Navigating Normal Ultrastructure: A Comprehensive Guide to PCD Diagnosis and Genetic Resolution
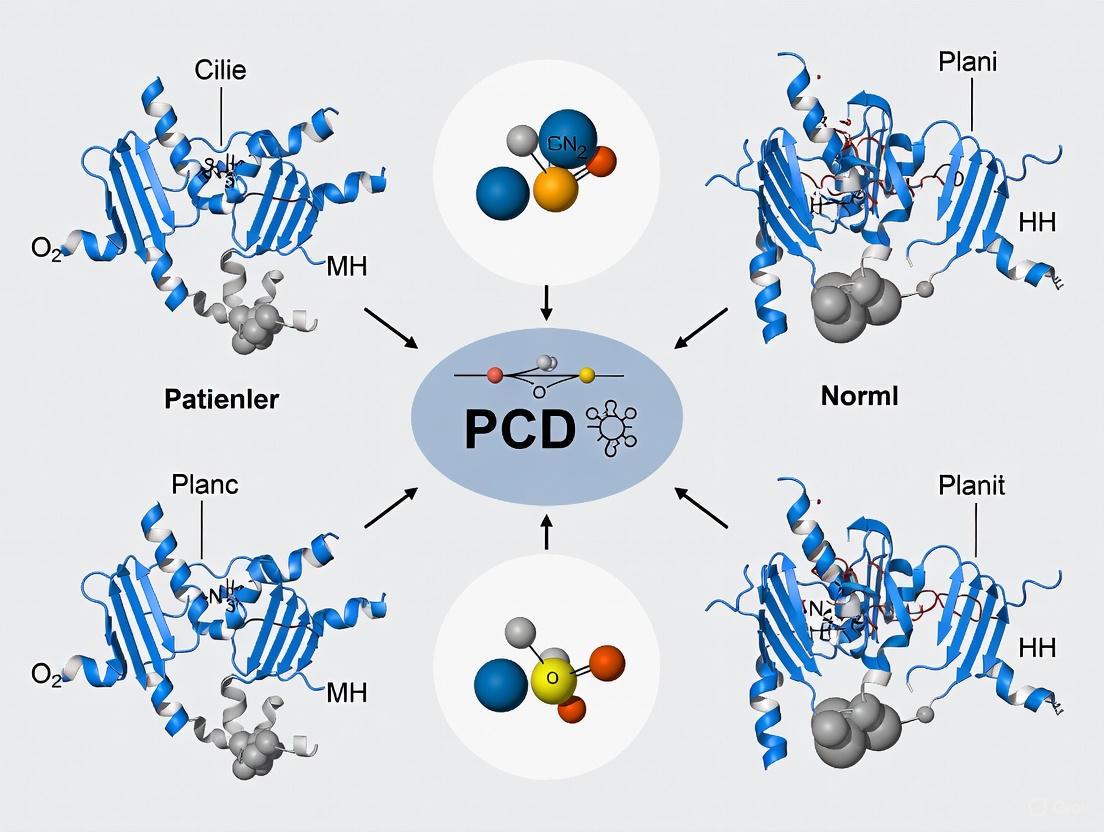
Diagnosing Primary Ciliary Dyskinesia (PCD) in patients with normal ciliary ultrastructure presents a significant challenge, requiring a shift from traditional diagnostic paradigms.
Navigating Normal Ultrastructure: A Comprehensive Guide to PCD Diagnosis and Genetic Resolution
Abstract
Diagnosing Primary Ciliary Dyskinesia (PCD) in patients with normal ciliary ultrastructure presents a significant challenge, requiring a shift from traditional diagnostic paradigms. This article provides a comprehensive framework for researchers and drug development professionals, addressing the foundational genetics, advanced multi-modal diagnostic methodologies, strategies for optimizing diagnostic yield, and the validation of patient-reported outcomes. It synthesizes current knowledge on genes like DNAH11 that cause PCD without ultrastructural defects, explores the integration of genetic testing with high-speed video microscopy and nasal nitric oxide measurement, and discusses the implications for clinical trial design and the development of targeted therapies, including gene-based treatments.
Decoding the Genetic Basis of PCD with Normal Ultrastructure
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: What percentage of genetically-confirmed PCD cases present with normal ciliary ultrastructure under TEM, and what are the primary genetic culprits?
A1: Current research indicates that up to 30% of patients with clinically and genetically confirmed PCD display normal ciliary ultrastructure when analyzed by standard Transmission Electron Microscopy (TEM) [1] [2]. This significant subset of cases presents a major diagnostic challenge. The primary genetic associations for this phenotype include mutations in genes such as Dynein Axonemal Heavy Chain 11 (DNAH11) and HYDIN [2]. In these cases, the cilia possess all the normal structural components (e.g., dynein arms, microtubules) but are functionally impaired due to defects in the molecular mechanisms that govern ciliary beat, which are not visible with conventional ultrastructural analysis.
Q2: Our lab has identified a patient with a strong clinical phenotype of PCD, but TEM results are normal. What is the recommended diagnostic pathway?
A2: When faced with a classic PCD phenotype and normal TEM findings, the diagnostic pathway should pivot to alternative and complementary modalities. The recommended workflow is:
- Genetic Testing: Pursue a comprehensive PCD genetic panel to identify mutations in genes known to cause PCD with normal ultrastructure (e.g., DNAH11, HYDIN) [2] [3]. This is now considered a primary diagnostic method.
- Functional Ciliary Assessment: Employ High-Speed Video Microscopy Analysis (HSVA) to evaluate ciliary beat pattern and frequency. Cilia in these cases often exhibit abnormal, dyskinetic, or stiff beating patterns despite normal appearance [4] [3].
- Nasal Nitric Oxide (nNO) Measurement: Use nNO as a screening tool. Patients with PCD, including those with normal ultrastructure, typically have very low levels of nasal nitric oxide. This serves as a strong supportive indicator [4] [5]. A combination of these approaches is essential for a definitive diagnosis when TEM is inconclusive [1] [4].
Q3: In a resource-limited setting where only TEM is available, how should we interpret "suggestive" ultrastructural defects like isolated inner dynein arm (IDA) absence or microtubular disorganization?
A3: In settings with limited access to genetic or functional tests, interpreting TEM findings requires caution. Defects such as isolated IDA absence or microtubular disorganization are categorized as Class 2 defects and are not considered confirmatory for PCD on their own [1]. These findings can be secondary to epithelial damage from infections, pollutants, or inflammation [1] [2]. The consensus guideline is to:
- Repeat the nasal brushing after a period of clinical stability and aggressive medical management of infection and inflammation.
- If the Class 2 defects persist upon repeat testing, they are considered highly suggestive of PCD, but a definitive diagnosis ideally requires confirmation with another modality [1]. In these constrained environments, a "probable" diagnosis may be used to initiate early treatment while acknowledging the diagnostic uncertainty [1].
Q4: What are the key methodological pitfalls in TEM sample processing that can mimic primary ciliary defects, and how can we avoid them?
A4: Several technical artifacts can be misinterpreted as pathological defects. Key pitfalls and solutions include:
- Poor Sample Preservation: Inadequate or delayed fixation can cause microtubular disorganization and dynein arm loss that mimics true PCD. Solution: Immediately place the nasal brushing sample in buffered glutaraldehyde and refrigerate [1].
- Inadequate Ciliary Cross-Sections: Analyzing sections from the tip or base of the cilium, where the architecture naturally differs from the standard "9+2" pattern, leads to misdiagnosis. Solution: Ensure that quantitative analysis is performed on a sufficient number (e.g., >50) of high-quality, transverse sections from the mid-portion of the cilia [2].
- Insufficient Sample Size: A sample with too few ciliated cells or cilia can prevent a statistically valid assessment. Solution: Aim for samples with an adequate number of ciliated cells and report the proportion of cilia exhibiting the defect [1].
Diagnostic Test Performance & Quantitative Data
The following table summarizes the quantitative performance and characteristics of key diagnostic tests for PCD, particularly in the context of normal ultrastructure.
Table 1: Performance Metrics of Primary PCD Diagnostic Tests
| Test Method | Reported Sensitivity in PCD Diagnosis | Key Strengths | Key Limitations in Normal Ultrastructure Cases |
|---|---|---|---|
| Transmission Electron Microscopy (TEM) | ~70% [1] | Identifies hallmark structural defects (e.g., ODA/IDA loss); considered a traditional standard. | Fails to detect ~30% of PCD cases where ultrastructure appears normal [1] [2]. |
| Genetic Testing | >90% with advanced panels [5] | Provides a definitive molecular diagnosis; identifies pathogenic mutations regardless of ultrastructure. | Not all causative genes are known; variants of uncertain significance (VUS) can complicate interpretation [3]. |
| Nasal Nitric Oxide (nNO) | >95% as a screening tool [4] | Non-invasive, rapid, and highly sensitive for screening; low in most PCD patients. | Cannot differentiate between PCD genetic subtypes; requires patient cooperation [4] [3]. |
| High-Speed Video Microscopy (HSVA) | High for functional defects [4] | Assesses ciliary function directly; can detect beat pattern abnormalities even with normal structure. | Requires significant expertise; not widely standardized or available [4] [3]. |
Table 2: Distribution of Ultrastructural Findings in Suspected PCD Cohorts
| TEM Finding Category | Definition | Prevalence in a Study of 67 Patients [2] | Diagnostic Implication |
|---|---|---|---|
| Hallmark Defects (Class 1) | Confirmed ODA/IDA defects in >50% of cilia | 17.9% (12/67) | Confirmatory for PCD |
| Probable Criteria (Class 2) | Defects (e.g., IDA loss) in 25-50% of cilia or central pair defects | 16.4% (11/67) | Highly suggestive, requires confirmation |
| Normal Ultrastructure | No significant defects observed | 26.9% (18/67) | Does not rule out PCD |
| Secondary Defects | Compound cilia, extra tubules (often from infection) | 41.4% - 44.3% | Not diagnostic of PCD |
Experimental Protocols for Defining PCD with Normal Ultrastructure
Integrated Diagnostic Protocol
Objective: To provide a robust methodological framework for confirming a PCD diagnosis in patients with a strong clinical phenotype but normal ciliary ultrastructure upon initial TEM screening.
Workflow Diagram:
Methodology Details:
Patient Population & Clinical Phenotyping:
- Enrollment Criteria: Enroll patients with a strong clinical history indicative of PCD. Key features include: neonatal respiratory distress in term infants, daily perennial wet cough beginning in infancy, chronic sinusitis and otitis media, and any history of organ laterality defects (situs inversus or heterotaxy) [3] [5]. Tools like the PICADAR score can be used to quantify clinical likelihood [1].
Initial TEM Analysis:
- Sample Collection: A pulmonologist or ENT specialist should obtain nasal epithelial cells via brushing of the inferior surface of the nasal turbinates. The sample must be immediately placed in buffered glutaraldehyde (2.5%) and refrigerated to prevent artifactual degradation [1].
- Processing & Imaging: Process samples through standard dehydration, resin embedding, and ultra-thin sectioning (70 nm). Sections are double-stained with uranyl acetate and lead citrate and viewed under a TEM at 120kV [1].
- Quantitative Assessment: Analyze a minimum of 50 transverse ciliary sections. A diagnosis based on ultrastructure requires hallmark defects (e.g., absence of ODA/IDA) in >50% of the examined cilia [1] [2]. If results are normal or show only suggestive Class 2 defects, proceed to the next steps.
Genetic Testing:
- Sample & Method: Obtain a blood sample. Analysis should be performed using a next-generation sequencing (NGS) panel that encompasses all known PCD-associated genes (currently >40 genes) [6] [5].
- Interpretation: A definitive genetic diagnosis is made by identifying bi-allelic or X-linked hemizygous pathogenic mutations in a known PCD-causing gene [3]. The identification of mutations in genes like DNAH11 or HYDIN provides a clear explanation for normal ultrastructure.
Nasal Nitric Oxide (nNO) Measurement:
- Protocol: During a period of clinical stability, measure nNO using a chemiluminescence analyzer according to standardized guidelines. The patient should perform a breath-hold maneuver while gas is sampled from the nasal cavity.
- Interpretation: nNO levels in PCD patients, including those with normal ultrastructure, are typically very low compared to healthy controls. This serves as a powerful, non-invasive screening tool [4] [5].
High-Speed Video Microscopy Analysis (HSVA):
- Sample Preparation: Obtain a fresh nasal epithelial brushing and suspend it in cell culture medium.
- Imaging & Analysis: Record ciliary movement at high frame rates (≥500 frames per second). Analyze the videos for abnormal beat patterns, such as stiff, flickering, or circular motions, and reduced beat frequency, which are characteristic of functional ciliary defects despite normal structure [4] [3].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for PCD Diagnostic Research
| Item | Specific Example / Model | Function in Experiment |
|---|---|---|
| Nasal Brush | Flexible nylon laparoscopy brush (e.g., WS-1812XA3) [1] | Minimally invasive collection of ciliated epithelial cells from the nasal turbinates. |
| Primary Fixative | 2.5% EM-grade glutaraldehyde in 0.1M sodium cacodylate buffer [1] | Rapidly cross-links and preserves protein structure to prevent ultrastructural artifacts in TEM samples. |
| Resin for Embedding | Agar Scientific low viscosity resin [1] | Infiltrates and embeds fixed tissue for ultra-thin sectioning for TEM. |
| TEM Stains | Aqueous 4% uranyl acetate, Reynold's lead citrate [1] | Heavy metal stains that provide contrast to cellular structures (e.g., microtubules, dynein arms) under the electron beam. |
| nNO Analyzer | Chemiluminescence nitric oxide analyzer [4] [5] | Precisely measures the concentration of nitric oxide gas in a sampled airstream for diagnostic screening. |
| High-Speed Camera | Olympus Quemesa CCD camera [1] | Captures video at very high frame rates required for detailed analysis of rapid ciliary beat patterns. |
Beyond the Microscope: Key Genes Implicated in Normo-Ultrastructural PCD (e.g., DNAH11)
FAQs: Diagnosing Normo-Ultrastructural PCD
1. A patient has a strong clinical phenotype of PCD, including low nasal nitric oxide and situs inversus, but Transmission Electron Microscopy (TEM) is reported as normal. What is the most likely genetic cause, and how can I confirm it?
The most common genetic cause of PCD with normal ciliary ultrastructure is biallelic mutations in the DNAH11 gene [7]. One large cohort study found that 22% (13/58) of unrelated patients with a clinical PCD phenotype and normal ultrastructure had biallelic DNAH11 mutations [7].
Confirmation requires genetic testing. Sanger sequencing of the 82 exons of DNAH11 or its inclusion in a targeted next-generation sequencing (NGS) panel for PCD-related genes can identify pathogenic variants [7]. The majority of disease-causing DNAH11 mutations are nonsense, insertion/deletion, or loss-of-function splice-site mutations [7].
2. What is the functional consequence of DNAH11 mutations on ciliary function if the ultrastructure appears normal?
Despite normal appearance under conventional TEM, DNAH11 mutations cause a functional defect in ciliary beat. Instead of being immotile, cilia typically exhibit a hyperkinetic and dyskinetic beating pattern with a reduced waveform amplitude [7]. This abnormal motion is insufficient for effective mucociliary clearance, leading to the classic PCD symptoms. This is why high-speed video microscopy analysis (HSVMA) is a critical functional assay in these cases [7] [8].
3. We have identified a candidate variant in DNAH11. What in-silico and functional analyses are critical for determining its pathogenicity?
A multi-step approach is recommended to establish pathogenicity:
- In-Silico Prediction: Use programs like SIFT, PolyPhen-2, and MutationTaster to predict the impact of missense variants on protein function [9].
- Population Frequency: Filter against population databases (e.g., gnomAD, 1000 Genomes) to exclude common polymorphisms. Focus on rare variants (Minor Allele Frequency < 0.01%) [9].
- ACMG/AMP Guidelines: Classify variants according to the American College of Medical Genetics and Genomics and the Association for Molecular Pathology guidelines. A definitive genetic diagnosis typically requires two pathogenic variants in trans (either homozygous or compound heterozygous) [10].
- cDNA Analysis: If a variant affects a splice site, perform RT-PCR on RNA from patient-derived cells (e.g., nasal epithelial cells or lymphoblastoid cell lines) to confirm aberrant splicing [7].
4. Are there any advanced imaging techniques that can reveal ultrastructural defects in DNAH11-related PCD that are invisible to standard TEM?
Yes, electron tomography can detect subtle defects. While standard TEM provides 2D images, electron tomography produces 3D ultrastructural models with superior resolution. Studies show that DNAH11 mutations lead to a deficiency of >25% of the proximal outer dynein arm volume, a defect consistently visible only via this method [11]. This technique can be applied to existing araldite-embedded nasal cilia samples [11].
Troubleshooting Guide for Experimental Diagnosis
| Challenge | Potential Cause | Solution |
|---|---|---|
| Inconclusive Genetic Results | A patient with only one detected heterozygous pathogenic variant in a recessive PCD gene. | 1. Perform copy number variation (CNV) analysis to search for a second, large deletion/duplication that may be missed by NGS [10].2. Expand genetic analysis to a full whole-exome or whole-genome sequencing approach to identify variants in non-panel genes or deep intronic regions [8]. |
| Normal TEM & No Genetic Hits | Mutations in a PCD gene not included in your targeted panel; or a non-genetic mimic of PCD (e.g., secondary ciliary dyskinesia). | 1. Re-evaluate the clinical phenotype and history to exclude secondary causes [10].2. Utilize high-speed video microscopy analysis (HSVMA) to document the characteristic hyperkinetic, dyskinetic beat pattern [7] [8].3. Re-classify the case as "moderate suspicion" and consider re-screening as new PCD genes are discovered [10]. |
| Difficulty Interpreting TEM | Ciliary abnormalities are present but do not meet the quantitative threshold for a "Class I" hallmark defect. | Analyze samples according to the BEAT-PCD TEM criteria [10]. Look for "Class II" alterations (e.g., central complex defects, microtubular disorganization with inner dynein arms present) which, when combined with other supportive evidence like genetic findings, can confirm the diagnosis [10]. |
The Scientist's Toolkit: Research Reagent Solutions
| Essential Material | Function in PCD Research |
|---|---|
| Araldite-Embedded Ciliary Biopsies | Preserved nasal or bronchial epithelial samples for ultrastructural analysis via TEM and advanced 3D electron tomography [11]. |
| TruSeq Custom Amplicon Panel (Illumina) | A targeted NGS panel for sequencing the exonic regions of a defined set of PCD-related genes, including DNAH11, HYDIN, and CCDC65 [10]. |
| Anti-DNAH11 Antibody | For immunofluorescence staining to confirm the localization and absence of the DNAH11 protein in the proximal ciliary region (though its use in clinical diagnostics is not yet standard) [11]. |
| FlexiGene DNA Kit (Qiagen) | For reliable extraction of high-quality DNA from patient blood or buccal swabs for subsequent genetic analysis [10]. |
| Lymphoblastoid or iPSC Cell Lines | Creating stable cell lines from patient peripheral blood allows for a renewable source of DNA and RNA for genetic and transcriptomic studies, and iPSCs enable future functional correction experiments [12]. |
Experimental Workflow & Diagnostic Pathways
The following diagram illustrates the multi-modal diagnostic and research pathway for a suspected case of normo-ultrastructural PCD.
