Lipid Metabolite Signatures in Diabetic Complications: A Comparative Review of Pathophysiology, Biomarkers, and Clinical Applications
Diabetic microvascular complications, including kidney disease, retinopathy, and neuropathy, are major drivers of morbidity, yet their progression varies significantly among individuals.
Lipid Metabolite Signatures in Diabetic Complications: A Comparative Review of Pathophysiology, Biomarkers, and Clinical Applications
Abstract
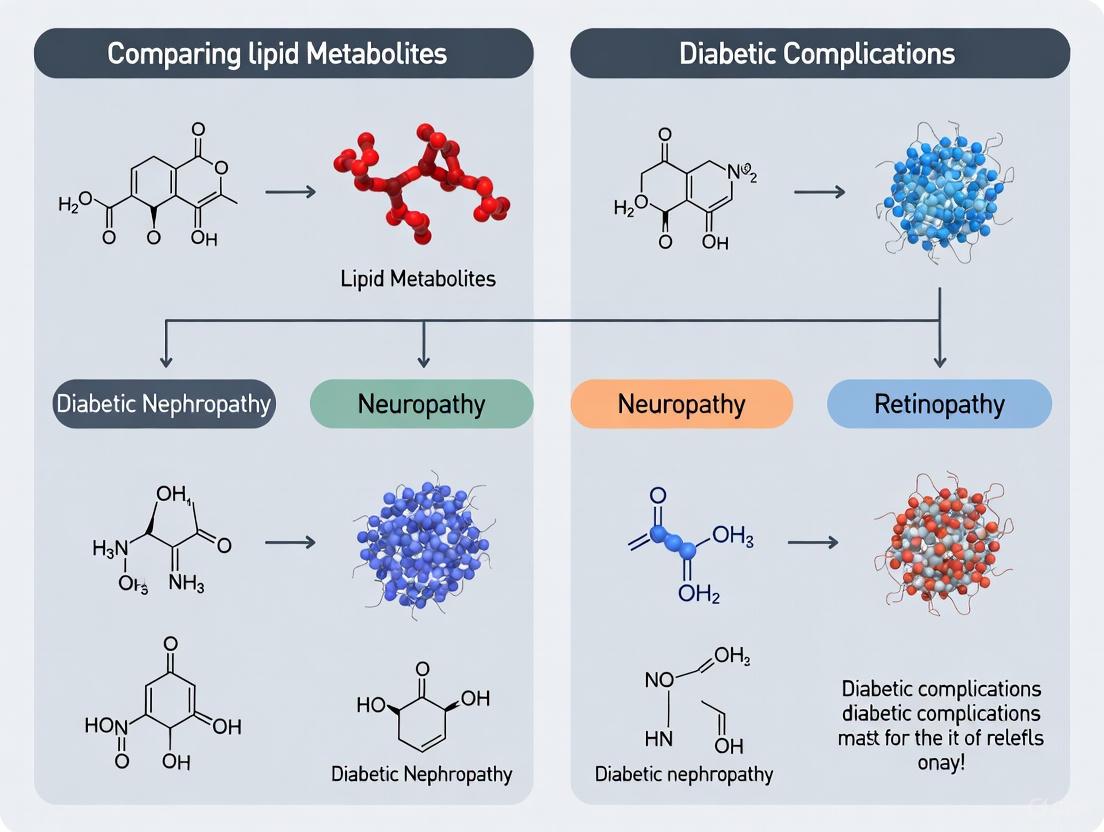
Diabetic microvascular complications, including kidney disease, retinopathy, and neuropathy, are major drivers of morbidity, yet their progression varies significantly among individuals. Emerging evidence underscores that distinct lipid metabolic reprogramming underpins each complication, offering a new layer of understanding beyond traditional risk factors. This article synthesizes recent findings from metabolomic and lipidomic studies to compare and contrast the specific lipid signatures associated with diabetic kidney disease, retinopathy, and neuropathy. We explore the pathophysiological roles of lipid droplet dynamics, lipotoxicity, and novel biomarkers like the Visceral Adiposity Index (VAI) and Lipid Accumulation Product (LAP). Furthermore, we evaluate advanced mass spectrometry methodologies for biomarker discovery, discuss the integration of machine learning for data stratification, and assess the translational potential of lipid metabolites for early diagnosis, risk stratification, and targeted therapeutic interventions. This comprehensive analysis aims to provide researchers and drug development professionals with a foundational resource for innovating in the prevention and management of diabetic complications.
The Landscape of Lipid Dysregulation in Diabetic Microvascular Complications
Lipid metabolic reprogramming, a fundamental adaptation of cellular metabolism under diabetic conditions, is increasingly recognized as a critical driver in the pathogenesis of diabetes and its complications. Under the persistent metabolic stress of diabetes, cells throughout the body—from pancreatic beta cells to renal cells—undergo significant alterations in their lipid handling, including increased lipid uptake, impaired fatty acid oxidation, and enhanced lipid synthesis [1] [2]. These changes result in the toxic accumulation of lipid species such as free fatty acids, diacylglycerol, and ceramides, a state known as lipotoxicity [1]. Lipotoxicity, in turn, triggers cascades of inflammation, fibrosis, and cellular dysfunction, accelerating damage in target organs like the kidneys, retina, and blood vessels [1] [3]. This article provides a comparative analysis of lipid metabolic alterations across major diabetic complications, synthesizing current molecular insights, profiling data, and experimental approaches that are shaping this frontier of metabolic research.
Comparative Data on Lipid Alterations in Diabetic Complications
The landscape of lipid dysregulation varies significantly across diabetic complications, both in the specific lipid species involved and their compartmentalization. The following tables synthesize key quantitative findings from recent clinical and omics studies.
Table 1: Comparison of Key Dysregulated Lipid Pathways in Diabetic Complications
| Diabetic Complication | Key Dysregulated Lipid Pathways | Accumulated Lipid Species | Major Cellular Consequences |
|---|---|---|---|
| Diabetic Kidney Disease (DKD) | Increased lipid influx (CD36, FATP2), Impaired fatty acid oxidation, Enhanced lipid synthesis (FASN, ACC) [1] [2] | Free Fatty Acids (FFAs), Diacylglycerol (DAG), Ceramides [1] [2] | Inflammation, Renal fibrosis, Podocyte & tubular cell dysfunction [1] [2] |
| Diabetic Retinopathy (DR) | Sphingomyelin-Ceramide pathway, Phosphatidylcholine metabolism, De novo lipogenesis [4] | Ceramides, Sphingomyelins, Lysophosphatidylcholine [4] | Retinal ganglion cell death, Neuroinflammation, Breakdown of blood-retinal barrier [4] |
| Pancreatic Beta Cell Dysfunction | Imbalanced esterification/oxidation, Enhanced lipid synthesis, LD dynamics disruption [3] [5] | Triglycerides (in LDs), DAG, Ceramides [3] [5] | Impaired GSIS, ER stress, Apoptosis, Dedifferentiation [5] |
Table 2: Quantitative Lipid Biomarker Performance for Predicting Complications
| Biomarker / Index | Calculation | Association with DKD (Weighted Mean Difference, WMD) | Predictive Performance for DKD |
|---|---|---|---|
| Lipid Accumulation Product (LAP) | [WC (cm) - 65] × TG (mmol/L) (Men); [WC (cm) - 58] × TG (mmol/L) (Women) [6] | WMD: 12.67 (95% CI: 7.83–17.51); P < .01 [6] | OR per 1-unit increase: 1.005 (95% CI: 1.003–1.006); P < .01 [6] |
| Atherogenic Index of Plasma (AIP) | log10(TG/HDL-C) [6] | WMD: 0.11 (95% CI: 0.03–0.19); P < .01 [6] | OR per 1-unit increase: 1.08 (95% CI: 1.04–1.12); P < .01 [6] |
| Visceral Adiposity Index (VAI) | (WC/39.68 + BMI/1.88) × (TG/1.03) × (1.31/HDL) (Men); (WC/36.58 + BMI/1.89) × (TG/0.81) × (1.52/HDL) (Women) [6] | WMD: 0.63 (95% CI: 0.38–0.89); P < .01 [6] | OR per 1-unit increase: 1.05 (95% CI: 1.03–1.07); P < .01 [6] |
Table 3: Urinary Lipid Metabolites Associated with Rapid DKD Progression [7]
| Metabolite Class | Specific Metabolites (Elevated in Fast Decliners) | Experimental Measurement | Key Finding |
|---|---|---|---|
| Ceramides | Multiple species identified | Targeted UPLC/TQMS | Strongly associated with the highest quartile of eGFR decline. |
| Diacylglycerols (DAG) | Multiple species identified | Targeted UPLC/TQMS | Baseline levels were significantly elevated in patients with subsequent rapid kidney function loss. |
| Other Complex Lipids | 21 significantly upregulated lipid metabolites in DKD vs. uncomplicated T2D | Targeted UPLC/TQMS | A panel of 8-9 candidate lipids predicted future decline better than albuminuria or eGFR alone. |
Experimental Protocols for Lipid Metabolic Research
Targeted Lipidomics for Biomarker Discovery
Objective: To identify and quantify specific lipid metabolites in biofluids (e.g., urine, serum) that predict the development or progression of diabetic complications.
Protocol Summary (as used in DKD studies [7]):
- Sample Collection: Collect fasting spot urine or serum samples. Standardize collection protocols to minimize pre-analytical variability.
- Sample Preparation: Mix a 20 μL aliquot of urine with 120 μL of a standard solution containing 508 targeted lipid metabolites. After centrifugation, derivatize the supernatant with freshly prepared reagents at 60°C for 1 hour.
- Instrumental Analysis: Analyze samples using Ultra-Performance Liquid Chromatography coupled with Targeted Quantification Mass Spectrometry (UPLC/TQMS). A Waters ACQUITY UPLC system with a XEVO TQ-S mass spectrometer is typically used.
- Data Processing: Process raw data files with specialized software (e.g., Targeted Metabolome Batch Quantification - TMBQ). Normalize all metabolite concentrations to urinary creatinine to correct for urine concentration.
- Quality Control: Apply stringent QC filters: signal-to-noise ratio >10, coefficient of variation <15% in pooled QC samples, and a detection rate >80% across all samples.
Bioinformatics Interrogation of Metabolic Reprogramming
Objective: To identify key metabolic reprogramming-related genes (MRRGs) and pathways from transcriptomic data of tissues affected by diabetic complications.
Protocol Summary (as applied to Diabetic Nephropathy [8] [9]):
- Data Acquisition: Source relevant transcriptome datasets (e.g., GSE30528, GSE96804) from public repositories like the Gene Expression Omnibus (GEO).
- Data Preprocessing: Perform batch effect correction on combined datasets using the
svaR package and the ComBat method. Normalize the expression matrix. - Identification of MRRGs: Obtain a list of MRRGs from the GeneCards database (search: "Metabolic Reprogramming," relevance score >4). Cross-reference these with differentially expressed genes (DEGs) from the processed datasets to find metabolic reprogramming-related DEGs (MRRDEGs).
- Enrichment and Network Analysis: Conduct functional enrichment analyses (GO, KEGG) on MRRDEGs using
clusterProfiler. Construct Protein-Protein Interaction (PPI) networks (e.g., via STRING database) and apply machine learning algorithms (e.g., random forest) or network tools (e.g., CytoHubba) to identify hub genes. - Validation: Validate the diagnostic value of hub genes using Receiver Operating Characteristic (ROC) analysis and confirm their expression patterns with experimental methods like qRT-PCR.
Signaling Pathways and Molecular Mechanisms
The pathological remodeling of lipid metabolism in diabetes is driven by interconnected signaling pathways that respond to the diabetic milieu. The core pathway linking hypoxia and inflammation to lipid accumulation in complications like Diabetic Kidney Disease is summarized below.
The typical workflow for a multi-omics study investigating lipid metabolic reprogramming, from sample collection to biomarker identification, is outlined below.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Reagents and Resources for Investigating Lipid Metabolic Reprogramming
| Tool / Reagent | Primary Function | Example Application in Diabetes Research |
|---|---|---|
| UPLC/TQMS Systems | High-sensitivity identification and quantification of lipid species in complex biological samples. | Targeted lipidomic profiling of 508 lipid metabolites in urine/serum for biomarker discovery [7]. |
| GeneCards Database | Collates information on human genes from multiple genomic data repositories. | Sourcing Metabolic Reprogramming-Related Genes (MRRGs) with relevance scores for transcriptomic studies [8] [9]. |
| STRING Database | Resource for predicting and analyzing Protein-Protein Interactions (PPI). | Constructing PPI networks from metabolic reprogramming-related DEGs to identify hub genes [9]. |
| sva R Package | Correction of batch effects in high-throughput genomic data. | Removing technical variability when integrating multiple transcriptomic datasets (e.g., GSE30528, GSE96804) [8] [9]. |
| limma R Package | Differential expression analysis for microarray and RNA-seq data. | Identifying genes significantly up- or down-regulated in diabetic nephropathy vs. control samples [8] [9]. |
| clusterProfiler R Package | Functional enrichment analysis of gene lists. | Performing GO and KEGG pathway analysis to interpret biological roles of MRRGs in diabetic complications [8] [9]. |
Lipid droplets (LDs) are dynamic, ubiquitous organelles central to cellular lipid and energy homeostasis. In metabolic health, they sequester and release lipids in response to nutrient fluctuations. However, in the context of type 2 diabetes mellitus (T2DM), dysregulated LD dynamics contribute significantly to ectopic lipid deposition and the development of lipotoxicity in non-adipose tissues [10] [11]. This pathophysiological process is a key driver of insulin resistance and the progression of diabetic complications across multiple organ systems [10] [12]. This guide provides a comparative analysis of LD dynamics and ectopic lipid deposition in target organs, framing the discussion within the broader context of lipid metabolites and diabetic complications research. It is designed to support researchers and drug development professionals by synthesizing current pathophysiological insights, experimental data, and methodologies.
Physiological and Pathological Roles of Lipid Droplets
Core Structure and Dynamics of Lipid Droplets
Lipid droplets possess a unique architecture, consisting of a neutral lipid core (composed of triglycerides and cholesteryl esters) enclosed by a phospholipid monolayer decorated with a specific set of proteins [11]. Their life cycle is governed by a coupled process of formation and degradation:
- Biogenesis: Occurs in the endoplasmic reticulum (ER) membrane, where neutral lipids synthesized by enzymes like DGAT1/2 accumulate to form an oil lens that subsequently buds off [10] [11].
- Degradation: Primarily occurs through two pathways: enzymatic hydrolysis (lipolysis) by lipases like ATGL and HSL, and selective autophagy (lipophagy) [10].
Lipid Droplet Dynamics in Metabolic Homeostasis and Disease
Under physiological conditions, LDs are protective. In pancreatic β-cells, they participate in lipid metabolism that regulates insulin secretion and isolate harmful lipids to protect against nutrient excess damage [10]. In adipose tissue, LDs respond to nutrient fluctuations, releasing free fatty acids (FFAs) and glycerol to influence systemic insulin sensitivity and glucose homeostasis [10].
Under the pathological conditions of T2DM, LD dynamics become dysregulated. Abnormal LD accumulation leads to ectopic lipid deposition in non-adipose tissues such as the liver, skeletal muscle, heart, kidneys, and pancreas [10] [12]. This exceeds the tissue's oxidative capacity, resulting in lipotoxicity—a process characterized by the accumulation of harmful lipid intermediates like diacylglycerol (DG) and ceramides, which induce cellular stress, inflammation, and impair insulin signaling [10] [12].
Comparative Analysis of Ectopic Lipid Deposition in Target Organs
The pathophysiology of ectopic lipid deposition exhibits distinct features across different target organs, as summarized in the table below.
Table 1: Organ-Specific Characteristics of Ectopic Lipid Deposition and LD Dynamics
| Target Organ | Key LD-Associated Proteins | Primary Pathophysiological Consequences | Major Diabetic Complication(s) |
|---|---|---|---|
| Liver | PLIN2, PLIN5 [12] [13] | Disrupted LD-regulated lipolysis and β-oxidation; hepatic insulin resistance; progression to metabolic dysfunction-associated steatotic liver disease (MASLD) [10] [12] | Hepatic Steatosis, MASLD [12] |
| Skeletal Muscle | PLIN2, PLIN5 [12] [13] | Intramyocellular lipid accumulation; impaired insulin-mediated glucose uptake; systemic insulin resistance [10] [12] | Insulin Resistance, Sarcopenia (indirectly) |
| Pancreas (β-cells) | PLINs (unspecified) [10] | Impaired glucose-stimulated insulin secretion; β-cell apoptosis via ER stress and oxidative stress [10] | β-cell Failure, Worsening Hyperglycemia |
| Heart | PLIN5 [10] [12] | Cardiac lipotoxicity; mitochondrial dysfunction; impaired contractility [10] | Diabetic Cardiomyopathy [10] |
| Kidney | Information not specified in search results | Information not specified in search results | Diabetic Kidney Disease (DKD) [10] [6] |
Key Signaling Pathways and Molecular Mechanisms
The regulation of LD dynamics and the progression to lipotoxicity involve complex inter-organellar communication and several key signaling pathways. The following diagram illustrates the core signaling pathways and pathological consequences associated with dysregulated LD dynamics in a metabolically stressed cell, such as a hepatocyte or myocyte.
A critical component of the pathway above is the interaction between lipid droplets and other organelles. The Perilipin (PLIN) family of proteins, particularly PLIN2 and PLIN5, are central gatekeepers of LD functions. Their tissue-specific roles and regulatory mechanisms are detailed in the following table.
Table 2: Key Functions of Select Perilipin (PLIN) Family Proteins in Lipid Metabolism
| Protein | Primary Tissue Expression | Core Functions in LD Dynamics | Regulatory Mechanisms |
|---|---|---|---|
| PLIN1 | White & Brown Adipose Tissue [12] | Major regulator of lipolysis; coats LD surface to isolate lipases at rest; phosphorylated by PKA to activate lipolysis during fasting/exercise [12]. | PKA-mediated phosphorylation [12]. |
| PLIN2 | Ubiquitous (Liver, Muscle, etc.) [12] | Promotes lipid storage & LD stability; inhibits lipolysis; also regulates LD-mediated lipophagy [12]. | Degraded via chaperone-mediated autophagy (CMA) during nutrient restriction [12]. |
| PLIN5 | Tissues with high aerobic metabolism (Heart, Muscle, Liver) [10] [12] | Regulates LD-mitochondria contact; suppresses lipolysis at rest; facilitates FA channeling to mitochondria for oxidation during energy demand [10] [12]. | PKA-mediated phosphorylation releases co-repressors, promoting lipolysis [12]. |
Experimental Models and Methodologies for Investigation
In Vivo Modeling of Ectopic Lipid Deposition
A common and robust method for inducing ectopic lipid deposition and studying insulin resistance is the diet-induced obesity (DIO) mouse model.
- Animal Model: C57BL/6J mice [13].
- Dietary Regimen: Mice are fed a high-fat diet (HFD), typically for 12-16 weeks, to induce obesity and metabolic dysfunction [13]. This model allows for the stratification of mice into diet-induced obese (DIO) and diet-induced obesity-resistant (DIO-R) phenotypes based on weight gain and the Lee index, enabling comparative studies [13].
- Key Readouts:
- Tissue Analysis: Histological examination of organs (e.g., liver, skeletal muscle) via Hematoxylin and Eosin (H&E) and Oil Red O staining to visualize lipid accumulation and steatosis [13].
- Systemic Metrics: Monitoring of body weight, fasting blood glucose, and insulin levels to assess glucose tolerance and insulin sensitivity [13].
In Vitro Modeling of Lipid Droplet Accumulation
Cultured cell lines exposed to free fatty acids (FFAs) are widely used to study the molecular mechanisms of LD dynamics and lipotoxicity.
- Cell Lines: HepG2 (liver) and C2C12 (skeletal muscle, requiring differentiation into myotubes) [13].
- Lipid Loading Protocol: Cells are treated with a mixture of fatty acids (e.g., 1 mM palmitic and oleic acid at a 1:2 ratio) complexed with fatty acid-free Bovine Serum Albumin (BSA) for 24 hours to induce LD formation [13].
- Genetic Manipulation: Transfection with siRNA (e.g., targeting FGF-21) to investigate the functional role of specific genes in LD regulation [13].
- Downstream Analysis:
The Scientist's Toolkit: Essential Research Reagents and Models
Table 3: Key Reagents and Models for Studying LD Dynamics and Ectopic Deposition
| Tool / Reagent | Category | Primary Function in Research | Example Application |
|---|---|---|---|
| C57BL/6J Mice | In Vivo Model | Gold-standard model for studying diet-induced obesity, insulin resistance, and organ-specific ectopic lipid deposition [13]. | Comparing DIO vs. DIO-R phenotypes to identify protective metabolic mechanisms [13]. |
| HepG2 & C2C12 Cells | In Vitro Model | Human liver and mouse skeletal muscle cell lines, respectively, for mechanistic studies of lipid metabolism and lipotoxicity [13]. | Investigating the impact of gene knockdown (e.g., FGF-21) on FFA-induced LD accumulation [13]. |
| Palmitic/Oleic Acid-BSA Conjugate | Metabolic Inducer | Mimics lipid overload in vitro; BSA conjugation facilitates FFA delivery to cells, inducing LD biogenesis and lipotoxicity [13]. | Standard protocol for creating cellular models of steatosis and insulin resistance [13]. |
| siRNA / shRNA | Genetic Tool | Silences specific gene expression to determine functional roles in LD dynamics (e.g., FGF-21, PLINs) [13]. | Elucidating gene function in regulated lipolysis, LD formation, and mitochondrial FA oxidation [13]. |
| Antibodies (PLIN2, PLIN5, FGF-21) | Analytical Reagent | Detects protein expression and localization via Western blot, immunofluorescence, and immunohistochemistry. | Quantifying tissue-specific PLIN expression changes under different metabolic states (e.g., fasting, exercise) [12]. |
| Oil Red O Stain | Histological/Cytological Dye | Stains neutral lipids (triglycerides, cholesteryl esters) in tissues and cells, allowing quantification of LD content [13]. | Visualizing and quantifying intramyocellular or intrahepatic lipid deposition in tissue sections or cultured cells [13]. |
Emerging Biomarkers and Therapeutic Targets
Beyond cellular proteins, novel lipid-based biomarkers are emerging for risk assessment in clinical and research settings.
- Atherogenic Index of Plasma (AIP): Calculated as log10(TG/HDL-C). It is a significant predictor of diabetic kidney disease (DKD) risk, with higher values indicating greater atherogenic potential and association with microvascular complications [14] [6].
- Triglyceride-Glucose Index (TyG): Calculated as ln[TG (mg/dL) × FPG (mg/dL)/2]. It is a reliable surrogate marker for insulin resistance and demonstrates superior predictive performance for T2D risk, even in individuals with a history of dyslipidemia [14].
Therapeutic strategies are increasingly focusing on restoring LD dynamics. These include lifestyle interventions like exercise, which modulates PLIN expression and promotes healthy LD turnover [12], and pharmacological agents that target specific nodes in the pathways, such as the cAMP/PKA signaling axis or directly enhancing mitochondrial function and MQC to alleviate lipotoxicity [10] [15].
Distinct Lipid Biomarker Profiles for Kidney Disease, Retinopathy, and Neuropathy
Lipid metabolism is increasingly recognized as a central player in the pathogenesis of diabetic microvascular complications. While diabetic kidney disease (DKD), diabetic retinopathy (DR), and diabetic neuropathy (DN) share hyperglycemia as a common underlying risk factor, emerging evidence reveals that distinct lipid biomarker profiles are associated with each complication. This divergence offers critical insights for developing targeted diagnostic and therapeutic strategies. Understanding these unique lipid signatures is essential for researchers and drug development professionals aiming to move beyond generic metabolic markers toward precision medicine approaches. This guide provides a comparative analysis of the specific lipid biomarkers, experimental methodologies, and pathophysiological mechanisms underlying these complications, synthesizing the most recent research findings to inform future investigation and therapeutic development.
Comparative Lipid Biomarker Profiles
The table below summarizes the distinct lipid biomarkers associated with each diabetic complication, highlighting their specific roles and research implications.
Table 1: Distinct Lipid Biomarker Profiles by Diabetic Complication
| Complication | Specific Lipid Biomarkers | Biological Sample | Associated Risk/Function |
|---|---|---|---|
| Kidney Disease (DKD) | • 21 specific lipids in urinary small extracellular vesicles (sEVs) [16]• Ceramides, Diacylglycerols [17]• Elevated LAP, AIP, VAI indices [6] | Urine, Blood [16] [6] [17] | Direct mediators of renal cell injury (lipotoxicity); predicts rapid eGFR decline [17]. |
| Retinopathy (DR) | • Specific lipidomes (e.g., Triacylglycerol) [18]• Glycolipids in retinal pigment epithelium (RPE) [19] | Blood, Retinal tissue [18] [19] | Causal relationship with DR onset/progression; altered metabolism drives RPE cell migration [18] [19]. |
| Neuropathy (DN) | • Lipid metabolism alterations in Schwann cells [20]• Perturbations in lipid rafts and signaling [20] | Peripheral nerve tissue [20] | Disruption of myelin integrity and axonal function; central to cellular dysfunction [20]. |
| General Complications | Lipid Droplet (LD) Dynamics [3] | Multiple organs (e.g., pancreas, kidney, retina) [3] | Ectopic lipid deposition and lipotoxicity exacerbate complications in target organs [3]. |
Experimental Protocols for Lipid Biomarker Analysis
Urinary sEV Lipidomics for Kidney Disease
Application: This protocol is designed for the discovery of lipid biomarkers in chronic kidney disease of unknown etiology (CKDu) and diabetic kidney disease (DKD) [16] [17].
Workflow:
- Sample Collection: Collect 15-20 mL of urine. For longitudinal studies, collect fasting spot urine at baseline and follow up for multiple years to track kidney function decline [16] [17].
- sEV Purification:
- Centrifuge urine at 1,000× g for 15 minutes at 4°C to remove particulates and cells [16].
- Filter the supernatant through a 0.22 µm PES filter [16].
- Perform ultracentrifugation of the filtered urine at 250,000× g for 2 hours at 4°C to pellet sEVs [16].
- Wash the pellet with phosphate-buffered saline (PBS) and repeat ultracentrifugation [16].
- Resuspend the final sEV pellet in 200 µL of PBS [16].
- sEV Characterization:
- Nanoparticle Tracking Analysis (NTA): Use an instrument (e.g., NanoSight NS300) to quantify the concentration and size distribution of sEVs by analyzing Brownian motion [16].
- Bead-Based Multiplex Flow Cytometry: Use a kit (e.g., MACSPlex Human EV Kit) to characterize surface protein profiles (e.g., CD9, CD63, CD81) to confirm sEV origin and identify tissue-specific markers [16].
- Lipidomics Analysis:
- Data Analysis:
- Use univariate statistical analysis to identify differentially expressed lipids with a threshold of |log2 fold change| ≥1.5 and p < 0.05 [17].
- Apply machine learning algorithms (e.g., random forest, Boruta) for feature selection to identify the most promising biomarker candidates from the lipid data [17].
Figure 1: Experimental workflow for urinary sEV lipidomics in kidney disease research.
Mendelian Randomization for Retinopathy Lipidomics
Application: This method is used to establish a causal relationship between specific lipidomes and diabetic retinopathy (DR), overcoming limitations of observational studies [18].
Workflow:
- Data Sourcing: Obtain summary-level data from large-scale genome-wide association studies (GWAS) for both the exposure (lipidomes) and the outcome (DR and its subtypes) from public repositories like the GWAS catalogue and biobanks (e.g., FinnGen) [18].
- Lipidome Profiling: Utilize high-resolution lipidomic techniques, such as shotgun lipidomics, to generate comprehensive lipidome data for the genetic analysis [18].
- Bidirectional MR Analysis:
- Select genetic variants (single nucleotide polymorphisms, SNPs) that are strongly associated with the specific lipidomes as instrumental variables [18].
- Perform a two-sample MR to estimate the causal effect of lipidomes on DR [18].
- Conduct a reverse-direction MR to test for causality from DR back to lipidomes, establishing the direction of the relationship [18].
- Mediation Analysis: Investigate whether circulating inflammatory proteins (e.g., interleukin-10) mediate the causal effect of protective lipids on DR. Calculate the mediation proportion to quantify this indirect effect [18].
