Optimizing Diagnostic Sensitivity: A Scientific Review of Nasal vs. Nasopharyngeal Swab Sampling
This article synthesizes current evidence on the diagnostic sensitivity of nasal (anterior nares) and nasopharyngeal swabs for respiratory pathogen detection, with a focus on SARS-CoV-2.
Optimizing Diagnostic Sensitivity: A Scientific Review of Nasal vs. Nasopharyngeal Swab Sampling
Abstract
This article synthesizes current evidence on the diagnostic sensitivity of nasal (anterior nares) and nasopharyngeal swabs for respiratory pathogen detection, with a focus on SARS-CoV-2. It explores the foundational rationale for sampling site selection, compares methodological performance across molecular and antigen tests, and provides evidence-based strategies for optimizing sensitivity. Key troubleshooting considerations, such as the impact of viral load and swab design, are reviewed. The content is validated through head-to-head clinical comparisons and an examination of novel pre-clinical models, offering researchers and drug development professionals a comprehensive framework for selecting and validating upper respiratory specimen collection strategies in both clinical and research settings.
The Gold Standard and Its Challengers: Anatomical and Practical Foundations of Respiratory Sampling
Frequently Asked Questions (FAQs)
1. Why are nasopharyngeal (NP) swabs considered the gold standard for SARS-CoV-2 detection? NP swabs are considered the gold standard because numerous studies have shown they provide the highest sensitivity for detecting respiratory viruses like SARS-CoV-2 compared to other upper respiratory specimens [1]. This is because the nasopharynx is a primary site of viral replication, and NP sampling collects respiratory secretions directly from this area [2].
2. What are the main limitations and complications associated with NP swabs? While generally safe, NP swabbing is an invasive procedure that can cause patient discomfort. Documented complications, though rare (occurring in approximately 0.0012% to 0.026% of procedures), include [2] [3]:
- Epistaxis (nosebleeds) [2].
- Retained swabs due to tip fracture [2].
- Cerebrospinal fluid (CSF) leakage, particularly in patients with undiagnosed skull base defects or prior surgery [2]. The procedure is also technically challenging and requires trained healthcare workers [4].
3. How does the sensitivity of anterior nasal (AN) swabs compare to NP swabs? Recent head-to-head studies have found that the diagnostic accuracy of AN swabs is becoming equivalent to that of NP swabs for SARS-CoV-2 antigen detection [5]. One large study reported sensitivities of 85.6% for AN swabs versus 83.9% for NP swabs for one test brand, and 79.5% for AN swabs versus 81.2% for NP swabs for another brand, with no statistically significant difference [5]. However, a different study on RT-PCR testing found nasal swab sensitivity to be lower at 82.4%, compared to 92.5% for NP swabs [4].
4. For the Omicron variant, is a throat swab better than a nasal swab? Research on the Omicron variant suggests that throat swabs may have higher PCR sensitivity than nose-only swabs. However, the most effective method remains the combined nose and throat swab. Viral concentration also appears to remain stable for a longer duration in nasal swabs compared to throat swabs [6].
5. What is the estimated real-world sensitivity of a single NP swab for SARS-CoV-2? One study assessing serial testing in patients with known COVID-19 estimated the overall sensitivity of a single NP swab to be 77% (95% CI, 73-81%). The sensitivity of the first follow-up NP swab was 79% (95% CI, 73-84%) [7].
Comparative Performance of Respiratory Swab Types
Table 1: Summary of key performance metrics from recent comparative studies.
| Study Focus | Swab Type | Sensitivity (%) | Specificity (%) | Notes |
|---|---|---|---|---|
| SARS-CoV-2 Ag-RDT (Sure-Status) [5] | Nasopharyngeal (NP) | 83.9 | 98.8 | Paired sampling in symptomatic patients. |
| Anterior Nares (AN) | 85.6 | 99.2 | High agreement with NP (κ=0.918). | |
| SARS-CoV-2 Ag-RDT (Biocredit) [5] | Nasopharyngeal (NP) | 81.2 | 99.0 | Paired sampling in symptomatic patients. |
| Anterior Nares (AN) | 79.5 | 100 | High agreement with NP (κ=0.833). | |
| SARS-CoV-2 RT-PCR [4] | Nasopharyngeal (NP) | 92.5 | - | Performed by otorhinolaryngologists. |
| Oropharyngeal (OP) | 94.1 | - | Sensitivity comparable to NP (p=1.00). | |
| Nasal Swab | 82.4 | - | Sensitivity lower than NP (p=0.07). | |
| SARS-CoV-2 RT-PCR (Rhinoswab) [8] | Combined OP/NP | (Reference) | - | Reference standard in the study. |
| Anterior Nasal (Rhinoswab) | 80.7 | 99.6 | Less invasive, patient-friendly method. |
Table 2: Documented complications and considerations for NP swabs.
| Aspect | Findings | Implications for Research & Practice |
|---|---|---|
| Complication Rate | 0.0012% - 0.026% of procedures [2] [3]. | Complications are rare but can be serious; requires proper training. |
| Common Complications | Epistaxis, retained swabs [2]. | Mostly manageable but can necessitate medical intervention. |
| Serious Complications | Cerebrospinal fluid (CSF) leakage [2]. | Often linked to pre-existing anatomical variances; underscores need for careful technique. |
| Patient Comfort | NP swabs are frequently described as uncomfortable or invasive [8]. | Anterior nasal sampling offers a better-tolerated alternative, potentially improving test adherence. |
Detailed Experimental Protocols
Protocol 1: Head-to-Head Comparison of AN and NP Swabs for Ag-RDT [5] This protocol is designed for a prospective diagnostic evaluation to compare the accuracy of different swab types.
- Sample Collection: Trained healthcare workers collect samples from symptomatic individuals. The NP swab is collected first in one nostril and placed in Universal Transport Media (UTM) for reference RT-qPCR testing. This is followed by collecting a second NP swab from the other nostril and finally an AN swab from both nostrils for the Ag-RDT under evaluation.
- Laboratory Analysis: The Ag-RDTs (e.g., Sure-Status, Biocredit) are performed strictly according to the manufacturers' instructions for use (IFU). To minimize bias, results are read by two operators who are blinded to each other's readings and the reference standard result. A third operator acts as a tiebreaker for discrepant results. The visual intensity of the test line can be scored on a quantitative scale (e.g., 1-10).
- Reference Standard: RNA is extracted from the first NP swab and tested via RT-qPCR (e.g., TaqPath COVID-19). A sample is considered positive if two of three target genes amplify with a cycle threshold (Ct) ≤40. Viral load can be quantified using a serial dilution standard curve.
- Statistical Analysis: Sensitivity and specificity for each swab type and Ag-RDT brand are calculated against the RT-qPCR reference standard. The agreement between AN and NP swabs is determined using Cohen's kappa (κ). The limit of detection (LoD) for each method can be compared using logistic regression.
Protocol 2: Comparison of NP, Oropharyngeal (OP), and Nasal Swabs for RT-PCR [4] This protocol uses a prospective design with samples collected by specialists to ensure high-quality sampling.
- Sample Collection: A consultant or registrar in otorhinolaryngology performs all swabs. The NPS is collected by inserting a flexible minitip flocked swab toward the earlobe until resistance is met (~8-11 cm deep). The OPS is collected by swabbing both palatine tonsils and the posterior oropharyngeal wall. The nasal swab is collected by inserting a rigid-shaft flocked swab only ~1-3 cm into the nasal cavity, brushing along the septum and inferior nasal concha.
- Laboratory Analysis: All samples from a single participant are tested using the same RT-PCR assay to ensure comparability. For a subset of samples tested with an identical platform, the mean Ct values for target genes (e.g., N gene) are calculated and compared to assess viral load.
- Statistical Analysis: The sensitivity of each swab type is calculated. The McNemar test is used to compare the differences in sensitivity between paired samples. Ct values are compared using the Wilcoxon matched-pairs signed-rank test.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key materials and reagents for respiratory swab research.
| Item | Specification / Example | Primary Function in Research |
|---|---|---|
| Flocked Swabs | COPAN FLOQSwabs [4] [9] | Superior sample collection and release for both NP and nasal sampling. Critical for high sensitivity. |
| Universal Transport Media (UTM) | Copan UTM [5] | Preserves viral integrity and nucleic acids during transport and storage prior to analysis. |
| RNA Extraction Kit | QIAamp 96 Virus QIAcube HT kit (Qiagen) [5] | Isolates viral RNA for downstream molecular detection via RT-PCR. |
| RT-PCR Assay | TaqPath COVID-19 (ThermoFisher) [5]; Allplex SARS-CoV-2 (Seegene) [4] | Gold-standard molecular method for detecting and quantifying SARS-CoV-2 RNA. |
| Ag-RDT Kits | Sure-Status (PMC, India); Biocredit (RapiGEN, South Korea) [5] | Rapid, point-of-care tests for antigen detection used in comparative accuracy studies. |
| Specialized Nasal Swab | Rhinoswab (Rhinomed, Australia) [8] | A novel ANS designed for simultaneous sampling of both nostrils, optimizing patient comfort and sample yield. |
Logical Workflow for Swab Sampling Research
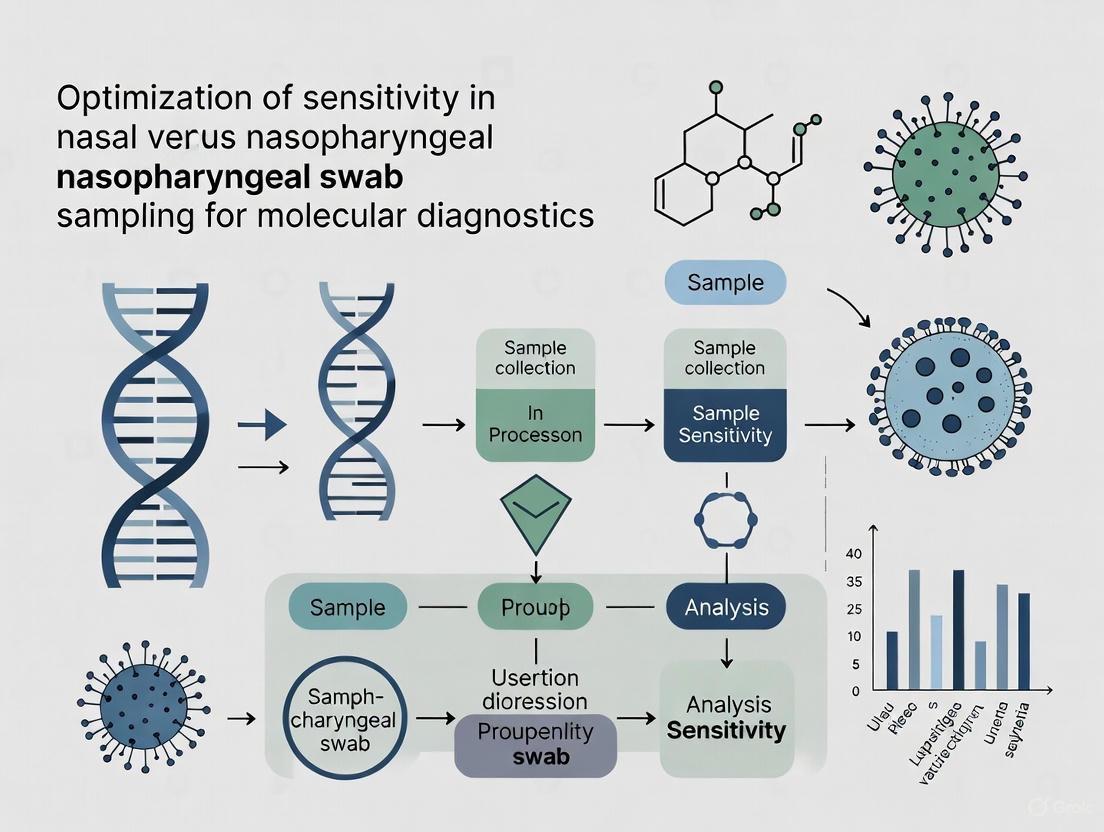
The diagram below visualizes the logical workflow and key decision points in designing a study to compare swab sampling methods.
Logical Workflow for Swab Sampling Research
Anatomical and Physiological Basis for Alternative Sampling Sites
For researchers and drug development professionals, selecting the optimal respiratory specimen type is a critical step in the accurate detection of pathogens like SARS-CoV-2 and other respiratory viruses. While the nasopharyngeal swab (NPS) has long been considered the gold standard, its invasive nature, requirement for skilled healthcare personnel, and patient discomfort have spurred significant research into alternative sampling sites. This technical guide is framed within the broader thesis of optimizing detection sensitivity. It synthesizes current evidence on the anatomical and physiological factors influencing the performance of nasal and saliva samples, providing troubleshooting guidance and standardized protocols to enhance the rigor and reproducibility of your research.
FAQs: Optimizing Sampling for Sensitivity
1. What is the anatomical rationale for using nasopharyngeal swabs, and what are its limitations?
The nasopharynx, the upper part of the throat behind the nose, is lined with respiratory epithelium and a high concentration of goblet cells and cilia. As the primary initial site of replication for many respiratory viruses, it is expected to harbor the highest viral loads [10]. Sampling this area involves inserting a flexible swab through the nostril along the nasal floor to a depth of approximately 7-11 cm until it contacts the posterior nasopharyngeal wall [11] [12]. This method is technically challenging, requires trained professionals, and is often described as uncomfortable for patients, which can limit testing compliance and scale [13] [4].
2. How do anterior nasal swabs compare to NPS in terms of sensitivity and viral concentration?
Anterior nasal swabs sample the mucosa within the first 1-3 cm of the nostril. While generally yielding slightly lower viral concentrations than NPS, they can be a highly viable alternative, especially when collection technique is optimized. One study found that NPS showed the lowest Cycle Threshold (Ct) values, indicating the highest virus concentrations, but that sufficiently rubbed nasal swabs could achieve similar concentrations [10]. The sensitivity of nasal swabs has been reported at 82.4%, compared to 92.5% for NPS in a head-to-head study [4]. The vigor and number of rubs are critical; one study demonstrated that swabs rotated 10 times inside the nostril yielded significantly lower Ct values (higher virus concentration) than those rotated only 5 times (Ct=24.3 vs. 28.9; P=0.002) [10].
3. Under what physiological conditions might saliva be a superior or comparable sample type?
Saliva's diagnostic value stems from the fact that the virus replicates in both the upper and lower respiratory tracts, and virus-containing secretions drain from the nasopharynx into the oropharynx, where they mix with saliva [14]. Studies have shown high positive percent agreement (94.0%) between saliva and nasal swabs in symptomatic individuals within the first 5 days of symptoms [14]. Saliva may be particularly advantageous for self-collection, reducing healthcare worker exposure and resource consumption [13] [14]. Furthermore, for the detection of mucosal immune markers like SARS-CoV-2 RBD-specific IgA, an expanding sponge method was found to have a significantly higher detection rate and antibody concentration compared to both nasopharyngeal and standard nasal swabs [15].
4. When is it not appropriate to use alternative-site sampling?
The primary concern with alternative sites, particularly in non-respiratory contexts like blood glucose monitoring, is the time lag in detecting rapid analyte changes. This principle can be extrapolated to respiratory virus dynamics. For example, alternate-site blood glucose testing is not recommended during periods of rapidly changing glucose levels (e.g., post-meal, after exercise, or during illness) because blood flow is slower in these areas compared to fingertips [16]. Similarly, for respiratory virus detection, alternative sites like anterior nasal or saliva may not reflect the very earliest stages of infection as accurately as NPS. Researchers should validate alternative sites against the gold standard during the acute phase of infection.
