CRISPR-Cas9 in Genetic Disorder Therapy: From Molecular Tools to Clinical Breakthroughs
This article provides a comprehensive overview of the transformative role of CRISPR-Cas9 gene-editing technology in treating genetic disorders.
CRISPR-Cas9 in Genetic Disorder Therapy: From Molecular Tools to Clinical Breakthroughs
Abstract
This article provides a comprehensive overview of the transformative role of CRISPR-Cas9 gene-editing technology in treating genetic disorders. Tailored for researchers, scientists, and drug development professionals, it explores the foundational mechanisms of CRISPR-Cas systems, details methodological advances and specific therapeutic applications for monogenic diseases, analyzes critical challenges such as off-target effects and delivery, and evaluates clinical validation through recent trials and comparative efficacy. The synthesis of current evidence highlights the paradigm shift from symptom management to curative potential, while also addressing the ongoing hurdles and future directions necessary for the widespread clinical translation of these innovative therapies.
The CRISPR-Cas9 Revolution: Understanding the Core Technology and Its Therapeutic Potential
From Bacterial Immunity to a Genome Engineering Revolution
The journey of CRISPR-Cas systems from a curious genetic sequence in bacteria to a revolutionary genome-editing toolkit represents one of the most significant advancements in modern biotechnology. Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) were first identified in 1987 in Escherichia coli as a set of unusual repetitive DNA sequences downstream of the iap gene [1]. For years, these sequences remained a molecular mystery until bioinformatics analyses revealed they were present in approximately 40% of bacteria and 90% of archaea [2]. The critical breakthrough came when researchers recognized that the spacer sequences between CRISPR repeats matched viral and plasmid DNA, suggesting a role in adaptive immunity [2] [1].
The functional validation of this hypothesis came in 2007 when Barrangou and colleagues demonstrated that Streptococcus thermophilus could acquire new spacers from invading viruses and that these spacers conferred resistance to subsequent viral attacks [2] [1]. This discovery confirmed CRISPR-Cas as a bacterial adaptive immune system. The system functions in three main stages: (1) adaptation, where new spacers are acquired from invading DNA; (2) expression, where CRISPR RNA (crRNA) is transcribed and processed; and (3) interference, where Cas proteins use crRNAs to identify and cleave matching foreign DNA sequences [1].
The transformation of this bacterial defense mechanism into a programmable gene-editing tool began with key discoveries elucidating the molecular components. Researchers found that in the Type II CRISPR system, the Cas9 protein is the sole enzyme responsible for DNA cleavage [2]. Critical work by the Charpentier group revealed the mechanism of crRNA biogenesis, showing that a trans-activating CRISPR RNA (tracrRNA) was essential for mature crRNA formation [2]. The pivotal moment came in 2012 when Doudna and Charpentier engineered the dual RNA guide (crRNA:tracrRNA) into a single-guide RNA (sgRNA) and demonstrated that Cas9 could be programmed to cleave any DNA sequence complementary to the sgRNA [3]. This simplification created the versatile CRISPR-Cas9 system that has revolutionized genetic research and therapeutic development.
Molecular Mechanism of the CRISPR-Cas9 System
The CRISPR-Cas9 gene-editing system operates as a precise molecular scissor guided by RNA-DNA recognition. The system consists of two fundamental components: the Cas9 endonuclease and the guide RNA (gRNA) [3]. The gRNA is a synthetic fusion of two natural RNA molecules - the CRISPR RNA (crRNA) that specifies the target sequence, and the trans-activating crRNA (tracrRNA) that serves as a scaffold for Cas9 binding [4] [3].
The mechanism of action begins with gRNA-Cas9 complex formation. The gRNA directs Cas9 to the target DNA sequence through Watson-Crick base pairing between its 20-nucleotide guide sequence and the complementary DNA strand [3] [1]. Target recognition requires the presence of a short Protospacer Adjacent Motif (PAM) sequence immediately adjacent to the target region [5] [1]. For the most commonly used Cas9 from Streptococcus pyogenes, the PAM sequence is 5'-NGG-3' [5].
Once the gRNA binds its complementary sequence and Cas9 recognizes the PAM, the enzyme undergoes a conformational change that activates its nuclease domains [3]. The HNH domain cleaves the DNA strand complementary to the gRNA, while the RuvC domain cleaves the non-complementary strand, resulting in a precise double-strand break (DSB) 3-4 nucleotides upstream of the PAM sequence [4] [3].
Cellular repair of these programmed DSBs occurs primarily through two pathways [5] [4]:
- Non-Homologous End Joining (NHEJ): An error-prone repair pathway that often results in small insertions or deletions (indels) that can disrupt gene function, enabling gene knockout.
- Homology-Directed Repair (HDR): A precise repair pathway that uses a homologous DNA template to repair the break, allowing for specific gene corrections or insertions.
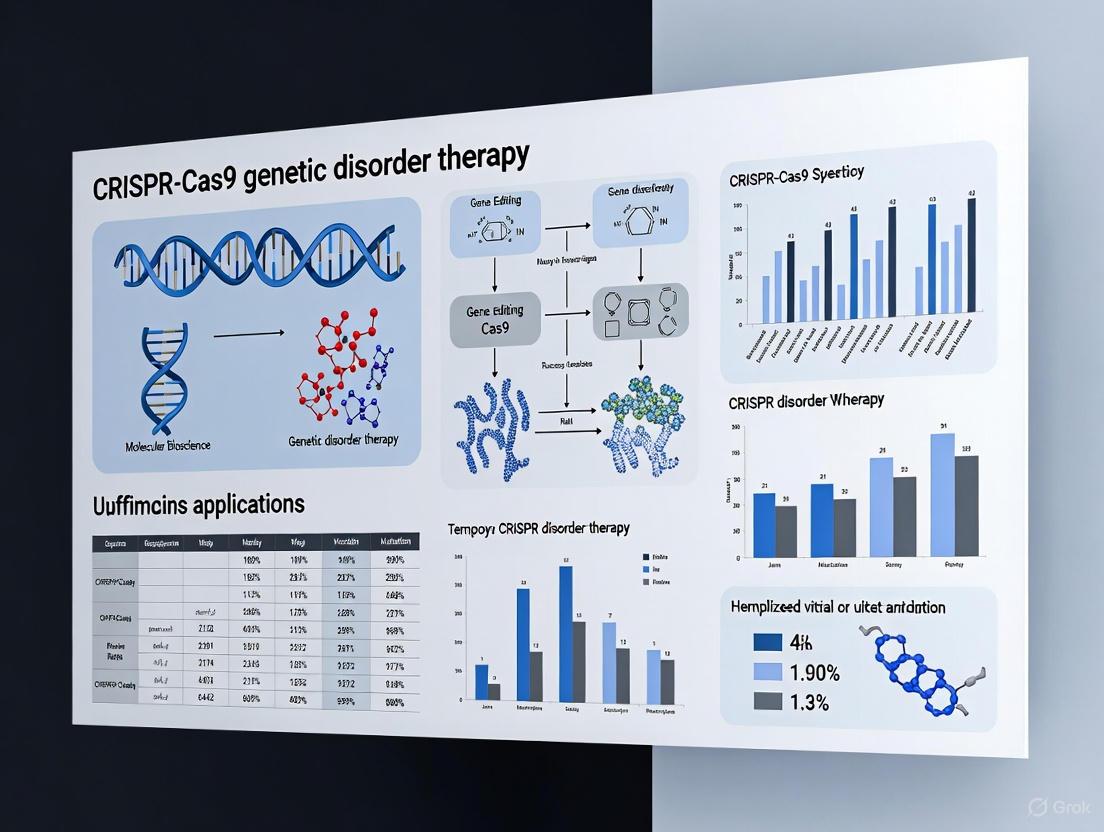
Figure 1: CRISPR-Cas9 Mechanism and DNA Repair Pathways. This workflow illustrates the sequential process from gRNA-Cas9 complex formation through target recognition, DNA cleavage, and cellular repair pathways.
Advanced CRISPR Toolkit: Beyond Basic Gene Editing
The fundamental CRISPR-Cas9 system has evolved into a diverse toolkit with capabilities extending far beyond simple gene disruption. These advanced derivatives have significantly expanded therapeutic applications:
Catalytically Impaired Cas9 Variants: The creation of dead Cas9 (dCas9), through point mutations in both nuclease domains, eliminates cleavage activity while retaining DNA-binding capability [6] [2]. dCas9 serves as a programmable DNA-targeting platform that can be fused to various effector domains for [6]:
- Gene regulation (CRISPRi/CRISPRa) when fused to transcriptional repressors or activators
- Epigenetic editing when fused to DNA methyltransferases or histone modifiers
- Chromatin imaging when fused to fluorescent proteins
Base Editing: Developed to overcome the limitations of HDR efficiency, base editors enable direct, irreversible conversion of one DNA base pair to another without requiring DSBs [5] [4]. These systems fuse dCas9 or Cas9 nickase to deaminase enzymes:
- Cytosine Base Editors (CBEs): Convert C•G to T•A base pairs
- Adenine Base Editors (ABEs): Convert A•T to G•C base pairs
Prime Editing: This more recent innovation uses a prime editing guide RNA (pegRNA) and a Cas9 nickase-reverse transcriptase fusion to directly write new genetic information into a target DNA site [4]. Prime editors can achieve all 12 possible base-to-base conversions, as well as small insertions and deletions, without requiring DSBs [4].
CRISPR-Based Diagnostics and Imaging: CRISPR systems have been adapted for diagnostic applications (e.g., SHERLOCK, DETECTR) and live-cell chromatin imaging using dCas9 fused to fluorescent proteins [6] [2].
Therapeutic Applications in Genetic Disorders
CRISPR-Cas9 technology has demonstrated remarkable potential for treating genetic disorders through diverse therapeutic approaches, with both ex vivo and in vivo applications showing promising results in clinical trials.
Table 1: Selected Clinical Trials of CRISPR-Cas9 Therapeutics for Genetic Disorders
| Disease | Target Gene | Intervention | Clinical Phase | Delivery Method | NCT Number |
|---|---|---|---|---|---|
| Sickle Cell Disease | BCL11A | CTX001 | Phase II/III | Electroporation (ex vivo) | NCT03745287 |
| Transfusion-Dependent Beta-Thalassemia | BCL11A | CTX001 | Phase II/III | Electroporation (ex vivo) | NCT03655678 |
| Leber Congenital Amaurosis | CEP290 | EDIT-101 | Phase I/II | AAV5 (in vivo) | NCT03872479 |
| Hereditary Transthyretin Amyloidosis | TTR | NTLA-2001 | Phase I | Lipid Nanoparticles (in vivo) | NCT04601051 |
| Hereditary Angioedema | KLKB1 | NTLA-2002 | Phase I/II | Lipid Nanoparticles (in vivo) | NCT05120830 |
Ex Vivo Therapeutic Approaches
Ex vivo genome editing involves modifying patient cells outside the body before transplanting them back into the patient. This approach has shown remarkable success for hematological disorders:
Sickle Cell Disease and Beta-Thalassemia: The therapies CTX001 target the BCL11A gene, a repressor of fetal hemoglobin [5]. By disrupting the BCL11A enhancer in autologous hematopoietic stem cells, these treatments reactivate fetal hemoglobin production, which compensates for the defective adult hemoglobin in sickle cell disease and beta-thalassemia [5] [7]. Clinical trials have reported successful transfusion independence in thalassemia patients and resolution of vaso-occlusive crises in sickle cell patients [5].
Cancer Immunotherapies: CRISPR-edited CAR-T cells have been developed for cancer treatment. Early-phase clinical trials have used CRISPR for multiple edits in T cells, including disrupting endogenous T-cell receptors and immune checkpoint genes to enhance antitumor activity [8].
In Vivo Therapeutic Approaches
In vivo delivery of CRISPR therapeutics involves directly administering the editing components to patients:
Hereditary Transthyretin Amyloidosis: NTLA-2001 uses lipid nanoparticles to deliver CRISPR components to the liver, targeting the TTR gene to reduce production of misfolded transthyretin protein [5]. Early clinical results demonstrated dose-dependent protein reduction up to 96% [5].
Leber Congenital Amaurosis: EDIT-101 uses an AAV5 vector to deliver CRISPR components to retinal cells, aiming to correct a mutation in the CEP290 gene that causes this inherited form of blindness [5].
Duchenne Muscular Dystrophy: Preclinical studies have successfully used CRISPR to restore dystrophin expression by excising mutation-containing exons in animal models [9].
Experimental Protocols for Genetic Disorder Research
Protocol: Ex Vivo Genome Editing of Hematopoietic Stem Cells for Hemoglobinopathies
This protocol outlines the methodology for editing hematopoietic stem cells (HSCs) to reactivate fetal hemoglobin for treating sickle cell disease and beta-thalassemia, based on successful clinical approaches [5] [7].
Materials and Reagents:
- Human CD34+ hematopoietic stem cells
- Cas9 protein or mRNA
- sgRNA targeting the BCL11A erythroid enhancer
- Electroporation buffer
- Stem cell culture media (StemSpan with cytokines)
- Homology-directed repair template (if using HDR)
Procedure:
- HSC Mobilization and Collection: Mobilize CD34+ cells from the patient using granulocyte colony-stimulating factor and collect via apheresis.
- Cell Preparation: Isulate CD34+ cells using immunomagnetic selection and culture overnight in StemSpan medium supplemented with cytokines (SCF, TPO, FLT3-L).
- Ribonucleoprotein Complex Formation: Incubate Cas9 protein with sgRNA targeting the BCL11A enhancer (molar ratio 1:2) for 10-20 minutes at room temperature.
- Electroporation: Wash cells and resuspend in electroporation buffer. Electroporate 1-2×10^6 cells/mL with RNP complex using appropriate settings (e.g., 1500V, 10ms pulse width).
- Recovery and Expansion: Immediately transfer electroporated cells to pre-warmed culture medium and incubate at 37°C, 5% CO2 for 48-72 hours.
- Quality Control: Assess editing efficiency by T7E1 assay or next-generation sequencing. Verify cell viability and phenotype.
- Transplantation: Infuse edited cells back into the patient after myeloablative conditioning.
Validation Methods:
- Measure indel frequency at the BCL11A enhancer
- Quantify fetal hemoglobin expression by FACS and HPLC
- Assess erythroid differentiation in vitro
- Verify absence of off-target edits at predicted sites
Protocol: In Vivo Genome Editing for Liver Disorders
This protocol describes the approach for in vivo genome editing using lipid nanoparticle delivery, as demonstrated in clinical trials for hereditary transthyretin amyloidosis [5] [4].
Materials and Reagents:
- LNP-formulated Cas9 mRNA
- LNP-formulated sgRNA targeting the TTR gene
- Saline for dilution
- Animal model of disease (e.g., transgenic mice expressing human TTR)
Procedure:
- LNP Formulation: Prepare LNPs containing Cas9 mRNA and sgRNA using microfluidic mixing technology with ionizable lipid, phospholipid, cholesterol, and PEG-lipid.
- Dose Preparation: Dilute LNP suspension in sterile saline to appropriate concentration for administration.
- Administration: Administer via intravenous injection at doses typically ranging from 0.1-1.0 mg/kg mRNA.
- Monitoring: Observe animals for potential adverse effects and monitor serum TTR levels over time.
- Tissue Collection: At endpoint, collect liver tissue and blood for analysis.
Validation Methods:
- Measure serum TTR reduction by ELISA
- Quantify editing efficiency in liver tissue by NGS
- Assess potential off-target effects by whole-genome sequencing
- Evaluate liver histology and function
Research Reagent Solutions for CRISPR Applications
Table 2: Essential Research Reagents for CRISPR-Cas9 Experiments
| Reagent Category | Specific Examples | Function & Applications |
|---|---|---|
| Nuclease Systems | Streptococcus pyogenes Cas9, Staphylococcus aureus Cas9, Campylobacter jejuni Cas9 | DNA cleavage with varying PAM requirements and molecular sizes |
| Guide RNA Systems | Synthetic sgRNA, crRNA:tracrRNA duplex, U6-driven expression vectors | Target sequence specification and Cas nuclease recruitment |
| Delivery Vehicles | AAV vectors (AAV2, AAV5, AAV9), Lentiviral vectors, Lipid Nanoparticles (LNPs), Electroporation systems | Intracellular delivery of CRISPR components |
| Editing Modalities | Wildtype Cas9, Cas9 nickase (D10A), dead Cas9 (dCas9), Base editors (CBE, ABE), Prime editors | Enable different types of genetic modifications (knockout, base conversion, precise editing) |
| Detection & Validation | T7 Endonuclease I assay, Tracking of Indels by Decomposition (TIDE), Next-generation sequencing, Western blot, Flow cytometry | Assessment of editing efficiency and functional outcomes |
Current Challenges and Future Perspectives
Despite the remarkable progress in CRISPR-based therapies, several challenges remain to be addressed for broader clinical application:
Delivery Efficiency: Efficient and specific in vivo delivery remains a significant hurdle. Current viral vectors (AAV) have packaging size constraints and can elicit immune responses, while non-viral methods (LNPs) need improved tissue targeting [5] [3]. Ongoing research focuses on developing novel delivery systems, including engineered AAV capsids and synthetic nanoparticles with enhanced tropism for specific tissues [4].
Off-Target Effects: Unintended editing at off-target sites with sequence similarity to the gRNA remains a safety concern [9] [10]. Strategies to mitigate this include:
- Using high-fidelity Cas9 variants with reduced off-target activity
- Careful gRNA design with computational prediction of potential off-target sites
- RNP delivery instead of plasmid DNA, which reduces exposure time
- Comprehensive off-target assessment using methods like CIRCLE-seq or GUIDE-seq
Immune Responses: Pre-existing immunity to bacterial Cas proteins in human populations and immune responses to delivery vectors may impact safety and efficacy [9] [3]. Approaches to address this include screening patients for pre-existing immunity, using Cas orthologs from less common bacteria, or employing transient delivery methods.
Ethical Considerations: The ability to perform germline editing raises significant ethical questions that require careful public discourse and regulatory frameworks [10] [7]. Most current clinical applications focus on somatic cell editing, which affects only the treated individual.
The future of CRISPR therapeutics lies in developing more precise, efficient, and safe systems. Next-generation editors with enhanced specificity, reduced immunogenicity, and broader targeting scope will expand therapeutic possibilities. As delivery technologies advance and long-term safety data accumulate, CRISPR-based therapies are poised to transform treatment for countless genetic disorders.
The CRISPR-Cas9 system, derived from an adaptive immune mechanism in bacteria, has revolutionized genome editing by providing researchers with a precise and programmable method for modifying DNA sequences [11] [12]. This technology centers on the ability of the Cas9 nuclease to create targeted double-stranded breaks (DSBs) in DNA when guided by a short RNA molecule [13]. For therapeutic research, this molecular complex offers unprecedented potential for correcting genetic mutations underlying hereditary disorders. The system's core components—the Cas9 enzyme and guide RNA (gRNA)—function together as a highly specific DNA-targeting complex that can be directed to virtually any genomic locus, making it particularly valuable for developing treatments for monogenic diseases such as sickle cell anemia and β-thalassemia [14] [12]. Understanding the precise mechanism by which these components achieve DNA cleavage is fundamental to advancing CRISPR-Cas9 applications in genetic therapy research.
Structural Components of the CRISPR-Cas9 System
The Cas9 Nuclease Architecture
The Cas9 protein possesses a bilobed architecture consisting of two primary lobes: the recognition (REC) lobe and the nuclease (NUC) lobe [11]. The REC lobe, comprised primarily of REC1, REC2, and REC3 domains, is responsible for binding the guide RNA and facilitating interactions with the target DNA [15]. The NUC lobe contains the catalytic core of the enzyme with two nuclease domains—HNH and RuvC—along with the PAM-interacting domain essential for initiating DNA binding [11] [16].
- HNH Domain: Cleaves the DNA strand complementary to the guide RNA (target strand) [11] [12]
- RuvC Domain: Cleaves the non-complementary DNA strand (non-target strand) [11] [12]
- PAM-Interacting Domain: Recognizes the protospacer adjacent motif (PAM), a short DNA sequence adjacent to the target site that serves as a binding signal [11] [13]
In eukaryotic cells, Cas9 requires nuclear localization signals (NLS) for transport into the nucleus where it can access genomic DNA [11]. Structural studies using cryo-electron microscopy have revealed that Cas9 undergoes significant conformational rearrangements upon binding to both guide RNA and target DNA, enabling its activation for DNA cleavage [15] [16].
Guide RNA: The Targeting Molecule
The guide RNA consists of two fundamental components that can be combined into a single-guide RNA (sgRNA) for experimental applications [11] [17]:
- crRNA (CRISPR RNA): A ~20 nucleotide sequence complementary to the target DNA that provides targeting specificity [11] [18]
- tracrRNA (trans-activating crRNA): A structural RNA that binds to Cas9 and facilitates complex formation [11]
The sgRNA forms a stable complex with Cas9, creating a ribonucleoprotein (RNP) complex capable of scanning the genome for complementary DNA sequences [13] [18]. The 5' end of the sgRNA contains the spacer sequence that determines DNA targeting through Watson-Crick base pairing, while the 3' end forms a scaffold that interacts with the Cas9 protein [17] [19].
Table 1: Key Components of the CRISPR-Cas9 System
| Component | Structure | Function |
|---|---|---|
| Cas9 Nuclease | Bilobed protein (REC and NUC lobes) | RNA-guided DNA endonuclease |
| HNH Domain | β-βα metal finger fold | Cleaves target DNA strand complementary to guide RNA |
| RuvC Domain | RNase H-like fold | Cleaves non-target DNA strand |
| PAM-Interacting Domain | Arg-rich motif | Recognizes NGG protospacer adjacent motif |
| crRNA | ~20 nt RNA sequence | Provides target specificity through DNA complementarity |
| tracrRNA | Structured RNA scaffold | Binds Cas9 and stabilizes crRNA |
Molecular Mechanism of Targeted DNA Cleavage
DNA Target Recognition and R-loop Formation
The process of targeted DNA cleavage begins with PAM recognition, where the Cas9-sgRNA complex scans the genome for the protospacer adjacent motif (typically 5'-NGG-3' for Streptococcus pyogenes Cas9) [11] [13]. The PAM sequence serves as an essential binding signal, and its recognition triggers local DNA melting, allowing the seed sequence (nucleotides 8-10 at the 3' end of the guide sequence) to initiate pairing with the target DNA [13] [15].
Following seed pairing, the R-loop expands as the sgRNA continues to hybridize with the target DNA in a 3' to 5' direction [13] [15]. Cryo-EM studies have revealed that this process occurs in distinct steps, with the REC2 and REC3 domains facilitating the accommodation of the emerging RNA-DNA heteroduplex [15]. The directional hybridization ensures that mismatches between the guide RNA and target DNA, particularly in the PAM-proximal seed region, are efficiently discriminated against, providing a critical checkpoint for target specificity [15] [16].
Conformational Activation and DNA Cleavage
Upon complete R-loop formation, Cas9 undergoes significant conformational changes that activate its nuclease domains [15] [16]. Structural studies have identified multiple conformational states of the HNH domain, with the active state positioning the catalytic residue H840 close to the scissile phosphate of the target DNA strand [16]. This conformational activation represents a critical checkpoint that monitors the integrity of the guide-target duplex before permitting DNA cleavage [15].
The cleavage event itself results in a blunt-ended double-strand break approximately 3-4 nucleotides upstream of the PAM sequence [13] [12]. The HNH domain cleaves the DNA strand complementary to the guide RNA, while the RuvC domain cleaves the opposite strand, with both domains functioning as metal-dependent nucleases [11] [16]. The resulting DSB then engages the cellular DNA repair machinery, enabling genome editing through either error-prone non-homologous end joining (NHEJ) or precise homology-directed repair (HDR) pathways [11] [18].
DNA Repair Pathways and Genome Editing Outcomes
Following Cas9-mediated DNA cleavage, cellular repair mechanisms determine the final genomic outcome. The two primary repair pathways—non-homologous end joining (NHEJ) and homology-directed repair (HDR)—offer distinct applications for genetic therapy research [11] [12].
Table 2: DNA Repair Pathways Following Cas9 Cleavage
| Repair Pathway | Mechanism | Editing Outcome | Therapeutic Applications |
|---|---|---|---|
| Non-homologous End Joining (NHEJ) | Error-prone ligation of broken ends without template | Small insertions or deletions (indels); gene disruption | Gene knockouts; disruption of pathogenic genes |
| Homology-Directed Repair (HDR) | High-fidelity repair using homologous donor template | Precise gene correction or insertion | Correction of point mutations; gene insertion therapy |
The NHEJ pathway is active throughout the cell cycle and represents the dominant repair mechanism in most mammalian cells [11] [18]. While efficient, this pathway often results in small random insertions or deletions (indels) at the cleavage site, which can disrupt gene function by introducing frameshift mutations or premature stop codons [13] [12]. For therapeutic applications, NHEJ is particularly valuable for disrupting pathogenic genes, such as those involved in genetic disorders driven by gain-of-function mutations [14].
In contrast, the HDR pathway utilizes a donor DNA template with homology to the sequences flanking the break site to enable precise genome editing [11] [18]. Although HDR occurs at lower frequencies than NHEJ and is restricted to specific cell cycle phases, it offers the potential for correcting disease-causing mutations with single-nucleotide precision [12]. Therapeutic strategies employing HDR typically provide an engineered donor template along with the CRISPR-Cas9 components, enabling the replacement of defective genomic sequences with functional ones [14].
Experimental Protocols for CRISPR-Cas9 Genome Editing
Ribonucleoprotein (RNP) Complex Delivery
The delivery of preassembled Cas9-gRNA ribonucleoprotein complexes represents a highly efficient and specific approach for genome editing applications [11]. The following protocol outlines a standard workflow for RNP-based editing:
sgRNA Design: Design sgRNA with optimal GC content (40-60%) and minimal off-target potential using bioinformatics tools [11] [17]. Ensure the target site is adjacent to a PAM (5'-NGG-3') and lacks significant homology to other genomic regions [11].
RNP Complex Assembly:
- Combine recombinant Cas9 protein (10-20 µM) with synthetic sgRNA at a 1:1.2-1.5 molar ratio in nuclease-free buffer
- Incubate at 25°C for 10-15 minutes to allow complex formation [11]
Cell Delivery:
Post-transfection Processing:
- Allow cells to recover for 24-72 hours in complete medium
- Assess editing efficiency using T7E1 assay, tracking of indels by decomposition (TIDE), or next-generation sequencing [11]
This RNP delivery method offers advantages including reduced off-target effects due to transient Cas9 activity, and minimal risk of genomic integration compared to plasmid-based approaches [11].
Validation and Analysis of Editing Outcomes
Comprehensive validation of CRISPR-Cas9 editing is essential for therapeutic applications:
Genomic DNA Extraction: Harvest cells 48-72 hours post-editing and extract genomic DNA using standard protocols
Editing Efficiency Analysis:
- PCR Amplification: Amplify target region using flanking primers (amplicon size: 300-500 bp)
- Next-generation Sequencing: Sequence amplicons to precisely quantify indels and verify HDR events
- Alternative Methods: T7E1 assay or SURVEYOR assay for initial screening of editing efficiency [11]
Off-target Assessment:
- Use computational prediction tools (e.g., Cas-OFFinder) to identify potential off-target sites
- Perform targeted sequencing of top predicted off-target loci with sequence similarity to the sgRNA
- Consider using high-fidelity Cas9 variants (e.g., SpCas9-HF1, eSpCas9(1.1) to minimize off-target editing [11] [13]
Advanced Cas9 Engineering for Enhanced Specificity
Wild-type Cas9 can tolerate mismatches between the guide RNA and target DNA, potentially leading to off-target effects that pose challenges for therapeutic applications [11] [13]. Several engineered Cas9 variants have been developed to address this limitation:
Table 3: Engineered Cas9 Variants for Improved Specificity
| Cas9 Variant | Engineering Strategy | Key Features | Therapeutic Advantages |
|---|---|---|---|
| High-fidelity Cas9 (SpCas9-HF1) | Structure-guided mutagenesis to reduce non-specific DNA contacts | ~500-fold reduction in off-target editing while maintaining on-target efficiency | Enhanced safety profile for clinical applications |
| Enhanced Specificity Cas9 (eSpCas9) | Weakened interactions with non-target DNA strand | Reduced off-target effects without compromising on-target activity | Improved target specificity for precision medicine |
| Hyper-accurate Cas9 (HypaCas9) | Enhanced proofreading capability through allosteric regulation | Improved discrimination against mismatched targets | Reduced risk of unintended genomic alterations |
| Cas9 Nickase (nCas9) | Inactivation of either HNH or RuvC domain (D10A or H840A mutation) | Creates single-strand breaks instead of DSBs; requires paired gRNAs for DSB formation | Significantly reduced off-target effects when used as paired nickases |
Additional engineering efforts have focused on altering PAM specificity to expand the targeting range of Cas9. Variants such as xCas9 and SpCas9-NG recognize alternative PAM sequences (NG, GAA, and GAT for xCas9), thereby increasing the number of targetable genomic sites for therapeutic applications [13].
Research Reagent Solutions for CRISPR-Cas9 Experiments
Table 4: Essential Reagents for CRISPR-Cas9 Research
| Reagent Category | Specific Examples | Research Applications | Considerations |
|---|---|---|---|
| Cas9 Expression Systems | Wild-type SpCas9, High-fidelity variants (SpCas9-HF1, eSpCas9) | General genome editing, applications requiring high specificity | Choose based on specificity requirements and delivery method |
| Guide RNA Formats | Synthetic sgRNA, crRNA:tracrRNA duplex, plasmid-encoded sgRNA | Flexible experimental designs; synthetic RNAs offer immediate activity | Synthetic RNAs reduce off-target risks; plasmid formats enable stable expression |
| Delivery Vehicles | Electroporation systems, lipid nanoparticles (LNPs), viral vectors (AAV, lentivirus) | Cell type-specific delivery optimization | LNPs ideal for primary cells; viral vectors for hard-to-transfect cells |
| Detection & Validation | T7E1 assay, next-generation sequencing, digital PCR, flow cytometry | Assessment of editing efficiency and specificity | Multiplexed approaches recommended for comprehensive validation |
| HDR Donor Templates | Single-stranded DNA oligos, double-stranded DNA plasmids, AAV vectors | Precision genome editing, gene correction | Optimize design with long homology arms (≥800 bp) for efficient HDR |
Clinical Applications and Therapeutic Outlook
The mechanistic understanding of Cas9 DNA cleavage has enabled remarkable advances in therapeutic development for genetic disorders. Recent clinical trials demonstrate the potential of CRISPR-Cas9 for treating monogenic diseases:
Sickle Cell Disease and β-Thalassemia: The FDA-approved therapy Casgevy utilizes ex vivo CRISPR-Cas9 editing of hematopoietic stem cells to reactivate fetal hemoglobin production, effectively compensating for the defective adult hemoglobin in these disorders [14].
Hereditary Transthyretin Amyloidosis (hATTR): Intellia Therapeutics has demonstrated successful in vivo genome editing using LNP-delivered CRISPR-Cas9 to reduce levels of disease-causing transthyretin protein in the liver, with clinical trials showing ~90% reduction in serum TTR levels that remains durable over time [14].
Rare Genetic Disorders: The landmark case of a personalized CRISPR treatment for an infant with CPS1 deficiency established a regulatory precedent for rapidly developed bespoke therapies for ultra-rare genetic conditions [14]. This approach, developed and delivered in just six months, illustrates the potential for CRISPR-based interventions for previously untreatable disorders.
Emerging delivery technologies, particularly lipid nanoparticles (LNPs), have enabled efficient in vivo delivery of CRISPR components to target tissues, opening new avenues for therapeutic development [14]. Additionally, the integration of artificial intelligence tools like CRISPR-GPT is accelerating experimental design and optimization, potentially reducing development timelines for CRISPR-based therapies [20].
