Oropharyngeal vs. Nasal Swab Sampling: A Comparative Analysis of Sensitivity for Respiratory Pathogen Detection
This article provides a comprehensive, evidence-based review for researchers and drug development professionals on the comparative sensitivity of oropharyngeal (OP) and nasal swab sampling methods for detecting respiratory pathogens, with...
Oropharyngeal vs. Nasal Swab Sampling: A Comparative Analysis of Sensitivity for Respiratory Pathogen Detection
Abstract
This article provides a comprehensive, evidence-based review for researchers and drug development professionals on the comparative sensitivity of oropharyngeal (OP) and nasal swab sampling methods for detecting respiratory pathogens, with a significant focus on SARS-CoV-2 and Mycoplasma pneumoniae. It synthesizes findings from recent clinical studies to explore the foundational principles of viral load distribution, analyzes methodological protocols and their impact on diagnostic yield, discusses strategies for optimizing sensitivity and addressing sampling challenges, and validates findings through head-to-head comparative studies. The analysis aims to inform robust diagnostic development and effective testing strategies in both clinical and research settings.
Understanding Viral Tropism and Anatomical Distribution of Pathogens
The declaration of nasopharyngeal (NP) swabs as the gold standard for SARS-CoV-2 detection at the onset of the COVID-19 pandemic was less a product of comparative scientific validation and more a historical precedent from other upper respiratory tract pathogens [1]. This default designation occurred amidst a cascading collapse of supply chains, worsening shortages of personal protective equipment, and an urgent global need for mass testing [1]. However, as the crisis evolved, this initial standard was rigorously challenged. The inherent discomfort of the procedure, its technical complexity, and the significant risk of aerosol exposure for healthcare workers catalyzed a widespread search for less invasive, simpler, and safer alternatives such as oropharyngeal (OP) and nasal swabs [2] [1]. This initiated a critical scientific debate concerning diagnostic sensitivity, patient tolerability, and operational feasibility that continues to inform respiratory pathogen testing protocols.
This guide objectively compares the performance of NP, OP, and nasal swab sampling methods through the lens of published experimental data. It is framed within the broader thesis of understanding comparative sensitivity in respiratory specimen collection, providing researchers, scientists, and drug development professionals with a synthesized overview of methodological protocols and performance metrics essential for diagnostic development and clinical study design.
Comparative Performance Analysis of Swabbing Techniques
Extensive head-to-head studies have generated robust data on the relative sensitivities of different upper respiratory sampling methods. The table below summarizes key comparative findings from recent clinical studies.
Table 1: Comparative Sensitivity of Upper Respiratory Specimens for SARS-CoV-2 Detection
| Specimen Type | Reported Sensitivity (%) | 95% Confidence Interval (%) | Comparative Context (vs. NP) | Key Study Findings |
|---|---|---|---|---|
| Nasopharyngeal (NP) | 92.5 | 85 to 99 | Reference Standard | Considered gold standard but technically challenging [2] |
| Oropharyngeal (OP) | 94.1 | 87 to 100 | Comparable (p=1.00) | Equivalent alternative; well-tolerated [2] |
| Nasal Swab (Anterior) | 82.4 | 72 to 93 | Lower (p=0.07) | Less sensitive alone but valuable in combination [2] |
| Combined OP/NP | 100.0 | Not Reported | Superior | Maximum sensitivity from combining specimens [2] |
| Combined OP/Nasal | 96.1 | 90 to 100 | Superior to Nasal alone (p=0.03) | Significantly enhances nasal swab sensitivity [2] |
| Anterior Nasal (Rhinoswab) | 80.7 | 73.8 to 86.2 | Lower | New standardized method; suitable for self-sampling [3] |
Further analysis of viral load, as indicated by RT-PCR Cycle Threshold (Ct) values, provides a quantitative dimension to these comparisons. Lower Ct values indicate higher viral concentrations in the specimen.
Table 2: Comparative Viral Load (Mean Ct Value) by Specimen Type
| Specimen Type | Mean Ct Value (N Gene) | Statistical Significance (vs. NP) | Interpretation |
|---|---|---|---|
| Nasopharyngeal (NP) | 24.98 | Reference | Highest viral load |
| Oropharyngeal (OP) | 26.63 | Not Significant (p=0.084) | Comparable viral load |
| Nasal Swab | 30.60 | Significant (p=0.002) | Significantly lower viral load |
The data reveals that while NP swabs generally yield the highest viral loads, the sensitivity of OP swabs can be statistically comparable in well-conducted studies [2]. The significantly higher Ct values for nasal swabs explain their lower individual sensitivity [2]. However, the combination of different specimen types, such as OP with a nasal swab, can achieve near-perfect sensitivity, offering a powerful strategy for high-accuracy testing scenarios [2]. It is crucial to note that real-world performance can diverge significantly from controlled studies, with one analysis of over 31,000 patients finding positivity rates could drop from 38.1% to 2.3% when switching from NP to OP sampling in practice, highlighting the impact of operational factors [4].
Experimental Protocols and Methodological Insights
Standardized Swab Collection Procedures
The accuracy of SARS-CoV-2 testing is profoundly dependent on correct specimen collection. The following protocols, derived from CDC guidelines and prospective clinical trials, detail the standardized procedures for each method [2] [5].
Nasopharyngeal (NP) Swab Collection Protocol
- Swab Type: Use a flexible, mini-tip flocked swab with a plastic or wire shaft. Calcium alginate or wooden-shaft swabs are not acceptable as they may inhibit tests [5].
- Patient Positioning: Tilt the patient's head back approximately 70 degrees [5].
- Insertion: Insert the swab through the nostril parallel to the palate (not upward) until resistance is encountered, indicating contact with the nasopharynx. The depth is typically equivalent to the distance from the nostrils to the outer opening of the ear [2] [5].
- Specimen Collection: Leave the swab in place for several seconds to absorb secretions. Gently rub and roll the swab, then slowly remove it while rotating [5].
- Post-Collection: Place the swab tip-first into a sterile tube containing viral transport medium and break the applicator stick [5].
Oropharyngeal (OP) Swab Collection Protocol
- Swab Type: A rigid-shaft flocked swab is typically used [2].
- Visualization: Use a tongue depressor to improve visualization of the posterior oropharynx.
- Swabbing Technique: Swab the posterior pharynx and tonsillar areas, rubbing the swab over both tonsillar pillars and the posterior oropharynx. Avoid touching the tongue, teeth, or gums to avoid contaminating the specimen with oral flora [2] [5].
- Post-Collection: Place the swab into viral transport media as above [2].
Anterior Nasal Swab Collection Protocol
- Swab Type: A tapered swab is used, such as the specialized Rhinoswab with a double-loops nylon-flocked tip [3] [5].
- Insertion: Insert the entire collection tip of the swab (approximately 1-1.5 cm) inside the nostril [5]. For the Rhinoswab, insert until slight resistance is met [3].
- Specimen Collection: Firmly sample the nasal wall by rotating the swab in a circular path against the nasal wall at least 4 times, taking approximately 15 seconds to collect the specimen. Repeat in the other nostril using the same swab [3] [5]. Some protocols leave the swab in place for 60 seconds for enhanced absorption [3].
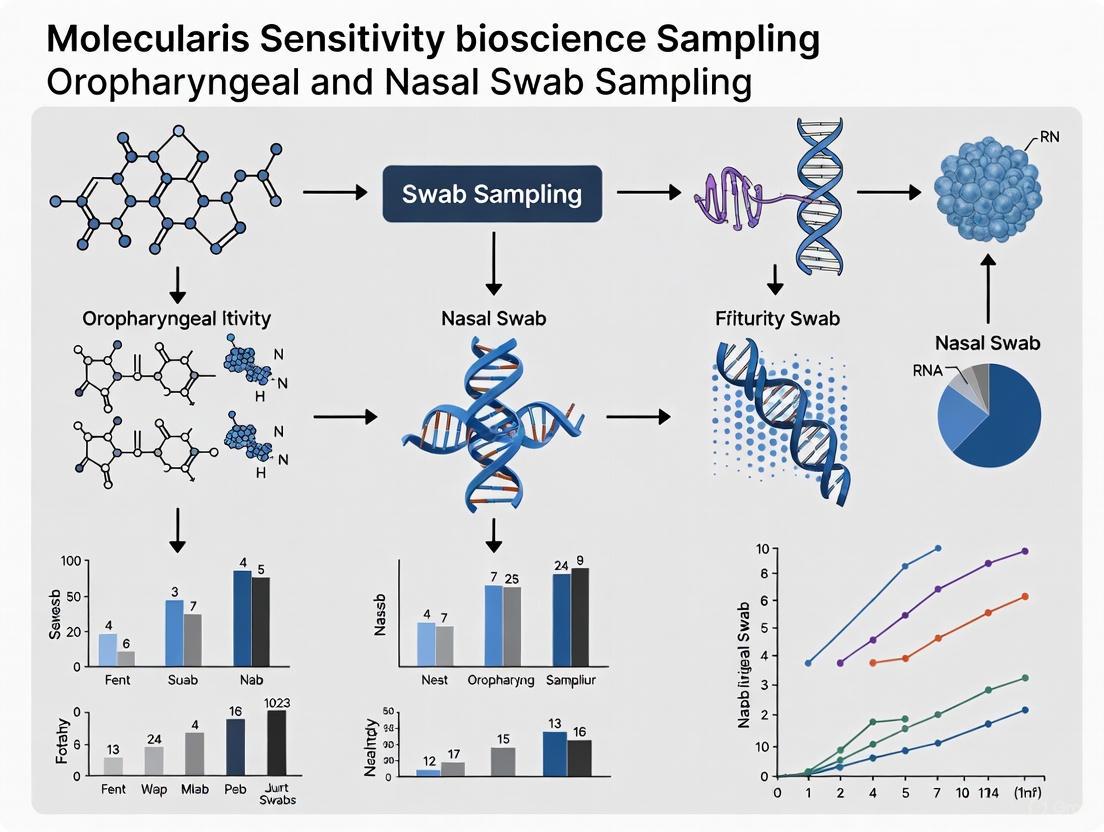
Visualizing the Comparative Diagnostic Workflow
The following diagram illustrates the logical relationship and comparative performance outcomes of the different sampling strategies, based on head-to-head clinical study data.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful execution of respiratory specimen studies requires specific materials and reagents. The following table details key components of the research toolkit for this field.
Table 3: Essential Research Reagents and Materials for Respiratory Specimen Studies
| Item Name | Specification / Example | Primary Function in Research |
|---|---|---|
| Flocked Swabs | Flexible minitip (e.g., COPAN A305CS01) [2] [6] | NP specimen collection; optimized cell elution |
| Rigid-Shaft Swabs | Flocked design (e.g., Meditec A/S) [2] | OP and anterior nasal specimen collection |
| Specialized Nasal Swabs | Rhinoswab (Rhinomed) [3] | Bilateral anterior nasal sampling with large surface area |
| Viral Transport Medium (VTM) | Universal Transport Medium (e.g., Copan UTM) [7] | Preserves viral RNA integrity during transport/storage |
| Alternative Transport Media | Dulbecco’s Modified Eagle Medium (DMEM) [6] | Validated alternative during VTM shortages |
| RNA Extraction Kits | Viral RNA Isolation Kits [8] | Nucleic acid purification for downstream molecular assays |
| RT-PCR Master Mixes | Fast Viral Master mix (Life Technologies) [3] | Amplification and detection of SARS-CoV-2 RNA targets |
| Validated Assays | Allplex SARS-CoV-2 Assay (Seegene) [2] | Multi-target RT-PCR for sensitive detection |
The choice of swab is particularly critical. Synthetic fibers (e.g., nylon flocked) are preferred over calcium alginate or cotton as they release collected material more efficiently, improving test sensitivity [5]. Similarly, swabs with plastic or wire shafts are mandated, as wooden shafts may contain substances that inactivate viruses and inhibit molecular tests [5].
The debate over the "gold standard" for respiratory pathogen sampling has progressed from a default designation to an evidence-based evaluation. The body of research demonstrates that NP swabs generally provide the highest single-site sensitivity and viral load [2] [8]. However, OP swabs demonstrate comparable sensitivity in well-controlled, prospective studies and offer advantages in patient comfort and procedural safety [2]. While anterior nasal swabs are less sensitive when used alone, their performance is significantly enhanced when combined with OP swabs, making combined sampling a powerful strategy for maximizing detection rates [2]. Furthermore, the emergence of novel, standardized anterior nasal swabs like the Rhinoswab shows promise for reliable diagnosis, particularly in outpatient or self-sampling contexts [3].
Future directions in this field point toward greater standardization and the exploration of non-swab-based methods. Saliva testing, for instance, has emerged as a highly scalable and patient-friendly alternative, with numerous studies reporting comparable sensitivity to NP swabs when optimal collection and processing methods are employed [1]. For researchers and drug developers, the choice of sampling method must be guided by a balanced consideration of diagnostic accuracy, patient acceptability, operational feasibility, and the specific objectives of the clinical or surveillance study. The historical context of the NP swab as a default standard has given way to a more nuanced understanding, where the optimal specimen type may be context-dependent, and combination approaches often provide the most robust solution for accurate pathogen detection.
Respiratory pathogen diagnostics rely on the fundamental principle of pathogen tropism, the propensity of a virus or bacterium to infect specific anatomical sites within the respiratory tract. The comparative sensitivity of oropharyngeal versus nasal swab sampling is a critical area of research, as the choice of sampling site can significantly impact detection accuracy and subsequent clinical and public health decisions. This guide synthesizes recent experimental data to objectively compare how SARS-CoV-2, Influenza viruses, and Mycoplasma pneumoniae (M. pneumoniae) loads vary across different respiratory sites, providing researchers with a evidence-based framework for selecting optimal sampling protocols.
Comparative Pathogen Detection Across Anatomical Sites
The following tables consolidate key experimental findings on the detection sensitivity of various respiratory pathogens across different sampling sites.
Table 1: Comparative Sensitivity of Swab Types for SARS-CoV-2 Detection
| Swab Type | Sensitivity (%) | Comparative Notes | Study Details |
|---|---|---|---|
| Oropharyngeal (OP) | 94.1% | Comparable to Nasopharyngeal (NP); not statistically different (p=1.00) | Prospective study of 51 confirmed cases [9] |
| Nasopharyngeal (NP) | 92.5% | Considered the clinical gold standard | Same study as above [9] |
| Nasal Swab | 82.4% | Significantly lower sensitivity (p=0.07) | Same study as above [9] |
| Combined OP/NP | 100% | Highest sensitivity; all cases detected | Same study as above [9] |
| Combined Nose & Throat | Benchmark (100%) | Used as reference for other methods | Study of 815 participants [10] |
| Throat Only | 97% | Higher than nose-only relative to combined | Same study as above [10] |
| Nose Only | 91% | Lower than throat-only relative to combined | Same study as above [10] |
Table 2: Detection of Influenza Viruses and M. pneumoniae by Sampling Site
| Pathogen | Swab Type | Detection Performance | Study Details |
|---|---|---|---|
| SARS-CoV-2/Influenza A+B/RSV | Oropharyngeal-Nasal (ON) & NP | Similar detection rates on BioFire RP2.1 | 358 pediatric sample pairs [11] |
| Mycoplasma pneumoniae | Oropharyngeal-Nasal (ON) | Sensitivity: 94% | Significantly higher than NP (p=0.0020) [11] |
| Mycoplasma pneumoniae | Nasopharyngeal (NP) | Sensitivity: 64% | Significantly lower than ON (p=0.0020) [11] |
| Influenza D Virus (in ferrets) | Upper Respiratory Tract | D/OK clade replicated mostly in URT; higher transmission | Study of tissue tropism [12] |
| Influenza D Virus (in ferrets) | Lower Respiratory Tract | D/OK660HEF clade replicated in URT and trachea; lower transmission | Study of tissue tropism [12] |
Key Insights from Comparative Data
The data reveals distinct pathogen-specific tropism patterns with direct implications for diagnostic sampling:
- SARS-CoV-2: For the Omicron variant, throat swabs may offer superior sensitivity compared to nasal swabs alone, though combined sampling remains the most reliable method [10]. The viral concentration in nasal samples demonstrates greater consistency over time than in throat samples [10].
- Mycoplasma pneumoniae: Shows a strong preference for the oropharyngeal region, with combined oropharyngeal-nasal (ON) swabs demonstrating a dramatic 30% higher sensitivity compared to traditional nasopharyngeal (NP) swabs [11]. This finding is particularly relevant for diagnosing childhood pneumonia.
- Influenza Viruses: Evidence from influenza D virus studies in ferret models indicates that even subtle genetic differences, such as six amino acid mutations in the HEF protein, can influence tissue tropism and subsequently alter transmission efficiency between the upper and lower respiratory tract [12].
Detailed Experimental Protocols and Workflows
Standardized Swab Collection Procedures
The following workflow outlines the standardized collection methods used in key comparative studies, which are crucial for ensuring consistent and reliable results.
Diagram 1: Experimental workflow for comparative swab sensitivity studies.
Nasopharyngeal (NP) Swab Collection
- Procedure: The patient's head is tilted slightly back. A flexible minitip flocked swab is inserted into the nasal cavity and directed toward the earlobe, following the nasal floor. The swab is inserted approximately 8-11 cm deep until resistance is met at the posterior nasopharyngeal wall. The swab remains in place for several seconds, is rotated three times, and is then withdrawn [9].
- Materials: Flexible minitip flocked swab (e.g., COPAN diagnostics Inc.) [9].
Oropharyngeal (OP) Swab Collection
- Procedure: A tongue depressor is used to improve visualization. A rigid-shaft flocked swab is used to collect specimen from both palatine tonsils and the posterior oropharyngeal wall using a painting and rotating motion, taking care to avoid touching the cheeks, teeth, or gums [9].
- Materials: Rigid-shaft flocked swab (e.g., Meditec A/S) [9].
Nasal Swab Collection
- Procedure: Similar to NP swab collection, but the swab is inserted only 1-3 cm into the nasal cavity. It is brushed along the septum and inferior nasal concha and rotated three times before withdrawal [9].
- Materials: Rigid-shaft flocked swab [9].
Combined Oropharyngeal-Nasal (ON) Swab Collection
- Procedure: This method uses a single flocked swab. The swab is first used to collect a sample from the oropharyngeal area (tonsils and posterior pharynx), and then the same swab is inserted into the nostril to collect a nasal sample [11]. For parent-collected samples, instructional videos and written materials are provided to ensure proper technique.
