Mastering SOX9 Detection in Immune Cells: A Comprehensive Guide for Biomarker Discovery and Therapeutic Targeting
This article provides a definitive resource for researchers and drug development professionals on the critical techniques and considerations for detecting the transcription factor SOX9 within diverse immune cell subpopulations.
Mastering SOX9 Detection in Immune Cells: A Comprehensive Guide for Biomarker Discovery and Therapeutic Targeting
Abstract
This article provides a definitive resource for researchers and drug development professionals on the critical techniques and considerations for detecting the transcription factor SOX9 within diverse immune cell subpopulations. SOX9 is a janus-faced regulator with a complex and dual role in immunology, influencing processes from tumor immune escape to tissue repair. We cover the foundational biology of SOX9 in immunity, explore and compare state-of-the-art methodological approaches from single-cell RNA sequencing to flow cytometry, address common troubleshooting and optimization challenges, and outline rigorous validation frameworks. By synthesizing the latest research, this guide aims to empower the development of robust detection protocols, accelerating the validation of SOX9 as a diagnostic, prognostic, and therapeutic target in cancer and immune-related diseases.
SOX9 in the Immune Landscape: From Basic Biology to Dual-Role Functions
The Structural and Functional Biology of the SOX9 Transcription Factor
SOX9 FAQs: Structure and Function
What is the primary structure and functional organization of the SOX9 protein?
SOX9 is a 509-amino acid protein belonging to the SOXE subgroup of SRY-related HMG-box transcription factors. Its functional domains are organized from N- to C-terminus as follows: a dimerization domain (DIM), the HMG box DNA-binding domain, two nuclear localization signals (NLS1 and NLS2), a central transactivation domain (TAM), a proline/glutamine/alanine (PQA)-rich domain, and a C-terminal transactivation domain (TAC). The HMG domain facilitates sequence-specific DNA binding to the consensus motif AGAACAATGG, while the transactivation domains interact with transcriptional co-activators like MED12, CBP/p300, TIP60, and WWP2 to regulate target gene expression [1] [2].
Why is SOX9 considered essential in organogenesis and disease?
SOX9 is a master regulator of development for multiple organs including cartilage, testis, nervous system, retina, lung, heart valve, pancreas, and intestine. Heterozygous mutations in SOX9 cause campomelic dysplasia, a haploinsufficiency disorder characterized by skeletal malformations and frequent 46,XY sex reversal. SOX9 plays additional critical roles in stem cell maintenance, tumor progression, and immune regulation, making it a significant factor in both development and disease pathogenesis [1] [2].
What makes SOX9 detection challenging in immune cell subpopulations?
Detecting SOX9 in immune cell subpopulations presents technical challenges due to its context-dependent expression, nuclear localization requirements, and potential post-translational modifications. In neuropathic pain models, nerve injury induces abnormal SOX9 phosphorylation at site 181, triggering nuclear translocation and altered transcriptional activity. Furthermore, SOX9 exists in different oligomerization states (monomer vs. dimer) depending on cell type, which can affect antibody recognition and functional assessments [1] [3].
SOX9 Detection Troubleshooting Guide
Weak or No Signal
| Possible Cause | Solution | Recommended Optimization |
|---|---|---|
| Inefficient protein transfer | Verify transfer efficiency using Ponceau S staining or reversible protein stains. For low MW antigens (<25 kDa), add 20% methanol to transfer buffer; for high MW antigens, add 0.01-0.05% SDS [4] [5]. | Increase transfer time; use nitrocellulose with 0.2 µm pores for low MW targets [6]. |
| Insufficient antigen | Load 20-30 µg protein per lane for whole cell extracts; increase to 100 µg for modified targets in tissue extracts [6]. | Concentrate sample using immunoprecipitation; include protease/phosphatase inhibitors [5] [6]. |
| Sub-optimal antibody concentration | For WB, start with 1:1,000 dilution; for IHC/ICC use 1:50-1:200 [7]. | Perform dot-blot assay for antibody titration; use freshly diluted antibodies [5] [6]. |
| Antigen masking by blocking buffer | Compare different blocking buffers (BSA vs. milk); reduce blocking time [4] [5]. | For phospho-protein detection, use BSA instead of milk to avoid casein interference [6]. |
| Sodium azide contamination | Eliminate sodium azide from buffers when using HRP-conjugated antibodies [4] [5]. | Use alternative preservatives in antibody storage buffers. |
High Background and Non-specific Bands
| Possible Cause | Solution | Recommended Optimization |
|---|---|---|
| Antibody concentration too high | Optimize and decrease primary and/or secondary antibody concentration [4] [5]. | Perform checkerboard titration to determine optimal signal-to-noise ratio. |
| Incomplete blocking | Increase protein concentration in blocking buffer; extend blocking to 2 hours at RT or overnight at 4°C [4] [5]. | Add 0.05% Tween-20 to blocking and antibody dilution buffers [4]. |
| Insufficient washing | Increase wash number and volume; include 0.05% Tween-20 in wash buffers [4] [5]. | Perform 5x 5-minute washes with agitation between incubation steps. |
| Antibody aggregation | Filter secondary antibody through 0.2µm filter before use; use fresh aliquots [5]. | Centrifuge antibodies briefly before dilution to remove aggregates. |
| Non-specific cross-reactivity | Use species-appropriate pre-immune sera as control; validate with KO cell lines [6]. | Ensure secondary antibody is cross-adsorbed against host species proteins. |
Multiple or Diffuse Bands
| Possible Cause | Solution | Recommended Optimization |
|---|---|---|
| Protein degradation | Use fresh protease inhibitor cocktails; sonicate samples to shear DNA [4] [6]. | Prepare fresh samples; avoid repeated freeze-thaw cycles. |
| Post-translational modifications | Research expected PTMs using databases like PhosphoSitePlus [6]. | Treat samples with phosphatases or glycosidases to confirm PTM identity. |
| SOX9 isoforms or oligomerization | SOX9 can function as monomer or dimer depending on cell type [1]. | Use non-reducing conditions to detect oligomerization states. |
| Alternative splicing | Check UniProt for known isoforms; run longer gels for better resolution [6]. | Use antibodies targeting specific isoforms when available. |
Optimized Protocols for SOX9 Detection
Western Blot Protocol for SOX9 Detection in Immune Cells
Sample Preparation:
- Harvest immune cells (1-5×10⁶ cells) and lyse in RIPA buffer containing protease/phosphatase inhibitors
- Sonicate samples with microtip probe (3×10 second bursts at 15W on ice) to shear DNA and ensure complete lysis [6]
- Centrifuge at 12,000×g for 10 minutes at 4°C and collect supernatant
- Determine protein concentration by BCA assay
- Prepare samples in Laemmli buffer (final concentration: 50mM DTT or 2.5% β-mercaptoethanol)
- Heat samples at 70°C for 10 minutes (avoid boiling to prevent proteolysis) [4]
Electrophoresis and Transfer:
- Load 20-50 µg protein per lane on 10% SDS-PAGE gel
- For low abundance targets, load up to 100 µg protein [6]
- Electrophorese at 100V until dye front reaches bottom
- Transfer to PVDF membrane using wet transfer system (70V for 2 hours at 4°C in Tris-glycine buffer with 20% methanol) [6]
- For high molecular weight SOX9 complexes, reduce methanol to 5-10% and extend transfer to 3-4 hours [6]
Immunodetection:
- Block membrane with 5% BSA in TBST for 1 hour at room temperature
- Incubate with anti-SOX9 primary antibody (1:1,000 in 5% BSA/TBST) overnight at 4°C [7]
- Wash 5×5 minutes with TBST
- Incubate with HRP-conjugated secondary antibody (1:2,000-1:10,000 in 5% non-fat dry milk/TBST) for 1 hour at room temperature
- Wash 5×5 minutes with TBST
- Detect with enhanced chemiluminescence substrate (2-minute exposure recommended) [6]
SOX9 Immunofluorescence in Immune Cell Subpopulations
Cell Preparation:
- Culture immune cells on poly-L-lysine coated coverslips
- Fix with 4% paraformaldehyde for 15 minutes at room temperature
- Permeabilize with 0.25% Triton X-100/PBS for 10 minutes [7]
- Block with 5% normal serum from secondary antibody host species for 1 hour
Immunostaining:
- Incubate with anti-SOX9 antibody (1:50-1:200 in blocking buffer) overnight at 4°C [7]
- Wash 3×5 minutes with PBS
- Incubate with fluorophore-conjugated secondary antibody (1:500-1:1,000) for 1 hour at room temperature in darkness
- Wash 3×5 minutes with PBS
- Counterstain nuclei with DAPI (1 µg/mL) for 5 minutes
- Mount with anti-fade mounting medium
Imaging and Analysis:
- Image using confocal microscopy with appropriate filter sets
- For nuclear localization quantification, use image analysis software to calculate nuclear-to-cytoplasmic ratio
- Include isotype controls and secondary-only controls to assess specificity
SOX9 Signaling Pathways in Immune Regulation
The SOX9-HK1 pathway illustrates how nerve injury induces SOX9 phosphorylation, triggering nuclear translocation and transcriptional activation of hexokinase 1 (HK1). This enhances glycolytic flux and lactate production, leading to histone lactylation (H3K9la) that drives pro-inflammatory gene expression while reducing beneficial astrocyte populations, ultimately promoting neuropathic pain conditions [3].
Research Reagent Solutions
| Reagent | Function/Application | Specification/Validation |
|---|---|---|
| Anti-SOX9 Antibody (A00177-1) | Detection of SOX9 in WB, IHC, ICC, IP, Flow Cytometry [7] | Rabbit polyclonal; reactive with human, mouse, rat; validated for 56.1 kDa band [7] |
| Protease/Phosphatase Inhibitor Cocktail | Preserve protein integrity and phosphorylation states during extraction [6] | 100X concentration; include PMSF, leupeptin, sodium orthovanadate [6] |
| PVDF/Nitrocellulose Membranes | Protein immobilization for immunodetection | 0.2 µm pore for low MW targets; 0.45 µm for standard applications [4] |
| Enhanced Chemiluminescence Substrate | Signal detection for HRP-conjugated antibodies | Femto-level sensitivity for low abundance targets [4] |
| Recombinant SOX9 Protein | Positive control for antibody validation | Verify antibody specificity and establish detection limits |
Frequently Asked Questions & Troubleshooting Guides
Antibody and Staining Issues
Q: My flow cytometry results for SOX9 in immune cells show high background or non-specific staining. What could be the cause?
- Potential Cause: Inappropriate permeabilization buffer or incorrect antibody concentration.
- Solution:
- Use the Correct Permeabilization Buffer: BD Phosflow Perm Buffer III (Cat. No. 558050) is specifically recommended for intracellular SOX9 staining. Using BD Perm/Wash Buffer (Cat. No. 554723) is not recommended and can lead to poor results [8].
- Titrate Your Antibody: Always titrate the antibody to determine the optimal concentration for your specific experimental setup. The purified mouse anti-SOX9 antibody has been validated at concentrations ranging from 0.06 µg/ml to 2.5 µg/ml for various applications [8].
- Include Proper Controls: Use an isotype control (e.g., Purified Mouse IgG1 κ Isotype Control, Cat. No. 554121) at the same concentration as your primary antibody to distinguish specific from non-specific binding [8].
- Potential Cause: Suboptimal cell lysis, protein transfer, or antibody detection conditions.
- Solution:
- Verify Antibody Specificity: The BD Pharmingen Purified Mouse Anti-Sox9 (Clone T32-668) specifically identifies SOX9 as a band of 62 kDa in Hep G2 cell lysates [8].
- Check Antibody Concentration: For western blot, probe the membrane with the antibody at concentrations of 0.25, 0.125, and 0.06 µg/ml to find the optimal signal-to-noise ratio [8].
- Confirm Detection System: Use an appropriate secondary antibody, such as HRP Goat Anti-Mouse Ig (Cat. No. 554002), for detection [8].
Biological Interpretation and Experimental Design
Q: In my cancer model, SOX9 appears to have opposing roles. How can I interpret this?
- Explanation: SOX9 is a "double-edged sword" or "Janus-faced" regulator, a concept central to its function. Its role is highly context-dependent [2].
- Oncogenic Role: In most solid cancers (e.g., liver, lung, breast, gastric), SOX9 is frequently overexpressed and acts as a proto-oncogene. It promotes tumor proliferation, metastasis, drug resistance, and is associated with poor prognosis [2] [9].
- Tumor-Suppressive Role: In specific contexts like melanoma (SKCM) and testicular germ cell tumors (TGCT), SOX9 expression is significantly decreased and can inhibit tumorigenicity, functioning as a tumor suppressor [9].
Q: How does SOX9 influence the tumor immune microenvironment?
- Explanation: SOX9 expression is strongly correlated with specific patterns of immune cell infiltration, which can create an immunosuppressive niche [2].
- Negative Correlations: High SOX9 often correlates with reduced infiltration of B cells, resting mast cells, monocytes, plasma cells, and eosinophils [2].
- Positive Correlations: It can correlate with increased infiltration of neutrophils, macrophages, and activated mast cells [2].
- Functional Impact: In cancers like prostate cancer, SOX9 can contribute to an "immune desert" microenvironment by decreasing effector immune cells (e.g., CD8+ T cells) and increasing immunosuppressive cells (e.g., Tregs, M2 macrophages), thereby promoting immune escape [2].
SOX9 Expression and Prognostic Value in Pan-Cancer Analysis
The following table summarizes the expression patterns and prognostic significance of SOX9 across various human cancers, based on data from The Cancer Genome Atlas (TCGA) and the Gene Expression Profile Interaction Analysis (GEPIA) database [9].
Table 1: SOX9 Expression and Prognosis in Pan-Cancer
| Cancer Type (Abbreviation) | SOX9 Expression vs. Matched Healthy Tissue | Correlation with Overall Survival (OS) |
|---|---|---|
| Liver cancer (LIHC) | Significantly Increased | Varies |
| Lung cancer (LUSC) | Significantly Increased | Varies |
| Breast cancer | Increased (Oncogene) [2] | Varies |
| Glioblastoma (GBM) | Significantly Increased | Varies |
| Low-Grade Glioma (LGG) | Significantly Increased | Shorter OS (Worst Prognosis) |
| Cervical Cancer (CESC) | Significantly Increased | Shorter OS (Worst Prognosis) |
| Thymoma (THYM) | Significantly Increased | Shorter OS (Worst Prognosis) |
| Stomach Cancer (STAD) | Significantly Increased | Varies |
| Colorectal Cancer (COAD/READ) | Significantly Increased | Varies |
| Melanoma (SKCM) | Significantly Decreased | Varies (Tumor Suppressor) |
| Testicular Cancer (TGCT) | Significantly Decreased | Varies (Tumor Suppressor) |
| Adrenocortical Carcinoma (ACC) | Information Missing | Longer OS (Better Prognosis) |
Essential Protocols for SOX9 Research
Protocol 1: Flow Cytometric Analysis of Intracellular SOX9
This protocol is adapted from the validated methodology using BD Biosciences reagents [8].
Key Reagent Solutions:
- Fixation Buffer: BD Cytofix Fixation Buffer (Cat. No. 554655)
- Permeabilization Buffer: BD Phosflow Perm Buffer III (Cat. No. 558050) - Critical
- Primary Antibody: Purified Mouse Anti-Sox9 (Cat. No. 565492)
- Isotype Control: Purified Mouse IgG1 κ Isotype Control (Cat. No. 554121)
- Cell Stain Buffer: For washing and resuspending cells (e.g., Cat. No. 554656 or 554657)
Step-by-Step Workflow:
- Harvest and Wash Cells: Collect your cell suspension (e.g., immune cells or cultured cell lines like Hep G2) and wash with cold stain buffer.
- Fix Cells: Resuspend cell pellet in BD Cytofix Fixation Buffer. Incubate for 10-20 minutes at room temperature.
- Permeabilize Cells: Wash cells thoroughly, then resuspend in BD Phosflow Perm Buffer III. Incubate for 30 minutes on ice.
- Stain with Antibody: Wash cells with perm/wash or stain buffer. Divide cells into aliquots for your test antibody and isotype control. Stain with the pre-titrated concentration of Anti-SOX9 antibody or isotype control for 30-60 minutes at room temperature in the dark.
- Wash and Analyze: Wash cells twice to remove unbound antibody. Resuspend in stain buffer and analyze immediately on a flow cytometer (e.g., BD FACSCanto II).
Protocol 2: Targeting SOX9 with Small Molecule Inhibitors
This protocol outlines the use of Cordycepin (CD), an adenosine analog, to inhibit SOX9 expression in cancer cell lines [9].
Key Reagent Solutions:
- Small Molecule Inhibitor: Cordycepin (CD)
- Cell Lines: Validated in prostate cancer (22RV1, PC3) and lung cancer (H1975) cells.
- Culture Media: RPMI 1640 or DMEM, supplemented with 10-15% FBS.
Step-by-Step Workflow:
- Cell Culture: Maintain cells in appropriate media at 37°C with 5% CO₂.
- Seed Cells: Inoculate cells into 12-well plates and allow them to adhere.
- Drug Treatment: Treat cells with Cordycepin at final concentrations of 0, 10, 20, and 40 µM for 24 hours.
- Downstream Analysis:
- Protein Analysis: Collect cell lysates for Western blotting to detect SOX9 protein levels (∼62 kDa).
- mRNA Analysis: Extract total RNA for RT-qPCR to quantify changes in SOX9 transcript levels.
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for SOX9 Detection and Modulation
| Reagent Name | Catalog Number (Example) | Function/Brief Explanation |
|---|---|---|
| Purified Mouse Anti-Sox9 | 565492 (BD) [8] | Primary antibody for detection in WB, FC, IF, IHC. Clone T32-668. |
| BD Cytofix Fixation Buffer | 554655 (BD) [8] | For cell fixation prior to intracellular staining for flow cytometry. |
| BD Phosflow Perm Buffer III | 558050 (BD) [8] | Essential for permeabilizing cells for intracellular SOX9 staining. |
| Mouse IgG1 κ Isotype Control | 554121 (BD) [8] | Critical negative control to distinguish non-specific binding. |
| HRP Goat Anti-Mouse Ig | 554002 (BD) [8] | Secondary antibody for Western blot detection. |
| Cordycepin (CD) | N/A [9] | Small molecule adenosine analog that inhibits SOX9 expression in a dose-dependent manner. |
| Biotin Goat Anti-Mouse Ig | 550337 (BD) [8] | Secondary antibody for immunohistochemistry staining workflows. |
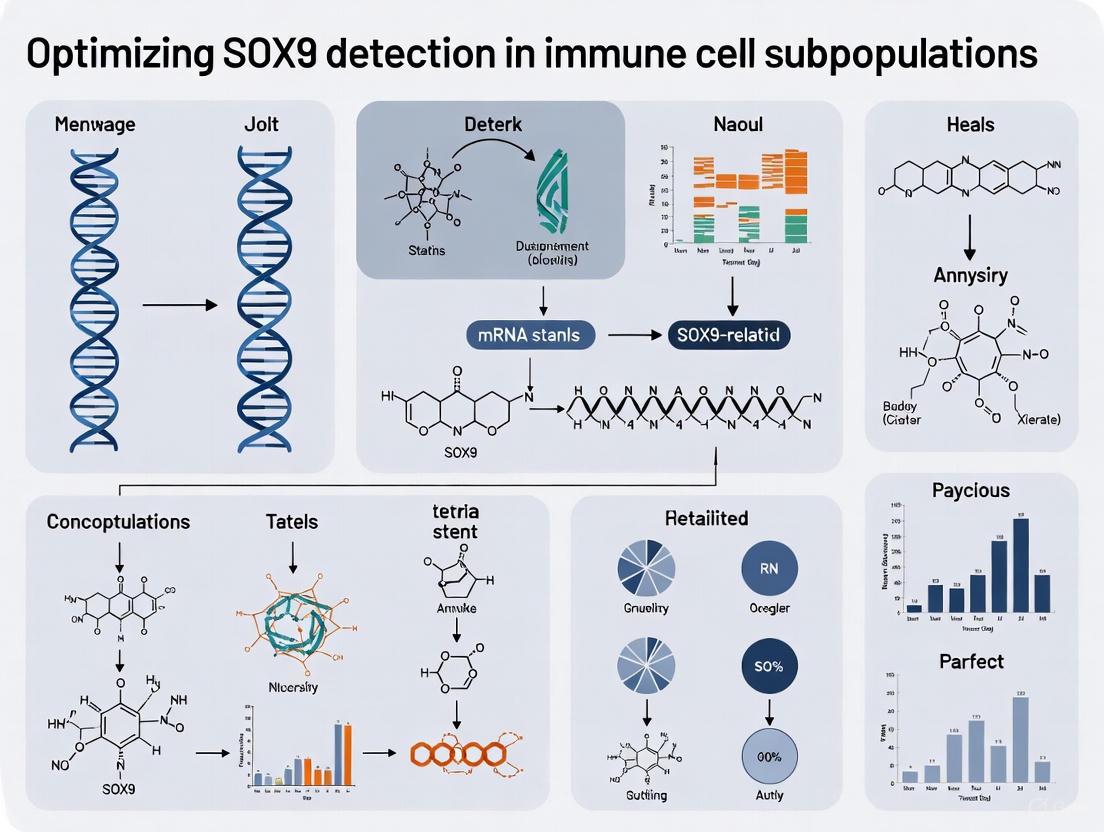
SOX9 Signaling and Experimental Workflow Diagrams
Diagram 1: The dual role of SOX9 in immunology. SOX9 can act as an oncogene promoting tumor progression and immune suppression (red arrows), while also playing a beneficial role in tissue repair and regeneration (green arrows) [2].
Diagram 2: Experimental workflow for inhibiting SOX9 using Cordycepin. Treatment of cancer cell lines with Cordycepin leads to a dose-dependent reduction in both SOX9 mRNA and protein levels, mediating anticancer roles [9].
Mapping SOX9 Expression Across Innate and Adaptive Immune Cell Lineages
The transcription factor SOX9 (SRY-related HMG-box 9) is increasingly recognized as a pivotal regulator in both development and disease, with emerging roles in immunology that position it as a "double-edged sword" in immune regulation [2]. This technical resource addresses the critical need for optimized detection and analysis methodologies specific to immune cell populations. SOX9's function varies dramatically by cellular context—it can promote immune escape in cancer by impairing immune cell function while simultaneously maintaining macrophage function to support tissue repair [2]. This complexity necessitates precise, cell-type-specific detection approaches for researchers investigating SOX9 in immunological contexts, from basic research to therapeutic development.
SOX9 in Immune Cell Development and Function: Key Mechanisms
SOX9 in T Cell Biology
SOX9 plays a significant role in T cell development and differentiation. During thymic development, SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (including Il17a and Blk), thereby modulating the lineage commitment of early thymic progenitors and influencing the balance between αβ T cell and γδ T cell differentiation [2]. This function positions SOX9 as a determinant in T cell fate decisions with potential implications for immune responses.
SOX9 in Innate Immunity and Macrophages
Beyond adaptive immunity, SOX9 contributes significantly to innate immune function. Increased SOX9 levels help maintain macrophage function, contributing to cartilage formation, tissue regeneration, and repair processes [2]. This protective function contrasts with its role in cancer contexts, highlighting the context-dependent nature of SOX9 activity across different immune cell types and physiological states.
SOX9 in Tumor Microenvironment and Immune Evasion
In cancer biology, SOX9 expression correlates strongly with altered immune cell infiltration within the tumor microenvironment. Bioinformatics analyses integrating multi-omics data reveal that SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [2]. Furthermore, SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with memory CD4+ T cells [2]. This reprogramming of the immune landscape ultimately creates an "immune desert" microenvironment that promotes tumor immune escape.
