In Vivo vs Ex Vivo CRISPR-Cas9 Therapy: 2025 Clinical Approaches, Challenges, and Future Directions
This article provides a comprehensive analysis of in vivo and ex vivo CRISPR-Cas9 therapeutic approaches for researchers and drug development professionals.
In Vivo vs Ex Vivo CRISPR-Cas9 Therapy: 2025 Clinical Approaches, Challenges, and Future Directions
Abstract
This article provides a comprehensive analysis of in vivo and ex vivo CRISPR-Cas9 therapeutic approaches for researchers and drug development professionals. Covering foundational mechanisms to cutting-edge clinical applications, we examine the distinct methodologies, delivery systems, and optimization strategies for each approach. The content explores current clinical trial outcomes, including recently approved ex vivo therapies and emerging in vivo applications, while addressing critical safety considerations and technical hurdles. Through comparative analysis of therapeutic efficacy, scalability, and clinical translation challenges, this review synthesizes key insights to guide strategic development decisions in CRISPR-based therapeutics.
CRISPR-Cas9 Fundamentals: From Bacterial Immunity to Therapeutic Genome Editing
CRISPR-Cas9 technology has revolutionized genome engineering by providing an unprecedented ability to perform precise, targeted modifications to DNA sequences. This in-depth technical guide examines the core mechanisms of CRISPR-Cas9 systems, from their origins as bacterial adaptive immune systems to their current applications as powerful gene-editing tools. The fundamental operating principle involves a Cas nuclease directed by a guide RNA to a specific DNA sequence, where it introduces a double-strand break (DSB) that activates cellular DNA repair pathways [1] [2]. Understanding these mechanisms is paramount for researchers and drug development professionals working to advance therapeutic applications, particularly in the context of comparing in vivo versus ex vivo delivery approaches. This guide provides a comprehensive technical foundation of CRISPR-Cas9 mechanisms, detailed experimental methodologies, and essential research tools to support therapeutic development.
Fundamental CRISPR-Cas9 Mechanisms
Historical Context and Natural Biological Function
The CRISPR-Cas system was originally discovered as an adaptive immune mechanism in bacteria and archaea that provides protection against invading mobile genetic elements (MGEs) such as bacteriophages and plasmids [3] [2]. The system operates through a sequence-specific targeting mechanism that relies on RNA-DNA complementarity. The natural system consists of two key components: CRISPR arrays (short DNA repeats interspersed with "spacer" sequences derived from previous MGE invasions) and Cas proteins that facilitate the immune response [3]. The groundbreaking 2012 publication by Dr. Jennifer Doudna and Dr. Emmanuelle Charpentier demonstrated that this bacterial immune system could be repurposed as a programmable gene-editing tool, earning them the 2020 Nobel Prize in Chemistry [1].
Molecular Components and Mechanism
The repurposed CRISPR-Cas9 gene-editing system consists of two fundamental molecular components:
- Guide RNA (gRNA): A customizable RNA sequence that directs the nuclease to a specific target DNA sequence through Watson-Crick base pairing [1].
- Cas9 Nuclease: An enzyme that creates double-stranded breaks (DSBs) in the target DNA at the location specified by the gRNA [1].
The targeting specificity requires the presence of a Protospacer Adjacent Motif (PAM), a short DNA sequence adjacent to the target site that is essential for Cas9 recognition and activation [3] [2]. The most commonly used nuclease is CRISPR Cas9, though other variants include Cas12, Cas13, and Cas14, each with distinct properties and applications [1].
The following diagram illustrates the core CRISPR-Cas9 mechanism and its relationship to DNA repair pathways:
DNA Repair Pathways in CRISPR-Cas9 Editing
After Cas9 creates a double-strand break, cellular DNA repair mechanisms are activated to resolve the damage. The two primary pathways are Non-homologous end joining (NHEJ) and Homology-directed repair (HDR), each resulting in distinct genetic outcomes with important implications for therapeutic applications [1].
Non-Homologous End Joining (NHEJ)
NHEJ is the dominant DNA repair pathway in human cells and is active throughout the cell cycle. This pathway directly ligates the broken DNA ends without requiring a repair template. NHEJ is often error-prone, frequently resulting in small insertions or deletions (indels) at the cleavage site [1]. When these indels occur within the coding region of a gene, they can cause frameshift mutations that disrupt the reading frame and generate premature stop codons, effectively resulting in gene knockout [1]. This pathway is particularly useful for creating gene knockouts in functional genomics, pathway analysis, and therapeutic applications where disrupting gene function is desired.
Homology-Directed Repair (HDR)
HDR is a more precise repair pathway that uses a DNA template with homologous regions flanking the cut site to repair the break. This pathway is active primarily during the S and G2 phases of the cell cycle and enables precise genetic modifications, including nucleotide substitutions or insertion of entire genes (gene knock-in) [1]. HDR is less frequent than NHEJ and presents greater technical challenges for efficient implementation, but it is essential for therapeutic applications requiring precise gene correction [1]. Experimental strategies to enhance HDR efficiency include cell cycle synchronization and using small molecule inhibitors of key NHEJ pathway components [1].
Table 1: Comparison of DNA Repair Pathways in CRISPR-Cas9 Genome Editing
| Parameter | Non-Homologous End Joining (NHEJ) | Homology-Directed Repair (HDR) |
|---|---|---|
| Repair Mechanism | Direct ligation of broken ends | Uses homologous DNA template |
| Template Requirement | Not required | Required (donor DNA template) |
| Cell Cycle Phase | Active throughout all phases | Primarily S/G2 phases |
| Editing Outcome | Indels (insertions/deletions) | Precise nucleotide changes or insertions |
| Primary Application | Gene knockouts | Gene knock-ins or precise corrections |
| Efficiency in Postmitotic Cells | High | Limited |
| Common Experimental Results | Frameshift mutations creating gene knockouts | Precise edits with donor template sequence incorporation |
CRISPR-Cas Applications in Therapeutic Contexts
CRISPR-Cas9 technologies enable three primary types of genetic modifications, each with distinct mechanisms and therapeutic applications. The choice of editing strategy depends on the therapeutic goal, target cell type, and available delivery methods.
Table 2: CRISPR-Cas9 Gene Editing Applications and Outcomes
| Editing Type | Molecular Mechanism | Repair Pathway | Therapeutic Applications | Technical Considerations |
|---|---|---|---|---|
| Gene Knockout | Indels causing frameshift mutations | NHEJ | Sickle cell disease (BCL11A targeting), Cancer immunotherapy (CAR-T cells) | High efficiency; potential for "knockout escaping" with residual functional proteins [1] |
| Gene Knock-in | Insertion of new DNA sequence | HDR | Correcting genetic mutations, inserting therapeutic genes | Lower efficiency than knockouts; requires donor template; cell cycle synchronization beneficial [1] |
| Gene Expression Regulation | dCas9 fusion with transcriptional regulators | N/A (no DNA cleavage) | Developmental biology, infectious disease management, functional genomics | CRISPRa for activation, CRISPRi for interference; precise control without permanent DNA changes [1] |
In Vivo versus Ex Vivo Therapeutic Approaches
The delivery of CRISPR-Cas9 therapeutics occurs through two primary approaches, each with distinct advantages, limitations, and technical considerations for drug development professionals.
Ex Vivo Gene Editing involves harvesting cells from the patient, editing the cells with CRISPR outside the body, and then returning the modified cells to the patient. The first approved CRISPR-based therapy, exagamglogene autotemcel (exa-cel, marketed as Casgevy), utilizes this approach for treating sickle cell disease and transfusion-dependent beta-thalassemia [1]. Exa-cel uses CRISPR-Cas9 gene editing to increase fetal hemoglobin production by disrupting the BCL11A gene in hematopoietic stem cells [1]. This approach allows for precise quality control, selection of successfully edited cells, and comprehensive safety testing before reinfusion.
In Vivo Gene Editing involves directly administering the CRISPR-Cas9 therapeutic agents to the patient, where editing occurs inside the body. This approach typically uses viral vectors (such as AAV) or lipid nanoparticles (LNPs) to deliver the editing components [4]. Recent advances include the first personalized in vivo CRISPR treatment for an infant with CPS1 deficiency, which was developed and delivered in just six months [4]. Lipid nanoparticles are particularly promising for liver-targeted therapies, as they naturally accumulate in hepatic tissue after systemic administration [4].
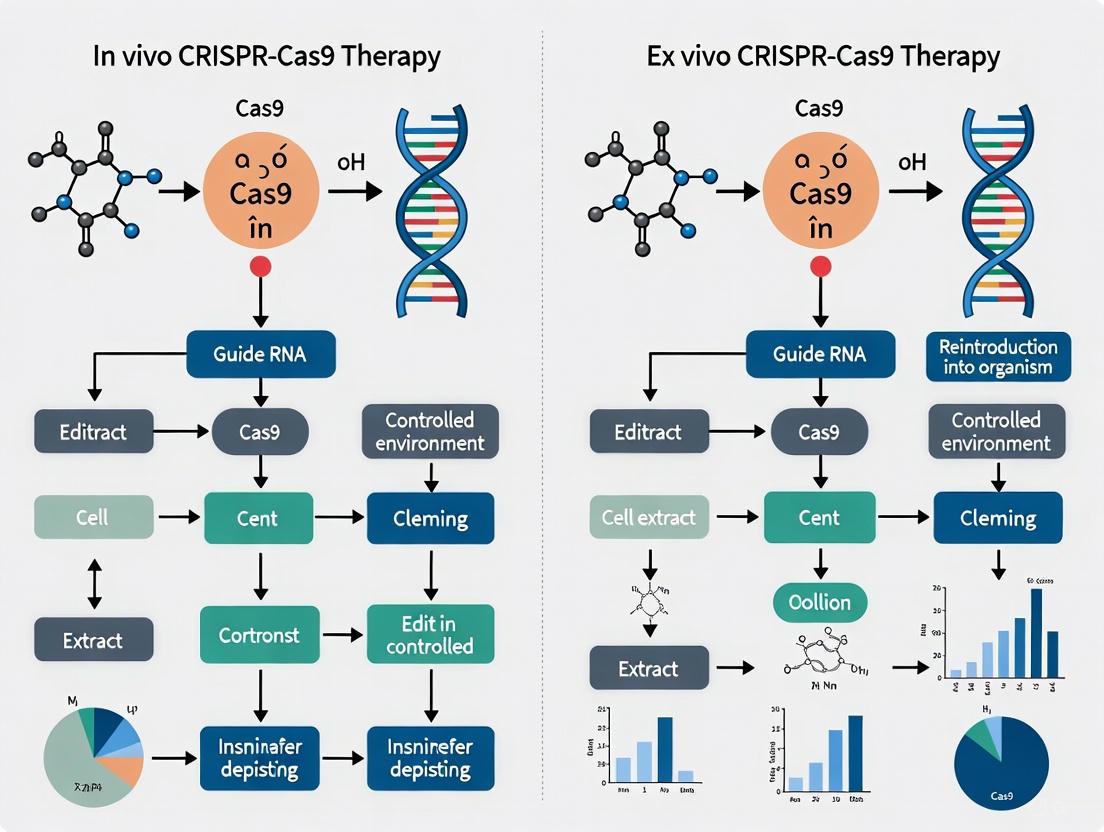
The following diagram illustrates the key differences between these two therapeutic approaches:
Experimental Protocols and Methodologies
ArrayEdit: High-Content Analysis of CRISPR-Edited Cells
The ArrayEdit protocol enables efficient gene editing and analysis of human embryonic stem cells (hESCs) using arrayed surface-modified multiwell plates. This approach decreases the time and cost of gene editing while enabling automated, live, high-content imaging and analysis [5].
Protocol Steps:
- One-pot sgRNA Transcription: Rapidly transcribe single-guide RNAs, which can be multiplexed to edit multiple targets simultaneously [5].
- Surface Modification: Prepare multiwell plates with surface modifications to separate thousands of edited cell populations [5].
- Cell Seeding and Editing: Seed hESCs onto the arrayed plates and introduce CRISPR-Cas9 components.
- High-Content Imaging: Perform automated live-cell imaging to monitor editing outcomes in complex structures generated by human cells [5].
- In Situ Analysis: Analyze editing efficiency and select edited populations without destroying initial samples, enabling optical and molecular perturbations in the editing workflow [5].
ORANGE Toolkit for Endogenous Protein Tagging in Neurons
The ORANGE (Open Resource for the Application of Neuronal Genome Editing) toolkit enables CRISPR-Cas9-mediated targeted genomic integration of epitope tags in rodent dissociated neuronal culture, organotypic slices, and in vivo [6]. This methodology addresses the challenge of efficient genome editing in postmitotic cells.
Protocol Steps:
- HITI Vector Design: Utilize the homology-independent targeted integration (HITI) method based on NHEJ, which outperforms HDR-based methods in postmitotic neurons [6].
- Knock-in Construct Assembly: Employ the pORANGE template vector containing: U6-driven gRNA expression cassette, donor sequence with fluorescent tag, and Cas9 expression cassette driven by β-actin promoter [6].
- Target Sequence Selection: Design gRNA to target specific genomic loci with inverted orientation of target sequence and PAM sites flanking the donor [6].
- Validation: Confirm accurate integration and functionality using live-cell and superresolution imaging to resolve protein localization and dynamics at nanoscale resolution [6].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for CRISPR-Cas9 Experiments
| Reagent/Solution | Function | Example Applications | Technical Notes |
|---|---|---|---|
| Cas9 Nuclease | Creates double-strand breaks at target DNA sequences | Gene knockout, knock-in, and editing | Multiple variants available (HiFi Cas9 for reduced off-target effects) [7] |
| Guide RNA (gRNA) | Targets Cas nuclease to specific genomic loci | All CRISPR applications | Design critical for efficiency and specificity; multiplexing possible [1] |
| Donor DNA Template | Provides homologous sequence for HDR | Precise gene correction, knock-in | Homology arm design affects HDR efficiency [1] |
| Lipid Nanoparticles (LNPs) | In vivo delivery of CRISPR components | Liver-targeted therapies (hATTR, HAE) [4] | Enables redosing; natural liver tropism [4] |
| AAV Vectors | In vivo delivery of CRISPR components | Tissue-specific targeting | Potential immune response concerns limit redosing [4] |
| DNA-PKcs Inhibitors | Enhances HDR efficiency by suppressing NHEJ | Improving precise editing outcomes | Risk of increased structural variations; use requires caution [7] |
| pORANGE Vector System | Endogenous protein tagging in neurons | Studying protein localization and dynamics | Based on HITI method; effective in postmitotic cells [6] |
Safety Considerations and Genomic Integrity
As CRISPR-based therapies advance clinically, understanding and mitigating potential genotoxic risks is paramount. Beyond well-documented off-target effects at sites with sequence similarity to the intended target, recent studies reveal more pressing concerns regarding large structural variations (SVs) [7]. These include:
- Kilobase- to megabase-scale deletions at the on-target site [7]
- Chromosomal translocations between heterologous chromosomes [7]
- Chromosomal losses or truncations [7]
- On-target genomic aberrations that may delete critical cis-regulatory elements [7]
Notably, strategies to enhance HDR efficiency through inhibition of key NHEJ pathway components like DNA-PKcs may exacerbate these genomic aberrations. DNA-PKcs inhibitors can increase the frequency of megabase-scale deletions and cause a thousand-fold increase in chromosomal translocations [7]. These findings highlight the critical need for comprehensive genomic integrity assessment in therapeutic development, utilizing methods capable of detecting large structural variations that conventional short-read sequencing might miss.
Risk mitigation strategies include using high-fidelity Cas9 variants, carefully evaluating the necessity of HDR-enhancing compounds, and implementing robust analytical methods like CAST-Seq and LAM-HTGTS to detect structural variations [7]. For therapeutic applications, even low or moderate editing levels may suffice if corrected cells gain a selective advantage, potentially reducing the need for aggressive HDR-enhancement strategies that compromise genomic integrity [7].
The advent of programmable nucleases has revolutionized genetic engineering, providing researchers with unprecedented tools for precise genome modification. These technologies have evolved through three distinct generations: Zinc-Finger Nucleases (ZFNs), Transcription Activator-Like Effector Nucleases (TALENs), and the Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 system. Each platform represents a significant leap in our ability to understand and manipulate gene function, moving from challenging and time-consuming processes to highly flexible and efficient editing capabilities.
These systems function by creating targeted double-strand breaks (DSBs) in the DNA, which harnesses the cell's innate DNA repair mechanisms—primarily non-homologous end joining (NHEJ) or homology-directed repair (HDR). The NHEJ pathway is error-prone, often leading to small insertions or deletions (indels) that disrupt gene function, making it ideal for gene knockouts. In contrast, HDR uses a donor DNA template to facilitate precise gene corrections or insertions [1] [8]. The core difference between these platforms lies in their mechanism for achieving DNA recognition: ZFNs and TALENs rely on protein-DNA interactions, whereas CRISPR-Cas9 utilizes a guide RNA for DNA recognition via Watson-Crick base pairing, simplifying design and scaling [9] [10].
Historical Development and Technological Comparisons
First and Second Generation Editors: ZFNs and TALENs
Zinc-Finger Nucleases (ZFNs) were among the first engineered nucleases to enable targeted genome editing. A ZFN is a chimeric protein composed of a customizable zinc-finger DNA-binding domain, where each zinc-finger module recognizes approximately three base pairs, and the non-specific FokI endonuclease cleavage domain. A critical feature is that the FokI domain must dimerize to become active, which necessitates the design of two ZFN proteins that bind to opposite DNA strands at sites separated by a short spacer [9] [10]. While pioneering, the development of ZFNs was hampered by technical challenges. The DNA recognition code of zinc fingers can be context-dependent, meaning that the specificity of individual fingers can be influenced by their neighbors, making the rational design of long, specific arrays complex and laborious [9].
Transcription Activator-Like Effector Nucleases (TALENs) emerged as a powerful alternative, offering a more straightforward design principle. TALENs are also fusions of a customizable DNA-binding domain and the FokI nuclease. Their DNA-binding domain is derived from TALE proteins of plant pathogenic Xanthomonas bacteria. A key discovery was that TALE DNA-binding specificity is determined by a simple code: each TALE repeat domain recognizes a single DNA base pair through two hypervariable amino acids known as Repeat-Variable Diresidues (RVDs) [9] [10]. This one-to-one recognition code made TALEN design more modular and predictable than ZFNs. Similar to ZFNs, TALENs also require dimerization of the FokI nuclease, which enhances their target specificity [10].
The CRISPR-Cas9 Revolution
The development of the CRISPR-Cas9 system marked a paradigm shift in genome editing. Originally discovered as an adaptive immune system in bacteria and archaea, it was repurposed into a highly versatile gene-editing tool by Charpentier and Doudna, who were awarded the Nobel Prize in Chemistry in 2020 for this work [1] [8]. The system comprises two key components: the Cas9 nuclease and a guide RNA (gRNA). The gRNA is a synthetic fusion of two natural RNAs—CRISPR RNA (crRNA) and trans-activating crRNA (tracrRNA)—and contains a ~20 nucleotide sequence that directs Cas9 to a specific genomic locus through complementary base pairing. Cas9 cleaves the target DNA only if it is adjacent to a short DNA sequence known as the Protospacer Adjacent Motif (PAM), which for the commonly used Streptococcus pyogenes Cas9 is 5'-NGG-3' [1] [8] [10].
The primary advantage of CRISPR-Cas9 over ZFNs and TALENs is its simplicity and programmability. Designing new gRNAs to target different genomic sites is significantly easier and faster than engineering new protein-based DNA-binding domains, enabling high-throughput genetic screening and multiplexed editing (targeting multiple genes simultaneously) [10].
Comparative Analysis of Editing Platforms
Table 1: Comparative Analysis of Major Genome Editing Platforms
| Feature | ZFNs | TALENs | CRISPR-Cas9 |
|---|---|---|---|
| DNA Recognition Mechanism | Protein-DNA interaction | Protein-DNA interaction | RNA-DNA interaction (Watson-Crick base pairing) |
| Recognition Target Length | 9-18 bp | 30-40 bp | 22 bp + PAM sequence |
| Cleavage Mechanism | FokI dimerization (double-strand break) | FokI dimerization (double-strand break) | Cas9 nuclease (double-strand break) |
| Molecular Design | Challenging due to context-dependent finger specificity | Easy due to modular, one-to-one TALE repeat code | Very easy; requires only gRNA sequence design |
| Multiplexing Potential | Low | Low | High (multiple gRNAs can be used simultaneously) |
| Protein Engineering Required | For each new target | For each new target | No; the Cas9 protein is constant |
| Typical Mutation Profile | Small indels at target site | Small indels at target site | Small indels, with potential for larger structural variations [7] |
In vivo versus Ex vivo CRISPR Therapy Approaches
The translation of CRISPR-Cas9 technology into clinical therapies primarily follows two strategic pathways: in vivo and ex vivo gene editing. The choice between these approaches has profound implications for manufacturing, delivery, safety, and therapeutic application.
Ex Vivo Gene Editing
Ex vivo gene editing involves harvesting cells from a patient, genetically modifying them outside the body using CRISPR, and then reinfusing the edited cells back into the patient [1]. This approach offers greater control over the editing process, as the conditions can be meticulously optimized, and the edited cells can be analyzed for quality and safety (e.g., assessing on-target and off-target edits) before administration.
- Therapeutic Example: The first and only CRISPR-based therapy to receive regulatory approval internationally, exagamglogene autotemcel (exa-cel, marketed as Casgevy), is an ex vivo treatment for sickle cell disease and transfusion-dependent beta-thalassemia [1] [4].
- Workflow: Hematopoietic stem cells are collected from the patient and sent to a manufacturing facility. There, CRISPR-Cas9 is used to disrupt the BCL11A gene's erythroid-specific enhancer, a step that promotes the production of fetal hemoglobin. Meanwhile, the patient undergoes chemotherapy to clear out their native bone marrow stem cells, creating space for the reinfused, edited cells to engraft and regenerate a new blood cell population that ameliorates the disease [1].
- Advantages: Includes precise control over the editing environment, ability to perform rigorous quality control, and reduced concern about delivery vehicle immunogenicity.
- Challenges: The process is complex, costly, and requires sophisticated manufacturing infrastructure and logistics. It also subjects the patient to conditioning chemotherapy, which carries its own risks [1] [11].
In Vivo Gene Editing
In vivo gene editing involves directly administering the CRISPR-Cas9 therapeutic agents (e.g., as mRNA, protein, or encoded in a viral vector) into the patient's body to edit cells in situ [1]. This strategy is necessary for tissues that cannot be easily removed, manipulated, and reimplanted, such as the liver or brain.
- Therapeutic Example: Intellia Therapeutics has pioneered systemic in vivo CRISPR trials. In a Phase I trial for hereditary transthyretin amyloidosis (hATTR), CRISPR components were packaged into Lipid Nanoparticles (LNPs) and administered intravenously. The LNPs naturally accumulated in the liver, where they edited the TTR gene in hepatocytes, resulting in a sustained, deep reduction (~90%) of the disease-causing protein in the blood [4].
- Landmark Case: In a landmark 2025 case, a personalized in vivo CRISPR therapy was developed for an infant with CPS1 deficiency. The treatment, delivered via LNP, was developed and administered in just six months, establishing a proof-of-concept for rapid, bespoke in vivo gene therapy [4].
- Advantages: Avoids complex cell manufacturing and the need for patient conditioning regimens. Potentially applicable to a wider range of diseases, especially those affecting solid organs.
- Challenges: The major hurdle is delivery—getting the CRISPR machinery efficiently and specifically to the target cells while avoiding off-target tissues. Immune responses to the delivery vehicle or the bacterial-derived Cas9 protein itself can also be a significant concern [12] [4] [13].
Table 2: Comparison of In Vivo and Ex Vivo Therapeutic Approaches
| Parameter | Ex Vivo Editing | In Vivo Editing |
|---|---|---|
| Definition | Cells are edited outside the body and then transplanted back into the patient. | The genome-editing system is delivered directly into the patient to edit cells inside the body. |
| Key Delivery Vehicles | Electroporation, viral vectors (e.g., lentivirus) | Lipid Nanoparticles (LNPs), Adeno-Associated Viruses (AAVs) |
| Therapeutic Examples | Casgevy (for sickle cell disease, beta-thalassemia); CAR-T cell engineering | Intellia's NTLA-2001 (for hATTR); personalized therapy for CPS1 deficiency |
| Major Advantages | High control over editing process; enables pre-transplant quality control; avoids systemic delivery challenges. | Less invasive and complex manufacturing; applicable to non-removable tissues and organs. |
| Major Challenges | Complex, costly, and lengthy cell manufacturing process; often requires patient conditioning (e.g., chemotherapy). | Significant delivery challenges (efficiency, specificity, immunogenicity); more difficult to assess and control editing outcomes. |
The following diagram illustrates the core workflows for both therapeutic approaches.
Delivery Methods for CRISPR-Cas9 Systems
Effective delivery is arguably the greatest challenge in CRISPR-based therapeutics, particularly for in vivo applications. The delivery vehicle must protect the CRISPR cargo (which can be DNA, mRNA, or preassembled Ribonucleoprotein (RNP)), facilitate its entry into target cells, and ultimately release it into the cytoplasm or nucleus to perform its function, all while minimizing immune activation and off-target effects [12] [13].
Viral Vectors
Viral vectors are engineered viruses that have been stripped of their pathogenic genes and repurposed to deliver genetic material.
- Adeno-Associated Viruses (AAVs): These are small, non-pathogenic viruses with a low immunogenicity profile, making them a popular choice for in vivo gene therapy. A key limitation is their small packaging capacity (~4.7 kb), which is insufficient for the standard SpCas9 coding sequence plus gRNAs. Strategies to overcome this include using smaller Cas9 orthologs (e.g., from S. aureus) or splitting the Cas9 and gRNA expression cassettes into two separate AAVs [13].
- Lentiviral Vectors (LVs): LVs are capable of delivering larger genetic payloads and can infect both dividing and non-dividing cells. A significant safety consideration is that they integrate into the host genome, which carries a risk of insertional mutagenesis [13].
Non-Viral Vectors
Non-viral methods are gaining traction due to their improved safety profiles, reduced immunogenicity, and potential for large-scale production.
- Lipid Nanoparticles (LNPs): LNPs are synthetic, spherical vesicles that have become a leading platform for in vivo delivery, as demonstrated by their success in mRNA COVID-19 vaccines. They efficiently encapsulate and protect CRISPR cargo (especially mRNA and RNPs) and have a natural tropism for the liver after intravenous administration. Recent advances include Selective Organ Targeting (SORT) LNPs, which can be engineered to target tissues beyond the liver [4] [13]. A major advantage of LNPs is that they enable transient expression of CRISPR components, reducing the risk of long-term off-target effects, and they allow for potential re-dosing, as they do not elicit a strong neutralizing immune response like viral vectors [4].
- Electroporation: This physical method uses an electrical field to create temporary pores in the cell membrane, allowing CRISPR cargo (most commonly RNPs) to enter the cell directly. It is highly efficient for ex vivo editing of a wide range of cell types, including immune cells and stem cells [13].
- Other Non-Viral Vectors: Research is ongoing into other delivery systems, including extracellular vesicles (EVs), which are natural lipid nanoparticles derived from cells; cell-penetrating peptides (CPPs); and various inorganic nanoparticles [12] [13].
Table 3: Key Delivery Methods for CRISPR-Cas9 Systems
| Delivery Method | Cargo Type | Primary Application | Pros | Cons |
|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | DNA | In vivo | Low immunogenicity; long-term expression | Small payload capacity; potential for pre-existing immunity |
| Lentivirus (LV) | DNA | Ex vivo, In vitro | Large payload; infects non-dividing cells | Integrative; raises safety concerns for in vivo use |
| Lipid Nanoparticles (LNP) | mRNA, RNP | In vivo, Systemic | Clinically validated; transient expression; targetable (e.g., SORT); allows re-dosing [4] | Limited tissue targeting beyond liver without engineering; endosomal escape can be inefficient |
| Electroporation | RNP, mRNA | Ex vivo | High efficiency for hard-to-transfect cells; transient RNP activity | Cytotoxicity; not suitable for in vivo use |
| Virus-Like Particles (VLP) | Protein, RNP | In vivo, Ex vivo | Non-integrative; no viral genome; transient | Manufacturing challenges; cargo size limitations [13] |
Experimental Protocols and Workflows
A Representative Protocol for Ex Vivo Gene Editing (e.g., Hematopoietic Stem Cells)
This protocol outlines the key steps for creating a therapy analogous to Casgevy.
- Guide RNA Design and Preparation: Design a gRNA targeting the specific regulatory element or gene of interest (e.g., the BCL11A enhancer for sickle cell disease). The gRNA sequence should be selected using established algorithms to maximize on-target efficiency and minimize potential off-target sites [1] [8].
- CRISPR-Cas9 RNP Complex Formation: Complex the purified Cas9 protein with the synthesized gRNA at an optimal molar ratio in a suitable buffer. Incubate to allow the formation of the preassembled Ribonucleoprotein (RNP) complex. Using RNP complexes, as opposed to DNA plasmids, reduces the duration of nuclease activity inside the cell, which can lower off-target effects and improve editing precision [13].
- Cell Harvesting and Activation: Isolate CD34+ hematopoietic stem and progenitor cells (HSPCs) from a patient's apheresis product. Culture the cells in a cytokine-rich medium to promote a healthy, activated state prior to editing.
- Electroporation: Wash the HSPCs and resuspend them in an electroporation buffer. Mix the cell suspension with the preformed RNP complex and transfer to an electroporation cuvette. Electroporate using an optimized electrical waveform and parameters specific for primary human HSPCs.
- Post-Editing Culture and Analysis: After electroporation, immediately transfer the cells to recovery medium. A small aliquot of cells can be taken 48-72 hours post-electroporation to extract genomic DNA and assess editing efficiency at the target locus, typically by T7 Endonuclease I assay or TIDE sequencing analysis.
- Cell Expansion and Quality Control: Expand the edited cells in culture under defined conditions. Prior to reinfusion, the final cell product must undergo rigorous quality control (QC) and release testing, which includes assessments of viability, sterility, potency, and purity, as well as more comprehensive genomic analyses to check for potential off-target edits [1].
- Reinfusion: The patient undergoes myeloablative conditioning (e.g., with busulfan) to create niche space in the bone marrow. The validated, edited HSPC product is then infused back into the patient [1].
A Representative Protocol for Systemic In Vivo Gene Editing (e.g., LNP Delivery)
This protocol is based on the approach used in clinical trials for targeting genes expressed in the liver, such as TTR [4].
- Cargo Selection and gRNA Design: For LNP delivery, the CRISPR machinery is typically encoded as mRNA. Produce in vitro transcribed (IVT) mRNA encoding the Cas9 protein (often a smaller ortholog like SaCas9 to fit packaging constraints) and a separate IVT mRNA for the gRNA targeting the gene of interest.
- LNP Formulation and Encapsulation: Formulate the Cas9 mRNA and gRNA mRNA into LNPs using a microfluidic device. This process involves mixing an aqueous phase containing the mRNA with an ethanol phase containing ionizable lipids, phospholipid, cholesterol, and PEG-lipid. The components rapidly mix, precipitating to form stable, mRNA-loaded LNPs. The surface properties of the LNPs can be modified (e.g., with SORT molecules) to influence their tropism [13].
- LNP Purification and Characterization: Purify the formulated LNPs via tangential flow filtration (TFF) to remove residual ethanol and non-encapsulated mRNA. Characterize the final LNP product for critical quality attributes, including particle size (e.g., via dynamic light scattering), polydispersity index (PDI), encapsulation efficiency, and concentration.
- In Vivo Administration and Biodistribution: Administer the LNP formulation to the subject via a single intravenous injection. LNPs typically accumulate predominantly in the liver due to absorption by hepatocytes. The dose is calculated based on the subject's body weight.
