review of Indian studies (3,817 patients). | 79-93% reduction in VOC frequency. | Variable across 27 studies. |
| CASGEVY (exa-cel) [64] | CLIMB-121 and CLIMB-131 trials (evaluable patients, N=45). | 95.6% (43/45) free of VOCs for ≥12 consecutive months. | Mean duration VOC-free: 35.0 months (max 66.2). |
| CASGEVY (exa-cel) [89] | CLIMB-121 and CLIMB-131 trials (evaluable patients, N=42). | 93% (39/42) free of VOCs for ≥12 consecutive months. | Mean duration VOC-free: 30.9 months (max 59.6). |
Transfusion Independence
For patients with TDT, freedom from chronic transfusions is the definitive marker of therapeutic success. Transfusion independence (TI) is rigorously defined as maintaining a weighted average hemoglobin of at least 9 g/dL without any red blood cell transfusions for at least 12 consecutive months (TI12) [64].
Table 3: Achievement of Transfusion Independence in Beta Thalassemia
| Therapy | Study / Context | Transfusion Independence Rate | Additional Hematologic Outcomes |
|---|---|---|---|
| CASGEVY (exa-cel) [64] | CLIMB-111 and CLIMB-131 trials (evaluable patients, N=55). | 98.2% (54/55) achieved TI12. | Mean duration of TI: 40.5 months (max 70.8); 69.6% stopped iron chelation therapy. |
| CASGEVY (exa-cel) [89] | CLIMB-111 and CLIMB-131 trials (evaluable patients, N=54). | 98% (53/54) achieved TI12. | Mean duration of TI: 34.5 months (max 64.1). |
CRISPR-Cas9 Experimental Strategies and Protocols
CRISPR-based approaches for hemoglobinopathies primarily involve ex vivo editing of autologous hematopoietic stem and progenitor cells (HSPCs). The two dominant strategies are HbF reactivation and direct gene correction.
Strategy 1: HbF Reactivation via BCL11A Gene Knockout
This is the mechanism underpinning the approved therapy CASGEVY. The erythroid-specific enhancer of BCL11A, a master transcription factor that represses γ-globin expression, is targeted for knockout.
Diagram: BCL11A Knockout Workflow
Detailed Experimental Protocol [64] [89]:
- HSPC Collection (Apheresis): Patients undergo mobilization with plerixafor (a CXCR4 antagonist) to move CD34+ HSPCs from the bone marrow into the peripheral blood. Cells are collected via apheresis. A backup portion of unmanipulated cells is cryopreserved as a "rescue" product.
- Ex Vivo Manufacturing:
- The apheresis product is shipped to a manufacturing facility.
- CD34+ HSPCs are isolated and transfected with CRISPR-Cas9 components (e.g., as ribonucleoprotein complexes) targeting the erythroid-specific enhancer in the BCL11A gene.
- The process uses non-viral delivery, creating a precise double-strand break in the DNA. The cell's own repair mechanism, non-homologous end joining (NHEJ), introduces insertions or deletions (indels) that disrupt the enhancer.
- Myeloablative Conditioning: Patients receive busulfan conditioning for several days to clear bone marrow niches and enable engraftment of the edited HSPCs.
- Reinfusion: The CRISPR-edited HSPCs (the final drug product) are thawed and administered via a single intravenous infusion.
- Engraftment and Recovery: Patients remain hospitalized for monitoring until neutrophil and platelet counts recover. The entire process, from cell collection to infusion, can take up to 6 months.
Strategy 2: Direct HBB Gene Correction
This investigational strategy aims to correct the causative point mutation in the HBB gene itself, preserving physiologic regulation.
Diagram: HBB Gene Correction Workflow
Detailed Experimental Protocol [3]:
- HSPC Collection: Plerixafor-mobilized CD34+ HSPCs are collected from patients or healthy donors.
- Gene Editing:
- HSPCs are electroporated with a high-fidelity Cas9 ribonucleoprotein (RNP) complex designed to create a double-strand break near the SCD point mutation.
- A recombinant adeno-associated virus serotype 6 (rAAV6) vector is used as the donor template, providing a homologous DNA sequence containing the correct HBB sequence.
- The cell's homology-directed repair (HDR) pathway uses this template to precisely correct the E6V mutation.
- Engraftment and Safety Testing: Preclinical studies involve transplanting the corrected HSPCs into immunodeficient NSG mice to assess long-term engraftment and multi-lineage differentiation. Edited human cells are retrieved from the mouse bone marrow and analyzed for the frequency of gene correction and potential genotoxicity.
Strategy 3: HbF Reactivation via LRF Repressor Disruption
An alternative HbF reactivation strategy targets the binding sites for the lymphoma-related factor (LRF) repressor within the γ-globin gene promoters [4]. The experimental protocol is similar to the BCL11A knockout approach, but the CRISPR-Cas9 system is designed to disrupt LRF binding sites, directly leading to HBG gene derepression and HbF synthesis. This strategy has shown high editing efficiency and potent HbF production in pre-clinical models, with evidence suggesting even higher efficiency in SCD patient-derived HSPCs compared to healthy donor cells [4].
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Reagents for CRISPR-based Hemoglobinopathy Research
| Research Reagent / Tool | Function in Experimental Protocol | Specific Application Example |
|---|---|---|
| Plerixafor (Mozobil) [3] | CXCR4 antagonist that mobilizes CD34+ HSPCs from bone marrow to peripheral blood for collection. | Used for HSPC mobilization in both CASGEVY clinical trials and pre-clinical HBB correction studies. |
| CRISPR-Cas9 Ribonucleoprotein (RNP) [3] | The core gene-editing machinery. A complex of Cas9 enzyme and guide RNA (gRNA). Direct RNP delivery is rapid and reduces off-target effects. | Used in HBB gene correction [3] and LRF disruption [4] protocols for high-efficiency editing. |
| rAAV6 Donor Template [3] | Recombinant adeno-associated virus serotype 6. Serves as a highly efficient delivery vector for the homologous DNA donor template in HDR-based strategies. | Used to deliver the corrective HBB sequence for precise gene correction in HSPCs [3]. |
| Busulfan [64] [89] | Myeloablative conditioning agent. Clears the bone marrow to create niches for the engraftment of infused, edited HSPCs. | Standard conditioning regimen prior to infusion of CASGEVY and other ex vivo gene-edited HSPC products. |
| Immunodeficient NSG Mice [3] | A mouse model (NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ) that lacks an adaptive immune system, enabling engraftment of human cells. | Critical for pre-clinical in vivo studies to assess long-term engraftment and differentiation potential of edited human HSPCs. |
The advent of CRISPR-Cas9 gene editing has revolutionized the therapeutic landscape for genetic disorders, with sickle cell disease (SCD) serving as a pioneering validation case following the regulatory approval of Casgevy (exa-cel). This therapy corrects the beta-globin mutation through ex vivo editing of hematopoietic stem cells (HSCs) to disrupt the BCL11A gene, thereby reactivating fetal hemoglobin (HbF) production [100]. While demonstrating remarkable efficacy, comprehensive safety assessment remains paramount for clinical translation. This technical guide provides an in-depth analysis of three critical safety considerations—off-target effects, immunogenicity, and long-term risks—within the specific context of SCD therapy development, offering researchers and drug development professionals methodologies and frameworks for rigorous safety evaluation.
