Fetal Hemoglobin Reactivation: From Genomic Mechanisms to Next-Generation Therapies for Sickle Cell and Thalassemia
This article provides a comprehensive analysis of fetal hemoglobin (HbF) reactivation as a therapeutic strategy for β-hemoglobinopathies.
Fetal Hemoglobin Reactivation: From Genomic Mechanisms to Next-Generation Therapies for Sickle Cell and Thalassemia
Abstract
This article provides a comprehensive analysis of fetal hemoglobin (HbF) reactivation as a therapeutic strategy for β-hemoglobinopathies. It explores the foundational biology of globin switching, evaluates cutting-edge methodologies from CRISPR-based gene editing to novel pharmacological and oligonucleotide approaches, and addresses critical optimization challenges including safety and accessibility. Through comparative validation of different molecular targets and therapeutic platforms, we synthesize a roadmap for developing effective, scalable treatments for sickle cell disease and β-thalassemia, addressing both scientific and implementation barriers for research and drug development professionals.
The Molecular Basis of Globin Switching: From Developmental Biology to Therapeutic Insight
In humans, the composition of hemoglobin undergoes two critical developmental transitions. The final switch, from fetal hemoglobin (HbF, α2γ2) to adult hemoglobin (HbA, α2β2), represents a fundamental paradigm of developmental gene regulation and a pivotal therapeutic target for the β-hemoglobinopathies [1] [2]. This switch, which occurs perinatally and is largely complete by approximately six months of age, is of profound clinical importance because the persistence or reactivation of HbF can significantly ameliorate the clinical manifestations of both sickle cell disease (SCD) and β-thalassemia [1] [2]. In SCD, HbF inhibits the polymerization of sickle hemoglobin (HbS), thereby reducing red blood cell sickling. In β-thalassemia, increased HbF compensates for the deficient or absent production of adult β-globin chains [3] [4]. Consequently, understanding the molecular machinery that silences γ-globin gene expression is a central focus of modern hematology research, with the goal of developing targeted therapies to reverse this developmental switch.
Molecular Regulation of Globin Gene Switching
The fetal-to-adult hemoglobin switch is orchestrated by a complex network of transcriptional regulators, chromatin remodeling, and three-dimensional genome architecture. The core principle involves the coordinated silencing of the fetal γ-globin genes (HBG1 and HBG2) and the activation of the adult β-globin gene (HBB) within the β-globin locus on chromosome 11.
Key Transcriptional Repressors
Research over the past decade has identified several key transcriptional repressors that are essential for γ-globin silencing.
Table 1: Major Transcriptional Repressors in Globin Switching
| Repressor | Function & Mechanism | Therapeutic Relevance |
|---|---|---|
| BCL11A [3] | A zinc-finger protein that acts as a master repressor of HBG1/2. Its expression is controlled by a critical erythroid-specific enhancer. | A primary target for gene therapy. Disruption of its enhancer via CRISPR/Cas9 effectively reactivates HbF. |
| ZBTB7A/LRF [5] | A zinc-finger and BTB domain transcription factor that binds directly to the γ-globin promoters to mediate repression. | CRISPR-mediated disruption of its binding site in the γ-globin promoter potently reactivates HbF. |
| MBD2-NuRD [6] | A methyl-DNA binding protein that recruits the NuRD co-repressor complex, establishing a repressive chromatin state at the γ-globin promoters. | Genetic ablation of MBD2, but not its homolog MBD3, robustly induces HbF with minimal impact on erythropoiesis. |
Chromatin and 3D Genome Architecture
The β-globin locus is regulated by a distal super-enhancer known as the Locus Control Region (LCR). The LCR is essential for high-level expression of all β-like globin genes and communicates with gene promoters through chromatin looping [1] [7]. A pivotal discovery is that the BCL11A erythroid enhancer forms a specific three-dimensional "chromatin rosette" structure, which brings multiple regulatory elements into close proximity to ensure high-level BCL11A expression [3]. CRISPR-Cas9-mediated gene therapy introduces a double-strand break in this enhancer, which disrupts the rosette structure. This disruption allows repressive proteins to access the locus, leading to BCL11A silencing and subsequent HbF reactivation [3]. The formation and maintenance of this structure also depend on a special class of enhancer-derived RNA (eRNA), offering another potential therapeutic node [3].
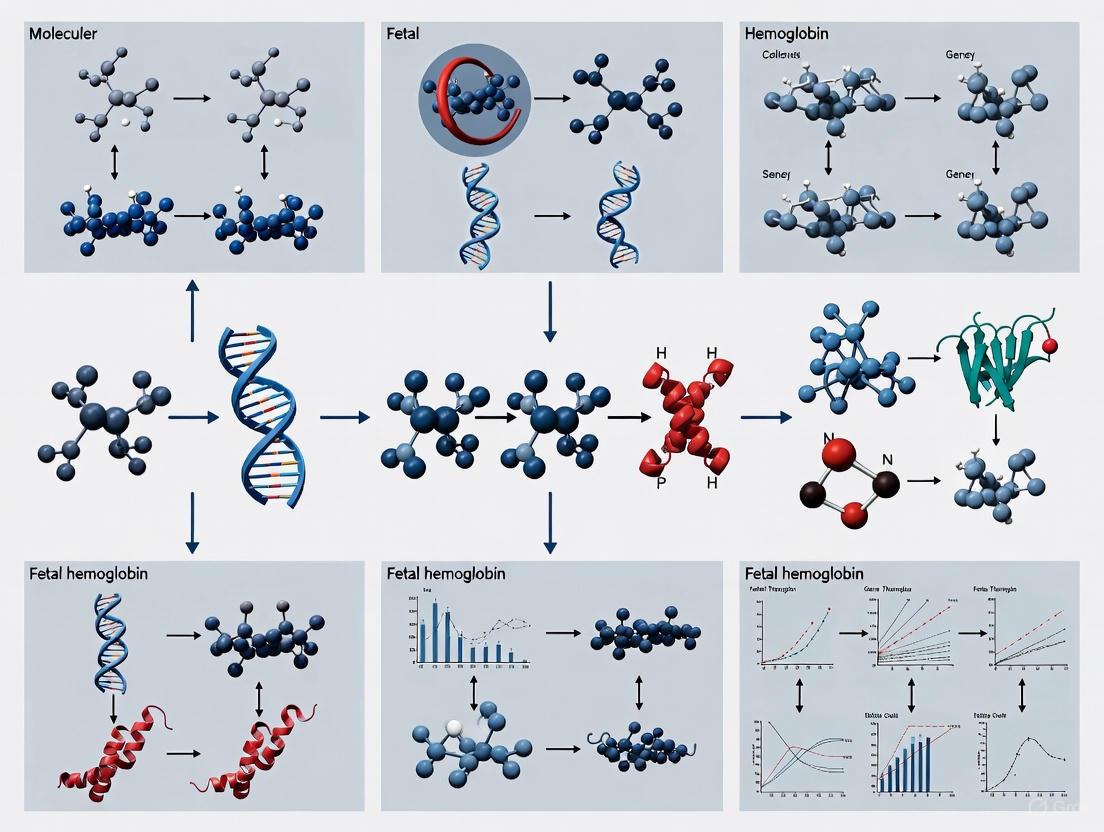
The following diagram illustrates the core regulatory pathway governing the fetal-to-adult hemoglobin switch and the primary therapeutic intervention strategies.
Quantitative Data from Therapeutic Strategies
Multiple therapeutic strategies have been developed to reactivate fetal hemoglobin by targeting the repressors outlined above. The following table summarizes quantitative data from recent experimental and clinical approaches.
Table 2: Efficacy of HbF Reactivation Strategies in Preclinical/Clinical Studies
| Therapeutic Approach | Target | Model System | Editing Efficiency (Indels) | Resulting HbF Increase |
|---|---|---|---|---|
| ZFN Editing [8] | BCL11A Erythroid Enhancer | Healthy Donor HSPCs | 75.3% | ~3-fold increase in γ-globin protein |
| ZFN Editing [8] | BCL11A Erythroid Enhancer | SCD Donor HSPCs | 64.2% | ~2-3-fold increase in γ-globin protein |
| CRISPR/Cas9 [5] | BCL11A site in HBG Promoter (-115) | Healthy Donor HSPCs | 84.9% ± 17.1% | 26.2% ± 1.4% of total Hb |
| CRISPR/Cas9 [5] | ZBTB7A site in HBG Promoter (-197) | Healthy Donor HSPCs | 69.4% ± 7.4% | 27.9% ± 1.5% of total Hb |
| CRISPR/Cas9 [5] | BCL11A site in HBG Promoter (-115) | β0-thalassemia/HbE HSPCs | 88.5% ± 3.1% | 62.7% ± 0.9% of total Hb |
| CRISPR/Cas9 [5] | ZBTB7A site in HBG Promoter (-197) | β0-thalassemia/HbE HSPCs | 68.2% ± 12.2% | 64.0% ± 1.6% of total Hb |
Abbreviations: ZFN: Zinc Finger Nuclease; HSPCs: Hematopoietic Stem and Progenitor Cells; SCD: Sickle Cell Disease; Indels: Insertions/Deletions.
Experimental Workflows for HbF Reactivation
To facilitate research replication and development, this section outlines detailed protocols for key experiments in the field.
Protocol: CRISPR-Cas9-Mediated Disruption of Repressor Binding Sites
This protocol is adapted from studies that successfully reactivated HbF by editing the HBG promoter [5].
- Isolation of CD34+ HSPCs: Collect hematopoietic stem/progenitor cells from healthy donors or patients via bone marrow harvest or mobilization of peripheral blood using an approved agent like plerixafor (especially for SCD patients, where G-CSF is contraindicated).
- Electroporation with RNP Complex: Electroporate the CD34+ HSPCs with a pre-formed ribonucleoprotein (RNP) complex. The complex consists of:
- Cas9 Nuclease: Purified recombinant protein.
- sgRNA: Synthetic single-guide RNA targeting the desired site (e.g., for the ZBTB7A binding site at -197:
sg-LRF; for the BCL11A binding site at -115:sg-BCL11A).
- In Vitro Erythroid Differentiation: Culture the edited HSPCs in a staged, serum-free erythroid differentiation medium. A standard protocol involves:
- Phase 1 (Expansion): Culture for 7-8 days with cytokines (SCF, IL-3, EPO).
- Phase 2 (Differentiation): Culture for an additional 10-12 days with EPO to enucleate the cells.
- Assessment of Outcomes:
- Editing Efficiency: Genomic DNA is harvested post-editing. The target site is amplified by PCR and analyzed by deep sequencing to quantify the frequency of insertions and deletions (indels).
- HbF Expression: Differentiated erythroid cells are analyzed using:
- HPLC: Cation-exchange HPLC to quantify the percentage of HbF relative to total hemoglobin.
- qRT-PCR: To measure the fold-increase in γ-globin mRNA transcripts.
- Flow Cytometry: Using an antibody against HbF to determine the frequency of F-cells.
Protocol: Targeting Enhancer RNA with Antisense Oligonucleotides (ASOs)
This protocol is based on the discovery that the BCL11A enhancer produces a functional RNA [3].
- Cell Culture: Maintain human erythroid progenitor cells (e.g., derived from CD34+ HSPCs or an erythroid cell line like HUDEP-2) in appropriate culture medium.
- ASO Transfection: Transfect cells with chemically modified antisense oligonucleotides (ASOs) designed to be complementary and induce degradation of the specific BCL11A enhancer-derived RNA. Scrambled or non-targeting ASOs should be used as a negative control.
- Functional Analysis:
- Molecular Confirmation: Use qRT-PCR to confirm the reduction in the target enhancer RNA levels and a subsequent decrease in BCL11A mRNA.
- Phenotypic Readout: After allowing for erythroid differentiation, measure HbF protein levels via HPLC or flow cytometry, as described in the previous protocol.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for Globin Switching Research
| Reagent / Tool | Function in Research | Example Application |
|---|---|---|
| Mobilized CD34+ HSPCs | Primary human cells that can be differentiated into erythroid lineage; the target for ex vivo gene therapy. | In vitro studies of editing efficacy and erythroid differentiation [8] [5]. |
| Plerixafor | CXCR4 antagonist used to mobilize CD34+ HSPCs from bone marrow to peripheral blood for collection. | Safe mobilization agent for SCD patients, avoiding G-CSF [4] [8]. |
| CRISPR-Cas9 RNP | Pre-complexed Cas9 protein and sgRNA for highly efficient and specific genome editing with reduced off-target effects. | Disruption of BCL11A enhancer or ZBTB7A/BCL11A binding sites in the HBG promoter [5]. |
| Zinc Finger Nuclease (ZFN) mRNA | Alternative gene-editing platform using engineered zinc-finger proteins to create sequence-specific DNA breaks. | Clinical development of BIVV003 therapy targeting the BCL11A enhancer [8]. |
| Erythroid Differentiation Media | Serum-free media with staged cytokine cocktails (SCF, EPO, IL-3) to drive CD34+ HSPCs to mature erythroid cells. | Generating enucleated red blood cells in culture for hemoglobin analysis [8] [5]. |
| Antisense Oligonucleotides (ASOs) | Synthetic nucleic acids designed to bind and degrade a specific RNA target. | Targeting BCL11A enhancer RNA as a non-genetic editing therapeutic strategy [3]. |
The developmental switch from fetal to adult hemoglobin is a precisely orchestrated biological process governed by repressors like BCL11A and ZBTB7A, chromatin modifications, and dynamic 3D genome structures. The detailed elucidation of these mechanisms has been directly translated into revolutionary therapeutic strategies for sickle cell disease and β-thalassemia. The recent approval of the first CRISPR-based gene therapies targeting BCL11A marks a new era. Future research is poised to expand these successes by developing next-generation in vivo gene therapies, small-molecule inhibitors of repressors like MBD2, and other innovative approaches. The ultimate goal is to make safe, effective, and accessible curative treatments available to the global population affected by these severe hemoglobin disorders.
The developmental switch from fetal hemoglobin (HbF) to adult hemoglobin (HbA) represents a critical therapeutic target for the β-hemoglobinopathies sickle cell disease (SCD) and β-thalassemia. Reactivation of HbF through disruption of its transcriptional repressors can compensate for defective or deficient adult β-globin. This whitepaper provides a comprehensive technical analysis of three key repressor systems—BCL11A, ZBTB7A/LRF, and the MBD2-NuRD complex—that collectively silence γ-globin expression. We examine their molecular mechanisms, integrated functions, and experimental approaches for their therapeutic targeting, framing this discussion within the context of developing novel genetic and small-molecule therapies.
The transition from fetal to adult hemoglobin production is orchestrated by a complex network of transcriptional and epigenetic regulators that silence the genes encoding γ-globin (HBG1 and HBG2). BCL11A, ZBTB7A (also known as LRF), and the MBD2-NuRD complex have emerged as potent silencers of HbF expression [9] [10]. These factors operate within a coordinated framework, recruiting chromatin-modifying enzymes and remodeling complexes to establish a repressive chromatin state at the γ-globin promoters. Their independent and combined actions ensure robust silencing of HbF in adult erythroid cells, making them prime targets for therapeutic intervention aimed at reversing this process to ameliorate SCD and β-thalassemia.
Molecular Mechanisms of Key Transcriptional Repressors
BCL11A: A Master Regulator of Hemoglobin Switching
BCL11A is a zinc-finger transcription factor and a critical developmental stage-specific repressor of γ-globin.
- DNA Binding Mechanism: BCL11A binds to the TGACCA motif at positions -118 to -113 in the γ-globin promoter via its C-terminal triple zinc finger domain (ZnF456) [11]. Structural analyses reveal that while zinc fingers 4 and 5 (ZnF4, ZnF5) bind the DNA major groove, ZnF6 interacts non-specifically with the minor groove, providing a positive entropic contribution that stabilizes the complex and is crucial for full repressive activity [11].
- Erythroid-Specific Regulation: BCL11A expression in erythroid cells is controlled by a dedicated enhancer in intron 2, which contains a critical GATA-binding site and forms a specific chromatin "rosette" structure essential for high-level expression [9] [3].
- Therapeutic Targeting: CRISPR-Cas9 disruption of this enhancer disrupts the three-dimensional chromatin structure, leading to BCL11A silencing, HbF reactivation, and successful clinical outcomes for SCD and β-thalassemia [9] [3]. Recent investigations also explore targeting enhancer-derived RNAs with antisense oligonucleotides as a alternative therapeutic strategy [3].
ZBTB7A/LRF: A Partner in Repression
ZBTB7A functions as a complementary repressor to BCL11A within the hemoglobin switching regulatory network.
- Complex Formation: Evidence suggests that ZBTB7A interacts with or is part of a NuRD complex, specifically the MBD3-NuRD variant, to facilitate γ-globin silencing [10]. This places it in a parallel but distinct pathway from BCL11A.
- Coordinated Silencing: While both are potent repressors, ZBTB7A and BCL11A appear to operate through partially independent mechanisms, as the loss of one does not completely abolish the other's function, suggesting a multi-faceted repression system.
MBD2-NuRD Complex: An Epigenetic Silencer
The MBD2-NuRD complex provides a critical link between DNA methylation, chromatin remodeling, and γ-globin silencing.
- Recruitment to the Promoter: The MBD2a isoform binds specifically to methylated CpG dinucleotides in the γ-globin promoter through its methyl-cytosine-binding domain (MBD), with its N-terminal arginine-rich (GR) domain recruiting additional repressive components [12].
- Chromatin Remodeling and Repression: MBD2-NuRD occupancy positions a nucleosome over the γ-globin transcription start site (-110 to +36), creating a closed chromatin configuration that physically excludes the transcriptional activator NF-Y from binding to its CCAAT box motif at position -89 [12].
- Interaction with BCL11A: MBD2-NuRD and BCL11A function as co-factors within a unified silencing complex that also includes the arginine methyltransferase PRMT5, which places the repressive histone mark H3K8me2 at the promoter [12].
Table 1: Core Transcriptional Repressors of Fetal Hemoglobin
| Repressor | Type | Binding Site / Recruitment | Primary Mechanism of Action |
|---|---|---|---|
| BCL11A | Zinc finger transcription factor | TGACCA motif at -118 to -113 of HBG promoter [11] | Direct promoter repression; recruits chromatin modifiers [9] |
| ZBTB7A (LRF) | Transcription factor (POK family) | Not fully characterized | Recruits MBD3-NuRD complex for repression [10] |
| MBD2-NuRD | Methyl-DNA binding complex | Methylated CpGs in HBG promoter [12] | Nucleosome positioning to exclude NF-Y activator; chromatin compaction [12] |
Table 2: Quantitative Effects of Repressor Disruption in Model Systems
| Experimental Manipulation | Model System | Key Outcomes | Reference |
|---|---|---|---|
| BCL11A enhancer editing | Human CD34+ HSPCs | HbF reactivation sufficient to ameliorate SCD phenotype in mice | [9] [3] |
| MBD2 knockout | HUDEP-2 cells | Chromatin opening at HBG promoters; NF-Y binding despite BCL11A presence | [12] |
| BCL11A enhancer disruption | Xenotransplantation into mice | Impaired erythroid expansion; dysregulation of 94 erythroid genes | [13] |
Integrated Model of Repressor Function
The repressors BCL11A, ZBTB7A, and MBD2-NuRD do not function in isolation but form a coordinated, multi-layered silencing network at the γ-globin promoters. A unified model emerges where:
- DNA methylation provides the initial epigenetic signal through methylated CpG dinucleotides in the γ-globin promoter.
- MBD2a-NuRD binds these methylated sites via its MBD domain, while its GR domain recruits PRMT5.
- This complex positions a nucleosome over the transcription start site, creating a closed chromatin state that physically excludes the NF-Y activator.
- BCL11A binds to its cognate site nearby and stabilizes the repressive complex, potentially through direct or indirect interactions with MBD2-NuRD components.
- ZBTB7A functions in a parallel pathway, likely through recruitment of MBD3-NuRD, to ensure redundant silencing control.
This integrated mechanism ensures robust, developmentally appropriate γ-globin silencing in adult erythroid cells, and explains why targeting individual components can partially, but not always completely, reverse silencing.
Experimental Approaches and Methodologies
CRISPR-Based Functional Genomics
CRISPR-Cas9 has enabled precise dissection of repressor functions through several key approaches:
- Enhancer Targeting: Disruption of the BCL11A erythroid enhancer via CRISPR-Cas9 in CD34+ hematopoietic stem and progenitor cells (HSPCs) followed by xenotransplantation into immunodeficient mice to assess erythropoiesis and HbF reactivation [3] [13].
- Saturating Mutagenesis: Systematic mutagenesis of regulatory elements to identify critical transcription factor binding sites, such as the GATA site within the BCL11A enhancer [9].
- Gene Knockout: Complete disruption of repressor genes (e.g., MBD2, BCL11A) in human erythroid cell lines (HUDEP-2) to characterize molecular consequences on chromatin structure and gene expression [12].
Table 3: Key Methodologies for Studying Hemoglobin Repressors
| Methodology | Application | Key Insights Generated |
|---|---|---|
| CRISPR-Cas9 Gene Editing | Disruption of BCL11A enhancer or coding sequence | Demonstrated therapeutic HbF reactivation; revealed essential role in erythropoiesis [9] [13] |
| Chromatin Immunoprecipitation (ChIP) | Mapping transcription factor binding (BCL11A, MBD2, NF-Y) | Defined direct promoter occupancy and nucleosome positioning [12] |
| ATAC-seq | Assessing chromatin accessibility | Revealed closed chromatin at HBG promoters in wild-type vs. open in MBD2KO cells [12] |
| NOMe-seq | Nucleosome positioning and DNA methylation | Showed nucleosome occlusion of TSS in wild-type cells lost in MBD2KO [12] |
| X-ray Crystallography & NMR | Structural analysis of BCL11A DNA-binding domain | Revealed ZnF456 architecture and ZnF6's role in DNA binding [11] |
Protocol: Assessing Chromatin Changes Upon Repressor Disruption
Objective: To evaluate changes in chromatin accessibility and nucleosome positioning at the γ-globin promoter following CRISPR-mediated knockout of MBD2.
Workflow:
- Cell Line: Utilize HUDEP-2 cells (human erythroid progenitor cell line).
- Genetic Modification: Create MBD2 knockout using CRISPR-Cas9 with guides targeting essential exons.
- ATAC-seq Library Preparation:
- Harvest 50,000 viable cells from both wild-type and MBD2KO populations.
- Perform tagmentation using Tr5 transposase (Illumina Tagment DNA TDE1 Enzyme and Buffer Kits).
- Purify and amplify libraries with barcoded primers for multiplexing.
- NOMe-seq Library Preparation:
- Treat nuclei with GpC methyltransferase M.CviPI to mark accessible regions.
- Extract genomic DNA and perform bisulfite conversion.
- Amplify γ-globin promoter region with bisulfite-converted primers and sequence.
- Data Analysis:
- Map ATAC-seq reads to reference genome and call accessible peaks.
- Analyze NOMe-seq data to determine nucleosome positioning patterns.
- Compare wild-type vs. MBD2KO profiles to identify changes in chromatin architecture.
Expected Results: MBD2KO cells should show increased accessibility at HBG promoters and disrupted nucleosome positioning at the transcription start site, allowing NF-Y binding [12].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Studying Hemoglobin Repressors
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| HUDEP-2 cells | Immortalized human erythroid progenitor cell line | In vitro modeling of terminal erythropoiesis and globin regulation [12] |
| CD34+ HSPCs from umbilical cord blood | Primary human hematopoietic stem/progenitor cells | Xenotransplantation studies; therapeutic gene editing validation [13] |
| BCL11A ZnF456 recombinant protein | Structural and DNA-binding studies | X-ray crystallography and NMR to determine DNA-binding mechanism [11] |
| Anti-BCL11A antibody (ab191401) | Chromatin immunoprecipitation | Mapping BCL11A occupancy at γ-globin promoter [11] |
| Anti-MBD2 antibody | Chromatin immunoprecipitation | Demonstrating direct MBD2 occupancy at HBG promoters [12] |
| CRISPR-Cas9 with enhancer-targeting gRNAs | Functional genomic disruption | Targeting BCL11A intron 2 enhancer for HbF reactivation [9] [3] |
| MBD2-specific shRNAs | Knockdown studies | Functional assessment of MBD2 loss in erythroid differentiation [12] |
Therapeutic Implications and Future Directions
The mechanistic understanding of BCL11A, ZBTB7A, and MBD2-NuRD has directly enabled the development of novel therapeutic strategies for β-hemoglobinopathies.
- FDA-Approved Gene Therapy: CRISPR-Cas9 editing of the BCL11A erythroid enhancer in autologous CD34+ HSPCs (exa-cel) represents the first approved genetic therapy for SCD and transfusion-dependent β-thalassemia [10]. This approach disrupts the three-dimensional chromatin structure of the enhancer, leading to BCL11A downregulation and HbF reactivation [3].
- Alternative Molecular Strategies: Research continues into:
- Antisense oligonucleotides targeting BCL11A enhancer RNA [3]
- Small molecule inhibitors disrupting repressor function or complex formation
- Protein degradation approaches such as PROTACs targeting BCL11A
- Considerations and Challenges: Recent findings that BCL11A-deficient erythropoiesis shows impaired expansion in vitro and after xenotransplantation highlight potential clinical consequences of its disruption beyond γ-globin regulation, emphasizing the need for careful therapeutic targeting [13].
The continued elucidation of the intricate relationships between these repressors and their associated complexes will undoubtedly reveal new therapeutic opportunities for safe and effective HbF reactivation in patients with SCD and β-thalassemia.
Hereditary Persistence of Fetal Hemoglobin (HPFH) as a Natural Disease Modifier
Hereditary Persistence of Fetal Hemoglobin (HPFH) is a benign genetic condition characterized by the continued production of fetal hemoglobin (HbF) into adulthood, bypassing the typical developmental switch to adult hemoglobin. This persistent γ-globin expression compensates for defective β-globin chains in sickle cell disease (SCD) and β-thalassemia, significantly ameliorating clinical severity. This whitepaper examines HPFH's molecular genetics, its role as a natural disease modifier, and how this biological mechanism informs the development of CRISPR-based and other therapeutic strategies aimed at HbF reactivation for treating β-hemoglobinopathies.
Hereditary Persistence of Fetal Hemoglobin (HPFH) is a genetically heterogeneous, benign condition in which significant fetal hemoglobin production continues well into adulthood, disregarding the normal shutoff point after which only adult-type hemoglobin should be produced [14] [15]. In healthy individuals, HbF (α2γ2) typically constitutes less than 1% of total hemoglobin after infancy, replaced predominantly by HbA (α2β2) [14]. In HPFH, the percentage of incorrect HbF expression might be as low as 10%–15% or as high as 100% of the total hemoglobin, usually higher in homozygotes than in heterozygotes [14].
The condition is primarily asymptomatic and typically discovered incidentally during screening for other hemoglobin disorders [15] [16]. Its profound clinical significance emerges when co-inherited with SCD or β-thalassemia, where elevated HbF levels inhibit polymerization of HbS in sickle cell disease and compensate for absent or deficient β-globin chains in thalassemia, substantially reducing disease severity [14] [15] [16].
Molecular Genetics and Pathophysiology
Genetic Basis of HPFH
HPFH arises from mutations that disrupt the normal developmental γ-to-β-globin switch. These genetic alterations primarily occur in two categories:
- Deletional HPFH: Large deletions in the β-globin gene cluster (HBB, HBD, HBBP, and HBG1) that remove adult globin genes and their regulatory elements [17].
- Non-deletional HPFH: Point mutations in the promoter regions of fetal γ-globin genes (HBG1 and HBG2) that create binding sites for transcriptional activators (e.g., GATA1, TAL1, KLF1) or disrupt repressor binding sites (e.g., BCL11A, ZBTB7A) [18].
Specific single-nucleotide polymorphisms (SNPs) associated with HPFH have been identified at positions -113, -114, -117, -175, -195, -196, -197, -198, -201, and -202 upstream of HBG1/HBG2 transcription start sites [18]. For instance, mutations at -113A>G create de novo binding sites for GATA1, while -175T>C creates sites for TAL1, and -198T>C for KLF1 [18]. Other mutations, including -114C>T, -117G>A, and -195C>G, disrupt binding sites for the HbF repressors BCL11A and ZBTB7A [18].
The BCL11A Regulatory Axis
BCL11A has emerged as a master transcription factor responsible for fetal hemoglobin silencing during development [3]. This repressor functions within a sophisticated three-dimensional genome architecture where enhancer regions form a chromatin 'rosette' structure, making multiple contacts with critical regulatory elements of the gene to ensure high-level BCL11A expression and prevent its silencing in red blood cell precursors [3]. Disruption of this structure, either naturally in HPFH or therapeutically in CRISPR-based interventions, allows repressive proteins to enter and silence the BCL11A gene, leading to HbF reactivation [3].
Figure 1: Molecular Mechanism of HPFH and HbF Regulation. HPFH mutations disrupt the BCL11A enhancer and chromatin structure, reducing BCL11A expression and subsequent γ-globin repression, thereby increasing HbF production.
HPFH as a Disease Modifier: Quantitative Impact
Modifying Sickle Cell Disease
In sickle cell disease, elevated HbF levels directly inhibit the polymerization of HbS, the fundamental pathophysiological process underlying this disorder [14] [15]. The protective effect is substantial – even modest increases in HbF can significantly ameliorate clinical severity. Individuals with sickle cell trait who inherit HPFH demonstrate approximately 40% HbS with the remainder as normal HbA, where the HbA form interferes with HbS polymerization [14]. A study of a black family with a unique form of HPFH producing 3%-8% HbF in heterozygotes revealed that a sickle cell homozygote who had apparently inherited the HPFH determinant had 20.3% HbF, substantially modifying disease expression [19].
Modifying β-Thalassemia
In β-thalassemia, HPFH compensates for deficient β-globin synthesis by maintaining γ-globin production, which pairs with excess α-globin chains to form functional HbF tetramers. This reduces the α:non-α-globin chain imbalance that drives ineffective erythropoiesis and hemolysis [14] [17]. The quantitative effect is dramatic – homozygous HPFH individuals typically have HbF levels approaching 100% with only mild erythrocytosis as compensation [14]. Case reports describe individuals with homozygous HPFH exhibiting HbF levels of 94.90% while remaining completely asymptomatic [14].
Table 1: HPFH Genetic Profiles and Associated HbF Levels
| Genetic Profile | Average HbF Percentage | Clinical Impact | Population Prevalence |
|---|---|---|---|
| Heterozygous HPFH | 10%-30% [14] | Asymptomatic, benign [16] | ~0.1% in African populations [14] |
| Homozygous HPFH | Up to 100% [14] | Asymptomatic, mild erythrocytosis [14] | Extremely rare [14] |
| HPFH with Sickle Cell Trait | 3%-8% in heterozygotes, 20.3% in homozygotes [19] | Significant reduction in sickling [19] | Uncommon [19] |
| HPFH with β-thalassemia | Varies by mutation | Ameliorates anemia severity [17] | Depends on population prevalence |
Table 2: Therapeutic Approaches Leveraging the HPFH Mechanism
| Therapeutic Approach | Molecular Target | Mechanism of Action | Development Status |
|---|---|---|---|
| CRISPR/AAV6-mediated HPFH mutation introduction | HBG1/HBG2 promoters | Introduces natural HPFH mutations via homologous recombination [18] | Preclinical validation in HUDEP-2 cells and primary HSPCs [18] |
| BCL11A enhancer editing | BCL11A erythroid enhancer | Disrupts 3D chromatin structure, silences BCL11A [3] | Approved therapy (2024) [20] |
| Delete-to-recruit technology | Genomic distance between enhancer and fetal genes | Brings fetal globin genes closer to enhancers [20] | Early research stage [20] |
| Antisense oligonucleotides | BCL11A enhancer RNA | Degrades enhancer RNA, silences BCL11A [3] | Preclinical research [3] |
Experimental Models and Research Methodologies
Recent advances have enabled researchers to precisely recreate natural HPFH mutations in model systems to study their therapeutic potential. The following protocol outlines a representative methodology for introducing HPFH mutations in hematopoietic stem and progenitor cells (HSPCs):
Experimental Protocol: Introduction of HPFH Mutations in HSPCs
Guide RNA Design: Design synthetic sgRNAs targeting the BCL11A binding site in HBG1/HBG2 promoters, using chemically modified sgRNAs for enhanced stability and on-target efficiency [18].
Donor Template Construction: Design single-stranded AAV6 homology repair vectors (HBG1 AAV6 and HBG2 AAV6) containing approximately 800-bp homologous arms flanking the Cas9 RNP-induced cut site, incorporating HPFH mutations -113A>G, -114C>T, -117G>A, -175T>C, -195C>G, and -198T>C [18].
Cell Transfection:
- Use a Neon Transfection System for electroporation
- Electroporate approximately 5×10^5 CD34+ cells with Cas9-ribonucleoprotein (RNP) complexes
- Immediately add AAV6 homology donor vectors post-electroporation [18]
Efficiency Validation:
- Measure insertion/deletion (InDel) frequencies and homologous recombination efficiency via next-generation sequencing (NGS)
- Validate using fluorescent markers (GFP/mCherry) incorporated in donor vectors [18]
Functional Assessment:
- Differentiate edited HSPCs toward erythroid lineage
- Quantify γ-globin/β-like globin mRNA expression using RT-qPCR
- Measure HbF percentage via ion-exchange high-performance liquid chromatography (HPLC) [18]
In Vivo Validation:
- Transplant edited CD34+ cells into immunodeficient B-NDG hTHPO mice
- Analyze bone marrow for human cell chimerism and multi-lineage differentiation 16 weeks post-transplantation [18]
This approach has demonstrated efficient editing, with studies reporting 62.75% ± 0.93% InDel formation and successful homologous recombination leading to significantly increased γ-globin expression during erythroid differentiation [18].
