Evaluating Cathepsin B Inhibition Models: From Computational Screening to Therapeutic Applications in Cancer and Neurodegenerative Diseases
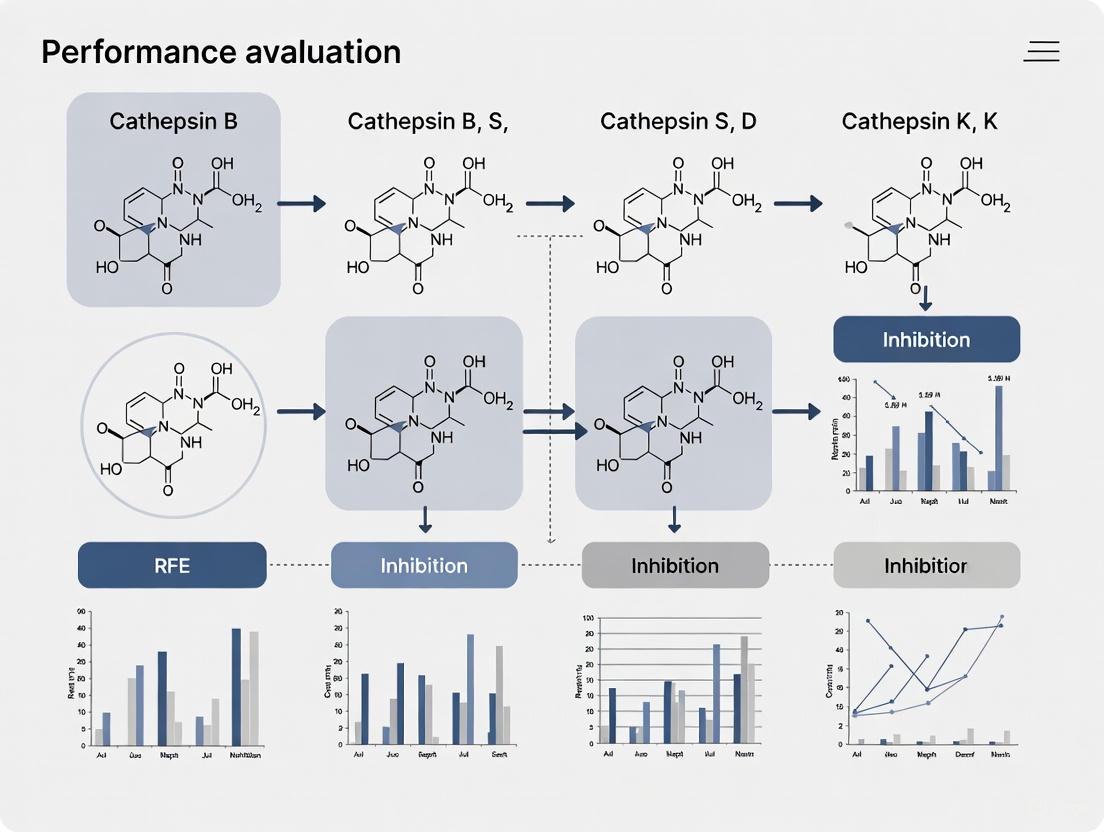
This comprehensive review systematically evaluates the performance of Recursive Feature Elimination (RFE) models in identifying and optimizing Cathepsin B inhibitors.
Evaluating Cathepsin B Inhibition Models: From Computational Screening to Therapeutic Applications in Cancer and Neurodegenerative Diseases
Abstract
This comprehensive review systematically evaluates the performance of Recursive Feature Elimination (RFE) models in identifying and optimizing Cathepsin B inhibitors. Cathepsin B, a cysteine protease implicated in cancer progression, Alzheimer's disease, and Parkinson's disease, represents a promising therapeutic target. This article explores foundational biological roles of Cathepsin B across pathological contexts, examines computational and experimental methodologies for inhibitor screening, addresses critical optimization challenges including selectivity and pH-dependent activity, and validates approaches through comparative analysis of emerging therapeutic candidates. Designed for researchers, scientists, and drug development professionals, this work integrates structural biology, machine learning, and clinical translation to advance targeted inhibition strategies.
Cathepsin B as a Multifaceted Therapeutic Target: Biological Roles and Disease Implications
Cathepsin B (CTSB), a lysosomal cysteine protease of the papain family, is a key player in tumor progression. While it normally functions in intracellular protein turnover within the acidic lysosomal environment, its dysregulation in cancer contexts contributes significantly to malignant transformation. In various human cancers, CTSB undergoes overexpression, altered trafficking, and secretion into the extracellular space, where it facilitates critical tumor-promoting processes including extracellular matrix (ECM) degradation, angiogenesis, and metastasis [1] [2]. This review synthesizes current mechanistic understanding of CTSB in cancer progression, compares its roles across different cancer models, and details the experimental approaches used to evaluate CTSB function and inhibition, providing a resource for therapeutic development.
Molecular Regulation and Trafficking of Cathepsin B in Cancer
Transcriptional and Post-transcriptional Regulation
The CTSB gene, located on chromosome 8p22, is regulated by multiple promoters rich in GC content but lacking TATA and CAAT boxes [1]. Key transcription factors including Ets1, Sp1, and Sp3 bind to these promoter regions and activate transcription [1]. Ets1, a proto-oncogene that enhances invasiveness, is frequently overexpressed in cancers such as breast cancer [1]. Upstream stimulatory factors (USFs) that bind to the E-box in the promoter can either increase or repress CTSB expression, providing a link to stress-responsive pathways [1]. Post-transcriptionally, alternative splicing generates variants like CB(-2) and CB(-2,3). The CB(-2) variant translates more efficiently, while CB(-2,3) produces a truncated protein that may be mislocalized to mitochondria and involved in cell death pathways [1].
Altered Trafficking and Localization
In normal physiology, CTSB is synthesized as a preproenzyme and traffics through the endoplasmic reticulum and Golgi apparatus to lysosomes [1]. In cancer cells, this trafficking is disrupted, leading to CTSB secretion and association with the plasma membrane [1]. This redistribution is facilitated by binding to the annexin II heterotetramer, which localizes CTSB to caveolae, specialized membrane microdomains [1] [3]. This pericellular localization positions CTSB to degrade ECM components and activate proteolytic cascades critical for invasion.
The following diagram illustrates the key regulatory and trafficking pathways of Cathepsin B in a cancer cell:
Mechanisms of Action in Cancer Progression
Facilitation of Invasion and Metastasis
CTSB promotes invasion through direct degradation of ECM components and activation of other proteases [2]. As a cysteine protease with both endopeptidase and exopeptidase activities, CTSB can cleave various structural proteins in the basement membrane and interstitial matrix [1]. In colorectal cancer models, CTSB silencing reduced invasion capacity and metastatic spread in immunodeficient mice [4]. Furthermore, CTSB can process and activate other proteolytic enzymes, including urokinase-type plasminogen activator (uPA), thereby amplifying the overall proteolytic cascade that enables cancer cell dissemination [1].
Regulation of Angiogenesis
CTSB modulates the angiogenic switch through multiple mechanisms. In endothelial cells, suppression of CTSB activity increased VEGF mRNA and protein levels, correlating with elevated HIF-1α, while also reducing the anti-angiogenic protein endostatin [5]. This suggests CTSB helps balance pro- and anti-angiogenic factors. Additionally, CTSB can inactivate tissue inhibitors of matrix metalloproteinases (TIMPs), specifically TIMP-1 and TIMP-2, thereby releasing their inhibition of MMPs and creating a pro-angiogenic environment [6]. This TIMP inactivation represents an indirect mechanism whereby CTSB promotes blood vessel formation to support tumor growth.
Role in Programmed Cell Death
CTSB localizes to the cytosol under pathological conditions due to lysosomal membrane permeabilization, where it participates in multiple programmed cell death (PCD) pathways [3]. In apoptosis, CTSB can cleave Bid to its active form (tBid), triggering mitochondrial cytochrome c release and caspase activation [3]. CTSB also contributes to pyroptosis by promoting NLRP3 inflammasome activation, though the specific substrates remain unclear [3]. The dual role of CTSB in both promoting and inhibiting cell death depending on cellular context adds complexity to its functions in tumor progression.
Experimental Models and Data Comparison
Research into CTSB function employs diverse experimental approaches, from in vitro enzyme assays to complex in vivo models. The table below summarizes key experimental findings and methodologies across different cancer models.
Table 1: Comparative Experimental Data on Cathepsin B in Cancer Models
| Cancer Type/Model | Experimental Approach | Key Findings | Molecular Mechanisms |
|---|---|---|---|
| Colorectal Cancer [4] | CTSB silencing (RNAi) in human CRC cells; Xenograft models | Inhibited growth in soft agar; Reduced invasion and metastatic spread; Increased p27Kip1 levels | Lysosomal degradation of p27Kip1 cell cycle inhibitor |
| Glioma [1] | Transgenic models; Protease targeting studies | Single CTSB targeting less effective than multi-protease targeting | Part of proteolytic pathway with other proteases/receptors |
| Pancreatic & Mammary Carcinoma [1] | Transgenic murine models | Causal roles in initiation, growth, angiogenesis, invasion, and metastasis | Promotion of tumor cell proliferation; Involvement in tumor-associated macrophages |
| Endothelial Cells & Angiogenesis [5] | Tube formation assay in collagen; CTSB inhibition (CA-074-Me) | Eliminated dependence on exogenous VEGF; Increased HIF-1α and VEGF; Reduced endostatin | Regulation of intrinsic angiogenic threshold; Balance of pro/anti-angiogenic factors |
Detailed Experimental Protocols
Tube Formation Assay for Angiogenesis Studies
The tube formation assay evaluates endothelial cell morphogenesis into capillary-like structures, simulating early stages of angiogenesis [5].
Materials:
- Collagen gel mixture: 80% VITROGEN, 0.02 N NaOH, 20 mM HEPES, 2 mg/ml NaHCO₃, 0.5 μg/ml fibronectin, 0.5 μg/ml laminin, and 10.5 mg/ml RPMI powder [5].
- Cells: Bovine Retinal Endothelial Cells (BRECs) or Human Umbilical Vein Endothelial Cells (HUVECs) [5].
- Inhibitors: Cathepsin B inhibitor (CA-074-Me) [5].
Methodology:
- Lower gel layer: Add 400 μL of collagen gel mixture per well to a 24-well plate. Incubate at 37°C for 2 hours for polymerization [5].
- Cell seeding: Seed 1 × 10⁵ BRECs or 7 × 10⁴ HUVECs per well in appropriate medium. Incubate for 24 hours at 37°C [5].
- Upper gel layer: Remove medium and add 150 μL of fresh collagen gel mixture on top of the cell layer [5].
- Treatment: Add test compounds (e.g., VEGF, CTSB inhibitors) in culture medium.
- Analysis: After incubation (typically 24-48 hours), quantify tube formation by measuring total tube length, number of branch points, or enclosed areas using microscopy and image analysis software [5].
RNA Interference and Xenograft Studies
Gene silencing followed by xenograft implantation assesses the role of CTSB in tumorigenesis and metastasis in vivo [4].
Materials:
- Cells: Human colorectal cancer (CRC) cell lines (e.g., HCT116, HT-29) [4].
- Animals: Immunodeficient mice (e.g., CD1 nu/nu, SCID) [4].
- Reagents: CTSB-specific shRNA/siRNA, transfection reagent, Matrigel [4].
Methodology:
- CTSB knockdown: Transfect CRC cells with CTSB-specific RNAi constructs using standard protocols (e.g., lipofection) [4].
- Validation: Confirm knockdown efficiency via Western blotting or qPCR [4].
- Xenograft establishment: Subcutaneously inject control and CTSB-deficient cells (e.g., 5 × 10⁶ cells in Matrigel) into flanks of mice [4].
- Metastasis models: For spontaneous metastasis, use orthotopic implantation; for experimental metastasis, use intravenous injection [4].
- Monitoring: Measure primary tumor volume weekly with calipers. For metastasis, image organs (e.g., lungs, liver) ex vivo after sacrifice and count metastatic nodules [4].
- Tissue analysis: Process tumors for immunohistochemistry (IHC) or Western blotting to analyze proliferation markers (e.g., Ki-67), apoptosis (e.g., cleaved caspase-3), and pathway components (e.g., p27Kip1) [4].
Cathepsin B Inhibition as a Therapeutic Strategy
Inhibiting CTSB has emerged as a promising therapeutic approach. The diagram below illustrates the mechanistic strategy for selective CTSB inhibition in the pathogenic cytosolic environment, a novel approach for conditions like traumatic brain injury and Alzheimer's disease that may also inform cancer therapeutic development [7].
The pH-dependent inhibitor strategy leverages the different microenvironments where CTSB operates. Under normal conditions, CTSB functions in acidic lysosomes (pH ~4.6). In pathology, lysosomal leakage releases CTSB into the neutral cytosol (pH ~7.2) [7] [3]. Inhibitors like Z-Arg-Lys-AOMK are designed to be selective for the neutral pH form of CTSB, potentially targeting the disease-associated pool of the enzyme while sparing its normal physiological function [7]. In cancer, the extracellular tumor microenvironment can also be slightly acidic, which may influence the efficacy of such pH-sensitive agents.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Research Reagents for Cathepsin B Studies
| Reagent / Tool | Primary Function / Mechanism | Example Applications |
|---|---|---|
| CA-074 / CA-074Me [5] [4] | Selective, potent cathepsin B inhibitor (CA-074Me is cell-permeable prodrug) | Inhibiting extracellular vs. intracellular CTSB; Studying CTSB loss-of-function in vitro and in vivo |
| E64d [7] | Broad-spectrum cysteine protease inhibitor (prodrug of E64c) | General cysteine protease inhibition; Assessing overall class contribution to pathology |
| Z-Arg-Lys-AOMK [7] | Neutral pH-selective cathepsin B inhibitor | Selective targeting of cytosolic (pathogenic) CTSB without affecting lysosomal CTSB |
| CTSB-specific siRNA/shRNA [4] | RNA interference for targeted gene knockdown | Establishing stable CTSB-deficient cell lines; Determining long-term functional consequences |
| Anti-Cathepsin B Antibodies [4] | Detection of CTSB protein levels and localization | Immunohistochemistry, Western blotting, immunofluorescence for expression analysis |
| Activity-Based Probes [1] | Covalently bind active enzyme forms, enabling detection | Labeling active CTSB on tumor cell surfaces; Identifying compensatory proteases |
Cathepsin B emerges as a multifunctional protease that significantly contributes to cancer progression through diverse mechanisms, including direct ECM degradation, regulation of angiogenesis, modulation of cell death pathways, and control of cell cycle progression. Its value as a therapeutic target is supported by evidence from genetic knockout and pharmacological inhibition studies across multiple cancer models. The development of sophisticated tools, such as pH-selective inhibitors and activity-based probes, continues to refine our understanding of CTSB's pathophysiological roles and promises to enable more targeted therapeutic interventions. Future research should focus on clarifying context-specific functions of CTSB in different cancer types and stages, and exploring combination therapies that simultaneously target CTSB and complementary proteolytic pathways.
The intricate interplay between protein aggregation pathways represents a central frontier in neurodegenerative disease research. Alzheimer's disease (AD) and Parkinson's disease (PD), the two most prevalent neurodegenerative disorders, are characterized by the accumulation of specific pathological proteins—amyloid-β (Aβ) and tau in AD, and α-synuclein (α-syn) in PD [8] [9]. Emerging evidence reveals that these proteins operate within a connected pathological network, where cross-talk between Aβ and α-syn accelerates cognitive decline and disease progression [8] [9]. Within this complex protein interplay, lysosomal proteases—particularly cathepsins—have emerged as critical regulators of both Aβ processing and α-syn clearance mechanisms.
This review examines the dual role of cathepsin B as a nexus between AD and PD pathophysiology, focusing on its dual functions in amyloid-beta processing and alpha-synuclein clearance. We synthesize current experimental evidence to evaluate cathepsin B's potential as a therapeutic target, providing researchers with structured experimental data, methodological approaches, and analytical frameworks for investigating lysosomal pathways in neurodegenerative proteinopathies.
Cathepsin B at the Crossroads of Neurodegenerative Pathways
Cathepsin B is a lysosomal cysteine protease belonging to the papain family, normally localized to the lysosomal lumen where it maintains cellular homeostasis through protein degradation [10] [11]. Beyond its classical lysosomal functions, cathepsin B operates extracellularly under pathological conditions and participates in multiple signaling pathways relevant to neurodegeneration [11]. Genetic studies have identified variants in the CTSB gene encoding cathepsin B that are associated with increased PD risk, particularly through mechanisms that reduce enzyme expression or function [10].
The enzyme demonstrates a complex, context-dependent relationship with neurodegenerative processes. Cathepsin B can cleave both monomeric and fibrillar forms of α-syn, and its inhibition impairs autophagy, reduces glucocerebrosidase activity, and leads to accumulation of lysosomal content [10]. Simultaneously, cathepsin B interacts with Aβ metabolism, though these relationships remain less fully characterized than its functions in α-syn clearance. This dual involvement positions cathepsin B as a potentially significant modulator at the intersection of AD and PD pathology.
Table 1: Cathepsin B Functions in Neurodegenerative Protein Processing
| Biological Context | Effect on α-Synuclein | Effect on Amyloid-β | Net Pathological Impact |
|---|---|---|---|
| Normal Lysosomal Function | Cleaves monomeric and fibrillar α-syn [10] | Limited data; potential cleavage of Aβ species | Protective through aggregate clearance |
| Reduced Expression/Activity | Impaired α-syn fibril degradation; increased p-α-syn inclusions [10] | Predicted increased Aβ accumulation based on parallel pathways | Pathogenic through reduced clearance |
| Inflammatory Milieu | Potential enhanced cleavage generating aggregation-prone truncations [10] | Possible altered processing | Context-dependent: protective or pathogenic |
| Genetic Risk Variants | Reduced clearance capacity; increased Lewy body pathology risk [10] | Theoretical increased plaque deposition risk | Increased overall neurodegenerative risk |
Experimental Models and Methodologies for Cathepsin B Functional Analysis
Genetic Manipulation Approaches
Investigations into cathepsin B function have employed sophisticated genetic models to establish causal relationships between enzyme activity and protein clearance. Both knockout and activation models have been developed across different cellular systems:
CRISPR-Cas9 Knockout Generation: CTSB-knockout induced pluripotent stem cell (iPSC) lines are created using single-guide RNA (gRNA) targeting exon 4 with a single-stranded DNA repair template to introduce a stop codon. Transfected iPSCs are selected via puromycin resistance, with edited clones verified by digital PCR and Western blot confirmation of protein loss [10].
Gene Activation Strategies: CTSB gene activation utilizes CRISPR-based synergistic activation mediators (SAM) to enhance endogenous expression. This approach increases cathepsin B transcription without overexpression artifacts, providing a physiologically relevant model to study enhanced clearance capacity [10].
iPSC-Derived Neuronal Models: Human iPSCs are differentiated into dopaminergic neurons using patterned growth factors (e.g., bFGF, heregulin, activin A, IGF-1) with ciliary neurotrophic factor (CNTF) added during final maturation stages. These models recapitulate disease-relevant vulnerability and allow assessment of α-syn clearance in human neuronal populations [10] [12].
Pharmacological Modulation Protocols
Complementing genetic approaches, pharmacological tools enable acute manipulation of cathepsin B activity:
Cathepsin B Inhibitors: CA-074Me is a cell-permeable cathepsin B-specific inhibitor administered at concentrations ranging from 10-100 μM for 24-72 hours. Treatment efficacy is validated through fluorometric activity assays using Z-Arg-Arg-AMC substrates [10] [11].
Lysosomal Function Assessment: Concomitant evaluation of lysosomal integrity is performed using LysoTracker staining for lysosomal acidity and immunoblotting for LAMP1/LAMP2 to assess lysosomal membrane stability [10].
Protein Aggregation and Clearance Assays
Standardized methodologies for generating and quantifying protein aggregates are essential for clearance studies:
α-Syn Preformed Fibrils (PFF) Production: Recombinant monomeric α-syn (5mg/ml in PBS) is agitated at 1000 rpm for 7 days at 37°C. Fibrils are sonicated (20% amplitude, 1s on/off for 30s) before use to ensure uniform fragmentation [10] [12].
Aβ Fibril Generation: Synthetic Aβ42 monomers are dissolved in 10mM NaOH/PBS (2mg/ml) and agitated at 1500 rpm for 4 days at 37°C. Cy3-labeling enables fluorescence-based quantification [12].
Clearance Quantification: Cells are exposed to sonicated fibrils (1-5μg/ml) for 24-72 hours. Internalized aggregates are quantified via ELISA, immunocytochemistry, or fluorescence-activated cell sorting (FACS) [10] [12]. Clearance rates are calculated as the percentage reduction in intracellular aggregates over time.
Cathepsin B in α-Synuclein Clearance: Mechanisms and Experimental Evidence
The role of cathepsin B in α-synuclein clearance exemplifies the complex balance between protective and potentially detrimental effects in protein quality control. Evidence from multiple experimental systems indicates that cathepsin B promotes the lysosomal degradation of α-syn aggregates through several interconnected mechanisms.
Genetic and pharmacological studies demonstrate that cathepsin B reduction impairs autophagy, decreases glucocerebrosidase activity, and leads to accumulation of lysosomal content, ultimately reducing clearance of α-syn fibrils [10]. Conversely, CTSB gene activation enhances fibril clearance capacity, supporting a protective role. In midbrain organoids and iPSC-derived dopaminergic neurons, cathepsin B inhibition potentiates the formation of phosphorylated α-syn inclusions following exposure to preformed fibrils [10]. This clearance function occurs within the broader context of the autophagy-lysosomal pathway, where fibrillar α-syn is primarily targeted by autophagy while monomeric or prefibrillar species are handled by the ubiquitin-proteasome system and chaperone-mediated autophagy [13].
The cellular context significantly influences cathepsin B's effects. In microglia, cathepsin B participates in P62-mediated selective autophagy of α-syn fibrils, while in astrocytes, different mechanisms predominate [13]. Importantly, crosstalk between these cell types enhances overall clearance capacity. Co-cultures of astrocytes and microglia demonstrate significantly reduced intracellular α-syn deposits compared to monocultures, with live imaging revealing that microglia can attract and clear protein deposits from astrocytes through direct membrane contacts and tunneling nanotubes [12].
Table 2: Experimental Findings on Cathepsin B in α-Synuclein Clearance
| Experimental System | Intervention | Key Findings | Reference |
|---|---|---|---|
| iPSC-derived dopaminergic neurons | CTSB knockout vs. activation | KO: impaired fibril clearance; Activation: enhanced clearance | [10] |
| Neuroglioma cells | CTSB siRNA knockdown | Reduced degradation of α-syn preformed fibrils | [10] |
| Midbrain organoids | CA-074Me inhibition | Increased phosphorylated α-syn inclusions | [10] |
| Astrocyte-microglia co-culture | None (comparative analysis) | Enhanced aggregate clearance compared to monocultures | [12] |
| In vitro enzymatic assays | Recombinant cathepsin B | Cleaves both monomeric and fibrillar α-syn | [10] |
Cathepsin B in Alpha-Synuclein Clearance Pathways
Cathepsin B in Amyloid-Beta Processing: Emerging Connections
While cathepsin B's role in α-synuclein clearance is relatively well-established, its involvement in amyloid-beta processing represents an emerging frontier with significant implications for AD pathophysiology and the interconnection between neurodegenerative processes. The current understanding of these relationships, though less comprehensive, points to complex interactions within the protein triumvirate of Aβ, tau, and α-syn [8] [9].
Protein interactome analyses reveal that Aβ, tau, and α-syn operate within a connected network, where each can influence the aggregation and toxicity of the others [9]. Within this framework, cathepsin B emerges as a potential modulator of Aβ pathology through several hypothesized mechanisms. As a lysosomal protease, cathepsin B likely participates in Aβ degradation through the endosomal-lysosomal system, similar to its role in α-syn clearance. Additionally, cathepsin B may indirectly influence Aβ generation through its interactions with other proteases involved in amyloid precursor protein (APP) processing [9].
The crosstalk between Aβ and α-syn pathologies provides another dimension to cathepsin B's potential involvement. Studies indicate that Aβ plaque deposition can dramatically accelerate both the seeding and spreading of α-syn aggregation in the brain [9]. This synergistic relationship may create a feed-forward cycle of protein aggregation that cathepsin B could potentially modulate through its dual substrate specificity. Furthermore, the observed co-existence of Aβ and α-syn pathologies in a majority of autopsied AD brains suggests the possible involvement of shared clearance mechanisms, with cathepsin B as a plausible candidate [14] [8].
Table 3: Cathepsin B and Amyloid-β: Evidence and Potential Mechanisms
| Evidence Type | Findings | Implications for Aβ Processing |
|---|---|---|
| Protein Interactome Analysis | APP, MAPT, and SNCA share common interactors and pathways [9] | Cathepsin B may operate at intersection of Aβ and α-syn pathologies |
| Pathological Co-existence | Aβ/α-syn/tau co-pathology in >50% of AD brains [14] [8] | Suggests shared clearance mechanisms potentially involving cathepsin B |
| Cross-promotion of Aggregation | Aβ accelerates α-syn seeding and spreading [9] | Cathepsin B may modulate this synergistic toxicity |
| Therapeutic Targeting | Multi-target approaches needed for mixed proteinopathies [8] | Supports cathepsin B as potential target for combined pathology |
Integrated Experimental Workflow for Cathepsin B Functional Analysis
A comprehensive approach to evaluating cathepsin B in neurodegenerative protein processing requires the integration of methodological streams across cellular models, functional assays, and analytical endpoints. The following workflow provides a structured framework for investigating cathepsin B's dual roles in Aβ and α-syn pathology.
Cathepsin B Investigation Workflow
Research Reagent Solutions for Cathepsin B Studies
Table 4: Essential Research Tools for Cathepsin B Investigation
| Reagent/Category | Specific Examples | Research Application | Experimental Notes |
|---|---|---|---|
| Cell Models | iPSC-derived dopaminergic neurons [10], Human iPSC-derived astrocytes [12], Microglia [12] | Physiological relevance for neurodegenerative studies | Co-culture systems enhance physiological mimicry [12] |
| Genetic Tools | CRISPR-Cas9 CTSB knockout constructs [10], CTSB activation systems [10], siRNA/shRNA | Mechanistic studies of CTSB function | Verify edits with sequencing and Western blot [10] |
| Pharmacological Modulators | CA-074Me (CTSB inhibitor) [10] [11], Cathepsin B activators | Acute modulation of enzyme activity | Validate efficacy with activity assays [10] |
| Protein Aggregates | α-Syn preformed fibrils [10] [12], Aβ fibrils [12] | Substrate for clearance assays | Standardize sonication protocols for reproducibility [12] |
| Activity Assays | Z-Arg-Arg-AMC substrate [10], Lysotracker staining [10], LAMP1/2 immunoblotting | Functional assessment of lysosomes | Multiplex approaches recommended [10] |
| Detection Methods | Phospho-α-syn antibodies [10], ELISA for protein quantification [12], Live-cell imaging [12] | Quantification of pathology and clearance | Combine methods for validation |
Cathepsin B occupies a critical position at the intersection of Alzheimer's disease amyloid-beta processing and Parkinson's disease alpha-synuclein clearance pathways. The experimental evidence demonstrates that cathepsin B promotes clearance of α-synuclein aggregates through lysosomal degradation mechanisms, with reduced activity impairing autophagy and increasing pathological inclusions. While direct evidence for cathepsin B's role in amyloid-beta processing remains more limited, its position within the interconnected network of neurodegenerative proteinopathies suggests broader involvement in protein homeostasis.
The complex, context-dependent nature of cathepsin B function—with both protective and potentially detrimental effects—highlights the importance of sophisticated experimental approaches that capture the intricacies of protein clearance pathways. The integrated methodological framework presented here provides researchers with a systematic approach for investigating cathepsin B in neurodegenerative processes, with particular utility for evaluating therapeutic strategies targeting lysosomal function in protein aggregation disorders. Future research elucidating the precise mechanisms governing cathepsin B's dual roles may yield valuable insights for developing targeted interventions for Alzheimer's, Parkinson's, and related neurodegenerative conditions characterized by mixed proteinopathies.
Cathepsin B (CatB) is a lysosomal cysteine protease belonging to the papain superfamily that plays crucial roles in both physiological and pathological processes. Unlike other members of this family, cathepsin B possesses a unique structural feature—a 20-residue insertion called the occluding loop—that enables its dual endopeptidase and exopeptidase (peptidyldipeptidase) activities [15]. This loop, which blocks the primed terminus of the active site cleft, contains two adjacent histidine residues (H110 and H111) that provide positive charges to anchor the negatively-charged C-terminal carboxylate of exo-substrates [16]. The structural versatility of cathepsin B, particularly its sensitivity to pH changes and the dynamic nature of its occluding loop, makes it a compelling target for drug development in conditions ranging from cancer and Alzheimer's disease to traumatic brain injury [17] [16] [18].
The enzyme's active site comprises the canonical catalytic triad of cysteine proteases (C29, H199, and N219), with the interdomain interface forming the active site cleft that accommodates substrate binding [16]. Cathepsin B's activity is strongly pH-dependent, with optimal function in acidic environments (pH 4.5-5.5) but significant activity preservation possible at neutral pH under certain conditions, particularly when stabilized by interactions with molecules like heparin [16]. This pH sensitivity is governed by protonation state changes in key residues, including those in the active site and occluding loop, which alter electrostatic potential and structural dynamics [16]. Understanding these structural features is essential for developing effective inhibitors that can target cathepsin B in various disease contexts.
Active Site Architecture and Occluding Loop Mechanism
Structural Components of the Catalytic Machinery
The active site of cathepsin B is formed at the interface between two distinct domains that create a large polar surface area. The catalytic residues C29, H199, and N219 project their side chains into this interface, forming the essential machinery for peptide bond hydrolysis [16]. The cysteine residue (C29) acts as a nucleophile, while the histidine (H199) functions as a general base/acid during the catalytic cycle. Asparagine (N219) helps orient the histidine residue for optimal catalysis. This active site cleft runs the length of the enzyme surface and is partially obstructed on its prime side by the unique occluding loop, which confers cathepsin B with its distinctive exopeptidase capability [15].
The occluding loop represents a 20-residue insertion not found in other papain-family enzymes, with the 12 central residues being particularly critical for function. This structural element controls access to the active site for larger substrates while providing the molecular architecture necessary for dipeptidyl carboxypeptidase activity [15]. Site-directed mutagenesis studies have confirmed that deletion of the entire occluding loop or its central portion completely abolishes exopeptidase activity while preserving endopeptidase function [15] [16]. Additionally, the occluding loop contributes to thermal stability and provides resistance against endogenous inhibitors like cystatin C, which shows 40-fold higher affinity for cathepsin B when the occluding loop is modified or deleted [15].
