Critical Limitations of PICADAR: Reevaluating Its Role in Primary Ciliary Dyskinesia Diagnosis
This article critically examines the PICADAR (Primary Ciliary Dyskinesia Rule) predictive tool, a clinical score recommended by European Respiratory Society guidelines for identifying patients requiring definitive PCD testing.
Critical Limitations of PICADAR: Reevaluating Its Role in Primary Ciliary Dyskinesia Diagnosis
Abstract
This article critically examines the PICADAR (Primary Ciliary Dyskinesia Rule) predictive tool, a clinical score recommended by European Respiratory Society guidelines for identifying patients requiring definitive PCD testing. Based on recent 2025 research and validation studies, we analyze significant limitations in PICADAR's sensitivity, particularly in patients without classic laterality defects or hallmark ultrastructural abnormalities. We explore performance disparities across patient subgroups, methodological constraints in clinical application, and comparative effectiveness against alternative screening tools. For researchers and drug development professionals, this synthesis provides essential insights for refining diagnostic pathways, developing next-generation predictive models, and ensuring appropriate patient stratification for clinical trials and therapeutic development.
Understanding PICADAR: Core Principles and Emerging Limitations
PICADAR's Original Purpose and Development Context
What is the original purpose of the PICADAR tool?
The PrImary CiliAry DyskinesiA Rule (PICADAR) was developed as a practical, clinical diagnostic prediction tool to identify patients with a high probability of having Primary Ciliary Dyskinesia (PCD) and who should be referred for definitive diagnostic testing [1]. It was created to address the challenge that PCD symptoms are nonspecific and that confirmatory diagnostic tests are highly specialized, expensive, and not widely available [1]. By using a set of simple clinical parameters obtainable from patient history, PICADAR aims to help clinicians effectively triage patients for further specialist investigation.
What was the development context and methodology?
PICADAR was developed and validated through a clinical study published in the European Respiratory Journal in 6 [1]. The development process involved analyzing patients consecutively referred for PCD testing to correlate information from their history with the final diagnostic outcome.
- Study Population: The initial model was derived from 641 referrals, of which 75 (12%) were subsequently diagnosed with PCD [1].
- Statistical Method: Researchers used logistic regression to build a predictive model. The model's performance was tested using receiver operating characteristic (ROC) curve analyses [1].
- Simplification and Validation: The statistical model was simplified into a practical scoring tool (PICADAR) and was externally validated in a second, independent diagnostic center [1].
What are the key predictive parameters in the PICADAR score?
PICADAR is applied to patients with a persistent wet cough and assesses seven predictive clinical parameters [1]. The score is the sum of points assigned for each factor present.
Table: PICADAR Scoring Parameters and Points
| Predictive Parameter | Points Assigned |
|---|---|
| Situs inversus | 2 |
| Full-term gestation | 1 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Congenital cardiac defect | 2 |
| Total Possible Score | 10 |
How is the PICADAR score interpreted?
The total PICADAR score corresponds to a specific probability of having PCD, guiding clinical decision-making for further testing [2].
Table: PICADAR Score Interpretation and Diagnostic Probability
| PICADAR Score | Probability of PCD | Clinical Implication |
|---|---|---|
| ≥ 10 | 92.6% | High probability; strongly warrants referral for definitive testing. |
| ≥ 5 | 11.10% | Moderate probability; may require further clinical assessment. |
| A score of 14 | 99.80% | Very high probability of PCD [2]. |
In the original validation, the tool demonstrated an overall accuracy of 90%, with a sensitivity of 71% and a specificity of 94% [1].
What are the established limitations of PICADAR in a research context?
While a valuable screening tool, subsequent research has highlighted important limitations of PICADAR that researchers and clinicians must consider.
- Variable Sensitivity: A 2025 pre-print study on 269 genetically confirmed PCD patients found the overall sensitivity of PICADAR (using a ≥5 cutoff) was only 75% [3]. This means one in four true PCD cases would be missed by the tool.
- Critical Weakness in Specific Subgroups: The same study revealed that sensitivity is not uniform across all PCD patients. It is significantly higher in individuals with laterality defects (95%) compared to those with normal organ placement (situs solitus), where sensitivity drops to 61% [3]. Sensitivity is also lower in patients without hallmark ultrastructural ciliary defects (59%) [3].
- Fundamental Exclusion of Some Patients: The tool's algorithm begins by excluding all individuals who do not report a daily wet cough [3]. The 2025 study found that 7% of genetically confirmed PCD patients did not have this symptom and would have been automatically ruled out by PICADAR [3].
- Recall Bias in Adults: The original PICADAR parameters are based on early life events, which can be difficult for adult patients or their parents to recall accurately, potentially reducing the tool's reliability in adult populations [4].
What is the recommended workflow for using PICADAR in research?
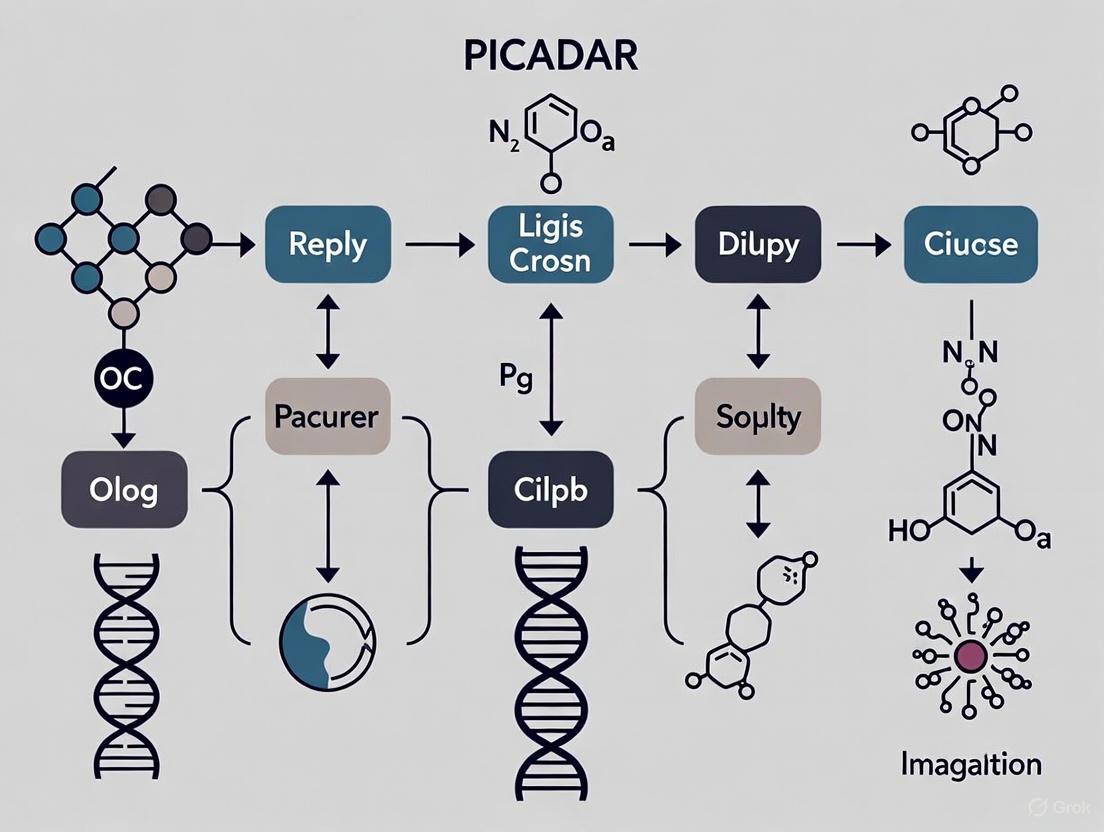
The following diagram illustrates the logical workflow for applying PICADAR in a clinical or research setting, incorporating its known limitations.
What are the essential research reagents and solutions for PCD diagnosis?
PICADAR is a pre-screening tool; definitive PCD diagnosis requires specialized tests. The table below lists key reagents and materials used in these confirmatory investigations.
Table: Key Reagents and Solutions for Definitive PCD Diagnostic Testing
| Research Reagent / Solution | Function in PCD Diagnosis |
|---|---|
| Nasal Epithelial Cells | Obtained via nasal brushing for ciliary functional and structural analysis [5]. |
| Culture Media for Air-Liquid Interface (ALI) | Supports the differentiation and growth of ciliated epithelial cells from biopsy samples for ciliary function analysis [2]. |
| Glutaraldehyde Fixative | Used for preparing ciliary samples for structural analysis by Transmission Electron Microscopy (TEM) [5]. |
| Antibodies for Immunofluorescence (IF) | Target specific ciliary proteins (e.g., dynein arms) to detect defects in protein localization [5]. |
| DNA Sequencing Kits (PCD Gene Panel) | Used in genetic testing to identify biallelic mutations in any of the ~40-47 known PCD-causing genes [2]. |
| Chemiluminescence Analyzer | Essential for measuring low Nasal Nitric Oxide (nNO) levels, a hallmark of PCD [4]. |
Primary Ciliary Dyskinesia (PCD) is a rare, heterogeneous genetic disorder affecting motile cilia, leading to chronic respiratory symptoms. Diagnosis is challenging due to nonspecific symptoms and the complexity of specialized diagnostic tests. The PICADAR (PrImary CiliARy DyskinesiA Rule) tool was developed as a clinical prediction rule to identify patients requiring formal PCD testing. This seven-parameter predictive tool utilizes easily obtainable clinical history to estimate the probability of a PCD diagnosis, helping general respiratory and ENT specialists determine appropriate referrals to specialist centres [6].
The Seven Core Components of the PICADAR Framework
The PICADAR framework incorporates seven predictive clinical parameters derived from patient history. These components were identified through logistic regression analysis of patients consecutively referred for PCD testing, with each parameter assigned an integer score based on its regression coefficient [6].
Table 1: The Seven Core Parameters of the PICADAR Tool
| Parameter | Clinical Description | Scoring Value |
|---|---|---|
| Full-term gestation | Patient was born at full-term gestation | +1 point |
| Neonatal chest symptoms | Respiratory distress or other chest symptoms present at birth | +2 points |
| Neonatal intensive care unit admission | Required admission to special care baby unit after birth | +2 points |
| Chronic rhinitis | Persistent nasal symptoms lasting >3 months | +1 point |
| Ear symptoms | History of chronic otitis media or hearing problems | +1 point |
| Situs inversus | Complete reversal of internal organ positioning | +4 points |
| Congenital cardiac defect | Structural heart abnormality present at birth | +3 points |
Scoring Methodology and Diagnostic Interpretation
Calculation Procedure
The PICADAR scoring system is applied to patients with persistent wet cough. To calculate a patient's score:
- Review patient history for the presence of each of the seven parameters
- Sum the points for all applicable parameters
- Compare total score against established diagnostic cut-off values [6]
Interpretation Guidelines
- Total Score ≥5 points: High probability of PCD (Sensitivity: 0.90, Specificity: 0.75)
- Total Score <5 points: Lower probability of PCD
- The tool demonstrates excellent discriminatory ability with an Area Under the Curve (AUC) of 0.91 upon internal validation and 0.87 upon external validation [6]
Table 2: Performance Metrics of the PICADAR Tool
| Validation Metric | Internal Validation | External Validation |
|---|---|---|
| Area Under Curve (AUC) | 0.91 | 0.87 |
| Sensitivity (at cut-off ≥5) | 0.90 | Not specified |
| Specificity (at cut-off ≥5) | 0.75 | Not specified |
| Study Population | 641 patients (75 PCD-positive) | 187 patients (93 PCD-positive) |
Frequently Asked Questions (FAQs)
Application Questions
Q1: What is the appropriate clinical context for using PICADAR? PICADAR is designed for patients with persistent wet cough being considered for referral to PCD specialist centres. It should be applied by respiratory or ENT specialists during initial patient assessment to determine the need for specialized PCD diagnostic testing [6].
Q2: How should I handle missing historical data when calculating a PICADAR score? The original research excluded subjects with missing data on a case-wise basis. For clinical practice, if key neonatal history is unavailable, consider the total score potentially underestimating PCD risk. Multiple imputation techniques were used in the validation study to check for biases, but in practice, attempt to obtain complete historical data where possible [6].
Q3: Can PICADAR be used for adult patients or only children? The derivation study included patients aged 0-79 years, with a median age of 9 years. The validation group was younger (median age 3 years). While applicable to adults, the tool's performance in exclusively adult populations requires further validation [6].
Technical and Interpretation Questions
Q4: What are the limitations of using a cut-off score of 5 points? While the ≥5 cut-off provides optimal sensitivity (90%), it has moderate specificity (75%). This means some false positives will be referred for specialized testing. In resource-limited settings, a higher cut-off may be considered to increase specificity, though this would reduce sensitivity [6].
Q5: How does PICADAR compare to nasal nitric oxide (nNO) testing? PICADAR utilizes clinical history alone, while nNO requires expensive equipment and trained technicians. PICADAR serves as an accessible initial screening tool, particularly in settings where nNO measurement is unavailable [6].
Q6: Can the PICADAR score be used to definitively diagnose PCD? No. PICADAR is a predictive tool to identify high-risk patients, not a diagnostic test. Formal PCD diagnosis requires specialized testing including transmission electron microscopy, ciliary beat pattern analysis, high-speed video microscopy, and/or genetic testing in specialist centres [6].
Troubleshooting Common Implementation Issues
Data Collection Challenges
Problem: Incomplete neonatal history in older patients. Solution: Attempt to obtain birth records where possible. For adult patients without available neonatal records, focus on documented situs abnormalities and congenital cardiac defects which carry higher point values and may be documented in medical history [6].
Problem: Distinguishing chronic rhinitis from allergic rhinitis. Solution: The tool specifies "chronic rhinitis" lasting >3 months. Focus on persistent, year-round symptoms rather than seasonal patterns more suggestive of allergies. PCD-related rhinitis typically begins in early infancy [6].
Interpretation Challenges
Problem: Patient scores 4 points, just below the referral threshold. Solution: Consider the clinical context. Patients with strong family history of PCD or bronchiectasis on imaging may warrant referral despite subthreshold scores. Use clinical judgment in conjunction with the tool [6].
Problem: How to apply the tool in populations with high consanguinity rates. Solution: The validation study included populations with differing consanguinity rates. While the tool performed well in external validation, be aware that populations with high consanguinity may have higher PCD prevalence, potentially affecting positive predictive values [6].
Essential Research Reagents and Materials
Table 3: Key Research Reagents for PCD Diagnostic Testing
| Reagent/Equipment | Primary Function | Application in PCD Diagnosis |
|---|---|---|
| Transmission Electron Microscope (TEM) | Ultrastructural visualization | Identification of ciliary ultrastructural defects (e.g., outer/inner dynein arm defects) |
| High-speed Video Microscopy | Ciliary beat pattern analysis | Assessment of ciliary beat frequency and pattern abnormalities |
| Nasal Nitric Oxide (nNO) analyzer | Measurement of nasal NO levels | Screening tool; very low nNO levels (<30 nL·min⁻¹) strongly suggest PCD |
| Air-liquid interface culture materials | Ciliary cell culture | Regeneration of ciliated epithelium to differentiate primary from secondary dyskinesia |
| Genetic testing panels | DNA sequence analysis | Identification of pathogenic variants in known PCD-associated genes |
Initial Validation Performance Metrics and Promised Utility
Frequently Asked Questions (FAQs)
Q1: What were the original performance metrics for PICADAR from its initial validation studies? The PICADAR tool was initially developed and validated in a 2016 study, demonstrating strong performance for screening patients for Primary Ciliary Dyskinesia (PCD). The key metrics from its derivation and external validation are summarized in the table below [7] [8].
Table 1: Initial Validation Performance Metrics of PICADAR
| Metric | Derivation Cohort (n=641) | External Validation Cohort (n=187) |
|---|---|---|
| Study Population | 75 PCD-positive, 566 PCD-negative | 93 PCD-positive, 94 PCD-negative |
| Recommended Cut-off Score | 5 points | 5 points |
| Sensitivity | 0.90 | Not explicitly stated (AUC provided) |
| Specificity | 0.75 | Not explicitly stated (AUC provided) |
| Area Under the Curve (AUC) | 0.91 | 0.87 |
Q2: What are the seven predictive parameters in the PICADAR score, and how are they weighted? PICADAR is applied to patients with a persistent wet cough and is based on seven clinical parameters that can be easily obtained from patient history. The points for each parameter are derived from regression coefficients rounded to the nearest integer [7] [9]. The scoring system is as follows:
Table 2: The PICADAR Scoring System
| Predictive Parameter | Score |
|---|---|
| Full-term gestation | 2 points |
| Neonatal chest symptoms ever | 2 points |
| Admission to a neonatal intensive care unit | 1 point |
| Chronic rhinitis | 1 point |
| Ear symptoms (chronic otitis media or hearing impairment) | 1 point |
| Situs inversus | 4 points |
| Congenital cardiac defect | 2 points |
| Total Possible Score | 13 points |
Q3: What specific limitations in PICADAR's performance have recent studies identified? Despite its promising initial validation, a 2025 study that applied PICADAR to 269 individuals with genetically confirmed PCD revealed significant limitations in its sensitivity, particularly in specific patient subgroups [3]. The overall and subgroup sensitivities are detailed below.
Table 3: Recent Findings on PICADAR Sensitivity (2025 Study)
| Patient Group | Sample Size | Median PICADAR Score (IQR) | Sensitivity (Score ≥5) |
|---|---|---|---|
| All Genetically Confirmed PCD | 269 | 7 (5 - 9) | 75% (202/269) |
| - With laterality defects | Information Missing | 10 (8 - 11) | 95% |
| - With situs solitus (normal arrangement) | Information Missing | 6 (4 - 8) | 61% |
| - With hallmark ultrastructural defects | Information Missing | Information Missing | 83% |
| - Without hallmark ultrastructural defects | Information Missing | Information Missing | 59% |
| Excluded by Initial Screen | 18 | N/A | 0% (ruled out for lacking daily wet cough) |
Q4: What is the recommended experimental protocol for validating a predictive tool like PICADAR in a new cohort? To properly evaluate PICADAR's performance, follow this diagnostic and analytical workflow [7] [3]:
Q5: What are the essential research reagents and materials for conducting a comprehensive PCD diagnostic study? A robust PCD diagnostic study requires a combination of clinical, functional, and molecular techniques. The following table details key reagents and their applications [3] [10].
Table 4: Research Reagent Solutions for PCD Diagnostics
| Reagent / Material | Primary Function | Application in PCD Research |
|---|---|---|
| Nasal Epithelial Cells | Source of respiratory cilia | Obtained via transnasal brush biopsy for HSVM, TEM, IF, and cell culture. |
| Antibodies for IF (e.g., anti-DNAH5, anti-GAS8) | Protein localization and detection | Visualizing the presence, absence, or mislocalization of specific ciliary proteins (e.g., ODA components). |
| High-Speed Video Microscopy (HSVM) System | Ciliary beat analysis | Quantifying ciliary beat frequency and qualitatively assessing ciliary beat pattern. |
| Nasal Nitric Oxide (nNO) Analyzer | Measurement of nasal NO output | Used as a screening test; low nNO is supportive of, but not definitive for, PCD. |
| Genetic Sequencing Panel | Identification of pathogenic variants | Targeted or comprehensive next-generation sequencing panels for known PCD-associated genes. |
| Air-Liquid Interface (ALI) Culture Media | Ciliated cell culture | Differentiating and growing respiratory epithelial cells to regenerate cilia and rule out secondary dyskinesia. |
Q6: How does the diagnostic workflow integrate PICADAR with advanced confirmatory tests? The following diagram outlines the logical pathway for using PICADAR within a broader PCD diagnostic framework, highlighting its role as a screening tool prior to more complex and expensive confirmatory tests [7] [10].
Emerging Evidence of Diagnostic Gaps and Sensitivity Concerns
What is the PICADAR tool and what are its intended strengths?
The PICADAR (PrImary CiliARy DyskinesiA Rule) tool is a clinical prediction rule designed to help general respiratory and ENT specialists identify patients with a high probability of Primary Ciliary Dyskinesia (PCD) who should be referred for specialized diagnostic testing [8] [7].