Figure 2: Experimental Workflow for Introducing HPFH Mutations. This diagram outlines the key steps in CRISPR/Cas9-mediated introduction of natural HPFH mutations into hematopoietic stem cells for therapeutic development.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for HPFH and HbF Reactivation Studies
| Reagent / Tool | Function | Example Application |
|---|---|---|
| CRISPR/Cas9 RNP complexes | Site-specific DNA cleavage | Disrupting BCL11A binding sites in HBG promoters [18] |
| AAV6 homology donors | Delivery of HPFH mutation templates | Introducing specific HPFH mutations via homologous recombination [18] |
| CD34+ hematopoietic stem cells | Primary human target cells | Evaluating editing efficiency and HbF reactivation in relevant models [18] |
| HUDEP-2 cells | Immortalized erythroid precursor cell line | Initial testing of editing strategies [18] |
| B-NDG hTHPO mice | Immunodeficient humanized mouse model | In vivo assessment of edited HSPC engraftment and differentiation [18] |
| Ion-exchange HPLC | Quantification of hemoglobin variants | Precise measurement of HbF percentages [18] |
| Next-generation sequencing | Analysis of editing efficiency and specificity | Quantifying InDel formation and HDR rates [18] |
| Flow cytometry with HbF antibodies | Detection of F-cells | Measuring proportion of HbF-producing erythrocytes [19] |
Emerging Therapeutic Strategies Inspired by HPFH
CRISPR-Based BCL11A Targeting
The first approved CRISPR-based therapy for SCD leverages the HPFH mechanism by targeting the BCL11A enhancer region in blood stem cells [3]. This approach induces double-strand breaks that disrupt the three-dimensional chromatin 'rosette' structure required for maintaining high-level BCL11A expression [3]. Without this structure, repressive proteins silence BCL11A, leading to HbF reactivation that compensates for defective adult hemoglobin in sickle cell disease and β-thalassemia [3].
Novel Genome Editing Approaches
Beyond BCL11A disruption, several innovative strategies are emerging:
Enhancer RNA targeting: Using antisense oligonucleotides to selectively degrade BCL11A enhancer RNA, achieving effects similar to gene therapy without permanent genome modification [3].
"Delete-to-recruit" technology: Employing CRISPR-Cas9 to remove intervening DNA sequences, physically bringing fetal globin genes closer to enhancers to reactivate their expression [20].
Base editing and prime editing: Utilizing newer CRISPR platforms that enable more precise nucleotide conversions without double-strand breaks, potentially offering safer therapeutic profiles [21].
Clinical Implications and Diagnostic Considerations
The diagnostic recognition of HPFH is crucial in genetic counseling, particularly in populations with high prevalence of hemoglobinopathies. Cases have been reported where a pregnant woman presented with elevated HbF (14.5%), initially creating diagnostic challenges until comprehensive molecular investigation revealed heterozygosity for HPFH in the mother and beta thalassemia trait in the father [17]. Prenatal diagnosis in such cases requires sophisticated techniques like multiplex ligation-dependent probe amplification (MLPA) and hemoglobinopathy gene panel sequencing to distinguish HPFH from other conditions with elevated HbF, such as δβ-thalassemia [17].
While HPLC efficiently screens for hemoglobinopathies, comprehensive molecular investigations are essential for precise diagnosis and optimal medical management, particularly in reproductive planning and prenatal diagnosis [17].
HPFH represents a powerful natural proof-of-concept for therapeutic HbF reactivation in β-hemoglobinopathies. The molecular characterization of this condition has fundamentally advanced our understanding of globin gene regulation and hemoglobin switching, directly enabling the development of transformative genetic therapies. Current research continues to refine these approaches, with efforts focused on improving precision, safety, and accessibility.
Future directions include optimizing delivery systems such as lipid nanoparticles and engineered exosomes [21], enhancing the specificity of gene editing platforms like base editors and prime editors [21], and developing non-viral delivery methods to reduce costs and broaden availability [3] [20]. As these technologies mature, the natural phenomenon of HPFH will continue to illuminate the path toward curative treatments for sickle cell disease and β-thalassemia worldwide.
Three-Dimensional Genome Architecture in γ-Globin Gene Regulation
The three-dimensional (3D) organization of the genome plays a pivotal role in the spatiotemporal control of gene expression, with profound implications for developmental processes and disease therapeutics. In the context of hemoglobinopathies, understanding the architectural regulation of the β-globin locus has emerged as a critical frontier for developing novel treatments. This technical review examines how nuclear architecture governs the developmental switching from fetal (γ-globin) to adult (β-globin) hemoglobin expression. We synthesize current evidence demonstrating that chromatin looping, topological domains, and nuclear compartmentalization create precise regulatory environments that control γ-globin gene silencing and reactivation potential. Within the framework of therapeutic strategies for sickle cell disease and β-thalassemia, this review highlights how recent advances in 3D genomics are revealing novel molecular targets for fetal hemoglobin reactivation through targeted disruption of repressive chromatin structures.
The human genome is packaged into a sophisticated 3D architecture within the nucleus, far beyond a simple linear arrangement of genetic elements. This organization encompasses hierarchical structural features including chromatin loops, topologically associating domains (TADs), and nuclear compartments that collectively regulate gene expression patterns by modulating physical interactions between genomic elements [22] [23]. In erythroid cells, this architectural framework is particularly crucial for the coordinated expression of globin genes during development, as it enables precise communication between distant regulatory elements and gene promoters across the β-globin locus.
The β-globin locus spans approximately 100 kb on chromosome 11 and contains five functional genes (ε, Gγ, Aγ, δ, and β) that are expressed in a developmental stage-specific manner, alongside a master locus control region (LCR) located upstream of the cluster [22] [24]. The LCR contains multiple DNase I hypersensitive sites (HSs) that function as powerful enhancers essential for high-level globin gene expression. Traditional linear models of gene regulation failed to fully explain how the LCR specifically activates different globin genes during development. It is now established that the 3D architecture of this locus facilitates stage-specific interactions between the LCR and active globin gene promoters through chromatin looping, while excluding silent genes from these regulatory hubs [22] [24].
Methodological Approaches for Studying 3D Genome Architecture
Investigating chromatin architecture requires specialized molecular and computational approaches that capture spatial proximity information between genomic elements. The following table summarizes key methodologies employed in studying 3D genome organization with particular relevance to the β-globin locus:
Table 1: Key Methodologies for 3D Genome Analysis
| Method | Principle | Application in Globin Research | Resolution |
|---|---|---|---|
| 3C (Chromosome Conformation Capture) | Crosslinking, digestion, ligation, and quantification of interaction frequency between two specific loci [22] | Validation of specific LCR-promoter interactions [22] | 1-vs-1 |
| 4C (Circular Chromosome Conformation Capture) | Inverse PCR-based method to identify all genomic regions interacting with a single "bait" sequence [22] | Uncovering genome-wide interaction partners of the β-globin LCR [24] | 1-vs-all |
| Hi-C | Genome-wide version of 3C that captures all-vs-all chromatin interactions [22] [24] | Mapping global chromatin architecture in fetal versus adult erythroblasts [24] | Genome-wide |
| ChIA-PET (Chromatin Interaction Analysis with Paired-End Tag Sequencing) | Combines chromatin immunoprecipitation with proximity ligation to map interactions mediated by specific protein factors [22] | Identifying transcription factor-mediated loops (e.g., ERα) [22] | Protein-specific |
| Capture-C | Multiplexed 3C derivative using oligonucleotide capture for high-resolution interaction profiling [24] | High-resolution mapping of the β-globin locus architecture [24] | Targeted high-resolution |
| ATAC-seq (Assay for Transposase-Accessible Chromatin with Sequencing) | Maps open chromatin regions using hyperactive Tn5 transposase [25] | Identifying accessible regulatory elements in fetal versus adult erythroblasts [25] | Chromatin accessibility |
Figure 1: Experimental workflow for 3D genomics technologies. Common chromosome conformation capture (3C) methods begin with formaldehyde crosslinking to preserve chromatin interactions, followed by restriction enzyme digestion, proximity ligation, and high-throughput sequencing to map genome architecture at different resolutions and specificities.
Architectural Proteins and Chromatin Looping in Globin Regulation
Chromatin looping represents a fundamental mechanism whereby distal regulatory elements physically interact with target gene promoters through protein-mediated bridges. At the β-globin locus, multiple protein factors have been identified as critical mediators of chromatin architecture:
CTCF and Cohesin: The architectural protein CTCF, frequently in complex with cohesin, plays a pivotal role in establishing chromatin loop boundaries and facilitating long-range interactions. CTCF binding sites flanking the β-globin locus help define its structural domain and facilitate LCR-promoter looping [22]. Genome-wide studies reveal CTCF bound at cohesin binding sites across the mammalian genome, suggesting cohesin's involvement in maintaining long-range chromatin structures [22].
Transcription Factors: Erythroid-specific transcription factors including GATA1, TAL1, LMO2, and LDB1 form multi-protein complexes that mediate enhancer-promoter interactions. LDB1 is particularly crucial as it functions as a scaffold protein that stabilizes looping interactions [26]. Forced recruitment of LDB1 to the γ-globin promoter can sustain active chromatin looping even in adult erythroid cells [26].
BCL11A: A master repressor of γ-globin expression that functions partly through architectural reorganization. BCL11A facilitates the formation of repressive chromatin loops that exclude the LCR from γ-globin promoters in adult erythroid cells [24]. Deletion of BCL11A or its binding sites results in profound reconfiguration of locus topology resembling fetal-stage architecture [24].
NFIX: Recently identified as a novel fetal hemoglobin repressor through ATAC-seq comparisons of fetal and adult erythroid cells [25]. NFIX expression is significantly elevated in adult versus fetal erythroblasts, and its knockdown robustly reactivates γ-globin expression by altering chromatin accessibility and DNA methylation at the HBG promoter [25].
The dynamic nature of chromatin looping is exemplified during the fetal-to-adult hemoglobin switch. In fetal erythroblasts, the LCR preferentially interacts with the active γ-globin promoters, while in adult erythroblasts, these contacts shift to the β-globin promoter [24]. This developmental switching of loop configurations is orchestrated by coordinated changes in the composition and binding of architectural protein complexes.
Comparative Chromatin Architecture in Fetal versus Adult Erythroblasts
Global chromatin architecture is remarkably conserved between fetal and adult erythroblasts, with only approximately 5% of the genome switching between active (A) and inactive (B) compartments during this developmental transition [24]. This stands in stark contrast to the more dramatic architectural reorganization observed during lineage specification, where 28-36% of compartments switch states [24]. However, at the local scale of the β-globin locus, significant architectural differences emerge that correlate with developmental gene expression patterns.
Table 2: Chromatin Architectural Features in Fetal versus Adult Erythroblasts
| Architectural Feature | Fetal Erythroblasts | Adult Erythroblasts | Functional Consequence |
|---|---|---|---|
| LCR Contact Preferences | Preferentially contacts γ-globin promoters [24] | Primarily contacts β-globin promoter [24] | Directs enhancer activity to stage-appropriate genes |
| HBBP1-BGLT3 Region Contacts | Contacts with HS5 and 3'HS1 flanking regions [24] | Contacts with embryonic ε-globin region [24] | Separation of fetal genes from enhancer in adult stage |
| BCL11A-Mediated Loops | Absent or diminished [24] | Prominent repressive loops [24] | γ-globin silencing in adult cells |
| TAD Boundaries | Largely conserved [24] | Largely conserved [24] | Stability of genomic neighborhood |
| Compartment Status | ~5% different from adult [24] | ~5% different from fetal [24] | Minor changes in general activity status |
Hi-C and Capture-C analyses have revealed distinctive folding patterns at the developmentally controlled β-globin locus between fetal and adult stages [24]. Specifically, the intergenic region between Aγ- and δ-globin genes (containing HBBP1 pseudogene and BGLT3 noncoding RNA) exhibits stage-specific contact patterns. In fetal cells, this region contacts two distal sites (HS5 and 3'HS1) that flank the locus, while in adult cells, it instead contacts the embryonic ε-globin gene region, effectively separating the fetal globin genes from the LCR [24].
Deletion of the HBBP1 region in adult erythroid cells alters contact landscapes to more closely resemble fetal patterns, with increased LCR-γ-globin contacts and strong reactivation of γ-globin transcription [24]. Notably, the architectural changes and γ-globin reactivation following HBBP1 deletion closely mimic those observed after deletion of the fetal globin repressor BCL11A, suggesting functional interconnection between these elements [24].
Figure 2: Developmental switching of chromatin architecture at the β-globin locus. In fetal erythroblasts, the LCR preferentially loops to active γ-globin genes, while the HBBP1 region contacts flanking sites (HS5, 3'HS1). In adult erythroblasts, BCL11A-mediated repressive complexes reorganize locus architecture, directing LCR contacts to the β-globin gene and creating different HBBP1 interactions that contribute to γ-globin silencing.
Therapeutic Genome Editing Targeting 3D Architecture
The critical role of 3D genome architecture in γ-globin gene regulation has revealed multiple promising targets for therapeutic genome editing in hemoglobinopathies. CRISPR/Cas9-based approaches are being employed to disrupt key regulatory elements and mimic natural hereditary persistence of fetal hemoglobin (HPFH) mutations:
Promoter-Focused Editing: Direct disruption of repressor binding sites in the γ-globin promoters can prevent recruitment of repressive complexes. Editing the ZBTB7A/LRF binding site at position -197 and the BCL11A binding site at position -115 in the γ-globin promoters significantly increases fetal hemoglobin production in both healthy donor cells (to 26-28% HbF) and β0-thalassemia/HbE patient cells (to 62-64% HbF) [5]. The most frequent indels observed are 6-bp deletions at the ZBTB7A/LRF site and 13-bp deletions at the BCL11A site, both effectively disrupting transcription factor binding [5].
HPFH-Mimicking Mutations: Introduction of natural HPFH-associated point mutations can create de novo binding sites for transcriptional activators. The -175T>C HPFH mutation creates a novel E-Box motif that recruits the activator TAL1 along with its cofactors LMO2 and LDB1 to the γ-globin promoter [26]. This recruitment promotes chromatin looping between the LCR and γ-globin promoter, resulting in reactivated fetal globin expression.
Architectural Element Editing: Deleting or modifying structural elements that facilitate repressive chromatin looping can shift locus architecture toward fetal-like configurations. Deletion of the HBBP1 region in adult erythroid cells alters chromatin contact landscapes to more closely resemble fetal patterns, with increased LCR-γ-globin interactions and strongly reactivated γ-globin transcription [24]. Similarly, disruption of BCL11A expression or its enhancer elements produces analogous architectural and transcriptional effects.
Table 3: Therapeutic Genome Editing Strategies for HbF Reactivation
| Editing Strategy | Molecular Target | Mechanism of Action | Efficacy (HbF Increase) |
|---|---|---|---|
| ZBTB7A/LRF Site Disruption | -197 bp in HBG promoter [5] | Prevents repressor binding, reduces transcriptional repression | 27.9% in healthy cells [5] |
| BCL11A Site Disruption | -115 bp in HBG promoter [5] | Disrupts repressive complex formation | 26.2% in healthy cells [5] |
| BCL11A Enhancer Editing | +55, +58, +62 DHSs [5] | Reduces BCL11A expression specifically in erythroid lineage | Variable depending on specific enhancer targeted |
| HPFH Mutation Introduction | -175 position (T>C) [26] | Creates de novo TAL1 binding site, activates γ-globin | 16-41% in natural carriers [26] |
| HBBP1 Region Deletion | Intergenic region between HBG and HBD [24] | Alters chromatin architecture, increases LCR-HBG contacts | Strong γ-globin reactivation [24] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Essential Research Reagents for 3D Genomic Studies of Globin Regulation
| Reagent/Cell Model | Specifications | Research Application | Key References |
|---|---|---|---|
| HUDEP-1 Cell Line | Human umbilical cord blood-derived erythroid progenitor line [25] | Models fetal-type hemoglobin expression; ~85% HbF [25] | [25] |
| HUDEP-2 Cell Line | Adult peripheral blood-derived erythroid progenitor line [25] | Models adult-type hemoglobin expression; ~3% HbF [25] | [25] |
| MEL-BAC Cell Model | Murine erythroleukemia cells with human β-globin BAC [26] | Globin switching studies with fluorescent reporters (dsRED, EGFP) [26] | [26] |
| Primary CD34+ HSPCs | Hematopoietic stem/progenitor cells from BM, PB, or CB [24] [5] | Primary human erythroid differentiation models | [24] [5] |
| CRISPR/Cas9 Systems | RNP complexes with sgRNAs targeting regulatory elements [5] | Genome editing to disrupt repressor binding sites | [5] |
| TAL1/LDB1/LMO2 Antibodies | High-quality ChIP-grade reagents [26] | Chromatin immunoprecipitation of looping complexes | [26] |
| Hi-C & ATAC-seq Kits | Commercial kits for 3D genomics and chromatin accessibility [24] [25] | Mapping chromatin architecture and open chromatin regions | [24] [25] |
The comprehensive understanding of 3D genome architecture in γ-globin gene regulation represents a paradigm shift in our approach to therapeutic intervention for hemoglobinopathies. Rather than targeting single linear elements, current strategies aim to reconfigure the spatial organization of entire genomic loci to achieve therapeutic fetal hemoglobin reactivation. The dynamic and protein-mediated nature of chromatin looping provides multiple entry points for therapeutic manipulation, from disrupting repressor binding sites to introducing activating mutations that rewire enhancer-promoter communications.
Future directions in this field will likely focus on enhancing the specificity and efficacy of architectural editing approaches. This includes developing more precise methods to manipulate chromatin loops without off-target effects, identifying additional structural regulators beyond the known factors like BCL11A and ZBTB7A/LRF, and understanding how cooperative interactions between multiple architectural proteins coordinate locus topology. The recent identification of NFIX as a novel fetal hemoglobin repressor through integrated chromatin accessibility and expression analyses demonstrates the power of multi-omics approaches to reveal new therapeutic targets [25].
As CRISPR-based therapies advance toward clinical application for hemoglobinopathies, incorporating 3D genomic principles will be essential for optimizing therapeutic outcomes. The remarkable success of early clinical trials targeting BCL11A highlights the therapeutic potential of manipulating the nuclear architecture to reactivate fetal hemoglobin. With ongoing advances in genome editing technologies and nuclear imaging, the coming years promise to yield even more sophisticated approaches for therapeutically reprogramming gene expression through targeted reorganization of the 3D genome.
β-hemoglobinopathies, including sickle cell disease and β-thalassemia, represent a major global health burden caused by defects in the adult β-globin gene. The severity of these genetic disorders is profoundly influenced by the natural persistence of fetal hemoglobin (HbF), a compensatory mechanism that can effectively dilute the pathogenic adult hemoglobin. Hereditary Persistence of Fetal Hemoglobin (HPFH), a benign genetic condition, demonstrates that sustained HbF expression beyond the fetal period can significantly ameliorate clinical symptoms [27]. Consequently, research has focused on understanding and therapeutically reversing the developmental switch from fetal to adult hemoglobin, with epigenetic mechanisms emerging as central regulators of this process. Unlike genetic mutations, epigenetic modifications – including DNA methylation and histone modifications – are reversible and control gene expression without altering the underlying DNA sequence, making them particularly attractive therapeutic targets [28] [29]. This whitepaper examines the intricate epigenetic landscape governing HbF silencing and outlines how its targeted manipulation heralds a transformative approach for treating β-hemoglobinopathies.
Molecular Mechanisms of HbF Silencing
The silencing of the γ-globin genes (HBG1 and HBG2), which encode the globin chains of HbF, is orchestrated by a complex interplay of transcriptional repressors and epigenetic machinery. This process ensures the developmental switch from fetal to adult hemoglobin, but can be therapeutically disrupted.
Key Transcriptional Repressors and Their Binding Sites
Two principal transcriptional repressors, BCL11A and ZBTB7A (also known as LRF), are paramount for γ-globin gene silencing [5]. These proteins bind to specific sites within the γ-globin gene promoters:
- The BCL11A binding site is located at approximately -115 nucleotides upstream from the transcription start site.
- The ZBTB7A/LRF binding site is situated at approximately -197 nucleotides upstream from the transcription start site.
Naturally occurring HPFH mutations disrupt these binding sites, preventing repressor attachment and leading to sustained HbF production in adulthood [5]. Furthermore, a novel mechanism involving three-dimensional genome structure has been identified. The enhancer region of BCL11A forms a specific chromatin "rosette" structure that maintains high-level BCL11A expression in red blood cell precursors. Disruption of this structure silences BCL11A and reactivates HbF [3].
Epigenetic Layers of Silencing
The repressors do not function in isolation; they recruit epigenetic modifiers that establish a repressive chromatin state at the γ-globin promoters.
- DNA Methylation: This process involves the addition of a methyl group to cytosine residues in CpG dinucleotides, typically leading to gene silencing. Research demonstrates that DNA methylation directly influences hemoglobin expression, and targeted DNA demethylation of the fetal hemoglobin genes can facilitate HbF reactivation [27].
- Histone Modifications: DNA is wrapped around histone proteins to form chromatin. The addition of repressive histone marks, such as certain types of histone methylation (e.g., H3K27me3), helps maintain the γ-globin genes in a transcriptionally inactive state [21]. Conversely, active genes are associated with histone acetylation.
Table 1: Key Epigenetic Modifications and Their Effects on HbF Expression
| Epigenetic Modification | Effect on Chromatin State | Result on HbF Expression |
|---|---|---|
| DNA Hypermethylation at γ-globin promoters | Condensed, inactive | Silenced |
| DNA Hypomethylation at γ-globin promoters | Open, accessible | Reactivated |
| Repressive Histone Methylation (e.g., H3K27me3) | Condensed, inactive | Silenced |
| Histone Acetylation | Open, accessible | Reactivated |
The following diagram illustrates the coordinated mechanism by which transcriptional repressors and epigenetic machinery silence the fetal hemoglobin genes:
Therapeutic Strategies for Epigenetic Reactivation of HbF
Several innovative therapeutic strategies are being developed to reverse the epigenetic silencing of HbF, ranging from small molecule drugs to precision gene and epigenetic editing.
Small Molecule Epigenetic Drugs
Small molecule inhibitors target the enzymes responsible for writing or reading repressive epigenetic marks. Histone deacetylase inhibitors (HDACi) and DNA methyltransferase inhibitors (DNMTi) have shown potential in reactivating HbF [30] [29]. These drugs can broadly alter the epigenetic landscape, leading to the re-expression of silenced tumor suppressor genes in cancer and HbF in erythroid cells. Several HDACi, such as Vorinostat and Panobinostat, are already FDA-approved for specific cancers, providing a foundation for their potential repurposing [29].
CRISPR-Based Genome Editing
CRISPR-based therapies represent a curative, one-time treatment approach. The first approved CRISPR-based therapy for β-hemoglobinopathies, CASGEVY, disrupts a BCL11A enhancer in hematopoietic stem cells (HSCs) [3] [31]. This disruption occurs not by correcting the mutated HBB gene itself, but by indirectly reactivating HbF. Clinical trials have reported transformative outcomes, with a high percentage of patients achieving transfusion independence for over 5.5 years [31]. The precise mechanism involves CRISPR-Cas9 making a DNA break in the enhancer, which disrupts the critical chromatin rosette structure required for high-level BCL11A expression, leading to its silencing and consequent HbF reactivation [3].
Precision Epigenome Editing
A promising alternative to conventional genome editing is epigenome editing. This strategy aims to reprogram gene expression by rewriting epigenetic signatures without editing the DNA sequence itself, thereby avoiding the risk of unintended mutations [32] [27]. This is typically achieved using a catalytically inactive Cas9 (dCas9) fused to epigenetic effector domains (e.g., a demethylase or acetyltransferase). Research from the Institut Imagine has demonstrated that targeting these tools to the γ-globin promoters can achieve HbF reactivation in hematopoietic stem cells from patients with β-hemoglobinopathies, offering a potentially safer therapeutic avenue [27]. A significant advantage of this approach is its potential reversibility, as epigenetic marks can change over time, unlike permanent DNA sequence changes.
Table 2: Comparison of HbF Reactivation Strategies Targeting Epigenetics
| Therapeutic Strategy | Mechanism of Action | Development Stage | Key Advantages | Key Challenges |
|---|---|---|---|---|
| Small Molecule Inhibitors (e.g., HDACi, DNMTi) | Broad inhibition of epigenetic enzymes | Approved for cancers; preclinical for hemoglobinopathies | Non-invasive; can be administered systemically | Lack of specificity; potential off-target effects |
| CRISPR Genome Editing (e.g., CASGEVY) | Disrupts DNA sequence of repressor binding sites/silencers | Approved therapy | One-time, durable cure | Risk of off-target mutations; complex delivery |
| CRISPR Epigenome Editing | Uses dCas9-effector fusions to modify epigenetic marks | Preclinical research | Does not alter DNA sequence; potentially reversible | Ensuring stability and persistence of epigenetic changes |
The workflow below delineates the key steps involved in developing and implementing an ex vivo epigenome editing therapy for HbF reactivation:
Experimental Protocols for Epigenetic Analysis and Editing
This section provides detailed methodologies for key experiments cited in this whitepaper, enabling researchers to replicate and build upon current findings.
Protocol: CRISPR/Cas9-Mediated Disruption of Repressor Binding Sites
This protocol is adapted from a study that disrupted ZBTB7A or BCL11A binding sites in CD34+ hematopoietic stem/progenitor cells (HSPCs) from healthy donors and β0-thalassemia/HbE patients [5].
- sgRNA Design: Use previously validated sgRNA sequences targeting the ZBTB7A binding site at HBG-197 (sg-LRF: 5'-GAGTCTGGCAAAAGTCAGGC-3') or the BCL11A binding site at HBG-115 (sg-BCL11A: 5'-GCCCAATTCTATCCCCAAGA-3').
- Ribonucleoprotein (RNP) Complex Formation: Complex purified Cas9 protein with the sgRNA at a molar ratio of 1:2 (e.g., 60 pmol Cas9:120 pmol sgRNA) and incubate at 25°C for 10 minutes.
- Electroporation: Electroporate 1-2 x 10^5 mobilized CD34+ HSPCs using the Neon Transfection System (Thermo Fisher Scientific) with the following parameters: 1400 V, 10 ms, 3 pulses.
- Erythroid Differentiation: Culture edited HSPCs in a three-phase erythroid differentiation medium containing SCF, EPO, and IL-3 for 18-21 days.
- Efficiency Assessment:
- Indel Frequency: Analyze editing efficiency 48-72 hours post-electroporation by deep sequencing of the targeted genomic region (e.g., Illumina MiSeq). The study reported editing efficiencies of 57-60% for the ZBTB7A site and 75-92% for the BCL11A site [5].
- HbF Measurement: After differentiation, perform hemoglobin analysis by cation exchange-high-performance liquid chromatography (HPLC) to quantify HbF levels. The cited study reported HbF increases to ~27% in healthy donor cells and ~63% in β0-thalassemia/HbE cells [5].
Protocol: Assessing Epigenetic Marks at the γ-Globin Locus
To correlate HbF reactivation with changes in the epigenetic landscape, the following analyses can be performed on edited or drug-treated erythroblasts.
- DNA Methylation Analysis (Bisulfite Sequencing):
- Treat 500 ng of genomic DNA with sodium bisulfite to convert unmethylated cytosines to uracils.
- Amplify the γ-globin promoter region of interest by PCR using bisulfite-specific primers.
- Clone the PCR products and sequence multiple clones, or perform deep sequencing to determine the percentage of methylation at individual CpG sites.
- Histone Modification Analysis (Chromatin Immunoprecipitation - ChIP):
- Cross-link proteins to DNA in cells using 1% formaldehyde for 10 minutes.
- Lyse cells and sonicate chromatin to shear DNA to fragments of 200-500 bp.
- Immunoprecipitate the chromatin-protein complexes using antibodies specific for the histone modification of interest (e.g., anti-H3K27ac for active marks, anti-H3K27me3 for repressive marks).
- Reverse cross-links, purify DNA, and quantify the enrichment of the γ-globin promoter region relative to a control region via qPCR.
The Scientist's Toolkit: Essential Research Reagents
The table below catalogues key reagents and tools essential for conducting research in HbF epigenetic reactivation.
Table 3: Research Reagent Solutions for HbF Epigenetics Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| CD34+ Hematopoietic Stem/Progenitor Cells | Primary model system for ex vivo editing and differentiation | Source for CRISPR editing and subsequent erythroid differentiation [5] |
| Validated sgRNAs (e.g., sg-LRF, sg-BCL11A) | Target specific genomic loci for CRISPR/Cas9 cutting or dCas9 targeting | Disruption of ZBTB7A or BCL11A binding sites in the γ-globin promoter [5] |
| Recombinant Cas9 and dCas9 Proteins | CRISPR nuclease or epigenetic effector platform | Formation of RNP complexes for electroporation to minimize off-target effects and immune responses [5] |
| dCas9-Epigenetic Effector Fusions | Precision epigenome editing (e.g., dCas9-DNMT3A for methylation, dCas9-p300 for acetylation) | Targeted rewriting of epigenetic marks at the γ-globin locus to reactivate HbF [32] [27] |
| Erythroid Differentiation Media | In vitro culture system to generate mature red blood cells from HSPCs | Functional assessment of HbF production post-editing via HPLC [5] |
| HDAC & DNMT Inhibitors | Small molecule modulators of global epigenetic state | Testing pharmacological reactivation of HbF (e.g., Vorinostat, Panobinostat) [29] |
| HPLC System | Quantitative analysis of hemoglobin subtypes | Precise measurement of HbF levels in differentiated erythroblasts [5] |
| Antibodies for Histone Modifications | Detection and enrichment of specific histone marks via ChIP | Mapping active (H3K27ac) and repressive (H3K27me3) marks at the β-globin locus [21] |
Therapeutic Platforms for HbF Induction: From Genome Editing to Pharmaceutical Intervention
β-hemoglobinopathies, primarily sickle cell disease (SCD) and β-thalassemia, represent the most common monogenic disorders worldwide and are caused by defects in the adult β-globin gene [33] [34]. SCD results from a single nucleotide substitution in the β-globin gene (HBB), replacing glutamic acid with valine at position 6 (p.Glu6Val), which produces hemoglobin S (HbS) that polymerizes under deoxygenated conditions, leading to sickled red blood cells, chronic hemolysis, vaso-occlusive crises, and end-organ damage [33] [35]. β-thalassemia is characterized by either reduced or absent synthesis of β-globin chains, causing an imbalance in the α- and β-globin ratio, precipitation of excess α-globin, ineffective erythropoiesis, and hemolytic anemia [33] [36]. For decades, treatment options have been limited to symptomatic management, hydroxyurea to induce fetal hemoglobin (HbF), chronic blood transfusions, and allogeneic hematopoietic stem cell transplantation (HSCT)—the only curative option but restricted by donor availability and graft-versus-host disease risks [35] [34].
A transformative therapeutic strategy involves reactivating fetal hemoglobin (HbF), a developmentally silenced form of hemoglobin composed of two α-globin and two γ-globin chains (α2γ2) [33] [36]. HbF exhibits potent anti-sickling properties and can functionally compensate for the deficient or abnormal adult β-globin in both SCD and β-thalassemia [36]. Naturally occurring hereditary persistence of fetal hemoglobin (HPFH), a benign condition where individuals maintain elevated HbF levels into adulthood, convincingly demonstrates that high HbF levels correlate with reduced clinical severity in SCD and β-thalassemia [33] [26]. This genetic evidence validated HbF reactivation as a powerful therapeutic goal, galvanizing research into methods to reverse γ-globin silencing in adult erythroid cells [34].
The discovery of BCL11A as a master transcriptional repressor of γ-globin provided a pivotal molecular target [33]. Genome-wide association studies (GWAS) identified BCL11A as a quantitative trait locus for HbF levels, and subsequent functional studies confirmed that BCL11A directly binds to the γ-globin promoters and suppresses their expression in adult erythroid cells [33] [5]. Furthermore, erythroid-specific deletion of BCL11A in mice de-represses γ-globin and reverses the sickling phenotype without perturbing erythropoiesis, establishing BCL11A inhibition as a promising therapeutic strategy [33]. Simultaneously, research identified repressive transcription factor binding sites in the γ-globin promoters for BCL11A and ZBTB7A/LRF, disruption of which can mimic natural HPFH mutations [5] [26]. These foundational insights have paved the way for CRISPR-Cas9 gene editing to engineer durable HbF reactivation by targeting these key regulatory nodes, heralding a new era of autologous, cell-based therapies for hemoglobinopathies [37] [34].
Core Mechanisms and Signaling Pathways
The Molecular Basis of Hemoglobin Switching and Fetal Hemoglobin Repression
Hemoglobin expression is developmentally regulated, with the β-like globin genes (ε, Gγ, Aγ, δ, β) arranged in a cluster on chromosome 11 and expressed in a spatiotemporal manner [33]. The transition from fetal to adult hemoglobin, known as hemoglobin switching, occurs around birth when expression of the γ-globin genes (HBG1 and HBG2) is silenced and the β-globin gene (HBB) is activated [33]. This switch is clinically critical because β-hemoglobinopathies manifest postnatally as γ-globin silencing occurs; thus, inhibiting this switch provides a therapeutic window [33]. The repression of γ-globin in adult erythroid cells is orchestrated by a complex interplay of transcription factors, chromatin modifiers, and three-dimensional genome architecture. The key repressors include:
- BCL11A: A zinc-finger transcription factor that serves as a master repressor. It is recruited to the γ-globin promoters, particularly at the -115 region, where it binds and facilitates transcriptional silencing [33] [5]. BCL11A expression is itself under tight regulation, with a critical erythroid-specific enhancer cluster located in its intron 2 [3] [38].
- ZBTB7A/LRF: Another potent repressor that binds to the γ-globin promoter at the -197 site, collaborating with BCL11A and other co-repressors to maintain γ-globin silencing [5].
- The NuRD Complex: Co-repressor complexes such as the nucleosome remodeling and deacetylase (NuRD) complex, including LSD1, are recruited to the γ-globin promoters, leading to repressive chromatin modifications [36].
A recent groundbreaking discovery revealed that the three-dimensional genome structure is fundamental to BCL11A's regulation and function. The erythroid-specific enhancer within BCL11A intron 2 forms a multi-contact chromatin "rosette" structure, bringing together critical regulatory elements to ensure high-level BCL11A expression and prevent its silencing in red blood cell precursors [3] [38]. Disruption of this enhancer, as achieved in CRISPR-based therapies, destabilizes this rosette, allowing repressive proteins to invade and silence BCL11A, thereby reactivating HbF [3].
