m6A-Related lncRNA Signatures: Predictive Biomarkers for Immunotherapy Response in Cancer
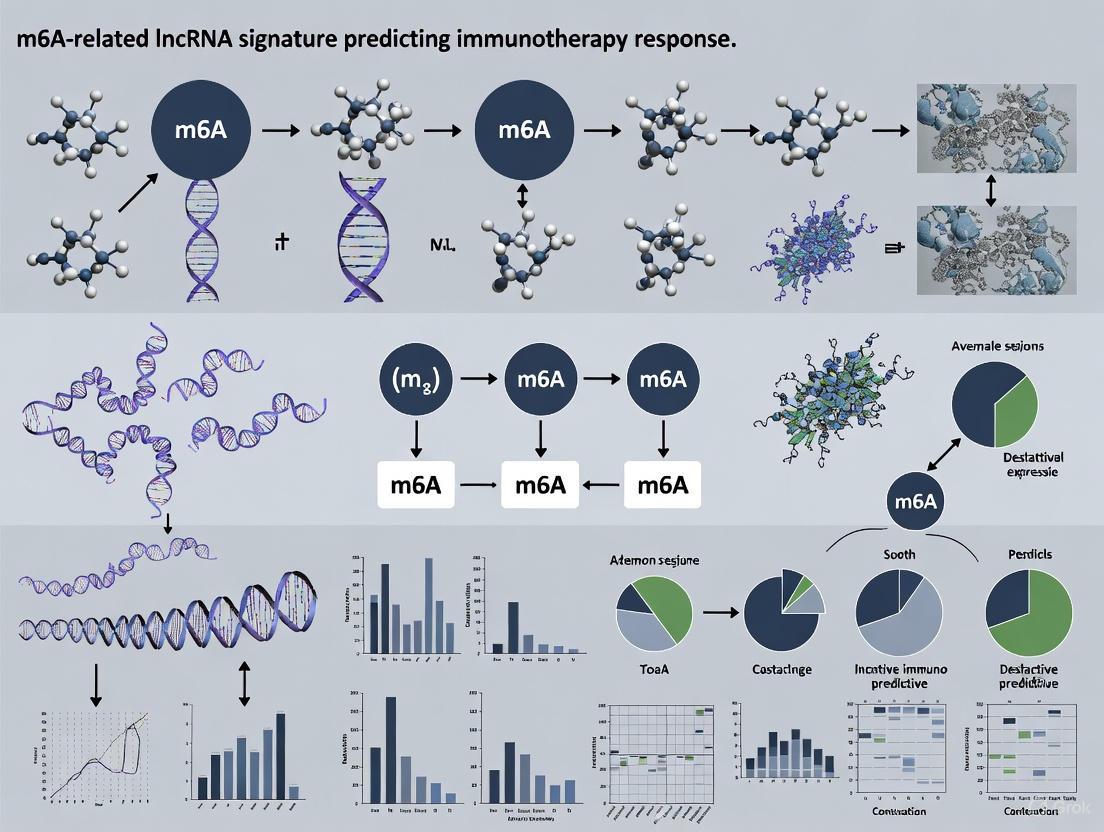
This comprehensive review explores the emerging role of m6A-related long non-coding RNA (lncRNA) signatures as powerful prognostic tools and predictors of immunotherapy efficacy across multiple cancer types.
m6A-Related lncRNA Signatures: Predictive Biomarkers for Immunotherapy Response in Cancer
Abstract
This comprehensive review explores the emerging role of m6A-related long non-coding RNA (lncRNA) signatures as powerful prognostic tools and predictors of immunotherapy efficacy across multiple cancer types. We synthesize recent evidence demonstrating how these epitranscriptomic biomarkers, derived from large-scale genomic analyses like TCGA, stratify patients into distinct risk groups with significant differences in overall survival, tumor immune microenvironment composition, and immune checkpoint inhibitor response. The article details the bioinformatics methodologies for signature development, validates their independent prognostic value, and examines their clinical utility in predicting sensitivity to immunotherapies and chemotherapeutic agents. For researchers and drug development professionals, this work provides a framework for integrating m6A-lncRNA biomarkers into precision oncology strategies to optimize immunotherapy outcomes.
The Convergence of m6A RNA Modification and lncRNAs in Cancer Immunology
N6-methyladenosine (m6A) is the most prevalent, abundant, and conserved internal post-transcriptional modification found in eukaryotic RNAs, including mRNAs, miRNAs, lncRNAs, and circRNAs [1]. This chemical modification occurs primarily within the RRACH consensus sequence (R = G or A; H = A, C, or U) and is particularly enriched in the 3' untranslated regions (3' UTRs), near stop codons, and within long internal exons [1] [2]. The m6A modification exerts comprehensive effects on RNA metabolism, including RNA stability, splicing, nuclear export, translation efficiency, and subcellular localization [1] [3]. In recent years, research has revealed that m6A plays a significant role in various physiological processes and diseases, particularly in cancer progression, metastasis, drug resistance, and immunotherapy response [1] [4].
The dynamic and reversible nature of m6A modification is regulated by three specialized classes of proteins: writers (methyltransferases), erasers (demethylases), and readers (m6A-binding proteins) [1] [5]. This application note details the fundamental biology of these regulatory components and provides experimental protocols for investigating m6A modifications, with particular emphasis on applications in m6A-related lncRNA signature research for predicting immunotherapy response.
The m6A Regulatory Machinery
Writers: m6A Methyltransferases
The writers constitute the methyltransferase complex (MTC) responsible for installing m6A modifications on target RNAs. The core complex functions as a multimeric unit with specialized components [1] [2].
Table 1: m6A Writer Proteins and Their Functions
| Regulator | Gene Name | Primary Function | Key Characteristics |
|---|---|---|---|
| METTL3 | Methyltransferase Like 3 | Catalytic subunit | Primary catalytic component; binds ~22% of all m6A sites; can function as oncogene or tumor suppressor [1] |
| METTL14 | Methyltransferase Like 14 | RNA-binding platform | Forms heterodimer with METTL3; enhances catalytic activity; provides structural scaffold [1] [2] |
| WTAP | Wilms Tumor 1 Associated Protein | Regulatory subunit | Guides localization to nuclear speckles; non-catalytic [1] [2] |
| VIRMA/KIAA1429 | Vir Like m6A Methyltransferase Associated | Scaffold protein | Recruits complex to 3'UTR and stop codon regions; enables region-specific methylation [1] |
| RBM15/RBM15B | RNA Binding Motif Protein 15/15B | Recruitment factor | Binds and recruits WTAP-METTL3 complex to specific sites like XIST [1] [2] |
| ZC3H13 | Zinc Finger CCCH-Type Containing 13 | Nuclear localization | Bridges RBM15 to WTAP-VIRMA complex; maintains complex in nucleus [1] [2] |
| METTL16 | Methyltransferase Like 16 | Independent methyltransferase | Methylates U6 snRNA and MAT2A mRNA; functions independently of MTC [1] |
The METTL3-METTL14 heterodimer forms the catalytic core, with METTL3 providing methyltransferase activity and METTL14 primarily serving as an RNA-binding platform that allosterically activates METTL3 [2]. This core complex associates with regulatory proteins including WTAP, which directs localization to nuclear speckles, and VIRMA (KIAA1429), which guides region-specific methylation toward the 3'UTR [1]. Additional components such as RBM15/RBM15B and ZC3H13 facilitate recruitment to specific RNA targets and maintain proper nuclear localization of the complex [2].
Erasers: m6A Demethylases
The erasers are demethylase enzymes that catalyze the removal of m6A modifications, enabling dynamic regulation of the epitranscriptome [1] [5].
Table 2: m6A Eraser Proteins and Their Functions
| Regulator | Gene Name | Primary Function | Regulatory Role in Cancer | Key Targets |
|---|---|---|---|---|
| FTO | Fat Mass and Obesity-Associated Protein | Demethylase | Oncogenic in AML, liver, lung, breast cancer; Tumor-suppressive in kidney, pancreatic cancer [1] | ASB2, RARA [1] |
| ALKBH5 | AlkB Homolog 5 | Demethylase | Context-dependent oncogene/tumor suppressor [1] | PD-L1, FOXM1, NEAT1 [1] |
FTO was the first identified m6A demethylase and has been shown to play critical roles in various cancers. For instance, in acute myeloid leukemia (AML), FTO reduces m6A levels on ASB2 and RARA transcripts, inhibiting ATRA-induced differentiation and promoting leukemia progression [1]. ALKBH5, the second confirmed demethylase, regulates diverse targets including PD-L1, where its deletion increases m6A abundance in the 3'UTR of PD-L1 mRNA, promoting degradation in a YTHDF2-dependent manner and thereby influencing the tumor immune microenvironment [1].
Readers: m6A Recognition Proteins
The readers are RNA-binding proteins that recognize and bind to m6A-modified RNAs, directing downstream functional consequences including RNA processing, translation, and decay [1] [5].
Table 3: m6A Reader Proteins and Their Functions
| Regulator | Gene/Family Name | Primary Function | Mechanism of Action |
|---|---|---|---|
| YTHDF1 | YTH N6-Methyladenosine RNA Binding Protein 1 | Translation promotion | Accelerates translation of m6A-modified transcripts [5] |
| YTHDF2 | YTH N6-Methyladenosine RNA Binding Protein 2 | mRNA decay | Promotes degradation of m6A-modified mRNAs [5] |
| YTHDF3 | YTH N6-Methyladenosine RNA Binding Protein 3 | Coordination | Coordinates with YTHDF1 and YTHDF2 [5] |
| YTHDC1 | YTH Domain Containing 1 | Splicing and export | Mediates nuclear processing and export of m6A-modified RNAs [5] |
| YTHDC2 | YTH Domain Containing 2 | Translation and decay | Enhances translation efficiency and decreases mRNA abundance [5] |
| IGF2BP1/2/3 | Insulin Like Growth Factor 2 mRNA Binding Protein | Stability and translation | Promotes mRNA stability and translation [1] [5] |
| HNRNPA2B1 | Heterogeneous Nuclear Ribonucleoprotein A2/B1 | pri-miRNA processing | Mediates processing of primary miRNAs [5] |
The YTHDF family proteins constitute the primary m6A readers, with YTHDF1 promoting translation, YTHDF2 facilitating RNA decay, and YTHDF3 cooperating with both [5]. Nuclear readers like YTHDC1 regulate splicing and nuclear export, while IGF2BP proteins generally stabilize target transcripts and enhance translation [1]. HNRNPA2B1 represents a specialized reader that recognizes m6A modifications on primary miRNAs and facilitates their processing into mature miRNAs [5].
m6A-LncRNA Interactions in Cancer Immunotherapy
The interaction between m6A modification and long non-coding RNAs (lncRNAs) represents a crucial regulatory axis in cancer biology and therapeutic response. m6A modifications can alter the structure, stability, and function of lncRNAs, while lncRNAs can reciprocally regulate m6A machinery components, creating complex feedback loops [5] [6].
Research has demonstrated that m6A-related lncRNA signatures can stratify cancer patients into distinct prognostic groups and predict response to immunotherapy [4] [6]. In lung adenocarcinoma (LUAD), a novel m6A-related lncRNA signature successfully classified patients into clusters with different immune phenotypes—immune-excluded, immune-inflamed, and immune-desert—which corresponded to differential responses to anti-PD-1/L1 immunotherapy [4]. Patients with high lncRNA scores showed significantly better overall survival, enhanced response to immunotherapy, and greater sensitivity to targeted therapies like erlotinib and axitinib [4].
Similarly, in esophageal squamous cell carcinoma (ESCC), a risk score model based on ten m6A/m5C-related lncRNAs effectively predicted survival outcomes and immunotherapy response [6]. Patients in the low-risk group demonstrated better prognosis, higher abundance of immune cells (CD4+ T cells, CD4+ naive T cells, class-switched memory B cells, and Tregs), and enhanced expression of most immune checkpoint genes, suggesting they would derive greater benefit from immune checkpoint inhibitor treatment [6].
Experimental Protocols for m6A Research
Protocol 1: m6A Sequencing (m6A-seq) for Transcriptome-Wide m6A Mapping
Purpose: To identify and quantify m6A modifications across the transcriptome [7].
Workflow:
Detailed Steps:
RNA Isolation and Quality Control: Extract total RNA using TRIzol reagent or column-based methods. Assess RNA integrity using Bioanalyzer or TapeStation (RIN > 8.0 recommended) [8].
RNA Fragmentation: Fragment 1-5 μg of total RNA using magnesium-based fragmentation buffer (e.g., 10 mM ZnCl2) at 94°C for 15-30 minutes to generate 100-200 nucleotide fragments. Purify using RNA clean-up beads [8].
Immunoprecipitation: Incubate fragmented RNA with anti-m6A antibody (5 μg per sample) in IP buffer (50 mM Tris-HCl pH 7.4, 150 mM NaCl, 0.1% NP-40) for 2 hours at 4°C with rotation. Add protein A/G magnetic beads and incubate for additional 2 hours. Wash beads 3-5 times with IP buffer [8].
Elution and RNA Recovery: Elute RNA from beads using elution buffer (6.7 mM m6A nucleotide in IP buffer) or directly extract with TRIzol. Purify IP RNA and input RNA simultaneously [8].
Library Preparation and Sequencing: Use standard RNA-seq library preparation kits for both IP and input samples. Perform quality control and sequence on Illumina platform (recommended depth: 40-50 million reads per sample) [8].
Bioinformatic Analysis:
- Quality control of raw reads (FastQC)
- Alignment to reference genome (STAR, HISAT2)
- Peak calling using MACS2 or exomePeak
- Differential peak analysis with MeTDiff or similar tools
- Motif analysis (HOMER) for RRACH validation [8]
Critical Considerations: The reproducibility of MeRIP-seq varies between 30-60% across studies, even within the same cell type. Biological replicates (minimum n=3) are essential for robust differential methylation analysis. Sufficient sequencing depth (minimum 10-50X mean gene coverage) is required to avoid false negatives [8].
Protocol 2: DART-FISH for In Situ Visualization of m6A Modifications
Purpose: To visualize m6A-modified and unmodified transcripts at single-cell resolution with spatial context [3].
Workflow:
Detailed Steps:
Cell Preparation and Transgene Expression:
- Plate cells on poly-d-lysine coated coverslips at appropriate density
- Generate stable cell lines expressing APOBEC1-YTH fusion protein (or APOBEC1-YTHmut control) using lentiviral infection
- Induce transgene expression with 1 μg/ml doxycycline for 24 hours [3]
Fixation and Permeabilization:
- Wash cells with PBS and fix with 4% formaldehyde for 10 minutes at room temperature
- Permeabilize with 0.5% Triton X-100 in PBS for 10 minutes
- Wash 3 times with PBS [3]
Padlock Probe Hybridization:
- Design padlock probes targeting C-to-U editing sites created by APOBEC1-YTH adjacent to m6A residues
- Hybridize probes (50 nM each) in hybridization buffer with target-specific oligonucleotides
- Incubate at 37°C for 2-16 hours [3]
Ligation and Amplification:
- Perform ligation reaction with Circligase II ssDNA ligase
- Amplify signals using rolling circle amplification with phi29 DNA polymerase
- Hybridize fluorescently labeled detection probes [3]
Imaging and Analysis:
- Image using fluorescence microscopy or confocal microscopy
- Quantify fluorescence signals to identify m6A-modified (DART-FISH positive) and unmodified transcripts
- Analyze subcellular localization patterns [3]
Applications: DART-FISH enables investigation of m6A stoichiometry at single-cell resolution, examination of differential localization of modified and unmodified transcripts, and validation of m6A dependence through METTL3/METTL14 knockdown controls [3].
Protocol 3: Developing m6A-Related LncRNA Signatures for Immunotherapy Prediction
Purpose: To construct prognostic signatures based on m6A-related lncRNAs for predicting immunotherapy response in cancer patients [4] [6].
Workflow:
Detailed Steps:
Data Acquisition and Processing:
Identification of m6A-Related LncRNAs:
- Compile list of established m6A regulators (writers, erasers, readers)
- Perform co-expression analysis between m6A regulators and lncRNAs using Spearman correlation
- Select lncRNAs with |correlation coefficient| > 0.3 and p-value < 0.05 as m6A-related lncRNAs [6]
Consensus Clustering and Survival Analysis:
- Perform consensus clustering of patient samples based on m6A-related lncRNA expression
- Determine optimal cluster number using cumulative distribution function (CDF)
- Compare overall survival between clusters using Kaplan-Meier analysis and log-rank test [4]
Construction of RiskScore Model:
Validation and Immunotherapy Response Assessment:
- Validate RiskScore model in independent datasets
- Analyze correlation between RiskScore and immune cell infiltration (CIBERSORT, xCell)
- Evaluate association with immune checkpoint gene expression (PD-1, PD-L1, CTLA-4)
- Assess predictive value for immunotherapy response using TIDE algorithm or validated immunotherapy cohorts [4] [6]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for m6A Studies
| Category | Reagent/Resource | Specific Example | Application/Function |
|---|---|---|---|
| Cell Lines | Inducible APOBEC1-YTH | HeLa, NIH3T3, Neuro2a, U-2 OS G3BP1-GFP | DART-FISH for m6A visualization [3] |
| Antibodies | Anti-m6A | Synaptic Systems 202003 | MeRIP-seq, m6A immunoprecipitation [8] |
| Inhibitors | METTL3/METTL14 Inhibitor | STM2457 (30 μM, 72h) | Writer inhibition controls [3] |
| siRNAs | METTL3/METTL14 siRNA | Qiagen (1027417:SI04317096) | Knockdown for validation experiments [3] |
| Plasmids | APOBEC1-YTH Construct | Addgene #178949 | DART-FISH implementation [3] |
| Databases | TCGA, GEO | GSE53622, TCGA-ESCC | Clinical and transcriptomic data for signature development [4] [6] |
| Software | Peak Callers | MACS2, exomePeak, MeTDiff | m6A peak identification from sequencing data [8] |
| Analysis Tools | Immune Deconvolution | CIBERSORT, xCell, TIDE | Immune cell infiltration analysis and immunotherapy prediction [4] [6] |
The fundamental biology of m6A modification—orchestrated by writers, erasers, and readers—represents a critical layer of post-transcriptional regulation with profound implications for cancer biology and therapeutic response. The experimental protocols detailed herein provide robust methodologies for investigating m6A modifications, with particular relevance for developing m6A-related lncRNA signatures that predict immunotherapy outcomes. As research in this field advances, standardized protocols and reagents will be essential for translating these findings into clinically applicable biomarkers for cancer immunotherapy.
LncRNAs as Key Regulators of Tumor Immune Microenvironment
Long non-coding RNAs (lncRNAs) have emerged as pivotal regulators of gene expression, playing critical roles in shaping the tumor immune microenvironment (TIME). Their interaction with RNA modifications, particularly N6-methyladenosine (m6A), creates a complex regulatory layer that influences cancer progression and response to immunotherapy [9] [10]. The dynamic and reversible nature of m6A modification, governed by writers, erasers, and readers, adds a crucial dimension to lncRNA function, enabling rapid responses to microenvironmental cues [11]. This interplay significantly impacts immune cell function, immune checkpoint expression, and the overall immunosuppressive landscape, making m6A-related lncRNAs promising biomarkers and therapeutic targets [9] [12]. This application note provides detailed protocols for constructing m6A-related lncRNA signatures and experimentally validating their function in modulating tumor immunity, providing a practical framework for researchers investigating this rapidly evolving field.
Computational Identification of m6A-Related lncRNA Signatures
Data Acquisition and Preprocessing
Purpose: To uniformly process raw transcriptomic and clinical data from public databases for subsequent analysis.
- Input Data Sources:
- The Cancer Genome Atlas (TCGA): Primary source for RNA-seq data (FPKM or TPM format) and corresponding clinical information (overall survival, TNM stage, etc.) [9] [10] [12].
- Gene Expression Omnibus (GEO): Independent validation cohorts (e.g., GSE53622 for ESCC) [6].
- ImmPort Database: Repository for immune-related genes [11].
- Preprocessing Workflow:
- Gene Annotation: Use Ensembl Genome Browser (e.g., GRCh38.p13) or GENCODE to classify genes as mRNA or lncRNA [9].
- Data Normalization: Convert raw counts to Transcripts Per Million (TPM) to facilitate cross-sample comparison. Use the R package
svato correct for batch effects [11] [13]. - Clinical Data Curation: Merge transcriptomic data with cleaned clinical data, ensuring consistent formatting of survival time and status variables.
Identification of m6A-Related lncRNAs
Purpose: To identify lncRNAs significantly correlated with known m6A regulators.
- m6A Regulator List: Compile a list of well-established m6A regulators. A typical set includes:
- Correlation Analysis:
Construction of a Prognostic Risk Model
Purpose: To build a multi-lncRNA signature that stratifies patients into risk groups with distinct clinical outcomes.
- Prognostic LncRNA Screening:
- Model Building with LASSO Regression:
- Risk Score Calculation:
- Model Validation:
- Internal Validation: Use Kaplan-Meier (K-M) survival analysis and log-rank test to compare OS between risk groups. Assess predictive accuracy with time-dependent Receiver Operating Characteristic (ROC) curves (e.g., 1-, 3-, 5-year AUC) [9] [13].
- External Validation: Validate the model's performance in an independent cohort (e.g., from GEO or a separate clinical dataset) [14].
- Multivariate Cox Regression: Confirm the risk score is an independent prognostic factor by adjusting for clinical variables like age and stage [10].
Table 1: Exemplary m6A-Related lncRNA Signatures Across Cancers
| Cancer Type | Signature Size | Example LncRNAs | Associated m6A Regulators | Prognostic Value | Immune Context |
|---|---|---|---|---|---|
| Colorectal Cancer [9] | 11 | Not specified | Writers, Erasers, Readers | Independent predictor of OS | High-risk: ↑ PD-1, PD-L1, CTLA4; ↑ T cell infiltration |
| Lung Adenocarcinoma [10] | 8 | FAM83A-AS1, AL606489.1, COLCA1 | METTL14, FTO, YTHDC1 | Independent predictor of OS | Associated with immune cell infiltration & drug sensitivity |
| Cervical Cancer [12] | 4 | AL139035.1, AC015922.2 | Not specified | Independent predictor of OS | Predicts immunotherapy response & drug sensitivity |
| Hepatocellular Carcinoma [14] | 2 | LINC00839, MIR4435-2HG | TSPAN4, NDST1 (Migrasome-related) | Independent predictor of OS | High-risk: ↑ Immunosuppression, ↑ PD-L1, ↓ CD8+ T cells |
Analysis of Tumor Immune Microenvironment Association
Purpose: To decipher the relationship between the m6A-lncRNA signature and the immune landscape.
- Immune Cell Infiltration Estimation:
- Immune Checkpoint and Immunotherapy Response Analysis:
- Functional Enrichment Analysis:
- Perform Gene Set Enrichment Analysis (GSEA) on genes differentially expressed between risk groups to identify enriched immune-related pathways (e.g., cytokine-cytokine receptor interaction, JAK-STAT signaling) [10].
The following workflow summarizes the key computational steps for building and validating the m6A-related lncRNA signature.
Experimental Validation of m6A-Related lncRNA Function
Functional Assays In Vitro
Purpose: To experimentally validate the oncogenic or tumor-suppressive roles of key lncRNAs identified in the signature.
- Cell Culture: Use relevant human cancer cell lines (e.g., A549 for lung adenocarcinoma, HeLa for cervical cancer) and maintain them according to ATCC guidelines [10].
- Gene Knockdown:
- Transfection: Design and synthesize small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) targeting the lncRNA of interest. Transfect cells using Lipofectamine RNAiMAX or similar reagents [10] [14].
- Validation: Confirm knockdown efficiency 48-72 hours post-transfection using quantitative RT-PCR (qRT-PCR).
- Phenotypic Assays:
- Proliferation: Assess using Cell Counting Kit-8 (CCK-8) or colony formation assay.
- Migration/Invasion: Evaluate via Transwell assay with or without Matrigel coating.
- Apoptosis: Quantify using flow cytometry with Annexin V/PI staining [10].
- Mechanistic Investigation - EMT and Immune Evasion:
- Western Blot: Analyze expression changes in epithelial-mesenchymal transition (EMT) markers (E-cadherin, N-cadherin, Vimentin) and immune checkpoint protein PD-L1 after lncRNA knockdown [14].
- RNA Immunoprecipitation (RIP): Validate direct interaction between the lncRNA and suspected m6A readers (e.g., YTHDF2) or other RBPs using a RIP kit and antibodies against the target protein [10].
Validation in Clinical Specimens
Purpose: To confirm the clinical relevance and expression pattern of signature lncRNAs.
- Tissue Collection: Obtain paired tumor and adjacent normal tissues from patients with informed consent, under approved ethical guidelines.
- RNA Extraction and qRT-PCR:
- Homogenize tissues, extract total RNA using TRIzol reagent.
- Synthesize cDNA using a reverse transcription kit.
- Perform qRT-PCR with SYBR Green mix and gene-specific primers for the target lncRNAs (e.g., ILF3-DT, PPP1R14B-AS1, RUSC1-AS1). Use GAPDH or β-actin as an internal control [13].
- Immunohistochemistry (IHC):
- To link lncRNA signature with immune context, perform IHC on formalin-fixed paraffin-embedded (FFPE) tissue sections using antibodies against PD-L1, CD8 (cytotoxic T cells), and CD68 (macrophages) [11]. Correlate staining intensity and patterns with lncRNA expression levels.
The following diagram illustrates the core experimental workflow for functional validation.
Table 2: Key Research Reagent Solutions for m6A-lncRNA Studies
| Category / Reagent | Specific Example / Product | Function and Application in Research |
|---|---|---|
| Data Resources | ||
| Transcriptomic Data | TCGA Database, GEO Datasets | Primary source for RNA-seq data and clinical correlations [9] [6]. |
| Immune Gene Sets | ImmPort Database | Reference for immune-related genes used in functional enrichment [11]. |
| Bioinformatics Tools | ||
| Clustering & Model Building | R: ConsensusClusterPlus, glmnet |
Unsupervised clustering and LASSO regression for signature construction [11] [12]. |
| Immune Deconvolution | CIBERSORT, ESTIMATE | Quantify immune cell infiltration from bulk RNA-seq data [10] [11]. |
| Immunotherapy Prediction | TIDE Algorithm | Predict potential response to immune checkpoint blockade [14]. |
| Experimental Reagents | ||
| Gene Knockdown | siRNAs, shRNAs, Lipofectamine RNAiMAX | Functional loss-of-function studies to probe lncRNA mechanism [10] [14]. |
| qRT-PCR Reagents | TRIzol, SYBR Green kits, Primers | Validate lncRNA expression in cell lines and clinical tissues [13] [14]. |
| Protein Interaction | RNA Immunoprecipitation (RIP) Kits | Investigate direct binding between lncRNAs and m6A regulators/other proteins [10]. |
| Antibodies for IHC | Anti-PD-L1, Anti-CD8, Anti-CD68 | Characterize immune contexture in the tumor microenvironment [11]. |
Concluding Remarks
The integrated computational and experimental framework outlined herein enables the systematic discovery and validation of m6A-related lncRNA signatures that govern the tumor immune landscape. These signatures demonstrate significant potential as robust biomarkers for prognostic stratification and for predicting which patients may benefit from immune checkpoint inhibitor therapy [9] [12] [6]. Future research should focus on elucidating the precise molecular mechanisms by which specific m6A-modified lncRNAs recruit immune cells and modulate checkpoint expression. Translating these findings into clinical practice requires the development of standardized assays and prospective clinical trials to validate the utility of these signatures in personalizing cancer immunotherapy.
Mechanistic Links Between m6A-Modified lncRNAs and Immune Evasion
Immune evasion represents a fundamental challenge in oncology, enabling tumors to persist and progress despite host immune responses. Recent research has illuminated the crucial role of epigenetic regulation, particularly N6-methyladenosine (m6A) modification of long non-coding RNAs (lncRNAs), in orchestrating immune escape mechanisms. As the most prevalent internal mRNA modification in mammalian cells, m6A methylation dynamically regulates RNA processing, including splicing, stability, translation, and localization [15] [16]. When this modification occurs on lncRNAs, it creates a powerful regulatory layer that influences tumor immune surveillance and response. Understanding these mechanistic links provides critical insights for developing novel immunotherapeutic strategies and biomarkers for predicting treatment response.
The integration of m6A and lncRNA biology represents a paradigm shift in cancer immunology. LncRNAs, once considered "transcriptional noise," are now recognized as pivotal regulators of gene expression through various mechanisms, including chromatin modification, transcriptional and post-transcriptional regulation, and the formation of ceRNA networks [10] [17]. The addition of m6A modification adds further complexity to their regulatory potential, particularly within the tumor microenvironment (TME) where they mediate critical interactions between cancer cells and immune components. This application note examines the established and emerging mechanisms through which m6A-modified lncRNAs facilitate immune evasion and provides detailed protocols for investigating these processes in cancer research and drug development.
Established Mechanisms of m6A-lncRNA Mediated Immune Evasion
Regulation of Immune Checkpoint Expression
m6A-modified lncRNAs utilize sophisticated molecular strategies to control the expression of critical immune checkpoint proteins, thereby enabling tumor cells to evade T-cell mediated destruction:
ceRNA Network Mechanisms: Multiple lncRNAs function as competing endogenous RNAs (ceRNAs) that sequester microRNAs, preventing these miRNAs from repressing immune checkpoint transcripts. In colorectal cancer (CRC), SNHG14 acts as a molecular sponge for miR-200a-3p, relieving miR-200a-3p-mediated suppression of immune checkpoint genes including PDCD1 (PD-1), CTLA-4, and CD274 (PD-L1) [17]. Similarly, MIR4435-2HG targets miR-500a-3p to regulate PDCD1, CD274, and CTLA-4 expression, while LINC00460 upregulates CD47 and PD-L1 through ceRNA mechanisms [17].
Protein Interaction Pathways: Some lncRNAs directly interact with key regulatory proteins to stabilize immune checkpoint expression. The lncRNA SNHG29 stabilizes YAP (Yes-associated protein) by preventing its phosphorylation and degradation, leading to enhanced PD-L1 transcription [17]. Meanwhile, CDR1-AS increases the abundance of CMTM4 and CMTM6 proteins, which promote PD-L1 stability on cancer cell membranes [17].
m6A-Dependent Regulation: The m6A modification itself directly influences lncRNA function in immune checkpoint regulation. m6A readers and writers can determine the stability, localization, and molecular interactions of lncRNAs involved in immune checkpoint expression, creating a dynamic regulatory system that responds to changing conditions in the TME [15] [9].
Modulation of Immune Cell Function and Polarization
m6A-modified lncRNAs significantly alter the function and polarization states of various immune cells within the TME:
Macrophage Polarization: LINC00543 expression in CRC induces M2 polarization of macrophages, promoting an immunosuppressive phenotype that supports tumor progression [17]. This transition from pro-inflammatory M1 to anti-inflammatory M2 macrophages represents a critical immune evasion mechanism facilitated by m6A-modified lncRNAs.
T-cell Regulation: The m6A machinery directly impacts T-cell biology, with METTL3 regulating SOCS expression in T-cells to maintain naive T-cell homeostasis, proliferation, and differentiation [15]. Additionally, RBM15 inhibits macrophage infiltration and phagocytosis, further limiting anti-tumor immunity [15].
Myeloid-derived Suppressor Cell (MDSC) Recruitment: Tumors exploit m6A-modified lncRNAs to actively attract regulatory immune cells including MDSCs and T-regulatory cells (Tregs), which inhibit anti-tumor immune responses through multiple mechanisms including production of immunosuppressive cytokines and nutrient depletion in the TME [18].
Metabolic Reprogramming of the Tumor Microenvironment
The TME undergoes significant metabolic alterations that suppress immune function, and m6A-modified lncRNAs play instrumental roles in this process:
Acidic Microenvironment Formation: Tumor cells frequently undergo aerobic glycolysis, leading to lactate accumulation and subsequent acidification of the TME. This acidic environment directly inhibits the function of immune cells including T cells, macrophages, dendritic cells, and NK cells [18]. Lactic acid impairs T-cell activation and proliferation by disrupting key signaling pathways, reduces proliferation and cytokine production of cytotoxic T lymphocytes (CTLs), and induces immunosuppressive M2 macrophage polarization [18].
Ammonia-mediated T-cell Death: Recently identified as an immune suppressive mechanism, ammonia induces a unique form of cell death in effector T cells. Through glutaminolysis, rapidly proliferating T cells produce ammonia that accumulates in lysosomes, causing alkalization, mitochondrial damage, and ultimately T-cell death [18].
Glycolytic Pathway Regulation: m6A-modified lncRNAs regulate key glycolytic enzymes and pathways, establishing metabolic competition between tumor cells and immune cells within the TME. This competition for essential nutrients creates a metabolically hostile environment for anti-tumor immune cells [15].
