PICADAR in Focus: A Critical Analysis of Sensitivity and Specificity for PCD Diagnosis
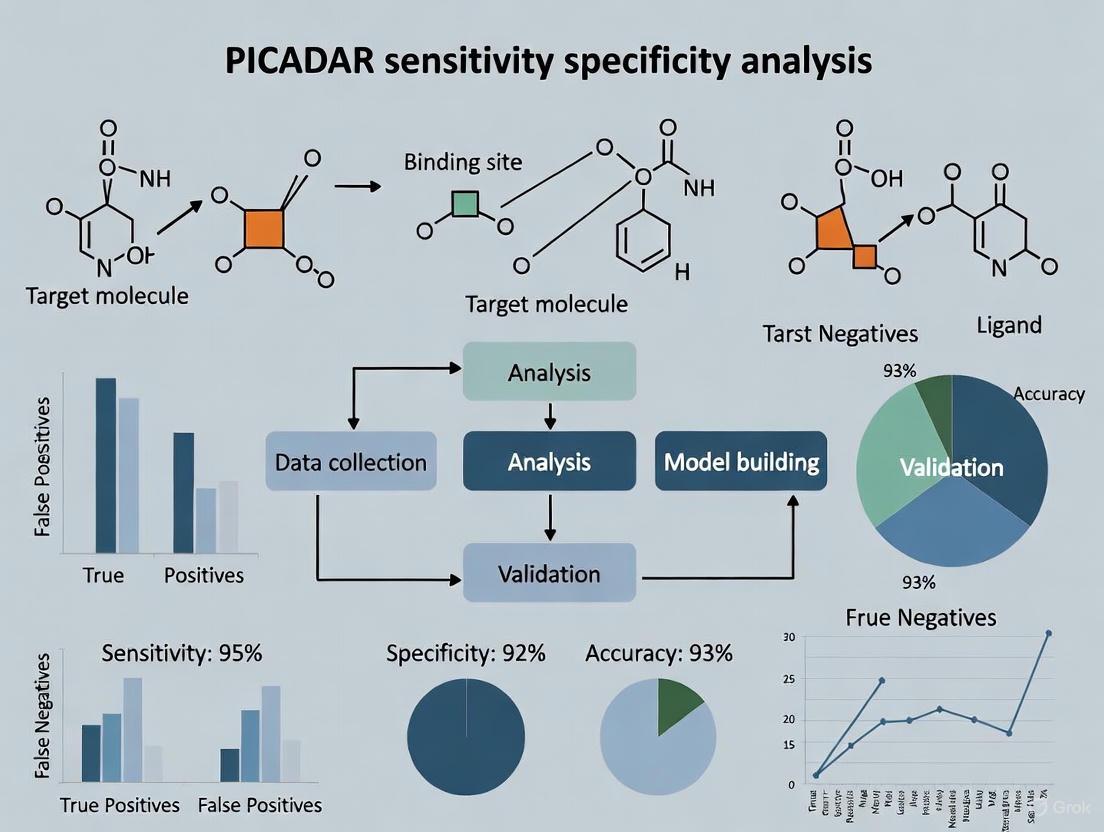
This article provides a comprehensive analysis of the PICADAR score, a clinical prediction tool for Primary Ciliary Dyskinesia (PCD).
PICADAR in Focus: A Critical Analysis of Sensitivity and Specificity for PCD Diagnosis
Abstract
This article provides a comprehensive analysis of the PICADAR score, a clinical prediction tool for Primary Ciliary Dyskinesia (PCD). It explores the foundational concepts of diagnostic test accuracy, details PICADAR's methodology, and presents recent evidence on its performance limitations, particularly its variable sensitivity across patient subgroups. Aimed at researchers and clinicians, the content evaluates PICADAR against emerging alternatives and discusses its implications for optimizing diagnostic pathways and patient selection in clinical practice and drug development.
Understanding Diagnostic Accuracy and the PICADAR Tool
This guide provides an objective analysis of the performance metrics of diagnostic tools, focusing on the PrImary Ciliary DyskinesiA Rule (PICADAR) within the context of primary ciliary dyskinesia (PCD) diagnosis. We examine the foundational principles of sensitivity, specificity, and predictive values, and apply these to compare PICADAR's established benchmarks against recent validation studies. Quantitative data are synthesized to reveal critical limitations in test sensitivity across patient subgroups, providing researchers and drug development professionals with evidence-based insights for diagnostic protocol selection and evaluation.
Diagnostic test accuracy is fundamental to clinical decision-making and therapeutic development. The performance of any diagnostic tool is quantified by its sensitivity—the ability to correctly identify individuals with the disease—and specificity—the ability to correctly identify those without the disease [1]. These metrics, along with positive predictive value (PPV) and negative predictive value (NPV), provide a framework for evaluating a test's real-world utility and limitations [2]. Sensitivity represents the proportion of true positives detected by the test among all individuals with the condition, calculated as True Positives / (True Positives + False Negatives) [1]. Conversely, specificity represents the proportion of true negatives among all disease-free individuals, calculated as True Negatives / (True Negatives + False Positives) [1]. In screening contexts, these metrics must be interpreted with an understanding of their inherent trade-offs and their relationship to disease prevalence in the target population [2].
The diagnostic landscape for rare diseases presents particular challenges, where imperfect reference standards and phenotypic heterogeneity can significantly impact measured test performance [3]. This analysis uses PICADAR, a predictive tool for primary ciliary dyskinesia (PCD), to illustrate these core diagnostic principles with empirical data, highlighting how test performance varies across patient populations and clinical settings.
Core Diagnostic Metrics: Definitions and Calculations
Foundational Formulas and Relationships
The validity of a diagnostic test is determined through direct comparison with a reference standard, which represents the best available assessment of the true disease status [2]. The interrelationships between diagnostic metrics are visualized through a standard 2x2 contingency table, from which all accuracy calculations derive.
Diagram 1: Diagnostic Test Calculation Framework. PPV: Positive Predictive Value; NPV: Negative Predictive Value.
Critical Distinctions in Metric Interpretation
Healthcare providers must recognize crucial distinctions between these metrics. Sensitivity and specificity are considered stable test attributes that describe its performance relative to a reference standard, while predictive values determine the probability that a test result correctly classifies a patient's condition and are influenced by disease prevalence [1] [2]. This prevalence dependence means that even tests with high sensitivity and specificity can yield misleading predictive values when applied to populations with drastically different disease prevalence than the original validation cohort.
A critical and often misunderstood relationship exists between sensitivity and PPV. Sensitivity describes a test's performance among people known to have the disease (reference standard positive), whereas PPV describes the test's performance among people who test positive on the screening test [2]. This distinction fundamentally impacts how test results should be interpreted in both clinical practice and research settings, particularly for disorders like PCD where prevalence varies across populations and healthcare settings.
PICADAR: Original Development and Validation
Tool Development and Methodology
The Primary Ciliary Dyskinesia Rule (PICADAR) was developed as a practical clinical tool to identify patients requiring specialized PCD testing [4]. Developed through analysis of 641 consecutive referrals to a PCD diagnostic center, the tool aims to streamline referral pathways by utilizing readily obtainable clinical history rather than specialized equipment. The original study employed logistic regression to identify predictive parameters from 27 potential variables, ultimately selecting seven key clinical features for inclusion in the final model [4].