Understanding Off-Target Effects in CRISPR Editing
Mechanisms and Biological Consequences
Off-target editing refers to non-specific CRISPR-Cas9 activity at genomic sites other than the intended target, leading to unintended double-strand breaks (DSBs) [69]. These events occur primarily due to the natural tolerance of Cas9 nucleases for mismatches between the guide RNA (gRNA) and genomic DNA; the wild-type Streptococcus pyogenes Cas9 (SpCas9) can tolerate 3-5 base pair mismatches, enabling cleavage at sites with sequence similarity to the target, provided they contain the correct protospacer adjacent motif (PAM) sequence [69].
The biological impact of off-target effects depends largely on their genomic location. Edits in non-coding regions may have minimal consequences, while mutations in protein-coding regions, tumor suppressor genes, or oncogenes can confound experimental results, compromise therapeutic safety, and potentially drive malignant transformation [69] [101]. In clinical applications, off-target effects pose significant safety risks, as they may result in genotoxic events that could delay clinical development or cause patient harm [69].
Detection and Analysis Methodologies
Comprehensive off-target assessment requires integrated computational prediction and experimental validation approaches. The table below summarizes the primary methodologies employed in off-target profiling:
Table 1: Methods for CRISPR Off-Target Prediction and Detection
| Method Type | Specific Method | Key Characteristics | Advantages | Limitations |
|---|---|---|---|---|
| In silico Prediction | Cas-OFFinder | Adjustable sgRNA length, PAM type, mismatch/bulge tolerance | Widely applicable, comprehensive scanning | Biased toward sgRNA-dependent effects; misses epigenomic factors |
| FlashFry | High-throughput analysis with GC content scoring | Rapid processing of large sgRNA sets | Computational prediction requires experimental validation | |
| DeepCRISPR | Incorporates sequence and epigenetic features | More comprehensive prediction model | Complex implementation requiring specialized expertise | |
| Experimental Detection (Cell-Free) | Digenome-seq | Digests purified genomic DNA with Cas9-gRNA RNP followed by whole-genome sequencing | Highly sensitive | Expensive; requires high sequencing coverage |
| CIRCLE-seq | Circularizes sheared DNA, incubates with RNP, linearizes for sequencing | Low background noise; high sensitivity | Does not account for cellular context | |
| Experimental Detection (Cell-Based) | GUIDE-seq | Integrates double-stranded oligodeoxynucleotides (dsODNs) into DSBs | Highly sensitive; cost-effective; low false-positive rate | Limited by transfection efficiency |
| LAM-HTGTS | Detects DSB-induced chromosomal translocations via bait-prey junction sequencing | Specifically identifies chromosomal rearrangements | Only detects translocations, not all off-target events | |
| DISCOVER-Seq | Utilizes DNA repair protein MRE11 for ChIP-seq | Highly sensitive in cellular contexts | Potential for false positives | |
| Comprehensive Analysis | Whole Genome Sequencing (WGS) | Sequences entire genome before and after editing | Most comprehensive; detects all mutation types | Extremely expensive; limited clone analysis |
Experimental Protocol 1: GUIDE-seq for Comprehensive Off-Target Profiling
- Transfection: Co-transfect cells with Cas9-gRNA ribonucleoprotein (RNP) complexes and dsODN tags using appropriate delivery methods (electroporation for hematopoietic stem cells).
- Integration: Allow dsODN tags to integrate into DSB sites generated by Cas9 activity (48-72 hours post-transfection).
- Genomic DNA Extraction: Harvest cells and extract high-quality genomic DNA using standardized protocols.
- Library Preparation & Sequencing: Amplify integration sites with PCR using tags-specific primers, prepare sequencing libraries, and perform high-throughput sequencing.
- Bioinformatic Analysis: Map sequenced reads to reference genome, identify dsODN integration sites, and validate potential off-target sites through targeted sequencing.
Experimental Protocol 2: CIRCLE-seq for Sensitive In Vitro Detection
- DNA Isolation & Shearing: Extract genomic DNA from relevant cell types and fragment to 300-500bp using controlled enzymatic or mechanical shearing.
- Circularization: Ligate fragmented DNA into circular molecules using circligase enzyme.
- RNP Treatment: Incubate circularized DNA with pre-complexed Cas9-gRNA RNP complexes under optimal reaction conditions.
- Linearization & Purification: Treat RNP-digested DNA with exonuclease to degrade non-edited linear DNA, preserving only linearized fragments from Cas9 cleavage events.
- Library Preparation & Sequencing: Prepare sequencing libraries from purified linear DNA and sequence using appropriate platforms.
- Data Analysis: Map sequencing reads to reference genome, identifying sites with read start/end clusters indicating Cas9 cleavage.
Minimization Strategies
Multiple strategies exist to reduce off-target activity in therapeutic contexts:
High-Fidelity Cas Variants: Engineered Cas9 nucleases (e.g., HiFi Cas9) demonstrate reduced off-target cleavage while maintaining on-target efficiency [101] [102]. These variants incorporate mutations that decrease tolerance for gRNA-DNA mismatches.
gRNA Optimization: Careful gRNA design is crucial for minimizing off-target risk. Computational tools (CRISPOR, etc.) evaluate potential off-target sites and rank gRNAs based on predicted specificity. Optimal gRNAs typically feature higher GC content (40-60%) and minimal similarity to off-target genomic sites [69]. Chemical modifications (2'-O-methyl analogs, 3' phosphorothioate bonds) can further enhance specificity and stability [69].
Alternative Editing Platforms: Base editors and prime editors can achieve therapeutic effects without creating DSBs, significantly reducing off-target risks [69] [101]. Similarly, Cas9 nickase (nCas9) systems requiring paired gRNAs for DSB formation offer enhanced specificity through dual recognition requirements [69].
Delivery Optimization: Transient delivery of CRISPR components (e.g., as RNP complexes) limits exposure time and reduces off-target editing compared to stable vector-based expression [69].
Immunogenicity of CRISPR Components
Immune Recognition and Clinical Implications
CRISPR-Cas9 components, particularly bacterial-derived Cas nucleases, can trigger both innate and adaptive immune responses in human recipients [103]. Pre-existing immunity to Cas proteins, potentially acquired through natural bacterial exposures, poses significant challenges for in vivo therapies by potentially compromising efficacy and causing adverse inflammatory responses [103]. Immune recognition can occur through multiple mechanisms:
- Pattern Recognition Receptors detect conserved microbial motifs in Cas proteins
- MHC-mediated presentation of Cas-derived peptides activates Cas-specific T cells
- Antibody-mediated clearance of Cas9-expressing cells reduces editing efficiency
The clinical implications are particularly significant for in vivo applications, where immune responses can eliminate edited cells or cause inflammatory pathology. For ex vivo SCD therapies like Casgevy, immunogenicity risks are reduced but not eliminated, as residual immune responses may impact engraftment or long-term persistence of edited HSCs [103].