Research Reagent Solutions
Table: Essential Reagents for SOX9 Detection in Immune Cells
| Reagent Type | Specific Product/Clone | Applications | Species Reactivity | Key Features |
|---|---|---|---|---|
| Primary Antibody | Sox9 (D8G8H) Rabbit Monoclonal #82630 [10] | WB, IHC, Simple Western | Human, Mouse, Rat | IHC-optimized (1:300-1:1200 dilution) |
| Primary Antibody | Anti-SOX9 [EPR14335-78] (ab185966) [11] | WB, ICC/IF, IHC-P, Flow Cytometry | Human, Mouse, Rat | Most cited clone; validated in multiple applications |
| Reporter Cell Line | SOX9-IRES-tdTomato knockin [12] | Lineage tracing, FACS sorting | Human | Enables isolation of SOX9+ progenitors |
| SUMOylation Reporter | NanoBiT Sox9-SUMOylation reporter [13] | Live-cell SUMOylation detection | Human, Mouse | Quantitative detection of post-translational modifications |
Experimental Design and Workflow Optimization
Sample Preparation Considerations
Proper sample preparation is critical for accurate SOX9 detection in immune cells. For intracellular staining in flow cytometry, use 0.1% Triton X-100 for permeabilization with 1% BSA/10% normal goat serum/0.3M glycine in 0.1% PBS-Tween for blocking [11]. For tissue sections, heat-mediated antigen retrieval in citrate buffer provides optimal results for IHC applications [11].
Controls and Validation
Essential controls for SOX9 experiments include:
- CRISPR-Cas9 edited SOX9 knockout cells as negative controls [11]
- Tissue-specific positive controls (colon, cartilage, developing eye) [11]
- Isotype controls for antibody-specific staining validation
Troubleshooting Guides
FAQ: SOX9 Detection in Immune Cell Subpopulations
Q: Why do I detect multiple bands in Western blot for SOX9? A: SOX9 can be ubiquitinated or SUMOylated, resulting in higher molecular weight bands (50-70kDa range) [11]. Additionally, truncated isoforms like mini-SOX9 may be present. Always include appropriate positive controls (SW480 cell lysate) and validate with CRISPR-Cas9 knockout lines to confirm specificity [11].
Q: How can I improve SOX9 detection in rare immune cell populations? A: Implement pre-enrichment strategies using surface markers prior to intracellular staining. For extremely rare populations, consider using the SOX9 reporter cell lines that allow direct FACS sorting of SOX9+ cells without antibody staining [12]. Amplification methods in IHC may also enhance detection sensitivity.
Q: What methods can detect SOX9 activity beyond protein expression? A: The NanoBiT SUMOylation reporter system enables quantitative detection of SOX9 modification in live cells [13]. Additionally, chromatin immunoprecipitation (ChIP) assays can determine SOX9 binding to target genes in specific immune cell types.
Q: How does SOX9 expression vary between immune cell types? A: SOX9 shows cell-type-specific expression patterns: it modulates γδ T cell differentiation [2], is overexpressed in B-cell lymphomas like DLBCL [2], and maintains macrophage function [2]. Always include multiple immune cell controls in your experiments.
Q: Why do I get variable SOX9 staining in tumor-infiltrating immune cells? A: SOX9 expression is highly context-dependent and influenced by the local microenvironment [2]. In tumors, SOX9 correlates with specific immune infiltration patterns and may be induced by chemotherapy [14]. Standardize fixation times and include internal positive controls on each slide.
Advanced Methodologies
Single-Cell Analysis of SOX9 in Immune Cells
Single-cell RNA sequencing has revealed that SOX9 is consistently upregulated in epithelial cancer cells following platinum-based chemotherapy [14]. This approach can be adapted to characterize SOX9 expression across immune cell subtypes in complex tissues. The methodology involves:
- Tissue dissociation and single-cell suspension preparation
- scRNA-seq library preparation and sequencing
- Bioinformatic analysis of SOX9 expression across cell clusters
- Validation of findings using flow cytometry or immunofluorescence
Non-Invasive Detection Methods
Recent advances enable non-invasive SOX9 detection using deep learning approaches applied to CT images [15]. This method uses deep reinforcement learning to identify image regions highly correlated with SOX9 expression, achieving 91% AUC in predicting SOX9 status in hepatocellular carcinoma [15]. While developed for tumor cells, this approach may have applications for monitoring SOX9 in immune contexts.
Diagram: Experimental Workflow for SOX9 Detection in Immune Cells
Data Presentation and Analysis
Table: SOX9 Expression Patterns Across Immune Contexts
| Biological Context | SOX9 Expression/Function | Detection Method | Key Associations |
|---|---|---|---|
| Tumor Microenvironment [2] | Overexpressed | IHC, RNA-seq | Negative correlation with CD8+ T cells, NK cells, M1 macrophages |
| Colorectal Cancer [2] | High expression | Bioinformatics | Altered immune cell infiltration patterns |
| Ovarian Cancer Post-Chemotherapy [14] | Chemotherapy-induced | scRNA-seq | Associated with chemoresistance and stem-like state |
| Glioblastoma [16] | Highly expressed | RNA-seq, IHC | Correlated with immune infiltration and checkpoints |
| Normal Development [12] | Progenitor marker | Lineage tracing | Sclerotomal progenitors, cartilage formation |
Optimizing SOX9 detection in immune cell subpopulations requires careful consideration of context-dependent expression patterns, appropriate controls, and method validation. The dual nature of SOX9 in immunity—functioning as both a promoter of immune escape and a maintainer of protective immune functions—demands precise analytical approaches. By implementing the standardized protocols, troubleshooting guides, and reagent recommendations outlined in this technical resource, researchers can enhance the reliability and reproducibility of their SOX9 studies in immunological contexts, ultimately advancing our understanding of this multifaceted transcription factor in health and disease.
The Critical Role of SOX9 in Tumor Immune Cell Infiltration and the Tumor Microenvironment
FAQs: SOX9 in Tumor Immunology
Q1: What is the fundamental role of SOX9 in the tumor microenvironment? SOX9 is a transcription factor that plays a critical oncogenic role in many cancers by driving tumor progression and shaping an immunosuppressive tumor microenvironment (TME). It promotes tumor cell proliferation, invasion, and metastasis, while simultaneously modulating immune cell infiltration to favor immune escape [17] [18] [2]. Key mechanisms include the suppression of cytotoxic immune cells like CD8+ T cells and Natural Killer (NK) cells, and the alteration of the physical TME through increased collagen deposition and tumor stiffness [17].
Q2: In which cancer types is SOX9 typically overexpressed? SOX9 is significantly upregulated in a wide array of malignant tumors. Pan-cancer analyses reveal that SOX9 expression is significantly increased in fifteen cancer types, including lung adenocarcinoma (LUAD), glioblastoma (GBM), colorectal cancer (COAD/READ), and liver cancer (LIHC) [9]. In contrast, SOX9 expression is decreased in only a few cancers, such as skin cutaneous melanoma (SKCM) and testicular germ cell tumors (TGCT), where it can act as a tumor suppressor [9].
Q3: How does SOX9 expression correlate with patient prognosis? The prognostic impact of SOX9 is cancer-type dependent. High SOX9 expression is generally associated with shorter overall survival in cancers like LUAD, CESC, and THYM, making it a valuable prognostic biomarker for poor outcomes [17] [9] [18]. However, in specific contexts such as IDH-mutant glioblastoma and its lymphoid invasion subgroup, high SOX9 expression has been surprisingly linked to a better prognosis [19].
Q4: What is the relationship between SOX9 and immune checkpoints? Research indicates that SOX9 expression is closely correlated with the expression of key immune checkpoints. In glioblastoma, for example, SOX9 expression is correlated with the levels of immune checkpoints like PD-1, suggesting a potential for combined therapeutic strategies [19]. Its role in creating an "immune desert" TME further underscores its connection to pathways that may be targeted with immune checkpoint blockade therapies [2].
Troubleshooting Guides
Issue 1: Inconsistent SOX9 Detection in Immune Cell Populations
Problem: Difficulty in obtaining consistent and reproducible results when detecting SOX9 protein or mRNA levels across different immune cell subpopulations.
Solutions:
- Validate Antibody Specificity: Ensure the antibody used for detection (e.g., via Western Blot, IHC, or Flow Cytometry) is validated for the specific sample type (e.g., human vs. mouse, tissue lysate vs. cell lysate). Use positive and negative controls as recommended in the kit datasheet [20].
- Optimize Sample Lysis: For protein detection, use a validated cell lysis buffer that effectively extracts nuclear proteins. The Human SOX9 ELISA Kit, for instance, includes a 5X Cell Extraction Buffer PTR that is optimized for this purpose [20].
- Employ a Sensitive Detection Method: If working with low cell numbers, consider using a highly sensitive ELISA. The Human SOX9 ELISA Kit has a sensitivity of 22.8 pg/mL and a recovery rate of 94-100% in cell lysates, making it suitable for quantifying SOX9 in precious samples [20].
- Corroborate with mRNA Data: Use RT-qPCR to measure SOX9 mRNA levels as a complementary method to confirm protein expression data, as demonstrated in multiple studies [17] [9].
Issue 2: Variable Immune Cell Infiltration Data in SOX9-High Tumors
Problem: High intra- and inter-tumor heterogeneity leads to variable results when analyzing immune cell infiltration in SOX9-high tumor models.
Solutions:
- Utilize Computational Deconvolution: Employ bioinformatics tools like CIBERSORT or ESTIMATE to analyze bulk RNA-sequencing data. These methods can infer the proportions of 22 immune cell types and calculate overall immune/stromal scores, which have been used to establish ICI clusters and scores in colorectal cancer [21].
- Implement Consensus Clustering: Use algorithms like ConsensusClusterPlus to robustly group samples based on their immune cell infiltration (ICI) patterns before comparing SOX9-high and SOX9-low groups. This helps in managing heterogeneity [21].
- Confirm with Orthogonal Techniques: Validate bioinformatics findings with flow cytometry or immunohistochemistry on tumor tissue sections. For example, the finding that SOX9 suppresses CD8+ T and NK cell infiltration was confirmed by flow cytometry in mouse LUAD models [17].
Issue 3: Modeling SOX9-Driven Immunosuppression In Vivo
Problem: Challenges in recapitulating the SOX9-mediated immunosuppressive tumor microenvironment in animal models.
Solutions:
- Use Immunocompetent Models: Conduct tumor grafting experiments in immunocompetent (syngeneic) mice rather than immunocompromised models. Research shows that SOX9-promoted tumor growth is significantly attenuated in immunocompromised mice, highlighting the critical role of the immune system in SOX9's oncogenic function [17].
- Leverage Genetically Engineered Models: Utilize conditional knockout mouse models (e.g., KrasLSL-G12D; Sox9flox/flox) to study the specific impact of Sox9 loss on tumor development and the immune landscape in an endogenous setting [17].
- Analyze Multiple Immune Parameters: Use a combination of methods to fully characterize the TME. This includes flow cytometry for immune cell populations, gene expression analysis for cytokines and checkpoint markers, and histology for collagen deposition, as SOX9 is known to elevate collagen-related gene expression and increase collagen fibers [17].
Data Presentation
Table 1: Correlation Between High SOX9 Expression and Immune Cell Infiltration in Human Cancers
| Cancer Type | Correlation with Key Immune Cells | Impact on Survival | Primary Experimental Methods |
|---|---|---|---|
| Lung Adenocarcinoma (LUAD) [17] | Suppresses CD8+ T cells, NK cells, and Dendritic Cells. Increases collagen fibers. | Shorter Overall Survival | Flow Cytometry, IHC, RNA-Seq (Mouse & Human) |
| Colorectal Cancer (CRC) [21] [2] | Negatively correlates with B cells, resting mast cells, and monocytes. Positively correlates with neutrophils and macrophages. | Varies by ICI Subtype | CIBERSORT, ESTIMATE, RNA-Seq (Human) |
| Glioblastoma (GBM) [19] | Correlated with immune checkpoint expression (e.g., PD-1). Linked to specific immune infiltration subgroups. | Better prognosis in IDH-mutant and lymphoid invasion subgroups | TCGA/GTEx RNA-Seq Analysis, Immunohistochemistry |
| Pan-Cancer Analysis [9] [2] | Negatively correlates with CD8+ T cell, NK cell, and M1 macrophage function. Positively correlates with memory CD4+ T cells. | Shorter OS in LGG, CESC, THYM; Long in ACC | Bioinformatics Analysis of TCGA Data |
Table 2: Essential Research Reagent Solutions for SOX9-Immune Research
| Reagent / Kit | Function / Application | Key Specifications | Example Product |
|---|---|---|---|
| SOX9 ELISA Kit | Quantitative measurement of SOX9 protein in cell and tissue lysates. | Sensitivity: 22.8 pg/mL. Range: 62.5-4000 pg/mL. 90-minute protocol [20]. | Human SOX9 ELISA Kit (ab253226) |
| SOX9 Antibodies (Validated) | Detection of SOX9 via Western Blot, Immunohistochemistry (IHC), and Flow Cytometry. | Specific for SOX9 transcription factor. Critical for confirming protein localization and expression [17]. | Various commercial providers |
| Cell Extraction Buffer | Lysis of cells for protein analysis, optimized for nuclear transcription factors. | Component of ELISA kits; ensures efficient SOX9 extraction [20]. | 5X Cell Extraction Buffer PTR |
| CRISPR/Cas9 System | For Sox9 knockout studies to validate its functional role in vitro and in vivo. | Used with pSECC system for somatic gene editing in mouse models [17]. | sgRNA targeting Sox9 (e.g., sgSox9.2-pSECC) |
Experimental Protocols
Protocol 1: Quantifying SOX9 Protein from Cell Lysates Using ELISA
This protocol is adapted from the methodology used with the Human SOX9 ELISA Kit [20].
Sample Preparation:
- Lyse cells using the provided 5X Cell Extraction Buffer PTR, diluted to 1X in PBS.
- Add the 50X Cell Extraction Enhancer Solution to the lysis buffer for improved protein recovery.
- Incubate the lysate on ice for 20 minutes, then centrifuge at 18,000 x g for 20 minutes at 4°C.
- Collect the supernatant and determine total protein concentration. Dilute the lysate to fall within the assay's range (62.5-4000 pg/mL) using the provided Sample Diluent NS.
ELISA Procedure:
- Add the prepared samples and SOX9 standard to the pre-coated wells.
- Simultaneously add the Capture and Detector Antibodies to each well.
- Incubate for 1 hour at room temperature on a plate shaker.
- Wash the plate once with 1X Wash Buffer.
- Add TMB Development Solution and incubate for 10 minutes in the dark.
- Stop the reaction with Stop Solution and read the absorbance immediately at 450 nm.
Protocol 2: Analyzing SOX9-Dependent Immune Cell Infiltration via Flow Cytometry
This protocol is based on methods used to characterize the TME in KrasG12D-driven LUAD models [17].
Tumor Dissociation:
- Harvest tumor tissue and process it into a single-cell suspension using a mechanical and enzymatic dissociation kit suitable for tough tissues.
Cell Staining:
- Count the cells and aliquot up to 1x10^7 cells per staining condition.
- Block Fc receptors to prevent non-specific antibody binding.
- Stain the cells with a panel of fluorescently conjugated antibodies against immune cell surface markers. A core panel for TME analysis should include:
- CD45 (pan-immune cell marker)
- CD3 (T cells)
- CD8 (cytotoxic T cells)
- CD4 (helper T cells)
- NK1.1/CD49b (Natural Killer cells)
- CD11c (Dendritic cells)
- F4/80 (Macrophages)
- Include a viability dye to exclude dead cells.
Acquisition and Analysis:
- Acquire data on a flow cytometer.
- Analyze the data using flow cytometry software. Gate on live, single cells, then on CD45+ immune cells, and subsequently on the specific immune cell populations of interest. Compare the proportions and absolute numbers of these cells between SOX9-high and SOX9-low (or knockout) tumor models.
Signaling Pathways and Workflow Visualizations
SOX9 in the Tumor Immune Microenvironment
Workflow for SOX9 Immune Role Analysis
Frequently Asked Questions (FAQs)
Q1: Why is SOX9 considered a high-value target in cancer research? SOX9 is a transcription factor frequently dysregulated in cancers. It drives key tumorigenic processes like cell proliferation, metastasis, and drug resistance. Its expression is a negative prognostic biomarker in numerous cancers, and it plays a role in shaping the immunosuppressive tumor microenvironment, making it a promising therapeutic target [18] [22] [23].
Q2: I am getting inconsistent SOX9 detection in immune cell subpopulations. What could be the cause? SOX9 expression is highly context-dependent. Inconsistent detection can stem from:
- Cell State and Differentiation: SOX9 is crucial for progenitor cell development and its levels fluctuate with cell differentiation state [24] [2].
- Post-Translational Modifications (PTMs): Phosphorylation at residues like S64 and S181 can alter SOX9's nuclear localization and stability, affecting antibody binding and detection [24].
- Epigenetic Regulation: DNA methylation of the SOX9 promoter can silence its expression in a cell-type-specific manner [24].
Q3: What is the relationship between SOX9 and cancer drug resistance? High SOX9 expression is a established biomarker for resistance to various therapies. Mechanistically, SOX9 can:
- Activate pathways like Wnt/β-catenin to induce Epithelial-Mesenchymal Transition (EMT) [22].
- Regulate the expression of specific miRNAs (e.g., miR-613, miR-190) to promote survival under drug treatment [22].
- Upregulate drug efflux pumps and aldehyde dehydrogenase (ALDH) activity, enriching for cancer stem cell populations that are inherently therapy-resistant [18] [22].
Q4: Does SOX9 always act as an oncogene? No, SOX9 function is tissue and context-specific. While it acts as an oncogene in most cancers (e.g., prostate, lung, liver), it can function as a tumor suppressor in others, such as melanoma, where its expression inhibits tumorigenicity [9].
Troubleshooting Guides
Guide 1: Optimizing SOX9 Detection and Quantification
Problem: Low or variable signal in Western Blot or qPCR.
| Step | Potential Issue | Solution |
|---|---|---|
| Sample Prep | Protein Degradation / RNA Degradation | Use fresh protease and phosphatase inhibitors. For RNA, use RNase inhibitors and work in an RNase-free environment. |
| Lysis | Incomplete nuclear lysis | SOX9 is a nuclear protein. Use a lysis buffer with a strong detergent and consider a sonication step to ensure complete nuclear disruption. |
| Antibody Selection | Poor antibody specificity | Validate antibodies in a SOX9-knockdown cell line. Use antibodies validated for Chromatin Immunoprecipitation (ChIP) if working with DNA-binding studies. |
| qPCR | Inefficient primer design | Design primers that span an exon-exon junction to avoid genomic DNA amplification. Verify primer efficiency with a standard curve. |
| Data Normalization | Use of unstable reference genes | Do not use GAPDH or β-actin universally. Validate stable reference genes (e.g., TBP, HPRT1) for your specific cell type and experimental conditions. |
Guide 2: Investigating SOX9-Mediated Drug Resistance
Problem: Establishing a causal link between SOX9 and drug resistance in a new cancer model.
| Step | Action | Protocol Detail |
|---|---|---|
| 1. Correlation | Confirm SOX9 is overexpressed in resistant cells. | Isolate drug-resistant cell populations. Perform qPCR and Western Blot to compare SOX9 levels vs. parental sensitive cells. |
| 2. Perturbation | Modulate SOX9 expression. | Knockdown: Use siRNA or shRNA. Knockout: Use CRISPR/Cas9. Overexpress: Use a SOX9 plasmid. Include empty vector controls. |
| 3. Functional Assay | Test if SOX9 modulation affects resistance. | Treat modified cells with the drug. Perform cell viability assays (e.g., MTT, CellTiter-Glo) and clonogenic survival assays. |
| 4. Mechanism | Identify the downstream pathway. | Perform RNA-Seq or ChIP-Seq on SOX9-modulated cells to identify target genes (e.g., stemness factors, EMT markers, survival genes). |
Summarized Data Tables
Table 1: SOX9 Expression and Prognostic Value in Pan-Cancer Analysis
Data derived from public databases (TCGA, GTEx) reveals SOX9's differential expression and clinical impact [9].
| Cancer Type | SOX9 Expression vs. Normal | Correlation with Overall Survival (OS) | Potential Clinical Utility |
|---|---|---|---|
| Glioblastoma (GBM) | Increased | Shorter OS (in IDH-wildtype contexts) | Diagnostic & Prognostic Biomarker [19] |
| Colon Adenocarcinoma (COAD) | Increased | Shorter OS | Prognostic Biomarker & Drug Resistance Marker [9] [22] |
| Lung Adenocarcinoma (LUAD) | Increased | Shorter OS | Prognostic Biomarker & Therapeutic Target [2] [22] |
| Liver Cancer (LIHC) | Increased | Shorter OS | Prognostic Biomarker [9] [22] |
| Skin Cutaneous Melanoma (SKCM) | Decreased | Varies (Tumor Suppressor Role) | Context-Dependent Biomarker [9] |
| Thymoma (THYM) | Increased | Shorter OS | Prognostic Biomarker [9] |
Table 2: Experimental Modulators of SOX9 Expression and Activity
A list of research reagents used to study SOX9 function [9] [24] [22].
| Reagent / Method | Function / Target | Experimental Outcome |
|---|---|---|
| Cordycepin | Adenosine analog; inhibits SOX9 mRNA and protein | Dose-dependent downregulation of SOX9; reduced cancer cell viability [9] |
| siRNA / shRNA | RNAi-mediated SOX9 mRNA knockdown | Reduces tumor growth, invasion, and reverses chemoresistance [22] [23] |
| CRISPR/Cas9 | SOX9 gene knockout | Ablates tumor initiation and confirms SOX9 as a key driver gene [25] |
| PKA / ERK1/2 Activators | Induces phosphorylation at S64, S181 | Enhances SOX9 nuclear import and transcriptional activity [24] |
| EZH2 Inhibitors | Inhibits H3K27 methyltransferase | Prevents epigenetic repression of SOX9, potentially increasing its expression [24] |
The Scientist's Toolkit: Key Research Reagent Solutions
| Item | Function / Application | Example & Notes |
|---|---|---|
| SOX9 Antibody (ChIP-grade) | Chromatin Immunoprecipitation | Identifies direct genomic binding sites of SOX9. Critical for mapping its transcriptional network. |
| SOX9 KO Cell Line | Functional loss-of-function studies | Validates specificity of antibodies and phenotypic results from siRNA studies. |
| Cordycepin | Small-molecule inhibitor of SOX9 | Used to probe SOX9-dependent mechanisms in vitro; a starting point for therapeutic development [9]. |
| Luciferase Reporter with SOX9 Response Element | Measuring SOX9 transcriptional activity | Contains tandem repeats of the SOX9 binding motif (e.g., AGAACAATGG). |
| Phospho-specific SOX9 Antibodies (e.g., pS64, pS181) | Detecting post-translational activation | Essential for studying SOX9 regulation by kinase pathways like PKA and ERK [24]. |
Experimental Protocol: Inhibiting SOX9 with Cordycepin and Assessing Functional Impact
Objective: To determine the effect of SOX9 inhibition on cancer cell viability and gene expression.
Materials:
- Cancer cell lines (e.g., 22RV1, PC3, H1975) [9]
- Cordycepin (Chengdu Must Bio-Technology or equivalent)
- RPMI 1640 or DMEM culture medium with 10% FBS
- Cell viability assay kit (e.g., MTS, CellTiter-Glo)
- RNA extraction kit, cDNA synthesis kit, qPCR reagents
- SOX9 and GAPDH primers
- RIPA lysis buffer, SDS-PAGE equipment, Western blot transfer apparatus
- SOX9 antibody, HRP-conjugated secondary antibody
Method:
- Cell Culture and Treatment:
- Culture cells in appropriate medium at 37°C with 5% CO₂.
- Seed cells in 12-well plates at a density of 2-5 x 10⁴ cells/well and allow to adhere overnight.
- Treat cells with cordycepin at a range of concentrations (e.g., 0, 10, 20, 40 µM) for 24-48 hours [9].
Viability Assessment (48 hours post-treatment):
- Aspirate medium and add fresh medium containing a cell viability reagent.
- Incubate for 1-4 hours and measure absorbance/luminescence according to the manufacturer's instructions.
SOX9 Expression Analysis (24 hours post-treatment):
- RNA Extraction and qPCR: Extract total RNA, synthesize cDNA, and perform qPCR. Calculate relative SOX9 mRNA expression using the 2^–ΔΔCt method normalized to GAPDH.
- Protein Extraction and Western Blot: Lyse cells in RIPA buffer. Separate proteins by SDS-PAGE, transfer to PVDF membrane, and immunoblot with anti-SOX9 and anti-GAPDH antibodies [9].