Table 1: Original PICADAR Predictive Parameters and Scoring System
| Predictive Parameter | Points |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms | 1 |
| Neonatal intensive care admission | 2 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 4 |
| Total Possible Score | 12 |
PICADAR incorporates an initial gatekeeping question about persistent wet cough. Patients without this symptom are excluded from further scoring, while those with persistent wet cough proceed through the seven-item evaluation [5] [6]. The total score determines the probability of PCD, with the originally recommended referral threshold set at ≥5 points [4].
Original Performance Claims
In its original validation, PICADAR demonstrated strong diagnostic performance in both derivation and external validation cohorts, supporting its adoption into clinical guidelines.
Table 2: Originally Reported PICADAR Performance Metrics
| Metric | Derivation Cohort | External Validation |
|---|---|---|
| Sensitivity | 0.90 | 0.90 |
| Specificity | 0.75 | 0.75 |
| Area Under Curve (AUC) | 0.91 | 0.87 |
| Population | 641 referrals (75 PCD+) | 187 patients (93 PCD+) |
The original research reported excellent discrimination with area under the receiver operating characteristic curve (AUC) of 0.91 in the derivation group and 0.87 in external validation [4]. Based on these findings, the European Respiratory Society incorporated PICADAR into diagnostic guidelines as a recommended tool for estimating PCD likelihood prior to specialized testing.
Contemporary Analysis of PICADAR Performance
Recent Validation Study Methodology
A 2025 study led by Schramm et al. conducted a rigorous re-evaluation of PICADAR's sensitivity in a genetically confirmed PCD cohort [5] [6]. The investigation analyzed 269 individuals with definitive genetic diagnoses of PCD, applying the standard PICADAR scoring protocol to calculate sensitivity based on the recommended ≥5 point threshold. Subgroup analyses examined how test performance varied by the presence of laterality defects (situs inversus or heterotaxy) and hallmark ultrastructural ciliary defects [5].
The experimental protocol followed these key steps:
- Patient Selection: 269 individuals with genetically confirmed PCD provided the reference standard
- Data Collection: Clinical history necessary for PICADAR scoring obtained from medical records
- Scoring Application: PICADAR scores calculated according to published algorithms
- Sensitivity Calculation: Proportion of patients with scores ≥5 points determined
- Stratified Analysis: Performance calculated across subgroups based on laterality and ultrastructural status
This methodology provided a robust framework for assessing real-world PICADAR performance against a genetic gold standard, particularly in patient subgroups that may not exhibit classic PCD phenotypes.
Revealed Limitations in Test Sensitivity
The 2025 validation revealed significant limitations in PICADAR's sensitivity, particularly in key patient subgroups. The overall sensitivity of 75% (202/269) fell substantially below originally reported values [5] [6]. Most notably, 7% (18/269) of genetically confirmed PCD patients were excluded by PICADAR's initial gatekeeping question due to absence of daily wet cough [5].
Table 3: Stratified Sensitivity Analysis of PICADAR in Genetically Confirmed PCD
| Patient Subgroup | Sensitivity | Median Score (IQR) |
|---|---|---|
| Overall Cohort | 75% (202/269) | 7 (5-9) |
| With Laterality Defects | 95% | 10 (8-11) |
| Situs Solitus (Normal Laterality) | 61% | 6 (4-8) |
| Hallmark Ultrastructural Defects | 83% | Not reported |
| Normal Ultrastructure | 59% | Not reported |
The stratified analysis demonstrated dramatically different performance across phenotypic presentations. While sensitivity reached 95% in patients with laterality defects, it dropped to just 61% in those with normal organ arrangement (situs solitus) [5] [6]. Similarly, patients without hallmark ultrastructural defects on transmission electron microscopy showed significantly lower sensitivity (59%) compared to those with definitive ultrastructural abnormalities (83%) [5].
Comparative Performance Analysis
PICADAR Versus Alternative Diagnostic Approaches
PCD diagnosis typically employs a multi-test algorithm rather than reliance on a single modality. The comparative performance characteristics of available diagnostic methods reveal complementary strengths and limitations.
Table 4: Comparative Diagnostic Modalities in PCD Evaluation
| Diagnostic Method | Typical Sensitivity | Key Limitations |
|---|---|---|
| PICADAR Score | 75% (61-95% by subgroup) | Low sensitivity in situs solitus and normal ultrastructure cases |
| Nasal Nitric Oxide (nNO) | High (variable by genotype) | Requires expensive equipment and patient cooperation |
| Genetic Testing | >90% for known genes | Limited by unidentified genes; expensive; complex interpretation |
| Transmission Electron Microscopy | ~70% | Misses ultrastructurally normal PCD; requires expertise |
| High-Speed Video Microscopy | High for motile cilia | Limited availability; secondary dyskinesia confounds |
The tabular comparison illustrates that PICADAR serves as an accessible initial screening tool but requires supplementation with more specialized testing for definitive diagnosis, particularly given its variable sensitivity across genotypic and phenotypic presentations [7]. This comprehensive diagnostic approach acknowledges the absence of a single gold standard test for PCD, instead relying on congruent findings across multiple modalities to establish diagnosis [7].
Impact of Phenotypic and Genotypic Diversity
The performance variations observed in PICADAR highlight a fundamental challenge in rare disease diagnostics: the influence of population heterogeneity on test accuracy. The tool demonstrates substantially different performance across ethnic populations, as illustrated by a Japanese study where only 25% of PCD patients exhibited situs inversus compared to approximately 50% in Western cohorts [8]. This discrepancy reflects differences in the distribution of causative genetic mutations across populations, with corresponding impacts on phenotypic presentation and, consequently, on PICADAR scores [8].
The dependency on laterality features creates particular challenges for diagnosing PCD in patients with normal organ arrangement, who represent a growing proportion of identified cases as genetic testing expands. These findings underscore the necessity of considering local genotype-phenotype correlations when implementing diagnostic prediction rules across diverse populations and healthcare settings.
Essential Research Reagents and Methodologies
Research Reagent Solutions for PCD Diagnostic Research
Table 5: Essential Research Materials for PCD Diagnostic Development
| Reagent/Technology | Primary Function | Research Application |
|---|---|---|
| Genetic Sequencing Panels | Detection of mutations in >50 PCD-associated genes | Definitive diagnosis; genotype-phenotype correlation |
| Transmission Electron Microscopy | Visualization of ciliary ultrastructure | Identification of hallmark defects (ODA, IDA, MTD) |
| High-Speed Video Microscopy | Analysis of ciliary beat pattern and frequency | Functional assessment of ciliary motility |
| Nasal Nitric Oxide Systems | Measurement of nNO production | Screening; typically low nNO in PCD |
| Immunofluorescence Assays | Protein localization in ciliary apparatus | Detection of missing axonemal proteins |
| Air-Liquid Interface Cell Culture | Ciliary differentiation and regeneration | Exclusion of secondary dyskinesia |
The research reagents and technologies outlined in Table 5 represent essential components for comprehensive PCD diagnostic development and validation [7]. These tools enable multimodal assessment that accounts for the genetic and phenotypic heterogeneity characteristic of PCD, providing orthogonal verification methods necessary for robust test validation.
Diagnostic Workflow Integration
The following diagram illustrates how diagnostic modalities integrate within a comprehensive PCD evaluation pathway, highlighting decision points and complementary test relationships:
Diagram 2: Comprehensive PCD Diagnostic Pathway. NO: nitric oxide.