Diagram: Mechanism of Fetal Hemoglobin Regulation and CRISPR-Cas9 Therapeutic Intervention. In normal adulthood, a chromatin rosette structure maintains high BCL11A expression, which represses the γ-globin promoter. CRISPR-Cas9 therapy disrupts the BCL11A enhancer, collapsing the rosette, silencing BCL11A, and reactivating γ-globin expression.
Targeting the γ-Globin Promoters: Mimicking Natural HPFH Mutations
An alternative to targeting the BCL11A gene is to directly engineer the HBG promoters to disrupt the binding sites for transcriptional repressors, thereby mimicking natural HPFH-associated mutations [5] [26]. Naturally occurring point mutations in the γ-globin promoters at positions -115 and -175 are associated with elevated HbF levels:
- -115 (HPFH): This cluster of mutations disrupts the BCL11A binding site in the HBG promoter [5].
- -175 (HPFH): This T>C substitution creates a de novo binding site (E-Box) for the transcriptional activator TAL1 [26]. This recruits TAL1 and its cofactors LMO2 and LDB1, promoting chromatin looping between the Locus Control Region (LCR) and the γ-globin promoter, thereby enhancing its transcription [26].
- -197 (HPFH): Mutations at this site disrupt the binding site for the repressor ZBTB7A/LRF [5].
CRISPR-Cas9 can be deployed to introduce indels that disrupt the -115 BCL11A site or the -197 ZBTB7A site, effectively preventing repressor binding and leading to durable HbF reactivation [5]. A more precise strategy involves using base editors or prime editors to install specific HPFH point mutations (e.g., -175T>C) without creating double-strand DNA breaks, offering a potentially safer editing profile [39] [26].
Experimental Approaches and Methodologies
Detailed Protocol: Disrupting the BCL11A Erythroid Enhancer
This protocol outlines the procedure for reactivating HbF by targeting the +58 DNase I hypersensitive site (DHS) within the BCL11A intronic enhancer in human hematopoietic stem and progenitor cells (HSPCs), a strategy underpinning approved therapies [3] [37] [38].
- 1. Source and Isolation of HSPCs: Obtain human CD34+ HSPCs from mobilized peripheral blood, bone marrow, or umbilical cord blood from a patient (for autologous therapy) or healthy donor (for research). Isolate CD34+ cells using clinical-grade magnetic-activated cell sorting (MACS) kits. Maintain cells in serum-free expansion media (e.g., StemSpan) supplemented with cytokines (SCF, TPO, FLT3-L, IL-3) at 37°C and 5% CO₂ [34].
- 2. Design and Preparation of CRISPR-Cas9 Components:
- sgRNA Design: Design a synthetic sgRNA targeting the +58 DHS region in intron 2 of BCL11A (e.g., target sequence per clinical trial designs). A validated sequence is critical.
- RNP Complex Formation: Complex high-fidelity Cas9 protein with the synthetic sgRNA at a molar ratio of 1:2 (e.g., 100 pmol Cas9: 200 pmol sgRNA) in a nuclease-free buffer. Incubate at room temperature for 10-20 minutes to form the ribonucleoprotein (RNP) complex [5].
- 3. Electroporation of CD34+ HSPCs: Pre-stimulate the isolated CD34+ cells in cytokine-containing media for 24-48 hours. Wash and resuspend 1x10⁵ to 1x10⁶ cells in electroporation buffer. Transfer the cell suspension to a cuvette, add the pre-formed RNP complex, and electroporate using a certified device (e.g., Lonza 4D-Nucleofector) with an optimized program (e.g., EO-115 for human CD34+ cells). Include a non-electroporated control and an RNP-free electroporation control to assess viability and editing specificity [34] [5].
- 4. Post-Editing Culture and Transplantation:
- In vitro differentiation: For analytical purposes, culture a portion of the edited cells in erythroid differentiation medium (e.g., containing EPO, SCF, holotransferrin) for 14-18 days to generate erythroblasts for downstream HbF analysis [5].
- In vivo transplantation: For preclinical validation, transplant the edited CD34+ cells into immunodeficient mice (e.g., NSG) via tail vein injection after sublethal irradiation. Monitor engraftment and human chimerism in bone marrow for 16-24 weeks to assess long-term, multi-lineage repopulating potential of edited hematopoietic stem cells (HSCs) [34].
- 5. Analytical and Functional Assessments:
- Editing Efficiency: Genomic DNA is extracted from edited cells. The BCL11A enhancer target site is PCR-amplified and analyzed by deep sequencing (Illumina MiSeq) to quantify indel frequencies and spectra [5].
- HbF Quantification: In differentiated erythroblasts, perform:
- Off-Target Analysis: Perform whole-genome sequencing (WGS) or targeted sequencing of predicted off-target sites to assess the safety profile of the editing strategy [39].
Detailed Protocol: Engineering the γ-Globin Promoter
This protocol describes the disruption of transcriptional repressor binding sites in the HBG promoter to reactivate HbF, suitable for both research and therapeutic development [5].
- 1. Cell Source and Culture: Utilize human CD34+ HSPCs from healthy donors or patients with β-hemoglobinopathies, as described in section 3.1.
- 2. CRISPR-Cas9 Targeting of HBG Promoter:
- sgRNA Selection: Design and validate sgRNAs targeting the -115 region (for BCL11A binding disruption, e.g.,
sg-BCL11A) and/or the -197 region (for ZBTB7A/LRF disruption, e.g.,sg-LRF). These sequences are available in published studies [5]. - RNP Electroporation: Form RNP complexes as in section 3.1. Electroporate CD34+ HSPCs using the same optimized conditions.
- sgRNA Selection: Design and validate sgRNAs targeting the -115 region (for BCL11A binding disruption, e.g.,
- 3. Erythroid Differentiation and Analysis: Differentiate the edited HSPCs into erythroblasts in vitro. After 14-18 days, harvest cells for analysis.
- Molecular Analysis: Extract total RNA, synthesize cDNA, and perform quantitative RT-PCR (qPCR) to measure γ-globin mRNA expression, normalized to housekeeping genes (e.g., GAPDH). Compare to unedited controls [5].
- Hemoglobin Analysis: Use HPLC to quantify the percentage of HbF in the total hemoglobin pool. Edited β-thalassemia/HbE cells have shown HbF levels increasing from a baseline to over 60% post-editing [5].
- 4. Assessment of Erythroid Differentiation and Off-Targets: Use flow cytometry to track the expression of erythroid surface markers (e.g., CD235a, CD71) to ensure that editing does not impair differentiation. Perform targeted deep sequencing of the top in silico predicted off-target sites for the chosen sgRNAs [5].
Comparative Data Analysis of Editing Strategies
The quantitative outcomes of different CRISPR-Cas9 strategies for HbF reactivation are summarized in the tables below, providing a basis for comparing their efficacy and safety profiles.
Table 1: Quantitative Outcomes of BCL11A Enhancer Editing in Clinical and Preclinical Studies
| Cell Type / Study Model | Editing Efficiency (Indel %) | Therapeutic Outcome: HbF Elevation | Key Clinical Endpoint | Source |
|---|---|---|---|---|
| SCD Patient HSPCs (Clinical Trial) | High (Data specific %) | Significant HbF reactivation | Repression of vaso-occlusive crises | [37] |
| β-thalassemia Patient HSPCs (Clinical Trial) | High (Data specific %) | Significant HbF reactivation | Transfusion independence | [37] |
| Human HSPCs (Preclinical) | N/A | HbF reactivation compensating for defective Hb | N/A | [3] |
Table 2: Quantitative Outcomes of γ-Globin Promoter Editing in Preclinical Studies
| Target Site | Cell Type | Editing Efficiency (Indel %) | HbF Level Post-Editing | Off-Target Effects | Source |
|---|---|---|---|---|---|
| BCL11A (-115) | Healthy Donor HSPCs | 75–92% | 26.2 ± 1.4% | Absent | [5] |
| ZBTB7A/LRF (-197) | Healthy Donor HSPCs | 57–60% | 27.9 ± 1.5% | Observed at low frequencies | [5] |
| BCL11A (-115) | β0-thal/HbE HSPCs | 84.9–88.5% | 62.7 ± 0.9% | Absent | [5] |
| ZBTB7A/LRF (-197) | β0-thal/HbE HSPCs | 68.2–69.4% | 64.0 ± 1.6% | Observed at low frequencies | [5] |
| BCL11A-binding motif (tBE base editing) | β-thalassemia HSPCs | N/A | Potent HbF expression | No detectable DNA/RNA off-target | [39] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Resources for BCL11A and HBG Promoter Editing Experiments
| Reagent / Resource | Function / Application | Example Details / Specifications |
|---|---|---|
| Human CD34+ HSPCs | Primary cell source for editing and transplantation. | Sourced from mobilized peripheral blood, bone marrow, or cord blood. |
| CRISPR-Cas9 System | Precision genome editing machinery. | High-fidelity SpCas9 protein complexed with target-specific synthetic sgRNA as RNP. |
| Electroporator System | Delivery of RNP complexes into HSPCs. | Lonza 4D-Nucleofector System with specific cell kit (e.g., P3 Kit). |
| Erythroid Differentiation Media | In vitro generation of erythroblasts from edited HSPCs. | Serum-free media with cytokines: EPO, SCF, IL-3, holotransferrin, dexamethasone. |
| Cation-Exchange HPLC | Quantitative analysis of hemoglobin types (HbA, HbF, HbS). | Validated clinical-grade HPLC systems and protocols. |
| Deep Sequencer | Assessing on-target editing efficiency and screening for off-target effects. | Illumina MiSeq for targeted amplicon sequencing. |
| Flow Cytometer | Analysis of F-cells (HbF+) and erythroid differentiation markers. | Antibodies: anti-HbF, CD235a (Glycophorin A), CD71 (Transferrin receptor). |
| Immunodeficient Mice | In vivo assessment of HSC engraftment and long-term safety/efficacy. | NOD-scid-IL2Rγc⁻¹/⁻ (NSG) mouse model. |
CRISPR-Cas9-mediated editing of the BCL11A enhancer and γ-globin promoter has transitioned from a compelling genetic concept to a transformative clinical reality, offering a one-time, potential functional cure for SCD and β-thalassemia [37]. The direct disruption of the BCL11A erythroid enhancer has proven highly effective in clinical trials, leading to sustained HbF reactivation, transfusion independence in thalassemia, and repression of vaso-occlusive crises in SCD [37]. The recent elucidation of its mechanism—disrupting a critical chromatin rosette structure—not only explains its efficacy but also opens new avenues for therapeutic intervention, such as using antisense oligonucleotides to target enhancer RNAs [3] [38].
Simultaneously, direct engineering of the HBG promoters to disrupt repressor binding sites has demonstrated comparable efficacy in preclinical models, with HbF levels rising to over 60% in edited β-thalassemia/HbE cells [5]. The emergence of next-generation editing tools like base editors (BEs) and prime editors (PEs) further refines this approach, enabling the precise installation of beneficial HPFH point mutations without double-strand breaks, thereby minimizing the risk of genotoxicity and off-target indels [35] [39]. For instance, transformer Base Editor (tBE)-mediated disruption of the BCL11A-binding motif in the HBG promoter achieved potent HbF expression with no detectable DNA or RNA off-target mutations in human HSCs, highlighting a path toward even safer therapies [39].
Despite these remarkable advances, challenges remain. The high cost and complexity of current autologous HSPC transplantation protocols limit global accessibility [3]. Research into in vivo gene editing, where editing components are delivered directly to a patient's HSCs via lipid nanoparticles or viral vectors, aims to bypass the need for myeloablation and complex cell manufacturing, potentially enabling more scalable and affordable treatments [34]. As the field progresses, the continued optimization of editing efficiency, safety, and delivery will be paramount. The pioneering work on BCL11A and γ-globin promoter engineering has unequivocally validated HbF reactivation as a powerful therapeutic paradigm, establishing a robust foundation for the next generation of genetic medicines for hemoglobinopathies and beyond.
The reactivation of fetal hemoglobin (HbF) presents a transformative therapeutic strategy for treating β-hemoglobinopathies, including sickle cell disease and β-thalassemia. These conditions stem from defects in the adult β-globin gene, but naturally occurring hereditary persistence of fetal hemoglobin (HPFH) mutations demonstrate that sustained γ-globin expression can compensate for dysfunctional adult hemoglobin, significantly ameliorating disease severity [40]. Prime editing has emerged as a particularly suitable technology for recapitulating these beneficial HPFH mutations, enabling precise, multiplexed genome editing without introducing double-strand DNA breaks, thus avoiding the large deletions and complex on-target rearrangements that can occur with conventional CRISPR-Cas9 nucleases in the highly homologous γ-globin promoter regions [41] [40].
Prime Editing Platform Optimization for Hematopoietic Cells
Recent advances have substantially improved prime editing efficiency, making therapeutic application in hematopoietic stem and progenitor cells (HSPCs) feasible. Key optimizations include the development of enhanced systems like PEmax and the use of engineered pegRNAs (epegRNAs) with stabilizing motifs such as tevopreQ1, which increase editing efficiency [42]. Furthermore, disrupting the DNA mismatch repair (MMR) pathway, particularly by targeting MLH1, has been shown to dramatically boost precise editing outcomes, with studies reporting up to 95% precise editing in MMR-deficient cell lines [42]. Stable expression of the prime editor components, rather than transient delivery, allows editing to accumulate over time, further increasing the proportion of successfully modified cells [42].
Table: Optimized Components for High-Efficiency Prime Editing in Hematopoietic Cells
| Component | Optimal Version | Function | Impact on Editing Efficiency |
|---|---|---|---|
| Prime Editor | PEmax | Cas9 H840A nickase fused to engineered reverse transcriptase | Higher efficiency than foundational PE2 system [42] |
| Guide RNA | epegRNA (with tevopreQ1 motif) | Specifies target site and encodes the desired edit; engineered for stability | Increases editing efficiency and reliability compared to standard pegRNAs [42] |
| MMR Status | MLH1-disrupted (MMR-deficient) | Disruption of DNA mismatch repair | Dramatically increases precise editing rates (e.g., from ~2% to >80% for some edits) [42] |
| Delivery Method | Stable, constitutive expression | Maintains persistent editor presence in cells | Enables accumulation of edits over time, improving final efficiency [42] |
Target Selection: HPFH-like Mutations in the γ-Globin Promoters
Tiling the proximal promoters of the HBG1 and HBG2 genes using base editors has identified several key regulatory regions where point mutations can potently reactivate γ-globin expression [40]. While established targets include the -115 and -200 regions that disrupt binding sites for repressors BCL11A and ZBTB7A/LRF, recent screens have uncovered novel, potent HPFH-like mutations.
Notably, adenine base editing at positions -123 and -124 of the HBG promoter to create -123T>C and -124T>C mutations has been shown to drive γ-globin expression to levels higher than those achieved by disrupting the known BCL11A binding site [40]. Mechanistically, these mutations create a de novo binding site for the erythroid activator KLF1, illustrating how prime editing can be used not only to disrupt repressors but also to install novel binding elements for transcriptional activators [40]. This highlights the advantage of a multiplexed editing approach, as introducing multiple HPFH-like mutations combinatorially can produce a synergistic increase in γ-globin levels, significantly surpassing the effect of individual mutations [41] [43].
Diagram 1: Mechanism of Prime Editing for Installing HPFH-like Mutations. The prime editor complex, consisting of the PEmax protein and an epegRNA, introduces precise point mutations into the γ-globin promoter through a multi-step process that avoids double-strand breaks [42] [44].
Experimental Workflow and Protocol for HSPCs
A standardized protocol for introducing HPFH-like mutations into patient-derived HSPCs involves several critical steps, from editor delivery to functional validation.
Diagram 2: Experimental Workflow for Prime Editing of Hematopoietic Stem/Progenitor Cells (HSPCs). The process involves isolating target cells, delivering editing components, allowing time for editing, and then differentiating the cells to assess the functional outcome of the edits on fetal hemoglobin production [41] [44].
Detailed Methodologies
Editor Delivery into HSPCs: Electroporate approximately 1x10^5 CD34+ HSPCs (in single-cell suspension) with 250 ng of pegRNA-encoding plasmid and 83 ng of nicking sgRNA-encoding plasmid (for PE3 systems) using a Neon electroporation system (1050V, 30ms, two pulses). Seed transfected cells in erythroid expansion medium supplemented with 10 μM Y-27632 (ROCK inhibitor) for 24 hours [44].
Erythroid Differentiation and HbF Quantification: Culture edited HSPCs in a multi-phase erythroid differentiation medium. Initially, use serum-free expansion media with stem cell factor (SCF), thrombopoietin (TPO), and FLT3 ligand, followed by differentiation media containing erythropoietin (EPO), insulin, and holotransferrin. After 18-21 days of differentiation, harvest erythroblasts for analysis [40]. Quantify HbF-positive cells using flow cytometry with HbF-specific antibodies. Precisely measure γ-globin chain levels via reverse-phase high-performance liquid chromatography (RP-HPLC) [40].
Analysis of Editing Efficiency and Specificity: Extract genomic DNA from cultured cells 3-5 days post-editing. Amplify target loci via PCR and sequence using Sanger or next-generation sequencing (NGS). For Sanger data, use tools like Synthego's ICE (Inference of CRISPR Edits) to quantify indel percentage and knockout scores [45]. Perform off-target analysis using methods such as GUIDE-seq to profile potential off-target sites and whole-genome sequencing (WGS) to confirm the absence of guide RNA-independent mutations, a key advantage of prime editors over base editors [44].
Table: Key Quantitative Outcomes from Prime Editing Studies for HbF Reactivation
| Experimental Setting | Editing Target | Editing Efficiency | γ-globin/HbF Outcome | Key Finding |
|---|---|---|---|---|
| Hematopoietic Cell Line | Multiplexed γ-globin promoter edits | ~50% precise editing | Significantly elevated | High efficiency achieved with optimized parameters [41] |
| Patient HSPCs (Donor Variable) | Multiplexed HPFH-like mutations | Variable among donors | Significantly higher in clones with multiple vs. single mutations | Confirms therapeutic potential of combined strategy [41] [43] |
| MMR-deficient PEmaxKO cells + epegRNA | Model loci (HEK3, DNMT1) | Up to 95% precise editing | Not Applicable | Validates platform optimization for maximal efficiency [42] |
| Base Editing Screen (HUDEP-2 cells) | Novel -123/-124 HBG targets | 59-73% (CBE) | Higher than BCL11A disruption | Identifies potent novel HPFH-like mutations [40] |
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagent Solutions for Prime Editing HPFH-like Mutations
| Reagent / Tool | Function / Description | Example or Note |
|---|---|---|
| PEmax System | Optimized prime editor protein (Cas9 nickase-RT fusion) | Confers higher editing efficiency than PE2 [42] |
| epegRNA | Engineered pegRNA with 3' tevopreQ1 motif | Increases RNA stability and editing efficiency [42] |
| MMR-Inhibited Cell Line | MLH1-knockout or MMR-deficient background | Dramatically improves precise editing yields [42] |
| HUDEP-2 Cells | Immortalized human erythroid progenitor cell line | Useful for initial screening of gRNAs and editing efficiency [40] |
| CD34+ HSPCs | Primary human hematopoietic stem/progenitor cells | Clinically relevant cell type for therapeutic development [41] [40] |
| Erythroid Differentiation Media | Cytokine cocktails for ex vivo RBC production | Contains SCF, EPO, TPO, IL-3, holotransferrin [40] |
| ICE Analysis Tool | Software for analyzing CRISPR edits from Sanger data | Quantifies indel %, KO score, and editing efficiency [45] |
Prime editing represents a powerful and precise method for introducing therapeutic HPFH-like mutations into the γ-globin promoters to reactivate fetal hemoglobin. With optimized systems combining PEmax, epegRNAs, and MMR inhibition, researchers can achieve high-efficiency multiplexed editing in clinically relevant HSPCs. The continued identification of novel potent mutations, such as those at the -123/-124 sites, coupled with robust experimental workflows for delivery and validation, positions prime editing as a leading strategy for developing next-generation therapies for sickle cell disease and β-thalassemia.
Antisense Oligonucleotides (ASOs) Targeting Enhancer RNAs
Enhancer RNAs (eRNAs) are a subclass of non-coding RNAs transcribed from enhancer regions that have emerged as critical regulators of gene expression in health and disease [46] [47]. Unlike traditional drug targets, eRNAs represent a previously underexplored layer of transcriptional control that can be targeted with high specificity. These RNAs are typically bidirectional, lack polyadenylation, and function through mechanisms including stabilization of enhancer-promoter looping, recruitment of transcriptional coactivators, and modulation of chromatin accessibility [46] [47]. The discovery that eRNAs are essential for the formation and maintenance of three-dimensional genome structures, particularly in the context of fetal hemoglobin regulation, has positioned them as promising therapeutic targets for genetic disorders like sickle cell disease and β-thalassemia [3] [38].
The therapeutic targeting of eRNAs with Antisense Oligonucleotides (ASOs) represents a paradigm shift in drug development, moving beyond protein inhibition to upstream transcriptional regulation. ASOs are short, synthetic, single-stranded DNA or RNA molecules (typically 12-30 nucleotides in length) designed to bind complementary RNA sequences through Watson-Crick base pairing [48]. This binding enables precise modulation of gene expression through multiple mechanisms, including RNA degradation, splicing modification, and translation blocking [48]. For eRNA targeting, ASOs function primarily by marking these non-coding RNAs for degradation, thereby disrupting the enhancer-dependent regulatory mechanisms they facilitate [3] [46] [49].
Molecular Mechanisms: How eRNA-Targeted ASOs Reactivate Fetal Hemoglobin
The BCL11A Enhancer and Chromatin Rosette Structure
The reactivation of fetal hemoglobin (HbF) represents a promising therapeutic strategy for β-hemoglobinopathies, as HbF compensates for defective adult hemoglobin in sickle cell disease and β-thalassemia [3] [50]. The transcription factor BCL11A is a genetically and clinically validated master regulator of the fetal-to-adult hemoglobin switch, acting as a repressor of HbF expression in adult erythroid cells [3] [38] [5]. Recently approved CRISPR-based therapies for these disorders target a specific enhancer within the BCL11A gene to reactivate HbF [3] [49].
Critical research has revealed that the remarkable efficacy of CRISPR-mediated enhancer editing stems from its disruption of a sophisticated three-dimensional genome architecture. Scientists at St. Jude Children's Research Hospital and Northwestern University discovered that the BCL11A enhancer forms a specific "chromatin rosette" structure – a flower-like arrangement where the enhancer makes multiple contacts with critical regulatory elements of the gene [3] [38]. This structure functions as an epigenetic insulator, ensuring high-level BCL11A expression and preventing its silencing in red blood cell precursors [38]. The formation and stability of this essential rosette structure depend on a special type of RNA: enhancer RNAs (eRNAs) produced by the BCL11A enhancer itself [3] [38].
ASO-Mediated Disruption of Epigenetic Insulation
Targeting BCL11A eRNAs with ASOs presents a non-genome-editing approach to silence BCL11A and reactivate HbF. The mechanistic workflow involves:
Diagram 1: ASO-mediated disruption of the BCL11A chromatin rosette. The process shows how ASOs target eRNAs, disrupting the epigenetic insulation and leading to HbF reactivation.
When ASOs are delivered to red blood cell precursors, they bind to complementary BCL11A eRNA sequences and trigger their degradation [3] [49]. This degradation prevents the formation of the chromatin rosette structure, impairing epigenetic insulation. Without this insulation, repressive proteins gain access to the BCL11A locus, leading to transcriptional silencing of BCL11A [38]. With BCL11A repression lifted, fetal hemoglobin production is reactivated, providing functional hemoglobin that compensates for the defective adult hemoglobin in sickle cell disease and β-thalassemia [3]. This mechanism mirrors the outcome of CRISPR-based gene editing but achieves it through a reversible, non-mutagenic approach that does not permanently alter the DNA [49].
Experimental Protocols for ASO Targeting of eRNAs
Identification and Validation of Functional eRNAs
The first critical step in developing eRNA-targeted ASO therapies is the comprehensive identification of functional eRNAs associated with your target gene of interest. The following integrated multi-omics approach has been successfully employed in recent studies [46] [47]:
- Chromatin Accessibility Profiling: Perform ATAC-seq (Assay for Transposase-Accessible Chromatin using sequencing) on relevant cell types (e.g., erythroid precursors for hemoglobinopathy research) under both baseline and stimulated conditions. Identify accessible chromatin regions using stringent peak detection criteria (p < 0.05, peak length < 500 bp, occurrence in multiple biological replicates) [47].
- Enhancer-Specific Histone Mark Detection: Conduct chromatin immunoprecipitation sequencing (ChIP-seq) for enhancer-associated histone marks, particularly H3K27ac (marking active enhancers) and H3K4me1 (marking primed enhancers). Integrate these data with ATAC-seq results to refine enhancer predictions [46] [47].
- Transcriptomic Analysis of eRNAs: Perform total RNA-seq with a focus on early time points after cellular stimulation (e.g., 1-hour post-erythroid differentiation induction). Identify bidirectionally transcribed regions characteristic of eRNA production. Intersect these with enhancer regions identified through epigenetic mapping [46].
- Functional Enhancer-Gene Linking: Utilize activity-by-contact (ABC) models and similar computational approaches to link candidate enhancers with their target genes. Enhancements with chromatin conformation capture techniques (e.g., Hi-C) can validate physical interactions [46].
- Differential Expression Analysis: Identify eRNAs that are differentially expressed between disease and normal states, or in response to relevant stimuli, using appropriate statistical thresholds (e.g., |fold change| > 1.5, p-value < 0.05) [47].
ASO Design, Testing, and Functional Validation
Once target eRNAs are identified, proceed with ASO development and testing using this established workflow:
Diagram 2: Comprehensive workflow for developing and testing ASOs targeting eRNAs.
Detailed ASO Design and Screening Protocol
ASO Design Considerations [48]:
- Sequence Selection: Design 15-20 nucleotide ASOs with complete complementarity to the target eRNA sequence. Perform BLAST analysis against the transcriptome to minimize off-target binding.
- Chemical Modifications: Incorporate 2'-O-methoxyethyl (2'-MOE) modifications at the wing regions to enhance nuclease resistance and binding affinity. Use phosphorothioate (PS) linkages in the backbone to improve stability and enable protein binding for enhanced pharmacokinetics.
- Delivery Optimization: For erythroid-specific delivery, consider conjugation approaches or optimized electroporation protocols for hematopoietic stem and progenitor cells (HSPCs).
In Vitro Screening Pipeline:
- Primary Screening: Transfect a panel of ASOs (typically 5-20 designs) into relevant cell models (e.g., HUDEP-2 cells for erythroid studies, primary human erythroblasts) at concentrations ranging from 1-100 μM.
- Initial Efficacy Assessment: 48 hours post-transfection, measure:
- Target eRNA levels using RT-qPCR with primers specific to the eRNA sequence
- Expression of the enhancer's target gene (e.g., BCL11A for HbF reactivation)
- Desired functional outcome (e.g., γ-globin mRNA for HbF studies)
- Dose-Response Analysis: Test lead ASO candidates across a concentration gradient (0.1-50 μM) to establish IC₅₀ values for eRNA suppression and therapeutic effect.
Functional Validation in Disease-Relevant Models
For hemoglobinopathy research, employ the following validation cascade:
- Primary Human Erythroblast Models: Isolate CD34+ hematopoietic stem/progenitor cells from healthy donors and β-thalassemia/SCD patients. Differentiate towards the erythroid lineage using established cytokine cocktails (EPO, SCF, IL-3). Introduce ASOs via electroporation at the progenitor stage (typically day 4-6 of differentiation) [3] [5].
- Endpoint Analyses (assess at maturation day 12-14):
- Molecular Efficacy: Quantify eRNA suppression, BCL11A mRNA and protein levels, and γ-globin transcript expression using RT-qPCR and Western blotting.
- Hemoglobin Analysis: Perform cation-exchange HPLC to quantify fetal hemoglobin percentage. Successful BCL11A suppression typically yields HbF levels of 20-30% in healthy donor cells and >60% in β-thalassemia cells [5].
- Phenotypic Rescue: In SCD models, assess sickling propensity under hypoxic conditions. In thalassemia models, evaluate improved erythroid enucleation and reduced apoptosis.
- Specificity Assessment: Perform RNA-seq to identify off-target transcriptional effects. Compare expression profiles between ASO-treated and control cells, with particular attention to genes with partial sequence complementarity to the ASO.
Quantitative Data and Comparative Analysis
Efficacy Metrics for eRNA-Targeting Approaches
Table 1: Quantitative outcomes of eRNA-targeting therapies for fetal hemoglobin reactivation
| Therapeutic Approach | Target | Model System | eRNA Reduction | BCL11A Silencing | HbF Induction | Reference |
|---|---|---|---|---|---|---|
| ASO targeting BCL11A eRNA | BCL11A enhancer RNA | Primary human erythroblasts (healthy) | ~70-80% | ~60-70% protein reduction | 20-30% of total Hb | [3] [49] |
| ASO targeting BCL11A eRNA | BCL11A enhancer RNA | Primary human erythroblasts (SCD/β-thal) | Similar to healthy | Similar to healthy | >60% of total Hb | [3] |
| CRISPR editing of BCL11A enhancer | BCL11A enhancer DNA | Primary human erythroblasts | Not measured | ~70-80% protein reduction | 25-40% of total Hb | [3] [5] |
| ASO targeting TNF-9 eRNA | TNFα enhancer RNA | Mouse macrophages | ~60-70% | Not applicable | Not applicable (TNFα reduced) | [46] |
Comparison with Alternative Gene-Targeting Approaches
Table 2: Comparison of eRNA-targeting ASOs with other genetic therapies for hemoglobinopathies
| Parameter | eRNA-Targeting ASOs | CRISPR Gene Editing | Lentiviral Gene Addition | Small Molecule Inducers |
|---|---|---|---|---|
| Molecular Mechanism | eRNA degradation leading to epigenetic changes | DNA cleavage and repair errors | Functional gene insertion | Protein-targeted inhibition |
| Permanence | Transient, requiring redosing | Permanent | Permanent | Transient, requiring redosing |
| Manufacturing Complexity | Moderate (chemical synthesis) | High (viral delivery, ex vivo) | High (viral production, ex vivo) | Low (chemical synthesis) |
| Therapeutic Specificity | High (sequence-specific RNA targeting) | Moderate (potential off-target editing) | Low (random integration) | Low (broad protein binding) |
| Delivery Method | In vivo or ex vivo possible | Primarily ex vivo | Ex vivo | In vivo |
| Development Timeline | 2-4 years | 5-7 years | 5-7 years | 4-6 years |
| Regulatory Precedent | Established (multiple ASO approvals) | Emerging (recent approvals) | Established (multiple approvals) | Well-established |
| Cost Considerations | Moderate | Very high (>$2M per treatment) | Very high (>$2M per treatment) | Low |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key reagents and resources for eRNA-targeted ASO research
| Research Tool Category | Specific Examples | Primary Applications | Technical Considerations |
|---|---|---|---|
| Cell Models | Primary human CD34+ HSPCs, HUDEP-2 cells, Patient-derived iPSCs | Functional validation of ASOs in physiologically relevant systems | Primary cells require specific cytokine cocktails for erythroid differentiation; HUDEP-2 cells need stem cell factor maintenance |
| Epigenomic Profiling Reagents | ATAC-seq kits, H3K27ac/H3K4me1 antibodies for ChIP, Total RNA-seq kits | Identification of functional eRNAs and their associated enhancers | ATAC-seq requires careful titration of transposase; enhancer RNA detection benefits from total RNA-seq with ribosomal RNA depletion |
| ASO Chemical Modifications | 2'-MOE modifications, Phosphorothioate backbones, GalNAc conjugates | Enhancing ASO stability, binding affinity, and cellular delivery | 2'-MOE modifications improve nuclease resistance but may increase toxicity; PS backbones promote plasma protein binding |
| Delivery Systems | Electroporation systems (e.g., Neon, Amaxa), Lipid nanoparticles | Introducing ASOs into hard-to-transfect primary cells | Electroporation parameters must be optimized for each cell type; LNPs can enable in vivo delivery but require formulation optimization |
| Analytical Tools | HPLC for hemoglobin quantification, Digital droplet PCR for eRNA detection, Western blot for BCL11A protein | Quantifying therapeutic efficacy and molecular endpoints | HbF quantification by HPLC requires careful standardization; eRNA detection benefits from highly sensitive PCR methods due to low abundance |
| Specificity Assessment Platforms | RNA-seq for transcriptome-wide profiling, PRImerize algorithm for off-target prediction | Evaluating off-target effects and ASO specificity | RNA-seq should be performed at sufficient depth (≥30M reads) to detect subtle expression changes; computational prediction helps guide ASO design |
Targeting enhancer RNAs with antisense oligonucleotides represents a cutting-edge therapeutic strategy that combines the precision of genetic medicine with the reversibility and tunability of traditional pharmaceuticals. The demonstrated success of this approach in reactivating fetal hemoglobin for hemoglobinopathy treatment underscores its potential to address a significant unmet medical need [3] [49]. Unlike genome-editing approaches that permanently alter DNA, ASO-mediated eRNA targeting offers a controllable, dose-titratable intervention that may present a superior safety profile for certain patient populations.
The broader implications of eRNA-targeting ASOs extend well beyond hemoglobinopathies. Research has already demonstrated similar approaches for modulating chronic inflammatory diseases by targeting eRNAs that regulate TNFα expression [46], and in oncology, where eRNAs such as LTFe have been identified as tumor suppressors in prostate cancer [47]. The programmable nature of ASOs enables rapid development of treatments for diverse conditions by simply modifying the nucleotide sequence to target different eRNAs [48].
As the field advances, key challenges remain in optimizing delivery to specific tissues, minimizing off-target effects through improved bioinformatics and chemical modifications, and establishing standardized efficacy and safety assessment protocols [51] [48]. The anticipated growth of the antisense oligonucleotides market to USD 2.5 billion in 2025, with a projected CAGR of 15%, reflects strong confidence in this therapeutic platform [52]. With continued innovation in delivery technologies and our expanding understanding of enhancer biology, eRNA-targeted ASOs are poised to become a major therapeutic modality for addressing previously undruggable disease targets.