Troubleshooting Common Experimental Issues
| Issue | Possible Cause | Solution |
|---|---|---|
| Low viral concentration in nasal swabs. | Insufficient rubbing or swab contact time. | Standardize protocol to include at least 5-10 firm rubs while rotating the swab against the nasal wall [10]. |
| Low sample volume from saliva. | Patient dehydration or difficulty in expectorating. | For expectoration, encourage the patient to imagine smelling a sour lemon to stimulate saliva production. For younger children, use a sponge-based collection kit placed in the buccal cavity [13]. |
| Inconsistent Ct values across sample types. | Anatomical and physiological variation in viral shedding. | Collect paired samples from the same individual to control for inter-patient variability. Consider using a combined approach (e.g., OPS/NPS) to maximize sensitivity [4]. |
| Sample collection is painful, leading to low participant enrollment. | Use of overly invasive NPS technique. | For NPS, ensure the swab follows the nasal floor parallel to the palate, not upwards. Evidence suggests that rotating the swab after insertion may not increase nucleic acid yield but does increase discomfort [11]. |
| Low detection rate of mucosal antibodies. | Inefficient sampling method failing to collect sufficient mucosal lining fluid. | Transition from swabs to an expanding sponge method, which was shown to be superior for collecting nasal SARS-CoV-2 WT-RBD IgA [15]. |
Comparative Performance Data of Sampling Methods
Table 1: Comparison of SARS-CoV-2 Detection Sensitivity Across Different Sample Types
| Sample Type | Sensitivity (%) | Notes / Comparative Context | Source |
|---|---|---|---|
| Nasopharyngeal Swab (NPS) | 92.5 - 100% | Considered the reference standard; consistently shows the lowest Ct values (highest viral load). | [10] [4] |
| Oropharyngeal Swab (OPS) | 94.1% | Sensitivity comparable to NPS (p=1.00); can be a equivalent alternative. | [4] |
| Anterior Nasal Swab | 82.4 - 88.3% | Sensitivity improves with vigorous rubbing (10 rubs vs. 5 rubs). | [10] [4] |
| Saliva | 94.0% PPA | Positive Percent Agreement with nasal swabs within first 5 days of symptoms. | [14] |
| Combined OPS/NPS | 100% | Maximizes sensitivity but uses more resources. | [4] |
Table 2: Viral Load (Ct Value) and Antibody Recovery by Sampling Method
| Sample Type | Metric | Median Value / Finding | Source | |
|---|---|---|---|---|
| NPS | Mean Ct Value (N gene) | 24.98 | [4] | |
| OPS | Mean Ct Value (N gene) | 26.63 (p=0.084 vs. NPS) | [4] | |
| Nasal Swab | Mean Ct Value (N gene) | 30.60 (p=0.002 vs. NPS) | [4] | |
| Nasal Swab (10 rubs) | Median Ct Value (E gene) | 24.3 | Not significantly different from NPS. | [10] |
| Nasal Swab (5 rubs) | Median Ct Value (E gene) | 28.9 (p=0.002 vs. 10 rubs) | [10] | |
| Expanding Sponge (M3) | SARS-CoV-2 RBD IgA | 171.2 U/mL | Significantly outperformed swab methods. | [15] |
Standardized Experimental Protocols
Protocol 1: Anterior Nasal Swab Collection for Viral Detection
This protocol is optimized for high viral recovery based on comparative studies [10] [12].
- Materials: Sterile synthetic fiber swab (e.g., flocked swab) with plastic or wire shaft, viral transport medium (VTM), transport tube.
- Procedure:
- Tilt the patient's head back slightly (approximately 70 degrees).
- Gently insert the swab into one nostril, approximately 1-2 cm deep (or ½ to ¾ of an inch), parallel to the palate.
- Firmly rub the swab against the nasal wall (septum and inferior concha) while rotating it. Perform this action at least 5-10 times to ensure sufficient contact.
- Slowly withdraw the swab while continuing to rotate it.
- Repeat the process in the other nostril using the same swab.
- Place the swab into the VTM tube, snap the applicator shaft at the score line, and cap the tube tightly.
- Key Consideration: The number of rubs significantly impacts viral yield. Standardize this variable in your study protocol [10].
Protocol 2: Saliva Collection for Molecular Detection
This protocol outlines methods for expectoration and sponge-based collection [13] [14].
- Materials: For expectoration: sterile, leak-proof screw-cap collection tube (e.g., DNA Genotek OM-505). For sponge-based: oral sponge kit (e.g., DNA Genotek ORE-100).
- Procedure (Expectoration):
- Instruct the participant not to eat, drink, or smoke for at least 30 minutes prior to collection.
- Have the participant pool saliva in their mouth and then passively drool 1-2 mL of saliva through the funnel into the collection tube.
- Cap the tube securely.
- Procedure (Sponge-Based, for young children or those who cannot expectorate):
- Place a small, sterile sponge between the patient's cheek and gum.
- Leave the sponge in place for at least 1-3 minutes to allow for saturation.
- Remove the sponge and place it into the provided transport container or medium.
- Key Consideration: Saliva samples can be transported at room temperature and are stable for up to 48 hours before processing, simplifying logistics [14].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials for Respiratory Sample Collection and Analysis
| Item | Function & Rationale | Example(s) |
|---|---|---|
| Flocked Swabs | Sample collection. Synthetic fibers create a micro-brush that efficiently traps and releases cellular material and viruses, improving yield over traditional wound-fiber swabs. | Copan FLOQSwabs [4], Puritan UniTranz-RT [11] |
| Viral Transport Medium (VTM) | Preserves viral integrity and viability during transport from collection site to laboratory. | Copan UTM [15], Various commercial VTM formulations |
| Proteinase K / Lysis Buffer | For saliva pre-processing; inactivates virus and degrades nucleases, stabilizing viral RNA for RT-PCR without the need for nucleic acid extraction. | Used in SalivaDirect protocol [14] |
| Expanding Polyvinyl Alcohol Sponge | For superior collection of mucosal lining fluid, particularly for antibody detection; expands in the nasal cavity for increased surface area contact. | PVF-J Sponge (Beijing Yingjia) [15] |
| Validated ELISA Kit | Quantitative detection of mucosal immunoglobulins (e.g., IgA) in nasal samples; critical for evaluating mucosal immune responses. | In-house validated assays per ICH guidelines [15] |
Experimental Workflow and Decision Pathways
Comparative Discomfort, Technical Difficulty, and Safety Profiles
Comparative Performance and Tolerability of Swab Types
The choice between nasal and nasopharyngeal swabs involves balancing test sensitivity against patient tolerability and safety. The data below summarizes key comparative studies.
| Swab Type | Reported Sensitivity/Detection Rate | Reported Discomfort & Tolerability | Key Safety Considerations |
|---|---|---|---|
| Nasopharyngeal Swab (NPS) | Considered the gold standard [10] [17]. Higher virus concentrations (lower Ct values) than nasal swabs or saliva [10]. 97% detection rate for RSV [18]. | More frequently associated with discomfort and pain [19] [17]. Less comfortable for the patient [18]. | Rare but serious risks include CSF leakage, epistaxis, and retained swabs, especially in patients with skull base defects [2]. |
| Anterior Nasal Swab | Lower detection rate for RSV (76%) compared to NPS [18]. Sensitivity of 82.4% for SARS-CoV-2, improved with vigorous rubbing [10] [17]. | Better tolerated in children [19] and less invasive [18]. Ideal for self-testing [18]. | Generally very low risk. Potential for minor discomfort or epistaxis if inserted too forcefully [20]. |
| Oropharyngeal Swab (OPS) | Sensitivity comparable to NPS (94.1% vs. 92.5%) for SARS-CoV-2 [17]. Applying excessive force during collection does not improve sensitivity [21]. | More comfortable for patients than NPS [21]. | Generally safe. |
Detailed Experimental Protocols from Cited Studies
Protocol 1: Comparison of Nasopharyngeal, Anterior Nasal, and Saliva Samples in Children
This methodology was used to generate data found in [19].
- Study Population: Pediatric patients (0–15 years) presenting at an emergency department with respiratory symptoms.
- Sample Collection:
- Nasopharyngeal Swab (NPS): Collected by a nurse using a nylon-flocked dry swab inserted through one nostril to the nasopharynx. This was the reference sample for clinical care.
- Anterior Nasal Swab: Collected by a nurse or research nurse by rotating a nylon-flocked dry swab in both nostrils.
- Saliva Sample: Collected from the buccal mucosa with a wrapped polyester swab or by having older children spit into a container.
- Virus Analysis: All samples were analyzed using the BioFire Respiratory Panel 2.1 plus multiplex PCR test.
- Tolerability Assessment: Guardians and patients (≥4 years) evaluated the tolerance of each sampling method on a scale from 1 (pleasant) to 5 (unpleasant).
Protocol 2: Head-to-Head Comparison of Oropharyngeal, Nasopharyngeal, and Nasal Swabs
This methodology was used to generate data found in [17].
- Study Population: Adults with a recently confirmed SARS-CoV-2 infection.
- Sample Collection by Otorhinolaryngologists:
- Nasopharyngeal Swab (NPS): A flexible minitip flocked swab was inserted towards the patient's earlobe until resistance was met (approx. 8–11 cm), rotated three times, and withdrawn.
- Oropharyngeal Swab (OPS): Using a tongue depressor, both palatine tonsils and the posterior oropharyngeal wall were swabbed with a rigid-shaft flocked swab.
- Nasal Swab: A rigid-shaft flocked swab was inserted 1–3 cm into the nasal cavity, brushed along the septum and inferior nasal concha, and rotated three times.
- Laboratory Methods: All samples were tested for SARS-CoV-2 using RT-PCR, and Cycle Threshold (Ct) values were compared.
Protocol 3: Effect of Applied Force on Oropharyngeal Swab Quality
This methodology was used to generate data found in [21].
- Objective: To determine the correlation between swabbing force, collected cell count, and SARS-CoV-2 detection sensitivity.
- Method: A force-feedback device was used to collect oropharyngeal samples from healthy and SARS-CoV-2-positive individuals at controlled forces of 1.5 N, 2.5 N, and 3.5 N.
- Analysis: Cell counts were calculated based on the human RNase P gene, and SARS-CoV-2 RNA was quantified via RT-PCR.
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: Which swab type should I choose for a population where tolerability is a primary concern, such as in pediatric studies? A: Anterior nasal swabs are the most suitable choice. Studies show they are better tolerated than nasopharyngeal swabs in children while still providing a feasible sample type for detecting respiratory viruses via PCR [19]. Their use also enables self-collection, which minimizes discomfort and exposure risk.
Q2: Our research requires the highest possible sensitivity for virus detection. Is NPS always the best option? A: While NPS is generally considered the gold standard and yields the highest virus concentrations [10], a combined approach can be optimal. Research shows that combining an Oropharyngeal Swab (OPS) with an NPS can achieve a 100% detection rate in confirmed positive cases [17]. If NPS is not feasible, a vigorously collected nasal swab (e.g., 10 rubs) can yield viral concentrations similar to an NPS [10].
Q3: We are training staff on NPS collection. What are the critical safety points to emphasize? A: Safe NPS collection requires proper technique and anatomical knowledge [2]. Key points include:
- Insertion Angle: Keep the swab within 30° of the nasal floor (the line from the nostril to the external ear canal) [2].
- Path: Gently insert the swab along the nasal septum just above the nasal floor [2].
- Action: Do not use forceful insertion. Rotate the swab upon reaching the nasopharynx and hold it in place for several seconds before withdrawal [2].
- Contraindications: Be aware of high-risk factors, including severe septal deviation, pre-existing skull base defects, or a history of sinus or pituitary surgery [2].
Q4: Does applying more pressure during swab collection improve sample quality and test sensitivity? A: No. Studies on oropharyngeal swabs show that while increased force (e.g., 3.5 N) collects more cells, it results in higher (worse) Ct values in SARS-CoV-2 testing, indicating poorer diagnostic sensitivity compared to a standard 1.5 N force [21]. The technique should be firm and standardized, but excessive force is counterproductive.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function/Application | Examples from Literature |
|---|---|---|
| Nylon Flocked Swabs | Designed for efficient sample collection and release. Often used for NP and nasal sampling. | Copan FLOQSwabs [19] [17] |
| Polyester Swabs | Used for saliva or oropharyngeal sampling. | Wrapped polyester swabs for buccal collection [19] |
| Universal Transport Medium (UTM) | Preserves viral integrity for transport and subsequent PCR analysis. | Copan UTM [19] [15] |
| Multiplex PCR Panels | Enable simultaneous detection of a broad panel of respiratory pathogens from a single sample. | BioFire Respiratory Panel 2.1 plus [19]; Allplex Respiratory Panels & SARS-CoV-2 assay [10] [17] |
| Force-Feedback Device | Allows for standardized and quantitative application of force during swab collection for methodological studies. | Used to apply controlled forces of 1.5N, 2.5N, and 3.5N [21] |
Experimental Workflow and Decision Pathway
Diagram Title: Swab Type Selection Workflow for Research
Safety and Complication Profile of Nasopharyngeal Swabs
While generally safe, NPS procedures carry a low risk of complications that researchers must recognize. Documented adverse events from the literature include [2]:
- Most Frequent: Retained swabs (due to fracture) and epistaxis (nosebleeds).
- Most Serious: Cerebrospinal fluid (CSF) leakage, typically in individuals with undiagnosed anatomical anomalies like skull base defects or encephaloceles.
The overall rate of complications requiring medical evaluation is very low, ranging from 0.0012% to 0.026% [2]. Adherence to correct anatomical insertion techniques is the primary method of risk mitigation.
Technical Support Center
Troubleshooting Guides
Q1: Our AN swab samples consistently yield lower viral RNA concentrations compared to historical NP swab data. What are the primary factors we should investigate? A1: Focus on these critical parameters:
- Swab Technique: AN sampling is highly technique-dependent. Ensure the swab is inserted approximately 2 cm (or until resistance is met) and is firmly rotated against the nasal wall for 10-15 seconds. Inadequate contact time or depth is a common cause of low yield.
- Swab Material: Confirm you are using swabs with synthetic tips (e.g., flocked nylon) and plastic/wire shafts. Calcium alginate swabs or those with wooden shafts can inhibit PCR and should be avoided.
- Transport Media Volume: Using excessive volume of viral transport media (VTM) can dilute the sample. Ensure the volume is appropriate for the swab type and elution protocol (typically 1-3 mL).
Q2: We are observing high Ct values and inconsistent results from OP swabs. What could be causing this variability? A2: Inconsistency in OP sampling is often due to:
- Sampling Site Inaccuracy: The target is the posterior pharynx and tonsillar pillars, not the tongue, cheeks, or saliva. Use a tongue depressor and ensure the swab does not touch other oral surfaces during insertion and withdrawal.
- Gag Reflex: This can lead to rapid, shallow sampling. Train participants to breathe slowly through the mouth to suppress the reflex.
- Sample Degradation: OP samples may have higher nuclease activity. Ensure immediate placement into VTM and cold chain storage/freezing after collection to preserve nucleic acid integrity.
Q3: When comparing AN and NP swabs in a study, what are the key experimental controls to include? A3: To ensure valid comparison, implement these controls:
- Sample Order Randomization: Counterbalance the order of swab collection (AN vs. NP) to control for carry-over effects or discomfort affecting subsequent samples.
- Split-Sample Validation: For a subset of participants, split the eluent from a single swab and run duplicates to confirm assay precision.
- Standardized Elution Protocol: Use identical vortexing, incubation times, and centrifugation steps for all swab types to minimize processing variability.
Frequently Asked Questions (FAQs)
Q: What is the primary driver for the shift from NP to AN swabs in clinical research? A: The key drivers are improved patient comfort and tolerability, which enhances recruitment and allows for repeated self-sampling in longitudinal studies. This must be balanced against potential sensitivity differences, which is an active area of optimization.
Q: Can AN swabs be used for all respiratory viruses with the same efficacy as NP swabs? A: No. Efficacy is virus-dependent. For SARS-CoV-2, AN swabs show high concordance with NP swabs, especially in symptomatic individuals. For other viruses like influenza or RSV, the data is more variable, and NP may still be the gold standard. Always consult literature specific to your pathogen of interest.
Q: What is the recommended storage condition for AN/OP swab samples prior to nucleic acid extraction? A: If extraction cannot be performed within 48-72 hours, store samples at -70°C to -80°C. Avoid repeated freeze-thaw cycles, which degrade RNA.
Data Presentation: Comparative Swab Performance
Table 1: Summary of Reported Sensitivity for SARS-CoV-2 Detection by Swab Type
| Swab Type | Relative Sensitivity vs. NP (Range) | Key Advantages | Key Limitations |
|---|---|---|---|
| Nasopharyngeal (NP) | 100% (Reference) | Considered gold standard; deep sampling site. | Invasive, requires trained personnel, poor patient tolerance. |
| Anterior Nares (AN) | 85% - 98% | High patient tolerance, suitable for self-swabbing. | Technique-sensitive, viral load may be lower. |
| Oropharyngeal (OP) | 80% - 90% | Easily accessible, minimal training required. | High variability, susceptible to gag reflex, may contain PCR inhibitors. |
Table 2: Essential Reagent Solutions for Swab-Based Viral Research
| Research Reagent | Function & Importance |
|---|---|
| Flocked Nylon Swabs | Swabs with frayed ends for superior sample absorption and release. Critical for maximizing elution efficiency. |
| Universal Transport Media (UTM) | Maintains viral integrity and prevents bacterial overgrowth during transport and storage. |
| RNA Stabilization Buffer | Protects labile viral RNA from degradation by nucleases, especially critical for OP samples. |
| Nucleic Acid Extraction Kits (Magnetic Bead) | High-throughput, automated purification of viral RNA with consistent yield and purity. |
| PCR Master Mix with UDG | Contains Uracil-DNA glycosylase to prevent carryover contamination from previous PCR amplicons. |
Experimental Protocols
Protocol 1: Standardized Paired Swab Collection for Comparative Sensitivity Objective: To directly compare viral load recovery between AN and NP swabs from the same participant.
- Participant Preparation: Tilt participant's head back 70 degrees.
- NP Swab Collection: Gently insert a flocked NP swab along the nasal septum to the nasopharynx. Rotate swab and hold for 10-15 seconds to absorb secretions.
- AN Swab Collection: Using a fresh flocked swab, insert into the anterior naris ~2 cm. Rotate the swab firmly against the nasal wall for 10-15 seconds. Repeat in the second naris using the same swab.
- Processing: Immediately place each swab into separate tubes containing 3 mL of UTM. Vortex vigorously for 15 seconds. Store at -80°C until nucleic acid extraction.
