Cross-Validation of Lipidomic Biomarkers Across Diverse Populations: From Discovery to Clinical Application
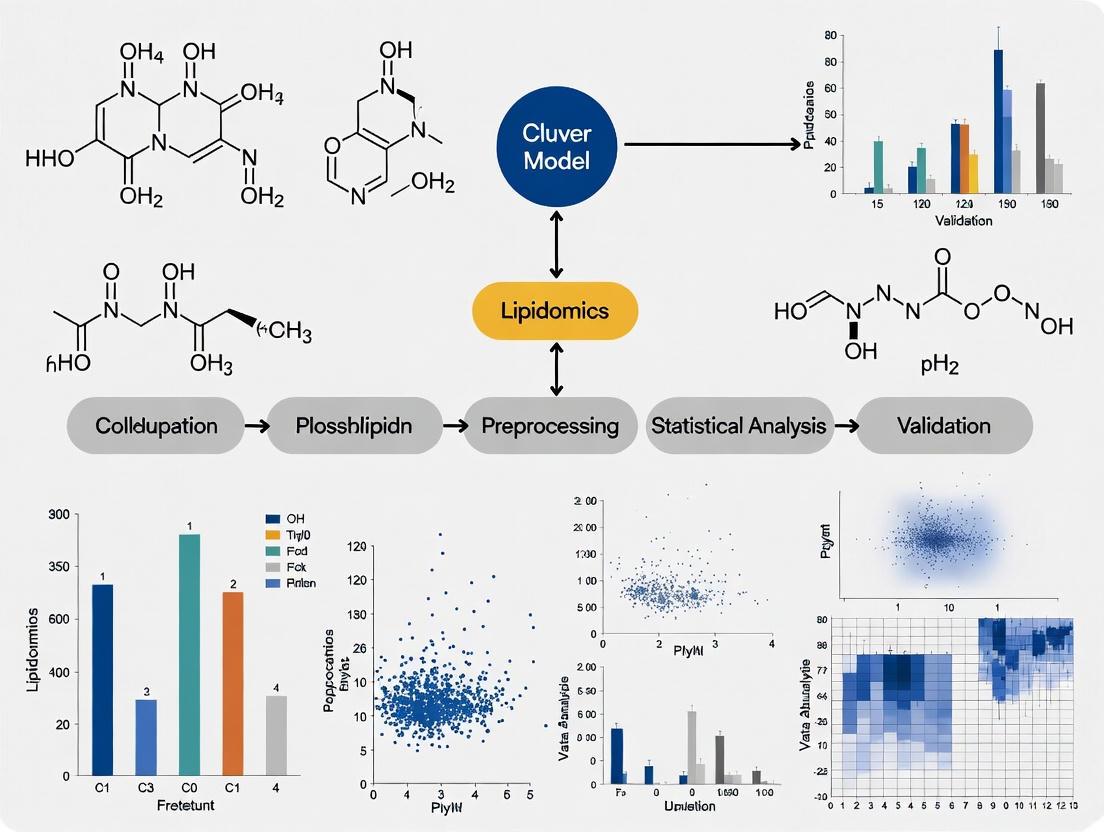
This article provides a comprehensive framework for the cross-validation of lipidomic findings across different populations, a critical step for translating lipid biomarkers into clinical practice.
Cross-Validation of Lipidomic Biomarkers Across Diverse Populations: From Discovery to Clinical Application
Abstract
This article provides a comprehensive framework for the cross-validation of lipidomic findings across different populations, a critical step for translating lipid biomarkers into clinical practice. We explore the foundational sources of lipidomic variation—including ethnicity, sex, age, and developmental stage—that necessitate rigorous cross-population validation. The review details advanced methodological approaches from large-scale cohort studies and automated platforms that enhance reproducibility, while addressing key troubleshooting challenges in standardization and data harmonization. Finally, we examine successful validation strategies employing machine learning and independent cohort replication, offering researchers and drug development professionals actionable insights for developing robust, clinically relevant lipidomic biomarkers with broad applicability.
Understanding Lipidomic Diversity: The Biological Imperative for Cross-Population Validation
Cardiovascular diseases (CVDs) represent the leading cause of death worldwide, imposing a substantial burden on healthcare systems. Dyslipidemia, a condition characterized by abnormal lipid metabolism, serves as a primary risk factor for CVDs. Research has consistently demonstrated that susceptibility to dyslipidemia and its cardiovascular consequences varies significantly across ethnic populations. South Asians (SAs)—individuals originating from India, Pakistan, Bangladesh, Sri Lanka, Nepal, Bhutan, and the Maldives—experience a disproportionately higher risk of developing dyslipidemia and subsequent CVDs compared to white Europeans (WEs). This review synthesizes evidence from comparative studies to elucidate the distinct lipid profiles, genetic underpinnings, and physiological responses that contribute to these ethnic disparities, providing a foundation for targeted therapeutic strategies and future research directions.
Comparative Lipid Profiles: South Asians vs. White Europeans
Epidemiological and clinical studies have identified a characteristic dyslipidemic pattern among South Asians, often termed "atherogenic dyslipidemia." This profile differs qualitatively and quantitatively from that typically observed in white European populations [1] [2]. The table below summarizes the key differences in lipid parameters between these ethnic groups.
Table 1: Comparative Lipid Profiles in South Asians and White Europeans
| Lipid Parameter | Pattern in South Asians vs. White Europeans | Clinical Implications |
|---|---|---|
| LDL Cholesterol | Similar or slightly lower circulating levels, but composed of denser, smaller particles [1]. | Smaller, denser LDL particles are more atherogenic and penetrate the endothelium more easily, contributing to CVD risk at lower serum concentrations [1]. |
| Triglycerides | Significantly higher levels; hypertriglyceridemia affects up to 70% of the SA population [1]. | Drives the formation of atherogenic, small dense LDL and reduces HDL levels, amplifying overall CVD risk [1] [2]. |
| HDL Cholesterol | Lower serum levels of HDL-C, and its protective effect against CVD is weaker [1] [3]. | The functionality of HDL is impaired, diminishing its role in reverse cholesterol transport and vascular protection [1]. |
| Lipoprotein(a) | Higher levels compared to white Europeans [1] [2]. | An independent, genetically determined risk factor for atherosclerosis and thrombogenesis [2]. |
This distinct lipid phenotype in South Asians is not fully captured by standard lipid panels, which measure total LDL cholesterol but not particle size or density. This underscores the need for more refined lipid assessment in this high-risk group.
Genetic and Molecular Basis of Disparities
The ethnic differences in lipid metabolism and CVD risk are rooted in genetic variations that influence key proteins and enzymes in the lipid pathway.
Key Genetic Variations
Mendelian randomization and genetic association studies have identified several genes with polymorphisms that exhibit different frequencies and effects in South Asian populations [1] [4]. These include:
- PCSK9 (Proprotein Convertase Subtilisin/Kexin Type 9): A regulator of LDL receptor degradation. Notably, genetically proxied PCSK9 levels demonstrate a significantly weaker association with LDL-C in South Asians (β = 0.16) compared to Europeans (β = 0.37) [4]. This suggests that PCSK9 inhibitors, while effective, might have a different magnitude of effect in South Asians.
- CELSR2: A gene involved in lipoprotein metabolism, which has been linked to both dyslipidemia and coronary artery disease in South Asians [4].
- ANGPTL3 (Angiopoietin-Related Protein 3): An inhibitor of lipoprotein lipase, identified as a potential causal protein for lipid traits in South Asians [4].
- Other Genes: Variations in Apolipoprotein H, Lipoprotein Lipase, MBOAT7, SGPP1, and SPTLC3 have also been associated with the unique SA lipid profile [1] [3].
Protein Targets and Therapeutic Implications
The identification of these genetically validated proteins provides a roadmap for targeted therapies. Proteins like PCSK9, ANGPTL3, and Apolipoprotein(a) are the targets of existing or developing lipid-lowering drugs [4]. The evidence of population-specific effects highlights the importance of tailoring drug development and clinical trials to include diverse genetic backgrounds to ensure efficacy across populations.
Experimental Evidence: Physiological Responses to Metabolic Stress
Controlled intervention studies provide compelling evidence for the heightened metabolic susceptibility of South Asians. The GlasVEGAS study, a key experimental model, directly compared the metabolic consequences of weight gain in SA and WE men.
Experimental Protocol: The GlasVEGAS Study
- Objective: To compare the effects of induced weight gain on body composition, metabolic responses, and adipocyte morphology in SA versus WE men without overweight or obesity.
- Participants: 14 South Asian and 21 white European men.
- Intervention: A 4–6 week overfeeding regimen designed to induce a 5–7% gain in body weight.
- Pre-/Post-Intervention Assessments:
- Body Composition: Measured via whole-body MRI to quantify adipose tissue (subcutaneous, visceral) and lean tissue volumes.
- Metabolic Function: Assessed via a mixed-meal tolerance test, measuring glucose, insulin, and triglyceride levels over 300 minutes. Insulin sensitivity was calculated using the Matsuda index and HOMA-IR.
- Adipocyte Morphology: A subcutaneous abdominal adipose tissue biopsy was taken to analyze adipocyte size and size distribution [5].
Key Findings and Quantitative Data
The study revealed profound ethnic differences in the metabolic response to weight gain, with South Asians experiencing significantly greater adverse effects.
Table 2: Metabolic and Body Composition Responses to Weight Gain in the GlasVEGAS Study
| Parameter | South Asian Men | White European Men | P-value for Interaction |
|---|---|---|---|
| Weight Gain | +6.5% ± 0.3% | +6.3% ± 0.2% | 0.62 |
| Δ Matsuda Index | -38% | -7% | 0.009 |
| Δ Fasting Insulin | +175% | No significant change | 0.02 |
| Δ Lean Tissue Mass | Lower increase | Greater increase | Not specified |
| Baseline Mean Adipocyte Volume | 76% larger | Reference | 0.006 |
| Baseline Large Adipocytes | 60% of total volume | 9.1% of total volume | 0.005 |
The data demonstrates that despite equivalent weight gain, South Asian men suffered a dramatically greater decline in insulin sensitivity and a more pronounced increase in insulin resistance. This was coupled with a baseline adipocyte morphology characterized by larger, lipid-filled cells and a reduced population of small adipocytes, suggesting a limited capacity for safe lipid storage in subcutaneous fat depots [5]. This "adipocyte dysfunction" is hypothesized to lead to ectopic fat deposition and greater metabolic dysfunction in SAs, even with modest weight gain.
Methodologies for Advanced Lipid Research
Understanding ethnic disparities requires sophisticated technologies that move beyond traditional bulk lipid measurements.
Single-Cell Lipidomics
Single-cell lipidomics represents a transformative approach for capturing cellular heterogeneity in lipid metabolism that is obscured in bulk tissue analysis [6].
- Core Technology: Ultra-sensitive high-resolution mass spectrometry (e.g., Orbitrap, FT-ICR) enables the identification and quantification of lipid molecules at the attomole level in individual cells [6].
- Workflow: Individual cells are isolated, their lipidomes are profiled via MS, and the data is computationally analyzed to identify cell-type-specific lipid signatures and metabolic states.
- Application: This technique can reveal how different cell types (e.g., adipocytes, macrophages) within adipose tissue from various ethnic groups contribute to overall lipid metabolism and inflammatory responses [6].
Mass Spectrometry Imaging
Spatial distribution of lipids within tissues is critical for understanding localized effects.
- Core Technology: Matrix-Assisted Laser Desorption/Ionization Mass Spectrometry Imaging allows for the visualization of the spatial distribution of hundreds of lipids directly from thin tissue sections [6].
- Workflow: A tissue section is coated with a matrix and irradiated with a laser, which desorbs and ionizes molecules from discrete locations. A mass spectrum is acquired at each pixel, generating a spatial map of lipid abundance.
- Application: MSI can be used to map lipid heterogeneity in atherosclerotic plaques or liver sections, identifying ethnic-specific patterns of lipid accumulation associated with disease progression [6].
The following table details key reagents and databases essential for conducting rigorous lipidomics research in diverse populations.
Table 3: Essential Research Reagents and Resources for Cross-Population Lipidomics
| Research Reagent / Resource | Function and Application | Relevance to Ethnic Disparity Research |
|---|---|---|
| Stable Isotope-Labeled Lipid Standards | Internal standards for absolute quantification of lipid species in MS-based workflows [7]. | Ensures accurate and comparable quantification of lipid profiles across different study cohorts. |
| LIPID MAPS Database | A curated database providing reference on lipid structures, nomenclature, and metabolic pathways [6]. | Essential for the consistent identification and annotation of lipid species discovered in diverse populations. |
| NIST Plasma Reference Material | A standardized reference plasma used for quality control to monitor batch-to-batch reproducibility [7]. | Critical for maintaining data quality and allowing valid comparisons in multi-center or longitudinal studies. |
| Antibodies for Lipid-Associated Proteins | Proteins like PCSK9, ANGPTL3, and Apo(a) for validating genetic findings via Western Blot or ELISA [4]. | Allows for the functional validation of genetically identified protein targets in plasma or tissue samples from different ethnic groups. |
Visualizing Experimental and Metabolic Pathways
The diagrams below illustrate the core experimental workflow and a key metabolic pathway relevant to the discussed ethnic disparities.
Experimental Workflow for Metabolic Phenotyping
Genetic & Metabolic Pathway in Dyslipidemia
The evidence from genetic, clinical, and experimental studies consistently demonstrates that South Asians possess a unique lipid phenotype and a heightened metabolic susceptibility compared to white Europeans. This is characterized by a more atherogenic lipid profile (featuring small dense LDL, high triglycerides, and dysfunctional HDL), genetic variations in key lipid-regulating genes, and a pronounced deterioration in metabolic health upon weight gain. These findings underscore that ethnicity is a critical biological variable in lipid metabolism and CVD risk. Future research must leverage advanced tools like single-cell lipidomics and mass spectrometry imaging to further unravel the cellular mechanisms of these disparities. Ultimately, this knowledge must inform the development of population-specific risk assessment tools, treatment guidelines, and therapeutic agents to achieve equitable cardiovascular health outcomes.
Lipidomics, the large-scale study of lipid pathways and networks, has revealed significant sexual dimorphism in human lipid metabolism, providing crucial insights for precision medicine. The circulatory lipidome demonstrates high individuality and sex specificity, constituting fundamental prerequisites for next-generation metabolic health monitoring [7]. Specific lipid classes, particularly sphingomyelins and ether-linked phospholipids, consistently exhibit pronounced sex-specific patterns that persist across diverse populations and disease states. These sex-specific lipidomic fingerprints influence aging trajectories, disease susceptibility, and therapeutic responses, forming an essential context for cross-validation of lipidomic findings across different populations.
Understanding these dimorphic patterns requires integrating analytical lipidomics with systems biology approaches. This guide objectively compares lipidomic performance data across multiple studies, providing researchers with validated signatures and methodologies for investigating sex-specific lipid metabolism in both basic research and drug development contexts.
Key Lipid Classes in Sexual Dimorphism
Comparative Analysis of Sex-Specific Lipid Patterns
Table 1: Sex-Specific Lipid Signatures Across Multiple Studies
| Lipid Class | Specific Lipid Species | Sex-Bias | Concentration Difference | Biological Context | Study Population |
|---|---|---|---|---|---|
| Sphingomyelins | Multiple species | Female-biased | Significantly higher in females [7] | Healthy aging | Lausanne population (N=1,086) [7] |
| Ether-linked phospholipids | Plasmalogens | Female-biased | Significantly higher in females [7] | Healthy aging | Lausanne population (N=1,086) [7] |
| Ceramides | Multiple species | Dynamic with aging | Age-associated increases in both sexes [8] | Aging "crests" | Aging cohort (N=1,030) [8] |
| Hexosylceramides | Hex1Cer | Female-specific | Increased with age only in women [9] | Aging dynamics | Aging cohort (N=1,030) [9] |
| Lysophosphatidylethanolamine | LPE | Female-specific | Global increase with aging [9] | Aging dynamics | Aging cohort (N=1,030) [9] |
| Phosphatidylcholine | PC(18:0p/22:6) | Disease-associated | Decreased in pediatric IBD [10] | Inflammatory bowel disease | Pediatric cohort (N=263) [10] |
| Lactosyl ceramide | LacCer(d18:1/16:0) | Disease-associated | Increased in pediatric IBD [10] | Inflammatory bowel disease | Pediatric cohort (N=263) [10] |
Temporal Dynamics in Sex-Specific Lipid Metabolism
The aging process reveals non-linear dynamics in lipid metabolism, with specific "aging crests" where lipidomic changes accelerate. Research has identified three distinct aging crests at 55-60, 65-70, and 75-80 years, with the 65-70 years crest dominant in men and the 75-80 years crest in women [8]. These temporal patterns highlight the importance of considering age as a critical variable when validating lipidomic findings across populations.
During these transitional periods, ether lipids and sphingolipids drive sex-specific aging dynamics, with functional indices indicating compositional shifts in lipid species that suggest impairment of lipid functional categories [8]. These include loss of dynamic properties, alterations in bioenergetics, antioxidant defense, cellular identity, and signaling platforms.
Experimental Methodologies for Lipidomic Profiling
Standardized Lipidomic Workflow Protocols
Table 2: Experimental Protocols for Sex-Specific Lipidomic Studies
| Methodological Component | Standard Protocol | Technical Variations | Quality Control Measures |
|---|---|---|---|
| Sample Preparation | Semiautomated using stable isotope dilution approach [7] | Manual extraction for specific tissues [11] | Use of reference materials (NIST SRM 1950) [7] [9] |
| Lipid Separation | Hydrophilic interaction liquid chromatography (HILIC) [7] | Reversed-phase C18 columns [12] | Internal standards for each lipid class [13] |
| Mass Spectrometry Analysis | LC-MS/MS with targeted approach [9] | High-resolution TOF/MS [12] | Batch-to-batch reproducibility monitoring (median 8.5% RSD) [7] |
| Data Processing | Targeted processing with internal standard normalization [7] | Untargeted with chemometrics [11] [14] | Peak area RSD <7.8%, mass accuracy <500 ppb [12] |
| Statistical Analysis | Linear and non-linear modeling [9] | PCA, PLS-DA, random forest [11] | Cross-validation across independent cohorts [10] |
Cross-Validation Approaches Across Populations
Robust validation of sex-specific lipidomic findings requires multiple cohort designs and advanced statistical modeling. The integration of machine learning algorithms has significantly enhanced the identification of reproducible lipid signatures across populations. For instance, in pediatric inflammatory bowel disease, a diagnostic lipidomic signature comprising only lactosyl ceramide (d18:1/16:0) and phosphatidylcholine (18:0p/22:6) was validated across independent cohorts, demonstrating consistent performance [10].
Similarly, in breast cancer research, lipidomic profiling of patients categorized by HR and HER2 status revealed distinct lipid compositions across groups, with triglycerides such as TG(16:0-18:1-18:1)+NH4 showing significant differences, validated through principal component analysis (PCA), partial least squares-discriminant analysis (PLS-DA), and random forest classification [11].
Signaling Pathways and Metabolic Networks
Hormonal Regulation of Lipid Metabolism
The sexual dimorphism observed in lipidomic profiles is fundamentally regulated by hormonal influences, with estrogen playing a particularly significant role in shaping female-specific lipid patterns. Estrogen signaling impacts multiple aspects of lipid metabolism, including sphingolipid biosynthesis, peroxisomal ether lipid synthesis, and mitochondrial fatty acid oxidation.
In breast cancer research, lipidomic profiles correlate strongly with hormone receptor status, with specific triglycerides and phosphatidylinositol phosphates serving as crucial features for accurate tumor classification [11]. This demonstrates how hormonal signaling directly influences lipid composition in both physiological and pathological states.
Ether Lipid and Sphingolipid Interrelationships
The diagram illustrates the coordinated regulation of ether lipids and sphingolipids by hormonal signaling, particularly estrogen. These lipid networks collectively influence membrane properties, cellular signaling platforms, and antioxidant defense mechanisms—all of which demonstrate sex-specific characteristics and contribute to differential disease susceptibility between males and females.
The Researcher's Toolkit: Essential Reagents and Platforms
Core Lipidomics Research Solutions
Table 3: Essential Research Tools for Sex-Specific Lipidomics
| Tool Category | Specific Solution | Application Context | Performance Characteristics |
|---|---|---|---|
| Mass Spectrometry | Xevo MRT Mass Spectrometer [12] | High-resolution lipidomic profiling | 100,000 FWHM resolution, <500 ppb mass accuracy [12] |
| Chromatography | ACQUITY Premier UPLC CSH C18 [12] | Lipid separation | 1.7 µm particle size, 2.1 × 50 mm dimensions [12] |
| Quality Control | NIST SRM 1950 [7] [9] | Inter-laboratory standardization | Reference for 'normal' human plasma lipid concentrations [9] |
| Internal Standards | EquiSPLASH [12] | Quantification normalization | Contains multiple stable isotope-labeled lipid species [12] |
| Data Processing | LipoStar2 Software [12] | Lipid identification and statistical analysis | Enables database searching and pathway profiling [12] |
| Statistical Analysis | Random Forest Classification [11] | Pattern recognition in lipidomic data | Identifies significant lipid features in complex datasets [11] |
Analytical Performance Standards
Reproducible sex-specific lipidomics requires stringent quality control measures. High-performance instruments should demonstrate mass accuracy <500 ppb and peak area RSD <7.8% across hundreds of injections to ensure detection of subtle sex-specific differences [12]. Between-batch reproducibility should target median CV <8.5% across all quantified lipid species, with biological variability significantly exceeding analytical variability [7].
For sex-specific analyses, the implementation of sex-stratified quality control pools is recommended, as general reference materials may not capture the full spectrum of sex-specific lipid variation. Additionally, the use of stable isotope internal standards for each lipid class improves quantitative accuracy when comparing concentrations between sexes [13].
The consistent identification of sex-specific lipidomic fingerprints across diverse populations and disease contexts underscores the fundamental importance of considering biological sex as a critical variable in lipidomics research. The robust patterns observed for sphingomyelins and ether-linked phospholipids highlight their roles as key mediators of sexual dimorphism in metabolic health and disease susceptibility.
Cross-validation of these findings across independent cohorts—from aging populations to specific disease contexts—strengthens the evidence for biologically significant sex differences in lipid metabolism. As lipidomics continues to transition toward clinical applications [13], the integration of sex-specific reference ranges and analytical frameworks will be essential for realizing the full potential of precision medicine approaches targeting lipid metabolism.
For researchers investigating sex-specific lipidomics, the consistent implementation of standardized protocols, rigorous quality control measures, and validation across independent populations will ensure the continued advancement of this critical field at the intersection of lipid biology and sexual dimorphism.
Lipidomics, the large-scale study of lipid molecules, has emerged as a powerful tool for understanding metabolic health and disease risk across the human lifespan. Mounting evidence suggests that in utero and early life exposures may predispose individuals to metabolic disorders in later life, with dysregulation of lipid metabolism playing a critical role in such outcomes [15]. The developmental origins of health and disease (DOHaD) paradigm suggests that prenatal, perinatal, and postnatal influences result in long-term developmental, physiological, and metabolic changes that can contribute to later life disease risk, including cardiovascular diseases and related cardiometabolic conditions [15]. While large population-based studies have established specific lipids to be associated with cardiometabolic disorders in adults, little is known about lipid metabolism in early life until recently [15]. Understanding the key determinants of early life lipid metabolism will inform the development of risk-stratification and early interventions for metabolic diseases. This review synthesizes current evidence on lipidomic trajectories from gestation through childhood and their implications for long-term health outcomes, with particular emphasis on cross-population validation of findings.
