Optimizing m6A-Related lncRNA Prognostic Models: A Comprehensive Guide to Enhancing ROC Curve Performance
This article provides a comprehensive framework for researchers and bioinformaticians aiming to develop and optimize prognostic models based on m6A-related long non-coding RNAs (lncRNAs).
Optimizing m6A-Related lncRNA Prognostic Models: A Comprehensive Guide to Enhancing ROC Curve Performance
Abstract
This article provides a comprehensive framework for researchers and bioinformaticians aiming to develop and optimize prognostic models based on m6A-related long non-coding RNAs (lncRNAs). It covers the entire pipeline from foundational biology and data acquisition to advanced model construction, performance troubleshooting, and rigorous validation. Focusing specifically on enhancing the predictive accuracy as measured by Receiver Operating Characteristic (ROC) curve analysis, the guide synthesizes current methodologies, including LASSO Cox regression and deep learning approaches, and emphasizes the critical link between model performance and clinical applicability in cancer prognosis and therapeutic response prediction.
Laying the Groundwork: Understanding m6A-lncRNA Biology and Data Acquisition for Robust Model Development
The Critical Role of m6A Modifications in Regulating lncRNA Function in Cancer
FAQ: m6A-lncRNA Model Troubleshooting
Q1: My prognostic risk model based on m6A-related lncRNAs shows poor performance in ROC curve analysis. What could be wrong?
- Insufficient lncRNA Selection Rigor: The initial identification of m6A-related lncRNAs may have used weak correlation thresholds. Ensure you use |Pearson R| > 0.4 and p < 0.01 as a minimum standard, with some studies recommending |R| > 0.5 for stronger associations [1] [2] [3].
- Inadequate Validation Cohort: The model may be overfitted. Always split your dataset into training and testing cohorts (typically 70:30 ratio) and validate findings in both sets [1] [3].
- Suboptimal Cut-off Selection: For dichotomizing continuous risk scores, use the Maximum Absolute Youden Index (MAYI) method rather than maximally selected chi-square statistics, as it provides more meaningful p-values and better performance with RNA-seq data distributions [4].
Q2: How can I experimentally validate that an lncRNA is genuinely regulated by m6A modification?
- Knockdown Approach: Genetically inhibit key m6A writers (e.g., METTL3, RBM15) or erasers (e.g., FTO, ALKBH5) in your cancer cell lines. A true m6A-regulated lncRNA should show significant expression changes upon perturbation of these regulators [5] [2].
- m6A-Specific RIP-qPCR: Perform RNA immunoprecipitation using anti-m6A antibodies followed by quantitative PCR targeting your specific lncRNA. This directly confirms m6A modification presence [6].
- Stability Assays: Compare lncRNA half-life after transcriptional inhibition (using Actinomycin D) in control versus m6A regulator-knockdown cells. m6A modification often affects RNA stability [6].
Q3: My m6A-lncRNA risk model performs well in training data but fails in clinical specimen validation. What might explain this discrepancy?
- Sample Preservation Issues: Improper RNA preservation can degrade lncRNAs and affect m6A modification patterns. Ensure immediate freezing of clinical samples at -80°C and use appropriate RNA stabilization reagents [7].
- Tumor Heterogeneity: Bulk tissue analysis may mask important subpopulations. Consider laser-capture microdissection or single-cell approaches to ensure you're analyzing pure tumor cell populations [7] [8].
- Normalization Problems: Use multiple reference genes (not just 18S RNA) for qRT-PCR normalization, and validate their stability in your specific sample types [7].
Q4: How can I improve the clinical relevance of my m6A-lncRNA signature?
- Incorporate Clinical Parameters: Integrate your molecular signature with established clinical factors (TNM stage, grade) using nomograms to enhance predictive power [1] [2].
- Validate in Multiple Cancer Types: Test your signature across different cancer types to determine if it has pan-cancer utility or is tissue-specific [7] [1] [5].
- Assess Immune Microenvironment Correlations: Evaluate whether your m6A-lncRNA signature correlates with immune cell infiltration patterns, as this significantly impacts clinical outcomes and therapy response [7] [8] [3].
Experimental Protocols for m6A-lncRNA Research
Protocol: Constructing an m6A-lncRNA Prognostic Model
Table 1: Key Steps in m6A-lncRNA Prognostic Model Development
| Step | Procedure | Tools/Packages | Key Parameters | ||
|---|---|---|---|---|---|
| 1. Data Acquisition | Download RNA-seq data and clinical information | TCGAbiolinks R package | HTSeq-FPKM or TPM values [7] [1] | ||
| 2. Identify m6A-related lncRNAs | Calculate correlation between lncRNAs and m6A regulators | Pearson correlation | R | > 0.4, p < 0.01 [1] [2] | |
| 3. Initial Screening | Univariate Cox regression | survival R package | p < 0.05 for significance [7] [2] | ||
| 4. Model Construction | LASSO Cox regression | glmnet R package | 10-fold cross-validation [1] [3] | ||
| 5. Risk Score Calculation | Apply formula: Σ(Coefi × Expressioni) | Custom R script | Median risk score as cutoff [1] [2] [3] | ||
| 6. Model Validation | ROC analysis, survival curves | timeROC, survminer R packages | AUC > 0.7 acceptable [7] [1] |
Protocol: Experimental Validation of m6A-modified lncRNAs
Cell Culture and Transfection
- Culture relevant cancer cell lines (e.g., Caki-1/OS-RC-2 for renal cancer [1], bladder cancer lines [5])
- Transfect with siRNAs targeting m6A regulators (METTL3, RBM15, FTO, etc.) using appropriate transfection reagents
- Include appropriate negative controls (scrambled siRNA)
Functional Assays
- CCK-8/EdU Assays: Seed 2-3×10^3 cells/well in 96-well plates after transfection. Measure proliferation at 0, 24, 48, and 72 hours [1]
- Transwell Migration/Invasion: Seed 5×10^4 cells in serum-free medium in upper chamber. Count migrated cells after 24-48 hours [1] [5]
- Colony Formation: Seed 500-1000 cells/well in 6-well plates, culture for 10-14 days, stain with crystal violet, and count colonies [5] [6]
Molecular Validation
- RNA Extraction and qRT-PCR: Use Trizol method for RNA extraction, reverse transcribe with PrimeScript kit, perform qPCR with SYBR Green [7]
- m6A Immunoprecipitation: Fragment RNA to 100-500 nt, incubate with anti-m6A antibody, pull down with protein A/G beads, and detect target lncRNA by qRT-PCR [6]
Research Reagent Solutions
Table 2: Essential Reagents for m6A-lncRNA Research
| Reagent/Category | Specific Examples | Function/Application | Validation Approach |
|---|---|---|---|
| m6A Writers | METTL3, METTL14, RBM15 | Catalyze m6A modification; knockdown validates m6A dependence | siRNA/shRNA knockdown; assess lncRNA expression changes [5] [2] |
| m6A Erasers | FTO, ALKBH5 | Remove m6A modifications; inhibition stabilizes m6A-modified lncRNAs | Pharmacological inhibitors or genetic knockout [9] [2] |
| m6A Readers | HNRNPC, YTHDF1-3, IGF2BP1-3 | Recognize/bind m6A-modified RNAs; affect stability and function | RIP-qPCR to confirm binding to specific lncRNAs [9] [6] |
| Detection Reagents | Anti-m6A antibodies | Identify m6A modification sites via MeRIP/CLIP | Use positive control RNAs with known m6A sites [6] |
| Cell Function Assays | CCK-8, EdU, Transwell | Assess proliferation, migration after lncRNA manipulation | Include appropriate controls and multiple time points [1] [2] |
Signaling Pathways and Workflows
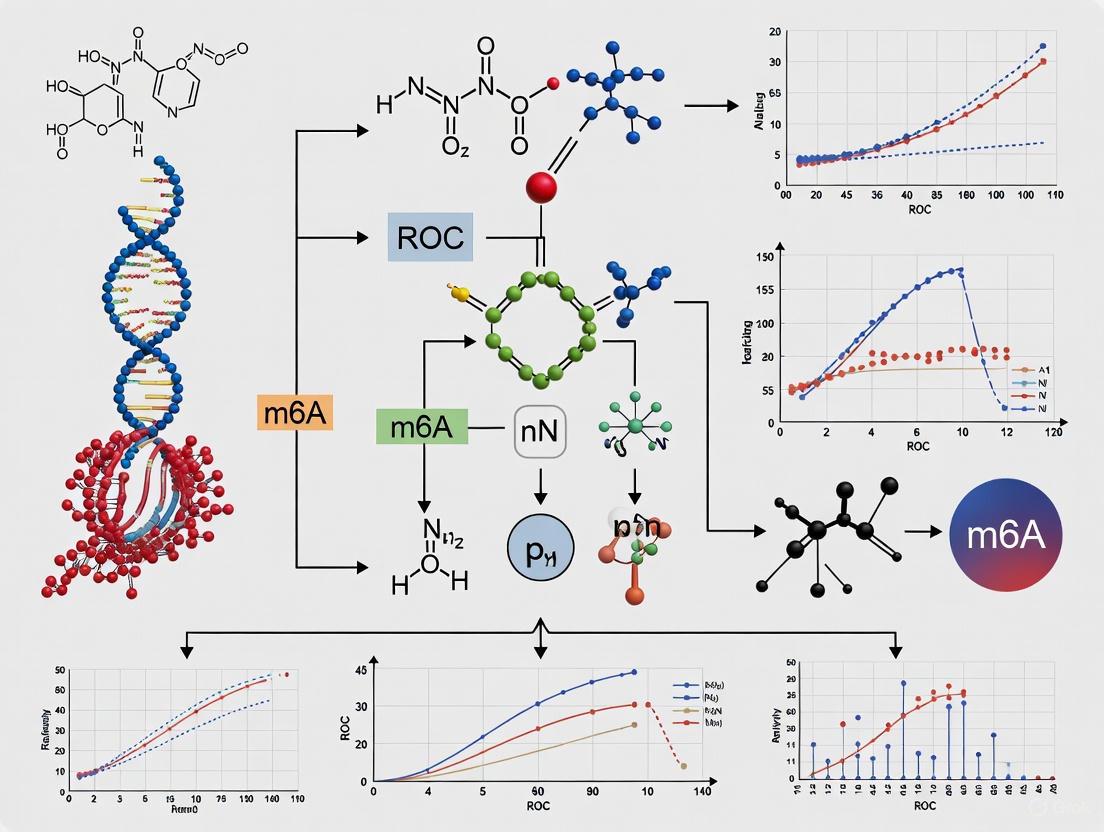
Visual Guide 1: m6A Regulation of lncRNA in Cancer. This diagram illustrates how m6A machinery components (writers, erasers, readers) collectively influence lncRNA stability and function, ultimately driving cancer phenotypes through multiple cellular pathways.
Visual Guide 2: m6A-lncRNA Research Workflow. This workflow outlines the key steps in developing and validating m6A-lncRNA models, from bioinformatics analysis to experimental validation, with associated computational tools for each step.
For researchers investigating the complex relationships between m6A modifications and long non-coding RNAs (lncRNAs) in cancer biology, access to high-quality transcriptomic data is paramount. The ability to construct robust prognostic models and generate reliable ROC curve analyses depends fundamentally on properly sourced and processed data. This guide provides essential technical support for navigating major data repositories, with a specific focus on applications in m6A-lncRNA research, to enhance model performance and analytical rigor.
Frequently Asked Questions (FAQs)
Q1: What types of data in TCGA are most relevant for building m6A-lncRNA prognostic models? TCGA provides comprehensive multi-omics data ideally suited for m6A-lncRNA research. For prognostic model development, you will primarily need:
- Transcriptomic data: RNA-Seq data for identifying lncRNA expression profiles [10] [11]
- Clinical data: Overall survival, disease stage, and treatment response information for survival analysis [10] [12]
- Molecular characterization data: Including mutation and methylation data for integrative analysis [13] Recent studies have successfully utilized these TCGA data types to construct m6A-related lncRNA signatures for various cancers including colorectal, bladder, and esophageal cancer [10] [5] [11].
Q2: What is the difference between TCGA harmonized data and legacy data? TCGA data exists in two main forms with important distinctions:
- Harmonized data: Processed using standardized pipelines, aligned to GRCh38, and available through the GDC portal [13] [14]
- Legacy data: The original data generated by TCGA sequencing centers, available through Broad's Firehose or cBioPortal [13] For new analyses, the harmonized data is recommended as it ensures consistency across different cancer types through uniform processing protocols [13].
Q3: How can I handle the computational challenges of processing large TCGA datasets? Working with TCGA data requires substantial computational resources. Consider these approaches:
- NIH Biowulf HPC cluster: Recommended for large-scale analyses, memory-intensive tasks, and when working with millions of sequences [13]
- GDC Data Transfer Tool: Essential for efficiently downloading large numbers of files or datasets exceeding 5GB [13]
- Pre-processed datasets: Resources like MLOmics provide TCGA data that is already processed for machine learning applications, which can significantly reduce preprocessing burdens [14].
Q4: What are common pitfalls in lncRNA identification from TCGA data and how can I avoid them? Accurate lncRNA identification requires careful computational handling:
- Use updated annotations: Cross-reference gene IDs with Ensembl Genome Browser (GRCh38.p13) from GENCODE to properly distinguish lncRNAs from mRNAs [10]
- Apply correlation filters: Identify m6A-related lncRNAs using Pearson correlation thresholds (e.g., |R| > 0.3, p < 0.001) with known m6A regulators [10] [12]
- Account for dynamic nature: Remember that lncRNA localization and function can be cell-type specific and influenced by experimental conditions [15]
Q5: Are there alternative resources if I need TCGA data pre-processed for machine learning? Yes, several resources offer pre-processed TCGA data:
- MLOmics: Provides 8,314 patient samples across 32 cancer types with four omics types, featuring multiple processed versions (Original, Aligned, Top) suitable for machine learning [14]
- cBioPortal: Offers user-friendly access to TCGA data with visualization tools [13]
- LinkedOmics: Contains multi-omics data with additional analysis capabilities [14]
Troubleshooting Guides
Issue: Difficulty Accessing Controlled Data
Problem: Some TCGA data requires dbGaP authorization, creating access barriers.
Solution:
- Determine access level: Identify whether your required data is open-access or controlled [13]
- Obtain authorization: For controlled data (e.g., germline variants, primary sequence BAM files), complete the dbGaP authorization process through eRA Commons [13]
- Use alternative resources: For preliminary analysis, consider using MLOmics or cBioPortal which may provide derived datasets without access restrictions [14]
Issue: Inconsistent Gene Nomenclature and Annotation
Problem: Discrepancies in gene naming conventions across platforms affect lncRNA identification.
Solution:
- Standardize identifiers: Use unified gene IDs to resolve naming variations caused by different sequencing methods or reference standards [14]
- Leverage annotation resources: Cross-reference with Ensembl Genome Browser 99 (GRCh38.p13) from GENCODE [10]
- Apply consistent filters: Implement a standardized pipeline for all samples, as demonstrated in recent m6A-lncRNA studies [10] [12]
Issue: Technical Variation Affecting Model Performance
Problem: Batch effects and technical artifacts compromise model robustness and ROC analysis.
Solution:
- Utilize harmonized data: Access data through GDC which has been processed using standardized pipelines [13]
- Implement normalization: Apply appropriate normalization methods (e.g., z-score, log transformation) as used in MLOmics processing pipelines [14]
- Select significant features: Use ANOVA-based feature selection to filter out noisy genes, retaining only those with significant variance across samples [14]
Research Reagent Solutions
Table: Essential Computational Tools for m6A-lncRNA Research
| Resource/Tool | Function | Application in m6A-lncRNA Research |
|---|---|---|
| GDC Data Portal | Primary access point for TCGA data | Download harmonized transcriptomic and clinical data [13] |
| Ensembl Genome Browser | Gene annotation reference | Properly identify and classify lncRNAs vs. mRNAs [10] |
| MLOmics | Pre-processed TCGA for ML | Access cancer multi-omics data ready for prognostic modeling [14] |
| GDC Data Transfer Tool | Bulk data download | Efficiently transfer large genomic datasets [13] |
| R/Bioconductor Packages | Data analysis and visualization | Perform differential expression, survival analysis, and ROC curve generation [10] [12] |
Experimental Protocols
Protocol: Downloading TCGA Data via GDC Portal
This protocol outlines the systematic process for acquiring TCGA data appropriate for m6A-lncRNA prognostic model development.
Materials:
- GDC Data Portal access (portal.gdc.cancer.gov)
- GDC Data Transfer Tool (for large datasets)
- Computational resources (local or HPC cluster)
Procedure:
- Navigate to GDC: Access the GDC Data Portal at https://portal.gdc.cancer.gov/ [13]
- Select cohort: Use "Cohort Builder" or "Projects" tab to select your cancer type of interest (e.g., TCGA-BRCA for breast cancer) [13]
- Apply filters: Refine your cohort using clinical or molecular filters (e.g., gender, tumor stage) as needed for your research question [13]
- Access repository: Navigate to "Repository" to filter files by data type (e.g., RNA-Seq, gene quantification files) [13]
- Review file metadata: Examine file properties, associated cases, and processing methods for each file of interest [13]
- Download data: For datasets <5GB and <10,000 files, use direct download; for larger datasets, use the GDC Data Transfer Tool with the manifest file [13]
- Download associated data: Ensure you obtain clinical data (TSV/JSON), biospecimen information, and sample sheets for complete analysis [13]
Protocol: Identifying m6A-Related lncRNAs from Transcriptomic Data
This methodology is adapted from multiple recent studies that successfully constructed m6A-lncRNA prognostic models [10] [11] [12].
Materials:
- TCGA transcriptome data (RNA-Seq)
- List of m6A regulators (writers, readers, erasers)
- Computational environment (R statistical software)
- R packages: limma, glmnet, survival
Procedure:
- Data preparation:
lncRNA identification:
- Cross-reference gene IDs with Ensembl Genome Browser to distinguish lncRNAs from mRNAs [10]
- Apply quality control filters to remove low-expression transcripts
Co-expression analysis:
Prognostic model construction:
- Conduct univariate Cox regression to identify m6A-related lncRNAs with prognostic significance [10] [12]
- Apply LASSO-Cox regression to refine the lncRNA signature and prevent overfitting [10] [11]
- Calculate risk scores using the formula:
riskScore = Σ(Coefficient(gene_i) * mRNA Expression(gene_i))[12]
Model validation:
Key Considerations for Enhancing Model Performance
When working with TCGA data for m6A-lncRNA prognostic models, several factors significantly impact ROC curve analysis and overall model performance:
- Data Quality: Prioritize harmonized data over legacy data to minimize technical artifacts [13] [14]
- Feature Selection: Implement rigorous feature selection methods (e.g., ANOVA-based) to reduce dimensionality and focus on biologically relevant lncRNAs [14]
- Validation Strategy: Always validate findings in independent datasets when possible, and perform comprehensive survival and ROC analyses [10] [12]
- Multi-omics Integration: Consider incorporating additional data types (methylation, mutation) to enhance model predictive power [14]
By following these guidelines and leveraging the resources outlined, researchers can effectively source high-quality transcriptomic data to build robust m6A-lncRNA prognostic models with improved performance metrics.
Core m6A Regulators: A Reference Table
The machinery governing N6-methyladenosine (m6A) modification is categorized into three functional classes: writers (methyltransferases), erasers (demethylases), and readers (binding proteins). The table below summarizes the key components and their primary functions.
Table 1: Core m6A Regulatory Proteins and Their Functions
| Regulator Class | Component Name | Primary Function | Key Characteristics | Subcellular Localization |
|---|---|---|---|---|
| Writers | METTL3 | Catalytic subunit of methyltransferase complex [16] [17] | Installs m6A modification; essential for embryonic development [16] | Nucleus [17] |
| METTL14 | RNA-binding scaffold in methyltransferase complex [16] [17] | Enhances METTL3 catalytic activity; lacks independent catalytic function [16] | Nucleus [17] | |
| WTAP | Regulatory subunit [16] [18] | Directs complex to nuclear speckles and mRNA targets [17] [18] | Nucleus [17] | |
| KIAA1429 (VIRMA) | Scaffold protein for methyltransferase complex [16] [19] | Guides region-selective m6A methylation, particularly in 3'UTR [16] [19] | Nucleus | |
| Erasers | FTO | Demethylase [19] [18] | Removes m6A; preferentially demethylates m6Am [18] | Nucleus [18] |
| ALKBH5 | Demethylase [19] [18] | Major m6A demethylase; influences tumor immune microenvironment [19] | Nucleus [18] | |
| Readers | YTHDF1 | Binds m6A-modified RNA [17] [18] | Promotes translation efficiency [17] [18] | Cytoplasm [18] |
| YTHDF2 | Binds m6A-modified RNA [17] [18] | Promotes mRNA decay and regulates stability [17] [18] | Cytoplasm [18] | |
| YTHDC1 | Binds m6A-modified RNA [17] [18] | Regulates alternative splicing [17] [18] | Nucleus [18] | |
| IGF2BP1/2/3 | Binds m6A-modified RNA [19] [18] | Enhances mRNA stability and storage [19] [18] | Cytoplasm [18] |
The m6A Regulatory Network
The following diagram illustrates the functional relationships between the core m6A regulators and their impact on RNA metabolism.
Diagram Title: m6A Regulator Network and Functional Outcomes
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: My m6A-related lncRNA risk model has a low Area Under the Curve (AUC) value in ROC analysis. What could be the cause? A low AUC value suggests limited diagnostic ability of your model [20]. An AUC of 0.5 indicates performance equivalent to random chance, while values below 0.8 are considered to have limited clinical utility [20]. Potential causes and solutions include:
- Insufficient Feature Selection: The initial set of m6A-related lncRNAs may not be prognostic enough. Re-evaluate your univariate and multivariate Cox regression analyses with stricter significance thresholds (e.g., P < 0.01) to identify the most robust lncRNA signatures [10] [21].
- Overfitting: Using too many lncRNAs in your signature relative to your sample size can lead to a model that performs poorly on new data. Employ regularization techniques like LASSO Cox regression, which helps penalize model complexity and select the most relevant features [10].
- Lack of Validation: Always validate your model's performance in an independent patient cohort. This confirms that the model generalizes and is not tailored to the specific quirks of your initial dataset [10].
Q2: How do I interpret the AUC value from my model's ROC curve? The AUC value is a key metric for evaluating the diagnostic performance of your model [20] [22]. It represents the probability that your model will rank a randomly chosen positive instance (e.g., a patient with poor outcome) higher than a randomly chosen negative instance (e.g., a patient with good outcome) [22]. The following table provides a standard interpretation guide:
Table 2: Interpreting Area Under the Curve (AUC) Values
| AUC Value | Interpretation |
|---|---|
| 0.9 ≤ AUC | Excellent discrimination |
| 0.8 ≤ AUC < 0.9 | Considerable/good discrimination |
| 0.7 ≤ AUC < 0.8 | Fair discrimination |
| 0.6 ≤ AUC < 0.7 | Poor discrimination |
| 0.5 ≤ AUC < 0.6 | Fail (no better than chance) |
Adapted from [20]
Q3: I've identified a candidate m6A-related lncRNA. How can I experimentally validate its functional role and effect on the tumor immune microenvironment?