The analysis of PICADAR within the framework of diagnostic test principles reveals both utility and significant limitations. While offering an accessible initial screening method with good specificity, its variable sensitivity—particularly in patients with situs solitus (61%) or normal ciliary ultrastructure (59%)—limits its reliability as a standalone tool [5] [6]. These findings underscore the necessity of context-specific test interpretation and the importance of understanding how phenotypic and genotypic variations impact diagnostic performance.
For researchers and drug development professionals, these insights highlight several critical considerations: the imperative of population-specific validation, the limitations of clinical prediction rules in genetically heterogeneous disorders, and the necessity of multimodal diagnostic approaches when no single gold standard test exists. Future diagnostic development should focus on creating complementary tools that address PICADAR's sensitivity gaps, particularly for patients without classic laterality defects, to ensure equitable diagnostic access across all PCD phenotypes and genotypes.
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disease characterized by abnormal ciliary function, leading to impaired mucociliary clearance and subsequent chronic infections of the upper and lower airways [9]. With an estimated prevalence of 1:10,000-1:20,000 and over 50 identified causative genes, PCD presents substantial diagnostic challenges [9] [7]. The disease manifests with heterogeneous clinical presentations, often combining persistent wet cough, chronic rhinosinusitis, recurrent otitis media, bronchiectasis, and laterality defects such as situs inversus (present in approximately 50% of patients) [9] [7]. A critical challenge is that the vast majority of PCD patients remain undiagnosed, creating a major obstacle to delivering appropriate care [9]. This diagnostic gap persists despite advances in understanding the genetic basis and pathophysiology of PCD, highlighting the urgent need for effective screening strategies and standardized diagnostic protocols.
Diagnostic delays remain significant, with patients often experiencing over 40 medical visits for PCD-related symptoms before referral for specialized testing [9]. The median age at diagnosis is 13 years, with a four-year gap between initial suspicion and confirmatory testing [10]. This delay is particularly problematic as late diagnosis associates with decreased lung function and poorer prognosis due to irreversible structural lung damage [10]. Early identification and treatment are therefore essential to prevent bronchiectasis and preserve lung function, underscoring the clinical imperative for effective screening methodologies in at-risk populations.
The Complex Diagnostic Landscape: Available Tools and Their Limitations
PCD diagnosis lacks a single gold standard test, requiring instead a combination of technically demanding investigations [11] [7]. The European Respiratory Society (ERS) guidelines recommend a multi-test algorithm incorporating clinical features, nasal nitric oxide (nNO) measurement, high-speed video microscopy analysis (HSVA), transmission electron microscopy (TEM), and genetic testing [11]. This combinatorial approach is necessary because each test has distinct limitations in sensitivity, specificity, and technical requirements. The diagnostic landscape is further complicated by variations in test availability across different healthcare systems, with limited access to specialized PCD diagnostic centers in many regions [9] [10]. Centralized care facilities managing over 20 PCD patients have demonstrated diagnosis at earlier ages, emphasizing the importance of specialized expertise and high patient throughput [9].
Table 1: Diagnostic Tests for PCD and Their Performance Characteristics
| Diagnostic Test | Sensitivity | Specificity | Key Limitations |
|---|---|---|---|
| Nasal Nitric Oxide (nNO) | 91% [12] | 96% [12] | Less reliable in children <5-6 years; requires patient cooperation; not disease-specific [11] [12] |
| High-Speed Video Microscopy Analysis (HSVA) | 100% [12] | 93% [12] | Requires significant expertise; secondary ciliary dyskinesia can mimic PCD [9] [12] |
| Transmission Electron Microscopy (TEM) | ~79% [13] | 100% [12] | Misses 15-30% of PCD cases with normal ultrastructure; technical complexity [9] [13] |
| Genetic Testing | 60-70% (for known genes) [9] | High (varies) | Incomplete knowledge of all PCD genes; variants of uncertain significance [9] [10] |
Technical Challenges and Standardization Issues
Each diagnostic modality faces significant technical challenges that impact its reliability and implementation. For nNO measurement, cut-off values vary considerably between centers due to differences in equipment, techniques, and patient age [9]. Although a cut-off of 77 nL·min⁻¹ has shown disease-specific discriminatory value in multiple sites when using standardized protocols, consensus on appropriate thresholds for children under 6 years remains lacking [9]. For HSVA, ciliary beat pattern analysis is observer-dependent, and standardizing terminology for different beat patterns presents ongoing challenges [9]. Subtle ciliary abnormalities are difficult to differentiate from secondary defects caused by infection or inflammation, often requiring repeat testing or air-liquid interface (ALI) culture to confirm primary defects [11] [12].
TEM faces quantitative challenges in determining the minimal number of cilia that must be scored and standardized terminology for ultrastructural defects [9]. Furthermore, 15-20% of confirmed PCD cases have normal ciliary ultrastructure despite causative genetic mutations, limiting TEM's sensitivity as a standalone test [9] [13]. Genetic testing continues to evolve as new PCD-related genes are discovered, but current panels identify mutations in only 60-70% of clinically confirmed cases [9]. The absence of a gold standard creates circularity in validating new genetic discoveries, as case definition typically requires abnormal HSVA or TEM findings [9].
PICADAR: A Validated Clinical Tool for Targeted Screening
Development and Implementation
The PCD Rule (PICADAR) is a clinical predictive tool developed to identify patients at high risk for PCD who should be referred for specialized diagnostic testing [9] [11]. This validated scoring system uses seven clinical features to calculate a probability score for PCD: neonatal chest symptoms, neonatal respiratory support, situs inversus, congenital cardiac defect, persistent perennial rhinitis, chronic ear symptoms, and chronic nasal symptoms [14]. PICADAR was developed through systematic analysis of clinical features in genetically confirmed PCD cases and validated in consecutive referrals for PCD testing [9]. The tool provides a simple, evidence-based method for general practitioners and pediatricians to identify appropriate candidates for specialist referral, potentially reducing diagnostic delays and unnecessary testing in low-probability cases.
The European Respiratory Society guidelines suggest using predictive tools like PICADAR in combination with distinct PCD symptoms to identify patients for diagnostic testing [11]. This recommendation acknowledges that no single clinical feature is pathognomonic for PCD, but specific combinations can strongly suggest the diagnosis. For neonates, the combination of lobar collapse, situs inversus, and/or persistent oxygen therapy for over 2 days in term newborns with respiratory distress can accurately predict PCD [9]. The diagnosis should also be considered in term neonates with normal situs but unexplained respiratory distress, as over 70% of PCD patients suffer from neonatal respiratory symptoms [9].
Performance and Comparative Analysis
PICADAR demonstrates robust performance characteristics as a screening tool. In validation studies, it effectively stratifies patients by disease probability, helping to prioritize specialist referrals in resource-constrained settings [9]. The tool's structured approach standardizes the clinical assessment for PCD suspicion, reducing reliance on individual clinician experience and awareness. When compared to other screening methods, PICADAR offers the advantage of being rapidly applicable during routine clinical encounters without requiring specialized equipment or technical expertise, making it particularly valuable in primary and secondary care settings where access to nNO, HSVA, TEM, and genetic testing may be limited.