- Sensitivity Analysis: Perform a battery of sensitivity tests (e.g., MR-Egger, MR-PRESSO) to validate the reliability of the findings and ensure they are not biased by pleiotropy [18].
Investigating Lipid Dynamics in Neuropathy
Application: This approach focuses on understanding the role of lipid metabolism alterations in peripheral neurons and Schwann cells in diabetic neuropathy [20].
Workflow:
- Model Systems: Use both inherited (e.g., Charcot-Marie-Tooth disease models) and acquired peripheral neuropathy models to study lipid-centric mechanisms [20].
- Focus Areas:
- Lipid Rafts: Investigate the role of lipid rafts—specialized membrane microdomains—in Schwann cell signaling and myelin integrity [20].
- Lipid Storage and Signaling: Analyze changes in lipid storage and the function of lipids as signaling molecules in peripheral neurons [20].
- Genetic and Environmental Links: Explore how genetic mutations and environmental factors known to cause neuropathy converge on pathways affecting lipid metabolism in peripheral nerves [20].
- Techniques: A combination of omics technologies (lipidomics, transcriptomics), histological analysis, and functional nerve conduction studies are typically employed to correlate lipid changes with cellular dysfunction and clinical phenotypes [20].
Pathophysiological Pathways and Mechanisms
The pathophysiological pathways linking lipid metabolism to each complication are distinct, yet interconnected through the overarching theme of lipotoxicity.
Figure 2: Distinct pathological mechanisms of lipid dysregulation in microvascular complications.
Kidney Disease Pathogenesis: Lipids contribute to DKD primarily through lipotoxicity. Specific lipid species like ceramides and diacylglycerols act as direct mediators of renal cell injury [17]. Urinary sEVs serve as vehicles for lipid trafficking and signaling, and their lipid content is significantly altered in early CKD. These sEVs also express surface proteins indicative of early inflammation, suggesting a combined lipid and inflammatory insult in the kidneys [16]. Furthermore, calculated indices like LAP, AIP, and VAI, which reflect visceral adiposity and atherogenic dyslipidemia, are significantly elevated in patients with DKD, providing a link between systemic lipid metabolism and renal damage [6].
Retinopathy Pathogenesis: In AMD and DR, lipid dysregulation manifests prominently in the retinal pigment epithelium (RPE). Research using imaging mass spectrometry has shown that migrating RPE cells undergo a change in lipid metabolism, particularly involving glycolipids [19]. This altered metabolism drives a process of transdifferentiation, where RPE cells change their identity, migrate, and form hyperreflective foci—a known biomarker for disease progression [19]. Furthermore, MR studies have established a causal relationship between specific lipidomes and DR, with inflammatory factors like interleukin-10 acting as key mediators in the protective mechanisms of certain lipids [18].
Neuropathy Pathogenesis: The integrity of the myelin sheath—a lipid-rich structure—is critical for axonal function in the peripheral nervous system. Alterations in lipid metabolism in Schwann cells and neurons disrupt this integrity [20]. The mechanisms involve perturbations in lipid rafts (signaling platforms), impaired lipid storage, and dysregulated lipid signaling. These changes, whether from genetic or acquired causes, are central to cellular dysfunction in peripheral neuropathies, making lipid balance a key therapeutic target [20].
The Scientist's Toolkit: Essential Research Reagents
The following table lists key reagents and technologies used in the featured lipid biomarker research.
Table 2: Essential Research Reagents and Solutions for Lipid Biomarker Studies
| Reagent / Technology | Function / Application | Example Use Case |
|---|---|---|
| Ultracentrifugation | Isolation and purification of small extracellular vesicles (sEVs) from biofluids. | Pelleting sEVs from urine for subsequent lipid profiling [16]. |
| MACSPlex Human EV Kit | Bead-based multiplex flow cytometry for characterizing sEV surface markers. | Detecting CD9, CD63, CD81 and kidney-specific markers on urinary sEVs [16]. |
| NanoSight NS300 (NTA) | Nanoparticle Tracking Analysis to quantify the size and concentration of vesicles. | Determining the concentration and size distribution of isolated sEVs [16]. |
| UPLC/TQMS | Ultra-Performance Liquid Chromatography/Tandem Quadrupole Mass Spectrometry for targeted lipid quantification. | Precise identification and quantification of hundreds of lipid species in urine or tissue [17]. |
| Imaging Mass Spectrometry (IMS) | Spatial mapping of molecular distributions directly in tissue sections at near single-cell resolution. | Identifying the specific glycolipid composition of migrating RPE cells in the retina [19]. |
| Shotgun Lipidomics | A high-resolution, comprehensive approach to profile the entire lipidome of a sample. | Generating lipidome data for causal inference studies in retinopathy [18]. |
| GWAS Summary Data | Publicly available genetic data used for Mendelian Randomization analysis. | Sourcing instrumental variables for lipids and diabetic retinopathy from biobanks [18]. |
The landscape of lipid biomarkers in diabetic microvascular complications is characterized by both disease-specific profiles and shared pathophysiological themes like lipotoxicity. Kidney disease research is advancing with non-invasive urinary sEV lipidomics, retinopathy studies are leveraging causal genetic tools like Mendelian Randomization, and neuropathy investigations are focusing on lipid-centric mechanisms in Schwann cells and myelin. These distinct approaches underscore the necessity of precision medicine. For researchers and drug developers, this means that therapeutic strategies targeting lipids will likely need to be complication-specific. Future research should focus on integrating these multi-omics biomarkers with artificial intelligence to improve early detection, risk stratification, and the development of targeted lipid-modulating therapies.
In the evolving landscape of metabolic disease research, the identification of reliable biomarkers for predicting complication risk in diabetes mellitus remains a critical scientific challenge. Traditional lipid profiles and anthropometric measurements often fail to capture the complex interplay between visceral adiposity, dyslipidemia, and microvascular pathology. Within this context, novel composite indices—specifically the Visceral Adiposity Index (VAI), Lipid Accumulation Product (LAP), and Atherogenic Index of Plasma (AIP)—have emerged as integrated measures that may offer superior predictive capability for diabetic complications. These calculated indices synthesize routine clinical measurements into powerful risk assessment tools that reflect underlying pathophysiological processes, including visceral adipose tissue dysfunction, systemic insulin resistance, and atherogenic lipid patterning. This review provides a comprehensive comparison of these three indices' predictive performance across multiple diabetic complications, supported by experimental data and mechanistic insights to guide researchers and drug development professionals in their translational applications.
Comparative Analysis of Predictive Performance
Diagnostic Accuracy for Diabetic Kidney Disease (DKD)
A recent systematic review and meta-analysis comprising 23 studies demonstrated that all three indices significantly predict diabetic kidney disease risk in diabetic populations [6]. The analysis revealed markedly elevated biomarker levels in patients with DKD compared to those without nephropathy.
Table 1: Biomarker Levels in DKD vs. Non-DKD Patients
| Biomarker | Weighted Mean Difference (WMD) | 95% Confidence Interval | P-value |
|---|---|---|---|
| LAP | 12.67 | 7.83 to 17.51 | < 0.01 |
| AIP | 0.11 | 0.03 to 0.19 | < 0.01 |
| VAI | 0.63 | 0.38 to 0.89 | < 0.01 |
For each unit increase in these indices, the associated risk of developing DKD rose significantly, with AIP showing the strongest association per unit change [6].
Table 2: Odds Ratios for DKD Risk per 1-Unit Increase
| Biomarker | Odds Ratio (OR) | 95% Confidence Interval | P-value |
|---|---|---|---|
| LAP | 1.005 | 1.003 to 1.006 | < 0.01 |
| AIP | 1.08 | 1.04 to 1.12 | < 0.01 |
| VAI | 1.05 | 1.03 to 1.07 | < 0.01 |
Predictive Value for Diabetic Retinopathy (DR)
Research findings regarding diabetic retinopathy show conflicting results. While the comprehensive meta-analysis found no significant associations between these biomarkers and DR [6], a large cross-sectional study using NHANES 2005-2008 data (n=2,591) demonstrated positive associations after full covariate adjustment [21] [22].
Table 3: Association Between Indices and Diabetic Retinopathy
| Biomarker | Odds Ratio (OR) | 95% Confidence Interval | P-value |
|---|---|---|---|
| LAP | 1.004 | 1.002 to 1.006 | < 0.0001 |
| VAI | 1.090 | 1.037 to 1.146 | 0.0007 |
| AIP | 1.802 | 1.240 to 2.618 | 0.0020 |
This discrepancy highlights the need for further prospective studies but suggests these indices may have value in DR risk stratification, particularly in specific populations.
Cardiovascular Disease Prediction
Beyond microvascular complications, these indices demonstrate significant predictive capacity for cardiovascular diseases. A 6-year prospective study of 9,704 individuals found AIP, LAP, and VAI significantly associated with CVD incidence after adjusting for confounding factors [23]. The decision tree analysis identified AIP ≥ 0.94 as a critical threshold for CVD risk in men, while VAI remained significant in multivariate models for women [23].
Type 2 Diabetes Incidence Prediction
In a large Japanese cohort study (n=195,989), all three indices strongly predicted new-onset T2DM over a mean follow-up of 4.61 years [24]. The areas under the receiver operating characteristic curves (AUC) for AIP, LAP, and VAI ranged between 0.821 and 0.844, indicating excellent predictive capability [24].
Experimental Protocols and Methodologies
Calculation Formulas
The indices are calculated using standardized formulas incorporating routine clinical and laboratory measurements:
Lipid Accumulation Product (LAP)
- Males: LAP = [WC (cm) - 65] × TG (mmol/L)
- Females: LAP = [WC (cm) - 58] × TG (mmol/L)
Visceral Adiposity Index (VAI)
- Males: VAI = (WC/39.68 + BMI/1.88) × (TG/1.03) × (1.31/HDL-C)
- Females: VAI = (WC/36.58 + BMI/1.89) × (TG/0.81) × (1.52/HDL-C)
Atherogenic Index of Plasma (AIP)
Key Population Studies
The evidence base for these indices derives from several methodological approaches:
- Systematic Reviews/Meta-Analyses: The foundational evidence comes from a comprehensive analysis of 23 studies following PRISMA guidelines, synthesizing data across multiple research designs and populations [6] [25].
- Large Prospective Cohorts: Studies like the Fukushima Health Database (n=195,989) and MASHAD study (n=9,704) provide longitudinal data on disease incidence with multivariable adjustment for confounders [23] [24].
- Cross-Sectional Population Studies: NHANES analyses provide generalizable population-level estimates of association between indices and complications [21] [22].
- Multivariable Regression Models: Studies typically employ multiple adjusted models, progressively controlling for demographic, clinical, and metabolic confounders to isolate independent effects [21].
Research Methodology Workflow
Pathophysiological Mechanisms and Signaling Pathways
The predictive capacity of these indices stems from their reflection of underlying pathological processes linking dyslipidemia, visceral adiposity, and complication risk.
Lipid Droplet Dynamics and Visceral Adipose Tissue Dysfunction
Visceral adipose tissue exhibits distinct pathological behavior in diabetes, with enhanced lipolytic activity and increased inflammatory cell infiltration compared to subcutaneous fat [6]. VAI specifically captures this dysfunction by integrating measures of visceral fat distribution with lipid parameters. Under insulin-resistant conditions, lipid droplet dynamics become impaired, leading to ectopic lipid accumulation in tissues vulnerable to diabetic complications, including kidneys, retina, and vascular endothelium [3].
Excessive lipid accumulation beyond compensatory capacity initiates lipotoxicity through several mechanisms:
- Elevated free fatty acids induce endoplasmic reticulum stress and mitochondrial dysfunction [3]
- Altered perilipin protein expression disrupts lipid mobilization [3]
- Impaired lipophagy reduces lipid turnover and promotes cytotoxic lipid intermediate accumulation [3]
Pathophysiological Pathways to Complications
Atherogenic Dyslipidemia and Insulin Resistance
AIP captures the atherogenic lipid pattern characterized by elevated triglycerides and low HDL-C that frequently accompanies insulin resistance [6] [21]. This lipid profile promotes vascular dysfunction through multiple mechanisms:
- Increased triglyceride-rich lipoproteins and their remnants penetrate the vascular wall, initiating atherosclerotic plaque formation [23]
- HDL dysfunction impairs reverse cholesterol transport and reduces vasoprotective effects [23]
- Altered lipoprotein composition enhances oxidation and glycation, increasing immunogenicity and inflammatory responses [26]
LAP integrates both anthropometric and lipid parameters to reflect the interplay between abdominal obesity and dyslipidemia in driving complication risk [24] [21]. The strong correlation between LAP and diabetic kidney disease suggests this index captures pathways relevant to renal pathology, potentially through lipid-induced podocyte injury, tubular damage, and glomerular sclerosis [6] [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for Investigating VAI, LAP, and AIP
| Reagent/Instrument | Research Function | Application Context |
|---|---|---|
| Enzymatic Colorimetric Assays | Quantitative measurement of TG and HDL-C | Core lipid parameter quantification for index calculation |
| Standardized Anthropometric Tools | Precise measurement of waist circumference | Critical for LAP and VAI computation with minimal measurement error |
| Automated Clinical Chemistry Analyzers | High-throughput lipid profiling | Large cohort studies requiring standardized measurements across participants |
| ELISA Kits for Adipokines | Quantification of leptin, adiponectin | Validation of visceral adipose dysfunction correlates |
| Lipoprotein Fractionation Systems | Separation and analysis of lipoprotein subclasses | Mechanistic studies linking AIP to atherogenic particle distribution |
| Liquid Chromatography-Mass Spectrometry | Comprehensive lipidomic profiling | Advanced investigation of lipid species underlying index associations |
The comprehensive comparison of VAI, LAP, and AIP reveals distinct patterns of predictive capacity across diabetic complications. While all three indices demonstrate significant associations with diabetic kidney disease and cardiovascular outcomes, their performance varies by complication type and population. AIP shows particularly strong associations with both microvascular and macrovascular complications, potentially reflecting its capture of atherogenic lipid patterning. LAP excels in abdominal obesity-related risk stratification, while VAI specifically addresses visceral adipose tissue dysfunction. Despite promising diagnostic characteristics, current evidence indicates these indices offer complementary rather than redundant information, suggesting potential utility in multi-marker prediction panels. For drug development professionals, these indices provide valuable intermediate endpoints for clinical trials targeting metabolic pathways in diabetes complications. Future research should focus on standardizing cut-off values across populations, validating these indices in diverse ethnic groups, and exploring their utility in guiding targeted therapeutic interventions.
Lipotoxicity refers to the process by which excess lipids accumulate in non-adipose tissues, leading to cellular dysfunction and cell death. The term was first coined in 1994 when researchers observed that lipid overload in pancreatic β-cells led to loss of function and the onset of type 2 diabetes mellitus in rats [27] [28]. Since this seminal discovery, research has revealed that lipotoxicity represents a fundamental pathological mechanism connecting obesity to metabolic disease, affecting multiple organs including the pancreas, liver, skeletal muscles, heart, and kidneys [27] [29]. While initial research focused on general lipid accumulation, recent advances have identified specific lipid metabolites—Free Fatty Acids (FFAs), Diacylglycerol (DAG), and ceramides—as the primary molecular mediators of lipotoxic damage [29] [30]. These bioactive lipids disrupt cellular signaling pathways, promote inflammation, induce oxidative stress, and ultimately contribute to insulin resistance and diabetic complications [31] [30]. This review systematically compares the distinct and overlapping mechanisms through which FFAs, DAG, and ceramides drive cellular dysfunction, providing a comprehensive analysis of their roles as key pathological agents in metabolic disease.
Comparative Pathophysiology of Key Lipotoxic Mediators
Free Fatty Acids (FFAs): Initiators of Lipotoxic Stress
Free Fatty Acids, particularly saturated fatty acids like palmitic acid, serve as fundamental precursors to lipotoxic damage. When FFA delivery exceeds the metabolic capacity of non-adipose tissues, they initiate a cascade of cellular stress responses [29]. The mechanisms of FFA-induced lipotoxicity include:
Reactive Oxygen Species (ROS) Generation: Elevated FFA levels stimulate ROS production through protein kinase C-dependent activation of NAD(P)H oxidase in vascular cells and through mitochondrial electron transport chain inefficiencies [28] [30]. This oxidative stress damages cellular components including lipids, proteins, and DNA.
Endoplasmic Reticulum (ER) Stress: Chronic lipid overload disrupts ER function, engaging the unfolded protein response which, when prolonged, transitions from adaptive to pro-apoptotic signaling [28] [29].
Inflammatory Pathway Activation: FFAs activate toll-like receptors (particularly TLR4) and the NLRP3 inflammasome, triggering the production of pro-inflammatory cytokines such as TNF-α, IL-1β, and IL-6 [29] [30].
Mitochondrial Dysfunction: Excessive FFAs overwhelm mitochondrial β-oxidation capacity, leading to incomplete fatty acid oxidation and accumulation of toxic lipid intermediates [29] [30]. This is particularly detrimental in pancreatic β-cells, where mitochondrial function is crucial for glucose-stimulated insulin secretion.
Interestingly, not all FFAs exert equally detrimental effects. Saturated fatty acids (e.g., palmitate) are strongly lipotoxic, while monounsaturated fatty acids (e.g., oleate) can actually protect against lipotoxic stress by promoting triglyceride storage in lipid droplets and reducing ceramide synthesis [29].
Diacylglycerol (DAG): The Insulin Signaling Disruptor
Diacylglycerol accumulates as an intermediate in lipid metabolism and functions as a potent signaling molecule that directly impairs insulin action through:
Protein Kinase C (PKC) Activation: DAG activates several PKC isoforms, predominantly the novel (δ, ε, θ) and conventional (βII) forms. PKCθ activation in skeletal muscle and PKCε activation in the liver phosphorylate insulin receptor substrate (IRS) proteins on inhibitory serine residues, impairing insulin signal transduction [30].
Disruption of Insulin Receptor Signaling: By activating PKC, DAG interferes with the tyrosine phosphorylation of IRS-1, reducing its ability to activate downstream effectors in the PI3K/Akt pathway [31]. This ultimately impairs GLUT4 translocation to the cell membrane and reduces glucose uptake.
Tissue-Specific Effects: DAG accumulation in the liver promotes hepatic insulin resistance and increases gluconeogenesis, while in skeletal muscle it reduces glucose disposal capacity [30]. The subcellular localization of DAG pools is critical, with plasma membrane-associated DAG exhibiting the greatest impact on insulin signaling.
The table below summarizes the distinct mechanisms through which DAG species contribute to insulin resistance across different tissues:
Table 1: Tissue-Specific Mechanisms of DAG-Induced Insulin Resistance
| Tissue | Primary DAG Species | PKC Isoform Activated | Downstream Effects |
|---|---|---|---|
| Skeletal Muscle | C18:0, C18:1 | PKCθ | Reduced IRS-1 tyrosine phosphorylation; Impaired GLUT4 translocation |
| Liver | C16:0, C18:0 | PKCε | Increased gluconeogenic gene expression; Reduced glycogen synthesis |
| Heart | C16:0, C18:1 | PKCβII | Reduced glucose oxidation; Preferential fatty acid utilization |
Ceramides: The Apoptotic and Inflammatory Mediators
Ceramides, a class of sphingolipids, have emerged as particularly potent lipotoxic agents with dual roles in promoting insulin resistance and cellular apoptosis. Ceramide synthesis occurs through three major pathways: de novo synthesis, sphingomyelin hydrolysis, and the salvage pathway [27] [31]. Their mechanisms of action include:
Direct Inhibition of Insulin Signaling: Ceramides inhibit the PI3K/Akt pathway through multiple mechanisms, including activation of protein phosphatase 2A (PP2A) which dephosphorylates Akt, and promotion of Akt ubiquitination and degradation [27] [31]. Specific ceramide species (particularly C16 and C18) exhibit the strongest associations with insulin resistance [32].
Mitochondrial Dysfunction: Ceramides accumulate in mitochondrial membranes where they inhibit electron transport chain complexes (particularly III and IV), increase reactive oxygen species production, and enhance mitochondrial membrane permeability, promoting cytochrome c release and apoptosis [27] [33].
Inflammatory Signaling: Ceramides activate NF-κB signaling and promote the production of pro-inflammatory cytokines including TNF-α, IL-1β, and IL-6 [27]. They also form lipid rafts that facilitate inflammatory receptor clustering and signaling.
β-Cell Apoptosis: In pancreatic β-cells, ceramides induce apoptosis through both extrinsic (death receptor) and intrinsic (mitochondrial) pathways, contributing to the progressive β-cell loss observed in type 2 diabetes [31].
The six ceramide synthase isoforms (CerS1-6) produce ceramide species with different fatty acyl chain lengths, each with distinct biological functions and tissue distributions [27]. For example, CerS1 generates C18-ceramide predominantly in muscle tissue, while CerS6 produces C16-ceramide in adipose tissue [27]. This specificity has important implications for tissue-specific lipotoxicity and presents potential therapeutic targets.
Table 2: Ceramide Synthase Isoforms and Their Roles in Metabolic Disease
| Ceramide Synthase | Primary Ceramide Species | Tissue Expression | Metabolic Functions |
|---|---|---|---|
| CerS1 | C18:0 | Skeletal muscle, brain | Regulates insulin sensitivity in muscle; Promotes neuronal survival |
| CerS2 | C22:0, C24:0 | Liver, kidney | Maintains normal hepatic and renal function; Elevated in NAFLD |
| CerS3 | Ultra-long chain | Skin, testis | Primarily structural role in skin barrier |
| CerS4 | C20:0, C22:0 | Skin, liver, leukocytes | Limited role in metabolic disease |
| CerS5 | C16:0 | Ubiquitous | Promotes hepatic insulin resistance; Associated with CVD risk |
| CerS6 | C16:0 | Adipose tissue, ubiquitous | Adipose tissue inflammation; Systemic insulin resistance |
Integrated Signaling Pathways in Lipotoxicity
The following diagram illustrates the key molecular pathways through which FFAs, DAG, and ceramides induce cellular dysfunction and inflammation:
Lipotoxicity Signaling Network. This diagram illustrates the convergent and distinct pathways through which FFAs, DAG, and ceramides promote insulin resistance and cellular dysfunction. Yellow nodes represent FFA-mediated pathways, red indicates DAG-specific mechanisms, blue shows ceramide actions, and green denotes common downstream effects.
Experimental Models and Methodologies for Lipotoxicity Research
In Vitro Models and Treatment Protocols
Cell Culture Systems: Primary hepatocytes, skeletal myocytes (C2C12), pancreatic β-cell lines (MIN6, INS-1), and cardiomyocytes are commonly used. Treatment with pathophysiological concentrations of palmitate (0.25-0.75 mM) for 6-24 hours reliably induces lipotoxicity [31] [29]. BSA-conjugated palmitate preparations ensure proper solubility and delivery.
Lipotoxicity Assessment: Key endpoints include insulin signaling (IRS-1 tyrosine phosphorylation, Akt phosphorylation), glucose uptake assays, mitochondrial function (Seahorse analyzer), apoptosis markers (caspase-3 activation, TUNEL staining), and inflammatory cytokine secretion (ELISA) [31] [29].
In Vivo Models and Dietary Interventions
Genetic Models: db/db mice (leptin receptor deficiency), ob/ob mice (leptin deficiency), and Zucker diabetic fatty rats represent gold standard models that develop severe obesity and diabetes with characteristic tissue lipid accumulation [28] [34].
Dietary Models: High-fat diets (45-60% kcal from fat) administered for 8-24 weeks induce obesity, insulin resistance, and tissue lipid accumulation in C57BL/6J mice and other strains [33].
Intervention Studies: Alternate-day fasting protocols (24-hour fast followed by 24-hour ad libitum feeding) for extended durations (e.g., 6 months in db/db mice) effectively reduce hepatic ceramides and improve metabolic parameters without weight loss [34].
The table below summarizes key experimental approaches for studying lipotoxic metabolites:
Table 3: Experimental Models for Investigating Lipotoxic Metabolites
| Research Goal | Preferred Model | Key Readouts | Experimental Duration |
|---|---|---|---|
| FFA-induced IR | Primary hepatocytes; H4IIEC3 hepatoma cells | PKCε translocation; Akt phosphorylation; Glucose output | 6-24 hours |
| DAG signaling | Skeletal muscle strips; L6 myotubes | Membrane DAG content; PKCθ activation; 2-deoxyglucose uptake | 2-6 hours |
| Ceramide effects | Pancreatic β-cell lines; C2C12 myotubes | Ceramide species (LC-MS/MS); PP2A activity; Apoptosis markers | 12-48 hours |
| Whole-body metabolism | HFD-fed C57BL/6J mice; db/db mice | Glucose tolerance; Tissue lipidomics; Insulin signaling | 8-24 weeks |
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 4: Key Research Reagents for Lipotoxicity Studies
| Reagent/Method | Application | Key Features |
|---|---|---|
| Palmitate-BSA conjugates | Induction of lipotoxicity in vitro | Physiological relevance; Controllable concentrations |
| Myriocin | Ceramide synthesis inhibition | Specific inhibitor of serine palmitoyltransferase (SPT) |
| Fumonisin B1 | Ceramide synthase inhibition | Broad-spectrum CerS inhibitor |
| LC-MS/MS lipidomics | Comprehensive lipid analysis | Quantitative measurement of lipid species; High sensitivity |
| Seahorse Analyzer | Mitochondrial function assessment | Real-time OCR and ECAR measurements |
| C16-ceramide antibodies | Ceramide detection | Immunohistochemistry and Western blot applications |
| AdipoRon | Adiponectin receptor agonist | Activates AdipoR1/2 ceramidase activity |
Therapeutic Implications and Future Directions
The understanding of lipotoxicity mechanisms has opened several promising therapeutic avenues:
Ceramide-Lowering Approaches: Pharmacological inhibition of ceramide synthesis with myriocin or fumonisin B1 improves insulin sensitivity and reduces atherosclerosis in animal models [27] [33]. Adiponectin receptor agonists that activate receptor ceramidase activity represent another promising strategy [33].
Lifestyle Interventions: Alternate-day fasting and time-restricted feeding protocols significantly reduce ceramide levels and improve glucose homeostasis, even in the absence of weight loss [34]. These interventions enhance mitochondrial function and promote beneficial shifts in lipid metabolism.
Precision Targeting: Isoform-specific ceramide synthase inhibitors (e.g., targeting CerS6 for C16-ceramide production) may provide therapeutic benefits with reduced side effects [27] [32]. Similarly, tissue-specific approaches to modulate DAG-sensitive PKC isoforms offer potential for targeted intervention.
Future research should focus on delineating the specific roles of different ceramide species in disease pathogenesis, developing more precise pharmacological tools to modulate specific lipotoxic pathways, and conducting human trials to validate interventions that successfully target these mechanisms in clinical populations.
Advanced Analytical Techniques for Lipidomic Profiling and Biomarker Discovery
Liquid chromatography-mass spectrometry (LC-MS) technologies have become foundational tools in modern life sciences research, particularly in the field of metabolomics and lipidomics for studying complex diseases such as diabetes and its complications [35]. Among these platforms, Ultra-High Performance Liquid Chromatography coupled with Tandem Mass Spectrometry (UHPLC-MS/MS) and Liquid Chromatography with High-Resolution Mass Spectrometry (LC-HRMS) represent two sophisticated approaches with complementary strengths and applications [36] [37]. The selection between these platforms involves careful consideration of resolution, sensitivity, throughput, and analytical goals, especially when investigating subtle metabolic alterations in diabetic progression [38] [4]. This guide provides an objective comparison of these methodologies, focusing on their performance characteristics and applications in lipid metabolite research for diabetic complications.
Technical Fundamentals and Comparison
Core Principles and Instrumentation
UHPLC-MS/MS typically employs triple quadrupole (QqQ) or similar tandem mass analyzers operating at unit mass resolution. This platform excels in targeted analyses using techniques like Multiple Reaction Monitoring (MRM), where specific precursor-to-product ion transitions are monitored for precise quantification [37]. The UHPLC component provides superior chromatographic separation with sub-2μm particles, resulting in higher peak capacity, improved resolution, and reduced analysis times compared to conventional HPLC [37].