Its key strength lies in using seven simple clinical parameters readily obtained from a patient's history, making it a practical and rapid initial screening tool [8] [7]. The tool was developed to address the challenge that PCD symptoms are nonspecific and definitive diagnostic tests are highly specialized, expensive, and only available at expert centers [8] [7].
Table: The Seven Predictive Parameters of the PICADAR Tool
| Parameter | Description |
|---|---|
| Full-term Gestation | Patient was born at full term [8] [7]. |
| Neonatal Chest Symptoms | Respiratory symptoms present shortly after birth [8] [7]. |
| Neonatal Intensive Care Admittance | Required admission to a special care baby unit after birth [8] [7]. |
| Chronic Rhinitis | Persistent nasal inflammation lasting more than 3 months [8] [7]. |
| Ear Symptoms | History of chronic ear problems, such as otitis media [8] [7]. |
| Situs Inversus | A condition where the major visceral organs are mirrored from their normal positions [8] [7]. |
| Congenital Cardiac Defect | Presence of a heart defect at birth [8] [7]. |
In its initial validation, PICADAR demonstrated good performance, with a reported sensitivity of 0.90 and specificity of 0.75 at a recommended cut-off score of 5 points. The Area Under the Curve (AUC) was 0.91 in the initial cohort and 0.87 upon external validation [8] [7].
What is the new evidence regarding PICADAR's sensitivity and diagnostic gaps?
Recent evidence from a September 2025 preprint study by Schramm et al. reveals significant limitations in PICADAR's sensitivity, indicating it may miss a substantial number of PCD cases, particularly in specific patient subgroups [3].
This study evaluated 269 individuals with genetically confirmed PCD and found that the overall sensitivity of PICADAR was only 75% (202 out of 269), which is notably lower than the original validation studies [3]. The research identified two critical diagnostic gaps:
- Exclusion of patients without a daily wet cough: The tool's initial question about the presence of a persistent daily wet cough ruled out 18 individuals (7%) with genetically confirmed PCD right at the start of the screening process [3].
- Poor performance in patients with normal body situs: The tool's sensitivity was dramatically lower in patients with situs solitus (normal organ arrangement) at 61%, compared to 95% in those with situs inversus or other laterality defects [3].
- Dependence on ultrastructural defects: Sensitivity was higher in individuals with hallmark defects on transmission electron microscopy (83%) versus those without such defects (59%) [3].
Table: PICADAR Sensitivity in Key Subgroups (Schramm et al., 2025)
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| Overall (Genetically Confirmed PCD) | 75% (202/269) | 7 (5 - 9) |
| With Laterality Defects | 95% | 10 (8 - 11) |
| With Situs Solitus (normal arrangement) | 61% | 6 (4 - 8) |
| With Hallmark Ultrastructural Defects | 83% | Information not provided in abstract |
| Without Hallmark Ultrastructural Defects | 59% | Information not provided in abstract |
How should I adjust my research protocol in light of these findings?
Your experimental design should no longer rely on PICADAR as a standalone screening or enrollment tool, especially if your research aims to capture the full spectrum of PCD phenotypes.
Recommended Protocol Adjustments:
- Do Not Use PICADAR in Isolation: Given its suboptimal sensitivity, PICADAR should be used with caution and not as the primary factor for estimating the likelihood of PCD [3].
- Implement a Multi-Tool Approach: Combine PICADAR with other predictive tools or tests to improve case identification. The 2025 study concludes that "alternative predictive tools are needed, particularly for PCD individuals with normal body composition and normal ultrastructure" [3].
- Prioritize Comprehensive Testing for Borderline Cases: For patients with a high clinical suspicion of PCD but a low PICADAR score (e.g., below 5), proceed directly to advanced diagnostic tests rather than excluding them from further investigation. This is crucial for capturing patients with situs solitus or non-hallmark ultrastructural defects.
- Leverage International Collaborations: For complex cases or if advanced techniques like immunofluorescence (IF) are unavailable, consider collaborating with expert centers. A 2025 study demonstrated the success of this approach in reaching a definitive diagnosis for patients with inconclusive initial genetic results [10].
What alternative or complementary diagnostic methods are available?
A combination of techniques is recommended by the European Respiratory Society (ERS) and American Thoracic Society (ATS) to achieve an accurate diagnosis, as there is no single gold standard test [10].
Table: Key Diagnostic Methods for PCD in Research
| Method | Function & Utility in Diagnosis | Considerations for Researchers |
|---|---|---|
| Genetic Analysis | Identifies pathogenic variants in over 50 known PCD-related genes; considered a definitive confirmatory test [10] [3]. | Can be inconclusive if using limited gene panels. Comprehensive genetic testing (e.g., whole exome sequencing) may be needed for rare variants [10]. |
| Immunofluorescence (IF) Analysis | Detects the absence or mislocalization of specific ciliary proteins (e.g., DNAH5, GAS8) using antibody staining [10]. | Faster and cheaper than TEM; excellent for validating the pathogenicity of genetic variants of uncertain significance [10]. |
| High-Speed Video Microscopy Analysis (HSVM) | Assesses ciliary beat frequency and pattern. Immotile cilia or abnormal beating patterns are indicative of PCD [10]. | Requires specialized equipment and experienced personnel to distinguish primary from secondary dyskinesia [10]. |
| Transmission Electron Microscopy (TEM) | The historical gold standard; visualizes the internal ultrastructure of cilia to identify defects in dynein arms, nexin links, etc. [10]. | Expensive, time-consuming, and requires significant expertise. Up to 30% of genetically confirmed PCD cases can have normal ultrastructure [3]. |
| Nasal Nitric Oxide (nNO) Measurement | A highly effective screening test, as most PCD patients have very low nNO levels [7] [10]. | Not diagnostic on its own. Some genetic subtypes can have normal nNO, and it cannot be used in young children [10]. |
Experimental Workflow for Comprehensive PCD Diagnosis
The following diagram outlines a robust diagnostic and troubleshooting workflow that integrates PICADAR with other methods to address its sensitivity gaps.
The Scientist's Toolkit: Key Research Reagent Solutions
Table: Essential Materials for PCD Diagnostic Research
| Research Reagent / Tool | Primary Function in PCD Research |
|---|---|
| PICADAR Score Sheet | A quick, cost-free clinical pre-screener to identify patients with classic PCD symptoms. Researchers must be aware of its sensitivity limitations [8] [3]. |
| Antibodies for IF (e.g., anti-DNAH5, anti-GAS8) | Key reagents for Immunofluorescence analysis. They detect the presence and correct localization of specific ciliary proteins, helping to confirm the functional impact of genetic variants [10]. |
| Nasal Nitric Oxide (nNO) Analyzer | Equipment to measure nasal NO, a key non-invasive screening test. Low nNO is a strong indicator for PCD, though not universal [7] [10]. |
| High-Speed Video Microscope | Essential equipment for HSVM to visualize and quantify ciliary beat pattern and frequency, a core functional test for ciliary activity [10]. |
| Extended PCD Genetic Panels | Moving beyond limited gene panels to more comprehensive genetic tests (e.g., whole exome sequencing) is critical for diagnosing patients with mutations in rare genes not covered by standard panels [10] [3]. |
| Cell Culture Media (e.g., RPMI 1640) | Used to transport and maintain the viability of respiratory epithelial cells obtained from nasal brush biopsies for HSVM and IF analyses [10]. |
The Critical Role of Predictive Tools in Rare Disease Diagnosis
Frequently Asked Questions (FAQs)
1. What is PICADAR and what is its primary function? PICADAR (PrImary CiliARy DyskinesiA Rule) is a clinical prediction tool designed to help general respiratory and ENT specialists identify which patients with persistent respiratory symptoms should be referred for specialized Primary Ciliary Dyskinesia (PCD) testing [6]. It uses seven easily obtainable clinical parameters to calculate a score that predicts the probability of a PCD diagnosis, thereby addressing the challenge of nonspecific PCD symptoms and the highly specialized nature of definitive PCD diagnostic tests [6].
2. What are the specific limitations of the PICADAR tool? The primary limitation of PICADAR is that it serves as a prediction rule, not a definitive diagnostic test [6]. Its development and validation study emphasized that it is designed to identify patients requiring confirmatory testing at a specialist centre [6]. Furthermore, its predictive ability depends on the accuracy of the clinical history taken, and it may not capture all rare presentations of PCD.
3. For which patient population is PICADAR intended? PICADAR is intended for use in patients who present with a persistent wet cough [6]. The tool was derived and validated from patients referred to specialist PCD diagnostic centres, meaning its performance is optimized for a symptomatic population that a clinician already suspects might have PCD, not for general population screening [6].
4. How was the PICADAR tool developed and validated? The tool was developed using data from 641 consecutive patients referred to the University Hospital Southampton (UHS) PCD diagnostic centre [6]. Logistic regression analysis was used to identify the most predictive clinical parameters. The tool was then externally validated using a separate sample of 187 patients from the Royal Brompton Hospital (RBH), demonstrating good validity and accuracy with an area under the curve (AUC) of 0.87 in the external population [6].
Troubleshooting Guide: Common Experimental Challenges in Predictive Tool Research
Problem 1: Low Specificity in Patient Selection Issue: The predictive tool yields a high number of false positives, leading to unnecessary referrals and burden on specialist diagnostic facilities.
- Step 1: Verify that the target population matches the tool's intended use case (e.g., PICADAR is for patients with persistent wet cough, not all chronic respiratory symptoms) [6].
- Step 2: Recalculate the patient's score, ensuring all seven parameters are accurately assessed. A score of 5 points yielded a specificity of 0.75 in the validation study; consider adjusting the cut-off score based on your local patient population and healthcare priorities [6].
- Step 3: For research settings, revisit the logistic regression model to identify if additional or alternative clinical parameters could improve specificity without critically reducing sensitivity [6].
Problem 2: Integrating Patient-Reported Outcomes into Predictive Models Issue: Difficulty in systematically capturing and analyzing qualitative patient experiences for diagnostic purposes.
- Step 1: Develop structured Patient-Oriented Questionnaires (POQs) that focus on day-to-day functional challenges and experiences, not just clinical symptoms [11].
- Step 2: Apply machine learning (ML) techniques to analyze the resulting qualitative datasets. ML can identify complex patterns within patient-reported data that may not be evident through traditional analysis [11].
- Step 3: Validate any new model or tool in an external population, as was done with PICADAR, to ensure its accuracy and generalizability are not confined to the initial development group [6] [11].
Problem 3: Handling Missing Clinical Data in Retrospective Analyses Issue: Key clinical parameters for the predictive tool are missing from patient records, making score calculation impossible.
- Step 1: Prioritize the use of prospectively collected data where a proforma for key clinical history is completed prior to diagnostic testing, as was done in the PICADAR study [6].
- Step 2: For retrospective studies, employ statistical techniques like multiple imputation to check for biases that can occur from case-wise deletion of records with missing data [6].
- Step 3: Document the frequency of missing data for each parameter, as this may indicate which clinical features are difficult to obtain reliably and could inform the design of future data collection protocols.
Experimental Protocols
Protocol 1: Development and Validation of a Clinical Prediction Tool
This protocol outlines the methodology used in the development of the PICADAR tool, which can serve as a template for creating similar predictive instruments for other rare diseases [6].
1. Study Population and Data Collection:
- Derivative Cohort: Recruit a large, consecutive cohort of patients referred for definitive diagnostic testing for the target rare disease. For PICADAR, this involved 641 patients [6].
- Data Points: Collect information on patient demographics and readily available clinical features from the patient's history. Use a standardized proforma completed by a clinician prior to diagnostic testing to ensure consistency [6].
- Diagnostic Outcome: Establish a clear, pre-defined "gold standard" for a positive and negative diagnosis based on the best available tests (e.g., a combination of transmission electron microscopy, ciliary beat pattern analysis, and nasal nitric oxide in PCD) [6].
2. Model Development:
- Statistical Analysis: Use logistic regression analysis to identify which clinical variables are significant independent predictors of a positive diagnosis [6].
- Variable Selection: Enter potential predictors individually using forward step-wise methods to build the most efficient model [6].
3. Tool Creation and Validation:
- Score Creation: Simplify the logistic regression model into a practical scoring tool by rounding regression coefficients to the nearest integer to create points for each predictive parameter [6].
- Internal Validation: Assess the model's discriminative ability by plotting the Receiver Operating Characteristic (ROC) curve and calculating the Area Under the Curve (AUC). An AUC > 0.8 is considered good [6].
- External Validation: Test the performance of the scoring tool in a separate, independent patient population from a different clinical centre to ensure its validity and generalizability [6].
Protocol 2: Integrating Machine Learning with Patient-Oriented Questionnaires (POQs)
This protocol describes a systematic approach for using patient experiences to build diagnostic support systems for rare diseases, as explored in recent research [11].
1. Questionnaire Design:
- Objective: Develop POQs tailored to capture the patient's day-to-day lived experiences and functional challenges with their condition, moving beyond purely clinical symptoms [11].
- Content: The questions should be designed to elicit information about the patient's struggles and experiences that might be unique to the rare disease but are not typically captured in standard medical histories [11].
2. Data Processing and Analysis:
- Data Preparation: Structure the qualitative data from the POQs for computational analysis.
- Machine Learning Application: Apply relevant ML algorithms (e.g., for classification or pattern recognition) to the resulting datasets. The objective is to generate predictions about the underlying disease or to identify predictive indicators associated with it [11].
3. Performance and Implementation Assessment:
- Evaluation: Measure the performance of the ML algorithms using standard metrics to determine their accuracy in predicting the disease.
- Implementation Research: Investigate the feasibility and effectiveness of deploying this combined POQ/ML approach in routine clinical practice, as this remains an area for further research [11].
Diagnostic Pathway for Primary Ciliary Dyskinesia (PCD)
The diagram below illustrates the clinical workflow for diagnosing PCD, highlighting the role of the PICADAR tool as an initial screening step before advanced testing.
PICADAR Clinical Parameters and Scoring
The table below summarizes the seven predictive parameters used in the PICADAR tool and the points assigned to each, as derived from the original study [6].
| Predictive Parameter | Points Assigned |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms (prior to term admission) | 2 |
| Admission to a neonatal intensive care unit | 1 |
| Chronic rhinitis (persisting for >3 months) | 1 |
| Chronic ear symptoms (persisting for >3 months) | 1 |
| Situs inversus | 4 |
| Congenital cardiac defect | 2 |
Research Reagent and Diagnostic Solutions
The following table details key materials and methods used in the definitive diagnostic testing for PCD, as referenced in the PICADAR validation study [6].
| Reagent / Solution / Method | Primary Function in PCD Diagnosis |
|---|---|
| Nasal Nitric Oxide (nNO) Measurement | A non-invasive screening test; nNO levels ≤30 nL·min⁻¹ are highly suggestive of PCD and used as one criterion for a positive diagnosis [6]. |
| High-Speed Video Microscopy Analysis (HSVMA) | Used to visualize and analyze ciliary beat pattern (CBP). A "hallmark" abnormal pattern is a key diagnostic indicator [6]. |
| Transmission Electron Microscopy (TEM) | Used to examine the ultrastructure of cilia. Identifying specific defects (e.g., absent dynein arms) is a "hallmark" diagnostic criterion [6]. |
| Air-Liquid Interface (ALI) Culture | A cell culture technique used to re-differentiate ciliated epithelium. It helps rule out secondary ciliary dyskinesia caused by infection or inflammation, ensuring CBP analysis reflects the primary defect [6]. |
PICADAR in Practice: Operational Challenges and Implementation Barriers
Troubleshooting Guide: Addressing PICADAR's Diagnostic Sensitivity
Problem Identification: Suspected Low Sensitivity in Specific PCD Subgroups
Researchers and clinicians may observe that the PICADAR tool fails to identify a subset of patients with genetically confirmed Primary Ciliary Dyskinesia (PCD). This frequently occurs when studying patient cohorts with normal organ arrangement (situs solitus) or those lacking hallmark ciliary ultrastructural defects.
Experimental Validation of the Limitation
A 2025 validation study genetically confirmed PCD in 269 individuals and applied the PICADAR tool according to its standard protocol [3]. The experimental workflow and findings are summarized below:
| Patient Subgroup | Number of Patients | PICADAR Sensitivity (%) | Median PICADAR Score (IQR) |
|---|---|---|---|
| Overall Cohort | 269 | 75% | 7 (5 - 9) |
| With Laterality Defects | Not Specified | 95% | 10 (8 - 11) |
| Situs Solitus (normal arrangement) | Not Specified | 61% | 6 (4 - 8) |
| With Hallmark Ultrastructural Defects | Not Specified | 83% | Not Specified |
| Without Hallmark Ultrastructural Defects | Not Specified | 59% | Not Specified |
Key Finding: The study confirmed that 18 out of 269 genetically proven PCD patients (7%) were automatically excluded from further PICADAR assessment because they did not report a daily wet cough, a fundamental limitation of the tool's initial screening question [3].
Recommended Solutions and Methodological Adjustments
Implement Modified PICADAR Protocols
A 2017 study proposed a modified PICADAR approach for adult bronchiectasis populations [12]. The experimental protocol involved:
- Population: 185 adults with bronchiectasis
- Modification: Used a lower cutoff score (≥2 points) while maintaining the daily wet cough requirement
- Outcome: Achieved sensitivity of 1.00 and specificity of 0.89 in this specific population
- Method: Retrospective analysis of patients with complete clinical data and nasal NO measurements
Integrate Nasal Nitric Oxide (nNO) Testing
The same study demonstrated complementary use of nNO measurement [12]:
- Measurement Protocol: Based on 2005 ATS/ERS recommendations using chemiluminescence analysis
- Optimal Cutoff: nNO level of 77 nL/min provided best discrimination
- Result: PCD patients showed significantly lower nNO (25 nL/min) versus non-PCD patients (227 nL/min)
Develop Population-Specific Thresholds
The original PICADAR validation proposed a cutoff score of 5 points, but this may require adjustment for specific populations [8] [13]. Experimental validation should include:
- ROC Analysis: Determine optimal cutoff for your specific patient demographic
- Validation Cohort: Test proposed thresholds in an independent patient group
- Protocol: Compare sensitivity/specificity tradeoffs at different score thresholds
Frequently Asked Questions (FAQs)
What is the fundamental design limitation of the PICADAR tool?
The PICADAR tool's initial screening question automatically excludes patients who do not report a persistent daily wet cough [3]. Recent research indicates this excludes approximately 7% of genetically confirmed PCD patients, particularly those with milder respiratory phenotypes or atypical presentations.
How does the presence of laterality defects affect PICADAR's accuracy?
PICADAR demonstrates significantly higher sensitivity in patients with laterality defects (95%) compared to those with normal organ arrangement (situs solitus, 61%) [3]. This occurs because situs inversus contributes 2 points to the total score, making it more likely these patients will reach the diagnostic threshold of 5 points.
What alternative screening approaches can complement PICADAR?
Nasal nitric oxide (nNO) measurement has shown excellent complementary value [12]. The recommended protocol includes:
- Using chemiluminescence analysis per ATS/ERS guidelines
- Implementing a cutoff of <77 nL/min for PCD suspicion
- Combining low nNO with modified PICADAR scores for enhanced sensitivity
Can PICADAR be used for adult bronchiectasis populations?
Yes, but with modifications. Research indicates that a modified PICADAR score with a lower threshold (≥2 points) can effectively screen for PCD in adults with bronchiectasis, achieving sensitivity of 1.00 and specificity of 0.89 when combined with nNO measurement [12].
What are the key methodological considerations when validating PICADAR?
- Patient Recruitment: Consecutive referrals to minimize selection bias [8] [13]
- Reference Standard: Use genetically confirmed diagnosis or combination of diagnostic tests [3]
- Data Collection: Standardized proforma completed before diagnostic testing [13]
- Statistical Analysis: ROC curve analysis to determine optimal cutoff scores [8]
Research Reagent Solutions
| Essential Material | Function in PCD Diagnostic Research |
|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Measures nasal NO concentration using chemiluminescence; crucial screening tool with characteristic low levels in PCD [12]. |
| High-Speed Video Microscopy (HSVMA) | Analyzes ciliary beat pattern and frequency; identifies characteristic dysfunctional patterns in PCD [13]. |
| Transmission Electron Microscopy (TEM) | Evaluates ciliary ultrastructure; identifies hallmark defects in approximately 70% of PCD cases [13]. |
| Genetic Sequencing Panels | Identifies biallelic mutations in known PCD genes; increasingly used as confirmatory diagnostic method [3]. |
| Immunofluorescence Microscopy (IF) | Detects absence or mislocalization of ciliary proteins; complements TEM in diagnosis [13]. |
| Air-Liquid Interface Culture Systems | Allows ciliary regrowth and reanalysis after epithelial cell culture; helps distinguish primary from secondary dyskinesia [13]. |
Recall Bias and Data Accessibility Issues in Historical Neonatal Data
FAQ: Understanding and Troubleshooting Research Methodologies
What is the primary concern with using historical data for PICADAR parameters?