Protocol 2: RNA Extraction and RT-qPCR for Viral Quantification Objective: To quantify viral RNA load from swab eluents.
- Sample Thaw: Thaw UTM samples on ice or at 4°C.
- Nucleic Acid Extraction: Use a commercial magnetic bead-based RNA extraction kit. Process 200 µL of UTM sample, eluting in 60 µL of nuclease-free water.
- RT-qPCR Setup: Prepare a one-step RT-qPCR reaction mix targeting a conserved viral gene (e.g., SARS-CoV-2 E gene). Include a standard curve of known copy number for absolute quantification and no-template controls.
- Amplification: Run on a real-time PCR system using the following cycling conditions: 50°C for 15 min (reverse transcription); 95°C for 2 min (polymerase activation); 45 cycles of 95°C for 15 sec and 60°C for 1 min (amplification).
Mandatory Visualization
Diagram 1: Swab Comparison Workflow
Diagram 2: Factors Influencing Swab Sensitivity
From Theory to Practice: Sampling Protocols and Performance Across Testing Modalities
Standardized Procedures for NP, AN, and Oropharyngeal Swab Collection
This technical support guide provides detailed, evidence-based protocols for the collection of nasopharyngeal (NP), anterior nares (AN), and oropharyngeal (OP) swabs. Proper specimen collection is the most critical pre-analytical factor influencing the sensitivity and specificity of downstream severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) detection assays [22]. Inadequate sampling technique directly contributes to false-negative results, compromising research integrity and diagnostic accuracy [23]. This document, framed within a broader thesis on optimizing sensitivity in nasal versus nasopharyngeal sampling, standardizes procedures for researchers, scientists, and drug development professionals to ensure the highest quality data generation in clinical and research settings.
Standardized Swab Collection Procedures
The following table summarizes the key steps for each standardized swab collection procedure, based on guidelines from the U.S. Centers for Disease Control and Prevention (CDC) and clinical studies [12] [23].
Table 1: Standardized Procedures for NP, AN, and Oropharyngeal Swab Collection
| Swab Type | Patient/Subject Positioning | Swab Insertion & Path | Sampling Technique & Duration | Final Swab Handling |
|---|---|---|---|---|
| Nasopharyngeal (NP) | Seated, head tilted back 70 degrees [12]. Ideally, use a reclining chair to align operator with target area [23]. | Insert swab through nostril parallel to the palate (hard palate floor), aiming toward the ear. Insert until resistance is met (~7-9 cm depth) [12] [23]. | Gently rub and roll the swab [12]. Leave in place for several seconds (e.g., 5-10 seconds) to absorb secretions [11] [12]. Slowly remove while rotating it. | Place swab tip-first into sterile transport tube containing viral transport media (VTM). Break or cut swab shaft as needed [12]. |
| Anterior Nares (AN) | Seated, head tilted back 70 degrees [12]. | Insert the entire collection tip of the swab (½ to ¾ of an inch, or 1-1.5 cm) inside the nostril [12]. | Firmly sample the nasal wall by rotating the swab in a circular path against the nasal wall at least 4 times [12]. Take approximately 15 seconds to collect the specimen. Repeat in the other nostril using the same swab. | Place swab tip-first into sterile transport tube containing VTM [12]. |
| Oropharyngeal (OP) | Seated, facing the collector with mouth wide open. Use a tongue depressor if necessary for better visualization [23]. | Insert swab into the posterior pharynx and tonsillar areas [12]. | Rub swab over both tonsillar pillars and the posterior oropharynx. Avoid touching the tongue, teeth, and gums to avoid contaminant introduction [12]. | Place swab tip-first into sterile transport tube containing VTM [12]. |
Experimental Protocols for Comparative Sensitivity
To support the thesis on optimizing sensitivity, the following section details key experimental methodologies from cited studies that directly compare the performance of different swab types.
Head-to-Head Diagnostic Accuracy Evaluation
This protocol is adapted from a prospective study comparing AN and NP swabs for SARS-CoV-2 antigen detection [5].
- Objective: To conduct a head-to-head diagnostic accuracy evaluation of AN and NP swabs for SARS-CoV-2 antigen detection using rapid diagnostic tests (Ag-RDTs).
- Study Population: Symptomatic individuals presenting at a testing center. For statistical power, the study should proceed until at least 100 Ag-RDT positives are obtained using AN swabs, per WHO recommendations [5].
- Sample Collection (Paired Design):
- NP Swab (for Reference Standard): A trained healthcare worker collects an NP swab from one nostril and places it in Universal Transport Medium (UTM) for RT-qPCR analysis.
- NP Swab (for Index Test): A second NP swab is collected from the other nostril for the Ag-RDT.
- AN Swab (for Index Test): Finally, an AN swab is collected from both nostrils for the Ag-RDT, following the manufacturer's instructions [5].
- Laboratory Analysis:
- Reference Standard: RNA is extracted from the UTM sample and tested via RT-qPCR (e.g., TaqPath COVID-19). A positive result is defined as amplification of ≥2 SARS-CoV-2 target genes with a cycle threshold (Ct) ≤40 [5].
- Index Test: Both the NP and AN swabs for the Ag-RDT are processed immediately according to the manufacturer's Instructions for Use (IFU). Results should be read by two operators blinded to each other's readings and the RT-qPCR result to minimize bias. The test line intensity can be scored on a quantitative scale (e.g., 1-10) [5].
- Data Analysis: Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for both AN and NP swabs against the RT-qPCR reference standard. The level of agreement between swab types can be determined using Cohen’s kappa (κ). Logistic regression can be used to analyze sensitivity relative to viral load (RNA copy numbers) [5].
Evaluating the Impact of Sampling Force on Quality
This protocol is based on a study investigating pre-analytical factors, specifically the force applied during oropharyngeal sampling [21].
- Objective: To examine the effect of applied force during oropharyngeal sampling on sample quality, specifically assessing host cell count and SARS-CoV-2 NAT cycle threshold (Ct) values.
- Sample Collection with Controlled Force:
- A force-feedback device is used to standardize the application of force during swab collection.
- Swabs are collected from SARS-CoV-2 positive patients using controlled forces (e.g., 1.5 N, 2.5 N, and 3.5 N) in a randomized sequence.
- Laboratory Analysis:
- Swabs are vortexed to suspend cells in the transport medium.
- Nucleic acids are extracted from an aliquot of the medium.
- SARS-CoV-2 RNA is quantified using a validated NAT assay (e.g., Abbott RealTime SARS-CoV-2 Assay) to obtain Ct values.
- Host cell count is quantified by measuring the number of copies of a human reference gene (e.g., RNase P) via PCR [21].
- Data Analysis: Compare mean Ct values and mean calculated cell counts across the different force groups using non-parametric statistical tests (e.g., Wilcoxon test). A statistically significant difference is defined as p < 0.05 [21].
Research Reagent Solutions
The following table lists essential materials and reagents required for conducting swab collection and processing in a research context.
Table 2: Essential Research Reagents and Materials for Swab-Based Studies
| Item | Specification / Function | Key Considerations |
|---|---|---|
| Swabs | Synthetic fiber (e.g., polyester, flocked) swabs with thin plastic or wire shafts [12]. | Critical: Do not use calcium alginate swabs or swabs with wooden shafts, as they may contain substances that inactivate viruses and inhibit molecular tests [12]. |
| Transport Media | Universal Transport Medium (UTM) or Viral Transport Medium (VTM) [5]. | Contains compounds to stabilize viral nucleic acids and inhibit bacterial growth during transport. Essential for maintaining sample integrity [22]. |
| Nucleic Acid Extraction Kits | e.g., QIAamp 96 Virus QIAcube HT kit (Qiagen) [5] or Roche MagNA Pure 96 Kit [21]. | For purifying viral RNA from swab media for downstream RT-qPCR or NAT analysis. Automation increases throughput and consistency. |
| RT-qPCR / NAT Assays | e.g., TaqPath COVID-19 (ThermoFisher) [5] or Abbott RealTime SARS-CoV-2 Assay [21]. | Targets specific SARS-CoV-2 genes (N, ORF1ab, S). Must include an internal control to monitor extraction and amplification. |
| Ag-RDT Kits | e.g., Sure-Status (PMC, India) or Biocredit (RapiGEN, South Korea) [5]. | Used for rapid antigen detection. Performance must be validated for the specific swab type (AN vs. NP) being used. |
Troubleshooting Guide & FAQs
Diagram: Troubleshooting Logic for Swab Collection Issues
Frequently Asked Questions (FAQs)
Q1: For SARS-CoV-2 detection, which swab type offers the highest sensitivity? The nasopharyngeal (NP) swab is historically considered the gold standard for respiratory virus detection, including SARS-CoV-2, as it samples the site of active viral replication [22]. However, recent head-to-head studies of rapid antigen tests found that anterior nares (AN) swabs can have equivalent diagnostic accuracy to NP swabs, with one study reporting sensitivities of 85.6% for AN vs. 83.9% for NP for one brand, and 79.5% for AN vs. 81.2% for NP for another [5]. For PCR, a combined nose and throat swab has shown the highest sensitivity for detecting the Omicron variant [6]. The choice depends on the specific test, variant, and context, balancing sensitivity with invasiveness and feasibility.
Q2: Does applying more force during swab collection improve sample quality and test sensitivity? No. Evidence indicates that while higher force (e.g., 3.5 Newtons) during oropharyngeal swab collection can increase host cell count, it actually leads to higher (worse) Ct values in nucleic acid testing, reducing sensitivity [21]. Excessive force may cause discomfort and does not improve diagnostic yield. A gentle but firm technique, ensuring proper contact with the mucosal surface, is sufficient.
Q3: Is rotating the swab after insertion into the nasopharynx necessary? Evidence suggests it may not be necessary and can increase patient discomfort. A study comparing an "in-out" technique (no rotation) with a "rotation" technique (rotating for 10 seconds) found no significant difference in the recovery of human nucleic acids, a marker of sample quality [11]. The CDC guideline recommends to "gently rub and roll" the swab, which occurs during insertion and/or removal, but prolonged rotation in place may not add benefit [12].
Q4: What are the most common anatomical pitfalls during NP swab collection and how can they be avoided?
- Incorrect Angle: Directing the swab upward (toward the skull base) instead of parallel to the palate. This causes pain and misses the nasopharynx.
- Septal Contact: Pressing the swab against the medial nasal septum, which is highly sensitive and can cause significant pain and sneezing. The swab should be directed laterally, toward the inferior turbinate [23].
- Insufficient Depth: Not inserting the swab far enough (~7-9 cm in adults) to reach the nasopharynx. The distance can be estimated by holding the swab from the nostril to the tragus of the ear [23].
Q5: Our research involves self-collected swabs. What are the key considerations to ensure data quality? Only certain swab types are appropriate for self-collection. AN and nasal mid-turbinate (NMT) swabs are approved for self-collection, while NP and OP swabs are not, as they require professional training to perform safely and effectively [12]. It is critical to provide subjects with clear, visual, and simple-to-follow instructions. For AN swabs, specifically instruct to rotate the swab against the nasal wall in a circular path multiple times in both nostrils [12]. Note that self-interpretation of rapid tests using AN swabs can be challenged by weaker test line intensity, potentially leading to false negatives if users misread the result [5].
Swab Type Comparison: Nasopharyngeal vs. Nasal vs. Oropharyngeal
Multiple clinical studies have directly compared the sensitivity of different upper respiratory swab types for SARS-CoV-2 detection using RT-PCR. The table below summarizes key findings from recent head-to-head comparisons.
Table 1: Clinical Sensitivity of Different Swab Types for SARS-CoV-2 Detection by RT-PCR
| Swab Type | Reported Sensitivity (95% CI) | Comparative Reference | Study Details |
|---|---|---|---|
| Oropharyngeal (OP) | 94.1% (87-100%) | vs. NPS [4] | Prospective study of 51 confirmed positive participants [4] |
| Nasopharyngeal (NP) | 92.5% (85-99%) | Gold Standard [4] | Same study as above; considered benchmark [4] |
| Nasal Swab | 82.4% (72-93%) | vs. NPS [4] | Anterior nasal or mid-turbinate sampling [4] |
| Combined OP/NP | 100% | Self-comparison [4] | Positive if one or both swabs were positive [4] |
| Combined OP/Nasal | 96.1% (90-100%) | vs. Nasal swab alone [4] | Significantly increased sensitivity vs. single nasal swab [4] |
| Throat Only | 97% | vs. Combined Nose & Throat [6] | Study of 815 participants during Omicron wave [6] |
| Nose Only | 91% | vs. Combined Nose & Throat [6] | Same study as above [6] |
Key Experimental Protocol: Swab Collection
The following methodology is adapted from a prospective diagnostic study comparing swab types [4].
- Participant Recruitment: Enroll adults (≥18 years) with a recent (e.g., <10 days) initial positive SARS-CoV-2 test. Exclude participants if all subsequent swabs (NPS, OPS, nasal) test negative.
- Sample Collection: A trained healthcare professional (e.g., otorhinolaryngologist) should collect all swabs for consistency.
- Nasopharyngeal Swab (NPS): Use a flexible minitip flocked swab. Tilt the patient's head back, insert the swab into the nasal cavity toward the earlobe, following the nasal floor. Insert until resistance is met at the nasopharynx (approx. 8-11 cm), leave for a few seconds, rotate 3 times, and withdraw [4].
- Oropharyngeal Swab (OPS): Use a rigid-shaft flocked swab. Use a tongue depressor for visualization. Swab both palatine tonsils and the posterior oropharyngeal wall with a painting, rotating motion, avoiding the cheeks, teeth, and gums [4].
- Nasal Swab: Use a rigid-shaft flocked swab. Insert the swab ~1-3 cm into the nasal cavity, brush along the septum and inferior nasal concha, and rotate 3 times before withdrawal [4].
- Sample Processing: Place each swab into a separate sterile tube containing viral transport medium.
- Laboratory Analysis: Test all samples from a single participant using the same RT-PCR assay. Common targets include the E, N, and RdRP/S genes. A cycle threshold (Ct) cut-off value of ≤40 is typically used to define positivity [4].
- Data Analysis: Calculate sensitivity for each swab type against a composite gold standard (e.g., a participant is considered positive if one or more of their swabs are positive). Compare sensitivities using statistical tests like the McNemar test and compare Ct values using the Wilcoxon matched-pairs signed-rank test [4].
PCR Troubleshooting Guide
Table 2: Common PCR Issues and Recommended Solutions
| Observation | Possible Cause | Recommended Solution |
|---|---|---|
| No Product | Incorrect annealing temperature | Recalculate primer Tm; test a gradient starting 5°C below the lower Tm [24] [25]. |
| Poor template quality or inhibitors | Repurify template DNA via ethanol precipitation or commercial clean-up kits; dilute template to dilute inhibitors [26] [24] [25]. | |
| Insufficient number of cycles | Increase cycle number (e.g., by 3-5, up to 40 cycles) [25]. | |
| Multiple or Non-Specific Bands | Low annealing temperature | Increase annealing temperature in 2°C increments [26] [25]. |
| Excess primer or template | Optimize primer concentration (0.1–1 µM); reduce template amount by 2–5 fold [26] [25]. | |
| Non-hot-start polymerase | Use a hot-start polymerase to prevent activity at room temperature and reduce non-specific amplification [26] [24]. | |
| Smear on Gel | Overcycling | Reduce the number of PCR cycles [25]. |
| Contamination | Include a negative (no-template) control; use dedicated pre- and post-PCR work areas and equipment [25]. | |
| Excessively long extension time | For certain enzymes, long extensions can cause smearing; follow manufacturer's guidelines [25]. | |
| Sequence Errors | Low fidelity polymerase | Switch to a high-fidelity polymerase [24]. |
| Unbalanced dNTP concentrations | Use fresh, equimolar dNTP mixes [26] [24]. | |
| Excessive Mg2+ concentration | Optimize and reduce Mg2+ concentration in the reaction [26] [24]. |
Frequently Asked Questions (FAQs)
Q: What is the single most important step to prevent PCR contamination? A: Physically separating pre-PCR and post-PCR work areas. No reagents, equipment, or materials from the post-PCR area (where amplified DNA is handled) should ever be brought into the pre-PCR area (where reaction mixtures are set up). Using dedicated pipettes, tips, and lab coats for each area is critical [25].
Q: My template has high GC content. How can I improve amplification? A: Use a polymerase specifically formulated for GC-rich templates. You can also add PCR co-solvents or additives like DMSO, GC enhancer, or formamide to help denature the stubborn secondary structures. Increasing the denaturation temperature and/or time may also be beneficial [26] [24] [25].
Q: I have a low abundance target. What can I adjust? A: First, ensure you are using a polymerase with high sensitivity. You can increase the number of PCR cycles (up to 40) and increase the amount of template DNA, provided it does not introduce inhibitors. Using nested PCR in a second round of amplification can significantly improve detection [26] [25].