LC-HRMS utilizes mass analyzers such as Time-of-Flight (TOF) or Orbitrap technologies capable of resolution ≥20,000 full width at half maximum (FWHM) [39]. This enables exact mass measurement with accuracy typically <5 ppm, allowing determination of elemental compositions and discrimination of isobaric compounds [40] [39]. Common configurations include Q-TOF and Q-Orbitrap hybrid systems that combine MS and MS/MS capabilities [35].
Performance Characteristics Comparison
Table 1: Direct Comparison of UHPLC-MS/MS and LC-HRMS Performance Characteristics
| Parameter | UHPLC-MS/MS | LC-HRMS |
|---|---|---|
| Mass Resolution | Unit mass resolution (±1 Da) [39] | High resolution (≥20,000 FWHM) with mass accuracy <5 ppm [39] |
| Primary Strength | High sensitivity for targeted quantification [37] | Untargeted screening and retrospective analysis [37] |
| Selectivity | Relies on retention time and MRM transitions; may yield false positives for isobaric compounds [40] | High selectivity via exact mass measurement; can resolve isobaric interferences [40] [39] |
| Data Acquisition | Targeted (MRM) or limited multi-analyte methods [36] | Full-scan data with data-dependent or data-independent MS/MS [36] |
| Dynamic Range | Typically wider dynamic range [39] | Historically narrower, though improving with recent instruments [39] |
| Throughput | Excellent for routine targeted analysis [37] | Suitable for untargeted screening; data processing can be more time-intensive [37] |
| Ideal Application | Quantitative analysis of known metabolites [37] | Discovery research, unknown identification, retrospective analysis [37] |
Experimental Evidence for Selectivity Differences
A comprehensive comparison study demonstrated the superior selectivity of LC-HRMS (at 50,000 FWHM) over LC-MS/MS in analyzing complex biological samples [40]. Researchers monitored dummy exact masses and transitions in blank matrix extracts (fish, pork kidney, pork liver, honey) and found LC-HRMS provided higher selectivity at corresponding mass windows [40].
The practical implication was demonstrated in honey analysis, where LC-MS/MS produced a false positive for a banned nitroimidazole drug due to an interfering matrix compound with identical retention time and MRM transitions [40]. LC-HRMS clearly resolved the interference, unmasking the false finding [40]. This demonstrates the critical advantage of high-resolution platforms in regulatory and research contexts where result confidence is paramount.
Applications in Diabetic Complications Research
Lipidomics in Diabetes and Hyperuricemia
UHPLC-MS/MS has been effectively employed to investigate lipid metabolic disorders in diabetes mellitus combined with hyperuricemia (DH) [41]. An untargeted lipidomic analysis using UHPLC-MS/MS revealed significant alterations in 1,361 identified lipid molecules across 30 subclasses when comparing DH patients, diabetes mellitus (DM) patients, and healthy controls [41].
Table 2: Lipid Metabolites Identified in Diabetes with Hyperuricemia Using UHPLC-MS/MS
| Lipid Category | Specific Metabolites | Alteration Trend | Biological Significance |
|---|---|---|---|
| Triglycerides (TGs) | TG(16:0/18:1/18:2) and 12 other TGs | Significantly upregulated | Indicates disrupted neutral lipid metabolism |
| Phosphatidylethanolamines (PEs) | PE(18:0/20:4) and 9 other PEs | Significantly upregulated | Suggests membrane lipid remodeling |
| Phosphatidylcholines (PCs) | PC(36:1) and 6 other PCs | Significantly upregulated | Reflects alterations in major phospholipid species |
| Phosphatidylinositol (PI) | Not specified | Significantly downregulated | Indicates potential signaling pathway disruptions |
Multivariate analyses confirmed distinct lipidomic profiles among the groups, with pathway analysis identifying glycerophospholipid metabolism (impact value: 0.199) and glycerolipid metabolism (impact value: 0.014) as the most significantly perturbed pathways in DH patients [41].
Lipidomic Stratification of Diabetic Retinopathy Stages
LC-HRMS has demonstrated exceptional utility in stratifying stages of diabetic retinopathy (DR) through comprehensive serum lipidomic profiling [4]. Using liquid chromatography-high-resolution mass spectrometry (LC-HRMS), researchers analyzed serum from 167 participants including non-diabetic retinopathy (NDR) controls, non-proliferative diabetic retinopathy (NPDR) patients, and proliferative diabetic retinopathy (PDR) patients [4].
The MTBE/methanol extraction method was employed for its effectiveness in extracting both polar and nonpolar metabolites while providing excellent reproducibility [4]. Machine learning approaches applied to the LC-HRMS data enabled effective classification of DR stages based on lipidomic profiles, highlighting the potential of HRMS-derived data for developing predictive biomarkers in diabetic complications [4].
Experimental Protocols and Methodologies
Standardized UHPLC-MS/MS Protocol for Lipidomics
Sample Preparation (Based on [41]):
- Collect fasting blood samples and centrifuge at 3,000 rpm for 10 minutes at room temperature
- Aliquot 0.2 mL of upper plasma layer into 1.5 mL centrifuge tubes
- Store at -80°C until analysis
- Thaw samples on ice and vortex
- Extract lipids using methyl tert-butyl ether (MTBE)/methanol method: Add 200 μL of 4°C water to 100 μL plasma, mix, then add 240 μL of pre-cooled methanol
- Add 800 μL MTBE, mix, and sonicate in low-temperature water bath for 20 minutes
- Let stand at room temperature for 30 minutes
- Centrifuge at 14,000 g for 15 minutes at 10°C
- Collect upper organic phase and dry under nitrogen
- Reconstitute in 100 μL isopropanol for analysis
Chromatographic Conditions (Based on [41]):
- Column: Waters ACQUITY UPLC BEH C18 (2.1 × 100 mm, 1.7 μm)
- Mobile Phase: A: 10 mM ammonium formate in water; B: 10 mM ammonium formate in acetonitrile-isopropanol
- Gradient: Optimized for comprehensive lipid separation
- Temperature: Maintained at constant temperature appropriate for lipid stability
Mass Spectrometry Parameters:
- Ionization: Electrospray ionization (ESI) in positive and negative modes
- Acquisition: Multiple reaction monitoring (MRM) for targeted lipids or data-dependent acquisition for untargeted approaches
- Collision energies: Optimized for specific lipid classes
Representative LC-HRMS Protocol for Metabolic Profiling
Sample Preparation (Based on [42]):
- Collect fasting plasma using EDTA anticoagulation
- Precipitate proteins with methanol under vigorous shaking for 2 minutes
- Centrifuge and divide resulting extract into fractions for different analysis modes
- Implement rigorous quality control with pooled matrix samples
Chromatographic Conditions (Based on [42]):
- Utilize different chromatographic columns for hydrophilic and hydrophobic compounds
- Employ HILIC chromatography for polar metabolites under basic conditions
- Use reversed-phase C18 columns for hydrophobic compounds
- Mobile phases may include water and acetonitrile with 10 mmol/L ammonium formate
Mass Spectrometry Parameters (Based on [42] [4]):
- Instrumentation: Q-Exactive or similar high-resolution/accurate mass spectrometer
- Resolution: ≥20,000 FWHM for precise mass measurement
- Ionization: Heated electrospray ionization (HESI-II)
- Acquisition: Full-scan MS with data-dependent MS/MS for top N ions
- Mass accuracy: Maintain <5 ppm with regular calibration
Visualized Workflows and Pathways
Experimental Workflow for Lipidomics in Diabetic Complications
Perturbed Lipid Pathways in Diabetic Complications
Essential Research Reagent Solutions
Table 3: Key Research Reagents and Materials for LC-MS Based Lipidomics
| Reagent/Material | Function | Application Examples |
|---|---|---|
| MTBE/Methanol Extraction System | Simultaneous extraction of polar and nonpolar metabolites with high reproducibility and recovery [4] | Serum lipidomics in diabetic retinopathy [4] |
| QuEChERS Kits | Quick, Easy, Cheap, Effective, Rugged and Safe sample preparation for multi-analyte extraction [37] | Pesticide analysis in food; adaptable to biological samples [37] |
| UHPLC BEH C18 Columns (2.1 × 100 mm, 1.7 μm) | High-resolution chromatographic separation with sub-2μm particles for complex lipid separations [41] [42] | Lipid class separation in diabetes-hyperuricemia studies [41] |
| Ammonium Formate Buffers | Mobile phase additive providing improved ionization efficiency and chromatographic performance [41] [42] | Lipidomic profiling in various biological matrices [41] |
| Quality Control Pooled Matrix | Monitoring analytical performance and correcting instrumental drift across large sample sets [42] | Long-term metabolomic studies in diabetic complications [42] |
Platform Selection Guidelines
Decision Framework
The choice between UHPLC-MS/MS and LC-HRMS should be guided by specific research objectives:
Select UHPLC-MS/MS when:
- Analyzing predefined lipid targets with required high sensitivity
- Conducting high-throughput quantitative analyses in clinical cohorts
- Working within established regulatory frameworks requiring validated MRM methods
- Studying known metabolic pathways with well-characterized biomarkers [37]
Select LC-HRMS when:
- Conducting discovery-phase research without predefined targets
- Suspecting unknown or unexpected metabolites in diabetic complications
- Requiring retrospective data analysis without re-extracting samples
- Needing to differentiate isobaric compounds in complex matrices [40] [37]
Emerging Trends and Future Directions
The distinction between these platforms is blurring with technological advancements. Modern HRMS instruments are addressing previous limitations in sensitivity and dynamic range [39]. There is growing interest in combined approaches using HRMS for discovery and MS/MS for validation [36]. Additionally, integrated ion mobility separation adds another dimension of resolution for complex lipid analyses [37].
Future applications in diabetic complications research will likely leverage the complementary strengths of both platforms through tiered analytical approaches, with LC-HRMS for comprehensive profiling and UHPLC-MS/MS for focused validation in large clinical cohorts.
The identification and verification of robust biomarkers are paramount for understanding the pathogenesis of diabetic complications. In the specific context of lipid metabolites and diabetic complications, this guide provides a comparative analysis of targeted and untargeted metabolomics strategies. It details how a cross-validated framework, which integrates the discovery power of untargeted methods with the precision of targeted assays, can enhance the rigor and translational potential of biomarker research for conditions such as diabetic kidney disease (DKD).
Metabolomics, the comprehensive study of small molecules, is crucial for elucidating the biochemical landscape of diabetic complications [43]. The two primary methodologies—untargeted and targeted metabolomics—offer complementary insights. Untargeted metabolomics is a global, hypothesis-generating approach that aims to capture all measurable metabolites in a sample, including unknown compounds [44] [45]. Conversely, targeted metabolomics is a hypothesis-driven approach focused on the precise identification and absolute quantification of a predefined set of metabolites [44] [45].
In the field of diabetic complications research, particularly concerning lipid metabolites, each approach has a distinct role. Untargeted methods can reveal novel lipid species and pathways associated with disease progression, while targeted methods are indispensable for validating these findings and establishing clinically applicable assays. A cross-validated approach that sequentially employs both strategies mitigates the limitations of each, creating a more robust pipeline for biomarker verification [44] [45].
Comparative Analysis: Targeted vs. Untargeted Metabolomics
The choice between targeted and untargeted metabolomics hinges on the research objective. The table below summarizes the core differences, providing a framework for selection.
Table 1: Core Methodological Differences Between Targeted and Untargeted Metabolomics
| Feature | Untargeted Metabolomics | Targeted Metabolomics |
|---|---|---|
| Goal | Comprehensive detection of known and unknown metabolites [44] [45] | Precise measurement of predefined metabolites [44] [45] |
| Scope | Broad (100s to 1000s of compounds) [46] | Narrow (dozens to ~100 compounds) [46] |
| Approach | Exploratory, hypothesis-generating [45] | Confirmatory, hypothesis-driven [45] |
| Quantification | Semi-quantitative (relative) [44] [45] | Absolute quantification [44] [45] |
| Standards | Not strictly required [45] | Isotopically labeled internal standards essential [44] [45] |
| Ideal Use Case | Biomarker discovery, pathway analysis [47] | Biomarker validation, clinical assay development [44] |
Advantages and Disadvantages
Untargeted Metabolomics
- Advantages: Its primary strength is its unbiased nature, allowing for the discovery of novel biomarkers and unexpected metabolic relationships without prior knowledge of the metabolome [44] [45]. It provides extensive coverage, enabling the systematic measurement of thousands of metabolites in a single analysis [44].
- Disadvantages: It generates complex data that requires extensive processing and sophisticated statistical analysis [44] [45]. The identification of unknown metabolites is challenging without reference standards, and the method suffers from decreased precision due to relative quantification and a bias toward detecting higher-abundance metabolites [44] [45].
Targeted Metabolomics
- Advantages: This approach offers high sensitivity, specificity, and precision by using isotopically labeled standards for absolute quantification, which minimizes false positives and analytical artifacts [44] [45]. It is optimized for quantifying specific metabolites of interest with high accuracy and reproducibility.
- Disadvantages: Its focused nature means it is limited to a predefined set of metabolites, creating a high risk of missing relevant biomarkers outside the target panel [44] [45]. It is dependent on prior knowledge and the commercial availability of validated standards [45].
Cross-Validated Workflow for Biomarker Verification
A synergistic, cross-validated workflow leverages the strengths of both untargeted and targeted methods to deliver verified, high-confidence biomarkers. The following diagram and protocol outline this integrated approach.
Diagram 1: Integrated cross-validation workflow for biomarker verification, combining untargeted discovery and targeted validation phases.
Experimental Protocols
Phase 1: Untargeted Discovery for Candidate Biomarker Identification
- Sample Preparation: Employ a global metabolite extraction protocol suitable for a wide range of lipid species. A biphasic liquid-liquid extraction using methanol and chloroform (e.g., Folch or Bligh & Dyer methods) is widely used to simultaneously extract polar and non-polar metabolites [43]. For lipid-focused studies, methyl tert-butyl ether (MTBE) is also an effective non-polar solvent [43].
- Data Acquisition: Utilize high-resolution mass spectrometry (MS) platforms, such as Fourier Transform Ion Cyclotron Resonance (FT-ICR-MS) or Quadrupole Time-of-Flight (Q-TOF) mass analyzers [48]. FT-ICR-MS offers unmatched mass resolution and accuracy, enabling precise molecular formula assignment and differentiation of thousands of compounds in complex biological samples, which is critical for discovering unknown lipid metabolites [48]. Coupling with Liquid Chromatography (LC) or direct infusion can be used.
- Data Processing and Analysis: Process raw data using software tools (e.g., XCMS, MZmine) for peak picking, alignment, and normalization [47]. Subsequently, apply multivariate statistical analyses (e.g., PCA, PLS-DA) to identify metabolite features that significantly differentiate sample groups (e.g., diabetic patients with complications vs. those without) [47]. This yields a list of candidate biomarkers for validation.
Phase 2: Targeted Validation for Absolute Quantification
- Sample Preparation: Perform specific extraction procedures optimized for the candidate lipid metabolites. A key step is the addition of isotopically labeled internal standards for each target analyte prior to extraction. This controls for variability in extraction efficiency and ionization, enabling absolute quantification [44] [43].
- Data Acquisition: Use tandem mass spectrometry systems, typically triple quadrupole (QQQ) instruments operating in Multiple Reaction Monitoring (MRM) mode [44]. This setup provides high sensitivity, specificity, and a broad dynamic range for the precise quantification of the predefined metabolite panel.
- Cross-Validation and Statistical Assessment: According to ICH M10 guidelines for bioanalytical method validation, a cross-validation between the untargeted screening results and the targeted quantitative assay is essential when combining data for regulatory submission [49]. This involves analyzing a set of samples (n>30 recommended) with both methods and assessing the agreement. Statistical measures may include calculating the 90% confidence interval (CI) of the mean percent difference to evaluate bias and using Deming regression or Concordance Correlation Coefficient (CCC) to quantify agreement [49]. This step confirms that the semi-quantitative data from the discovery phase reliably predicts the absolute concentrations obtained in validation.
Application in Diabetic Complications Research
Dysregulated lipid metabolism is a hallmark of type 2 diabetes and its microvascular complications [3]. Research has highlighted the role of ectopic lipid deposition and lipotoxicity in organs like the kidneys, retina, and nerves [3]. In this context, metabolomics is instrumental in identifying specific lipid species and pathways involved.
Key Lipid Biomarkers and Experimental Data
Novel lipid-related indices such as the Visceral Adiposity Index (VAI), Lipid Accumulation Product (LAP), and Atherogenic Index of Plasma (AIP) have shown promise as biomarkers. A 2025 meta-analysis synthesized evidence on their association with diabetic microvascular complications [6].
Table 2: Association of Novel Lipid Biomarkers with Diabetic Kidney Disease (DKD) - Meta-Analysis Data [6]
| Biomarker | Calculation Formula | Weighted Mean Difference (WMD) in DKD vs. Control | Odds Ratio (OR) for DKD Risk per 1-unit increase |
|---|---|---|---|
| Lipid Accumulation Product (LAP) | Men: [WC (cm)-65] × TG (mmol/L)Women: [WC (cm)-58] × TG (mmol/L) |
WMD: 12.67 (95% CI: 7.83, 17.51; P<.01) | OR: 1.005 (95% CI: 1.003, 1.006; P<.01) |
| Atherogenic Index of Plasma (AIP) | log10(TG/HDL-C) |
WMD: 0.11 (95% CI: 0.03, 0.19; P<.01) | OR: 1.08 (95% CI: 1.04, 1.12; P<.01) |
| Visceral Adiposity Index (VAI) | Men: (WC/39.68 + BMI/1.88) × (TG/1.03) × (1.31/HDL)Women: (WC/36.58 + BMI/1.89) × (TG/0.81) × (1.52/HDL) |
WMD: 0.63 (95% CI: 0.38, 0.89; P<.01) | OR: 1.05 (95% CI: 1.03, 1.07; P<.01) |
Abbreviations: WC, Waist Circumference; TG, Triglycerides; HDL-C, High-Density Lipoprotein Cholesterol; BMI, Body Mass Index; CI, Confidence Interval.
The data in Table 2 demonstrates that patients with DKD have significantly higher levels of LAP, AIP, and VAI compared to those without DKD, and each unit increase in these biomarkers is associated with a elevated risk of DKD [6]. However, the same meta-analysis found no significant association between these biomarkers and Diabetic Retinopathy (DR), and the overall diagnostic accuracy for DKD was modest, underscoring the need for more specific lipid metabolite panels and the application of the cross-validated workflow to discover and verify superior biomarkers [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagents and Materials for Metabolomics Workflows
| Item | Function & Application |
|---|---|
| Methanol/Chloroform | A classic biphasic solvent system for global metabolite extraction, separating polar metabolites (methanol phase) from non-polar lipids (chloroform phase) [43]. |
| Methyl tert-Butyl Ether (MTBE) | A non-polar solvent effective for the specialized extraction of lipophilic metabolites, including triglycerides and cholesterol esters [43]. |
| Isotopically Labeled Internal Standards | (e.g., 13C, 2H-labeled metabolites). Added to samples before processing in targeted metabolomics to correct for losses during preparation and ion suppression/enhancement during MS analysis, enabling absolute quantification [44] [43]. |
| Solid-Phase Extraction (SPE) Cartridges | Used for sample clean-up to remove salts and other interfering matrix components, thereby reducing ion suppression and improving MS detection sensitivity, especially in untargeted analysis [48]. |
| Quality Control (QC) Pools | A pooled sample created from aliquots of all study samples. Run repeatedly throughout the analytical sequence to monitor instrument stability and for data normalization to ensure data quality [43]. |
In the search for reliable lipid biomarkers for diabetic complications, the journey from collecting a blood sample to generating a robust dataset is fraught with potential variability. Pre-analytical factors—including the choice of blood collection tube, processing methodology, and participant characteristics—introduce significant variability and bias that can compromise data integrity if not properly controlled [50]. For researchers investigating lipid metabolites in diabetic complications such as diabetic retinopathy (DR) and diabetic kidney disease (DKD), standardized protocols are not merely optional but essential for producing comparable, reproducible results across studies and laboratories.
The growing emphasis on large-scale lipidomics studies demands increased attention to these pre-analytical variables. While high-throughput technologies have revolutionized lipidomics by enabling large-sample detection, performing large-scale sample processing introduces challenges related to consistency [50]. This guide provides a comprehensive comparison of sample processing methodologies and data processing approaches, with specific application to lipid biomarker discovery in diabetic complications research.
Blood Sample Processing: Serum vs. Plasma in Diabetes Research
Fundamental Differences and Preparation Protocols
The choice between serum and plasma begins with different blood collection and processing methods, each with distinct implications for the resulting lipidomic profile.
- Plasma Preparation: Blood is collected into tubes containing anticoagulants such as EDTA, sodium heparin, or lithium heparin. Tubes are gently inverted several times to mix, then centrifuged at approximately 3,000 rpm for 10 minutes at 4°C. The resulting supernatant is plasma [51].
- Serum Preparation: Blood is collected into tubes without anticoagulants, often containing a serum separation gel and coagulants. Tubes stand at room temperature for 30-60 minutes to allow complete coagulation, after which they are centrifuged at 3,000 rpm for 10 minutes at 4°C. The supernatant (serum) is carefully collected [51].
The coagulation process fundamentally alters the composition. Serum has a lower protein concentration than plasma (by approximately 3-4%), primarily due to the removal of fibrinogen and other proteins trapped in the fibrin clot [51]. This removal can also extend to lipids associated with these proteins or with platelets, which are more activated during serum preparation.
Comparative Lipidomic Profiles: Implications for Diabetic Complications
Targeted metabolomics studies reveal consistent, measurable differences between serum and plasma lipid profiles that researchers must account for.
Table 1: Comparison of Serum and Plasma for Lipidomics Studies
| Feature | Plasma | Serum | Implication for Diabetic Complications Research |
|---|---|---|---|
| Preparation | Requires anticoagulant | Requires clotting time | Plasma offers simpler, more standardized processing [51] |
| Fibrinogen Content | Present | Removed during clotting | May affect lipid-protein interactions; plasma more closely represents in-vivo state |
| Platelet Activation | Minimal | Significant | Serum more affected by platelet-derived lipids [51] |
| Reported Lipid Differences | Reference medium | 4 amino acid/driver metabolites lower; 5 other compounds higher [50] | Confounding if studies mix sample types |
| Throughput Consideration | Clotting time not required | Extended clotting time (30-60 mins) | Plasma more efficient for high-throughput studies |
| Lipidomic Stability | Generally more stable profile | Subject to clot formation variability | Plasma often preferred for biomarker discovery |
Evidence from diabetic complications research underscores the practical impact of this choice. Studies investigating lipid biomarkers for diabetic retinopathy [52] [53] and diabetic kidney disease [54] typically utilize serum, establishing a substantial body of literature against which new findings must be compared. However, this does not inherently make serum superior. The consistency of the protocol within and across studies is paramount.
Experimental Protocols in Diabetic Complications Lipidomics
Standardized Lipid Extraction and Analysis
Robust lipidomic profiling in diabetes research relies on consistent methodology. The following protocol summarizes common approaches used in recent studies of diabetic complications:
- Sample Collection and Storage: Collect fasting blood samples. For serum, allow coagulation; for plasma, use appropriate anticoagulants. Centrifuge at 1,500-3,000 rpm for 10-20 minutes at 4°C. Aliquot and store supernatant at -80°C until analysis [52] [53].
- Lipid Extraction: Thaw samples on ice. For a 100 μL serum sample, add 300 μL of ice-cold isopropanol containing internal standards (e.g., SPLASH LIPIDOMIX Mass Spec Standard). Vortex thoroughly, then incubate at -20°C for several hours or overnight. Centrifuge at 4°C at high speed (e.g., 4,000 rcf for 20 minutes) [53]. Collect the supernatant for analysis. Some protocols use a modified Folch or Bligh-Dyer method with methanol/chloroform mixtures [52].
- LC-MS/MS Analysis:
- Chromatography: Use UPLC systems with CSH C18 or similar reversed-phase columns (e.g., 1.7 μm, 2.1 × 100 mm). Mobile phases often consist of (A) acetonitrile-water (e.g., 60:40) and (B) isopropanol-acetonitrile (e.g., 90:10), both with 10 mM ammonium formate and 0.1% formic acid [52] [53].
- Mass Spectrometry: Perform analysis using triple quadrupole (QQQ) or Q-TOF mass spectrometers. Use both positive and negative ionization modes. For targeted analysis, use Multiple Reaction Monitoring (MRM) to quantify specific lipid species [54] [53].
- Quality Control: Pool aliquots of all samples to create a quality control (QC) sample. Run QC samples repeatedly at the beginning of the sequence to equilibrate the system and then periodically throughout the run to monitor instrument stability [53].
Workflow Visualization: From Sample to Data
The following diagram illustrates the comprehensive workflow for a lipidomics study in diabetic complications research, integrating both laboratory and computational steps:
Data Processing Tools for Lipidomics
Software Solutions for Lipidomic Data
The complexity of lipidomic datasets necessitates specialized software tools for processing, identification, and statistical analysis. The LIPID MAPS consortium provides a comprehensive guide to available solutions [55].
Table 2: Key Data Processing Tools for Lipidomics of Diabetic Complications
| Tool Name | Primary Function | Application in Diabetic Complications Research | Platform |
|---|---|---|---|
| LipidFinder [56] [55] | Distinguishes lipid-like features from contaminants in HR LC/MS data | Data clean-up for identifying low-abundance lipid biomarkers | Windows, Linux, Web |
| LipidXplorer [55] | Lipid identification and quantification from shotgun MS data | Determining lipid class alterations in disease progression | Web-based |
| MS-DIAL [55] | Comprehensive pipeline for untargeted MS data (deconvolution, identification, alignment) | Discovery of novel lipid signatures in DR/DKD | Windows, Linux |
| XCMS [55] | Peak picking, retention time correction, and statistical analysis | Identifying significantly altered lipids between patient groups | Online, R-based |
| Lipid Data Analyzer (LDA) [55] | Targeted and untargeted analysis of lipidomic LC-MS data | Quantitative analysis of specific lipid classes of interest | Platform-independent |
| LIPID MAPS Structure Database (LMSD) [56] [55] | Reference database of lipid structures | Structural identification of differentially expressed lipids | Web-based |
Normalization and Integration Strategies
When combining datasets—especially those from different sample types (serum vs. plasma) or studies—normalization becomes critical. A recent proteomics study demonstrated a viable approach for normalizing data between serum and plasma using protein-specific transformation factors derived from linear models [57]. While developed for proteomics, this conceptual framework is highly relevant to lipidomics.
Key steps for cross-dataset normalization include:
- Identify Correlated Lipids: Determine which lipid species show strong linear relationships between sample types or batches.
- Develop Cohort-Specific Models: Use linear modeling on paired samples to establish transformation factors.
- Validate Factors: Test transformation factors in independent cohorts with diverse disease phenotypes [57].
Lipid Biomarkers in Diabetic Complications: Case Studies
Diabetic Retinopathy (DR) Lipidomics
Targeted lipidomic profiling of serum samples has revealed specific lipid alterations associated with diabetic retinopathy:
- Ceramides and Sphingomyelins: A study of 622 T2DM patients found significantly lower levels of specific ceramides (Cer)—including Cer(d18:0/22:0) and Cer(d18:0/24:0)—and sphingomyelins in the DR group compared to diabetic controls without retinopathy, even after matching for traditional risk factors [53]. Multifactorial logistic regression indicated that decreased levels of these ceramides were an independent risk factor for DR.
- Diagnostic Models: Another study identified a four-lipid combination diagnostic model (including TAG58:2-FA18:1) that effectively distinguished patients without DR from those with non-proliferative DR [52].
Diabetic Kidney Disease (DKD) Lipidomics
Lipidomic studies of DKD reveal progressive alterations throughout disease development:
- Early Transition Markers: The transition from diabetes mellitus (DM) to DKD is characterized by elevated levels of certain lysophosphatidylethanolamines (LPEs), phosphatidylethanolamines (PEs), ceramides (Cers), and diacylglycerols (DAGs) [54].
- Advanced Stage Markers: Progression from early DKD (DKD-E) to advanced DKD (DKD-A) shows further increases in most LPEs, lysophosphatidylcholines (LPCs), along with several monoacylglycerols (MAGs) and triacylglycerols (TAGs) [54].