- Functional Validation (In Vitro): Perform knockdown or overexpression of the lncRNA in relevant cancer cell lines (e.g., A549 for lung adenocarcinoma) [21]. Assess subsequent changes in:
- Proliferation, invasion, and migration: Using assays like CCK-8, transwell, and wound healing.
- Apoptosis and drug resistance: Using flow cytometry and IC50 measurements for chemotherapeutics like cisplatin [21].
- Immune Microenvironment Analysis (In Silico/Bioinformatics): Leverage transcriptomic data to analyze correlations between your lncRNA signature and:
- Immune Cell Infiltration: Use tools like CIBERSORT to estimate abundances of member cell populations (e.g., T cells, macrophages) [10] [21].
- Immune Checkpoint Expression: Evaluate the expression levels of key immune checkpoints like PD-1, PD-L1, and CTLA-4 between high-risk and low-risk patient groups defined by your model [10]. Studies have shown that high-risk groups can exhibit significantly higher checkpoint expression, suggesting potential for immunotherapy response prediction [10].
Q4: How can I improve the stability and reliability of my siRNA for knocking down lncRNAs in functional experiments?
- Use Chemically Modified siRNA: Chemically modified siRNA duplexes (e.g., Stealth RNAi) offer increased stability in serum, which is crucial for both in vitro and in vivo experiments [23].
- Optimize Transfection Conditions: Run a transfection reagent-only control to assess cellular sensitivity. Systematically test different cell densities and siRNA concentrations (e.g., between 5 nM and 100 nM) to find optimal conditions that minimize toxicity and maximize knockdown efficiency [23].
- Include Proper Controls: Always use a validated positive control siRNA (e.g., targeting GAPDH) to confirm transfection efficiency and a negative control siRNA to account for non-specific effects [23].
Experimental Protocols for m6A-Related lncRNA Model Development
Protocol 1: Constructing an m6A-Related lncRNA Prognostic Signature
This protocol is adapted from established methodologies used in cancer research [10] [21].
- Data Acquisition: Obtain transcriptomic RNA-seq data (e.g., FPKM values) and corresponding clinical information (especially overall survival data) from a public database such as The Cancer Genome Atlas (TCGA).
- Identify m6A Regulators and lncRNAs: Extract a known set of m6A regulator genes (writers, erasers, readers; approximately 19-23 genes) from literature [10] [21]. Use an annotation file (e.g., from GENCODE) to distinguish and extract lncRNAs from the transcriptomic data.
- Define m6A-Related lncRNAs (mRLs): Perform co-expression analysis between the expression of m6A regulators and all lncRNAs. Identify mRLs using a correlation threshold (e.g., |Pearson R| > 0.3) and a significance threshold (e.g., P < 0.001) [10].
- Screen Prognostic mRLs: Conduct univariate Cox regression analysis on the mRLs to identify those significantly associated with patient overall survival (OS). A common threshold is P < 0.01 [10].
- Model Construction with LASSO Cox Regression: To prevent overfitting, subject the significant prognostic mRLs from step 4 to Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression. This will further refine the lncRNA list and calculate a coefficient for each. The final risk score for each patient is calculated using the formula:
Risk Score = Σ (Expression of mRLn * Coefficient of mRLn) - Patient Stratification: Divide patients into high-risk and low-risk groups based on the median risk score or an optimal cut-off value determined from the data.
- Model Validation:
- Kaplan-Meier Analysis: Plot survival curves for the high and low-risk groups and assess significance with a log-rank test.
- ROC Analysis: Evaluate the model's predictive accuracy by plotting time-dependent Receiver Operating Characteristic (ROC) curves and calculating the Area Under the Curve (AUC) for 1-, 3-, and 5-year overall survival [10].
Protocol 2: Assessing Association with Tumor Immune Microenvironment
- Immune Cell Infiltration Estimation: For each tumor sample in your cohort, use a computational tool like CIBERSORT in conjunction with the LM22 signature matrix to estimate the relative fractions of 22 human immune cell types [21].
- Immune Checkpoint Analysis: Extract the expression data for key immune checkpoint genes (e.g., PD-1, PD-L1, CTLA-4) from your transcriptomic dataset.
- Correlation with Risk Score: Compare the immune cell infiltration scores and immune checkpoint expression levels between the high-risk and low-risk groups defined by your m6A-lncRNA signature. Use statistical tests like the Wilcoxon test to determine significance [10]. This can reveal whether your model is associated with an immunosuppressive or immunoreactive microenvironment.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for m6A and lncRNA Research
| Reagent / Tool Type | Specific Example | Primary Function in Research |
|---|---|---|
| Validated Antibodies | Anti-METTL3, Anti-FTO, Anti-YTHDF2 [18] | Protein detection via Western Blot (WB), Immunohistochemistry (IHP), or Immunoprecipitation (IP) to validate regulator expression. |
| siRNA / RNAi Tools | Stealth RNAi, In Vivo siRNA [23] | Chemically modified duplexes for potent and stable knockdown of target lncRNAs or m6A regulators in vitro and in vivo. |
| In Vivo Transfection Reagent | Invivofectamine 3.0 [23] | Lipid-based reagent for systemic delivery of siRNA molecules in animal models. |
| Bioinformatics Tools | CIBERSORT [10] [21] | Deconvolutes transcriptomic data to infer immune cell infiltration levels in tumor samples. |
| Sequencing Kits | MeRIP-seq / miCLIP Kits [18] | High-resolution mapping of m6A modifications across the transcriptome. |
Frequently Asked Questions (FAQs) & Troubleshooting Guides
FAQ: How do I initially identify m6A-related lncRNAs from transcriptomic data?
Q: What is the standard methodological workflow for the initial identification of m6A-related long non-coding RNAs?
A: The initial identification involves a multi-step bioinformatic screening process using transcriptomic data, typically from sources like The Cancer Genome Atlas (TCGA). The core of this method is a correlation analysis between the expression levels of known m6A regulators and all detected lncRNAs [24] [25].
- Step 1: Data Acquisition and Preparation. Obtain RNA sequencing data that includes both normal and diseased tissues (e.g., tumor samples). Annotate the transcripts to distinguish lncRNAs from mRNAs [26] [25].
- Step 2: Define m6A Regulator Gene Set. Compile a list of known writers, erasers, and readers. Studies often use a set of 23-29 well-established m6A genes, such as METTL3, METTL14, FTO, ALKBH5, YTHDF1/2/3, and IGF2BP1/2/3 [24] [25].
- Step 3: Perform Correlation Analysis. Calculate the correlation coefficient (e.g., Pearson or Spearman) between the expression of each m6A regulator and each lncRNA across all samples [24] [25].
- Step 4: Set a Significance Threshold. Apply thresholds to identify statistically significant and biologically relevant associations. A common threshold is an absolute correlation coefficient > 0.4 with a p-value < 0.001 [25]. LncRNAs passing this filter are considered "m6A-related."
Troubleshooting Tip: Low Number of Significant lncRNAs
- Problem: The analysis yields very few m6A-related lncRNAs.
- Solution: Consider using a less stringent correlation coefficient threshold (e.g., >0.3) or adjusting the p-value cutoff. Ensure your dataset has a sufficient sample size, as statistical power is highly dependent on the number of observations [27].
FAQ: How can I improve the performance of a prognostic model based on m6A-related lncRNAs?
Q: What strategies can be employed to enhance the predictive accuracy and robustness of an m6A-lncRNA risk model, as reflected in the ROC curve analysis?
A: Improving model performance involves careful feature selection, validation, and integration of clinical variables.
- Strategy 1: Employ Advanced Feature Selection. Use the Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression analysis on your initial list of m6A-related lncRNAs. This technique penalizes the model for having too many features, helping to select the most prognostic lncRNAs and prevent overfitting [28] [24] [25]. This step is crucial for building a robust model with a high Area Under the ROC Curve (AUC).
- Strategy 2: Construct a Multi-lncRNA Signature. A model combining multiple m6A-related lncRNAs (a "risk signature") consistently shows better predictive performance than single lncRNA markers [24] [25]. The risk score is calculated using the formula:
Risk score = Σ(Coef_i * Exp_i), whereCoef_iis the regression coefficient from the LASSO analysis, andExp_iis the expression level of each lncRNA [25]. - Strategy 3: Build a Integrated Nomogram. Combine the m6A-lncRNA risk score with established clinical factors like pathologic stage to create a nomogram. This integrated approach has been shown to enhance prognostic prediction accuracy for 1-, 3-, and 5-year overall survival, as confirmed by calibration plots [25].
Troubleshooting Tip: Poor Validation in an Independent Cohort
- Problem: Your model performs well in the training dataset but poorly in the testing dataset.
- Solution: This indicates overfitting. Revisit the LASSO regression parameters and ensure 10-fold cross-validation was used during the model building phase. Also, verify that the training and testing datasets are from the same source and processed identically [25].
FAQ: How do I move from a list of lncRNAs to understanding their functional role?
Q: After identifying key m6A-related lncRNAs, what experimental and bioinformatic methods are used to decipher their biological function and regulatory mechanisms?
A: Functional characterization typically involves constructing regulatory networks and validating specific molecular interactions.
- Method 1: Construct a Competing Endogenous RNA (ceRNA) Network. This is a common mechanism of action for lncRNAs. The workflow is:
- Predict microRNAs (miRNAs) that bind to your key m6A-related lncRNAs using tools like TargetScan and miRanda [28] [29].
- Identify the target mRNAs of these miRNAs.
- Construct a visual network (e.g., using Cytoscape) comprising the lncRNAs, miRNAs, and mRNAs [28]. This network hypothesizes a functional pathway where the lncRNA "sponges" miRNA to regulate mRNA expression.
- Method 2: Functional Enrichment Analysis. Use the list of genes (mRNAs) from your ceRNA network or genes co-expressed with your m6A-related lncRNA to perform Gene Ontology (GO) and Kyoto Encyclopedia of Genes and Genomes (KEGG) analyses. This reveals enriched biological processes and signaling pathways (e.g., MAPK signaling, PPAR signaling), providing insight into the lncRNA's potential role in disease [29] [26] [25].
- Method 3: Experimental Validation of the m6A Modification.
- methylated RNA immunoprecipitation sequencing (MeRIP-Seq/qPCR): This is the gold standard for confirming m6A modification on a specific lncRNA. It uses an anti-m6A antibody to immunoprecipitate methylated RNA fragments, which are then sequenced or quantified via qPCR [29] [30] [31].
- Functional Assays: Perform in vitro or in vivo experiments (e.g., cell proliferation, migration, colony formation assays) after knocking down or overexpressing the lncRNA to observe phenotypic changes [6].
Troubleshooting Tip: ceRNA Network is Too Large and Unwieldy
- Problem: The predicted ceRNA network contains hundreds of molecules, making it difficult to interpret.
- Solution: Increase the stringency of your prediction parameters (e.g., context++ score in TargetScan, energy threshold in miRanda). Focus the subsequent analysis on the top-ranked interactions or only include molecules that are differentially expressed in your dataset [29].
The Scientist's Toolkit: Key Research Reagent Solutions
The table below outlines essential reagents and tools used in the featured methodologies.
| Item Name | Function / Explanation | Example from Literature |
|---|---|---|
| Anti-m6A Antibody | Immunoprecipitation of m6A-modified RNA fragments in MeRIP-Seq/qPCR experiments. | Rabbit polyclonal antibody (Synaptic Systems, 202003) used to pull down methylated LncRNAs [29]. |
| m6A Regulator Gene Set | A pre-defined list of writer, eraser, and reader genes for correlation analysis. | A set of 23 genes (e.g., METTL3/14, FTO, ALKBH5, YTHDF1-3, IGF2BPs) used to find correlated lncRNAs [25]. |
| TCGA/CEO Datasets | Publicly available transcriptomic and clinical data for bioinformatic discovery and validation. | SKCM and COAD data from TCGA used to identify prognostic m6A-related lncRNA signatures [28] [24] [25]. |
| LASSO Cox Regression | A statistical method for selecting the most relevant prognostic genes and building a predictive model. | Used to narrow down dozens of m6A-related lncRNAs to a final prognostic signature of 12 lncRNAs [25]. |
| Cytoscape Software | An open-source platform for visualizing complex molecular interaction networks. | Used to construct and visualize the lncRNA-m6A regulator-mRNA co-expression network [26]. |
Experimental Workflow & Network Diagrams
Diagram 1: m6A-lncRNA Identification Workflow
The diagram below illustrates the core bioinformatic pipeline for identifying and modeling m6A-related lncRNAs.
Diagram 2: m6A-lncRNA Regulatory Network
This diagram visualizes the core regulatory network involving m6A-modified lncRNAs, showing how different players interact.
Integrating Clinical Phenotype Data for Meaningful Outcome Association
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: Why does my disulfidptosis-related LncRNA risk model have high AUC but fails to stratify patient survival in Kaplan-Meier analysis?
This discrepancy often arises from incorrect risk score cut-off selection or violation of the proportional hazards assumption. Use the survminer R package to determine the optimal risk score cut-point using the "maxstat" method. If survival curves cross, restrict your analysis to time periods before the crossover and re-run the log-rank test [8].
Q2: How can I improve ROC curve analysis when my sample size is limited?
With smaller sample sizes, nonparametric ROC curves may appear jagged and yield biased AUC estimates. Consider using the parametric method if your data meets normality assumptions, or apply 10-fold cross-validation to obtain more reliable performance metrics. The pROC R package can smooth curves and calculate confidence intervals for AUC [32].
Q3: What is the minimum correlation coefficient threshold for identifying disulfidptosis-related LncRNAs?
Research indicates that setting a Pearson correlation coefficient threshold of |R| > 0.4 with a significance of p < 0.001 effectively filters for biologically relevant LncRNAs while reducing false positives. Validate co-expression patterns using RT-qPCR on at least 7 patient-matched tissue samples [33] [34].
Q4: How do I handle missing clinical phenotype data when building integrated models?
Implement multiple phenotype capture methods: collect structured data via HPO terms, unstructured clinical notes, and automated NLP extraction from EHRs. The PhenoTips platform facilitates structured phenotype entry, while manual curation of clinic notes remains the most reliable method for WGS analysis [35].
Troubleshooting Common Experimental Issues
Table 1: Troubleshooting m6A LncRNA Model Performance Issues
| Problem | Potential Causes | Solutions |
|---|---|---|
| Poor model generalizability | Overfitting on training data | Apply LASSO-Cox regression with 10-fold cross-validation; use λ_1se for higher penalty [33] [8] |
| Low AUC in validation cohort | Batch effects between datasets | Normalize RNA-seq data using TPM transformation; apply ComBat batch correction [8] |
| Inconsistent immune infiltration results | Different deconvolution algorithms | Compare CIBERSORT, ESTIMATE, and ssGSEA results; use consistent method across analyses [33] |
| Weak clinical correlation | Inadequate phenotype annotation | Implement multi-source phenotyping: HPO terms, EHR extraction, and specialist notes [35] |
Experimental Protocols
Protocol 1: Constructing a Disulfidptosis-Related LncRNA Prognostic Signature
Purpose: Develop and validate a multi-LncRNA signature for outcome prediction in cancer patients [33] [34].
Materials:
- RNA-seq data from TCGA (cancer samples) and GTEx (normal controls)
- Clinical follow-up data (overall survival, disease-free survival)
- R packages:
limma,survival,glmnet,timeROC
Procedure:
- Data Acquisition and Preprocessing
- Download transcriptomic data and clinical information from TCGA (e.g., TCGA-AML, TCGA-SKCM)
- Normalize count data to TPM or FPKM and apply log2 transformation
- Merge with clinical variables: age, stage, treatment history, survival status
Identify Disulfidptosis-Related LncRNAs
- Compile established disulfidptosis-related genes (DRGs: FLNA, FLNB, MYH9, MYH10, NDUFA11, NDUFS1, NUBPL, SLC7A11, TLN1)
- Calculate Pearson correlation between all LncRNAs and DRGs
- Filter for |R| > 0.4 and p < 0.001
- Visualize relationships using Sankey diagrams (
ggalluvialpackage)
Prognostic Model Construction
- Perform univariate Cox regression to identify survival-associated DRLs (p < 0.05)
- Apply LASSO-Cox regression with 10-fold cross-validation to prevent overfitting
Calculate risk score using the formula:
Risk Score = Σ(coefficientlncRNA × expressionlncRNA)Stratify patients into high/low-risk groups using median risk score
Model Validation
- Assess predictive performance with time-dependent ROC curves (1-, 3-, 5-year)
- Validate in independent datasets using the same risk score calculation
- Perform multivariate Cox regression adjusting for clinical covariates
Protocol 2: Integrated Single-Cell Analysis of Disulfidptosis Microenvironment
Purpose: Characterize disulfidptosis-related gene expression at single-cell resolution and intercellular communication [34].
Materials:
- Single-cell RNA-seq data (e.g., GSE135337 for BLCA)
- R packages:
Seurat,CellChat,singleR - Computational resources: 16GB+ RAM, multi-core processor
Procedure:
- Quality Control and Cell Filtering
- Filter cells with >500 and <2500 expressed genes
- Exclude cells with >5% mitochondrial content
- Normalize data using
NormalizeDatafunction - Identify 3000 highly variable genes for downstream analysis
Cell Clustering and Annotation
- Perform PCA and select top 20 principal components
- Cluster cells using
FindClustersfunction (resolution = 0.5) - Annotate cell types using
singleRwith manual refinement via known markers - Visualize with UMAP/t-SNE plotting
Disulfidptosis Module Scoring
- Calculate disulfidptosis scores using
AddModuleScorefunction - Compare scores across cell types and conditions
- Identify cell populations with elevated disulfidptosis activity
- Calculate disulfidptosis scores using
Cell-Cell Communication Analysis
- Input annotated single-cell data to
CellChatpackage - Identify significantly enriched ligand-receptor pairs
- Visualize communication networks and key signaling pathways
- Input annotated single-cell data to
Signaling Pathways & Experimental Workflows
Diagram 1: Prognostic Model Development Workflow
Diagram 2: Clinical Phenotype Integration Framework
Research Reagent Solutions
Table 2: Essential Research Reagents and Resources for m6A LncRNA Studies
| Reagent/Resource | Type | Function | Example Sources |
|---|---|---|---|
| TCGA Datasets | Data Resource | Provides RNA-seq and clinical data for model training | TCGA-AML, TCGA-SKCM [33] [8] |
| GTEx Normal Controls | Data Resource | Normal tissue expression baseline for differential analysis | GTEx Portal [33] |
| GEO Series | Data Resource | Validation datasets and single-cell RNA-seq data | GSE135337, GSE8401, GSE15605 [8] [34] |
| Disulfidptosis-Related Genes | Gene Set | Core genes for LncRNA correlation analysis | FLNA, SLC7A11, MYH9, etc. [33] [34] |
| Human Phenotype Ontology | Annotation System | Standardized phenotype capture and analysis | HPO Database [35] |
| CIBERSORT Algorithm | Computational Tool | Immune cell infiltration quantification | CIBERSORT Web Portal [33] |
| CellChat Package | Computational Tool | Cell-cell communication analysis from scRNA-seq | R/Bioconductor [34] |
| glmnet Package | Computational Tool | LASSO-Cox regression implementation | R CRAN [33] [8] |
Building the Signature: From Feature Selection to Model Construction and ROC Evaluation
In the field of cancer research, particularly in studies focusing on m6A-related lncRNAs, building robust prognostic models is crucial for advancing personalized medicine. The performance of these models heavily depends on effective feature selection techniques that identify the most biologically relevant biomarkers from high-dimensional genomic data. Univariate Cox regression and LASSO (Least Absolute Shrinkage and Selection Operator) regression represent two powerful approaches for this purpose, serving as critical steps in the pipeline to improve model performance and ROC curve analysis. This technical support guide addresses common challenges researchers encounter when implementing these techniques in their experiments.
FAQs & Troubleshooting Guides
FAQ 1: Why is feature selection necessary before building an m6A-lncRNA prognostic model?
Answer: Feature selection is a critical preprocessing step in high-dimensional genomic studies where the number of features (genes, lncRNAs) far exceeds the number of observations (patients). This "n << p" problem makes standard regression models prone to overfitting, where models perform well on training data but generalize poorly to new datasets [36]. Proper feature selection:
- Reduces model complexity and enhances generalizability
- Identifies truly informative m6A-related lncRNAs from thousands of candidates
- Improves computational efficiency
- Enhances biological interpretability of the final model
In m6A-lncRNA research, studies typically begin with thousands of lncRNA candidates, which must be refined to a manageable signature (often 6-11 key markers) using rigorous statistical methods [10] [37] [38].
FAQ 2: When should I choose Univariate Cox versus LASSO Cox regression for feature selection?
Answer: These methods serve complementary purposes in the feature selection pipeline:
Univariate Cox Regression:
- Purpose: Initial filtering of features based on individual prognostic strength
- When to use: First-step screening to reduce feature space
- Advantages: Computationally efficient, easy to interpret
- Limitations: Ignores interactions between features
LASSO Cox Regression:
- Purpose: Multivariate feature selection that accounts for correlations between features
- When to use: After univariate analysis to build the final prognostic signature
- Advantages: Handles multicollinearity, produces sparse models
- Limitations: More computationally intensive
Table 1: Comparison of Feature Selection Methods in Survival Analysis
| Method | Implementation | Key Characteristics | Best Use Cases |
|---|---|---|---|
| Univariate Cox | Separate Cox model for each feature | Uses Wald test statistic; filters features by p-value (typically <0.05) | Initial screening of thousands of lncRNAs |
| LASSO Cox | Penalized multivariate Cox regression | Applies L1 penalty; shrinks coefficients of irrelevant features to zero | Building final prognostic signature from pre-filtered features |
| Multivariate Cox | Standard Cox regression with multiple features | No built-in feature selection; requires pre-selected features | Validating final feature set |
FAQ 3: How do I implement Univariate Cox regression for initial lncRNA screening?
Experimental Protocol:
Data Preparation:
- Format data as (Ti, δi, xi) where Ti is observed time, δi is censoring indicator, and xi is the lncRNA expression vector [36]
- Normalize lncRNA expression values (e.g., log transformation, standardization)
- Ensure sufficient events (deaths) per variable (EPV ≥ 10-15)
Statistical Implementation:
- Extract hazard ratios, confidence intervals, and p-values for each lncRNA
- Apply multiple testing correction (Bonferroni or FDR) to account for false discoveries
- Select lncRNAs with p-value < 0.05 (or more stringent threshold) for further analysis
Validation:
- Check proportional hazards assumption for selected lncRNAs
- Ensure clinical relevance of selected features
FAQ 4: What are the key parameters and implementation steps for LASSO Cox regression?
Experimental Protocol:
Data Preparation:
- Use lncRNAs pre-filtered by univariate analysis (p < 0.05)
- Ensure no missing data in the selected feature set
- Create training (70-80%) and validation (20-30%) sets
LASSO Implementation:
Parameter Optimization:
- Use k-fold cross-validation (typically 5- or 10-fold) to select optimal λ (lambda)
- Choose λ that minimizes partial likelihood deviance (λ.min) or most regularized model within 1 standard error (λ.1se)
- Ensure stability of selected features through bootstrap validation
FAQ 5: How can I troubleshoot poor ROC performance after feature selection?