- Efficacy and Safety Assessment: After a predetermined period, collect blood and tissue samples to assess therapeutic efficacy. For example, in hATTR trials, blood serum is analyzed for a reduction in TTR protein levels. To assess safety, monitor subjects for adverse events, particularly infusion-related reactions, and measure standard clinical pathology markers. Tissue samples can be further analyzed using advanced sequencing methods (e.g., CAST-Seq, LAM-HTGTS) to detect any potential on-target structural variations or off-target chromosomal translocations [4] [7].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Kits for CRISPR-based Research
| Reagent / Kit | Function | Key Considerations |
|---|---|---|
| CRISPR Nuclease (e.g., WT SpCas9, HiFi Cas9) | The enzyme that performs the DNA cleavage. | High-fidelity variants (e.g., HiFi Cas9) are preferred to reduce off-target effects [7]. |
| Synthetic Guide RNA (sgRNA) | Directs the Cas nuclease to the specific genomic target. | Chemical modifications can enhance stability and reduce immunogenicity, especially for in vivo use. |
| Preassembled RNP Complex | Cas9 protein pre-complexed with gRNA. | The preferred cargo for many ex vivo applications due to rapid activity and reduced off-target effects [13]. |
| Lipid Nanoparticles (LNPs) | A delivery vehicle for in vivo mRNA or RNP delivery. | Liver-tropic LNPs are standard; SORT-LNPs enable targeting of other tissues (lung, spleen) [13]. |
| Adeno-Associated Virus (AAV) | A viral vector for in vivo or ex vivo delivery of CRISPR machinery. | Serotype determines tissue tropism; payload capacity is a major limitation for large Cas9 orthologs [13]. |
| Electroporation System/Kit | A physical method for delivering CRISPR cargo into cells ex vivo. | Optimization of cell type-specific electroporation parameters is critical for high efficiency and low toxicity. |
| HDR Donor Template | A DNA template (single or double-stranded) for precise gene insertion or correction. | Can be delivered as a single-stranded oligodeoxynucleotide (ssODN) for small edits or as a plasmid/donor AAV for larger insertions. |
| Off-Target Analysis Kit (e.g., CAST-Seq) | A method for genome-wide detection of structural variations and translocations induced by CRISPR editing. | Crucial for comprehensive safety assessment, as it can detect large deletions and rearrangements missed by amplicon sequencing [7]. |
Safety Considerations and Genomic Integrity
As CRISPR-based therapies advance clinically, a thorough understanding of potential safety risks is paramount. While early concerns focused primarily on off-target mutations (edits at unintended genomic sites with sequence similarity to the target), recent studies have revealed a potentially more significant challenge: on-target structural variations (SVs) [7].
These unintended on-target consequences can include:
- Large Deletions: Kilobase- to megabase-scale deletions originating from the on-target cut site [7].
- Chromosomal Rearrangements: Including translocations between homologous or heterologous chromosomes, which can occur when two DSBs are present simultaneously in the genome [7].
- Chromothripsis: A catastrophic event where a chromosome is shattered and then stitched back together incorrectly, a phenomenon linked to cancer [7].
A critical finding is that strategies used to enhance HDR efficiency, such as the use of DNA-PKcs inhibitors (e.g., AZD7648), can dramatically increase the frequency of these large SVs. Furthermore, traditional short-read amplicon sequencing, a common method for assessing editing outcomes, often fails to detect these large deletions if they remove the primer binding sites, leading to an overestimation of HDR efficiency and an underestimation of genotoxic risk [7]. Therefore, comprehensive safety assessment for therapeutic genome editing must now incorporate specialized, genome-wide methods like CAST-Seq or LAM-HTGTS to accurately profile the full spectrum of editing outcomes [7].
The journey of therapeutic gene editing from ZFNs and TALENs to CRISPR-Cas9 systems represents a remarkable convergence of basic biological discovery and transformative technological application. The unique advantages of the CRISPR-Cas9 platform—particularly its simplicity, programmability, and versatility—have accelerated both basic research and the development of a new class of medicines, as evidenced by the approved ex vivo therapy Casgevy and the promising in vivo candidates in clinical trials.
The central strategic dichotomy of ex vivo versus in vivo delivery defines the current landscape of CRISPR therapeutics, each with distinct advantages and hurdles. The primary challenge for ex vivo therapies lies in scaling complex and costly manufacturing processes. For in vivo therapies, the defining challenge remains the development of safe, efficient, and tissue-specific delivery vectors. Looking forward, the field must address the emerging safety concerns regarding on-target structural variations with robust analytical methods. Continued innovation in delivery technologies, high-fidelity editors, and comprehensive safety profiling will be critical to fully realizing the potential of these powerful platforms, ultimately enabling therapies for a broader range of genetic diseases.
The advent of CRISPR-Cas9 technology marked a revolutionary leap in our ability to modify genomes, yet its reliance on double-strand breaks (DSBs) introduced significant limitations including unintended insertions/deletions (indels) and chromosomal rearrangements [14]. The emergence of base editing and prime editing represents a paradigm shift toward precision genome editing, enabling targeted nucleotide changes without requiring DSBs. These technologies are particularly crucial for therapeutic applications where precision and safety are paramount, and they offer distinct advantages and considerations within both in vivo and ex vivo therapeutic frameworks [15]. This evolution from cutting to rewriting the genetic code expands the potential for treating a vast array of genetic disorders caused by point mutations, which constitute a significant portion of known human genetic diseases [16].
Technical Foundations of Precision Editing
Base Editing Mechanics
Base editors are sophisticated molecular machines that combine a catalytically impaired Cas protein with a single-strand DNA-modifying enzyme [16]. They operate through a precise mechanism that avoids double-strand DNA breaks, significantly reducing unintended mutations compared to traditional CRISPR-Cas9 editing [17].
Core Components:
- Catalytically Impaired Cas Protein: Uses either dead Cas9 (dCas9, completely inactive) or nickase Cas9 (nCas9, cuts only one DNA strand) as a DNA-targeting module [16].
- Deaminase Enzyme: Chemically modifies specific DNA bases within a defined "editing window" [16].
- Guide RNA (gRNA): Directs the complex to the target genomic locus [16].
The base editing process can be visualized as follows, showing how these components work together to achieve precise DNA modification:
Figure 1: Base Editor Architecture and Mechanism. The base editor complex uses a guide RNA to position itself at the target DNA site, where the deaminase enzyme performs a chemical conversion of a specific nucleotide.
Prime Editing Architecture
Prime editing represents a more recent advancement that further expands editing capabilities beyond what base editors can achieve. This "search-and-replace" technology can install virtually any point mutation, small insertion, or deletion without requiring donor DNA templates or causing double-strand breaks [18].
Prime Editor Components:
- Cas9 Nickase (nCas9): A Cas9 variant that cuts only one DNA strand, fused to a reverse transcriptase enzyme [18] [19].
- Reverse Transcriptase (RT): An enzyme that synthesizes DNA using an RNA template, typically derived from Moloney Murine Leukemia Virus (M-MLV) [18] [19].
- Prime Editing Guide RNA (pegRNA): A specially engineered guide RNA that both specifies the target site and encodes the desired edit [18].
The prime editing process involves multiple coordinated steps, as illustrated in the following workflow:
Figure 2: Prime Editing Workflow. The prime editor uses a pegRNA to target the DNA, nick one strand, and template reverse transcription to copy edited sequence information into the genome.
Comparative Analysis of Editing Technologies
The selection of appropriate genome editing technology depends on the specific application requirements, target sequence constraints, and desired outcomes. The table below provides a comprehensive comparison of the key characteristics of base editing versus prime editing:
Table 1: Technical Comparison of Base Editing and Prime Editing Platforms
| Feature | Base Editing | Prime Editing |
|---|---|---|
| DNA Break Mechanism | No DSBs; single-strand nicking possible with nCas9 [16] | No DSBs; uses targeted nicking [18] |
| Editing Efficiency | High (can exceed 50% in optimized systems) [19] | Variable (typically 20-50%, optimized systems higher) [19] |
| Editing Window | Narrow (typically 4-5 nucleotides within protospacer) [16] | Flexible (PAM-to-edit distance can be >30 bp) [19] |
| Indel Formation | Low (with proper design) [17] | Very low (1-10% with PE2, reduced with PE3b) [18] |
| Theoretical Target Coverage | Corrects ~25% of known pathogenic SNPs [14] | Could correct up to 89% of known genetic variants [14] |
| PAM Constraints | Dependent on Cas variant [14] | Less constrained; edits possible far from PAM [19] |
| Bystander Editing | Possible within editing window [19] | Minimal; highly specific to target base [19] |
| Delivery Challenges | Moderate (BE size ~5.2 kb for ABE8e) | Significant (PE size ~6.3 kb for PEmax) |
Editing Scope and Versatility: While base editors can perform four transition mutations (C→T, T→C, A→G, and G→A), prime editors can accomplish all 12 possible base-to-base conversions, plus targeted insertions and deletions [14] [19]. This significantly expands the therapeutic applications of prime editing, though often at the cost of lower efficiency compared to base editing for simple transitions.
Byproduct Profiles: Base editors can produce bystander edits when multiple targetable bases fall within the editing window, which can be advantageous for some applications but problematic for others requiring single-base precision [19]. Prime editors demonstrate exceptional precision with minimal bystander activity, making them preferable for applications requiring exact single-base changes [18].
Therapeutic Applications in In Vivo and Ex Vivo Contexts
The therapeutic implementation of base editing and prime editing follows two primary paradigms: in vivo editing, where modifications occur directly within the patient's body, and ex vivo editing, where cells are modified outside the body before transplantation back into the patient.
In Vivo Therapeutic Approaches
In vivo delivery represents the most direct approach for therapeutic genome editing, particularly for tissues that are difficult to extract and transplant. Recent advances have demonstrated the remarkable potential of this approach:
Table 2: In Vivo Precision Editing Clinical Applications
| Therapeutic Area | Target Gene | Technology | Delivery Method | Clinical Status |
|---|---|---|---|---|
| Hereditary Transthyretin Amyloidosis (hATTR) | TTR | CRISPR-Cas9 LNP (Knockout) | LNP Intravenous [4] | Phase 3 (Trials paused due to toxicity) [20] |
| Hereditary Angioedema (HAE) | Kallikrein | CRISPR-Cas9 LNP (Knockout) | LNP Intravenous [4] | Phase 1/2 (86% protein reduction) [4] |
| Dyslipidemia/CVD | ANGPTL3 | CRISPR-Cas9 LNP (Knockout) | LNP Intravenous [21] | Phase 1 (73% protein reduction, 55% triglyceride reduction) [21] |
| Familial Hypercholesterolemia | PCSK9 | Base Editing (VERVE-101) | LNP [17] | Phase 1 (First in vivo base editing trial) [17] |
| Personalized Rare Disease | CPS1 | Bespoke CRISPR | LNP Intravenous [4] | Proof-of-concept (Infant treated) |
The landmark case of an infant with CPS1 deficiency treated with a personalized in vivo CRISPR therapy demonstrates the potential for rapid development of customized editing therapies, with the entire process—from development to delivery—completed in just six months [4]. This case also established the feasibility of redosing with LNP-del editors, as the patient safely received three doses with improved symptoms after each administration [4].
Ex Vivo Therapeutic Approaches
Ex vivo editing involves modifying patient-derived cells in controlled laboratory conditions before reinfusion, offering advantages in editing efficiency, safety validation, and quality control:
- CAR-T Cell Engineering: Base editing has been successfully employed to create allogeneic CAR-T cells by knocking out genes that cause host-versus-graft reactions. In a groundbreaking application, base editing was used to make four single-nucleotide changes to create a CAR-T cell therapy for a child with treatment-resistant leukemia [17].
- Hematopoietic Stem Cell (HSC) Therapies: In sickle cell disease models, base editing of hematopoietic stem cells has demonstrated higher editing efficiency and reduced genotoxicity concerns compared to traditional CRISPR-Cas9 approaches [20].
- Epidermolysis Bullosa: Prime editing has achieved up to 60% efficiency in correcting pathogenic COL17A1 variants in patient keratinocytes, with corrected cells showing a selective advantage in xenograft models [20].
Experimental Protocols and Methodologies
Base Editing Experimental Workflow
Step 1: Target Selection and gRNA Design
- Identify the target nucleotide within the genomic context
- Ensure the target base falls within the editing window (typically positions 4-8 in the protospacer for SpCas9-based editors) [16]
- Design gRNAs with optimal on-target efficiency and minimal off-target potential using computational tools
- Verify PAM availability for the chosen Cas variant
Step 2: Base Editor Selection
- Choose appropriate base editor: CBE for C•G to T•A conversions or ABE for A•T to G•C conversions [16]
- Select Cas variant based on PAM requirements and delivery constraints (SpCas9, SaCas9, or compact variants for AAV delivery) [14]
Step 3: Delivery Method Optimization
- For in vivo applications: Formulate LNPs with optimized lipid compositions for target tissue tropism [4] [21]
- For ex vivo applications: Use electroporation or nucleofection for RNP or mRNA delivery
- For viral delivery: Package split-intein systems or use compact editors to overcome AAV size limitations [14]
Step 4: Validation and Analysis
- Sequence target locus to assess editing efficiency and precision
- Screen for potential off-target edits using specialized methods (e.g., GUIDE-seq, CIRCLE-seq)
- Evaluate functional outcomes through protein analysis and phenotypic assays
Prime Editing Experimental Workflow
Step 1: pegRNA Design
- Design the spacer sequence (20 nt) to target the desired genomic locus
- Optimize the primer binding site (PBS) length (typically 8-15 nt)
- Define the reverse transcriptase template (RTT) to encode the desired edit
- Consider using engineered pegRNAs (epegRNAs) with RNA pseudoknots to enhance stability [19]
Step 2: Prime Editor Selection
- Choose appropriate PE system based on application: PE2 for basic editing, PE3 for enhanced efficiency with additional nicking sgRNA, or PE4/PE5 with MMR suppression [19]
- Consider specialized PE6 variants for specific edit types or delivery constraints [19]
Step 3: Delivery Optimization
- For in vivo delivery: Utilize dual AAV systems or non-viral methods (LNP-mRNA) to overcome packaging limitations [18]
- For ex vivo delivery: Employ plasmid, mRNA, or RNP delivery methods
- Co-deliver MMR-suppressing components (e.g., dominant-negative MLH1) when using PE4/5 systems [19]
Step 4: Analysis and Validation
- Quantify editing efficiency and purity using next-generation sequencing
- Assess indel formation rates at target sites
- Evaluate heteroduplex resolution and editing outcomes
Research Reagent Solutions
Successful implementation of precision editing requires carefully selected reagents and tools. The following table outlines essential components for base editing and prime editing research:
Table 3: Essential Research Reagents for Precision Editing
| Reagent Category | Specific Examples | Function | Considerations |
|---|---|---|---|
| Base Editors | BE4, ABE8e, AccuBase CBE [16] | Catalyze specific base conversions | Choose based on target mutation; consider size constraints for delivery |
| Prime Editors | PE2, PEmax, PE6 variants [19] | Enable search-and-replace editing | PE3/PE5 require additional sgRNA; PE4/PE5 need MMR suppression |
| Cas Variants | SpCas9, SaCas9, Cas12f [14] [20] | DNA targeting with PAM specificity | Smaller variants (SaCas9, Cas12f) enable AAV packaging |
| Delivery Systems | LNPs [4] [21], AAV [14], Electroporation | Deliver editing components to cells | LNP preferred for in vivo liver delivery; AAV for other tissues |
| Guide RNAs | Custom gRNAs, pegRNAs, epegRNAs [19] | Target specificity and edit encoding | epegRNAs show enhanced stability and efficiency |
| Validation Tools | NGS assays, DISCOVER-Seq [20] | Assess on-target efficiency and off-target effects | Essential for therapeutic development |
Current Challenges and Future Directions
Despite remarkable progress, several challenges remain in the widespread clinical implementation of base editing and prime editing technologies:
Delivery Limitations: The relatively large size of editing enzymes presents significant packaging challenges for viral delivery vectors [18]. Creative solutions such as split-intEin systems [18] and the development of compact editors like Cas12f-based systems [20] are actively being pursued to overcome these limitations.
Efficiency Optimization: Particularly for prime editing, efficiency can vary significantly based on genomic context, cell type, and the specific edit being made [19]. Ongoing engineering efforts focus on improving nuclear localization, codon optimization, and adding DNA-binding domains to enhance editing efficiency [18].
Safety Considerations: While precision editors significantly reduce off-target effects compared to traditional CRISPR-Cas9, comprehensive profiling remains essential. New detection methods like AutoDISCO enable clinically feasible off-target detection with minimal patient tissue [20].
The future of precision editing will likely see increased personalization of therapies, expanded in vivo applications beyond the liver, and integration with artificial intelligence for improved guide RNA design and outcome prediction [20]. As these technologies mature, they will continue to blur the line between genetic therapy and genetic cure, offering new hope for patients with previously untreatable genetic disorders.
The advent of CRISPR-Cas9 technology has revolutionized the field of genetic engineering, offering unprecedented precision in modifying DNA sequences within living organisms [22]. As this powerful technology transitions from basic research to clinical applications, two distinct methodological paradigms have emerged: in vivo and ex vivo gene editing. The fundamental distinction lies in the location where genetic modification occurs. In vivo editing involves delivering CRISPR components directly into the patient's body to edit cells inside their natural biological environment [1] [23]. In contrast, ex vivo editing entails extracting cells from the patient, genetically modifying them in a controlled laboratory setting, and then reinfusing the edited cells back into the patient [1]. Understanding the core principles, technical requirements, and applications of each approach is essential for researchers and drug development professionals working to advance CRISPR-based therapies. This whitepaper delineates these paradigms within the broader context of therapeutic development, providing a technical framework for selecting appropriate strategies based on therapeutic goals, target tissues, and clinical constraints.
Conceptual Foundations and Key Distinctions
The conceptual divide between in vivo and ex vivo CRISPR therapies originates from fundamental differences in biological context, delivery logistics, and manufacturing complexity. Both approaches utilize the same core CRISPR mechanism—where a guide RNA (gRNA) directs the Cas9 nuclease to a specific DNA sequence, inducing a double-strand break (DSB) that is subsequently repaired by cellular machinery via either Non-Homologous End Joining (NHEJ) or Homology-Directed Repair (HDR) [24] [22]. However, their operational frameworks differ significantly.
In vivo gene editing requires sophisticated delivery vehicles to transport CRISPR components (typically as DNA, mRNA, or Ribonucleoprotein complexes) through the body to the target organ [13]. This approach must overcome numerous biological barriers, including immune system recognition, cellular uptake, and endosomal escape, to achieve efficient editing in the correct cell type [24]. Successful applications often leverage natural tropisms of delivery vectors, such as the propensity of Lipid Nanoparticles (LNPs) to accumulate in the liver [23] [4]. The process is administered systemically (e.g., via intravenous infusion) or locally (e.g., via subretinal injection) and is typically a one-time intervention [23] [25].
Ex vivo gene editing offers greater control over the editing process. Cells of interest (e.g., hematopoietic stem cells or T-cells) are harvested from the patient and cultured in a Good Manufacturing Practice (GMP) facility. CRISPR components are then introduced into these cells, often using physical methods like electroporation [24]. This controlled environment allows for precise optimization of editing efficiency, thorough quality control checks, and even selection of successfully modified cells before they are expanded and reinfused into the patient [1]. This paradigm transforms the therapy into an autologous cell transplant, often requiring patients to undergo conditioning chemotherapy (e.g., bone marrow ablation) to make room for the new, edited cells [1].
Table 1: Core Conceptual Distinctions Between In Vivo and Ex Vivo CRISPR Therapies
| Parameter | In Vivo Approach | Ex Vivo Approach |
|---|---|---|
| Site of Editing | Inside the patient's body [1] | Outside the body, in a laboratory setting [1] |
| Biological Context | Complex, systemic environment with biological barriers [24] | Controlled, sterile cell culture system [1] |
| Typical Delivery Vehicles | Viral vectors (AAV), Lipid Nanoparticles (LNPs) [24] [23] | Electroporation, viral vectors (Lentivirus) [24] |
| Manufacturing & Logistics | Single-dose administration; complex vector manufacturing [23] | Multi-step process involving cell harvest, culture, editing, and reinfusion [1] |
| Level of Control | Lower control over editing efficiency and specificity in the target tissue [24] | High control over editing conditions and ability for pre-infusion quality control [1] |
| Patient Conditioning | Generally not required | Often requires conditioning (e.g., chemotherapy) [1] |
Methodological Approaches and Workflows
The experimental and therapeutic workflows for in vivo and ex vivo CRISPR therapies involve distinct protocols, equipment, and validation steps. The following diagrams and detailed methodologies outline the standard operating procedures for each paradigm.
In Vivo CRISPR Therapy Workflow
The in vivo workflow centers on the design, production, and systemic delivery of CRISPR-cargo vectors. Key considerations include the selection of the appropriate Cas nuclease and gRNA, the choice of delivery vehicle based on the target tissue, and the route of administration.
Detailed Protocol for LNP-Mediated In Vivo Liver Editing
This protocol is based on methods used in clinical trials for targeting genes like ANGPTL3 and TTR in the liver [23] [4].
- CRISPR Component Preparation: Formulate a cocktail containing mRNA encoding the Cas9 protein (e.g., SpyCas9) and a synthetic single-guide RNA (sgRNA) targeting the gene of interest. The sgRNA sequence must be designed to minimize off-target effects using specialized bioinformatics tools [24] [13].
- LNP Formulation: Encapsulate the CRISPR mRNA and sgRNA into ionizable lipid nanoparticles using a microfluidic mixer. The LNP composition should be optimized for stability, endosomal escape, and hepatocyte tropism. The final product must be sterile-filtered and undergo quality control for particle size, encapsulation efficiency, and endotoxin levels [23] [13].
- In Vivo Administration and Validation:
- Systemic Delivery: Administer the LNP formulation to the patient via a single intravenous infusion. The typical dose is calculated based on mRNA mass per kilogram of body weight [4].
- Efficacy Assessment: After a predetermined period (e.g., 4-8 weeks), collect blood samples to quantify the reduction of the target protein (e.g., TTR for hATTR amyloidosis) using ELISA or mass spectrometry. A successful edit is indicated by a significant and sustained reduction (>80%) in protein levels [4].
- Safety Monitoring: Use next-generation sequencing (NGS)-based methods, such as CAST-Seq or LAM-HTGTS, on biopsies of the target tissue (e.g., liver) to detect potential large-scale structural variations (e.g., chromosomal translocations, megabase-scale deletions) at the on-target site and known off-target sites [7].
Ex Vivo CRISPR Therapy Workflow
The ex vivo workflow is a multi-stage process that focuses on the efficient and precise genetic modification of patient-derived cells outside the body, followed by the reinfusion of those edited cells.
Detailed Protocol for Ex Vivo Hematopoietic Stem Cell (HSC) Editing
This protocol is modeled on the manufacturing process for Casgevy (exa-cel), the first approved CRISPR therapy for sickle cell disease and beta-thalassemia [1].
- Cell Collection and Isolation:
- Collect hematopoietic stem and progenitor cells (HSPCs) from the patient via apheresis.
- Isate CD34+ HSPCs from the apheresis product using immunomagnetic beads. Confirm cell viability and purity using flow cytometry [1].
- CRISPR Transfection:
- Resuspend the CD34+ cells in an electroporation buffer.
- Combine the cells with a pre-complexed Ribonucleoprotein (RNP) complex comprising a high-fidelity Cas9 protein and a synthesized sgRNA targeting the BCL11A erythroid enhancer.
- Electroporate the cell-RNP mixture using a clinical-grade electroporator (e.g., Lonza 4D-Nucleofector) with an optimized electrical pulse program for HSCs [1] [13].
- Post-Transfection Processing and Quality Control:
- Immediately after electroporation, transfer the cells into pre-warmed culture media supplemented with cytokines (SCF, TPO, FLT3-L) to support cell survival and maintenance.
- Culture the cells for a short period (typically 48 hours) to allow for gene editing to occur.
- Quality Control Assays: Harvest a sample of cells for critical quality control tests.
- On-target Efficiency: Use next-generation sequencing (NGS) of PCR amplicons spanning the BCL11A target site to quantify the percentage of alleles with the intended deletion.
- Karyotyping/Structural Variation Analysis: Perform assays to rule out large, unintended chromosomal abnormalities at the target locus [7].
- Reinfusion and Engraftment:
- The final edited cell product is washed, formulated for infusion, and cryopreserved.
- The patient undergoes myeloablative conditioning (e.g., with busulfan) to clear the bone marrow niche.
- The thawed, edited CD34+ cells are infused back into the patient. Successful engraftment is monitored by tracking neutrophil and platelet recovery, followed by measurement of fetal hemoglobin (HbF) levels, which indicate therapeutic efficacy [1].
Clinical Applications and Trial Data
The distinct advantages of each paradigm have steered them toward different therapeutic areas. Ex vivo approaches have seen the first regulatory approvals, while in vivo therapies are rapidly advancing through clinical trials for a range of conditions.
Table 2: Key Clinical Applications and Representative Trials of CRISPR Therapies
| Therapeutic Area | In Vivo Approach | Ex Vivo Approach |
|---|---|---|
| Hematologic Disorders | Sickle Cell Disease/ Beta-Thalassemia (Casgevy)• Target: BCL11A enhancer• Intervention: Edit patient HSCs to reactivate fetal hemoglobin [1]. | |
| Genetic Metabolic Diseases | Hereditary ATTR Amyloidosis• Target: TTR gene in hepatocytes• Intervention: LNP delivery to knock out TTR, reducing pathogenic protein by ~90% [4]. | |
| Ophthalmic Diseases | Leber Congenital Amaurosis (LCA10)• Target: CEP290 IVS26 mutation• Intervention: Subretinal AAV5 delivery of CRISPR to restore splicing (EDIT-101 trial) [25]. | |
| Infectious Disease / Oncology | CRISPR-Enhanced Phage Therapy• Target: Bacterial genome in chronic infections• Intervention: Phages engineered with CRISPR-Cas to selectively eliminate antibiotic-resistant bacteria [4]. | CAR T-Cell Immunotherapy• Target: Endogenous T-cell receptors• Intervention: Edit patient T-cells to generate potent CAR-T cells for cancer treatment [1]. |
| Cardiovascular Risk Reduction | Elevated Lp(a) and ANGPTL3• Target: LPA or ANGPTL3 genes in liver• Intervention: LNP-based knockout to permanently reduce key cholesterol and triglyceride regulators [23]. |
Technical Challenges and Safety Considerations
Each paradigm presents a unique set of technical hurdles and potential safety concerns that must be addressed during therapeutic development.
In Vivo Challenges
- Delivery Efficiency and Specificity: The primary challenge is achieving efficient delivery of CRISPR components to the desired organ and cell type while avoiding off-target tissues. Vectors like AAV and LNP have inherent tropisms (e.g., LNPs for the liver), making it difficult to target other organs effectively [24] [23].
- Immune Responses: The patient's immune system may recognize and mount a response against the bacterial-derived Cas9 protein or the viral capsid (in AAV delivery), potentially reducing efficacy and causing adverse effects. Pre-existing immunity in patients is a significant concern [24] [25].
- Cargo Size Limitations: Adeno-associated viruses (AAVs), a common delivery vector, have a strict packaging limit of ~4.7 kb. This is too small for the widely used SpCas9 nuclease (~4.2 kb) plus its gRNA and regulatory elements. Solutions include using smaller Cas orthologs (e.g., SaCas9, CjCas9) or splitting the system across two AAVs [24] [25].
- Persistent Nuclease Activity: Long-term expression of Cas9 from viral vectors can increase the risk of off-target edits. Using transient delivery methods like LNP-mRNA can mitigate this risk [13].
Ex Vivo Challenges
- Manufacturing Complexity: The process is logistically complex, expensive, and time-sensitive. It requires specialized GMP facilities and can take weeks from cell collection to reinfusion, which may not be feasible for all patients [1].
- Cell Viability and Function: The processes of cell extraction, manipulation in vitro (especially electroporation), and expansion can stress cells, reducing viability and potentially impairing their long-term functional capacity, such as the engraftment potential of HSCs [1] [26].
- Genomic Instability in Cultured Cells: The use of CRISPR in rapidly dividing cells ex vivo can lead to mosaicism (where only a subset of cells is edited) and large-scale structural variations (SVs), including chromosomal translocations and megabase-scale deletions, which pose significant safety risks [26] [7].
The Scientist's Toolkit: Essential Research Reagents
The following table details key reagents and materials critical for conducting research in both in vivo and ex vivo CRISPR therapy development.
Table 3: Essential Research Reagents for CRISPR Therapy Development
| Reagent / Material | Function | Application Notes |
|---|---|---|
| High-Fidelity Cas9 Nuclease | Engineered Cas9 variant with reduced off-target activity while maintaining high on-target efficiency (e.g., HiFi Cas9) [7]. | Critical for both paradigms to minimize genotoxic risk. Available as protein for RNP formation (ex vivo) or encoded in DNA/mRNA (in vivo). |
| Ionizable Lipid Nanoparticles (LNPs) | Synthetic nanoparticles that encapsulate and deliver CRISPR mRNA and sgRNA; particularly effective for liver-targeted in vivo delivery [23] [13]. | The ionizable lipid component enables endosomal escape. Commercially available from several specialty chemical and biotech suppliers. |
| Adeno-Associated Virus (AAV) Vectors | Viral vectors for in vivo delivery of CRISPR machinery. Offer long-term expression and broad tissue tropism depending on serotype (e.g., AAV5 for retina, AAV9 for CNS) [25]. | Packaging capacity is a major limitation. Requires use of compact Cas enzymes or dual-vector systems. |
| Clinical-Grade Electroporator | Instrument for delivering electrical pulses to transiently open pores in cell membranes, allowing for RNP or nucleic acid entry (e.g., Lonza 4D-Nucleofector) [24] [13]. | Essential for ex vivo editing of hard-to-transfect primary cells like HSCs and T-cells. Optimization of buffer and pulse code is required for each cell type. |
| Next-Generation Sequencing (NGS) Assays for SVs | Specialized NGS-based assays (e.g., CAST-Seq, LAM-HTGTS) to detect large, unintended on-target and off-target structural variations post-editing [7]. | A crucial safety QC tool, especially for ex vivo therapies and for assessing the genotoxic impact of new in vivo delivery methods. |
The choice between in vivo and ex vivo CRISPR therapy paradigms is foundational to therapeutic design, dictated by the target disease, biological constraints, and practical considerations. The ex vivo approach offers superior control over the editing process and has paved the way with the first approved therapies, proving indispensable for conditions requiring the modification of cells that can be manipulated outside the body. Conversely, the in vivo approach represents the frontier of therapeutic simplicity and potential scalability, aiming to transform complex genetic disorders into manageable conditions with a single treatment. Its success is intrinsically tied to advancements in delivery technologies, such as LNPs and novel AAV vectors. Both pathways must continuously address the dual challenges of efficiency and safety, particularly concerning unanticipated genomic alterations. Future progress will hinge on interdisciplinary innovations—including the development of more precise nucleases, smarter delivery vectors, and more sensitive safety assays—to fully realize the promise of CRISPR-based gene therapy across the spectrum of human disease.
Delivery Systems and Clinical Applications: From Bench to Bedside
Ex vivo gene therapy represents a foundational approach in the rapidly advancing field of CRISPR-Cas9-based therapeutics. This methodology involves the extraction of specific cells from a patient, their genetic modification outside the body (ex vivo), and the subsequent reinfusion of the edited cells back into the patient [1]. In the broader context of comparing in vivo versus ex vivo delivery approaches, the ex vivo strategy offers distinct advantages, including precise control over the editing process and the ability to conduct comprehensive quality control checks on the modified cells before reinfusion, thereby enhancing safety profiles [1]. Furthermore, it avoids the complex delivery challenges associated with targeting specific tissues inside the body.
The ex vivo approach is particularly well-suited for editing hematopoietic stem cells (HSCs) and immune cells such as T cells, which can be conveniently harvested from blood or bone marrow, manipulated in controlled laboratory settings, and then returned to the patient to engraft and produce the desired therapeutic effect [1] [27]. The first-ever approved CRISPR-based therapy, Casgevy (exagamglogene autotemcel or exa-cel) for sickle cell disease and transfusion-dependent beta thalassemia, successfully utilized this ex vivo paradigm, establishing a robust clinical proof-of-concept [4] [1].
Ex Vivo versus In Vivo Therapeutic Approaches
The choice between ex vivo and in vivo gene editing strategies is fundamental to therapeutic design, hinging on the biological context of the target disease, the nature of the target cells, and the specific clinical objectives. The table below summarizes the core characteristics of each approach.
Table 1: Comparison of Ex Vivo and In Vivo CRISPR-Cas9 Therapeutic Approaches
| Feature | Ex Vivo Approach | In Vivo Approach |
|---|---|---|
| Process | Cells are extracted, edited outside the body, and reinfused [1]. | Gene-editing components are delivered directly into the patient's body [1]. |
| Key Advantage | High control over editing; enables complex manipulations like CAR-T generation; lower risk of immune reaction to editing tools [1] [27]. | Applicable to tissues that cannot be easily removed (e.g., liver, brain, muscle); less complex manufacturing logistics [25] [23]. |
| Delivery System | Often uses electroporation or viral vectors (e.g., lentivirus) in the lab [27]. | Relies on viral vectors (e.g., rAAV) or non-viral nanoparticles (e.g., LNPs) for in vivo delivery [25] [23]. |
| Therapeutic Examples | Casgevy (for SCD/TDT), CAR-T cell therapies for cancer [4] [1] [27]. | NTLA-2001 (for hATTR), VERVE-101/102 (for cardiovascular disease) [4] [28]. |
| Primary Challenge | Complex, costly manufacturing; requires myeloablation for stem cell engraftment [1]. | Delivery efficiency to target tissues; potential for immune responses to delivery vectors or Cas protein [25] [12]. |
The following workflow diagram illustrates the fundamental steps of the ex vivo gene editing process, from cell extraction to patient reinfusion.