Q: Why are my Ct values for nasal swabs consistently higher than for NP swabs? A: This is a common finding in clinical studies and suggests a lower viral load in the anterior nares compared to the nasopharynx. Studies consistently report higher mean Ct values (indicating less viral RNA) for nasal swabs compared to NPS and OPS [4] [27]. This biological variation is a key reason nasal swabs may exhibit lower clinical sensitivity.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Materials for Swab Comparison and PCR Studies
| Item | Function / Application |
|---|---|
| Flocked Swabs | Sample collection; superior release of cellular material compared to spun-fiber swabs. Minitip for NPS, standard for OPS [4]. |
| Viral Transport Medium (VTM) | Preserves viral integrity and inactivates pathogens for safe transport and storage of swab samples [4]. |
| Hot-Start High-Fidelity DNA Polymerase | Reduces non-specific amplification and minimizes misincorporation of nucleotides, crucial for sensitive and accurate RT-PCR [26] [24]. |
| RNA Extraction Kit | Isolates high-purity viral RNA free of PCR inhibitors from swab samples in VTM [4]. |
| PCR Additives (e.g., DMSO, GC Enhancer) | Aids in denaturing complex templates (e.g., high GC-content, secondary structures) to improve amplification efficiency and yield [26] [24]. |
| Synthetic RNA Controls | Acts as an external positive control to monitor the efficiency of the entire RT-PCR process, from extraction to amplification. |
Experimental Workflow and Decision Pathway
The following diagram illustrates the logical workflow for a head-to-head clinical comparison of swab types and subsequent troubleshooting steps.
Diagram 1: Swab Study and Troubleshooting Workflow
Diagram 2: PCR Troubleshooting Decision Tree
FAQs on Swab Sampling and Test Sensitivity
What is the primary factor influencing the sensitivity of Ag-RDTs?
Viral load is the most important factor determining SARS-CoV-2 antigen test sensitivity [28]. Test sensitivity is significantly higher in individuals with high viral loads, which often occur early in infection. One study demonstrated that the sensitivity of a nasal Ag-RDT was 100% for samples with Ct values <15, but dropped to 57.1% for Ct values between 25-29.9, and 0% for Ct values ≥30 [29].
How does the sensitivity of nasal swabs compare to nasopharyngeal (NP) swabs for Ag-RDTs?
Nasal swabs generally show comparable, though slightly lower, sensitivity to NP swabs, making them an adequate alternative [29] [30]. One study reported an overall sensitivity of 88.0% for nasal swabs compared to NP swabs confirmed by RT-PCR [29]. Another head-to-head comparison found sensitivities of 70.2% for NP swabs and 67.3% for nasal swabs, with a 99.4% agreement between the methods [30].
Does combining different swab types improve detection sensitivity?
Yes, combining swabs from different anatomical sites can enhance sensitivity. Research indicates that a combined nose and throat swab provides higher viral concentration and is the most effective method for SARS-CoV-2 detection via PCR [6]. One study found that combining oropharyngeal and nasal swab results significantly increased sensitivity to 96.1% compared to nasal swab alone (82.4%) [4].
How should a negative Ag-RDT result be interpreted?
A negative Ag-RDT result should be considered presumptive. The FDA and CDC recommend repeat testing after a negative result. For symptomatic individuals, test again 48 hours after the first negative test. For asymptomatic individuals, test again 48 hours after the first negative test, and then 48 hours after the second negative test, for a total of at least three tests [31] [32].
Troubleshooting Common Experimental Issues
Issue: Lower-than-expected sensitivity in Ag-RDT results
Potential Causes and Solutions:
Cause: Testing outside the optimal viral load window.
- Solution: Ensure testing is performed during the peak viral load phase, typically within the first 5-7 days of symptom onset [28].
Cause: Inadequate specimen collection technique.
- Solution: For nasal swabs: Insert the swab approximately 1-3 cm into the nasal cavity and brush along the septum and inferior nasal concha, rotating at least three times [4]. For nasopharyngeal swabs: Insert the swab until resistance is met (approximately 8-11 cm deep), point towards the earlobe, and rotate about three times [4].
Cause: Improper specimen handling and storage.
- Solution: Perform tests in an environment between 15-30°C (59-86°F). If test kits have been exposed to extreme temperatures, bring the package inside and leave it unopened at room temperature for at least two hours before use [31].
Issue: Inconsistent results between technical replicates
Potential Causes and Solutions:
Cause: Variable sample collection depth or technique.
- Solution: Standardize collection protocols and ensure all personnel are trained in consistent swab collection methods. Using swabs with depth markers can improve consistency [4].
Cause: Uneven viral distribution in the respiratory tract.
Comparative Performance Data of Swab Modalities
Table 1: Sensitivity Comparison Across Sampling Methods
| Swab Type | Sensitivity (%) | Specificity (%) | Test Platform | Study Population |
|---|---|---|---|---|
| Nasopharyngeal (NP) | 92.5 [4] | N/P | RT-PCR | Confirmed SARS-CoV-2 positive |
| Oropharyngeal (OP) | 94.1 [4] | N/P | RT-PCR | Confirmed SARS-CoV-2 positive |
| Nasal | 82.4 [4] | N/P | RT-PCR | Confirmed SARS-CoV-2 positive |
| Combined OP/Nasal | 96.1 [4] | N/P | RT-PCR | Confirmed SARS-CoV-2 positive |
| Nasopharyngeal | 70.2 [30] | 97.9 [30] | Ag-RDT (SD Biosensor) | Symptomatic/Exposed |
| Nasal | 67.3 [30] | 97.9 [30] | Ag-RDT (SD Biosensor) | Symptomatic/Exposed |
| Combined NP/Nasal | 74.4 [30] | 97.5 [30] | Ag-RDT (SD Biosensor) | Symptomatic/Exposed |
N/P: Not Provided in the source material
Table 2: Impact of Viral Load on Ag-RDT Sensitivity
| Cycle Threshold (Ct) Range | Sensitivity of Nasal Ag-RDT (%) |
|---|---|
| <15 | 100.0 [29] |
| 15-19.9 | 94.0 [29] |
| 20-24.9 | 80.5 [29] |
| 25-29.9 | 57.1 [29] |
| ≥30 | 0.0 [29] |
Experimental Protocols for Swab Comparison Studies
Protocol 1: Standardized Swab Collection for Head-to-Head Comparison
Purpose: To compare the sensitivity of different swab types for SARS-CoV-2 detection using Ag-RDT [4].
Materials:
- Flexible minitip flocked swab for nasopharyngeal sampling
- Rigid-shaft flocked swab for oropharyngeal and nasal sampling
- Sterile tubes with viral transport medium
- Personal protective equipment (PPE)
Procedure:
- Nasopharyngeal Swab: Tilt patient's head slightly back. Insert swab into nasal cavity pointing towards the earlobe, following the nasal floor. Insert approximately 8-11 cm deep until resistance is met. Leave for a few seconds, rotate three times, and withdraw [4].
- Oropharyngeal Swab: Use a tongue depressor for visualization. Collect specimen from both palatine tonsils and the posterior oropharyngeal wall with a painting and rotating movement, avoiding cheeks, teeth, and gums [4].
- Nasal Swab: Insert swab approximately 1-3 cm into nasal cavity. Brush along the septum and inferior nasal concha, rotating three times before withdrawal [4].
- Place each specimen into separate sterile tubes with transport medium.
- Process samples according to Ag-RDT manufacturer instructions.
Protocol 2: Viral Load Stratification Analysis
Purpose: To evaluate Ag-RDT performance across different viral load ranges [29].
Materials:
- Paired nasopharyngeal and nasal swabs
- Ag-RDT test kits (e.g., Abbott Panbio COVID-19 Ag)
- RT-PCR equipment
- Viral transport media
Procedure:
- Collect paired NP and nasal swabs from participants.
- Perform Ag-RDT according to manufacturer instructions for both swab types.
- Process NP swab in viral transport media for RT-PCR analysis.
- Stratify results based on RT-PCR cycle threshold (Ct) values.
- Calculate sensitivity and specificity for each Ct range category (<15, 15-19.9, 20-24.9, 25-29.9, ≥30).
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Swab Sensitivity Research
| Item | Function | Example/Specifications |
|---|---|---|
| Flexible Minitip Flocked Swabs | NP sample collection; designed to reach nasopharynx and maximize cell/viral particle collection | COPAN diagnostics Inc, Italy [4] |
| Rigid-Shaft Flocked Swabs | OP and anterior nasal sample collection | Meditec A/S, Denmark [4] |
| Viral Transport Medium (VTM) | Preserve viral integrity during transport and storage | 2 mL tubes (Meditec A/S, Denmark) [4] |
| Ag-RDT Test Kits | Rapid antigen detection | Abbott Panbio COVID-19 Ag Test [29] or SD Biosensor STANDARD Q [30] |
| RT-PCR Assays | Reference standard for confirmatory testing and viral load quantification | Allplex SARS-CoV-2 Assay (Seegene) [4] or similar |
Experimental Workflows and Diagnostic Pathways
Diagram 1: Swab Comparison Study Workflow
Diagram 2: Diagnostic Result Interpretation Algorithm
For researchers studying mucosal immunity, particularly against respiratory pathogens like SARS-CoV-2, the choice of sampling method is a critical determinant of data quality and reliability. The "expanding sponge technique" has emerged as a superior method for collecting nasal mucosal lining fluid, significantly outperforming traditional swab-based methods in detection rates and immunoglobulin concentration measurements [15] [33].
This technical resource center provides detailed methodologies, troubleshooting guidance, and reagent solutions to support implementation of this advanced technique in your research on optimizing sensitivity in nasal versus nasopharyngeal sampling.
Quantitative Comparison: Expanding Sponge vs. Traditional Methods
Recent systematic comparisons demonstrate clear performance advantages of the expanding sponge method over conventional approaches for mucosal immunity detection [15] [33].
Table 1: Performance Comparison of Nasal Sampling Methods for SARS-CoV-2 RBD-Specific IgA Detection
| Sampling Method | Single-Day Detection Rate (%) | 5-Day Consecutive Detection Rate (%) | Median IgA Concentration (U/mL) |
|---|---|---|---|
| Expanding Sponge (M3) | 95.5 | 88.9 | 171.2 |
| Nasal Swab (M2) | 88.3 | 77.3 | 93.7 |
| Nasopharyngeal Swab (M1) | 68.8 | 48.7 | 28.7 |
Statistical analysis revealed the expanding sponge method significantly outperformed nasopharyngeal swabs (p<0.0001) and nasal swabs (p<0.05) across all measured parameters [15]. This enhanced performance is attributed to the sponge's superior ability to absorb mucosal lining fluid throughout the nasal cavity, providing a more comprehensive sample of the mucosal immune environment.
Experimental Protocol: Standardized Expanding Sponge Methodology
Materials and Equipment
Table 2: Essential Research Reagent Solutions for Expanding Sponge Protocol
| Item | Specification/Supplier | Function in Protocol |
|---|---|---|
| Expanding Sponge | Polyvinyl alcohol sponge (e.g., cat no.: PVF-J, Beijing Yingjia Medic Medical Materials Co., Ltd) | Core sampling material that expands to absorb mucosal lining fluid |
| Transport Medium | UTM universal transport medium (Copan Diagnostics) | Preserves sample integrity during transport and processing |
| Syringe | 10 mL disposable syringe | Facilitates fluid expulsion from sponge after collection |
| ELISA Kit | Validated SARS-CoV-2 WT-RBD specific IgA detection assay | Standardized detection of target immunoglobulin |
Step-by-Step Sampling Procedure
Sponge Preparation: Soak the polyvinyl alcohol sponge in 50 mL of physiological saline to allow complete expansion [15] [33].
Sponge Loading: Place the expanded sponge into a 10 mL disposable syringe and push the plunger to the 4 mL mark to expel excess fluid [33].
Sponge Division: Using sterile scissors, divide the dehydrated sponge into two equal parts, and cut each part into three equal pieces [15].
Sample Collection: Insert one sponge piece into the nostril and leave in place for 5 minutes to allow absorption of mucosal lining fluid [15] [33].
Sample Recovery: Place the sponge with absorbed sample into 1.5 mL UTM universal transport medium [33].
Processing: Within 4 hours of sampling, expel the sponge's absorbed liquid using a syringe, followed by centrifugation (room temperature, 1000 rpm, 3 min) and aliquoting of supernatant [15].
Detection Method Validation
The expanding sponge method is compatible with various detection platforms, but optimal results require standardized detection protocols:
ELISA Validation: Establish a validated ELISA for nasal SARS-CoV-2 WT-RBD specific IgA detection following ICH guidelines Q14 and Q2(R2) for analytical procedure development [15].
Quality Parameters: Ensure intermediate precision <17% and relative bias <±4% to meet Analytical Target Profile requirements [15].
Concordance Testing: Verify strong concordance with reference methods (concordance correlation coefficient of 0.87 for quantitative results) [15].
Troubleshooting Guide: Common Technical Challenges and Solutions
Table 3: Troubleshooting Common Issues with Expanding Sponge Technique
| Problem | Potential Causes | Solution | Prevention |
|---|---|---|---|
| Low sample volume recovery | Incomplete sponge expansion; insufficient absorption time | Ensure proper saline soaking pre-expansion; maintain full 5-minute in-situ time | Standardize sponge preparation protocol across all operators |
| Inconsistent IgA measurements | Variable sponge insertion depth; improper processing timeline | Train operators on consistent placement; process within 4-hour window | Use anatomical landmarks for consistent placement; strict adherence to processing timeline |
| Sample contamination | Non-sterile technique during sponge handling | Implement aseptic technique; use single-use sterile instruments | Establish clean handling protocol; use pre-sterilized sponge materials |
| High inter-operator variability | Lack of standardized training for sponge insertion | Develop detailed SOP with visual guides; conduct inter-operator concordance testing | Regular training refreshers; periodic quality control checks |
FAQs: Addressing Researcher Questions on Sponge Sampling
Q1: How does the expanding sponge achieve superior performance compared to flocked swabs?
The expanding sponge creates significantly greater surface area contact with the nasal mucosa and absorbs the mucosal lining fluid more effectively than swab methods. Traditional swabs primarily collect surface cells, while the sponge physically absorbs the fluid layer containing secreted immunoglobulins, providing a more comprehensive representation of the mucosal immune environment [15] [33].
Q2: What is the evidence supporting the expanding sponge's superior detection rates?
Clinical comparison studies demonstrated the expanding sponge method achieved a 95.5% single-day detection rate for SARS-CoV-2 WT-RBD IgA, significantly higher than nasal swabs (88.3%) and nasopharyngeal swabs (68.8%). The 5-day consecutive detection rate was 88.9% for the sponge versus 77.3% for nasal swabs and 48.7% for nasopharyngeal swabs [15].
Q3: Can this method be adapted for detecting other respiratory pathogens?
Yes, the standardized nasal detection system established for SARS-CoV-2 can be adapted with appropriate modifications for clinical evaluation of other respiratory mucosal vaccines and pathogens. The fundamental principle of mucosal lining fluid absorption is applicable across respiratory immunology research [15].
Q4: How critical is the 5-minute placement time for sample quality?
The 5-minute placement is critical for optimal absorption of mucosal lining fluid. Shorter times may not allow complete absorption, while longer times may increase participant discomfort without significant improvement in sample quality. This timing was validated in comparative studies [15] [33].
Q5: What quality control measures should be implemented when establishing this technique?
Key QC measures include: (1) validation of IgA detection assay with intermediate precision <17% and relative bias <±4%; (2) operator training to minimize technical variability; (3) strict adherence to processing timelines (<4 hours from collection); and (4) periodic validation of sponge absorption capacity [15].
Theoretical Framework: Mucosal Sampling in Research Context
The expanding sponge technique addresses fundamental challenges in mucosal immunity research by providing standardized methodology that enhances detection sensitivity and reliability. This approach is particularly valuable for evaluating mucosal vaccines, where accurate measurement of antigen-specific IgA at the portal of entry is essential for assessing vaccine efficacy [15] [34] [35].
The method's superior performance stems from its ability to overcome the limitations of swab-based techniques, which often yield inconsistent results due to variable collection efficiency and limited absorption capacity. By implementing this technique with proper standardization, researchers can significantly improve cross-study comparability and advance the development of mucosal vaccines against respiratory pathogens [15] [33] [36].
Maximizing Detection: Critical Factors Influencing Swab Sensitivity and Accuracy
Core Concepts: Understanding Ct Values and Viral Load
What is a Cycle Threshold (Ct) Value? The Cycle Threshold (Ct) value is a crucial result from a real-time reverse transcription-polymerase chain reaction (RT-PCR) test. It represents the number of amplification cycles required for the target viral gene's signal to cross a predetermined fluorescent threshold. This threshold is set within the exponential phase of the PCR amplification, where the reaction is most efficient and reproducible [37].
What is the fundamental relationship between Ct value and viral load? The Ct value is inversely correlated with viral load. A lower Ct value indicates a higher viral load, as fewer amplification cycles were needed to detect the virus. Conversely, a higher Ct value indicates a lower viral load [38] [37] [39]. Each unit decrease in Ct value corresponds to an approximate doubling of the viral genetic material.
What is a "Reasonable Range" for Ct Values? In diagnostic qPCR, a sample is typically considered positive if the Ct value is below 40 [38]. For quantitative results, the generally accepted effective range for Ct values is between 15 and 35 [40]. Values below 15 may fall within the baseline phase, while results above 35 may indicate a very low initial template quantity that is statistically less reliable.