- Materials: Copan FLOQSwab placed in Universal Transport Medium [11].
Laboratory Analysis Methods
Table 3: Key Research Reagent Solutions and Laboratory Methods
| Reagent/Instrument | Primary Function | Example Application in Studies |
|---|---|---|
| Copan FLOQSwab + UTM | Sample collection & transport | Standardized collection for viral PCR [11] |
| Real-time RT-PCR | Pathogen nucleic acid detection | Gold standard for SARS-CoV-2, influenza detection [9] [13] |
| BioFire Respiratory Panel 2.1 | Multiplex PCR for respiratory pathogens | Detected 15 viral and 4 bacterial targets in ON/NP comparison [11] |
| GeneXpert Xpress Assay | Rapid automated PCR testing | Used for SARS-CoV-2/Influenza A+B/RSV testing [11] |
| Metagenomic Next-Generation Sequencing (mNGS) | Unbiased pathogen detection | Comprehensive detection in immunocompromised hosts [14] |
Discussion and Research Implications
Anatomical Tropism and Diagnostic Optimization
The observed variations in pathogen detection across sampling sites reflect fundamental differences in anatomical tropism. The superior detection of M. pneumoniae in oropharyngeal-na sal swabs suggests this pathogen may preferentially colonize or infect both the oropharynx and the anterior nares more effectively than the nasopharynx [11]. For SARS-CoV-2, particularly the Omicron variant, the higher sensitivity of throat swabs may indicate a shift in viral replication dynamics toward more proximal respiratory tissues compared to earlier variants [10].
The positivity rate for respiratory pathogens can change dramatically based on sampling methodology. One study found that switching from oropharyngeal to nasopharyngeal sampling in the same clinical setting increased the positivity rate from 2.3% to 38.11% [4], highlighting the critical importance of site selection.
Acceptability and Implementation Considerations
Beyond pure sensitivity, the acceptability of sampling methods is crucial for implementation, particularly in pediatric populations. Caregivers rated combined oropharyngeal-nasal (ON) swabs as significantly more acceptable than nasopharyngeal (NP) swabs (median score 4.5 vs. 2 on a 5-point Likert scale, p<0.0001) [11]. This improved tolerability, combined with comparable or superior sensitivity for several pathogens, makes ON swabs a viable patient-centered alternative, especially for home-based or repeated testing scenarios.
Advanced Detection Technologies
For complex cases, particularly in immunocompromised patients such as persons living with HIV (PLWH), metagenomic next-generation sequencing (mNGS) demonstrates remarkable utility. mNGS of bronchoalveolar lavage fluid (BALF) achieved a pathogen detection sensitivity of 98.0%, significantly higher than the 32.1% sensitivity of traditional cultures [14]. This technology is particularly valuable for detecting mixed infections, which were present in 94.2% of PLWH with pulmonary infections in one study [14].
Pathogen-specific tropism significantly influences the detection sensitivity of respiratory pathogens across different anatomical sampling sites. The evidence compiled in this guide demonstrates that:
- Combined oropharyngeal-nasal swabs offer an excellent balance of high sensitivity and patient acceptability, proving particularly effective for detecting M. pneumoniae and comparable to nasopharyngeal swabs for common respiratory viruses.
- Throat swabs may be more sensitive than nasal swabs alone for detecting the SARS-CoV-2 Omicron variant.
- Nasopharyngeal swabs remain a sensitive gold standard for many applications but are less acceptable to patients, especially children.
- Pathogen-specific factors, including genetic variations in influenza viruses, directly influence tissue tropism and should inform sampling strategy selection.
These findings provide researchers and clinicians with an evidence-based framework for optimizing respiratory pathogen detection protocols based on the target pathogen, patient population, and clinical context. Future research should continue to elucidate the molecular mechanisms driving pathogen tropism to further refine diagnostic approaches.
The accurate detection of pathogens like SARS-CoV-2 in upper respiratory specimens is a cornerstone of modern molecular diagnostics in public health and clinical practice. For researchers and drug development professionals, evaluating the performance of different sampling methods is critical for guiding diagnostic protocols, surveillance studies, and clinical trial designs. This guide provides an objective comparison between two common sampling techniques—oropharyngeal (OP) swabs and nasal swabs—by analyzing the key experimental metrics of diagnostic sensitivity, cycle threshold (Ct) values, and viral RNA load. Framed within the broader thesis of comparative sensitivity research, this analysis synthesizes data from controlled studies to inform evidence-based decision-making.
Core Diagnostic Metrics Explained
In the comparison of respiratory specimen types, three quantitative metrics are paramount:
- Diagnostic Sensitivity: This measures the proportion of actual positive cases that are correctly identified by the test. It is expressed as a percentage, with a higher percentage indicating a lower rate of false negatives [2] [8].
- Cycle Threshold (Ct) Value: In real-time reverse transcription–polymerase chain reaction (rRT-PCR), the Ct value indicates the number of amplification cycles required for the target pathogen's signal to exceed a background threshold. A lower Ct value correlates with a higher amount of target nucleic acid in the original specimen [2] [8].
- Viral RNA Load: This is a quantitative measure of the viral material present in a sample, often reported as copies per milliliter (copies/mL). It can be absolutely quantified using a standard curve or relatively inferred from Ct values [15] [16].
Direct Comparison of Oropharyngeal and Nasal Swabs
The following tables consolidate quantitative data from recent peer-reviewed studies to facilitate a direct comparison of OP and nasal swabs.
Table 1: Comparison of Diagnostic Sensitivity
| Specimen Type | Reported Sensitivity (%) | Study Details |
|---|---|---|
| Oropharyngeal (OP) Swab | 94.1% | Prospective study of 51 confirmed COVID-19 patients [2] |
| 10.0% | Prospective study of 120 inpatients (Earlier pandemic strain) [8] | |
| Nasal Swab | 82.4% | Prospective study of 51 confirmed COVID-19 patients [2] |
| Combined OP/Nasal Swab | 96.1% | Paired sampling from 51 patients [2] |
| 92.7% | Evaluation in hospitalized patients (n=28) [17] |
Table 2: Comparison of Viral Load and Ct Values
| Specimen Type | Mean/Median Ct Value | Viral Load (Inferred from Ct) | Total RNA Concentration |
|---|---|---|---|
| Oropharyngeal (OP) Swab | Mean Ct: 26.63 [2] | Lower than NPS [8] | Median: 3.20 ng/μl [15] |
| Nasal Swab | Mean Ct: 30.60 [2] | Lower than OP swab and NPS [2] | Information Not Available |
| Nasopharyngeal (NPS) - Reference | Mean Ct: 24.98 [2] | Highest among swab types [2] [16] | Median: 5.05 ng/μl [15] |
Table 3: Key Research Reagent Solutions for Specimen Testing
| Reagent / Material | Function in Experimental Workflow | Example Product |
|---|---|---|
| Flocked Swab | Specimen collection; superior release of cellular material [2] | Flexible minitip flocked swab (COPAN) [2] |
| Viral Transport Medium (VTM) | Preservation of viral RNA integrity during transport [2] | BioVTM (Biofarma) [15] |
| RNA Extraction Kit | Isolation of pure viral RNA for downstream analysis [2] [15] | PureLink Viral RNA Mini Kit (Thermo Fisher) [15] |
| One-Step RT-PCR Kit | Reverse transcription and PCR amplification in a single reaction [17] | Qiagen One Step RT-PCR Kit [17] |
| Real-Time PCR Assay | Qualitative and quantitative detection of SARS-CoV-2 RNA [2] | Allplex SARS-CoV-2 Assay (Seegene) [2] |
Experimental Protocols for Key Studies
The comparative data presented above are derived from rigorously controlled experiments. The following outlines the core methodologies employed in these studies.
Protocol for Head-to-Head Prospective Comparison
A 2023 prospective study directly compared OP swabs, nasopharyngeal (NPS) swabs, and nasal swabs collected from the same 51 confirmed SARS-CoV-2-positive individuals [2].
- Specimen Collection: A consultant in otorhinolaryngology performed all swabbings. NPS was collected by inserting a flexible minitip flocked swab approximately 8–11 cm into the nostril until resistance was met. OP swab was collected by wiping both palatine tonsils and the posterior oropharyngeal wall. The nasal swab was inserted only 1–3 cm into the nasal cavity and brushed along the septum [2].
- Laboratory Analysis: Specimens were stored at 2–6°C before RNA extraction and rRT-PCR analysis. For a subset of participants tested with the same assay (Allplex SARS-CoV-2), the mean Ct values for the N gene were calculated and compared [2].
- Statistical Analysis: Sensitivity comparisons used McNemar's test, while Ct value comparisons used the Wilcoxon matched-pairs signed-rank test [2].
Protocol for Viral Load and Total RNA Quantification
A 2024 cross-sectional study evaluated the total RNA and viral loads from different swab types, addressing the potential for normalization using an internal control [15].
- Specimen Collection: The study used 111 positive specimens collected from different patients: 41 oropharyngeal swabs, 34 nasopharyngeal swabs, and 36 combined naso-oropharyngeal swabs, all stored in the same viral transport medium [15].
- Laboratory Analysis: RNA was extracted from 200 μL of specimen. The total RNA concentration (ng/μL) of the extract was measured via NanoDrop. Quantitative rRT-PCR was performed using a standard curve (AMPLIRUN SARS-CoV-2 RNA CONTROL) to determine viral load in copies/mL, and the RNase P gene was simultaneously amplified as an internal control [15].
- Statistical Analysis: The Kruskal-Wallis test and ANOVA were used to compare median total RNA and mean RNase P Ct values between the three swab groups, respectively [15].
Visualizing the Comparative Analysis Workflow
The following diagram illustrates the logical workflow for a head-to-head comparison study of respiratory swabs, from participant enrollment to data analysis.
Visualizing Viral Load Quantification
This diagram outlines the key steps involved in the quantitative analysis of viral load from respiratory swab specimens, a critical process for objective comparison.
In molecular diagnostics and drug development, the selection of a sampling site is far from a trivial decision; it is a critical variable that directly influences the sensitivity, specificity, and ultimate success of detection strategies. The prevailing assumption that one sampling method can be universally applied across different diseases, stages of infection, and patient populations represents a significant evidence gap in medical research. This guide objectively compares the performance of oropharyngeal and nasal swab sampling, focusing primarily on SARS-CoV-2 diagnostics as a well-researched model, to demonstrate how sampling efficacy is context-dependent.
Robust evidence now indicates that optimal sampling site varies based on multiple factors including the pathogen's replication dynamics, time since symptom onset, and specific patient characteristics [18] [19]. The transition to an endemic phase for respiratory viruses like SARS-CoV-2 has further highlighted the need for less invasive, more acceptable testing methods that can be widely adopted for personal decision-making and public health surveillance [18]. Through a detailed examination of comparative performance data, experimental methodologies, and underlying biological mechanisms, this analysis provides researchers and drug development professionals with evidence-based insights for selecting appropriate sampling modalities based on specific research objectives and clinical contexts.
Comparative Performance Data: Quantitative Analysis of Sampling Efficacy
Substantial clinical studies have directly compared the diagnostic performance of different sampling methods, revealing significant variations in sensitivity, specificity, and viral load dynamics. The tables below summarize key quantitative findings from recent research.
Table 1: Overall Diagnostic Performance of Saliva/Oropharyngeal vs. Nasal Swab Sampling for SARS-CoV-2 Detection
| Performance Measure | Saliva/Oropharyngeal | Nasal Swab (Anterior) | Nasopharyngeal Swab (NPS) | Study Details |
|---|---|---|---|---|
| Sensitivity (Overall) | 69.2% (95% CI: 57.2–79.5%) | Not Reported | Reference Standard | Longitudinal study; sensitivity varied by infection phase [19] |
| Sensitivity (Early Infection) | 82.0% | Not Reported | Reference Standard | Highest sensitivity during early infection [19] |
| Sensitivity (Mid-Phase) | 40.0% | Not Reported | Reference Standard | Lowest sensitivity during mid-phase infection [19] |
| Positive Percent Agreement (PPA) | 94.0% (95% CI: 88.9–99.1%) | Reference Standard | Not Applicable | Symptomatic participants within first 5 days of symptoms [18] |
| Specificity | 96.6% (95% CI: 92.9–98.7%) | Not Reported | Reference Standard | Longitudinal study in symptomatic individuals [19] |
| Negative Percent Agreement (NPA) | 99.0% (95% CI: 98.1–99.9%) | Reference Standard | Not Applicable | Symptomatic participants within first 5 days of symptoms [18] |
Table 2: Viral Load Dynamics and Practical Considerations Across Sampling Methods
| Parameter | Saliva/Oropharyngeal | Nasal Swab | Nasopharyngeal Swab (NPS) | Sources |
|---|---|---|---|---|
| Mean Ct Value (Viral Load) | 28.75 (Higher load) | 26.75 (Lower load) | Not Reported | Lower Ct value indicates higher viral load [19] |
| Viral Load Peak | Day 1 of symptoms | Day 4 of symptoms | Not Reported | Study in symptomatic individuals [18] |
| Patient Acceptability (Pediatric) | Not Reported | Low | Very Low | 83.9% refusal rate for NPS/OPS in children [20] |
| Key Advantages | Less invasive, fewer resources, self-collection potential | Less invasive than NPS | Established "gold standard," high sensitivity | [18] [20] |
| Key Limitations | Variable sensitivity | Lower acceptability than saliva | Highly invasive, requires trained personnel, low acceptability | [19] [20] |
Experimental Protocols and Methodologies
Standardized Sample Collection Procedures
The reliability of comparative data hinges on standardized collection protocols. The following methodologies are cited from peer-reviewed studies providing the performance metrics in Section 2.
- Saliva Collection: Participants provided 1-2 mL of saliva (drool) into a preservative-free collection tube without any stimulants. After collection, the funnel was removed, the tube was capped, and samples were transported at room temperature to the laboratory for processing within 48 hours, leveraging the demonstrated stability of SARS-CoV-2 in raw saliva during this timeframe [18].
- Nasal Swab Collection: Participants used a standardized swab (e.g., Roche cobas PCR Uni swab) inserted approximately one inch (2.5 cm) inside the nostril. The swab was rubbed in a circle five times for 10-15 seconds per nostril, using the same swab for both nostrils. The swab was then placed in the transport medium, the handle snapped off, and the tube capped [18].
- Nasopharyngeal Swab (NPS) Collection: A nylon flocked swab was inserted into the nostril to the nasopharyngeal region, rotated once, and held in place for 15 seconds to ensure adequate sampling [7]. This method is more invasive than anterior nasal swabbing.
Laboratory Processing and Analysis
- Saliva Processing (covidSHIELD Protocol): Saliva samples underwent heat inactivation at 95°C for 30 minutes. A 1:1 ratio of 2× Tris/borate/EDTA/Tween20 buffer was added to the sample. Testing targeted three SARS-CoV-2 specific genes (ORF, N, and S) using the Thermo Fisher Scientific TaqPath COVID-19 Combo Kit on RT-qPCR platforms [18].
- Swab Sample Processing: Swabs in viral transport media were vortexed. RNA extraction was performed using automated systems like the MGISP-960 instrument with the MGI Easy Nucleic Acid Extraction Kit. Subsequent detection of viral RNA was performed using approved RT-qPCR kits, such as the SARS-CoV-2 EDx kit (Bio-Manguinhos-FIOCRUZ) targeting the E gene [19].
Mechanistic Insights: Visualizing Sampling Site Efficacy
The differential performance of sampling sites is not arbitrary but is governed by the underlying biological and temporal dynamics of respiratory infections. The following diagram synthesizes findings from the research to illustrate the key factors and relationships that determine efficacy.
Interpretation of Mechanistic Relationships
The diagram above illustrates the complex interplay between fundamental factors and the resulting biological evidence that collectively determine sampling efficacy:
- Temporal Dynamics: The shifting sensitivity of saliva throughout infection phases and the different viral load peaks between saliva and nasal sites demonstrate that optimal sampling is time-dependent [18] [19]. This evidence challenges static testing approaches.
- Methodological Impact: Significant differences in analyte recovery between standard swabs and alternative methods like expanding sponges highlight how collection technology directly influences test sensitivity [7].
- Population Considerations: The extremely high refusal rate for invasive swabbing in pediatric populations creates a practical barrier that can override theoretical diagnostic sensitivity, necessitating alternative approaches [20].
These relationships collectively support the central conclusion that site selection must be a deliberate, context-dependent decision rather than a default to traditional methods.
The Scientist's Toolkit: Essential Research Reagents and Materials
Selecting appropriate collection materials is paramount to ensuring sample quality and assay reliability. The following table details key solutions and their applications in sampling research.
Table 3: Essential Research Reagents and Sampling Materials
| Reagent/Material | Function & Application | Examples & Specifications |
|---|---|---|
| Universal Transport Medium (UTM) | Preserves viral integrity during transport for molecular analysis. | Copan UTM; used for storing swabs/sponges after collection [7]. |
| Flocked Swabs | Improved sample release and cellular collection for enhanced sensitivity. | Nylon flocked swabs (e.g., Copan Diagnostics) for nasopharyngeal sampling [7]. |
| Expanding Sponges | Absorbs mucosal lining fluid more effectively than swabs for antibody detection. | Polyvinyl alcohol sponge (e.g., PVF-J, Beijing Yingjia) [7]. |
| Proteinase K & Lysis Buffers | Digest proteins and inactivate nucleases for nucleic acid extraction from saliva. | Component of saliva processing kits (e.g., SalivaDirect) [18]. |
| Nucleic Acid Extraction Kits | Isolate and purify viral RNA/DNA from complex sample matrices. | MGI Easy Nucleic Acid Extraction Kit [19]; Magmax Viral/Pathogen Kit [21]. |
| RT-qPCR Master Mixes | Enable reverse transcription and amplification of viral targets for detection. | Thermo Fisher TaqPath COVID-19 Combo Kit [18]; SARS-CoV-2 EDx kit [19]. |
The comparative analysis of oropharyngeal and nasal swab sampling reveals a landscape far more complex than a simple hierarchical ranking. The evidence consistently demonstrates that sampling efficacy is not one-size-fits-all but is influenced by a constellation of factors including pathogen kinetics, disease stage, collection methodology, and patient population. Saliva emerges as a superior option for early infection detection and in settings prioritizing patient comfort and self-collection, while nasal sampling may provide complementary value at different disease stages.