Table 2: Comparison of Screening and Diagnostic Approaches for PCD
| Method | Primary Use | Advantages | Limitations |
|---|---|---|---|
| PICADAR | Clinical screening | No specialized equipment needed; rapid application; validated predictive value | Relies on accurate history; less effective without classic symptoms |
| Nasal NO | Screening/Diagnostic | High specificity in children >6 years; non-invasive | Limited in young children; requires specialized equipment; false negatives in some genotypes |
| HSVA | Diagnostic | Direct functional assessment; high sensitivity | Requires expertise; secondary changes affect interpretation |
| TEM | Diagnostic | High specificity; identifies structural defects | Misses normal ultrastructure cases; invasive sampling |
| Genetic Testing | Diagnostic/Confirmatory | Definitive when pathogenic mutations identified; enables family screening | 30-40% of cases have no identified mutation; cost and accessibility |
Analytical Frameworks: Experimental Protocols and Methodologies
Standardized Diagnostic Protocols
Comprehensive PCD diagnostic testing follows standardized protocols to ensure accurate and reproducible results. For nNO measurement, the ERS guidelines recommend using a chemiluminescence analyzer with a velum closure technique during breath-hold in children over 6 years and adults, while suggesting tidal breathing measurements for children under 6 years [11]. Measurements should be performed when patients are free of acute respiratory infections, typically waiting at least 4 weeks after infection resolution [12]. For HSVA, ciliated epithelial samples obtained via nasal brush biopsy are analyzed using high-speed cameras recording at 500 frames per second, with qualitative assessment of ciliary beat pattern and quantitative measurement of ciliary beat frequency [12]. Expert microscopists analyze at least six healthy strips of ciliated epithelium, with abnormal patterns including static, uncoordinated, rotational, or reduced amplitude beating [12].
TEM analysis requires examination of at least 100 cilia in transverse section at 60,000x magnification, with quantitative assessment of axonemal structure using center-specific normative data [12]. Hallmark ultrastructural defects include outer dynein arm (ODA) absence, combined ODA and inner dynein arm (IDA) absence, and microtubular disorganization with IDA defects [10]. When initial results are inconclusive or show secondary dyskinesia, repeat testing following air-liquid interface (ALI) culture is recommended to exclude acquired defects and confirm primary ciliary abnormalities [11] [12]. Genetic testing approaches have evolved from candidate gene analysis to next-generation sequencing panels covering all known PCD-related genes, with classification of identified variants according to American College of Medical Genetics and Genomics guidelines [10].
Research Reagent Solutions for PCD Investigation
Table 3: Essential Research Reagents and Materials for PCD Diagnostic Studies
| Reagent/Material | Application | Function | Technical Notes |
|---|---|---|---|
| Chemiluminescence NO Analyzer | nNO measurement | Quantifies nasal nitric oxide concentration | Use velum closure technique; establish center-specific reference values |
| High-Speed Camera System | HSVA | Records ciliary beating for pattern and frequency analysis | Minimum 500 fps; requires specialized analysis software |
| Transmission Electron Microscope | TEM | Visualizes ciliary ultrastructure at high resolution | Analyze ≥100 cilia cross-sections; quantitative assessment |
| Air-Liquid Interface Culture System | Ciliary culture | Differentiates primary from secondary ciliary defects | 3-4 week culture period; allows ciliary regeneration |
| Genetic Sequencing Panels | Genetic testing | Identifies mutations in PCD-associated genes | NGS panels should cover >50 known genes; confirm bi-allelic mutations |
| Glutaraldehyde Fixative | TEM sample preparation | Preserves ciliary ultrastructure for electron microscopy | 3% concentration; immediate fixation after sampling |
Visualizing Diagnostic Pathways and Genetic Relationships
PCD Diagnostic Decision Algorithm
PCD Diagnostic Decision Algorithm
Genetic Landscape of PCD Ultrastructural Defects
Genetic Associations with Ultrastructural Defects
The diagnostic landscape for PCD remains complex, requiring integration of multiple complementary approaches to achieve accurate diagnosis. PICADAR provides a valuable evidence-based screening tool to identify high-risk patients who warrant specialized testing, potentially reducing diagnostic delays and improving resource allocation. However, even with optimal screening, definitive diagnosis requires sophisticated testing available only at specialized centers. The limitations of individual diagnostic modalities—including the inability of TEM to detect 15-30% of PCD cases with normal ultrastructure, the technical challenges of HSVA interpretation, and the incomplete coverage of current genetic panels—necessitate a combinatorial diagnostic approach.
Future directions in PCD diagnostics include the standardization of testing protocols across centers, validation of novel screening biomarkers, expansion of genetic panels as new disease genes are discovered, and development of targeted genetic testing for populations with founder mutations. Immunofluorescence staining of ciliary proteins shows promise as an emerging diagnostic adjunct that may help identify cases with normal ultrastructure [11] [7]. For researchers and clinicians, understanding the performance characteristics, limitations, and appropriate applications of each diagnostic tool is essential for accurate PCD diagnosis and for advancing the development of more effective screening strategies. As genetic knowledge expands and technologies evolve, the diagnostic paradigm for PCD will continue to refine, hopefully leading to earlier diagnosis and improved clinical outcomes for patients with this heterogeneous genetic disorder.
The PrImary CiliAry DyskinesiA Rule (PICADAR) is a clinical prediction tool developed to identify patients at high probability of having Primary Ciliary Dyskinesia (PCD) before proceeding with complex, costly, and invasive diagnostic testing. This objective comparison guide details PICADAR's original development, stated objectives, and current performance metrics against other diagnostic approaches, providing researchers and clinicians with synthesized experimental data and methodological protocols essential for evaluating its utility in both clinical and research settings.
Original Development and Objectives
PICADAR was developed to serve as an accessible, evidence-based screening instrument for PCD, a rare genetic disease affecting approximately 1 in 7,500 to 1 in 20,000 live births [7]. The tool was created to address the significant diagnostic challenges posed by PCD, which requires specialized testing methods—such as nasal nitric oxide (nNO) measurement, high-speed video microscopy analysis (HSVA), transmission electron microscopy (TEM), and genetic testing—that are not universally available and can be technically demanding [7].
The primary stated objective of PICADAR is to provide a systematic method for general practitioners and pediatricians to quantify the pre-test probability of PCD, thereby guiding appropriate referral to specialized centers. By identifying high-risk individuals efficiently, PICADAR aims to reduce diagnostic delays, which are common in PCD due to its nonspecific clinical presentation overlapping with more common respiratory conditions like asthma and recurrent bronchitis [7].