Detailed Ex Vivo Protocol for Hematopoietic Stem and Progenitor Cells (HSPCs)
This protocol provides a detailed technical guide for the genetic modification of human HSPCs using CRISPR-Cas9, incorporating key optimizations to preserve the long-term functionality of these critical stem cells [29].
Stage 1: Cell Harvesting and Initial Culture
- Cell Source: Obtain HSPCs via leukapheresis from a mobilized donor or via direct bone marrow harvest. The target cell population is CD34+ HSPCs [29].
- Thawing and Washing: Rapidly thaw cryopresened vials of CD34+ HSPCs in a 37°C water bath. Immediately transfer the cell suspension to a pre-warmed medium containing DNase (e.g., 50 µg/mL). Centrifuge and carefully remove the supernatant [29].
- Initial Culture: Resuspend the washed HSPCs in a pre-optimized serum-free culture medium. Supplement the medium with a specific combination of cytokines essential for HSPC viability and initial activation, typically including SCF, TPO, and FLT3-L. The initial cell density should be maintained at approximately 1-2 x 10^6 cells/mL [29].
Stage 2: Pre-Conditioning and Gene Editing
- Pre-Conditioning for Editing: To enhance gene editing efficiency while preserving stemness, integrate a p38 inhibitor (e.g., 1-5 µM) into the culture medium. This step is critical for reducing detrimental stress responses in HSPCs triggered by ex vivo manipulation, thereby safeguarding their long-term repopulating capacity [29].
- CRISPR Complex Delivery: For CRISPR-Cas9 delivery, the ribonucleoprotein (RNP) electroporation method is preferred. This involves pre-complexing the purified Cas9 protein with synthetic guide RNA (sgRNA) to form the RNP complex. This complex is then delivered into the pre-conditioned HSPCs using a specialized electroporation system (e.g., Neon or Lonza 4D-Nucleofector) [29].
- Editing for Knockout vs. Knock-in:
- Gene Knockout: To disrupt a gene, the non-homologous end joining (NHEJ) repair pathway is harnessed following the Cas9-induced double-strand break. This requires only the delivery of the RNP complex [1].
- Gene Knock-in: For precise insertion of a therapeutic transgene, the homology-directed repair (HDR) pathway must be engaged. This necessitates the co-delivery of the RNP complex along with a donor DNA template containing the desired sequence flanked by homologous arms during the electroporation step. HDR is inherently less efficient than NHEJ and occurs only in specific cell cycle stages, making this a more challenging process to optimize [1].
Stage 3: Post-Editing Processing and Reinfusion
- Post-Editing Recovery and Expansion: Immediately after electroporation, transfer the cells into a recovery medium, again supplemented with cytokines and the p38 inhibitor. Continue the culture for a defined period (e.g., 48 hours) to allow for cell recovery and the expression of the edited gene product [29].
- Quality Control (QC) Testing: Before reinfusion, perform critical QC assays on an aliquot of the final product. These must include:
- Cell Viability and Count: Assessed using trypan blue exclusion or flow cytometry.
- Editing Efficiency: Quantified using next-generation sequencing (NGS) or digital PCR to determine the percentage of alleles with the intended modification.
- Sterility Tests: Conduct rapid microbiological tests to ensure the product is free from bacterial and fungal contamination [29].
- Patient Conditioning and Reinfusion: The patient must undergo a myeloablative conditioning regimen, typically with busulfan, to create space in the bone marrow for the incoming edited cells. Once conditioned, the final formulated cell product is administered to the patient via intravenous infusion, analogous to a blood transfusion [1].
Key Research Reagents and Solutions
Successful execution of an ex vivo editing protocol relies on a suite of specialized reagents and tools. The table below details essential components for an HSPC editing workflow.
Table 2: Essential Research Reagent Solutions for Ex Vivo HSPC Editing
| Reagent/Solution | Function | Technical Notes |
|---|---|---|
| CD34+ Cell Isolation Kit | Immunomagnetic positive selection of target HSPCs from a heterogeneous cell source. | Critical for obtaining a pure starting population. Kits from Miltenyi Biotec or Stemcell Technologies are commonly used. |
| Serum-Free Medium (e.g., StemSpan) | Provides a defined, xeno-free environment for HSPC culture and expansion. | Supplements with cytokines (SCF, TPO, FLT3-L) are essential for cell survival and proliferation [29]. |
| p38 MAPK Inhibitor | A small molecule added to culture medium to reduce cellular stress and improve the long-term engraftment potential of edited HSPCs. | A key protocol optimization to prevent "culture shock" and preserve stemness [29]. |
| CRISPR-Cas9 RNP Complex | The active gene-editing machinery. Comprises purified Cas9 protein complexed with synthetic guide RNA (sgRNA). | RNP delivery is favored for its rapid activity and reduced off-target effects compared to plasmid DNA. |
| Donor DNA Template | A single-stranded or double-stranded DNA molecule containing the therapeutic gene flanked by homology arms. | Used for HDR-mediated knock-in. Can be a single-stranded oligodeoxynucleotide (ssODN) or an AAV6 vector [1]. |
| Electroporation System | A device that uses a controlled electrical pulse to create transient pores in the cell membrane, allowing the RNP complex to enter the cell. | The Neon Transfection System (Thermo Fisher) and the 4D-Nucleofector (Lonza) are standard platforms. |
Analysis of Current Clinical and Technological Trends
The ex vivo therapy landscape is dominated by applications in oncology and rare genetic diseases, driven by clear biological rationales and maturing manufacturing processes.
- Therapeutic Dominance: An analysis of 1,491 ex vivo gene therapy products revealed that neoplasms (cancers) are the target for 79.78% of therapies, with T cells being the primary cell type (75.26%) [27]. The most common genetic modification in these T cells is the chimeric antigen receptor (CAR), present in 83.19% of products, highlighting the massive impact of CRISPR-engineered CAR-T cell therapies [27].
- Editing Platform Evolution: While lentiviral vectors remain the dominant platform (40.12%) for delivering genetic cargos in ex vivo settings, CRISPR-based modifications are rapidly expanding and now account for 25.66% of products, reflecting a strong shift towards more precise and versatile gene editing tools [27].
- Clinical Momentum: The field's maturity is underscored by the fact that 22 ex vivo products have advanced to pre-registration or registration phases, indicating a pipeline of viable treatments nearing clinical approval and commercialization [27].
Ex vivo CRISPR-Cas9 therapy represents a powerful and clinically validated modality for treating a range of human diseases. Its core strength lies in the controlled and precise engineering of patient-derived cells, such as HSPCs and T lymphocytes, which can be rigorously validated before being returned to the patient to exert a durable therapeutic effect. While the methodology demands a complex and costly logistical chain, its successful implementation in therapies like Casgevy and numerous CAR-T products has irrevocably established its value.
Future progress in this field will be driven by continued optimization of protocols to enhance the engraftment potential of edited stem cells, the development of more efficient and safer knock-in strategies for large transgenes, and the scaling of manufacturing processes to improve accessibility. As the technology matures, ex vivo gene editing is poised to move beyond rare diseases and oncology, potentially offering one-time curative treatments for a broader spectrum of common genetic disorders.
The therapeutic application of CRISPR-Cas9 gene editing represents a paradigm shift in modern medicine, offering potential cures for genetic disorders that were previously considered untreatable. The efficacy of this technology hinges entirely on one critical factor: the efficient delivery of CRISPR components into the nucleus of target cells in vivo [30] [12]. While ex vivo approaches, exemplified by Casgevy for sickle cell disease and β-thalassemia, involve editing cells outside the body before reinfusion, in vivo delivery presents substantially greater challenges [1] [4]. It requires navigation of complex biological barriers, avoidance of immune surveillance, and achieving precise tissue targeting—all while maintaining editing efficiency and ensuring patient safety [13] [31].
This technical guide provides a comprehensive analysis of the three primary vehicle categories for in vivo CRISPR delivery: viral vectors, lipid nanoparticles (LNPs), and physical methods. We examine their fundamental mechanisms, present comparative performance data, detail experimental protocols, and discuss their integration within the broader context of therapeutic development. As the field progresses toward treating more complex diseases, understanding these delivery platforms becomes paramount for researchers and drug development professionals aiming to translate CRISPR technology from laboratory breakthroughs to clinical realities [32].
Cargo Formats for CRISPR-Cas9 Delivery
The choice of cargo format significantly influences the kinetics, specificity, and safety profile of in vivo gene editing. The three predominant cargo types each present distinct advantages and limitations for therapeutic development [13] [30].
Plasmid DNA (pDNA) was among the earliest cargo formats employed. It involves delivering a DNA plasmid encoding both the Cas9 nuclease and the guide RNA. While cost-effective to produce, pDNA necessitates nuclear entry for transcription, which can limit its efficiency in non-dividing cells. Furthermore, prolonged expression from persistent plasmids increases the potential for off-target effects and raises safety concerns due to possible genomic integration [13] [30].
Messenger RNA (mRNA) combined with a separate guide RNA offers a transient expression profile. The mRNA is translated into Cas9 protein in the cytoplasm, leading to a rapid but short-lived editing window that minimizes off-target activity. However, the inherent instability of RNA molecules requires sophisticated delivery systems to protect them from degradation in vivo, and unmodified RNA can stimulate innate immune responses [30] [32].
Ribonucleoprotein (RNP) complexes, consisting of preassembled, purified Cas9 protein and guide RNA, represent the most recently adopted format. RNPs are immediately active upon delivery and are cleared rapidly, offering the highest specificity with minimal off-target effects. The primary challenges for RNP delivery in vivo involve the large size and relative instability of the protein complex, requiring advanced encapsulation technologies to ensure functional delivery to target tissues [13] [30] [33].
Table 1: Comparison of CRISPR-Cas9 Cargo Formats
| Cargo Format | Key Advantages | Key Limitations | Ideal Use Cases |
|---|---|---|---|
| Plasmid DNA (pDNA) | Cost-effective production, stable storage [30] | Requires nuclear entry; prolonged expression increases off-target risk [13] [30] | Early-stage proof-of-concept studies |
| mRNA + gRNA | Rapid expression; transient activity reduces off-target effects [30] [32] | Potential immunogenicity; requires protection from degradation [30] [32] | In vivo therapies requiring a short editing window |
| Ribonucleoprotein (RNP) | Immediate activity; highest specificity; minimal off-target effects [13] [30] [33] | Complex large-scale manufacturing; limited in vivo stability [13] [33] | Applications demanding maximal precision and safety |
Viral Vector Delivery Systems
Viral vectors exploit the natural efficiency of viruses to transport genetic material into cells. They are among the most common vehicles used in gene therapy trials, with several classes being adapted for CRISPR delivery [13] [12].
Types of Viral Vectors and Their Characteristics
Adeno-Associated Viruses (AAVs) are small, non-pathogenic viruses that have become a leading platform for in vivo CRISPR delivery. Their primary advantage is an excellent safety profile, with low immunogenicity and non-integrative behavior, reducing the risk of insertional mutagenesis. The most significant limitation is their constrained packaging capacity (~4.7 kb), which is insufficient for the standard Streptococcus pyogenes Cas9 (SpCas9) and its associated expression elements. Strategies to overcome this include using dual AAV systems or engineering smaller Cas9 orthologs, such as those from Staphylococcus aureus (SaCas9) [13].
Adenoviral Vectors (AdVs) offer a major advantage in their large packaging capacity (up to ~36 kb), enabling them to carry full-length Cas9, multiple gRNAs, and even donor DNA templates for homology-directed repair. Similar to AAVs, they do not integrate into the host genome. However, their high prevalence in the human population often leads to pre-existing immunity, which can neutralize the vector and trigger potent inflammatory responses, posing a significant challenge for clinical application [13] [12].
Lentiviral Vectors (LVs) are capable of delivering large genetic payloads and can infect both dividing and non-dividing cells. A critical distinction from AAVs and AdVs is their propensity to integrate into the host genome, which supports long-term transgene expression but carries the risk of oncogenesis if integration occurs near proto-oncogenes. For this reason, their use in in vivo CRISPR therapy is more limited compared to non-integrating vectors [13].
Quantitative Comparison of Viral Vectors
Table 2: Performance Metrics of Viral Vector Systems for In Vivo CRISPR Delivery
| Vector Type | Packaging Capacity | Integration Profile | Immunogenicity | Tropism | Reported Editing Efficiency In Vivo |
|---|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | ~4.7 kb [13] | Non-integrative [13] | Low to Moderate [13] | Broad, serotype-dependent [13] | High in liver, muscle, eye (e.g., EDIT-101 trial) [4] |
| Adenovirus (AdV) | Up to ~36 kb [13] | Non-integrative [13] | High [13] [12] | Broad | Efficient in multiple tissues, but limited by immunity [13] |
| Lentivirus (LV) | ~8 kb [13] | Integrating [13] | Moderate [13] | Broad, can be pseudotyped [13] | Primarily used for ex vivo editing (e.g., CAR-T cells) [13] [31] |
Protocol: Production and Purification of AAV Vectors for CRISPR Delivery
This protocol outlines the production of AAV vectors encoding a CRISPR component, such as a SaCas9 and gRNA expression cassette, using the HEK293T cell system [13].
Step 1: Plasmid Transfection
- Culture HEK293T cells in a multi-layer flask or bioreactor to ~70% confluence.
- Co-transfect the cells with three plasmids using a polyethylenimine (PEI) protocol:
- Rep/Cap Plasmid: Provides AAV replication (Rep) and capsid (Cap) proteins.
- pHelper Plasmid: Provides essential adenoviral genes (E2A, E4, VA RNA).
- ITR Plasmid: Contains the transgene of interest (e.g., SaCas9-gRNA) flanked by AAV Inverted Terminal Repeats (ITRs).
- Incubate the transfected cells for 48-72 hours to allow for viral particle assembly [13].
Step 2: Harvest and Lysis
- Harvest the cells and media.
- Lyse the cell pellet via repeated freeze-thaw cycles or detergent treatment to release the viral particles.
- Clarify the lysate by centrifugation to remove cell debris [13].
Step 3: Purification and Formulation
- Purify the crude AAV preparation using iodixanol density gradient centrifugation or affinity chromatography.
- Concentrate the purified AAV using centrifugal filters.
- Dialyze the final product into a physiological buffer (e.g., PBS with surfactants) and filter-sterilize.
- Quantify the viral titer (genome copies/mL) using quantitative PCR (qPCR) and assess purity via SDS-PAGE [13].
Non-Viral Delivery: Lipid Nanoparticles (LNPs)
Lipid Nanoparticles have emerged as a leading non-viral platform for in vivo CRISPR delivery, validated by their successful application in mRNA COVID-19 vaccines and the first in vivo personalized CRISPR therapy [32] [4].
Composition, Mechanism, and Advantages
LNPs are typically 50-120 nm particles composed of four key lipid components: ionizable lipids, phospholipids, cholesterol, and PEG-lipids [32]. The ionizable lipid is the most critical functional component; it is positively charged at low pH during formulation to enable efficient encapsulation of nucleic acids, but neutral in the bloodstream to minimize toxicity. Following systemic administration, LNPs naturally accumulate in the liver due to apolipoprotein E adsorption and receptor-mediated uptake by hepatocytes [32]. Upon cellular uptake via endocytosis, the acidification of the endosome protonates the ionizable lipid, disrupting the endosomal membrane and facilitating the release of the CRISPR cargo into the cytoplasm [32].
The advantages of LNPs over viral vectors are substantial. They exhibit lower immunogenicity, which allows for repeat dosing—a critical feature for achieving therapeutic levels of editing, as demonstrated in the personalized treatment for infant CPS1 deficiency [32] [4]. Their transient nature limits the duration of Cas9 expression, thereby reducing the risk of off-target effects. Furthermore, LNP manufacturing is highly scalable and can be completed in days, offering significant advantages in production flexibility and speed compared to the complex and lengthy process of manufacturing viral vectors [32].
Protocol: Formulating LNPs for RNP Delivery via Microfluidic Mixing
While LNPs are most commonly used for mRNA delivery, encapsulating RNP complexes is an area of intense research. This protocol describes a method for formulating RNP-loaded LNPs.
Step 1: Lipid Preparation
- Prepare an ethanol-phase lipid mixture containing the ionizable lipid (e.g., ALC-0315), phospholipid (e.g., DSPC), cholesterol, and PEG-lipid (e.g., DMG-PEG) at a defined molar ratio (e.g., 50:10:38.5:1.5) [32].
Step 2: RNP Complex Preparation
- Complex purified Cas9 protein with synthetic guide RNA at a predetermined molar ratio in an appropriate buffer to form the RNP. Incubate to allow for complex formation [30] [33].
Step 3: Microfluidic Mixing
- Use a microfluidic device (e.g., NanoAssemblr) to mix the ethanolic lipid stream with an aqueous stream containing the RNP complexes at a defined flow rate and ratio.
- The rapid mixing induces nanoparticle self-assembly, encapsulating the RNP cargo within the forming LNP [32].
Step 4: Downstream Processing
- Dialyze the formed LNPs against a suitable buffer (e.g., PBS) to remove ethanol and exchange the buffer.
- Concentrate the LNPs using centrifugal filters.
- Characterize the final formulation for particle size (e.g., DLS), polydispersity, encapsulation efficiency, and concentration [32].
Physical Delivery Methods
Physical methods utilize physical forces to transiently disrupt the cell membrane and facilitate the direct intracellular delivery of CRISPR components. While predominantly used for ex vivo applications, some advanced techniques show promise for localized in vivo use.
Electroporation applies short, high-voltage electrical pulses to create transient pores in the cell membrane. It is highly efficient for ex vivo editing of hematopoietic stem cells, as demonstrated in the Casgevy therapy, where it achieved up to 90% indel formation in the BCL11A enhancer [30] [1]. Its application in vivo is limited to accessible tissues and can cause significant cytotoxicity and muscle contraction [30].
Microinjection involves the direct mechanical injection of CRISPR reagents into a single cell or nucleus using a fine glass needle. It offers precision and high efficiency for editing single-cell embryos or specific cells in vitro, with one study reporting around 40% editing efficiency in HepG2 cells [30]. However, it is a low-throughput, technically demanding process unsuitable for systemic or whole-tissue therapy.
Other Physical Techniques include sonoporation (using ultrasound) and magnetofection (using magnetic fields to direct nucleic acids), which are under investigation for deeper tissue targeting in vivo but remain largely in the research phase [30].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Developing and Testing In Vivo CRISPR Delivery Vehicles
| Reagent / Material | Function | Example Use Case |
|---|---|---|
| Ionizable Lipids (e.g., ALC-0315) | Core component of LNPs; enables encapsulation and endosomal escape [32] | Formulating mRNA-LNPs for liver-targeted editing [32] [4] |
| PEG-Lipids (e.g., ALC-0159) | Stabilizes LNP surface; modulates pharmacokinetics and biodistribution [32] | Improving LNP circulation time and reducing non-specific uptake [32] |
| AAV Serotype Library (e.g., AAV8, AAV9) | Provides a range of tissue tropisms for targeted delivery [13] | Selecting optimal AAV capsid for targeting central nervous system (e.g., AAV9) [13] |
| VSV-G Glycoprotein | Pseudotyping agent for LV and other vesicles; broadens cellular tropism [33] | Enhancing the budding and gene editing efficiency of engineered extracellular vesicles (ARMMs) [33] |
| Designed Ankyrin Repeat Proteins (DARPins) | Targeting ligands conjugated to LNP surface [32] | Redirecting LNPs from the liver to T cells (achieving ~90% expression in human CD8+ T cells) [32] |
Visualization of Workflows and System Relationships
In Vivo CRISPR Delivery Workflow
LNP Formulation via Microfluidics
The development of effective in vivo delivery vehicles is the critical path forward for unlocking the full potential of CRISPR-Cas9 therapeutics. Viral vectors, particularly AAVs, offer high transduction efficiency and persistence but are constrained by immunogenicity and payload size. LNPs present a versatile, scalable, and transient alternative with a favorable safety profile that enables redosing, though their natural tropism for the liver remains a primary limitation [32] [4].
Future progress hinges on overcoming key challenges. Tissue-specific targeting beyond the liver is a major focus, with strategies like SORT molecules and DARPin conjugates showing promise for redirecting LNPs to specific cell types [13] [32]. Mitigating immunogenicity remains paramount for both viral and non-viral systems to allow for safe and effective treatments. Finally, the ability to administer multiple doses safely, as demonstrated in recent clinical cases, will be essential for treating a wider range of diseases, particularly those requiring high editing thresholds [32] [4].
As the field matures, the convergence of these technologies—such as the engineering of hybrid systems and the application of machine learning to vector design—will likely yield the next generation of delivery platforms. This will expand the scope of in vivo gene editing from monogenic liver disorders to complex diseases affecting the central nervous system, musculoskeletal system, and beyond, ultimately fulfilling the promise of CRISPR as a revolutionary therapeutic modality.
The advent of CRISPR-Cas9 gene-editing technology has ushered in a transformative era for therapeutic development, creating a clear paradigm shift in how genetic diseases are treated. This whitepaper examines the clinical success of ex vivo CRISPR therapies, with a primary focus on CASGEVY (exagamglogene autotemcel), the first CRISPR-based medicine to receive regulatory approval for sickle cell disease (SCD) and transfusion-dependent beta thalassemia (TBT) [4] [1]. The analysis is framed within the broader context of comparing ex vivo and in vivo therapeutic approaches, two distinct strategies with differing technical challenges, clinical applications, and developmental pathways. Ex vivo editing, exemplified by CASGEVY, involves genetically modifying a patient's own cells outside the body before reinfusion, offering precise control over the editing process. In vivo editing, in contrast, delivers CRISPR components directly into the patient's body to edit cells in their natural niche. While the ex vivo approach has achieved landmark approvals, the field is rapidly advancing toward a future where in vivo therapies may address a wider range of genetic disorders. This document provides an in-depth technical analysis of the clinical evidence, experimental protocols, and mechanistic data underpinning these successes, and explores the evolving pipeline that will define the next generation of CRISPR-based medicines.
Clinical Evidence and Efficacy Data
The approval of CASGEVY is grounded in robust clinical data from pivotal trials demonstrating significant and sustained clinical benefits for patients with severe hemoglobinopathies.
CASGEVY for Sickle Cell Disease (SCD)
The efficacy of CASGEVY for SCD was evaluated in an ongoing open-label, single-arm trial [34]. The study enrolled 44 patients aged 12 to 35 with severe SCD, defined by having at least two severe vaso-occlusive crises (VOCs) per year in the two years prior to enrollment. A severe VOC was defined as a pain event requiring a visit to a medical facility and pain medication, a red blood cell transfusion, or events such as acute chest syndrome, priapism, or splenic sequestration [34].
Table 1: Key Efficacy Endpoints from CASGEVY SCD Clinical Trial
| Endpoint Measure | Result | Follow-up Period |
|---|---|---|
| Patients free of severe VOCs for ≥12 consecutive months | 93.5% (29 out of 31 patients) | Minimum 12 months post-infusion |
| Patients free of hospitalization for severe VOCs for ≥12 consecutive months | 100% (30 out of 30 patients) | Minimum 12 months post-infusion |
| Median duration of freedom from severe VOCs | 22.2 months | Ongoing trial |
| Hemoglobin F (HbF) levels | Increased and sustained | Up to 24 months |
The interim results, with the longest patient follow-up exceeding five years, show a profound treatment effect. The near-total elimination of severe VOCs, which are the primary cause of morbidity and mortality in SCD, represents a functional cure for the majority of treated participants [4] [34].
CASGEVY for Transfusion-Dependent Beta Thalassemia (TBT)
In parallel clinical trials for TBT, CASGEVY demonstrated similarly transformative results. The therapy was evaluated in patients who required regular red blood cell transfusions due to their disease. The primary efficacy measure was transfusion independence, defined as maintaining a weighted average hemoglobin level of at least 9 g/dL without any red blood cell transfusions for at least 12 consecutive months [1].
Manufacturer-presented interim results for 56 patients with TBT showed that the vast majority achieved transfusion independence, with the longest patient follow-up also being more than five years post-treatment [1]. This data underscores the therapy's potential to liberate patients from a lifelong dependence on transfusions.
Broader Ex Vivo Clinical Impact
Beyond CASGEVY, the ex vivo platform is proving successful in other domains. Clinical success stories are emerging from ongoing trials. For instance, one report highlights a young patient named Ashanti who received a CRISPR-based ex vivo therapy for SCD through the Ruby clinical trial sponsored by Editas Medicine. Following the treatment, she became asymptomatic for her sickle cell disease, a outcome her physician described as transformative [35].
Furthermore, companies like CRISPR Therapeutics are advancing a broad pipeline of ex vivo cell therapies, including allogeneic CAR-T cell therapies (e.g., CTX112) for oncology and autoimmune diseases, which have shown promising early clinical results [36].
Experimental Protocols and Workflows
The development and administration of ex vivo CRISPR therapies involve complex, multi-step protocols. Below is a detailed breakdown of the standard methodology for an ex vivo therapy like CASGEVY.
CASGEVY Treatment Protocol
Step 1: Hematopoietic Stem Cell (HSC) Mobilization and Apheresis
- Objective: To collect a sufficient quantity of the patient's own CD34+ hematopoietic stem cells for editing.
- Procedure:
- The patient receives a mobilization medicine (typically granulocyte colony-stimulating factor, G-CSF) to stimulate the bone marrow to release HSCs into the peripheral blood.
- Through a process called apheresis, the patient's blood is passed through a machine that separates and collects the HSCs, returning the remainder of the blood to the body.
- This process may be repeated multiple times over up to a week to collect the required cell dose.
- Rescue cells (a portion of the unedited collected cells) are cryopreserved and stored as a backup in case of manufacturing failure or failure of the edited cells to engraft [34].
Step 2: Ex Vivo CRISPR Gene Editing and Manufacturing
- Objective: To precisely edit the patient's HSCs to produce therapeutic levels of fetal hemoglobin.
- Procedure:
- The collected CD34+ HSCs are transported to a specialized Good Manufacturing Practice (GMP) facility.
- Cells are transfected with the CRISPR-Cas9 system—specifically, the ribonucleoprotein (RNP) complex of Cas9 nuclease and a synthetic guide RNA (gRNA).
- The gRNA is designed to target the BCL11A gene, a key transcriptional repressor of fetal hemoglobin (HbF).
- The CRISPR-Cas9 complex induces a double-strand break (DSB) in the BCL11A gene enhancer region.
- The cell repairs this break via the error-prone non-homologous end joining (NHEJ) pathway, which results in insertions or deletions (indels) that disrupt the enhancer sequence.
- This knockout of the BCL11A enhancer leads to de-repression of HbF production in the resulting red blood cells [1] [36].
- The entire manufacturing, including quality control testing, can take up to six months [34].
Step 3: Patient Conditioning and Myeloablation
- Objective: To clear the patient's bone marrow of native HSCs to create space for the engraftment of the edited cells.
- Procedure:
- After manufacturing is complete, the patient is admitted to the hospital.
- The patient receives a myeloablative conditioning regimen (e.g., busulfan) for several days. This chemotherapy eliminates the existing bone marrow stem cells.
- This step is critical for enabling the engineered cells to engraft but results in a period of severely low blood cell counts (cytopenia), requiring intensive supportive care [34].
Step 4: Reinfusion and Engraftment
- Objective: To administer the edited cells and support their engraftment and repopulation of the bone marrow.
- Procedure:
- The CASGEVY product is thawed and administered via a simple intravenous (IV) infusion over a short period.
- The patient remains in the hospital for close monitoring for approximately 4-6 weeks post-infusion.
- During this time, clinicians manage the side effects of conditioning and monitor blood counts for signs of engraftment, which is confirmed by the recovery of neutrophil and platelet counts.
- Successful engraftment leads to the production of red blood cells that express high levels of HbF, which does not sickle and provides therapeutic benefit [34].
Figure 1: Ex Vivo CRISPR Therapy Workflow. This diagram illustrates the multi-step process for autologous ex vivo therapies like CASGEVY, from cell collection to patient reinfusion and recovery.
In Vivo vs. Ex Vivo CRISPR Approaches
The distinction between in vivo and ex vivo delivery is fundamental to understanding the current state and future direction of CRISPR therapies.
Figure 2: In Vivo vs. Ex Vivo Therapy Comparison. A direct comparison of the core advantages and challenges associated with each major therapeutic delivery approach.
Ex Vivo Gene Editing: A Deeper Dive
Ex vivo editing involves extracting specific cells from a patient, genetically modifying them outside the body, and then reinfusing them back into the patient [1] [37]. This approach is also referred to as cell therapy.
- Mechanism: As detailed in the CASGEVY protocol, the editing is performed under controlled conditions in a manufacturing facility. This allows for quality control, precise optimization of the editing process, and the possibility of selecting successfully edited cells before reinfusion [1].
- Therapeutic Targets: This approach is ideally suited for diseases affecting cells that can be easily extracted, manipulated, and functionally engrafted upon reinfusion. Its primary successes to date are in hematopoietic stem cells (HSCs) for genetic blood disorders like SCD and TBT, and in T-cells for engineered CAR-T cancer immunotherapies [1] [36] [37].
- Key Challenges: The process is logistically complex, time-consuming, and extremely costly. It requires specialized GMP facilities and carries the risks associated with myeloablative conditioning, including prolonged cytopenia and infertility [34] [37].
In Vivo Gene Editing: The Frontier of Delivery
In vivo editing involves the direct administration of CRISPR components into the patient to modify the DNA of target cells inside the body [1] [37].
- Mechanism: The CRISPR system (typically as mRNA or as a protein complex) is packaged into a delivery vector and administered systemically or locally. The vector must protect the payload, navigate biological barriers, and deliver it specifically to the target cells [4] [8].
- Delivery Vectors: Lipid Nanoparticles (LNPs) have emerged as a leading non-viral vector for in vivo delivery, particularly for targeting the liver. Their success is demonstrated in clinical trials for diseases like hereditary transthyretin amyloidosis (hATTR) and hereditary angioedema (HAE), where they are used to systemically deliver CRISPR to knock down disease-causing genes in hepatocytes [4]. Adeno-Associated Viruses (AAVs) are also used but have limitations such as limited packaging capacity and potential immunogenicity [8].
- Key Challenges: The paramount challenge is delivery—achieving efficient, specific, and safe targeting of the desired tissues and cells while avoiding off-target effects and immune system clearance [4] [8]. The long-term activity and potential immunogenicity of the editing machinery are also areas of active investigation.
Table 2: Comparative Analysis of In Vivo vs. Ex Vivo CRISPR Therapies
| Feature | In Vivo Therapy | Ex Vivo Therapy |
|---|---|---|
| Definition | CRISPR components delivered directly into the patient's body [1]. | Cells are edited outside the body and then reinfused [1]. |
| Delivery Vectors | Lipid Nanoparticles (LNPs), Adeno-Associated Virus (AAV) [4] [8]. | Electroporation (common for RNP delivery) [1]. |
| Therapeutic Examples | Intellia's NTLA-2001 for hATTR, CTX310 for cardiovascular disease [4] [36]. | CASGEVY for SCD/TBT, CAR-T cell therapies for cancer [34] [36]. |
| Key Advantages | Single administration; potential to target inaccessible tissues; simpler patient journey [4]. | Precise control over editing; ability to select and quality-check edited cells; validated clinical success [1]. |
| Major Challenges | Delivery efficiency and specificity; immune responses; limited payload capacity of vectors [8]. | Complex, costly manufacturing; requires myeloablative conditioning; limited to certain cell types [34] [37]. |
| Dosing | Potential for redosing (with LNP delivery) [4]. | Typically a one-time infusion (but requires conditioning). |
The Scientist's Toolkit: Research Reagent Solutions
The development and implementation of CRISPR therapies rely on a suite of specialized reagents and tools.