Molecular Mechanism of the Occluding Loop
The occluding loop functions as a structural gatekeeper that regulates substrate access and enzyme specificity. The two histidine residues (H110 and H111) located on this loop create a positively charged patch that specifically interacts with the C-terminal carboxylate group of peptide substrates, facilitating the exopeptidase activity by which cathepsin B removes dipeptides from the C-terminus of proteins [16]. This mechanism is unique to cathepsin B within the papain family and expands its functional repertoire beyond the endopeptidase activity characteristic of other cysteine cathepsins.
During proenzyme activation, the occluding loop undergoes significant reorientation to accommodate binding of the propeptide, which itself is a potent inhibitor of the enzyme [15]. This structural rearrangement is essential for the transition from zymogen to active enzyme, with the propeptide binding affinity increasing 50-fold when the occluding loop is altered, indicating strong interactions between these structural elements [15]. The flexibility and dynamic motions of the occluding loop, particularly under different pH conditions, contribute importantly to regulating cathepsin B activity and inhibition.
Figure 1: Occluding Loop Functional Relationships. The occluding loop, containing H110-H111, regulates exopeptidase activity, while the active site residues (C29-H199-N219) mediate endopeptidase function.
pH-Dependent Structural Dynamics and Activity Regulation
Molecular Basis of pH Sensitivity
Cathepsin B exhibits remarkable sensitivity to pH changes, which significantly impacts its structural stability and catalytic efficiency. The enzyme is normally active within acidic lysosomes (pH ~4.6-5.5) but can also function in neutral environments (pH ~7.2) under certain pathological conditions [16] [19]. This pH-dependent behavior stems from alterations in the protonation states of key titratable residues, particularly at the interdomain interface and within the active site. Computational pKa calculations have identified six key residues that display distinct protonation states under different pH conditions: E36, H199, E171, H110, H97, and H190 [16].
At alkaline pH, the catalytic histidine (H199) undergoes deprotonation, which subsequently affects the ionization state of the catalytic cysteine (C29), shifting its pKa from approximately 3.7 at pH 5.5 to 7.3 at pH 8.0 [16]. This coupling between H199 and C29 ionization states directly impacts catalytic efficiency. Similarly, H110 in the occluding loop shows altered protonation states with pH changes, affecting its ability to anchor substrate C-terminal and thereby modulating exopeptidase activity. These protonation changes collectively alter the electrostatic potential at the cathepsin B surface, influencing substrate binding, inhibitor affinity, and overall structural stability.
pH-Mediated Structural Changes and Heparin Stabilization
Under alkaline conditions, cathepsin B undergoes significant structural destabilization characterized by increased overall flexibility, loss of interactions between active site residues, decreased helical content, and domain separation [16]. Molecular dynamics simulations reveal that the occluding loop exhibits particularly high-amplitude motions at neutral/alkaline pH, compromising its gatekeeping function and contributing to enzyme inactivation [16]. These structural changes explain the rapid inactivation of cathepsin B observed at physiological pH when not stabilized by co-factors or specific interactions.
Heparin and heparan sulfate glycosaminoglycans (GAGs) can prevent pH-induced inactivation by binding to basic surface regions on cathepsin B and restricting enzyme flexibility [16]. This interaction promotes rearrangement of contacts between cathepsin B domains, maintains helical content, and stabilizes the active site configuration. Molecular docking studies have identified two primary heparin-binding sites on cathepsin B, through which heparin exerts an allosteric stabilizing effect that modulates large-amplitude motions, particularly in the occluding loop [16]. This protective mechanism explains how membrane-associated forms of cathepsin B resist alkaline inactivation in physiological environments.
Figure 2: pH-Dependent Activity Regulation. Cathepsin B remains stable and active at acidic pH but becomes unstable at alkaline pH unless stabilized by heparin binding.
Comparative Analysis of Cathepsin B Inhibitor Classes
Performance Comparison of Inhibitor Strategies
Table 1: Comparative Analysis of Cathepsin B Inhibitor Classes
| Inhibitor Class | Representative Compounds | Mechanism of Action | pH Selectivity | Key Molecular Interactions | Experimental IC₅₀/Ki |
|---|---|---|---|---|---|
| Occluding Loop-Targeted | E-64 derivatives [20] | Binds occluding loop His pairs | Poor above pH 5.5 | Ionic interaction with H110-H111 | ~nM range at pH ≤5.5 [20] |
| pH-Selective Inhibitors | Z-Arg-Lys-AOMK [19] | Irreversible active site binding | 100-fold selective for pH 7.2 | Catalytic C29, occluding loop residues | Low nM at pH 7.2 [19] |
| Natural Product Inhibitors | Nicandrenone, Picrasidine M [18] | Competitive active site binding | Variable | Trp30, Trp221, catalytic residues | Superior binding affinity in silico [18] |
| Repurposed Drugs | Lurasidone, Paliperidone [21] | Catalytic pocket binding | Under investigation | Multiple active site residues | Stable complexes in 500ns MD [21] |
| Peptidic Inhibitors | CA-074Me [18] [21] | Irreversible active site inhibitor | Limited | Gln23, Cys29, His199, Trp221 | Reference compound [18] |
Structural Basis for Inhibitor Efficacy
The comparative analysis of cathepsin B inhibitors reveals distinct structure-activity relationships governed by interactions with both the active site and occluding loop. Inhibitors targeting the occluding loop, such as E-64 derivatives, show strong pH dependence with dramatically reduced efficacy (decreased kinact/KI) as pH increases from 4 to 7.8, corresponding to a single ionization event with pKa 4.4 [20]. This limitation has prompted the development of pH-selective inhibitors like Z-Arg-Lys-AOMK, which was rationally designed based on cathepsin B's preference for cleaving peptides with Arg in the P2 position at neutral pH, contrasted with its preference for Glu in P2 at acidic pH [19].
Natural products and repurposed drugs represent promising avenues for cathepsin B inhibition, with compounds like Nicandrenone and Picrasidine M demonstrating superior binding affinities and robust interactions with catalytic residues in molecular dynamics simulations [18]. Similarly, repurposed antipsychotics Lurasidone and Paliperidone form stable complexes with cathepsin B throughout 500ns MD simulations, suggesting their potential as lead compounds for further development [21]. These inhibitors typically engage key residues including Trp30, Cys29, His110, His111, and His199, leveraging both the active site machinery and occluding loop interactions for selective inhibition.
Experimental Methodologies for Cathepsin B Research
Key Experimental Protocols
Site-Directed Mutagenesis and Deletion Analysis: Fundamental insights into occluding loop function have been obtained through deletion mutagenesis studies where all or part of the 20-residue occluding loop was removed [15]. Experimental protocols involve generating human procathepsin B variants with specific deletions, expressing them in yeast systems like Pichia pastoris, and comparing autoprocessing kinetics and enzymatic activities of mutant versus wild-type enzymes. These studies have confirmed that deletion of the 12 central residues abolishes exopeptidase activity while maintaining endopeptidase function, and significantly increases affinity for inhibitors like cystatin C and the propeptide [15].
Molecular Dynamics Simulations of pH Effects: Detailed protocols for assessing pH-dependent structural changes involve molecular dynamics simulations using different protonation states corresponding to acidic (pH 5.5) and alkaline (pH 8.0) conditions [16]. Simulations typically run for 40ns or longer, analyzing parameters such as hydrogen bond occupancy, helical content preservation, domain separation, and occluding loop mobility. These studies incorporate pKa predictions from tools like PROPKA to determine appropriate protonation states for titratable residues under different pH conditions [16]. MD simulations have also been used to validate the stabilizing effect of heparin binding on cathepsin B structure at alkaline pH.
Virtual Screening for Inhibitor Identification: Computational screening approaches employ structure-based virtual screening of large compound libraries (e.g., IMPPAT 2 with ~18,000 phytochemicals or DrugBank with ~3,500 FDA-approved drugs) [18] [21]. Standard protocols include molecular docking with tools like AutoDock or InstaDock, followed by molecular dynamics simulations of 100-500ns to assess complex stability [18] [21]. Additional filtering includes pharmacokinetic profiling, ADMET prediction, and binding free energy calculations using MM-GBSA/PBSA methods [17] [18]. These workflows have successfully identified novel natural product inhibitors and repurposed drug candidates with high binding affinity and specificity for cathepsin B.
Quantitative Structure-Activity Relationship (QSAR) Approaches
QSAR modeling represents a powerful tool for investigating correlations between chemical structures and anti-cathepsin B activity [22]. Experimental protocols involve calculating molecular descriptors representing physical, chemical, structural, and geometric properties of compounds, followed by data preprocessing and feature selection to reduce descriptor complexity. Key preprocessing methods include filtering approaches like Recursive Feature Elimination (RFE) and wrapping methods such as Forward Selection (FS), Backward Elimination (BE), and Stepwise Selection (SS) [22]. These methods, particularly when coupled with nonlinear regression models, have demonstrated promising performance in predicting IC₅₀ values for anti-cathepsin B compounds, enabling more efficient lead compound optimization.
Figure 3: Virtual Screening Workflow. Computational pipeline for identifying cathepsin B inhibitors from large compound libraries.
Research Reagent Solutions for Cathepsin B Studies
Table 2: Essential Research Reagents for Cathepsin B Investigation
| Reagent/Category | Specific Examples | Research Application | Key Features/Benefits |
|---|---|---|---|
| Expression Systems | Pichia pastoris [15] | Recombinant cathepsin B production | Proper folding, post-translational modifications |
| Reference Inhibitors | CA-074Me, E-64 [18] [21] | Experimental controls, validation | Well-characterized specificity, potency |
| Activity Assays | Z-Phe-Arg-AMC [19] | Enzymatic activity measurement | Fluorogenic substrate, continuous monitoring |
| Structural Biology Resources | PDB IDs: 1GMY, 1CSB [18] [23] | Molecular docking, structure analysis | High-resolution crystal structures |
| Computational Tools | AutoDock, InstaDock [23] [21] | Virtual screening, binding pose prediction | Automated workflows, high throughput |
| MD Simulation Software | AMBER, GROMACS [16] | Dynamics, stability assessment | pH-dependent protonation states |
| Specialized Substrates | Z-Arg-Lys-AMC [19] | pH-dependent activity profiling | Selective for neutral pH activity |
The structural biology of cathepsin B reveals a sophisticated enzymatic machinery whose function is intricately regulated by its unique occluding loop and sensitive to pH-induced conformational changes. The occluding loop serves as a structural determinant for exopeptidase activity and modulates inhibitor access to the active site, while pH-dependent protonation states of key residues govern catalytic efficiency and structural stability. These insights have enabled the development of increasingly sophisticated inhibitor strategies, from early occluding loop-targeted compounds to advanced pH-selective inhibitors that capitalize on cathepsin B's differential cleavage preferences at neutral versus acidic pH.
Future research directions should focus on leveraging these structural insights to develop context-specific inhibitors that target cathepsin B in particular cellular compartments or disease states without disrupting its physiological functions. The promising results from natural product screening and drug repurposing efforts provide diverse chemical starting points for optimization. As structural characterization methods continue to advance, particularly in capturing dynamic enzyme states and protein-ligand interactions under physiologically relevant conditions, our understanding of cathepsin B biology will further deepen, enabling more precise therapeutic targeting of this multifunctional protease in cancer, neurodegenerative disorders, and other pathological conditions.
Cysteine cathepsins are a family of lysosomal proteolytic enzymes that play critical roles in protein turnover, antigen presentation, and various other physiological processes. As members of the papain-like protease family, their activity must be precisely regulated to prevent inappropriate tissue damage and maintain cellular homeostasis. Unregulated cathepsin activity has been implicated in numerous pathological conditions, including cancer, neurodegenerative diseases, and inflammatory disorders. The primary endogenous regulators of these enzymes are protein inhibitors known as cystatins, which comprise a superfamily of tight-binding, reversible inhibitors that control cysteine protease activity in intracellular and extracellular environments.
The cystatin superfamily is classified into three types based on their structural characteristics and subcellular localization. Type 1 cystatins (stefins A and B) are intracellular proteins of approximately 100 residues that lack disulfide bonds and secretion signal peptides. Type 2 cystatins (C, D, E, F, S, SA, and SN) are secreted proteins of about 120 amino acids that contain two conserved disulfide crosslinks and a secretion signal sequence. Type 3 cystatins are the kininogens, which are multidomain plasma proteins containing three type-2 cystatin-like domains, one of which is inactive as a protease inhibitor [24]. This review will focus specifically on the comparative analysis of Stefin A (cystatin A) and cystatin C, two prominent members of this inhibitor family that play crucial yet distinct roles in regulating cysteine cathepsin activity in physiological and pathological contexts, with particular emphasis on their performance in cathepsin B, S, D, and K inhibition models relevant to current research.
Comparative Structural and Functional Characteristics
Molecular Structures and Inhibition Mechanisms
Stefin A and cystatin C share a common evolutionary origin and structural fold despite their different subcellular localizations and biological functions. Both inhibitors feature a conserved five-stranded antiparallel β-sheet wrapped around a five-turn α-helix, forming a wedge-shaped structure that inserts into the active site of target cysteine cathepsins [24]. However, they differ significantly in their precise mechanisms of interaction with various cathepsins.
The molecular mechanism of inhibition involves three distinct contact regions that contribute differently to the binding energy. Kinetic studies with natural and recombinant variants reveal that for chicken cystatin (homologous to human cystatin C), the N-terminal segment contributes approximately 36% of the binding energy for papain complexes, while the first hairpin loop contributes 51%, and the second hairpin loop contributes 13% [25]. The essential nature of the N-terminal region is demonstrated by the dramatic 10,000-fold reduction in affinity for papain when this segment is removed from chicken cystatin. Interestingly, Stefin B (closely related to Stefin A) remains a tight-binding inhibitor of papain and actinidin even without its N-terminal segment, suggesting structural and functional differences in the inhibition mechanisms between type 1 and type 2 cystatins [25].
Structural analyses of complexes reveal that Stefin A binds deeper in the active site cleft of cathepsin H than Stefin B does in papain [24]. The N-terminal residues of Stefin A form a short turn that creates a hook structure, which pushes away the mini-chain in the active site cleft of cathepsin H, resulting in an "S-shaped" bend instead of the extended conformation observed in cathepsin H alone. This binding interaction induces significant conformational changes in cathepsin H, including disordered structure in a short insertion that normally forms a loop in the free enzyme [24].
Table 1: Structural and Functional Characteristics of Stefin A and Cystatin C
| Characteristic | Stefin A (Cystatin A) | Cystatin C |
|---|---|---|
| Classification | Type 1 cystatin (stefin) | Type 2 cystatin |
| Molecular Weight | ~100 residues (11 kDa) | ~120 residues (13 kDa) |
| Structural Features | Single chain, no disulfide bonds | Two conserved disulfide crosslinks |
| Subcellular Localization | Intracellular | Extracellular, secreted |
| Signal Peptide | Absent | Present (26 amino acids) |
| Tissue Distribution | Restricted (mainly epidermal cells) | Ubiquitous (all nucleated cells) |
| Binding Regions | N-terminus and two hairpin loops | N-terminus and two hairpin loops |
| Inhibition Mechanism | Competitive, tight-binding | Competitive, tight-binding |
Tissue Distribution and Expression Patterns
The tissue distribution of Stefin A and cystatin C reflects their distinct biological roles. Stefin A demonstrates a restricted tissue distribution, being found mainly in epidermal cells and exhibiting limited expression patterns. In contrast, cystatin C is widely expressed across virtually all nucleated cells in the body and is constitutively produced at a constant rate [24] [26]. This ubiquitous expression pattern aligns with cystatin C's role as a general extracellular regulator of cysteine protease activity.
The differential expression extends to pathological conditions. In colorectal cancer, Stefin A and cystatin C levels are moderately increased in patient sera (1.4-fold and 1.6-fold respectively compared to healthy controls), while Stefin B levels remain statistically unchanged [27]. In squamous cell carcinoma of the head and neck (SCCHN), cystatin C levels in tumor tissue were found to be 1.18 times lower than in corresponding normal mucosa, with the degree of reduction correlating with disease progression [26].
Inhibitory Performance Against Key Cathepsins
Quantitative Inhibition Profiles
The inhibitory efficacy of Stefin A and cystatin C varies significantly across different cysteine cathepsins, reflecting their specialized biological functions. Both inhibitors display distinctive affinity profiles for cathepsins B, H, L, and S, with important implications for their physiological roles and potential therapeutic applications.
Table 2: Inhibition Constants (Kᵢ) of Stefin A and Cystatin C for Various Cysteine Cathepsins
| Target Enzyme | Stefin A Kᵢ (M) | Cystatin C Kᵢ (M) | Experimental Context |
|---|---|---|---|
| Cathepsin B | Weaker inhibitor [24] | Weaker inhibitor [24] | Mouse stefins A & B comparison |
| Cathepsin H | 0.31 × 10⁻⁶ [24] | < 1.0 × 10⁻¹⁰ [24] | Human liver-derived inhibitors |
| Cathepsin L | Variable inhibition [24] | Potent inhibition [24] | General characteristic |
| Cathepsin S | Limited data | Potent inhibition [28] | Specific interaction |
| Papain | 10000-fold lower affinity without N-terminal segment [25] | Tight-binding [25] | Recombinant variant studies |
The data reveals that cystatin C generally demonstrates higher affinity for most cathepsins compared to Stefin A, particularly for cathepsin H where cystatin C exhibits sub-nanomolar inhibition (Kᵢ < 1.0 × 10⁻¹⁰ M) compared to Stefin A's micromolar range inhibition (Kᵢ = 0.31 × 10⁻⁶ M) [24]. This approximately 3000-fold difference in inhibitory potency highlights the specialized functions of these inhibitors, with cystatin C serving as a potent extracellular regulator, while Stefin A functions primarily in intracellular compartments.
For cathepsin B, both Stefin A and cystatin C demonstrate relatively weaker inhibition compared to their effects on other cathepsins. Studies indicate that inhibition of cathepsin B by stefins A and B follows a slow-binding mechanism, with stefin B exhibiting a two-step mechanism involving slow isomerization of the enzyme-inhibitor complex [25]. This relatively weaker inhibition of cathepsin B may reflect this enzyme's unique structural features, including its occluding loop that potentially interferes with inhibitor binding.
Specificity and Binding Affinity Considerations
The specificity of Stefin A and cystatin C for different cathepsins is influenced by structural variations in both the enzymes and inhibitors. For instance, the first hairpin loop plays a critical role in determining binding specificity, as demonstrated by a Val48→Asp mutant of stefin B that exhibited a 240-fold lower affinity for papain [25]. Similarly, single amino acid substitutions in Stefin A can significantly impact its inhibitory capacity, with the E94K mutation in Stefin A decreasing binding affinity for cathepsin B by approximately 8% and resulting in complex instability during molecular dynamics simulations [29].
The S2 and S3 pockets of cathepsins represent key determinants of inhibitor specificity. These structural features are particularly important for distinguishing between highly similar cathepsins such as S, K, and L, which share more than 57% amino acid sequence identity [28]. While detailed structural studies of Stefin A and cystatin C with these specific cathepsins are limited, the general principle that the S2 and S3 pockets govern inhibitor selectivity underscores the importance of these regions for understanding the differential inhibitory profiles of physiological cystatins.
Experimental Methodologies for Inhibitor Characterization
Kinetic Characterization Protocols
The determination of inhibition constants and mechanisms for Stefin A and cystatin C typically employs well-established enzymological approaches. The standard methodology involves incubating fixed concentrations of cysteine cathepsins with varying concentrations of inhibitors across appropriate pH ranges (typically pH 5.0-7.5 for most cathepsins), using fluorogenic or chromogenic substrates to monitor residual enzyme activity.
For determination of inhibition constants (Kᵢ values), the general experimental workflow follows these key steps:
- Enzyme Activation: Pre-incubate procathepsins in activation buffer (e.g., 100 mM sodium acetate, 1 mM EDTA, 2.5 mM DTT, pH 5.5) at 37°C for 15-30 minutes to generate mature enzymes.
- Inhibitor Titration: Prepare serial dilutions of purified Stefin A or cystatin C in appropriate assay buffer.
- Reaction Setup: Incubate activated enzyme with different inhibitor concentrations for a fixed time period (typically 15-60 minutes) to allow complex formation.
- Activity Measurement: Add specific substrate (e.g., Z-FR-AMC for cathepsin B or Z-VVR-AMC for cathepsin S) and monitor product formation continuously using a fluorometer or spectrophotometer.
- Data Analysis: Calculate residual enzyme activity and determine Kᵢ values using appropriate inhibition models (competitive, non-competitive, or mixed-type) through nonlinear regression analysis of dose-response data [25] [24].
Slow-binding inhibition, as observed for stefins A and B with cathepsin B, requires more specialized kinetic approaches involving pre-incubation of enzyme and inhibitor for extended time periods followed by measurement of reaction progress curves to determine association and dissociation rate constants [25].
Structural Analysis Techniques
Structural characterization of Stefin A and cystatin C complexes with target cathepsins employs both X-ray crystallography and nuclear magnetic resonance (NMR) spectroscopy. The crystallographic analysis of human Stefin A in complex with cathepsin H revealed the deep binding mode of Stefin A within the active site cleft and the associated conformational changes in both molecules [24].
The standard protocol for structural analysis includes:
- Protein Purification: Recombinant expression in E. coli or eukaryotic systems followed by affinity and size-exclusion chromatography.
- Complex Formation: Incubation of purified cathepsins with stoichiometric amounts of inhibitors under controlled conditions.
- Crystallization: Screening of numerous crystallization conditions using robotic systems and optimization of initial hits.
- Data Collection and Structure Determination: X-ray diffraction data collection at synchrotron sources followed by molecular replacement or experimental phasing and iterative model building and refinement [24] [29].
For dynamic studies of inhibitor binding, molecular dynamics simulations provide complementary information about complex stability and flexibility, as demonstrated in the analysis of Stefin A mutants with reduced affinity for cathepsin B [29].
Figure 1: Experimental Workflow for Characterizing Cystatin-Cathepsin Interactions
Research Reagent Solutions and Essential Tools
Table 3: Essential Research Reagents for Studying Cystatin-Cathepsin Interactions
| Reagent Category | Specific Examples | Research Applications | Key Characteristics |
|---|---|---|---|
| Recombinant Proteins | Human recombinant cystatin C [26], Stefin A variants [29] | Kinetic studies, structural biology, cellular assays | High purity (>95%), confirmed activity, endotoxin-free for cellular studies |
| Activity Assays | Fluorogenic substrates (Z-FR-AMC, Z-VVR-AMC) [28] | Enzyme activity measurements, inhibition constant determination | Cathepsin-specific, sensitive fluorescence detection, suitable for continuous assays |
| Antibodies | Monoclonal anti-cystatin C (1A2) [26], polyclonal anticystatin C IgG | ELISA, Western blot, immunohistochemistry | Specific for native and complexed forms, no cross-reactivity with related inhibitors |
| Cell-Based Models | iPSC-derived neurons [30], cancer cell lines | Functional validation, pathological relevance | Disease-relevant context, reproducible phenotype, tractable for manipulation |
| Clinical Samples | Paired tumor-normal tissues [26], patient sera [27] | Correlation with disease progression, prognostic significance | Well-annotated clinical data, proper preservation, ethical approval |
The selection of appropriate research reagents is critical for generating reliable data on cystatin-cathepsin interactions. The monoclonal antibody 1A2 specifically recognizes both recombinant and native human cystatin C without cross-reactivity to closely related inhibitors like stefins A and B, making it invaluable for immunoassays [26]. For kinetic studies, recombinant proteins expressed in E. coli systems maintain proper folding and inhibitory function while allowing production of mutant variants for structure-function studies [29] [26].
Pathological Implications and Therapeutic Applications
Role in Disease Pathogenesis
Dysregulation of the balance between cysteine cathepsins and their endogenous inhibitors contributes significantly to various pathological conditions. In cancer progression, altered expression of Stefin A and cystatin C correlates with clinical outcomes across multiple cancer types. In colorectal cancer, high serum levels of stefin B and cystatin C are associated with significantly increased risk of death (hazard ratio = 1.6 and 1.3, respectively) [27]. For squamous cell carcinoma of the head and neck (SCCHN), low tumor levels of cystatin C predict poor disease-free survival (P = 0.013) and disease-specific survival (P = 0.013) in univariate analysis [26].
In neurodegenerative disorders, the cystatin-cathepsin axis plays important roles in protein aggregation clearance. Recent research demonstrates that recombinant cathepsins B and L promote α-synuclein clearance and restore lysosomal function in human and murine models with α-synuclein pathology, suggesting therapeutic potential for Parkinson's disease and other synucleinopathies [30]. Interestingly, muscle-derived cathepsin B has been shown to improve motor coordination, memory function, and adult hippocampal neurogenesis in an Alzheimer's Disease mouse model, highlighting the complex interplay between different proteolytic systems across tissues [31].
Diagnostic and Therapeutic Potential
The consistent production rate of cystatin C by all nucleated cells has established it as a superior biomarker for glomerular filtration rate (GFR) compared to creatinine, particularly in special populations like children with posterior urethral valves where muscle mass and nutritional status vary considerably [32]. Creatinine-based formulas consistently yield slightly higher eGFR values (median differences of 1.5 to 2.6 mL/min/1.73 m²) compared to cystatin C-based methods, potentially reflecting creatinine's susceptibility to extrarenal factors like muscle mass [32].
Therapeutic targeting of the cystatin-cathepsin axis represents an emerging frontier in drug development. For cathepsin S, involved in various disease pathophysiologies including autoimmune disorders, cardiovascular diseases, and cancer, extensive efforts have been made to develop specific inhibitors [28]. The development of selective cathepsin inhibitors must address the challenge of significant structural similarities between different cathepsin family members, particularly in the S2 and S3 substrate binding pockets that determine inhibitor specificity [28].
Figure 2: Physiological and Pathological Consequences of Cystatin-Cathepsin Balance
Stefin A and cystatin C represent two essential components of the physiological regulatory system for cysteine cathepsin activity, each with distinct structural characteristics, inhibitory profiles, and biological functions. While both inhibitors employ a conserved structural fold to block the active sites of their target enzymes, they demonstrate marked differences in specificity and affinity across the cathepsin family. Cystatin C generally exhibits higher affinity for most cathepsins and serves as the primary extracellular regulator, while Stefin A functions predominantly in intracellular compartments with a more restricted tissue distribution.
The performance evaluation of these physiological inhibitors reveals a sophisticated regulatory network where relatively small structural differences translate into significant functional specialization. The differential expression patterns and distinct inhibitory profiles of Stefin A and cystatin C enable precise spatial and temporal control of cathepsin activity under physiological conditions. Dysregulation of this balance contributes to various pathological processes, particularly in cancer and neurodegenerative diseases, highlighting the therapeutic potential of targeting these natural regulatory pathways. Future research directions should focus on elucidating the precise structural determinants of inhibitor specificity and developing therapeutic strategies that restore the natural balance between cysteine cathepsins and their physiological inhibitors in disease states.
Cathepsin B (CTSB), a lysosomal cysteine protease, is a pivotal enzyme in cellular homeostasis and a significant player in cancer progression. Its role, however, is not monolithic; it exhibits profound context-dependency, varying across cancer types, cell lines, and physiological conditions. Understanding these expression patterns and the intricate balance between CTSB and its endogenous inhibitor, Stefin A (STFA), is crucial for developing effective therapeutic strategies. This guide objectively compares CTSB expression and function across various cancer models, providing a foundation for evaluating CTSB-targeted inhibition models in oncological research and drug development.
Comparative Analysis of CTSB/STFA Expression and Function
The interplay between CTSB and its natural inhibitor, Stefin A (STFA), is a critical determinant of proteolytic activity and tumor progression. The table below summarizes the expression patterns and functional outcomes of the CTSB/STFA axis across different cellular contexts.
Table 1: CTSB/STFA Expression Patterns and Functional Correlations Across Cell Lines
| Cell Line / Cancer Type | CTSB Expression & Activity | STFA Expression & Regulation | Key Phenotypic Outcomes | Clinical/Experimental Correlation |
|---|---|---|---|---|
| Renal Cancer (769-P) | High expression and activity [33] [34]. | Impaired regulatory feedback; CTSB overexpression alters STFA levels [33]. | Promotes invasion and metastasis [33]. | Correlates with advanced tumor stages and poor prognosis [34]. |
| Prostate Cancer (Du145) | High expression and activity [33] [34]. | Impaired regulatory feedback [33]. | Promotes tumor aggressiveness [34]. | Associated with disease progression. |
| Triple-Negative Breast Cancer (MDA-MB-231) | High expression associated with better outcomes [35]. | Information not specified in search results. | Knockout increases 3D invasion and chemosensitivity [35]. | Cell-line specific role; effects are not generalizable [35]. |
| Triple-Negative Breast Cancer (MDA-MB-468) | High expression associated with better outcomes [35]. | Information not specified in search results. | Knockout increases cell viability and drives chemoresistance [35]. | Cell-line specific role; differential mTOR/Akt activation [35]. |
| Oral Squamous Cell Carcinoma (OSCC) | Cytoplasmic expression in 34.6% of patients; correlated with migration [36]. | Information not specified in search results. | Promotes migration and invasion [36]. | Independent unfavorable prognostic factor in buccal mucosa carcinoma [36]. |
| Glioblastoma (GBM) | Commonly overexpressed [37]. | Information not specified in search results. | Contributes to angiogenesis, tumor progression, and pharmacological resistance [37]. | Targeted in drug delivery systems; silencing enhances radiosensitivity [37]. |
| Non-Cancerous (Hek293T Embryonic Kidney) | Lower basal activity; distinct regulatory response [33] [34]. | Normal regulatory feedback maintained [33]. | Silencing STFA decreases cell viability [34]. | Represents a non-malignant regulatory baseline [33] [34]. |
A key finding across studies is the fundamental disruption of the CTSB-STFA regulatory loop in cancer cells compared to non-cancerous cells. In embryonic renal cells (Hek293T), CTSB and STFA exist in a tightly regulated balance. However, in renal cancer cells (769-P) and prostate cancer cells (Du145), this feedback mechanism is impaired. Research demonstrates that exogenously increasing CTSB levels can significantly alter STFA expression in cancer cells, suggesting a corrupted feedback mechanism influenced by CTSB's enzymatic activity [33]. This dysregulation creates a proteolytic environment conducive to invasion and metastasis.
Detailed Experimental Protocols for Key Findings
Protocol 1: Investigating the CTSB-STFA Regulatory Interplay
This methodology is central to understanding the expression patterns summarized in Table 1.
- 1. Cell Culture and Transfection: Non-cancerous embryonic renal cells (Hek293T), renal cancer cells (769-P), and prostate cancer cells (Du145) are cultured. Cells are transfected with plasmids for CTSB gain-of-function (overexpression), loss-of-function (silencing), or treated with biochemical inhibitors [33].