Methodological Approaches in Developmental Lipidomics
Analytical Technologies and Protocols
The advances in lipidomic profiling have been driven primarily by technological innovations in mass spectrometry. Most large-scale population studies now utilize ultra-high-performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) for comprehensive lipid profiling [15] [16]. The typical workflow involves lipid extraction using organic solvents such as butanol:methanol (1:1) with 10 mM ammonium formate containing deuterated internal standards, followed by chromatographic separation and mass spectrometric analysis [15].
For lipid extraction, 10 µL of plasma is typically mixed with 100 µL of butanol:methanol (1:1) with 10 mM ammonium formate containing a mixture of internal standards. Samples are vortexed, sonicated for an hour, and then centrifuged before transferring the supernatant for analysis [15]. Liquid chromatography is commonly performed using C18 columns with solvent gradients ranging from aqueous to organic phases, and mass spectrometry analysis is conducted in both positive and negative ion modes with dynamic scheduled multiple reaction monitoring (MRM) [15].
Quality control procedures are critical for ensuring data reliability. Most studies incorporate pooled quality control samples extracted alongside the study samples at regular intervals (typically 1 QC per 20 samples) to monitor technical variation, with additional technical QCs to account for instrument performance [15]. The inclusion of reference materials such as NIST 1950 SRM samples allows for alignment across different datasets and laboratories [15].
Cross-Study Methodological Consistency
A comparative analysis of major developmental lipidomics studies reveals consistent methodological approaches across research groups, which enables cross-population validation:
Table 1: Methodological Comparison Across Major Developmental Lipidomics Studies
| Study | Cohort | Sample Size | Lipid Species | Analytical Platform | Age Points |
|---|---|---|---|---|---|
| BIS [15] | Australian (Caucasian) | 1074 mother-child dyads | 776 features, 39 classes | UHPLC-MS/MS | 28wk gestation, birth, 6mo, 12mo, 4yr |
| GUSTO [16] | Singaporean (Asian) | 1247 mother-child pairs | 480 species | LC-MS/MS | 26-28wk gestation, birth, 4-5yr postpartum, 6yr |
| HOLBAEK [17] | Danish (Caucasian) | 1331 children | 227 annotated lipids | MS-based lipidomics | Cross-sectional (6-16yr) |
| MDC-CC [18] | Swedish (Caucasian) | 4067 participants | 184 lipid species | Shotgun lipidomics | Adult baseline + 23yr follow-up |
| PROTECT [19] | Puerto Rican | 259 mother-child pairs | Bioactive lipids | HPLC-MS/MS | 26wk gestation, 1-3yr childhood |
Developmental Lipidomic Trajectories from Gestation to Childhood
The Prenatal and Perinatal Period
The lipid environment during gestation plays a crucial role in fetal development. Comprehensive lipid profiling of mother-child dyads in the Barwon Infant Study revealed that the lipidome differs significantly between mother and newborn, with cord serum enriched with long chain poly-unsaturated fatty acids (LC-PUFAs) and corresponding cholesteryl esters relative to maternal serum [15]. This selective transfer mechanism ensures adequate LC-PUFAs for fetal brain and nervous system development.
A striking finding from the GUSTO cohort was that levels of 36% of profiled lipids were significantly higher (absolute fold change > 1.5) in antenatal maternal circulation compared to the postnatal phase, with phosphatidylethanolamine levels changing the most [16]. Compared to antenatal maternal lipids, cord blood showed lower concentrations of most lipid species (79%) except lysophospholipids and acylcarnitines [16], suggesting selective placental transfer or fetal metabolism priorities.
The Barwon Infant Study also identified specific associations between antenatal factors and cord serum lipids. The majority of cord serum lipids were strongly associated with gestational age and birth weight, with most lipids showing opposing associations for these two parameters [15]. Each mode of birth showed an independent association with cord serum lipids, indicating that the labor process itself influences neonatal lipid metabolism [15].
Postnatal Development and Early Childhood
The transition from intrauterine to extrauterine life involves dramatic metabolic adaptations, with the lipidome undergoing significant reorganization. In the Barwon Infant Study, researchers observed marked changes in the circulating lipidome with increasing child's age. Specifically, alkenylphosphatidylethanolamine species containing LC-PUFAs increased with child's age, whereas the corresponding lysophospholipids and triglycerides decreased [15].
The GUSTO cohort provided additional insights by comparing changes from birth to 6 years of age with changes between a 6-year-old child and an adult. Changes in lipid concentrations from birth to 6 years were much higher in magnitude (log2FC = -2.10 to 6.25) than the changes observed between a 6-year-old child and an adult (postnatal mother) (log2FC = -0.68 to 1.18) [16]. This indicates that early childhood represents a period of particularly dynamic lipidomic reorganization.
Nutritional influences, particularly breastfeeding, had a significant impact on the plasma lipidome in the first year of life. The Barwon Infant Study reported up to 17-fold increases in a few species of alkyldiaclylglycerols at 6 months of age associated with breastfeeding [15], highlighting how early nutritional exposures can dramatically shape lipid metabolism.
Childhood to Adolescence: Emergence of Cardiometabolic Risk Signatures
As children grow older, specific lipid patterns begin to associate with cardiometabolic risk. The HOLBAEK study, which included children and adolescents with normal weight, overweight, or obesity, identified distinct lipid signatures associated with adiposity and metabolic health [17]. Their analysis revealed that ceramides, phosphatidylethanolamines, and phosphatidylethanolamines were associated with insulin resistance and cardiometabolic risk, whereas sphingomyelins showed inverse associations [17].
Notably, the study found that a panel of three lipids predicted hepatic steatosis as effectively as liver enzymes, suggesting the potential for lipidomic signatures in early detection of metabolic complications [17]. The interaction between obesity and age revealed that pubertal development stages showed different lipidomic patterns in normal weight versus overweight/obesity groups, indicating that obesity may disrupt typical developmental lipid trajectories [17].
Table 2: Key Lipid Classes and Their Developmental Associations
| Lipid Class | Gestational Trends | Postnatal Trends | Association with Health Outcomes |
|---|---|---|---|
| Long-chain PUFAs | Enriched in cord serum vs maternal [15] | Variable based on diet | Essential for neurodevelopment [19] |
| Lysophospholipids | Higher in cord blood vs other lipids [16] | Decrease with age [15] | Signaling molecules; associated with inflammation |
| Ceramides | Not prominently featured in gestation | Increase with obesity [17] | Cardiometabolic risk, insulin resistance [17] |
| Sphingomyelins | Not prominently featured in gestation | Protective inverse associations [17] | Inverse association with cardiometabolic risk [17] |
| Phosphatidylethanolamines | Most changed in pregnancy vs postpartum [16] | Alkenyl species increase with age [15] | Associated with cardiometabolic risk [17] |
| Triglycerides | Lower in cord blood [16] | Decrease with age in early childhood [15] | Traditional cardiometabolic risk markers |
Cross-Population Validation of Lipidomic Findings
The generalizability of lipidomic discoveries requires validation across diverse populations. Several studies have undertaken such cross-population comparisons, with consistent findings emerging despite ethnic and geographic differences.
The GUSTO study validated its findings in the independent Barwon Infant Study cohort, noting that associations of cord blood lipidomic profiles with birth weight displayed distinct trends compared to lipidomic profiles associated with child BMI at 6 years [16]. This suggests that different stages of development may have unique lipidomic determinants of growth and adiposity.
When comparing pediatric versus maternal obesity signatures, researchers found similarities in association with consistent trends (R² = 0.75) between child and adult BMI [16]. However, a larger number of lipids were associated with BMI in adults (67%) compared to children (29%) [16], indicating that the lipidomic signature of adiposity becomes more pronounced with age.
The Malmö Diet and Cancer-Cardiovascular Cohort study demonstrated that lipidomic risk scores showed only marginal correlation with polygenic risk scores, indicating that the lipidome and genetic variants may constitute largely independent risk factors for type 2 diabetes and cardiovascular disease [18]. This finding has important implications for risk prediction models, suggesting that lipidomic profiling provides complementary information to genetic testing.
Pathway Visualization: Lipid Metabolism in Early Development
The following diagram illustrates key lipid metabolic pathways and their changes throughout early development, based on findings from multiple cohort studies:
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful lipidomic research requires specific reagents and materials to ensure accurate, reproducible results. The following table details key research reagent solutions used across the cited studies:
Table 3: Essential Research Reagents for Developmental Lipidomics
| Reagent/ Material | Function | Example Specifications | Notes |
|---|---|---|---|
| Internal Standards | Quantification reference | Deuterated or non-physiological IS mixture [15] | Critical for accurate quantification |
| Butanol:Methanol (1:1) | Lipid extraction | With 10 mM ammonium formate [15] | Efficient extraction of diverse lipid classes |
| C18 UHPLC Columns | Lipid separation | ZORBAX eclipse plus C18 (2.1 × 100 mm, 1.8 μm) [15] | High-resolution separation |
| Reference Plasma | Quality control | NIST 1950 SRM sample [15] | Cross-laboratory standardization |
| Ammonium Formate | Mobile phase additive | 10 mM in mobile phases [15] | Enhances ionization efficiency |
| SPE Columns | Sample cleanup | Strata-X Polymeric SPE [19] | Bioactive lipid isolation |
| Deuterated Standards | Bioactive lipid quant | Oxylipins and parent PUFAs [19] | Essential for oxylipin analysis |
Implications for Drug Discovery and Biomarker Development
The longitudinal trajectories of lipid species from gestation through childhood offer valuable insights for both biomarker and therapeutic development. Lipidomics is increasingly being recognized as an important tool for the identification of druggable targets and biochemical markers [20]. Several promising avenues have emerged from recent developmental studies:
Predictive Biomarkers for Metabolic Disease
The Malmö Diet and Cancer-Cardiovascular Cohort study demonstrated that lipidomic risk scores could stratify participants into risk groups with a 168% increase in type 2 diabetes incidence rate in the highest risk group and a 77% decrease in the lowest risk group compared to average case rates [18]. Notably, this lipidomic risk assessment required only a single mass spectrometric measurement that is relatively cheap and fast compared to genetic testing [18].
In pediatric populations, the HOLBAEK study identified specific lipid signatures that could predict hepatic steatosis as effectively as liver enzymes [17], suggesting opportunities for non-invasive monitoring of metabolic liver disease in children. Their finding that ceramides, phosphatidylethanolamines, and phosphatidylinositols were associated with insulin resistance while sphingomyelins showed protective associations [17] points to potential biomarkers for early detection of metabolic dysfunction.
Intervention Monitoring and Personalized Approaches
Lipidomic profiling also shows promise for monitoring intervention responses. In the PREVIEW study, researchers identified serum lipids that could serve as evaluative or predictive biomarkers for individual glycemic changes following diet-induced weight loss [21]. They found that dietary intervention significantly reduced diacylglycerols, ceramides, lysophospholipids, and ether-linked phosphatidylethanolamine, while increasing acylcarnitines, short-chain fatty acids, and organic acids [21].
The HOLBAEK intervention study further demonstrated that family-based, nonpharmacological obesity management reduced levels of ceramides, phospholipids, and triglycerides, indicating that lowering the degree of obesity could partially restore a healthy lipid profile in children and adolescents [17]. This suggests that lipidomic profiling could be used to monitor response to lifestyle interventions in pediatric populations.
The comprehensive profiling of lipidomic changes from gestation through childhood has revealed dynamic developmental trajectories that reflect both normal metabolic maturation and early signs of disease predisposition. Cross-population studies have consistently demonstrated that early life factors including gestational age, birth weight, mode of delivery, and infant feeding practices leave discernible imprints on the lipidome that may influence long-term health outcomes.
Future research directions should include expanded longitudinal sampling across the entire developmental spectrum, from gestation through older age, to better understand critical transition periods. Additionally, integration of lipidomics with other omics technologies—including genomics, proteomics, and metabolomics—will provide more comprehensive insights into the complex interplay between genetic predisposition, environmental exposures, and metabolic health across the lifespan.
The demonstrated utility of lipidomic signatures for risk prediction and intervention monitoring suggests strong potential for clinical translation. However, standardization of analytical protocols and validation in diverse populations will be essential before widespread clinical implementation. As these methods become more accessible and cost-effective, lipidomic profiling may become an valuable tool for personalized prevention and management of metabolic diseases from early life.
Impact of Lifestyle and Environmental Factors on Population-Specific Lipid Profiles
Lipidomics, the large-scale study of cellular lipids, has evolved into a powerful tool for understanding metabolic health and disease risk. While genetic predispositions establish baseline lipid levels, a growing body of evidence underscores that lifestyle and environmental factors are potent modulators of the lipid profile, contributing to significant variations across different populations. These influences range from broad geographical and climatic conditions to specific dietary and physical activity patterns. Framing lipidomic findings within this context is crucial for cross-population research, as it helps disentangle the complex interplay of inherent and external factors shaping lipid metabolism. This guide objectively compares lipid profile data from diverse populations and details the experimental protocols that enable robust, comparable findings essential for drug development and public health strategies.
Comparative Analysis of Lipid Profiles Across Populations
Environmental and lifestyle factors produce distinct lipid profile signatures in different populations. The following tables synthesize quantitative findings from key studies, highlighting these disparities.
Table 1: Prevalence of Dyslipidemia and Lipid Abnormalities Across Populations
| Population / Study Cohort | Dyslipidemia Prevalence | Key Lipid Abnormalities (Prevalence or Mean Levels) | Primary Associated Environmental/Lifestyle Factors |
|---|---|---|---|
| Islamabad & Rawalpindi, Pakistan [22] | 86% | High TG (50%), Low HDL (48%), High LDL (31%), High TC (29%) | Urbanization, dietary shifts |
| Peruvian Cohort (Rural Areas) [23] | High Non-HDL-C: 88.0% | Hypertriglyceridemia: Lower prevalence vs. urban (PR=0.75) | Rural lifestyle, diet high in carbohydrates, high physical activity [23] |
| Peruvian Cohort (Semi-Urban Areas) [23] | High Non-HDL-C: 96.0% | High LDL-C: Higher prevalence vs. highly urban (PR=1.37) | Transitional economy, changing dietary patterns |
| Chinese Middle-Aged & Elderly [24] | Not Specified | Nonlinear associations with TC, TG, LDL-C, HDL-C | Air pollutants (PM~2.5~, NO~2~, O~3~), meteorological factors (temperature, humidity) |
| Metabolic Syndrome Patients (India) [25] | 91% (≥1 abnormal lipid) | TC: 220.6 ± 38.5 mg/dL, TG: 186.9 ± 54.3 mg/dL, LDL-C: 140.4 ± 31.2 mg/dL, HDL-C: 38.7 ± 8.9 mg/dL | Central obesity, insulin resistance, dietary habits |
Table 2: Lipid Profile Ratios and Cardiovascular Risk Indicators
| Lipid Ratio | Pakistan Study Cohort [22] | Ideal / Low-Risk Ratio | Clinical Interpretation |
|---|---|---|---|
| LDL-C to HDL-C Ratio | 2.7 | < 2.0 | Higher than ideal, indicating elevated cardiovascular disease risk [22] |
| Triglyceride to HDL-C Ratio | 4.7 | < 2.0 | Higher than ideal, indicating elevated risk of insulin resistance and cardiovascular disease [22] |
| Cholesterol to LDL-C Ratio | 1.8 | ~1.0 - 3.0 (Context dependent) | Within normal range [22] |
Detailed Experimental Protocols for Cross-Population Lipidomics
To ensure findings are valid and comparable across different studies and populations, rigorous and standardized experimental protocols are mandatory. The following sections detail key methodologies.
Protocol 1: Blood Collection and Standard Lipid Profile Analysis
This protocol is foundational for clinical lipidology and was used in studies such as the Pakistani dyslipidemia investigation and the Metabolic Syndrome study in India [22] [25].
- Objective: To accurately measure standard lipid panel components (Total Cholesterol, Triglycerides, LDL-C, and HDL-C) from blood serum.
- Sample Collection:
- Sample Processing:
- Collected blood samples are allowed to clot.
- Samples are centrifuged at 5000 rpm for 5 minutes to separate serum from blood cells [22].
- Biochemical Analysis:
- Serum is analyzed on automated clinical chemistry analyzers (e.g., Cobas e-311) [22].
- Enzymatic colorimetric methods are employed to quantify Total Cholesterol, Triglycerides, and HDL-C [25].
- LDL-C is often calculated using the Friedewald formula (provided TG levels are <400 mg/dL): LDL-C = Total Cholesterol - HDL-C - (Triglycerides/5) [25].
- Quality Control: Analysis batches include standard calibrators and control samples to ensure accuracy and reproducibility [22] [25].
Protocol 2: Advanced MS-Based Lipidomics for Biomarker Discovery
This protocol leverages mass spectrometry for deep phenotyping and is critical for studies exploring predictive biomarkers and subtle metabolic shifts, such as the PREVIEW sub-study [26] [27].
- Objective: To identify and quantify a wide panel of lipid species (hundreds to thousands) for discovery of evaluative or predictive biomarkers.
- Sample Preparation:
- A stable isotope dilution approach is used for robust quantification, where known amounts of isotope-labeled lipid standards are added to the samples prior to extraction [7].
- Semiautomated or manual liquid-liquid extraction (e.g., using methyl-tert-butyl ether) is performed to isolate lipids from serum or plasma [7].
- Lipid Separation and Analysis:
- Technique: Liquid Chromatography coupled to Tandem Mass Spectrometry (LC-MS/MS).
- Chromatography: Hydrophilic Interaction Liquid Chromatography (HILIC) is often used for class-specific separation, while Reversed-Phase Chromatography (RPLC) separates lipids by acyl chain length and saturation [26].
- Mass Spectrometry: A high-resolution mass spectrometer operates in data-dependent acquisition (DDA) or multiple reaction monitoring (MRM) modes to measure the mass-to-charge ratio (m/z) of intact lipid ions and their characteristic fragments [26] [27].
- Data Processing:
- Quality Control:
Protocol 3: Statistical and Pathway Analysis for Interpretation
This protocol outlines the analytical workflow for deriving biological meaning from complex lipidomics datasets, particularly in cross-population and intervention studies [24] [28].
- Objective: To identify statistically significant lipid alterations and place them in a biological context.
- Data Preprocessing:
- Normalization: Data is normalized to correct for variations in sample concentration and instrument sensitivity.
- Batch Effect Correction: Methods like ComBat are applied to remove technical artifacts from different processing batches [28].
- Statistical Analysis:
- Univariate Analysis: T-tests (for two groups) or ANOVA (for multiple groups) are used to identify lipids with significant abundance changes, with False Discovery Rate (FDR) correction for multiple testing [28].
- Multivariate Analysis: Principal Component Analysis (PCA) and Partial Least Squares-Discriminant Analysis (PLS-DA) are used to visualize group separations and identify lipids driving the differences [28].
- Machine Learning: For complex datasets, Random Forest models can be used to rank the importance of environmental factors (e.g., air pollutants, temperature) and identify nonlinear associations with lipid levels [24].
- Pathway Analysis:
- Differentially abundant lipids are input into tools like MetaboAnalyst.
- Over-Representation Analysis (ORA) or Pathway Topology Analysis is performed to identify enriched metabolic pathways (e.g., glycerophospholipid metabolism, sphingolipid signaling), providing mechanistic insights [28].
The following diagram visualizes the integrated workflow from sample collection to biological insight.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Lipidomics Research
| Item | Function / Application |
|---|---|
| Serum Separator Tubes (SST) | Collects and preserves blood samples; gel barrier separates serum during centrifugation for clinical lipid profiling [22]. |
| Stable Isotope-Labeled Lipid Standards | Added to samples before extraction; enables absolute quantification by correcting for losses during preparation and ion suppression in MS [7]. |
| NIST Plasma Reference Material | Quality control material analyzed across batches to monitor and correct for instrumental drift and ensure reproducibility in large-scale studies [7]. |
| Chromatography Columns (HILIC & RPLC) | HILIC columns separate lipids by class (polar head group); RPLC columns separate by acyl chain hydrophobicity, providing comprehensive lipidome coverage [26]. |
| Enzymatic Assay Kits | Reagent kits for colorimetric or fluorometric measurement of specific lipid classes (e.g., total cholesterol, triglycerides) on automated analyzers [25]. |
The impact of lifestyle and environmental factors on lipid profiles is profound and varies significantly across populations, driven by factors such as urbanization, diet, altitude, and air pollution. Cross-validation of lipidomic findings demands rigorous, standardized experimental protocols—from meticulous blood collection and advanced mass spectrometry to sophisticated statistical and pathway analysis. For researchers and drug development professionals, acknowledging and controlling for these population-specific influences is paramount. It ensures the discovery of robust biomarkers, facilitates the development of targeted therapies, and ultimately paves the way for more effective, personalized cardiovascular and metabolic disease interventions on a global scale.
Advanced Lipidomic Platforms and Study Designs for Multi-Center Validation
High-Throughput HILIC and RPLC-MS/MS Platforms for Large-Scale Cohort Analysis
Liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) serves as the cornerstone of modern large-scale lipidomic and metabolomic studies. For comprehensive analysis of complex biological samples, no single chromatographic technique can sufficiently capture the entire metabolome. Reversed-Phase Liquid Chromatography (RPLC) and Hydrophilic Interaction Liquid Chromatography (HILIC) have emerged as complementary techniques that, when combined, significantly expand metabolome coverage [29]. This guide provides an objective comparison of these platforms, focusing on their performance characteristics, implementation protocols, and applications in large-scale cohort studies, framed within the context of cross-validating lipidomic findings across different populations.
Technical Comparison of HILIC and RPLC Platforms
Fundamental Separation Mechanisms
Reversed-Phase Liquid Chromatography (RPLC) employs hydrophobic stationary phases (typically C18 or C8) with a polar mobile phase. Separation occurs primarily through hydrophobic interactions, where analytes are retained based on their hydrophobicity. Non-polar compounds with longer alkyl chains and higher molecular weight exhibit stronger retention, while polar compounds elute quickly, often with inadequate separation from the void volume [30] [31].
Hydrophilic Interaction Liquid Chromatography (HILIC) utilizes hydrophilic stationary phases (e.g., bare silica, amide, or zwitterionic materials) with a mobile phase consisting of a high proportion of organic solvent (typically acetonitrile) with a small amount of aqueous buffer. The separation mechanism involves partition of analytes between the organic-rich mobile phase and a water-enriched layer immobilized on the stationary phase, supplemented by secondary electrostatic interactions and hydrogen bonding [32]. This mechanism provides excellent retention for polar and ionizable compounds that are poorly retained in RPLC.