For researchers and drug development professionals, these findings carry significant implications:
- Protocol Design: Studies must explicitly justify sampling site selection based on the research question rather than defaulting to historical standards.
- Method Standardization: Cross-study comparability requires detailed reporting of collection techniques, including swab type, duration, and anatomical precision.
- Future Development: Investment in novel sampling technologies like expanding sponges and standardized mucosal antibody assays is crucial to advancing diagnostic and therapeutic development [7].
Addressing these evidence gaps with rigorous, context-aware sampling strategies will enhance the validity of research outcomes and accelerate the development of more effective diagnostics and therapeutics for respiratory pathogens and beyond.
Standardized Protocols for Oropharyngeal and Nasal Swab Collection
The accurate diagnosis of respiratory infections relies heavily on the quality of specimen collection. Within the context of comparative sensitivity research for oropharyngeal (throat) versus nasal swab sampling, the oropharyngeal (OP) swab represents a less invasive, often more tolerable alternative for patients, particularly in pediatric populations [11]. While the nasopharyngeal (NP) swab is often considered the clinical standard for respiratory virus testing, its collection can be uncomfortable and requires trained healthcare personnel [22] [23]. This guide objectively compares the performance of oropharyngeal swabs with other sampling methods, presenting supporting experimental data to inform researchers, scientists, and drug development professionals.
Evidence suggests that the diagnostic yield of oropharyngeal samples can be comparable to, and in some cases superior for certain pathogens, than other sampling methods. For instance, one study found that for the detection of Mycoplasma pneumoniae, a common and treatable cause of childhood pneumonia, oropharyngeal-nasal (ON) swabs demonstrated a sensitivity of 94%, significantly higher than the 64% sensitivity of nasopharyngeal swabs [11]. Furthermore, the acceptability of the procedure is markedly higher; parents and caregivers rated oropharyngeal-nasal swabs as more acceptable than nasopharyngeal swabs (median score of 4.5 vs. 2 on a 5-point Likert scale) [11]. This combination of patient comfort and robust diagnostic performance for specific pathogens positions the oropharyngeal swab as a critical tool in the respiratory pathogen diagnostic arsenal.
Comparative Experimental Data: Oropharyngeal vs. Alternative Methods
The following tables summarize key experimental data from recent studies comparing the performance of oropharyngeal-inclusive swabs against the standard nasopharyngeal swab for detecting various respiratory pathogens.
Table 1: Diagnostic Sensitivity and Specificity of Oropharyngeal-Inclusive Swabs vs. Nasopharyngeal (NP) Swabs
| Pathogen | Swab Type | Sensitivity (95% CI) | Specificity (95% CI) | Study Details |
|---|---|---|---|---|
| Influenza (A & B) | Self-collected Oral-Nasal [22] | 0.67 (0.49–0.81) | 0.96 (0.89–0.99) | Reference: HCW-collected NP swab |
| RSV | Self-collected Oral-Nasal [22] | 0.75 (0.43–0.95) | 0.99 (0.93–1.00) | Reference: HCW-collected NP swab |
| Mycoplasma pneumoniae | Caregiver-collected Oropharyngeal-Nasal (ON) [11] | 0.94 (0.86–0.98) | Not Reported | Composite reference standard used |
| SARS-CoV-2 | Self-collected Nasal & Rhinoswab [24] | 0.90–0.95 | >0.95 | Reference: HCW-collected combined nose/throat swab |
Table 2: Acceptability and Agreement Metrics Across Swab Types
| Swab Type | Patient Acceptability (Median Score) | Agreement with NP (Kappa) | Key Findings | Source |
|---|---|---|---|---|
| Caregiver-collected ON | 4.5 (IQR 4-5) [11] | Not Reported | Superior detection of M. pneumoniae; high feasibility in children. | [11] |
| HCW-collected NP | 2 (IQR 1-3) [11] | N/A | Current clinical standard but less acceptable. | [11] |
| Self-collected Oral-Nasal for RSV | Feasible, minimal instruction [22] | 0.79 (0.56–0.92) | Not a substitute for NP swab primarily due to suboptimal Influenza sensitivity. | [22] |
| Self-collected Oral-Nasal for Influenza | Feasible, minimal instruction [22] | 0.68 (0.52–0.80) | Not a substitute for NP swab primarily due to suboptimal Influenza sensitivity. | [22] |
Detailed Experimental Protocols for Comparative Studies
To ensure the reproducibility of comparative sensitivity studies, the following details the methodologies employed in key cited research.
Protocol 1: Validation of Self-Collected Oral-Nasal Swabs
This study aimed to validate a self-collected oral-nasal swab for detecting Influenza and RSV against a provider-collected NP swab [22].
- Study Population & Design: Consecutive adults presenting to an emergency department with suspected viral upper respiratory tract infections were included. Participants self-collected an oral-nasal swab, which was compared to a provider-collected NP swab taken as part of routine care [22].
- Specimen Collection:
- Self-collected Oral-Nasal Swab: Individuals used a disposable flocked swab to self-swab the anterior aspect of both nares, the buccal mucosa, and the tongue [22].
- Provider-collected NP Swab: Collected by a healthcare worker following standard clinical procedures.
- Laboratory Analysis: All specimens were placed in universal transport media. Nucleic acid extraction was performed using an automated instrument with a viral nucleic acid kit. Detection of viral targets (Influenza A, Influenza B, RSV, SARS-CoV-2) was performed using a laboratory-developed real-time reverse-transcription PCR (RT-PCR) assay [22].
- Statistical Analysis: Performance characteristics (sensitivity and specificity) were calculated for each virus using the NP swab as the reference standard. The kappa coefficient was used to estimate agreement between the two methods [22].
Protocol 2: Evaluation of Parent-Collected Oropharyngeal-Nasal (ON) Swabs in Children
This study evaluated the diagnostic yield and acceptability of parent-collected ON swabs compared to HCW-collected NP swabs in symptomatic children [11].
- Study Population & Design: Symptomatic children (0–4 years) presenting to a pediatric emergency department provided a HCW-collected NP swab and a caregiver-collected ON swab [11].
- Specimen Collection:
- Caregiver-collected ON Swab: Parents/caregivers collected the ON swab using written instructions. The method involved swabbing both tonsillar pillars and the posterior oropharynx, followed by both anterior nares, using a single flocked swab [11].
- HCW-collected NP Swab: Collected by a healthcare worker following standard clinical procedures.
- Laboratory Analysis: In the research phase, NP swabs were tested using the BioFire RP2.1 respiratory panel. Both ON and NP swabs were tested using the GeneXpert SARS-CoV-2/Influenza A+B/RSV assay. In a subsequent implementation phase, both sample types were tested on the BioFire RP2.1 panel [11].
- Acceptability Assessment: After collection, parents/caregivers rated the acceptability of each method using a 5-point Likert scale (1=unacceptable, 5=acceptable) [11].
Step-by-Step Oropharyngeal Swab Collection Procedure
Proper technique is critical for obtaining a quality specimen. The following procedure, synthesizing best practices from clinical guidelines and study protocols, should be performed by a trained healthcare provider [5] [23].
Table 3: Research Reagent Solutions and Essential Materials
| Item | Function/Description |
|---|---|
| Flocked or Synthetic Fiber Swab | Swabs with synthetic tips and plastic or wire shafts are recommended. Calcium alginate or swabs with wooden shafts should be avoided as they may contain substances that inactivate viruses and inhibit molecular tests [5]. |
| Universal Transport Media (UTM) | A liquid viral transport medium that preserves virus viability and nucleic acids for transport to the laboratory. |
| Sterile Leak-Proof Specimen Container | A tube designed to contain the swab and transport media, ensuring specimen integrity and biohazard safety during transport [25]. |
| Personal Protective Equipment (PPE) | Includes gloves, gown, eye protection, and an N95 or higher-level respirator (or face mask) to protect the healthcare collector from exposure [5]. |
- Preparation: Confirm the patient's identity. Wash hands thoroughly and don appropriate personal protective equipment (PPE). Assemble the swab in its sterile packaging, the specimen tube containing transport media, and a biohazard bag [25] [5].
- Positioning: Ask the patient to sit upright and open their mouth wide. For better visualization, especially in patients with a difficult-to-see oropharynx, use a tongue depressor to gently hold the tongue down [23].
- Swab Insertion: Carefully remove the swab from its packaging, handling it only by the distal end to maintain sterility. Insert the swab into the patient's oral cavity [25].
- Sample Collection: Systematically swab the target areas to ensure adequate cellular collection [23]:
- Posterior Oropharynx: Rub the swab over the mucosal surface of the posterior wall of the throat.
- Tonsillar Areas: Swab both tonsillar pillars (the anterior and posterior folds) and the tonsils themselves (if present). Swab the area behind the tonsillar pillars as well.
- Base of Tongue: Gently swab the base of the tongue.
- Avoid touching the patient's teeth, gums, tongue, or cheeks, as this can contaminate the specimen with bacteria and inhibit PCR reactions [25] [23].
- Specimen Placement: Remove the swab from the mouth without touching any other surfaces. Open the transport media tube and insert the swab tip-first. Break the swab's shaft at the scored breakpoint against the tube's rim, allowing the swab head to remain in the media. Discard the broken handle and close the tube tightly [25].
- Labeling and Storage: Label the tube with the patient's identifying information, date, time, and specimen source (e.g., "OP"). Place the tube into a biohazard bag. Store and transport the specimen at the temperature recommended by the testing laboratory, typically 2-8°C, and ensure it is tested as soon as possible after collection [25] [5].
Workflow and Technical Considerations
The following diagram illustrates the logical workflow and key decision points in a comparative study design for evaluating oropharyngeal swabs.
Comparative Study Workflow
Technical Pitfalls and Anatomical Considerations
- Inadequate Sampling: A primary reason for false-negative results is failing to swab the correct anatomical sites. Swabbing only the oral mucosa, tongue, or tonsils in isolation is insufficient. The swab must make contact with the posterior oropharynx and bilateral tonsillar regions [23].
- Contamination: The swab tip contacting the tongue, teeth, or gums introduces contaminants that can interfere with nucleic acid amplification tests, potentially leading to false negatives or inhibition of the PCR reaction [25] [23].
- Gag Reflex: The procedure can stimulate the gag reflex, causing the patient to cough or gag. This can lead to the production of aerosols and discomfort. Instructing the patient to breathe slowly and deeply through the nose can help mitigate this response. Using a swift but thorough technique is also beneficial [23].
- Variable Viral Shedding: The sensitivity of oropharyngeal swabs can be influenced by the pathogen and the stage of infection. Some viruses may replicate and shed more in the nasopharynx than in the oropharynx, which can explain performance differences observed in comparative studies [22].
The accurate detection of respiratory pathogens like SARS-CoV-2 relies heavily on proper specimen collection techniques. Anterior nasal (AN) and nasal mid-turbinate (NMT) swabs have emerged as less invasive alternatives to nasopharyngeal (NP) swabs, balancing patient comfort with diagnostic sensitivity. Within the broader research on comparative sensitivity of oropharyngeal versus nasal swab sampling, understanding the standardized procedures for these nasal methods is fundamental. These sampling sites are particularly relevant for detecting pathogens that replicate in the nasal epithelium, and their performance is a critical variable in diagnostic test evaluations and clinical trial outcomes [26] [3]. This guide details the best practices for AN and NMT swab collection, providing researchers with standardized protocols to ensure specimen quality and data reliability.
Comparative Performance of Nasal Swab Types
Extensive research has evaluated the diagnostic performance of different upper respiratory specimen types. The table below summarizes key comparative data from recent clinical studies.
Table 1: Diagnostic Performance of Anterior Nasal and Nasal Mid-Turbinate Swabs
| Swab Type | Reference Standard | Sensitivity (%) | Specificity (%) | Study Details |
|---|---|---|---|---|
| Anterior Nasal (AN) | NP RT-PCR | 80.7 [3] | 99.6 [3] | RT-PCR testing with Rhinoswab [3] |
| Anterior Nares (AN) | NP RT-PCR | 85.6 (Sure-Status Ag-RDT) [26] | 99.2 (Sure-Status Ag-RDT) [26] | Symptomatic participants, drive-through test center [26] |
| Anterior Nares (AN) | NP RT-PCR | 79.5 (Biocredit Ag-RDT) [26] | 100 (Biocredit Ag-RDT) [26] | Symptomatic participants, drive-through test center [26] |
| Nasal Mid-Turbinate (NMT) | NP Swab | Sensitivity considered "equivalent" to NP for Ag-RDTs [5] | Specificity considered "equivalent" to NP for Ag-RDTs [5] | CDC recommendation based on clinical evaluations [5] |
Table 2: Anatomical and Procedural Characteristics of Nasal Swab Types
| Characteristic | Anterior Nasal (AN) Swab | Nasal Mid-Turbinate (NMT) Swab | Nasopharyngeal (NP) Swab |
|---|---|---|---|
| Insertion Depth | 1-1.5 cm [5] [27] | ~2 cm or until resistance is met [5] [27] | ~7 cm or until resistance [28] [27] |
| Collection Site | Nasal wall (anterior nares) [5] | Middle of the inferior turbinate [27] | Posterior nasopharynx [28] |
| Typical Procedure Time | ~15 seconds per nostril [5] | Several rotations against nasal wall [5] | Several seconds to absorb secretions [5] |
| Patient Discomfort | Generally low | Moderate | Higher, can be uncomfortable [28] |
| Suitability for Self-Collection | Yes [5] [3] | Yes, with instruction [5] | No, requires trained healthcare provider [5] |
Research indicates that while the diagnostic accuracy of AN swabs is high and often equivalent to NP swabs for antigen tests, some studies note a lower test line intensity on rapid antigen tests when using AN swabs compared to NP swabs. This highlights the importance of proper technique to maximize viral material collection and could potentially influence result interpretation by lay users [26].
Step-by-Step Collection Procedures
Anterior Nasal (AN) Swab Collection
The anterior nasal swab samples the mucosal surface within the anterior nares (nostrils). The CDC and clinical studies outline the following procedure, which can be performed by a healthcare provider or a patient after reviewing instructions [5].
Detailed Protocol:
- Patient Positioning: Instruct the patient to sit comfortably with their head tilted slightly back at approximately 70 degrees [5].
- Swab Selection: Use a sterile synthetic fiber swab (e.g., polyester, nylon, or Dacron). Avoid swabs with wooden shafts or calcium alginate tips, as they may contain substances that inactivate viruses or inhibit molecular tests [5]. The Rhinoswab, a double-loops nylon-flocked swab, is an example of a specialized device for this purpose [3].
- Swab Insertion: Gently insert the entire collection tip of the swab (typically ½ to ¾ of an inch, or 1 to 1.5 cm) into one nostril, parallel to the palate (not upwards) [5] [27].
- Specimen Collection: Firmly sample the nasal wall by rotating the swab in a circular path against the nasal wall at least 4 times. The collection process should take approximately 15 seconds to ensure adequate saturation of the swab. Be sure to collect any nasal drainage that may be present [5].
- Repeat Procedure: Using the same swab, repeat the identical collection process (steps 3-4) in the other nostril [5].
- Specimen Placement: Carefully place the swab, tip first, into the transport tube provided. Ensure the tube contains the appropriate transport medium for the subsequent test (e.g., viral transport media for RT-PCR) [5].
- Packaging and Transport: Follow laboratory-specific instructions for packaging and transporting the specimen, maintaining the cold chain if required.
Nasal Mid-Turbinate (NMT) Swab Collection
The NMT swab is inserted deeper than the AN swab to sample the middle region of the inferior turbinate. The mean endoscopic insertion depth to this site is approximately 4.2 cm from the vestibulum nasi, though this can vary with anatomy [27].
Detailed Protocol:
- Patient Positioning: Have the patient sit with their head tilted back at a 70-degree angle [5].
- Swab Selection: Use a tapered swab designed for nasal mid-turbinate sampling. The swab should have a flexible shaft (plastic or wire) and a synthetic tip [5].
- Swab Insertion: While gently rotating the swab, insert it less than 1 inch (about 2 cm) into one nostril, following the path parallel to the palate (not angled upwards) until resistance is met at the turbinates [5].
- Specimen Collection: Rotate the swab several times against the nasal wall at the point of resistance to ensure adequate specimen collection from the mucosal surface.
- Repeat Procedure: Withdraw the swab slightly, then gently advance it into the other nostril using the same swab. Repeat the rotation against the nasal wall in the second nostril [5].
- Specimen Placement: Place the swab, tip first, into the designated transport tube and snap or cut the applicator stick to secure the lid, if applicable [5].
- Packaging and Transport: Package the specimen according to testing laboratory requirements for transport.
Key Differences in Technique
The primary distinctions between the two methods lie in the depth of insertion and the specific anatomical site being sampled. The AN swab collects from the readily accessible anterior nares, while the NMT swab requires deeper insertion to contact the turbinate, a bony structure lined with respiratory epithelium that projects into the nasal cavity [29]. Proper training is essential for NMT collection to ensure the swab reaches the intended site without causing discomfort or trauma.
Experimental Protocols for Comparative Studies
To ensure the validity of research comparing nasal swab sensitivities, especially against oropharyngeal or NP standards, a rigorous and standardized protocol must be followed. The following workflow, derived from published methodologies, outlines a robust framework for such evaluations [26] [3].
Diagram: Experimental Workflow for Comparative Swab Studies
Detailed Methodology:
Study Population and Ethics:
- Recruit a cohort of symptomatic individuals presenting for testing (e.g., at a drive-through test center or emergency department) [26] [3].
- Obtain informed consent and record demographic and clinical data, including symptom onset and vaccination status. The study must be approved by an institutional review board or ethics committee [26] [3].
Specimen Collection Workflow (Critical for Validity):
- To avoid contamination of the nasal site by viral material from the nasopharynx, always collect the AN or NMT sample before the OP/NP sample [3].
- Collect all swabs from a single participant within a short timeframe. Trained healthcare workers should perform the collection, or supervise self-collection, to ensure protocol adherence [26].
- For head-to-head comparisons of swab types for the same test (e.g., Ag-RDT), collect paired swabs—one AN and one NP—from the same participant. The NP swab for the reference standard should be collected from one nostril, and the swab for the index test (e.g., AN or another NP) from the other nostril [26].