Performance Comparison with Alternative Diagnostic Approaches
The following tables synthesize quantitative performance data for PICADAR and alternative PCD diagnostic methods, compiled from recent validation studies.
| Diagnostic Tool | Reported Sensitivity | Reported Specificity | Target Population | Study Sample Size |
|---|---|---|---|---|
| PICADAR (Score ≥5) | 75% (202/269) [6] | Not fully evaluated in recent studies | Genetically confirmed PCD patients | 269 [6] |
| PICADAR (Situs Solitus subgroup) | 61% [6] | N/A | PCD patients without laterality defects | Subgroup of 269 [6] |
| PICADAR (No hallmark ultrastructural defects) | 59% [6] | N/A | PCD patients with normal ultrastructure | Subgroup of 269 [6] |
| Nasal Nitric Oxide (nNO) | High (varies by method) [7] | High (varies by method) [7] | Patients with clinical suspicion of PCD | Variable across studies [7] |
| Genetic Testing | Evolving (>40-50 known genes) [7] | ~100% (for confirmed pathogenic variants) [7] | Patients with clinical suspicion of PCD | Variable across studies [7] |
Table 2: Subgroup Performance Analysis of PICADAR
| Patient Subgroup | Median PICADAR Score (IQR) | Sensitivity | Statistical Significance (p-value) |
|---|---|---|---|
| All Genetically Confirmed PCD | 7 (IQR: 5-9) [6] | 75% (202/269) [6] | Reference |
| With Laterality Defects | 10 (IQR: 8-11) [6] | 95% [6] | p < 0.0001 [6] |
| With Situs Solitus (normal arrangement) | 6 (IQR: 4-8) [6] | 61% [6] | p < 0.0001 (vs. with laterality defects) [6] |
| With Hallmark Ultrastructural Defects | Not specified | 83% [6] | p < 0.0001 [6] |
| Without Hallmark Ultrastructural Defects | Not specified | 59% [6] | p < 0.0001 (vs. with hallmark defects) [6] |
| Japanese PCD Cohort | Mean: 7.3 (range: 3-14) [8] | Not specified | Different patient demographics [8] |
Experimental Protocols and Methodologies
Recent Validation Study Protocol
A 2025 multi-center study conducted by Schramm et al. provides the most recent robust evaluation of PICADAR's performance, using the following methodological approach [6]:
- Study Population: 269 individuals with genetically confirmed PCD, ensuring an objective diagnostic standard.
- PICADAR Application: Researchers calculated PICADAR scores retrospectively based on clinical data. The tool consists of an initial gatekeeping question about the presence of daily wet cough, followed by seven additional questions for those who screen positive [6].
- Scoring Interpretation: A score of ≥5 points was used as the positive cutoff threshold as recommended in the original PICADAR development study.
- Statistical Analysis: Sensitivity was calculated as the proportion of genetically confirmed PCD patients who scored ≥5 on PICADAR. Subgroup analyses examined the impact of laterality defects (situs inversus versus situs solitus) and predicted hallmark ultrastructural defects on test performance [6].
PICADAR's Original Scoring Criteria
The PICADAR tool assesses the following clinical features, which reflect the typical presentation of PCD [7]:
- Initial Screening Question: Presence of daily wet cough (if negative, rules out PCD according to the tool's logic)
- Additional Scored Features:
- Neonatal respiratory symptoms at term birth
- Chest symptoms in the neonatal period
- Chronic rhinitis
- Persistent perennial rhinitis
- Hearing impairment or serous otitis media
- Situs inversus
- Congenital cardiac defect
PICADAR in the PCD Diagnostic Pathway
The diagnostic pathway for PCD illustrates how PICADAR serves as an initial clinical screening tool before advanced testing.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for PCD Diagnostic Research
| Reagent/Material | Primary Function in PCD Research | Specific Application Examples |
|---|---|---|
| Transmission Electron Microscopy (TEM) | Ultrastructural analysis of ciliary defects [7] | Identifying ODA, IDA, microtubular disorganization, and central pair defects [7] |
| High-Speed Video Microscopy (HSVA) | Functional analysis of ciliary beat pattern and frequency [7] | Detecting dyskinetic, immotile, or uncoordinated ciliary motion [7] |
| Nasal Nitric Oxide (nNO) Measurement | Non-invasive screening with high negative predictive value [7] | Differentiating PCD from other respiratory conditions (consistently low nNO in PCD) [7] |
| Next-Generation Sequencing Panels | Genetic confirmation of PCD diagnosis [7] | Identifying mutations in >50 known PCD-associated genes (e.g., DNAH5, DNAH11, CCDC39, CCDC40) [7] |
| Immunofluorescence Assays | Protein localization and analysis [7] | Detecting absence or mislocalization of specific ciliary proteins resulting from genetic mutations [7] |
Genetic Signaling Pathways in PCD
The genetic complexity of PCD underpins the challenges faced by clinical prediction tools like PICADAR, as different genetic subtypes present with varying clinical features.
Critical Analysis and Research Implications
While PICADAR provides a valuable structured approach to PCD suspicion, recent evidence reveals significant limitations that researchers must consider when incorporating it into study designs or clinical protocols [6]:
Critical Sensitivity Gap: The finding that 7% of genetically confirmed PCD patients were ruled out by the initial "daily wet cough" question alone highlights a fundamental limitation in the tool's design, potentially missing atypical presentations [6].
Demographic and Genetic Variability: The Japanese cohort study revealed a much lower rate of situs inversus (25% versus approximately 50% in Western populations), indicating that PICADAR's performance may vary significantly across different ethnic and genetic backgrounds [8]. This is particularly important for international clinical trials and genetic studies.
Ultrastructural Dependency: The significantly lower sensitivity (59%) in patients without hallmark ultrastructural defects indicates PICADAR may preferentially identify certain PCD genotypes over others, potentially introducing selection bias in research studies [6].
These limitations underscore the need for continued refinement of PCD prediction tools and the importance of using PICADAR as one component in a comprehensive diagnostic approach rather than as a definitive screening mechanism, particularly in research settings seeking to understand the full spectrum of PCD presentation.
The PrImary CiliAry DyskinesiA Rule (PICADAR) is a clinical predictive tool designed to identify patients at high probability of primary ciliary dyskinesia (PCD) who should be referred for specialized diagnostic testing [15]. This review deconstructs the PICADAR scorecard by examining its seven predictive parameters, analyzes its performance against subsequent validation studies, and details the experimental methodologies used in its development and evaluation. Evidence synthesized from foundational and recent critical studies demonstrates that while PICADAR provides a valuable structured screening approach, its sensitivity varies significantly across patient subgroups, particularly those without laterality defects or hallmark ultrastructural defects [5] [6]. This objective comparison provides researchers and clinicians with a comprehensive evidence-based framework for implementing PCD predictive tools in both research and clinical settings.
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous, autosomal recessive disorder caused by mutations in over 50 genes encoding proteins essential for ciliary structure and function [7]. The disease impairs mucociliary clearance, leading to recurrent respiratory tract infections, chronic rhinosinusitis, otitis media, and bronchiectasis; approximately half of patients exhibit laterality defects including situs inversus or heterotaxy [15] [7]. With an estimated prevalence of 1:7,500–1:20,000 live births, PCD remains challenging to diagnose due to its nonspecific clinical presentation and the requirement for complex, expensive diagnostic tests available only at specialized centers [7]. These tests include nasal nitric oxide (nNO) measurement, high-speed video microscopy analysis (HSVA), transmission electron microscopy (TEM), and genetic testing, none of which alone serves as a standalone gold standard [7]. The PICADAR tool was developed to address this diagnostic challenge by providing a evidence-based method to triage patients for specialized testing using readily available clinical information [15].