- 2. Gene Expression Analysis: Total RNA is extracted 48 hours post-transfection. mRNA expression levels of CTSB and STFA are quantified using reverse transcription quantitative polymerase chain reaction (RT-qPCR) [33] [34].
- 3. Protein Expression and Activity Assay: Protein lysates are analyzed by Western Blot to detect CTSB and STFA protein levels. CTSB enzymatic activity is measured using fluorogenic substrates (e.g., Z-Phe-Arg-AMC) [34].
- 4. Subcellular Localization: Immunocytochemistry and confocal microscopy are used to determine the cytoplasmic and nuclear distribution of CTSB and STFA. Colocalization analysis confirms direct protein interaction [34].
Protocol 2: Assessing CTSB in Cell Migration and Invasion
- 1. Gene Knockdown: Oral cancer cell lines (e.g., OC2, CAL27) are treated with CTSB-specific small interfering RNA (siRNA) or a non-targeting control siRNA for 48 hours. Knockdown efficiency is confirmed by Western Blot [36].
- 2. Transwell Migration Assay: After knockdown, cells are harvested and seeded into the upper chamber of a Transwell insert in serum-free medium. The lower chamber contains medium with serum as a chemoattractant. Cells are incubated for 48 hours to allow migration [36].
- 3. Analysis: Migrated cells on the lower surface of the membrane are fixed, stained, and counted under a microscope. A significant reduction in migrated cells in the CTSB-knockdown group indicates its role in promoting migration [36].
Signaling Pathways and Experimental Workflows
The following diagrams visualize the key regulatory pathways and experimental workflows described in the research.
Diagram 1: CTSB-STFA regulatory interplay in cancerous vs. non-cancerous contexts. In non-cancerous cells, a homeostatic balance is maintained. In cancer, this feedback is impaired, leading to a proteolytic imbalance that drives invasion and metastasis [33] [34].
Diagram 2: A generalized experimental workflow for analyzing CTSB function. Studies typically involve genetic manipulation of CTSB (knockdown or overexpression), followed by validation at molecular and functional levels to assess its impact on cancer phenotypes [34] [35] [36].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and their applications in CTSB research, as utilized in the cited studies.
Table 2: Key Research Reagents for Cathepsin B Investigation
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| CTSB siRNA / shRNA | Knocks down CTSB gene expression to study loss-of-function phenotypes. | Used to inhibit oral cancer cell (OC2, CAL27) migration [36] and to study TNBC cell invasion and chemosensitivity [35]. |
| CTSB Expression Plasmids | Overexpresses CTSB to study gain-of-function effects and regulatory mechanisms. | Employed to demonstrate the feedback regulation of STFA in cancer cell lines [33]. |
| Fluorogenic Substrates (e.g., Z-Phe-Arg-AMC) | Measures CTSB enzymatic activity. The substrate emits fluorescence upon cleavage. | Used to quantify CTSB activity in various cell lines following STFA modulation [34] [38]. |
| Specific Inhibitors (e.g., CA074, E-64) | Irreversibly or reversibly inhibits CTSB activity to probe its catalytic function. | CA074 used for structural studies and specificity profiling [39]. E-64 used in inhibition kinetics with immobilized CTSB [38]. |
| Anti-Cathepsin B Antibodies | Detects CTSB protein levels and localization via Western Blot, immunohistochemistry, and immunofluorescence. | Used for protein level validation in knockdown/overexpression experiments and for subcellular localization studies [34] [36]. |
| Transwell Chambers | Assesses cell migration and invasion capabilities in vitro. | Demonstrated that CTSB knockdown reduces the migratory capacity of oral cancer cells [36]. |
Computational and Experimental Approaches for Cathepsin B Inhibitor Discovery
Virtual screening has emerged as an indispensable computational tool in modern drug discovery, enabling researchers to rapidly identify potential hit compounds from vast chemical libraries. Among the most effective strategies are ligand-based pharmacophore modeling and structure-based molecular docking. These approaches are particularly valuable for targets like cathepsin B, a cysteine protease whose inhibition is a promising therapeutic strategy for conditions including Alzheimer's disease [23] [40]. Ligand-based methods extract essential chemical features from known active compounds, while structure-based techniques leverage three-dimensional protein structures to predict binding interactions. When integrated, these complementary approaches form a powerful workflow for identifying novel bioactive molecules with greater efficiency and lower costs than traditional high-throughput screening methods.
Theoretical Foundations and Comparative Analysis
Ligand-Based Pharmacophore Modeling
Pharmacophore models abstract the essential steric and electronic features responsible for a molecule's biological activity, providing a template for virtual screening. These features typically include hydrogen bond acceptors (HBA), hydrogen bond donors (HBD), hydrophobic regions (H), aromatic rings (AR), and ionizable groups [41]. The model development process involves identifying common chemical features from a set of known active compounds and optimizing the model to maximize its ability to discriminate between active and inactive molecules [41].
In a study targeting 17β-hydroxysteroid dehydrogenase 2 (17β-HSD2), researchers developed three complementary pharmacophore models using structurally diverse training compounds. These models collectively achieved 87% sensitivity in retrieving known active compounds while excluding inactive ones, demonstrating the power of well-validated pharmacophore approaches [41]. The models consisted of 6-7 chemical features with exclusion volumes defining steric constraints, and when applied to screen over 200,000 compounds, they identified 1,531 hits (0.75% of the database), illustrating effective enrichment [41].
Structure-Based Molecular Docking
Molecular docking predicts the preferred orientation of a small molecule when bound to a protein target, estimating binding affinity through scoring functions. This method requires knowledge of the protein's three-dimensional structure, either from experimental methods (X-ray crystallography, NMR) or homology modeling [23] [42]. Docking algorithms typically employ search algorithms (e.g., Lamarckian Genetic Algorithm in AutoDock) to explore possible binding conformations and scoring functions to rank them by predicted binding energy [23].
For cathepsin B inhibition studies, docking simulations have revealed critical interactions with active site residues including Gln23, Cys29, His110, His111, His199, and Trp221 [23]. These precise molecular insights enable rational inhibitor design and optimization beyond what ligand-based methods alone can provide.
Integrated Virtual Screening Workflow
The most effective virtual screening strategies combine both approaches in a sequential workflow to leverage their complementary strengths as shown in Figure 1.
Figure 1. Integrated virtual screening workflow combining ligand-based pharmacophore modeling (green) and structure-based docking (blue) with key filtering steps.
Table 1: Comparative analysis of virtual screening approaches
| Feature | Ligand-Based Pharmacophore | Structure-Based Docking |
|---|---|---|
| Structural Requirement | Known active ligands | Target protein 3D structure |
| Key Advantages | Does not require protein structure; Can identify diverse chemotypes | Provides atomic-level binding insights; Can design novel scaffolds |
| Limitations | Dependent on quality/ diversity of known actives | Limited by scoring function accuracy; Computationally intensive |
| Typical Hit Rate | 0.1-1.0% of screened database [41] | 1-10% of pre-filtered compounds [42] |
| Key Software Tools | LigandScout, MOE, Discovery Studio | AutoDock Vina, Glide, GOLD |
| Best Applications | Target with known ligands but no structure; Scaffold hopping | Structure-rich targets; Binding mode prediction |
Experimental Protocols and Methodologies
Ligand-Based Pharmacophore Model Development
The development of a high-quality pharmacophore model requires careful curation of training compounds and rigorous validation as shown in Figure 2.
Step 1: Training Set Compilation
- Select 5-30 known active compounds with structural diversity and potency data (e.g., IC₅₀ values)
- Include confirmed inactive compounds for model validation [41]
- For cathepsin B models, 24 known inhibitors of both natural and synthetic origin were used [23]
Step 2: Molecular Feature Alignment
- Use software such as LigandScout or MOE to identify common chemical features
- Align conformations of training compounds to maximize feature overlap
- Define feature tolerances and exclusion volumes based on molecular superimposition [43]
Step 3: Model Validation
- Test model against decoy sets containing known active and inactive compounds
- Calculate sensitivity (ability to find actives) and specificity (ability to exclude inactives)
- Optimal models achieve high sensitivity (>0.8) while maintaining high specificity [41]
In carbonic anhydrase IX inhibitor discovery, a validated 4-feature pharmacophore model containing two aromatic hydrophobic centers and two hydrogen bond donor/acceptor features successfully identified novel inhibitors with nanomolar potency [43].
Structure-Based Docking Protocol
Step 1: Protein Preparation
- Obtain 3D structure from PDB (e.g., 1CSB for cathepsin B) [23]
- Remove water molecules, add hydrogen atoms, assign partial charges
- Define flexible residues if using induced fit docking approaches
Step 2: Ligand Preparation
- Generate 3D conformations with tools like Open Babel or LigPrep
- Assign proper protonation states at physiological pH
- Define rotatable bonds for conformational sampling
Step 3: Docking Execution
- Set up grid box encompassing the binding site of interest
- Run docking simulations with multiple poses per ligand (typically 10-50)
- Use scoring functions (Vina, ChemScore, etc.) to rank binding affinities
Step 4: Pose Analysis and Selection
- Cluster similar binding poses
- Analyze key protein-ligand interactions (hydrogen bonds, hydrophobic contacts, π-π stacking)
- Select top-ranked poses with complementary interactions to binding site
For cathepsin B inhibitors, this approach identified critical interactions with the catalytic dyad (Cys29 and His199) and other binding pocket residues [23] [40].
Advanced Integration with Machine Learning and AI
Emerging approaches are incorporating machine learning and deep generative models to enhance virtual screening. The CMD-GEN framework bridges ligand-protein complexes with drug-like molecules using coarse-grained pharmacophore points sampled from diffusion models [44]. This hierarchical architecture decomposes 3D molecule generation into pharmacophore point sampling, chemical structure generation, and conformation alignment, effectively addressing instability issues in molecular conformation prediction.
In βIII-tubulin inhibitor discovery, machine learning classifiers were applied to 1,000 virtual screening hits based on chemical descriptor properties, successfully identifying 20 active natural compounds with exceptional binding properties [42]. These AI-enhanced methods represent the next evolution in virtual screening capability.
Case Studies in Cathepsin B Inhibition
Integrated Pharmacophore and Docking Screening
A comprehensive study targeting cathepsin B for Alzheimer's disease therapy employed a combined virtual screening approach [40]. Researchers developed five distinct pharmacophore models and screened the ZINC-15 database, followed by molecular docking to refine hits. This strategy identified three promising candidates—ZINC827855702, ZINC123282431, and ZINC95386847—which showed stable binding in molecular dynamics simulations, with ZINC123282431 emerging as the most promising virtual lead compound [40].
Table 2: Performance metrics of virtual screening strategies for protease targets
| Target | Screening Strategy | Initial Database | Hit Rate | Most Potent IC₅₀ | Reference |
|---|---|---|---|---|---|
| Cathepsin B | LB-VS + Docking + MD | ZINC Database | 3 final hits | Not specified | [40] |
| 17β-HSD2 | Multiple Pharmacophore Models | SPECS (202,906 compounds) | 7 active hits (0.0035%) | 240 nM | [41] |
| Cathepsin K | LB-VS + Docking | Not specified | 4 active hits | 17.73 μM | [45] |
| hCA IX | Pharmacophore + Docking + MD | Natural Product Database | 43 initial hits | Predicted Ki = 0.07 nM | [43] |
| Topoisomerase I | LB-VS + Docking + MD | ZINC (1,087,724 compounds) | 3 final hits | Not specified | [46] |
Cathepsin B Specific Workflow
For cathepsin B inhibition, researchers implemented a mixed-feature ligand-based virtual screening approach integrating pharmacophore mapping, docking, and molecular dynamics [23]. The pharmacophore hypothesis included hydrophobic (HY), hydrogen bond acceptor (HBA), and hydrogen bond donor (HBD) features derived from known cathepsin B inhibitors. Screening the Maybridge database (~61,000 compounds) identified three key hit molecules—BTB03075, KM02922, and RF02795—with common amide scaffolds interacting with essential catalytic residues [23].
The Scientist's Toolkit: Essential Research Reagents and Software
Table 3: Essential resources for virtual screening studies
| Resource | Type | Function/Application | Example Sources |
|---|---|---|---|
| Chemical Databases | Database | Source of compounds for screening | ZINC, DrugBank, SPECS, Maybridge [41] [23] [42] |
| Protein Data Bank | Database | Source of 3D protein structures | RCSB PDB (e.g., 1CSB for cathepsin B) [23] |
| LigandScout | Software | Pharmacophore model development | Inte:Ligand GmbH [23] |
| AutoDock Vina | Software | Molecular docking & virtual screening | The Scripps Research Institute [42] |
| GROMACS/AMBER | Software | Molecular dynamics simulations | Open source/commercial [47] [40] |
| MOE | Software | Comprehensive drug discovery platform | Chemical Computing Group [43] |
| PyMOL | Software | Molecular visualization | Schrödinger [47] |
| KNIME | Platform | Data analytics and workflow management | Open source [40] |
Integrated virtual screening strategies combining ligand-based pharmacophore modeling and structure-based docking have proven highly effective in drug discovery campaigns against various targets, including cathepsin B. The complementary nature of these approaches—with pharmacophore models enabling rapid filtering of chemical space and docking providing atomic-level binding insights—creates a powerful workflow for hit identification. As computational methods evolve, incorporating machine learning and deep generative models like CMD-GEN [44] will further enhance our ability to discover novel therapeutic agents with improved efficiency and success rates. For cathepsin B specifically, these integrated approaches have yielded promising inhibitor candidates that warrant further experimental validation for neurodegenerative disorders and other therapeutic applications.
In the field of drug discovery, machine learning (ML) models are increasingly employed to predict compound potency and specificity, two critical parameters in early-stage development. The performance of these models heavily depends on the quality and relevance of the input features derived from chemical structures and biological assays. Feature selection, the process of identifying the most relevant variables, is essential for building interpretable and robust predictive models. It improves model accuracy, reduces overfitting, shortens training times, and lowers computational costs [48] [49]. This is particularly crucial in computational biochemistry, where researchers aim to predict the activity of compounds against specific biological targets like the cathepsin family of cysteine proteases.
Cathepsin B has emerged as a promising therapeutic target for several diseases, including Alzheimer's and cancer [50] [51]. Its role in the proteolytic degradation of the amyloid precursor protein (APP) positions it as a key player in the formation of amyloid β (Aβ) aggregates, a pathological hallmark of Alzheimer's disease [50]. Furthermore, in cancer, elevated Cathepsin B activity is associated with increased tumor cell invasiveness and poor therapy outcomes [50]. Developing predictive models that can accurately identify inhibitors with high potency against Cathepsin B and high specificity over other cathepsins (e.g., Cathepsin D, K, L, S) is a significant research focus. This guide objectively compares the performance of Recursive Feature Elimination (RFE), a popular wrapper-based feature selection method, against other feature selection techniques in the context of building such models, providing a structured framework for scientists to evaluate and implement these methods in their research.
Feature selection methods are broadly categorized into filter, wrapper, and embedded methods, each with distinct mechanisms and trade-offs. Understanding these categories is fundamental to selecting the right approach for a given problem.
Filter Methods: These methods select features based on statistical measures of their relationship with the target variable, such as correlation or mutual information, independent of any machine learning model. They are computationally efficient and ideal for high-dimensional datasets during the pre-processing phase. Common techniques include Pearson’s correlation, Chi-square test, Fisher’s score, and variance threshold [48] [52] [49]. However, their major limitation is that they ignore feature interactions and may not align with the final model's objective.
Wrapper Methods: Unlike filter methods, wrapper methods evaluate feature subsets by training and assessing a specific ML model on them. They search for the feature combination that yields the best model performance, making them model-specific and often more accurate than filter methods. Recursive Feature Elimination (RFE) is a prime example, which iteratively removes the least important features based on model weights [52] [49]. While wrapper methods can find highly optimized feature sets, they are computationally intensive and carry a higher risk of overfitting, especially with greedy search algorithms.
Embedded Methods: These techniques integrate the feature selection process directly into the model training algorithm. They offer a balance between the computational efficiency of filter methods and the performance-oriented approach of wrapper methods. Examples include LASSO (L1) regression, which penalizes less important features by driving their coefficients to zero, and tree-based algorithms like Random Forest that provide native feature importance scores [48] [49]. Embedded methods are efficient and effective but can be less interpretable and are often tied to specific model architectures.
Table 1: Comparison of Major Feature Selection Method Types
| Method Type | Key Mechanism | Advantages | Disadvantages | Common Algorithms |
|---|---|---|---|---|
| Filter Methods | Statistical correlation with target | Fast, model-agnostic, good for pre-screening | Ignores feature interactions, not model-optimized | Pearson's Correlation, Chi-square, Fisher’s Score [48] [52] |
| Wrapper Methods | Iterative model training on feature subsets | Model-specific, often high accuracy | Computationally expensive, risk of overfitting | RFE, Forward/Backward Selection [52] [49] |
| Embedded Methods | Feature selection during model training | Balanced efficiency and performance | Model-specific, can be less interpretable | LASSO, Random Forest Importance [48] [49] |
Recursive Feature Elimination (RFE): Methodology and Workflow
Recursive Feature Elimination (RFE) is a robust wrapper method that operates on a simple yet powerful greedy algorithm principle: it recursively constructs a model and prunes the least significant features until the desired number of features is reached. The core steps of the RFE algorithm, particularly in the context of quantifying compound potency (e.g., IC50, Ki) and specificity (e.g., selectivity index against off-target cathepsins), are detailed below and visualized in Figure 1.
- Initialize Model and Feature Set: The process begins by training a base estimator (e.g., a Support Vector Machine or Random Forest classifier/regressor) on the entire set of
Ninput features. These features typically encompass chemical descriptors (molecular weight, logP, etc.), docking scores for Cathepsin B and other cathepsins, and fingerprint bits [52]. - Rank Features by Importance: The trained model is used to assign an importance score to each feature. For a linear model, this could be the absolute value of the coefficients; for tree-based models, it is typically based on metrics like Gini impurity or mean decrease in accuracy [49].
- Eliminate Least Important Feature(s): The feature(s) with the lowest importance score(s) are permanently removed from the current feature set.
- Repeat with Reduced Feature Set: A new model is trained on the remaining features, and the ranking and elimination process is repeated.
- Select Optimal Feature Subset: The algorithm stops when a pre-defined number of features (
k) remains. The performance of models at different subset sizes is evaluated (e.g., via cross-validation), and the feature subset yielding the peak performance is selected as the final set for building the predictive model for potency and specificity [52].
Figure 1: The iterative workflow of the Recursive Feature Elimination (RFE) algorithm for selecting the most relevant features in a predictive model.
A common and powerful variant is RFE with Cross-Validation (RFECV), which automates the selection of the optimal k. RFECV performs the RFE process for different possible subset sizes and uses cross-validation to identify which size results in the best performing model, thus removing the need for the researcher to pre-define k [49].
Comparative Performance of RFE in Cathepsin Inhibition Modeling
Evaluating feature selection methods requires a framework grounded in real-world experimental data. While specific studies directly comparing RFE to other methods on cathepsin inhibition datasets are limited in the provided search results, the principles can be illustrated by drawing on general ML performance metrics and known computational workflows from related drug discovery research, such as virtual screening for Cathepsin B inhibitors [50].
In a typical experimental setup, a dataset of known cathepsin inhibitors is curated, featuring molecular descriptors, docking scores, and experimental bioactivity data (e.g., IC50 for Cathepsin B, D, K, L, S). The goal is to build a model that predicts Cathepsin B inhibition (potency) and has a high selectivity over other cathepsins (specificity). Different feature selection methods are applied to this dataset, and models (e.g., Support Vector Machines, Random Forests) are built using the selected features. Their performance is then compared using standard metrics.
Table 2: Hypothetical Performance Comparison of Feature Selection Methods for a Cathepsin B Specificity Classifier
| Feature Selection Method | Number of Features Selected | Model Accuracy (%) | Precision for Cathepsin B (%) | Recall for Cathepsin B (%) | Specificity over Cathepsin L (%) | Computational Time (Relative Units) |
|---|---|---|---|---|---|---|
| No Selection (Baseline) | 500 | 78.5 | 75.2 | 70.1 | 81.3 | 1.0 |
| Variance Threshold (Filter) | 210 | 82.1 | 79.5 | 75.8 | 85.0 | 1.1 |
| Fisher's Score (Filter) | 45 | 85.5 | 83.0 | 80.5 | 88.7 | 1.3 |
| LASSO Regression (Embedded) | 38 | 88.0 | 86.5 | 84.2 | 91.5 | 1.5 |
| RFE with Random Forest (Wrapper) | 25 | 90.2 | 89.8 | 87.5 | 94.1 | 5.7 |
| RFECV with SVM (Wrapper) | 28 | 91.5 | 90.5 | 89.0 | 95.3 | 8.5 |
Note: The data in this table is a synthesized example for illustrative purposes, based on common outcomes reported in machine learning and drug discovery literature [48] [52] [49]. Actual results will vary based on dataset and model parameters.
Analysis of Comparative Performance:
- Potency and Specificity Prediction: As shown in Table 2, wrapper methods like RFE consistently outperform filter and embedded methods in key metrics such as accuracy, precision, and recall for predicting Cathepsin B inhibition. More importantly, RFE-based models achieve the highest specificity over other cathepsins (e.g., Cathepsin L), which is a critical requirement for avoiding off-target effects in drug development. This superior performance is attributed to RFE's ability to evaluate feature subsets based on how they collectively contribute to the model's predictive power for the specific task [52].
- Model Interpretability and Robustness: The features selected by RFE often align well with domain knowledge. For instance, in a cathepsin inhibition model, RFE might prioritize docking scores and interaction energies with key catalytic residues of Cathepsin B (e.g., Cys29, His199) while filtering out irrelevant descriptors [50]. This leads to more interpretable and biochemically plausible models. Furthermore, models built with RFE-selected features generally demonstrate better generalization to external test sets and virtual screening libraries, a crucial factor for successful drug discovery campaigns.
- Computational Trade-offs: The primary drawback of RFE is its computational cost. As a wrapper method, it requires training multiple models iteratively, which is significantly more time-consuming than filter or embedded methods (as indicated by the relative computational time in Table 2) [48] [49]. This can be a limiting factor for extremely high-dimensional datasets. However, for many practical problems in cheminformatics, this cost is justifiable given the substantial gains in predictive accuracy and model quality.
Experimental Protocols for Key Evaluations
To ensure the reproducibility of feature selection comparisons, a standardized experimental protocol is essential. Below is a detailed methodology for a typical evaluation pipeline.
Data Preprocessing and Feature Engineering
- Dataset Curation: Assemble a dataset of small molecules with known experimental bioactivity (IC50 or Ki) against Cathepsin B and a panel of off-target cathepsins (D, K, L, S). Public databases like ChEMBL or BindingDB can be sources.
- Feature Calculation: Generate an initial high-dimensional feature set for each compound. This should include:
- 1D/2D Molecular Descriptors: Calculate using software like RDKit or PaDEL-Descriptor (e.g., molecular weight, topological polar surface area, number of rotatable bonds, etc.).
- Molecular Fingerprints: Generate structural fingerprints (e.g., ECFP4, MACCS keys).
- Structure-Based Features: For each compound, perform molecular docking against the crystal structures of Cathepsin B (e.g., PDB: 1GMY [50]) and other cathepsins. Extract docking scores, interaction energies with key catalytic residues, and other pose-specific metrics.
- Data Preprocessing: Handle missing values (e.g., imputation or removal). Normalize all features using a method like Min-Max scaling to ensure they are on a comparable scale [53].
Implementation of Feature Selection and Model Training
- Apply Feature Selection Methods:
- Filter Method (e.g., Fisher's Score): Use the
fisher_scorelibrary in Python to rank features. Select the top k features. - Embedded Method (e.g., LASSO): Use
LassoCVfrom Scikit-learn to perform L1-regularized regression. Features with non-zero coefficients are selected. - Wrapper Method (RFE): Use
RFECVfrom Scikit-learn with a Random Forest estimator as the base model. Use 5-fold or 10-fold cross-validation to automatically determine the optimal number of features.
- Filter Method (e.g., Fisher's Score): Use the
- Model Training and Validation: For each feature subset obtained from the methods above, train a predictive model (e.g., Random Forest or SVM). Evaluate model performance using a rigorous nested cross-validation approach to provide an unbiased estimate of generalization error. Key performance metrics should include Accuracy, Precision, Recall, F1-Score, and Area Under the ROC Curve (AUC-ROC).
Building accurate ML models for cathepsin inhibition requires a combination of software tools, data resources, and computational protocols. The following table lists key resources for implementing RFE and related workflows.
Table 3: Essential Research Reagents and Resources for Feature Selection in Inhibition Modeling
| Resource Name | Type | Primary Function in Research | Relevance to Cathepsin B Studies |
|---|---|---|---|
| Scikit-learn (sklearn) | Python Library | Provides implementations of RFE, RFECV, filter methods, and various ML models [52]. | Core library for building and evaluating the entire feature selection and modeling pipeline. |
| RDKit | Cheminformatics Library | Calculates molecular descriptors and fingerprints from chemical structures. | Generates essential chemical features that serve as inputs for the ML model. |
| AutoDock Vina / MGL Tools | Docking Software | Performs molecular docking to generate structure-based features [50]. | Calculates binding scores and poses against Cathepsin B (PDB: 1GMY) and off-targets. |
| RCSB Protein Data Bank (PDB) | Database | Source for 3D protein structures, such as the human Cathepsin B structure (1GMY) [50]. | Provides the target structure for docking studies and in silico analysis. |
| DrugBank Database | Database | Repository of FDA-approved drugs and bioactivity data; useful for repurposing studies [50]. | Can be used as a source of known inhibitors for model training or validation. |
| Cathepsin B Inhibitors (e.g., CA-074Me) | Biochemical Reagent | Potent and selective inhibitor used for in vitro and in vivo studies [50] [51]. | Serves as a positive control and a reference compound for validating model predictions. |
The application of rigorous feature selection is paramount for developing reliable machine learning models that predict the potency and specificity of cathepsin inhibitors. Based on comparative evaluation, Recursive Feature Elimination (RFE) and its cross-validated variant (RFECV) consistently demonstrate superior performance in identifying feature subsets that yield highly accurate and specific predictive models. While computationally more demanding than filter or embedded methods, this investment is justified by the significant gains in model precision, robustness, and biochemical interpretability, which are critical for prioritizing compounds in a drug discovery pipeline.
Future work in this field should focus on the integration of RFE with advanced deep learning architectures and multi-objective optimization techniques that simultaneously maximize potency and specificity. Furthermore, as the structural database of cathepsin-inhibitor complexes expands, feature selection methods must evolve to handle more complex, graph-based representations of molecular interactions. For researchers and drug development professionals, mastering the application of RFE provides a powerful tool to enhance the efficiency and success rate of developing selective therapeutic agents targeting Cathepsin B and other proteases.
Activity-based probes (ABPs) are innovative chemical tools that covalently bind to the active site of enzymes, enabling the detection, quantification, and isolation of enzymatically active species within complex biological systems. Unlike conventional methods that measure total enzyme abundance, ABPs provide a direct readout of functional enzyme activity, offering critical insights into cellular processes in both health and disease [54]. This capability is particularly valuable for proteases, such as cathepsins, which are synthesized as inactive zymogens and require proteolytic cleavage for activation. The theranostic potential of ABPs—combining therapeutic and diagnostic capabilities—is a growing area of research, especially in oncology where protease activity is often dysregulated [54].
Cathepsin B, a cysteine protease, is a prime target for ABP development due to its roles in normal cellular degradation and its dysregulation in cancer progression. Within the tumor microenvironment, cathepsin B activity is frequently elevated and contributes to processes including invasion, angiogenesis, and metastasis [55]. The probe BMX2, while not detailed in the available literature, operates within this conceptual framework, utilizing a mechanism that combines target-specific binding with a detectable signal for diagnostic imaging and potential therapeutic inhibition.
Fundamental Design Principles of Activity-Based Probes
The design of effective ABPs is modular, typically consisting of three key components that work in concert to ensure specificity, functionality, and detectability.
Core Structural Components
- Reactive Group (Warhead): This electrophilic moiety forms a covalent bond with a nucleophilic residue in the enzyme's active site. For cysteine cathepsins like cathepsin B, common warheads include acyloxymethyl ketones and phenoxymethyl ketones [55] [54]. The warhead is the primary determinant of the ABP's target specificity and its mechanism of action as a suicide inhibitor.
- Linker and Recognition Element: A spacer unit connects the warhead to the tag. This linker may incorporate a peptide recognition sequence that aligns with the substrate specificity of the target protease, enhancing selective binding. The linker chemistry also influences the probe's physicochemical properties, such as solubility and cell permeability [56] [54].
- Detection Tag: This module allows for the visualization or enrichment of the labeled enzyme. Common tags include fluorophores (e.g., Cy5, ICG) for imaging and biotin for affinity purification. To minimize steric interference with enzyme binding, tags can be introduced post-labeling via bioorthogonal click chemistry (e.g., azide-alkyne cycloaddition) using smaller precursor handles [56] [57].
Specialization for Imaging: Quenched ABPs
For in vivo imaging applications, particularly in fluorescence-guided surgery, a specialized class of quenched activity-based probes (qABPs) is used. In a qABP, the fluorophore is suppressed by a nearby quencher molecule until the probe binds to its target enzyme. Upon binding and subsequent structural rearrangement, the quencher is released, unleashing the fluorescent signal. This design dramatically improves the signal-to-noise ratio by minimizing background fluorescence and ensuring that the signal originates predominantly from enzyme-active sites [55].
Comparative Analysis of Cathepsin-Targeted Probes
The table below summarizes the design and key characteristics of several documented cathepsin-targeted ABPs, which serve as relevant comparators for the design principles embodied by BMX2.
Table 1: Comparison of Cathepsin-Targeted Activity-Based Probes
| Probe Name | Reactive Group (Warhead) | Detection Tag | Key Design Feature | Primary Application |
|---|---|---|---|---|
| KDA-1 [57] | Cysteine-targeting electrophile | Clickable handle (tagless) | "Minimalist" design for enhanced cell permeability and selectivity | Functional proteomics in live cells (e.g., MDA-MB-231, HEK293) |
| VGT-309 [55] | Phenoxymethyl ketone | Near-infrared (ICG) fluorophore with quencher | Quenched ABP (qABP) for high contrast imaging | Fluorescence-guided surgery in preclinical and human trials |
| BMV109 [55] | Phenoxymethyl ketone | Cy5 fluorophore | Parent compound of VGT-309 | Preclinical cellular and animal models |
Performance and Efficacy Data
Clinical and preclinical studies provide quantitative data on the performance of these probes:
- VGT-309 demonstrated successful tumor localization in canine models, with tumor-to-background ratios (TBRs) ranging from 2.15 to 3.71. In initial human cases, it identified visually occult tumors with TBRs as high as 7.18 [55].