Table 1: Prognostic m6A-related lncRNA Signatures Across Various Cancers
| Cancer Type | Signature Name/Components | Number of lncRNAs | Prognostic Value | Immune Correlations | Therapeutic Predictions |
|---|---|---|---|---|---|
| Lung Adenocarcinoma | m6ARLSig (AL606489.1, COLCA1, etc.) | 8 | Independent predictor of OS; stratifies low/high-risk patients | Associations with immune cell infiltration; distinct immune microenvironments between risk groups | Differential drug sensitivity; FAM83A-AS1 knockdown attenuates cisplatin resistance [10] |
| Colorectal Cancer | m6A-immune-related lncRNA signature | 11 | Strong predictive performance for OS; independent prognostic factor | HRG: higher immune infiltration (CD4+ T cells, macrophages); elevated checkpoints (PD-1, PD-L1, CTLA-4) | Distinct immunotherapy responses; guides immunosuppressant selection [9] |
| Esophageal Cancer | m6aCRLncs (ELF3-AS1, HNF1A-AS1, LINC00942, etc.) | 5 | Predicts survival outcomes; significant differences in cluster distribution | Correlations with naive B cells, resting CD4+ T cells, plasma cells, macrophages M0/M1 | Identified candidate drugs: Bleomycin, Cisplatin, Erlotinib, Gefitinib [16] |
| Cervical Cancer | mfrlncRNA signature (AC016065.1, AC096992.2, etc.) | 6 | Predicts prognosis; independent prognostic factor (RiskScore + stage) | Low-risk group: more active immunotherapy response | Sensitive to chemotherapeutic drugs (e.g., imatinib) [19] |
| Cervical Cancer | m6A-related lncRNA model (AL139035.1, AC015922.2, etc.) | 4 | Independent prognostic predictor | Enables screening of patients with potential immunotherapy benefits | Predicts immunotherapy response; informs individualized treatment [12] |
Table 2: Experimentally Validated m6A-modified lncRNAs in Immune Evasion
| lncRNA | Cancer Type | Validation Method | Molecular Mechanism | Functional Outcome | Reference |
|---|---|---|---|---|---|
| FAM83A-AS1 | Lung Adenocarcinoma | Knockdown in A549 and A549/DDP cells | Not fully characterized | Repressed proliferation, invasion, migration, EMT; increased apoptosis; attenuated cisplatin resistance | [10] |
| ELF3-AS1 | Esophageal Cancer | RT-qPCR in KYSE-30 and KYSE-180 cell lines | Part of m6A-cuproptosis related signature | Significantly upregulated in EC cell lines; prognostic stratification | [16] |
| FOXD1-AS1 | Cervical Cancer | qPCR in clinical tumor samples | Component of m6A-ferroptosis signature | Upregulated expression in tumor samples; prognostic prediction | [19] |
| AP000695.2 | Gastric Cancer | Knockdown in MKN-45 cells (in vitro and in vivo) | ceRNA network: sponges miR-144-3p and miR-7-5p to upregulate CDH11, COL5A2, COL12A1, VCAN | Promotes tumor growth; associated with poor prognosis and higher T stage; VCAN correlates with reduced anti-PD-1 response | [20] |
| SNHG14 | Colorectal Cancer | Literature synthesis | ceRNA: sponges miR-200a-3p to inhibit PCOLCE2 suppression | Upregulates PDCD1, CTLA-4, CD274; facilitates immune evasion | [17] |
Detailed Experimental Protocols
Protocol 1: Constructing an m6A-related lncRNA Prognostic Signature
Purpose: To develop a risk stratification model based on m6A-related lncRNAs for predicting patient survival, immune microenvironment characteristics, and therapeutic response.
Materials and Reagents:
- RNA-seq data and clinical information from TCGA database
- R statistical software (version 4.0.3 or later)
- R packages: limma, survival, glmnet, survminer, timeROC, rms, clusterProfiler
- List of m6A regulators (writers: METTL3, METTL14, METTL16, WTAP, RBM15, etc.; erasers: FTO, ALKBH5; readers: YTHDF1-3, YTHDC1-2, IGF2BP1-3, etc.)
Procedure:
- Data Acquisition and Preprocessing:
- Download RNA-seq data (FPKM or TPM normalized) and corresponding clinical information for your cancer of interest from TCGA.
- Filter samples to include only those with complete survival information and survival time >30 days.
- Annotate the transcriptome using GENCODE or Ensembl to identify lncRNAs.
Identification of m6A-related lncRNAs:
- Extract expression data for known m6A regulators.
- Perform co-expression analysis between m6A regulators and all detected lncRNAs using Pearson correlation.
- Apply filtering thresholds (commonly |Pearson R| >0.3 or 0.4 and p < 0.001) to identify m6A-related lncRNAs.
Prognostic lncRNA Screening:
- Perform univariate Cox regression analysis on all m6A-related lncRNAs.
- Select lncRNAs with significant association with overall survival (p < 0.05 or more stringent p < 0.01) for further analysis.
Signature Construction:
- Randomly divide patients into training and testing cohorts (typically 50:50 or 70:30 ratio).
- Apply Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to the training cohort to prevent overfitting and select the most relevant lncRNAs.
- Perform multivariate Cox regression analysis to calculate risk coefficients for each selected lncRNA.
- Construct risk score formula: Risk score = Σ(expression of lncRNAi × coefficienti).
Model Validation:
- Stratify patients into high-risk and low-risk groups based on median risk score or optimal cut-off value.
- Perform Kaplan-Meier survival analysis with log-rank test to compare overall survival between risk groups in both training and testing cohorts.
- Assess model accuracy using time-dependent receiver operating characteristic (ROC) curves at 1, 3, and 5 years.
- Conduct univariate and multivariate Cox regression to determine whether the risk score is an independent prognostic factor when adjusted for clinical variables (age, stage, etc.).
Clinical Application:
- Construct a nomogram incorporating the risk score and clinical parameters to predict individual patient survival probability.
- Validate predictive accuracy of the nomogram using calibration curves.
Protocol 2: Evaluating Immune Microenvironment and Therapy Response
Purpose: To characterize differences in immune infiltration and therapeutic sensitivity between risk groups defined by m6A-related lncRNA signatures.
Materials and Reagents:
- Risk groups stratified by m6A-lncRNA signature
- R packages: CIBERSORT, xCell, ESTIMATE, GSVA, pRRophetic, ggplot2
- CIBERSORT LM22 signature matrix
- Hallmark gene sets from MSigDB
Procedure:
- Immune Cell Infiltration Analysis:
- Utilize multiple algorithms (CIBERSORT, xCell, ESTIMATE) to quantify immune cell subsets in each tumor sample.
- Compare immune cell infiltration scores between high-risk and low-risk groups using Wilcoxon rank-sum test.
- Apply false discovery rate (FDR) correction for multiple comparisons.
Immune Checkpoint Assessment:
- Extract expression data of key immune checkpoint genes (PD-1, PD-L1, CTLA-4, LAG3, TIM-3, etc.).
- Compare expression levels between risk groups using appropriate statistical tests (t-test or Mann-Whitney U test).
- Visualize results using violin plots or boxplots.
Functional Enrichment Analysis:
- Perform Gene Set Variation Analysis (GSVA) using Hallmark gene sets to identify differentially activated pathways between risk groups.
- Conduct Gene Set Enrichment Analysis (GSEA) to further characterize biological processes and signaling pathways.
- Set significance thresholds (NOM p < 0.05 and FDR < 0.25 for GSEA).
Therapy Response Prediction:
- Use the pRRophetic R package to predict IC50 values for common chemotherapeutic agents in each sample.
- Compare drug sensitivity between risk groups to identify potential therapeutic vulnerabilities.
- Apply Tumor Immune Dysfunction and Exclusion (TIDE) algorithm to predict response to immune checkpoint inhibitors.
Experimental Validation (Optional):
- Select key lncRNAs from the signature for experimental validation.
- Perform RT-qPCR in relevant cell lines and/or clinical samples to confirm differential expression.
- Conduct functional studies (knockdown or overexpression) to validate the role of selected lncRNAs in immune modulation.
Visualizing m6A-lncRNA Mechanisms in Immune Evasion
Figure 1: m6A-Modified lncRNAs Drive Immune Evasion Through Multiple Integrated Mechanisms
Table 3: Key Research Reagent Solutions for Investigating m6A-lncRNAs in Immune Evasion
| Category | Reagent/Resource | Specific Examples | Function/Application |
|---|---|---|---|
| Bioinformatics Tools | TCGA Database | RNA-seq data & clinical information | Primary data source for model development and validation [10] [9] [16] |
| R Packages | limma, survival, glmnet, CIBERSORT, ESTIMATE | Statistical analysis, model construction, immune infiltration estimation [10] [9] [19] | |
| Algorithms | CIBERSORT, xCell, ESTIMATE, TIDE | Immune cell deconvolution, TME scoring, immunotherapy response prediction [10] [9] [19] | |
| Molecular Biology Reagents | m6A Regulator Lists | 21-23 m6A regulators (writers, erasers, readers) | Core reference set for identifying m6A-related lncRNAs [16] [19] [21] |
| Cell Lines | Disease-relevant models (e.g., A549, KYSE-30, MKN-45) | Functional validation of lncRNA mechanisms [10] [16] [20] | |
| qPCR/Knockdown Tools | shRNAs, lentiviral vectors, RT-qPCR reagents | Experimental validation of lncRNA expression and function [16] [19] [20] | |
| Therapeutic Response Predictors | Drug Sensitivity Databases | PRISM, GDSC, CTRP | Correlation of risk signatures with therapeutic vulnerabilities [10] [16] [19] |
| Immunotherapy Predictors | TIDE algorithm, immune checkpoint gene sets | Assessment of potential response to immune checkpoint inhibitors [9] [19] [21] |
The mechanistic links between m6A-modified lncRNAs and immune evasion represent a transformative frontier in cancer biology and therapeutic development. Through integrated regulation of immune checkpoint expression, immune cell function, and metabolic programming of the TME, these epigenetic regulators establish multiple layers of immunosuppression that facilitate tumor progression and therapy resistance. The protocols and resources outlined in this application note provide a systematic framework for investigating these mechanisms across cancer types. The developing prognostic signatures based on m6A-related lncRNAs hold significant promise for personalized cancer immunotherapy, enabling improved patient stratification and treatment selection. As research in this field advances, targeting specific m6A-lncRNA axes may yield novel therapeutic opportunities to overcome immune evasion and enhance anti-tumor immunity.
Computational Identification of m6A-Related lncRNAs from TCGA and GEO Databases
Within the field of cancer epitranscriptomics, the integration of N6-methyladenosine (m6A) modifications with long non-coding RNA (lncRNA) biology has emerged as a critical area for biomarker discovery and therapeutic targeting. This protocol details a computational framework for identifying m6A-related lncRNA signatures from publicly available genomic databases, specifically designed to predict patient response to immunotherapy. The establishment of such signatures enables risk stratification and prognostic assessment across various cancers, providing insights into the complex interplay between RNA methylation, lncRNA regulation, and anti-tumor immunity [22] [6]. The reproducibility of this approach has been demonstrated across multiple malignancies, including head and neck squamous cell carcinoma (HNSCC) [22], bladder cancer [23], esophageal squamous cell carcinoma (ESCC) [6], and cervical cancer [19], highlighting its broad applicability in cancer research.
Data Acquisition and Preprocessing
The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO) serve as the foundational resources for transcriptomic data and clinical information. The following table summarizes the essential data components and their sources:
Table 1: Essential Data Components and Sources
| Data Type | Description | Source | Key Considerations |
|---|---|---|---|
| RNA-seq Data | Raw count or FPKM/TPM normalized data | TCGA | Harmonize normalization methods across datasets |
| Clinical Data | Overall survival, age, gender, stage, treatment response | TCGA/GEO | Ensure consistent follow-up time across patients |
| m6A Regulators | 21-23 well-established writers, erasers, readers | Published literature [21] [23] | Use consistent gene symbols across studies |
| lncRNA Annotations | Genomic coordinates and biotypes | Ensembl, GENCODE | Apply uniform filtering criteria for lncRNA identification |
Data Preprocessing Pipeline
Raw sequencing data requires rigorous preprocessing to ensure analytical reliability. The standard workflow includes:
- Data Cleaning: Remove genes with zero expression in >50% of samples and filter out patients lacking essential clinical information (particularly overall survival data) [21].
- LncRNA Identification: Annotate transcripts using reference databases (e.g., Ensembl) to distinguish lncRNAs from protein-coding genes [22] [6].
- Normalization: Transform raw counts to transcripts per million (TPM) or log2(TPM+1) to enable cross-sample comparison [6].
- Batch Effect Correction: Address technical variations between different sequencing batches or datasets using established normalization methods when integrating multiple cohorts [6].
Identification of m6A-Related lncRNAs
Correlation Analysis
The core of the identification process involves correlating lncRNA expression patterns with known m6A regulators:
- Compile m6A Regulator List: Assemble a comprehensive list of m6A regulators, typically including writers (METTL3, METTL14, WTAP, RBM15, RBM15B, ZC3H13, CBLL1), erasers (FTO, ALKBH5), and readers (YTHDF1-3, YTHDC1-2, IGF2BP1-3, HNRNPA2B1, HNRNPC) [23].
- Calculate Correlation Coefficients: Perform correlation analysis (Pearson or Spearman) between each lncRNA and each m6A regulator across all samples in the dataset.
- Apply Significance Thresholds: Identify m6A-related lncRNAs using stringent statistical thresholds, commonly set at correlation coefficient > 0.4 and p-value < 0.001 [22] [6].
Functional Characterization of m6A-Related lncRNAs
Once identified, characterize the potential functional roles of m6A-related lncRNAs through:
- Co-expression Network Analysis: Construct correlation networks to identify functionally related lncRNA-mRNA pairs and potential regulatory modules using tools such as WGCNA [21].
- Genomic Localization Analysis: Determine the genomic context of significant lncRNAs (e.g., intergenic, antisense, sense-overlapping) to infer potential regulatory mechanisms [24].
- Cellular Localization Prediction: Utilize online tools such as lncATLAS and lncSLdb to predict the subcellular localization of identified lncRNAs, which provides insights into their potential molecular functions [6].
The following diagram illustrates the logical relationships and workflow for the identification and functional characterization of m6A-related lncRNAs:
Development of Prognostic Signatures
Unsupervised Clustering for m6A Modification Patterns
Utilize consensus clustering to identify distinct m6A modification patterns based on the expression of m6A-related lncRNAs:
- Algorithm Selection: Apply the Partitioning Around Medoids (PAM) algorithm with Spearman correlation as the distance metric [19].
- Cluster Number Determination: Use the ConsensusClusterPlus R package with k-values ranging from 2 to 10. Select the optimal k based on consensus cumulative distribution function (CDF) and tracking plots [6] [19].
- Subtype Validation: Validate clusters by assessing survival differences between subtypes using Kaplan-Meier analysis and log-rank tests [19].
Construction of Prognostic Risk Models
Develop a quantitative risk score model to predict patient survival outcomes:
- Prognostic lncRNA Identification: Perform univariate Cox regression analysis on m6A-related lncRNAs to identify those significantly associated with overall survival (p < 0.05) [23].
- Feature Selection: Apply Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to reduce overfitting and select the most relevant lncRNAs for the final model [21] [22] [23].
Risk Score Calculation: Construct a multivariate Cox proportional hazards model to calculate risk scores using the formula:
Risk Score = Σ(Expression of lncRNAi × Coefficienti)
where coef_i represents the regression coefficient derived from multivariate Cox analysis [22] [6].
- Patient Stratification: Dichotomize patients into high-risk and low-risk groups using the median risk score as the cutoff point [22] [23].
Table 2: Example m6A-Related lncRNA Signatures from Various Cancers
| Cancer Type | Number of lncRNAs | Example lncRNAs in Signature | Validation Method | Clinical Application |
|---|---|---|---|---|
| Head and Neck Squamous Cell Carcinoma | 9 | SNHG16, JPX, AL450384.2 | Training/validation split (7:3) | Prognosis prediction, immunotherapy response [22] |
| Bladder Cancer | 26 | RASAL2-AS1, ARHGAP22-IT1, RNF217-AS1 | Independent cohort validation | Prognostic stratification, immune infiltration analysis [23] |
| Esophageal Squamous Cell Carcinoma | 10 | Not specified in detail | GEO dataset (GSE53622) | Predicting immunotherapy efficacy [6] |
| Cervical Cancer | 6 | AC016065.1, FOXD1_AS1, AC133644.1 | TCGA-CESC and GTEx data | Forecasting treatment response, survival prediction [19] |
Analysis of Tumor Microenvironment and Immunotherapy Response
Immune Infiltration Profiling
Quantify the immune contexture within the tumor microenvironment using multiple computational approaches:
- Cellular Deconvolution: Apply established algorithms (CIBERSORT, xCell, MCP-counter, EPIC, TIMER, QUANTISEQ) to estimate abundances of specific immune cell populations from bulk RNA-seq data [22] [19].
- Immune Function Analysis: Conduct single-sample gene set enrichment analysis (ssGSEA) to evaluate the activity of immune-related pathways and functions [22] [23].
- Immune Checkpoint Expression: Examine the expression levels of critical immune checkpoint molecules (PD-1, PD-L1, CTLA-4) across risk groups [22] [6].
Predicting Immunotherapy Response
Evaluate the potential clinical utility of the risk model for predicting immunotherapy outcomes:
- Tumor Mutational Burden (TMB) Calculation: Determine TMB by counting non-synonymous mutations per megabase of exonic sequence [21] [22].
- TIDE Analysis: Utilize the Tumor Immune Dysfunction and Exclusion (TIDE) platform to simulate patient response to immune checkpoint inhibitors [21] [22].
- Immunophenoscore Assessment: Calculate MHC expression, immunomodulator levels, and effector cell infiltration to generate composite response scores [6].
The following workflow diagram outlines the key steps from data acquisition to clinical application:
Experimental Validation and Clinical Translation
Laboratory Validation of Signature lncRNAs
While computational predictions provide valuable insights, experimental validation remains essential for clinical translation:
- RNA Extraction: Isolate total RNA from patient tissue samples (approximately 100mg) using TRIzol reagent following manufacturer protocols [21] [25].
- Quantitative RT-PCR: Validate the expression of signature lncRNAs using quantitative reverse transcription polymerase chain reaction (RT-qPCR) [21] [19].
- Direct RNA Sequencing: For comprehensive m6A modification profiling, employ direct RNA long-read sequencing to identify m6A sites at single-base resolution [26] [25].
Clinical Application and Drug Sensitivity Analysis
Translate computational findings into clinically actionable insights:
- Nomogram Development: Construct a composite nomogram integrating the lncRNA risk score with clinical variables (age, stage) to predict individual patient survival probabilities at 1, 3, and 5 years [21] [23].
- Drug Sensitivity Prediction: Calculate half-maximal inhibitory concentration (IC50) values for common chemotherapeutic agents using the R package "oncoPredict" to identify potential treatment options specific to risk groups [22] [23].
- Decision Curve Analysis (DCA): Evaluate the clinical utility of the risk model by quantifying net benefits across different threshold probabilities compared to traditional clinical factors [22] [23].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Category | Tool/Reagent | Specific Function | Application in Protocol |
|---|---|---|---|
| Data Resources | TCGA Database | Provides RNA-seq and clinical data for various cancers | Primary data source for model development [21] [23] |
| GEO Database | Repository of independent expression datasets | Validation cohort for model performance [21] [6] | |
| Computational Tools | ConsensusClusterPlus | Unsupervised clustering for subtype identification | Defining m6A modification patterns [21] [19] |
| glmnet R package | LASSO Cox regression analysis | Feature selection for prognostic signatures [22] [23] | |
| CIBERSORT/xCell | Deconvolution of immune cell populations | Tumor microenvironment analysis [22] [19] | |
| TIDE algorithm | Predicting response to immune checkpoint inhibitors | Immunotherapy response assessment [21] [22] | |
| Wet Lab Reagents | TRIzol Reagent | Total RNA isolation from tissue samples | Experimental validation of signature lncRNAs [21] [25] |
| Dynabeads mRNA DIRECT Kit | Poly-A RNA enrichment for sequencing | m6A modification analysis [26] [25] |
Correlation Analysis Strategies for Linking lncRNAs with m6A Regulators
The interplay between N6-methyladenosine (m6A) regulators and long non-coding RNAs (lncRNAs) has emerged as a critical regulatory layer in cancer biology, particularly in shaping the tumor immune microenvironment and predicting immunotherapy response. This Application Note provides a comprehensive methodological framework for identifying and validating m6A-related lncRNAs, detailing computational strategies for correlation analysis and experimental protocols for functional characterization. We present standardized workflows for constructing prognostic signatures and demonstrate their utility in predicting patient survival and therapeutic efficacy across multiple cancer types, with special emphasis on immunotherapeutic applications for researchers and drug development professionals.
N6-methyladenosine (m6A) modification, the most abundant internal RNA modification in eukaryotic cells, dynamically regulates RNA metabolism through writer, eraser, and reader proteins. Long non-coding RNAs (lncRNAs), defined as transcripts longer than 200 nucleotides with limited protein-coding potential, serve as key regulators of gene expression at epigenetic, transcriptional, and post-transcriptional levels. Emerging evidence indicates that m6A modifications can directly regulate lncRNA structure, stability, and function, while lncRNAs can reciprocally modulate m6A regulator expression, creating complex regulatory networks that significantly influence cancer progression and therapy resistance. Within the context of cancer immunotherapy research, establishing robust correlation analysis strategies for linking lncRNAs with m6A regulators enables the construction of predictive signatures for patient stratification, prognosis assessment, and treatment response prediction.
Computational Identification of m6A-Related lncRNAs
Data Acquisition and Preprocessing
The foundation of reliable correlation analysis begins with comprehensive data acquisition from publicly available repositories.
Table 1: Essential Data Sources for m6A-Related lncRNA Analysis
| Data Type | Sources | Key Specifications | Preprocessing Steps |
|---|---|---|---|
| RNA-seq Data | TCGA (https://portal.gdc.cancer.gov/) | FPKM or TPM normalized data | Batch effect correction, log2 transformation |
| Clinical Data | TCGA, GEO (https://www.ncbi.nlm.nih.gov/geo/) | Overall survival, disease stage, treatment history | Data cleaning, variable coding |
| m6A Regulators | Published literature [27] [28] | 23 well-established writers, erasers, readers | Expression matrix extraction |
| lncRNA Annotation | GENCODE (https://www.gencodegenes.org/) [27] | GRCh38 assembly | LncRNA identification and classification |
Correlation Analysis Methodologies
Multiple statistical approaches enable the identification of lncRNAs involved in m6A regulation (LI-m6As) based on coordinated expression patterns with established m6A regulators.
Pearson Correlation Analysis: Calculate Pearson correlation coefficients (PCC) between all lncRNAs and m6A regulators across patient samples. Apply thresholds of |PCC| > 0.4 and p-value < 0.01 to identify significant associations, as validated in ovarian cancer studies [27].
Spearman Correlation Analysis: Implement Spearman's rank correlation for non-parametric relationships, particularly useful for non-normally distributed expression data. Employ thresholds of |ρ| > 0.3-0.5 and p-value < 0.05, as demonstrated in esophageal squamous cell carcinoma and pancreatic cancer research [6] [29].
Co-expression Network Construction: Build weighted gene co-expression networks using algorithms such as WGCNA to identify modules of lncRNAs and m6A regulators with highly correlated expression patterns [4].
Prognostic Signature Development
Once LI-m6As are identified, prognostic models can be constructed through the following workflow:
- Univariate Cox Regression: Filter LI-m6As significantly associated with overall survival (p-value < 0.05) [27]
- LASSO Cox Regression: Perform least absolute shrinkage and selection operator regression to prevent overfitting and select the most predictive lncRNAs [27] [12]
Risk Score Calculation: Apply the formula:
Risk Score = Σ(Coefficienti × Expressioni)
where Coefficienti represents the LASSO-derived coefficient for each lncRNA, and Expressioni represents its normalized expression value [27] [29]
- Stratification: Divide patients into high-risk and low-risk groups based on median risk score
Table 2: Exemplary m6A-Related lncRNA Signatures in Various Cancers
| Cancer Type | Key m6A-Related lncRNAs | Signature Performance | Clinical Utility |
|---|---|---|---|
| Ovarian Cancer | AC010894.3, ACAP2-IT1, CACNA1G-AS1, UBA6-AS1 [27] | Independent prognostic predictor | Predicts chemotherapy response |
| Lung Adenocarcinoma | 9-lncRNA signature [4] | Stratifies immune phenotypes | Predicts anti-PD-1/L1 response |
| Cervical Cancer | AL139035.1, AC015922.2, AC073529.1, AC008124.1 [12] | Nomogram with high accuracy | Immunotherapy benefit screening |
| Breast Cancer | 18-lncRNA signature including OTUD6B-AS1, ITGA6-AS1 [30] | Independent prognostic factor | Drug sensitivity prediction |
| Colorectal Cancer | 23 prognostic lncRNAs [31] | Classifies tumor microenvironment | Predicts immunotherapy efficacy |
Experimental Validation Protocols
Functional Characterization of LI-m6As
Gene Set Enrichment Analysis (GSEA):
- Input: Differentially expressed genes between high-risk and low-risk patient groups
- Parameters: 1000 gene permutations, significance threshold FDR < 0.25
- Output: Enriched pathways and biological processes [27]
Competing Endogenous RNA (ceRNA) Network Construction:
- Predict miRNAs targeted by LI-m6As using starBase and NPInter databases [27] [32]
- Identify miRNA-targeted mRNAs using miRTarBase and TargetScan
- Construct lncRNA-miRNA-mRNA networks using Cytoscape (v3.6.1 or higher) [32]
Immune Infiltration Analysis:
- Utilize CIBERSORT or ESTIMATE algorithms to quantify tumor-infiltrating immune cells [29]
- Correlate risk scores with immune checkpoint gene expression (PD-1, PD-L1, CTLA-4) [4] [31]
- Apply Tumor Immune Dysfunction and Exclusion (TIDE) scoring to predict immunotherapy response [29]
In Vitro Validation Experiments
Cell Culture and Treatment:
- Maintain relevant cancer cell lines (e.g., HUVECs for diabetic endothelial dysfunction studies [32]) in appropriate media supplemented with 10% FBS
- For high-glucose treatment: Apply 25 mM glucose for 48 hours with 5.5 mM glucose as control [32]
- For cytokine stimulation: Treat with 5 ng/mL TNF-α to model inflammatory conditions [32]
m6A-sequencing (MeRIP-seq) Protocol:
- Total RNA Extraction: Use TRIzol reagent following manufacturer's protocol
- RNA Quality Control: Assess integrity via Nanodrop and gel electrophoresis
- Immunoprecipitation: Perform m6A RNA immunoprecipitation using GenSeqTM m6A-MeRIP Kit
- Library Preparation: Prepare sequencing libraries from both input and immunoprecipitated samples
- Sequencing: Run on Illumina NovaSeq 6000 with 150bp paired-end reads [32]
Data Analysis Pipeline:
- Quality Control: FastQC (v0.11.7) for raw read quality assessment
- Adapter Trimming: Cutadapt (v2.5) for adapter removal
- Alignment: HISAT2 (v2.1.0) aligned to reference genome (GRCh38/hg38)
- Peak Calling: exomePeak (v2.13.2) for differentially m6A-methylated regions
- Motif Analysis: HOMER (v4.10.4) for de novo motif discovery [32]
Functional Assays:
- LncRNA Knockdown: Utilize siRNA or shRNA to target candidate lncRNAs (e.g., CACNA1G-AS1 in ovarian cancer [27])
- Proliferation Assessment: Perform Cell Counting Kit-8 (CCK-8) assays at 0, 24, 48, and 72 hours post-transfection
- Validation: Confirm lncRNA expression changes via qRT-PCR with GAPDH as internal control [27]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for m6A-lncRNA Studies
| Reagent/Resource | Function/Application | Example Specifications | References |
|---|---|---|---|
| m6A-MeRIP Kit | m6A RNA immunoprecipitation | GenSeqTM m6A-MeRIP Kit | [32] |
| Cell Culture Models | Disease modeling | HUVECs for endothelial dysfunction | [32] |
| siRNA/shRNA | LncRNA knockdown | Target-specific sequences | [27] |
| Cell Viability Assays | Proliferation measurement | Cell Counting Kit-8 (CCK-8) | [27] |
| RNA Extraction Reagents | Total RNA isolation | TRIzol reagent | [32] |
| Bioinformatics Tools | Differential expression analysis | limma R package | [27] |
| Immune Deconvolution Algorithms | Immune cell quantification | CIBERSORT, ESTIMATE | [29] |
| Pathway Analysis Tools | Functional enrichment | clusterProfiler R package | [27] |
Application in Immunotherapy Response Prediction
The integration of m6A-related lncRNA signatures with immunotherapy response prediction represents a transformative approach in precision oncology. Research across multiple cancer types demonstrates that these signatures effectively stratify patients likely to benefit from immune checkpoint inhibitors.
In lung adenocarcinoma, patients with high lncRNA scores exhibited enhanced response to anti-PD-1/L1 immunotherapy and showed significant therapeutic advantages [4]. Similarly, in colorectal cancer, patients with low-risk scores based on m6A/m5C-related lncRNAs demonstrated improved response to anti-PD-1/L1 treatment [31]. Pancreatic cancer studies further validated that high-risk patients derived greater benefit from immune checkpoint inhibitors based on m6A/m5C/m1A-associated lncRNA profiles [29].
The mechanistic basis for these predictive capabilities lies in the association between m6A-related lncRNA signatures and tumor immune microenvironment characteristics. These signatures correlate with immune cell infiltration patterns, immune checkpoint expression, and cancer stemness features that collectively determine immunotherapy efficacy. For drug development professionals, these signatures offer valuable tools for patient stratification in clinical trials and development of combination therapies targeting both m6A modification and immune checkpoint pathways.
This Application Note outlines comprehensive strategies for correlating lncRNAs with m6A regulators, from computational identification to experimental validation. The standardized protocols enable researchers to construct robust prognostic signatures that predict immunotherapy response across diverse cancer types. As the field advances, integrating multi-omics approaches including m5C and m1A modifications with m6A-related lncRNA analysis will provide increasingly sophisticated tools for personalized cancer immunotherapy. The methodological framework presented here serves as a foundation for developing predictive biomarkers that can guide therapeutic decisions and improve patient outcomes in the era of cancer immunotherapy.
Building Predictive Risk Models: From Bioinformatics to Clinical Application
In the evolving landscape of cancer immunotherapy, accurately predicting patient response remains a significant challenge. The development of molecular signatures that can stratify patients based on their likelihood of treatment benefit is crucial for advancing personalized medicine. Among the most promising approaches are signatures based on m6A-related lncRNAs (long non-coding RNAs), which sit at the intersection of epitranscriptomic regulation and immune modulation [22].
This protocol details the computational framework for constructing a prognostic signature using univariate and multivariate Cox regression analyses. The methodology outlined below has been successfully applied across multiple cancer types, including head and neck squamous cell carcinoma (HNSCC), cervical cancer, and esophageal squamous cell carcinoma, to predict immunotherapy response and overall survival [22] [12] [6]. By following this structured approach, researchers can develop robust biomarkers that integrate molecular features with clinical outcomes.
Background and Significance
m6A Modifications and Cancer Immunotherapy
N6-methyladenosine (m6A) represents the most prevalent RNA modification in eukaryotic cells, influencing virtually every aspect of RNA metabolism, including splicing, stability, translocation, and translation [22] [33]. This dynamic modification is regulated by three classes of proteins: writers (methyltransferases), erasers (demethylases), and readers (binding proteins) [33]. The dysregulation of m6A modification has been implicated in various cancers, affecting tumorigenesis, metastasis, and treatment response.
Long non-coding RNAs (lncRNAs) exceeding 200 nucleotides in length play crucial regulatory roles in cellular processes despite lacking protein-coding potential. When modified by m6A, these lncRNAs demonstrate distinct expression patterns and functions in cancer progression [22] [33]. For instance, LNCAROD stabilizes through m6A methylation mediated by METTL3 and METTL14, formulating ternary complexes that drive HNSCC progression [22].
Cox Regression in Survival Analysis
The Cox proportional hazards model is a semi-parametric statistical method that evaluates the effect of multiple risk factors on survival time simultaneously [34]. Unlike Kaplan-Meier analysis which is limited to categorical predictors, Cox regression accommodates both continuous and categorical variables, making it ideal for molecular signature development [34].
The model is expressed by the hazard function: ( h(t) = h0(t) \times \exp(b1x1 + b2x2 + ... + bpxp) ), where ( h(t) ) represents the hazard rate at time ( t ), ( h0(t) ) is the baseline hazard function, ( xi ) are the predictor variables, and ( bi ) are the coefficients measuring the impact of each covariate [34]. The exponentiated coefficients ( \exp(b_i) ) represent hazard ratios (HR), which quantify the relative risk associated with each predictor variable [34].