- Machine Learning Panels: A biomarker panel termed "Lipid9"—consisting of nine lipid species (LPC(18:2), LPC(20:5), LPE(16:0), LPE(18:0), LPE(18:1), LPE(24:0), PE(34:1), PE(34:2), and PE(36:2))—accurately distinguished DKD from DM (AUC: 0.78). When combined with clinical indexes (serum creatinine and blood urea nitrogen) in a "Lipid9-SCB" model, the accuracy improved further (AUC: 0.83), demonstrating the power of integrating lipidomic and clinical data [54].
Pathway Visualization: Lipid Dysregulation in Diabetic Complications
The following diagram summarizes key lipid pathways implicated in the progression of diabetic complications, based on current lipidomic findings:
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful lipidomics requires specific reagents and materials at each processing stage. The following toolkit summarizes essentials for diabetic complications research:
Table 3: Essential Research Reagent Solutions for Lipidomics
| Category | Item | Specific Function | Application Notes |
|---|---|---|---|
| Sample Collection | EDTA/Lithium Heparin tubes (Plasma) | Prevents coagulation by chelating calcium/inhibiting thrombin | Preferred for minimizing platelet activation [51] |
| Serum separation gel tubes (Serum) | Promotes clot formation and separation | Traditional medium for diabetic complication studies [52] | |
| Lipid Extraction | Isopropanol (IPA) / Methanol / Chloroform | Protein precipitation and lipid solubilization | IPA effective for direct serum/plasma precipitation [53] |
| SPLASH LIPIDOMIX Internal Standard | Quantification normalization across samples | Corrects for extraction efficiency and MS variability [53] | |
| LC-MS Analysis | CSH C18 UPLC Columns | Chromatographic separation of complex lipid mixtures | Provides high-resolution separation of lipid classes [52] [53] |
| Ammonium Formate/Acetate with Formic/Acetic Acid | Mobile phase additives for LC-MS | Enhances ionization efficiency and adduct formation consistency | |
| Data Processing | LIPID MAPS Structure Database | Structural identification of lipid species | Essential reference for annotuting lipid species [56] [55] |
| Lipidomics Software (e.g., MS-DIAL, XCMS) | Peak alignment, identification, and statistical analysis | Enables high-throughput processing of large sample sets [55] |
Generating robust lipidomic datasets for diabetic complications research requires meticulous attention to both sample preparation and data processing. The choice between serum and plasma must be deliberate, considering that each matrix yields systematically different lipid profiles. For longitudinal studies or when combining datasets from multiple sources, normalization strategies and consistent processing protocols are non-negotiable.
The emerging consensus suggests that plasma may offer advantages in standardization and reduced platelet activation, while serum has a more extensive established literature in diabetic complications research. Regardless of the choice, consistency within a study and transparent reporting of methodologies are paramount. When integrated with sophisticated data processing tools and validated against clinical outcomes, lipidomics holds tremendous promise for delivering novel biomarkers that can improve early detection and management of diabetic retinopathy, nephropathy, and other complications.
Diabetic complications represent a significant burden on global healthcare systems, driven by complex metabolic dysregulations that extend beyond chronic hyperglycemia. Among these, abnormalities in lipid metabolism are increasingly recognized as central players in the pathogenesis of diabetic nephropathy, cardiovascular disease, and other diabetes-related sequelae. Recent advances in lipidomics and machine learning have created unprecedented opportunities to decode these complex relationships and develop sophisticated diagnostic tools for early detection. The integration of computational biology with experimental validation provides a powerful framework for identifying lipid biomarkers and constructing predictive models with clinical utility. This guide objectively compares the performance of two primary machine learning algorithms—LASSO regression and SVM-RFE—in building diagnostic models based on multi-lipid panels, with a specific focus on their application in diabetic complications research.
Experimental Protocols: Methodological Approaches for Lipid Biomarker Discovery
Bioinformatics and Lipidomics Workflows
The identification of lipid biomarkers for diabetic complications follows a structured analytical pipeline that integrates multiple data modalities. A typical workflow begins with sample preparation and lipid extraction from relevant biological specimens (serum, plasma, or tissue), followed by lipid profiling using mass spectrometry-based techniques such as UPLC-ESI-MS/MS. [58] [59] This analytical approach enables the comprehensive characterization of lipid classes and subclasses, having identified 35 lipid subclasses encompassing 564 lipid molecules in recent studies. [58] Subsequent data preprocessing includes normalization, batch effect correction, and quality control to ensure analytical robustness.
For transcriptomic analyses, researchers typically obtain gene expression datasets from public repositories like the Gene Expression Omnibus (GEO), followed by differential expression analysis using the limma R package with thresholds commonly set at |log2FC| > 0.5-1 and adjusted p-value < 0.05. [60] [8] [61] Lipid metabolism-related genes (LMRGs) are identified from databases such as MsigDB, GeneCards, or Reactome, then intersected with differentially expressed genes to pinpoint lipid-specific alterations. [60] [61] Functional enrichment analysis via GO and KEGG pathways reveals the biological processes and signaling pathways implicated in diabetic complications, with common enrichments including phospholipid metabolic processes, lysosome function, and glycerophospholipid metabolism. [61] [59]
Machine Learning Algorithm Implementation
The core analytical phase employs multiple machine learning algorithms to identify optimal biomarker panels:
LASSO Regression: Implemented using the glmnet R package, LASSO performs variable selection and regularization through L1 penalty to enhance prediction accuracy and interpretability. [61] [62] The algorithm applies a penalty parameter (λ) that shrinks coefficients of less relevant variables to zero, effectively selecting only the most predictive features. [63]
SVM-RFE: The Support Vector Machine-Recursive Feature Elimination algorithm, implemented via the e1071 R package, recursively removes features with the smallest ranking criteria based on support vector weight magnitude. [60] [62] This approach typically employs 5- or 10-fold cross-validation to evaluate classification performance and minimize overfitting. [64] [63]
Random Forest: As a complementary algorithm, Random Forest constructs multiple decision trees and outputs the mode of their classes, providing robust feature importance metrics through Gini index or permutation importance. [60] [63]
These algorithms are often used in combination, with their intersections taken to identify the most robust biomarker candidates. [61] [58] Model performance is typically evaluated through receiver operating characteristic (ROC) analysis, with area under the curve (AUC) values >0.7 considered diagnostically informative. [61] [64]
Validation Approaches
Rigorous validation is essential for establishing clinical relevance:
- External Validation: Candidate biomarkers are validated in independent datasets to assess generalizability. [60] [65]
- Experimental Validation: RT-qPCR analysis of candidate genes in disease models (e.g., dextran sulfate sodium-induced colitis mice, AP mouse models) confirms expression patterns observed in computational analyses. [65] [62]
- Single-Cell RNA Sequencing: Reveals cell-type-specific expression of biomarkers across different immune and tissue-resident cells. [60] [65]
- Immune Infiltration Analysis: CIBERSORT algorithm assesses correlations between biomarker expression and immune cell populations in the tissue microenvironment. [60] [61] [64]
The following diagram illustrates the complete experimental workflow for building diagnostic models using these methodologies:
Figure 1: Experimental workflow for diagnostic model development integrating lipidomics, transcriptomics, and machine learning approaches.
Comparative Performance of LASSO and SVM-RFE in Lipid Biomarker Discovery
Algorithm Performance Across Diabetic Complications
The application of LASSO and SVM-RFE algorithms has demonstrated variable performance across different diabetic complications, with each exhibiting distinct strengths in biomarker identification.
Table 1: Performance Comparison of LASSO and SVM-RFE Across Diabetic Complications
| Disease Context | Algorithm | Biomarkers Identified | Diagnostic Performance (AUC) | Key Advantages | Reference |
|---|---|---|---|---|---|
| Diabetic Kidney Disease | LASSO + SVM-RFE | Lysophosphatidylethanolamines | 0.78-0.85 | Handles correlated lipid features | [59] |
| Atherosclerosis in Diabetes | LASSO | TYROBP, CSF1R, LCP2, C1QA | 0.72-0.89 | Effective dimension reduction | [60] |
| Acute Pancreatitis | LASSO + SVM-RFE | Amacr, Cyp39a1, Echs1, Gpd2 | 0.71-0.83 | Identifies metabolic pathway genes | [62] |
| Diabetic Nephropathy | SVM-RFE | CXCR2, NAMPT, CUEDC2 | 0.68-0.75 | Robust to high-dimensional data | [8] |
| Ulcerative Colitis | LASSO + RF + SVM-RFE | EIF5A2, IDO1, CDH5, MYL5 | 0.81-0.87 | Ensemble approach improves accuracy | [65] |
In diabetic kidney disease, the combination of LASSO and SVM-RFE has proven particularly effective, identifying lysophosphatidylethanolamines as significant biomarkers with AUC values ranging from 0.78 to 0.85. [59] The complementary strengths of both algorithms—LASSO's effectiveness in handling correlated lipid features and SVM-RFE's robustness in high-dimensional data spaces—enable comprehensive biomarker discovery. For atherosclerosis in diabetes, LASSO regression alone identified key regulatory genes (TYROBP, CSF1R, LCP2, C1QA) with AUC values up to 0.89, demonstrating exceptional diagnostic potential for this cardiovascular complication. [60]
Technical Comparison of Algorithm Characteristics
Beyond diagnostic performance, the selection between LASSO and SVM-RFE involves important technical considerations that influence their applicability to different research scenarios.
Table 2: Technical Comparison of LASSO and SVM-RFE Algorithms
| Characteristic | LASSO Regression | SVM-RFE |
|---|---|---|
| Variable Selection | L1 regularization shrinks coefficients to zero | Recursive feature elimination based on weight magnitude |
| Handling Correlated Features | Selects one representative from correlated groups | More stable with correlated features |
| Computational Complexity | Lower computational requirements | Higher due to iterative model rebuilding |
| Model Interpretability | High - provides coefficient values | Moderate - feature rankings without effect direction |
| Data Type Suitability | Effective with continuous lipid concentration data | Handles both continuous and categorical data well |
| Implementation | glmnet R package | e1071 R package with custom RFE |
LASSO regression provides superior model interpretability through coefficient values that indicate both the direction and magnitude of each feature's effect, which is particularly valuable for understanding lipid metabolism pathways in diabetic complications. [62] [63] In contrast, SVM-RFE offers enhanced stability with correlated features, making it suitable for lipidomic datasets where many lipid species are biologically interrelated. [8] [64] The computational intensity of SVM-RFE's iterative process can be mitigated through parallel processing and appropriate cross-validation strategies.
Lipid Panels and Pathophysiological Insights in Diabetic Complications
Disease-Specific Lipid Metabolic Signatures
Different diabetic complications exhibit distinct alterations in lipid metabolism, yielding complication-specific biomarker panels with varying diagnostic and prognostic utility.
In diabetic kidney disease (DKD), lipidomic analyses have revealed significant alterations in lysophosphatidylethanolamines (LPEs), with specific decreases in LPE(16:0), LPE(18:0), and LPE(18:1) concentrations correlating with disease progression. [59] These lipid species are implicated in membrane integrity and inflammatory signaling pathways, providing a mechanistic link between lipid dysregulation and renal dysfunction. Additionally, research has identified key metabolic reprogramming genes including CXCR2, NAMPT, and CUEDC2 through SVM-RFE algorithms, highlighting the intersection of lipid metabolism and immune responses in DKD pathogenesis. [8]
For cardiovascular complications in diabetes, studies have identified ferroptosis-related lipid peroxidation pathways as central mechanisms, with key regulatory genes including CYBB, HMOX1, and IL1B. [60] These genes, identified through integrated machine learning approaches, participate in iron-dependent lipid peroxidation that drives endothelial cell damage and macrophage-mediated inflammatory responses in atherosclerotic lesions. The inhibition of ferroptosis using compounds like Ferrostatin-1 has demonstrated therapeutic potential by attenuating ox-LDL-induced gene upregulation and improving mitochondrial function. [60]
In acute pancreatitis associated with diabetic hyperlipidemia, LASSO and SVM-RFE algorithms have identified seven core lipid metabolism genes: Amacr, Cyp39a1, Echs1, Gpd2, Osbpl9, Acsl4, and Mcee. [62] These genes collectively impact fatty acid metabolism, cholesterol homeostasis, and mitochondrial function, with ACSL4 particularly implicated in cell membrane lipid synthesis and inflammatory cytokine activation. [62]
Signaling Pathways in Lipid-Mediated Diabetic Complications
The pathophysiological mechanisms linking lipid metabolism dysregulation to diabetic complications involve complex signaling networks that can be visualized as follows:
Figure 2: Signaling pathways linking lipid metabolism dysregulation to diabetic complications through specific molecular and cellular events.
Research Reagent Solutions for Lipid Biomarker Discovery
The experimental workflows for building diagnostic models require specialized reagents and computational resources that ensure reproducibility and analytical robustness.
Table 3: Essential Research Reagents and Resources for Lipid Biomarker Studies
| Category | Specific Product/Resource | Application in Research | Technical Considerations |
|---|---|---|---|
| Lipid Extraction | Methyl-tert-butyl ether (MTBE) method | Comprehensive lipid extraction from biological samples | Provides high recovery of diverse lipid classes |
| Chromatography | UPLC systems (Waters, Thermo) | Lipid separation prior to mass spectrometry | Enables resolution of isobaric lipid species |
| Mass Spectrometry | Q-TOF and Orbitrap platforms | High-resolution lipid identification and quantification | Requires appropriate internal standards |
| RNA Isolation | RNAprep Pure Hi-Blood Kit | Extraction from blood samples for transcriptomics | Maintains RNA integrity for accurate expression |
| Gene Expression | PrimeScript RT Reagent Kit | cDNA synthesis for qRT-PCR validation | Ensures faithful reverse transcription |
| Bioinformatics | limma R package | Differential expression analysis | Handles multiple comparison corrections |
| Machine Learning | glmnet, e1071, randomForest R packages | Implementation of LASSO, SVM-RFE, and Random Forest | Requires careful parameter tuning |
| Pathway Analysis | clusterProfiler R package | GO and KEGG enrichment analysis | Provides functional context for biomarkers |
The integration of wet laboratory reagents with computational packages creates a seamless pipeline from sample collection to diagnostic model building. Mass spectrometry platforms, particularly UPLC-ESI-MS/MS systems, enable the comprehensive lipid profiling necessary for generating high-quality input data for machine learning algorithms. [58] [59] Bioinformatics packages like limma and clusterProfiler provide the statistical foundation for identifying significant alterations, while machine learning libraries including glmnet and e1071 facilitate the implementation of LASSO and SVM-RFE algorithms for biomarker selection. [60] [62]
The comparative analysis of LASSO and SVM-RFE algorithms for building diagnostic models based on multi-lipid panels reveals a complex landscape with significant opportunities for advancing early detection of diabetic complications. LASSO regression demonstrates particular strength in creating interpretable models with direct clinical applicability, while SVM-RFE offers robustness in high-dimensional data environments typical of lipidomic studies. The integration of both approaches, complemented by Random Forest and other machine learning techniques, provides a powerful framework for identifying biomarkers with both diagnostic accuracy and biological relevance.
Future research directions should focus on several key areas: (1) longitudinal validation of identified lipid biomarkers in prospective cohort studies to establish temporal relationships; (2) integration of multi-omics data layers including proteomics and metabolomics to create comprehensive pathophysiological models; (3) development of standardized protocols for lipidomic analyses to enhance reproducibility across research centers; and (4) translation of computational findings into clinically implementable diagnostic panels that can improve risk stratification and early intervention strategies for diabetic complications.
The systematic comparison of experimental approaches and algorithmic performance presented in this guide provides researchers with a foundation for selecting appropriate methodologies based on specific research questions, available resources, and intended clinical applications. As lipidomics and machine learning continue to evolve, their integration will undoubtedly yield increasingly sophisticated tools for understanding and addressing the complex metabolic disruptions in diabetes and its complications.
Diabetic retinopathy (DR), a prevalent microvascular complication of diabetes, remains a leading cause of visual impairment and blindness among working-age adults globally [4]. The traditional classification system divides DR into two primary stages: non-proliferative diabetic retinopathy (NPDR), characterized by microaneurysms, hemorrhages, and intraretinal microvascular abnormalities; and proliferative diabetic retinopathy (PDR), defined by preretinal neovascularization [4]. Current diagnostic methods primarily rely on fundus imaging, which can only detect the condition after structural damage to the retina has occurred [52]. This limitation underscores the critical need for molecular-based approaches that can identify at-risk patients earlier in the disease process.
Integrated metabolomic and lipidomic profiling represents a transformative approach in DR research, enabling comprehensive analysis of metabolic alterations throughout disease progression. As terminal products of cellular regulatory processes, metabolites and lipids provide a direct readout of physiological activity and disease-induced perturbations [4]. The integration of these omics technologies with advanced machine learning algorithms has created unprecedented opportunities for biomarker discovery, disease stratification, and elucidation of underlying molecular mechanisms in DR pathophysiology [66] [67]. This case study examines how this integrated approach is revolutionizing our understanding and clinical management of diabetic retinopathy.
Comparative Analysis of Metabolomic and Lipidomic Studies in DR
Key Studies and Their Experimental Designs
Recent advances in mass spectrometry have enabled detailed characterization of metabolic alterations across DR stages. The table below summarizes the experimental designs of three pivotal studies investigating metabolomic and lipidomic profiles in diabetic retinopathy.
Table 1: Experimental Designs of Key DR Metabolomic-Lipidomic Studies
| Study Focus | Participant Groups & Sample Size | Analytical Platform | Key Measured Molecules | Statistical & Machine Learning Approaches |
|---|---|---|---|---|
| DR Stage Stratification [66] | 167 total: 45 NDR, 69 NPDR (varying severity), 53 PDR | LC-HRMS | 962 molecules (653 lipids + 309 polar metabolites) | Statistical models; 10 ML algorithms including K-nearest neighbor |
| Early DR Biomarkers [52] | 62 total: 31 NDR, 31 NPDR | UHPLC-MS/MS (targeted lipidomics) | 102 significantly altered lipids | LASSO; SVM-RFE; ROC analysis |
| T2DM Lipidomics [68] | 60 total: 30 T2DM, 30 healthy controls | UPLC-MS | 1162 lipid metabolites (267 significantly altered) | PLS-DA; PCA; VIP scores; Pearson correlation |
Metabolic Alterations Across DR Progression
The studies identified consistent patterns of metabolic dysregulation throughout DR progression. In the comprehensive analysis by Fang et al., purine metabolism and sphingolipid metabolism were significantly disrupted in both NPDR and PDR stages [66] [4]. Tyrosine metabolism was specifically disturbed in non-proliferative disease, while glycine-serine-threonine metabolism alterations became prominent in proliferative disease [66]. Disease progression was particularly associated with marked reductions in sphingomyelins, phosphatidylcholines, and lysophosphatidylcholines [66] [4].
The lipidomic study focusing on early DR identified four lipid metabolites with superior diagnostic capability: TAG58:2-FA18:1, and three additional lipid species [52]. These biomarkers demonstrated robust performance in distinguishing NDR from NPDR patients in both discovery and validation cohorts, suggesting their potential utility for early detection before visible retinal changes occur [52].
Table 2: Key Metabolic Alterations Across Diabetic Retinopathy Stages
| Disease Stage | Most Significantly Altered Pathways | Key Lipid Alterations | Potential Biomarker Molecules |
|---|---|---|---|
| NPDR | Purine metabolism; Sphingolipid metabolism; Tyrosine metabolism [66] | Reduced sphingomyelins, phosphatidylcholines, and lysophosphatidylcholines [66] | Four-lipid panel including TAG58:2-FA18:1 [52] |
| PDR | Purine metabolism; Sphingolipid metabolism; Glycine-serine-threonine metabolism [66] | Continued reduction in complex phospholipids; specific ceramide species alterations [66] | Lipid ST 24:1;O4; beta-hydroxyisovaleric acid [66] |
| Advanced PDR | Mitochondrial dysfunction; Fatty acid oxidation [4] | Accumulation of specific fatty acids including FA(16:1), FA(20:1) [69] | Acetylcarnitine; specific ceramide species [69] |
Machine Learning Performance in DR Stratification
The integration of machine learning with omics data has significantly enhanced DR classification accuracy. In the study by Fang et al., ten different machine learning models were evaluated, with the K-nearest neighbor algorithm demonstrating the highest performance for stage classification [66]. The lipid species ST 24:1;O4 and the metabolite beta-hydroxyisovaleric acid were identified as the top contributors to this classification model [66].
Similarly, in a broader diabetes classification study, the Extra Trees Classifier achieved remarkable performance (AUC: 0.9985) in stratifying patients across four health states: healthy, prediabetes, T2DM without complications, and T2DM with complications [67]. The top contributing features included three molecular markers (miR342, NFKB1, and miR636) and two biochemical markers (albumin-to-creatinine ratio and HDLc) [67].
Table 3: Machine Learning Performance in Diabetes and DR Classification
| Study | Best Performing Algorithm | Classification Performance | Top Discriminatory Features |
|---|---|---|---|
| DR Stage Stratification [66] | K-nearest neighbor | Highest classification performance among 10 ML models | Lipid ST 24:1;O4; beta-hydroxyisovaleric acid |
| Diabetes Staging [67] | Extra Trees Classifier | AUC: 0.9985 (95% CI: [0.994–1.000]) | miR342, NFKB1, miR636, albumin-to-creatinine ratio, HDLc |
Experimental Protocols and Methodologies
Sample Collection and Preparation
Standardized sample collection and preparation protocols are critical for reproducible metabolomic and lipidomic analyses. Across studies, fasting venous blood is typically collected in EDTA-coated tubes or vacuum serum tubes [68] [70]. Samples are centrifuged at 3,000 × g for 10-15 minutes at 4°C to separate plasma or serum, with aliquots stored at -80°C until analysis [68] [70].
For metabolomic analysis, the preferred protein precipitation and metabolite extraction method involves mixing 100-200μL serum with 400μL cold methanol/acetonitrile (1:1, v/v) solution [70] [69]. The mixture is vortexed, sonicated for 10 minutes at 4°C, then centrifuged at 13,000-14,000 × g for 15-20 minutes at 4°C [70]. The supernatant is collected and dried using a vacuum centrifuge or nitrogen stream, with residues reconstituted in 100μL acetonitrile/water (1:1, v/v) for LC-MS analysis [69].
For lipidomic analysis, the methyl-tert-butyl ether (MTBE) method is widely employed [68] [69]. Typically, 22-50μL serum is mixed with 200μL methanol, then 800μL MTBE is added [69]. After vortexing and sonication for 20 minutes at 4°C, the mixture rests at room temperature for 30 minutes before adding 200μL MS-grade water [69]. Following centrifugation at 14,000 rpm for 15 minutes at 4°C, the upper organic layer is collected and evaporated under nitrogen [69]. The residue is reconstituted in 100-200μL isopropanol/acetonitrile (9:1, v/v) for LC-MS analysis [69].
LC-MS/MS Analytical Conditions
Liquid chromatography-tandem mass spectrometry (LC-MS/MS) represents the gold standard for comprehensive metabolomic and lipidomic profiling. For metabolomic analysis, separation is typically performed using HILIC columns with mobile phases comprising (A) 0.1% formic acid in water and (B) 0.1% formic acid in acetonitrile [70]. For lipidomic analysis, C8 or C18 columns are preferred, with mobile phases consisting of (A) methanol-acetonitrile-water (1:1:1) with 5mmol/L ammonium acetate and (B) isopropanol with 5mmol/L ammonium acetate [68].
Mass spectrometric detection is commonly performed using Q Exactive HF-X or TripleTOF systems [68] [70]. Typical ion source parameters include ion spray voltage of +5500V (positive) and -4500V (negative), source temperature of 350-500°C, and curtain gas flow of 25-35 psi [68]. Data acquisition typically employs information-dependent acquisition (IDA) to collect MS/MS spectra for molecular identification [68].
Data Processing and Statistical Analysis
Raw LC-MS/MS data processing represents a critical step in the analytical pipeline. Most studies utilize software such as XCMS (v3.18.0) and MS-DIAL (v4.9) for peak alignment, annotation, and normalization [70]. Features with >80% missing values are typically excluded, with remaining missing values imputed using k-nearest neighbors (k=10) [70]. Batch effects are corrected via Combat algorithm in the sva R package [70].
Multivariate statistical analyses including Principal Component Analysis (PCA) and Partial Least Squares-Discriminant Analysis (PLS-DA) are employed to identify group-discriminant metabolites and lipids [68]. Features with variable importance in projection (VIP) >1.0, p<0.05, and fold change >1.2 or <0.83 are typically considered statistically significant [68] [70]. Machine learning algorithms such as Random Forest (with 1000 trees) and LASSO regression are subsequently applied for feature selection and biomarker identification [70].
Diagram 1: Integrated Metabolomic and Lipidomic Workflow for DR Stratification. This diagram illustrates the comprehensive experimental pipeline from sample preparation through data analysis used in DR metabolomic-lipidomic studies.
Signaling Pathways in Diabetic Retinopathy Progression
Integrated metabolomic and lipidomic analyses have identified several key pathways consistently dysregulated throughout DR progression. Sphingolipid metabolism emerges as a central pathway, with specific ceramide species progressively altered from early to advanced stages [66] [52]. Purine metabolism demonstrates significant disruption across both NPDR and PDR stages, reflecting alterations in energy metabolism and cellular stress responses [66]. Mitochondrial dysfunction, evidenced by disrupted fatty acid oxidation and carnitine metabolism, becomes increasingly prominent in advanced disease [69].
Stage-specific pathway alterations provide insights into disease mechanisms. Tyrosine metabolism disturbances characterize the NPDR stage, potentially influencing neurotransmitter synthesis and vascular function [66]. The transition to PDR involves a shift toward glycine-serine-threonine metabolism alterations, which may reflect increased collagen turnover and extracellular matrix remodeling associated with neovascularization [66]. The mTORC1 signaling pathway, identified as significantly dysregulated in related metabolic studies, may represent a convergent node integrating these metabolic disturbances [70].
Diagram 2: Metabolic Pathways in Diabetic Retinopathy Pathogenesis. This diagram illustrates the key metabolic disturbances and signaling pathways implicated in DR progression, from initial metabolic insults to clinical manifestations.
Research Reagent Solutions for DR Metabolomic-Lipidomic Studies
Table 4: Essential Research Reagents for DR Metabolomic-Lipidomic Studies
| Reagent Category | Specific Products | Application in DR Studies | Key Functions |
|---|---|---|---|
| Chromatography Columns | Kinetex C18 (2.6 μm, 2.1 × 100 mm); HILIC columns; BEH C8 columns [68] [52] | Metabolite and lipid separation | Molecular separation based on hydrophobicity (C8/C18) or polarity (HILIC) |
| Mass Spectrometry Systems | AB SCIEX TripleTOF 5500; Q Exactive HF-X; UPLC-MS/MS systems [68] [70] | High-resolution metabolite and lipid detection | Accurate mass measurement; structural characterization via MS/MS |
| Lipid Extraction Solvents | Methyl-tert-butyl ether (MTBE); Methanol; Acetonitrile; Isopropyl alcohol [68] [69] | Comprehensive lipid extraction from serum | Efficient extraction of both polar and non-polar lipid species |
| Internal Standards | 15:0–18:1-d₇-phosphatidylcholine; 18:1-d₇-cholesteryl ester; d₁₈:1–18:1-d₉-sphingomyelin; L-carnitine-d₉ [69] | Quantification accuracy | Correction for extraction and ionization efficiency variations |
| Data Analysis Software | XCMS (v3.18.0); MS-DIAL (v4.9); MetaboAnalyst 5.0 [70] | Data processing and pathway analysis | Peak alignment, statistical analysis, pathway mapping |
Integrated metabolomic and lipidomic profiling has demonstrated significant potential for transforming diabetic retinopathy management through precise stage stratification and early risk detection. The consistent identification of sphingolipid metabolism disruptions, specific phospholipid alterations, and stage-specific metabolic pathway perturbations provides a robust molecular framework for understanding DR progression [66] [4] [52]. The successful application of machine learning algorithms to these complex datasets further enhances the translational potential of these findings, enabling accurate classification of disease stages based on molecular signatures rather than solely on structural retinal changes [66] [67].