Mitigation Approaches
Several strategies have emerged to address Cas9 immunogenicity:
Epitope Engineering: Computational and experimental identification and removal of immunodominant T cell and B cell epitopes from Cas proteins while maintaining enzymatic activity [103].
Delivery System Optimization: Lipid nanoparticles (LNPs) demonstrate reduced immunogenicity compared to viral vectors and enable redosing, as evidenced by the successful multiple administrations in recent clinical cases [104] [6]. LNPs avoid the pre-existing immunity and strong immune activation associated with adenoviral or AAV vectors.
Nucleic Acid Modifications: Incorporating modified nucleotides in mRNA or gRNA components can reduce innate immune recognition by Toll-like receptors [103].
Immunosuppressive Regimens: Transient immunosuppression around the time of treatment can mitigate immune responses to CRISPR components, particularly for ex vivo applications where limited duration suppression is feasible [103].
Long-Term Risks and Genomic Instability
Structural Variations and Chromosomal Aberrations
Beyond small indels, CRISPR editing can induce large structural variations (SVs) including kilobase- to megabase-scale deletions, chromosomal translocations, and chromothripsis [101] [105]. These undervalued genomic alterations raise substantial safety concerns for clinical translation, particularly in the context of SCD therapies targeting the BCL11A locus [101].
Studies have demonstrated that large deletions at the on-target site occur more frequently than previously recognized, with the use of DNA-PKcs inhibitors to enhance homology-directed repair (HDR) exacerbating these aberrations [101]. In one investigation, DNA-PKcs inhibition resulted in a thousand-fold increase in translocation frequency and significantly increased megabase-scale deletions [101]. Chromosomal translocations can occur between the target site and off-target sites, or between two off-target sites, with potentially oncogenic consequences if tumor suppressor genes are disrupted or oncogenes activated [101].
Assessment Methods for Genomic Integrity
Specialized methodologies are required to detect these large-scale alterations:
Table 2: Methods for Detecting Structural Variations and Chromosomal Aberrations
| Method | Targeted Aberrations | Key Features | Therapeutic Application |
|---|---|---|---|
| CAST-Seq | Chromosomal translocations, large deletions | Amplification-based detection of rearrangement junctions; validated for clinical applications | Used in safety assessment for Casgevy and other therapies |
| LAM-HTGTS | Chromosomal translocations, structural variations | High-throughput genome-wide translocation sequencing; comprehensive translocation profiling | Detects DSB-induced translocations across the genome |
| Single-Cell Sequencing | Chromosome loss, large deletions | Analyses genomic integrity at single-cell level; identifies heterogeneous editing outcomes | Used to detect chromosome loss in edited T cells and HSCs |
| Karyotyping/ FISH | Gross chromosomal abnormalities | Traditional cytogenetic methods; detects large-scale rearrangements | Complementary validation for sequencing-based methods |
Experimental Protocol 3: CAST-Seq for Translocation Detection
- Editing & DNA Extraction: Edit target cells (e.g., CD34+ HSCs) with CRISPR system and extract high-molecular-weight genomic DNA after 72 hours.
- Adapter Ligation: Fragment DNA and ligate with platform-specific adapters containing sample barcodes.
- Nested PCR: Perform two rounds of PCR with primers specific to the on-target site and universal adapters to amplify potential translocation junctions.
- Library Preparation & Sequencing: Prepare sequencing libraries and run on high-throughput platform with sufficient coverage for rare event detection.
- Bioinformatic Analysis: Map chimeric reads to identify translocation partners, annotate genomic features of breakpoints, and quantify translocation frequency.
Recent investigations utilizing single-cell analysis have revealed that CRISPR-Cas9 editing can result in chromosome loss across various genomic targets and cell types, including clinical samples [105]. This finding highlights the need for comprehensive genomic integrity assessment beyond conventional off-target analysis in therapeutic development.
Mitigation Strategies for Genomic Instability
Alternative Repair Modulation: Avoiding DNA-PKcs inhibition in favor of more targeted HDR enhancement approaches that demonstrate better safety profiles, such as transient 53BP1 inhibition, which does not increase translocation frequency [101].
p53 Pathway Considerations: Transient p53 suppression has been shown to reduce large chromosomal aberrations, though this approach requires careful evaluation due to oncogenic concerns [101].
Nuclease Selection: High-fidelity Cas variants or nickase-based systems reduce but do not eliminate on-target structural variations, indicating that all platforms require thorough genomic integrity assessment [101].
Editing Control Optimization: Limiting nuclease exposure through RNP delivery and titrating to the minimum effective dose can reduce complex rearrangement formation [69] [101].
Integrated Safety Assessment Framework for SCD Therapies
Preclinical Safety Assessment Workflow
A comprehensive safety assessment strategy for SCD therapies should incorporate multiple orthogonal approaches:
Diagram 1: Safety Assessment Workflow. This diagram outlines the sequential approach for comprehensive CRISPR safety evaluation, from initial gRNA design to final risk assessment.
Essential Research Reagents and Tools
Table 3: Essential Research Reagents for CRISPR Safety Assessment
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Cas Nuclease Variants | SpCas9, HiFi Cas9, Cas12a | Comparison of specificity profiles; therapeutic nuclease selection | HiFi variants reduce off-targets but may lower on-target efficiency |
| gRNA Design Tools | CRISPOR, FlashFry | In silico specificity prediction and gRNA ranking | Multiple algorithms provide consensus prediction; experimental validation required |
| Detection Kits | GUIDE-seq kit, CIRCLE-seq kit | Experimental off-target profiling | Varying sensitivities and biases; orthogonal methods recommended |
| Control gRNAs | Validated high-specificity and low-specificity gRNAs | Assay validation and experimental controls | Essential for establishing detection sensitivity thresholds |
| Bioinformatics Pipelines | CRISPR-SURF, CRISPResso2 | Data analysis and quantification of editing outcomes | Standardized pipelines enable cross-study comparisons |
| Cell Line Models | HSPCs, HEK293, HUDEP-2 | Specificity assessment in relevant cellular contexts | Primary HSPCs most relevant for SCD therapy development |
Risk Management in Clinical Translation
For SCD therapies specifically, several risk mitigation strategies should be implemented:
Patient-Specific Considerations: FDA guidance notes that individuals carrying rare genetic variants may be at higher risk for off-target editing, emphasizing the need for personalized risk assessment [69].
Comprehensive Off-Target Profiling: Regulatory agencies require thorough characterization of both on-target and off-target effects, including evaluation of structural genomic integrity [101].
Long-Term Follow-Up: Monitoring edited cell populations over time to assess clonal dynamics and potential selection of cells with detrimental edits [101].
Alternative Editing Approaches: Base editing and prime editing strategies for SCD are demonstrating favorable safety profiles with reduced genotoxicity concerns compared to nuclease-based approaches [106].