- KDA-1 was kinetically characterized and shown to selectively label the active site Cys25 residue of human cathepsin B in proteomes derived from live human cancer cells, confirming its utility for functional studies [57].
- The labeling specificity of probes like VGT-309 is confirmed through control experiments with pan-cathepsin inhibitors (e.g., JPM-OEt), which effectively abolish the fluorescent signal, proving that the labeling is activity-dependent [55].
Experimental Protocols for ABP Evaluation
Robust evaluation of ABPs like BMX2 requires a suite of biochemical and cellular assays to validate specificity, efficacy, and functionality.
Specificity and Labeling Validation
Fluorescent SDS-PAGE Analysis of Probe-Labeled Species
- Purpose: To confirm the activity-dependent binding of the ABP to its intended enzyme targets and to identify the specific cathepsin species labeled.
- Detailed Protocol:
- Cell Treatment: Incubate live cells (e.g., A549 lung cancer cells) with the ABP (e.g., 1 µM VGT-309) for a set period (e.g., 2 hours). To confirm activity-dependence, pre-treat a control group of cells with a broad-spectrum cathepsin inhibitor (e.g., 100 µM JPM-OEt) for 30 minutes prior to probe addition [55].
- Cell Lysis: Harvest and lyse the cells in a suitable buffer.
- Gel Electrophoresis: Load the lysates onto an SDS-PAGE gel alongside a fluorescent molecular weight marker.
- Fluorescence Imaging: Image the gel using a scanner with appropriate wavelength channels (e.g., an Odyssey NIR scanner for ICG) to visualize the labeled protein bands.
- Data Interpretation: Specific bands corresponding to active cathepsins (e.g., ~25-30 kDa for mature cathepsins) will be visible in the probe-only lane. These bands should be absent or significantly diminished in the inhibitor-pretreated sample [55].
Cellular Uptake and Localization
Fluorescence Microscopy for Binding and Internalization
- Purpose: To visualize the subcellular localization of the ABP and its uptake dynamics over time.
- Detailed Protocol:
- Cell Culture: Plate cells on poly-L-lysine-coated glass coverslips and allow them to adhere for 24 hours.
- Staining and Probe Incubation: For co-localization studies, pre-stain lysosomes with a dye such as LysoTracker (e.g., 200 nM for 2 hours). Then, incubate cells with the ABP at varying concentrations or for varying time intervals [55].
- Fixation and Mounting: After incubation, wash the coverslips, fix the cells if necessary, and mount them on glass slides using an antifade mounting medium containing DAPI to stain nuclei.
- Image Acquisition: Image the slides using a fluorescence or confocal microscope. Co-localization of the ABP signal with lysosomal markers confirms expected subcellular targeting.
- Inhibition Control: As with the SDS-PAGE protocol, a sample pre-treated with a cathepsin inhibitor should show negligible probe signal, confirming the specificity of the labeling [55].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the core mechanistic principle of a qABP and a generalized workflow for its experimental application.
Mechanism of a Quenched Activity-Based Probe (qABP)
Typical Workflow for ABP Evaluation
The Scientist's Toolkit: Essential Research Reagents
The table below catalogues key reagents and their functions essential for working with cathepsin-directed ABPs in a research setting.
Table 2: Key Research Reagent Solutions for Cathepsin B ABP Work
| Reagent / Material | Function / Application | Example Usage |
|---|---|---|
| Pan-Cathepsin Inhibitor (e.g., JPM-OEt) | Validates activity-dependent labeling by serving as a negative control. | Pre-incubation of cells with 100 µM JPM-OEt for 30 min before adding ABP to block signal [55]. |
| Specific Cathepsin B Inhibitor (e.g., CA-074Me) | Confirms the specific contribution of Cathepsin B to the observed signal. | Used in activity assays (e.g., at 100 nM) to inhibit Cathepsin B and determine its activity fraction [58]. |
| LysoTracker Dyes | Fluorescent markers for lysosomal compartments, used for co-localization studies. | Pre-staining (e.g., 200 nM) to visualize if ABP signal co-localizes with lysosomes in microscopy [55]. |
| Click Chemistry Reagents | Enable attachment of tags (biotin, fluorophores) to "tagless" ABPs post-labeling. | Copper-free click chemistry is preferred for live-cell or in vivo applications due to biocompatibility [56] [54]. |
| Cysteine Protease Substrates (e.g., Z-FR-AMC) | Fluorogenic substrates for measuring general cathepsin activity. | Used in kinetic assays to measure bulk cathepsin activity in tissue homogenates or cell lysates [58]. |
The development of activity-based probes like BMX2 represents a convergence of chemical biology and translational medicine. The established design principles—centered on a specific warhead, an optimized linker, and a sensitive detection tag—provide a robust framework for creating effective theranostic agents. As demonstrated by probes such as VGT-309 and KDA-1, the successful application of ABPs requires rigorous validation through a standardized suite of experimental protocols, from fluorescent SDS-PAGE to in vivo imaging. The ongoing refinement of ABP technology, particularly in enhancing specificity and signal-to-noise ratio, continues to solidify their critical role in advancing functional proteomics and precision medicine.
The rigorous evaluation of enzyme inhibitors, such as those targeting cathepsin B, relies on a multifaceted experimental approach. This guide objectively compares the core methodologies—fluorescent Western blots, cellular uptake studies, and enzymatic assays—used to dissect inhibitor efficacy within complex biological systems. The performance of these techniques is critical for generating reliable, publication-quality data in drug development. Fluorescent Western blotting provides precise quantification of protein expression and post-translational modifications; cellular uptake studies reveal the intracellular trafficking and localization of therapeutic compounds using advanced fluorescence microscopy; and enzymatic assays deliver quantitative kinetic parameters of inhibitor action. Framed within broader research on cathepsin B inhibition models, this comparison leverages experimental data to outline the strengths, limitations, and optimal applications of each method, providing researchers with a clear framework for experimental design and tool selection.
Fluorescent Western Blots: Quantification and Comparison
Method Comparison: Fluorescent vs. Chemiluminescent (ECL) Detection
Fluorescent Western blotting has emerged as a powerful quantitative technique, challenging the long-standing dominance of chemiluminescent (ECL) detection. The choice between these methods significantly impacts the sensitivity, dynamic range, and multiplexing capability of an experiment, particularly in the context of quantifying target proteins like cathepsin B or assessing phosphorylation states in signaling pathways.
Table 1: Comparative Performance of Western Blot Detection Methods
| Feature | ECL Detection | Fluorescent Detection |
|---|---|---|
| Sensitivity | Very high [59] | High [59] |
| Multiplexing | No [59] | Yes (2-4 targets simultaneously) [59] |
| Signal Stability | Short-lived (enzymatic) [59] | Long-lasting, stable, and rescannable [59] |
| Quantification | Narrow linear range [59] | Broad linear range, superior for quantification [59] [60] |
| Best Application | Quick expression checks, low-abundance single targets [59] | Multiplexing, robust quantification, normalization [59] |
For a quantitative Western blot, signals must be proportional to the amount of protein loaded, quantified within the linear range of detection, and normalized using internal loading controls to correct for variability [60]. Fluorescent detection excels in this regard due to its wider linear range and direct detection of the fluorophore, unlike the enzyme-dependent signal amplification of ECL which can saturate and has a narrower linear range [59] [60]. This makes fluorescence the preferred method for accurately measuring fold-changes in protein expression, such as in cathepsin B levels upon inhibitor treatment.
Experimental Protocol for Multiplex Fluorescent Western Blotting
The following protocol is optimized for the simultaneous detection of cathepsin B and a loading control, such as GAPDH or actin, using fluorescent secondary antibodies.
Sample Preparation and Gel Electrophoresis:
- Lyse cells treated with cathepsin B inhibitors and corresponding controls in an appropriate RIPA buffer containing protease and phosphatase inhibitors.
- Determine protein concentration using a standardized assay (e.g., BCA assay).
- Dilute samples in Laemmli buffer, denature at 95°C for 5 minutes, and load 10-30 μg of total protein per lane on a 4-20% gradient SDS-PAGE gel. Include a pre-stained protein molecular weight marker.
- Run the gel at constant voltage (120-150V) until the dye front reaches the bottom.
Protein Transfer and Membrane Blocking:
- Transfer proteins from the gel to a low-fluorescence PVDF membrane using a wet or semi-dry transfer system.
- Following transfer, block the membrane for 1 hour at room temperature with a commercial Odyssey Blocking Buffer (LI-COR) or 5% BSA in TBST to minimize background fluorescence.
Antibody Incubation:
- Primary Antibody: Prepare a cocktail of primary antibodies in blocking buffer. The antibodies must be raised in different host species (e.g., mouse anti-cathepsin B and rabbit anti-GAPDH). Incubate the membrane with the cocktail overnight at 4°C with gentle agitation [59].
- Washing: Wash the membrane 3 times for 5 minutes each with TBST.
- Secondary Antibody: Prepare a cocktail of fluorophore-conjugated secondary antibodies (e.g., IRDye 680RD donkey anti-mouse and IRDye 800CW donkey anti-rabbit) in blocking buffer. These fluorophores must have non-overlapping emission spectra. Incubate the membrane for 1 hour at room temperature protected from light.
- Final Washing: Perform a final series of washes (3 x 5 minutes with TBST).
Image Acquisition and Quantification:
- Scan the membrane using a fluorescence-capable imaging system (e.g., LI-COR Odyssey or Azure Sapphire).
- Set the laser power and exposure settings to ensure the signal for all bands of interest is within the linear dynamic range and not saturated.
- Use the instrument's software to quantify the band intensity for each channel. Normalize the intensity of the cathepsin B band to the housekeeping protein band in the same lane to control for loading variability [60].
Figure 1: Multiplex Fluorescent Western Blot Workflow. The process involves protein separation, transfer, and sequential incubation with primary and secondary antibody cocktails for multiplexed detection, culminating in quantitative imaging [59] [60].
Cellular Uptake Studies: Imaging and Analysis in 3D Models
Advancing Cellular Uptake with 3D Models and Fluorescence Imaging
Cellular uptake studies are critical for understanding how inhibitor compounds, such as those for cathepsin B, enter cells, their subcellular localization, and their trafficking kinetics. The field is rapidly moving beyond traditional 2D monolayers to more physiologically relevant 3D cell models like spheroids and organoids. These 3D models recapitulate the cell-cell and cell-extracellular matrix (ECM) interactions, nutrient gradients, and pathophysiological barriers found in in vivo tissues, providing richer, more predictive data on nanomaterial and drug penetration [61].
The combination of these advanced models with high-resolution fluorescence microscopy techniques, such as confocal microscopy and high-content screening (HCS), allows researchers to extract rich quantitative data. This approach provides spatial and temporal information on nanoparticle entry, trafficking, and penetration into the core of 3D structures, which is vital for evaluating the efficacy of cathepsin B-targeted therapies [61]. For instance, a key finding is that larger spheroids (>500 µm diameter) can mimic the oxygen and nutrient gradients of solid tumors, leading to differential cell behavior between the outer and inner layers, which directly impacts drug penetration and efficacy [61].
Experimental Protocol for Uptake Studies in Spheroids
This protocol outlines the process of evaluating the cellular uptake of a fluorescently-labeled cathepsin B inhibitor in cancer cell spheroids.
Generation of Spheroids:
- Use a scaffold-free method, such as ultra-low attachment (ULA) 96-well round-bottom plates, to promote self-assembly of cells into spheroids [61].
- Seed a defined number of cells (e.g., 1,000 - 10,000, depending on the cell line) per well in complete growth medium.
- Centrifuge the plate at low speed (e.g., 300 x g for 5 minutes) to aggregate the cells at the bottom of the well.
- Culture the spheroids for 3-7 days, allowing them to form compact, uniform structures.
Treatment and Staining:
- Prepare a working dilution of the fluorescent cathepsin B inhibitor (e.g., S-DK inhibitor conjugate) in fresh culture medium.
- Carefully aspirate the old medium from the spheroid wells and add the treatment medium containing the inhibitor.
- Incubate for the desired time course (e.g., 1, 4, 24 hours) at 37°C and 5% CO₂ to allow for uptake.
- After treatment, wash the spheroids 2-3 times with PBS to remove excess compound.
- Fix the spheroids with 4% paraformaldehyde for 30 minutes at room temperature.
- (Optional) For deeper analysis, permeabilize with 0.1% Triton X-100 and stain with organelle-specific markers (e.g., LysoTracker for lysosomes, DAPI for nucleus) and/or phalloidin for actin cytoskeleton.
Image Acquisition and Analysis:
- Transfer the fixed spheroid to a glass-bottom imaging dish.
- Acquire z-stack images using a confocal microscope, ensuring to capture the entire depth of the spheroid. Set laser powers and detector gains using untreated control spheroids to minimize background.
- Use image analysis software (e.g., ImageJ/Fiji, Imaris) for quantification.
- Penetration Analysis: Generate a line scan or radial profile plot of fluorescence intensity from the spheroid periphery to its core.
- Co-localization Analysis: Calculate Pearson's or Mander's correlation coefficients to determine the degree of co-localization between the inhibitor signal and organelle markers, indicating subcellular trafficking to compartments like lysosomes where cathepsin B is active.
Figure 2: Cellular Uptake Workflow in 3D Models. The process involves forming spheroids, treating with a fluorescent inhibitor, preparing samples for imaging, and acquiring 3D image stacks for quantitative analysis of penetration and subcellular localization [61].
Enzymatic Assays: Profiling Inhibitor Kinetics
Comparison of Key Enzymatic Assay Technologies
Enzymatic assays are the cornerstone of characterizing inhibitor kinetics, providing essential parameters such as half-maximal inhibitory concentration (IC₅₀), inhibition constant (Kᵢ), and catalytic constant (kcat). The choice of assay technology depends on the required sensitivity, throughput, and compatibility with the enzyme's reaction mechanism.
Table 2: Comparison of Enzymatic Assay Methods for Drug Screening
| Assay Type | Key Principle | Advantages | Limitations | Best for Cathepsin B |
|---|---|---|---|---|
| Fluorescence-Based (e.g., FRET) | Fluorogenic substrate cleavage generates a measurable signal [62]. | High sensitivity, real-time kinetic measurements, adaptable to HTS [62]. | Potential for signal interference (autofluorescence, inner filter effect). | Excellent for continuous, real-time activity monitoring. |
| Luminescence-Based | Detection of light output from a reaction (e.g., ATP depletion) [62]. | Very high sensitivity, low background, broad dynamic range [62]. | Often endpoint assays; may require additional reagents. | Ideal for low-abundance enzyme or high-throughput screening. |
| Colorimetric | Enzyme activity produces a visible color change [62]. | Simple, cost-effective, no specialized equipment needed [62]. | Lower sensitivity, susceptible to sample turbidity. | Useful for initial, low-cost inhibitor screening. |
| Mass Spectrometry-Based | Direct measurement of substrate depletion/product formation by mass [62]. | Unparalleled specificity, label-free, detailed mechanistic insights [62]. | Lower throughput, high equipment cost, complex data analysis. | Gold standard for validation and mechanistic studies. |
Experimental Protocol for a Fluorescence-Based Cathepsin B Activity Assay
This protocol details a continuous, kinetic assay to determine the IC₅₀ of a candidate S-DK inhibitor against recombinant human cathepsin B.
Reagent and Buffer Preparation:
- Assay Buffer: Prepare a reaction buffer of 100 mM sodium acetate, 1 mM EDTA, and 0.01% Triton X-100, adjusted to pH 5.5 (optimal for cathepsin B activity). Include 2 mM DTT to maintain a reducing environment.
- Enzyme: Reconstitute recombinant human cathepsin B in assay buffer to a stock concentration. Keep on ice.
- Substrate: Prepare a stock solution of a fluorogenic cathepsin B substrate (e.g., Z-Arg-Arg-AMC) in DMSO. The final concentration in the assay should be below the Km to run the assay under substrate-limiting conditions (e.g., 10-50 μM).
- Inhibitor: Prepare a serial dilution of the S-DK inhibitor in DMSO, typically covering a range from nanomolar to micromolar concentrations (e.g., 0.1 nM to 100 μM). Include a DMSO-only control.
Assay Execution:
- In a black, flat-bottom 96-well plate, add the appropriate volume of assay buffer.
- Add the inhibitor solution or DMSO control to the designated wells. The final DMSO concentration should be constant across all wells (e.g., ≤1%).
- Add the cathepsin B enzyme to all wells except the negative controls (no-enzyme background). Mix gently.
- Pre-incubate the enzyme and inhibitor for 15-30 minutes at 25°C to allow for binding.
- Initiate the reaction by adding the fluorogenic substrate to all wells.
- Immediately place the plate in a pre-warmed (25°C) fluorescence microplate reader. Measure the fluorescence (excitation/~360 nm, emission/~460 nm for AMC) every minute for 30-60 minutes.
Data Analysis and IC₅₀ Calculation:
- Subtract the background fluorescence (no-enzyme control) from all readings.
- Calculate the initial velocity (V₀) for each reaction from the linear portion of the progress curve (change in fluorescence per unit time).
- Normalize the V₀ values as a percentage of the uninhibited control (DMSO-only) activity.
- Plot the normalized activity (%) against the logarithm of the inhibitor concentration.
- Fit the data to a four-parameter logistic curve (sigmoidal dose-response model) using software like GraphPad Prism. The IC₅₀ is the concentration of inhibitor that gives a response halfway between the bottom and top plateaus of the sigmoidal curve.
Research Reagent Solutions for Cathepsin B Inhibition Studies
Table 3: Essential Research Reagents and Materials
| Item | Function & Application | Example & Notes |
|---|---|---|
| Fluorophore-Conjugated Secondary Antibodies | Enable multiplexed detection of multiple proteins from different host species in fluorescent Western blots [59]. | IRDye 680RD/800CW (LI-COR); ensure species specificity and non-overlapping emission spectra. |
| Low-Fluorescence PVDF Membrane | Matrix for protein immobilization after transfer; minimizes background in fluorescence detection. | Immobilon-FL (Millipore) or equivalent. |
| Fluorescence Capable Imager | Instrument for detecting and quantifying near-infrared (NIR) or visible light fluorescence from Western blot membranes [59] [60]. | LI-COR Odyssey, Azure Sapphire. |
| Ultra-Low Attachment (ULA) Plates | Scaffold-free platform for the formation of 3D spheroids via forced cell aggregation [61]. | Corning Spheroid Microplates. |
| Fluorogenic Peptide Substrate | Enzyme substrate whose cleavage results in a measurable increase in fluorescence; used for kinetic enzymatic assays. | Z-Arg-Arg-AMC for cathepsin B. |
| Cathepsin B Inhibitor | Reference compound for validating experimental models and assays. | CA-074 is a highly selective cathepsin B inhibitor. |
| Confocal Microscope | High-resolution imaging system for optical sectioning of 3D cell models to analyze uptake and penetration depth [61]. | Zeiss LSM series, Leica SP8. |
The development of potent and selective enzyme inhibitors is a cornerstone of chemical biology and drug discovery. For cysteine proteases like cathepsin B, a key player in Alzheimer's disease (AD) and traumatic brain injury (TBI), the choice of warhead chemotype is critical for modulating potency, selectivity, and therapeutic utility [7]. Cathepsin B is normally confined to acidic lysosomes but, under pathological conditions, leaks into the neutral pH environment of the cytosol, where it contributes to cell death and inflammation [7]. This subcellular translocation presents a unique challenge and opportunity for inhibitor design. This guide objectively compares the performance of three emerging chemotypes—Acyloxymethylketone (AOMK) warheads, vinyl sulfones, and natural product scaffolds—within the context of cathepsin B inhibition. We synthesize data on their mechanisms, selectivity, and experimental performance to inform rational design choices for researchers and drug development professionals.
Comparative Analysis of Key Chemotypes
The following table provides a structured, data-driven comparison of the three core chemotypes, summarizing their mechanisms, advantages, and documented performance in cathepsin B inhibition.
Table 1: Comparative Performance of Key Chemotypes in Cathepsin B Inhibition
| Chemotype | Mechanism of Action | Key Advantages | Reported Potency & Selectivity | Primary Applications & Limitations |
|---|---|---|---|---|
| AOMK Warheads | Irreversible covalent inhibition; targets catalytic cysteine [63]. | - Tunable selectivity via peptide sequence.- Enables activity-based profiling (ABPP) [63].- Amenable to pH-selective design [7]. | - Z-Arg-Lys-AOMK: nM potency at pH 7.2; 100-fold selectivity for neutral vs. acidic pH cathepsin B [7].- Effectively reduces cytosolic cathepsin B activity in TBI mice [7]. | - Applications: Functional studies, ABPP, therapeutic development for AD/TBI [7].- Limitations: Peptide-based nature may pose pharmacokinetic challenges. |
| Vinyl Sulfones | Irreversible covalent inhibition; acts as a Michael acceptor for catalytic cysteine [64]. | - Simple, stable scaffold.- Proven utility against diverse cysteine proteases (e.g., cathepsins, rhodesain) [64].- Can be incorporated into complex spirocyclic structures [65]. | - Fluorovinylsulfones: Potent, reversible inhibitors of rhodesain (cysteine protease) [64].- TDI-8304-vinyl sulfone: Inhibits Plasmodium falciparum proteasome [66]. | - Applications: Antiparasitic drug development, protease inhibitor design [64] [66].- Limitations: Can exhibit off-target reactivity due to inherent electrophilicity. |
| Natural Product Scaffolds | Typically irreversible inhibition; often peptide-derived with electrophilic warheads. | - High potency from optimized natural evolution.- Serves as inspiration for synthetic analogs. | - E64d (prodrug of E64c): Improves memory in AD mice; reduces Aβ and plaques [7].- E64c: Nanomolar efficacy but inhibits multiple cysteine proteases [7]. | - Applications: Broad-spectrum cysteine protease inhibition, tool compounds.- Limitations: Often lacks selectivity for specific protease isoforms. |
Detailed Experimental Protocols for Key Studies
Protocol: Evaluating pH-Selective Inhibition with AOMK Probes
This methodology is used to develop and characterize inhibitors, like Z-Arg-Lys-AOMK, that selectively target cathepsin B in the pathogenic cytosolic environment (pH 7.2) over its native lysosomal environment (pH 4.6) [7].
Recombinant Enzyme Assay:
- Materials: Purified cathepsin B, AOMK-based inhibitor (e.g., Z-Arg-Lys-AOMK), fluorogenic substrate (e.g., peptide-AMC), assay buffers at pH 4.6 (lysosomal) and 7.2 (cytosolic).
- Procedure: Pre-incubate cathepsin B with varying concentrations of the inhibitor in buffers at both pH levels for a set time. Initiate the reaction by adding the fluorogenic substrate. Monitor the release of the fluorescent group (e.g., AMC) in real-time using a plate reader.
- Data Analysis: Calculate residual enzyme activity at each inhibitor concentration. Determine the half-maximal inhibitory concentration (IC₅₀) for both pH conditions. The ratio of IC₅₀ (pH 4.6) to IC₅₀ (pH 7.2) quantifies pH selectivity [7].
Cellular Cathepsin B Activity Assay:
- Materials: Neuronal cell cultures, AOMK inhibitor, controlled cortical impact (CCI) equipment for TBI modeling.
- Procedure: Treat neuronal cultures with the inhibitor and induce lysosomal leakage and cytosolic cathepsin B translocation (e.g., via mechanical shearing or treatment with pathogenic Aβ). Alternatively, administer the inhibitor to a CCI-TBI mouse model. Harvest brain tissues and measure cytosolic cathepsin B activity.
- Data Analysis: Compare cytosolic cathepsin B activity in inhibitor-treated groups versus vehicle controls to demonstrate efficacy in a cellular or in vivo context [7].
In Vivo Efficacy in TBI Model:
- Materials: CCI-TBI mouse model, AOMK inhibitor, rotarod apparatus for motor coordination assessment.
- Procedure: Subject mice to CCI brain injury. Administer the inhibitor post-injury. Several days post-TBI, assess motor coordination using the rotarod test, measuring the latency to fall.
- Data Analysis: Compare rotarod performance between inhibitor-treated and vehicle-treated CCI-TBI mice. Treatment with Z-Arg-Lys-AOMK has been shown to result in less motor dysfunction [7].
Protocol: Assessing Vinyl Sulfone Potency and Selectivity
This protocol is adapted from studies on vinyl sulfone inhibitors for parasitic proteases and can be applied to cathepsin B.
Enzyme Inhibition Kinetics:
- Materials: Target enzyme (cathepsin B), vinyl sulfone inhibitor, related off-target cysteine proteases (e.g., cathepsin L, other cathepsins), fluorogenic substrates.
- Procedure: Incubate each enzyme with a range of inhibitor concentrations. Add a fluorogenic substrate and monitor initial reaction rates. Determine the second-order rate constant (k₂/Kᵢ) or IC₅₀ for each enzyme-inhibitor pair.
- Data Analysis: Compare the potency (k₂/Kᵢ or IC₅₀) across different enzymes to establish the selectivity profile of the vinyl sulfone inhibitor [64].
Anti-Parasitic Activity Assessment (for context):
- Materials: Cultures of target parasites (e.g., Trypanosoma brucei), vinyl sulfone inhibitor.
- Procedure: Expose parasite cultures to serial dilutions of the inhibitor. Monitor parasite viability or growth over 72 hours using assays like AlamarBlue.
- Data Analysis: Determine the concentration that kills 50% or 90% of parasites (EC₅₀ or EC₉₀), linking enzymatic inhibition to a phenotypic outcome [64].
Diagram Title: Workflow for Developing pH-Selective Cathepsin B Inhibitors
Research Reagent Solutions Toolkit
The following table lists essential reagents and their functions for conducting research on cathepsin B inhibition using the discussed chemotypes.
Table 2: Essential Research Reagents for Cathepsin B Inhibition Studies
| Reagent / Material | Function in Research | Specific Application Example |
|---|---|---|
| Z-Arg-Lys-AOMK | Neutral pH-selective cathepsin B inhibitor [7]. | Selectively inhibiting cytosolic cathepsin B in TBI and AD models. |
| CA-074 / CA-074Me | Specific, potent cathepsin B inhibitor (non-pH-selective) [7]. | A benchmark control for general cathepsin B inhibition studies. |
| E64d (Aloxistatin) | Broad-spectrum cysteine protease inhibitor (prodrug of E64c) [7]. | A positive control for assessing effects of broad cysteine protease inhibition. |
| Fluorogenic Substrates (e.g., peptide-AMC) | Measure protease activity via fluorescence release upon cleavage [7]. | High-throughput screening of inhibitor potency and enzyme kinetics. |
| Activity-Based Probes (ABPs) | Covalently label active enzymes in complex proteomes for detection/identification [67] [63]. | Profiling active cathepsin B populations and target engagement studies. |
| Cellular Models (Neuronal Cultures) | Model lysosomal leakage and cytosolic cathepsin B translocation [7]. | Evaluating inhibitor efficacy in a physiologically relevant cellular environment. |
| In Vivo Models (e.g., CCI-TBI, APP/PS1 AD mice) | Recapitulate human disease pathology for therapeutic testing [31] [7]. | Assessing behavioral and neuropathological outcomes of inhibitor treatment. |
The comparative data and protocols presented herein underscore that the choice of chemotype is fundamental to defining the performance profile of a cathepsin B inhibitor. AOMK warheads currently lead in sophistication, enabling the design of pH-selective inhibitors that specifically target the pathogenic pool of cathepsin B, a strategy with immense therapeutic potential for neurological conditions [7]. Vinyl sulfones offer a robust and versatile scaffold with proven efficacy against cysteine proteases, though their application for selective cathepsin B inhibition requires further refinement [64] [65]. Natural product scaffolds like E64 provide potent inhibition but serve more as foundational tools due to their inherent lack of selectivity [7]. Future research will likely focus on integrating AI-assisted design to generate novel scaffolds and optimize the pharmacological properties of these warheads, further accelerating the translation of targeted cathepsin B inhibitors from the bench to the clinic [67] [68].
Diagram Title: Mechanism of pH-Selective Cathepsin B Inhibition in Disease
Addressing Selectivity, pH-Dependency, and Translational Challenges in Inhibition
Within the intricate landscape of cysteine cathepsins, achieving precise specificity for Cathepsin B (CatB) over other structurally similar proteases like Cathepsins S (CatS), K (CatK), and L (CatL) is a fundamental challenge in biochemical research and drug development. These enzymes share overlapping roles in lysosomal protein degradation, but their distinct and specialized functions in health and disease necessitate highly selective targeting strategies. Abnormal CatB activity is implicated in a range of pathological conditions, including cancer metastasis, neurodegenerative diseases like Alzheimer's, and rheumatoid arthritis [21] [69] [3]. Accurately distinguishing its activity from that of CatS, CatK, and CatL is therefore not merely an academic exercise but a critical prerequisite for developing effective diagnostics and therapeutics. This guide provides a comprehensive comparison of the biochemical properties of these cathepsins and details the experimental strategies—from substrate design to inhibitor use—that enable researchers to achieve the specificity required for rigorous scientific discovery.
Comparative Analysis of Cathepsin Properties
The distinct enzymatic profiles of CatB, CatS, CatK, and CatL provide the foundation for developing specific detection and inhibition protocols. A thorough understanding of their unique cleavage preferences, pH activity ranges, and sensitivity to inhibitors is essential for designing specific experiments.
Table 1: Key Biochemical and Functional Properties of Cysteine Cathepsins
| Property | Cathepsin B | Cathepsin L | Cathepsin S | Cathepsin K |
|---|---|---|---|---|
| Primary Substrate Specificity | Prefers dibasic sequences (e.g., -Arg-Arg-) [70] | Prefers bulky hydrophobic residues at P2 position [70] | Prefers residues with large aromatic side chains at P2 position [70] | Prefers Pro at P2 and Arg at P1' positions [70] |
| pH Activity Profile | Bimodal activity at both acidic (pH ~4.6) and neutral pH (pH ~7.2) [70] [3] | Optimal activity in acidic pH range (pH ~5.5-6.0) [70] | Retains significant activity at neutral pH [70] | Optimal activity in acidic pH range [70] |
| Key Distinguishing Inhibitor | CA-074 (and its cell-permeable form CA-074Me) [71] [69] | Cathepsin L Inhibitor II (Z-FY-CHO) [71] | Not specified in results | Not specified in results |
| Role in Disease | Cancer progression, Alzheimer's disease, rheumatoid arthritis, epilepsy pathogenesis [21] [69] [3] | Implicated in cancer and other diseases, but inhibition did not significantly reduce melanoma cell invasiveness in one study [71] | Implicated in cancer and other diseases, but inhibition did not significantly reduce melanoma cell invasiveness in one study [71] | Implicated in cancer and other diseases, but inhibition did not significantly reduce melanoma cell invasiveness in one study [71] |
| Notable Characteristic | Can function in extralysosomal spaces (cytosol, nuclei) due to broad pH activity [70] [3] | Compensatory networks with other cathepsins; double knockout of CatB/CatL is lethal [3] | Expressed in antigen-presenting cells; stable at neutral pH [70] | Potent elastase and collagenase activity [70] |
The data in Table 1 highlights key differentiating factors. CatB's unique ability to remain active from acidic to neutral pH allows it to function in diverse cellular compartments, a property not shared by all cathepsins [70]. Furthermore, its specific inhibition by CA-074 provides a powerful tool for functional studies, as this inhibitor did not impede the activity of CatL or CatD in melanoma cell models [71]. Genetic ablation studies further underscore its non-redundant role; for instance, removing CatB, but not CatL or CatS, partially rescued pathological apoptosis in a cystatin B-deficient mouse model of epilepsy [72].