Future research directions should focus on validating these metabolic biomarkers in larger, multi-center cohorts and diverse populations. The development of standardized protocols for metabolomic and lipidomic profiling will be essential for clinical implementation [68] [70]. Additionally, longitudinal studies tracking metabolic changes throughout DR progression and in response to interventions will provide crucial insights into disease mechanisms and therapeutic response monitoring. The integration of metabolomic-lipidomic data with other omics approaches (genomics, proteomics) and clinical imaging data represents the next frontier in developing comprehensive predictive models for personalized DR management [71]. As these technologies continue to advance, molecular-based stratification of diabetic retinopathy promises to enable earlier intervention and more targeted therapies, ultimately reducing the global burden of diabetes-related vision loss.
Addressing Analytical Challenges and Translating Biomarkers to Clinical Utility
The investigation of lipid metabolites has become a central focus in the quest to understand, predict, and prevent the microvascular complications of diabetes mellitus. Diabetic kidney disease (DKD), diabetic retinopathy (DR), and diabetic neuropathy (DN) collectively represent a massive burden, affecting millions of patients worldwide and contributing significantly to diabetes-related morbidity and mortality [72]. While hyperglycemia has long been recognized as a key driver, it fails to fully explain complication risk, prompting increased attention to the role of dyslipidemia and altered lipid metabolism [72].
This research field faces significant methodological challenges. The accurate measurement and interpretation of lipid biomarkers are complicated by substantial sample variability across study populations and individual patients. Furthermore, the absence of standardized methodologies for measuring both novel and traditional lipid parameters threatens the reproducibility of research findings, potentially slowing clinical translation [73]. This guide objectively compares the performance of various lipid biomarkers and analytical approaches, providing researchers with the experimental data and protocols needed to navigate these challenges.
Comparative Analysis of Lipid Biomarkers for Diabetic Complications
Established vs. Novel Lipid Biomarkers
Research has evolved from examining traditional lipid profiles to developing novel composite biomarkers that better reflect pathophysiological processes like visceral adiposity and atherogenicity.
Table 1: Comparison of Traditional and Novel Lipid Biomarkers in Diabetic Complications
| Biomarker Category | Specific Marker | Association with DKD | Association with DR | Association with DN | Key Findings from Meta-Analyses |
|---|---|---|---|---|---|
| Traditional Lipids | Triglycerides (TG) | Positive [74] [75] | Not Significant [75] | Positive [74] | Higher TG levels increase the odds of DN (OR: 1.36; 95% CI: 1.20–1.54) [74]. |
| HDL Cholesterol | Inverse [74] [75] | Not Significant [75] | Inverse [74] | Higher HDL reduces DN risk (OR: 0.85; 95% CI: 0.75–0.96) [74]. | |
| LDL Cholesterol | Positive [75] | Not Significant [75] | Positive [74] | Higher LDL increases DN risk (OR: 1.10; 95% CI: 1.02–1.19) [74]. LDL variability linked to nephropathy [75]. | |
| Novel Composite Indices | Lipid Accumulation Product (LAP) | Positive [6] | Not Significant [6] | Data Limited | Patients with DKD have significantly higher LAP (WMD: 12.67; 95% CI: 7.83–17.51) [6]. |
| Atherogenic Index of Plasma (AIP) | Positive [6] | Not Significant [6] | Data Limited | Each 1-unit increase in AIP elevates DKD risk (OR: 1.08; 95% CI: 1.04–1.12) [6]. | |
| Visceral Adiposity Index (VAI) | Positive [6] | Not Significant [6] | Data Limited | Significantly higher VAI in DKD patients (WMD: 0.63; 95% CI: 0.38–0.89) [6]. |
The Emerging Challenge: Lipid Variability
Beyond absolute levels, intra-individual visit-to-visid lipid variability has emerged as a novel and independent risk factor.
Table 2: Impact of Lipid Variability on Microvascular Complications in Diabetes
| Lipid Component | Impact on Diabetic Nephropathy | Impact on Diabetic Neuropathy | Impact on Diabetic Retinopathy | Supporting Evidence |
|---|---|---|---|---|
| HDL Variability | Adverse Effect [75] | Adverse Effect [75] | No Apparent Relationship [75] | Higher HDL variability increases risk of nephropathy and neuropathy [75]. |
| LDL Variability | Adverse Effect [75] | Adverse Effect [75] | No Apparent Relationship [75] | Associated with development of albuminuria and eGFR decline [75]. |
| TG Variability | Adverse Effect [75] | Adverse Effect [75] | No Apparent Relationship [75] | Associated with microalbuminuria incidence and GFR decline [75]. |
Experimental Protocols and Methodologies
Core Methodologies for Systematic Reviews and Meta-Analyses
The evidence presented in the tables above is largely derived from systematic reviews and meta-analyses, which follow rigorous, predefined protocols to ensure reproducibility.
- Protocol Registration: The study protocol is registered in a prospective database like PROSPERO (e.g., CRD42024596607 [6]) or the Open Science Framework [75] before commencing. This pre-specifies the research question, eligibility criteria, and analytical approach to minimize bias.
- Search Strategy: A comprehensive, systematic search is performed across multiple electronic databases (e.g., PubMed, Scopus, Embase, Web of Science) using a combination of keywords and Medical Subject Headings (MeSH) related to the population, exposure, and outcomes. Searches are often restricted to "title/abstract" fields and may have language limitations (e.g., English-only studies) [6] [74] [75].
- Eligibility Criteria & Study Selection: Studies are included based on predefined PICO (Population, Intervention, Comparison, Outcome) criteria. For example, population must be patients with diabetes mellitus, and the study must evaluate microvascular complications in relation to specific lipid biomarkers [6]. The selection process is typically performed by two independent investigators to reduce error, with disagreements resolved by a third reviewer [6] [75].
- Data Extraction & Quality Assessment: Data is extracted using a standardized template. The methodological quality of included studies is assessed using tools like the Joanna Briggs Institute (JBI) Critical Appraisal tools or the Newcastle-Ottawa Scale (NOS) [74] [75].
- Statistical Synthesis: Data is synthesized using meta-analytic techniques. For continuous outcomes (e.g., biomarker levels), pooled weighted mean differences (WMDs) or standardized mean differences (SMDs) with 95% confidence intervals (CIs) are calculated. For dichotomous outcomes (e.g., complication risk), pooled odds ratios (ORs) are calculated. Random-effects or fixed-effects models are chosen based on heterogeneity, which is quantified using I² statistics [6] [74] [76].
Formulas for Novel Lipid Biomarkers
The calculation of novel composite indices is a key source of methodological variation that requires standardization.
- Lipid Accumulation Product (LAP):
- For men:
[WC (cm) − 65] × TG (mmol/L) - For women:
[WC (cm) − 58] × TG (mmol/L)[6]
- For men:
- Atherogenic Index of Plasma (AIP):
AIP = log₁₀(TG / HDL-C)where TG and HDL-C are in mg/dL or converted to consistent units [6]
- Visceral Adiposity Index (VAI):
- For men:
(WC / 39.68 + (BMI / 1.88)) × (TG / 1.03) × (1.31 / HDL-C) - For women:
(WC / 36.58 + (BMI / 1.89)) × (TG / 0.81) × (1.52 / HDL-C)[6] - Note: TG units must be mmol/L in the standard VAI formula.
- For men:
Visualizing Metabolic Pathways and Research Workflows
Tissue-Specific Lipid Flux in Diabetic Complications
The diagram below illustrates the tissue-specific differences in glucose and lipid metabolism in complication-prone tissues, as revealed by stable isotope tracing studies in a murine model of type 2 diabetes [72].
Systematic Review Workflow for Lipid Biomarker Research
The following workflow diagram outlines the standard methodology for conducting a systematic review and meta-analysis in this field, as per PRISMA guidelines [6] [75].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successfully navigating the challenges of sample variability and standardization requires a carefully selected toolkit of reagents and methodologies.
Table 3: Essential Research Reagents and Materials for Lipid Biomarkers Research
| Category / Item | Specific Examples / Formats | Primary Function in Research |
|---|---|---|
| Blood Collection & Processing | EDTA or heparinized tubes; Centrifuges | Standardized collection and separation of plasma/serum to prevent pre-analytical variability. |
| Automated Clinical Chemistry Analyzers | Platforms from Roche, Siemens, Abbott | High-throughput, standardized measurement of traditional lipids (TG, HDL-C, LDL-C, TC). |
| Anthropometric Measurement Tools | Seca 201 measuring tape; calibrated stadiometers and scales | Accurate measurement of Waist Circumference (WC) and Height/Weight for BMI calculation, critical for LAP and VAI. |
| Statistical Analysis Software | STATA; R (with 'metafor' package); Comprehensive Meta-Analysis | Performing complex meta-analyses, calculating pooled effect sizes, and assessing heterogeneity. |
| Reference Materials for Standardization | CDC-certified lipid standards; NIST SRMs | Calibrating equipment to ensure measurement consistency and reproducibility across labs and studies. |
The comparative analysis presented in this guide reveals a nuanced landscape for lipid biomarkers in diabetic complications research. While novel indices like LAP, VAI, and AIP show significant promise, particularly for predicting DKD, their diagnostic accuracy remains modest and their utility for DR is limited [6]. Traditional lipids, especially TG and HDL, retain significant value, particularly for DN, but their variability over time adds a new layer of complexity to risk assessment [74] [75].
The path forward requires a concerted effort to overcome the hurdles of sample variability and a lack of standardization. Researchers must adopt rigorous, pre-registered methodologies, clearly report units and formulas for composite indices, and utilize standardized reagents to enhance the reproducibility of findings. By doing so, the research community can accelerate the translation of lipid biomarkers into clinical tools that improve outcomes for patients with diabetes.
The rising global burden of diabetic microvascular complications necessitates advanced diagnostic strategies for early detection and risk stratification. Current clinical biomarkers, including HbA1c and albuminuria, often identify complications only after established organ damage has occurred, limiting opportunities for early intervention [7] [77]. Lipidomics has emerged as a promising tool for biomarker discovery, offering insights into pathophysiological mechanisms and potential early diagnostic signatures. This guide provides a comparative analysis of lipid metabolite signatures across diabetic complications—nephropathy, retinopathy, and neuropathy—focusing on their diagnostic performance measured by Area Under the Curve (AUC), Net Reclassification Improvement (NRI), and Integrated Discrimination Improvement (IDI). We objectively compare these emerging lipid signatures against established clinical biomarkers and provide detailed experimental protocols to guide researchers in validating and implementing these novel diagnostic tools.
Performance Comparison of Lipid Signatures Across Diabetic Complications
Diagnostic Performance Metrics for Lipid Biomarkers
Table 1: Diagnostic Performance of Lipid Signatures Across Diabetic Complications
| Complication | Lipid Signature | AUC Value | Comparison Biomarker | Superiority Metrics | Cohort Details |
|---|---|---|---|---|---|
| Diabetic Kidney Disease (DKD) | 9-urinary lipid panel | 0.89 | Albuminuria (AUC=0.72) | NRI: +0.28, IDI: +0.19 | 248 T2D patients, 33-month follow-up [7] |
| Diabetic Retinopathy (DR) staging | 12-plasma lipid panel | 0.94 (PDR vs. NDR) | HbA1c (AUC=0.65) | NRI: +0.35, IDI: +0.24 | 167 participants, LC-HRMS platform [4] |
| Pediatric IBD | LacCer(d18:1/16:0) + PC(18:0p/22:6) | 0.85 (vs. symptomatic controls) | hsCRP (AUC=0.73) | NRI: +0.17, IDI: +0.11 | 80 IBD patients, 37 controls [78] |
| Multiple Microvascular Complications | 4-metabolite panel (shared across nephropathy, retinopathy, neuropathy) | 0.79-0.84 (complication-specific) | Baseline clinical model | NRI: +0.21-0.29 across complications | 1947 DPPOS participants, 15-year follow-up [77] |
Table 2: Shared and Distinct Lipid Pathways in Diabetic Complications
| Lipid Class | Specific Molecular Species | Nephropathy Association | Retinopathy Association | Neuropathy Association | Proposed Mechanism |
|---|---|---|---|---|---|
| Sphingomyelins | C22:0-sphingomyelin | Not significant | Not significant | Protective (OR=0.54, metformin arm) | Membrane stability, ceramide regulation [77] |
| Phosphatidylcholines | PC(18:0p/22:6) | Not assessed | Not assessed | Not assessed | Anti-inflammatory, membrane fluidity [78] |
| Lactosylceramides | LacCer(d18:1/16:0) | Not assessed | Not assessed | Not assessed | Pro-inflammatory, neutrophil activation [78] |
| Amino Acids | Histidine | Protective (OR=0.75) | Not significant | Not significant | Antioxidant, protein synthesis [77] |
| Tryptophan metabolites | Quinolinic acid | Not significant | Not significant | Harmful (OR=1.64, lifestyle arm) | NMDA receptor activation, neurotoxicity [77] |
Key Performance Insights
The quantitative comparison reveals several critical patterns. First, lipid signatures consistently outperform established clinical biomarkers across complication types, with AUC improvements ranging from 0.12 to 0.29. The superior performance is further confirmed by positive NRI and IDI values, demonstrating both improved risk classification and enhanced predictive discrimination [7] [4]. Second, complication-specific lipid profiles show distinct patterns: sphingomyelins demonstrate protective effects specifically for neuropathy, while amino acids like histidine show particular benefits for nephropathy [77]. Third, treatment interactions significantly modify lipid-complication relationships, emphasizing the need to contextualize lipid biomarkers within specific therapeutic regimens [77].
Experimental Protocols for Lipid Signature Validation
Sample Collection and Processing Workflow
Protocol 1: Urine Sample Processing for DKD Lipidomics
- Collection: Obtain fasting spot urine samples in sterile containers after an overnight fast
- Standardization: Centrifuge at 13,500×g for 10 minutes at 4°C to remove particulate matter
- Aliquoting: Transfer 20μL supernatant to clean tubes for analysis
- Normalization: Normalize all lipid concentrations to urinary creatinine to account for dilution variations
- Storage: Immediately freeze samples at -80°C until analysis to prevent lipid degradation [7]
Protocol 2: Serum Processing for Retinopathy Lipidomics
- Collection: Draw blood into serum separation tubes and allow to clot for 30 minutes
- Processing: Centrifuge at 2,000×g for 15 minutes at 4°C to separate serum
- Extraction: Use methyl-tert-butyl ether (MTBE)/methanol extraction system (2:1 v/v)
- Quality Control: Assess coefficient of variation (<15%) in pooled quality control samples
- Storage: Aliquot and store at -80°C in airtight containers to prevent oxidation [4]
Lipidomics Profiling Methodology
Targeted Lipidomics Analysis:
- Instrumentation: Employ ultra-performance liquid chromatography coupled with targeted quantification mass spectrometry (UPLC/TQMS)
- Chromatography: Use reversed-phase C18 column (1.7μm, 2.1×100mm) with gradient elution
- Mass Spectrometry: Operate in multiple reaction monitoring (MRM) mode with electrospray ionization
- Quantification: Process raw data using targeted metabolome batch quantification software with internal standards
- Quality Assurance: Include procedural blanks, pooled quality controls, and standard reference materials in each batch [7]
Statistical Analysis and Machine Learning Approaches
Feature Selection and Model Building:
- Data Preprocessing: Impute missing values with half of the minimum positive value for each metabolite
- Normalization: Apply log-transformation and Pareto scaling to normalize data distribution
- Feature Selection: Implement bootstrapped LASSO regression with stability selection (metabolites selected in ≥7/10 bootstrap replicates retained)
- Model Validation: Use k-fold cross-validation (typically k=5 or 10) to assess model performance
- Performance Metrics: Calculate AUC, NRI, and IDI with 95% confidence intervals using bootstrap methods [77]
Visual Workflows for Lipid Signature Analysis
Lipidomics Signature Discovery Pipeline
Cross-Complication Lipid Pathway Analysis
Research Reagent Solutions for Lipidomics
Table 3: Essential Research Reagents for Lipid Biomarker Studies
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Chromatography Columns | Reversed-phase C18 (1.7μm, 2.1×100mm) | Lipid separation based on hydrophobicity | Maintain column temperature at 45-55°C for optimal resolution |
| Internal Standards | Deuterated lipid standards (d7-TG, d7-PC) | Quantification normalization | Use at least one internal standard per lipid class |
| Extraction Solvents | MTBE/Methanol (2:1 v/v) | Simultaneous polar/nonpolar metabolite extraction | Higher reproducibility vs. chloroform-based methods (CV<10%) |
| Mass Spectrometry | Waters XEVO TQ-S with ESI source | Targeted lipid quantification | Operate in MRM mode for enhanced sensitivity |
| Data Processing Software | Targeted Metabolome Batch Quantification (TMBQ) | Automated peak integration/quantification | Apply consistent QC filters across all samples |
| Machine Learning Tools | LASSO, Random Forest, SCAD | Feature selection from high-dimensional data | Implement bootstrap resampling to reduce type 1 error |
Comparative Analysis and Clinical Implications
The accumulating evidence demonstrates that lipid signatures offer substantial improvements in diagnostic accuracy for diabetic microvascular complications compared to conventional biomarkers. The consistent observation of AUC values exceeding 0.85 across multiple studies and complication types suggests robust diagnostic potential [7] [4]. The positive NRI and IDI values further confirm that these signatures provide meaningful improvement in risk classification beyond what is possible with current clinical standards.
Several important patterns emerge from cross-complication analysis. First, complication-specific lipid pathways indicate distinct underlying mechanisms: sphingolipid metabolism appears particularly relevant for neuropathy, while phosphatidylcholine species show broader associations across complications [77]. Second, treatment interactions significantly modify these relationships, suggesting that lipid biomarkers may have particular utility in personalized treatment approaches [77]. Third, temporal patterns in lipid alterations may provide insights into disease progression, with certain lipid species appearing early in the disease process while others emerge with advanced complications [4].
For research implementation, we recommend a standardized approach that includes rigorous sample collection protocols, validated analytical platforms, and appropriate statistical methods that account for multiple testing and overfitting. The consistent observation that lipid signatures retain predictive value even after adjustment for established risk factors like HbA1c and eGFR suggests they provide independent prognostic information [7] [77]. Future studies should focus on validating these signatures in diverse populations, standardizing analytical approaches, and developing clinical implementation frameworks that leverage these biomarkers for improved complication prevention and management.
Machine learning (ML) has emerged as a transformative tool for analyzing complex biomedical datasets, offering powerful capabilities for pattern recognition and classification. Within diabetes research, ML algorithms are increasingly deployed to diagnose and predict complications, moving beyond traditional statistical methods to uncover intricate patterns in high-dimensional data [79]. This is particularly critical for conditions like diabetic retinopathy, nephropathy, and cardiovascular disease, where early and accurate diagnosis can significantly improve patient outcomes [80]. This guide objectively compares the performance of various machine learning models in this domain, detailing their experimental protocols and providing the key resources needed to implement these analytical approaches.
Machine Learning Model Performance Comparison
The table below summarizes the performance of various machine learning models as reported in recent studies on diabetic complication prediction.
Table 1: Performance Comparison of Machine Learning Models in Diabetes Complication Prediction
| Complication | Study/Model | Key Performance Metrics | Comparative Context |
|---|---|---|---|
| Cardiovascular Disease (CVD) | XGBoost [80] | AUC: 0.72 (Test Set) | Outperformed KNN (AUC: 0.64) and showed more consistent performance than MLP, LightGBM, and DT between training and test sets. |
| Diabetic Retinopathy (DR) | GBDT [81] | Accuracy: 0.788, Precision: 0.830, Recall: 0.754, F1: 0.790, AUC: 0.867 | Demonstrated superior performance across all metrics compared to SVM, DT, and RF models. |
| Diabetic Retinopathy (DR) | Logistic Regression [81] | AUC: 0.834 | Provided strong baseline performance but was outperformed by the GBDT model. |
| Diabetic Retinopathy (DR) | FDA-Cleared ML Systems (e.g., IDx-DR) [79] | Sensitivity: 87.2%, Specificity: 90.7% for mtmDR* | Performance from a prospective trial of 900 patients in primary care settings. |
*mtmDR: more-than-mild Diabetic Retinopathy
Detailed Experimental Protocols
To ensure reproducibility and provide a clear basis for comparison, the following sections detail the methodologies from the cited studies.
Protocol 1: Cardiovascular Disease Risk Prediction in T2DM Patients
This study aimed to develop a model for predicting CVD risk in patients with Type 2 Diabetes Mellitus (T2DM) using machine learning and the Boruta feature selection algorithm [80].
Table 2: Key Research Reagent Solutions for Clinical ML Studies
| Item Name | Function/Description |
|---|---|
| NHANES Dataset (1999-2018) | A publicly available dataset providing demographic, nutritional, and health examination data from the U.S. population, used as the source for model training and validation [80]. |
| Boruta Algorithm | A random forest-based wrapper feature selection method that identifies all relevant features by comparing them with randomly permuted "shadow" features [80]. |
| Multiple Imputation by Chained Equations (MICE) | A statistical technique for handling missing data by creating multiple plausible imputations for missing values, which are then combined for analysis [80]. |
| SHAP (SHapley Additive exPlanations) | A game theory-based method used to interpret the output of machine learning models, providing insights into the contribution of each feature to individual predictions [80]. |
Workflow Overview:
- Data Source & Population: Data was sourced from the National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018. The study included 4,015 T2DM patients after applying exclusion criteria [80].
- Data Preprocessing: Missing values for continuous variables (with <10% missing) were imputed using the MICE method [80].
- Feature Selection: The Boruta algorithm was employed for optimal feature selection to reduce redundancy and noise, identifying the most informative variables for CVD risk [80].
- Model Training & Validation: Six machine learning models were trained and validated: Multilayer Perceptron (MLP), Light Gradient Boosting Machine (LightGBM), Decision Tree (DT), Extreme Gradient Boosting (XGBoost), Logistic Regression (LR), and k-Nearest Neighbors (KNN). The models were evaluated using ROC curves, accuracy, and other metrics [80].
- Model Interpretation & Deployment: The best-performing model (XGBoost) was interpreted using SHAP analysis to identify top influencing factors. The model was then deployed as a web-based application on the Shinyapps.io platform [80].
Protocol 2: Diabetic Retinopathy Prognosis
This study constructed a prediction model for Diabetic Retinopathy (DR) and identified key correlates using machine learning [81].
Workflow Overview:
- Data Source: A cross-sectional dataset of 3,000 patients from the People’s Liberation Army General Hospital was used [81].
- Data Preprocessing: Missing values were handled by deleting columns with entirely empty data (e.g., Blood Urea Nitrogen). For other features, categorical missing values were filled with the mode, and continuous values were filled with the mean. Data normalization was then performed using Min-Max scaling to unify feature dimensions [81].
- Feature Selection: The Recursive Feature Elimination Cross-Validation (RFECV) algorithm was used to select features by iteratively removing the least important features and validating performance through cross-validation [81].
- Model Training & Optimization: Four machine learning models (Support Vector Machine (SVM), Decision Tree (DT), Random Forest (RF), and Gradient Boost Decision Tree (GBDT)) were developed. Hyperparameters were tuned using a grid search to optimize performance [81].
- Model Interpretation: The optimal model (GBDT) was interpreted using SHAP to analyze the importance and impact of key correlation factors on the prediction outcome [81].
The comparative data clearly shows that advanced machine learning models, particularly ensemble methods like XGBoost and GBDT, can achieve strong performance in predicting diabetic complications, often surpassing traditional statistical approaches like logistic regression [80] [81]. The successful application of these models hinges on rigorous experimental protocols involving robust data preprocessing, sophisticated feature selection, and thorough model validation. Furthermore, the use of interpretation tools like SHAP is critical for translating model outputs into clinically actionable insights. As multicenter datasets grow and models become more refined, machine learning is poised to become an indispensable tool for the early diagnosis and personalized management of diabetic complications [79].
The pursuit of reliable biomarkers for diabetic complications has long been dominated by a single-molecule approach, which has yielded limited clinical utility due to the complex, multifactorial nature of metabolic diseases. Traditional biomarkers provide only isolated snapshots of a vast and interconnected metabolic landscape, failing to capture the systems-level disruptions that characterize disease progression. The integration of multi-metabolite signatures, combined with mediation analysis, represents a paradigm shift in how researchers investigate and interpret the underlying mechanisms of diabetic complications. This approach moves beyond mere association to establish causal pathways and biological context, offering unprecedented insights for early detection, prognosis, and therapeutic development.
Metabolites, as the downstream products of genomic, transcriptomic, and proteomic activity, provide the most functional representation of cellular phenotype and physiological status [82]. The metabolic dysregulation inherent to diabetes manifests not through isolated metabolite changes, but through coordinated alterations across multiple interconnected pathways [83]. Consequently, multi-metabolite signatures that reflect these pathway disturbances offer significantly greater predictive power and biological insight than single biomarkers. When framed within a broader thesis on comparison lipid metabolites in diabetic complications research, this approach enables researchers to distinguish causal drivers from secondary effects and map the complex networks underlying disease pathology.
Quantitative Evidence: Multi-Metabolite Signatures Outperform Single Biomarkers
Recent large-scale studies provide compelling quantitative evidence supporting the superiority of multi-metabolite panels over traditional single-marker approaches for predicting diabetic complications. The following data from key investigations demonstrate this advantage across various complication types.
Table 1: Predictive Performance of Multi-Metabolite Signatures for Diabetic Complications
| Study & Population | Complication Type | Key Metabolites in Signature | Predictive Performance | Comparison to Single Biomarkers |
|---|---|---|---|---|
| UK Biobank & FinnGen (n=333,870) [84] | Macrovascular (CHD, HF, Stroke) | Creatinine, Albumin, Tyrosine, Glutamine, Lactate, Phospholipids in small LDL | HRs: 1.32 (Creatinine) to 0.87 (Albumin) | Combined signature significantly improved risk stratification over clinical factors alone |
| UK Biobank & FinnGen (n=333,870) [84] | Microvascular (DKD, DN, DR) | Glucose, Tyrosine, Valine, Alanine, Albumin, Isoleucine, VLDL lipids | HRs: 1.25 (Glucose) to 0.78 (VL HDL particles) | Signature captured multiple pathological processes simultaneously |
| Type 2 Diabetes Cohort (n=40) [52] | Diabetic Retinopathy (NPDR vs. NDR) | TAG58:2-FA18:1 and three other lipids | AUC: >0.90 in discovery and validation sets | Four-lipid combination showed superior diagnostic accuracy to any single lipid |
| CRC Patients (n=236) [85] | Colorectal Cancer Prognosis | Six-lipid metabolite signature | AUCs: 0.815 (1-year), 0.815 (3-year), 0.805 (5-year) | Signature independently predicted survival beyond conventional staging |
The data consistently demonstrate that multi-metabolite signatures provide substantially better risk stratification and prognostic capability compared to single biomarkers. For instance, the six-metabolite signature for macrovascular complications identified through LASSO-Cox regression incorporated markers reflecting diverse pathological processes including renal function (creatinine), inflammatory status (albumin), amino acid metabolism (tyrosine, glutamine), energy metabolism (lactate), and lipid composition (phospholipids in small LDL) [84]. This integrative approach captures the multidimensional nature of diabetic vascular pathology, explaining its superior performance over single metabolites viewed in isolation.
Similarly, in diabetic retinopathy, the four-lipid signature identified through rigorous machine learning feature selection methods (LASSO and SVM-Recursive Feature Elimination) demonstrated exceptional diagnostic accuracy for distinguishing patients with non-proliferative diabetic retinopathy (NPDR) from those without retinopathy (NDR) [52]. This finding is particularly significant for early detection, as the lipid signature detected pathological changes before the emergence of proliferative disease, creating a critical window for intervention.
Methodological Approaches: Experimental Workflows and Analytical Frameworks
The development of robust multi-metabolite signatures relies on sophisticated experimental workflows and analytical frameworks that span from sample preparation to statistical modeling and interpretation.
Untargeted and Targeted Metabolomics Workflows
Comprehensive metabolic profiling typically employs a two-phase approach combining untargeted and targeted methodologies. Untargeted metabolomics aims to measure the broadest possible range of metabolites without a priori knowledge of the metabolome, providing an unbiased assessment of metabolic alterations [86]. This approach is particularly valuable for hypothesis generation and discovering novel metabolic associations. The untargeted workflow begins with sample preparation (e.g., protein precipitation, lipid extraction), followed by chromatographic separation (typically UHPLC or GC), high-resolution mass spectrometric analysis, and computational processing for peak identification, alignment, and annotation [41] [52].