Swab Sampling Comparison: Nasopharyngeal vs. Nasal
The choice of sampling method can significantly impact sensitivity and Ct values. The following table summarizes key performance metrics from head-to-head comparisons.
Table 1: Sensitivity and Ct Value Comparison of Upper Respiratory Specimens for SARS-CoV-2 Detection
| Specimen Type | Sensitivity (vs. Gold Standard) | Mean/Median Ct Value (vs. NPS) | Key Study Findings |
|---|---|---|---|
| Nasopharyngeal Swab (NPS) | Gold Standard (92.5-100%) [4] [41] | Reference (24.98) [4] | Considered the gold standard due to high sensitivity. |
| Oropharyngeal Swab (OPS) | 94.1% [4] | 26.63 (p=0.084) [4] | Statistically comparable sensitivity to NPS. |
| Mid-Nasal Swab (Self-collected) | 99.2% (Baseline); 72.8% (Day 7) [41] | 22.90 (Baseline); 33.95 (Day 7) [41] | High correlation with NPS at high viral loads; performance drops at lower viral loads (Ct >30). |
| Nasal Swab | 82.4% [4] | 30.60 (p=0.002) [4] | Significantly lower sensitivity and higher Ct values than NPS. |
| Saliva (Self-collected) | 90.0% (Baseline); 42.4% (Day 7) [41] | 29.56 (Baseline); 36.69 (Day 7) [41] | Fair correlation with NPS; sensitivity drops significantly at lower viral loads. |
Experimental Protocol for Comparative Swab Studies
The following workflow, derived from prospective diagnostic studies, outlines the methodology for head-to-head comparison of different swab types [4] [41]:
Key Takeaways for Sensitivity Optimization
- Combined Approaches: Using a combination of OPS and NPS can achieve 100% detection sensitivity in confirmed positive cases [4].
- Viral Load Dependence: The performance of alternative swabs (like nasal or saliva) is highly dependent on viral load. They show excellent sensitivity when NPS Ct values are low (high viral load) but perform poorly when NPS Ct values are high (low viral load) [41].
- Procedural Rigor: High-quality, standardized collection procedures by trained personnel are critical for obtaining reliable and comparable results [4].
Troubleshooting Guide: Abnormal Ct Values
Ct values that fall outside the expected range can indicate issues with the experiment. The table below outlines common problems and solutions.
Table 2: Troubleshooting Abnormal Ct Values in qPCR Experiments
| Problem | Potential Causes | Recommended Solutions |
|---|---|---|
| Ct Value Too High (Low Signal) | Low template concentration or degradation [40].Presence of PCR inhibitors [40].Low amplification efficiency due to poor primer design or suboptimal reaction conditions [40]. | Increase template concentration or re-extract nucleic acids [40].Dilute the template to reduce inhibitors; use purification kits [40].Re-design primers; optimize annealing temperature; use a two-step protocol [40]. |
| Ct Value Too Low (High Background) | High template concentration leading to non-specific amplification [40].Contamination in reagents (No Template Control, NTC, is positive) [40]. | Dilute the template to an appropriate concentration [40].Prepare fresh reagents; use dedicated equipment; employ UDGase anti-contamination protocols [40]. |
| High Variability Between Replicates | Pipetting errors [40].Inhomogeneous mixing of reaction components [40].Inconsistent sample quality or collection. | Calibrate pipettes; use master mixes for consistency [40].Vortex and centrifuge all reagents thoroughly before use [40].Standardize sample collection and nucleic acid extraction protocols. |
The Impact of Biological and Technical Factors on Ct Values
Ct values are not only a diagnostic marker but also a source of valuable clinical and epidemiological information. It is crucial to remember that Ct values are semi-quantitative and can be influenced by numerous pre-analytical and analytical factors, from sample collection to RNA extraction and the PCR assay itself.
Key Biological and Epidemiological Correlates Research has identified several factors that correlate with Ct values:
- Vaccination: Being vaccinated is associated with higher Ct values (lower viral load) [38].
- Age: Older age has been linked to lower Ct values (higher viral load) [38].
- Viral Variants: Different variants of concern (e.g., Delta, Omicron) can exhibit different typical Ct values, reflecting their evolving characteristics [39] [42]. One study found median Ct values decreased from 31.71 in early pandemic phases to 21.27 during the Omicron period, indicating higher viral loads [39].
- Disease Severity: Some studies, including one in children, found that hospitalized symptomatic patients had lower Ct values than asymptomatic patients, suggesting a link between higher viral load and more severe disease [42].
Advanced Applications: Quantitative Analysis with Double Delta Ct
For gene expression analysis, the Double Delta Ct (ΔΔCt) method is a common approach to calculate relative fold changes in target abundance [37] [43]. This method normalizes the Ct value of the target gene to a reference ("housekeeping") gene and then to a control group.
The logical workflow and calculation for this method are as follows:
Research Reagent Solutions
The following table details key reagents and kits used in the studies cited, which are essential for conducting similar research.
Table 3: Essential Research Reagents for SARS-CoV-2 RT-PCR and Sequencing
| Reagent / Kit Name | Primary Function | Specific Application / Target |
|---|---|---|
| BioGerm 2019-nCoV Kit [38] | RT-PCR Detection | Targets ORF1ab and N genes of SARS-CoV-2. |
| Allplex SARS-CoV-2 Assay [4] [39] | Multiplex RT-PCR Detection | Targets E, RdRP/S, and N genes; used for variant identification. |
| TaqPath COVID-19 Combo Kit [42] | Multiplex RT-PCR Detection | Targets ORF1ab, S, and N genes; provides Ct values for viral load correlation. |
| Applied Biosystems MagMAX Viral/Pathogen II Nucleic Acid Isolation Kit [42] | Nucleic Acid Extraction | Automated RNA extraction on KingFisher Flex System. |
| COPAN flocked swab [4] | Specimen Collection | Used for Nasopharyngeal Swab (NPS) collection. |
| DANASALIVA collection kit [41] | Specimen Collection | Standardized collection and preservation of saliva samples. |
Frequently Asked Questions (FAQs)
Q1: Can a single Ct value determine patient infectiousness or disease severity? No. While a lower Ct value (indicating higher viral load) is correlated with increased infectiousness and has been associated with a higher risk of severe disease in some studies, it should not be used as a sole determinant [38] [42]. Clinical symptoms, symptom onset date, and other patient factors are critical for a comprehensive assessment.
Q2: Why is a housekeeping gene included in RT-PCR assays? A housekeeping gene (e.g., RNAse P) serves as an internal control for sample quality and nucleic acid extraction efficiency. It verifies that a negative result for the target virus is truly negative and not due to a failed sample collection, extraction, or the presence of PCR inhibitors [38] [37].
Q3: Our lab is considering switching from nasopharyngeal to anterior nasal swabs. What is the key trade-off? The primary trade-off is a potential loss in sensitivity, especially in patients with low viral loads. While nasopharyngeal swabs remain the gold standard, self-collected mid-nasal swabs show high sensitivity in patients with high viral loads (low Ct values) but this sensitivity decreases significantly later in the infection when viral loads drop [4] [41]. The decision should be based on your testing goals: nasal swabs may be sufficient for mass screening of symptomatic individuals, but NPS is superior for diagnostic confirmation or testing asymptomatic contacts.
Q4: How do viral variants impact the interpretation of Ct values? The emergence of new variants can shift the population distribution of Ct values. For example, the Delta and Omicron variants were associated with significantly lower median Ct values (higher viral loads) compared to earlier variants [39] [42]. This underscores the importance of ongoing genomic surveillance and caution when comparing Ct value trends over long periods without variant context.
Within the critical field of respiratory pathogen diagnostics, the performance of specimen collection swabs is a fundamental pre-analytical variable that directly impacts assay sensitivity. This technical resource examines the core scientific principles and performance characteristics of two predominant swab types: traditional flocked swabs and emerging injection-molded swabs. Framed within the broader objective of optimizing sensitivity in nasal versus nasopharyngeal sampling research, this guide provides researchers and drug development professionals with actionable troubleshooting protocols and comparative data to inform experimental design and diagnostic development.
Technical Performance Comparison
The design and material composition of collection swabs directly influence their sample collection, retention, and release capabilities. The following table summarizes key performance metrics derived from preclinical and clinical validation studies.
Table 1: Quantitative Performance Comparison of Flocked and Injection-Molded Swabs
| Performance Metric | Flocked Swabs | Injection-Molded Swabs | Experimental Context & Notes |
|---|---|---|---|
| Sample Collection Capacity | Superior [44] | Moderate [44] | Flocked swabs collected 1.8x more synthetic mucus than injection-molded (Heicon) swabs in a nasopharyngeal cavity model [44]. |
| Sample Release Efficiency | Variable (25.9% - 69.4%) [44] | Superior (68.8% - 82.5%) [44] | Release percentage is model-dependent. Injection-molded swabs consistently show higher release rates [44]. |
| Viral RNA Detection (Ct Value) | Comparable to injection-molded [45] [46] | Comparable to flocked [45] [46] | Both swab types yield similar Ct values in RT-qPCR for SARS-CoV-2, indicating comparable detection sensitivity [45] [47]. |
| Impact of Mucus Viscosity | High impact [45] | High impact [45] | Both swab types show significantly different Ct values between asymptomatic (low viscosity) and symptomatic (high viscosity) mucus conditions [45]. |
| Cell Count Collection | Higher in some clinical studies [46] | Lower in some clinical studies [46] | One preclinical human sampling study reported flocked swabs (Copan) released more cells than ClearTip injection-molded swabs [46]. |
| Key Material/Design Principle | Absorbent, nylon fibers for high surface area [48] [49] | Non-absorbent, hydrophobic polymer [46] [47] | Flocked swabs rely on capillary action; injection-molded swabs use surface tension and grooves for sample retention [46] [48]. |
Troubleshooting Guides & FAQs
Common Experimental Challenges and Solutions
Q1: Our RT-qPCR results show unacceptably high Cycle Threshold (Ct) values with injection-molded swabs, suggesting poor viral recovery. What could be the cause?
- Potential Cause 1: Inefficient sample elution due to swab polymer hydrophobicity.
- Solution: Optimize the elution protocol. Extend vortexing time (e.g., 60 seconds instead of 30), incorporate a 1-minute sonication step, and follow with a second vortexing. This rigorous process has been shown to significantly improve viral RNA release from injection-molded swabs [46].
- Potential Cause 2: Mucus viscosity interfering with sample release.
- Solution: Account for mucus properties in your model. Use a synthetic mucus with physiologically relevant viscosities (e.g., Poly(ethylene oxide) at 0.5% w/v for asymptomatic and 3.0% w/v for symptomatic conditions) during preclinical validation [45]. Higher viscosity mucus can hinder release from all swab types.
Q2: Our flocked swabs collect a large sample volume, but a significant portion is retained on the swab and not released into the transport media. How can we improve release?
- Potential Cause: The absorbent nature of flocked fibers leads to sample entrapment.
- Solution: While optimizing the elution protocol (as in Q1) helps, the core design may limit improvement. Consider switching to a non-absorbent injection-molded swab for applications where maximum release is critical. Studies show injection-molded swabs can have over 2.5x the release efficiency of flocked swabs in anatomically accurate models [44].
Q3: How does the sampling location (e.g., anterior nasal vs. nasopharyngeal) interact with swab design choice?
- Consideration: Anatomical constraints and target cell/virus location.
- Solution: For nasopharyngeal sampling, which remains the clinical gold standard for many pathogens, standard flocked swabs are well-established [15] [50]. For anterior nasal sampling, which is more comfortable and suitable for self-sampling, both swab types are used. However, note that one clinical study found an expanding sponge method superior to both nasopharyngeal and standard nasal swabs for collecting nasal IgA, indicating that the sampling device must be matched to the analyte and anatomical site [15].
Q4: We are developing a new in vitro model for swab validation. How can we ensure it provides clinically relevant results?
- Potential Cause: Over-reliance on simple benchtop models like dipping swabs into a tube of saline.
- Solution: Implement a 3D-printed nasal tissue model that recapitulates key physiological features:
- Architecture: Use CT-derived 3D-printed nasal cavities that mimic the nasal passage, turbinates, and nasopharynx [45] [44].
- Soft Tissue: Line the model with a soft material like a silk fibroin sponge or cellulose sponge to mimic the compliance of nasal tissue [45] [46].
- Mucosal Environment: Use a shear-thinning hydrogel (e.g., SISMA hydrogel or PEO solutions) to simulate the viscosity and rheology of native mucus [45] [44]. This model will provide more reproducible and clinically predictive results than a simple tube.
- Solution: Implement a 3D-printed nasal tissue model that recapitulates key physiological features:
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials for Swab Performance and Sampling Research
| Item | Function/Description | Example Use in Research |
|---|---|---|
| Synthetic Mucus (PEO) | Mimics the viscosity of asymptomatic and symptomatic nasal fluid for standardized in vitro testing [45]. | Used to saturate nasal tissue models to study the effect of mucus viscosity on swab pick-up and release [45] [46]. |
| Silk Fibroin Sponge | A biocompatible, soft substrate used to line 3D-printed nasal models, mimicking the mechanical properties of nasal soft tissue [45]. | Provides a physiologically relevant surface for swab interaction in benchtop validation models [45]. |
| SISMA Hydrogel | A shear-thinning hydrogel with viscosity parameters nearly identical to actual nasopharyngeal mucus [44]. | Serves as a mucosa equivalent in advanced nasopharyngeal cavity models for swab validation [44]. |
| Heat-Inactivated SARS-CoV-2 | A safe, non-infectious surrogate for the live virus, used to spike samples and validate detection sensitivity via RT-qPCR [46]. | Spiked into synthetic mucus to quantify viral RNA recovery and release efficiency of different swabs [46]. |
| 3D-Printed Nasal Cavity Model | An anatomically accurate model of the human nasal passages, created from CT scans, for physiologically relevant swab testing [45] [44]. | Serves as the core platform for preclinical swab validation, bridging the gap between simple benchtop and clinical studies [45]. |
Experimental Workflow & Logical Relationships
The following diagram illustrates the logical workflow for the preclinical validation of swab performance, as described in the cited methodologies.
FAQs and Troubleshooting Guides
Frequently Asked Questions
1. How does sampling force specifically affect the sensitivity of SARS-CoV-2 diagnostic tests? Excessive sampling force is a critical pre-analytical variable that can compromise test sensitivity. While not directly quantified in the studies reviewed, its impact is inferred from sample quality assessments. Excessive force may cause patient discomfort, leading to improper technique or early termination of sampling, thereby reducing the collection of viral material. Furthermore, aggressive force can cause tissue trauma, potentially introducing inhibitors or blood that may interfere with assay chemistry. The consistency of sample collection, which is disrupted by variable force, is a known factor affecting the reliable detection of viral loads, particularly in samples with low pathogen concentration [5].
2. When comparing anterior nares (AN) and nasopharyngeal (NP) swabs, which method is more susceptible to variations in sampling force? Anterior nares (nasal) swabs are generally less invasive and may be less susceptible to significant variations caused by sampling force, as they do not require deep insertion. However, one study noted that test line intensity on Ag-RDTs was lower when using AN swabs, suggesting that the sample quality or viral load collected might be more easily influenced by sub-optimal technique, including insufficient force or contact time [5]. In contrast, NP swabbing is a more technically demanding procedure where excessive force can cause significant patient discomfort and injury, potentially leading to inadequate sampling if not performed correctly.
3. What is the observed diagnostic performance difference between nasal and nasopharyngeal sampling? Multiple head-to-head studies have found that the diagnostic accuracy of anterior nares (AN) and nasopharyngeal (NP) swabs is largely equivalent for SARS-CoV-2 detection using RT-PCR and certain Ag-RDTs. The table below summarizes key comparative data:
Table 1: Head-to-Head Comparison of AN and NP Swab Diagnostic Accuracy
| Evaluation Focus | Swab Type | Sensitivity | Specificity | Citation |
|---|---|---|---|---|
| SARS-CoV-2 Ag-RDT (Sure-Status) | NP Swab | 83.9% (95% CI 76.0–90.0) | 98.8% (95% CI 96.6–9.8) | [5] |
| AN Swab | 85.6% (95% CI 77.1–91.4) | 99.2% (95% CI 97.1–99.9) | [5] | |
| SARS-CoV-2 Ag-RDT (Biocredit) | NP Swab | 81.2% (95% CI 73.1–87.7) | 99.0% (95% CI 94.7–86.5) | [5] |
| AN Swab | 79.5% (95% CI 71.3–86.3) | 100% (95% CI 96.5–100) | [5] | |
| RT-PCR (Rhinoswab vs. OP/NP) | AN Swab | 80.7% (95% CI 73.8–86.2) | 99.6% (95% CI 97.3–100) | [8] |
4. What are the best practices to standardize sampling force and technique? To minimize variability and optimize sensitivity, adhere to these protocols:
- Follow Manufacturer's Instructions for Use (IFU): Strictly adhere to specified swab insertion depth, rotation steps (e.g., three complete turns), and contact time (e.g., leaving the swab in place for 60 seconds) as detailed in the test's IFU [5] [8] [51].