Table 2: Selective Substrates for Differentiating Cathepsin Activity
| Substrate | Cathepsin B Activity | Cathepsin L Activity | Cathepsin S/K Activity | Application Notes |
|---|---|---|---|---|
| Z-Phe-Arg-AMC | High | High | High | A general cathepsin substrate; lacks specificity and should be used with inhibitors for distinction [70]. |
| Z-Arg-Arg-AMC | High at neutral pH, minimal at acidic pH [70] | Low | Low | Historically used as a specific substrate for CatB, but its pH-dependent activity is a major limitation [70]. |
| Z-Nle-Lys-Arg-AMC | High specific activity across acidic to neutral pH [70] | Low | Low | A novel, rationally designed substrate that allows specific monitoring of CatB activity over a broad pH range [70]. |
| Abz-Gly-Ile-Val-Arg~Ala-Lys(Dnp)-OH | High (Fluorogenic) | Not specified | Not specified | A sensitive fluorogenic substrate specific for CatB used in activity assays [71]. |
Experimental Protocols for Specific Detection
Leveraging the comparative biochemical data requires robust and reproducible experimental methodologies. The following sections outline detailed protocols for distinguishing CatB activity using substrate-based assays and selective inhibition.
Protocol 1: Differentiating Cathepsins Using Selective Substrates and pH Profiling
This protocol uses a combination of novel specific substrates and pH manipulation to accurately quantify CatB activity.
- Workflow Overview: The following diagram illustrates the key decision points and steps in the experimental workflow for differentiating cathepsin activity using substrates.
Materials & Reagents:
- Recombinant Cathepsins: Human recombinant CatB, CatL, CatS, CatK (from commercial sources like R&D Systems or Abcam) [70].
- Substrates: Z-Phe-Arg-AMC (general substrate), Z-Arg-Arg-AMC (CatB, pH-sensitive), and Z-Nle-Lys-Arg-AMC (novel specific CatB substrate). These can be custom-synthesized or purchased from suppliers like Bachem [70].
- Assay Buffers: Citrate-phosphate buffer for acidic pH (e.g., pH 4.6) and phosphate-buffered saline or HEPES for neutral pH (e.g., pH 7.2). Include EDTA (1 mM) to chelate metals and DTT (1-5 mM) to maintain a reducing environment for cysteine protease activity [70].
- Detection Instrument: A fluorometer or fluorescence plate reader capable of excitation at ~355-380 nm and detection of emission at ~460 nm for AMC liberation.
Step-by-Step Procedure:
- Prepare Reaction Mixtures: In a low-binding microtube or plate well, combine the assay buffer (for the desired pH), the cathepsin enzyme (e.g., 10-100 nM), and the substrate (e.g., 10-50 µM). Include a negative control without enzyme.
- Incubate and Monitor: Incubate the reaction mixture at 37°C and monitor the increase in fluorescence (ex/em ~380/460 nm for AMC) over time (e.g., 30-60 minutes).
- Compare Substrate Specificity: Perform the assay in parallel for all cathepsins (B, L, S, K) using the panel of substrates (Z-Phe-Arg-AMC, Z-Arg-Arg-AMC, Z-Nle-Lys-Arg-AMC).
- Profile pH Dependence: For each enzyme, repeat the activity measurement at both acidic (pH 4.6) and neutral (pH 7.2) conditions.
- Data Analysis: Calculate the initial rates of substrate hydrolysis. CatB activity will be uniquely identified by high activity with Z-Nle-Lys-Arg-AMC across both pH conditions and with Z-Arg-Arg-AMC primarily at neutral pH. Other cathepsins will show minimal cleavage of these specific substrates [70].
Protocol 2: Validating Functional Role with Selective Inhibitors
This protocol uses potent and selective chemical inhibitors to confirm the functional contribution of CatB in complex biological systems, such as cell-based models.
- Workflow Overview: The logical flow of the inhibitor-based validation protocol is shown below, from initial observation to functional confirmation.
Materials & Reagents:
- Cell Line: Relevant model, such as metastatic melanoma cell lines (e.g., MM1, LM) or rheumatoid arthritis fibroblast-like synoviocytes (RA-FLS) [71] [69].
- Selective Inhibitors:
- Phenotypic Assay Kits: Reagents for cell viability (e.g., CCK-8), migration/invasion (e.g., Transwell), or apoptosis/ferroptosis detection (e.g., lipid ROS, glutathione assays) [69].
Step-by-Step Procedure:
- Pre-treat Cells: Culture cells and pre-treat experimental groups with specific inhibitors. Typical concentrations are 10 µM for CA-074/CA-074Me and Cathepsin L Inhibitor II, and 100 µM for Pepstatin A, for a suitable period (e.g., 1-2 hours) [71]. Include a vehicle control (e.g., DMSO).
- Induce Phenotype: Subject the pre-treated cells to a relevant challenge (e.g., a phagocytic challenge with E. coli bioparticles, or a growth factor stimulus) [73].
- Measure Functional Output: Quantify the phenotypic endpoint of interest. For instance:
- Invasion/Migration: Use a Boyden chamber assay to count invading cells.
- Cell Death/Survival: Use a CCK-8 assay to measure viability.
- Ferroptosis Markers: Measure accumulation of lipid ROS and ferrous ions [69].
- Data Analysis: Compare the results across inhibitor treatments. A significant reduction in the phenotype (e.g., invasion, cell survival) specifically in the CA-074/CA-074Me groups, but not in the CatL or Pepstatin A groups, provides strong evidence for a CatB-specific mechanism [71] [69].
The Scientist's Toolkit: Essential Research Reagents
Successful execution of the aforementioned protocols relies on a curated set of high-quality reagents. The following table lists essential tools for probing Cathepsin B specificity.
Table 3: Key Research Reagents for Cathepsin B Specificity Research
| Reagent Name | Type/Category | Primary Function in Research | Key Characteristic |
|---|---|---|---|
| CA-074 / CA-074Me [71] [69] | Irreversible Chemical Inhibitor | Selectively inhibits Cathepsin B activity; CA-074Me is cell-permeable. Used to confirm CatB's functional role in cellular and animal models. | Gold-standard for functional distinction; shown to reduce metastasis and induce ferroptosis in RA-FLS. |
| Z-Nle-Lys-Arg-AMC [70] | Fluorogenic Peptide Substrate | Monitors Cathepsin B enzymatic activity with high specificity across a broad pH range (acidic to neutral). | Rationally designed to overcome the pH-limitations of older substrates like Z-Arg-Arg-AMC. |
| GB111-NH₂ / YBN14 [74] | Activity-Based Probe (ABP) / Theranostic Probe | Covalently binds to active Cathepsins (B, L, S). Allows detection, imaging, and (in the case of YBN14) photodynamic therapy. | Provides a direct readout of active enzyme populations, not just protein abundance. |
| Lurasidone / Paliperidone [21] | Repurposed Drug Candidate (Predicted) | Identified via virtual screening as potential CatB inhibitors. Candidates for anti-Alzheimer's and anticancer drug development. | Example of how computational screening can identify novel, potent, and drug-like CatB inhibitors. |
Distinguishing Cathepsin B from the related cathepsins S, K, and L is a multi-faceted problem that can be effectively addressed by a strategic combination of tools. Researchers can achieve high specificity by leveraging the unique bimodal pH activity of CatB, employing novel substrates like Z-Nle-Lys-Arg-AMC that perform reliably across pH ranges, and using the potent and selective inhibitor CA-074/CA-074Me for functional validation in complex models. The integration of these well-defined biochemical properties with robust experimental protocols provides a clear roadmap for scientists to accurately attribute observed proteolytic and phenotypic effects to Cathepsin B, thereby enhancing the validity and impact of their research in disease mechanisms and therapeutic development.
The cysteine protease cathepsin B has emerged as a significant target in the pathophysiology of brain disorders such as traumatic brain injury (TBI) and Alzheimer's disease (AD). Under normal physiological conditions, cathepsin B is confined to the acidic environment of lysosomes (pH ~4.6), where it contributes to protein catabolism and cellular homeostasis. However, in pathological states, lysosomal membrane permeabilization enables the translocation of cathepsin B to the neutral-pH cytosol (pH ~7.2), where it initiates cell death and inflammation pathways [75] [76]. This subcellular relocation presents a unique therapeutic opportunity: the development of pH-selective inhibitors that specifically target the pathogenic cytosolic pool of cathepsin B while sparing its normal lysosomal function, thereby minimizing potential side effects and enhancing therapeutic efficacy.
The design of such pH-selective probes represents an innovative approach in drug discovery that considers the biological pH environment of the target in the disease process. Traditional screening methods conducted at optimal enzyme pH conditions fail to distinguish between enzymes in their physiological versus pathological compartments. By developing inhibitors selective for cathepsin B at cytosolic pH, researchers can achieve precise targeting of the disease-relevant enzyme pool. This review comprehensively compares current pH-selective inhibition strategies, experimental methodologies for evaluating inhibitor efficacy, and the therapeutic potential of these approaches in relevant disease models.
Pathophysiological Context: Cytosolic Cathepsin B in Disease
Evidence from Traumatic Brain Injury Models
Research using the controlled cortical impact (CCI) mouse model of TBI has demonstrated that brain injury increases cytosolic cathepsin B activity in the cerebral cortex of the ipsilateral hemisphere, with a concomitant decrease in the lysosomal fraction [75]. Cellular imaging reveals a shift from the normal discrete lysosomal distribution of cathepsin B to a diffuse cytosolic pattern following CCI-TBI. These molecular changes correlate with functional deficits, as CCI-TBI results in significant motor impairment measured by rotarod performance and causes visible brain tissue lesions and hippocampal disorganization [75]. The causal role of cathepsin B in these deficits is supported by evidence that cathepsin B gene knockout ameliorates TBI-induced motor dysfunction in mouse models [75].
Connections to Neurodegenerative Diseases
Beyond TBI, cathepsin B dysregulation has been implicated in Alzheimer's disease pathology, with elevated levels observed in AD patients that correlate with cognitive deficits [75]. Interestingly, while cytosolic cathepsin B appears to drive pathology in these conditions, recent research has revealed that enhancing lysosomal cathepsin B function may have therapeutic benefits in other protein aggregation disorders. For example, treatment with recombinant cathepsin B promotes α-synuclein clearance and restores lysosomal function in models of Parkinson's disease [30]. This dichotomy underscores the importance of subcellular localization and context in determining cathepsin B's role in health and disease.
Table 1: Dual Roles of Cathepsin B in Brain Disorders
| Condition | Pathogenic Role of Cytosolic Cathepsin B | Potential Therapeutic Role of Lysosomal Cathepsin B |
|---|---|---|
| Traumatic Brain Injury | Increased cytosolic activity correlates with motor deficits and tissue damage [75] | Not demonstrated |
| Alzheimer's Disease | Elevated levels correlate with cognitive deficits; inhibition reduces pathology [75] | Not demonstrated |
| Parkinson's Disease | Not reported | Recombinant cathepsin B enhances α-synuclein clearance [30] |
pH-Selective Inhibition Strategies and Experimental Assessment
Rational Design of pH-Selective Inhibitors
The substantial pH difference between lysosomes (pH 4.6) and cytosol (pH 7.2) enables the development of environment-sensitive inhibitors. The design strategy for pH-selective cathepsin B inhibitors leverages the pH-dependent substrate preferences of the enzyme, which were identified through cleavage profiling analysis using diverse peptide substrates [76]. This approach led to the development of Z-Arg-Lys-AMC as a neutral-pH-selective substrate and Z-Glu-Lys-AMC as an acid-pH-selective substrate for monitoring cathepsin B activity under different pH conditions [76].
The most promising inhibitor emerging from this rational design approach is Z-Arg-Lys-AOMK, a compound that specifically inhibits cathepsin B at neutral pH (7.2) with nanomolar potency while showing no significant inhibition at acidic pH (4.6) at similar concentrations [75] [76]. This remarkable pH selectivity enables precise targeting of cathepsin B that has translocated to the cytosol in pathological conditions while sparing the enzyme remaining in lysosomes, thus preserving normal cellular functions dependent on lysosomal cathepsin B.
Natural Product-Derived Inhibitors with pH Selectivity
Screening of marine and plant natural product libraries at both acidic and neutral pH conditions has identified additional compounds with pH-dependent inhibition profiles. Unlike Z-Arg-Lys-AOMK, which selectively inhibits at neutral pH, natural products such as GER-12 (Crossbyanol B) and GER-24 ((7Z,9Z,12Z)-octadeca-7,9,12-trien-5-ynoic acid) preferentially inhibit cathepsin B at acidic pH (4.6) with IC50 values of 3 μM and 16 μM, respectively [76]. GER-12 acts as a reversible inhibitor, while GER-24 functions through an irreversible mechanism [76].
Table 2: Characteristics of pH-Selective Cathepsin B Inhibitors
| Inhibitor | Selectivity Profile | IC50 Value | Mechanism of Action | Source |
|---|---|---|---|---|
| Z-Arg-Lys-AOMK | Neutral pH (7.2) selective | Nanomolar range | Covalent inhibition | Synthetic peptide [75] [76] |
| GER-12 (Crossbyanol B) | Acidic pH (4.6) selective | 3 μM | Reversible inhibition | Marine natural product [76] |
| GER-24 | Acidic pH (4.6) selective | 16 μM | Irreversible inhibition | Marine natural product [76] |
Experimental Models and Assessment Methodologies
In Vitro Screening Approaches
The identification and validation of pH-selective cathepsin B inhibitors rely on carefully designed in vitro screening protocols. These assays typically involve pre-incubating the test compound with cathepsin B at both pH 4.6 and 7.2 for a standardized period (e.g., 30 minutes), followed by addition of pH-selective substrates to monitor proteolytic activity [76]. The use of pH-selective substrates is crucial for accurate assessment, with Z-Arg-Lys-AMC employed for neutral pH conditions and Z-Glu-Lys-AMC for acidic pH conditions [76].
Initial screening identifies compounds showing at least 50% inhibition at one pH but not the other, which are then advanced to concentration-response studies to determine IC50 values. Further characterization includes assessing the reversibility of inhibition through dialysis experiments and evaluating specificity by testing against other cysteine cathepsins [76].
Cellular and Animal Models of Disease
The therapeutic potential of pH-selective cathepsin B inhibitors has been evaluated in several disease models:
Controlled Cortical Impact TBI Model: Daily administration of Z-Arg-Lys-AOMK beginning one day before CCI-TBI injury significantly reduced increased cytosolic cathepsin B activity and ameliorated motor function deficits in the rotarod assay [75]. This model demonstrates the functional benefits of selectively inhibiting cytosolic cathepsin B.
Alzheimer's Disease Models: While not yet tested with pH-selective inhibitors, cathepsin B gene knockout reduces memory loss and decreases amyloid-β in AD mouse models [75], suggesting potential utility for pH-selective inhibitors in this context.
Parkinson's Disease Models: Treatment with recombinant procathepsin B enhances α-synuclein clearance and restores lysosomal function in human and murine models with α-synuclein pathology [30], highlighting the therapeutic potential of modulating cathepsin B activity in protein aggregation disorders.
Diagram 1: pH-selective inhibition strategy for pathogenic cytosolic cathepsin B. Under pathological conditions, cathepsin B translocates from lysosomes to the cytosol. Neutral-pH selective inhibitors (Z-Arg-Lys-AOMK) specifically target the pathogenic cytosolic pool, while acidic-pH selective inhibitors (GER-12/GER-24) target lysosomal cathepsin B.
Research Reagent Solutions for Lysosomal and Cathepsin B Studies
Table 3: Essential Research Reagents for Lysosomal Function and Cathepsin B Studies
| Reagent Category | Specific Products/Assays | Research Application |
|---|---|---|
| Lysosomal pH Detection | Lysosomal Acidic pH Detection Kit (pHLys Green/Red with LysoPrime) [77] | Simultaneous measurement of lysosomal pH and mass |
| Lysosomal Tracking Probes | LysoTracker dyes (Various colors), CellLight Lysosomes-GFP/RFP [78] | Live-cell imaging of lysosomes and acidic compartments |
| Cathepsin B Activity Assays | Z-Nle-Lys-Arg-AMC, Z-Arg-Lys-AMC (pH 7.2), Z-Glu-Lys-AMC (pH 4.6) [75] [76] | Selective detection of cathepsin B activity at different pH values |
| Lysosomal Ion Detection | MQAE-MP chloride ion-selective probe [79] | Measurement of lysosomal chloride concentrations |
| Autophagy/Mitophagy Assays | Autophagic Flux Assay Kit, Mitophagy Detection Kit [77] | Monitoring autophagy-related processes |
| Cellular Viability Assays | Cell Counting Kit-8, Cytotoxicity LDH Assay [77] | Assessment of cell health and compound toxicity |
Diagram 2: Experimental workflow for developing pH-selective cathepsin B inhibitors. The process begins with sample preparation and progresses through primary screening, hit confirmation, cellular validation, and functional assessment in disease models.
The development of pH-selective inhibitors represents a sophisticated approach to targeting subcellularly localized enzyme pools in disease. For cathepsin B, the neutral pH-selective inhibitor Z-Arg-Lys-AOMK has demonstrated significant efficacy in reducing cytosolic cathepsin B activity and improving functional outcomes in TBI models [75]. This strategy offers the potential for enhanced therapeutic specificity by selectively targeting the pathogenic pool of the enzyme while preserving its physiological functions in lysosomes.
Future directions in this field should include the optimization of inhibitor pharmacokinetics and brain penetration for neurological applications, exploration of combination therapies with other protease modulators, and expansion of the pH-selectivity concept to other targets involved in lysosomal membrane permeabilization and cellular stress responses. The continued development and refinement of research tools for monitoring lysosomal function, subcellular enzyme localization, and pH-dependent activity will be crucial for advancing this promising therapeutic strategy.
The lysosomal cysteine protease Cathepsin B (CTSB) is a key player in both cellular homeostasis and cancer pathology, where its dysregulation contributes significantly to tumor aggressiveness. CTSB is synthesized as a preproenzyme in the endoplasmic reticulum and matures through several steps into a 31 kDa active form, functioning as both an exopeptidase in acidic lysosomes and an endopeptidase in neutral environments. Its activity supports critical processes including autophagy, apoptosis, and extracellular matrix (ECM) remodeling. In cancer, however, excessive CTSB expression promotes invasion and metastasis by degrading ECM components like collagen IV and laminin, activating oncogenic pathways such as MMP-9 and NF-κB, and facilitating immune evasion. This enzymatic activity is meticulously regulated by endogenous inhibitors, most notably Stefin A (STFA), which belongs to the cytosolic cystatin superfamily and inhibits papain-like cysteine proteases through a tripartite wedge mechanism.
The balance between CTSB and its endogenous inhibitor STFA represents a critical regulatory node in cancer progression. Recent investigations have revealed a complex feedback relationship between this protease and its inhibitor that extends beyond simple enzymatic inhibition. In renal cell carcinoma (RCC), the most common form of kidney cancer, CTSB shows notable upregulation that correlates with advanced tumor stages, metastasis, and poor prognosis. Understanding the precise nature of the CTSB-STFA regulatory interplay is essential for developing effective therapeutic strategies that can overcome inherent compensatory mechanisms in cancer cells. This guide provides a comprehensive comparison of current experimental models and approaches for investigating this dynamic relationship, with particular focus on their implications for therapeutic inhibition strategies.
Comparative Analysis of CTSB Inhibition Models
Performance Comparison of CTSB-Targeting Approaches
Table 1: Comparison of major CTSB inhibition strategies and their effects on STFA regulation
| Inhibition Model | Mechanism of Action | Effects on CTSB Activity | Effects on STFA Expression | Compensatory Cellular Responses | Therapeutic Potential |
|---|---|---|---|---|---|
| STFA Overexpression (Genetic) | Increases endogenous inhibitor levels | Significant reduction in activity [80] | Directly increased via plasmid transfection [80] | Alters CTSB subcellular distribution; reduces nuclear CTSB [80] | High for targeted intervention |
| STFA Silencing (Genetic) | Reduces endogenous inhibition | Significant increase in cancer cells [80] | Directly decreased via shRNA [80] | Increases CTSB protein levels 3-fold in cancer cells [80] | Research tool only |
| Small-Molecule Inhibitors (CA074) | Directly binds and inhibits CTSB enzymatic site | Significant reduction in pericellular proteolysis [81] | Not documented in results | Disrupts caveolae-associated proteolysis without compensatory STFA changes [81] | Established experimental inhibitor |
| Cathepsin-B Responsive Nanoparticles | Enzyme-activated drug release | Exploits elevated CTSB for targeted release [82] | Not applicable | Enhanced cellular uptake at acidic pH where CTSB is active [82] | Promising for targeted therapy |
Quantitative Analysis of CTSB-STFA Interplay Across Cell Models
Table 2: Experimental data from modulation studies across different cell lines
| Cell Line | Experimental Condition | CTSB mRNA Change | CTSB Protein Change | CTSB Activity | Viability Impact | Nuclear CTSB Localization |
|---|---|---|---|---|---|---|
| Hek293T (Embryonic Kidney) | STFA Overexpression | Slight decrease [80] | Significant decrease [80] | Reduced [80] | Not significant [80] | Decreased [80] |
| Hek293T (Embryonic Kidney) | STFA Silencing | Decreased [80] | Comparable to control [80] | No change [80] | Statistically significant decrease [80] | Similar to control [80] |
| 769P (Renal Cancer) | STFA Overexpression | Slight decrease [80] | Significant decrease [80] | Reduced [80] | Not significant [80] | Decreased [80] |
| 769P (Renal Cancer) | STFA Silencing | >15-fold increase [80] | 3-fold increase [80] | Significant increase [80] | Increased [80] | Cytoplasmic accumulation [80] |
| Du145 (Prostate Cancer) | STFA Overexpression | Slight decrease [80] | Significant decrease [80] | Reduced [80] | Not significant [80] | Decreased [80] |
| Du145 (Prostate Cancer) | STFA Silencing | >4-fold increase [80] | 3-fold increase [80] | Significant increase [80] | Increased [80] | Cytoplasmic accumulation [80] |
| SUM149 (IBC) | CA074 Inhibition | Not measured | Not significantly changed | Significant reduction [81] | Reduced invasiveness [81] | Disrupted pericellular localization [81] |
Experimental Models and Methodologies
Genetic Manipulation Protocols
The foundational methodology for investigating CTSB-STFA interplay involves genetic manipulation of expression levels in various cell models. The standard protocol utilizes plasmid-based overexpression and silencing systems (pSTFA and pShSTFA respectively), with experiments typically conducted 48 hours post-transfection to allow for full protein turnover and system equilibration. For overexpression studies, researchers employ a plasmid vector carrying the STFA cDNA sequence (pSTFA), while silencing approaches use shRNA constructs specifically targeting STFA expression (pShSTFA). Transfection efficiency is validated through simultaneous measurement of STFA mRNA and protein levels, with successful transfections typically showing 13-100 fold increases in mRNA and 3-4 fold increases in protein for overexpression, and 10-20 fold decreases in mRNA with significant protein reduction for silencing approaches.
Cell viability assessments are conducted in parallel using standard assays (e.g., MTT, WST-1) to distinguish specific regulatory effects from general toxicity. The critical methodological consideration is the differential response observed between cancerous (769P, Du145) and non-cancerous (Hek293T, EA.hy926) cell lines, which must be analyzed separately to identify cancer-specific mechanisms. Subcellular fractionation followed by Western blotting or immunofluorescence is essential for evaluating compartment-specific redistribution of both CTSB and STFA following genetic manipulation.
Activity and Localization Assessment Methods
The functional assessment of the CTSB-STFA relationship requires integrated methodological approaches that evaluate both enzymatic activity and spatial distribution. CTSB activity is typically measured using fluorogenic substrates specific for cysteine cathepsins, with activity normalized to total cellular protein. For localization studies, researchers employ confocal microscopy with specific antibodies against CTSB and STFA, followed by quantitative colocalization analysis using Pearson's correlation coefficient or similar metrics.
Advanced methodologies include the use of live-cell proteolysis assays to evaluate pericellular degradation of matrix components like type IV collagen, which is particularly relevant for understanding invasion mechanisms. Fractionation techniques isolating caveolae-enriched membrane domains have proven valuable, as CTSB localization to these microdomains is functionally significant for invasion. These specialized fractions can be obtained through both non-detergent (sodium carbonate-based) and detergent-based (Triton X-100) protocols followed by sucrose density gradient ultracentrifugation.
CTSB-STFA Regulatory Network: This diagram illustrates the core feedback regulation between Cathepsin B and its inhibitor Stefin A, highlighting the opposing effects of STFA manipulation on CTSB function and localization.
Research Reagent Solutions Toolkit
Table 3: Essential research reagents for investigating CTSB-STFA biology
| Reagent Category | Specific Examples | Research Application | Key Features |
|---|---|---|---|
| Expression Plasmids | pSTFA (overexpression), pShSTFA (silencing) [80] | Genetic manipulation of STFA levels | High efficiency (100-fold increase in 769p cells); validated shRNA |
| Cell Lines | 769P (renal cancer), Du145 (prostate cancer), Hek293T (embryonic kidney) [80] | Comparative studies across malignant/non-malignant contexts | Differential responses highlight cancer-specific mechanisms |
| Activity Assays | Fluorogenic substrates (e.g., Z-Arg-Arg-AMC) | Quantification of CTSB enzymatic activity | Sensitive detection of functional changes beyond expression |
| Small Molecule Inhibitors | CA074 (cell-impermeable) [81] | Selective inhibition of extracellular CTSB | Highly selective cathepsin B inhibitor; reduces invasion |
| Localization Tools | Anti-CTSB/Caveolin-1 antibodies [81] | Subcellular localization studies | Identifies caveolae-associated proteolytic complexes |
| Proteolysis Assays | Type IV collagen degradation assays [81] | Functional assessment of ECM degradation | Measures pericellular proteolysis relevant to invasion |
Experimental Workflow for CTSB-STFA Studies
CTSB-STFA Research Workflow: This experimental pathway outlines the key methodological stages for comprehensive investigation of the protease-inhibitor relationship, from initial genetic manipulation to integrated data analysis.
Implications for Therapeutic Development
The comparative analysis of CTSB inhibition models reveals critical considerations for therapeutic development. The differential response between cancerous and non-cancerous cells to STFA manipulation suggests cancer-specific vulnerabilities that could be exploited therapeutically. Notably, STFA silencing increases viability in cancer cells while decreasing it in embryonic cells, indicating a fundamental difference in how cancer cells utilize the CTSB-STFA axis. The discovery that STFA not only inhibits CTSB activity but also regulates its expression and subcellular distribution reveals multiple regulatory layers that must be considered when designing intervention strategies.
The most promising therapeutic approaches appear to be those that either mimic STFA's multifaceted inhibition (simultaneously targeting activity, expression, and localization) or exploit elevated CTSB levels for targeted drug delivery, as demonstrated by cathepsin B-responsive nanoparticles. However, the compensatory increase in CTSB expression following STFA silencing in cancer cells highlights a significant challenge: single-dimensional approaches may trigger adaptive resistance mechanisms. Successful therapeutic strategies will likely require combination approaches that simultaneously target multiple aspects of the CTSB-STFA regulatory network to prevent compensatory escape mechanisms and achieve sustained pathway suppression.
The blood-brain barrier (BBB) represents one of the most selective and formidable physiological barriers in the human body, serving as a sophisticated interface between the central nervous system (CNS) and the circulatory system. This highly specialized structure functions as a protective membrane that effectively isolates the brain from potentially harmful substances in the bloodstream while simultaneously maintaining the delicate homeostasis required for optimal neural function [83]. From a clinical perspective, the BBB's exceptional selectivity presents a major obstacle for neurological therapeutics, as it excludes over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from entering the brain [83] [84]. This profound limitation significantly complicates the treatment of a wide spectrum of neurological disorders, including Alzheimer's disease (AD), Parkinson's disease, and other neurodegenerative conditions where targeted drug delivery to the brain is essential for therapeutic efficacy.
The BBB's core anatomical structure consists of cerebral microvascular endothelial cells interconnected by intricate tight junctions that drastically limit paracellular transport [83] [84]. These specialized endothelial cells differ markedly from their peripheral counterparts, exhibiting no fenestrations, minimal transcellular vesicular transport, and an abundance of energy-producing mitochondria to support active transport mechanisms [83]. This cellular barrier is further reinforced through dynamic interactions with surrounding pericytes, astrocytes, and the basement membrane, collectively forming a neurovascular unit that precisely regulates molecular exchange between blood and brain tissue [85] [83] [84]. Understanding the fundamental biology of this sophisticated barrier system provides the essential foundation for developing innovative strategies to overcome its formidable resistance to therapeutic intervention.
Physiological Structure and Function of the BBB
Core Cellular Components
The BBB's remarkable barrier properties emerge from the coordinated functions of multiple specialized cell types that collectively constitute the neurovascular unit. Brain microvascular endothelial cells form the primary physical barrier, lining cerebral blood vessels and connecting through extensive tight junctions that eliminate ordinary paracellular pathways for substance exchange [83] [84]. These endothelial cells display a characteristic net negative surface charge that further restricts negatively charged compounds and exhibit markedly reduced expression of leukocyte adhesion molecules, thereby limiting immune cell infiltration into the CNS under physiological conditions [83].
Pericytes, embedded within the basement membrane and positioned abluminally to endothelial cells, play a pivotal role in BBB development, maintenance, and regulation [83]. These mural cells cover nearly 100% of the CNS endothelium and communicate intimately with endothelial cells through direct physical contact and paracrine signaling [83]. The PDGF-B signaling pathway represents one crucial communication mechanism, whereby endothelial cell-derived PDGF-B binds to PDGFRβ receptors on pericytes, facilitating pericyte recruitment to developing vessels [83]. Reductions in pericyte coverage directly correlate with increased BBB permeability through diminished tight junction integrity [83].