Quantitative Data on DNAH11 in PCD
Table 1: Frequency of DNAH11 Mutations in a Selected PCD Cohort [7]
| Patient Cohort | Number of Unrelated Patients | Patients with Biallelic DNAH11 Mutations | Percentage |
|---|---|---|---|
| PCD with normal ultrastructure | 58 | 13 | 22% |
| PCD with outer dynein arm defects | 76 | 0 | 0% |
| PCD with radial spoke/central pair defects | 6 | 0 | 0% |
| Isolated situs abnormalities (no PCD) | 13 | 0 | 0% |
Table 2: Spectrum and Predicted Impact of DNAH11 Mutations [7] [9]
| Mutation Type | Proportion of Mutant Alleles (in one study) | Functional Consequence |
|---|---|---|
| Nonsense / Frameshift / Splice-site | 24/35 (69%) | Loss-of-function, premature termination |
| Missense | 11/35 (31%) | Amino acid substitution; requires pathogenicity prediction |
Primary ciliary dyskinesia (PCD) is a genetically heterogeneous, typically autosomal recessive disorder caused by impaired motile ciliary function [13]. Establishing a definitive PCD diagnosis is contingent upon a multi-faceted approach that integrates clinical symptoms with specialized testing [14]. A significant diagnostic challenge arises in patients with strong clinical evidence of PCD but normal ciliary ultrastructure on transmission electron microscopy (TEM). In these cases, the ciliary axoneme appears structurally intact despite clear functional deficiencies, a scenario now explained by mutations in specific PCD-related genes that do not disrupt the core 9+2 microtubule architecture [15]. This technical support guide provides methodologies for correlating genotypes with clinical presentations in these complex cases, focusing on the integration of advanced genetic and functional assays to resolve diagnostic uncertainties.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: A patient has a classic PCD clinical phenotype, including neonatal respiratory distress and laterality defects, but TEM shows normal ultrastructure. What is the most efficient diagnostic path?
A1: Proceed directly to genetic testing using a comprehensive PCD gene panel. Several genetic defects, particularly those in DNAH11, HYDIN, CCDC164, and CCDC65, are known to cause PCD with normal TEM findings [15] [16]. In one study, genetic testing confirmed PCD in 50.7% of clinically suspected cases, whereas TEM alone would have identified defects in only 40.5% of those confirmed cases, highlighting the limited sensitivity of TEM for all PCD genotypes [15].
Q2: Genetic testing identified a single heterozygous pathogenic variant in a recessive PCD gene. What are the next steps to confirm or rule out PCD?
A2: This is a common diagnostic dilemma. Current research indicates that noncoding DNA variants may account for a significant number of these incomplete genetic diagnoses.
- Recommended Action: If available, pursue end-to-end gene sequencing of the relevant PCD gene, focusing on intronic regions, to identify potential splice-altering variants [16]. One study found that this approach successfully identified a second pathogenic (intronic) variant in 38% of patients with a single previously identified heterozygous mutation, thereby confirming the diagnosis [16].
- Alternative Approach: Perform cDNA analysis from nasal epithelial cells to validate the impact of the variant on splicing and gene expression [16].
Q3: How reliable is nasal nitric oxide (nNO) as a screening tool for PCD genotypes with normal ultrastructure?
A3: nNO measurement remains a valuable screening tool, as levels are typically very low in most PCD patients [17] [13] [18]. However, be aware that some genetic variants may show discrepancies with nNO measurements [18]. It should not be used as a standalone test but as part of a multi-modal diagnostic strategy to target patients for advanced genetic testing [13].
Troubleshooting Common Experimental and Diagnostic Scenarios
| Challenge | Possible Cause | Recommended Solution |
|---|---|---|
| Inconclusive Genetic Test (Single heterozygous variant) | Variant in non-coding region (intron); Poorly characterized VUS [16] | Perform end-to-end gene sequencing; conduct cDNA analysis to confirm splicing defects; share variant data via ClinGen/CiliaVar databases [16]. |
| Strong Clinical Phenotype, Normal TEM, Negative Genetics | Mutations in novel PCD genes not on standard panels; non-ciliopathy genetic disorder mimicking PCD (e.g., WFDC2 deficiency) [16] | Utilize whole-exome/genome sequencing; consider functional ciliary studies like high-speed video microscopy analysis (HSVA) [15] [16]. |
| Poor Quality Nasal Biopsy for TEM/IF | Acute infection, improper sample handling/processing [1] | Repeat biopsy 4-8 weeks after resolution of acute illness; ensure immediate fixation in buffered glutaraldehyde; use standardized processing protocols [1]. |
| Discrepancy between nNO and Clinical Picture | Specific genotype affecting NO synthesis; technical issues with measurement [18] | Use nNO as a screening tool only; rely on genetic testing and other functional assays (e.g., HSVA) for diagnostic confirmation [15] [18]. |
Quantitative Data: Genotype-Phenotype Correlations in PCD
Understanding the distribution of genetic defects and their associated clinical outcomes is crucial for prognosis and management. The tables below synthesize key quantitative findings from recent studies.
Table 1: Distribution of Ultrastructural and Genetic Defects in Confirmed PCD Cases
| Defect Category | Subtype | Percentage of Cases | Common Associated Gene(s) |
|---|---|---|---|
| Ultrastructural Defects (via TEM) [15] | Outer Dynein Arm (ODA) | 32% | DNAH5, DNAI1 [17] [13] |
| Central Apparatus | 19% | RSPH4A, RSPH9 [15] | |
| Radial Spokes | 16% | RSPH1 [15] | |
| Ciliogenesis Defects | 14% | CCDC40, CCDC39 [15] | |
| Nexin-Dynein Regulatory Complex | 11% | CCDC65, GAS8 [15] | |
| Normal Ultrastructure [15] | (Normal on TEM) | ~30% | DNAH11, HYDIN, CCDC164 [15] [16] |
Table 2: Clinical Presentation Frequencies in Genetically Confirmed PCD Cohorts
| Clinical Feature | Frequency in PCD Patients | Notes / Genotype Correlations |
|---|---|---|
| Chronic Wet Cough [15] [19] | 100% | Universal finding, typically beginning in first year of life [15]. |
| Neonatal Respiratory Distress [13] | "Most patients" [13] | A history in term infants is a major clinical criterion [15]. |
| Bronchiectasis [15] [19] | 70.3% | Demonstrated on CT scan; prevalence increases with age [15]. |
| Situs Inversus Totalis [15] | ~50% | Hallmark of Kartagener's syndrome [13]. |
| Situs Abnormalities (total) [15] | 24.3% | Includes situs inversus and heterotaxy [15]. |
| Chronic Rhinitis/Nasal Congestion [15] | 97.3% | Daily and year-round from early life [15]. |
| Chronic Otitis Media [15] | 75.7% | Leads to hearing impairment in some cases [15]. |
Experimental Protocols for Advanced PCD Diagnostics
Protocol 1: Transmission Electron Microscopy for Ciliary Ultrastructure
Principle: This protocol details the standardized processing and analysis of nasal brush biopsies to visualize the ciliary axonemal structure via TEM, which is critical for identifying hallmark defects [1].
Methodology:
- Sample Collection: Obtain nasal brushings from the inner turbinates using a flexible nylon laparoscopy brush. Immediately place the sample in fresh, cold buffered glutaraldehyde (2.5%) [1].
- Sample Cleaning: Under a dissecting microscope, gently clean the brush of adherent mucus and debris while immersed in fixative [1].
- Processing:
- Rinse in buffer (3 x 30 min).
- Post-fix in 1% buffered osmium tetroxide for 1 hour.
- Rinse again in buffer and then pure water.
- Dehydrate in a graded ethanol series (10% to 100%).
- Infiltrate with low-viscosity resin (e.g., Agar Scientific) using resin:ethanol mixtures, culminating in pure resin overnight.
- Embed in capsules and polymerize at 70°C [1].
- Sectioning and Staining: Section the polymerized blocks at 70 nm thickness. Double-stain grids with aqueous uranyl acetate (4%, 15 min) and Reynold's lead citrate (10 min) [1].
- Imaging and Analysis: View grids at 120 kV. Capture micrographs of ciliary cross-sections. Analyze a minimum of 50 cilia from different cells, following international consensus guidelines [1]. Defects in >50% of cilia are considered diagnostic for PCD for specific ultrastructural abnormalities (Class 1 defects) [1].
Protocol 2: Next-Generation Sequencing and Variant Interpretation
Principle: To identify pathogenic sequence variants in known PCD-associated genes from patient-derived DNA.
Methodology:
- DNA Extraction: Extract genomic DNA from peripheral blood leukocytes or other suitable tissues using standard protocols [15] [19].
- Library Preparation & Sequencing: Prepare sequencing libraries from the DNA. Use a targeted multigene panel for PCD or whole-exome sequencing. Perform sequencing on an NGS platform [15].
- Bioinformatic Analysis: Map sequence reads to a reference genome. Call and annotate variants (SNPs, indels). Filter against population frequency databases (e.g., gnomAD) to remove common polymorphisms [15] [19].
- Variant Assessment: Interpret the pathogenicity of remaining variants according to American College of Medical Genetics and Genomics (ACMG/AMP) guidelines. Use in silico prediction tools (e.g., SIFT, PolyPhen2, MutationTaster) and databases (e.g., ClinVar) [15] [19]. For cases with a single identified variant, consider end-to-end sequencing to find noncoding (e.g., intronic) variants [16].
- Segregation Analysis: Confirm compound heterozygosity or homozygosity by Sanger sequencing of the variant(s) in available family members [15].
Protocol 3: Immunofluorescence Analysis of Ciliary Proteins
Principle: To confirm the pathogenicity of genetic variants by visualizing the presence, absence, or mislocalization of specific ciliary proteins.
Methodology:
- Sample Preparation: Obtain nasal brushings and place the cells in appropriate culture medium or process immediately [15].
- Slide Preparation and Fixation: Spread cells onto glass slides and allow to adhere. Fix cells, typically with methanol or paraformaldehyde, depending on antibody requirements [15].
- Antibody Staining:
- Permeabilize and block cells to reduce non-specific binding.
- Incubate with primary antibodies (e.g., mouse anti-DNAH5, rabbit anti-GAS8) diluted in blocking buffer.
- Wash thoroughly.
- Incubate with fluorophore-conjugated secondary antibodies (e.g., anti-mouse IgG-Alexa Fluor 488, anti-rabbit IgG-Alexa Fluor 594) [15].
- Microscopy and Analysis: Mount slides with an anti-fade medium containing DAPI to stain nuclei. Image using a fluorescence or confocal microscope. Compare the staining pattern and intensity in patient cells to healthy controls to identify protein deficiencies [15].
Diagnostic Pathways & Genetic Analysis
The following diagrams illustrate the logical workflow for diagnosing PCD, particularly in complex cases with normal ultrastructure, and the process for resolving variants of uncertain significance.
Diagram 1: Diagnostic workflow for PCD, integrating multiple testing modalities to resolve cases with normal ultrastructure or inconclusive genetics. nNO: nasal nitric oxide; TEM: transmission electron microscopy; NGS: next-generation sequencing; VUS: variant of uncertain significance.
Diagram 2: A stepwise pipeline for resolving the clinical significance of a genetic variant of uncertain significance (VUS).
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for PCD Diagnostic and Research Experiments
| Reagent / Material | Function / Application | Example / Specification |
|---|---|---|
| Flexible Nylon Brushes | Collection of ciliated nasal epithelial cells for TEM, IF, or cell culture. | WS-1812XA3 laparoscopy brush; cervix brush with trimmed fibres [1]. |
| Buffered Glutaraldehyde | Primary fixative for TEM; preserves ultrastructural details of cilia. | 2.5% EM grade glutaraldehyde in 0.1 M sodium cacodylate buffer, osmotically adjusted [1]. |
| Low-Viscosity Resin | Embedding medium for TEM samples; allows for precise thin-sectioning. | Agar Scientific low viscosity resin [1]. |
| Primary Antibodies for IF | Visualize specific ciliary proteins to confirm genetic findings (e.g., absence of protein). | Mouse anti-DNAH5; Rabbit anti-GAS8; used at 1:500 dilution [15]. |
| PCD Multigene NGS Panel | Targeted sequencing of all known PCD-related genes for efficient molecular diagnosis. | Panels should include >50 genes, e.g., DNAH5, DNAH11, RSPH4A, CCDC genes [15] [19] [16]. |
| Whole Exome/Genome Sequencing | Hypothesis-free genetic testing to identify novel variants or genes, especially in unsolved cases. | Used when targeted NGS panels are negative [16]. |
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder affecting motile cilia, with significant implications for patient morbidity and mortality. Understanding the epidemiology and disease trajectory is crucial for researchers and clinicians developing targeted therapies. The estimated prevalence of PCD ranges from 1:7,500 to 1:20,000 live births, though the true prevalence is likely higher due to diagnostic challenges and underrecognition [20]. Prognosis varies considerably based on genotypic and phenotypic factors, with certain genetic subtypes experiencing more severe disease progression and poorer outcomes [21]. This technical guide provides researchers with essential troubleshooting and methodological frameworks for investigating PCD prevalence and prognostic determinants, with particular emphasis on diagnostically challenging cases with normal ultrastructure.
Prevalence and Diagnostic Statistics
Table 1: Epidemiological and Diagnostic Characteristics of PCD
| Parameter | Statistical Range | Context & Notes |
|---|---|---|
| Prevalence | 1:7,500 - 1:20,000 live births | True prevalence likely higher due to underdiagnosis [20] |
| Genetic Heterogeneity | >50 associated genes | Number continues to grow with ongoing research [20] [22] |
| Cases with Normal Ultrastructure | ~30% | Normal TEM findings despite clinical PCD (e.g., DNAH11 mutations) [11] [23] |
| Diagnostic Sensitivity of TEM Alone | ≤70% | Limited by normal ultrastructure cases; requires complementary tests [23] |
| Neonatal Respiratory Distress | >80% of neonates | Requiring respiratory support within first day of life [20] |
| Laterality Defects | ~50% of patients | Situs inversus or heterotaxy [20] |
Prognostic Indicators and Clinical Outcomes
Table 2: Prognostic Factors and Disease Outcomes in PCD
| Factor | Impact on Prognosis | Evidence & Notes |
|---|---|---|
| Genotype | Variable severity | CCDC39/CCDC40 mutations associated with poorer outcomes and rapid lung function decline [21] |
| Lung Function (FEV1) | Progressive decline | Similar decline course to cystic fibrosis; stabilizes in middle age possibly due to survivor bias [21] |
| Early Diagnosis | Morbidity reduction | Some benefit from diagnosis <1 year; no significant difference in annual lung function decline post-diagnosis [21] |
| PCD vs. CF Outcomes | Worse in PCD pre-modulators | Children with PCD had worse health outcomes than those with CF before CFTR modulator therapies [21] |
| Bronchiectasis | Common complication | Children with MTD/IDA defects (CCDC39, CCDC40) have greater tendency to bronchiectasis [20] |
Troubleshooting Guide: PCD Research Challenges & Solutions
Diagnostic Challenges in Normal Ultrastructure PCD
Problem: How to confirm PCD diagnosis in patients with normal ciliary ultrastructure on transmission electron microscopy (TEM)?
- Background: Approximately 30% of PCD cases, particularly those with DNAH11 mutations, display normal ciliary ultrastructure with standard TEM, creating diagnostic challenges [11] [23].
- Solution Protocol: Implement electron tomography for enhanced ultrastructural analysis.
- Sample Preparation: Collect nasal cilia biopsies and embed in araldite resin per standard TEM protocols [11].
- Data Collection: Acquire dual-axis tomograms from embedded cilia samples.
- Image Processing: Reconstruct 3D ultrastructural models using IMOD and Chimera software [11].
- Quantitative Analysis: Measure proximal outer dynein arm volume; deficiency of >25% is indicative of DNAH11-related PCD [11].
- Validation: This method successfully identified proximal outer dynein arm deficiencies in all studied patients with DNAH11 mutations (n=7) despite normal standard TEM [11].
Problem: How to identify appropriate candidates for PCD testing amid nonspecific respiratory symptoms?
- Solution Protocol: Apply the PICADAR (PCD Rule) clinical prediction tool.
- Inclusion Criteria: Patients with persistent wet cough [24].
- Parameter Scoring: Assign points for seven clinical features:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care admission
- Chronic rhinitis
- Ear symptoms
- Situs inversus
- Congenital cardiac defect [24]
- Interpretation: Score ≥5 points indicates high probability of PCD (sensitivity 0.90, specificity 0.75) [24].
Technical and Methodological Challenges
Problem: How to diagnose PCD in resource-limited settings with restricted access to advanced testing?
- Background: Many settings lack access to genetic testing, nNO measurement, or high-speed video microscopy [23].
- Solution Protocol: Optimize TEM as a primary diagnostic tool with standardized reporting.
- Sample Collection: Obtain nasal brushings from inner turbinates using flexible nylon laparoscopy brushes [23].
- Processing: Immediate fixation in buffered glutaraldehyde, followed by standard TEM processing [23].
- Analysis: Evaluate transverse sections of ≥50 cilia for hallmark ultrastructural defects [23].
- Classification:
- Limitations: TEM alone cannot detect 30% of PCD cases with normal ultrastructure [23].
Problem: How to correlate genotype with disease prognosis for drug development targeting?
- Solution Protocol: Establish genotype-phenotype correlations through natural history studies.
- Patient Stratification: Group patients by confirmed genetic mutations [20] [21].
- Longitudinal Monitoring: Track lung function decline (FEV1), bronchiectasis progression via CT imaging, and microbiology patterns [20] [21].
- Outcome Analysis: Compare disease severity trajectories across genotypic groups.
- Key Findings: CCDC39 and CCDC40 mutations are associated with more severe lung disease and earlier bronchiectasis development compared to ODA defects (e.g., DNAH5, DNAI1) [20] [21].
Research Workflow: Diagnostic Pathway for Normal Ultrastructure PCD
The following diagram illustrates the integrated diagnostic and research pathway for investigating PCD cases with normal ultrastructure:
Research Reagent Solutions for PCD Investigations
Table 3: Essential Research Materials for PCD Studies
| Reagent/Resource | Primary Application | Research Utility |
|---|---|---|
| Nasal Brush Biopsy Kits | Ciliary sample acquisition | Obtain ciliated epithelial cells for TEM, genetic analysis, and culture [23] |
| Glutaraldehyde Fixative (2.5%) | TEM sample preservation | Maintain ciliary ultrastructure for electron microscopy studies [23] |
| PCD Genetic Panels | Mutation detection | Identify pathogenic variants across >50 known PCD-associated genes [20] [3] |
| IMOD & Chimera Software | 3D electron tomography | Reconstruct and analyze ciliary ultrastructure from tomographic data [11] |
| Antibodies for Ciliary Proteins | Immunofluorescence staining | Visualize specific protein localization and defects (e.g., DNAH11) [20] [3] |
| PICADAR Scoring Tool | Patient screening | Identify high-probability PCD cases for research enrollment [24] |
FAQs on PCD Prevalence and Prognosis Research
Q1: Why is PCD considered underdiagnosed, and how does this affect prevalence studies? A: PCD is underdiagnosed due to several factors: nonspecific clinical presentation overlapping with more common respiratory conditions, limited access to specialized diagnostic centers, and the absence of a single standalone diagnostic test with 100% sensitivity. Current prevalence estimates of 1:7,500-1:20,000 likely represent underestimates, and true prevalence may be higher. Research accounting for diagnostic limitations suggests genomic screening of bronchiectasis populations reveals significant underdiagnosis [20] [22].
Q2: What are the key prognostic differences between major genetic subtypes of PCD? A: Genotype significantly influences disease progression:
- CCDC39/CCDC40 mutations: Associated with more severe lung disease, earlier bronchiectasis development, and poorer lung function outcomes [20] [21].
- DNAH5/DNAI1 mutations (ODA defects): Typically follow a milder disease course with slower progression [20].
- DNAH11 mutations: Often show preserved lung function despite typical PCD symptoms, with normal ultrastructure on standard TEM [20]. Natural history studies for different genetic subtypes remain a research priority [21].
Q3: What methodological approaches are essential for investigating PCD with normal ultrastructure? A: Research on normal ultrastructure PCD requires:
- Advanced imaging: Electron tomography to detect subtle defects missed by standard TEM [11].
- Genetic sequencing: Comprehensive panels or whole exome sequencing to identify mutations in genes like DNAH11 [11].
- Functional assays: High-speed video microscopy analysis to characterize ciliary beat patterns [20].
- Protein localization: Immunofluorescence staining to visualize protein distribution abnormalities [3].
Q4: How do outcomes for PCD compare to cystic fibrosis, and why does this matter for drug development? A: Evidence shows children with PCD had worse health outcomes than those with CF before the advent of CFTR modulators. With the development of highly effective CF modulators like Trikafta, this outcome gap is widening significantly. This disparity highlights the urgent need for targeted PCD therapies and justifies increased research investment in disease-modifying treatments for PCD [21].