The safety profile of CRISPR-based therapies for sickle cell disease encompasses a complex landscape of off-target effects, immunogenicity, and long-term genomic risks. A comprehensive assessment strategy integrating computational prediction, advanced experimental detection, and rigorous genomic integrity evaluation is essential for therapeutic development. As the field advances, emerging technologies including high-fidelity nucleases, improved delivery systems, and alternative editing platforms continue to enhance the safety of genetic medicines. For SCD researchers and therapy developers, implementing the structured safety assessment framework outlined in this document will be crucial for balancing therapeutic efficacy with patient safety in bringing new treatments to the clinic.
The advent of Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-based gene therapies for sickle cell disease (SCD) represents a watershed moment in medicine, introducing unprecedented therapeutic possibilities alongside profound economic challenges. SCD, caused by a point mutation in the β-globin gene (HBB) that leads to production of sickle hemoglobin (HbS), affects millions globally and imposes significant lifetime healthcare costs exceeding $550,000 per person [107]. The recent FDA approval of Casgevy (exagamglogene autotemcel) and Lyfgenia (lovotibeglogene autotemcel) heralds a new era of potentially curative treatments, yet their multimillion-dollar price tags necessitate rigorous economic evaluation [108] [109]. This technical analysis examines the cost-benefit profile and healthcare system impact of these transformative therapies within the broader context of CRISPR-mediated β-globin mutation correction, providing researchers and drug development professionals with frameworks for assessing value and accessibility.
Economic Evaluation of CRISPR SCD Therapies
Current Pricing and Cost-Effectiveness Landscape
The landmark approval of CRISPR-based therapies for SCD has established new benchmarks for therapeutic pricing, with Casgevy priced at $2.2 million and Lyfgenia at $3.1 million per treatment [109]. Economic evaluations utilize sophisticated modeling approaches to determine whether these prices align with the value delivered, considering both health system and societal perspectives.
Table 1: Cost-Effectiveness Analysis of SCD Gene Therapies
| Analysis Parameter | Casgevy (exa-cel) | Lyfgenia (lovo-cel) | Standard of Care |
|---|---|---|---|
| Acquisition Cost | $2.2 million [109] | $3.1 million [109] | N/A |
| Health Care Sector ICER | $193,000/QALY (UW-MEASURE) [109] | Similar range as exa-cel [108] | Reference |
| Societal Perspective ICER | $126,000/QALY (UW-MEASURE) [109] | Similar range as exa-cel [108] | Reference |
| Value-Based Price Range | $2.2M - $3.1M (ICER) [109] | $2.2M - $3.1M (ICER) [109] | N/A |
| Undiscounted Life-Years Gained | 17.4 years [109] | 17.4 years [109] | Reference |
The Institute for Clinical and Economic Review (ICER) determined that both Casgevy and Lyfgenia would be cost-effective within conventional thresholds if priced between $1.35 million and $2.05 million [109]. Current prices therefore exceed these ranges, though advanced modeling frameworks that account for disease severity and societal benefits provide more favorable assessments.
Budget Impact on Healthcare Systems
The budget impact of SCD gene therapies extends beyond individual patient treatment costs to substantial system-wide financial implications. A Belgian budget impact analysis projected a five-year cumulative impact of €30,024,968, with 91% attributed to drug acquisition costs, of which CTX001 (Casgevy) accounted for €25,575,150 [110]. Similarly, a US Medicaid analysis estimated a mean one-year budget impact of $29.96 million per state Medicaid program, equating to a $1.91 per member per month increase in spending [107].
Table 2: Budget Impact Analysis Across Healthcare Systems
| Healthcare System | Time Horizon | Total Budget Impact | Key Cost Drivers |
|---|---|---|---|
| Belgian Healthcare | 5 years | €30,024,968 [110] | Drug acquisition (91% of total) [110] |
| US Medicaid (10 states) | 1 year | $29.96 million per state [107] | Treatment price, eligible population size [107] |
| Alternative Financing Model | 5 years | 63% reduction vs. base case [110] | Managed entry agreements, outcome-based contracts [110] |
The disproportionate SCD prevalence in Medicaid populations (approximately 55,000 enrolled nationally) creates particular affordability challenges for public payers [107]. Sensitivity analyses indicate that patient population size, number of treated patients, and drug costs most significantly influence budget impact, while discontinuation, acute crisis, and adverse event rates have comparatively minimal impact [110].
Global Accessibility and Value-Based Pricing Considerations
The economic viability of CRISPR SCD therapies varies dramatically across healthcare systems, particularly affecting low- and middle-income countries (LMICs) where SCD prevalence is highest. A multi-country modeling analysis demonstrated that value-based prices (VBP) ranged from $3.6 million in the United States to just $700 in Uganda, reflecting vast differences in healthcare funding and cost-effectiveness thresholds [111].
The Generalized Risk-Adjusted Cost-Effectiveness (GRACE) model offers a more nuanced approach to valuation by accounting for disease severity, risk aversion, and differential valuation of quality-adjusted life years (QALYs) for severely ill populations [108]. Implementing GRACE for SCD therapies reduces incremental cost-effectiveness ratios (ICERs) by approximately 6% and increases willingness-to-pay thresholds by about 50% compared to traditional cost-effectiveness analysis [108].
Experimental and Methodological Framework
CRISPR Therapeutic Mechanisms for SCD
CRISPR-based approaches for SCD correction employ distinct mechanistic strategies targeting the fundamental pathophysiology of hemoglobin dysfunction:
BCL11A Gene Knockout (Casgevy Approach): This method utilizes CRISPR-Cas9 to disrupt an erythroid-specific enhancer of BCL11A, a transcriptional repressor of fetal hemoglobin (HbF) [27] [26]. Knockout of BCL11A promotes persistent expression of HbF (α₂γ₂), which does not polymerize like HbS and effectively compensates for the defective adult hemoglobin [26]. Induction of ≥30% HbF is sufficient to prevent HbS polymerization and ameliorate disease symptoms [27].
Gene Addition/Correction Strategies: Alternative approaches include lentiviral vector-mediated addition of functional β-globin genes (Lyfgenia) or precise CRISPR-mediated correction of the causative β-globin mutation via homology-directed repair (HDR) [27]. The gene correction strategy introduces a donor template with the normal HBB sequence to precisely correct the E6V mutation through HDR, restoring production of normal adult hemoglobin [26].