Sample Processing and Laboratory Analysis:
- Place swabs immediately into viral transport media (VTM) [26] [3].
- Transport samples to the laboratory in cooler bags and process them promptly, often within 24 hours, freezing at -20°C or -80°C if analysis is delayed [3] [30].
- Analyze all samples using a validated RT-PCR assay as the reference standard. The RNA extraction and PCR protocols should be consistent across all samples [26] [3]. A common approach is to use systems like the MagNa Pure96 for RNA extraction and LightCycler 480 II for RT-PCR, with a cycle threshold (Ct) value below 40 defined as positive [3].
- For Ag-RDT evaluations, perform the rapid tests according to the manufacturer's instructions, ideally with two blinded operators reading the results to minimize bias. A third operator can act as a tiebreaker for discrepant readings [26].
Data Analysis and Statistics:
- Calculate sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) for the index test (AN/NMT) against the reference standard (OP/NP RT-PCR), including 95% confidence intervals [26] [3].
- Assess the level of agreement between different swab types using Cohen’s kappa (κ) statistic [26].
- Perform sub-analyses based on viral load (Ct-value ranges), days since symptom onset, and vaccination status using appropriate statistical tests (e.g., Mann-Whitney U test, chi-square test) [26] [3].
- Determine the limit of detection (LoD) for different swab types using logistic regression with RNA copy numbers [26].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Research Reagents and Materials for Nasal Swab Studies
| Item | Function/Description | Example Brands/Types |
|---|---|---|
| Sterile Synthetic Swabs | Collects specimen without inhibiting tests; type depends on site (AN, NMT, NP). | Puritan UniTranz-RT; Rhinoswab; Cyto-Soft brush for specialized RNA collection [3] [28] [30] |
| Viral Transport Media (VTM) | Preserves viral integrity and nucleic acids during transport. | Copan UTM; Mantacc VTM; Universal Transport Media [26] [3] |
| RNA Extraction Kit | Isolates viral and human RNA from the specimen for RT-PCR. | QIAamp 96 Virus QIAcube HT kit; miRNeasy Mini Kit; easyMAG system [26] [3] [30] |
| RT-PCR Assay Master Mix | Amplifies and detects target viral RNA sequences. | TaqPath COVID-19; Fast Viral Master mix; One-Step RT-ddPCR Advanced Kit [26] [3] [28] |
| Ag-RDT Test Kits | For rapid antigen detection performance comparisons. | Sure-Status COVID-19 Antigen Card Test; Biocredit COVID-19 Antigen Test [26] |
| Droplet Digital PCR (ddPCR) | Provides absolute quantification of viral load with high precision, used for LoD studies. | BioRad QX200 Droplet Reader and related reagents [28] |
| Next-Generation Sequencing (NGS) | For comprehensive genomic studies (e.g., host response, variant detection). | TruSeq RNA Access Library Prep; Illumina NextSeq instruments [30] |
Mastering the step-by-step procedures for anterior nasal and nasal mid-turbinate swab collection is fundamental for diagnostic researchers and clinicians. The experimental data demonstrate that when performed correctly, these less invasive methods can achieve diagnostic accuracy comparable to nasopharyngeal swabbing for SARS-CoV-2 detection, particularly with RT-PCR and certain Ag-RDTs [26] [3]. Adherence to the detailed protocols for specimen collection, paired with the rigorous experimental design outlined for comparative studies, ensures the generation of high-quality, reliable data. This evidence base is crucial for informing public health testing strategies and for the development of future diagnostic solutions for respiratory pathogens.
The critical need for widespread diagnostic testing during the COVID-19 pandemic exposed significant limitations of traditional nasopharyngeal (NP) swab collection, including healthcare worker (HCW) exposure risk, supply chain shortages, and patient discomfort [31] [32]. These challenges accelerated the validation of patient-collected methods, with saline gargle and combined oropharyngeal/nares (OP/N) swabs emerging as promising alternatives. This review synthesizes evidence from comparative clinical studies to evaluate the performance characteristics of these methods against the reference standard NP swab, providing researchers and clinicians with objective data on their diagnostic reliability and implementation feasibility.
Comparative Performance Data
Sensitivity Relative to Nasopharyngeal Swabs
Multiple studies have directly compared the sensitivity of alternative specimen types to NP swabs for SARS-CoV-2 detection using nucleic acid amplification testing. The table below summarizes pooled sensitivity estimates from meta-analyses and individual comparative studies:
Table 1: Comparative sensitivity of alternative specimen types for SARS-CoV-2 detection
| Specimen Type | Collection Method | Sensitivity (95% CI) | Reference Standard |
|---|---|---|---|
| Saline Gargle | Self-collected | 90% (86-94%) | NP Swab [31] |
| Saline Gargle | Self-collected | 93.8-96.9%* | HCW-collected OP/N [33] |
| OP/N Swab | Self-collected | 100% (92.6-100%) | HCW-collected OP/N [33] |
| OP/N Swab | Self-collected | 87% (77-93%) | NP Swab [31] |
| Oral Swab | Self-collected | 82% (72-89%) | NP Swab [31] |
| Nasal Swab | HCW-collected | 82% (73-90%) | NP Swab [34] |
| Oropharyngeal Swab | HCW-collected | 84% (57-100%) | NP Swab [34] |
| Combined OP/NS | HCW-collected | 97% (90-100%) | NP Swab [34] |
*Sensitivity range varies by molecular platform: 93.8% for LDT, 96.8% for Cobas 6800, 96.7% for Panther assay
Cycle Threshold Value Comparisons
Viral load measurements provide additional insights into test performance characteristics:
Table 2: Cycle threshold (Ct) value comparisons between specimen types
| Specimen Type | Concordant Specimens Median Ct | Discordant Specimens Median Ct | P-value |
|---|---|---|---|
| Saline Gargle | 17 | 31 | < 0.001 [31] |
| Oral Swab | 17 | 28 | < 0.001 [31] |
| Oral-Anterior Nasal Swab | 18 | 31 | 0.007 [31] |
Higher Ct values in discordant specimens (those testing negative despite a positive NP swab) suggest that sensitivity is strongly associated with viral load, with alternative methods performing best in cases with higher viral loads.
Detailed Experimental Protocols
Self-Collection Protocol for Saline Gargle
The saline gargle method follows a standardized protocol to ensure consistency and diagnostic performance:
Patient Preparation: Patients should abstain from eating, drinking, smoking, chewing gum, and brushing teeth for at least one hour prior to collection [33].
Collection Process:
- Patients empty a 5 mL container of 0.9% sterile saline into the mouth
- Perform three alternating cycles of:
- Swishing saline in cheeks (5 seconds each cycle)
- Gargling in the posterior oropharynx (5 seconds each cycle)
- Total collection time is approximately 30 seconds [33]
Specimen Handling: The gargle is expelled into a sterile specimen container and refrigerated until processing, ideally within 12 hours of collection [33].
This protocol demonstrated high sensitivity (93.8-96.9% across platforms) compared to HCW-collected OP/N swabs, with slightly increased Ct values (1.2-1.6 cycles) suggesting marginally lower viral recovery but maintaining clinical utility [33].
Combined Oropharyngeal/Nares (OP/N) Swab Collection
The OP/N swab protocol enables comprehensive sampling of both oral and nasal compartments:
Figure 1: Workflow for combined oropharyngeal/nares (OP/N) swab collection
Both self-collected and HCW-collected OP/N swabs demonstrate equivalent sensitivity (100% in direct comparisons), making this method particularly suitable for unsupervised self-collection scenarios [33]. The dual-site sampling strategy likely contributes to its robust performance by capturing virus from multiple anatomical sites where SARS-CoV-2 replicates.
Method Selection Framework
The choice between saline gargle and OP/N swab methods depends on research objectives, population characteristics, and resource constraints:
Figure 2: Decision framework for selecting between saline gargle and OP/N swab methods
Research Reagent Solutions
Successful implementation of these methods requires specific reagents and collection materials:
Table 3: Essential research reagents and materials for alternative collection methods
| Reagent/Material | Specification | Function | Method Compatibility |
|---|---|---|---|
| Sterile Saline | 0.9% sodium chloride | Gargle medium; maintains viral integrity | Saline Gargle |
| Foam-tipped Swabs | Polyurethane foam head, plastic shaft | Dual-site sampling without trauma | OP/N Swab |
| Transport Medium | Phosphate-buffered saline (PBS) pH 7.4 | Preserves viral RNA during transport | OP/N Swab |
| Specimen Containers | Sterile, leak-proof containers | Secure specimen transport | Both Methods |
| RNA Stabilization Buffer | Guanidinium thiocyanate-based | Preserves nucleic acids for delayed processing | Both Methods |
The validation of saline gargle and combined OP/N swab methods represents a significant advancement in respiratory pathogen detection methodologies. Both approaches demonstrate favorable sensitivity profiles compared to NP swabs while offering distinct advantages in terms of patient comfort, reduced healthcare worker exposure, and suitability for self-collection. The choice between methods should be guided by specific research requirements, population characteristics, and laboratory processing capabilities. As molecular diagnostics continue to evolve, these alternative collection methods provide valuable tools for pandemic preparedness and broader respiratory pathogen surveillance.
The accurate detection of pathogens like SARS-CoV-2 relies on a complex chain of laboratory procedures, beginning the moment a sample is collected. For researchers and drug development professionals, understanding the nuances of this workflow—from the initial choice of sampling site to the final amplification of nucleic acids—is critical for interpreting data, designing assays, and developing new diagnostics. This guide objectively compares the performance of two common sampling methods, oropharyngeal swabs (OPS) and nasal swabs (including nasopharyngeal/NPS and anterior nasal), within the context of a broader thesis on comparative sensitivity. We present supporting experimental data and detailed methodologies to provide a clear, evidence-based resource for the scientific community.
Comparative Performance of Oropharyngeal and Nasal Swabs
The choice between oropharyngeal and nasal swabs can significantly impact the sensitivity and reliability of downstream molecular tests. The following table summarizes key performance metrics from recent clinical studies.
Table 1: Comparative Diagnostic Performance of Swab Types for SARS-CoV-2 Detection
| Study & Population | Swab Type | Sensitivity (%) | Specificity (%) | Agreement with Reference | Key Findings |
|---|---|---|---|---|---|
| Symptomatic Patients (2023, n=737) [18] | Anterior Nasal (RT-qPCR) | Reference | - | - | A total of 120 participants tested positive in at least one test. |
| Saliva (RT-qPCR) | 94.0 PPA* (95% CI: 88.9–99.1) | 99.0 NPA (95% CI: 98.1–99.9) | High within 5 days of symptom onset | Viral load in saliva decreased beyond day 1 of symptoms. | |
| Symptomatic Patients in Brazil (2021-2022, n=72) [19] | Nasopharyngeal (NPS) | Reference | - | - | Longitudinal study analyzing 285 paired samples. |
| Saliva (RT-qPCR) | 69.2 overall (95% CI: 57.2–79.5); 82.0 in early infection | 96.6 (95% CI: 92.9–98.7) | 91.6% (κ = 0.78) | Sensitivity varied by infection phase (40%-82%). Saliva detected late-stage infections missed by NPS. | |
| Hospitalized COVID-19 Patients (2020, n=120) [8] | Nasopharyngeal (NPS) | 46.7 (Detection Rate) | - | - | Prospective study of inpatients. |
| Oropharyngeal (OPS) | 10.0 (Detection Rate) | - | Poor | NPS had significantly higher detection rate and viral load (lower mean Ct) than OPS. | |
| Patients in China (2020, n=353) [35] | Nasopharyngeal (NPS) | 19.0 (Detection Rate) | - | - | Review of medical records from inpatients and outpatients. |
| Oropharyngeal (OPS) | 7.6 (Detection Rate) | - | Poor (Kappa = 0.308) | NPS showed a higher positive rate, especially in inpatients. Combining both swabs slightly increased the detection rate. |
PPA: Positive Percent Agreement; *NPA: Negative Percent Agreement
Experimental Protocols for Key Studies
Protocol: Prospective Comparison of Saliva vs. Nasal Swab in Symptomatic Individuals
This 2023 study provides a direct, head-to-head comparison in a symptomatic population during the endemic phase [18].
- Sample Collection: Matched saliva and anterior nasal swab samples were collected from 737 symptomatic participants. Saliva (1-2 mL) was collected first via drool into a preservative-free tube. Subsequently, a nasal swab was collected using a Roche cobas PCR Uni swab by inserting it approximately one inch inside the nostril, rotating five times for 10-15 seconds per nostril [18].
- Sample Transport & Storage: Saliva samples were transported at room temperature and tested within 48 hours, leveraging the demonstrated stability of SARS-CoV-2 in raw saliva during this window [18].
- Sample Pre-processing: Saliva samples were heated at 95°C for 30 minutes. A Tris/borate/EDTA/Tween20 buffer was then added at a 1:1 ratio [18].
- Nucleic Acid Amplification: Processed samples were tested using the Thermo Fisher Scientific TaqPath COVID-19 Combo Kit, targeting three SARS-CoV-2 genes (ORF, N, and S) via RT-qPCR [18].
Protocol: Longitudinal Diagnostic Accuracy of Saliva vs. NPS
This longitudinal study in Brazil tracked symptomatic individuals across multiple time points to capture dynamic changes in test performance [19].
- Sample Collection: Participants provided paired NPS and saliva specimens. For saliva, individuals were asked to bring up saliva from the back of the throat and spit at least 3 mL into a sterile tube. NPS were collected by rubbing and rotating a swab in the nasopharynx for 10 seconds [19].
- Sample Transport: All samples were refrigerated immediately after collection and transported to the testing laboratory within 24 hours [19].
- Nucleic Acid Extraction: Total viral RNA was extracted from a 200 µL input volume of each sample using an MGISP-960 automated system and the MGI Easy Nucleic Acid Extraction Kit. RNA was eluted in 30 µL of ultrapure H₂O [19].
- Nucleic Acid Amplification: Extracted RNA was detected using the SARS-CoV-2 EDx RT-qPCR kit (Bio-Manguinhos-FIOCRUZ), which targets the SARS-CoV-2 E gene [19].
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the featured studies, highlighting their critical functions in the laboratory workflow.
Table 2: Essential Research Reagents and Materials for SARS-CoV-2 RT-qPCR Workflow
| Item | Function/Description | Example Products/Studies |
|---|---|---|
| Swab Types | Sample collection from specific anatomical sites. Material and design impact collection and release efficiency. | Polyester-tipped swabs [36], Nylon flocked swabs [37], Synthetic fiber swabs [8] |
| Transport Medium | Preserves viral integrity during transport from collection site to laboratory. | Viral Transport Medium (VTM) [36], Viral lysis buffer [38] |
| Automated Nucleic Acid Extraction System | Isolates and purifies viral RNA from the sample matrix, removing inhibitors. | MGISP-960 system [19], Tianlong PANA9600 system [35] |
| Nucleic Acid Extraction Kit | Contains lysing buffers and purification reagents optimized for the extraction system. | MGI Easy Nucleic Acid Extraction Kit [19], QIAamp Viral RNA Mini Kit [36] |
| RT-qPCR Master Mix | Provides enzymes, dNTPs, and buffers for the reverse transcription and amplification reactions. | AgPath-ID One-Step RT-PCR Kit [36], TaqPath COVID-19 Combo Kit [18] |
| Primers & Probes | Target-specific oligonucleotides that define the assay's specificity and enable fluorescent detection. | Targets: ORF1ab, N, S, E genes [18] [19] [8] |
Workflow Diagram: Comparative Swab Testing Pathway
The following diagram illustrates the logical workflow for a comparative study of oropharyngeal and nasal swab sampling, from participant enrollment through final data analysis.
Maximizing Diagnostic Yield: Overcoming Sampling Challenges and Variables
In molecular diagnostics, particularly for respiratory pathogens like SARS-CoV-2, the analytical phase of testing receives significant attention for quality control. However, the pre-analytical phase—encompassing sample collection, handling, and processing—introduces substantial variability that can critically impact test results [39]. For researchers and drug development professionals, understanding and controlling these variables is not merely procedural but fundamental to ensuring reliable, reproducible data for clinical trials and diagnostic development.
This guide examines the impact of three key pre-analytical variables: swab type, transport medium, and operator skill. The analysis is framed within the context of comparative sensitivity research for oropharyngeal (OP) versus nasal swab sampling, a subject of intense investigation during the COVID-19 pandemic. Variations in these factors can alter analyte stability, affect biomarker integrity, and ultimately determine the success or failure of downstream analytical processes [40]. Standardizing these elements is therefore a critical prerequisite for any robust diagnostic or research protocol.
Comparative Sensitivity of Oropharyngeal vs. Nasal Swab Sampling
The choice of sampling site is a primary pre-analytical decision. While nasopharyngeal swabs (NPS) have long been the gold standard for respiratory virus detection, their discomfort and technical requirement prompted the evaluation of alternatives.
Head-to-Head Diagnostic Sensitivity
A 2023 prospective study compared the sensitivity of oropharyngeal swabs (OPS), NPS, and nasal swabs performed by otorhinolaryngologists on 51 confirmed SARS-CoV-2-positive participants [2].
Table 1: Diagnostic Sensitivity of Different Swab Types for SARS-CoV-2 Detection
| Swab Type | Sensitivity (%) | 95% Confidence Interval | p-value vs. OPS |
|---|---|---|---|
| Oropharyngeal (OPS) | 94.1% | 87% to 100% | (Reference) |
| Nasopharyngeal (NPS) | 92.5% | 85% to 99% | 1.00 |
| Nasal Swab | 82.4% | 72% to 93% | 0.07 |
The study concluded that OPS achieved a sensitivity comparable to NPS, suggesting it is an equivalent alternative [2]. The lower sensitivity of nasal swabs alone indicates a potential limitation for this less invasive site.
The Case for Combined Sampling
Evidence strongly supports combined sampling to maximize sensitivity. The same study found that combining OPS and NPS detected SARS-CoV-2 in 100% of cases [2]. Another large study focusing on the Omicron variant reinforced this, finding that combined nose & throat samples had higher viral concentration and better sensitivity than either site alone [10]. If a single swab must be used, throat swab has a higher sensitivity than nose swabs for detecting the Omicron variant [10].