Performance Characteristics in Cohort Studies
Table 1: Quantitative Performance Comparison of HILIC and RPLC Platforms
| Performance Metric | HILIC Platform | RPLC Platform | Combined Approach |
|---|---|---|---|
| Reproducibility (Intrabatch CV) | <12% [29] | Similar to HILIC [29] | Maintains performance of individual methods |
| Reproducibility (Interbatch CV) | <22% (over 40 days) [29] | Similar to HILIC [29] | Maintains performance of individual methods |
| Polar Compound Coverage | Excellent for logD < 0 [30] | Limited for polar compounds [30] | Up to 108% more features in plasma [29] |
| Non-polar Compound Coverage | Limited | ~90% for logD > 0 [30] | Comprehensive coverage |
| Peak Width | ~7 seconds [30] | ~4 seconds [30] | Platform-dependent |
| Analysis Time | ~25 minutes [30] | ~20-24 minutes [30] | Combined runtime ~45 minutes |
Table 2: Compound Class Coverage by Chromatographic Platform
| Compound Class | HILIC Performance | RPLC Performance | Remarks |
|---|---|---|---|
| Phospholipids | Class-based separation [31] | Species-based separation [31] | HILIC co-elutes by class; RPLC separates by fatty acyl chains |
| Sphingolipids | Excellent for glycosphingolipids [10] | Good for ceramides [13] | Complementary coverage |
| Lyso-phospholipids | Effective retention [31] | Moderate retention [31] | Both suitable with different selectivity |
| Acylcarnitines | Excellent retention [33] | Limited retention | HILIC preferred |
| Cholesteryl Esters | Poor retention | Excellent retention [13] | RPLC preferred |
| Triacylglycerols | Limited retention | Excellent retention [10] | RPLC preferred |
| Organic Acids | Good with anion exchange [30] | Limited retention | IC complementary to both |
Experimental Protocols for Large-Scale Cohort Analysis
Sample Preparation Workflow
For comprehensive lipidomic profiling, a standardized sample preparation protocol is essential for maintaining reproducibility across large cohorts:
- Protein Precipitation: Add 375 μL ice-cold methanol to 50 μL plasma, vortex thoroughly [31].
- Lipid Extraction: Add 1250 μL methyl tert-butyl ether (MTBE), vortex, and incubate for 1 hour at 4°C with shaking [31].
- Phase Separation: Add 375 μL water, vortex, centrifuge (10 min, 4°C, 1000×g) [31].
- Organic Phase Collection: Transfer the upper organic phase to a new tube.
- Re-extraction: Repeat extraction of aqueous phase with 500 μL MTBE/MeOH/H2O (4/1.2/1, v/v) [31].
- Combination and Evaporation: Combine organic phases and evaporate to dryness under vacuum [31].
- Reconstitution: Reconstitute in 200 μL pure isopropanol with vigorous vortexing [31].
- Dilution: Dilute with isopropanol to final concentration of 0.03 μL plasma/μL isopropanol [31].
HILIC-MS/MS Methodology
Optimal Stationary Phase: Zwitterionic sulfobetaine (ZIC-HILIC) column (e.g., SeQuant ZIC-HILIC, 2.1 × 100 mm, 1.7 μm) operated at neutral pH provides optimal performance for diverse hydrophilic metabolites [29].
Mobile Phase Composition:
- Eluent A: 95% acetonitrile with 5% water containing 5-10 mM ammonium formate or acetate [30] [29]
- Eluent B: 95% water with 5% acetonitrile containing 5-10 mM ammonium formate or acetate [30] [29]
Gradient Program:
- 0-20 min: 0-40% B (curve linear or slightly convex)
- 20-22 min: 40-100% B
- 22-25 min: 100% B (wash)
- 25-25.1 min: 100-0% B
- 25.1-30 min: 0% B (re-equilibration) [30] [32]
MS Parameters:
- Ionization: ESI positive/negative switching
- Mass Analyzer: Q-TOF or Orbitrap for untargeted; TQ-SIM for targeted
- Scan Range: m/z 100-1500
- Source Temperature: 300°C
- Drying Gas Flow: 10 L/min [30] [29]
RPLC-MS/MS Methodology
Optimal Stationary Phase: C18 columns with aqueous stability (e.g., Hypersil GOLD for urine, Zorbax SB aq for plasma) [29].
Mobile Phase Composition:
- Eluent A: Acetonitrile/water (1:1, v/v) with 5 mM ammonium formate and 0.1% formic acid [31]
- Eluent B: Isopropanol/acetonitrile/water (85:10:5, v/v) with 5 mM ammonium formate and 0.1% formic acid [31]
Gradient Program:
- 0-20 min: 10-86% B (curve 4)
- 20-22 min: 86-100% B
- 22-25 min: 100% B (wash)
- 25-25.1 min: 100-10% B
- 25.1-30 min: 10% B (re-equilibration) [31]
MS Parameters:
- Ionization: ESI positive/negative switching
- Mass Analyzer: Q-TOF or Orbitrap
- Scan Range: m/z 200-2000
- Source Temperature: 300°C
- Drying Gas Flow: 12 L/min [31]
Quality Control Procedures
For large-scale cohort analysis, implement rigorous quality control:
- Pooled QC Samples: Create from aliquots of all samples; analyze regularly throughout batch [7]
- Reference Materials: Include NIST SRM 1950 plasma with each batch [7]
- Internal Standards: Use deuterated lipid standards for quantification (e.g., SPLASH LIPIDOMIX) [31]
- System Suitability Tests: Monitor retention time stability, peak width, and intensity of reference compounds [7]
Figure 1: Integrated HILIC and RPLC-MS/MS Workflow for Large-Scale Cohort Analysis
Cross-Validation of Lipidomic Findings Across Populations
The combination of HILIC and RPLC platforms enables robust cross-validation of lipidomic signatures across diverse populations. This orthogonal approach verifies that identified biomarkers represent true biological signals rather than method-specific artifacts.
Case Study: Cardiovascular Risk Stratification
In a large-scale CAD cohort (n = 1,057), untargeted lipidomics revealed characteristic lipid signatures associated with adverse cardiovascular events [33]. The most prominent upregulated lipids in patients with cardiovascular events belonged to phospholipids and fatty acyls classes. The orthogonal separation by HILIC and RPLC confirmed these findings, with the platelet lipidome identifying 767 lipids with characteristic changes in patients with adverse CV events [33].
Statistical models incorporating both HILIC and RPLC data demonstrated improved risk prediction. The CERT2 score, incorporating ceramides (better separated by RPLC) and phosphatidylcholines (well-separated by both techniques), yielded hazard ratios of 1.44-1.69 for cardiovascular mortality across multiple cohorts [13].
Case Study: Pediatric Inflammatory Bowel Disease (IBD)
A blood-based diagnostic lipidomic signature for pediatric IBD was identified and validated across multiple cohorts using combined chromatographic approaches [10]. The signature comprised:
- Increased lactosyl ceramide (d18:1/16:0) - well-separated by HILIC
- Decreased phosphatidylcholine (18:0p/22:6) - separated by both techniques
This signature achieved an AUC of 0.85 (95% CI 0.77-0.92) in discriminating IBD from symptomatic controls, significantly outperforming hsCRP (AUC = 0.73) [10]. The combination of HILIC and RPLC provided complementary coverage that enhanced diagnostic performance.
Biological Variability and Analytical Reproducibility
In population studies (n = 1,086), HILIC-based methodology demonstrated robust measurement of 782 circulatory lipid species spanning 22 lipid classes [7]. The median between-batch reproducibility was 8.5% across 13 independent batches. Critically, biological variability per lipid species significantly exceeded batch-to-batch analytical variability, confirming that technical performance adequately captures biological signals [7].
Figure 2: Cross-Validation Framework for Lipidomic Findings Across Populations
Essential Research Reagent Solutions
Table 3: Essential Research Reagents for HILIC and RPLC-MS/MS Lipidomics
| Reagent Category | Specific Products | Function & Application | Considerations |
|---|---|---|---|
| Internal Standards | SPLASH LIPIDOMIX [31] | Quantification normalization | "One ISTD-per-lipid class" approach |
| Reference Materials | NIST SRM 1950 [7] | Quality control, inter-lab standardization | Provides consensus values |
| HILIC Columns | ZIC-HILIC [29], BEH Amide [30] | Polar compound separation | Zwitterionic for broad coverage |
| RPLC Columns | Accucore C18 [31], Hypersil GOLD [29] | Non-polar compound separation | Aqueous-stable for lipidomics |
| Extraction Solvents | MTBE, methanol, isopropanol [31] | Lipid extraction from biological matrices | MTBE method provides high recovery |
| Mobile Phase Additives | Ammonium formate, ammonium acetate [32] | MS-compatible buffering | Volatile for MS detection |
HILIC and RPLC-MS/MS platforms offer complementary strengths for large-scale cohort lipidomic analysis. RPLC provides excellent coverage for non-polar to moderately polar lipids (~90% for logD > 0), while HILIC effectively captures polar metabolites poorly retained by RPLC. When combined, these platforms expand metabolome coverage by 44-108% compared to RPLC alone [29], enabling more comprehensive biomarker discovery.
The orthogonal separation mechanisms facilitate cross-validation of lipidomic findings across different populations, strengthening the biological significance of identified signatures. Implementation of standardized protocols with rigorous quality control enables reproducible measurement of hundreds of lipid species across large cohorts, with between-batch reproducibility of <10% achievable [7].
For large-scale cohort studies aiming to discover and validate lipidomic biomarkers, a combined HILIC and RPLC approach provides the most comprehensive coverage and strongest validation framework, ultimately enhancing the translation of lipidomic findings into clinically useful applications.
Reproducibility is a fundamental pillar of scientific research, yet it remains a significant challenge in lipidomics, especially in multi-center studies where protocol variations can lead to inconsistent results [34]. The integration of lipidomic profiles into clinical and precision medicine hinges on the ability to cross-validate findings across diverse populations reliably. Automated sample preparation has emerged as a critical technological solution, minimizing manual handling errors and standardizing protocols to enhance data reproducibility [35] [36]. This guide objectively compares the performance of automated and manual sample preparation methods, providing researchers and drug development professionals with experimental data to inform their analytical strategies for large-scale, multi-population lipidomic studies.
The Role of Standardization in Cross-Validation Lipidomics
Cross-validation of lipidomic findings across different populations requires exceptionally high levels of analytical consistency. Biological lipidomes are highly dynamic and influenced by genetics, diet, and environment, introducing substantial inter-individual variability that can obscure genuine biomarker signals [26]. In multi-center studies, this inherent biological variation is compounded by pre-analytical inconsistencies arising from differences in sample handling, extraction techniques, and operator skill across sites [34].
Automated sample preparation directly addresses these challenges by implementing standardized, protocol-driven workflows that are consistently replicated across instruments and laboratories. This standardization is crucial for reducing operational variances, thereby ensuring that observed lipid differences reflect true biological phenomena rather than technical artifacts [35]. The resulting improvement in data quality strengthens the statistical power of studies exploring lipidomic variations across demographic and geographic populations, ultimately accelerating the translation of lipid biomarkers into clinical practice [37].
Performance Comparison: Automated vs. Manual Sample Preparation
Direct comparative studies provide compelling evidence for the advantages of automation in lipidomic sample preparation. The following data, synthesized from cross-validation studies, highlights key performance metrics.
Table 1: Performance comparison between manual and automated sample preparation for lipidomics
| Performance Metric | Manual Preparation | Automated Preparation | Implications for Multi-Center Studies |
|---|---|---|---|
| Precision (CV%) | Majority < 15% [38] | Majority < 15%; occasional species >20% [38] | Good overall precision; automation requires method optimization for specific lipids |
| Throughput | Limited by manual pipetting | High; 96-well or 384-well plate formats [35] [36] | Essential for processing thousands of samples in large biobanks [38] |
| Calibration Accuracy (Mean Bias%) | Mostly between -10% to +10% [38] | Mostly between -20% to +20% [38] | Automated methods meet acceptance criteria but may show slightly higher variability |
| Sample-to-Sample Variation | Higher due to human intervention | 1.8-fold reduction reported in proteomics [36] | Directly enhances reproducibility across study sites |
| Operator Dependency | High | Minimal after initial programming | Critical for standardizing protocols across multiple research centers |
Case Study: Phosphatidylethanol (PEth) Analysis in Whole Blood
A robust comparison between an optimized automated method and a manual method for quantifying the alcohol biomarker PEth 16:0/18:1 in whole blood demonstrates automation's practical benefits. The automated method used a liquid handler for a 96-well plate format with blood samples pre-treated by freezing to reduce viscosity and clogging. The manual method involved traditional tube-based liquid-liquid extraction [39].
Both methods were validated and showed good agreement, with coefficients of variation (CV) below 15% and accuracy within 15% of the target value. A key finding was that the automated method effectively eliminated pipetting challenges associated with viscous whole blood, improving operational robustness. Furthermore, the automated 96-well format significantly increased throughput, enabling rapid processing of large sample volumes received by the laboratory [39].
Case Study: Cross-Validation of a High-Throughput Lipidomics Platform
In another systematic comparison, a manual protein precipitation protocol was cross-validated against an automated procedure using a Hamilton Microlab STAR liquid handling system for the analysis of multiple lipid classes in plasma.
The results demonstrated that both methods produced CVs mostly below 15% across a set of internal standards (n=40). While the manual preparation yielded slightly better accuracy for back-calculated standard concentrations (majority within ±10% vs. ±20% for automation), the automated procedure satisfactorily met method acceptance criteria. The authors concluded that automation offers a cost-effective solution for large-scale lipidomic studies, despite manual preparation in glass vials potentially providing marginally superior precision for smaller datasets [38].
Detailed Experimental Protocols
To ensure experimental reproducibility, this section outlines the specific methodologies from the cited comparison studies.
- Sample Pretreatment: For the automated method, all whole blood samples (calibrators, quality controls, and clinical samples) were frozen at -80 °C for at least 60 minutes to induce hemolysis. This step reduces viscosity and prevents pipette tip clogging.
- Automated Extraction (96-well plate):
- An automated liquid handler was used to transfer 50 µL of pre-treated frozen blood and 200 µL of 2-propanol (containing internal standard) to a 96-well plate.
- The aspirating and dispensing parameters for the blood and solvent were specifically optimized for the robot.
- The plate was sealed, mixed, and then centrifuged.
- The supernatant was directly transferred to an analysis plate for UHPLC-MS/MS.
- Manual Extraction (Tube-based):
- 50 µL of untreated whole blood was manually pipetted into a tube.
- 200 µL of 2-propanol (with internal standard) was added.
- The tube was vortex-mixed and then centrifuged.
- The supernatant was manually transferred to a vial for UHPLC-MS/MS.
- UHPLC-MS/MS Analysis: Chromatographic separation was performed, and PEth 16:0/18:1 was detected and quantified using mass spectrometry in multiple reaction monitoring (MRM) mode.
- Sample Preparation: The study used a simple protein precipitation method suitable for automation.
- Manual Protocol: One part plasma (25 µL) was transferred to a low-protein-binding Eppendorf tube, and five parts of an isopropanol/acetonitrile (1:2, v/v) solution containing a cocktail of deuterated internal standards were added. Samples were vortexed, shaken for two hours at 5°C, and then centrifuged. The supernatant was transferred to glass vials for LC-MS/MS analysis.
- Automated Protocol: The above steps were replicated using a Hamilton Microlab STAR liquid handling system in a 96-well plate format. After centrifugation, the supernatant was automatically transferred to a 96-well analysis plate.
- LC-MS/MS Analysis (LipidQuan Workflow):
- Instrumentation: Waters ACQUITY UPLC I-Class PLUS System coupled to a Xevo TQ-XS Mass Spectrometer.
- Chromatography: An ACQUITY UPLC BEH Amide Column (2.1 mm x 100 mm, 1.7 µm) was used. Lipids were separated over an 8-minute gradient.
- Mass Spectrometry: Data acquisition was performed in both positive and negative ionization modes using targeted multiple reaction monitoring (MRM).
- Data Analysis: Lipid identification and quantification were performed using TargetLynx software, comparing back-calculated concentrations of standards and QC replicates between the two preparation methods.
Essential Research Reagent Solutions
The following reagents and materials are critical for implementing robust and reproducible lipidomics sample preparation, whether manual or automated.
Table 2: Key research reagents and materials for lipidomic sample preparation
| Reagent/Material | Function in Workflow | Example Use Case |
|---|---|---|
| Deuterated Internal Standards (e.g., Splash Lipidomix) | Corrects for extraction efficiency and instrument variability; essential for quantification [40] [38] | Added to plasma/serum before protein precipitation to monitor performance of each sample [38] |
| Isopropanol/Acetonitrile Solvent System | Precipitates proteins and efficiently extracts a broad range of lipid classes [38] | Used in a 1:2 (v/v) ratio with plasma for simple and automatable protein crash [38] |
| Chlorinated Solvents (e.g., Dichloromethane) | Facilitates liquid-liquid extraction for comprehensive lipid recovery [40] | Used in a modified Bligh & Dyer method (DCM/MeOH/water 2:2:1) for wide lipid coverage [40] |
| 96-Well Plates (Polypropylene) | Standardized format for high-throughput automated processing | Used in robotic systems for holding samples, reagents, and final extracts [39] [38] |
| Calibrator Solutions (e.g., Odd-Chained Lipidomix) | Enables construction of calibration curves for absolute quantification | Spiked into control matrix to create a standard curve for concentration calculations [38] |
Workflow and Impact Visualization
The logical progression from sample collection to data acquisition, and the comparative impact of manual versus automated methods on data quality, can be visualized through the following diagrams.
Diagram 1: Comparative sample preparation workflow.
Diagram 2: Impact on multi-center study objectives.
The consistent implementation of automated sample preparation is a critical success factor for cross-validating lipidomic findings across different populations. While manual methods can achieve excellent precision on a small scale, the operational superiority of automation in reducing human error, standardizing protocols, and enabling high-throughput is undeniable for multi-center research [39] [36] [38]. As the field moves toward integrating lipidomics into precision medicine, the adoption of these robust, scalable workflows will be indispensable for generating reproducible and clinically actionable data from diverse global cohorts.
Crossover study designs represent a powerful methodological approach in clinical research, enabling investigators to compare interventions with greater precision by having each participant serve as their own control. This design significantly reduces inter-individual variability—a major confounding factor in parallel-group trials—particularly valuable in emerging fields like lipidomics where biological variability can obscure treatment effects. By minimizing the influence of confounding variables and reducing sample size requirements, crossover trials offer distinct advantages for detecting subtle intervention effects. However, these designs require careful implementation to address potential carryover effects and other methodological challenges. This review examines the fundamental principles, applications, and methodological considerations of crossover designs, with emphasis on their growing importance in nutritional science, pharmacology, and biomarker research.
Crossover studies are randomized, repeated measurement designs where participants receive multiple interventions in sequential periods, typically separated by washout phases [41]. In the most basic 2x2 crossover design, participants are randomly allocated to one of two sequences: receiving treatment A followed by B, or treatment B followed by A [42]. This design enables direct within-participant comparison of interventions, effectively controlling for inherent biological variability that often confounds parallel-group studies where each participant receives only one treatment [43].
The fundamental strength of crossover designs lies in their ability to separate within-participant variability from between-participant variability [43]. In traditional parallel-group designs, between-participant variability inflates standard errors, potentially masking true treatment effects. By using each participant as their own control, crossover designs eliminate between-participant variability from treatment effect estimates, resulting in greater statistical power and precision [43]. This advantage is particularly valuable when studying heterogeneous populations or interventions with modest effect sizes, as it allows researchers to detect differences with smaller sample sizes—in some cases reducing participant requirements by 60-70% compared to parallel designs [41].
Crossover designs have evolved significantly since their initial application in agricultural experiments in the mid-nineteenth century [43]. Today, they are extensively used in pharmaceutical development (particularly bioequivalence studies), nutritional science, psychology, and biomarker research [43]. Their utility continues to expand with the growing emphasis on personalized medicine and understanding of individual differences in treatment response.
Fundamental Principles and Mechanisms
Core Components and Terminology
Understanding crossover designs requires familiarity with several key components:
- Treatments: The interventions being compared, typically denoted by capital letters (A, B, etc.) [42]
- Sequence: The order in which treatments are administered to participant groups (e.g., AB or BA) [41]
- Period: The time during which a specific treatment is administered and outcomes are measured [41]
- Washout: A critical interval between treatment periods where no intervention is administered, allowing treatment effects to dissipate [41]
The most fundamental crossover design is the 2x2 crossover (2 treatments, 2 sequences, 2 periods), though more complex designs exist for comparing multiple treatments across multiple periods [43]. The design's structure enables researchers to distinguish several effects: direct treatment effects, period effects (where outcomes differ based on timing regardless of treatment), and sequence effects (where the order of administration influences results) [42].
Statistical Foundation
The statistical advantage of crossover designs becomes apparent when comparing their model to parallel-group designs. In a parallel-group trial, the response for the k-th subject in the i-th group is represented as:
Yik = μ + τd*(i) + E_ik
where Eik includes both between-subject variability (σs²) and within-subject variability (σ²) [43]. This combination inflates standard errors for treatment effect estimates. In contrast, crossover designs enable estimation of treatment effects through within-subject differences, effectively eliminating between-subject variability and resulting in smaller standard errors and greater statistical power [43].
Table 1: Key Advantages and Disadvantages of Crossover Designs
| Advantages | Disadvantages |
|---|---|
| Each participant serves as own control, reducing confounding [44] | Potential for carryover effects from previous treatments [41] |
| Requires smaller sample sizes (60-70% reduction in some cases) [41] | Not suitable for acute or curable conditions [41] |
| Increased statistical power for detecting treatment differences [43] | Longer study duration may increase dropout rates [41] |
| All participants receive active treatment at some point [41] | Complex statistical analysis requiring specialized expertise [45] |
| Ideal for detecting individual response variability [46] | Cannot be used for treatments with permanent effects [44] |
Experimental Evidence and Comparative Data
Exercise Physiology Application
A rigorous crossover study examined individual variability in responses to different exercise training protocols [46]. Twenty-one recreationally active adults completed three weeks of both endurance training (END: 30 minutes at ~65% VO₂peak) and sprint interval training (SIT: eight 20-second intervals at ~170% VO₂peak) in randomized order with a three-month washout period between interventions [46].
The study demonstrated significant inter-individual variability in training responses. While group-level analyses showed main effects of training for VO₂peak, lactate threshold, and submaximal heart rate, individual patterns differed substantially between END and SIT protocols [46]. Using typical error (TE) measurement to define non-response (failing to demonstrate changes greater than 2×TE), researchers identified non-responders for VO₂peak (TE: 0.107 L/min), lactate threshold (TE: 15.7 W), and submaximal heart rate (TE: 10.7 bpm) following both END and SIT [46].
Table 2: Response Rates to Different Exercise Training Modalities [46]
| Outcome Measure | Non-Responders to END | Non-Responders to SIT | Consistent Responders to Both |
|---|---|---|---|
| VO₂peak | Observed | Observed | Pattern differed between protocols |
| Lactate Threshold | Observed | Observed | Pattern differed between protocols |
| Submaximal Heart Rate | Observed | Observed | Pattern differed between protocols |
| Key Finding | All individuals responded in at least one variable when exposed to both END and SIT |
Notably, the study found no significant positive correlations between individual responses to END versus SIT across any measured variable, suggesting that non-response to one training modality does not predict non-response to another [46]. This highlights the value of crossover designs for detecting individual-specific intervention effects that would be obscured in group-level analyses.