Table 1: Key Components of Cox Proportional Hazards Model
| Component | Description | Interpretation |
|---|---|---|
| Baseline Hazard (( h_0(t) )) | Underlying hazard function when all predictors are zero | Non-parametric component that cancels out in hazard ratios |
| Regression Coefficients (( b_i )) | Measure of each predictor's effect on survival | Estimated via partial likelihood maximization |
| Hazard Ratio (( \exp(b_i) )) | Ratio of hazard rates between predictor levels | HR > 1: Poor prognosis; HR < 1: Good prognosis |
| Partial Likelihood | Method for estimating coefficients without specifying baseline hazard | Uses ranking of event times rather than actual values |
Materials and Methods
Research Reagent Solutions
Table 2: Essential Research Reagents and Resources
| Category | Specific Resource | Function/Application |
|---|---|---|
| Data Resources | The Cancer Genome Atlas (TCGA) | Source of RNA-seq data, clinical information, and mutation data [22] |
| Gene Expression Omnibus (GEO) | Independent validation dataset source [6] | |
| Computational Tools | R Statistical Software | Primary platform for statistical analysis and model building [34] |
| survival R package | Implementation of Cox regression models [34] | |
| limma R package | Differential expression analysis [22] | |
| ConsensusClusterPlus | Consensus clustering of samples [6] | |
| m6A Regulators | Writers: METTL3, METTL14, WTAP | Catalyze m6A RNA modification [33] |
| Erasers: FTO, ALKBH5 | Remove m6A modifications [33] | |
| Readers: YTHDF1-3, IGF2BP1-3 | Recognize and bind m6A-modified RNAs [33] |
The following diagram illustrates the comprehensive workflow for signature development:
Data Collection and Preprocessing
Data Acquisition: Download RNA-seq data, corresponding clinical information (including survival times and event status), and gene mutation data from public repositories such as TCGA . Ensure datasets include normal samples for comparison where possible [22].
Data Filtering: Remove duplicate samples and those with incomplete clinical information, particularly missing follow-up data or survival outcomes [22].
Expression Matrix Organization: Annotate the expression profiles based on the Ensembl database to separate mRNAs from lncRNAs. Extract expression values and transform to appropriate formats (e.g., transcripts per million - TPM) for downstream analysis [22] [6].
m6A Gene Compilation: Curate a comprehensive list of m6A regulators (writers, erasers, and readers) from published literature. Typically, this includes 20-30 well-characterized m6A genes [22] [33].
Identification of m6A-Related lncRNAs
Co-expression Analysis: Calculate correlation coefficients between all lncRNAs and m6A regulators using Spearman or Pearson methods. Apply thresholds (typically |correlation coefficient| > 0.4 and p-value < 0.001) to identify significantly associated lncRNA-m6A pairs [22] [6].
Visualization: Generate network diagrams to visualize relationships between m6A genes and associated lncRNAs using R packages such as "circlize" [33].
Univariate Cox Regression Analysis
Setup: For each m6A-related lncRNA identified in the previous step, perform univariate Cox regression analysis with overall survival as the dependent variable.
Implementation in R:
Significance Filtering: Identify lncRNAs with significant prognostic value (typically p-value < 0.05) for further analysis. In the HNSCC study, this step reduced 468 m6A-related lncRNAs to 35 with prognostic significance [22].
LASSO Regression for Variable Selection
Purpose: Least Absolute Shrinkage and Selection Operator (LASSO) regression addresses overfitting by penalizing the absolute size of regression coefficients, effectively selecting the most relevant predictors [22] [6].
Implementation:
Output: The LASSO analysis typically reduces the number of candidate lncRNAs substantially. In the HNSCC example, 35 prognostic lncRNAs were reduced to 17 candidates [22].
Multivariate Cox Regression Analysis
Purpose: Establish the final prognostic model by evaluating the independent contribution of each LASSO-selected lncRNA while controlling for other factors.
Implementation:
Risk Score Calculation: Compute risk scores for each patient using the formula:
( \text{RiskScore} = \sum{i=1}^{n} (\text{Expression of lncRNA}i \times \text{Coefficient}_i) )
where ( n ) represents the number of lncRNAs in the final signature [22] [6].
Patient Stratification: Divide patients into high-risk and low-risk groups based on the median risk score or optimal cutoff determined through survival analysis [22].
Risk Model Validation
Internal Validation:
- Split dataset into training and testing sets (typically 70:30 ratio) [22]
- Perform Kaplan-Meier survival analysis with log-rank test to compare high-risk and low-risk groups
- Generate time-dependent receiver operating characteristic (ROC) curves to assess predictive accuracy
- Calculate area under the curve (AUC) values for 1-, 3-, and 5-year survival [22]
External Validation: Validate the signature in independent cohorts from GEO or other sources to ensure generalizability [6].
Statistical Assessment:
Advanced Analytical Techniques
Stratified Cox Models
When the proportional hazards assumption is violated for certain variables, stratified Cox models can be employed. This approach allows different baseline hazard functions across strata while estimating common effects for predictors [35] [36].
Immunological Characterization
Immune Infiltration Analysis: Estimate immune cell abundances using algorithms such as CIBERSORT, EPIC, XCELL, TIMER, or MCPCOUNTER [22] [33].
Immune Checkpoint Expression: Compare expression of immune checkpoint genes (PD-1, PD-L1, CTLA-4) between risk groups [22].
Tumor Immune Dysfunction and Exclusion (TIDE) Analysis: Predict immunotherapy response based on tumor immune evasion signatures [22].
Tumor Mutational Burden (TMB) Assessment: Calculate TMB from mutation data and correlate with risk scores [22] [37].
Therapeutic Sensitivity Prediction
Drug Sensitivity Analysis: Compute half inhibitory concentration (IC50) values for various compounds using R packages such as "pRRophetic" [22].
Candidate Drug Identification: Identify potential therapeutic agents with differential effectiveness between risk groups. For example, bladder cancer patients in high-risk groups showed increased sensitivity to Talazoparib [33].
Case Study Application
HNSCC m6A-Related lncRNA Signature
A study on head and neck squamous cell carcinoma identified 468 m6A-related lncRNAs, of which 35 had prognostic value. LASSO and multivariate Cox analyses yielded a final 9-lncRNA signature (including SNHG16, JPX, and AL450384.2) that effectively stratified patients into high-risk and low-risk groups [22]. The signature demonstrated:
- Predictive Power: 5-year AUC values of 0.774 in training set and 0.740 in validation set
- Immunological Insights: High-risk patients showed distinct immune infiltration patterns and higher TIDE scores, suggesting poorer immunotherapy response
- Clinical Utility: The signature outperformed traditional clinical features in prognostic accuracy [22]
Mechanistic Insights
The following diagram illustrates the biological relationship between m6A modification and lncRNA function in cancer progression:
Troubleshooting and Technical Considerations
Addressing Common Issues
Proportional Hazards Assumption Violation:
- Check using Schoenfeld residuals
- Implement stratified Cox models for variables violating the assumption [35]
- Consider time-dependent covariates in the model
Data Quality Control:
- Remove outliers that disproportionately influence results
- Ensure adequate sample size - minimum of 10 events per predictor variable
- Address missing data through appropriate imputation methods
Model Overfitting:
Interpretation Guidelines
Table 3: Interpretation of Cox Regression Results
| Statistical Output | Interpretation | Clinical Relevance |
|---|---|---|
| Hazard Ratio (HR) | HR > 1: Increased risk event; HR < 1: Decreased risk event | Identifies risk factors and protective factors |
| P-value | Statistical significance of the predictor | Determines whether to include lncRNA in final signature |
| Regression Coefficient | Direction and magnitude of effect | Used in risk score calculation formula |
| Confidence Interval | Precision of hazard ratio estimate | Wider intervals suggest less reliable estimates |
The systematic development of m6A-related lncRNA signatures through univariate and multivariate Cox regression provides a powerful framework for predicting cancer immunotherapy response. This methodology leverages the crucial role of epitranscriptomic regulation in immune modulation while employing robust statistical approaches to create clinically actionable biomarkers.
The resulting signatures not only stratify patients based on prognosis but also offer insights into underlying biological mechanisms, potential therapeutic targets, and personalized treatment strategies. As demonstrated across multiple cancer types, this approach represents a significant advancement in precision oncology with potential to improve patient outcomes through better treatment selection.
LASSO Penalized Regression for Optimal lncRNA Selection
Long non-coding RNAs (lncRNAs) have emerged as crucial regulators in carcinogenesis and therapeutic response. In the specific context of m6A-related lncRNA signatures predicting immunotherapy response, selecting the most biologically relevant biomarkers from high-dimensional transcriptomic data presents significant statistical challenges. LASSO (Least Absolute Shrinkage and Selection Operator) penalized regression addresses this challenge by performing simultaneous variable selection and regularization, enhancing both prediction accuracy and model interpretability [38] [39]. This protocol details the application of LASSO regression for identifying optimal lncRNA signatures within m6A-related research, enabling researchers to construct robust prognostic models that can predict immunotherapy outcomes across various malignancies.
The integration of m6A modification data with lncRNA expression profiles creates a high-dimensional dataset where the number of potential features (p) often exceeds the number of observations (n). LASSO regression effectively handles this "curse of dimensionality" by forcing the sum of the absolute values of the regression coefficients to be less than a fixed value, thereby shrinking less important coefficients to exactly zero and effectively selecting only the most relevant m6A-related lncRNAs for inclusion in the final model [10] [38]. This property makes it particularly valuable for developing parsimonious biomarker signatures with maximal predictive power for immunotherapy response.
Theoretical Foundation of LASSO Regression
Mathematical Formulation
LASSO regression modifies the ordinary least squares objective function by adding an L1-norm penalty term. Given a dataset with N cases, where yi represents the outcome and xi = (x1, x2, ..., xp)i represents the covariates for the i-th case, the LASSO estimates are defined by:
Objective Function:
minβ0,β{1N‖y−β0−Xβ‖22+λ‖β‖1}
where β0 is the intercept term, β = (β1, β2, ..., βp) represents the coefficient vector, λ is the tuning parameter that controls the strength of the penalty, and ‖β‖1 = Σ|βj| is the L1-norm of the coefficient vector [38] [39]. The tuning parameter λ determines the degree of shrinkage applied to the coefficients; as λ increases, more coefficients are shrunk to zero, resulting in a sparser model.
Comparison to Other Regularization Methods
Table 1: Comparison of Regularization Methods in High-Dimensional Transcriptomic Data
| Method | Penalty Term | Variable Selection | Coefficient Behavior | Suitability for lncRNA Data |
|---|---|---|---|---|
| LASSO | λ‖β‖1 | Yes | Shrinks coefficients and sets some to exactly zero | Excellent for sparse lncRNA signatures |
| Ridge Regression | λ‖β‖22 | No | Shrinks coefficients proportionally without setting to zero | Suitable for correlated lncRNAs but less interpretable |
| Elastic Net | λ(α‖β‖1 + (1-α)‖β‖22) | Yes | Balances between LASSO and ridge | Useful when lncRNAs are highly correlated |
Unlike ridge regression, which shrinks coefficients proportionally but retains all variables in the model, LASSO performs variable selection by forcing some coefficients to exactly zero [38]. This property is particularly valuable in lncRNA biomarker discovery, where researchers aim to identify a compact set of non-redundant biomarkers with strong predictive power for immunotherapy response.
Workflow for LASSO-Based lncRNA Signature Development
The following diagram illustrates the comprehensive workflow for developing an m6A-related lncRNA signature using LASSO regression:
Figure 1: Comprehensive Workflow for LASSO-Based m6A-Related lncRNA Signature Development. This diagram outlines the key steps in developing a prognostic lncRNA signature, from data preparation through clinical application.
Experimental Protocols
Data Collection and Preprocessing
4.1.1 RNA-Seq Data Acquisition
- Obtain lncRNA expression data from public repositories such as The Cancer Genome Atlas (TCGA) or Gene Expression Omnibus (GEO) [10] [40]. For m6A-related studies, include data from at least 50-100 patients per cohort to ensure sufficient statistical power.
- Collect corresponding clinical data, including survival outcomes, treatment history, and immunotherapy response metrics [10].
- For m6A-specific analyses, obtain expression profiles of known m6A regulators (writers, erasers, readers) and identify m6A-related lncRNAs through correlation analysis [10].
4.1.2 Data Preprocessing and Quality Control
- Perform normalization using the R "limma" package to adjust for technical variations between samples [41].
- Conduct differential expression analysis using DESeq2 with screening criteria of |log2FoldChange| > 1 and p < 0.05 to identify DE lncRNAs [41] [42].
- Remove batch effects when integrating multiple datasets using the ComBat algorithm or similar approaches [41].
- Assess RNA-seq quality using FastQC and filter raw reads to remove adapter sequences, low-quality reads, and reads with high proportion of uncertain bases using Cutadapt or Trimmomatic [42].
LASSO Implementation for lncRNA Selection
4.2.1 Algorithm Implementation
- Utilize the R "glmnet" package for LASSO Cox regression analysis [41] [43] [40].
- Standardize all lncRNA expression values to have mean zero and unit variance before model fitting to ensure equal penalty application across features [39].
- For survival outcomes, employ the Cox proportional hazards model with LASSO penalty, which uses a partial likelihood approach to handle censored data [40].
4.2.2 Parameter Tuning and Model Selection
- Perform 10-fold cross-validation repeated 100 times to determine the optimal λ value [40].
- Select the λ value that minimizes the cross-validated partial likelihood deviance (lambda.min) or the largest λ within one standard error of the minimum (lambda.1se) for a more parsimonious model [41] [40].
- Use the coordinate descent algorithm for efficient computation, which optimizes the objective function with respect to one parameter at a time while keeping others fixed [39].
4.2.3 Risk Score Calculation
- Calculate risk scores for each patient using the formula:
Risk score = Σ(coefficient(lncRNAi) × expression(lncRNAi))[10] [40]. - Dichotomize patients into high-risk and low-risk groups based on the median risk score or optimal cutpoint determined using survival analysis [40].
- Validate the prognostic performance in independent internal and external validation cohorts using the same risk formula and predetermined cutpoints [40].
Validation and Functional Characterization
4.3.1 Experimental Validation
- Validate the expression of selected lncRNAs using quantitative real-time PCR (qRT-PCR) [41] [44].
- Collect human tissue samples (cancer and adjacent normal tissues) with appropriate ethical approval and patient informed consent [41].
- Extract total RNA using Trizol reagent and conduct qRT-PCR with TB Green Premix Ex Taq kit following manufacturer instructions [41].
- Use GAPDH as normalization control and calculate gene expression using the 2-ΔΔCT method with each test performed in triplicate [41].
4.3.2 Functional Annotation of Selected lncRNAs
- Predict miRNAs that interact with the selected lncRNAs using miRcode, starbase, and lncRNABase V.2 databases [41].
- Identify target mRNAs of the miRNAs using Targetscan, miRDB, and miTarBase databases [41].
- Construct competing endogenous RNA (ceRNA) networks using Cytoscape_v3.10.2 software to visualize lncRNA-miRNA-mRNA interactions [41].
- Perform gene set enrichment analysis (GSEA) to identify biological processes and pathways associated with the lncRNA signature [10].
Case Studies and Applications
LASSO for lncRNA Selection in Colorectal Cancer
A 2025 study demonstrated the application of LASSO regression for identifying CRC-associated lncRNAs. Researchers initially screened 3028 CRC-related lncRNAs from GEO databases, identified 55 differentially expressed lncRNAs through differential analysis, and then applied LASSO alongside Random Forest to select the most relevant biomarkers [41]. The study identified five key lncRNAs (NCAL1, CRNDE, HMGA1P4, EPIST, and MT1JP) with AUC values greater than 0.7, indicating good diagnostic performance [41].
m6A-Related lncRNA Signature in Lung Adenocarcinoma
In lung adenocarcinoma research, LASSO regression was employed to develop an m6A-related lncRNA signature (m6ARLSig) for prognostic stratification. The study identified eight m6A-related lncRNAs significantly associated with patient outcomes, with AL606489.1 and COLCA1 functioning as independent adverse prognostic biomarkers, while six other lncRNAs served as favorable predictors [10]. The risk model effectively stratified patients into low-risk and high-risk categories with marked divergence in overall survival and showed associations with immune cell infiltration and therapeutic responses [10].
Six-lncRNA Signature for Ovarian Cancer Recurrence
A study focused on ovarian cancer recurrence developed a six-lncRNA signature (RUNX1-IT1, MALAT1, H19, HOTAIRM1, LOC100190986, and AL132709.8) using LASSO penalized regression [40]. The signature was validated in internal and external validation cohorts and maintained significance after adjusting for clinical factors such as age, tumor stage, and grade [40]. The lncRNAs in this signature were found to be involved in cancer-related biological processes including cell adhesion, inflammatory response, and immune response [40].
Table 2: LASSO-Derived lncRNA Signatures in Cancer Studies
| Cancer Type | Selected lncRNAs | Sample Size | Validation Approach | AUC/Performance | Functional Role |
|---|---|---|---|---|---|
| Colorectal Cancer | NCAL1, CRNDE, HMGA1P4, EPIST, MT1JP | 73 patients | qRT-PCR in CRC tissues | AUC > 0.7 | Candidate biomarkers for diagnosis |
| Lung Adenocarcinoma | Eight m6A-related lncRNAs including AL606489.1, COLCA1 | 526 patients | TCGA validation, in vitro assays | Independent prognostic factor | Associated with immune infiltration and therapy response |
| Ovarian Cancer | RUNX1-IT1, MALAT1, H19, HOTAIRM1, LOC100190986, AL132709.8 | 311 patients | Internal and external validation | AUC = 0.813 at 3 years | Involved in cell adhesion and immune response |
Technical Considerations and Optimization
Addressing Computational Challenges
LASSO regression for lncRNA selection presents specific computational challenges, particularly with high-dimensional transcriptomic data. The coordinate descent algorithm has emerged as the most efficient approach for optimizing the LASSO objective function, as it doesn't require differentiability of the entire function [39]. Implementation involves:
Soft Threshold Function Implementation:
Coordinate Descent Algorithm:
The algorithm iteratively updates each coefficient while keeping others fixed:
βj = S(ρj, λ) / zj
where S is the soft thresholding function, ρj is the partial residual, and zj is a normalizing constant [39].
Model Stability and Reproducibility
Ensuring the stability and reproducibility of LASSO-selected lncRNA signatures requires:
- Performing bootstrap resampling to assess the frequency with which individual lncRNAs are selected across different subsets of the data [40].
- Using independent validation cohorts that were not involved in the feature selection process [40] [44].
- Applying stability selection methods to identify lncRNAs that are consistently selected across different penalty parameters [41].
- Reporting complete methodological details including normalization procedures, parameter tuning approaches, and validation strategies to enable replication [45].
Research Reagent Solutions
Table 3: Essential Research Reagents and Tools for LASSO-based lncRNA Studies
| Reagent/Tool | Specification | Application | Example Sources/Protocols |
|---|---|---|---|
| RNA Extraction | Trizol reagent | Total RNA isolation from tissues | Thermo Fisher Scientific [41] |
| qRT-PCR Validation | TB Green Premix Ex Taq kit | Expression validation of selected lncRNAs | Takara [41] |
| Sequencing Library Prep | rRNA removal kits, strand-specific library construction | lncRNA sequencing | Illumina TruSeq, Strand-specific protocols [42] |
| Computational Tools | R "glmnet" package | LASSO implementation | CRAN repository [41] [43] |
| Differential Expression | DESeq2, limma packages | Identification of DE lncRNAs | Bioconductor [41] [42] |
| Pathway Analysis | DAVID, GSEA | Functional annotation of lncRNA signatures | [10] [40] |
| Network Visualization | Cytoscape_v3.10.2 | ceRNA network construction | [41] |
Integration with m6A Immunotherapy Response Research
The application of LASSO regression in developing m6A-related lncRNA signatures for immunotherapy response prediction requires specific methodological adjustments. The following diagram illustrates the integrated analytical pipeline:
Figure 2: Integrated Pipeline for m6A-Related lncRNA Signature Development in Immunotherapy Response Research. This workflow specifically addresses the integration of m6A modification data with lncRNA expression for predicting immunotherapy outcomes.
Key considerations for m6A-focused applications include:
- Prioritizing lncRNAs that show significant correlations with established m6A regulators (writers, erasers, readers) before applying LASSO regression [10].
- Incorporating immune cell infiltration data from tools such as CIBERSORT to validate the relationship between the lncRNA signature and tumor microenvironment [10].
- Evaluating the association between the lncRNA signature and immune checkpoint inhibitor gene expression to establish relevance to immunotherapy response [10].
- Conducting in vitro functional validation using approaches such as gene knockdown in relevant cell lines (e.g., A549 for lung cancer) to confirm the biological role of selected lncRNAs in drug resistance and treatment response [10].
LASSO penalized regression represents a powerful statistical approach for developing optimal lncRNA signatures in the context of m6A-related immunotherapy response research. By effectively handling high-dimensional transcriptomic data and selecting the most relevant features, LASSO enables the construction of parsimonious models with strong prognostic and predictive capabilities. The integration of this methodological approach with experimental validation and functional characterization provides a comprehensive framework for advancing our understanding of lncRNAs in cancer biology and treatment response. As research in this field evolves, LASSO-derived lncRNA signatures hold significant promise for guiding personalized immunotherapeutic strategies and improving patient outcomes across various malignancies.
Risk Score Calculation and Patient Stratification Methodologies
Risk stratification has emerged as a cornerstone of personalized medicine, enabling the classification of patients based on their health status, genetic makeup, and likelihood of clinical outcomes. In oncology, this technique allows researchers and clinicians to systematically categorize cancer patients based on their molecular profiles, prognosis, and predicted treatment response [46] [47]. The fundamental goal of risk stratification is to facilitate risk-stratified care management, in which patients are managed according to their assigned risk level to optimize resource allocation, anticipate clinical needs, and proactively manage patient populations [46]. This approach is particularly valuable in the context of immunotherapy, where identifying likely responders can significantly improve outcomes while avoiding unnecessary treatments and side effects in non-responders.
The emergence of complex, multimodal profiling using biological data (genomic, epigenomic, transcriptomic, etc.) has revolutionized patient stratification, gradually replacing subgroup identification based on limited determinants [47]. In this context, m6A-related long non-coding RNAs (lncRNAs) have garnered significant attention as potential biomarkers for predicting cancer prognosis and therapeutic response. RNA methylation modifications, particularly N6-methyladenosine (m6A), have been implicated in the development and progression of various cancers, including lung adenocarcinoma (LUAD), head and neck squamous cell carcinoma (HNSCC), and cervical cancer [10] [22] [12]. These modifications are regulated by three groups of enzymes: "writers" (methyltransferases like METTL3 and METTL14), "erasers" (demethylases like FTO and ALKBH5), and "readers" (proteins that recognize m6A modifications) [10] [6].
Computational Framework for Risk Signature Development
Data Acquisition and Preprocessing
The development of an m6A-related lncRNA risk signature begins with comprehensive data acquisition from publicly available databases such as The Cancer Genome Atlas (TCGA). Typically, RNA-seq data, clinical information, and gene mutation data are downloaded and processed [22] [12]. For a study on head and neck squamous cell carcinoma, researchers collected data from 498 tumor and 44 normal samples, from which 14,086 lncRNAs were retrieved [22]. Similarly, in lung adenocarcinoma research, data from 526 LUAD patients were acquired, with subsequent analyses focusing on 480 individuals with adequate follow-up details [10].
Table 1: Data Sources and Specifications for m6A-related lncRNA Studies
| Cancer Type | Data Source | Sample Size | Number of lncRNAs Identified | Reference |
|---|---|---|---|---|
| Lung Adenocarcinoma (LUAD) | TCGA | 526 patients (480 with follow-up) | 8 prognostic lncRNAs | [10] |
| Head and Neck Squamous Cell Carcinoma (HNSCC) | TCGA | 498 tumor, 44 normal samples | 468 m6A-related lncRNAs | [22] |
| Cervical Cancer | TCGA | 4-lncRNA signature developed | 79 prognostic m6A-related lncRNAs | [12] |
| Esophageal Squamous Cell Carcinoma (ESCC) | TCGA and GEO | 81 ESCC samples in training set | 606 m6A/m5C-related lncRNAs | [6] |
The process continues with the identification of m6A-related lncRNAs through co-expression analysis with known m6A regulators. This typically involves calculating correlation coefficients between lncRNA expression profiles and m6A regulator expression levels. For instance, in HNSCC research, lncRNAs with a correlation coefficient >0.4 and P-value <0.001 were selected as m6A-related lncRNAs [22]. A similar approach was used in esophageal squamous cell carcinoma research, where Spearman's correlation analysis identified m6A/m5C-lncRNA pairs with an absolute correlation coefficient greater than 0.3 and a p-value less than 0.05 [6].
Risk Model Construction and Validation
The core of risk stratification involves developing a computational model that integrates the expression levels of selected m6A-related lncRNAs into a risk score formula. This process typically employs univariate Cox regression analysis to identify prognostic lncRNAs, followed by Least Absolute Shrinkage and Selection Operator (LASSO) regression to refine the selection, and multivariate Cox regression to establish the final model [22] [12].
The fundamental formula for risk score calculation is:
[ \text{Risk Score} = \sum{i=1}^{n} ( \text{Expression of lncRNA}i \times \text{Coefficient of lncRNA}_i ) ]
Where gene i represents the ith lncRNA in the signature, and coefficient (gene i) represents the estimated regression coefficient derived from multivariate Cox analysis [48] [6]. This formula has been applied across multiple cancer types with different lncRNA signatures:
In lung adenocarcinoma, a signature termed m6ARLSig incorporated eight m6A-related lncRNAs, with AL606489.1 and COLCA1 functioning as independent adverse prognostic biomarkers, while six others served as favorable predictors [10]. For head and neck squamous cell carcinoma, a nine-lncRNA signature was developed, including SNHG16, JPX, and AL450384.2, among others [22]. Cervical cancer research identified a four-lncRNA signature (AL139035.1, AC015922.2, AC073529.1, AC008124.1) that effectively stratified patients into high- and low-risk groups [12].
Following model development, validation is conducted by dividing the dataset into training and testing cohorts, typically in a 7:3 ratio [22]. The predictive performance of the model is assessed using Kaplan-Meier survival analysis, receiver operating characteristic (ROC) curves, principal component analysis (PCA), and decision curve analysis (DCA) [10] [22]. The model's independence from other clinical variables is evaluated through univariate and multivariate Cox regression analyses.
Figure 1: Workflow for Developing m6A-lncRNA Risk Signatures
Experimental Protocols for Signature Development
Bioinformatics Analysis Protocol
Objective: To identify m6A-related lncRNAs and construct a prognostic signature for cancer immunotherapy response prediction.
Materials and Software:
- RNA-seq data and clinical information from TCGA
- R statistical software (version 4.0.3 or higher)
- R packages: survival, glmnet, limma, clusterProfiler, ggplot2
- Cytoscape software (version 3.7.2 or higher) for network visualization
Procedure:
- Data Preprocessing:
- Download RNA-seq data (FPKM or TPM values), clinical information, and mutation data from TCGA.
- Annotate lncRNAs and mRNAs using Ensembl database or GENCODE.
- Filter samples with incomplete clinical information or survival data.
Identification of m6A-related lncRNAs:
- Compile a list of m6A regulators (writers, erasers, readers) from literature.
- Calculate correlation coefficients between lncRNA expression and m6A regulator expression.
- Apply filtering criteria (e.g., cor > 0.4 and P < 0.001) to identify m6A-related lncRNAs.
Prognostic Model Construction:
- Randomly divide dataset into training and validation cohorts (typically 70:30 ratio).
- Perform univariate Cox regression analysis on m6A-related lncRNAs in training cohort.
- Apply LASSO Cox regression to select the most prognostic lncRNAs.
- Conduct multivariate Cox regression to establish final model and calculate coefficients.
- Compute risk score for each patient using the formula: Risk Score = Σ(ExpressionlincRNA × CoefficientlincRNA).
Model Validation:
- Stratify patients into high-risk and low-risk groups based on median risk score.
- Perform Kaplan-Meier survival analysis with log-rank test.
- Generate time-dependent ROC curves to assess predictive accuracy.
- Conduct univariate and multivariate Cox regression to evaluate independence from other clinical variables.
Functional Analysis:
- Perform Gene Set Enrichment Analysis (GSEA) to identify signaling pathways.
- Analyze immune cell infiltration using CIBERSORT, EPIC, or other algorithms.
- Evaluate tumor mutation burden (TMB) and tumor immune dysfunction and exclusion (TIDE) scores.
In Vitro Validation Protocol
Objective: To functionally validate the oncogenic role of specific m6A-related lncRNAs identified in the signature.
Materials:
- Human cancer cell lines (e.g., A549 for lung cancer)
- Normal cell lines for comparison (e.g., 16-HBE for lung)
- Small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) for knockdown
- Quantitative real-time PCR equipment and reagents
- Transfection reagents
- Functional assay kits (proliferation, apoptosis, migration, invasion)
Procedure:
- Cell Culture and Transfection:
- Maintain cancer cell lines and normal counterparts in appropriate media.
- Design and synthesize siRNAs targeting candidate lncRNAs.
- Transfect cells using lipid-based transfection reagents.
- Validate knockdown efficiency using qRT-PCR after 24-48 hours.
Functional Assays:
- Proliferation: Perform MTT or CCK-8 assays at 0, 24, 48, and 72 hours post-transfection.
- Apoptosis: Analyze using Annexin V-FITC/PI staining and flow cytometry.
- Migration and Invasion: Conduct Transwell assays with or without Matrigel coating.
- Drug Sensitivity: Treat transfected cells with chemotherapeutic agents (e.g., cisplatin) and measure IC50 values.
Mechanistic Studies:
- Subcellular fractionation to determine lncRNA localization.
- RNA immunoprecipitation to identify binding proteins.
- Luciferase reporter assays to validate regulatory relationships.
Analytical Tools for Risk Model Assessment
Statistical Evaluation Methods
The validation of risk models requires multiple statistical approaches to ensure robustness and clinical applicability. Key methods include:
Survival Analysis: Kaplan-Meier curves with log-rank tests are used to compare overall survival between high-risk and low-risk groups. In LUAD, this analysis revealed a marked divergence in overall survival between risk groups, substantiating the prognostic utility of the m6ARLSig signature [10].
ROC Analysis: Time-dependent receiver operating characteristic curves assess the predictive sensitivity and specificity of the risk signature. For the HNSCC nine-lncRNA signature, the 5-year AUC value was 0.774 in the training set, 0.740 in the validation set, and 0.731 in the entire set, indicating high predictive accuracy [22].
Principal Component Analysis (PCA): PCA is employed to visualize the distribution pattern of patients based on different gene sets. Studies have shown that while the distributions of whole gene expression profiles and m6A genes between high- and low-risk groups were relatively scattered, the m6A-related lncRNAs in the signature showed clear separation between risk groups [22].
Decision Curve Analysis (DCA): DCA evaluates the clinical utility of the risk model by quantifying the net benefits at different threshold probabilities, allowing comparison with traditional clinical features [22].
Table 2: Performance Metrics of m6A-lncRNA Risk Signatures Across Cancers
| Cancer Type | Signature Size | Statistical Method | AUC (5-Year) | P-value (Survival) | Reference |
|---|---|---|---|---|---|
| HNSCC | 9 lncRNAs | ROC Analysis | 0.731 (entire set) | <0.001 | [22] |
| LUAD | 8 lncRNAs | Kaplan-Meier | Not specified | Significant divergence | [10] |
| Cervical Cancer | 4 lncRNAs | Multivariate Cox | Independent predictor | <0.001 | [12] |
| ESCC | 10 lncRNAs | LASSO-Cox | Validated in GEO | Independent predictor | [6] |
Clinical Application Framework
The transition of risk signatures from computational tools to clinical applications requires additional validation steps:
Nomogram Development: Integrate the risk signature with clinical parameters (age, tumor stage, etc.) to create a quantitative tool for predicting individual patient survival probability. For LUAD, a nomogram incorporating m6ARLSig and clinicopathological parameters was developed, providing a clinically adaptable tool for survival probability estimation [10].
Immunotherapeutic Response Prediction: Evaluate the correlation between risk scores and immune checkpoint inhibitor response. In ESCC, patients with low RiskScore showed enhanced expression of most immune checkpoint genes and were more likely to benefit from immune checkpoint inhibitor treatment [6].
Drug Sensitivity Analysis: Compare IC50 values of chemotherapeutic drugs and targeted therapies between risk groups. In HNSCC, the risk model was used to evaluate the sensitivity of various novel compounds for clinical treatment [22].
Figure 2: Clinical Implications of Risk Stratification Based on m6A-lncRNA Signatures
Table 3: Key Research Reagent Solutions for m6A-lncRNA Studies
| Reagent/Resource | Function/Application | Specifications | Example Sources |
|---|---|---|---|
| TCGA Datasets | Provides RNA-seq and clinical data for model development | Various cancer types, standardized processing | The Cancer Genome Atlas |
| Cell Lines | In vitro validation of lncRNA function | A549 (lung), other cancer-specific lines | ATCC, commercial vendors |
| siRNA/shRNA | Knockdown of candidate lncRNAs | Sequence-specific, validated efficiency | Commercial synthesis services |
| CIBERSORT Algorithm | Immune cell infiltration analysis | LM22 reference matrix, requires specific input format | https://cibersort.stanford.edu/ |
| R Statistical Packages | Data analysis and visualization | survival, glmnet, limma, clusterProfiler | Comprehensive R Archive Network |
| Cytoscape Software | Network visualization and analysis | Version 3.7.2 or higher, with plugins | http://www.cytoscape.org/ |
| TIDE Algorithm | Immunotherapy response prediction | Web-based or standalone implementation | http://tide.dfci.harvard.edu/ |
Risk score calculation and patient stratification methodologies based on m6A-related lncRNA signatures represent a powerful approach for predicting cancer prognosis and immunotherapy response. The standardized workflow involving data acquisition, lncRNA identification, model construction, and validation provides a robust framework for translating molecular signatures into clinically useful tools. The integration of these computational approaches with functional validation experiments creates a comprehensive strategy for advancing personalized cancer immunotherapy. As research in this field progresses, these methodologies are expected to become increasingly refined, potentially incorporating additional molecular features and clinical parameters to enhance predictive accuracy and clinical utility.