The PICADAR Scorecard: Parameters and Scoring System
The PICADAR scorecard was derived from a prospective study of 641 consecutive patients referred for PCD testing, of whom 75 (12%) received a positive diagnosis [15]. Through logistic regression analysis of 27 potential clinical variables, seven predictive parameters were identified that can be readily obtained through patient history [15] [16]. The scoring system applies specifically to patients with persistent wet cough and assigns points as follows:
Table 1: The Seven Predictive Parameters of the PICADAR Scorecard
| Predictive Parameter | Score |
|---|---|
| Full-term gestation (≥37 weeks) | 2 points |
| Neonatal chest symptoms (within first month of life) | 2 points |
| Neonatal intensive care unit admission | 1 point |
| Chronic rhinitis (>3 months) | 1 point |
| Chronic ear symptoms | 1 point |
| Situs inversus | 2 points |
| Congenital cardiac defect | 2 points |
The following diagram illustrates the logical workflow for calculating a patient's PICADAR score and interpreting the result:
Performance Analysis: Validation and Limitations
Since its original development, multiple studies have evaluated PICADAR's performance in different populations, revealing both its utility and significant limitations.
Table 2: PICADAR Performance Across Validation Studies
| Study Population | Sensitivity | Specificity | AUC | Key Findings |
|---|---|---|---|---|
| Original derivation (n=641) [15] | 0.90 | 0.75 | 0.91 | Cut-off score of 5 points optimized performance |
| External validation (n=187) [15] | N/A | N/A | 0.87 | Good discriminative ability in independent cohort |
| Genetically confirmed PCD (n=269) [5] | 0.75 | N/A | N/A | 7% with no daily wet cough automatically excluded |
| PCD with laterality defects [5] | 0.95 | N/A | N/A | High sensitivity in this subgroup |
| PCD with situs solitus (normal arrangement) [5] [6] | 0.61 | N/A | N/A | Significantly reduced sensitivity |
| PCD with hallmark ultrastructural defects [5] [6] | 0.83 | N/A | N/A | Moderate sensitivity |
| PCD without hallmark ultrastructural defects [5] [6] | 0.59 | N/A | N/A | Substantially limited sensitivity |
| Japanese cohort (n=67) [8] | N/A | N/A | N/A | Mean score: 7.3; only 25% with situs inversus |
A critical 2025 study by Schramm et al. evaluating 269 genetically confirmed PCD patients revealed important limitations [5] [6]. The study found that 18 individuals (7%) reported no daily wet cough, automatically ruling out PCD according to PICADAR's initial screening question [5]. The overall sensitivity was 75%, significantly lower than the original derivation study [5] [6]. Subgroup analysis demonstrated dramatically different performance: sensitivity reached 95% in patients with laterality defects but dropped to 61% in those with situs solitus (normal organ arrangement) [5] [6]. Similarly, sensitivity was substantially higher in patients with hallmark ultrastructural defects (83%) compared to those without (59%) [5] [6]. These findings highlight significant limitations in detecting PCD patients without classic laterality defects or ultrastructural abnormalities.
Ethnic variations further complicate PICADAR's performance. A Japanese study of 67 PCD patients found only 25% had situs inversus, substantially lower than the approximately 50% typically reported in other populations [8]. This difference was attributed to variations in prevalent causative genes across ethnic groups [8]. With a mean PICADAR score of 7.3 points, the tool remained useful in this population, but the dramatically lower rate of situs inversus—a high-scoring parameter—could impact its performance in non-European populations [8].
Experimental Methodologies
Original Derivation Study Protocol
The original PICADAR derivation study employed a rigorous methodological approach [15]. The research analyzed data from 641 consecutive patients with definitive diagnostic outcomes from the University Hospital Southampton PCD diagnostic center between 2007-2013 [15]. A standardized proforma was used to collect patient data through clinical interviews prior to diagnostic testing [15]. Diagnostic criteria required a typical clinical history with at least two abnormal specialized tests: "hallmark" transmission electron microscopy (TEM) findings, "hallmark" ciliary beat pattern (CBP) on high-speed video microscopy analysis, or nasal nitric oxide (nNO) ≤30 nL·min⁻¹ [15]. Statistical analysis involved comparing characteristics of positive and negative referrals using parametric (t-test) and nonparametric (Mann-Whitney) tests, chi-squared tests, or Fisher's exact tests as appropriate [15]. Logistic regression analysis identified significant predictors, with model performance assessed through receiver operating characteristic (ROC) curve analysis and area under the curve (AUC) calculations [15]. The model was simplified into a practical scoring tool by rounding regression coefficients to the nearest integer [15].
External Validation Methodology
External validation followed a similar protocol using a sample of 187 patients (93 PCD-positive, 94 PCD-negative) referred to the Royal Brompton Hospital between 1983-2013 [15]. An equal number of positive and negative referrals were randomly selected from the overall population [15]. Using a similar protocol to the derivation group, clinical history proformas were completed before diagnostic testing [15]. The discriminative ability of the PICADAR scores in this validation population was assessed using ROC curve analysis [15]. This external validation cohort was younger and more likely to be non-white and from consanguineous backgrounds compared to the derivation group, reflecting different population characteristics and testing the tool's generalizability [15].
Genetic Validation Study Design
The 2025 validation study by Schramm et al. employed a distinct methodology focused on genetically confirmed PCD cases [5] [6]. The research evaluated 269 individuals with genetically confirmed PCD, using the initial PICADAR question about daily wet cough as a gatekeeper [5]. The study calculated test sensitivity based on the proportion of individuals scoring ≥5 points as recommended in the original tool [5] [6]. Subgroup analyses specifically examined the impact of laterality defects and predicted hallmark ultrastructural defects on test performance [5] [6]. This genetic confirmation approach provided an independent assessment of PICADAR's performance against a molecular gold standard, revealing important limitations not apparent in the original validation against composite diagnostic standards [5] [6].
Essential Research Toolkit for PCD Diagnostic Prediction Research
Table 3: Essential Reagents and Materials for PCD Diagnostic Prediction Research
| Research Tool | Application in PCD Research | Key Function |
|---|---|---|
| High-speed video microscopy (HSVA) | Ciliary beat pattern analysis | Visualizes and quantifies ciliary motion abnormalities [7] |
| Transmission electron microscopy (TEM) | Ciliary ultrastructural assessment | Identifies defects in dynein arms, microtubule organization [7] |
| Nasal nitric oxide (nNO) measurement | Screening and diagnostic testing | Low nNO levels support PCD diagnosis [15] [7] |
| Genetic testing panels | Mutation identification in >50 PCD-associated genes | Confirms diagnosis, establishes genotype-phenotype correlations [5] [7] |
| Clinical data collection proformas | Standardized symptom documentation | Ensures consistent data collection for predictive tool application [15] |
| Immunofluorescence microscopy | Protein localization in cilia | Detects absence or mislocalization of ciliary proteins [7] |
The following diagram illustrates how these research tools integrate into a comprehensive PCD diagnostic workflow:
The PICADAR scorecard represents an important advancement in systematizing the clinical assessment of patients with suspected PCD, providing a structured approach to prioritizing specialized testing. Its seven predictive parameters effectively identify classic PCD presentations, particularly in patients with laterality defects and characteristic ultrastructural abnormalities [15] [5]. However, evidence from recent studies indicates significant limitations in sensitivity, especially for patients without situs inversus (61%) or those lacking hallmark ultrastructural defects (59%) [5] [6]. The tool's dependency on daily wet cough as an initial screening question automatically excludes approximately 7% of genetically confirmed PCD cases [5]. Furthermore, ethnic variations in clinical presentation, such as the lower prevalence of situs inversus in Japanese populations (25%), may impact its performance across different genetic backgrounds [8]. These limitations underscore the need for complementary predictive tools and careful clinical judgment when implementing PICADAR in research protocols or clinical practice. Future development of PCD predictive tools should focus on capturing the full phenotypic spectrum of this genetically heterogeneous disorder, particularly patients with normal body laterality and ultrastructure.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary function, leading to impaired mucociliary clearance of the airways. The diagnosis of PCD is challenging due to the non-specific nature of its symptoms and the requirement for highly specialized, expensive diagnostic testing available only at specialized centers [15]. To address this challenge, the PrImary CiliARy DyskinesiA Rule (PICADAR) was developed as a clinical predictive tool to identify patients who should be referred for definitive PCD testing [15] [16]. This diagnostic predictive tool aggregates easily obtainable clinical features into a single numerical score, with a critical cut-off point that stratifies patients based on their probability of having PCD. The selection of an appropriate score threshold balances the competing needs of identifying true positive cases while avoiding unnecessary specialist referrals. This guide provides a comprehensive analysis of the score of 5 within the PICADAR framework, examining its original validation, comparative performance against other tools, and important limitations that researchers and clinicians must consider when implementing this tool in practice.