Q5: What are the limitations of current PCD diagnostic tests in research settings? A: Major limitations include:
- TEM: Cannot detect approximately 30% of PCD cases with normal ultrastructure [23].
- Genetic testing: May not identify definitive causal variants in all patients, as not all PCD genes are known [11].
- nNO measurement: Requires patient cooperation and specialized equipment, with limited availability [20].
- HSVA: Needs specialized expertise for interpretation and may be normal in some PCD cases [20]. The diagnostic golden standard requires a combination of these modalities [20] [22].
Advanced Diagnostic Toolkit: A Multi-Modal Approach for Complex Cases
Frequently Asked Questions (FAQs)
Q1: What is the diagnostic yield of extended genetic panels compared to Whole-Exome Sequencing (WES) for PCD?
Genetic testing strategies vary in their diagnostic sensitivity. The table below summarizes the reported diagnostic yields from key studies.
Table 1: Diagnostic Yield of Genetic Testing Strategies for PCD
| Testing Method | Reported Diagnostic Yield | Key Study Findings |
|---|---|---|
| Extended Gene Panel (26 genes) | 80% sensitivity in definite PCD cases [25] | 20% false-negative rate in a multicenter study of 534 children with high clinical suspicion [25]. |
| Whole-Exome Sequencing (WES) | 76% overall molecular genetic yield [26] | WES followed by targeted CNV analysis identified diagnoses in 34 of 45 families (76%) [26]. |
| Combined WES & CNV Analysis | 55% increased diagnosis in unsolved cases [26] | Applied to 20 previously unsolved families, this approach identified clinically significant findings in 11 (55%) [26]. |
Q2: Which PCD genes are associated with normal ciliary ultrastructure, and why is their identification important?
A significant number of PCD-causing genes do not produce the hallmark ultrastructural defects visible under transmission electron microscopy (TEM). Identifying these genotypes is critical to avoid misdiagnosis.
Table 2: PCD Genes Associated with Normal Ciliary Ultrastructure [26] [20]
| Gene | Primary Ciliary Defect |
|---|---|
| DNAH11 | Outer dynein arm (ODA) defects that do not alter ultrastructure but impair motility [26] [20]. |
| HYDIN | Absence of central pair projection proteins; TEM appears normal due to technical limitations in visualizing the defect [26] [20]. |
| CCDC164/DRC1 | Defects in the nexin-dynein regulatory complex (N-DRC) [26]. |
| CCDC65/DRC2 | Defects in the nexin-dynein regulatory complex (N-DRC) [26]. |
Q3: What are the common pitfalls in interpreting genetic test results for PCD?
Researchers should be vigilant about several common issues:
- Variants of Uncertain Significance (VUS): Sequence changes whose clinical impact is unknown. A VUS is not a diagnostic result and should not be used to confirm or rule out PCD [27].
- False Negatives: These can occur due to variants in non-coding regions, copy number variations (CNVs) not detected by sequencing, or novel genes not yet associated with PCD [25] [26].
- Complex Genetic Results: Misinterpretation of benign variants as pathogenic can lead to misdiagnosis and inappropriate management, as seen in other genetic disorders [27].
Troubleshooting Guides
Problem: Inconclusive Genetic Results in a Patient with Strong Clinical Phenotype and Low nNO
Scenario: A patient has classic PCD symptoms and repeatedly low nasal nitric oxide (nNO), but initial genetic testing (panel or WES) does not identify biallelic pathogenic mutations.
Solution: Implement a systematic re-analysis protocol.
- Interim Diagnosis: Classify the case as "probable PCD" based on clinical phenotype and low nNO [25].
- Data Re-analysis: Re-analyze the raw sequencing data (e.g., VCF files) from the initial test. Focus on:
- Novel Genes: The list of known PCD-associated genes has grown to over 50 [20]. Regular re-analysis can uncover mutations in genes discovered after the initial test was run.
- Copy Number Variations (CNVs): Perform targeted CNV analysis on suspected genes. CNVs account for a significant number of cases and are not always detected by standard sequencing [26].
- Research Pathways: If clinically available testing remains inconclusive, consider enrolling the patient in a research study focused on gene discovery.
The following workflow diagram illustrates this troubleshooting process:
Problem: Differentiating PCD from Other Hereditary Bronchiectasis Causes
Scenario: A patient presents with diffuse bronchiectasis and chronic respiratory symptoms. Genetic testing is needed to distinguish between PCD, Cystic Fibrosis (CF), and other genetic causes.
Solution: Deploy a multi-test diagnostic algorithm that integrates WES with functional assays.
- Initial Simultaneous Testing:
- Integrated Interpretation: Correlate the genetic findings with functional test results.
- A low nNO with biallelic mutations in a PCD gene confirms PCD.
- An elevated sweat chloride level with biallelic CFTR mutations confirms CF.
- WES may identify mutations in genes such as those causing Immunodeficiency-21 [28].
Experimental Protocols
Protocol: Whole-Exome Sequencing and Analysis for PCD
This protocol outlines the key steps for using WES in a PCD research or diagnostic pipeline.
1. Sample Preparation & Sequencing
- DNA Source: Extract genomic DNA from peripheral blood leukocytes [26] [28].
- Exome Capture: Use a clinical-grade exome capture kit (e.g., Agilent SureSelectXT) to enrich for protein-coding regions [26].
- Sequencing Platform: Sequence the library on an Illumina platform (e.g., HiSeq 2500) to achieve a mean depth of coverage >100x, with >95% of target bases covered [26].
2. Bioinformatic Analysis
- Alignment: Align sequence reads to the reference human genome (hg19) using a tool like Burrows-Wheeler Aligner (BWA) [26].
- Variant Calling: Identify single nucleotide variants (SNVs) and small insertions/deletions (indels) using a pipeline like GATK [26].
- Variant Filtering & Prioritization:
- Filter for variants with a minor allele frequency (MAF) <0.01 in population databases (e.g., gnomAD, 1000 Genomes).
- Prioritize loss-of-function variants (nonsense, frameshift, splice-site) and missense variants predicted to be damaging by in silico tools (e.g., SIFT, PolyPhen-2).
- Focus on genes known to be associated with PCD and other motile ciliopathies [26] [28].
3. Copy Number Variation (CNV) Analysis
- Perform targeted CNV analysis on the WES data or using complementary methods like array comparative genomic hybridization (aCGH) to detect exon-level deletions or duplications [26].
4. Validation & Reporting
- Confirm pathogenic or likely pathogenic variants by an independent method (e.g., Sanger sequencing).
- Report findings according to ACMG guidelines, stating clearly if biallelic mutations in a PCD gene were identified [28].
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for PCD Genetic Research
| Item | Function in Research |
|---|---|
| Agilent SureSelectXT Human All Exon V4+ Capture Kit | A commercial kit used to enrich for the exonic regions of the genome prior to sequencing [26]. |
| Illumina HiSeq 2500/4000 Systems | Next-generation sequencing platforms used for high-throughput WES [26]. |
| Burrows-Wheeler Aligner (BWA) | Open-source software for aligning sequencing reads to a reference genome [26]. |
| Genome Analysis Toolkit (GATK) | A structured software package for variant discovery in high-throughput sequencing data [26]. |
| Franklin by Genoox | A commercial genomic analysis platform used for the interpretation and clinical reporting of genetic variants [28]. |
| TaqMan Copy Number Assays | Used for targeted validation of specific CNVs (e.g., exon 7 deletions in DYX1C1) identified in WES data [26]. |
Technical Troubleshooting Guide
This guide addresses common challenges encountered during HSVA experiments for Primary Ciliary Dyskinesia (PCD) research.
Table 1: Troubleshooting Common HSVA Experimental Issues
| Problem Phenomenon | Potential Causes | Recommended Solutions |
|---|---|---|
| Abnormal ciliary beat pattern/frequency in samples | Secondary damage (infection, smoking, drugs) [29] | Repeat brush biopsy at a different time; confirm identical aberration across at least two tests [29] |
| Low specificity; inconsistent results | Investigator inexperience; low sample throughput [30] | Limit HSVA to expert centres with high sample volume; utilize post-cell culture analysis [30] |
| Poor sample viability or yield | Sample processing delays; suboptimal brush biopsy [29] | Use nasal brush biopsy; suspend cells in medium; perform analysis immediately after sampling [29] |
| Difficulty identifying circular ciliary movements | Limited analysis perspective [29] | Analyze cilia from both side and top views during video evaluation [29] |
| Inability to exclude PCD despite normal HSVM | PCD variants with near-normal ciliary beating [29] [20] | Use HSVA as an adjunct test only; confirm diagnosis with TEM, genetic testing, or nNO [30] [31] |
Frequently Asked Questions (FAQs)
What is the primary diagnostic value of HSVA in PCD research, especially for patients with normal ultrastructure?
HSVA is a cornerstone for detecting functional PCD variants with normal ultrastructure, which methods like transmission electron microscopy (TEM) might miss [29]. Whereas TEM detects only 60-70% of PCD cases, HSVA can identify abnormalities in ciliary beating even when the ciliary structure appears normal under TEM, such as in cases caused by mutations in the DNAH11 gene [29] [20]. This makes it a crucial functional assay to complement structural and genetic analyses.
Why is my HSVA yielding inconsistent or non-specific results, and how can I improve accuracy?
Inconsistencies often arise from secondary ciliary damage or investigator inexperience [29] [30]. Cilia are highly sensitive to damage from infections, smoking, or other insults, which can alter the beat pattern and impair specificity [29]. To improve accuracy:
- Perform post-cell culture analysis whenever possible, as it has higher specificity compared to pre-culture testing [30].
- Ensure the analysis is conducted at a specialist centre with a high throughput of samples to maintain expertise [30].
- Repeat the test at least twice at different times to confirm persistent abnormalities [29].
What are the critical technical specifications for a valid HSVA?
A valid HSVA requires adherence to specific technical standards:
- Recording Speed: Use a high-speed video camera recording at >100 frames per second [29].
- Analysis Mode: Evaluation must be performed in real time and slow motion to qualitatively and quantitatively characterize the beat pattern, including frequency, amplitude, and waveform [29].
- Sample Type: Nasal brush biopsies are recommended for the best yield [29].
- Analysis Perspective: It is critical to observe cilia from both the side and top views to correctly identify circular movements [29].
My patient has a strong clinical phenotype, but HSVA shows normal ciliary beating. Does this rule out PCD?
No, a normal HSVM result does not exclude PCD [30]. Several PCD variants are known to have increased ciliary beat frequency or an almost normal beat pattern [29]. Therefore, HSVA should not be used as a stand-alone diagnostic test. The diagnosis must be confirmed through a combination of other methods, such as genetic testing, TEM, immunofluorescence (IF), or demonstrating reduced nasal nitric oxide (nNO) [29] [30] [31].
Experimental Protocols & Workflows
Core HSVA Protocol for Ciliary Beat Analysis
Below is a standardized workflow for measuring ciliary beat frequency (CBF) and mucociliary transport (MCT) in human airway epithelial cells, integrating key steps from current methodologies [29] [32] [33].
Protocol Details:
- Sample Collection: Obtain respiratory ciliated cells via brush biopsy from the inferior nasal turbinate. Nasal samples provide the best yield and can be easily obtained [29] [34].
- Sample Preparation: Suspend the brushed cells in culture medium and place them on a slide. The analysis should be performed as soon as possible after sampling to preserve ciliary function [29].
- High-Speed Video Recording: Record ciliary motion using a high-speed video camera connected to a microscope, capturing sequences at a frame rate of >100 frames per second [29].
- Post-Acquisition Analysis: Analyze the recorded videos in real time and slow motion. Characterize the ciliary beat pattern both quantitatively (frequency) and qualitatively (amplitude, waveform). It is crucial to observe cilia from both side and top views to identify abnormal, circular movements [29]. Utilize image processing and particle imaging velocimetry for precise quantification of CBF and MCT [32] [33].
- Data Interpretation: Compare the observed beat pattern and frequency against known pathological patterns. A diagnosis of PCD should be supported by other tests (genetics, TEM, nNO) or by demonstrating identical aberrations in repeated HSVA tests [29] [30].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for HSVA Experiments
| Item | Function/Application in HSVA |
|---|---|
| Brush Biopsy Kit | Minimally invasive collection of ciliated epithelial cells from the nasal turbinate [29]. |
| Cell Culture Medium | Suspension medium for sampled cells to maintain viability prior to and during analysis [29]. |
| High-Speed Video Microscope | Core system for capturing ciliary motion at frame rates >100 fps for detailed beat pattern analysis [29]. |
| Differential Interference Contrast (DIC) Optics | Enhances contrast in unstained, transparent ciliated samples for clearer visualization [34]. |
| Image Processing & PIV Software | For post-acquisition analysis, enabling precise quantification of ciliary beat frequency (CBF) and mucociliary transport (MCT) velocity [32] [33]. |
Frequently Asked Questions (FAQs)
Q1: What is the primary diagnostic role of nNO measurement in PCD? nNO measurement serves as a highly sensitive and specific screening tool for Primary Ciliary Dyskinesia (PCD). In cooperative patients (generally over 5 years old) with a high clinical suspicion for PCD, meta-analyses have shown that nNO testing using velum closure maneuvers has a summary sensitivity of 97.6% and specificity of 96.0% compared to the reference standards of electron microscopy (EM) and/or genetic testing. This makes it a powerful initial test in the diagnostic pathway [35].
Q2: Which respiratory manoeuvres are used for nNO sampling, and how do I choose? There are three main respiratory manoeuvres, selected based on patient age and cooperation level [36]:
- Exhalation Against Resistance (ER-nNO): The gold-standard method. It provides feedback on sustained exhalation and velum closure. Suitable for cooperative patients, generally over 5-6 years old.
- Breath-Hold (BH-nNO): An alternative method for patients who can voluntarily close their velum. It shows similar repeatability to the ER method if velum closure is achieved.
- Tidal Breathing (TB-nNO): A non-velum closure method used when patients cannot perform the other manoeuvres, such as in infants, young children (under 5-6 years), or adults with poor lung function. Note that results from this method are typically lower due to dilution from lower airway air [36].
Q3: What factors can lead to falsely low or high nNO measurements? Several patient and environmental factors can influence nNO levels and must be considered before testing [36]:
| Factor Type | Specific Factor | Impact on nNO Level |
|---|---|---|
| Patient Factors | Acute viral infection or upper/lower airway exacerbation | Falsely Low |
| Recent nasal or sinus surgery | Falsely Low | |
| Nose bleeds or recent nasal biopsy/brushing | Falsely Low | |
| Nasal obstruction (e.g., polyps, severe congestion) | Falsely Low | |
| Environmental Factors | High ambient NO levels | Falsely High |
| Technical Factors | Sampling line obstruction | Falsely Low |
| Poor seal with the nasal olive | Variable |
Q4: My patient has a strong clinical phenotype for PCD but a normal nNO level. What should I do? A normal nNO level does not completely rule out PCD. Some genetic variants, particularly those affecting ciliary central apparatus components, can present with a PCD phenotype but have nNO levels within the normal or borderline range [37] [18]. In such cases, and in all cases where clinical suspicion remains high, you should proceed with confirmatory diagnostic tests. The European Respiratory Society (ERS) guidelines recommend a multi-step diagnostic process, which includes high-speed video microscopy analysis (HSVA), transmission electron microscopy (TEM), and genetic testing [20].
Q5: What are the key differences between chemiluminescence and electrochemical nNO analyzers? The choice of analyzer is fundamental. The table below summarizes the pros and cons of each technology [36]:
| Feature | Chemiluminescence Analyzers | Electrochemical Analyzers |
|---|---|---|
| Accuracy & Precision | High accuracy and reliability [36] | Good performance [36] |
| Data Output | Real-time display of NO curve; allows for manual plateau selection and validation [36] | Results are displayed after a fixed sampling time; some models may display a non-real-time curve [36] |
| Validation | Rigorously tested with published, validated cut-off values [36] | Less published validation data available [36] |
| Ease of Use | Requires rigorous operator training and expertise [36] | Simple to use; consistent training provided [36] |
| Portability & Cost | Less portable; more expensive to purchase and maintain [36] | Smaller, portable, and more cost-effective [36] |
| Maintenance | Requires regular calibration [36] | Requires no calibration or preventative maintenance [36] |
Troubleshooting Common nNO Measurement Issues
Problem 1: Inability to Achieve a Stable Plateau during Exhalation Against Resistance
- Potential Causes: The patient may not be exhaling steadily, the resistance may be incorrect, or there could be a velum closure issue.
- Solutions:
- Ensure the patient is exhaling against the resistor (e.g., a party blower) at a pressure of 5-10 cm H₂O.
- Provide the patient with thorough coaching and a demonstration.
- Verify that the equipment (mouth resistor, sampling tube) is not blocked.
- If a stable plateau still cannot be achieved, consider switching to the breath-hold manoeuvre if the patient is able [36].
Problem 2: Consistently Low nNO Readings in a Patient Without a Typical PCD Phenotype
- Potential Causes: Refer to the table in FAQ #3. Common causes include recent respiratory infection, undetected nasal bleeding, or cystic fibrosis (CF).
- Solutions:
- Clinical History: Carefully re-evaluate the patient's recent history for signs of infection and delay testing for 2-4 weeks post-illness.
- Exclude CF: Ensure cystic fibrosis has been ruled out before interpreting low nNO as indicative of PCD [35].
- Nasal Inspection: Examine the nasal passages for obstruction, polyps, or signs of recent bleeding. Refer to an ENT specialist if obstruction is suspected [36].
- Repeat Testing: Schedule a repeat measurement on a separate day when confounding factors are minimized.
Problem 3: High Variability Between Measurements on the Same Patient
- Potential Causes: Inconsistent technique, nasal cycle variations, or equipment issues.
- Solutions:
- Standardize Technique: Ensure the same operator performs the test using a consistent protocol. The manoeuvre should be repeated twice in each nostril to assess repeatability [36].
- Patient Preparation: Instruct the patient to blow their nose thoroughly before testing. Gentle saline lavage may be used if needed, taking care not to injure the mucosa [36].
- Check Equipment: Inspect the nasal olive and sampling lines for blockages or leaks. Ensure a good seal is formed in the nostril.
nNO Diagnostic Accuracy Data
The following table summarizes the diagnostic accuracy of nNO measurement from a large meta-analysis, comparing different reference standards [35].
Table 1: Summary of nNO Diagnostic Accuracy for PCD Diagnosis [35]
| Reference Standard | Number of Studies | Sensitivity (95% CI) | Specificity (95% CI) | Positive Likelihood Ratio (95% CI) | Negative Likelihood Ratio (95% CI) |
|---|---|---|---|---|---|
| EM alone or EM/Genetic | 12 | 97.6% (92.7–99.2) | 96.0% (87.9–98.7) | 24.3 (7.6–76.9) | 0.03 (0.01–0.08) |
| EM and/or Genetic | 7 | 96.3% (88.7–98.9) | 96.4% (85.1–99.2) | 26.5 (5.9–119.1) | 0.04 (0.01–0.12) |
Experimental Protocol: nNO Measurement via Exhalation Against Resistance
This protocol is based on ERS technical standards and manufacturer guidelines for devices like the NIOX VERO [38] [36].
Principle: To aspirate air from the nasal cavity while the velum is closed, preventing contamination from low-NO air from the lower airways and providing a representative sample of nasal NO.
Equipment and Reagents:
- Chemiluminescence or approved electrochemical nNO analyzer (e.g., NIOX VERO)
- Nasal sampling kit (including nasal olives in adult and pediatric sizes)
- Disposable patient filters and mouth resistors/party blowers
- Computer with associated software for data analysis (if applicable)
Procedure:
- Patient Preparation:
- Contraindications: Do not perform if there is evidence of active nasal bleeding.
- Have the patient blow their nose thoroughly to clear nasal passages.
- Delay testing for 2-4 weeks after a respiratory infection or nasal surgery.
- The patient should avoid nitrogen-rich foods and strenuous exercise for 2 hours prior to testing [39].
Equipment Setup:
- Connect the nasal olive to the analyzer's sampling port.
- For the exhalation against resistance method, attach a new patient filter to the breathing handle. Insert a nasal restrictor into the filter.