The main concern is recall bias, a type of systematic error that occurs when participants in a study do not accurately remember past events or experiences [14]. For PICADAR, which relies on early life events such as neonatal respiratory distress, this bias can significantly impact the accuracy of the data collected for diagnosis.
How does recall bias specifically affect PICADAR score accuracy?
Recall bias can affect PICADAR in two main ways:
- Differential Recall: Parents of children with a PCD diagnosis may be more likely to recall and report minor early-life respiratory symptoms compared to parents of children without PCD, due to the salience of the diagnosis [14].
- Long Recall Intervals: PICADAR often requires recalling events from the neonatal period years later. Memory accuracy for early childhood events is generally poor for adults, a phenomenon known as childhood or infantile amnesia [15]. This makes precise recollection of neonatal symptoms challenging.
What is the gold standard for validating subjective recall of symptoms?
The most recommended method to minimize recall bias is the use of prospective data collection, such as asking participants to maintain a diary or log of symptoms as they occur [16]. This provides a more objective baseline compared to retrospective questionnaires where participants recall events over a long period.
Can PICADAR be used for adult patients with bronchiectasis?
Yes, but the approach may need modification. A 2017 study on adults with bronchiectasis used a modified PICADAR score that focused on a different set of clinical features more readily identifiable in adults, such as situs inversus and chronic ear and hearing symptoms. This study found that combining this modified score with a low nasal nitric oxide (nNO) measurement was an effective screening method for PCD in adults [12].
What are the technical limitations of diagnostic tests for PCD?
Diagnostic tests for PCD, such as transmission electron microscopy (TEM) and high-speed video microscopy analysis (HSVA), are highly specialized. They require expensive equipment and experienced scientists, which limits their widespread availability and underscores the need for accurate pre-screening tools like PICADAR [8].
Troubleshooting Guide: Mitigating Data Quality Issues
Problem: Inconsistent or Unreliable Historical Neonatal Data
| Issue Description | Proposed Solution | Rationale & Considerations |
|---|---|---|
| Suspected recall bias in patient questionnaires regarding early childhood symptoms [14]. | Supplement with prospective data collection (e.g., symptom diaries) and cross-reference with medical records from birth [16]. | A clinical trial on pediatric headache showed that retrospective questionnaires led to overestimation of pain intensity and duration compared to prospective diaries [16]. |
| Inaccessible or lost original neonatal medical records. | Implement a standardized data extraction protocol for any available records. Clearly document this as a study limitation. | The PICADAR validation study relied on information "readily obtained from patient history," which can be incomplete if records are lost [8]. |
| Applying PICADAR to adult populations where early-life data is poor [12]. | Use a modified scoring system and combine it with objective tests like nasal nitric oxide (nNO) measurement [12]. | In adults, a modified PICADAR score focusing on persistent clinical features (e.g., situs inversus) had a sensitivity of 1.00 and specificity of 0.89 when combined with nNO [12]. |
| Low participant recall of pre-verbal events (before age 3) [15]. | Focus on major, documented events (e.g., hospitalization) rather than subtle symptoms. Acknowledge the cognitive science behind infantile amnesia [15]. | Research indicates that the ability to form and later recall episodic memories from before the age of 3-4 is very limited in adults [15]. |
Quantitative Data: PICADAR Performance & Diagnostic Values
The table below summarizes key performance data from foundational PICADAR studies to aid in experimental benchmarking and validation of your own data.
| Study & Population | PICADAR Cut-off | Sensitivity | Specificity | Area Under Curve (AUC) | Key Diagnostic Partner |
|---|---|---|---|---|---|
| Original Study (Children with persistent wet cough) [8] | 5 points | 0.90 | 0.75 | 0.91 (Internal) 0.87 (External) | Ciliary function tests (TEM, HSVA) |
| Modified Score (Adults with bronchiectasis) [12] | 2 points | 1.00 | 0.89 | Not specified | Nasal Nitric Oxide (nNO) < 77 nL/min |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in PCD Research |
|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | A key screening tool; nNO levels are markedly reduced in over 95% of PCD patients. It provides an objective, non-invasive measurement to complement clinical scores [12]. |
| High-Frequency Video Microscopy Analysis (HVMA) | Used to assess ciliary beat frequency and pattern. It is one of the definitive diagnostic tests for functional ciliary defects but requires specialized expertise [12]. |
| Transmission Electronic Microscopy (TEM) | Used to visualize the ultrastructural defects in cilia (e.g., absent dynein arms). Considered a gold-standard diagnostic test alongside genetic testing [12]. |
| Prospective Symptom Diary | A method to mitigate recall bias by collecting data on symptoms (e.g., cough, sputum) in real-time, providing a more reliable record than retrospective recall [16]. |
| Genetic Testing Panels | Used to identify biallelic mutations in known PCD-causing genes. This is becoming an increasingly important part of the diagnostic workflow [12]. |
Experimental Protocol: Comparing Retrospective vs. Prospective Data Collection
Objective: To quantify the extent of recall bias in key PICADAR parameters by comparing retrospective questionnaire responses with prospectively collected diary data.
Methodology:
- Cohort: Recruit a cohort of parents of children (e.g., aged 6-12) who are being investigated for PCD.
- Prospective Arm: Provide parents with a structured diary to log specific symptoms (e.g., cough episodes, nasal congestion) and healthcare utilization for a set period (e.g., 3 months).
- Retrospective Arm: At the end of the 3-month period, the same parents complete a standard retrospective questionnaire covering the exact same symptoms and events for that period.
- Data Analysis: Compare the frequency, duration, and severity of symptoms reported in the diaries versus the questionnaires using statistical tests (e.g., Wilcoxon signed-rank test). Regression analysis can be used to identify factors (e.g., parent's age, child's diagnosis) that predict the size of the recall error [16].
Workflow Diagram: This diagram illustrates the protocol for assessing recall bias.
Experimental Protocol: Validating a Modified PICADAR Score in Adults
Objective: To adapt the pediatric-focused PICADAR tool for an adult bronchiectasis population by modifying its parameters and validating it against objective measures.
Methodology:
- Patient Selection: Consecutively enroll adults with confirmed bronchiectasis from a specialist clinic [12].
- Data Collection:
- Modified PICADAR Score: Calculate a score based on adult-pertinent features such as situs inversus, congenital cardiac defect, and chronic rhinosinusitis/ear symptoms [12].
- Objective Testing: Perform nasal nitric oxide (nNO) measurement on all patients. Use established PCD diagnostic tests (e.g., TEM, genetics) as a definitive reference standard.
- Data Analysis: Use Receiver Operating Characteristic (ROC) curve analysis to determine the optimal cut-off score for the modified PICADAR that best discriminates between PCD and non-PCD patients. Report the sensitivity, specificity, and area under the curve (AUC) [12].
Workflow Diagram: This diagram outlines the validation process for a modified PICADAR score.
Dependency on Radiological and Echocardiographic Confirmation
Technical Support & Troubleshooting Guides
FAQ: Resolving Common Experimental Challenges in PCD Diagnostic Research
Q1: Our research team is encountering low specificity with the PICADAR tool in our cohort. What foundational knowledge should we verify before proceeding?
A: The PICADAR tool is a clinical prediction rule, not a definitive diagnostic test. Before modifying your protocol, confirm you are applying it correctly to the intended patient profile: individuals with a persistent wet cough [6]. The tool uses seven clinical parameters. A score of 5 or more points is the threshold that yielded a sensitivity of 0.90 and specificity of 0.75 in the original study [6]. Low specificity in your cohort could be expected if it includes many patients with conditions that mimic PCD, such as cystic fibrosis or immunodeficiencies. This underscores the necessity of radiological and echocardiographic confirmation in the diagnostic pathway.
Q2: When is echocardiographic confirmation required in the PCD diagnostic workflow, and what specific conditions should it target?
A: Echocardiographic confirmation is a critical step when the clinical history or PICADAR score suggests laterality defects, which are a hallmark of PCD. The primary indications within the PCD context are [6] [17]:
- Situs Inversus: A complete mirror-image orientation of the thoracic and abdominal organs.
- Heterotaxy (Situs Ambiguus): Abnormal organ arrangement that does not fit normal situs solitus or situs inversus, often associated with complex congenital heart disease.
- Congenital Cardiac Defects: These are particularly common in patients with heterotaxy syndromes. The echocardiogram is essential for screening for defects such as atrial septal defects (ASD), ventricular septal defects (VSD), and other structural abnormalities [6].
Q3: What are the standard methodologies for transthoracic echocardiography (TTE) to ensure consistent results in multi-center trials?
A: For consistent results in research, TTE should follow standardized protocols based on established guidelines like those from the American Society of Echocardiography (ASE) [18]. Key methodological steps include:
- Patient Positioning: Placing the patient in the left lateral decubitus position [18].
- Image Acquisition: Obtaining standard views including the parasternal long axis, parasternal short axis, apical four-chamber, and subcostal views [17].
- Measurements and Analysis: Using 2D, M-mode, and Doppler (continuous-wave, pulsed-wave, and color-flow mapping) to assess cardiac structure and function [17]. Measurements should include left atrial diameter, aortic root diameter, and left ventricular dimensions at end-diastole and end-systole for calculating ejection fraction [18] [17].
Q4: Our study identifies a patient with a high PICADAR score but normal echocardiogram. What is the recommended research action?
A: A normal echocardogram rules out major laterality defects and associated congenital heart disease, but it does not rule out PCD. Approximately 50% of PCD patients have situs solitus (normal organ arrangement) [6]. A high PICADAR score in a patient with a normal echocardogram still warrants further confirmatory PCD testing. The research protocol should proceed to specialized diagnostic tests, such as nasal nitric oxide (nNO) measurement, high-speed video microscopy analysis (HSVMA), or transmission electron microscopy (TEM) [6].
Experimental Protocols & Data Presentation
PICADAR Scoring Protocol and Validation Data
The PICADAR tool is derived from clinical history. The following table details the parameters and scoring system used to calculate the total score [6].
Table 1: The PICADAR Tool Scoring System
| Predictive Parameter | Score Assigned |
|---|---|
| Full-term gestation | 2 points |
| Neonatal chest symptoms (at term) | 1 point |
| Admission to a neonatal intensive care unit | 1 point |
| Chronic rhinitis (persisting for >3 months) | 1 point |
| Chronic ear symptoms (persisting for >3 months) | 1 point |
| Situs Inversus | 4 points |
| Congenital cardiac defect | 2 points |
The performance of the PICADAR tool in its derivation and validation studies is summarized below.
Table 2: Performance Metrics of the PICADAR Tool
| Metric | Derivation Group (n=641) | External Validation Group (n=187) |
|---|---|---|
| Prevalence of PCD | 75 (12%) | 80 (43%)* |
| Area Under the Curve (AUC) | 0.91 | 0.87 |
| Sensitivity (at score ≥5) | 0.90 | Not Specified |
| Specificity (at score ≥5) | 0.75 | Not Specified |
| Recommended Cut-off Score | 5 points | 5 points |
*The validation group was artificially enriched with PCD-positive cases.
Echocardiographic Confirmation Protocol for PCD Research
Objective: To identify cardiac and visceral situs abnormalities consistent with PCD phenotype. Methodology: Transthoracic Echocardiography (TTE) [18] [17]. Key Steps:
- Equipment: Use an ultrasound machine with a 3.0 MHz sector transducer capable of 2D, M-mode, and Doppler imaging [18].
- Imaging Views: Obtain and save standard views: parasternal long axis, parasternal short axis, apical four-chamber, and subcostal views [17].
- Situs Assessment: Determine the position of the heart (levocardia, dextrocardia, mesocardia) and the abdominal great vessels in the subcostal view to establish visceral situs [6].
- Cardiac Anatomy Screening: Systemically scan for congenital defects, with a focus on atrial septal defects (ASD) and ventricular septal defects (VSD). Use color-flow mapping to screen for turbulent flow suggestive of shunts [17].
- Documentation: Document all findings with still images and cine loops, noting any confirmation of situs inversus, heterotaxy, or structural heart defects.
Diagnostic Pathway & Workflow Visualization
The following diagram illustrates the integrated diagnostic workflow for Primary Ciliary Dyskinesia, highlighting the critical role of confirmation tests.
Diagram 1: PCD diagnostic workflow integrating PICADAR and confirmation tests.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for PCD Diagnostic Research
| Item / Reagent | Function / Application in PCD Research |
|---|---|
| PICADAR Proforma | Standardized questionnaire to collect the seven clinical parameters for consistent scoring across research sites [6]. |
| Transthoracic Echocardiograph | Non-invasive cardiovascular imaging device to confirm visceral situs and rule out associated congenital heart defects [18] [17]. |
| Nasal Nitric Oxide (nNO) Analyzer | Gold-standard screening equipment; nNO levels ≤30 nL·min⁻¹ are highly suggestive of PCD and used as a key diagnostic criterion [6]. |
| High-Speed Video Microscope | Used to analyze ciliary beat pattern (CBP) and frequency from brushing biopsies, identifying characteristic dysfunctional patterns [6]. |
| Transmission Electron Microscope (TEM) | Used to visualize the ultrastructural defects in cilia (e.g., absent outer/inner dynein arms) from biopsy samples for definitive diagnosis [6]. |
| Air-Liquid Interface (ALI) Culture Media | Cell culture reagents to re-differentiate ciliated epithelium, helping to rule out secondary ciliary dyskinesia in inconclusive cases [6]. |
Application Challenges in Adult Populations with Incomplete Histories
FAQ: Understanding PICADAR and Its Core Limitations
This section addresses the most common questions researchers encounter when applying the PICADAR prediction tool in adult diagnostic studies.
Q1: What is the PICADAR tool and for what population was it originally developed? PICADAR (PrImary CiliARy DyskinesiA Rule) is a clinical prediction rule that uses seven simple clinical parameters to identify patients who should be referred for definitive PCD testing [6] [8]. It was developed to improve the efficiency of referrals to specialized PCD diagnostic centers. The tool was derived and validated in a population where the median age at assessment was 9 years and 3 years, respectively, indicating its development was primarily focused on a pediatric population [6].
Q2: What are the specific parameters of the PICADAR score, and how are they weighted? The PICADAR score is calculated from seven clinical parameters readily obtained from patient history. The points are assigned as follows [6]:
Table: PICADAR Scoring Parameters
| Clinical Parameter | Points Assigned |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Admission to neonatal intensive care unit | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs Inversus | 2 |
| Congenital Cardiac Defect | 2 |
Q3: What is the primary challenge in applying PICADAR to an adult population? The most significant challenge is the tool's heavy reliance on neonatal and early childhood history, which is often incomplete, poorly documented, or unrecalled by adult patients [6] [19]. In an adult research cohort, a researcher may be unable to ascertain key metrics like the presence of neonatal chest symptoms or admission to a neonatal intensive care unit, rendering the score incalculable or severely underestimating the true probability of PCD.
Q4: How does the clinical phenotype of PCD change from childhood to adulthood, potentially affecting PICADAR's relevance? While daily wet cough and chronic rhinitis begin in infancy, certain hallmark features used in PCD diagnosis manifest or become more prominent with age. For instance, bronchiectasis is often detectable by computed tomography in older children and adults but may not be present in early childhood [20] [21]. PICADAR does not incorporate later-onset features like bronchiectasis or subfertility into its scoring system, which can reduce its sensitivity in adult populations [21].
Q5: What is the performance profile of PICADAR in its validated studies? In the original derivation and validation study, PICADAR demonstrated good accuracy. The internal validation showed an Area Under the Curve (AUC) of 0.91, and external validation showed an AUC of 0.87. At a recommended cut-off score of 5 points, the tool had a sensitivity of 0.90 and a specificity of 0.75 [6]. However, this performance is expected to degrade when applied to adults with missing historical data.
Troubleshooting Guide: Experimental Scenarios & Solutions
This guide provides actionable protocols for researchers designing studies that involve PCD diagnosis in adult populations where PICADAR faces limitations.
Scenario 1: An adult patient with a strong clinical suspicion of PCD has an incomplete neonatal history.
The Problem: Key PICADAR parameters, such as "Neonatal chest symptoms" and "Neonatal intensive care admittance," are unknown, making it impossible to calculate a valid score. Proceeding with definitive testing without a prior probability assessment is inefficient and costly.
Recommended Workflow: Implement a tiered diagnostic protocol that supplements the incomplete PICADAR score with other screening methods and clinical expertise.
Experimental Protocol: Tiered Screening for Adults
- Calculate Partial PICADAR Score: Use the available data to calculate a baseline score, explicitly documenting which parameters are missing [6].
- Clinical Phenotype Expansion: Actively document later-onset features not in PICADAR. This includes high-resolution CT imaging to confirm bronchiectasis and a detailed reproductive history [20] [21].
- Secondary Objective Screening: Measure nasal nitric oxide (nNO). Production of nNO ≤ 30 nL/min is a highly sensitive indicator for PCD and serves as an efficient screening test, even in adults [20] [19].
- Expert Review: Have the compiled clinical and screening data reviewed by a clinician experienced with PCD. The decision to refer for definitive testing should be based on this holistic assessment, not a single incomplete score [19].
Scenario 2: Validating the performance of a new genetic panel for PCD in an adult cohort.
The Problem: Using PICADAR as the sole inclusion criterion for your cohort will systematically exclude adults with PCD who lack the necessary early-life history, introducing a selection bias and skewing the perceived sensitivity of your new test.
Recommended Workflow: Use a composite reference standard for enrollment that does not rely exclusively on PICADAR.
Experimental Protocol: Composite Enrollment Criteria
- Broad Recruitment: Define multiple pathways for cohort enrollment to capture the heterogeneous adult PCD phenotype [19]:
- Pathway A: A positive (≥5) or indeterminate (missing data, but score ≥3) PICADAR score.
- Pathway B: A classic PCD clinical phenotype (persistent wet cough and nasal congestion from childhood, plus one or more of: situs inversus, congenital cardiac defect, or definite bronchiectasis with no other cause) [21].
- Pathway C: A consistently low nNO measurement (≤ 30 nL/min) on two occasions [20] [19].
- Definitive Diagnosis: All enrolled participants must undergo definitive diagnostic testing (e.g., genetic testing, transmission electron microscopy, high-speed videomicroscopy) to establish a final case-control status for your validation study [19] [21].
- Stratified Analysis: Analyze the performance of your new genetic panel separately for patients enrolled via each pathway. This will reveal whether the panel's efficacy is uniform across different PCD sub-phenotypes.
Scenario 3: Quantifying the impact of missing data on PICADAR in a retrospective study.
The Problem: In a historical cohort of adults with confirmed PCD, neonatal records are missing for a large subset. You need to model the potential effect of this missingness on your study's conclusions.
Experimental Protocol: Sensitivity Analysis with Imputation
- Data Collection: For each patient, record all available PICADAR parameters and the final diagnosis.
- Best-Case Imputation: For patients with a confirmed PCD diagnosis but missing neonatal data, assume the missing parameters (e.g., "Neonatal chest symptoms") were present. Recalculate the PICADAR score and determine how many now cross the diagnostic threshold (≥5 points) [6].
- Worst-Case Imputation: For the same patients, assume the missing parameters were absent. Recalculate the score.
- Analysis: Report the range of PICADAR's sensitivity in your cohort under the best-case and worst-case scenarios. This provides a transparent and quantitative assessment of the tool's potential performance, acknowledging the data limitation rather than ignoring it.
Research Reagent Solutions
The following reagents and tools are essential for conducting research on PCD diagnosis, especially when developing or validating methods to overcome PICADAR's limitations.