- Utilize Standardized Tools: Consider using specially designed swabs, such as the Rhinoswab, which is engineered for consistent bilateral anterior nasal sampling and can help standardize the process [8].
- Implement Comprehensive Training: Ensure all healthcare workers and research personnel performing sample collection are uniformly trained on the correct pressure, motion, and sequence for different swab types to reduce operator-dependent variability [5].
Troubleshooting Guide
Problem: Inconsistent sensitivity results across sampling operators.
- Potential Cause: High inter-operator variability in sampling technique, including differences in applied force, swab rotation, and contact time with the mucosal surface.
- Solution: Implement a standardized training and certification program for all operators. This should include practical demonstrations and, if possible, the use of anatomical models to practice consistent force and technique. Utilizing less invasive AN swabs can also help reduce variability stemming from operator hesitation with the more uncomfortable NP procedure [5] [8].
Problem: Low viral load detection in samples despite patient symptoms.
- Potential Cause: Sub-optimal sampling force or technique failing to collect sufficient viral material. This is particularly critical for detecting the Omicron variant, where viral concentration may differ between sampling sites [6].
- Solution: Ensure that the correct anatomical site is being sampled thoroughly. For nasal swabs, this includes both nostrils. If sensitivity is paramount, consider a combined sampling approach. One study found that combined nose & throat swabs had higher viral concentrations and better sensitivity for detecting the Omicron variant than either site alone [6].
Problem: Invalid results or assay interference.
- Potential Cause: Excessive sampling force causing tissue trauma and bleeding. Blood can contain PCR inhibitors or interfere with the chemical reactions in antigen tests.
- Solution: Train personnel to apply firm but gentle pressure. If bleeding is observed, discard the swab and wait for bleeding to stop before collecting a new sample with a new swab from an alternative nostril or site.
Experimental Protocols & Data
Detailed Methodology for a Head-to-Head Swab Comparison Study
The following protocol is adapted from published studies to directly evaluate the impact of sampling variables on sensitivity [5] [52].
1. Sample Collection:
- Population: Recruit symptomatic participants. Sample collection should be performed by trained healthcare workers.
- Swab Order: To prevent cross-contamination, collect the NP swab first from one nostril for the reference standard test (e.g., RT-PCR). Then, collect the index test swabs (e.g., for Ag-RDT) from the other nostril: first an NP swab, followed by an AN swab [5].
- Standardized Technique:
- NP Swab: Insert a flexible mini-tip flocked swab through the nasal passage into the nasopharynx. Rotate the swab several times and remove it after several rotations [8].
- AN Swab: Insert the swab into both nostrils until slight resistance is met. Follow the specific protocol, which may involve leaving the swab in place for 60 seconds with or without subsequent side-to-side movements for 15 seconds [8].
- Sample Processing: Place swabs in appropriate transport media, transport under controlled conditions, and process in a suitable laboratory setting.
2. Laboratory Analysis:
- RT-PCR Analysis: Perform RNA extraction and RT-PCR using a validated assay (e.g., TaqPath COVID-19). Define a positive result based on the amplification of specific target genes (e.g., Ct ≤40 for two targets) [5].
- Ag-RDT Analysis: Perform the Ag-RDT according to the manufacturer's IFU. Have results read by two operators blinded to each other's results and to the RT-PCR outcome to prevent bias. A third operator can act as a tiebreaker for discrepant readings [5].
3. Data Analysis:
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for each swab type and test brand against the RT-PCR reference standard.
- Determine the level of agreement between AN and NP swabs using Cohen’s kappa (κ).
- Use logistic regression to analyze the relationship between Ag-RDT sensitivity and viral RNA copy numbers.
Table 2: Key Research Reagent Solutions for Swab Comparison Studies
| Item | Function/Description | Example from Literature |
|---|---|---|
| Flocked Swabs | Swabs with perpendicular fibers for superior sample collection and release. Essential for both NP and AN sampling. | Flexible mini-tip flocked swab (e.g., Copan 481C) for NP; Rhinoswab for bilateral AN sampling [8] [51]. |
| Viral Transport Media (VTM) | Preserves viral integrity for transport and subsequent RT-PCR analysis. | Universal Transport Media (UTM, e.g., Copan) [5]. |
| RT-PCR Assay Kit | The reference standard test for detecting SARS-CoV-2 RNA. | TaqPath COVID-19 (ThermoFisher) kit [5]. |
| Ag-RDT Kits | Rapid tests for detecting SARS-CoV-2 antigens; the index tests under evaluation. | Sure-Status (PMC, India) and Biocredit (RapiGEN, South Korea) tests [5]. |
| RNA Extraction Kit | For purifying viral RNA from swab samples prior to RT-PCR. | QIAamp 96 Virus QIAcube HT kit (Qiagen) [5]. |
Workflow and Relationship Visualizations
Swab Comparison Experimental Workflow
Decision Guide for Swab Selection
In the field of diagnostic and research sampling, particularly for respiratory pathogens like SARS-CoV-2, the choice of sampling method is a critical determinant of test sensitivity. This technical support center resource addresses a key optimization strategy: the use of combined swab approaches to maximize detection sensitivity. For researchers and scientists focused on nasal versus nasopharyngeal swab sampling, understanding how to leverage combined methods can significantly enhance experimental outcomes and diagnostic accuracy. The following guides and FAQs provide detailed, evidence-based protocols and troubleshooting advice to support your work in assay development and diagnostic optimization.
Frequently Asked Questions (FAQs)
Q1: What is the scientific basis for the superior sensitivity of combined swab approaches?
Combined swab approaches, typically integrating nose and throat samples, capitalize on complementary viral shedding patterns across different anatomical sites. Research indicates that viral concentration and presence can vary between the nose and throat during different stages of infection. A 2023 prospective clinical study found that while viral concentration in nose samples remains more consistent over time, it declines in throat samples during later infection stages [6]. By combining samples from both sites, the method compensates for these temporal variations, ensuring a higher probability of pathogen capture regardless of infection stage. This approach effectively creates a more comprehensive anatomical profile of pathogen presence than any single site can provide [6] [17].
Q2: In what specific research scenarios should I prioritize combined swab methods?
Combined swab methods are particularly valuable in these key research scenarios:
- Early Variant Research: When investigating new or emerging pathogen variants where tropism and shedding patterns are not yet fully characterized [6].
- Low Viral Load Studies: In studies focusing on asymptomatic infections, post-treatment monitoring, or late infection phases where viral loads may be approaching detection limits [17].
- Diagnostic Validation: When serving as a reference standard against which new diagnostic platforms or simplified sampling methods are being validated [14] [17].
- Therapeutic Efficacy Trials: In clinical trials for antivirals or vaccines where maximizing detection sensitivity is crucial for accurate endpoint measurement [14].
Q3: What are the primary limitations of single-swab methods that combined approaches address?
Single-swab methods face several limitations that combined approaches effectively mitigate:
Table: Limitations of Single-Swab Sampling Methods
| Limitation Type | Impact on Research | How Combined Swabs Help |
|---|---|---|
| Anatomical Restricted Sampling | May miss localized infection foci | Broader anatomical coverage |
| Temporal Variance in Shedding | Inconsistent detection across infection timeline | Compensates for phase-dependent shedding patterns |
| Technical Variability | Operator-dependent collection efficiency | Reduces false negatives from technique variance |
| Suboptimal Sample Volume | Limited material for replicate assays | Increases total biological material for analysis |
Additionally, swab-based methods inherently face challenges with inconsistent sample recovery due to technique variation, sample entrapment in swab materials leading to incomplete elution, and dependence on transport media that can introduce variability [53]. Combined approaches provide a robustness that partially offsets these methodological weaknesses.
Troubleshooting Guides
Issue: Inconsistent Recovery Rates Between Different Swab Types
Problem: Your experiments show significant variability in analyte recovery when using different swab materials or designs for nasal versus nasopharyngeal sampling.
Solution:
- Standardize Swab Materials: Use the same swab type across all sampling sites. Flocked nylon swabs generally demonstrate superior sample release properties compared to traditional cotton swabs, which can retain samples [17] [54].
- Validate Recovery Efficiency: Conduct controlled recovery studies for each swab type with your target analytes. The recovery efficiency is defined as the transfer effectiveness from a sampled surface to the extraction solution [54].
- Optimize Extraction Protocols: For difficult-to-release samples, implement enhanced extraction methods such as vibratory shaking or ultrasonic bath treatment to improve recovery [55].
Prevention: Develop standardized operating procedures that specify swab material, pressure application (slight bending indicates correct pressure), and elution techniques across all experimental conditions [55] [56].
Issue: Low Analytical Sensitivity in Late-Stage Infection Samples
Problem: Sensitivity drops significantly in samples collected more than 5-7 days post-symptom onset, particularly with single-site sampling.
Solution:
- Implement Dual-Site Sampling: Combine nasal and throat swabs in a single collection tube to maximize viral material [6] [17].
- Time Collection Strategically: For longitudinal studies, schedule collections based on known viral dynamics - nasal sampling may be more productive later in infection [6].
- Concentrate Samples: Use sample processing methods that concentrate analytes prior to analysis to overcome low viral loads.
Prevention: Design studies with frequent sampling intervals and multiple sites to characterize temporal and spatial dynamics of your target pathogen throughout the infection cycle.
Experimental Protocols & Data
Protocol: Standardized Procedure for Combined Nose and Throat Swab Collection
This protocol is adapted from prospective comparative studies of SARS-CoV-2 sampling methods [6] [17].
Materials Needed:
- Flexible minitip flocked swabs for nasopharyngeal sampling
- Rigid-shaft flocked swabs for oropharyngeal sampling
- Sterile transport medium tubes
- Tongue depressors
- Personal protective equipment
Step-by-Step Procedure:
Nasopharyngeal Swab Collection:
- Tilt the patient's head back approximately 70 degrees.
- Insert a flexible minitip flocked swab gently into the nostril, following the floor of the nose toward the earlobe.
- Advance the swab approximately 8-11 cm deep until resistance is encountered at the nasopharynx.
- Leave the swab in place for 2-3 seconds, then rotate it slowly 3-5 times.
- Withdraw the swab carefully and place it in transport media.
Oropharyngeal Swab Collection:
- Using a tongue depressor to ensure proper visualization, swab both palatine tonsils and the posterior oropharyngeal wall with a painting and rotating motion.
- Avoid touching the cheeks, teeth, or gums to prevent contamination.
- Place the swab in the same transport media container as the nasopharyngeal swab.
Sample Processing:
- Transport samples to the laboratory at 2-6°C within 2 hours of collection.
- Process samples within 24-48 hours for optimal analyte stability.
Comparative Performance Data of Swab Modalities
Research studies have directly compared the sensitivity of different swabbing approaches:
Table: Comparative Sensitivity of Different Swab Methods for SARS-CoV-2 Detection [6] [17]
| Swab Method | Sensitivity (%) | 95% Confidence Interval | Mean Ct Value | Statistical Significance |
|---|---|---|---|---|
| Combined Nose & Throat | 100% | N/A | Lowest | Reference standard |
| Throat Only | 97% | 94-100% | 26.63 | p=1.00 (vs. NPS) |
| Nasopharyngeal Only | 92.5% | 85-99% | 24.98 | Reference |
| Nasal Only | 82.4% | 72-93% | 30.60 | p=0.002 (vs. NPS) |
Research Reagent Solutions
Table: Essential Materials for Swab-Based Sampling Research
| Item | Function | Technical Considerations |
|---|---|---|
| Flocked Nylon Swabs | Sample collection | Superior collection and release properties; minimal sample retention [17] [54] |
| Transport Media | Sample preservation and transport | Must maintain analyte stability; compatible with downstream assays [53] |
| Proteinase K | Sample pre-processing | Digests nucleases and enhances nucleic acid recovery [14] |
| Nucleic Acid Extraction Kits | Target isolation | Selection critical for yield and purity; magnetic bead systems often preferred [14] |
| PCR Reagents | Target amplification | Should be validated for compatibility with swab materials and transport media [17] |
Workflow Diagram
The following diagram illustrates the strategic decision pathway for selecting optimal swab approaches in research settings:
Swab Method Selection Workflow
Key Technical Considerations
Swab Material Selection
The choice of swab material significantly impacts recovery efficiency. Key material properties to consider:
- Nylon-Flocked Swabs: Feature short nylon fibers attached to a plastic shaft, creating a hydrophilic open-fiber morphology that enhances sample collection and release [54].
- Cotton Swabs: Traditional choice but can retain samples through hydrogen bonding with cellulose hydroxyl groups, reducing elution efficiency [54].
- Polyester Swabs: Exhibit good collection and release characteristics but have less open structure than flocked swabs [54].
- Foam Swabs: Have sponge-like open structure but may be hydrophobic, causing aqueous solutions to remain on the surface rather than penetrating the foam [54].
Methodological Standardization
To ensure reproducible results in swab-based research:
- Establish consistent swab pressure application (slight bending indicates appropriate pressure) [55]
- Use overlapping lanes when swabbing surfaces with defined sampling patterns [55]
- Maintain consistent swab rotation (typically 3-5 rotations during collection) [17]
- Control surface contact time (typically 10-15 seconds per site) [17]
- Standardize elution procedures (volume, duration, and agitation methods) [55]
For researchers and drug development professionals optimizing sensitivity in nasal versus nasopharyngeal swab sampling, the evidence consistently demonstrates that combined swab approaches provide superior detection capability compared to any single-site method. By implementing the standardized protocols, troubleshooting guides, and strategic workflows outlined in this technical resource, scientists can significantly enhance the sensitivity and reliability of their sampling methodologies, ultimately leading to more robust research outcomes and diagnostic applications.
Evidence and Innovation: Validating Performance Through Clinical and Pre-Clinical Models
This technical support center provides troubleshooting guides and FAQs for researchers conducting comparative studies on nasal and nasopharyngeal swab sampling methods.
Frequently Asked Questions
Q1: In a head-to-head comparison, which swab type demonstrates superior sensitivity for SARS-CoV-2 antigen detection? Multiple prospective diagnostic evaluations have found that the diagnostic accuracy of anterior nares (AN) swabs is equivalent to that of nasopharyngeal (NP) swabs for SARS-CoV-2 antigen detection using rapid diagnostic tests (Ag-RDTs) [5]. The sensitivity and specificity between the two swab types were not statistically significantly different across the test brands evaluated [5].
Q2: What is a key methodological consideration that could impact result interpretation when using anterior nares swabs? Although the overall sensitivity is equivalent, a key observation is that the test line intensity on Ag-RDTs can be lower when using AN swabs compared to NP swabs [5]. This requires careful attention during interpretation by laboratory personnel, as a faint line is still a positive result. Ensuring adequate training and using standardized reading guides can mitigate the risk of misinterpreting weak positive results.
Q3: For molecular testing (RT-PCR), how do alternative swab types compare to the nasopharyngeal gold standard? A prospective study comparing upper respiratory specimens for SARS-CoV-2 molecular testing found that oropharyngeal (OP) swabs achieved a sensitivity comparable to NP swabs [4]. Nasal swabs (distinct from deep AN swabs) demonstrated the lowest sensitivity among the types tested [4]. Combining swab types, such as OP/NP or OP/nasal swab, significantly increased detection sensitivity compared to using a nasal swab alone [4].
Q4: What are the primary pre-analytical factors that can affect swab test performance? Factors influencing test sensitivity include [22]:
- Specimen collection quality: The technique and thoroughness of the healthcare professional.
- Patient viral load: Varies over the infection course and may differ between anatomical sites.
- Specimen transport conditions: Delays or inappropriate transport media can degrade the sample.
Troubleshooting Guides
Issue: Inconsistent sensitivity results between paired AN and NP swabs.
- Potential Cause: Suboptimal collection technique for the AN swab. The AN swab requires firm sampling of both nostrils by rotating the swab several times against the nasal wall [5] [22].
- Solution: Implement and verify standardized training for all sample collectors. The procedure for AN swabs should follow manufacturer instructions, which typically involve inserting the swab approximately 1-2 cm into the nostril and rotating it multiple times against the nasal septum and inferior concha [4] [22].
Issue: Low viral load recovery from swab samples.
- Potential Causes:
- Inferior swab material: Some materials may not release the sample efficiently into the transport media or during test processing.
- Sample viscosity: High viscosity, sometimes encountered with saliva or nasal lining fluid, can interfere with automated pipetting and assay performance [22].
- Solution: Use flocked swabs, which are designed to maximize sample absorption and release [57]. For difficult samples, consider protocol adjustments such as sample dilution or the use of additives to reduce viscosity, while being mindful of the potential for diluting the target analyte [22].