Troubleshooting Guide:
Table 2: Common ROC Performance Issues and Solutions
| Problem | Potential Causes | Diagnostic Steps | Solutions |
|---|---|---|---|
| Low AUC (<0.7) | Weak prognostic features; over-aggressive feature selection; small sample size | Check univariate HRs; verify sample size adequacy; examine validation performance | Increase sample size; relax univariate p-value threshold; incorporate clinical variables |
| Overfitting (training AUC >> test AUC) | Too many features relative to samples; inadequate regularization | Compare training vs. validation performance; use nested cross-validation | Strengthen LASSO penalty (use λ.1se); implement repeated cross-validation; reduce feature set |
| Unstable feature selection | High correlation between lncRNAs; small sample effects | Check correlation matrix; bootstrap feature selection stability | Use elastic net (alpha = 0.5-0.9); pre-filter highly correlated features; increase sample size |
Additional Solutions:
- Implement nested cross-validation for unbiased performance estimation [36]
- Combine multiple feature selection methods (e.g., random forest + LASSO)
- Validate findings in independent external datasets when possible
- Consider alternative metrics like precision-recall curves for imbalanced data [39] [40]
FAQ 6: What validation steps are essential after feature selection?
Answer: Comprehensive validation is crucial for ensuring model reliability:
Internal Validation:
- Bootstrap validation (200-500 replicates)
- Calculate optimism-corrected performance metrics
- Time-dependent ROC analysis at clinically relevant timepoints [36]
Clinical Validation:
Biological Validation:
Research Reagent Solutions
Table 3: Essential Research Materials for m6A-lncRNA Studies
| Reagent/Tool | Function | Example Applications |
|---|---|---|
| TCGA Database | Source of lncRNA expression and clinical data | Obtain RNA-seq data and survival information for various cancers [10] [37] |
| CIBERSORT/xCell/ESTIMATE | Immune cell infiltration analysis | Characterize tumor immune microenvironment in risk groups [10] [38] |
| qRT-PCR Reagents | Experimental validation of lncRNA expression | Verify expression of signature lncRNAs in clinical samples [37] [38] |
| R Survival Package | Implementation of Cox regression models | Perform univariate and multivariate survival analysis [36] |
| glmnet Package | LASSO and elastic net regularization | Implement penalized Cox regression for feature selection [36] |
Workflow Visualization
Feature Selection Workflow for m6A-lncRNA Signature Development
ROC Curve Analysis and AUC Interpretation
This guide provides technical support for constructing and validating a risk score formula, specifically within the context of building prognostic models for m6A-related lncRNA research. A well-constructed risk score is a numerical value that reflects the severity or likelihood of a specific outcome, such as disease progression or patient survival [41]. In cancer research, these models help stratify patients into risk groups, enabling personalized treatment strategies [10] [21].
The following sections offer a detailed, step-by-step methodology and troubleshooting guide to help you build a robust model and correctly perform the essential ROC curve analysis to evaluate its performance.
Step-by-Step Experimental Protocol
Step 1: Data Acquisition and Definition of m6A-Related lncRNAs
The first step involves gathering the necessary genomic and clinical data.
- Data Source: Obtain RNA-sequencing data and corresponding clinical information (e.g., overall survival time and status) from public repositories like The Cancer Genome Atlas (TCGA). For a typical analysis, you might work with a dataset comprising hundreds of patient samples (e.g., 611 CRC and 51 normal specimens, or 526 LUAD patients) [10] [21].
- Data Processing: Use an annotation database, such as the Ensembl Genome Browser, to distinguish lncRNAs from mRNAs in your dataset [10].
- Identify m6A-Related lncRNAs (mRLs):
- Compile a list of known m6A regulatory genes ("writers" like METTL3/14, "readers" like YTHDF1/2/3, and "erasers" like FTO and ALKBH5) [10] [21].
- Perform a co-expression analysis between the expression profiles of these m6A regulators and all lncRNAs in your dataset.
- Identify m6A-related lncRNAs (mRLs) by applying a correlation threshold (e.g., |Pearson R| > 0.3 and a statistical significance of p < 0.001) [10].
Step 2: Construction of the Risk Score Formula
The core of the model is a formula that combines the expression levels of key prognostic mRLs.
- Identify Prognostic mRLs: Perform univariate Cox regression analysis on the mRLs to identify those significantly associated with patient overall survival (OS) [10] [21].
- Build the Multivariate Model: Input the significant mRLs from the univariate analysis into a multivariate Cox regression analysis. This determines the independent contribution of each lncRNA to survival.
- Develop the Risk Formula: The risk score for each patient is calculated using the following formula [21]:
Risk Score = Σ(Coefficient<sub>lncRNA1</sub> × Expression<sub>lncRNA1</sub>) + (Coefficient<sub>lncRNA2</sub> × Expression<sub>lncRNA2</sub>) + ... + (Coefficient<sub>lncRNAn</sub> × Expression<sub>lncRNAn</sub>)- Coefficient: Derived from the multivariate Cox regression, it represents the weight or contribution of each lncRNA to the risk.
- Expression: The normalized expression level of each lncRNA in a patient's sample.
The workflow below summarizes the key stages of model development and validation.
Step 3: Model Validation via ROC Curve Analysis
The Receiver Operating Characteristic (ROC) curve and the Area Under the Curve (AUC) are fundamental for assessing your model's discriminative ability [42].
- The ROC Curve is a plot of the True Positive Rate (Sensitivity) against the False Positive Rate (1 - Specificity) across all possible risk score cut-off points [42].
- The AUC quantifies the overall ability of the risk score to distinguish between two outcome groups (e.g., short-term vs. long-term survivors). An AUC of 0.5 indicates no discriminative power (like random chance), while an AUC of 1.0 represents perfect discrimination [43] [42].
Troubleshooting & FAQs
FAQ 1: My ROC curve is in the lower right half, and the AUC is less than 0.5. What went wrong?
- Problem: A realistic diagnostic test should have an AUC of at least 0.5. An AUC significantly below 0.5 indicates the test's accuracy is worse than random guessing [44].
- Solution: This error almost always results from an incorrect "test direction" setting in your statistical software. When setting up the ROC analysis, you must correctly specify whether a larger or a smaller risk score indicates a higher likelihood of the event (e.g., patient death). If you get an AUC < 0.5, reverse this setting [44].
FAQ 2: The ROC curves for my two models intersect. Can I just compare the full AUCs?
- Problem: Simply comparing the full Area Under the Curve (AUC) is only valid when one ROC curve is consistently above the other. If the curves cross, the full AUC can be misleading because one test might be better in a specific region (e.g., high-sensitivity range) while the other is better elsewhere [44].
- Solution:
- Use the partial AUC (pAUC) to compare the areas under specific, clinically relevant regions of the curves (e.g., where False Positive Rates are between 0 and 0.1, if high specificity is crucial for your context) [43] [44].
- Supplement your analysis with other metrics like accuracy, precision, and recall (sensitivity) to provide a comprehensive assessment of model performance [44].
FAQ 3: I have two models with similar AUCs. How do I determine if one is statistically better?
- Problem: A visual inspection or simple comparison of AUC values is not sufficient to claim a statistically significant difference between two models.
- Solution: You must perform a formal statistical test for comparing ROC curves.
FAQ 4: My ROC curve has only one cut-off point and two straight lines. Is this normal?
- Problem: This "single cut-off" ROC shape typically appears when the input variable for the ROC analysis is binary, not continuous [44].
- Solution: Ensure you are using the continuous risk score to generate the ROC curve, not a previously dichotomized version (e.g., a binary high/low risk label). The ROC curve is designed to evaluate a continuous or multi-class variable across all its potential thresholds [44].
The Scientist's Toolkit: Research Reagent Solutions
Table 1: Essential reagents, tools, and datasets for constructing an m6A-lncRNA risk model.
| Item | Function / Application |
|---|---|
| TCGA Database | Primary source for RNA-seq data and clinical information (e.g., survival, stage) for various cancers [10] [21]. |
| Ensembl Genome Browser | Used to annotate and differentiate lncRNAs from mRNAs in the transcriptomic data [10]. |
| m6A Regulator List | A curated list of known "writer," "reader," and "eraser" genes (e.g., METTL3, FTO, YTHDF1) to identify m6A-related lncRNAs [10]. |
| Cox Regression Model | A statistical method to identify factors (lncRNAs) associated with survival time and to calculate their coefficients for the risk formula [10]. |
| CIBERSORT Tool | An algorithm used to estimate the abundance of specific immune cell types in a tissue sample based on gene expression data, allowing for analysis of immune infiltration [10] [21]. |
| R packages: 'survival', 'pROC', 'rms' | Essential software tools for performing survival analyses, ROC curve analysis, and constructing nomograms [10] [21]. |
Data Presentation and Interpretation
Table 2: Key metrics for evaluating the performance of a prognostic risk model.
| Metric | Definition | Interpretation in m6A-lncRNA Model Context |
|---|---|---|
| Risk Score | A numerical value calculated from the risk formula. | Used to rank patients; a higher score indicates a poorer predicted prognosis [10]. |
| Hazard Ratio (HR) | The ratio of the hazard rates between two groups (e.g., High vs. Low Risk). | An HR > 1 for the high-risk group indicates a higher risk of death over time [21]. |
| Area Under Curve (AUC) | The probability that the model ranks a random positive case higher than a random negative case. | Measures the model's ability to discriminate between patients with good and poor outcomes. An AUC of 0.75 means a 75% chance of correct ranking [42]. |
| Sensitivity (Recall) | True Positive Rate: Proportion of actual positives correctly identified. | In a prognostic model, it is the ability to correctly identify patients who will have a poor outcome [42] [44]. |
| Specificity | True Negative Rate: Proportion of actual negatives correctly identified. | The model's ability to correctly identify patients who will have a good outcome [42] [44]. |
| p-value (Cox Model) | The statistical significance of a variable's association with survival. | A p < 0.05 for a lncRNA suggests it is a significant prognostic factor [10]. |
The Role of Nomograms in Integrating Risk Scores with Clinical Variables
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of using a nomogram over a simple risk score? A nomogram integrates multiple types of information—including risk scores from molecular signatures (like m6A-lncRNA models) and traditional clinical variables—into a single, easy-to-use visual tool. This allows for individualized risk prediction and superior clinical utility compared to using any single predictor alone [45] [46] [47]. For example, a nomogram for predicting intracranial infection combined a risk score based on six predictors (including pneumonia and procalcitonin levels) into a model with an AUC of 0.91 [45].
Q2: My m6A-lncRNA risk model has a good AUC. Why should I build a nomogram? While a high AUC indicates strong discriminative ability, it does not necessarily translate into clinical utility. A nomogram quantifies the individual patient's risk, helping clinicians answer the critical question: "What is the specific probability of an event for this patient?" Decision Curve Analysis (DCA) often demonstrates that a nomogram provides a greater net clinical benefit across a wide range of risk thresholds than the risk score or clinical variables alone [45] [46].
Q3: What are the essential components I need to build a nomogram for my m6A-lncRNA model? You will need three key components:
- A validated m6A-lncRNA risk signature with a calculated risk score for each patient [10] [21].
- Clinically relevant variables that are independently prognostic, such as age, disease stage, or other laboratory findings [46] [47].
- A multivariate regression model (typically Cox or logistic) that identifies the independent predictors and their coefficients, which form the foundation of the nomogram [45] [21].
Q4: How do I validate that my nomogram is robust? A robust validation process includes:
- Internal Validation: Using bootstrapping (e.g., 1000 resamples) to calculate a bias-corrected C-index and generate calibration plots [46].
- External Validation: Testing the nomogram's performance (discrimination and calibration) on a separate, independent patient cohort from a different institution [45] [47].
- Clinical Validation: Employing Decision Curve Analysis (DCA) to evaluate whether using the nomogram for clinical decisions provides a net benefit over alternative strategies [45] [46].
Troubleshooting Guides
Issue 1: Poor Calibration of the Nomogram
Problem: The calibration curve shows that the predicted probabilities from your nomogram systematically deviate from the observed outcomes (e.g., predictions are consistently too high or too low).
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Overfitting | Check if the number of events is too low relative to the number of predictors included. | Use regularization techniques (like LASSO regression) during variable selection to prevent overfitting. Perform internal validation with bootstrapping to assess optimism [10]. |
| Spectrum Bias | Verify if the validation cohort has a different case-mix (e.g., different disease stages) than the training cohort. | Recalibrate the nomogram for the new population or ensure the model is validated in a cohort that reflects the target population [45]. |
| Incorrect Model Assumptions | Test the linearity assumption for continuous variables. | Transform non-linear variables (e.g., using splines) before including them in the model [45]. |
Issue 2: Suboptimal Discriminatory Performance (Low C-index/AUC)
Problem: The nomogram's ability to distinguish between patients with and without the event is weak.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Weak Predictors | Check the effect sizes (Hazard Ratios/Odds Ratios) of the included variables. | Re-evaluate the variable selection process. Consider incorporating more powerful molecular markers or novel clinical biomarkers [48] [5]. |
| Redundant Variables | Check for high correlation (multicollinearity) between the m6A-lncRNA risk score and other clinical variables. | Remove one of the highly correlated variables or combine them into a composite score to improve model stability [10]. |
| Data Quality | Audit the source data for the m6A-lncRNA signature and clinical variables. | Ensure accurate quantification of lncRNA expression and consistent measurement of clinical variables across patients [48]. |
Issue 3: ROC Curve Analysis Errors
Problem: Common pitfalls when evaluating the nomogram or its components using ROC analysis.
| Error Type | How to Identify | Prevention & Correction |
|---|---|---|
| AUC < 0.5 | The ROC curve descends below the diagonal. | This usually indicates an incorrect "test direction" in the statistical software. Specify whether a larger or smaller test result indicates a more positive test [44]. |
| Intersecting ROC Curves | The ROC curves of two models cross. | Do not rely solely on the full AUC. Compare partial AUC (pAUC) in a clinically relevant FPR range (e.g., high-sensitivity region for screening). Use DeLong's test for statistical comparison [44]. |
| Single Cut-off ROC Curve | The ROC curve is V-shaped with only one inflection point. | This occurs if a continuous variable (like a risk score) was incorrectly treated as a binary variable. Ensure the original continuous values are used for ROC analysis [44]. |
Experimental Protocols
Protocol 1: Developing and Validating an m6A-lncRNA Risk Signature
This protocol outlines the foundational step for obtaining the molecular risk score to be integrated into a nomogram [10] [21] [5].
- Data Acquisition: Obtain RNA-seq data and corresponding clinical information (especially overall survival or other relevant endpoints) from a public database like TCGA.
- Identify m6A-related lncRNAs (mRLs):
- Compile a list of known m6A regulators (Writers: METTL3, METTL14, WTAP, etc.; Erasers: FTO, ALKBH5; Readers: YTHDF1-3, etc.).
- Construct a co-expression network between the expression of these regulators and all lncRNAs.
- Define mRLs using a correlation threshold (e.g., |Pearson R| > 0.3 and p < 0.001).
- Build a Prognostic Signature:
- Perform univariate Cox regression analysis to identify mRLs significantly associated with survival.
- Use LASSO-Cox regression to penalize coefficients and select the most robust lncRNAs for the final signature to avoid overfitting.
- Calculate the risk score for each patient using the formula:
Risk Score = Σ (Coefficient<sub>lncRNAi</sub> × Expression<sub>lncRNAi</sub>)
- Validate the Signature: Stratify patients into high-risk and low-risk groups based on the median risk score. Validate the prognostic power using Kaplan-Meier survival analysis and time-dependent ROC curves in both training and validation cohorts.
Protocol 2: Constructing and Validating the Integrated Nomogram
This protocol details the process of combining the m6A-lncRNA risk score with clinical variables [45] [46] [47].
- Data Preparation: Merge the m6A-lncRNA risk scores with curated clinical data for each patient.
- Univariate and Multivariate Analysis:
- Perform univariate logistic (for binary outcomes) or Cox (for time-to-event outcomes) regression analysis on all candidate variables, including the risk score and clinical factors.
- Enter significant variables from the univariate analysis into a multivariate regression model to identify independent predictors.
- Nomogram Construction: Using the
rmspackage in R (or similar), construct the nomogram based on the final multivariate model. Each predictor is assigned a points scale, and the total points correspond to a predicted probability of the clinical event. - Performance Assessment:
- Discrimination: Calculate the Harrell's C-index and plot the ROC curve to assess the model's ability to distinguish between outcomes.
- Calibration: Plot calibration curves (predicted probability vs. observed frequency); a 45-degree line indicates perfect calibration.
- Clinical Utility: Perform Decision Curve Analysis (DCA) to evaluate the net benefit of using the nomogram for clinical decision-making across different probability thresholds.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Description | Example Application in m6A-lncRNA Research |
|---|---|---|
| TCGA Database | A public repository of cancer genomics data, providing RNA-seq and clinical data. | Sourcing transcriptomic data and clinical information to identify and validate m6A-related lncRNA signatures [10] [21]. |
| LASSO-Cox Regression | A statistical method that performs variable selection and regularization to enhance prediction accuracy. | Shrinking coefficients of non-essential lncRNAs to build a parsimonious and prognostic risk signature [10] [5]. |
| CIBERSORT Algorithm | A computational tool for estimating immune cell infiltration from bulk tissue gene expression data. | Characterizing the tumor immune microenvironment (TIME) in high-risk vs. low-risk groups defined by the m6A-lncRNA signature [10] [21]. |
| SHAPE/DMS Probing | Experimental techniques for determining RNA secondary structure at nucleotide resolution. | Investigating the structure-function relationship of prognostic lncRNAs, as their function is often dictated by structure [48] [49]. |
| METTL3/RBM15 siRNA | Small interfering RNA to knock down the expression of specific m6A "writer" genes. | Functionally validating the role of m6A regulators in controlling the expression and modification of prognostic lncRNAs [5]. |
Workflow Diagram: From Data to Clinical Nomogram
The diagram below visualizes the logical workflow for developing a nomogram that integrates an m6A-lncRNA risk score with clinical variables.
Frequently Asked Questions (FAQs) on ROC Curve Analysis
FAQ 1: What does the Area Under the Curve (AUC) value actually tell me about my model's performance?
The AUC, or Area Under the ROC Curve, is a single scalar value that summarizes the overall ability of your diagnostic test or binary classification model to discriminate between two classes (e.g., high-risk vs. low-risk patients) [50]. It is equivalent to the probability that a randomly chosen positive instance will be ranked higher than a randomly chosen negative instance [22]. The following table interprets the range of AUC values:
Table 1: Interpretation of AUC Values for Model Performance
| AUC Value Range | Interpretation of Discriminatory Power |
|---|---|
| 0.9 - 1.0 | Outstanding |
| 0.8 - 0.9 | Excellent |
| 0.7 - 0.8 | Acceptable |
| 0.5 - 0.7 | Poor |
| 0.5 | No discrimination (equivalent to random guessing) |
FAQ 2: How do I interpret an ROC curve for a time-to-event outcome, like overall survival at 1, 3, and 5 years?
For survival analysis, a separate ROC curve can be constructed for each pre-specified time point (e.g., 1, 3, and 5 years) [51] [52]. This is known as time-dependent ROC analysis. The resulting AUC at each time point (AUC(t)) tells you how well your model's risk score (e.g., from an m6A-lncRNA signature) can distinguish between patients who experienced an event (like death) by time t and those who did not. Comparing the AUCs across time points helps you understand if your model's predictive performance is consistent over the entire follow-up period or if it diminishes for long-term predictions.
FAQ 3: My model's AUC is less than 0.5. What does this mean and how can I fix it?
An AUC significantly less than 0.5 is incorrect for a realistic diagnostic test and indicates that your model's predictions are worse than random guessing [44]. This error most commonly arises from an incorrect "test direction" selected in the statistical software. For example, if a higher risk score is associated with a higher likelihood of being in the positive group (e.g., poor survival), you must select 'larger test result indicates more positive test'. Conversely, if a lower score indicates a positive outcome, you should select 'smaller test result indicates more positive test' [44]. Correcting this setting will typically resolve the issue.
FAQ 4: Two of my compared models have similar AUCs, but their ROC curves cross. Which one is better?
Simply comparing the total AUC values can be misleading when ROC curves intersect [44]. In such cases, the models may perform differently in specific regions of the curve that are critical for your application. Instead of relying on the total AUC, you should:
- Calculate the partial AUC (pAUC) for the range of False Positive Rates (FPRs) that are clinically relevant for your study [44].
- Compare other metrics like accuracy, precision, and recall at the operational threshold you plan to use [44].
- Use statistical tests like the DeLong test (for correlated ROC curves from the same subjects) to determine if the difference in AUCs is statistically significant [44].
FAQ 5: How do I choose the optimal cut-off value from my ROC curve for clinical stratification?
The point on the ROC curve that is farthest from the diagonal line of no-discrimination (the top-left corner) often represents the best balance between sensitivity and specificity [22] [50]. A common method to find this point is to maximize Youden's J statistic (J = Sensitivity + Specificity - 1) [22]. However, the "optimal" threshold ultimately depends on the clinical context. If missing a positive case (e.g., a high-risk patient) is very costly, you might choose a threshold that favors higher sensitivity, even if it means a lower specificity.
Troubleshooting Common ROC Analysis Errors
Table 2: Common ROC Curve Errors and Solutions
| Error | Description | Prevention & Solution |
|---|---|---|
| Error 1: AUC < 0.5 [44] | The ROC curve falls significantly below the diagonal, indicating performance worse than random guessing. | Check and correctly set the "test direction" in your statistical software (e.g., SPSS, R) to define what constitutes a "positive" test result [44]. |
| Error 2: Intersecting ROC Curves [44] | Two ROC curves from different models cross each other, making a simple AUC comparison insufficient. | Do not rely solely on total AUC. Use partial AUC (pAUC) for clinically relevant FPR regions and compare secondary metrics like precision and recall [44]. |
| Error 3: Ignoring Statistical Comparison [44] | Concluding one model is better than another based on a trivial difference in AUC values without statistical testing. | For models tested on the same subjects, use the DeLong test. For independent sample sets, use methods like the Dorfman and Alf method [44]. |
| Error 4: Single Cut-off ROC Curve [44] | The ROC curve is not smooth but appears as a single inflection point with two straight lines, providing no information on other thresholds. | This happens when the test variable is incorrectly treated as binary. Ensure you use the original continuous variable (e.g., the raw risk score) to plot the ROC curve, not a pre-determined binary classification [44]. |
Experimental Protocol: Validating an m6A-Related lncRNA Prognostic Signature with Time-Dependent ROC Analysis
The following workflow outlines the key steps for developing and validating a prognostic model, as used in studies on colorectal and pancreatic cancer [10] [51] [52].
Step-by-Step Methodology:
Data Acquisition and Preprocessing:
- Obtain RNA-Sequencing (RNA-seq) data and corresponding clinical survival data (overall survival or progression-free survival) from public databases like The Cancer Genome Atlas (TCGA) and Gene Expression Omnibus (GEO). Use data in FPKM or count formats [51] [52].
- Annotate the transcriptome using a reference like GENCODE to differentiate between mRNAs and lncRNAs [51] [52].
Identification of m6A-Related lncRNAs:
- Compile a list of known m6A regulators (writers, readers, erasers) from literature [10] [51].
- Perform co-expression analysis between the expression of these m6A regulators and all lncRNAs in the dataset. Identify m6A-related lncRNAs (mRLs) using a Pearson correlation threshold (e.g., |R| > 0.4) and a significance level (e.g., p < 0.001) [51] [52].