Sickle cell disease (SCD) and β-thalassemia are among the most common inherited monogenic disorders worldwide, representing a significant global health burden [6] [53]. For the millions affected, the reactivation of fetal hemoglobin (HbF) presents a promising therapeutic strategy by compensating for defective adult β-globin function [54] [55]. HbF, composed of two α-globin and two γ-globin chains, is the predominant hemoglobin during fetal development but is largely silenced after birth through a process known as hemoglobin switching [53] [56]. In SCD, increased HbF inhibits the polymerization of deoxygenated hemoglobin S, thereby reducing disease severity [6]. In β-thalassemia, γ-globin chains compensate for the deficiency in β-globin synthesis, alleviating the imbalance of globin chains [53] [56].
Pharmacological induction of HbF represents a cornerstone approach for treating these hemoglobinopathies [53]. While hydroxyurea (HU) remains the only FDA-approved drug for SCD that increases HbF, its efficacy is variable, and a significant number of patients show incomplete response [57] [6]. Consequently, research has focused on epigenetic modulators—compounds that target the enzymatic machinery responsible for γ-globin gene silencing [55] [56]. This whitepaper provides an in-depth technical review of histone deacetylase (HDAC) inhibitors and other epigenetic modulators for HbF reactivation, detailing their mechanisms, experimental evidence, and protocols for preclinical assessment.
Epigenetic Regulation of γ-Globin Expression
The developmental switch from fetal to adult hemoglobin involves the acquisition of repressive epigenetic marks at the γ-globin gene promoters, leading to transcriptional silencing in adult erythroid cells [6] [58]. Key repressor complexes containing epigenetic-modifying enzymes are recruited to the γ-globin promoters by transcription factors such as BCL11A, ZBTB7A, and TR2/TR4 [6] [58]. These enzymes establish a repressive chromatin environment through:
- DNA methylation: Catalyzed by DNA methyltransferases (DNMTs), leading to cytosine methylation at CpG islands in the γ-globin promoter region [53] [56].
- Histone deacetylation: Mediated by histone deacetylases (HDACs), which remove acetyl groups from histone tails, promoting chromatin condensation [57] [55].
- Histone methylation: Facilitated by enzymes such as euchromatic histone methyltransferases (EHMT1/2) and lysine-specific histone demethylase 1 (LSD1) [55].
Pharmacological inhibition of these enzymes can reverse γ-globin silencing, providing the rational basis for using epigenetic modulators to induce HbF [55] [56].
Key Epigenetic Targets for HbF Induction
Table 1: Major Epigenetic Regulators Targeted for HbF Induction
| Epigenetic Regulator | Class/Type | Role in γ-Globin Regulation | Inhibitors/Modulators |
|---|---|---|---|
| HDAC 1, 2, 3 | Class I HDAC | Transcriptional repression through histone deacetylation | CT-101, Valproic Acid, Sodium Phenylbutyrate [57] |
| DNMT1 | DNA methyltransferase | DNA methylation-mediated silencing | Decitabine, 5-Azacytidine, GSK3482364 [53] |
| LSD1 (KDM1A) | Histone demethylase | Demethylation of H3K4me1/2 at γ-globin promoter | Not specified in results [55] |
| EHMT1/2 (G9a) | Histone methyltransferase | H3K9 methylation for heterochromatin formation | Not specified in results [55] |
| MBD2-NuRD | Methyl-DNA binding complex | Recruits repressive complexes to methylated DNA | Potential target for small molecules [6] [58] |
Figure 1: Epigenetic Regulation of γ-globin Expression and Pharmacological Reactivation Strategy. Transcription factors recruit co-repressor complexes containing epigenetic enzymes that establish repressive chromatin. Inhibitors target these enzymes to reverse silencing.
HDAC Inhibitors for HbF Induction
Class I-Selective HDAC Inhibitors
Histone deacetylase inhibitors represent a rational molecularly targeted approach for HbF induction. Early pan-HDAC inhibitors like valproic acid, sodium phenylbutyrate, and arginine butyrate demonstrated proof-of-concept but were limited by administration routes or side effects [57]. Recent efforts have focused on developing class I-selective HDAC inhibitors with improved potency and specificity.
CT-101, a novel Class I-restricted HDAC inhibitor derived from Largazole, has shown promising results [57]. The prodrug CT-101 is converted to the active free thiol form (CT-101S) by plasma esterases and lipases, enabling potent inhibition of HDAC isoforms at nanomolar concentrations by binding to their critical zinc cofactor [57].
Table 2: Experimental Profile of HDAC Inhibitor CT-101
| Parameter | Experimental Findings |
|---|---|
| HDAC Inhibition Profile | Selective for Class I HDACs (HDAC 1, 2, 3, 8) [57] |
| Potency | Nanomolar concentrations [57] |
| γ-globin mRNA Induction | Significant increase in SCD-derived erythroid progenitors [57] |
| HbF Protein Induction | Increased HbF expression; additive effect with hydroxyurea [57] |
| Chromatin Changes | Increased acetylated histone H3 levels; open chromatin conformation at γ-globin promoter [57] |
| Cytotoxicity | No significant cytotoxicity observed at effective concentrations [57] |
Experimental Protocol: Evaluating HDAC Inhibitors in Erythroid Progenitors
Primary Cell Culture from SCD Patients
- Collect peripheral blood mononuclear cells (PBMCs) from consented SCD patients [57].
- Isate CD34+ hematopoietic stem and progenitor cells using immunomagnetic selection.
- Culture cells in a three-phase erythroid differentiation system:
- Phase 1 (Days 0-7): Expand progenitor cells in serum-free medium containing SCF, FLT3-L, IL-3, and IL-6.
- Phase 2 (Days 7-14): Induce erythroid differentiation with erythropoietin (EPO), insulin, and dexamethasone.
- Phase 3 (Days 14-21): Complete maturation in medium with EPO and insulin [57].
Drug Treatment and Analysis
- Add HDAC inhibitors (e.g., CT-101) during the differentiation phase (typically from day 7 onward) [57].
- Include hydroxyurea alone and in combination to test additive effects.
- Harvest cells at different time points for:
- HbF Analysis: Flow cytometry for F-cells and intracellular HbF.
- Molecular Analysis: qRT-PCR for γ-globin mRNA.
- Chromatin Studies: Chromatin immunoprecipitation (ChIP) for histone modifications at γ-globin promoter.
Other Epigenetic Modulators
DNA Methyltransferase Inhibitors
DNA hypomethylating agents were among the first epigenetic drugs shown to induce HbF. Decitabine, a potent DNMT1 inhibitor, has demonstrated efficacy in clinical studies. A pilot study administering decitabine subcutaneously (0.2 mg/kg twice weekly for 12 weeks) increased total hemoglobin from 78.8 to 90.4 g/L and absolute HbF levels from 36.4 to 42.9 g/L in β-thalassemia intermedia patients [53]. To overcome oral bioavailability challenges, decitabine has been combined with tetrahydrouridine (THU), a cytosine deaminase inhibitor, resulting in F-cell increases up to 80% in clinical trials [53].
A novel orally bioavailable DNMT1-selective inhibitor, GSK3482364, offers advantages over traditional cytidine analogs. Its inhibitory mechanism does not require DNA incorporation and is reversible. In vitro erythropoiesis models showed that GSK3482364 and decitabine led to comparable increases in HbF-positive cells, but GSK3482364 resulted in a larger proportion of cells maturing into HbF-expressing reticulocytes [53].
Emerging Target: MBD2-NURD Complex
Recent research has identified the methyl-CpG-binding domain protein 2 (MBD2) as a critical specific regulator of γ-globin silencing. CRISPR/Cas9 knockout studies demonstrated that disruption of MBD2, but not its homolog MBD3, reactivates HbF expression to high levels in human erythroid cells (HUDEP-2) and primary human erythroid cultures [6] [58]. Importantly, MBD2 knockout did not affect erythroid differentiation or expression of other known γ-globin repressors like BCL11A [6].
Key functional domains of MBD2 essential for γ-globin repression include:
- Coiled-coil (CC) domain: Mediates interactions with GATAD2A and recruitment of chromatin-modifying protein CHD4.
- Intrinsically disordered region (IDR): Necessary for interaction with an HDAC core complex [6] [58].
Since MBD2 knockout mice show minimal phenotypic effects, small molecule inhibitors targeting MBD2's functional domains represent a promising therapeutic strategy with potentially fewer side effects [6] [58].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for HbF Induction Studies
| Reagent/Cell Line | Function/Application | Key Features |
|---|---|---|
| HUDEP-2 cells | Immortalized human erythroid progenitor cell line | Capable of terminal erythroid differentiation; model for human erythropoiesis [6] |
| Primary human CD34+ cells | Hematopoietic stem/progenitor cells from peripheral blood or bone marrow | Gold standard for ex vivo erythroid differentiation studies [57] |
| β-YAC transgenic mouse model | Contains human β-globin locus | In vivo model for studying γ-globin gene regulation and drug responses [57] |
| BERK1 sickle mouse | SCD mouse model | In vivo evaluation of HbF inducers in sickle cell context [57] |
| HDAC inhibition assays | Measure inhibition of specific HDAC isoforms | Fluorescence-based or colorimetric assays using recombinant HDAC proteins [57] |
| Chromatin Immunoprecipitation (ChIP) | Analyze histone modifications at specific genomic loci | Antibodies against acetylated histones (H3K9ac, H3K27ac) for γ-globin promoter [57] |
Experimental Protocol: Epigenetic Modifier Screening
Comprehensive Workflow for Evaluating Epigenetic Modulators
Figure 2: Experimental Workflow for Evaluating Epigenetic Modulators. The process begins with in vitro cell systems, progresses through molecular and cellular analyses, and culminates in functional validation.
Phase 1: In Vitro Screening
- Cell Culture: Maintain HUDEP-2 cells in expansion medium (StemSpan with dexamethasone, SCF, and EPO). For differentiation, switch to medium containing EPO, doxycycline, and estrogen [6].
- Compound Treatment: Add epigenetic modulators at beginning of differentiation phase. Include positive controls (hydroxyurea) and vehicle controls.
- Endpoint Analyses:
- qRT-PCR: Measure γ-globin, β-globin, and housekeeping gene expression.
- Flow Cytometry: Analyze HbF production using intracellular staining.
- Western Blot: Detect histone modifications (e.g., acetylated H3) and globin proteins.
Phase 2: Mechanism of Action Studies
- Chromatin Immunoprecipitation (ChIP):
- Cross-link proteins to DNA with formaldehyde.
- Sonicate chromatin to 200-500 bp fragments.
- Immunoprecipitate with antibodies against acetylated histones or other epigenetic marks.
- Analyze γ-globin promoter enrichment using qPCR [57].
- HDAC Inhibition Assay:
- Incubate recombinant HDAC isoforms with fluorogenic substrates.
- Add inhibitors at various concentrations.
- Measure fluorescence to determine IC50 values [57].
Phase 3: In Vivo Validation
- Utilize human β-globin YAC transgenic mice or BERK1 sickle mice.
- Administer compounds via appropriate routes (oral gavage, intraperitoneal injection).
- Monitor hematological parameters and HbF levels periodically.
- Assess organ toxicity and compound pharmacokinetics [57].
HDAC inhibitors and other epigenetic modulators represent a promising therapeutic strategy for reactivating fetal hemoglobin in β-hemoglobinopathies. Class I-selective HDAC inhibitors like CT-101 demonstrate targeted epigenetic effects with potential for clinical application, while emerging targets such as the MBD2-NURD complex offer new avenues for drug development with potentially fewer side effects. The continued elucidation of molecular mechanisms governing γ-globin silencing, coupled with advances in epigenetic drug discovery, holds significant promise for developing more effective and targeted therapies for sickle cell disease and β-thalassemia. The experimental frameworks and technical approaches outlined in this review provide researchers with comprehensive methodologies for evaluating novel HbF-inducing compounds.
The therapeutic reactivation of fetal hemoglobin (HbF) represents a cornerstone in the treatment of β-hemoglobinopathies, including sickle cell disease (SCD) and β-thalassemia. By compensating for defective adult β-globin, increased HbF levels inhibit hemoglobin S polymerization and ameliorate disease severity [4] [54]. The central challenge lies in efficiently delivering genetic cargo to hematopoietic stem cells (HSCs), the self-renewing progenitors of the erythroid lineage. This technical review examines the two dominant paradigms for achieving this goal: established ex vivo HSC editing and rapidly emerging in vivo approaches. Ex vivo methods involve extracting, modifying, and re-infusing a patient's HSCs, while in vivo strategies aim to deliver editing machinery directly to HSCs within the bone marrow niche via systemic administration [4] [59]. We provide a comparative analysis of their underlying mechanisms, technical workflows, and performance metrics, contextualized within the framework of HbF reactivation for a research audience.
Ex Vivo HSC Editing: Methodology and Current Landscape
Ex vivo editing requires a multi-step process where patient-derived HSCs are genetically modified outside the body before transplantation.
Core Experimental Protocol
The standard workflow for ex vivo HSC gene therapy for HbF reactivation is as follows [4] [60] [50]:
- HSC Collection and Mobilization: CD34+ hematopoietic stem and progenitor cells (HSPCs) are collected from a patient via bone marrow harvest or apheresis of mobilized peripheral blood. For SCD patients, the CXCR4 antagonist plerixafor is the preferred mobilization agent, as granulocyte colony-stimulating factor (G-CSF) is contraindicated due to the risk of vaso-occlusive crises [4].
- Ex Vivo Culture and Genetic Modification: The collected CD34+ cells are placed in culture systems optimized for HSC maintenance. Genetic modification is performed using one of two primary strategies:
- Lentiviral Vector (LV) Transduction: Cells are transduced with a lentiviral vector carrying a therapeutic transgene, such as a short hairpin RNA (shRNA) targeting the HbF repressor BCL11A [60] [61].
- CRISPR-Cas9 Genome Editing: Cells are electroporated with Cas9 nuclease complexed with a guide RNA (gRNA) as a ribonucleoprotein (RNP). Common targets for HbF induction include the BCL11A erythroid-specific enhancer or the repressor binding sites in the γ-globin promoters (e.g.,
HBG1/2promoter at -115 for BCL11A or -197 for ZBTB7A/LRF) [5] [62].
- Myeloablative Conditioning: The patient receives a myeloablative conditioning regimen, typically with busulfan, to create space in the bone marrow niche for the engraftment of the modified cells [4] [50].
- Reinfusion and Engraftment: The genetically modified CD34+ HSCs are infused back into the patient. Successful engraftment leads to the reconstitution of a hematopoietic system capable of producing red blood cells with elevated HbF [4].
Quantitative Performance of Ex Vivo Platforms
The following table summarizes key efficacy data from clinical and pre-clinical ex vivo studies targeting HbF reactivation.
Table 1: Efficacy Metrics of Ex Vivo HSC Editing Platforms for HbF Reactivation
| Therapy/Platform | Editing Target | Modality | Efficiency/Indel Rate | HbF Increase | Source |
|---|---|---|---|---|---|
| Exa-cel (CASGEVY) | BCL11A Erythroid Enhancer | CRISPR-Cas9 | N/A (Clinical) | ~40% of total Hb (sustained) [62] | |
| Pre-clinical (β0-thal/HbE) | HBG1/2 BCL11A site (-115) |
CRISPR-Cas9 RNP | 75-92% Indel | 62.7% ± 0.9% in erythroblasts [5] | |
| Pre-clinical (β0-thal/HbE) | HBG1/2 ZBTB7A site (-197) |
CRISPR-Cas9 RNP | 57-60% Indel | 64.0% ± 1.6% in erythroblasts [5] | |
| BCH-BB694 | BCL11A mRNA | LV-shRNA | N/A | Robust HbF induction (Clinical) [61] |
Emerging In Vivo Delivery Platforms
In vivo gene editing seeks to bypass the complex logistics of ex vivo manipulation by delivering genetic tools directly to a patient's HSCs.
Core Experimental Protocol
The in vivo approach is an actively developing field. A representative protocol, based on recent pre-clinical studies, involves [59]:
- Delivery Vehicle Formulation: The gene-editing cargo (e.g., Cas9 mRNA and gRNA) is encapsulated within a targeted non-viral delivery vehicle. The most advanced current platform is targeted Lipid Nanoparticles (tLNPs). These tLNPs are engineered with specific surface ligands to bind receptors on HSCs, enhancing tropism and cellular uptake [59].
- Systemic Administration: A single intravenous dose of the formulated tLNPs is administered to the patient or animal model.
- In Vivo Transduction and Editing: The tLNPs travel through the bloodstream to the bone marrow, where they are internalized by HSCs. The editing cargo is released into the cell cytoplasm, and the Cas9/gRNA complex enters the nucleus to perform the genomic edit—for example, disrupting the
HBG1/2promoter to reactivate HbF [59]. - Monitoring and Analysis: Engraftment and editing efficiency in the bone marrow are monitored over time. In animal models, this is typically assessed via flow cytometry of bone marrow aspirates and next-generation sequencing of edited genomic sites [59].
Quantitative Performance of In Vivo Platforms
While no in vivo HSC therapy is yet approved, recent pre-clinical data demonstrate rapid progress.
Table 2: Efficacy Metrics of Emerging In Vivo HSC Editing Platforms for HbF Reactivation
| Therapy/Platform | Editing Target | Delivery System | Model | Editing Efficiency | Source |
|---|---|---|---|---|---|
| Editas MED | HBG1/2 Promoter |
Proprietary tLNP (AsCas12a) | Non-Human Primate | Up to 47% in HSCs | [59] |
| Editas MED | HBG1/2 Promoter |
Proprietary tLNP (AsCas12a) | Humanized Mice | 48% in LT-HSCs | [59] |
Comparative Workflow Visualization
The diagram below illustrates the fundamental procedural differences between the ex vivo and in vivo delivery pathways.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of these therapies in a research setting relies on specialized reagents and materials.
Table 3: Key Research Reagents for HSC Gene Therapy Development
| Reagent/Material | Function | Application Notes |
|---|---|---|
| CD34+ HSPCs | Target cell population for genetic modification. | Sourced from mobilized peripheral blood, bone marrow, or cord blood. Purity and viability are critical [4] [63]. |
| Plerixafor | CXCR4 antagonist for HSC mobilization. | Preferred mobilizing agent for SCD patients instead of G-CSF [4]. |
| Lentiviral Vectors | Gene delivery vehicle for stable transgene integration. | Self-inactivating (SIN) designs with erythroid-specific promoters are standard for globin gene therapy [60] [62]. |
| CRISPR-Cas9 RNP | Precision genome editing complex. | Electroporation of pre-complexed RNP increases editing efficiency and reduces off-target effects compared to plasmid delivery [5]. |
| Targeted LNPs (tLNPs) | Non-viral delivery vehicle for in vivo cargo delivery. | Engineered with surface ligands for HSC tropism. Encapsulates mRNA and gRNA [59]. |
| Liproxstatin-1 (Lip-1) | Ferroptosis inhibitor. | Added to ex vivo culture media at 10 µM to significantly enhance HSC survival and expansion by preventing iron-dependent cell death [63]. |
| Busulfan | Myeloablative alkylating agent. | Used for conditioning to clear bone marrow niches, enabling engraftment of modified HSCs in ex vivo protocols [4] [50]. |
Discussion and Future Directions
The choice between ex vivo and in vivo delivery systems involves critical trade-offs. Ex vivo editing, exemplified by approved therapies like CASGEVY and LYFGENIA, offers proven efficacy and direct control over the editing process [50] [62]. However, it is inherently complex, requiring sophisticated manufacturing facilities (GMP), and is associated with high costs and patient burden from myeloablation [4]. In contrast, in vivo editing promises a streamlined "one-and-done" treatment, potentially lower costs, and broader accessibility [59] [62]. Its success hinges on overcoming significant technical hurdles, including achieving high editing efficiency in enough HSCs for a durable effect and ensuring superior safety and specificity of the delivery vehicle.
Future research will focus on optimizing in vivo delivery vectors, improving HSC tropism, and developing less toxic or non-myeloablative conditioning regimens suitable for both platforms. The ultimate goal is to make curative HbF-reactivating therapies accessible to the global population burdened by SCD and β-thalassemia.
Overcoming Technical and Clinical Hurdles in HbF-Targeted Therapies
Minimizing Off-Target Effects in CRISPR-Based Genome Editing
The recent approval of the first CRISPR-based gene therapies for sickle cell disease and β-thalassemia represents a watershed moment for genomic medicine. These therapies function by reactivating fetal hemoglobin (HbF), a developmental form of hemoglobin that can compensate for defective adult hemoglobin in these inherited blood disorders [3]. The therapeutic strategy involves using CRISPR-Cas9 to disrupt repressive regulatory elements or their binding sites, thereby silencing BCL11A, a master transcriptional repressor of fetal hemoglobin, and resulting in HbF reactivation [3] [5]. Despite this clinical success, a significant challenge remains: the potential for off-target effects—unintended, spurious edits at genomic sites similar to the intended target. These effects pose substantial safety concerns, including the risk of initiating oncogenic mutations, and can confound experimental results [64] [65]. For therapies involving in vivo editing, where corrected cells cannot be selected post-delivery, minimizing off-targets is particularly critical [65]. This guide provides an in-depth technical framework for predicting, detecting, and mitigating off-target effects, with a specific focus on applications in fetal hemoglobin reactivation for hemoglobinopathy research and therapy.
The Biological Mechanism of HbF Reactivation and Associated Off-Target Risks
Understanding the biological context is essential for designing specific editing strategies. The therapeutic goal is to reactivate fetal hemoglobin by disrupting the repression of γ-globin genes. Two primary genomic targets have been identified, both successfully advanced into clinical trials:
- BCL11A Enhancer Disruption: The first approach involves targeting a specific enhancer region that controls the expression of the BCL11A gene. Research from St. Jude Children's Research Hospital and Northwestern University revealed that CRISPR editing disrupts a critical three-dimensional chromatin "rosette" structure necessary for high-level BCL11A expression in red blood cell precursors [3]. Breaking this structure allows repressive complexes to silence BCL11A, leading to HbF reactivation.
- γ-Globin Promoter Editing: The second strategy directly targets the binding sites of transcriptional repressors (ZBTB7A/LRF or BCL11A) within the γ-globin gene promoters (e.g., HBG1 and HBG2). Disrupting these sites via CRISPR/Cas9 prevents repressor binding, thereby reactivating fetal hemoglobin synthesis [5].
The following diagram illustrates the core logic behind targeting these two pathways to achieve therapeutic HbF reactivation.
While highly effective, both strategies carry an inherent risk of off-target effects. The Cas9 nuclease can tolerate mismatches between the guide RNA (gRNA) and genomic DNA, potentially leading to cleavage at unintended sites that bear sequence similarity to the on-target site [64] [65]. A 2025 study directly comparing these two targeting approaches in β-thalassemia/HbE cells found that while editing the BCL11A binding site exhibited no detectable off-target effects, editing the ZBTB7A/LRF site resulted in low-frequency off-target mutations, underscoring the variable risk profile of different gRNAs [5].
Prediction and Detection of Off-Target Effects
A robust off-target analysis strategy combines computational prediction with experimental validation. Proactive prediction enables the selection of optimal gRNAs, while thorough post-editing detection characterizes the safety profile of a given editing experiment.
Computational Prediction Tools and Workflows
In silico prediction is the first and most critical step in gRNA design. Numerous algorithms and online tools are available to nominate potential off-target sites based on sequence homology. These tools can be broadly categorized as follows [64] [66]:
- Alignment-based models: Tools like Cas-OFFinder and CasOT perform exhaustive searches of a reference genome to find sites with high sequence similarity to the gRNA, allowing for a user-defined number of mismatches and bulges. They are highly customizable in terms of gRNA length and PAM type [64].
- Scoring-based models: Tools such as CCTop and Cutting Frequency Determination (CFD) employ more sophisticated scoring systems that weight factors like the position of mismatches relative to the PAM sequence. DeepCRISPR incorporates both sequence and epigenetic features into its predictions using machine learning [64].
The typical workflow for gRNA selection and initial risk assessment is outlined below.
Best practice dictates selecting gRNAs with not only high predicted on-target activity but also a high number of mismatches required for the most similar off-target sites. gRNAs with a GC content between 40-60% are generally preferred, as this stabilizes the DNA:RNA hybrid [65]. Furthermore, it is crucial to check that the chosen gRNA does not have highly similar sequences near or within oncogenes or tumor suppressor genes.
Experimental Detection and Analysis Methods
Computational prediction has limitations, as it is inherently biased toward sgRNA-dependent off-targets and may miss sites affected by chromatin structure or other cellular factors [64]. Therefore, experimental validation is mandatory, especially for preclinical therapeutic development. The following table summarizes the primary methods used for detecting off-target effects.
Table 1: Experimental Methods for Detecting CRISPR Off-Target Effects
| Method | Principle | Advantages | Disadvantages | Best For |
|---|---|---|---|---|
| Candidate Site Sequencing [65] | Sanger or NGS of sites nominated by in silico tools. | Low cost, simple, accessible. | Incomplete; misses unpredicted sites. | Initial validation, low-risk experiments. |
| GUIDE-seq [64] | Captures double-strand breaks (DSBs) via integration of double-stranded oligodeoxynucleotides. | Highly sensitive, low false-positive rate, genome-wide. | Limited by transfection efficiency. | Comprehensive profiling in cell culture. |
| CIRCLE-seq [64] [65] | In vitro Cas9 cleavage of circularized, sheared genomic DNA followed by NGS. | Ultra-sensitive, works on any DNA source, no background noise. | Purely in vitro; may not reflect cellular context. | Highest sensitivity screening without live cells. |
| DISCOVER-seq [64] | Uses DNA repair protein MRE11 to mark DSB sites via ChIP-seq. | Works in vivo, high precision in cells. | Can have false positives, requires specific antibodies. | Identifying off-targets in animal models or primary cells. |
| Whole Genome Sequencing (WGS) [64] [65] | Comprehensive sequencing of the entire genome before and after editing. | Truly unbiased, detects all types of variants and chromosomal aberrations. | Very expensive, requires high sequencing depth, complex data analysis. | Gold-standard for final safety assessment of clinical candidates. |
For most preclinical therapeutic applications, a combination of GUIDE-seq (for comprehensive in vitro mapping) followed by WGS on a clonal population is considered the most rigorous approach to characterize an editing platform's safety [65].
Strategies for Minimizing Off-Target Effects
Minimizing off-target activity requires a multi-faceted strategy that encompasses the choice of editing machinery, the design of the guide RNA, the mode of delivery, and the control of editing duration.
Selection of High-Fidelity Editing Systems
Moving beyond the wild-type Streptococcus pyogenes Cas9 (SpCas9) is a fundamental step toward improving specificity. Several engineered alternatives now exist:
- High-Fidelity Cas9 Variants: Mutants such as eSpCas9(1.1) and SpCas9-HF1 were designed to reduce non-specific interactions between the Cas9 protein and the DNA backbone, thereby increasing the stringency for perfect gRNA:DNA pairing. While they significantly reduce off-target cleavage, some may exhibit reduced on-target efficiency [64] [65].
- Alternative Cas Nucleases: Cas12a (Cpf1) has a different PAM requirement and creates staggered DNA ends, which can alter its off-target profile compared to SpCas9 [64].
- Anti-CRISPR Proteins: A groundbreaking 2025 development from MIT and Harvard introduced a cell-permeable anti-CRISPR protein system (LFN-Acr/PA). This system can be delivered after successful editing to rapidly shut down residual Cas9 activity, reducing off-target effects and boosting editing specificity by up to 40% [67].
- Advanced Editors that Avoid Double-Strand Breaks (DSBs): Base editors (BEs) and prime editors (PEs) do not create DSBs. Instead, they use a catalytically impaired Cas9 fused to other enzymes to directly convert one base to another or to write new sequences, respectively. These systems demonstrate substantially lower off-target effects [21].
gRNA Engineering and Delivery Optimization
The design and delivery of the gRNA itself are levers for enhancing specificity.
- Chemical Modifications: Synthetic gRNAs can be modified with 2'-O-methyl analogs (2'-O-Me) and 3' phosphorothioate bonds (PS) to increase their stability and reduce off-target binding while potentially enhancing on-target efficiency [65].
- Truncated gRNAs: Using gRNAs shorter than the standard 20 nucleotides can reduce off-target activity, albeit sometimes at the cost of on-target potency [65].
- Optimal Cargo and Delivery: The form in which CRISPR components are delivered profoundly impacts their intracellular lifetime and thus the window for off-target activity. RNA-based delivery (e.g., Cas9 mRNA + synthetic gRNA) leads to transient expression and is superior to DNA-based delivery (e.g., plasmids), which results in prolonged expression and a higher risk of off-target effects [65]. For in vivo therapy, lipid nanoparticles (LNPs) are an effective non-viral method for delivering RNA cargo [68].
Experimental Protocol: Off-Target Assessment for HbF Reactivation
This section provides a detailed protocol for a key experiment: assessing the efficiency and specificity of CRISPR-mediated disruption of the BCL11A binding site in the γ-globin promoter, based on a 2025 study [5].
Materials and Reagents
Table 2: Essential Research Reagents for CRISPR Off-Target Assessment
| Reagent / Tool | Function / Description | Example or Specification |
|---|---|---|
| CD34+ Hematopoietic Stem/Progenitor Cells (HSPCs) | Primary cells for modeling hemoglobinopathy therapy. | Mobilized from healthy donors or β-thalassemia patients [5]. |
| sgRNA Targeting BCL11A site | Guides Cas9 to the specific repressor binding site in the HBG promoter. | Sequence: sg-BCL11A (from previously validated studies) [5]. |
| High-Fidelity Cas9 Nuclease | Engineered Cas9 protein with reduced off-target activity. | eSpCas9(1.1) or SpCas9-HF1. |
| Electroporation System | Method for delivering RNP complexes into hard-to-transfect HSPCs. | Neon or Amaxa Nucleofector [5]. |
| Erythroid Differentiation Media | Culture conditions to drive HSPCs to become red blood cells. | Multi-step protocol with SCF, EPO, IL-3, and dexamethasone [5]. |
| High-Throughput Sequencing Platform | For indel analysis and off-target detection. | Illumina MiSeq for on-target; GUIDE-seq or WGS for off-target. |
| Cation-Exchange HPLC | To quantify fetal hemoglobin (HbF) protein levels. | For measuring therapeutic efficacy [5]. |
| CRISPOR or Cas-OFFinder | Web-based tool for gRNA design and off-target prediction. | Essential for pre-experimental design and risk assessment [66]. |
Step-by-Step Methodology
- gRNA Design and In Silico Analysis: Design gRNAs targeting the HBG promoter BCL11A binding site (e.g., -115). Use CRISPOR to select candidates with high on-target and low off-target scores. Run Cas-OFFinder to generate a list of potential off-target sites for later validation [66] [5].
- Ribonucleoprotein (RNP) Complex Formation: Complex purified, high-fidelity Cas9 protein with synthetic, chemically modified sgRNA at a molar ratio of 1:2. Incubate for 10-20 minutes at room temperature to form active RNP complexes [5].
- Cell Electroporation: Electroporate mobilized CD34+ HSPCs from healthy donors or β-thalassemia patients using the pre-formed RNP complexes. Include a non-treated control and a mock-electroporated control [5].
- Erythroid Differentiation: After editing, culture the cells in a multi-phase erythroid differentiation medium for 14-16 days to generate mature erythroblasts [5].
- On-Target Efficiency Analysis:
- Genomic DNA Extraction: Harvest cells at day 3-5 post-editing and extract genomic DNA.
- PCR and Sequencing: Amplify the on-target region by PCR and analyze editing efficiency (indel percentage) using Sanger sequencing analyzed with the Inference of CRISPR Edits (ICE) tool or by deep sequencing [65] [5].
- Therapeutic Efficacy Assessment:
- HbF Quantification: At the end of the differentiation period, analyze hemoglobin types in cell lysates using cation-exchange HPLC to measure the percentage of HbF [5].
- Off-Target Analysis:
- Perform GUIDE-seq on a separate aliquot of cells harvested 3 days post-editing to identify potential off-target sites genome-wide [64].
- For the top 10-15 potential off-target sites identified in silico and via GUIDE-seq, perform targeted deep sequencing (amplicon sequencing) on the final differentiated cell population to quantify the frequency of any off-target mutations [5].
This integrated protocol ensures a comprehensive assessment of both the efficacy and safety of the CRISPR editing strategy for HbF reactivation.
The minimization of off-target effects is not merely a technical hurdle but a prerequisite for the safe and effective clinical application of CRISPR-based therapies for sickle cell disease and β-thalassemia. A robust framework combines rational gRNA selection using advanced computational tools, the employment of high-fidelity editing systems like base editors or anti-CRISPR-controlled Cas9, and rigorous experimental profiling with methods such as GUIDE-seq and WGS. As the field progresses, the integration of machine learning for improved gRNA design and the continued development of next-generation editors promise to further enhance the precision of genomic medicine. By adhering to these stringent design and validation principles, researchers and drug developers can advance transformative therapies for hemoglobinopathies with an unwavering commitment to patient safety.
Addressing Variable Editing Efficiencies and Donor-Specific Responses
The reactivation of fetal hemoglobin (HbF) represents a transformative therapeutic strategy for sickle cell disease (β-thalassemia) [21]. Advanced gene editing technologies, including CRISPR/Cas9, base editing, and prime editing, enable precise manipulation of the fetal-to-adult hemoglobin switch by targeting specific genetic pathways [21] [69]. However, the transition from promising preclinical results to reliable clinical applications is hampered by significant variability in editing efficiencies and heterogeneous donor-specific responses [41] [70]. This variability presents a critical challenge for the consistent and predictable application of these therapies across diverse patient populations. The underlying causes are multifactorial, stemming from biological differences between donors, technical aspects of the editing process, and the complex cellular repair mechanisms that respond to genetic interventions [41] [71]. This technical guide examines the core factors contributing to this variability and outlines systematic experimental approaches to identify, quantify, and mitigate these donor-specific responses, thereby supporting the development of more robust and equitable therapeutic protocols.
Core Strategies for HbF Reactivation and Their Associated Variability
Current approaches to HbF reactivation primarily function by disrupting the repression of γ-globin expression. The table below summarizes the key strategies, their molecular targets, and the documented sources of variability associated with each.