As the field advances, ongoing challenges include optimizing delivery efficiency, minimizing off-target effects, and ensuring equitable access to these transformative therapies. Continued research into the fundamental mechanisms of Cas9 function will further refine this powerful technology, ultimately expanding its potential for treating a broad spectrum of genetic disorders.
The advent of CRISPR-Cas systems has revolutionized biological research and therapeutic development by providing unprecedented ability to manipulate genomes. While the initial CRISPR-Cas9 system functions as programmable "genetic scissors" that create double-strand breaks (DSBs), recent innovations have dramatically expanded the CRISPR toolkit beyond this foundational mechanism [21] [22]. Base editors and prime editors represent the next generation of precision genome editing tools that overcome fundamental limitations of conventional CRISPR-Cas9, particularly for therapeutic applications where precision and safety are paramount [23].
These advanced editors are particularly valuable in the context of genetic disorder therapy research, where many diseases are caused by specific point mutations that require precise correction rather than gene disruption [21]. Over 75,000 pathogenic genetic variants have been identified in humans, and previously developed genome editing methods could only correct a minority of these variants [24]. This application note provides a comparative analysis of Cas9 nucleases, base editors, and prime editors, with specific experimental protocols and resource guidance to enable researchers to select and implement the optimal tool for their genetic correction objectives.
Technology Comparison: Mechanisms and Capabilities
Core Mechanisms of Action
CRISPR-Cas9 Nucleases utilize a complex of Cas9 enzyme and guide RNA (gRNA) to create targeted double-strand breaks in DNA [21]. The system relies on recognition of a protospacer adjacent motif (PAM) sequence adjacent to the target site [21]. Once DSBs are generated, cellular repair mechanisms are harnessed to achieve the desired genetic change: error-prone non-homologous end joining (NHEJ) typically results in insertions or deletions (indels) that disrupt gene function, while homology-directed repair (HDR) can incorporate donor DNA templates for precise changes [21] [23]. However, HDR efficiency is generally low, especially in non-dividing cells, and the process frequently produces a mixture of outcomes including undesirable indels [21] [23].
Base Editors represent the first major evolution beyond standard CRISPR nucleases, enabling direct chemical conversion of one DNA base to another without creating DSBs [21] [22]. These fusion proteins combine a catalytically impaired Cas protein (nCas9) with a deaminase enzyme [23]. Two primary classes have been developed: Cytosine Base Editors (CBEs) convert cytosine to thymine (C→T) through a cytidine deaminase, while Adenine Base Editors (ABEs) convert adenine to guanine (A→G) using an engineered adenosine deaminase [21] [23]. Base editors operate within a defined "editing window" where all susceptible bases are modified, which can lead to bystander edits when multiple target bases are present in this window [24].
Prime Editors constitute the most versatile precision editing system, capable of installing all 12 possible base-to-base conversions, as well as small insertions and deletions, without requiring DSBs or donor DNA templates [21] [24]. The system employs a prime editing guide RNA (pegRNA) that both specifies the target site and encodes the desired edit, along with a fusion protein consisting of Cas9 nickase fused to an engineered reverse transcriptase [25] [24]. After nicking the target DNA, the pegRNA's primer binding site anneals to the nicked strand, and the reverse transcriptase synthesizes new DNA containing the edited sequence using the pegRNA's template region [24] [26].
Quantitative Performance Comparison
Table 1: Performance Characteristics of CRISPR Editing Technologies
| Parameter | CRISPR-Cas9 Nuclease | Base Editors | Prime Editors |
|---|---|---|---|
| Editing Precision | Low (mixed outcomes) | Moderate (editing window) | High (specific change) |
| Efficiency for Point Mutations | Typically <10% (HDR) [24] | High (typically 50-80%) [22] | Variable (1-50%) [24] |
| Indel Formation | High (∼50-90% of events) [23] | Low (<1-10%) [23] | Low (typically 1-10%) [24] |
| Theoretical Targeting Scope | ∼37.5% of pathogenic SNPs [21] | ∼25% of pathogenic SNPs [21] | ∼89% of pathogenic SNPs [21] |
| Primary Editing Byproducts | Indels, translocations [23] | Bystander edits within window [24] | Low complexity outcomes [24] |
| Typical Edit Size | Large deletions/insertions | Single base changes | Up to ∼20 bp edits [25] |
Table 2: Molecular Capabilities of CRISPR Editing Technologies
| Edit Type | CRISPR-Cas9 Nuclease | Base Editors | Prime Editors |
|---|---|---|---|
| C→T | Possible via HDR | Yes (CBE) [21] | Yes [24] |
| A→G | Possible via HDR | Yes (ABE) [21] | Yes [24] |
| Transversions | Possible via HDR | No | Yes [24] |
| Small Insertions | Possible via HDR | No | Yes (∼20 bp max) [25] |
| Small Deletions | Yes (via NHEJ) | No | Yes [24] |
| Multiple Simultaneous Edits | Challenging | No | Possible [24] |
| Gene Disruption | Excellent | Possible | Less efficient [25] |
Therapeutic Applications and Experimental Evidence
Application-Specific Technology Selection
The choice of CRISPR technology depends heavily on the specific genetic correction objective. For disease modeling where gene disruption is desired, conventional CRISPR-Cas9 nuclease remains highly effective [23]. For therapeutic correction of point mutations, base editors offer high efficiency when the desired change is a transition mutation (C→T, G→A, A→G, or T→C) and the target base is optimally positioned within the editing window [22]. Prime editors provide the broadest capabilities for precise edits, particularly when the required change involves transversions, small insertions or deletions, or when bystander editing must be avoided [24].
Sickle Cell Disease Case Study: Research demonstrates how both base editing and prime editing can effectively address the same genetic disorder through different approaches. A base editing strategy successfully converted the sickle cell disease mutation (A→T in β-globin) to a nonpathogenic variant known as hemoglobin G Makassar using a custom adenine base editor, achieving 68% editing efficiency in mouse models with stable correction over 16 weeks [22]. Alternatively, a prime editing approach directly reverted the mutation to the normal sequence with 42% efficiency in erythroid precursors after 17 weeks in humanized mice [22]. The base editing approach benefited from higher efficiency, while the prime editing approach achieved the exact natural sequence with potentially fewer off-target effects.
Hereditary Transthyretin Amyloidosis (hATTR): Intellia Therapeutics' phase I clinical trial demonstrated the in vivo therapeutic potential of CRISPR-Cas9 delivered via lipid nanoparticles (LNPs) to target the TTR gene in the liver [14]. This treatment achieved approximately 90% reduction in disease-related protein levels sustained over two years, with functional improvement in symptoms [14]. This success highlights the movement of CRISPR technologies toward therapeutic reality.
Decision Framework for Technology Selection
Experimental Protocols and Workflows
Base Editing Experimental Protocol
Objective: Precise correction of a point mutation using adenine or cytosine base editing.
Materials Required:
- Base editor plasmid (ABE8e for A→G or BE4max for C→T conversions)
- Target-specific sgRNA plasmid or synthetic sgRNA
- Appropriate delivery system (lipofection, electroporation, AAV)
- Target cells with known mutation
- PCR reagents for amplification of target region
- Next-generation sequencing platform for efficiency analysis
Step-by-Step Workflow:
Target Site Identification: Identify target sequence containing the pathogenic mutation. Verify that the target base falls within the optimal editing window (typically positions 4-8 for SpCas9-based editors) and check for potential bystander bases that might be unintentionally modified [23].
sgRNA Design and Preparation: Design sgRNA with 20-nt spacer sequence complementary to target site adjacent to appropriate PAM (NGG for SpCas9). Synthesize as plasmid expression construct or chemically modified synthetic sgRNA for improved stability.
Base Editor Delivery:
- For plasmid transfection: Co-transfect base editor and sgRNA plasmids at 3:1 ratio using appropriate transfection reagent.
- For RNP delivery: Pre-complex purified base editor protein with sgRNA at 3:1 molar ratio in Cas9 reaction buffer, incubate 15 minutes at room temperature, then deliver via electroporation.
- Include appropriate controls: sgRNA-only, base editor-only, and untreated cells.
Editing Efficiency Analysis:
- Harvest cells 48-72 hours post-delivery.
- Extract genomic DNA and amplify target region by PCR.
- Perform next-generation sequencing (minimum 10,000x coverage) or Sanger sequencing with decomposition analysis.
- Calculate editing efficiency as percentage of sequencing reads containing desired edit.
Off-Target Assessment:
- Analyze top predicted off-target sites by in silico prediction tools.
- Perform targeted sequencing of potential off-target loci.
- For therapeutic applications, conduct whole-genome sequencing to identify unexpected edits.
Troubleshooting Notes: Low editing efficiency may require optimization of sgRNA sequence, testing different base editor variants, or adjusting delivery conditions. High bystander editing may necessitate redesign to alternative target sites or switching to prime editing approach.
Prime Editing Experimental Protocol
Objective: Precise installation of specific point mutations, small insertions, or deletions.
Materials Required:
- Prime editor plasmid (PEmax recommended)
- pegRNA expression plasmid or synthetic pegRNA
- Optional: nicking sgRNA for PE3/PE3b systems
- Delivery system (electroporation recommended for hard-to-transfect cells)
- Target cells
- PCR and sequencing reagents
Step-by-Step Workflow:
pegRNA Design:
- Design pegRNA with 20-nt spacer sequence targeting desired locus.
- Engineer reverse transcriptase template (RTT) to encode desired edit with 8-15 nt of homologous sequence flanking both sides.
- Include primer binding site (PBS) of 10-15 nt complementary to DNA 3' of nick site.
- Consider using epegRNA designs with 3' RNA pseudoknots to enhance stability [24].
pegRNA Validation: Test multiple pegRNA designs for each target as efficiency varies significantly based on sequence context. Computational tools are available to predict optimal pegRNA designs.
Prime Editor Delivery:
- For plasmid transfection: Co-transfect prime editor and pegRNA plasmids at 1:3 ratio.
- For RNP delivery: Complex purified PEmax protein with in vitro transcribed pegRNA.
- For PE3/PE3b systems: Include additional nicking sgRNA plasmid or synthetic RNA.
- Include essential controls: pegRNA-only, prime editor-only, and untreated cells.
Editing Efficiency Optimization:
- Test various PBS lengths (10-15 nt) and RTT lengths.
- Evaluate different architectures (PE2, PE3, PE3b, PE5).
- Consider temporary mismatch repair inhibition (PE4/PE5 systems) to improve efficiency [24].
- Allow sufficient time for editing - analyze at 72-96 hours post-delivery.
Analysis and Validation:
- Amplify target region by PCR and sequence by next-generation sequencing.
- Calculate prime editing efficiency as percentage of reads with exact desired edit.
- Screen for byproducts including undesired insertions, deletions, or point mutations.
- For clonal applications, isolate single-cell clones and expand for comprehensive genotyping.
Troubleshooting Notes: Prime editing efficiency is highly variable across targets. If efficiency remains low after optimization, consider alternative pegRNA designs, testing specialized PE6 variants for specific edit types, or using dual-pegRNA strategies. Delivery optimization is often critical for success.
Research Reagent Solutions
Table 3: Essential Reagents for CRISPR Editing Experiments
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Editor Plasmids | PEmax, ABE8e, BE4max [24] | Express editor proteins | Choose size-optimized versions for viral delivery |
| Guide RNA Systems | pegRNA, sgRNA, epegRNA [24] | Target specification and edit template | Chemical modification improves stability |
| Delivery Vehicles | Lipid nanoparticles (LNPs), AAV, electroporation [14] | Deliver editing components to cells | LNPs enable redosing [14] |
| Validation Tools | NGS assays, Sanger sequencing, T7E1 assay | Assess editing efficiency and specificity | NGS provides quantitative accuracy |
| Cell Culture | Stem cell media, cytokines, transfection reagents | Maintain and edit target cells | Optimization needed for primary cells |
| Control Reagents | Off-target prediction algorithms, control gRNAs | Establish experimental specificity | Include multiple negative controls |
The CRISPR toolkit has evolved substantially from the initial Cas9 nuclease to increasingly sophisticated base editing and prime editing systems. Each technology offers distinct advantages and limitations, making them complementary rather than competing solutions. Conventional CRISPR-Cas9 remains ideal for gene disruption applications, base editors provide highly efficient point mutation correction for transition mutations within their editing windows, and prime editors offer unprecedented versatility for precise genetic manipulations including transversions, insertions, and deletions [24] [22].
Current research focuses on addressing the remaining limitations of these technologies, including further improving editing efficiency, expanding targeting scope through engineered Cas variants with altered PAM requirements, enhancing specificity to minimize off-target effects, and developing optimized delivery systems capable of transporting these large molecular machines to target tissues in vivo [23] [24]. The successful clinical translation of CRISPR-based therapies for sickle cell disease and beta thalassemia, along with promising ongoing clinical trials for conditions like hereditary transthyretin amyloidosis and hereditary angioedema, underscore the tremendous therapeutic potential of these technologies [14] [27].
As the field continues to advance, researchers should maintain a flexible approach to technology selection, choosing the most appropriate tool based on their specific genetic correction objective rather than defaulting to familiar methods. The protocols and comparisons provided in this application note offer a foundation for making informed decisions and implementing these powerful genome engineering technologies in both basic research and therapeutic development contexts.
Monogenic disorders, resulting from mutations in a single gene, represent a class of over 7,000 known human diseases that collectively affect approximately 300 million people worldwide [28]. Historically, treatment for these conditions has focused primarily on symptom management due to the inherent challenges in addressing their genetic roots. The advent of CRISPR-Cas9 gene editing technology has fundamentally shifted this therapeutic paradigm, enabling direct correction of pathogenic mutations at the DNA level [29] [30]. This powerful technology functions as a programmable molecular scissor, utilizing a Cas nuclease guided by a single-guide RNA (sgRNA) to create precise double-strand breaks at specific genomic loci, which are then repaired by the cell's endogenous DNA repair mechanisms [29] [31].
The applications of CRISPR-based therapies have expanded dramatically, with the first FDA-approved CRISPR therapy (Casgevy for sickle cell disease and transfusion-dependent beta thalassemia) marking a watershed moment for the field [14] [32]. Current research has further advanced beyond traditional CRISPR-Cas9 to include more precise genetic modification tools such as base editing and prime editing, which can directly convert one DNA base to another without creating double-strand breaks, thereby reducing potential off-target effects [28] [33]. This review provides a comprehensive overview of the spectrum of monogenic disorders amenable to CRISPR therapy, detailed experimental protocols for researchers, and essential tools advancing this revolutionary therapeutic approach.
The Expanding Spectrum of Addressable Monogenic Disorders
CRISPR-based therapeutic strategies are being actively investigated for a wide range of monogenic diseases, with approaches tailored to the specific genetic mutation and pathological mechanism. The table below summarizes key disease targets, therapeutic strategies, and current development status.
Table 1: Monogenic Diseases Amenable to CRISPR Therapy
| Disease Category | Specific Disorders | Target Gene(s) | CRISPR Strategy | Development Stage |
|---|---|---|---|---|
| Hematological | Sickle Cell Disease (SCD) [31] | HBB, BCL11A | BCL11A enhancer disruption to reactivate fetal hemoglobin [32] | FDA-Approved (Casgevy) [14] |
| Transfusion-Dependent Beta Thalassemia (TDT) [31] | HBB, BCL11A | BCL11A enhancer disruption [31] | FDA-Approved (Casgevy) [14] | |
| Hemophilia A & B [31] [32] | F8, F9 | Gene correction/insertion to restore clotting factor expression [31] | Clinical Trials | |
| Neuromuscular | Duchenne Muscular Dystrophy (DMD) [30] | DMD | Exon skipping/deletion to restore reading frame [30] | Preclinical (mice, dog models) |
| Spinal Muscular Atrophy (SMA) [28] | SMN2 | Base editing to convert SMN2 into SMN1-like function [28] [33] | Preclinical | |
| Metabolic | Hereditary Transthyretin Amyloidosis (hATTR) [14] | TTR | Gene disruption to reduce pathogenic protein production [14] | Phase III Trials |
| Ornithine Transcarbamylase (OTC) Deficiency [30] | OTC | In vivo gene correction in hepatocytes [30] | Preclinical (mouse models) | |
| Glycogen Storage Disease Type Ia [33] | G6PC | Base editing to correct metabolic abnormalities [33] | Preclinical (humanized mouse model) | |
| Phenylketonuria (PKU) [30] | PAH | Gene correction in hepatocytes [30] | Preclinical (mouse, pig models) | |
| Other | Hereditary Angioedema (HAE) [14] | KLKB1 | Gene disruption to reduce kallikrein protein [14] | Phase I/II Trials |
| Cystic Fibrosis (CF) [30] | CFTR | Correction of ΔF508 mutation in epithelial cells [30] | Preclinical (cell, sheep, rabbit models) |
The diversity of strategies highlights CRISPR's versatility. For loss-of-function disorders, the goal is often gene correction or insertion, while for gain-of-function or dominant-negative disorders, gene disruption or silencing is a viable path [31]. The recent success of Casgevy exemplifies a creative indirect strategy: instead of correcting the mutated HBB gene itself, it disrupts the enhancer of BCL11A, a repressor of fetal hemoglobin (HbF), thereby reactivating HbF production to compensate for the defective adult hemoglobin [32].
Quantitative Outcomes of Leading Clinical Candidates
The efficacy of these therapies is demonstrated by robust clinical and preclinical data. The following table summarizes key quantitative outcomes from prominent studies.
Table 2: Efficacy Outcomes from Key CRISPR Therapy Studies
| Therapy / Target | Disease Model | Key Efficacy Metric | Result |
|---|---|---|---|
| Casgevy (SCD/TDT) [32] | Human Patients | Proportion of HbF in total hemoglobin | 43.9% at 6 months, sustained for ≥24 months |
| hATTR Therapy [14] | Human Patients (Phase I) | Reduction in disease-related TTR protein | ~90% reduction, sustained for 2 years |
| HAE Therapy [14] | Human Patients (Phase I/II) | Reduction in kallikrein protein and attacks | 86% kallikrein reduction; 8/11 patients attack-free |
| DMD Therapy [30] | mdx mouse model | Dystrophin-positive muscle fibers | Up to 70% of myogenic area |
| OTC Deficiency Therapy [30] | spf^(ash) mouse model | Hepatocyte correction rate | ~10% of hepatocytes corrected |
Experimental Protocols for CRISPR-Based Therapeutic Development
Protocol 1: Ex Vivo Editing of Hematopoietic Stem Cells (HSCs) for Hemoglobinopathies
This protocol outlines the methodology used in the development of Casgevy, an autologous ex vivo CRISPR-Cas9-edited cell therapy for SCD and TDT [32].
Workflow Overview:
Materials:
- Patient-derived CD34+ HSPCs: Sourced from bone marrow aspiration or apheresis after mobilization with granulocyte colony-stimulating factor (G-CSF) [31] [32].
- CRISPR Reagents: Cas9 nuclease (e.g., SpCas9) and synthetic sgRNA designed to target the erythroid-specific enhancer region of the BCL11A gene [32].
- Electroporation System: Such as the Lonza 4D-Nucleofector, for efficient delivery of ribonucleoprotein (RNP) complexes into HSCs [31].
- Cell Culture Media: Serum-free expansion media supplemented with cytokines (SCF, TPO, FLT3-L) to maintain stem cell viability and proliferation during editing [31].
Step-by-Step Methodology:
- HSC Mobilization and Collection: Mobilize hematopoietic stem cells from the patient's bone marrow into the peripheral blood using G-CSF. Collect CD34+ cells via leukapheresis and purify using immunomagnetic selection [32].
- CRISPR RNP Complex Formation: Complex purified, high-fidelity Cas9 protein with synthetic sgRNA at a predetermined molar ratio in an appropriate electroporation buffer. Incubate for 10-15 minutes at room temperature to form the RNP complex [31].
- Electroporation: Resuspend the CD34+ cells in the RNP-containing buffer and electroporate using a pre-optimized protocol for HSCs. Immediate rescue of cells into pre-warmed culture media is critical for viability [32].
- Myeloablative Conditioning: While edited cells are in culture, administer a myeloablative conditioning regimen (e.g., busulfan) to the patient to create marrow space for the engraftment of the edited HSCs [14].
- Cell Reinfusion and Engraftment: After a brief ex vivo culture period (typically 1-2 days), wash and cryopreserve the edited cells. Thaw and infuse the final product back into the patient via intravenous infusion. Monitor for engraftment (neutrophil and platelet recovery) and subsequent tracking of HbF levels [14] [32].
Protocol 2: In Vivo Gene Editing via Lipid Nanoparticles (LNPs) for Liver Disorders
This protocol describes the methodology for systemic in vivo gene editing, as exemplified by therapies for hATTR and the landmark case of a personalized treatment for CPS1 deficiency [14].
Workflow Overview:
Materials:
- LNP Formulation: CRISPR-Cas9 mRNA and sgRNA encapsulated in lipid nanoparticles with ionizable cationic lipids, phospholipids, cholesterol, and PEG-lipid components. LNPs are preferred for liver-targeted delivery due to natural tropism and lower immunogenicity compared to viral vectors [14].
- Animal Model: Validated murine or larger animal model of the target disease (e.g., Agxt1^-/- mice for primary hyperoxaluria type I) [30].
- Analytical Reagents: Antibodies for Western blot/ELISA to quantify target protein reduction, and primers for next-generation sequencing (NGS) to assess editing efficiency and off-target profiling [14] [30].
Step-by-Step Methodology:
- LNP Formulation and QC: Formulate CRISPR-Cas9 mRNA and guid sgRNA into LNPs using microfluidic mixing techniques. Characterize LNPs for size (typically 70-100 nm), polydispersity, encapsulation efficiency, and endotoxin levels [14].
- Dose Determination and Administration: Establish a dosing regimen based on preclinical animal studies. Administer the LNP formulation via a single intravenous injection (e.g., tail vein in mice, peripheral IV in larger animals and humans) [14].
- Biodistribution and Efficacy Analysis: At predetermined time points post-injection, sacrifice a cohort of animals to analyze biodistribution. The liver is the primary target organ. Analyze editing efficiency in genomic DNA extracted from hepatocytes using NGS. Quantify the reduction of the pathogenic protein (e.g., TTR) in plasma by ELISA [14].
- Safety and Off-Target Analysis: Evaluate potential immunogenicity by measuring cytokine levels. Perform broad off-target analysis using in silico prediction followed by CIRCLE-seq or similar unbiased methods on genomic DNA from treated liver tissue [29] [14].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful development of CRISPR therapies relies on a suite of specialized reagents and tools. The following table catalogs key solutions for researchers in this field.
Table 3: Essential Research Reagents for CRISPR Therapeutic Development
| Reagent Category | Specific Examples | Function & Importance |
|---|---|---|
| Editing Machinery | High-fidelity SpCas9 protein [29], ABE8e adenine base editor [28], CBE4 cytosine base editor [28] | Engineered proteins with improved specificity and expanded editing windows to minimize off-target effects and broaden targetable sites. |
| Delivery Vehicles | AAV vectors (e.g., AAV8 for liver) [30], Lipid Nanoparticles (LNPs) [14], Electroporation systems [31] | Enable transport of CRISPR components to target cells (in vivo) or facilitate efficient intracellular delivery (ex vivo). |
| sgRNA Tools | Chemically modified sgRNAs [31], sgRNA libraries for screening [29] | Modified sgRNAs enhance stability and reduce immunogenicity; libraries enable functional genomics and target discovery. |
| Cell Culture Systems | CD34+ HSPC expansion media [31], Human iPSCs [32] | Specialized media maintains stemness during editing; iPSCs provide a versatile patient-specific model for disease modeling and therapy development. |
| Analysis & QC Kits | NGS-based editing efficiency assays (e.g., Illumina), Off-target detection kits (e.g., GUIDE-seq) [29], ELISA for protein quantification [14] | Critical for quantifying primary editing outcomes, identifying potential off-target sites, and measuring functional phenotypic correction. |
The therapeutic landscape for monogenic diseases is being fundamentally reshaped by CRISPR-based gene editing. From the first FDA approvals for hemoglobinopathies to the rapid advancement of in vivo base editing and personalized therapies, the field is demonstrating tangible clinical success. The protocols and tools outlined herein provide a framework for researchers to advance new therapies. Future progress will hinge on overcoming persistent challenges in delivery efficiency, ensuring long-term safety, and expanding the reach of these potentially curative treatments to all patients in need.
From Bench to Bedside: Therapeutic Strategies and Clinical Applications for Genetic Diseases
The emergence of CRISPR-Cas9 technology has revolutionized the therapeutic landscape for genetic disorders, presenting two fundamental strategic paradigms: ex vivo and in vivo gene editing [29] [30]. Ex vivo therapy involves the genetic modification of patient-derived cells outside the body followed by reinfusion, while in vivo therapy delivers editing machinery directly to target cells inside the patient [34]. For hematopoietic disorders such as sickle cell disease and β-thalassemia, ex vivo editing of hematopoietic stem and progenitor cells (HSPCs) has demonstrated remarkable clinical success [35] [36]. Conversely, in vivo approaches show increasing promise for treating solid organ disorders like Duchenne muscular dystrophy and cystic fibrosis, where target tissues are not readily accessible for extraction [30] [37]. This application note delineates detailed protocols and strategic considerations for both approaches within the broader context of CRISPR-Cas9 applications for genetic disorder therapy, providing researchers with essential methodologies for therapeutic development.
Comparative Analysis of Strategic Approaches
Table 1: Strategic Comparison of Ex Vivo and In Vivo Therapy Approaches
| Parameter | Ex Vivo Therapy | In Vivo Therapy |
|---|---|---|
| Target Cells | Hematopoietic stem and progenitor cells (HSPCs), T-cells, other immunocytes [35] [36] | Hepatocytes, myocytes, neuronal cells, respiratory epithelial cells [30] |
| Therapeutic Workflow | Cell extraction → Ex vivo editing → Expansion → Reinfusion [36] | Direct systemic or localized administration of editing components [38] |
| Editing Efficiency | High (30-90% in HSPCs) [35] | Variable (5-70% depending on delivery system) [37] |
| Key Advantages | Controlled editing conditions, precise quality control, reduced immune responses, transient editor exposure [35] [36] | Non-invasive, potential for multi-tissue editing, no cell manipulation artifacts [38] [39] |
| Major Challenges | Complex cell processing, risk of cell differentiation during culture, need for conditioning regimens [35] | Delivery efficiency, immune clearance, potential off-target effects in inaccessible tissues [38] [40] |
| Ideal Disorder Types | Hematological disorders (SCD, β-thalassemia, SCID), immunodeficiencies [35] [36] | Monogenic disorders affecting solid organs (DMD, CF, OTC deficiency) [30] |
| Clinical Stage | Multiple Phase I/II/III trials (e.g., CTX001 for SCD and β-thalassemia) [36] | Early-phase clinical trials (e.g., NTLA-2001 for ATTR amyloidosis) [39] |
Table 2: Quantitative Comparison of Editing Outcomes in Preclinical Models
| Disease Model | Editing Approach | Target | Efficiency | Functional Outcome |
|---|---|---|---|---|
| Sickle Cell Disease [35] | Ex vivo (HSPCs) | HBB | >90% indel frequency | Increased HbF levels, reduced sickling |
| β-thalassemia [35] [30] | Ex vivo (HSPCs) | HBB | 93% indel frequency | Improved hemoglobin levels |
| Duchenne Muscular Dystrophy [30] | In vivo (AAV-CRISPR) | Dystrophin | Up to 70% myogenic area | Dystrophin restoration, improved force generation |
| Ornithine Transcarbamylase Deficiency [30] | In vivo (AAV-CRISPR) | OTC | 10% hepatocyte correction | Improved protein tolerance, survival |
| Phenylketonuria [30] | In vivo (AAV-CRISPR) | PAH | Partial hepatocyte correction | Reduced blood phenylalanine |
| Atherosclerosis [30] | In vivo (AAV-CRISPR) | LDLR | Partial rescue | Reduced cholesterol, smaller plaques |
Diagram 1: Comparative workflows for ex vivo and in vivo CRISPR-Cas9 therapeutic approaches.
Ex Vivo Therapy: Applications and Protocols for Hematopoietic Disorders
Ex vivo CRISPR-Cas9 therapy has demonstrated remarkable success for hematopoietic disorders, with clinical trials showing transformative outcomes for sickle cell disease and β-thalassemia [35] [36]. This approach leverages the accessibility and engraftment potential of hematopoietic stem and progenitor cells (HSPCs) to establish durable therapeutic effects.
Strategic Advantages for Hematopoietic Disorders
The hematopoietic system presents unique advantages for ex vivo editing: (1) HSPCs can be relatively easily accessed via mobilization and apheresis; (2) edited HSPCs possess the capacity to engraft and reconstitute the entire blood system; (3) ex vivo manipulation avoids systemic delivery challenges; and (4) quality control can be performed pre-infusion [35]. Furthermore, the transient exposure of cells to editing components ex vivo minimizes the risk of persistent off-target effects and immune recognition [36].
Detailed Experimental Protocol: HSPC Editing for Hemoglobinopathies
Table 3: Key Research Reagent Solutions for Ex Vivo HSPC Editing
| Reagent Category | Specific Examples | Function & Application Notes |
|---|---|---|
| Cell Isolation | CD34+ immunomagnetic selection kits (e.g., CliniMACS) | Isolation of target HSPC population with >90% purity [35] |
| Editing Machinery | SpCas9 RNPs with target-specific sgRNA | Direct delivery of precomplexed ribonucleoprotein for rapid editing with minimal off-target effects [40] |
| Delivery Method | Electroporation systems (e.g., Neon, 4D-Nucleofector) | High-efficiency RNP delivery with optimized programs for HSPCs [35] |
| Culture Media | Serum-free expansion media with cytokines (SCF, TPO, FLT3-L) | Maintenance of stemness and viability during ex vivo culture [36] |
| Quality Control | NGS-based off-target assays, flow cytometry, CFU assays | Assessment of editing efficiency, viability, and functional potential [35] |
Protocol: HSPC Editing for Hemoglobinopathies
Step 1: HSPC Mobilization and Collection
- Mobilize HSPCs using granulocyte colony-stimulating factor (G-CSF) or plerixafor [35]
- Collect cells via apheresis (yield: typically 5-20 × 10^6 CD34+ cells/kg patient weight)
- Critical Note: Patients with sickle cell disease may experience vaso-occlusive crises during mobilization - require careful monitoring [35]
Step 2: CD34+ Cell Selection and Culture
- Isplicate CD34+ cells using immunomagnetic selection (purity >90%)
- Culture cells in serum-free medium (StemSpan) supplemented with:
- Culture duration: 24-48 hours pre-editing to activate cells
Step 3: RNP Complex Formation and Delivery
- Design sgRNA targeting therapeutic locus (e.g., BCL11A erythroid enhancer for SCD)
- Complex high-fidelity SpCas9 protein with sgRNA at molar ratio 1:2
- Incubate 10-20 minutes at room temperature to form RNP complexes
- Electroporate using optimized parameters (e.g., Neon System: 1600V, 10ms, 3 pulses)
- Cell density: 1-2 × 10^6 cells per electroporation reaction [35]
Step 4: Post-Editing Culture and Quality Control
- Culture edited cells for 48 hours in expansion medium
- Assess editing efficiency: T7E1 assay or NGS (expect 30-90% indels)
- Evaluate cell viability (expect >70% recovery)
- Perform CFU assays to confirm differentiation potential [35] [36]
Step 5: Patient Conditioning and Reinfusion
- Administer myeloablative conditioning (busulfan 4-6 mg/kg)
- Thaw and wash edited cells in infusion medium
- Infuse via central venous catheter (target dose: >2 × 10^6 CD34+ cells/kg)
- Monitor for engraftment (neutrophils >500/μL by day +21, platelets >20,000/μL by day +28) [36]
In Vivo Therapy: Applications and Protocols for Solid Organ Disorders
In vivo delivery of CRISPR-Cas9 therapeutics represents a promising approach for genetic disorders affecting solid organs where ex vivo manipulation is impractical [38] [30]. This strategy requires sophisticated delivery systems to transport editing components to target tissues.