Nutritional Intervention Application
A replicate crossover trial investigating dietary nitrate supplementation provides another exemplary application [47]. Fifteen healthy males participated in a double-blind, placebo-controlled trial where they consumed either nitrate-rich beetroot juice (~14.0 mmol nitrate) or nitrate-depleted beetroot juice (~0.03 mmol nitrate) on four separate laboratory visits, with each condition administered twice in randomized order [47].
The replicate design (multiple administrations of each condition) enabled formal quantification of participant-by-treatment interaction variance, a robust approach for characterizing true inter-individual response differences beyond random within-subject variability [47]. Results showed that nitrate-rich supplementation significantly reduced systolic blood pressure by a mean of -7 mmHg (95% CI: -3 to -11) and diastolic blood pressure by -6 mmHg (95% CI: -2 to -9) versus placebo [47].
Crucially, the researchers identified substantial inter-individual variability in these responses, with participant-by-condition interaction variability of ±7 mmHg (95% CI: 3 to 9) for systolic blood pressure [47]. Between-replicate correlations were moderate-to-large for plasma nitrate (r=0.55-0.91), nitrite (r=0.55-0.91), and systolic blood pressure (r=0.55-0.91), indicating consistent individual responses across repeated administrations [47].
Methodological Implementation
Design Considerations
Successful implementation of crossover designs requires careful attention to several methodological factors:
Participant Selection: Crossover designs are most appropriate for stable chronic conditions where symptoms return to baseline after treatment withdrawal [41]. They are unsuitable for acute conditions or diseases that are curable through intervention [44]. Participants should have conditions that are relatively stable over the study period, as rapidly progressing diseases may confound treatment effects [41].
Washout Period Determination: The washout period between treatments must be sufficiently long to eliminate carryover effects (where effects of the first treatment persist into the second period) [41]. The appropriate duration depends on the pharmacological properties of interventions or the persistence of physiological effects. Washout periods should be justified based on known kinetics of the interventions being studied [45].
Randomization and Blinding: Proper randomization of treatment sequences is essential to minimize confounding [45]. Blinding both participants and investigators to treatment sequence helps prevent bias, particularly given the potential for participants to detect treatment effects that could unmask their assignment [41].
Diagram 1: 2x2 Crossover Study Workflow
Statistical Analysis Approaches
Appropriate statistical analysis of crossover trials requires specialized approaches that account for the design's structure:
Primary Analysis Model: For continuous outcomes, a linear mixed model incorporating fixed effects for treatment, period, and sequence, with random participant effects, is often appropriate [43]. This approach can accommodate missing data under plausible assumptions and provide valid treatment effect estimates.
Handling Carryover Effects: Testing and adjusting for potential carryover effects remains controversial in statistical literature. Some statisticians recommend testing for carryover effects using treatment-by-period interaction terms, while others advocate for designs that minimize carryover risk through adequate washout periods rather than statistical adjustment [43].
Replicate Designs for Response Heterogeneity: Conventional crossover designs cannot distinguish true inter-individual response variability from random within-subject variation [47]. Replicate crossover designs, where each treatment is administered multiple times, enable formal quantification of participant-by-treatment interaction variance through within-participant linear mixed models or meta-analytic approaches [47].
Diagram 2: Statistical Model Components
Application to Lipidomics and Biomarker Research
Special Value for Lipidomic Studies
Crossover designs offer particular advantages for lipidomic research and biomarker validation for several reasons:
Reducing Biological Variability: Lipid profiles exhibit substantial natural inter-individual variation influenced by genetics, diet, microbiome composition, and other factors [37]. Crossover designs control for this baseline variability, enhancing ability to detect intervention-induced lipid changes that might otherwise be obscured [37].
Biomarker Response Characterization: The ability to detect individual response patterns makes crossover designs ideal for identifying lipidomic biomarkers that predict therapeutic response [37]. This aligns with precision medicine approaches seeking to match interventions to individual biochemical phenotypes.
Methodological Alignment: Lipidomic technologies, particularly mass spectrometry-based platforms, demonstrate technical variability that can be better controlled in within-participant designs [37]. Crossover designs reduce the impact of both biological and technical variability on treatment effect estimation.
Lipidomic-Specific Methodological Adaptations
Implementing crossover designs in lipidomics research requires specific methodological considerations:
Washout Period Determination: For nutritional interventions affecting lipid metabolism, washout periods must account for the turnover rates of relevant lipid species, which can range from hours to weeks depending on lipid classes [37]. Pilot studies may be necessary to establish appropriate washout durations.
Baseline Assessment: Comprehensive lipidomic profiling at baseline enables examination of whether baseline lipid patterns moderate intervention responses, potentially identifying biomarkers predictive of treatment success [37].
Response Definition: Lipidomic studies typically examine multiple lipid species simultaneously, requiring careful definition of response endpoints and appropriate multiple testing corrections [37].
Table 3: Essential Research Reagents for Crossover Lipidomic Studies
| Reagent/Category | Primary Function | Application Notes |
|---|---|---|
| Mass Spectrometry Systems | Lipid identification and quantification | LC-MS/MS platforms recommended for broad lipid coverage [37] |
| Internal Standards | Quantification normalization | Stable isotope-labeled standards essential for accurate quantification [37] |
| Lipid Extraction Solvents | Lipid isolation from biological samples | Methyl-tert-butyl ether (MTBE) methods often preferred [37] |
| Chromatography Columns | Lipid separation | C18 and HILIC columns provide complementary separation mechanisms [37] |
| Quality Control Pools | Monitoring analytical performance | Pooled reference samples critical for assessing run-to-run variability [37] |
Current Challenges and Reporting Standards
Methodological Limitations
Despite their advantages, crossover designs face several implementation challenges:
Carryover Effects: Persistent effects of previous treatments remain the primary concern [41]. While adequate washout periods can minimize this risk, some interventions may have prolonged or permanent effects that preclude crossover designs entirely [44].
Missing Data: Participant dropout between periods poses greater threats to validity in crossover than parallel designs, as participants who complete only one period contribute little to the analysis [41]. Statistical approaches like mixed models that accommodate missing data are often necessary.
Period and Sequence Effects: Temporal changes in participant status unrelated to treatment (period effects) or interaction between treatment order and response (sequence effects) can complicate interpretation if not properly accounted for in design and analysis [42].
Reporting Quality and Guidelines
Current reporting of crossover trials shows significant deficiencies. A comprehensive review found that only 17% of published crossover trials reported allocation concealment, 7% described sequence generation, and 29% addressed carryover issues in their methods [45]. Furthermore, only 20% reported sample size calculations, and just 31% of these considered the paired nature of data in their calculations [45].
To improve reporting quality, researchers should:
- Clearly describe randomization methods and allocation concealment
- Justify washout period duration based on intervention pharmacokinetics/pharmacodynamics
- Pre-specify methods for testing and handling carryover and period effects
- Report appropriate variance estimates to enable future meta-analyses
- Use CONSORT flow diagrams to document participant progression through all study periods
Crossover study designs offer a powerful approach for reducing inter-individual variability in clinical trials, particularly valuable for detecting subtle intervention effects and individual response differences. Their efficiency and sensitivity make them ideally suited for emerging research areas like lipidomics, where controlling biological variability is essential for identifying robust biomarkers and treatment responses.
Successful implementation requires careful attention to design elements—particularly adequate washout periods and appropriate statistical analysis—to address potential carryover effects and other limitations. As precision medicine advances, the ability of crossover designs to characterize individual response heterogeneity will become increasingly valuable for understanding variable treatment effects and developing personalized intervention strategies.
Future methodological developments, particularly in replicate crossover designs and sophisticated mixed modeling approaches, will further enhance our ability to distinguish true inter-individual response differences from random variability. Improved reporting standards will also increase the validity and utility of published crossover studies across biomedical research domains.
Lipidomics, the large-scale study of lipid pathways and networks, is a rapidly developing field with diverse applications in clinical and health biomarker discovery [48]. However, the absence of community-wide established guidelines, protocols, or best practices presents a significant challenge for measurement comparability and data quality [48]. This methodological diversity was starkly illustrated in the National Institute of Standards and Technology (NIST) Lipidomics Interlaboratory Comparison Exercise (NIST-ILCE), where no two lipidomics workflows were the same among the 31 participating laboratories [49]. Such variability complicates the cross-validation of lipidomic findings across different populations and research sites, undermining the reproducibility of biological interpretations.
The strategic implementation of Standard Reference Materials (SRMs) and robust batch correction techniques forms the cornerstone of a quality control framework designed to overcome these challenges. SRMs provide a benchmark to assess the validity of diverse lipidomics workflows, enabling harmonization across platforms and laboratories—the essential first step toward full standardization [49]. This guide objectively compares the performance of NIST reference materials and analytical tools in bridging methodological gaps, providing researchers with experimental data and protocols to ensure their lipidomic measurements are accurate, reproducible, and comparable across studies.
The NIST Lipidomics Reference Material: SRM 1950
NIST Standard Reference Material (SRM) 1950, "Metabolites in Frozen Human Plasma," is a cornerstone for quality control in both metabolomics and lipidomics applications [49]. Developed as a "normal" human plasma reference material, SRM 1950 was constructed from 100 fasting individuals, ages 40-50, who represented the average U.S. population as defined by race, sex, and health [49]. This composition makes it particularly valuable for studies aiming to cross-validate findings across diverse human populations.
SRM 1950 is primarily used as a matrix-matched quality control material, extracted alongside test plasma samples to monitor analytical performance [49]. Its key function is to help laboratories assess the reproducibility and quality of their datasets, which directly affects the biochemical interpretation of results [49]. While certified values for SRM 1950 are available only for selected metabolites (e.g., amino acids, vitamins, carotenoids), fatty acids, and total cholesterol, it also provides "reference" and "information" values that, although not metrologically traceable, are highly useful when assessing measurements from similar analytical systems [49].
Consensus Values from Interlaboratory Comparison
To address the need for robust benchmark values reflecting the diversity of the lipidome, NIST established consensus mean concentrations for SRM 1950 through its Lipidomics Interlaboratory Comparison Exercise (NIST-ILCE) involving 31 diverse national and international laboratories [49]. These consensus values provide a critical resource for harmonizing results across different analytical platforms.
Table 1: Lipid Categories and Classes with Consensus Values in SRM 1950
| Lipid Category | Lipid Classes Covered | Consensus Value Type |
|---|---|---|
| Fatty Acyls (FA) | Free Fatty Acids (FFA), Eicosanoids | MEDM, DSL estimates |
| Glycerolipids (GL) | Diacylglycerols (DAG), Triacylglycerols (TAG) | MEDM, DSL estimates |
| Glycerophospholipids (GP) | Lysophosphatidylcholines (LPC), Phosphatidylcholines (PC), Lysophosphatidylethanolamines (LPE), Phosphatidylethanolamines (PE), Phosphatidylglycerols (PG), Phosphatidylinositols (PI), Phosphatidylserines (PS) | MEDM, DSL estimates |
| Sphingolipids (SP) | Ceramides (CER), Dihydroceramides (CerOH), Hexosylceramides (HexCer), Lactosylceramides (LacCer), Sphingomyelin (SM), Sphingosine-1-phosphate (S1P), Sphinganine-1-phosphate (dhS1P) | MEDM, DSL estimates |
| Sterols (ST) | Cholesteryl Esters (CE), Free Cholesterol/Cholesterol Derivatives (FC/CHOL), Bile Acids (BA) | MEDM, DSL estimates |
The consensus means were calculated using two statistical approaches. For lipid species measured by five or more laboratories with coefficient of dispersion (COD) values ≤40%, the Median of Means (MEDM) estimation method was used [49]. To expand lipidome coverage, the DerSimonian Laird (DSL) estimation method was applied for lipid species measured by three or four laboratories with CODs ≤40% and a ≤20% percent difference between MEDM and DSL estimations [49]. All consensus mean estimates, uncertainties, and calculations are provided in the NIST Internal Report [49].
Comparative Performance: LipidQC vs. Alternative Quantitation Approaches
The LipidQC Visualization Tool
LipidQC is a semiautomated visualization tool that addresses the harmonization challenge in lipid quantitation by providing a platform-independent method for comparing experimental results of SRM 1950 against the benchmark consensus mean concentrations derived from the NIST-ILCE [49]. This open-source tool enables researchers to rapidly compare their measured lipid concentrations (nmol/mL) with community-derived consensus estimates and corresponding uncertainties, independent of their specific sample preparation methods, MS instruments, or lipid adduct formation [49].
LipidQC supports a wide array of lipid nomenclature conventions, including sum composition annotations (e.g., PC 34:2), fatty acid position level with known fatty acyl position [PC(16:0/18:1)], and fatty acid level with unknown fatty acyl position [PC(16:0_18:1)] [49]. The tool automatically parses user-provided lipid species names to determine: (1) lipid class, (2) sum composition of each lipid species using methodology employed in LipidPioneer, and (3) sum concentration of isobaric lipid species of the same lipid class [49]. This functionality is particularly valuable for handling the complex isomeric relationships in lipidomics data.
Performance Comparison with Other Quantitation Methods
Table 2: Performance Comparison of Lipid Quantitation and QC Approaches
| Method/Approach | Traceability | Lipidome Coverage | Interlaboratory Validation | Ease of Implementation |
|---|---|---|---|---|
| LipidQC with SRM 1950 | Consensus values from 31 labs | Broad: 5 major categories, 22 classes | Extensive (NIST-ILCE) | Moderate (requires data input) |
| Traditional Internal Standards | Instrument response | Limited to available standards | Laboratory-specific | High |
| LIPID MAPS Targeted Analysis | Single laboratory reference | 588 abundant species | Limited to targeted workflows | High for specified lipids |
| In-house QC Materials | Laboratory-specific | Variable | None | Variable |
When compared to alternative quantitation strategies, the LipidQC/SRM 1950 combination demonstrates distinct advantages. The 2011 LIPID MAPS consortium quantified 588 of the more abundant lipid species in SRM 1950 using a targeted triple quadrupole mass spectrometry platform [49] [48]. However, these values were obtained by a single laboratory and are primarily comparable only to targeted lipidomics workflows, limiting their utility for untargeted lipidomics studies [49]. In contrast, the NIST-ILCE consensus values reflect measurements from 31 diverse laboratories employing both global and targeted lipidomic methodologies across academia, industry, and core facilities [49].
The top five challenges perceived by the lipidomics community, identified through a comprehensive NIST questionnaire, were: (1) lack of standardization amongst methods/protocols, (2) lack of lipid standards, (3) software/data handling, (4) quantification challenges, and (5) over-reporting/false positives [48]. The LipidQC/SRM 1950 framework directly addresses four of these five critical challenges.
Experimental Protocols for Implementing NIST SRM 1950
Sample Preparation Methodologies
The following protocols have been successfully applied for lipid extraction from SRM 1950 and can be implemented with common laboratory equipment:
Method A: Standard Bligh-Dyer Extraction
- Use 30 μL of SRM 1950 plasma for lipid extraction [49]
- Employ the classic Bligh-Dyer protocol using chloroform:methanol:water mixture (1:2:0.8 v/v/v) [49]
- Vortex mixture thoroughly and centrifuge to separate phases
- Collect organic (lower) phase containing lipids
- Evaporate under nitrogen stream and reconstitute in appropriate MS-compatible solvent
Method B: Modified Bligh-Dyer Extraction
- Use 25 μL of SRM 1950 plasma [49]
- Implement modifications appropriate for your specific analytical platform
- Adjust solvent ratios to optimize recovery for your target lipid classes
- Include internal standards as needed for quantification
Instrumental Analysis Conditions
The extracted lipids can be analyzed using various instrumental platforms, with the following conditions providing representative examples:
High-Resolution LC-MS Platform (Used with Method A)
- Instrument: High-resolution orbitrap mass spectrometer coupled to UHPLC system [49]
- Column: Waters Acquity C18 BEH (2.1 mm × 100 mm, 1.7 μm particle size) at 60°C [49]
- Injection Volume: 5 μL (positive ion mode) and 10 μL (negative ion mode) [49]
- Mobile Phase:
- Phase C: acetonitrile/water (60:40, v/v)
- Phase D: isopropanol/acetonitrile/water (90:8:2, v/v/v)
- Both containing 10 mmol/L ammonium formate and 0.1% formic acid [49]
- Gradient: Optimized for comprehensive lipid separation
- Detection: Full scan and data-dependent MS/MS (m/z 150-2000) [49]
Triple Quadrupole LC-MS Platform (Used with Method B)
- Instrument: Triple quadrupole mass spectrometer coupled to LC system for direct flow injection [49]
- Injection Volume: 50 μL (two injections) [49]
- Ionization: ESI positive and negative mode with MRM transitions
- Data Acquisition: Multiple Reaction Monitoring (MRM) for targeted lipid classes including FFA, TAG, DAG, CE, PC, LPC, PE, LPE, SM, and CER [49]
Data Processing with LipidQC
After instrumental analysis, implement the following workflow to assess data quality:
- Convert raw data to concentration values (nmol/mL) for lipids identified in SRM 1950
- Format data according to LipidQC requirements (supported nomenclature)
- Input concentration data into LipidQC for comparison with NIST-ILCE consensus values
- Generate visual output to identify systematic biases or variability in your workflow
- Adjust calibration or methodology based on discrepancies identified
Visualizing the Quality Control Workflow
The following diagram illustrates the integrated workflow for implementing NIST reference materials and batch correction in lipidomics studies:
Diagram 1: Quality Control Workflow for Lipidomics - Integrating SRM 1950 and LipidQC for cross-validation.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for Lipidomics QC
| Material/Reagent | Function in QC Workflow | Example Source/Product |
|---|---|---|
| SRM 1950: Metabolites in Frozen Human Plasma | Matrix-matched reference material for assessing measurement accuracy and precision | NIST Office of Reference Materials |
| NISTmAb (RM 8671) | IgG1κ monoclonal antibody standard for system suitability in protein-lipid interaction studies | NIST Biomanufacturing Program [50] |
| NISTCHO (RM 8675) | Living cell reference material for evaluating bioprocesses in lipid metabolism studies | NIST Biomanufacturing Program [50] |
| Chloroform, Methanol, Water (HPLC grade) | Lipid extraction solvents for sample preparation | Various commercial suppliers |
| Ammonium Formate, Formic Acid | Mobile phase additives for LC-MS analysis | Various commercial suppliers |
| Internal Standard Mixtures | Isotopically-labeled lipid standards for quantification | Various commercial suppliers |
| SRM 1989: Monodisperse Particles | Particle size standard for instrument qualification in automated systems | NIST Store [51] |
Implementing a robust quality control framework centered on NIST reference materials and batch correction strategies is essential for generating reliable, comparable lipidomics data. The combination of SRM 1950 and the LipidQC visualization tool provides an objectively validated solution that outperforms laboratory-specific approaches and single-laboratory reference values. This framework directly addresses the most critical challenges identified by the lipidomics community, particularly the lack of standardization and quantification issues [48].
For researchers focused on cross-validating lipidomic findings across different populations, this QC framework offers a standardized approach to ensure that observed biological differences reflect true variation rather than methodological artifacts. The consensus values derived from the NIST Interlaboratory Comparison Exercise create a common reference point that transcends individual methodological choices, enabling meaningful comparison of data generated across different platforms, laboratories, and study populations. By adopting these practices, the lipidomics community can advance toward greater harmonization, ultimately strengthening the biological insights gained from lipid profiling in diverse human populations.
Addressing Analytical and Biological Challenges in Multi-Population Lipidomics
In biomedical research, particularly in fields like clinical lipidomics and cell-free DNA (cfDNA) analysis, the journey from sample collection to data generation is fraught with potential variables that can compromise data integrity. The pre-analytical phase—encompassing sample collection, handling, transportation, temporary storage, processing, and extraction—represents a critical juncture where standardization is paramount for generating reliable, reproducible results. Studies indicate that pre-analytical variables account for up to 75% of laboratory errors in diagnostic testing, highlighting their profound impact on data quality and study outcomes [52] [53].
The challenge is particularly acute in cross-validation lipidomic studies across different populations, where inconsistencies in pre-analytical procedures can introduce artifacts that obscure true biological signals. Without rigorous standardization, distinguishing between actual biological differences and procedural artifacts becomes challenging, potentially invalidating cross-population comparisons [54] [26]. This guide objectively compares the effects of various pre-analytical approaches on sample integrity and analytical results, providing researchers with evidence-based protocols to enhance data reliability.
Critical Pre-Analytical Variables and Their Standardization
Sample Collection and Initial Handling
Sample collection constitutes the first and perhaps most crucial step in the pre-analytical workflow. The methods and materials used during collection can significantly influence downstream analyses.
Blood Collection Tubes: The choice of anticoagulant in blood collection tubes systematically impacts downstream analyses. EDTA tubes are widely recommended for cfDNA studies, while specialized cell-free DNA collection tubes containing preservation reagents demonstrate superior performance for maintaining sample integrity over extended processing delays [54]. Heparin should be avoided for molecular studies due to its inhibitory effect on PCR amplification [53].
Urine Sample Considerations: Urine cfDNA presents unique challenges due to its sensitivity to environmental conditions such as temperature and pH. Without appropriate preservation solutions, urine cfDNA degrades rapidly, resulting in inadequate concentrations for downstream analysis compared to blood-derived cfDNA [54].
Tissue Sample Preservation: Tissue samples requiring subsequent processing must be maintained in metabolically active states after excision. Collection in specialized media or custodial solutions like Histidine-Tryptophan-Ketoglutarate (HTK) allows tissues to remain viable briefly outside the body [53]. Immediate preservation with reagents such as RNAlater is essential for RNA studies.
The time-to-processing represents one of the most critical variables. Standard protocols recommend preparing serum and plasma within 2-4 hours of blood collection [53]. When immediate processing is impossible, maintaining consistent handling conditions across all samples within a study is essential to minimize variability [53].
Transportation and Temporary Storage Conditions
Transportation conditions and temporary storage parameters significantly influence sample integrity, particularly for temperature-sensitive analytes.
Temperature Control: Temperature fluctuations during transport can accelerate sample degradation. Plasma and serum samples should be maintained at 4°C during temporary storage when processing delays occur [55]. For lipidomics, repeated freeze-thaw cycles can degrade lipid profiles, making temperature stability paramount [52].
Standardization Across Sites: In multi-center studies, variability in transportation protocols between collection sites can introduce significant inconsistencies. Implementing standardized shipping protocols with temperature monitoring ensures uniform sample quality across all sites [52].
Processing and Extraction Methodologies
Sample processing and extraction methodologies represent another source of potential variation that must be controlled.
Centrifugation Protocols: Variations in centrifugation speed, duration, and temperature can affect sample composition. For plasma preparation, a consistent centrifugation protocol is essential to prevent cellular contamination that could alter lipid profiles or introduce genomic DNA into cfDNA samples [54] [53].
Extraction Kits and Reagents: Different nucleic acid or lipid extraction kits demonstrate varying efficiencies and biases. Some kits may preferentially recover longer DNA fragments or specific lipid classes, potentially skewing results [54]. Using the same lot of extraction reagents across a study enhances reproducibility.