Signaling Pathway and Experimental Workflow Diagrams
Advanced Techniques for SOX9 Profiling: From Single-Cell Resolution to High-Throughput Screening
Leveraging Single-Cell RNA Sequencing for Unbiased SOX9+ Immune Cell Discovery
The transcription factor SOX9 (SRY-box transcription factor 9) plays a complex, context-dependent role in immune regulation. It functions as a "double-edged sword" in immunology, capable of both promoting tumor immune escape and contributing to tissue repair and regeneration [2]. Its expression is significantly upregulated in numerous cancers, where it can influence immune cell infiltration and function [9]. Traditionally, studying such rare immune subpopulations has been challenging due to technological limitations.
Single-cell RNA sequencing (scRNA-seq) has revolutionized this field by enabling the unbiased dissection of cellular heterogeneity at unprecedented resolution. This powerful technology allows researchers to profile the transcriptomes of individual cells within a complex mixture, making it ideally suited for discovering and characterizing rare SOX9+ immune cell subsets and understanding their functional roles in health and disease [26]. This technical support guide provides optimized protocols and troubleshooting advice to overcome common challenges in detecting SOX9 in immune cells using scRNA-seq.
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Common Experimental Challenges and Solutions
Table: Troubleshooting Common scRNA-seq Issues for SOX9+ Immune Cell Research
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Low cDNA yield | Low RNA content per cell; inhibition of reverse transcription by buffer components [27]. | - Perform a pilot experiment to determine RNA content for your specific immune cell type [27].- Wash and resuspend cells in EDTA-, Mg2+-, and Ca2+-free PBS or a validated sorting buffer [27]. |
| High background in negative controls | Contamination from amplicons or environment; insufficient bead cleanup [27]. | - Maintain separate pre- and post-PCR workspaces [27].- Use a strong magnetic device for bead cleanups and allow complete separation before supernatant removal [27]. |
| Poor SOX9 protein detection despite high mRNA | Epitope damage from enzymatic digestion; suboptimal antibody titration [28]. | - Test antibody clone sensitivity to your dissociation enzyme cocktail [28].- Use CITE-seq and optimize antibody concentrations via flow cytometry titrations [28]. |
| Mis-annotation of SOX9+ immune cells | Reliance solely on transcriptional data for clustering; low mRNA abundance of key markers [28]. | - Integrate protein expression data via CITE-seq to accurately identify immune lineages [28].- Validate findings with orthogonal methods like fluorescence-activated cell sorting (FACS). |
| Low cell viability after sorting | Extended processing time; stressful dissociation protocols [27]. | - Work quickly. Snap-freeze samples after collection or process immediately [27].- Optimize tissue dissociation to minimize stress on primary immune cells. |
Frequently Asked Questions
Q1: Can I treat individual cells as biological replicates for statistical testing? A: No. Treating individual cells as replicates leads to sacrificial pseudoreplication, which confounds within-sample and between-sample variation and drastically increases false-positive rates [29]. Always include multiple biological replicates (samples from different donors or animals). During analysis, use methods like "pseudobulking" to account for sample-to-sample variation before performing differential expression tests [29].
Q2: My immune cells are fragile. What is the ideal sample preparation for 10x Genomics workflows? A: The ideal sample has >90% viability and is suspended in a buffer like PBS with 0.04% BSA that is free of reverse transcription inhibitors (e.g., high EDTA) [29]. Aim for a concentration of 1,000-1,600 cells/μL and deliver a minimum of 100,000-150,000 total cells to the sequencing facility to ensure adequate cell recovery [29].
Q3: SOX9 seems to have opposing roles in different cancers. How can scRNA-seq help clarify this? A: scRNA-seq can dissect the tumor microenvironment at a cellular level. It allows you to determine whether SOX9 is expressed in the tumor cells, specific immune subpopulations, or stromal cells. By coupling this with gene expression profiling, you can correlate SOX9 expression with specific pathways, like cytokine signaling (e.g., CXCL3/5) or immune checkpoint molecules, providing mechanistic insight into its dual roles [26] [2].
Key Experimental Protocols and Workflows
Optimized Protocol for scRNA-seq of SOX9+ Cells from Tissues
This protocol is adapted from studies investigating SOX9 in bronchoalveolar lavage fluid (BALF) and kidney models [26] [30].
Step 1: Tissue Dissociation and Single-Cell Suspension
- Tissue Processing: Mechanically dissociate tissue using a gentleMACS Dissociator or similar device [28].
- Enzymatic Digestion: Use a validated enzyme cocktail (e.g., Collagenase-based). Critical: Test the impact of digestion on your immune cell surface markers of interest beforehand [28].
- Filtration and Lysis: Pass the cell suspension through a 70-micron cell strainer [26]. Lyse red blood cells if present.
Step 2: Cell Quality Control and Sorting
- Viability Assessment: Use trypan blue exclusion to assess cell viability. Only proceed if viability exceeds >80% [26] [29].
- Cell Sorting: FACS-sort cells into an appropriate collection buffer (see Reagent Table). For SOX9 pre-enrichment, sort cells based on viability dyes and/or specific surface markers.
- Buffer Compatibility: Ensure the sort buffer is compatible with your scRNA-seq kit (e.g., Mg2+- and Ca2+-free PBS for many kits) [27].
Step 3: scRNA-seq Library Preparation
- Follow the manufacturer's instructions for your chosen platform (e.g., 10x Genomics 3' or 5' Gene Expression kit) [29].
- For immune cell profiling, the 10x Genomics 5' Gene Expression kit is advantageous as it allows for concurrent V(D)J sequencing of T and B cell receptors [29].
- If performing CITE-seq, stain the single-cell suspension with the validated antibody panel before loading onto the platform [28].
Step 4: Sequencing and Data Analysis
- Sequence libraries to a minimum depth of 50,000 reads per cell.
- For data preprocessing, use tools like CeleScope for alignment to the GRCh38 genome and quantification of UMIs and genes [26].
- Perform quality control, normalization, and clustering using standard packages (e.g., Scanpy in Python or Seurat in R) [26].
- Identify SOX9-expressing clusters and perform differential expression analysis to define their unique molecular signatures.
Diagram Title: scRNA-seq Workflow for SOX9+ Cell Discovery
Protocol for CITE-seq to Enhance SOX9+ Immune Cell Detection
This protocol is crucial for accurately identifying immune cell types, especially when protein markers do not correlate well with mRNA levels [28].
Antibody Titration and Validation:
- Titrate each TotalSeq-C antibody using flow cytometry on a representative sample (e.g., splenocytes) to determine the optimal concentration that provides the best signal-to-noise ratio [28].
- Validate that the antibody clones are resistant to the enzymatic digestion process used in your tissue dissociation protocol [28].
Cell Staining:
- Create a single-cell suspension as described in Section 3.1.
- Resuspend up to 10^6 cells in a master mix containing the titrated, pooled TotalSeq-C antibodies in cell staining buffer.
- Incubate for 30 minutes on ice, protected from light.
- Wash cells twice with cold PBS + 0.04% BSA to remove unbound antibody.
Combining with scRNA-seq:
- Proceed immediately with the standard scRNA-seq protocol for your chosen platform (e.g., 10x Genomics 5' Gene Expression with Feature Barcoding technology), loading the stained cells as the input [29].
The Scientist's Toolkit: Essential Research Reagents
Table: Key Reagents for scRNA-seq Analysis of SOX9+ Immune Cells
| Reagent / Tool | Function / Description | Example / Specification |
|---|---|---|
| Collagenase Enzyme Cocktail | Digests extracellular matrix to create single-cell suspensions from tissues. | Collagenase Gold, Liberase [28] |
| FACS Buffer | Protects cell viability and surface epitopes during sorting; must be RT-compatible. | EDTA-, Mg2+-, Ca2+-free PBS; BD FACS Pre-Sort Buffer [27] |
| Viability Dye | Distinguishes live from dead cells during FACS, critical for data quality. | Propidium Iodide, 7-AAD |
| scRNA-seq Kit | Platform for generating barcoded single-cell libraries. | 10x Genomics 3' or 5' Gene Expression Kit [29] |
| CITE-seq Antibodies | Oligo-tagged antibodies for simultaneous surface protein detection. | TotalSeq-C antibodies from BioLegend; must validate clones [28] |
| SOX9 Antibody (IHC) | Validates SOX9 protein expression and localization in tissue context. | Recombinant Rabbit monoclonal, e.g., MSVA-709R [31] |
| Bioinformatics Tools | Software for processing, analyzing, and visualizing scRNA-seq data. | Scanpy (Python), Seurat (R), CellChat [26] |
Visualizing SOX9-Associated Signaling in Immune Cells
ScRNA-seq data from severe checkpoint inhibitor-related pneumonitis (CIP) revealed a pro-inflammatory role for SOX9 in aberrant basaloid cells. The proposed signaling pathway illustrates how SOX9 may drive immune activation [26].
Diagram Title: SOX9-Linked Pro-Inflammatory Pathway in CIP
This technical support center provides targeted troubleshooting guides and FAQs to help researchers optimize the detection and quantification of SOX9 protein in immune cell subpopulations, a critical focus in immunology and drug development research.
Troubleshooting Guide: Flow Cytometry
Weak or No Signal in SOX9 Detection
Problem: You are getting a weak or no fluorescence signal when detecting SOX9 in immune cell populations.
Possible Causes & Solutions: [32]
| Possible Cause | Recommendation |
|---|---|
| Inadequate fixation/permeabilization | For intracellular SOX9, use ice-cold 90% methanol added drop-wise to the cell pellet while vortexing. Alternatively, use formaldehyde fixation with Saponin or Triton X-100. |
| Dim fluorochrome for low-abundance target | Use a bright fluorochrome (e.g., PE) conjugated to your anti-SOX9 antibody for best detection of low-density targets. |
| Suboptimal instrument settings | Ensure the flow cytometer's laser wavelength and PMT settings match the excitation/emission wavelengths of your fluorochrome. |
| Low target expression | Include positive controls. For phospho-specific or low-abundance targets, use cell treatments known to induce expression to confirm antibody functionality. |
High Background in Immune Cell Populations
Problem: High background or non-specific staining is obscuring your SOX9 signal, particularly in complex immune cell mixtures.
Possible Causes & Solutions: [33] [32]
| Possible Cause | Recommendation |
|---|---|
| Fc receptor binding | Block cells with BSA, a commercial Fc receptor blocking reagent, or normal serum from the secondary antibody host prior to staining. |
| Dead cells | Use a viability dye (e.g., PI, 7-AAD for live cells; fixable viability dyes for fixed cells) to gate out dead cells. |
| High autofluorescence | Use fluorochromes that emit in red-shifted channels (e.g., APC instead of FITC). Use bright fluorochromes (e.g., Alexa Fluor 488) to overpower background. |
| Antibody concentration too high | Titrate your anti-SOX9 antibody to find the optimal concentration. High concentrations increase non-specific binding. |
Troubleshooting Guide: Immunohistochemistry (IHC)
Weak or No Staining for SOX9 in Tissue Sections
Problem: You are observing little to no specific staining for SOX9 in your tissue sections.
Possible Causes & Solutions: [34] [35]
| Possible Cause | Recommendation |
|---|---|
| Suboptimal antigen retrieval | Use heat-induced epitope retrieval (HIER). A microwave oven is often preferred; for some targets, a pressure cooker may yield stronger signals. Use the recommended buffer (e.g., 10 mM sodium citrate, pH 6.0). |
| Antibody dilution or diluent | Use the primary antibody diluent specified on the datasheet. Titration may be required if using a different diluent. |
| Loss of antibody potency | Ensure the antibody is stored correctly and avoid repeated freeze-thaw cycles. Include a known positive control tissue to confirm antibody activity. |
| Slide storage issues | Use freshly cut slides whenever possible. If slides must be stored, keep them at 4°C. |
High Background Staining in IHC
Problem: High background staining results in a poor signal-to-noise ratio, making it difficult to interpret SOX9 localization.
Possible Causes & Solutions: [34] [35]
| Possible Cause | Recommendation |
|---|---|
| Endogenous enzyme activity | Quench endogenous peroxidases by incubating slides in 3% H2O2 for 10 minutes prior to primary antibody incubation. |
| Endogenous biotin | For biotin-based detection systems, use a commercial avidin/biotin blocking solution, especially in tissues like liver and kidney. |
| Insufficient blocking | Block tissue sections with 1X TBST with 5% normal serum from the species of your secondary antibody for at least 30 minutes. |
| Secondary antibody cross-reactivity | Always include a control slide stained without the primary antibody to identify background from the secondary antibody. |
| Inadequate washing | Wash slides 3 times for 5 minutes with TBST after both primary and secondary antibody incubations. |
Frequently Asked Questions (FAQs)
Q1: My SOX9 antibody works in Western blot but not in flow cytometry for my immune cell study. Why?
This is common and often due to application-specific antibody validation. An antibody validated for Western blot recognizes denatured proteins, whereas flow cytometry requires recognition of the native protein, often in a different cellular context. [32] [36]
- Solution: First, confirm the antibody is validated for flow cytometry on the manufacturer's datasheet. If it is, the issue may be with your protocol. Ensure your fixation and permeabilization steps (critical for the nuclear protein SOX9) are optimized and do not destroy the epitope. Test the antibody with a known positive control cell line to confirm performance. [32]
Q2: How can I validate that my flow cytometry signal for SOX9 is specific?
Rigorous antibody validation is crucial for accurate data interpretation. Consider these approaches: [36] [37]
- Genetic Validation: Use CRISPR-Cas9 knockout or siRNA knockdown of SOX9 in your cell model. A specific antibody will show a clear reduction in signal.
- Orthogonal Correlation: Compare your flow cytometry data with RNA expression data from the same cell populations. A positive correlation between protein signal (flow) and mRNA level (RNA-seq) increases confidence.
- Cell Treatment: Use a cell treatment known to modulate SOX9 expression. The antibody signal should reflect the expected change.
- Independent Antibodies: Use two different antibody clones that recognize different epitopes on SOX9. A similar staining pattern supports specificity.
Q3: In IHC, my SOX9 staining is patchy and uneven. What could be the cause?
This is frequently a result of inadequate deparaffinization of your formalin-fixed, paraffin-embedded (FFPE) tissue sections. [35]
- Solution: Repeat the experiment with new tissue sections and use fresh xylene during the deparaffinization step to ensure all paraffin is completely removed.
Q4: How can I reduce autofluorescence in my IHC samples for clearer SOX9 detection?
Tissue autofluorescence is a common challenge, especially in FFPE sections. Several strategies can help: [34]
- Chemical Quenching: Treat tissue sections with dyes that quench fluorescence, such as Sudan black or Pontamine sky blue.
- Alternative Fluorophores: Choose fluorescent markers whose emission is in the near-infrared range (e.g., Alexa Fluor 647, Alexa Fluor 750), as most tissue autofluorescence occurs at lower wavelengths.
- Fixative Adjustment: If using aldehyde-based fixatives, treat the sample with ice-cold sodium borohydride (1 mg/mL) to reduce fixative-induced autofluorescence.
Experimental Protocol: Key Workflows
Standard Workflow for SOX9 Detection via Flow Cytometry in Immune Cells
This protocol is critical for analyzing SOX9 protein levels in different immune cell subpopulations. [32]
- Cell Preparation: Harvest your immune cells (e.g., from blood, spleen, or cultured cells) and wash with a suitable buffer like PBS.
- Viability Staining (Optional but Recommended): If staining surface markers, use a viability dye to label and later gate out dead cells.
- Surface Staining: Incubate cells with fluorochrome-conjugated antibodies against surface markers (e.g., CD45, CD3, CD19) to define your immune subpopulations. Do this before fixation.
- Fixation: Add 4% methanol-free formaldehyde to the cell pellet to cross-link and preserve the cells. Fix immediately after treatment to inhibit phosphatase activity.
- Permeabilization: For the nuclear protein SOX9, permeabilize the cells to allow antibody access. Add ice-cold 90% methanol drop-wise to the cell pellet while gently vortexing. Alternatively, use a detergent like Saponin or Triton X-100.
- Intracellular Staining: Incubate the fixed and permeabilized cells with your validated, fluorochrome-conjugated anti-SOX9 antibody at the optimal dilution.
- Analysis: Resuspend cells in buffer and acquire data on the flow cytometer. Use a low flow rate setting for optimal resolution. Analyze SOX9 expression within your gated immune cell populations.
Standard Workflow for SOX9 Detection via IHC in FFPE Tissues
This protocol is essential for visualizing the spatial localization of SOX9 protein within tissue microenvironments. [34] [35]
- Sectioning and Deparaffinization: Cut thin sections (4-6 µm) from your FFPE tissue block. Deparaffinize by immersing slides in fresh xylene, then rehydrate through a graded series of ethanol to water.
- Antigen Retrieval: Perform Heat-Induced Epitope Retrieval (HIER) to break cross-links and expose antigens. A common method is heating slides in 10 mM sodium citrate buffer (pH 6.0) using a microwave oven or pressure cooker for optimal results.
- Blocking and Peroxidase Quenching: Block the tissue with 3% H2O2 to inhibit endogenous peroxidase activity. Then, block with 5% normal serum to prevent non-specific binding of antibodies.
- Primary Antibody Incubation: Apply the optimized dilution of your anti-SOX9 antibody in a recommended diluent. Incubate overnight at 4°C in a humidified chamber to ensure specific binding.
- Detection: Use a sensitive, polymer-based detection system (HRP-conjugated) followed by incubation with DAB chromogen. The polymer system provides high signal amplification with low background.
- Counterstaining and Mounting: Counterstain with hematoxylin to visualize cell nuclei. Dehydrate the sections through ethanol and xylene, and mount with a permanent mounting medium for long-term preservation.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Application |
|---|---|
| Methanol-free Formaldehyde | A superior fixative for flow cytometry and IHC; prevents over-permeabilization and loss of intracellular proteins. [32] |
| SignalStain Antibody Diluent | A optimized diluent for primary antibodies in IHC; using the manufacturer's recommended diluent is critical for optimal signal-to-noise ratio. [35] |
| Polymer-Based Detection Reagents | Used in IHC for signal amplification; more sensitive than traditional avidin-biotin systems and avoid background from endogenous biotin. [35] |
| Sodium Citrate Buffer (pH 6.0) | A standard buffer for heat-induced antigen retrieval (HIER) in IHC; essential for unmasking many epitopes, including SOX9, in FFPE tissues. [34] [35] |
| Viability Dye (e.g., 7-AAD) | A critical dye for flow cytometry to identify and gate out dead cells, which non-specifically bind antibodies and contribute to high background. [32] |
| Fc Receptor Blocking Reagent | Used prior to antibody staining in flow cytometry to block non-specific binding of antibodies to Fc receptors on immune cells, reducing background. [32] |
FAQs: Circulating SOX9 Analysis in PBMCs
Q1: What is the biological significance of detecting SOX9 in PBMCs? SOX9 is a transcription factor that acts as a cancer stem cell (CSC) marker, maintaining cells in an undifferentiated state and promoting their renewal and differentiation [38]. Assessing its levels in circulating PBMCs provides a non-invasive method for understanding tumor biology, as circulating SOX9 levels correlate with local tumor SOX9 expression. Research shows simultaneous up-regulation of circulating SOX9 in patients with bone cancer compared to healthy individuals, accompanying overexpression in malignant tumors [38] [39].
Q2: How does SOX9 expression in PBMCs correlate with clinical features? Circulating SOX9 expression shows significant correlation with several important clinical parameters [38] [39]:
| Clinical Feature | SOX9 Expression Correlation |
|---|---|
| Tumor Malignancy | Higher in malignant vs. benign tumors (P < 0.0001) |
| Tumor Grade | Up-regulated in high-grade tumors |
| Metastasis | Elevated in metastatic tumors |
| Treatment Response | Higher in patients with poor response to therapy |
| Recurrence | Increased in recurrent tumors |
| Chemotherapy | Up-regulated in patients receiving chemotherapy |
Q3: What are the key technical considerations for SOX9 detection in PBMCs? For reliable SOX9 detection in PBMCs, these technical aspects are crucial [38]:
- Sample Collection: Collect fresh peripheral blood (6mL used in referenced study) and process promptly for PBMC separation
- Cell Processing: Isolate PBMCs using appropriate density gradient centrifugation
- Sample Preservation: Fresh tissues and cells are preferred; if using frozen samples, optimize protocols as freezing can affect viability and antigen preservation
- Controls: Include healthy donor samples as controls (60 healthy blood samples used as reference in bone cancer study)
Troubleshooting Guides
Weak or No SOX9 Fluorescence Signal in Flow Cytometry
| Possible Cause | Solution |
|---|---|
| Antibody degradation or expiration | Ensure proper storage per manufacturer's instructions; verify products are not expired [40] |
| Low antibody concentration | Titrate antibodies before use to determine optimal concentration; use appropriate positive and negative controls [40] |
| Low target antigen expression | Use freshly isolated PBMCs rather than frozen samples; optimize cell culture/stimulation protocols [40] [41] |
| Suboptimal antigen-antibody binding | Optimize antibody incubation time and temperature; consider biotinylated primary antibodies with streptavidin amplification [40] |
| Incompatible laser/PMT settings | Ensure proper instrument settings are loaded; use suitable positive and negative controls to optimize settings [40] |
| Weak antigen paired with dim fluorochrome | Pair low-expressing antigens with bright fluorochromes like PE or APC [40] [41] |
High Background or Non-Specific Staining
| Possible Cause | Solution |
|---|---|
| Unbound antibodies in sample | Wash cells adequately after every antibody incubation step [40] |
| Non-specific cell targeting | Include isotype control; block Fc receptors with BSA or FBS prior to antibody incubation [40] [41] |
| High autofluorescence | Include unstained control; use fluorochromes emitting in red channel (e.g., APC) where autofluorescence is minimal [40] |
| Presence of dead cells | Include viability dyes (PI, 7-AAD) to gate out dead cells; use freshly isolated cells when possible [40] |
| Excessive antibody concentration | Titrate antibodies to find optimal concentration; use recommended antibody dilutions [41] |
Abnormal Cell Scatter Profiles or Event Rates
| Issue | Possible Cause | Solution |
|---|---|---|
| Low event rate | Low cell number | Maintain cell count at ~1×10⁶/mL; ensure gentle pipetting to mix cells [40] |
| Sample clumping | Sieve cells before acquisition to remove debris; ensure gentle mixing [40] | |
| High event rate | Concentrated sample | Dilute cell count to ~1×10⁶/mL [40] |
| Abnormal scatter | Cell damage or lysis | Optimize sample preparation to avoid cell lysis; avoid vortexing or high-speed centrifugation [40] |
| Presence of un-lysed RBCs | Ensure complete RBC lysis; use fresh RBC lysis buffer [40] |
Experimental Protocols
PBMC Collection and SOX9 Expression Analysis
Workflow for SOX9 Analysis in PBMCs
Detailed Protocol [38]:
- Blood Collection and PBMC Isolation
- Collect peripheral blood (6mL used in referenced study) in appropriate anticoagulant tubes
- Separate PBMCs using density gradient centrifugation (e.g., Ficoll-Paque)
- Wash cells with phosphate-buffered saline (PBS)
- Count cells and assess viability
RNA Extraction
- Use appropriate RNA extraction kits following manufacturer's protocols
- Determine RNA concentration and quality using spectrophotometry
- Ensure RNA integrity before proceeding to cDNA synthesis
cDNA Synthesis and Real-Time PCR
- Perform reverse transcription using commercial kits
- Use specific SOX9 primers (sequences not provided in search results)
- Perform Real-Time PCR with appropriate cycling conditions
- Normalize SOX9 expression to housekeeping genes (e.g., GAPDH, β-actin)
Data Analysis
- Calculate ΔCt values (Ct[SOX9] - Ct[housekeeping])
- Use ΔΔCt method for relative quantification comparing patient samples to healthy controls
- Correlate SOX9 expression levels with clinical parameters
Protein-Level SOX9 Detection in PBMCs
For protein-level analysis, Western blotting can be performed on PBMC lysates [38]:
- Cell Lysis: Use appropriate lysis buffers with protease inhibitors
- Protein Quantification: Determine protein concentration using BCA or Bradford assay
- Western Blotting: Separate proteins by SDS-PAGE, transfer to PVDF membranes, and probe with SOX9-specific antibodies
- Detection: Use appropriate secondary antibodies and detection methods
The Scientist's Toolkit: Essential Research Reagents
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| SOX9 Antibodies | Anti-SOX9 (MSVA-709R) [31]; sc-20095 (specific for SOX9 without SOX10 cross-reactivity) [42] | Detection of SOX9 protein in IHC, Western blot, flow cytometry |
| Cell Separation | Ficoll-Paque density gradient medium | Isolation of PBMCs from peripheral blood |
| Nucleic Acid Analysis | RNA extraction kits; reverse transcription kits; Real-Time PCR reagents | SOX9 gene expression analysis in PBMCs |
| Flow Cytometry | Viability dyes (PI, 7-AAD); fixation/permeabilization buffers; fluorescent-conjugated antibodies | Analysis of SOX9 expression in immune cell subpopulations |
| Protein Analysis | RIPA lysis buffer; protease inhibitors; PVDF membranes; ECL detection reagents | Western blot analysis of SOX9 protein levels |
SOX9 Detection Quality Control Workflow
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ 1: What is the biological and clinical significance of SOX9 in pan-cancer analysis?