The PICADAR Tool: Composition and Calculation
The PICADAR tool is designed for patients with persistent wet cough and incorporates seven key clinical parameters obtained from patient history [15]. Each parameter is assigned a specific point value based on regression coefficients from the original derivation study. When summed, these points generate a total score that corresponds to the probability of a PCD diagnosis.
PICADAR Scoring Parameters
| Predictive Parameter | Points Assigned |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 2 |
Table 1: The seven predictive parameters of the PICADAR tool and their assigned point values [15].
The PICADAR evaluation process follows a specific clinical workflow. It is crucial to note that the tool is only applied to patients who present with a persistent wet cough, which serves as an initial screening question [6]. Patients without this symptom are not considered for further PICADAR evaluation, representing an inherent limitation in its design.
Figure 1: The clinical workflow for applying the PICADAR tool, beginning with the assessment for persistent wet cough [15] [6].
Performance Data for the PICADAR Score of 5
Original Validation Studies
In the original 2016 derivation and validation study by Behan et al., which analyzed 641 consecutive referrals to a PCD diagnostic center, a PICADAR score of 5 emerged as the optimal cut-off value [15]. At this threshold, the tool demonstrated a sensitivity of 0.90 and a specificity of 0.75 for predicting a positive PCD diagnosis, with an Area Under the Curve (AUC) of 0.91 upon internal validation [15]. External validation at a second diagnostic center showed maintained performance with an AUC of 0.87 [15]. This balance between sensitivity and specificity meant that the tool correctly identified 90% of true PCD cases while correctly excluding 75% of non-PCD cases.
Comparative Performance Against Other Predictive Tools
Subsequent studies have compared PICADAR's performance against other predictive tools, notably the Clinical Index (CI) and the North American Criteria Defined Clinical Features (NA-CDCF). A 2021 study by Tabs et al. evaluated all three tools in 1,401 patients with suspected PCD [17].
| Predictive Tool | Area Under Curve (AUC) | Key Advantages | Key Limitations |
|---|---|---|---|
| PICADAR (Score ≥5) | 0.91 (original) [15] | High sensitivity in classic phenotype | Not applicable without chronic wet cough [17] |
| Clinical Index (CI) | Larger than NA-CDCF (p=0.005) [17] | Does not require assessment of laterality [17] | Less validated in diverse populations |
| NA-CDCF | No significant difference from PICADAR [17] | Simple, four-item criteria | May miss atypical presentations |
| nNO Measurement | N/A | Further improves all predictive tools when combined [17] | Requires expensive equipment [15] |
Table 2: Comparative performance of PCD predictive tools based on validation studies.
The study found that while all three scores were significantly higher in the PCD group (p < 0.001), the CI demonstrated potential advantages in certain clinical scenarios [17]. Importantly, the researchers noted that PICADAR could not be assessed in 6.1% of patients because they did not have chronic wet cough, a mandatory prerequisite for using the tool [17].
Critical Limitations and Population-Specific Performance
Sensitivity Concerns in Genetically Confirmed PCD
A critical 2025 pre-print study by Omran et al. evaluated PICADAR's performance in 269 individuals with genetically confirmed PCD, revealing significant limitations in test sensitivity [6] [18]. The study reported an overall sensitivity of only 75% at the recommended cut-off score of ≥5, meaning the tool would miss approximately one in four confirmed PCD cases [6]. Even more concerning were the subgroup analyses, which demonstrated markedly variable performance:
- 95% sensitivity in patients with laterality defects (median score: 10) [6]
- 61% sensitivity in patients with situs solitus (normal organ arrangement; median score: 6) [6]
- 83% sensitivity in patients with hallmark ultrastructural defects [6]
- 59% sensitivity in patients without hallmark ultrastructural defects [6]
These findings indicate that PICADAR performs excellently for classic PCD presentations with laterality defects but misses nearly 40% of cases with normal organ arrangement or normal ciliary ultrastructure.
Geographical and Genetic Variability
The performance of PICADAR also appears to vary across different ethnic and geographical populations. A study of Japanese PCD patients found that only 25% exhibited situs inversus [8], compared to the approximately 50% typically reported in other populations [15]. This difference reflects variations in prevalent genetic mutations across populations and directly impacts PICADAR scores, as situs inversus contributes 2 points toward the total score. Consequently, PICADAR may systematically underscore patients from populations with lower prevalence of laterality defects.
Experimental Protocols for PICADAR Validation
Original Derivation Study Methodology
The original PICADAR derivation and validation followed a rigorous methodological protocol [15]:
- Study Population: 641 consecutive patients with definitive diagnostic outcomes from the University Hospital Southampton PCD diagnostic center (2007-2013).
- Data Collection: A proforma was used to collect patient data through clinical interview prior to diagnostic testing, including gestational age, neonatal symptoms, admittance to special care units, respiratory support needs, chronic cough, rhinitis, sinusitis, ear problems, situs abnormalities, and congenital cardiac defects.
- Statistical Analysis: Logistic regression analysis identified significant predictors from 27 potential variables. The model's discrimination was assessed using Receiver Operating Characteristic (ROC) curve analysis and Area Under the Curve (AUC) calculations. A Hosmer-Lemeshow goodness-of-fit test assessed calibration.
- Validation: External validation was performed using data from 187 patients (93 PCD-positive, 94 PCD-negative) from Royal Brompton Hospital.
Comparative Validation Protocol
The 2021 comparative study by Tabs et al. employed the following methodology [17]:
- Population: 1,401 patients with suspected PCD referred for high-speed video microscopy testing.
- Assessment: CI, PICADAR, and NA-CDCF scores were calculated retrospectively from medical records.
- Diagnostic Confirmation: PCD diagnosis followed ERS guidelines, incorporating nNO measurement, HSVM, transmission electron microscopy, and genetic testing.
- Statistical Comparison: Predictive characteristics were analyzed using ROC curves and AUC comparisons between tools.