Inhibitor Removal: Incomplete removal of PCR inhibitors during nucleic acid extraction can lead to false negatives or quantification inaccuracies. Incorporating appropriate controls and validation steps is essential [54].
Comparative Analysis of Pre-Analytical Approaches
Quantitative Comparison of Pre-Analytical Variables
The table below summarizes the impact of different pre-analytical variables on sample integrity based on current research findings:
Table 1: Impact of Pre-Analytical Variables on Sample Integrity
| Pre-Analytical Variable | Recommended Standard | Deviation Impact | Evidence Source |
|---|---|---|---|
| Blood Processing Time | Process within 2-4 hours at RT [53] | Increased cfDNA concentration & genomic DNA contamination [54] | Plasma/Serum Proteomics |
| Centrifugation Delay | Immediate processing or consistent delay [55] | Hemoglobin protein release in plasma; altered protein distributions [55] | Plasma Proteomics |
| Freeze-Thaw Cycles | Minimize (≤3 cycles); single freeze-thaw ideal [55] | Protein degradation; altered lipid profiles [52] [55] | Plasma Proteomics & Lipidomics |
| Collection Tube Type | EDTA or specialized cfDNA tubes [54] | PCR inhibition (heparin); analyte degradation [54] [53] | cfDNA Studies |
| Urine Sample Preservation | Preservation solution; pH control [54] | Rapid cfDNA degradation; inadequate concentrations [54] | Urine cfDNA Studies |
| Long-Term Storage | -80°C with monitoring [52] | Loss of sample viability & molecular integrity [52] | Biobanking Studies |
Cross-Study Comparison of Lipidomic Analytical Performance
The table below compares key methodological factors across lipidomic studies that influence cross-study validation:
Table 2: Comparison of Lipidomic Methodologies Affecting Cross-Study Validation
| Analytical Factor | Untargeted Lipidomics Approach | Targeted Lipidomics Approach | Impact on Cross-Validation |
|---|---|---|---|
| Chromatography | RPLC: separates by hydrophobicity [26] | HILIC: class-specific separation [26] | Different lipid coverage; complementary data |
| HILIC: separates by polarity [26] | RPLC or HILIC [26] | ||
| MS Resolution | High resolution (TOF, Orbitrap) [56] | MRM on triple quadrupole [56] | Variable identification confidence |
| Identification Confidence | Accurate mass + RT + CCS (ion mobility) [26] | RT matching to pure standards [57] | Higher in targeted with authentic standards |
| Quantitation Approach | Relative quantitation; isotope-labeled standards [57] | Absolute quantitation with calibration curves [57] | Targeted enables absolute comparison |
| Data Deposition | Metabolomics Workbench; LIPID MAPS [57] | Specific datasets with internal standards [57] | Essential for meta-analysis |
Experimental Protocols for Key Analyses
Standardized Plasma Processing Protocol for Lipidomics
The protocol below ensures reproducible plasma sample preparation for lipidomic analyses:
- Collection: Draw blood into EDTA tubes and invert gently 8-10 times for mixing [54].
- Transport: Maintain samples at 4°C and process within 2 hours of collection [53].
- Centrifugation: Centrifuge at 2,000 × g for 10 minutes at 4°C to separate plasma from cellular components [54].
- Secondary Centrifugation: Transfer supernatant to a new tube and centrifuge at 14,000 × g for 10 minutes at 4°C to remove remaining platelets and debris [53].
- Aliquoting: Immediately aliquot plasma into pre-labeled cryovials to avoid repeated freeze-thaw cycles [52].
- Storage: Flash-freeze aliquots in liquid nitrogen and store at -80°C until analysis [52] [53].
Bile Sample Processing for Lipidomic Analysis
For specialized samples like bile in cholangiocarcinoma research, specific protocols are required:
- Collection: Collect bile via endoscopic retrograde cholangiography (ERCP) into sterile containers [56].
- Processing: Centrifuge at 3,000 × g for 15 minutes at 4°C to remove insoluble particles and cellular debris [56].
- Preservation: Add antioxidant preservatives if analyzing oxidation-sensitive lipids [56].
- Aliquoting: Aliquot supernatant into cryovials, minimizing headspace to prevent oxidation [56].
- Storage: Flash-freeze in liquid nitrogen and store at -80°C for long-term preservation [56].
Urine cfDNA Extraction and Preservation
For urine cfDNA studies, specialized handling is required due to its susceptibility to degradation:
- Collection: Collect mid-stream urine into sterile containers with prescribed preservation solutions [54].
- Processing: Process within 4 hours of collection or use preservation tubes that stabilize cfDNA [54].
- Centrifugation: Centrifuge at 2,000 × g for 10 minutes to remove cells and debris [54].
- cfDNA Extraction: Use specialized cfDNA extraction kits that optimize recovery of short fragments [54].
- Storage: Store extracted cfDNA at -80°C in low-binding tubes to prevent adsorption [54].
Visualizing Pre-Analytical Workflows
Sample Collection to Analysis Workflow
Sample Journey from Collection to Analysis This workflow illustrates the critical pre-analytical steps where standardization is essential. The dashed line indicates that samples may be retrieved from long-term storage for future analysis, requiring maintained integrity [54] [52].
Crossover Study Design for Lipidomics
Crossover Design for Lipidomics Studies This diagram visualizes the AB/BA crossover design where subjects serve as their own controls, reducing inter-individual variability in lipidomic studies [26]. The washout period eliminates carry-over effects between interventions.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Essential Research Reagents for Pre-Analytical Standardization
| Reagent/Solution | Primary Function | Application Examples |
|---|---|---|
| EDTA Blood Collection Tubes | Anticoagulant; inhibits coagulation | Plasma preparation for lipidomics; cfDNA studies [54] |
| Cell-Free DNA Collection Tubes | Stabilizes nucleases; prevents degradation | Blood collection for liquid biopsy; extends processing window [54] |
| RNAlater Stabilization Solution | RNA stabilization; inhibits RNases | Tissue and cell samples for transcriptomics [53] |
| Protease Inhibitor Cocktails | Inhibits protein degradation | Protein extraction from tissues; plasma proteomics [53] |
| Custodial HTK Solution | Tissue preservation; maintains metabolic activity | Organ and tissue samples for metabolic studies [53] |
| Specialized cfDNA Extraction Kits | Optimized short fragment recovery | Liquid biopsy; urine cfDNA extraction [54] |
| Lipid Extraction Solvents | Lipid solubilization; class-specific extraction | Chloroform-methanol for comprehensive lipidomics [26] [56] |
| Synthetic Lipid Standards | Quantitation reference; retention time marker | Targeted lipid quantification; method validation [57] |
Standardizing pre-analytical variables is not merely a procedural concern but a fundamental requirement for generating valid, comparable data in cross-population lipidomic research. The evidence presented demonstrates that inconsistencies in sample collection, processing, and storage introduce significant variability that can obscure true biological signals and compromise cross-study comparisons.
By implementing the standardized protocols, comparative frameworks, and reagent solutions outlined in this guide, researchers can significantly enhance the reliability of their findings. Particularly for cross-validation studies across diverse populations, meticulous attention to pre-analytical standardization ensures that observed differences reflect genuine biological variation rather than methodological artifacts. As lipidomics continues to evolve as a tool for understanding disease mechanisms and identifying biomarkers, robust pre-analytical practices will remain the foundation upon which meaningful scientific insights are built.
Lipidomics, the large-scale study of lipids, has become an indispensable tool for discovering biomarkers and understanding disease mechanisms in biomedical research. However, the reproducibility of lipid identification across different mass spectrometry-based platforms and laboratories remains a significant challenge. Inconsistent identifications can lead to incorrect biological conclusions and hinder the translation of research findings, especially in critical areas like drug development. This guide objectively compares the performance of popular lipidomics software platforms, presents experimental data on their agreement rates, and provides detailed methodologies to help researchers cross-validate findings across different populations and study designs.
The Reproducibility Gap in Lipid Identification
Quantitative Evidence of Platform Discrepancies
A direct cross-platform comparison of two leading lipidomics software packages, MS DIAL and Lipostar, processing identical liquid chromatography-mass spectrometry (LC-MS) spectral data from a human pancreatic adenocarcinoma cell line (PANC-1) revealed a critical reproducibility issue.
The table below summarizes the alarming discrepancy in their identification outputs:
Table 1: Lipid Identification Agreement Between MS DIAL and Lipostar
| Data Type Used for Identification | Identification Agreement | Experimental Conditions |
|---|---|---|
| Default Settings (MS1) | 14.0% | Positive mode, default libraries |
| Fragmentation Data (MS2) | 36.1% | Positive mode, default libraries |
When using only MS1 data and default settings, the agreement was strikingly low at just 14.0% [58]. Even when utilizing more specific MS2 fragmentation data, the concordance remained poor at 36.1% [58]. This demonstrates that the choice of software alone can be a major source of variability, potentially overshadowing true biological signals.
Underlying Causes of Inconsistency
Several factors contribute to these platform discrepancies:
- Different Spectral Processing Algorithms: Each software uses unique approaches for peak picking, baseline correction, and noise reduction [58].
- Varying Lipid Libraries: Platforms utilize different in-silico spectral libraries (e.g., LipidBlast, LipidMAPS, ALEX123) with distinct contents and annotation rules [58].
- Co-elution and Co-fragmentation: MS2 spectra can be confounded by closely related lipids or multiple species eluting simultaneously [58].
- Inconsistent Use of Retention Time (tR): Many software tools do not fully leverage retention time information, a rich source of identification confidence [58].
- Over-reporting of Structural Details: Some platforms annotate lipids with a structural resolution (e.g., specific double bond positions) not fully supported by the available fragmentation data [59].
Experimental Protocols for Cross-Platform Comparison
Case Study Methodology: PANC-1 Lipid Extraction and LC-MS Analysis
The experimental data in Table 1 was generated using a standardized protocol suitable for cross-laboratory studies:
Table 2: Key Experimental Protocols for Lipidomics Workflow
| Protocol Step | Detailed Methodology |
|---|---|
| Cell Line & Culture | Human pancreatic adenocarcinoma cells (PANC-1, Merck, cat no. 87092802) [58] [60]. |
| Lipid Extraction | Modified Folch extraction using chilled methanol/chloroform (1:2 v/v) supplemented with 0.01% butylated hydroxytoluene (BHT) to prevent oxidation [58]. |
| Internal Standard | Avanti EquiSPLASH LIPIDOMIX quantitative MS internal standard (deuterated lipids) added to a final concentration of 16 ng/mL [58]. |
| Chromatography | Microflow LC (8 µL/min) using Luna Omega 3 µm polar C18 column (50 × 0.3 mm). Binary gradient: eluent A (60:40 acetonitrile/water) and B (85:10:5 isopropanol/water/acetonitrile), both with 10 mM ammonium formate and 0.1% formic acid [58]. |
| Mass Spectrometry | ZenoToF 7600 mass spectrometer (Sciex) in positive ionization mode [58]. |
| Data Processing | Identical raw spectral files processed independently in MS DIAL (v4.9.221218) and Lipostar (v2.1.4) using default settings and libraries to simulate a typical user scenario [58]. |
| Data Comparison | Lipid identifications considered in agreement only if formula, lipid class, and aligned retention time (within 5 seconds) were identical between platforms [58]. |
Complementary Platform Comparisons
Other studies have compared untargeted LC-MS with targeted platforms like the Lipidyzer. While not focusing on software disagreement, they reveal complementary insights:
- In a comparison of untargeted LC-MS versus the targeted Lipidyzer platform in aging mouse plasma, only 35-57% of lipid species overlapped between the platforms, despite both detecting over 300 lipids [61].
- The untargeted approach identified a broader range of lipid classes and could unambiguously identify all three fatty acids in triacylglycerols, while the targeted platform provided better absolute quantification [61].
- Technical repeatability was high for both platforms (median CV of 4.7-6.9%), indicating that the platforms are precise internally, but disagree on identities [61].
Figure 1: Workflow illustrating how identical spectral data processed through different software platforms leads to divergent lipid identifications.
Strategies to Overcome Platform Discrepancies
Analytical Best Practices for Improved Reproducibility
To enhance agreement rates and generate more robust lipidomic data, researchers should implement the following strategies:
- Multi-Mode Validation: Acquire data in both positive and negative ionization modes for the same sample to increase confidence in identifications [58].
- Manual Curation: Manually inspect MS2 spectra, particularly for potential biomarker candidates, to verify software annotations against known fragmentation patterns [58].
- Retention Time Prediction: Utilize Support Vector Machine (SVM) regression with leave-one-out cross-validation or other machine learning approaches to predict lipid retention times and flag outliers that may be false positives [58].
- Standardized Annotation: Adopt rule-based identification software like LipidMatch that prevents over-reporting of structural details not supported by fragmentation data [59].
- Cross-Platform Validation: Process critical samples through at least two different software platforms and focus on lipids consistently identified by both [58].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagent Solutions for Robust Lipid Identification
| Reagent/Material | Function in Lipidomics Workflow | Example Product/Source |
|---|---|---|
| Quantitative Internal Standards | Normalization of extraction efficiency, ionization variability, and quantitative concentration estimation. | Avanti EquiSPLASH LIPIDOMIX [58] |
| Stable Isotope-Labeled Lipids | Act as internal standards for specific lipid classes, correcting for technical variability during sample preparation and MS analysis. | Deuterated lipid standards [7] |
| Quality Control (QC) Materials | Monitor instrument performance and batch effects. Pooled quality control samples should be analyzed intermittently throughout the batch. | National Institute of Standards and Technology (NIST) plasma reference material [7] |
| Chromatography Columns | Separate lipid species prior to MS analysis to reduce ion suppression and isobaric interferences. | Luna Omega 3 µm polar C18 (e.g., 50 × 0.3 mm) [58] |
| Lipid Spectral Libraries | In-silico databases for matching experimental MS2 spectra to lipid identities. Using multiple libraries can improve coverage. | LipidBlast, LipidMAPS, ALEX123, METLIN [58] |
| Specialized Software Platforms | Process raw LC-MS data into lipid identifications and abundances. Using multiple platforms is recommended for critical findings. | MS DIAL, Lipostar, LipidMatch [58] [59] |
Figure 2: Key strategies to overcome platform discrepancies and achieve robust lipid identifications for reliable cross-population research.
The significant discrepancies in lipid identification between software platforms underscore the critical need for rigorous cross-validation in lipidomics research. The low agreement rates between commonly used platforms like MS DIAL and Lipostar (14.0-36.1%) reveal that software choice alone can dramatically influence research outcomes and potentially lead to false biomarker discovery. This reproducibility gap is particularly concerning for drug development and clinical applications, where findings must be translatable across different laboratories and patient populations.
Researchers should adopt a multi-pronged strategy to mitigate these issues: implementing multi-mode validation, manual curation of spectra, retention time prediction, and standardized annotation protocols. Furthermore, processing data through multiple software platforms and focusing on consensus identifications can significantly enhance confidence in results. As lipidomics continues to play an expanding role in understanding disease mechanisms and developing therapeutic interventions, addressing these platform discrepancies is essential for generating robust, reproducible data that can be reliably compared across different populations and research settings.
Managing Batch Effects and Technical Variability in Longitudinal Multi-Center Studies
Batch effects represent a fundamental challenge in large-scale omics studies, referring to technical variations introduced during experimental processes that are unrelated to the biological factors of interest [62]. These non-biological variations can arise from multiple sources, including differences in experimental conditions over time, utilization of equipment from different laboratories, or variations between analytical pipelines [62]. In the specific context of lipidomics—the comprehensive analysis of lipids within biological systems—batch effects are particularly problematic due to the structural complexity and diversity of lipid molecules and their sensitivity to technical processing variations [63].
The implications of uncorrected batch effects are severe and far-reaching. In the most benign scenarios, batch effects increase variability and decrease statistical power to detect genuine biological signals. In more critical cases, they can lead to incorrect conclusions, irreproducible findings, and even retracted scientific publications [62]. The problem is especially pronounced in longitudinal multi-center studies, where samples are collected and processed across different locations and timepoints, creating complex hierarchical structures of technical variability that can confound biological interpretations [64]. For lipidomic studies aiming to cross-validate findings across different populations, effectively managing these technical artifacts is not merely advantageous—it is essential for generating scientifically valid and clinically meaningful results.
Technical variability in lipidomic studies can emerge at virtually every stage of the experimental workflow. During study design, improper randomization of samples or confounded arrangements where batch effects correlate with biological outcomes can introduce systematic biases that are exceptionally challenging to correct during data analysis [62]. The sample preparation and storage phase introduces multiple potential sources of variation, including differences in protocol procedures, reagent lots, and storage conditions [62]. Specifically for lipidomics, the choice of extraction method (e.g., Folch vs. Matyash/MTBE methods) significantly impacts both the number of lipid species detected and the quantitative reproducibility of measurements [63].
During instrumental analysis, batch effects can arise from fluctuations in instrument performance over time, differences between platforms or laboratories, and variations in analytical conditions [65]. Finally, during data processing, variations in peak picking, integration algorithms, and normalization approaches can introduce additional technical artifacts that obscure biological signals [65]. In longitudinal multi-center designs, these sources of variability compound across time and location, creating complex hierarchical structures where cells are nested within samples, samples within subjects, and subjects within study centers [64].
Documented Impacts on Research Outcomes
The consequences of unaddressed batch effects have been demonstrated across multiple studies. In one clinical trial, a change in RNA-extraction solution resulted in a shift in gene-based risk calculations, leading to incorrect classification outcomes for 162 patients, 28 of whom received inappropriate or unnecessary chemotherapy regimens [62]. In cross-species comparative studies, apparent differences between human and mouse gene expression profiles were initially attributed to biological factors but were later shown to be driven primarily by batch effects related to different subject designs and data generation timepoints separated by three years [62].
In lipidomics specifically, the high individuality and sex specificity of circulatory lipidomes means that technical variability can easily obscure biologically meaningful patterns if not properly controlled [7]. The profound negative impact of batch effects extends beyond individual studies to contribute to the broader reproducibility crisis in scientific research, with one Nature survey finding that 90% of respondents believe there is a significant reproducibility crisis in science [62].
Strategic Approaches for Managing Batch Effects
Pre-Study Planning and Experimental Design
Strategic study design represents the first and most crucial line of defense against batch effects. Proper randomization of samples across processing batches ensures that technical variability does not systematically correlate with biological factors of interest. Incorporating quality control samples throughout the analytical sequence is essential for monitoring technical performance and facilitating later batch effect correction. Two primary types of quality controls are recommended: pooled quality controls (QCs) created by combining small aliquots of all biological samples, and standard reference materials (SRMs) such as the NIST SRM 1950 for plasma-based lipidomics [65].
For longitudinal multi-center studies, standardized protocols across all participating sites are essential. This includes harmonizing sample collection procedures, storage conditions, and documentation practices. Additionally, planning for balanced processing across timepoints and centers ensures that technical variability is distributed evenly across biological groups, preventing confounding between batch effects and factors of interest [62].
Selection and Optimization of Analytical Methods
The choice of lipid extraction methodology significantly influences both the extent of technical variability and the ability to detect biologically relevant signals. Recent research demonstrates that method selection should be based not only on the number of features detected but, more importantly, on the capacity to capture meaningful biological variability while minimizing technical noise [63].
Table 1: Comparison of Lipid Extraction Methods for Statistical Power and Feature Detection
| Method | Total Features | High-Quality Features | Biological Variability Capture | Technical Variability | Recommended Use Cases |
|---|---|---|---|---|---|
| Folch (Fresh Tissue) | Moderate | High | Excellent | Low | Maximizing statistical power for group discrimination |
| Folch (Dry Tissue) | Low | Moderate | Moderate | Moderate | Resource-limited settings |
| Matyash/MTBE (Fresh Tissue) | High | Moderate | Good | Moderate | Comprehensive lipid coverage |
| Matyash/MTBE (Dry Tissue) | Moderate | Low | Poor | High | Specialized applications only |
The incorporation of extraction quality controls provides a robust mechanism for monitoring variability introduced during sample preparation, enabling researchers to distinguish between technical artifacts and genuine biological signals [63].
Computational Approaches for Batch Effect Correction
Multiple computational strategies exist for identifying and correcting batch effects in lipidomic data. Exploratory data analysis techniques, including Principal Component Analysis and hierarchical clustering, can reveal systematic patterns associated with processing batches rather than biological groups. Formal batch effect correction algorithms implement statistical models to remove technical variability while preserving biological signals [65].
The effectiveness of any batch correction approach depends critically on the inclusion of appropriate quality control samples throughout the analytical sequence. These QCs enable monitoring of technical performance and provide a basis for normalization methods that can remove unwanted variation while retaining biological signals of interest [65].
Comparative Analysis of Batch Effect Management Strategies
Experimental Protocols for Batch Effect Assessment
Protocol 1: Quality Control Sample Integration
- Prepare pooled QC samples by combining equal aliquots from all biological samples
- Analyze QCs at regular intervals throughout the analytical sequence (e.g., every 6-10 samples)
- Monitor QC performance using multivariate statistics (e.g., PCA) to identify technical drift
- Implement system suitability criteria based on QC stability to determine data acceptability
- Apply normalization algorithms (e.g., quality control-based robust spline correction) to correct for identified batch effects [65]
Protocol 2: Extraction Method Evaluation for Biological Relevance
- Process representative sample subsets using multiple extraction methods (e.g., Folch, Matyash)
- For each method, calculate within-group and between-group relative standard deviations
- Compute statistical power for detecting known biological differences using each method
- Select the extraction protocol that maximizes between-group differences while minimizing within-group technical variability [63]
- Implement the selected method across all study sites with standardized protocols
Protocol 3: Cross-Validation Framework for Multi-Center Lipidomics
- Establish harmonized sample collection and processing protocols across all centers
- Implement a centralized quality assurance program with standardized reference materials
- Conduct periodic cross-center sample exchanges to assess inter-laboratory reproducibility
- Apply consistent data preprocessing and batch correction algorithms across all datasets
- Validate findings through independent replication in subset of centers [10]
Performance Comparison of Management Approaches
Table 2: Batch Effect Management Strategy Performance Comparison
| Management Strategy | Batch Effect Reduction | Statistical Power Preservation | Implementation Complexity | Suitability for Multi-Center Studies |
|---|---|---|---|---|
| Quality Control-Based Normalization | High | Moderate | Moderate | Excellent |
| Harmonized Protocols | Moderate | High | High | Excellent |
| Combat and Other Model-Based Methods | High | Variable | High | Good |
| Extraction Method Optimization | Moderate | High | Moderate | Good (with centralized training) |
| Cross-Validation Framework | High | High | High | Excellent |
Cross-Validation of Lipidomic Findings Across Populations
The integration of effective batch effect management strategies enables robust cross-validation of lipidomic findings across diverse populations. This approach has been successfully demonstrated in several recent studies. In pediatric inflammatory bowel disease research, a diagnostic lipidomic signature comprising lactosyl ceramide and phosphatidylcholine was initially identified in a discovery cohort and subsequently validated in an independent inception cohort, demonstrating consistent performance across different patient populations [10].