Table 3: Essential Research Reagents for CRISPR-Based Therapy Development
| Reagent / Tool | Function | Example in Clinical Use |
|---|---|---|
| CRISPR-Cas9 Nuclease | Creates double-strand breaks (DSBs) in DNA at a site specified by the guide RNA. The core enzyme of the editing system [1]. | SpCas9 is the nuclease used in the majority of early clinical programs, including CASGEVY [1]. |
| Guide RNA (gRNA) | A synthetic RNA sequence that binds to Cas9 and directs it to a specific genomic locus via complementary base pairing [1]. | In CASGEVY, the gRNA targets the enhancer region of the BCL11A gene in hematopoietic stem cells [1] [36]. |
| Ribonucleoprotein (RNP) Complex | A preassembled complex of the Cas9 protein and gRNA. Direct delivery of RNP is a common strategy for ex vivo editing due to its high efficiency and reduced off-target effects compared to plasmid DNA delivery [1]. | The RNP complex is used in the ex vivo manufacturing process of CASGEVY [1]. |
| Lipid Nanoparticles (LNPs) | A non-viral delivery vector comprising lipid bilayers that encapsulate CRISPR payloads (mRNA, gRNA, RNP). Protects the payload and facilitates cellular uptake [4] [8]. | Used in Intellia's in vivo therapies (e.g., for hATTR and HAE) to deliver Cas9 mRNA and gRNA to the liver [4]. |
| Viral Vectors (e.g., AAV) | Engineered viruses used to deliver CRISPR machinery in vivo. Effective at transducing certain cell types but has packaging size constraints and can elicit immune responses [8]. | Commonly used in gene therapy and in vivo editing research; however, LNPs are often preferred for CRISPR nuclease delivery due to larger capacity and transient expression [8]. |
| Hematopoietic Stem Cell Media | Specialized, serum-free cell culture media formulations designed to maintain the viability and stemness of HSCs during the ex vivo editing and expansion process. | Used in GMP manufacturing of CASGEVY and other ex vivo HSC therapies. Optimized media is critical for high engraftment efficiency [38]. |
Beyond CASGEVY: The Expanding Therapeutic Pipeline and Future Directions
The success of CASGEVY has validated the ex vivo CRISPR platform and catalyzed the development of a diverse pipeline of next-generation therapies.
Next-Generation Ex Vivo Therapies
- Allogeneic ("Off-the-Shelf") Therapies: The current paradigm for CAR-T and some HSC therapies is autologous (using the patient's own cells). The field is rapidly moving toward allogeneic therapies, which use healthy donor cells. CRISPR is used to edit these cells to evade host immune rejection (e.g., by knocking out HLA genes) and to enhance their therapeutic function. CRISPR Therapeutics' CTX112, an allogeneic anti-CD19 CAR-T cell therapy for autoimmune diseases and immuno-oncology, is a prime example [36].
- Multiplexed Editing: Researchers are moving beyond single gene knockouts. For instance, the creation of "universal" regulatory T cells (Tregs) involves using CRISPR to disrupt both HLA class I and II genes while simultaneously inserting an HLA-E fusion protein, a process requiring multiple precise edits [38].
Advanced In Vivo Applications
The in vivo pipeline is expanding beyond liver-targeted gene knockout. Clinical-stage programs are now targeting common diseases like cardiovascular disease (e.g., CTX310, CTX320) and refractory hypertension (CTX340) through in vivo knockout of disease-associated genes in the liver using LNP delivery [36]. Furthermore, advanced editing tools like base editing and prime editing are being advanced into the clinic. These technologies allow for precise single-base changes without creating double-strand breaks, potentially improving safety. A 2025 report highlighted the use of prime editing to correct a pathogenic mutation causing inherited retinal disease in human stem cells, demonstrating the potential for precise correction of point mutations [38].
Addressing Technical and Safety Hurdles
The field is proactively addressing challenges such as off-target effects and complex editing outcomes. Research has shown that CRISPR-Cas9 editing can sometimes lead to structural variants (SVs), including large deletions and chromosomal rearrangements [39]. The community is responding with improved analytical methods (e.g., long-read sequencing) to detect these events and engineering strategies to create more precise editors with reduced off-target activity [39] [38]. As one review notes, "Overcoming these delivery obstacles is essential for translating the promise of in vivo gene editing into effective clinical treatments" [38].
The approval and clinical success of CASGEVY represent a watershed moment for molecular medicine, definitively proving that ex vivo CRISPR gene editing can provide a functional cure for devastating genetic diseases like sickle cell disease and beta thalassemia. This success is built upon a foundation of robust clinical data, a well-defined and controlled manufacturing protocol, and a clear biological mechanism of action. While the ex vivo approach has established itself as a validated platform for blood and immune disorders, the rapid advancement of in vivo delivery technologies, particularly LNPs for liver-directed therapy, promises to extend the benefits of CRISPR to a much wider array of indications. The future of the field lies not in a competition between these two approaches, but in their parallel development, each suited to different therapeutic needs. The ongoing evolution of the CRISPR toolkit—including base editing, prime editing, and improved delivery systems—coupled with rigorous safety assessments, ensures that the next decade will see an accelerated expansion of CRISPR-based therapies from targeted genetic corrections to mainstream treatments for common diseases.
The liver has emerged as a premier organ for pioneering in vivo CRISPR-Cas9 therapies, representing a paradigm shift from ex vivo approaches where cells are edited outside the body before reinfusion. This strategic focus is largely due to the liver's unique anatomical and physiological characteristics. Its sinusoidal vasculature contains fenestrated endothelium that permits efficient uptake of systemically administered therapeutic vectors, particularly lipid nanoparticles (LNPs), which show a natural tropism for hepatic tissue [4]. Furthermore, the liver's immense regenerative capacity enables selectively edited hepatocytes to repopulate the organ, potentially yielding a durable therapeutic effect from a single treatment [40].
The transition from ex vivo to in vivo editing marks a critical evolution in gene therapy. Ex vivo strategies, exemplified by Casgevy for sickle cell disease and beta-thalassemia, involve complex, multi-step processes of cell extraction, external manipulation, and reinfusion [1]. In vivo approaches, by contrast, aim to deliver CRISPR components directly into the patient's body, offering a less invasive and potentially more scalable solution for treating genetic disorders [4]. This technical guide explores the cutting-edge applications, delivery technologies, and experimental frameworks defining the current landscape of liver-directed in vivo CRISPR therapies.
Clinical Landscape of Liver-Directed In Vivo CRISPR Therapies
Substantial clinical progress has been made with in vivo CRISPR therapies targeting monogenic liver disorders. These approaches primarily utilize systemic administration of LNP-formulated CRISPR components to achieve therapeutic gene editing within hepatocytes.
Table 1: Key Clinical-Stage In Vivo CRISPR Therapies for Liver Disorders
| Disease Target | CRISPR Mechanism | Delivery System | Key Clinical Outcomes | Development Stage |
|---|---|---|---|---|
| Hereditary Transthyretin Amyloidosis (hATTR) [4] | Knockout of TTR gene | LNP | ~90% sustained reduction in serum TTR protein [4] | Phase III Global Trials |
| Hereditary Angioedema (HAE) [4] | Knockout of kallikrein gene | LNP | 86% reduction in kallikrein; 8/11 patients attack-free [4] | Phase I/II Trial |
| Personalized CPS1 Deficiency [4] | Bespoke gene correction | LNP | Symptom improvement with multiple dosing [4] | Proof-of-Concept Case |
A landmark case reported in 2025 demonstrated the feasibility of ultra-personalized in vivo CRISPR medicine. An infant with a rare, life-threatening CPS1 deficiency received a bespoke LNP-delivered CRISPR therapy developed and approved by the FDA in just six months [4]. Crucially, the use of LNP delivery enabled multiple doses to be administered safely to increase the proportion of edited cells—a flexibility typically not possible with viral vectors due to immunogenicity concerns [4]. This case establishes a regulatory and technical precedent for "on-demand" CRISPR therapies for rare genetic diseases.
Advanced Delivery Systems for Organ-Specific Targeting
Effective delivery remains the foremost challenge for in vivo CRISPR therapies. The ideal delivery system must protect nucleic acids from degradation, traverse biological barriers, and achieve efficient editing in target cells with minimal off-target effects or immune activation [41] [42].
Non-Viral Delivery Platforms
Lipid Nanoparticles (LNPs) have become the leading non-viral delivery vehicle for hepatic CRISPR targeting. Their efficacy stems from a natural affinity for the liver following systemic administration, where they accumulate and edit hepatocytes with high efficiency [4]. Standard LNPs are effective for liver targeting but face biodistribution limitations for extrahepatic tissues. Recent innovations focus on engineering next-generation LNPs with enhanced targeting capabilities:
- Peptide-Ionizable Lipids: Incorporation of artificial and natural amino acids creates nanoparticles capable of targeting specific tissues, including lungs, liver, spleen, thymus, and bone [43].
- Peptide-Encoded Organ-Selective Targeting (POST): This method uses specific amino acid sequences to modify LNP surfaces, forming distinct protein coronas that enable precise delivery to extrahepatic organs following systemic administration [43].
- LNP-Spherical Nucleic Acids (LNP-SNAs): These structures incorporate LNPs surrounded by a dense DNA shell, demonstrating 2-3-fold higher cellular uptake and superior gene-editing performance compared to standard LNPs across multiple cell lines [43].
Viral Vector Delivery Systems
Adeno-associated viruses (AAVs) remain valuable for their ability to mediate long-term transgene expression. Ongoing capsid engineering efforts aim to enhance liver tropism, reduce immunogenicity, and increase packaging capacity for CRISPR machinery [44]. However, their limited cargo capacity often necessitates dual-vector systems for delivering larger CRISPR nucleases, and pre-existing immunity in human populations can limit their applicability [45].
Table 2: Comparison of CRISPR Delivery Vehicles for Liver-Directed Therapy
| Characteristic | Lipid Nanoparticles (LNPs) | Adeno-Associated Virus (AAV) |
|---|---|---|
| Packaging Capacity | Higher capacity for CRISPR components [41] | Limited capacity (~4.5kb) [45] |
| Immunogenicity | Lower risk; enables redosing [4] | Higher risk; limits redosing [4] |
| Manufacturing | Scalable synthetic production [44] | Complex biological production [44] |
| Editing Persistence | Transient activity (days-weeks) | Potentially prolonged expression |
| Tropism | Natural liver affinity; engineerable [4] [43] | Native and engineered liver tropism [44] |
Experimental Protocols and Workflows
In Vivo Gene Editing with Selective Advantage
A groundbreaking experimental strategy termed "Repair Drive" addresses the fundamental challenge of achieving therapeutic levels of gene correction in the liver, where only about 1% of hepatocytes are actively dividing and accessible to homology-directed repair (HDR) [40].
Table 3: Research Reagent Solutions for CRISPR Liver Editing
| Reagent/Category | Specific Examples | Function in Experimental Workflow |
|---|---|---|
| CRISPR Nuclease | hfCas12Max, eSpOT-ON, SaCas9 [45] | Creates DNA break or edit at precise genomic location |
| Delivery Vehicle | Liver-tropic LNPs, AAVs [4] [44] | Packages and delivers CRISPR components to hepatocytes |
| Selective Agent | FAH-targeting siRNA [40] | Creates selective pressure favoring growth of edited cells |
| Donor Template | HDR donor with siRNA-resistant FAH [40] | Provides correct DNA sequence for repair of disease gene |
| Validation Tool | NGS assays for on/off-target editing [40] | Confirms precision and specificity of editing outcomes |
Experimental Workflow:
- Design and Synthesis: Design CRISPR guide RNAs and donor DNA templates. Select an appropriate nuclease (e.g., SaCas9 for AAV delivery due to small size) [45].
- Vector Packaging: Package CRISPR machinery into selected delivery vehicles (LNPs or AAVs) [41].
- Animal Model Administration: Systemically administer vectors to mouse models of liver disease via intravenous injection [40].
- Selective Pressure Application: Administer small interfering RNA (siRNA) to temporarily inhibit an essential gene (FAH), creating a competitive advantage for hepatocytes that have received the therapeutic edit [40].
- Validation and Assessment: Harvest liver tissue at predetermined endpoints. Analyze editing efficiency via next-generation sequencing, assess off-target effects, and evaluate phenotypic correction through functional assays and biomarker measurement [40].
This protocol dramatically increased the proportion of correctly repaired hepatocytes from approximately 1% to over 25% in mouse models, enabling edited cells to divide and regenerate a healthy liver [40].
Advanced Nuclease Engineering for Enhanced Safety
To address safety concerns such as off-target effects and double-stranded break (DSB) risks, researchers are developing engineered nucleases with improved precision profiles:
- High-Fidelity Variants: Nucleases like hfCas12Max and eSpOT-ON demonstrate robust on-target editing with significantly reduced off-target activity, as validated in primary human T-cells and mouse models [45].
- Staggered-Cut Nucleases: Unlike SpCas9 which creates blunt-ended DSBs, hfCas12Max and eSpOT-ON create staggered DNA ends ("sticky ends") that reduce the risk of chromosomal translocations and promote more accurate repair [45].
- Compact Nucleases: Smaller Cas proteins like SaCas9 and Cas12a (approximately 1kb smaller than SpCas9) fit more easily into delivery vehicles with limited capacity, such as AAVs [45].
Emerging Applications in Hepatocellular Carcinoma and Complex Diseases
While monogenic diseases represent the most straightforward targets, CRISPR applications are expanding toward complex liver conditions, including hepatocellular carcinoma (HCC) and metabolic disorders. The extensive heterogeneity of HCC at both genetic and molecular levels presents significant challenges for developing effective therapies [46].
Molecular Diagnostics and Personalized Therapy
Next-generation sequencing technologies enable comprehensive molecular characterization of HCC tumors, identifying distinct subtypes with implications for prognosis and treatment selection [46]. Liquid biopsy approaches analyzing circulating tumor DNA (ctDNA) and circulating tumor cells (CTCs) provide minimally invasive biomarkers for early detection, monitoring treatment response, and tracking clonal evolution [46]. These molecular diagnostics create opportunities for personalized CRISPR interventions targeting driver mutations in individual patients.
CRISPR Screens for Target Discovery
CRISPR-based functional genomics screens are identifying novel therapeutic targets and resistance mechanisms in HCC. For example, a recent CRISPR screen in primary macrophages revealed how tumor-associated macrophages develop diverse functional phenotypes in response to tumor-derived factors [43]. This approach identified a TGF-β-induced long non-coding RNA (LIMD1-AS1) that enhances cancer cell plasticity, suggesting new therapeutic strategies to restrain TGF-β-induced epithelial-mesenchymal transition and breast cancer progression [43].
The field of liver-directed in vivo CRISPR therapies is progressing at an accelerated pace, transitioning from proof-of-concept studies to validated clinical applications. The convergence of multiple technological advances—including optimized non-viral delivery systems, engineered nucleases with enhanced precision, and innovative strategies for selective expansion of edited cells—positions in vivo liver editing as a transformative modality for treating genetic diseases.
Future development will focus on overcoming remaining challenges, particularly expanding applications beyond monogenic disorders to complex conditions like HCC and metabolic liver diseases. Key research priorities will include refining organ-specific targeting to enable extrahepatic applications, mitigating immune responses to enable redosing where necessary, and establishing robust safety profiles through long-term follow-up of treated patients. As these technologies mature, in vivo CRISPR therapies promise to redefine treatment paradigms across a broad spectrum of liver disorders, ultimately fulfilling the promise of personalized genomic medicine.
The advent of CRISPR-Cas systems has revolutionized biomedical research and therapeutic development, offering unprecedented precision in genome editing. However, the efficient and safe delivery of these molecular tools remains a significant bottleneck, particularly for in vivo applications. The central challenge stems from the packaging limitations of adeno-associated virus (AAV), the leading vector for in vivo gene therapy, which has a constrained capacity of <4.7 kb [47]. This limitation severely restricts the clinical application of most CRISPR-Cas systems, as commonly used nucleases like Streptococcus pyogenes Cas9 (SpCas9) approach or exceed this size when combined with their guide RNAs and regulatory elements [48].
The field has responded to this challenge through two complementary innovative strategies: the identification and engineering of compact Cas orthologs that can be packaged alongside their guide RNAs into single AAV vectors, and the development of sophisticated dual AAV systems that split larger Cas proteins across two vectors for reconstitution in target cells. These advances are crucial for enabling both in vivo gene therapy (where editing components are delivered directly into the patient's body) and ex vivo approaches (where cells are edited outside the body before transplantation) [1] [37]. This technical guide examines the latest developments in both strategies, providing researchers with a comprehensive resource for selecting and implementing these systems in their therapeutic development pipelines.
Compact CRISPR-Cas Orthologs for Single AAV Delivery
The Size Advantage of Compact Cas Proteins
Compact Cas orthologs are naturally occurring or engineered variants that are sufficiently small to be packaged into a single AAV vector alongside their guide RNA and regulatory elements. This section details the most promising compact Cas systems currently advancing the field.
Table 1: Comparison of Compact Cas Orthologs for AAV Delivery
| Cas Protein | Size (aa/kb) | PAM Sequence | Editing Efficiency | Key Advantages | Primary Applications |
|---|---|---|---|---|---|
| EbCas12a | 1158 aa/~3.47 kb | 5'-TTTV-3' (V = A, G, C) | ~1.9x higher than wild-type EbCas12a | Smallest Cas12a ortholog; T-rich PAM | All-in-one AAV delivery for gene therapy |
| enEbCas12a (D141R) | 1158 aa/~3.47 kb | 5'-TTTV-3' (V = A, G, C) | Comparable to AsCas12a and LbCas12a | Enhanced activity with high specificity | High-fidelity genome editing in mammalian cells |
| SpaCas9 | ~3.3 kb | 5'-NNGYRA-3' | Efficient disruption in mouse embryos | Distinct PAM recognition from other small Cas9s | Base editing (CBE, ABE) in adult mouse liver |
| Cas9d (MG34-1) | 747 aa | NGG | Up to 22% base editing efficiency | High-fidelity nuclease with novel sgRNA scaffold | Single AAV delivery for diverse editing applications |
Enhanced EbCas12a: A Case Study in Ortholog Engineering
The engineering of EbCas12a from an unclassified Erysipelotrichia species represents a landmark achievement in compact nuclease development. With only 1158 amino acids (~3.47 kb), it is the smallest known Cas12a ortholog identified to date [47]. Initial characterization revealed that wild-type EbCas12a possesses DNA cleavage activity both in vitro and in mammalian cells, recognizing a T-rich PAM sequence (5'-TTTV-3') that complements the G-rich PAMs of many Cas9 variants.
To enhance its therapeutic potential, researchers introduced a single point mutation (D141R) to create enhanced EbCas12a (enEbCas12a). This variant demonstrates approximately 1.9-fold higher editing efficiency than the wild-type enzyme, with comparable performance to AsCas12a and LbCas12a at multiple genomic loci in mammalian cells [47]. GUIDE-seq analysis confirmed that enEbCas12a maintains high specificity with low off-target effects, addressing a critical concern for therapeutic applications.
The compact size of enEbCas12a enables the development of an all-in-one AAV delivery system where the nuclease and its crRNA can be packaged into a single AAV vector. This system has demonstrated efficient editing in both in vitro and in vivo models, representing a significant advancement for Cas12a-based therapeutics [47].
SpaCas9 and Cas9d: Expanding the PAM Diversity of Compact Systems
Beyond EbCas12a, other compact Cas orthologs offer distinct PAM specificities that expand the targetable genomic landscape. SpaCas9, derived from Streptococcus pasteurianus, recognizes a unique 5'-NNGYRA-3' PAM, distinct from other small Cas9 orthologs [49]. This PAM preference enables targeting of genomic sites inaccessible to other compact systems. SpaCas9 has been successfully deployed for both knockout and base editing applications in adult mouse liver, demonstrating its therapeutic potential for metabolic disorders.
Similarly, Cas9d (MG34-1) represents a particularly compact type II-D Cas9 ortholog from Deltaproteobacteria. At only 747 amino acids, it employs a novel sgRNA scaffold that coordinates with its REC domain to form a specialized "RNA-coordinated target Engagement Module" (REM) [50]. This unique architecture contributes to its high fidelity and precise mismatch discrimination, making it an attractive option for therapeutic applications where off-target editing must be minimized.
Dual AAV Systems for Delivering Large Payloads
Overcoming Packaging Limitations Through Split Systems
For Cas proteins that exceed AAV packaging constraints even in their compact forms, dual AAV approaches provide an effective alternative. These systems split the coding sequence of large nucleases between two separate AAV vectors, which recombine or reconstitute in target cells to produce functional proteins. The three primary strategies for dual AAV systems include DNA trans-splicing, protein trans-splicing (intein-based), and mRNA trans-splicing.
Table 2: Comparison of Dual AAV System Approaches
| Approach | Mechanism | Reconstitution Efficiency | Advantages | Limitations |
|---|---|---|---|---|
| DNA Trans-splicing | Homologous recombination between two AAV genomes | Low to moderate | Simple design | Efficiency depends on homologous recombination rates |
| Protein Trans-splicing (Intein) | Protein splicing via split intein domains | High | Potentially high efficiency | Limited by split site availability; produces intein fragments |
| mRNA Trans-splicing (REVeRT) | Splicing of separate mRNA transcripts | High (up to 44% in vitro) | Flexible split site selection; no foreign protein fragments | Requires optimized splice sites and binding domains |
REVeRT: mRNA Trans-Splicing for Flexible Reconstitution
The REVeRT (Reconstitution Via mRNA Trans-splicing) technology represents a significant advancement in dual AAV systems. This approach utilizes optimized splice sites and complementary binding domains to facilitate trans-splicing between two separate mRNA molecules, resulting in reconstitution of the full-length protein [51].
Key optimization parameters for REVeRT include:
- Binding Domains: Modified lacZ sequences without homology to human or mouse genomes minimize off-target effects while enhancing reconstitution efficiency (up to 44% in flow cytometry and 53.5% in western blot quantifications) [51].
- Splice Site Selection: The strength and composition of splice acceptor sites significantly impact reconstitution efficiency, with CAG|GT identified as an optimal split site sequence.
- Promoter Requirements: Both 5' and 3' fragments require independent promoters, confirming that reconstitution occurs at the mRNA level rather than through DNA recombination.
REVeRT has successfully reconstituted large genes including ABCA4 (implicated in Stargardt disease) and various CRISPRa modules in multiple mouse tissues following different administration routes [51]. This flexibility and efficiency make it particularly valuable for both basic research and clinical applications.
Split-Cas9 Systems for Epigenome Engineering
Dual AAV systems have also enabled epigenome engineering applications using catalytically dead Cas9 (dCas9) fused to transcriptional effector domains. By splitting dCas9 between two vectors, researchers have created modular platforms for targeted gene repression (CRISPRi) and activation (CRISPRa) [52].
This system was applied to target retinitis pigmentosa in a mouse model through repression of the Nrl gene, a master regulator of rod photoreceptor determination. Nrl knockdown mediated reprogramming of rod cells into cone-like cells resistant to disease-specific mutations, demonstrating the therapeutic potential of this approach [52]. The dual AAV format accommodated not only the split-dCas9 but also additional effector domains (KRAB for repression, VP64+rTA for activation) that would exceed the packaging capacity of a single vector.
Experimental Protocols for Key Applications
Protocol: All-in-One AAV Delivery of enEbCas12a
Objective: To achieve efficient genome editing in mammalian cells using a single AAV vector delivering enEbCas12a and its crRNA.
Materials:
- enEbCas12a expression cassette (including crRNA sequence)
- AAV packaging system (e.g., AAV-DJ or AAV8 serotypes)
- HEK293T cells or target primary cells
- Transfection reagents (for initial validation)
- T7E1 assay or targeted deep sequencing reagents for efficiency assessment
Methodology:
- Vector Construction: Clone the enEbCas12a coding sequence (with D141R mutation) and crRNA expression cassette into an AAV transfer plasmid, ensuring the total size remains under 4.7 kb.
- Virus Production: Package the construct into AAV particles using standard AAV production protocols.
- Cell Transduction: Transduce target cells with AAV-enEbCas12a at appropriate MOI (typically 10^4-10^5 vg/cell).
- Editing Assessment: Harvest cells 72-96 hours post-transduction and extract genomic DNA.
- Efficiency Quantification:
- Perform T7E1 assay on PCR-amplified target regions
- Confirm results with targeted deep sequencing (recommended for off-target assessment)
- Functional Validation: Assess phenotypic consequences of editing as appropriate for your target gene.
Key Optimization Parameters:
- crRNA spacer length should be 21-25 nt for optimal activity [47]
- Utilize the cognate direct repeat or Lb2 direct repeat for highest efficiency
- Validate PAM requirement (5'-TTTV-3') for your target sequence
Protocol: Dual AAV REVeRT for Large Gene Reconstitution
Objective: To reconstitute large Cas effectors or therapeutic genes using the REVeRT dual AAV system.
Materials:
- 5' and 3' split fragments with optimized binding domains and splice sites
- AAV vectors (serotype selected for your target tissue)
- Target cells or animal model
- Luciferase or fluorescent reporter systems for efficiency monitoring
Methodology:
- Split Site Selection: Identify potential split sites containing AGG minimal consensus sequence; synonymous codons can be used to create optimal split sites without altering the protein sequence.
- Vector Construction:
- Clone 5' fragment with promoter, complementary binding domain, and splice donor
- Clone 3' fragment with complementary binding domain, splice acceptor, and polyA signal
- System Validation:
- Co-transfect split constructs into HEK293T cells
- Assess reconstitution efficiency via western blot or functional assays
- AAV Production: Package optimized constructs into AAV vectors.
- In Vivo Delivery: Co-administer both AAVs to target tissue (e.g., subretinal injection for retinal applications, intravenous for hepatic targets).
- Efficiency Assessment: Quantify reconstitution 2-4 weeks post-injection using:
- Western blot for protein expression
- Functional assays (editing efficiency, gene activation/repression)
- Immunohistochemistry for tissue-specific expression
Critical Considerations:
- The splice acceptor site strength significantly impacts efficiency; use the optimized SAS identified in [51]
- Both split fragments require independent promoters for efficient reconstitution
- Binding domains should be devoid of homology to the target species genome to minimize off-target effects
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Compact Cas and Dual AAV Systems
| Reagent/Category | Specific Examples | Function/Application | Technical Notes |
|---|---|---|---|
| Compact Cas Orthologs | EbCas12a, enEbCas12a, SpaCas9, Cas9d | Genome editing in size-constrained contexts | Select based on PAM availability and editing requirements |
| Dual AAV Systems | REVeRT Vectors, Split-Intein Systems, DNA Trans-splicing Vectors | Delivery of large genetic payloads | REVeRT offers greatest flexibility in split site selection |
| AAV Serotypes | AAV8, AAV-DJ, AAV8(Y733F) | Tissue-specific targeting in vivo | AAV8 for liver; AAV8(Y733F) for retinal applications |
| Efficiency Reporters | Split-Luciferase, Split-Fluorophores (Cerulean, Citrine) | Quantifying reconstitution efficiency | Enable rapid optimization of delivery parameters |
| Editing Assessment Tools | T7E1 Assay, Targeted Deep Sequencing, GUIDE-seq | Quantifying on-target and off-target editing | GUIDE-seq provides genome-wide off-target profiling |
Comparative Analysis of Delivery Approaches
The selection between compact single-AAV systems and dual-AAV approaches involves careful consideration of multiple factors. Compact orthologs offer simplicity and potentially higher efficiency due to single-vector delivery, but may have limitations in PAM availability or editing efficiency compared to larger counterparts. Dual AAV systems enable the use of optimized, larger Cas proteins with potentially superior characteristics, but introduce complexity in production and potential efficiency losses due to reconstitution requirements.
For target tissues with high AAV uptake, such as liver and retina, dual AAV systems have demonstrated robust efficacy. For applications where delivery efficiency is limiting, compact single-AAV systems may provide advantages. Recent advances in both strategies have significantly narrowed the performance gap between these approaches and traditional plasmid-based delivery.
Visualizing Experimental Workflows and System Architectures
Diagram Title: CRISPR Delivery System Architectures
The development of compact Cas orthologs and dual AAV systems represents significant progress in overcoming the critical delivery challenges that have limited the clinical translation of CRISPR-based therapies. These innovations have expanded the therapeutic window for both in vivo and ex vivo applications, enabling researchers to address previously inaccessible genomic targets.
Future developments in this field will likely focus on further optimizing the efficiency and specificity of both compact nucleases and reconstitution systems, expanding the PAM diversity of compact variants, and developing next-generation delivery vectors with enhanced tissue specificity and packaging capacity. As these technologies mature, they will continue to blur the distinction between what is possible in vitro versus in vivo, ultimately enabling more effective and accessible CRISPR-based therapies for a broad range of human diseases.
The integration of these delivery innovations with emerging editing modalities, particularly base editing and prime editing, represents a particularly promising direction for next-generation therapeutics that can achieve precise genomic modifications without requiring double-strand breaks. Through continued refinement of both the molecular tools and their delivery vehicles, the field moves closer to realizing the full potential of precision genetic medicine.
Technical Hurdles and Optimization Strategies for Clinical Translation
The advent of CRISPR-Cas9 genome editing has revolutionized biomedical research and therapeutic development, offering unprecedented potential for treating genetic disorders. However, this powerful technology carries inherent safety considerations that must be thoroughly addressed for successful clinical translation. Off-target effects and structural variations represent two critical classes of unintended genomic alterations that pose significant challenges for therapeutic applications [53] [7]. These genotoxic events can disrupt normal gene function and regulation, with potential consequences including oncogenic transformation [54]. The safety profile of CRISPR-based therapies must be evaluated within the context of their application, as the balance of risks and benefits differs considerably between in vivo approaches (where editing occurs directly within the patient's body) and ex vivo strategies (where cells are edited outside the body before transplantation) [55]. This technical guide examines the mechanisms, detection methodologies, and mitigation strategies for these unintended editing outcomes, providing a framework for researchers and drug development professionals to advance CRISPR therapies with enhanced safety profiles.
Defining the Problem: Off-Target Effects and Structural Variations
Off-Target Effects (OTEs)
Off-target effects occur when the CRISPR-Cas9 system recognizes and cleaves genomic loci with sequence similarity to the intended target site. This phenomenon arises from the inherent biochemical flexibility of the Cas9-gRNA complex, which can tolerate mismatches, bulges, and non-canonical PAM sequences [54]. The mismatch tolerance of the Cas9-gRNA-DNA interaction allows for binding at sites with up to 5-7 base pair mismatches relative to the intended target, particularly when these mismatches are distributed in the distal region of the protospacer sequence [54]. Off-target activity is influenced by multiple factors including gRNA sequence composition, chromatin accessibility, epigenetic landscape, and cellular context [7] [54].
Structural Variations (SVs)
Beyond small indels, CRISPR-Cas9 editing can induce larger-scale genomic rearrangements collectively termed structural variations. These include:
- Large deletions (kilobase- to megabase-scale) at on-target sites [7] [56]
- Chromosomal translocations between simultaneously cleaved target and off-target sites [7]
- Chromosomal losses or truncations [7]
- Complex rearrangements including inversions and chromothripsis [7]
Recent evidence suggests that structural variations may represent a more pressing safety concern than traditional off-target mutations, particularly in therapeutic contexts where large numbers of cells are edited [7]. The use of DNA-PKcs inhibitors to enhance HDR efficiency has been shown to dramatically increase the frequency of these events, with one study reporting a thousand-fold increase in chromosomal translocations [7].
Table 1: Classification of Unintended CRISPR Editing Outcomes
| Category | Subtype | Definition | Potential Functional Impact |
|---|---|---|---|
| Off-Target Effects | Mismatch-mediated | Editing at sites with sequence similarity to target | Disruption of coding or regulatory elements |
| PAM-relaxed | Editing at sites with non-canonical PAM sequences | Alteration of tumor suppressor or oncogenes | |
| Structural Variations | Large deletions (>50 bp) | Removal of large genomic segments | Loss of regulatory elements or multiple genes |
| Chromosomal translocations | Exchange of genetic material between chromosomes | Generation of oncogenic fusion proteins | |
| Complex rearrangements | Multiple simultaneous rearrangements | Chromosomal instability |
Detection and Quantification Methodologies
Off-Target Detection assays
Comprehensive assessment of off-target activity requires a combination of in silico prediction and experimental validation. The following experimental approaches represent the current state-of-the-art for off-target profiling:
GUIDE-seq (Genome-wide, Unbiased Identification of DSBs Enabled by sequencing) employs double-stranded oligodeoxynucleotides to tag DNA double-strand breaks, enabling genome-wide mapping of CRISPR-Cas9 cleavage sites [57]. The experimental workflow involves: (1) Co-delivery of Cas9-gRNA RNP with dsODN tag into cells; (2) Integration of dsODN tags at DSB sites; (3) Tag-specific PCR amplification and next-generation sequencing; (4) Bioinformatics analysis to identify integration sites. This method provides sensitive, genome-wide detection of off-target sites but requires efficient delivery of the dsODN tag, which can be challenging in primary cells [57].
CIRCLE-seq (Circularization for In vitro Reporting of Cleavage Effects by Sequencing) is an in vitro approach that offers ultra-sensitive detection of potential off-target sites [57]. The protocol includes: (1) Isolation of genomic DNA and fragmentation; (2) Circularization of DNA fragments; (3) In vitro cleavage with Cas9-gRNA RNP; (4) Linearization of cleaved circles and sequencing library preparation. CIRCLE-seq provides exceptional sensitivity but may identify sites without cellular relevance due to the absence of chromatin structure [57].