Astrocytes, the most abundant glial cells in the CNS, extend specialized end-feet processes that envelop approximately 99% of the brain's capillary surface area [83] [84]. Through the release of various growth factors and signaling molecules, astrocytes promote endothelial cell differentiation, enhance tight junction stability, and help maintain the barrier's selective permeability properties [83] [84]. The basement membrane, composed primarily of collagen, laminin, and other extracellular matrix proteins, provides structural support for the endothelial cells and pericytes while serving as a critical interface for cell-matrix signaling interactions that regulate barrier function [85] [84].
Functional Transport Mechanisms
The BBB maintains CNS homeostasis through sophisticated transport mechanisms that selectively permit the passage of essential nutrients while excluding potentially harmful substances. The principal transport pathways across the BBB include:
- Paracellular diffusion: Tightly restricted by tight junction complexes, allowing only very small, hydrophilic molecules under limited circumstances [83] [84].
- Transcellular passive diffusion: The primary pathway for small (<400-600 Da), lipid-soluble molecules with favorable lipophilicity (LogP>2) and limited hydrogen bonding capacity (<6 bonds) [83] [84].
- Carrier-mediated transcytosis (CMT): Utilizes specific transporter proteins (e.g., GLUT1 for glucose, LAT1 for large neutral amino acids) to facilitate the uptake of essential nutrients and structurally similar drug analogs [84].
- Receptor-mediated transcytosis (RMT): Enables selective uptake of specific macromolecules through vesicular trafficking initiated by ligand-receptor binding (e.g., transferrin receptor, insulin receptor) [86] [84].
- Adsorptive-mediated transcytosis (AMT): A non-specific charge-based mechanism triggered by electrostatic interactions between cationic molecules and the negatively charged endothelial cell surface [86] [84].
- Cell-mediated transcytosis: Involves the migration of certain cells (e.g., leukocytes) across the BBB, potentially carrying therapeutic cargo [83] [84].
Additionally, ATP-binding cassette (ABC) transporters such as P-glycoprotein (P-gp) actively efflux many foreign compounds back into the bloodstream, further limiting brain penetration of therapeutic agents [83] [84].
Table 1: Primary Transport Mechanisms at the Blood-Brain Barrier
| Mechanism | Key Features | Substrate Characteristics | Examples |
|---|---|---|---|
| Passive Transcellular Diffusion | Concentration gradient driven; non-saturable | Small size (<500 Da), lipophilic (LogP>2), limited H-bond donors (<6) | Alcohol, steroid hormones, dexamethasone |
| Carrier-Mediated Transcytosis (CMT) | Utilizes specific nutrient transporters; saturable | Structural similarity to endogenous substrates | Glucose (via GLUT1), L-DOPA (via LAT1) |
| Receptor-Mediated Transcytosis (RMT) | Ligand-receptor binding initiates vesicular transport | Macromolecules with specific receptor ligands | Insulin, transferrin, lipoproteins |
| Adsorptive-Mediated Transcytosis (AMT) | Electrostatic interactions with cell surface | Cationic charges | Cationized albumin, cell-penetrating peptides |
| Active Efflux Transport | ATP-dependent export against concentration gradient | Diverse substrates recognized by efflux pumps | Many chemotherapeutic agents, antibiotics |
BBB Penetration Strategies for CNS-Targeted Therapeutics
Physicochemical Optimization and Passive Diffusion
Enhancing passive diffusion through strategic molecular modification represents a fundamental approach to improving BBB penetration. Compounds with molecular weights below 500 Da, moderate lipophilicity (LogP 2-5), reduced hydrogen bonding capacity (<6-8 bonds), and polar surface areas below 60-70 Ų generally demonstrate superior passive diffusion across the BBB [83] [84]. Structural modification to increase lipophilicity has proven successful for some therapeutics, as exemplified by Crizotinib derivatives where fluorination enhanced brain penetration while maintaining target activity [83]. However, this strategy must be carefully balanced against potential increases in plasma protein binding, non-specific tissue distribution, and metabolic clearance, which can ultimately reduce brain exposure despite improved permeability [83].
Active Targeting Strategies
Active targeting approaches leverage the BBB's endogenous transport systems to facilitate therapeutic entry into the CNS. Receptor-mediated transcytosis (RMT) has emerged as a particularly promising strategy, employing ligands that bind to receptors abundantly expressed on brain endothelial cells. Nanoparticles functionalized with transferrin, lactoferrin, insulin, or lipoprotein receptor ligands have demonstrated significantly enhanced brain uptake through this mechanism [86] [83]. Similarly, adsorptive-mediated transcytosis (AMT) utilizes cationic molecules (e.g., cell-penetrating peptides, cationized proteins) that interact electrostatically with the negatively charged endothelial cell surface, inducing vesicular uptake and transcellular transport [86] [84]. While generally less specific than RMT, AMT offers higher capacity and can accommodate diverse cargoes.
Table 2: Comparison of Blood-Brain Barrier Penetration Strategies
| Strategy | Mechanism | Advantages | Limitations | Therapeutic Examples |
|---|---|---|---|---|
| Physicochemical Optimization | Enhanced passive diffusion through increased lipophilicity | Simple implementation, maintains small molecule properties | Increased off-target distribution, potential metabolic instability | Crizotinib derivatives [83] |
| Receptor-Mediated Transcytosis | Ligand-receptor binding initiates vesicular transport | High specificity, suitable for large molecules | Potential receptor competition, limited carrying capacity | Transferrin receptor-targeted nanoparticles [86] [83] |
| Adsorptive-Mediated Transcytosis | Electrostatic interactions with anionic cell surface | High capacity, versatile cargo compatibility | Reduced specificity, potential cytotoxicity | Cationized albumin, cell-penetrating peptides [86] [84] |
| Nanoparticle Carriers | Multiple mechanisms depending on surface properties | Protection of cargo, tunable properties, multifunctionality | Complexity of manufacture, potential long-term toxicity concerns | Liposomes, polymeric nanoparticles [85] [86] |
| BBB Disruption | Temporary opening of tight junctions | Enables broad-spectrum drug entry | Risk of neurotoxicity, limited temporal control | Focused ultrasound with microbubbles [85] |
Nanoparticle-Based Delivery Systems
Nanoparticle (NP) technologies represent a versatile platform for overcoming BBB limitations, offering customizable size, surface properties, and functionalization options to enhance brain delivery. Lipid-based NPs, including liposomes and solid lipid nanoparticles, provide biocompatible carriers capable of encapsulating both hydrophilic and hydrophobic therapeutics [86] [84]. Polymeric nanoparticles, particularly those fabricated from biodegradable materials like polylactic acid (PLA) and poly(lactic-co-glycolic acid) (PLGA), enable sustained release kinetics and surface modification with targeting ligands [85] [86]. Inorganic nanoparticles (e.g., gold, silica, magnetic particles) offer unique properties for theragnostic applications but require careful evaluation of long-term safety profiles [83].
Strategic surface modification through PEGylation prolongs systemic circulation time by reducing opsonization and reticuloendothelial clearance, while conjugation of targeting ligands (e.g., antibodies, peptides, aptamers) enhances BBB-specific interactions and transport [86] [83]. The optimal nanoparticle characteristics—including size (typically <100 nm for effective penetration), surface charge (slightly cationic for AMT), and ligand density—must be carefully balanced to maximize brain delivery efficiency while minimizing off-target accumulation and potential toxicity [86].
Cathepsin B as a Therapeutic Target in Neurological Disorders
Pathophysiological Role of Cathepsin B in Neurodegeneration
Cathepsin B (CTSB), a lysosomal cysteine protease belonging to the papain family, has emerged as a significant therapeutic target for multiple neurological disorders, particularly Alzheimer's disease (AD) and various lysosomal storage diseases (LSDs) [23] [87]. Under physiological conditions, CTSB participates in intracellular protein degradation and autophagy regulation, but pathologically elevated levels and aberrant subcellular localization contribute to disease progression through several mechanisms. In Alzheimer's disease, CTSB catalyzes the proteolytic degradation of amyloid precursor protein (APP), promoting the formation and accumulation of amyloid-β (Aβ) aggregates and plaques that represent pathological hallmarks of the disease [23].
Recent studies have demonstrated that CTSB levels are elevated 3- to 5-fold in the cortices of mouse models of neurological LSDs, including mucopolysaccharidoses and sialidosis, with similar elevations observed in human patient cortical samples [87]. Crucially, CTSB exhibits abnormal cytoplasmic localization in pyramidal neurons of cortical layers IV-V, indicating lysosomal leakage and suggesting a mechanism for its aberrant interaction with APP and other substrates [87]. This pathological redistribution coincides with the accumulation of thioflavin-S+, β-amyloid+ aggregates, establishing a direct link between CTSB dysregulation and amyloidogenesis in neurological disorders [87].
Therapeutic Inhibition of Cathepsin B
Targeted inhibition of CTSB represents a promising therapeutic strategy for mitigating amyloidogenesis in neurological disorders. Both genetic and pharmacological approaches have demonstrated efficacy in preclinical models. Genetic inactivation of CTSB in mucopolysaccharidosis (MPS IIIC) mouse models completely abolishes accumulation of β-amyloid aggregates in pyramidal cortical neurons [87]. Similarly, chronic treatment with the irreversible brain-penetrable CTSB inhibitor E64 produces comparable effects in both MPS IIIC and sialidosis mice, significantly reducing neuronal thioflavin-S+/APP+ deposits and restoring autophagy function [87]. These interventions not only ameliorate pathological hallmarks but also rescue behavioral abnormalities, including hyperactivity and reduced anxiety, in MPS IIIC mouse models [87].
Structure-based drug design approaches have identified novel chemotypes with potent CTSB inhibitory activity. Mixed-feature ligand-based virtual screening has yielded compounds featuring pyridine, acetamide, and benzohydrazide scaffolds that demonstrate important interactions with key residues in the CTSB active site, including Gln23, Cys29, His110, His111, Glu122, His199, and Trp221 [23]. These inhibitors effectively block the proteolytic activity of CTSB, thereby reducing amyloidogenic processing of APP and potentially slowing disease progression in AD and related disorders [23].
Table 3: Experimental Models for Cathepsin B Inhibition Studies
| Model System | Experimental Approach | Key Findings | Reference |
|---|---|---|---|
| MPS IIIC Mouse Model (HgsnatP304L) | Genetic CTSB inactivation (HgsnatP304L/Ctsb−/−) | Complete abolition of β-amyloid aggregate accumulation in cortical neurons | [87] |
| MPS IIIC & Sialidosis Mouse Models | Pharmacological inhibition with E64 (brain-penetrable CTSB inhibitor) | Drastic reduction in neuronal thioflavin-S+/APP+ deposits; restored autophagy | [87] |
| In Silico Screening & Biochemical Assays | Mixed-feature ligand-based virtual screening of Maybridge database | Identification of pyridine, acetamide, and benzohydrazide compounds as potent CTSB inhibitors | [23] |
| Alzheimer's Disease Models | Molecular docking, pharmacophore mapping, and molecular dynamics | Compounds interact with key active site residues (Gln23, Cys29, His110, His111, His199) | [23] |
Experimental Protocols for Evaluating BBB Penetration and Target Engagement
Virtual Screening Protocol for Cathepsin B Inhibitors
The identification of novel cathepsin B inhibitors through computational approaches involves a multi-step workflow that integrates pharmacophore modeling, molecular docking, and molecular dynamics simulations [23]. The protocol begins with the generation of a mixed-feature, ligand-based three-dimensional pharmacophore hypothesis using known CTSB inhibitors as training sets. Critical chemical features including hydrophobic (HY), hydrogen bond acceptor (HBA), and hydrogen bond donor (HBD) properties are mapped to create a validated pharmacophore model (e.g., Hypo III) [23]. This model subsequently screens chemical databases such as the Maybridge library (~61,000 compounds) to identify potential hits with complementary feature alignment.
Promising candidates undergo molecular docking against the crystal structure of cathepsin B (PDB ID: 1CSB) using AutoDock tools with a Lamarckian genetic algorithm [23]. Docking parameters typically include 20 different runs terminating after a maximum of 2,500,000 energy evaluations or 27,000 generations, with a population size of 150. Cluster analysis groups docking solutions with atomic root-mean-square deviations (RMSDs) within 2.0 Å, ranked by their lowest energy conformations [23]. Final prioritization incorporates binding free energy calculations using MM-PBSA and MM-GBSA methodologies, followed by molecular dynamics simulations over 20-ns timeframes to evaluate complex stability and interaction persistence [23].
In Vivo Validation of BBB-Penetrant Cathepsin B Inhibitors
In vivo validation of brain-penetrant CTSB inhibitors employs well-characterized animal models of neurological disorders, particularly murine models of mucopolysaccharidosis and sialidosis [87]. The experimental protocol typically involves chronic administration of the candidate inhibitor (e.g., E64) to diseased mice at the age corresponding to advanced pathology stages (e.g., 6 months for MPS IIIC models, 4 months for sialidosis) [87]. Treatment efficacy is evaluated through multiple endpoints, including quantification of neuronal amyloid aggregates via immunohistochemistry using antibodies against β-amyloid and thioflavin-S staining, assessment of lysosomal integrity through LAMP-1 co-localization studies, and measurement of autophagy markers (P62, LC3) [87].
Behavioral phenotyping using standardized tests for hyperactivity, anxiety-like behaviors, and cognitive function provides functional correlates to pathological improvements [87]. Post-mortem biochemical analyses include immunoblotting to measure levels of mature CTSB and its activity using fluorogenic substrates (e.g., Z-Arg-Arg-AMC), providing direct evidence of target engagement and enzymatic inhibition [87]. This comprehensive approach validates both BBB penetration and therapeutic efficacy of CTSB inhibitors in relevant disease models.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Advancing research in BBB penetration and cathepsin B inhibition requires specialized reagents and methodologies carefully selected for their specific applications. The following toolkit summarizes critical resources for investigators in this field:
Table 4: Essential Research Reagents and Resources
| Reagent/Resource | Specifications | Research Application | Key Features |
|---|---|---|---|
| Cathepsin B Protein | Human recombinant, active form (25 kDa mature enzyme) | Enzymatic inhibition assays, binding studies | High purity, confirmed activity with fluorogenic substrates [23] |
| CTSB Fluorogenic Substrate | Z-Arg-Arg-AMC | Enzymatic activity measurements in tissue homogenates | Specific cleavage by CTSB, sensitive detection [87] |
| Cathepsin B Antibodies | Specific for mature (25 kDa) and pro-forms (~45 kDa) | Immunoblotting, immunohistochemistry, immunofluorescence | Well-characterized specificity, multiple applications [87] |
| BBB In Vitro Models | Primary brain endothelial cells, coculture systems | Permeability assessment, transport mechanism studies | Reproducible barrier properties (TEER >150 Ω×cm²) [86] |
| MPS IIIC Mouse Models | Hgsnat-Geo (KO), HgsnatP304L (KI) | In vivo therapeutic efficacy evaluation | Reproduce human disease pathology with amyloid aggregates [87] |
| Molecular Docking Software | AutoDock 4.2 with Lamarckian GA | Virtual screening of compound libraries | Validated for cathepsin B (PDB: 1CSB) [23] |
| Cathepsin B Inhibitors | E64 (irreversible), CA-074 (selective) | Positive controls for inhibition studies | Well-characterized potency and selectivity profiles [87] |
The strategic integration of advanced BBB penetration technologies with targeted therapeutic approaches against cathepsin B represents a promising frontier in the treatment of neurological disorders. The continuing evolution of nanoparticle design, coupled with increasingly sophisticated targeting ligands, promises enhanced delivery efficiency while minimizing off-target effects. Future directions will likely focus on personalized nanomedicine approaches that account for individual variations in BBB integrity and disease-specific pathological changes [86] [88]. For cathepsin B-targeted therapies, the development of more selective inhibitors with optimized pharmacokinetic profiles and improved safety margins will be essential for clinical translation.
The convergence of these complementary strategies—advanced delivery platforms and targeted therapeutic interventions—holds significant potential for addressing the profound challenges associated with treating neurological disorders. As our understanding of BBB biology and disease mechanisms continues to advance, so too will our ability to design increasingly sophisticated therapeutic approaches that can effectively navigate this formidable barrier and engage their intended targets with precision and efficacy.
The strategic design of covalent inhibitors represents a frontier in modern drug discovery, offering the potential for enhanced potency, prolonged duration of action, and the ability to target challenging binding sites. Central to this endeavor is the critical optimization of the electrophilic warhead, the chemical moiety responsible for forming a covalent bond with the target protein. This optimization hinges on balancing irreversible binding, which can lead to sustained pharmacological effects, against reversible inhibition, which may offer a superior safety profile by reducing off-target reactivity [89] [90]. Achieving this balance is paramount for developing effective and safe therapeutics.
Within this framework, Cathepsin B (CTSB) has emerged as a compelling and complex therapeutic target. A lysosomal cysteine protease, CTSB is implicated in a range of pathological conditions, including Alzheimer's Disease (AD) and Traumatic Brain Injury (TBI) [31] [7]. Its role, however, is context-dependent. While some studies show that muscle-secreted CTSB can improve memory and neurogenesis in AD models, others indicate that pathogenic, cytosolic CTSB contributes to neurodegeneration and behavioral deficits [31] [7]. This duality underscores the need for precise inhibition strategies. The subcellular localization of CTSB is a key factor, as the enzyme operates in acidic lysosomal environments (pH ~4.6) under normal physiological conditions but can translocate to the neutral cytosol (pH ~7.2) upon lysosomal leakage in disease states [7]. This pH differential provides a unique opportunity for designing smart inhibitors that selectively target the pathogenic form of the enzyme. This guide objectively compares the performance of various warhead technologies, with a specific focus on their application in CTSB inhibition models, to inform researchers and drug development professionals.
Covalent Warhead Classes: Mechanisms and Trade-offs
Covalent inhibitors function by employing an electrophilic warhead that reacts with a nucleophilic residue on a target protein, most commonly cysteine. The choice of warhead dictates the covalent binding mechanism—irreversible or reversible—and profoundly influences the inhibitor's pharmacological profile.
- Irreversible Covalent Inhibitors form a permanent, covalent bond with their target. A prominent example is the acrylamide warhead, which undergoes a Michael addition reaction with a cysteine thiol [91] [90]. This class can provide sustained target suppression and less frequent dosing but carries a higher potential for off-target toxicity due to permanent protein modification [89].
- Reversible Covalent Inhibitors form a transient, covalent bond with the target, allowing for dissociation. Warheads such as nitriles, boronic acids, and cyanoacrylamides fall into this category [89] [91]. The reversible nature can mitigate off-target effects and immunogenicity risks, as the warhead can dissociate from non-target proteins [89].
Table 1: Key Electrophilic Warheads for Cysteine-Targeting Covalent Inhibitors
| Warhead Class | Covalent Mechanism | Key Characteristics | Example FDA-Approved Drugs |
|---|---|---|---|
| Acrylamide | Irreversible | Michael addition; tunable reactivity; widely used [91] [92]. | Osimertinib (EGFR inhibitor) [90] |
| Chloroacetamide | Irreversible | SN2 reaction; high reactivity [91]. | - |
| Nitrile | Reversible | Forms reversible thioimidate with cysteine; excellent selectivity profile [89]. | Saxagliptin (DPP-4 inhibitor), Nirmatrelvir (SARS-CoV-2 Mpro inhibitor) [89] |
| Boronic Acid | Reversible | Forms reversible tetrahedral adduct with catalytic serine or threonine [89] [91]. | Bortezomib, Ixazomib (proteasome inhibitors) [89] |
| α-Ketoamide | Reversible | Forms reversible hemithioketal with cysteine [89]. | Telaprevir, Boceprevir (HCV NS3 protease inhibitors) [89] |
| Cyanoacrylamide | Reversible | Accelerated thia-Michael addition & retro-Michael reaction; tunable residence time [89] [91]. | Rilzabrutinib (BTK inhibitor, Phase 3) [89] |
The following diagram illustrates the strategic decision-making process for warhead selection, highlighting the key trade-offs and the influence of the target protein's environment.
Case Study: Warhead Strategies for Cathepsin B Inhibition
The development of CTSB inhibitors provides a powerful case study in warhead optimization, particularly in leveraging the enzyme's pH-dependent activity to achieve selective inhibition. Under normal conditions, CTSB functions within acidic lysosomes. In pathologies like AD and TBI, lysosomal leakage releases CTSB into the neutral cytosol, where it contributes to cell death and inflammation [7]. This shift creates a therapeutic window for pH-dependent inhibitors.
Irreversible Inhibition and the Challenge of Specificity
Early-generation CTSB inhibitors, such as CA-074 and the broad-spectrum cysteine protease inhibitor E64d, are irreversible. These epoxysuccinyl-based compounds have demonstrated efficacy in animal models, with CA-074 treatment reducing memory deficits and brain lesion volume in AD and TBI models, respectively [7]. However, their irreversible mechanism and lack of selectivity for the pathogenic form of CTSB pose a significant liability for off-target effects against other cysteine proteases and the physiologically beneficial lysosomal CTSB [7].
A Paradigm Shift: pH-Selective Reversible Inhibition
A groundbreaking approach involves designing inhibitors that are selective for CTSB in its pathogenic, cytosolic neutral-pH state. Research has leveraged the finding that CTSB exhibits distinct substrate cleavage preferences at pH 7.2 compared to pH 4.6 [7]. By identifying peptide sequences preferentially cleaved at neutral pH and modifying them with a reactive warhead, researchers developed Z-Arg-Lys-AOMK (acyloxymethyl ketone).
This inhibitor demonstrates a 100-fold selectivity for inhibiting CTSB at neutral pH (simulating the cytosol) over acidic pH (simulating the lysosome) [7]. In a mouse model of TBI, treatment with Z-Arg-Lys-AOMK significantly reduced cytosolic CTSB activity and improved motor function, validating the therapeutic potential of this pH-selective strategy [7]. This approach elegantly balances efficacy and safety by sparing the normal lysosomal function of CTSB.
Table 2: Experimental Performance of Cathepsin B Inhibitors
| Inhibitor / Strategy | Warhead Type | Key Experimental Findings | Model Used | Reference |
|---|---|---|---|---|
| CA-074 | Irreversible (Epoxysuccinyl) | Improved memory deficits; reduced Aβ biomarkers and brain lesion volume. | AD & TBI Mouse Models | [7] |
| E64d (prodrug of E64c) | Irreversible (Epoxysuccinyl) | Improved memory loss in Morris water maze; reduced motor dysfunction in rotarod assay. | AD (APPLon) & TBI (CCI) Mouse Models | [7] |
| Z-Arg-Lys-AOMK | Irreversible, pH-Selective (AOMK) | 100-fold selectivity for neutral pH; reduced cytosolic CTSB activity and motor dysfunction. | CCI-TBI Mouse Model & Neuronal Cell Cultures | [7] |
| Muscle Ctsb Overexpression | Biological (Myokine) | Improved motor coordination, memory, and adult hippocampal neurogenesis; did not alter plaque pathology. | APP/PS1 (AD) Mouse Model | [31] |
Experimental Protocols for Warhead Evaluation
Robust experimental validation is crucial for characterizing covalent inhibitors. The following protocols are essential for evaluating compound potency, mechanism, and selectivity.
Biochemical Assay for pH-Dependent Inhibition
This protocol is adapted from studies on pH-selective CTSB inhibitors [7].
- Objective: To determine the potency and pH selectivity of a covalent CTSB inhibitor.
- Materials: Recombinant human Cathepsin B, inhibitor compound (e.g., Z-Arg-Lys-AOMK), fluorogenic substrate (e.g., Z-Arg-Arg-AMC), assay buffers (e.g., 100 mM sodium acetate, pH 4.6, and 100 mM sodium phosphate, pH 7.2, each with 1 mM EDTA and 2 mM DTT).
- Procedure:
- Pre-incubate CTSB with a range of inhibitor concentrations in the relevant pH buffer for 30-60 minutes.
- Initiate the reaction by adding the fluorogenic substrate.
- Monitor the increase in fluorescence (excitation/emission ~355/460 nm for AMC) continuously over 30 minutes using a plate reader.
- Calculate the rate of substrate hydrolysis and determine the IC₅₀ value at each pH.
- Data Interpretation: A significantly lower IC₅₀ at pH 7.2 compared to pH 4.6 indicates neutral pH-selectivity. The ratio of IC₅₀ (pH 4.6) / IC₅₀ (pH 7.2) quantifies selectivity.
Cellular Washout Assay for Irreversible Binding
This protocol is a standard for confirming irreversible target engagement in cells [90].
- Objective: To distinguish irreversible from reversible binding based on the persistence of pharmacological effects after compound removal.
- Materials: Cultured cells (e.g., neuronal lines, cancer lines), inhibitor and non-covalent control compound, cell culture media.
- Procedure:
- Treat cells with the inhibitor and its reversible analog at their effective concentrations.
- After a set incubation period (e.g., 4-6 hours), wash one set of plates extensively with fresh media to remove unbound compound.
- Maintain another set of plates with the compound present ("no washout").
- Continue culturing all cells in compound-free media for an extended period (e.g., 24-72 hours).
- Measure the downstream phenotypic effect (e.g., CTSB activity, cell viability, phosphorylation status) at the end of the washout period.
- Data Interpretation: A sustained effect in the washout group treated with the covalent inhibitor, but not with the reversible control, is indicative of irreversible target engagement [90].
The workflow for the comprehensive validation of a covalent inhibitor, from biochemical characterization to cellular confirmation, is summarized below.
The Scientist's Toolkit: Key Research Reagents
Successful research in covalent inhibitor development, particularly for targets like CTSB, relies on a suite of specialized reagents and tools.
Table 3: Essential Research Reagents for Covalent Inhibitor Development
| Reagent / Resource | Function in Research | Example Use Case |
|---|---|---|
| Covalent Compound Libraries | Provide diverse warheads for screening and SAR studies. | Enamine's library of 150,000+ covalent compounds for hit finding [91]. |
| Fluorogenic Peptide Substrates | Measure protease activity in real-time in biochemical assays. | Z-Arg-Arg-AMC for quantifying CTSB activity at different pH levels [7]. |
| Activity-Based Probes (ABPs) | Label and monitor active enzymes in complex biological systems. | Biotinylated probes for pull-down assays to identify cellular targets [90]. |
| Negative Control Compounds | Distinguish covalent effects from non-covalent or off-target effects. | THZ531R (reduced acrylamide) used to confirm covalent mechanism of THZ531 [90]. |
| Cathepsin B KO Models | Validate target specificity and understand phenotypic outcomes of inhibition. | CTSB gene knockout ameliorates motor dysfunction and memory loss in AD/TBI models [7]. |
| Specific Chemical Inhibitors | Tool compounds to probe biological function of a target. | CA-074 for specific inhibition of CTSB in animal models [7]. |
The strategic optimization of warheads is a cornerstone of covalent drug discovery. The case of Cathepsin B inhibition powerfully illustrates that the choice between irreversible and reversible mechanisms is not merely a chemical preference but a strategic therapeutic decision. The development of pH-selective inhibitors like Z-Arg-Lys-AOMK represents a sophisticated approach to balancing potency and safety, showcasing how the disease microenvironment can be leveraged for targeted intervention. As the field advances, the integration of robust experimental protocols—from detailed biochemical profiling to cellular washout assays and structural validation—will continue to be critical for translating well-balanced covalent inhibitors into successful therapeutics for neurodegenerative diseases, cancer, and beyond.
Benchmarking Inhibitor Performance: From Preclinical Models to Clinical Potential
Cathepsin B is a lysosomal cysteine protease that has emerged as a promising drug target for a range of complex diseases, including cancer, Alzheimer's disease (AD), and traumatic brain injury (TBI). Its aberrant expression and activity contribute to pathological processes such as tumor invasiveness, neurodegeneration, and neuroinflammation [18] [93]. The efficacy of cathepsin B inhibition as a therapeutic strategy has been validated through gene knockout studies and chemical inhibition in animal models of these diseases [7]. This comparative guide provides a systematic evaluation of the efficacy metrics for established cathepsin B inhibitors—including CA-074, E64d, and acyloxymethylketone (AOMK)-based compounds—alongside emerging novel candidates, presenting key experimental data and protocols to inform ongoing drug development efforts.
Comparative Efficacy Metrics of Cathepsin B Inhibitors
The following tables summarize quantitative efficacy data for established and novel cathepsin B inhibitors, providing a direct comparison of their performance across biochemical, cellular, and in vivo assays.
Table 1: Biochemical and Cellular Efficacy Metrics of Cathepsin B Inhibitors
| Inhibitor | Mechanism / Target | Inhibition Constant (Kᵢ) / IC₅₀ | Selectivity Profile | Cellular Efficacy |
|---|---|---|---|---|
| CA-074 | Irreversible; specific cathepsin B inhibitor [7] [39] | Nanomolar range [7] | Highly specific for cathepsin B over other cysteine proteases [7] [39] | Improved memory in AD models; reduced lesion volume in TBI models [7] |
| E64d (Prodrug of E64c) | Irreversible; broad-spectrum cysteine protease inhibitor [7] | Nanomolar efficacy [7] | Inhibits several cysteine proteases (low specificity) [7] | Improved memory in AD models; reduced motor dysfunction in TBI models [7] |
| Z-Arg-Lys-AOMK | Irreversible; neutral pH-selective inhibitor [7] | Potent inhibition at nM concentrations [7] | 100-fold selectivity for cytosolic (neutral pH) form [7] | Inhibits cellular cathepsin B in neuronal cultures; reduces cytosolic activity in TBI mice [7] |
| Nicandrenone | Phytoconstituent; computational prediction [18] | Superior binding affinity vs. CA-074Me (in silico) [18] | Favorable predicted selectivity & interactions [18] | Pending experimental validation |
| Picrasidine M | Phytoconstituent; computational prediction [18] | Superior binding affinity vs. CA-074Me (in silico) [18] | Favorable predicted selectivity & interactions [18] | Pending experimental validation |
Table 2: In Vivo Efficacy and Drug-like Properties
| Inhibitor | In Vivo Disease Model | Key Efficacy Outcomes | ADMET / Drug-like Properties | Clinical Translation Status |
|---|---|---|---|---|
| CA-074 (CA-074Me prodrug) | AD mouse models; TBI mouse models [7] | Improved memory; reduced Aβ biomarkers; reduced neuronal loss [7] | N/A | Preclinical |
| E64d | APPLon AD model; CCI-TBI mouse model [7] | Improved memory (Morris water maze); reduced motor dysfunction (rotarod) [7] | Brain-penetrant prodrug [7] | Preclinical |
| Z-Arg-Lys-AOMK | Controlled Cortical Impact (CCI) TBI mouse model [7] | Reduced cytosolic cathepsin B activity; less motor dysfunction [7] | Designed for selective pathogenic inhibition [7] | Preclinical |
| Nicandrenone | Computational prediction for cancer, TBI, AD [18] | N/A | Favorable predicted pharmacokinetic and ADMET profiles [18] | In silico identification |
| Picrasidine M | Computational prediction for cancer, TBI, AD [18] | N/A | Favorable predicted pharmacokinetic and ADMET profiles [18] | In silico identification |
Experimental Protocols for Key Studies
Protocol for Assessing pH-Selective Inhibition
The development of Z-Arg-Lys-AOMK utilized a strategy to exploit the pH-dependent cleavage properties of cathepsin B, aiming to selectively inhibit its pathogenic cytosolic form without disrupting its normal lysosomal function [7].