Table 1: Key Genome Editing Strategies for Fetal Hemoglobin Reactivation and Sources of Variability
| Strategy | Molecular Target | Mechanism of Action | Reported Efficiency Range | Sources of Variability |
|---|---|---|---|---|
| Prime Editing of γ-globin promoters [41] | HBG1/HBG2 promoters | Introduces multiple gain-of-function mutations to enhance promoter activity. | ~50% precise edits in cell lines; variable in patient HSPCs [41] | Donor-specific HSPC response; DNA repair mechanism heterogeneity [41] |
| Adenine Base Editing (ABE) [70] | HBG1/HBG2 promoter (e.g., -123, -175) or BCL11A erythroid enhancer | A-to-G conversions to disrupt repressor binding sites or create activator sites. | 49.4% - 66.8% editing efficiency; 23.3% - 41.2% HbF+ cells [70] | gRNA:ABE ratio; electroporation timing; Cas9/TadA variant and UTR design [70] |
| CRISPR/Cas9 Nuclease-Mediated Disruption [5] | BCL11A binding site (HBG -115) or ZBTB7A/LRF binding site (HBG -197) | Creates indels to disrupt transcription factor binding sites in the γ-globin promoter. | 75-92% (BCL11A site) vs. 57-60% (ZBTB7A site) editing; 26-64% HbF [5] | Target site accessibility; differential indel profiles (e.g., 13-bp vs. 6-bp deletions) [5] |
| BCL11A Enhancer Targeting [3] | BCL11A erythroid-specific enhancer (+55, +58, +62) | Disrupts a 3D chromatin "rosette" structure, leading to BCL11A silencing. | Preclinical validation; high HbF reactivation [3] | Efficiency in disrupting chromatin architecture; cellular levels of repressive complexes [3] |
The following diagram illustrates the logical workflow for investigating and mitigating the sources of variability in editing outcomes, from initial observation to mechanistic insight and protocol optimization.
Biological Determinants of Donor-Specific Responses
The inherent biological variation between individual donors is a primary source of differential editing outcomes. Research indicates that the complex DNA repair mechanisms involved in prime editing are a significant factor, though their exact role can be context-dependent [41]. For instance, while mismatch repair (MMR) is known to influence editing outcomes in some systems, studies in human Hematopoietic Stem and Progenitor Cells (HSPCs) have shown that transient inhibition of MMR via MLH1dn expression did not consistently improve prime editing efficiency, suggesting that cellular MMR may not be the primary limiting factor in these primary cells [71]. Beyond repair pathways, the baseline epigenetic state of the target cells is crucial. The three-dimensional genome structure, particularly the chromatin "rosette" formed by the BCL11A enhancer, is essential for maintaining high BCL11A expression, and its disruption is a key mechanism of HbF reactivation [3]. Variability in this architecture or in the expression of epigenetic co-repressors like the MBD2-NURD complex—which has been definitively shown to mediate γ-globin silencing, unlike the MBD3-NURD complex—can lead to differential responses to editing [58].
Technical and Protocol-Dependent Factors
Experimental parameters play a major role in determining the efficiency and consistency of gene editing. The choice of editing platform itself is critical; for example, prime editing (PE) systems have evolved into more efficient architectures like PEmax, which confer 1.3- to 3.5-fold average increases in editing efficiency over the original PE in HSPCs [71]. The design of guide RNAs is equally important. The use of engineered pegRNAs (epegRNAs) that incorporate a 3' structured motif protects the reverse transcriptase template from degradation and can significantly enhance prime editing outcomes [71]. Furthermore, the delivery method and its timing are key sources of variability. For base editing in CD34+ HSPCs, critical optimizations included adjusting the gRNA-to-editor ratio and the timing of electroporation, which boosted both editing efficiency and HbF expression without impairing the clonogenic potential of the cells [70]. The specific target site within a regulatory region also dictates outcomes. Disruption of the BCL11A binding site (HBG -115) in the γ-globin promoter consistently resulted in higher editing efficiencies (75-92%) compared to disruption of the ZBTB7A/LRF site (HBG -197; 57-60%), and the distribution of resultant indel mutations (e.g., predominant 13-bp vs. 6-bp deletions) varied between sites, potentially influencing the functional consequence of the edit [5].
Experimental Protocols for Investigating Variability
Protocol 1: Quantifying Prime Editing Efficiency and By-products in HSPCs
This protocol is designed to assess the on-target efficiency and safety of prime editing strategies in patient-derived hematopoietic cells, which is crucial for understanding donor-to-donor variability [71].
- Isolation and Culture of HSPCs: Isolate CD34+ HSPCs from mobilized peripheral blood or cord blood of multiple donors. Maintain cells in a cytokine-rich serum-free medium (e.g., StemSpan SFEM II supplemented with SCF, TPO, FLT3-L) to preserve stemness.
- Prime Editor Delivery: Electroporate HSPCs with in vitro-transcribed mRNA encoding the optimized prime editor (e.g., PEmax) complexed with synthetic epegRNA and nicking sgRNA as a ribonucleoprotein (RNP) complex. Include a non-targeting control.
- Assessment of Editing Efficiency: Harvest genomic DNA from edited and control cells 72-96 hours post-electroporation. Amplify the target locus by PCR and perform deep sequencing (NGS) to quantify the percentage of reads with the precise intended edit.
- Analysis of Editing By-products: From the NGS data, analyze the spectrum and frequency of undesired outcomes, including small insertions and deletions (indels) and other point mutations, at the target locus.
- In Vivo Engraftment and Persistence Analysis: Transplant edited HSPCs from different donors into immunodeficient mice (e.g., NSG). After 17+ weeks, analyze bone marrow for human cell engraftment (CD45+), lineage differentiation, and persistence of the prime edit in myeloid and erythroid cells to evaluate long-term stability [71].
Protocol 2: Evaluating Functional HbF Reactivation via Erythroid Differentiation
This protocol outlines a functional assay to measure the ultimate phenotypic outcome of gene editing—HbF protein production—in a context that mimics human erythropoiesis.
- Erythroid Differentiation of Edited HSPCs: After editing, culture the HSPCs in a multi-phase erythroid differentiation system. Initiate with expansion media (SCF, EPO, IL-3), then transition to differentiation media with high EPO concentrations to promote maturation over 21-28 days.
- Flow Cytometry for F-cells: At terminal differentiation (days 18-21), harvest erythroblasts. Fix and permeabilize cells, then stain with a fluorescently labeled antibody against HbF. Analyze by flow cytometry to determine the percentage of F-cells (HbF-positive cells).
- Hemoglobin Analysis by HPLC: Lysate the erythroid cells and analyze the soluble hemoglobin content by Cation-Exchange High-Performance Liquid Chromatography (HPLC). This quantifies the relative percentages of HbF, adult hemoglobin (HbA), and sickle hemoglobin (HbS), providing a precise measurement of HbF induction [5].
- Hypoxic Sickling Assay: To functionally validate the therapeutic effect, culture edited erythrocytes under low oxygen tension (1-2% O2) for several hours. Fix the cells and visualize by microscopy to quantify the percentage of cells that maintain a normal biconcave shape versus those that sickle. Edited cells with sufficient HbF should show significant resistance to sickling [71].
The Scientist's Toolkit: Key Research Reagents and Solutions
The consistent execution of the protocols above relies on a standardized set of high-quality reagents. The following table details essential materials and their functions for investigating editing variability.
Table 2: Essential Research Reagents for Investigating Editing Variability in HbF Reactivation
| Reagent / Material | Function / Application | Example / Key Consideration |
|---|---|---|
| CD34+ HSPCs | Primary cell model for ex vivo editing and transplantation. | Source (mobilized peripheral blood, cord blood), donor age, and genetic background are critical variables to track [70] [5]. |
| PEmax mRNA [71] | Optimized prime editor protein expression. | Confers higher editing efficiency than first-generation PE; delivered via electroporation. |
| epegRNA [71] | Synthetic guide RNA for prime editing. | Contains a 3' structured RNA motif (e.g., EvoPre-seq validated) to enhance stability and efficiency. |
| Cas9-gRNA RNP [5] | Pre-complexed ribonucleoprotein for nuclease editing. | Direct delivery of active complex; reduces off-target effects and enables rapid editing. |
| Erythroid Differentiation Media | Induces maturation of HSPCs into erythrocytes. | Multi-phase, serum-free media kits with staged cytokine addition (SCF, EPO, IL-3) are essential for robust differentiation [70]. |
| Anti-HbF Antibody | Detection of HbF protein in cells for flow cytometry. | Critical for quantifying the population of F-cells; clone and conjugate (e.g., FITC) should be validated for intracellular staining. |
| Cation-Exchange HPLC | Quantitative analysis of hemoglobin variants. | Provides precise measurement of HbF%, HbA%, and HbS% from cell lysates [5]. |
| NGS Library Prep Kit | Preparation of amplicon libraries for deep sequencing. | Used for on-target efficiency analysis and indel profiling; must have high accuracy for low-frequency variant calling. |
Addressing the challenges of variable editing efficiencies and donor-specific responses is not merely a technical hurdle but a fundamental requirement for the successful clinical translation of HbF reactivation therapies. A comprehensive understanding of the interplay between biological determinants—such as genetic background, epigenetic landscape, and DNA repair dynamics—and technical parameters—including editor choice, gRNA design, and delivery protocol—is paramount. By adopting the standardized experimental frameworks and reagents outlined in this guide, researchers can systematically deconstruct the sources of variability. This rigorous approach will accelerate the optimization of robust, next-generation editing platforms and delivery methods, ultimately paving the way for highly effective and accessible genetic cures for all patients suffering from β-hemoglobinopathies.
Optimizing Multiplexed Editing Strategies for Enhanced γ-Globin Reactivation
The reactivation of fetal hemoglobin (HbF) represents a cornerstone in the development of curative therapies for β-hemoglobinopathies, including sickle cell disease (SCD) and β-thalassemia. These monogenic disorders, affecting millions globally, stem from mutations in the adult β-globin gene that disrupt hemoglobin function or production, leading to severe anemia, organ damage, and reduced life expectancy [62]. The therapeutic principle underpinning HbF reactivation is that increased levels of γ-globin, the fetal subunit of HbF, can effectively compensate for defective β-globin. In SCD, γ-globin exerts an anti-sickling effect by competing with the pathological sickle β-globin (βs) for incorporation into hemoglobin tetramers, thereby reducing the formation of sickle hemoglobin (HbS) polymers responsible for vaso-occlusive crises [72]. In β-thalassemia, γ-globin pairs with excess α-globin chains, forming functional HbF and ameliorating the ineffective erythropoiesis caused by α-globin precipitation [62].
While the FDA has approved CRISPR-Cas9-based therapies like CASGEVY that target the BCL11A enhancer to reactivate HbF, clinical outcomes reveal limitations, including variable HbF induction among individuals and often incomplete phenotypic rescue [72] [73]. To address these challenges, the field is increasingly advancing beyond single-gene targeting toward multiplexed editing strategies. These approaches simultaneously target multiple regulatory nodes within the globin switch network—such as the γ-globin promoters and multiple enhancers of the repressor BCL11A—to achieve synergistic and more potent HbF reactivation. This technical guide explores the optimization of these multiplexed editing strategies, detailing the latest platforms, methodologies, and quantitative outcomes that are pushing the boundaries of therapeutic efficacy and safety for β-hemoglobinopathies.
Technical Approaches to Multiplexed Editing
The evolution from single to multiplex genome editing has been enabled by advances in CRISPR-based precision tools. The core objective is to disrupt the transcriptional machinery that silences γ-globin expression after birth, primarily by targeting key repressive domains or installing naturally occurring persistence mutations.
Prime Editing of γ-Globin Promoters
Prime editing represents a precise "search-and-replace" technology that enables the installation of targeted point mutations without generating double-strand breaks (DSBs). A recent groundbreaking study applied this technology to rewrite the fetal γ-globin promoters (HBG1 and HBG2) by introducing multiple mutations associated with hereditary persistence of fetal hemoglobin (HPFH) [41].
- Strategic Goal: The research aimed to replicate combined HPFH-associated mutations in the γ-globin promoters, which are expected to synergistically increase promoter activity and thus γ-globin expression.
- Optimization Workflow: The team systematically tested multiple prime editing target sites and optimized a variety of parameters, including the design of prime editing guide RNAs (pegRNAs) and the conditions for delivering the prime editing machinery into hematopoietic stem and progenitor cells (HSPCs).
- Key Outcome: Through rigorous optimization, they achieved approximately 50% precise editing efficiency in a hematopoietic cell line, with minimal off-target effects observed. This work also provided new insights into the complex DNA repair mechanisms that govern prime editing outcomes [41].
- Therapeutic Validation: When tested in patient-derived HSPCs, editing efficiency varied among donors. However, a critical finding was that erythroid clones carrying multiple combined mutations expressed significantly higher γ-globin levels than cells with only individual mutations. This confirms the superior therapeutic potential of a multiplex prime editing strategy over single-editing approaches [41].
Table 1: Key Outcomes of a Prime Editing Strategy for γ-Globin Promoter Rewriting
| Metric | Outcome | Significance |
|---|---|---|
| Editing Efficiency | ~50% precise edits in cell line [41] | Demonstrates feasibility of high-efficiency multiplex mutation installation. |
| Donor Variability | Variable editing in patient HSPCs [41] | Highlights need for further process optimization. |
| γ-globin Expression | Highest in clones with combined mutations [41] | Validates the synergistic effect of multiplex editing. |
| Safety Profile | Minimal off-target effects [41] | Suggests a favorable safety profile for prime editing. |
Multiplex Base Editing of BCL11A Enhancers
An alternative strategy focuses on disrupting the erythroid-specific enhancers of BCL11A, a major transcriptional repressor of γ-globin. While CRISPR-Cas9 nuclease disruption of the +58 kb enhancer is the mechanism of the approved therapy Casgevy, new research explores multiplex base editing to simultaneously target both the +58 kb and +55 kb enhancers for superior efficacy [72] [73].
- Technology: Base editors (BEs) are used, including cytosine base editors (CBEs), adenine base editors (ABEs), and dual base editors (DBEs). These tools catalyze precise C-to-T (or T-to-C) or A-to-G (or G-to-A) nucleotide conversions without inducing DSBs, thereby minimizing the risk of genomic rearrangements [72].
- Target Identification: Researchers first dissected the critical DNA motifs within the GATA1 (at +58 kb) and ATF4 (at +55 kb) binding sites that are recognized by transcriptional activators. By using different BEs and sgRNAs, they generated specific editing profiles (e.g., +58 CBEI, +58 ABEIII, +55 CBEII) to disrupt these motifs and reduce enhancer activity [72].
- Multiplexing Advantage: The simultaneous editing of both the +58 kb and +55 kb enhancers via multiplex base editing resulted in stronger BCL11A downregulation and consequently higher HbF reactivation than editing either enhancer alone. This synergistic effect demonstrates the power of coordinated multipoint disruption [72].
- Efficacy and Safety: This approach achieved HbF levels of approximately 29% of total hemoglobin—a therapeutically beneficial level—while generating virtually no large genomic rearrangements (e.g., 3.2 kb deletions) that were frequently observed with multiplexed CRISPR-Cas9 nuclease editing [72] [73].
Table 2: Performance Comparison of Editing Strategies for HbF Reactivation
| Strategy | Editing Tool | Key Target(s) | Therapeutic Outcome | Key Safety Findings |
|---|---|---|---|---|
| Prime Editing | Prime Editor (PE) | HBG1/HBG2 promoters [41] | High γ-globin in multi-mutant clones [41] | Minimal off-target effects [41] |
| Multiplex Base Editing | CBE, ABE | +58 kb & +55 kb BCL11A enhancers [72] | ~29% HbF; superior to single editing [73] | Few DSBs; no large rearrangements [72] [73] |
| CRISPR-Cas9 Nuclease | Cas9 Nuclease | +58 kb BCL11A enhancer (Casgevy) [72] | Variable HbF; substantial HbS remains [72] | Large genomic rearrangements possible [72] |
Diagram 1: Strategic Pathways for HbF Reactivation. This workflow compares the core methodologies and outcomes of prime editing, multiplex base editing, and standard CRISPR-Cas9 nuclease approaches.
Experimental Protocols and Workflows
Successful multiplexed editing requires optimized protocols from guide RNA design through final functional assessment. Below is a detailed methodology for a typical multiplex base editing experiment in hematopoietic stem and progenitor cells (HSPCs), as exemplified by recent studies [72].
Cell Source and Culture
- Cell Type: Mobilized peripheral blood or bone marrow-derived CD34+ HSPCs from healthy donors or SCD patients.
- Pre-culture: Maintain cells in a suitable medium (e.g., SFEM II) supplemented with cytokines (SCF, TPO, FLT3-L, IL-3) for 24-48 hours to promote cell cycling and enhance editing efficiency.
Guide RNA Design and Complex Formation
- Target Selection: Identify specific nucleotides within the GATA1 binding site of the BCL11A +58 kb enhancer (e.g., sequence: GTGATAAA) and the ATF4 binding site of the +55 kb enhancer (e.g., sequence: TTGCATCATCC) [72].
- sgRNA Design: Design and synthesize sgRNAs with high on-target and minimal predicted off-target activity. For enhanced specificity, truncating the sgRNA binding sequence to 18-19 bp can be considered [74].
- RNP Complex Formation: For delivery, pre-complex the sgRNAs with the base editor protein (e.g., BE4max for CBE, ABE8e for ABE) to form ribonucleoprotein (RNP) complexes. Using RNP delivery is associated with reduced off-target effects and lower cytotoxicity compared to plasmid or viral delivery [74].
Cell Transfection and Editing
- Transfection Method: Electroporate the pre-formed RNP complexes into HSPCs using optimized electroporation parameters (e.g., Lonza 4D-Nucleofector).
- Post-Transfection Care: Immediately after electroporation, transfer cells to pre-warmed medium. To improve cell viability, consider adding a pan-caspase inhibitor like Z-Vad-FMK to the culture for 24 hours to mitigate apoptosis [74].
Assessment of Editing Efficiency
- Genomic Analysis: Extract genomic DNA from edited cells 3-5 days post-electroporation.
- On-Target Editing: Assess editing efficiency at the +58 kb and +55 kb target sites by PCR amplification of the genomic regions, followed by next-generation sequencing (NGS) to quantify the percentage of intended base conversions and identify any insertions or deletions (indels).
- Off-Target Analysis: Perform assays such as GUIDE-seq or whole-exome sequencing to profile potential off-target editing events across the genome [72] [73].
Differentiation and Functional Validation
- Erythroid Differentiation: Culture a portion of the edited HSPCs in a multi-phase erythroid differentiation medium containing EPO, SCF, IL-3, and hydrocortisone for approximately 13-18 days to generate mature erythroblasts [72] [74].
- Molecular Phenotyping:
- HbF Quantification:
- Protein Level: Use flow cytometry to detect HbF-positive cells (F-cells) and perform high-performance liquid chromatography (HPLC) to quantify the percentage of HbF relative to total hemoglobin [72].
- RNA Level: Use RT-qPCR to measure HBG mRNA expression, normalized to housekeeping genes.
- BCL11A Downregulation: Use RT-qPCR or western blot to assess the reduction of BCL11A expression in differentiated erythroid cells compared to controls.
- Functional Rescue (Sickling Assay): For SCD models, subject differentiated erythroid cells to hypoxic conditions and measure the reduction in the frequency of sickled cells compared to untreated SCD controls [72].
- HbF Quantification:
Diagram 2: Experimental Workflow for Multiplex Base Editing in HSPCs. This detailed protocol outlines the key steps from cell preparation through functional validation of edited hematopoietic stem and progenitor cells.
The Scientist's Toolkit: Essential Research Reagents
Implementing multiplexed editing strategies requires a suite of specialized reagents and tools. The following table catalogs essential components for conducting these advanced experiments.
Table 3: Research Reagent Solutions for Multiplexed Genome Editing
| Reagent / Tool | Function / Description | Example Application |
|---|---|---|
| CD34+ HSPCs | Primary human hematopoietic stem/progenitor cells; the therapeutic cell product. | Sourced from mobilized peripheral blood or bone marrow; used for all ex vivo editing [72] [74]. |
| Base Editors (BEs) | Engineered proteins (e.g., BE4max-CBE, ABE8e) that catalyze specific base conversions without DSBs. | Disruption of key nucleotides in BCL11A enhancers (GATA1/ATF4 sites) [72]. |
| Prime Editors (PEs) | Fusion proteins that use a pegRNA to template the installation of desired edits without DSBs. | Introducing multiple HPFH-like point mutations into the γ-globin promoters [41]. |
| sgRNAs / pegRNAs | Synthetic guide RNAs that direct the editing machinery to specific genomic loci. | Designed for BCL11A +58 kb/+55 kb enhancers or HBG promoter regions [41] [72]. |
| Electroporation System | Device (e.g., Lonza 4D-Nucleofector) for delivering RNP complexes into HSPCs. | High-efficiency, transient delivery of editors with reduced cytotoxicity [74]. |
| Erythroid Differentiation Media | Cytokine cocktails (EPO, SCF, IL-3, etc.) to drive HSPCs to mature erythroblasts. | Generating red blood cells for functional assessment of HbF reactivation [72] [74]. |
| NGS Assays | Next-generation sequencing for on-target efficiency and off-target profiling. | Quantifying base conversion rates and identifying potential off-target sites via GUIDE-seq [72]. |
| HPLC / Flow Cytometry | Analytical tools for quantifying HbF at the protein and single-cell level. | Measuring therapeutic efficacy: HbF% by HPLC, F-cells by flow cytometry [72]. |
The strategic shift from single-point to multiplexed genome editing marks a significant evolution in the quest to achieve curative levels of γ-globin reactivation for β-hemoglobinopathies. The emerging data is compelling: prime editing can install multiple HPFH-like mutations in the γ-globin promoters to synergistically enhance their activity [41], while multiplex base editing of the +58 kb and +55 kb BCL11A enhancers produces a more potent downregulation of this repressor and a consequent greater HbF induction than targeting a single site [72]. A critical advantage shared by these advanced platforms is their improved safety profile, as they largely avoid the double-strand breaks that can lead to genotoxic chromosomal rearrangements—a noted concern with traditional CRISPR-Cas9 nuclease approaches [73].
Despite the promise, challenges remain. Donor-to-donor variability in editing efficiency and the technical complexity of delivering large editor constructs to HSPCs at high efficiency are current bottlenecks that require further optimization of delivery platforms and editor architecture [41] [74]. Furthermore, while phenotypic rescue is robust, it can be incomplete, underscoring the need to push HbF levels even higher. Future research directions will likely focus on combining these strategies—for example, simultaneously editing the BCL11A enhancers and the γ-globin promoters—to unlock the full therapeutic potential of the fetal globin switch. As these refined multiplexed editing strategies progress from the bench to the clinic, they hold the promise of delivering safer, more effective, and universally applicable cures for sickle cell disease and β-thalassemia.
Scalability and Manufacturing Challenges for Global Accessibility
The reactivation of fetal hemoglobin (HbF) represents a transformative therapeutic strategy for sickle cell disease (SCD) and β-thalassemia, monogenic disorders affecting millions worldwide. While recently approved CRISPR-based therapies like CASGEVY demonstrate remarkable efficacy, their global impact remains limited by significant scalability and manufacturing hurdles. This whitepaper examines the core technical challenges—including viral vector production constraints, ex vivo manufacturing complexity, and high costs—that restrict patient access. Furthermore, we analyze emerging alternative approaches, such as antisense oligonucleotides (ASOs) and novel delivery systems, that offer potential pathways toward more scalable, affordable, and globally accessible therapies. By synthesizing current research findings and experimental data, this review provides researchers and drug development professionals with a technical framework for advancing next-generation HbF reactivation strategies that balance precision with practicality.
β-hemoglobinopathies, including SCD and β-thalassemia, are among the most prevalent monogenic disorders globally, with over 300,000 infants born with severe forms annually [62]. These conditions stem from mutations in the β-globin gene (HBB), leading to defective adult hemoglobin production, ineffective erythropoiesis, and multisystem complications. The natural persistence or reactivation of fetal hemoglobin (HbF), which contains γ-globin chains instead of β-globin chains, substantially ameliorates disease severity by compensating for defective adult hemoglobin [3] [62].
The molecular basis for HbF reactivation therapies centers on disrupting the physiological silencing of γ-globin genes that occurs postnatally. Key repressors identified include BCL11A and ZBTB7A/LRF, which act through binding sites in the γ-globin promoters and through higher-order chromatin structures [3] [5]. Recently approved gene therapies such as CASGEVY (exagamglogene autotemcel) utilize CRISPR/Cas9 to disrupt a BCL11A enhancer in hematopoietic stem and progenitor cells (HSPCs), resulting in sustained HbF reactivation and transformative outcomes for patients [3] [75].
However, these advanced therapies face profound scalability and manufacturing challenges that severely limit global accessibility. The ex vivo gene editing process requires complex facilities, lengthy manufacturing timelines, and specialized expertise. Additionally, the reliance on viral vectors for delivery presents production bottlenecks, immunogenicity concerns, and substantial cost barriers [21] [62]. With current gene therapies costing over $2 million per patient and available only at specialized centers, they remain inaccessible to most patients worldwide, particularly in low- and middle-income countries where the disease burden is highest [3] [75].
This whitepaper examines the technical foundations of these challenges and explores innovative approaches under development to overcome them, with particular focus on their implications for researchers and drug development professionals working to expand global access to HbF-directed therapies.
Current HbF Reactivation Approaches: Mechanisms and Limitations
CRISPR-Based Genome Editing Strategies
CRISPR-based technologies have evolved into a diverse toolkit for HbF reactivation, each with distinct mechanisms and technical considerations:
BCL11A Enhancer Disruption: The mechanism of recently approved therapies involves CRISPR/Cas9-mediated disruption of an erythroid-specific enhancer of the BCL11A gene. Research reveals this enhancer forms a three-dimensional chromatin "rosette" structure essential for maintaining high-level BCL11A expression. CRISPR targeting disrupts this structure, allowing repressive proteins to silence BCL11A, thereby reactivating HbF production [3].
γ-Globin Promoter Editing: An alternative approach directly targets transcriptional repressor binding sites in the γ-globin promoters. Disruption of ZBTB7A/LRF or BCL11A binding sites at positions -197 and -115 upstream of the transcription start site effectively reactivates HbF. Editing efficiency is higher for the BCL11A site (75-92%) compared to the ZBTB7A/LRF site (57-60%), with both strategies achieving significant HbF increases in β-thalassemia/HbE patient cells [5].
Advanced CRISPR Systems: Next-generation editors including base editors (BEs) and prime editors (PEs) enable more precise genetic modifications without double-strand breaks. Base editors facilitate single-nucleotide conversions, while prime editors support targeted insertions, deletions, and all point mutation types with reduced off-target risks [21].
Table 1: Comparison of CRISPR-Based HbF Reactivation Approaches
| Approach | Molecular Target | Editing Efficiency | HbF Induction | Key Advantages | Technical Challenges |
|---|---|---|---|---|---|
| BCL11A Enhancer Editing | Erythroid-specific enhancer region | 80.5±9.8% (healthy donors); 85.8±14.7% (SCD patients) [75] | 19.0-26.8% of total Hb [75] | High specificity; mimics natural HPFH | Complex 3D genome disruption; delivery challenges |
| γ-Globin Promoter Editing (BCL11A site) | HBG promoter at -115 | 75-92% [5] | 26.2±1.4% (healthy); 62.7±0.9% (β-thal/HbE) [5] | Direct targeting of repressor binding | Potential off-target effects at homologous sites |
| γ-Globin Promoter Editing (ZBTB7A site) | HBG promoter at -197 | 57-60% [5] | 27.9±1.5% (healthy); 64.0±1.6% (β-thal/HbE) [5] | Alternative pathway for HbF induction | Lower editing efficiency compared to BCL11A site |
| Base Editors | Specific nucleotides in regulatory regions | Varies by system | Preclinical validation ongoing | Reduced indel formation; no DSBs | Limited editing window; potential bystander edits |
| Prime Editors | Targeted sequences with pegRNA templates | Varies by system | Preclinical validation ongoing | Broad editing capabilities; no DSBs | Lower efficiency; complex reagent design |
Lentiviral Gene Addition Strategies
An alternative to gene editing is lentiviral vector-mediated addition of functional β-globin genes or modified antisickling globin variants. LYFGENIA (lovotibeglogene autotemcel) utilizes the BB305 lentiviral vector to encode HbAT87Q, a modified β-globin with an amino acid substitution (threonine to glutamine at position 87) that inhibits sickle hemoglobin polymerization [75]. This approach requires careful vector design incorporating "mini-LCR" elements (HS2, HS3, and HS4) from the β-globin locus control region to achieve erythroid-specific expression, typically resulting in 1.0-1.2 vector copies per transduced cell [75].
Diagram 1: CRISPR-based HbF reactivation pathways. The diagram illustrates the different molecular approaches to reactivate fetal hemoglobin using CRISPR technology, showing both direct promoter editing and enhancer disruption strategies.
Scalability and Manufacturing Challenges
Viral Vector Production Limitations
The manufacturing of viral vectors represents perhaps the most significant bottleneck in scaling HbF reactivation therapies globally:
Lentiviral Vector Production Constraints: Lentiviral vectors used in gene addition therapies require complex production systems involving multiple plasmid transfections into packaging cell lines. The current manufacturing capacity remains limited, with challenges in achieving consistent high titers, appropriate purity, and compliance with regulatory standards. Vector yields from current production methods are insufficient to meet global demand for β-hemoglobinopathies [21] [62].
Packaging Capacity Limitations: Lentiviral vectors have limited packaging capacity (~8-10 kb), constraining the size of regulatory elements that can be included. While "mini-LCR" designs (2.6-3.4 kb) have been developed to overcome this, they may not fully recapitulate native regulation, potentially leading to position effects and variable expression [62] [75].
Immunogenicity and Safety Concerns: Viral vectors can elicit immune responses that reduce efficacy or cause adverse events. Additionally, insertional mutagenesis remains a concern, though newer self-inactivating (SIN) designs have mitigated this risk [21].
Ex Vivo Manufacturing Complexity
The current paradigm of ex vivo gene therapy presents multiple logistical and technical hurdles:
Cell Processing Challenges: Ex vivo therapies require extraction of patient CD34+ hematopoietic stem cells via apheresis, followed by complex processing, stimulation, genetic modification, and quality testing before reinfusion. This process necessitates specialized facilities with Good Manufacturing Practice (GMP) compliance and highly trained personnel [62] [75].
Myeloablative Conditioning Requirements: Patients must undergo myeloablative conditioning with busulfan before reinfusion of modified cells, creating additional toxicity risks and requiring specialized inpatient care [75].
Stability and Storage Considerations: Cryopreservation of modified cells during quality testing and transport adds complexity and cost, with risks of cell viability loss during freeze-thaw cycles [62].
Table 2: Scalability Challenges of Current HbF Reactivation Therapies
| Challenge Category | Specific Limitations | Impact on Global Accessibility |
|---|---|---|
| Viral Vector Production | Limited manufacturing capacity; batch-to-batch variability; high production costs | Constrains patient slots; increases costs to >$2M per treatment |
| Ex Vivo Processing | Requirement for GMP facilities; specialized expertise; lengthy manufacturing time | Limits treatment to specialized centers; complex logistics |
| Cell Collection & Transport | Apheresis requirements; cryopreservation needs; viability maintenance | Creates geographical barriers for remote patients |
| Conditioning Regimens | Myeloablation-related toxicity; need for inpatient care | Increases treatment risks and healthcare infrastructure demands |
| Quality Control & Testing | Extensive safety and potency assays; regulatory validation | Extends manufacturing timeline; requires advanced laboratory capabilities |
Economic and Infrastructure Barriers
The economic reality of current HbF reactivation therapies creates profound accessibility challenges:
Prohibitive Costs: At over $2 million per treatment, currently approved gene therapies are beyond reach for most healthcare systems, particularly in low- and middle-income countries where the disease burden is concentrated [3] [75].
Specialized Center Requirements: The complex administration process requires specialized academic medical centers with expertise in stem cell transplantation, genetic therapies, and supportive care, which are unavailable in many regions [62].
Limited Manufacturing Capacity: Global production capacity for viral vectors and ex vivo cell processing can currently serve only a tiny fraction of the eligible patient population, creating multi-year waiting lists even in high-income countries [21].
Emerging Solutions and Alternative Approaches
Non-Viral Delivery Systems
Innovative non-viral delivery approaches offer promising alternatives to overcome viral vector limitations:
Lipid Nanoparticles (LNPs): LNPs have emerged as versatile carriers for CRISPR components, demonstrating efficacy in preclinical models. They offer advantages including reduced immunogenicity, larger payload capacity, and simpler manufacturing scalability compared to viral vectors. Current research focuses on optimizing LNP formulations for hematopoietic stem cell targeting [21].
Engineered Exosomes: Naturally occurring extracellular vesicles show potential as delivery vehicles for gene editing tools. They can be engineered with specific surface markers to enhance cell-type specificity and have demonstrated efficient cargo delivery in preliminary studies [21].
Electroporation Enhancements: Improved electroporation technologies enable more efficient delivery of ribonucleoprotein (RNP) complexes to hematopoietic stem cells while maintaining cell viability. Recent advances include cell-type specific parameters and closed-system electroporation devices suitable for GMP manufacturing [5].
In Vivo Gene Editing Approaches
In vivo delivery strategies could potentially revolutionize the treatment paradigm by eliminating ex vivo manufacturing:
Direct Administration: Preclinical research demonstrates the feasibility of directly administering gene editing components to patients, potentially simplifying treatment to a single infusion. Early success in animal models shows efficient editing of hematopoietic stem cells in their native bone marrow niche [62].
Targeted Delivery Systems: Advances in tissue-specific targeting ligands, such as antibodies against CD117 (c-Kit) on hematopoietic stem cells, enable more precise delivery of editing tools to target cells while minimizing off-target effects [62].
Alternative Therapeutic Modalities
Novel molecular approaches offer potentially more scalable paths to HbF reactivation:
Antisense Oligonucleotides (ASOs): Recent research has identified that the therapeutic effects of BCL11A enhancer editing can be replicated using ASOs that target enhancer-derived RNAs (eRNAs). In preclinical models, ASO-mediated degradation of BCL11A eRNAs prevented epigenetic insulation, silenced BCL11A, and reactivated HbF production without permanent genome modification [3] [49]. This approach could offer a more affordable, accessible, and scalable alternative to current gene therapies.