DISCOVER-Seq (Discovery of In Situ Cas Off-Targets with Verification and Sequencing) leverages the endogenous DNA repair protein MRE11 to identify CRISPR-Cas9 cleavage sites in cellular contexts [57]. The method involves: (1) Editing of target cells; (2) Immunoprecipitation of MRE11-bound DNA fragments; (3) Sequencing and analysis. DISCOVER-Seq enables in situ identification of off-target sites while preserving native chromatin context [57].
Structural Variation Detection
Traditional short-read sequencing approaches frequently fail to detect large structural variations due to limited read length and amplification biases. Advanced methodologies have been developed to address this limitation:
CAST-Seq (CRISPR Affinity Selection in Sequencing) enables comprehensive detection of structural variations, including translocations, resulting from CRISPR-Cas9 cleavage [7]. The technique: (1) Uses biotinylated Cas9 to capture target and off-target regions; (2) Employs long-range PCR to amplify captured fragments; (3) Utilizes next-generation sequencing for identification; (4) Incorporates specialized bioinformatics pipelines to identify complex rearrangements.
Long-read sequencing technologies (PacBio SMRT sequencing and Oxford Nanopore) provide direct detection of structural variations without amplification biases [56]. These approaches: (1) Generate long reads (kb to Mb range) capable of spanning complex rearrangements; (2) Preserve epigenetic information; (3) Enable phased variant calling. A study in zebrafish using PacBio Sequel sequencing revealed that structural variants represented 6% of editing outcomes in founder larvae and could be inherited by subsequent generations [56].
Table 2: Detection Methods for Unintended CRISPR Edits
| Method | Detection Scope | Sensitivity | Advantages | Limitations |
|---|---|---|---|---|
| GUIDE-seq | Genome-wide DSBs | High (0.1-1%) | Unbiased, works in cells | Requires dsODN delivery |
| CIRCLE-seq | In vitro cleavage sites | Very High (<0.1%) | Ultra-sensitive, no delivery needed | No chromatin context |
| DISCOVER-Seq | Cellular DSBs | Moderate | In situ, native chromatin | Lower sensitivity |
| CAST-Seq | Structural variations | Moderate-High | Detects translocations, complex SVs | Targeted approach |
| Long-read sequencing | All variant types | Varies | Comprehensive SV detection | Higher cost, computational demand |
Diagram 1: DNA Repair Pathways and Outcomes. This diagram illustrates how CRISPR-induced double-strand breaks are processed through different DNA repair pathways, resulting in various editing outcomes. The diagram also shows how experimental modulation of DNA repair components can influence the generation of structural variations.
In Vivo vs. Ex Vivo Therapeutic Approaches: Comparative Safety Considerations
The safety considerations for off-target effects and structural variations differ significantly between in vivo and ex vivo therapeutic approaches, with implications for risk assessment and mitigation strategies.
Ex Vivo Editing Safety Profile
Ex vivo genome editing involves extracting cells from a patient, modifying them in controlled laboratory conditions, and then reinfusing the edited cells back into the patient. This approach offers several safety advantages:
- Selection capability: Edited cells can be screened and selected based on desired genetic and functional characteristics before transplantation [7] [4]
- Comprehensive characterization: Extensive molecular analyses can be performed to assess on-target efficiency, off-target effects, and structural variations
- Dose control: The exact number and purity of edited cells can be determined before administration
- Limited expansion: Only successfully edited cells are expanded, potentially reducing the impact of mosaic editing
The recently approved ex vivo therapy Casgevy (exa-cel) for sickle cell disease and β-thalassemia demonstrates this approach, where hematopoietic stem cells are edited to target the BCL11A gene [7] [4]. However, studies have revealed that editing at the BCL11A locus can produce frequent kilobase-scale deletions, warranting careful monitoring [7]. The mosaic nature of editing in founder cells presents a significant challenge, with zebrafish studies showing that adult founders are highly mosaic in their germ cells, and 26% of their offspring can carry off-target mutations [56].
In Vivo Editing Safety Profile
In vivo editing delivers CRISPR components directly to target tissues within the patient's body, presenting distinct safety challenges:
- Limited characterization: Comprehensive assessment of editing outcomes is challenging without tissue biopsy
- Delivery-associated toxicity: Viral vectors and lipid nanoparticles can induce immune responses and tissue-specific toxicity [4]
- Heterogeneous editing: Variable delivery efficiency across cell populations leads to mosaic editing
- Persistence concerns: Sustained expression of editing components increases the window for off-target activity
Recent clinical developments highlight both the promise and challenges of in vivo editing. Intellia Therapeutics' Phase I trial for hereditary transthyretin amyloidosis (hATTR) demonstrated successful in vivo editing using LNP delivery, with sustained reduction of TTR protein levels [4]. However, the recent pause in their Phase III trials due to a case of severe liver toxicity underscores the importance of continued safety evaluation [20]. The ability to redose LNP-based therapies (as demonstrated in both the hATTR trial and the personalized treatment for CPS1 deficiency) offers potential advantages for achieving therapeutic efficacy with lower individual doses [4].
Table 3: Safety Considerations in Ex Vivo vs. In Vivo Therapeutic Approaches
| Parameter | Ex Vivo Editing | In Vivo Editing |
|---|---|---|
| Off-target assessment | Comprehensive pre-transplant analysis possible | Limited to biopsy samples or surrogate tissues |
| Structural variation risk | Can be characterized before administration | Difficult to monitor in real-time |
| Mosaicism | Can be minimized through clonal selection | Inevitable due to delivery heterogeneity |
| Delivery concerns | Primarily electroporation or viral transduction | LNP, viral vectors with tissue tropism |
| Immune response | Limited to reinfused cells | Systemic immune activation possible |
| Mitigation strategies | Cell sorting, clonal selection, deep sequencing | Tissue-specific promoters, transient expression, dosing optimization |
| Clinical example | Casgevy for sickle cell disease [4] | Intellia's hATTR program [4] |
Mitigation Strategies and Safety by Design
gRNA Design and Selection
Careful gRNA design represents the first line of defense against off-target effects. Computational tools have been developed to predict both on-target efficiency and off-target potential:
- CRISPOR integrates multiple scoring algorithms and off-target prediction based on mismatch tolerance [57]
- DeepCRISPR employs deep learning to model gRNA on-target and off-target activities [57]
- Elevation uses a hierarchical Bayesian model to rank gRNAs based on specificity [57]
Best practices include selecting gRNAs with minimal sequence similarity to other genomic regions, avoiding stretches of high GC content, and considering genetic variation across populations that might create novel off-target sites [54].
High-Fidelity Cas Variants
Engineering of Cas9 nucleases with enhanced specificity has produced several high-fidelity variants:
- HiFi Cas9 maintains robust on-target activity while significantly reducing off-target cleavage [7] [57]
- eSpCas9(1.1) and SpCas9-HF1 incorporate mutations that destabilize non-specific DNA binding [57]
- Cas12a (Cpf1) offers an alternative nuclease with different PAM requirements and reduced off-target activity in some contexts [57]
While these variants reduce off-target activity, they do not eliminate the risk of structural variations and may still introduce substantial on-target aberrations [7].
Alternative Editing Platforms
Novel editing platforms that avoid double-strand breaks offer potential safety advantages:
- Base editors enable direct chemical conversion of one DNA base to another without DSBs [58]
- Prime editors use a reverse transcriptase-Cas9 nickase fusion to copy edited information from a template [58]
- Epigenetic editors modulate gene expression through targeted chromatin modifications without altering DNA sequence [20]
While these systems reduce the formation of indels and structural variations, they still exhibit off-target activity, including RNA off-target effects in the case of base editors [7].
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Assessing CRISPR Safety
| Reagent/Category | Function | Example Products/Assays |
|---|---|---|
| Off-target Prediction Tools | In silico gRNA design and specificity assessment | CRISPOR, ChopChop, Cas-OFFinder [57] |
| High-Fidelity Nucleases | Engineered Cas variants with reduced off-target activity | HiFi Cas9, eSpCas9(1.1), SpCas9-HF1 [7] [57] |
| Detection Kits | Experimental validation of off-target editing | GUIDE-seq, CIRCLE-seq, DISCOVER-Seq kits [57] |
| Structural Variation Assays | Detection of large genomic rearrangements | CAST-Seq, LAM-HTGTS, long-read sequencing [7] |
| Alternative Editors | Editing without double-strand breaks | ABE, CBE base editors; Prime editors [58] |
| Delivery Tools | Controlled expression of editing components | LNP formulations, AAV vectors with tissue-specific promoters [4] |
The therapeutic application of CRISPR-Cas9 genome editing requires careful consideration of off-target effects and structural variations. While significant progress has been made in detection methodologies and mitigation strategies, comprehensive safety assessment remains challenging, particularly for in vivo applications. The field is moving toward a safety-by-design approach, where gRNA selection, nuclease engineering, and delivery optimization are integrated from the earliest stages of therapeutic development. As the clinical experience with CRISPR therapies expands, continued refinement of safety assessment frameworks will be essential to balance therapeutic benefit with genomic risk. Regulatory agencies including the FDA and EMA now require comprehensive assessment of both on-target and off-target effects as well as evaluation of structural genomic integrity, emphasizing the critical importance of these safety considerations for clinical translation [7].
The therapeutic application of CRISPR-Cas9 gene editing fundamentally hinges on the efficient delivery of macromolecular complexes—the Cas nuclease and guide RNA—to specific target cells. The choice of delivery vector not only determines editing efficiency but also profoundly influences the host immune response and subsequent therapeutic flexibility. Within the broader context of in vivo versus ex vivo CRISPR therapy approaches, this dichotomy becomes paramount: ex vivo editing involves harvesting patient cells, modifying them outside the body, and reinfusing them (as seen with Casgevy for sickle cell disease), while in vivo editing delivers the CRISPR components directly into the patient's body [1]. The core challenge is that the vectors enabling in vivo delivery, particularly viral vectors, often trigger immune reactions that can compromise efficacy and safety, while non-viral alternatives like lipid nanoparticles (LNPs) offer a path to circumvent these limitations and enable novel treatment strategies, including redosing [59] [60].
Immune Responses to Viral Vectors
Viral vectors, evolved from naturally occurring viruses, are efficient gene transfer vehicles but are perceived by the host immune system as foreign invaders, leading to complex immune challenges.
Mechanisms of Immunity Against Viral Vectors
The immune response to viral vectors is a two-stage process, involving both innate and adaptive immunity.
- Innate Immune Activation: Upon systemic administration, viral vector components are recognized by pattern recognition receptors (PRRs) on immune cells. This triggers inflammatory signaling pathways, leading to the production of type I interferons (IFN-α/β) and other cytokines, which can create an antiviral state in surrounding tissues, reducing transduction efficiency [59]. For instance, adenoviral (Ad) vectors can induce potent innate responses within hours, including thrombocytopenia, endothelial cell activation, and fever [59].
- Adaptive Immune Activation: This antigen-specific response involves both T cells and B cells. Dendritic cells (DCs) play a pivotal role by engulfing vector particles or transduced cells, processing viral and transgene proteins, and presenting them to T cells. This can lead to:
- CD8+ Cytotoxic T Lymphocyte (CTL) Activation: These T cells can identify and lyse cells expressing viral capsid/envelope proteins or the therapeutic transgene product, eliminating the edited cells and curtailing long-term gene expression [59].
- CD4+ T Helper Cell Activation: These cells provide crucial signals for optimal CTL activation and B cell help.
- Neutralizing Antibody (NAB) Production: B cells produce antibodies specifically targeting the viral vector's capsid or envelope proteins. These NABs can bind to subsequent vector doses, preventing them from reaching target cells and rendering redosing ineffective [59].
Table 1: Comparative Immune Profiles of Major Viral Vector Platforms
| Vector | Innate Immunity | Pre-existing Immunity in Humans | Adaptive Immune Responses |
|---|---|---|---|
| Adenovirus (Ad) | Potent; triggers inflammatory cytokines, endothelial activation, thrombocytopenia [59] | High prevalence to common serotypes (e.g., AdHu5) [59] | Strong CD8+ T cell responses to viral genes/capsid; efficient NAB formation [59] |
| Adeno-Associated Virus (AAV) | Comparatively weak and transient; TLR9 signaling can promote CD8+ T cell responses [59] | Varies by serotype and geographic location; can be high [59] | CD8+ T cell responses to capsid; NAB formation; less efficient transgene immunity vs. Ad/LV [59] |
| Lentivirus (LV) | Strong IFN-α/β response limits transduction and drives adaptive immunity [59] | Generally low [59] | Efficient inducer of B and T cell responses to transgene; NABs to envelope [59] |
Consequences for In Vivo Gene Therapy
These immune responses present significant hurdles. Pre-existing immunity from natural infections can neutralize a vector before it delivers its payload. More importantly, the adaptive immune response to the capsid or transgene can lead to the elimination of transduced cells, resulting in a loss of therapeutic effect and posing a safety risk. This immune-mediated clearance is a primary reason why redosing with viral vectors is typically not feasible [59].
LNP Delivery and the Potential for Redosing
Lipid nanoparticles represent a non-viral alternative that has gained prominence, particularly for delivering RNA payloads, as demonstrated by their successful use in mRNA COVID-19 vaccines [61].
LNP Composition and Function
LNPs are sophisticated, multi-component systems where each lipid has a distinct role, as detailed in the table below.
Table 2: Core Components of CRISPR-Loaded Lipid Nanoparticles and Their Functions
| Lipid Component | Primary Function | Key Examples & Characteristics |
|---|---|---|
| Ionizable Lipid | - Encapsulates nucleic acids via charge interaction at low pH- Mediates endosomal escape via membrane fusion [61] | - ALC-0315 (Pfizer/BioNTech), SM-102 (Moderna)- pKa determines endosomal escape efficiency [61] |
| Phospholipid | - Provides structural integrity to the particle- Can influence membrane fusion (e.g., DOPE) [61] | - DSPC: Saturated, high melting temp (Tm), stable structure- DOPE: Unsaturated, cone-shaped, fusogenic [61] |
| Cholesterol | - Enhances membrane integrity and particle stability- Promotes endosomal release [61] | - Content (typically 30-50 mol %) critical for transfection [61] |
| PEGylated Lipid | - Shields LNP surface, reduces aggregation, extends circulation half-life- Modulates immunogenicity and tropism [61] | - ALC-0159 (Pfizer/BioNTech), PEG-DMG (Moderna)- Can impact liver tropism and uptake by immune cells [61] |
Clinical Proof-of-Concept for Redosing
The critical advantage of LNPs in the context of immune responses is their low immunogenicity profile. Unlike viral vectors, they do not typically elicit a strong, memory T cell or neutralizing antibody response against the particle itself. This inherent property opens the door for redosing.
Landmark clinical data from Intellia Therapeutics in June 2024 provided the first-ever clinical proof-of-concept for redosing an in vivo CRISPR therapy [60]. In their Phase 1 trial of NTLA-2001 for transthyretin (ATTR) amyloidosis, three patients who initially received a low dose (0.1 mg/kg) and achieved a 52% median reduction in serum TTR were later given a follow-on 55 mg dose. The results were groundbreaking:
- Efficacy: The redosing led to a 90% median reduction in serum TTR at day 28, achieving the target therapeutic effect that was missed with the initial low dose. The combined reduction from the original baseline was 95% [60].
- Safety: The 55 mg follow-on dose was well tolerated, with a safety profile consistent with the single-dose administration. Only one patient experienced a mild infusion-related reaction [60].
This demonstrates that LNP-based CRISPR delivery can enable an additive pharmacodynamic effect without triggering prohibitive immune responses against the delivery vehicle. This paradigm is further supported by the case of an infant with CPS1 deficiency who safely received three personalized LNP-CRISPR doses, with symptomatic improvement after each administration [4].
Figure 1: Immune Pathways and Redosing Potential of Viral Vectors vs. LNPs. Viral vectors often trigger adaptive immune responses that prevent effective redosing, while LNPs, with their lower immunogenicity, enable repeated administration for additive effects.
Quantitative Data Comparison: Viral Vectors vs. LNPs
The distinct biological behaviors of viral and LNP vectors translate into directly comparable quantitative outcomes, crucial for therapeutic decision-making.
Table 3: Comparative Quantitative Outcomes of Viral Vector and LNP-Based In Vivo Therapies
| Therapy / Vector | Therapeutic Indication | Key Efficacy Metric | Reported Outcome | Immune / Redosing Limitation |
|---|---|---|---|---|
| Exa-cel (Casgevy) [1]Ex vivo CRISPR | Sickle Cell Disease, Beta-Thalassemia | Patients free of severe vaso-occlusive crises | 59% (26 of 44) with ≥3 crises/year were crisis-free post-treatment [1] | N/A (Ex vivo) |
| Adenovirus Vector [59] | In vivo gene transfer (historical) | Durability of transgene expression | Transient expression; elimination of transduced cells by CTLs [59] | Redosing ineffective due to NABs |
| NTLA-2001 (Intellia) [60]LNP-CRISPR | hATTR Amyloidosis | Reduction in Serum TTR protein | ~90% reduction sustained at 2 years; 95% with redosing [60] | Redosing demonstrated; mild infusion reactions |
Experimental Protocols for Assessing Immune Responses
Robust preclinical assessment is critical for evaluating the immunogenicity and safety of CRISPR delivery vectors.
Protocol: Evaluating Adaptive Immune Responses to Viral Vectors
This protocol is designed to assess the potential for cell-mediated immunity against the vector and transgene in a murine model [59].
- Animal Dosing: Administer the viral vector (e.g., AAV, Ad) to immunocompetent mice via the intended clinical route (e.g., intravenous, intramuscular).
- Immune Cell Isolation: At a predetermined timepoint (e.g., 14-21 days post-dosing), harvest the spleen and draining lymph nodes.
- Antigen Re-stimulation: Isolate splenocytes and stimulate them in culture with overlapping peptide pools covering the viral capsid proteins or the therapeutic transgene product.
- T Cell Response Analysis:
- ELISpot Assay: Measure interferon-gamma (IFN-γ) production to quantify the number of antigen-specific T cells.
- Intracellular Cytokine Staining (ICS) with Flow Cytometry: Identify and characterize the specific T cell subsets (CD4+ vs. CD8+) responding to the antigens and the cytokines they produce (e.g., IFN-γ, TNF-α, IL-2).
- Humoral Response Analysis: Collect serum samples pre- and post-dosing to measure anti-capsid and anti-transgene neutralizing antibody (NAB) titers using a cell-based neutralization assay.
Protocol: Validating LNP Redosing Potential
This protocol evaluates whether an LNP formulation can be successfully readministered to achieve an enhanced or sustained therapeutic effect [60].
- Study Design: Implement a multi-arm, dose-escalation study in a relevant animal model of the disease.
- Arm 1: Single high dose of LNP-CRISPR.
- Arm 2: Initial low dose, followed by a higher secondary dose after a defined interval (e.g., 4-8 weeks).
- Control Arm: Placebo or control formulation.
- Pharmacodynamic (PD) Monitoring: Throughout the study, repeatedly measure a direct biomarker of the CRISPR editing effect. For liver-targeted therapies, this could be:
- Plasma protein levels (e.g., TTR for hATTR [60]).
- Target gene mRNA expression in biopsy samples.
- Direct sequencing of target tissue to quantify editing rates.
- Immunogenicity Assessment: Monitor for anti-LNP and anti-Cas9 antibodies in serum before and after each dose.
- Data Interpretation: Successful redosing is demonstrated if the second dose leads to a significant and additive improvement in the PD biomarker (e.g., a further 40-50% reduction in TTR [60]) without a loss of efficacy relative to the single high dose, and in the absence of high-titer neutralizing antibodies.
Figure 2: Integrated Workflow for Evaluating Vector Immunity and Redosing Potential. A strategic flowchart for profiling immune responses and determining the feasibility of redosing during therapeutic development.
The Scientist's Toolkit: Key Research Reagents and Materials
Advancing research in this field relies on a suite of specialized reagents and tools, as detailed below.
Table 4: Essential Research Reagents for Investigating Vector Immunity and LNP Performance
| Reagent / Tool | Primary Function | Application Example |
|---|---|---|
| Ionizable Lipids | Core component of LNPs for RNA encapsulation and endosomal escape [61] | SM-102, ALC-0315; used in clinical-stage LNP formulations [61]. |
| PEGylated Lipids | Stabilize LNPs, modulate pharmacokinetics and biodistribution [61] | ALC-0159, PEG-DMG; critical for controlling liver tropism and preventing rapid clearance [61]. |
| IFN-γ ELISpot Kit | Quantify antigen-specific T cell responses ex vivo [59] | Measure T cell reactivity to Cas9 protein or viral capsid peptides in splenocytes from dosed animals [59]. |
| Neutralization Assay | Titrate neutralizing antibodies (NABs) against viral vectors in serum [59] | Assess pre-existing immunity and NAB induction post-dosing using a vector encoding a reporter gene (e.g., luciferase) [59]. |
| CAST-Seq | Detect structural variations (SVs) and chromosomal translocations from CRISPR editing [7] | Comprehensive genotoxicity profiling for on-target and off-target analysis in preclinical development [7]. |
The CRISPR-Cas9 system has revolutionized genome engineering by providing researchers with an unprecedented ability to induce targeted double-strand breaks (DSBs) in the genome. The core of this technology centers on the Cas9 nuclease, which is directed by a single-guide RNA (sgRNA) to a specific genomic locus where it creates a DSB [62]. However, the ultimate editing outcome is not determined by the cleavage event itself, but by the cell's subsequent endogenous DNA repair machinery. Two primary pathways compete to repair these breaks: the error-prone non-homologous end joining (NHEJ) and the precise homology-directed repair (HDR) [62] [63]. The balance between these pathways fundamentally shapes the efficiency and fidelity of genome editing, making its understanding and modulation critical for both basic research and therapeutic applications, particularly within the context of developing in vivo versus ex vivo CRISPR-Cas9 therapies.
NHEJ operates throughout the cell cycle and functions by directly ligating the broken DNA ends, a process often accompanied by small insertions or deletions (indels) that can disrupt gene function [62] [64]. In contrast, HDR is largely restricted to the S and G2 phases of the cell cycle and utilizes a homologous DNA template to achieve precise, error-free repair, enabling specific nucleotide changes or gene insertions [63]. A major challenge in the field is that NHEJ is the predominant and more efficient pathway in most cellular contexts, while HDR remains relatively inefficient, especially in non-dividing cells such as neurons or photoreceptors [62] [65]. This technical brief provides an in-depth analysis of the mechanisms governing the HDR/NHEJ balance, quantitative assessments of editing efficiencies, and detailed methodologies for pathway modulation, specifically framed for scientists developing next-generation CRISPR therapies.
Molecular Mechanisms of DNA Repair Pathway Choice
The cellular decision to repair a Cas9-induced DSB via NHEJ or HDR is a highly regulated process involving a complex interplay of repair proteins, cell cycle checkpoints, and chromatin dynamics.
The Non-Homologous End Joining (NHEJ) Pathway
NHEJ is often described as the cell's "first responder" to DSBs. The process initiates when the Ku70/Ku80 heterodimer recognizes and binds to the broken DNA ends, forming a ring that encircles the DNA [62] [63]. This binding event serves two critical functions: it protects the DNA ends from excessive resection, and it recruits downstream NHEJ factors. The Ku complex subsequently promotes the binding of XRCC4 and DNA ligase IV, which catalyze the ligation of the DNA ends [62]. In many cases, the ends are not perfectly ligatable and require further processing. The DNA-dependent protein kinase catalytic subunit (DNA-PKcs) is recruited and activates the Artemis endonuclease to trim overhanging nucleotides, while polymerases Pol μ and Pol λ can fill in small gaps [62] [63]. This processing inherently makes NHEJ error-prone, frequently resulting in indels. NHEJ is active throughout all phases of the cell cycle, making it the default pathway in most cells, particularly in post-mitotic tissues targeted by in vivo therapies [64].
The Homology-Directed Repair (HDR) Pathway
HDR is a more complex, high-fidelity pathway that requires a template for repair. The initial step involves 5' to 3' end resection of the DNA break, a decisive event that commits the repair to a homology-based pathway [63]. The MRN complex (MRE11-RAD50-NBS1) and CtIP initiate the resection, which is then extended by nucleases like EXO1 and the BLM helicase [63]. This creates 3' single-stranded DNA (ssDNA) overhangs that are rapidly coated by Replication Protein A (RPA). The key HDR factor, RAD51, then displaces RPA to form a nucleoprotein filament that performs a homology search and invades the sister chromatid or an exogenously provided donor template, forming a D-loop structure [63]. DNA synthesis then occurs using the homologous sequence as a template, followed by resolution of the resulting structures to complete the precise repair. Crucially, HDR is highly dependent on the cell cycle, as it requires a sister chromatid template and is therefore primarily active in the S and G2 phases [63] [64].
Pathway Competition and Alternative Routes
The choice between NHEJ and HDR is not passive but involves active competition and reciprocal inhibition. Key regulatory proteins act as molecular switches. 53BP1 and RIF1 protect DNA ends from resection, thereby promoting NHEJ, whereas BRCA1 and CtIP antagonize 53BP1 to initiate resection and favor HDR [63] [64]. Beyond these two primary pathways, alternative repair mechanisms exist. Microhomology-Mediated End Joining (MMEJ), also known as Polymerase Theta-Mediated End-Joining (TMEJ), requires short microhomologies (2-20 bp) and is characterized by larger deletions [63]. MMEJ shares the initial resection step with HDR but then follows a distinct, error-prone repair process mediated by Polymerase θ (POLQ) and PARP1 [63]. The following diagram illustrates the key steps and regulatory nodes in these competing pathways.
Diagram: Competing DNA Repair Pathways after a CRISPR-Cas9-Induced Double-Strand Break (DSB). The cellular response to a DSB involves a critical decision point between end protection (favoring NHEJ) and end resection (favoring HDR or MMEJ). Key regulatory proteins like 53BP1 and BRCA1 act as molecular switches to control this balance [62] [63] [64].
Quantitative Analysis of HDR vs. NHEJ Efficiencies
The inherent competition between DNA repair pathways results in starkly different efficiencies for precise versus error-prone editing. The following table summarizes key quantitative data and factors influencing HDR and NHEJ outcomes, essential for planning both ex vivo and in vivo therapeutic strategies.
Table 1: Quantitative Comparison of HDR and NHEJ Editing Efficiencies
| Parameter | HDR (Homology-Directed Repair) | NHEJ (Non-Homologous End Joining) |
|---|---|---|
| Typical Efficiency | Generally low (often <10-30% in optimal conditions) [65] | High (can often exceed 70-80% in many cell types) [66] |
| Cell Cycle Dependence | Restricted to S/G2 phases [63] [64] | Active throughout all cell cycle phases (G0, G1, S, G2) [62] |
| Primary Applications | Precise gene correction, knock-in of tags/transgenes, nucleotide substitutions [62] [67] | Gene knock-out, functional gene disruption, frameshift mutation introduction [66] |
| Key Limiting Factors | Low efficiency in post-mitotic cells; competition from NHEJ/MMEJ; need for donor template delivery [62] [65] | Error-prone nature unsuitable for precise correction; can generate a spectrum of indels [62] |
| Impact of Modulation | Small molecules (e.g., RS-1) can enhance HDR 2-3 fold; NHEJ inhibition can boost HDR efficiency [62] [63] | Small molecules (e.g., Repsox) can enhance NHEJ efficiency 1.5-3 fold in some systems [66] |
The data in Table 1 underscores the fundamental challenge in precision genome editing: HDR is intrinsically less efficient than NHEJ. This is particularly problematic for in vivo therapies targeting post-mitotic cells like neurons or photoreceptors, where the cell cycle restriction of HDR presents a major barrier [65]. In contrast, ex vivo applications allow for cell cycle synchronization to enrich for HDR-permissive cells, providing a significant strategic advantage for precise editing.
Experimental Modulation of the HDR/NHEJ Balance
A primary focus of CRISPR research is developing methods to skew the DNA repair balance toward the desired pathway. The strategies below represent the most current and effective approaches, complete with experimental considerations.
Strategies for Enhancing HDR Efficiency
1. Pharmacological Inhibition of NHEJ Key Proteins The transient inhibition of core NHEJ factors is a widely used strategy to reduce competition and enhance HDR.
- Target: DNA-PKcs, a critical kinase in the NHEJ pathway.
- Reagents: Small molecule inhibitors such as AZD7648 and NU7441.
- Protocol: Treat cells with the inhibitor (e.g., 1 µM AZD7648) at the time of or shortly after CRISPR-Cas9 delivery. Maintain the inhibitor in the culture medium for 12-24 hours post-transfection [63].
- Considerations: A critical safety warning is necessary here. Recent studies reveal that DNA-PKcs inhibitors, while boosting HDR, can lead to severe unintended consequences, including kilobase- to megabase-scale deletions and a marked increase in chromosomal translocations [7]. These findings, detectable only with long-read sequencing or specialized assays like CAST-Seq, suggest that the use of these inhibitors, particularly for therapeutic applications, requires extreme caution and comprehensive genomic integrity assessment.
2. Pharmacological Activation of HDR and Cell Cycle Synchronization
- Target: HDR pathway proteins and cell cycle regulation.
- Reagents: RS-1 (a RAD51 stimulator); CR8 (a CDK inhibitor for cell cycle synchronization in S/G2).
- Protocol: For CR8 synchronization, treat cells with 10 µM CR8 for 16-24 hours prior to transfection/electroporation. Transfect cells while still in the presence of the drug. For RS-1, use a concentration range of 5-10 µM during or after Cas9 delivery [63].
- Efficacy: These strategies can yield a 2- to 3-fold increase in HDR efficiency, though results are highly cell-type dependent [62].
3. Engineered Cas9 Fusion Proteins This strategy involves fusing Cas9 to proteins that directly recruit or enhance HDR factors, creating a localized effect.
- Protocol: Utilize plasmids or mRNA encoding fusion proteins such as Cas9-DN1S (a dominant-negative 53BP1 fragment) or Cas9-RAD51 [63]. Co-deliver the fusion construct along with the sgRNA and donor template.
- Advantage: This approach provides spatial and temporal control over repair modulation, potentially reducing genome-wide risks associated with small molecule inhibitors.
Strategies for Enhancing NHEJ Efficiency
For applications requiring gene knock-out, enhancing NHEJ efficiency is desirable.
- Target: TGF-β signaling and other regulatory nodes.
- Reagents: Repsox (a TGF-β signaling inhibitor).
- Protocol: Add Repsox at its optimal concentration (e.g., 5-10 µM) to the cell culture medium immediately after electroporation of CRISPR components (RNP or plasmid). Continue treatment for 48-72 hours [66].
- Efficacy: In porcine PK15 cells, Repsox increased NHEJ-mediated editing efficiency by up to 3.16-fold in RNP delivery systems. Mechanistic studies showed it acts by reducing the expression of SMAD2, SMAD3, and SMAD4 in the TGF-β pathway [66].
The following workflow diagram integrates these modulation strategies into a coherent experimental plan.
Diagram: Experimental Workflow for Modulating DNA Repair Pathways. This workflow guides researchers in selecting the appropriate modulation strategy based on their editing goal, highlighting the critical safety consideration when using potent NHEJ inhibitors to enhance HDR [66] [63] [7].
The Scientist's Toolkit: Key Reagents for Repair Pathway Modulation
Table 2: Essential Research Reagents for HDR and NHEJ Modulation
| Reagent / Tool | Primary Function | Key Considerations & Applications |
|---|---|---|
| AZD7648 | DNA-PKcs inhibitor; suppresses NHEJ to enhance HDR [63] [7] | High-Risk Alert: Associated with increased genomic structural variations (SVs); requires long-read sequencing for safety validation. Use with caution. |
| Repsox | TGF-β signaling inhibitor; enhances NHEJ efficiency [66] | Shown to increase NHEJ efficiency >3-fold in porcine cells. Ideal for robust gene knockout projects. |
| RS-1 | RAD51 stimulator; enhances the strand invasion step of HDR [62] [63] | Can provide a modest HDR boost. Often used in combination with other HDR-enhancing strategies. |
| Cas9-DN1S Fusion | Engineered Cas9 fused to a dominant-negative 53BP1 fragment; locally inhibits NHEJ [63] | Offers a more targeted approach to HDR enhancement, potentially reducing off-target genomic effects. |
| CR8 | CDK inhibitor; synchronizes cells in S/G2 phase where HDR is active [63] | Highly effective for ex vivo editing. Not applicable for in vivo therapies targeting non-dividing cells. |
| ssODN | Single-stranded oligodeoxynucleotide; serves as a donor template for HDR [64] | Optimal for introducing point mutations or short tags. Must contain homologous arms (typically 60-90 nt). |
Therapeutic Implications: In Vivo vs. Ex Vivo Perspectives
The choice between HDR and NHEJ strategies, and the ability to modulate them, has profound implications for therapeutic development, directly influencing the decision to pursue in vivo or ex vivo therapy paradigms.