Delivery System Selection and Optimization
Table 4: Delivery Systems for In Vivo CRISPR-Cas9 Therapy
| Delivery System | Cargo Format | Advantages | Limitations | Target Tissues |
|---|---|---|---|---|
| Adeno-Associated Virus (AAV) [38] [37] | Plasmid DNA | High transduction efficiency, tissue-specific serotypes, long-term expression | Limited packaging capacity (<4.7kb), immunogenicity, potential genotoxicity | Liver, muscle, CNS, retina |
| Lipid Nanoparticles (LNP) [38] [37] | mRNA, sgRNA | Modular design, high payload capacity, transient expression, reduced immunogenicity | Primarily hepatic tropism, optimization required for other tissues | Liver, immune cells |
| Virus-Like Particles (VLP) [40] [37] | RNP | Transient activity, reduced off-target effects, modular targeting | Lower editing efficiency compared to viral vectors, complex production | Broad potential |
| Extracellular Vesicles [40] | RNP, mRNA | Native biological carrier, low immunogenicity, natural targeting | Heterogeneous composition, standardization challenges | Broad potential |
Diagram 2: Decision framework for in vivo CRISPR-Cas9 delivery system selection.
Detailed Experimental Protocol: LNP-Mediated In Vivo Delivery
Protocol: LNP-Mediated In Vivo Genome Editing for Liver Disorders
Step 1: CRISPR-Cas9 Payload Design and Preparation
- For targeted gene disruption: Format Cas9 as mRNA with co-encapsulated sgRNA
- For base editing: Format base editor as mRNA with sgRNA
- For prime editing: Format prime editor as mRNA with pegRNA [35] [37]
- Critical Consideration: Optimize codon usage for target species and incorporate modified nucleotides (e.g., N1-methylpseudouridine) to reduce immunogenicity and enhance stability [38]
Step 2: LNP Formulation and Characterization
- Utilize ionizable cationic lipids (e.g., DLin-MC3-DMA, SM-102)
- Prepare lipid mixture in ethanol:
- Ionizable lipid (50 mol%)
- Phospholipid (10 mol%)
- Cholesterol (38.5 mol%)
- PEG-lipid (1.5 mol%)
- Prepare aqueous phase containing CRISPR mRNA/sgRNA in citrate buffer (pH 4.0)
- Use microfluidic mixer for precise nanoprecipitation (flow rate ratio 3:1 aqueous:ethanol)
- Dialyze against PBS (pH 7.4) to remove ethanol and establish neutral pH [38] [37]
- Characterize LNP properties:
- Size: 70-100 nm (dynamic light scattering)
- PDI: <0.2
- Encapsulation efficiency: >90% (RiboGreen assay)
- Endotoxin: <5 EU/mL
Step 3: In Vivo Administration and Biodistribution
- Administration route: Intravenous injection via tail vein (mice) or peripheral vein (large animals)
- Dosage: 1-3 mg mRNA/kg body weight
- Critical Note: Pre-dose with antihistamines or corticosteroids if immunogenicity concerns exist
- Assess biodistribution via quantitative PCR or bioimaging
- Expected liver tropism: >80% of administered dose [38]
Step 4: Editing Efficiency and Safety Assessment
- Collect tissue samples at peak expression (24-72 hours post-injection)
- Quantify editing efficiency:
- NGS of target locus (expect 5-70% depending on target and delivery)
- Sanger sequencing with TIDE decomposition analysis
- Assess potential off-target effects:
- GUIDE-seq or CIRCLE-seq for unbiased off-target identification
- NGS of predicted off-target sites
- Monitor immune responses:
Step 5: Functional Efficacy Evaluation
- Measure phenotypic correction:
- Protein restoration (western blot, immunohistochemistry)
- Metabolic or functional assays specific to target disease
- Physiological improvement in disease models
- Assess durability of effect:
- Short-term (1-2 weeks): Peak editing
- Long-term (4-12 weeks): Stable phenotypic correction [30]
Advanced Genome Editing Tool Selection
Beyond standard CRISPR-Cas9 systems, advanced editors offer specialized capabilities for different therapeutic contexts.
Table 5: Advanced Genome Editing Systems for Therapeutic Applications
| Editing System | Mechanism | Therapeutic Advantages | Format Considerations | Ideal Applications |
|---|---|---|---|---|
| Base Editors [35] [37] | Chemical conversion of single bases without DSBs | Reduced indel formation, efficient in non-dividing cells | BE4max with additional nuclear localization signals | Point mutation corrections (e.g., sickle cell disease) |
| Prime Editors [35] [37] | Reverse transcriptase template-guided editing | Versatile (all transition/transversion mutations, small insertions/deletions), no DSB requirement | Dual-AAV system for packaging or smaller Cas9 orthologs | Diseases requiring precise sequence rewriting |
| CRISPR-Activated Transposases [37] | Transposase-mediated gene insertion | Large DNA insertion (>5kb) without host repair mechanisms | Optimized transposon donor design | Gene insertion therapies (e.g., factor VIII in hemophilia) |
The strategic selection between ex vivo and in vivo therapeutic approaches depends fundamentally on target tissue accessibility, disease pathophysiology, and available delivery technologies. Ex vivo editing offers precise control for hematopoietic disorders, while in vivo approaches present transformative potential for solid organ diseases. As delivery technologies continue to advance and editing precision improves, both strategies will expand their therapeutic reach. Future developments should focus on enhancing delivery efficiency to non-hepatic tissues, reducing immunogenicity, and improving safety profiles through more sophisticated editing systems and thorough preclinical assessment.
The treatment of monogenic hematologic disorders has been transformed by the advent of precise gene-editing technologies. Among these, the CRISPR-Cas9 system represents a paradigm shift in therapeutic development for severe inherited hemoglobinopathies, specifically sickle cell disease (SCD) and transfusion-dependent β-thalassemia (TDT). These conditions stem from mutations in the β-globin gene (HBB) on chromosome 11, leading to defective hemoglobin synthesis, chronic anemia, and significant morbidity and mortality [41] [42]. For decades, clinical management has relied primarily on supportive care, including chronic red blood cell transfusions and iron chelation therapy, with the only curative option being allogeneic hematopoietic stem cell transplantation (HSCT)—a procedure limited by donor availability and significant associated risks [43] [42].
The year 2023 marked a historic turning point, as regulatory agencies in the United Kingdom, United States, and European Union granted the first approvals for CRISPR-Cas9-based therapies, Casgevy (exagamglogene autotemcel) and Lyfgenia (lovotibeglogene autotemcel) [41] [44]. This review details the experimental protocols, mechanistic basis, and clinical data underpinning these advances, framing them within the broader thesis that CRISPR-Cas9 technology offers a viable, one-time functional cure for these debilitating genetic disorders.
Pathophysiological Basis and Therapeutic Targets
Sickle cell disease and β-thalassemia, while both β-hemoglobinopathies, have distinct pathophysiological mechanisms. SCD is caused by a point mutation (Glu6Val) in the HBB gene, resulting in the production of hemoglobin S (HbS). Under deoxygenated conditions, HbS polymerizes, causing erythrocytes to assume a sickled shape. This leads to hemolytic anemia, vaso-occlusive crises (VOCs), and end-organ damage [41] [42]. An estimated 100,000 Americans, predominantly of African descent, live with SCD [41].
In contrast, TDT results from over 350 different mutations in the HBB gene that reduce (β+) or eliminate (β0) the synthesis of the β-globin chain. This leads to an excess of unpaired α-globin chains, which form aggregates that precipitate in erythroid precursors, causing ineffective erythropoiesis and severe anemia. Patients require lifelong transfusions, with a global prevalence of carriers estimated at 80-90 million [41] [43].
A key physiological insight underpinning CRISPR therapies is the role of fetal hemoglobin (HbF). HbF (α2γ2) is the primary hemoglobin during fetal development but is largely replaced by adult hemoglobin (HbA, α2β2) after birth. However, elevated HbF levels can ameliorate the symptoms of both SCD and TDT. In SCD, HbF interferes with HbS polymerization, while in TDT, γ-globin chains can pair with excess α-globin chains to form functional hemoglobin, compensating for the lack of β-globin [45] [42]. The transcription factor BCL11A is a known repressor of γ-globin expression and HbF production. Therefore, a primary therapeutic strategy is to disrupt the BCL11A gene or its erythroid-specific enhancer to reactivate HbF synthesis [45] [46].
Approved CRISPR-Cas9 Therapeutics: Mechanisms and Protocols
Casgevy (Exagamglogene Autotemcel)
Casgevy, developed by Vertex Pharmaceuticals and CRISPR Therapeutics, is an autologous ex vivo CRISPR-Cas9 gene-edited therapy. Its mechanism of action involves the disruption of a cis-acting enhancer element within the BCL11A gene, specifically in erythroid cells, to de-repress HbF production [41] [45].
Experimental and Manufacturing Protocol:
The following workflow details the standard operating procedure for Casgevy treatment, from cell collection to patient follow-up.
Table 1: Key Reagents and Materials for Casgevy Manufacturing
| Research Reagent / Material | Function in Experimental Protocol |
|---|---|
| CD34+ Hematopoietic Stem/Progenitor Cells (HSPCs) | Autologous patient-derived cells serving as the starting material for ex vivo editing; capable of reconuting the entire hematopoietic system [45] [47]. |
| CRISPR-Cas9 Ribonucleoprotein (RNP) | Pre-complexed complex of Cas9 enzyme and synthetic guide RNA (sgRNA); directs specific cleavage in the BCL11A erythroid enhancer region. Minimizes off-target effects compared to plasmid delivery [45] [42]. |
| Electroporation System | Physical method (e.g., Nucleofector) for transiently permeabilizing cell membranes to enable efficient RNP delivery into CD34+ HSPCs with high viability [45]. |
| Myeloablative Busulfan | Conditioning chemotherapy administered to the patient prior to infusion to create marrow "space" and facilitate engraftment of the edited HSPCs [41] [44]. |
| Cell Culture Media & Cytokines | Specified serum-free media supplemented with cytokines (e.g., SCF, TPO, Fit3-L) to maintain HSPC viability and potency during the ex vivo editing process [45]. |
Lyfgenia (Lovotibeglogene Autotemcel)
Lyfgenia, developed by bluebird bio, is also an autologous cell-based gene therapy but employs a different mechanism. It uses a lentiviral vector to introduce a functional gene encoding HbAT87Q, a hemoglobin variant designed to be anti-sickling, into patient HSPCs [41] [44]. While not a CRISPR-based therapy, its concurrent approval and similar ex vivo autologous stem cell transplant protocol position it as a key pillar of the new era of gene therapy for SCD.
Quantitative Clinical Outcomes
Robust data from clinical trials demonstrate the high efficacy of these therapies, summarized in the table below.
Table 2: Summary of Efficacy Outcomes from Key Clinical Trials
| Therapy / Clinical Trial | Patient Population | Primary Efficacy Endpoint | Efficacy Results | Key Biomarker Changes |
|---|---|---|---|---|
| Casgevy (CLIMB SCD-121) [41] | SCD (n=31, age ≥12) | Freedom from severe VOC for ≥12 consecutive months | 29/31 (93.5%) of patients met the primary endpoint [41] | Robust, pancellular HbF distribution; increased total Hb |
| Casgevy (CLIMB THAL-111) [41] [43] | TDT (n=35, mean age 18.1) | Transfusion independence for ≥12 consecutive months | 32/35 (91.4%) of patients achieved transfusion independence [43] | Mean HbF: 11.9 g/dl; Mean Total Hb: 13.1 g/dl [43] |
| Lyfgenia [44] | SCD | Elimination of severe VOC (6-18 mo. post-infusion) | 94% of evaluable patients free of severe VOC [44] | Production of functional HbAT87Q |
| Reni-cel (EDIT-301) [44] | SCD (n=28) | Freedom from VOC post-infusion | 27/28 (96.4%) patients free of VOC [44] | Robust increases in HbF and total Hb |
| BEAM-101 [44] | SCD (n=17) | Increased HbF, reduced sickling | Durable increases in HbF, reductions in HbS [44] | Normalized markers of hemolysis |
The efficacy is further supported by long-term follow-up data. A systematic review of 101 patients across four trials reported a mean age of 18.1 years and showed that TDT patients achieved sustained transfusion independence, while SCD patients experienced a profound reduction or complete absence of vaso-occlusive events [43]. The elevation of HbF is a critical biomarker of success, effectively correcting the chronic anemia in TDT and preventing sickling in SCD.
Safety and Tolerability Profile
The safety profile of Casgevy is consistent with that of autologous HSCT following myeloablative conditioning with busulfan. The most common adverse events (AEs) are related to the conditioning regimen and the period of cytopenia preceding engraftment.
- Common Adverse Events: The most frequently reported AEs include febrile neutropenia, nausea, mouth ulcers, musculoskeletal pain, abdominal pain, and reduced levels of platelets and white blood cells [41].
- Serious Adverse Events: A systematic review noted that grade ≥3 adverse events were reported in 87.1% of patients, with febrile neutropenia being the most common [43]. This highlights the intensive nature of the therapy and the critical importance of managing the peri-transplant period in specialized centers.
- Engraftment and Survival: Notably, across trials, all patients achieved successful neutrophil and platelet engraftment, with no reported cases of graft failure or rejection [41] [45]. No deaths related to the therapy have been reported in the cited studies.
The diagram below illustrates the risk-benefit assessment for CRISPR-Cas9 therapy in hemoglobinopathies, contextualizing the observed safety profile.
The Evolving Therapeutic Pipeline and Future Directions
The success of first-generation therapies has accelerated the development of next-generation gene-editing approaches.
- Novel CRISPR Platforms: Reni-cel (EDIT-301) from Editas Medicine uses the CRISPR-Cas12a enzyme to edit the promoter regions of the gamma-globin genes (HBG1/HBG2) directly to increase HbF. Updated data shows 27 of 28 patients were free of vaso-occlusive events post-infusion [44].
- Base Editing: BEAM-101 from Beam Therapeutics is a base editing therapy that chemically converts a single DNA base in the HBG promoters to inhibit BCL11A binding without creating a double-strand break in DNA, potentially offering a safer profile. Recent data from 17 patients show robust increases in HbF [44].
- In Vivo Gene Editing: The field is actively pursuing in vivo delivery methods, where the CRISPR therapeutic is delivered directly into the patient via viral or non-viral vectors, eliminating the need for complex ex vivo stem cell harvesting and conditioning [48] [42].
Despite the promise, challenges remain. The high cost of therapy, complex manufacturing, and need for specialized medical centers limit accessibility [44] [48]. Furthermore, ensuring long-term safety and stability of the edits requires ongoing monitoring. However, with over 40 CRISPR-based medicines in active trials worldwide and a projected market growth to USD 26.22 billion by 2034, the future of CRISPR-based therapies for hematologic and other genetic disorders is exceptionally bright [48] [49].
The clinical approval of CRISPR-Cas9 therapies for sickle cell disease and β-thalassemia represents a landmark achievement in molecular medicine. By leveraging a sophisticated understanding of hemoglobin biology to target specific genetic loci like BCL11A, these therapies offer a one-time, potentially curative treatment for patients with severe disease. The robust clinical data confirm high efficacy, with the majority of patients achieving transfusion independence or freedom from vaso-occlusive crises, alongside a manageable safety profile primarily defined by the conditioning chemotherapy. As research progresses, next-generation editors and improved delivery systems are poised to broaden the application, improve safety, and enhance the accessibility of this revolutionary class of therapeutics, firmly establishing gene editing as a cornerstone for treating genetic disorders.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-CRISPR-associated protein 9 (Cas9) system has revolutionized the therapeutic landscape for genetic disorders, enabling precise modification of DNA sequences to correct pathogenic mutations [9]. This RNA-guided genome-editing technology has progressed from a bacterial adaptive immune system to a versatile therapeutic platform with applications across a broad spectrum of human diseases [9]. The fundamental mechanism involves a complex of the Cas9 nuclease and a single guide RNA (sgRNA) that induces double-stranded breaks at predefined genomic loci, leveraging cellular repair mechanisms to achieve gene correction, disruption, or replacement [9] [50]. For researchers and drug development professionals, understanding the current preclinical and clinical progress across different disease domains is essential for guiding therapeutic development. This application note provides a detailed analysis of CRISPR-Cas9 advancements in liver, neurological, and muscular diseases, featuring structured experimental data, methodological protocols, and visual workflow representations to facilitate research in this rapidly evolving field.
Application Note: Liver Diseases
Clinical Trial Landscape and Quantitative Outcomes
The liver has emerged as a primary target for in vivo CRISPR-Cas9 therapies due to the organ's accessibility to lipid nanoparticle (LNP) delivery systems and its central role in metabolic regulation [14] [51]. Several programs have reached advanced clinical development, demonstrating durable target protein reduction after a single administration.
Table 1: Clinical-Stage CRISPR-Based Therapies for Liver Diseases
| Therapy | Target Gene | Indication | Phase | Key Efficacy Findings | Delivery System |
|---|---|---|---|---|---|
| NTLA-2001 [14] [52] | TTR | Transthyretin Amyloidosis (ATTR) | Phase 3 | ~90% reduction in TTR protein sustained at 2 years | LNP |
| NTLA-2002 [14] [52] | KLKB1 | Hereditary Angioedema (HAE) | Phase 1/2 | 86% kallikrein reduction; 8/11 patients attack-free at 16 weeks | LNP |
| CTX310 [53] [52] | ANGPTL3 | Dyslipidemias, Familial Hypercholesterolemia | Phase 1 | Preclinical: Durable ANGPTL3 & triglyceride reduction in NHPs | LNP |
| CTX320 [53] [52] | LPA | Elevated Lipoprotein(a) | Phase 1 | Preclinical: Durable Lp(a) reduction in NHPs | LNP |
| VERVE-101 [52] | PCSK9 | Heterozygous Familial Hypercholesterolemia | Phase 1b | Trial paused; enrollment suspended | LNP |
| VERVE-102 [52] | PCSK9 | Heterozygous FH, Coronary Artery Disease | Phase 1b | Well-tolerated in initial cohorts; no serious adverse events | GalNAc-LNP |
| VERVE-201 [52] | ANGPTL3 | Homozygous FH, Refractory Hyperlipidemia | Phase 1b | First patient dosed November 2024 | GalNAc-LNP |
Experimental Protocol: LNP-MediatedIn VivoGenome Editing
Protocol Title: Lipid Nanoparticle (LNP) Formulation and In Vivo Delivery of CRISPR-Cas9 Components for Liver-Directed Gene Editing
Principle: LNPs encapsulating CRISPR-Cas9 ribonucleoprotein (RNP) complexes or mRNA/sgRNA formulations preferentially accumulate in hepatocytes following systemic administration, enabling efficient in vivo genome editing without ex vivo manipulation [14].
Materials:
- CRISPR-Cas9 Components: Cas9 mRNA or recombinant Cas9 protein; synthetic sgRNA targeting gene of interest
- Lipid Formulation: Ionizable cationic lipid, phospholipid, cholesterol, PEG-lipid (e.g., ALC-0315, DLin-MC3-DMA)
- Formulation Apparatus: Microfluidic mixer (e.g., NanoAssemblr)
- Animal Model: Wild-type or disease-model mice (e.g., C57BL/6), non-human primates (NHPs)
- Analytical Tools: Next-generation sequencing for indel analysis; ELISA for protein quantification; immunohistochemistry
Procedure:
- LNP Formulation:
- Prepare an aqueous phase containing Cas9 mRNA (50-100 µg) and sgRNA (30-60 µg) in citrate buffer (pH 4.0).
- Prepare lipid phase in ethanol containing ionizable lipid, phospholipid, cholesterol, and PEG-lipid at molar ratios optimized for hepatocyte transfection.
- Combine aqueous and lipid phases using microfluidic mixer at 1:3 volumetric flow rate ratio with total flow rate 12 mL/min.
- Dialyze formed LNPs against PBS (pH 7.4) for 24 hours to remove ethanol and buffer exchange.
- Concentrate LNPs using centrifugal filters (100 kDa MWCO) to final concentration of 1-2 mg/mL total RNA.
- Characterize LNP size (Z-average 70-100 nm) by dynamic light scattering and encapsulation efficiency (>90%) by RiboGreen assay.
In Vivo Administration:
- Administer LNP formulation via intravenous injection (tail vein in mice, peripheral vein in NHPs) at dose of 1-3 mg/kg total RNA.
- For non-human primates, utilize dose escalation study design (e.g., 0.5, 1.0, 2.0 mg/kg) with n=3-6 animals per cohort.
Efficacy Assessment:
- Collect serial blood samples at baseline, 1, 2, 4, 8, and 12 weeks post-administration for plasma protein analysis (e.g., TTR, ANGPLT3, Lp(a)).
- Sacrifice subset of animals at 2-4 weeks for liver collection and genomic DNA isolation.
- Amplify target genomic region and perform next-generation sequencing to quantify editing efficiency (% indels).
- For disease-relevant endpoints, monitor physiological parameters (e.g., lipid panels, disease symptoms) through 6-12 month follow-up.
Troubleshooting:
- Low Editing Efficiency: Optimize sgRNA design using validated algorithms; increase LNP dose while monitoring toxicity.
- Liver Toxicity: Monitor serum transaminases (ALT, AST); adjust lipid composition to improve therapeutic index.
- Immune Activation: Include immunosuppressive regimens (e.g., corticosteroids) if elevated cytokines observed.
Research Reagent Solutions for Liver-Directed Editing
Table 2: Essential Reagents for Liver-Directed CRISPR-Cas9 Research
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| CRISPR-Cas9 Components | Cas9 mRNA, recombinant Cas9 protein, synthetic sgRNA | Genome editing payload | High-purity, endotoxin-free; chemical modifications enhance sgRNA stability |
| Lipid Nanoparticles | Ionizable lipids (DLin-MC3-DMA, ALC-0315), PEG-lipids | In vivo delivery vehicle | Optimized ratios for hepatocyte tropism; scalable manufacturing |
| Animal Models | Wild-type mice/rats, non-human primates, disease-specific models (e.g., ApoE-/-) | Therapeutic efficacy & safety | Species-specific sgRNA design; relevant disease phenotypes |
| Analytical Tools | NGS for indel analysis, ELISA for protein quantification, LNP characterization equipment | Efficacy & biodistribution assessment | Multiplexed NGS panels enable simultaneous on-/off-target analysis |
Application Note: Neurological Diseases
Preclinical Advances in Neurodegenerative Disorders
CRISPR-Cas9 applications in neurological diseases primarily focus on neurodegenerative conditions such as Alzheimer's disease (AD), Parkinson's disease (PD), Huntington's disease (HD), and amyotrophic lateral sclerosis (ALS) [54] [9]. Unlike liver diseases, most neurological applications remain in preclinical development due to challenges with blood-brain barrier (BBB) penetration and efficient delivery to neuronal cells.
Key Preclinical Targets:
- Alzheimer's Disease: Targeting genes involved in amyloid-β production (APP, BACE1) and tau pathology (MAPT) [54] [9]. CRISPR-Cas9 has been used to correct ancestral mutations in presenilin 1 (PSEN1) and presenilin 2 (PSEN2) genes associated with early-onset AD [9].
- Parkinson's Disease: Focused on reducing α-synuclein (SNCA) accumulation and addressing mutations in LRRK2 and PARK2 genes [54].
- Huntington's Disease: Selective suppression of mutant huntingtin (HTT) allele while preserving wild-type function [9]. CRISPR-Cas9 has been used to suppress mHTT gene expression in mouse models [9].
- Amyotrophic Lateral Sclerosis: Targeting SOD1 and C9orf72 mutations; CRISPR screens identifying novel therapeutic targets [54].
Experimental Protocol:Ex VivoEditing of Neural Stem Cells
Protocol Title: CRISPR-Cas9-Mediated Gene Editing in Neural Stem Cells for Neurodegenerative Disease Modeling
Principle: Neural stem cells (NSCs) can be genetically modified ex vivo using CRISPR-Cas9 to introduce disease-relevant mutations or correct existing mutations, followed by differentiation into neuronal subtypes for disease modeling and therapeutic testing [54].
Materials:
- Cell Culture: Human neural stem cells (e.g., H9-derived NSCs)
- CRISPR Delivery: Electroporation system (e.g., Neon Transfection System)
- CRISPR Components: Cas9 ribonucleoprotein complex (Cas9 protein + sgRNA)
- Differentiation Media: Neural differentiation kits with specific patterning factors
- Analysis: Immunocytochemistry, Western blot, RNA-seq, electrophysiology
Procedure:
- NSC Culture Maintenance:
- Maintain NSCs in neural expansion medium on poly-ornithine/laminin-coated plates.
- Passage cells at 70-80% confluence using enzymatic dissociation.
CRISPR-Cas9 Electroporation:
- Design sgRNAs targeting gene of interest (e.g., APP, SNCA, HTT) with high on-target efficiency.
- Complex purified Cas9 protein (30 µg) with sgRNA (60 pmol) to form RNP complexes (15 min, room temperature).
- Harvest 1×10^6 NSCs, resuspend in R solution with RNP complexes.
- Electroporate using 1400V, 20ms, 1 pulse parameters.
- Plate transfected cells in recovery medium for 24 hours before selection.
Clonal Selection and Validation:
- Apply appropriate antibiotic selection 48 hours post-electroporation.
- Isolate single cells by FACS into 96-well plates.
- Expand clonal lines and validate edits by Sanger sequencing and Western blot.
Neuronal Differentiation:
- Differentiate validated NSC clones using neural differentiation protocols with specific patterning factors (e.g., BDNF, GDNF, ascorbic acid).
- For disease modeling, differentiate into relevant neuronal subtypes (cortical neurons, motor neurons, dopaminergic neurons).
Phenotypic Screening:
- Assess disease-relevant phenotypes: protein aggregation (immunostaining), neuronal function (calcium imaging, MEA), transcriptomic changes (RNA-seq).
Application Note: Muscular Diseases
Progress in Muscular Dystrophy Therapies
Duchenne Muscular Dystrophy (DMD) represents the most advanced application of CRISPR-Cas9 for muscular diseases, with multiple therapeutic approaches entering clinical development. The primary strategy involves restoring the dystrophin reading frame through exon skipping or specific mutation correction.
Table 3: CRISPR-Based Therapies for Muscular Diseases
| Therapy | Target | Approach | Development Stage | Key Findings |
|---|---|---|---|---|
| HG-302 [52] | DMD exon 51 | In vivo exon skipping using hfCas12Max | Phase 1 (First patient dosed 2024) | Compact nuclease enables single AAV delivery; preclinical efficacy in humanized mice & monkeys |
| Research Approaches [9] | Dystrophin | Ex vivo and in vivo correction | Preclinical | CRISPR-Cas9 used to fix DMD gene mutations in patient-derived cells and animal models |
Experimental Protocol: AAV-MediatedIn VivoMuscle Editing
Protocol Title: AAV Delivery of CRISPR-Cas9 Components for In Vivo Genome Editing in Skeletal Muscle
Principle: Adeno-associated virus (AAV) vectors provide efficient transduction of skeletal muscle cells, enabling durable expression of CRISPR-Cas9 components for correction of muscular dystrophy mutations [52].
Materials:
- AAV Vectors: AAV9 or other muscle-tropic serotypes encoding SaCas9 or compact Cas variants
- Animal Model: MDX mouse (DMD model) or humanized DMD models
- Delivery Method: Intravenous or intramuscular injection
- Analysis: Western blot for dystrophin, immunohistochemistry, muscle function assays
Procedure:
- Vector Design and Production:
- Select muscle-tropic AAV serotype (AAV9, AAVrh74) with high skeletal muscle tropism.
- For compact Cas variants (SaCas9, Cas12Max), package entire editing system in single vector.
- For SpCas9, utilize dual-vector system (one for Cas9, one for sgRNA).
- Produce AAV vectors using triple transfection in HEK293 cells, purify by iodixanol gradient.
In Vivo Administration:
- Administer AAV via tail vein injection (systemic) or intramuscular injection (local) in DMD model mice.
- Use dose range of 1×10^13 to 1×10^14 vg/kg for systemic delivery.
- Include control groups receiving empty vector or sham injection.
Efficacy Assessment:
- Monitor dystrophin expression by Western blot and immunohistochemistry at 4, 8, and 12 weeks post-injection.
- Assess functional improvement by grip strength, treadmill exhaustion, and forced wire hang tests.
- Evaluate histological improvements in muscle fiber architecture and reduction in fibrosis.
Safety Evaluation:
- Assess off-target editing in top predicted off-target sites by NGS.
- Monitor immune responses to Cas9 and AAV capsid.
- Evaluate overall animal health and muscle histology.
Research Reagent Solutions for Muscular Disease Applications
Table 4: Essential Reagents for Muscle-Directed CRISPR-Cas9 Research
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| AAV Vectors | AAV9, AAVrh74, engineered capsids | In vivo muscle delivery | Serotype determines tropism; compact Cas variants enable single-vector delivery |
| Animal Models | MDX mice, humanized DMD models | Therapeutic efficacy testing | Species-specific sgRNA design; functional outcomes crucial |
| Functional Assays | Grip strength test, treadmill, electrophysiology | Functional improvement assessment | Standardized protocols enable cross-study comparisons |
| Histological Tools | Dystrophin antibodies, H&E staining, Masson's trichrome | Structural improvement assessment | Quantitative image analysis enhances objectivity |
Comparative Analysis and Future Directions
The application of CRISPR-Cas9 across liver, neurological, and muscular diseases demonstrates distinct technological challenges and developmental timelines. Liver-directed therapies have progressed most rapidly to clinical validation, benefiting from efficient LNP delivery systems and accessible biomarkers for monitoring therapeutic response [14]. Neurological applications remain predominantly preclinical due to formidable delivery barriers, though innovative approaches using engineered AAV capsids and focused ultrasound are emerging to enhance blood-brain barrier penetration [54]. Muscular diseases represent an intermediate case, where AAV delivery has enabled promising preclinical results and initial clinical translation, particularly for DMD [52].
The field is evolving toward next-generation editing technologies including base editing and prime editing, which offer enhanced precision by avoiding double-strand breaks and reducing off-target effects [55]. Prime editing, in particular, has demonstrated proof-of-concept for sickle cell disease in animal models and received FDA clearance for clinical trials in chronic granulomatous disease [55]. For all disease areas, delivery remains the primary bottleneck, with ongoing research focused on improving tissue specificity, editing efficiency, and safety profiles of CRISPR-Cas9 delivery platforms.
Table 5: Technology Readiness Level Across Disease Domains
| Disease Domain | Delivery Challenges | Lead Delivery Platform | Clinical Stage | Key Limitations |
|---|---|---|---|---|
| Liver Diseases | Low (excellent LNP uptake) | LNP | Phase 3 (multiple programs) | Primarily suitable for liver-expressed targets |
| Neurological Diseases | High (blood-brain barrier) | AAV, ex vivo approaches | Preclinical | Limited biodistribution; immune concerns |
| Muscular Diseases | Medium (efficient with AAV) | AAV (serotypes 9, rh74) | Phase 1 | Immune response to AAV; payload size limitations |
CRISPR-Cas9 technology has established a robust therapeutic platform with applications spanning diverse genetic disorders. Liver-directed therapies lead clinical translation with multiple programs in advanced trials, demonstrating durable target protein reduction after single administrations [53] [14]. Neurological and muscular applications, while earlier in development, show substantial preclinical promise with continued innovation in delivery systems and editing precision. The field is rapidly evolving toward next-generation editors that offer enhanced safety profiles, while parallel advances in delivery technologies promise to expand the therapeutic scope to additional tissues and disease targets. For research and drug development professionals, understanding these domain-specific advances, methodological approaches, and reagent solutions provides a foundation for advancing new CRISPR-based therapeutics through preclinical development and into clinical application.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 system has revolutionized biological research and therapeutic development by enabling precise genome editing. However, the safe and efficient delivery of CRISPR components (plasmid DNA, mRNA, or ribonucleoprotein) to target cells in living organisms remains a significant translational challenge [56] [57]. Delivery systems must navigate complex biological barriers, protect their cargo from degradation, achieve specific tissue targeting, and minimize off-target effects and immune responses [58] [59]. This application note provides a comprehensive overview of viral and non-viral delivery platforms for in vivo CRISPR-Cas9 gene editing, with structured experimental data, detailed protocols, and essential resource guidance for therapeutic development.