Construction of the Prognostic Signature:
- Univariate Cox Regression: Identify mRLs significantly associated with patient survival (p < 0.05) [10] [52].
- LASSO Cox Regression: Apply the least absolute shrinkage and selection operator (LASSO) method with tenfold cross-validation to the significant mRLs from the previous step. This penalizes the coefficients of less important variables, reducing overfitting and selecting the most parsimonious set of lncRNAs for the model [10] [52].
- Multivariate Cox Regression: Perform a multivariate Cox regression on the lncRNAs selected by LASSO to establish the final model and calculate the regression coefficients (β) for each lncRNA [52].
- Calculate Risk Score: For each patient, compute a risk score using the formula:
Risk Score = (β1 * Exp1) + (β2 * Exp2) + ... + (βn * Expn)where β is the coefficient from the multivariate Cox model and Exp is the expression value of the corresponding lncRNA [52].
Model Validation using ROC Analysis:
- Stratify patients into high-risk and low-risk groups based on the median risk score from the training cohort (e.g., TCGA) [51] [52].
- Use Kaplan-Meier survival analysis with the log-rank test to visualize and assess the survival difference between the two groups.
- Perform time-dependent ROC curve analysis to evaluate the model's predictive accuracy at 1, 3, and 5 years. Calculate the AUC for each time point [51] [52]. The model's performance is considered robust if the AUC values are consistently above 0.7 across these time points.
- Validate the model's performance in an independent external cohort (e.g., from ICGC or a GEO dataset) using the same risk score formula and cut-off value [52].
Table 3: Key Reagents and Computational Tools for m6A-lncRNA Model Development
| Item / Resource | Function / Description | Example Use in Protocol |
|---|---|---|
| TCGA & ICGC Databases | Public repositories providing standardized cancer genomic, transcriptomic, and clinical data. | Source for training (TCGA) and independent validation (ICGC) of the prognostic signature [51] [52]. |
| GENCODE Annotation | A high-quality reference gene annotation. | Used to differentiate mRNA from lncRNA in the transcriptome data [51] [52]. |
| R Statistical Software | A programming language and environment for statistical computing and graphics. | Platform for performing all statistical analyses, including Cox regression, LASSO, and ROC curve generation [10] [51]. |
R package: glmnet |
Implements LASSO regression models. | Used for performing LASSO Cox regression to select the most relevant lncRNAs [10] [51]. |
R package: survivalROC |
Calculates time-dependent ROC curves for censored survival data. | Essential for calculating and plotting the AUC at specific time points (1, 3, 5 years) [52]. |
R package: pRRophetic |
Predicts clinical drug response and chemosensitivity from gene expression data. | Used to correlate the m6A-lncRNA risk score with potential response to chemotherapy, adding functional relevance [52]. |
| Cox Regression Model | A statistical method for investigating the effect of several variables on the time until an event. | The core algorithm for building the prognostic model by weighting the contribution of each lncRNA [10] [52]. |
| ssGSEA/ESTIMATE Algorithm | Algorithms for quantifying immune cell infiltration and tumor microenvironment composition from gene expression data. | Used to correlate the m6A-lncRNA signature with the immune context of the tumor, providing biological insights [10] [52]. |
How are high-performing m6A-related lncRNA models currently benchmarked in oncology?
Benchmarking of m6A-related lncRNA models involves evaluating their performance across multiple cancer types using standardized metrics and validation frameworks. The table below summarizes key performance indicators from recently published models in colorectal cancer (CRC), lung adenocarcinoma (LUAD), and gastric cancer (GC).
Table 1: Benchmarking Performance of m6A-Related lncRNA Models Across Cancer Types
| Cancer Type | Model Components | Performance Metrics | Validation Methods | Key Clinical Applications |
|---|---|---|---|---|
| Colorectal Cancer (CRC) | 11-mRL signature [10] | Strong predictive performance for OS; ROC analysis; Significant survival divergence between HRG/LRG [10] | Kaplan-Meier analysis; ROC curves; Multivariate Cox regression; Immune infiltration analysis [10] | Prognosis prediction; Immunotherapy response guidance; Immune checkpoint expression (PD-1, PD-L1, CTLA4) assessment [10] |
| Lung Adenocarcinoma (LUAD) | 8-lncRNA signature (m6ARLSig) including FAM83A-AS1, AL606489.1, COLCA1 [21] | Significant survival divergence; ROC curve validation; Multivariate modeling as independent prognostic predictor [21] | Principal component analysis; Nomogram; CIBERSORT for immune infiltration; Drug sensitivity prediction [21] | Survival probability estimation; Therapeutic response prediction; Immune cell infiltration assessment; Cisplatin resistance evaluation [21] |
| Gastric Cancer (GC) * | MSI status prediction using foundation models [53] | State-of-the-art performance on MSI status prediction benchmark [53] | Multiple instance learning; Cross-validation; Benchmarking against leading pathology foundation models [53] | Microsatellite instability status prediction; Immunotherapy candidate identification [53] |
Note: While the search results do not contain a specific m6A-lncRNA model for GC, they include benchmarking data for MSI status prediction in GC, which represents a related biomarker discovery application.
What experimental protocols and workflows ensure reproducible model development?
A standardized workflow for m6A-related lncRNA model development encompasses multiple phases from data acquisition to clinical application. The following diagram illustrates this comprehensive process:
Diagram 1: Comprehensive Workflow for m6A-lncRNA Model Development
Detailed Experimental Protocols:
Data Acquisition and Preprocessing:
- Obtain RNA-seq data and clinical information from TCGA database (e.g., 611 CRC samples and 51 normal controls) [10]
- Cross-reference gene IDs with Ensembl Genome Browser 99 (GRCh38.p13) from GENCODE to distinguish mRNAs and lncRNAs [10]
- Collect m6A regulatory genes including writers (METTL3/14, KIAA1429, RBM15, WTAP, ZC3H13), readers (YTHDC1/2, YTHDF1/2/3, HNRNPA2B1, HNRNPC, IGF2BP1/2/3), and erasers (ALKBH3/5, FTO) [10] [21]
Identification of m6A-Related lncRNAs:
- Perform co-expression analysis between lncRNAs and m6A regulators using Pearson correlation with threshold of |R| > 0.3 and p < 0.001 [10] [21]
- Conduct univariate Cox regression analysis to identify prognostic m6A-related lncRNAs (p < 0.01) [10] [21]
- Apply LASSO Cox regression to select most predictive lncRNAs and construct risk signature [10] [54]
Model Validation Framework:
- Perform Kaplan-Meier survival analysis with log-rank test to compare high-risk and low-risk groups [10] [21] [54]
- Conduct time-dependent ROC curve analysis to assess model sensitivity and specificity [10] [21] [55]
- Execute multivariate Cox regression to confirm independent prognostic value [10] [21]
- Validate using external datasets when available (e.g., ICGC for PDAC models) [54]
What are the common troubleshooting challenges in ROC curve analysis for biomarker models?
Table 2: Troubleshooting Guide for ROC Curve Analysis in m6A-lncRNA Models
| Challenge | Root Cause | Solution | Preventive Measures |
|---|---|---|---|
| Poor AUC (<0.7) | Overfitting due to small sample size; Inadequate feature selection [56] [57] | Apply LASSO or ridge regression for feature selection; Use cross-validation [10] [54] | Ensure adequate sample size; Apply stringent correlation thresholds (|R|>0.3, p<0.001) [10] |
| Over-optimistic performance | Data leakage between training and test sets; Inappropriate validation strategies [56] | Implement strict separation of training/test data; Use external validation cohorts [56] [57] | Apply k-fold cross-validation; Use independent datasets for final validation [58] |
| Limited clinical utility | Focus on statistical rather than clinical significance [56] [57] | Integrate clinical parameters into nomograms; Assess decision curve analysis [10] [21] | Define clinically relevant effect sizes during study design; Incorporate clinical expertise [57] |
| Poor generalizability | Batch effects; Biological heterogeneity; Cohort-specific biases [56] | Apply batch correction methods; Validate across multiple cancer types [56] [57] | Use diverse patient cohorts; Document preprocessing steps thoroughly [53] [57] |
How do I improve ROC performance in m6A-lncRNA risk models?
Strategic Approaches for ROC Enhancement:
Feature Selection Optimization:
- Combine biological relevance with statistical criteria by selecting lncRNAs strongly correlated with m6A regulators (|R| > 0.3, p < 0.001) [10]
- Employ LASSO Cox regression to reduce overfitting while maintaining predictive features [10] [54]
- Implement multi-step selection: univariate Cox (p < 0.01) followed by multivariate analysis [21]
Model Integration and Validation:
- Develop nomograms combining m6A-lncRNA signatures with clinicopathological variables [10] [21]
- Validate using multiple approaches: temporal validation (time-dependent ROC), internal validation (bootstrap), and external validation [10] [21]
- Assess performance across patient subgroups stratified by clinical characteristics [21]
Biological Context Integration:
- Correlate risk scores with immune infiltration patterns using CIBERSORT or ESTIMATE algorithms [10] [21] [54]
- Evaluate association with immune checkpoints (PD-1, PD-L1, CTLA-4) to establish clinical relevance [10]
- Connect signature performance to functional validation (e.g., in vitro assays for key lncRNAs) [21] [54]
What key reagents and computational tools are essential for developing m6A-lncRNA models?
Table 3: Research Reagent Solutions for m6A-lncRNA Model Development
| Resource Category | Specific Tools/Databases | Application in Model Development | Key Features |
|---|---|---|---|
| Data Resources | The Cancer Genome Atlas (TCGA) [10] [21] | Source of RNA-seq data and clinical information | Standardized processing; Multiple cancer types; Clinical outcome data |
| Genotype-Tissue Expression (GTEx) [54] | Normal tissue controls for differential expression | Normal tissue reference; Expanded sample diversity | |
| Computational Tools | CIBERSORT [10] [21] [54] | Immune cell infiltration analysis | Deconvolution algorithm; LM22 reference matrix |
| R packages: survival, pheatmap, scatterplot3D, rms, ggalluvial [10] [21] | Statistical analysis and visualization | Comprehensive statistical functions; Specialized visualization capabilities | |
| Cytoscape [21] | Co-expression network visualization | Network analysis and visualization; Plugin architecture | |
| Validation Resources | Cell lines (A549, BxPC-3, PANC-1) [21] [54] | Functional validation of key lncRNAs | Well-characterized models; Genetic manipulation capability |
| siRNA/lentiviral vectors [21] [54] | Knockdown studies for functional analysis | Efficient gene silencing; Stable expression modulation |
The field continues to evolve with emerging technologies such as foundation models like H-optimus-1, which has demonstrated state-of-the-art performance on various cancer classification tasks including MSI status prediction in gastric cancer [53]. Additionally, machine learning frameworks like MarkerPredict show promise in classifying potential predictive biomarkers using Random Forest and XGBoost algorithms with high accuracy (0.7-0.96 LOOCV) [58]. These advanced computational approaches may enhance future m6A-lncRNA model development by integrating additional data modalities and improving predictive performance.
Beyond Baseline Performance: Advanced Strategies to Boost ROC-AUC and Model Generalizability
In the field of m6A-related lncRNA biomarker research, where models are often built on high-dimensional transcriptomic data with limited patient samples, overfitting presents a critical challenge. Overfitting occurs when a machine learning model learns not only the underlying patterns in the training data but also its noise and random fluctuations, essentially "memorizing" the training set instead of learning to generalize [59] [60]. This results in a model that performs almost perfectly on training data but fails significantly when presented with new, unseen data [59] [61]. For researchers developing prognostic signatures for colorectal cancer or other malignancies, an overfit model can lead to misleading biological conclusions and clinically unreliable biomarkers that fail in validation cohorts [10] [51]. This guide provides essential troubleshooting protocols to diagnose, prevent, and remediate overfitting specifically within the context of m6A-lncRNA model development.
➤ Frequently Asked Questions (FAQs)
Q1: How can I quickly determine if my m6A-lncRNA prognostic signature is overfit?
The most reliable indicator is a significant performance gap between training and validation datasets. If your model shows near-perfect discrimination on training data (e.g., high AUC during ROC analysis) but performance drops substantially on a held-out test set or external validation cohort, it is likely overfit [59] [60]. For example, an AUC of 0.98 on training data that falls to 0.65 on an independent GEO dataset strongly suggests overfitting [51].
Q2: My m6A-lncRNA risk model has high variance. Should I collect more patient samples?
Gathering more high-quality, representative data is one of the most effective strategies against overfitting [59] [62]. However, when prospective sample collection is infeasible, alternatives exist. Data augmentation techniques, leveraging synthetic data generation, or utilizing public repositories like TCGA and GEO to expand your training cohort can help [59]. If these options are exhausted, focus on reducing model complexity and increasing regularization [61].
Q3: What is the practical difference between L1 (Lasso) and L2 (Ridge) regularization for lncRNA selection?
L1 regularization (Lasso) is particularly valuable for feature selection in high-dimensional spaces, as it can shrink the coefficients of less important lncRNAs to exactly zero, effectively removing them from your model [51] [63]. This is ideal for creating sparse, interpretable prognostic signatures. L2 regularization (Ridge) shrinks coefficients but rarely zeroes them out, retaining all features while penalizing extreme values. For m6A-lncRNA studies aiming to identify a concise biomarker panel, L1 regularization is often preferred [51].
Q4: Can a model be both overfit and underfit?
Not simultaneously for the same data, but a model can oscillate between these states during training. This is why monitoring performance on a validation set throughout the training process is crucial [62]. A model might start underfit (high bias), then improve, and eventually become overfit (high variance) if training continues for too long.
Q5: Why does my model's AUC remain high on the test set, but the clinical stratification fails?
A high AUC indicates good ranking ability (separating high-risk from low-risk patients) but does not guarantee that the risk groups are clinically distinct at a specific operating threshold [39] [64]. The chosen probability threshold might be suboptimal. Use your ROC curve to find a threshold that balances sensitivity and specificity for your clinical goal, and validate stratification with Kaplan-Meier survival analysis [10] [51].
➤ Troubleshooting Guides
Problem: Performance Discrepancy Between Training and Validation Sets
Symptoms: High training accuracy/AUC (>0.95) but significantly lower validation accuracy/AUC (drop >0.15) [59] [60].
Diagnosis Protocol:
- Plot Learning Curves: Graph model performance (e.g., loss or AUC) for both training and validation sets against the amount of training data or training epochs. A large, persistent gap between the two curves indicates overfitting [59].
- Implement k-Fold Cross-Validation: Divide your data into k subsets (e.g., k=5 or k=10). Iteratively train on k-1 folds and validate on the remaining fold. A high variance in cross-validation scores suggests the model is sensitive to the specific data split, a sign of overfitting [59] [60].
- Validate on External Datasets: Test your finalized model on a completely independent dataset (e.g., from GEO, such as GSE39582 or GSE17538 for CRC). This is the gold standard for assessing generalizability [51].
Solutions:
- Apply Regularization:
- L1/L2 Regularization: Add a penalty term to your loss function. For logistic regression or Cox models in
scikit-learnorR, set thepenaltyandCparameters. L1 (Lasso) can help with feature selection by driving coefficients of irrelevant lncRNAs to zero [60] [61]. - Code Example (Python with
sklearn):
- L1/L2 Regularization: Add a penalty term to your loss function. For logistic regression or Cox models in
- Simplify the Model:
- For random forests or gradient boosting, reduce
max_depth, increasemin_samples_leaf, or lower the number of trees (n_estimators). - For neural networks, reduce the number of layers or units per layer [61].
- For random forests or gradient boosting, reduce
- Use Early Stopping: When training iterative models (e.g., neural networks), monitor the validation loss. Stop training as soon as the validation loss stops improving and begins to increase [59] [60].
- Employ Ensemble Methods: Use bagging techniques like Random Forests, which build multiple decorrelated trees on random subsets of the data, to reduce variance [60].
Problem: Optimal ROC Curve but Poor Clinical Stratification
Symptoms: High AUC value on the test set, but Kaplan-Meier survival curves for predicted high-risk and low-risk groups are not statistically significant (log-rank p-value >0.05) [10] [51].
Diagnosis Protocol:
- Analyze the ROC Curve: Identify the point on the ROC curve closest to the top-left corner (0,1). This point often represents a better balance of True Positive Rate (sensitivity) and False Positive Rate (1-specificity) than the default 0.5 threshold [39] [64].
- Calibration Assessment: Check if the predicted probabilities align with the observed event rates. A well-calibrated model that predicts a 20% risk of mortality should have approximately 20% of those patients die. Use calibration plots for this purpose.
Solutions:
- Adjust Classification Threshold: Don't rely on the default 0.5 threshold. Based on your ROC curve and clinical needs (e.g., prioritizing sensitivity to avoid missing high-risk patients), select a new operating point [39].
- Cost-Sensitive Learning: If your data is imbalanced (e.g., few death events), assign higher misclassification costs to the minority class during training to make the model more sensitive to it.
- Refine Feature Set: Re-evaluate your m6A-lncRNA signature. Some lncRNAs might be technically predictive but not biologically relevant to disease progression. Incorporate domain knowledge or use more stringent feature selection (like LASSO Cox regression) to refine the signature [10] [51] [63].
Problem: Handling High-Dimensional Data with Limited Samples
Symptoms: Your dataset contains expression levels of hundreds or thousands of lncRNAs but only dozens or hundreds of patient samples, making the model prone to learning noise [10] [63].
Diagnosis Protocol: Examine the feature-to-sample ratio. A very high ratio (many more features than samples) is a classic setup for overfitting.
Solutions:
- Aggressive Regularization: Prioritize L1 regularization (LASSO) to force a sparse solution. This is the technique used in m6A-lncRNA studies to whittle down thousands of candidates to a concise, prognostic signature of 5-11 lncRNAs [10] [51] [63].
- Dimensionality Reduction: Before modeling, use techniques like Principal Component Analysis (PCA) to transform your high-dimensional lncRNA data into a smaller set of uncorrelated components that capture most of the variance.
- Feature Selection First: Apply univariate statistical tests (e.g., Cox regression for survival data) to filter out the most significant lncRNAs before feeding them into a multivariate model [10] [51].
Table 1: Quantitative Comparison of Regularization Techniques for m6A-lncRNA Models
| Technique | Mechanism | Best For | Impact on Model | Key Parameter(s) |
|---|---|---|---|---|
| L1 (Lasso) | Adds absolute value of coefficients to loss function; can zero out features. | Feature selection, creating sparse, interpretable signatures [51] [63]. | Reduces variance, increases bias. | C (inverse of regularization strength), penalty='l1'. |
| L2 (Ridge) | Adds squared value of coefficients to loss function; shrinks all coefficients. | Handling correlated features, general variance reduction. | Reduces variance, increases bias. | C, penalty='l2'. |
| Elastic Net | Combines L1 and L2 penalties. | When you have many correlated features but still desire sparsity. | Balances feature selection and coefficient shrinkage. | C, l1_ratio. |
| Dropout (Neural Networks) | Randomly drops neurons during training. | Preventing complex co-adaptations in neural networks [59] [62]. | Reduces variance, acts as an ensemble. | dropout_rate. |
| Early Stopping | Halts training when validation performance degrades. | All iterative models (NNs, GBM) [59] [60]. | Prevents model from over-optimizing on training data. | patience (epochs to wait before stopping). |
➤ Experimental Protocols for Robust m6A-lncRNA Models
Protocol 1: Building a Regularized Prognostic Signature with LASSO Cox Regression
This methodology is widely adopted in recent m6A-lncRNA research [10] [51] [63].
- Data Preparation: Obtain transcriptomic data (e.g., from TCGA) and clinical survival data. Identify m6A-related lncRNAs via co-expression analysis with known m6A regulators (e.g., |Pearson R| > 0.4, p < 0.05).
- Initial Filtering: Perform univariate Cox regression on the m6A-related lncRNAs to identify candidates significantly associated with overall survival (OS) or progression-free survival (PFS). Use a liberal p-value (e.g., p < 0.05) to retain potential features.
- LASSO Cox Regression:
- Use the
glmnetpackage in R (orscikit-learnin Python). - Input the expression matrix of candidate lncRNAs and survival data.
- The algorithm applies a penalty that shrinks coefficients, and with sufficient penalty, sets less important lncRNA coefficients to zero.
- Use k-fold cross-validation (
cv.glmnet) to find the optimal penalty parameterlambdathat minimizes the cross-validated error.
- Use the
- Signature Construction: The lncRNAs with non-zero coefficients at the optimal
lambdaform your prognostic signature. The risk score for a patient is calculated as:Risk Score = Σ (LncRNA_Expression_i * Lasso_Coefficient_i)[51] [63]. - Validation: Stratify patients into high-risk and low-risk groups based on the median risk score. Validate the stratification using Kaplan-Meier survival analysis and log-rank test in both training and independent validation cohorts [10] [51].
Protocol 2: k-Fold Cross-Validation for Model Evaluation
- Data Splitting: Randomly shuffle your dataset and split it into k (e.g., 5 or 10) mutually exclusive folds of approximately equal size.
- Iterative Training and Validation: For each iteration i (from 1 to k):
- Reserve the i-th fold as the validation set.
- Train your model on the remaining k-1 folds.
- Evaluate the model on the i-th validation fold, recording the performance metric (e.g., AUC).
- Performance Averaging: Calculate the average and standard deviation of the k performance scores. The average gives a robust estimate of your model's expected performance on unseen data, while a small standard deviation indicates stability [59] [60].
➤ Visualizing the Strategy: A Workflow for Preventing Overfitting
The following diagram illustrates a systematic workflow for diagnosing and addressing overfitting in m6A-lncRNA research, integrating the key concepts from this guide.
Systematic Workflow for Diagnosing and Addressing Overfitting
Table 2: Key Resources for m6A-lncRNA Model Development and Validation
| Resource Category | Specific Examples | Function & Application |
|---|---|---|
| Public Data Repositories | The Cancer Genome Atlas (TCGA), Gene Expression Omnibus (GEO) | Source of transcriptomic data and clinical information for model training and external validation [10] [51] [63]. |
| Bioinformatics Tools | R glmnet package, Python scikit-learn |
Implementation of regularized models (LASSO, Ridge) and evaluation metrics (ROC, AUC) [51]. |
| Validation Datasets | GEO datasets (e.g., GSE17538, GSE39582 for CRC) | Independent cohorts for rigorously testing the generalizability of a developed prognostic signature [51]. |
| Molecular Databases | M6A2Target, lncATLAS, GENCODE | Identify m6A-related lncRNAs and annotate their potential functions and localizations [51] [63]. |
| Clinical Validation Reagents | Custom qPCR assays for signature lncRNAs (e.g., for SLCO4A1-AS1, H19) | Wet-lab validation of the computational model in an in-house patient cohort [51]. |
Leveraging Ensemble and Deep Learning Models for Enhanced Accuracy
Frequently Asked Questions (FAQs) and Troubleshooting
FAQ 1: What are the most effective deep learning architectures for building a predictive model for m6A sites in lncRNAs, and how do I choose between them?
Different deep learning architectures capture distinct aspects of biological sequences. Your choice should be guided by the specific characteristics of your data and the biological question.