Similarly, research on type 2 diabetes in Asian Indian populations identified distinctive lipidomic alterations, including upregulated free fatty acids and lysophosphatidylcholines, along with decreased sphingomyelins and phosphatidylcholines in diabetic individuals [66]. These findings revealed population-specific lipid patterns while also confirming conserved metabolic disruptions observed in other ethnic groups. The study further identified significant gender differences in age-associated lipid patterns, with sphingomyelins increasing in men after 40 years, while lysophosphatidylcholine 22:6 rapidly increased after menopause in women [66].
The clinical lipidomics analysis of the Lausanne population study provided further evidence of high individuality and sex specificity of circulatory lipidomes, establishing that biological variability significantly exceeds analytical variability when appropriate quality control measures are implemented [7]. These findings collectively highlight the importance of effective batch effect management for distinguishing genuine biological patterns from technical artifacts when comparing lipidomic profiles across different populations.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents and Materials for Batch-Effect Controlled Lipidomics
| Reagent/Material | Function | Considerations for Batch Effect Control |
|---|---|---|
| Standard Reference Materials (e.g., NIST SRM 1950) | Quality control for instrumental performance | Use identical lot across all centers; analyze at regular intervals |
| Internal Standard Mixture | Normalization of extraction efficiency | Use stable isotope-labeled standards covering multiple lipid classes |
| Pooled Quality Control Samples | Monitoring technical variability | Prepare from representative pool of all samples; use throughout sequence |
| Pre-characterized Plasma Pools | Cross-batch normalization | Aliquot and store at -80°C; use for between-batch normalization |
| Standardized Extraction Kits | Consistent sample preparation | Use identical lot numbers across all study sites |
| Quality Control Materials for Extraction | Monitoring extraction variability | Include extraction quality controls with each batch |
Workflow Diagrams for Batch Effect Management
Comprehensive Batch Effect Management Workflow
Multi-Center Cross-Validation Framework
Effective management of batch effects and technical variability represents a fundamental requirement for generating scientifically valid and reproducible lipidomic data, particularly in longitudinal multi-center studies aiming to cross-validate findings across different populations. The integration of strategic experimental design, appropriate analytical method selection, robust quality control procedures, and computational batch correction approaches provides a comprehensive framework for distinguishing technical artifacts from genuine biological signals.
As lipidomics continues to evolve as a tool for biomarker discovery and metabolic phenotyping, the implementation of these batch effect management strategies will be essential for establishing robust, clinically relevant lipid signatures that transcend individual studies and population boundaries. The consistent demonstration of high individuality and sex specificity in circulatory lipidomes, coupled with the successful cross-validation of diagnostic lipid signatures across diverse cohorts, highlights both the challenges and opportunities in this rapidly advancing field.
Bioinformatic Strategies for Correcting Isotopic Overlap and Signal Drift
In mass spectrometry-based lipidomics and metabolomics, the accurate identification and quantification of analytes are fundamental to deriving biologically relevant conclusions. Two pervasive analytical challenges that complicate this process are isotopic overlap and signal drift. Isotopic overlap occurs when the isotopic envelopes of different molecules, or different forms of the same molecule, coincide in the m/z dimension, convoluting their individual signals [67] [68]. Signal drift refers to unwanted, non-biological fluctuations in instrument response over time, introduced by factors such as batch effects or variations in sample preparation [65] [69]. Within the broader context of cross-validating lipidomic findings across different populations, the ability to correct for these artifacts is not merely a technical detail but a prerequisite for generating reproducible and comparable data. This guide objectively compares the performance of several bioinformatic strategies designed to resolve these issues, providing researchers with a clear framework for selecting appropriate tools.
Comparison of Deconvolution Strategies for Isotopic Overlap
Isotopic overlap is a common issue in the analysis of complex biological samples. It can arise from the co-elution of different lipid species, the presence of metabolically labeled pairs, or from post-translational modifications like deamidation that introduce small mass shifts [68] [70]. The following table compares the performance, underlying algorithms, and optimal use cases for three distinct computational strategies that address this challenge.
Table 1: Performance Comparison of Isotopic Overlap Correction Strategies
| Strategy Name | Underlying Algorithm | Reported Accuracy/Performance | Best For | Software/Tool |
|---|---|---|---|---|
| OIE_CARE [67] | Relative deviation between ideal and observed abundance | 95.6% isotopic peaks interpreted; 99.2% abundance interpreted in myoglobin HCD spectra | Intact protein analysis; high-resolution MS data | ProteinGoggle |
| Isotopic Envelope Mixture Modeling (IEMM) [68] | Linear mixture modeling of theoretical isotopic envelopes | R² = 0.96 for deamidation quantification; accurate 16O/18O ratios from 10:1 to 1:10 | Quantifying overlapping peptides (e.g., deamidation, 18O labeling) | MICIT (Java application) |
| IPPD [71] | Non-negative least squares/least absolute deviation regression | Effectively disentangles complicated pattern overlaps; robust to noise | High-noise spectra; challenging overlaps in peptide MS | IPPD (R/Bioconductor package) |
Experimental Protocols for Key Strategies
OIECARE Workflow: The OIECARE method was validated using Higher-energy Collisional Dissociation (HCD) tandem mass spectra of myoglobin and an intact E. coli proteome [67]. The core protocol involves:
- Theoretical Envelope Calculation: For all product ions, the exact theoretical isotopic envelope is computed from the elemental composition of their actual amino acids, moving beyond generic "Averagine" models [67].
- Ideal Abundance Calculation: For a given overlapping isotopic peak (OIP), the ideal experimental abundance is calculated for every overlapping isotopic envelope (OIE) that shares it.
- Relative Deviation (RD) and Correction: The relative deviation (RD) of the overall observed experimental abundance of the OIP from the summed ideal value is computed. The final, deconvoluted abundance for each OIE's OIP is its individual ideal abundance multiplied by (1 + RD) [67].
- Search Parameters: A typical database search using this method employs tolerances such as an isotopic peak abundance cutoff (IPACO) of 20%, an isotopic peak m/z deviation (IPMD) of 15 ppm, and an isotopic peak-abundance deviation (IPAD) of 50% [67].
Isotopic Envelope Mixture Modeling (IEMM) Protocol: The IEMM method, implemented in the MICIT software, was tested for quantifying deamidation and 18O-labeled peptides [68]. A standard validation experiment involves:
- Sample Preparation: Synthetic peptides and their deamidated forms are mixed at precise known ratios (e.g., 1:0, 1:2, 2:1, 4:1, 10:1, 20:1). For 18O labeling, BSA digests are prepared in H216O and H218O and then mixed at various ratios [68].
- LC-MS Analysis: Peptide mixtures are analyzed by reverse-phase liquid chromatography coupled to a high-resolution Q-TOF mass spectrometer.
- Data Deconvolution: The MICIT software uses theoretically predicted isotopic distributions and an instrument response function to model the observed signal as a linear mixture of the light and heavy envelopes. The model fits the data to determine the ratio of the components that best explains the observed spectrum [68].
Diagram 1: A workflow comparison of three core computational strategies for resolving isotopic overlap in mass spectrometry data.
Signal Drift Correction and Data Standardization
Signal drift poses a significant threat to the longitudinal reliability of lipidomics data, particularly in multi-batch studies or when cross-validating findings across different populations. Correction strategies are essential for distinguishing true biological variation from technical artifact.
Handling Unwanted Variation
A typical lipidomics dataset is a matrix of lipid concentrations across many samples, characterized by heteroscedasticity, non-normal distributions, and the presence of missing values and outliers [65]. Quality Control (QC) samples, created by pooling small aliquots of all biological samples, are critical for monitoring and correcting signal drift. These QCs are analyzed at regular intervals throughout the measurement sequence, allowing for the detection of technical variation over time [65]. The data normalization process aims to remove this unwanted variation, focusing the final dataset on biological information.
Managing Missing Data
The approach to missing values is a key part of data standardization. These values are categorized as Missing Completely at Random (MCAR), Missing at Random (MAR), or Missing Not at Random (MNAR), with the latter often resulting from analyte abundance falling below the detection limit [65]. Best practices involve:
- Filtering: Removing lipid species with a high percentage of missing values (e.g., >35%) [65].
- Imputation: Applying specialized methods to replace missing values. Studies suggest that k-nearest neighbors (kNN)-based imputation performs well for both MCAR and MNAR data in lipidomics, while random forest-based imputation is also highly effective. For MNAR, a common practice is imputation with a small constant, such as a percentage of the lowest measured concentration [65].
Table 2: Essential Research Reagent Solutions for Lipidomics Workflows
| Reagent/Category | Function in Workflow | Example & Rationale |
|---|---|---|
| QC Samples | Monitoring technical variation and signal drift; normalization | Pooled biological samples or NIST SRM 1950; enables batch effect correction [65]. |
| Chloroform Substitutes | Sustainable lipid extraction | Cyclopentyl methyl ether (CPME) showed comparable/superior performance to chloroform in Folch protocol [72]. |
| Internal Standards | Quality control for extraction & quantification | EquiSPLASH LIPIDOMIX Mass Spec Standard; used to evaluate extraction efficiency and normalize data [72]. |
| Data Imputation Tools | Handling missing values | k-nearest neighbors (kNN) or random forest algorithms; replace missing values based on dataset structure [65]. |
Integrated Workflow for Cross-Validation Studies
To ensure lipidomic findings are robust and reproducible across different populations, an integrated analytical workflow that proactively addresses both isotopic overlap and signal drift is essential. The following diagram outlines a recommended protocol from sample preparation to data processing.
Diagram 2: An integrated experimental and computational workflow for lipidomics studies requiring cross-validation, highlighting critical steps for correcting signal drift and isotopic overlap.
The choice of a bioinformatic strategy for correcting isotopic overlap is not one-size-fits-all and should be guided by the specific analytical challenge and data type. OIE_CARE is highly effective for the complex overlapping product ions encountered in intact protein analysis [67]. For precise quantification of specific peptide modifications or labeling, the IEMM approach provides high accuracy [68]. In contrast, the IPPD method offers superior robustness in the face of significant spectral noise and complex overlaps [71].
Similarly, mitigating signal drift requires a proactive, two-pronged approach: rigorous experimental design incorporating QC samples and standardized extraction protocols, followed by computational data cleaning that includes intelligent missing value imputation and batch effect correction [72] [65].
In conclusion, the reliability of cross-population lipidomic findings is inextricably linked to the rigor of the underlying data processing. By objectively comparing the performance of these bioinformatic strategies and providing detailed experimental protocols, this guide empowers researchers to build a more robust analytical foundation. The integration of these correction methods into standardized workflows, as outlined, is paramount for generating lipidomic data that is not only statistically significant but also truly reproducible and biologically meaningful.
Validation Strategies and Machine Learning for Clinically Actionable Biomarkers
The transgenerational transmission of Type 2 Diabetes (T2D) risk is a major public health challenge, with maternal diabetes history being a particularly significant factor. [73] Understanding the precise mechanisms and validating genetic and biochemical markers through independent cohort replication is essential for advancing predictive diagnostics and personalized prevention strategies. This guide objectively compares findings from key studies that have investigated this phenomenon in different populations, focusing on their methodologies, results, and the cross-validation of findings, particularly in the context of lipidomics and metabolic health.
Case Study 1: Parental Origin of T2D Risk in a Northern Chinese Cohort
Experimental Protocol & Cohort Design
This prospective, family-based cohort study aimed to elucidate the differential impact of maternal versus paternal T2D on offspring risk. [73]
- Population: The study recruited 4,508 adults free of diabetes at baseline from the Beijing Fangshan family-based cohort. Participants were followed for a median of 7.32 years.
- Exposure Assessment: Parental T2D status was determined via offspring self-report, categorized into: neither parent with T2D, only mother with T2D, only father with T2D, or both parents with T2D.
- Outcome Ascertainment: Offspring T2D was defined by a documented diagnosis (ICD-10 code E11), HbA1c ≥ 6.5%, fasting blood glucose ≥ 7.0 mmol/L, or use of glucose-lowering medications.
- Statistical Analysis: Family-based multilevel Cox regression models were used to calculate hazard ratios (HRs), adjusting for age, sex, BMI, lifestyle factors (smoking, alcohol, diet, exercise), and metabolic covariates.
Key Findings and Quantitative Data
The study provided clear data on the parent-of-origin effect, summarized in the table below.
Table 1: Parent-of-Origin Effect on Offspring T2D Risk from the Northern Chinese Cohort [73]
| Parental T2D Status | Adjusted Hazard Ratio (HR) | 95% Confidence Interval | P-value |
|---|---|---|---|
| Any Parental T2D | 1.82 | 1.44 – 2.30 | - |
| Maternal T2D Only | 2.55 | 1.87 – 3.50 | 4.70 × 10-9 |
| Paternal T2D Only | 1.27 | 0.88 – 1.84 | Not Significant |
| Both Parents with T2D | 1.89 | 1.47 – 2.43 | - |
A critical finding was that lifestyle factors significantly modified the risk associated with maternal T2D. A healthy diet (diet score >2) and regular exercise substantially attenuated the inherited risk, with the hazard ratio dropping from 2.76 to 1.34 for diet, and from 2.10 to 1.13 for exercise. [73]
Case Study 2: GDM Genetics and Early Prediction in Chinese Pregnancies
Experimental Protocol & Cohort Design
This study focused on the genetic architecture of Gestational Diabetes Mellitus (GDM) and its utility for early prediction, leveraging large-scale genomic data. [74]
- Population: A massive cohort of 116,144 Chinese pregnant women, utilizing their non-invasive prenatal test (NIPT) sequencing data and detailed prenatal records. This included 12,024 GDM cases and 67,845 non-diabetes controls.
- Genomic Analysis: Genome-wide association studies (GWAS) were conducted on GDM and five glycemic traits (e.g., fasting plasma glucose, OGTT values, HbA1c). Three analytical methods (PLINK2, REGENIE, BOLT-LMM) were used for robustness.
- Risk Prediction Model: A machine learning model was developed to predict GDM before 20 weeks of gestation. It integrated a polygenic risk score (PRS) derived from the GWAS with common biomarkers and electronic health records from early pregnancy.
Key Findings and Replication Data
The study significantly advanced the understanding of GDM genetics and demonstrated a clinically applicable prediction model.
Table 2: Genetic Discoveries and Model Performance from the GDM Cohort [74]
| Metric | Study Findings |
|---|---|
| Novel GDM Loci Identified | 13 |
| Novel Glycemic Trait Loci | 111 |
| SNP Heritability (GDM) | 6.9% (s.e. 0.7%) |
| Genetic Correlation with East Asian T2D | rg = 0.525 |
| Prediction Model AUC | 0.729 |
| Prediction Model Accuracy | 0.835 |
The machine learning model offered a cost-effective strategy for early GDM prediction using existing clinical NIPT data. Shapley value analysis identified the polygenic risk score as a key contributor to the model's predictive power. [74]
Cross-Validation of Mechanistic Insights
Independent studies provide converging evidence on the biological mechanisms underlying maternal transmission of diabetes risk, moving from genetics to functional biology and epigenetics.
Beta Cell Dysfunction as a Core Mechanism
Recent reviews of human studies place pancreatic beta cell dysfunction at the centre of early T2D pathogenesis. [75] Evidence from the Human Pancreas Analysis Program (HPAP) indicates that in impaired glucose tolerance (a prediabetic state), there are reduced levels of proteins critical for insulin granule docking and exocytosis (e.g., STX1A, VAMP2, UNC13A). This functional deficit in insulin secretion is a primary driver of hyperglycaemia, often preceding measurable changes in beta cell mass. [75]
Epigenetic Programming in Offspring
A separate study provided direct evidence for an epigenetic mechanism. Researchers found that both gestational diabetes and maternal obesity were associated with epigenome-wide DNA methylation changes in children. [76] These alterations in the epigenetic landscape represent a plausible molecular mechanism for the long-term metabolic programming observed in offspring exposed to maternal diabetes in utero.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key reagents and materials essential for research in this field.
Table 3: Essential Research Reagents for Cohort and Lipidomics Studies in T2D
| Research Solution | Function & Application |
|---|---|
| UPLC-ESI-MS/MS | Ultra-Performance Liquid Chromatography coupled to Electrospray Ionization Tandem Mass Spectrometry is a high-sensitivity platform for comprehensive lipidomics, enabling the identification and quantification of hundreds of lipid species from biological samples. [26] [77] |
| activPAL & Actiwatch | Objective monitoring devices used in cohort studies for 24-hour assessment of physical activity, sedentary behavior, and sleep patterns, providing gold-standard data on modifiable lifestyle factors. [78] |
| GWAS & PRS Panels | Genotyping arrays and computational tools for conducting Genome-Wide Association Studies and calculating Polygenic Risk Scores, which are vital for assessing genetic susceptibility to T2D and GDM. [74] |
| NIPT Sequencing Data | Utilizing existing Non-Invasive Prenatal Test sequencing data from clinical practice provides a cost-effective resource for large-scale genetic studies in pregnant populations. [74] |
| CRISPR Screens (e.g., in human beta cells) | Functional genomics tool for validating the role of candidate genes (e.g., CALCOCO2) identified by GWAS in disease-relevant cell types, bridging the gap between genetic association and biological mechanism. [75] |
Visualizing Key Workflows and Pathways
The following diagrams illustrate the core experimental workflow and a key biological pathway relevant to the discussed research.
Cohort Study and Lipidomics Analysis Workflow
Maternal Diabetes and Offspring Risk Pathway
Lipidomics, a specialized field within metabolomics, comprehensively studies the structure and function of the complete set of lipids (the lipidome) in biological systems. The lipidome consists of thousands of chemically distinct lipids, which the Lipid Metabolites and Pathways Strategy (LIPID MAPS) classifies into eight major categories: fatty acyls (FA), glycerolipids (GL), glycerophospholipids (GP), sphingolipids (SP), sterol lipids (ST), prenol lipids (PR), saccharolipids (SL), and polyketides (PK) [37]. These molecules are not merely structural components but play vital roles in cellular signaling, energy storage, and maintaining structural membrane integrity. The molecular structures of lipids largely determine their biological functions, and alterations in lipid metabolism have been implicated in numerous disease pathways [37].
The integration of mass spectrometry (MS) with advanced computational approaches has revolutionized lipidomics research, enabling the identification and quantification of hundreds to thousands of lipid species from minimal biological samples. MS-based lipidomics platforms typically utilize liquid chromatography (LC) coupled with MS, with reverse-phase chromatography separating lipids by hydrophobicity (acyl chain length, sn-positional isomers, and double bond positions), while hydrophilic interaction liquid chromatography (HILIC) separates lipids by polarity in a class-specific fashion [26]. Recent technological advances have further enhanced lipid profiling capabilities through techniques such as ion mobility MS, which separates lipid ions based on their drift time in buffer gas phase according to charge, size, and shape, providing collision cross section (CCS) values as an additional dimension for lipid identification [26].
Machine learning (ML), a subset of artificial intelligence, has emerged as a powerful companion to lipidomics by developing systems that can learn and improve from data without explicit programming [79]. The combination of ML with lipidomics is particularly powerful for discovering candidate prognostic and predictive biomarkers because it can identify complex, non-linear patterns in high-dimensional data that traditional statistical methods might miss. This integration is especially valuable for identifying robust lipid signatures that hold across diverse populations, addressing a critical challenge in translational lipidomics research [37].
Current Landscape of ML-Driven Lipidomics Research
Key Studies and Findings Across Populations
Table 1: Representative ML-Lipidomics Integration Studies Across Disease Types
| Disease Area | Study Population | Key Lipid Alterations Identified | ML Approach | Performance |
|---|---|---|---|---|
| Infectious Disease (COVID-19) [80] | 126 COVID-19+, 45 COVID-19- hospitalized, 50 healthy | • COVID-19 vs Healthy: ↑ Acylcarnitines, Lysophosphatidylethanolamines, Arachidonic acid, Oxylipins• COVID-19+ vs COVID-19-: Lysophosphatidylcholine 22:6-sn2, Phosphatidylcholine 36:1, Secondary bile acids | Machine learning interpretation of lipidomics data | Distinct signatures identified with clinical decision-making potential |
| Ovarian Cancer [79] | DKO mouse model (faithfully recapitulates human HGSC) | • Early stage: ↑ Phosphatidylcholines, Phosphatidylethanolamines• Later stages: ↑ Fatty acids, Triglycerides, Ceramides, Hexosylceramides, Sphingomyelins, Lysophosphatidylcholines, Phosphatidylinositols | Unsupervised learning, Hierarchical clustering, Multiple ML algorithms, Survival analysis | Time-resolved lipidome evolution mapped throughout cancer progression |
| Osteosarcoma [81] | Multicenter cohorts: TARGET-OS, GSE21257, GSE39058, GSE16091 | • C1 subtype: ↑ Cholesterol, Fatty acid synthesis, Ketone metabolism• C2 subtype: ↑ Steroid hormone biosynthesis, Arachidonic acid, Glycerolipid, Linoleic acid metabolism | Consensus clustering, Univariate Cox, StepAIC, Multiple ML algorithms | Lipid Metabolism-Related Signature (LMRS) robustly predicted prognosis across cohorts |
The application of ML-driven lipidomics has yielded significant insights across diverse pathological conditions and populations. In infectious disease research, a 2022 study demonstrated that machine learning could identify distinct serum lipid signatures that not only differentiate COVID-19-positive patients from healthy controls but, more importantly, distinguish COVID-19-specific inflammation from other infectious/inflammatory diseases [80]. This finding is particularly significant for pan-population research as it suggests that while many lipid alterations represent general inflammatory responses, specific lipid signatures may be disease-specific.
In oncology, lipidomics research has revealed profound temporal dynamics in lipidome remodeling during disease progression. A longitudinal study of high-grade serous ovarian cancer (HGSC) in a mouse model demonstrated that early cancer progression was marked by increased levels of phosphatidylcholines and phosphatidylethanolamines, while later stages featured more diverse lipid alterations including fatty acids, triglycerides, ceramides, and sphingomyelins [79]. These temporal patterns highlight the importance of considering disease stage when identifying lipid signatures across populations.
Similarly, research on osteosarcoma has identified distinct molecular subtypes based on lipid metabolism genes, with significantly different survival outcomes and metabolic characteristics [81]. The C1 subtype showed enrichment in cholesterol, fatty acid synthesis, and ketone metabolism, while the C2 subtype focused on steroid hormone biosynthesis, arachidonic acid, and glycerolipid metabolism. This subtyping approach, validated across multiple cohorts, demonstrates how ML can identify biologically meaningful subgroups within broader populations, potentially enabling more personalized therapeutic approaches.
Analytical Methodologies in Cross-Population Lipidomics
Table 2: Comparison of Lipidomics Methodological Approaches
| Methodological Aspect | Approaches | Advantages | Challenges in Pan-Population Studies |
|---|---|---|---|
| Study Design [26] | Parallel, Crossover, Longitudinal | Crossover reduces inter-individual variability by using subjects as own controls | Carry-over effects, Requires washout periods, Complex statistical analysis |
| MS Acquisition [26] | Targeted, Untargeted, Pseudotargeted | Untargeted: Comprehensive coverage; Targeted: Better quantification | Untargeted: Structural annotation challenges; Inter-laboratory reproducibility |
| Chromatography [26] | RPLC, HILIC, Shotgun, Ion Mobility | RPLC: Separates by hydrophobicity; HILIC: Class-specific separation | Complementary approaches needed for comprehensive coverage; Isobaric separation challenges |
| Data Analysis [26] | Univariate, Multivariate, ML | ML: Captures complex patterns; Traditional: More interpretable | Overfitting risk with high-dimension data; Requires large sample sizes for validation |
The search for robust pan-population lipid signatures employs diverse methodological approaches, each with distinct advantages for cross-population research. Study design significantly impacts the ability to identify generalizable lipid signatures, with crossover designs offering particular advantages for reducing inter-individual variability—a critical challenge in lipidomics due to the strong influence of genotype, daily activity, diet, and gut flora on the human lipidome [26]. In such designs, participants serve as their own controls, potentially reducing the required sample size and enhancing the detection of true treatment or disease effects amidst substantial biological variability.