Measurement:
- Seat the patient comfortably.
- Select the appropriate sized nasal olive and ensure an airtight seal in the nostril. Align the sampling hole with the nasal passage.
- Pass the breathing handle with the attached resistor to the patient.
- Instruct the patient to: a. Inhale deeply to total lung capacity. b. Seal their lips tightly around the patient filter. c. Exhale steadily and continuously for the duration required by the device (e.g., 30 seconds).
- Initiate the measurement on the analyzer.
- The device will aspirate nasal air for a set period (e.g., 30 seconds) and then analyze the sample.
Data Analysis:
- For chemiluminescence analyzers: Observe the real-time tracing. A valid plateau is defined as a stable exhalation for ≥3 seconds with ≤10% variation. Manually select this plateau for the final value [36].
- For electrochemical analyzers: The device may provide a result automatically. If the software allows, visualize the curve to check for a stable exhalation profile.
Reporting:
- Report the nNO value in parts per billion (ppb) or nanoliters per minute (nL/min).
- Note the measurement method (e.g., ER-nNO), the nostril tested, and the ambient NO level if recorded.
nNO Testing Workflow
The diagram below outlines the logical workflow for utilizing nNO measurement in the PCD diagnostic pathway.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials for nNO Measurement in Research
| Item | Function / Application |
|---|---|
| Chemiluminescence Analyzer (e.g., CLD 88 sp, Sievers NOA) | High-accuracy device considered the gold-standard for nNO measurement in research settings; allows real-time curve visualization [36]. |
| Electrochemical Analyzer (e.g., NIOX VERO) | Portable, cost-effective device suitable for clinical settings; simpler to operate but with limitations in real-time data inspection [38] [36]. |
| Nasal Sampling Kit | Includes tubing and disposable nasal olives of various sizes to create an airtight seal in the nostril during aspiration [38]. |
| Mouth Resistor / Party Blower | Used during the exhalation against resistance manoeuvre to generate back pressure, ensuring velum closure [36]. |
| Disposable Patient Filters | Hygienic barrier placed between the breathing handle/mouthpiece and the patient to prevent cross-contamination [38]. |
Frequently Asked Questions (FAQs)
1. What is an integrated diagnostic approach for PCD, and why is it necessary? An integrated diagnostic approach for Primary Ciliary Dyskinesia (PCD) uses a combination of tests rather than relying on a single method. This is necessary because no single test is sufficient for a definitive diagnosis in all cases. Genetic testing can identify known mutations, but up to 30% of patients with a clinical PCD picture have no identifiable mutations in known genes. Conversely, Transmission Electron Microscopy (TEM) has a diagnostic sensitivity of only about 70-75%, as a significant proportion of genetically confirmed PCD cases show normal ciliary ultrastructure [1] [40]. Integrating multiple methods maximizes sensitivity and diagnostic confidence.
2. How can we diagnose PCD when TEM results are normal? A normal TEM result does not rule out PCD. In cases of strong clinical suspicion but normal ultrastructure, the diagnostic process should proceed with other modalities. Key steps include:
- Genetic Testing: This is crucial for identifying mutations in genes known to cause PCD with normal ultrastructure, such as DNAH11 and DRC1 [40].
- Immunofluorescence (IF) Microscopy: This technique can detect the absence or mislocalization of specific ciliary proteins, which can confirm a diagnosis even when the structure appears normal under TEM [40].
- Functional Tests: High-speed video microscopy (HSVM) to analyze ciliary beat pattern and frequency, alongside nasal nitric oxide (nNO) measurement, provides functional data to support the diagnosis [40].
3. What are the common pitfalls in interpreting TEM results, and how can we avoid them? Common pitfalls include misinterpreting secondary ciliary defects (caused by infection or inflammation) as primary defects and a lack of standardized evaluation. To avoid these:
- Follow International Guidelines: Adhere to the international consensus guidelines for TEM diagnosis, which classify defects as Class 1 (confirmatory, e.g., outer dynein arm defects) or Class 2 (suggestive but requiring confirmation) [1] [40].
- Quantitative Analysis: Evaluate a sufficient number of ciliary cross-sections (e.g., >50) and report defects as a percentage. Defects in <10% of cilia are often within the normal range, while Class 1 defects are typically present in >50% of cilia [1].
- Repeat Testing: In cases of acute infection, consider repeating the nasal brushing after the infection has resolved to distinguish primary from secondary defects [1].
4. How do you validate a new integrated diagnostic algorithm in a research setting? Validation involves a prospective comparison of the algorithm's performance against a robust clinical gold standard. The process, as demonstrated in other medical fields, includes [41] [42]:
- Defining a Gold Standard: The final diagnosis is made by a panel of specialists based on a comprehensive review of all available data, including history, all test results, and imaging.
- Calculating Performance Metrics: The algorithm's diagnoses are compared to the gold standard to calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV).
- Identifying Limitations: The validation study should identify specific conditions that lead to false positives or false negatives, allowing for further refinement of the algorithm.
Troubleshooting Guides
Issue 1: Inconclusive Results from a Multi-Test Diagnostic Workflow
| Symptoms | Possible Causes | Corrective Actions |
|---|---|---|
| Conflicting results between tests (e.g., genetic variant of uncertain significance (VUS) and normal TEM). | A rare or novel genetic mutation not previously associated with PCD; secondary ciliary damage masking a primary defect. | 1. Functional Corroboration: Prioritize functional tests like HSVM and nNO. An abnormal ciliary beat pattern strongly supports a PCD diagnosis.2. Immunofluorescence: Perform IF staining targeted by the genetic result to see if the protein product is affected.3. Segregation Analysis: Test parents/siblings for the genetic variant to help determine its pathogenicity. |
| All test results are borderline or normal, but clinical phenotype is highly suggestive. | The patient may have a PCD-causing gene not covered by the genetic panel or a non-genetic mimic of PCD. | 1. Expand Genetic Analysis: Consider whole-exome or whole-genome sequencing.2. Expert Review: Have TEM images and HSVM videos re-evaluated by a central reference laboratory.3. Clinical Follow-up: Monitor disease progression and re-evaluate after a period of time or after an infection has cleared. |
Issue 2: Poor-Quality Nasal Brush Biopsy for TEM
| Symptoms | Possible Causes | Corrective Actions |
|---|---|---|
| Few or no ciliated cells in the sample. | Insufficient brushing technique; sample taken from a non-ciliated area; sample processing artifacts. | 1. Standardize Collection: Ensure the brush scrapes the inferior surface of the inferior turbinate firmly.2. Immediate Fixation: Place the brush immediately in buffered glutaraldehyde to preserve ultrastructure [1].3. Proper Handling: Gently clean the brush of adherent mucus under a dissecting microscope before processing to avoid loss of cells. |
| Poor preservation of ciliary ultrastructure (e.g., disrupted microtubules). | Delay in fixation; use of incorrect fixative or buffer; osmotic imbalance during processing. | 1. Optimize Fixative: Use 2.5% EM-grade glutaraldehyde in a 0.1 M sodium cacodylate buffer, osmotically adjusted with sucrose [1].2. Minimize Delay: Process the sample from collection to resin embedding as quickly as possible.3. Expert Processing: Ensure the TEM processing protocol, including dehydration and resin embedding, is performed by an experienced technician. |
Performance of Diagnostic Modalities in PCD
The following table summarizes the key characteristics of major PCD diagnostic tests, highlighting the need for an integrated approach.
| Diagnostic Method | Primary Function | Key Strengths | Inherent Limitations | Reported Sensitivity/Success |
|---|---|---|---|---|
| Transmission Electron Microscopy (TEM) | Visualizes ciliary ultrastructure | Identifies specific structural defects (e.g., ODA/IDA loss); considered a definitive test when Class 1 defects are found [40]. | Cannot detect functional defects; ~30% of PCD cases have normal ultrastructure; requires expertise and expensive infrastructure [1] [40]. | ~70-75% [1] [40] |
| Genetic Testing | Identifies mutations in PCD-associated genes | High specificity; can provide a definitive diagnosis and inform genotype-phenotype correlations. | ~20-30% of patients have no identified mutations; variants of uncertain significance (VUS) can be difficult to interpret [40]. | ~70-80% [40] |
| High-Speed Video Microscopy (HSVM) | Analyzes ciliary beat pattern and frequency | Directly assesses ciliary function; can diagnose PCD in cases with normal ultrastructure. | Requires specialized equipment and expert analysis; results can be affected by secondary inflammation. | Varies by center and expertise |
| Nasal Nitric Oxide (nNO) | Measures nasal NO levels | Excellent screening tool; very low nNO is highly suggestive of PCD. | Not diagnostic on its own; requires patient cooperation; can be falsely normal in some PCD cases. | High sensitivity for screening |
Experimental Protocol: Standardized TEM Analysis for PCD Diagnosis
Principle: This protocol outlines the standardized processing and evaluation of nasal brush biopsies for the ultrastructural diagnosis of PCD, based on international consensus guidelines [1] [40].
Materials:
- Nasal cytology brush (e.g., flexible nylon laparoscopy brush)
- 2.5% EM-grade glutaraldehyde in 0.1M sodium cacodylate buffer (with osmotic adjustment)
- 1% buffered osmium tetroxide
- Graded ethanol series (10%, 30%, 50%, 70%, 90%, 100%)
- Agar Scientific low viscosity resin
- Ultramicrotome
- Transmission Electron Microscope
Methodology:
- Sample Collection: After obtaining informed consent, perform a nasal brush biopsy from the inferior surface of the inferior turbinate.
- Immediate Fixation: Immediately place the brush into cold 2.5% glutaraldehyde fixative for a minimum of 2 hours.
- Sample Cleaning: Under a dissecting microscope, gently clean the brush fibers in fresh fixative to remove mucus and collect cell fragments.
- Post-fixation and Processing:
- Rinse samples 3 times in buffer (30 min each).
- Post-fix in 1% buffered osmium tetroxide for 1 hour.
- Rinse in buffer (3 x 30 min) and then in pure water for 5 min.
- Dehydrate in a graded ethanol series (10% to 100%), 30 minutes per step.
- Resin Infiltration and Embedding:
- Infiltrate with low viscosity resin using a resin:ethanol series (1:3, 1:1, 3:1) and then pure resin (overnight).
- Embed samples in fresh resin in BEEM capsules and polymerize at 70°C.
- Sectioning and Staining: Cut 70 nm ultrathin sections using an ultramicrotome. Double-stain sections with aqueous uranyl acetate (15 min) and Reynold's lead citrate (10 min).
- Imaging and Analysis:
- Examine grids under the TEM at 120kV.
- Systematically capture images of multiple ciliary cross-sections.
- Evaluate a minimum of 50-100 ciliary cross-sections per patient.
- Classify defects according to international guidelines [40]:
- Class 1 Defects (Confirmatory): Hallmark defects (e.g., ODA, ODA+IDA loss) in >50% of cilia.
- Class 2 Defects (Suggestive): Defects requiring confirmation by another method (e.g., defects in 25-50% of cilia, central complex defects).
Diagnostic Workflow and Research Reagents
Integrated PCD Diagnostic Algorithm
The following diagram illustrates the logical workflow for diagnosing PCD, emphasizing how methods are combined to achieve maximum sensitivity, especially for patients with normal ultrastructure.
Research Reagent Solutions
This table details essential materials and reagents used in the TEM and genetic diagnostic protocols.
| Item | Function/Application in PCD Research | Specific Example / Note |
|---|---|---|
| Glutaraldehyde (EM-grade) | Primary fixative for TEM; cross-links proteins to preserve ultrastructure. | Use at 2.5% in 0.1M sodium cacodylate buffer, osmotically adjusted [1]. |
| Osmium Tetroxide | Post-fixative for TEM; stabilizes lipids and provides electron density. | Typically used at 1% concentration after aldehyde fixation [1]. |
| Low Viscosity Resin | Embedding medium for TEM; allows for cutting of ultra-thin sections. | Agar Scientific low viscosity resin is a common choice [1]. |
| Nasal Cytology Brush | For obtaining ciliated epithelial cell samples from the nasal mucosa. | A flexible nylon brush with a twisted wire shaft (e.g., WS-1812XA3) [1]. |
| PCD Genetic Panel | Targeted next-generation sequencing to identify mutations in known PCD genes. | Panels should include common genes (e.g., DNAH5, CCDC39/40) and genes associated with normal ultrastructure (e.g., DNAH11, DRC1) [40]. |
| Antibodies for IF | For immunofluorescence microscopy to localize specific ciliary proteins. | Antibodies against proteins like DNAH5 (ODA) or GAS8 (nexin link) can confirm absent/mislocalized proteins [40]. |
Overcoming Diagnostic Hurdles and refining the Diagnostic Pathway
Primary Ciliary Dyskinesia (PCD) diagnosis presents significant challenges, particularly in cases with normal ultrastructure where false negatives frequently occur. International guidelines recommend a multi-faceted diagnostic approach since no single test provides 100% certainty [3]. The limitations of individual modalities become particularly problematic in research settings where accurate phenotyping is essential for valid results. This technical support center provides troubleshooting guidance for researchers encountering false negatives in PCD diagnostic assays, with special emphasis on patients with normal ultrastructure who may be misclassified as disease-negative.
Understanding False Negatives in PCD Diagnostics
The Scope of the Problem
False negatives in PCD research occur when patients with the disease receive negative test results, potentially excluding them from studies or leading to incorrect conclusions. Several factors contribute to this problem:
- Normal Ultrastructure Cases: Approximately 15-30% of genetically-confirmed PCD cases exhibit normal ciliary ultrastructure on transmission electron microscopy (TEM) [8] [43] [23]. One study of 200 confirmed PCD subjects found 67 (33.5%) had normal ultrastructure (NU) but abnormal ciliary motility [43].
- Genetic Heterogeneity: Over 40 PCD-associated genes have been identified, but current genetic panels account for only 60-70% of cases [8]. Furthermore, clinical testing is available for only about 6,000 of an estimated 20,000 human genes [44].
- Technical Limitations: Each diagnostic modality has specific limitations that can produce false negatives, particularly when used in isolation.
Table 1: Diagnostic Test Limitations in PCD Research
| Diagnostic Method | Reported False Negative Rate | Primary Limitations |
|---|---|---|
| Transmission Electron Microscopy (TEM) | 15-30% [8] [23] | Normal ultrastructure in known genetic variants (e.g., DNAH11, GAS8) |
| Genetic Testing | 30-40% [8] [44] | Incomplete gene coverage, variants of unknown significance, novel genes |
| Nasal Nitric Oxide (nNO) | Not quantified | Requires cooperation, age-dependent, not specific to PCD |
| High-Speed Video Microscopy Analysis (HSVMA) | Not quantified | Secondary damage mimics PCD, requires expertise |
Key Biological Concepts
The diagram below illustrates the relationship between genetic defects, protein expression, ciliary structure/function, and clinical presentation in PCD, highlighting points where diagnostic methods may fail:
PCD Diagnostic Challenge Pathway
Troubleshooting Guides
Genetic Testing False Negatives
Problem:
Genetic testing fails to identify biallelic mutations in patients with strong clinical phenotype of PCD.
Investigation Protocol:
- Review Test Methodology: Verify whether next-generation sequencing panels cover all known PCD genes (minimum 40 genes recommended) [45].
- Analyze Coverage: Check for low-coverage regions that might miss exonic deletions or duplications.
- Assess Variant Interpretation: Re-evaluate variants of unknown significance (VUS) using updated databases and functional prediction tools.
- Check for Technical Artifacts: Review aligned sequence data for systematic errors in GC-rich regions or homopolymer stretches.
Solutions:
- Expand Genetic Analysis: Use whole-exome or whole-genome sequencing to identify mutations in genes not included in standard panels.
- Functional Validation: Employ bioinformatic tools to assess the potential impact of VUS on protein function.
- Segregation Analysis: Confirm compound heterozygosity in family members when possible.
- Complement with Other Methods: Use immunofluorescence microscopy to detect abnormal protein localization even when genetic results are inconclusive.
TEM False Negatives in Normal Ultrastructure Cases
Problem:
Patients with strong clinical PCD phenotype show normal ciliary ultrastructure on TEM.
Investigation Protocol:
- Quantitative Analysis: Ensure evaluation of at least 50-100 ciliary cross-sections per sample [23].
- Review Sampling Technique: Verify proper nasal brushing technique from multiple sites of the nasal mucosa.
- Assess Tissue Viability: Check for secondary epithelial damage from inflammation or infection.
- Confirm Expertise: Verify that electron microscopists are specifically trained in PCD diagnosis.
Solutions:
- Ciliogenesis Culture: Establish air-liquid interface (ALI) cultures to regenerate cilia and eliminate secondary damage [43]. This method was crucial for diagnosing 39 subjects with PCD and normal ultrastructure in one study.
- Repeat Testing: Perform repeat brushings after treating secondary infections or inflammation.
- Complement with HSVMA: Use high-speed video microscopy to identify functional defects despite normal structure.
- Immunofluorescence Testing: Employ antibody staining to detect specific protein mislocalization.
Functional Assay False Negatives
Problem:
High-speed video microscopy analysis (HSVMA) fails to detect ciliary dysfunction in genetically-confirmed PCD cases.
Investigation Protocol:
- Review Sample Quality: Assess ciliary vitality and presence of secondary damage.
- Analyze Multiple Fields: Ensure examination of ciliary function from different areas of the sample.
- Verify Expertise: Confirm that analysts are trained to recognize subtle beat pattern abnormalities.
- Check Equipment Specifications: Validate that video capture rates are sufficient (typically ≥500 frames/second).
Solutions:
- Standardized Analysis Protocols: Implement quantitative ciliary beat frequency and pattern analysis software.
- Temperature Control: Maintain samples at 37°C during analysis to preserve native ciliary function.
- Multiple Sampling: Collect samples from different anatomical sites if initial results are inconclusive.
- Expert Consultation: Utilize international PCD diagnostic networks for second opinions on ambiguous cases.
Frequently Asked Questions
Q: What percentage of PCD cases have normal ultrastructure, and how does this impact diagnostic accuracy?
A: Studies indicate that 15-30% of confirmed PCD cases have normal ciliary ultrastructure on TEM [8] [23]. One center reported that 33.5% (67/200) of their diagnosed PCD patients had normal ultrastructure [43]. This significantly impacts diagnostic accuracy as TEM alone would falsely exclude these patients, highlighting the necessity of a multi-modal diagnostic approach.
Q: Why might genetic testing return false negative results in patients with classic PCD symptoms?
A: False negatives in genetic testing occur due to several factors: (1) current genetic panels cover only 60-70% of known PCD cases [8]; (2) technical limitations in detecting certain variant types (copy number variations, deep intronic mutations); (3) variants of unknown significance that are not classified as pathogenic; and (4) potentially novel PCD genes not yet associated with the disease [44].
Q: What is the role of ciliogenesis culture in reducing false negatives, and how is it implemented?
A: Ciliogenesis culture involves growing ciliated epithelial cells at air-liquid interface to regenerate cilia without secondary inflammatory damage [43]. This technique allows for analysis of primary ciliary defects by eliminating acquired abnormalities from infection or inflammation. Implementation requires:
- Establishing nasal epithelial cell cultures
- Allating cells to differentiate and form new cilia
- Re-testing ciliary ultrastructure and function after culture This method has been shown to unequivocally diagnose PCD in patients with normal ultrastructure when standard methods fail [43].
Q: How can researchers optimize patient selection to reduce false negatives in PCD studies?
A: Use validated clinical prediction tools like PICADAR (Primary Ciliary Dyskinesia Rule), which has high sensitivity (0.97) for identifying patients who require diagnostic testing [46]. Include patients with suggestive clinical features even when initial screening tests are negative, particularly those with:
- Unexplained neonatal respiratory symptoms in term infants
- Daily year-round wet cough starting in infancy
- Laterality defects (situs inversus or heterotaxy)
- Chronic otosinopulmonary symptoms despite appropriate treatment [3]
Q: What quality control measures should be implemented for HSVMA to minimize false negatives?