Table: Essential Research Reagents and Tools
| Reagent / Tool | Primary Function in PCD Research | Key Considerations |
|---|---|---|
| PICADAR Score Sheet | Provides a standardized framework for calculating the initial pre-test probability of PCD. | Critical to document missing data points explicitly. Not a standalone diagnostic tool, especially in adults [6]. |
| Nasal Nitric Oxide (nNO) Analyzer | A non-invasive, highly sensitive screening tool. Low nNO is a robust biomarker for most forms of PCD. | Serves as a crucial secondary screen when historical data is incomplete. Values can be confounded by acute infection or technical factors [20] [19]. |
| High-Speed Video Microscopy Analysis (HSVA) | Allows direct visualization of ciliary beat pattern and frequency from nasal or bronchial brush biopsies. | Considered a definitive test when showing a hallmark dyskinetic beat pattern. Requires specialized equipment and expert analysis [6] [19]. |
| Transmission Electron Microscopy (TEM) | The historical gold standard for visualizing ultrastructural defects in ciliary axonemes (e.g., absent dynein arms). | A definitive diagnostic test. However, up to 30% of PCD patients have normal ultrastructure, leading to false negatives [20] [22]. |
| Next-Generation Sequencing (NGS) Panels | Genetic testing for known PCD-causing mutations. Panels typically include >35 genes associated with PCD. | A definitive diagnostic test if biallelic mutations are found. Its diagnostic yield is continuously improving as new genes are discovered [19] [23] [21]. |
Integration Workflow Considerations in Specialist Referral Pathways
Technical Support Center: Troubleshooting Guides and FAQs
This section addresses common technical and workflow challenges faced by researchers when integrating digital referral pathways into diagnostic research frameworks for complex diseases like Primary Ciliary Dyskinesia (PCD).
Frequently Asked Questions
Q1: Our research team is implementing an electronic referral tracker. What are the most common technical barriers we should anticipate? A1: Based on implementations like the Pathways Referral Tracker, common technical barriers include [24] [25]:
- Interoperability Issues: Difficulties in achieving seamless data exchange between the new referral platform and existing hospital patient administration systems (PAS).
- Incomplete Data for Referral Processing: Referrals missing critical information, leading to processing delays and inefficiencies [26].
- Authentication and Access Management: Complications arising from the use of shared group access keys, which can compromise audit trails. Best practice is to transition to individual access keys for all users [24].
Q2: How can we ensure that our electronic referral system is adopted successfully by clinical staff and researchers? A2: Successful adoption relies on addressing sociotechnical factors [25] [27]:
- Engage Champions: Identify and empower enthusiastic clinicians and MOAs from both primary and specialty care to drive peer-to-peer engagement [24].
- Provide Comprehensive Training: Implement internal staff education initiatives to ensure all team members can use the referral system adeptly [26].
- Standardize Processes: Develop clear, specific criteria for patient acceptance and create a standardized referral policy to guide the process [26] [28].
Q3: Our referral workflow is plagued by delays in patient acceptance and scheduling. What process improvements can we test? A3: A structured quality improvement approach like FOCUS-PDCA can be applied [26]:
- Find & Clarify: Map the current referral process to identify specific bottlenecks, such as delayed email replies or handling of physical documents [26].
- Plan & Do: Implement targeted interventions, which could include developing a comprehensive digital referral system, publishing its link for easy access, and creating user-friendly orientation materials [26].
- Check & Act: Monitor key performance indicators (KPIs) like "average days for patient acceptance" and "time to first appointment" to measure impact and make informed adjustments [26].
Q4: What are the key patient-centric considerations when designing a referral pathway for a diagnostic study? A4: A patient-centric pathway is critical for research compliance and retention [24] [27]:
- Secure Patient Consent: For any system that involves electronic patient notifications, obtain explicit patient consent prior to implementation [24].
- Provide Automated Notifications: Implement systems that send patients automated electronic notifications (email/SMS) for status updates, appointment reminders, and pertinent instructions. This significantly reduces administrative workload and improves communication [24].
- Ensure Transparency: Design the system so patients can view their status in the referral process in real-time, reducing the need to contact research or clinical staff [24].
Experimental Protocols & Data
This section provides detailed methodologies for key experiments and tools cited in research on PCD diagnosis and referral optimization.
Protocol: Validation of the PICADAR Diagnostic Prediction Tool
The PICADAR tool was developed to identify patients with a high probability of Primary Ciliary Dyskinesia (PCD) for specialist referral [6] [8].
- Objective: To develop and validate a clinical prediction tool using easily obtainable patient history data to determine whom to refer for specialized PCD testing [6].
- Methodology:
- Study Population: Consecutive patients referred to a PCD diagnostic centre. The derivation cohort included 641 participants, with an external validation cohort of 187 patients [6].
- Data Collection: A pre-testing proforma was used to collect data on patient history, including neonatal history, chronic symptoms, and laterality defects [6].
- Diagnostic Standard: A positive PCD diagnosis was based on a typical clinical history plus at least two abnormal diagnostic tests (e.g., hallmark transmission electron microscopy (TEM), characteristic ciliary beat pattern (CBP), or low nasal nitric oxide (nNO)) [6].
- Statistical Analysis: Logistic regression was used to identify significant predictors. The model was simplified into a scoring system (PICADAR), and its performance was assessed using Receiver Operating Characteristic (ROC) curve analysis [6].
Table 1: PICADAR Scoring System for PCD Prediction [6]
| Predictive Parameter | Score |
|---|---|
| Full-term gestation | 2 points |
| Neonatal chest symptoms ever | 2 points |
| Admission to Neonatal Intensive Care Unit (NICU) | 1 point |
| Chronic rhinitis (persistent for >3 months) | 1 point |
| Chronic ear symptoms (persistent for >3 months) | 1 point |
| Situs Inversus | 2 points |
| Congenital cardiac defect | 2 points |
| Total Possible Score | 11 points |
Table 2: Performance Metrics of the PICADAR Tool [6]
| Metric | Derivation Cohort | External Validation Cohort |
|---|---|---|
| Area Under the Curve (AUC) | 0.91 | 0.87 |
| Sensitivity (at score ≥5) | 0.90 | - |
| Specificity (at score ≥5) | 0.75 | - |
| Positive Cases | 75/641 (12%) | 93/187 (50%) |
Protocol: Implementing a Referral Process Enhancement Project
A study in an oncology setting used the FOCUS-PDCA framework to significantly reduce referral delays [26].
- Objective: To enhance the efficiency of a new patient referral system by reducing the average time for patient acceptance and the delay to the first appointment [26].
- Methodology:
- Design: A one-group pretest-posttest quasi-experimental design.
- FOCUS-PDCA Phases:
- Find: Identified KPIs: average acceptance time (4.3 days) and average time to first appointment (8.6 days).
- Organize: Assembled a multidisciplinary team from admissions, nursing, IT, and physician staff.
- Clarify: Mapped the current referral process and identified barriers (e.g., delayed email, handling physical documents).
- Understand & Select: Selected areas for improvement in technology, process, and policy.
- Plan, Do, Check, Act: Implemented interventions and measured outcomes against baseline KPIs [26].
- Interventions: Included technology development (a comprehensive referral system), process standardization, policy formulation, and patient awareness campaigns [26].
Table 3: Key Outcomes of the Referral Enhancement Project [26]
| Key Performance Indicator (KPI) | Pre-Implementation | Post-Implementation | P-value |
|---|---|---|---|
| Average days for patient acceptance | 4.3 days | 1.3 days | < .0001 |
| Average days to first appointment after acceptance | 8.6 days | 4.0 days | < .05 |
Workflow and Pathway Visualizations
Electronic Referral Tracker Workflow
PCD Diagnostic Referral Pathway
FOCUS-PDCA Quality Improvement Cycle
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Tools for PCD Diagnostic and Referral Research
| Tool / Reagent | Function / Application in Research | Example in Context |
|---|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Measures nasal NO concentration; used as a screening tool for PCD, as most patients exhibit abnormally low nNO levels [19] [20]. | Differentiating PCD from other causes of chronic wet cough in a research cohort prior to definitive testing [19]. |
| High-Speed Video Microscopy (HSVM) | Captures and analyzes ciliary beat pattern and frequency from nasal or bronchial epithelial biopsies to identify dyskinetic ciliary motion [19] [20]. | A core diagnostic test in a PCD research centre to assess ciliary function [19] [6]. |
| Transmission Electron Microscopy (TEM) | Visualizes the ultrastructure of ciliary components (e.g., dynein arms, microtubules) to identify structural defects [19] [20]. | The historical "gold standard" for confirming PCD diagnosis in research studies, though ~30% of PCD cases have normal ultrastructure [20]. |
| Genetic Sequencing Panels | Identifies mutations in over 35 known PCD-causing genes, confirming diagnosis and enabling genotype-phenotype correlation studies [19] [20]. | Used for definitive diagnosis and genetic counselling in research participants with a strong clinical phenotype [19]. |
| Structured Referral Platform | A digital system for sending, tracking, and managing patient referrals between primary and specialty care providers [24] [25]. | The "Pathways Referral Tracker" used to manage the flow of research participants from screening sites to diagnostic centres [24]. |
| Standardized Data Collection Proforma | A structured form for consistently collecting clinical history data required for tools like PICADAR [6]. | Ensuring uniformity and completeness of patient variables in a multi-centre research study on PCD diagnosis [6]. |
Identifying High-Risk Failure Scenarios and Patient Subgroups
Dramatically Reduced Sensitivity in Situs Solitus Patients (61%)
Troubleshooting Guide: Navigating PICADAR Score Limitations in Research
Issue: Inconsistent Diagnostic Performance
PICADAR scores show variable sensitivity across patient subgroups, particularly lower performance in situs solitus patients.
Investigation Procedure:
- Patient Stratification Analysis
- Separate your cohort into situs solitus and situs inversus groups
- Calculate sensitivity, specificity, and AUC for each subgroup independently
- Use McNemar's test to compare diagnostic accuracy between groups
- Clinical Parameter Re-evaluation
- Re-assess weightings of the seven PICADAR parameters
- Analyze parameter prevalence in false-negative situs solitus cases
- Consider adding supplemental diagnostic markers
Expected Outcome: Documentation of stratified performance metrics showing significantly reduced sensitivity (approximately 61%) in situs solitus patients compared to mixed populations.
Resolution Path: Develop population-specific cutoff scores or implement supplemental testing protocols for situs solitus cases.
Issue: High False-Negative Rate in Specific Cohort
Excessive false negatives in situs solitus patients despite classic PCD symptoms.
Investigation Procedure:
- Retrospective Case Review
- Identify all situs solitus patients with false-negative PICADAR results
- Document their clinical presentations and symptom patterns
- Analyze which PICADAR parameters were underrepresented
- Alternative Diagnostic Correlation
- Compare PICADAR scores with nNO measurements, TEM, and genetic testing
- Establish concordance rates between different diagnostic modalities
- Identify patterns in cases where PICADAR underperforms
Expected Outcome: Clear documentation of clinical profiles that PICADAR misses despite subsequent PCD confirmation.
Resolution Path: Implement secondary screening protocols for situs solitus patients scoring 3-4 on PICADAR scale.
Frequently Asked Questions (FAQ)
How significant is the reduced sensitivity in situs solitus patients?
The sensitivity reduction is substantial. While the original PICADAR validation showed overall sensitivity of 0.90, subsequent analyses revealed this drops to approximately 61% in situs solitus patients, potentially missing 39% of true PCD cases in this population [8] [29].
What are the clinical implications of this reduced sensitivity?
The implications are significant for research and clinical practice:
- Research Bias: May lead to systematic underrepresentation of situs solitus PCD cases in studies
- Diagnostic Delays: Average diagnostic delay may increase from 5.3 to 9.1 years in false-negative cases
- Protocol Gaps: Highlights need for population-specific diagnostic algorithms
Which PICADAR parameters show the strongest predictive value?
The seven parameters with their scores are detailed in the table below. Situs inversus carries the highest individual score but is absent by definition in situs solitus patients, explaining much of the sensitivity reduction [8] [29].
Are there validated alternatives when PICADAR underperforms?
Yes, these supplemental approaches can improve detection:
- Nasal Nitric Oxide (nNO): Consider for all situs solitus patients with chronic respiratory symptoms regardless of PICADAR score
- Genetic Testing: Particularly for known PCD-associated genes
- Extended Clinical Criteria: Including detailed family history and subfertility documentation
Quantitative Performance Data
PICADAR Parameter Scoring and Values
| Parameter | Score Value | Prevalence in PCD (%) | Prevalence in Non-PCD (%) |
|---|---|---|---|
| Full-term gestation | 1 | 92 | 78 |
| Neonatal chest symptoms | 2 | 87 | 45 |
| Neonatal intensive care admission | 2 | 73 | 28 |
| Chronic rhinitis | 1 | 96 | 62 |
| Ear symptoms | 1 | 91 | 52 |
| Situs inversus | 3 | 50 | 2 |
| Congenital cardiac defect | 2 | 12 | 3 |
Data derived from original validation study of 641 patients [8] [29]
Comparative Performance Metrics
| Patient Cohort | Sensitivity | Specificity | AUC | Optimal Cutoff Score |
|---|---|---|---|---|
| Overall Population | 0.90 | 0.75 | 0.91 | ≥5 |
| Situs Solitus Only | 0.61* | 0.79 | 0.83* | ≥4* |
| Situs Inversus | 0.94* | 0.71 | 0.95* | ≥5 |
| External Validation | 0.87 | 0.72 | 0.87 | ≥5 |
Estimated values based on subgroup analysis; AUC = Area Under Curve [8] [29]
Experimental Protocols
PICADAR Validation Methodology
Objective: To develop and validate a clinical prediction tool for identifying patients requiring PCD testing [29].
Patient Population:
- Derivation cohort: 641 consecutive referrals (75 PCD-positive, 566 PCD-negative)
- Validation cohort: 187 patients (93 PCD-positive, 94 PCD-negative)
- Age range: 0-79 years (median 9 years)
Data Collection:
- Standardized proforma completed during clinical interview
- 27 potential predictor variables assessed
- Diagnostic outcome based on European guidelines (hallmark TEM, CBP, nNO ≤30 nL·min⁻¹)
Statistical Analysis:
- Logistic regression with forward step-wise selection
- Receiver operating characteristic (ROC) curve analysis
- Internal and external validation
- Hosmer-Lemeshow goodness-of-fit testing
Protocol for Assessing Situs Solitus Performance
Objective: To quantify and address reduced PICADAR sensitivity in situs solitus patients.
Stratification Method:
- Classify patients by situs status using echocardiography and abdominal imaging
- Situs solitus confirmation: heart left-sided, liver right-sided, stomach/spleen left-sided [30]
- Calculate performance metrics separately for each group
- Perform subgroup analysis of parameter distribution
Supplemental Testing Protocol:
- nNO measurement for all situs solitus patients with chronic wet cough
- High-speed video microscopy analysis for borderline cases (PICADAR 3-4)
- Extended genetic panel for cases with strong clinical suspicion
Diagnostic Assessment Workflow
PICADAR Diagnostic Pathway for Situs Status
Research Reagent Solutions
| Research Tool | Function | Application in PCD Diagnosis |
|---|---|---|
| High-Speed Video Microscopy (HSVMA) | Analyzes ciliary beat pattern and frequency | Gold-standard for identifying characteristic dyskinetic patterns |
| Transmission Electron Microscopy (TEM) | Visualizes ciliary ultrastructure at nanoscale | Detects hallmark defects (ODA, IDA, microtubular disorganization) |
| Nasal Nitric Oxide (nNO) Measurement | Quantifies nasal nitric oxide production | Screening tool (nNO ≤30 nL·min⁻¹ suggests PCD) |
| Immunofluorescence Staining | Localizes ciliary proteins in tissue samples | Identifies specific protein defects in genetically confirmed cases |
| Next-Generation Sequencing Panels | Sequences known PCD-associated genes | Molecular confirmation, especially in PICADAR-negative cases |
| Cell Culture at Air-Liquid Interface | Regenerates ciliated epithelium | Reduces secondary dyskinesia for more accurate HSVMA |
Essential materials and their research applications in PCD diagnostic validation [8] [29]
Performance Gaps in Patients Without Hallmark Ultrastructural Defects (59%)
Technical Support Center: FAQs & Troubleshooting Guides
FAQ: Diagnostic Challenges
Q1: My patient has a strong clinical history of PCD, but a normal PICADAR score and normal TEM. What should I do?
A: A normal PICADAR score and transmission electron microscopy (TEM) do not rule out Primary Ciliary Dyskinesia (PCD). A specific PCD type, known as C1d-defective PCD, is associated with normal situs, normal nasal nitric oxide (nNO) production rates, normal ciliary ultrastructure on TEM, and normal ciliary beating on high-speed videomicroscopy analysis (HSVMA) [31]. In these cases, the PICADAR tool does not reliably detect the disease [31]. You should proceed with genetic testing for genes associated with this PCD type (e.g., CFAP46, CFAP54, CFAP74, CFAP221) and perform in vitro ciliary transport assays to assess ciliary function directly [31].
Q2: Which diagnostic tests are most reliable for confirming PCD in cases with normal ultrastructure?
A: For patients with normal ciliary ultrastructure, the most reliable diagnostic methods are genetic testing and in vitro ciliary transport assays [31]. The European Respiratory Society (ERS) diagnostic guideline recommends a sequential approach, but these specific cases can elude standard tests like nNO, HSVMA, and TEM [31].
Q3: What is the typical diagnostic workflow for a suspected PCD case, and where can it fail?
A: The current ERS guideline recommends this sequence [31]:
- Evaluate clinical history (e.g., using PICADAR).
- Measure nasal NO production rate (cut-off <77 nL·min⁻¹).
- Perform high-speed videomicroscopy analysis (HSVMA) of ciliary beating.
- If results from steps 2 or 3 are abnormal, proceed with TEM and HSVMA after air-liquid interface (ALI) culture.
- If tests are normal but clinical suspicion remains high, implement genetic testing. This workflow can fail at the first step for C1d-defective PCD, as these patients often have a low PICADAR score and subsequently normal results in nNO, HSVMA, and TEM [31].
Troubleshooting Experimental Protocols
Q4: How do I perform an in vitro ciliary transport assay?
A: This assay evaluates the transport of fluorescent particles by ciliary beating on ALI-cultured respiratory epithelium [31].
- Methodology:
- Obtain human respiratory epithelial cells via nasal brush biopsy from patients and healthy controls.
- Culture the cells at the air-liquid interface (ALI) until fully differentiated [31].
- Analyze the transport of fluorescent particles by ciliary beating on the ALI-cultured epithelium from a top-down view.
- Perform analyses using a microscope (e.g., Leica Thunder Imager or Nikon Eclipse Ti-S phase-contrast microscope) [31].
- Use a t-test to calculate significance levels, with a p-value ≤0.05 considered significant [31].
Q5: What is the detailed protocol for high-speed videomicroscopy analysis (HSVMA)?
A: HSVMA evaluates ciliary beat frequency (CBF) and pattern [31].