MS-based lipidomics platforms continue to evolve, with current approaches including targeted methods (focusing on predefined lipid panels), untargeted methods (comprehensively detecting all measurable lipids), and pseudotargeted approaches (combining elements of both) [37]. Chromatographic separation techniques similarly offer complementary advantages: RPLC separates lipids by hydrophobicity, revealing differences in acyl chain characteristics, while HILIC separates by polarity in a class-specific manner [26]. The emerging incorporation of ion mobility MS provides an additional separation dimension based on the structural shape of lipid ions, characterized by collision cross section (CCS) values, which can help distinguish isobaric species that are challenging to resolve with MS alone [26].
The analytical workflow for cross-population lipidomics must carefully address multiple challenges, including batch effects, platform variability, and the need for appropriate normalization. Studies integrating multiple cohorts, such as the osteosarcoma research that combined TARGET-OS, GSE21257, GSE39058, and GSE16091, often employ strategies like binary transformation of expression values (categorizing as 0 or 1 based on median expression) to mitigate batch effects when merging datasets [81]. Such approaches are particularly valuable for pan-population research, as they enhance the comparability of data derived from different sources or populations.
Experimental Protocols and Methodologies
Standardized Lipidomics Workflow for Multi-Cohort Studies
Figure 1: Comprehensive Lipidomics Workflow for Pan-Population Studies
The experimental workflow for identifying pan-population lipid signatures integrates robust laboratory protocols with computational approaches. Sample collection begins with multi-cohort recruitment, carefully considering demographic factors, clinical characteristics, and potential confounding variables. For biofluid-based studies, serum and plasma are commonly used matrices, with standardized collection protocols essential for cross-study comparisons [37]. Sample preparation typically involves lipid extraction using methods like liquid-liquid extraction, with the addition of internal standards for quantification normalization. Quality control pools—created by combining small aliquots from all samples—are analyzed throughout the sequence to monitor instrument performance and correct for technical variability [26].
LC-MS analysis employs complementary chromatographic separations to maximize lipid coverage. As demonstrated in the ovarian cancer study, reverse-phase UHPLC-MS enables the separation and detection of thousands of lipid features across positive and negative ionization modes [79]. MS data acquisition typically alternates between data-dependent acquisition (DDA) for lipid identification and data-independent acquisition (DIA) for comprehensive quantification. Identification confidence is enhanced through matching to MS/MS spectral libraries and the incorporation of additional dimensions such as retention time and collision cross section values where available [26].
Data processing transforms raw MS data into a structured quantitative matrix, involving feature detection, de-isotoping, and alignment across samples. Lipid identification leverages databases such as LIPID MAPS, with annotation levels following the Metabolomics Standards Initiative guidelines [37]. The resulting data matrix undergoes rigorous quality assessment, including evaluation of signal drift, batch effects, and missing value patterns, before proceeding to statistical and ML analysis.
Machine Learning Protocols for Robust Signature Identification
Machine learning approaches for lipid signature discovery must address the high-dimensionality of lipidomics data, where the number of lipid features often vastly exceeds the number of samples. Dimensionality reduction techniques, such as principal component analysis (PCA), t-distributed stochastic neighbor embedding (t-SNE), and uniform manifold approximation and projection (uMAP), are commonly employed for exploratory data analysis and visualization, as demonstrated in the HGSC mouse model study [79]. However, for predictive modeling, more sophisticated feature selection approaches are typically employed.
The osteosarcoma study exemplifies a rigorous feature selection protocol, employing a multi-step process that included: (1) Fisher's exact test to identify lipid metabolism genes differentially expressed between molecular subtypes; (2) univariate Cox proportional hazards analysis to evaluate prognostic significance; and (3) stepwise Akaike Information Criterion (stepAIC) to select the most informative genes while mitigating overfitting risks [81]. Such multi-stage approaches help identify lipid signatures with both biological relevance and predictive power.
For predictive modeling, studies typically compare multiple ML algorithms with varying inductive biases to identify the most performant approach for a given dataset. Commonly employed algorithms include support vector machines (SVM), random forests, gradient boosting machines, and regularized Cox regression, with performance evaluated using metrics appropriate to the research question (e.g., C-index for survival prediction, accuracy for classification) [81]. Crucially, model performance must be validated in independent cohorts to assess generalizability across populations, as demonstrated by the osteosarcoma study that validated its Lipid Metabolism-Related Signature in three independent datasets [81].
Technical Specifications and Research Toolkit
Essential Research Reagent Solutions
Table 3: Essential Research Reagents and Platforms for Lipidomics Studies
| Category | Specific Products/Platforms | Research Application | Considerations for Pan-Population Studies |
|---|---|---|---|
| MS Platforms [6] | Orbitrap, FT-ICR, Q-TOF | High-resolution lipid detection | FT-ICR offers highest resolution; Orbitrap balances sensitivity and resolution |
| Chromatography [26] | RPLC, HILIC, Ion Mobility | Lipid separation | RPLC for hydrophobic separation; HILIC for class separation; Complementary use |
| Lipid Standards [26] | Stable isotope-labeled internal standards | Quantification normalization | Should cover multiple lipid classes; Essential for cross-study comparisons |
| Sample Preparation [26] | Liquid-liquid extraction kits | Lipid extraction from biofluids | Standardized protocols critical for multi-center studies |
| Databases [37] [6] | LIPID MAPS, LipidBlast, HMDB | Lipid identification & annotation | LIPID MAPS provides standardized nomenclature and classification |
| Software Tools [37] | MS-DIAL, Lipostar, XCMS | Lipidomics data processing | Low agreement (14-36%) between tools necessitates consistency in multi-cohort studies |
The experimental toolkit for pan-population lipidomics research requires carefully selected reagents and platforms that ensure reproducibility and comparability across studies. MS platforms form the foundation of lipid detection, with high-resolution instruments such as Orbitrap and Fourier-transform ion cyclotron resonance (FT-ICR) mass spectrometers enabling the identification of lipid molecules at attomole levels, capturing even subtle alterations in lipid species [6]. The exceptional sensitivity of these systems is particularly crucial for single-cell lipidomics applications and for detecting low-abundance lipid mediators in clinical samples.
Chromatographic separation techniques represent another critical component, with RPLC and HILIC providing complementary separation mechanisms. The choice between these approaches depends on the specific research questions—RPLC offers superior separation within lipid classes based on acyl chain characteristics, while HILIC enables class-specific separation that simplifies data interpretation [26]. Emerging technologies such as ion mobility MS add another dimension of separation based on the structural shape of lipid ions, characterized by collision cross section values, which helps distinguish challenging isobaric species [26].
For data processing and analysis, numerous software tools are available, including MS-DIAL, Lipostar, and XCMS. However, studies have demonstrated concerningly low agreement rates (as low as 14-36%) between different platforms when processing identical datasets [37]. This variability underscores the importance of maintaining consistent data processing protocols throughout pan-population studies and transparently reporting software parameters and versions to enable meaningful cross-study comparisons.
Visualization Approaches for Lipidomics Data
Figure 2: ML-Driven Signature Discovery and Validation Workflow
Effective visualization of lipidomics data and analytical workflows is essential for interpreting complex relationships and communicating findings. The ML-driven signature discovery process follows an iterative workflow that begins with multi-cohort lipidomics data integration, requiring careful attention to batch effect correction methods when combining datasets from different sources or populations [81]. Feature selection techniques then identify the most informative lipid species, balancing predictive power with biological interpretability and clinical applicability.
ML model training typically employs multiple algorithms with different inductive biases, selecting the best-performing approach based on appropriate validation strategies [81]. The resulting models must undergo rigorous validation in independent cohorts to assess their generalizability across populations, with performance metrics tailored to the specific clinical or biological question. For survival prediction, the C-index provides a measure of prognostic discrimination [81], while for classification tasks, metrics such as accuracy, sensitivity, and specificity are more appropriate.
This process is often iterative, with initial results informing refinement of feature selection or model parameters. The ultimate goal is a robust pan-population lipid signature that maintains predictive performance across diverse cohorts and demonstrates biological plausibility through enrichment analysis and pathway mapping [81].
Cross-Validation of Lipidomic Findings Across Populations
The validation of lipid signatures across diverse populations represents the most significant challenge in translational lipidomics research. Several strategies have emerged to strengthen the generalizability of findings, including multi-cohort validation, cross-disciplinary integration, and advanced statistical approaches that explicitly account for population heterogeneity.
Multi-cohort validation, as demonstrated in the osteosarcoma study that integrated TARGET-OS, GSE21257, GSE39058, and GSE16091 datasets, provides the strongest evidence for pan-population applicability [81]. Such approaches typically involve discovery-validation frameworks, where signatures identified in an initial cohort are tested in one or more independent populations. When combining cohorts, batch effect correction methods—such as the binary transformation approach used in the osteosarcoma study—are essential to minimize technical artifacts that could obscure true biological signals [81].
Cross-disciplinary integration enhances the biological interpretability of lipid signatures and strengthens their validity. The COVID-19 study exemplifies this approach by contextualizing lipid findings within immunological mechanisms, noting that specific lysophosphatidylcholines, phosphatidylcholines, and secondary bile acids best discriminated COVID-19-positive from COVID-19-negative patients [80]. Such integration helps distinguish disease-specific alterations from general physiological responses, a critical consideration for pan-population biomarker development.
Advanced statistical approaches that explicitly consider study design can further enhance cross-population validation. For crossover-designed studies, which reduce inter-individual variability by using participants as their own controls, specialized statistical models that account for repeated longitudinal measurements are essential for appropriate inference [26]. Mixed-effects models can accommodate both fixed effects (e.g., treatment, disease status) and random effects (e.g., individual variability), providing more accurate effect estimation in heterogeneous populations.
Despite these advances, significant challenges remain in achieving true pan-population applicability. Biological variability, lipid structural diversity, inconsistent sample processing, and a lack of standardized procedures continue to hamper reproducibility and clinical validation [37]. Agreement between different lipidomics platforms can be alarmingly low, with one report noting concordance rates as low as 14-36% between popular software tools when processing identical LC-MS data [37]. These limitations highlight the need for continued methodological refinement and standardization in the pursuit of robust, clinically applicable lipid signatures that perform reliably across diverse human populations.
Clinical reference intervals (RIs) are fundamental tools for interpreting laboratory test results, enabling researchers and clinicians to distinguish health from disease. These intervals are critically influenced by two distinct types of variance: biological variability (differences between individuals) and analytical variability (measurement imprecision). This guide examines the methodologies for establishing RIs that effectively separate these variability components, with a specific focus on lipidomics applications in cross-population research. We compare experimental approaches, provide quantitative data on variability metrics, and detail essential protocols for RI development, offering drug development professionals a framework for validating biochemical findings across diverse populations.
Reference intervals (RIs) are defined as the central 95% of laboratory test results obtained from a healthy reference population, serving as the primary interpretive tool for clinical laboratory data [82]. The construction of reliable RIs requires careful consideration of two fundamental variability sources: biological variability, which encompasses physiological differences between individuals within a population, and analytical variability, which represents the technical imprecision of measurement systems [83]. Understanding the relationship between these variability components is essential for developing clinically meaningful RIs, particularly in emerging fields like lipidomics where comprehensive population-specific data may be limited.
The conceptual foundation of RIs has evolved significantly from historical "normal ranges" based on ill-defined populations to current standardized approaches endorsed by international organizations like the International Federation of Clinical Chemistry (IFCC) and the Clinical and Laboratory Standards Institute (CLSI) [84]. This evolution reflects growing recognition that biological variability typically exceeds analytical variability for most measurands, necessitating rigorous statistical approaches to distinguish true physiological differences from measurement noise [7]. In lipidomics research, this distinction becomes particularly critical when comparing findings across populations with potentially different genetic backgrounds, environmental exposures, and lifestyle factors that may influence lipid metabolism.
Comparative Analysis of Variability in Lipidomics Studies
Quantitative Comparison of Biological and Analytical Variability
Table 1: Biological vs. Analytical Variability Metrics in Clinical Lipidomics
| Variability Component | Description | Typical Magnitude in Lipidomics | Impact on RI Establishment |
|---|---|---|---|
| Biological Variability | Natural physiological variation between individuals and within individuals over time [83] | Significantly higher than analytical variability; shows high individuality and sex specificity [7] | Primary driver of RI width; necessitates population partitioning (e.g., by sex, age) |
| Within-Subject Biological Variability | Physiological variation within the same individual over time [7] | Lower than between-subject variability in lipidomics studies [7] | Impacts RI utility for longitudinal monitoring; enables personalized RIs |
| Between-Subject Biological Variability | Physiological differences between different individuals [7] | Significantly higher than within-subject variability for most lipid species [7] | Determines population-based RI width; reflects true biological diversity |
| Analytical Variability | Measurement imprecision from technical processes and instrumentation [83] | Median between-batch reproducibility of 8.5% in quantitative LC-MS/MS lipidomics [7] | Determves RI reliability; must be minimized through quality control |
| Between-Batch Analytical Variability | Measurement differences across independent analytical runs [7] | 8.5% median in lipidomics (across 13 batches, 1,086 samples) [7] | Controlled through reference materials and standardized protocols |
Implications for Cross-Population Lipidomics Research
The quantitative relationship between biological and analytical variability has profound implications for cross-population lipidomics research. When biological variability significantly exceeds analytical variability—as demonstrated in large-scale lipidomics studies where biological variation per lipid species was "significantly higher than the batch-to-batch analytical variability"—researchers can confidently attribute profile differences to true physiological distinctions rather than technical artifacts [7]. This statistical reality enables meaningful comparisons between populations, provided that analytical variability remains well-characterized and controlled.
The high individuality and sex specificity observed in circulatory lipidomes constitutes an important prerequisite for applying lipidomics in next-generation metabolic health monitoring [7]. Specifically, significantly lower between-subject than within-subject variability, combined with unsupervised sample clustering, demonstrates that lipid profiles maintain characteristic individual patterns despite temporal fluctuations. This biological pattern has direct implications for RI establishment: it supports the feasibility of personalized reference intervals while simultaneously validating population-based approaches when properly partitioned by relevant biological factors.
Methodological Approaches for Establishing Reference Intervals
Direct versus Indirect Methods for RI Establishment
Table 2: Comparison of Direct and Indirect Methods for Reference Interval Establishment
| Parameter | Direct Approach | Indirect Approach |
|---|---|---|
| Definition | New data generated from specifically recruited reference individuals [82] | Uses existing data from specimens collected for routine purposes [82] |
| Sample Size Requirements | Minimum 120 reference individuals per partition [85] [86] | Large datasets (e.g., 1,000-10,000 samples) [82] |
| Cost Implications | Higher cost to perform [82] | Lower cost to perform [82] |
| Preanalytical Conditions | May not match routine conditions [82] | Matches routine operational conditions [82] |
| Ethical Considerations | Requires informed consent and ethical approval [86] | No additional ethical issues beyond data usage permissions [82] |
| Statistical Complexity | Requires basic statistical knowledge [82] | Requires significant statistical expertise [82] |
| Risk of Pathological Contamination | Low probability with proper screening [87] | High without proper statistical separation [87] |
| Population Representation | May not reflect service population if recruitment is biased [87] | Inherently reflects laboratory service population [87] |
| Implementation Examples | Prospective population studies with health screening [86] | Data mining of laboratory information systems [87] |
Experimental Protocols for RI Development
Direct Method Protocol for Lipidomics RI Establishment
The direct approach for establishing lipidomics reference intervals follows a standardized protocol based on CLSI guidelines [82] [86]:
Reference Individual Selection: Recruit participants through health screening questionnaires and examinations. Implement specific inclusion/exclusion criteria based on factors known to influence lipid metabolism (e.g., medication use, recent illnesses, smoking status). Obtain written informed consent and ethical approval [86].
Sample Collection and Preparation: Standardize pre-analytical conditions including fasting status, time of day, physical activity, and sample processing protocols. For lipidomics, use stable isotope dilution approaches for quantification and incorporate alternate analysis of reference materials (e.g., National Institute of Standards and Technology plasma) as quality control [7].
Analytical Measurements: Employ high-throughput quantitative methods such as LC-MS/MS lipidomics with robust measurement of multiple lipid species across concentration ranges spanning several orders of magnitude. Maintain between-batch reproducibility benchmarks (<10% median CV) through standardized protocols [7].
Statistical Analysis and Outlier Handling: Apply statistical methods to determine reference limits:
- Remove outliers using established methods (e.g., Dixon's Q test or Tukey fence method)
- Assess data distribution normality
- Calculate nonparametric RIs as the central 95% between 2.5th and 97.5th percentiles
- Partition by biologically relevant factors (e.g., sex) when standard deviation ratio between subgroups exceeds 1.5 [82]
Verification Protocol for Transferred Reference Intervals
For laboratories adopting established RIs rather than developing new ones, CLSI guidelines provide a verification protocol [88] [82]:
- Sample Collection: Obtain 20 samples from reference individuals representative of the laboratory's service population.
- Analysis and Interpretation: Analyze samples using standardized methods. If no more than 2 of the 20 results (≤10%) fall outside the proposed reference limits, the interval can be considered verified for local use.
- Escalation Procedure: If 3 or more results fall outside the proposed limits, collect 20 additional reference samples. If again 3 or more results fall outside the limits, the laboratory should establish population-specific RIs [82].
Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for Lipidomics RI Studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Stable Isotope Internal Standards | Quantitative accuracy through isotope dilution | Multiple lipid class-matched standards for absolute quantification [7] |
| Reference Control Materials | Quality control and reproducibility monitoring | National Institute of Standards and Technology (NIST) plasma reference material [7] |
| LC-MS/MS Lipidomics Platform | High-throughput lipid separation and quantification | Quantitative hydrophilic interaction liquid chromatography; measurement of 782 lipid species across 22 classes [7] |
| Sample Preparation Kits | Standardized lipid extraction | Semiautomated platforms for reproducible sample processing [7] |
| Quality Control Materials | Monitoring analytical performance | Between-batch control materials with established reproducibility targets (e.g., <10% CV) [7] |
| Data Analysis Software | Statistical determination of reference intervals | Nonparametric methods for RI calculation with outlier detection algorithms [82] |
Workflow Visualization
Reference Interval Establishment Workflow
Impact of Variability Components on RI Validity
The establishment of clinically relevant reference intervals in lipidomics research requires meticulous attention to the distinct contributions of biological and analytical variability. Through implementation of standardized direct or indirect methodologies, utilization of appropriate research reagents, and application of rigorous statistical approaches, researchers can develop RIs that reliably distinguish true physiological differences from measurement noise. This foundation enables meaningful cross-population comparisons and enhances the translational potential of lipidomic profiling in both clinical practice and drug development. As lipidomics continues to evolve toward personalized medicine applications, understanding these fundamental variability components will remain essential for validating biomarkers and interpreting metabolic profiles across diverse human populations.
The translation of lipidomic discoveries into FDA-approved clinical biomarkers represents a critical frontier in precision medicine. Lipids, encompassing thousands of distinct molecular species, offer profound insights into cellular metabolism, signaling pathways, and disease mechanisms. This guide objectively compares the current performance of lipid biomarker translation strategies, evaluating technological platforms, analytical methodologies, and validation frameworks. Despite the identification of numerous promising lipid signatures associated with cardiovascular, neurodegenerative, and oncological pathologies, the journey from research findings to clinically implemented diagnostics faces substantial hurdles. These include analytical standardization, biological variability, and regulatory validation across diverse populations. By examining successful translation cases alongside persistent gaps, this analysis provides researchers and drug development professionals with a comprehensive resource for advancing robust lipid biomarkers through the development pipeline to FDA approval.
Lipidomics, a specialized branch of metabolomics, comprehensively analyzes lipid pathways and networks in biological systems [37] [28]. The human lipidome comprises thousands of chemically distinct lipids classified into eight major categories: fatty acyls (FA), glycerolipids (GL), glycerophospholipids (GP), sphingolipids (SP), sterol lipids (ST), prenol lipids (PR), saccharolipids (SL), and polyketides (PK) [37]. These molecules perform vital cellular functions including energy storage, membrane structure, and signal transduction, making their dysregulation informative for disease pathophysiology [37] [13].
The transition of lipid research from bench to bedside hinges on discovering biomarkers that are clinically reliable, repeatable, and validated across various populations [37]. Early identification of metabolic and other diseases through lipid biomarkers enables timely interventions that can reduce morbidity through pharmacological means [37]. Currently, clinical lipid measurements primarily focus on total triglycerides, total cholesterol, LDL-C, and HDL-C [13]. While these established markers provide valuable information, they represent only a tiny fraction of the metabolically informative lipidome, leaving substantial diagnostic potential untapped [13].
The path toward FDA-approved lipid biomarkers requires navigating a complex development pipeline spanning basic discovery, analytical validation, clinical validation, and regulatory approval. This process demands interdisciplinary collaboration among lipid biologists, clinicians, bioinformaticians, and regulatory scientists to fully leverage lipidomics in personalized medicine [37].
Success Stories: Translated Lipid Biomarkers
The Ceramide-Based Cardiovascular Risk Assessment
The development and clinical implementation of a ceramide-based cardiovascular risk assessment represents a pioneering success in lipid biomarker translation. This assay originated from work by Laaksonen et al., who demonstrated that specific serum ceramide species predict cardiovascular death in patients with stable coronary heart disease and acute coronary syndrome [13].
Development Pipeline: The translational pathway progressed through several critical stages:
- Initial Discovery: Identification of specific ceramide species (Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/24:0), and their ratios) associated with CVD mortality.
- Assay Development: Creation of a high-throughput ceramide assay using a 96-well plate format with LC-MS/MS analysis.
- Multi-Cohort Validation: Validation of the ceramide associations across several independent cohorts.
- Clinical Implementation: Translation of the assay into clinical practice at the Mayo Clinic [13].
Enhanced Risk Model: The biomarker evolved into a more sophisticated risk score (CERT2) that incorporates ceramides with phosphatidylcholine-based cardiovascular risk markers. Developed using lipidomic data from the Western Norway Coronary Angiography Cohort (N=3,789), the model was successfully validated in two additional large studies: the LIPID trial (N=5,991) and the Langzeiterfolge der KARdiOLogischen Anschlussheilbehandlung study (N=1,023) [13]. The CERT2 score demonstrated significant predictive power for CVD mortality, with hazard ratios of 1.44, 1.47, and 1.69 across the validation cohorts, respectively.
Commercial Translation: This technology was subsequently licensed to Quest Diagnostics for further development into a clinical laboratory-developed test, marking a significant milestone in lipid biomarker commercialization [13].