Comparative Analysis of Delivery Systems
The selection of an appropriate delivery vector is critical for successful in vivo gene editing. The table below provides a quantitative comparison of the primary viral and non-viral systems.
Table 1: Quantitative Comparison of CRISPR-Cas9 Delivery Systems for In Vivo Applications
| Delivery System | Payload Capacity | Editing Efficiency | Immune Response | Integration Risk | Stability/Storage | Key Applications |
|---|---|---|---|---|---|---|
| AAV | ~4.7 kb [60] | Moderate [61] | Low [61] [62] | Low (mostly episomal) [61] [59] | Moderate (-80°C for ~1 year) [61] | In vivo delivery to CNS, retina, liver, muscle [61] [63] [62] |
| Lentivirus | 8-10 kb [59] | High [61] | Moderate [61] | Moderate (WT virus insertional mutagenesis) [61] | Low (-80°C for ~6 months) [61] | In vitro and ex vivo editing (e.g., CAR-T cells) [61] |
| Lipid Nanoparticles (LNPs) | High [56] [64] | 70-97% (in specific models) [59] | Minimal [59] | None [59] | Variable; formulation-dependent | Liver-targeted in vivo editing, mRNA delivery [56] [59] |
| Polymer-based Nanoparticles | High [56] [57] | Variable; can be high with optimized polymers [56] [57] | Minimal to low [56] [57] | None [57] | Variable; formulation-dependent | Experimental in vivo delivery to various tissues [56] [64] |
Viral Vector Delivery Systems
Adeno-Associated Virus (AAV) Vectors
AAVs are among the most widely used viral vectors for in vivo CRISPR delivery due to their low immunogenicity, high transduction efficiency in non-dividing cells, and the availability of serotypes with distinct tissue tropisms [60] [62].
Table 2: AAV Serotypes and Their Tissue Tropisms
| AAV Serotype | Primary Tissue Tropism | Recommended Promoters | Applications in CRISPR Delivery |
|---|---|---|---|
| AAV8 | Liver [60] | TBG, ApoE [60] | Treatment of liver-specific metabolic disorders |
| AAV9 | Heart, muscle, CNS [60] [62] | CAG, EF1α [60] | Targeting CNS disorders (e.g., Alzheimer's, Parkinson's) [62] |
| AAV2 | Retina [60] [63] | Synapsin, CaMKIIα [60] | Retinal disease therapy (e.g., Leber congenital amaurosis) [63] |
Protocol 3.1.1: Dual AAV Strategy for Delivering Large CRISPR Constructs
Background: The limited packaging capacity of AAV (~4.7 kb) presents a challenge for delivering the commonly used Streptococcus pyogenes Cas9 (SpCas9, ~4.2 kb) along with gRNA and regulatory elements. A dual AAV system overcomes this by splitting components [60].
Materials:
- Transfer Plasmids: AAV plasmid containing SaCas9 (or split SpCas9) and a separate AAV plasmid containing gRNA expression cassette.
- Packaging System: AAV rep/cap plasmid (select serotype based on target tissue), adenoviral helper plasmid.
- Cell Line: HEK293T cells for virus production.
- Purification & Titration Kits: DNase I, RNase A, qPCR kit for genome titer determination.
Method:
- Vector Design and Cloning:
- For SaCas9 (3.2 kb): Clone SaCas9 driven by a tissue-specific promoter (e.g., TBG for liver) into one AAV transfer plasmid. Clone the gRNA expression cassette (U6 promoter) into a second AAV plasmid [60].
- For SpCas9 splitting: Use intein-based splitting strategies to divide SpCas9 into N-terminal and C-terminal fragments, each packaged into separate AAVs [60].
Virus Production (Triple Transfection in HEK293T cells):
- Day 1: Seed HEK293T cells at 70% confluency in cell factories or multi-layer flasks.
- Day 2: Co-transfect cells with three plasmids: i) AAV transfer plasmid (for Cas9 OR gRNA), ii) AAV rep/cap plasmid (providing serotype-specific capsid), and iii) adenoviral helper plasmid using PEI transfection reagent.
- Day 5: Harvest cells and supernatant. Pellet cells by centrifugation and lyse via freeze-thaw cycles. Purify AAV vectors from the lysate using iodixanol density gradient centrifugation or affinity chromatography.
Vector Purification and Quality Control:
- Concentrate purified AAV using centrifugal filters.
- Determine genomic titer (vg/mL) via qPCR with primers targeting the ITR region.
- Assess purity via SDS-PAGE and silver staining.
In Vivo Administration and Analysis:
- Administer a 1:1 mixture of the two AAVs (total dose ~1x10^12 - 1x10^13 vg per animal) to adult mice via intravenous (for systemic delivery) or intracranial (for CNS delivery) injection [62].
- After 4-6 weeks, analyze editing efficiency by extracting genomic DNA from the target tissue and performing T7E1 assay or next-generation sequencing of the target locus.
Lentiviral Vectors
Lentiviral vectors (LVs) offer advantages of a larger payload capacity (8-10 kb) and stable integration, making them suitable for delivering larger CRISPR constructs or for applications requiring long-term expression [61] [59]. However, the risk of insertional mutagenesis limits their in vivo use. Non-integrating lentiviral vectors (NILVs) provide a safer alternative by enabling transient expression with minimal integration [61] [59].
Protocol 3.2.1: Production of Non-Integrating Lentiviral Vectors (NILVs) for CRISPR Delivery
Background: NILVs are engineered with mutations in the integrase enzyme (e.g., D64V mutation), leading to circularization of the viral DNA in the nucleus and transient gene expression, thereby reducing the risk of insertional mutagenesis [61].
Materials:
- Packaging Plasmids: psPAX2-D64V (integrase-deficient), pMD2.G (VSV-G envelope).
- Transfer Plasmid: LVX vector containing Cas9 and gRNA expression cassettes.
- Cell Line: HEK293T cells.
- Reagents: Polyethylenimine (PEI), PEG-it Virus Precipitation Solution, 0.45 μm PVDF filter.
Method:
- Day 1: Seed HEK293T cells in 10 cm dishes to reach 70-80% confluency at the time of transfection.
- Day 2: Triple Transfection:
- Prepare DNA mix: 10 μg LVX-transfer plasmid, 7.5 μg psPAX2-D64V, 5 μg pMD2.G in Opti-MEM.
- Add PEI (60 μL of 1 mg/mL stock), vortex, incubate 15 min at room temperature.
- Add complex dropwise to cells.
- Day 3: Replace medium 8-12 hours post-transfection with fresh DMEM + 10% FBS.
- Day 4 & 5: Harvest supernatant at 48 and 72 hours post-transfection. Pool harvests, filter through a 0.45 μm PVDF filter.
- Concentrate virus via ultracentrifugation (50,000 x g for 2 hours) or using PEG-it solution per manufacturer's instructions.
- Resuspend pellet in PBS, aliquot, and store at -80°C. Determine titer via p24 ELISA or by transducing HEK293T cells and quantifying integration-deficient vector copies by qPCR.
Non-Viral Nanoparticle Delivery Systems
Lipid Nanoparticles (LNPs)
LNPs have emerged as a leading non-viral platform for in vivo delivery of CRISPR components, building on their success with mRNA vaccines [56] [59]. They offer high payload capacity, low immunogenicity, and no risk of genomic integration [57] [59].
Protocol 4.1.1: Formulation of LNPs for CRISPR RNP Delivery
Background: Direct delivery of preassembled Cas9 ribonucleoprotein (RNP) complexes enables rapid editing with reduced off-target effects and transient activity. LNPs protect the RNP from proteolytic degradation and facilitate cellular uptake [61] [57].
Materials:
- Lipids: Ionizable lipid (e.g., DLin-MC3-DMA), DSPC, Cholesterol, DMG-PEG2000.
- Aqueous Phase: 25 mM Sodium acetate buffer, pH 4.0.
- Organic Phase: Ethanol.
- CRISPR RNP: Precomplexed Cas9 protein and sgRNA (incubate at 37°C for 10 min before use).
- Equipment: Microfluidic mixer (e.g., NanoAssemblr).
Method:
- Prepare Lipid Mix:
- Dissolve lipids in ethanol at molar ratio: Ionizable lipid (50%), DSPC (10%), Cholesterol (38.5%), DMG-PEG2000 (1.5%). Total lipid concentration: 10-20 mM.
- Prepare Aqueous Phase:
- Dialyze precomplexed Cas9 RNP into sodium acetate buffer. Final concentration: 20-50 μg/μL.
- Formulate LNPs via Microfluidic Mixing:
- Set total flow rate (TFR) to 12 mL/min and flow rate ratio (FRR) to 3:1 (aqueous:organic).
- Load lipid mix (ethanol) and RNP solution (aqueous buffer) into separate syringes.
- Mix streams in the microfluidic device. Collect LNP formulation in a vial.
- Dialyze and Characterize:
- Dialyze against 1X PBS (pH 7.4) for 2 hours to remove ethanol and buffer exchange.
- Filter through a 0.22 μm sterile filter.
- Measure particle size and PDI via dynamic light scattering (target: 80-100 nm). Determine encapsulation efficiency using Ribogreen assay.
Table 3: Key Research Reagent Solutions for CRISPR Delivery Development
| Reagent/Category | Specific Examples | Function & Application Notes |
|---|---|---|
| CRISPR Enzymes | SpCas9, SaCas9, Cas12f [60] [56] | SpCas9 is standard but large; SaCas9 and ultra-small Cas12f are preferred for AAV packaging due to smaller size [60]. |
| Viral Packaging Systems | AAVpro Helper Free System (Takara), Lenti-X Packaging Single Shots (Clontech) | Simplify production of high-titer, clinical-grade AAV and lentiviral vectors with reduced safety concerns. |
| LNP Formulation Components | Ionizable lipids (DLin-MC3-DMA), PEGylated lipids (DMG-PEG2000) [56] [59] | Core components for assembling stable LNPs; ionizable lipids enable endosomal escape, PEG-lipids enhance stability and circulation time. |
| Tissue-Specific Promoters | TBG (liver), Synapsin (neuron), MHCK7 (muscle) [60] | Restrict Cas9/gRNA expression to target tissues, minimizing off-target editing and potential toxicity. |
| gRNA Cloning & Production | U6 promoter vectors, in vitro transcription kits | U6 is a strong Pol III promoter for gRNA expression. Commercial kits enable rapid production of sgRNAs for RNP formation. |
| Analytical & QC Tools | T7 Endonuclease I assay, NGS for off-target analysis, ddPCR for viral titering | Critical for quantifying editing efficiency (on-target and off-target) and determining vector potency and quality. |
The optimal delivery system for in vivo CRISPR-Cas9 gene editing is highly dependent on the specific therapeutic application, target tissue, and desired duration of editing. Viral vectors like AAV offer high transduction efficiency and tissue specificity, while non-viral systems like LNPs provide superior safety profiles and larger cargo capacity. The protocols and resources outlined in this application note provide a foundational framework for researchers to develop and optimize CRISPR-based therapies for genetic disorders. Future directions will focus on engineering next-generation vectors with enhanced tissue specificity, reduced immunogenicity, and the ability to deliver increasingly sophisticated CRISPR machinery such as base and prime editors [64] [65].
The advent of CRISPR-Cas9 genome editing has ushered in a transformative era for therapeutic intervention in genetic disorders, moving from theoretical concept to clinical reality [4]. This case study examines the landmark first-in-human trial of CTX310, a CRISPR-Cas9 therapy targeting lipid disorders, which demonstrated unprecedented efficacy in reducing LDL cholesterol and triglycerides by nearly 50% with a single administration [66] [67]. This development represents a significant advancement in the application of gene editing technologies for common, complex diseases beyond rare monogenic disorders, particularly in the field of cardiovascular medicine where long-term medication adherence presents a major clinical challenge [68]. The therapy exemplifies the strategic shift from conventional protein-targeted approaches to direct genomic modification, offering the potential for a one-time treatment that durably addresses the underlying genetic contributors to dyslipidemia [69].
Experimental Data and Results
The Phase I clinical trial for CTX310 employed an open-label, ascending-dose design to evaluate the safety, tolerability, and preliminary efficacy of this investigational CRISPR-Cas9 therapy in patients with refractory lipid disorders [66] [68].
Study Population Characteristics
The trial enrolled 15 adult participants aged 18-75 years (median age 53; 87% male) with various difficult-to-treat lipid conditions despite maximal tolerated lipid-lowering therapy [66] [68]. The cohort included patients with heterozygous familial hypercholesterolemia (n=5), homozygous familial hypercholesterolemia (n=1), mixed dyslipidemia (n=1), and severe hypertriglyceridemia (n=2) [66]. Baseline lipid parameters reflected the refractory nature of their conditions, with mean directly measured LDL cholesterol level of 155 mg/dL and median triglyceride level of 192 mg/dL [68]. Most participants were receiving background lipid-lowering therapy including statins (60%), ezetimibe (53%), or PCSK9 inhibitors (40%) [68].
Efficacy Outcomes
The efficacy results demonstrated substantial, dose-dependent reductions in key lipid parameters within two weeks of treatment, with effects sustained through at least 60 days of follow-up [66] [67]. The table below summarizes the percentage reductions in lipid parameters observed across different dose levels:
Table 1: Lipid Parameter Reductions Following CTX310 Administration
| Dose Level (mg/kg) | LDL Cholesterol Reduction (%) | Triglyceride Reduction (%) | ANGPTL3 Reduction (%) | Non-HDL Cholesterol Reduction (%) |
|---|---|---|---|---|
| 0.1 | Minimal change | Minimal change | +9.6 | Minimal change |
| 0.3 | Minimal change | Minimal change | +9.4 | Minimal change |
| 0.6 | ~30% | ~35% | -32.7 | ~35% |
| 0.7 | ~45% | ~50% | -79.7 | ~45% |
| 0.8 | 48.9 | 55.2 | -73.2 | 49.8 |
At the highest dose (0.8 mg/kg), reductions of up to 60% in both LDL cholesterol and triglycerides were observed in some participants [66]. Additionally, significant reductions were noted in other atherogenic lipids, including apolipoprotein B (33.4%) and HDL cholesterol (24.1%) [68].
Safety Profile
The trial demonstrated a generally favorable safety profile for CTX310 with no dose-limiting toxic effects or treatment-related serious adverse events reported [68]. Key safety observations included:
- Infusion-related reactions occurred in three participants (fever, nausea, back pain) at the 0.6 and 0.8 mg/kg doses, which resolved with temporary infusion interruption and symptomatic medication [66] [68]
- One participant with baseline elevated liver enzymes experienced a transient increase in aminotransferases (3-5 times upper limit of normal) that peaked at day 4 and returned to baseline by day 14 without clinical sequelae [68]
- One patient with a history of familial hypercholesterolemia and multiple cardiovascular interventions died suddenly 179 days after receiving the lowest dose (0.1 mg/kg), which was not considered treatment-related by investigators [68]
- No evidence of off-target editing effects was reported within the follow-up period, though long-term monitoring continues as per FDA recommendations for CRISPR-based therapies [66]
Biological Mechanism and Therapeutic Approach
CTX310 employs a sophisticated mechanism that combines advanced genome editing technology with insights from human genetics to achieve therapeutic effects [68].
ANGPTL3 as a Therapeutic Target
Angiopoietin-like protein 3 (ANGPTL3) is a hepatocyte-derived protein that inhibits lipoprotein lipase and endothelial lipase, key enzymes involved in the metabolism of triglyceride-rich lipoproteins and HDL cholesterol [68]. The selection of ANGPTL3 as a therapeutic target is grounded in human genetic evidence demonstrating that individuals born with natural loss-of-function mutations in the ANGPTL3 gene exhibit lifelong reductions in LDL cholesterol and triglyceride levels, with a corresponding reduced risk of atherosclerotic cardiovascular disease without apparent harmful effects [66] [68]. This human validation made ANGPTL3 an ideal candidate for a gene-editing therapeutic approach aimed at replicating this protective phenotype.
CRISPR-Cas9 Therapeutic Construct
CTX310 consists of a lipid nanoparticle (LNP) formulation encapsulating two key components [68]:
- CRISPR-Cas9 messenger RNA encoding the Cas9 nuclease
- Single guide RNA (sgRNA) specifically designed to target the ANGPTL3 gene in hepatocytes
The LNP delivery system exhibits natural tropism for hepatocytes following intravenous administration, facilitating efficient delivery of the CRISPR components to the target tissue [14]. This delivery approach represents a significant advancement in in vivo gene editing, eliminating the need for ex vivo manipulation of cells.
Figure 1: Mechanism of Action of CTX310 CRISPR Therapy
Gene Editing Process
Upon delivery to hepatocytes, the therapeutic components facilitate a precise genome editing process [70] [4]:
- Cas9 protein translation from the delivered mRNA
- Formation of ribonucleoprotein complex between Cas9 and the sgRNA
- Identification of target sequence in the ANGPTL3 gene guided by sgRNA complementarity
- Cas9-mediated double-strand DNA break at the target site
- Cellular DNA repair via non-homologous end joining (NHEJ), introducing insertion/deletion mutations that disrupt ANGPTL3 function
This process results in durable reduction of ANGPTL3 protein production, thereby releasing the inhibition of lipoprotein lipase and promoting clearance of atherogenic lipoproteins from circulation [68].
Experimental Protocol
The clinical implementation of CTX310 required meticulous protocol development and execution, representing a model for future in vivo CRISPR-based therapies.
Therapeutic Administration Protocol
Table 2: CTX310 Administration Protocol
| Protocol Step | Specifications | Rationale |
|---|---|---|
| Patient Pre-screening | Eligibility confirmation: elevated lipids despite maximal tolerated therapy; exclusion of significant hepatic impairment | Ensures appropriate patient selection and risk mitigation |
| Pre-medication | Corticosteroids and antihistamines 30-60 minutes pre-infusion | Prevents or minimizes infusion-related reactions |
| Dose Preparation | CTX310 reconstitution per manufacturer specifications; five dose levels (0.1, 0.3, 0.6, 0.7, 0.8 mg/kg) | Ensures accurate dosing and maintains product integrity |
| Infusion Administration | Single intravenous infusion over maximum 4.5 hours; gradual rate escalation with monitoring | Allows for controlled administration and early reaction detection |
| In-Infusion Monitoring | Vital signs every 30 minutes; assessment for infusion reactions | Enables prompt intervention if adverse events occur |
| Post-Infusion Observation | Minimum 2-hour monitoring post-completion; longer if reactions occurred | Ensures patient stability before discharge |
Assessment and Monitoring Schedule
The trial incorporated comprehensive monitoring aligned with FDA recommendations for CRISPR-based therapies [66]:
- Lipid parameters: Measured at baseline, days 15, 30, 60, and every 30 days thereafter
- ANGPTL3 levels: Quantified at same intervals as lipid measurements to confirm target engagement
- Liver function tests: Assessed at baseline, days 1, 2, 4, 7, 15, 30, and 60 to monitor for hepatotoxicity
- Immunological assessments: Evaluation of immune responses to Cas9 or LNPs
- Long-term safety monitoring: Planned for 15 years post-administration as per FDA guidance for gene therapies
All participants had at least 60 days of safety follow-up for the primary analysis, with ongoing monitoring continuing [66].
The Scientist's Toolkit: Research Reagent Solutions
The development and implementation of CRISPR-based therapies like CTX310 requires specialized reagents and materials that meet rigorous regulatory standards for clinical application [71].
Table 3: Essential Research Reagents for CRISPR Therapeutic Development
| Reagent/Material | Specifications | Application in CTX310 Development |
|---|---|---|
| Guide RNA (gRNA) | High-purity, synthetic sgRNA with GMP-grade manufacturing; sequence specificity verified for ANGPTL3 target | Directs Cas9 to specific genomic locus with minimal off-target potential [71] |
| Cas9 mRNA | Modified nucleotide composition to reduce immunogenicity; codon-optimized for human hepatocyte expression | Encodes the Cas9 nuclease enzyme; LNP-protected for efficient delivery [68] |
| Lipid Nanoparticles (LNPs) | Optimized lipid composition for hepatocyte tropism; stable encapsulation of nucleic acid payload | Protects CRISPR components and enables targeted delivery to liver [14] [68] |
| Analytical Tools for Off-Target Assessment | Computational prediction algorithms; next-generation sequencing for genome-wide off-target screening | Verifies specificity of gene editing and identifies potential unintended cleavage sites [71] |
| Cell-Based Assay Systems | Primary human hepatocytes; hepatocyte-like cells derived from iPSCs | Enables in vitro assessment of editing efficiency and functional effects prior to clinical trials [71] |
| Animal Models | Mice with humanized ANGPTL3 locus; non-human primates for toxicology studies | Provides preclinical proof-of-concept and safety data for IND submission [71] |
The transition from research-grade to clinically applicable reagents requires strict adherence to Good Manufacturing Practice (GMP) guidelines and comprehensive documentation for regulatory submissions [71]. For CRISPR-based therapeutics, the FDA typically recommends using high-quality gRNAs with extensive documentation to support their purity and appropriate Good Laboratory Practice (GLP) for nonclinical studies [71].
The successful first-in-human trial of CTX310 represents a paradigm shift in the therapeutic approach to lipid disorders, demonstrating that a single administration of CRISPR-Cas9 therapy can achieve substantial and sustained reductions in atherogenic lipids [66] [67]. This proof-of-concept extends the application of gene editing beyond rare monogenic disorders to common conditions affecting millions worldwide, potentially offering a solution to the challenge of long-term medication adherence in chronic diseases [68].
Future development will require larger Phase 2 and 3 trials with more diverse patient populations and longer follow-up to fully establish the safety and efficacy profile of this approach [66]. The transient liver enzyme elevations observed in one participant and the serious liver injury reported in a trial of a different CRISPR therapy for transthyretin amyloidosis highlight the importance of vigilant safety monitoring as these therapies advance [68]. Furthermore, the economic considerations of widespread implementation of high-cost gene therapies will need to be addressed through innovative payment models and careful patient selection [14].
As the field progresses, CRISPR-based interventions for cardiovascular disease may expand to target multiple genetic pathways simultaneously, potentially offering combination approaches that address complex polygenic risk factors [68]. The CTX310 trial establishes a foundational framework for such future developments, marking a significant milestone in the evolution of precision genetic medicine for common chronic diseases.
Navigating Technical Hurdles: Off-Target Effects, Delivery, and Safety Optimization
The CRISPR-Cas9 system has revolutionized genetic research and holds transformative potential for treating genetic disorders. This powerful technology functions as precise molecular scissors, using a guide RNA (gRNA) to direct the Cas9 nuclease to a specific DNA sequence, where it creates a double-strand break (DSB) [72]. The cell's subsequent repair of this break via non-homologous end joining (NHEJ) or homology-directed repair (HDR) enables targeted gene disruption, correction, or insertion [73] [74]. However, a significant challenge impedes its seamless transition to the clinic: off-target effects [75] [76]. These occur when the Cas9 nuclease cleaves DNA at sites other than the intended target, leading to unintended mutations that can compromise experimental results and, critically, pose serious safety risks in therapeutic contexts, including the potential disruption of essential genes or activation of oncogenes [77] [78]. This application note defines the challenge of CRISPR-Cas9 off-target effects within the context of genetic disorder therapy research, providing a detailed overview of their mechanisms, methods for their quantification, and strategies for their mitigation.
Mechanisms and Consequences of Off-Target Editing
Molecular Mechanisms Leading to Off-Target Cleavage
Understanding the origins of off-target activity is the first step toward its control. Several factors contribute to unintended cleavage by the CRISPR-Cas9 system:
- Mismatch Tolerance: The Cas9-sgRNA complex can tolerate up to 3 mismatches between the guide RNA and the target DNA sequence, allowing it to bind and cleave sites with partial complementarity [73] [74]. Mismatches in the "seed region" (the 8-12 nucleotides proximal to the Protospacer Adjacent Motif or PAM) are particularly consequential for off-target activity [77].
- Role of the PAM Sequence: Cleavage requires recognition of a short PAM sequence (e.g., 5'-NGG-3' for standard S. pyogenes Cas9) adjacent to the target site. While this requirement adds a layer of specificity, off-target cleavage can occur at sites with canonical PAMs and, in some cases, non-canonical PAMs [77].
- Cellular Environment Factors: The physical accessibility of the DNA, governed by chromatin structure and epigenetic modifications (e.g., histone marks, DNA methylation), significantly influences Cas9 binding and cleavage efficiency. Regions of open chromatin are generally more susceptible to both on-target and off-target editing [79] [78].
- sgRNA and Cas9-Specific Factors: The sequence and structure of the sgRNA itself are critical. Guides with high GC content or those targeting repetitive genomic regions are more prone to promiscuous activity [77]. Furthermore, the duration and level of Cas9 expression in cells correlate with the likelihood of off-target events [78].
Functional Consequences of Unintended Edits
The downstream effects of off-target mutations are a primary concern for therapeutic development:
- Genomic Instability: Unintended DSBs can lead to small insertions or deletions (indels), as well as larger structural variations such as chromosomal translocations, inversions, and large deletions (up to thousands of base pairs) [80] [78].
- Oncogenic Risk: Unintended mutations in genes controlling cell growth, such as tumor suppressor genes or oncogenes, could theoretically initiate carcinogenesis, representing a critical safety hurdle for in vivo therapies [77].
- Persistence in Cell Therapies: In ex vivo edited cell therapies (e.g., hematopoietic stem and progenitor cells - HSPCs), studies show that large deletion events induced by Cas9 cutting can persist through cell differentiation, carrying the risk of altered biological function in the final therapeutic product [80].
- Germline Considerations: For potential germline editing applications, off-target mutations would raise profound ethical concerns as they could become heritable, affecting future generations [77].
Quantitative Profiling of Off-Target Effects: Methods and Protocols
Accurately quantifying the scope and frequency of off-target effects is essential for profiling the safety of a CRISPR-based therapeutic candidate. The following section outlines key methodologies, which are often used in combination for a comprehensive risk assessment.
In silico Prediction Tools
Computational prediction represents the first and most accessible line of screening for potential off-target sites. These tools scan a reference genome to identify loci with sequence similarity to the sgRNA.
Table 1: Classification of In silico Off-Target Prediction Tools
| Tool Category | Representative Tools | Key Features | Primary Utility |
|---|---|---|---|
| Alignment-Based | Cas-OFFinder, CasOT, FlashFry, Crisflash [73] [74] [78] | Exhaustively searches for sites with user-defined mismatches and bulges; fast and customizable. | Initial screening to identify all potential off-target candidate loci. |
| Scoring-Based | MIT Scoring Model, CCTop, CROP-IT, CFD Score [73] [74] | Applies weighting or machine learning models to rank off-target sites by likelihood of cleavage. | Prioritizing the most probable off-target sites for experimental validation. |
| Deep Learning & Multi-Modal | DeepCRISPR, Elevation, DNABERT-Epi [73] [79] | Integrates sequence data with epigenetic features (e.g., chromatin accessibility) for improved accuracy. | State-of-the-art prediction that accounts for the cellular environment. |
Application Note: While indispensable, in silico tools primarily predict sgRNA-dependent off-targets and may miss events caused by cellular factors or unusual sgRNA conformations. Their predictions must be validated experimentally [74] [78].
A novel approach, DNABERT-Epi, demonstrates the next generation of prediction tools. It integrates a deep learning model pre-trained on the human genome (DNABERT) with epigenetic features such as H3K4me3, H3K27ac, and ATAC-seq data. This integration of sequence context and chromatin accessibility has been shown to significantly enhance predictive accuracy [79].
Experimental Detection Protocols
Experimental methods are required to identify the full spectrum of off-target effects, including sgRNA-independent events. These can be broadly categorized into cell-free and cell-based methods.
Protocol 1: CIRCLE-seq (Cell-free)
CIRCLE-seq is a highly sensitive in vitro method for genome-wide identification of off-target sites.
Principle: Genomic DNA is sheared, circularized, and incubated with Cas9-sgRNA ribonucleoprotein (RNP). Cleaved DNA fragments are linearized, amplified, and sequenced, providing a comprehensive profile of Cas9's cleavage propensity without cellular constraints [73] [74] [78].
Detailed Workflow:
- DNA Preparation: Extract high-molecular-weight genomic DNA from relevant cell types (e.g., HEK293, primary HSPCs).
- Fragmentation & Circularization: Shear the gDNA to ~300 bp fragments using ultrasonication. Ligate the fragments into circular molecules using a DNA circligase.
- Cas9 RNP Cleavage: Incubate the circularized DNA library with pre-complexed Cas9-sgRNA RNP. The RNP cleaves its target sites, linearizing the corresponding circles.
- Library Preparation for Sequencing: Treat the reaction with an exonuclease to degrade non-circular (non-cleaved) DNA. Amplify the linearized, cleaved fragments via PCR, adding sequencing adapters and barcodes.
- Sequencing & Analysis: Perform high-throughput sequencing (Illumina). Map the sequenced reads back to the reference genome to identify all cleavage sites.
Advantages & Limitations:
- Advantages: Extremely high sensitivity; low false-positive rate from background DSBs; requires minimal cellular material.
- Limitations: Lacks cellular context (chromatin, DNA repair machinery); may overpredict off-targets that do not occur in live cells [74] [78].
Protocol 2: GUIDE-seq (Cell-based)
GUIDE-seq is a robust, cell-based method that directly captures DSBs in living cells.
Principle: A short, double-stranded oligodeoxynucleotide (dsODN) tag is co-delivered with the Cas9-sgRNA complex into cells. This tag is integrated into DSBs as they occur. The genomic locations of these breaks are then identified by sequencing the tagged sites [74] [78].
Detailed Workflow:
- Cell Transfection/Electroporation: Co-deliver the Cas9 (plasmid, mRNA, or RNP) and sgRNA along with the GUIDE-seq dsODN tag into the target cells.
- Tag Integration & DNA Extraction: Allow cells to recover for 48-72 hours to permit DSB generation and tag integration. Extract genomic DNA.
- Library Preparation: Fragment the gDNA and perform an enrichment step (e.g., using biotinylated primers against the dsODN tag) to pull down tag-integrated fragments. Prepare a sequencing library from the enriched fragments.
- Sequencing & Data Analysis: Sequence the library (Illumina). Bioinformatics pipelines are used to identify genomic locations flanking the integrated tag, revealing the landscape of Cas9-induced DSBs.
Advantages & Limitations:
- Advantages: Performed in a cellular context with native chromatin; genome-wide and unbiased; higher validation rate than cell-free methods.
- Limitations: Dependent on transfection/electroporation efficiency; the dsODN tag can be toxic to some primary cells [74].
Table 2: Comparison of Key Experimental Off-Target Detection Methods
| Method | Type | Key Principle | Sensitivity | Key Considerations |
|---|---|---|---|---|
| CIRCLE-seq [73] [74] | Cell-free | Cleavage of circularized genomic DNA in vitro. | Very High (detects low-frequency events) | High sensitivity but lacks cellular context. |
| GUIDE-seq [74] [78] | Cell-based | Capture of DSBs via integration of a dsODN tag. | High | Works in living cells; tag toxicity can be an issue. |
| Digenome-seq [73] [74] | Cell-free | Whole-genome sequencing of Cas9-digested purified DNA. | High | Requires high sequencing coverage; expensive. |
| SITE-seq [74] [78] | Cell-free | Biotin-based enrichment of Cas9-cleaved ends from gDNA. | Moderate | Lower background; minimal read depth required. |
| LAM-HTGTS [74] [78] | Cell-based | Sequencing of bait-prey DSB junctions. | Targeted | Excellent for detecting structural variations like translocations. |
The Scientist's Toolkit: Essential Reagents and Materials
Successful off-target assessment relies on a suite of specialized reagents and tools.