- Convolutional Neural Networks (CNNs) are excellent at identifying local, position-invariant sequence motifs and patterns that are indicative of m6A modification [65].
- Bidirectional Long Short-Term Memory Networks (BiLSTMs) are designed to learn long-range dependencies and contextual information across the entire RNA sequence, which can be crucial for understanding regulatory contexts [65] [66].
- Transformers utilize self-attention mechanisms to weigh the importance of different nucleotide positions relative to each other, effectively capturing both short and long-range interactions without the sequential processing constraints of RNNs [65] [66]. Models like DNABERT, which are pre-trained on large-scale genomic data, have shown superior performance in m6A prediction tasks [65].
Troubleshooting Guide: If your model performance plateaus, try the following:
- Symptom: High training accuracy but low validation accuracy.
- Potential Cause: Overfitting due to the high dimensionality of sequence data and limited training samples.
- Solution: Integrate regularization techniques such as dropout layers into your network. Alternatively, employ an ensemble of different architectures (e.g., CNN-BiLSTM) to leverage their complementary strengths and improve generalization [65] [66].
- Symptom: Poor performance across all metrics.
- Potential Cause: Suboptimal input sequence window size or inadequate data preprocessing.
- Solution: Systematically benchmark different input window sizes (e.g., 21bp, 51bp, 101bp) to find the optimal context for m6A prediction, as the flanking sequences are critical [65].
FAQ 2: My model's performance seems random when applied to lncRNA sequences from different subcellular localizations or disease contexts. How can I improve its generalizability?
This is a common challenge arising from the structural flexibility of RNA and the scarcity of high-quality, context-specific ground truth data [67]. A key strategy is to move beyond sequence-only features.
- Incorporate Multi-Source Features: Enhance your model's input by integrating:
- Physicochemical Properties: Features like ring structure, hydrogen chemical properties, and position-specific data have been used successfully in models like M6APred-EL [65].
- Genomic Context: Tools like WHISTLE have shown that integrating genomic-derived features alongside sequence features significantly boosts prediction accuracy [65].
- Subcellular Localization Data: Since lncRNA function is tightly linked to its location in the cell, incorporating subcellular localization information can provide critical contextual signals [66].
- Adopt a Network-Based Framework: Construct a global interaction network (GIN) that integrates lncRNA-lncRNA, lncRNA-protein coding gene (PCG), and PCG-PCG interactions. You can then use algorithms like Random Walk with Restart on this network to quantify association strengths and annotate lncRNA function more robustly, as demonstrated by the ncFN tool [68].
FAQ 3: How can I reliably benchmark my model's performance, particularly using ROC curve analysis, when my dataset has a significant class imbalance?
While the Area Under the ROC Curve (AUC) is a standard metric, it can be optimistic with imbalanced data. A comprehensive evaluation strategy is essential.
- Use Multiple Metrics: Always report the Area Under the Precision-Recall Curve (AUPR) alongside AUC. AUPR is more informative than AUC for imbalanced datasets because it focuses on the performance of the positive (minority) class [69].
- Compare Against Established Baselines: Benchmark your model's AUC and AUPR against a diverse set of existing methods. The table below provides a performance summary of various models on m6A prediction tasks for easy comparison.
Table 1: Performance Benchmarking of Selected m6A Prediction Models
| Model Name | Core Methodology | Key Features | Reported AUC | Key Insight |
|---|---|---|---|---|
| DNABERT [65] | Transformer | Pre-trained on large DNA sequences | Superior Performance | Excels at capturing long-range context. |
| adaptive-m6A [65] | CNN-BiLSTM-Attention | Identifies m6A in multiple species | 0.990 | Attention mechanism improves interpretability. |
| WHISTLE [65] | SVM (Traditional ML) | Integrates 35 genomic features | 0.948 (full transcript) | Shows power of feature integration. |
| EMDLP [65] | Ensemble Deep Learning | Combines multiple encodings & models | 0.852 | Ensemble improves robustness. |
FAQ 4: What is the most straightforward way to boost the AUC of my existing m6A-lncRNA model without designing a completely new architecture?
Implementing an ensemble learning approach is one of the most effective strategies to enhance predictive accuracy and robustness.
- "Wisdom of Crowds" Ensemble: Instead of relying on a single model, train multiple different models (e.g., a CNN, a BiLSTM, and a Transformer). You can then average their predictions (for regression) or take a majority vote (for classification). This "wisdom of crowds" approach has been proven remarkably robust in bioinformatics, often outperforming the best single model in a given task [70].
- Stacking Ensemble: For a more sophisticated setup, use the predictions of multiple base models (e.g., SVM, KNN, Random Forest, CNN) as input features for a final "meta-learner" model (like a neural network) that makes the ultimate prediction. This stacking method has achieved accuracy up to 98% in multi-omics cancer classification, demonstrating its power [71].
- Ablation Study: To confirm the value of each component in your ensemble, perform an ablation study. Systematically remove one component at a time and observe the drop in performance (e.g., AUC and AUPR). This validates that each model in the ensemble contributes to the final, superior result [66] [69].
Experimental Protocols for Key Cited Experiments
Protocol 1: Implementing a Benchmarking Study for Deep Learning Models on m6A Data
This protocol is adapted from a study that benchmarked six deep learning models for m6A site prediction [65].
Dataset Preparation:
- Source: Obtain a curated m6A dataset, such as the one constructed by Song et al. [65].
- Format: The dataset should contain sequences (e.g., 1001 bp) with a central adenine (A). Ensure a balanced set of positive (m6A-modified) and negative samples.
- Preprocessing: Partition the data into training and test sets (e.g., 9:1 ratio). Adjust the input window size (e.g., 21 bp, 51 bp, 101 bp) centered on the candidate adenine.
Model Selection and Training:
- Select Architectures: Choose a diverse set of deep learning models, including BiLSTM, GRU, TextCNN, and Transformer-based models like DNABERT [65].
- Encoding: Convert RNA sequences into numerical representations using one-hot encoding or more advanced embedding techniques.
- Training: Train each model on the training set using standard deep learning frameworks (e.g., TensorFlow, PyTorch). Employ cross-validation to tune hyperparameters.
Performance Evaluation and Visualization:
- Metrics Calculation: Generate ROC and PR curves for each model on the held-out test set. Calculate the AUC and AUPR values.
- WebLogo Plot: Create a WebLogo plot to visualize the nucleotide conservation and probability at each position in your positive and negative sequences, which can reveal important motifs [65].
- Comparison: Compare the AUC/AUPR of all models in a consolidated table or graph to identify the best-performing architecture for your specific data.
Protocol 2: Building a Stacking Ensemble for Enhanced Classification
This protocol outlines the methodology for creating a stacking ensemble, as applied in multi-omics cancer classification [71].
Base Model Selection: Choose five to seven diverse, well-established models as base learners. Suitable examples include Support Vector Machine (SVM), k-Nearest Neighbors (KNN), Random Forest, Artificial Neural Network (ANN), and Convolutional Neural Network (CNN) [71].
Data Preprocessing and Feature Extraction:
- Normalization: Normalize the input data (e.g., RNA-seq data using TPM normalization).
- Dimensionality Reduction: For high-dimensional data, use an autoencoder or similar technique for feature extraction. The autoencoder can be structured with multiple dense layers (e.g., 5 layers with 500 nodes) and a dropout rate (e.g., 0.3) to prevent overfitting [71].
Training the Stacking Ensemble:
- Step 1 - Base Model Training: Train all base models on the full training set.
- Step 2 - Prediction Generation: Use the trained base models to generate prediction probabilities on a validation set or via cross-validation on the training data. These predictions become the new input features for the meta-learner.
- Step 3 - Meta-learner Training: Train a final classifier (the meta-learner), such as a neural network or logistic regression model, on the new feature set generated from the base models' predictions.
Evaluation: Finally, evaluate the performance of the entire stacking ensemble on a completely independent test set by calculating AUC, AUPR, and accuracy.
Workflow and Relationship Diagrams
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Computational Tools and Resources for m6A-lncRNA Research
| Item / Resource | Type | Function / Application |
|---|---|---|
| RNAInter & RNALocate [67] [66] | Database | Provides large-scale, experimentally validated RNA-protein interaction and subcellular localization data for model training. |
| GEO & SRA [72] | Database | Public repositories for downloading RNA-seq and functional genomics data to build custom training datasets. |
| ENCODE [72] | Database | Source of quality-controlled, uniformly processed functional genomics data (e.g., eCLIP, RAMPAGE). |
| ncFN [68] | Software Tool | A framework for functional annotation of ncRNAs using a global interaction network, useful for feature generation. |
| Autoencoder [71] | Algorithm | A deep learning technique for non-linear dimensionality reduction of high-dimensional omics data (e.g., RNA-seq). |
| TPM Normalization [71] | Data Preprocessing | A method for normalizing RNA-seq data to eliminate technical variation and enable cross-sample comparison. |
| DNABERT [65] | Pre-trained Model | A transformer model pre-trained on genomic sequences, which can be fine-tuned for m6A prediction tasks. |
| One-hot Encoding [65] | Data Encoding | A fundamental method for converting nucleotide sequences (A, C, G, U/T) into a numerical matrix. |
| Graphviz | Software | A tool for visualizing complex workflows and network relationships, as used in the diagram above. |
Integrating Multi-Omics Data to Refine Predictive Signals
Frequently Asked Questions
FAQ: Our model's performance plateaus. How can multi-omics data help? A common reason for performance plateaus is relying on a single data type (e.g., transcriptomics) which provides an incomplete picture. Integrating multi-omics data (e.g., genomics, proteomics, metabolomics) can reveal how genes, proteins, and metabolites interact to drive disease, uncovering novel predictive signals and pathways that single-omics analyses miss [73]. For instance, combining m6A lncRNA data with proteomics can validate if RNA modifications translate to functional protein-level changes.
FAQ: We have data from different platforms and batches. How do we handle technical variation? Technical variation from different labs, platforms, or batches is a major challenge. It can be addressed through:
- Data Normalization and Harmonization: Use methods like TPM for RNA-seq or intensity normalization for proteomics to make datasets comparable [73].
- Batch Effect Correction: Apply statistical methods like ComBat to remove systematic noise introduced by technical factors [73].
- Data Imputation: Use robust methods like k-nearest neighbors (k-NN) to handle missing data points that are common in multi-modal datasets [73].
FAQ: What is the most practical strategy for integrating our diverse data types? The choice of integration strategy depends on your data and computational resources. Here is a comparison of common approaches [73]:
| Integration Strategy | Description | Best Use Case |
|---|---|---|
| Early Integration | Combines all raw data features into a single dataset before analysis. | Capturing all possible interactions when computational power is sufficient. |
| Intermediate Integration | Transforms each data type before combination, often using networks. | Incorporating biological context; useful when data types have different structures. |
| Late Integration | Analyzes each data type separately and combines the results at the end. | Handling missing data efficiently and for a more robust, computationally efficient analysis. |
FAQ: Our multi-omics model is complex. How can we ensure it is biologically interpretable? To maintain interpretability:
- Use methods like Similarity Network Fusion (SNF), which integrates data by creating and fusing patient-similarity networks, making the results more intuitive for biological subtyping [73].
- Apply Bayesian models that incorporate existing biological knowledge from pathway databases as prior information, grounding your model in known biology [73].
- Perform Gene Set Enrichment Analysis (GSEA) on your results to link predictive features to established biological pathways and functions [27].
FAQ: How can we visually compare results across multiple omics layers or model configurations? For three-way comparisons (e.g., control vs. two treatments), consider an HSB (Hue, Saturation, Brightness) color-coding approach. This method assigns specific hues to each dataset and calculates a composite color that intuitively shows which datasets are similar or different, helping to pinpoint consistent signals across modalities [74].
Troubleshooting Guides
Problem: Poor Model Performance and Low AUC in ROC Analysis
- Potential Cause 1: Isolated Data Types. The model is trained on a single type of omics data, lacking a holistic view.
- Solution: Employ an intermediate integration approach. Use a Graph Convolutional Network (GCN) to map different omics data (e.g., m6A lncRNA, proteomics) onto a unified biological network. This allows the model to learn from the interactions between genes and proteins [73].
- Potential Cause 2: High-Dimensional Data and Overfitting. The number of features (genes, proteins) far exceeds the number of samples.
- Solution: Implement dimensionality reduction. Use Autoencoders (AEs) to compress high-dimensional omics data into a lower-dimensional latent space that retains the most important biological signals before building your predictive model [73].
- Potential Cause 3: Spurious Correlations from Noisy Data. Technical noise or batch effects are being learned by the model instead of true biological signals.
Problem: Inconsistent lncRNA-Disease Association Predictions
- Potential Cause: Sparse or Low-Quality Known Associations. Many computational models for lncRNA-disease association rely on known interaction data, which is often limited and incomplete [75].
- Solution: Utilize methods that do not require known lncRNA-disease associations. For example, the LFMP model predicts associations by integrating other data sources, such as lncRNA-miRNA and miRNA-disease interactions, which can be more abundant. This circumvents the sparsity issue of direct association data [75].
Problem: Difficulty in Translating Model Findings to Biological Mechanisms
- Potential Cause: The model is a "black box." Complex AI models can identify patterns but fail to provide insights into the underlying biology.
- Solution:
- Prioritize HUBgenes: After identifying key genes (e.g., via LASSO analysis as in [27]), perform functional enrichment analysis (GSEA) to determine the biological pathways they are involved in (e.g., cytokine production, mitochondrial membrane) [27].
- Validate Experimentally: Use the Quantitative Real-time PCR (qRT-PCR) wet-lab method to confirm the expression levels of key predicted genes like
ZNF595andRRAS2in your disease model [27]. - Infer Function via Co-expression: For lncRNAs, infer their potential function based on the protein-coding genes they are co-expressed with (the "guilt by association" principle) [76].
- Solution:
Experimental Protocols
Protocol 1: A Workflow for Identifying and Validating m6A-Related Key Genes
This protocol is adapted from a study investigating m6A-related ferroptosis genes in intervertebral disc degeneration [27].
Data Acquisition and Preprocessing:
- Obtain transcriptome datasets from public repositories like GEO (e.g., GSE150408, GSE124272).
- Perform batch correction between datasets using the
limmapackage in R to remove non-biological technical variations. - Verify batch effect removal with Principal Component Analysis (PCA).
Identify Key Module Genes:
- Perform Weighted Gene Co-expression Network Analysis (WGCNA) to cluster genes into modules based on their expression patterns.
- Correlate modules with the disease phenotype (e.g., IDD vs. Normal) and select the most relevant module(s) for further analysis.
Differential Expression and Integration:
- Identify Differentially Expressed Genes (DEGs) using the
limmapackage (common thresholds: \|log2FC\| > 0.5, p-value < 0.05). - Obtain lists of m6A regulators and Ferroptosis-Related Genes (FRGs) from literature and specialized databases (e.g., FerrDb V2).
- Intersect the key module genes, DEGs, and m6A-FRGs to obtain a refined list of candidate genes.
- Identify Differentially Expressed Genes (DEGs) using the
Predictive Model Building:
- Apply Least Absolute Shrinkage and Selection Operator (LASSO) regression to the candidate gene list to select the most predictive features and avoid overfitting. These are your HUBgenes.
Functional and Immune Context Analysis:
- Conduct Gene Set Enrichment Analysis (GSEA) on the HUBgenes to identify associated biological pathways and functions.
- Use Single-sample GSEA (ssGSEA) to quantify the relative abundance of immune cell populations in your samples and compare them between disease and control groups.
Experimental Validation:
- Design primers for your HUBgenes (e.g.,
ZNF595,RRAS2). - Isolate RNA from your patient or model samples (both disease and control).
- Perform Quantitative Real-time PCR (qRT-PCR) to measure and validate the expression levels of the HUBgenes.
- Design primers for your HUBgenes (e.g.,
Overview of m6A Key Gene Analysis
Protocol 2: Constructing a Robust lncRNA Signature for Prognosis
This protocol is based on a study that developed a five-lncRNA signature for predicting breast cancer recurrence [76].
Data Collection and Re-annotation:
- Obtain multiple gene expression datasets from GEO measured on the same platform (e.g., Affymetrix HU133 Plus 2.0).
- Re-annotate the microarray probes by uniquely mapping them to the human genome (hg19). Select probes that fall completely within lncRNA exons and do not overlap with protein-coding genes.
- Construct the lncRNA expression matrix by taking the median value of probes mapping to the same lncRNA. Log2-transform and quantile-normalize the data.
Identify Survival-Related lncRNAs:
- Using the largest dataset as a training cohort, perform univariate Cox proportional hazards regression analysis on the lncRNAs, with Disease-Free Survival (DFS) as the endpoint.
- Select lncRNAs with a significant p-value (e.g., p < 0.05) as candidates.
Infer lncRNA Function and Refine Signature:
- For each candidate lncRNA, identify highly co-expressed protein-coding genes (Pearson correlation ≥ 0.8).
- Perform GO and KEGG pathway enrichment analysis on these co-expressed genes to infer the lncRNA's biological function.
- Manually curate a list of "disease-related functions" from literature.
- Intersect the survival-related lncRNAs with lncRNAs linked to these key functions.
- Use a forward stepwise selection method to find a minimal set of lncRNAs (e.g., 5) that provides the best predictive model.
Validate the Signature:
- Test the performance of the final lncRNA signature in multiple independent validation cohorts.
- Assess its prognostic power using Kaplan-Meier survival analysis and the log-rank test. Show that it is independent of other clinical variables (e.g., subtype, treatment).
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function / Application |
|---|---|
| Gene Expression Omnibus (GEO) | A public repository for high-throughput gene expression and other functional genomics datasets. Used as a primary source for transcriptomic data [27] [76]. |
| FerrDb V2 | A specialized database for ferroptosis regulators and marker genes. Used to obtain a curated list of Ferroptosis-Related Genes (FRGs) [27]. |
| LASSO Regression | A statistical method used for variable selection and regularization in predictive modeling. It helps prevent overfitting by shrinking less important coefficients to zero, ideal for identifying HUBgenes from a large candidate list [27]. |
| WGCNA R Package | An R package for performing Weighted Gene Co-expression Network Analysis. Used to find clusters (modules) of highly correlated genes and link them to clinical traits [27]. |
| Single-sample GSEA (ssGSEA) | An extension of Gene Set Enrichment Analysis that calculates separate enrichment scores for each sample and gene set. Used to quantify immune cell infiltration or other pathway activity in individual samples [27]. |
| Comparative Toxicogenomics Database (CTD) | A public database that curates interactions between chemicals, genes, and diseases. Can be used to predict potential drugs or molecular compounds that modulate your genes of interest [27]. |
| DAVID | The Database for Annotation, Visualization, and Integrated Discovery. A tool for functional annotation and enrichment analysis of gene lists, such as those co-expressed with key lncRNAs [76]. |
| Similarity Network Fusion (SNF) | A computational method that integrates multiple omics data types by constructing and fusing patient similarity networks. Useful for disease subtyping and clustering [73]. |
| Graph Convolutional Networks (GCNs) | A type of neural network that operates on graph-structured data. Powerful for integrating multi-omics data by learning from biological networks (e.g., protein-protein interactions) [73]. |
Optimizing Input Data and Feature Engineering for m6A Site Prediction
What are the most informative input features to improve m6A prediction model performance?
Integrating diverse and biologically relevant input features is crucial for enhancing the performance of m6A site prediction models, as measured by ROC curve analysis. The table below summarizes the key feature categories and their contributions.
Table 1: Key Input Features for m6A Prediction Models
| Feature Category | Specific Descriptors | Biological Significance | Impact on Model Performance |
|---|---|---|---|
| Primary Sequence | One-hot encoding, k-mer frequencies, RRACH/DRACH motifs | Captures conserved methylation motifs and nucleotide composition | Foundation for most models; essential but insufficient alone [77] [78] |
| RNA Secondary Structure | Base-pairing interactions represented as adjacency matrices, loop regions | m6A modifications frequently occur in loop regions of stem-loop structures; affects site accessibility [77] | Enables identification of structurally conserved methylation regions; improves accuracy [77] |
| Evolutionary Conservation | Phylogenetic conservation patterns | RNA structures are often more conserved than nucleotide sequences [77] | Enhances generalizability across species and tissues [77] [78] |
| Cell/Tissue-Specific Context | Expression patterns across different cell lines and tissues | A subset of m6A modifications is tissue-specific [79] | Reduces false positives; improves biological relevance of predictions [79] |
How can I troubleshoot poor model performance (low AUROC/AUPRC) despite using standard sequence features?
Poor model performance often stems from inadequate feature engineering or ignoring critical biological context. Below are common issues and their solutions.
Table 2: Troubleshooting Guide for Poor m6A Prediction Performance
| Problem | Root Cause | Solution | Expected Outcome |
|---|---|---|---|
| Low AUROC/AUPRC | Using only primary sequence features without structural context | Integrate RNA secondary structure predictions using tools like RNAfold [77] | ~16-18% increase in AUROC and ~44-46% increase in AUPRC as demonstrated in advanced frameworks [80] |
| Poor Generalizability | Training on limited cell lines/tissues without accounting for context-specificity | Implement cell line/tissue-specific models; use datasets spanning multiple biological contexts [79] | Improved portability across similar cross-cell line/tissue datasets [79] |
| Limited Interpretability | Black-box models without mechanistic insights | Employ interpretable architectures like invertible neural networks (INNs) or motif analysis [77] [79] | Identification of conserved methylation-related regions and biological motifs [77] |
| Insufficient Context | Ignoring the influence of m6A modifiers (writers, readers, erasers) | Incorporate binding region information for various m6A modifiers under cis-regulatory mechanisms [77] | More accurate prediction of regional specificity in m6A modifications [77] |
Experimental Protocol: Integrating RNA Secondary Structure Features
Input Data Preparation: Extract 201-nucleotide RNA sequences with adenine in the center for each candidate site [79].
Secondary Structure Prediction:
Feature Representation:
Model Integration:
Which model architectures specifically address feature integration challenges for m6A prediction?
Advanced deep learning architectures have been developed to optimally integrate diverse feature types for m6A site prediction.
Invertible Neural Networks (m6A-IIN): This architecture uses a cross-structural coupling framework with two dedicated channels for primary and secondary structure information. Through reversible blocks with additive coupling flows, it enables bijective mapping between different feature representations, preserving information flow in both forward and inverse transformations [77].
Combined Framework (deepSRAMP): Integrating Transformer architecture with recurrent neural networks allows the model to capture both long-range dependencies through self-attention mechanisms and sequential patterns through RNN components. This hybrid approach effectively leverages both sequence-based and genome-derived features [80].
Cell Line-Specific CNN (CLSM6A): A convolutional neural network framework designed specifically for single-nucleotide-resolution m6A prediction across multiple cell lines and tissues. It incorporates motif discovery and interpretation strategies to identify critical sequence patterns contributing to predictions [79].
Table 3: Advanced Model Architectures for m6A Prediction
| Model Architecture | Key Innovation | Optimal Use Case | Performance Advantage |
|---|---|---|---|
| m6A-IIN [77] | Invertible neural networks with cross-structural coupling | Scenarios requiring high interpretability with integrated structural features | State-of-the-art performance across 11 benchmark datasets from different species and tissues |
| deepSRAMP [80] | Hybrid Transformer-RNN framework | Mammalian m6A epitranscriptome mapping under diverse cellular conditions | 16.1-18.3% increase in AUROC and 43.9-46.4% increase in AUPRC over existing methods |
| CLSM6A [79] | Cell line/tissue-specific CNN models | Single-nucleotide-resolution prediction across diverse biological contexts | Superior performance across 8 cell lines and 3 tissues with enhanced interpretability |
What experimental validation strategies confirm the biological relevance of model predictions?