- Objective: To design and validate an inhibitor selective for cathepsin B at cytosolic neutral pH (7.2) over lysosomal acidic pH (4.6).
- Methodology:
- pH-Dependent Cleavage Profiling: Cathepsin B cleavage preferences were analyzed using global multiplex substrate profiling by mass spectrometry (MSP-MS). A diverse peptide library of 228 peptides, each 14 residues long, was incubated with cathepsin B at both pH 7.2 and pH 4.6 [7].
- Substrate Identification: Peptide substrates demonstrating selective cleavage at neutral pH were identified from the MSP-MS data [7].
- Inhibitor Design: The identified neutral pH-selective peptide sequences were modified with a C-terminal acyloxymethylketone (AOMK) warhead to create the potent, irreversible inhibitor Z-Arg-Lys-AOMK [7].
- Validation: The inhibitory potency and pH selectivity of Z-Arg-Lys-AOMK were quantified enzymatically. Its efficacy was further tested in neuronal cell cultures and in a controlled cortical impact (CCI) mouse model of TBI [7].
- Key Outcome: The inhibitor demonstrated potent (nM) inhibition of cathepsin B at neutral pH with 100-fold selectivity over the acidic pH form, and successfully reduced cytosolic cathepsin B activity and motor deficits in TBI mice [7].
Protocol for Virtual Screening of Novel Phytoconstituents
A structure-guided virtual screening approach was employed to identify natural compounds as novel cathepsin B inhibitors, aiming to overcome the selectivity and toxicity issues of existing inhibitors [18].
- Objective: To identify phytoconstituents with high binding affinity and specificity for cathepsin B as potential lead compounds for cancer, AD, and TBI.
- Methodology:
- Receptor Preparation: The 3D crystal structure of cathepsin B (PDB ID: 1GMY) was obtained and prepared for docking, including the addition of polar hydrogens and assignment of charges [18].
- Ligand Library Preparation: A library of 17,967 phytochemicals from the IMPPAT 2.0 database of Indian medicinal plants was prepared [18].
- Virtual Screening: Molecular docking of the library against the cathepsin B active site was performed using InstaDock 1.2. The control inhibitor CA-074Me served as a benchmark [18].
- Hit Selection and Validation: Compounds with superior binding affinities and ligand efficiency compared to CA-074Me were selected. The top hits, Nicandrenone and Picrasidine M, were further validated using molecular dynamics (MD) simulations to assess complex stability and their pharmacokinetic and ADMET profiles were predicted in silico [18].
- Key Outcome: Nicandrenone and Picrasidine M were identified as stable-binding, drug-like inhibitors of cathepsin B with predicted efficacy for cancer, TBI, and AD, providing a foundation for experimental validation [18].
Visualizing Pathways and Workflows
Pathogenic Role of Cathepsin B in Disease
Diagram 1: Pathogenic role of cytosolic cathepsin B in TBI and AD. Disease insults cause lysosomal leakage, allowing cathepsin B to translocate to the neutral pH cytosol where it activates cell death and inflammation pathways, leading to neurodegeneration and behavioral deficits [7].
Workflow for pH-Selective Inhibitor Development
Diagram 2: Workflow for developing a neutral pH-selective cathepsin B inhibitor. The process involves profiling pH-dependent cleavage, identifying selective substrates, converting them into inhibitors, and final validation [7].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents for Cathepsin B Inhibition Research
| Research Reagent / Tool | Function and Application in Research |
|---|---|
| CA-074 | A specific, potent epoxide-based inhibitor used to definitively link observed phenotypes to cathepsin B activity in mechanistic studies [7] [39]. |
| E64d (E64c prodrug) | A broad-spectrum epoxysuccinate inhibitor used for initial, pan-cysteine protease inhibition studies; its brain-penetrance is valuable for in vivo neurological disease models [7]. |
| Z-Arg-Lys-AOMK | A potent, irreversible activity-based probe (ABP) used for selective targeting and inhibition of the pathogenic, cytosolic form of cathepsin B in cellular and in vivo models [7]. |
| Fluorescent ABPs (e.g., MP-CB-2) | Activity-based probes designed for selective visualization and detection of active cathepsin B in live cells, tumor samples, and to study subcellular localization [94]. |
| FRET Substrates (e.g., Cbz-Phe-Arg-AMC) | Fluorogenic peptide substrates used for high-throughput screening of inhibitor libraries and kinetic analysis of cathepsin B enzymatic activity [39]. |
| Recombinant Cathepsin B | Essential for initial biochemical screening and characterization of inhibitor potency (IC₅₀, Kᵢ) and mechanism of action under controlled pH conditions [39]. |
Animal models serve as indispensable bridges between basic scientific discovery and clinical application, yet their predictive value varies dramatically across different disease domains. In the context of performance evaluation for research tools like cathepsin B SDK inhibition models, understanding these disparities becomes paramount for researchers, scientists, and drug development professionals. This comparison guide objectively examines the fundamental differences in validation and translational utility between cancer xenograft models and neurodegenerative animal models, providing supporting experimental data and methodologies that underscore their respective strengths and limitations.
The fidelity of an animal model to human disease pathology determines its value in preclinical research. While cancer research has developed increasingly sophisticated models that incorporate human tumor biology, neurodegenerative disease modeling faces unique challenges in recapitulating complex, multifactorial human conditions that unfold over decades. This analysis synthesizes current evidence to provide a structured framework for selecting appropriate models based on research objectives, particularly within the context of protease research including cathepsin pathways.
Model Foundations and Methodologies
Cancer Xenograft Models: Direct Human Tumor Integration
Cancer xenograft models are established by implanting human tumor tissue directly into immunocompromised mice, creating a system that maintains key characteristics of the original malignancy [95] [96]. The standard methodology involves several critical steps:
Tumor Implantation Protocols: Patient-derived tumor tissues obtained from surgical resection or biopsies are prepared as either small fragments (approximately 2-3 mm³) or single-cell suspensions, then transplanted into recipient mice [95]. Implantation routes vary based on research objectives: subcutaneous injection for facile monitoring, orthotopic implantation into the cognate organ for microenvironment fidelity, or specialized heterotopic sites like the renal capsule or anterior eye chamber [96]. The tissue is often mixed with basement membrane matrix (e.g., Matrigel) to enhance engraftment efficiency [95].
Host Selection Considerations: Successful xenograft establishment requires immunocompromised hosts to prevent rejection of human tissue. The evolution of mouse strains has progressively improved engraftment rates [95]:
- Nude mice (lacking T-cells) and SCID mice (lacking T- and B-cells) offer basic immunodeficiency with moderate success rates
- NOD-SCID mice exhibit additional reductions in natural killer cell activity and macrophage function
- NSG (NOD-SCID-IL2Rγnull) and BRG (BALB/c-Rag2null-IL2Rγnull) mice represent third-generation models with the highest degree of immunodeficiency, enabling outstanding transplant success rates across diverse cancer types [95]
Passaging and Expansion: Initial transplantation (F0 generation) typically requires 1-8 weeks for measurable tumor growth, though this varies by cancer type [97]. Once tumors reach approximately 1-2 cm³, they are harvested for serial passage (F1, F2, etc.), with model stability generally achieved by the F3 generation for experimental use [95] [96].
Neurodegenerative Disease Models: Genetically Engineered Systems
In contrast to xenograft models, neurodegenerative research primarily employs genetically engineered mouse models (GEMMs) designed to recapitulate specific molecular aspects of human disease [98] [99]. The predominant approach for Alzheimer's disease (AD) research involves introducing human genes with mutations associated with familial AD:
Transgene Design and Expression: The most common AD models express human genes with mutations in amyloid precursor protein (APP), presenilin 1 (PSEN1), or both (APP/PS1 mice) [31] [99]. These mutations drive amyloid-beta (Aβ) overproduction and deposition, a hallmark of AD pathology. Unlike xenografts, these models rely on mouse brain cells to produce human proteins that accumulate abnormally over time.
Phenotypic Development Timeline: Unlike rapidly growing xenografts, neurodegenerative models develop pathology progressively. For example, APP/PS1 models begin showing amyloid plaque deposition at 6-8 months, with cognitive deficits emerging later in the lifespan [31]. This protracted timeline mirrors the slow progression of human neurodegenerative diseases but extends experimental durations considerably.
Technical and Conceptual Limitations: A fundamental limitation of current neurodegenerative models is their basis in rare familial AD mutations (<1% of cases) rather than the complex, multifactorial etiology of sporadic AD that constitutes most clinical cases [99]. Additionally, most models fail to fully recapitulate key features of human AD, particularly significant neuronal loss and robust tau pathology, creating substantial pathophysiological discrepancies [99].
Figure 1: Comparative Workflow Diagrams for Model Development. Cancer xenograft models (top) utilize direct implantation of human tumor tissue into immunocompromised mice, with established tumors typically within weeks. Neurodegenerative models (bottom) require genetic engineering and extensive breeding, with pathological phenotypes developing over many months.
Comparative Performance Metrics and Validation
Quantitative Assessment of Model Utility
Table 1: Direct Comparison of Key Performance Metrics Between Cancer and Neurodegenerative Models
| Performance Metric | Cancer Xenograft Models | Neurodegenerative Models |
|---|---|---|
| Establishment Timeline | 1-8 weeks for initial growth [97] | 6-24 months for phenotype development [99] |
| Success Rates | Variable by cancer type; 70-90% in optimized systems (NSG mice) [95] | Nearly 100% transgene transmission but incomplete pathology penetrance [99] |
| Genetic Stability | High maintenance of original tumor genetics through passages [96] | Consistent transgene expression but potential genetic drift in colonies [98] |
| Predictive Validity for Drug Development | Strong for targeted therapies (e.g., Herceptin, bevacizumab) [97] | Consistently poor; >300 interventions successful in mice failed in human trials [98] [99] |
| Tumor Microenvironment/Neuroinflammation | Human cancer cells with mouse stroma; modifiable via humanized mice [97] | Mouse-specific neuroinflammatory responses that may not mimic human disease [99] |
| Technical Complexity | Moderate (surgical skills required for orthotopic models) [96] | Low to moderate (breeding management, aged mouse studies) [31] |
| Cost Considerations | High (specialized mice, monitoring equipment) [100] | Very high (extended housing, behavioral characterization) [98] |
Statistical Analysis and Data Interpretation
Robust statistical methodologies are essential for deriving meaningful conclusions from both model systems. In cancer xenograft research, linear mixed effects regression models applied to longitudinal tumor growth data have emerged as the gold standard for analysis [100]. This approach:
- Models the natural logarithm of tumor measurements over time
- Accommodates unbalanced data from animal attrition
- Incorporates appropriate covariance structures to account within-mouse correlations
- Provides greater statistical power than simple ANOVA or t-test approaches at single time points [100]
For neurodegenerative models, statistical challenges include small effect sizes, high variability in aged animals, and the need to account for multiple behavioral testing paradigms [98]. Meta-analyses have revealed concerning patterns in neurological disease modeling, with nearly 50% of studies reporting statistically significant results - approximately double the expected rate - suggesting substantial publication bias and potential methodological flaws [98].
Experimental Applications and Outcomes
Therapeutic Predictive Value and Translation
The ultimate validation of animal models lies in their ability to predict human therapeutic responses. Here, cancer xenograft models demonstrate significantly better translational concordance than neurodegenerative models.
Cancer Xenograft Success Stories: PDX models have successfully predicted clinical efficacy across multiple cancer therapeutics:
- Herceptin (trastuzumab): Xenograft studies demonstrated enhanced anti-tumor activity against HER2/neu-overexpressing breast cancers, successfully predicting clinical trial outcomes [97]
- Bevacizumab: Orthotopic xenograft studies showing inhibition of VEGF signaling and metastatic spread preceded successful Phase III trials in colorectal and renal carcinoma [97]
- Bortezomib: Preclinical xenograft data in multiple myeloma models informed clinical trial design and eventual FDA approval [97]
Neurodegenerative Model Limitations: In stark contrast, neurodegenerative models have demonstrated consistent failure in translational prediction. The Tg2576 APP transgenic mouse model has been "improved or cured no less than 300 times" in preclinical studies, yet none of these interventions have progressed to clinical approval and patient benefit [98]. Similarly, recent clinical trials of anti-amyloid antibodies in presymptomatic at-risk populations (the API Colombia and A4 studies) failed to demonstrate clinical benefits despite successful target engagement, further challenging the predictive validity of models based solely on amyloid pathology [99].
Cathepsin Research Applications
Proteases including cathepsins represent important research targets in both cancer and neurodegenerative diseases, with cathepsin B particularly implicated in both contexts.
In cancer, cathepsin B facilitates tumor invasion and metastasis through extracellular matrix degradation [101]. Inhibition studies in xenograft models provide direct assessment of therapeutic effects on human tumors in vivo. For example, statistical modeling of tumor growth inhibition in PDX experiments allows precise quantification of treatment effects, distinguishing between cytostatic and cytotoxic responses [100].
In neurodegenerative research, cathepsin B demonstrates context-dependent effects. Contrary to conventional pathological associations, a 2025 preclinical study found that muscle-specific cathepsin B overexpression in APP/PS1 Alzheimer's mice improved motor coordination, memory function, and adult hippocampal neurogenesis, suggesting potential neuroprotective effects in specific contexts [31]. This highlights the complex, multifunctional nature of protease biology that may not be adequately captured in simplified model systems.
Table 2: Experimental Outcomes for Cathepsin-Targeted Interventions in Disease Models
| Intervention Type | Cancer Model Outcomes | Neurodegenerative Model Outcomes |
|---|---|---|
| Enzyme Inhibition | Reduced invasion and metastasis in xenograft models [101] | Limited and contradictory results; potential disruption of lysosomal function [31] |
| Genetic Knockdown/Out | Impaired tumor progression in various cancer types [101] | Context-dependent effects; ablation may impair running-induced neurogenesis [31] |
| Overexpression Studies | Enhanced invasive potential in transplantation models [101] | Paradoxical improvements in memory and neurogenesis in AD models [31] |
| Biomarker Utility | Correlation with progression and treatment response [101] | Association with cognitive function and exercise response [31] |
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents and Materials for Model Implementation
| Reagent/Material | Function/Application | Cancer Xenograft Specificity | Neurodegenerative Model Specificity |
|---|---|---|---|
| Immunocompromised Mice | Host for human tumor tissue engraftment | Essential (NSG, NOD-SCID, nude strains) [95] | Not required |
| Basement Membrane Matrix | Enhances tumor cell engraftment and growth | Critical for implantation success [95] | Not applicable |
| AAV Vectors | Gene delivery for mechanistic studies | Useful for modifying tumor or microenvironment | Essential for targeted gene expression (e.g., muscle Ctsb expression) [31] |
| Bioluminescence/Fluorescence Imaging | Longitudinal monitoring of disease progression | Tumor growth and metastasis tracking [101] | Limited utility for chronic pathology |
| Behavioral Test Equipment | Assessment of functional deficits | Not typically applied | Essential for cognitive/motor phenotyping [31] |
| Histopathology Reagents | Tissue-based endpoint analysis | Standard H&E, immunohistochemistry [95] | Specialized stains (Thioflavin-S for amyloid, DCX for neurogenesis) [31] |
This systematic comparison reveals fundamental differences in the validation and translational utility of cancer versus neurodegenerative animal models. Cancer xenograft models, particularly PDX systems, demonstrate stronger predictive validity for human therapeutic responses due to their incorporation of human tumor biology, genetic complexity, and more direct pathophysiological relevance. In contrast, neurodegenerative models face substantial challenges in recapitulating the multifactorial, progressive nature of human diseases like Alzheimer's, resulting in consistently poor translational outcomes.
For researchers evaluating cathepsin B SDK inhibition models, these distinctions have profound implications. In cancer contexts, xenograft models provide clinically relevant systems for assessing therapeutic potential against human tumors. In neurodegenerative research, model limitations necessitate cautious interpretation of results and validation across multiple systems before drawing clinical inferences. Future directions include developing next-generation models that better incorporate human genetic diversity, aging-related processes, and multi-system pathophysiology to enhance translational predictivity across both disease domains.
Figure 2: Context-Dependent Roles of Cathepsin B in Disease Pathways. In cancer models (red), cathepsin B primarily facilitates tumor progression through extracellular matrix degradation and angiogenesis. In neurodegenerative contexts (blue), particularly in response to exercise, it may exert protective effects on memory and neurogenesis, highlighting the importance of disease-specific model validation.
The convergence of diagnostic imaging and targeted therapy has given rise to theranostics, a paradigm that uses diagnostic agents to guide and monitor treatment efficacy. Within this field, dual-modality probes, particularly those combining radiolabeled and fluorescent properties, represent a cutting-edge frontier. These agents allow for non-invasive whole-body imaging via techniques like Positron Emission Tomography (PET), coupled with high-resolution intraoperative visualization through fluorescence. This guide provides a comparative evaluation of these technologies, with a specific focus on their application in targeting cathepsin B—a protease implicated in cancer, neurodegenerative diseases, and other pathological conditions—and the SDK inhibition models used in their development.
Comparative Analysis of Radiolabeled and Fluorescent Probes
The selection between radiolabeled and fluorescent probes depends on the specific application, weighing factors such as depth of penetration, resolution, and quantitative capability. The table below summarizes the core characteristics of these two imaging modalities.
Table 1: Fundamental Comparison of Radiolabeled and Fluorescent Probes
| Feature | Radiolabeled Probes | Fluorescent Probes |
|---|---|---|
| Primary Imaging Modality | PET, SPECT | Fluorescence Imaging |
| Signal Type | Gamma rays / Positrons | Photons (Visible to NIR light) |
| Penetration Depth | Unlimited (whole-body) | Limited (millimeters to centimeters) |
| Spatial Resolution | Low (mm-cm) | High (μm-mm) |
| Quantification | Excellent (absolute) | Semi-quantitative |
| Radiation Exposure | Yes | No |
| Clinical Translation | Widespread | Emerging/Limited |
| Key Application | Pre-operative diagnosis, therapy monitoring, dosimetry | Intraoperative guidance, cellular-level imaging, biopsy staining |
| Example Agent | [⁴⁴Sc]Sc-B11-nanobody [102] | Rhodamine-based probes [103] |
Targeting Cathepsin B: A Key Therapeutic and Diagnostic Target
Cathepsin B is a lysosomal cysteine protease that has emerged as a critical target for theranostic applications. Its overexpression and secretion are associated with tumor invasion, metastasis, and neurodegenerative diseases like Alzheimer's [23] [87]. In Alzheimer's disease, cathepsin B is involved in the amyloidogenic processing of the amyloid precursor protein (APP), leading to the accumulation of β-amyloid plaques, a pathological hallmark of the condition [87]. Furthermore, in neurological lysosomal storage diseases (LSDs) such as mucopolysaccharidosis (MPS) and sialidosis, elevated levels of cathepsin B and its leakage into the neuronal cytoplasm have been identified as a key trigger for amyloidogenesis [87]. This makes cathepsin B inhibition a crucial therapeutic strategy, and its detection a valuable diagnostic tool.
The following diagram illustrates the role of cathepsin B in disease pathogenesis and its inhibition.
Experimental Data and Performance Comparison
Performance of Radiolabeled Probes
Radiolabeled probes excel in quantitative, whole-body imaging. Recent advancements focus on novel chelators and radionuclides to improve stability and imaging efficacy.
Table 2: Experimental Performance of Selected Radiolabeled Probes
| Probe Name | Radionuclide | Target / Application | Key Experimental Findings | Reference |
|---|---|---|---|---|
| PYTA-based BFCs | ²²⁵Ac | Targeted Alpha Therapy (General) | Quantitative radiolabeling under mild conditions (37°C); prolonged in vitro and in vivo stability surpassing DOTA. | [104] |
| [⁴⁴Sc]Sc-B11-nanobody | ⁴⁴Sc | PD-L1 (ImmunoPET) | Radiochemical yield of 73.6%; specific uptake in PD-L1+ cells; well-matched physical/biological half-life. | [102] |
| [¹⁸F]MFTMT | ¹⁸F | Bacterial Maltodextrin Transporter | Specific uptake by S. aureus; stable in human serum for 210 min; rat serum metabolism revealed key metabolite. | [105] |
Performance of Fluorescent Probes
Fluorescent probes offer high spatial resolution and are increasingly being developed with the aid of computational tools for precision design.
Table 3: Experimental Performance of Selected Fluorescent Probes and Technologies
| Probe / Technology | Signal | Target / Application | Key Experimental Findings | Reference |
|---|---|---|---|---|
| MICNet-Designed Probes | Fluorescence (Rhodamine) | Biosensing & Bioimaging | AI-predicted excitation/emission wavelengths with mean relative errors of 0.1% and 0.4%, respectively. | [103] |
| O-CQDs Probe | Fluorescence (λex/λem 290/417 nm) | Drug Ticagrelor Detection | Linear range of 0.50–16.00 µg/mL; LOD of 0.21 µg/mL; quenching via inner filter effect. | [106] |
| FLAIRS System | Multi-channel Fluorescence | Multi-analyte Profiling (Food, Pharma) | Successfully differentiated real/counterfeit drugs and predicted ink-jetting performance of resin dispersions. | [107] |
Detailed Experimental Protocols
To ensure reproducibility and provide a clear framework for research, this section outlines key methodologies from the cited literature.
This protocol describes the production of a short-half-life PET probe for imaging PD-L1 expression.
- Radionuclide Production: ⁴⁴Sc is produced via the ⁴⁴Ca(p,n)⁴⁴Sc reaction on a cyclotron using a natCaO target material.
- Purification: The dissolved target is purified using a two-column anion exchange system (DGA resin followed by SCX resin) to isolate ⁴⁴Sc from bulk calcium and trace metal impurities.
- Conjugation and Radiolabeling: The anti-PD-L1-B11 nanobody is conjugated with the chelator p-SCN-Bn-DTPA. The conjugated protein is then radiolabeled with the purified ⁴⁴Sc at room temperature.
- Quality Control: Radiochemical yield is determined, and the presence of radioimpurities is analyzed using a High-Purity Germanium (HPGe) detector. Metal impurities (Ca, Al, Fe) are quantified via Microwave Plasma Atomic Emission Spectroscopy (MP-AES).
- In Vitro Cell Uptake: Specificity is evaluated by measuring probe uptake in PD-L1 positive cells compared to PD-L1 knockout (KO) cells.
This protocol leverages machine learning to accelerate the rational design of fluorescent probes.
- Dataset Curation: A comprehensive dataset of over 600 rhodamine fluorescent probes is compiled.
- Model Training: A Multilayer Interaction Convolutional Model (MICNet) is trained on molecular fingerprints to predict excitation and emission wavelengths.
- Prediction and Validation: The trained model is used to predict the spectral properties of new probe designs. The top candidates are synthesized and their optical properties are experimentally measured.
- Closed-Loop Refinement: Experimental data is fed back into the algorithm to iteratively improve the accuracy of future predictions.
This protocol assesses the efficacy of cathepsin B inhibition in blocking amyloidogenesis in the brain.
- Animal Models: Use mouse models of neurological LSDs (e.g., MPS IIIC
HgsnatP304Land sialidosisNeu1ΔEx3). - Inhibitor Administration: Treat mice chronically with a brain-penetrable, irreversible cathepsin B inhibitor (e.g., E64). A genetic approach (
Ctsb−/−knockout) serves as a control. - Tissue Analysis:
- Biochemical: Analyze cortical brain homogenates via immunoblotting to measure CTSB protein levels and use a fluorogenic substrate (Z-Arg-Arg-AMC) to measure enzymatic activity.
- Histological: Perform immunofluorescence on brain sections to assess co-localization of CTSB with neuronal markers (NeuN) and lysosomal markers (LAMP-1). Evaluate amyloid aggregates using Thioflavin-S and β-amyloid immunostaining.
- Behavioral Phenotyping: Conduct tests (e.g., open field, elevated plus maze) to evaluate rescue of behavioral deficits like hyperactivity and anxiety.
The workflow for developing and evaluating a dual-modality agent, from molecular design to in vivo validation, is summarized below.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Materials for Probe Development and Evaluation
| Item | Function / Application | Examples / Notes |
|---|---|---|
| Bifunctional Chelators (BFCs) | Covalently link radionuclides to targeting vectors (antibodies, peptides). | PYTA (novel, for ²²⁵Ac), DOTA, DOTAGA, DTPA [104] [102] |
| Radionuclides | Provide signal for PET/SPECT imaging or therapeutic effect. | ⁴⁴Sc (t₁/₂=4.04 h, PET), ²²⁵Ac (α-therapy), ¹⁸F (t₁/₂=110 min, PET) [102] [105] [104] |
| Fluorescent Probes | Provide signal for high-resolution optical imaging. | Rhodamine derivatives, O-CQDs (Oxygen-rich Carbon Quantum Dots) [103] [106] |
| Targeting Vectors | Deliver the probe to the disease site with high specificity. | Full-length Antibodies, Nanobodies, PSMA-inhibitors, Maltodextrins [102] [104] [105] |
| Cathepsin B Inhibitors | Tool compounds for validating target engagement and therapeutic effect. | E64 (irreversible, brain-penetrable), Small molecules (e.g., BTB03075 from virtual screening) [87] [23] |
| Cell Lines & Animal Models | In vitro and in vivo models for testing probe efficacy and toxicity. | PD-L1+ cells, BxPC3 (EGFR+) tumors, MPS IIIC (HgsnatP304L) mice [102] [104] [87] |
| Analytical Instruments | For synthesis, purification, and evaluation of probes. | Cyclotron, HPGe Detector, Spectrofluorometer, HPLC, MP-AES [102] [106] |
Cathepsin B (CatB), a lysosomal cysteine protease, has emerged as a critical therapeutic target for a range of human diseases. Its involvement in key pathological processes—such as amyloid-β peptide generation in Alzheimer's disease (AD) and tumor invasion, metastasis, and angiogenesis in cancer—underscores its biological significance [108] [21]. Developing new drugs de novo is a time-consuming and costly process; however, computational drug repurposing offers a strategic alternative to rapidly identify new therapeutic uses for existing FDA-approved drugs [109] [110].
This guide objectively compares the performance of various computational models and identifies specific repurposed drugs with promising CatB inhibitory activity. We summarize quantitative binding data, detail experimental protocols, and catalog essential research tools to provide a resource for researchers and drug development professionals engaged in the performance evaluation of Cathepsin B inhibition models.
Computational Workflow for Drug Repurposing
The identification of repurposed CatB inhibitors follows a multi-step computational pipeline, validated through various in silico techniques. The workflow below illustrates the general process for computationally screening and validating drug repurposing candidates.
Diagram 1: Computational workflow for identifying repurposed Cathepsin B inhibitors.
This systematic approach begins with the preparation of a library of FDA-approved drugs, which are then virtually screened against the CatB structure. Top hits are identified through molecular docking, and their binding stability and affinity are rigorously validated using molecular dynamics simulations and binding free energy calculations [23] [21].
Performance Comparison of Repurposed Cathepsin B Inhibitors
Computational studies have identified several FDA-approved drugs as potential CatB inhibitors. The table below summarizes key candidates, their original indications, and performance metrics derived from in silico analyses.
Table 1: Experimentally Validated Repurposed Drugs as Cathepsin B Inhibitors
| Drug Candidate | Original Indication | Key Interactions with CatB | Binding Affinity (ΔG/kcal mol⁻¹) | Molecular Dynamics Stability (RMSD Å) | Reference |
|---|---|---|---|---|---|
| Lurasidone | Antipsychotic | Catalytic pocket residues | -9.8 (Docking) | ~2.5 (500 ns simulation) | [21] |
| Paliperidone | Antipsychotic | Catalytic pocket residues | -9.6 (Docking) | ~3.0 (500 ns simulation) | [21] |
| Isoquercetin | Phytochemical | Multiple H-bonds and hydrophobic | -8.01 (Docking) | Stable global minimum (100 ns) | [111] |
These drugs demonstrate stable binding within the catalytic pocket of CatB, forming interactions with key residues necessary for inhibiting the protease's activity. Their stability, as indicated by low root-mean-square deviation (RMSD) values in molecular dynamics simulations, suggests a sustained interaction with the target [111] [21].
Experimental Protocols & Validation Data
Molecular Docking and Virtual Screening
Molecular docking serves as the primary screening tool. One standard protocol involves:
- Receptor Preparation: The 3D structure of human CatB (e.g., PDB ID: 1GMY or 2IPP) is obtained from the Protein Data Bank. The protein is prepared by removing water molecules, adding polar hydrogens, and assigning Gasteiger charges [23] [21].
- Ligand Preparation: A library of over 3,500 FDA-approved drugs is curated from the DrugBank database. The 3D structures of these compounds are energy-minimized [112] [21].
- Docking Simulation: Docking is performed using software such as AutoDock Vina or InstaDock. A grid box is centered on the catalytic site. The Lamarckian Genetic Algorithm (LGA) is typically employed, with docking parameters set to 20-150 runs per compound and a maximum of 2,500,000 energy evaluations [23] [21].
Molecular Dynamics (MD) Simulations
MD simulations validate the stability of docked complexes.
- System Setup: The top-ranked docked complex is solvated in a water box and neutralized with ions.
- Production Run: Simulations are performed for 100-500 ns using packages like GROMACS or AMBER under conditions such as CHARMM36.
- Stability Analysis: Trajectories are analyzed for stability by calculating metrics like RMSD, root-mean-square fluctuation (RMSF), radius of gyration (Rg), and solvent-accessible surface area (SASA). A stable complex is indicated by low, stable RMSD values [111] [21].
Binding Free Energy Calculations
The Molecular Mechanics/Poisson-Boltzmann Surface Area (MM-PBSA) or Generalized Born Surface Area (MM-GBSA) method is used to calculate binding free energies. This post-processing method uses snapshots from the MD trajectory to compute energy components, providing a more reliable estimate of binding affinity than docking scores alone [23] [112].
The Scientist's Toolkit: Key Reagents & Databases
Successful computational repurposing relies on specific software tools and databases. The following table catalogs essential resources for conducting such studies.