SOX9 (SRY-box transcription factor 9) is a transcription factor involved in developmental pathways and cell differentiation. Its clinical significance in cancer is complex and context-dependent [9].
- Role as an Oncogene: In the majority of cancer types (15 out of 33 analyzed), SOX9 expression is significantly upregulated compared to matched healthy tissues. Cancers with high SOX9 expression include CESC (cervical squamous cell carcinoma and endocervical adenocarcinoma), COAD (colon adenocarcinoma), GBM (glioblastoma), LIHC (liver hepatocellular carcinoma), and PAAD (pancreatic adenocarcinoma). This upregulation suggests SOX9 often acts as a proto-oncogene [9].
- Role as a Tumor Suppressor: In a minority of cancers, notably SKCM (skin cutaneous melanoma) and TGCT (testicular germ cell tumors), SOX9 expression is significantly decreased. In melanoma models, restoring SOX9 expression actually inhibited tumorigenicity, indicating a tumor-suppressive role in specific contexts [9].
- Prognostic Value: High SOX9 expression is associated with the worst overall survival in cancers like LGG (lower grade glioma), CESC, and THYM (thymoma), making it a potential prognostic biomarker [9].
FAQ 2: How do I properly define "normal" tissue controls when analyzing SOX9 expression in TCGA?
A critical and often overlooked step is the definition of "normal" control tissue. TCGA provides two main types of normal samples: true healthy tissues from non-cancerous organ donors and "Normal Adjacent to Tumor" (NAT) tissues [43].
- The Problem: NAT tissues, while histologically normal, are not biologically equivalent to healthy tissues from non-diseased individuals. Transcriptomic analyses reveal that NAT presents a unique intermediate state between healthy and tumor tissues. They exhibit molecular alterations related to wound response, extracellular matrix remodeling, and inflammation, a phenomenon linked to "field cancerization" [43].
- The Solution: For the most accurate assessment of SOX9 dysregulation, compare tumor samples against true healthy tissues from sources like GTEx whenever possible. If using NAT from TCGA, explicitly state this in your methodology and interpret results with the understanding that these tissues may already have undergone molecular changes, which could dilute the observed effect size of SOX9 dysregulation [43].
Table 1: SOX9 Expression Patterns Across Selected Cancers
| Cancer Type | SOX9 Expression vs. Normal | Proposed Role in Cancer | Prognostic Association |
|---|---|---|---|
| GBM (Glioblastoma) | Increased [19] | Oncogene [19] | Conflicting data; potential biomarker in IDH-mutant cases [19] |
| CESC (Cervical cancer) | Increased [44] | Oncogene [44] | High expression linked to poorer prognosis [9] |
| COAD (Colon adenocarcinoma) | Increased [9] | Oncogene [9] | Information missing |
| LIHC (Liver cancer) | Increased [9] | Oncogene [9] | Information missing |
| SKCM (Melanoma) | Decreased [9] | Tumor Suppressor [9] | Information missing |
False correlations can arise from technical and biological artifacts.
- Tissue Contamination and Cellular Heterogeneity: A bulk RNA-seq sample is a mixture of many cell types. A strong correlation between SOX9 and an immune gene signature could mean that SOX9 is highly expressed in cancer cells within a tumor rich in immune cells, not that SOX9 is expressed in the immune cells themselves. This is a false positive at the cellular level.
- Troubleshooting Guide:
- Problem: Observed correlation between SOX9 and a T-cell signature.
- Potential Cause: Cellular heterogeneity; the sample contains both SOX9-high cancer cells and many T-cells.
- Solution: Validate findings using single-cell RNA sequencing (scRNA-seq) data if available, which can isolate expression signals to individual cells. Alternatively, use deconvolution algorithms (e.g., CIBERSORT, EPIC) to estimate cell-type proportions and perform partial correlation analysis that controls for this heterogeneity.
- Biological Context: SOX9 can have opposing roles in different cancers. For example, in thymoma, high SOX9 is negatively correlated with PD-L1 expression and T-cell receptor signaling, potentially facilitating immune escape. In lung adenocarcinoma, it may suppress the tumor microenvironment. Ensure your interpretation aligns with the known biology of your cancer of interest [9] [19].
FAQ 4: Which tools and databases are essential for SOX9-immune correlation analysis?
A robust bioinformatics pipeline relies on specific, curated tools.
Table 2: Essential Bioinformatics Tools for SOX9-Immune Analysis
| Tool Name | Primary Function | Application in SOX9 Research |
|---|---|---|
| cBioPortal | Visualize and analyze multidimensional cancer genomics data [9] | Assess SOX9 genomic alterations (mutations, copy-number changes) across TCGA cohorts. |
| GEPIA2 | Analyze RNA expression data from TCGA and GTEx [9] | Compare SOX9 expression between tumor and normal tissues; perform survival analysis; generate correlation plots. |
| TIMER2.0 | Systematically analyze immune infiltrates [44] | Investigate the correlation between SOX9 expression and abundance of immune cell types (e.g., cancer-associated fibroblasts). |
| LinkedOmics | Analyze multi-omics data within and across TCGA cancers [19] | Identify genes co-expressed with SOX9 and perform functional enrichment analysis on these gene sets. |
| STRING | Construct Protein-Protein Interaction (PPI) networks [19] | Identify potential functional partners of SOX9 to hypothesize mechanisms of action. |
FAQ 5: How can I experimentally validate my bioinformatics findings on SOX9?
Computational predictions must be confirmed with wet-lab experiments.
- Validating SOX9 Expression:
- Protein Level: Perform Western Blot or Immunohistochemistry (IHC) on patient-derived tissue samples (tumor vs. normal). IHC results from the Human Protein Atlas (HPA) can serve as a preliminary reference [44].
- mRNA Level: Use quantitative PCR (qPCR) on the same tissue samples to confirm transcript-level changes observed in TCGA/GTEx [44].
- Validating Immune Correlations:
- In Vitro Models: Treat cancer cell lines (e.g., prostate cancer 22RV1, PC3, or lung cancer H1975) with compounds that modulate SOX9. Cordycepin, an adenosine analog, has been shown to inhibit SOX9 expression in a dose-dependent manner in these cells [9].
- Methodology: Treat cells with varying doses of Cordycepin (e.g., 0, 10, 20, 40 µM) for 24 hours. Collect protein and RNA to measure SOX9 levels via Western Blot and qPCR. Subsequent co-culture experiments with immune cells (e.g., T cells) can then test if SOX9 inhibition alters immune cell activation or cytotoxicity [9].
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Resources for SOX9-Immune Research
| Reagent/Resource | Function/Description | Example in Context |
|---|---|---|
| TCGA & GTEx Datasets | Foundational transcriptomic data for pan-cancer and normal tissue analysis. | Used as the primary data source for initial discovery of SOX9 dysregulation and correlation with immune signatures [9] [45]. |
| Cordycepin | An adenosine analog that inhibits SOX9 expression. | Used in in vitro experiments to probe the functional role of SOX9 and its downstream effects on the immune response [9]. |
| SOX9 Antibodies | For detection and localization of SOX9 protein. | Critical for validating bioinformatics predictions via Western Blot (quantification) and IHC (spatial localization in tissue sections) [44]. |
| Cancer Cell Lines | In vitro models for functional validation. | Lines like 22RV1 (prostate), PC3 (prostate), and H1975 (lung) are used to test the effects of SOX9 modulation on cellular phenotypes and immune-relevant pathways [9]. |
| Single-Cell RNA-Seq Datasets | For resolving cell-type-specific expression in complex tissues. | Used to confirm whether SOX9 expression and its correlated immune genes originate from the tumor, immune, or stromal compartments, avoiding false positives from bulk data [46]. |
Workflow Visualization
Diagram 1: SOX9-Immune Correlation Analysis Workflow
Diagram 2: SOX9 in Cancer and Immune Signaling
Integrating Spatial Transcriptomics to Contextualize SOX9 Expression in Tissue Architecture
FAQs: Experimental Design and Platform Selection
What are the key considerations when choosing a spatial transcriptomics platform for studying a transcription factor like SOX9? Your choice should balance spatial resolution, gene coverage, and sample quality requirements. For identifying SOX9 expression in specific immune cell subpopulations, high cellular resolution is critical. Table 1 summarizes the core trade-offs. If your goal is to discover novel SOX9-regulated genes or pathways, a whole-transcriptome, sequencing-based platform like Visium is appropriate, though its resolution (55-100 µm) may capture multiple cells per spot. To precisely localize SOX9 expression to specific immune cell types, imaging-based platforms like Xenium, MERSCOPE, or CosMx offer subcellular resolution but require you to pre-define a gene panel, including SOX9 and immune cell markers [47] [48].
How many samples and sequencing reads are required for a robust study of SOX9 in the tumor immune microenvironment? Spatial transcriptomics is highly sensitive to tissue heterogeneity. Underpowered studies risk missing rare but biologically critical SOX9-expressing cell populations [47].
- Biological Replicates: A minimum of 3-5 biological replicates per condition is recommended to account for biological variability.
- Sequencing Depth: While manufacturer guidelines often suggest 25,000–50,000 reads per spot, recent empirical data from over 1,000 samples indicates that for complex tissues or FFPE samples, 100,000–120,000 reads per spot significantly improves gene detection sensitivity, which is crucial for detecting transcription factors like SOX9 that may be expressed at moderate levels [47].
- Region of Interest (ROI) Selection: For a heterogeneous tissue like a tumor, analyzing multiple ROIs per sample is advised to capture the variability in SOX9 expression and immune cell infiltration [47].
Our sample is a large tissue section. How can we profile SOX9 contextually across the entire architecture? Conventional ST platforms have limited capture areas (e.g., 6.5 x 6.5 mm for Visium), which can be a constraint for large tissues [48]. Emerging methods like iSCALE address this by using machine learning. This approach involves obtaining a small set of ST "daughter captures" from the large "mother" tissue section. A model is trained to learn the relationship between H&E-stained image features and gene expression patterns from these captures. This model can then predict gene expression, including SOX9, across the entire large tissue section at near-cellular resolution (8 µm x 8 µm superpixels), providing an unbiased, comprehensive view of its expression landscape [48].
FAQs: Sample Preparation and Quality Control
What sample preparation method is optimal for preserving SOX9 mRNA? The choice between Fresh-Frozen (FF) and Formalin-Fixed Paraffin-Embedded (FFPE) tissue depends on your study context and the need for morphological integrity [47].
- Fresh-Frozen (FF) Tissue: Generally yields higher RNA integrity and is preferred for full-transcriptome analysis. It requires rapid freezing and careful cryosectioning.
- Formalin-Fixed Paraffin-Embedded (FFPE) Tissue: Superior for preserving tissue morphology and is standard in clinical pathology. While RNA is more fragmented, modern ST protocols (like Visium for FFPE) have been optimized for it, making it suitable for targeted panels that include SOX9.
What QC metrics should we use to ensure our samples are viable for SOX9 detection? Rigorous QC is non-negotiable [47].
- RNA Quality: For FF samples, an RNA Integrity Number (RIN) > 7 is ideal. For FFPE, a DV200 value (percentage of RNA fragments > 200 nucleotides) above 50-70% is a key indicator of suitability. However, recent evidence suggests that even samples below these thresholds can sometimes yield biologically meaningful data, but the risk of failure is higher [47].
- Tissue Morphology: Always involve a pathologist to assess H&E images for tissue and cellular integrity and to annotate Regions of Interest (e.g., tumor core, invasive margin, tertiary lymphoid structures) to guide downstream analysis.
Troubleshooting Guides
Issue: Weak or No SOX9 Signal
| Potential Cause | Solution |
|---|---|
| Poor RNA integrity | Verify RNA quality (RIN/DV200) from an adjacent section. Optimize tissue preservation and handling to minimize RNase degradation [47]. |
| Low sequencing depth | Increase sequencing depth to 100,000-120,000 reads per spot for FFPE samples to enhance detection sensitivity for moderately expressed genes like SOX9 [47]. |
| SOX9 not in gene panel | For targeted imaging platforms (Xenium, CosMx), confirm that SOX9 is included in your custom gene panel design. |
| Biological reality | SOX9 may be expressed only in rare cell populations. Ensure adequate sequencing depth and replicate number, and use high-resolution platforms to find these niches [14]. |
Issue: Difficulty Integrating Multiple ST Slices to Reconstruct SOX9 Expression Patterns
Challenge: Aligning and integrating multiple tissue slices (from the same sample or across conditions) is complex due to tissue heterogeneity and lack of z-axis information [49]. Solutions:
- Leverage Computational Tools: Utilize specialized tools for ST data alignment and integration. Table 2 categorizes available tools by methodology [49].
- Plan Experiment for 3D Reconstruction: If the goal is a 3D model of SOX9 expression, plan to collect consecutive tissue sections. Tools like PASTE, GPSA, and STaCker are designed for this purpose [49].
- Use a Common Coordinate Framework: Align your ST data to a public or custom tissue atlas to contextualize SOX9 expression against a known architectural background.
Table 2: Categories of Computational Tools for ST Data Alignment and Integration [49]
| Methodology Category | Representative Tools | Best Suited For |
|---|---|---|
| Statistical Mapping | PASTE, GPSA, PRECAST, Eggplant | Aligning slices with homogeneous or well-defined spatial domains. |
| Image Processing & Registration | STalign, STUtility, STIM | Leveraging H&E images to guide alignment, including heterogeneous tissues. |
| Graph-Based | SpatiAlign, STAligner, SLAT | Integrating data across samples and experiments, dealing with complex batch effects. |
Issue: Distinguishing SOX9-Related Expression from Background in the Tumor Microenvironment
Challenge: The tumor microenvironment is a complex admixture of cell types. A spot in sequencing-based ST often contains multiple cells, making it hard to determine if SOX9 expression originates from tumor cells or adjacent stromal or immune cells. Solutions:
- Computational Deconvolution: Use tools like Cell2location, RCTD, or SpatialDWLS to estimate the proportion of different cell types within each spot and deconvolute the expression signal. This helps attribute SOX9 expression to specific subpopulations [47].
- Single-Cell + Spatial Integration: Combine your ST data with a paired single-cell RNA-seq (scRNA-seq) dataset from the same tissue type. The scRNA-seq data provides a high-resolution reference to infer cell type-specific expression in the spatial data, clarifying the cellular source of SOX9 [47] [50].
- Leverage High-Resolution Platforms: For definitive results, use a high-resolution imaging platform (e.g., Xenium) that allows you to visually co-localize SOX9 mRNA with marker genes for specific cell lineages at a subcellular level.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for SOX9 Spatial Transcriptomics
| Item | Function | Example/Note |
|---|---|---|
| 10x Genomics Visium | Whole-transcriptome, sequencing-based spatial mapping. | Ideal for discovery; spot size limits single-cell resolution [47]. |
| 10x Genomics Xenium | Targeted, imaging-based in situ analysis. | Subcellular resolution; requires a pre-designed gene panel [47] [48]. |
| iSCALE Software | Predicts gene expression on large tissues from H&E images. | Overcomes platform size limitations; requires training with smaller ST captures [48]. |
| STalign | Computational tool for image-based alignment of ST slices. | Aligns ST data using H&E morphology, critical for multi-sample studies [49]. |
| Cell2location | Bayesian model for cell type deconvolution. | Maps cell types onto ST data using scRNA-seq as a reference [47]. |
| SOX9 Antibody (for IHC) | Orthogonal validation of protein expression. | Confirms that mRNA signals translate to protein in the same spatial context. |
| Custom Gene Panel | Defines targets for imaging-based platforms. | Must include SOX9, pan-immune cell markers (PTPRC/CD45), and lineage-specific markers (CD3E, CD19, etc.). |
Experimental Protocols & Workflows
Detailed Protocol: Integrating scRNA-seq with ST to Resolve SOX9 Expression in Immune Cells
This protocol is designed to deconvolute the cellular source of SOX9 expression in complex tissues.
Step 1: Generate a High-Quality scRNA-seq Reference.
- Isolate single cells from the same tissue type being studied with ST.
- Perform scRNA-seq using a platform like 10x Chromium to create a comprehensive transcriptome profile.
- Annotate cell types by clustering and identifying canonical markers (e.g., T cells: CD3D, CD3E; B cells: CD79A, MS4A1; Macrophages: CD68, AIF1). Identify which clusters express SOX9.
Step 2: Acquire Spatial Transcriptomics Data.
- Section adjacent tissue onto your chosen ST platform (e.g., Visium).
- Follow manufacturer protocols for library preparation. For FFPE, use the dedicated Visium protocol.
- Sequence at a depth of 100,000 reads per spot for FFPE samples [47].
Step 3: Computational Integration via Cell2location.
- Inputs: Your ST count matrix and the scRNA-seq reference with annotated cell types.
- Process: Cell2location uses a Bayesian model to learn the reference cell type signatures and then estimates the abundance and location of each cell type in the ST data.
- Output: A spatial map of estimated cell type abundances for each spot.
Step 4: Contextualize SOX9 Expression.
- Overlay the deconvoluted cell type maps with the spatial expression map of SOX9.
- Statistically test for correlation between SOX9 expression levels and the abundance of specific immune cell types across all spots to objectively identify which subpopulations are associated with SOX9.
Workflow for SOX9 Contextualization
Conceptual Framework: The Translation-Integration Axis for SOX9 Analysis
Understanding how morphological features relate to gene expression is key to advanced analysis. A proposed framework categorizes this relationship into four quadrants based on feature relevance and information shared with gene expression [51]. For SOX9 research:
- Translation (Quadrant I): Morphological features highly predictive of SOX9 expression. This allows for predicting SOX9 expression from standard H&E images, a cost-effective strategy for large cohorts [51] [48].
- Integration (Quadrant II): Morphological features provide complementary information not captured by SOX9 expression alone. This is ideal for identifying spatial domains where SOX9's downstream effects on tissue structure are manifest [51].
Morphology-Gene Expression Framework [51]
Overcoming Detection Challenges: Pitfalls, Standardization, and Assay Optimization
Addressing Context-Dependent and Low-Abundance SOX9 Expression in Rare Immune Subsets
Technical Troubleshooting Guide
Q1: My flow cytometry experiment shows a weak or absent SOX9 signal in rare immune cell subsets. What could be the cause?
A: Weak or absent signals for a low-abundance transcription factor like SOX9 can stem from multiple sources in the experimental workflow. The table below outlines common issues and their solutions.
| Potential Source of Issue | Recommended Solution |
|---|---|
| Suboptimal Antibody Concentration [52] | Titrate the anti-SOX9 antibody concentration specifically for your cell type and experimental conditions. |
| Inadequate Permeabilization [52] | Use vigorous detergents (e.g., 0.1–1% Triton X-100) for nuclear targets. For high background, consider alcohol permeabilization (noted to be compatible with Alexa Fluor conjugates). |
| Inaccessible Target [52] | Ensure fixation and permeabilization methods are appropriate for a nuclear protein. Keep cells on ice during surface staining to prevent internalization. |
| Photobleaching [52] | Protect all samples, including single-stained controls, from light during staining and storage. |
| Poor Panel Design [52] | Pair low-abundance SOX9 with the brightest fluorochrome in your panel. Use a spectra viewer to minimize spillover spreading. |
| Low Cell Number/Density [52] | For very low-density populations, ensure sufficient events are collected; techniques like single-cell Westerns may complement your data. |
Q2: How can I reduce high background fluorescence that is obscuring my SOX9-positive population?
A: High background can be particularly problematic when analyzing rare subsets. The following steps can help improve your signal-to-noise ratio.
| Potential Source of Issue | Recommended Solution |
|---|---|
| Cell Autofluorescence [52] | Use fresh cells or cells fixed for a short time. Include unstained and viability dye controls to gate out dead cells and autofluorescent populations. |
| Non-specific Antibody Binding [52] | Use Fc receptor blocking reagents. Titrate your antibody to find the optimal dilution and increase wash steps. |
| Poor Compensation [52] | Ensure single-stained controls are brighter than the experimental sample and collect at least 5,000 positive events for an accurate calculation. |
| Spillover Spreading [52] | Redesign your panel to use fluorochromes with non-overlapping emission spectra for parameters co-expressed with SOX9. |
Researcher's FAQs
Q3: Should I stain for surface markers before or after intracellular SOX9 staining?
A: Always perform extracellular surface staining first [52]. The reagents used for the subsequent fixation and permeabilization steps required for SOX9 detection can decrease surface antigen availability and epitope recognition, leading to weak or lost surface marker signals.
Q4: What are the critical controls needed to confidently gate SOX9-positive immune cells?
A: Proper controls are non-negotiable for validating SOX9 expression in rare subsets. The essential controls are listed below.
| Control Type | Purpose |
|---|---|
| Fluorescence-Minus-One (FMO) [52] | To accurately set gates for SOX9 positivity, especially when its expression is dim or the population is rare. |
| Isotype Control [52] | To determine the contribution of non-specific antibody binding. It must match the SOX9 antibody's species, isotype, fluorochrome, and conjugation ratio. |
| Unstained Cells [52] | To assess cellular autofluorescence and set negative populations. |
| Compensation Controls [52] | Single-stained samples (cells or beads) for every fluorochrome in the panel are required to correct for spectral overlap. |
| Biological Control | A cell line or population with known SOX9 expression (e.g., certain breast cancer cell lines [53]) serves as a positive control for the staining protocol. |
Q5: My experimental treatment might alter SOX9 levels. How can I ensure my detection method is sensitive enough?
A: For detecting subtle changes in a low-abundance target, consider these strategies:
- Indirect Detection: If your direct-conjugated anti-SOX9 antibody is not sensitive enough, use an unconjugated primary antibody followed by a bright, fluorochrome-conjugated secondary antibody. This can amplify the signal but requires careful control for cross-reactivity [52].
- Optimized Fixation: Over-fixation can diminish signals. If 4% formaldehyde reduces signal, test lower concentrations (0.5-1%) [52].
- Functional Assays: Since SOX9 can drive the expression of specific targets like the immune checkpoint B7x, measuring downstream proteins can provide indirect validation of SOX9 activity [53].
Experimental Protocols & Workflows
Detailed Protocol: Simultaneous Surface Marker and Intracellular SOX9 Staining for Flow Cytometry
This protocol is designed for the detection of nuclear SOX9 in defined immune cell subsets.
Key Research Reagent Solutions [52] [53]
| Reagent / Material | Function / Note |
|---|---|
| Fc Receptor Blocking Reagent | Reduces non-specific antibody binding, crucial for low-abundance targets. |
| Viability Dye (e.g., PI, DAPI) | Distinguishes live/dead cells; dead cells contribute to high background. |
| Fluorochrome-conjugated Surface Antibodies | To define immune subsets (e.g., CD3, CD14, CD19, CD56). |
| Fixation Buffer (e.g., 1-4% Formaldehyde) | Cross-links and preserves cellular proteins. |
| Permeabilization Buffer (e.g., 0.1-1% Triton X-100) | Dissolves nuclear membrane for anti-SOX9 antibody access. |
| Anti-SOX9 Antibody | Titrated and conjugated to a bright, compatible fluorochrome. |
| Compensation Beads | Used to create consistent single-stained compensation controls. |
Procedure:
- Harvest and Wash: Harvest your single-cell suspension (from peripheral blood, tissue, or culture) and wash with a cold FACS buffer (e.g., PBS with 1-2% FBS).
- Fc Receptor Blocking: Incubate cells with an Fc receptor blocking reagent for 10-15 minutes on ice.