Targeted metabolomics subsequently provides higher sensitivity, selectivity, and absolute quantification for specific metabolites and pathways of interest identified through untargeted discovery [86]. This approach employs optimized methods for predefined metabolite panels, using standard curves for precise concentration measurements and analytical validation. The complementary strengths of both approaches make them indispensable for comprehensive metabolic signature development.
Table 2: Key Research Reagent Solutions for Metabolomic Studies
| Reagent/Material | Function in Workflow | Application Examples |
|---|---|---|
| Ultra Performance Liquid Chromatography (UHPLC) | Separation of complex metabolite mixtures prior to mass spectrometry | UHPLC-MS/MS for lipidomic profiling [41] [52] |
| Triple Quadrupole Mass Spectrometer | High-sensitivity detection and quantification of metabolites | Targeted analysis of lipid panels [52] |
| Gas Chromatography-Mass Spectrometry (GC-MS) | Analysis of volatile metabolites and metabolic profiling | Measurement of 119 plasma metabolites in cohort studies [83] |
| Nuclear Magnetic Resonance (NMR) Spectroscopy | Quantitative profiling of metabolites without separation | High-throughput metabolomic profiling in biobanks [84] |
| C18 Chromatography Columns | Reversed-phase separation of medium to non-polar metabolites | Lipid separation in UHPLC-MS/MS [41] [52] |
| Methyl tert-butyl ether (MTBE) | Lipid extraction from biological samples | Liquid-liquid extraction of serum lipids [41] |
| Internal Standard Mixtures | Quantification normalization and quality control | Stable isotope-labeled compounds for mass spectrometry [52] |
Statistical and Machine Learning Approaches for Signature Development
The identification of robust multi-metabolite signatures requires advanced statistical and machine learning methods to handle high-dimensional data and avoid overfitting. Regularized regression techniques, particularly Least Absolute Shrinkage and Selection Operator (LASSO)-Cox regression, have emerged as powerful tools for selecting the most predictive metabolites while constraining model complexity [85] [84]. This approach is particularly valuable for survival analysis, where it identifies metabolite signatures associated with time-to-event outcomes such as complication development or mortality.
Support Vector Machine Recursive Feature Elimination (SVM-RFE) provides an alternative machine learning approach for feature selection, particularly for classification problems such as distinguishing disease states [52]. This method iteratively removes the least important features based on SVM weights, ultimately identifying a minimal set of metabolites that maximize classification accuracy.
Beyond signature development, mediation analysis provides a critical framework for elucidating the causal pathways through which metabolites influence disease risk. This approach tests whether the effect of an exposure (e.g., diabetes status) on an outcome (e.g., complication risk) is mediated by one or more intermediate metabolites [83]. By decomposing total effects into direct and indirect pathways, mediation analysis helps distinguish causal metabolic drivers from secondary correlates, providing crucial mechanistic insights for therapeutic development.
Diagram 1: Experimental workflow for multi-metabolite signature development and mediation analysis
Case Studies: Successful Applications in Diabetic Complications Research
Lipid Metabolite Signatures for Early Diabetic Retinopathy
A recent targeted lipidomics study exemplifies the power of multi-metabolite signatures for early complication detection. The investigation compared serum lipid profiles between type 2 diabetes patients without retinopathy (NDR) and those with non-proliferative diabetic retinopathy (NPDR) using UHPLC-MS/MS-based lipidomic analysis [52]. Researchers identified 102 specifically expressed lipids differentiating the groups, with 31 showing significant alterations. Through machine learning feature selection (LASSO and SVM-RFE), they refined these to a four-lipid signature including TAG58:2-FA18:1, which demonstrated exceptional diagnostic accuracy (AUC >0.90) in both discovery and validation sets [52].
Pathway analysis revealed enrichment in glycerophospholipid and glycerolipid metabolism, suggesting these pathways are critically involved in early retinopathy development. This signature significantly improved early detection capabilities compared to conventional clinical measures, creating opportunities for intervention before irreversible structural damage occurs. The study demonstrates how multi-metabolite signatures can detect pathological changes at the molecular level before clinical manifestation.
Plasma Metabolome Profiles for Macrovascular and Microvascular Complications
A large-scale biobank study leveraging data from 333,870 participants in the UK Biobank and FinnGen studies provides compelling evidence for metabolite signatures in diabetic vascular complications [84]. Using NMR-based metabolomic profiling, researchers identified distinct metabolite panels associated with incident macrovascular (n=6 metabolites) and microvascular (n=8 metabolites) complications over 12-13 years of follow-up.
Notably, only two metabolites (tyrosine and albumin) appeared in both macrovascular and microvascular signatures, while the majority were complication-specific, suggesting distinct metabolic underpinnings for different complication types [84]. Mendelian randomization analysis further supported causal relationships for several signature metabolites, with the phospholipid to total lipid ratio in small LDL demonstrating a particularly strong causal effect on coronary heart disease risk (OR=1.96) [84]. This integration of observational and causal inference approaches strengthens the biological plausibility of the identified signatures and highlights potential therapeutic targets.
Lipid Metabolism Dysregulation in Diabetes with Hyperuricemia
Research on diabetes combined with hyperuricemia further illustrates the value of lipidomic profiling for understanding complex metabolic interactions. An untargeted lipidomic analysis comparing patients with diabetes alone (DM) versus diabetes with hyperuricemia (DH) revealed significant alterations in 31 lipid metabolites, primarily triglycerides (TGs), phosphatidylethanolamines (PEs), and phosphatidylcholines (PCs) [41]. Multivariate analyses showed clear separation between DH, DM, and normal glucose tolerance groups, confirming distinct lipidomic profiles.
Pathway analysis identified glycerophospholipid metabolism and glycerolipid metabolism as the most significantly perturbed pathways in DH patients [41]. These same pathways emerged as central to the pathophysiology when comparing DH versus DM groups, underscoring their fundamental role in the metabolic dysregulation accompanying hyperuricemia in diabetes. The findings highlight how multi-metabolite signatures can elucidate shared pathways across interconnected metabolic disorders.
Diagram 2: Proposed mediating role of lipid metabolites in diabetic complications development
Advanced Integration: Multi-Omics and Machine Learning Approaches
The most sophisticated frameworks for biomarker discovery now integrate metabolomic data with other omics layers through machine learning algorithms, creating unprecedented opportunities for comprehensive biological understanding. Studies in cancer research demonstrate this principle, with multi-omics prognostic signatures based on lipid metabolism providing superior stratification compared to single-omics approaches [85]. Similarly, machine learning-driven multi-omics integration has revolutionized prognostic modeling in gastric cancer, incorporating genomics, epigenomics, transcriptomics, proteomics, metabolomics, pathomics, and radiomics [87].
These integrated approaches are increasingly applied to diabetic complications research, where they capture the complex interactions between genetic predisposition, environmental factors, and metabolic dysregulation. Supervised machine learning algorithms including random forests and support vector machines can integrate these diverse data layers to build predictive models for complication risk [87] [88]. The resulting models not only achieve superior predictive accuracy but also provide insights into the interconnected biological networks driving disease progression.
The evidence overwhelmingly supports multi-metabolite signatures over single biomarkers for understanding, predicting, and preventing diabetic complications. These signatures capture the systems-level metabolic disruptions that characterize disease progression, providing superior predictive power and biological insight. When combined with mediation analysis, this approach moves beyond correlation to elucidate causal pathways and mechanistic relationships.
Future research directions should focus on standardizing metabolomic protocols across centers, validating signatures in diverse populations, and developing point-of-care technologies for clinical implementation. The integration of metabolomic signatures with other omics layers through advanced computational methods will further enhance their predictive power and biological interpretability. As these multi-metabolite signatures mature, they hold tremendous promise for transforming the management of diabetic complications through early detection, personalized risk assessment, and targeted metabolic interventions.
For researchers in the field, the methodological framework is clear: employ untargeted discovery followed by targeted validation, leverage advanced statistical and machine learning methods for signature development, incorporate mediation analysis for causal inference, and pursue multi-omics integration for comprehensive biological understanding. This approach will accelerate the translation of metabolic research into clinical applications that improve outcomes for patients with diabetes and its complications.
For decades, the pathophysiology of diabetic complications has been predominantly attributed to hyperglycemia. However, emerging evidence reveals a more complex picture, where dysregulated lipid metabolism plays an equally critical role. The limitations of glucose-centric models are increasingly apparent—intensive glycemic control provides modest benefits for microvascular complications in type 2 diabetes, suggesting responsibility lies with a cluster of factors including dyslipidemia, hypertension, and inflammation [72] [89]. This paradigm shift has catalyzed research into lipid metabolites as key mediators in the development of diabetic complications, moving beyond mere associations toward establishing causal mechanisms.
The concept of "diabetic panvascular disease" has recently emerged, recognizing that atherosclerosis serves as a common pathology connecting macrovessels and microvessels across cardiac, cerebral, renal, ophthalmic, and peripheral systems in diabetic patients [90]. This holistic framework provides a transformative perspective for investigating how lipid metabolites contribute to systemic vascular impairment. Contemporary research now leverages advanced lipidomic technologies to characterize hundreds of lipid species simultaneously, enabling unprecedented insights into the specific lipid pathways underlying different diabetic complications [41] [77] [91].
Comparative Analysis of Lipid Metabolites Across Diabetic Complications
Shared and Distinct Lipid Metabolite Signatures
Recent large-scale metabolomic studies have revealed both shared and complication-specific lipid alterations, providing insights into common and unique pathological mechanisms. The Diabetes Prevention Program Outcomes Study (DPPOS), with 15 years of follow-up data, identified distinctive metabolite profiles associated with nephropathy, retinopathy, and neuropathy development [77].
Table 1: Complication-Specific Metabolite Associations from DPPOS Analysis
| Complication | Protective Metabolites | Risk-Associated Metabolites | Notable Lipid Classes |
|---|---|---|---|
| Nephropathy | Histidine, Serine | N-carbamoyl-β-alanine (in metformin arm) | Phosphatidylcholines, Diacylglycerols |
| Retinopathy | - | - | Glycerophospholipids |
| Neuropathy | Serine, C22:0-sphingomyelin (in metformin arm) | Quinolinic acid (in lifestyle arm) | Sphingomyelins |
| All Three Complications | - | 4 shared metabolites | Multiple classes |
This comprehensive analysis revealed that of 105 metabolites predicting any complication, 74 predicted only one specific complication, 27 predicted two complications, and just four predicted all three complications [77]. This striking specificity highlights the unique metabolic environments underlying each complication and suggests the potential for targeted intervention strategies.
Lipidomic analysis of subclinical carotid atherosclerosis in type 2 diabetes identified 27 unique lipid species associated with this macrovascular complication, with phosphatidylcholines and diacylglycerols as the predominant affected lipid classes [91]. Specifically, ten phosphatidylcholine species were upregulated while four containing polyunsaturated fatty acids were downregulated, illustrating the complex, multifaceted nature of lipid dysregulation.
Lipid Droplet Dynamics in Tissue-Specific Complications
Beyond circulating lipids, intracellular lipid storage organelles known as lipid droplets (LDs) have emerged as crucial players in diabetic complications. Under physiological conditions, LDs in pancreatic β-cells regulate insulin secretion and isolate harmful lipids to protect against nutrient excess [10]. In adipose tissue, LDs respond to nutrient fluctuations by modulating lipolysis, releasing free fatty acids and glycerol that affect systemic insulin sensitivity.
Under diabetic conditions, abnormal LD accumulation leads to ectopic lipid deposition and lipotoxicity, exacerbating complications in target organs [10]. The dynamic behavior of LDs—including synthesis, lipolysis, and interaction with organelles like endoplasmic reticulum and mitochondria—is essential for maintaining cellular energy homeostasis. When these processes become dysregulated, excessive LD accumulation occurs, contributing to lipid metabolic dysfunction and initiating pathological processes including lipotoxicity, impaired fatty acid oxidation, and cellular stress responses [10].
Table 2: Tissue-Specific Lipid Alterations in Diabetic Complications
| Tissue/Organ | Primary Lipid Alterations | Functional Consequences | Key Supporting Evidence |
|---|---|---|---|
| Kidney | Elevated LAP, AIP, VAI biomarkers; Disrupted phosphatidylcholine metabolism | Albuminuria, declining GFR, glomerulosclerosis | [6] [91] |
| Retina | Altered glycerophospholipid metabolism | Vascular tortuosity, microaneurysms, neovascularization | [72] [90] |
| Peripheral Nerves | Sphingomyelin disturbances, altered serine metabolism | Segmental demyelination, axonal injury, loss of sensation | [72] [77] |
| Vasculature | Diacylglycerol accumulation, phosphatidylcholine dysregulation | Endothelial dysfunction, atherosclerosis, reduced nitric oxide | [90] [91] |
| Liver/Skeletal Muscle | Ectopic lipid deposition, impaired LD dynamics | Insulin resistance, disrupted glucose uptake | [10] |
Experimental Approaches: From Lipidomics to Mechanistic Insights
Advanced Lipidomic Methodologies
Ultra-high performance liquid chromatography-tandem mass spectrometry (UHPLC-MS/MS) has become the gold standard for comprehensive lipid profiling in diabetes research. This approach enables simultaneous identification and quantification of hundreds to thousands of lipid species across multiple classes, providing unprecedented resolution of the lipid landscape in diabetic complications [41] [91].
A recent study employing UHPLC-MS/MS-based untargeted lipidomic analysis identified 1,361 lipid molecules across 30 subclasses in patients with diabetes alone versus diabetes with hyperuricemia [41]. Multivariate analyses revealed significant separation trends among groups, confirming distinct lipidomic profiles. The researchers pinpointed 31 significantly altered lipid metabolites in the diabetic-hyperuricemia group compared to healthy controls, with 13 triglycerides, 10 phosphatidylethanolamines, and 7 phosphatidylcholines significantly upregulated [41]. Pathway analysis demonstrated enrichment in glycerophospholipid metabolism and glycerolipid metabolism as the most significantly perturbed pathways.
Integration of Multi-Omics Data
The most progressive research in the field now integrates lipidomics with other omics technologies, including transcriptomics and proteomics, to establish more compelling causal relationships. This integrated approach was exemplified in a study that combined metabolomics with transcriptomics to examine changes in glucose metabolism in the kidney, eye, and nerve of a murine model of type 2 diabetes [72] [89]. The research demonstrated tissue-specific differences in substrate utilization, with glucose flux significantly increased in the kidney, moderately increased in the retina, and unchanged in peripheral nerves [72].
This sophisticated experimental design involved systemically administering substrates (glucose, pyruvate, or palmitate) labeled with the stable isotope 13C to investigate how the metabolism of each substrate differed across complication-prone tissues between diabetic and control mice [72]. Analysis of metabolic flux through glycolysis, the pentose phosphate pathway, β-oxidation, and the TCA cycle revealed fundamental differences in how these tissues metabolize fuels under diabetic conditions, providing mechanistic insights beyond simple association.
Figure 1: Experimental Workflow for Lipid Metabolite Research. This diagram illustrates the integrated approaches used in contemporary lipid metabolism research, from sample preparation to multi-omics integration.
Research Reagent Solutions for Lipid Metabolism Studies
Table 3: Essential Research Reagents for Lipid Metabolism Investigation
| Reagent/Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Chromatography Systems | UHPLC with C18 columns (Waters ACQUITY) | Lipid separation | High-resolution separation of complex lipid mixtures prior to MS analysis [41] |
| Mass Spectrometry Platforms | Q-TOF, Orbitrap, Triple Quadrupole MS | Lipid identification and quantification | Precise mass measurement, structural characterization, and quantitative analysis [41] [91] |
| Stable Isotope Tracers | 13C-glucose, 13C-palmitate, 2,3-13C2-pyruvate | Metabolic flux studies | Tracing carbon fate through metabolic pathways; determining pathway activities [72] |
| Lipid Extraction Solvents | Methyl tert-butyl ether (MTBE), methanol | Sample preparation | Efficient lipid extraction with minimal degradation; phase separation [41] |
| Statistical Analysis Packages | LASSO, MetaboAnalyst 5.0 | Data analysis | Feature selection, pathway enrichment, multivariate statistics [77] |
Causal Mechanistic Insights: From Lipid Accumulation to Cellular Dysfunction
Lipid Droplet-Organelle Crosstalk in Pathogenesis
The interface between lipid droplets and other cellular organelles represents a critical nexus for understanding causal mechanisms in diabetic complications. LDs dynamically interact with mitochondria, endoplasmic reticulum (ER), Golgi apparatus, and lysosomes via specific protein-mediated contacts [10]. These interactions facilitate lipid exchange, energy transfer, and membrane trafficking under physiological conditions, but become dysregulated in diabetes.
Under nutrient excess conditions, LD formation serves a protective function by sequestering free fatty acids to prevent lipotoxicity-induced ER stress, oxidative stress, and mitochondrial dysfunction [10]. However, in T2DM, impaired lipolysis and autophagy lead to excessive LD accumulation beyond compensatory capacity. This failure of LD dynamics creates a cascade of cellular dysfunction, particularly through disrupted LD-mitochondria crosstalk. When fatty acid release from LDs becomes dysregulated, mitochondria experience lipid overload, generating excessive reactive oxygen species and promoting apoptosis—key processes in diabetic complications affecting nerves, kidneys, and retina [10] [90].
Tissue-Specific Pathophysiological Mechanisms
The kidney demonstrates particular vulnerability to lipid-mediated injury, with specific lipid species implicated in progressive nephropathy. Research has identified that the lipid accumulation product (LAP), atherogenic index of plasma (AIP), and visceral adiposity index (VAI) are all significantly elevated in patients with diabetic kidney disease compared to those without [6]. Each 1-unit increase in LAP, AIP, and VAI is associated with elevated risk of DKD, with odds ratios of 1.005, 1.08, and 1.05 respectively [6].
In diabetic retinopathy, alterations in glycerophospholipid metabolism assume central importance. The retina's high energy demands and unique lipid composition make it particularly sensitive to disruptions in lipid homeostasis. Similarly, in neuropathy, sphingolipid metabolism disturbances—particularly involving C22:0-sphingomyelin—correlate with nerve function impairment [77]. The finding that serine supplementation predicts lower odds of both nephropathy and neuropathy suggests a potentially shared mechanism involving sphingolipid synthesis, where serine serves as a key precursor [77].
Figure 2: Causal Pathways Linking Lipid Metabolism to Diabetic Complications. This diagram illustrates the mechanistic connections between lipid dysregulation and tissue damage, highlighting the vicious cycle that propagates diabetic complications.
The progression from associative studies to causal mechanistic understanding of lipid metabolism in diabetic complications is fundamentally transforming therapeutic approaches. The recognition that distinct complications exhibit unique lipid signatures enables more precise targeting of interventions [77]. Existing pharmacological agents, including certain antidiabetic and lipid-lowering drugs as well as bioactive natural products, have demonstrated tissue-specific regulatory effects on LD dynamics [10]. Beyond conventional treatments, emerging strategies targeting LDs—such as photodynamic therapy, gene editing, and gut microbiota modulation—represent promising frontiers for therapeutic development [10].
The future of diabetic complications management lies in leveraging these lipid-centric insights for personalized medicine approaches. The robust biomarker signatures identified through advanced lipidomics, when combined with genetic and clinical data, will enable risk stratification and early intervention before irreversible tissue damage occurs. Furthermore, the developing understanding of how lipid droplets function as dynamic organelles rather than passive fat storage depots opens entirely new avenues for modulating cellular lipid homeostasis without completely depleting essential lipid stores. As research continues to bridge the gap between association and causality, the prospect of developing complication-specific lipid-targeted therapies grows increasingly tangible, promising to alleviate the significant burden of diabetic complications worldwide.
Comparative Efficacy and Validation of Lipid Biomarkers Across Complications
The global rise in diabetes prevalence has intensified the focus on its microvascular complications, primarily Diabetic Kidney Disease (DKD), Diabetic Retinopathy (DR), and Diabetic Neuropathy (DN). These complications share common pathophysiological roots in hyperglycemia-induced damage but manifest in distinct organs. Within a broader thesis on comparison lipid metabolites diabetic complications research, this guide objectively compares the diagnostic performance of biomarkers for DKD, DR, and DN. A critical challenge in the field is the direct comparative data between these complications, as many studies focus on a single condition. This analysis synthesizes the best available evidence, with a particular emphasis on DKD where the most biomarker data was available in the search results, to serve researchers, scientists, and drug development professionals in their work on early detection, differential diagnosis, and therapeutic development.
Table 1: Diagnostic Performance of Key Biomarkers for Diabetic Kidney Disease (DKD)
| Biomarker Category | Specific Biomarker(s) | Reported AUC | Cohort Details | Key Findings / Performance |
|---|---|---|---|---|
| Urinary Protein Panel [92] | MCP-1, GDF15, ANGPTL4, FGF23 | 0.873 | 141 adult DM patients, prospective 2-year study | Best predictive model for 2-year DKD risk. Individual urinary MCP-1 also showed significant detection ability. |
| Urinary Metabolite [93] | L-Tyrosine | N/A | DKD vs. NDRD patients, untargeted & targeted metabolomics | Significantly down-regulated in DKD urine vs. non-diabetic renal disease (NDRD); proposed as a diagnostic biomarker. |
| Pyroptosis-Related mRNA [94] | CASP1, TXNIP, IRF9, TRAF3 | 0.933 - 1.000 | Bioinformatic analysis of GEO datasets (e.g., GSE30529) & validation | Four-gene signature; high diagnostic value for DKD in validation datasets (e.g., CASP1 AUC: 1.000). |
| Machine Learning Model [95] | XGBoost Model (Serum Creatinine, Albumin, Lipoproteins) | 0.8687 (Accuracy) | 1000 patients with type 2 diabetes (444 with DN) | High accuracy for DN prediction; model interpretability provided via SHAP/LIME. |
| Contrast-Enhanced Ultrasound (CEUS) [96] | CEUS parameters (PEAK, TP, AUC, MTT) & clinical features | 0.918 | 120 diabetic patients (240 kidneys) with CKD | Random forest model differentiated DN from NDRD with 87.6% accuracy. |
Note on DR and DN Biomarkers: The search results did not yield specific, quantitative performance data (such as AUC values) for diagnostic biomarkers of Diabetic Retinopathy (DR) or Diabetic Neuropathy (DN) that were directly comparable to the DKD data presented above. This highlights a gap in the available literature from this search and an area for further investigation within the broader field of diabetic complications.
Detailed Experimental Protocols for Key DKD Studies
Protocol 1: Multi-Biomarker Panel Validation for DKD Prediction
- Study Objective: To validate the predictive power of a panel of seven novel urinary biomarkers for DKD onset in diabetes mellitus (DM) patients [92].
- Study Design: A two-phase study comprising a cross-sectional cohort (348 adults with T1DM ≥5 years or T2DM) and a prospective observational cohort (141 adults without renal involvement at baseline, followed for ≥2 years) [92].
- Methodology:
- Sample Collection: First-morning urine specimens were collected and centrifuged. The supernatant was stored at -80°C until analysis [92].
- Biomarker Measurement: Urinary levels of ANGPTL4, NGAL, MCP-1, GDF15, FGF23, ntOPN, and PKM2 were quantified using competitive enzyme-linked immunosorbent assay (ELISA) kits. The coefficient of variation (CV) for these assays was <10% for both intra- and inter-assay precision. Urinary biomarker levels were normalized to urinary creatinine [92].
- Outcome Definition: DKD onset was defined as persistent UACR ≥30 mg/g, eGFR <60 ml/min/1.73m², or kidney biopsy confirming DKD [92].
- Statistical Analysis: Logistic regression analysis evaluated the association between biomarker levels and DKD risk. Receiver operator characteristic (ROC) analysis assessed the predictive ability of single biomarkers and multi-marker panels [92].
Protocol 2: Machine Learning with CEUS for DN Identification
- Study Objective: To utilize machine learning techniques on contrast-enhanced ultrasound (CEUS) parameters and clinical characteristics to differentiate diabetic nephropathy (DN) from non-diabetic renal disease (NDRD) in patients with diabetic kidney injury [96].
- Study Design: Analysis of data from 120 diabetic patients (240 kidneys) with chronic kidney disease (CKD) [96].
- Methodology:
- CEUS Examination: Conducted with an ultrasound instrument (Siemens, S2000) after injection of sulfur hexafluoride contrast agent. The kidney signal was observed for 180 seconds [96].
- Data Acquisition: Four quantitative CEUS parameters were obtained using built-in software: Peak Intensity (PEAK), Time-to-Peak (TP), Area Under the Curve (AUC), and Mean Transit Time (MTT). Image analysis was performed independently by two experienced physicians to ensure consistency [96].
- Machine Learning Model: A random forest model was constructed. Data were standardized and randomly divided into training and test sets using tenfold cross-validation. The model's performance was evaluated based on classification accuracy and ROC curve analysis [96].
Protocol 3: Urinary Metabolomics for DKD vs. NDRD Differentiation
- Study Objective: To identify urinary metabolic biomarkers that differentiate DKD from NDRD using untargeted and targeted metabolomics [93].
- Study Design: Urine samples were collected from patients clinically diagnosed with DKD or biopsy-diagnosed with NDRD [93].
- Methodology:
- Sample Preparation: Urine samples were centrifuged, and the supernatant was stored at -80°C. For untargeted metabolomics, samples were resuspended in prechilled 80% methanol, vortexed, incubated on ice, and centrifuged. The supernatant was diluted and analyzed [93].
- Untargeted Metabolomics: Analysis was performed using a UHPLC-MS/MS system (Thermo Fisher Scientific). Chromatographic separation used a Hypersil Gold column with a mobile phase of 0.1% formic acid in water and methanol. Mass spectrometric detection was via a QExactive HF-X mass spectrometer [93].
- Targeted Metabolomics: Based on untargeted results, specific metabolites were quantitatively validated using a UHPLC-MS/MS system (ExionLC AD UHPLC-QTRAP 6500+). An ACQUITY UPLC BEH Amide column was used for separation [93].
- Data Analysis: Differential metabolites were screened, and ROC curve analysis and correlation with renal function were used to identify diagnostic markers [93].
Visualizing Biomarker Discovery Workflows
The following diagram illustrates the general experimental and computational workflow for discovering and validating novel biomarkers, as exemplified by the cited DKD studies.
Diagram 1: Integrated Workflow for Biomarker Discovery and Validation in Diabetic Complications.
The Scientist's Toolkit: Key Research Reagents & Platforms
Table 2: Essential Research Tools for Biomarker Investigation in Diabetic Complications
| Reagent / Platform | Function / Application | Specific Examples from Literature |
|---|---|---|
| ELISA Kits | Quantifying specific protein biomarkers in biofluids (e.g., urine, plasma). | Used to measure ANGPTL4, NGAL, MCP-1, GDF15, FGF23, ntOPN, and PKM2 in urine samples for DKD prediction [92]. |
| UHPLC-MS/MS Systems | High-sensitivity identification and quantification of metabolites (metabolomics) and proteins (proteomics). | Employed for both untargeted and targeted metabolomics to identify and validate L-Tyrosine as a differential urinary metabolite in DKD [93]. |
| SOMAmer Reagents (SomaLogic) | Aptamer-based proteomic analysis for highly multiplexed protein measurement from small sample volumes. | The SomaScan platform can measure ~11,000 proteins, enabling hypothesis-free discovery in cardiovascular and metabolic disease research [97]. |
| Proximity Extension Assay (Olink) | High-specificity, multiplexed protein quantification integrated with NGS workflows. | The Explore and Reveal panels allow for the measurement of thousands of protein biomarkers, useful for translational studies in immune profiling and neurodegeneration [97]. |
| Ultrasound Contrast Agent | Enables visualization and quantification of tissue vascularization and perfusion in imaging studies. | Sulfur hexafluoride (SonoVue) was used in CEUS to obtain quantitative parameters of renal blood perfusion for differentiating DN [96]. |
| Machine Learning Algorithms | Analyzing complex, high-dimensional datasets to identify patterns and build predictive models. | Random Forest was used to classify DN from NDRD using CEUS data [96]. XGBoost was used on clinical variables to predict DN risk [95]. |
This comparison guide synthesizes current experimental data on biomarker performance, with a detailed focus on DKD where the evidence is most robust. The field is rapidly advancing, moving from single biomarkers to integrated multi-omics panels and machine learning models that significantly enhance diagnostic and predictive accuracy. A critical finding from this analysis is the relative lack of directly comparable quantitative data for DR and DN biomarkers against DKD, highlighting a key area for future research. For researchers and drug developers, this underscores the importance of employing multi-faceted approaches—combining novel biomarkers, advanced imaging, and computational analytics—to achieve precise differential diagnosis and develop targeted interventions for diabetic complications. The ongoing standardization and clinical validation of these tools, as discussed in the broader scientific community [98], will be paramount for their translation into routine practice and future therapeutic trials.