Ex Vivo Gene Therapy: This approach involves editing cells outside the patient's body, followed by autologous transplant. It is highly amenable to HDR-based strategies because it allows for precise control over the editing environment. Researchers can use cell cycle synchronization, small molecule modulators, and, most importantly, clonal selection to isolate and expand the rare cells that have undergone a perfect HDR event [65]. This is the basis for therapies like exa-cel (Casgevy), where hematopoietic stem cells are edited ex vivo to reactivate fetal hemoglobin.
In Vivo Gene Therapy: This approach involves delivering CRISPR components directly to the patient's body to edit cells in situ. For most tissues, this paradigm heavily favors NHEJ-based strategies. The reasons are twofold: First, the majority of target cells for adult-onset diseases (e.g., photoreceptors in retinal dystrophy, neurons in neurological disorders) are post-mitotic, rendering HDR largely inaccessible [65]. Second, the safety concerns associated with systemic delivery of NHEJ-inhibiting small molecules like AZD7648, which can cause widespread genomic instability, are currently prohibitive [7]. Consequently, in vivo therapies are currently focused on NHEJ-mediated gene knock-out (e.g., ablation of a dominant mutant allele like RHO P23H in retinitis pigmentosa) or HDR-independent methods like base and prime editing [65].
A critical consideration for both approaches is the risk of structural variations (SVs). Techniques that rely on DSBs, particularly when combined with repair modulators, can result in large, on-target deletions and chromosomal translocations that are invisible to standard short-read sequencing [7]. Therefore, comprehensive off-target and, crucially, on-target analysis using SV-detection methods is non-negotiable for clinical translation.
The balance between HDR and NHEJ is a central determinant of success in CRISPR-Cas9 genome editing. While significant progress has been made in developing strategies to modulate this balance, the current state of the field reveals a clear divergence in therapeutic application. Ex vivo therapies, with their capacity for environmental control and clonal selection, are the primary beneficiaries of advanced HDR-enhancing techniques. In contrast, in vivo therapies currently rely on the inherent efficiency of NHEJ or on the development of DSB-free editing technologies. As our understanding of tissue-specific DNA repair mechanisms deepens [64], and as safer, more precise modulation tools emerge—such as cell cycle-independent HDR enhancers or more localized Cas9 fusions—the gap between these two paradigms may narrow. For now, a meticulous and context-aware approach to manipulating the HDR/NHEJ axis, coupled with rigorous genomic safety assessment, remains the cornerstone of responsible and effective CRISPR-based therapeutic development.
The transition from personalized therapies to scalable platform technologies represents a central challenge in CRISPR-Cas9 clinical development. This paradigm spans two distinct approaches: ex vivo therapies, where patient cells are edited outside the body and reinfused, and in vivo therapies, where editing components are delivered directly into the patient's body [4] [22]. While the first approved CRISPR-based therapy, Casgevy (exa-cel) for sickle cell disease and transfusion-dependent beta thalassemia, demonstrates the remarkable potential of ex vivo editing, its personalized nature presents significant manufacturing complexities [4]. Conversely, in vivo approaches aim for a more streamlined "off-the-shelf" model but face substantial delivery and safety hurdles. The emerging landscape in 2025 reflects both significant progress and sobering challenges, where scientific advancement intersects with market forces that have reduced venture capital investment in biotechnology, leading companies to narrow their pipelines and focus on getting a smaller set of products to market quickly [4]. This review examines the technical and manufacturing considerations for scaling both therapeutic paradigms, providing researchers and drug development professionals with a comprehensive analysis of current methodologies, quantitative comparisons, and future directions.
Technical Comparison: Ex Vivo versus In Vivo Therapeutic Approaches
The fundamental distinction between ex vivo and in vivo CRISPR therapies dictates their respective manufacturing workflows, scalability potential, and clinical applications.
Ex Vivo Manufacturing involves harvesting specific cell types (typically hematopoietic stem cells or T-cells) from a patient, genetically modifying them in a controlled laboratory environment, and then reinfusing the edited cells back into the patient [4] [31]. This approach offers precise control over editing efficiency and thorough quality control testing before patient administration. The ex vivo process is inherently personalized, as each batch is manufactured from a single patient's cells, creating significant scalability challenges and high costs [4]. Casgevy exemplifies this approach, requiring complex logistics including cell collection, shipment to manufacturing facilities, editing, expansion, and reinfusion.
In Vivo Manufacturing involves delivering CRISPR components directly to target cells inside the patient's body, typically using viral vectors or lipid nanoparticles (LNPs) [4] [13] [24]. This approach aims for a more traditional pharmaceutical model where a standardized therapy can be administered to multiple patients, offering greater potential for scalability and reduced costs. However, in vivo delivery presents substantial challenges in targeting specificity, immune response management, and ensuring efficient editing in the correct tissues [24] [22]. A landmark 2025 case demonstrated the potential of personalized in vivo therapy, where researchers developed a bespoke CRISPR treatment for an infant with CPS1 deficiency in just six months, delivered via lipid nanoparticles [4].
Table 1: Comparative Analysis of Ex Vivo vs. In Vivo CRISPR Therapies
| Characteristic | Ex Vivo Approach | In Vivo Approach |
|---|---|---|
| Manufacturing Process | Cells edited outside body, then reinfused | CRISPR components delivered directly to target cells in body |
| Scalability Potential | Lower (patient-specific) | Higher (standardized therapy) |
| Key Delivery Methods | Electroporation, viral transduction [24] | Lipid nanoparticles (LNPs), viral vectors (AAV) [4] [13] |
| Editing Control | High (controlled environment) | Moderate (influenced by host biology) |
| Major Challenges | Complex logistics, high cost, cell viability [4] | Delivery specificity, immune responses, off-target concerns [24] [22] |
| Therapeutic Examples | Casgevy (SCD, TBT), CAR-T cell therapies [4] [68] | Intellia's hATTR program, personalized CPS1 deficiency treatment [4] |
Quantitative Data Analysis: Manufacturing and Clinical Outcomes
Recent clinical data provides critical insights into the efficiency and scalability of both therapeutic approaches. The following table summarizes key quantitative metrics from prominent clinical programs and trials.
Table 2: Quantitative Manufacturing and Clinical Outcomes of CRISPR Therapies
| Therapy/Platform | Therapeutic Area | Editing Efficiency/Reduction | Dosing Regimen | Manufacturing Timeline | Key Scalability Metrics |
|---|---|---|---|---|---|
| Casgevy (exa-cel) | SCD, TBT [4] | Not specified in results | Single infusion of edited cells | Several weeks (personalized) | 50 active treatment sites globally; challenges with reimbursement and cost [4] |
| Nexiguran ziclumeran (nex-z) | hATTR amyloidosis [4] | ~90% reduction in TTR protein levels [4] | Single IV infusion (potential for redosing) | Standard pharmaceutical manufacturing | Phase 3 trials initiated; global recruitment of 500+ participants planned [4] |
| Personalized CPS1 Therapy | Rare genetic disorder (CPS1 deficiency) [4] | Improvement with each dose (quantitative data not specified) | Three LNP doses via IV infusion | 6 months from development to delivery | Proof-of-concept for rapid personalized in vivo therapy [4] |
| HAE Therapy (Intellia) | Hereditary angioedema [4] | 86% reduction in kallikrein; 8 of 11 patients attack-free at 16 weeks [4] | Single IV infusion (higher dose group) | Not specified in results | Phase I/II trial demonstrates potential for one-time treatment [4] |
| SyNTase Editor (AATD) | Alpha-1 Antitrypsin Deficiency [69] | Up to 95% editing in vitro; >70% mRNA correction in vivo [69] | Single IV dose (≤0.5 mg/kg) | Not specified in results | AI-guided platform with potential for multiple monogenic disorders [69] |
Diagram 1: Manufacturing workflows for ex vivo and in vivo CRISPR therapies illustrate the fundamental differences between personalized and platform approaches.
Experimental Protocols and Methodologies
Ex Vivo CAR-T Cell Manufacturing Protocol
The development of non-viral PD1-integrated CAR-T therapy (BRL-201) demonstrates an efficient ex vivo manufacturing protocol that has produced durable remissions in lymphoma patients [68]:
- Leukapheresis: Isolate peripheral blood mononuclear cells (PBMCs) from patient blood.
- T-cell Activation: Activate T-cells using anti-CD3/CD28 antibodies in X-VIVO 15 media supplemented with 5% human AB serum and 300 IU/mL IL-2.
- CRISPR Editing:
- Prepare CRISPR-Cas9 ribonucleoprotein (RNP) complex by combining 60 µg of high-fidelity Cas9 protein with 30 µg of synthetic sgRNA targeting the PD1 locus.
- Transfect activated T-cells via electroporation (Neon Transfection System, 1600V, 10ms, 3 pulses).
- Simultaneously introduce AAV6 donor vector containing anti-CD19 CAR cassette.
- Cell Expansion: Culture edited cells in G-Rex bioreactors for 10-14 days with continuous cytokine support.
- Quality Control:
- Assess editing efficiency via flow cytometry for PD1 knockout and CAR expression.
- Perform targeted deep sequencing (≥5000x coverage) to profile potential off-target effects.
- Validate functional activity through cytokine release and cytotoxicity assays against CD19+ target cells.
- Formulation and Infusion: Harvest cells, formulate in Lactated Ringer's solution, and reinfuse into lymphodepleted patients.
In Vivo LNP Delivery Protocol
Intellia Therapeutics' Phase I trial for hereditary transthyretin amyloidosis (hATTR) established a standardized protocol for systemic in vivo CRISPR delivery [4]:
- LNP Formulation:
- Encapsulate CRISPR-Cas9 mRNA and sgRNA targeting the TTR gene in ionizable lipid nanoparticles (LNPs) comprising proprietary lipid, DSPC, cholesterol, and PEG-lipid at molar ratio 50:10:38.5:1.5.
- Adjust total RNA concentration to 0.5 mg/mL in phosphate-buffered saline, pH 7.4.
- Filter sterilize through 0.22 µm membrane and store at -80°C until use.
- Characterization:
- Determine particle size (target: 70-100 nm) and polydispersity index (<0.2) via dynamic light scattering.
- Measure encapsulation efficiency (>95%) using RiboGreen assay.
- Administration:
- Premedicate patients with glucocorticoid, antihistamine, and acetaminophen to mitigate infusion-related reactions.
- Administer LNP formulation via intravenous infusion over 2-4 hours at dose levels ranging from 0.1-0.5 mg/kg.
- Monitor vital signs continuously during infusion and for 24 hours post-infusion.
- Efficacy Assessment:
- Quantify serum TTR protein levels monthly via immunoturbidimetric assay.
- Evaluate clinical outcomes using neuropathy impairment scores and quality of life measures.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for CRISPR Therapy Development
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| CRISPR Nucleases | SpCas9, hfCas12Max [13], Cas12f1Super, TnpBSuper [20] | DNA cleavage; compact variants enable viral packaging |
| Delivery Systems | Lipid nanoparticles (LNPs) [4] [13], AAV vectors [13] [24], Electroporation systems [24] | Deliver CRISPR components to target cells |
| Editing Enhancers | Alt-R HDR Enhancer Protein [68], SyNTase editors [69] | Improve homology-directed repair efficiency; enable gene correction |
| Cell Culture Media | X-VIVO 15, StemSpan [68] | Support ex vivo cell growth and maintenance |
| Analytical Tools | Flow cytometry, NGS off-target screening [68], ISS for spatial editing tracking [20] | Assess editing efficiency, purity, and safety |
Diagram 2: Key delivery platforms for CRISPR therapies with their respective advantages, highlighting technical considerations for manufacturing and scalability.
Implementation Roadmap: Navigating Technical Challenges
Scalability Optimization Strategies
Process Intensification: For ex vivo therapies, implement closed automated systems like the Cocoon Platform to reduce manual operations and facility footprint. For in vivo approaches, focus on high-yield LNP production processes (>80% encapsulation efficiency) with scalable tangential flow filtration purification [13].
Analytical Development: Implement rapid potency assays (e.g., droplet digital PCR for editing efficiency) to reduce quality control timelines. Utilize machine learning algorithms for gRNA design to minimize off-target effects and enhance editing efficiency [24] [20].
Supply Chain Resilience: Establish dual sourcing for critical raw materials, particularly lipids for LNP formulations and single-use bioprocess containers. Implement cold chain monitoring with real-time tracking for both starting materials and final products.
Emerging Solutions for Manufacturing Bottlenecks
Allogeneic (Off-the-Shelf) Approaches: Develop healthy donor-derived cell therapies with CRISPR-mediated knockout of endogenous TCR and HLA genes to prevent graft-versus-host disease, potentially transforming ex vivo therapies from autologous to allogeneic models [68].
Novel Delivery Platforms: Engineered virus-like particles (VLPs) and protein nanoparticle systems based on endogenous human proteins show promise for expanding in vivo delivery beyond the liver, potentially addressing a key limitation of current LNP systems [13] [68].
Redosable Systems: The demonstration that LNP-delivered CRISPR systems can be redosed without significant immune response (as shown in Intellia's hATTR trial and the CPS1 deficiency case) enables titration to therapeutic effect and potentially improves clinical outcomes [4].
The CRISPR therapy landscape is evolving toward hybrid models that incorporate both personalized and platform approaches. The emergence of rapid personalized in vivo therapies (exemplified by the 6-month development timeline for the CPS1 deficiency treatment) demonstrates the potential for accelerated bespoke solutions for ultra-rare diseases [4]. Simultaneously, platform technologies like SyNTase editors with AI-guided design are streamlining development for more common genetic disorders [69]. The convergence of CRISPR with artificial intelligence and machine learning is enhancing gRNA design, predicting off-target effects, and optimizing manufacturing parameters [24] [20]. As the field addresses current challenges in delivery efficiency and manufacturing scalability, the distinction between personalized and platform therapies will likely blur, yielding a new generation of precision genetic medicines that balance individualized needs with scalable production. The ongoing clinical successes and setbacks (such as the recent pause in Intellia's Phase 3 trials due to liver toxicity) provide crucial learning opportunities that will ultimately enhance the safety, efficacy, and accessibility of CRISPR-based therapies [20].
Clinical Evidence and Strategic Decision Framework
The clinical landscape for CRISPR-Cas9 therapies has dramatically evolved since the first approvals in 2023, solidifying gene editing's transition from research tool to therapeutic reality. As of 2025, the field is characterized by a dynamic tension between remarkable scientific progress and increasing economic pressures [4]. The clinical pipeline now encompasses over 250 gene-editing therapeutic candidates, with more than 150 trials currently active across multiple therapeutic areas [70]. This growth has been accompanied by increasing methodological sophistication, with the field now divided between two dominant technological approaches: in vivo editing (where modifications occur directly inside the patient's body) and ex vivo editing (where cells are modified outside the body before reinfusion) [28]. The distinction between these approaches has profound implications for therapeutic development, manufacturing logistics, and clinical implementation. This review provides a comprehensive 2025 update on the clinical trial landscape, with a specific focus on comparing the progress, outcomes, and technical requirements of in vivo versus ex vivo CRISPR-Cas9 therapeutic approaches.
Methodology: Analyzing the 2025 Clinical Trial Landscape
This analysis synthesizes data from multiple sources to present a current view of the CRISPR clinical landscape. We examined clinical trial databases, peer-reviewed publications, company announcements, and scientific reviews from 2024-2025. The primary focus was on interventional clinical trials with reported outcomes, with data extracted on trial design, patient population, editing methodology, delivery systems, efficacy endpoints, and safety outcomes. Trials were categorized by therapeutic area and editing approach (in vivo vs. ex vivo). Quantitative data on editing efficiency, biomarker changes, and clinical outcomes were tabulated for direct comparison. Given the rapid evolution of the field, we prioritized recently reported results from active trials over historical data to provide the most current assessment of the landscape.
Current Status of CRISPR Clinical Trials
Therapeutic Area Distribution
The clinical application of CRISPR technologies has expanded beyond initial focus areas into diverse disease domains. As of February 2025, the field spans multiple therapeutic categories, with notable concentrations in several key areas [70]:
- Blood disorders continue to lead the field, with the majority of Phase 3 trials targeting sickle cell disease and/or beta thalassemia.
- Oncology applications, particularly for hematological malignancies, represent a major focus area with multiple CAR-T and other cell therapy approaches.
- Cardiovascular diseases, especially familial hypercholesterolemia and other lipid disorders, have emerged as a prominent target for in vivo approaches.
- Rare genetic diseases including hereditary amyloidosis, immunodeficiencies, and muscular dystrophies are being addressed through both ex vivo and in vivo strategies.
- Autoimmune diseases such as systemic lupus erythematosus and multiple sclerosis represent newer application areas with growing trial activity.
- Infectious diseases including bacterial infections (E. coli, UTIs) and viral diseases are being targeted with CRISPR-based antimicrobial approaches.
Phase 3 trials are currently underway not only in blood disorders but also in hereditary amyloidosis and immunodeficiencies, indicating the maturation of the field across multiple therapeutic areas [70].
Analysis of Editing Approaches: In Vivo vs. Ex Vivo
The division between in vivo and ex vivo editing approaches represents a fundamental strategic distinction in clinical development. Each approach presents unique advantages, limitations, and technical requirements, as detailed in Table 1.
Table 1: Comparison of In Vivo vs. Ex Vivo CRISPR Therapy Approaches
| Parameter | In Vivo Editing | Ex Vivo Editing |
|---|---|---|
| Delivery System | Lipid nanoparticles (LNPs), viral vectors (AAV) | Electroporation, viral vectors (lentiviral, retroviral) |
| Therapeutic Examples | NTLA-2001 (hATTR), VERVE-101/102 (hypercholesterolemia), CTX310 (dyslipidemia) | CASGEVY (SCD/TDT), CAR-T therapies (ALL, NHL, multiple myeloma) |
| Key Advantages | Single administration, non-invasive, potential for multi-organ targeting | Controlled editing conditions, quality control pre-infusion, lower immune response risk |
| Major Challenges | Delivery efficiency, immunogenicity, off-target effects in situ | Complex manufacturing, high cost, conditioning chemotherapy required |
| Clinical Scale-up | More straightforward manufacturing, lower cost of goods | Complex logistics, specialized facilities required |
| Editing Assessment | Indirect biomarkers (protein levels), tissue biopsies | Direct sequencing of edited cells pre-infusion |
| Therapeutic Durability | Potentially lifelong for non-dividing cells | Lifelong for hematopoietic stem cells |
| Dosing Strategy | Weight-based, titratable | Cell number-based, fixed |
In vivo approaches have gained significant momentum in 2024-2025, with multiple clinical programs demonstrating proof-of-concept for direct administration of CRISPR therapies. The development of sophisticated delivery systems, particularly lipid nanoparticles (LNPs) optimized for specific tissue targeting, has enabled this progress [4]. Intellia Therapeutics' NTLA-2001 for hereditary transthyretin amyloidosis (hATTR) represents a landmark program for in vivo editing, demonstrating sustained reduction of disease-causing TTR protein levels for up to two years after a single administration [4]. The cardiovascular space has been particularly active, with Verve Therapeutics' VERVE-101 and VERVE-102 (for heterozygous familial hypercholesterolemia) and CRISPR Therapeutics' CTX310 (for dyslipidemia) all reporting positive Phase 1 results [28] [21]. These programs utilize base editing and knockout approaches respectively to target genes in the liver (PCSK9 and ANGPTL3) responsible for cholesterol regulation.
Ex vivo approaches continue to demonstrate therapeutic value, particularly in hematological diseases and oncology. The approval of CASGEVY (exagamglogene autotemcel) for sickle cell disease and transfusion-dependent beta thalassemia in 2023 established a regulatory pathway for ex vivo CRISPR therapies [4] [70]. The oncology field has seen extensive activity with allogeneic and autologous CAR-T therapies targeting various hematological malignancies including B-cell acute lymphoblastic leukemia, non-Hodgkin lymphoma, and multiple myeloma [70]. Recent progress has extended to autoimmune diseases, with Fate Therapeutics reporting promising Phase 1 data for FT819, an off-the-shelf CAR T-cell therapy for systemic lupus erythematosus [20]. Ex vivo editing provides greater control over the editing process and enables comprehensive quality assessment before patient administration, but requires complex manufacturing capabilities and patient conditioning regimens.
Key Clinical Trials and Outcomes: 2024-2025 Updates
In Vivo Editing Trials
Table 2: Key In Vivo CRISPR Clinical Trials with 2024-2025 Results
| Therapy/Indication | Developer | Phase | Editing Approach | Key Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|---|
| NTLA-2001 (hATTR) | Intellia Therapeutics | 3 | CRISPR-Cas9 knockout (LNP) | ~90% sustained TTR reduction at 2 years; functional stability/improvement [4] | Mild/moderate infusion reactions; generally well-tolerated |
| CTX310 (Dyslipidemia) | CRISPR Therapeutics | 1 | CRISPR-Cas9 knockout (LNP) of ANGPTL3 | -73% ANGPTL3, -55% TG, -49% LDL at highest dose; durable effect [21] | Well-tolerated; no treatment-related SAEs; mild-mod infusion reactions |
| VERVE-102 (HeFH/CAD) | Verve Therapeutics | 1b | Base editing (GalNAc-LNP) of PCSK9 | 53% avg LDL-C reduction (up to 69% at higher doses) [71] | Well-tolerated in initial cohorts; no serious adverse events |
| NTLA-2002 (HAE) | Intellia Therapeutics | 1/2 | CRISPR-Cas9 knockout (LNP) of KLKB1 | 86% kallikrein reduction; 8/11 attack-free (16 weeks) [4] | Favorable; ongoing evaluation |
The past year has yielded significant clinical data for in vivo CRISPR therapies, particularly for genetic diseases amenable to liver-directed editing. Intellia Therapeutics' NTLA-2001 continues to demonstrate durable protein reduction in hereditary transthyretin amyloidosis, with all 27 participants who reached two years of follow-up showing sustained response with no evidence of effect weakening over time [4]. CRISPR Therapeutics' CTX310 has emerged as a promising approach for dyslipidemia, demonstrating robust, dose-dependent reductions in both triglycerides and LDL cholesterol following a single-course IV administration [21]. At the highest dose (0.8 mg/kg), mean reductions of -73% in ANGPTL3, -55% in triglycerides, and -49% in LDL were observed, with some participants achieving reductions as high as 89%, 84%, and 87% respectively [21]. These effects are particularly notable given that 40% of participants were concurrently receiving PCSK9 inhibitor therapy [21].
Beyond these late-stage programs, the field has witnessed significant technical innovations in in vivo editing. A landmark case reported in May 2025 demonstrated the first personalized in vivo CRISPR treatment for an infant with CPS1 deficiency, developed and delivered in just six months [4]. This bespoke therapy was delivered via lipid nanoparticles and administered by IV infusion, with the patient safely receiving multiple doses to increase editing efficiency—an approach enabled by the favorable immunogenicity profile of LNP delivery compared to viral vectors [4]. The case establishes a regulatory precedent for rapid development of personalized CRISPR therapies for ultrarare genetic diseases.
Ex Vivo Editing Trials
Table 3: Key Ex Vivo CRISPR Clinical Trials with 2024-2025 Results
| Therapy/Indication | Developer | Phase | Editing Approach | Key Efficacy Outcomes | Safety Profile |
|---|---|---|---|---|---|
| CASGEVY (SCD/TDT) | CRISPR Therapeutics/Vertex | Approved | CRISPR-Cas9 (CD34+ HSCs) | Elimination of VOCs in SCD; transfusion independence in TDT [4] [70] | Manageable adverse events; conditioning-related toxicity |
| FT819 (SLE) | Fate Therapeutics | 1 | Gene-edited CAR-T | Significant disease improvement in 10/10 patients; complete renal responses in LN [20] | Favorable; minimal/no conditioning chemo; same-day discharge possible |
| PM359 (CGD) | Prime Medicine | Preclinical (IND cleared) | Prime editing (CD34+ HSCs) | IND cleared 2024; trial expected 2025 [28] | Preclinical evaluation ongoing |
| CTX211 (Type 1 Diabetes) | CRISPR Therapeutics | 1/2 | CRISPR-Cas9 (allogeneic PEC210A cells) | Ongoing; estimated completion August 2025 [28] | Ongoing evaluation |
Ex vivo editing approaches have demonstrated substantial progress across multiple disease areas in 2024-2025. In autoimmune diseases, Fate Therapeutics presented promising Phase 1 data for FT819, an off-the-shelf CAR T-cell therapy for systemic lupus erythematosus [20]. The therapy achieved significant disease improvements in all 10 treated patients, including complete renal responses in patients with lupus nephritis, with one patient maintaining drug-free remission at 15 months [20]. The favorable safety profile enabled same-day discharge in some cases and demonstrated effective immune remodeling with minimal or no conditioning chemotherapy [20].
The ex vivo landscape has also been expanded through the application of next-generation editing technologies. Prime Medicine received IND clearance for PM359, the first prime editing candidate to enter clinical development for chronic granulomatous disease [28] [71]. This ex vivo approach uses prime editors to correct mutations in the NCF1 gene in patient CD34+ hematopoietic stem cells, with a phase I trial predicted to begin in early 2025 [28]. Similarly, CRISPR Therapeutics is advancing CTX211 (VCTX210A), an immune-evasive, stem cell-derived beta-cell replacement therapy for Type 1 diabetes that uses CRISPR-Cas9 to edit healthy donor cells to enhance their fitness and allow them to evade the host immune system before transplantation [28].
The ex vivo manufacturing process typically involves several critical steps, as illustrated in the following workflow:
Diagram 1: Ex Vivo CRISPR Therapy Manufacturing and Treatment Workflow (53 characters)
Technical and Methodological Advances
Delivery System Innovations
Delivery remains the primary challenge for CRISPR therapeutics, particularly for in vivo applications. The past year has seen significant refinements in both viral and non-viral delivery systems:
Lipid Nanoparticles (LNPs) have emerged as the leading platform for in vivo delivery, particularly for liver-directed therapies. LNPs offer several advantages over viral vectors, including lower immunogenicity, the potential for redosing, and larger payload capacity [4]. The favorable safety profile of LNP delivery was demonstrated in the personalized CPS1 deficiency treatment, where the infant patient safely received three separate doses to increase editing efficiency—an approach that would be contraindicated with viral vectors due to immune reaction concerns [4]. Intellia Therapeutics has similarly reported redosing in their hATTR trial, with three participants who initially received the lowest dosage opting to receive a second infusion at higher doses after demonstrating safety and efficacy at those levels [4].
Virus-Like Particles (VLPs) represent an emerging delivery approach that combines advantages of viral and non-viral systems. Recent research has demonstrated that VLPs pseudotyped with VSVG and/or BaEVRless envelope proteins can achieve up to 97% transduction efficiency in human iPSC-derived neurons, enabling efficient Cas9 RNP delivery to postmitotic cells [72]. This delivery platform has enabled the study of DNA repair mechanisms in clinically relevant non-dividing cells, revealing that CRISPR repair outcomes differ dramatically in neurons compared to genetically identical dividing cells [72].
Cell-Type Specific Targeting remains an active area of innovation. Researchers are developing versions of LNPs with affinity for different organs beyond the liver, though these have not yet reached clinical trials [4]. The natural tropism of current LNP systems for the liver has made it an attractive target for initial in vivo applications, with multiple clinical programs focusing on liver-expressed proteins involved in metabolic diseases [4].
Next-Generation Editing Platforms
Beyond standard CRISPR-Cas9 systems, several enhanced editing platforms have advanced clinically in 2024-2025:
Base Editing has demonstrated significant therapeutic potential, with multiple programs in clinical development. Beam Therapeutics is advancing a base editing therapy for alpha-1 antitrypsin deficiency that corrects (rather than disrupts) a disease-causing mutation, representing "the first example you can point to where there has been direct correction of a disease-causing mutation in the body of a patient" [71]. Verve Therapeutics' VERVE-101 and VERVE-102 programs for familial hypercholesterolemia utilize adenine base editors to disrupt the PCSK9 gene in hepatocytes, with VERVE-102 demonstrating LDL-C reductions of 53-69% in Phase 1b trials [71]. Base editors offer advantages over conventional CRISPR-Cas9 by creating single-base changes without generating double-strand breaks, potentially reducing unwanted editing outcomes [71].
Prime Editing has entered clinical development with Prime Medicine's PM359 for chronic granulomatous disease receiving IND clearance in 2024 [28]. This ex vivo approach corrects disease-causing mutations using prime editors that can directly write new genetic information into a specified DNA site, offering greater precision and versatility than earlier editing approaches [71]. The first clinical results from two patients treated ex vivo for chronic granulomatous disease demonstrated promising efficacy, with the therapy working "really well at treating the disease" according to investigators [71].
Epigenetic Editing represents another frontier, with CRISPR-based therapies designed to modulate gene expression without altering the DNA sequence itself. Epicrispr Biotechnologies has initiated a first-in-human clinical trial for facioscapulohumeral muscular dystrophy using a compact nuclease-dead Cas9 fused to epigenetic effectors to silence a toxic gene (DUX4) in skeletal muscle [71]. This approach leverages the understanding that "all the cells in our body share the same code, yet they are very different cells with different functions, and that is epigenetics" [71].
The following diagram illustrates the molecular mechanisms of these next-generation editing technologies:
Diagram 2: Next-Gen CRISPR Editing Mechanism Comparison (53 characters)
Enhanced Analytical Methods
Advanced analytical methods have emerged to support the development of more precise editing technologies:
qEva-CRISPR represents a significant advancement in editing efficiency quantification. This method overcomes limitations of earlier techniques by detecting all mutation types (including point mutations and large deletions) with sensitivity independent of mutation type [73]. Unlike mismatch cleavage assays that can overlook single-nucleotide changes and larger deletions, qEva-CRISPR provides quantitative, multiplex capability for parallel analysis of target and off-target sites [73]. This methodology is particularly valuable for evaluating experimental conditions that affect genome editing and distinguishing between homology-directed repair and non-homologous end joining outcomes.
DNA Repair Mechanism Studies have provided crucial insights into cell-type-specific editing outcomes. Recent research comparing human iPSCs and iPSC-derived neurons has revealed that "CRISPR editing outcomes differ dramatically in neurons compared to genetically identical dividing cells" [72]. Neurons take longer to fully resolve DNA damage and upregulate non-canonical DNA repair factors in the process [72]. These differences have important implications for therapeutic editing in non-dividing cells, which constitute many clinically relevant targets for neurological disorders.
The Scientist's Toolkit: Essential Research Reagents and Methods
The advancing CRISPR clinical landscape has driven development of specialized research tools and methodologies essential for preclinical and clinical development:
Table 4: Essential Research Reagents and Methods for CRISPR Clinical Development
| Tool/Reagent | Function | Application in Clinical Development |
|---|---|---|
| Lipid Nanoparticles (LNPs) | In vivo delivery of CRISPR components | Liver-directed therapies (NTLA-2001, CTX310, VERVE-102) |
| Virus-Like Particles (VLPs) | Protein-based delivery of Cas9 RNP | Efficient transduction of difficult cells (neurons, cardiomyocytes) |
| qEva-CRISPR Assay | Quantitative evaluation of editing efficiency | Multiplex analysis of target/off-target editing; sgRNA screening |
| Modified sgRNA Scaffolds | Multiplexed genomic imaging | Dual-color tracking of genomic loci; study of chromatin dynamics |
| iPSC-Derived Neurons/Cardiomyocytes | Model systems for postmitotic cells | Study of DNA repair mechanisms in clinically relevant non-dividing cells |
| Base Editor Screening Platforms | Identification of editing determinants | Optimization of editing efficiency and specificity (e.g., Lig3, MutS-alpha) |
These tools have become essential for addressing the unique challenges of therapeutic genome editing. LNPs have emerged as the delivery vehicle of choice for liver-directed in vivo therapies, with multiple clinical programs demonstrating their utility for achieving therapeutic levels of editing [4] [21]. VLPs offer an alternative delivery strategy that efficiently transduces difficult-to-transfect cells, including neurons and cardiomyocytes, enabling the study of DNA repair mechanisms in clinically relevant postmitotic cells [72]. Advanced analytical methods like qEva-CRISPR provide robust quantification of editing outcomes, while modified sgRNA scaffolds enable visualization of editing consequences in living cells [73] [74].