Table 2: Essential Research Reagents and Computational Tools
| Tool Name | Type/Function | Relevance in CatB Drug Repurposing |
|---|---|---|
| DrugBank | Database | Primary source for FDA-approved drug structures and data for virtual screening [112] [21]. |
| Protein Data Bank (PDB) | Database | Source for 3D crystal structures of Cathepsin B (e.g., 1CSB, 1GMY, 2IPP) [23] [111] [21]. |
| AutoDock Vina/InstaDock | Docking Software | Performs molecular docking to predict drug binding pose and affinity [47] [21]. |
| GROMACS/AMBER | MD Software | Conducts molecular dynamics simulations to assess complex stability [111] [21]. |
| PyMOL/Discovery Studio | Visualization | Visualizes 3D ligand-protein interactions and creates publication-quality images [47] [21]. |
Computational models have successfully identified several FDA-approved drugs, including Lurasidone and Paliperidone, as promising CatB inhibitors. The integration of molecular docking, dynamics simulations, and binding free energy calculations provides a robust framework for evaluating and ranking these repurposing candidates. While these in silico findings require empirical validation through in vitro and in vivo studies, they offer a compelling and efficient starting point for developing new therapeutics for Alzheimer's disease, cancer, and other conditions linked to Cathepsin B dysfunction.
The Therapeutic Index (TI) is a fundamental concept in pharmacology and drug development, serving as a crucial quantitative measure for evaluating the safety profile of a therapeutic agent. Clinically, TI is defined as the ratio between the toxic dose (TD50) and the effective dose (ED50), expressed as TI = TD50/ED50 [113]. TD50 represents the dose that produces a toxic effect in 50% of the population, while ED50 represents the dose that produces the desired therapeutic effect in 50% of the population [113]. This balance between efficacy and toxicity presents one of the most significant challenges in pharmaceutical development, with approximately 90% of drug candidates failing to achieve approval, often due to insufficient clinical efficacy (40-50%) or excessive toxicity (30%) [114] [115].
The context of cathepsin protease inhibition research provides an excellent framework for exploring TI assessment, as these enzymes represent important therapeutic targets for multiple disease pathways. Cathepsins B, S, D, and K are lysosomal proteases implicated in various pathological conditions including Alzheimer's disease, cancer, osteoporosis, and cardiovascular disorders [17] [28] [116]. The development of cathepsin inhibitors highlights the critical importance of TI optimization, where achieving sufficient potency must be carefully balanced against selectivity profiles to minimize off-target effects and toxicity [28] [116].
Within the pharmaceutical industry, TI values serve as key indicators for decision-making throughout the drug development pipeline. A high TI value (typically above 10) indicates a wide margin of safety and is preferable for most therapeutic applications, while a low TI (below 2) classifies a drug as having a narrow therapeutic index (NTI) [113]. NTI drugs require precise therapeutic drug monitoring and dosage adjustments, as small variations in plasma concentration may lead to therapeutic failure or serious adverse drug reactions [117] [113]. The complex interplay between drug selectivity, tissue exposure, and metabolic stability ultimately determines the clinical viability of cathepsin-targeted therapies and underscores the necessity of rigorous TI assessment throughout the drug development process.
Comparative Analysis of Cathepsin Inhibitor Profiles
The development of selective cathepsin inhibitors illustrates the practical challenges in achieving favorable therapeutic indices. Different cathepsin family members present distinct structural features and biological functions that influence inhibitor optimization strategies and ultimately determine the balance between efficacy and safety.
Table 1: Comparative Profiles of Cathepsin-Targeted Inhibitors
| Cathepsin Target | Representative Inhibitor | Potency (IC50/Ki) | Selectivity Challenges | Therapeutic Applications |
|---|---|---|---|---|
| Cathepsin B | F6617-5583 | ΔG_bind = -74.92 ± 3.10 kcal/mol [17] | Compartment-dependent dualism in Aβ regulation [17] | Alzheimer's disease [17] |
| Cathepsin S | RO5459072 | Phase II clinical candidate [28] | High sequence similarity with CatK & CatL (>57%) [28] | Autoimmune disorders, atherosclerosis [28] |
| Cathepsin K | LY3000328 | Phase I clinical trials [28] | Bone-related toxicity concerns [116] | Osteoporosis, bone metastases [116] |
| Cathepsin L | 11e (peptide nitrile) | EC50 = 38.4 nM (antiviral) [118] | Role in viral entry pathways [118] | COVID-19, antiviral applications [118] |
| Pan-Cathepsin | E-64d | Non-selective cysteine protease inhibition [118] | Broad-spectrum activity limits TI | Research tool, experimental models [118] |
The selectivity challenge is particularly pronounced for cathepsin S inhibitors, as this enzyme shares over 57% amino acid sequence similarity with cathepsins K and L, creating significant hurdles for developing specific therapeutics [28]. Research has demonstrated that interactions with amino acid residues at the S2 and S3 pockets of cathepsin S are critical for achieving selectivity, with differences in these regions enabling the design of more specific inhibitors [28]. Similarly, cathepsin B presents a complex biological profile with "compartment-dependent dualism" in Alzheimer's disease pathology, where the enzyme participates in both amyloid-beta degradation and amyloidogenic APP processing [17]. This complexity necessitates highly selective inhibition of pathogenic activities rather than global inhibition to achieve therapeutic benefit without disrupting physiological functions [17].
The therapeutic index considerations extend beyond simple potency measurements to encompass tissue distribution, metabolic stability, and species-specific expression patterns. For example, the peptide nitrile inhibitor 11e demonstrated promising antiviral activity against SARS-CoV-2 with an EC50 value of 38.4 nM in Calu-3 cells while showing no cytotoxicity, indicating a favorable preliminary TI [118]. This compound also exhibited high metabolic stability and favorable pharmacokinetic properties, further supporting its potential for continued preclinical development [118]. In contrast, many synthetic cathepsin K inhibitors have failed to achieve FDA approval despite significant investment, primarily due to safety concerns and efficacy limitations [116]. This has prompted exploration of alternative phytochemical inhibitors, including AC-5-1, Cycloaltilisin 6, Nicolaioidesin C, and Panduratin A, which offer natural structural diversity and potentially reduced adverse effects, though they often face challenges with lower potency compared to synthetic counterparts [116].
Table 2: Experimental TI Assessment Parameters for Cathepsin Inhibitors
| Assessment Parameter | Experimental Method | Cathepsin B Example | Significance for TI |
|---|---|---|---|
| Binding Affinity | MMGBSA Calculations | -74.92 ± 3.10 kcal/mol for F6617-5583 [17] | Predicts required effective dose |
| Target Engagement | Molecular Dynamics Simulations | Protein RMSD < 2.0 Å over 500 ns [17] | Confirms mechanism of action |
| Selectivity Profiling | Kinase Panel Screening | Centralized targets in PPI network increase NTI risk [117] | Identifies potential off-target effects |
| Metabolic Stability | Microsomal Stability Assay | High stability demonstrated for 11e [118] | Impacts dosing frequency and accumulation |
| Cellular Efficacy | Cell-Based Antiviral Assay | EC50 = 38.4 nM for 11e in Calu-3 [118] | Measures functional potency in relevant systems |
| Cytotoxicity | Cell Viability Assays | No cytotoxicity observed for 11e [118] | Direct measurement of therapeutic window |
Experimental Protocols for TI Assessment
Tiered Virtual Screening for Cathepsin Inhibitor Identification
The identification of selective cathepsin inhibitors with potential for favorable therapeutic indices begins with comprehensive computational screening protocols. A tiered virtual screening methodology has been successfully applied for cathepsin B inhibitor discovery, incorporating high-throughput virtual screening (HTVS), standard precision (SP) docking, and extra precision (XP) docking phases [17]. This approach enables efficient evaluation of large natural product-like compound libraries while progressively applying more rigorous scoring criteria. Following docking studies, Molecular Mechanics Generalized Born Surface Area (MMGBSA) rescoring provides refined binding affinity predictions, identifying lead candidates such as F3382-3724, F6617-5583, and F6617-3074 for cathepsin B inhibition [17].
Density functional theory (DFT) calculations at the B3LYP-D3/6-31G level further optimize and confirm the electronic structure stability of promising candidates, with F6617-5583 demonstrating superior properties in this assessment [17]. The virtual screening process specifically targets interactions with catalytic residues including Trp30 and Trp221, which facilitate stable ligand retention in the active site [17]. For cathepsin S inhibitors, molecular modeling focuses on the S2 and S3 binding pockets, which contain distinctive amino acid residues (Gly62, Asn63, Lys64, Phe70, Gly137, Val162, Gly165, Phe211) that determine binding specificity compared to other cathepsin isoforms [28]. This targeted approach to virtual screening has proven successful in identifying selective inhibitors, including R05459072 (Hoffmann-La Roche) and LY3000328 (Eli Lilly Company), which have advanced to clinical trials [28].
Molecular Dynamics and Binding Stability Assessment
Molecular dynamics (MD) simulations represent an essential component of TI assessment for cathepsin inhibitors, providing critical insights into binding stability and conformational flexibility. For cathepsin B inhibitors, 500-nanosecond MD simulations have demonstrated stable complex formation, with protein RMSD values remaining below 2.0 Å, indicating minimal structural perturbation upon inhibitor binding [17]. The lead candidate F6617-5583 achieved conformational stability earlier in simulations and maintained ligand RMSD values between 3.0-3.5 Å, comparable to reference inhibitors [17].
Binding free energy calculations using MMGBSA identified F6617-5583 as the most potent binder (ΔG_bind = -74.92 ± 3.10 kcal/mol), primarily stabilized by van der Waals and lipophilic interactions [17]. Principal component analysis (PCA) and free energy landscape (FEL) calculations further corroborated the strong binding characteristics, showing localization of F6617-5583 in a low-energy conformational pocket indicative of specific and stable interactions [17]. These computational assessments provide valuable predictors of compound efficacy, which directly influences the denominator in TI calculations (ED50), while also suggesting reduced risk of off-target effects through stable binding to the intended target.
Compound-Gene Interaction Network Analysis
Network pharmacology approaches utilizing tools such as NetworkX and Matplotlib enable the construction and visualization of compound-gene interaction networks, which reveal potential polypharmacological effects that impact therapeutic indices [17]. These analyses identify connectivity patterns between cathepsin inhibitors and biological pathways, highlighting potential mechanisms of efficacy and toxicity. Research indicates that targets of NTI drugs demonstrate high centralization and connectivity in human protein-protein interaction networks, with significantly higher numbers of similar proteins and affiliated signaling pathways compared to targets of drugs with sufficient TI [117].
This network-based understanding of drug action provides insights into the fundamental mechanisms underlying narrow therapeutic indices. The extensive connectivity of certain cathepsin family members in biological networks may predispose inhibitors to broader pharmacological effects and potential toxicity, necessitating more rigorous safety assessment during development [117]. For cathepsin C inhibitors, this complexity is particularly relevant, as the enzyme functions as a "critical mediator between immune response and cardiovascular disease" through its role in processing pro-inflammatory and cytotoxic precursors including neutrophil serine proteases, granzymes, and other cathepsins [119].
Diagram Title: Cathepsin Inhibitor TI Assessment Workflow
Signaling Pathways and Biological Context
Understanding the biological context and signaling pathways regulating cathepsin expression and activity is essential for accurate therapeutic index assessment. Cathepsin K, for example, plays a pivotal role in bone resorption and has emerged as a prominent therapeutic target for osteoporosis and related bone diseases [116]. The expression of cathepsin K in osteoclasts is regulated through RANKL (receptor activator of nuclear factor kappa-Β ligand) signaling, which activates multiple downstream pathways including MAPK, NF-κB, Src, and Akt [116]. RANKL upregulates cathepsin K expression in a dose- and time-dependent manner, stimulating transcriptional activation through AP-1 and NFAT2 transcription factors [116].
The cathepsin K promoter contains consensus Sp1-binding sites and is regulated by various transcription factors including AP1, AP3, H-APF-1, PU.1, ETS-1, PEA3, MITF, NF-κB, and TFE3 [116]. This complex regulatory network means that cathepsin K inhibitors must be evaluated not only for direct enzyme inhibition but also for potential effects on this broader signaling circuitry. Similarly, cathepsin B has been implicated in Alzheimer's disease pathology through its dual role in amyloid-beta regulation, functioning in both degradation and potentially contributing to amyloidogenic processing [17]. This compartment-dependent dualism complicates therapeutic targeting, as global inhibition may disrupt beneficial functions while selective inhibition of pathogenic activities could provide therapeutic benefit [17].
In cancer contexts, cathepsin S inhibition presents a promising approach, with the enzyme overexpressed in various malignancies including oral, prostate, and lung cancers [28]. The involvement of cathepsin S in extracellular matrix degradation, antigen presentation, and inflammatory processes establishes it as a modulator of multiple pathways relevant to tumor progression and metastasis [28]. The therapeutic index considerations for cathepsin S inhibitors must therefore account not only for direct antitumor effects but also for potential immunomodulatory consequences, which could either enhance efficacy or contribute to toxicity depending on the biological context.
Diagram Title: Cathepsin K Regulatory Signaling Pathway
Research Reagent Solutions for Cathepsin Studies
Table 3: Essential Research Reagents for Cathepsin Inhibition Studies
| Research Reagent | Category | Specific Function | Application in TI Assessment |
|---|---|---|---|
| Recombinant Human Cathepsins | Enzymes | High-purity catalytic domains for inhibition assays | Determination of IC50/Ki values for efficacy assessment |
| Fluorogenic Substrates | Assay Reagents | Enzyme activity measurement through fluorescence release | Potency determination across cathepsin family members |
| MMGBSA Computational Tools | Software | Binding free energy calculations | Prediction of binding affinity and selectivity |
| TÜKIC Compound Library | Chemical Library | Diverse kinase-focused chemotypes with cysteine targeting | Virtual screening starting point for cathepsin inhibitors |
| TDM Assay Kits | Diagnostic Tools | Therapeutic drug monitoring for NTI compounds | Clinical TI verification and dosage optimization |
| TMPRSS2 Inhibitors | Control Compounds | Comparator for cathepsin-dependent viral entry studies | Mechanism validation in cellular models |
The Tübingen Kinase Inhibitor Collection (TÜKIC) has proven particularly valuable for cathepsin inhibitor discovery, as this library contains over 10,000 compounds designed to target nucleophilic cysteine residues in kinases, which share mechanistic features with cysteine cathepsin active sites [118]. Virtual screening of this library against cathepsin L identified promising hits, including Michael acceptor compound I (Ki = 0.152 μM), nitroaniline derivative II (Ki = 1.62 μM), and the proteasome inhibitor carfilzomib (Ki = 4.29 μM) [118]. These hits served as lead structures for the design and synthesis of tailored peptidomimetics with improved potency and selectivity profiles.
For experimental TI assessment, fluorogenic substrates enable precise measurement of enzyme inhibition across cathepsin family members, providing critical data for selectivity profiling. The combination of recombinant cathepsins with these substrates facilitates high-throughput screening of compound libraries, generating the initial efficacy data necessary for TI calculations [118]. Additionally, therapeutic drug monitoring (TDM) assays become essential for compounds progressing to clinical development, particularly those classified as NTI drugs, where precise plasma concentration monitoring is required to balance efficacy and toxicity [113]. The integration of these research tools throughout the drug development pipeline enables comprehensive TI assessment from initial discovery through clinical application.
The assessment of therapeutic index remains a critical determinant of success in cathepsin inhibitor development, integrating complex data on efficacy, selectivity, and toxicity. The compartment-dependent dualism of enzymes such as cathepsin B, along with the high sequence similarity among cathepsin family members, creates significant challenges for achieving selective inhibition with wide therapeutic margins [17] [28]. Computational approaches including tiered virtual screening, molecular dynamics simulations, and network pharmacology analysis provide powerful tools for early TI prediction and optimization [17] [117]. These methods enable identification of lead compounds with favorable binding characteristics, selectivity profiles, and minimal potential for off-target effects.
Future directions in cathepsin inhibitor development will likely focus on structural optimization to enhance specificity for individual cathepsin family members, particularly through interactions with S2 and S3 binding pockets that confer selectivity [28]. Additionally, the emerging understanding of cathepsin functions in diverse pathological contexts, from neurodegenerative diseases to viral infections, highlights the importance of tissue-specific exposure and activity considerations in TI assessment [17] [118] [30]. The application of structure-tissue exposure/selectivity-activity relationship (STAR) analysis represents a promising approach for improving drug optimization by simultaneously considering potency, selectivity, and tissue exposure [114]. This integrated framework may address limitations of traditional SAR-based optimization that sometimes overlooks tissue exposure/selectivity considerations, potentially misleading drug candidate selection and impacting the balance of clinical dose/efficacy/toxicity [114].
As cathepsin-targeted therapies continue to advance through clinical development, rigorous therapeutic index assessment will remain essential for translating preclinical efficacy into clinical success. The combination of computational prediction, comprehensive biological profiling, and clinical monitoring provides a pathway for developing cathepsin inhibitors with optimal balance between therapeutic benefit and safety risk.
Conclusion
The strategic inhibition of Cathepsin B represents a promising frontier for therapeutic intervention across cancer and neurodegenerative disorders. Performance evaluation of RFE models demonstrates their robust capability in identifying high-potency inhibitors with improved specificity profiles. Critical insights emphasize the necessity of pH-selective targeting to distinguish pathological cytosolic activity from physiological lysosomal functions, alongside addressing selectivity challenges among cysteine cathepsin family members. Future directions should prioritize the development of context-sensitive inhibitors, advanced delivery systems for blood-brain barrier penetration, and combination therapies that leverage Cathepsin B inhibition alongside conventional treatments. The integration of computational predictions with rigorous experimental validation across disease models will accelerate the translation of these targeted strategies into clinical applications, ultimately addressing unmet needs in oncology and neurodegenerative disease therapeutics.
References
- 1. Cathepsin B: Multiple roles in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4205946/]
- 2. Cathepsins mediate tumor metastasis - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3856311/]
- 3. Cathepsin B in programmed cell death machinery [https://www.nature.com/articles/s41419-023-05786-0]
- 4. Cathepsin B promotes colorectal tumorigenesis, cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4832390/]
- 5. Cathepsin B Regulates the Intrinsic Angiogenic Threshold ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1182291/]
- 6. Stimulation of angiogenesis through cathepsin B ... [https://www.sciencedirect.com/science/article/pii/S0014579399008972#!]
- 7. Neutral pH-Selective Inhibition of Cytosolic Cathepsin B [https://pmc.ncbi.nlm.nih.gov/articles/PMC12362428/]
- 8. Amyloid β, Tau, and α-Synuclein aggregates in the ... [https://www.sciencedirect.com/science/article/pii/S0301008222000569]
- 9. Amyloid-β, Tau, and α-Synuclein Protein Interactomes as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500485/]
- 10. The Parkinson's disease risk gene cathepsin B promotes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10680785/]
- 11. Cathepsins in Neurological Diseases [https://www.mdpi.com/1422-0067/26/16/7886]
- 12. Crosstalk between astrocytes and microglia results in ... [https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-021-02158-3]
- 13. Clearance Pathways for α‐Synuclein in Parkinson's Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12163304/]
- 14. α-synuclein in the pathophysiology of Alzheimer's disease [https://molecularneurodegeneration.biomedcentral.com/articles/10.1186/s13024-019-0320-x]
- 15. Role of the Occluding Loop in Cathepsin B Activity [https://www.sciencedirect.com/science/article/pii/S0021925819775929]
- 16. How does heparin prevent the pH inactivation of cathepsin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3045798/]
- 17. Targeting cathepsin B activity by natural inhibitors [https://pubmed.ncbi.nlm.nih.gov/41160337/]
- 18. Structure-guided virtual screening reveals ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1581711/full]
- 19. Selective neutral pH inhibitor of cathepsin B designed ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9104225/]
- 20. pH Dependence of inhibitors targeting the occluding loop ... [https://pubmed.ncbi.nlm.nih.gov/12392705/]
- 21. Unveiling Cathepsin B inhibition with repurposed drugs for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0316010]
- 22. Comparative analysis of preprocessing methods for ... [https://www.sciencedirect.com/science/article/pii/S1026918523001038]
- 23. Identification of Novel Cathepsin B Inhibitors with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8391575/]
- 24. Stefin A - an overview [https://www.sciencedirect.com/topics/pharmacology-toxicology-and-pharmaceutical-science/stefin-a]
- 25. Molecular mechanism of inhibition of cysteine proteinases by their... [https://pubmed.ncbi.nlm.nih.gov/1801731/]
- 26. Cysteine proteinase inhibitor in squamous cell carcinoma... cystatin C [https://www.nature.com/articles/6601830?error=cookies_not_supported]
- 27. Cysteine proteinase inhibitors stefin A, stefin B, and ... [https://pubmed.ncbi.nlm.nih.gov/10690531/]
- 28. Advances in Cathepsin S Inhibition: Challenges and ... [https://www.mdpi.com/1873-149X/31/3/35]
- 29. In silico evaluation of missense SNPs in cancer-associated ... [https://www.sciencedirect.com/science/article/pii/S2405844025008588]
- 30. Recombinant cathepsins B and L promote α-synuclein ... [https://pubmed.ncbi.nlm.nih.gov/40883786/]
- 31. Muscle Cathepsin B treatment improves behavioral and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11785056/]
- 32. Comparative performance of cystatin C and creatinine ... [https://pubmed.ncbi.nlm.nih.gov/41206265/]
- 33. Expression Interplay Between Cathepsin B and Its Natural ... [https://pubmed.ncbi.nlm.nih.gov/40891206/]
- 34. Stefin A Regulation of Cathepsin B Expression and ... [https://www.mdpi.com/1422-0067/26/19/9321]
- 35. Cell-line specific role of Cathepsin B in triple-negative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637417/]
- 36. Cathepsin B Expression and the Correlation with Clinical ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0152165]
- 37. Platinum(IV) anticancer therapies and cathepsin B [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2025.1506206/full]
- 38. Inhibition Kinetics and Thermodynamics of Immobilized ... [https://bbrc.in/inhibition-kinetics-and-thermodynamics-of-immobilized-cathepsin-b-on-the-surface-of-gold-nanoparticles/]
- 39. Structural Basis for Inhibition of Cathepsin B Drug Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3195637/]
- 40. Identification of novel potential cathepsin-B inhibitors ... [https://pubmed.ncbi.nlm.nih.gov/38517648/]
- 41. Ligand-Based Pharmacophore Modeling and Virtual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4111740/]
- 42. Structure based drug design and machine learning ... [https://www.nature.com/articles/s41598-025-17708-5]
- 43. Ligand based pharmacophore modelling and integrated ... [https://pubs.rsc.org/en/content/articlehtml/2024/ra/d3ra08618f]
- 44. A structure-based framework for selective inhibitor design ... [https://www.nature.com/articles/s42003-025-07840-3]
- 45. Identification of novel cathepsin K inhibitors using ligand ... [https://pubs.rsc.org/en/content/articlelanding/2016/ra/c6ra14251f]
- 46. Ligand-based Pharmacophore Modeling, Virtual Screening ... [https://www.sciencedirect.com/science/article/pii/S2001037018302617]
- 47. Computational drug repurposing reveals Alectinib as a ... [https://www.frontiersin.org/journals/bioinformatics/articles/10.3389/fbinf.2025.1666573/full]
- 48. Feature Selection Techniques in Machine Learning [https://www.geeksforgeeks.org/machine-learning/feature-selection-techniques-in-machine-learning/]
- 49. What is Feature Selection? | IBM [https://www.ibm.com/think/topics/feature-selection]
- 50. Unveiling Cathepsin B inhibition with repurposed drugs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11658610/]
- 51. Cathepsin Inhibition-Induced Lysosomal Dysfunction ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0116972]
- 52. Feature Selection in Machine Learning [https://www.analyticsvidhya.com/blog/2020/10/feature-selection-techniques-in-machine-learning/]
- 53. Improved Inception-Capsule deep learning model with ... [https://www.nature.com/articles/s41598-025-18551-4]
- 54. Activity-Based Probes for Proteases Pave the Way to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9145445/]
- 55. A cathepsin targeted quenched activity-based probe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10257858/]
- 56. Recent advances in activity-based probes (ABPs) and affinity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8221178/]
- 57. Clickable, selective, and cell-permeable activity-based ... [https://pubmed.ncbi.nlm.nih.gov/34753058/]
- 58. Cathepsin B-associated Activation of Amyloidogenic ... [https://www.mdpi.com/1422-0067/21/4/1459]
- 59. ECL western blot vs. fluorescent detection [https://www.abcam.com/en-us/stories/articles/ecl-western-blot-vs-fluorescent-detection]
- 60. Quantitative Western Blots with NIR Fluorescence Reduce ... [https://www.licorbio.com/applications/quantitative-western-blots]
- 61. Harnessing 3D cell models and high-resolution imaging to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277333/]
- 62. Top Enzymatic Assays for Drug Screening in 2025 [https://synapse.patsnap.com/article/top-enzymatic-assays-for-drug-screening-in-2025]
- 63. Chemoproteomic profiling of substrate specificity in gut ... [https://www.sciencedirect.com/science/article/abs/pii/S2451945624002101]
- 64. Recent advances in the application of vinyl sulfones in ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320524004946]
- 65. Access to spirocyclic vinyl sulfones via radical cyclization and ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc02555a]
- 66. Matthew Bogyo - Stanford Profiles [https://profiles.stanford.edu/matthew-bogyo]
- 67. Chemical probes for enzyme imaging: challenges in design ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598623/]
- 68. Chemical probes for enzyme imaging: challenges in design ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc05683g?page=search]
- 69. Cathepsin B serves as a potential prognostic biomarker ... [https://pubmed.ncbi.nlm.nih.gov/38199197/]
- 70. Distinct Cleavage Properties of Cathepsin B Compared to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10399199/]
- 71. Cathepsin B inhibition interferes with metastatic potential of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2925371/]
- 72. Cathepsin B but not cathepsins L or S contributes to ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/12918016/]
- 73. Cathepsin B Is Up-Regulated and Mediates Extracellular ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0068668]
- 74. Photodynamic Quenched Cathepsin Activity Based Probes ... [https://www.thno.org/v05p0847.htm]
- 75. Activation of Cytosolic Cathepsin B Activity in the Brain by Traumatic... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11969537/]
- 76. Discovery of pH-Selective Marine and Plant Natural Product ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9330179/]
- 77. Lysosome Function Analysis - Selection Guide for Detection and... [https://www.dojindo.com/contents/lysosomal_function_analysis.html]
- 78. for Lysosomes, Peroxisomes... | Thermo Fisher Scientific - RU Probes [https://www.thermofisher.com/ru/ru/home/references/molecular-probes-the-handbook/probes-for-organelles/probes-for-lysosomes-peroxisomes-and-yeast-vacuoles.html]
- 79. A lysosomal chloride ion- selective fluorescent probe for biological... [https://pubs.rsc.org/en/content/articlelanding/2019/sc/c8sc04084b]
- 80. Stefin A Regulation of Cathepsin B Expression and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12524445/]
- 81. Inhibition of cathepsin B activity attenuates extracellular matrix ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3326557/]
- 82. Investigating the performance of a novel pH and cathepsin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8551370/]
- 83. The blood–brain barrier: Structure, regulation and drug ... [https://www.nature.com/articles/s41392-023-01481-w]
- 84. Strategies for delivering drugs across the blood-brain ... [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 85. Drug Delivery Across the Blood–Brain Barrier: A New Strategy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11677317/]
- 86. Targeted Nanoparticles for Drug Delivery Across the Blood ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12627166/]
- 87. Cathepsin B inhibition blocks amyloidogenesis in the mouse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11910108/]
- 88. Pathology-directed drug delivery strategies [https://www.sciencedirect.com/science/article/pii/S2211383525006938]
- 89. An update on the discovery and development of reversible ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10148018/]
- 90. Recent Advances in Selective and Irreversible Covalent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6886688/]
- 91. Covalent Compounds [https://enamine.net/compound-collections/covalent-compounds]
- 92. Factors affecting irreversible inhibition of EGFR and ... [https://www.nature.com/articles/s42004-025-01501-6]
- 93. The Role of Cysteine Cathepsins in Cancer Progression ... [https://www.mdpi.com/1422-0067/20/14/3602]
- 94. Fluorescent probes towards selective cathepsin B ... [https://www.sciencedirect.com/org/science/article/pii/S2041652023046916]
- 95. Patient-derived xenograft models: Current status, challenges ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12179623/]
- 96. Patient-derived xenograft models in cancer therapy [https://www.nature.com/articles/s41392-023-01419-2]
- 97. Mouse xenograft models vs GEM models for human cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2562196/]
- 98. All (animal) models (of neurodegeneration) are wrong. Are ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6279414/]
- 99. Lost in translation: Inconvenient truths on the utility of ... [https://elifesciences.org/articles/90633]
- 100. Statistical analysis of comparative tumor growth repeated ... [https://www.nature.com/articles/s41598-021-87470-x]
- 101. Approaches to modeling cancer metastasis: from bench to ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1602489/full]
- 102. Synthesis and In Vitro Evaluation of a Scandium-44 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12196724/]
- 103. Enhancing fluorescent design through multilayer interaction... probe [https://pubs.rsc.org/en/content/articlelanding/2025/sc/d4sc08695c]
- 104. Versatile Bifunctional PYTA Derivatives for 225Ac Radiolabeling [https://jnm.snmjournals.org/content/early/2025/07/10/jnumed.125.270234]
- 105. Synthesis, radiolabeling, and biological evaluation of methyl 6 ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra00693g]
- 106. Blue Shifted Carbon Dots-Based Fluorescent for Determination... Probe [https://link.springer.com/article/10.1007/s10895-025-04618-y]
- 107. Article: Applicability and Prospects of FLAIRS... | Konica Minolta [https://research.konicaminolta.com/en/report/2025/technical-papers/applicability-and-prospects-of-flairs-a-highly-advanced-multidimensional-data-analysis-technology-utilizing-fluorescent-probes/]
- 108. Computational analysis of the cathepsin B inhibitors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2735608/]
- 109. Validation approaches for computational drug repurposing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10785886/]
- 110. Computational Drug Repurposing: Approaches and Case ... [https://www.drugpatentwatch.com/blog/computational-drug-repurposing-approaches-and-case-studies/?srsltid=AfmBOorHkW4lvrL9Kef25xXaV2-hmOCYOWsp60J7uDqUd36WfS6jRa5Q]
- 111. Computational characterization of phytochemical inhibitors ... [https://www.sciencedirect.com/science/article/abs/pii/S0167732225005902]
- 112. Computational drug repurposing reveals Alectinib as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12504298/]
- 113. Use of Drug Sensitisers to Improve Therapeutic Index in ... [https://www.mdpi.com/1999-4923/16/7/928]
- 114. Why 90% of clinical drug development fails and how to ... [https://www.sciencedirect.com/science/article/pii/S2211383522000521]
- 115. Advancing Drug Safety in Drug Development - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11187637/]
- 116. Review of Cathepsin K Inhibitor Development and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11721202/]
- 117. Determining the Balance Between Drug Efficacy and Safety by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6220079/]
- 118. Cathepsin-Targeting SARS-CoV-2 Inhibitors - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10863444/]
- 119. Cathepsin C: a critical mediator between immune response ... [https://pubmed.ncbi.nlm.nih.gov/41065194/]