Table 3: Research Reagent Solutions for Off-Target Analysis
| Item/Category | Function/Description | Example Use Case |
|---|---|---|
| High-Fidelity Cas9 | Engineered Cas9 variants with reduced mismatch tolerance. | Improving on-target specificity in therapeutic RNP formulations [78]. |
| Chemically Modified sgRNA | sgRNAs with modified backbones (e.g., 2'-O-methyl) to enhance stability and specificity. | Reducing off-target effects while maintaining on-target activity [78]. |
| GUIDE-seq dsODN Tag | A short, double-stranded oligodeoxynucleotide that integrates into DSBs. | Tagging and identifying CRISPR-induced breaks in living cells [74]. |
| CIRCLE-seq Library Prep Kit | Optimized reagents for DNA circularization and cleavage-specific amplification. | Performing sensitive, cell-free, genome-wide off-target screening [73]. |
| Epigenetic Data (e.g., ATAC-seq) | Public or newly generated datasets on chromatin accessibility. | Informing sgRNA design and improving in silico prediction accuracy with DNABERT-Epi [79]. |
The journey from research tool to approved therapy necessitates a rigorous, multi-faceted approach to off-target risk assessment. Regulatory agencies like the FDA and EMA require comprehensive evaluations that typically combine in silico prediction with orthogonal experimental methods to profile the safety of a CRISPR-based therapeutic [78]. For example, the first approved CRISPR-based medicine, exagamglogene autotemcel (exa-cel) for sickle cell disease and beta-thalassemia, undoubtedly underwent such exhaustive scrutiny.
The quantification of not just small indels but also large gene modifications is critical. Recent studies using long-read sequencing technologies (e.g., PacBio SMRT-seq) have revealed that Cas9 can induce large deletions (>200 bp) and complex rearrangements at on-target sites with frequencies ranging from 11.7% to 35.4% in HSPCs edited at the HBB locus [80]. These unintended on-target consequences are as important as distant off-target effects and must be quantified for a complete safety profile.
In conclusion, defining and quantifying CRISPR-Cas9 off-target effects is a complex but surmountable challenge. By leveraging a structured workflow that integrates advanced in silico prediction, sensitive experimental detection, and the use of high-fidelity reagents, researchers can thoroughly characterize and mitigate these risks. This diligent approach is foundational to realizing the full therapeutic potential of CRISPR-Cas9 for treating genetic disorders, ensuring that new therapies are not only effective but also safe for patients.
The application of CRISPR-Cas9 in therapeutic research for genetic disorders demands extreme precision to correct disease-causing mutations without introducing unintended genomic alterations. While the wild-type Streptococcus pyogenes Cas9 (WT-SpCas9) nuclease has revolutionized genome editing, concerns regarding off-target activity present significant barriers to clinical translation [81]. High-fidelity Cas9 variants and sophisticated guide RNA (gRNA) design strategies have emerged as crucial solutions to enhance editing precision. This protocol details integrated approaches for achieving superior specificity in CRISPR-Cas9 experiments, particularly within the context of genetic disorder therapy development. The following sections provide comprehensive methodologies for selecting high-fidelity enzymes, designing optimal gRNAs, implementing experimental workflows, and utilizing key reagents to maximize on-target efficiency while minimizing off-target effects.
High-Fidelity Cas9 Variants: Mechanisms and Performance Characteristics
High-fidelity Cas9 variants are engineered versions of the wild-type enzyme designed to reduce non-specific interactions with DNA, thereby decreasing off-target editing while maintaining robust on-target activity. These variants typically contain point mutations that destabilize Cas9's interaction with the DNA backbone outside the intended target sequence, enforcing stricter reliance on correct guide RNA:DNA hybridization [81].
Table 1: Comparison of High-Fidelity Cas9 Variants
| Variant | Key Mutations | Mechanism of Action | Reported On-Target Efficiency | Reported Off-Target Reduction |
|---|---|---|---|---|
| eSpCas9(1.1) | K848A, K1003A, R1060A | Weakenes non-specific Cas9-DNA interactions, reducing tolerance to mismatches | 47-73% of WT-SpCas9 activity [82] | >10-fold to >100-fold reduction [81] |
| SpCas9-HF1 | N497A, R661A, Q695A, Q926A | Alters key residues interacting with DNA phosphate backbone | ~50% of WT-SpCas9 activity for many targets [82] | >85% reduction at known off-target sites [81] |
| HypaCas9 | K848A, K1003A, R1060A + N692A, M694A, H698A | Combines eSpCas9 mutations with additional fidelity-enhancing mutations | Improved activity over eSpCas9 while maintaining high fidelity [82] | Undetectable off-target activity at sites where WT shows cleavage [82] |
These high-fidelity variants address the critical challenge of off-target effects, which remain a primary safety concern for therapeutic applications. However, their enhanced specificity often comes with varying degrees of reduced on-target activity compared to WT-SpCas9, necessitating complementary strategies to boost editing efficiency [83].
Advanced gRNA Design Strategies for Enhanced Specificity
Guide RNA design represents the most critical determinant of CRISPR-Cas9 editing success. Optimal gRNA selection influences both on-target efficiency and off-target potential, with specific considerations for high-fidelity variants.
Key Parameters for gRNA Design
- Sequence-Unique Target Sites: Select target sites with minimal sequence homology elsewhere in the genome. Computational analysis should confirm fewer than 3 potential off-target sites with ≤3 nucleotide mismatches [81].
- gRNA Sequence Composition: Avoid homopolymer stretches (>4 identical consecutive nucleotides) and maintain GC content between 40-80% [84]. The 5' terminus of the gRNA should ideally begin with a G nucleotide when using the human U6 promoter for transcription initiation [82].
- Structural Considerations: gRNAs with stable secondary structures or minimum folding energies (MFE) < -7.5 kcal/mol typically show reduced activity due to impaired Cas9 binding [84].
- gRNA-DNA Binding Energy (ΔGB): The binding free energy between gRNA and target DNA represents a key feature for predicting on-target efficiency, with more negative ΔGB values generally correlating with higher activity [84].
Computational Tools for gRNA Design
Several deep learning-based algorithms have been specifically developed for predicting gRNA activity in high-fidelity Cas9 variants:
Table 2: Computational Tools for gRNA Efficiency Prediction
| Tool Name | Compatible Cas9 Variants | Algorithm Type | Key Features | Access URL |
|---|---|---|---|---|
| DeepHF | WT-SpCas9, eSpCas9(1.1), SpCas9-HF1 | Recurrent Neural Network (RNN) + biological features | Predicts activity for high-fidelity variants specifically | http://www.DeepHF.com/ [85] |
| CRISPRon | WT-SpCas9 | Deep learning | Integrates gRNA-DNA binding energy (ΔGB) for improved predictions | https://rth.dk/resources/crispr/ [84] |
Integrated Experimental Protocols
Protocol 1: tRNA-sgRNA Fusion System to Enhance High-Fidelity Cas9 Activity
Background: High-fidelity Cas9 variants often exhibit reduced editing efficiency. This protocol utilizes a tRNA-processing system to boost activity while maintaining specificity [83].
Reagents Required:
- Plasmid expressing high-fidelity Cas9 variant (eSpCas9(1.1), SpCas9-HF1, or HypaCas9)
- tRNA-sgRNA fusion construct (see diagram below)
- HEK-293 cells (or other relevant cell line)
- Flow cytometry reagents for analysis
- T7E1 assay or deep sequencing reagents for indel quantification
Procedure:
- Design tRNA-sgRNA Fusion: Fuse the 5' end of the GN20 sgRNA sequence to the 3' end of a tRNAGln gene using overlapping PCR or synthesis.
- Clone Construct: Insert the tRNA-sgRNA fusion into an appropriate expression vector with RNA Polymerase III promoter.
- Transfect Cells: Co-transfect the tRNA-sgRNA plasmid with high-fidelity Cas9 expression vector into target cells using preferred transfection method.
- Analyze Editing Efficiency: At 48-72 hours post-transfection, harvest cells and quantify indel frequencies using T7E1 assay or targeted deep sequencing.
- Validate Specificity: Perform off-target analysis at predicted off-target sites using targeted sequencing.
Expected Results: The tRNA-sgRNA system typically yields 6- to 8-fold improvement in editing efficiency for high-fidelity variants compared to standard sgRNA designs, as demonstrated in correction of pathogenic mutations in the retinoschisin 1 (RS1) gene model [83].
Diagram 1: Workflow for enhancing high-fidelity Cas9 activity using a tRNA-sgRNA fusion system.
Protocol 2: Genome-Wide gRNA Activity Profiling for High-Fidelity Variants
Background: This protocol enables large-scale screening of gRNA activity for high-fidelity Cas9 variants, generating datasets for training predictive algorithms [82].
Reagents Required:
- Array-synthesized oligonucleotide pool (12,000-80,000 gRNAs)
- Lentiviral backbone vector
- HEK-293T cells expressing high-fidelity Cas9 variant
- Puromycin selection antibiotic
- Deep sequencing platform and reagents
Procedure:
- Library Design: Design gRNAs targeting coding genes and non-coding regions using established criteria. Include gRNAs with both A and G as first nucleotide where possible.
- Library Cloning: Amplify oligonucleotide pool by PCR and clone into lentiviral vector via Gibson assembly.
- Lentiviral Production: Package lentiviral gRNA library in HEK-293T cells using standard packaging plasmids.
- Cell Transduction: Transduce Cas9-expressing cells at low MOI (0.3) to ensure single gRNA integration per cell.
- Selection and Expansion: Apply puromycin selection (2-5 μg/mL) for 3-5 days to eliminate untransduced cells.
- Genomic DNA Extraction and Sequencing: Extract genomic DNA at day 8-10 post-transduction. Amplify integrated target regions with barcoded primers for deep sequencing.
- Data Analysis: Calculate indel frequencies for each gRNA by comparing to pre-edited control library. Filter out synthesis errors present in original library.
Expected Results: This approach typically yields valid gRNA activity data for >50,000 gRNAs, enabling comprehensive analysis of sequence features influencing efficiency in high-fidelity variants [82].
Diagram 2: Genome-wide gRNA activity profiling workflow for high-fidelity Cas9 variants.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for High-Fidelity CRISPR Applications
| Reagent/Category | Specific Examples | Function/Application | Considerations for Use |
|---|---|---|---|
| High-Fidelity Cas9 Expression Plasmids | eSpCas9(1.1), SpCas9-HF1, HypaCas9 | Provides the nuclease with reduced off-target activity | Select based on balance of specificity and efficiency requirements |
| gRNA Cloning Vectors | Lentiviral gRNA vectors with mU6/hU6 promoters | Enables gRNA expression; mU6 expands targeting to GN19NGG and AN19NGG sites | mU6 promoter allows greater target range than hU6 [82] |
| tRNA-sgRNA Fusion Systems | tRNAGln-processing system | Enhances activity of high-fidelity Cas9 variants | Can improve efficiency 6-8 fold for pathogenic mutation correction [83] |
| Delivery Vehicles | Lentiviral particles, lipid nanoparticles (LNPs) | Enables efficient intracellular delivery of CRISPR components | LNPs preferred for in vivo therapeutic applications; avoid immune response [14] |
| Off-Target Detection Kits | GUIDE-seq, Digenome-seq, BLESS | Identifies and quantifies off-target editing events | Each method has different sensitivity, scalability, and technical requirements [81] |
The strategic integration of high-fidelity Cas9 variants with optimized gRNA design represents a powerful approach for achieving the precision required in therapeutic genome editing for genetic disorders. While these engineered nucleases significantly reduce off-target effects, their sometimes-reduced efficiency can be mitigated through tRNA-sgRNA fusion systems and computational gRNA design tools trained on variant-specific activity data. The protocols and reagents outlined here provide researchers with a comprehensive framework for implementing these enhanced precision strategies in both basic research and therapeutic development contexts. As CRISPR-based therapies advance toward clinical application, continued refinement of these approaches will be essential for ensuring both safety and efficacy in treating genetic diseases.
The CRISPR-Cas9 system has revolutionized genetic engineering, offering unprecedented potential for treating genetic disorders. However, a significant challenge impeding its clinical translation is the occurrence of off-target effects, where unintended genomic locations are cleaved. These effects pose substantial safety risks, as they can disrupt vital genes or regulatory sequences, potentially leading to adverse outcomes like oncogenesis [74] [73]. Consequently, rigorous assessment of off-target activity is a critical step in the therapeutic development pipeline. This review provides a comparative analysis of the two cornerstone approaches for off-target assessment: in silico prediction tools and experimental detection methods. Framed within the context of developing therapies for genetic disorders, we detail their methodologies, applications, and protocols, providing researchers with a practical guide for ensuring the specificity and safety of CRISPR-Cas9-based treatments.
In Silico Off-Target Prediction: Principles and Tools
In silico prediction tools are computationally efficient methods for nominating potential off-target sites during the guide RNA (gRNA) design phase. These algorithms primarily identify sites in the genome with sequence similarity to the intended on-target site, tolerating a limited number of mismatches or small insertions and deletions (indels) [74] [73]. They are classified into distinct categories based on their underlying algorithms, each with strengths and limitations.
Table 1: Categories and Characteristics of In Silico Off-Target Prediction Tools
| Category | Principle | Representative Tools | Key Features | Limitations |
|---|---|---|---|---|
| Alignment-Based | Identifies genomic sites with high sequence similarity to the sgRNA, allowing for mismatches and bulges. | Cas-OFFinder [74], CHOPCHOP [86], CasOT [74], Crisflash [74] | Fast genome-wide scanning; adjustable PAM and mismatch/indel parameters. | Purely sequence-based; does not predict cleavage likelihood. |
| Scoring-Based | Assigns a weighted score based on mismatch position/type relative to the PAM to estimate cleavage probability. | CCTop [86] [74], MIT Score [74] [87] | Provides a quantitative score to prioritize potential off-targets. | Early models did not consider epigenetic factors. |
| Energy-Based | Models the binding energy of the Cas9-gRNA-DNA complex. | CRISPRoff [88] | Provides a biophysical basis for prediction. | Computationally intensive. |
| Learning-Based | Uses machine/deep learning on large experimental datasets to predict cleavage activity. | DeepCRISPR [74], CCLMoff [88], CRISPR-Net [88] | High accuracy; can incorporate epigenetic features (e.g., chromatin accessibility). | Requires large training datasets; performance depends on data quality. |
The practical application of these tools reveals significant variability. A study aiming to correct the p.Trp402* variant in the IDUA gene for Mucopolysaccharidosis type I (MPS I) used five popular predictors and found starkly different numbers of potential off-targets, with Cas-OFFinder predicting 13,352 sites while COSMID predicted only 15. This highlights a lack of consensus and the importance of using multiple tools [86]. Furthermore, the consideration of genetic variability is crucial. The same study identified 84 polymorphic sites within the potential off-target sequences, which can alter the sequence enough to either create new off-target sites or eliminate predicted ones, underscoring the need for population-specific analysis in gRNA design for inclusive therapies [86].
Protocol: Implementing a Standard In Silico Workflow for gRNA Design
Application Note: This protocol is designed for the initial assessment of a candidate sgRNA's specificity during the design phase for a genetic disorder therapy.
Research Reagent Solutions:
- sgRNA Sequence: The 20-nucleotide target sequence.
- Reference Genome: The appropriate reference genome (e.g., GRCh38/hg38).
- Computational Tools: Access to a suite of web-based or command-line tools (e.g., CCTop, Cas-OFFinder, DeepCRISPR).
Methodology:
- Sequence Input: Start with the candidate sgRNA sequence (e.g., 5'-GCTCTAGGCCGAAGTGTCGCAGG-3' as used in the MPS I study [86]).
- Tool Selection and Execution: Run the sgRNA sequence against at least two tools from different categories (e.g., one alignment-based like Cas-OFFinder and one learning-based like CCLMoff) using the standard human reference genome.
- Parameter Setting: Configure parameters to allow for up to 6 nucleotide mismatches and up to 2 indels, based on empirical evidence that sites with this level of divergence can still be cleaved [86] [88].
- Data Integration and Prioritization: Compile results from all tools. Prioritize off-target sites based on:
- Consensus across multiple predictors.
- High CFD (Cutting Frequency Determination) score (e.g., >0.023 [86]) or other relevant model-specific scores.
- Fewer mismatches, especially in the "seed" region proximal to the PAM sequence.
- Location within genic or regulatory regions.
- Polymorphism Screening: Cross-reference the final list of high-priority off-target sites with population genetic databases (e.g., 1000 Genomes) to identify polymorphic sites that may affect off-target risk [86].
Figure 1: A standard workflow for in silico off-target prediction, integrating multiple tools and population data.
Experimental Detection of Off-Target Effects
While in silico tools are excellent for initial screening, they can produce false positives and negatives as they may not fully capture the complexity of the intracellular environment, including chromatin structure and accessibility [74] [73]. Therefore, experimental validation is indispensable for a comprehensive off-target profile. These methods can be broadly classified into cell-free and cell-based techniques.
Table 2: Experimental Methods for Genome-Wide Off-Target Detection
| Method | Category | Principle | Key Advantages | Key Disadvantages |
|---|---|---|---|---|
| Digenome-seq [74] [73] | Cell-free | Purified genomic DNA is digested with Cas9 RNP in vitro and sequenced via WGS to find cleavage ends. | Highly sensitive; can detect low-frequency indels. | High sequencing coverage required; expensive; ignores chromatin state. |
| CIRCLE-seq [74] [88] | Cell-free | Genomic DNA is circularized, digested with Cas9 RNP, linearized, and sequenced. Extremely sensitive. | Very high sensitivity; low background. | Purely in vitro; may identify sites not accessible in cells. |
| GUIDE-seq [74] [88] | Cell-based | DSBs are tagged by integration of a double-stranded oligodeoxynucleotide (dsODN), which is then sequenced. | Highly sensitive; low false-positive rate; captures cellular context. | Limited by transfection efficiency. |
| DISCOVER-seq [88] | Cell-based | Uses the DNA repair protein MRE11 as a bait to perform ChIP-seq on Cas9-induced DSBs. | Can detect off-targets in primary cells and in vivo; uses endogenous repair machinery. | Potential for false positives. |
| SMRT-OTS / Nano-OTS [89] | Cell-free / Long-read | Amplification-free long-read sequencing detects Cas9 cleavage patterns on native genomic DNA. | Reveals off-targets in "dark" genomic regions missed by short-reads. | Emerging technology; requires specialized long-read sequencing. |
The evolution of these methods aims to better recapitulate the intracellular environment. For instance, DIG-seq was developed as an improvement over Digenome-seq by using cell-free chromatin instead of purified DNA, thereby incorporating aspects of chromatin accessibility and achieving a higher validation rate [73]. Furthermore, long-read sequencing methods like SMRT-OTS have uncovered unforeseen off-target activities in genomic regions that are difficult to map with short-read sequencing, including those with multiple mismatches or indels that were not predicted by computational tools [89].
Protocol: Experimental Off-Target Validation Using GUIDE-seq
Application Note: This protocol is a widely adopted cell-based method for identifying off-target sites in a relevant cellular model, a critical step pre-clinical safety assessment.
Research Reagent Solutions:
- Cas9 Delivery System: Plasmid expressing Cas9 nuclease or purified Cas9 protein.
- sgRNA: The candidate therapeutic sgRNA.
- GUIDE-seq dsODN: A short, double-stranded oligodeoxynucleotide tag with a specific sequence for PCR enrichment.
- Cells: A relevant cell line (e.g., HEK293) or primary cell model for the genetic disorder.
- Next-Generation Sequencing (NGS) Platform.
Methodology:
- Co-transfection: Co-deliver the following into the target cells:
- Cas9 (as plasmid, mRNA, or RNP).
- The candidate sgRNA.
- The GUIDE-seq dsODN tag.
- Genomic DNA Extraction: Allow 2-3 days for editing and tag integration. Then, harvest cells and extract genomic DNA.
- Library Preparation and Sequencing:
- Fragment the genomic DNA.
- Perform PCR enrichment using primers specific to the GUIDE-seq dsODN tag to selectively amplify fragments that have incorporated the tag at a DSB.
- Prepare an NGS library from the amplified products and sequence.
- Bioinformatic Analysis:
- Map the sequenced reads to the reference genome.
- Identify genomic locations where the dsODN tag has been integrated. These sites represent Cas9-induced DSBs, both on-target and off-target.
- Filter and annotate the list of off-target sites.
Figure 2: Key experimental steps for off-target detection using the GUIDE-seq method.
Integration and Future Perspectives for Therapeutic Applications
For clinical development, a synergistic approach combining in silico and experimental methods is paramount. A robust strategy involves using multiple computational tools for initial gRNA screening, followed by exhaustive experimental validation in the most physiologically relevant models available, such as patient-derived iPSCs or animal models [86] [89]. The field is rapidly advancing with the development of more precise CRISPR systems (e.g., high-fidelity Cas9 variants, base editors) and improved delivery methods like lipid nanoparticles (LNPs), which have shown success in recent clinical trials for hereditary transthyretin amyloidosis (hATTR) [14].
The future of off-target prediction lies in sophisticated deep learning models. Tools like CCLMoff incorporate pre-trained RNA language models and are trained on comprehensive datasets from multiple detection technologies, enabling them to capture complex patterns and generalize well across different conditions [88]. These models are beginning to integrate epigenetic data, such as DNA methylation and chromatin accessibility, to further enhance prediction accuracy within a therapeutic context [74] [88]. As CRISPR therapeutics progress—evidenced by the first FDA-approved treatment, Casgevy, for sickle cell disease and beta-thalassemia, and the first personalized in vivo CRISPR therapy [14]—the stringent and integrated application of these detection and mitigation strategies will be the cornerstone of developing safe and effective gene therapies for a broader range of genetic disorders.
{Article Content Start}
Overcoming Immunogenicity and Delivery Barriers to Efficient In Vivo Editing
The advent of CRISPR-Cas9 genome editing has inaugurated a new era in therapeutic research for genetic disorders, offering the potential for precise, permanent correction of disease-causing mutations. However, the transition from in vitro success to effective in vivo therapies is critically dependent on overcoming two interconnected major hurdles: the immunogenicity of the CRISPR system components and the development of safe, efficient in vivo delivery vehicles [38] [90] [91]. The Cas9 nuclease, being of bacterial origin, is recognized as foreign by the human immune system, which can lead to neutralization of the therapy and serious inflammatory adverse effects [90] [59]. Concurrently, delivering the large Cas9 protein and its guide RNA to the correct tissues and into the nuclei of target cells in vivo presents a monumental biophysical challenge [38] [92]. This application note, framed within a broader thesis on advancing CRISPR-Cas9 for genetic disorders, details the most recent progress in understanding these barriers and provides actionable, detailed protocols for researchers and drug development professionals to develop safer and more effective in vivo gene editing therapies.
Decoding and Mitigating Cas9 Immunogenicity
A significant proportion of the human population possesses pre-existing immunity to Cas9 proteins. Pre-existing anti-Cas9 antibodies are found in approximately 5% of individuals, and T-cell responses have been detected in 57% to 95% of healthy subjects [59]. This high prevalence is attributed to past common bacterial infections, such as those caused by Streptococcus pyogenes and Staphylococcus aureus [59]. Upon administration, Cas9 can trigger both innate and adaptive immune responses, potentially leading to rapid clearance of the editing machinery, reduced therapeutic efficacy, and dangerous inflammatory reactions [90] [59].
Table 1: Strategies to Overcome CRISPR-Cas9 Immunogenicity
| Strategy | Mechanism of Action | Key Advantages | Considerations for Implementation |
|---|---|---|---|
| Epitope Engineering [90] | Modifying surface amino acids of Cas9 to eliminate immunodominant T-cell epitopes. | Reduces immune recognition while retaining nuclease activity. | Requires detailed mapping of epitopes and functional validation of engineered variants. |
| Use of Cas9 RNP Complexes [38] [91] | Direct delivery of pre-formed Ribonucleoprotein (Cas9 protein + gRNA). | Transient presence in cells minimizes exposure to the immune system. | Large size and positive charge of Cas9 complicate delivery vehicle design [91]. |
| Immunosuppressive Regimens [59] | Pre-treatment with glucocorticoids and histamine blockers. | Clinically tractable; has enabled sustained editing in trials. | Does not address pre-existing immunity; carries general risks of immunosuppression. |
| Adoptive Treg Transfer [59] | Co-administration of regulatory T cells (Tregs) to induce tolerance. | Potentially induces long-term tolerance to Cas9. | Complex and still an emerging experimental approach. |
| Exploitation of Immune-Privileged Sites [38] | Local delivery to tissues like the eye or brain. | Minimizes systemic immune exposure. | Limited to a specific subset of diseases. |
Navigating the Delivery Vehicle Landscape
Selecting an appropriate delivery vehicle is equally critical for successful in vivo editing. The ideal vector must protect its nucleic acid or protein cargo from degradation, navigate to the target tissue, facilitate cellular uptake, escape the endosomal compartment, and finally, enable nuclear entry [93] [92]. The cargo itself can be delivered in multiple formats: DNA (plasmid), RNA (mRNA + gRNA), or as a pre-complexed Ribonucleoprotein (RNP) [38] [92]. RNP delivery is increasingly favored for its rapid onset of action, short cellular residence time, and reduced off-target effects, though it requires advanced delivery solutions [38] [92] [91].
Table 2: Comparison of Primary In Vivo CRISPR Delivery Systems
| Delivery System | Payload Capacity | Immunogenicity | Integration Risk | Key Strengths | Primary Limitations |
|---|---|---|---|---|---|
| Adeno-Associated Virus (AAV) [92] [59] | Limited (~4.7 kb) | Low | Low (mostly episomal) | Excellent tissue targeting via serotypes; proven clinical safety profile. | Limited cargo capacity necessitates smaller Cas9 orthologs or dual-vector systems. |
| Lentiviral Vector (LV) [92] [59] | Higher (8-10 kb) | Low | Moderate (mitigated by NILVs*) | High transduction efficiency; sustains long-term expression. | Safety concerns around insertional mutagenesis with integrating versions. |
| Lipid Nanoparticle (LNP) [93] [59] | High | Minimal | None | Proven success with mRNA vaccines; tunable for organ targeting; scalable production. | Requires optimization for endosomal escape and nuclear import; can induce transient inflammation. |
| Virus-Like Particle (VLP) [92] [94] | Moderate | Minimal | None | Combines high transduction efficiency of viruses with safety of non-viral systems; transient expression. | Complex manufacturing and stability issues. |
NILVs: Non-Integrating Lentiviral Vectors
The following diagram illustrates the logical decision-making pathway for selecting an appropriate delivery vehicle based on therapeutic goals and constraints.
The Scientist's Toolkit: Essential Reagents and Materials
Table 3: Research Reagent Solutions for In Vivo CRISPR Delivery
| Item | Function | Example & Notes |
|---|---|---|
| Ionizable Lipid Nanoparticles [93] [59] | Core component of LNPs; encapsulates nucleic acid/protein cargo and enables endosomal escape. | Proprietary ionizable lipids (e.g., in Intellia's NTLA-2002); DOPE for liver targeting, DSPC for splenic cells [93] [59]. |
| Engineered Cas9 Variants [90] [92] | Reduces immunogenicity and/or fits within AAV cargo size limit. | SaCas9 (smaller size); hfCas12Max (1080aa, high-fidelity); Epitope-deimmunized variants [90] [92]. |
| Cell-Penetrating Peptides (CPPs) [92] | Covalently linked to Cas9 RNP to facilitate cellular uptake without a delivery vehicle. | Various peptide sequences (e.g., TAT); used in non-viral, direct RNP delivery approaches. |
| Targeting Ligands [93] [59] | Conjugated to delivery vehicle (LNP, VLP) to direct it to specific cell surface receptors. | Antibody fragments, peptides, or small molecules (e.g., Hyaluronic Acid for CD44 receptors) [93]. |
| Cationic Polymers [92] [91] | Complex with nucleic acids to form polyplexes; enhance stability and cellular uptake. | Polyethylenimine (PEI), used in DNA nanoclew coatings for endosomal escape [91]. |
Detailed Experimental Protocols
Protocol: Formulating CRISPR-Cas9 RNP for LNP Delivery
This protocol outlines the preparation of Lipid Nanoparticles (LNPs) encapsulating Cas9 Ribonucleoprotein (RNP) for in vivo liver-targeted editing, based on successful preclinical studies [93] [59].
I. Materials
- Cas9 Protein: Purified, E-tagged SpCas9 or high-fidelity variant.
- sgRNA: Chemically modified, HPLC-purified synthetic sgRNA.
- Lipids: Ionizable lipid (e.g., DLin-MC3-DMA), DSPC, Cholesterol, DMG-PEG 2000.
- Buffers: Sodium Acetate (pH 4.0), Tris-EDTA (pH 8.0).
- Equipment: Microfluidics mixer (e.g., NanoAssemblr), PD-10 Desalting Columns, Dynamic Light Scattering (DLS) instrument.
II. Procedure
- RNP Complex Formation:
- Dilute the Cas9 protein and sgRNA in nuclease-free PBS to a final concentration of 100 µg/µL and 50 µg/µL, respectively.
- Mix the Cas9 and sgRNA at a 1:1.2 molar ratio (Cas9:sgRNA) and incubate at room temperature for 10 minutes to form the RNP complex.
Lipid Stock Preparation:
- Prepare an ethanolic lipid mixture containing the ionizable lipid, DSPC, Cholesterol, and DMG-PEG 2000 at a molar ratio of 50:10:38.5:1.5. The total lipid concentration should be 10 mM in ethanol.
LNP Formulation via Microfluidics:
- Set the flow rate ratio of the aqueous phase (RNP complex in PBS) to the organic phase (ethanolic lipid mix) to 3:1.
- Using the microfluidics device, rapidly mix the two streams to form blank LNPs.
- Immediately after mixing, dilute the resulting LNP formulation in 5x volume of PBS to quench the reaction.
Buffer Exchange and Purification:
- Use a PD-10 desalting column or dialysis against PBS (pH 7.4) to remove ethanol and exchange the buffer. Sterile-filter the final formulation through a 0.22 µm filter.
Quality Control:
- Size and PDI: Measure by DLS. Acceptable parameters: 70-100 nm, PDI < 0.2.
- Encapsulation Efficiency: Quantify using RiboGreen assay for RNA. Aim for >90% encapsulation.
- Sterility: Perform sterility testing according to institutional guidelines.
Protocol: Assessing Cas9 Immunogenicity In Vitro
This protocol describes a method to evaluate the potential immunogenicity of a Cas9 protein using human peripheral blood mononuclear cells (PBMCs) [90] [59].
I. Materials
- Cells: Cryopreserved human PBMCs from multiple healthy donors.
- Antigens: Candidate Cas9 protein (e.g., engineered variant), wild-type Cas9 protein (positive control), and an irrelevant protein (negative control).
- Media: RPMI-1640 supplemented with 10% human AB serum, L-glutamine, and penicillin/streptomycin.
- Assay Kits: IFN-γ ELISpot kit or flow cytometry panels for T-cell activation markers (CD69, CD25, CD137).
II. Procedure
- PBMC Thawing and Resting:
- Rapidly thaw PBMCs and wash twice in complete media.
- Rest the cells overnight at 37°C in a humidified 5% CO2 incubator.
Antigen Stimulation:
- Seed PBMCs (2-4 x 10^5 cells per well) in a 96-well U-bottom plate.
- Stimulate cells with candidate Cas9 proteins, wild-type Cas9, and negative control (all at 10 µg/mL). Include a positive control (e.g., PHA at 5 µg/mL).
- Incubate for 24-48 hours for early activation marker analysis by flow cytometry, or for 5-7 days for ELISpot.
Immune Response Detection:
- Option A (Flow Cytometry): Harvest cells after 24-48 hours, stain for surface markers (CD3, CD4, CD8, CD69, CD137) and analyze by flow cytometry. The frequency of activated (CD69+CD137+) T-cells indicates a response.