Comparative Performance Data
Table 1: Head-to-Head Comparison of Swab Types for SARS-CoV-2 Ag-RDT Detection [5]
| Ag-RDT Brand | Swab Type | Sensitivity (%) | Specificity (%) | Inter-Rater Reliability (κ) |
|---|---|---|---|---|
| Sure-Status | Nasopharyngeal (NP) | 83.9 (76.0–90.0) | 98.8 (96.6–9.8) | 0.918 |
| Anterior Nares (AN) | 85.6 (77.1–91.4) | 99.2 (97.1–99.9) | ||
| Biocredit | Nasopharyngeal (NP) | 81.2 (73.1–87.7) | 99.0 (94.7–86.5) | 0.833 |
| Anterior Nares (AN) | 79.5 (71.3–86.3) | 100 (96.5–100) |
Table 2: Head-to-Head Comparison of Swab Types for SARS-CoV-2 Molecular Detection (RT-PCR) in 51 Positive Participants [4]
| Swab Type | Sensitivity (%) | Mean Ct Value (N Gene) |
|---|---|---|
| Oropharyngeal (OP) | 94.1 | 26.63 |
| Nasopharyngeal (NP) | 92.5 | 24.98 |
| Nasal Swab | 82.4 | 30.60 |
| Combined OP/NP | 100.0 | N/A |
| Combined OP/Nasal | 96.1 | N/A |
Table 3: Key Research Reagent Solutions for Swab-Based Respiratory Pathogen Detection
| Item | Function/Description | Example Brands/Types |
|---|---|---|
| Flocked Swabs | Sample collection; nylon fibers perpendicular to shaft maximize cellular absorption and elution [57]. | COPAN FLOQSwabs [4] [57], Puritan Medical Products [57] |
| Universal Transport Media (UTM) | Preserves specimen integrity during transport and inactivates potential contaminants [5]. | Copan UTM [5] |
| RNA Extraction Kits | Isolates viral RNA for downstream molecular detection (e.g., RT-PCR) [5]. | QIAamp 96 Virus QIAcube HT Kit (Qiagen) [5] |
| SARS-CoV-2 Ag-RDTs | Rapid, point-of-care tests detecting viral antigens; used for evaluating swab performance [5]. | Sure-Status (PMC, India), Biocredit (RapiGEN, South Korea) [5] |
| RT-PCR Assays | Gold-standard molecular test for sensitive viral RNA detection; used as a reference standard [5] [4]. | TaqPath COVID-19 (ThermoFisher) [5], Allplex SARS-CoV-2 Assay (Seegene) [4] |
Experimental Protocols
Protocol 1: Standardized Paired Swab Collection for Method Comparison [5] This protocol is designed for a head-to-head diagnostic accuracy study.
- Participant Recruitment: Recruit symptomatic individuals. Obtain informed consent as per ethical guidelines.
- Swab Collection Order: Trained healthcare workers should collect swabs in this sequence to prevent cross-contamination and ensure sample quality:
- NP Swab (for Reference Standard): Insert a swab into one nostril until reaching the nasopharynx. Rotate and place in Universal Transport Media (UTM).
- NP Swab (for Index Test): Insert a second swab into the other nostril for the test being evaluated.
- AN Swab (for Index Test): Insert a swab into both nostrils (~1-2 cm), rotating against the nasal wall as per manufacturer's instructions.
- Sample Processing: Transport samples to the lab in cooler bags. Process in an appropriate biosafety cabinet (e.g., CL3 for SARS-CoV-2).
- Testing: Perform the index test (e.g., Ag-RDT) and reference standard test (e.g., RT-PCR) according to their respective instructions for use.
- Blinded Interpretation: Have two operators read the Ag-RDT results independently, blinded to each other's readings and the reference standard result. A third operator can act as a tie-breaker for discrepant readings.
Protocol 2: Quantitative Analysis of Test Line Intensity and Viral Load [5] This supplemental protocol helps investigate the relationship between signal strength and viral load.
- Image Capture: Photograph all Ag-RDT results under standardized lighting conditions.
- Intensity Scoring: Score the visual read-out of the test band on a quantitative scale (e.g., from 1 [weak positive] to 10 [strong positive]).
- Viral Load Quantification: Using the reference RT-PCR, determine the viral load in the sample (e.g., in RNA copies/mL) via a standard curve.
- Correlation Analysis: Statistically analyze the correlation between test line intensity scores and viral loads using methods like the Pearson correlation coefficient.
Experimental Workflow Visualization
Diagram 1: Paired swab evaluation workflow.
Frequently Asked Questions (FAQs)
FAQ 1: For a multi-virus respiratory study, which sample type offers the highest sensitivity for PCR detection?
Nasopharyngeal swabs (NPS) remain the gold standard for the detection of a broad range of respiratory viruses. A 2023 comparative study confirmed that NPS samples consistently showed the lowest PCR cycle threshold (Ct) values, indicating the highest virus concentrations, for viruses including SARS-CoV-2, influenza, RSV, parainfluenza, human metapneumovirus, and rhinovirus [10]. The study reported a 100% positivity rate for NPS samples using real-time PCR panels, outperforming nasal swabs and saliva samples [10].
FAQ 2: Can nasal swabs be a viable alternative to nasopharyngeal swabs?
Yes, under specific conditions. While slightly less sensitive than NPS, nasal swabs provide an adequate and more comfortable alternative, particularly when high viral loads are present. One study found that self-collected foam nasal swabs used with a saline nasal spray had a sensitivity of 96% for detecting various respiratory viruses in immunocompetent, symptomatic individuals [58]. The key to performance is sufficient sampling; nasal swabs collected with 10 rotations showed significantly lower Ct values (higher viral load) than those collected with only 5 rotations [10].
FAQ 3: How does the stage of illness or viral load impact swab sensitivity?
The sensitivity of all swab types is highly dependent on viral load, which is often highest early in the illness. Rapid antigen tests (RATs) and other detection methods show significantly higher sensitivity in samples with high viral loads (typically corresponding to PCR Ct values ≤ 25) [29] [59]. As viral load decreases later in the infection, the sensitivity gap between NPS and other sample types like nasal swabs or saliva may widen [60]. The following table summarizes how sensitivity changes with viral load for a common RDT.
Table 1: Sensitivity of a Combined Rapid Antigen Test (Alltest) at Different Viral Loads [59]
| Virus | Overall Sensitivity (Ct ≤ 35) | Sensitivity at High Viral Load (Ct ≤ 25) |
|---|---|---|
| SARS-CoV-2 | 60.0% | 100% |
| Influenza A/B | 54.3% | 100% |
| RSV | 60.0% | 100% |
FAQ 4: What is the role of saliva in detecting respiratory viruses beyond SARS-CoV-2?
Saliva can detect respiratory viruses but generally with lower sensitivity compared to NPS. The 2023 study found that saliva samples (both swab and undiluted) yielded positive results for SARS-CoV-2 and other respiratory viruses, but with higher Ct values than paired NPS samples [10]. For non-SARS-CoV-2 viruses, saliva's performance is more variable and is not generally recommended as a first-choice sample type for broad respiratory virus testing when the highest sensitivity is required.
Troubleshooting Guides
Issue 1: Low viral yield from self-collected nasal swabs.
- Potential Cause: Insufficient sampling technique or lack of nasal saline spray.
- Solution: Implement a standardized collection protocol.
- Step 1: Instruct participants to blow their nose before collection to clear mucus.
- Step 2: Instill 5 sprays (approximately 0.5 mL) of saline into the naris. Research shows this "wet" collection method significantly improves sensitivity for many respiratory viruses [58].
- Step 3: The participant should insert a foam or flocked swab into the naris and rotate it vigorously against the nasal wall for at least 5 seconds, aiming for 10 full rotations to maximize cell collection [10].
- Preventative Measure: Provide participants with visual aids or video demonstrations of the proper technique.
Issue 2: Inconsistent results between sample types in a validation study.
- Potential Cause: Discrepancies are often due to differences in viral load, which can vary between anatomical sites and over the course of infection.
- Solution:
- Step 1: Stratify your results by PCR Ct value. Discordant results (e.g., NPS positive, nasal swab negative) are significantly more likely to occur in samples with higher Ct values (lower viral loads) [29] [59].
- Step 2: Use the residual buffer from rapid test devices for confirmatory RT-PCR. One study demonstrated that RT-PCR on the residual buffer from both NPS and nasal swab Ag-RDTs had sensitivities of 100% and 98.7%, respectively, streamlining confirmation without recollection [29].
- Step 3: Ensure all paired samples are collected at the same time point in the illness, as sensitivity declines for all sample types later in the infection [60].
Experimental Protocols
Protocol 1: Standardized Paired Swab Collection for Method Comparison
This protocol is designed for studies directly comparing the sensitivity of nasopharyngeal (NP) and nasal (NA) swabs.
- Sample Collection Order: To prevent cross-contamination, collect the NPS sample first, followed by the nasal swab from the opposite nostril.
- Nasopharyngeal Swab (NPS):
- Use a flocked or foam swab.
- Tilt the patient's head back 70 degrees.
- Gently insert the swab along the nasal septum to the nasopharynx until resistance is met.
- Rotate the swab 2-3 times and hold for 5 seconds to absorb secretions.
- Place the swab in recommended transport media [10].
- Nasal Swab (Self-Collected or Assisted):
- Use a foam swab (e.g., Puritan Medical Products #25-1805 or equivalent).
- Instill 0.5 mL of saline spray into the nostril.
- Insert the swab approximately 2 cm into the naris.
- Firmly rub the swab against the nasal wall while rotating it 10 times.
- Place the swab in dry sterile tube or universal transport medium [58] [10].
- Sample Transport and Storage: Transport samples at 4°C or room temperature and process within 24-48 hours. Before nucleic acid extraction, add 0.5-1 mL of transport media (e.g., Hank's Balanced Salt Solution) to dry-collected swab tubes and vortex vigorously [58].
Protocol 2: PCR Confirmation from Rapid Test Residual Buffer
This protocol allows for confirmatory testing without collecting a second sample.
- Perform Rapid Test: Conduct the antigen-based rapid diagnostic test (Ag-RDT) according to the manufacturer's instructions using either NP or NA swabs.
- Buffer Retention: After applying the swab to the test device, do not discard the extraction tube containing the residual test buffer (RTB).
- Direct RT-PCR: Use 200 μL of the RTB for nucleic acid extraction. This buffer can be subjected to real-time RT-PCR using standard protocols and primers for the target respiratory viruses. Studies have shown this method to be highly sensitive (98.7-100%) compared to traditional swabs in viral transport media [29].
Research Reagent Solutions
Table 2: Essential Materials for Respiratory Virus Swab Studies
| Item | Function & Rationale | Example Products & Specifications |
|---|---|---|
| Flocked NPS | Sample collection from nasopharynx. Minimizes specimen retention for higher elution efficiency. | Copan FLOQSwabs [10] |
| Foam Nasal Swab | For anterior nasal sampling. Softer and more comfortable for self-collection. | Puritan Medical Products #25-1805 1PF [58] |
| Universal Transport Medium (UTM) | Preserves virus viability and nucleic acids during transport. | Copan UTM [59] [58] |
| Saline Nasal Spray | Enhances viral recovery in self-collected nasal swabs by loosening secretions. | Polyethylene metered spray bottle (0.5 mL per 5 sprays) [58] |
| Multiplex RT-PCR Panels | Simultaneous detection of multiple respiratory viruses from a single sample, streamlining workflow. | Allplex Respiratory Panels 1/2/3 (Seegene) [10] |
Experimental Workflow and Data Analysis
The following diagram illustrates the logical workflow for a study comparing swab performance, from participant enrollment to data interpretation.
Diagram 1: Swab performance study workflow.
Troubleshooting Guides
Print Quality and Model Fidelity Issues
Problem: My printed model lacks the necessary anatomical detail for realistic swab practice.
- Cause & Solution: Low-resolution printing settings or incorrect technology choice. Use Stereolithography (SLA) printing for high-detail models with intricate features like turbinates and the nasopharyngeal passage. Ensure your source medical scan data (CT/MRI) is high-resolution with thin slices for accurate segmentation [61].
Problem: The model's surface is rough, has holes, or is not watertight.
- Cause & Solution: An unrepaired mesh from the segmentation process. Import your generated STL file into mesh repair software to patch holes, remove intersecting surfaces, and ensure the model is a single, "watertight" object before printing [61].
Problem: Printed layers are shifting, resulting in a misaligned nasal cavity.
- Cause & Solution: Loose printer belts or excessive print speed. Tighten all belts on the X and Y axes and ensure pulleys are firmly attached. Reduce the print speed to minimize vibrations and sudden movements [62].
Problem: Filament stringing creates "hairs" inside the nasal passage, interfering with swab insertion.
- Cause & Solution: Incorrect retraction settings or high print temperature. Enable and calibrate retraction in your slicer software. Lower the nozzle temperature in 5°C increments to reduce oozing [62].
Functional and Material Issues
Problem: The model does not provide feedback on correct swab placement.
- Cause & Solution: Missing functional component for feedback. Integrate a replaceable colored pad on the posterior wall of the nasopharynx. Correct swab insertion will color the swab tip, providing real-time feedback [63].
Problem: The model material cracks or breaks during use.
- Cause & Solution: Low infill density or incorrect material selection. Increase the infill percentage in your slicer settings and choose a more durable material like nylon (for SLS printing) or a tough resin (for SLA) to withstand repeated swab insertions [64] [61].
Problem: Swab insertion feels unrealistic or offers incorrect resistance.
- Cause & Solution: Model material is too rigid or soft. For FDM printing, consider using a flexible filament like TPU to simulate soft tissue. For SLA, use a flexible or soft-touch resin to better mimic mucosal tissue response [61] [65].
Frequently Asked Questions (FAQs)
Q1: What file format should I use to ensure color data for my model is preserved? For full-color or multi-color models, use the 3D Manufacturing Format (.3MF). Unlike STL, 3MF can retain color, texture, and material information in a single file [66].
Q2: How many practice sessions on the simulator are typically needed for proficiency? Research indicates that technical fluency can be acquired quickly. The mean number of nasopharyngeal swab (NPS) conducts on the simulator for operators to feel at ease was two [63].
Q3: My institution only has an FDM printer. Can I still create a useful simulator? Yes. While other technologies like SLA offer higher detail, FDM is a cost-effective solution for creating large, durable anatomical models. Using a well-calibrated FDM printer with PLA or PETG is suitable for producing functional nasopharyngeal swab simulators [61].
Q4: How can I add color to a model to highlight different anatomical structures?
- Color by Mesh: Assign different colors to entire sub-meshes (e.g., nasal bones in one color, soft palate in another) in your CAD software before exporting [66].
- Pause at Height: For single-extruder printers, use your slicer's "Pause at Height" function to change filament color at a specific layer [67].
- Dual Extruder: Use a printer with two extruders to print with two different colored materials simultaneously [67].
Q5: What is the evidence that these simulators actually improve sampling technique? In a multicenter study, 589 participants assessed a 3D-printed NPS simulator. After training, 72% felt their future NPS would be more reliable, 70% expected them to be less painful, and 90% felt they would be carried out more serenely [63].
Experimental Protocols & Data
Detailed Methodology: Simulator Training and Assessment
The following protocol is adapted from a multicenter study evaluating a 3D-printed nasopharyngeal swab collection simulator [63].
1. Objective: To standardize the learning and improvement of NPS collection technique using a 3D-printed anatomical simulator. 2. Materials: - 3D-printed NPS simulator (designed to include nasal bones, turbinates, nasopharynx, hard palate). - Replaceable colored pads for placement feedback. - Standard nasopharyngeal swabs. 3. Procedure: - Session Initiation: A dedicated trainer provides oral explanations on simulator use. A descriptive video is viewed by participants. - Hands-On Training: Participants practice on the simulator until they feel comfortable with the procedure. - Data Collection: Participants independently complete a 16-item questionnaire assessing the simulator's realism, utility, and its impact on their perceived future performance. 4. Statistical Analysis: - Data analyzed descriptively as percentages or mean estimations with 95% confidence intervals. - Qualitative variables compared using two-tailed χ2 tests with Yates' correction or Fisher's exact tests. - Quantitative variables compared using a two-tailed Mann-Whitney-Wilcoxon test. A P-value of < 0.05 is considered significant.
The table below summarizes key quantitative findings from the simulator assessment study [63].
| Evaluation Metric | Result (Mean or Percentage) |
|---|---|
| Overall Satisfaction (0-10 scale) | 9.0 [8.9 - 9.1] |
| Considered Simulator Very Realistic | 95% |
| Considered Simulator Easy to Use | 97% |
| Useful for Understanding Anatomy | 89% |
| Useful for Understanding NPS Technique | 93% |
| Considered Tool Essential | 93% |
| Felt Future NPS Would Be More Reliable | 72% |
| Felt Future NPS Would Be Less Painful | 70% |
| Felt Future NPS Would Be Easier to Perform | 88% |
| Would Carry Out NPS More Serenely | 90% |
| Mean NPS on Simulator to Feel at Ease | 1.8 [1.7 - 1.9] |
Workflow Visualization
Anatomical Simulator Production Workflow
Research Reagent Solutions
The table below lists key materials and reagents essential for developing and utilizing 3D-printed anatomical simulators for swab validation research.
| Item | Function / Application |
|---|---|
| 3D Printable Biocompatible Resins | Used in SLA/PolyJet printing to create safe, high-detail models simulating tissue properties [61] [65]. |
| PLA, PETG, Nylon Filaments | Thermoplastics for FDM/SLS printing; balance durability, cost, and simulation of bony/soft structures [61]. |
| Replaceable Colored Pads | Integrated into the simulator to provide immediate visual feedback on correct swab placement [63]. |
| Auxetic Structure Designs | Advanced swab designs that shrink laterally under axial load, reducing patient discomfort during sampling [68]. |
| Pantone-Validated Color System | Ensures color accuracy and consistency in full-color models for distinguishing anatomical features [65]. |
| Multi-Material Photopolymers | PolyJet materials that simulate a range of durometers (soft to rigid) in a single print for anatomical realism [65]. |
This technical support guide addresses a key challenge in SARS-CoV-2 testing research: optimizing sensitivity when comparing nasal (NA) and nasopharyngeal (NP) swab sampling methods. A significant innovation in this field is performing confirmatory RT-PCR directly from the residual test buffer (RTB) of antigen-based rapid diagnostic tests (Ag-RDTs), eliminating the need for cumbersome and time-consuming specimen recollection [29]. This approach streamlines validation workflows and enhances the efficiency of large-scale asymptomatic screening studies, which are crucial for public health containment measures [29].