Comprehensive Model Validation in Training and Testing Cohorts
Within the broader research on m6A-related lncRNA signatures for predicting immunotherapy response, the phase of comprehensive model validation is a critical determinant of clinical translatability. A prognostic signature's value is not determined by its performance on a single dataset but by its robustness and generalizability across multiple, independent patient cohorts. This document outlines detailed application notes and protocols for establishing a rigorous validation framework, ensuring that developed models provide reliable and clinically actionable insights.
The process involves distinct stages: initially, data is partitioned into training and testing cohorts to build and preliminarily assess the model. Subsequently, external validation using completely independent datasets from different institutions or studies is essential to confirm generalizability. Furthermore, multi-cohort validation strategies, which integrate data from several sources during the model development phase, are increasingly recognized for producing more robust and stable predictive tools [49]. This protocol synthesizes best practices from recent studies on m6A-related lncRNA signatures in cancer [10] [50] [19] and machine learning applications in biomedicine [51] [52] [49].
Performance Metrics for Model Validation
Table 1: Key Quantitative Metrics for Prognostic Model Validation
| Metric Category | Specific Metric | Interpretation and Validation Role |
|---|---|---|
| Predictive Accuracy | Area Under the Curve (AUC) of Receiver Operating Characteristic (ROC) | Evaluates the model's ability to distinguish between risk groups (e.g., high-risk vs. low-risk) over time. AUC values of 0.7-0.8 are considered acceptable, 0.8-0.9 excellent, and >0.9 outstanding [50] [51]. |
| Time-Dependent AUC (e.g., 1-, 3-, 5-year) | Assesses accuracy at specific clinical timepoints, crucial for prognostic survival models [50]. | |
| Prognostic Separation | Kaplan-Meier Survival Analysis with Log-Rank Test | Visually and statistically compares the survival curves between risk groups. A significant log-rank p-value (<0.05) indicates strong prognostic separation [10] [50] [19]. |
| Hazard Ratio (HR) | Quantifies the magnitude of difference in risk between groups. An HR > 1 with a 95% Confidence Interval (CI) not crossing 1 indicates a significant independent prognostic factor [10] [51]. | |
| Model Robustness & Calibration | Concordance Index (C-index) | Measures the model's ability to provide a concordant prognostic ranking for all pairs of patients; commonly used for survival data. A C-index of 0.5 is random, 0.7 is good [49]. |
| Calibration Plot | Graphs the relationship between predicted probabilities and observed outcomes. A slope close to 1 indicates good calibration [10]. | |
| Clinical Utility | Nomogram | Provides a user-friendly graphical tool for clinicians to calculate an individual patient's probability of survival or response based on the model [10] [50] [19]. |
| Decision Curve Analysis (DCA) | Evaluates the net clinical benefit of using the model for decision-making across different risk thresholds. |
Table 2: Example Performance of Validated m6A-Related lncRNA Signatures in Oncology
| Cancer Type | Signature Composition | Training Cohort Performance | Testing/Validation Cohort Performance | Primary Clinical Endpoint |
|---|---|---|---|---|
| Lung Adenocarcinoma (LUAD) [10] | 8-lncRNA signature (m6ARLSig) | Developed from TCGA (n=480). Multivariate Cox confirmed independent prediction. | Risk score stratified patients into low/high-risk with significant OS divergence (p<0.001). | Overall Survival (OS) |
| Colorectal Cancer (CRC) [50] | 8-lncRNA signature | Constructed from TCGA data via LASSO-Cox. | AUC for 1, 3, 5-year OS: 0.753, 0.682, 0.706. High-risk group had poorer prognosis (p<0.05). | Overall Survival (OS) |
| Cervical Cancer [12] | 4-lncRNA signature (AL139035.1, AC015922.2, etc.) | Identified from TCGA. LASSO regression used for model construction. | Validated in a separate testing cohort. Signature was an independent prognostic predictor. | Overall Survival (OS) |
| Cervical Cancer [19] | 6-lncRNA signature (e.g., AC119427.1, FOXD1_AS1) | Prognostic signature developed from public datasets. | Nomogram (RiskScore + stage) accurately forecast OS. Low-risk group had more active immunotherapy response. | Overall Survival & Immunotherapy Response |
| Esophageal Squamous Cell Carcinoma [6] | 10 m6A/m5C-lncRNA signature (RiskScore) | Constructed from TCGA-ESCC cohort (n=81) via lasso Cox. | Validated in GEO dataset (GSE53622, n=120). Low-RiskScore group had better prognosis and higher immune cell abundance. | Overall Survival & Immunotherapy Response |
Experimental Protocols for Validation
Protocol 1: Cohort Partitioning and Internal Validation
Objective: To split the primary dataset into training and testing cohorts for initial model development and internal performance assessment.
Materials: Unified transcriptomic data (e.g., RNA-seq from TCGA) with matched clinical follow-up data.
Procedure:
- Data Preprocessing: Filter out genes with zero expression values in >80% of samples. For genes with multiple entries, calculate the average expression value across each sample [19]. Annotate and extract lncRNA expression profiles.
- Cohort Randomization: Randomly partition the entire dataset (e.g., TCGA-CESC) into a training cohort (typically 70%) and a testing cohort (30%). Ensure the partitioning is stratified by critical clinical variables (e.g., survival status, cancer stage) to maintain similar distribution of outcomes between the two sets [12].
- Model Construction in Training Cohort:
- Identify prognostic m6A-related lncRNAs via univariate Cox regression analysis (p < 0.05) [10].
- Apply Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression analysis to the training cohort to prevent overfitting and select the most robust lncRNAs for the signature [50] [12].
- Calculate the risk score for each patient using the formula:
Risk Score = Σ(coefficient(lncRNAi) × expression(lncRNAi))[10] [6].
- Internal Validation in Testing Cohort:
- Apply the model and risk score calculation formula derived from the training cohort to the held-out testing cohort.
- Stratify patients in the testing cohort into high- and low-risk groups using the median risk score from the training cohort as the cutoff.
- Perform Kaplan-Meier survival analysis with log-rank test to evaluate prognostic separation.
- Generate time-dependent ROC curves (e.g., 1, 3, 5-year) and calculate AUC values to assess predictive accuracy [50].
Protocol 2: External and Multi-Cohort Validation
Objective: To validate the prognostic model's generalizability using completely independent datasets and to enhance robustness through multi-cohort analysis.
Materials: Independent external datasets (e.g., from GEO or other consortiums), which may have been generated using different sequencing platforms or protocols.
Procedure:
- Dataset Acquisition: Source independent datasets with relevant transcriptomic and clinical data. For example, use the GEO database (e.g., GSE53622 for ESCC) for validation [6].
- Data Harmonization:
- Cross-Study Normalization: Address batch effects and platform-specific biases using normalization methods. Compare performance of normalized vs. unnormalized models to determine the optimal approach for the data [49].
- Model Application: Apply the exact same model (i.e., the same lncRNAs and their coefficients) to the external validation set. Do not re-train the model on this new data.
- Performance Assessment:
- Calculate risk scores for each patient in the external cohort and perform risk stratification.
- Evaluate prognostic separation via Kaplan-Meier curves and predictive accuracy via AUC, as in Protocol 1.
- Conduct multivariate Cox regression analysis that includes the risk score and key clinicopathological parameters (e.g., age, stage, grade) to confirm the risk score is an independent prognostic factor [10] [12].
- Multi-Cohort Validation (Advanced):
- Integrate several independent cohorts (e.g., NHANES, CHARLS, etc.) for model development and validation [52] [49].
- Use a "leave-one-cohort-out" approach: iteratively train the model on all but one cohort and validate on the held-out cohort.
- This strategy improves model stability, reduces cohort-specific biases, and increases the reliability of clinical predictions [49].
Protocol 3: Validation of Immunotherapy Response Prediction
Objective: To assess the model's utility in predicting response to immunotherapy, a key translational application.
Materials: Risk scores for patients, immunogenomic data (e.g., immune checkpoint gene expression), and (if available) immunotherapy response data.
Procedure:
- Immune Infiltration Analysis:
- Use algorithms such as CIBERSORT [10] [19], xCell [19], or ESTIMATE [19] to quantify the abundance of various immune cell types in the tumor microenvironment (TME) from transcriptomic data.
- Compare the immune infiltration scores between the high- and low-risk groups defined by the lncRNA signature using Wilcoxon tests [19].
- Immune Checkpoint Analysis:
- Immunotherapy Response Prediction:
- Utilize the Tumor Immune Dysfunction and Exclusion (TIDE) algorithm or similar frameworks to predict the likelihood of response to immune checkpoint blockade therapy in the high- and low-risk groups.
- Compare the predicted response rates or TIDE scores between the groups. A lower TIDE score in the low-risk group suggests a potentially better immunotherapy response [12] [6].
- Drug Sensitivity Prediction:
- Use R packages such as "pRRophetic" or data from the Genomics of Drug Sensitivity in Cancer (GDSC) to estimate the half-maximal inhibitory concentration (IC50) of common chemotherapeutic drugs or targeted therapies.
- Identify differential drug sensitivity between the risk groups, which can inform personalized treatment strategies [10] [19].
Workflow Visualization
Figure 1: Comprehensive Workflow for Model Validation in Training and Testing Cohorts. The process flows from internal validation, through external and multi-cohort validation, to functional and translational assessment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Resources for m6A-lncRNA Signature Research
| Resource Category | Specific Item / Tool | Function and Application Note |
|---|---|---|
| Data Resources | The Cancer Genome Atlas (TCGA) | Primary source for transcriptomic (RNA-seq) data and clinical data for various cancers for model development [10] [50] [19]. |
| Gene Expression Omnibus (GEO) | Repository for independent validation datasets. Use the GEOquery package in R for data acquisition [6]. | |
| FerrDB Database | Source for ferroptosis-related genes, used in multi-modal signature studies [19] [53]. | |
| Computational Tools & Algorithms | R Statistical Software | Core platform for data analysis, model construction (using 'survival', 'glmnet' packages), and visualization [10] [19]. |
| CIBERSORT/xCell/ESTIMATE | Algorithms for deconvoluting transcriptomic data to infer immune cell infiltration in the tumor microenvironment [10] [19]. | |
| TIDE (Tumor Immune Dysfunction and Exclusion) | Computational framework to model tumor immune evasion and predict response to checkpoint inhibitors [12] [6]. | |
| Wet-Lab Validation Reagents | A549 and A549/DDP cell lines | Human lung adenocarcinoma and cisplatin-resistant derivative cell lines for functional validation of lncRNAs (e.g., proliferation, invasion, drug resistance assays) [10]. |
| Specific siRNAs or shRNAs | For knocking down the expression of target lncRNAs (e.g., FAM83A-AS1) to investigate their oncogenic functions in vitro [10]. | |
| qPCR Reagents | For quantitative PCR validation of the expression levels of signature lncRNAs in clinical samples or cell lines [19] [53]. |
Prognostic prediction is a critical component of oncology research and clinical practice, enabling risk stratification and personalized treatment planning. The integration of molecular biomarkers with established clinical parameters has revolutionized survival prediction models, particularly through the development of nomograms that provide individualized probabilistic estimates. Within this context, m6A-related long non-coding RNAs (lncRNAs) have emerged as powerful prognostic biomarkers across various cancers, reflecting the essential role of epigenetic regulation in tumor progression and therapeutic response [10] [12] [54].
This protocol outlines the methodology for constructing nomograms that integrate m6A-related lncRNA signatures with standard clinical parameters to predict survival outcomes in cancer patients. The approach leverages computational biology, statistical modeling, and clinical validation to create tools that outperform traditional staging systems, ultimately supporting clinical decision-making for researchers, scientists, and drug development professionals working in immuno-oncology [55] [54].
Key m6A-Related lncRNA Signatures in Cancer Prognosis
Research across multiple malignancies has established that m6A-related lncRNA signatures provide significant prognostic value beyond conventional clinical parameters. The table below summarizes validated signatures from recent studies:
Table 1: Validated m6A-related lncRNA Signatures in Various Cancers
| Cancer Type | Number of lncRNAs in Signature | Risk Model Performance | Clinical Utility | Citation |
|---|---|---|---|---|
| Lung Adenocarcinoma (LUAD) | 8 | Independent prognostic predictor; Significant survival divergence between risk groups | Predicts immune cell infiltration and therapeutic response; Associated with cisplatin resistance | [10] |
| Cervical Cancer | 4 | Independent prognostic predictor | Predicts immunotherapy response and drug sensitivity | [12] |
| Hepatocellular Carcinoma (HCC) | 14 | C-index: 0.65-0.72; Superior to TP53 mutation or TMB alone | Stratifies survival and predicts sorafenib and immunotherapy responses | [54] |
| Esophageal Squamous Cell Carcinoma (ESCC) | 10 | Effectively stratifies patients into distinct risk categories | Predicts immune microenvironment and immunotherapy benefit | [6] |
| Cervical Cancer (m6A/ferroptosis-related) | 6 | High performance in prognosis prediction | Forecasts treatment response; Validated in clinical samples | [19] |
These signatures consistently demonstrate that patients classified as high-risk exhibit significantly poorer overall survival compared to low-risk patients across cancer types, establishing their fundamental prognostic value [10] [12] [54].
Computational Methodology for Signature Development
Data Acquisition and Preprocessing
The foundation of robust nomogram construction begins with comprehensive data collection and processing:
- Data Sources: Utilize public repositories including The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO), and other cancer genomics databases [10] [6] [54].
- RNA-seq Data Processing: Convert raw sequencing data to transcripts per million (TPM) or fragments per kilobase million (FPKM) values for normalization. Filter out genes with expression values of zero in >80% of samples [54] [19].
- Clinical Data Integration: Merge molecular data with comprehensive clinical information including survival time, survival status, age, gender, TNM stage, and tumor grade [10] [55].
- m6A Regulator Compilation: Compile known m6A regulators (typically 23 genes) categorized as "writers" (METTL3, METTL14, WTAP, etc.), "erasers" (FTO, ALKBH5), and "readers" (YTHDF family, IGF2BPs, HNRNPs) [10] [54] [19].
Identification of m6A-Related lncRNAs
The correlation-based identification of m6A-related lncRNAs follows a systematic approach:
- Correlation Analysis: Calculate correlation coefficients (Pearson or Spearman) between lncRNA expression and m6A regulator expression profiles [6] [54].
- Significance Thresholding: Apply statistical thresholds (typically |R| > 0.4-0.6 and p < 0.001) to identify significantly correlated lncRNA-m6A pairs [6] [54].
- LncRNA Annotation: Use human reference genome GTF annotation files to classify RNA molecules, retaining only those annotated as lncRNAs for further analysis [19].
Prognostic Signature Construction
The development of the m6A-related lncRNA prognostic signature employs rigorous statistical approaches:
- Univariate Cox Regression: Identify lncRNAs significantly associated with overall survival (p < 0.05) [10] [54].
- LASSO-Penalized Cox Regression: Apply least absolute shrinkage and selection operator (LASSO) regression to prevent overfitting and select the most prognostic lncRNAs [12] [54] [56].
- Risk Score Calculation: Compute risk scores using the formula: Risk Score = Σ(coefficient(lncRNAi) × expression(lncRNAi)) [10] [54].
- Risk Stratification: Dichotomize patients into high-risk and low-risk groups using median risk score or optimal cut-off value determined by survival analysis [10] [12] [54].
Table 2: Statistical Methods for Prognostic Model Development
| Analytical Step | Primary Method | Software/Tools | Key Parameters |
|---|---|---|---|
| Survival Analysis | Cox Proportional Hazards Regression | R survival package | Hazard ratios, confidence intervals |
| Variable Selection | LASSO Regression | R glmnet package | λ value determined by cross-validation |
| Model Validation | ROC Analysis | R timeROC package | AUC for 1-, 3-, 5-year survival |
| Group Stratification | Kaplan-Meier Analysis | R survminer package | Log-rank test p-value |
Nomogram Construction Protocol
Integration of Clinical Parameters
The nomogram integrates the m6A-related lncRNA signature with established clinical prognostic factors:
- Variable Selection: Include clinically relevant parameters such as age, TNM stage, tumor grade, and treatment history alongside the lncRNA risk score [55] [12] [54].
- Multivariate Cox Regression: Confirm independent prognostic value of each variable through multivariate analysis [10] [55].
- Proportional Hazards Assumption: Verify that all included variables satisfy the proportional hazards assumption required for Cox modeling.
Nomogram Development
The practical construction of the nomogram utilizes specialized statistical packages:
- R Package Implementation: Employ the 'rms' (regression modeling strategies) package in R to construct the nomogram [57] [54].
- Scale Definition: Assign point scales for each variable based on their relative contribution to the prognostic model, with total points corresponding to prediction outcomes [57].
- Survival Probability Functions: Incorporate survival functions for 1-, 3-, and 5-year overall survival using the
Survival()function from thermspackage [57] [54].
Model Validation
Comprehensive validation ensures the nomogram's reliability and clinical applicability:
- Discrimination: Evaluate using Harrell's concordance index (C-index) or time-dependent receiver operating characteristic (ROC) curves [55] [54] [56].
- Calibration: Assess agreement between predicted and observed outcomes using calibration plots [55] [58] [59].
- Clinical Utility: Perform decision curve analysis (DCA) to evaluate net benefit across threshold probabilities [56].
Research Reagent Solutions
Table 3: Essential Research Reagents and Resources for m6A-related lncRNA Studies
| Reagent/Resource | Specification | Application | Example Sources |
|---|---|---|---|
| TCGA Datasets | RNA-seq data and clinical information | Primary data for signature development | TCGA Portal [10] [54] |
| Cell Lines | A549, 16-HBE, cancer-specific lines | Functional validation of lncRNAs | ATCC, Chinese Academy of Sciences [10] |
| siRNA/shRNA | Sequence-specific knockdown constructs | Functional investigation of lncRNAs | Commercial suppliers [10] |
| R Statistical Software | Version 4.0 or higher | Data analysis and model construction | R Project [57] |
| R Packages | survival, rms, glmnet, ggplot2 | Specific analytical procedures | CRAN Repository [57] [54] |
| CIBERSORT | Leukocyte deconvolution algorithm | Immune infiltration analysis | https://cibersort.stanford.edu/ [10] |
Workflow Visualization
The following diagram illustrates the complete workflow for nomogram development and application:
Functional Validation Protocols
In Vitro Investigation of m6A-related lncRNAs
Experimental validation of identified lncRNAs follows established molecular biology protocols:
- Gene Knockdown: Implement siRNA or shRNA-mediated knockdown of target lncRNAs in cancer cell lines (e.g., A549 for lung cancer) [10].
- Phenotypic Assays: Evaluate functional consequences through:
- Proliferation: CCK-8, MTT, or colony formation assays
- Apoptosis: Annexin V/PI staining with flow cytometry
- Migration/Invasion: Transwell and wound healing assays
- Drug Resistance: IC50 determination for chemotherapeutic agents (e.g., cisplatin) [10]
- Mechanistic Studies: Investigate molecular mechanisms through RNA immunoprecipitation (RIP), RNA-protein pull-down, and luciferase reporter assays to identify interacting partners and regulatory networks.
Immunotherapy Response Assessment
The predictive value for immunotherapy response can be evaluated through:
- Immune Cell Infiltration: Quantify immune cell populations using CIBERSORT, xCell, or ESTIMATE algorithms [10] [54] [19].
- Immune Checkpoint Analysis: Examine expression of PD-1, PD-L1, CTLA-4, and other checkpoint molecules across risk groups [6] [54].
- Immunophenoscore (IPS): Utilize IPS as a predictor of response to immune checkpoint inhibitors [54].
- Drug Sensitivity Prediction: Apply R package "pRRophetic" to estimate IC50 values for various chemotherapeutic and targeted agents [54].
The integration of m6A-related lncRNA signatures with clinical parameters through nomogram construction provides a powerful approach for personalized survival prediction in cancer patients. This protocol outlines a comprehensive framework spanning computational analysis, statistical modeling, and experimental validation to develop clinically applicable prognostic tools. As research in epitranscriptomics advances, these integrated models will play an increasingly important role in stratifying patients for tailored immunotherapy approaches and optimizing therapeutic outcomes in oncology.
Practical Application in Treatment Decision-Making and Patient Stratification
m6A-related long non-coding RNA (lncRNA) signatures are emerging as powerful tools in clinical oncology, enabling refined patient stratification and prediction of immunotherapy responses. These signatures, derived from the interplay between RNA methylation and lncRNA function, provide critical insights into tumor microenvironment (TME) composition and therapeutic vulnerabilities. This protocol details the methodology for implementing an m6A-related lncRNA signature framework to guide treatment decisions, with particular emphasis on predicting response to immune checkpoint inhibitors (ICIs) across multiple cancer types, including lung adenocarcinoma (LUAD), head and neck squamous cell carcinoma (HNSCC), and cervical cancer.
The N6-methyladenosine (m6A) modification represents the most abundant internal RNA modification in eukaryotic cells, dynamically regulating RNA processing, stability, translation, and degradation. This modification is orchestrated by three classes of regulators: "writer" methyltransferases (e.g., METTL3/14, WTAP), "eraser" demethylases (FTO, ALKBH5), and "reader" binding proteins (YTHDF1-3, IGF2BP1-3) that recognize m6A marks [10] [60].
Long non-coding RNAs (lncRNAs) are transcripts longer than 200 nucleotides with limited protein-coding potential that regulate gene expression through diverse mechanisms. When modified by m6A, lncRNAs experience altered stability, localization, and function, ultimately influencing key cancer-related processes including proliferation, metastasis, drug resistance, and immune evasion [10] [61]. The integration of m6A and lncRNA biology provides a novel dimension for understanding cancer heterogeneity and developing precision medicine approaches.
Computational Framework for Signature Development
Data Acquisition and Preprocessing
- Data Sources: Obtain RNA-seq data and corresponding clinical information (including overall survival, disease stage, and treatment history) from public repositories such as The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO).
- Gene Annotation: Annotate the transcriptome data using reference databases (e.g., Ensembl) to distinguish lncRNAs from coding mRNAs.
- m6A Regulator List: Curate a comprehensive list of m6A regulators (typically 21-23 genes) from literature, including writers, erasers, and readers [60] [62].
Identification of m6A-Related lncRNAs
- Correlation Analysis: Calculate correlation coefficients (Pearson or Spearman) between the expression of all lncRNAs and each m6A regulator.
- Selection Threshold: Identify m6A-related lncRNAs using stringent thresholds (commonly |R| > 0.4 and p < 0.001) [22] [63]. This generates a co-expression network linking m6A regulators to functionally relevant lncRNAs.
Prognostic Model Construction
- Univariate Cox Regression: Identify m6A-related lncRNAs significantly associated with overall survival from the training cohort.
- LASSO-Penalized Cox Regression: Apply Least Absolute Shrinkage and Selection Operator (LASSO) regression to prevent overfitting and select the most robust prognostic lncRNAs.
Multivariate Cox Regression: Construct the final prognostic model and calculate risk scores using the formula:
Risk Score = Σ (Coefficienti × Expressioni)
where Coefficient_i represents the regression coefficient for each selected lncRNA, and Expression_i represents its normalized expression value [60] [22] [12].
Table 1: Representative m6A-Related lncRNA Signatures Across Cancers
| Cancer Type | Signature Components | Prognostic Value | Immunotherapy Prediction |
|---|---|---|---|
| Lung Adenocarcinoma (LUAD) | 8-12 lncRNAs (e.g., AL606489.1, COLCA1) [10] [60] | High-risk = poorer overall survival [10] | High-risk associated with immune-excluded phenotype [61] |
| Head and Neck Squamous Cell Carcinoma (HNSCC) | 9 lncRNAs (e.g., SNHG16, JPX) [22] | High-risk = shorter survival time (p < 0.001) [22] | High-risk linked to higher TIDE score, suggesting immunotherapy resistance [22] |
| Cervical Cancer | 4-6 lncRNAs (e.g., AC015922.2, FOXD1_AS1) [12] [19] | High-risk = independent poor prognostic factor [12] | Low-risk group shows enhanced response to anti-PD-1/L1 [19] |
| Gastric Cancer | 11 lncRNAs (e.g., LINC00454, LASTR) [63] | AUC for 5-year survival = 0.850 [63] | Low-risk group has higher immune infiltration and checkpoint expression [63] |
Patient Stratification
- Risk Score Calculation: Compute the risk score for each patient in the cohort using the established formula.
- Stratification Threshold: Dichotomize patients into high-risk and low-risk groups based on the median risk score or an optimized cut-off value determined from the training set.
- Validation: Confirm the prognostic performance of the signature in internal validation sets and external independent cohorts using Kaplan-Meier survival analysis and time-dependent receiver operating characteristic (ROC) curves.
Experimental Validation Protocols
In Vitro Functional Validation of Signature lncRNAs
This protocol uses the example of FAM83A-AS1, an m6A-related lncRNA identified as oncogenic in LUAD [10].
- Cell Culture: Maintain human LUAD cell lines (e.g., A549 and cisplatin-resistant A549/DDP) and normal bronchial epithelial cells (e.g., 16-HBE) in recommended media with 10% fetal bovine serum.
- Gene Knockdown:
- Design and synthesize small interfering RNAs (siRNAs) or short hairpin RNAs (shRNAs) targeting FAM83A-AS1.
- Transfect cells using appropriate transfection reagents (e.g., Lipofectamine RNAiMAX). Include non-targeting siRNA as a negative control.
- Phenotypic Assays:
- Proliferation: Assess using Cell Counting Kit-8 (CCK-8) or colony formation assays at 0, 24, 48, and 72 hours post-transfection.
- Apoptosis: Quantify using flow cytometry with Annexin V/propidium iodide staining 48 hours post-transfection.
- Migration/Invasion: Evaluate using Transwell assays with or without Matrigel coating, fixing and staining migrated cells after 24-48 hours.
- Drug Sensitivity: Treat transfected cells with a concentration gradient of chemotherapeutic agents (e.g., cisplatin) for 48-72 hours and calculate IC₅₀ values from dose-response curves.
- Mechanistic Studies:
- Analyze epithelial-mesenchymal transition (EMT) by measuring marker expression (E-cadherin, N-cadherin, Vimentin) via Western blot.
- Confirm m6A modification of the lncRNA using methylated RNA immunoprecipitation (MeRIP) with an anti-m6A antibody.
Diagram Title: m6A-lncRNA Signature Development and Application Workflow
Analysis of Tumor Immune Microenvironment
- Immune Cell Infiltration:
- Utilize computational tools (CIBERSORT, EPIC, xCell, MCP-counter, etc.) with RNA-seq data to estimate the abundance of various immune cell types in the TME of high-risk and low-risk patients [60] [61] [63].
- Compare immune cell infiltration patterns between risk groups using statistical tests (Wilcoxon rank-sum test).
- Immune Checkpoint Expression:
- Extract expression data of key immune checkpoint genes (PD-1, PD-L1, CTLA-4, LAG-3, etc.) from the transcriptomic dataset.
- Compare expression levels between risk groups and correlate with risk scores.
- Immunotherapy Response Prediction:
- Calculate Tumor Immune Dysfunction and Exclusion (TIDE) scores for each patient (http://tide.dfci.harvard.edu/). A lower TIDE score suggests a higher likelihood of responding to ICIs [22] [61].
- Evaluate Tumor Mutational Burden (TMB) from somatic mutation data. High TMB is often associated with better ICI response.
- Validate predictions using external immunotherapy cohorts (e.g., IMvigor210 for anti-PD-L1) when available [61] [62].
Table 2: Characteristic Features of High-Risk vs. Low-Risk Patient Groups
| Parameter | High-Risk Group | Low-Risk Group |
|---|---|---|
| Overall Survival | Significantly Shorter [10] [60] [22] | Significantly Longer [10] [60] [22] |
| TME Immune Infiltration | Generally "Cold"; Immunosuppressive [61] [62] | Generally "Hot"; Immunologically Active [61] [62] |
| Key Immune Features | Increased Tregs, Myeloid-derived suppressor cells (MDSCs); M2 Macrophage polarization [61] | Increased CD8+ T cells, NK cells, M1 Macrophages [61] [63] |
| Immune Checkpoint Expression | Variable, but often lower PD-L1 [61] | Often higher, but context-dependent [63] |
| Predicted ICI Response | Poor / Resistant [22] [61] | Favorable / Sensitive [61] [19] |
| Tumor Mutational Burden (TMB) | Lower in some studies [60] | Higher in some studies [60] |
| Drug Sensitivity (Examples) | More sensitive to certain chemotherapies (context-dependent) [10] | More sensitive to erlotinib, axitinib [61]; Sensitive to imatinib in cervical cancer [19] |
Clinical Application and Integration
Development of Clinical Decision Tools
- Nomogram Construction: Integrate the m6A-lncRNA risk score with standard clinical variables (age, stage, etc.) into a visual nomogram to provide a quantitative tool for predicting individual patient probability of 1-, 3-, and 5-year survival [10] [22].
- Drug Sensitivity Prediction (pRRophetic Algorithm):
- Use the R package "pRRophetic" to predict the half-maximal inhibitory concentration (IC₅₀) for a panel of chemotherapeutic and targeted drugs based on the tumor's gene expression profile.
- Compare IC₅₀ values between high-risk and low-risk groups to identify candidate therapeutics for each subgroup [60] [61] [19].
Diagram Title: m6A-lncRNA Mechanisms Influencing Cancer Immunotherapy
Therapeutic Implications and Patient Stratification Strategy
Based on the m6A-lncRNA risk stratification, distinct therapeutic pathways are recommended:
For Low-Risk Patients:
- Priority: Immune Checkpoint Inhibitors (anti-PD-1/PD-L1, anti-CTLA-4). These patients have an immune-inflamed TME, making them ideal candidates for immunotherapy [61] [64].
- Alternative/Combination: Consider combination with specific targeted therapies (e.g., erlotinib, axitinib) for which low-risk patients show increased sensitivity [61].
For High-Risk Patients:
- Challenge: Immunosuppressive, "cold" TME, suggesting inherent resistance to ICIs.
- Strategy: Focus on conventional therapies (chemotherapy, radiation) or investigate novel combinations aimed at converting "cold" tumors to "hot". This may include strategies to target the specific m6A-modified lncRNAs (e.g., using antisense oligonucleotides) or their downstream effectors [10] [22].
- Emerging Approach: Preclinical evidence suggests that targeting m6A regulators (e.g., with FTO or ALKBH5 inhibitors) can enhance ICI efficacy, presenting a potential combination strategy for this subgroup [64] [62].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for m6A-lncRNA Studies
| Reagent / Resource | Function / Application | Examples / Specifications |
|---|---|---|
| Public Data Repositories | Source of transcriptomic and clinical data for model development | TCGA (https://portal.gdc.cancer.gov/), GEO (https://www.ncbi.nlm.nih.gov/geo/) |
| Bioinformatics Tools | Immune deconvolution, pathway analysis, drug prediction | CIBERSORT, xCell, ESTIMATE, GSVA, GSEA, pRRophetic R package |
| Cell Lines | In vitro functional validation of signature lncRNAs | A549 (LUAD), A549/DDP (cisplatin-resistant), 16-HBE (normal control) [10] |
| siRNAs/shRNAs | Knockdown of target lncRNAs to study function | ON-TARGETplus siRNA, Mission shRNA (Sigma-Aldrich) |
| qPCR Reagents | Validation of lncRNA expression levels | iTaq Universal SYBR Green Supermix (Bio-Rad), TaqMan assays |
| m6A-Specific Antibodies | Confirmation of m6A modification on RNA | Anti-m6A antibody for MeRIP (Merck Millipore, Abcam) |
| Flow Cytometry Antibodies | Analysis of apoptosis and immune cell markers | Annexin V/PI kits, Anti-CD3, CD8, CD4, CD45, etc. (BioLegend, BD Biosciences) |
| In Vivo Models | Preclinical validation of therapeutic strategies | Patient-derived xenografts (PDX), syngeneic mouse models |
The stratification of cancer patients using m6A-related lncRNA signatures provides a robust, biologically grounded framework for personalizing therapy. This approach effectively predicts prognosis and response to immunotherapy, thereby addressing a critical challenge in medical oncology. The outlined protocols for computational modeling and experimental validation provide a comprehensive roadmap for researchers and clinicians to implement this strategy, with the ultimate goal of improving patient outcomes by matching the right therapy to the right patient. Future work will focus on standardizing these signatures across platforms and prospectively validating them in clinical trials.
Addressing Analytical Challenges and Enhancing Predictive Performance
Optimizing Correlation Coefficients and Statistical Thresholds for lncRNA Identification
Within the expanding field of cancer research, the identification of m6A-related long non-coding RNAs (lncRNAs) has emerged as a crucial area of investigation for predicting immunotherapy response. The efficacy of this research is fundamentally dependent on the initial, critical step of accurately identifying these lncRNAs from complex transcriptomic data. This protocol details a standardized methodology for optimizing the key statistical parameters—specifically, correlation coefficients and statistical thresholds—to ensure the robust and reproducible discovery of m6A-related lncRNAs. The procedures outlined herein are designed to be integrated into a broader research workflow aimed at constructing prognostic signatures that can forecast patient survival and response to immune checkpoint inhibitors in various cancers.