Diagram 1: CRISPR therapeutic mechanisms for sickle cell disease
Experimental Workflow for CRISPR SCD Therapy
The development and implementation of CRISPR-based SCD therapies follows a standardized experimental and clinical workflow with distinct stages from target identification to patient monitoring:
Diagram 2: Experimental workflow for ex vivo CRISPR SCD therapy
Research Reagent Solutions for SCD Gene Editing
Table 3: Essential Research Reagents for CRISPR SCD Investigations
| Reagent/Category | Function | Application Example |
|---|---|---|
| CRISPR-Cas9 System | RNA-guided DNA endonuclease for precise gene editing | BCL11A enhancer disruption or HBB gene correction [26] |
| Lentiviral Vectors | Delivery of CRISPR components or therapeutic transgenes | Expression of therapeutic β-globin (HbAT87Q) in Lyfgenia [27] |
| Lipid Nanoparticles (LNPs) | Non-viral delivery vehicle for CRISPR components | In vivo delivery of editing machinery; enables redosing [6] |
| Hematopoietic Stem Cells (CD34+) | Target cells for genetic modification | Autologous transplantation after ex vivo editing [32] |
| Homology-Directed Repair (HDR) Donor Template | DNA template for precise gene correction | Repair of E6V mutation in HBB gene [26] |
| Base Editors/Prime Editors | Precision genome editing without double-strand breaks | Conversion of sickle allele to non-pathogenic Makassar variant [26] |
Healthcare System Implementation Challenges
Manufacturing and Infrastructure Barriers
The complex ex vivo manufacturing process for current CRISPR SCD therapies presents significant scalability challenges. The procedure requires specialized facilities for hematopoietic stem cell (HSC) collection, CD34+ cell isolation, CRISPR editing, and quality control testing before reinfusion [32]. This resource-intensive process creates bottlenecks in patient throughput and limits widespread accessibility, particularly in resource-constrained settings. The requirement for myeloablative conditioning with busulfan further complicates treatment administration due to associated toxicities including infections, mucosal damage, and risk of infertility [32].
Emerging in vivo gene editing approaches, utilizing lipid nanoparticle (LNP) delivery systems, promise to circumvent many ex vivo manufacturing challenges by enabling direct administration of CRISPR components to patients [6]. Early-phase trials have demonstrated the feasibility of LNP-mediated in vivo editing, with potential for redosing and simplified treatment protocols [6].
Alternative Payment Models and Financing Solutions
The substantial upfront costs of SCD gene therapies have stimulated development of innovative payment models designed to align financial risk with therapeutic outcomes:
Annuity Payments: Spreading therapy costs over multiple years (e.g., 5 years) to reduce short-term budget impact [107]. This model decreases immediate financial burden on payers while ensuring continued payment for durable therapies.
Outcome-Based Risk Sharing Agreements: Linking payment to achievement of predefined clinical endpoints (e.g., sustained VOC reduction, hemoglobin stabilization) [110]. These arrangements protect payers from paying for treatments that prove ineffective in real-world settings.
Population-Based Financing Models: Establishing dedicated funding streams for high-cost therapies through mechanisms such as state-based reinsurance programs or federal cost-sharing initiatives [107].
CRISPR-based gene therapies for sickle cell disease represent a remarkable scientific achievement with complex economic implications. While these interventions offer potential lifelong benefits including complete remission of debilitating symptoms, their current cost structure presents substantial challenges for healthcare systems, particularly public payers serving disproportionately affected populations. Comprehensive economic evaluations demonstrate that value-based pricing must account for both conventional cost-effectiveness metrics and additional factors such as disease severity, caregiver impact, and societal benefits. Future directions should focus on simplifying manufacturing processes through in vivo delivery approaches, developing sustainable financing models, and implementing equitable access strategies to ensure these transformative therapies reach global populations most affected by sickle cell disease.
The approval of Casgevy (exagamglogene autotemcel) in December 2023 marked a historic milestone as the first FDA-approved CRISPR/Cas9-based therapy for sickle cell disease (SCD), establishing a foundational regulatory pathway for genetically modified biologics [44] [112]. This approval demonstrated the FDA's capacity to evaluate innovative gene editing products and created a precedent for future CRISPR-based therapeutics targeting monogenic diseases. The regulatory landscape for these advanced therapy medicinal products (ATMPs) is characterized by evolving guidance documents and specialized review offices designed to address their unique scientific and technical considerations [113].
The Center for Biologics Evaluation and Research (CBER) oversees the regulation of CRISPR-based therapies through the Office of Therapeutic Products (OTP), a "super office" established to enhance review capabilities for complex biologics [113]. This office includes six specialized sub-offices focusing on gene therapy chemistry, manufacturing, and controls (CMC); cellular therapy; clinical evaluation; pharmacology/toxicology; and review management. To manage the increasing number of cell and gene therapy applications, the FDA has recruited additional staff with specialized expertise, with the OTP reaching approximately 75-80% of its staffing goals by early 2024 [113].
FDA Approval Pathways and Designations
Primary Regulatory Pathways
CRISPR-based products for sickle cell disease can access several regulatory pathways designed to accelerate development and review of promising therapies:
Table 1: FDA Expedited Programs for CRISPR Therapies
| Program | Purpose | Eligibility Criteria | Benefits |
|---|---|---|---|
| Fast Track | Facilitates development and expedites review | Therapies for serious conditions with unmet medical need | Early and frequent communication with FDA, rolling review of BLA |
| Breakthrough Therapy | Expedites development and review | Preliminary clinical evidence demonstrates substantial improvement over available therapies | Intensive FDA guidance, organizational commitment |
| Regenerative Medicine Advanced Therapy (RMAT) | Accelerates approval of regenerative medicine products | Cell/gene therapies for serious conditions with preliminary clinical evidence | Early interactions on surrogate endpoints, potential accelerated approval |
| Priority Review | Shortens FDA review timeline | Therapies that would provide significant improvement in safety/efficacy | Review timeline reduced from 10 to 6 months |
Casgevy utilized multiple expedited programs, receiving Priority Review, Orphan Drug, Fast Track, and RMAT designations, which collectively streamlined its development and regulatory assessment process [44] [112]. The RMAT designation, specifically created for regenerative medicine products, proved particularly valuable by enabling ongoing dialogue regarding the use of sustained freedom from vaso-occlusive crises (VOCs) as evidence of effectiveness [112].
Clinical Trial Design and Submission Requirements
The FDA has published specific guidance for cell and gene therapy sponsors regarding clinical trial design and submission requirements:
- Umbrella Trial Designs: The FDA's 2022 guidance "Studying Multiple Versions of a Cellular or Gene Therapy Product in an Early-Phase Clinical Trial" enables sponsors to evaluate different versions of a CRISPR therapy under a single master protocol [113]. This approach employs a Primary IND containing the master protocol and information for one product version, with secondary INDs for other versions that cross-reference the primary submission.
- IND Structure: Investigational New Drug applications for CRISPR products must include comprehensive information on chemistry, manufacturing, and controls (CMC); pharmacology and toxicology; and clinical trial protocols [113]. For genome editing products, the FDA's final guidance "Human Gene Therapy Products Incorporating Human Genome Editing" provides specific recommendations on the information required in IND filings.
- Product Comparability: The FDA recognizes that changes in manufacturing processes may occur during development. The guidance clarifies that certain changes (e.g., transitioning from adherent to suspension cell culture) do not constitute different product versions requiring separate INDs, while modifications to critical components (e.g., viral capsid proteins for delivery) do represent distinct versions [113].