- Surface Staining: Add titrated cocktails of fluorochrome-conjugated antibodies against your surface markers (e.g., CD45, CD3, CD4, CD8). Incubate for 30 minutes on ice or at 4°C, protected from light.
- Viability Staining: Wash cells twice with cold FACS buffer. If using a viability dye compatible with fixation, stain according to the manufacturer's instructions. Wash again.
- Fixation: Resuspend the cell pellet in a formaldehyde-based fixation buffer (e.g., 4% PFA). Incubate for 20-30 minutes at room temperature. Do not exceed recommended fixation times.
- Permeabilization: Wash cells twice with a permeabilization buffer. Resuspend in a vigorous permeabilization buffer (e.g., 0.5% Triton X-100) for intracellular nuclear targets. Incubate for 15-30 minutes at room temperature.
- Intracellular SOX9 Staining: Add the titrated, directly conjugated anti-SOX9 antibody. Incubate for 45-60 minutes at room temperature, protected from light.
- Final Washes and Acquisition: Wash cells twice with permeabilization buffer, then once with FACS buffer. Resuspend in FACS buffer for acquisition on a flow cytometer. Keep samples on ice and protected from light.
- Controls: Process unstained, FMO, isotype, and single-stained compensation controls in parallel with your experimental samples.
Workflow Diagram: SOX9 Staining & Analysis
The following diagram illustrates the logical flow of the experiment from sample preparation to data analysis, highlighting key decision points.
Data Presentation & Analysis
Quantitative Data from Literature: Immune Cell Associations
The following table summarizes key quantitative findings from recent studies that successfully identified SOX9 or associated immune cell subsets, providing a reference for expected outcomes.
| Observation / Finding | Associated Cell Population | Quantitative Measure / Correlation | Source / Context |
|---|---|---|---|
| SOX9 upregulation induces immune checkpoint B7x expression [53] | Dedifferentiated tumor cells (Breast Cancer) | Correlation between SOX9 and B7x expression; associated with reduced CD8+ T cell infiltration. | In vitro & mouse models |
| High Systemic Immune-Inflammation Index (SII) correlates with specific immune shifts [54] | Neutrophils; T-cells | SII ≥ 1003 associated with higher neutrophil % and lower lymphocyte % (driven by T-cells). | Germ cell tumor patients |
| Identification of a disease-associated monocyte subset [55] | EGR1+ CD14+ monocytes | Significant enrichment in SRC patients (median log2-fold change: +1.9). | Systemic sclerosis patients |
This technical support document is framed within the broader thesis of "Optimizing SOX9 detection in immune cell subpopulations research." The protocols and troubleshooting advice herein are designed to empower researchers to overcome the significant challenges of context-dependent expression and low protein abundance, thereby enabling more reliable and reproducible findings in the field.
Optimizing Antibody Specificity and Antigen Retrieval for Immunoassays
This technical support center provides targeted guidance for researchers optimizing the detection of the transcription factor SOX9, a critical yet complex target in immune and glial cell research. SOX9 plays context-dependent roles, functioning as an oncogene in numerous cancers while also maintaining essential functions in astrocyte-mediated brain protection and tissue homeostasis [2]. Its detection is complicated by its nuclear localization, post-translational modifications, and the challenging environment of formalin-fixed paraffin-embedded (FFPE) tissues. The following FAQs, troubleshooting guides, and optimized protocols are designed to address the specific challenges encountered when studying SOX9 in immune cell subpopulations and neurological research.
Frequently Asked Questions (FAQs)
1. Why is antigen retrieval particularly critical for SOX9 detection? SOX9 is a nuclear transcription factor, and its epitopes become masked during standard formalin fixation due to methylene bridge cross-linking. Effective antigen retrieval is essential to reverse these cross-links and make the epitopes accessible to antibodies. Without proper retrieval, even a high-affinity antibody may yield false-negative results [56].
2. What are the key considerations for validating SOX9 antibody specificity? Specificity validation should include multiple approaches:
- Knockout/Knockdown Controls: Using SOX9 CRISPR-Cas9 edited cell lines (e.g., HCT 116) to confirm the absence of the target band in Western blot [57].
- Band Pattern Analysis: SOX9 can appear as multiple bands (e.g., 50-70 kDa) due to ubiquitination, SUMOylation, or the presence of truncated isoforms like mini-SOX9. Recognizing these patterns is crucial for correct interpretation [57].
- Cell Line Selection: Using control cell lines with known SOX9 expression (e.g., SW480 - positive; HeLa - very low expression) confirms antibody performance [57].
3. How does the biological context of my sample affect SOX9 detection? SOX9 expression and function are highly context-dependent. In Alzheimer's disease models, astrocytic SOX9 overexpression is associated with beneficial plaque clearance [58] [59]. In contrast, in most cancers, SOX9 acts as an oncogene, and its expression is significantly upregulated [9]. This variability means optimization might be needed for different tissue types or disease states.
Troubleshooting Common Issues
Problem: Weak or Absent Staining
| Possible Cause | Solution |
|---|---|
| Insufficient Epitope Unmasking | Optimize Heat-Induced Epitope Retrieval (HIER) by testing different buffer pH levels (e.g., pH 6.0 vs. pH 9.0) [56] [60]. |
| Over-fixation | Limit formalin fixation time to 24 hours maximum. For immersion fixation, use tissue pieces <10 mm and fix for 2-24 hours at room temperature [61]. |
| Low Antibody Concentration | Perform a titration experiment to determine the optimal primary antibody concentration. A cited example uses 0.1 µg/ml for IHC on a Ventana platform [57]. |
Problem: High Background/Non-Specific Staining
| Possible Cause | Solution |
|---|---|
| Non-specific Antibody Binding | Increase the concentration of blocking agent (e.g., 1% BSA/10% normal goat serum) and extend blocking time to 1 hour [57]. |
| Over-retrieval | Empirically optimize HIER incubation time. Test a range from 1 to 20 minutes to find the ideal balance between signal and background [60]. |
| Antibody Cross-Reactivity | Ensure proper validation using a knockout control. Check the antibody datasheet for confirmed species reactivity (e.g., Human, Mouse, Rat) [57]. |
Problem: Inconsistent Results Between Experiments
| Possible Cause | Solution |
|---|---|
| Variable Retrieval Conditions | Standardize the HIER method across all experiments. A pressure cooker is often preferred over a domestic microwave for even heating and to prevent section dissociation [56]. |
| Inconsistent Sample Prep | Adopt a uniform fixation and embedding protocol. For perfusion fixation, follow with immersion fixation for complete tissue preservation [61]. |
| Improper Antibody Handling | Aliquot antibodies to avoid freeze-thaw cycles. Use carrier-free formulations where possible and store according to manufacturer specifications. |
Optimized Experimental Protocols
Protocol 1: Heat-Induced Epitope Retrieval (HIER) for SOX9 in FFPE Tissues
This is a detailed methodology for achieving consistent SOX9 unmasking, based on cited best practices [56] [60].
Materials Required:
- Sodium citrate buffer (10 mM, pH 6.0) or Tris-EDTA buffer (10 mM, pH 9.0)
- Domestic stainless steel pressure cooker or scientific microwave
- Hot plate
- Slide rack
Step-by-Step Method:
- Dewaxing and Rehydration: Deparaffinize and rehydrate the FFPE tissue sections using standard xylene and ethanol series.
- Buffer Preparation: Add a sufficient volume of antigen retrieval buffer to the pressure cooker to cover the slides by a few centimeters. Pre-heat the buffer until it reaches a boil.
- Retrieval: Transfer the slides to the boiling buffer. Secure the lid and allow the cooker to reach full pressure.
- Incubation: Start timing once full pressure is reached. A common starting point is 3 minutes in a pressure cooker or 20 minutes in a scientific microwave or vegetable steamer at 95-100°C [56].
- Cooling: After incubation, immediately depressure and cool the cooker by running cold tap water over it for about 10 minutes. This gradual cooling helps the antigenic sites re-form into their native conformation.
- Staining: Proceed with the standard immunohistochemical staining protocol.
Optimization Note: The optimal buffer and incubation time must be determined empirically. Create an optimization matrix testing different buffer pHs (acidic, neutral, basic) against various incubation times (1, 5, 15 minutes) [60].
Protocol 2: Validating SOX9 Antibody Specificity via Western Blot
This protocol outlines a method for confirming antibody specificity, as demonstrated in search results [57].
Materials Required:
- Validated anti-SOX9 antibody (e.g., Recombinant Rabbit Monoclonal [EPR14335])
- Control cell lysates: SOX9-positive (e.g., SW480), SOX9-low/negative (e.g., HeLa), and SOX9-knockout (e.g., CRISPR-edited HCT116)
- SDS-PAGE and Western Blotting equipment
Step-by-Step Method:
- Protein Extraction: Lyse cells in an appropriate buffer (e.g., EBC buffer) to collect total protein.
- Electrophoresis and Transfer: Boil protein samples in SDS loading buffer, separate via SDS-PAGE, and transfer to a PVDF membrane under ice-cold conditions.
- Blocking and Incubation: Block the membrane in 5% non-fat dry milk in TBST. Incubate with the primary anti-SOX9 antibody (e.g., at a 1/1000 dilution) overnight at 4°C [57].
- Detection: Wash the membrane, incubate with an HRP-conjugated secondary antibody (e.g., at 1/20,000 dilution) for 1 hour at room temperature, and detect using a chemiluminescent substrate.
- Interpretation:
- A specific signal should be present in SOX9-positive lysates (SW480) and absent in the knockout control (HCT116).
- Expect bands between 50-70 kDa. The presence of additional bands may indicate post-translational modifications or truncated isoforms and should be investigated [57].
Research Reagent Solutions
The following table details essential reagents for SOX9-focused research, as cited in the search results.
| Item | Function/Description | Example & Specification |
|---|---|---|
| Anti-SOX9 Antibody | Recombinant monoclonal antibodies offer high specificity and lot-to-lot consistency for detecting SOX9 in applications like IHC, WB, and IF [57]. | Clone EPR14335; Validated for Human, Mouse, Rat; working dilution for IHC-P: 1/2000 [57]. |
| Antigen Retrieval Buffers | Critical for breaking formaldehyde-induced cross-links in FFPE tissues to expose hidden SOX9 epitopes. | - Sodium Citrate (10 mM, pH 6.0) [56]- Tris-EDTA (10 mM, pH 9.0) [56] |
| Control Cell Lysates | Essential experimental controls for verifying antibody specificity in Western blot assays. | - Positive Control: SW480 cell lysate (colorectal adenocarcinoma) [57]- Negative Control: SOX9 CRISPR-Cas9 edited HCT116 cell lysate [57] |
| Blocking Serum | Reduces non-specific background staining by occupying hydrophobic binding sites on tissues. | A solution containing 1% BSA and 10% normal goat serum is effective for IHC/IF [57]. |
SOX9 Detection Workflow and Validation
The diagram below outlines the critical steps and decision points for optimizing SOX9 detection, from sample preparation to specificity validation.
SOX9 Detection and Validation Workflow
SOX9 Biological Context in Research
Understanding the dual role of SOX9 is vital for interpreting experimental results. The diagram below summarizes its key functions in different pathological contexts, as identified in recent research.
SOX9 Functions in Disease Contexts
Standardization and Normalization Strategies for Cross-Study Comparability
This technical support guide provides standardized protocols and troubleshooting advice for researchers studying the transcription factor SOX9 within immune cell subpopulations. The context is a broader thesis on optimizing SOX9 detection, acknowledging that SOX9 expression and function vary significantly across biological systems—from driving fibrosis in various organs to acting as an oncogene or tumor suppressor in different cancers, and recently being identified as a key regulator in Alzheimer's disease pathology through its role in astrocyte function. These guidelines address the critical technical challenges in achieving reproducible and comparable SOX9 data across different experimental platforms and research institutions.
Frequently Asked Questions (FAQs)
Q1: Why does SOX9 detection yield inconsistent results across different research studies?
A: Inconsistencies in SOX9 detection primarily stem from biological and technical variability. Biologically, SOX9 expression exhibits significant context-dependence—it functions as a proto-oncogene in 15 cancer types (including COAD, GBM, LIHC) while acting as a tumor suppressor in others like SKCM and TGCT [9]. Technically, variations in sample processing, antibody validation, and normalization methods introduce further discrepancies. Standardizing these technical aspects is crucial for cross-study comparability.
Q2: What are the major biological factors affecting SOX9 expression that complicate cross-study comparisons?
A: Several biological factors critically influence SOX9 expression patterns:
- Tissue and Cell Type Specificity: SOX9 shows differential expression across normal tissues, with high protein expression in 13 organs and no expression in only two organs [9].
- Disease Context: SOX9 is significantly upregulated in fifteen cancer types but shows opposite expression patterns in melanoma and testicular germ cell tumors [9].
- Immune Microenvironment: SOX9 expression in tumor cells can drive immune evasion by helping cells avoid immune surveillance [62] [63].
- Post-translational Modifications: Phosphorylation at serine residues (S64, S181, S211) and other PTMs significantly regulate SOX9 activity and stability [64].
Q3: What normalization strategies are most effective for single-cell RNA sequencing data of SOX9 in immune cells?
A: For scRNA-seq data analysis, particularly in complex tissues like bone microenvironment or adipose tissue, implement these normalization strategies:
- Employ Robust Preprocessing Pipelines: Use standardized workflows specifically designed for metabolically active tissues, which address lipid content, structural fragility, and ambient RNA contamination [65].
- Apply Consensus Cell Type Annotation: Follow established marker gene panels for immune cell identification, using canonical markers (e.g., CD3D/CD3E/CD3G for T cells; CD79A/CD79B for B cells; HLA-DRA/CD14/CD68 for macrophages) [66].
- Utilize Cross-Platform Normalization: When integrating datasets, apply batch correction methods to account for platform-specific technical variations while preserving biological signals of SOX9 expression [65].
Troubleshooting Guides
Issue 1: Inconsistent SOX9 Protein Detection via Western Blot
Problem: Variable SOX9 band patterns or intensities across experiments.
Solutions:
- Sample Preparation: Lyse cells in EBC buffer with 2×SDS loading buffer. Boil protein samples at 100°C for 5 minutes before electrophoresis [9].
- Electrophoresis Conditions: Use Bio-Rad Mini PROTEAN Tetra System or equivalent with consistent buffer conditions [9].
- Transfer Optimization: Perform protein transfer to PVDF membrane under ice bath conditions to prevent overheating and ensure complete transfer [9].
- Antibody Validation: Always include positive controls (e.g., prostate cancer cell lines PC3 or 22RV1 which express SOX9) and negative controls to confirm antibody specificity [9].
Prevention:
- Maintain consistent cell culture conditions, as SOX9 expression can be regulated by various factors including cordycepin (an adenosine analog) which inhibits SOX9 in a dose-dependent manner [9].
- Use the same protein quantification method across all experiments to ensure equal loading.
Issue 2: Low SOX9 Signal in Immunofluorescence of Immune Cells
Problem: Weak or absent SOX9 staining in immune cell populations.
Solutions:
- Epitope Retrieval Optimization: For formalin-fixed paraffin-embedded samples, test multiple antigen retrieval methods (citrate buffer, EDTA, enzymatic) to determine optimal conditions for SOX9 epitope exposure.
- Signal Amplification: Implement tyramide signal amplification (TSA) systems for low-abundance SOX9 detection in immune cell subpopulations.
- Cross-Validation: Confirm findings with multiple detection methods (e.g., RNAscope for SOX9 mRNA coupled with protein detection).
Prevention:
- Use fresh tissue samples when possible, as SOX9 protein degradation can occur with prolonged storage.
- Include known positive control tissues (e.g., cartilage, testis) to validate staining protocols.
Issue 3: High Background in SOX9 Immunohistochemistry
Problem: Excessive non-specific staining obscuring specific SOX9 signal.
Solutions:
- Antibody Titration: Perform checkerboard titration of primary antibody to determine optimal dilution that maximizes signal-to-noise ratio.
- Blocking Enhancement: Extend blocking time (1-2 hours) with appropriate serum matching secondary antibody host species.
- Stringency Washes: Increase wash buffer stringency (e.g., higher salt concentrations) to reduce non-specific binding.
Prevention:
- Include no-primary-antibody controls in every experiment to identify background from secondary antibody or detection system.
- Use validated SOX9 antibodies with published applications in your specific tissue type.
Data Standardization Tables
Table 1: SOX9 Expression Patterns Across Biological Systems
| Biological Context | SOX9 Expression Level | Functional Role | Key Regulatory Factors |
|---|---|---|---|
| Alzheimer's Disease Models | Increased in astrocytes | Promotes Aβ plaque phagocytosis, preserves cognitive function | MEGF10 phagocytic receptor [67] [58] |
| Pan-Cancer Analysis (15 cancer types) | Significantly upregulated | Proto-oncogene role in tumor progression | Varies by cancer type [9] |
| Melanoma (SKCM) | Significantly decreased | Tumor suppressor role | PGD2 increases SOX9, restores retinoic acid sensitivity [9] |
| Testicular Germ Cell Tumors (TGCT) | Significantly decreased | Tumor suppressor role | Not specified in search results [9] |
| Breast Cancer | Frequently overexpressed | Promotes tumor initiation, proliferation, immune evasion | AKT signaling, Bmi1 promoter activation [62] |
| Organ Fibrosis | Upregulated | Promotes ECM accumulation in heart, liver, kidney, lung | Multiple signaling pathways [64] |
Table 2: Recommended Positive Controls for SOX9 Detection
| Experimental Method | Recommended Positive Controls | Alternative Controls |
|---|---|---|
| Western Blot | Prostate cancer cells (22RV1, PC3), Lung cancer cells (H1975) | Chondrocytes, Testicular tissue extracts |
| Immunohistochemistry | Cartilage tissue, Testis, Breast cancer tissue with known SOX9 expression | Tonsil tissue, Intestinal crypts |
| scRNA-seq | Chondrocyte clusters, Known SOX9-high cell populations | Spiked control RNAs |
| Flow Cytometry | SOX9-overexpressing cell lines, Intracellular staining controls | Compensation controls |
Experimental Protocols for Key Methodologies
Protocol 1: SOX9 Detection via Western Blot in Immune Cells
Materials:
- Cell lysis buffer: EBC buffer
- Loading buffer: 2×SDS loading buffer
- Electrophoresis system: Bio-Rad Mini PROTEAN Tetra System
- Transfer system: Standard wet transfer apparatus
- Membrane: PVDF
- Primary antibody: Validated anti-SOX9 antibody
- Secondary antibody: HRP-conjugated species-specific antibody
Method:
- Lyse cells in EBC buffer supplemented with 2×SDS loading buffer.
- Boil samples at 100°C for 5 minutes to denature proteins.
- Perform electrophoresis using the Bio-Rad system at constant voltage (100-120V) until proper separation is achieved.
- Transfer proteins to PVDF membrane under ice bath conditions to maintain low temperature.
- Block membrane with 5% non-fat milk in TBST for 1 hour at room temperature.
- Incubate with primary anti-SOX9 antibody (dilution as validated) overnight at 4°C.
- Wash membrane 3×10 minutes with TBST.
- Incubate with appropriate HRP-conjugated secondary antibody for 1 hour at room temperature.
- Wash membrane 3×10 minutes with TBST.
- Develop using enhanced chemiluminescence substrate and image.
Troubleshooting Note: If SOX9 signal is weak, consider treating cells with proteasome inhibitors before lysis, as SOX9 can be rapidly degraded [9].
Protocol 2: scRNA-seq Analysis Pipeline for SOX9+ Immune Subpopulations
Materials:
- Software: Seurat package, Monocle 3, pySCENIC
- Reference datasets: Human Cell Atlas Adipose Bionetwork consensus markers
- Computational resources: Adequate RAM and processing power for large datasets
Method:
- Quality Control: Filter cells based on nFeature, nCount, and mitochondrial gene percentage (recommended cutoff: >10% mitochondrial genes) [66].
- Normalization: Normalize data using SCTransform or LogNormalize method in Seurat.
- Integration: If multiple datasets, use integration methods (e.g., CCA, Harmony) to correct for batch effects.
- Clustering: Perform PCA followed by graph-based clustering using FindNeighbors and FindClusters functions in Seurat.
- Cell Type Annotation: Annotate immune cell populations using canonical markers:
- T cells: CD3D, CD3E, CD3G
- B cells: CD79A, CD79B, CD19
- Macrophages: HLA-DRA, CD14, CD68
- Neutrophils: CEACAM8, FCGR3B, CEACAM1 [66]
- SOX9 Expression Analysis: Subset immune cell populations and analyze SOX9 expression patterns across subclusters.
- Trajectory Analysis: Use Monocle 3 to construct pseudotime trajectories for SOX9+ immune cells.
- Regulatory Networks: Apply pySCENIC to identify transcription factors co-regulated with SOX9 in immune subpopulations.
Troubleshooting Note: For tissues with high lipid content (e.g., adipose tissue), use specialized pipelines that account for lipid-associated gene contamination [65].
Signaling Pathway and Experimental Workflow Visualizations
Diagram 1: SOX9 Regulatory Network in Disease Contexts
Diagram 2: Standardized SOX9 Detection Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for SOX9 Research
| Reagent | Function | Example Applications | Key Considerations |
|---|---|---|---|
| Validated Anti-SOX9 Antibodies | Specific detection of SOX9 protein | Western blot, IHC, IF, Flow cytometry | Validate for specific applications and species |
| Cordycepin (Adenosine analog) | Inhibits SOX9 expression | Dose-dependent SOX9 inhibition studies | Use concentrations 10-40μM for 24h treatment [9] |
| CRISPR/Cas9 System | SOX9 gene editing | Knockout, knockin, or overexpression models | AAVS1 safe harbor locus for stable expression [68] |
| Tet-off Inducible System | Regulatable SOX9 expression | Controlled overexpression studies | Temporal control of transgene expression [68] |
| scRNA-seq Platforms | Single-cell transcriptomics | Immune cell subpopulation analysis | Follow standardized analytical pipelines [65] [66] |
| ChIP-grade SOX9 Antibodies | Chromatin immunoprecipitation | SOX9 target gene identification | Verify specificity for DNA-binding applications |
Navigating the Complexities of SOX9 Isoforms and Post-Translational Modifications
SOX9 (SRY-box transcription factor 9) is a pivotal transcription factor involved in embryonic development, cell differentiation, and stem cell maintenance. For researchers studying immune cell subpopulations, accurate detection of SOX9 is complicated by its various isoforms, numerous post-translational modifications (PTMs), and context-dependent expression. This technical guide addresses common experimental challenges and provides validated protocols to ensure reliable SOX9 detection in your research.
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: Why do I observe multiple bands (e.g., ~62 kDa) when running a SOX9 western blot, and how can I confirm the correct one?
A: Multiple bands often arise from post-translational modifications or alternative isoforms of SOX9.
- Cause: The theoretical molecular weight of the canonical SOX9 protein is approximately 56 kDa [69] [9]. However, common PTMs like phosphorylation, sumoylation, and acetylation can increase its apparent molecular weight [69] [70]. A band at ~62 kDa is frequently observed and validated in protocols [8].
- Troubleshooting:
- Validate with a positive control: Use a cell lysate from a known SOX9-expressing cell line, such as Hep G2 (human hepatocellular carcinoma), which shows a clear band at 62 kDa [8].
- Check antibody specification: Ensure your antibody is raised against a specific epitope of SOX9. For example, the clone T32-668 is validated for western blot and detects a 62 kDa band [8].
- Use siRNA knockdown: Confirm specificity by showing band disappearance upon SOX9-specific siRNA transfection [71].
Q2: My SOX9 immunohistochemistry (IHC) results are inconsistent across different tissue types. What could be the reason?
A: SOX9 expression is highly tissue-specific, and its detection is sensitive to pre-analytical conditions.
- Cause: SOX9 has a defined expression pattern. For instance, in the colon, it is strongly expressed in crypt base epithelial cells but absent in surface epithelium, while in the brain, protein can be undetectable by IHC despite the presence of RNA [31]. This discrepancy can be due to prolonged formalin fixation, which masks epitopes [31].
- Troubleshooting:
- Include validated controls: Always run a positive control tissue section, such as human colon or testis, where Sertoli cells show strong nuclear staining [8] [31].
- Optimize antigen retrieval: For IHC, use heat-induced antigen retrieval at 121°C for 5 minutes in a pH 7.8 buffer [31].