Application Notes: Core Principles and Parameter Optimization
Definition and Rationale for Key Statistical Parameters
The accurate identification of m6A-related lncRNAs relies on establishing a statistically significant co-expression relationship between lncRNAs and known m6A regulators. The following parameters are fundamental:
- Correlation Coefficient (|R|): This metric quantifies the strength and direction of the linear relationship between the expression levels of a lncRNA and an m6A regulator. A higher absolute value indicates a stronger relationship. The choice of threshold balances discovery sensitivity with specificity.
- P-value: This metric determines the statistical significance of the observed correlation. A low p-value (typically < 0.05) indicates that the observed correlation is unlikely to be due to random chance.
- False Discovery Rate (FDR): When testing thousands of lncRNAs simultaneously, the FDR correction (e.g., Benjamini-Hochberg procedure) controls for the expected proportion of false positives among the identified significant correlations. An FDR < 0.05 is a standard stringency level.
The table below summarizes the correlation and significance thresholds successfully employed in recent cancer studies for identifying m6A-related lncRNAs, serving as a practical reference for parameter selection.
Table 1: Empirical Statistical Thresholds for m6A-related lncRNA Identification from Published Studies
| Cancer Type | Correlation Coefficient (|R|) | Statistical Significance (P-value) | Primary Analysis Goal | Citation |
|---|---|---|---|---|
| Lung Adenocarcinoma (LUAD) | Not Specified | P < 0.05 (Correlation Test) | Prognostic Signature | [10] |
| Breast Cancer (BC) | |R| > 0.3 | P < 0.001 | Prognostic Signature & Immune Infiltration | [65] |
| Papillary Renal Cell Carcinoma (pRCC) | |R| > 0.4 | P < 0.001 | Prognostic Model & Immunotherapy Response | [66] |
| Colorectal Cancer (CRC) | |R| > 0.2 | P < 0.05 | Signature for Progression-Free Survival | [67] |
Protocol for Determining m6A-related lncRNAs
The following workflow outlines the step-by-step process for identifying m6A-related lncRNAs from public transcriptomic databases, such as The Cancer Genome Atlas (TCGA).
Procedure:
- Data Acquisition: Download RNA-seq transcriptome data (e.g., in FPKM or TPM format) and corresponding clinical data for your cancer of interest from a repository like TCGA.
- LncRNA Annotation: Filter the transcriptome data to separate lncRNAs from coding genes. This is typically done using an annotation file from sources like GENCODE. As described in one protocol, "the final assembled transcripts were compared with the reference gene, and the fragments that were roughly identical to the known transcripts were removed" to isolate novel and known lncRNAs [68].
- Define m6A Regulators: Compile a list of established m6A regulator genes. These are categorized as writers (e.g., METTL3, METTL14, WTAP), erasers (e.g., FTO, ALKBH5), and readers (e.g., YTHDF1, YTHDC1, IGF2BP1-3). A set of 20-23 regulators is commonly used [65] [67].
- Correlation Analysis: Perform a pairwise correlation analysis (e.g., Pearson correlation) between the expression levels of all annotated lncRNAs and each m6A regulator across the patient samples.
- Apply Statistical Thresholds: Filter the results based on pre-defined correlation coefficient (|R|) and p-value thresholds. For instance, a study on breast cancer applied |R| > 0.3 and p < 0.001 to define m6A-related lncRNAs [65]. The optimal threshold can be adjusted based on the initial results and the desired balance between the number of identified lncRNAs and the confidence of the association.
- Output: Generate a final list of lncRNAs that meet the specified criteria for use in subsequent prognostic model construction and immunotherapy response analysis.
Advanced Computational and Experimental Validation
Advanced Correlation Methodologies
Beyond simple Pearson correlation, more sophisticated methods can be employed to refine the identification process.
- Heuristic Correlation Optimization: Methods like ImReLnc integrate both direct correlation coefficients and partial correlation coefficients using a logistic function. This approach accounts for both direct and indirect relationships within the complex regulatory network, providing a more robust ranking score for immune-related enrichment analysis [69].
- Integration with ceRNA Networks: LncRNAs can be identified within a competitive endogenous RNA (ceRNA) network. In this context, correlations are also assessed between lncRNAs and microRNAs (miRNAs), with a threshold such as |R| > 0.3 and a significance of P < 0.05 used to define regulatory pairs in cancers like lung squamous cell carcinoma [70].
Protocol for Experimental Validation of Identified lncRNAs
Computational identification must be followed by experimental validation to confirm both the expression and functional role of candidate m6A-related lncRNAs.
Table 2: Key Research Reagent Solutions for Experimental Validation
| Reagent / Material | Function / Application | Example Protocol Details |
|---|---|---|
| Specific siRNAs | Gene knockdown to assess functional impact of lncRNA. | Transfect into human cancer cell lines (e.g., pRCC) using lipid-based transfection reagents [66]. |
| qRT-PCR Assays | Quantify lncRNA expression in patient tissues and cell lines. | Use SYBR Green Master Mix on a real-time PCR system; primers designed for target lncRNAs [65] [67]. |
| CCK-8 Assay | Measure cell proliferation after lncRNA knockdown. | Incubate cells with CCK-8 reagent and measure absorbance at 450nm to assess viability [66]. |
| Transwell Assays | Evaluate cell migration and invasion capabilities. | Seed transfected cells in upper chamber; count cells that migrate through membrane [66]. |
| Immunohistochemistry (IHC) | Validate protein expression of m6A regulators and immune markers. | Stain tissue sections with primary antibodies (e.g., anti-METTL3); detect with HRP-conjugated secondary antibodies [65]. |
Procedure:
Expression Validation:
- Tissue Samples: Collect paired tumor and adjacent normal tissues from patients (e.g., 55 CRC patients as in one study [67]). Total RNA is extracted using Trizol reagent.
- qRT-PCR: Synthesize cDNA and perform quantitative real-time PCR using gene-specific primers for the target lncRNAs. Normalize expression to an internal control (e.g., GAPDH). An up-regulation in tumors compared to normal tissues validates the computational finding [67].
Functional Assays (In Vitro):
- Cell Culture: Use relevant human cancer cell lines (e.g., A549 for LUAD, pRCC cell lines).
- Gene Knockdown: Transfert cells with specific small interfering RNAs (siRNAs) targeting the lncRNA of interest. A non-targeting siRNA serves as a negative control.
- Phenotypic Assessment:
- Proliferation: Use the CCK-8 assay to measure cell viability at 24, 48, and 72 hours post-transfection [66].
- Migration and Invasion: Perform Transwell assays with or without Matrigel coating. Count the number of cells that migrate through the membrane after a set incubation period [66].
- Apoptosis and Drug Resistance: Assess apoptosis via flow cytometry (Annexin V staining). To study drug resistance, treat transfected cells with chemotherapeutic agents like cisplatin and measure IC50 values, as demonstrated with FAM83A-AS1 in A549/DDP cells [10].
Integration with Immunotherapy Response Prediction
The ultimate application of identifying m6A-related lncRNAs lies in predicting immunotherapy response. The validated lncRNAs are incorporated into a multi-step analytical pipeline.
Protocol for Constructing a Prognostic Immunotherapy Signature
Procedure:
- Prognostic lncRNA Selection: From the list of validated m6A-related lncRNAs, perform univariate Cox regression analysis on patient survival data (Overall Survival or Progression-Free Survival) to identify lncRNAs significantly associated with outcome.
- Signature Construction: Use LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression to further refine the lncRNA set and prevent overfitting. This yields a minimal set of genes with the strongest prognostic power, as demonstrated in studies identifying 4-8 lncRNA signatures [12] [66].
- Risk Model Calculation: Calculate a risk score for each patient using a formula based on the lncRNA expression levels weighted by their regression coefficients. For example:
Risk score = (coefficient_lncRNA1 × expression_lncRNA1) + (coefficient_lncRNA2 × expression_lncRNA2) + ...[10] [65]. Stratify patients into high-risk and low-risk groups based on the median risk score. - Immune Context Evaluation:
- Immune Infiltration: Analyze differences in immune cell infiltration between risk groups using tools like CIBERSORT, which deconvolutes transcriptome data to estimate abundances of 22 immune cell types [10] [66]. Studies consistently show significant differences in macrophages and T-cell subsets between risk groups.
- Immune Checkpoints: Compare the expression of key immune checkpoint inhibitor genes (e.g., PD-1, PD-L1, CTLA-4) between risk groups. High-risk scores are often associated with increased checkpoint expression [10] [12].
- Tumor Mutation Burden (TMB): Analyze TMB from genomic data. High-risk groups often correlate with higher TMB and specific mutations (e.g., SETD2 in pRCC), which can influence immunotherapy response [66].
- Drug Sensitivity: Predict IC50 values for common chemotherapeutic agents and targeted therapies between risk groups to guide treatment selection [10].
- Clinical Translation: Construct a nomogram that integrates the lncRNA risk score with standard clinicopathological variables (e.g., age, TNM stage) to provide a quantitative tool for clinicians to predict individual patient survival probability at 1, 3, and 5 years [10] [66].
The precise optimization of correlation coefficients and statistical thresholds is a foundational step in the reliable identification of m6A-related lncRNAs. By adhering to the standardized protocols and validation workflows outlined in this document—from initial bioinformatic filtering with thresholds like |R| > 0.4 and p < 0.001 to rigorous functional assays—researchers can construct robust, clinically relevant prognostic signatures. These signatures not only elucidate the intricate mechanisms of cancer progression but also hold significant promise for enhancing the prediction of patient responses to immunotherapy, ultimately paving the way for more personalized and effective cancer treatments.
Managing Overfitting in Multivariate Models Through Regularization Techniques
In the development of multivariate prognostic models, such as those based on m6A-related lncRNA signatures for predicting immunotherapy response, a primary challenge is ensuring that the model generalizes effectively to new, unseen patient data. Overfitting occurs when a model learns the training data too well, including its noise and random fluctuations, leading to poor performance on validation or test datasets [71] [72]. This phenomenon is particularly prevalent in high-dimensional biological data where the number of features (e.g., expression levels of thousands of lncRNAs) can be large relative to the number of patient samples [10] [12]. An overfit model may appear to have perfect predictive power during training but fails to provide accurate prognostic stratification when applied to independent cohorts, severely limiting its clinical utility [72] [73].
The consequences of overfitting are far-reaching in translational research. In the context of m6A-related lncRNA signatures, which aim to forecast patient survival and treatment response, an overfit model could lead to incorrect identification of biomarker candidates, inaccurate risk stratification, and ultimately, misguided clinical decisions [10] [19]. The paradox of overfitting lies in the fact that increasingly complex models contain more information about the training data but less information about future testing data [72]. Therefore, managing model complexity through regularization techniques becomes indispensable for building robust, reliable prognostic tools that can truly inform personalized treatment strategies in oncology.
Theoretical Foundation of Regularization Techniques
The Bias-Variance Tradeoff
Regularization techniques are fundamentally grounded in the bias-variance tradeoff, a core concept in statistical learning theory. Bias refers to the error introduced when a real-world problem is approximated by a simplified model, while variance refers to the model's sensitivity to fluctuations in the training data [72] [73]. Complex models with numerous parameters typically have low bias but high variance, making them prone to overfitting. Conversely, simple models have high bias but low variance, which may lead to underfitting [72].
In multivariate prognostic modeling, the goal is to strike an optimal balance between bias and variance [74]. This balance ensures that the m6A-related lncRNA signature captures the true underlying biological relationships between RNA modifications and cancer outcomes without being unduly influenced by sample-specific noise [10] [12]. Regularization achieves this balance by adding constraints to the model's optimization process, explicitly controlling the tradeoff between fitting the training data well and maintaining model simplicity [71] [75].
Mathematical Formulation of Regularization
Regularization works by adding a penalty term to the loss function that the model minimizes during training. The general form of a regularized loss function can be represented as:
Loss = Loss_data + λ × Penalty
Where Loss_data is the original loss function (e.g., mean squared error for regression, log-loss for classification), λ is the regularization parameter that controls the strength of penalty, and Penalty is a function of the model coefficients that increases with their magnitude [71] [75]. This additional penalty term discourages the model from assigning excessively large values to coefficients, thereby controlling complexity and reducing overfitting [71].
Table 1: Comparison of Regularization Techniques in Multivariate Models
| Technique | Mathematical Formulation | Key Characteristics | Best Suited Scenarios |
|---|---|---|---|
| L1 (Lasso) | Loss + λ × Σ|w| | Promotes sparsity; performs feature selection | High-dimensional data with many irrelevant features [71] [76] |
| L2 (Ridge) | Loss + λ × Σw² | Shrinks coefficients evenly; retains all features | Correlated features; multicollinearity present [71] [75] |
| Elastic Net | Loss + λ₁ × Σ|w| + λ₂ × Σw² | Balance between L1 and L2 benefits | Many correlated features with some irrelevant ones [76] |
| Dropout | Randomly omits units during training | Prevents co-adaptation of features | Deep neural networks; complex architectures [74] [76] |
| Early Stopping | Stops training when validation performance degrades | Prevents overfitting without changing model | Iterative algorithms; neural networks [75] [76] |
Regularization Techniques: Principles and Applications
L1 Regularization (Lasso)
L1 regularization, also known as Lasso (Least Absolute Shrinkage and Selection Operator), adds a penalty equal to the absolute value of the magnitude of coefficients [71] [77]. This technique is particularly valuable in m6A-related lncRNA signature development because it performs automatic feature selection by driving less important coefficients to exactly zero [71] [76]. In practice, this means that from hundreds or thousands of potentially relevant lncRNAs, L1 regularization can identify a subset that most strongly contributes to prognostic prediction [71].
The mathematical formulation of L1 regularization for a linear model is: Loss = MSE + α × Σ|w| Where 'w' represents the model's coefficients, 'α' is the regularization strength, and MSE is the mean squared error [71]. A key advantage of L1 regularization in biomarker discovery is its ability to produce sparse models that are more interpretable for clinical researchers, as only the most relevant lncRNAs retain non-zero coefficients in the final model [71] [76].
L2 Regularization (Ridge)
L2 regularization, also known as Ridge regression, adds a penalty equal to the square of the magnitude of coefficients [71] [75]. Unlike L1 regularization, L2 does not force coefficients to exactly zero but rather shrinks them toward zero, with the degree of shrinkage controlled by the regularization parameter λ [75]. This approach is particularly beneficial when dealing with correlated features, a common scenario in transcriptomic data where lncRNAs may exhibit co-expression patterns [75].
In the context of m6A-related lncRNA signatures, L2 regularization helps to stabilize model predictions when multiple biologically relevant lncRNAs are moderately correlated [75]. By keeping all features in the model while reducing their collective variance, L2 regularization maintains the potential contribution of multiple related biomarkers while still mitigating overfitting [71] [75]. The L2 penalty is calculated as the sum of squared weights: L2 regularization = w₁² + w₂² + ... + wₙ² [75].
Advanced and Hybrid Techniques
Elastic Net regularization combines the penalties of both L1 and L2 methods, offering a balanced approach that benefits from both feature selection (L1) and handling of correlated variables (L2) [76]. This hybrid technique is particularly advantageous in m6A-lncRNA research where both irrelevant features and correlated relevant features are likely present [76].
Dropout is a regularization technique specifically designed for neural networks, which randomly drops units (along with their connections) from the network during training [74] [76]. This prevents units from co-adapting too much and forces the network to learn more robust features that are useful in combination with many different random subsets of other units [74].
Early Stopping is a simple yet effective form of regularization that monitors the model's performance on a validation set during training and halts the training process when performance begins to degrade [75] [76]. This approach prevents the model from over-optimizing on the training data and is particularly useful for complex models like deep neural networks that have high capacity for memorization [75].
Experimental Protocols for Regularization Implementation
Protocol 1: Implementing Regularized Cox Regression for Survival Analysis
Purpose: To develop a prognostic m6A-related lncRNA signature for predicting overall survival in cancer patients while controlling for overfitting.
Materials and Reagents:
- Computational Environment: R Statistical Software (v4.0.3+) or Python (v3.8+)
- Bioinformatic Packages: R 'glmnet' package for Lasso/Cox regression or Python 'scikit-survival'
- Data: Processed lncRNA expression matrix from RNA-seq data (e.g., TCGA-CESC, TCGA-LUAD)
- Clinical Data: Annotated survival data (overall survival time, vital status)
Procedure:
- Data Preprocessing: Normalize lncRNA expression data using variance stabilizing transformation or TPM normalization. Remove lncRNAs with zero expression in >80% of samples [10] [12].
- Training-Test Split: Randomly partition the dataset into training (70%) and test (30%) cohorts, ensuring balanced distribution of clinical characteristics [12].
- Feature Preselection: Perform univariate Cox regression on training data to identify lncRNAs with p<0.05 for further analysis [10].
- Regularization Parameter Tuning:
- Implement k-fold cross-validation (typically k=10) on the training set
- Evaluate a range of λ values (e.g., 10^-5 to 10^1 on logarithmic scale)
- Select the λ value that minimizes the partial likelihood deviance [10]
- Model Training: Fit a regularized Cox proportional hazards model using the optimal λ on the entire training set.
- Risk Score Calculation: For each patient, compute risk score using the formula: Risk score = Σ(coefficient(lncRNAi) × expression(lncRNAi))
- Model Validation:
Protocol 2: Cross-Validation Framework for Model Selection
Purpose: To objectively evaluate model performance and select optimal regularization parameters without overfitting.
Procedure:
- Stratified k-Fold Setup: Divide the dataset into k folds (typically k=5 or k-10), preserving the event rate proportion in each fold [74].
- Iterative Validation:
- For each fold iteration:
- Designate one fold as validation set and remaining k-1 folds as training set
- Train regularized models with varying hyperparameters on training set
- Evaluate model performance on the validation set
- Repeat until each fold has served as the validation set [74]
- For each fold iteration:
- Performance Aggregation: Calculate average performance metrics across all folds for each hyperparameter setting.
- Hyperparameter Selection: Choose the hyperparameter values that yield the best average performance.
- Final Model Training: Train the model with selected hyperparameters on the entire dataset.
Table 2: Research Reagent Solutions for m6A-related lncRNA Signature Development
| Reagent/Resource | Function | Example Sources/Platforms |
|---|---|---|
| TCGA Data Portal | Provides RNA-seq data and clinical annotations for cancer patients | The Cancer Genome Atlas [10] [12] |
| CIBERSORT Tool | Quantifies immune cell infiltration from expression data | https://cibersort.stanford.edu/ [10] |
| GTEx Database | Normal tissue expression reference for comparison | Genotype-Tissue Expression Project [19] |
| glmnet R Package | Implements Lasso and Ridge regularization for various models | CRAN Repository [10] |
| ConsensusClusterPlus | Performs unsupervised clustering for molecular subtypes | Bioconductor [19] |
| UCSC Xena Browser | Integrative analysis of multi-omics and clinical data | https://xenabrowser.net/ [19] |
Case Study: Regularization in m6A-Related lncRNA Signature Development
Application in Cervical Cancer Prognostics
In a recent study developing an m6A-related lncRNA signature for cervical cancer, researchers employed Lasso regularization to identify a prognostic signature from 79 candidate lncRNAs [12]. Through 10-fold cross-validation with Lasso-penalized Cox regression, they derived a final signature comprising four lncRNAs (AL139035.1, AC015922.2, AC073529.1, AC008124.1) that significantly stratified patients into high-risk and low-risk groups with distinct overall survival outcomes [12]. The regularization parameter λ was selected to minimize the cross-validation error, ensuring optimal balance between model complexity and predictive accuracy.
The implementation of regularization in this study prevented overfitting to the training data (n=304 patients), which was particularly important given the high dimensionality of the feature space relative to sample size [12]. The resulting model maintained its prognostic value in validation cohorts, demonstrating the effectiveness of regularization in developing generalizable biomarkers. Furthermore, the signature was independently associated with prognosis in multivariate analysis after adjusting for clinical factors including age, tumor stage, and grade [12].
Application in Lung Adenocarcinoma
A similar approach was applied in lung adenocarcinoma (LUAD), where researchers developed an m6A-related lncRNA signature using regularized Cox regression [10]. From an initial set of candidates, the method identified eight lncRNAs significantly associated with patient outcomes, with two functioning as independent adverse prognostic biomarkers and six as favorable predictors [10]. The risk score derived from this signature effectively stratified patients into prognostic categories and was significantly associated with immune cell infiltration patterns and therapeutic responses [10].
The incorporation of regularization enabled the researchers to build a parsimonious model that captured the essential biological signal without being overwhelmed by noise. This resulted in a clinically relevant tool that could potentially guide immunotherapy decisions in LUAD patients [10]. The study further validated the functional relevance of one signature lncRNA (FAM83A-AS1) through in vitro experiments, demonstrating its role in promoting proliferation, invasion, and drug resistance [10].
Visualization of Regularization Concepts and Workflows
Regularization Technique Selection Algorithm
Regularized Prognostic Model Development Workflow
Regularization techniques provide an essential methodological foundation for developing robust multivariate prognostic models in cancer research, particularly for high-dimensional m6A-related lncRNA signatures. By strategically controlling model complexity, these techniques mitigate overfitting and enhance generalizability, ultimately producing more reliable biomarkers for clinical translation. The integration of L1, L2, Elastic Net, dropout, and early stopping into the analytical pipeline represents best practices in computational biology for biomarker discovery. As research in m6A-related lncRNAs continues to evolve, appropriate implementation of regularization will be crucial for transforming high-throughput omics data into clinically actionable diagnostic and prognostic tools that can genuinely inform personalized immunotherapy approaches.
Resolving Discrepancies in lncRNA Annotation Across Platforms
The pursuit of reliable molecular signatures for predicting cancer immunotherapy response has increasingly focused on m6A-related long non-coding RNAs (lncRNAs). These signatures show significant promise for stratifying patients in cancers such as esophageal squamous cell carcinoma (ESCC), hepatocellular carcinoma (HCC), and lung adenocarcinoma (LUAD) [78] [79] [80]. However, a critical yet often overlooked challenge undermines the reproducibility and clinical translation of these findings: substantial discrepancies in lncRNA annotation across different databases and analysis platforms. These inconsistencies arise from several factors, including the complex and dynamic nature of lncRNA structures, the prevalence of non-orthologous lncRNAs in primate lineages, and the use of diverse computational identification pipelines [81] [82]. This protocol provides a standardized framework to resolve these annotation discrepancies, ensuring robust and reproducible identification of m6A-related lncRNAs in immunotherapy research.
Understanding the root causes of annotation variability is essential for developing effective solutions. Key challenges include:
- Structural Heterogeneity and Dynamic Folding: LncRNAs exhibit significant conformational flexibility, exploring expansive landscapes rather than adopting single, static structures. Experimental techniques like SHAPE and DMS probing have false negative rates around 17% and false discovery rates near 21%, while computational predictions struggle with RNA's dynamic nature and energy degeneracy [81].
- Evolutionary and Species-Specific Differences: Approximately one-third of lncRNAs have emerged within the primate lineage, with about 40% being brain-specific. Genomic features differ significantly between shared orthologous and non-orthologous lncRNAs, particularly in transcript length and exon number [82].
- Platform-Specific Identification Pipelines: Different databases and tools employ varied criteria for lncRNA classification, gene symbol assignment, and interaction prediction, leading to substantial integration challenges [83].
Standardized Experimental Framework
Database Integration and Identifier Reconciliation
Effective reconciliation begins with integrating multiple, high-confidence data sources while standardizing molecular identifiers.
Table 1: Essential Databases for lncRNA Annotation Integration
| Database Category | Database Name | Primary Utility | Key Consideration |
|---|---|---|---|
| Reference Annotation | GENCODE | Comprehensive lncRNA catalog; benchmark for novel predictions | Use most recent version for updated annotations [82] |
| Interaction Evidence | starBase, LncBase | Experimentally validated miRNA-lncRNA and RBP-lncRNA interactions | Apply stringent filters (e.g., CLIP-seq and degradome support) [84] |
| Functional Annotation | ncFN | Heterogeneous network-based functional inference | Integrates PCG-PCG, ncRNA-PCG, and ncRNA-ncRNA interactions [84] |
| m6A Integration | MeT-DB, RMBase | m6A modification sites and methylation patterns | Correlate with lncRNA expression for m6A-related signature discovery [78] |
Protocol Steps:
- Data Retrieval: Download lncRNA annotation and interaction data from Table 1 sources.
- Identifier Standardization: Convert all gene identifiers to authoritative standards:
- Orthology Mapping: For cross-species studies, distinguish between shared orthologous and non-orthologous lncRNAs using tools like OrthoMCL or Ensembl Compare [82].
m6A-Related lncRNA Identification and Signature Development
This core protocol details the identification of m6A-related lncRNAs and construction of prognostic signatures for immunotherapy response prediction.
Table 2: Key Research Reagent Solutions for m6A-lncRNA Studies
| Research Reagent | Function/Application | Example Use Case |
|---|---|---|
| m6A Regulators (Writers, Erasers, Readers) | Define m6A modification patterns for co-expression analysis [80] | Identify m6A-related lncRNAs via WGCNA [80] |
| Chemical Probing Reagents (DMS, DMS-MaPseq) | Nucleotide-resolution RNA structural probing in vitro and in vivo [81] | Determine lncRNA secondary structure and protein-binding regions [81] |
| Immune Cell Deconvolution Algorithms (TIMER, ESTIMATE) | Infer immune cell infiltration from bulk transcriptome data [85] | Characterize tumor immune microenvironment (TIME) of lncRNA subtypes [85] |
| LASSO-Cox Regression Model | Select most prognostic lncRNAs and construct risk signature [86] | Develop parsimonious prognostic model (e.g., 3-10 lncRNAs) [78] [86] |
Protocol Steps:
- Define m6A-Related Genes: Compile a reference list of m6A regulators, typically including:
- Writers: METTL3, METTL14, RBM15, WTAP, ZC3H13
- Erasers: FTO, ALKBH5
- Readers: YTHDF1, YTHDF2, YTHDF3, YTHDC1, HNRNPA2B1 [85]
- Identify m6A-Related lncRNAs:
- Calculate co-expression relationships (e.g., Pearson correlation) between m6A regulators and all lncRNAs in your transcriptomic dataset (e.g., from TCGA).
- Apply stringent thresholds (e.g., |R| > 0.3 or 0.4 and p-value < 0.001) to define significant m6A-related lncRNAs [85].
- Construct Prognostic Signature:
- Perform univariate Cox regression to identify m6A-related lncRNAs associated with overall survival.
- Apply LASSO-Cox regression for dimensionality reduction and select the most prognostic lncRNAs to avoid overfitting [86].
- Calculate a risk score for each patient using the formula:
Risk Score = Σ(Expression of LncRNA_i × Coefficient_i)[86]. - Stratify patients into high-risk and low-risk groups using the median risk score as cutoff [78].
The following workflow diagram illustrates the core analytical process for developing and validating an m6A-lncRNA signature:
Functional Validation and Clinical Translation
After developing a signature, functional validation and clinical correlation are essential.
Protocol Steps:
- Characterize Tumor Immune Microenvironment (TIME):
- Use algorithms like ESTIMATE to calculate Immune, Stromal, and tumor Purity scores [85].
- Apply TIMER or similar deconvolution tools to quantify abundances of specific immune cells (B cells, CD4+ T cells, CD8+ T cells, macrophages, neutrophils, dendritic cells) [85].
- Correlate risk scores with immune checkpoint gene expression (PD-1, PD-L1, CTLA-4) [79] [85].
- Predict Immunotherapy Response:
- Experimental Validation:
- Employ gene silencing (e.g., siRNA or CRISPRi) against signature lncRNAs in relevant cancer cell lines.
- Assess functional impact through proliferation, invasion, and apoptosis assays [86].
- For structural studies, use in vivo SHAPE or DMS-MaPseq under physiologically relevant magnesium concentrations to capture native conformations [81].
Integrated Analysis Framework
The ncFN framework provides a powerful approach for functional annotation that transcends individual platform limitations by leveraging a global interaction network.
Protocol Steps:
- Network Construction: Build a heterogeneous Global Interaction Network (GIN) integrating:
- Association Strength Calculation: For a query lncRNA, use Random Walk with Restart (RWR) on the GIN to quantify Association Strengths (ASs) with all PCGs [84].
- Functional Annotation: Perform pre-ranked Gene Set Enrichment Analysis (GSEA) using PCGs ranked by their ASs against functional gene sets (e.g., KEGG pathways) [84].
This protocol provides a comprehensive framework for resolving lncRNA annotation discrepancies in the context of m6A-related immunotherapy signature development. By implementing these standardized procedures for database integration, identifier reconciliation, signature construction, and functional validation, researchers can significantly enhance the reliability, reproducibility, and clinical translatability of their findings. The integration of computational network-based approaches with experimental validation creates a robust pipeline for advancing lncRNA research from descriptive association to mechanistic understanding and therapeutic application.
Standardizing Immune Infiltration Analysis Using CIBERSORT, TIMER, and xCell
The tumor immune microenvironment (TIME) is a critical determinant of cancer progression and patient response to immunotherapy. The composition and abundance of tumor-infiltrating immune cells profoundly influence immunotherapy efficacy, with T-cell-inflamed tumors typically showing improved responses to immune checkpoint inhibitors compared to T-cell-depleted tumors [87]. In the context of researching m6A-related lncRNA signatures and their ability to predict immunotherapy response, precisely characterizing the immune context becomes indispensable for validating these biomarkers.
Computational deconvolution of bulk tumor transcriptomes has emerged as a powerful approach for systematically quantifying immune infiltration, overcoming limitations of traditional methods like flow cytometry and immunohistochemistry [88]. This application note provides standardized protocols for three widely used deconvolution tools—CIBERSORT, TIMER, and xCell—enabling researchers to generate consistent, reproducible immune infiltration data that can correlate m6A-related lncRNA expression patterns with immune context, ultimately refining predictive models of immunotherapy response.
Tool Selection: Comparative Analysis of Deconvolution Methods
Technical Specifications and Applications
Table 1: Comparison of Key Immune Deconvolution Tools
| Tool | Algorithm Type | Cell Types Quantified | Output Type | Tissue Specificity | Key Strengths |
|---|---|---|---|---|---|
| CIBERSORT | Support Vector Regression (SVR) | 22 human hematopoietic subsets (LM22 matrix) [88] | Relative proportions (can be converted to absolute) [87] | No (Pan-tissue) | Excellent for closely related immune subsets; provides confidence measure [88] |
| TIMER | Linear Least Square Regression | 6 immune cell types (B, CD4+ T, CD8+ T, Neutrophils, Macrophages, Dendritic) [89] | Relative abundances | Yes (Cancer-type specific) | Incorporates tumor purity adjustment; cancer-specific signatures [90] |
| xCell | ssGSEA Enrichment | 64 immune and stromal cell types [87] | Enrichment scores | No (Pan-tissue) | Broadest cell type coverage; includes stromal populations [89] |
Performance Characteristics in Tumor Contexts
Each algorithm demonstrates unique performance characteristics. CIBERSORT implements ν-support vector regression (ν-SVR) to deconvolve relative fractions of 22 immune cell types from bulk tissue gene expression profiles (GEPs) [88]. Its absolute mode, which incorporates a scaling factor reflecting total immune content, enables more accurate inter-sample comparisons [87]. TIMER uses cancer-specific signatures selected based on their correlation with tumor purity in The Cancer Genome Atlas (TCGA) data, making it particularly suited for oncology applications where tumor purity significantly confounds analysis [90] [89]. xCell employs a signature-based method that calculates single-sample gene set enrichment analysis (ssGSEA) scores, providing the most extensive cellular coverage including stromal cells, though it performs best with heterogeneous samples and has limitations in intra-cell type comparisons [89].