Validation strategies should bridge computational predictions and biological significance, particularly for lncRNA m6A modifications.
Direct RNA Sequencing: Utilize long-read direct RNA sequencing (e.g., Oxford Nanopore Technologies) to profile epitranscriptome-wide m6A modifications within lncRNAs at single-site resolution. This allows validation without antibodies or chemical treatments [81].
Consensus Motif Analysis: Verify that predicted sites enrich for known m6A consensus motifs (RRACH/DRACH). Although only a subset of these motifs is actually methylated, this provides initial validation of sequence-level plausibility [77] [81].
Cross-cell-line Validation: Test model predictions across multiple cell lines and tissues to distinguish universally predictive features from context-specific ones. This helps identify biologically conserved versus condition-specific methylation patterns [79].
Functional Association Analysis: Correlate predicted m6A sites with functional genomic data, such as expression quantitative trait loci (eQTLs), splicing patterns, or protein binding data, to assess potential functional impact [82] [81].
Table 4: Key Research Reagents and Computational Tools for m6A Prediction
| Resource Category | Specific Tools/Databases | Function | Application Context |
|---|---|---|---|
| Secondary Structure Prediction | RNAfold (ViennaRNA Package) [77] | Computes optimal RNA secondary structures | Feature engineering for structural context integration |
| Benchmark Datasets | m6A-Atlas [79] | High-confidence m6A sites from base-resolution technologies | Model training and validation across cell lines/tissues |
| Detection Techniques | MeRIP-seq, miCLIP, DART-seq, direct RNA sequencing [83] [81] | Experimental validation of m6A sites | Ground truth data generation for model training |
| Computational Frameworks | m6A-IIN, deepSRAMP, CLSM6A [77] [79] [80] | Pre-trained models for m6A site prediction | Baseline implementations and transfer learning |
| Motif Analysis | MEME Suite, STREME | Discovers enriched sequence patterns | Interpretation of model predictions and biological validation |
How can I adapt existing m6A models specifically for lncRNA targets?
Adapting mRNA-focused m6A prediction models for lncRNAs requires addressing several unique challenges, as lncRNAs exhibit distinct modification patterns compared to mRNAs.
Consider Reduced Abundance: Account for the fact that only ~1.16% of m6A-modified RRACH motifs are present within lncRNAs compared to 98.5% in mRNA transcripts [81]. This class imbalance may require specialized sampling strategies during training.
Leverage Tissue Specificity: Capitalize on the finding that m6A modifications in lncRNAs show strong tissue specificity, particularly in brain tissues [81]. Implement tissue-specific models when predicting lncRNA m6A modifications.
Incorporate Structural Prioritization: Place greater emphasis on RNA secondary structure features, as lncRNAs often function through structural mechanisms, and m6A can significantly alter lncRNA secondary structures and protein-binding capabilities [81].
Validate with lncRNA-Specific Data: Utilize emerging lncRNA-specific m6A datasets, such as those from glioma transcriptomes, which have identified differentially methylated lncRNAs across cancer grades [81] [51].
Troubleshooting Common Pitfalls in Immune and Therapy Response Prediction
Frequently Asked Questions (FAQs)
FAQ 1: Why does my m6A-lncRNA prognostic model have high training accuracy but poor performance on independent validation datasets?
This is often due to overfitting, where your model learns noise and dataset-specific patterns instead of biologically generalizable signals.
- Solution: Implement rigorous validation. Use Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to reduce the number of lncRNAs in your signature and prevent overfitting [10] [84]. Always validate your model on multiple independent cohorts from databases like GEO; for example, a five-lncRNA signature for CRC was validated on six independent datasets totaling 1,077 patients [84].
FAQ 2: How can I account for tumor heterogeneity in my predictive model?
Tumor heterogeneity creates multimodal distributions in genomic data, which violate the unimodal assumption of standard machine learning models [85].
- Solution: Use a heterogeneity-optimized framework. Before building your main prediction model, apply
K-means clustering(e.g., K=2) to stratify patients into biologically distinct subgroups, such as "hot-tumor" and "cold-tumor" subtypes. Then, train separate, optimized models (e.g., a Support Vector Machine for hot-tumor and a Random Forest for cold-tumor) on each subgroup [85].
FAQ 3: My model's risk score is significant, but how do I know if it's an independent prognostic factor?
A significant risk score might be confounded by other established clinical variables like tumor stage.
- Solution: Perform multivariate Cox regression analysis. Include your risk score along with key clinicopathological variables such as age, gender, and AJCC TNM stage. If the risk score remains a statistically significant predictor in this combined model, it can be considered an independent prognostic factor [84] [54].
FAQ 4: What is the best way to present the clinical utility of my prognostic model?
Beyond risk groups and survival curves, you can create a tool for individualized prognosis prediction.
- Solution: Develop a nomogram. Integrate your m6A-lncRNA signature with other independent prognostic factors into a nomogram. This provides a visual tool to calculate a numerical probability of survival (e.g., 1-year or 3-year overall survival) for individual patients, which is highly valuable for clinical decision-making [10] [54].
Troubleshooting Guides
Issue 1: Low Area Under the Curve (AUC) in ROC Analysis
A low AUC indicates that your model has a limited ability to discriminate between patient outcomes (e.g., high-risk vs. low-risk).
| Potential Cause | Diagnostic Check | Corrective Action |
|---|---|---|
| Weak Predictors | Check p-values from univariate Cox regression of candidate lncRNAs. | Start with lncRNAs significantly associated with prognosis (p < 0.01) [10]. Use LASSO to select the most robust predictors [54]. |
| Incorrect Risk Stratification | Verify that Kaplan-Meier curves for your high/low-risk groups are well-separated (log-rank p < 0.05). | Adjust the risk score cut-off. While the median is common, you may need to use optimal cut-off values determined from ROC analysis or other methods. |
| Ignoring Tumor Immune Context | Analyze the correlation between your risk score and immune cell infiltration (e.g., via CIBERSORT) or immune checkpoint gene expression [54]. | Integrate immune-related features. If your risk score is strongly correlated with the tumor immune microenvironment, this can bolster its biological plausibility and predictive power. |
Issue 2: Failure to Predict Response to Immune Checkpoint Blockade (ICB)
Predicting response to immunotherapy involves factors beyond traditional prognostic markers.
| Potential Cause | Diagnostic Check | Corrective Action |
|---|---|---|
| Over-reliance on a Single Biomarker | Check the distribution of features like TMB in your cohort; it often has a bimodal distribution [85]. | Combine tumor immunogenicity with immune response profiles. Use a framework like EaSIeR, which integrates systems biology traits (immune cell fractions, pathway signaling) and can be combined with TMB for better ICB response classification [86]. |
| Using a Monolithic Model | Test if your patient cohort can be split into distinct subgroups using clustering algorithms. | Build subtype-specific models. Stratify patients into hot and cold tumors, then train separate classifiers for each subgroup [85]. |
| Lack of Direct Immunogenicity Data | Determine if your model is based solely on computational predictions. | Incorporate immunopeptidomics. Use mass spectrometry (MS) to directly identify peptides presented by MHC molecules on tumor cells, validating neoantigens that computational methods might miss [87]. |
Experimental Protocols for Key Validation Steps
Protocol 1: In Vitro Validation of Candidate LncRNAs
This protocol outlines the functional validation of a prognostic lncRNA (e.g., FAM225B from PDAC study [54]) to bolster the mechanistic basis of your model.
- Cell Culture: Use relevant human cancer cell lines (e.g., PDAC lines BxPC-3 and PANC-1). Culture them in RPMI 1640 medium supplemented with 10% FBS and 1% penicillin–streptomycin at 37°C with 5% CO₂ [54].
- Gene Knockdown: Transfect cells with lncRNA-specific siRNA (50 nM final concentration) using a transfection reagent like Lipofectamine 2000. Include a non-targeting siRNA as a negative control.
- RNA Isolation and qRT-PCR: 48 hours post-transfection, extract total RNA using Trizol reagent. Perform reverse transcription, then quantitative RT-PCR using SYBR Green mix. Calculate relative expression using the 2^−ΔΔCt method, normalized to a housekeeping gene (e.g., GAPDH).
- Functional Assays:
- Cell Proliferation: Perform MTT assay. Seed transfected cells in 96-well plates and measure absorbance at 570nm daily for 5 days.
- Cell Invasion: Use Matrigel-coated Transwell chambers. Seed transfected cells in serum-free medium in the upper chamber, with medium containing 30% FBS in the lower chamber. After 24 hours, stain and count cells that invade through the membrane.
Protocol 2: Validating Immune Microenvironment Associations
This protocol describes how to computationally validate the relationship between your m6A-lncRNA risk score and the tumor immune landscape.
- Data Acquisition: Download RNA-seq data and clinical information for your cancer of interest from TCGA.
- Immune Cell Infiltration Estimation: Use computational tools like CIBERSORT or ssGSEA to estimate the relative fractions of various immune cell types (e.g., CD8+ T cells, macrophages, Tregs) in each tumor sample [54].
- Immune Checkpoint Analysis: Compile a list of immune checkpoint genes (e.g., PD-1, PD-L1, CTLA-4) [10] [54]. Compare their expression levels between the high-risk and low-risk groups defined by your model using statistical tests (t-test or Mann-Whitney U test).
- Statistical Correlation: Perform Pearson or Spearman correlation analysis between the continuous risk score and immune cell infiltration scores. A significant correlation provides evidence that your model captures features of the immune microenvironment.
Key Signaling Pathways and Workflows
Diagram: m6A-lncRNA Prognostic Model Development Workflow
Diagram: Heterogeneity-Optimized ICB Prediction Framework
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Resource | Function in Research | Example Application |
|---|---|---|
| LASSO Cox Regression (glmnet R package) | Performs variable selection and regularization to enhance prediction accuracy and prevent overfitting in prognostic models [10] [84]. | Developing a succinct 5-lncRNA signature for predicting progression-free survival in colorectal cancer [84]. |
| CIBERSORT/ssGSEA | Computational methods for deconvoluting bulk tumor RNA-seq data to estimate relative abundances of member cell types in the tumor immune microenvironment [54]. | Demonstrating that high-risk PDAC patients have significantly different immune cell infiltration profiles compared to low-risk patients [54]. |
| Univariate Cox Regression | A statistical method to identify individual variables (e.g., lncRNAs) significantly associated with survival outcomes (e.g., Overall Survival, Progression-Free Survival). | Screening for m6A-related lncRNAs with potential prognostic value before multi-variable model construction [84] [54]. |
| Mass Spectrometry (MS) | Used in immunopeptidomics to directly identify and sequence peptides presented by MHC molecules on the surface of tumor cells [87]. | Experimentally validating neoantigens predicted by genomic pipelines, overcoming limitations of purely computational prediction [87]. |
Ensuring Clinical Relevance: Robust Validation, Comparative Analysis, and Functional Insights
Frequently Asked Questions
Q1: Our m6A-lncRNA model shows an AUC of 0.65 on external data, down from 0.92 internally. What happened? This performance drop often indicates overfitting or a covariate shift between your development and validation datasets. An AUC of 0.65, while potentially statistically significant, suggests very limited clinical utility according to standard interpretation guidelines [20]. To diagnose:
- Check dataset similarity: Differences in patient demographics, sample collection methods, or sequencing protocols between cohorts can cause this discrepancy [88].
- Review internal validation: Models developed on small samples (median ~445 subjects in many studies) are high-risk for overfitting. Performance estimates from internal validation alone are often severely optimistic [89].
Q2: Should I use a simple data split or bootstrapping for internal validation of my m6A model? For most biomarker studies, bootstrapping is strongly preferred over a single random split [89].
- Avoid random split-sample approaches (e.g., 70/30 splits) in small development samples. This leads to unstable models and validation findings, as it effectively reduces your sample size for development [89].
- Use bootstrapping to resample your dataset with replacement hundreds of times, repeating the entire model building process each time. This provides a more honest assessment of model performance and accounts for overfitting [89].
Q3: How do I choose the optimal cut-point for my m6A-lncRNA risk score? The Youden index (J = Sensitivity + Specificity - 1) is a common method to identify the cut-point that maximizes both sensitivity and specificity [20] [90].
- Clinical Context Matters: The "optimal" threshold can depend on your clinical goal. If identifying high-risk patients for aggressive intervention is critical, you might prioritize high sensitivity. For confirming a diagnosis, high specificity may be preferred [90].
- Alternative Methods: Other statistical methods like the Euclidean index and Product index can also be used. It's best practice to compare results from multiple methods for consistency [90].
Q4: What is the difference between internal and external validation?
- Internal Validation assesses model performance using data derived from the same source as the development data, through methods like bootstrapping or cross-validation. It primarily checks for overfitting [89] [88].
- External Validation tests the model on entirely new data collected from different populations, centers, or time periods. It evaluates the model's generalizability and transportability to new settings, which is the ultimate test for clinical application [88].
Troubleshooting Guides
Problem: Model Fails to Generalize in External Validation
Symptoms:
- Significant drop in AUC, sensitivity, or specificity on the external dataset.
- Poor model calibration where predicted probabilities do not match observed outcome rates.
Investigation and Solution Steps:
- Analyze Data Similarity: Systematically compare the distributions of key clinical variables (e.g., age, disease stage, sex) and technical factors (e.g., RNA sequencing batch) between your development and external validation cohorts. Significant differences suggest a covariate shift [88].
- Test for Heterogeneity: Use statistical tests to check for heterogeneity in predictor effects. This can involve including interaction terms (e.g.,
predictor * cohort) in your model to see if the effect of your m6A-lncRNAs differs significantly between cohorts [89]. - Consider Model Updating: If the model's structure is sound but performance is degraded, you may update the model's intercept or recalibrate it on the new data, rather than abandoning it entirely.
Problem: Selecting the Wrong Internal Validation Method
Symptoms:
- Highly optimistic performance estimates from internal validation that are never replicated.
- Unstable model with different variables being selected in different data splits.
Investigation and Solution Steps:
- Audit Your Sample Size: Check the number of events (e.g., patients with poor outcome) relative to the number of candidate predictors. A low events-per-variable (EPV) ratio increases overfitting risk [89].
- Implement Bootstrapping: Use bootstrap resampling to internally validate your model. This process should include all modeling steps (including any variable selection) repeated in each bootstrap sample to give a realistic estimate of model performance [89].
- Explore Internal-External Validation: If you have data from multiple centers or collected over a long time period, use a form of internal-external cross-validation. Leave out one center (or time period) for validation, and build the model on the rest. Repeat for all centers. This gives a better impression of external validity even at the development stage [89].
Experimental Protocols for Robust m6A-lncRNA Model Development
Protocol 1: Rigorous Internal Validation via Bootstrapping
This protocol provides a robust framework for internal validation of your m6A-lncRNA prognostic signature, minimizing over-optimism [89].
- Model Development: Develop your initial model (e.g., a Cox regression model based on 11 m6A-lncRNAs) on the entire development dataset (
Dataset D) [10]. - Bootstrap Sampling: Generate a large number (e.g., 500-1000) of bootstrap samples by randomly sampling
Nsubjects fromDataset Dwith replacement. - Repeat Model Building: For each bootstrap sample, repeat the entire model development process, including any steps for variable selection or tuning parameter estimation.
- Test on Original Data: Apply the model developed on the bootstrap sample to the original
Dataset Dto calculate a performance measure (e.g., AUC). - Calculate Optimism: Calculate the difference between the performance on the bootstrap sample and the performance on the original data. This is the "optimism".
- Compute Optimism-Corrected Performance: Average the optimism over all bootstrap samples and subtract it from the apparent performance (the performance of the model developed on
Dataset Dand tested onDataset D) to get an optimism-corrected estimate.
Protocol 2: Designing an External Validation Study
This protocol outlines the key steps for a methodologically sound external validation of a published or pre-existing m6A-lncRNA model [88].
- Define Validation Cohort: Acquire or collect a new dataset (
Dataset V). This should be from a distinct population, institution, or time period, with pre-specified inclusion/exclusion criteria. - Implement the Existing Model: Apply the exact, pre-specified model (including the same lncRNAs, coefficients, and cut-points) to
Dataset V. Do not re-fit the model. - Assess Performance: Calculate key performance metrics:
- Discrimination: The ability to distinguish between outcomes. Report the Area Under the ROC Curve (AUC) and its confidence interval [20].
- Calibration: The agreement between predicted probabilities and observed outcomes. Use a calibration plot or statistical test.
- Clinical Utility: The value of the model for clinical decision-making, which can be assessed via decision curve analysis.
- Report with Context: Clearly report the performance metrics and provide a "Table 1" comparing the clinical characteristics of the development and validation cohorts to help readers assess generalizability.
Data Presentation
Table 1: Interpretation of AUC Values for Diagnostic and Prognostic Tests
| AUC Value | Interpretation | Clinical Usability |
|---|---|---|
| 0.9 ≤ AUC | Excellent | High clinical utility |
| 0.8 ≤ AUC < 0.9 | Considerable | Good clinical utility |
| 0.7 ≤ AUC < 0.8 | Fair | Limited clinical utility |
| 0.6 ≤ AUC < 0.7 | Poor | Very limited clinical utility |
| 0.5 ≤ AUC < 0.6 | Fail | No better than chance |
Source: Adapted from [20].
Table 2: Comparison of Methods for Determining Optimal Cut-Points
| Method | Formula | Interpretation | Advantages/Limitations |
|---|---|---|---|
| Youden Index [20] [90] | J = Sensitivity + Specificity - 1 | Maximizes the sum of sensitivity and specificity. | Simple, widely used. May not agree with other methods in skewed distributions [90]. |
| Euclidean Index [90] | Minimizes the Euclidean distance to the top-left corner (0,1) of the ROC curve. | Finds the point on the ROC curve closest to perfect discrimination. | A geometric approach. Can produce similar results to the Youden index [90]. |
| Diagnostic Odds Ratio (DOR) [90] | DOR = (LR+) / (LR-) | Maximizes the odds of positivity in the diseased group compared to the non-diseased. | Can produce extreme, less informative cut-points [90]. |
| Clinical Utility | Based on clinical consequence (e.g., cost of false negative). | Selects a threshold that aligns with clinical priorities. | Most relevant for practice, but requires expert input and may not be statistically "optimal." |
The Scientist's Toolkit: Research Reagent Solutions
| Category / Item | Function in m6A-lncRNA Research |
|---|---|
| Data Sources | |
| The Cancer Genome Atlas (TCGA) | Provides large-scale transcriptomic data (RNA-seq) and corresponding clinical information for model development and validation, e.g., for colorectal or gastric cancer [10] [91]. |
| Gene Expression Omnibus (GEO) | A public repository for transcriptomic datasets, useful for finding independent data for external validation [92]. |
| Bioinformatics Software | |
| R Statistical Software | The primary environment for statistical analysis; essential for performing Cox regression, LASSO, bootstrapping, and generating ROC curves [10] [91]. |
| Key R Packages | |
pheatmap |
Used to generate heatmaps illustrating the connection between lncRNA expression and clinicopathological features [10]. |
limma |
Used for differential expression analysis to identify m6A-related lncRNAs that are differentially expressed between diseased and normal tissues [91] [92]. |
glmnet |
Used to implement the LASSO Cox regression algorithm for variable selection and model construction [10] [91]. |
Workflow Visualization
Diagram 1: m6A-lncRNA Model Development & Validation Workflow
Diagram 2: Internal-External Cross-Validation Logic
FAQs: Troubleshooting Your Benchmarking Analysis
Q1: How do I determine if my m6A-lncRNA model's performance is statistically significant compared to traditional staging systems?
A: To statistically validate that your model's improvement over traditional staging is significant, employ the following methods:
- Delong's Test: Use this statistical test to formally compare the Area Under the Curve (AUC) of your m6A-lncRNA model's ROC curve with the AUC of the traditional staging system's ROC curve. A p-value < 0.05 indicates a statistically significant difference in predictive performance [93].
- Decision Curve Analysis (DCA): This method evaluates the clinical utility and net benefit of your model against traditional staging across a range of risk thresholds. It demonstrates whether using your model for clinical decisions would provide better outcomes than using the traditional system or treating all/no patients [94].
- Concordance Index (C-Index) Calculation: The C-index is a measure of discriminative power for survival models, analogous to the AUC. Report the C-index for both your model and the traditional staging in multivariate analysis to show which is a stronger independent prognostic factor [94] [95].
Q2: My m6A-lncRNA signature has a high AUC but poor calibration in some patient subgroups. How can I improve this?
A: Poor calibration indicates that the predicted probabilities from your model do not align well with observed outcomes. Address this by:
- Constructing a Nomogram: Integrate your m6A-lncRNA signature with key clinical variables (e.g., age, TNM stage) into a nomogram. This visual tool improves individualized risk estimation and clinical applicability by combining the strengths of molecular and clinical predictors [95] [37].
- Assessing Calibration Plots: After building your model, create calibration curves to compare predicted versus actual survival probabilities. A well-calibrated model should closely follow the 45-degree line. Significant deviations, especially in high-risk or low-risk subgroups, indicate a need for model recalibration [51].
- Subgroup Stratification Analysis: Perform ROC and survival analysis within predefined clinical subgroups (e.g., by age, gender, cancer stage). If performance varies significantly across subgroups, consider developing subgroup-specific models or risk-adjustment factors [94].
Q3: What are the key steps to ensure a fair comparison when benchmarking my new m6A-lncRNA signature against established molecular signatures?
A: Ensuring a fair and unbiased comparison is critical for validating your model's advancement:
- Use Consistent Datasets: Validate all models—your new m6A-lncRNA signature and established benchmarks—on the same testing dataset. This eliminates performance variability due to different patient populations or data processing methods [51].
- Apply Identical Validation Metrics: Compare models using the same set of metrics beyond just AUC, including time-dependent ROC analysis, Kaplan-Meier survival differences between risk groups, and clinical net benefit (via DCA) [93] [94].
- Implement Proper Cross-Validation: When comparing multiple models on the same dataset, use identical cross-validation splits (e.g., the same random seed for training/testing splits) to ensure the comparison is based on identical data partitions [96].
Q4: How can I validate that my m6A-lncRNA signature is truly capturing biological signal rather than just technical artifacts?
A: Technical validation is crucial for establishing biological relevance:
- Experimental Validation with qRT-PCR: Select 2-3 key lncRNAs from your signature and validate their expression levels in an independent patient cohort using quantitative RT-PCR. Correlation between sequencing data and qRT-PCR results confirms technical reproducibility [51] [37].
- Correlation with m6A Regulator Expression: Test whether your m6A-related lncRNAs show significant correlation (e.g., Pearson |R| > 0.3, p < 0.001) with known m6A regulators (writers, erasers, readers). This confirms the biological link to m6A modification processes [37] [95].
- Immunohistochemical Co-localization: In high-risk versus low-risk patient tissues, perform IHC staining for key m6A regulators (e.g., METTL3, METTL14). Co-localization of m6A regulators with your signature's risk stratification provides spatial biological validation [37].