- Titrate your antibody: For clone MSVA-709R, a dilution range of 1:50 to 1:75 is recommended for IHC [31].
Q3: How do post-translational modifications (PTMs) affect SOX9 function and detection in immune cells?
A: PTMs finely regulate SOX9's activity, stability, and localization, which is crucial in dynamic environments like the tumor immune microenvironment [70].
- Key Modifications:
- Phosphorylation: (e.g., by MAPK/ERK at Ser181) can enhance SOX9's nuclear localization and transcriptional activity [69].
- Sumoylation: (e.g., at Lys61 and Lys398) generally represses SOX9's transactivation potential [69].
- Acetylation: by p300 can facilitate SOX9's recruitment to chromatin and activate target genes [69].
- Ubiquitination: targets SOX9 for proteasomal degradation, regulating its turnover [69] [70].
- Impact on Research: Altered PTM states in different cell types or conditions can affect antibody binding and interpretation of SOX9 expression levels.
Q4: What is the best method to analyze SOX9 expression in specific immune cell populations?
A: Intracellular flow cytometry is the most suitable technique for this purpose.
- Validated Protocol:
- Cell Fixation and Permeabilization: Fix cells with BD Cytofix Fixation Buffer and permeabilize with BD Phosflow Perm Buffer III. Note that BD Perm/Wash buffer is not recommended for use with the T32-668 antibody [8].
- Staining: Use a directly conjugated antibody against your immune cell surface markers (e.g., CD45 for leukocytes) alongside an intracellular SOX9 antibody (e.g., Purified Mouse Anti-Sox9). Use an isotype control at the same concentration for gating [8].
- Compensation is Critical: When performing multi-color flow cytometry, you must perform electronic compensation using single-color stained controls to correct for spectral overlap between fluorochromes [72]. Use compensation beads, especially when working with tandem dyes [72].
Table: Key Post-Translational Modifications of SOX9 and Their Functional Consequences
| Modification Type | Example Residues / Enzymes | Primary Functional Consequence | Consideration for Detection |
|---|---|---|---|
| Phosphorylation | Ser181 (MAPK/ERK, PKA) [69] | Enhances nuclear localization and transcriptional activity [69] | May alter electrophoretic mobility; phospho-specific antibodies can detect active state. |
| Sumoylation | Lys61, Lys398 [69] | Represses transactivation potential [69] | Can cause higher molecular weight shifts on western blots. |
| Acetylation | Mediated by p300/CBP [69] [70] | Promotes chromatin recruitment and gene activation [69] | Can influence protein-protein interactions and stability. |
| Ubiquitination | Targets for proteasomal degradation [69] [70] | Controls protein stability and turnover [69] [70] | Treatment with proteasome inhibitors (e.g., MG132) can increase detectable SOX9 levels. |
Experimental Protocols
Protocol 1: Western Blot for SOX9 Detection
This protocol is adapted from the validation data for the BD Pharmingen Anti-Sox9 antibody (Clone T32-668) [8].
- Sample Preparation: Lyse cells (e.g., Hep G2) in RIPA or SDS-sample buffer. Boil samples at 100°C for 5 minutes.
- Gel Electrophoresis: Load lysate onto a Tris-Glycine polyacrylamide gel and run SDS-PAGE.
- Transfer: Transfer proteins to a PVDF membrane.
- Blocking: Block the membrane with 5% non-fat milk or BSA in TBST.
- Primary Antibody Incubation: Probe membrane with Purified Mouse Anti-Sox9 at a concentration of 0.06 - 0.25 µg/ml. Incubate overnight at 4°C with gentle shaking [8].
- Washing: Wash membrane 3 times for 5 minutes each with TBST.
- Secondary Antibody Incubation: Incubate with an HRP-conjugated Goat Anti-Mouse Ig antibody for 1 hour at room temperature [8].
- Detection: Develop using an enhanced chemiluminescence (ECL) substrate. The expected band for SOX9 is at ~62 kDa [8].
Protocol 2: Immunohistochemistry (IHC) for SOX9 on Formalin-Fixed Paraffin-Embedded (FFPE) Tissues
This protocol is based on the manufacturer's instructions for the MSVA-709R antibody [31].
- Sectioning: Use freshly cut sections (cut less than 10 days before staining to prevent epitope degradation) [31].
- Deparaffinization and Rehydration: Follow standard xylene and ethanol series.
- Heat-Induced Antigen Retrieval: Perform in an autoclave at 121°C for 5 minutes using a pH 7.8 Target Retrieval Solution buffer [31].
- Blocking: Block endogenous peroxidases and apply a protein block serum.
- Primary Antibody Incubation: Apply the SOX9 antibody (MSVA-709R) at a dilution of 1:50. Incubate at 37°C for 60 minutes [31].
- Visualization: Use the EnVision Kit (Dako, Agilent) according to the manufacturer's directions for detection [31].
- Counterstaining and Mounting: Counterstain with hematoxylin, dehydrate, and mount.
Table: Essential Research Reagent Solutions for SOX9 Detection
| Reagent / Material | Specific Example / Clone | Function / Application | Validation Note |
|---|---|---|---|
| Anti-SOX9 Antibody for Western Blot | Purified Mouse Anti-Sox9 (Clone T32-668) [8] | Detects SOX9 at ~62 kDa in western blot, flow cytometry, and immunofluorescence [8]. | Routinely tested for intracellular flow cytometry and developed for western blot [8]. |
| Anti-SOX9 Antibody for IHC | Recombinant Rabbit Anti-SOX9 (Clone MSVA-709R) [31] | For IHC on FFPE tissues; shows strong nuclear staining in colon crypts, Sertoli cells, etc. [31]. | Specificity validated by orthogonal strategy (RNA data) and comparison with independent antibodies [31]. |
| Positive Control Cell Line | Hep G2 (Human Hepatocellular Carcinoma) [8] | Provides a reliable positive control for western blot and flow cytometry experiments. | Used in the validation of the T32-668 antibody; shows clear SOX9 expression [8]. |
| Positive Control Tissue | Human Colon or Testis [31] | Provides a reliable positive control for IHC/IFF experiments. | Colon crypt base cells and testis Sertoli cells show strong, specific nuclear staining [8] [31]. |
| Flow Cytometry Permeabilization Buffer | BD Phosflow Perm Buffer III [8] | Permeabilization of cells for intracellular SOX9 staining in flow cytometry. | Recommended for use with the T32-668 antibody; other buffers may not be optimal [8]. |
| Small Molecule Inhibitor | Cordycepin (Adenosine Analog) [9] | Used in research to downregulate SOX9 expression in cancer cell lines (e.g., 22RV1, PC3, H1975). | Inhibits both SOX9 mRNA and protein expression in a dose-dependent manner (10-40 µM) [9]. |
Visual Guide: SOX9 Molecular Regulation and Detection Workflow
The following diagrams summarize the key regulatory mechanisms of SOX9 and a generalized workflow for its optimal detection.
SOX9 Regulation by PTMs
SOX9 Detection Workflow
Panel Design and Gating Strategies for Multicolor Flow Cytometry in Heterogeneous Samples
The accurate identification of specific cell populations, such as SOX9+ cells, within complex samples like immune cells or neural tissue presents several technical hurdles. Successful multicolor flow cytometry requires careful panel design to overcome spectral overlap and sensitive detection methods for intracellular targets like transcription factors.
A major challenge in detecting SOX9, a key transcription factor, is that its antibody labeling traditionally requires extensive paraformaldehyde (PFA) fixation, which significantly compromises RNA quality and yield for subsequent transcriptomic analysis [73]. The glyoxal-fixed astrocyte nuclei transcriptomics (GFAT) protocol provides an alternative by using glyoxal fixation, which preserves RNA quality comparable to fresh tissue while enabling successful SOX9 antibody detection [73].
Panel Design Principles
Fluorochrome Selection and Spectra Management
Modern spectral flow cytometry has expanded panel capabilities, allowing differentiation of fluorochromes with significant emission spectrum overlap. This enables the use of previously incompatible fluorochrome pairs [74].
Table 1: Compatible Fluorochrome Pairs in Spectral Flow Cytometry
| Fluorochrome Pair | Traditional Compatibility | Spectral Compatibility |
|---|---|---|
| Brilliant Blue 515 & FITC | Not recommended | Compatible |
| BV421 & Pacific Blue | Not recommended | Compatible |
| PerCP & Brilliant Blue 700 & PerCP-eFluor710 | Not recommended | Compatible |
| CF555 & PE & CF568 | Not recommended | Compatible |
| APC & Alexa Fluor 647 | Not recommended | Compatible |
Panel Design Strategy
When designing panels for heterogeneous samples targeting SOX9+ populations:
- Assign brightest fluorochromes to lowest-density targets: Use PE conjugates for low-density targets (e.g., CD25) and dimmer fluorochromes (e.g., FITC) for high-density targets (e.g., CD8) [75].
- Leverage spectral capabilities: With spectral cytometry, previously incompatible combinations like BV510 with eFluor506 can be used in the same panel [74].
- Consider intracellular requirements: For nuclear targets like SOX9, larger fluorochromes may not penetrate efficiently; choose smaller, more stable fluorochromes for intracellular staining [75].
Gating Strategies for Heterogeneous Samples
Sequential Gating for SOX9+ Population Identification
The following diagram illustrates a robust gating strategy for identifying SOX9+ cell populations in heterogeneous samples:
Key Gating Considerations
- Doublet discrimination: Essential for accurate population identification, using FSC-A versus FSC-H [76].
- Viability gating: Critical for excluding dead cells which show increased autofluorescence and nonspecific antibody binding [75].
- Background reduction: For SOX9 detection, include NeuN staining to exclude neuronal populations (SOX9+NeuN-) when studying astrocytic populations [73].
- Autofluorescence management: Certain cell types naturally exhibit higher autofluorescence; use red-shifted fluorochromes (e.g., APC) which show less autofluorescence compared to FITC or Pacific Blue [75].
Research Reagent Solutions
Table 2: Essential Reagents for SOX9 Flow Cytometry
| Reagent | Function | Example Specifications |
|---|---|---|
| Anti-SOX9 Antibody | Primary detection | Rabbit anti-Sox9 (1:100 dilution) [73] |
| Glyoxal Fixative | Nuclear fixation | 3% glyoxal acidic solution, fresh preparation [73] |
| Permeabilization Buffer | Nuclear membrane permeabilization | 0.1% Triton X-100 in NIM [73] |
| Nuclear Isolation Media (NIM) | Nuclei purification | Sucrose-based buffer with KCl, MgCl₂, Tris-Cl [73] |
| Fc Blocking Reagent | Reduce nonspecific binding | Bovine Serum Albumin or normal serum [75] |
| Viability Dye | Exclude dead cells | SYTOX Blue, DAPI, or fixable viability dyes [74] [75] |
Troubleshooting Common Issues
FAQ 1: How can I reduce high background and non-specific staining in my SOX9 assay?
Possible Causes and Solutions:
- Fc receptor binding: Block cells with Bovine Serum Albumin, Fc receptor blocking reagents, or normal serum prior to staining [75].
- Antibody concentration too high: Titrate antibodies to determine optimal concentration; commercial recommended dilutions are typically optimized for 10⁵-10⁶ cells [75].
- Dead cells in sample: Use a viability dye (e.g., PI, 7-AAD, or fixable viability dyes) to gate out dead cells [75].
- Incomplete red blood cell lysis: Perform additional washes to eliminate red blood cell debris [75].
FAQ 2: Why is my SOX9 signal weak or absent despite confirmed expression?
Possible Causes and Solutions:
- Suboptimal fixation: For SOX9 detection, use glyoxal fixation instead of PFA for better epitope preservation and RNA quality [73].
- Inadequate permeabilization: For nuclear targets, ensure sufficient permeabilization with Triton X-100; however, note that over-permeabilization can damage cells [73] [75].
- Dim fluorochrome on low-abundance target: SOX9 is a transcription factor with limited copy numbers; pair with bright fluorochromes (e.g., PE, Brilliant Violet conjugates) rather than dim fluorochromes like FITC [75].
- Fixation compromising epitopes: Test how the SOX9 epitope responds to your fixative; glyoxal fixation has shown better results for SOX9 detection compared to PFA [73].
FAQ 3: How can I improve resolution of SOX9+ subpopulations in heterogeneous samples?
Possible Causes and Solutions:
- Insufficient panel validation: Include appropriate controls - unstimulated/untreated, isotype, unstained, and positive controls [75].
- Spectral spillover: Use spectral flow cytometry when possible to better resolve fluorochromes with overlapping emission spectra [74].
- High sample flow rate: Use lower flow rates (particularly for cell cycle analysis) to reduce coefficients of variation and improve resolution [75].
- Combine with neuron exclusion: Include NeuN staining to exclude neuronal populations (SOX9+NeuN-) for cleaner astrocyte population identification [73].
Experimental Workflow for SOX9 Detection
The following diagram outlines the complete GFAT protocol workflow for SOX9 detection and transcriptomic analysis:
Advanced Applications
The GFAT protocol enables several advanced applications:
- Parallel astrocyte and neuron profiling: Simultaneous sorting of SOX9+ astrocytes and NeuN+ neurons from the same sample [73].
- Transcriptomic analysis: High-quality RNA sequencing from sorted nuclei due to glyoxal's RNA preservation properties [73].
- Cross-regional and age comparisons: Applicable to different brain regions (cortex, cerebellum) and age ranges (adult, aged) [73].
- Transgenic-line-free approach: Does not require specialized mouse lines or viral injection for cell-type-specific profiling [73].
By implementing these panel design principles, gating strategies, and optimized protocols, researchers can significantly improve the resolution and reliability of SOX9+ cell population identification in heterogeneous samples.
Validating SOX9 as a Robust Biomarker: Diagnostic, Prognostic, and Clinical Relevance
Establishing SOX9 as a Diagnostic and Prognostic Biomarker in Glioblastoma and Other Cancers
SOX9 in Cancer: Expression & Prognostic Significance
Table 1: SOX9 Expression and Prognostic Value Across Cancers
| Cancer Type | SOX9 Expression vs. Normal Tissue | Prognostic Association | Key Correlations & Notes |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly increased [16] [9] | Better prognosis in specific subgroups; independent prognostic factor for IDH-mutant cases [16] | Correlated with immune cell infiltration and immune checkpoint expression [16] |
| Pan-Cancer Overview (15 types) | Significantly increased in 15 cancer types including CESC, COAD, ESCA, etc. [9] [77] | Shorter Overall Survival (OS) in LGG, CESC, and THYM [9] [77] | Acts primarily as a proto-oncogene [9] |
| Skin Cutaneous Melanoma (SKCM) | Significantly decreased [9] [77] | Not specified | Functions as a tumor suppressor in this context [9] |
| Testicular Germ Cell Tumors (TGCT) | Significantly decreased [9] [77] | Not specified | Functions as a tumor suppressor in this context [9] |
| Colorectal Cancer (CRC) | Information missing from search results | Poor prognosis; associated with tumor relapse [78] | Expression negatively correlates with infiltration of B cells, resting mast cells, and monocytes [2] |
| Prostate Cancer | Information missing from search results | Poor prognosis [78] | Promotes cell proliferation and tumor growth [9] [78] |
| Non-Small Cell Lung Cancer (NSCLC) | Information missing from search results | Poor prognosis [78] | Associated with resistance to EGFR-tyrosine kinase inhibitors [78] |
Essential Research Reagent Solutions
Table 2: Key Reagents for SOX9 Research
| Reagent / Resource | Function / Application | Example Details / Specifications |
|---|---|---|
| SOX9 Recombinant Monoclonal Antibody | Immunohistochemistry (IHC), Immunofluorescence (IF), Western Blot (WB) for protein detection and localization. | Clone 5H12; recommended IHC dilution: 1:50-1:200; reacts with human SOX9 protein [79]. |
| IHC/IF Assay Kits | Visualization of antibody binding in tissue sections. | DAB detection system for IHC; fluorophore-conjugated secondary antibodies (e.g., Alexa 546) for IF [80]. |
| Primary Cell Lines & Culture Reagents | In vitro functional studies (e.g., gene regulation, drug response). | Prostate cancer cells (PC3, 22RV1), lung cancer cell (H1975); cultured in RPMI 1640 or DMEM with 10-15% FBS [9] [77]. |
| Small Molecule Inhibitors (e.g., Cordycepin) | Investigating SOX9 inhibition and therapeutic potential. | Adenosine analog; inhibits SOX9 mRNA and protein expression in a dose-dependent manner (e.g., 10-40 µM for 24h) [9] [77]. |
| Online Databases | Bioinformatics analysis of SOX9 expression, mutations, and prognosis. | The Human Protein Atlas (HPA), TCGA, GTEx, GEPIA2, cBioPortal, UCSC Xena [16] [9] [77]. |
Experimental Protocols & Methodologies
Protocol 1: Immunohistochemical (IHC) Detection of SOX9 in Formalin-Fixed Paraffin-Embedded (FFPE) Tissues
This protocol is critical for validating SOX9 protein expression and localization in patient tissue samples, a cornerstone of biomarker studies [80].
- Sectioning: Cut FFPE tissue sections to 4 µm thickness and mount on glass slides.
- Deparaffinization & Rehydration: Deparaffinize slides and rehydrate through a graded alcohol series.
- Endogenous Peroxidase Blocking: Incubate sections in a solution of 80% alcohol containing 4 mL of 30% hydrogen peroxide for 30 minutes at room temperature to quench endogenous peroxidase activity.
- Antigen Retrieval: Perform heat-induced epitope retrieval (HIER) by incubating slides in sodium citrate buffer (pH 6.0) at 96–99 °C for 20 minutes.
- Blocking: Block non-specific binding with phosphate-buffered saline (PBS) containing 3% bovine serum albumin (BSA) for 20 minutes at room temperature.
- Primary Antibody Incubation: Incubate sections with the anti-SOX9 primary antibody (e.g., diluted 1:100 in 1% BSA) overnight at 4°C in a humidified chamber.
- Secondary Antibody Incubation: Apply a compatible HRP-conjugated secondary antibody (e.g., EnVision+ Single Reagent) for 30 minutes at room temperature.
- Detection: Visualize immunoreactivity using a diaminobenzidine (DAB) detection system.
- Counterstaining & Mounting: Counterstain with haematoxylin, dehydrate, and cover slides with a mounting medium.
- Analysis: Quantify staining intensity and the percentage of positive cells using light microscopy. For cell-type-specific analysis (e.g., in immune infiltrates), determine the number of SOX9-positive cells per area or per total cell count [80].
Protocol 2: Analyzing SOX9 Expression and Immune Correlations Using Bioinformatics
This methodology outlines the comprehensive bioinformatics pipeline used to establish SOX9 as a diagnostic and prognostic biomarker, particularly its role in the immune microenvironment [16].
- Data Acquisition:
- Obtain RNA-seq data (e.g., HTSeq-FPKM, HTSeq-Count) for your cancer of interest (e.g., GBM) from public databases like The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) [16].
- Differential Expression Analysis:
- Use the R package
DESeq2to compare SOX9 expression between tumor and normal tissues. Generate volcano plots to visualize significantly differentially expressed genes (DEGs) [16].
- Use the R package
- Functional Enrichment Analysis:
- Immune Infiltration & Checkpoint Analysis:
- Use the
GSVAR package withssGSEAandESTIMATEalgorithms to analyze the correlation between SOX9 expression and levels of various immune cell infiltration [16]. - Analyze the correlation between SOX9 expression and the expression levels of key immune checkpoint genes (e.g., PD-1, CTLA-4) using statistical tests like the Wilcoxon rank-sum test [16].
- Use the
- Prognostic Model Building:
- Perform survival analysis (Kaplan-Meier curves) and univariate/multivariate Cox regression analysis to assess the prognostic value of SOX9.
- Use LASSO Cox regression to select the most significant prognostic genes and integrate them with SOX9 and clinical features (e.g., IDH status) to build a nomogram model for predicting overall survival [16].
Frequently Asked Questions & Troubleshooting
Q1: My IHC staining for SOX9 is weak or non-specific in glioblastoma samples. What could be the issue?
- Problem: The most common issues are related to sample preparation and antibody specificity.
- Solution:
- Antigen Retrieval Optimization: Ensure heat-induced antigen retrieval is performed correctly. The citrate buffer pH (6.0 is standard) and heating time (20 min at 96-99°C) are critical. Try different pH buffers or enzymatic retrieval if results are suboptimal [80].
- Antibody Validation: Confirm the antibody's specificity for SOX9. Use a recombinant monoclonal antibody if possible, and always include a positive control (e.g., a known SOX9-positive tissue like colon) and a negative control (omitting the primary antibody) in your experiment [79].
- Blocking: Increase the concentration of the blocking agent (e.g., BSA to 3-5%) and extend the blocking time to reduce non-specific background [80].
Q2: We are finding contradictory roles for SOX9 in our cancer model versus published literature. How can a single biomarker have dual functions?
- Problem: SOX9 appears to act as an oncogene in some cancers (e.g., GBM, prostate) but as a tumor suppressor in others (e.g., melanoma).
- Solution: This is a recognized characteristic of SOX9, making it a "Janus-faced" regulator. The function is highly context-dependent, influenced by:
- Cell and Tissue Type: Its role is defined by the cellular microenvironment and the network of co-factors present [9] [2].
- Genetic Background: Mutations in key signaling pathways (e.g., IDH status in glioma) can alter SOX9's function [16].
- Tumor Immune Microenvironment (TIME): SOX9 can have immunopromotive or immunosuppressive effects depending on the tumor type, influencing immune cell infiltration and function [2]. Always interpret your results within the specific biological context of your model.
Q3: Our analysis shows no significant correlation between SOX9 expression and patient survival, contrary to published data. What should we check?
- Problem: Discrepancy in prognostic validation.
- Solution:
- Cohort Stratification: Do not analyze the cohort as a whole. Re-analyze your data after stratifying patients based on key molecular or clinical subtypes. For example, high SOX9 expression is remarkably associated with better prognosis specifically in the lymphoid invasion subgroups of GBM and is an independent prognostic factor for IDH-mutant cases [16].
- Data Source and Normalization: Ensure the RNA-seq or microarray data from public repositories (TCGA, etc.) is processed and normalized consistently. Differences in batch effects or normalization methods can lead to varying results.
- Threshold for Grouping: The cut-off value for defining "high" vs. "low" SOX9 expression groups (e.g., median vs. quartile) can significantly impact survival analysis results. Experiment with different validated cut-offs.
Q4: How can I experimentally modulate SOX9 expression in cancer cell lines to study its function?
- Problem: Need for reliable methods to manipulate SOX9 levels.
- Solution:
- Knockdown: Use siRNA or shRNA targeting SOX9 mRNA for loss-of-function studies.
- Overexpression: Use plasmid vectors or lentiviruses carrying the SOX9 coding sequence for gain-of-function studies.
- Pharmacological Inhibition: Treat cells with small molecules like Cordycepin (CD), an adenosine analog that has been shown to inhibit both SOX9 protein and mRNA expression in a dose-dependent manner in cancer cell lines (e.g., 10-40 µM for 24 hours) [9] [77].
SOX9 Immunometabolic Signaling in Pathogenesis
The following diagram illustrates the key immunometabolic signaling pathway involving SOX9, as identified in neuropathic pain models with relevance to cancer biology [3].
Correlating SOX9 Detection Levels with Clinical Outcomes and Immune Cell Infiltration Scores
SOX9 (SRY-box transcription factor 9) is a transcription factor involved in various developmental pathways, including cell differentiation and progenitor cell development [9]. Recently, research has highlighted its significant role in cancer biology and tumor immunology. SOX9 expression is dysregulated in numerous cancer types and has been correlated with clinical outcomes and immune cell infiltration in the tumor microenvironment [9]. This technical support document provides comprehensive guidelines for optimizing SOX9 detection and analyzing its correlation with clinical parameters and immune infiltration scores, addressing common experimental challenges faced by researchers.
Key Clinical Correlations: SOX9 Expression and Patient Outcomes
Understanding the clinical significance of SOX9 detection requires correlation with patient outcome data. The table below summarizes documented relationships between SOX9 expression levels and clinical parameters across various cancer types, serving as a reference for interpreting your experimental results.