Table 2: Practical Considerations for Tool Selection
| Analysis Scenario | Recommended Tool | Rationale | Data Requirements |
|---|---|---|---|
| Detailed T-cell subset analysis | CIBERSORT | Resolves 7 T-cell types including naive, memory, follicular helper, and regulatory T cells [88] | TPM, FPKM, or non-log microarray data |
| Pan-cancer TCGA analysis | TIMER | Built-in cancer-type specific signatures and purity adjustment [90] | RNA-seq TPM values |
| Stromal-immune interactions | xCell | Includes fibroblasts, endothelial cells, and immune subsets [89] | Gene expression matrix |
| Cross-sample comparison | CIBERSORT (absolute) or EPIC/quanTIseq | Absolute scores enable valid inter-sample comparisons [87] | Appropriate normalization |
| Consensus analysis | Multiple tools (TIMER2.0/3.0) | TIMER platforms integrate 6-15 algorithms for robust results [90] [91] | Varies by platform |
Integrated Protocol for Immune Deconvolution
Input Data Preparation and Quality Control
Gene Expression Profiling Requirements
- Platform compatibility: RNA-sequencing (TPM, FPKM recommended) or microarray data (non-log linear space) [88]
- Data formatting: Tab-delimited text files with genes as rows and samples as columns
- Gene identifier consistency: Uniform gene symbols or Ensembl IDs across mixture and signature files
- Missing data: Complete matrix without missing values
- For CIBERSORT with LM22: 547-gene signature matrix for 22 hematopoietic cell types [88]
Preprocessing for m6A-lncRNA Studies
- When correlating with m6A-related lncRNAs, ensure consistent normalization across all samples
- For TCGA data analysis, utilize RSEM-derived TPM values as processed by TIMER platforms [90]
- Batch effect correction crucial when integrating multiple datasets (e.g., TCGA with GEO data) [67]
Execution Protocols
CIBERSORT Implementation
- Access: Register for academic use at CIBERSORT Stanford website [88]
- Signature selection: Use LM22 matrix (547 genes, 22 immune cell types) or create custom matrix
- Upload mixture file: Tab-delimited format with gene column header "Name"
- Parameter setting: Select "Absolute mode" for cross-sample comparisons [87]
- Output interpretation: Check p-values for deconvolution confidence (p < 0.05 recommended) [89]
TIMER/TIMER2.0 Web Server Protocol
- Access: Navigate to http://timer.cistrome.org/ (TIMER2.0) [90]
- Module selection: Choose "Immune" component for association analysis
- Gene input: Input m6A-related lncRNA of interest (e.g., ELFN1-AS1, H19, PCAT6) [92] [67]
- Adjustment: Select "purity adjustment" for tumor samples (except with EPIC/quanTIseq) [90]
- Output: Functional heatmap table displays correlations across multiple cancer types
xCell Through R Implementation
Output Interpretation and Integration
Normalization for Cross-Study Comparison
- CIBERSORT absolute scores and quanTIseq/EPIC fractions enable direct comparison across samples [89]
- xCell scores require within-cell type comparison only
- For correlation with m6A-lncRNA signatures, use consistent normalization across all samples
Quality Assessment Metrics
- CIBERSORT: Examine p-values for each sample (recommended < 0.05) [89]
- Check correlation between methods for consensus (e.g., CD8+ T cells across algorithms)
- Compare with expected biological patterns (e.g., higher lymphocyte infiltration in MSI-high tumors)
Integration Framework for m6A-lncRNA Studies
Analytical Workflow for Biomarker Validation
The integration of immune deconvolution in m6A-related lncRNA research follows a systematic workflow to establish connections between epigenetic regulation, immune context, and therapeutic response.
Application in Diffuse Large B-Cell Lymphoma Research
In DLBCL, a recent study established an m6A-related lncRNA risk model incorporating three lncRNAs (including ELFN1-AS1) that could differentiate patient response to immunotherapy [92]. Through computational analysis of immune infiltration, researchers demonstrated that the risk model effectively stratified patients into distinct immune microenvironments, with the high-risk group exhibiting immune-suppressive characteristics that may inform combination therapy approaches.
Correlation Analysis Protocol
Standardized Association Testing
- Calculate m6A-lncRNA signature score (e.g., m6A-LncScore = 0.32SLCO4A1-AS1 + 0.41MELTF-AS1 + 0.44SH3PXD2A-AS1 + 0.39H19 + 0.48*PCAT6) [67]
- Compute immune cell abundances using 2+ deconvolution tools for consensus
- Apply appropriate statistical tests:
- Spearman correlation for continuous immune scores vs. lncRNA expression
- Cox proportional hazards for survival outcomes with immune covariates
- Logistic regression for binary immunotherapy response outcomes
- Adjust for tumor purity, especially when using relative abundance estimates [90]
- Validate findings in multiple cohorts (e.g., TCGA + independent GEO datasets)
Research Reagent Solutions
Table 3: Essential Research Resources for Immune Deconvolution Studies
| Resource Category | Specific Solution | Application Context | Access Information |
|---|---|---|---|
| Signature Matrices | LM22 (22 immune cell types) | CIBERSORT deconvolution of human samples [88] | Academic registration required |
| Integrated Platforms | TIMER2.0 / TIMER3.0 | Multi-algorithm analysis (6-15 methods) [90] [91] | http://timer.cistrome.org/ |
| R Packages | immunedeconv | Unified interface for 6 algorithms including CIBERSORT, xCell, EPIC [90] | CRAN/Bioconductor |
| Reference Datasets | TCGA RNA-seq data | Pan-cancer analysis with clinical annotations [90] | https://portal.gdc.cancer.gov/ |
| Validation Tools | mMCP-counter | Mouse model infiltration analysis [90] | Included in immunedeconv |
Troubleshooting and Quality Assurance
Common Technical Challenges
Platform-Specific Limitations
- CIBERSORT: Academic license required; LM22 matrix optimized for microarray data [88]
- xCell: Performance decreases with homogeneous samples; not for intra-cell type comparisons [89]
- TIMER: Limited to 6 immune cell types; cancer-type specific [90]
- Solution: Use multiple algorithms through TIMER2.0/3.0 or immunedeconv R package [90]
Data Interpretation Pitfalls
- Relative vs. absolute scores: CIBERSORT relative proportions measure immune composition, while absolute scores measure abundance relative to total sample [87]
- Tumor purity confounding: Always adjust for purity in solid tumor analyses (except with EPIC/quanTIseq) [90]
- Cross-algorithm discrepancies: Validate key findings with multiple methods and orthogonal validation when possible
Validation Strategies
Technical Validation
- Compare results across multiple deconvolution algorithms
- Correlate with orthogonal methods (IHC, flow cytometry) when feasible
- Assess consistency with expected biological patterns
Biological Validation
- Replicate findings in independent cohorts
- Confirm associations with known immune markers (e.g., CD8A for cytotoxic T cells)
- Test predictive performance in held-out datasets using ROC analysis [67]
Standardized implementation of CIBERSORT, TIMER, and xCell provides a robust framework for quantifying tumor immune infiltration in m6A-related lncRNA studies. By following these detailed application notes and protocols, researchers can generate consistent, reproducible immune context data that strengthens the validation of m6A-related lncRNA signatures as predictors of immunotherapy response. The integration of computational immune deconvolution with epigenetic biomarker research represents a powerful approach for advancing precision immuno-oncology and identifying patient subgroups most likely to benefit from specific immunotherapeutic strategies.
Improving Immunotherapy Response Prediction with TIDE and TMB Integration
Immune checkpoint blockade (ICB) has revolutionized cancer treatment, yet patient response rates remain variable, underscoring the urgent need for robust predictive biomarkers [93]. While tumor mutation burden (TMB) has emerged as a prominent genomic biomarker, its predictive power is limited by technical confounders and biological complexity [94]. Similarly, transcriptomic biomarkers like Tumor Immune Dysfunction and Exclusion (TIDE) offer insights into tumor microenvironment but may lack genomic context. This protocol details integrated methodologies that synergize TMB's assessment of tumor immunogenicity with TIDE's evaluation of pre-existing immune evasion mechanisms, framed within the emerging context of m6A-related lncRNA signatures as potential modulators of immunotherapy response.
Background and Significance
Limitations of Single-Modality Biomarkers
Traditional biomarkers for ICB response prediction have inherent limitations. TMB, measured as nonsynonymous mutations per megabase, shows variable predictive power across cancer types with no universal threshold [93]. Technically, TMB estimation is confounded by tumor purity—samples with low tumor content yield inaccurate TMB measurements [94]. Biologically, high TMB does not guarantee response, as mutations may not generate immunogenic neoantigens or may occur in immunosuppressive contexts.
Transcriptomic biomarkers like TIDE model tumor immune dysfunction and exclusion signatures but may overlook genomic determinants of response [95]. The TIDE web platform (http://tide.dfci.harvard.edu/) integrates data from over 33,000 samples across 188 tumor cohorts, 998 tumors from 12 ICB clinical studies, and eight CRISPR screens, enabling comprehensive assessment of immune evasion phenotypes [95].
Emergence of m6A-Related lncRNAs in Immunotherapy Response
Recent evidence implicates m6A-related long non-coding RNAs (lncRNAs) in modulating ICB response. These epigenetic regulators influence immune cell infiltration, checkpoint expression, and drug resistance [10]. In lung adenocarcinoma (LUAD), prognostic models incorporating m6A-related lncRNAs significantly predict patient survival and immunotherapy outcomes [96]. Similarly, in cervical cancer, a 4-m6A-related-lncRNA signature (AL139035.1, AC015922.2, AC073529.1, AC008124.1) independently predicts prognosis and immunotherapy benefit [12].
Table 1: Established m6A-Related lncRNA Signatures in Cancer Immunotherapy
| Cancer Type | Signature Components | Predictive Value | Reference |
|---|---|---|---|
| Lung Adenocarcinoma (LUAD) | 8-lncRNA signature (m6ARLSig) | Prognostic prediction; immune infiltration assessment | [10] |
| Lung Adenocarcinoma (LUAD) | 6-lncRNA signature (NFYC-AS1, OGFRP1, MIR4435-2HG, TDRKH-AS1, DANCR, TMPO-AS1) | Survival prediction; therapy guidance | [97] |
| Cervical Cancer | 4-lncRNA signature (AL139035.1, AC015922.2, AC073529.1, AC008124.1) | Independent prognostic predictor | [12] |
Integrated Computational Methodology
TMB Calculation and Correction
Procedure:
- Sequence Data Processing: Process whole-exome or targeted sequencing data through standardized pipelines (GATK4) for somatic mutation calling [93].
- Mutation Annotation: Annotate somatic mutations using Ensembl VEP, retaining nonsynonymous variants (missense, inframe indels, frameshift, splice-site, start/stop lost) [93].
- Raw TMB Calculation: Compute TMB as the number of nonsynonymous mutations per megabase of coding region.
- Tumor Purity Correction: Apply purity-adjusted TMB correction using the following approach:
- Estimate tumor purity from sequencing data or histopathology
- Reference the correction table developed by Anagnostou et al. [94]
- Multiply observed TMB by purity-specific coefficients (e.g., for 20-30% purity, apply correction factor of 1.8)
Table 2: Tumor Purity Correction Factors for TMB Calculation
| Tumor Purity Range | Correction Factor | Application Notes |
|---|---|---|
| 10-20% | 2.5-3.0 | Use with caution; consider re-biopsy |
| 20-30% | 1.8-2.2 | Standard correction for low-purity samples |
| 30-50% | 1.3-1.6 | Moderate correction |
| >50% | 1.0-1.2 | Minimal correction needed |
Pathway-Derived TMB (P-TMB) Computation
Procedure:
- Pathway Selection: Curate 209 biological pathways including KEGG pathways, ImmPort immune pathways, and DNA repair pathways [93].
- Mutation Frequency Matrix: Generate mutation frequency matrix (samples × genes) for each dataset.
- Gene Set Variation Analysis: Apply GSVA algorithm to calculate normalized enrichment scores (NES) of mutated genes in each pathway per sample.
- Pathway Categorization: Identify positive pathways (PP) enriched in responders and negative pathways (NP) enriched in non-responders using Mann-Whitney U test (p<0.05) across multiple datasets [93].
- P-TMB Calculation: Compute pathway-derived TMB score incorporating only mutations in genes from significant pathways.
TIDE Analysis Protocol
Procedure:
- Data Input: Prepare pre-treatment tumor RNA-seq or microarray data (normalized counts or FPKM).
- TIDE Score Calculation:
- Access TIDE web platform (http://tide.dfci.harvard.edu/)
- Upload expression matrix with proper gene identifiers
- Select cancer type for appropriate model application
- Execute TIDE algorithm modeling T cell dysfunction and exclusion
- Output Interpretation:
- Negative TIDE scores indicate low immune evasion likelihood
- Positive scores suggest active dysfunction/exclusion mechanisms
- Review subcomponent scores (MDSC, CAF infiltration) for mechanistic insights
Integrated Biomarker Consensus
Procedure:
- Multi-Modal Data Integration: Combine corrected TMB, P-TMB, TIDE scores, and m6A-lncRNA risk scores (if available) into unified data structure.
- Response Prediction Algorithm:
- Apply random forest or logistic regression classifier
- Train on cohort with known ICB response (e.g., 287 patients with melanoma/NSCLC) [93]
- Weight biomarkers by validated predictive power
- Consensus Calling:
- Favorable prediction: Negative TIDE + high corrected TMB + favorable P-TMB + low m6A-lncRNA risk
- Unfavorable prediction: Positive TIDE + low corrected TMB + unfavorable P-TMB + high m6A-lncRNA risk
Experimental Validation Protocols
m6A-Related lncRNA Signature Validation
Cell Line Assay Protocol:
- Cell Culture: Maintain A549 and A549/DDP (cisplatin-resistant) LUAD cells in RPMI-1640 with 10% FBS [10].
- lncRNA Modulation:
- Design siRNA targeting specific m6A-related lncRNAs (e.g., FAM83A-AS1)
- Transfect using Lipofectamine 3000 per manufacturer protocol
- Include non-targeting siRNA as negative control
- Phenotypic Assessment:
- Proliferation: MTT assay at 24, 48, 72 hours post-transfection
- Apoptosis: Annexin V/PI staining with flow cytometry
- Invasion: Transwell Matrigel invasion assay
- Drug resistance: IC50 determination for cisplatin/immunotherapy agents
Longitudinal Liquid Biopsy Profiling
Procedure for Dynamic Immune Monitoring:
- Sample Collection: Collect peripheral blood at pre-treatment (Day 0) and early on-treatment (Day 9-14) timepoints [98].
- Single-Cell RNA/TCR Sequencing:
- Isolate PBMCs using Ficoll density gradient
- Process through 10X Genomics platform for scRNA-seq + scTCR-seq
- Sequence on Illumina NovaSeq with minimum 50,000 reads/cell
- Computational Analysis:
- Cell type identification: Unsupervised clustering with Seurat
- T/B cell repertoire analysis: Clonal expansion metrics
- Differential abundance testing: Wilcoxon rank-sum for responders vs. non-responders
Visualization and Data Interpretation
Integrated Biomarker Workflow
Immune Dynamics in ICB Response
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Category | Item | Specification/Function | Application |
|---|---|---|---|
| Wet Lab Reagents | TRIzol Reagent | RNA isolation and preservation | m6A-lncRNA extraction |
| Lipofectamine 3000 | siRNA transfection reagent | lncRNA knockdown studies | |
| Annexin V-FITC/PI Apoptosis Kit | Apoptosis detection by flow cytometry | Therapeutic response assessment | |
| Matrigel Matrix | Basement membrane extract for invasion assays | Cell invasion measurement | |
| Computational Tools | TIDE Web Platform | Tumor Immune Dysfunction and Exclusion analysis | Immune evasion phenotype scoring |
| GATK4 | Genome Analysis Toolkit for mutation calling | Somatic variant detection for TMB | |
| CIBERSORT | Digital cytometry for immune cell quantification | Immune infiltration analysis | |
| GSVA R Package | Gene Set Variation Analysis | Pathway enrichment scoring for P-TMB | |
| Databases | TCGA | The Cancer Genome Atlas database | Clinical-genomic validation cohorts |
| ImmPort | Immunology database and analysis portal | Immune pathway definitions | |
| m6AVar Database | m6A-associated variants database | m6A methylation site annotation |
Anticipated Results and Interpretation
Performance Metrics
When properly implemented, the integrated TIDE-TMB approach demonstrates superior prediction accuracy compared to individual biomarkers. The pathway-derived TMB (P-TMB) component alone achieves prediction AUC of 0.74-0.82 across multiple datasets [93]. Incorporating m6A-lncRNA signatures further enhances stratification, with established lncRNA risk models showing significant separation in overall survival (p<0.001) [10] [97].
Clinical Application Guidance
For clinical translation, the following interpretation framework is recommended:
- High Priority for ICB: Negative TIDE + high corrected TMB (>10 muts/Mb) + low m6A-lncRNA risk score
- Intermediate Priority: Discordant biomarkers - consider combination therapy or clinical trial
- Low Priority: Positive TIDE + low corrected TMB (<5 muts/Mb) + high m6A-lncRNA risk score
Longitudinal liquid biopsy assessment at early on-treatment (Day 9-14) provides dynamic validation, with expansion of effector memory T cells and specific B cell populations indicating likely response [98].
This integrated protocol synergizes genomic, transcriptomic, and epigenetic biomarkers to optimize ICB response prediction. The methodology addresses critical limitations of single-modality approaches while incorporating emerging determinants of immunotherapy efficacy, particularly m6A-related lncRNA signatures. Implementation requires multidisciplinary expertise but offers substantially improved patient stratification for precision immuno-oncology.
Benchmarking Performance Against Existing Clinical Parameters and Traditional Biomarkers
The emergence of N6-methyladenosine (m6A)-related long non-coding RNA (lncRNA) signatures represents a significant advancement in the pursuit of prognostic biomarkers for cancer immunotherapy. As these novel molecular signatures transition toward clinical application, rigorous benchmarking against established clinical parameters and traditional biomarkers becomes imperative. This application note provides a standardized protocol for the comprehensive evaluation of m6A-related lncRNA signatures, enabling researchers to quantitatively assess their prognostic and predictive performance relative to conventional clinical tools. The protocols outlined herein facilitate the direct comparison of these multi-lncRNA signatures against established factors such as TNM staging, tumor grade, and single molecular biomarkers, ensuring robust validation of their clinical utility.
Performance Benchmarking: m6A-Related lncRNA Signatures Across Cancers
Table 1: Comparative Performance of m6A-Related lncRNA Signatures in Predicting Immunotherapy Response
| Cancer Type | Signature Components | Benchmark Against Clinical Parameters | Statistical Performance | Key Superior Findings |
|---|---|---|---|---|
| Pancreatic Cancer [99] [100] | 5-lncRNA (LINC01091, AC096733.2, AC092171.5, AC015660.1, AC005332.6) | TNM stage, tumor grade | Independent prognostic factor in multivariate analysis (HR: 1.252, 95% CI: 1.093-1.434, P<0.001) [100] | Superior prediction of immune cell infiltration and response to drugs (WZ8040, selumetinib) [99] |
| Cervical Cancer [12] | 4-lncRNA (AL139035.1, AC015922.2, AC073529.1, AC008124.1) | Age, clinical stage, TNM stage | Nomogram C-index: 0.75 (combined signature & clinical factors) [12] | Improved accuracy in predicting overall survival versus clinical factors alone |
| Lung Adenocarcinoma [10] | 8-lncRNA signature (including FAM83A-AS1) | Tumor stage, metastasis status | Risk score as independent prognostic factor (P<0.001) [10] | Stronger correlation with tumor microenvironment and cisplatin resistance than stage alone |
| Esophageal Cancer [16] | 5-lncRNA (ELF3-AS1, HNF1A-AS1, LINC00942, LINC01389, MIR181A2HG) | Clinical stage, N stage | Significant difference in cluster distribution and disease stage (P<0.05) [16] | Better stratification of patients for targeted therapies (Bleomycin, Cisplatin) |
| Bladder Cancer [33] | 11-lncRNA signature | Pathologic tumor stage, age | AUC for 1-, 3-, 5-year survival: 0.75, 0.78, 0.80 respectively [33] | Enhanced prediction of tumor mutation burden and Talazoparib response |
Table 2: Benchmarking Against Single-Parameter Biomarkers in the Tumor Microenvironment
| Biomarker Category | Traditional Biomarker | m6A-LncRNA Signature Advantage | Experimental Evidence |
|---|---|---|---|
| Immune Checkpoints | PD-L1 IHC expression | Captures broader immune landscape; predicts non-responders with high PD-L1 [101] [33] | Identified CD274, CTLA4, TNFRSF14, LGALS9 correlations simultaneously [16] [85] |
| Tumor Mutational Burden | Whole-exome sequencing | Lower-cost prediction; integrates TMB with immune context [33] | Significant TMB differences between risk groups (P<0.05); high TMB + high risk = poorest survival [100] |
| Immune Cell Infiltration | CD8+ T-cell IHC | Quantifies multiple immune cell populations simultaneously [85] | Specific correlations with naive B cells, resting CD4+ T cells, plasma cells, macrophages M0/M1 [16] |
| Stemness Indices | Functional assays | RNA-based stemness score calculation [33] | Significant differences in mRNA expression-based stemness indices between risk groups (P<0.001) [33] |
Experimental Protocols for Benchmarking Studies
Protocol 1: Development and Validation of m6A-Related lncRNA Signatures
Purpose: To construct a prognostic risk model based on m6A-related lncRNAs and validate its performance against established clinical parameters.
Materials:
- RNA-seq data and clinical information from TCGA database
- R statistical software (version 4.2.1 or later)
- Bioinformatics packages: limma, survival, glmnet, timeROC, clusterProfiler
Procedure:
- Data Acquisition and Preprocessing
- Download RNA-seq data and corresponding clinical information for target cancer type from TCGA (https://portal.gdc.cancer.gov/)
- Annotate lncRNAs using GENCODE database (https://www.gencodegenes.org)
- Normalize expression data using TPM or FPKM methods
Identification of m6A-Related lncRNAs
- Obtain 23 established m6A regulators from literature (writers: METTL3/14, WTAP, RBM15; erasers: FTO, ALKBH5; readers: YTHDF1/2/3, IGF2BP1/2/3)
- Calculate Pearson correlation coefficients between lncRNAs and m6A regulators
- Identify m6A-related lncRNAs with |R| > 0.4 and p < 0.001 [101]
Prognostic Signature Construction
- Perform univariate Cox regression to identify survival-associated m6A-related lncRNAs
- Apply LASSO Cox regression to prevent overfitting and select most prognostic features
- Conduct multivariate Cox regression to establish final model
- Calculate risk score: RiskScore = Σ(ExpressionLncRNAi × CoefficientLncRNAi)
Model Validation
- Divide dataset into training and testing cohorts (typically 70:30 ratio)
- Validate risk model in both cohorts using Kaplan-Meier analysis and log-rank test
- Assess predictive accuracy using time-dependent ROC curves at 1, 3, and 5 years
- Compare ROC curves of risk score versus clinical parameters alone [12]
Protocol 2: Direct Comparison Against Clinical Parameters
Purpose: To quantitatively evaluate whether the m6A-related lncRNA signature provides prognostic value beyond standard clinical parameters.
Materials:
- Clinical data including age, gender, TNM stage, tumor grade
- R packages: rms, regplot, survminer
Procedure:
- Univariate and Multivariate Cox Regression
- Perform univariate Cox regression with individual clinical parameters
- Conduct multivariate Cox regression including both risk score and clinical parameters
- Calculate hazard ratios (HR) and 95% confidence intervals for each variable
- Consider p < 0.05 as statistically significant [100]
Stratified Survival Analysis
- Stratify patients by clinical parameters (e.g., early vs. late stage)
- Within each stratum, divide patients into high- and low-risk using lncRNA signature
- Compare survival between risk groups within each clinical stratum
- Test significance with log-rank test [10]
Nomogram Construction
Prognostic Accuracy Assessment
- Calculate Harrell's C-index for clinical model alone versus combined model
- Compare AUC values for different models using Delong's test
- Evaluate net reclassification improvement (NRI) and integrated discrimination improvement (IDI) [33]
Signaling Pathways and Molecular Interactions
(Diagram 1: Integrative Model of m6A-lncRNA Signature in Prognostication. The diagram illustrates how m6A modifications regulate lncRNA expression to form prognostic signatures that interact with the immune microenvironment, ultimately contributing to a combined model that enhances prediction of immunotherapy response.)
Table 3: Key Research Reagent Solutions for m6A-lncRNA Studies
| Category | Specific Resource | Function/Application | Key Features |
|---|---|---|---|
| Data Resources | TCGA Database (portal.gdc.cancer.gov) | Primary source of RNA-seq and clinical data | Standardized multi-omics data across 33 cancer types [99] [12] [16] |
| m6A Regulators | 23-gene m6A regulator set | Defining m6A-related lncRNAs | Comprehensive coverage of writers, erasers, readers [19] [101] |
| Computational Tools | CIBERSORT (cibersort.stanford.edu) | Immune cell infiltration estimation | Deconvolution algorithm for 22 immune cell types [33] |
| Immunotherapy Prediction | TIDE (tide.dfci.harvard.edu) | Immunotherapy response modeling | Computational framework simulating tumor immune escape [100] |
| Drug Sensitivity | GDSC/PRISM Databases | Chemotherapeutic response prediction | Large-scale pharmacogenomic screening data [10] [100] |
| Pathway Analysis | MSigDB (gsea-msigdb.org) | Functional enrichment analysis | Curated gene sets for GSEA [10] [100] |
| Validation Tools | RT-qPCR Assays | Experimental validation of signature lncRNAs | Confirm differential expression in cell lines/tissues [16] [19] |
The comprehensive benchmarking protocols outlined in this application note provide a rigorous framework for evaluating m6A-related lncRNA signatures against established clinical parameters and traditional biomarkers. The consistent demonstration of these signatures as independent prognostic factors across multiple cancer types, with superior performance in predicting immunotherapy response and characterizing the tumor immune microenvironment, highlights their potential clinical utility. Standardized implementation of these protocols will facilitate the validation and eventual clinical translation of m6A-related lncRNA signatures as valuable tools for personalized cancer immunotherapy.
Cross-Cancer Validation and Comparative Analysis of m6A-lncRNA Signatures
Independent Prognostic Validation Through Multivariate Cox Regression Analysis
In the evolving landscape of cancer biomarker discovery, the identification of molecular signatures requires rigorous statistical validation to establish clinical utility. Multivariate Cox proportional hazards regression analysis serves as the statistical cornerstone for demonstrating that a putative biomarker provides independent prognostic value beyond established clinical parameters [102] [103]. This protocol details the application of this methodology within the context of validating m6A-related lncRNA signatures for predicting immunotherapy response, a burgeoning research area with significant implications for personalized cancer treatment [10] [19] [85].
The core principle of this approach involves determining whether an m6A-related lncRNA signature retains a statistically significant association with patient survival outcomes after adjusting for known clinical confounders such as age, disease stage, and performance status. When successfully validated, such signatures can stratify patients into distinct risk categories, potentially guiding therapeutic decisions, including immunotherapy selection [10] [85].
Application Notes: Key Concepts and Considerations
The Role of Multivariate Cox Regression in Prognostic Validation
Prognostic factor analysis distinguishes between variables that are merely associated with an outcome and those that provide independent predictive information. Multivariate Cox regression achieves this by simultaneously evaluating the effect of multiple predictor variables on a time-to-event outcome, typically overall survival (OS) or cancer-specific survival (CSS) [102] [104]. In the context of an m6A-related lncRNA signature, the analysis tests the null hypothesis that the signature's hazard ratio (HR) is equal to 1.0 after controlling for other significant clinical variables. Rejection of this hypothesis (commonly at p < 0.05) provides evidence that the signature is an independent prognostic factor [102] [103].
Comparison with Machine Learning Approaches
While Cox regression is the traditional workhorse for survival analysis, machine learning (ML) methods like Random Survival Forests (RSF) and DeepSurv are increasingly applied. A recent systematic review and meta-analysis found that ML models and Cox regression generally demonstrate comparable performance in predicting cancer survival outcomes [105]. The choice between methodologies often depends on the research context: Cox regression provides easily interpretable hazard ratios and is well-suited for smaller datasets with pre-specified hypotheses, while certain ML methods may excel with complex, high-dimensional data but can function as "black boxes" [105] [106].
Handling Time-Dependent Covariates
Standard Cox models assume that the effect of a covariate is constant over time. For biomarkers whose values change during follow-up, a time-dependent Cox regression is more appropriate. This approach incorporates longitudinal data, allowing the dynamic changes in a patient's clinical status to be reflected in the analysis, thereby providing a more accurate assessment of prognostic impact [107].
Experimental Protocol: Independent Validation of an m6A-related lncRNA Signature
Data Acquisition and Preprocessing
- Data Sources: Utilize large-scale public databases such as The Cancer Genome Atlas (TCGA) for transcriptomic data and corresponding clinical information [10] [19] [85]. For the study of m6A-related lncRNAs, gather RNA-seq data and clinical survival data for the cancer type of interest (e.g., TCGA-CESC for cervical cancer, TCGA-CRC for colorectal cancer).
- LncRNA Identification: Map Ensembl IDs to gene symbols using an annotation file (e.g., from GENCODE). Filter out genes with expression values of zero in >80% of samples. Calculate average expression for genes with multiple entries to create a final lncRNA expression matrix [19].
- m6A-related LncRNA Signature: The specific m6A-related lncRNA signature (e.g., an 11-lncRNA signature for colorectal cancer [85] or a 6-lncRNA signature for cervical cancer [19]) should be defined a priori from a training cohort. This protocol covers the subsequent validation step.
Statistical Analysis Workflow
- Risk Score Calculation: For each patient in the validation cohort, calculate a risk score based on the predefined signature formula. The formula is typically:
risk score = Σ(coefficient(lncRNA_i) × expression(lncRNA_i))for all lncRNAs in the signature [10] [85]. - Cohort Stratification: Dichotomize patients into high-risk and low-risk groups using the median risk score or an optimal cut-off value determined from the training cohort.
- Univariate Cox Regression: Perform univariate Cox regression for each variable, including the lncRNA risk score and potential clinical confounders (e.g., age, gender, TNM stage, tumor grade). The goal is to identify variables with a preliminary association with survival (typically p < 0.10 or p < 0.05) for inclusion in the multivariate model [103] [85].
- Multivariate Cox Regression:
- Include the lncRNA risk score (as a continuous or categorical variable) and all significant clinical covariates from the univariate analysis in a single multivariate Cox proportional hazards model.
- Check for multicollinearity among variables. Exclude variables with a Variance Inflation Factor (VIF) > 4 to ensure model stability [103].
- Assess the proportional hazards assumption using Schoenfeld residuals [107].
- The output will provide Hazard Ratios (HR), 95% Confidence Intervals (CI), and p-values for each variable, indicating their independent effect on survival.
Performance and Validation
- Model Discrimination: Evaluate the model's ability to distinguish between patients with different outcomes using Harrell's Concordance Index (C-index). A C-index > 0.70 is generally considered acceptable, and > 0.75 indicates good discriminatory power [104] [103].
- Model Calibration: Assess the agreement between predicted and observed survival probabilities using calibration plots [104] [103].
- Clinical Utility: Evaluate the potential net benefit of using the model for clinical decision-making using Decision Curve Analysis (DCA) [103] [85].
Data Presentation
Table 1: Example Output of Multivariate Cox Regression Analysis for an m6A-related lncRNA Signature in a Hypothetical Cohort
| Variable | Hazard Ratio (HR) | 95% Confidence Interval | P-value |
|---|---|---|---|
| m6A-lncRNA Risk Score (High vs. Low) | 2.11 | 1.71 - 2.61 | < 0.001 |
| Age (≥65 vs. <65 years) | 1.35 | 1.02 - 1.78 | 0.036 |
| TNM Stage (III/IV vs. I/II) | 2.18 | 1.49 - 3.20 | < 0.001 |
| Tumor Size (≥5cm vs. <5cm) | 1.58 | 1.20 - 2.08 | 0.001 |
Table 2: Comparison of Cox Regression vs. Machine Learning for Survival Prediction (Based on Meta-Analysis Findings) [105] [106]
| Feature | Cox Regression Model | Machine Learning Models (e.g., RSF, DeepSurv) |
|---|---|---|
| Primary Strength | Interpretability, provides explicit hazard ratios | Handles complex, non-linear interactions without pre-specified assumptions |
| Model Performance | Stable and robust performance (e.g., C-index ~0.75) [106] | Similar performance to Cox in direct comparisons (SMD in C-index: 0.01) [105] |
| Data Assumptions | Proportional hazards, linearity | Fewer statistical assumptions |
| Output | Well-defined statistical parameters (HR, CI) | Often less interpretable ("black box") |
| Ideal Use Case | Confirmatory analysis with predefined hypotheses | Exploratory analysis with high-dimensional data |
Visualized Workflow
Figure 1. Logical workflow for the independent prognostic validation of an m6A-related lncRNA signature using multivariate Cox regression.
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for m6A-related lncRNA Prognostic Studies
| Item / Resource | Function / Application | Example / Source |
|---|---|---|
| TCGA/GTEx Datasets | Provides transcriptomic data and corresponding clinical information for model development and validation. | UCSC Xena database [19] [85] |
| R Statistical Software | Open-source platform for all statistical analyses, including survival analysis and visualization. | R Foundation (version 4.0.3 or later) [102] [107] |
| R Survival Package | Core package for performing Cox regression and Kaplan-Meier survival analysis. | survival R package [102] [10] |
| CIBERSORT/xCell/ESTIMATE | Computational algorithms for deconvoluting immune cell infiltration and analyzing the tumor immune microenvironment. | [10] [19] [85] |
| ConsensusClusterPlus | R package for unsupervised clustering to identify distinct m6A-lncRNA subtypes. | [19] |
| TIMEOR Database | Web resource for analyzing correlations between genes and immune cell infiltration levels. | [85] |
| FerrDB Database | Repository for retrieving ferroptosis-related genes for integrated analysis. | [19] |
In the rapidly evolving field of cancer genomics, the development of molecular signatures for predicting treatment response and patient survival requires robust statistical evaluation. For m6A-related lncRNA signatures predicting immunotherapy outcomes, standard binary classification metrics fall short because they cannot account for the dynamic nature of survival outcomes where event times are censored. Time-dependent Receiver Operating Characteristic (ROC) curves and the Concordance Index (C-index) address this critical need by providing tools to assess how well a prognostic signature discriminates between patients at different time points throughout the follow-up period [108] [109]. These metrics are particularly valuable in immunotherapy research where the timing of disease progression or recurrence significantly impacts clinical decision-making.