Chemistry, Manufacturing, and Controls (CMC) Considerations
CRISPR-based therapies present unique CMC challenges that require careful attention throughout development and regulatory review:
Critical Quality Attributes
Table 2: CMC Considerations for CRISPR Sickle Cell Therapies
| Component | Key Considerations | Testing Methods |
|---|---|---|
| CRISPR Editing System | Purity, potency, identity, specificity | NGS, Sanger sequencing, in vitro cleavage assays |
| Stem Cell Source | Viability, purity, differentiation potential | Flow cytometry, colony-forming unit assays |
| Delivery Method | Efficiency, safety, scalability | Vector titer, transduction efficiency, copy number assays |
| Final Product | Viability, editing efficiency, sterility, purity | Flow cytometry, NGS, mycoplasma testing, endotoxin testing |
For ex vivo therapies like Casgevy, the manufacturing process involves mobilization and apheresis to collect autologous CD34+ hematopoietic stem and progenitor cells, followed by electroporation to deliver the CRISPR-Cas9 ribonucleoprotein complex, and finally reinfusion after myeloablative conditioning [26] [112]. The editing process specifically targets the BCL11A gene's erythroid-specific enhancer region to disrupt its expression and reactivate fetal hemoglobin production [26].
Analytical Development and Potency Assays
Developing validated potency assays represents a particular challenge for CRISPR therapies. For Casgevy, critical quality attributes include:
- On-target editing efficiency (reported as 80.5±9.8% in healthy donors and 85.8±14.7% in SCD patients) [84]
- Fetal hemoglobin induction capacity (resulting in 19.0-26.8% of total hemoglobin post-treatment) [84]
- Cell viability and proliferation potential following editing
- Absence of residual CRISPR components in the final product
Preclinical and Clinical Development Requirements
Preclinical Proof of Concept
Preclinical studies for CRISPR-based SCD therapies must demonstrate:
- Proof of concept in relevant animal models (e.g., transgenic SCD mice)
- Editing efficiency in target cell populations
- Durability of effect through long-term engraftment studies
- Safety profile including assessment of off-target editing
The Casgevy development program utilized humanized mouse models to demonstrate that edited CD34+ cells could engraft and produce erythrocytes with increased fetal hemoglobin levels before progressing to clinical trials [18].
Clinical Trial Endpoints
Clinical trials for CRISPR SCD therapies typically employ multiple endpoints to demonstrate safety and efficacy:
Table 3: Primary Efficacy Endpoints in CRISPR SCD Trials
| Endpoint Category | Specific Metrics | Casgevy Results | Traditional Gene Therapy Results |
|---|---|---|---|
| Hemoglobin Response | F-cell percentage, HbF levels, total hemoglobin | 69.7-87.8% F-cells, 19.0-26.8% HbF [84] | HbAT87Q ≥40% of total hemoglobin [84] |
| Clinical Outcomes | Freedom from vaso-occlusive crises (VOCs), hospitalization reduction | 93.5% free of severe VOCs for ≥12 months [44] [112] | 88% with complete VOC resolution [84] |
| Patient-Reported Outcomes | Quality of life measures, pain scores | Improved functional assessments [6] | Stability or improvement in symptoms [6] |
For Casgevy, the primary efficacy outcome in the Phase III trial was freedom from severe vaso-occlusive crises for at least 12 consecutive months during the 24-month follow-up period. Of the 31 evaluable patients, 29 (93.5%) achieved this endpoint, with all achieving successful engraftment and no cases of graft failure or rejection [44].
Post-Market Surveillance Requirements
Regulatory Framework for Post-Approval Monitoring
The FDA has established comprehensive post-market surveillance requirements for cell and gene therapy products, detailed in the September 2025 draft guidance "Postapproval Methods to Capture Safety and Efficacy Data for Cell and Gene Therapy Products" [114]. This guidance emphasizes that given the potential for long-lasting effects of CGT products and the limited number of participants in pre-approval clinical trials, post-approval monitoring is crucial for gathering additional safety and effectiveness data over time.
The FDA requires patients treated with CRISPR gene therapies to be monitored for up to 15 years to assess potential late-onset adverse events [112]. For Casgevy, this translated into two specific post-marketing requirement (PMR) safety studies focusing on:
- Assessment of hematologic malignancies
- Monitoring for unintended off-target genome edits [112]
These requirements align with the FDA's industry-wide guidance on long-term follow-up after administration of human gene therapies and reflect concerns about theoretical risks associated with genome editing.
Safety Monitoring and Risk Management
The post-market surveillance framework for CRISPR therapies includes:
The diagram above illustrates the comprehensive approach to post-market surveillance for CRISPR therapies, encompassing clinical monitoring, regulatory requirements, and manufacturing surveillance.
Special Considerations for CRISPR-Based Products
Genome Editing-Specific Regulations
The FDA has established specific guidelines for products incorporating human genome editing, including:
- Off-Target Analysis: Comprehensive assessment of potential off-target editing events using computational prediction followed by experimental validation [113]
- On-Target Editing Efficiency: Demonstration of consistent and precise editing at the intended genomic locus
- Long-Term Stability: Evidence that the edited cells maintain their genetic modifications and function over time
- Product Characterization: Detailed analysis of editing outcomes, including distribution of insertions/deletions (indels) and presence of unintended genetic rearrangements
Emerging Regulatory Science
As CRISPR technology evolves, the FDA is developing new regulatory approaches to address:
- Novel Editing Platforms: Base editors, prime editors, and epigenome editors that don't create double-strand breaks require adapted safety assessment frameworks [26]
- Delivery System Advancements: Lipid nanoparticles (LNPs) and novel viral vectors present distinct characterization challenges compared to established delivery methods [6]
- In Vivo vs. Ex Vivo Applications: The regulatory requirements for in vivo genome editing (e.g., direct administration of editing components) differ significantly from ex vivo approaches [6]
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Tools for CRISPR SCD Therapy Development
| Research Tool | Function | Application in SCD Therapy |
|---|---|---|
| CRISPR-Cas9 RNPs | Precise genome editing | BCL11A enhancer disruption for HbF reactivation |
| Lentiviral Vectors | Gene delivery | Traditional gene addition approaches (e.g., HbAT87Q) |
| Lipid Nanoparticles (LNPs) | In vivo delivery | Liver-targeted editing for alternative approaches |
| CD34+ Cell Isolation Kits | Stem cell purification | Patient stem cell collection for ex vivo editing |
| Flow Cytometry Panels | Cell characterization | Assessment of editing efficiency and differentiation |
| Next-Generation Sequencing | Off-target analysis | Comprehensive safety profiling |
| Colony-Forming Unit Assays | Stem cell potency | Functional assessment of edited hematopoietic cells |
| GMP-Grade Culture Media | Cell expansion | Manufacturing scale-up under regulatory compliance |
The FDA has established a comprehensive regulatory framework for CRISPR-based therapies for sickle cell disease, balancing accelerated access for patients with serious conditions against the need for robust evidence of safety and efficacy. The approval of Casgevy demonstrates that the existing pathways can accommodate the unique challenges of genome editing products when supported by compelling clinical data. As the field advances, regulatory science continues to evolve to address emerging technologies such as base editing, prime editing, and novel delivery systems. The successful navigation of this landscape requires early and ongoing engagement with regulatory agencies, careful attention to CMC considerations, and commitment to long-term safety monitoring.