Small Molecule Therapies: High-throughput screening approaches have identified small molecules that can disrupt the BCL11A complex or interfere with γ-globin repression. While still in early development, these approaches could ultimately provide orally administered, cost-effective treatments [76].
Diagram 2: Challenges and emerging solutions for scalable HbF therapies. This diagram maps the primary scalability challenges against innovative approaches under development to improve global accessibility of HbF reactivation treatments.
Experimental Protocols for HbF Reactivation Research
CRISPR Editing of BCL11A Enhancer in HSPCs
This protocol outlines the key methodology for investigating BCL11A enhancer editing, based on approaches used in developing CASGEVY:
Cell Collection and Preparation: Collect mobilized CD34+ hematopoietic stem/progenitor cells from healthy donors or patients via apheresis. Isulate CD34+ cells using immunomagnetic selection, achieving >90% purity. Culture cells in serum-free expansion medium supplemented with SCF, TPO, FLT3-L, and IL-3 for 24-48 hours before editing [3] [75].
RNP Complex Formation: Combine Streptococcus pyogenes Cas9 protein (100 pmol) with single-guide RNA (gRNA-68, 120 pmol) targeting the BCL11A erythroid-specific enhancer region. Incubate at room temperature for 10-20 minutes to form ribonucleoprotein (RNP) complexes [75].
Electroporation Conditions: Electroporate 1×10^5 CD34+ cells using the Lonza 4D-Nucleofector system with program DZ-100 and P3 primary cell solution. Use 10-20 μg RNP complex per 100 μL reaction volume. Immediately transfer cells to pre-warmed recovery medium post-electroporation [5] [75].
Erythroid Differentiation and Analysis: Culture edited cells in erythroid differentiation medium containing SCF, EPO, and dexamethasone for 14-21 days. Analyze HbF production using flow cytometry (F-cells), HPLC (HbF percentage), and γ-globin mRNA expression by RT-qPCR [5].
ASO-Mediated BCL11A eRNA Targeting
This protocol describes the alternative approach of targeting BCL11A enhancer RNAs with antisense oligonucleotides:
ASO Design and Preparation: Design antisense oligonucleotides complementary to the BCL11A enhancer-derived RNA sequences. Incorporate chemical modifications (e.g., 2'-O-methoxyethyl, phosphorothioate backbone) to enhance stability and cellular uptake. Resuspend ASOs in nuclease-free water at 100 μM stock concentration [3] [49].
Cell Culture and Treatment: Culture human erythroid progenitors from peripheral blood or CD34+ cells in erythroid differentiation medium. At day 7 of differentiation, transfer cells to 24-well plates at 2×10^5 cells/well. Transfert ASOs using lipid-based transfection reagents at 10-100 nM final concentration. Include scrambled ASO controls and untreated controls [49].
eRNA Detection and Analysis: Harvest cells 24-48 hours post-transfection. Isolate total RNA using TRIzol reagent. Perform RT-qPCR using primers specific for BCL11A eRNAs, normalizing to GAPDH or β-actin. Assess BCL11A mRNA expression to confirm silencing efficacy [3].
Functional Assessment: Continue erythroid differentiation for 14-21 days total. Analyze HbF production by HPLC and flow cytometry. Perform chromatin conformation capture (3C) assays to evaluate disruption of the chromatin rosette structure in the BCL11A locus [3].
Research Reagent Solutions
Table 3: Essential Research Reagents for HbF Reactivation Studies
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Gene Editing Tools | S. pyogenes Cas9, gRNA-68, Base editors (ABE, CBE), Prime editors | CRISPR-mediated disruption of BCL11A enhancer or γ-globin promoter | RNP delivery preferred for reduced off-target effects; validate editing efficiency by NGS |
| Delivery Systems | Lonza 4D-Nucleofector, Lipid nanoparticles (LNPs), Engineered exosomes | Efficient delivery of editing components to HSPCs | Optimize delivery parameters for cell viability and editing efficiency |
| Cell Culture Supplements | StemSpan SFEM, SCF, TPO, FLT3-L, EPO, IL-3, Dexamethasone | HSPC expansion and erythroid differentiation | Maintain cytokine concentrations throughout differentiation protocol |
| Analytical Tools | HPLC with cation exchange columns, Flow cytometry antibodies (HbF, CD235a), NGS platforms | Assessment of HbF induction and editing efficiency | Include appropriate controls for gating and quantification |
| ASO Reagents | 2'-MOE-modified phosphorothioate ASOs, Lipid transfection reagents | BCL11A eRNA targeting studies | Optimize ASO concentration and transfection timing in differentiation |
| Specialized Assays | Chromatin Immunoprecipitation (ChIP), 3C/4C, RNA-seq, ATAC-seq | Mechanistic studies of chromatin structure and gene expression | Include spike-in controls and sufficient replicates for statistical power |
The reactivation of fetal hemoglobin continues to demonstrate remarkable therapeutic potential for sickle cell disease and β-thalassemia, yet realizing its global impact requires overcoming profound scalability and manufacturing challenges. Current CRISPR-based approaches achieve unprecedented efficacy but face limitations in viral vector production, ex vivo processing complexity, and economic viability that restrict accessibility to a small fraction of patients.
Promising emerging strategies—including non-viral delivery systems, in vivo editing approaches, and alternative modalities like ASOs—offer pathways toward more scalable solutions. The recent discovery that ASOs can target BCL11A enhancer RNAs to disrupt chromatin structure and reactivate HbF provides a particularly compelling direction for future research, potentially enabling more affordable and accessible therapies.
For researchers and drug development professionals, priority areas include optimizing delivery efficiency, streamlining manufacturing processes, developing predictive safety models, and establishing scalable production platforms. By addressing these technical challenges through collaborative innovation, the field can advance toward the ultimate goal: safe, effective, and globally accessible HbF reactivation therapies for all patients suffering from β-hemoglobinopathies.
Mitigating Immunogenicity and Long-Term Safety Monitoring
Fetal hemoglobin (HbF) reactivation represents a transformative therapeutic strategy for sickle cell disease (SCD) and β-thalassemia, genetic disorders caused by defects in the adult β-globin gene [77]. The cornerstone of this approach involves reversing the developmental switch from fetal to adult hemoglobin, thereby compensating for dysfunctional β-globin chains through increased γ-globin production [76]. While CRISPR-based gene editing technologies have demonstrated remarkable clinical success, their translational application faces two paramount challenges: mitigating immunogenicity associated with therapeutic delivery systems and establishing comprehensive long-term safety monitoring protocols [21] [78]. These challenges are particularly critical for advanced therapies like exagamglogene autotemcel (exa-cel), a CRISPR-Cas9-edited cellular therapy that has shown robust and sustained improvements in quality of life for patients with severe SCD or transfusion-dependent beta thalassemia [79]. This technical guide examines current strategies and methodologies for addressing these challenges within the context of HbF-reactivating therapies, providing a framework for researchers and drug development professionals engaged in translating these innovative approaches to clinical practice.
Immunogenicity Challenges in HbF Reactivation Therapies
The immunogenic potential of HbF-reactivating therapies varies significantly based on their therapeutic modality. Understanding these differences is crucial for selecting appropriate delivery strategies and designing effective mitigation approaches.
Table 1: Immunogenicity Profiles of Delivery Systems for HbF Reactivation Therapies
| Delivery System | Immunogenic Components | Primary Concerns | Mitigation Strategies |
|---|---|---|---|
| Viral Vectors (Lentiviruses, AAVs) | Viral capsid proteins, transgenic products | Pre-existing immunity, cell-mediated immune responses, insertional mutagenesis [21] | Pseudotyping, promoter optimization, proteasome inhibition [80] |
| CRISPR-Cas9 Components | Bacterial Cas9 nuclease, guide RNA | Anti-Cas9 antibodies, T-cell responses, off-target editing [78] | Ex vivo delivery, Cas9 protein/RNA delivery versus DNA, immunosuppression [21] |
| Lipid Nanoparticles (LNPs) | Ionizable lipids, PEG-lipids | Anti-PEG antibodies, complement activation, accelerated blood clearance [21] | Novel lipid design, PEG alternatives, dose optimization [21] [80] |
| Engineered Exosomes | Surface proteins, cargo | Minimal compared to other systems [21] | Autologous sources, surface engineering [21] |
Viral Vector Immunogenicity
Viral vectors, particularly adeno-associated viruses (AAVs) and lentiviruses, present significant immunogenicity challenges. Pre-existing immunity to AAV serotypes is prevalent in human populations and can neutralize systemically administered vectors, reducing therapeutic efficacy [21]. Additionally, cell-mediated immune responses against transduced cells can lead to loss of therapeutic effect over time. Lentiviral vectors, while less immunogenic than AAVs, raise concerns regarding insertional mutagenesis due to their integrating nature [80]. Mitigation strategies include pseudotyping with alternative viral envelopes, using tissue-specific promoters to limit transgene expression to target cells, and transient immunosuppression during initial vector exposure [80].
CRISPR-Cas9 Immunogenicity
The CRISPR-Cas9 system, derived from bacterial immune systems, introduces foreign proteins that can elicit both humoral and cellular immune responses. Anti-Cas9 antibodies have been detected in human sera, and pre-existing T-cell responses against Cas9 orthologs may lead to rapid clearance of edited cells or inflammatory toxicity [78]. Ex vivo delivery approaches, where hematopoietic stem and progenitor cells (HSPCs) are edited outside the body, significantly reduce but do not eliminate these concerns, as residual Cas9 expression may persist in some edited cells [21]. Delivery of Cas9 as ribonucleoprotein (RNP) complexes rather than DNA plasmids reduces persistence time and consequently may lower immunogenic potential [5].
Safety Monitoring Frameworks and Protocols
Comprehensive long-term safety monitoring is essential for HbF reactivation therapies, particularly for genome-editing approaches that induce permanent genetic modifications. Monitoring protocols must address both general gene therapy risks and specific concerns related to the therapeutic mechanism.
Table 2: Long-Term Safety Monitoring Parameters for HbF Reactivation Therapies
| Monitoring Category | Specific Parameters | Recommended Duration | Detection Methods |
|---|---|---|---|
| Genotoxicity | Off-target editing, chromosomal abnormalities, insertional mutagenesis | 15+ years [78] | WGS, LAM-PCR, Digenome-seq, GUIDE-seq |
| Immunological Safety | Graft-versus-host disease (allogeneic), anti-Cas9 immunity, vector immunity | 5+ years [81] [78] | ELISA, ELISpot, flow cytometry, immune cell counts |
| Therapeutic Persistence | HbF levels, F-cells, edited cell population, transfusion requirements | Lifetime [79] | HPLC, flow cytometry, vector copy number, engraftment analysis |
| Organ Function | Hepatic, renal, cardiac, pulmonary function | 5+ years [81] | Standard clinical chemistry, imaging, functional tests |
Genotoxicity Assessment
Genotoxicity assessment focuses on identifying unintended genetic alterations resulting from gene-editing procedures. For CRISPR-based therapies, this includes comprehensive evaluation of off-target editing at sites with sequence similarity to the guide RNA target sequence [78]. Recommended methodologies include:
- Whole Genome Sequencing (WGS): Provides unbiased assessment of genomic integrity but requires sophisticated bioinformatic analysis to distinguish meaningful variants from background noise [78].
- Linear Amplification-Mediated PCR (LAM-PCR): Used for monitoring vector integration sites in lentiviral-based therapies, identifying potential genotoxic hotspots near oncogenes [80].
- GUIDE-seq and Digenome-seq: In vitro methods for profiling genome-wide off-target activity of CRISPR nucleases, often employed during therapeutic development [5].
Long-term monitoring should include regular assessment for clonal hematopoiesis, which may indicate selective expansion of edited cells with potentially deleterious mutations [80].
Immunological Safety Monitoring
Immunological safety monitoring encompasses both the response to therapeutic components and immune-related adverse events:
- Anti-Cas9 Immunity: Serial assessment of Cas9-specific antibodies and T-cell responses using ELISA and ELISpot assays, respectively [78].
- Graft-versus-Host Disease (GVHD): For allogeneic approaches, standardized grading of acute and chronic GVHD using established criteria [81].
- Vector-Specific Immunity: Monitoring for neutralizing antibodies against viral vectors, particularly important for in vivo delivery approaches [21].
Immunological monitoring should be particularly intensive during the first year post-treatment when most immune-mediated adverse events manifest.
Experimental Protocols for Immunogenicity and Safety Assessment
Robust experimental protocols are essential for generating clinically relevant data on immunogenicity and safety profiles of HbF reactivation therapies.
Protocol: Off-Target Editing Analysis Using GUIDE-seq
GUIDE-seq (Genome-wide, Unbiased Identification of DSBs Enabled by Sequencing) provides a comprehensive method for identifying off-target CRISPR-Cas9 activity [5]:
- Cell Transfection: Co-transfect 1×10^6 HEK293T cells or primary CD34+ HSPCs with 5μg of Cas9-gRNA RNP complex and 100pmol of GUIDE-seq oligonucleotide using electroporation.
- Genomic DNA Extraction: Harvest cells 72 hours post-transfection and extract genomic DNA using silica membrane-based kits.
- Library Preparation: Fragment DNA to 400bp, end-repair, and ligate with adaptors. Perform PCR enrichment with primers specific to the GUIDE-seq oligonucleotide.
- Sequencing and Analysis: Sequence libraries on Illumina platforms. Align sequences to reference genome and identify off-target sites using validated bioinformatic pipelines (e.g., GUIDEs-seq analysis software).
This protocol should be validated in relevant cell types, including primary hematopoietic stem cells, as off-target profiles can vary between cell types [5].
Protocol: Anti-Cas9 T-Cell Response Assay
Assessment of T-cell responses against Cas9 provides critical immunogenicity data:
- PBMC Isolation: Isolate peripheral blood mononuclear cells (PBMCs) from patient blood samples at baseline and multiple timepoints post-treatment (e.g., days 14, 30, 90, 180).
- Antigen Stimulation: Culture 2×10^5 PBMCs per well with overlapping peptide pools covering the full Cas9 protein sequence (15-mer peptides with 11-amino acid overlap) for 24 hours.
- Cytokine Detection: Detect T-cell activation using IFN-γ ELISpot or intracellular cytokine staining with flow cytometry.
- Data Interpretation: Compare post-treatment responses to baseline values. Responses exceeding 2-fold increase over background and 50 spot-forming cells per million PBMCs are generally considered significant.
This assay helps identify patients at risk for cell-mediated immune responses against CRISPR-edited cells [78].
Visualization of Key Concepts
Immunogenicity Mitigation Strategies
Safety Monitoring Framework
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Immunogenicity and Safety Assessment
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| CRISPR Components | Cas9 nuclease, sgRNAs, RNP complexes | Genome editing efficiency assessment, off-target profiling [5] | High-purity grades reduce immune activation; chemical modifications enhance stability |
| Cell Isolation Kits | CD34+ selection kits, PBMC isolation kits | Target cell population purification, immunogenicity assays [5] | Purity impacts editing efficiency; endotoxin-free reagents critical for clinical applications |
| Immunogenicity Assays | IFN-γ ELISpot kits, cytokine detection arrays, flow cytometry panels | Detection of cellular and humoral immune responses [78] | Validated reagents essential for reproducible results; consider species reactivity |
| Sequencing Reagents | WGS kits, LAM-PCR reagents, targeted sequencing panels | Genotoxicity assessment, tracking edited clones [5] [80] | Depth of coverage critical for off-target detection; standardized bioinformatic pipelines |
| Hemoglobin Analysis | HPLC columns, HbF antibodies, flow cytometry kits | Therapeutic efficacy monitoring, F-cell quantification [5] [79] | Standardized protocols enable cross-study comparisons; sensitivity thresholds important |
Mitigating immunogenicity and establishing robust long-term safety monitoring protocols represent critical components in the development pathway of HbF reactivation therapies. The strategies and methodologies outlined in this technical guide provide a framework for addressing these challenges across diverse therapeutic modalities, from viral vector-mediated gene addition to CRISPR-based genome editing. As evidenced by recent clinical successes, including the approval of exa-cel for SCD and β-thalassemia, comprehensive approaches to safety and immunogenicity can enable the successful translation of these transformative therapies [79]. Continued refinement of these approaches, particularly through the development of increasingly sensitive detection methods and novel mitigation strategies, will be essential for expanding the therapeutic index of HbF reactivation therapies and ensuring their accessibility to diverse patient populations worldwide.
Comparative Efficacy Analysis and Preclinical-to-Clinical Translation
The reactivation of fetal hemoglobin (HbF) represents a paramount therapeutic objective for treating β-hemoglobinopathies, including sickle cell disease (SCD) and β-thalassemia. These common monogenic disorders are caused by defects in the adult β-globin gene (HBB); elevating HbF compensates for the absent or dysfunctional adult β-globin, alleviating disease pathology [82]. A profound understanding of the developmental switch from fetal (γ-globin, HBG) to adult (β-globin, HBB) hemoglobin has unveiled key transcriptional repressors, namely BCL11A and ZBTB7A (also known as LRF), which silence HBG expression in adult erythroid cells [82] [83]. Consequently, disrupting the function of these repressors has emerged as a leading gene-editing strategy.
While multiple approaches exist to inhibit these repressors—such as targeting their upstream regulators or enhancers—this whitepaper focuses on a direct, promoter-centric comparison: the disruption of their specific binding sites within the γ-globin gene promoter. This document provides an in-depth technical guide, synthesizing recent and direct experimental evidence to compare the efficiency, efficacy, and safety of CRISPR/Cas9-mediated disruption of the BCL11A binding site at position -115 versus the ZBTB7A/LRF binding site at position -200. The data and protocols herein are intended to inform the experimental design of researchers and drug development professionals working towards curative genetic therapies.
Molecular Basis of Fetal Hemoglobin Silencing
The transition from HbF to adult hemoglobin around birth is a tightly regulated process governed by the coordinated action of transcriptional repressors that bind directly to the HBG promoters. Two zinc-finger proteins are established as the principal direct repressors:
- BCL11A: This repressor binds a
5′-TGACCA-3′element at approximately -115 nucleotides upstream of the HBG transcription start site. Its expression is notably higher in adult erythroid cells compared to fetal cells, a key mechanism for developmental silencing [82] [83]. - ZBTB7A/LRF: This repressor binds a pyrimidine-rich
5′-CCCCTTCCCC-3′element at the -200 site. Structural analyses reveal that its DNA-binding domain, consisting of four zinc fingers, recognizes eight C:G base pairs within this element. Naturally occurring mutations in this site that impair ZBTB7A binding are linked to the benign condition Hereditary Persistence of Fetal Hemoglobin (HPFH) [83].
These repressors function additively; neither is sufficient for complete HBG silencing without the other, and disruption of either can lead to significant HbF reactivation [82]. The following diagram illustrates their direct role in silencing the γ-globin gene.
Figure 1: Direct repression of γ-globin gene expression. The transcriptional repressors ZBTB7A/LRF and BCL11A bind to their specific sites at the -200 and -115 positions, respectively, on the γ-globin promoter, leading to gene silencing and low fetal hemoglobin (HbF) levels.
Quantitative Comparison of Disruption Efficiencies and Outcomes
A pivotal 2025 study provided a head-to-head comparison of CRISPR/Cas9 editing for both repressor binding sites in hematopoietic stem/progenitor cells (HSPCs) from both healthy donors and β⁰-thalassemia/HbE patients [5] [84] [85]. The following tables summarize the key quantitative findings from this investigation.
Table 1: Comparison of Genome Editing Efficiency and Molecular Outcomes
| Parameter | BCL11A Binding Site (-115) Disruption | ZBTB7A/LRF Binding Site (-200) Disruption |
|---|---|---|
| Target Site | HBG -115 | HBG -197 |
| Editing Efficiency | 75–92% [5] | 57–60% [5] |
| Most Common Indel | 13-bp deletion (21.1 ± 0.6% in healthy; 21.6 ± 2.1% in patient cells) [5] | 6-bp deletion (10.8 ± 1.5% in healthy; 11.1 ± 0.3% in patient cells) [5] |
| γ-Globin mRNA Fold Change | Healthy: 6.1–11.2x; β⁰-thal/HbE: 2.7–3.2x [5] | Healthy: 7.5–11.4x; β⁰-thal/HbE: 4.0–5.3x [5] |
| Impact on Repressor Gene Expression | No significant change in BCL11A mRNA [5] | No significant change in ZBTB7A mRNA [5] |
Table 2: Comparison of Functional and Safety Outcomes
| Parameter | BCL11A Binding Site (-115) Disruption | ZBTB7A/LRF Binding Site (-200) Disruption |
|---|---|---|
| HbF Induction (HPLC) | Healthy: 26.2 ± 1.4%;β⁰-thal/HbE: 62.7 ± 0.9% [5] | Healthy: 27.9 ± 1.5%;β⁰-thal/HbE: 64.0 ± 1.6% [5] |
| Erythroid Differentiation | Not significantly affected [5] | Not significantly affected [5] |
| Off-Target Effects | None detected [5] | Observed at low frequencies [5] |
Key Comparative Insights
- Higher Editing Efficiency for BCL11A Site: The BCL11A binding site was consistently edited with higher efficiency (75-92%) compared to the ZBTB7A site (57-60%) across cell types [5].
- Comparable Functional Efficacy: Despite the difference in editing efficiency, both strategies produced remarkably similar and robust increases in HbF protein levels, normalizing to ~26-28% in healthy donor cells and to over 60% in β⁰-thalassemia/HbE cells [5] [85].
- Divergent Safety Profile: A critical distinction was observed in off-target effects. Editing the BCL11A site resulted in no detectable off-target mutations, whereas editing the ZBTB7A site led to low-frequency off-target effects [5].
- Preserved Erythropoiesis: Neither intervention significantly impaired the normal differentiation of edited HSPCs into mature erythroid cells, a crucial indicator for therapeutic applicability [5].
Detailed Experimental Protocol
The following workflow and detailed methodology are based on the core 2025 study, which offers a directly comparable experimental framework for evaluating these two targets [5].
Figure 2: Core experimental workflow for comparing BCL11A and ZBTB7A binding site disruptions, from cell source to functional analysis.
Critical Reagents and Equipment
Table 3: The Scientist's Toolkit: Key Research Reagent Solutions
| Reagent/Equipment | Function/Description | Critical Notes |
|---|---|---|
| Mobilized CD34+ HSPCs | Primary human hematopoietic stem/progenitor cells; therapeutically relevant cell source. | Source from healthy donors and patient cohorts (e.g., β⁰-thalassemia/HbE) for comparative studies [5]. |
| sgRNAs for RNP Complex | sg-BCL11A: Targets HBG -115 site.sg-LRF: Targets HBG -197 site. | Use chemically synthesized, high-purity sgRNAs. Sequences should be validated from prior studies (e.g., [5]). |
| Cas9 Nuclease | High-purity, recombinant Cas9 protein. | Complex with sgRNA to form Ribonucleoprotein (RNP) for delivery, reducing off-target risk and enabling rapid activity. |
| Electroporation System | For efficient RNP delivery into CD34+ HSPCs (e.g., Neon, Lonza 4D-Nucleofector). | Optimize protocol for primary CD34+ cells to maintain high viability and editing efficiency. |
| Erythroid Differentiation Media | cytokine cocktail to support CD34+ cell expansion and terminal erythroid differentiation. | Typically includes SCF, EPO, and IL-3. Standardize conditions to allow direct comparison between edited and control cells. |
| Cation-Exchange HPLC | Gold-standard method for quantifying hemoglobin types (HbF, HbA). | Essential for measuring the primary functional outcome—HbF protein levels [5]. |
Step-by-Step Workflow Description
- Cell Source Preparation: Isolate and purify CD34+ hematopoietic stem/progenitor cells. The cited study used mobilized peripheral blood from healthy donors and β⁰-thalassemia/HbE patients [5]. Ensure all necessary ethical approvals are in place for working with primary human samples.
- RNP Complex Formation and Delivery:
- Design sgRNAs: Use previously validated guide RNA sequences targeting the -115 site for BCL11A and the -197 site for ZBTB7A [5].
- Form RNP: Pre-complex the sgRNA with Cas9 protein to form the ribonucleoprotein (RNP) complex.
- Electroporation: Introduce the RNP complexes into the CD34+ HSPCs using a optimized electroporation protocol. Include a non-edited control (NEC) electroporated without RNP.
- Design sgRNAs: Use previously validated guide RNA sequences targeting the -115 site for BCL11A and the -197 site for ZBTB7A [5].
- In Vitro Erythroid Differentiation: Culture the edited and control cells for approximately 21 days in a serum-free medium supplemented with a cytokine cocktail (e.g., StemSpan with EPO, SCF, IL-3, dexamethasone) to drive differentiation into mature erythroblasts [5].
- Downstream Analysis:
- Editing Efficiency: Harvest a portion of cells 48-72 hours post-electroporation. Extract genomic DNA and perform PCR amplification of the targeted regions. Analyze indel frequency and spectrum using deep sequencing [5].
- Functional Assessment:
- Gene Expression: At the terminal stage of differentiation (e.g., day 21), extract total RNA. Perform quantitative RT-PCR (qRT-PCR) to measure γ-globin mRNA levels, normalized to housekeeping genes [5].
- HbF Protein Quantification: Analyze lysates from differentiated erythroblasts using cation-exchange High-Performance Liquid Chromatography (HPLC) to precisely measure the percentage of HbF [5].
- Safety and Specificity:
- Erythroid Differentiation: Use flow cytometry to track the expression of erythroid surface markers (e.g., CD235a/GPA, CD71) throughout the culture to ensure differentiation is not impaired.
- Off-Target Analysis: Employ unbiased methods like GUIDE-seq or CIRCLE-seq on edited samples to identify and quantify potential off-target editing events [5].
The direct, side-by-side comparison reveals that disrupting either the BCL11A or ZBTB7A/LRF binding site in the γ-globin promoter is a potent strategy for HbF reactivation, with the potential to cure β-hemoglobinopathies. The choice between these two targets involves a strategic trade-off.
Disrupting the BCL11A binding site at -115 offers a superior safety profile with no detected off-target effects and the highest editing efficiency. This makes it a compelling candidate for clinical translation, as it may present a lower risk of unintended genomic consequences. In contrast, disrupting the ZBTB7A/LRF site at -200 is equally effective in raising HbF to therapeutic levels but is associated with lower editing efficiency and detectable, albeit low-frequency, off-target events [5].
For researchers and therapy developers, this comparison underscores that there is no single "best" target, but rather a decision guided by priorities. If maximizing on-target editing and minimizing theoretical safety concerns are paramount, the BCL11A site is advantageous. However, the robust HbF induction from ZBTB7A site disruption confirms its validity as a therapeutic target, and further optimization of guide RNA design may mitigate its off-target profile. Ultimately, both approaches represent a paradigm shift from disease management to a one-time curative treatment, and both warrant continued investigation as promising avenues for gene therapy.
The reactivation of fetal hemoglobin (HbF) represents a cornerstone therapeutic strategy for the treatment of β-hemoglobinopathies, including sickle cell disease (SCD) and β-thalassemia [86]. These inherited disorders, among the most common monogenic diseases worldwide, stem from defects in the adult β-globin gene, leading to the production of dysfunctional hemoglobin or a complete lack of it [87]. The only available curative treatments, allogeneic hematopoietic stem cell transplantation and, more recently, gene therapy, face significant limitations in terms of donor availability, high cost, complex procedures, and potential risks [87] [88]. Consequently, therapeutic approaches focused on HbF induction offer a promising alternative by targeting a endogenous physiological process. The biological rationale for this approach is well-established: HbF (α2γ2) dilutes the concentration of pathological adult hemoglobin (HbS in SCD) and, due to its superior inhibitory effect on HbS polymerization, effectively reduces disease severity and associated complications [86] [89]. This whitepaper provides an in-depth technical analysis and comparison of the three leading platforms for HbF induction—CRISPR-based genome editing, Antisense Oligonucleotides (ASOs), and small molecules—framed within the context of therapeutic development for SCD and thalassemia.
Molecular Basis of the Fetal-to-Adult Hemoglobin Switch
Understanding the mechanistic basis of HbF silencing is fundamental to developing targeted reactivation strategies. The fetal-to-adult hemoglobin switch is a tightly regulated developmental process that occurs shortly after birth, whereby expression shifts from the γ-globin genes (HBG1 and HBG2) to the β-globin gene (HBB) [86]. This switch is orchestrated by a complex network of transcriptional regulators.
A key repressor identified is BCL11A, a zinc-finger transcription factor that serves as a master regulator of γ-globin silencing [3]. BCL11A functions by binding to specific sites in the β-globin gene cluster, facilitating the repression of HBG genes. Recent research has elucidated that a specific enhancer region of BCL11A folds into a three-dimensional chromatin "rosette" structure in red blood cell precursors, which is critical for maintaining high-level BCL11A expression [3]. Disruption of this structure, whether by CRISPR-Cas9-mediated DNA cleavage or ASO-mediated degradation of enhancer-derived RNA, leads to silencing of BCL11A and consequent HbF reactivation [3]. Other significant transcriptional repressors include MYB and KLF1, which also contribute to the suppression of γ-globin gene expression in adult erythroid cells [86].
The following diagram illustrates the core regulatory pathway governing the hemoglobin switch and the points of intervention for different therapeutic platforms.
Platform #1: CRISPR-Based Genome Editing
Mechanism of Action and Experimental Protocols
CRISPR-based genome editing facilitates HbF induction through precise, permanent modifications to the genome of hematopoietic stem and progenitor cells (HSPCs). The primary strategies involve:
- Disruption of the BCL11A Erythroid Enhancer: The most clinically advanced approach utilizes the CRISPR-Cas9 system to create a double-strand break in a specific enhancer region within the BCL11A gene that is critical for its expression in the erythroid lineage [3] [88]. The repair of this break via error-prone non-homologous end joining (NHEJ) introduces mutations that disrupt the enhancer's function. This disruption prevents the formation of a critical chromatin rosette structure, leading to epigenetic silencing of BCL11A and subsequent HbF reactivation [3].
- Direct Editing of γ-Globin Promoters: An alternative strategy involves using prime editing to install specific mutations in the γ-globin gene promoters. This method, which does not require double-strand breaks, can rewrite promoter sequences to mimic natural hereditary persistence of fetal hemoglobin (HPFH)-associated mutations, thereby increasing γ-globin gene activity [41] [90].
- Correction of Underlying β-Globin Mutations: While not an HbF-induction approach per se, CRISPR-Cas9 can also be used to directly correct mutations in the β-globin gene itself, leading to de novo production of functional adult hemoglobin (HbA) [91]. This strategy can be considered in parallel for comprehensive therapeutic development.
A generalized workflow for BCL11A enhancer editing is as follows:
- HSPC Collection: Mobilize and collect autologous CD34+ HSPCs from the patient.
- Ex Vivo Editing: Electroporate the HSPCs with CRISPR-Cas9 components (e.g., Cas9 ribonucleoprotein complex and sgRNA targeting the BCL11A enhancer).
- Quality Control: Assess editing efficiency and cell viability.
- Reinfusion: After myeloablative conditioning, infuse the edited CD34+ cells back into the patient.
- Engraftment: The edited HSPCs engraft in the bone marrow and reconstitute an erythroid system capable of producing HbF [87] [88].
Efficacy and Clinical Data
CRISPR-based disruption of the BCL11A enhancer has demonstrated transformative outcomes in clinical trials.
Table 1: Efficacy of CRISPR-Based HbF Induction in Clinical Trials
| Therapy Type | Target | Study Phase | Patient Population | HbF Induction Level / Key Outcome | Source |
|---|---|---|---|---|---|
| exa-cel (Casgevy) | BCL11A Enhancer | Phase 3 | Transfusion-Dependent β-Thalassemia (TDT) | 91% (32/35) achieved transfusion independence | [88] |
| exa-cel (Casgevy) | BCL11A Enhancer | Phase 3 | Severe Sickle Cell Disease (SCD) | Elimination of vaso-occlusive crises in >90% of patients | [87] [88] |
| BCL11A shmiR | BCL11A mRNA (Lentiviral) | Phase 1/2 | Severe SCD | Median HbF% = 27.9%; significant reduction in HbS% | [89] |
A detailed single-cell analysis comparing CRISPR-mediated BCL11A silencing with hydroxyurea treatment revealed that the genetic approach led to a more favorable hemoglobin profile, with fewer red blood cells containing high levels of HbS and greater resistance to HbS polymerization at low oxygen tension [89].
Platform #2: Antisense Oligonucleotides (ASOs) and RNA Interference (RNAi)
Mechanism of Action and Experimental Protocols
ASOs and RNAi technologies achieve HbF induction through post-transcriptional gene silencing. They are designed to target and degrade mRNA molecules, preventing the translation of specific proteins.
- ASOs against BCL11A Enhancer RNA: A novel application involves designing ASOs to target and degrade a specific enhancer RNA (eRNA) produced by the BCL11A enhancer [3]. As depicted in the pathway diagram, this eRNA is essential for the formation of the active chromatin rosette. Its degradation by ASOs disrupts the enhancer's three-dimensional structure, leading to epigenetic silencing of BCL11A and HbF reactivation, mirroring the effect of CRISPR without altering the DNA sequence itself [3].
- RNAi for BCL11A Knockdown: An alternative method uses lentiviral vectors to deliver a short hairpin RNA (shRNA) embedded in a microRNA architecture (shmiR) into HSPCs. This shmiR mediates the degradation of BCL11A mRNA, leading to reduced BCL11A protein levels and HbF reactivation [89].
The experimental protocol for the ASO/eRNA approach involves:
- Identification of Target eRNA: Pinpoint the specific eRNA transcript essential for the BCL11A enhancer activity.
- ASO Design and Synthesis: Chemically synthesize single-stranded ASOs complementary to the target eRNA sequence.
- In Vitro/Ex Vivo Delivery: Deliver ASOs into human erythroid precursor cells or CD34+ HSPCs using standard transfection or electroporation techniques.
- Outcome Assessment: Measure the reduction in eRNA and BCL11A mRNA levels, HbF production (%HbF and F-cells), and the impact on HbS polymerization [3].
Efficacy and Preclinical/Clinical Data
While CRISPR therapies are already approved, ASO/RNAi approaches show significant promise in clinical trials.