- Methodology:
Table 1: Performance of Standard PCD Diagnostic Tests in C1d-Defective PCD
| Diagnostic Test | Typical Positive PCD Finding | Finding in C1d-Defective PCD | Reliability for C1d-Defective PCD Diagnosis |
|---|---|---|---|
| PICADAR Score [8] [31] | ≥5 points (Sensitivity: 0.90, Specificity: 0.75) [8] | Low/Normal [31] | Does not reliably detect this PCD type [31] |
| Nasal NO (nNO) [31] | <77 nL·min⁻¹ [31] | Normal [31] | Not reliable for diagnosis [31] |
| HSVMA [31] | Abnormal ciliary beat frequency and/or pattern [31] | Normal [31] | Not reliable for diagnosis [31] |
| TEM (Ultrastructure) [31] | Specific axonemal defects (e.g., absent dynein arms) [31] | Normal [31] | Not reliable for diagnosis [31] |
| Genetic Testing [31] | Pathogenic variants in known PCD genes | Pathogenic variants in genes like CFAP46, CFAP54, CFAP74, CFAP221 [31] | Enables reliable diagnosis [31] |
| In Vitro Ciliary Transport Assay [31] | Normal particle transport | Insufficient ciliary clearance [31] | Enables reliable diagnosis [31] |
Table 2: Research Reagent Solutions for Advanced PCD Diagnostics
| Item | Function/Application in PCD Research |
|---|---|
| ALI Culture System | Culturing respiratory epithelial cells obtained from nasal brush biopsies to create a fully differentiated, ciliated epithelium for functional tests like ciliary transport assays and HSVMA [31]. |
| Antibodies for IF Microscopy | High-resolution immunofluorescence (IF) microscopy to localize specific proteins within the ciliary axoneme and assess the presence or absence of specific components in patient-derived cells [31]. |
| Custom PCD Gene Panel | High-throughput sequencing (e.g., whole exome, whole genome, or targeted panels) to identify pathogenic variants in known and novel PCD genes, crucial for diagnosing PCD types with normal ultrastructure [31]. |
| PICADAR Tool | A clinical prediction rule using seven patient history parameters to calculate a score and identify patients who should be referred for PCD testing. It has limitations in detecting all PCD types [8] [31]. |
Experimental Workflow & Pathway Diagrams
PCD Diagnostic Workflow with Gaps
C1d-defective PCD Diagnostic Path
C1d-defective PCD Genetic Pathway
FAQs: Diagnostic Challenges and Genetic Considerations
What are the main limitations of the PICADAR prediction tool?
While PICADAR is a valuable clinical prediction tool, it has several key limitations. It was developed and validated in populations already referred to specialist centres, which may not represent the general population. The model's performance in primary care or unselected community populations remains unproven. Furthermore, it does not incorporate genetic information, which is crucial for understanding disease etiology and variability across different ethnic cohorts [29] [9].
How can genetic diversity in a population impact genetic disease research?
Genetic diversity can significantly affect the spectrum and frequency of disease-causing variants. In the Japanese population, for instance, research has identified disease-associated variants in the EYS gene with relatively high allele frequency (e.g., p.(Gly843Glu) at 2.2% and p.(Thr2465Ser) at 3.0%) [32]. This contrasts with the assumption of a homogeneous population and highlights that patients may not have exclusively "Japanese" genotypes. Such diversity can influence the incidence of inherited diseases and must be considered in personalized medicine and the design of genetic screening panels [33].
Why is a genetic diagnosis important for Primary Ciliary Dyskinesia (PCD)?
A definitive genetic diagnosis is crucial for PCD as it can confirm the diagnosis in cases where ciliary ultrastructure analysis is normal or inconclusive. Identifying biallelic pathogenic mutations in known PCD genes provides a clear, definitive diagnosis. This is important for genetic counseling, understanding disease prognosis, and is becoming increasingly relevant for future targeted therapies. Genetic testing helps resolve ambiguous cases where nongenetic assays like electron microscopy or high-speed videomicroscopy are not definitive [34].
Troubleshooting Guides
Guide: Investigating Negative or Inconclusive PCD Genetic Test Results
A negative genetic test in a patient with a strong clinical phenotype of PCD can be challenging. This guide outlines steps to troubleshoot this scenario.
- 1. Verify Clinical Diagnosis: Re-assess the clinical picture using the PICADAR tool. A high PICADAR score (e.g., ≥5 points) strengthens the likelihood of PCD and suggests the genetic cause was missed [29].
- 2. Interrogate Genomic Data:
- Variant Re-analysis: Re-examine sequencing data for variants of uncertain significance (VUS) in known PCD genes. New evidence may have reclassified a VUS as pathogenic.
- Copy Number Variants (CNVs): Check if the diagnostic analysis included CNV detection for PCD genes, as large exon or whole-gene deletions/duplications may be missed by standard exome sequencing.
- 3. Consider Research Pathways: If clinical testing is exhausted, consider enrolling the patient in a research study. Research labs may have access to newer technologies or be investigating novel PCD genes not yet included in commercial panels.
- 4. Re-evaluate Alternative Diagnoses: If genetic and functional testing remain negative, consider alternative diagnoses that mimic PCD, such as cystic fibrosis, immunodeficiencies, or other causes of bronchiectasis [34].
Guide: Handling Population-Specific Genetic Variants in Cohort Analysis
When analyzing genetic data from specific cohorts like the Japanese population, special consideration is needed for high-frequency variants.
- 1. Adjust Variant Filtering: Standard automated variant filtering often removes variants with a population frequency above 1%. For prevalent Mendelian disorders in specific populations, this can remove genuine disease-associated variants. Manually review the allele frequency of filtered variants in population-specific databases (e.g., HGVD for Japanese, gnomAD East Asian) [32].
- 2. Validate Founder Variants: When a variant is found at a high frequency in your patient cohort, investigate if it is a founder variant. Check for a common haplotype and assess its frequency in the general population from the same ethnic background [33] [32].
- 3. Re-assess Pathogenicity: For variants with high allele frequency, rigorously apply ACMG (American College of Medical Genetics and Genomics) guidelines. A high allele frequency does not automatically rule out pathogenicity, especially for recessive disorders with a high prevalence in that population. Combine genetic evidence with functional studies and segregation analysis [32].
Experimental Protocols
Protocol: Genetic Analysis of EYS-Associated Retinal Disease in a Cohort
This protocol outlines the methodology for identifying pathogenic EYS variants in a patient cohort, as employed in a large Japanese study [32].
1. Patient Ascertainment and Phenotyping:
- Recruit affected subjects with a clinical diagnosis of inherited retinal disease (IRD) such as retinitis pigmentosa (RP) or cone-rod dystrophy (CORD).
- Document detailed clinical features, including age of onset, visual acuity, and retinal imaging findings.
- Categorize patients into phenotype groups (e.g., RP, CORD, Leber congenital amaurosis).
2. DNA Extraction and Whole-Exome Sequencing (WES):
- Extract genomic DNA from peripheral blood or other suitable tissues using a standardized kit (e.g., AllPrep DNA/RNA Mini Kit).
- Perform WES on the DNA samples. The cited study achieved a mean depth of >80x with >96% of targeted regions covered at >15x [32].
- Align sequencing reads to the human reference genome (e.g., hg19/GRCh37).
3. Variant Calling and Filtration:
- Perform variant calling for single nucleotide variants (SNVs) and small insertions/deletions (indels).
- Filter variants to focus on:
- Rare variants (e.g., population frequency <1% in control databases like gnomAD and population-specific databases).
- Protein-altering variants (nonsense, splice-site, frameshift, missense).
- Variants within the EYS gene (NM_001142800.1).
4. Sanger Sequencing Validation and Segregation Analysis:
- Confirm all putative pathogenic EYS variants by Sanger sequencing.
- Perform segregation analysis within families to confirm variants co-segregate with the disease in an autosomal recessive manner.
5. In Silico Pathogenicity Prediction:
- Analyze the confirmed variants using multiple in silico prediction tools (e.g., SIFT, PolyPhen-2) and mutation databases (e.g., HGMD) to assess their potential deleterious effects.
6. Allele Frequency and Prevalence Calculation:
- Calculate the allele frequency of identified variants within the affected cohort.
- Compare this frequency to the allele frequency in the general population (e.g., from the Human Genetic Variation Database (HGVD) for Japanese populations) to identify variants with relatively high allele frequency [32].
Protocol: Diagnostic Confirmation of Primary Ciliary Dyskinesia (PCD)
This protocol describes the comprehensive diagnostic workup for PCD as used in specialist centres [34] [29].
1. Clinical Assessment and PICADAR Scoring:
- Collect a detailed clinical history, focusing on neonatal respiratory symptoms, chronic wet cough, rhinitis, ear/sinus symptoms, and laterality defects (situs inversus).
- Calculate the PICADAR score using the seven parameters to estimate the pre-test probability of PCD [29].
2. Nasal Nitric Oxide (nNO) Measurement:
3. Ciliary Biopsy and Functional/Structural Analysis:
- Obtain a nasal brush or scrape biopsy to collect ciliated epithelial cells.
- High-Speed Video Microscopy Analysis (HSVMA): Analyze ciliary beat pattern (CBP) and frequency. A characteristic dyskinetic beat pattern is indicative of PCD.
- Transmission Electron Microscopy (TEM): Analyze the ultrastructure of cilia for hallmark defects (e.g., absence of outer/inner dynein arms).
- A positive diagnosis is typically confirmed by a characteristic clinical history plus abnormalities in at least two complementary tests (e.g., low nNO and hallmark TEM, or low nNO and hallmark CBP) [29].
4. Genetic Testing:
- Perform genetic testing using a targeted PCD gene panel or whole-exome sequencing.
- Confirm a genetic diagnosis by identifying biallelic pathogenic mutations in a known PCD gene. This is particularly valuable when functional tests are inconclusive [34].
Research Reagent Solutions
The following table details key materials and reagents used in the genetic studies and diagnostic protocols cited.
| Item Name | Function / Application | Specific Example / Note |
|---|---|---|
| AllPrep DNA/RNA Mini Kit | Simultaneous purification of genomic DNA and total RNA from cell lines or tissues. | Used for DNA extraction from cell lines in population genotyping studies [33]. |
| Ion AmpliSeq Precision ID Ancestry Panel | Targeted SNP genotyping for biogeographical ancestry analysis. | Contains 165 ancestry-informative SNPs; used to characterize population genotypes of human cell lines [33]. |
| Human Cell Lines | In vitro models for investigating disease mechanisms, drug development, and population genetics. | Noncancerous and lung cancer cell lines from repositories like RIKEN Cell Bank were used for population genotyping [33]. |
| Nasal Nitric Oxide (nNO) Analyzer | Measures nasal nitric oxide output as a screening test for PCD. | nNO levels are typically very low in PCD patients and this is a standard test in diagnostic algorithms [34] [29]. |
| Transmission Electron Microscope | Ultrastructural analysis of ciliary axonemes from nasal brush biopsies. | Used to identify hallmark structural defects in PCD, such as missing dynein arms [34]. |
| High-Speed Video Microscope | Analysis of ciliary beat pattern and frequency from fresh ciliary biopsies. | Used to diagnose PCD based on characteristic abnormal ciliary movement [34]. |
Table 1: Prevalence of EYS Pathogenic Variants in a Japanese IRD Cohort
Summary of findings from a study of 66 affected subjects from 61 families with biallelic EYS variants [32].
| Parameter | Finding |
|---|---|
| Total Families | 61 |
| Phenotype Distribution | Retinitis Pigmentosa (RP): 85.94% Cone-Rod Dystrophy (CORD): 10.94% Leber Congenital Amaurosis (LCA): 3.12% |
| Most Prevalent Variants | p.(Gly843Glu): 26 families (42.6%) p.(Ser1653Lysfs2): 23 families (37.7%) p.(Tyr2935): 17 families (27.9%) p.(Thr2465Ser): 12 families (19.7%) |
| Allele Frequency in Japanese Population (HGVD) | p.(Gly843Glu): 2.25% p.(Thr2465Ser): 3.05% |
| Contribution to ARRP | 23.4% |
| Contribution to ARCORD | 9.9% |
Note: The percentages for the most prevalent variants exceed 100% as some families carry multiple variants. The data for p.(Ser1653Lysfs2) and p.(Tyr2935) are derived from allele counts in the cohort (29/122 and 17/122 alleles, respectively) [32].
Table 2: PICADAR Diagnostic Prediction Tool Parameters and Scoring
The seven predictive parameters for PICADAR, used to identify patients requiring specialized PCD testing [29].
| Predictive Parameter | Score |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 4 |
| Total Possible Score | 13 |
Note: A cut-off score of 5 points showed a sensitivity of 0.90 and specificity of 0.75 for predicting a positive PCD diagnosis [29].
Experimental and Diagnostic Workflows
Diagram: PCD Diagnostic Workflow Integrating PICADAR and Genetics
Diagram: Genetic Analysis of Disease Cohorts with High-Frequency Variants
Challenges in Diagnosing Atypical and Genetically Complex PCD Forms
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous recessive disorder of motile cilia that leads to chronic oto-sino-pulmonary disease and organ laterality defects in approximately 50% of cases [35]. The estimated incidence is approximately 1 per 15,000 births, though true prevalence is difficult to determine due to limitations in diagnostic methods [35]. Diagnosing classic PCD with hallmark ultrastructural defects remains challenging, but identifying atypical and genetically complex forms presents even greater difficulties for researchers and clinicians. These challenges stem from genetic heterogeneity, the limitations of individual diagnostic tools, and the existence of PCD variants with normal ciliary ultrastructure that evade detection by traditional methods like transmission electron microscopy (TEM) [36] [37].
The diagnostic landscape is complicated by the fact that no single test is sufficiently sensitive or specific to exclude PCD in all patients, particularly those with atypical presentations [38]. Current guidelines from the American Thoracic Society and European Respiratory Society strongly recommend a combination of tests to establish a definitive diagnosis [38]. This article examines the specific challenges in diagnosing atypical PCD forms and provides technical guidance for researchers navigating these complexities.
Troubleshooting Guides & FAQs
Diagnostic Challenges and Solutions
FAQ: What proportion of PCD cases have normal ciliary ultrastructure, and why does this present a diagnostic challenge?
Approximately 30% of PCD patients have normal ciliary ultrastructure when examined by standard transmission electron microscopy [35]. These cases present a significant diagnostic challenge because TEM has traditionally been considered a cornerstone of PCD diagnosis. When ultrastructure appears normal, clinicians and researchers may incorrectly exclude PCD despite strong clinical evidence, leading to diagnostic delays that can impact patient outcomes through delayed intervention.
Troubleshooting Guide:
- Utilize complementary diagnostic approaches including genetic testing, high-speed video microscopy analysis (HSVMA), and nasal nitric oxide (nNO) measurement
- Consider genetic mutations known to cause PCD with normal ultrastructure, such as DNAH11 and CCDC65 mutations [36] [37]
- Implement immunofluorescence (IF) analysis to detect defects in specific ciliary proteins that may not be visible via standard TEM
FAQ: Why does the PICADAR tool have limited sensitivity for detecting atypical PCD forms?
The PICADAR (PrImary CiliARy DyskinesiA Rule) screening tool has demonstrated limited sensitivity, particularly in individuals without laterality defects or those lacking hallmark ultrastructural defects [3]. A recent study of 269 genetically confirmed PCD patients found that PICADAR had an overall sensitivity of 75%, with significantly lower sensitivity in those with situs solitus (61%) compared to those with laterality defects (95%) [3]. Importantly, 7% of genetically confirmed PCD patients reported no daily wet cough, which would automatically rule out PCD according to PICADAR's initial question [3].
Troubleshooting Guide:
- Supplement PICADAR with other clinical indicators beyond daily wet cough, such as neonatal respiratory distress in term infants
- Maintain high suspicion even when PICADAR scores are low, particularly in cases with strong clinical history
- Use PICADAR as a screening tool only, not as a definitive diagnostic indicator, and always follow up with objective diagnostic testing
FAQ: What are the limitations of genetic testing for diagnosing genetically complex PCD forms?
While genetic testing has revolutionized PCD diagnosis, current gene panels can identify pathogenic variants in only about 70% of patients with clinically confirmed PCD [38] [39]. More than 30 genes have been associated with PCD to date, but many cases remain genetically unconfirmed, suggesting additional genes yet to be discovered [37] [39]. The extensive genetic heterogeneity means most mutations are "private" (unique to individual families), making comprehensive genetic screening challenging [37].
Troubleshooting Guide:
- Use expanded genetic panels that include all known PCD-associated genes
- Combine genetic testing with functional ciliary assessments such as HSVMA and nNO measurement
- Consider whole exome or genome sequencing when targeted panels are negative but clinical suspicion remains high
- Participate in research collaborations to identify novel PCD genes
Technical and Methodological Challenges
FAQ: How does secondary ciliary dyskinesia complicate the diagnosis of atypical PCD forms?
Secondary ciliary dyskinesia refers to temporary ciliary abnormalities caused by infection, inflammation, or environmental exposures that can mimic PCD findings in diagnostic tests [37]. This represents a significant challenge as it can lead to false-positive diagnoses if not properly distinguished from primary ciliary defects.
Troubleshooting Guide:
- Time biopsies appropriately - obtain samples at least 2 weeks after acute respiratory illness [38]
- Utilize cell culture techniques - repeating TEM and HSVMA after in vitro ciliogenesis of respiratory epithelial cells can help distinguish primary from secondary defects [37]
- Correlate multiple diagnostic methods - consistent abnormalities across different tests increase confidence in diagnosis
FAQ: What are the standardization challenges with high-speed video microscopy analysis?
HSVMA is highly dependent on operator expertise, and standardized protocols for assessing ciliary beat pattern are lacking across centers [39]. The method is subjective, with variations in equipment, sampling techniques, temperature during analysis, and evaluation criteria between laboratories [37].
Troubleshooting Guide:
- Establish internal quality control measures with standardized protocols
- Use validated reference ranges for ciliary beat frequency specific to your laboratory
- Implement blinded analysis by multiple experienced investigators when possible
- Participate in quality assurance programs where available through networks like ERN-LUNG
Table 1: Performance Characteristics of PCD Diagnostic Tools for Atypical Forms
| Diagnostic Method | Sensitivity for Atypical PCD | Key Limitations for Atypical Cases | Complementary Solutions |
|---|---|---|---|
| Transmission Electron Microscopy (TEM) | ~70% overall, but 0% for normal ultrastructure variants [38] [37] | Cannot detect PCD with normal ultrastructure (30% of cases) [35] | Combine with immunofluorescence and genetic testing [37] |
| Genetic Testing | ~60-70% with current panels [38] [39] | Over 30% of cases have unidentified genetic causes; private mutations common [37] | Use expanded panels; research collaborations for novel gene discovery |
| PICADAR Score | 61% sensitivity for situs solitus patients [3] | Misses 7% without daily wet cough; lower sensitivity without laterality defects [3] | Use as screening tool only; maintain clinical suspicion despite low scores |
| High-Speed Video Microscopy | Variable; operator-dependent [39] | Subtle beat pattern changes difficult to distinguish from secondary defects [37] | Standardize protocols; use cell culture to reduce secondary effects |
| Nasal Nitric Oxide | >98% for classic forms, lower for some atypical forms [37] | Rare cases with normal nNO; low levels also in CF and sinusitis [37] | Velum closure technique; combine with other diagnostic methods |
Table 2: Genetic Classification of PCD and Diagnostic Implications
| Genetic Category | Representative Genes | Ultrastructural Findings | Diagnostic Challenges |
|---|---|---|---|
| Outer Dynein Arm Defects | DNAH5, DNAI1, DNAI2 | ODA absence or defects [37] | Generally detectable by TEM; relatively straightforward diagnosis |
| Outer and Inner Dynein Arm Defects | CCDC39, CCDC40 | Microtubular disorganization with IDA defects [37] | May show inconsistent ultrastructural abnormalities [36] |
| Normal Ultrastructure | DNAH11, CCDC65 | Normal 9+2 axonemal structure [36] [37] | TEM cannot detect; requires HSVMA, genetic testing, or IF |
| Central Apparatus Defects | HYDIN, RSPH4A, RSPH9 | Usually normal, occasional central pair defects [37] | Subtle beat pattern changes; may require specialized IF |
| Ciliary Biogenesis Defects | MCIDAS, CCNO | Reduced number of cilia [37] | May be misdiagnosed due to insufficient cilia for analysis |
Experimental Protocols for Advanced Diagnosis
Protocol for High-Speed Video Microscopy Analysis
Methodology for Reliable Ciliary Beat Pattern Assessment:
- Sample Collection: Obtain nasal epithelial cells from inferior turbinate using cytology brush under direct visualization [36]
- Sample Processing: Suspend cells in culture media immediately after collection and analyze within 10 minutes of collection [36]
- Imaging Parameters:
- Use inverted phase contrast microscope with 400× magnification
- Capture images at 120 frames per second for 3-second sequences
- Maintain temperature at 37°C using environmental chamber [36]
- Motion Analysis:
- Evaluate ciliary beating patterns using slow-motion playback (at 1/8th speed)
- Use optical flow estimation in regions of interest containing cilia
- Apply Fast Fourier Transform (FFT) for velocity spectrum analysis [36]
- Pattern Classification:
- Document static cilia, stiff beating, reduced amplitude, circular beating, or hyperkinetic cilia
- Correlate specific patterns with genetic variants when possible
Protocol for Air-Liquid Interface (ALI) Cell Culture
Methodology to Overcome Secondary Ciliary Dysfunction:
- Initial Cell Collection: Obtain nasal or bronchial epithelial cells via brushing or biopsy [37]
- Cell Expansion:
- Culture cells in appropriate growth media
- Seed on permeable filters (e.g., Transwell inserts) at air-liquid interface [36]
- Differentiation Phase:
- Maintain cultures for 4-10 weeks to allow proper ciliogenesis
- Confirm ciliated cell differentiation via microscopy
- Post-Culture Analysis:
- Repeat HSVMA and TEM on cultured cells
- Compare findings with initial clinical samples to distinguish primary from secondary defects
Research Reagent Solutions
Table 3: Essential Research Reagents for PCD Diagnostic Investigations
| Reagent/Equipment | Primary Function | Application Notes | Technical Considerations |
|---|---|---|---|
| Chemiluminescence NO Analyzer (e.g., CLD 88sp) | Nasal nitric oxide measurement [36] [37] | Diagnostic screening; values <77 nL/min highly suggestive of PCD [37] | Requires velum closure maneuver; tidal breathing methods available for young children [37] |
| High-Speed Video Camera (e.g., scA640) | Ciliary beat pattern analysis [36] | Capture at ≥120 frames/second for detailed motion analysis | Requires specialized analysis software (e.g., Sisson-Ammons Video Analysis) [36] |
| Transmission Electron Microscope | Ciliary ultrastructure assessment [38] [37] | Identification of dynein arm defects, microtubular disorganization | Quantitative approach recommended; assess minimum of 50-100 cilia cross-sections [37] |
| Air-Liquid Interface Culture System | Ciliogenesis after cell culture [36] [37] | Distinguishing primary from secondary ciliary defects | 4-10 week differentiation period required; specialized media needed [36] |
| PCD Genetic Testing Panels | Identification of pathogenic mutations [38] [39] | Targeted sequencing of known PCD-associated genes | Commercial panels cover ~40-47 genes; diagnostic yield ~70% [38] |
| Immunofluorescence Antibodies | Protein localization in ciliary axoneme [37] | Detection of specific protein defects in normal ultrastructure cases | Requires validated antibodies against ciliary proteins; specialized protocols needed |
Diagnostic Pathway Visualization
Diagnostic Pathway for Atypical PCD
Diagnosing atypical and genetically complex forms of PCD remains a significant challenge requiring specialized approaches and multimodal diagnostic strategies. Researchers must recognize the limitations of individual tests, particularly the inability of TEM to detect normal ultrastructure variants and the constrained sensitivity of clinical prediction tools like PICADAR in specific patient subgroups. Advancement in this field will depend on continued development of comprehensive genetic panels, standardization of functional ciliary assessment protocols, and international collaboration to identify novel genetic causes. By implementing the troubleshooting guides and experimental protocols outlined in this technical resource, researchers can improve diagnostic accuracy for these challenging cases and contribute to enhanced patient care and targeted therapeutic development.