Viral Dynamics and Site-Specific Considerations
The optimal sampling site can be influenced by viral dynamics. Research on the Omicron variant showed that viral concentration (VC) in nose samples is more consistent over time than in throat samples, where VC declines faster in later infection stages [10]. This highlights the complexity of viral shedding patterns and suggests that the timing of sample collection relative to symptom onset may interact with the choice of sampling site.
The Impact of Swab Type on Sample Integrity
The physical design and material of the collection swab are critical pre-analytical variables that influence the amount of biological material collected and released for testing.
Swab Material and Design
Swabs are not interchangeable. They vary in tip material (e.g., flocked nylon, flocked polyester, foam, injection molded) and shaft design (flexible vs. rigid), which affect their performance [2] [41].
Performance Characteristics of Different Swabs
A 2023 study quantitatively compared the performance of several commercially available swabs using a benchtop anterior nasal cavity tissue model [41].
Table 2: Performance Characteristics of Different Swab Types
| Swab Type | Mass Uptake (Relative Performance) | Cellular-Mimicking Release (Relative Performance) | Volume Retention |
|---|---|---|---|
| Injection Molded | Low | High | Low |
| Nylon Flocked | High | Intermediate | High |
| Polyester Flocked | Intermediate | Low | High |
| Foam | Statistically Different from others | High | Low |
The study demonstrated statistically significant differences in performance across the different swab types [41]. Characteristics like low volume retention and high release capacity, as seen with the injection molded swabs, contributed to more consistent and reliable detection of viral material in pooled testing scenarios.
The Role of Transport Medium and Sample Stability
The transport medium and conditions following collection are essential for preserving the integrity of the analyte until testing.
Stability and Pre-Analytical Handling
The pre-analytical journey—including transportation, temporary storage, and processing—is intricate, and each step introduces variables that can affect the stability of the target analyte [42]. For molecular tests, this means preserving the integrity of nucleic acids like RNA from SARS-CoV-2. Delays in processing or exposure to adverse temperatures can lead to degradation and false-negative results. One review on cell-free DNA (cfDNA) highlights that variations in biospecimen processing (e.g., centrifuge models, spin speeds, spin times) can dramatically affect sample quality and composition [40]. While specific data on SARS-CoV-2 RNA stability in transport media is not detailed in the results, the fundamental principle is that establishing and adhering to validated stability conditions is mandatory.
Operator Skill and Standardized Protocols
The skill of the individual performing the sample collection is a human factor that can override the quality of all other materials used.
The Need for Standardization
Variations in sample collection technique directly impact diagnostic yield. To provide high-quality, standardized specimens, the 2023 study on OPS/NPS comparison used consultants or registrars in otorhinolaryngology to perform all swabs [2]. Their detailed, standardized protocols ensure consistency and are provided below.
Detailed Experimental Protocol for Swab Collection
The following methodology, adapted from a prospective diagnostic study [2], outlines the proper procedure for collecting upper respiratory specimens.
- Nasopharyngeal Swab (NPS): The patient's head is tilted slightly back. A flexible minitip flocked swab is inserted into the nasal cavity and pointed towards the earlobe of the patient following the floor of the nose. The swab is inserted approximately 8–11 cm deep until resistance is met at the posterior wall of the nasopharynx. The swab is left for a few seconds, rotated about three times, and withdrawn [2].
- Oropharyngeal Swab (OPS): A tongue depressor is used to improve visualization. A rigid-shaft flocked swab is used to collect specimen from both palatine tonsils and the posterior oropharyngeal wall with a painting and rotating movement, avoiding contact with the cheeks, teeth, or gums [2].
- Nasal Swab: The swab is inserted approximately 1–3 cm into the nasal cavity (not reaching the nasopharynx) and brushed along the septum and the inferior nasal concha, rotating about three times before withdrawal [2].
Diagram 1: Standardized workflow for upper respiratory specimen collection and processing.
Essential Research Reagent Solutions
The following table details key materials and their functions, as derived from the cited experimental protocols [2] [41].
Table 3: Research Reagent Solutions for Respiratory Specimen Collection
| Item | Function | Examples / Specifications |
|---|---|---|
| Flocked Swabs | Sample collection; superior release of cellular material compared to traditional wound fiber swabs. | Flexible minitip (for NPS), rigid-shaft (for OPS) [2]. |
| Viral Transport Medium (VTM) | Stabilizes virus and preserves nucleic acid integrity during transport and storage. | Typically contains proteins, antibiotics, and buffers [2]. |
| Nucleic Acid Extraction Kit | Isolves viral RNA from the sample matrix for downstream molecular analysis. | QIAamp Viral RNA Mini Kit [36]. |
| RT-PCR Master Mix | Performs reverse transcription and amplification of target viral genes. | Allplex SARS-CoV-2 Assay, AgPath-ID One-Step RT-PCR Kit [2] [36]. |
| Positive Controls | Validates the entire testing process, from extraction to amplification. | Synthetic or inactivated viral targets for genes like E, N, and RdRP [2] [36]. |
The body of evidence demonstrates that pre-analytical variables exert a profound influence on the outcomes of respiratory pathogen testing. The comparative sensitivity of oropharyngeal versus nasal sampling is not an absolute metric but is modulated by factors such as swab design, the use of combined sampling approaches, and the strict adherence to standardized collection protocols by trained operators. For researchers and drug development professionals, a meticulous focus on standardizing the entire pre-analytical workflow—from the patient to the laboratory—is not merely a matter of procedure but a fundamental requirement for generating reliable, reproducible, and clinically meaningful data.
The accurate detection of SARS-CoV-2, the virus responsible for the COVID-19 pandemic, has been a cornerstone of public health efforts worldwide. Real-time reverse-transcriptase-polymerase chain reaction (rRT-PCR) performed on upper respiratory tract specimens remains the most common confirmatory method. Historically, nasopharyngeal (NP) swabs have been considered the gold standard for sample collection due to the high viral load in the nasopharynx. However, NP sampling is technically challenging, requires trained healthcare personnel, causes significant patient discomfort, and has faced international supply shortages. These limitations have accelerated the search for effective alternatives and combination strategies that can maintain high diagnostic sensitivity while improving practicality and patient tolerance [43] [2].
This guide objectively examines the evidence for a powerful diagnostic strategy: combining swabs from different anatomical sites. We focus specifically on the comparative sensitivity of oropharyngeal (OP) swabs and nasal swabs against the NP standard, and critically evaluate the data demonstrating that combined approaches—such as OP/NP or oropharyngeal/nasal (OP/N)—can achieve superior detection rates. The synthesis of quantitative data and experimental protocols presented herein is designed to inform researchers, scientists, and drug development professionals in their diagnostic development and testing strategies.
Comparative Performance Data: Single vs. Combined Swab Strategies
Quantitative Synthesis of Diagnostic Sensitivity
The following tables consolidate key performance metrics from recent clinical studies, enabling a direct comparison of the sensitivity of various sampling methods and their combinations.
Table 1: Comparative sensitivity of different swab types for SARS-CoV-2 detection.
| Swab Type | Sensitivity (%) | Specificity (%) | Study Population (n) | Citation |
|---|---|---|---|---|
| Nasopharyngeal (NP) | 92.5 | - | 51 confirmed positive cases | [2] |
| Oropharyngeal (OP) | 94.1 | - | 51 confirmed positive cases | [2] |
| Nasal Swab | 82.4 | - | 51 confirmed positive cases | [2] |
| Combined OP/NP | 100.0 | - | 51 confirmed positive cases | [2] |
| Combined OP/Nasal | 96.1 | - | 51 confirmed positive cases | [2] |
| Combined Oropharyngeal/Nasal (OP/N) | 92.7* | - | 28 hospitalized patients | [43] |
| Nasopharyngeal (NP) | 89.3* | - | 28 hospitalized patients | [43] |
| Throat Only | 97.0 | - | 815 participants | [10] |
| Nose Only | 91.0 | - | 815 participants | [10] |
Sensitivity relative to bronchoalveolar lavage (BAL) fluid as a confirmatory test. *Sensitivity relative to a combined nose & throat swab as the reference standard.
Table 2: Discordance analysis between NP and OP swabs in a large cohort study (n=1125).
| Category | Concordant Positive Pairs | NP+/OP- Pairs | NP-/OP+ Pairs | Overall Concordance |
|---|---|---|---|---|
| All Participants | 306 (27.2%) | 217 (19.3%) | 187 (16.6%) | 64.1% |
| Age <20 years | Not specified | 49 (22.1%) | 30 (13.5%) | 143 (64.4%) |
| Age 21-40 years | Not specified | 112 (20.9%) | 103 (19.3%) | 320 (59.8%) |
| Age 41-60 years | Not specified | 40 (15.2%) | 40 (15.2%) | 183 (69.5%) |
Interpreting the Data Patterns
The evidence reveals several key patterns. First, single swab methods show variable performance. While one head-to-head study found OP swabs (94.1%) had a slightly higher sensitivity than NP swabs (92.5%), nasal swabs were less sensitive (82.4%) [2]. Another study found a "fair" agreement (kappa = 0.275) between individual NP and OP swabs, with a significant proportion of samples being positive on one type but negative on the other [44]. This inherent variability and discordance between single-site samples forms the rationale for combination strategies.
Second, and most critically, combining swabs from different sites significantly enhances detection. As shown in Table 1, the combination of OP and NP swabs achieved 100% sensitivity in one study, while the combination of OP and nasal swabs significantly boosted sensitivity to 96.1% compared to a nasal swab alone (82.4%) [2]. This is because the combined approach captures viral material from multiple independent reservoirs, mitigating the risk of a false negative that can occur if the virus is preferentially located in one site at a given time. A large study of 815 participants confirmed this principle, finding that a combined nose and throat swab had a higher viral concentration and was more effective than either swab type alone [10].
Experimental Protocols and Methodologies
To ensure the validity and reproducibility of comparative swab studies, standardized protocols for sample collection and processing are paramount. The following section details the methodologies employed in the key studies cited.
Sample Collection Procedures
Trained healthcare personnel, including otorhinolaryngologists, performed sample collections in many studies to minimize technical variability [44] [2].
- Nasopharyngeal (NP) Swab: The patient's head is tilted slightly back. A flexible minitip flocked swab is inserted into the nasal cavity and advanced along the floor of the nose towards the earlobe until resistance is met at the nasopharynx (approximately 8-11 cm deep). The swab is left in place for a few seconds, rotated 3 complete turns, and then withdrawn [2].
- Oropharyngeal (OP) Swab: A tongue depressor is used to improve visualization. A rigid-shaft flocked swab is used to rub the posterior oropharyngeal wall and both palatine tonsils in a painting and rotating movement, taking care to avoid touching the teeth, gums, or cheeks [2].
- Combined Oropharyngeal/Nasal (OP/N) Swab: The same swab is used sequentially. First, the oropharyngeal space is rubbed on both sides of the uvula. Then, without changing the swab, it is inserted into both nasal cavities until slight resistance is felt (mid-turbinate level), rotating it three complete turns [43]. The order of collection is critical; OP sampling should be performed before nasal sampling to avoid contaminating the oropharynx with viral material from the nasopharynx.
- Nasal Swab: A swab is inserted approximately 1-3 cm into the nasal cavity (anterior nares) and brushed along the nasal septum and inferior nasal concha, rotating it about three times before withdrawal [2].
Laboratory Analysis and rRT-PCR
After collection, swabs are placed in viral transport media (VTM) and transported to the laboratory under cold chain conditions [44].
- Nucleic Acid Extraction: Automated systems, such as the Kingfisher Flex Purification System with the MagMAX viral/Pathogen Nucleic Acid isolation kit, are commonly used for RNA extraction. An extraction control is often spiked into the sample to monitor extraction efficiency [44].
- rRT-PCR Assay: Extracted RNA is amplified using platforms like the Bio-Rad CFX 96. Commercial kits (e.g., Allplex 2019-nCoV Assay, Seegene) targeting SARS-CoV-2 genes (E, N, RdRp) are standard. The cycle threshold (Ct) cut-off for positivity is typically set at ≤40 cycles. The internal control (e.g., RNase P) is used to assess specimen quality and nucleic extraction integrity [44] [2].
The following diagram illustrates the logical relationship and workflow for determining a positive SARS-CoV-2 diagnosis using a combined sampling strategy.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key materials and reagents for respiratory swab studies.
| Item | Specification / Example | Primary Function |
|---|---|---|
| NP Swab | Flexible mini-tip flocked swab (e.g., Copan 481CE) | Accesses the nasopharynx for sample collection. |
| OP Swab | Rigid-shaft flocked swab (e.g., Copan 480CE, Meditec) | Samples the oropharyngeal tonsils and posterior wall. |
| Viral Transport Media (VTM) | Hi Viral TM (HiMedia) or Universal Transport Media (UTM) | Preserves viral integrity during transport and storage. |
| Nucleic Acid Extraction Kit | MagMAX Viral/Pathogen NA Isolation Kit (Thermo Fisher) | Isolates and purifies viral RNA from the specimen. |
| Automated Extraction System | Kingfisher Flex System (Thermo Fisher) | Automates the nucleic acid extraction process for consistency. |
| rRT-PCR Kit | Allplex SARS-CoV-2 Assay (Seegene) | Amplifies and detects specific SARS-CoV-2 gene targets. |
| rRT-PCR Instrument | CFX96 Touch Real-Time PCR Detection System (Bio-Rad) | Performs thermal cycling and fluorescence detection for PCR. |
| Internal Control | RNase P gene | Monitors sample collection, extraction, and amplification efficiency. |
The collective evidence firmly supports the superior diagnostic performance of combined swab strategies for SARS-CoV-2 detection. The fundamental principle is that anatomical distribution of the virus can vary between individuals and during the course of infection. Relying on a single sampling site risks false negatives if the viral load is low or absent at that specific location at the time of collection [44] [10]. Combined OP/NP or OP/Nasal sampling mitigates this risk by casting a wider net, thereby increasing the probability of capturing viral material.
For researchers and public health strategists, the choice of method involves a trade-off between ultimate sensitivity and practical constraints. The OP/NP combination, while achieving the highest theoretical sensitivity, still requires a somewhat invasive NP procedure. The OP/Nasal combination presents a compelling alternative; it is less invasive, potentially suitable for self-sampling, and has been shown to be equivalent to NP sampling and significantly better than a nasal swab alone [43] [2]. This makes it an excellent candidate for large-scale screening programs where comfort, speed, and resource availability are critical factors.
In conclusion, the "power of combination" is a robust diagnostic concept validated by multiple clinical studies. Moving forward, the adoption of combined swab strategies, particularly the OP/Nasal approach, can enhance the accuracy of SARS-CoV-2 detection and provide a more flexible toolkit for managing current and future respiratory virus outbreaks. Future research should focus on standardizing combined sampling protocols and further validating their performance in asymptomatic and pauci-symptomatic populations.
In the field of diagnostic testing, particularly during the COVID-19 pandemic, the comparative sensitivity of oropharyngeal (OP) swabs versus nasal swabs has been a significant area of research. While the gold standard has traditionally been nasopharyngeal sampling, the exploration of less invasive methods with comparable sensitivity has become crucial for widespread testing adoption [18]. Understanding the variables that affect test sensitivity is not merely an academic exercise but a practical necessity for optimizing diagnostic strategies, especially as we move into the endemic phase of diseases like COVID-19. The broader thesis of comparative sensitivity research seeks to evaluate how different sampling sites perform under varying physiological and patient-specific conditions, thereby guiding clinical practice and public health policy.
This guide objectively compares the performance of oropharyngeal and nasal swab sampling by synthesizing current experimental data, with a specific focus on three critical factors: the timing of sample collection relative to symptom onset, the age of the patient, and the influence of prior medication use. The high dimensionality of molecular profiles compared to limited samples presents challenges, but knowledge-based approaches leveraging biological insights can improve both prediction and interpretability [45]. By examining these factors through robust experimental data and sensitivity analyses, this guide aims to provide researchers, scientists, and drug development professionals with evidence-based insights to refine diagnostic protocols and therapeutic interventions.
Comparative Data: Oropharyngeal vs. Nasal Swab Performance
The diagnostic yield of different sampling methods is not absolute but is significantly influenced by temporal and individual patient factors. The following table synthesizes key comparative findings from recent studies.
Table 1: Comparative Sensitivity of Oropharyngeal and Nasal Swab Sampling
| Study Focus / Comparative Metric | Oropharyngeal (OP) Swab Findings | Anterior Nasal (AN) Swab Findings | Key Implications |
|---|---|---|---|
| Overall Diagnostic Yield | No singular preferred sample type was identified in a 2022 cross-sectional study [46]. | Similarly, no dominant sample type was found; a composite of positive MT (nasal) or OP swab trended toward higher yield [46]. | A combined approach (OP + Nasal) may maximize diagnostic sensitivity, though this was not statistically significant [46]. |
| Sensitivity Relative to Symptom Onset | Data specific to OP swab sensitivity over time was not highlighted in the search results. | Viral load increased up to day 4 of symptoms before declining, as per a 2023 study on symptomatic individuals [18]. | The optimal window for nasal swab testing appears to be within the first 4 days of symptom onset for highest sensitivity [18]. |
| Impact of Symptom Type on Yield | Apparent OP swab predominance was associated with specific patient symptoms [46]. | Apparent MT (nasal) swab predominance was also associated with specific patient symptoms [46]. | The dominant sample type for detection may vary based on the symptomatic presentation of the individual [46]. |
| Comparison to Saliva | A composite OP/MT (nasal) assay trended toward higher diagnostic yield than either alone [46]. | Higher concentrations of virus were observed in the nares in a familial cohort study [46]. | Saliva-based testing demonstrated a 94.0% Positive Percent Agreement (PPA) with nasal tests within the first 5 days of symptoms [18]. |
Detailed Experimental Protocols and Methodologies
Protocol 1: Longitudinal Comparison of Saliva and Nasal Swabs in Symptomatic Individuals
This protocol is derived from a 2023 study comparing an Emergency Use Authorized direct saliva-to-RT-qPCR test against an FDA-authorized nasal swab RT-qPCR assay [18].
- Objective: To compare the sensitivity of saliva and anterior nasal swab sampling for SARS-CoV-2 detection in symptomatic individuals, with analysis relative to days since symptom onset.