Frequently Asked Questions (FAQs)
1. How does the sensitivity of nasal swab collection compare to nasopharyngeal swabs when used with Ag-RDTs? In asymptomatic populations, bilateral nasal swab sampling with the Panbio Ag-RDT demonstrates a sensitivity of 88.0% compared to confirmed cases initially detected by NP-based Ag-RDT [29]. This performance makes NA swabs an adequate and more comfortable alternative, particularly in individuals with high viral loads [29].
2. Can RT-PCR be reliably performed directly from the used rapid test buffer? Yes. Research shows that RT-PCR testing on the residual buffer from Ag-RDTs is highly sensitive. One study reported 100% sensitivity for NP swab RTB and 98.7% sensitivity for NA swab RTB, making it a viable and streamlined approach for confirmatory testing without recollection [29].
3. What is the impact of viral load on Ag-RDT sensitivity? The sensitivity of Ag-RDTs is highly dependent on viral load, as measured by RT-PCR cycle threshold (CT) values. The table below details how the sensitivity of nasal swab Ag-RDT decreases as the CT value increases (indicating lower viral load) [29]:
| CT Value Range | Ag-RDT Sensitivity (%) |
|---|---|
| < 15 | 100.0 |
| 15.0 - 19.9 | 94.0 |
| 20.0 - 24.9 | 80.5 |
| 25.0 - 29.9 | 57.1 |
| ≥ 30 | 0.0 |
Source: [29]
4. What are the advantages of a one-step RT-PCR system for this type of research? A one-step RT-PCR system, which pre-mixes reverse transcriptase and DNA polymerase in a single tube, simplifies setup, minimizes pipetting steps, and reduces the chance of contamination [69]. Modern systems can complete the reverse transcription step in as few as 10 minutes, significantly accelerating the workflow [69].
Troubleshooting Guides
Problem: Low Sensitivity in Nasal Swab Ag-RDT Results
Potential Causes and Solutions:
- Cause: Low viral load in the sample.
- Solution: Correlate results with RT-PCR CT values. Ag-RDT sensitivity is expected to be lower in samples with CT values above 20 [29]. Confirm low-positive or negative Ag-RDT results with a more sensitive RT-PCR test.
- Cause: Suboptimal swab collection technique.
- Solution: Ensure proper bilateral nasal swab collection according to manufacturer and study protocols. Training for consistent technique is essential.
- Cause: Improper storage or handling of the Ag-RDT device or buffer.
- Solution: Adhere strictly to manufacturer guidelines for storage temperature and device handling to maintain test integrity.
Problem: Pipetting Errors During RT-PCR Setup
Potential Causes and Solutions:
- Cause: Loss of track of which reaction tubes have been mixed during repetitive pipetting.
- Solution: Utilize a one-step RT-PCR system with a color-changing buffer. These innovative buffers contain red and blue tracking dyes that form purple when reaction components are successfully combined, providing a visual confirmation of proper mixing [69].
Problem: Inconsistent Confirmatory RT-PCR Results from Residual Test Buffer
Potential Causes and Solutions:
- Cause: Presence of inhibitors from the rapid test device or buffer that may affect the PCR reaction.
- Solution: Use RT-PCR enzymes engineered for high processivity and increased template affinity, which perform better in the face of routine inhibitors and sample impurities [69].
- Cause: Incorrect annealing temperature in the RT-PCR protocol.
- Solution: Employ a RT-PCR system with universal annealing (e.g., 60°C). This allows you to skip Tm calculations, standardizes the protocol, and helps ensure optimal yield and specificity without temperature optimization [69].
Experimental Protocols
Protocol: Validating Ag-RDT Results with Direct RT-PCR from Residual Buffer
Methodology: This protocol is adapted from a study comparing NA and NP swabs in asymptomatic individuals [29].
- Sample Collection: Collect specimens from asymptomatic individuals using both NP and bilateral NA swabs as per the study design.
- Ag-RDT Testing: Process the NP swab first using the standard procedure for the Ag-RDT (e.g., Abbott Panbio). Repeat the Ag-RDT with the NA swab for comparison.
- Residual Buffer Storage: After performing the Ag-RDT, carefully store the residual test buffer (RTB) from the specimen processing tube for both NP and NA samples. Do not discard.
- Confirmatory RT-PCR:
- Data Analysis: Compare the RT-PCR results from the RTB to those from the VTM sample to calculate sensitivity and agreement.
Workflow Visualization
Protocol: One-Step RT-PCR with Color-Changing Buffers
Methodology: This protocol leverages a modern one-step RT-PCR system to minimize errors and save time [69].
- Reaction Setup: Thaw all premixed reaction components (reverse transcriptase, DNA polymerase, buffers, nucleotides) and keep them on ice.
- Master Mix Preparation: Combine the required volumes of each premixed component into a single tube. The buffer will contain red and blue tracking dyes.
- Visual Verification: As the components are combined, observe the color change to a uniform purple, confirming successful and complete mixing [69].
- Plate/Tube Setup: Aliquot the master mix into the PCR plate or tubes.
- Sample Addition: Add the template RNA (e.g., from VTM or residual test buffer) to each reaction.
- RT-PCR Run: Place the plate in a thermal cycler and run the optimized program. A typical one-step protocol may include:
- Analysis: Analyze the results based on your detection method (e.g., gel electrophoresis, real-time fluorescence).
Workflow Visualization
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Benefit |
|---|---|
| One-Step RT-PCR Kit | Pre-mixed enzymes and buffers simplify setup, reduce contamination, and shorten hands-on time [69]. |
| Color-Changing Buffer | Provides visual confirmation of proper pipetting and mixing of reaction components, reducing setup errors [69]. |
| Panbio COVID-19 Ag Rapid Test | An example Ag-RDT device authorized for use with both NP and NA swabs, enabling comparative studies [29]. |
| Universal Annealing Primers/System | Allows all reactions to be run at a single, optimized annealing temperature (e.g., 60°C), streamlining protocol development and execution [69]. |
| Viral Transport Media (VTM) | Preserves specimen viability for standard RT-PCR confirmation, serving as a reference method [29]. |
Conclusion
The evidence confirms that while nasopharyngeal swabs remain a highly sensitive method, anterior nasal and oropharyngeal swabs present viable, less invasive alternatives with only a marginal trade-off in sensitivity under most conditions, particularly when viral loads are high. Optimization hinges on understanding key factors such as viral load dynamics, swab design, and sampling technique. The future of respiratory pathogen testing lies in context-specific application—leveraging the practical advantages of nasal swabs for mass screening and self-testing, while reserving nasopharyngeal sampling for high-stakes diagnostics. For researchers, this underscores the need for continued innovation in swab design, the development of standardized, anatomically accurate pre-clinical validation models, and the expansion of robust clinical data across diverse pathogen targets and patient populations to further refine these critical diagnostic tools.
References
- 1. Recent Study Finds Nasopharyngeal (NP) Swabs Remain the ... [https://www.copanusa.com/blogs/recent-study-finds-nasopharyngeal-np-swabs-remain-the-gold-standard-for-diagnosis-of-covid-19/]
- 2. Complications of Nasopharyngeal Swabs and Safe ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8938608/]
- 3. Complications of nasal and pharyngeal swabs [https://publications.ersnet.org/content/erj/57/4/2004004]
- 4. Head-to-Head Comparison of Nasopharyngeal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9857511/]
- 5. Head-to-head comparison of anterior nares and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934397/]
- 6. Comparative evaluation of swabbing sites for Omicron ... [https://www.sciencedirect.com/science/article/pii/S0732889324004024]
- 7. Sensitivity of SARS-CoV-2 Detection With Nasopharyngeal ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2020.593491/full]
- 8. Evaluation of a New Standardized Nasal Sampling Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10820932/]
- 9. Olfactory swab sampling optimization for α-synuclein ... [https://translationalneurodegeneration.biomedcentral.com/articles/10.1186/s40035-022-00311-3]
- 10. Comparison of Nasal Swabs, Nasopharyngeal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10151282/]
- 11. Evaluation of Nasopharyngeal Swab Collection Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7665666/]
- 12. Interim Guidelines for Collecting and Handling of Clinical ... [https://www.cdc.gov/covid/hcp/clinical-care/clinical-specimen-guidelines.html]
- 13. Nasopharyngeal swabs vs. saliva sampling for SARS-CoV-2 ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0270929]
- 14. Saliva Has High Sensitivity and Specificity for Detecting SARS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346843/]
- 15. Exploring the standardized detection and sampling ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1571418/full]
- 16. Alternate-Site Testing Tips - How to Manage Your Diabetes [https://www.diabetesselfmanagement.com/managing-diabetes/blood-glucose-management/alternate-site-testing-2/]
- 17. Head-to-Head Comparison of Nasopharyngeal ... [https://www.mdpi.com/2075-4418/13/2/283]
- 18. Nasopharyngeal Swab vs Nasal Swab: Comparing Methods [https://blog.puritanmedproducts.com/nasopharyngeal-swab-vs-nasal-swab]
- 19. Saliva and Anterior Nasal Samples for Detecting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12606524/]
- 20. Nasopharyngeal Swab vs. Nasal Swab - iProcess [https://iprocess.net/nasopharyngeal-swab-vs-nasal-swab/]
- 21. the relationship between force applied and SARS-CoV-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12060361/]
- 22. Comparison of SARS-CoV-2 Specimen Types [https://health.ucdavis.edu/blog/lab-best-practice/comparison-of-sars-cov-2-specimen-types-nasal-swabs-nasopharyngeal-swabs-and-beyond/2021/09]
- 23. Proper Procedures for Performing Nasopharyngeal and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8015770/]
- 24. PCR Troubleshooting Guide [https://www.neb.com/en-us/tools-and-resources/troubleshooting-guides/pcr-troubleshooting-guide?srsltid=AfmBOoqLC0b2N_ZU9F5VV9SICGAsWTmhHqQfOJnf5Anw60hgDdcGt2DD]
- 25. Troubleshooting your PCR [https://www.takarabio.com/learning-centers/pcr/faq/troubleshooting?srsltid=AfmBOooHg6xareGcf81FNBsgg7uvDTXbSUpmveK9pnuklO2wpcCVyF93]
- 26. PCR Troubleshooting Guide | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/life-science/cloning/cloning-learning-center/invitrogen-school-of-molecular-biology/pcr-education/pcr-reagents-enzymes/pcr-troubleshooting.html]
- 27. Comparison of RT-PCR and antigen test sensitivity across ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10945130/]
- 28. Factors that Influence the Reported Sensitivity of Rapid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8524138/]
- 29. Comparison between Nasal and Nasopharyngeal Swabs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8849095/]
- 30. Head-to-head comparison of nasal and nasopharyngeal ... [https://pubmed.ncbi.nlm.nih.gov/36862684/]
- 31. At-Home COVID-19 Diagnostic Tests: Frequently Asked ... [https://www.fda.gov/medical-devices/coronavirus-covid-19-and-medical-devices/home-covid-19-diagnostic-tests-frequently-asked-questions]
- 32. Considerations for SARS-CoV-2 Antigen Testing ... [https://archive.cdc.gov/www_cdc_gov/coronavirus/2019-ncov/lab/resources/antigen-tests-guidelines.html]
- 33. Exploring the standardized detection and sampling methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12129971/]
- 34. Mucosal immunity and vaccination strategies: current insights ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12364801/]
- 35. Mucosal immune response in biology, disease prevention ... [https://www.nature.com/articles/s41392-024-02043-4]
- 36. COVID-19 and Mucosal Immunization: Assessing Current ... [https://link.springer.com/article/10.1007/s40588-025-00262-z]
- 37. Understanding Ct Values in Real-Time PCR [https://www.thermofisher.com/blog/behindthebench/understanding-ct-values/]
- 38. The association of cycle threshold value with clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12002790/]
- 39. Long-term trends in cycle threshold values [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2024.1394565/full]
- 40. The Reasonable Range of Ct Values in qPCR Experiments [https://www.yeasenbio.com/blogs/molecular-biology/the-reasonable-range-of-ct-values-in-qpcr-experiments]
- 41. Self-collected mid-nasal swabs and saliva specimens ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8444446/]
- 42. SARS-CoV-2 Disease Severity and Cycle Threshold ... [https://wwwnc.cdc.gov/eid/article/30/6/23-1427_article]
- 43. qPCR Double Delta Ct Analysis in 4 Easy Steps [https://bitesizebio.com/24894/4-easy-steps-to-analyze-your-qpcr-data-using-double-delta-ct-analysis/]
- 44. A new in vitro pre-clinical method for testing SARS-CoV-2 ... [https://www.nature.com/articles/s41598-025-21107-1]
- 45. In Vitro Nasal Tissue Model for the Validation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9016850/]
- 46. Preclinical Validation of a Novel Injection-Molded Swab for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8775180/]
- 47. Preclinical Validation of a Novel Injection-Molded Swab for ... [https://www.mdpi.com/2075-4418/12/1/206]
- 48. Advantages of flocked swabs in medical IVD sampling [https://www.chenyanglobal.com/advantages-of-flocked-swabs-in-medical-ivd-sampling.html]
- 49. Everything to Know About Flocked Swabs [https://blog.puritanmedproducts.com/why_you_need_flock_swabs]
- 50. Comparison of nasopharyngeal flocked swabs and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4655598/]
- 51. Combined oropharyngeal/ nasal is equivalent to... swab [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-021-02087-4]
- 52. Head-to-head performance comparison of self-collected nasal ... versus [https://pubmed.ncbi.nlm.nih.gov/34028625/]
- 53. The Hidden Weaknesses of Swab-Based Sampling [https://readygotest.com/news/the-hidden-weaknesses-of-swab-based-sampling]
- 54. What Are the Limitations and Challenges of Swab-Based ... [https://www.mdpi.com/2673-6756/4/1/6]
- 55. What Errors can occur with Swab Sampling during ... [https://www.gmp-compliance.org/gmp-news/what-errors-can-occur-with-swab-sampling-during-cleaning-validation]
- 56. Troubleshooting Cleaning Validation Swab Failures [https://www.cleanmo.com/a-news-troubleshooting-cleaning-validation-swab-failures-common-pitfalls-to-avoid.html]
- 57. Top Nasal Sampling Swab Factories: 2025 Global Review [https://hanheng-medical.com/nasal-sampling-swab0402/]
- 58. Self-Collection of Foam Nasal Swabs for Respiratory Virus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3536199/]
- 59. Diagnostic Performance of a Combined Rapid Antigen Test for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12265398/]
- 60. Sensitivity of Nasopharyngeal Swabs and Saliva for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7337630/]
- 61. Master 3D Printing Anatomical Models: Complete Workflow ... [https://pycad.co/3-d-printing-anatomical-models/]
- 62. Common 3D Printing Issues & How to Fix Them [https://additiveplus.com/3d-printing-troubleshooting-common-3d-printing-issues-and-how-to-fix-them/?srsltid=AfmBOoqLq2GaXZIAfGlxhTtqaqmPGkrLnrEa5-vZs8ndaMbSMMdsZjOu]
- 63. 3D-printed simulator for nasopharyngeal swab collection for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8824092/]
- 64. 3D Printer Troubleshooting Guide [https://www.matterhackers.com/articles/3d-printer-troubleshooting-guide?srsltid=AfmBOoo4T7bFFrG0G-bI2shKqAQGSz0w8GiLmbpzhBtGTYNqQWOaAay0]
- 65. Advanced Multi-Color and Full-Color 3D Printing [https://www.stratasys.com/en/resources/blog/full-color-3d-printing/]
- 66. Full Color 3D Printing Best Practices [https://www.xometry.com/resources/3d-printing/full-color-3d-printing/]
- 67. 4.6 Use of Colour [https://tactiles.eu/guideline/4-6-use-of-colour/]
- 68. 3D printed auxetic nasopharyngeal swabs for COVID-19 ... [https://www.sciencedirect.com/science/article/abs/pii/S1751616120307177]
- 69. Single-Tube Analysis Can Help You Avoid These 5 ... [https://www.thermofisher.com/blog/life-in-the-lab/single-tube-analysis-can-help-you-avoid-these-5-common-rt-pcr-challenges/]