- Option B (ELISpot): After 5-7 days of stimulation, transfer cells to an IFN-γ ELISpot plate and follow manufacturer's instructions. Count spot-forming units (SFUs) representing antigen-reactive T-cells.
Data Analysis:
- Compare the T-cell response to the candidate Cas9 against the wild-type control. A significant reduction in activation markers or SFUs indicates successful deimmunization.
The following workflow diagram maps the key stages and decision points in the translational pipeline for developing an in vivo CRISPR therapy, integrating the strategies and protocols detailed above.
The path to realizing the full therapeutic potential of in vivo CRISPR-Cas9 gene editing is being paved by concerted efforts to engineer solutions to the dual challenges of immunogenicity and delivery. As detailed in these application notes, the field is moving beyond wild-type Cas9 and first-generation viral vectors towards a sophisticated toolkit that includes deimmunized proteins, versatile non-viral platforms like LNPs, and highly specific targeting strategies. The experimental protocols provided offer a practical starting point for researchers to characterize and advance their own therapeutic candidates. By systematically applying these strategies—selecting the appropriate cargo and delivery vehicle for the specific clinical indication and rigorously assessing both efficacy and immune profile—scientists and drug developers can accelerate the transition of transformative in vivo CRISPR therapies from the laboratory to the clinic.
{Article Content End}
Addressing Genotoxicity and Long-Term Safety in Clinical Applications
The therapeutic application of CRISPR-Cas9 gene editing represents a paradigm shift in treating genetic disorders, with approved therapies like Casgevy for sickle cell disease and β-thalassemia demonstrating remarkable clinical success [95]. However, this revolutionary technology introduces potential genotoxic risks that must be systematically addressed to ensure patient safety. CRISPR-Cas9-induced DNA double-strand breaks (DSBs) can lead to a spectrum of unintended genetic consequences, including off-target mutations at sites with sequence similarity to the intended target, and complex on-target rearrangements that often evade conventional detection methods [96] [97]. These genotoxic effects raise legitimate concerns about long-term risks, including potential tumorigenesis, particularly when editing occurs in therapeutic contexts involving hematopoietic stem/progenitor cells (HSPCs) or in vivo administration [95] [97].
Understanding these risks is particularly crucial for therapeutic development for genetic disorders, where the goal is to provide lifelong benefit without introducing new health complications. This Application Note provides a structured framework for identifying, quantifying, and mitigating genotoxicity risks throughout the therapeutic development pipeline, with specific protocols and analytical methods tailored to meet regulatory standards for clinical translation.
Quantitative Profiling of CRISPR-Cas9 Genotoxicity
Comprehensive risk assessment requires understanding the frequency and nature of genotoxic events across different editing contexts. The data below summarize key quantitative findings from preclinical and clinical studies.
Table 1: Spectrum and Frequency of CRISPR-Cas9-Induced Genetic Alterations
| Genotoxicity Type | Detection Method | Reported Frequency | Biological Context | Reference |
|---|---|---|---|---|
| Short indels (on-target) | Standard PCR + sequencing | Varies by target (often >80% efficiency) | Multiple cell types | [95] |
| Large deletions (100bp - several kb) | FAMReD, LR-PCR, aCGH | ~1/1000 edited cells | Human fibroblasts, stem cells | [98] [97] |
| Megabase-scale rearrangements (CN-LOH, CL-LOH) | FAMReD, aCGH, SNP array | ~0.1% of edited cells | p53-proficient human fibroblasts | [97] |
| Off-target editing (known sites) | GUIDE-seq, CIRCLE-seq | Highly gRNA-dependent | Various primary cells | [96] |
| Translocations | Cytogenetics, FISH | Rare | Cancer cell lines, stem cells | [97] |
| Chromothripsis | Cytogenetics, aCGH | Very rare | Stem cells, embryos | [97] |
Table 2: Factors Influencing Genotoxicity Risk and Mitigation Strategies
| Risk Factor | Impact on Genotoxicity | Risk Mitigation Approach | Experimental Evidence | |
|---|---|---|---|---|
| p53 status | p53 deficiency increases large deletions 5-10 fold | Prioritize p53-wildtype cells for editing; monitor p53 status | Human iPSCs, fibroblasts | [97] |
| Cell division rate | Higher division increases rearrangement risk | Cell cycle synchronization during editing | Human stem/progenitor cells | [97] |
| gRNA specificity | Determines off-target profile | In silico prediction + empirical validation | Multiple clinical programs | [96] |
| Delivery method | Viral vectors cause additional integration risks | Optimize non-viral delivery (RNP, LNPs) | Clinical trials (e.g., CTX310) | [66] [14] |
| Editor type | DSB-inducing nucleases have highest risk | Use base/prime editors when possible | Preclinical studies | [95] [96] |
| Target locus chromatin | Accessible regions have higher editing efficiency | Consider epigenetic context in gRNA design | Various cell types | [96] |
The quantitative assessment reveals that while standard indels represent the majority of editing outcomes, more complex rearrangements occur at lower but biologically significant frequencies. Critically, the detection method profoundly influences which genotoxic events are observed, with specialized approaches like FAMReD (Fluorescence-Assisted Megabase-scale Rearrangements Detection) required to identify large-scale rearrangements that escape conventional PCR-based analyses [97].
Experimental Protocols for Genotoxicity Assessment
Protocol: Comprehensive On-Target Genotoxicity Assessment
Principle: Standard PCR-based genotyping methods significantly underestimate large-scale on-target rearrangements. This protocol employs complementary techniques to fully characterize the spectrum of on-target editing outcomes, including megabase-scale events.
Materials:
- Edited cell populations (≥15 days post-editing for stable rearrangement assessment)
- ALA (5-aminolevulinic acid) for FAMReD system
- FACS capability for cell sorting
- aCGH or SNP array platform
- Long-range PCR reagents
- Next-generation sequencing capability
Procedure:
Cell Preparation and Editing
- Perform CRISPR editing on target cell population using clinically relevant delivery method
- Culture cells for minimum of 15 days to allow stabilization of chromosomal rearrangements
- Include appropriate controls (non-edited, transfection-only)
FAMReD Analysis for Megabase-Scale Rearrangements [97]
- Implement fluorescence-based detection system for loss of heterozygosity (LOH)
- For endogenous detection: Expose cells to ALA precursor and detect fluorescent red porphyrin accumulation in UROS-deficient cells via flow cytometry
- Sort fluorescent (LOH+) and non-fluorescent populations for separate analysis
- Culture sorted populations for additional 40 days to assess stability of rearrangements
Molecular Characterization of Sorted Populations
- Perform array Comparative Genomic Hybridization (aCGH) on sorted LOH+ and LOH- populations
- Conduct SNP array analysis to identify copy-neutral LOH events
- Implement long-range PCR (amplicons >5kb) spanning the cut site to detect large deletions
- Validate findings with Sanger sequencing of junction sites
Data Analysis and Risk Quantification
- Calculate frequency of LOH+ events as percentage of total edited population
- Map breakpoints for all identified rearrangements
- Classify events by type: terminal copy-loss LOH, copy-neutral LOH, interstitial duplications
- Assess potential functional consequences of identified rearrangements
Technical Notes: The FAMReD system requires engineering of reporter cell lines, which can be adapted to different chromosomal locations. For therapeutic applications, analyze at least 10^5 edited cells to achieve statistical significance for rare events (frequency <0.1%). Cell division rate and p53 status should be documented as they significantly influence rearrangement frequency [97].
Protocol: Off-Target Editing Assessment
Principle: CRISPR-Cas9 can cleave genomic sites with sequence similarity to the intended target, particularly those with mismatches in the distal region from the PAM sequence. This protocol provides a comprehensive approach for off-target assessment.
Materials:
- CIRCLE-seq or GUIDE-seq reagents
- Next-generation sequencing platform
- In vitro transcribed Cas9 protein and gRNA
- Genomic DNA extraction kit
- Bioinformatics pipeline for off-target analysis
Procedure:
In Silico Prediction
- Identify potential off-target sites using multiple algorithms (e.g., Cas-OFFinder, CCTop)
- Include sequences with up to 5 nucleotide mismatches and/or RNA bulges
- Prioritize sites in coding regions, promoter elements, and known tumor suppressor/oncogenes
Biochemical Off-Target Prediction (CIRCLE-seq) [96]
- Ispute genomic DNA and fragment to 300-500bp
- Circularize DNA fragments and incubate with Cas9-gRNA RNP complex
- Linearize cleaved fragments and prepare NGS library
- Sequence and identify enriched cleavage sites throughout the genome
Cell-Based Off-Target Validation (GUIDE-seq)
- Transfect cells with Cas9-gRNA RNP along with GUIDE-seq oligonucleotide tag
- Allow 48-72 hours for editing and tag integration
- Extract genomic DNA and perform tag-specific PCR amplification
- Sequence amplified products and map integration sites to genome
Functional Validation
- Design PCR primers flanking predicted top 10-20 off-target sites
- Amplify regions from edited cell genomic DNA
- Perform deep sequencing (≥10,000X coverage) to detect indels
- Quantify editing frequency at each site
Technical Notes: CIRCLE-seq provides comprehensive, bias-free identification of potential off-target sites but may overpredict biologically relevant sites. GUIDE-seq identifies off-targets in actual cellular context but may miss sites in inaccessible chromatin. For clinical applications, both methods should be employed complementarily [96].
Safety Workflow and Risk Mitigation Pathway
The following workflow integrates genotoxicity assessment throughout therapeutic development, from gRNA selection to clinical monitoring.
Figure 1: Integrated workflow for genotoxicity risk assessment and mitigation throughout therapeutic development. The pathway emphasizes early risk mitigation through careful gRNA selection and editor choice, comprehensive preclinical assessment using complementary methods, and long-term clinical monitoring.
Table 3: Research Reagent Solutions for Genotoxicity Assessment
| Reagent/Resource | Function | Application Context | Key Considerations |
|---|---|---|---|
| FAMReD System [97] | Detection of megabase-scale LOH events | Preclinical safety assessment in relevant cell types | Requires engineered reporter cell line; enables detection of CN-LOH and CL-LOH |
| CIRCLE-seq Kit [96] | Biochemical identification of off-target sites | Early gRNA screening | Comprehensive but may overpredict biologically relevant sites |
| GUIDE-seq Reagents [96] | Cell-based off-target identification | Preclinical validation in therapeutic cell types | Reflects cellular context but limited by delivery efficiency |
| HiFi-Cas9 Variants | Reduced off-target editing | Therapeutic editing applications | Improved specificity with potentially reduced on-target efficiency |
| Base/Prime Editors [95] [96] | DSB-free editing; reduced genotoxicity | Point mutation correction | Limited to specific mutation types; potential bystander edits |
| Long-range PCR Kits | Detection of large deletions | On-target characterization | Amplicons >5kb required for comprehensive assessment |
| aCGH/SNP Array Platforms | Genome-wide structural variation detection | Comprehensive on-target assessment | Identifies copy number changes and copy-neutral LOH |
Concluding Remarks and Future Directions
Addressing genotoxicity and long-term safety concerns is not merely a regulatory hurdle but an essential component of responsible therapeutic development. The approaches outlined herein enable researchers to comprehensively characterize CRISPR-based therapies, from expected on-target edits to rare, complex rearrangements that may have profound clinical implications. The field continues to evolve rapidly, with emerging technologies like CRISPR-Cas12a offering alternative editing platforms with different specificity profiles [99], and lipid nanoparticle delivery systems enabling redosable in vivo editing with improved safety profiles [66] [14]. As clinical experience grows - with ongoing trials in diverse conditions from hematological disorders to amyloidosis and cholesterol management - the long-term safety data collected will further refine our understanding and management of genotoxic risks [66] [14]. By implementing robust, comprehensive safety assessment protocols throughout therapeutic development, researchers can maximize the transformative potential of CRISPR technologies while ensuring patient safety remains the highest priority.
Clinical Validation and Comparative Analysis: Efficacy, Safety, and Market Landscape
The advent of CRISPR-Cas9 gene-editing technology has initiated a transformative era in the therapeutic landscape for genetic disorders. From the first approved CRISPR-based therapy to an expanding pipeline of late-stage investigational treatments, the field is rapidly advancing toward addressing previously untreatable conditions. This progression from conceptual research to clinical application represents a pivotal shift in medical science, offering potential cures for monogenic diseases through precise genomic interventions. The technology's journey from laboratory discovery to approved medicine marks a milestone in biomedical innovation, demonstrating the tangible clinical impact of gene editing [53] [14].
This article reviews pivotal clinical trial data for both approved and late-stage CRISPR therapies, providing detailed experimental protocols and analytical frameworks for researchers and drug development professionals. We synthesize quantitative outcomes across multiple trials, delineate standardized methodologies for critical experiments, and visualize complex biological pathways and workflows. Within the broader thesis of CRISPR-Cas9 applications in genetic disorder therapy, this analysis aims to serve as both a technical reference and a strategic overview of the current clinical landscape and its future directions [100] [95].
Approved CRISPR Therapies: Efficacy and Safety Profiles
CASGEVY (exagamglogene autotemcel)
CASGEVY (exa-cel), developed through collaboration between CRISPR Therapeutics and Vertex Pharmaceuticals, represents the pioneering FDA-approved CRISPR-based therapy for sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TDT). This ex vivo CRISPR-Cas9 gene-edited cell therapy targets the BCL11A gene to enhance fetal hemoglobin production, effectively addressing the pathological mechanisms of both hemoglobinopathies [53].
Table 1: Clinical Trial Outcomes for CASGEVY
| Parameter | Sickle Cell Disease | Transfusion-Dependent Beta Thalassemia |
|---|---|---|
| Primary Endpoint | Proportion of patients free of severe vaso-occlusive crises for ≥12 consecutive months | Proportion of patients maintaining weighted average Hb ≥9 g/dL without red blood cell transfusions for ≥12 consecutive months |
| Efficacy Rate | >94% (achieved primary endpoint) | >90% (achieved primary endpoint) |
| Follow-up Duration | Median 22.4 months (clinical trials) | Median 23.5 months (clinical trials) |
| Key Safety Observations | Myeloablative conditioning-related adverse events; no off-target editing concerns | Myeloablative conditioning-related adverse events; no off-target editing concerns |
| Commercial Status | >50 authorized treatment centers globally; >50 patients initiated cell collection | >50 authorized treatment centers globally; >50 patients initiated cell collection |
The global launch of CASGEVY continues to gain momentum throughout 2025, with strong patient demand and robust payer support systems. As of early 2025, over 50 authorized treatment centers have been activated worldwide, and more than 50 patients have initiated cell collection. The therapy has received regulatory approval across multiple jurisdictions, including the United States, United Kingdom, European Union, and United Arab Emirates. The recent voluntary agreement between Vertex and the Centers for Medicare & Medicaid Services (CMS) in the U.S. establishes a groundbreaking outcomes-based arrangement for CASGEVY, ensuring broad and equitable access for patients across state Medicaid programs [53].
Late-Stage Clinical Pipeline: Emerging Candidates
In Vivo CRISPR Therapies for Cardiovascular and Metabolic Diseases
The CRISPR therapeutic pipeline has expanded significantly beyond ex vivo applications to include in vivo gene editing approaches, particularly for cardiovascular and metabolic diseases. Lipid nanoparticle (LNP) delivery systems have enabled targeted CRISPR-Cas9 delivery to hepatocytes, opening new treatment paradigms for common chronic conditions [53] [101].
Table 2: Late-Stage In Vivo CRISPR Therapies for Cardiovascular and Metabolic Diseases
| Therapy | Target | Indication | Phase | Key Efficacy Findings | Safety Profile |
|---|---|---|---|---|---|
| CTX310 (CRISPR Therapeutics) | ANGPTL3 | Homozygous/heterozygous familial hypercholesterolemia, severe hypertriglyceridemia, mixed dyslipidemias | Phase 1 | 50% reduction in LDL cholesterol; 55% reduction in triglycerides at highest dose (0.8 mg/kg) | No serious adverse events; minor infusion reactions (back pain, nausea) resolved with medication |
| CTX320 (CRISPR Therapeutics) | LPA | Elevated lipoprotein(a) | Phase 1 | Preclinical NHP studies show durable Lp(a) reduction | Ongoing trials; no serious safety concerns reported |
| VERVE-102 (Verve Therapeutics) | PCSK9 | Heterozygous familial hypercholesterolemia, coronary artery disease | Phase 1b | Well-tolerated in initial cohorts; preliminary efficacy data expected H1 2025 | No serious adverse events or laboratory anomalies in initial cohorts |
| NTLA-2001 (Intellia Therapeutics) | TTR | Transthyretin amyloidosis with cardiomyopathy (ATTR-CM) and polyneuropathy (ATTRv-PN) | Phase 3 | ~90% reduction in TTR protein sustained through 2+ years; functional improvement or stability | Mild to moderate infusion-related events common; no long-term safety concerns |
Recent Phase 1 clinical trial results for CTX310 demonstrate promising safety and efficacy data. Presented at the American Heart Association's Scientific Sessions 2025 and simultaneously published in the New England Journal of Medicine, the first-in-human trial included 15 patients with lipid disorders resistant to conventional medications. Participants received a single intravenous infusion of CTX310 at doses ranging from 0.1 to 0.8 mg/kg. The therapy achieved substantial reductions in both LDL cholesterol and triglyceride levels within two weeks, with effects maintained for at least 60 days. Future Phase 2 studies are planned to begin in 2026, focusing on broader patient populations and longer-term outcomes [101].
Oncology and Autoimmune Disease Applications
The application of CRISPR technology in oncology and autoimmune diseases represents another advancing frontier, with allogeneic CAR T-cell therapies demonstrating significant potential across multiple indications [53].
CTX112, a next-generation, wholly-owned, allogeneic CAR T product candidate targeting CD19, is being developed for both hematologic malignancies and autoimmune indications. Recent data from the ongoing Phase 1/2 trial in relapsed or refractory CD19+ B-cell malignancies demonstrates strong efficacy comparable to autologous therapies, with a tolerable safety profile and robust cell expansion. Notably, responses were observed in all six patients who had received prior T-cell engager-based therapies, including three with large B-cell lymphoma who had either relapsed post-TCE treatment or were refractory to TCEs. Based on these encouraging oncology data, CRISPR Therapeutics is expanding trials for CTX112 in systemic lupus erythematosus to include patients with systemic sclerosis and inflammatory myositis in a basket study, with updates expected in mid-2025 [53].
The therapy has received regenerative medicine advanced therapy (RMAT) designation from the FDA based on strong preliminary data, potentially accelerating its development timeline. The company plans to engage with regulatory authorities to align on the path forward for CTX112 in B-cell malignancies, with a comprehensive update expected in mid-2025 [53].
Experimental Protocols and Methodologies
Ex Vivo Hematopoietic Stem Cell Editing Protocol
The following detailed protocol outlines the standardized methodology for ex vivo CRISPR-Cas9 editing of hematopoietic stem cells (HSCs), as employed in CASGEVY manufacturing and similar investigational therapies for genetic blood disorders [53] [95].
Diagram Title: Ex Vivo HSC Editing and Transplantation Workflow
Key Reagents and Materials:
- CRISPR-Cas9 Ribonucleoprotein (RNP) Complex: Purified Cas9 protein complexed with synthetic single-guide RNA (sgRNA) targeting the specific genomic locus
- CD34+ Cell Selection Kit: Immunomagnetic beads for positive selection of hematopoietic stem/progenitor cells
- Electroporation System: Device for efficient RNP delivery into cells
- Stem Cell Culture Medium: Serum-free medium supplemented with cytokines (SCF, TPO, FLT3-L)
- Myeloablative Conditioning Agent: Busulfan for bone marrow clearance pre-transplant
Critical Quality Control Assessments:
- Editing Efficiency: T7 Endonuclease I assay or next-generation sequencing to quantify indels at target site
- Cell Viability: Flow cytometry with Annexin V/PI staining post-electroporation
- Sterility Testing: BacT/ALERT microbial culture system
- Vector Copy Number: qPCR to confirm absence of viral vector integration
- Karyotyping: Chromosomal analysis to detect potential large-scale abnormalities
In Vivo LNP Delivery and Liver-Targeted Editing
For in vivo CRISPR therapies such as CTX310 and CTX320, the following protocol details the LNP formulation, administration, and monitoring approach that has demonstrated efficacy in clinical trials [101] [102].
Diagram Title: In Vivo LNP Delivery and Monitoring Workflow
Key Reagents and Materials:
- CRISPR-Cas9 mRNA: Modified nucleotide mRNA encoding SpCas9 protein
- Single-Guide RNA (sgRNA): Chemically modified sgRNA targeting therapeutic gene
- Ionizable Lipid Nanoparticles: Proprietary LNP formulation with hepatic tropism
- Pre-medication Regimen: Corticosteroids and antihistamines to prevent infusion reactions
Critical Parameters for LNP Formulation:
- Particle Size: 70-100 nm optimized for hepatocyte uptake
- Polydispersity Index: <0.2 indicating uniform size distribution
- Encapsulation Efficiency: >90% RNA encapsulation
- Endotoxin Levels: <5 EU/mL per regulatory guidelines
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for CRISPR Clinical Trial Applications
| Reagent/Material | Function | Example Applications | Critical Quality Attributes |
|---|---|---|---|
| CRISPR-Cas9 RNP Complex | Directs specific DNA cleavage | Ex vivo HSC editing (CASGEVY); T-cell engineering | High purity; specificity; minimal off-target activity |
| Ionizable Lipid Nanoparticles | In vivo delivery to hepatocytes | CTX310, CTX320, NTLA-2001 programs | Hepatic tropism; high encapsulation efficiency; tolerable safety profile |
| CD34+ Cell Selection Kits | Hematopoietic stem cell isolation | Ex vivo therapies for hemoglobinopathies, immunodeficiencies | High purity (>90%); maintained cell viability; sterility |
| Electroporation Systems | Non-viral delivery of editing components | Ex vivo cell processing across multiple platforms | High efficiency; optimal viability; scalability |
| Cell Culture Media Formulations | Supports cell expansion and maintenance | All ex vivo editing protocols | Serum-free; defined composition; cytokine supplements |
| Next-Generation Sequencing Assays | Assessing on-target editing and off-target effects | All clinical trials for comprehensive safety evaluation | Comprehensive genome coverage; sensitive variant detection |
The clinical development of CRISPR-Cas9 therapies has progressed from proof-of-concept to validated therapeutic approach within a remarkably short timeframe. The approval and successful commercialization of CASGEVY for sickle cell disease and beta thalassemia demonstrates the transformative potential of gene editing for addressing monogenic disorders. Meanwhile, the expanding pipeline of late-stage investigational therapies across cardiovascular, metabolic, autoimmune, and oncological indications highlights the versatility and broadening applications of this technology platform [53] [14] [101].
Substantial challenges remain in optimizing delivery systems, ensuring long-term safety, and expanding access to these potentially curative treatments. However, the continued innovation in gene-editing tools—including base editing, prime editing, and retron-based systems—promises to address many current limitations. The retron system developed at UT Austin, which enables correction of multiple disease-causing mutations simultaneously, represents one such advancement that could dramatically improve the inclusivity of gene therapies for patients with diverse mutations in conditions like cystic fibrosis [103].
As the field advances, the establishment of standardized experimental protocols, comprehensive safety monitoring frameworks, and robust manufacturing processes will be critical for translating these technologies to broader patient populations. The ongoing clinical trials and emerging data throughout 2025 and beyond will further refine our understanding of both the potential and limitations of CRISPR-based therapies, ultimately determining their place in the therapeutic arsenal for genetic disorders [100] [95].
CRISPR vs. Traditional Gene Therapy and Other Gene-Editing Platforms (ZFNs, TALENs)
Gene editing has become a cornerstone of modern molecular biology, enabling precise modifications to DNA sequences for research, therapeutic, and agricultural applications [104]. The field has evolved from early homologous recombination techniques to programmable nucleases, including Zinc Finger Nucleases (ZFNs), Transcription Activator-Like Effector Nucleases (TALENs), and the more recent CRISPR-Cas systems [104] [105]. While traditional gene therapy aims to introduce new genetic material to compensate for defective genes, modern gene-editing platforms directly correct the underlying DNA sequence, offering the potential for permanent cures [106].
This document provides a technical comparison of these platforms, with detailed protocols and application notes framed within CRISPR-Cas9 applications for genetic disorder therapy research.
Platform Comparison: Mechanisms and Technical Specifications
The core distinction between platforms lies in their DNA recognition mechanisms: CRISPR uses RNA-DNA base pairing, while ZFNs and TALENs rely on protein-DNA interactions [107] [108].
Comparative Analysis of Gene-Editing Platforms
Table 1: Technical comparison of major gene-editing platforms.
| Feature | CRISPR-Cas9 | TALENs | ZFNs |
|---|---|---|---|
| Mechanism of Target Recognition | RNA-DNA interaction (Watson-Crick base pairing) [107] | Protein-DNA interaction [107] | Protein-DNA interaction [107] |
| DNA-Binding Domain | Guide RNA (gRNA, ~20 bp) [107] | TALE repeats (one repeat per nucleotide) [107] [105] | Zinc finger arrays (each recognizes 3 bp) [105] |
| Cleavage Domain / Nuclease | Cas9 (or variants) [104] | FokI dimer [107] [105] | FokI dimer [107] [105] |
| Target Site Requirement | Protospacer Adjacent Motif (PAM, e.g., 5'-NGG-3' for SpCas9) [107] | No PAM requirement; requires a 5' T [107] | No PAM requirement |
| Ease of Design & Cloning | Simple (design of gRNA sequence) [104] [107] | Moderate (cloning of TALE repeats) [104] [107] | Complex (engineering of zinc finger arrays) [104] [105] |
| Multiplexing Capacity | High (multiple gRNAs) [104] [108] | Low [104] | Low [104] |
| Typical Delivery Format | Plasmid, RNA, or RNP complex [107] | Plasmid DNA [107] [108] | Plasmid DNA [108] |
| Relative Cost | Low [104] | High [104] | High [104] |
| Key Advantages | User-friendly, highly versatile, cost-effective, suitable for high-throughput screening [104] | High specificity, flexible target design [104] [107] | High specificity, smaller size than TALENs for viral delivery [108] |
| Key Limitations | Off-target effects, PAM sequence dependency [104] [107] | Large size impedes viral delivery, time-consuming assembly [104] [108] | Difficult and time-consuming to design, potential cytotoxicity [104] [105] |
CRISPR vs. Traditional Gene Therapy
Traditional gene therapy introduces a functional copy of a gene into a cell's genome using a viral vector (e.g., Adeno-Associated Virus) to compensate for a defective gene, but it does not correct the underlying mutation [106]. This can lead to unpredictable expression and poses risks if the new gene inserts into an unfavorable genomic location. In contrast, CRISPR gene editing directly corrects the disease-causing mutation at the native genomic locus, offering the potential for permanent, physiological regulation of the corrected gene [106].
Application Notes: CRISPR in Therapeutic Development
CRISPR's versatility has accelerated its translation from basic research to clinical applications, particularly for genetic disorders.
Clinical Trial Landscape and Key Therapeutic Areas
As of early 2025, the gene-editing clinical landscape includes over 150 active trials, with CRISPR-based therapies dominating the pipeline [27]. Key therapeutic areas include [27]:
- Blood Disorders: Sickle Cell Disease (SCD) and β-thalassemia (e.g., Casgevy, the first FDA-approved CRISPR therapy) [14] [109].
- Genetic Metabolic Disorders: Hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE) [14].
- Cardiovascular Diseases: Heterozygous familial hypercholesterolemia (HeFH) and hypercholesterolemia [101] [27].
- Oncology: Various B-cell malignancies and acute lymphoblastic leukaemia [27].
- Infectious Diseases: CRISPR-enhanced phage therapies for E. coli and urinary tract infections [14].
- Autoimmune Diseases: Lupus and multiple sclerosis [27].
Quantitative Clinical Outcomes
Table 2: Efficacy data from select CRISPR clinical trials (2024-2025).
| Therapy / Target | Condition | Key Result | Trial Phase | Reference |
|---|---|---|---|---|
| Casgevy (Exagamglogene autotemcel) | Sickle Cell Disease (SCD) & Transfusion-Dependent Beta Thalassemia (TBT) | FDA and EMA approved; prevents vaso-occlusive crises in SCD [14] [109] | Approved (2023-2024) | [14] [109] |
| NTLA-2001 (Intellia Therapeutics) | Hereditary Transthyretin Amyloidosis (hATTR) | ~90% sustained reduction in serum TTR protein levels at 2 years [14] | Phase III | [14] |
| NTLA-2002 (Intellia Therapeutics) | Hereditary Angioedema (HAE) | 86% reduction in kallikrein; 8 of 11 high-dose participants were attack-free over 16 weeks [14] | Phase I/II | [14] |
| CTX310 (CRISPR Therapeutics) | Hypercholesterolemia (ANGPTL3 gene) | 50% reduction in LDL cholesterol; ~55% reduction in triglycerides [101] | Phase I | [101] |
Experimental Protocols
Protocol: CRISPR-Cas9 Knockout in Hematopoietic Stem Cells (HSCs) for SCD Therapy
This protocol outlines the key steps for generating a knockout of the BCL11A gene in HSCs to reactivate fetal hemoglobin (γ-globin) as a therapeutic strategy for Sickle Cell Disease (SCD), based on the approach used in Casgevy [109].
I. Research Reagent Solutions Table 3: Essential reagents for HSC gene editing.
| Reagent / Material | Function / Description |
|---|---|
| Mobilized CD34+ HSCs | Primary cells isolated from patient peripheral blood after granulocyte colony-stimulating factor (G-CSF) mobilization. |
| CRISPR RNP Complex | Pre-complexed recombinant Cas9 protein and synthetic gRNA targeting the BCL11A erythroid enhancer region. |
| Electroporation System | Device for delivering RNP complexes into cells via electrical pulses (e.g., Neon or Lonza 4D-Nucleofector). |
| StemSpan SFEM II Medium | Serum-free, cytokine-supplemented medium for ex vivo HSC culture. |
| Cytokine Cocktail | Recombinant human SCF, TPO, FLT-3L to maintain stemness and promote survival during editing. |
| ClonaCell-TCS Medium | Semi-solid methylcellulose medium for Colony-Forming Unit (CFU) assays to assess editing efficiency and differentiation. |
II. Step-by-Step Workflow
- HSC Harvest & Isolation: Isolate CD34+ hematopoietic stem and progenitor cells (HSPCs) from a leukapheresis product of a mobilized donor using clinical-grade CD34+ immunomagnetic selection. Culture cells in StemSpan SFEM II medium supplemented with the cytokine cocktail (SCF, TPO, FLT-3L) for 24-48 hours prior to editing.
- RNP Complex Formation: Resuspend synthetic gRNA (targeting the BCL11A enhancer) and recombinant Cas9 protein in nuclease-free buffer. Incubate at room temperature for 10-20 minutes to form the Ribonucleoprotein (RNP) complex.
- Electroporation: Harvest pre-stimulated CD34+ cells. Resuspend 1-5 x 10^5 cells in the RNP complex solution. Transfer the cell-RNP suspension to an electroporation cuvette and electroporate using a pre-optimized protocol (e.g., 1600 V, 10 ms, 3 pulses). Immediately after electroporation, transfer cells to pre-warmed, cytokine-supplemented medium.
- Post-Editing Culture & Analysis:
- Viability Assessment: At 24 hours post-electroporation, determine cell viability using Trypan Blue exclusion.
- Editing Efficiency: At 48-72 hours, extract genomic DNA. Assess indel frequency at the target locus using T7 Endonuclease I assay or TIDE (Tracking of Indels by Decomposition) analysis. Confirm on-target editing and screen for potential off-target sites via next-generation sequencing (NGS).
- Functional CFU Assay: Plate 500-1000 cells per dish in methylcellulose-based ClonaCell medium. Incubate for 14 days. Score myeloid (CFU-GM) and erythroid (BFU-E) colonies. Pick individual colonies for genomic DNA extraction and sequencing to confirm biallelic editing and measure fetal hemoglobin (HbF) levels via HPLC.