Experimental Protocols for Key Benchmarking Analyses
Protocol 1: Time-Dependent ROC Curve Analysis for Survival Prediction
Purpose: To evaluate the predictive performance of your m6A-lncRNA signature for prognosis over time, rather than at a single time point.
Procedure:
- Data Preparation: Organize your dataset with survival time, event status (e.g., death/recurrence), and risk scores from your m6A-lncRNA signature.
- Software Implementation: Use R statistical software with the
timeROCpackage or equivalent. - Define Time Points: Select clinically relevant time points for evaluation (e.g., 1, 3, and 5 years).
- Calculate Time-Dependent Sensitivity/Specificity:
- Apply incident/dynamic (I/D) definitions where cases are individuals with events at time t, and controls are event-free at time t [93].
- Use the Kaplan-Meier method to estimate sensitivity and specificity at each time point.
- Plot ROC Curves: Generate time-dependent ROC curves for each time point of interest.
- Compute AUC Values: Calculate the area under each time-dependent ROC curve to quantify predictive accuracy over time.
Table 1: Comparison of Time-Dependent AUC Values for Prognostic Models
| Model Type | 1-Year AUC | 3-Year AUC | 5-Year AUC |
|---|---|---|---|
| m6A-lncRNA Signature | 0.82 | 0.77 | 0.73 |
| Traditional Staging | 0.71 | 0.69 | 0.66 |
| Published lncRNA Signature | 0.75 | 0.72 | 0.68 |
Protocol 2: Decision Curve Analysis for Clinical Utility Assessment
Purpose: To evaluate the clinical net benefit of using your m6A-lncRNA signature for medical decision-making compared to alternatives.
Procedure:
- Define Risk Thresholds: Identify a range of clinically reasonable risk thresholds (e.g., 10% to 50% probability of event).
- Calculate Net Benefit:
- For each threshold, compute net benefit = (True Positives/n) - (False Positives/n) × (pt/(1-pt)), where p_t is the threshold probability.
- Calculate net benefit for four strategies: your model, treat all, treat none, and traditional staging.
- Plot Decision Curves: Graph net benefit across all risk thresholds for each strategy.
- Interpret Results: The model with highest net benefit across the most relevant thresholds is clinically most useful [94].
Essential Research Reagent Solutions
Table 2: Key Experimental Reagents for m6A-lncRNA Research
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| m6A Antibodies | Millipore (ABE572, MABE1006), Cell Signaling Technology (#56593) | Immunoprecipitation of m6A-modified RNA fragments in MeRIP-seq; optimal performance varies by tissue type [97]. |
| m6A Regulators (Writer Targets) | METTL3, METTL14, WTAP, VIRMA (KIAA1429) | Core methyltransferase complex components; key targets for validating m6A mechanism [98] [37]. |
| m6A Regulators (Eraser Targets) | FTO, ALKBH5 | m6A demethylases; important for understanding reversible nature of modifications [95] [98]. |
| m6A Regulators (Reader Targets) | YTHDF1-3, YTHDC1-2, HNRNPC | m6A binding proteins; mediate functional effects of m6A modification [51] [95]. |
| Library Prep Kits | SMARTer Stranded Total RNA-Seq Kit v2 (Pico Input Mammalian) | Library construction for low-input RNA samples, crucial for limited clinical specimens [97]. |
Workflow Visualization
Diagram 1: Benchmarking Workflow for m6A-lncRNA Models
Diagram 2: Model Comparison Framework
Frequently Asked Questions (FAQs) and Troubleshooting Guides
Model Development and Statistical Validation
FAQ 1: How can I improve the prognostic performance of my m6A-related lncRNA signature? A common and validated approach is to use a multi-step statistical process to identify the most potent lncRNA biomarkers and construct a robust risk model [10] [21].
Recommended Workflow:
- Identification: Correlate lncRNA expression profiles with known m6A regulators (e.g., METTL3, FTO, YTHDF1) from TCGA data. Identify m6A-related lncRNAs (mRLs) using a Pearson correlation threshold (e.g., |R| > 0.3 or 0.6, p < 0.001) [10] [11] [38].
- Prognostic Screening: Perform univariate Cox regression analysis to select mRLs significantly associated with overall survival (OS) [10] [21].
- Model Construction: Apply Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to the prognostic mRLs to prevent overfitting and build a concise signature [10] [54] [21].
- Validation: Calculate a risk score for each patient and stratify them into high- and low-risk groups. Validate the model using Kaplan-Meier survival analysis and time-dependent Receiver Operating Characteristic (ROC) curves [10] [54].
Troubleshooting Guide:
- Problem: Poor separation in Kaplan-Meier curves between risk groups.
- Solution: Re-evaluate the correlation thresholds and the coefficients from the LASSO regression. Consider incorporating a larger cohort or additional validation from a separate database (e.g., ICGC) to strengthen the model [54].
FAQ 2: What are the key statistical metrics to report for model validation? Beyond a significant log-rank p-value in survival analysis, it is crucial to report metrics that quantify the model's predictive accuracy over time [10] [21].
- Essential Metrics:
- Time-dependent ROC curves: Report the Area Under the Curve (AUC) at 1, 3, and 5 years to demonstrate predictive consistency [10] [21].
- Hazard Ratio (HR): Provide the HR from multivariate Cox regression to confirm the risk score is an independent prognostic factor after adjusting for clinical variables like age and stage [54] [21].
- C-index: The concordance index is a measure of the model's overall predictive performance.
The table below summarizes quantitative data from published studies employing these strategies.
Table 1: Performance Metrics of m6A-Related lncRNA Prognostic Models in Various Cancers
| Cancer Type | Signature Size (lncRNAs) | ROC AUC (e.g., 1/3/5-year) | Key Validation Methods | Source Study |
|---|---|---|---|---|
| Colorectal Cancer | 11 | Strong predictive performance (specific values not stated) | Kaplan-Meier, ROC, Multivariate Cox | [10] |
| Lung Adenocarcinoma | 8 | High performance (specific values not stated) | Kaplan-Meier, ROC, PCA | [21] |
| Pancreatic Ductal Adenocarcinoma | 4 | Strong performance in survival prediction | Kaplan-Meier, ROC, Multivariate Analysis | [54] |
| Esophageal Cancer | 5 | Robustness confirmed via ROC curves | Survival Analysis, Risk Stratification, ROC | [11] |
| Cervical Cancer | 6 | High performance in prognosis prediction | Survival Analysis, ROC, Nomogram | [38] |
Biological Relevance and Immune Microenvironment
FAQ 3: My model has a good ROC, but how do I link it to the tumor immune microenvironment? A high-performing model gains biological credibility when correlated with immune landscape features. This involves computational deconvolution of immune cell populations and analysis of immune checkpoint expression [10] [21] [11].
Experimental Protocol: Assessing TIME Correlation
- Immune Cell Infiltration Analysis: Use algorithms like CIBERSORT, ssGSEA, or xCell on your cohort's transcriptome data to estimate the abundance of various immune cells (e.g., CD8+ T cells, macrophages, naive B cells) in each sample [10] [21] [11].
- Compare Risk Groups: Statistically compare the infiltration scores of specific immune cell types between the high-risk and low-risk groups defined by your model. For example, high-risk scores are frequently associated with increased M2 macrophage infiltration and reduced CD8+ T cell abundance [11].
- Immune Checkpoint Analysis: Extract and compare the expression levels of critical immune checkpoint genes (e.g., PD-1, PD-L1, CTLA-4, LAG3) between the risk groups. Elevated checkpoint expression in the high-risk group can suggest a potential for immune evasion [10] [21].
Troubleshooting Guide:
- Problem: No significant differences in immune cell infiltration between risk groups are found.
- Solution: Verify the input data quality and normalization. Try an alternative deconvolution algorithm (e.g., switch from CIBERSORT to EPIC or quanTIseq) to confirm the results. The biological context of the cancer type should also be considered.
The following diagram illustrates the logical workflow for connecting a computational model to features of the immune microenvironment.
Model to Immune Microenvironment Workflow
Table 2: Key Research Reagents and Computational Tools for Immune Microenvironment Analysis
| Reagent/Tool | Function/Explanation | Example Use in Context |
|---|---|---|
| CIBERSORT | Computational algorithm to estimate immune cell type abundances from bulk RNA-seq data. | Quantifying differences in CD4+ T cells and macrophages between m6A-lncRNA risk groups [10] [21]. |
| ESTIMATE | Algorithm to infer stromal and immune scores in tumor samples from transcriptome data. | Characterizing overall immune enrichment in the tumor microenvironment of different risk groups [54] [38]. |
| ssGSEA | Gene set enrichment analysis method that calculates separate enrichment scores for each sample. | Evaluating the activity of specific immune pathways or cell type signatures in high-risk vs. low-risk patients [11] [38]. |
| Immune Checkpoint Panel | A curated list of genes (PDCD1, CD274, CTLA4, etc.) for expression analysis. | Identifying which immune checkpoints are upregulated in the high-risk group to guide immunotherapy predictions [10] [11]. |
Drug Sensitivity and Therapeutic Prediction
FAQ 4: How can I use my m6A-lncRNA model to predict response to therapy? The risk score can be leveraged to investigate differential sensitivity to both chemotherapy and targeted drugs, providing actionable clinical insights [21] [11].
Experimental Protocol: In Silico Drug Sensitivity Analysis
- Data Source: Utilize public pharmacogenomic databases such as the Genomics of Drug Sensitivity in Cancer (GDSC) or patient-derived xenograft (PDX) models [99].
- Prediction Method: Employ computational tools (e.g., R package
pRRophetic) or machine learning models to predict the half-maximal inhibitory concentration (IC50) of various drugs for each patient in your cohort based on their gene expression profiles [21]. - Group Comparison: Compare the predicted IC50 values for common chemotherapeutic and targeted agents between the high-risk and low-risk groups. A lower IC50 in a group indicates higher predicted sensitivity [11] [38].
Troubleshooting Guide:
- Problem: The drug sensitivity predictions are inconsistent with the clinical prognosis of the risk groups.
- Solution: Remember that a high-risk score is often linked to aggressive disease and treatment resistance. Validate the predictions using independent drug response datasets or through in vitro experiments in cell lines. Consider the specific biology of the lncRNAs in your signature.
FAQ 5: What is the best way to present my findings for clinical translation? Integrating your model into a clinically intuitive tool is a powerful way to demonstrate utility [10] [21] [38].
- Recommended Tool: Construct a Nomogram A nomogram is a graphical calculation tool that integrates the m6A-lncRNA risk score with standard clinical parameters (e.g., TNM stage, age) to generate an individualized probability of survival or treatment response at specific time points (e.g., 1, 3, 5 years) [10] [21] [38].
- Validation: Assess the nomogram's accuracy using calibration curves, which plot the predicted probabilities against the actual observed outcomes [54] [38].
The diagram below outlines the key steps for performing and validating a drug sensitivity analysis.
Drug Sensitivity Analysis Workflow
In Vitro and In Vivo Functional Validation of Key Signature lncRNAs
The development of prognostic models based on m6A-related long non-coding RNAs (lncRNAs) has significantly advanced cancer research, particularly in colorectal cancer (CRC) and lung adenocarcinoma (LUAD) [10] [100] [21]. These models, validated through Receiver Operating Characteristic (ROC) curve analysis with Area Under the Curve (AUC) values often exceeding 0.75 for 1-, 3-, and 5-year survival, demonstrate remarkable clinical predictive potential [100] [101] [21]. However, the transition from computational identification to biological and therapeutic relevance requires rigorous functional validation of signature lncRNAs through both in vitro and in vivo experiments. This technical guide addresses the key methodologies and troubleshooting approaches for establishing the functional significance of your m6A-related lncRNA signatures, thereby enhancing model performance and biological credibility.
FAQ: Functional Validation of m6A-Related lncRNAs
Q1: What are the primary steps for validating m6A-related lncRNAs after identifying a prognostic signature?
After establishing a prognostic signature (e.g., an 11-lncRNA model in CRC or an 8-lncRNA model in LUAD) [10] [21], the validation pipeline involves sequential steps:
- Expression Verification: Confirm the expression levels of your signature lncRNAs in relevant cell lines and patient tissues compared to normal controls using qRT-PCR or RNA-seq.
- In Vitro Functional Screening: Perform loss-of-function (LOF) or gain-of-function (GOF) studies in disease-relevant cell models to assess phenotypes like proliferation, migration, invasion, and apoptosis. For instance, FAM83A-AS1 knockdown in A549 lung cancer cells repressed proliferation, invasion, migration, and epithelial-mesenchymal transition (EMT) [21].
- Mechanistic Investigation: Identify the molecular mechanism of action, which may include encoding micropeptides [102] [103], acting as competing endogenous RNAs (ceRNAs) [21], or regulating transcription.
- In Vivo Confirmation: Validate the oncogenic or tumor-suppressive role using animal models, such as xenografts in immunodeficient mice or humanized mouse models for non-conserved human lncRNAs [104].
Q2: Which loss-of-function techniques are most effective for lncRNA functional screening?
The choice of LOF technique depends on your target lncRNA's location and mechanism. The table below compares the primary methods:
| Technique | Principle | Key Applications | Throughput | Key Considerations |
|---|---|---|---|---|
| CRISPR/Cas9 Knockout [105] | Genomic deletion via paired sgRNAs (pgRNAs) targeting promoter/exons. | Complete gene ablation; studies relying on DNA-level alteration. | High | High efficacy but variable deletion efficiency; requires careful sgRNA design. |
| CRISPR Interference (CRISPRi) [105] | dCas9 fused to repressor domain (e.g., KRAB) blocks transcription. | Transcriptional repression; essential for loci with regulatory DNA elements. | High | High specificity; minimal off-target effects; requires knowledge of TSS. |
| RNA Interference (RNAi) [105] | siRNA or shRNA mediates transcript degradation. | Post-transcriptional knockdown; rapid screening. | High | Potential off-target effects; transient effect (siRNA). |
| Antisense Oligonucleotides (ASOs) [105] | Gapmers induce RNase H-mediated degradation of RNA-DNA heteroduplex. | Knockdown nuclear lncRNAs; high specificity. | Medium | Effective for nuclear-retained lncRNAs; can be used therapeutically. |
| CRISPR/Cas13 [105] | RNA-targeting Cas protein cleaves lncRNA transcript. | Transcript degradation; high specificity. | High | Emerging technology; requires optimization. |
Q3: How can I validate the expression of a lncRNA-encoded micropeptide?
The discovery that some lncRNAs encode functional micropeptides (lncPEPs) adds a layer of complexity to functional validation [102] [103]. A multi-technique approach is required:
- Ribosome Profiling (Ribo-seq): This is the primary method to identify actively translated regions, including small open reading frames (sORFs) within lncRNAs [102] [103]. It provides genome-wide evidence of translation.
- Mass Spectrometry (MS): Used to directly detect and validate the translated micropeptide. Stable Isotope Labeling with Amino Acids in Cell Culture (SILAC) and Data-Independent Acquisition (DIA) MS have improved the detection of these low-abundance peptides [102].
- Genetic Validation: Use CRISPR/Cas9 to mutate the start codon of the sORF or employ antisense oligonucleotides to block translation. The functional phenotype should be abolished if the micropeptide is responsible [103].
- Biochemical Assays: Techniques like co-immunoprecipitation (Co-IP) and RNA pull-down assays can identify the micropeptide's interaction partners and its molecular function [103].
Q4: What are the best practices for moving fromin vitrotoin vivolncRNA validation?
In vivo validation is crucial for establishing physiological relevance. Key considerations include:
- Model Selection: For conserved lncRNAs, standard mouse xenograft models are suitable. For non-conserved human lncRNAs, humanized mouse models are essential, as they provide a human-specific context. For example, a humanized TK-NOG mouse model with liver repopulated by human hepatocytes has been successfully used to study the function of a human-specific lncRNA, LINC01018, in regulating fatty acid oxidation [104].
- Phenotypic Endpoints: Common readouts include tumor growth, metastasis, survival analysis, and analysis of relevant signaling pathways in the tumor tissue.
- Delivery Methods: In vivo LOF can be achieved using in vivo-ready siRNA, ASOs, or viral vectors (e.g., lentivirus, AAV) encoding shRNA or CRISPR components for stable knockdown/knockout.
Experimental Protocols for Key Validation Assays
Protocol 1: CRISPR/dCas9-Based Interference (CRISPRi) for LncRNA Knockdown
This protocol is ideal for transcript-specific knockdown without altering the genome [105].
Materials:
- dCas9-KRAB expression plasmid
- sgRNA expression plasmid/library targeting the lncRNA transcription start site (TSS)
- Lentiviral packaging system (psPAX2, pMD2.G)
- Target cell line
- Polybrene
- Puromycin or other appropriate selection antibiotic
Method:
- sgRNA Design: Design 3-5 sgRNAs targeting the TSS (within -50 to +300 bp relative to TSS) of your target lncRNA. Include non-targeting sgRNAs as negative controls.
- Virus Production: Co-transfect HEK-293T cells with the dCas9-KRAB plasmid, sgRNA plasmid, and packaging plasmids using a standard transfection reagent. Collect the lentivirus-containing supernatant at 48 and 72 hours post-transfection.
- Cell Infection: Infect your target cells with the collected lentivirus in the presence of 8 µg/mL Polybrene. Spinoculation (centrifugation at 800-1000 x g for 30-60 minutes at 32°C) can enhance infection efficiency.
- Selection: Begin antibiotic selection (e.g., 1-2 µg/mL Puromycin) 48 hours post-infection. Maintain selection for at least 5-7 days to generate a stable pool.
- Validation: Harvest cells and validate lncRNA knockdown using qRT-PCR. Proceed to phenotypic assays.
Protocol 2: Validating LncRNA-Derived Micropeptides
This protocol outlines steps to confirm the existence and function of a putative lncPEP [102] [103].
Materials:
- Antibody against the putative micropeptide (can be custom-made)
- Plasmids for epitope-tagged (e.g., FLAG, HA) lncRNA sORF expression
- Control plasmid with mutated sORF start codon (ATG -> GTG)
- Mass spectrometry system (e.g., LC-MS/MS)
- Ribo-seq library preparation kit
Method:
- Confirm Translation:
- Ribo-seq: Perform ribosome profiling on your cell line or tissue of interest. Align the ribosome-protected fragments to the genome and look for a clear 3-nucleotide periodicity within the sORF of your lncRNA, indicating active translation [102].
- Epitope Tagging: Transfert cells with a plasmid expressing the lncRNA sORF fused to a C-terminal FLAG or HA tag. Perform western blot on the cell lysates using an anti-FLAG/HA antibody to detect the peptide. The negative control (mutated start codon) should show no band.
- Detect Endogenous Peptide:
- Use a custom-generated antibody against the micropeptide for western blot or immunofluorescence. Alternatively, perform immunoprecipitation of the epitope-tagged peptide and subject the eluate to mass spectrometry for direct identification [103].
- Functional Linkage:
- Use CRISPR/Cas9 to precisely mutate the start codon of the sORF within the genomic context. The phenotype observed from full-lncRNA knockdown should be recapitulated by this sORF-specific mutation if the micropeptide is functional.
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Tool | Function | Example Application |
|---|---|---|
| dCas9-KRAB & sgRNAs [105] | Transcriptional repression (CRISPRi). | Knockdown of nuclear lncRNAs with high specificity. |
| Paired sgRNAs (pgRNAs) [105] | Genomic deletion of lncRNA loci. | Complete knockout of a lncRNA gene, including its promoter. |
| siRNA/shRNA Pools [105] | Post-transcriptional degradation of lncRNAs. | Rapid, transient (siRNA) or stable (shRNA) knockdown for initial screening. |
| Antisense Oligonucleotides (ASOs) [105] | RNase H-mediated degradation of target RNA. | Effective knockdown of nuclear-retained lncRNAs; potential for in vivo use. |
| Humanized Mouse Models [104] | In vivo study of non-conserved human lncRNAs. | Validating the physiological function of human-specific lncRNAs in a relevant microenvironment. |
| Ribo-seq Kits [102] [103] | Genome-wide mapping of translated regions. | Identifying sORFs within lncRNAs and providing evidence of their translation. |
| Cox Regression & LASSO Analysis [10] [100] [101] | Statistical method for prognostic model building. | Constructing a multi-lncRNA signature and calculating a risk score for prognosis prediction. |
Troubleshooting Common Experimental Issues
Problem: Inconsistent Phenotypes Between Different Loss-of-Function Techniques
- Potential Cause 1: Transcriptional vs. Post-transcriptional Effects. CRISPRi and genomic knockout can affect the act of transcription itself, which may have cis-regulatory effects on neighboring genes, a common lncRNA mechanism. RNAi/ASOs only target the transcript.
- Solution: Carefully design controls. If possible, perform "rescue" experiments by re-expressing the lncRNA cDNA (for RNAi/ASO) or from an exogenous promoter (for CRISPRi/KO) in the knockdown cells. Monitor the expression of neighboring genes to rule out cis-effects.
- Potential Cause 2: Inefficient Knockdown/Knockout.
- Solution: Always validate the efficiency of your LOF method using qRT-PCR (for knockdown) or genomic PCR and sequencing (for knockout). Use multiple independent sgRNAs/siRNAs to ensure the phenotype is consistent and not due to off-target effects.
Problem: Inability to Detect a Putative lncRNA-Encoded Micropeptide
- Potential Cause 1: Low Abundance and Stability. Micropeptides are often expressed at very low levels and can be unstable.
- Solution: Use proteasome inhibitors (e.g., MG132) before cell lysis to prevent peptide degradation. Concentrate your protein lysate and use highly sensitive mass spectrometry techniques like DIA-SWATH or TMT labeling [102]. Overexpression of an epitope-tagged version is a reliable first step to confirm translatability.
- Potential Cause 2: The sORF is Not Translated.
- Solution: Ribo-seq is the gold standard to confirm active translation. Without Ribo-seq evidence, claims of a functional micropeptide are weak [102] [103].
Problem: Poor Performance of the Prognostic Model in Independent Datasets
- Potential Cause 1: Batch Effects and Technical Variability. Differences in RNA-seq platforms, library preparation protocols, and data processing pipelines can introduce noise.
- Solution: Use standardized normalization methods (e.g., TPM, FPKM) and consider batch effect correction algorithms (e.g., ComBat) when integrating datasets. Validate your model using qRT-PCR in an independent patient cohort.
- Potential Cause 2: Biological Heterogeneity. The model may not generalize well across different patient populations or disease subtypes.
- Solution: Perform subgroup analysis (e.g., by stage, gender, molecular subtype) to identify populations where your signature is most robust. Incorporate more biologically relevant lncRNAs through functional screening prior to model construction [10] [21].
Visualization of Experimental Workflows
Diagram: Integrated Workflow for lncRNA Functional Validation
Diagram: Decision Workflow for Selecting a Loss-of-Function Technique
In the evolving landscape of precision oncology, models based on N6-methyladenosine (m6A)-related long non-coding RNAs (lncRNAs) have emerged as powerful tools for predicting patient prognosis and therapeutic response. These models analyze the intricate relationships between RNA modification, gene expression, and the tumor immune microenvironment (TIME). A primary method for quantifying the predictive performance of these binary classification models is the Receiver Operating Characteristic (ROC) curve and its associated Area Under the Curve (AUC) metric. The ROC curve visually represents the trade-off between a model's sensitivity (True Positive Rate) and its specificity (1 - False Positive Rate) across all possible classification thresholds. The AUC provides a single scalar value summarizing this performance, where an AUC of 1.0 indicates a perfect classifier, 0.5 is equivalent to random guessing, and values above 0.7 are generally considered clinically useful [64] [106]. This technical resource center is designed to help researchers troubleshoot common challenges and optimize the performance of their m6A-lncRNA risk models.