A: For reliable HSVMA results:
- Establish standardized protocols for sample acquisition and processing
- Implement blinded analysis by multiple experienced personnel
- Use calibrated equipment with appropriate frame rates (≥500 fps)
- Analyze multiple ciliated edges from different areas of the sample
- Correlate findings with clinical phenotype and other diagnostic tests
- Participate in external quality control programs when available [46] [8]
Research Reagent Solutions
Table 2: Essential Research Reagents for Comprehensive PCD Diagnosis
| Reagent/Resource | Application | Technical Considerations |
|---|---|---|
| Expanded PCD Gene Panels (40+ genes) | Genetic diagnosis | Essential for comprehensive screening; covers 60-70% of known cases [45] |
| Air-Liquid Interface Culture System | Ciliogenesis studies | Critical for differentiating primary from secondary ciliary defects [43] |
| Transmission Electron Microscopy Facilities | Ultrastructural analysis | Requires expertise in PCD-specific defects; quantitative analysis of 50+ cilia [23] |
| High-Speed Video Microscopy System | Ciliary function analysis | Minimum 500 fps capture rate; temperature control at 37°C essential [46] |
| Immunofluorescence Antibodies | Protein localization | Targets key ciliary proteins (DNAH5, DNAI1, GAS8) absent in specific genotypes [8] |
| Nasal Nitric Oxide Analyzer | Screening tool | Velum closure technique; age-specific reference values needed [8] |
Integrated Diagnostic Workflow
The following diagram illustrates a recommended diagnostic workflow to minimize false negatives in PCD research:
PCD Diagnostic Decision Pathway
This technical support resource provides researchers with specific methodologies to address the challenge of false negatives in PCD diagnostics, with particular emphasis on cases with normal ultrastructure. By implementing these troubleshooting guides, FAQs, and integrated workflows, research teams can improve diagnostic accuracy and ensure appropriate inclusion of patients in research studies.
Interpreting Variants of Uncertain Significance (VUS) in PCD Genes
FAQs: Navigating VUS Challenges in PCD Genetic Analysis
Q1: What constitutes a Variant of Uncertain Significance (VUS) in PCD genetics? A VUS is a genetic change whose effect on disease risk is currently unknown. In PCD, this typically occurs when a variant is identified in a known disease-associated gene, but there is insufficient evidence to classify it as clearly pathogenic or benign. This is a particular challenge in PCD, where over 50 genes are known to be involved, and approximately 20-30% of patients with clinically confirmed PCD lack identifiable pathogenic variants in known genes [47] [48].
Q2: Why is VUS interpretation particularly challenging in PCD compared to other genetic disorders? PCD presents unique interpretation challenges due to its extensive genetic heterogeneity, with mutations in more than 50 genes identified to date [20] [47]. Additionally, the absence of a gold standard diagnostic test means genetic findings cannot always be validated against a definitive clinical benchmark [49]. Furthermore, ethnic-specific variations in common pathogenic variants mean population frequency databases may not accurately reflect variant prevalence across different populations [48].
Q3: What functional evidence can help reclassify a VUS in PCD genes? Multiple lines of evidence can support reclassification:
- Transcript analysis: Demonstrating aberrant splicing through methods like minigene assays or RNA sequencing [50] [51].
- Functional ciliary studies: Using transmission electron microscopy (TEM) to show ultrastructural defects (e.g., absent dynein arms) or high-speed video microscopy analysis (HSVA) to confirm abnormal ciliary beat patterns in patient-derived cells [50] [49].
- Segregation analysis: Confirming biallelic inheritance in compound heterozygotes or homozygous states in affected individuals [50].
- In silico predictions: Computational evidence supporting a deleterious effect on the gene or gene product, though this evidence alone is typically insufficient for definitive classification [52].
Q4: How do I approach a case with a single heterozygous VUS in a PCD-associated gene? The identification of a single heterozygous VUS in an autosomal recessive disorder like PCD is often insufficient for diagnosis. In such cases:
- Pursue comprehensive genetic testing to identify a potential second variant in the same gene or in another PCD-associated gene.
- Consider copy number variation (CNV) analysis, as large deletions or duplications may not be detected by standard sequencing [51].
- Integrate results with other diagnostic methods, such as nasal nitric oxide (nNO) measurement and TEM, to build a complete clinical picture [49] [47].
Q5: What resources are available for standardizing VUS interpretation for PCD? The ClinGen Motile Ciliopathy Variant Curation Expert Panel (VCEP) is actively working to adapt and validate ACMG/AMP guidelines for specific PCD genes, starting with DNAH5. The VCEP aims to resolve variants with conflicting interpretations and develop gene-specific classification rules [53].
Troubleshooting Guides: Resolving VUS Interpretation Challenges
Table 1: Common VUS Scenarios and Recommended Actions
| Scenario | Challenge | Recommended Troubleshooting Steps | Key Analytical Tools |
|---|---|---|---|
| Missense VUS with uncertain protein impact | Inconclusive in silico predictions; no functional data. | 1. Perform segregation analysis in family members.2. Utilize protein structure modeling if available.3. Seek cross-species conservation data.4. Pursue functional studies in patient-derived cells. | PolyPhen-2, SIFT, CADD; Alamut Visual; Familial segregation |
| Non-canonical splice site VUS | Difficulty predicting impact on mRNA splicing. | 1. Conduct transcript analysis (RT-PCR) from patient nasal epithelial cells or respiratory ciliated cells.2. Employ minigene splicing assays to validate splicing defects [50] [51]. | RNA sequencing; RT-PCR; Minigene assay (e.g., in HEK293T cells) |
| Single heterozygous VUS in a recessive gene | Incomplete genetic explanation; uncertain diagnosis. | 1. Search for a second variant via CNV analysis or deep intronic sequencing.2. Correlate with functional ciliary studies (TEM, HSVA).3. Rule out other genetic mimics (e.g., cystic fibrosis, immunodeficiency). | MLPA; aCGH; Whole-genome sequencing; nNO measurement; TEM |
| VUS in a gene associated with normal ultrastructure | TEM results cannot confirm or refute variant pathogenicity. | 1. Prioritize genetic and bioinformatic evidence.2. Use high-speed video microscopy to assess ciliary beat pattern and frequency.3. Perform immunofluorescence (IF) for specific protein localization [49]. | HSVA; Immunofluorescence staining; Genetic linkage |
Table 2: Research Reagent Solutions for Key VUS Functional Assays
| Research Reagent | Application in VUS Resolution | Function & Utility |
|---|---|---|
| Nasal Epithelial Cells | Primary culture for functional ciliary analysis. | Provides patient-derived material for direct assessment of ciliary function (HSVA), ultrastructure (TEM), and transcript analysis [50] [49]. |
| HEK293T Cell Line | Model system for minigene splicing assays. | Allows for in vitro investigation of a variant's potential impact on mRNA splicing when patient RNA is unavailable [50]. |
| Anti-Dynein Antibodies (e.g., DNAH5, DNAI1) | Immunofluorescence (IF) microscopy. | Determines if a VUS causes mislocalization or absence of specific ciliary proteins, supporting a loss-of-function mechanism [49]. |
| Transmission Electron Microscope | Ultrastructural analysis of ciliary axonemes. | Identifies hallmark defects (e.g., ODA/IDA loss, microtubule disorganization) that provide strong functional evidence for pathogenicity [20] [50]. |
| High-Speed Video Microscope | Analysis of ciliary beat frequency and pattern. | Detects functional ciliary impairments even when ultrastructure appears normal, crucial for genes like DNAH11 [49] [51]. |
Experimental Protocols for VUS Resolution
Protocol 1: Minigene Splicing Assay for Splice-Site VUS
Purpose: To experimentally determine the impact of a VUS on pre-mRNA splicing.
Methodology (adapted from [50]):
- Vector Cloning: Clone genomic DNA fragments containing the VUS of interest (e.g., the exon and flanking intronic regions) into a splicing-competent vector (e.g., pSPL3).
- Site-Directed Mutagenesis: If necessary, introduce the specific nucleotide change to create the mutant construct. The wild-type sequence serves as a control.
- Cell Transfection: Transfect the wild-type and mutant minigene constructs into a suitable cell line (e.g., HEK293T cells).
- RNA Isolation and RT-PCR: After 24-48 hours, isolate total RNA from transfected cells, perform reverse transcription (RT), and amplify the resulting cDNA using vector-specific primers.
- Product Analysis: Analyze the RT-PCR products by agarose gel electrophoresis and Sanger sequencing to identify and characterize any aberrantly spliced transcripts.
Protocol 2: Integrated Functional Phenotyping for VUS
Purpose: To correlate a VUS with the cellular PCD phenotype using patient-derived cells.
Methodology (adapted from [50] [49]):
- Sample Collection: Obtain nasal epithelial cells from the patient and a healthy control using a cytobrush.
- High-Speed Video Microscopy Analysis (HSVA):
- Suspend cells in culture medium (e.g., DMEM with serum).
- Record ciliary motion using a high-speed video microscope within 1 hour of collection.
- Analyze recordings for ciliary beat frequency (CBF) and, more critically, beat pattern (CBP). Aberrations like immotility, stiff beating, or circular patterns are indicative of PCD [50] [49].
- Transmission Electron Microscopy (TEM):
- Fix the cell sample in glutaraldehyde.
- Process through post-fixation (osmium tetroxide), dehydration, and embedding.
- Section and stain with uranyl acetate and lead citrate.
- Image using TEM to assess the 9+2 microtubule ultrastructure and identify defects in dynein arms (ODA/IDA), nexin links, or radial spokes [50].
- Data Integration: Correlate the genetic finding (VUS) with the functional (HSVA) and structural (TEM) outcomes. Concordant abnormal results provide strong evidence for pathogenicity.
Case Study: Successful VUS Reclassification
Background: A 16-year-old male presented with classic PCD symptoms, including year-round productive cough, rhinosinusitis, otitis media, and situs inversus totalis. Nasal NO levels were significantly low [50].
Genetic Finding: Whole exome sequencing identified two compound heterozygous variants in DNAAF3: a missense variant c.557G>A (p.G186E) and a novel missense variant c.1364G>A (p.G455D) located at the terminal nucleotide of exon 10 [50].
VUS Resolution Strategy:
- Initial Challenge: The c.1364G>A variant was a VUS with uncertain impact.
- Functional Experiment: A minigene assay demonstrated that this variant caused aberrant splicing, leading to a four-nucleotide skipping event in exon 10.
- Phenotypic Correlation: TEM of the patient's cilia revealed the absence of both outer and inner dynein arms, and HSVA showed cilia were almost immotile.
- Outcome: The functional data provided strong evidence for pathogenicity, enabling reclassification of the VUS and confirming the molecular diagnosis of PCD [50]. This case highlights the critical role of functional assays in resolving VUS.
For researchers investigating Primary Ciliary Dyskinesia (PCD), particularly in patients with normal ultrastructure, clinical predictive tools provide essential frameworks for standardizing patient identification and recruitment. These tools help address the significant diagnostic challenge posed by PCD's genetic and clinical heterogeneity, with over 50 known associated genes and varying phenotypic presentations [20] [54]. In studies focusing on patients with normal ciliary ultrastructure—where transmission electron microscopy (TEM) fails to detect hallmark defects—these clinical instruments become particularly valuable for ensuring research cohorts include appropriately classified participants.
The diagnostic complexity of PCD stems from its multisystem involvement affecting respiratory function, organ laterality, and fertility [55] [56]. Without a single gold-standard diagnostic test, researchers must employ a combination of approaches including nasal nitric oxide (nNO) measurement, genetic testing, high-speed video microscopy analysis (HSVMA), and TEM [20] [56]. Clinical predictive tools serve as the initial stratification step in this multi-layered diagnostic process, enabling more efficient allocation of specialized diagnostic resources.
Frequently Asked Questions for Researchers
FAQ 1: Which clinical predictive tool demonstrates superior performance for research cohort identification?
Recent comparative studies indicate that the Clinical Index (CI) may outperform other tools in certain research settings. A 2021 study evaluating 1401 patients found that CI demonstrated a larger area under the ROC curve (AUC) compared to NA-CDCF, while PICADAR and NA-CDCF showed statistically equivalent performance [57]. However, tool selection should align with specific research objectives, as each instrument has distinct strengths and limitations detailed in the performance metrics table below.
FAQ 2: What are the key limitations of PICADAR when studying PCD patients with normal ultrastructure?
A 2025 pre-print study revealed significant limitations in PICADAR's sensitivity, particularly in patient subgroups relevant to normal ultrastructure research. The study of 269 genetically confirmed PCD patients found PICADAR's overall sensitivity was 75%, but this dropped substantially to 59% in patients without hallmark ultrastructural defects [58]. Additionally, PICADAR cannot be calculated for the 7% of PCD patients who do not present with daily wet cough, potentially excluding important phenotypic variants from research cohorts [58].
FAQ 3: How can researchers optimize patient stratification when using these clinical tools?
Combining clinical predictive tools with nasal nitric oxide (nNO) measurement significantly enhances predictive power for all major instruments [57]. The 2021 study demonstrated that nNO measurement improved diagnostic accuracy when used alongside CI, PICADAR, and NA-CDCF. For research protocols, implementing a sequential approach—using clinical tools for initial screening followed by nNO measurement—can optimize resource allocation while maintaining comprehensive phenotyping.
FAQ 4: What methodological considerations are crucial when applying these tools in adult populations?
Recall bias presents a significant challenge when using these tools in adult populations, particularly for PICADAR which requires accurate neonatal history including gestational age, NICU admission, and specific neonatal respiratory symptoms [57]. NA-CDCF may offer practical advantages in adult research settings as it doesn't require detailed neonatal history for application.
Performance Metrics of Major Clinical Predictive Tools
Table 1: Comparative Performance Characteristics of PCD Clinical Predictive Tools
| Tool | Sensitivity | Specificity | AUC | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| PICADAR | 90% [59] (derivation), 75% [58] (validation) | 75% [59] (derivation) | 0.91 (derivation) [59], 0.87 (validation) [59] | Good overall performance in derivation cohort; includes specific neonatal parameters | Requires detailed neonatal history; excludes patients without daily wet cough (7% of PCD) [58]; lower sensitivity in normal ultrastructure (59%) [58] |
| NA-CDCF | 80% (2 features), 21% (4 features) [56] | 72% (2 features), 99% (4 features) [56] | Not specified | Simple application; high specificity with 4 features | Low sensitivity with 4 features; may miss many true PCD cases |
| Clinical Index (CI) | Varies by cutoff (5-point scale) [57] | Varies by cutoff (5-point scale) [57] | Larger than NA-CDCF (p=0.005) [57] | No need for laterality assessment; all data from patient history | Less validation in diverse populations; limited use in infants |
Table 2: Component Analysis of PCD Clinical Predictive Tools
| Tool | Number of Items | Neonatal Components | Laterality Assessment | Respiratory Components | ENT Components |
|---|---|---|---|---|---|
| PICADAR | 7 plus initial daily wet cough requirement [59] | Gestational age, neonatal chest symptoms, NICU admission [59] | Situs inversus, congenital cardiac defect [59] | Persistent wet cough [59] | Chronic rhinitis, ear symptoms [59] |
| NA-CDCF | 4 [56] | Unexplained neonatal respiratory distress [56] | Laterality defects [56] | Early-onset year-round wet cough [56] | Early-onset year-round nasal congestion [56] |
| Clinical Index (CI) | 7 [57] | Significant respiratory difficulties after birth [57] | None [57] | Pneumonia, recurrent bronchitis, antibiotic use [57] | Early rhinitis, nasal discharge/obstruction, otitis media [57] |
Experimental Protocols for Tool Implementation
Protocol 1: Implementing PICADAR in Research Settings
Methodology: PICADAR application requires a structured approach beginning with the initial screening question about persistent daily wet cough. For patients meeting this criterion, seven parameters are assessed: full-term gestation, neonatal chest symptoms, neonatal intensive care admission, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defects [59]. Each parameter is assigned a points value, with a recommended cutoff score of ≥5 points indicating high PCD probability [59].
Technical Considerations: Researchers should standardize neonatal history collection methods, recognizing that retrospective data may be subject to recall bias. For situs assessment, documentation of method (physical exam, imaging) should be consistently recorded. Congenital cardiac defect verification should distinguish between clinical diagnosis and echocardiogram confirmation.
Validation Steps: In research protocols, all patients should undergo definitive diagnostic testing regardless of PICADAR scores to avoid verification bias. For studies focusing on normal ultrastructure PCD, researchers should anticipate lower sensitivity and plan for supplemental recruitment strategies.
Protocol 2: Integrating nNO with Clinical Predictive Tools
Methodology: Nasal nitric oxide measurement should be performed using standardized protocols with chemiluminescence analyzers. The tidal breathing technique is appropriate for younger children, while velum closure techniques can be used in cooperative patients ≥5 years old [56]. Consistent sampling flow rates (5 mL·s⁻¹) and equipment calibration are essential for reproducible results.
Interpretation Framework: The American Thoracic Society recommends nNO <77 nL·min⁻¹ on two separate occasions as diagnostic in high-probability patients [56]. For research classification, consider tiered interpretation: definitive (<77 nL·min⁻¹), indeterminate (77-200 nL·min⁻¹), and unlikely (>200 nL·min⁻¹), with adjustments for age and technical factors.
Integration with Clinical Tools: For optimal efficiency, implement sequential testing: clinical tool application first, followed by nNO measurement in intermediate-probability patients. High-probability patients on clinical tools can proceed directly to definitive diagnostic testing, while nNO can help stratify intermediate-probability patients.
Research Reagent Solutions for PCD Diagnostic Confirmation
Table 3: Essential Research Materials for PCD Diagnostic Confirmation
| Reagent/Equipment | Primary Function | Research Application | Technical Notes |
|---|---|---|---|
| Transmission Electron Microscope | Ultrastructural analysis of ciliary components [20] | Identification of hallmark defects (ODA, IDA, MTD, CP defects) [20] | Requires specialized expertise; normal ultrastructure does not exclude PCD [56] |
| High-Speed Video Microscope | Ciliary beat pattern and frequency analysis [20] | Functional assessment of ciliary motility | Should be repeated after air-liquid interface culture to exclude secondary dyskinesia [56] |
| Nasal Nitric Oxide Analyzer (chemiluminescence) | Measurement of nNO production [56] | Screening and diagnostic support | Values <77 nL·min⁻¹ supportive of PCD in cooperative patients ≥5 years [56] |
| Next-Generation Sequencing Panel (>39 PCD genes) [57] | Genetic confirmation of PCD [20] | Definitive diagnosis, particularly in normal ultrastructure cases | Essential for patients with normal ultrastructure; panels should include recently discovered genes |
| Immunofluorescence Assays | Protein localization in ciliary structure [20] | Secondary confirmation of genetic findings | Particularly valuable when genetic variants are of uncertain significance |
Diagnostic Pathway for PCD Research
The following workflow illustrates the integrated application of clinical predictive tools within a comprehensive PCD diagnostic research framework:
Troubleshooting Guide for Research Implementation
Challenge: Low sensitivity of PICADAR in normal ultrastructure cohort
- Root Cause: PICADAR's development emphasized classic PCD presentations with laterality defects and hallmark ultrastructural abnormalities [58]
- Solution: Implement complementary recruitment strategies using multiple clinical tools, particularly focusing on patients with strong respiratory phenotype but normal situs
Challenge: Incomplete neonatal history in adult research participants
- Root Cause: PICADAR requires specific neonatal parameters that may be poorly documented in adult medical records [57]
- Solution: Utilize NA-CDCF or Clinical Index as alternative tools, or develop study-specific criteria that acknowledge this limitation
Challenge: Discordant results between clinical tools and definitive testing
- Root Cause: PCD's phenotypic heterogeneity means some patients lack classic clinical features [55] [58]
- Solution: Maintain multidisciplinary adjudication process with consideration of all available clinical, microscopic, and genetic data
Challenge: Verification bias in study recruitment
- Root Cause: Selective application of definitive testing only to high-probability patients
- Solution: Implement consecutive recruitment with uniform diagnostic testing regardless of clinical tool scores
FAQs: Troubleshooting mRNA Analysis in PCD Diagnostics
1. How can I ensure the integrity and purity of my mRNA samples for accurate diagnostic analysis?
Ensuring mRNA integrity is critical. Use capillary gel electrophoresis (CGE) or a fragment bioanalyzer to assess RNA length and size distribution. Your sample should show a clear peak for full-length mRNA. For purity, utilize ion-pair reversed-phase liquid chromatography (IP-RP LC) to separate mRNA from impurities like truncated RNA species or abortive transcripts. Double-stranded RNA (dsRNA) impurities, which can trigger unwanted immune responses, should be detected using gel electrophoresis or enzyme-linked immunosorbent assays (ELISA) [60].