Diagram 1: HSC CRISPR editing workflow.
Protocol: In Vivo CRISPR Therapy for Lipid Disorders
This protocol describes the key steps for the development and administration of CTX310, an LNP-formulated CRISPR therapy that inactivates the ANGPTL3 gene in the liver to treat hypercholesterolemia [101].
I. Research Reagent Solutions Table 4: Essential reagents for LNP-formulated CRISPR therapy.
| Reagent / Material | Function / Description |
|---|---|
| CRISPR Plasmid DNA | Plasmid encoding Cas9 nuclease and a gRNA targeting the ANGPTL3 gene. |
| LNP Formulation Components | Ionizable lipid, phospholipid, cholesterol, and PEG-lipid for encapsulating CRISPR machinery. |
| Pre-treatment Medications | Corticosteroids and antihistamines to preempt infusion-related reactions. |
| Animal Model | Non-human primate or mouse model with diet-induced hypercholesterolemia. |
| Clinical Chemistry Analyzer | Platform for measuring LDL-C, triglycerides, and liver enzymes (ALT/AST) in serum/plasma. |
II. Step-by-Step Workflow
- gRNA Design and Validation: Design gRNAs targeting the ANGPTL3 gene. Validate cleavage efficiency and specificity in relevant hepatocyte cell lines (e.g., HepG2) using the RNP delivery method described in Protocol 4.1. Select the lead candidate with high on-target and minimal off-target activity.
- LNP Formulation and Encapsulation: Prepare a nucleic acid payload containing Cas9 mRNA and the validated ANGPTL3 gRNA. Use microfluidic mixing to encapsulate the payload into LNPs composed of the ionizable lipid, phospholipid, cholesterol, and PEG-lipid. Purify the formulated LNPs via tangential flow filtration and characterize for size, polydispersity, and encapsulation efficiency.
- In Vivo Dosing and Monitoring:
- Pre-treatment: Administer corticosteroids and antihistamines to the patient approximately 1 hour before the LNP infusion to mitigate potential infusion-related reactions [101].
- Administration: Administer a single intravenous infusion of the LNP-formulated CRISPR therapy (e.g., CTX310) at a defined dose (e.g., 0.8 mg/kg) [101].
- Efficacy and Safety Monitoring:
- Biochemical Efficacy: Monitor serum levels of ANGPTL3 protein, LDL cholesterol, and triglycerides at baseline, 2 weeks, 4 weeks, and 8 weeks post-infusion. Expect significant reductions (e.g., ~50% LDL-C, ~55% triglycerides) [101].
- Safety Monitoring: Perform comprehensive metabolic panels to monitor liver function (ALT, AST), renal function, and complete blood counts. Monitor for and document any infusion-related reactions.
Diagram 2: In vivo LNP-CRISPR therapy workflow.
Advanced CRISPR Technologies and Future Directions
The field is rapidly advancing beyond standard CRISPR-Cas9 to enhance safety and precision.
- Base Editing: Allows for direct, irreversible chemical conversion of one DNA base into another (e.g., C•G to T•A) without requiring a DSB, thereby minimizing indel formation [104]. This is ideal for correcting single-nucleotide polymorphisms (SNPs).
- Prime Editing: A "search-and-replace" technology that can mediate all 12 possible base-to-base conversions, as well as small insertions and deletions, without requiring DSBs or donor DNA templates, further expanding the scope of editable mutations [104].
- AI-Powered Experimental Design: Tools like CRISPR-GPT, an AI agent trained on over a decade of CRISPR experimental data, can assist researchers in generating optimized experimental designs, predicting off-target effects, and troubleshooting, significantly accelerating the therapeutic development pipeline [20].
CRISPR-Cas9 has democratized gene editing due to its simplicity, cost-effectiveness, and versatility, largely superseding ZFNs and TALENs for most research and therapeutic applications [104] [108]. Its success in clinical trials for diseases like SCD and hATTR underscores its transformative potential [14] [109] [101]. However, challenges remain, including the potential for off-target effects, efficient in vivo delivery to non-liver tissues, and immune responses to bacterial Cas proteins [104] [106]. The choice of editing platform ultimately depends on the specific research goal, with traditional methods like TALENs retaining value for applications requiring exceptionally high specificity with minimal off-target risk [104]. The continued evolution of CRISPR technologies, including base editing and AI-assisted design, promises to further refine its precision and expand its therapeutic potential.
Analyzing Durability of Effect and Long-Term Patient Follow-Up Data
The advent of CRISPR-Cas9 gene editing has ushered in a new era for the treatment of genetic disorders. While initial efficacy results from clinical trials are promising, a critical component for the successful translation of these therapies is a rigorous analysis of the durability of effect and the implementation of comprehensive long-term patient follow-up protocols. The permanent nature of genomic edits necessitates extended monitoring to confirm that therapeutic benefits are sustained and to identify any delayed adverse events [110]. This document provides detailed application notes and experimental protocols to standardize the assessment of long-term outcomes in CRISPR-based clinical trials and preclinical studies, supporting the broader research objective of developing safe and durable genetic therapies.
Current Clinical Data on Durability and Follow-Up
Recent clinical trials provide the first insights into the durability of CRISPR-based therapies. Summarized below are quantitative data from key trials, highlighting the initial evidence of sustained effect.
Table 1: Long-Term Follow-Up Data from Select CRISPR Clinical Trials
| Therapy / Trial | Target Condition | Key Durability Metric | Reported Durability | Long-Term Follow-Up Plan |
|---|---|---|---|---|
| CTX310 (Phase 1) [69] | Mixed Dyslipidemia | Reduction in LDL Cholesterol & Triglycerides | Sustained reduction through at least 60 days | Patients monitored for 1 year in-trial; Long-term safety follow-up for 15 years as per FDA guidance |
| Intellia's hATTR Therapy (Phase 1) [14] | Hereditary Transthyretin Amyloidosis | Reduction in TTR Protein | ~90% reduction sustained for 2+ years in all 27 participants | Ongoing; long-term follow-up is standard |
| CASGEVY (Approved) [111] [14] | Sickle Cell Disease, Beta-Thalassemia | Fetal Hemoglobin Level | Sustained production post-treatment, leading to functional cure | 15-year follow-up required post-infusion to monitor long-term safety |
Key Observations from Clinical Data
- Rapid and Sustained Onset: Therapies often show effects within weeks, which then plateau and are maintained over time. For example, CTX310 reduced cholesterol levels within two weeks, and this effect persisted for the 60-day observation period [69].
- Durability of One-Time Treatment: The "one-and-done" treatment approach has demonstrated sustained effects over multiple years in trials for conditions like hATTR, validating the potential for durable cures from a single intervention [69] [14].
- Regulatory Mandates for Long-Term Follow-Up: Given the permanent nature of DNA edits, the U.S. Food and Drug Administration (FDA) recommends, and often requires, long-term safety monitoring for up to 15 years for all participants in CRISPR-based therapy trials [69] [110]. This is a critical consideration for clinical trial design.
Core Principles and Key Concepts
Defining Durability in Genome Editing
In the context of CRISPR-Cas9 therapies, "durability of effect" refers to the stable, long-term presence of the therapeutic genetic modification and its associated phenotypic outcome. This durability hinges on the permanent alteration of the DNA sequence in the target cell population, which can then be passed to daughter cells through cell division [112].
Mechanisms Affecting Long-Term Stability
The persistence of the edited cell population is a primary factor influencing durability. This is influenced by:
- Cell Turnover Rate: Therapies targeting long-lived cells (e.g., neurons, hematopoietic stem cells) are more likely to yield permanent effects compared to those targeting short-lived cells [112].
- Immune Response: An immune reaction against the bacterial-derived Cas9 protein or the delivery vector (e.g., AAV) can clear edited cells, potentially undermining durability. The use of lipid nanoparticles (LNPs) appears to mitigate this risk and may even allow for re-dosing, as evidenced in recent trials [14].
- Genomic Instability: Unwanted editing outcomes, such as large deletions or chromosomal rearrangements, may manifest over time and potentially lead to adverse events like malignancy, underscoring the need for long-term surveillance [110] [112].
Experimental Protocols for Assessing Durability
A multi-faceted approach is required to comprehensively evaluate the durability and safety of CRISPR interventions.
Protocol 1: Longitudinal Tracking of Editing Outcomes in Patient Samples
This protocol details the process for monitoring the stability and heterogeneity of genomic edits over time using sequencing-based methods.
1. Sample Collection:
- Materials: Cell separation tubes, DNA extraction kits.
- Procedure: Collect longitudinal samples (e.g., peripheral blood mononuclear cells, tissue biopsies) at predetermined time points (e.g., baseline, 1 month, 6 months, 1 year, then annually). For blood-based therapies, isolate the relevant cell population (e.g., CD34+ cells, T cells) using density gradient centrifugation or magnetic-activated cell sorting (MACS).
2. Genomic DNA Extraction and Target Amplification:
- Materials: DNeasy Blood & Tissue Kit (or equivalent), PCR reagents, primers flanking the on-target and predicted off-target sites.
- Procedure: Extract high-quality genomic DNA from sorted cells. Amplify the target genomic regions using polymerase chain reaction (PCR). Ensure amplification of unedited control samples for comparison.
3. Sequencing and Analysis:
- Materials: Next-generation sequencing (NGS) platform, Sanger sequencing reagents, computational analysis tools (e.g., ICE, TIDE).
- Procedure:
- For a comprehensive view, use targeted amplicon sequencing (NGS). This provides deep, quantitative data on the spectrum of indels (insertions/deletions) and their relative abundances over time, allowing researchers to track the clonal stability of the edited cell population [113] [114].
- For a more cost-effective and rapid analysis, use Sanger sequencing followed by computational decomposition with tools like Inference of CRISPR Edits (ICE) or Tracking of Indels by Decomposition (TIDE). These tools quantify editing efficiency and indel distributions from chromatogram data [113].
4. Data Interpretation:
- A stable or increasing percentage of desired edits indicates good durability.
- A shift in the distribution of indel types or a decline in editing percentage may indicate selective pressure against certain edits or immune-mediated clearance of edited cells.
Protocol 2: Long-Term Safety and Off-Target Monitoring
This protocol outlines strategies to identify and monitor potential off-target editing events throughout a study.
1. In Silico Prediction:
- Materials: Bioinformatics software (e.g., Cas-OFFinder).
- Procedure: Before initiating the study, computationally predict potential off-target sites across the genome based on sequence similarity to the guide RNA, including mismatches and bulges [114].
2. Experimental Off-Target Screening:
- Materials: In vitro cleavage assays (e.g., SITE-seq, CIRCLE-seq), cellular assays (e.g., GUIDE-seq if applicable).
- Procedure:
- Employ sensitive in vitro methods like CIRCLE-seq or SITE-seq. These assays use purified genomic DNA and the CRISPR ribonucleoprotein (RNP) complex to identify potential off-target sites in a controlled, high-sensitivity context [114].
- The top predicted and in vitro-identified off-target sites are then tracked in all longitudinal patient samples using targeted NGS, similar to the on-target analysis in Protocol 1 [114].
3. Monitoring for Gross Rearrangements and Genomic Instability:
- Materials: Karyotyping kits, FISH probes, PCR for fusion transcripts.
- Procedure: Periodically analyze edited cells for large-scale genomic alterations using karyotyping or fluorescence in situ hybridization (FISH). The presence of oncogenic fusion transcripts can be assessed via RT-PCR.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Durability and Follow-Up Analysis
| Reagent / Tool | Function | Application in Durability Studies |
|---|---|---|
| Lipid Nanoparticles (LNPs) [69] [14] | In vivo delivery vehicle for CRISPR components. | Enables efficient liver-directed editing and may allow for re-dosing due to low immunogenicity, directly impacting durability strategies. |
| Next-Generation Sequencing (NGS) [113] [114] | High-throughput, deep sequencing of DNA. | Gold standard for quantifying on-target editing efficiency, tracking indel spectra, and monitoring predicted off-target sites over time. |
| ICE (Inference of CRISPR Edits) Software [113] | Computational tool for analyzing Sanger sequencing data. | A cost-effective and accurate (R² = 0.96 vs. NGS) method to quantify editing efficiency and indel patterns from longitudinal samples. |
| CIRCLE-seq / SITE-seq [114] | In vitro assays for genome-wide off-target identification. | Provides a sensitive, unbiased profile of potential off-target sites to be monitored in long-term patient samples. |
| Guide RNA (gRNA) with High Specificity | Targets the Cas9 nuclease to the DNA locus of interest. | Using computationally optimized and validated high-fidelity gRNAs minimizes the risk of off-target effects, a primary long-term safety concern. |
| Cas9 Protein Variants (e.g., High-Fidelity Cas9) [110] [114] | Engineered nuclease with reduced off-target activity. | Employing high-fidelity Cas9 variants (e.g., eSpCas9, SpCas9-HF1) is a critical strategy to improve the long-term safety profile of a therapy. |
Visualization of Workflows and Relationships
The following diagrams illustrate the core protocols and decision-making processes for long-term follow-up.
Long-Term Monitoring Workflow
CRISPR Analysis Method Selection
The successful translation of CRISPR-Cas9 therapies from bench to bedside is intrinsically linked to a deep and systematic understanding of their long-term behavior. By implementing the standardized application notes and detailed protocols outlined herein—focusing on longitudinal molecular tracking, comprehensive safety monitoring, and adherence to regulatory follow-up timelines—researchers and drug developers can generate the robust data required to ensure that these revolutionary therapies are not only effective but also durable and safe for a patient's lifetime. This rigorous approach to analyzing durability is foundational to fulfilling the promise of CRISPR as a definitive treatment for genetic disorders.
The advent of CRISPR-Cas9 gene-editing technology has revolutionized the therapeutic landscape, offering unprecedented potential for curing genetic disorders that were once considered untreatable. Derived from a bacterial immune system, this groundbreaking technology enables scientists to make precise alterations to DNA sequences in living organisms with remarkable efficiency and relative simplicity [115]. The system operates through a guide RNA (gRNA) that directs the Cas9 enzyme—functioning as "molecular scissors"—to specific locations in the genome, where it creates double-stranded breaks in the DNA. These breaks then trigger the cell's natural repair mechanisms, allowing for targeted genetic modifications [115] [116].
The therapeutic potential of this technology is vast, with clinical trials demonstrating remarkable success in treating inherited blood disorders such as sickle cell disease and beta-thalassemia [5] [117]. For instance, in a landmark clinical trial, all 31 sickle cell patients receiving CRISPR-based treatment became free of symptoms, despite previous diagnoses with severe cases of the disease [117]. Similarly, 42 of 44 beta-thalassemia patients were able to discontinue the transfusions that had been essential to their survival [117]. These breakthroughs represent a paradigm shift in medicine, transitioning from chronic disease management to potential one-time cures.
However, this revolutionary therapeutic promise is accompanied by a formidable challenge: extraordinarily high costs that threaten to limit patient access and exacerbate health disparities. The first generation of genomic therapies has entered the market with price tags reaching up to $3.5 million per treatment [118], with the recently approved CRISPR-based therapy Casgevy priced at $2.2 million per patient [119]. This cost paradox—unprecedented therapeutic potential coupled with potentially prohibitive pricing—represents a critical challenge that must be addressed to ensure that the genomic medicine revolution benefits all who need it, not only the affluent.
Quantitative Landscape of Current Therapeutic Costs
The high cost of curative therapies is not merely theoretical but is already manifesting in the market, with significant implications for healthcare systems and patients. The table below summarizes the pricing landscape for recently approved genomic therapies:
Table 1: Approved Genomic Therapies and Their Pricing
| Therapy | Date Approved | Disease | Price (USD) |
|---|---|---|---|
| ZOLGENSMA | May 2019 | Spinal muscular atrophy | $2.125 million [118] |
| ZYNTEGLO | August 2022 | β-thalassemia | $2.8 million [118] |
| SKYSONA | September 2022 | Cerebral adrenoleukodystrophy | $3.0 million [118] |
| HEMGENIX | November 2022 | Hemophilia B | $3.5 million [118] |
| Casgevy | 2023 | Sickle cell disease | $2.2 million [119] |
These prices pose substantial challenges to healthcare systems, particularly for conditions that disproportionately affect marginalized communities. For example, sickle cell disease (SCD) primarily affects individuals of African ancestry, while Artemis Severe Combined Immunodeficiency (SCID) is highly prevalent in Navajo and Apache communities [118]. The financial impact on public insurance systems could be staggering; one estimate suggests that if a sickle cell disease genomic therapy came to market at $1 million per patient, it would cost Medicaid $55 billion—roughly 85% of Medicaid's total spending on outpatient drugs in 2017 [118].
The economic burden extends beyond the therapy itself. Even when drugs are provided at low cost or for free, patients may still face "very high affordability concerns related to the hospital bill, which don't get written off as easily" [120]. This creates a situation where even medically successful treatments remain practically inaccessible to many patients, raising profound questions about health equity and distributive justice in the genomic medicine era.
Analysis of Cost Drivers in CRISPR-Based Therapies
Research, Development, and Manufacturing Complexities
The development of CRISPR-based therapies involves substantial upfront investment and complex manufacturing processes that contribute significantly to their high costs. Developing a gene therapy can cost an estimated $5 billion—more than five times the average cost of developing traditional drugs [120]. These elevated costs reflect the technical challenges and specialized infrastructure required for advanced therapy medicinal products (ATMPs).
Several key factors drive these development costs:
Preclinical Research: CRISPR therapy development requires extensive target validation, guide RNA design and optimization, and in vitro and in vivo testing to demonstrate efficacy and safety.
Vector Development and Production: Most gene therapies rely on viral vectors (such as adeno-associated viruses or lentiviruses) for efficient delivery of CRISPR components. These vectors are complex and expensive to produce at clinical grade [5].
Manufacturing Challenges: CRISPR therapies often involve autologous approaches, where a patient's own cells are harvested, genetically modified ex vivo, and then reinfused. This process requires sophisticated good manufacturing practice (GMP) facilities and stringent quality control measures [118].
Characterization and Analytics: Extensive testing is required to ensure product safety, potency, and purity, including assessments for on-target editing efficiency and potential off-target effects.
Clinical Trial and Regulatory Expenses
Clinical development of CRISPR therapies presents unique challenges that increase costs compared to conventional drugs:
Specialized Trial Designs: Gene therapy trials often require complex protocols with long-term follow-up to assess durability of response and potential late-onset adverse events.
Small Patient Populations: Many genetic disorders targeted by CRISPR therapies are rare diseases, resulting in small clinical trials with high per-patient costs to achieve statistical significance.
Regulatory Complexity: The novel nature of CRISPR therapies means regulatory pathways are often evolving, requiring extensive interactions with regulatory agencies and additional data collection.
Long-Term Follow-Up: Regulatory requirements typically mandate long-term patient monitoring (often 5-15 years) to assess persistence of therapeutic effect and monitor for delayed adverse events, adding substantial cost.
Economic and Market Factors
Beyond technical and clinical factors, market dynamics play a significant role in pricing decisions:
Limited Patient Populations: For rare diseases, the small number of eligible patients means that development costs must be recouped from a limited market. For example, Zolgensma for spinal muscular atrophy is only approved for use in children under two years old, with an estimated 700 eligible patients in the U.S. [120].
Value-Based Pricing: Pharmaceutical companies often justify high prices based on the lifetime value of curative therapies. As one analysis notes, "the high cost of these therapies is often justified on the basis that genomic therapies are one-time, potentially curative treatments that offer high value to patients and health systems by negating future costs related to treating the disease" [118].
Patent Protections and Limited Competition: The current intellectual property landscape for CRISPR technology and the limited number of developers for specific genetic disorders reduces competitive pressure that might otherwise drive down prices [120].
Ethical Imperatives and Equity Considerations
Health Equity Implications
The high cost of CRISPR-based cures raises profound ethical concerns regarding equitable access to medical breakthroughs. As these therapies emerge, there is a significant risk that they will primarily benefit affluent patients in well-resourced healthcare systems, potentially widening existing health disparities [121]. This is particularly problematic for diseases like sickle cell disease, which "primarily affects individuals of African ancestry or Central and South American descent" [121], communities that have historically faced barriers to accessing advanced medical care.
The ethical imperative for affordable pricing is underscored by the fact that early research and development of many gene therapies received substantial public funding. As noted in the literature, "governments and philanthropies fund early-stage research at academic institutions" [118], meaning that the public often bears the initial financial risk, yet private companies subsequently set prices that limit access. This creates what has been termed a "double payment" problem, where taxpayers fund basic research and then face prohibitive prices for the resulting therapies.
Community Engagement and Representation
Addressing health equity concerns requires meaningful engagement with affected communities throughout the research and development process. Minority populations remain gravely underrepresented in genomics research, which may lead to "less effective and accepted CRISPR tools and therapies for these groups" [121]. This underrepresentation creates a vicious cycle where therapies may be less optimized for diverse populations, potentially reducing their efficacy and further discouraging investment in conditions that disproportionately affect marginalized groups.
The principle of justice in healthcare demands that the benefits of scientific progress be distributed fairly. As one analysis argues, "the approval of CRISPR transforms our obligations of justice and compels us to bring future gene therapies to the maximum possible number of patients with serious genetic diseases at affordable prices" [119]. This perspective suggests that the revolutionary nature of CRISPR technology carries with it a corresponding responsibility to ensure broad access.
Alternative Models for Affordable and Accessible Therapies
Novel Payment and Reimbursement Structures
Innovative financing models are being explored to address the affordability challenge while ensuring sustainable development of CRISPR therapies:
Table 2: Alternative Payment Models for High-Cost Curative Therapies
| Model Type | Key Mechanism | Potential Benefits | Implementation Challenges |
|---|---|---|---|
| Outcome-Based Spread Payments | Payments spread over time and adjusted based on therapeutic outcomes [122] | Reduces initial budget impact; aligns payment with value | Complex administration; requires outcome measurement infrastructure |
| Subscription Models | Flat fee for unlimited access to a therapy for a defined population [120] | Predictable costs for payers; guaranteed revenue for manufacturers | Risk assessment for both parties; potential for over- or under-utilization |
| Health Care Utility Model | Purchasers (health systems) collectively finance and own therapy development [118] | Aligns incentives around patient access rather than profit maximization | Requires unprecedented collaboration among health systems |
| Public Benefit Corporation | For-profit entity legally permitted to prioritize social goals alongside shareholder value [118] | Attracts impact investment while maintaining commercial viability | May face tension between social mission and financial sustainability |
Alternative Organizational and Development Models
Beyond payment reforms, structural changes to therapy development and distribution are being explored:
Nonprofit Drug Development: Organizations like CivicaRx are pioneering nonprofit models that address "generic drug pricing and shortage issues" [118], providing a template that could be adapted for CRISPR therapies. This model replaces the traditional separation between investors and customers with a structure where purchasers have a direct stake in therapy development.
Public-Private Partnerships: These collaborations can distribute risk and align incentives across sectors. By leveraging public funding for early-stage research and private sector expertise for development and commercialization, such partnerships can "reduce drug development risks for companies" [118] while maintaining some public influence over pricing and access.
Academic-Industry Consortia: Structures that maintain academic involvement throughout the development process can help ensure that public health priorities influence decision-making. For example, the Innovative Genomics Institute (IGI) has launched an expert Affordability Task Force to "investigate the underlying drivers of high prices and explore alternative pathways to development" [118].
Experimental Protocols and Research Applications
Research Reagent Solutions for CRISPR-Based Therapy Development
Table 3: Essential Research Reagents for CRISPR Therapy Development
| Reagent/Material | Function | Application Notes |
|---|---|---|
| Cas9 Enzyme Variants | DNA cleavage at target sites | High-fidelity variants (eSpCas9, SpCas9-HF1) reduce off-target effects [115] |
| Guide RNA (gRNA) | Target specificity | Chemically modified gRNAs enhance stability and reduce immune responses [115] |
| Delivery Vectors | Intracellular delivery of CRISPR components | AAV vectors common for in vivo use; lentivirus for ex vivo approaches [5] |
| Electroporation Systems | Physical delivery method | Efficient for ex vivo editing of hematopoietic stem cells [5] |
| Lipid Nanoparticles (LNPs) | Non-viral delivery vehicle | Emerging approach for in vivo delivery, as used in NTLA-2001 trial [5] |
| Cell Culture Media | Maintenance and expansion of primary cells | Specialized formulations required for different cell types (e.g., HSPCs, T-cells) |
| CRISPR Screening Libraries | Genome-wide functional genomics | Arrayed or pooled formats for target identification and validation |
Detailed Protocol: Ex Vivo Genome Editing for Hematopoietic Disorders
The following protocol outlines the key steps for ex vivo CRISPR-Cas9 editing of hematopoietic stem and progenitor cells (HSPCs) for therapeutic applications in disorders like sickle cell disease and beta-thalassemia, based on successful clinical trials [5] [117]:
Step 1: Patient-Specific HSPC Collection and Isolation
- Collect autologous CD34+ HSPCs via apheresis after mobilization with granulocyte colony-stimulating factor (G-CSF)
- Isulate CD34+ cells using immunomagnetic selection
- Quality control assessments: viability (>95%), purity (>90% CD34+), and sterility
Step 2: CRISPR-Cas9 RNP Complex Formation
- Design and synthesize gRNA targeting the BCL11A erythroid enhancer region (for sickle cell/thalassemia) or other therapeutic target
- Complex high-fidelity Cas9 protein with sgRNA at molar ratio of 1:2 in appropriate buffer
- Incubate 10-15 minutes at room temperature to form ribonucleoprotein (RNP) complexes
Step 3: Electroporation and Genome Editing
- Suspend HSPCs in electroporation buffer at concentration of 1-2×10^6 cells/mL
- Combine cells with RNP complexes and transfer to electroporation cuvette
- Electroporate using optimized parameters (e.g., 1500V, 10ms pulse width)
- Immediately transfer cells to recovery medium supplemented with cytokines
Step 4: Cell Expansion and Quality Assessment
- Culture edited cells in serum-free medium with SCF, TPO, and Flt-3 ligand
- Maintain at 37°C, 5% CO2 for 48-72 hours
- Assess editing efficiency: T7E1 assay or next-generation sequencing for on-target editing
- Perform off-target assessment: GUIDE-seq or similar method
- Confirm viability and sterility before infusion
Step 5: Patient Conditioning and Cell Reinfusion
- Administer myeloablative conditioning (busulfan) to create niche for engraftment
- Thaw and infuse edited HSPCs via intravenous injection
- Monitor for engraftment and hematopoietic recovery
This protocol successfully resulted in "effective and long-term engraftment of CRISPR-edited HSPCs" in clinical trials, with efficacy of CCR5 disruption increasing "from 5.2% to 8.3% in bone marrow cells over 19 months" in one HIV trial [5], and complete resolution of symptoms in sickle cell patients [117].
Visualization of Key Concepts
The Affordability Challenge Framework
Diagram 1: Affordability challenge framework showing how high costs create access barriers and potential solutions.
Alternative Payment Model Implementation
Diagram 2: Implementation pathways for alternative models that address therapy affordability.
The development of CRISPR-Cas9 based therapies represents one of the most significant medical breakthroughs of our time, offering the potential to cure genetic diseases that have plagued humanity for generations. However, without deliberate intervention, this revolutionary therapeutic potential may remain inaccessible to many patients who need it most. The affordability challenge is not merely an economic issue but an ethical imperative that demands multidisciplinary solutions.
Addressing this challenge will require collaborative efforts across academia, industry, government, and patient advocacy groups to implement innovative pricing models, alternative development structures, and policies that prioritize patient access alongside therapeutic innovation. As research continues to advance the technical capabilities of CRISPR technology, parallel progress must be made in developing sustainable models that ensure these life-changing therapies can reach all patients, regardless of socioeconomic status or geographic location.
The success of CRISPR as a therapeutic platform will ultimately be measured not only by its technical achievements but by its ability to deliver cures to the patients who need them. By addressing the affordability challenge directly, the scientific community can fulfill the promise of gene editing as a truly transformative force in medicine.
Regulatory Landscape and Path to Market for CRISPR-Based Therapeutics
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR) and CRISPR-associated protein 9 (Cas9) system has emerged as a revolutionary genome-editing tool with transformative potential for treating genetic disorders. Derived from a natural prokaryotic adaptive immune system, the CRISPR-Cas9 system enables precise modification of DNA sequences through RNA-guided DNA targeting and cleavage [3]. This technology has superior precision and efficiency compared to previous gene-editing methods like Zinc-Finger Nucleases (ZFNs) and Transcription Activator-Like Effector Nucleases (TALENs), offering researchers an unprecedented ability to address the genetic root causes of human diseases [123] [4].
The core CRISPR-Cas9 system consists of two fundamental components: the Cas9 endonuclease enzyme, which creates double-strand breaks in DNA, and a guide RNA (gRNA) molecule that directs Cas9 to specific genomic sequences through complementary base pairing [3]. The system requires a Protospacer Adjacent Motif (PAM) sequence adjacent to the target site for recognition and cleavage. Once the DNA is cleaved, the cell's natural repair mechanisms—either Non-Homologous End Joining (NHEJ) or Homology-Directed Repair (HDR)—are harnessed to achieve the desired genetic modification [4].
For therapeutic applications, CRISPR-Cas9 technology has evolved beyond the standard CRISPR-Cas9 system to include more precise approaches such as base editing and prime editing, which allow for single-nucleotide changes without creating double-strand breaks in DNA [55] [4]. These advancements are particularly valuable for correcting point mutations that underlie many genetic disorders while minimizing potential genotoxic risks.
Current Regulatory and Clinical Trial Landscape
Approved CRISPR Therapies and Global Regulatory Status
The regulatory landscape for CRISPR-based therapeutics reached a historic milestone in 2023-2024 with the first regulatory approvals of a CRISPR-Cas9 therapy. Casgevy (exagamglogene autotemcel), developed by CRISPR Therapeutics and Vertex Pharmaceuticals, received approval for the treatment of sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TDT) in multiple jurisdictions [14] [53]. This approval marked a watershed moment for the entire gene therapy field, demonstrating that CRISPR-based medicines could successfully navigate the complex regulatory pathway from concept to commercial product.
Table 1: Global Regulatory Approvals for Casgevy (as of 2025)
| Region/Country | Approval Date | Indications | Key Regulatory Aspects |
|---|---|---|---|
| United States | 2023 | SCD, TDT | First FDA-approved CRISPR therapy |
| United Kingdom | 2023 | SCD, TDT | MHRA approval via innovative licensing pathway |
| European Union | 2024 | SCD, TDT | EMA approval based on clinical trial results |
| Saudi Arabia | 2024 | SCD, TDT | Approval for high-prevalence markets |
| United Arab Emirates | 2024 | SCD, TDT | Regulatory clearance in Middle East |
By 2025, Casgevy had secured regulatory clearance in at least nine countries, with over 75 authorized treatment centers activated globally to administer the therapy [124]. The rapid global expansion of Casgevy approvals demonstrates how regulatory agencies worldwide have adapted to accommodate the unique characteristics of gene-editing therapies while maintaining rigorous safety and efficacy standards.
The clinical development pipeline for CRISPR-based therapeutics has expanded significantly, with approximately 250 clinical trials involving gene-editing therapeutic candidates tracked as of February 2025, including more than 150 currently active trials [27]. These trials span multiple therapeutic areas and utilize various gene-editing platforms, including CRISPR-Cas, base editors, prime editors, and other editing technologies.