- Participant Recruitment: The study enrolled 737 symptomatic participants who self-elected to test at community testing sites or a walk-in clinic due to respiratory symptoms. Recruitment occurred between March and September 2023.
- Sample Collection:
- Saliva Sample: Participants provided 1–2 mL of saliva (drool) into a preservative-free collection tube. Samples were transported at room temperature and tested within 48 hours, leveraging the known stability of SARS-CoV-2 in raw saliva during this period [18].
- Nasal Swab: Immediately after saliva collection, participants self-collected an anterior nasal swab using a Roche cobas PCR Uni swab sample tube. The swab was inserted approximately one inch inside each nostril and rubbed in a circle five times for 10–15 seconds per nostril.
- Laboratory Analysis: Saliva samples were processed per EUA (202555) protocol, which involved heating at 95°C for 30 minutes, followed by the addition of a Tris/borate/EDTA/Tween20 buffer. Testing was performed using the Thermo Fisher Scientific TaqPath COVID-19 Combo Kit to detect three SARS-CoV-2 specific genes (ORF, N, and S) via RT-qPCR [18].
- Data Analysis: Positive Percent Agreement (PPA) and Negative Percent Agreement (NPA) were calculated with 95% confidence intervals. Viral load dynamics were analyzed by correlating cycle threshold (Ct) values with self-reported dates of symptom onset.
Protocol 2: Cross-Sectional Analysis of Multiple Sample Types
This protocol summarizes a 2022 study aimed at understanding differences in SARS-CoV-2 Omicron variant viral load across sample types [46].
- Objective: To compare viral load concentrations and assay sensitivity between nasopharyngeal (NP) swabs, mid-turbinate/anterior nasal (MT) swabs, oropharyngeal (OP) swabs, and saliva.
- Study Cohorts: The analysis included a cross-sectional cohort of 39 symptomatic cases from Atlanta, GA, in January 2022, and a separate longitudinal familial cohort.
- Sample Collection and Testing: Matched NP, MT, OP, and saliva samples were collected from participants. All samples were tested by both RT-PCR and ultrasensitive antigen assays to provide a comprehensive comparison of detection capabilities across different technologies.
- Data Analysis: The diagnostic yield of each sample type was assessed individually and in composite (e.g., considering a test positive if either MT or OP was positive). The association between the predominant sample type (MT or OP) and specific patient symptoms was also investigated [46].
Visualizing Research Workflows and Biological Relationships
Diagnostic Sensitivity Research Workflow
The following diagram illustrates the logical flow and key decision points in a comparative diagnostic sensitivity study, from participant enrollment to data interpretation.
Patient Factors Influencing Test Sensitivity and Drug Response
This diagram conceptualizes the complex interplay between patient-specific factors, diagnostic sensitivity, and medication response, which are key areas of investigation in precision medicine.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential materials and reagents used in the featured experiments for comparative sensitivity research.
Table 2: Essential Research Reagents and Materials for Diagnostic Sensitivity Studies
| Item Name | Function / Application in Research | Example from Search Results |
|---|---|---|
| Roche cobas PCR Uni Swab | Standardized collection of anterior nasal swab samples for consistent nucleic acid recovery and downstream RT-qPCR analysis. | Used for participant-collected nasal swabs in the symptomatic cohort study [18]. |
| Preservative-Free Saliva Collection Tube | Enables collection of 'raw' saliva (drool) for assays that use heat or proteinase K for pre-processing, minimizing inhibitory substances. | Used for saliva sample collection in the 2023 study; samples were stable at room temperature for 48h [18]. |
| Thermo Fisher TaqPath COVID-19 Combo Kit | RT-qPCR kit for the detection of multiple SARS-CoV-2 genes (ORF, N, S). Provides Emergency Use Authorization for defined diagnostic protocols. | Used for the definitive detection and quantification of viral RNA in saliva samples [18]. |
| Ultrasensitive Antigen Assay | Provides an alternative detection method to RT-PCR, potentially offering faster results and correlating viral antigen presence with infectivity. | Used alongside RT-PCR in the 2022 cross-sectional study to compare diagnostic yield across sample types [46]. |
| Anatomical Therapeutic Chemical (ATC) Code System | International standard for classifying medications, enabling systematic study of medication use patterns in relation to disease onset or test sensitivity. | Used in a register-based study to categorize prescription medication use prior to young-onset Alzheimer's diagnosis [47]. |
Discussion: Implications for Research and Clinical Practice
The experimental data underscore that the timing of sample collection is a paramount factor influencing sensitivity. The finding that nasal swab viral load peaks around day 4 of symptoms [18] provides a critical evidence-based window for maximizing test sensitivity in clinical and research settings. This temporal dynamic necessitates careful study design that accounts for and meticulously records the time since symptom onset.
Furthermore, the association between symptom type and the predominance of virus in a particular sample type (OP vs. nasal) [46] suggests that the pathophysiology of infection—such as viral tropism and replication sites—may vary between individuals. This highlights a need for a more personalized diagnostic approach rather than a one-size-fits-all model. The concept that a composite of OP and nasal sampling could enhance diagnostic yield, while not yet conclusive, points toward a potential strategy for increasing sensitivity in high-stakes scenarios.
Beyond infectious disease diagnostics, the principles of sensitivity extend to pharmacogenomics and drug development. The trait of Sensory Processing Sensitivity (SPS) has been shown to correlate with self-reported medication sensitivity, independent of negative affectivity [48]. This suggests that inherent biological traits can influence an individual's response to pharmaceuticals, impacting optimal dosing and the likelihood of adverse drug reactions [48]. Similarly, large-scale observational studies have linked the use of specific medication classes, such as those acting on the nervous system (e.g., antidepressants, antipsychotics), to a subsequent diagnosis of conditions like young-onset Alzheimer's disease, potentially serving as early indicators of underlying pathology [47]. These findings collectively argue for the integration of patient factors—including biological traits, medication history, and genetic makeup—into the broader framework of sensitivity research to advance personalized medicine.
The accurate diagnosis of respiratory pathogens, such as SARS-CoV-2, hinges on the collection of high-quality specimens. For researchers and clinicians, selecting a sampling method involves balancing critical factors: diagnostic sensitivity, patient tolerance, and safety for healthcare personnel. The global SARS-CoV-2 pandemic underscored the urgent need for sampling strategies that mitigate the risk of aerosol transmission to healthcare workers while maintaining high sensitivity and ensuring patient compliance, particularly in serial testing scenarios. This guide objectively compares the performance of various upper respiratory tract sampling methods—including nasopharyngeal, nasal, and oropharyngeal swabs, as well as saliva collection—framed within the broader research on comparative sensitivity. We synthesize current experimental data to provide a clear analysis of the trade-offs between comfort, safety, and analytical performance, supported by detailed protocols and quantitative findings.
Comparative Analysis of Sampling Methods
The following table summarizes key performance metrics, including patient tolerance and aerosol risk, for the primary respiratory specimen collection methods, as established by contemporary research.
Table 1: Comparative Overview of Respiratory Specimen Collection Methods
| Sampling Method | Reported Discomfort / Tolerance | Aerosol Generation Risk | Typical Collector | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| Nasopharyngeal (NP) Swab [5] [49] | Higher discomfort; less comfortable for patient [49] | Lower risk when performed correctly; not classified as aerosol-generating [5] | Healthcare Worker only [5] [49] | Considered a gold standard for many pathogens; high specimen yield [49] | Requires trained personnel; patient discomfort can limit repeat testing |
| Nasal Swabs (Anterior Nares/Mid-Turbinate) [5] [49] | More comfortable; "less invasive" [49] | Low risk; suitable for self-collection, eliminating close contact [5] [50] | Healthcare Worker or Patient (self) [5] [50] | Enables self-collection, reducing healthcare worker exposure; better patient acceptance | Specimen yield may be marginally lower than NP swabs [50] |
| Oropharyngeal (Throat) Swab [10] [5] | Can induce gagging; generally tolerable | Lower risk; not classified as aerosol-generating | Healthcare Worker only [5] | High sensitivity for certain variants (e.g., Omicron) [10] | Requires a healthcare worker; sensitivity can vary with pathogen and timing [10] |
| Saliva Collection [51] [19] [52] | Very low discomfort; "non-invasive" [51] | Low risk, especially with unsupervised self-collection [5] | Primarily Patient (self) | Excellent patient tolerance, ideal for paediatric and large-scale testing [51] | Sensitivity can be variable and may be lower than NP swabs in some studies [19] |
| Combined Nose & Throat Swab [10] | Combines discomfort of nasal/oropharyngeal swabbing | Low risk; involves swabbing without aerosol-generation | Healthcare Worker or Patient (self for anterior nasal) | Highest sensitivity for SARS-CoV-2 Omicron detection [10] | Invasive nature may reduce patient willingness for repeated sampling |
Quantitative data from large-scale studies reinforce the viability of self-collection methods. One study with 3,990 participants found no significant difference in sensitivity and specificity between self-collected (anterior nasal and oral) and healthcare worker-collected (nasopharyngeal and oropharyngeal) swabs, showing an "almost perfect agreement" (κ = 0.87) [50]. This demonstrates that self-collection, which inherently reduces close contact and aerosol risk for healthcare workers, does not sacrifice diagnostic accuracy.
Detailed Experimental Protocols and Data
To ensure reproducibility and critical evaluation, this section details the methodologies from key cited studies.
Protocol 1: Comparative Evaluation of Swabbing Sites for Omicron
This study directly compared the sensitivity of different swabbing sites for detecting the Omicron variant [10].
- Objective: To evaluate the sensitivity of detecting SARS-CoV-2 Omicron across nose-only, throat-only, and combined nose-and-throat swabs.
- Study Population: 815 participants undergoing testing at NHS Test and Trace sites in England.
- Sample Collection: Participants provided self-collected samples using all three swab types (nose, throat, combined). All samples were analyzed by real-time PCR.
- Key Metrics: Viral concentration (VC) and sensitivity relative to the combined swab approach.
- Results Summary: The data below illustrate the performance of single-site swabs relative to the combined method. Table 2: Sensitivity and Viral Concentration by Swab Site [10]
| Swab Type | Sensitivity Relative to Combined Swab | Viral Concentration (VC) Dynamics |
|---|---|---|
| Nose Only | 91% | More consistent over time |
| Throat Only | 97% | Declined faster in later infection stages |
| Combined Nose & Throat | (Reference) | Highest overall VC and sensitivity |
Protocol 2: Longitudinal Accuracy of Saliva vs. Nasopharyngeal Swabs
This longitudinal study provides a robust comparison of a non-invasive method against the traditional gold standard [19].
- Objective: To evaluate the diagnostic accuracy of saliva against nasopharyngeal swabs (NPS) in symptomatic individuals over time.
- Study Design: Longitudinal study involving 72 symptomatic participants across six visits from July 2021 to May 2022, analyzing 285 paired RT-qPCR samples.
- Sample Collection: Saliva was collected by having participants bring up saliva from the back of the throat and spit at least 3 mL into a sterile tube. NPS were collected by trained healthcare workers using standard techniques [19].
- Key Metrics: Sensitivity, specificity, agreement, and Cycle threshold (Ct) values.
- Results Summary: The findings highlight the performance of saliva over the course of infection. Table 3: Diagnostic Performance of Saliva vs. NPS [19]
| Metric | Overall Result | Notes by Infection Phase |
|---|---|---|
| Sensitivity | 69.2% (95% CI 57.2–79.5%) | Ranged from 82% (early) to 40% (mid-phase) |
| Specificity | 96.6% (95% CI 92.9–98.7%) | High specificity confirms utility for rule-out testing |
| Overall Agreement | 91.6% (κ = 0.78) | Indicates substantial agreement with NPS |
| Mean Ct Value | Saliva: 28.75; NPS: 26.75 | Slightly higher viral load in NPS (mean ΔCt = 0.79) |
Protocol 3: Feasibility of Non-Invasive Paediatric Saliva Sampling
This study protocol evaluates a novel saliva collection device designed for vulnerable populations [51].
- Objective: To assess the feasibility of implementing the CandyCollect lollipop device for saliva self-sampling among paediatric patients compared to standard mouth swabs.
- Study Setting & Population: Field study conducted at Steve Biko Academic Hospital, South Africa, focusing on paediatric patients.
- Sample Collection: Saliva is collected using the CandyCollect lollipop device, where the spiral groove captures pathogens as the child uses it. This is compared to standard mouth swabs collected by healthcare workers or caregivers.
- Analysis: Samples are analyzed using quantitative PCR and rapid antigen tests targeting key paediatric pathogens (e.g., RSV, influenza, SARS-CoV-2).
- Additional Metrics: User experience and acceptability are assessed via child-friendly and caregiver surveys.
Visualizing the Comparative Evaluation Workflow
The following diagram illustrates the logical workflow for a comparative evaluation of sampling methods, from participant enrollment and specimen collection to laboratory analysis and key outcome assessment.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogs key materials and reagents required for executing the specimen collection and analysis protocols described in this guide.
Table 4: Essential Reagents and Materials for Respiratory Pathogen Sampling Research
| Item | Specification / Example | Primary Function in Protocol |
|---|---|---|
| Swabs | Synthetic fiber (flocked polyester, foam); thin plastic/wire shaft [5]. | Effective specimen collection and release. Wooden shafts or calcium alginate are prohibited as they may inhibit tests [5]. |
| Universal Transport Media (UTM) | Copan UTM [7]. | Preserves viral integrity during transport and storage. |
| Nucleic Acid Extraction Kit | MGI Easy Nucleic Acid Extraction Kit [19]; Roche MagNA Pure 96 system reagents [50]. | Isolates viral RNA for downstream molecular detection. |
| RT-qPCR Master Mix | SARS-CoV-2 EDx kit (Bio-Manguinhos-FIOCRUZ) [19]; Allplex SARS-CoV-2 Assay (Seegene) [50]. | Amplifies and detects target viral genes via reverse transcription quantitative PCR. |
| Saliva Collection Device | CandyCollect lollipop device [51]; preservative-free collection tube with funnel [52]. | Enables non-invasive and user-friendly saliva specimen collection, crucial for paediatric studies. |
| Internal Positive Controls | Included in commercial qPCR kits or added separately. | Monitors for PCR inhibition and verifies the integrity of each reaction. |
| Viral Load Standard | Serial dilutions of SARS-CoV-2 RNA (e.g., NCCP-43330 strain) [50]. | Enables quantification of viral load from Ct values by generating a standard curve. |
The choice of a respiratory specimen collection method is a multifaceted decision that significantly impacts diagnostic accuracy, user safety, and patient comfort. Evidence indicates that no single method is superior in all aspects. Nasopharyngeal swabs, while often considered the sensitivity gold standard, present challenges in comfort and require skilled personnel. Combined swabs offer the highest sensitivity for certain pathogens like the Omicron variant but are the most invasive. In contrast, self-collected anterior nasal swabs demonstrate performance comparable to healthcare worker-collected specimens while dramatically reducing exposure risk and resource burden. Saliva emerges as a highly comfortable and safe alternative, with high specificity making it particularly valuable for public health screening and paediatric populations, despite potentially variable sensitivity.
The optimal method depends on the specific research or clinical context, including the target pathogen, population, available resources, and the balance between maximum sensitivity and the practicalities of large-scale, repeat testing. The continued development and validation of non-invasive, self-collected methods represent a critical step toward sustainable, patient-centred, and safe diagnostic systems.
Head-to-Head Clinical Validation and Comparative Sensitivity Analysis
The accurate detection of SARS-CoV-2 is a cornerstone of public health efforts to control the COVID-19 pandemic. Real-time quantitative reverse transcriptase-polymerase chain reaction (RT-qPCR) remains the most extensively used diagnostic method, which can be performed on various respiratory samples [53]. The selection of an appropriate sampling site is critical, as it directly influences test sensitivity, patient comfort, and healthcare worker safety. This guide provides an objective comparison of the three common upper respiratory tract sampling methods—oropharyngeal swabs (OPS), nasopharyngeal swabs (NPS), and anterior nasal swabs (Nasal Swab)—by synthesizing current experimental data and methodologies. The broader context frames this comparison within ongoing research into optimizing SARS-CoV-2 detection protocols for researchers and drug development professionals.
Comparative Sensitivity Data Analysis
The diagnostic sensitivity of SARS-CoV-2 tests varies significantly depending on the sample type, viral load, symptom status, and the specific variant of concern. The following tables summarize key quantitative findings from recent clinical studies.
Table 1: Overall Comparative Sensitivity of Different Sample Types for SARS-CoV-2 Detection
| Sample Type | Reported Sensitivity Range (%) | Key Influencing Factors | Best Application Context |
|---|---|---|---|
| Oropharyngeal Swab (OPS) | 71.4% - 94.1% [53] | Lower sensitivity when collected >7 days after symptom onset [53] | Early symptom onset (≤7 days) |
| Nasopharyngeal Swab (NPS) | 92.5% - 100% [53] | Consistently high sensitivity across disease stages [53] | Reference standard; high sensitivity required |
| Anterior Nares (Nasal Swab) | 79.5% - 85.6% [26] | Equivalent to NPS in Ag-RDTs; lower test line intensity [26] | Rapid antigen testing; self-testing |
| Saliva | 40.0% - 94.0% [54] [18] [19] | High variability; depends on symptom status and variant [55] | Non-invasive community screening |
Table 2: Impact of Viral Load and Variant on Sample Sensitivity
| Study Factor | Sample Type | Findings | Source | |
|---|---|---|---|---|
| High Viral Load (Ct < 25) | Saliva (vs. NP RT-PCR) | Sensitivity: ~94.0% in first 5 days of symptoms [18] | Vaz et al., 2025 | |
| High Viral Load (Ct < 25) | Rapid Antigen Test (RAT) | Sensitivity increased to 71-97% [56] | BMC Infect Dis, 2025 | |
| Variant Dependence | Saliva (vs. NPS) | Delta: 79.6% | Omicron: 61.5% [55] | J Appl Lab Med, 2024 |
| Symptom Dependence | Saliva (vs. NPS) | Symptomatic: 78.7-100% | Asymptomatic: 48.3-72.5% [55] | J Appl Lab Med, 2024 |
Detailed Experimental Protocols
To ensure the reproducibility of comparative sensitivity studies, the following details key methodological aspects from cited research.
Sample Collection Protocols
Standardized collection procedures are vital for sample quality and result comparability.