2. What are the key quality attributes to check for in vitro transcribed (IVT) mRNA?
A comprehensive quality control check should include [60]:
- Integrity: Confirm the sample contains full-length mRNA with minimal degradation products.
- Identity: Verify the correct mRNA sequence via RT-PCR-Sanger sequencing or direct RNA sequencing.
- Capping Efficiency: Ensure a high percentage of mRNA molecules possess the 5' cap, essential for translation, typically measured by HPLC-UV/MS.
- Poly(A) Tail Length: Analyze the length of the poly(A) tail, crucial for stability, also via HPLC-UV/MS.
- Functionality: Validate protein translation efficiency through in vitro translation assays or Western blotting.
3. My mRNA samples are degrading rapidly. What steps can I take to improve stability?
mRNA is inherently unstable and prone to degradation by ribonucleases (RNases). To improve stability [60]:
- Use Modified Nucleosides: Incorporate stable nucleosides like pseudouridine (Ψ) or 5-methylcytidine (5mC) during transcription.
- Ensure Proper Capping: A complete 5' cap structure is vital for protecting the mRNA from exonuclease degradation.
- Maintain Cold Chain: Always store and handle mRNA samples on ice or at frozen temperatures.
- Use Nuclease-Free Reagents: Ensure all buffers, water, and plasticware are certified nuclease-free.
FAQs: Troubleshooting Immunofluorescence (IF) for PCD Protein Localization
1. I am getting high background fluorescence in my IF samples. How can I reduce this?
High background is a common issue. Address it by [61]:
- Optimize Blocking: Use an appropriate blocking buffer (e.g., Bovine Serum Albumin or normal serum from the host species of your secondary antibody) for a sufficient time (typically 30-60 minutes) to cover non-specific binding sites.
- Titrate Antibodies: High concentrations of primary or secondary antibodies are a frequent cause of background. Perform a dilution series to find the optimal concentration.
- Improve Washing: Increase the number and duration of washes with an appropriate buffer (e.g., PBS with a mild detergent like Tween-20) after each antibody incubation step.
- Check Antibody Specificity: Ensure your primary antibody is specific for the target antigen in your sample type (e.g., human respiratory cells).
2. My IF signal is weak or absent, even though my target is expected to be present. What should I do?
A weak signal can result from several factors [61]:
- Antigen Retrieval: For formalin-fixed paraffin-embedded (FFPE) samples, epitopes are often masked. Implement a Heat-Induced Epitope Retrieval (HIER) method using a high-pH buffer (e.g., Tris-EDTA) to break cross-links and unmask the antigen.
- Fixation Issues: Over-fixation can destroy epitopes. Optimize fixation time and method. For IF, 4% paraformaldehyde is often preferred.
- Antibody Validation: Confirm that your antibody is compatible with IF and works for your specific application and species. Check the manufacturer's datasheet.
- Signal Amplification: Consider using a tyramide-based signal amplification system or a polyclonal secondary antibody, which can bind multiple epitopes on the primary antibody to enhance the signal [61].
3. When should I choose confocal microscopy over standard epifluorescence microscopy for my IF analysis?
The choice depends on your experimental needs and the availability of resources [62]:
- Use Epifluorescence (EF) Microscopy for routine analysis of bright, abundant targets and for high-throughput imaging. It is faster and more cost-effective. A study comparing RNAScope (mRNA) and IHC analysis found EF sufficient for quantifying mRNA expression with relatively low puncta per cell [62].
- Use Confocal Microscopy when you need higher resolution, reduced background blur, and the ability to create Z-stacks for 3D reconstruction. It is preferable for targets with low abundance, for detailed subcellular localization, and when imaging thicker samples. The same study noted that confocal microscopy provided clearer definition for protein relationships and was better at detecting statistically significant changes in some low-abundance protein targets [62].
Advanced Applications: Integrating mRNA and Protein Analysis
1. How can I simultaneously analyze mRNA and protein expression in the same PCD patient sample?
The immunoFISH technique allows for the simultaneous in situ analysis of specific mRNA transcripts and proteins within a single cell or tissue sample [63].
- Workflow: The sample is first processed for immunofluorescence to detect the protein of interest (e.g., a ciliary protein). Subsequently, the same sample is subjected to RNA fluorescence in situ hybridization (FISH) using labeled oligonucleotide probes that target the mRNA of interest (e.g., the mRNA transcript of the same ciliary protein or a mutated gene) [63].
- Troubleshooting Tip: The order of protocols and fixation conditions are critical. Ensure the IF protocol is compatible with the subsequent FISH procedure to preserve both protein antigenicity and RNA integrity.
Quantitative Data for Diagnostic Assay Development
Table 1: Key Analytical Techniques for mRNA Quality Control in Diagnostics [60]
| Quality Attribute | Analytical Technique | Key Performance Metric |
|---|---|---|
| Integrity & Purity | Capillary Gel Electrophoresis (CGE) | Percentage of full-length mRNA |
| Identity | RT-PCR-Sanger Sequencing / Direct RNA Sequencing | 100% sequence verification |
| Capping Efficiency | High-Performance Liquid Chromatography (HPLC-UV/MS) | >90% capping efficiency |
| Poly(A) Tail Length | HPLC-UV/MS | Consistent, defined tail length |
| dsRNA Impurities | Gel Electrophoresis / ELISA | Below detection threshold |
Table 2: Comparison of Microscopy Modalities for Spatial Analysis [62] Data derived from a comparative study on RNAScope and IHC quantification in rat hindbrain.
| Microscopy Type | Best For | Relative Imaging Speed | Key Finding in Puncta Analysis |
|---|---|---|---|
| Epifluorescence | Abundant mRNA/protein targets; high-throughput | Fast | Sufficient for mRNA with relatively low puncta per cell |
| Confocal | Low-abundance targets; 3D structure; reduced background | Slow | Clearer protein definition; superior for low-producing targets |
Experimental Protocols
Protocol 1: Basic Immunofluorescence Staining for Cultured Respiratory Cells [61]
- Fixation: Culture cells on glass coverslips. Aspirate media and wash with PBS. Fix cells with 4% paraformaldehyde in PBS for 15 minutes at room temperature.
- Permeabilization: Permeabilize cells with 0.1% Triton X-100 in PBS for 10 minutes.
- Blocking: Incubate cells with a blocking solution (e.g., 1-5% BSA in PBS) for 30-60 minutes to prevent non-specific antibody binding.
- Primary Antibody Incubation: Apply the primary antibody diluted in blocking buffer onto the coverslip. Incubate in a humidified chamber for 1-2 hours at room temperature or overnight at 4°C.
- Washing: Wash the coverslip 3 times for 5 minutes each with PBS.
- Secondary Antibody Incubation: Apply the fluorophore-conjugated secondary antibody (specific to the host species of the primary antibody) diluted in blocking buffer. Incubate for 1 hour at room temperature in the dark.
- Final Wash and Mounting: Wash 3 times for 5 minutes with PBS. Counterstain nuclei with DAPI if desired. Mount the coverslip onto a glass slide using an antifade mounting medium.
Protocol 2: Integrated immunoFISH for Concurrent mRNA and Protein Detection [63]
- Perform Immunofluorescence: First, complete steps 1-7 of the basic IF protocol above.
- Post-Fixation: After the final IF wash, post-fix the cells with 4% PFA for 10 minutes to stabilize the antibodies during the FISH procedure.
- Hybridize FISH Probes: Apply the labeled oligonucleotide FISH probes (designed against your target mRNA) in a hybridization buffer to the sample. Incubate overnight at 37°C in a dark, humidified chamber.
- Stringency Washes: The next day, perform stringent washes with a saline-sodium citrate (SSC) buffer to remove unbound or non-specifically bound probes.
- Final Mounting and Imaging: Mount the sample and image using an appropriate fluorescence microscope (epifluorescence or confocal).
Visualizing the Diagnostic and Experimental Workflow
Diagram 1: PCD Diagnostic Pathway for Normal Ultrastructure
Diagram 2: Integrated mRNA & Protein Analysis Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for mRNA and Immunofluorescence Analysis
| Reagent / Material | Function / Application | Example Use in PCD Research |
|---|---|---|
| Anti-DNAH5 / DNAI1 Antibodies | Detect outer dynein arm proteins via IF | Localize ODA proteins in respiratory cilia; confirm absence in specific PCD genotypes [20]. |
| Oligonucleotide FISH Probes | Target specific mRNA transcripts for visualization | Quantify transcripts from PCD-associated genes (e.g., DNAH11, HYDIN) in situ, even when ultrastructure is normal [20] [63]. |
| High-Speed Video Microscopy | Analyze ciliary beat frequency and pattern | Functional assessment of ciliary motion, which can be abnormal even with normal TEM results [20] [8]. |
| Formalin-Fixed Paraffin-Embedded (FFPE) Tissue | Preserves tissue morphology for retrospective studies | Enables analysis of vast archives of patient samples using IF and RNA-FISH techniques [64]. |
| Multiplex Imaging Platforms (e.g., GeoMx DSP) | Simultaneously profile multiple RNA and/or protein targets from a single tissue section | Comprehensive profiling of the respiratory epithelium to study cell-specific expression of PCD-related molecules [64]. |
Benchmarking Success: Validating Tools and Comparing Therapeutic Implications
Patient-Reported Outcome (PRO) instruments are essential tools in clinical research that capture the patient's own perspective on their health status. For individuals with Primary Ciliary Dyskinesia (PCD), a rare genetic respiratory disorder, the Quality of Life-Primary Ciliary Dyskinesia (QOL-PCD) instrument serves as the first disease-specific health-related quality of life measure developed specifically for this population [65]. The validation of such instruments is particularly crucial for research involving patients with PCD who present with normal ciliary ultrastructure – a diagnostic challenge where patient-reported symptoms may provide critical insights not revealed through structural analysis alone.
The development and validation of PROs like QOL-PCD follow rigorous methodological guidelines to ensure they reliably measure what they intend to measure [66]. For PCD research, especially studies focusing on patients without hallmark ultrastructural defects, properly validated PROs become indispensable for evaluating treatment effectiveness, monitoring disease progression, and capturing the full impact of the condition on patients' lives.
Instrument Validation and Psychometric Properties
The QOL-PCD instrument was developed in multiple versions for different age groups and underwent comprehensive validation to establish its psychometric properties. The validation process followed established guidelines for patient-reported outcome measures [66] and demonstrated that QOL-PCD performs reliably across diverse clinical settings.
Quantitative Validation Data
Table 1: Psychometric Properties of QOL-PCD Instruments Across Age Groups
| Age Version | Number of Items | Internal Consistency (Cronbach's α) | Test-Retest Reliability (ICC) | Domains Measured |
|---|---|---|---|---|
| Adult [65] | 40 items | 0.74-0.94 | 0.73-0.96 | Physical, emotional, role and social functioning, treatment burden, vitality, health perceptions, upper respiratory, lower respiratory, and ears/hearing symptoms |
| Adolescent [67] | 34-38 items | Good internal consistency (specific ranges not provided) | 0.71-0.89 | Physical, emotional & social functioning, treatment burden, role, vitality, upper respiratory, lower respiratory, ears and hearing symptoms |
| Child [67] | 34-38 items | Good internal consistency (specific ranges not provided) | Stability demonstrated across all scales | Physical, emotional & social functioning, treatment burden, role, vitality, upper respiratory, lower respiratory, ears and hearing symptoms |
| Parent-Proxy [67] | 34-38 items | 0.62-0.86 | Stability demonstrated across all scales | Physical, emotional & social functioning, treatment burden, role, vitality, upper respiratory, lower respiratory, ears and hearing symptoms |
Validation Methodology
The validation of QOL-PCD followed a rigorous multi-step process:
Initial Item Development: The prototype instruments contained 49 items for adults and slightly different numbers for other age groups, based on comprehensive development work [65] [67].
Multitrait Analysis: Researchers used multitrait analysis to evaluate how items loaded on hypothesized scales. This analysis led to the removal of 9 items from the adult version and 3-6 items from pediatric versions, resulting in the final instruments [65] [67].
Reliability Testing:
Validity Assessment:
- Convergent validity was established by demonstrating strong correlations between QOL-PCD scales and similar constructs on established generic questionnaires (e.g., lower respiratory symptoms and SGRQ-C [r=0.72, p<0.001]) [65].
- Divergent validity was shown through weak correlations between measures of different constructs [65].
- Known-groups validity was evidenced by significant correlations between QOL-PCD scores and clinical parameters like age and FEV₁ [65].
QOL-PCD Validation Workflow Diagram
Troubleshooting Guides and FAQs for Researchers
Implementation in Clinical Trials
Q: What are the specific considerations when implementing QOL-PCD in clinical trials involving PCD patients with normal ultrastructure?
A: When studying PCD patients with normal ciliary ultrastructure, particular attention should be paid to the respiratory symptoms domains of QOL-PCD. These patients often have preserved lung function but still experience significant symptoms [20]. Researchers should:
- Ensure adequate sample size to detect meaningful differences in this subgroup
- Pay particular attention to the upper and lower respiratory symptoms scales
- Consider more frequent administration to capture symptom variability
- Correlate PRO data with objective measures like nasal NO and lung function tests
Q: How should researchers handle missing data in QOL-PCD assessments?
A: The multitrait analysis during validation provides guidance on how items cluster within domains. If limited missing data occurs within a scale, imputation methods can be considered based on the strong internal consistency of each scale (Cronbach's α: 0.74-0.94) [65]. However, protocols should prioritize complete data collection through:
- Training site staff on proper administration
- Implementing electronic data capture with required fields
- Establishing clear stopping rules for when assessments become invalid due to missing items
Q: What is the minimal clinically important difference (MCID) for QOL-PCD scales?
A: While specific MCID values for QOL-PCD require further research, researchers can interpret changes in context with other measures. The strong correlations between QOL-PCD scales and established instruments like SGRQ-C (r=0.72) provide preliminary benchmarks [65]. For trial planning, conservative estimates of 0.3-0.5 standard deviations per scale are recommended until disease-specific MCIDs are established.
Technical and Methodological Issues
Q: How does the validation of pediatric versions differ from the adult QOL-PCD?
A: Pediatric versions (child, adolescent, and parent-proxy) underwent similar but developmentally appropriate validation processes [67]. Key differences include:
- Age-appropriate wording and response formats
- Inclusion of parent-proxy reporting to capture observer perspective
- Slightly different scale structures reflecting developmental differences
- Validation against pediatric-specific generic measures rather than adult instruments
Q: What cultural adaptation is needed when implementing QOL-PCD in international trials?
A: The initial validation studies were conducted across multiple centers in the UK and North America, demonstrating cross-cultural performance [67]. For broader international use:
- Forward-backward translation following ISPOR guidelines is recommended
- Cognitive debriefing with patients in new cultural contexts
- Verification of measurement invariance across language versions
- Potential recalibration of symptom frequency descriptors that may vary culturally
Q: How should researchers analyze and interpret multi-domain QOL-PCD data?
A: The instrument's multi-domain structure requires specific analytical approaches:
- Consider both individual domain scores and overall patterns
- Account for multiple comparisons when testing across domains
- Utilize multivariate methods to capture correlated changes across domains
- Pre-specify primary domains of interest in trial protocols to avoid selective reporting
Application in PCD with Normal Ultrastructure Research
Diagnostic Challenges and PRO Integration
PCD patients with normal ciliary ultrastructure present particular diagnostic challenges, as standard transmission electron microscopy (TEM) fails to identify structural defects despite clinical symptoms [20] [40]. In these cases, PRO instruments like QOL-PCD provide essential complementary data for both diagnosis and monitoring disease progression.
Table 2: Correlating QOL-PCD Domains with Diagnostic Findings in Normal Ultrastructure PCD
| QOL-PCD Domain | Relevance to Normal Ultrastructure PCD | Correlative Diagnostic Tests |
|---|---|---|
| Upper Respiratory Symptoms | Captures chronic rhinosinusitis symptoms despite normal ciliary structure | Nasal nitric oxide measurement, sinus imaging |
| Lower Respiratory Symptoms | Documents bronchiectasis symptoms and cough frequency | Chest CT, pulmonary function tests |
| Ears and Hearing Symptoms | Tracks otitis media impact and hearing fluctuations | Audiometry, tympanometry |
| Treatment Burden | Quantifies healthcare utilization and treatment adherence | Medication records, healthcare visits |
| Emotional Functioning | Assesses psychological impact of diagnostic uncertainty | Psychological assessments |
Research Protocol for PRO Implementation
For researchers studying PCD with normal ultrastructure, the following detailed protocol ensures proper implementation of QOL-PCD:
Subject Recruitment and Eligibility
- Include patients with confirmed PCD diagnosis despite normal ultrastructure based on genetic testing or functional assessments
- Document specific genetic mutations (e.g., DNAH11) associated with normal ultrastructure
- Record prior diagnostic journey including failed TEM diagnoses
Assessment Timeline
- Baseline: Administer QOL-PCD at study entry alongside comprehensive clinical assessment
- Follow-up: Schedule administrations at regular intervals (3-6 months) consistent with the instrument's test-retest reliability parameters
- Endpoint: Ensure final assessment captures intervention effects or natural history progression
Data Collection Procedures
- Train site staff in standardized administration using manual and training materials
- Use consistent mode of administration (electronic or paper) throughout study
- Implement quality checks for completeness at time of administration
- Document concurrent clinical events that might influence PRO scores
Analysis Plan
- Pre-specify primary QOL-PCD domains of interest based on study objectives
- Account for multiple domains in statistical power calculations
- Include appropriate covariates in models (age, disease duration, genetic subtype)
- Plan sensitivity analyses for missing data and different scoring approaches
PRO Integration in Normal Ultrastructure Research
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Methods for QOL-PCD Research
| Research Tool | Specification/Function | Application in PCD Research |
|---|---|---|
| QOL-PCD Adult Version | 40-item validated instrument with 10 domains | Primary outcome measure in adult clinical trials and observational studies |
| QOL-PCD Pediatric Versions | Age-adapted forms for children, adolescents, and parent-proxy | Pediatric clinical trials and natural history studies |
| Generic PRO Comparators | SF-36, SGRQ-C, SNOT-20 | Validation of convergent validity and comparison with other respiratory diseases |
| Clinical Data Forms | Standardized case report forms | Collection of concomitant clinical data for correlation with PRO scores |
| Electronic Data Capture | REDCap or similar validated systems | Efficient administration, data management, and quality control |
| Statistical Analysis Packages | R, SAS, or SPSS with appropriate licenses | Psychometric analysis and interpretation of multi-domain data |
| Translation Protocols | ISPOR PRO Translation Guidelines | Cross-cultural adaptation for international studies |
The QOL-PCD instrument represents a significant advancement in PCD research, providing a validated disease-specific measure that is particularly valuable for studying patients with normal ciliary ultrastructure. Its robust psychometric properties, including high internal consistency, test-retest reliability, and demonstrated validity, support its use as an endpoint in clinical trials and observational studies.
For the specific context of PCD with normal ultrastructure research, QOL-PCD addresses critical gaps in traditional diagnostic approaches by quantifying the patient experience of this complex disease. As research in this field evolves, particularly with emerging genetic understandings and therapeutic developments [20], properly validated PRO instruments will play an increasingly important role in capturing treatment benefits and documenting the natural history of this challenging condition.