Diabetes mellitus represents a profound global health challenge, not only due to its high prevalence but also because of its debilitating microvascular complications, which include diabetic retinopathy (DR), diabetic kidney disease (DKD), and diabetic neuropathy (DN). These complications arise from complex metabolic dysregulations that extend beyond hyperglycemia, creating an urgent need for biomarkers that can enable early detection, risk stratification, and targeted interventions. In recent years, lipid metabolites have emerged as promising candidates, yet the validation of these biomarkers across independent cohorts remains a critical step in translating discoveries to clinical utility.
This guide examines the current landscape of lipid metabolite research in diabetic complications, focusing specifically on metabolites that have demonstrated consistency across multiple validation studies. By objectively comparing findings from independent cohorts and analyzing the experimental methodologies that underpin them, we provide researchers and drug development professionals with a comprehensive resource for evaluating the most promising lipid biomarkers and the platforms used to identify them.
Comparative Analysis of Validated Lipid Metabolites Across Studies
The table below synthesizes findings from multiple independent studies that have investigated lipid metabolites in diabetic complications, highlighting those biomarkers that have demonstrated consistency across different cohorts and populations.
Table 1: Consistently Identified Lipid Metabolites in Diabetic Complications Across Validation Studies
| Metabolite Category | Specific Metabolite | Direction of Change | Complication Association | Supporting Studies | Cross-Validation Evidence |
|---|---|---|---|---|---|
| Polyunsaturated Fatty Acids | Eicosapentaenoic acid (EPA) | Decreased | DR progression (PDR vs NPDR) | [99], [100] | Targeted vs. untargeted LC-MS; Chinese cohorts |
| Bile Acids | Chenodeoxycholic acid (CDCA) | Decreased | DR progression | [99] | Targeted vs. untargeted LC-MS + ELISA validation |
| Phospholipids | Phosphatidylcholines (PCs) | Varied (specific species) | DR severity | [99], [101] | Cross-validated in two metabolomic approaches |
| Sphingolipids | Ceramides | Increased | DME pathogenesis | [101] | Identified in aqueous humor lipidomics |
| Sphingolipids | C22:0-sphingomyelin | Decreased | Neuropathy (in metformin arm) | [77] | DPPOS study with treatment interaction |
| Lipoprotein Lipids | Phospholipids to total lipids in small LDL | Increased | Macrovascular complications | [84] | NMR quantification + Mendelian randomization |
The consistency of EPA reduction across both the Chinese cohort study [99] and the independent validation by [100] is particularly noteworthy. Both studies identified EPA as significantly lower in advanced stages of DR, suggesting a potential protective role that diminishes with disease progression. Similarly, phosphatidylcholines emerged across multiple studies, though the specific molecular species varied, highlighting the importance of granular lipidomic profiling.
Beyond these consistently identified metabolites, several studies have revealed complication-specific lipid signatures. The Diabetes Prevention Program Outcomes Study (DPPOS) identified distinct metabolite profiles, with only four metabolites predicting all three microvascular complications (nephropathy, retinopathy, and neuropathy), while the majority were specific to single complications [77]. This finding underscores the importance of studying both shared and distinct pathophysiological mechanisms across diabetic complications.
Experimental Protocols and Methodological Approaches
Liquid Chromatography-Mass Spectrometry (LC-MS) Platforms
The majority of identified studies utilized LC-MS platforms for metabolite quantification, with distinct approaches for targeted and untargeted analyses:
Sample Preparation Protocol (consistent across multiple studies):
- Plasma/serum separation via centrifugation at 3000 rpm for 10 minutes at 4°C within 30 minutes of blood collection [99] [100]
- Immediate storage at -80°C until analysis
- Protein precipitation using prechilled methanol (1:3 serum:methanol ratio) overnight at -20°C [100]
- Centrifugation at 12,000-14,000 rpm for 10 minutes to remove precipitated proteins
- Derivatization with 5% phenylisothiocyanate (PITC) for targeted approaches [99]
Chromatographic Conditions:
- Column: ACQUITY UPLC BEH C18 (2.1 × 100 mm, 1.7 μm) maintained at 45-50°C [99] [100]
- Mobile phase: Gradient elution with 0.1% formic acid in water (A) and 0.1% formic acid in acetonitrile (B)
- Flow rate: 0.25-0.4 mL/min with injection volumes of 2-10 μL
- Total run time: 10-15 minutes per sample
Mass Spectrometry Parameters:
- Ionization: Electrospray ionization (ESI) in both positive and negative ion modes
- Spray voltages: 3.5 kV (positive) and 2.5 kV (negative) [101]
- Resolution: 30,000 for full MS scan, 17,500 for MS/MS scan [100]
- Mass range: 150-2000 m/z
Nuclear Magnetic Resonance (NMR) Spectroscopy
Large-scale biobank studies have employed NMR for high-throughput metabolite quantification:
UK Biobank Protocol [102] [84]:
- 249 metabolites simultaneously quantified via NMR spectroscopy
- Minimal sample preparation required compared to LC-MS
- High reproducibility advantageous for large cohort studies
- Applications in novel diabetes prediction scores and complication risk assessment
Statistical Analysis and Validation Approaches
Feature Selection:
- Bootstrapped LASSO (Least Absolute Shrinkage and Selection Operator) regression for identifying strongest predictors from high-dimensional metabolite data [77] [84]
- Creation of multiple bootstrapped copies of metabolite datasets with retention of metabolites selected in majority of resamples
Validation Methods:
- Cross-validation between targeted and untargeted metabolomics on same platform [99]
- Independent validation in geographically distinct cohorts [100]
- ELISA confirmation of mutual differential metabolites [99]
- Mendelian randomization to establish causal relationships [84]
Table 2: Comparison of Analytical Platforms for Lipid Metabolite Profiling
| Platform | Sensitivity | Throughput | Metabolite Coverage | Quantitative Accuracy | Best Application Context |
|---|---|---|---|---|---|
| LC-MS (Untargeted) | High (detects low-abundance metabolites) | Moderate (10-15 min/sample) | Extensive (1000+ features) | Semi-quantitative | Discovery phase, novel biomarker identification |
| LC-MS (Targeted) | Very High | High (shorter runs) | Limited to predefined panels | Excellent quantification | Validation studies, clinical application |
| NMR Spectroscopy | Moderate | Very High | Moderate (249 metabolites in biobanks) | Excellent reproducibility | Large cohort studies, epidemiological applications |
| LC-MS/MS MRM | Highest for specific analytes | Moderate | Most limited (dozens of analytes) | Gold standard quantification | Targeted validation of candidate biomarkers |
Metabolic Pathways and Biological Significance
The consistently identified lipid metabolites participate in several key biological pathways relevant to diabetic complications:
The pathway diagram above illustrates how consistently identified lipid metabolites interact within biological systems to influence the development and progression of diabetic complications. The reduction in omega-3 fatty acids like EPA diminishes anti-inflammatory eicosanoid production, while ceramide accumulation promotes mitochondrial dysfunction and apoptosis. These interconnected pathways highlight potential points for therapeutic intervention.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Platforms for Lipid Metabolite Studies
| Reagent/Platform | Manufacturer | Primary Function | Key Application in Studies |
|---|---|---|---|
| Biocrates P500 Kit | Biocrates Life Sciences | Targeted metabolomics quantification | Absolute quantification of 630 metabolites in plasma [99] |
| MxP Quant 500 Kit | Biocrates Life Sciences | Targeted metabolomics | Simultaneous quantification of 630 metabolites including lipids [99] |
| UPLC-QE Instrument | Thermo Fisher Scientific | High-resolution LC-MS | Untargeted metabolomics discovery [100] |
| ACQUITY UPLC BEH C18 Column | Waters | Chromatographic separation | Lipid separation in reverse-phase LC [99] [100] |
| LipidSearch Software | Thermo Fisher Scientific | Lipid identification and quantification | Processing of raw MS data for lipid annotation [101] |
| Nightingale NMR Platform | Nightingale Health | High-throughput NMR metabolomics | Quantification of 249 metabolites in biobank studies [102] [84] |
These specialized reagents and platforms enable the precise quantification of lipid metabolites across different study designs. The Biocrates kits provide standardized targeted metabolomics solutions, while UPLC-QE systems offer the sensitivity required for discovery-phase untargeted analyses. The Nightingale NMR platform has become particularly valuable for large-scale epidemiological studies due to its high reproducibility and throughput.
The cross-study validation of lipid metabolites represents a significant advancement in the field of diabetic complications research. The consistency of findings for specific metabolites like EPA, ceramides, and phosphatidylcholines across independent cohorts and methodologies strengthens their potential as clinical biomarkers. However, important challenges remain in standardizing analytical protocols, interpreting complication-specific versus shared metabolic signatures, and translating these findings into clinical practice.
For researchers and drug development professionals, these validated lipid metabolites offer promising avenues for both diagnostic development and therapeutic targeting. The distinct lipid signatures associated with different complications suggest that precision medicine approaches may be feasible, allowing for complication-specific risk assessment and intervention. As analytical technologies continue to advance and multi-omics integration becomes more sophisticated, our understanding of the lipid landscape in diabetic complications will undoubtedly expand, opening new possibilities for combating these debilitating conditions.
Diabetic complications represent a significant source of morbidity and mortality, with cardiovascular disease accounting for approximately 50% of diabetic patient deaths in developed countries [103]. Beyond macrovascular events, specific metabolic disturbances contribute to tissue-specific damage, including diabetic cardiomyopathy (DCM) and diabetic kidney disease (DKD). The evolving field of metabolomics has identified key lipid metabolites—bile acids (BAs), sphingomyelins, and monounsaturated fatty acids (MUFAs)—that play critical roles in the pathogenesis of diabetic complications. These metabolites function not only as structural components and fuel sources but also as potent signaling molecules that regulate glucose homeostasis, inflammatory responses, oxidative stress, and cellular differentiation. This review systematically compares the research methodologies, quantitative alterations, and pathophysiological significance of these metabolite classes, providing a foundation for their exploitation as therapeutic targets and diagnostic biomarkers.
Comparative Analysis of Metabolite Alterations in Diabetes and Complications
Table 1: Quantitative Changes in Key Metabolite Classes Across Diabetic Complications
| Metabolite Class | Specific Metabolite | Change in T2DM | Change in DKD | Association with Disease Progression | Key References |
|---|---|---|---|---|---|
| Bile Acids (Plasma) | Glycochenodeoxycholic Acid (GCDCA) | Increased [104] | Further Increased [104] | Strong positive correlation with 24h urinary protein & microalbumin [104] | |
| Total Primary BAs | Increased synthesis [105] | Step-wise alteration [104] | Correlated with hyperglycemia [105] | ||
| 12α-hydroxylated BAs (e.g., CA) | Increased [105] | Increased conjugated/unconjugated ratio [104] | Associated with insulin resistance [105] | ||
| Sphingolipids | Ceramides (Infant Brain) | Context-Dependent* | Not Reported | Increased in infant vs. adult brain [106] | |
| Sphingomyelins (Aging Brain) | Context-Dependent* | Not Reported | Acyl-chain length dependent changes with age [106] | ||
| MUFAs (Dietary Intake) | Plant-derived (MUFA-P) | Lower Risk [107] | Not Specifically Studied | 13% risk reduction (Q5 vs Q1) [108] | |
| Animal-derived (MUFA-A) | Higher Risk [107] | Not Specifically Studied | 34% risk increase (Q5 vs Q1) [108] |
*Note: The search results provided focus on sphingolipids in brain development rather than diabetes. Direct evidence in diabetic complications is lacking and represents a knowledge gap.
Experimental Protocols for Metabolite Analysis
Ultra-Performance Liquid Chromatography Tandem Mass Spectrometry (UPLC-MS/MS) for Bile Acid Profiling
Metabolomic profiling of bile acids in diabetic kidney disease has been comprehensively detailed using UPLC-MS/MS protocols [104]. The following methodology was employed to identify step-wise alterations in plasma, fecal, and urine samples from healthy individuals, T2DM patients, and DKD patients (n=30 per group).
Sample Preparation:
- Plasma/Urine: 50 μL of thawed sample was mixed with 50 μL of an isotopically-labeled internal standard (IS) mix and 200 μL of methanol for protein precipitation [104].
- Feces: 20 mg of fecal sample was homogenized with 50 μL IS and 200 μL methanol at 4°C for 10 minutes [104].
- All mixtures were vortexed, centrifuged, and the supernatant was evaporated to dryness. The residue was reconstituted in 100 μL of 50% methanol/water (v/v) for LC-MS injection [104].
Chromatographic Separation:
- Column: Waters ACQUITY UPLC HSS T3 C18 (100 mm × 2.1 mm, 1.8 μm particle size) [104].
- Mobile Phase: A) Water with 0.01% acetic acid and 5 mM ammonium acetate; B) Acetonitrile with 0.01% acetic acid [104].
- Gradient: An isocratic gradient elution program was used (detailed in supplementary materials of the original study) [104].
Mass Spectrometric Detection:
- System: AB 6500+ QTRAP LC-MS/MS System with an ESI Turbo Ion-Spray Interface [104].
- Ion Mode: Negative [104].
- Data Acquisition: Multiple Reaction Monitoring (MRM) mode controlled by Analyst 1.6.3 software. Declustering potentials and collision energies were optimized for each of the 50 quantified BA species [104].
Data Analysis:
- Multivariate Statistics: Orthogonal Projections to Latent Structures Discriminant Analysis (OPLS-DA) in SIMCA-P v16.0.2 to discriminate between patient groups [104].
- Model Validation: Goodness-of-fit (R2) and predictive ability (Q2) parameters. Variable Importance in Projection (VIP) >1.2 considered statistically significant for group discrimination [104].
- Biomarker Potential: Receiver-operating characteristic (ROC) curves generated to evaluate the predictive performance of key BAs for DKD (AUC >0.7 considered significant) [104].
Prospective Cohort Study Design for MUFA Intake Assessment
The associations between MUFA intake and type 2 diabetes risk were evaluated in three large prospective cohorts using a standardized nutritional epidemiology protocol [107] [108].
Cohort Description:
- Nurses' Health Study (NHS): 121,700 female nurses aged 30-55, recruited in 1976 [108].
- Nurses' Health Study II (NHSII): 116,430 female nurses aged 25-44, recruited in 1989 [108].
- Health Professionals Follow-up Study (HPFS): 51,529 male health professionals aged 40-75, recruited in 1986 [108].
- Analysis Baseline: 1990 for NHS and HPFS, 1991 for NHSII (first years with olive oil consumption data) [108].
Dietary Assessment:
- Tool: Validated semi-quantitative Food Frequency Questionnaires (FFQs) administered every 4 years [108].
- Nutrient Calculation: USDA and Harvard University food composition databases used to calculate intake of total MUFAs, plant-based MUFAs (MUFA-Ps), and animal-based MUFAs (MUFA-As) [108].
- Covariate Assessment: Biennial questionnaires collected data on anthropometrics, lifestyle, medical history, and disease diagnoses [108].
Case Ascertainment and Statistical Analysis:
- T2D Diagnosis: Participants self-reporting physician-diagnosed T2D received supplementary questionnaires. Cases were confirmed using National Diabetes Data Group criteria (pre-1998) or American Diabetes Association criteria (post-1998), including HbA1c ≥6.5% from 2010 onward [108].
- Statistical Modeling: Time-dependent Cox proportional hazards models used to calculate hazard ratios (HRs). Analyses were conducted per cohort and pooled via inverse-variance weighted meta-analysis [108].
- Substitution Analysis: Models evaluated the effect of isocalorically replacing 5% of energy from saturated fatty acids (SFAs) or animal-based MUFAs with plant-based MUFAs [108].
Pathophysiological Roles and Signaling Pathways
Bile Acid Signaling in Glucose Homeostasis and Diabetic Complications
Bile acids regulate glucose metabolism through multiple receptor-dependent and independent mechanisms. Their signaling is integral to understanding their role in diabetic complications.
Figure 1: Bile Acid Signaling Pathways in Glucose Homeostasis. BAs exert pleiotropic effects on glucose metabolism primarily through activation of the nuclear receptor FXR and membrane receptor TGR5. Intestinal FXR activation stimulates FGF19 release, which promotes hepatic glycogen synthesis. Hepatic FXR activation induces SHP, which suppresses gluconeogenic enzymes (G6Pase, PEPCK). TGR5 activation stimulates GLP-1 secretion, enhancing insulin sensitivity. FXR inhibition can also suppress inflammatory responses [103] [109].
The pathogenesis of Diabetic Kidney Disease is associated with specific alterations in bile acid metabolism. A comprehensive metabolomic study revealed step-wise alterations in BA pools from healthy status to T2DM and onward to DKD [104]. Key changes include:
- Plasma BAs: Increased levels of glycochenodeoxycholic acid (GCDCA) strongly correlated with clinical indicators of DKD progression, including estimated glomerular filtration rate (eGFR), 24-hour urinary protein, and 24-hour urinary microalbumin [104].
- Conjugation Patterns: Increased conjugated/unconjugated ratios of primary BAs including cholic acid (CA), chenodeoxycholic acid (CDCA), and deoxycholic acid (DCA) in plasma and feces of DKD patients [104].
- Synthesis Rates: Insulin resistance and T2DM are associated with increased bile acid synthesis, potentially driven by glucose induction of the rate-limiting enzyme CYP7A1 [105].
Sphingolipid Metabolism in Neurological Complications
While the provided search results focus on brain development rather than diabetes, sphingolipid biology offers plausible mechanisms for neurological complications of diabetes.
Figure 2: Sphingolipid Biogenesis and Recycling Pathways. Ceramides, the central building blocks of sphingolipids, are generated via three main pathways: (1) de novo synthesis in the endoplasmic reticulum initiated by serine palmitoyltransferase (SPT); (2) sphingomyelinase pathway hydrolyzing complex sphingolipids; (3) salvage pathway recycling sphingosine. Six mammalian ceramide synthases (Cers) show specificity toward different acyl-CoA chains, generating molecular diversity [106].
Lipidomic studies reveal dynamic changes in sphingolipids during development and aging:
- Acyl-Chain Length: Aging mouse brains show increased longer acyl-chain (C20-C26) sphingolipids and decreased shorter chains [106].
- Human Brain Evolution: Human brains show the most distinct lipid composition divergence from non-neural tissue among species, with accelerated evolution of brain-enriched lipids in primates [106].
- Ceramide Abundance: Higher concentrations of ceramides are found in infant human brains compared to adult brains [106].
The biological effects of monounsaturated fatty acids are significantly influenced by their dietary sources, explaining previously conflicting evidence in the literature.
Table 2: Hazard Ratios for Type 2 Diabetes by MUFA Source and Substitution Analysis
| Dietary Fat Manipulation | Hazard Ratio (HR) | 95% Confidence Interval | P-Value/Interpretation |
|---|---|---|---|
| Highest vs. Lowest Quintile (Q5 vs. Q1) | |||
| Total MUFA Intake | 1.10 | (1.01, 1.22) | Associated with higher risk |
| Plant-based MUFAs (MUFA-Ps) | 0.87 | (0.81, 0.94) | 13% risk reduction |
| Animal-based MUFAs (MUFA-As) | 1.34 | (1.23, 1.45) | 34% risk increase |
| Substitution Analysis (per 5% energy) | |||
| MUFA-Ps replacing MUFA-As | 0.72 | (0.66, 0.78) | 28% risk reduction |
| MUFA-Ps replacing SFAs+MUFA-As | 0.82 | (0.77, 0.88) | 18% risk reduction |
| MUFA-Ps replacing trans fats (per 2%) | 0.92 | (0.86, 0.99) | 8% risk reduction |
| MUFA-As replacing SFAs | 1.43 | (1.33, 1.54) | 43% risk increase |
| MUFA-As replacing refined carbohydrates | 1.33 | (1.25, 1.43) | 33% risk increase |
Data derived from prospective cohorts of NHS, NHSII, and HPFS [107] [108].
The differential effects of MUFA sources may be mediated through several mechanisms:
- Food Matrix Effects: Animal-based MUFAs typically co-exist with saturated fats and heme iron, which may counteract potential benefits [108].
- Impact on Lipoproteins: High-MUFA diets favorably influence triglyceride and HDL cholesterol levels compared to high-carbohydrate diets, and are associated with less atherogenic, buoyant LDL particles compared to the dense LDL particles promoted by low-fat diets [110].
- Ancillary Benefits: MUFA-rich diets have demonstrated favorable effects on blood pressure, coagulation, endothelial activation, inflammation, and thermogenic capacity in limited experimental evidence [110].
Table 3: Key Research Reagent Solutions for Metabolite Analysis
| Reagent/Resource | Specific Application | Function/Rationale | Example from Literature |
|---|---|---|---|
| UPLC-MS/MS Systems | Bile acid quantification & profiling | High-resolution separation & detection of diverse BA species | AB 6500+ QTRAP System [104] |
| C18 Chromatography Columns | Lipid metabolite separation | Hydrophobic interaction chromatography for lipid separation | Waters ACQUITY UPLC HSS T3 C18 [104] |
| Stable Isotope-Labeled Standards | Metabolite quantification | Internal standards for correction of matrix effects & recovery | Isotope-labeled BA mix (9 kinds) [104] |
| Validated Food Frequency Questionnaires (FFQs) | Nutritional epidemiology | Assessment of habitual dietary intake in large cohorts | Harvard FFQ [107] [108] |
| Food Composition Databases | Nutrient intake calculation | Conversion of food intake to nutrient values | USDA & Harvard University databases [108] |
| Multivariate Statistical Software | Metabolomic data analysis | Pattern recognition & biomarker identification | SIMCA-P v16.0.2 [104] |
The comparative analysis of PCs, sphingomyelins, MUFAs, and bile acids reveals a complex metabolic landscape in diabetic complications. Bile acids demonstrate the most robust step-wise alterations from health to T2DM and onward to specific complications like DKD, with distinct signaling pathways through FXR and TGR5 receptors. Sphingolipids, while less studied in the context of diabetes in the available literature, represent promising targets given their fundamental roles in membrane structure and cellular signaling. Most notably, monounsaturated fatty acids exhibit source-dependent effects, with plant-derived MUFAs conferring protection against T2DM while animal-derived MUFAs increase risk—a critical distinction for nutritional guidance. The experimental approaches detailed herein, particularly advanced metabolomic profiling and prospective nutritional epidemiology, provide robust methodologies for continued investigation into these metabolite classes. Future research should focus on elucidating the specific mechanisms linking these metabolic disturbances to end-organ damage and exploring their potential as targets for novel therapeutic interventions.
In the field of diabetic complications research, the discovery and validation of lipid metabolites and protein biomarkers have become pivotal for understanding disease progression and developing diagnostic tools. Diabetic microvascular complications, including diabetic kidney disease (DKD) and diabetic retinopathy (DR), represent a significant burden, with chronic hyperglycemia inflicting damage on small blood vessels [6]. The identification of reliable biomarkers enables early detection and risk assessment, potentially improving patient outcomes through timely intervention. Emerging lipid-related biomarkers such as the Visceral Adiposity Index (VAI), Lipid Accumulation Product (LAP), and Atherogenic Index of Plasma (AIP) have demonstrated potential in predicting metabolic disorders and associated complications [6]. Similarly, protein biomarkers like irisin and metabolomic profiles show promise in reflecting disease severity and progression [111] [99]. This guide objectively compares the performance of enzyme-linked immunosorbent assay (ELISA) with other analytical methodologies in validating these key biomarkers, providing researchers with experimental data and protocols to inform their study designs.
Analytical Methodologies: Principles and Protocols
ELISA Technology and Validation Standards
The enzyme-linked immunosorbent assay (ELISA) remains a gold-standard tool for quantifying biomolecules in biological matrices such as serum, plasma, or cell supernatant [112]. This immunoassay technique relies on the specific binding between an antigen and antibody, with an enzyme conjugate producing a measurable signal proportional to the analyte concentration. For regulatory compliance in quantitative analyses, ELISA methods require rigorous validation against parameters including accuracy, precision, sensitivity, linearity, matrix effects, and reproducibility [112]. The validation process must confirm that the method fulfills requirements for its specific intended use, whether for pharmacokineti c (PK) studies, immunogenicity detection, or diagnostic biomarker quantification [113].
Standard operating procedures for full method validation include assessment of robustness, precision, trueness, uncertainty, limits of quantification, dilutional linearity, parallelism, recovery, selectivity, and sample stability [113]. For commercial assays, a partial validation may suffice, typically including all parameters except robustness, which should be covered by the manufacturer during method development [113]. The step-by-step validation approach generally involves: defining the analytical purpose, establishing linearity and calibration curves, determining sensitivity (LOD and LOQ), evaluating precision and reproducibility, assessing matrix compatibility and interference, and conducting quality control and stability testing [112].
Alternative Analytical Platforms
While ELISA maintains widespread use, alternative platforms offer different advantages for specific applications:
Chemiluminescence Immunoassay (CLIA) utilizes chemiluminescence-related substances to label antigens or antibodies, followed by separation of free markers after specific antigen-antibody reaction. The addition of chemiluminescence system substances generates light emission for qualitative or quantitative detection [114]. CLIA advantages include rapid detection, ease of operation, high sensitivity, and specificity, positioning it as a leading alternative to ELISA [114].
Liquid Chromatography-Mass Spectrometry (LC-MS) platforms, particularly when configured for targeted metabolomics, provide highly specific quantification of metabolite panels. The Biocrates P500 platform using the MxP Quant kit, for instance, enables targeted quantitative analysis of numerous metabolites simultaneously [99]. This approach uses target compound standards as reference to detect and analyze specific metabolites in biological samples with high accuracy [99].
Comparative Method Performance: Experimental Data
Method Comparison Studies
Recent studies have directly compared the performance of ELISA with alternative methodologies for biomarker quantification:
Table 1: Comparison of CLIA vs. ELISA for Autoantibody Detection in Type 1 Diabetes
| Parameter | GADA | IA-2A | ZnT8A |
|---|---|---|---|
| Correlation Coefficient (r) | >0.96 | >0.96 | >0.96 |
| Cohen's κ | >0.8 | >0.8 | >0.8 |
| Proportional Bias | CLIA underestimation | CLIA overestimation | CLIA underestimation |
| Intra-assay CV | ≤10% | ≤10% | ≤10% |
| Inter-assay CV | ≤15% | ≤15% | ≤15% |
Data adapted from a study comparing MAGLUMI 800 CLIA with ELISA for detection of islet autoantibodies [114].
Table 2: Metabolomic Validation in Diabetic Retinopathy Using Multiple Platforms
| Metabolite | LC-MS Finding (DR vs. T2DM) | ELISA Confirmation | Biological Significance |
|---|---|---|---|
| L-Citrulline (Cit) | Decreased in DR | Confirmed decrease | Related to nitric oxide metabolism |
| Indoleacetic acid (IAA) | Increased in DR | Confirmed increase | Tryptophan derivative, potential toxin |
| Chenodeoxycholic acid (CDCA) | Lower in PDR vs. NPDR | Confirmed decrease | Primary bile acid |
| Eicosapentaenoic acid (EPA) | Lower in PDR vs. NPDR | Confirmed decrease | Omega-3 fatty acid |
| Hexanoylcarnitine | Altered in DR progression | Not validated | Fatty acid oxidation marker |
Data synthesized from a study comparing targeted and untargeted metabolomics with ELISA validation in diabetic retinopathy [99].