- Nasopharyngeal Swab (NPS): A flexible, fine-shafted swab is inserted into the nostril parallel to the palate until resistance is met (reaching the nasopharynx). The swab is rubbed and rotated gently for several seconds (e.g., 10 seconds) to absorb secretions. The procedure is typically performed on one nostril. The swab is immediately placed into a tube containing viral transport medium (VTM) [54] [53].
- Oropharyngeal Swab (OPS): A swab is used to collect samples from the posterior pharynx and tonsillar areas. The patient is asked to open their mouth wide, and the swab is rubbed against the posterior oropharyngeal wall and the right and left tonsillar arches, avoiding contact with the tongue, teeth, and gums. The swab is then placed in VTM [54] [53].
- Anterior Nares Swab (Nasal Swab): A swab is inserted approximately 1-2 centimeters (about 1 inch) into the nostril and firmly rubbed against the nasal wall in a circular motion for the time specified by the test manufacturer (e.g., 10-15 seconds per nostril). This process is repeated in the other nostril using the same swab [26] [18].
Laboratory Analysis Workflow
The central workflow for RT-qPCR analysis, the gold standard for SARS-CoV-2 detection, involves several critical steps as illustrated below. This process is largely consistent across sample types, though pre-processing may differ.
Key Methodologies from Cited Studies
- Head-to-Head Ag-RDT Comparison (PMC11934397): This prospective evaluation collected paired AN (anterior nares) and NP swabs from symptomatic individuals. NP swabs were collected first in one nostril for reference RT-qPCR, followed by an NP swab in the other nostril and finally an AN swab in both nostrils for Ag-RDT testing. Sure-Status and Biocredit Ag-RDTs were performed per manufacturer instructions, with results read by two blinded operators. Test line intensity was scored quantitatively [26].
- Longitudinal Saliva Accuracy Study (s41598-025-20841-w): This study collected paired NPS and saliva samples from 72 symptomatic individuals across six longitudinal visits. Saliva was self-collected by having participants bring up saliva from the back of the throat and spit at least 3 mL into sterile tubes. Viral RNA was extracted using an MGISP-960 instrument and detected using the SARS-CoV-2 EDx kit (Bio-Manguinhos-FIOCRUZ) [54] [19].
- Variant-Dependent Saliva Sensitivity (J Appl Lab Med, 2024): Paired NPS and saliva specimens were collected from individuals with acute symptoms or known exposure. SARS-CoV-2 RT-PCR was performed using the CDC protocol, and viral genome sequencing of NPS specimens was conducted to determine the infecting variant. Saliva sensitivity was calculated using NPS-positive RT-PCR as the reference standard [55].
Specimen Collection Pathway and Selection Logic
The following diagram illustrates the decision-making pathway for selecting an appropriate respiratory specimen based on testing objectives, patient population, and available resources.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing studies on SARS-CoV-2 sampling sensitivity, the following key reagents and materials are essential.
Table 3: Essential Research Reagents and Materials for Comparative Sensitivity Studies
| Reagent/Material | Function/Application | Examples/Notes |
|---|---|---|
| Swabs | Sample collection from respiratory mucosa | Sterile polyester or foam swabs; flocked swabs often enhance elution [53]. |
| Viral Transport Medium (VTM) | Preserves viral integrity during transport | Typically contains protein stabilizers and antimicrobial agents [26] [55]. |
| RNA Extraction Kits | Purification of viral RNA for RT-qPCR | QIAamp Viral RNA Mini Kit (QIAGEN) or automated systems like eMAG (bioMérieux) [26] [55]. |
| RT-PCR Master Mix | Enzymatic amplification of viral RNA | 1-Step TaqPath Master Mix (Thermo Fisher); targets include N, E, ORF1ab genes [26] [55]. |
| SARS-CoV-2 Primers/Probes | Specific detection of viral sequences | CDC N1 & N2 gene targets; RNase P (RNP) as internal control [18] [55]. |
| Rapid Antigen Tests (Ag-RDTs) | Point-of-care detection of viral nucleocapsid protein | Sure-Status (PMC, India), Biocredit (RapiGEN, South Korea) [26]. |
| Automated Extraction/PCR Platforms | High-throughput, standardized processing | cobas 6800 systems (Roche), MGISP-960 instruments (MGI Tech) [19] [56]. |
Accurate and timely diagnosis of Mycoplasma pneumoniae (MP) is a critical challenge in managing respiratory infections. As a cell wall-deficient bacterium insensitive to beta-lactam antibiotics, its precise identification directly impacts therapeutic decisions and patient outcomes. The ongoing debate regarding optimal sampling sites for molecular detection has significant implications for diagnostic accuracy. This guide objectively compares the performance of oropharyngeal versus nasopharyngeal swabbing for MP detection, presenting recent experimental data to inform researchers and clinical development professionals. Contemporary studies now provide compelling evidence that sampling methodology substantially influences detection sensitivity, with oropharyngeal sampling demonstrating marked superiority in head-to-head comparisons.
Comparative Performance Analysis
Diagnostic Sensitivity by Sample Type
Recent rigorous comparative studies have quantified significant differences in MP detection rates between oropharyngeal and nasopharyngeal samples. The data, summarized in Table 1, reveal consistent patterns across different patient populations and testing methodologies.
Table 1: Comparative Sensitivity of Oropharyngeal vs. Nasopharyngeal Sampling for M. pneumoniae Detection
| Study Population | Testing Method | Oropharyngeal Sensitivity | Nasopharyngeal Sensitivity | Reference Standard | Citation |
|---|---|---|---|---|---|
| 422 children with suspected MP | Commercial PCR (Smart Gene Myco) | 96.2% (92.3–98.4%) | 74.9% (67.9–81.0%) | RT-PCR on oropharyngeal residuals | [57] |
| 326 children with ARTI | Suspension microarray | 84% detection rate | 29% detection rate | Parallel testing of paired samples | [58] |
| 440 hospitalized children | GeXP-based multiplex PCR | Lower detection rate* | Higher detection rate* | Parallel testing with sputum as comparator | [59] |
Note: The study by Wang et al. (2019) found sputum superior to both swab types but observed substantially higher MP detection in sputum versus oropharyngeal swabs. [59]
The most compelling evidence comes from a 2025 study of 422 children with suspected MP infection, which demonstrated a 21.3% absolute difference in sensitivity favoring oropharyngeal samples (96.2% vs. 74.9%) when using commercially available PCR tests. This difference was statistically significant and maintained when using real-time PCR of residual extracts as a reference standard. [57]
An independent 2026 study corroborated these findings, reporting dramatically higher MP detection rates in oropharyngeal swabs (84%) compared to nasopharyngeal swabs (29%) in children with acute respiratory tract infections. [58]
Methodological Considerations for Optimal Detection
The superior performance of oropharyngeal sampling for MP detection is theorized to stem from the bacterium's biological preference for the lower respiratory tract and bronchial epithelium. During infection, MP attaches to respiratory epithelial cells using specialized adhesion proteins, and higher bacterial concentrations may be present in secretions from the oropharynx compared to the nasopharynx. [60]
Several factors influencing detection rates deserve consideration:
- Prior antimicrobial therapy: Fluoroquinolone use demonstrates a negative correlation with oropharyngeal DNA loads (P = 0.004), potentially impacting detection sensitivity. [57]
- Sample collection technique: Proper technique involving firm swabbing of both tonsillar pillars and the posterior oropharynx is essential for adequate specimen collection. [59]
- Transport and storage conditions: Immediate freezing at -80°C or -18°C and avoidance of thawing during transport preserve nucleic acid integrity. [57]
Experimental Protocols and Methodologies
Paired Sample Collection and Processing
The seminal 2025 study employed a rigorous paired-sample design where both nasopharyngeal and oropharyngeal samples were collected simultaneously from each participant by trained physicians. This approach controlled for inter-patient variability and enabled direct comparison. [57]
Figure 1: Experimental Workflow for Comparative Sampling Study
Molecular Detection Methods
Studies utilized various PCR-based methodologies with different performance characteristics:
Table 2: Molecular Assays Used in Comparative Studies
| Assay Name | Platform Type | Target Gene | Limit of Detection | Special Capabilities | Citation |
|---|---|---|---|---|---|
| SpotFire Respiratory Panel | Multiplex PCR | Multiple respiratory pathogens | 2.1 copies/μL for MP | Syndromic pathogen detection | [57] |
| FilmArray Respiratory Panel 2.1 | Multiplex PCR | Multiple respiratory pathogens | 0.46 copies/μL for MP | Syndromic pathogen detection | [57] |
| Smart Gene Myco | QProbe PCR | MP-specific and macrolide resistance | 10 copies/μL | Detects 23S rRNA mutations | [57] |
| In-house RT-PCR | Real-time PCR | CARDS toxin gene | N/A | Quantitative DNA load measurement | [57] |
| GeXP-based Multiplex PCR | Capillary electrophoresis | 11 pathogen targets | N/A | Multiple pathogen detection | [59] |
The 2025 study validated commercial test results using an in-house real-time PCR assay targeting the CARDS toxin gene with the following parameters: forward primer 5'-TTTGGTAGCTGGTTACGGGAAT-3', reverse primer 5'-GGTCGGCACGAATTTCATATAAG-3', and probe 5'-FAM-TGTACCAGAGCACCCCAGAAGGGCT-BHQ1-3'. Thermal cycling conditions included 45 cycles of 15 seconds at 95°C and 1 minute at 60°C following initial activation steps. [57]
Statistical Analysis Approaches
Studies employed comprehensive statistical methods to ensure robust conclusions:
- Sensitivity and specificity calculations with 95% confidence intervals using McNemar's tests for comparing paired proportions [57]
- DNA load comparisons using Wilcoxon signed-rank tests and Spearman's rank correlation [57]
- Multivariate analysis using generalized linear models to assess impact of prior antimicrobial treatment and resistance mutations [57]
- Concordance assessment using Kappa statistics (κ values) for agreement between sample types [59]
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for M. pneumoniae Sampling and Detection
| Reagent/Kit | Manufacturer | Primary Function | Application Notes | Citation |
|---|---|---|---|---|
| UTM Nasopharyngeal Sample Collection Kit | Copan | Sample preservation for nasopharyngeal swabs | Maintains specimen integrity during transport | [57] |
| Nipro Sponge Swab TYPE L | Nipro | Oropharyngeal sample collection | Optimized for nucleic acid recovery | [57] |
| Smart Gene Myco | MIZUHO MEDY | Detection of MP and macrolide resistance | Point-of-care capable; 23S rRNA mutation detection | [57] |
| QIAamp DNA Mini Kit | Qiagen | Nucleic acid extraction | Efficient DNA purification from respiratory samples | [57] |
| TaqMan Universal PCR Master Mix | Thermo Fisher | Real-time PCR amplification | Compatible with multiple detection chemistries | [61] |
| Respiratory Pathogens Multiplex Kit | Health Gene Tech | Multiplex pathogen detection | GeXP platform; detects 11 respiratory pathogens | [59] |
Research Implications and Future Directions
The demonstrated superiority of oropharyngeal sampling for MP detection has significant implications for clinical practice and research. The consistently higher sensitivity across studies suggests that diagnostic guidelines should potentially be revised to recommend oropharyngeal sampling as the preferred method for MP detection via PCR. [57] [58]
For researchers, these findings highlight the critical importance of sample selection in study design, particularly when comparing diagnostic platforms or establishing epidemiological prevalence. The 21.3% sensitivity difference observed between sampling methods exceeds the marginal improvements often reported between assay generations, suggesting that optimization of pre-analytical factors may yield greater diagnostic gains than analytical refinements alone. [57]
Future research should explore whether similar advantages exist for oropharyngeal sampling in adult populations and investigate the potential for dual-site sampling to further enhance detection rates. Additionally, the relationship between bacterial load quantification from oropharyngeal samples and disease severity warrants further investigation to establish prognostic value.
Compelling evidence from recent well-designed studies demonstrates the clear superiority of oropharyngeal over nasopharyngeal sampling for PCR-based detection of Mycoplasma pneumoniae. The consistent finding of significantly higher sensitivity (96.2% vs. 74.9%) across multiple study populations and testing platforms provides a robust evidence base for recommending oropharyngeal sampling as the optimal approach for MP detection. Researchers and clinicians should prioritize specimen collection from the oropharynx to maximize diagnostic accuracy, guide appropriate antimicrobial therapy, and enhance epidemiological surveillance capabilities.
Within the broader context of comparative sensitivity research for SARS-CoV-2 detection, understanding viral load quantification across different sample types is fundamental for diagnostic accuracy, epidemiological monitoring, and clinical management. The cycle threshold (Ct) value from reverse transcription quantitative polymerase chain reaction (RT-qPCR) serves as a semi-quantitative proxy for viral load, with lower Ct values indicating higher viral RNA concentrations [62]. However, comparability across studies is challenging due to variations in measurement units, sample collection methods, and viral transport media [63]. This analysis objectively compares viral load quantification, expressed through both Ct values and genome copies/mL, across major sample types including nasopharyngeal, nasal, oropharyngeal, and saliva specimens, providing researchers with consolidated experimental data and methodologies to inform study design and interpretation.
Comparative Performance of Different Sample Types
Quantitative Comparison of Viral Load Across Specimens
Table 1: Comparative Viral Load Across Respiratory Specimens from Hospitalized Symptomatic COVID-19 Patients
| Specimen Type | Comparative Viral Load | Detection Sensitivity | Key Findings | Study Reference |
|---|---|---|---|---|
| Nasopharyngeal Swab (NPS) | Highest RNA concentration | Reference standard | Considered highest sensitivity for hospitalized patients; gold standard for initial diagnosis | [16] [62] |
| Anterior Nasal Swab | ~2.5 log10 copies/mL lower than NPS | Comparable to throat swabs | Viral load comparable to throat swabs; suitable for self-collection | [16] |
| Saliva | Mean Ct 28.75 (vs. NPS 26.75) | 69.2% overall sensitivity (40-82% range) | Variable sensitivity across infection phases; higher in early infection (82%) | [19] |
| Pharyngeal Swab | Lower than NPS | Lower than NPS | Often combined with other specimens to improve sensitivity | [16] |
| Stool | 89.1% positivity at admission | 45.7% positivity at outcome | Clearance more efficient than respiratory specimens; higher diversity | [63] |
Table 2: Temporal Dynamics of Viral Load in Different Sample Types
| Sample Type | Peak Viral Load Timing | Clearance Patterns | Notes | Study Reference |
|---|---|---|---|---|
| Nasal Swab | Increases up to day 4 post-symptom onset | Gradual decline after peak | Viral load trend distinct from saliva | [18] |
| Saliva | Day 1 post-symptom onset | Decreases after day 1 | Earlier peak than nasal swabs | [18] |
| Nasopharyngeal | Highest in first 5 days post-symptom | Detectable for extended periods | 67.4% remained positive at clinical outcome in ICU patients | [63] |
| Stool | Variable | Faster clearance than respiratory specimens | 45.7% positivity at clinical outcome vs. 67.4% for NP | [63] |
Diagnostic Performance Metrics
Table 3: Diagnostic Accuracy of Alternative Specimens Versus Nasopharyngeal Swab
| Specimen Type | Sensitivity (%) | Specificity (%) | Overall Agreement | Optimal Use Conditions | Study Reference |
|---|---|---|---|---|---|
| Saliva | 69.2 (57.2-79.5) | 96.6 (92.9-98.7) | 91.6% (κ=0.78) | Early infection phase (82% sensitivity) | [19] |
| Saliva (first 5 days symptomatic) | 94.0 (88.9-99.1) | 99.0 (98.1-99.9) | High agreement | Early symptomatic phase | [18] |
| Self-collected nasal/oral | 86.3-89.2 | High (exact NS) | κ=0.87 | Large-scale community sampling | [50] |
| Anterior nasal swabs | Lower than NPS | High | Moderate | Late phase infection less reliable | [16] |
Methodological Approaches for Viral Load Quantification
Standard RT-qPCR Methodology
The gold standard for SARS-CoV-2 RNA detection uses RT-qPCR targeting specific viral genes, most commonly the nucleocapsid (N1, N2), envelope (E), RNA-dependent RNA polymerase (RdRp), and spike (S) genes [63] [18] [50]. The CDC 2019-nCoV RT-qPCR assay protocol implemented by multiple studies includes:
- Primers/Probes: N1 and N2 primer/probe sets for SARS-CoV-2 detection, RNase P (RP) as internal control [63] [64]
- Reaction Setup: 20μL reaction volume using 5μL of template RNA [64]
- Cycling Conditions: 55°C for 10 min (reverse transcription), 95°C for 1 min (initial denaturation), followed by 45 cycles of 95°C for 10 sec and 60°C for 30 sec [64]
- Quantification: External standard curves with serial dilutions of known SARS-CoV-2 RNA copies (e.g., 2.0 × 100–2.0 × 10^5 copies/μL) to convert Ct values to absolute copy numbers [63]
Extraction-Free Saliva Testing
Recent methodologies have developed extraction-free approaches for high-throughput testing:
- Sample Processing: Heat treatment at 95°C for 30 minutes followed by addition of Tris/borate/EDTA/Tween20 buffer [18]
- Limit of Detection: 4 GE/μL in raw saliva with precision (CV < 5%) at viral loads ≥10 GE/μL [64]
- Sample Stability: Saliva samples stable at room temperature for 48 hours with minimal Ct value impact (mean increase 1.56 at 4°C over 2 weeks) [64]
Digital Droplet PCR (ddPCR) for Absolute Quantification
For precise viral load measurement without standard curves:
- Technology: Bio-Rad SARS-CoV-2 ddPCR kit with 2019-nCoV CDC ddPCR triplex probe assay [64]
- Sensitivity: LoD of 0.150 copies/μL [64]
- Correlation: Ct values between 20-30 correlated with viral loads between 10-1,500 copies/μL in saliva [64]
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Viral Load Quantification Studies
| Reagent/Kit | Primary Function | Application Notes | Study Reference |
|---|---|---|---|
| QIAamp Viral RNA Mini Kit | RNA extraction from swabs/stool | Standardized extraction for various sample types | [63] |
| PureLink Viral RNA/DNA Mini Kit | RNA extraction from NP swabs | Alternative extraction methodology | [63] |
| CDC 2019-nCoV RT-qPCR Assay | Viral RNA detection | Targets N1, N2 genes with RNase P internal control | [63] [64] |
| Allplex SARS-CoV-2 Assay | Multiplex RT-qPCR | Detects E, RdRP, S, N genes simultaneously | [50] |
| TaqPath COVID-19 Combo Kit | RT-qPCR detection | Targets ORF, N, S genes; used with EUA authorization | [18] |
| Bio-Rad SARS-CoV-2 ddPCR Kit | Absolute quantification | Gold standard for copy number determination | [64] |
| DNA Genotek Collection Devices | Sample collection | Standardized self-collection anterior nasal and saliva | [64] |
Factors Influencing Viral Load Quantification
Biological and Temporal Considerations
Viral load dynamics follow distinct temporal patterns across sample types. Nasal swabs typically show increasing viral loads up to day 4 post-symptom onset, while saliva peaks earlier around day 1 [18]. This compartmentalization suggests different viral replication dynamics in various anatomical sites.