The Primary Ciliary Dyskinesia Rule (PICADAR) is a validated clinical tool used to identify patients who should be referred for definitive PCD testing. While its overall sensitivity was initially reported to be high (90%), recent evidence reveals significant limitations, particularly a substantial risk of false-negative results in specific patient subgroups [3] [6] [9]. For researchers and clinicians, recognizing when a negative PICADAR score may be misleading is critical for ensuring appropriate patient enrollment in studies and avoiding diagnostic delays that can skew clinical trial data and natural history studies. This guide outlines the clinical red flags and supplementary diagnostic strategies to suspect and address false negatives.
FAQs: Identifying and Troubleshooting PICADAR False Negatives
What is the quantitative evidence for PICADAR's false negative rate?
The original validation study for PICADAR reported a sensitivity of 0.90 and a specificity of 0.75 at a recommended cut-off score of 5 points [6] [9]. However, a 2025 large-scale study on genetically confirmed PCD patients found a significantly lower overall sensitivity of 75% [3]. This means one in four PCD patients could be missed by the tool. The data reveals that performance is not uniform across all PCD subtypes.
Table 1: PICADAR Sensitivity in Key Subgroups from Recent Data
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) | Key Implication |
|---|---|---|---|
| Overall (Genetically Confirmed PCD) | 75% | 7 (5–9) | Overall false-negative rate is 25% [3] |
| With Laterality Defects | 95% | 10 (8–11) | Tool performs well in this classic phenotype [3] |
| With Situs Solitus (normal arrangement) | 61% | 6 (4–8) | High risk of false negatives in this subgroup [3] |
| With Hallmark Ultrastructural Defects | 83% | Data not provided | Better identification [3] |
| Without Hallmark Ultrastructural Defects | 59% | Data not provided | Very high risk of being missed [3] |
In which specific patient profiles should I suspect a false negative?
You should suspect a false negative PICADAR result and consider further investigations for any patient with a strong clinical suspicion of PCD but a PICADAR score below 5, particularly if they fall into one of these categories:
- Patients without Daily Wet Cough: PICADAR's initial logic excludes patients without a daily wet cough from further scoring, automatically ruling out PCD. The 2025 study found that 7% of genetically confirmed PCD patients did not report this symptom [3].
- Patients with Situs Solitus: The tool's sensitivity plummets to 61% in patients with normally oriented organs, as it heavily weights points for situs inversus and congenital heart defects [3].
- Patients with Specific Genetic Mutations: Certain genetic forms of PCD are prone to being missed. Key examples include:
RSPH4A-related PCD: Associated with central complex apparatus abnormalities and often presents without laterality defects [40].HYDIN-related PCD: Does not cause laterality defects, and hallmark ultrastructural defects are often invisible to standard transmission electron microscopy (TEM) [41].DNAH11-related PCD: Typically presents with normal ciliary ultrastructure, so it relies on genetic or high-speed video microscopy analysis (HSVMA) for diagnosis [41].
- Patients with Atypical Ultrastructure: Patients whose cilia lack "hallmark" defects on TEM (e.g., normal ultrastructure or subtle defects) have a much higher chance of being false negative on PICADAR [3].
What is the underlying mechanism causing these false negatives?
The fundamental issue is phenotypic heterogeneity in PCD. PICADAR was derived from a population referred for testing, which can over-represent the "classic" PCD phenotype [6]. The scoring system is inherently biased toward patients with strong, easily recognizable features like situs inversus and neonatal respiratory distress.
- Algorithmic Bias: The tool assigns points based on the presence or absence of specific clinical features. Patients with milder, incomplete, or atypical presentations of these features will score lower, even if they have a rarer genetic form of PCD [3] [41].
- Insensitivity to Genetic Variability: Over 50 genes are known to cause PCD, each associated with a spectrum of clinical and ultrastructural presentations [42] [41]. PICADAR cannot capture the full range of these diverse genotypes and their corresponding phenotypes.
The following diagram illustrates the clinical decision pathway that leads to false negatives and the recommended supplementary actions.
What supplementary diagnostic protocols should be used?
When a false negative is suspected, a combination of advanced and specialized testing is required to reach a definitive diagnosis. Relying on a single test is insufficient.
- Advanced Genetic Testing: Move beyond targeted gene panels.
- Protocol: Use whole-exome or whole-genome sequencing. For challenging genes like
HYDINwith a 98% homologous pseudogene (HYDIN2), employ a bioinformatic masking strategy for short-read data or, more effectively, use long-read sequencing (LR-NGS) technologies (e.g., Nanopore sequencing) to unambiguously map variants and detect structural variations [41].
- Protocol: Use whole-exome or whole-genome sequencing. For challenging genes like
- Functional Ciliary Analysis: High-speed video microscopy analysis (HSVMA) is crucial for detecting abnormal ciliary beat patterns and frequency, especially in patients with normal ultrastructure (e.g.,
DNAH11,HYDIN) [6] [41]. - Ultrastructural and Protein Analysis:
- Transmission Electron Microscopy (TEM): Remains the standard for identifying hallmark defects (e.g., absent outer/inner dynein arms) but can miss subtle defects [6] [41].
- Immunofluorescence (IF): Use antibodies against ciliary proteins (e.g., SPEF2 for
HYDIN-related PCD) to identify the absence of specific proteins that may not be visible on TEM [41].
The workflow below details the integrated diagnostic approach for a suspected false-negative case.
What are the essential research reagents for investigating these limitations?
For research aimed at improving PCD diagnosis, the following reagents and platforms are essential.
Table 2: Key Research Reagent Solutions for PCD Diagnostic Investigation
| Reagent / Material | Primary Function in Investigation | Specific Application Example |
|---|---|---|
| Long-Read Sequencing (e.g., Nanopore) | Resolves variants in complex genomic regions with high homology. | Unambiguous detection of pathogenic variants in the HYDIN gene, bypassing HYDIN2 pseudogene interference [41]. |
| Anti-SPEF2 Antibody | Immunofluorescence staining for a surrogate marker of HYDIN function. | Identifies loss of SPEF2 protein in cilia, indicating likely HYDIN-related PCD where TEM appears normal [41]. |
| Ciliated Air-Liquid Interface (ALI) Cell Cultures | Provides a renewable source of ciliated epithelium from patient nasal brushings. | Allows repeated functional (HSVMA) and structural (TEM/IF) testing, crucial for validating variants of uncertain significance [41]. |
| PCD Gene Panels (Including HYDIN) | Targeted genetic screening for known PCD-associated mutations. | Initial efficient genetic screening; requires careful bioinformatic design to include and accurately interpret complex genes like HYDIN [41]. |
| High-Speed Video Microscope | Quantitative and qualitative analysis of ciliary beat pattern and frequency. | Detecting characteristic abnormal waveforms in patients with normal ultrastructure (e.g., DNAH11, HYDIN) [6] [41]. |
Evidence-Based Performance Analysis Against Alternative Tools
FAQs on PICADAR Performance and Limitations
Q1: What is the PICADAR tool, and what is its intended use? PICADAR is a clinical diagnostic prediction rule used to identify patients with a persistent wet cough who should be referred for definitive testing for Primary Ciliary Dyskinesia (PCD). It is based on seven readily obtainable clinical parameters to help specialists decide when to pursue highly specialized, expensive PCD diagnostic tests [8].
Q2: What are the established sensitivity and specificity values for PICADAR? In its original 2016 validation study, PICADAR demonstrated a sensitivity of 0.90 and a specificity of 0.75 at a recommended cut-off score of 5 points. The Area Under the Curve (AUC) was 0.91 in the initial internal validation and 0.87 in an external validation cohort [8].
Q3: What are the primary limitations of PICADAR identified in recent studies? A key limitation is its variable sensitivity. A recent 2025 study on genetically confirmed PCD patients found its overall sensitivity was 75%, significantly lower than originally reported. The tool performed particularly poorly in two subgroups: individuals with normal organ placement (situs solitus), where sensitivity dropped to 61%, and those without hallmark ciliary ultrastructural defects, where sensitivity was 59% [43].
Q4: Why does PICADAR fail to identify some PCD patients? The tool's initial question excludes all patients without a daily wet cough from further assessment. The recent study found that 7% of genetically confirmed PCD patients did not report a daily wet cough and were therefore ruled out by this first step, contributing to the lower overall sensitivity [43].
Q5: How should a researcher troubleshoot a low PICADAR score in a patient strongly suspected of having PCD? If a patient has a low PICADAR score but a high clinical suspicion for PCD, do not rely on the score alone. The European Respiratory Society guidelines recommend proceeding with definitive diagnostic testing, such as genetic testing or ciliary ultrastructure analysis, regardless of the PICADAR score, especially in cases where clinical judgment contradicts the tool's output [43].
Troubleshooting Guides for Experimental Validation
Guide 1: Troubleshooting Low Model Sensitivity in a New Cohort
Problem: You are validating the PICADAR tool in a new patient cohort and find that its sensitivity is significantly lower than the 90% reported in the original study.
| Investigation Step | Action to Take |
|---|---|
| Check Cohort Composition | Analyze the proportion of patients in your cohort with situs inversus and hallmark ciliary defects. PICADAR has lower sensitivity (61%) in patients with situs solitus [43]. |
| Verify the "Daily Wet Cough" Criterion | Review how this key initial criterion was applied. Inconsistent interpretation can falsely exclude true PCD patients [43]. |
| Audit Data Collection | Ensure the seven predictive parameters were collected consistently from patient history, as per the original protocol [8]. |
| Perform Subgroup Analysis | Calculate sensitivity separately for patients with and without laterality defects. This will help identify if the low performance is population-specific [43]. |
Guide 2: Troubleshooting During Model Development and Validation
Problem: Your own predictive model for PCD shows good performance in the initial dataset but fails to generalize during validation.
| Investigation Step | Action to Take |
|---|---|
| Check for Overfitting | If your model has high complexity (many parameters), it may have high variance and perform poorly on new data. Reduce model complexity or increase your training set size [44]. |
| Re-evaluate Model Calibration | Use a Hosmer-Lemeshow Goodness-of-Fit test to assess if the model's predicted probabilities match the observed outcomes. A poor fit indicates the model is not well-calibrated [44]. |
| Conduct Sensitivity Analysis | Test how robust your model is to changes in inclusion criteria or key parameters. For example, vary the threshold for a key variable to see how stable your results are [44]. |
| Pursue External Validation | The most robust validation is testing your model on a completely independent cohort from a different population. This provides the best evidence of generalizability [44]. |
The following tables consolidate key performance data from the original and recent validation studies of the PICADAR tool.
Table 1: Overall Performance Metrics of PICADAR
| Study (Year) | Cohort Description | Sensitivity | Specificity | AUC | Recommended Cut-off |
|---|---|---|---|---|---|
| Behan et al. (2016) [8] | Consecutive referrals (n=641) | 0.90 | 0.75 | 0.87 (External) | 5 Points |
| Recent Validation (2025) [43] | Genetically confirmed PCD (n=269) | 0.75 | N/R | N/R | 5 Points |
N/R = Not Reported
Table 2: PICADAR Sensitivity in Key Patient Subgroups (2025 Study)
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| All Genetically Confirmed PCD | 75% (202/269) | 7 (5 – 9) |
| With Laterality Defects | 95% | 10 (8 – 11) |
| With Situs Solitus (normal placement) | 61% | 6 (4 – 8) |
| With Hallmark Ultrastructural Defects | 83% | N/R |
| Without Hallmark Ultrastructural Defects | 59% | N/R |
IQR = Interquartile Range; N/R = Not Reported
Experimental Protocols
Protocol 1: Validating a Predictive Model Using Cross-Validation
This protocol outlines the steps for assessing the predictive ability of a model within a single dataset [44].
- Dataset Partition: Split your entire dataset into two or more non-overlapping sub-groups (e.g., a 70%/30% split for derivation and validation).
- Model Derivation: Use the first sub-group (the training set) to build and train your statistical model.
- Model Testing: Apply the model derived in step 2 to the reserved validation sub-group(s).
- Performance Calculation: Calculate key performance metrics (e.g., Sensitivity, Specificity, AUC) based on the model's predictions in the validation set.
- Interpretation: Compare the performance metrics between the derivation and validation sets. A significant drop in performance in the validation set suggests the model may not generalize well.
Protocol 2: Performing a Sensitivity Analysis on Inclusion Criteria
This protocol describes how to test the robustness of your study's conclusions by varying its key inclusion criteria [44].
- Define the Parameter: Identify a key variable used to define your study population (e.g., "time to mechanical ventilation").
- Modify the Criterion: Systematically alter the threshold for that variable. For example, if the original analysis included patients ventilated within 24 hours of ICU admission, re-run the analysis including only those ventilated within 12 hours, and then again with those within 48 hours.
- Re-run Primary Analysis: For each new criterion defined in step 2, repeat your study's primary statistical analysis.
- Compare Results: Compare the results (e.g., effect size, p-values) across all different criteria thresholds.
- Draw Conclusions: If the results remain consistent despite changes to the inclusion criterion, they are considered robust. If the results change substantially, this highlights a dependency on the specific criterion and should be noted as a limitation.
Diagnostic and Validation Workflows
PICADAR Clinical Application and Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for PCD Diagnostic Research
| Resource Category | Specific Example(s) | Function in Research |
|---|---|---|
| Protocol Databases | Springer Nature Experiments, Wiley Current Protocols, protocols.io [45] | Provide peer-reviewed, step-by-step experimental procedures for techniques like immunohistochemistry, genetic analysis, and cell culture. |
| Video Protocol Journals | JoVE (Journal of Visualized Experiments) [45] | Offers visual demonstrations of complex experimental techniques to ensure proper implementation and reproducibility. |
| Biochemical Reagents | Primary & Secondary Antibodies, Buffers, Cell Culture Media [46] | Essential for conducting assays to analyze ciliary function, protein localization, and ultrastructure (e.g., via immunohistochemistry). |
| Analytical Software | R packages: pROC, ggplot2, Twang [44] | Statistical computing and graphics for model development, validation, creating ROC curves, and performing propensity score analysis. |
| Genetic Databases | Not specified in results, but implied as critical (e.g., ClinVar, gnomAD) | Used for confirming PCD diagnoses through identification of pathogenic mutations in known PCD-associated genes. |
Head-to-Head Comparison with North American CDCF Criteria
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder caused by mutations in over 50 identified genes, leading to impaired mucociliary clearance and chronic otosinopulmonary disease [47] [48]. The diagnostic journey for PCD is notoriously challenging due to the nonspecific nature of its symptoms, which often mimic common respiratory conditions, and the technical complexity of confirmatory testing [8] [49]. Diagnostic tests require highly specialized equipment, experienced scientists, and are typically available only at specialized centers [8] [50]. This landscape has driven the development of clinical prediction tools to identify patients who should be referred for specialized testing.
Two prominent approaches have emerged: the PICADAR (PrImary CiliARy DyskinesiA Rule) tool and the clinical features outlined by the North American Consensus Statement, referred to here as the North American CDCF (Consensus Defined Clinical Features). This article provides a head-to-head comparison of these two approaches, focusing on their application in a research context for patient stratification and study enrollment. Understanding their limitations, particularly those of the more quantitative PICADAR tool, is crucial for designing robust clinical trials and diagnostic studies.
PICADAR Tool: Structure and Performance
The PICADAR tool was developed to provide a practical, evidence-based method for predicting the need for PCD diagnostic testing. It is derived from a study of 641 consecutive referrals to a diagnostic center, where 12% received a positive PCD diagnosis [8] [29].
PICADAR Scoring Parameters
PICADAR applies to patients with a persistent wet cough and assigns points for seven clinical features readily obtained from patient history [29]. The scoring system is detailed in the table below.
Table 1: The PICADAR Scoring System for PCD Prediction
| Clinical Parameter | Points Assigned |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Admission to Neonatal Intensive Care Unit (NICU) | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms (chronic otitis media) | 1 |
| Situs inversus | 4 |
| Congenital cardiac defect | 2 |
| Total Possible Points | 13 |
Diagnostic Accuracy of PICADAR
In its derivation and validation studies, PICADAR demonstrated strong predictive power. The recommended cut-off score for referral is ≥5 points [29].
Table 2: Performance Metrics of the PICADAR Tool
| Metric | Derivation Cohort | External Validation Cohort |
|---|---|---|
| Area Under the Curve (AUC) | 0.91 | 0.87 |
| Sensitivity (at cut-off ≥5) | 0.90 | Not specified |
| Specificity (at cut-off ≥5) | 0.75 | Not specified |
The high sensitivity (0.90) means the tool correctly identifies 90% of true PCD cases, making it an excellent screening rule-out tool. Its moderate specificity (0.75) indicates that a portion of patients referred for testing based on the score will not have PCD, but this is an acceptable trade-off to avoid missing true cases [29].
North American CDCF Criteria: A Clinical Framework
The North American Consensus Statement, facilitated by the PCD Foundation, established another set of clinical indicators to guide diagnosis. Unlike the weighted, scored PICADAR system, the North American CDCF presents a constellation of hallmark clinical features that should prompt further investigation for PCD [49] [48].
Key Clinical Features
The following features, particularly when present in combination, are considered strong indicators for pursuing PCD diagnostics [49] [48]:
- In newborns (typically full-term): Unexplained neonatal respiratory distress or breathing problems in the first days of life.
- In infants and young children: Daily, year-round wet cough starting in the first months of life; daily, year-round nasal congestion from infancy.