Table 1: SOX9 Expression Correlations with Clinical Outcomes in Various Cancers
| Cancer Type | SOX9 Expression Pattern | Correlation with Clinical Outcomes | Prognostic Value |
|---|---|---|---|
| Oesophageal Squamous Cell Carcinoma (ESCC) | Significantly increased in 62.9% of samples [81] | Positive correlation with depth of invasion, advanced stage, lymphatic & venous invasion [81] | Shorter postoperative survival (univariate analysis) [81] |
| Intrahepatic Cholangiocarcinoma (iCCA) | High expression in a subset of patients [82] | Shorter survival time, especially in chemotherapy-treated patients (22 vs. 62 months) [82] | Independent biomarker for chemoresistance and poor survival [82] |
| Pan-Cancers (15 types including COAD, PAAD, LIHC) | Significantly upregulated in 15/33 cancer types [9] | Varies by cancer type; generally associated with worse prognosis [9] | Worst overall survival in LGG, CESC, THYM; prognostic potential [9] |
| Glioblastoma (GBM) | Highly expressed in tumor tissue [19] | Better prognosis in lymphoid invasion subgroups; independent factor for IDH-mutant [19] | Diagnostic and prognostic biomarker, particularly in IDH-mutant cases [19] |
SOX9 and Immune Cell Infiltration: Analytical Workflows
The relationship between SOX9 expression and the tumor immune microenvironment is a critical area of investigation. The following diagram outlines a core workflow for analyzing these correlations using modern high-dimensional techniques.
Key Considerations for Immune Infiltration Analysis:
- Technology Selection: Mass cytometry (CyTOF) is particularly valuable for high-dimensional immune profiling at single-cell resolution, allowing simultaneous detection of SOX9 and multiple immune cell markers [83]. Single-cell RNA sequencing (scRNA-seq) can provide complementary transcriptomic data.
- Data Normalization: Ensure proper normalization across samples when comparing SOX9 expression levels. Batch effects can significantly impact correlation measurements.
- Validation: Correlate protein and mRNA level detection of SOX9 where possible, as discrepancies can occur due to post-transcriptional regulation.
Essential Research Reagents and Tools
Successful SOX9 detection requires specific, validated reagents. The table below lists essential materials and their applications in SOX9 research protocols.
Table 2: Key Research Reagents for SOX9 Detection and Analysis
| Reagent / Tool | Specifications | Recommended Application | Function in Experiment |
|---|---|---|---|
| Anti-SOX9 Antibody | Monoclonal, Mouse Anti-Human [84] | Western Blotting [84] | Primary antibody for SOX9 protein detection |
| Anti-SOX9 Antibody (IHC) | Polyclonal Rabbit [82] | Immunohistochemistry (IHC) [82] | Primary antibody for SOX9 detection in FFPE tissues |
| SOX9 siRNA | siRNA targeting human SOX9 [82] | Functional loss-of-function studies [82] | Knockdown of SOX9 expression to study functional impact |
| Cordycepin (CD) | Adenosine analog [9] | Small molecule inhibitor study | Inhibition of SOX9 expression in cancer cell lines |
Troubleshooting Common Experimental Challenges
Q1: Why do I get high background noise in my SOX9 immunohistochemistry staining?
A: High background often results from non-specific antibody binding or insufficient blocking. Implement these specific fixes:
- Optimize antigen retrieval by testing different conditions (citrate buffer, pH, heating time) [81].
- Increase blocking time using 3% skim milk or appropriate serum to 1 hour at room temperature.
- Titrate your primary antibody to find the optimal concentration; for SOX9 IHC, a 1:100 dilution has been used successfully [82].
- Include proper controls: PBS instead of primary antibody as a negative control, and known SOX9-positive tissue as a positive control [81].
Q2: How can I reliably quantify SOX9 expression levels across different patient samples?
A: Consistent quantification requires standardized scoring systems:
- For IHC, use a semi-quantitative scoring system that considers both intensity and proportion of positive cells [82].
- Intensity score: 0 (negative), 1 (weak-yellow), 2 (medium-brown), 3 (strong-black).
- Proportion score: 0 (≤1%), 1 (>1-10%), 2 (>10-33%), 3 (>33-66%), 4 (>66%).
- Calculate final score as: intensity × proportion. Define "high expression" using a validated cutoff (e.g., >10) [82].
- For transcriptomic data, use normalized counts (e.g., FPKM) from RNA-seq and establish percentiles based on control populations.
Q3: What is the best method to correlate SOX9 expression with immune cell infiltration scores?
A: A multi-modal approach yields the most reliable correlations:
- Utilize computational tools like ssGSEA and ESTIMATE algorithm to calculate immune infiltration scores from transcriptomic data [19].
- For single-cell resolution, employ CITE-seq (Cellular Indexing of Transcriptomes and Epitopes by Sequencing) which simultaneously measures transcriptome and surface proteins [55].
- Apply differential abundance analysis with specialized tools (e.g., milo) to identify SOX9-associated immune subpopulations while adjusting for covariates like age [55].
- Validate findings with orthogonal methods such as immunofluorescence co-staining for SOX9 and immune cell markers (CD8, CD4, CD14).
Q4: My SOX9 Western blot shows multiple bands or no signal. What could be wrong?
A: SOX9 detection by Western blot requires optimized conditions:
- Use a validated anti-SOX9 antibody specifically confirmed for Western blot applications [84].
- Ensure proper protein loading (35μg/lane minimum) and transfer conditions [84].
- Include appropriate cell line controls (e.g., K562 cells show detectable SOX9) [84].
- Check antibody concentration: for monoclonal mouse anti-human SOX9, follow manufacturer's recommendations and empirically determine optimal dilution.
- Pre-treat cells with proteasome inhibitors if degradation is suspected, as transcription factors can have rapid turnover.
Standardized Experimental Protocol: SOX9 IHC and Scoring
Materials:
- Formalin-fixed, paraffin-embedded tissue sections
- Anti-SOX9 antibody (e.g., HPA001758, Sigma-Aldrich)
- Citrate buffer (1mM EDTA, pH 8.4) for antigen retrieval
- Hydrogen peroxidase blocking solution
- Normal serum matching secondary antibody host
- HRP-conjugated secondary antibody
- DAB substrate solution
- Haematoxylin counterstain
Procedure:
- Deparaffinize and rehydrate tissue sections through xylene and graded ethanol series.
- Perform heat-induced antigen retrieval with citrate buffer at 98°C for 10 minutes [82].
- Block endogenous peroxidase activity with 3% hydrogen peroxidase for 5 minutes at room temperature.
- Block nonspecific binding with 3% skim milk or appropriate serum for 30 minutes.
- Incubate with primary anti-SOX9 antibody at 1:100 dilution overnight at 4°C [82].
- Wash with PBS 3 times for 5 minutes each.
- Incubate with HRP-conjugated secondary antibody for 1 hour at room temperature.
- Detect with DAB substrate for 7 minutes, then counterstain with haematoxylin.
- Dehydrate, clear, and mount slides for microscopy.
Scoring and Interpretation:
- Evaluate nuclear staining in tumor cells; SOX9 is primarily a nuclear protein [81] [82].
- Score according to the semi-quantitative system described in the troubleshooting section.
- Have at least two independent evaluators score the staining blinded to clinical data.
- Classify samples as "high SOX9" or "low SOX9" using a pre-defined cutoff validated for your cancer type.
Accurate detection and quantification of SOX9 is essential for investigating its roles in clinical outcomes and immune regulation. The protocols and troubleshooting guides provided here address the most common challenges in SOX9 research. As the field advances, standardization of detection methods and scoring systems will be crucial for comparing findings across studies and translating SOX9 as a diagnostic and prognostic biomarker into clinical practice.
FAQs on SOX9 Detection
What is the primary advantage of using SOX9 as an astrocyte marker compared to GFAP or S100β? SOX9 is a nuclear transcription factor, making it an excellent nuclear marker for the definitive identification of astrocytes in the adult central nervous system (CNS). Unlike cytoplasmic markers like GFAP, which can be regulated developmentally and functionally, SOX9 expression remains nuclear in mature astroglia, does not decrease with aging, and is upregulated in reactive astrocytes. This facilitates a more precise and reliable assignment of individual cell identity [85].
Our lab is new to SOX9 detection. Which method is most suitable for initial validation and localization? Immunohistochemistry (IHC) is highly recommended for initial experiments. It allows for the spatial localization of SOX9 within specific cell types, such as astrocytes in the spinal cord or limbal stem cells in the eye, in the context of tissue architecture. The nuclear localization of SOX9 simplifies the interpretation of staining patterns. A wide range of antibodies validated for IHC are commercially available [85] [86] [87].
We are studying heterogeneous cell populations. How can we quantify SOX9-positive cells and co-stain with other markers? For heterogeneous populations, Flow Cytometry combined with Immunocytochemistry (ICC) is ideal. Flow cytometry provides quantitative data on the percentage of SOX9-positive cells within a population. ICC can then be used to validate this data and investigate co-localization with other cytoplasmic or membrane markers, providing both quantitative and visual confirmation [85] [87].
We need to confirm the specificity of our SOX9 antibody. What is the gold-standard validation method? The most rigorous proof of antibody specificity comes from Knockout-Validated Antibodies. Many commercial providers now offer antibodies whose specificity has been confirmed using knockdown or knockout cell lines or tissues, ensuring that the detected signal is truly from SOX9. Always consult the manufacturer's validation data for this information [87].
Why might we detect SOX9 in non-astrocyte cell types? It is crucial to remember that SOX9 is a marker for astrocytes outside of the neurogenic regions. In areas like the subventricular zone (SVZ) and the hippocampal subgranular zone, SOX9 is also expressed by neural progenitor cells. Furthermore, it is expressed in ependymal cells. Therefore, the brain region being analyzed must be considered when interpreting results [85].
Troubleshooting Common Experimental Issues
| Issue | Possible Cause | Solution |
|---|---|---|
| High Background in IHC/ICC | Non-specific antibody binding or over-fixation. | Optimize antibody dilution and include a relevant isotype control. Try an antigen retrieval step for over-fixed tissues [87]. |
| Weak or No Signal | Low SOX9 expression in the cell type, inefficient epitope exposure, or antibody degradation. | Use a positive control (e.g., chondrocytes or known astrocyte sample). Optimize fixation and permeabilization protocols. Ensure fresh antibody aliquots are used [86] [88]. |
| Inconsistent Western Blot Results | Improper nuclear protein extraction or protein degradation. | Ensure use of a rigorous nuclear extraction protocol. Include protease and phosphatase inhibitors in all buffers. Confirm sample integrity [14] [87]. |
| Failure to Detect SOX9 in Astrocytes | The specific astrocyte subpopulation may have low or altered SOX9. | Note that SOX9 expression and phosphorylation state can change with cellular activation (e.g., in neuropathic pain), which might affect detection. Consider using multiple markers for astrocytes [3] [85]. |
Comparison of SOX9 Detection Methodologies
The table below summarizes the key characteristics of common SOX9 detection methods to aid in experimental design.
| Method | Key Application | Key Advantage | Key Limitation | Typical Sample Type |
|---|---|---|---|---|
| Immuno-histochemistry (IHC) | Localization in tissue context | Preserves spatial and structural information; identifies specific cell types (e.g., astrocytes). | Semi-quantitative at best. | Tissue sections [85] [86] |
| Western Blot (WB) | Protein expression validation | Semi-quantitative; confirms protein size. | Loses cellular and subcellular localization. | Cell or tissue lysates [14] [87] |
| Immuno-cytochemistry (ICC) | Cellular localization and co-staining | Provides subcellular (nuclear) localization in single cells. | Requires single-cell suspension or culture. | Cultured cells [87] |
| Flow Cytometry | Quantification in mixed populations | High-throughput, quantitative analysis of SOX9+ cell populations. | Loses tissue architecture context. | Single-cell suspensions [85] [87] |
| Chromatin Immuno-precipitation (ChIP) | Identification of DNA binding sites | Determines direct transcriptional targets of SOX9. | Technically challenging; requires high-quality antibodies. | Cross-linked cells [88] [87] |
Detailed Experimental Protocols
Protocol 1: Immunohistochemical Detection of SOX9 in Spinal Cord Tissue This protocol is adapted from methods used to identify SOX9-positive astrocytes in the CNS [85].
- Tissue Preparation: Perfuse-fix mice with 4% paraformaldehyde (PFA). Dissect and post-fix the spinal cord in 4% PFA for 24 hours, followed by cryopreservation in 30% sucrose.
- Sectioning: Embed tissue in OCT compound and section on a cryostat to obtain 10-20 µm thick sections.
- Antigen Retrieval: Perform antigen retrieval using citrate buffer (pH 6.0) heated to 95-100°C for 20 minutes.
- Blocking: Block sections with 5% normal donkey or goat serum in PBS containing 0.3% Triton X-100 for 1 hour at room temperature.
- Primary Antibody Incubation: Incubate sections with a validated rabbit anti-SOX9 monoclonal antibody (e.g., Cat # MA5-41174) diluted in blocking buffer overnight at 4°C.
- Secondary Antibody Incubation: Wash and incubate with a species-appropriate fluorescently-labeled secondary antibody (e.g., Alexa Fluor 488) for 1-2 hours at room temperature.
- Counterstaining and Mounting: Counterstain nuclei with DAPI and mount sections with an anti-fade mounting medium.
- Imaging: Image using a confocal or fluorescence microscope. SOX9 signal will be localized to the nucleus of astrocytes.
Protocol 2: Validating SOX9 Antibody Specificity by Knockout This is a critical control, as referenced in commercial antibody validations [87].
- Generate Control and KO Cells: Use CRISPR/Cas9 technology with a SOX9-targeting sgRNA to create a SOX9 knockout cell line in your model system (e.g., a chondrocyte or astrocyte line). A non-targeting sgRNA serves as the control.
- Protein Lysate Preparation: Lyse both control and KO cell populations in RIPA buffer supplemented with protease inhibitors.
- Western Blot: Separate proteins via SDS-PAGE and transfer to a PVDF membrane.
- Probing: Probe the membrane with the anti-SOX9 antibody being validated.
- Validation: A specific antibody will produce a band at the expected molecular weight (~60-70 kDa) in the control lane and show a complete absence of this band in the SOX9-KO lane. Any remaining bands are non-specific.
SOX9 Detection Workflow
The following diagram illustrates a logical workflow for selecting and validating a SOX9 detection method based on your experimental goals.
Research Reagent Solutions
The following table lists essential reagents for SOX9 research, as utilized in the cited studies.
| Reagent | Function / Target | Example Specification | Key Application |
|---|---|---|---|
| SOX9 Monoclonal Antibody | Binds SOX9 protein for detection | Rabbit Recombinant Monoclonal [e.g., MA5-41174] [87] | IHC, WB, ICC, Flow Cytometry |
| SOX9 Polyclonal Antibody | Binds multiple SOX9 epitopes | Rabbit Polyclonal [e.g., PA5-81966] [87] | WB, IHC, ICC |
| Phospho-SOX9 (S181) Antibody | Detects pathologically relevant phosphorylation | Specific for phosphorylated Serine 181 [3] | Investigation in disease models (e.g., neuropathic pain) |
| SOX9-EGFP Reporter Mouse | Labels SOX9-expressing cells in vivo | Transgenic reporter strain [85] | Lineage tracing and cell fate mapping |
| CRISPR/Cas9 SOX9 KO Kit | Generates SOX9 knockout cells | SOX9-targeting sgRNA [14] | Essential control for antibody validation and functional studies |
Linking SOX9 Expression to Immune Checkpoint Status and Therapy Response
Scientific Foundation: The SOX9-Immune Checkpoint Axis
SOX9 is a transcription factor that plays a complex, dual role in tumor immunology, acting as a key regulator of the tumor immune microenvironment [2]. Its expression is significantly correlated with immune checkpoint activity and therapy response.
Table 1: SOX9 and Immune Checkpoint Correlations in Human Cancers
| Cancer Type | Correlated Immune Checkpoint | Relationship to SOX9 | Impact on TILs | Therapeutic Implication |
|---|---|---|---|---|
| Basal-like Breast Cancer (BLBC) | B7x (B7-H4/VTCN1) | SOX9 induces expression via STAT3 and direct transcription [53] | Reduced CD8+ T cell infiltration [53] | Target for overcoming anti-PD-L1 resistance [53] |
| Glioblastoma (GBM) | Multiple Checkpoints | Expression is closely correlated [16] | Correlated with immune cell infiltration patterns [16] | Potential prognostic and therapeutic target [16] |
| Colorectal Cancer (CRC) | N/A | SOX9 expression is a diagnostic marker [2] | Negatively correlates with B cells, resting mast cells, and monocytes [2] | N/A |
| Lung Adenocarcinoma (LUAD) | Various Checkpoints | Mutually exclusive with checkpoints [16] | N/A | Indicates involvement in immunosuppressive TME [16] |
The relationship between SOX9 and the immune checkpoint B7x is a critical, recently elucidated pathway. The following diagram illustrates this signaling axis.
Troubleshooting Guide: SOX9 Detection & Functional Analysis
This section addresses common experimental challenges in linking SOX9 to immune responses.
Table 2: Troubleshooting SOX9 Flow Cytometry in Immune Context
| Problem | Possible Cause | Solution |
|---|---|---|
| Weak or No SOX9 Signal | Low antigen expression; suboptimal antibody concentration; inefficient permeabilization [89]. | Titrate antibody; use bright fluorochromes (e.g., PE, APC); optimize permeabilization (use Phosflow Perm Buffer III) [8] [89]. |
| High Background/ Non-specific Staining | Unbound antibodies; Fc receptor binding; dead cells; autofluorescence [89]. | Include Fc block; use isotype control; add viability dye (e.g., PI, 7-AAD); gate out dead cells/debris [89]. |
| Loss of Epitope | Over-fixation; sample not kept on ice [89]. | Use only 1% PFA; fix for <15 mins; keep samples on ice to prevent protease activity [89]. |
| Discrepancy with Functional Assays (e.g., T cell suppression) | SOX9's biological role is context-dependent [2]. | Correlate protein levels with functional readouts (e.g., T cell co-culture assays) [53]. Validate in relevant disease models. |
Frequently Asked Questions (FAQs)
Q1: Why does SOX9 correlate with both better and worse patient prognosis? A1: SOX9 is a "Janus-faced regulator" [2]. Its impact depends on the cancer type and immune context. For instance, in IDH-mutant glioblastoma, high SOX9 is associated with better prognosis, whereas in other cancers like ovarian cancer, it drives chemoresistance and is linked to poorer survival [16] [14]. The specific immune cell subsets it influences (e.g., CD8+ T cells vs. Tregs) determine the outcome.
Q2: How can I experimentally validate that SOX9 is directly regulating an immune checkpoint in my model? A2: The study on breast cancer provides a robust methodological blueprint [53]:
- Genetic Manipulation: Use Sox9 conditional knockout (cKO) models or CRISPR/Cas9 to delete SOX9 in tumor cells.
- Immune Phenotyping: Analyze resulting tumors via flow cytometry for changes in TILs (CD3+, CD4+, CD8+) and immunohistochemistry for Granzyme B+ cells.
- Checkpoint Analysis: Evaluate expression of target checkpoints like B7x via qPCR and Western blot in SOX9-knockout vs. control cells.
- Functional T-cell Assays: Perform co-culture experiments with human T cells to confirm that SOX9-expressing tumor cells suppress T-cell proliferation and cytotoxicity.
Q3: My intracellular staining for SOX9 is inconsistent. What are the critical steps for optimization? A3: Based on validated protocols [8] [89]:
- Fixation: Use BD Cytofix Fixation Buffer.
- Permeabilization: This is critical. BD Phosflow Perm Buffer III is recommended for SOX9 [8]. Avoid BD Perm/Wash buffer for this target.
- Antibody Titration: The Purified Mouse Anti-Sox9 (Clone T32-668) should be titrated for optimal results. A starting concentration of 0.25 µg/ml is suggested for Western blot, but flow cytometry may require different optimization [8] [89].
- Controls: Always include an isotype control and a viability dye to gate out dead cells.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for SOX9-Immune Research
| Reagent / Assay | Specific Example / Clone | Function & Application | Considerations |
|---|---|---|---|
| Anti-SOX9 Antibody [8] | Purified Mouse Anti-Sox9 (Clone T32-668) | Detects human and rat SOX9 (62 kDa) via Flow Cytometry, Western Blot, Immunofluorescence, IHC. | Requires specific permeabilization buffer (BD Phosflow Perm Buffer III) for intracellular staining. |
| In Vivo Tumor Model [53] | C3-TAg; MMTV-iCre;Sox9Fl/Fl | Mouse model of basal-like breast cancer to study SOX9's role in immune evasion and tumor progression. | T cell depletion (anti-CD4/CD8) restores tumor progression in Sox9-cKO models. |
| T-cell Functional Assay [53] | Antigen-Specific Cytotoxicity Co-culture | Co-culture SOX9-OE tumor cells with engineered CD8+ T cells (e.g., NY-ESO-1 TCR) to quantify suppression of T-cell killing. | Measures the direct functional impact of tumor cell SOX9 on T-cell activity. |
| Immune Cell Analysis Panel | CD45, CD3, CD8, CD4, FoxP3 | Standard flow cytometry panel to assess tumor-infiltrating lymphocyte populations in response to SOX9 expression. | Correlate SOX9 levels with abundance of specific immune subsets. |
Detailed Experimental Workflow: From Detection to Validation
The most comprehensive approach to linking SOX9 with immune checkpoint status involves a multi-step process, summarized in the workflow below.
Step 1: SOX9 Detection & Quantification
- Method Details: For flow cytometry, use the validated antibody clone T32-668. Cells must be fixed and permeabilized, with a specific note that BD Phosflow Perm Buffer III is effective, while BD Perm/Wash is not recommended for this particular antibody [8]. Always include an isotype control and titrate the antibody to determine the optimal signal-to-noise ratio [89].
Step 2: Immune Correlate Analysis
- Method Details: Utilize datasets like TCGA and GTEx for initial bioinformatic correlation between SOX9 expression and immune gene signatures [16]. Experimentally, perform multiplex staining or flow cytometry on tumor tissues to quantify immune checkpoint proteins (e.g., B7x, PD-L1) and characterize tumor-infiltrating immune cells (CD8+ T cells, Tregs, macrophages) [53] [90]. This identifies potential immune partners for SOX9.
Step 3: Genetic Perturbation
- Method Details: Use CRISPR/Cas9 or lentiviral shRNA (e.g., targeting sequences: GCATCCTTCAATTTCTGTATA) to create stable SOX9-knockout or knockdown cell lines [91] [14]. Conversely, generate SOX9-overexpressing lines. These engineered cells are the foundation for establishing causality.
Step 4: Functional Validation
- Method Details: Co-culture control and SOX9-modified tumor cells with activated T cells. Isolate CD4+ and CD8+ T cells from human PBMCs and stimulate them with anti-CD3/CD28 antibodies [53]. Measure T-cell proliferation via dye dilution and assess cytotoxicity using assays that measure specific lysis of target tumor cells. This directly tests the functional consequence of SOX9 expression on immune cell activity.
Step 5: Translational Confirmation
- Method Details: Validate findings in clinically relevant models. Use patient-derived xenografts in immunocompetent or humanized mice. Analyze paired patient tumor biopsies taken before and after chemotherapy, as treatment can induce SOX9 expression [14], allowing you to correlate its upregulation with changes in the immune microenvironment and therapy response.
Developing and Validating Integrated Prognostic Models and Nomograms Incorporating SOX9
SOX9 Technical Support Center
This guide provides targeted troubleshooting and methodological support for researchers developing prognostic models that incorporate SOX9, with a specific focus on its role within immune cell subpopulations.
Frequently Asked Questions
Q1: Why does our SOX9 immunohistochemistry staining show high background noise in immune cell-rich tumor regions? A1: High background in immune cell regions often stems from non-specific antibody binding or insufficient blocking.
- Solution: Validate your anti-SOX9 antibody using a SOX9-knockdown cell control. Include a non-immune IgG isotope control in your IHC/IF protocol. For flow cytometry of immune cells, titrate your antibody to determine the optimal concentration that minimizes background while preserving signal. Pre-incubate tissue sections with a blocking solution containing sera from the same species as your secondary antibody and 2-5% BSA. If using archival tissue, consider antigen retrieval optimization, as over-fixed tissue can increase background [92] [93].