The fundamental challenge in evaluating prognostic signatures for time-to-event data stems from the fact that both the marker value (e.g., risk score) and the disease status change over time [108]. Individuals who are event-free earlier may experience the event later due to longer study follow-up. Furthermore, the occurrence of censoring—where the exact event time is unknown for some patients beyond their last follow-up—complicates traditional ROC analysis. Time-dependent ROC curve analysis and the C-index overcome these limitations, providing researchers with powerful tools to validate the clinical utility of m6A-related lncRNA signatures for immunotherapy response prediction [110] [22].
Theoretical Foundations of Time-Dependent ROC Analysis
Core Definitions and Framework
In the context of censored survival data, Heagerty and Zheng proposed three primary definitions for time-dependent sensitivity and specificity that form the basis for time-dependent ROC analysis [108] [111]:
Cumulative Sensitivity and Dynamic Specificity (C/D): At each time point t, a case is defined as any individual experiencing the event between baseline and time t (cumulative case), while a control is an individual remaining event-free at time t (dynamic control). The C/D definitions are particularly relevant when there's a specific time of interest for clinical decision-making.
Incident Sensitivity and Dynamic Specificity (I/D): A case is defined as an individual with an event at exactly time t (incident case), while a control remains an event-free individual at time t. This approach focuses on predicting new incident cases at specific time points.
Incident Sensitivity and Static Specificity (I/S): This approach defines cases as incident cases at time t, while controls are those who remain event-free through a fixed, pre-specified time period (e.g., 5 years).
For a continuous marker X (such as an m6A-related lncRNA risk score) and threshold c, the time-dependent sensitivity and specificity for the C/D definition are formulated as [108]:
- Sensitivity: Se(c,t) = P(Xi > c | Ti ≤ t)
- Specificity: Sp(c,t) = P(Xi ≤ c | Ti > t)
The corresponding time-dependent AUC is defined as the probability that the marker values for a randomly selected case (with Ti ≤ t) are greater than the marker values for a randomly selected control (with Tj > t): AUC(t) = P(Xi > Xj | Ti ≤ t, Tj > t) for i ≠ j [108].
Concordance Index (C-index)
The Concordance Index (C-index) provides a global summary of a prognostic model's discrimination power across all available time points [110]. It estimates the probability that, for two randomly selected patients, the patient with the higher risk score will experience the event first. A C-index of 0.5 indicates no predictive discrimination, while a value of 1.0 indicates perfect discrimination.
Unlike time-dependent AUC which evaluates discrimination at specific time points, the C-index provides an overall measure of a model's ability to rank patients by their risk. In practice, the C-index is particularly useful for comparing multiple prognostic models, as it captures the model's performance across the entire follow-up period rather than at isolated time points [110].
Table 1: Comparison of Performance Metrics for Prognostic Signatures
| Metric | Interpretation | Range | Strengths | Limitations |
|---|---|---|---|---|
| Time-dependent AUC | Probability that a randomly selected case has a higher risk score than a randomly selected control at specific time t | 0-1 | Evaluates discrimination at clinically relevant time points; Handles censored data | Varies over time; Requires selection of time points |
| C-index | Probability that the model correctly orders the event times for two random patients | 0-1 | Global summary of discrimination; Does not require selecting time points | Does not capture time-varying performance; Can be dominated by early events |
| Traditional AUC | Discrimination at a fixed time point ignoring censoring | 0-1 | Simple interpretation | Inappropriate for censored data; Excludes censored observations |
Application in m6A-Related lncRNA Signature Research
Current Practices in Prognostic Model Evaluation
Recent studies developing m6A-related lncRNA signatures for cancer prognosis and immunotherapy response prediction have increasingly adopted time-dependent ROC analysis for comprehensive model validation. These approaches are essential for establishing clinical utility across multiple cancer types:
In hepatocellular carcinoma (HCC), a 4-m6A-related lncRNA signature (ZEB1-AS1, MIR210HG, BACE1-AS, SNHG3) was evaluated using time-dependent ROC curves, demonstrating AUC values that validated the model's predictive accuracy for patient survival [112]. Similarly, in head and neck squamous cell carcinoma (HNSCC), a 9-m6A-related lncRNA signature showed 5-year AUC values of 0.774 in the training set and 0.740 in the validation set, confirming the model's robust discriminatory power [22].
For pancreatic ductal adenocarcinoma (PDAC), researchers established a prognostic signature based on 9 m6A-related lncRNAs and assessed its predictive capacity using time-dependent ROC curve analysis, which confirmed that high-risk patients exhibited significantly worse prognosis than low-risk patients [113]. The same approach was applied in gastric cancer, where an 11-m6A-related lncRNA signature achieved an impressive AUC of 0.879 for risk stratification [114].
Table 2: Exemplary Applications of Time-Dependent ROC Analysis in m6A-lncRNA Research
| Cancer Type | Signature Size | AUC Values | Clinical Application | Reference |
|---|---|---|---|---|
| Head and Neck Squamous Cell Carcinoma | 9 lncRNAs | 5-year AUC: 0.774 (training), 0.740 (validation) | Prognostic prediction and immunotherapy response | [22] |
| Gastric Cancer | 11 lncRNAs | AUC: 0.879 for risk stratification | Predicting prognosis and monitoring immunotherapy | [114] |
| Breast Cancer | 6 lncRNAs | Not specified | Prognostic prediction and immune infiltration analysis | [65] |
| Hepatocellular Carcinoma | 4 lncRNAs | Not specified | Prognostic prediction | [112] |
| Esophageal Squamous Cell Carcinoma | 10 m6A/m5C-lncRNAs | Not specified | Predicting survival and immunotherapy response | [6] |
Connection to Immunotherapy Response Prediction
The evaluation of m6A-related lncRNA signatures extends beyond overall survival prediction to encompass immunotherapy response stratification. Time-dependent ROC analysis plays a crucial role in validating these applications:
In non-small cell lung cancer (NSCLC), a random forest model incorporating routine blood test parameters was developed to predict response to immune checkpoint inhibitors (ICIs). The model demonstrated a C-index of 0.803 in the training cohort and 0.712 in the validation cohort, significantly outperforming traditional prognostic scores like the Lung Immune Prognostic Index (LIPI) and Systemic Inflammatory Score (SIS) [110]. This highlights how modern machine learning approaches combined with appropriate performance metrics can enhance immunotherapy beneficiary selection.
Similarly, in HNSCC, m6A-related lncRNA signatures have been used to stratify patients according to their likely response to immunotherapy by evaluating the association between risk scores and markers of immune cell infiltration, immune checkpoint expression, and tumor immune dysfunction and exclusion (TIDE) scores [22]. The time-dependent AUC values provided critical evidence of the signature's ability to maintain discriminatory power over extended follow-up periods.
Experimental Protocols for Performance Evaluation
Protocol 1: Time-Dependent ROC Curve Analysis
Purpose: To evaluate the discriminative ability of an m6A-related lncRNA signature at specific prediction time points.
Materials and Software:
- R statistical software (version 4.0 or higher)
- R packages:
survivalROC,timeROC,survival - Dataset containing: event time, censoring indicator, and m6A-lncRNA risk scores
Procedure:
- Data Preparation: Organize your dataset to include:
- Patient identification variables
- Overall survival (OS) or progression-free survival (PFS) time
- Event indicator (1 for event, 0 for censored)
- Calculated risk score from m6A-lncRNA signature
- Relevant clinical covariates (optional for adjustment)
Select Time Points: Choose clinically relevant time points for evaluation (e.g., 1, 3, and 5 years based on the cancer type and follow-up duration).
Execute Analysis: Use the
survivalROCortimeROCpackage in R to calculate time-dependent AUC values. The key function in thesurvivalROCpackage is:Where:
Stime= survival timestatus= event indicator (1 for event, 0 for censored)marker= risk score from m6A-lncRNA signaturepredict.time= time point of interestmethod= "NNE" (nearest neighbor estimation) or "KM" (Kaplan-Meier)
Interpret Results: Examine the AUC values at each time point. AUC > 0.7 indicates acceptable discrimination, > 0.8 indicates excellent discrimination.
Visualization: Plot ROC curves for each time point and create a plot of AUC over time to visualize how discrimination changes throughout the follow-up period.
Protocol 2: Concordance Index Calculation
Purpose: To compute the overall discriminative ability of the m6A-related lncRNA signature across all available time points.
Procedure:
- Data Preparation: Use the same dataset structure as for time-dependent ROC analysis.
Calculate C-index: Use the
coxphfunction in thesurvivalpackage or theconcordance.indexfunction in thesurvcomppackage:Bias Correction: For small sample sizes, consider using bootstrap resampling (1000 repetitions) to obtain a bias-corrected C-index estimate.
Confidence Intervals: Calculate 95% confidence intervals for the C-index to quantify estimation uncertainty.
Comparison: If evaluating multiple models, statistically compare C-indices using the
compareCfunction in thesurvcomppackage.
Protocol 3: Performance Comparison with Existing Biomarkers
Purpose: To determine whether the m6A-related lncRNA signature provides superior predictive performance compared to established clinical biomarkers.
Procedure:
- Reference Models: Identify established prognostic models for comparison (e.g., TNM staging, clinical nomograms, or published gene signatures).
Calculate Metrics: Compute time-dependent AUC values and C-index for both the new m6A-lncRNA signature and reference models.
Statistical Comparison: For time-dependent AUC, use the method proposed by Kang et al. (2015) for comparing correlated AUC curves. For C-index, use the
survcomppackage functions.Clinical Utility Assessment: Perform decision curve analysis (DCA) to evaluate the net benefit of the m6A-lncRNA signature across different threshold probabilities [22].
Workflow for Evaluating m6A-lncRNA Signature Performance
Table 3: Essential Computational Tools for Performance Metric Analysis
| Tool/Software | Primary Function | Application Context | Key Features |
|---|---|---|---|
| R survivalROC Package | Time-dependent ROC analysis | Calculating AUC at specific time points | Multiple estimation methods (NNE, KM); Handles censored data |
| R timeROC Package | Time-dependent ROC analysis | Comparative AUC analysis | Allows for cumulative/dynamic definitions; Computes confidence intervals |
| R survival Package | C-index calculation | Overall discrimination assessment | Integrated with Cox models; Standard error estimation |
| R survcomp Package | Performance comparison | Comparing multiple models | Statistical tests for C-index differences; Multiple testing correction |
| X-tile Software | Optimal cutpoint determination | Risk stratification | Determines optimal cutoff for high/low risk groups; Visualization capabilities [112] |
Troubleshooting and Technical Considerations
Addressing Common Analytical Challenges
Small Sample Sizes: For studies with limited patients (n < 100), time-dependent AUC estimates may exhibit substantial variability. Implement bootstrap resampling (1000 repetitions) to obtain bias-corrected confidence intervals. Consider using the incident/dynamic (I/D) approach which may provide more stable estimates with small samples [108].
Heavy Censoring: When more than 50% of observations are censored, the standard nonparametric estimation of time-dependent AUC may be biased. Apply inverse probability of censoring weighting (IPCW) to adjust for informative censoring patterns.
Multiple Time Points: When evaluating multiple time points, account for multiple testing using false discovery rate (FDR) correction rather than Bonferroni adjustment, which is overly conservative for correlated AUC estimates.
Model Overfitting: When developing and evaluating signatures on the same dataset, performance metrics will be optimistically biased. Always validate time-dependent AUC and C-index on independent datasets or using rigorous cross-validation approaches [113].
Interpretation Guidelines
Clinical Significance vs. Statistical Significance: A statistically significant AUC > 0.5 may not be clinically useful. Focus on the magnitude of improvement over existing biomarkers rather than statistical significance alone.
Time-Varying Performance: Note that discrimination often decreases with longer prediction horizons. A signature that maintains AUC > 0.7 over 3-5 years demonstrates robust performance [22] [113].
Context-Specific Benchmarks: Establish field-specific benchmarks for model performance. In oncology, AUC > 0.65 is generally considered acceptable, > 0.75 is good, and > 0.85 is excellent for prognostic models.
Time-dependent ROC curve analysis and the Concordance Index provide indispensable methodologies for rigorously evaluating m6A-related lncRNA signatures in cancer prognosis and immunotherapy response prediction. By appropriately accounting for censored observations and the time-varying nature of discrimination, these metrics enable researchers to establish robust evidence for the clinical utility of novel molecular signatures.
As the field advances toward more personalized cancer immunotherapy, the application of these sophisticated performance metrics will be crucial for translating m6A-related lncRNA research into clinically actionable tools that can guide treatment decisions and improve patient outcomes.
Comparative Analysis of Signature Performance Across LUAD, HNSCC, CRC, and ESCC
Within the field of cancer bioinformatics, the development of prognostic signatures based on m6A-related long non-coding RNAs (lncRNAs) represents a significant advancement for predicting patient survival and therapeutic response. These signatures leverage the crucial role of m6A RNA modification and lncRNAs in regulating gene expression, tumor progression, and the tumor immune microenvironment [10]. This application note provides a systematic comparison of the performance of these multi-lncRNA signatures across four major cancers: Lung Adenocarcinoma (LUAD), Head and Neck Squamous Cell Carcinoma (HNSCC), Colorectal Cancer (CRC), and Esophageal Squamous Cell Carcinoma (ESCC). Furthermore, we present detailed, standardized protocols to facilitate the construction and validation of such signatures, enabling their application in predictive oncology and drug development.
Comparative Performance of m6A and Immune-Related lncRNA Signatures
Analysis of published signatures reveals distinct prognostic lncRNA panels for various cancers, with consistent demonstration of independent predictive value for patient overall survival (OS).
Table 1: Comparative Overview of m6A and Immune-Related lncRNA Signatures
| Cancer Type | Signature Name/Components | Number of lncRNAs | Performance (AUC) | Independent Prognostic Value | Key Clinical Implications |
|---|---|---|---|---|---|
| LUAD | m6ARLSig (e.g., AL606489.1, COLCA1) [10] | 8 | Not Specified | Yes (p<0.05) | Predicts cisplatin resistance; associated with immune cell infiltration. |
| LUAD | 5-lncRNA Signature (AC068228.1, SATB2-AS1, LINC01843, AC026355.1, AL606489.1) [115] | 5 | > TNM stage | Yes (p<0.05) | More efficient and stable than TNM stage; shows sexual dimorphism (AL606489.1). |
| HNSCC | 3-lncRNA Signature [116] | 3 | Not Specified | Yes (p<0.05) | Stratifies patients into high/low-risk with significant survival difference (1.85 vs. 5.48 years). |
| CRC | 5 Immune-related lncRNA Signature [117] | 5 | Not Specified | Yes (p<0.05) | Correlates with tumor-infiltrating immune cells, immune status, and immunotherapy responsiveness. |
| CRC | 4-lncRNA Signature (SPRY4-IT1, LINC01133, Loc554202, RP11-727F15.13) [118] | 4 | 5-year OS: 0.727 [118] | Yes (p<0.05) | High-risk group had significantly shorter survival (median 18 vs. 24.5 months). |
| ESCC | 5-lncRNA Signature (AC007179.1, MORF4L2-AS1, etc.) [119] | 5 | Not Specified | Yes (p<0.05) | Superior to TNM stage for prognosis; validated in independent cohorts. |
| ESCC | m6A/m5C-related 10-lncRNA Signature [6] | 10 | Not Specified | Yes (p<0.05) | Low-risk group had better prognosis, higher immune cell abundance, and enhanced ICI benefit. |
Standardized Protocol for Constructing an m6A-Related lncRNA Prognostic Signature
Data Acquisition and Preprocessing
- Data Source: Obtain RNA-seq data (in FPKM or TPM format) and corresponding clinical data (survival time, status, and clinicopathological parameters) for the cancer of interest from public databases such as The Cancer Genome Atlas (TCGA) [10] [115] [118].
- Data Cleaning: Remove patients with incomplete clinical information or overall survival (OS) of less than 30 days to avoid bias from perioperative mortality [10]. Randomly divide the remaining cohort into a training set (e.g., 50-70% of patients) and a testing set (e.g., 30-50%), ensuring no significant differences in clinical characteristics between sets [120] [118].
Identification of m6A-Related lncRNAs
- Compile m6A Regulators: Curate a list of known m6A regulators (writers, erasers, readers) from literature, typically including genes such as METTL3, METTL14, FTO, ALKBH5, YTHDF1, and IGF2BP1 [10] [6].
- Co-expression Analysis: Calculate correlation coefficients (Pearson or Spearman) between the expression of all lncRNAs and the m6A regulators from the curated list. Identify m6A-related lncRNAs by applying a significance threshold (e.g., correlation coefficient > 0.4 or 0.5 and p-value < 0.001) [10] [121].
Construction of the Prognostic Signature
- Univariate Cox Regression: Perform this analysis on the training set to identify m6A-related lncRNAs significantly associated with overall survival (OS) [10] [120]. A p-value threshold of < 0.01 is commonly used to select candidate lncRNAs [120] [118].
- Multivariate Cox Regression & Model Fitting: Input the significant lncRNAs from the univariate analysis into a multivariate Cox regression analysis. Use a stepwise selection method based on the Akaike Information Criterion (AIC) to build the most parsimonious model with the best fit [120] [115].
- Risk Score Calculation: Construct a risk score formula for each patient based on the final model:
Risk Score = Σ (Coefficient_lncRNAi × Expression_lncRNAi)[10] [119] [115]. Calculate the risk score for every patient in the training set and use the median risk score as a cut-off to stratify patients into high-risk and low-risk groups [120] [115].
Validation of the Signature
- Survival Analysis: Use the Kaplan-Meier method and the log-rank test to compare overall survival between the high-risk and low-risk groups in the training, testing, and entire datasets. A significant p-value (p < 0.05) indicates good prognostic separation [10] [120] [116].
- ROC Analysis: Assess the predictive accuracy of the signature by plotting time-dependent receiver operating characteristic (ROC) curves and calculating the area under the curve (AUC) for 1, 3, and 5-year survival [120] [116] [118].
- Independence Test: Conduct univariate and multivariate Cox regression analyses that include the risk score and other clinical variables (e.g., age, gender, TNM stage). The risk score is an independent prognostic factor if it remains significantly associated with OS in the multivariate analysis [10] [115].
Functional and Clinical Correlation Analysis
- Immune Infiltration Analysis: Utilize algorithms such as CIBERSORT, QUANTISEQ, or ssGSEA to estimate the abundance of tumor-infiltrating immune cells in each sample. Correlate the risk scores with immune cell infiltration levels and the expression of immune checkpoint genes (e.g., PD-1, PD-L1, CTLA-4) [10] [117] [12].
- Drug Sensitivity Prediction: Use databases such as GDSC to estimate the half-maximal inhibitory concentration (IC50) of common chemotherapeutic drugs or targeted therapies between high- and low-risk groups to explore potential differences in treatment response [10].
- Functional Enrichment: Perform Gene Set Enrichment Analysis (GSEA) on high- and low-risk groups to identify signaling pathways and biological processes (e.g., from KEGG, GO) that are differentially activated [10].
Figure 1: Workflow for constructing and validating an m6A-related lncRNA prognostic signature.
Table 2: Key Reagents and Computational Tools for Signature Development
| Category/Item | Function/Description | Example Sources/Platforms |
|---|---|---|
| RNA-seq & Clinical Data | Provides standardized, large-scale omics and clinical data for model training and validation. | The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO) [10] [119]. |
| Immune Cell Deconvolution | Computational tool to estimate immune cell infiltration abundance from bulk RNA-seq data. | CIBERSORT, QUANTISEQ, XCELL, TIMER [10] [117] [121]. |
| Pathway Enrichment Analysis | Identifies biological pathways and processes significantly enriched in gene sets of interest. | Gene Set Enrichment Analysis (GSEA), clusterProfiler (for GO & KEGG) [10] [6]. |
| Statistical Computing | Primary software environment for all statistical analyses, modeling, and visualization. | R software with packages: survival, glmnet, survminer, timeROC, limma [120] [116] [117]. |
| In Vitro Functional Validation | Cell-based assays to confirm the oncogenic or tumor-suppressive roles of identified lncRNAs. | siRNA/shRNA knockdown, proliferation (CCK-8), migration (Transwell), apoptosis (flow cytometry) [10]. |
The consistent development and validation of m6A-related lncRNA signatures across LUAD, HNSCC, CRC, and ESCC underscore their robust potential as prognostic biomarkers. These signatures not only stratify patients more accurately than traditional staging systems but also provide insights into the tumor immune microenvironment and potential response to immunotherapy. The standardized protocols and toolkit outlined herein provide researchers and drug developers with a clear roadmap to construct, validate, and apply these powerful tools, ultimately paving the way for more personalized cancer therapy. Future efforts should focus on the technical validation of these signatures using targeted assays and their integration into prospective clinical trials.
This application note provides detailed protocols for analyzing correlations between a prognostic m6A-related long non-coding RNA (lncRNA) signature and the tumor immune microenvironment, specifically focusing on infiltrating immune cells and immune checkpoint expression. This analysis is situated within a broader research thesis investigating how m6A-related lncRNA signatures predict response to immunotherapy in cancer. The tumor immune microenvironment plays a critical role in therapeutic response, and understanding its composition and interaction with epigenetic regulators like m6A-modified lncRNAs is essential for developing predictive biomarkers and novel therapeutic strategies [10] [12]. This document provides standardized methodologies for researchers to validate these correlations in their experimental systems.
Key Research Reagent Solutions
The table below catalogues essential reagents and tools required for executing the protocols described in this document.
Table 1: Essential Research Reagents and Tools for Immune Microenvironment Analysis
| Reagent/Tool | Primary Function | Example Sources/Assays |
|---|---|---|
| RNA-seq Data | Source of lncRNA expression data and m6A regulator expression | The Cancer Genome Atlas (TCGA) [10] [6] |
| CIBERSORT Algorithm | Computational deconvolution of bulk tumor RNA-seq data to estimate relative abundances of 22 immune cell types [10] [122] [123] | LM22 signature matrix; Requires input of normalized gene expression data [10] [122] |
| ESTIMATE Algorithm | Calculation of immune, stromal, and estimate scores to infer tumor purity and presence of infiltrating non-tumor cells [124] | R package "estimate" |
| Multicolor IHC/mIHC | Simultaneous detection of multiple protein targets (e.g., PLCXD2, immune cell markers, checkpoint proteins) in formalin-fixed paraffin-embedded (FFPE) tissue samples [125] | Opal 7-Color mIHC Kit; Automated slide scanning systems (e.g., Vectra) |
| Immune Checkpoint Antibodies | Protein-level detection and quantification of key immune checkpoint molecules | Antibodies against PD-1, PD-L1, CTLA-4, CD80 [125] [124] |
| Cell Lines & Culture | In vitro functional validation of targets (e.g., proliferation, invasion, drug resistance assays) | A549 (LUAD), U87MG (glioma), 16-HBE (normal control) [10] [124] |
| siRNA/shRNA | Transient or stable knockdown of target genes (e.g., m6A-related lncRNAs, regulators) for functional studies [10] [124] | Commercially available sequences from suppliers (e.g., RiboBio) |
Quantitative Data Synthesis on m6A-lncRNA Signatures and Immune Correlations
Recent studies across multiple cancer types have established a strong link between m6A-related lncRNA signatures, patient prognosis, and the immune landscape. The following table synthesizes key quantitative findings from the literature.
Table 2: Correlation of m6A-related lncRNA Signatures with Prognosis and Immune Microenvironment in Human Cancers
| Cancer Type | m6A-lncRNA Signature | Prognostic Value | Key Immune Correlations | Therapeutic Prediction |
|---|---|---|---|---|
| Lung Adenocarcinoma (LUAD) [10] | 8-lncRNA signature (m6ARLSig); AL606489.1, COLCA1 (adverse); 6 others (favorable) | Independent predictor of overall survival (OS); High-risk group had worse OS [10] | Associated with specific immune cell infiltration patterns; Correlated with immune checkpoint inhibitor (ICI) gene expression [10] | High-risk score associated with attenuated cisplatin resistance in vitro (FAM83A-AS1 knockdown) [10] |
| Cervical Cancer [12] | 4-lncRNA signature (AL139035.1, AC015922.2, AC073529.1, AC008124.1) | Independent prognostic predictor | Low-risk group showed higher abundance of immune cells (e.g., CD4+ T cells, Tregs) and enhanced expression of most immune checkpoint genes [12] | Low-risk score predicted potential benefit from immune checkpoint inhibitor treatment (P < 0.05) [12] |
| Esophageal Squamous Cell Carcinoma (ESCC) [6] | 10 m6A/m5C-related lncRNA signature (RiskScore) | Validated independent prediction ability; Low-RiskScore associated with better prognosis [6] | Low-RiskScore group had higher abundance of CD4+ T cells, naive CD4+ T cells, class-switched memory B cells, and Tregs [6] | Patients with low-RiskScore were more likely to benefit from ICI treatment (P < 0.05) [6] |
Detailed Experimental Protocols
Protocol 1: Constructing an m6A-Related lncRNA Signature and Correlating with Clinical Outcome
This protocol outlines the bioinformatic pipeline for developing a prognostic m6A-related lncRNA signature from public transcriptomic data [10] [12] [6].
Procedure:
- Data Acquisition: Download RNA-seq data (in TPM or FPKM format) and corresponding clinical data (including overall survival time and status) for your cancer of interest from TCGA.
- Define m6A Regulators: Compile a list of known m6A "writer," "reader," and "eraser" genes (e.g., METTL3, YTHDF1, FTO) from literature [10] [6].
- Identify m6A-Related lncRNAs:
- Extract the expression matrix of all lncRNAs from the RNA-seq data.
- Perform Spearman's correlation analysis between the expression of each lncRNA and each m6A regulator.
- Identify m6A-related lncRNAs using a correlation coefficient threshold (e.g., |R| > 0.3) and a statistical significance threshold (e.g., P < 0.05) [6].
- Prognostic Signature Construction:
- Randomly split the patient cohort into training and testing sets.
- In the training set, perform univariate Cox regression analysis on the m6A-related lncRNAs to identify those significantly associated with overall survival.
- Subject the significant lncRNAs to Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression analysis to prevent overfitting and select the most robust features for the signature [12] [6].
- Calculate a risk score for each patient using the formula: Risk Score = Σ (Expression of lncRNAi × Lasso Coefficienti) [10].
- Validation: Stratify patients in the testing set and the entire cohort into high-risk and low-risk groups based on the median risk score. Validate the prognostic power of the signature using Kaplan-Meier survival analysis and log-rank test.
Protocol 2: Profiling Immune Cell Infiltration Using Computational Deconvolution
This protocol details the use of the CIBERSORT tool to infer immune cell composition from bulk tumor RNA-seq data, which can then be correlated with the m6A-lncRNA risk score [10] [122] [123].
Procedure:
- Data Preparation: Prepare a normalized gene expression matrix (e.g., TPM) for your tumor samples.
- CIBERSORT Analysis:
- Access the CIBERSORT web portal (https://cibersort.stanford.edu/) or use the corresponding R package.
- Upload the normalized expression matrix and the LM22 signature matrix, which defines gene expression signatures for 22 human immune cell types.
- Run the analysis with 1000 permutations for statistical analysis.
- Output Interpretation: The output provides the estimated proportion of each of the 22 immune cell types in each sample. The sum of all fractions equals 1 for each sample.
- Correlation Analysis:
- Compare the immune cell infiltration profiles between the high-risk and low-risk groups defined by the m6A-lncRNA signature using statistical tests (e.g., Wilcoxon rank-sum test).
- Perform Spearman's correlation analysis to directly assess the relationship between the continuous risk score and the infiltration level of specific immune cells (e.g., CD8+ T cells, Tregs, M2 macrophages) [122].
Protocol 3: Quantifying Immune Checkpoint Expression and Spatial Localization
This protocol describes methods for analyzing the expression of immune checkpoint genes and their correlation with the m6A-lncRNA signature, and for validating findings at the protein level.
Procedure: A. Gene Expression Analysis from RNA-seq Data:
- Extract the normalized expression values of key immune checkpoint genes (e.g., PDCD1/PD-1, CD274/PD-L1, CTLA-4, LAG-3, TIGIT) from the TCGA RNA-seq dataset [126] [124].
- Compare the expression levels of these checkpoint genes between the high-risk and low-risk groups.
- Perform Spearman's correlation analysis between the m6A-lncRNA risk score and the expression level of each checkpoint gene [10].
B. Protein-Level Validation via Multicolor Immunofluorescence (mIHC):
- Tissue Microarray (TMA) Staining: Use a TMA containing tumor and control tissues. Perform mIHC staining using the Opal kit according to the manufacturer's instructions [125].
- Antibody Panel Design: Select a panel of primary antibodies targeting:
- The protein of interest (e.g., a specific m6A regulator or a protein encoded by a candidate gene).
- Immune cell markers (e.g., CD8 for cytotoxic T cells, CD4 for helper T cells, CD68 for macrophages).
- Immune checkpoint proteins (e.g., PD-L1, CTLA-4).
- A tumor marker (e.g., Pan-cytokeratin) [125].
- Image Acquisition and Analysis:
- Scan stained TMA slides using a multispectral imaging system (e.g., Vectra).
- Use image analysis software (e.g., inForm) to perform cell segmentation and quantify the fluorescence signal for each marker on a single-cell basis.
- Calculate the density of specific immune cell subsets and their expression of checkpoint proteins within tumor nests and stromal regions.
- Correlation: Statistically correlate the protein expression levels of checkpoints and immune cell densities with the patient's m6A-lncRNA risk score or the expression of key signature lncRNAs.
Visualized Workflows and Signaling Pathways
Research Workflow for m6A-lncRNA and Immune Microenvironment Analysis
The diagram below illustrates the comprehensive research workflow integrating bioinformatic analysis with experimental validation.
Conceptual Framework of m6A-lncRNA in Immune Regulation
This diagram outlines the proposed mechanism by which m6A-related lncRNA signatures influence the tumor immune microenvironment and response to therapy.
Within the burgeoning field of cancer research, the prediction of patient response to therapy is a cornerstone of personalized medicine. A particularly promising avenue involves the study of m6A-related long non-coding RNAs (lncRNAs) and their role in determining tumor behavior and therapeutic susceptibility. These lncRNA molecules, modified by N6-methyladenosine (m6A) marks, are emerging as crucial regulators of cancer progression, immune evasion, and drug resistance [127] [128]. This protocol details the integration of an m6A-related lncRNA signature with IC50 value determination to predict chemotherapeutic response, providing a methodological framework for researchers aiming to translate these biomarkers into clinically actionable insights.
The core premise is that m6A-modified lncRNAs influence key cancer pathways and the tumor microenvironment. For instance, the lncRNA FAM83A-AS1 has been experimentally validated to promote cisplatin resistance in lung adenocarcinoma, while signatures comprising other m6A-related lncRNAs can stratify patients into risk categories with distinct survival outcomes and immune profiles [10] [12]. The half-maximal inhibitory concentration (IC50), a quantitative measure of a compound's potency, serves as a critical metric for evaluating drug sensitivity in vitro [129]. By coupling IC50 assays with m6A-related lncRNA profiling, researchers can build predictive models to identify patients who are likely to respond to conventional chemotherapy, thereby optimizing treatment strategies.
Key Concepts and Definitions
m6A Modification and Related lncRNAs
The m6A modification is a dynamic and reversible RNA methylation process regulated by three classes of enzymes:
- Writers: Complexes including METTL3, METTL14, and WTAP that install the m6A mark [127] [128].
- Erasers: Enzymes such as FTO and ALKBH5 that remove the m6A mark [127] [128].
- Readers: Proteins including YTHDF1-3 and IGF2BPs that recognize m6A and dictate the functional outcomes, influencing RNA stability, translation, and processing [128].
When lncRNAs are modified by m6A, their functions can be significantly altered, impacting crucial processes such as proliferation, invasion, and response to therapeutic agents [10] [127]. For example, m6A modification of the lncRNA NEAT1 has been linked to promoting bone metastasis in prostate cancer [127].
IC50 and Drug Sensitivity
The IC50 value is defined as the concentration of a drug required to reduce cell viability by 50% in vitro. It is a cornerstone of preclinical drug development and sensitivity testing [129]. However, a critical limitation is its time-dependent nature, as the evolving growth rates of treated and control populations over time can lead to varying IC50 values in the same assay [129]. To address this, newer parameters have been proposed:
- ICr0: The drug concentration at which the effective growth rate of the cell population is zero.
- ICrmed: The drug concentration that reduces the growth rate of the control population by half [129].
These parameters, derived from modeling cell proliferation as an exponential process, offer a more stable and biologically meaningful assessment of drug efficacy.
Protocol: Integrating an m6A-lncRNA Signature with IC50 Profiling
This protocol outlines a comprehensive workflow to establish and validate a prognostic m6A-related lncRNA signature and correlate it with drug sensitivity profiles derived from IC50 values.
Part A: Development of an m6A-Related lncRNA Prognostic Signature
Materials and Reagents
- RNA-seq Data: Publicly available data from repositories such as The Cancer Genome Atlas (TCGA) for the cancer type of interest [10] [12].
- Computational Environment: R programming language with packages for statistical analysis (e.g.,
survival,glmnet). - List of m6A Regulators: A curated list of known writer, eraser, and reader genes (e.g., METTL3, FTO, YTHDF1) from the scientific literature [10].