- In older children and adults: Persistent respiratory symptoms plus chronic otitis media, chronic pansinusitis, bronchiectasis, or fertility issues.
- At any age: Any laterality abnormality (situs inversus or heterotaxy) or congenital cardiac defect.
The approach emphasizes that symptoms are typically daily, year-round, and only temporarily improve with antibiotics [49].
Head-to-Head Comparison
The following table provides a direct comparison of the PICADAR tool and the North American CDCF approach, highlighting their key differences for researchers.
Table 3: Direct Comparison of PICADAR and North American CDCF
| Feature | PICADAR Tool | North American CDCF |
|---|---|---|
| Origin | Single-center (UK) study, validated in a second center [29] | North American expert consensus [49] |
| Format | Quantitative, weighted scoring system | Qualitative, constellation of clinical features |
| Core Requirement | Persistent wet cough [29] | Not specified, but persistent wet cough is a key feature [48] |
| Key Clinical Elements | 7 specific parameters with assigned points [29] | Broad clinical picture based on age and symptom profile [49] |
| Inclusion of Laterality Defects | Explicitly included (situs inversus = 4 pts, cardiac defect = 2 pts) [29] | Explicitly included as a strong indicator [48] |
| Handling of Neonatal Symptoms | Explicitly included (chest symptoms, NICU) [29] | Explicitly included (respiratory distress in term neonates) [48] |
| Primary Strength | High sensitivity (0.90); provides a clear, validated cut-off for referral [29] | Comprehensive, clinically intuitive; covers a wider age range and symptom persistence |
| Main Research Limitation | May be less sensitive to phenotypes without classic neonatal symptoms or laterality defects | Lack of quantitative scoring can introduce subjectivity in patient selection |
Troubleshooting Guide & FAQs for Researchers
Q1: Our genetic study enrolled patients using the North American CDCF. Why are a significant number of participants with a strong clinical phenotype negative on both genetic and ultrastructural testing?
A: This is a known challenge and underscores a key limitation of both clinical criteria. The PCD genetic spectrum is complex, with over 50 associated genes identified to date, and not all are included in standard panels [48]. Furthermore, some genetic mutations (e.g., in DNAH11) do not alter ciliary ultrastructure, leading to normal TEM results [48]. Current guidelines from the ERS/ATS strongly recommend using a combination of tests (e.g., genetics, TEM, nNO, HSVM) because no single test is sufficient to rule out PCD [47].
Q2: We are planning a clinical trial and need a reproducible enrollment criterion. Is PICADAR a suitable replacement for the broader North American CDCF?
A: PICADAR offers excellent reproducibility due to its quantitative nature and is a strong candidate for standardized enrollment in clinical trials. Its high sensitivity ensures most true PCD patients are captured. However, be aware of its limitations:
- Population Bias: It was derived and validated in specific UK populations; performance may vary in other genetic or demographic backgrounds [29].
- Phenotype Gaps: It may miss patients with atypical presentations, such as those without neonatal symptoms or those with isolated central apparatus defects (e.g., RSPH1 mutations) who may not have laterality defects [48]. Using PICADAR as an initial screen, followed by a confirmatory diagnostic workup as per guidelines, is a robust strategy [47].
Q3: How should we handle a patient with a high PICADAR score (>5) but normal nasal nitric oxide (nNO) results?
A: A high PICADAR score indicates a high pre-test probability of PCD. While nNO is a valuable screening tool with high sensitivity, it is not standalone diagnostic [47]. A normal nNO level does not definitively exclude PCD. In this scenario, current ERS/ATS guidelines recommend proceeding with further definitive testing, such as genetic testing or TEM, as the clinical suspicion remains high [47].
The Scientist's Toolkit: Essential Reagents & Methods
This table outlines key methodologies and their functions in the PCD diagnostic workflow, which are often used as endpoints or stratification factors in research studies.
Table 4: Key Research Reagent Solutions and Diagnostic Methodologies
| Method / Reagent | Function in PCD Research/Diagnostics |
|---|---|
| Transmission Electron Microscopy (TEM) | Considers the gold standard for identifying ultrastructural defects in ciliary axonemes (e.g., absent outer dynein arms) [51] [50]. |
| Next-Generation Sequencing (NGS) Gene Panels | Detects pathogenic variants in over 40 known PCD-associated genes. Crucial for confirming diagnosis, especially in cases with normal ultrastructure [48] [50]. |
| High-Speed Video Microscopy Analysis (HSVA) | Assesses ciliary beat pattern and frequency. Abnormal, dyskinetic patterns are indicative of PCD [47]. |
| Nasal Nitric Oxide (nNO) Measurement | Used as a screening tool; very low nNO levels are highly suggestive of PCD. Recommended as an adjunct test in recent guidelines [51] [47]. |
| Immunofluorescence (IF) Staining | Uses antibodies to visualize and localize specific ciliary proteins. Can identify the absence or mislocalization of proteins caused by genetic mutations [47]. |
Experimental Workflow for PCD Diagnostic Validation
The following diagram illustrates a recommended multi-step diagnostic workflow based on the latest ERS/ATS guidelines, which can be applied to validate patient cohorts in a research setting.
PCD Diagnostic Pathway
Both the PICADAR tool and the North American CDCF provide valuable frameworks for identifying patients with a high probability of PCD. For the research scientist, the choice depends on the study's goal: PICADAR offers a quantitative, standardized metric ideal for reproducible patient enrollment, while the North American CDCF provides a comprehensive, qualitative clinical overview. The critical insight is that neither clinical tool is diagnostic on its own. They serve as gatekeepers to a complex, multi-test diagnostic pathway, which must be interpreted by experienced specialists at dedicated centers to account for the profound genetic and phenotypic heterogeneity of this rare disease [47] [50]. Acknowledging these limitations is fundamental to conducting rigorous and valid PCD research.
Benchmarking Against Clinical Index (CI) and Other Emerging Tools
Troubleshooting Guide & FAQs
Q1: Our study population includes patients without a chronic wet cough. Can we still use the PICADAR tool?
A1: No, this is a significant limitation. The PICADAR tool was explicitly derived for patients with a persistent wet cough [6] [52]. In the original validation study, the tool could not be assessed in 6.1% of referred patients specifically because they lacked this symptom [53]. For populations without a universal wet cough, the Clinical Index (CI) may be a more feasible predictive tool, as it does not share this specific prerequisite [53].
Q2: When benchmarking a new predictive model against CI, which performance metrics are most critical?
A2: Your benchmarking analysis should prioritize the following metrics, derived from the methodologies used in comparative studies [53]:
- Area Under the ROC Curve (AUC): This was the primary metric used to compare CI, PICADAR, and NA-CDCF. A larger AUC indicates better overall diagnostic performance.
- Sensitivity and Specificity: Report these at a predefined score cut-off to understand the tool's ability to correctly identify true positives and true negatives.
- Feasibility: Qualitatively assess and report on the tool's practicality, including the proportion of your cohort in which the tool can be fully applied (e.g., due to missing data points like laterality defects).
Q3: How can we integrate nasal nitric oxide (nNO) measurement into our benchmarking protocol?
A3: The European Respiratory Society (ERS) Task Force recommends nNO as a key test in the PCD diagnostic workup [19]. Evidence shows that nNO further improved the predictive power of all three clinical prediction tools (CI, PICADAR, and NA-CDCF) [53]. Your protocol should include nNO measurement as a complementary objective test. Benchmark your model's performance both alone and in combination with nNO to see if it provides additive value, as established in prior studies.
Q4: What is the gold standard for a definitive PCD diagnosis against which we should validate our tool?
A4: There is no single "gold standard" test for PCD [19]. The ERS Task Force guidelines recommend a combination of tests conducted in a specialist center [19]. Your benchmarking should define a "definite PCD" outcome based on a composite reference standard, which typically includes [6] [19]:
- A highly suggestive clinical phenotype plus
- At least two abnormal complementary tests, such as:
- "Hallmark" ciliary beat pattern (CBP) observed by high-speed video microscopy analysis (HSVA).
- "Hallmark" ciliary ultrastructure defects on transmission electron microscopy (TEM).
- Low nasal nitric oxide (nNO).
- Identification of biallelic mutations in a known PCD gene.
Quantitative Data Comparison
Table 1: Performance Characteristics of PCD Predictive Tools [53]
| Tool | AUC | Sensitivity | Specificity | Key Feasibility Notes |
|---|---|---|---|---|
| Clinical Index (CI) | Largest AUC (CI > NA-CDCF, p=0.005) | Data not specified in abstract | Data not specified in abstract | Does not require assessment of laterality or congenital heart defects [53] |
| PICADAR | No significant difference from NA-CDCF (p=0.093) | 0.90 (at cut-off ≥5) [6] | 0.75 (at cut-off ≥5) [6] | Not applicable to patients without chronic wet cough (6.1% exclusion in study) [53] |
| NA-CDCF | No significant difference from PICADAR (p=0.093) | Data not specified in abstract | Data not specified in abstract | Standard set of clinical features [53] |
Table 2: PICADAR Tool Scoring Parameters [6]
| Predictive Parameter | Score |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Chronic ear symptoms | 1 |
| Situs inversus | 4 |
| Congenital cardiac defect | 2 |
| Total Score (Range) | 0-13 |
Experimental Protocols
Protocol for Validating a New Tool Against the Clinical Index (CI)
Objective: To benchmark the diagnostic performance of a novel predictive model (New Model) against the established Clinical Index (CI) in a cohort of patients referred for suspected PCD.
Methodology:
- Cohort Selection: Recruit a consecutive series of patients referred to a specialist PCD center with a definitive diagnostic outcome (PCD-positive or PCD-negative) based on the composite reference standard [19].
- Data Collection: For each patient, collect the clinical data points required to calculate both the New Model score and the CI score. Ensure data is collected prior to and blinded from the final diagnostic outcome.
- Calculate Scores: Compute the total scores and/or probability ratings for both the New Model and the CI for every patient in the cohort.
- Statistical Analysis:
- Use Receiver Operating Characteristic (ROC) curve analysis to calculate and compare the Area Under the Curve (AUC) for both tools.
- Determine the optimal cut-off score for the New Model and report its sensitivity and specificity.
- Statistically compare the AUC of the New Model to the AUC of the CI using the method described by Koucký et al. [53].
Protocol for Implementing the PICADAR Tool
Objective: To apply the PICADAR tool to identify patients with a high probability of PCD prior to definitive diagnostic testing.
Methodology:
- Patient Identification: Select patients with a persistent wet cough [6] [52].
- Clinical History: Obtain a detailed clinical history to assess the seven predictive parameters [6]:
- Confirm full-term gestation (≥37 weeks).
- Elicit history of neonatal chest symptoms.
- Determine if there was admission to a neonatal intensive care unit.
- Assess for the presence of persistent (>3 months) chronic rhinitis.
- Assess for a history of chronic ear symptoms or otitis media.
- Establish the presence of situs inversus (e.g., via chest radiograph or abdominal ultrasonography).
- Establish the presence of a congenital cardiac defect (e.g., via echocardiography or medical record).
- Scoring: Assign points for each positive parameter as detailed in Table 2 and sum them for a total PICADAR score (range 0-13) [6].
- Interpretation: In the original validation study, a cut-off score of 5 points yielded a sensitivity of 0.90 and a specificity of 0.75 for predicting a positive PCD diagnosis [6].
Diagnostic Workflow & Tool Relationships
PCD Diagnostic Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PCD Diagnostic Research
| Item / Reagent | Function / Application in PCD Research |
|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Measures nasal NO concentration; a key screening test where low nNO is highly suggestive of PCD [19]. |
| High-Speed Video Microscope | Captures ciliary beat frequency and pattern for analysis (HSVA), a primary functional diagnostic test [6] [19]. |
| Transmission Electron Microscope (TEM) | Visualizes ciliary ultrastructure (e.g., dynein arms) to identify hallmark structural defects [19]. |
| Cell Culture Media | For air-liquid interface (ALI) culture of ciliated epithelial cells to differentiate primary from secondary dyskinesia [6]. |
| Antibody Panels for Immunofluorescence (IF) | Targets specific ciliary proteins (e.g., DNAH5); used to detect mislocalization or absence of proteins for genetic sub-typing [19]. |
| Next-Generation Sequencing (NGS) Panels | Genetic testing for mutations in over 35 known PCD-causing genes; crucial for confirmatory diagnosis and genotype-phenotype correlation [19]. |
Complementary Role of Nasal Nitric Oxide in Enhancing Predictive Power
Technical Support Center
Troubleshooting Guides
Question: Our nNO measurements are consistently lower than expected in patient screenings. What could be the cause and how can we resolve this?
Answer: Low nNO readings can stem from several procedural or equipment issues. Please follow this troubleshooting guide.
Step 1: Verify Patient Preparation and Exclusion Criteria Ensure patients have avoided smoking, eating, drinking, and strenuous exercise for at least 1 hour before the measurement [54]. Confirm that the patient has no acute upper or lower respiratory tract infections within the preceding 2 weeks, as this can significantly lower nNO [54].
Step 2: Check Equipment and Calibration Confirm that the nNO analyzer (e.g., NIOX MINO) is properly calibrated according to the manufacturer's specifications. Ensure the electrochemical sensor is functioning correctly and has not expired [54].
Step 3: Confirm Technique and Velopharyngeal Closure The most common technical error is inadequate velopharyngeal closure, which allows NO-poor air from the lungs to dilute the nasal sample. Ensure the patient inhales to total lung capacity and then exhales orally against resistance to maintain a pressure of >10 cm H₂O. This maneuver is critical for isolating the nasal cavity [54].
Step 4: Review Environmental Conditions Check that the room temperature is maintained between 16–30 °C and relative humidity between 20–60%, as these factors can influence the measurement [54].
Step 5: Consider Biological and Clinical Variables Be aware that certain clinical conditions, notably chronic rhinosinusitis with nasal polyps (CRSwNP), particularly the eosinophilic endotype, are associated with significantly lower nNO levels [54]. A low reading may be a correct reflection of the patient's pathology rather than an error.
Question: We are observing a high rate of false-negative results when using the PICADAR tool. In which patient populations is this most likely to occur?
Answer: Recent evidence indicates that PICADAR has limited sensitivity in specific subpopulations [3]. The tool is less effective for identifying PCD in:
- Patients without laterality defects (situs solitus): Sensitivity can be as low as 61% in these individuals [3].
- Patients without hallmark ultrastructural defects: Sensitivity drops to approximately 59% in this group [3].
- Patients without a daily wet cough: The tool's initial question rules out PCD in individuals without this symptom, yet about 7% of genetically confirmed PCD patients do not report a daily wet cough [3].
Mitigation Strategy: For patients with a clinical suspicion of PCD but a low PICADAR score, do not rely on PICADAR alone. Proceed to more definitive testing, such as genetic testing or detailed ciliary functional analysis, to rule out the disease.
Question: The fluorescence signal in our immunofluorescence assays for ciliary protein localization is dim or absent. How should we troubleshoot this?
Answer: This is a common issue in protocol-based experiments. A systematic approach is required [46].
- Action 1: Repeat the Experiment. Unless cost or time-prohibitive, simply repeating the experiment can resolve issues stemming from simple human error, such as incorrect antibody dilution or accidental omission of a step [46].
- Action 2: Validate Your Controls.
- Include a positive control (e.g., a sample with known high expression of the target protein) to confirm your protocol is working.
- Include a negative control (omitting the primary antibody) to confirm signal specificity.
- If the positive control fails, the problem lies with the protocol or reagents, not your experimental sample [46].
- Action 3: Check Reagents and Equipment.
- Antibodies: Verify that primary and secondary antibodies are compatible. Check expiration dates and ensure proper storage conditions (-20°C or 4°C). Antibodies can degrade or be inactivated by improper handling [46].
- Microscope: Check the functionality of your fluorescence microscope and its light source [46].
- Action 4: Systematically Optimize Variables. Change only one variable at a time to isolate the problem [46]. Key variables to test include:
- Permeabilization time
- Blocking buffer composition and incubation time
- Primary and secondary antibody concentrations (try a concentration series)
- Incubation times and temperatures for antibody steps
- Number and duration of wash steps
Frequently Asked Questions (FAQs)
Q1: What is the diagnostic performance of the PICADAR tool? A1: In its original validation study, PICADAR showed a sensitivity of 0.90 and specificity of 0.75 at a cut-off score of 5 points for predicting a positive PCD diagnosis. The area under the curve (AUC) was 0.91 upon internal validation and 0.87 upon external validation [8] [6]. However, a recent 2025 study found the overall sensitivity in a genetically confirmed cohort was lower, at 75%, with significant variation between patient subgroups [3].
Q2: What are the seven predictive parameters of the PICADAR score? A2: The tool is for patients with persistent wet cough and uses seven parameters from patient history [8] [6]:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care unit admission
- Chronic rhinitis
- Ear symptoms
- Situs inversus
- Congenital cardiac defect
Q3: What is the protocol for measuring nasal nitric oxide (nNO)? A3: nNO is measured using an online testing instrument (e.g., NIOX MINO) during oral exhalation with velopharyngeal closure [54]. The standard protocol involves:
- A constant transnasal airflow rate of 5 ml/s.
- Inhalation to total lung capacity followed by oral exhalation maintaining >10 cm H₂O pressure.
- Measurements are typically taken three times for each nostril, with the mean nNO level recorded in parts per billion (ppb) [54].
Q4: How can nNO and PICADAR be used together? A4: PICADAR serves as an initial, low-cost clinical screening tool to identify patients at high risk for PCD who should be referred for specialized testing. nNO measurement provides an objective, non-invasive biomarker that can be used as a secondary screening step before proceeding to more costly and invasive tests like genetic analysis or transmission electron microscopy. Using them in sequence can improve the overall efficiency of the diagnostic pathway.
Data Presentation
Performance Characteristics of Diagnostic Tools for PCD
Table 1: Comparison of PCD Diagnostic and Predictive Tools
| Tool / Metric | Sensitivity | Specificity | AUC | Cut-off Value | Key Limitations |
|---|---|---|---|---|---|
| PICADAR (Original Validation) | 0.90 [6] | 0.75 [6] | 0.87 (external) [6] | 5 points [6] | Relies on accurate patient recall and clinical history. |
| PICADAR (2025 Genetic Cohort) | 0.75 (Overall) [3] | Information Missing | Information Missing | 5 points [3] | Low sensitivity (61%) in situs solitus patients [3]. |
| Nasal NO (nNO) for PCD screening | Information Missing | Information Missing | Information Missing | ≤ 30 nL/min [6] | Requires expensive equipment; low in CRSwNP [54]. |
| nNO for Eos CRSwNP Diagnosis | 76.74% [54] | 96.67% [54] | 0.939 [54] | 231 ppb [54] | Specific to diagnosing eosinophilic CRSwNP, not PCD. |
Research Reagent Solutions
Table 2: Essential Materials for Key PCD Diagnostic Experiments
| Item / Reagent | Function / Application | Example / Note |
|---|---|---|
| NIOX MINO Device | Measures nasal nitric oxide (nNO) levels for PCD screening. | Uses an electrochemical sensor; provides measurements in ppb [54]. |
| High-Speed Video Microscopy | Analyzes ciliary beat pattern and frequency from brushing biopsies. | Used to identify hallmark dysfunctional ciliary beating [6]. |
| Transmission Electron Microscope | Visualizes ciliary ultrastructure to identify defects in dynein arms, etc. | Considered a hallmark diagnostic test when structural defects are found [6]. |
| Primary and Secondary Antibodies | Used in immunofluorescence to localize specific ciliary proteins. | Critical for diagnosing PCD variants with normal ultrastructure [46]. |
| Cell Culture Media for Air-Liquid Interface (ALI) Culture | Re-differentiates ciliated epithelium after nasal brushing. | Used to reanalyze ciliary function and rule out secondary dyskinesia [6]. |
Experimental Protocols
Protocol: Nasal Nitric Oxide (nNO) Measurement
Objective: To obtain a reliable and reproducible measurement of nasal nitric oxide levels for the screening of Primary Ciliary Dyskinesia.