Conclusion
CRISPR-based correction of the beta-globin mutation represents a paradigm shift in sickle cell disease treatment, moving from symptomatic management to potentially curative genetic therapy. The approval of Casgevy validates the clinical feasibility of this approach, demonstrating durable production of fetal hemoglobin and significant reduction in vaso-occlusive crises. However, challenges remain in optimizing delivery efficiency, ensuring long-term safety, and improving accessibility of these complex therapies. Future directions should focus on developing next-generation editors with enhanced precision, establishing simplified in vivo delivery platforms to avoid myeloablative conditioning, and creating sustainable manufacturing processes to broaden global access. As the field advances, continued interdisciplinary collaboration between basic researchers, clinicians, and regulatory bodies will be essential to fully realize the therapeutic potential of CRISPR technology for sickle cell disease and other monogenic disorders.
References
- 1. HBB gene: MedlinePlus Genetics [https://medlineplus.gov/genetics/gene/hbb/]
- 2. Sickle Cell Disease—Genetics, Pathophysiology, Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7510211/]
- 3. Development of β-globin gene correction in human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8862191/]
- 4. Safety and efficacy studies of CRISPR-Cas9 treatment ... [https://pubmed.ncbi.nlm.nih.gov/39044427/]
- 5. Comprehensive regulation of γ-globin expression by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12535125/]
- 6. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 7. Correction of β-thalassemia by CRISPR/Cas9 editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7948300/]
- 8. Quarterly Industry Landscape Report | ASGCT [https://www.asgct.org/news-publications/landscape-report]
- 9. The vaso-occlusive pain crisis in sickle cell patients [https://www.sciencedirect.com/science/article/abs/pii/S2452318625000212]
- 10. Sickle Cell Disease: Role of Oxidative Stress and Antioxidant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919654/]
- 11. Vaso-occlusive crisis in sickle cell disease: a vicious cycle ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-021-03074-z]
- 12. Vaso-occlusion in sickle cell disease: pathophysiology and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3854110/]
- 13. High flow oxygen for vaso-occlusive crisis - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12458843/]
- 14. Advances in β-Thalassemia Gene Therapy: CRISPR/Cas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562837/]
- 15. Oxidative stress in sickle cell disease: An overview of ... [https://www.sciencedirect.com/science/article/abs/pii/S0891584913005844]
- 16. CRISPR/Cas9 Beta-globin Gene Targeting in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5898607/]
- 17. Gene Therapy Leads to Improved Quality of Life in Patients ... [https://www.hematology.org/newsroom/press-releases/2025/gene-therapy-leads-to-improved-quality-of-life]
- 18. Genome editing strategies for targeted correction of β- ... [https://www.sciencedirect.com/science/article/pii/S1525001625002217]
- 19. Barriers to hydroxyurea use from the perspectives of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9461276/]
- 20. Hydroxyurea Effective Long Term in Children Living With ... [https://www.hematology.org/newsroom/press-releases/2025/hydroxyurea-effective-long-term-in-children-living-with-scd]
- 21. Sickle cell disease: when and how to transfuse - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6142434/]
- 22. Global burden of transfusion in sickle cell disease [https://www.sciencedirect.com/science/article/pii/S1473050223001489]
- 23. Hematopoietic Stem Cell Transplantation in Sickle Cell Disease [https://www.ncbi.nlm.nih.gov/books/NBK538515/]
- 24. Undergoing Stem Cell Transplant for Sickle Cell Disease in ... [https://www.hematology.org/newsroom/press-releases/2024/undergoing-stem-cell-transplant-for-sickle-cell-disease-in-childhood]
- 25. Decision analysis of treatment strategies in children ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/19829150/]
- 26. Sickle Cell Gene Therapy Using CRISPR [https://www.synthego.com/crispr-sickle-cell-disease/]
- 27. Recent advancements in gene therapy for sickle cell ... [https://www.frontiersin.org/journals/hematology/articles/10.3389/frhem.2024.1468952/full]
- 28. CRISPR/Cas9 for the treatment of haematological diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC8118330/]
- 29. Dana-Farber Treats First Patient with Approved Gene ... [https://blog.dana-farber.org/insight/2025/09/dana-farber-treats-first-patient-with-approved-gene-therapy-for-beta-thalassemia/]
- 30. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-provides-business-update-and-reports-13]
- 31. crispr [https://en.wikipedia.org/wiki/CRISPR]
- 32. Hematopoietic stem cell therapy with gene modification to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12445678/]
- 33. How To Use ICE: A Detailed Guide for Analyzing CRISPR ... [https://www.synthego.com/guide/how-to-use-crispr/ice-analysis-guide/]
- 34. In Vivo Outcome of Homology-Directed Repair at the HBB ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6611979/]
- 35. Editing the Sickle Cell Disease Mutation in Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6697408/]
- 36. A differentiated β-globin gene replacement strategy uses ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11997512/]
- 37. Cas9-AAV6 gene correction of beta-globin in autologous ... [https://www.nature.com/articles/s41467-021-20909-x]
- 38. Efficient CRISPR-Cas9-based genome editing of β-globin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8091488/]
- 39. cutting-edge applications of base editing and prime editing in ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05957-3]
- 40. Disrupting ZBTB7A or BCL11A binding sites reactivates ... [https://www.nature.com/articles/s41598-025-10791-8]
- 41. Fetal Hemoglobin Induction by Epigenetic Drugs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6029722/]
- 42. BCL11A: a potential diagnostic biomarker and therapeutic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6851505/]
- 43. Multimeric transcription factor BCL11A utilizes two zinc ... [https://www.nature.com/articles/s41467-025-58998-7]
- 44. FDA Approves First Gene Therapies to Treat Patients with ... [https://www.fda.gov/news-events/press-announcements/fda-approves-first-gene-therapies-treat-patients-sickle-cell-disease]
- 45. Current and future treatments for sickle cell disease [https://www.sciencedirect.com/science/article/pii/S152500162500190X]
- 46. Therapeutically relevant engraftment of a CRISPR/Cas9- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8407476/]
- 47. CRISPR Therapeutics Highlights Strategic Priorities and ... [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-highlights-strategic-priorities-and]
- 48. Persistence of CRISPR/Cas9 gene edited hematopoietic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8235122/]
- 49. Emerging trends in prime editing for precision genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322275/]
- 50. Base editing shows potential superiority for curing sickle ... [https://www.stjude.org/media-resources/news-releases/2023-medicine-science-news/base-editing-shows-potential-superiority-for-curing-sickle-cell-disease.html]
- 51. Ex vivo prime editing of patient haematopoietic stem cells ... [https://www.nature.com/articles/s41551-023-01026-0]
- 52. Prime Editing as a Precision Gene Editing Tool [https://www.synthego.com/guide/crispr-methods/prime-editing/]