Researchers implementing QOL-PCD should adhere to the methodological considerations outlined in this guide to ensure data quality and interpretability, ultimately advancing both clinical care and therapeutic development for individuals with PCD.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder inherited predominantly in an autosomal recessive manner, affecting the structure and function of motile cilia [20]. This leads to impaired mucociliary clearance, resulting in recurrent respiratory tract infections, chronic rhinosinusitis, otitis media, bronchiectasis, and infertility [20]. A key diagnostic and pathological feature in PCD is the classification of cases based on whether they display ultrastructural defects (visible abnormalities in ciliary axoneme structure when viewed with transmission electron microscopy) or normo-ultrastructural defects (normal axoneme structure but impaired ciliary function) [20] [68]. This distinction has significant implications for disease progression, diagnostic approach, and potentially therapeutic strategies. The prevalence of PCD is estimated at 1:7,500–1:20,000 live births, though the true rate is likely higher due to diagnostic challenges [20]. Understanding the differences between these two forms is crucial for researchers and clinicians developing targeted interventions.
Genetic Foundations and Molecular Mechanisms
The genetic basis of PCD is highly complex, with mutations in over 50 identified genes encoding ciliary proteins [20] [69]. These genetic defects manifest differently in ultrastructural versus normo-ultrastructural PCD, driving distinct pathological mechanisms and clinical presentations.
Ultrastructural Defect Genetics
Ultrastructural PCD cases involve mutations in genes that encode structural components of the ciliary axoneme, leading to observable defects under transmission electron microscopy (TEM) [20]. These include:
- Outer Dynein Arm (ODA) Defects: Associated with mutations in DNAH5, DNAI1, DNAI2, DNAL1, CCDC114, CCDC151, ARMC4, TXNDC3, and TTC25 [20]. DNAH5 is the most frequently mutated gene and a leading genetic cause of PCD [20].
- Combined ODA and Inner Dynein Arm (IDA) Defects: Caused by mutations in DNAAF1-3, HEATR2, LRRC50, DYX1C1, ZMYND10, SPAG1, CCDC103, C21orf59, C11orf70, PIH1D3, and LRRC6 [20].
- IDA Defects: Associated with KTU mutations [20].
- Microtubule Disorganization (MTD): Linked to mutations in CCDC39, CCDC40, GAS8, RSPH9, and RSPH4A [20]. Mutations in CCDC39 and CCDC40 lead to more severe disease progression with greater tendency to bronchiectasis [20].
- Central Pair (CP) Defects: Associated with HYDIN mutations [20].
Normo-Ultrastructural Defect Genetics
Normo-ultrastructural PCD cases involve mutations in genes that affect ciliary function without disrupting the visible "9+2" microtubule arrangement. Key examples include:
- DNAH11 Mutations: These alterations do not alter cilia ultrastructure but impair motility, often presenting with relatively preserved lung function [20].
- CFAP54 Mutations: Recent research has identified CFAP54 as a novel PCD-related gene where compound heterozygous mutations cause PCD with normal ultrastructure [68]. A study demonstrated that patients with CFAP54 mutations presented with bronchiectasis, impaired lung function, and infertility, despite normal ciliary ultrastructure [68].
- GAS8 Mutations: Associated with microtubule disorganization but may present with subtle ultrastructural changes [20].
Table 1: Genetic Classification of PCD Based on Ultrastructural Phenotype
| Ultrastructural Category | Defect Type | Representative Mutated Genes | Key Functional Impact |
|---|---|---|---|
| Ultrastructural Defects | ODA | DNAH5, DNAI1, DNAI2 | Loss of motor protein function |
| ODA+IDA | DNAAF1-3, LRRC50, ZMYND10 | Disrupted dynein arm assembly | |
| IDA | KTU | Impaired inner arm function | |
| MTD | CCDC39, CCDC40 | Disorganized microtubule arrangement | |
| CP | HYDIN | Abnormal central pair structure | |
| Normo-Ultrastructural Defects | Normal EM appearance | DNAH11 | Abnormal ciliary beating pattern |
| Normal EM appearance | CFAP54 | Reduced ciliary beat frequency | |
| Subtle MTD | GAS8 | Mild structural disruption |
Clinical Progression and Disease Phenotypes
Disease progression differs significantly between ultrastructural and normo-ultrastructural PCD variants, impacting both the trajectory and severity of clinical manifestations across the patient's lifespan.
Respiratory Progression
The cycle of infection and inflammation drives progressive lung damage in all PCD forms, but the rate and pattern differ:
- Ultrastructural PCD with MTD Defects: Patients with mutations in CCDC39 and CCDC40 experience more rapid progression, with greater changes on chest CT scans and increased tendency to bronchiectasis compared to those with isolated ODA defects [20].
- Normo-Ultrastructural PCD with DNAH11 Mutations: Typically follows a milder course with relatively preserved lung function [20].
- General Progression Patterns: Children with PCD experience approximately 3.1 respiratory exacerbations per person annually, with the number increasing with age, disease severity, and chronic Pseudomonas aeruginosa infection [69]. Approximately 25% of children fail to recover baseline lung function within 3 months after an exacerbation [69].
Laterality and Extrapulmonary Manifestations
Laterality defects (situs inversus or heterotaxy) occur in approximately half of PCD patients due to dysfunction of embryonic nodal cilia [20]. The relationship between ultrastructural type and laterality defects varies:
- CP Defects: Mutations in RSPH9, RSPH4A, and HYDIN that cause central pair defects do not carry a risk of situs inversus, as embryonic nodal cilia naturally lack a central pair [20].
- Other Defect Types: Most other ultrastructural and normo-ultrastructural forms can present with laterality defects depending on their specific impact on nodal cilia function.
Fertility Implications
Infertility affects both males and females with PCD due to impaired function of sperm flagella and fallopian tube cilia [68] [70]. Research on CFAP54-related PCD demonstrated significant impacts on spermatogenesis, with mutant mice and human patients showing shortened or absent sperm flagella and disrupted axonemal assembly despite normal respiratory cilia ultrastructure [68].
Table 2: Comparative Clinical Progression in PCD Subtypes
| Clinical Feature | Ultrastructural PCD | Normo-Ultrastructural PCD |
|---|---|---|
| Lung Function Decline | Accelerated in MTD defects (~1.95% FEV1 decline per hospitalization) [69] | Milder progression in DNAH11 mutations [20] |
| Bronchiectasis Development | Earlier and more severe in CCDC39/CCDC40 mutations [20] | Later onset, slower progression [20] |
| Laterality Defects | Present in ~50% of cases, except CP defects [20] | Similar prevalence [20] |
| Fertility Impact | Severe in most forms affecting sperm flagella [68] | Similarly severe (e.g., CFAP54 mutations) [68] |
| Nasal NO Levels | Typically low [20] | Typically low [20] |
| Response to Exacerbations | 25% not recovering baseline after 3 months [69] | Similar exacerbation frequency [69] |
Diagnostic Approaches and Methodologies
Diagnosing PCD requires a multi-step approach given the absence of a single test with high sensitivity and specificity [20]. The diagnostic pathway differs significantly between ultrastructural and normo-ultrastructural forms.
Standard Diagnostic Toolkit
- Nasal Nitric Oxide (nNO) Measurement: nNO is typically low in PCD but cannot distinguish between ultrastructural and normo-ultrastructural forms [20] [70].
- High-Speed Video Microscopy Analysis (HSVA): Allows direct assessment of ciliary beat frequency and pattern [20] [68]. In CFAP54-related PCD, HSVA revealed significantly reduced ciliary beat frequency (6.2 Hz vs 8.2 Hz in wild-type) despite normal ultrastructure [68].
- Transmission Electron Microscopy (TEM): The gold standard for identifying ultrastructural defects but cannot detect normo-ultrastructural forms [20] [68].
- Genetic Testing: Essential for identifying mutations in all known PCD-associated genes, particularly crucial for diagnosing normo-ultrastructural forms [20] [68]. Next-generation sequencing panels covering >40 PCD genes are recommended.
Diagram 1: Diagnostic pathway for PCD
Advanced and Emerging Techniques
- Immunofluorescence (IF): Uses antibodies against ciliary proteins to detect specific defects; particularly useful when TEM is inconclusive [20].
- mRNA Expression Analysis: Quantifying transcript levels of mutant genes (e.g., demonstrating significantly reduced CFAP54 mRNA in patient bronchial tissue and sperm) [68].
- Mini-Gene Splicing Assays: In vitro functional assays to validate the pathogenicity of splice-site variants, as demonstrated in CFAP54 research [68].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for PCD Investigation
| Reagent/Resource | Application in PCD Research | Specific Examples from Literature |
|---|---|---|
| Transmission Electron Microscopy | Ultrastructural analysis of ciliary axonemes | Identification of ODA, IDA, MTD, and CP defects [20] |
| High-Speed Video Microscopy | Functional analysis of ciliary beat | Measuring ciliary beat frequency in CFAP54 mutants (6.2 Hz vs 8.2 Hz wild-type) [68] |
| Gene-Editing Tools (CRISPR/Cas9) | Generating animal models of PCD | Creation of Cfap54 knock-in mouse model [68] |
| Antibody Panels for IF | Detecting specific protein localization | Antibodies against DNAH5, DNAI2, GAS8 for specific defect identification [20] |
| RNAi/RNA Therapeutics | Investigating gene function and potential therapies | Experimental approaches to restore ciliary function [20] [69] |
| Next-Generation Sequencing Panels | Comprehensive genetic screening | Targeted panels covering >40 known PCD genes [20] [68] |
Experimental Models and Research Protocols
Animal Model Development
Animal models, particularly mice, are crucial for understanding PCD pathogenesis and testing therapeutic interventions:
- CFAP54 Knock-In Mouse Model: Researchers established a Cfap54 knock-in mouse model carrying the c.7535_7536delinCGCAGGCTGAATTCTTGGCA mutation (equivalent to human mutation) through CRISPR/Cas9 technology [68]. This model recapitulated key human PCD features including:
- Brain Ventricle Enlargement: 50% of homozygous mutants developed hydrocephalus with significant lateral ventricle enlargement [68].
- Sinusitis: MRI revealed mucus accumulation in nasal passages and sinuses, confirmed by AB-PAS staining [68].
- Male Infertility: Disrupted spermatogenesis with shortened or absent sperm flagella and disorganized axonemal structure [68].
- Pathophysiological Assessment: Mutant mice showed significantly reduced ciliary beat frequency (6.2 Hz vs 8.2 Hz in wild-type) when measured by high-speed video microscopy [68].
Molecular Validation Techniques
- Mini-Gene Splicing Assay: To validate the pathogenic effect of the CFAP54 c.2649_2657delinC mutation, researchers constructed minigene vectors containing wild-type and mutant exon 20 sequences, transfected them into HEK293T cells, and analyzed RNA expression by RT-PCR, showing reduced transcript levels for the mutant [68].
- qPCR Expression Analysis: Quantified CFAP54 mRNA levels in human patient bronchial tissues and sperm, demonstrating significant reduction compared to controls [68].
- Histopathological Techniques: Hematoxylin and eosin (H&E) staining of testicular sections and sperm smears, combined with TEM, revealed structural abnormalities in sperm flagella of both human patients and mouse models [68].
Diagram 2: Research pathway for novel gene discovery
FAQs: Troubleshooting PCD Research Challenges
Q1: How do we resolve discrepant results between TEM and genetic testing in PCD diagnosis?
A: Discrepancies often indicate normo-ultrastructural PCD. When genetic testing identifies pathogenic mutations (e.g., in DNAH11 or CFAP54) but TEM appears normal, employ functional assessments including high-speed video microscopy to analyze ciliary beat pattern and frequency [20] [68]. Immunofluorescence staining with antibodies against the protein product of the mutated gene can provide additional validation, as absent or reduced staining confirms the genetic findings despite normal ultrastructure [20].
Q2: What are the optimal methods for validating pathogenicity of novel genetic variants in PCD?
A: A multi-modal approach is essential:
- In silico prediction: Use SIFT, PolyPhen-2, and CADD to assess predicted functional impact [68].
- Family segregation analysis: Verify that variants follow expected inheritance patterns [68].
- Mini-gene splicing assays: For suspected splicing mutations, construct wild-type and mutant minigene vectors and transfert into suitable cell lines (e.g., HEK293T) to assess effects on RNA splicing [68].
- mRNA expression analysis: Quantify transcript levels in patient-derived tissues (e.g., bronchial epithelium or sperm) compared to controls [68].
- Animal model generation: Use CRISPR/Cas9 to create knock-in models with patient-specific mutations and characterize the phenotypic consequences [68].
Q3: How do we address the high phenotypic variability in PCD animal models?
A: Phenotypic variability in models (e.g., only 50% of CFAP54 KI mice developing hydrocephalus) reflects the human disease spectrum [68]. To address this:
- Increase sample sizes to account for incomplete penetrance
- Employ controlled environmental challenges (e.g., non-SF housing to assess sinusitis development)
- Use littermate controls and standardized phenotyping protocols
- Consider genetic background effects by backcrossing to inbred strains [68]
Q4: What are the key considerations when establishing ciliary functional assays?
A: For reliable ciliary functional assessment:
- Use fresh, non-confluent cell cultures (passage 1-3) from well-differentiated nasal or bronchial epithelial cells
- Maintain proper temperature (37°C) and pH (7.4) during analysis
- Analyze multiple fields (≥5) and cilia (≥50) per sample
- Include positive and negative controls in each experiment
- For high-speed video microscopy, ensure frame rates ≥500 frames per second for accurate beat frequency measurement [20] [68]
Therapeutic Implications and Future Directions
The distinction between ultrastructural and normo-ultrastructural PCD has significant implications for developing targeted therapies. Current management focuses on symptomatic treatment including airway clearance techniques, aggressive management of infections, and ENT care [20] [71]. However, emerging personalized approaches show promise:
- Gene and mRNA Therapies: Experimental approaches aim to restore ciliary function by delivering functional copies of mutated genes or correcting mRNA expression [20] [69]. These strategies may be particularly applicable to specific genetic subtypes.
- Small Molecule Interventions: Compounds that enhance mucociliary clearance or reduce neutrophilic inflammation are under investigation [69].
- Anti-inflammatory Strategies: Targeting neutrophilic inflammation and NETosis may break the cycle of infection and inflammation that drives disease progression [69].
Future research should focus on genotype-phenotype correlations, expanding the genetic spectrum of normo-ultrastructural PCD, and developing mutation-specific treatments that address the underlying molecular defects in both ultrastructural categories.
FAQs on Endpoint Selection for Heterogeneous Populations
Q1: Why is endpoint selection particularly challenging for clinical trials in heterogeneous populations, such as PCD patients?
In diseases like Primary Ciliary Dyskinesia (PCD), heterogeneity arises from genetic diversity (over 50 known causative genes) and variability in clinical presentation [12]. This complicates endpoint selection because a treatment might be effective only for a specific genetic subgroup or may manifest benefits differently across patients. A single endpoint may fail to capture the full treatment effect across all subgroups. Using a prioritized composite endpoint is one strategy to capture treatment effects across diverse clinical courses in such populations [72].
Q2: What are the main types of endpoints to consider for a heterogeneous population?
- Single Endpoint: Focuses on one specific outcome (e.g., rate of lung function decline). While simple, it may lack sensitivity in a heterogeneous population.
- Multiple Endpoints: Several endpoints are assessed simultaneously. This risks statistical challenges like inflation of Type I error due to multiple comparisons.
- Prioritized Composite Endpoint: A hierarchical ranking of multiple outcome measures. This approach allows a single, comprehensive assessment of treatment effect by analyzing the most clinically important outcome first, then moving to the next in sequence if the primary is not significant [72].
Q3: What does recent evidence suggest about the performance of different endpoint strategies?
Simulation studies show that in scenarios without heterogeneous treatment effects, analyses in the overall population generally have higher power. Time-to-recovery as a single endpoint can have relatively high power, while prioritized composite and multiple endpoints are comparable in performance [72]. However, in scenarios with treatment effect heterogeneity (e.g., where a treatment is effective on distinct endpoints in different patient subgroups), prioritized composite endpoints showed high power and are a preferable strategy [72].
Q4: How should we analyze data when population heterogeneity is anticipated?
When heterogeneity is expected, a stratified analysis that accounts for known sources of variation (e.g., disease severity, genetic variant) can be more powerful than an unstratified analysis. This approach should be considered for the primary analysis in the overall population [72].
Q5: How do diagnostic challenges in PCD impact trial design and participant selection?
A significant challenge is that up to 30% of patients with genetically confirmed PCD have normal ciliary ultrastructure on transmission electron microscopy (TEM) [1]. Relying solely on TEM for enrollment would incorrectly exclude these patients. Therefore, modern diagnostic criteria incorporate multiple modalities: clinical features, genetic testing, nasal nitric oxide (nNO), and TEM to define a "definite" PCD diagnosis [12]. Trials must clearly specify the combination of diagnostic criteria required for enrollment to ensure the correct population is studied.
Diagnostic Criteria & Methodologies for PCD
International guidelines recommend a multi-faceted approach for diagnosing PCD, as no single test is definitive for all cases [1]. The following table summarizes the key diagnostic criteria as per a 2024 practical guide, which can be used to define trial populations [12].
Table 1: Diagnostic Criteria for Primary Ciliary Dyskinesia (PCD)
| Category | Requirement for "Definite PCD" Diagnosis | Examples / Notes |
|---|---|---|
| Clinical Features | At least one of the six clinical features must be present. | - Unexplained neonatal respiratory distress in term infants- Chronic rhinosinusitis- Chronic otitis media with effusion- Persistent perennial rhinitis- Situs inversus- Bronchiectasis |
| Laboratory Findings | A positive result from at least one of the specified methods. | 1. Class 1 Defect on TEM2. Pathogenic PCD Gene Variant3. Ciliary Motility Repair in iPS Cells |
| Differential Diagnosis | Must exclude other conditions that can mimic PCD. | - Cystic Fibrosis- Primary Immunodeficiency |
| Genetic Testing | Identifies pathogenic or likely pathogenic variants in one of approximately 50 known PCD-related genes. | Used to confirm diagnosis, especially in cases with normal or inconclusive ultrastructure. |
Experimental Protocol: Transmission Electron Microscopy (TEM) for PCD Diagnosis
The following protocol is based on standardized international consensus guidelines for TEM-PCD diagnostic reporting [1].
1. Specimen Collection:
- Method: Nasal brushing taken from the inner turbinates.
- Tool: Flexible nylon laparoscopy brush or trimmed small cervix brush.
- Immediate Action: Place the brush immediately in buffered glutaraldehyde (2.5%) and store refrigerated.
2. Specimen Processing:
- Cleaning: Gently clean brushes of adherent matter under a dissecting microscope.
- Rinsing & Post-fixation: Rinse fragments in buffer (3x for 30 min), then post-fix in 1% buffered osmium tetroxide for one hour.
- Dehydration & Infiltration: Dehydrate in a graded ethanol series (10% to 100%). Infiltrate with low-viscosity resin using a resin:ethanol series (1:3, 1:1, 3:1) followed by pure resin.
- Polymerization: Transfer specimens to capsules and polymerize at 70°C.
3. Sectioning and Staining:
- Sectioning: Section polymerized blocks at 70 nm thickness using an ultramicrotome.
- Staining: Double-stain grids with aqueous 4% uranyl acetate (15 min) followed by Reynold's lead citrate (10 min).
4. Imaging and Analysis:
- Imaging: View grids at 120KV on a TEM and image with a CCD camera.
- Diagnostic Criteria (Consensus Guidelines):
- Class 1 Defect (Confirmatory): Hallmark ultrastructural defects in the outer dynein arms (ODA), both outer and inner dynein arms (O+IDA), or microtubular disarrangement with IDA loss, present in >50% of transverse sections. Analysis requires a minimum of 50 epithelial cilia [1].
- Class 2 Defect (Suggestive): Defects such as ODA+IDA defects in 25%-50% of cilia, central complex defects, or few/no cilia. These can be secondary to infection or inflammation and require confirmation by another PCD-testing modality [1].
Diagram 1: PCD Diagnostic Workflow Integrating TEM
Troubleshooting Guides for Clinical Trials
Guide: Addressing Poor Patient Recruitment in Rare Diseases
Problem: Inability to enroll a sufficient number of eligible patients, a common issue in rare diseases like PCD.
Corrective and Preventive Action (CAPA) Plan:
Corrective Action (Short-term):
- Broaden Eligibility Criteria: Review inclusion/exclusion criteria to ensure they are not overly strict without scientific justification [73].
- Partner with Patient Advocacy Groups: Leverage these groups to raise awareness and build trust within the PCD patient community [73].