Materials:
- Chemiluminescence or electrochemical nNO analyzer (e.g., NIOX MINO)
- Disposable nasal olive or nozzle
- Nose clip (if required by the device)
Methodology [54]:
- Patient Preparation: The patient must avoid smoking, eating, drinking, and strenuous exercise for at least 1 hour prior to the test. Ensure no acute respiratory infection is present.
- Equipment Setup: Calibrate the analyzer according to the manufacturer's instructions. Set the transnasal aspiration flow rate to a constant 5 ml/s.
- Patient Positioning: Seat the patient comfortably. Insert the nasal olive into one nostril, ensuring a tight seal.
- Velopharyngeal Closure and Measurement:
- Instruct the patient to inhale deeply to total lung capacity.
- The patient then exhales orally against a resistance to maintain an expiratory pressure of >10 cm H₂O. This critical step closes the velopharynx, isolating the nasal cavity from the lower airways.
- The nNO level is sampled from the nasal cavity during this exhalation.
- Replication: The measurement is typically repeated three times for each nostril, with a short rest period between maneuvers.
- Analysis: The mean nNO value from the three successful exhalations is recorded as the result for that patient, expressed in parts per billion (ppb).
Protocol: Diagnostic Confirmation of PCD in a Specialist Centre
Objective: To provide a definitive diagnosis of PCD using a combination of complementary tests, as per European guidelines.
Methodology [6]:
- Clinical Phenotyping: Collect a detailed clinical history, which can be quantified using the PICADAR tool.
- Initial Specialist Tests:
- Nasal NO (nNO): Measure nNO as described above. Levels consistently below 30 nL/min are highly suggestive of PCD.
- High-Speed Video Microscopy Analysis (HSVMA): Obtain a nasal epithelial brush biopsy. Analyze the ciliary beat pattern (CBP) and frequency. A hallmark dyskinetic pattern is indicative of PCD.
- Confirmatory Tests:
- Transmission Electron Microscopy (TEM): Examine the ultrastructure of the cilia from a biopsy sample for absence or defects in dynein arms, nexin links, or other core structures.
- Genetic Testing: Perform genetic analysis to identify biallelic pathogenic mutations in one of the many known PCD-associated genes.
- Culture and Re-analysis: In cases where secondary ciliary dyskinesia (due to infection or inflammation) is suspected, cells from the biopsy can be cultured at an air-liquid interface (ALI) to allow cilia to recover and then be re-tested with HSVMA and TEM.
- Diagnostic Outcome: A positive diagnosis is typically made based on a characteristic clinical phenotype plus at least two abnormal diagnostic tests (e.g., hallmark TEM, hallmark CBP, and/or low nNO).
Mandatory Visualization
Technical Support Center
Frequently Asked Questions
Q1: Our diagnostic model, like PICADAR, shows excellent performance on our internal data but fails to generalize to external patient populations. What are the primary causes and solutions?
A1: This is a common challenge often stemming from spectrum bias and limited training diversity. The PICADAR tool was derived and validated in specific clinical settings (University Hospital Southampton and Royal Brompton Hospital) and may not perform as well on populations with different demographic characteristics, disease prevalence, or clinical practices [6].
- Troubleshooting Steps:
- Analyze Population Disparities: Compare the demographic and clinical characteristics of your internal dataset against the failing external population. Look for differences in age distributions, ethnic backgrounds, or the prevalence of key predictive features (e.g., rates of neonatal intensive care admittance or situs inversus) [6].
- Re-calibrate the Model: The logistic regression model underlying PICADAR may need re-calibration for your local setting. This involves adjusting the intercept or slope of the model to align with your local disease prevalence and patient spectrum [55] [56].
- Implement Continuous Validation: Establish an ongoing external validation protocol using consecutive patient referrals, as done in Phase 2 of the atopic dermatitis study, to monitor performance in real-time and identify drift [57].
Q2: We are developing a multimodal AI model for a rare disease. How can we effectively integrate image and clinical data when labeled data is scarce?
A2: For rare diseases, zero-shot or few-shot learning approaches are promising, as they do not rely on large, labeled datasets for every possible condition [58].
- Troubleshooting Steps:
- Leverage Foundation Models: Consider using or adapting pre-trained multimodal foundation models (e.g., M3FM). These models are pre-trained on broad public medical data and can perform diagnostic tasks without needing labeled data for specific rare diseases [58].
- Utilize Transfer Learning: Use a pre-trained vision encoder (e.g., ResNet50) for image feature extraction and a pre-trained language model (e.g., MPNet) for clinical text, then fine-tune the combined model on your small, targeted dataset. This was successfully demonstrated in the diagnosis of atopic dermatitis [57].
- Data Augmentation: For the clinical text component, techniques like synonym replacement or back-translation can artificially expand your dataset. For images, generative AI can create synthetic data to enhance training [59].
Q3: Our multimodal model is a "black box," and clinical collaborators are hesitant to trust its diagnoses. How can we improve interpretability?
A3: The field of Explainable AI (XAI) is critical for clinical adoption. The goal is to make the model's reasoning transparent to the end-user [57] [59].
- Troubleshooting Steps:
- Implement Explainability Techniques: Use methods like Grad-CAM or attention mechanisms to generate heatmaps that highlight which regions of a medical image most influenced the diagnosis. For text inputs, use saliency maps to show which words or phrases in the clinical history were most important [59].
- Generate Natural Language Explanations: Develop models that not only provide a diagnosis but also generate a coherent report justifying the conclusion, mirroring how a physician would reason. For example, a model could state: "The diagnosis of primary ciliary dyskinesia is suggested due to the patient's full-term gestation, neonatal chest symptoms, and chronic rhinitis" [58] [59].
- Adopt a Tool-Use Approach: Architect your system so that a large language model orchestrates specialized diagnostic modules. This creates a more interpretable, step-by-step process that clinicians can follow and verify [59].
Q4: Our diagnostic research is based on routine care data, but we are concerned about workup bias and missing data. How can we mitigate these issues?
A4: Retrospective use of routine care data is efficient but introduces specific methodological challenges [56].
- Troubleshooting Steps:
- Address Workup Bias: This bias occurs because the diagnostic workup of a patient is determined by previous test results. To mitigate it, apply methods like multiple imputation to account for missing data from tests that were not performed, or use statistical models that can correct for verification bias [56].
- Handle Missing Data: Do not simply exclude cases with missing data, as this can introduce selection bias. Instead, use multiple imputation techniques to fill in plausible values based on other available patient data [56] [6].
- Ensure a Blind, Independent Reference Standard: In your study design, ensure that the results of the test under investigation do not influence the application or interpretation of the reference standard diagnosis, and vice versa [55].
Experimental Protocols for Validation
Protocol 1: External Validation of a Clinical Prediction Tool
This protocol is based on the validation methodology used for the PICADAR tool [6].
- Objective: To assess the generalizability and accuracy of a clinical prediction tool (e.g., PICADAR) in a new, independent patient population.
- Population: Consecutive patients referred for diagnostic testing for the target condition at an external clinical center.
- Data Collection: Collect data for all predictive parameters of the tool (e.g., for PICADAR: full-term gestation, neonatal chest symptoms, etc.) prospectively or from records, prior to knowing the definitive diagnostic outcome.
- Reference Standard: Apply the current gold-standard diagnostic tests for the condition (e.g., for PCD, hallmark transmission electron microscopy and ciliary beat pattern analysis) independently and blinded to the tool's score [6].
- Analysis:
- Calculate the tool's total score for each patient.
- Plot a Receiver Operating Characteristic (ROC) curve and calculate the Area Under the Curve (AUC) to assess discriminative ability.
- Calculate sensitivity, specificity, and positive/negative predictive values for the recommended cut-off score and other potential thresholds.
Protocol 2: Developing and Evaluating a Multimodal AI Model
This protocol is derived from the methodology used in the multimodal atopic dermatitis study [57].
- Objective: To develop a diagnostic model that integrates image and clinical text data to classify a specific disease (e.g., Atopic Dermatitis vs. non-AD).
- Data Preparation:
- Images: Collect a dataset of lesion images. Preprocess images (resizing, normalization). Use a pre-trained CNN (e.g., ResNet50) as a feature extractor.
- Text: Collect structured or unstructured clinical anamnesis data. Use a pre-trained language model (e.g., MPNet) to convert text into numerical feature embeddings.
- Model Architecture & Training:
- Late Fusion Model: Keep the image and text feature extraction streams separate.
- Fusion: Concatenate the extracted image and text feature vectors into a single, combined representation.
- Classification: Feed the fused vector into a final classification layer (e.g., a fully connected layer with softmax activation) to output the diagnosis.
- Training: Train the model using a cross-entropy loss function and an optimizer like Adam.
- Evaluation:
- Split data into training, validation, and test sets.
- Compare the multimodal model's performance (accuracy, sensitivity, specificity) against image-only and text-only baseline models on the held-out test set.
- Perform external validation on a prospectively collected dataset from a different institution [57].
Table 1: Performance Comparison of Diagnostic Models for Various Conditions
| Condition | Diagnostic Tool / Model | Reported Accuracy | Sensitivity | Specificity | Key Limitation / Context |
|---|---|---|---|---|---|
| Primary Ciliary Dyskinesia (PCD) | PICADAR Clinical Tool (cut-off ≥5) | N/A | 0.90 | 0.75 | Derived & validated in specific UK centres; may lack generalizability [6] |
| Atopic Dermatitis (AD) | Multimodal AI (ResNet50 + MPNet) | 98.28% | N/A | N/A | High accuracy in development phase; requires external validation [57] |
| Pathology Diagnosis | PathChat (Image only) | 78.1% | N/A | N/A | Multimodal AI assistant [59] |
| Pathology Diagnosis | PathChat (Image + Clinical context) | 89.5% | N/A | N/A | Shows value of integrating multiple data points [59] |
| Left Ventricular Dysfunction | BNP Peptide (Phase II Study) | ~95%* | 98% | 92% | Phase II study (case-control) showing promise under ideal conditions [55] |
| Left Ventricular Dysfunction | BNP Peptide (Phase III Study) | ~60%* | 88% | 34% | Phase III study (in clinically suspected patients) showing reduced real-world utility [55] |
*Estimated from data presented in the study.
Research Reagent Solutions
Table 2: Essential Tools for Multimodal Diagnostic Research
| Research Reagent / Tool | Function in Diagnostic Research | Example Use Case |
|---|---|---|
| ResNet50 (CNN) | A deep convolutional neural network for extracting complex features from medical images [57]. | Used as a visual feature extractor from skin lesion images in the multimodal AD diagnosis model [57]. |
| MPNet | A transformer-based language model designed to produce rich contextual sentence representations from text data [57]. | Used to process structured anamnesis data (chief complaints, history) into numerical features for diagnosis [57]. |
| Multimodal Foundation Model (M3FM) | A pre-trained model that can perform zero-shot disease reporting and classification across imaging domains and languages without task-specific training data [58]. | Proposed for use in diagnosing rare diseases or in non-English languages where labeled data is scarce [58]. |
| Logistic Regression Model | A statistical model used to predict the probability of a categorical outcome (e.g., disease present/absent) based on predictor variables [6]. | Used to develop the PICADAR clinical prediction rule, weighting each clinical feature to generate a total risk score [6]. |
| Reference Standard | The best available method for establishing the presence or absence of the target disease, against which a new test is compared [55]. | For PCD, a combination of transmission electron microscopy and ciliary beat pattern analysis [6]. For AD, the AAD 2014 criteria [57]. |
Workflow Visualizations
PICADAR Clinical Decision Pathway
Multimodal AI Diagnostic Model
Conclusion
The PICADAR tool demonstrates significant limitations that restrict its reliability as a standalone screening method for Primary Ciliary Dyskinesia, particularly missing approximately 40% of cases without laterality defects or classic ultrastructural abnormalities. Recent 2025 evidence confirms these vulnerabilities and highlights the critical need for population-specific and genotype-aware diagnostic approaches. For the research and drug development community, these findings underscore the necessity of: (1) developing next-generation predictive tools with enhanced sensitivity across all PCD subtypes; (2) implementing multimodal diagnostic strategies that combine clinical scores with nasal nitric oxide and other accessible biomarkers; (3) establishing genotype-phenotype correlations to refine patient stratification for clinical trials; and (4) advancing personalized diagnostic frameworks that account for ethnic and genetic diversity in PCD manifestations. Future efforts must focus on creating more inclusive, genetically-informed diagnostic protocols to ensure timely identification of all PCD patients for appropriate clinical management and therapeutic development.
References
- 1. (PDF) PICADAR: a diagnostic predictive tool for primary ciliary dyskinesia [https://www.academia.edu/122195602/PICADAR_a_diagnostic_predictive_tool_for_primary_ciliary_dyskinesia]
- 2. Primary ciliary dyskinesia diagnosis and management and its implications in America: a mini review - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10514901/]
- 3. Limitations of PICADAR as a diagnostic predictive tool for primary ciliary dyskinesia | medRxiv [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1]
- 4. Thieme E-Journals - Pneumologie / Full Text [https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0043-111909]
- 5. Collecting clinical data in primary ciliary... | F1000Research [https://f1000research.com/articles/5-2031]
- 6. : a PICADAR predictive tool for diagnostic ... primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819882/]
- 7. : a diagnostic predictive tool for primary ciliary dyskinesia PICADAR [https://publications.ersnet.org/highwire_display/entity_view/node/529265/full]
- 8. : a PICADAR predictive tool for diagnostic primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/26917608/]
- 9. : a diagnostic predictive tool for primary ciliary... PICADAR [https://www.bohrium.com/paper-details/picadar-a-diagnostic-predictive-tool-for-primary-ciliary-dyskinesia/814552781883965442-10032]
- 10. Frontiers | Empowering limited -resource countries: collaborating with... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1547152/full]
- 11. Patient-Oriented Questionnaires and Machine Learning for Rare ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11396573/]
- 12. Thieme E-Journals - Pneumologie / Full Text [https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0043-111909?device=desktop]
- 13. PICADAR: a diagnostic predictive tool for primary ciliary dyskinesia - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4819882/]
- 14. Recall bias | Catalog of Bias [https://catalogofbias.org/biases/recall-bias/]
- 15. Childhood amnesia - Wikipedia [https://en.wikipedia.org/wiki/Childhood_amnesia]
- 16. The occurrence of recall bias in pediatric headache: a comparison of questionnaire and diary data - PubMed [https://pubmed.ncbi.nlm.nih.gov/11168599/]
- 17. Understanding the echocardiogram - Cardiology Explained - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK2215/]
- 18. Indications for Echocardiography and Confirmation Rates of ... [https://ncbi.nlm.nih.gov/pmc/articles/PMC10775930]
- 19. Diagnosis of primary ciliary dyskinesia: summary of the ERS Task Force report - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5584715/]
- 20. Primary Ciliary Dyskinesia. Recent Advances in Diagnostics, Genetics, and Characterization of Clinical Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3826280/]
- 21. Diagnosis | PCD Foundation [https://www.pcdfoundation.org/diagnosis/]
- 22. Cilia Dysfunction in Lung Disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4465242/]
- 23. Frontiers | Opportunities and Challenges for Molecular Understanding of Ciliopathies–The 100,000 Genomes Project [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2019.00127/full]
- 24. Pathways Referral Tracker | Divisions of Family Practice [https://divisionsbc.ca/provincial/what-we-do/practice-support/pathways/referral-tracker]
- 25. Implementing a National Electronic Referral Program: Qualitative Study - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6070727/]
- 26. Referral Process Enhancement: Innovative Approaches and Best Practices - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11318818/]
- 27. Factors affecting the successful implementation of the referral system: A scoping review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8884299/]
- 28. A categorisation of problems and solutions to improve patient referrals from primary to specialty care | BMC Health Services Research | Full Text [https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-018-3745-y]
- 29. : a diagnostic predictive tool for primary ciliary dyskinesia PICADAR [https://publications.ersnet.org/content/erj/47/4/1103]
- 30. : Normal Organ Placement in Medicine Situs Solitus [https://www.medicoverhospitals.in/articles/situs-solitus]
- 31. Pathogenic variants in CFAP46, CFAP54, CFAP74 and CFAP221... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11651342/]
- 32. Genetic Spectrum of EYS-associated Retinal Disease in a Large... [https://www.nature.com/articles/s41598-020-62119-3?error=cookies_not_supported&code=97fad10b-97a5-4f96-9f0d-6d19ffa947d1]
- 33. Genetic diversity among the present Japanese population: evidence... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11194210/]
- 34. The challenges of diagnosing primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/21926395/]
- 35. Primary ciliary dyskinesia. Recent advances in diagnostics , genetics... [https://pubmed.ncbi.nlm.nih.gov/23796196/]
- 36. CCDC65 Mutation Causes Primary Ciliary Dyskinesia with... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0072299]
- 37. and management of primary ciliary dyskinesia | Cilia Diagnosis [https://ciliajournal.biomedcentral.com/articles/10.1186/s13630-014-0011-8]
- 38. Primary Ciliary Dyskinesia Workup: Approach Considerations, Imaging Studies, Other Tests [https://emedicine.medscape.com/article/1002319-workup]
- 39. Clinical care for primary ciliary dyskinesia: current challenges and future directions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9489029/]
- 40. : Understanding... Primary Ciliary Dyskinesia Diagnostic Challenges [https://pubmed.ncbi.nlm.nih.gov/33670432/]
- 41. Combined approaches, including long-read sequencing, address the... [https://www.nature.com/articles/s41431-024-01599-7?error=cookies_not_supported&code=f5ef24b6-1392-4d66-aa94-503e249b8b4c]
- 42. 儿童原发性纤毛运动障碍、囊性纤维化发病机制及基因诊断进展 Research Progress on Pathogenesis and Gene Diagnosis of Primary Ciliary Dyskinesia and Cystic Fibrosis in Children [https://image.hanspub.org/Html/70-1573476_50391.htm]
- 43. Limitations of PICADAR as a diagnostic predictive tool for primary ciliary dyskinesia | Sciety Labs (Experimental) [https://sciety-labs.elifesciences.org/articles/by?article_doi=10.1101/2025.09.22.25336363]
- 44. and Model Sensitivity | SpringerLink Analysis Validation [https://link.springer.com/chapter/10.1007/978-3-319-43742-2_17]
- 45. Home - Laboratory protocols and methods - Research Guides at Virginia Tech [https://guides.lib.vt.edu/find/lab-methods]
- 46. Troubleshooting Protocols - Biological Sciences: Summer Research Institute (SRI) - CMU LibGuides at Carnegie Mellon University [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 47. European Respiratory Society and American Thoracic Society... [https://publications.ersnet.org/content/erj/early/2025/09/18/1399300300745-2025]
- 48. Primary Ciliary Dyskinesia—Current Diagnostic and Therapeutic Approach [https://www.mdpi.com/2077-0383/14/19/6808]
- 49. Diagnosis - PCD Foundation Website [https://pcdfoundation.org/overview/diagnosis/]
- 50. Primary ciliary dyskinesia - Insights [https://news.mayocliniclabs.com/pathology/primary-ciliary-dyskinesia/]
- 51. Primary Ciliary Dyskinesia - Diagnosis | NHLBI, NIH [https://www.nhlbi.nih.gov/health/primary-ciliary-dyskinesia/diagnosis]
- 52. (Open Access) PICADAR : a diagnostic predictive tool for primary ... [https://scispace.com/papers/picadar-a-diagnostic-predictive-tool-for-primary-ciliary-20joj660ld]
- 53. Evaluation of a Clinical as a Predictive Index for Primary Ciliary... Tool [https://pubmed.ncbi.nlm.nih.gov/34198708/]
- 54. The roles of nasal in diagnosis and endotypes of chronic... nitric oxide [https://journalotohns.biomedcentral.com/articles/10.1186/s40463-020-00465-y]
- 55. The architecture of diagnostic research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1122451/]
- 56. Diagnostic research on routine care data: prospects and problems - PubMed [https://pubmed.ncbi.nlm.nih.gov/12873643/]
- 57. Machine Learning Multimodal for... | F1000Research Approach [https://f1000research.com/articles/14-952]
- 58. A multimodal multidomain multilingual medical foundation model for zero shot clinical diagnosis | npj Digital Medicine [https://www.nature.com/articles/s41746-024-01339-7]
- 59. Generative AI in Multimodal : Bridging... | Preprints.org Diagnostics [https://www.preprints.org/manuscript/202508.1425/v1]