The following experimental workflow illustrates a typical protocol for evaluating CRISPR editing outcomes in clinically relevant models:
Diagram 3: CRISPR Editing Evaluation Protocol (38 characters)
Challenges and Future Directions
Field-Wide Challenges
The CRISPR therapeutic landscape faces several significant challenges despite substantial clinical progress:
Financial Pressures have created headwinds for the broader field. Market forces have reduced venture capital investment in biotechnology, leading companies to narrow their pipelines and focus on getting a smaller set of products to market quickly rather than creating broader therapeutic pipelines [4]. This has resulted in significant layoffs in CRISPR-focused companies and increased pressure to pursue treatments for more common diseases that offer greater return on investment [4] [71]. Additionally, the first six months of 2025 saw major cuts in US government funding for basic and applied scientific research, with proposed cuts of 40% to the National Institute of Health budget that could dramatically impact the pace of biomedical research [4].
Safety Considerations remain paramount, as evidenced by Intellia Therapeutics pausing two Phase 3 trials of its CRISPR-Cas therapy for transthyretin amyloidosis after a patient experienced severe liver toxicity characterized by elevated enzymes and bilirubin [20]. While delivery vectors are not currently suspected, the event underscores the importance of ongoing safety monitoring even for advanced clinical programs [20].
Manufacturing and Scalability challenges persist, particularly for personalized approaches like the bespoke therapy developed for CPS1 deficiency. As IGI's Fyodor Urnov noted, the key challenge is how to "go from CRISPR for one to CRISPR for all" [4]. The resource-intensive nature of developing patient-specific therapies raises questions about broad applicability, though regulatory innovations may help address these challenges.
Emerging Solutions and Future Outlook
Several promising approaches are emerging to address these challenges:
Regulatory Innovation may help accelerate development of therapies for rare diseases. Researchers have proposed a model based on the rapid development of the personalized CPS1 deficiency treatment, where comprehensive studies for one variant could be supplemented with cellular studies of other variants followed by an umbrella clinical trial [71]. This approach could eventually support drug labels applicable to patients with multiple different genetic variants, improving commercial viability while addressing unmet medical needs [71].
Technical Advancements continue to address limitations in delivery and editing precision. The development of smaller Cas variants (such as Cas12f1Super and TnpBSuper) that are small enough for viral delivery yet show dramatically improved editing efficiency could overcome a significant hurdle in gene therapy by combining precision with practical size requirements for clinical delivery [20]. Similarly, the emergence of self-limiting genetic systems for population control of disease vectors represents an innovative application that balances efficiency with containment benefits [20].
Diagnostic Applications of CRISPR are expanding, with tools like bbCARMEN demonstrating the ability to identify multiple pathogens (SARS-CoV-2, respiratory syncytial virus, influenza A/B) from a single sample with 97.9% sensitivity for COVID-19 detection [71]. These applications leverage CRISPR's programmability for detection rather than therapeutic editing, expanding the technology's impact beyond medicine.
The field continues to evolve rapidly, with the ongoing clinical development reflecting both the remarkable progress and significant challenges that characterize this transformative therapeutic modality. The coming years will likely see additional approvals, further refinement of editing technologies, and continued navigation of the complex economic and regulatory landscape surrounding these innovative therapies.
The Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas9 system has revolutionized therapeutic development by enabling precise genomic modifications. This technology, derived from a bacterial adaptive immune system, utilizes a guide RNA (gRNA) to direct the Cas9 nuclease to specific DNA sequences, creating double-strand breaks that are repaired through nonhomologous end joining (NHEJ) or homology-directed repair (HDR) pathways [8] [75]. While both hematological and metabolic diseases represent promising application areas, they employ fundamentally distinct delivery approaches—ex vivo editing for hematological conditions and in vivo delivery for metabolic disorders—resulting in different efficacy profiles, safety considerations, and clinical development pathways.
This technical analysis compares the therapeutic efficacy of CRISPR-Cas9 across these disease domains, framed within the critical context of delivery methodology. The examination draws upon recent clinical evidence, including the first regulatory approvals for ex vivo applications and emerging in vivo trial data, to provide drug development professionals with a comprehensive assessment of the current landscape and future directions.
Comparative Efficacy Analysis: Clinical Evidence
Table 1: Efficacy Outcomes of Selected CRISPR-Cas9 Therapies in Hematological Diseases
| Therapeutic Application | Target Gene | Editing Approach | Patient Population | Key Efficacy Outcomes | Follow-up Duration | Citation |
|---|---|---|---|---|---|---|
| Exa-cel (Casgevy) | BCL11A | CRISPR-Cas9 knockout | Sickle cell disease (N=46) | Vaso-occlusive crisis resolution: 96% patients crisis-free; Significant HbF increase | >5 years (longest follow-up) | [1] |
| Exa-cel (Casgevy) | BCL11A | CRISPR-Cas9 knockout | Transfusion-dependent β-thalassemia (N=56) | Transfusion independence: 93% patients; Hemoglobin stabilization | >5 years (longest follow-up) | [1] |
| Experimental therapy | γ-globin promoters | LRF binding site disruption | Sickle cell disease | High editing efficiency; Potent HbF synthesis; Enhanced effect in SCD vs. healthy donor cells | Not specified | [76] |
Table 2: Efficacy Outcomes of Selected CRISPR-Cas9 Therapies in Metabolic Diseases
| Therapeutic Application | Target Gene | Delivery System | Patient Population | Key Efficacy Outcomes | Follow-up Duration | Citation |
|---|---|---|---|---|---|---|
| CTX310 (Phase 1) | ANGPTL3 | LNP (in vivo) | Dyslipidemia (N=15) | LDL-C: -48.9%; Triglycerides: -55.2% (0.8 mg/kg dose) | 60-90 days | [77] [78] |
| NTLA-2001 (Phase 1) | TTR | LNP (in vivo) | hATTR (N=27) | TTR reduction: ~90% sustained; Disease stabilization/improvement | 2 years | [4] |
| NTLA-2002 (Phase 1/2) | Kallikrein | LNP (in vivo) | HAE (N=11, high dose) | Kallikrein reduction: 86%; Attack-free: 73% (8/11 patients) | 16 weeks | [4] |
Hematological Disease Applications
Hematological diseases have demonstrated remarkable therapeutic responses to ex vivo CRISPR-Cas9 editing. The most advanced application targets sickle cell disease (SCD) and β-thalassemia through fetal hemoglobin (HbF) reactivation. Exagamglogene autotemcel (exa-cel, marketed as Casgevy) disrupts the BCL11A gene enhancer region in autologous hematopoietic stem and progenitor cells (HSPCs), thereby reducing repression of γ-globin expression and increasing HbF production [1]. Interim results from the CLIMB-121 trial demonstrated that 96% of SCD patients (44 of 46) achieved freedom from vaso-occlusive crises, with the longest follow-up exceeding five years [1]. Similarly, in transfusion-dependent β-thalassemia, 93% of patients achieved transfusion independence after treatment [1].
An alternative approach targeting lymphoma-related factor (LRF) binding sites in the γ-globin promoters has shown enhanced editing efficiency in SCD-derived HSPCs compared to healthy donor cells, suggesting disease-specific biological factors may influence therapeutic efficacy [76]. This strategy produced high frequencies of LRF binding site disruption and potent HbF synthesis in erythroid progeny without impairing HSPC engraftment capacity [76].
Metabolic Disease Applications
Metabolic diseases predominantly employ in vivo CRISPR-Cas9 editing, utilizing lipid nanoparticles (LNPs) to deliver therapeutic components directly to hepatocytes. Recent clinical trials have demonstrated promising efficacy in targeting genes involved in lipid metabolism and protein aggregation disorders.
The CRISPR-Cas9 trial evaluating CTX310, an LNP-formulated therapy targeting ANGPTL3, demonstrated dose-dependent reductions in atherogenic lipids, with the highest dose (0.8 mg/kg) reducing LDL cholesterol by 48.9% and triglycerides by 55.2% [77]. This approach represents a paradigm shift in dyslipidemia management by enabling single-dose administration rather than chronic therapy.
Similarly, Intellia Therapeutics' NTLA-2001 targeting transthyretin (TTR) for hereditary ATTR amyloidosis achieved approximately 90% sustained reduction in serum TTR levels—comparable to RNAi therapeutics but with potentially permanent effects from a single administration [4]. All 27 participants who reached two-year follow-up maintained this reduction with no evidence of diminished effect over time [4]. For hereditary angioedema (HAE), NTLA-2002 targeting kallikrein demonstrated 86% reduction in target protein and rendered 73% of high-dose recipients attack-free during the 16-week observation period [4].
Experimental Workflows and Methodologies
Ex Vivo Workflow for Hematological Diseases
Diagram 1: Ex vivo workflow for hematological diseases
The ex vivo editing paradigm for hematological diseases follows a standardized multi-step process. First, autologous CD34+ hematopoietic stem and progenitor cells (HSPCs) are collected from patients via apheresis following mobilization with granulocyte colony-stimulating factor [1]. These cells are then transported to a Good Manufacturing Practice (GMP) facility where they undergo CRISPR-Cas9 editing using electroporation to deliver ribonucleoprotein (RNP) complexes targeting specific genomic loci—typically the BCL11A erythroid enhancer or γ-globin promoter regions [76] [1]. Following editing, cells are expanded in culture media supplemented with cytokines (SCF, TPO, FLT3-L) to maintain stemness while allowing sufficient population expansion [76]. Meanwhile, patients receive myeloablative conditioning (typically busulfan) to create niche space in the bone marrow. Finally, edited cells are reinfused and engraft, with successful engraftment typically occurring within 2-4 weeks, followed by erythroid differentiation and HbF production [1].
In Vivo Workflow for Metabolic Diseases
Diagram 2: In vivo workflow for metabolic diseases
In vivo editing for metabolic diseases employs a fundamentally different approach centered on hepatic delivery. CRISPR-Cas9 components are encapsulated in liver-tropic lipid nanoparticles (LNPs) composed of ionizable lipids, phospholipids, cholesterol, and PEG-lipid conjugates [4] [78]. These LNPs typically contain Cas9 mRNA and single-guide RNA (sgRNA) targeting metabolic genes such as ANGPTL3, TTR, or kallikrein [77] [78]. Following intravenous administration, LNPs accumulate in hepatocytes via ApoE-mediated endocytosis [4]. After cellular uptake, LNPs escape endosomal compartments and release their payload into the cytoplasm, where Cas9 mRNA is translated and complexes with sgRNA to form functional ribonucleoproteins that translocate to the nucleus [75]. Once in the nucleus, Cas9 induces double-strand breaks at target genes, resulting in NHEJ-mediated knockout and permanent reduction of pathogenic proteins [77] [75].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR-Cas9 Therapeutic Development
| Reagent Category | Specific Examples | Research Function | Therapeutic Application |
|---|---|---|---|
| CRISPR Nucleases | SpCas9, SaCas9, Cas12a | Target gene disruption | Both hematological and metabolic |
| Delivery Systems | LNPs, AAVs, Electroporation systems | CRISPR component delivery | LNPs (in vivo), Electroporation (ex vivo) |
| Guide RNA Designs | sgRNAs targeting BCL11A, ANGPTL3, TTR | Target specificity | Disease-specific gene targets |
| Cell Culture Reagents | Cytokine cocktails (SCF, TPO, FLT3-L), Serum-free media | HSPC expansion | Ex vivo editing protocols |
| Analytical Tools | NGS off-target assays, ELISA for protein quantification, FACS for cell phenotyping | Efficacy and safety assessment | Both application areas |
| Animal Models | Humanized mouse models, Non-human primates | Preclinical validation | Both application areas |
Discussion
Efficacy Comparison and Therapeutic Implications
The comparative analysis reveals distinct efficacy patterns between hematological and metabolic disease applications. Ex vivo approaches for hematological diseases demonstrate potentially curative outcomes with sustained therapeutic effects beyond five years, as evidenced by exa-cel data [1]. This durability stems from permanent genetic modification of long-term repopulating HSPCs, creating a self-renewing reservoir of edited cells. In contrast, in vivo metabolic applications show impressive biomarker reduction (90% TTR reduction, 49% LDL-C lowering) but have shorter documented durability of approximately two years, though effects appear stable within this timeframe [4] [77].
The therapeutic index also differs substantially between approaches. Ex vivo editing enables comprehensive quality control, including off-target assessment, vector copy number analysis, and viability testing before patient infusion [76]. However, it requires myeloablative conditioning with associated risks of infertility, prolonged cytopenias, and infection [1]. In vivo editing eliminates conditioning-related toxicity but faces delivery challenges including preferential hepatocyte uptake, potential immune recognition of Cas9, and variable editing efficiency between patients [4] [75].
Technical Challenges and Safety Considerations
Off-target effects remain a concern for both approaches. Studies in SCD HSPCs detected off-target activity and chromosomal rearrangements, particularly in patient-derived samples, likely due to higher overall editing efficiency [76]. Transcriptomic analyses revealed that editing procedures upregulate genes involved in DNA damage and inflammatory responses, more evidently in SCD HSPCs [76]. For in vivo applications, the potential for off-target editing in non-hepatic tissues exists, though current LNP systems show strong hepatic tropism [4].
Immunogenicity presents another challenge. Preexisting Cas9 immunity has been detected in humans, potentially impacting therapeutic efficacy [75]. While ex vivo editing may allow immune profiling prior to treatment, in vivo approaches face greater uncertainty regarding immune reactions. Notably, LNP delivery appears less immunogenic than viral vectors, enabling redosing as demonstrated in trials where participants received multiple infusions [4].
Disease-specific biological factors also influence therapeutic outcomes. SCD HSPCs showed reduced engraftment capacity and myeloid bias compared to healthy donor cells, highlighting how disease pathophysiology can impact editing efficacy [76]. Additionally, inflammatory environments in certain diseases may affect CRISPR repair mechanisms, potentially favoring NHEJ over HDR pathways.
CRISPR-Cas9 therapeutics have demonstrated remarkable efficacy across both hematological and metabolic diseases, albeit through fundamentally distinct approaches. Ex vivo editing for hematological conditions offers potentially curative outcomes with sustained durability, while in vivo approaches for metabolic disorders provide transformative single-dose treatments with impressive biomarker reduction. The choice between approaches depends on multiple factors including disease pathophysiology, target tissue accessibility, and risk-benefit considerations.
Future directions will focus on enhancing safety profiles through novel Cas variants with reduced off-target effects, improving delivery efficiency for non-hepatic tissues, and potentially combining ex vivo and in vivo approaches for complex disorders. As the field matures, both therapeutic paradigms will likely continue to evolve, expanding the range of addressable diseases and improving patient access to these revolutionary therapies.
The therapeutic application of the CRISPR/Cas9 system represents a paradigm shift in the treatment of genetic disorders, with clinical successes already demonstrated for conditions like sickle cell disease and transfusion-dependent beta thalassemia [4]. The efficacy and safety of this powerful gene-editing tool, however, are profoundly influenced by the method used to deliver its molecular components into target cells. This analysis provides a comprehensive technical evaluation of the safety and risk-benefit profiles associated with the primary delivery modalities employed in CRISPR/Cas9 therapy, framed within the critical context of in vivo versus ex vivo therapeutic approaches. As the field advances toward treating more complex diseases, understanding these delivery parameters is essential for researchers and drug development professionals to design safer, more effective genetic therapies.
The choice of delivery system directly impacts critical safety parameters, including the duration of Cas9 nuclease activity, potential for off-target editing, and the host immune response [79]. Each delivery strategy presents a unique balance between editing efficiency and safety risks, requiring careful consideration based on the specific therapeutic application, target cell type, and desired genetic outcome.
Delivery Modalities: Technical and Safety Profiles
Viral Vector Systems
Viral vectors are engineered viruses that have been modified to deliver therapeutic genetic material while lacking the ability to replicate. They remain a cornerstone of CRISPR delivery due to their high transduction efficiency.
- Adeno-Associated Viruses (AAVs): AAVs are characterized by their low immunogenicity and long-term, stable gene expression in non-dividing cells. Their primary constraint is a limited packaging capacity (~4.7 kb), which is insufficient for the standard Streptococcus pyogenes Cas9 (SpCas9). This necessitates the use of smaller Cas9 orthologs or split-Cas9 systems [80] [31]. While AAVs are considered non-pathogenic, concerns regarding pre-existing immunity in human populations and the potential for immune activation upon administration remain [80].
- Adenoviruses (AdVs): Adenoviruses offer a larger packaging capacity than AAVs and can efficiently transduce both dividing and non-dividing cells. Their use is limited by a strong propensity to trigger host immune responses, which can lead to inflammation and rapid clearance of the transduced cells, making re-dosing challenging [81].
- Lentiviruses (LVs): Lentiviruses are capable of integrating into the host genome, facilitating stable, long-term transgene expression. This very characteristic poses a significant safety risk for CRISPR delivery, as random integration can lead to insertional mutagenesis, potentially disrupting tumor suppressor genes or activating oncogenes [81]. They are predominantly used in ex vivo settings where the risk of insertional mutagenesis can be carefully managed and edited cells can be screened prior to infusion [31].
Non-Viral Vector Systems
Non-viral methods have gained prominence for their improved safety profiles, including reduced immunogenicity and the ability to mediate transient Cas9 expression, which minimizes off-target risks.
- Lipid Nanoparticles (LNPs): LNPs are biocompatible, synthetic vesicles that encapsulate CRISPR cargo (RNP, mRNA, or plasmid DNA) and facilitate cellular entry through endocytosis. A key advantage is their potential for in vivo systemic administration and organ-specific targeting; for instance, they show a natural tropism for the liver [4]. Their transient expression profile and inability to integrate into the host genome make them a safer alternative to viral vectors. Recent clinical breakthroughs, including the first personalized in vivo CRISPR therapy for CPS1 deficiency, have successfully utilized LNP delivery, with patients safely receiving multiple doses [4].
- Electroporation: This physical method uses controlled electrical pulses to create transient pores in the cell membrane, allowing the direct passage of CRISPR cargo into the cytoplasm. It is highly efficient for ex vivo applications, particularly with RNP complexes, as it avoids the endosomal trapping that can plague other methods [82] [79]. A significant drawback is that it can induce cellular stress and apoptosis if parameters are not meticulously optimized, making it unsuitable for in vivo use with solid tissues [82].
Cargo Format Considerations
The format in which the CRISPR/Cas9 system is delivered is a critical determinant of its kinetic profile and, consequently, its safety.
- Plasmid DNA (pDNA): pDNA requires nuclear entry and transcription, leading to delayed and prolonged Cas9 expression. This increases the window for off-target activity and raises the risk of genomic integration, which can cause unpredictable mutagenesis [82] [79].
- mRNA: Delivery of in vitro transcribed mRNA eliminates the need for transcription and reduces the duration of Cas9 expression compared to pDNA. However, it still requires translation in the cytoplasm and can trigger innate immune responses, adding to the host's metabolic load [82] [79].
- Ribonucleoprotein (RNP) Complexes: RNP complexes, consisting of pre-assembled Cas9 protein and guide RNA, represent the safest cargo format. They are active immediately upon nuclear delivery and are rapidly degraded by cellular proteases, resulting in a short, defined pulse of nuclease activity. This transient presence dramatically reduces the probability of off-target editing [82] [79]. As one expert notes, "The longer Cas9 stays in the nucleus, the more likely it will find and accumulate off-target sites. That’s why the safest gene editing method is giving a very short Cas9 pulse through RNP" [79].
Table 1: Comparative Safety and Application Profile of Primary Delivery Modalities
| Delivery Modality | Cargo Compatibility | Primary Applications | Key Safety Advantages | Key Safety Risks |
|---|---|---|---|---|
| Adeno-Associated Virus (AAV) | DNA (requires small Cas9) | In vivo | Low immunogenicity; Non-pathogenic; Tissue-specific targeting | Pre-existing immunity; Limited packaging capacity; Risk of immune activation |
| Lentivirus (LV) | DNA | Ex vivo | High transduction efficiency; Stable expression | Insertional mutagenesis; Persistent expression increases off-target risk |
| Lipid Nanoparticle (LNP) | RNP, mRNA, DNA | In vivo & Ex vivo | Transient expression; Low immunogenicity; Redosable; No genomic integration | Variable encapsulation efficiency; Potential cytotoxicity at high doses |
| Electroporation | RNP, mRNA, DNA | Ex vivo | High efficiency for hard-to-transfect cells (e.g., stem cells); Direct cytoplasmic delivery | Cellular stress and toxicity; Not suitable for in vivo delivery |
Table 2: Safety and Kinetic Profile of CRISPR/Cas9 Cargo Formats
| Cargo Format | Mechanism of Action | Kinetic Profile | Off-Target Risk | Genomic Integration Risk | Immune Response |
|---|---|---|---|---|---|
| Plasmid DNA (pDNA) | Requires nuclear entry, transcription, and translation | Slow onset; Prolonged expression | High | High | Moderate |
| mRNA | Requires cytoplasmic translation | Faster onset; Medium duration | Moderate | Low | High (can trigger innate immunity) |
| Ribonucleoprotein (RNP) | Pre-formed complex; active upon nuclear entry | Immediate onset; Short duration | Low | None | Low |
Assessing and Mitigating Genotoxic Risks
A thorough safety assessment for CRISPR therapies must extend beyond standard off-target prediction algorithms to investigate a broader spectrum of genotoxic effects.
Beyond Off-Target Effects: Structural Variations and Genome Integrity
While off-target edits at sites with sequence similarity to the target have been a primary safety concern, recent evidence highlights a more pressing risk: on-target structural variations (SVs) [7]. These include large-scale genomic aberrations such as megabase-scale deletions, chromosomal translocations, and chromothripsis that occur at the intended target site.
These SVs are particularly concerning because they can delete critical genes and regulatory elements well beyond the immediate target locus, with profound consequences for cell viability and oncogenic potential [7]. Traditional short-read amplicon sequencing often fails to detect these large deletions, especially when they eliminate the primer binding sites used in the assay, leading to a dangerous overestimation of editing precision and HDR efficiency [7].
Experimental Protocols for Comprehensive Genotoxicity Assessment
To fully characterize the genomic impact of CRISPR editing, a combination of orthogonal assays is required.
Protocol 1: Detection of Large Structural Variations
- Objective: To identify large deletions and chromosomal rearrangements at the on-target site and across the genome.
- Methodology:
- Long-Range PCR & Long-Read Sequencing: Design primers flanking the target site (e.g., 5-10 kb apart). Amplify the region using a long-range PCR kit. Purify the amplicons and sequence them using long-read sequencing technologies (e.g., PacBio or Oxford Nanopore) to resolve complex structural variations [7].
- Karyotyping and FISH: Perform conventional G-banding karyotyping or Fluorescence In Situ Hybridization (FISH) with probes specific to the edited chromosomal region to visually identify large translocations and aneuploidy [7].
- CAST-Seq or LAM-HTGTS: Utilize specialized, genome-wide methods like CIRCLE-seq (in vitro) or DISCOVER-Seq (in vivo) to systematically profile off-target sites and translocations in an unbiased manner [57].
Protocol 2: Evaluating the Impact of HDR Enhancement Strategies
- Objective: To assess whether small molecule inhibitors used to enhance HDR efficiency exacerbate genomic instability.
- Methodology:
- Cell Treatment: Transfert cells with CRISPR RNP complexes. Divide the cells into two groups: one treated with an HDR-enhancing molecule (e.g., a DNA-PKcs inhibitor like AZD7648) and a vehicle control group [7].
- Analysis: Apply the detection methods from Protocol 1 to both groups. Compare the frequency and spectrum of SVs. Critical Finding: Studies indicate that DNA-PKcs inhibitors can increase the frequency of megabase-scale deletions and chromosomal translocations by up to a thousand-fold, suggesting that their clinical use requires careful re-evaluation [7].
The following diagram illustrates the critical safety challenge where common HDR-enhancing strategies can introduce hidden risks.
The Scientist's Toolkit: Essential Reagents and Methodologies
Table 3: Key Research Reagent Solutions for CRISPR Delivery and Safety Assessment
| Reagent / Solution | Function | Application Notes |
|---|---|---|
| High-Fidelity Cas9 Variants (e.g., HiFi Cas9) | Engineered nuclease with reduced off-target activity while maintaining robust on-target editing. | Crucial for therapies requiring high specificity; however, does not eliminate risk of on-target structural variations [7]. |
| Chemically Modified sgRNA | Enhances stability and reduces immunogenicity of the guide RNA. | Improves editing efficiency and can lessen innate immune responses, particularly for mRNA and RNP delivery [79]. |
| DNA Repair Pathway Inhibitors (e.g., AZD7648, SCR7) | Small molecules that inhibit NHEJ factors to skew repair toward HDR. | Warning: Use with caution. DNA-PKcs inhibitors are shown to dramatically increase the frequency of large structural variations and translocations [7]. |
| LNP Formulation Kits | Enable encapsulation of CRISPR RNPs or mRNA for in vivo delivery. | Essential for transitioning from in vitro to in vivo studies. Select kits optimized for nucleic acid/protein encapsulation. |
| ONE-seq / CHANGE-seq Kits | In vitro biochemical kits for genome-wide profiling of Cas9 nuclease off-target activity. | Provides an unbiased, cell-free method for initial off-target risk assessment before moving to cellular models [57]. |
| Long-Read Sequencing Services (PacBio, Nanopore) | Sequencing platforms capable of detecting large structural variations and complex rearrangements. | Non-negotiable for comprehensive safety assessment. Replaces or supplements standard short-read amplicon sequencing [7]. |
The selection of a delivery modality for a CRISPR/Cas9-based therapeutic is a fundamental decision that directly dictates its clinical safety and efficacy profile. The following decision framework synthesizes the critical risk-benefit analyses to guide researchers in aligning their delivery strategy with therapeutic goals.
For ex vivo therapies (e.g., engineered hematopoietic stem cells or T-cells), the gold standard for safety and efficiency is the delivery of pre-assembled RNP complexes via electroporation. This combination ensures a short nuclease pulse, minimizing off-target effects, and allows for comprehensive quality control, including genomic and functional validation of the edited cells before patient infusion [82] [79].
For in vivo therapies, LNPs have emerged as a leading platform due to their favorable safety profile, ability to be re-dosed, and transient expression kinetics. Their success in clinical trials for liver-based diseases underscores their therapeutic potential [4]. While AAVs are valuable for situations requiring sustained expression, their limitations regarding packaging capacity and immunogenicity must be rigorously addressed.
Ultimately, advancing CRISPR therapies into the clinic demands a holistic safety assessment that moves beyond simple off-target predictions. Researchers must employ a combination of advanced tools—including high-fidelity editors, RNP delivery, and long-read sequencing—to fully characterize and mitigate the risks of both off-target effects and on-target structural variations. This rigorous, evidential approach is paramount for translating the immense promise of CRISPR into safe and effective human therapeutics.
The transition of CRISPR-Cas9 therapies from research to clinical application introduces significant commercialization challenges, with manufacturing complexity and treatment costs representing pivotal considerations. Within the broader framework of in vivo versus ex vivo therapeutic approaches, these factors dictate scalability, market accessibility, and economic viability. Ex vivo therapies, involving cell extraction, external genetic modification, and reinfusion, require complex, personalized manufacturing processes that currently limit scalability and contribute to costs exceeding $1-2 million per treatment. In vivo approaches, where gene editing components are delivered directly into the patient's body, offer potential for scalable manufacturing but face significant biological barriers related to delivery efficiency and tissue-specific targeting. This whitepaper examines the technical foundations, manufacturing workflows, and economic implications of both platforms, providing researchers and drug development professionals with a structured analysis to guide strategic development decisions in the evolving CRISPR therapeutics landscape.
The fundamental distinction between in vivo and ex vivo CRISPR-Cas9 therapy approaches creates divergent pathways for commercialization, each with unique manufacturing considerations and cost structures. Ex vivo gene editing involves harvesting a patient's cells (typically T-cells or hematopoietic stem cells), genetically modifying them outside the body using CRISPR-Cas9 systems, and then reinfusing the edited cells back into the patient [83] [1]. This approach offers precise control over the editing process and enables quality control checks before administration, but generates inherently personalized therapeutics that are complex to manufacture at scale. In contrast, in vivo gene editing delivers CRISPR-Cas9 components directly into the patient's body using viral vectors (such as AAV) or non-viral nanoparticles (including LNPs), where genetic modification occurs internally [25] [4]. This approach facilitates off-the-shelf therapeutics with potentially simpler manufacturing but faces significant challenges in efficient delivery, tissue-specific targeting, and controlling immune responses.
The manufacturing complexity for both platforms stems from multiple factors: the biological nature of the products, the precision required for genetic modifications, the stability of editing components, and the stringent quality control necessary for human therapeutics [24] [84]. Treatment costs are consequently influenced by these technical challenges, with current pricing reflecting both the innovative nature of these therapies and the substantial infrastructure required for production. As the field advances with 6 approved CGT products in the U.S. as of 2024 and over 1,491 ex vivo gene therapy products in development, understanding the technical and economic distinctions between these platforms becomes increasingly critical for research direction and commercial planning [83] [85].
Manufacturing Complexity: Technical Comparison
Ex Vivo Manufacturing Workflows
Ex vivo CRISPR therapies require multi-step, cell-specific manufacturing processes that present significant technical challenges. For autologous therapies such as Casgevy (exagamglogene autotemcel), the process begins with leukapheresis to harvest the patient's own cells, which are then transported to specialized manufacturing facilities [1]. The core editing stage involves activating the cells, introducing CRISPR components (typically via electroporation), and expanding the successfully modified cells—a process requiring strict aseptic conditions and extensive quality control testing. The final cryopreserved product is shipped back to the treatment center for reinfusion after the patient receives conditioning chemotherapy [1] [4].
The manufacturing complexity for ex vivo therapies is substantially influenced by cell type characteristics. T-cells, representing 75.26% of ex vivo therapies in development, demonstrate robust expansion capabilities but require sophisticated activation steps prior to editing [83]. Hematopoietic stem cells (HSCs), used for genetic disorders like sickle cell disease and beta-thalassemia, present greater challenges due to their sensitivity to manipulation and difficulties maintaining stemness during expansion [1]. Process optimization must address multiple variables: cell culture conditions, editing efficiency, vector or delivery method selection, and comprehensive safety profiling including off-target analysis and sterility testing.
Manufacturing workflow for ex vivo CRISPR therapies:
In Vivo Manufacturing Workflows
In vivo CRISPR therapies utilize a more traditional biologic manufacturing approach centered on producing delivery vectors or nanoparticles containing gene editing components. The process involves creating master cell banks for viral vector production (HEK293T cells for AAV and lentiviral vectors) or synthesizing lipid nanoparticles (LNPs) for mRNA/protein delivery [25] [13]. For viral vectors, the manufacturing process includes transfection, harvest, purification, and concentration steps, with stringent quality control to assess vector potency, purity, and safety. Non-viral approaches like LNPs utilize microfluidic mixing to encapsulate CRISPR cargo, followed by purification and buffer exchange operations [13].
The primary technical challenge for in vivo manufacturing stems from the packaging constraints of delivery vectors, particularly adeno-associated viruses (AAVs) with their limited ~4.7 kb capacity [24] [25]. This constraint has driven development of multiple innovative solutions: compact Cas orthologs (SaCas9, CjCas9), dual AAV vector systems, and trans-splicing AAV vectors [25]. Additionally, different cargo formats (DNA, mRNA, or ribonucleoprotein complexes) present distinct manufacturing considerations—DNA plasmids allow longer expression but raise safety concerns, mRNA offers transient expression with reduced off-target risks, and RNPs provide immediate activity with high precision but complex manufacturing [13].
Manufacturing workflow for in vivo CRISPR therapies:
Comparative Analysis of Manufacturing Complexities
Table 1: Manufacturing Complexity Comparison Between Ex Vivo and In Vivo CRISPR Therapies
| Manufacturing Aspect | Ex Vivo Approach | In Vivo Approach |
|---|---|---|
| Production Timeline | 2-4 weeks (patient-specific) | 3-6 months (off-the-shelf) |
| Facility Requirements | Dedicated cleanrooms, multiple product suites | Single-product facility, bioreactor capacity |
| Personnel Expertise | Cell biology, GMP cell processing | Bioprocess engineering, virology/particle formulation |
| Quality Control Focus | Cell viability, editing efficiency, sterility, identity | Vector potency, purity, sterility, empty/full capsid ratio |
| Batch Definition | Patient-specific lot | Traditional multi-dose batch |
| Scalability Challenges | Parallel processing limitations, donor variability | Traditional bioprocess scaling, vector production yields |
| Storage & Distribution | Cryopreserved, complex cold chain | Typically stable at -60°C to -80°C |
| Key Technical Hurdles | Cell expansion, editing consistency, process automation | Delivery efficiency, tissue specificity, immunogenicity |
Treatment Cost Structures and Economic Considerations
Cost Drivers for Ex Vivo Therapies
Ex vivo CRISPR therapies face substantial cost pressures throughout their development and delivery lifecycle. Current pricing reflects these complexities, with approved therapies like Casgevy costing approximately $2.2 million per treatment [4] [84]. The patient-specific nature of these therapies creates inherent economic challenges, as manufacturing processes cannot benefit from traditional batch production economies of scale. Each treatment batch requires dedicated resources, personnel time, and facility utilization regardless of patient numbers, resulting in high fixed costs per unit [83].