- 53. Viral Vectors for the in Vivo Delivery of CRISPR Components [https://pmc.ncbi.nlm.nih.gov/articles/PMC9133430/]
- 54. Genome editing strategies for targeted correction of β-globin ... [https://pubmed.ncbi.nlm.nih.gov/?linkname=pubmed_pubmed_citedin&from_uid=40165374]
- 55. Delivery Strategies of the CRISPR-Cas9 Gene-Editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5723556/]
- 56. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 57. Viral Vectors for the in Vivo Delivery of CRISPR Components [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2022.895713/full]
- 58. Lipid nanoparticles: The game-changer in CRISPR-Cas9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10823087/]
- 59. AI-powered CRISPR could lead to faster gene therapies ... [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]
- 60. Emerging Gene Therapies in Sickle Cell Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599223/]
- 61. CASGEVY® Clinical Trial and Results [https://www.casgevy.com/sickle-cell-disease/study-information]
- 62. Gene therapy for sickle cell and β-thalassemia works by ... [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/gene-therapy-for-sickle-cell-and-beta-thalassemia-works-by-disrupting-three-dimensional-genome-structure.html]
- 63. CRISPR Cell and Gene Therapies: Key Challenges in ... [https://www.synthego.com/blog/crispr-cell-gene-therapy-obstacles/]
- 64. Vertex Presents Longer-Term Data at the 2025 European ... [https://investors.vrtx.com/news-releases/news-release-details/vertex-presents-longer-term-data-2025-european-hematology]
- 65. CRISPR/Cas9 Genome Editing for Tissue‐Specific In ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10323670/]
- 66. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 67. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://www.mdpi.com/1422-0067/26/9/4420]
- 68. Systemic nanoparticle delivery of CRISPR-Cas9 ... [https://www.nature.com/articles/s41467-020-17029-3]
- 69. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 70. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 71. CRISPR/Cas9 gene editing for curing sickle cell disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC8049447/]
- 72. Quantitative analysis of CRISPR/Cas9-mediated provirus ... [https://www.nature.com/articles/s41598-022-19861-7]
- 73. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 74. Optimizing CRISPR methodology for precise gene editing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12580712/]
- 75. Current Strategies for Increasing Knock-In Efficiency in ... [https://www.mdpi.com/1422-0067/25/5/2456]
- 76. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 77. Optimizing CRISPR methodology for precise gene editing ... [https://haematologica.org/article/view/12023]
- 78. CRISPR-Cas9 HDR optimization: RAD52, denatured, and 5 [https://pmc.ncbi.nlm.nih.gov/articles/PMC12616026/]
- 79. Genotoxic effects of base and prime editing in human ... [https://www.nature.com/articles/s41587-023-01915-4]
- 80. Recent advances in therapeutic gene-editing technologies [https://www.sciencedirect.com/science/article/pii/S152500162500200X]
- 81. Genotoxic Effects of Base and Prime Editing | The Scientist [https://www.the-scientist.com/genotoxic-effects-of-base-and-prime-editing-71587]
- 82. DNA repair pathway choices in CRISPR-Cas9 mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8187289/]
- 83. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 84. CRISPR vs Gene Therapy for Sickle Cell: Which Treatment ... [https://globalrph.com/2025/10/crispr-vs-gene-therapy-for-sickle-cell-which-treatment-works-better/]
- 85. Emerging Therapies for Sickle Cell Disease - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635507/]
- 86. Excellent outcome of stem cell transplantation for sickle ... [https://link.springer.com/article/10.1007/s00277-023-05447-4]
- 87. Severe inflammation and lineage skewing are associated ... [https://www.nature.com/articles/s41467-025-58321-4]
- 88. CASGEVY® Study and Results [https://www.casgevy.com/beta-thalassemia/study-information]
- 89. Vertex Presents Positive Long-Term Data On CASGEVY ... [https://news.vrtx.com/news-releases/news-release-details/vertex-presents-positive-long-term-data-casgevytm-0]
- 90. Vertex reports long-term results for Casgevy in sickle cell ... [https://www.clinicaltrialsarena.com/news/vertex-reports-long-term-results-for-casgevy-in-sickle-cell-and-thalassaemia/]
- 91. Efficacy of CASGEVY® (exagamglogene autotemcel) in Trial 1 ... [https://www.casgevyhcp.com/sickle-cell-disease/efficacy]
- 92. Safety profile in patients with SCD [https://www.casgevyhcp.com/sickle-cell-disease/safety]
- 93. Breaking: Base Editing Rescues Severe β-Thalassaemia ... [https://crisprmedicinenews.com/news/breaking-base-editing-rescues-severe-b-thalassaemia-mutations/]
- 94. Combination of lentiviral and genome editing technologies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8753569/]
- 95. 2 Comparative Analysis of CRISPR-Cas9, Lentiviral ... [https://www.sciencedirect.com/science/article/abs/pii/S2666636725000089]
- 96. CRISPR-Cas9-AAV versus lentivector transduction for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9846165/]
- 97. Viral or Nonviral: Which Is Better for CRISPR-Based ... [https://www.genengnews.com/topics/genome-editing/viral-or-nonviral-which-is-better-for-crispr-based-therapies/]
- 98. The Current Role of Hydroxyurea in the Treatment of Sickle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11546997/]
- 99. The Indian experience with hydroxyurea in sickle cell disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550388/]
- 100. CRISPR-Cas9基因编辑在镰状细胞病和β-地中海贫血中的 ... [https://www.ebiotrade.com/newsf/2025-9/20250920082948799.htm]
- 101. The hidden risks of CRISPR/Cas: structural variations and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325979/]
- 102. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 103. Peeling back the layers of immunogenicity in Cas9-based ... [https://www.sciencedirect.com/science/article/pii/S1525001625005350]
- 104. CRISPR 临床试验:2025 年更新- 创新基因组学研究所(IGI) [https://innovativegenomics.org/zh-CN/%E6%96%B0%E9%97%BB/Crispr-%E4%B8%B4%E5%BA%8A%E8%AF%95%E9%AA%8C-2025/]
- 105. 新论文指出了通过避免染色体丢失使CRISPR 更安全的方法 [https://innovativegenomics.org/zh-CN/%E6%96%B0%E9%97%BB/Crispr-%E6%9B%B4%E5%AE%89%E5%85%A8%E7%9A%84%E6%9F%93%E8%89%B2%E4%BD%93%E4%B8%A2%E5%A4%B1/]
- 106. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 107. A Budget Impact Analysis of Gene Therapy for Sickle Cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7985816/]
- 108. Implementing the Generalized Risk-Adjusted Cost ... [https://www.sciencedirect.com/science/article/pii/S1098301525023642]
- 109. Analysis Explores Gene Therapy's Potential to Be Cost- ... [https://www.ajmc.com/view/analysis-explores-gene-therapy-s-potential-to-be-cost-effective-in-scd]
- 110. Budget Impact of Disease-Modifying Treatments and a ... [https://pubmed.ncbi.nlm.nih.gov/39134876/]
- 111. The value-based price of transformative gene therapy for ... [https://www.nature.com/articles/s41598-024-53121-0]
- 112. FDA Approves exa-cel, the First CRISPR Gene Therapy ... [https://www.delveinsight.com/blog/vertex-crispr-gene-editing-therapy-exa-cel]
- 113. Understanding FDA Cell and Gene Therapy Guidance [https://www.synthego.com/blog/fda-cell-and-gene-therapy-guidance/]
- 114. Postapproval Methods to Capture Safety and Efficacy Data [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/postapproval-methods-capture-safety-and-efficacy-data-cell-and-gene-therapy-products]