Table 2: Efficacy of ASO/RNAi Platforms for HbF Induction
| Therapy Type | Target | Study Stage | Model / Population | Key Outcome | Source |
|---|---|---|---|---|---|
| ASOs | BCL11A Enhancer RNA | Preclinical | Normal & Sickle Erythroid Precursors | Selective eRNA degradation, BCL11A silencing, and HbF reactivation | [3] |
| shmiR (Lentiviral) | BCL11A mRNA | Phase 1/2 | Severe SCD (n=9) | Median HbF = 27.9%; fewer RBCs with high HbS% than hydroxyurea | [89] |
| ASOs | P2X3, TRPV1, Nav1.8 | Preclinical | Neuropathic Pain Models | Validation of ASO platform for gene silencing in neurological targets | [92] |
The clinical trial for the BCL11A shmiR demonstrated that this post-transcriptional silencing method not only increased HbF but also concurrently reduced HbS levels, resulting in a combinatorial anti-sickling effect [89].
Platform #3: Small Molecule Inducers
Mechanism of Action and Screening Protocols
Small molecules represent a pharmacological approach to HbF induction, offering potential advantages in terms of cost and administration. Their mechanisms are often pleiotropic and have historically been less defined.
- Hydroxyurea (HU): The only FDA-approved small molecule for SCD, HU is known to induce HbF. However, its mechanism of action is not fully elucidated and is believed to involve cellular stress and cytotoxicity, which may preferentially select for HbF-expressing erythroid progenitors [86] [93]. Its efficacy is variable, and a significant number of patients are non-responders or continue to experience symptoms [89] [93].
- Next-Generation Small Molecules (e.g., CLT-1081): Advanced screening techniques, such as pairing machine learning with high-resolution single-cell RNA sequencing maps of human erythropoiesis, are being employed to identify novel, more potent, and targeted small-molecule inducers [93]. These molecules are designed to trigger transcriptional signatures associated with fetal erythropoiesis. For instance, CLT-1081 was identified through such a platform and has been shown to reduce BCL11A expression among other transcriptional changes [93].
The experimental workflow for identifying novel small molecules is as follows:
- Data Generation: Create a high-resolution scRNA-seq map of both adult and fetal human erythropoiesis to define a "fetal" transcriptional signature.
- Computational Screening: Apply proprietary algorithms to this dataset to identify gene-network signatures that are targetable by small molecules.
- In Vitro Validation: Test predicted small molecules in a 14-day in vitro human erythroid differentiation system using mPB CD34+ HSPCs from healthy donors.
- Efficacy and Mechanistic Analysis: Measure HbF induction (%F-cells, %HbF by HPLC) and globin gene expression (HBG1, HBG2, HBB). Further characterize the mechanism using scRNA-seq to confirm the activation of the targeted gene signature [93].
Efficacy and Preclinical Data
Next-generation small molecules are demonstrating promising efficacy in preclinical models, potentially surpassing the current standard of care.
Table 3: Efficacy of Small Molecule HbF Inducers
| Molecule | Study Stage | Model / Population | HbF Induction Level | Comparison to Hydroxyurea (HU) | Source |
|---|---|---|---|---|---|
| Hydroxyurea | Clinical (Standard of Care) | SCD Patients (High Responders) | Median HbF = 27.0% | Reference | [89] |
| CLT-1081 | Preclinical | mPB CD34+ HSPCs (Healthy Donors) | 42.3% (±17.26) | Induced HbF >2.4x higher than HU | [93] |
| BCL11A CRISPR | Preclinical Control | mPB CD34+ HSPCs (Healthy Donors) | 32.58% (±10.66) | CLT-1081 induced HbF ~1.3x higher | [93] |
The data for CLT-1081 indicates that it not only induces robust HBG1 and HBG2 mRNA expression but also concomitantly reduces HBB transcript levels, similar to the effect of genetic BCL11A knockdown [93].
Comparative Analysis of HbF Induction Platforms
The following table provides a consolidated, direct comparison of the key technical and clinical characteristics of the three platforms for HbF induction.
Table 4: Comprehensive Comparison of HbF Induction Platforms
| Characteristic | CRISPR Genome Editing | ASOs / RNAi | Small Molecules |
|---|---|---|---|
| Molecular Target | DNA (BCL11A enhancer, HBG promoter) | RNA (BCL11A eRNA or mRNA) | Protein (Pleiotropic, e.g., BCL11A pathway) |
| Therapeutic Effect | Permanent, potentially curative | Transient (ASOs) to Long-term (Lentiviral RNAi) | Transient, requires continuous dosing |
| Mode of Action | Disrupts 3D chromatin structure or creates HPFH-like mutations | Degrades enhancer RNA or mRNA, disrupting repression | Modulates transcriptional networks, may reduce BCL11A |
| Delivery Method | Ex vivo electroporation of HSPCs | Ex vivo (Lentiviral) or In vivo (ASO infusion) | Oral administration |
| Clinical Status | FDA/EMA Approved (exa-cel) | Phase 1/2 Clinical Trials | Preclinical (Next-Gen) to Approved (HU) |
| Reported HbF Level | ~28% (Associated with transfusion independence) [89] | ~28% (shmiR) [89] | ~42% (CLT-1081, Preclinical) [93] |
| Key Advantages | One-time, durable treatment; high efficacy | ASOs offer a non-genotoxic alternative; scalable | Potentially low cost, oral, broad accessibility |
| Key Challenges | High cost, myeloablation risk, long-term safety monitoring | Immunogenicity, delivery efficiency (ASOs), viral vector risks (shmiR) | Off-target effects, variable patient response, toxicity (e.g., HU) |
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting experimental research in the field of HbF induction.
Table 5: Key Research Reagent Solutions for HbF Induction Studies
| Reagent / Material | Function in Research | Example Application |
|---|---|---|
| Mobilized Peripheral Blood CD34+ HSPCs | Primary human cells for ex vivo editing/differentiation; source of erythroid precursors. | In vitro erythroid differentiation assays to test CRISPR guides, ASOs, or small molecules [93] [90]. |
| CRISPR-Cas9 System (RNP) | Ribonucleoprotein complex for precise genome editing; allows for ex vivo manipulation of HSPCs. | Disruption of the BCL11A erythroid enhancer or installation of HPFH-associated mutations in the HBG promoter [87] [90]. |
| Prime Editors | CRISPR-based system that enables precise point mutations and small insertions without double-strand breaks. | Rewriting γ-globin promoters to reactivate HbF [41]. |
| Lentiviral Vectors (e.g., shmiR) | Delivery of genetic payloads (e.g., shRNAs) for stable gene knockdown in HSPCs. | Post-transcriptional silencing of BCL11A [89]. |
| In Vitro Erythroid Differentiation Media | Defined culture medium to support the proliferation and maturation of HSPCs into enucleated erythrocytes. | 14-day assay to evaluate the efficacy of HbF inducers [93]. |
| Flow Cytometry with Anti-HbF Antibody | Quantification of F-cells (HbF-positive RBCs) at the single-cell level. | Assessment of HbF distribution in cultured erythroid cells or patient samples [89] [93]. |
| HPLC for Hemoglobin | Separation and quantification of different hemoglobin types (HbA, HbF, HbS). | Precise measurement of the percentage of HbF in total hemoglobin from cell cultures or blood [91] [93]. |
| Single-Cell RNA Sequencing (scRNA-seq) | High-resolution analysis of transcriptional changes and heterogeneity during erythropoiesis. | Identifying fetal erythroid signatures and mechanism of action for novel inducers like CLT-1081 [93]. |
The therapeutic reactivation of fetal hemoglobin has matured from a compelling biological concept into a clinical reality. As this whitepaper details, CRISPR-based gene editing has led the way with approved therapies, demonstrating that precise genetic disruption of the BCL11A enhancer can achieve transformative, potentially curative outcomes for patients with SCD and TDT. The ASO/RNAi platform offers a powerful alternative that can achieve similar transcriptional silencing without permanent genomic alteration, showing significant efficacy in clinical trials. Finally, the emergence of next-generation small molecules, identified through sophisticated computational and screening platforms, promises a future where highly effective, oral, and accessible HbF induction could become a reality. The choice of platform involves a complex trade-off between durability, cost, scalability, and mode of administration. Future research may explore combinations of these modalities or further refine their safety and efficacy, ultimately expanding the arsenal of therapeutic options to alleviate the global burden of β-hemoglobinopathies.
Sickle cell disease (SCD) and β-thalassemia represent the most prevalent monogenic disorders worldwide, collectively affecting millions of individuals. While both conditions stem from mutations in the β-globin gene (HBB), their distinct molecular pathologies—structural hemoglobin aberration in SCD versus impaired β-globin production in β-thalassemia—create unique therapeutic landscapes for fetal hemoglobin (HbF) reactivation strategies. This technical review synthesizes current evidence on therapeutic outcomes of HbF-inducing interventions across disease models, highlighting efficacy measurements, safety considerations, and molecular response variations. Quantitative analyses reveal that comparable HbF induction yields differential phenotypic correction between these hemoglobinopathies, with SCD generally requiring lower HbF thresholds (≥30%) for clinical efficacy compared to β-thalassemia. Recent advances in gene editing technologies, including CRISPR-Cas9 and zinc finger nucleases (ZFNs), demonstrate robust HbF reactivation through BCL11A-targeted approaches, with emerging non-gene-editing alternatives showing promising preclinical results. This comprehensive assessment provides researchers with critical insights for optimizing therapeutic development and predicting clinical outcomes across hemoglobinopathies.
Comparative Disease Pathogenesis
SCD and β-thalassemia share an autosomal recessive inheritance pattern affecting the HBB gene on chromosome 11 but manifest distinct pathophysiological mechanisms. SCD results from a specific point mutation (HBB:c.20A>T) that substitutes valine for glutamic acid at codon 6 (Glu6Val), producing abnormal sickle hemoglobin (HbS) [94] [80]. Under hypoxic conditions, HbS polymerizes, causing erythrocyte deformation, hemolytic anemia, vaso-occlusion, and multiorgan damage [94]. In contrast, β-thalassemia arises from over 200 different mutations that reduce (β+) or eliminate (β0) β-globin chain synthesis, creating an α-/β-globin chain imbalance that leads to ineffective erythropoiesis, oxidative membrane damage, and accelerated apoptosis of erythroid precursors [62] [95].
Fetal Hemoglobin Reactivation as Therapeutic Strategy
The natural developmental switch from fetal hemoglobin (HbF, α2γ2) to adult hemoglobin (HbA, α2β2) shortly after birth provides a compelling therapeutic target for both disorders. HbF exerts protective effects through distinct mechanisms in each disease: in SCD, γ-globin chains incorporate into hemoglobin tetramers that resist polymerization with HbS, while in β-thalassemia, γ-globin chains pair with excess α-globin chains to form functional HbF, reducing α-globin precipitation and associated erythroid cytotoxicity [94] [62]. The hereditary persistence of fetal hemoglobin (HPFH) phenomenon, wherein individuals maintain elevated HbF levels postnatally, provides natural proof-of-concept for this approach, with HPFH carriers demonstrating markedly attenuated disease severity when co-inherited with either SCD or β-thalassemia mutations [62].
Quantitative Therapeutic Outcomes in Disease Models
Efficacy Thresholds and Hematological Parameters
Table 1: Comparative Therapeutic Efficacy thresholds for HbF Reactivation
| Parameter | Sickle Cell Disease | β-Thalassemia | Measurement Context |
|---|---|---|---|
| Minimum Therapeutic HbF Threshold | ≥30% [62] | ≥30% [62] | Percentage of total hemoglobin |
| HbF Distribution Requirement | Pancellular distribution preferred [94] | Heterocellular distribution may be sufficient [62] | Erythrocyte pattern |
| Impact on Primary Pathology | Prevents HbS polymerization [94] | Reduces α-globin precipitation [62] | Molecular effect |
| Clinical Outcome Measure | Reduction/elimination of vaso-occlusive crises [94] | Transfusion independence [62] | Primary endpoint |
| Therapeutic γ-globin Level | 2-3 fold increase from baseline [8] | 2-3 fold increase from baseline [8] | In erythroid progeny ex vivo |
Gene Editing Efficiency and Engraftment Outcomes
Table 2: Gene Editing Efficiency and Engraftment Across Disease Models
| Editing Platform | Target | Editing Efficiency (SCD) | Editing Efficiency (β-Thalassemia) | Engraftment Potential |
|---|---|---|---|---|
| CRISPR-Cas9 | BCL11A Erythroid Enhancer | 64.2% indel frequency [96] | 75.3% indel frequency [8] | Stable multilineage engraftment in NSG mice [8] |
| CRISPR-Cas9 | LRF/ZBTB7A BS in γ-globin promoters | Higher in SCD vs. healthy donor cells [96] | Not specifically reported | Reduced engraftment in SCD HSPCs [96] |
| Zinc Finger Nucleases (ZFN) | BCL11A GATAA motif | 64.2% indel frequency [8] | 75.3% indel frequency [8] | No impairment of engraftment [8] |
| Lentiviral Vector | β-globin gene addition | N/A (anti-sickling variant) [80] | 4-6 g/dL Hb per vector copy [62] | Stable long-term engraftment [80] |
Experimental Protocols for Therapeutic Assessment
In Vitro Erythroid Differentiation and HbF Analysis
Protocol: Erythroid Differentiation from Hematopoietic Stem/Progenitor Cells (HSPCs)
- HSPC Source: Isolate CD34+ cells from peripheral blood (mobilized with plerixafor for SCD patients; plerixafor plus granulocyte colony-stimulating factor for healthy donors and β-thalassemia patients) [8].
- Genetic Modification: Electroporate HSPCs with CRISPR-Cas9 ribonucleoprotein (RNP) complexes or ZFN mRNA targeting BCL11A enhancer regions [96] [8].
- Culture Conditions: Maintain cells in erythroid differentiation medium containing stem cell factor (SCF), erythropoietin (EPO), and dexamethasone for 18-20 days [8].
- HbF Quantification:
- Functional Assessment (SCD-specific): Subject differentiated erythrocytes to hypoxic conditions (2% O2) to assess sickling propensity via microscopy [8].
In Vivo Engraftment and Safety Studies
Protocol: NSG Mouse Model for Human Cell Engraftment
- Transplantation: Inject immunodeficient NOD scid gamma (NSG) mice with 0.5-1×10^6 gene-edited or control human CD34+ HSPCs via tail vein following sublethal irradiation [8].
- Monitoring: Track human cell chimerism in peripheral blood monthly via flow cytometry for human CD45+ cells [8].
- Lineage Analysis: At sacrifice (typically 16-20 weeks), assess editing persistence and HbF expression across hematopoietic lineages (myeloid CD33+, lymphoid CD19+, primitive CD34+CD38+ progenitors) from bone marrow [8].
- Off-Target Assessment: Perform whole-genome sequencing or targeted sequencing of predicted off-target sites to identify potential unintended edits [96].
- Genotoxicity Evaluation: Utilize specialized assays to detect chromosomal rearrangements, particularly in SCD samples which show higher susceptibility [96].
Single-Cell Clonal Analysis of Editing Outcomes
Protocol: Single-Cell Genotyping and Phenotypic Correlation
- Single-Cell Sorting: Sort ZFN-edited or CRISPR-edited HSPCs into individual wells containing erythroid differentiation medium [8].
- Colony Formation: Culture for 14 days to allow colony-forming unit (CFU) development [8].
- Genotype Analysis: Perform next-generation sequencing of the BCL11A target site from single-cell-derived colonies [8].
- Phenotype Correlation: Correlate specific indel patterns with HbF expression levels to determine genotype-phenotype relationships [8].
- Biallelic Editing Assessment: Calculate ratio of wild-type, monoallelic, and biallelic edited colonies; studies show enriched biallelic editing in both SCD and healthy donor HSPCs [8].
Signaling Pathways and Molecular Mechanisms
BCL11A-Mediated HbF Silencing Pathway
Figure 1: BCL11A-Mediated Fetal Hemoglobin Silencing Pathway
Therapeutic Intervention Mechanisms
Figure 2: Therapeutic Interventions for HbF Reactivation
Disease-Specific Therapeutic Responses and Safety Considerations
Differential Responses in SCD Versus β-Thalassemia Models
While HbF reactivation strategies demonstrate efficacy in both SCD and β-thalassemia, substantial differences emerge in disease-specific responses. CRISPR-Cas9 targeting of lymphoma-related factor (LRF) binding sites in the γ-globin promoters resulted in significantly higher editing efficiency in SCD-derived hematopoietic stem and progenitor cells (HSPCs) compared to those from healthy donors [96]. However, these same SCD HSPCs exhibited reduced engraftment capacity and displayed myeloid bias in xenotransplantation models [96]. Transcriptomic analyses further revealed that the editing procedure upregulates genes involved in DNA damage and inflammatory responses, with this effect being more pronounced in SCD HSPCs [96].
The search results indicate that β-thalassemia models generally show more robust editing efficiency compared to SCD models, with ZFN-mediated editing of the BCL11A erythroid enhancer achieving 75.3% indel frequency in β-thalassemia HSPCs versus 64.2% in SCD HSPCs [8]. This differential efficiency may reflect intrinsic biological differences in the hematopoietic cells between these disorders, possibly related to chronic inflammatory states and bone marrow stress in SCD.
Safety Profiles and Genotoxicity Assessment
Comprehensive safety assessment reveals disease-specific vulnerabilities. Chromosomal rearrangements and off-target editing activity are more frequently detected in SCD samples, likely reflecting higher overall editing efficiency in these cells [96]. Importantly, these aberrations did not significantly impact target gene expression or HSPC engraftment and differentiation in preclinical models [96]. Lentiviral vector-based approaches carry theoretical risks of insertional mutagenesis, with some clinical trials reporting cases of myeloid malignancies; however, evidence often attributes these events to conditioning regimen toxicity or pre-existing clonal hematopoiesis rather than vector integration itself [94].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for HbF Reactivation Studies
| Reagent/Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Gene Editing Platforms | CRISPR-Cas9 RNP complexes; ZFN mRNA [96] [8] | Targeted disruption of HbF repressors | ZFN editing shows enriched biallelic editing in HSPCs [8] |
| Delivery Systems | Electroporation (ex vivo); Lentiviral vectors [80] | Introducing editing machinery into HSPCs | Lentiviral vectors enable stable integration for gene addition [80] |
| HSPC Mobilization Agents | Plerixafor (SCD); Plerixafor + G-CSF (β-thalassemia) [8] | Harvesting target cells for modification | G-CSF contraindicated in SCD due to vaso-occlusive risk [8] |
| Cell Culture Supplements | Stem cell factor (SCF), Erythropoietin (EPO), Dexamethasone [8] | Ex vivo erythroid differentiation | Supports 18-20 day differentiation protocol to mature erythroid cells [8] |
| Analytical Tools | Anti-HbF antibodies for flow cytometry; HPLC systems; NGS panels [8] | Quantifying editing efficiency and HbF reactivation | Single-cell genotyping correlates indel patterns with HbF expression [8] |
| Antisense Oligonucleotides | eRNA-targeting ASOs [3] [49] | Non-gene-editing alternative for BCL11A suppression | Degrades enhancer RNA, disrupting chromatin structure [3] |
| Animal Models | Immunodeficient NSG mice [8] | In vivo engraftment and safety studies | Supports multilineage human hematopoiesis post-transplantation [8] |
Emerging Technologies and Future Directions
Non-Gene-Editing Approaches: Antisense Oligonucleotides
Recent investigations into the mechanistic basis of CRISPR therapies have revealed promising non-gene-editing alternatives. Research demonstrates that the BCL11A enhancer forms a three-dimensional chromatin "rosette" structure maintained by enhancer RNAs (eRNAs) [3] [49]. Targeting these eRNAs with antisense oligonucleotides (ASOs) effectively degrades them, disrupting the chromatin structure and silencing BCL11A expression, ultimately leading to HbF reactivation [3] [49]. This approach offers potential advantages in cost, accessibility, and scalability while avoiding permanent genome modification.
In Vivo Gene Therapy Approaches
Current ex vivo gene therapies requiring HSC harvesting, genetic modification, and transplantation present significant logistical and economic challenges. Next-generation approaches focus on in vivo delivery of gene therapy tools directly to patients' hematopoietic cells [80] [62]. This strategy could eliminate the need for complex manufacturing infrastructure and myeloablative conditioning, potentially expanding access to regions with high disease prevalence but limited medical resources [80]. Successful development would require overcoming barriers including targeted delivery to HSCs, minimization of immune responses, and ensuring precise editing efficiency [80].
Therapeutic HbF reactivation demonstrates substantial efficacy in both SCD and β-thalassemia disease models, with comparable target engagement but notable disease-specific differences in editing efficiency, engraftment potential, and safety profiles. Quantitative assessments establish that ≥30% HbF induction represents a key therapeutic threshold for both disorders, though the mechanisms of protection differ fundamentally. Emerging technologies—particularly non-gene-editing approaches using ASOs and in vivo delivery platforms—promise to enhance accessibility and reduce costs. Researchers should consider disease-specific biological differences when extrapolating findings between SCD and β-thalassemia models and prioritize comprehensive safety assessment, especially regarding genotoxicity and long-term engraftment stability. The continued refinement of these therapeutic strategies offers realistic prospects for durable remission or cure for both hemoglobinopathies.
Erythroid Differentiation Impact and Hematopoietic Function Preservation
Erythroid differentiation represents a critical biological process wherein hematopoietic stem cells undergo sophisticated maturation to form functional red blood cells. In hemoglobinopathies such as sickle cell disease (SCD) and β-thalassemia, this process becomes severely compromised, leading to ineffective erythropoiesis and profound anemia. Recent advances have illuminated the therapeutic potential of fetal hemoglobin (HbF) reactivation, which effectively counteracts the pathophysiological mechanisms underlying these disorders. This technical review examines the molecular basis of erythroid differentiation, the impact of hemoglobinopathies on this process, and the strategic preservation of hematopoietic function through HbF induction. We provide comprehensive experimental protocols, quantitative analyses, and visualization tools to support research and therapeutic development efforts aimed at targeting these mechanisms for clinical benefit.
Erythropoiesis is the highly regulated, multi-stage process through which hematopoietic stem cells (HSCs) differentiate into mature, enucleated erythrocytes, ensuring continuous oxygen transport throughout the body. This process evolves from primitive erythropoiesis in embryonic development to definitive erythropoiesis in adults, which occurs primarily in the bone marrow [97] [98]. The differentiation pathway follows a hierarchical structure: HSCs give rise to multipotent progenitors, which then differentiate into megakaryocyte-erythrocyte progenitors (MEPs), burst-forming unit-erythroid (BFU-E), colony-forming unit-erythroid (CFU-E), and finally progress through proerythroblast, basophilic, polychromatic, and orthochromatic erythroblast stages before enucleating to form reticulocytes and mature erythrocytes [97] [98].
In hemoglobinopathies such as β-thalassemia and sickle cell disease (SCD), this carefully orchestrated process becomes severely disrupted. β-thalassemia is characterized by reduced or absent synthesis of β-globin chains, leading to an imbalance in the α/β-globin ratio, accumulation of toxic free α-globin chains, and oxidative damage that triggers premature apoptosis of erythroid precursors [99]. Similarly, SCD results from a point mutation in the β-globin gene (Glu6Val), producing hemoglobin S (HbS) that polymerizes under hypoxic conditions, driving red blood cell sickling and subsequent vaso-occlusive pathology [100] [99]. Both conditions feature ineffective erythropoiesis as a central pathological mechanism, wherein erythroid maturation is impaired, leading to increased erythroblast apoptosis during terminal differentiation and ultimately contributing to chronic anemia [100] [99].
The reactivation of fetal hemoglobin (HbF, α2γ2) has emerged as a promising therapeutic strategy for these disorders. HbF effectively diminishes the pathological consequences of both conditions: in β-thalassemia, γ-globin chains substitute for deficient β-globin chains, restoring globin chain balance and reducing toxic α-globin precipitation; in SCD, HbF incorporation into hemoglobin tetramers inhibits HbS polymerization, thereby preventing sickling of red blood cells [100] [101]. Beyond these well-established mechanisms, recent evidence indicates that HbF also plays a crucial role in preserving effective erythropoiesis by rescuing erythroblasts from hypoxia-induced cell death during terminal differentiation, highlighting its multimodal therapeutic potential [100].
Molecular Mechanisms of Ineffective Erythropoiesis in Hemoglobinopathies
Pathophysiological Basis of Erythroid Defects
In hemoglobinopathies, the molecular defects in globin gene expression manifest as catastrophic failures in erythroid maturation. β-thalassemia is characterized by ineffective erythropoiesis driven by an accumulation of free α-globin chains that form toxic aggregates, leading to oxidative damage and premature apoptosis of erythroid precursors in the bone marrow [99]. This erythroid destruction occurs primarily during the final stages of terminal differentiation, comparable to the intramedullary apoptosis observed in SCD [100]. The resulting chronic severe anemia stimulates excessive erythropoietin (EPO) production, causing massive but ineffective expansion of the erythroid compartment and ultimately disrupting bone marrow homeostasis [99].
In SCD, the pathophysiology of erythroid impairment differs mechanistically but shares the hallmark of ineffective erythropoiesis. Under hypoxic conditions mimicking the bone marrow environment (0.1-6% O2), sickle erythroblasts demonstrate significant cell death beginning at the polychromatic stage, with evidence of HbS polymerization and cytoplasmic sequestration of heat shock protein 70 (HSP70) [100]. This hypoxic stress induces sickling of nucleated erythroblasts, triggering apoptotic pathways that disrupt normal maturation. Importantly, this erythroblast sickling and subsequent cell death creates a selective survival advantage for erythroid cells expressing higher levels of HbF, which confers protection against hypoxic damage [100].
Impact on Bone Marrow Microenvironment and Hematopoietic Function
The chronic stress of anemia and aberrant erythropoiesis in hemoglobinopathies extends beyond the erythroid lineage to disrupt the bone marrow microenvironment and overall hematopoietic function. The bone marrow niche—composed of mesenchymal stromal cells, endothelial cells, osteoblasts, and other supporting elements—normally provides critical signals that maintain HSC quiescence and regulate hematopoiesis [99] [102]. In both β-thalassemia and SCD, the consequences of severe anemia and ineffective erythropoiesis create chronic stress that alters this delicate microenvironment [99].
CXCL12-CXCR4 signaling, a key pathway for HSC retention and quiescence within the niche, becomes disrupted in hemoglobinopathies, potentially affecting HSC function and maintenance [102]. Additionally, the massive expansion of the erythroid compartment in β-thalassemia creates spatial competition within the bone marrow, potentially compromising niche support for other hematopoietic lineages. These alterations have profound implications for hematopoietic stem cell transplantation (HSCT) and gene therapy approaches, as both the quality of HSCs and the supporting capacity of the BM niche influence engraftment success and long-term outcomes [99].
Table 1: Characteristics of Ineffective Erythropoiesis in Hemoglobinopathies
| Feature | β-Thalassemia | Sickle Cell Disease |
|---|---|---|
| Primary molecular defect | Imbalanced α/β-globin chain synthesis | HbS polymerization under hypoxia |
| Main site of erythroid defect | Late stages of terminal differentiation | Polychromatic to orthochromatic transition |
| Key pathological process | Free α-globin chain accumulation & oxidative stress | HbS polymer formation & HSP70 sequestration |
| Erythroblast death mechanism | Apoptosis due to globin chain toxicity | Hypoxia-induced sickling and apoptosis |
| Impact of HbF | Restores globin chain balance | Inhibits HbS polymerization |
| Bone marrow niche alterations | Expanded erythroid compartment, oxidative stress | Hypoxic environment, vascular dysfunction |
Fetal Hemoglobin Reactivation Strategies
Genetic and Molecular Approaches
Multiple strategic approaches have been developed to reactivate fetal hemoglobin expression in erythroid cells, with recent advances in genetic technologies offering particularly promising therapeutic avenues:
CRISPR/Cas9-mediated genome editing has emerged as a powerful tool for HbF reactivation through targeted disruption of key transcriptional repressors. Research demonstrates that editing the γ-globin promoters to disrupt ZBTB7A/LRF or BCL11A binding sites effectively reactivates HbF production in erythroblasts from both healthy donors and β-thalassemia/HbE patients [5]. The editing efficiency for the BCL11A site (75-92%) is typically higher than for the ZBTB7A/LRF site (57-60%), with both approaches producing significant increases in HbF levels—approximately 26-28% in healthy donor cells and 62-64% in β-thalassemia/HbE cells [5]. These genetic modifications create permanent, hereditary persistence of fetal hemoglobin (HPFH)-like mutations that sustain γ-globin expression throughout the adult lifespan.
Lentiviral vector-mediated gene addition represents an alternative genetic approach. Vectors encoding a human γ-globin gene with erythroid-specific regulatory elements (e.g., V5m3 vector with β-globin LCR elements) have demonstrated the capacity to produce HbF levels of up to 21% per vector copy in erythroid progeny of normal CD34+ cells [101]. In β-thalassemic CD34+ cells, this approach achieves HbF production ranging from 45% to 60%, resulting in a 2.5 to 3-fold increase in total cellular hemoglobin content—sufficient to potentially ameliorate the disease phenotype [101].
Artificial transcription factors and RNA interference techniques offer additional mechanisms for HbF induction. A synthetic zinc-finger transcription factor (GG1-VP64) designed to interact with γ-globin gene promoters, as well as short-hairpin RNA targeting BCL11A expression, have both shown efficacy in enhancing HbF production in erythroid progeny of CD34+ cells [101]. These approaches directly target the natural repressors of γ-globin expression, mimicking the effect of natural HPFH mutations.
Table 2: Genetic Approaches for Fetal Hemoglobin Reactivation
| Approach | Mechanism | Efficiency | Advantages | Limitations |
|---|---|---|---|---|
| CRISPR/Cas9 editing of BCL11A site | Disrupts repressor binding at -115 position in γ-globin promoter | 75-92% indel frequency; 26-64% HbF depending on cell type | High efficiency; permanent effect | Potential off-target effects requires careful assessment |
| CRISPR/Cas9 editing of ZBTB7A/LRF site | Disrupts repressor binding at -197 position in γ-globin promoter | 57-60% indel frequency; 28-64% HbF depending on cell type | Permanent effect; comparable HbF induction to BCL11A editing | Lower efficiency than BCL11A editing; potential off-target effects |
| Lentiviral γ-globin gene addition | Adds functional γ-globin gene with LCR regulatory elements | 21% HbF per vector copy (normal cells); 45-60% HbF (thalassemic cells) | Well-established technology; high HbF production | Random integration; potential insertional mutagenesis |
| BCL11A shRNA knockdown | Reduces expression of γ-globin repressor BCL11A | Significant HbF increase demonstrated in vitro | Targets natural repressor mechanism; multiple delivery options | Transient effect with non-integrating vectors |
| Zinc-finger transcription factor GG1-VP64 | Binds γ-globin promoters to activate transcription | 3-fold HbF increase in thalassemic cultures | Specific targeting; artificial transcription factor design | Delivery challenges; potential immunogenicity |
Pharmacological and Cytokine-Based Approaches
Beyond genetic strategies, pharmacological and cytokine-based approaches offer alternative pathways for HbF reactivation:
Cytokine-mediated induction represents a promising non-genetic approach. Studies demonstrate that kit ligand (KL), alone or combined with dexamethasone, remarkably stimulates cell proliferation (3-4 logs more than control cultures) while decreasing the percentage of apoptotic and dyserythropoietic cells (<5%) in β-thalassemic erythroid cultures [103]. Importantly, these cytokine treatments induce a marked increase of γ-globin synthesis, reaching HbF levels 3-fold higher than in control cultures (e.g., from 27% to 75% or 81% in β-thalassemia major) [103]. This approach not only enhances HbF production but also promotes effective erythropoiesis and inhibits apoptosis, addressing multiple pathological aspects simultaneously.
Small molecule inducers of HbF continue to be investigated, though with varying clinical success. While hydroxyurea remains the only FDA-approved pharmacological agent for HbF induction in SCD, its efficacy in thalassemia has been inconsistent, prompting ongoing research into more targeted and potent compounds [103]. Novel therapeutic agents currently in development aim to modulate epigenetic regulators or key signaling pathways involved in globin gene regulation, offering the potential for more specific and effective HbF induction with reduced toxicity profiles.
Experimental Models and Methodologies
In Vitro Erythroid Differentiation Systems
Robust in vitro model systems are essential for studying erythroid differentiation and evaluating HbF reactivation strategies:
CD34+ cell liquid culture systems provide a physiologically relevant platform for investigating human erythropoiesis. The standard methodology involves isolating CD34+ hematopoietic stem and progenitor cells from peripheral blood or bone marrow sources using magnetic sorting systems (e.g., Miltenyi Biotec CD34 Progenitor cell isolation kit) [100] [101]. These cells are then cultured in a two-phase liquid culture system: an initial expansion phase with cytokines including stem cell factor (SCF), interleukin-3 (IL-3), and erythropoietin (EPO), followed by a differentiation phase with EPO and insulin to promote erythroid maturation [100] [98]. This system supports the complete differentiation of HSCs to enucleated erythrocytes over approximately 18-21 days, enabling stage-specific analysis and intervention.
Hypoxia modeling represents a critical technical consideration for studying sickle cell pathophysiology. To mimic the bone marrow microenvironment, erythroid cultures can be maintained at partial hypoxia (5% O2) starting from day 3 of the second phase of culture, when hemoglobin synthesis begins to increase markedly [100]. This hypoxic conditioning induces HbS polymerization in sickle erythroblasts, replicating the pathological features observed in vivo and providing a platform for evaluating protective interventions such as HbF induction.
Diagram 1: In Vitro Erythroid Differentiation Workflow. This experimental workflow outlines the key stages of CD34+ hematopoietic stem/progenitor cell culture, intervention points, and analytical endpoints for studying erythropoiesis and HbF induction strategies.
Assessment Methodologies for Erythroid Differentiation and HbF Production
Comprehensive assessment of erythroid differentiation and HbF induction requires multiple complementary analytical approaches:
Flow cytometry analysis enables quantitative evaluation of erythroid maturation stages using surface markers such as CD235a (glycophorin A), CD71 (transferrin receptor), and CD36, which exhibit dynamic expression patterns throughout differentiation [100] [101]. Additionally, intracellular staining for HbF with specific antibodies allows quantification of HbF-positive cells and the relative intensity of HbF expression at single-cell resolution. Apoptosis assays using Annexin V/7-AAD staining provide crucial information on erythroblast survival during differentiation, particularly relevant for assessing rescue from ineffective erythropoiesis [100] [103].