The cost structure for ex vivo therapies includes several significant components: (1) raw materials and reagents, particularly viral vectors for cell modification (lentivirus at 40.12% usage despite CRISPR-based modifications expanding to 25.66%) and cell culture media [83]; (2) specialized equipment for cell processing, editing, and quality control; (3) extensive personnel requirements for highly trained technical staff; (4) facility overhead for maintaining GMP-compliant cleanrooms; and (5) complex logistics including cryopreservation and cold chain management across the patient-to-factory-to-patient journey [83] [84]. Additionally, pretreatment conditioning chemotherapy and extended hospitalization further contribute to the total treatment cost, creating significant accessibility challenges despite the transformative potential of these therapies.
Cost Drivers for In Vivo Therapies
In vivo CRISPR therapies present a different economic model centered on scalable manufacturing with potential for traditional pharmaceutical production efficiencies. While still in earlier stages of commercialization with fewer approved products, their off-the-shelf nature offers potential for reduced costs per dose compared to personalized approaches [25] [4]. The manufacturing process for viral vectors and lipid nanoparticles, while technically complex, can be scaled to produce large batches serving multiple patients, distributing fixed costs across more units [13].
Key cost components for in vivo therapies include: (1) plasmid DNA production for vector manufacturing or mRNA synthesis; (2) cell culture systems and reagents for viral vector production; (3) purification and characterization processes, particularly challenging for AAV vectors with empty/full capsid separation requirements; (4) lipid nanoparticle formulation components and proprietary lipid mixtures; and (5) analytical development and quality control testing [25] [13]. Dose optimization presents a significant economic consideration, as higher doses increase material requirements but may improve efficacy—particularly relevant for tissues with low transfection efficiency. The emerging capability for redosing with LNP-based delivery systems (as demonstrated in Intellia's hATTR trial and Baby KJ's CPS1 deficiency treatment) introduces additional cost considerations but may improve therapeutic outcomes [4].
Cost-Benefit Considerations and Market Outlook
Table 2: Economic Comparison of Ex Vivo vs. In Vivo CRISPR Therapies
| Economic Factor | Ex Vivo Approach | In Vivo Approach |
|---|---|---|
| Development Costs | High (process optimization, analytics) | High (delivery system optimization, toxicology) |
| Manufacturing Cost/Dose | $100,000-$500,000+ | $1,000-$50,000 (projected at scale) |
| Therapeutic Pricing | $1-2.5 million per treatment | Unknown (potentially lower at scale) |
| Key Value Proposition | Curative potential, one-time treatment | Broader accessibility, scalable production |
| Reimbursement Challenges | High upfront cost vs. long-term savings | Outcomes-based agreements, demonstration of durability |
| Market Potential | $35 million (2024) to significant growth by 2030 | Expanding with pipeline progression to common diseases |
| Manufacturing Innovation Impact | Automation, allogeneic approaches, process intensification | Improved vector yields, selective organ targeting LNPs |
The CRISPR gene editing therapies market was estimated at $35 million in 2024, with projections suggesting substantial growth by 2030 [84]. The overall gene therapy platform market demonstrates similar expansion, calculated at $2.18 billion in 2024 and anticipated to reach $2.51 billion in 2025, potentially growing to $9.05 billion by 2034 at a CAGR of 15.3% [85]. This growth trajectory reflects both technological advances and increasing acceptance of gene therapies, though economic sustainability requires careful consideration of cost-benefit ratios across different disease areas.
Experimental Protocols and Methodologies
Ex Vivo Protocol: T-Cell Editing for CAR-T Therapy
This protocol outlines the manufacturing process for creating CRISPR-edited CAR-T cells, representing 75.26% of ex vivo gene therapies in development [83].
Materials:
- Patient leukapheresis product
- T-cell activation reagents (anti-CD3/CD28 antibodies)
- CRISPR editing components: Cas9 mRNA/protein and sgRNA targeting endogenous T-cell receptor genes
- Lentiviral vector carrying CAR transgene (for CD19-targeting, representing 16.01% of therapies)
- Cell culture media with cytokines (IL-2, IL-7, IL-15)
- Electroporation system
- Flow cytometry reagents for characterization
Method:
- T-Cell Isolation and Activation: Isolate T-cells from leukapheresis product using Ficoll density gradient centrifugation. Activate cells using anti-CD3/CD28 antibody-coated beads for 24-48 hours.
- CRISPR Editing: Electroporate activated T-cells with CRISPR-Cas9 ribonucleoprotein complex targeting TRAC locus to reduce graft-versus-host potential in allogeneic settings. Use optimized electroporation parameters: 1500V, 10ms pulse width, 3 pulses.
- Viral Transduction: Transduce edited cells with lentiviral vector carrying CAR transgene at MOI of 5-10 in the presence of 8μg/mL polybrene. Centrifuge at 1000×g for 90 minutes (spinoculation).
- Cell Expansion: Culture transduced cells in complete media with IL-2 (100IU/mL) for 10-14 days, maintaining cell density between 0.5-2×10^6 cells/mL.
- Quality Control: Assess editing efficiency (flow cytometry for TCR knockout), CAR expression (antigen-specific staining), sterility (mycoplasma, endotoxin), and functionality (cytokine release, cytotoxicity assays).
- Formulation and Cryopreservation: Harvest cells, wash, and resuspend in cryopreservation medium. Freeze using controlled-rate freezer and store in vapor phase liquid nitrogen.
In Vivo Protocol: LNP-Mediated Liver Editing
This protocol describes the methodology for LNP-formulated CRISPR delivery to hepatocytes, as used in clinical trials for hATTR and ongoing research for metabolic liver disorders [4].
Materials:
- Cas9 mRNA (modified with 5-methoxyuridine for reduced immunogenicity)
- Single-guide RNA targeting therapeutic gene (e.g., TTR for hATTR)
- Ionizable lipid (DLin-MC3-DMA), cholesterol, DSPC, DMG-PEG2000
- Microfluidic mixer (NanoAssemblr)
- Tangential flow filtration system
- Animal model (e.g., C57BL/6 mice or non-human primates)
Method:
- mRNA Production: Generate Cas9 mRNA via in vitro transcription from linearized DNA template, incorporating 5' cap analog and 3' polyA tail. Purify using HPLC or cellulose-based methods.
- LNP Formulation: Prepare lipid mixture in ethanol (ionizable lipid, cholesterol, DSPC, DMG-PEG at 50:38.5:10:1.5 molar ratio). Combine aqueous phase containing Cas9 mRNA and sgRNA in citrate buffer (pH 4.0). Use microfluidic mixer with total flow rate 12 mL/min and 3:1 aqueous-to-ethanol flow rate ratio to form LNPs.
- LNP Purification and Characterization: Dialyze LNP formulation against PBS (pH 7.4) using tangential flow filtration. Concentrate to target RNA concentration (1-2 mg/mL). Characterize particle size (70-100 nm target), polydispersity (<0.2), RNA encapsulation efficiency (>90%), and endotoxin levels.
- In Vivo Administration: Administer LNPs via intravenous injection at dosage of 1-3 mg RNA/kg. For non-human primates, use slow bolus injection with physiological monitoring.
- Efficacy Assessment: Quantify target protein reduction in serum (e.g., TTR by ELISA) at 7, 14, and 28 days post-administration. Analyze editing efficiency in liver tissue by next-generation sequencing of target locus.
- Safety Evaluation: Monitor liver enzymes (ALT, AST), inflammatory cytokines, and histopathology. Assess potential off-target editing through computational prediction followed by targeted sequencing.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for CRISPR Therapy Development
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| CRISPR Nucleases | SpCas9, SaCas9, CjCas9, Cas12a | Target gene disruption, precise editing | Size constraints (SaCas9: 3.16 kb), PAM requirements, editing efficiency |
| Editing Enhancers | HDR enhancers (RS-1, L755507), NHEJ inhibitors (SCR7) | Improving precise editing efficiency | Cytotoxicity, cell type-specific effects, timing of administration |
| Delivery Materials | AAV serotypes (AAV8, AAV9), ionizable lipids (MC3, SM-102), electroporation systems | In vivo and ex vivo delivery | Tropism, packaging capacity, transfection efficiency, cell viability |
| Cell Culture Supplements | IL-2, IL-7, IL-15, StemRegenin-1, UM171 | Maintaining cell function during expansion | Cell type-specific requirements, cost, GMP-grade availability |
| Analytical Tools | Flow cytometry antibodies, NGS off-target assays, ELISA kits | Quality control, safety assessment | Sensitivity, specificity, standardization across batches |
| Vector Production Systems | HEK293T cells, plasmid transfection reagents, packaging plasmids | Viral vector manufacturing | Transfection efficiency, vector yields, empty/full particle ratio |
The commercialization pathways for in vivo and ex vivo CRISPR therapies present distinct challenges in manufacturing complexity and treatment costs that will significantly influence their accessibility and application scope. Ex vivo approaches offer precise cellular engineering but face fundamental scalability limitations due to their personalized nature, resulting in costs exceeding $2 million per treatment that currently restrict broad patient access [1] [4]. In vivo strategies present potential for more traditional manufacturing scalability but encounter significant biological barriers in delivery efficiency and tissue-specific targeting that must be overcome to achieve therapeutic relevance [25] [13].
Future progress will depend on technological innovations addressing these core challenges. For ex vivo therapies, advances in automation, allogeneic ("off-the-shelf") approaches using multiplexed CRISPR editing to evade immune rejection, and process intensification could substantially reduce costs and increase throughput [83] [38]. In the in vivo space, development of novel delivery vectors with enhanced tissue specificity, improved LNP formulations enabling redosing regimens, and compact editing systems with reduced immunogenicity will be critical for expanding therapeutic applications [25] [4]. The ongoing evolution of the CRISPR toolkit—including base editing, prime editing, and epigenome modulation—may further influence manufacturing paradigms through improved safety profiles and editing precision [25] [38].
The economic sustainability of CRISPR therapies will ultimately depend on demonstrating long-term value to healthcare systems, optimizing manufacturing platforms to reduce production costs, and developing innovative payment models that balance innovation with accessibility. As the field progresses beyond rare diseases to more common conditions, the interplay between manufacturing complexity and treatment costs will increasingly determine which therapeutic approach achieves widespread clinical implementation and patient benefit.
The advent of CRISPR-Cas9 genome editing has ushered in a new era of therapeutic potential, capable of addressing the root causes of genetic diseases. Two fundamentally different paradigms have emerged for delivering these therapies: in vivo and ex vivo editing. The selection between these pathways is a critical early strategic decision that dictates every subsequent aspect of a therapeutic program's development, from manufacturing to clinical trial design. This guide provides a structured framework for researchers and drug development professionals to navigate this complex decision, grounded in current technological capabilities and clinical evidence.
Core Principles and Comparative Analysis
The fundamental distinction lies in the site of genetic modification. In vivo editing involves the direct administration of the CRISPR system into the patient's body to edit cells within their native physiological environment. In contrast, ex vivo editing is a multi-step process where target cells are extracted from the patient, genetically modified in a controlled laboratory setting, and then reinfused back into the patient [1].
The following table summarizes the core characteristics, advantages, and challenges of each approach.
Table 1: Strategic Comparison of In Vivo vs. Ex Vivo CRISPR Therapies
| Feature | In Vivo Approach | Ex Vivo Approach |
|---|---|---|
| Definition | CRISPR components delivered directly into the body to edit cells internally [86]. | Cells are collected from the patient, edited outside the body, and then reinfused [1]. |
| Key Advantage | Potential to treat a wider range of tissues and diseases; less complex patient logistics. | High precision and control over the editing process; easier to ensure quality and efficacy pre-infusion. |
| Primary Challenge | Delivery efficiency, immune responses to delivery vectors or Cas9, and potential off-target effects [86] [15]. | Complex, costly manufacturing; requires myeloablative conditioning chemotherapy [1]. |
| Manufacturing | Scalable production of delivery vectors (e.g., LNPs, AAVs); potentially simpler scale-up. | Complex, patient-specific (autologous) cell processing; significant quality control challenges. |
| Therapeutic Scope | Ideal for inaccessible tissues (e.g., liver, brain) or diseases affecting large cell populations. | Ideal for blood-borne diseases and engineered cell therapies (e.g., CAR-T, HSCs). |
| Clinical Example | Intellia's NTLA-2001 for hATTR (LNP delivery to liver) [4]. | CASGEVY (exa-cel) for Sickle Cell Disease and TDT (editing CD34+ HSCs) [87] [1]. |
| Regulatory Path | Evolving landscape for systemic gene editing; long-term monitoring for off-target effects is critical. | Established pathway for cell therapies; safety profile includes risks associated with cell manipulation and conditioning. |
Decision Framework: Key Selection Criteria
Choosing between in vivo and ex vivo approaches requires a systematic evaluation of biological, technical, and commercial factors. The following diagram illustrates the core decision-making workflow.
Biological and Technical Factors
- Target Cell Type and Accessibility: This is often the primary determinant. Ex vivo is the default choice for hematopoietic stem cells (HSCs) and T-cells, as they can be routinely harvested and reinfused with high engraftment efficiency [87] [1]. For tissues that cannot be easily removed or reintroduced, such as hepatocytes or neurons, in vivo delivery is the only feasible path [4].
- Complexity of the Genetic Edit: The choice of DNA repair mechanism—Non-Homologous End Joining (NHEJ) versus Homology-Directed Repair (HDR)—is a key technical driver. Ex vivo editing currently holds an advantage for HDR-mediated precise gene insertion or correction, as editing conditions can be optimized and clones can be selected pre-infusion [1]. While HDR is possible in vivo, it is significantly less efficient. For gene knockouts, which rely on the more efficient NHEJ pathway, in vivo approaches are highly effective, as demonstrated by the successful knockdown of the TTR and ANGPLT3 genes in the liver [4] [88].
- Safety and Immunogenicity Profile: Ex vivo editing allows for comprehensive off-target analysis and validation of the edited cell product before administration, mitigating some safety risks [15]. In vivo editing faces the challenge of potential immune reactions to the bacterial Cas9 protein or the viral/LNP delivery vectors, which can reduce efficacy or cause adverse events [86] [4]. Pre-existing immunity to AAV capsids, for instance, can exclude a significant portion of the patient population.
Clinical and Commercial Factors
- Manufacturing and Scalability: Ex vivo therapies like CASGEVY are autologous, leading to complex, costly, and patient-specific logistics. In vivo therapies are typically allogeneic (off-the-shelf), with a manufacturing model that more closely resembles traditional biologics, offering potential for broader and more economical distribution [4].
- Clinical Intervention Burden: Ex vivo therapies require myeloablative conditioning (e.g., chemotherapy) to clear space in the bone marrow for the edited cells, a process with significant toxicity and recovery time [1]. In vivo therapies, administered via infusion or injection, aim to be a one-time treatment without the need for such intensive pre-conditioning, representing a more favorable patient experience.
Experimental Protocols and Workflows
To ground the strategic framework in practical science, below are generalized protocols for each approach, reflecting current state-of-the-art methods.
Ex Vivo Workflow Protocol: HSC Editing (e.g., CASGEVY)
This protocol outlines the key steps for ex vivo editing of hematopoietic stem cells, based on the approved therapy for sickle cell disease [87] [1].
- Patient Mobilization and Apheresis: Administer granulocyte colony-stimulating factor (G-CSF) to mobilize CD34+ HSCs from the bone marrow into the peripheral blood. Collect these cells via leukapheresis.
- Cell Processing and Culture: Isolate and purify CD34+ HSCs from the apheresis product using immunomagnetic selection. Culture cells in a cytokine-rich medium (e.g., containing SCF, TPO, FLT-3L) to maintain viability and potency.
- CRISPR Delivery and Editing: Electroporation is the preferred method for its high efficiency in primary cells. Deliver the CRISPR-Cas9 ribonucleoprotein (RNP) complex—comprising purified Cas9 protein and synthetic sgRNA—directly into the cells. The RNP format enables rapid editing and minimizes off-target effects due to its transient activity [13]. The target for SCD/TDT is the BCL11A gene enhancer region.
- Quality Control and Release Testing: Perform rigorous testing on the final product. This includes:
- Viability and cell count.
- Potency assays (e.g., measurement of fetal hemoglobin production).
- Sterility, mycoplasma, and endotoxin testing.
- Assessment of editing efficiency (e.g., via NGS) and off-target profiling.
- Patient Conditioning and Reinfusion: While the cell product is being manufactured, the patient undergoes myeloablative conditioning with busulfan to eliminate native HSCs in the bone marrow. The cryopreserved, edited cell product is then thawed and administered via intravenous infusion.
- Post-Infusion Monitoring: Monitor patient for engraftment (neutrophil and platelet recovery), and track long-term efficacy (e.g., freedom from vaso-occlusive crises) and safety.
In Vivo Workflow Protocol: Liver-Directed Editing (e.g., NTLA-2001 or CTX310)
This protocol describes the process for systemic in vivo editing of hepatocytes, as used in clinical trials for transthyretin amyloidosis and dyslipidemias [4] [88].
- CRISPR Payload Design and Formulation:
- Cargo Selection: For a knockout strategy, use mRNA encoding the Cas9 protein and a separate sgRNA. This combination offers a balance of sufficient durability for editing and transient activity to limit off-targets [86].
- Vector Formulation: Encapsulate the mRNA and sgRNA into Liver-Targeting Lipid Nanoparticles (LNPs). LNPs protect the nucleic acids from degradation and facilitate delivery to hepatocytes after systemic administration [4] [13]. The ionizable lipid composition is critical for liver tropism.
- Preclinical Biodistribution and Safety:
- Conduct in vivo studies in relevant animal models to confirm predominant LNP uptake in the liver.
- Perform GLP toxicology studies to establish a safety profile and identify a starting dose for clinical trials.
- Use computational tools and empirical methods like CIRCLE-seq to predict and screen for potential off-target editing sites in the human genome.
- Clinical Administration and Monitoring:
- Administer a single intravenous infusion of the LNP formulation to patients.
- Monitor for infusion-related reactions and changes in liver enzymes (ALT, AST) as key safety parameters.
- Assess pharmacodynamic efficacy by repeatedly measuring the reduction in the target protein (e.g., TTR or ANGPLT3) in patient serum [4] [88].
- Conduct long-term follow-up to monitor the persistence of editing and long-term safety.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogs key reagents and their functions, as derived from the experimental protocols and current literature.
Table 2: Key Research Reagents for CRISPR Therapy Development
| Research Reagent / Tool | Function in Experimental Protocol |
|---|---|
| CRISPR Ribonucleoprotein (RNP) | The preassembled complex of Cas9 protein and sgRNA; used in ex vivo electroporation for transient, highly specific editing with reduced off-target effects [13]. |
| Lipid Nanoparticles (LNPs) | Synthetic delivery vector for in vivo therapy; encapsulates and protects CRISPR mRNA and sgRNA, facilitating targeted delivery to organs like the liver after IV infusion [86] [4]. |
| Adeno-Associated Virus (AAV) | A viral delivery vector for in vivo therapy; can deliver CRISPR DNA constructs for longer-term expression but has cargo size limitations and potential immunogenicity concerns [13]. |
| CD34+ Microbeads | Immunomagnetic cell separation reagent; critical for isolating pure populations of hematopoietic stem cells from apheresis product in ex vivo workflows [87] [1]. |
| Next-Generation Sequencing (NGS) | Platform for comprehensive quality control; used to quantify on-target editing efficiency and to conduct unbiased off-target analyses to assess product safety [15]. |
| Cytokine Cocktails (SCF, TPO, FLT-3L) | Cell culture supplements; essential for maintaining the viability and stemness of HSCs during the ex vivo editing and expansion process [87]. |
The strategic choice between in vivo and ex vivo CRISPR therapy is not a matter of superiority, but of context. The ex vivo approach, with its high level of control, remains the proven path for engineered cell therapies. The in vivo approach holds the promise of a simpler, more scalable treatment paradigm for a vast range of genetic diseases, contingent on overcoming delivery and immune hurdles. As vector technology and gene editing tools continue to advance—with novel LNPs, virus-like particles (VLPs), and more precise editors like base and prime editors—the boundaries of what is possible with each approach will continue to expand. A rigorous, systematic application of this strategic framework will enable researchers to select the most efficient and viable path to transform revolutionary science into life-changing medicines.
Conclusion
The differentiation between in vivo and ex vivo CRISPR-Cas9 therapies represents a fundamental strategic decision in therapeutic development, with each approach offering distinct advantages for specific clinical contexts. Ex vivo therapies have demonstrated groundbreaking success with approved products like CASGEVY®, offering controlled editing environments but facing manufacturing complexity. Meanwhile, in vivo approaches are showing remarkable progress in liver-directed therapies and personalized medicine, enabled by advancing LNP and viral vector technologies, though challenges in delivery precision and immune responses remain. Future directions will focus on developing next-generation editing tools like base and prime editors, expanding tissue tropism beyond the liver, optimizing redosing protocols, and addressing genomic safety concerns through improved detection methods. The convergence of CRISPR technology with artificial intelligence, enhanced delivery systems, and personalized therapeutic platforms promises to accelerate the development of safe, effective, and accessible genome editing treatments across a broader spectrum of human diseases.
References
- 1. CRISPR Technologies for In Vivo and Ex Vivo Gene Editing [https://www.ncbi.nlm.nih.gov/books/NBK609557/]
- 2. The CRISPR-Cas Mechanism for Adaptive Immunity and ... [https://www.frontiersin.org/journals/cellular-and-infection-microbiology/articles/10.3389/fcimb.2020.619763/full]
- 3. CRISPR-Cas adaptive immunity and the three Rs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5518543/]
- 4. CRISPR Clinical Trials: A 2025 Update [https://innovativegenomics.org/news/crispr-clinical-trials-2025/]
- 5. High-Content Analysis of CRISPR-Cas9 Gene-Edited ... [https://www.sciencedirect.com/science/article/pii/S2213671115003653]
- 6. ORANGE: A CRISPR/Cas9-based genome editing toolbox ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7176289/]
- 7. The hidden risks of CRISPR/Cas: structural variations and ... [https://www.nature.com/articles/s41467-025-62606-z]
- 8. CRISPR/Cas9 therapeutics: progress and prospects [https://www.nature.com/articles/s41392-023-01309-7]
- 9. ZFN, TALEN and CRISPR/Cas-based methods for genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3694601/]
- 10. CRISPR-Cas9, TALENs and ZFNs - the battle in gene editing [https://www.ptglab.com/news/blog/crispr-cas9-talens-and-zfns-the-battle-in-gene-editing/?srsltid=AfmBOoosO_qO0uTKBQH15vbjx9Wm9U6erCm1sOnqXKz1dH_bqPeTHeuP]
- 11. 2025伦敦·金斯瑞生物科技全球产业论坛圆满落幕:共话CGT ... [https://www.genscript.com.cn/genscript-biotech-global-forum-london-2025-concluded-successfully.html]
- 12. Overcoming the Delivery Challenges in CRISPR/Cas9 Gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12434829/]
- 13. CRISPR Delivery Methods: Cargo, Vehicles, and Challenges [https://www.synthego.com/blog/delivery-crispr-cas9/]
- 14. CRISPR-Cas9 DNA Base-Editing and Prime-Editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7503568/]
- 15. Advancing CRISPR genome editing into gene therapy clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094669/]
- 16. CRISPR Base Editing Explained | ABE & CBE in Gene ... [https://www.synthego.com/crispr-base-editing-guide/]
- 17. Base editing: What is it and what does it mean for ... [https://www.genomicseducation.hee.nhs.uk/blog/base-editing-what-is-it-and-what-does-it-mean-for-healthcare/]
- 18. Explainer: What Is Prime Editing and What Is It Used For? [https://crisprmedicinenews.com/news/explainer-what-is-prime-editing-and-what-is-it-used-for/]
- 19. Prime Editing: Adding Precision and Flexibility to CRISPR ... [https://blog.addgene.org/prime-editing-crisp-cas-reverse-transcriptase]
- 20. CMN Weekly (31 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-31-october-2025-your-weekly-crispr-medicine-news/]
- 21. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-announces-positive-phase-1-clinical-data]
- 22. Revolutionizing in vivo therapy with CRISPR/Cas genome ... [https://www.frontiersin.org/journals/genome-editing/articles/10.3389/fgeed.2024.1342193/full]
- 23. In Vivo [https://crisprtx.com/focus-areas/in-vivo]
- 24. Challenges and Opportunities in the Application of CRISPR ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12503735/]
- 25. innovations and challenges in rAAV vector-based CRISPR ... [https://www.nature.com/articles/s41434-025-00573-2]
- 26. CRISPR Genome Engineering: Advantages and Limitations [https://www.taconic.com/resources/crispr-genome-engineering-advantages-limitations]
- 27. Landscape of ex vivo gene therapies: Technological trends ... [https://www.sciencedirect.com/science/article/pii/S2329050125001755]
- 28. CRISPR Clinical Trials to Follow [https://www.synthego.com/blog/crispr-clinical-trials/]
- 29. Protocol for optimizing culture conditions for ex vivo ... [https://www.sciencedirect.com/science/article/pii/S2666166725001285]
- 30. CRISPR/Cas9 Delivery Systems to Enhance Gene Editing ... [https://www.mdpi.com/1422-0067/26/9/4420]
- 31. Overcoming the Delivery Challenges in CRISPR/Cas9 ... [https://www.medsci.org/v22p3625.htm]
- 32. Advancing gene editing: the role of lipid nanoparticles in ... [https://www.drugtargetreview.com/article/188056/advancing-gene-editing-the-role-of-lipid-nanoparticles-in-crispr-delivery/]
- 33. Engineering ARMMs for improved intracellular delivery of ... [https://www.sciencedirect.com/science/article/pii/S2773041725000186]
- 34. CASGEVY® Clinical Trial and Results [https://www.casgevy.com/sickle-cell-disease/study-information]
- 35. Sickle cell success stories: Why spring break will lead to a ... [https://web.musc.edu/about/news-center/2025/03/27/sickle-cell-success-stories-why-spring-break-will-lead-to-a-first-for-these-two]
- 36. Pipeline [https://crisprtx.com/pipeline]
- 37. Cell and gene therapy: In vivo and Ex vivo in comparison [https://www.susupport.com/blogs/knowledge/cell-and-gene-therapy-in-vivo-and-ex-vivo-in-comparison]
- 38. CMN Weekly (17 October 2025) [https://crisprmedicinenews.com/news/cmn-weekly-17-october-2025-your-weekly-crispr-medicine-news/]
- 39. Unintended CRISPR-Cas9 editing outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC10182114/]
- 40. Research achieves gene-editing breakthrough that could ... [https://www.sciencedaily.com/releases/2025/02/250213143552.htm]
- 41. CRISPR Delivery Systems for Organ-Specific Targeting [https://www.sciencedirect.com/science/article/pii/S2950482125000336]
- 42. Advancements in CRISPR/Cas systems for disease treatment [https://www.sciencedirect.com/science/article/pii/S2211383525003132]
- 43. CMN Weekly (5 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-5-september-2025-your-weekly-crispr-medicine-news/]
- 44. Nucleic acid therapeutics for liver diseases: A decade ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12496246/]
- 45. Alternatives to CRISPR-Cas9: Nucleases for Next-Gen ... [https://www.synthego.com/blog/alternatives-to-crispr-cas9-nucleases-for-next-gen-therapy/]
- 46. Emerging role of molecular diagnosis and personalized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12212695/]
- 47. Engineering of a compact, high-fidelity EbCas12a variant that ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11139299/]
- 48. CRISPR-Cas orthologues and variants - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC5569134/]
- 49. Versatile and efficient in vivo genome editing with compact ... [https://www.sciencedirect.com/science/article/pii/S1525001621003191]
- 50. Insights into the compact CRISPR–Cas9d system [https://www.nature.com/articles/s41467-025-57455-9]
- 51. mRNA trans-splicing dual AAV vectors for (epi)genome ... [https://www.nature.com/articles/s41467-023-42386-0]
- 52. In Situ Gene Therapy via AAV-CRISPR-Cas9-Mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6035733/]
- 53. Off-target effects in CRISPR-Cas genome editing for ... [https://www.sciencedirect.com/science/article/pii/S2162253125001908]
- 54. Off-target effects in CRISPR-Cas genome editing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12329535/]
- 55. Non-clinical safety considerations on genome editing using ... [https://www.sciencedirect.com/science/article/pii/S2352304225002740]
- 56. CRISPR-Cas9 induces large structural variants at on-target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8810904/]
- 57. Measurement and clinical interpretation of CRISPR off- ... [https://www.nature.com/articles/s41588-025-02428-3]
- 58. Recent advances in therapeutic CRISPR-Cas9 genome editing [https://pmc.ncbi.nlm.nih.gov/articles/PMC10080534/]
- 59. Immune Responses to Viral Gene Therapy Vectors - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7054714/]
- 60. Intellia Announces Positive Clinical Proof-of-Concept Data ... [https://ir.intelliatx.com/news-releases/news-release-details/intellia-announces-positive-clinical-proof-concept-data-redosing]
- 61. Lipid nanoparticles for delivery of RNA therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC9691360/]
- 62. CRISPR-Cas9-mediated homology-directed repair for precise gene editing - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11531618/]
- 63. Fine-Tuning Homology-Directed Repair (HDR) for Precision Genome Editing: Current Strategies and Future Directions [https://www.mdpi.com/1422-0067/26/9/4067]
- 64. Tissue Specific DNA Repair Outcomes Shape the ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.728520/full]
- 65. In vivo versus ex vivo CRISPR therapies for retinal dystrophy - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5289756/]
- 66. Improving the Efficiency of CRISPR/Cas9-Mediated Non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384319/]
- 67. CRISPR-Cas9-mediated homology-directed repair for ... [https://www.sciencedirect.com/science/article/pii/S2162253124002312]
- 68. CMN Weekly (26 September 2025) [https://crisprmedicinenews.com/news/cmn-weekly-26-september-2025-your-weekly-crispr-medicine-news/]
- 69. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-present-preclinical-data-alpha-1-antitrypsin]
- 70. Overview CRISPR Clinical Trials 2025 - Learn | Innovate [https://crisprmedicinenews.com/clinical-trials/]
- 71. Progress and Pressure: Taking Stock of the CRISPR ... [https://www.medscape.com/viewarticle/progress-and-pressure-taking-stock-crispr-landscape-2025a1000rzr]
- 72. Characterizing and controlling CRISPR repair outcomes in ... [https://www.nature.com/articles/s41467-025-66058-3]
- 73. qEva-CRISPR: a method for quantitative evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158505/]
- 74. Long-term dual-color tracking of genomic loci by modified ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4872083/]
- 75. Revolutionizing in vivo therapy with CRISPR/Cas genome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10867117/]
- 76. Safety and efficacy studies of CRISPR-Cas9 treatment ... [https://pubmed.ncbi.nlm.nih.gov/39044427/]
- 77. Phase 1 Trial of CRISPR-Cas9 Gene Editing Targeting ... [https://www.acc.org/Latest-in-Cardiology/Clinical-Trials/2025/11/23/20/14/CRISPR-Cas9]
- 78. CRISPR Therapeutics to Present Late-Breaking… [https://crisprtx.com/about-us/press-releases-and-presentations/crispr-therapeutics-to-present-late-breaking-data-at-the-american-heart-association-aha-scientific-sessions-2025]
- 79. CRISPR/Cas9 Gene Editing: Advancements Enhancing ... [https://www.moleculardevices.com/lab-notes/clone-screening/crispr-cas9-gene-editing]
- 80. Clinical applications of the CRISPR/Cas9 genome-editing ... [https://www.sciencedirect.com/science/article/pii/S235230422300079X]
- 81. Ex Vivo Cell-Based CRISPR/Cas9 Genome Editing for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7035593/]
- 82. Recent Advances in CRISPR/Cas9 Delivery Approaches for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10661828/]
- 83. Landscape of ex vivo gene therapies: Technological trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12547725/]
- 84. CRISPR Gene Editing Therapies Market [https://www.rootsanalysis.com/reports/crispr-based-therapeutics-market.html]
- 85. Gene Therapy Platform Market Size to Hit USD 9.05 Billion ... [https://www.biospace.com/press-releases/gene-therapy-platform-market-size-to-hit-usd-9-05-billion-by-2034-driven-by-advancements-in-crispr-and-personalized-medicine]
- 86. In vivo delivery of CRISPR-Cas9 therapeutics - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8424283/]
- 87. CRISPR Therapeutics Highlights Strategic Priorities and ... [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-highlights-strategic-priorities-and]
- 88. Press Release [https://ir.crisprtx.com/news-releases/news-release-details/crispr-therapeutics-provides-business-update-and-reports-13]