Biomarker Performance in Diabetic Complications
Independent cohort studies have established the clinical relevance of various biomarkers for diabetic complications:
Table 3: Lipid Biomarkers for Diabetic Kidney Disease Prediction
| Biomarker | Formula | WMD in DKD (95% CI) | OR for DKD (95% CI) | Diagnostic Performance |
|---|---|---|---|---|
| LAP | Men: [WC (cm)-65] × TG (mmol/L)Women: [WC (cm)-58] × TG (mmol/L) | 12.67 (7.83-17.51) | 1.005 (1.003-1.006) | Limited discriminatory power |
| AIP | log₁₀(TG/HDL-C) | 0.11 (0.03-0.19) | 1.08 (1.04-1.12) | Limited discriminatory power |
| VAI | Men: (WC/39.68 + BMI/1.88) × (TG/1.03) × (1.31/HDL-C)Women: (WC/36.58 + BMI/1.89) × (TG/0.81) × (1.52/HDL-C) | 0.63 (0.38-0.89) | 1.05 (1.03-1.07) | Limited discriminatory power |
Data from a systematic review and meta-analysis of 23 studies on lipid biomarkers and microvascular complications in diabetes [6].
For irisin in diabetic nephropathy, a meta-analysis of seven studies comprising 453 DN patients and 346 non-DN controls demonstrated significantly lower serum irisin levels in patients with diabetic nephropathy, particularly those with more advanced stages of albuminuria [111]. Pooled results showed significantly reduced irisin levels in patients with microalbuminuria (MD = 30.84, 95% CI: 7.81 to 53.87) and macroalbuminuria (MD = 30.84, 95% CI: 7.81 to 53.87) compared to those with normoalbuminuria [111].
Experimental Protocols for Method Validation
ELISA Validation Protocol
Robust ELISA validation requires a systematic approach with specific experimental protocols:
Step 1: Define Analytical Purpose - Clearly establish whether the assay is intended for PK studies, immunogenicity detection, small molecule quantification, or diagnostic biomarker detection, as each use case demands different validation depth [112].
Step 2: Linearity and Calibration Curve - Perform curve fitting with R² ≥ 0.98 using validated standards across the expected concentration range. For example, Denovo's DeQuanto ELISA kits validate linearity across ranges such as 5.2-200 ng/mL for Adalimumab and 0.1-3.1 µg/mL for Bevacizumab [112].
Step 3: Sensitivity Determination - Calculate Limit of Detection (LOD) using blank sample mean + 3 standard deviations, and confirm Limit of Quantification (LOQ) with CV ≤ 20%. Document sensitivity for each analyte-matrix combination [112].
Step 4: Precision and Reproducibility Assessment - Evaluate intra-assay precision (%CV across replicates within the same plate) and inter-assay precision (%CV across 3-5 days, analysts, or lots). Acceptance thresholds are typically ≤15% CV for medium/high QC and ≤20% CV for LLOQ samples [112].
Step 5: Matrix Compatibility and Interference - Validate assays in relevant biological matrices (e.g., human serum and plasma) using matrix blank and spike recovery, parallelism testing, and cross-reactivity evaluation [112].
Step 6: QC and Stability Testing - Test each ELISA kit for short-term stability, reagent storage conditions (2-8°C and -20°C), lot-to-lot consistency, and QC material traceability [112].
Cross-Validation Protocol Across Platforms
For biomarker verification across multiple analytical platforms:
Sample Preparation - After overnight fasting, collect venous blood samples and separate serum by centrifugation at 3000 rpm for 10 minutes at 4°C within 30 minutes [99]. Transfer plasma to sterile tubes and store at -80°C until analysis.
Targeted Metabolomics - Perform targeted quantitative analysis using platforms such as the Biocrates P500 with MxP Quant kit. Use 10 μL of plasma per well, dry under nitrogen stream, and derivatize with 5% phenylisothiocyanate (PITC) solution [99].
ELISA Confirmation - Select appropriate commercial ELISA kits for target metabolites or biomarkers. Follow manufacturer protocols while incorporating validation parameters. Include standards, controls, and samples in duplicate.
Data Analysis - Apply multiple linear regression analyses to adjust for the significance of different metabolites between groups. Use statistical methods such as Passing-Bablok regression, Spearman correlation, Bland-Altman analysis, and Cohen's kappa statistics for method comparison [114].
Signaling Pathways and Biological Workflows
Lipid Biomarker Pathway in DKD
Biomarker Discovery Workflow
Research Reagent Solutions
Table 4: Essential Research Reagents for Biomarker Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| PK ELISA Kits | Infliximab (PK1001), Adalimumab (PK1002), Bevacizumab (PK1005) | Quantification of therapeutic antibodies in biosimilar studies |
| Metabolite Standards | L-Citrulline, Indoleacetic acid, Chenodeoxycholic acid, Eicosapentaenoic acid | Reference standards for targeted metabolomics and assay calibration |
| Immunoassay Platforms | MAGLUMI 800 (CLIA), RSR and Medizym ELISA | Automated antibody detection for high-throughput screening |
| Sample Preparation Kits | Biocrates MxP Quant Kit | Standardized metabolite extraction for LC-MS analysis |
| Quality Control Materials | Human serum pools, Internal control materials | Monitoring assay performance and lot-to-lot consistency |
The external confirmation of key metabolites through ELISA and independent cohort studies provides critical validation for biomarkers implicated in diabetic complications. While emerging technologies like CLIA and LC-MS offer advantages in automation, throughput, and multiplexing, ELISA maintains its position as a reliable, accessible validation method. The experimental data presented demonstrates that biomarker panels including LAP, AIP, VAI, irisin, and specific metabolites show significant associations with diabetic kidney disease and retinopathy, though their diagnostic accuracy as stand-alone markers remains limited. Researchers should select analytical methodologies based on intended application, required throughput, and available resources, while incorporating rigorous validation protocols to ensure data reliability. The continued standardization of assays across platforms will enhance the comparability of research findings and accelerate the translation of biomarker discoveries into clinical applications.
In the evolving field of diabetic complications research, lipid metabolites have emerged as a promising frontier for predicting and understanding the microvascular damage that arises from diabetes. This guide provides a comparative analysis of the current evidence for two primary classes of lipid-based biomarkers: established clinical indices (VAI, LAP, AIP) and novel lipidomic species (e.g., specific ceramides, sphingomyelins). We objectively evaluate their performance, supported by experimental data, to assess their respective strengths, limitations, and readiness for clinical application. The evidence indicates that while traditional indices show significant associative strength with diabetic kidney disease (DKD), emerging lipidomic panels offer superior diagnostic accuracy for early-stage retinopathy, though they remain largely in the research domain.
Comparison of Lipid Biomarker Performance
The table below synthesizes quantitative data on the performance of various lipid biomarkers from recent meta-analyses and clinical studies.
Table 1: Comparative Performance of Lipid Biomarkers in Diabetic Complications
| Biomarker Category | Specific Biomarker | Associated Complication | Key Quantitative Data (vs. Control) | Diagnostic Performance (AUC) | Clinical Readiness |
|---|---|---|---|---|---|
| Clinical Indices [6] [115] | Lipid Accumulation Product (LAP) | Diabetic Kidney Disease (DKD) | WMD: 12.67 (95% CI: 7.83–17.51); OR for each 1-unit increase: 1.005 [6] | Limited / Modest [6] | Medium-High |
| Atherogenic Index of Plasma (AIP) | Diabetic Kidney Disease (DKD) | WMD: 0.11 (95% CI: 0.03–0.19); OR for each 1-unit increase: 1.08 [6] | Limited / Modest [6] | Medium-High | |
| Visceral Adiposity Index (VAI) | Diabetic Kidney Disease (DKD) | WMD: 0.63 (95% CI: 0.38–0.89); OR for each 1-unit increase: 1.05 [6] | Limited / Modest [6] | Medium-High | |
| Novel Lipidomic Species [52] | 4-Lipid Panel (e.g., TAG58:2-FA18:1) | Non-Proliferative Diabetic Retinopathy (NPDR) | N/A | Showed good predictive ability in discovery and validation sets [52] | Low |
| Ceramides (d18:1/18:0, d18:1/16:0) [116] | Type 2 Diabetes (T2DM) | Significantly increased in T2DM vs. healthy controls (P < 0.05) [116] | N/A | Low | |
| Sphingomyelins (d18:1/18:0, d18:1/18:1) [116] | Type 2 Diabetes (T2DM) | Significantly increased in T2DM vs. healthy controls (P < 0.05) [116] | N/A | Low |
Abbreviations: WMD: Weighted Mean Difference; OR: Odds Ratio; CI: Confidence Interval; AUC: Area Under the Receiver Operating Characteristic Curve.
Key Insights from Comparative Data:
- Clinical Indices (VAI, LAP, AIP) demonstrate a statistically significant associative strength with DKD, with elevated levels consistently observed in patients with this complication. However, their overall diagnostic accuracy remains modest, limiting their utility as standalone diagnostic tools [6] [115].
- Specificity of Complications: The same clinical indices show no significant association with diabetic retinopathy (DR), highlighting the tissue-specific nature of lipid metabolic disturbances [6]. This underscores a critical limitation and differentiates them from novel lipidomic panels, which show direct promise for DR.
- Therapeutic Response: Lipidomic profiling has proven valuable in monitoring therapeutic efficacy. For instance, levels of specific lipids like SM(d18:1/18:0) and LPC(16:0) were significantly reduced following exenatide treatment in T2DM patients, paralleling improvements in glycemic and lipid parameters [116]. This positions lipidomics as a powerful tool for drug development.
Detailed Experimental Protocols
Understanding the methodologies behind the data is crucial for critical appraisal. This section outlines the standard protocols for generating the evidence cited above.
Protocol for Clinical Index Meta-Analysis
This protocol details the methodology used to evaluate the clinical indices VAI, LAP, and AIP [6].
- 1. Search Strategy: A systematic search of electronic databases (PubMed, Scopus, Embase, Web of Science) is performed using keywords and MeSH terms related to "diabetic kidney disease," "retinopathy," "visceral adiposity index," etc., combined with Boolean operators.
- 2. Study Selection: Two independent investigators screen studies by title/abstract and then by full text against pre-defined eligibility criteria (PICOS model). Disagreements are resolved by a third reviewer.
- 3. Data Extraction: A structured data extraction sheet is used to collect information including study design, population characteristics, biomarker levels, and outcome measures (OR, WMD, AUC).
- 4. Quality Assessment: The quality of included studies is assessed using appropriate tools (e.g., Newcastle-Ottawa Scale for observational studies).
- 5. Statistical Synthesis: Pooled effect estimates (WMD, OR) with 95% confidence intervals are calculated. Heterogeneity is assessed using I² statistics. Meta-analysis is performed using random-effects or fixed-effects models depending on heterogeneity. Publication bias is evaluated via funnel plots and statistical tests.
Protocol for Lipidomics Analysis
This protocol describes the workflow for targeted lipidomics used to identify novel lipid biomarkers for diabetic retinopathy [52].
- 1. Sample Preparation: Serum is thawed on ice. An aliquot (e.g., 400 μL) is mixed with a lipid extraction solution (e.g., chloroform-methanol) and an internal standard mixture. The mixture is vortexed, sonicated in a cold water bath, and centrifuged. The supernatant is collected, dried under nitrogen gas, and reconstituted in a mobile phase.
- 2. Lipid Separation (UPLC): The extracted lipids are separated using an Ultrahigh-Performance Liquid Chromatography (UPLC) system, typically with a C18 reversed-phase column (e.g., Kinetex C18, 2.6 μm). A gradient of mobile phases (e.g., water-acetonitrile) is used to elute different lipid classes based on their hydrophobicity.
- 3. Lipid Detection (MS/MS): The eluted lipids are analyzed using tandem mass spectrometry (MS/MS), such as a triple quadrupole mass spectrometer. Detection occurs in Multiple Reaction Monitoring (MRM) mode for high sensitivity and specificity. Ion source parameters are set (e.g., Ion Spray Voltage: 5200 V (positive), -4500 V (negative); Temperature: 350°C).
- 4. Data Processing: Software (e.g., SCIEX OS) is used for peak identification, integration, and filtering. Data is normalized, and quality control (QC) samples are analyzed throughout the batch to ensure instrument stability.
- 5. Statistical & Biomarker Analysis: Univariate and multivariate statistical analyses (e.g., t-tests, LASSO, SVM-RFE) are applied to identify lipids that are significantly differentially expressed between groups (e.g., NDR vs. NPDR). A diagnostic model is built and validated in an independent cohort.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents used in the featured lipidomics experiments, providing a resource for replicating these studies [52] [116].
Table 2: Essential Research Reagents for Lipidomics in Diabetic Complications
| Item | Function / Role | Specific Examples / Properties |
|---|---|---|
| Ultrahigh-Performance Liquid Chromatography System (UPLC) | Separates the complex lipid extract into individual lipid components based on chemical properties prior to mass spectrometry detection. | Shimadzu LC-20AXR system; Uses C18 reversed-phase columns (e.g., Kinetex C18, 2.6 μm). |
| Tandem Mass Spectrometer (MS/MS) | Precisely identifies and quantifies individual lipid species based on their mass-to-charge ratio (m/z) and characteristic fragmentation patterns. | Triple quadrupole (e.g., AB SCIEX Triple Quad 6500+) or quadrupole time-of-flight (QTOF) mass spectrometers. |
| Internal Standard Mixture | A cocktail of stable isotope-labeled or non-natural lipid analogs added to the sample to correct for variations in extraction efficiency and instrument response, ensuring quantitative accuracy. | Mixture of deuterated or odd-chain lipids not naturally abundant in human serum. |
| Chromatographic Solvents | High-purity solvents used to prepare mobile phases for UPLC to separate lipids and to extract lipids from serum. | Acetonitrile, methanol, chloroform of LC-MS grade; water with 0.1% formic acid. |
| Standard Lipid Solutions | Commercially available pure lipid standards for instrument calibration and confirmation of lipid identities. | e.g., Sphingomyelin (d18:1/18:0), Ceramide (d18:1/16:0). |
Integrated Pathway and Conceptual Framework
The pathophysiological role of lipids in diabetic complications involves interconnected metabolic disturbances. The diagram below synthesizes these concepts from the reviewed literature [72] [89].
Conclusion
The comparative analysis of lipid metabolites across diabetic complications reveals a complex yet decipherable landscape of metabolic dysregulation. Key takeaways include the strong, specific association of novel indices like LAP and AIP with diabetic kidney disease, in contrast to their limited utility for retinopathy. Furthermore, sophisticated lipidomic profiling has successfully identified distinct, validated metabolite panels—including specific phosphatidylcholines, fatty acids, and bile acids—that can stratify patients by complication type and stage with promising accuracy. These findings underscore a paradigm shift towards understanding complications as disorders of specific lipid metabolism. Future research must focus on large-scale, prospective validation of these biomarkers, deeper mechanistic studies into how these lipid species directly contribute to pathogenesis, and the development of targeted therapies that can modulate these specific metabolic pathways. The ultimate goal is to integrate these lipid signatures into clinical practice for personalized risk assessment and early, mechanism-based intervention.
References
- 1. Targeting lipid metabolic reprogramming to alleviate ... [https://pubmed.ncbi.nlm.nih.gov/40352935/]
- 2. Targeting lipid metabolic reprogramming to alleviate ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1549484/full]
- 3. Lipid droplet dynamics in type 2 diabetes and its complications [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-025-02747-8]
- 4. Mass spectrometry-based metabolomic and lipidomic ... [https://www.sciencedirect.com/science/article/abs/pii/S0168822725004371]
- 5. Metabolic reprogramming of pancreatic beta cells in type 2 ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725002843]
- 6. Novel Lipid Biomarkers and Microvascular Complications ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12357997/]
- 7. Urinary lipid metabolites and progression of kidney ... [https://www.frontiersin.org/article/1650498]
- 8. Investigating the metabolic reprogramming mechanisms in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12426288/]
- 9. Identification of metabolic reprogramming-related genes as ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-024-01531-5]
- 10. Lipid droplet dynamics in type 2 diabetes and its complications [https://pmc.ncbi.nlm.nih.gov/articles/PMC12455809/]
- 11. Dynamics and functions of lipid droplets - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6746329/]
- 12. Perilipins: key targets for regulating lipid metabolism and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12522897/]
- 13. Increased FGF-21 Improves Ectopic Lipid Deposition in the ... [https://www.mdpi.com/2072-6643/16/9/1254]
- 14. Relationship between nontraditional lipid parameters and ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1610091/full]
- 15. Mitochondrial quality control in diabetes mellitus and ... [https://www.nature.com/articles/s41419-025-07936-y]
- 16. Novel Lipid Biomarkers of Chronic Kidney Disease of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12388243/]
- 17. Urinary lipid metabolites and progression of kidney ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1650498/full]
- 18. Novel High-Resolution Lipidomes Could Serve as New ... [https://pubmed.ncbi.nlm.nih.gov/40464192/]
- 19. New research points to lipids as possible culprit in age-related ... [https://medschool.vanderbilt.edu/basic-sciences/2025/08/14/new-research-points-to-lipids-as-possible-culprit-in-age-related-vision-loss/]
- 20. Lipid metabolism alterations in peripheral neuropathies [https://pubmed.ncbi.nlm.nih.gov/40311611/]
- 21. Association of diabetic retinopathy with plasma atherosclerotic ... [https://lipidworld.biomedcentral.com/articles/10.1186/s12944-024-02325-4]
- 22. Association of diabetic retinopathy with plasma atherosclerotic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11465674/]
- 23. Predictive properties of novel anthropometric and biochemical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11657368/]
- 24. Predictive value of obesity-related indices for incident type 2 ... [https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-025-01795-5]
- 25. Novel Lipid Biomarkers and Microvascular Complications ... [https://doaj.org/article/8a342e9434b94d1c81df33ae37b512c7]
- 26. Nutrient metabolism and complications of type 2 diabetes ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1699259/full]
- 27. Ceramides—Emerging Biomarkers of Lipotoxicity in ... [https://www.mdpi.com/2079-9721/12/9/195]
- 28. Lipotoxicity: Many Roads to Cell Dysfunction and Cell Death [https://pmc.ncbi.nlm.nih.gov/articles/PMC4959852/]
- 29. Molecular Mechanism of Lipotoxicity as an Interesting Aspect ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8909283/]
- 30. The role of mitochondrial function in the pathogenesis ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2025.1607641/full]
- 31. Role of ceramide in diabetes mellitus - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC3716967/]
- 32. are all saturated fatty acids to be blamed for ceramide- ... [https://pubmed.ncbi.nlm.nih.gov/39263838/]
- 33. The Role of Ceramides in Diabetes and Cardiovascular ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2020.569250/full]
- 34. Reshaping lipid metabolism with long-term alternate day ... [https://www.nature.com/articles/s44324-024-00039-w]
- 35. Recent Advances in Liquid Chromatography–Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204688/]
- 36. Advancing Food Analysis with Ultrahigh-Pressure Liquid ... [https://www.chromatographyonline.com/view/advancing-food-analysis-ultrahigh-pressure-liquid-chromatography-and-high-resolution-mass-spectrom-0]
- 37. Ultrahigh-pressure liquid chromatography-mass spectrometry [https://www.sciencedirect.com/science/article/abs/pii/S0165993619301700]
- 38. Metabolomics window into diabetic complications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5835462/]
- 39. Low-Resolution or High-Resolution Mass Spectrometry for ... [https://www.chromatographyonline.com/view/low-resolution-or-high-resolution-mass-spectrometry-for-clinical-and-forensic-toxicology-some-considerations-from-two-real-cases]
- 40. Comprehensive comparison of liquid chromatography ... [https://pubmed.ncbi.nlm.nih.gov/20630179/]
- 41. UHPLC-MS/MS-based plasma untargeted lipidomic ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1656458/full]
- 42. Ultra‐high performance liquid chromatography coupled to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10445193/]
- 43. Mass-spectrometry based metabolomics - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12105183/]
- 44. Targeted vs Untargeted vs Widely-targeted Metabolomics [https://www.metwarebio.com/targeted-vs-untargeted-metabolomics/]
- 45. Targeted vs Untargeted Metabolomics [https://www.metabolon.com/blog/targeted-vs-untargeted-metabolomics/]
- 46. Targeted vs Untargeted vs Semi-Targeted Metabolomics [https://www.arome-science.com/metabolomics/targeted-vs-untargeted-vs-semi-targeted-metabolomics/]
- 47. Evaluating Untargeted Metabolomics Pipelines for Sports ... [https://pubs.rsc.org/en/content/articlelanding/2025/ay/d5ay01484k]
- 48. Advancing Untargeted Metabolomics Through FT‐ICR‐MS [https://pmc.ncbi.nlm.nih.gov/articles/PMC12451246/]
- 49. Cross-Validations in Regulated Bioanalysis [https://labs.iqvia.com/blog/cross-validations-in-regulated-bioanalysis]
- 50. Plasma and serum metabolic analysis of healthy adults shows ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10943143/]
- 51. Protein sample preparation tips: Serum or Plasma? [https://www.metwarebio.com/protein-sample-preparation-serum-vs-plasma-proteomics/]
- 52. Clinical serum lipidomic profiling revealed potential lipid ... [https://www.nature.com/articles/s41598-024-66157-z]
- 53. Lipidomic studies revealing serological markers associated ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-024-05274-9]
- 54. Lipidomics reveals potential biomarkers and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11930151/]
- 55. Guiding the choice of informatics software and tools for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10263382/]
- 56. Lipid Analysis Software [https://www.lipidmaps.org/resources/tools/lm_software]
- 57. A Method for Comparing Proteins Measured in Serum and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12418474/]
- 58. Integrating lipidomics and machine learning to characterize ... [https://www.sciencedirect.com/science/article/pii/S003257912500481X]
- 59. Lipidomics reveals potential biomarkers and ... [https://www.sciencedirect.com/science/article/pii/S2589936825000106]
- 60. Abnormal lipid metabolism and atherosclerosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC12390804/]
- 61. Integrated multi-omics analysis identifies lipid metabolism ... [https://www.nature.com/articles/s41598-025-13703-y]
- 62. Identification of Key Biomarkers Related to Lipid Metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12467098/]
- 63. The Key Role and Mechanism of Oxidative Stress in ... [https://www.mdpi.com/2076-3921/14/5/557]
- 64. A comprehensive bioinformatics analysis of pathways and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1536551/full]
- 65. Multi-omics integration analysis based on plasma ... [https://www.frontiersin.org/articles/10.3389/fmolb.2025.1686282]
- 66. Mass spectrometry-based metabolomic and lipidomic ... [https://pubmed.ncbi.nlm.nih.gov/40850511/]
- 67. Machine learning-based stratification of prediabetes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12175357/]
- 68. Serum Lipidomic Analysis of T2DM Patients: A Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11847430/]
- 69. Integrated metabolomics and lipidomics reveal fatty acid ... [https://www.nature.com/articles/s41598-025-23667-8]
- 70. Integrated metabolomic-lipidomic profiling reveals novel ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1594313/full]
- 71. Early Detection and Severity Classification of Diabetic ... [https://link.springer.com/article/10.1007/s42979-025-04361-y]
- 72. New insights into the mechanisms of diabetic complications [https://pmc.ncbi.nlm.nih.gov/articles/PMC6679814/]
- 73. Conceptualizing, Measuring, and Studying Reproducibility [https://www.ncbi.nlm.nih.gov/books/NBK350355/]
- 74. A systematic review and meta-analysis of the serum lipid ... [https://www.nature.com/articles/s41598-020-79276-0]
- 75. Lipid variability and risk of microvascular complications in ... [https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-023-01526-9]
- 76. Sample Variability - an overview [https://www.sciencedirect.com/topics/psychology/sample-variability]
- 77. Shared and distinct metabolomics profiles associated with ... [https://link.springer.com/article/10.1007/s00125-025-06571-8]
- 78. Identification and validation of a blood- based diagnostic ... [https://www.nature.com/articles/s41467-024-48763-7]
- 79. Machine Learning to Diagnose Complications of Diabetes [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425951/]
- 80. Development and validation of a machine learning model ... [https://www.nature.com/articles/s41598-025-18443-7]
- 81. An enhanced machine learning algorithm for type 2 ... [https://www.nature.com/articles/s41598-024-75898-w]
- 82. Small molecule metabolites: discovery of biomarkers and ... [https://www.nature.com/articles/s41392-023-01399-3]
- 83. Metabolite Signatures of Metabolic Risk Factors and their ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4880163/]
- 84. Unveiling biomarkers via plasma metabolome profiling for ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-025-02899-y]
- 85. Multi-Omics Prognostic Signatures Based on Lipid Metabolism ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8874334/]
- 86. Metabolomics: beyond biomarkers and towards mechanisms [https://pmc.ncbi.nlm.nih.gov/articles/PMC5729912/]
- 87. Beyond Biomarkers: Machine Learning-Driven Multiomics for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12113022/]
- 88. Beyond single biomarkers: multi-omics strategies to predict ... [https://link.springer.com/article/10.1007/s10238-025-01902-w]
- 89. New insights into the mechanisms of diabetic complications [https://link.springer.com/article/10.1007/s00125-019-4959-1]
- 90. Diabetic vascular diseases: molecular mechanisms and ... [https://www.nature.com/articles/s41392-023-01400-z]
- 91. Lipidomic analysis reveals metabolism alteration ... [https://pubmed.ncbi.nlm.nih.gov/40176064/]
- 92. Performance of novel biomarkers for prediction of diabetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12466183/]
- 93. Analysis of potential biomarkers for diabetic kidney disease ... [https://bmcnephrol.biomedcentral.com/articles/10.1186/s12882-025-04544-y]
- 94. Bioinformatics analysis and validation of novel biomarkers ... [https://www.nature.com/articles/s41598-025-87854-3]
- 95. Interpretable Machine Learning Model for Predicting and ... [https://medinform.jmir.org/2025/1/e64979]
- 96. Reliable biomarkers for diabetic nephropathy using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578696/]
- 97. Best Biomarker Testing Companies in 2025 [https://infomeddnews.com/best-biomarker-testing-companies-in-2025/]
- 98. Insights from Biomarkers & Precision Medicine 2025 [https://www.signifyresearch.net/insights/biomarkers-billions-and-breakthroughs-insights-from-biomarkers-precision-medicine-2025/]
- 99. Metabolomic comparison followed by cross-validation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9492931/]
- 100. Metabolomic studies reveal and validate potential biomarkers ... [https://cardiab.biomedcentral.com/articles/10.1186/s12933-024-02535-1]
- 101. Lipid profile in the aqueous humor of diabetic macular ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1541360/full]
- 102. Novel type 2 diabetes prediction score based on traditional ... [https://www.sciencedirect.com/science/article/pii/S2589537024005509]
- 103. Bile Acids and Farnesoid X Receptor: Novel Target for the Treatment of Diabetic Cardiomyopathy - PubMed [https://pubmed.ncbi.nlm.nih.gov/31362653/]
- 104. Metabolomic profiling reveals the step-wise alteration of bile acid metabolism in patients with diabetic kidney disease | Nutrition & Diabetes [https://www.nature.com/articles/s41387-024-00315-0]
- 105. Bile acid metabolism in type 2 diabetes mellitus - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12053743/]
- 106. Sphingolipids and Ceramides in Brain Development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541296/]
- 107. Monounsaturated fatty acids from plant or animal sources and ... [https://pubmed.ncbi.nlm.nih.gov/39808307/]
- 108. Monounsaturated fatty acids from plant or animal sources and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12308698/]
- 109. Bile Acids and Type 2 Diabetes: Roles in Glucose ... [https://www.mdpi.com/2218-1989/15/6/401]
- 110. Dietary cis-monounsaturated fatty acids and metabolic ... [https://www.sciencedirect.com/science/article/pii/S0002916522033639]
- 111. Correlation of serum irisin levels with diabetic nephropathy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12420281/]
- 112. How to validate a Quantitative ELISA? [https://denovobiolabs.com/how-to-validate-a-quantitative-elisa/]
- 113. A Practical Guide to Immunoassay Method Validation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4541289/]
- 114. A Comparative Evaluation of the Chemiluminescence ... [https://www.mdpi.com/2075-4418/15/13/1695]
- 115. Novel Lipid Biomarkers and Microvascular Complications ... [https://pubmed.ncbi.nlm.nih.gov/40827201/]
- 116. The Changes of Lipidomic Profiles Reveal Therapeutic ... [https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2022.677202/full]