The correlation between RNA viral load and infectious virus presence varies throughout infection. While higher viral loads generally pose greater transmission risk, the relationship is not linear [62]. Detection of infectious virus is most likely during the first 5-8 days post-symptom onset, with decreasing probability despite persistent RNA detection [62].
Methodological Considerations for Cross-Study Comparisons
Several technical factors complicate direct comparison of viral load data across studies:
- Extraction Efficiency: Variable RNA recovery across different kits and sample types [64]
- Inhibition Effects: Differential PCR inhibition across sample matrices, particularly with extraction-free methods [64]
- Unit Disparities: Reporting in copies/mL, copies/swab, or Ct values without inter-laboratory standardization [63] [62]
- Storage Conditions: Sample stability variations affecting viral RNA integrity [64]
The implementation of WHO international standards for SARS-CoV-2 RNA has improved inter-laboratory comparability, but methodological differences remain significant confounding factors [62].
Viral load quantification across different sample types reveals significant variations in sensitivity, temporal dynamics, and absolute values. Nasopharyngeal swabs remain the gold standard for hospitalized patients, while saliva and anterior nasal swabs offer practical alternatives for community surveillance and self-collection. The choice of specimen should align with research objectives, considering that nasopharyngeal samples show highest sensitivity, particularly in advanced disease stages, while saliva demonstrates excellent performance in early infection with greater patient acceptance and scalability. Extraction-free methods and ddPCR quantification present promising approaches for high-throughput and precise viral load monitoring, respectively. Researchers should standardize viral load reporting in genome copies/mL with reference to international standards to enable meaningful cross-study comparisons and advance our understanding of SARS-CoV-2 pathogenesis and transmission dynamics.
The comparison of diagnostic methods sits at the intersection of controlled research environments and real-world clinical practice. Nowhere has this tension been more apparent than in the evaluation of sampling methods for SARS-CoV-2 detection during the COVID-19 pandemic. While nasopharyngeal swabs (NPS) have been widely regarded as the gold standard, supply chain limitations and patient discomfort prompted the investigation of alternatives including oropharyngeal swabs (OPS) and nasal swabs. This guide examines the convergence and divergence between controlled studies and real-world performance data for these sampling methods, providing researchers and drug development professionals with a structured analysis of their comparative sensitivity.
Experimental Approaches in Controlled Studies
Study Designs and Methodologies
Controlled studies comparing swab sampling methods typically employed prospective, head-to-head comparisons where multiple sample types were collected from the same participants simultaneously or in rapid succession. These studies minimized pre-analytical variables by using trained healthcare personnel for sample collection, often specialists such as otorhinolaryngologists [2].
The methodological rigor in these studies included:
- Paired sampling designs where all participants provided all sample types being compared
- Standardized collection techniques with precise anatomical descriptions and swab insertion depths
- Blinded laboratory analysis to prevent measurement bias
- Statistical power calculations to ensure adequate sample sizes
One particularly well-designed study published in 2023 enrolled 51 confirmed SARS-CoV-2-positive participants, with all swabs performed by otorhinolaryngologists following detailed protocols [2]. The NPS was inserted approximately 8-11 cm until resistance was met at the posterior wall of the nasopharynx, while the OPS collected sample from both palatine tonsils and the posterior oropharyngeal wall. The nasal swab was inserted only 1-3 cm into the nasal cavity [2].
Laboratory Analysis Methods
Laboratory methodologies across studies typically utilized real-time reverse transcription polymerase chain reaction (rRT-PCR) platforms. Most studies employed automated systems such as the Roche Cobas 6800, with target genes including E-gene, N-gene, and RdRP [2] [6]. The cycle threshold (Ct) values served as a semi-quantitative measure of viral load, with lower values indicating higher viral concentrations.
Comparative Performance Data
Sensitivity Across Sampling Methods
Table 1: Comparative Sensitivity of SARS-CoV-2 Detection Methods
| Sampling Method | Sensitivity (%) | 95% Confidence Interval | Study Population | Source |
|---|---|---|---|---|
| Oropharyngeal Swab (OPS) | 94.1 | 87.0-100.0 | 51 confirmed positive participants | [2] |
| Nasopharyngeal Swab (NPS) | 92.5 | 85.0-99.0 | 51 confirmed positive participants | [2] |
| Nasal Swab | 82.4 | 72.0-93.0 | 51 confirmed positive participants | [2] |
| Combined OPS/NPS | 100.0 | Not reported | 51 confirmed positive participants | [2] |
| Combined OPS/Nasal Swab | 96.1 | 90.0-100.0 | 51 confirmed positive participants | [2] |
| OPS (Hospitalized Patients) | 92.7 | Not reported | 28 hospitalized patients | [17] |
| NPS (Hospitalized Patients) | 89.3 | Not reported | 28 hospitalized patients | [17] |
Viral Load Measurements
Table 2: Mean Cycle Threshold (Ct) Values by Sample Type
| Sample Type | Mean Ct Value | Comparative P-value | Sample Size | Source |
|---|---|---|---|---|
| Nasopharyngeal Swab | 24.98 | Reference | 24 participants | [2] |
| Oropharyngeal Swab | 26.63 | P=0.084 | 24 participants | [2] |
| Nasal Swab | 30.60 | P=0.002 | 24 participants | [2] |
Methodological Workflow
The following diagram illustrates the typical experimental workflow for head-to-head comparison studies of sampling methods:
Analytical Considerations in Positivity Rate Comparisons
Statistical Approaches
The comparison of test positivity rates presents significant methodological challenges, particularly when rates are very similar. Research has identified important distinctions between frequentist tests (such as asymptotic z-tests and 'N-1' chi-square tests) and Bayesian methods for comparing proportions [65].
When test positivity rates are very small and of similar magnitude, frequentist tests with large sample sizes may indicate statistically significant differences despite trivial practical differences. In contrast, Bayesian approaches can identify practical equivalence, providing more clinically relevant interpretations [65]. For example, when comparing TP rates of 0.009 and 0.007, frequentist tests indicated a highly significant difference while Bayesian methods suggested practical equivalence [65].
Real-World Evidence vs. Randomized Controlled Trials
The broader methodological context contrasts Randomized Controlled Trials (RCTs) with Real-World Evidence (RWE) approaches [66]. While RCTs demonstrate highest reliability for efficacy under controlled conditions, RWE reflects actual clinical performance with heterogeneous populations and variable conditions [66].
Table 3: RCT vs. RWE Characteristics in Diagnostic Evaluation
| Variable | Randomized Controlled Trials | Real-World Evidence |
|---|---|---|
| Purpose | Efficacy | Effectiveness |
| Setting | Experimental setting | Real-world setting |
| Follow up | Designed | In actual practice |
| Treatment | Fixed pattern | Variable pattern |
| Study group | Homogenous | Heterogeneous |
| Attending physician | Investigator | Many practitioners |
| Patient monitoring | Continuous, per protocol | Changeable |
Essential Research Reagent Solutions
Table 4: Key Research Materials and Their Functions
| Reagent/Material | Function | Example Specifications |
|---|---|---|
| Flocked NPS Swab | Nasopharyngeal sample collection | Flexible minitip flocked swab (COPAN diagnostics) [2] |
| Rigid-shaft Flocked Swab | Oropharyngeal and nasal sample collection | Meditec A/S, Denmark [2] |
| Viral Transport Medium | Sample preservation during transport | Universal Transport Medium (UTM) or DMEM [6] |
| RNA Extraction System | Nucleic acid purification | NucliSens easyMag (bioMérieux) [17] |
| rRT-PCR Master Mix | Amplification and detection | Qiagen One Step RT-PCR Kit [17] |
| PCR Control Materials | Quality assurance | Diagenode RNA extraction and inhibition control [17] |
Discussion and Research Implications
The comparative sensitivity data demonstrate that oropharyngeal swabs achieve performance comparable to nasopharyngeal swabs, with OPS showing 94.1% sensitivity versus 92.5% for NPS in one rigorous comparison [2]. The minimal difference in Ct values between OPS and NPS (26.63 vs. 24.98, P=0.084) further supports their analytical equivalence [2].
The combined sampling approaches appear to enhance overall sensitivity, with OPS/NPS combination detecting 100% of cases and OPS/nasal swab combination reaching 96.1% sensitivity [2]. This suggests practical utility in situations where maximum detection sensitivity is critical.
From a research perspective, these findings highlight the importance of methodological alignment between study objectives and analytical approaches. The demonstration of OPS equivalence to NPS addresses both supply chain limitations (through alternatives to specialized NPS swabs) and patient comfort considerations without compromising diagnostic accuracy [2] [17].
For researchers and drug development professionals, these results underscore the value of real-world performance data to complement controlled studies, particularly for diagnostic methodologies that must perform across diverse clinical settings and operator skill levels. The convergence of findings from multiple controlled studies strengthens the evidence base for considering oropharyngeal swabs as equivalent alternatives for SARS-CoV-2 detection in many clinical and research scenarios.
Conclusion
The comparative analysis of oropharyngeal and nasal swab sampling reveals that a universal 'best' sample type is context-dependent. For SARS-CoV-2, oropharyngeal swabs demonstrate sensitivity equivalent to the traditional nasopharyngeal standard, while for pathogens like Mycoplasma pneumoniae, oropharyngeal sampling is significantly superior. The evidence strongly supports that combined sampling strategies (e.g., oropharyngeal/nasal) can achieve near-perfect sensitivity, mitigating the risk of false negatives. Key factors influencing success are rigorous technique and understanding pathogen-specific tropism. Future directions for biomedical research should focus on developing and validating non-invasive, patient-friendly methods like saline gargle and nasal strips, establishing pathogen-specific sampling guidelines, and integrating these optimized protocols into drug development trials and large-scale surveillance programs to enhance diagnostic accuracy and public health response.
References
- 1. Saliva as a gold-standard sample for SARS-CoV-2 detection [https://pmc.ncbi.nlm.nih.gov/articles/PMC8055204/]
- 2. Head-to-Head Comparison of Nasopharyngeal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9857511/]
- 3. Evaluation of a New Standardized Nasal Sampling Method ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10820932/]
- 4. Difference between real world practice and clinical ... [https://www.sciencedirect.com/science/article/pii/S1876034124003150]
- 5. Interim Guidelines for Collecting and Handling of Clinical ... [https://www.cdc.gov/covid/hcp/clinical-care/clinical-specimen-guidelines.html]
- 6. Sensitivity of nasopharyngeal, oropharyngeal, and nasal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7494432/]
- 7. Exploring the standardized detection and sampling ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1571418/full]
- 8. Nasopharyngeal Swabs Are More Sensitive Than ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2020.00334/full]
- 9. Head-to-Head Comparison of Nasopharyngeal ... [https://www.mdpi.com/2075-4418/13/2/283]
- 10. Comparative evaluation of swabbing sites for Omicron ... [https://www.sciencedirect.com/science/article/pii/S0732889324004024]
- 11. Combined oropharyngeal nasal (ON) swabs for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502526/]
- 12. Differential tissue tropism and transmission efficiency of two ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1013493]
- 13. Changes in the epidemic patterns of respiratory pathogens ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12210601/]
- 14. Metagenomic next-generation sequencing for pathogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12481790/]
- 15. Evaluation of SARS-CoV-2 quantification from oropharyngeal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10998208/]
- 16. Quantitative analysis of different respiratory specimens on ... [https://www.sciencedirect.com/science/article/pii/S0732889322001663]
- 17. Combined oropharyngeal/nasal swab is equivalent to ... [https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-021-02087-4]
- 18. Saliva Has High Sensitivity and Specificity for Detecting SARS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346843/]
- 19. Accuracy of saliva tests for SARS-CoV-2 diagnosis during ... [https://www.nature.com/articles/s41598-025-20841-w]
- 20. A descriptive study on feasibility of nasopharyngeal and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12185522/]
- 21. Evaluation of swabbing methods for culture and non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12422522/]
- 22. Validation of oral-nasal specimen collection for influenza ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12022927/]
- 23. Proper Procedures for Performing Nasopharyngeal and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8015770/]
- 24. A LABORATORY VALIDATION OF SELF-COLLECTED ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10186957/]
- 25. Nasal, Nasopharyngeal, & Oropharyngeal Swab Collection ... [https://clevelandcliniclabs.com/laboratory-resources/specimen-collection-transport/collection/nasal-nasopharyngeal-np-oropharyngeal-op-swab-collection-instructions/]
- 26. Head-to-head comparison of anterior nares and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11934397/]
- 27. Optimal Insertion Depth for Nasal Mid-Turbinate and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8306705/]
- 28. Evaluation of Nasopharyngeal Swab Collection Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7665666/]
- 29. The Nasal Cavity - Structure - Vasculature - Innervation [https://teachmeanatomy.info/head/organs/the-nose/nasal-cavity/]
- 30. Analytical validation of the Percepta Nasal Swab classifier [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13683-2]
- 31. Detection of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) in outpatients: A multicenter comparison of self-collected saline gargle, oral swab, and combined oral-anterior nasal swab to a provider collected nasopharyngeal swab - PubMed [https://pubmed.ncbi.nlm.nih.gov/33436122/]
- 32. Autonomous swab robot for naso- and oropharyngeal ... [https://www.nature.com/articles/s41598-023-50291-1]
- 33. Reliable detection of SARS-CoV-2 with patient-collected swabs and saline gargles: A three-headed comparison on multiple molecular platforms - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8141269/]
- 34. Performance of Saliva, Oropharyngeal Swabs, and Nasal Swabs for SARS-CoV-2 Molecular Detection: a Systematic Review and Meta-analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/33504593/]
- 35. Comparison of nasopharyngeal and oropharyngeal swabs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7166099/]
- 36. of Nasopharyngeal and Comparison for the... Oropharyngeal Swabs [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0021610]
- 37. A new in vitro pre-clinical method for testing SARS-CoV-2 ... [https://www.nature.com/articles/s41598-025-21107-1]
- 38. oropharyngeal swabs for covid 19 testing [https://www.datainsightsmarket.com/reports/oropharyngeal-swabs-for-covid-19-testing-1502808]
- 39. Preanalytical Variables and Their Influence on the Quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6238383/]
- 40. Why Pre-Analytical Variables Can Make or Break Your Assay [https://mtgroupbio.com/the-hidden-challenge-in-assay-development-why-pre-analytical-variables-can-make-or-break-your-assay/]
- 41. Underscoring the effect of swab type, workflow, and ... [https://www.nature.com/articles/s41598-023-34337-y]
- 42. The impact of preanalytical variables on the analysis of cell ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2024.1385041/full]
- 43. Combined oropharyngeal/nasal swab is equivalent to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7820523/]
- 44. Performance & clinical utility of oropharyngeal versus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10101371/]
- 45. Comparative evaluation of feature reduction methods for ... [https://www.nature.com/articles/s41598-024-81866-1]
- 46. Comparison of RT-PCR and antigen test sensitivity across ... [https://www.sciencedirect.com/science/article/pii/S2405844024032195]
- 47. Prescription medication use in the 10 years prior to diagnosis of... [https://alzres.biomedcentral.com/articles/10.1186/s13195-024-01523-7]
- 48. Frontiers | The relationship between sensory processing sensitivity ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2023.1320695/full]
- 49. Nasopharyngeal Swab vs Nasal Swab: Comparing Methods [https://blog.puritanmedproducts.com/nasopharyngeal-swab-vs-nasal-swab]
- 50. Performance Analysis of Self-Collected Nasal and Oral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9600397/]
- 51. Feasibility of implementing a non-invasive self-sampling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12530422/]
- 52. Saliva Has High Sensitivity and Specificity for Detecting ... [https://www.mdpi.com/2075-4418/15/15/1918]
- 53. Different Respiratory Samples for COVID-19 Detection by ... [https://brieflands.com/journals/ijpr/articles/124308]
- 54. Accuracy of saliva tests for SARS-CoV-2 diagnosis during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12546890/]
- 55. SARS-CoV-2 Variants May Affect Saliva RT-PCR Assay ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12001863/]
- 56. Diagnostic accuracy of non-invasive SARS-CoV-2 screening ... [https://bmcinfectdis.biomedcentral.com/articles/10.1186/s12879-025-11088-x]
- 57. PCR sensitivity for Mycoplasma pneumoniae detection in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345179/]
- 58. Higher detection rates of Mycoplasma pneumoniae in ... [https://pubmed.ncbi.nlm.nih.gov/40902551/]
- 59. Comparing the yield of oropharyngeal swabs and sputum for ... [https://virologyj.biomedcentral.com/articles/10.1186/s12985-019-1177-x]
- 60. Mycoplasma pneumoniae Antigen Detection: Rapid ... [https://vitrosens.com/mycoplasma-pneumoniae-antigen-detection-rapid-diagnosis-for-respiratory-infections/]
- 61. Implementation of a Laboratory-Developed Test for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12300490/]
- 62. SARS-CoV-2 viral load and shedding kinetics [https://www.nature.com/articles/s41579-022-00822-w]
- 63. SARS-CoV-2 Viral Load in Stool and Nasopharyngeal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12534152/]
- 64. SARS-Cov-2 Viral Load in Nasal Swab and Raw Saliva ... [http://fortuneonline.org/articles/sarscov2-viral-load-in-nasal-swab-and-raw-saliva-samples-from-covid19-patients.html]
- 65. Statistical methods for comparing test positivity rates between ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9760457/]
- 66. Real-world Evidence versus Randomized Controlled Trial [https://pmc.ncbi.nlm.nih.gov/articles/PMC6097073/]