Q2: Our prognostic model's performance degraded significantly upon external validation. What are the primary factors to check? A2: Model performance degradation typically indicates overfitting or population differences.
- Solution:
- Check Sample Size: For validation, ensure your sample has a sufficient number of events. A common "rule of thumb" is at least 100 events (e.g., disease progressions) and 100 non-events. For reliable calibration curves, at least 200 events and 200 non-events are recommended [94].
- Check Model Calibration: Assess the calibration slope and the observed vs. expected (O/E) ratio. A slope far from 1.0 or an O/E ratio far from 1.0 indicates the model needs updating or recalibration for the new population [95] [94].
- Check Predictor Measurements: Ensure the definition and measurement method of SOX9 (e.g., positive cell percentage, H-score) and other predictors are consistent with the model development phase [96].
Q3: How can we effectively analyze SOX9 expression in specific immune cell subpopulations from single-cell RNA sequencing data? A3: This requires precise cell type identification and analysis.
- Solution: Utilize established single-cell analysis toolkits.
- Cell Type Identification: Use tools like
Seuratfor clustering andSingleRorcelldexfor automated cell type annotation against reference datasets. Manually verify annotations using canonical markers (e.g., CD3E for T cells, CD79A for B cells, LYZ for monocytes) [97] [93]. - Subset and Analyze: Once all cell types are annotated, subset the immune cell populations (e.g., T cells, macrophages) and re-cluster to identify finer subpopulations. You can then calculate the average expression or percentage of SOX9-positive cells within these specific subsets [93].
- Cross-reference with Pathology: Correlate scRNA-seq findings with spatial techniques like immunofluorescence or in situ hybridization on matched tissue sections to confirm the localization of SOX9+ immune cells [92] [93].
- Cell Type Identification: Use tools like
Q4: What is the optimal method to integrate SOX9 with clinical variables in a nomogram? A4: The integration is done statistically during model building.
- Solution:
- Model Building: Use multivariate Cox proportional hazards regression (for time-to-event outcomes) or logistic regression (for binary outcomes). Include SOX9 and the selected clinical variables (e.g., age, disease stage) as co-variates in the model [98] [95].
- Nomogram Construction: The nomogram is a visual representation of this regression model. Each variable (including SOX9) is assigned a point scale based on its regression coefficient. The total points from all variables are then mapped to the probability of the outcome (e.g., 3-year survival). Ensure the predictors included have been shown to be statistically independent contributors to the outcome [98] [95].
Q5: Our analysis suggests SOX9 is associated with immune suppression, but how can we validate this functionally? A5: Functional validation requires in vitro or in vivo experiments.
- Solution: Based on recent literature, you can consider:
- NK Cell Cytotoxicity Assays: Co-culture SOX9-high and SOX9-low tumor cells with natural killer (NK) cells. Measure tumor cell death via assays like LDH release or flow cytometry for apoptosis (Annexin V/PI). Research has shown that SOX9 expression can confer resistance to NK cell-mediated killing [93].
- Conditioned Media Experiments: Culture immune cells (e.g., T cells, macrophages) with conditioned media from SOX9-overexpressing cells. Analyze the immune cells for expression of suppression markers (e.g., PD-1, LAG-3 on T cells; CD206 on macrophages) using flow cytometry [92].
- Animal Models: Use immune-competent mouse models to test if modulating SOX9 expression affects tumor growth and immune cell infiltration, which can be analyzed by flow cytometry or immunohistochemistry of the tumor mass [93].
Troubleshooting Guides
Issue: Poor Discrimination Power of the SOX9-Integrated Prognostic Model
A model with low discrimination power (e.g., C-statistic < 0.7) fails to separate patients with good and poor outcomes effectively.
- Step 1: Verify the Univariate Association. Check if SOX9 is significantly associated with the outcome (e.g., overall survival) in a univariate Cox model before building the multi-variable model. If not, it may be a weak predictor on its own [98].
- Step 2: Re-evaluate Predictor Selection. Avoid using only statistically significant predictors from univariate analysis. Use structured variable selection methods like LASSO regression or backward elimination based on the Akaike Information Criterion (AIC) to reduce overfitting and build a more robust model [99] [95].
- Step 3: Check for Non-linear Relationships. The relationship between SOX9 expression and risk may not be linear. Test for non-linearity using methods like restricted cubic splines. If found, transform the SOX9 variable appropriately for the model [95].
Issue: Inconsistent SOX9 Expression Measurement Between Techniques
Discrepancies are common between IHC, qPCR, and RNA-seq measurements.
- Step 1: Standardize the Quantification Method. For IHC, use a standardized scoring system like the H-score (which considers both staining intensity and percentage of positive cells) and ensure all slides are scored by at least two independent pathologists. For PCR, ensure normalization to appropriate housekeeping genes [92].
- Step 2: Correlate with a Gold Standard. If possible, use RNA-seq or qPCR data from the same samples as a quantitative benchmark to calibrate the IHC scoring system.
- Step 3: Define a Clinically Relevant Cut-off. Do not rely on median splits. Use data-driven methods like maximally selected rank statistics or X-tile software to find the cut-off point for SOX9 "high" vs. "low" that best separates survival curves [99].
Issue: The Prognostic Model is Well-Calibrated but Performs Poorly in a New Patient Cohort
This suggests transportability issues, often due to case-mix differences.
- Step 1: Recalibrate the Model. The model's baseline hazard may need adjustment. You can recalibrate the model by updating the intercept or using a more flexible approach like Cox regression with the original model's linear predictor as an offset term [95].
- Step 2: Perform Feature Engineering. The effect of SOX9 might be modified by other variables. Investigate if including interaction terms (e.g., between SOX9 and a key clinical stage variable) improves model performance in the new cohort [98].
- Step 3: Report Adherence to TRIPOD. Ensure your validation study follows the TRIPOD (Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis) reporting guidelines. This includes clearly describing the study design, participant eligibility, and details of the model being validated [96].
Research Reagent Solutions
The table below lists key reagents and tools for SOX9-focused research, as cited in recent literature.
Table: Essential Reagents and Tools for SOX9 and Immune Microenvironment Research
| Item Name | Function/Application | Example Usage in Research |
|---|---|---|
| Anti-SOX9 Antibody | Detection and localization of SOX9 protein | Immunofluorescence and IHC for spatial analysis in primary tumors and metastases [93]. |
| scRNA-seq Pipeline (10x Genomics, CellRanger, Seurat) | Characterization of cellular heterogeneity and SOX9 expression at single-cell resolution | Defining SOX9+ cell states and their association with immune cells in lung adenocarcinoma microenvironments [93]. |
| LASSO & Cox Regression | Statistical methods for building parsimonious prognostic models | Identifying a core set of SOX9-related prognostic genes (e.g., ADAMTS2, ARHGEF5) for liver fibrosis prediction [99] [95]. |
| CIBERSORT | Computational deconvolution of immune cell fractions from bulk RNA-seq data | Quantifying infiltration levels of 22 immune cell types and correlating them with SOX9 expression levels [99]. |
| NK Cell Cytotoxicity Assay | Functional validation of SOX9-mediated immune evasion | Demonstrating SOX9-dependent resistance to Natural Killer cell-mediated killing in cancer cells [93]. |
| RcisTarget / SCENIC | Inference of gene regulatory networks from scRNA-seq data | Identifying transcription factors and regulatory networks upstream and downstream of SOX9 [93]. |
| PhenoGraph | Graph-based clustering algorithm for high-dimensional single-cell data | Identifying distinct SOX9-high and SOX9-low cell subpopulations within a tumor [93]. |
| Spectral Flow Cytometry | High-parameter immunophenotyping and metabolic profiling of single cells | Comparing immunometabolic profiles of whole blood vs. PBMCs in health and disease contexts [97]. |
Experimental Protocols for Key Workflows
Protocol 1: Building a SOX9-Incorporated Prognostic Model using a Retrospective Cohort
This protocol outlines the steps for developing a clinical prediction model.
- Data Collection: Assemble a cohort with linked clinical data, outcome data (e.g., overall survival), and SOX9 measurement data (e.g., RNA-seq, IHC scores). Adhere to the TRIPOD statement for reporting [96].
- Data Cleaning: Handle missing data using multiple imputation methods. For continuous variables like SOX9 expression, avoid arbitrary dichotomization and consider non-linear transformations if needed [95].
- Variable Selection: Use penalized regression methods like LASSO to select the most relevant predictors from a pool of candidate variables (including SOX9 and clinical factors), preventing model overfitting [99] [95].
- Model Fitting: Fit a multivariate Cox proportional hazards model using the selected variables. For a diagnostic model, use logistic regression [95].
- Performance Assessment:
- Internal Validation: Use bootstrapping to estimate the model's optimism and calculate optimism-corrected performance metrics [95].
- Nomogram Construction: Translate the final Cox or logistic regression model into a nomogram for easy clinical use [95].
Protocol 2: Validating a SOX9-Based Prognostic Model in an External Cohort
This protocol is for assessing a model's generalizability.
- Sample Size Estimation: Calculate the required sample size for the validation study. For a binary outcome, tools like the
pmvalsampsizeR package can be used, which requires inputs like the expected event prevalence and the model's anticipated C-statistic [94]. - Data Application: Apply the exact same model (i.e., the same regression coefficients and linear predictor formula) to the new external cohort [96].
- Performance Evaluation: Recalculate the C-statistic for discrimination. For calibration, calculate the O/E ratio and plot the calibration curve. A slope of 1 and an O/E ratio of 1 indicate perfect calibration [95] [94].
- Model Update (if needed): If performance is poor, consider simple model recalibration (adjusting the intercept or baseline hazard) or more extensive model revision [95].
Experimental Workflow and Pathway Diagrams
The diagram below illustrates a generalized workflow for developing and validating a SOX9-integrated prognostic model.
Generalized Workflow for SOX9 Prognostic Model Development
The following diagram summarizes a key SOX9-related signaling pathway and its link to immune regulation, as identified in the tumor microenvironment.
SOX9-Associated Pathways in Immune Regulation
Conclusion
The precise detection and quantification of SOX9 within specific immune cell subpopulations is no longer a niche interest but a cornerstone for advancing immunology and oncology research. This synthesis of foundational knowledge, optimized methodologies, troubleshooting guides, and validation frameworks provides a clear path forward. Mastering SOX9 detection is paramount for unlocking its full potential as a biomarker for patient stratification, a predictor of treatment response, and a promising therapeutic target itself. Future efforts must focus on standardizing assays across laboratories, further exploring its functional roles in different immune contexts, and translating these robust detection protocols into clinical trials for SOX9-targeted therapies, ultimately paving the way for novel immunotherapeutic strategies in cancer and autoimmune diseases.
References
- 1. SOX9 in organogenesis: shared and unique transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482574/]
- 2. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 3. Sox9 regulation of hexokinase 1 controls ... [https://www.nature.com/articles/s41467-025-65092-5]
- 4. Western Blot Troubleshooting [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-gel-electrophoresis-information/western-blot-troubleshooting.html]
- 5. Western Blot Troubleshooting Guide | Boster Bio [https://www.bosterbio.com/protocol-and-troubleshooting/western-blot-troubleshooting?srsltid=AfmBOorUMVV4xCYDKMBl2G6UAPu8_Pl5MNoxZbpl1TtLTEy1Lne6H0ML]
- 6. Western Blotting Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/western-blot-troubleshooting-guide?srsltid=AfmBOoosU7sVPUFTdnG3ewhC8tZGbhCGS8j3P9r3ZlFD1olG2wlgE-Eq]
- 7. Anti-Transcription factor SOX-9 SOX9 Antibody [https://www.bosterbio.com/anti-transcription-factor-sox-9-sox9-antibody-a00177-1-boster.html?srsltid=AfmBOorjB6h7mIPs45ugch4TTWRmEtj2KOgImcTEnK4WcjdmsqQNkxCg]
- 8. BD Pharmingen™ Purified Mouse Anti-Sox 9 [https://www.bdbiosciences.com/en-us/products/reagents/flow-cytometry-reagents/research-reagents/single-color-antibodies-ruo/purified-mouse-anti-sox-9.565492]
- 9. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 10. Sox9 (D8G8H) Rabbit Monoclonal Antibody #82630 [https://www.cellsignal.com/products/primary-antibodies/sox9-d8g8h-rabbit-monoclonal-antibody/82630?srsltid=AfmBOopUGI6rXOvwsAzOXNPQFVtQzOGnG13ynAFEckWuL7h6ZAYIYgIm]
- 11. Anti-SOX9 antibody [EPR14335-78] (AB185966) [https://www.abcam.com/en-us/products/primary-antibodies/sox9-antibody-epr14335-78-ab185966]
- 12. Recapitulation of endochondral ossification by hPSC- ... [https://www.nature.com/articles/s41467-025-58122-9]
- 13. Generation of a Quantitative Luciferase Reporter for Sox9 ... [https://www.mdpi.com/1422-0067/21/4/1274]
- 14. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 15. Deep Reinforcement Learning for CT-Based Non-Invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110404/]
- 16. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 17. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 18. SOX9 as an emerging target for anticancer drugs and a ... [https://pubmed.ncbi.nlm.nih.gov/35636723/]
- 19. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 20. Human SOX9 ELISA Kit (AB253226) [https://www.abcam.com/en-us/products/elisa-kits/human-sox9-elisa-kit-ab253226]
- 21. Identification of immune cell infiltration landscape for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10089677/]
- 22. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/pii/S1359644622002136]
- 23. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 24. SOX9: a key transcriptional regulator in organ fibrosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11835943/]
- 25. Sox9 Controls Self-Renewal of Oncogene Targeted Cells ... [https://www.sciencedirect.com/science/article/pii/S1934590915002179]
- 26. Single-cell transcriptome sequencing reveals the immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11872840/]
- 27. 5 tips for successful single-cell RNA-seq [https://www.takarabio.com/about/bioview-blog/tips-and-troubleshooting/5-tips-to-make-your-single-cell-rna-seq-experiments-a-success?srsltid=AfmBOopQbhAypXxNn7mO3HqA5kDj-BK8J017dE7AoUu1yriSazj4BGcL]
- 28. Strategies for optimizing CITE-seq for human islets and ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1107582/full]
- 29. Guide to Getting Started with 10X Genomics Single Cell RNA ... [https://biotech.wisc.edu/guide-to-getting-started-with-10x-genomics-single-cell-rna-seq/]
- 30. Single-cell analysis highlights differences in druggable ... [https://www.nature.com/articles/s41467-022-31772-9]
- 31. SOX9 (MSVA-709R) [https://ms-validatedantibodies.com/product/sox9-msva-709r/]
- 32. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOormqMl82Lxr1RiFGjljp8kCvoeGj3WwNQtkkuabryd8tfDHRlPS]
- 33. Flow Cytometry Troubleshooting Guide [https://www.sigmaaldrich.com/US/en/technical-documents/technical-article/protein-biology/flow-cytometry/flow-cytometry-troubleshooting-guide?srsltid=AfmBOoqnc_gt6XRMyd4HJKTAGHFwpbZyaZH3r31x2t4b2c9bzSzU4uNH]
- 34. IHC Troubleshooting Guide [https://www.thermofisher.com/us/en/home/life-science/protein-biology/protein-biology-learning-center/protein-biology-resource-library/pierce-protein-methods/ihc-troubleshooting-guide.html]
- 35. Immunohistochemistry (IHC) Troubleshooting Guide & the ... [https://www.cellsignal.com/learn-and-support/troubleshooting/ihc-troubleshooting-guide?srsltid=AfmBOoqKwZM9fjPEwc-9ntMW8IARkju1MZNZZA_5IjkvVaf4WcsKSlY2]
- 36. Antibody Validation for Flow Cytometry [https://blog.addgene.org/antibody-validation-for-flow-cytometry]
- 37. Antibody Validation for Flow Cytometry [https://www.cellsignal.com/about-us/our-approach-process/antibody-validation-flow-cytometry?srsltid=AfmBOoqB2bUU1jisefab6ndjOiy_I7ousOjFYycvmcCw3rFLJ_K7PS2g]
- 38. The local and circulating SOX9 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292907/]
- 39. The local and circulating SOX9 as a potential biomarker for ... [https://pubmed.ncbi.nlm.nih.gov/32551218/]
- 40. Troubleshooting Flow Cytometry Issues [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-troubleshooting?srsltid=AfmBOopZCMqsqMsdz3d8CgnjjxJbRLD59-54VFVfruJJ6fNUx08uvYDi]
- 41. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOoqsljX1CMk0p0d4jJ4r5voKqYNgr9ne1k56QS0EICkaX1KBxebS]
- 42. Antagonistic Cross-Regulation between Sox9 and Sox10 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4309598/]
- 43. Comprehensive analysis of normal adjacent to tumor ... [https://www.nature.com/articles/s41467-017-01027-z]
- 44. Prognostic value of SOX9 in cervical cancer - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC9394184/]
- 45. Transcriptomic analysis reveals a tissue-specific loss of ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-023-09756-w]
- 46. A single-cell transcriptomic dataset of pluripotent stem ... [https://www.nature.com/articles/s41597-024-03823-x]
- 47. A practical guide to spatial transcriptomics: lessons from ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779925003579]
- 48. Scaling up spatial transcriptomics for large-sized tissues: uncovering cellular-level tissue architecture beyond conventional platforms with iSCALE | Nature Methods [https://www.nature.com/articles/s41592-025-02770-8]
- 49. A comprehensive review of spatial transcriptomics data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12199153/]
- 50. Exploring tissue architecture using spatial transcriptomics | Nature [https://www.nature.com/articles/s41586-021-03634-9]
- 51. Combining spatial transcriptomics with tissue morphology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12075478/]
- 52. Flow Cytometry Troubleshooting Guide [https://www.bio-techne.com/applications/flow-cytometry/flow-cytometry-troubleshooting-guide]
- 53. A SOX9-B7x axis safeguards dedifferentiated tumor cells from immune surveillance to drive breast cancer progression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842074/]
- 54. Detection of Specific Immune Cell Subpopulation Changes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9147028/]
- 55. Single-cell analysis reveals immune cell abnormalities ... [https://www.nature.com/articles/s41467-025-60034-7]
- 56. IHC antigen retrieval protocol [https://www.abcam.com/en-us/technical-resources/protocols/ihc-antigen-retrieval]
- 57. Anti-SOX9 antibody [EPR14335] - BSA and Azide free [https://www.abcam.com/en-us/products/primary-antibodies/sox9-antibody-epr14335-bsa-and-azide-free-ab220812]
- 58. Astrocytic Sox9 overexpression in Alzheimer's disease mouse ... [https://pubmed.ncbi.nlm.nih.gov/41272323/]
- 59. Boosting one protein helps the brain protect itself from ... [http://www.sciencedaily.com/releases/2025/11/251123085550.htm]
- 60. Optimizing HIER Antigen Retrieval for IHC [https://www.bosterbio.com/blog/post/protocol-for-optimizing-hier-antigen-retrieval-conditions?srsltid=AfmBOoraUkRi2n0roYRDbG5c5vNXiM_nobm6sn8z4ovDhvIXyKvLgCHP]
- 61. Immunohistochemistry (IHC): The Complete Guide [https://www.antibodies.com/applications/immunohistochemistry]
- 62. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 63. A SOX9-B7x axis safeguards dedifferentiated tumor cells ... [https://www.sciencedirect.com/science/article/pii/S1534580723005518]
- 64. SOX9: a key transcriptional regulator in organ fibrosis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1507282/full]
- 65. Building the adipose atlas: consensus guidelines and a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12238711/]
- 66. Single-cell RNA sequencing reveals multiple immune ... [https://www.nature.com/articles/s41598-024-80993-z]
- 67. Boosting one protein helps the brain protect itself from ... [https://www.sciencedaily.com/releases/2025/11/251123085550.htm]
- 68. Enhanced disc regeneration through CRISPR/Cas9-mediated ... [https://stemcellres.biomedcentral.com/articles/10.1186/s13287-025-04600-2]
- 69. SOX9 [https://grokipedia.com/page/SOX9]
- 70. Post-translational modification of SOX family proteins [https://pmc.ncbi.nlm.nih.gov/articles/PMC7703692/]
- 71. SOX9 - Wikipedia [https://en.wikipedia.org/wiki/SOX9]
- 72. Setting Compensation Multicolor Flow [https://www.bdbiosciences.com/en-us/resources/protocols/setting-compensation-multicolor-flow]
- 73. Protocol for the purification and transcriptomic analysis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10522990/]
- 74. Development of a 43 color panel for the characterization of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11497249/]
- 75. Flow Cytometry Troubleshooting Guide [https://www.cellsignal.com/learn-and-support/troubleshooting/flow-cytometry-troubleshooting-guide?srsltid=AfmBOorNBSCteELsKV-qb57NkEcK_Ehf57CJEoe183WRZFXsXPTpoTjq]
- 76. Guidelines for the use of flow cytometry and cell sorting in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9165548/]
- 77. Comprehensive analysis, immune, and cordycepin ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1149986/full]
- 78. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002136]
- 79. SOX9 Recombinant Monoclonal Antibody [https://www.cusabio.com/Recombinant_Antibodies/SOX9-Antibody-12929041.html?srsltid=AfmBOorLqqef7BDfnQUajnChcxXZuOSg5D5tywtCkpoCdiOLcQmCKyz-]
- 80. 4.7. Immunohistochemistry and Immunofluorescence [https://bio-protocol.org/exchange/minidetail?id=10398755&type=30]
- 81. Expression of SOX9 Is Related to Prognosis in Patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6117787/]
- 82. SOX9 expression decreases survival of patients with ... [https://www.nature.com/articles/s41416-018-0338-9]
- 83. Protocol to characterize immune cell subpopulations in ... [https://pubmed.ncbi.nlm.nih.gov/38678568/]
- 84. Anti-SOX9 Antibody [https://www.raybiotech.com/mouse-anti-human-sox9-102-10200]
- 85. SOX9 Is an Astrocyte-Specific Nuclear Marker in the Adult ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5413187/]
- 86. Sox9 prevents retinal degeneration and is required for ... [https://elifesciences.org/articles/102337]
- 87. Anti-SOX9 Antibodies | Invitrogen [https://www.thermofisher.com/antibody/primary/target/sox9]
- 88. SOX9 Governs Differentiation Stage-Specific Gene ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1002356]
- 89. Troubleshooting Flow Cytometry Issues [https://www.bosterbio.com/protocol-and-troubleshooting/flow-cytometry-troubleshooting?srsltid=AfmBOooXHxc9Fojyb6aUMUHLLe1bqL_1IGUmbsphx1vLi_rxDtZWndGZ]
- 90. Immune Biomarkers for Checkpoint Blockade in Solid Tumors [https://pmc.ncbi.nlm.nih.gov/articles/PMC12384685/]
- 91. Decreased expression of SOX9 indicates a better prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4637535/]
- 92. 胃癌免疫抑制微环境的异质性:对治疗发展的意义 [http://www.liangyihui.net/doc/148700]
- 93. IF 50+ 肺癌转移中的再生谱系和免疫介导的修剪原创 [https://blog.csdn.net/weixin_41368414/article/details/149436545]
- 94. 验证临床预测模型的样本量计算:pmvalsampsize包原创 [https://blog.csdn.net/weixin_49282401/article/details/147642331]
- 95. 临床预测模型研究方法与步骤 [http://www.liangyihui.net/doc/125478]
- 96. 临床预测模型建立、验证的报告规范:TRIPOD声明 [https://wj.iikx.com/thread-1430-1-1.html]
- 97. 全血与外周血单核细胞免疫代谢特征的比较 [https://www.ebiotrade.com/newsf/2025-11/20251122172807491.htm]
- 98. 肿瘤临床预后影响因素分析应该注意哪些因素? - 陈琼博士 [https://chenq.site/qsight/2023-03-21-%E8%82%BF%E7%98%A4%E4%B8%B4%E5%BA%8A%E9%A2%84%E5%90%8E%E5%BD%B1%E5%93%8D%E5%9B%A0%E7%B4%A0%E5%88%86%E6%9E%90%E5%BA%94%E8%AF%A5%E6%B3%A8%E6%84%8F%E5%93%AA%E4%BA%9B%E5%9B%A0%E7%B4%A0/index.html]
- 99. Identification of SOX9-related prognostic DEGs and a ... [https://pubmed.ncbi.nlm.nih.gov/39622395/]