High-performance liquid chromatography (HPLC) remains the gold standard for quantitative hemoglobin analysis, providing precise measurement of HbF percentages relative to other hemoglobin types (HbA, HbS, HbA2) in erythroid cell lysates [5]. Cation-exchange HPLC can reliably detect HbF levels as low as 1-2%, enabling sensitive quantification of induction following therapeutic interventions [5].
Molecular analyses including quantitative RT-PCR for globin gene expression (γ-, β-, and α-globin transcripts) and RNA sequencing provide insights into the transcriptional changes underlying HbF reactivation [5]. For genetic editing approaches, tracking of indels by decomposition (TIDE) analysis or next-generation sequencing is essential to verify editing efficiency and characterize the specific mutation spectrum at target sites [100] [5].
Table 3: Key Assessment Methods for Erythropoiesis and HbF Induction
| Method | Application | Key Parameters | Technical Considerations |
|---|---|---|---|
| Multiparameter flow cytometry | Erythroid maturation staging | CD235a, CD71, CD36 expression; apoptosis (Annexin V); cell cycle | Enables live cell analysis; requires appropriate marker panels |
| Intracellular HbF flow cytometry | HbF-positive cell quantification | Percentage of HbF+ cells; HbF intensity per cell | Requires cell permeabilization; antibody specificity critical |
| Cation-exchange HPLC | Hemoglobin variant quantification | Percentage of HbF, HbA, HbS, HbA2 | High precision; requires cell lysis and hemoglobin extraction |
| qRT-PCR for globin genes | Globin transcript quantification | γ-/β-globin mRNA ratio; absolute transcript levels | RNA quality critical; requires appropriate normalization |
| Western blot | Protein expression analysis | γ-globin protein; HSP70 localization; caspase cleavage | Subcellular fractionation may be needed (e.g., cytoplasmic/nuclear) |
| Next-generation sequencing | Editing efficiency and indel characterization | Indel frequency and spectrum; off-target effects | Comprehensive but computationally intensive |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Erythroid Differentiation and HbF Studies
| Reagent/Category | Specific Examples | Application/Function |
|---|---|---|
| Cell Sources | Primary human CD34+ HSPCs (mobilized peripheral blood, bone marrow) | Provide physiologically relevant models for human erythropoiesis |
| Cytokines/Growth Factors | Stem cell factor (SCF), erythropoietin (EPO), interleukin-3 (IL-3) | Support proliferation, survival, and differentiation of erythroid precursors |
| Culture Media/Supplements | IMDM, StemSpan, fetal bovine serum, penicillin/streptomycin, L-glutamine | Provide nutritional support and maintain sterility in culture systems |
| Genetic Modification Tools | CRISPR/Cas9 (RNP complexes), lentiviral vectors, shRNAs | Enable targeted genome editing or gene expression modulation |
| Antibodies for Flow Cytometry | CD34, CD71, CD235a, CD36, HbF | Allow identification and purification of specific erythroid populations |
| HbF Induction Compounds | Kit ligand, pomalidomide, dexamethasone, hydroxyurea | Pharmacological reactivation of fetal hemoglobin expression |
| Molecular Analysis Reagents | qPCR primers for globin genes, HbF antibodies for Western blot, HPLC standards | Enable quantification of HbF at transcriptional and protein levels |
| Apoptosis Detection Kits | Annexin V/7-AAD, caspase activity assays | Quantify cell death during erythroid differentiation |
The investigation of erythroid differentiation and development of strategies to preserve hematopoietic function represents a rapidly advancing frontier in the treatment of hemoglobinopathies. The evidence unequivocally demonstrates that HbF reactivation through genetic, epigenetic, or pharmacological approaches can effectively counteract the pathophysiological processes underlying both sickle cell disease and β-thalassemia. Beyond its well-established role in improving hemoglobin properties and red blood cell survival, HbF critically preserves effective erythropoiesis by rescuing erythroblasts from apoptosis during terminal differentiation [100].
Future research directions should focus on optimizing the specificity and safety of genome editing approaches, particularly in minimizing off-target effects while maximizing HbF induction levels. Additionally, the interplay between hematopoietic stem cells and the bone marrow niche in hemoglobinopathies warrants deeper investigation, as niche-directed therapies may complement HbF-focused approaches to more comprehensively address these complex disorders [99]. The integration of novel pharmacological agents with established and emerging genetic therapies offers promise for combination approaches that could yield synergistic benefits while minimizing individual treatment toxicities.
As these therapeutic strategies advance toward clinical application, continued refinement of experimental models—including improved in vitro systems that better recapitulate the bone marrow microenvironment and more sophisticated animal models of human hemoglobinopathies—will be essential for rigorous preclinical evaluation. With multiple therapeutic modalities now demonstrating substantial potential, the prospect of effective, accessible, and durable treatments for sickle cell disease and thalassemia appears increasingly attainable.
Diagram 2: Integrated Therapeutic Strategy for Hemoglobinopathies. This conceptual framework illustrates how combined approaches targeting HbF reactivation, effective erythropoiesis, and niche preservation can synergistically improve hematopoietic function in sickle cell disease and thalassemia.
Sickle cell disease (SCD) management has been transformed by therapies targeting the reactivation of fetal hemoglobin (HbF), a key modifier of disease severity. This whitepaper provides a technical benchmark of three approved SCD therapies—hydroxyurea, CASGEVY, and LYFGENIA—contrasting their molecular mechanisms, clinical efficacy, and experimental protocols. Hydroxyurea, a first-generation pharmacologic HbF inducer, is benchmarked against two advanced gene-based interventions: CASGEVY (exagamglogene autotemcel), a CRISPR-Cas9 gene-editing therapy disrupting the BCL11A repressor, and LYFGENIA (lovotibeglogene autotemcel), a lentiviral vector-mediated gene addition therapy producing an anti-sickling hemoglobin variant, HbA^T87Q^. This analysis, framed within a thesis on HbF reactivation strategies, delineates the evolution from systemic pharmacologic induction to targeted genomic intervention, providing researchers and drug development professionals with a foundational comparison of therapeutic paradigms, their associated methodologies, and translational outcomes.
Sickle cell disease is a monogenic disorder caused by a point mutation in the β-globin gene (HBB), leading to the production of abnormal hemoglobin S (HbS) [104] [105]. Upon deoxygenation, HbS polymerizes, causing erythrocyte sickling, hemolytic anemia, vaso-occlusion, and end-organ damage [104]. A principal genetic modifier of SCD severity is fetal hemoglobin (HbF), which is typically silenced after infancy. HbF does not incorporate the β-globin subunit and thus does not polymerize with HbS; its presence in erythrocytes significantly reduces sickling [104] [106].
The therapeutic reactivation of HbF synthesis represents a cornerstone of SCD management. This whitepaper benchmarks three approved therapies that operate on this principle via distinct mechanisms:
- Hydroxyurea: A cytostatic drug that pharmacologically augments HbF production.
- CASGEVY: A cell-based gene-editing therapy that disrupts the BCL11A gene, a transcriptional repressor of HbF.
- LYFGENIA: A cell-based gene addition therapy that introduces a gene encoding an anti-sickling β-globin variant (HbA^T87Q^) via a lentiviral vector.
The following sections provide a technical deep-dive into the mechanisms, efficacy, and experimental protocols of these therapies, contextualizing them within the broader research landscape of HbF reactivation for hemoglobinopathies.
Molecular Mechanisms and Signaling Pathways
HbF Silencing and Reactivation Pathways
The developmental switch from fetal to adult hemoglobin is orchestrated by complex genetic and epigenetic regulators. Understanding these pathways is critical for dissecting the mechanisms of action of the benchmarked therapies.
Figure 1: The core pathway of fetal hemoglobin (HbF) regulation. The BCL11A gene, activated by its erythroid-specific enhancer, produces a transcription factor that represses the γ-globin genes (HBG1/HBG2), leading to HbF silencing after birth. Therapeutic reactivation of HbF involves disrupting this repressive axis [75] [105] [49].
Comparative Therapeutic Mechanisms of Action
The three benchmarked therapies intervene at different nodes of the HbF regulatory network.
Hydroxyurea is a ribonucleotide reductase inhibitor whose precise mechanism of HbF induction remains partially elucidated. It is believed to cause cytotoxic stress, accelerating the turnover of late erythroid progenitors and selectively favoring the survival of erythroid precursor populations with a higher propensity for HbF production [104].
CASGEVY utilizes the CRISPR-Cas9 system to make a precise genomic modification. A guide RNA (gRNA-68) directs the Cas9 nuclease to create a double-strand break in the erythroid-specific enhancer region of the BCL11A gene. The cell's non-homologous end joining (NHEJ) repair mechanism introduces insertions or deletions (indels) that disrupt the enhancer, reducing BCL11A expression and thereby de-repressing γ-globin and HbF production [75] [105]. This mechanism mimics the natural hereditary persistence of fetal hemoglobin.
LYFGENIA employs a fundamentally different, gene addition strategy. Autologous CD34+ hematopoietic stem and progenitor cells (HSPCs) are transduced ex vivo with a BB305 lentiviral vector. This vector encodes a modified β-globin gene (β^A^T87Q) that produces an anti-sickling hemoglobin variant (HbA^T87Q^). This variant contains a single amino acid substitution (threonine to glutamine at position 87) that sterically inhibits the polymerization of HbS under deoxygenated conditions [75] [105]. Unlike CASGEVY, LYFGENIA does not reactivate endogenous HbF but instead introduces a novel, functional hemoglobin gene.
Figure 2: Comparative experimental workflows for CASGEVY and LYFGENIA. Both therapies begin with the collection of a patient's hematopoietic stem cells (apheresis). CASGEVY involves ex vivo gene editing via electroporation of a CRISPR-Cas9 ribonucleoprotein complex, while LYFGENIA involves ex vivo transduction with a lentiviral vector. The modified cells are then reinfused into the patient after myeloablative conditioning [75] [105] [107].
Clinical Efficacy and Safety Benchmarking
Quantitative data from pivotal clinical trials provide a basis for comparing the therapeutic potential of these agents.
Table 1: Benchmarking Clinical Efficacy of SCD Therapies
| Therapy Parameter | Hydroxyurea (Historical Trials) | CASGEVY (exa-cel) | LYFGENIA (lovo-cel) |
|---|---|---|---|
| Mechanism of Action | Pharmacologic HbF induction [104] | CRISPR-Cas9 disruption of BCL11A [75] [105] | Lentiviral addition of βA^T87Q^ globin gene [105] [108] |
| Efficacy Primary Endpoint | Increased HbF; reduced VOCs [104] | Freedom from severe VOCs for ≥12 months [109] [107] | Complete resolution of VOEs (6-18 months post-infusion) [108] |
| Efficacy Outcome | Variable HbF increase; reduced ACS & transfusion [104] | 93.5% (29/31) of patients met primary endpoint [109] [107] | 88% (28/32) of patients met primary endpoint [105] [108] |
| Hospitalization Freedom | Reduced frequency [104] | 100% (30/30) free of hospitalizations for severe VOCs for ≥12 months [109] | 94% (30/32) free of severe VOEs (hospitalizations) [108] |
| Hemoglobin Impact | Modest increase in total Hb [104] | Increased total Hb and HbF (≥12 g/dL total Hb sustained) [75] [107] | Increased total Hb; HbA^T87Q^ contributes ~40% of total Hb [75] |
| Key Safety Concerns | Myelosuppression, teratogenicity concerns (mitigated in later studies) [104] [106] | Myeloablation-related cytopenias, febrile neutropenia [105] [107] | Myeloablation-related cytopenias; Black box warning for hematologic malignancy [105] [110] |
Table 2: Technical and Logistical Comparison
| Parameter | Hydroxyurea | CASGEVY | LYFGENIA |
|---|---|---|---|
| Approval & Access | FDA-approved 1998; widely available, low cost [104] [106] | FDA-approved 2023; limited authorized treatment centers [110] | FDA-approved 2023; limited treatment centers [110] |
| Dosing Regimen | Chronic, daily oral administration [104] | One-time intravenous infusion [107] | One-time intravenous infusion [108] |
| Manufacturing | N/A (synthetic chemical) | Complex ex vivo editing; ~6 months [107] | Complex ex vivo transduction; 70-105 days [110] |
| Pre-conditioning | N/A | Myeloablative busulfan [107] | Myeloablative busulfan [108] |
| Price (WAC) | Low cost [106] | ~$2.2 million [110] | ~$3.1 million [110] |
Analysis of Clinical Data
- Hydroxyurea: The Multicenter Study of Hydroxyurea (MSH) established its efficacy in reducing the frequency of painful crises and acute chest syndrome. Long-term observational data suggest it reduces mortality. However, responses are heterogeneous, and its use, particularly in adults, remains suboptimal due to various factors including toxicity concerns and monitoring requirements [104] [106].
- CASGEVY: In the pivotal trial, the 93.5% efficacy was robust. Notably, one patient who initially achieved freedom from severe VOCs experienced an event at Month 22.8 associated with a parvovirus B19 infection, highlighting that external factors can precipitate events even after successful therapy [109]. Engraftment was successful in all patients, with a median time to neutrophil engraftment of 26-28 days [109].
- LYFGENIA: The 88% complete resolution rate of VOEs is compelling. However, the therapy carries a black box warning for hematologic malignancy. In clinical trials, two cases of acute myeloid leukemia were reported, though attributed to the prior manufacturing process [105] [110]. Post-infusion, patients must be monitored long-term for this potential risk.
Experimental and Methodological Protocols
Preclinical and Clinical Trial Designs
Hydroxyurea Clinical Trial Evolution:
- MSH Trial (Phase III): A randomized, double-blind, placebo-controlled trial in adults with moderate-to-severe SCD. Primary endpoint was the annual rate of painful crises. It demonstrated a significant reduction (44%) in crisis rate and a higher HbF level in the hydroxyurea group [104].
- Baby HUG Trial (Phase III): A randomized, double-blind, placebo-controlled trial in infants (9-18 months) with SCD. Primary endpoints were splenic and renal function. It confirmed the feasibility and safety of hydroxyurea in young children and showed beneficial effects on splenic function and VOC reduction [104].
CASGEVY Clinical Trial Protocol (NCT03745287):
- Design: Single-arm, open-label, multi-center, single-dose Phase 1/2/3 trial.
- Patient Population: Ages 12-35 with confirmed SCD and a history of ≥2 severe VOCs annually for the two prior years.
- Intervention: Patients underwent apheresis for CD34+ cell collection after mobilization with plerixafor. Cells were edited with CRISPR-Cas9 (CTX001 product) and cryopreserved. Patients received myeloablative busulfan conditioning followed by infusion of CASGEVY.
- Primary Efficacy Endpoint: Proportion of patients achieving freedom from severe VOCs for at least 12 consecutive months within the 24-month follow-up.
- Key Assessments: Engraftment (neutrophil and platelet recovery), HbF and total hemoglobin levels, VOC and hospitalization events, and safety monitoring for adverse events [109] [107].
LYFGENIA Clinical Trial Protocol (HGB-206):
- Design: Non-randomized, open-label, multi-site, single-dose Phase 1/2 trial.
- Patient Population: Ages 12-50 with SCD and a history of recurrent VOEs.
- Intervention: CD34+ cells were collected via apheresis after mobilization with plerixafor and transduced with the LentiGlobin BB305 vector. Patients received myeloablative busulfan conditioning followed by LYFGENIA infusion.
- Primary Efficacy Endpoint: Complete resolution of VOEs (VOC-CR) between 6 and 18 months post-infusion, with no VOEs between these time points.
- Key Assessments: HbA^T87Q^ levels, VOC and severe VOC events, vector copy number, integration site analysis, and long-term monitoring for malignancies [108].
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and analysis of these therapies rely on a suite of specialized research tools.
Table 3: Key Research Reagent Solutions for HbF Reactivation Studies
| Research Reagent / Tool | Function and Application in SCD Therapy R&D |
|---|---|
| CRISPR-Cas9 Ribonucleoprotein (RNP) | The core editing machinery for CASGEVY. Comprises purified Cas9 nuclease complexed with a synthetic single-guide RNA (gRNA-68). Used for precise, transient BCL11A enhancer editing in HSPCs without viral vector integration [75]. |
| Lentiviral Vectors (e.g., BB305) | Engineered viral delivery systems for stable gene integration. The BB305 vector in LYFGENIA contains a "mini-LCR" promoter to drive high-level, erythroid-specific expression of the βA^T87Q^ transgene in HSPCs [75]. |
| Antisense Oligonucleotides (ASOs) | Emerging tool to degrade enhancer RNA (eRNA). Preclinical studies show ASOs targeting BCL11A eRNA can disrupt epigenetic insulation, silence BCL11A, and reactivate HbF, offering a potential non-gene-editing therapeutic path [49]. |
| CD34+ Cell Selection Kits | Immunomagnetic bead-based kits for the positive selection of human CD34+ HSPCs from apheresis or marrow products. Critical for isolating the target cell population for ex vivo modification in both CASGEVY and LYFGENIA manufacturing [75] [107]. |
| HSPC Mobilization Agents (e.g., Plerixafor) | CXCR4 chemokine receptor antagonist used to mobilize CD34+ HSPCs from the bone marrow niche into the peripheral blood for collection via apheresis, a required first step for both gene therapies [108] [107]. |
| Myeloablative Conditioning Agents (e.g., Busulfan) | Cytotoxic alkylating agent used to create "space" in the bone marrow by clearing resident HSPCs. Essential pre-conditioning step to allow for engraftment and dominance of the re-infused, modified HSPCs [108] [107]. |
| Hemoglobin Electrophoresis/HPLC | Analytical techniques for quantifying different hemoglobin species (HbS, HbF, HbA, HbA^T87Q^). Used to monitor therapeutic efficacy and engraftment success in preclinical and clinical studies [75] [108]. |
| Digital PCR & Next-Generation Sequencing (NGS) | Molecular tools for quality control and safety monitoring. Used to measure on-target editing efficiency (CRISPR), vector copy number (lentivirus), and to profile viral integration sites and assess potential clonal dominance or oncogenic risk [75]. |
The benchmarked therapies—hydroxyurea, CASGEVY, and LYFGENIA—epitomize the evolution of HbF reactivation from a serendipitous pharmacologic effect to a precise genetic engineering feat. Hydroxyurea remains a foundational, accessible, and effective treatment, though with limitations in response variability and lifelong administration. CASGEVY and LYFGENIA represent a paradigm shift toward one-time, potentially curative treatments, each with distinct risk-benefit profiles. CASGEVY's gene-editing approach leverages endogenous regulatory mechanisms to reactivate HbF, while LYFGENIA's gene addition strategy introduces a novel therapeutic transgene.
For researchers and drug developers, this analysis highlights several critical considerations. The choice between a gene editing and a gene addition strategy involves trade-offs between mechanism (reactivating HbF vs. adding a β-globin variant), safety profile (malignancy risk associated with lentiviral integration vs. theoretical off-target editing risks), and manufacturing complexity. Future research directions include:
- Next-Generation HbF Inducers: Developing oral, targeted therapies that mimic the effects of genetic interventions, such as ASOs or small molecule inhibitors of BCL11A [49].
- Safety and Long-Term Monitoring: Establishing robust, long-term registries to monitor the durability of response and potential late effects of gene therapies, especially the risk of hematologic malignancies [105] [110].
- Access and Global Equity: Addressing the profound cost and logistical barriers (e.g., ~$2-3 million price tag, need for specialized centers, myeloablation) that currently limit these therapies to a small fraction of the global SCD population [106] [75] [110].
In conclusion, the field of HbF reactivation has progressed from systemic pharmacologic induction to targeted genomic intervention. The continued benchmarking of these and emerging therapies will be essential for guiding the next wave of innovation aimed at delivering safe, effective, and accessible cures for sickle cell disease and other hemoglobinopathies.
Conclusion
The therapeutic reactivation of fetal hemoglobin represents a paradigm shift in treating β-hemoglobinopathies, with multiple mechanistic approaches now demonstrating clinical potential. Foundational research has identified key repressors and 3D genomic structures that can be targeted through CRISPR editing, ASOs, and small molecules. While current gene therapies show remarkable efficacy, next-generation approaches focusing on precise editing, alternative molecular targets like MBD2, and non-gene-editing strategies offer promising paths toward overcoming cost, scalability, and safety limitations. Future success will require optimizing delivery platforms, validating long-term safety, and developing combinatorial approaches that ensure these transformative treatments reach the global patient population most in need.
References
- 1. Transcriptional regulation of fetal to adult hemoglobin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3087525/]
- 2. Advances in the understanding of haemoglobin switching - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4153468/]
- 3. Gene therapy for sickle cell and β-thalassemia works by ... [https://www.stjude.org/media-resources/news-releases/2025-medicine-science-news/gene-therapy-for-sickle-cell-and-beta-thalassemia-works-by-disrupting-three-dimensional-genome-structure.html]
- 4. Hematopoietic stem cell therapy with gene modification to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12445678/]
- 5. Disrupting ZBTB7A or BCL11A binding sites reactivates ... [https://www.nature.com/articles/s41598-025-10791-8]
- 6. A new target for fetal hemoglobin reactivation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6959183/]
- 7. Mechanisms of Globin Gene Regulation in Mammals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12452803/]
- 8. Zinc finger nuclease-mediated gene editing in ... [https://www.nature.com/articles/s41598-024-74716-7]
- 9. Transcriptional Repressor BCL11A in Erythroid Cells [https://pubmed.ncbi.nlm.nih.gov/39017845/]
- 10. Exploratory Review and In Silico Insights into circRNA and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11854342/]
- 11. Structural insights into the DNA-binding mechanism of ... [https://www.sciencedirect.com/science/article/abs/pii/S0969212624004222]
- 12. MBD2a–NuRD binds to the methylated γ-globin gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10288633/]
- 13. BCL11A-deficient human erythropoiesis is impaired in vitro ... [https://pubmed.ncbi.nlm.nih.gov/40020162/]
- 14. Hereditary persistence of fetal hemoglobin - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7983139/]
- 15. Hereditary persistence of fetal hemoglobin [https://en.wikipedia.org/wiki/Hereditary_persistence_of_fetal_hemoglobin]
- 16. Hereditary Persistence of Fetal Hemoglobin [https://together.stjude.org/en-us/conditions/blood-disorders/hereditary-persistence-of-fetal-hemoglobin.html]
- 17. Challenges in prenatal diagnosis and genetic counselling ... [https://www.sciencedirect.com/science/article/pii/S2468124525000282]
- 18. Induction of Fetal Hemoglobin by Introducing Natural ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.881937/full]
- 19. A New Form of Hereditary Persistence of Fetal Hemoglobin ... [https://www.sciencedirect.com/science/article/pii/S0006497120742205]
- 20. Scientists discover new approach to gene therapy [https://www.hubrecht.eu/new-approach-gene-therapy/]
- 21. Advances in β-Thalassemia Gene Therapy: CRISPR/Cas ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562837/]
- 22. 3D Shortcuts to Gene Regulation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2916936/]
- 23. 3D genomics and its applications in precision medicine [https://cmbl.biomedcentral.com/articles/10.1186/s11658-023-00428-x]
- 24. Comparative analysis of three-dimensional chromosomal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5647940/]
- 25. Erythroid lineage chromatin accessibility maps facilitate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10267139/]
- 26. Editing the genome to introduce a beneficial naturally ... [https://www.nature.com/articles/ncomms8085]
- 27. Epigenetic editing: a promising alternative to genome ... [https://www.institutimagine.org/en/epigenetic-editing-promising-alternative-genome-editing-treating-sickle-cell-disease-and-beta-1927]
- 28. Epigenetic reprogramming as a therapeutic strategy for ... [https://www.sciencedirect.com/science/article/abs/pii/S0014299925006077]
- 29. Epigenetic Modifiers in Cancer Therapy: Unlocking New ... [https://oncodaily.com/oncolibrary/375352]
- 30. Current trends in clinical trials and the development of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11233149/]
- 31. CMN Weekly (13 June 2025) - Your ... [https://crisprmedicinenews.com/news/cmn-weekly-13-june-2025-your-weekly-crispr-medicine-news/]
- 32. Epigenetic editing: from concept to clinic [https://www.nature.com/articles/s41573-025-01323-0]
- 33. Therapeutic gene editing strategies using CRISPR-Cas9 for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8038529/]
- 34. CRISPR/Cas9 gene editing for curing sickle cell disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC8049447/]
- 35. Gene Editing's breakthrough against sickle cell disease [https://www.sciencedirect.com/science/article/pii/S0268960X24000183]
- 36. Engineering Globin Gene Expression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6310746/]
- 37. CRISPR/Cas9 System as a Promising Therapy in ... [https://pubmed.ncbi.nlm.nih.gov/39794549/]
- 38. Silencing of BCL11A by Disrupting Enhancer-Dependent ... [https://pubmed.ncbi.nlm.nih.gov/41191525/]
- 39. Base editing of the HBG promoter induces potent fetal ... [https://www.sciencedirect.com/science/article/pii/S1934590923003697]
- 40. Identification of novel HPFH-like mutations by CRISPR ... [https://elifesciences.org/articles/65421]
- 41. A prime editing strategy to rewrite the γ-globin promoters ... [https://pubmed.ncbi.nlm.nih.gov/40857666/]
- 42. A benchmarked, high-efficiency prime editing platform for ... [https://www.nature.com/articles/s41592-024-02502-4]
- 43. A prime editing strategy to rewrite the γ-globin promoters ... [https://www.sciencedirect.com/science/article/pii/S0006497125020476]
- 44. Comprehensive analysis of prime editing outcomes in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8789035/]
- 45. How To Use ICE: A Detailed Guide for Analyzing CRISPR ... [https://www.synthego.com/guide/how-to-use-crispr/ice-analysis-guide/]
- 46. Targeting eRNA‐Producing Super‐Enhancers Regulates ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12533286/]
- 47. Enhancer transcription profiling reveals an enhancer RNA ... [https://www.nature.com/articles/s41392-025-02170-6]
- 48. Top 3 Opportunities Shaping Oligonucleotide Therapeutics [https://labtesting.wuxiapptec.com/2025/07/10/3-therapeutic-considerations-for-the-future-of-oligonucleotide-development/]
- 49. New method reactivates fetal hemoglobin without gene ... [https://sicklecellanemianews.com/news/new-method-reactivates-fetal-hemoglobin-without-gene-editing/]
- 50. Emerging Therapies for Sickle Cell Disease - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12635507/]
- 51. Off-target effects of oligonucleotides and approaches ... [https://www.sciencedirect.com/science/article/pii/S2472555225000474]
- 52. Antisense Oligonucleotides Market Trends Report 2025 ... [https://www.businesswire.com/news/home/20251003267905/en/Antisense-Oligonucleotides-Market-Trends-Report-2025-2035-Profiles-of-Antisense-Therapeutics-Biogen-Bio-Path-Ionis-ProQR-Sarepta-Sterna-Biologicals-Wave-Life-Sciences---ResearchAndMarkets.com]
- 53. Pharmacological Induction of Fetal Hemoglobin in β- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9227505/]
- 54. Reactivation of Fetal Hemoglobin for Treating β-Thalassemia ... [https://pubmed.ncbi.nlm.nih.gov/29127681/]
- 55. A critique review of fetal hemoglobin modulators through ... [https://pubmed.ncbi.nlm.nih.gov/40057227/]
- 56. Comprehensive regulation of γ-globin expression by ... [https://clinicalepigeneticsjournal.biomedcentral.com/articles/10.1186/s13148-025-01962-5]
- 57. Novel histone deacetylase inhibitor CT-101 induces γ ... [https://www.sciencedirect.com/science/article/abs/pii/S1079979621000929]
- 58. A new target for fetal hemoglobin reactivation [https://haematologica.org/article/view/9152]
- 59. Editas Medicine Reports New In Vivo Data Highlighting the ... [https://ir.editasmedicine.com/news-releases/news-release-details/editas-medicine-reports-new-vivo-data-highlighting-potential]
- 60. Ex vivo modification of hematopoietic stem and progenitor ... [https://www.sciencedirect.com/science/article/pii/S1525001625002679]
- 61. Emerging Gene Therapies in Sickle Cell Disease [https://www.dovepress.com/emerging-gene-therapies-in-sickle-cell-disease-a-comparative-review-of-peer-reviewed-fulltext-article-JBM]
- 62. Recent advancements in gene therapy for sickle cell ... [https://www.frontiersin.org/journals/hematology/articles/10.3389/frhem.2024.1468952/full]
- 63. Inhibiting ferroptosis enhances ex vivo expansion of ... [https://www.nature.com/articles/s41556-025-01814-7]
- 64. Off-target effects in CRISPR/Cas9 gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10034092/]
- 65. CRISPR Off-Target Editing: Prediction, Analysis, and More [https://www.synthego.com/blog/crispr-off-target-editing/]
- 66. Best practice for CRISPR design using current tools and ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202318303396]
- 67. A boost for the precision of genome editing [https://news.mit.edu/2025/boost-precision-genome-editing-0820]
- 68. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 69. Genome editing strategies for targeted correction of β- ... [https://www.sciencedirect.com/science/article/pii/S1525001625002217]
- 70. A NOVEL BASE-EDITING STRATEGY FOR THERAPEUTIC ... [https://www.htct.com.br/en-a-novel-base-editing-strategy-for-articulo-resumen-S2531137925003621]
- 71. Ex vivo prime editing of patient haematopoietic stem cells ... [https://www.nature.com/articles/s41551-023-01026-0]
- 72. Multiplex base editing of BCL11A regulatory elements to treat ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12629801/]
- 73. Multiplex Base Editing Safely Enhances Sickle Therapy [https://crisprmedicinenews.com/news/interview-multiplex-base-editing-safely-enhances-sickle-therapy/]
- 74. Optimization of CRISPR/Cas9 Delivery to Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6318785/]
- 75. CRISPR vs Gene Therapy for Sickle Cell: Which Treatment ... [https://globalrph.com/2025/10/crispr-vs-gene-therapy-for-sickle-cell-which-treatment-works-better/]
- 76. Elevating fetal hemoglobin: recently discovered regulators ... [https://www.sciencedirect.com/science/article/pii/S0006497124012916]
- 77. Fetal haemoglobin induction in sickle cell disease - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5898646/]
- 78. New Frontiers in Sickle Cell Disease: CRISPR-Based Cures [https://globalrph.com/2025/08/new-frontiers-in-sickle-cell-disease-crispr-based-cures/]
- 79. Gene Therapy Leads to Improved Quality of Life in Patients ... [https://www.hematology.org/newsroom/press-releases/2025/gene-therapy-leads-to-improved-quality-of-life]
- 80. Current and future treatments for sickle cell disease [https://www.sciencedirect.com/science/article/pii/S152500162500190X]
- 81. Hematopoietic Stem Cell Transplantation in Thalassemia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3331690/]
- 82. Elevating fetal hemoglobin: recently discovered regulators ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11830979/]
- 83. Structural basis for human ZBTB7A action at the fetal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8553545/]
- 84. Disrupting ZBTB7A or BCL11A binding sites reactivates ... [https://mahidol.elsevierpure.com/en/publications/disrupting-zbtb7a-or-bcl11a-binding-sites-reactivates-fetal-hemog]
- 85. Disrupting ZBTB7A or BCL11A binding sites reactivates ... [https://pubmed.ncbi.nlm.nih.gov/40665149/]
- 86. The Switch from Fetal to Adult Hemoglobin - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3530042/]
- 87. CRISPR-Based Gene Therapies: From Preclinical to ... [https://www.mdpi.com/2073-4409/13/10/800]
- 88. Successful treatment of transfusion-dependent β-thalassemia [https://pmc.ncbi.nlm.nih.gov/articles/PMC11830765/]
- 89. Genetic reversal of the globin switch concurrently ... [https://www.nature.com/articles/s41467-023-40923-5]
- 90. treatment with HbF inducers and CRISPR-Cas9 based ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2023.1204536/full]
- 91. Efficient CRISPR-Cas9-based genome editing of β-globin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8091488/]
- 92. Advances in Therapeutic Applications of CRISPR Genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12242737/]
- 93. Identification of Small Molecules That Induce Therapeutic ... [https://www.sciencedirect.com/science/article/pii/S0006497121039811]
- 94. Emerging Gene Therapies in Sickle Cell Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599223/]
- 95. Current and future alternative therapies for beta- ... [https://www.sciencedirect.com/science/article/pii/S2319417016000172]
- 96. Safety and efficacy studies of CRISPR-Cas9 treatment ... [https://pubmed.ncbi.nlm.nih.gov/39044427/]
- 97. Mechanisms of erythrocyte development and regeneration [https://pmc.ncbi.nlm.nih.gov/articles/PMC5825862/]
- 98. Erythropoiesis: insights from a genomic perspective [https://www.nature.com/articles/s12276-024-01311-1]
- 99. Targeting the Hematopoietic Stem Cell Niche in β ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9146437/]
- 100. Fetal hemoglobin rescues ineffective erythropoiesis in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8485663/]
- 101. Therapeutic levels of fetal hemoglobin in erythroid progeny of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3062294/]
- 102. Genetic and Epigenetic Mechanisms That Maintain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4699043/]
- 103. Effective erythropoiesis and HbF reactivation induced by kit ... [https://www.sciencedirect.com/science/article/pii/S0006497120485866]
- 104. Current and Future Therapeutics for Treating Patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11120250/]
- 105. FDA approval of Casgevy and Lyfgenia : a dual breakthrough in gene... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11374260/]
- 106. Sickle cell anaemia therapy in 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11886933/]
- 107. CASGEVY® Clinical Trial and Results [https://www.casgevy.com/sickle-cell-disease/study-information]
- 108. Clinical Trial Results | Vaso Occlusive Events Data [https://www.lyfgenia.com/clinical-trial-results]
- 109. Efficacy of CASGEVY® (exagamglogene autotemcel) in Trial 1 ... [https://www.casgevyhcp.com/sickle-cell-disease/efficacy]
- 110. vs. Lyfgenia : The Casgevy Treatment Showdown Sickle Cell [https://www.delveinsight.com/blog/lyfgenia-or-casgevy-for-sickle-cell-disease-treatment]