Procedure
- Identify m6A-Related lncRNAs: Correlate the expression of all annotated lncRNAs from the RNA-seq data with the expression of the known m6A regulators. LncRNAs with a significant correlation coefficient (e.g., |R| > 0.4 and p < 0.05) are classified as m6A-related [10] [130].
- Perform Univariate Cox Regression: Analyze the association between the expression of each m6A-related lncRNA and overall patient survival to identify prognostically significant lncRNAs [10] [131].
- Construct the Prognostic Signature:
a. Employ the Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression on the prognostic lncRNAs to prevent overfitting and select the most robust features for the model [12] [131].
b. Build a multivariate Cox regression model with the selected lncRNAs. The output is a risk score formula for each patient:
Risk Score = Σ (Coefficient_lncRNAi × Expression_lncRNAi)[10] [131]. - Validate the Signature: Stratify patients into high-risk and low-risk groups based on the median risk score. Validate the prognostic power of the signature using Kaplan-Meier survival analysis and time-dependent Receiver Operating Characteristic (ROC) curves [10] [12].
Part B: Experimental Determination of IC50 and Drug Sensitivity
Materials and Reagents
- Cell Lines: Relevant cancer cell lines (e.g., A549 for lung adenocarcinoma) and appropriate culture media [10] [129].
- Chemotherapeutic Agents: Drugs of clinical relevance, such as cisplatin, oxaliplatin, or paclitaxel [10] [129].
- Viability Assay Kit: MTT (Thiazolyl Blue Tetrazolium Bromide) assay or equivalent [129].
Procedure
- Cell Seeding and Treatment: Seed cells in 96-well plates at a density that ensures exponential growth throughout the assay duration. After cell attachment, treat the wells with a range of drug concentrations (typically a serial dilution series). Include untreated control wells [129].
- Cell Viability Measurement: After a defined incubation period (e.g., 72 hours), add MTT reagent to each well. Metabolically active cells will reduce MTT to purple formazan crystals. Solubilize the crystals with dimethyl sulfoxide (DMSO) and measure the absorbance at 570 nm [129].
- IC50 Calculation: Calculate the percentage of cell viability for each drug concentration, normalized to the untreated controls. Fit the dose-response data using non-linear regression to generate a curve and calculate the IC50 value [129].
- Optional: Advanced Growth Rate Analysis: For a more robust measurement, perform the MTT assay at multiple time points (e.g., 0, 24, 48, 72 hours). Calculate the effective growth rate for each drug concentration by fitting the absorbance data to an exponential growth model. Derive the ICr0 and ICrmed values from the curve of growth rate versus drug concentration [129].
Part C: Correlation and Functional Validation
- Correlate Risk Score with IC50: Using cell lines representing different risk groups (e.g., via gene manipulation), test their sensitivity to chemotherapeutics. A positive correlation between a high in silico risk score and elevated experimental IC50 values indicates the signature's predictive power for drug resistance [10].
- Functional Studies: To establish causality, perform gene knockdown of a signature lncRNA (e.g., FAM83A-AS1) in a resistant cell line using siRNA or shRNA. Subsequent IC50 assays should show a significant decrease in the IC50 value, indicating restored drug sensitivity [10].
The following diagram illustrates the complete experimental workflow, from data acquisition to functional validation.
Data Presentation and Analysis
Tabulating m6A-Related lncRNA Signature Components
The table below provides a hypothetical example of a finalized m6A-related lncRNA signature, as might be derived from multivariate Cox analysis.
Table 1: Example Components of a Prognostic m6A-Related lncRNA Signature
| lncRNA ID | Cox Coefficient | Hazard Ratio | Functional Role |
|---|---|---|---|
| AL606489.1 | 0.52 | 1.68 | Independent adverse prognostic biomarker [10] |
| COLCA1 | 0.41 | 1.51 | Independent adverse prognostic biomarker [10] |
| AC015922.2 | -0.63 | 0.53 | Favorable prognostic factor; potential tumor suppressor [12] |
| FAM83A-AS1 | 0.78 | 2.18 | Promotes proliferation, invasion, and cisplatin resistance [10] |
Presenting Drug Sensitivity (IC50) Data
The following table demonstrates how drug sensitivity data can be structured for comparison between different risk groups or genetic profiles.
Table 2: Example Drug Sensitivity Profiles in Cell Line Models
| Cell Line / Risk Group | Genetic Manipulation | Cisplatin IC50 (μM) | Oxaliplatin IC50 (μM) | Paclitaxel IC50 (nM) |
|---|---|---|---|---|
| A549 (Parental) | - | 12.5 ± 1.2 | 8.3 ± 0.9 | 45.2 ± 5.1 |
| A549 (High-Risk Model) | FAM83A-AS1 Overexpression | 28.7 ± 2.4 | 15.6 ± 1.5 | 52.1 ± 4.8 |
| A549 (Low-Risk Model) | FAM83A-AS1 Knockdown | 5.1 ± 0.6 | 4.2 ± 0.5 | 38.5 ± 3.7 |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Resources for m6A-lncRNA and Drug Sensitivity Studies
| Item | Function/Description | Example Sources/Assays |
|---|---|---|
| TCGA & GEO Datasets | Provides raw RNA-seq data and clinical information for signature discovery and validation [10] [130]. | UCSC Xena, GEOquery R package |
| m6A Regulator Gene List | A curated set of writer, eraser, and reader genes used to identify m6A-related lncRNAs. | Literature curation (e.g., METTL3, FTO, YTHDF1) [10] [128] |
| LASSO Cox Regression | A statistical method for variable selection and regularization to build a robust prognostic model with many potential predictors [12]. | glmnet R package |
| CIBERSORT/ESTIMATE | Computational algorithms to infer immune cell infiltration and tumor microenvironment scores from RNA-seq data [10] [131]. | CIBERSORT web portal, estimate R package |
| MTT Assay | A colorimetric assay for measuring cell metabolic activity, used as a surrogate for cell viability in IC50 calculations [129]. | Thiazolyl Blue Tetrazolium Bromide |
| siRNA/shRNA | Synthetic RNA molecules used for targeted knockdown of specific lncRNAs to validate their functional role in drug resistance [10]. | Commercial synthesis services |
Pathway and Mechanism Visualization
The predictive power of m6A-related lncRNAs stems from their involvement in core cancer pathways. The diagram below summarizes the key molecular mechanisms by which an m6A-modified lncRNA, such as FAM83A-AS1, can influence tumor progression and confer drug resistance.
Concluding Remarks
The integration of m6A-related lncRNA signatures with classical drug sensitivity metrics like IC50 provides a powerful, multi-dimensional approach to predicting chemotherapeutic response. The protocols outlined here—ranging from bioinformatic model construction to wet-lab validation—offer a roadmap for researchers to explore this promising field. Future efforts should focus on the standardization of these signatures across independent cohorts and the development of high-throughput functional screens to rapidly test their predictive value against libraries of therapeutic compounds, ultimately accelerating their translation into clinical decision support tools.
The discovery of m6A-related lncRNA signatures has emerged as a promising approach for predicting cancer prognosis and immunotherapy response [22] [80]. However, transitioning from computational identification to clinical application requires rigorous experimental validation. This document provides detailed application notes and protocols for validating m6A-related lncRNA signatures through clinical tissue correlation and in vitro functional studies, framed within the broader context of immunotherapy response research. The standardized methodologies outlined here are designed to help researchers establish reliable, reproducible validation pipelines that bridge bioinformatic discoveries with biological and clinical relevance.
Clinical Tissue Correlation Studies
Protocol: Clinical Specimen Collection and Processing
Purpose: To validate the expression patterns of identified m6A-related lncRNAs in clinical samples and correlate them with patient clinicopathological features and outcomes.
Materials and Reagents:
- Fresh tumor and matched adjacent normal tissues (stored in liquid nitrogen post-resection)
- TRIzol reagent for RNA isolation
- cDNA synthesis kit
- SYBR Green-based qPCR master mix
- Sequence-specific primers for target lncRNAs
- Institutional review board approval and informed patient consent
Procedure:
- Cohort Establishment: Recruit patients with appropriate sample size (e.g., 55-100 pairs of tumor/adjacent tissues) who underwent surgical resection without preoperative radiotherapy or chemotherapy [67] [132].
- RNA Extraction: Homogenize 30-50 mg tissue samples in TRIzol reagent following manufacturer's protocol. Assess RNA quality and quantity using spectrophotometry.
- cDNA Synthesis: Reverse transcribe 1-2 µg of total RNA using reverse transcriptase and random hexamers.
- Quantitative PCR: Perform triplicate reactions containing SYBR Green master mix, gene-specific primers, and cDNA template. Use the following cycling conditions: 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min.
- Data Analysis: Calculate relative expression using the 2^(-ΔΔCt) method with GAPDH or β-actin as endogenous control.
Validation Criteria: Signature lncRNAs should show significant differential expression between tumor and normal tissues (e.g., upregulation of SLCO4A1-AS1, MELTF-AS1, SH3PXD2A-AS1, H19, and PCAT6 in colorectal cancer) [67] [132].
Protocol: Immunohistochemical Validation of m6A Regulators
Purpose: To confirm the correlation between lncRNA signature and m6A modification machinery in clinical tissues.
Procedure:
- Tissue Sectioning: Cut 4-5 µm sections from formalin-fixed, paraffin-embedded tissue blocks.
- Antigen Retrieval: Perform heat-induced epitope retrieval in citrate buffer using a pressure cooker.
- Antibody Staining: Incubate sections overnight at 4°C with primary antibodies against m6A regulators (e.g., anti-METTL3 and anti-METTL14 at 1:100 dilution) [65].
- Detection: Apply HRP-conjugated secondary antibodies and visualize using DAB peroxidase substrate followed by hematoxylin counterstaining.
- Evaluation: Score staining intensity and percentage of positive cells. Correlate m6A regulator expression with lncRNA signature risk groups.
Table 1: Key Research Reagent Solutions for Clinical Validation
| Reagent Type | Specific Examples | Function/Application |
|---|---|---|
| RNA Stabilization Reagent | TRIzol | Preserves RNA integrity in fresh tissue specimens |
| Reverse Transcription Kit | 1st Strand cDNA Synthesis Kit | Converts RNA to cDNA for expression analysis |
| qPCR Master Mix | SYBR Green-based mixes | Enables quantitative measurement of lncRNA expression |
| Primary Antibodies | Anti-METTL3, Anti-METTL14 | Detects m6A regulator expression in tissue sections |
| Detection System | HRP-conjugated secondary antibodies with DAB | Visualizes antibody binding in immunohistochemistry |
In Vitro Functional Studies
Protocol: Functional Validation of Target lncRNAs in Cancer Cell Lines
Purpose: To investigate the oncogenic functions of signature lncRNAs identified through bioinformatic analysis.
Materials:
- Relevant cancer cell lines (e.g., A549 and A549/DDP for lung adenocarcinoma)
- Cell culture media and supplements
- Lipofectamine RNAiMAX or similar transfection reagent
- siRNA or shRNA targeting candidate lncRNAs
- Cell Counting Kit-8 (CCK-8) for proliferation assays
- Matrigel-coated Transwell inserts for invasion assays
- Annexin V-FITC/PI apoptosis detection kit
- Cisplatin or other relevant chemotherapeutic agents
Procedure:
- Cell Culture: Maintain appropriate cancer cell lines in recommended media with 10% FBS at 37°C with 5% CO₂.
- Gene Modulation: Transfect cells with 50-100 nM siRNA or shRNA targeting lncRNAs using Lipofectamine RNAiMAX. Include non-targeting siRNA as negative control.
- Proliferation Assay: Seed transfected cells in 96-well plates (3000 cells/well). Measure viability at 0, 24, 48, and 72 hours using CCK-8 reagent according to manufacturer's protocol [133].
- Invasion and Migration:
- For invasion assays: Place serum-starved cells in Matrigel-coated Transwell inserts with complete media in lower chamber as chemoattractant.
- After 24-48 hours, fix and stain migrated cells with crystal violet. Count cells in five random fields.
- Apoptosis Analysis: Harvest transfected cells after 48 hours, stain with Annexin V-FITC and propidium iodide, and analyze by flow cytometry.
- Drug Resistance Assessment: Treat lncRNA-modulated cells with increasing concentrations of chemotherapeutic agents (e.g., cisplatin) for 48 hours. Calculate IC50 values from dose-response curves [133].
Expected Results: Knockdown of oncogenic lncRNAs (e.g., FAM83A-AS1 in LUAD) should suppress proliferation, invasion, migration, epithelial-mesenchymal transition (EMT), and chemoresistance while increasing apoptosis [133].
Protocol: Investigating m6A Modification of lncRNAs
Purpose: To confirm whether identified lncRNAs are directly modified by m6A machinery and characterize the functional consequences.
Procedure:
- Methylated RNA Immunoprecipitation (MeRIP):
- Fragment cellular RNA to 100-500 nucleotides.
- Incubate with anti-m6A antibody or normal IgG (control) conjugated to magnetic beads.
- After washing, elute and purify bound RNA.
- Analyze lncRNA enrichment by qRT-PCR.
- RNA Stability Assay: Treat cells with actinomycin D (5 µg/mL) to inhibit transcription. Harvest cells at 0, 2, 4, and 8 hours post-treatment. Measure remaining lncRNA levels by qRT-PCR to determine half-life.
- Regulator Manipulation: Overexpress or knockdown specific m6A regulators (writers, erasers, readers) to assess their impact on lncRNA expression and function.
Figure 1: Experimental Validation Workflow for m6A-Related lncRNA Signatures. This diagram outlines the key stages in validating m6A-related lncRNA signatures, from initial identification through clinical correlation, functional studies, and mechanistic investigation.
Integration with Immunotherapy Response Assessment
Protocol: Validating Immunotherapeutic Predictive Value
Purpose: To experimentally verify whether the m6A-related lncRNA signature can predict response to immunotherapy.
Materials:
- Syngeneic mouse models or humanized mouse models
- Anti-PD-1/PD-L1 antibodies
- Flow cytometry antibodies for immune cell profiling (CD4, CD8, Treg markers)
- ELISA kits for cytokine detection
- Co-culture systems for T cell cytotoxicity assays
Procedure:
- In Vivo Validation:
- Implant control and lncRNA-knockdown cancer cells into immunocompetent mice.
- When tumors reach 100-150 mm³, treat mice with anti-PD-1/PD-L1 antibodies or isotype control (200 µg/dose, twice weekly for 3 weeks).
- Monitor tumor growth and survival daily.
- Harvest tumors for immune profiling by flow cytometry.
- Immune Cell Infiltration Analysis:
- Prepare single-cell suspensions from harvested tumors.
- Stain with fluorochrome-conjugated antibodies against CD45, CD3, CD4, CD8, FoxP3, and other immune markers.
- Analyze by flow cytometry to quantify tumor-infiltrating lymphocytes.
- T Cell Cytotoxicity Assay:
- Isolate T cells from mouse spleens or human donors.
- Activate with anti-CD3/CD28 beads for 72 hours.
- Co-culture activated T cells with target cancer cells at various effector:target ratios.
- Measure cancer cell killing using real-time cell analysis or LDH release assays.
Table 2: Key Assays for Immunotherapy Response Validation
| Assay Type | Measured Parameters | Interpretation |
|---|---|---|
| Flow Cytometry | Immune cell populations (CD8+ T cells, Tregs, macrophages) | Identifies changes in tumor immune microenvironment |
| Cytokine Profiling | IFN-γ, TNF-α, IL-2, IL-10 levels | Assesses immune activation or suppression |
| T cell Cytotoxicity | Specific lysis of target cells | Measures direct anti-tumor immune response |
| In vivo treatment | Tumor growth inhibition, survival prolongation | Evaluates therapeutic efficacy of ICB |
Figure 2: Immunotherapy Response Validation Pathway. This diagram illustrates the approach for validating the predictive value of m6A-related lncRNA signatures for immunotherapy response, connecting signature identification with immune profiling and therapeutic outcomes.
Data Analysis and Interpretation
Statistical Considerations
- Sample Size Calculation: For clinical correlation studies, ensure adequate power (typically ≥30 samples per group) based on preliminary effect size estimates.
- Multiple Testing Correction: Apply Bonferroni or False Discovery Rate (FDR) correction when testing multiple lncRNAs simultaneously.
- Correlation Analysis: Use Pearson or Spearman correlation to assess relationships between lncRNA expression, m6A regulator levels, and immune markers.
- Survival Analysis: Employ Kaplan-Meier curves with log-rank test to compare survival between high and low risk groups defined by lncRNA signature.
Interpretation Guidelines
- Clinical Relevance: Signature lncRNAs should demonstrate consistent differential expression across independent cohorts and correlate with established clinicopathological features.
- Functional Significance: Effective lncRNA modulation should alter key cancer hallmarks (proliferation, invasion, apoptosis, drug resistance).
- Immunotherapeutic Prediction: The signature should stratify patients according to likely immunotherapy benefit, supported by both computational predictions and experimental validations.
Troubleshooting Notes
- Low RNA Yield from Clinical Samples: Ensure immediate freezing of specimens in liquid nitrogen and minimize thawing cycles. Use RNA stabilization reagents if immediate processing isn't possible.
- Inefficient lncRNA Knockdown: Optimize siRNA sequences and transfection conditions. Consider using multiple siRNAs targeting different regions of the lncRNA.
- High Variability in Invasion Assays: Use consistent Matrigel lot and concentration. Pre-warm media and maintain uniform incubation times.
- Weak m6A Immunoprecipitation: Verify antibody specificity and optimize RNA fragmentation conditions. Include both positive and negative control RNAs.
The experimental validation frameworks outlined herein provide comprehensive methodologies for transitioning computational identifications of m6A-related lncRNA signatures toward clinically applicable biomarkers for immunotherapy response prediction. Through systematic implementation of these protocols, researchers can robustly verify both the biological significance and therapeutic relevance of their findings.
Conclusion
m6A-related lncRNA signatures represent a transformative approach in cancer immunotherapy, providing robust tools for prognosis prediction and treatment response assessment. The consistent validation of these signatures across multiple cancer types underscores their fundamental role in regulating tumor immune microenvironment and immune evasion mechanisms. These biomarkers successfully integrate epitranscriptomic regulation with immune profiling, enabling superior patient stratification compared to conventional clinical parameters. Future directions should focus on prospective clinical validation, standardization of analytical pipelines across institutions, and functional characterization of specific m6A-lncRNA mechanisms to identify novel therapeutic targets. The integration of these signatures into clinical trial designs promises to advance personalized immunotherapy and improve outcomes for cancer patients.
References
- 1. of Role , m and 6 in cancer | Experimental... A writers erasers readers [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-022-00298-7]
- 2. Dynamic transcriptomic m decoration: 6 , A , writers ... erasers readers [https://www.nature.com/articles/s41422-018-0040-8?error=cookies_not_supported&code=7e32fe9c-02c8-438a-a351-be0f3bddba2b]
- 3. In situ visualization of m6A sites in cellular mRNAs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10639046/]
- 4. A Novel m6A-Related LncRNA Signature for Predicting ... [https://pubmed.ncbi.nlm.nih.gov/35954243/]
- 5. Effects of writers , erasers and readers within miRNA‐related... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9816932/]
- 6. Identification of m6A/m5C-related lncRNA signature for ... [https://www.nature.com/articles/s41598-024-58743-y]
- 7. Protocol for measuring the auxin-induced changes of m6A ... [https://www.sciencedirect.com/science/article/pii/S2666166725000358]
- 8. Limits in the detection of m6A changes using MeRIP ... [https://www.nature.com/articles/s41598-020-63355-3]
- 9. Comprehensive analysis of m6A-related lncRNAs as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261012/]
- 10. Development of a Prognostic m6A-Related lncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495916/]
- 11. m6A regulators-based gene expression pattern is ... [https://www.nature.com/articles/s41598-025-26956-4]
- 12. Identification of m6A-related lncRNAs prognostic signature ... [https://www.sciencedirect.com/science/article/pii/S247263032400092X]
- 13. A novel disulfidptosis-related lncRNA signature to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12643716/]
- 14. Frontiers | A migrasome-related lncRNA signature predicts prognosis... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581122/full]
- 15. The Mechanism and Latest Progress of m6A Methylation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11781182/]
- 16. Subtype cluster analysis unveiled the correlation between ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1539630/full]
- 17. Functions and mechanisms of lncRNAs in immune escape ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06732-8]
- 18. Immune evasion in cancer: mechanisms and cutting-edge ... [https://www.nature.com/articles/s41392-025-02280-1]
- 19. Development of a m6A- and ferroptosis-related LncRNA ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13974-8]
- 20. Identification of a LncRNA based CeRNA network ... [https://www.nature.com/articles/s41598-025-05105-x]
- 21. Identification of a m6A-immune-related risk model for ... [https://www.nature.com/articles/s41598-025-22002-5]
- 22. m6A-related lncRNA signature for predicting prognosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9730119/]
- 23. Establishment of a m6 A-associated lncRNAs-derived risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12098242/]
- 24. Comprehensive analysis of lncRNAs N6-methyladenosine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7906145/]
- 25. m6A-lncRNA landscape highlights reduced levels of m6A ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01254-x]
- 26. m6A-lncRNA landscape highlights reduced levels of m6A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085027/]
- 27. Identification and validation of lncRNAs involved in m6A regulation for patients with ovarian cancer | Cancer Cell International | Full Text [https://cancerci.biomedcentral.com/articles/10.1186/s12935-021-02076-7]
- 28. Comprehensive analyses of m6A regulators and interactive coding and non-coding RNAs across 32 cancer types | Molecular Cancer | Full Text [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-021-01362-2]
- 29. Identification of m6A/m5C/m1A-associated LncRNAs for ... [https://www.nature.com/articles/s41598-023-30865-9]
- 30. Characteristics of m6A-related LncRNAs in breast cancer as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10539557/]
- 31. Frontiers | Cross-Talk Between m6A- and m5C-Related lncRNAs to Construct a Novel Signature and Predict the Immune Landscape of Colorectal Cancer Patients [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.740960/full]
- 32. Comprehensive analysis of m6A modification lncRNAs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9997758/]
- 33. m6A-immune-related lncRNA prognostic signature for ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-022-03711-1]
- 34. Cox Proportional-Hazards Model - Easy Guides - Wiki [https://www.sthda.com/english/wiki/cox-proportional-hazards-model]
- 35. A Visual Guide to the Stratified Cox Model in Survival ... [https://medium.com/@leushina.katya/when-cox-proportional-hazards-fails-a-visual-guide-to-the-stratified-cox-model-in-survival-0e690929c27d]
- 36. 20 Cox Proportional Hazards Regression Model [https://hbiostat.org/rmsc/cox]
- 37. Optimizing cancer immunotherapy response prediction by ... [https://www.nature.com/articles/s41698-023-00408-6]
- 38. Lasso (statistics) [https://en.wikipedia.org/wiki/Lasso_(statistics)]
- 39. LASSO Regression Step-by-Step Implementation Example [https://medium.com/@msoczi/lasso-regression-step-by-step-math-explanation-with-implementation-and-example-c37df7a7dc1f]
- 40. Identification of a six-lncRNA signature associated with ... [https://www.nature.com/articles/s41598-017-00763-y]
- 41. Screening and validation of long non-coding RNAs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12214067/]
- 42. Workflow of LncRNA Sequencing and Its Data Analysis [https://www.cd-genomics.com/workflow-of-lncrna-sequencing-and-its-data-analysis.html]
- 43. Identification and Evaluation of a Risk Assessment Model [https://bio-protocol.org/exchange/minidetail?id=7429862&type=30]
- 44. Identification and Validation of Long Noncoding RNA ... [https://www.sciencedirect.com/science/article/pii/S1556086415323674]
- 45. Discovery and Validation of Clinically Relevant Long Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405614/]
- 46. Risk Stratification: A Two-Step Process for Identifying Your ... [https://www.aafp.org/pubs/fpm/issues/2019/0500/p21.html]
- 47. Methods for Stratification and Validation Cohorts [https://pmc.ncbi.nlm.nih.gov/articles/PMC9144352/]
- 48. 2.3. Risk score calculation [https://bio-protocol.org/exchange/minidetail?id=7250740&type=30]
- 49. Multi-cohort machine learning identifies predictors of ... [https://www.nature.com/articles/s41746-025-01862-1]
- 50. Identification and Validation of a m6A-Related Long ... [https://pubmed.ncbi.nlm.nih.gov/39868645/]
- 51. Explainable machine learning model for predicting internal ... [https://pubmed.ncbi.nlm.nih.gov/40516245/]
- 52. Development and multi-cohort validation of a machine ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06728-4]
- 53. Identification and validation of m 6 A RNA methylation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1543517/full]
- 54. An N6-methyladenosine-associated lncRNA signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9096396/]
- 55. Construction and validation of a nomogram to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6745838/]
- 56. Construction and validation of a nomogram model for ... [https://bmcsurg.biomedcentral.com/articles/10.1186/s12893-023-02018-2]
- 57. Cox回归列线图(nomogram)的多种绘制方法原创 [https://blog.csdn.net/Ayue0616/article/details/126601816]
- 58. Construction and internal validation of a novel nomogram ... [https://www.nature.com/articles/s41598-022-22173-5]
- 59. Value and validation of a nomogram model based on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12406108/]
- 60. m6A-related lncRNAs are potential biomarkers for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8094594/]
- 61. A Novel m6A-Related LncRNA Signature for Predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9368324/]
- 62. Identification of an m6A Regulators-Mediated Prognosis ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.718912/full]
- 63. Identification of m 6 A-related long non-coding RNAs ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.1011716/full]
- 64. Targeting N6-methyladenosine RNA modification ... [https://www.sciencedirect.com/science/article/pii/S2001037022004202]
- 65. Identification and Validation of m6A-Related lncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8555664/]
- 66. Development and validation of a prognostic model based ... [https://www.nature.com/articles/s41598-024-83263-0]
- 67. Identification and Validation of an m6A-Related LncRNA ... [https://www.por-journal.com/journals/pathology-and-oncology-research/articles/10.3389/pore.2022.1610536/full]
- 68. lncRNA identification [https://bio-protocol.org/exchange/minidetail?id=7917741&type=30]
- 69. Frontiers | ImReLnc: Identifying Immune-Related LncRNA ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.792541/full]
- 70. Novel long noncoding RNA (lncRNA) panel as biomarkers ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8799182/]
- 71. Overfitting and Regularization in ML [https://www.geeksforgeeks.org/machine-learning/overfitting-and-regularization-in-ml/]
- 72. Overfitting, Model Tuning, and Evaluation of Prediction ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK583970/]
- 73. An Introduction to Regularization Techniques in Machine ... [https://www.certlibrary.com/blog/an-introduction-to-regularization-techniques-in-machine-learning/]
- 74. What is Overfitting in Deep Learning [+10 Ways to Avoid It] [https://www.v7labs.com/blog/overfitting]
- 75. Overfitting: L2 regularization | Machine Learning [https://developers.google.com/machine-learning/crash-course/overfitting/regularization]
- 76. 5 Regularization Techniques You Should Know [https://www.statology.org/5-regularization-techniques/]
- 77. Controlling Overfitting in Machine Learning | by Kiran vutukuri [https://medium.com/@kiranvutukuri/17-regularization-controlling-overfitting-in-machine-learning-204c8ef8cd7f]
- 78. Identification of m6A/m5C-related lncRNA signature for prediction of prognosis and immunotherapy efficacy in esophageal squamous cell carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/38589454/]
- 79. Identification of m6A methyltransferase-related lncRNA signature for predicting immunotherapy and prognosis in patients with hepatocellular carcinoma - PubMed [https://pubmed.ncbi.nlm.nih.gov/34027555/]
- 80. A Novel m6A-Related LncRNA Signature for Predicting Prognosis, Chemotherapy and Immunotherapy Response in Patients with Lung Adenocarcinoma [https://www.mdpi.com/2073-4409/11/15/2399]
- 81. Challenges and opportunities in technologies and methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492894/]
- 82. Long non-coding RNAs expression and regulation across ... [https://www.nature.com/articles/s41597-024-03380-3]
- 83. Exploring the landscape of tools and resources for ... [https://www.sciencedirect.com/science/article/pii/S2001037023003549]
- 84. ncFN: a comprehensive non-coding RNA function ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12550578/]
- 85. Comprehensive analysis of m6A-related lncRNAs as prognosis factors in the immune microenvironment of colorectal cancer - Lan - Journal of Gastrointestinal Oncology [https://jgo.amegroups.org/article/view/102152/html]
- 86. Cell-in-cell associated lncRNA signature predicts ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1597187/full]
- 87. Demographic and genetic factors influence the abundance ... [https://www.nature.com/articles/s41467-020-16097-9]
- 88. Profiling tumor infiltrating immune cells with CIBERSORT [https://pmc.ncbi.nlm.nih.gov/articles/PMC5895181/]
- 89. Chapter 6 Immune Infiltration | Tutorial of RNA-seq tumor ... [https://liulab-dfci.github.io/RIMA/Infiltration.html]
- 90. TIMER2.0 for analysis of tumor-infiltrating immune cells [https://pmc.ncbi.nlm.nih.gov/articles/PMC7319575/]
- 91. TIMER3 - Li Lab [https://compbio.cn/timer3/]
- 92. m6A‐related lncRNAs as potential biomarkers and the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10826449/]
- 93. Biological Pathway-Derived TMB Robustly Predicts the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496944/]
- 94. Multimodal Genomic Analyses Predict Response to ... [https://www.hopkinsmedicine.org/news/newsroom/news-releases/2020/01/multimodal-genomic-analyses-predict-response-to-immunotherapy-in-lung-cancer-patients]
- 95. Large-scale public data reuse to model immunotherapy ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-020-0721-z]
- 96. Development and Validation of Prognostic Model for Lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9243308/]
- 97. Construction and validation of a prognostic model of lncRNAs ... [https://tcr.amegroups.org/article/view/96787/html]
- 98. Longitudinal liquid biopsy identifies an early predictive ... [https://www.nature.com/articles/s41467-025-63538-4]
- 99. N6-Methylandenosine-related lncRNAs as potential ... [https://pubmed.ncbi.nlm.nih.gov/39833465/]
- 100. N6-Methylandenosine-related lncRNAs as potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11753445/]
- 101. N6-Methyladenosine (m6A)-Related lncRNAs Are Potential ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9462982/]
- 102. Multivariate Cox regression analysis of prognostic genes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11807035/]
- 103. The independent prognostic nomogram models for primary ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1642820/full]
- 104. Development and validation of a prognostic nomogram for ... [https://www.nature.com/articles/s41598-025-22760-2]
- 105. Comparison of machine learning methods versus traditional ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02694-z]
- 106. Comparison of machine learning and Cox regression ... [https://www.sciencedirect.com/science/article/pii/S2589845025000570]
- 107. Dynamic biomarkers and Cox regression with time ... [https://www.nature.com/articles/s41598-025-94416-0]
- 108. Time-dependent ROC curve analysis in medical research [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-017-0332-6]
- 109. Time-Dependent ROC Curve Analysis for Assessing the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10571898/]
- 110. A novel model for predicting immunotherapy response and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083170/]
- 111. Time-Dependent ROC [https://research.fredhutch.org/diagnostic-biomarkers-center/en/software/time-dependent-roc.html]
- 112. An m6A-Related lncRNA Signature Predicts the Prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9006777/]
- 113. Prognostic signature based on m6A-related lncRNAs to ... [https://www.nature.com/articles/s41598-022-07112-8]
- 114. A new risk model based on a 11-m6A-related lncRNA ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-021-09062-2]
- 115. An efficient five-lncRNA signature for lung adenocarcinoma ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.1052092/full]
- 116. A three-lncRNA expression signature predicts survival in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6246764/]
- 117. Identification of prognostic immune-related lncRNA ... [https://www.nature.com/articles/s41598-023-28305-9]
- 118. A long non-coding RNA signature for predicting survival in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5955136/]
- 119. Prognostic value of a five-lncRNA signature in esophageal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7419219/]
- 120. A five-long non-coding RNA signature with the ability to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6862666/]
- 121. Immune-Related lncRNA Signature for Predicting the ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.689224/full]
- 122. Investigating the Genetic Links Between Immune Cell Profiles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109282/]
- 123. Identification of potential biomarkers for Lyme disease ... [https://link.springer.com/article/10.1007/s10238-025-01803-y]
- 124. Cell division cycle 25 C (CDC25C) mediates cell-cycle ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12480179/]
- 125. PLCXD2 expression relates to the immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12605501/]
- 126. SLFN11 expression correlates with immune ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1607056/full]
- 127. The lncRNA epigenetics: The significance of m6A and m5C ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10033960/]
- 128. The role of N6-methyladenosine-modified non-coding ... [https://www.nature.com/articles/s41420-022-01113-2]
- 129. Assessment of Cell Viability in Drug Therapy: IC50 and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11859577/]
- 130. Enhanced multi-omics analysis reveals a lncRNA signature ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521086/]
- 131. Cuproptosis related lncRNA signature as a prognostic and ... [https://www.nature.com/articles/s41598-024-84024-9]
- 132. Identification and Validation of an m6A-Related LncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9407446/]
- 133. Integrative analysis of m6A-related lncRNAs reveals a ... [https://www.dovepress.com/development-of-a-prognostic-m6a-related-lncrna-signature-and-functiona-peer-reviewed-fulltext-article-OTT]