Frequently Asked Questions (FAQs)
1. What is the clinical significance of a high-AUC m6A-lncRNA model? A high-AUC model demonstrates a strong ability to distinguish between patient groups, such as those who will respond to immunotherapy versus those who will not. For example, a study on colorectal cancer (CRC) developed an 11-m6A-related lncRNA (mRL) signature that effectively stratified patients into high-risk and low-risk groups with distinct overall survival (OS) and responses to immune checkpoint inhibitors [10]. High-risk patients showed significantly higher infiltration of specific immune cells and elevated expression of checkpoints like PD-1, PD-L1, and CTLA-4, suggesting the model can identify candidates most likely to benefit from immunotherapy [10].
2. How are m6A-lncRNA signatures typically constructed and validated? The standard workflow, as utilized in studies on CRC and cervical cancer, involves several key stages [10] [38]:
- Data Acquisition: Transcriptomic data and clinical information are sourced from public databases like The Cancer Genome Atlas (TCGA).
- Identification of m6A-related lncRNAs: Correlation analysis (e.g., |Pearson R| > 0.3, P < 0.001) is performed between lncRNAs and known m6A regulators (writers, readers, erasers).
- Prognostic lncRNA Screening: Univariate Cox regression analysis identifies m6A-related lncRNAs significantly associated with patient survival.
- Model Construction: A multi-lncRNA signature is built using Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to prevent overfitting.
- Validation: The model's robustness is assessed through Kaplan-Meier survival analysis, time-dependent ROC curves, and independent cohort validation.
3. Beyond AUC, what other metrics are vital for a comprehensive model assessment? While AUC is excellent for overall performance, threshold-specific metrics are crucial for clinical application. These include [64] [106]:
- Sensitivity (Recall/True Positive Rate): The proportion of actual responders correctly identified.
- Specificity (True Negative Rate): The proportion of actual non-responders correctly identified.
- Precision: The proportion of patients identified as responders who are actual responders.
- F1-Score: The harmonic mean of precision and recall. The confusion matrix is the foundation for calculating these metrics [107]. Furthermore, the Precision-Recall curve is often a more informative tool than the ROC curve when working with imbalanced datasets [106].
4. How can I improve my model's AUC performance? Improving AUC often involves refining the feature selection and modeling process:
- Incorporate Multi-Omics Data: Integrate genomic, transcriptomic, and proteomic data. One study showed a ~15% improvement in predictive accuracy by using multi-omics with machine learning models [108].
- Advanced Feature Selection: Combine m6A with other regulatory processes like ferroptosis or cuproptosis to capture a more comprehensive biological picture [38] [11].
- Tune the Classification Threshold: The default threshold of 0.5 may not be optimal. Tuning can help balance sensitivity and specificity based on clinical need, for example, to minimize false negatives in a screening scenario [106].
- Compare Multiple Algorithms: Use ROC curves to visually compare the performance of different classifiers (e.g., Logistic Regression vs. Random Forest) on your validation set to select the best-performing model [106].
Troubleshooting Guides
Issue 1: Low or Stagnant AUC Score
Problem: Your m6A-lncRNA risk model's AUC is consistently at or below 0.7, indicating poor discriminative power.
Solution:
- Action 1: Re-evaluate Feature Selection.
- Description: The initial correlation and Cox regression filters may be too lenient.
- Protocol: Apply stricter significance thresholds (e.g., P < 0.01) in univariate Cox analysis. For LASSO regression, use k-fold cross-validation to ensure the penalty parameter (λ) is chosen to minimize out-of-sample error [10] [109].
- Action 2: Incorporate Tumor Microenvironment (TME) Features.
- Description: Prognosis and therapy response are heavily influenced by the TME.
- Protocol: Perform immune cell infiltration analysis (e.g., using CIBERSORT, xCell, or ESTIMATE algorithms) on your cohort [10] [38]. Check if your risk score correlates with known immune cell populations (e.g., CD8+ T cells, macrophages) or immune checkpoint expression. Integrating these features can enhance the model's biological relevance and predictive power [10] [11].
- Action 3: Validate with External Datasets.
- Description: A good performance on a single dataset might be due to overfitting.
- Protocol: Test your model's performance on an independent cohort from a different database (e.g., GEO). A significant drop in AUC on an external set is a classic sign of overfitting, necessitating a return to feature selection with more regularization [38].
Issue 2: Model Fails to Predict Immunotherapy Response
Problem: The model stratifies risk but does not correlate with observed responses to immune checkpoint inhibitors (ICIs).
Solution:
- Action 1: Analyze Immune Checkpoint Gene Expression.
- Description: Response to ICIs is directly linked to the expression of checkpoint proteins.
- Protocol: Extract and compare the expression levels of key immune checkpoint genes (e.g., PD-1, PD-L1, CTLA-4, LAG3) between your predicted high-risk and low-risk groups. A valid model should show significant upregulation in the high-risk group, as was demonstrated in the CRC study [10].
- Action 2: Interrogate the Tumor Mutational Burden (TMB).
- Description: TMB is a validated biomarker for immunotherapy response; high TMB generates more neoantigens, making tumors more visible to the immune system [108] [110].
- Protocol: Calculate TMB for your patient samples and analyze its correlation with your model's risk score. An ideal model will show that high-risk patients also have a high TMB, strengthening the biological rationale for their predicted response to ICIs [108].
- Action 3: Leverage Published Immunotherapy Signatures.
- Description: Validate your model against established immune signatures.
- Protocol: Use tools like TIDE (Tumor Immune Dysfunction and Exclusion) to score your samples. Compare your model's stratification with TIDE's prediction. Consistency with established frameworks adds credibility to your model's predictive capacity for immunotherapy [110].
Issue 3: Inconsistent ROC Curves Across Multiclass Problems
Problem: Your study involves multiple cancer subtypes or treatment response categories (e.g., complete response, partial response, stable disease, progressive disease), and the standard binary ROC analysis is not applicable.
Solution:
- Action: Implement a "One-vs-Rest" (OvR) ROC Strategy.
- Description: This approach extends ROC analysis to multi-class settings by treating one class as "positive" and the aggregate of all other classes as "negative," repeating this for every class [107] [106].
- Protocol: In Python, use
label_binarizefromsklearn.preprocessingto transform your multi-class labels into a binary format suitable for OvR. Then, compute the ROC curve and AUC for each class against all others. The final AUC can be reported as a macro-average (unweighted mean of all per-class AUCs) or a weighted average (weighted by class support) [107].
Experimental Protocols & Data Presentation
Key Experimental Workflow for m6A-lncRNA Model Development
The following diagram illustrates the standard end-to-end workflow for building and validating a prognostic m6A-lncRNA signature.
Quantitative Data from Key Studies
The table below summarizes the performance and clinical utility of m6A-lncRNA models from recent studies, providing a benchmark for researchers.
Table 1: Performance of m6A-lncRNA Prognostic Models Across Cancers
| Cancer Type | Signature Size | Key Performance Findings | Clinical Utility & Validation | Source Study |
|---|---|---|---|---|
| Colorectal Cancer (CRC) | 11 lncRNAs | ROC AUC for OS: Strong predictive performance confirmed by Kaplan-Meier analysis and Cox regression. | High-risk group (HRG) showed higher immune cell infiltration and elevated expression of PD-1, PD-L1, and CTLA4. Distinct immunotherapy response. | [10] |
| Cervical Cancer | 6 lncRNAs | High performance in predicting prognosis. Nomogram AUC for OS: High accuracy. | Low-risk group had more active immunotherapy response and sensitivity to chemotherapeutics like Imatinib. Validated by qPCR. | [38] |
| Esophageal Cancer (EC) | 5 lncRNAs | Risk model showed robust prognostic stratification via survival analysis and ROC curves. | Risk score correlated with specific immune cells (e.g., naive B cells, macrophages). Identified differential expression of 7 key immune checkpoints (e.g., CD44, HHLA2). | [11] |
| Ischemic Stroke (Non-Cancer Example) | 3 Genes (ABCA1, CPD, WDR46) | ROC AUCs: ABCA1: 0.88, CPD: 0.90, WDR46: 0.82. | Established diagnostic accuracy and confirmed via meta-analysis and RT-qPCR. Highlights generalizability of the analytical workflow. | [111] |
Interpreting Your ROC Curve
Understanding the ROC curve is critical for assessing your model's performance. The diagram below explains how to interpret different curve patterns and the impact of threshold selection.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Analytical Tools for m6A-lncRNA Research
| Item / Reagent | Function / Application | Example & Notes |
|---|---|---|
| Public Datasets | Source of transcriptomic and clinical data for model building and validation. | TCGA (The Cancer Genome Atlas): Primary source for cancer data [10] [38] [11]. GEO (Gene Expression Omnibus): Used for external validation [109]. GTEx: Provides normal tissue controls for differential expression analysis [38]. |
| m6A Regulator Gene List | A predefined set of genes to identify m6A-related lncRNAs via co-expression analysis. | Typically includes ~20-25 genes: Writers (METTL3, METTL14, WTAP), Erasers (FTO, ALKBH5), Readers (YTHDF1/2/3, HNRNPA2B1) [10] [38] [111]. |
| Bioinformatics R/Python Packages | Software tools for statistical analysis, model construction, and visualization. | R: limma (differential expression), survival (Cox regression), glmnet (LASSO), pROC/ROCit (ROC analysis) [10] [38]. Python: scikit-learn (metrics.roc_curve, metrics.auc) [64] [106]. |
| Immune Deconvolution Algorithms | Computational methods to quantify immune cell infiltration in the TME from bulk RNA-seq data. | CIBERSORT, xCell, ESTIMATE [10] [38]. Used to correlate risk scores with immune cell abundance and function. |
| qPCR Reagents | Experimental validation of signature lncRNA expression in cell lines or patient samples. | Reverse transcription and quantitative PCR kits. Used in multiple studies to confirm the differential expression of identified lncRNAs (e.g., in cervical and esophageal cancer) [38] [11]. |
Conclusion
The development of a high-performance m6A-related lncRNA prognostic model is a multi-stage process that hinges on robust biological foundations, meticulous statistical construction, and rigorous validation. Optimizing the ROC-AUC is not merely a statistical exercise but a pathway to creating clinically valuable tools for risk stratification and personalized therapy. Future directions should focus on the clinical translation of these signatures, the integration of single-molecule sequencing technologies for unparalleled resolution, and the exploration of m6A-lncRNA pathways as novel therapeutic targets themselves. This will ultimately pave the way for more precise and effective cancer management strategies.
References
- 1. Bioinformatics analysis and experimental validation of m6A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11128431/]
- 2. Identification and validation of lncRNAs involved in m6A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8268297/]
- 3. Identification of N6-Methyladenosine-Related LncRNAs for ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.742944/full]
- 4. Robust RNA-seq data analysis using an integrated method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9793859/]
- 5. Enhancing m6A modification of lncRNA through METTL3 ... [https://www.sciencedirect.com/science/article/pii/S2405844024041963]
- 6. HNRNPC stabilizes m6A-modified AC145207.5 to ... [https://www.sciencedirect.com/science/article/pii/S2468054025000411]
- 7. Investigating diagnostic potential of long non-coding RNAs ... [https://www.nature.com/articles/s41598-024-57987-y]
- 8. m6A RNA methylation regulator-associated genes drive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12574698/]
- 9. Research progress on N6-methyladenosine and non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12031709/]
- 10. Comprehensive analysis of m6A-related lncRNAs as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12261012/]
- 11. Subtype cluster analysis unveiled the correlation between ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1539630/full]
- 12. RNA methylated long non-coding RNAs as potential ... [https://link.springer.com/article/10.1007/s12672-025-02693-y]
- 13. Accessing and Downloading TCGA Data - BTEP Coding Club [https://bioinformatics.ccr.cancer.gov/docs/btep-coding-club/CC2024/TCGA/TCGA_download/]
- 14. Cancer Multi-Omics Database for Machine Learning [https://www.nature.com/articles/s41597-025-05235-x]
- 15. Challenges in LncRNA Biology: Views and Opinions [https://par.nsf.gov/biblio/10538686]
- 16. writers, erasers, readers and functions in RNA metabolism [https://www.nature.com/articles/s41422-018-0040-8]
- 17. m6A RNA Regulatory Diagram [https://www.cellsignal.com/pathways/m6a-rna-regulatory-diagram?srsltid=AfmBOopw_AugFQ3HXhzXbkUM7Zt7xUYpysftkfUjNpvZ4BkLpYjXN7de]
- 18. m6A writers, erasers, readers and their functions [https://www.abcam.com/en-us/technical-resources/pathways/m6a-functions-and-distribution]
- 19. Role of m6A writers, erasers and readers in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9361621/]
- 20. A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 21. Integrative analysis of m6A-related lncRNAs reveals a ... [https://www.dovepress.com/development-of-a-prognostic-m6a-related-lncrna-signature-and-functiona-peer-reviewed-fulltext-article-OTT]
- 22. What is a ROC Curve and How to Interpret It [https://www.displayr.com/what-is-a-roc-curve-how-to-interpret-it/]
- 23. Custom RNA, Stealth - FAQs [https://www.thermofisher.com/order/catalog/product/100002302/faqs]
- 24. Identification of m6A-related lncRNAs-based signature for ... [https://www.sciencedirect.com/science/article/pii/S2472630323000511]
- 25. Identification of an m6A-Related Long Noncoding RNA ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.910749/full]
- 26. Construction of lncRNA-m6A gene-mRNA regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10401877/]
- 27. Identification and immune characteristics of N6 ... [https://www.nature.com/articles/s41598-025-18011-z]
- 28. m6A RNA methylation regulator‑associated genes drive ... [https://www.spandidos-publications.com/10.3892/ol.2025.15350?text=fulltext]
- 29. M6A Modification and Transcription Analysis of LncRNA in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11470819/]
- 30. The functions of N6-methyladenosine modification in lncRNAs [https://pmc.ncbi.nlm.nih.gov/articles/PMC7729116/]
- 31. The role of N6-methyladenosine-modified non-coding ... [https://www.nature.com/articles/s41420-022-01113-2]
- 32. Receiver operating characteristic curve : overview and practical use for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8831439/]
- 33. A novel LncRNA risk model for disulfidptosis-related ... [https://www.nature.com/articles/s41598-025-01730-8]
- 34. Integrated single-cell analysis reveals the regulatory ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1527036/full]
- 35. Best practices for the interpretation and reporting of clinical ... [https://www.nature.com/articles/s41525-022-00295-z]
- 36. Unbiased Prediction and Feature Selection in High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4827277/]
- 37. Identification and Validation of m6A-Related lncRNA ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.745719/full]
- 38. Development of a m6A- and ferroptosis-related LncRNA ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13974-8]
- 39. Classification: ROC and AUC | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/roc-and-auc]
- 40. What Is ROC Curve in Machine Learning? [https://www.coursera.org/articles/what-is-roc-curve]
- 41. Calculating Risk Scores for Project Risk Analysis - Intaver [https://intaver.com/blog-project-management-project-risk-analysis/risk-scores-2/]
- 42. ROC curve analysis (AUC, Sensitivity, Specificity, etc.) [https://www.medcalc.org/en/manual/roc-curves.php]
- 43. Ready to ROC? A tutorial on simulation-based power ... [https://link.springer.com/article/10.3758/s13428-025-02646-x]
- 44. Four overlooked errors in ROC analysis: how to prevent ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171508/]
- 45. Development and validation of a nomogram for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12171118/]
- 46. Analysis of risk factors and construction of nomogram ... [https://www.nature.com/articles/s41598-025-22714-8]
- 47. Development and validation of a clinical risk score ... [https://www.sciencedirect.com/science/article/pii/S2405579425000622]
- 48. Challenges and opportunities in technologies and methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12492894/]
- 49. Structure–function-guided drug development efforts to ... [https://www.sciencedirect.com/science/article/abs/pii/S0165614725001385]
- 50. Receiver Operating Characteristic (ROC) Curve Analysis for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3755824/]
- 51. Identification and Validation of an m6A-Related LncRNA ... [https://www.por-journal.com/journals/pathology-and-oncology-research/articles/10.3389/pore.2022.1610536/full]
- 52. Prognostic signature based on m6A-related lncRNAs to ... [https://www.nature.com/articles/s41598-022-07112-8]
- 53. Bioptimus launches H-optimus-1: a state-of-the-art ... [https://www.bioptimus.com/news/bioptimus-launches-h-optimus-1]
- 54. Lactate-related lncRNAs assessment model predicts the ... [https://www.nature.com/articles/s41598-025-05486-z]
- 55. ROC Curve Analysis [https://www.cd-genomics.com/bmb/roc-curve-analysis.html]
- 56. A 2025 perspective on the role of machine learning for ... [https://pubmed.ncbi.nlm.nih.gov/40772544/]
- 57. Machine Learning in Biomarker Discovery for Precision ... [https://esmed.org/machine-learning-in-biomarker-discovery-for-precision-medicine/]
- 58. MarkerPredict: predicting clinically relevant ... [https://www.nature.com/articles/s41540-025-00603-0]
- 59. Overfitting and Underfitting 2025 Avoid the Biggest Mistakes [https://w3schools.cloud/avoid-the-biggest-overfitting-and-underfitting/]
- 60. Overfitting in Machine Learning Explained [https://aws.amazon.com/what-is/overfitting/]
- 61. ML | Underfitting and Overfitting [https://www.geeksforgeeks.org/machine-learning/underfitting-and-overfitting-in-machine-learning/]
- 62. How to Fix Overfitting and Underfitting | by Tahir | Oct, 2025 [https://medium.com/@tahirbalarabe2/how-to-fix-overfitting-and-underfitting-4cf8f383ea96]
- 63. Identification of m6A/m5C-related lncRNA signature for ... [https://www.nature.com/articles/s41598-024-58743-y]
- 64. Guide to AUC ROC Curve in Machine Learning [https://www.analyticsvidhya.com/blog/2020/06/auc-roc-curve-machine-learning/]
- 65. Computational models for prediction of m6A sites using ... [https://www.sciencedirect.com/science/article/abs/pii/S1046202325001082]
- 66. An ensemble deep learning framework for multi-class LncRNA ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-025-02148-4]
- 67. RNAtranslator: Modeling protein-conditional RNA design as ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12510665/]
- 68. ncFN: a comprehensive non-coding RNA function ... [https://www.sciencedirect.com/science/article/pii/S2468054025001106]
- 69. Decoding potential lncRNA and disease associations ... [https://www.nature.com/articles/s41598-025-16177-0]
- 70. Harnessing Unsupervised Ensemble Learning for ... [https://www.mdpi.com/2227-7390/13/3/420]
- 71. Stacked Deep Learning Ensemble for Multiomics Cancer Type ... [https://bioinform.jmir.org/2025/1/e70709]
- 72. Big data and deep learning for RNA biology [https://www.nature.com/articles/s12276-024-01243-w]
- 73. Integrating Multi-Omics for Precision Medicine: 2025 Guide [https://lifebit.ai/blog/integrating-multi-modal-genomic-and-multi-omics-data-for-precision-medicine/]
- 74. Visualization of three-way comparisons of omics data [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-8-72]
- 75. lncRNA-disease association prediction based on latent ... [https://www.nature.com/articles/s41598-021-99493-5]
- 76. Identification of a five-lncRNA signature for predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6519083/]
- 77. methyladenosine modification site prediction with invertible ... [https://www.nature.com/articles/s42003-025-08265-8]
- 78. From Detection to Prediction: Advances in m6A Methylation ... [https://www.mdpi.com/1422-0067/26/14/6701]
- 79. Interpretable prediction models for widespread m6A RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10697738/]
- 80. A combined deep learning framework for mammalian m6A ... [https://www.sciencedirect.com/science/article/pii/S2666979X24003264]
- 81. m6A-lncRNA landscape highlights reduced levels of m6A ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01254-x]
- 82. Integrated analysis of m6A regulator-mediated RNA ... [https://www.sciencedirect.com/science/article/pii/S2405844024046760]
- 83. From Detection to Prediction: Advances in m6A Methylation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294721/]
- 84. Identification and Validation of an m6A-Related LncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9407446/]
- 85. Heterogeneity-optimized method for predicting immune ... [https://www.nature.com/articles/s41598-025-17718-3]
- 86. Preview of "Interpretable systems biomarkers predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8369244/]
- 87. Advances and challenges in neoantigen prediction for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12198247/]
- 88. The importance of being external. methodological insights ... [https://www.sciencedirect.com/science/article/abs/pii/S016926072100362X]
- 89. Prediction models need appropriate internal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5578404/]
- 90. Methods of determining optimal cut-point of diagnostic ... [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-024-02198-2]
- 91. A new risk model based on a 11-m6A-related lncRNA ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-021-09062-2]
- 92. Identification and validation of m 6 A RNA methylation ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1543517/full]
- 93. Time-dependent ROC curve analysis in medical research [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-017-0332-6]
- 94. m6A-related lncRNA signature for predicting prognosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9730119/]
- 95. Identification of an m6A-Related lncRNA Signature for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8187870/]
- 96. Benchmarking of computational methods for m6A profiling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10818168/]
- 97. Comparative analysis of improved m6A sequencing based ... [https://www.nature.com/articles/s41598-025-85150-8]
- 98. LncRNAs and Chromatin Modifications Pattern m 6 A ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.866772/full]
- 99. Identifying meaningful drug response biomarkers from ... [https://www.sciencedirect.com/science/article/abs/pii/S1476927125003305]
- 100. Identification and Validation of a m6A-Related Long ... [https://pubmed.ncbi.nlm.nih.gov/39868645/]
- 101. Development and validation of a prognostic model based ... [https://www.nature.com/articles/s41598-024-83263-0]
- 102. LncRNA-Encoded Micropeptides: Expression Validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12192620/]
- 103. Unveiling the functional implications of long noncoding ... [https://www.sciencedirect.com/science/article/abs/pii/S2773044125000786]
- 104. In vivo functional analysis of non-conserved human ... [https://www.nature.com/articles/s41467-019-13688-z]
- 105. Functional Screening Techniques to Identify Long Non ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7763270/]
- 106. Explain The ROC Curve To Unlock ML Performance [https://www.acte.in/what-is-roc-curve-in-machine-learning]
- 107. Scoring metrics in the Splunk Machine Learning Toolkit [https://help.splunk.com/en/splunk-cloud-platform/apply-machine-learning/use-ai-toolkit/5.6.3/algorithms-and-scoring-metrics-in-mltk/scoring-metrics-in-the-splunk-machine-learning-toolkit]
- 108. Predictive Biomarkers in Cancer Immunotherapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12289453/]
- 109. Exploring the predictive “psycho-biomarkers” for ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1590670/full]
- 110. Longitudinal liquid biopsy identifies an early predictive ... [https://www.nature.com/articles/s41467-025-63538-4]
- 111. Integrated analysis of m6A regulator mediated RNA ... [https://www.nature.com/articles/s41598-025-16948-9]