Table 2: CRISPR Clinical Trials by Therapeutic Area (February 2025)
| Therapeutic Area | Number of Trials | Key Indications | Development Phase |
|---|---|---|---|
| Hematological Disorders | 50+ | SCD, TDT, hemophilia | Phase 1 to Phase 3 |
| Oncology | 70+ | Blood cancers, solid tumors | Phase 1 to Phase 2 |
| Metabolic Diseases | 20+ | ATTR amyloidosis, HAE | Phase 1 to Phase 3 |
| Cardiovascular Diseases | 15+ | Hypercholesterolemia, high Lp(a) | Phase 1 to Phase 2 |
| Autoimmune Diseases | 10+ | SLE, multiple sclerosis | Phase 1 to Phase 2 |
| Infectious Diseases | 10+ | E. coli infections, UTIs | Phase 1 to Phase 2 |
| Other Rare Diseases | 20+ | CGD, DMD, eye disorders | Phase 1 to Phase 2 |
The clinical trial landscape demonstrates a clear progression from early-phase safety studies to larger efficacy trials across multiple disease areas. Blood disorders continue to lead the field, with the majority of Phase 3 trials initially targeting sickle cell disease and beta-thalassemia [27]. However, the pipeline has diversified substantially, with Phase 3 trials now underway in additional indications including hereditary amyloidosis and immunodeficiencies [14].
Experimental Protocols and Methodologies
Ex Vivo Gene Editing Protocol: Hematopoietic Stem Cells
The ex vivo gene editing approach used in Casgevy represents a well-established protocol for CRISPR-based therapies. This methodology involves extracting patient cells, editing them outside the body, and reinfusing the modified cells back into the patient.
Materials and Reagents:
- Hematopoietic stem and progenitor cells (CD34+)
- CRISPR-Cas9 components (ribonucleoprotein complex)
- Cell culture media and cytokines
- Electroporation equipment
- Analytical reagents for quality control
Step-by-Step Protocol:
Cell Collection and Isolation: Collect hematopoietic stem and progenitor cells (CD34+ cells) from the patient via apheresis after mobilization from bone marrow. Isulate CD34+ cells using immunomagnetic selection to achieve high purity [53].
CRISPR Component Preparation: Formulate the CRISPR-Cas9 ribonucleoprotein (RNP) complex by combining purified Cas9 protein with synthetic guide RNA (sgRNA) targeting the BCL11A gene enhancer region. Use high-purity, research-grade components and verify targeting efficiency through prior validation [53] [52].
Electroporation and Gene Editing: Introduce the RNP complex into the isolated CD34+ cells using electroporation. Optimize electroporation parameters (voltage, pulse length, cell concentration) to maximize editing efficiency while maintaining cell viability [52].
Quality Control and Expansion: Culture the edited cells in appropriate media supplemented with cytokines to support cell viability and expansion. Perform rigorous quality control assessments including:
- Measurement of editing efficiency at on-target sites
- Assessment of potential off-target editing
- Evaluation of cell viability and potency
- Sterility testing for microbial contamination [53]
Patient Conditioning and Reinfusion: Administer myeloablative conditioning (busulfan) to the patient to create niche space in the bone marrow. Subsequently, reinfuse the edited CD34+ cells back into the patient via intravenous infusion [14] [53].
Post-Treatment Monitoring: Monitor patient for engraftment, potential adverse events, and therapeutic efficacy. Conduct long-term follow-up to assess persistence of edited cells and any delayed effects [14].
This ex vivo protocol offers advantages including controlled editing conditions, ability to perform comprehensive quality control before administration, and reduced risk of immune reactions to editing components. However, it requires complex manufacturing logistics and patient conditioning with chemotherapy [55].
In Vivo Gene Editing Protocol: Lipid Nanoparticle Delivery
In vivo CRISPR therapies represent the next frontier in gene editing, with several candidates in clinical development. These approaches deliver editing components directly to target cells within the patient's body, offering potential treatment options for a wider range of diseases.
Materials and Reagents:
- Lipid nanoparticles (LNPs) formulation components
- CRISPR-Cas9 mRNA and guide RNA
- Purification and filtration systems
- Analytical instruments for characterization
Step-by-Step Protocol:
Formulation of CRISPR-LNP Complex: Encapsulate CRISPR-Cas9 mRNA and sgRNA in lipid nanoparticles using microfluidic mixing technology. Optimize lipid composition for target tissue tropism (e.g., GalNAc-LNPs for liver targeting) and efficient intracellular delivery [14] [52].
Characterization and Quality Control: Characterize the final LNP product for parameters including:
- Particle size and size distribution
- Encapsulation efficiency of RNA components
- Endotoxin levels and sterility
- Potency through in vitro editing assays [14]
Administration and Dosing: Administer the LNP formulation to patients via intravenous infusion. Determine appropriate dosing based on preclinical pharmacokinetic and pharmacodynamic studies, considering factors such as target tissue distribution and anticipated therapeutic index [14] [52].
Pharmacodynamic Monitoring: Assess editing efficiency in target tissues through appropriate biomarkers. For liver-directed therapies, measure reduction in target protein levels (e.g., TTR for ATTR amyloidosis, kallikrein for HAE) in blood samples as a surrogate for editing efficiency [14].
Safety Monitoring: Implement comprehensive safety monitoring for potential adverse events including:
- Immune responses to LNPs or editing components
- Liver function tests for hepatic-directed therapies
- Assessment of potential off-target editing through sensitive assays
- Monitoring for any unexpected long-term effects [14]
The in vivo approach exemplified by Intellia Therapeutics' NTLA-2001 for transthyretin amyloidosis has demonstrated durable reduction of target protein levels by approximately 90% in clinical trial participants, validating this methodology for therapeutic application [14].
Signaling Pathways and Workflow Visualization
CRISPR-Cas9 Mechanism and DNA Repair Pathways
The therapeutic efficacy of CRISPR-Cas9 systems depends on their molecular mechanism of action and how cells respond to and repair the induced DNA changes. The following diagram illustrates the key pathways involved in CRISPR-Cas9 gene editing:
Therapeutic Development Workflow
The path from discovery to approved CRISPR therapy involves multiple stages with specific regulatory requirements and decision points. The following workflow illustrates this development pathway:
Research Reagent Solutions and Essential Materials
Successful development of CRISPR-based therapeutics requires specific research reagents and materials that ensure efficient editing, delivery, and safety assessment. The following table details key solutions used in CRISPR therapeutic development:
Table 3: Essential Research Reagents for CRISPR Therapeutic Development
| Reagent/Material | Function | Application Examples | Considerations |
|---|---|---|---|
| CRISPR-Cas9 RNP Complex | Direct gene editing | Ex vivo cell editing (e.g., Casgevy) | High purity reduces immune responses; precomplexing improves efficiency |
| Lipid Nanoparticles (LNPs) | In vivo delivery vehicle | Liver-directed therapies (e.g., NTLA-2001) | Composition affects tropism; optimize for target tissue |
| AAV Vectors | In vivo delivery vehicle | Tissue-specific delivery (e.g., muscle, eye) | Packaging size limitation; potential immunogenicity |
| Electroporation Systems | Physical delivery method | Ex vivo cell editing | Parameters vary by cell type; balance efficiency and viability |
| Guide RNA Libraries | Target specificity | Screening, multiplexed editing | Design affects specificity; chemical modifications enhance stability |
| Base Editors | Precise single-base changes | Correcting point mutations | Reduced indels compared to nuclease editing; specific window limitations |
| Prime Editors | Versatile precise editing | Small insertions, deletions, all base conversions | No double-strand breaks; more complex delivery |
| Off-Target Assays | Safety assessment | GUIDE-seq, CIRCLE-seq | Essential for therapeutic development; inform clinical trial design |
| Cell Culture Media | Cell maintenance and expansion | Ex vivo editing protocols | Serum-free formulations for clinical applications |
| Analytical Instruments | Quality control | NGS, HPLC, potency assays | Regulatory compliance requires validated methods |
Regulatory Considerations and Path to Market
Regulatory Framework and Requirements
The regulatory pathway for CRISPR-based therapeutics involves navigating complex requirements that address the unique characteristics of gene-editing products. Regulatory agencies including the U.S. Food and Drug Administration (FDA), European Medicines Agency (EMA), and other national authorities have developed specific frameworks for evaluating these innovative treatments.
Key Regulatory Considerations:
Demonstration of Specificity: Regulatory submissions must include comprehensive assessment of editing specificity, including evaluation of potential off-target effects using sensitive detection methods. This typically involves a combination of in silico prediction, biochemical assays, and cell-based methods to assess off-target potential, followed by targeted analysis of identified sites in preclinical and clinical samples [4].
Delivery System Safety: The safety profile of the delivery method (viral vectors, LNPs, electroporation) requires thorough characterization. For viral vectors, this includes assessment of integration potential, while for LNPs, evaluation of immunogenicity and distribution beyond target tissues is necessary [14] [3].
Long-Term Follow-Up: Regulatory agencies require long-term monitoring plans (typically 15 years) to assess persistence of edited cells and delayed adverse events. This is particularly important for therapies involving permanent genetic modifications [14].
Manufacturing and Quality Control: Robust manufacturing processes and comprehensive quality control are essential regulatory requirements. This includes demonstration of consistency in editing efficiency, cell viability (for ex vivo therapies), potency, purity, and identity across multiple batches [53].
Risk-Benefit Assessment: The regulatory review involves careful consideration of the therapy's risk-benefit profile in the context of the specific disease being treated. Treatments for severe, life-threatening diseases with limited alternatives may tolerate different risk profiles compared to therapies for less severe conditions [14] [53].
The FDA's new Platform Technology Designation Program, announced in 2024, provides a potentially streamlined pathway for CRISPR therapies that qualify as "well-understood and reproducible technologies" [55]. This program may allow developers to establish gene-editing platforms that can be more easily tailored to multiple diseases without repeating extensive preclinical safety testing for each new application.
Commercialization Challenges and Strategies
The path from regulatory approval to successful commercialization of CRISPR therapies involves addressing several significant challenges, including manufacturing scalability, reimbursement strategies, and healthcare system readiness.
Manufacturing Considerations:
- Scalability and Cost: Ex vivo therapies like Casgevy require complex, patient-specific manufacturing processes that present scaling challenges. Approaches to address this include:
- Quality Assurance: Implementing robust quality control systems that can accommodate patient-specific products while ensuring consistency and safety.
Market Access and Reimbursement:
- Pricing Strategies: CRISPR therapies command premium pricing (e.g., Casgevy at approximately $2 million per treatment) based on their potential for durable or curative benefits [125]. Successful pricing strategies must demonstrate long-term value to payers.
Outcomes-Based Agreements: Innovative contracting approaches, such as the outcomes-based arrangement negotiated for Casgevy with state Medicaid programs, help align cost with therapeutic performance and address payer concerns [53].
Global Access Planning: Strategic expansion into markets with high disease prevalence and establishing treatment centers in regions with significant patient populations [124].
The CRISPR therapeutics market is projected to grow substantially in the coming years, with estimates suggesting it could become a $15.92 billion industry by 2033 [125] [124]. This growth will be driven by an expanding pipeline, additional regulatory approvals, and expansion into new disease areas beyond the initial focus on rare genetic disorders.
The regulatory landscape for CRISPR-based therapeutics has evolved rapidly from theoretical concept to approved medicines, with Casgevy's approval representing a foundational milestone. The path to market for these innovative therapies involves navigating complex scientific, regulatory, and commercial considerations, with requirements for comprehensive preclinical characterization, rigorous clinical demonstration of safety and efficacy, and specialized manufacturing and quality control systems.
The field continues to advance rapidly, with several key trends shaping its future trajectory. These include the development of more precise editing systems (base and prime editors), improved delivery technologies, expansion into new therapeutic areas, and evolution of regulatory frameworks to accommodate the unique characteristics of gene-editing therapies. Additionally, the emergence of personalized CRISPR treatments, exemplified by the bespoke therapy developed for an infant with CPS1 deficiency, points toward a future of increasingly individualized genetic medicines [14].
For researchers and drug development professionals, success in navigating the path to market for CRISPR therapeutics will require interdisciplinary approaches that integrate advances in gene-editing technology, delivery systems, manufacturing science, and regulatory strategy. As the field matures, continued collaboration between industry, academia, regulators, and patient communities will be essential to fully realize the potential of CRISPR-based therapies to address the genetic root causes of human disease.
Conclusion
CRISPR-Cas9 technology has unequivocally ushered in a new era for genetic disorder therapy, demonstrating remarkable curative potential in a growing number of diseases, from blood disorders to lipid conditions. The synthesis of foundational science, advanced methodologies, rigorous safety optimization, and robust clinical validation confirms a paradigm shift from chronic disease management toward one-time, durable treatments. However, the path to broad clinical implementation requires overcoming significant hurdles, including ensuring absolute specificity, developing efficient and safe delivery vehicles, managing immune responses, and resolving profound affordability and access issues. Future progress will hinge on the continued refinement of editing precision through novel editors, expansion into more common polygenic diseases, the establishment of sustainable and equitable business models, and the accumulation of long-term patient safety data. For researchers and drug developers, the coming years present an unparalleled opportunity to translate these powerful tools into accessible and transformative medicines for patients worldwide.
References
- 1. Frontiers | CRISPR / Cas and Factors Affecting Its Precision... System [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.761709/full]
- 2. The CRISPR for tool ... | Nature Communications kit genome editing [https://www.nature.com/articles/s41467-018-04252-2?error=cookies_not_supported&code=9ce6e3bf-00cd-4f44-bc1e-4a1d5e204bf7]
- 3. Frontiers | CRISPR / Cas -Based therapeutics as a promising strategy... 9 [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1578138/full]
- 4. Advancing CRISPR genome editing into gene therapy clinical trials: progress and future prospects - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 5. of the Clinical / applications 9 genome-editing CRISPR ... Cas system [https://pmc.ncbi.nlm.nih.gov/articles/PMC10425811/]
- 6. The CRISPR for tool and beyond kit genome editing [https://pubmed.ncbi.nlm.nih.gov/29765029/]
- 7. – CRISPR Editing: Curing Cas by Inherited... 9 Gene Genetic Diseases [https://pmc.ncbi.nlm.nih.gov/articles/PMC10980556/]
- 8. Current Status of CRISPR/Cas9 Application in Clinical Cancer Research: Opportunities and Challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8870204/]
- 9. CRISPR-Cas9: A Preclinical and Clinical Perspective for the Treatment of Human Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7854284/]
- 10. CRISPR-Cas9 gene editing and its therapeutic applications: A literature review | Research, Society and Development [https://rsdjournal.org/rsd/article/view/46681]
- 11. : Structure, Cas & Genome Editing 9 Nuclease Mechanism [https://lifesciences.danaher.com/us/en/library/cas9-nuclease.html]
- 12. and Applications of CRISPR/ Mechanism - Cas -Mediated Genome... 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC8388126/]
- 13. Addgene: CRISPR Guide [https://www.addgene.org/guides/crispr/]
- 14. CRISPR Clinical Trials: A 2025 Update - Innovative Genomics Institute (IGI) [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 15. R-loop formation and conformational activation mechanisms of Cas 9 [https://www.nature.com/articles/s41586-022-05114-0?error=cookies_not_supported&code=5d0d4579-5c4e-4611-82ba-7060217ef536]
- 16. Structural insights into DNA cleavage activation of CRISPR-Cas9 system | Nature Communications [https://www.nature.com/articles/s41467-017-01496-2]
- 17. WU- CRISPR : characteristics of functional RNAs for the... guide [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-015-0784-0]
- 18. Nuclease CRISPR - Cas Genome Editing 9 RNA guided [https://www.sigmaaldrich.com/SB/en/technical-documents/protocol/genomics/advanced-gene-editing/crispr-cas9-genome-editing]
- 19. Regulating CRISPR / Cas through Conditional 9 ... Function Guide RNA [https://pmc.ncbi.nlm.nih.gov/articles/PMC7928076/]
- 20. AI-powered CRISPR could lead to faster gene therapies, Stanford Medicine study finds [https://med.stanford.edu/news/all-news/2025/09/ai-crispr-gene-therapy.html]
- 21. CRISPR-Cas9 DNA Base-Editing and Prime-Editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7503568/]
- 22. New kids on the block: Base and prime editors [https://www.asbmb.org/asbmb-today/science/011724/new-kids-on-the-block-base-and-prime-editors]
- 23. From bench to bedside: cutting-edge applications of base editing and prime editing in precision medicine | Journal of Translational Medicine | Full Text [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05957-3]
- 24. Prime Editing: Adding Precision and Flexibility to CRISPR Editing [https://blog.addgene.org/prime-editing-crisp-cas-reverse-transcriptase]
- 25. Prime Editing | ERS Genomics [https://ersgenomics.com/prime-editing/]
- 26. Prime Editing as a Precision Gene Editing Tool [https://www.synthego.com/guide/crispr-methods/prime-editing/]
- 27. Overview CRISPR Clinical Trials 2025 - Learn | Innovate | Access [https://crisprmedicinenews.com/clinical-trials/]
- 28. Frontiers | CRISPR -dependent base editing as a therapeutic strategy... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1553590/full]
- 29. CRISPR Gene Therapy: Applications, Limitations, and Implications for the Future - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7427626/]
- 30. The Potential of CRISPR/Cas9 Gene Editing as a Treatment Strategy for Inherited Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8715006/]
- 31. Treating genetic blood disorders in the era of CRISPR-mediated genome editing - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1525001625000358]
- 32. Gene therapy for polygenic or complex diseases | Biomarker Research | Full Text [https://biomarkerres.biomedcentral.com/articles/10.1186/s40364-024-00618-5]
- 33. CRISPR-dependent base editing as a therapeutic strategy for rare monogenic disorders - PubMed [https://pubmed.ncbi.nlm.nih.gov/40242216/]
- 34. CRISPR Therapeutics – Novel Use of CRISPR / Cas Technique in... 9 [https://ecampusontario.pressbooks.pub/bio16610w18/chapter/crispr-therapeutics-novel-use-of-crispr-cas9-technique-in-disease-therapy/]
- 35. Prime editing in hematopoietic stem cells—From ex to vivo ... in vivo [https://pmc.ncbi.nlm.nih.gov/articles/PMC10036844/]
- 36. (PDF) CRISPR - CAS -MEDIATED 9 gene editing for inherited... ex vivo [https://www.academia.edu/124271375/CRISPR_CAS9_MEDIATED_EX_VIVO_GENE_EDITING_FOR_INHERITED_HEMATOLOGICAL_DISORDERS_ADVANCEMENTS_CHALLENGES_AND_CLINICAL_POTENTIAL]
- 37. Applications and Research Advances in the Delivery of CRISPR/Cas9 Systems for the Treatment of Inherited Diseases [https://www.mdpi.com/1422-0067/24/17/13202]
- 38. In vivo delivery of CRISPR-Cas9 therapeutics: Progress and challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8424283/]
- 39. Frontiers | Revolutionizing in vivo therapy with CRISPR/Cas genome editing: breakthroughs, opportunities and challenges [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2024.1342193/full]
- 40. Recent Advances in CRISPR/Cas9 Delivery Strategies [https://www.mdpi.com/2218-273X/10/6/839]
- 41. Editorial: First Regulatory Approvals for CRISPR - Cas Therapeutic... 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10913280/]
- 42. Therapeutic promise of CRISPR-Cas9 gene editing in sickle cell disease and β-thalassemia: A current review - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S2452318625000224]
- 43. / Crispr gene editing in transfusion-dependent Cas - 9 and... β thalassemia [https://jmhg.springeropen.com/articles/10.1186/s43042-025-00806-4]
- 44. New treatment for sickle : cell pipeline highlights disease 2025 [https://www.labiotech.eu/in-depth/sickle-cell-disease-treatment/]
- 45. CRISPR-Cas9 Gene Editing for Sickle Cell Disease and β-Thalassemia - PubMed [https://pubmed.ncbi.nlm.nih.gov/33283989/]
- 46. / CRISPR System as a Promising Therapy in Cas and... 9 Thalassemia [https://link.springer.com/article/10.1007/s12033-025-01368-x]
- 47. Evaluation of Efficacy and Safety of a Single Dose... - Guideline Central [https://www.guidelinecentral.com/clinical-trial/?id=NCT05477563]
- 48. CRISPR Technology Market Size, Share, Trends & Growth Report, 2030 [https://www.mordorintelligence.com/industry-reports/crispr-technology-market---growth-trends-and-forecast-2019---2024]
- 49. CRISPR Technology Market Soars 16.54% CAGR by 2034 [https://www.towardshealthcare.com/insights/crispr-technology-market-sizing]
- 50. Recent applications, future perspectives, and limitations of the CRISPR-Cas system - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S216225312500188X]
- 51. Unlocking the Potential: CRISPR - Cas Gene Editing in 9 Liver Diseases [https://www.news-medical.net/health/Unlocking-the-Potential-CRISPR-Cas9-Gene-Editing-in-Liver-Diseases.aspx]
- 52. CRISPR Clinical Trials to Follow [https://www.synthego.com/blog/crispr-clinical-trials/]
- 53. Therapeutics Highlights Strategic Priorities and... - BioSpace CRISPR [https://www.biospace.com/press-releases/crispr-therapeutics-highlights-strategic-priorities-and-anticipated-2025-milestones]
- 54. Frontiers | CRISPR - Cas : bridging the gap between aging mechanisms... 9 [https://www.frontiersin.org/journals/cellular-neuroscience/articles/10.3389/fncel.2025.1681891/full]
- 55. : From Discovery To CRISPR —And Charting A Path Forward Clinic [https://www.forbes.com/councils/forbestechcouncil/2025/02/13/crispr-from-discovery-to-clinic-and-charting-a-path-forward/]
- 56. Advances in Nanoparticles as Non-Viral Vectors for Efficient Delivery of CRISPR/Cas9 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11434874/]
- 57. Challenges in delivery systems for CRISPR-based genome editing and opportunities of nanomedicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8316527/]
- 58. Overcoming the Delivery Challenges in CRISPR/Cas9 Gene Editing for Effective Cancer Treatment: A Review of Delivery Systems [https://www.medsci.org/v22p3625.htm]
- 59. Systems for In Vivo Gene Editing – MASI Longevity... CRISPR Delivery [https://masi.eu/blogs/longevity-news/crispr-delivery-systems-for-in-vivo-gene-editing]
- 60. -Mediated AAV : Tools, Mechanisms, and CRISPR Delivery Applications [https://www.atlantisbioscience.com/blog/aav-mediated-crispr-delivery-tools/]
- 61. This Way: Choosing Between CRISPR System | VectorBuilder Delivery [https://en.vectorbuilder.com/resources/vector-academy/lessons/crispr-delivery-systems.html]
- 62. Trends and challenges of AAV - delivered editing therapeutics for... gene [https://pubmed.ncbi.nlm.nih.gov/40799507/]
- 63. - Non of Viral /Cas Cargo to the Retina Using... Delivery CRISPR [https://pmc.ncbi.nlm.nih.gov/articles/PMC9503525/]
- 64. Intelligent nanotherapeutic strategies for the delivery of CRISPR system - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10326264/]
- 65. Frontiers | Unraveling the future of genomics: CRISPR, single-cell omics, and the applications in cancer and immunology [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1565387/full]
- 66. First-in-human trial of CRISPR gene-editing therapy safely lowered cholesterol, triglycerides | American Heart Association [https://newsroom.heart.org/news/first-in-human-trial-of-crispr-gene-editing-therapy-safely-lowered-cholesterol-triglycerides]
- 67. - First - in Suggests Human -Cas9 Therapy Targeting... Trial CRISPR [https://www.acc.org/Latest-in-Cardiology/Articles/2025/11/03/16/19/sat-956am-crispr-aha-2025]
- 68. CRISPR-Cas9 Gene-Editing Therapy Shows Early Promise for Dyslipidemia | tctmd.com [https://www.tctmd.com/news/crispr-cas9-gene-editing-therapy-shows-early-promise-dyslipidemia]
- 69. -time One therapy safely lowers cholesterol and triglycerides in... CRISPR [https://www.news-medical.net/news/20251110/One-time-CRISPR-therapy-safely-lowers-cholesterol-and-triglycerides-in-early-trial.aspx]
- 70. Current trends of clinical involving trials /Cas systems - PMC CRISPR [https://pmc.ncbi.nlm.nih.gov/articles/PMC10666174/]
- 71. Understanding CRISPR | Synthego Clinical Trials [https://www.synthego.com/blog/understanding-crispr-clinical-trials/]
- 72. CRISPR-Cas9 and Its Bioinformatics Tools: A Systematic Review [https://www.mdpi.com/1467-3045/47/5/307]
- 73. Frontiers | Off - target in effects / CRISPR gene editing Cas 9 [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1143157/full]
- 74. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 75. for detecting Methods - off of target / effects CRISPR Cas 9 [https://pubmed.ncbi.nlm.nih.gov/41213415/]
- 76. - Off in target / Effects -mediated Genome Engineering CRISPR Cas 9 [https://pubmed.ncbi.nlm.nih.gov/26575098/]
- 77. - CRISPR : Mechanisms and Solutions | Danaher Life... Off Target Effects [https://lifesciences.danaher.com/us/en/library/crispr-off-target-effects.html]
- 78. Frontiers | Beyond the promise: evaluating and mitigating off-target effects in CRISPR gene editing for safer therapeutics [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2023.1339189/full]
- 79. Improved CRISPR / Cas - 9 prediction with... | PLOS One off target [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0335863]
- 80. Comprehensive analysis and accurate quantification of unintended large gene modifications induced by CRISPR-Cas9 gene editing - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9586483/]
- 81. Methods for Optimizing CRISPR-Cas9 Genome Editing Specificity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4976696/]
- 82. Optimized CRISPR guide RNA design for two high - fidelity ... [https://www.nature.com/articles/s41467-019-12281-8?error=cookies_not_supported&code=1d4b6098-c14c-4862-9445-63998914ec0f]
- 83. Boosting activity of high - fidelity / CRISPR using... Cas 9 variants [https://pubmed.ncbi.nlm.nih.gov/31010827/]
- 84. Enhancing CRISPR-Cas9 gRNA efficiency prediction by data integration and deep learning | Nature Communications [https://www.nature.com/articles/s41467-021-23576-0]
- 85. Optimized CRISPR guide RNA design for two high - fidelity ... [https://pubmed.ncbi.nlm.nih.gov/31537810/]
- 86. analysis of potential In - silico sites to gene editing for... off target [https://pmc.ncbi.nlm.nih.gov/articles/PMC8786118/]
- 87. Using traditional machine learning and deep learning methods for on- and off-target prediction in CRISPR/Cas9: a review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10199778/]
- 88. A versatile CRISPR/Cas9 system off-target prediction tool using language model | Communications Biology [https://www.nature.com/articles/s42003-025-08275-6]
- 89. Amplification-free long-read sequencing reveals unforeseen... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-020-02206-w]
- 90. Peeling back the layers of immunogenicity in Cas9-based genomic medicine - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1525001625005350]
- 91. In Vivo Delivery of CRISPR/Cas9 for Therapeutic Gene Editing: Progress and Challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5846329/]
- 92. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 93. Nanotechnology-Based Delivery of CRISPR/Cas9 for Cancer Treatment: A Comprehensive Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346122/]
- 94. Recent Advances in CRISPR/Cas9 Delivery Strategies - PubMed [https://pubmed.ncbi.nlm.nih.gov/32486234/]
- 95. -Based Gene Therapies: From Preclinical to CRISPR ... Clinical [https://pmc.ncbi.nlm.nih.gov/articles/PMC11119143/]
- 96. Off-target effects in CRISPR-Cas genome editing for human therapeutics: Progress and challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12329535/]
- 97. Cell cycle arrest and p53 prevent ON-target megabase-scale rearrangements induced by CRISPR-Cas9 | Nature Communications [https://www.nature.com/articles/s41467-023-39632-w]
- 98. Efficacy and long-term safety of CRISPR/Cas9 genome editing in the SOD1-linked mouse models of ALS | Communications Biology [https://www.nature.com/articles/s42003-021-01942-4]
- 99. New CRISPR tool enables more seamless gene editing... | Yale News [https://news.yale.edu/2025/03/20/new-crispr-tool-enables-more-seamless-gene-editing-and-improved-disease-modeling]
- 100. Current progress in CRISPR-Cas systems for rare diseases - PubMed [https://pubmed.ncbi.nlm.nih.gov/39824580/]
- 101. Cleveland Clinic First-In-Human Trial of CRISPR Gene-Editing Therapy Shown to Safely Lower Cholesterol and Triglycerides [https://newsroom.clevelandclinic.org/2025/11/08/cleveland-clinic-first-in-human-trial-of-crispr-gene-editing-therapy-shown-to-safely-lower-cholesterol-and-triglycerides]
- 102. CRISPR Therapeutics to Present Late-Breaking Data at the American Heart Association (AHA) Scientific Sessions 2025 | CRISPR Therapeutics [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-present-late-breaking-data-american-heart]
- 103. Scientists just made gene editing far more powerful | ScienceDaily [https://www.sciencedaily.com/releases/2025/10/251025084545.htm]
- 104. Editing Platforms: Comparing . Gene Methods CRISPR vs Traditional [https://blog.crownbio.com/comparing-gene-editing-platforms-crispr-vs-traditional-methods]
- 105. Expanding the genetic editing tool kit: ZFNs , TALENs , and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4191047/]
- 106. Frontiers | CRISPR -Editing Models Geared Toward Gene for... Therapy [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2021.592571/full]
- 107. - CRISPR , Cas and 9 - the battle in gene editing TALENs ZFNs [https://www.ptglab.com/news/blog/crispr-cas9-talens-and-zfns-the-battle-in-gene-editing/]
- 108. Gene Editing Techniques: ZFNs , TALENs or CRISPR ? [https://www.news-medical.net/life-sciences/Gene-Editing-Techniques-ZFNs-TALENs-or-CRISPR.aspx]
- 109. /Cas9 in the treatment of sickle cell disease (SCD) and its... CRISPR [https://pmc.ncbi.nlm.nih.gov/articles/PMC11444630/]
- 110. Report on FDA Challenges for CRISPR -Based Therapies [https://www.linkedin.com/pulse/report-fda-challenges-crispr-based-therapies-mudassir-mohammed-ph-d--ms3xf]
- 111. Seven diseases that CRISPR technology could cure [https://www.labiotech.eu/in-depth/crispr-technology-cure-disease/]
- 112. Frontiers | The Potential of CRISPR/Cas9 Gene Editing as a Treatment Strategy for Inherited Diseases [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.699597/full]
- 113. How to Pick the Best CRISPR Data Analysis Method for Your Experiment [https://www.synthego.com/guide/how-to-use-crispr/analysis-methods/]
- 114. Technologies and Computational Analysis Strategies for CRISPR Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7497852/]
- 115. What is CRISPR - Cas ? Definition, 9 , and Future Applications [https://www.bajajfinserv.in/crispr-cas9]
- 116. - CRISPR In Gene Editing: Innovations, CAS and Ethical... 9 Applications [https://www.ijsrtjournal.com/article/CRISPRCAS+9+In+Gene+Editing+Innovations+Applications+and+Ethical+Challenges]
- 117. CRISPR gene-editing success for sickle cell raises new questions : Shots - Health News : NPR [https://www.npr.org/sections/health-shots/2023/03/16/1163104822/crispr-gene-editing-sickle-cell-success-cost-ethics]
- 118. Towards affordable CRISPR genomic therapies : a task force... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10678297/]
- 119. Affordable Pricing of CRISPR Treatments is a Pressing Ethical Imperative - PubMed [https://pubmed.ncbi.nlm.nih.gov/39392045/]
- 120. Paying for CRISPR Cures: The Economics of Genetic Therapies - Innovative Genomics Institute (IGI) [https://innovativegenomics.org/news/paying-for-crispr-cures/]
- 121. CRISPR in Public Health: The Health Equity Implications and Role of Community in Gene-Editing Research and Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10323846/]
- 122. Frontiers | Barriers and Opportunities for Implementation of... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.594446/full]
- 123. Frontiers | Mapping the therapeutic of landscape - CRISPR for... Cas 9 [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2025.1558432/full]
- 124. AG's Global Expansion of Casgevy in CRISPR ... Therapeutics 2025 [https://www.ainvest.com/news/crispr-therapeutics-ag-global-expansion-casgevy-2025-strategic-positioning-gene-editing-therapy-market-2509/]
- 125. Global CRISPR Opportunity & Clinical Trials Outlook... Cas 9 Market [https://finance.yahoo.com/news/global-crispr-cas9-market-opportunity-090200995.html]