- Use Real-World Data (RWD): Utilize RWD to identify potential candidates from electronic health records who meet specific criteria [73].
Preventive Action (Long-term):
- Implement Flexible Trial Designs: Consider decentralized trial elements to reduce patient burden, such as flexible visit scheduling and travel support [73].
- Community-Based Sites: Conduct trials in diverse communities or established PCD specialist centers to improve access and representation [73].
- Multilingual Outreach: Provide trial materials in multiple languages to overcome participation barriers [73].
Guide: Conducting Root Cause Analysis for Persistent Trial Issues
This guide uses the 5-Whys method to move beyond symptoms and identify the underlying root cause of a problem [74].
Problem: The clinical investigator's signature dates on the delegation log were changed, and some dates were recorded after staff began trial-related activities.
- Why? The investigator was busy and assumed the study coordinator was maintaining the log.
- Why? The investigator viewed this as an administrative task and deprioritized it.
- Why? The study coordinator was too busy with rapid subject enrollment and visits to follow up.
- Why? The department had no budget for additional staff, and the contract required a defined enrollment rate.
- Root Cause: Systemic resource constraints and contractual pressure led to poor task delegation and a lack of investigator oversight, compounded by poor communication between the monitor and the study manager [74].
Diagram 2: Root Cause Analysis with the 5-Whys
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Materials for PCD Diagnostic Research
| Item / Reagent | Function / Application | Example / Specification |
|---|---|---|
| Glutaraldehyde (EM grade) | Primary fixative for TEM specimens; preserves ultrastructure. | 2.5% in 0.1M sodium cacodylate buffer [1]. |
| Osmium Tetroxide | Post-fixation; stains and stabilizes lipids and membranes. | 1% solution in buffer [1]. |
| Low Viscosity Resin | Embedding medium for ultrathin sectioning. | Agar Scientific low viscosity resin [1]. |
| Uranyl Acetate | Heavy metal stain for TEM; enhances contrast of cellular components. | Aqueous 4% solution [1]. |
| Reynold's Lead Citrate | Heavy metal stain for TEM; further enhances contrast. | Used after uranyl acetate staining [1]. |
| Nasal Brushing Brush | Tool for obtaining ciliated epithelial cell samples. | Flexible nylon laparoscopy brush (e.g., WS-1812XA3) [1]. |
| Cell Culture Media for iPS | Reprogramming and maintenance of patient-derived iPS cells. | Used for ciliary motility functional assays [12]. |
FAQs: Genetic Diagnosis and Therapeutic Development for PCD
FAQ 1: Why is genetic testing crucial for PCD patients with normal ultrastructure? Transmission Electron Microscopy (TEM) can appear normal in a significant subset of Primary Ciliary Dyskinesia (PCD) patients, particularly those with pathogenic variants in genes like DNAH11 [75]. In these cases, genetic testing is the only definitive diagnostic method. Establishing a genetic diagnosis is the critical first step for enrolling patients in clinical trials and for the future development of mutation-specific therapies [76].
FAQ 2: What is the recommended genetic diagnostic workflow for a suspected PCD case? A sequential approach is often most efficient. A targeted PCD gene panel is a pragmatic first-tier test as it focuses on a predefined set of genes with deep coverage [77]. If this is inconclusive, Whole Exome Sequencing (WES) provides a broader analysis of all protein-coding regions and is valuable for identifying novel genes or variants in cases of high genetic heterogeneity [77] [78].
FAQ 3: How do I prioritize candidate variants from NGS data? Variant prioritization tools like Exomiser integrate multiple lines of evidence. Optimization is key; for WES data, parameter tuning can increase the rate of diagnostic variants ranked in the top 10 from 67.3% to 88.2% [78]. Critical filters include:
- Population frequency (e.g., gnomAD)
- In-silico predictions of pathogenicity
- Segregation analysis in the family
- The patient's phenotype encoded with Human Phenotype Ontology (HPO) terms [78]
FAQ 4: How does genotype influence phenotype and therapy selection in PCD? The specific genetic variant can predict disease manifestations and is essential for selecting the appropriate therapeutic modality. For instance, loss-of-function variants may require gene replacement, while missense mutations could be amenable to correction using gene editing [76]. The table below illustrates the correlation between genotype and the prevalence of neonatal respiratory distress (NRD) in PCD [75].
Table 1: Association between PCD Genotype/Ultrastructure and Neonatal Respiratory Distress (NRD)
| Ultrastructural Group / Gene | Example Gene | Prevalence of NRD | Odds Ratio (OR) for NRD |
|---|---|---|---|
| Outer Dynein Arm (ODA) Defect | DNAH5 | 63.7% - 66.7% | Reference |
| Inner Dynein Arm Defect with Microtubular Disorganization (IDA/MTD) | CCDC40 | 72.7% - 79.5% | Not Significant |
| Normal Ultrastructure | DNAH11 | 38.9% | 0.35 (95% CI: 0.16–0.76) |
Troubleshooting Guides
Challenge 1: Low Diagnostic Yield from Exome Sequencing
| Symptom | Possible Cause | Solution |
|---|---|---|
| No plausible candidate variants found. | Suboptimal HPO term selection; incomplete phenotypic description. | Action: Manually re-curate the patient's phenotype using the full HPO database. Include both positive and negative findings to improve the phenotype-driven ranking in tools like Exomiser [78]. |
| VUS (Variants of Uncertain Significance) identified, but pathogenicity is unclear. | Limited functional data or population frequency for rare variants. | Action: (1) Perform segregation analysis in the family. (2) Utilize tools like Genomiser to check for potential non-coding regulatory variants that may be compound heterozygous with a coding variant [78]. |
| High number of candidate variants, making manual review burdensome. | Use of default parameters in variant prioritization software. | Action: Systematically optimize parameters. For example, adjust gene-phenotype association algorithms and variant pathogenicity score thresholds. This can significantly improve the ranking of diagnostic variants [78]. |
Challenge 2: Interpreting Genotype-Phenotype Correlations in PCD
| Symptom | Possible Cause | Solution |
|---|---|---|
| A patient with a confirmed PCD genotype lacks a "classic" symptom like NRD. | Incomplete penetrance or variable expressivity; genotype-specific phenotypes. | Action: Consult genotype-phenotype association studies. For example, NRD is significantly less common in patients with DNAH11 mutations (~39%) compared to those with DNAH5 mutations (~67%) [75] [39]. This does not rule out the diagnosis. |
| Phenotypic variability among patients with the same gene mutated. | The type of genetic variant (e.g., loss-of-function vs. residual function) can influence severity. | Action: Classify variants beyond the gene level. In the DNAH5 group, patients with two loss-of-function variants had a 3.06 times higher odds of having NRD compared to those with possible residual function variants [75]. |
Experimental Protocols
Protocol 1: Optimized Variant Prioritization for Rare Disease Diagnosis
This protocol is based on an evidence-based framework for using Exomiser/Genomiser with WES or GS data [78].
1. Input Preparation:
- Sequencing Data: Multi-sample VCF file (proband and parents if available).
- Pedigree File: PED format specifying familial relationships.
- Phenotype Data: A comprehensive list of the proband's clinical features encoded as HPO terms (e.g., HP:0010520 "Neonatal respiratory distress").
2. Parameter Optimization in Exomiser:
- Gene-Phenotype Analysis: Use the
PHENIX_P_VALUEalgorithm. - Variant Pathogenicity: Apply a combined filter using
REVEL_score > 0.7andMVP_score > 0.8. - Variant Frequency: Set maximum allele frequency filter to
< 0.001(0.1%) for autosomal recessive disorders.
3. Post-Prioritization Refinement:
- Apply a p-value threshold (e.g.,
< 1x10^-3) to the Exomiser results to filter out genes with weak phenotypic matches. - Manually review the top 30 candidates, focusing on genes with established disease mechanisms.
The following workflow diagram visualizes this optimized process:
Protocol 2: Designing a Personalized mRNA Therapeutic Strategy
Once a genetic diagnosis is confirmed, the path towards a bespoke therapy can be mapped. This protocol outlines key considerations, inspired by the workflow used for a personalized mRNA-encoded base editor for a rare metabolic disease [79] [76].
1. Target Validation and Modality Selection:
- Gene/Mutation: Confirm the pathogenic variant and its functional consequence (e.g., loss-of-function, gain-of-function, missense).
- Therapeutic Modality:
2. mRNA Design and Production:
- Sequence Optimization: Design the mRNA sequence to encode the target antigen or corrected protein. Codon optimization can enhance protein expression.
- Modifications: Incorporate modified nucleosides (e.g., pseudouridine) to reduce innate immunogenicity and increase stability.
- Manufacturing: Produce the mRNA via in vitro transcription (IVT).
3. Formulation and Delivery:
- Lipid Nanoparticles (LNPs): Encapsulate the mRNA in LNPs for protection and efficient cellular delivery. Target-specific tissues by incorporating ligands (e.g., PD-L1 binding peptides for tumor targeting) [76].
- Dosing Regimen: Determine the dose and schedule based on preclinical models.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for PCD Genetic Research and Therapeutic Development
| Reagent / Tool | Function | Application in PCD Research |
|---|---|---|
| Targeted PCD Gene Panel | High-depth sequencing of a predefined set of known PCD genes. | Efficient first-tier diagnostic testing for patients with a classic PCD phenotype [77]. |
| Whole Exome Sequencing (WES) | Comprehensive analysis of the protein-coding exome. | Diagnostic tool for cases with atypical presentations or negative panel results; enables novel gene discovery [77] [39]. |
| Exomiser/Genomiser Software | Open-source tool for phenotype-driven variant prioritization. | Ranking candidate variants from WES/GS data by integrating HPO terms and genomic evidence [78]. |
| Human Phenotype Ontology (HPO) | Standardized vocabulary for clinical features. | Encoding patient phenotypes to computationally link them to genetic data in variant prioritization pipelines [78]. |
| Lipid Nanoparticles (LNPs) | Nanocarriers for nucleic acid delivery. | Formulating mRNA-based therapeutics for delivery to target cells in the airway or systemically [76]. |
Conclusion
The diagnosis of PCD in patients with normal ciliary ultrastructure is a rapidly evolving field that demands a sophisticated, multi-step approach. Moving beyond reliance on transmission electron microscopy alone is essential. Success hinges on the integrated application of advanced genetic testing, functional ciliary assessments, and careful clinical evaluation. This comprehensive strategy not only secures a diagnosis for elusive cases but also unlocks a deeper understanding of disease mechanisms and heterogeneity. For researchers and drug developers, these advances are pivotal. They enable more precise patient stratification for clinical trials, validate the use of quality-of-life measures as meaningful endpoints, and illuminate the path toward developing mutation-specific therapies, ultimately improving outcomes for all individuals with PCD.
References
- 1. Ultrastructure for the diagnosis of primary ciliary dyskinesia in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10461090/]
- 2. Transmission electron microscopy study of suspected ... [https://www.nature.com/articles/s41598-022-06370-w]
- 3. Diagnosing PCD [https://www.pcdfoundation.org/diagnosis/]
- 4. The challenges of diagnosing primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/21926395/]
- 5. CHEST Pulmonary Reviews Primary Ciliary Dyskinesia [https://www.sciencedirect.com/science/article/pii/S2949789223000041]
- 6. Primary Ciliary Dyskinesia - Diagnosis - NHLBI - NIH [https://www.nhlbi.nih.gov/health/primary-ciliary-dyskinesia/diagnosis]
- 7. Mutations of DNAH11 in Primary Ciliary Dyskinesia Patients ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3739700/]
- 8. Clinical care for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC9489029/]
- 9. DNAH11 variants and its association with congenital heart ... [https://www.nature.com/articles/s41598-019-43109-6]
- 10. Challenges in Diagnosing Primary Ciliary Dyskinesia in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9324289/]
- 11. Primary ciliary dyskinesia with normal ultrastructure [https://pubmed.ncbi.nlm.nih.gov/29467202/]
- 12. Practical guide for the diagnosis and management of ... [https://www.sciencedirect.com/science/article/pii/S0385814624000166]
- 13. Clinical and Genetic Aspects of Primary Ciliary Dyskinesia ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3739704/]
- 14. Primary ciliary dyskinesia: Aetiology, diagnosis and clinical ... [https://www.sciencedirect.com/science/article/pii/S1470211825000375]
- 15. Clinical, phenotype and genotype correlations in primary ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1641739/full]
- 16. Noncoding DNA Variants in Primary Ciliary Dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618996/]
- 17. Primary ciliary dyskinesia: clinical presentation, diagnosis ... [https://pubmed.ncbi.nlm.nih.gov/16203616/]
- 18. Primary ciliary dyskinesia: A review [https://www.sciencedirect.com/science/article/pii/S2950008725000420]
- 19. Analysis of Clinical Characteristics and Gene Variants ... [https://brieflands.com/journals/ijp/articles/132964]
- 20. Primary Ciliary Dyskinesia—Current Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525432/]
- 21. Improving Outcomes [https://pcdresearch.org/improving-outcomes/]
- 22. Primary ciliary dyskinesia: clinical manifestations and ... [https://pubmed.ncbi.nlm.nih.gov/40916971/]
- 23. Ultrastructure for the diagnosis of primary ciliary dyskinesia ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2023.1247638/full]
- 24. a diagnostic predictive tool for primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/26917608/]
- 25. Summary for Clinicians: Diagnosis of Primary Ciliary Dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC7336768/]
- 26. Whole-Exome Sequencing and Targeted Copy Number ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4528333/]
- 27. Missed diagnosis or misdiagnosis: common pitfalls in genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9979802/]
- 28. Whole exome sequencing enhances diagnosis of hereditary ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-03661-z]
- 29. High-speed Video Microscopy Analysis (HVMA) [https://www.medizin.uni-muenster.de/en/pcd/research/high-speed-video-microscopy-analysis-hvma.html]
- 30. Diagnosis of Primary Ciliary Dyskinesia [https://www.guidelinecentral.com/guideline/7172/]
- 31. Abstract - ERS Publications - European Respiratory Society [https://publications.ersnet.org/content/erj/early/2025/09/18/1399300300745-2025]
- 32. Protocol for characterizing airway epithelial ciliary beating ... [https://www.sciencedirect.com/science/article/pii/S2666166725000802]
- 33. Protocol for characterizing airway epithelial ciliary beating and ... [https://pubmed.ncbi.nlm.nih.gov/40053450/]
- 34. Analysis of ciliary beat pattern and beat frequency using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1745724/]
- 35. Accuracy of Nasal Nitric Oxide Measurement as a Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6137897/]
- 36. Nasal nitric oxide measurement for the diagnosis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171850/]
- 37. Primary Ciliary Dyskinesia. Recent Advances in Diagnostics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3826280/]
- 38. How can I use nNO testing with NIOX [https://www.niox.com/en-us/support/articles/using-nasal-nitric-oxide/]
- 39. Clinical features and genetic spectrum of children with ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1526675/full]
- 40. Diagnostic utility of standardized assessment of ciliary ... [https://www.sciencedirect.com/science/article/abs/pii/S2212534525001650]
- 41. Integrated diagnostic algorithm for acute vertigo combining ... [https://pubmed.ncbi.nlm.nih.gov/40659780/]
- 42. Integrated diagnostic algorithm for acute vertigo combining ... [https://www.nature.com/articles/s41598-025-11007-9]
- 43. PCD with normal ultrastructure is not rare - ERS Publications [https://publications.ersnet.org/content/erj/40/suppl56/2845]
- 44. Myths and realities about negative genetic testing [https://www.biron.com/en/education-center/myth-or-fact/negative-genetic-test/]
- 45. Primary ciliary dyskinesia - Insights - Mayo Clinic Labs [https://news.mayocliniclabs.com/pathology/primary-ciliary-dyskinesia/]
- 46. The Controversies and Difficulties of Diagnosing Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938149/]
- 47. Primary Ciliary Dyskinesia - GeneReviews® - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK1122/]
- 48. The challenge of diagnosing primary ciliary dyskinesia [https://www.nature.com/articles/s10038-023-01166-w]
- 49. ERS Task Force guideline for the diagnosis of primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6054534/]
- 50. Interpreting Variants of Uncertain Significance in PCD [https://pmc.ncbi.nlm.nih.gov/articles/PMC11705539/]
- 51. Transcript analysis for variant classification resolution in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7903884/]
- 52. Genetic Variant Interpretation Tool [https://www.medschool.umaryland.edu/genetic_variant_interpretation_tool1.html/]
- 53. Motile Ciliopathy Variant Curation Expert Panel [https://clinicalgenome.org/affiliation/50102/]
- 54. PCD Research – getting cilia moving [https://pcdresearch.org/]
- 55. , monitoring, and treatment of primary ciliary dyskinesia... Diagnosis [https://pmc.ncbi.nlm.nih.gov/articles/PMC4912005/]
- 56. ERS and ATS diagnostic guidelines for primary ciliary dyskinesia... [https://publications.ersnet.org/content/erj/54/3/1901066]
- 57. Evaluation of a Clinical Index as a Predictive Tool for Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232329/]
- 58. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1]
- 59. a diagnostic predictive tool for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819882/]
- 60. Current Analytical Strategies for mRNA-Based Therapeutics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11990077/]
- 61. An introduction to Performing Immunofluorescence Staining [https://pmc.ncbi.nlm.nih.gov/articles/PMC6918834/]
- 62. A comparison of confocal and epifluorescence microscopy ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10874114/]
- 63. Quantitative, in situ analysis of mRNAs and proteins with ... [https://www.nature.com/articles/s41598-017-16492-1]
- 64. What are immunofluorescence techniques? [https://nanostring.com/blog/what-are-immunofluorescence-techniques/]
- 65. Validation of a health-related quality of life ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/28246220/]
- 66. Guidelines for the development and validation of patient ... [https://pubmed.ncbi.nlm.nih.gov/38782559/]
- 67. Validation of pediatric health-related quality of life instruments ... [https://pubmed.ncbi.nlm.nih.gov/31475479/]
- 68. CFAP54缺失在小鼠模型和人类患者中引发原发性纤毛运动障碍 ... [https://paper.sciencenet.cn/htmlpaper/2025/9/2025929152537264140522.shtm]
- 69. Beyond the present: current and future perspectives on ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1564156/full]
- 70. 纖毛研究新突破揭示其在兒童疾病中的重要角色 [https://geneonline.news/%E7%BA%96%E6%AF%9B%E7%A0%94%E7%A9%B6%E6%96%B0%E7%AA%81%E7%A0%B4-%E6%8F%AD%E7%A4%BA%E5%85%B6%E5%9C%A8%E5%85%92%E7%AB%A5%E7%96%BE%E7%97%85%E4%B8%AD%E7%9A%84%E9%87%8D%E8%A6%81%E8%A7%92%E8%89%B2/]
- 71. Primary Cilia Dyskinesia: a National expert consensus ... [https://publications.ersnet.org/content/erjor/early/2025/08/14/2312054100466-2025]
- 72. Strategies to evaluate treatment effects in clinical trials for ... [https://pubmed.ncbi.nlm.nih.gov/40774424/]
- 73. Common Challenges in Clinical Research and Solutions [https://ccrps.org/clinical-research-blog/common-challenges-in-clinical-research-and-how-to-overcome-them]
- 74. Resolving and Preventing Repetitive Problems in Clinical ... [https://www.socra.org/blog/corrective-and-preventative-action/]
- 75. The Association of Neonatal Respiratory Distress With Ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12063519/]
- 76. The current and future landscape of RNA-based therapies ... [https://www.nature.com/articles/s43856-025-01166-1]
- 77. NGS Approaches in Clinical Diagnostics: From Workflow to ... [https://www.mdpi.com/1422-0067/26/19/9597]
- 78. An optimized variant prioritization process for rare disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12539062/]
- 79. Alliance for mRNA Medicines Welcomes New FDA ... [https://mrnamedicines.org/alliance-for-mrna-medicines-welcomes-new-fda-framework-to-accelerate-development-of-personalized-gene-therapies/]
- 80. Personalized mRNA Vaccines Will Revolutionize Cancer ... [https://www.scientificamerican.com/article/personalized-mrna-vaccines-will-revolutionize-cancer-treatment-if-federal/]