NMR-Based Lipoprotein Profiling
While mass spectrometry dominates discovery lipidomics, nuclear magnetic resonance (NMR) spectroscopy has achieved notable clinical translation for lipoprotein analysis:
Technology Foundation: NMR exploits the observation that 1H NMR signals from terminal methyl groups in lipid hydrocarbon chains of lipoprotein complexes systematically shift as particle size decreases [13]. This enables simultaneous quantification of VLDL, LDL, and HDL subclasses from a single measurement.
Commercial Implementation: The NMR method was developed into a commercial assay (LipoProfile) by LipoScience, requiring approximately one minute per sample [13]. The company further developed an FDA-cleared NMR-based LDL particle number diagnostic platform (Vantera Clinical Analyzer) in 2013.
Clinical Utility: Measurements of HDL and LDL particle number have proven superior to traditional total cholesterol measurements for cardiovascular risk assessment [13]. Another company, Nightingale Health, has commercialized an NMR platform capable of high-throughput analysis (~80,000 samples annually) for large-scale clinical trials and personalized health assessment.
Comparative Analysis of Lipid Biomarker Performance
The following tables summarize the current landscape of lipid biomarker research across various disease areas, highlighting both promising candidates and the validation gaps that remain.
Table 1: Performance of Lipid Biomarker Candidates in Disease Diagnosis
| Disease Area | Promising Lipid Biomarkers | Reported Performance (AUC) | Validation Status | Key Gaps |
|---|---|---|---|---|
| Pancreatic Cancer [89] | Panel of 18 phospholipids, 1 acylcarnitine, 1 sphingolipid | 0.9207 (increased to 0.9427 with CA19-9) | Single-center study, algorithm development | Requires multi-center validation; clinical practicality undefined |
| Cardiovascular Disease [13] | CERT2 score (ceramides + phosphatidylcholines) | HR: 1.44-1.69 for CVD mortality | Validated across multiple large cohorts | Limited FDA-approved assays beyond ceramide test |
| Critical Illness [90] | Phosphatidylethanolamines (PE), Triglycerides, Diacylglycerols, Ceramides | Prognostic for worse outcomes in trauma and COVID-19 | Identified in trauma cohort, validated in COVID-19 | Needs prospective intervention studies |
| Osteonecrosis of Femoral Head [91] | 11 lipid biomarkers identified via LASSO regression | AUC > 0.7 for diagnostic performance | Single-center case-control study | Requires external validation and mechanistic studies |
Table 2: Analytical Platforms for Lipid Biomarker Development
| Analytical Platform | Key Strengths | Limitations | Throughput | Quantitative Accuracy |
|---|---|---|---|---|
| LC-MS/MS (Targeted) [13] [89] | High sensitivity and specificity for predefined lipids | Limited to known targets | High | Excellent with internal standards |
| LC-MS (Untargeted) [37] | Comprehensive coverage of lipidome | Affected by matrix effects; complex data processing | Medium | Semi-quantitative without standards |
| 31P NMR [92] | Absolute quantification; structural information | Low sensitivity; high sample requirement | Low | Excellent with certified standards |
| ICP-MS [92] | Traceable quantification via phosphorus detection | Requires chromatographic separation; matrix effects | Medium-High | Excellent for phospholipids |
| NMR Spectroscopy [13] | High reproducibility; minimal sample preparation | Limited lipid species resolution | Very High | Good for lipoprotein subclasses |
Methodological Framework for Lipid Biomarker Development
Experimental Workflows for Lipid Biomarker Discovery and Validation
The path from lipid biomarker discovery to clinical validation requires multiple orthogonal approaches. The following diagram illustrates the integrated workflows and decision points in this process:
Detailed Experimental Protocols
Sample Preparation and Quality Control
Robust sample preparation is foundational to reliable lipidomic data. A standardized protocol includes:
Lipid Extraction: Modified methyl-tert-butyl ether (MTBE) method is widely employed. Briefly, 100 μL plasma is mixed with 0.75 mL methanol, vortexed, then supplemented with 2.5 mL MTBE and incubated for 1 hour at room temperature with shaking [91]. Phase separation is induced by adding 0.625 mL MS-grade water, followed by centrifugation at 1000× g for 10 minutes. The organic phase is collected, and the lower phase is re-extracted. Combined organic phases are dried and reconstituted in 100 μL isopropanol for analysis [91].
Quality Control Metrics:
- Signal Intensity: Consistent intensity across replicates indicates good data quality [28].
- Retention Time Alignment: Critical for accurate lipid identification in LC-MS; misalignment leads to incorrect peak assignments [28].
- Mass Accuracy: Regular mass spectrometer calibration ensures required precision [28].
- Batch Effect Correction: Techniques like ComBat or LOESS normalization address variations between analytical runs [28].
Mass Spectrometry Analysis
Instrumentation: High-resolution mass spectrometers (e.g., Orbitrap Q Exactive HF) coupled to UHPLC systems (e.g., Vanquish) provide the sensitivity and resolution needed for complex lipid separations [91].
Chromatography: Reversed-phase chromatography separates lipids by hydrophobicity, while hydrophilic interaction liquid chromatography (HILIC) separates by lipid class [92].
Quantification Approaches:
- Untargeted Analysis: Comprehensive profiling of all detectable lipids, providing hypothesis-generating data [37].
- Targeted Analysis: Focused quantification of predefined lipid panels using multiple reaction monitoring (MRM) for enhanced sensitivity and precision [13] [89].
- Pseudotargeted Approaches: Balance between coverage and quantification using including all ion fragmentation (AIF) [92].
Data Processing and Statistical Analysis
Preprocessing: Raw data processing includes peak alignment, peak picking, and quantification using software like Compound Discoverer, MS-DIAL, or LipidMatch [28] [91]. Normalization to total spectral intensity or internal standards corrects for technical variation.
Feature Selection: Machine learning approaches address high-dimensional data challenges:
- LASSO Regression: Performs both feature selection and regularization, identifying key lipid metabolites while preventing overfitting [91].
- Random Forests: Handle complex interactions between lipid species [28].
- Support Vector Machines: Effective for classification tasks in biomarker development [89].
Pathway Analysis: Tools like MetaboAnalyst and KEGG contextualize differentially expressed lipids within biological networks through over-representation analysis or pathway topology-based approaches [28].
Key Challenges in Lipid Biomarker Translation
Analytical and Standardization Gaps
The transition from research findings to clinically applicable biomarkers faces significant analytical hurdles:
Reproducibility Issues: Inconsistent results across platforms and laboratories present major obstacles. Studies show prominent software platforms (MS DIAL, Lipostar) agree on only about 14% of lipid identifications using identical LC-MS data and default settings [37]. This low concordance rate highlights the urgent need for standardized analytical protocols.
Quantification Challenges: Accurate absolute quantification remains difficult due to limited availability of certified reference materials and isotope-labeled internal standards for all lipid classes [92]. While traceable quantification using 31P NMR or ICP-MS provides validation, these techniques have limited accessibility [92].
Methodological Diversity: The field employs diverse platforms including targeted, untargeted, and pseudotargeted MS approaches, shotgun MS, and various chromatographic separations, each with different strengths and limitations that complicate cross-study comparisons [37] [92].
Biological and Clinical Validation Gaps
Beyond analytical challenges, biological and clinical factors impede translation:
Biological Variability: Lipid levels exhibit substantial inter-individual variation influenced by factors including age, sex, BMI, fasting status, and medication use [93]. This biological diversity necessitates validation in large, well-characterized cohorts.
Population Heterogeneity: Most lipid biomarker candidates are derived from single-center studies with limited demographic diversity [89] [91]. Cross-validation across different populations and ethnicities remains exceptional rather than routine [37].
Incomplete Regulatory Frameworks: Specific regulatory pathways for lipidomic biomarkers are underdeveloped compared to genomic or proteomic biomarkers [37]. The lack of defined regulatory frameworks and requirements creates uncertainty in the development process.
Integration and Implementation Gaps
Multi-Omics Integration: Lipid changes are frequently subtle and context-dependent, requiring integration with clinical, genomic, and proteomic data for meaningful interpretation [37]. Such integrated approaches remain computationally and methodologically challenging.
Clinical Workflow Integration: Most research protocols are not designed for continuous operation in clinical environments. Purpose-built clinical platforms capable of processing large sample volumes with rapid turnaround times are needed [13].
Table 3: Key Research Reagent Solutions for Lipid Biomarker Development
| Resource Category | Specific Examples | Function/Application |
|---|---|---|
| Reference Materials [92] [13] | NIST SRM 1950, SPLASH LipidoMix, Ceramide Internal Standards | Calibration and quantification accuracy |
| Analytical Platforms [92] [13] | LC-MS/MS systems, 31P NMR, ICP-MS, Vantera Clinical Analyzer | Lipid separation, detection, and quantification |
| Data Processing Software [37] [28] | MS-DIAL, LipidMatch, LipidQA, Compound Discoverer | Peak alignment, lipid identification, quantification |
| Statistical & Bioinformatics Tools [28] [91] | MetaboAnalyst, LASSO regression, Random Forests, SVM | Feature selection, model building, pathway analysis |
| Lipid Databases [28] [91] | LIPID MAPS, LipidBlast, HMDB, KEGG | Lipid identification, structural information, pathway mapping |
Emerging Technologies and Approaches
Innovative methodologies are poised to address current limitations in lipid biomarker translation:
Artificial Intelligence and Machine Learning: AI-based tools like MS2Lipid have demonstrated up to 97.4% accuracy in predicting lipid subclasses [37]. Machine learning frameworks are increasingly employed to uncover complex patterns and interactions that traditional statistical methods might miss [28] [94].
Advanced Integration Strategies: Multi-omics approaches that correlate lipid changes with alterations in gene expression and protein levels offer more comprehensive understanding of biological systems and disease mechanisms [28] [95].
Standardization Initiatives: Community-driven efforts to establish consensus protocols, reference materials, and data standards are critical for improving reproducibility. International ring trials have begun establishing consensus values for lipids in reference materials [92].
The translation of discovery findings to FDA-approved lipid biomarkers remains challenging yet promising. While significant gaps persist in analytical standardization, clinical validation across diverse populations, and regulatory frameworks, successful examples demonstrate the feasibility of this journey. The ceramide-based cardiovascular risk test and NMR lipoprotein profiling represent pioneering achievements that provide valuable roadmaps for future biomarker development.
As technologies advance, particularly in artificial intelligence and multi-omics integration, and as standardization efforts mature, the clinical landscape for lipid biomarkers is expected to expand rapidly. Researchers and drug development professionals should prioritize interdisciplinary collaboration, rigorous validation across diverse cohorts, and engagement with regulatory agencies to accelerate the translation of promising lipid biomarkers from discovery to clinical practice, ultimately enhancing personalized medicine through improved disease risk assessment, diagnosis, and monitoring.
Conclusion
The cross-validation of lipidomic findings across diverse populations is paramount for advancing precision medicine and requires addressing biological complexity through rigorous methodology. Key takeaways include the necessity of accounting for ethnic, sex, and developmental specificity in lipid metabolism, alongside implementing standardized, high-throughput platforms and robust statistical frameworks. Future directions should focus on establishing universal reference materials, developing AI-driven validation tools, and promoting data-sharing initiatives to build comprehensive lipidomic databases. Such efforts will ultimately enable the development of clinically actionable lipid biomarkers that are reproducible across global populations, thereby improving disease diagnosis, risk stratification, and therapeutic monitoring in diverse patient groups.
References
- 1. Patterns of lipid profile and genetic variations in South Asians [https://pmc.ncbi.nlm.nih.gov/articles/PMC12509405/]
- 2. Dyslipidemia and ASCVD in Non-White Ethnic, Racial, and ... [https://www.lipid.org/lipid-spin/spring-2024/clinical-feature-dyslipidemia-and-ascvd-non-white-ethnic-racial-and-ancestral]
- 3. Patterns of lipid profile and genetic variations in South Asians [https://pubmed.ncbi.nlm.nih.gov/41068856]
- 4. Identification of protein targets for dyslipidaemia and ... [https://www.sciencedirect.com/science/article/pii/S2772368225000927]
- 5. Weight gain leads to greater adverse metabolic responses ... [https://www.nature.com/articles/s42255-024-01101-z]
- 6. Unravelling lipid heterogeneity: Advances in single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270072/]
- 7. Clinical lipidomics reveals high individuality and sex ... [https://www.sciencedirect.com/science/article/pii/S0022227525000409]
- 8. Ether lipids and sphingolipids drive sex-specific human ... [https://pubmed.ncbi.nlm.nih.gov/40706291/]
- 9. Ether lipids and sphingolipids drive sex-specific human aging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12309944/]
- 10. Identification and validation of a blood- based diagnostic ... [https://www.nature.com/articles/s41467-024-48763-7]
- 11. Exploring lipidomic profiles and their correlation with hormone ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11542162/]
- 12. Optimizing lipidomic workflows [https://www.news-medical.net/whitepaper/20250519/Optimizing-lipidomic-workflows-with-high-performance-mass-spectrometry.aspx]
- 13. Clinical lipidomics: realizing the potential of lipid profiling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8528718/]
- 14. Determination and comparison of lipid profiles of Chinese green tea... [https://pubmed.ncbi.nlm.nih.gov/39999551/]
- 15. Ontogeny of circulating lipid metabolism in pregnancy and early childhood – a longitudinal population study | eLife [https://elifesciences.org/articles/72779]
- 16. Population-based plasma lipidomics reveals developmental changes in metabolism and signatures of obesity risk: a mother-offspring cohort study | BMC Medicine | Full Text [https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-022-02432-y]
- 17. Lipid profiling identifies modifiable signatures of ... [https://www.nature.com/articles/s41591-024-03279-x]
- 18. Lipidomic risk scores are independent of polygenic risk scores ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8893343/]
- 19. Maternal bioactive lipids during pregnancy and early childhood neurodevelopment and behavior | Pediatric Research [https://www.nature.com/articles/s41390-025-04465-4]
- 20. Lipidomics analysis in drug discovery and development [https://pubmed.ncbi.nlm.nih.gov/36586190/]
- 21. Deep serum lipidomics identifies evaluative and predictive ... [https://www.sciencedirect.com/science/article/pii/S0002916524007093]
- 22. Investigation of Dyslipidemia and Lipid Profile Ratios ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12208299/]
- 23. Urbanization, mainly rurality, but not altitude is associated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5624786/]
- 24. Nonlinear associations between environmental factors and ... [https://www.sciencedirect.com/science/article/abs/pii/S0048969722030595]
- 25. Lipid Profile Abnormalities in Metabolic Syndrome Patients [https://www.healthcare-bulletin.co.uk/article/lipid-profile-abnormalities-in-metabolic-syndrome-patients-a-comparative-cross-sectional-study-3539/]
- 26. Data analysis of MS-based clinical lipidomics studies with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8620525/]
- 27. Deep serum lipidomics identifies evaluative and predictive ... [https://pubmed.ncbi.nlm.nih.gov/39182617/]
- 28. How to Interpret Lipidomics Data: A Step-by-Step Guide [https://lipidomics.creative-proteomics.com/resource/how-to-interpret-lipidomics-data-a-step-by-step-guide.htm]
- 29. Optimized Analytical Procedures for the Untargeted ... [https://www.sciencedirect.com/science/article/pii/S1535947620331777]
- 30. Not One Method to Rule Them All: A Comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631722/]
- 31. Evaluation of lipid quantification accuracy using HILIC and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7220885/]
- 32. Applications of Hydrophilic Interaction Chromatography in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12430451/]
- 33. Large-scale lipidomics profiling reveals characteristic lipid ... [https://pubmed.ncbi.nlm.nih.gov/37470807/]
- 34. Research Reproducibility in Longitudinal Multi-Center Studies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5001777/]
- 35. Automated Sample Preparation Global Market Report 2025 [https://www.thebusinessresearchcompany.com/report/automated-sample-preparation-global-market-report]
- 36. Sample Preparation Market Size, Trends | Industry Share & ... [https://www.mordorintelligence.com/industry-reports/global-sample-preparation-market-industry]
- 37. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/pii/S0009898125005777?dgcid=rss_sd_all]
- 38. Cross Validation of an Automated LipidQuan Sample ... [https://www.waters.com/nextgen/in/en/library/application-notes/2020/cross-validation-of-an-automated-lipidquan-sample-preparation-procedure.html?srsltid=AfmBOoqNZS3iuA2yqmUzG7fvsu9ed1MqUsVcIWmORCN3lY9U0dQtdBHO]
- 39. A comparison of an optimized automated sample ... [https://www.sciencedirect.com/science/article/abs/pii/S0731708522000565]
- 40. A High Throughput Lipidomics Method Using Scheduled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9138805/]
- 41. Cross-over Studies - an overview [https://www.sciencedirect.com/topics/agricultural-and-biological-sciences/cross-over-studies]
- 42. How to analyze a 2x2 Crossover Study in Prism - FAQ 2162 [https://www.graphpad.com/support/faq/how-to-analyze-crossover-study-in-prism/]
- 43. A scientific review on advances in statistical methods for ... [https://arxiv.org/html/2410.08441v1]
- 44. Study designs [https://www.cebm.ox.ac.uk/resources/ebm-tools/study-designs]
- 45. , analysis, and presentation of Design | crossover | Full Text trials Trials [https://trialsjournal.biomedcentral.com/articles/10.1186/1745-6215-10-27]
- 46. - Inter in the Adaptive Responses to Endurance... Individual Variability [https://pmc.ncbi.nlm.nih.gov/articles/PMC5147982/]
- 47. - Inter differences in the blood pressure lowering effects of... individual [https://link.springer.com/article/10.1007/s00394-025-03616-x]
- 48. NIST lipidomics workflow questionnaire: an assessment of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11493135/]
- 49. LipidQC: Method Validation Tool for Visual Comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11493136/]
- 50. NIST Biomanufacturing Reference Materials: Development, ... [http://www.nae.edu/19579/19582/21020/338895/339009/NIST-Biomanufacturing-Reference-Materials-Development-Applications-and-Impact]
- 51. New NIST Reference Material to Strengthen Quality ... [https://www.nist.gov/news-events/news/2025/07/new-nist-reference-material-strengthen-quality-control-biological-drugs]
- 52. Expert Pre-Analytical Work Processing - Sampled [https://sampled.com/the-critical-role-of-pre-analytical-work/]
- 53. Pre-Analytical Sample Handling: What Can You Do Better? [https://bitesizebio.com/31073/pre-analytical-sample-handling/]
- 54. The impact of preanalytical variables on the analysis of cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11111958/]
- 55. The Effect of Preanalytical Variables on Plasma Samples ... [https://www.thermofisher.com/blog/biobanking/the-effect-of-preanalytical-variables-on-plasma-samples-stored-in-biobanks/]
- 56. Lipidomic profiling of human bile distinguishes ... [https://www.nature.com/articles/s41416-025-03144-9]
- 57. Steps Toward Minimal Reporting Standards for Lipidomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8376269/]
- 58. Challenges in Lipidomics Biomarker Identification [https://pmc.ncbi.nlm.nih.gov/articles/PMC11356033/]
- 59. LipidMatch: an automated workflow for rule-based lipid ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-017-1744-3]
- 60. Single-cell lipidomics: performance evaluation across four ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12462284/]
- 61. Cross-Platform Comparison of Untargeted and Targeted ... [https://www.nature.com/articles/s41598-018-35807-4]
- 62. Assessing and mitigating batch effects in large-scale omics ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-024-03401-9]
- 63. Enhancing statistical power and data reliability in Lipidomics [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25026943]
- 64. Simulating paired and longitudinal single-cell RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366488/]
- 65. Best practices and tools in R and Python for statistical ... [https://www.nature.com/articles/s41467-025-63751-1]
- 66. Circulating lipidome underpins gender differences in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12155659/]
- 67. Accurate and Efficient Resolution of Overlapping Isotopic Envelopes in Protein Tandem Mass Spectra - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4593959/]
- 68. Quantification of Isotopically Overlapping Deamidated and 18O Labeled Peptides Using Isotopic Envelope Mixture Modeling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2693468/]
- 69. Plasma lipidomics for biomarker identification in non-muscle ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-15019-6]
- 70. Matching isotopic distributions from metabolically labeled samples - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2718665/]
- 71. Isotope pattern deconvolution for peptide mass spectrometry by non-negative least squares/least absolute deviation template matching | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-13-291]
- 72. Towards sustainable lipidomics: computational screening ... [https://link.springer.com/article/10.1007/s00216-025-06136-z]
- 73. Parental Transmission of Type 2 Diabetes Risk in Offspring [https://pmc.ncbi.nlm.nih.gov/articles/PMC12030247/]
- 74. Genetic architecture and risk prediction of gestational ... [https://www.nature.com/articles/s41467-025-59442-6]
- 75. The role of the beta cell in type 2 diabetes: new findings ... [https://link.springer.com/article/10.1007/s00125-025-06499-z]
- 76. Gestational diabetes and maternal obesity are associated ... [https://insight.jci.org/articles/view/122572]
- 77. Integrating lipidomics and machine learning to characterize ... [https://www.sciencedirect.com/science/article/pii/S003257912500481X]
- 78. Study Design and Protocol of the Multisite Pregnancy 24/7 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11484610/]
- 79. Machine Learning Reveals Lipidome Remodeling Dynamics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9881992/]
- 80. Machine learning and semi-targeted lipidomics identify ... [https://pubmed.ncbi.nlm.nih.gov/35381232/]
- 81. Machine learning survival prediction using tumor lipid ... [https://www.nature.com/articles/s41598-024-63736-y]
- 82. Validation of reference intervals and reportable range [https://www.pathologyoutlines.com/topic/labadminreferenceintervals.html]
- 83. Biological versus technical variability [https://genomicsclass.github.io/book/pages/biological_versus_technical_var.html]
- 84. An introduction to reference intervals (1) - some theoretical ... [https://acutecaretesting.org/en/articles/an-introduction-to-reference-intervals-1--some-theoretical-considerations]
- 85. The Role and Limitations of the Reference Interval Within ... [https://www.frontierspartnerships.org/journals/british-journal-of-biomedical-science/articles/10.3389/bjbs.2024.12339/full]
- 86. Establishment of Population Specific Reference Intervals in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9644092/]
- 87. Modern Reference Intervals [https://myadlm.org/cln/articles/2021/july/modern-reference-intervals]
- 88. Reference Intervals: Practical Aspects - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4975204/]
- 89. Diagnostic Biomarker Candidates Proposed Using ... [https://www.mdpi.com/2072-6694/17/18/2988]
- 90. Lipidomic signatures align with inflammatory patterns and ... [https://www.nature.com/articles/s41467-022-34420-4]
- 91. Research on Lipidomic Profiling and Biomarker ... [https://www.mdpi.com/2227-9059/12/12/2827]
- 92. Achieving Absolute Molar Lipid Concentrations: A Phospholipidomics... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8792901/]
- 93. Current landscape of plasma proteomics from technical ... [https://www.nature.com/articles/s42004-025-01665-1]
- 94. Lipid-Lowering Effects Discovered in FDA-Approved Drugs ... [https://www.pharmacytimes.com/view/lipid-lowering-effects-discovered-in-fda-approved-drugs-using-machine-learning]
- 95. Advances in mass spectrometry of lipids for the investigation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308988/]