The Scientist's Toolkit: Essential Research Reagents and Materials
| Item | Function in PCD Research |
|---|---|
| High-Speed Video Microscopy (HSVM) | Analyzes ciliary beat frequency and pattern from nasal brushings [19] [17] |
| Transmission Electron Microscope (TEM) | Visualizes ultrastructural defects in ciliary architecture [19] |
| Nasal Nitric Oxide (nNO) Analyzer | Measures nNO levels (low nNO is a PCD screening marker) [15] [17] |
| Next-Generation Sequencing (NGS) | Identifies mutations in >50 known PCD genes [19] [17] |
| Immunofluorescence Assays | Detects specific protein localization in ciliary apparatus [19] |
| Cell Culture Systems | Allows ciliary re-differentiation for repeated functional testing [15] |
Table 3: Key reagents and equipment essential for PCD diagnostic research and predictive tool validation.
The PICADAR score of 5 represents a carefully validated cut-off that demonstrates good overall accuracy in the initial derivation studies. However, emerging evidence reveals significant limitations, particularly its substantially reduced sensitivity (61%) in PCD patients with normal organ arrangement [6] and its inapplicability to patients without persistent wet cough [17]. These limitations necessitate cautious implementation in clinical practice and research settings. For drug development professionals and researchers, these findings underscore that PICADAR should not be used as a standalone eligibility criterion for clinical trials or as the sole basis for estimating PCD prevalence in population studies. The tool works excellently for classic PCD presentations but systematically underestimates the likelihood of disease in patients with normal situs or non-classic genetic variants. Future research should focus on developing more inclusive predictive tools that incorporate genetic and ultrastructural data to better capture the full phenotypic spectrum of PCD, particularly as targeted therapies emerge that may benefit patients across all PCD subtypes.
Implementing PICADAR: Protocol, Calculation, and Clinical Workflow
Primary Ciliary Dyskinesia (PCD) is a rare genetic disorder characterized by impaired ciliary function, leading to chronic respiratory symptoms. Diagnosis is challenging due to nonspecific symptoms and the absence of a single gold-standard test. The PICADAR tool (Primary Ciliary Dyskinesia Rule) was developed as a clinical predictive tool to identify patients who should be referred for specialized PCD diagnostic testing [4]. This guide provides comprehensive instructions for administering the PICADAR questionnaire within research settings, alongside comparative performance data against other predictive tools.
Understanding the PICADAR Tool
Clinical Rationale and Development
PICADAR was developed to address the critical need for efficient patient triage in PCD diagnosis. Specialized diagnostic tests for PCD—including nasal nitric oxide (nNO) measurement, high-speed video microscopy (HSVM), transmission electron microscopy (TEM), and genetic testing—are technically complex, expensive, and limited to specialized centers [4] [7]. PICADAR utilizes easily obtainable clinical data to estimate the probability of PCD, enabling researchers and clinicians to identify high-risk patients efficiently.
The tool was derived from a study of 641 consecutive patients referred for PCD testing, with external validation in an independent cohort [4]. It applies specifically to patients with persistent wet cough and incorporates seven clinically significant parameters.
PICADAR Parameters and Scoring
The PICADAR questionnaire assesses seven predictive parameters, each assigned a specific point value [4] [20]. The total score determines the probability of PCD and corresponding referral recommendations.
Table 1: PICADAR Scoring Parameters
| Parameter | Description | Points |
|---|---|---|
| Situs inversus | Complete reversal of thoracic and abdominal organs | 2 |
| Congenital cardiac defect | Structural heart abnormality present at birth | 2 |
| Full-term gestation | Birth at ≥37 weeks gestation | 1 |
| Neonatal chest symptoms | Respiratory distress or requiring respiratory support in term newborn | 1 |
| Neonatal intensive care unit admission | Required NICU care after birth | 1 |
| Chronic rhinitis | Persistent nasal congestion/discharge beginning in infancy and lasting >3 months | 1 |
| Ear symptoms | Chronic otitis media or hearing impairment | 1 |
Scoring Interpretation
- Score ≥5 points: High probability of PCD (Sensitivity: 0.90, Specificity: 0.75) - Strongly recommend referral for specialized PCD testing [4]
- Score <5 points: Lower probability of PCD - Consider alternative diagnoses or continue monitoring
PICADAR Administration Protocol
Pre-Assessment Preparation
- Target Population: Patients with persistent wet cough of unknown etiology [4]
- Data Sources: Clinical interview, medical record review, or direct patient assessment
- Qualifications: Administered by healthcare professionals or trained research staff
- Timing: Typically administered during initial evaluation for chronic respiratory symptoms
Step-by-Step Administration Procedure
Figure 1: PICADAR Questionnaire Administration Workflow
- Confirm Gestational Age: Verify the patient was born at full-term (≥37 weeks gestation) [4]
- Assess Neonatal Respiratory History: Document whether the newborn experienced respiratory distress or required respiratory support at term gestation
- Establish NICU Admission: Confirm if the patient was admitted to a neonatal intensive care unit after birth
- Evaluate Chronic Rhinitis: Determine presence of persistent, year-round nasal congestion or discharge beginning in infancy and lasting >3 months
- Screen for Otologic Symptoms: Identify history of recurrent otitis media or hearing impairment
- Document Situs Status: Confirm presence of situs inversus through physical examination or review of prior imaging studies
- Identify Cardiac Abnormalities: Document any congenital heart defects through medical history or echocardiography reports
Data Collection Methodology
The original validation study utilized a structured proforma completed by clinicians through direct patient interview prior to diagnostic testing [4]. Data collection should be systematic and standardized:
- Clinical Interview: Conduct face-to-face structured interviews for comprehensive data collection [21]
- Medical Record Review: Supplement interview data with thorough chart review for objective parameters (e.g., gestational age, NICU admission)
- Standardized Coding: Record all parameters as binary outcomes (yes=1, no=0) [4]
Comparative Performance Analysis
Experimental Validation Data
PICADAR has been extensively validated against other predictive tools in multiple clinical studies. A 2021 study compared PICADAR with Clinical Index (CI) and North American Criteria Defined Clinical Features (NA-CDCF) in 1,401 patients with suspected PCD [17].
Table 2: Performance Comparison of PCD Predictive Tools
| Tool | AUC | Sensitivity | Specificity | Key Advantages | Key Limitations |
|---|---|---|---|---|---|
| PICADAR | 0.87 (external validation) [4] | 0.90 (at cut-off ≥5) [4] | 0.75 (at cut-off ≥5) [4] | Validated externally; good accuracy | Requires chronic wet cough; cannot assess in 6.1% without this symptom [17] |
| Clinical Index (CI) | Larger than NA-CDCF (p=0.005) [17] | Not specified | Not specified | No need to assess laterality or cardiac defects; feasible for all patients [17] | Less widely validated than PICADAR |
| NA-CDCF | No significant difference from PICADAR (p=0.093) [17] | Not specified | Not specified | Simple criteria; easy to remember | Limited predictive parameters |
| nNO Combined with PICADAR | Not specified | Improved when combined with PICADAR [17] | Improved when combined with PICADAR [17] | Enhanced predictive power | Requires specialized equipment |
Key Comparative Findings
- Diagnostic Accuracy: PICADAR demonstrated excellent discriminative ability with Area Under the Curve (AUC) of 0.91 in derivation and 0.87 in external validation [4]
- Clinical Utility: PICADAR significantly outperformed NA-CDCF in direct comparison (p=0.005), while showing equivalent performance to CI in some studies [17]
- Complementary Testing: Combining PICADAR with nasal nitric oxide (nNO) measurement further improved predictive power for all tools [17]
Research Implementation Framework
Integration with Diagnostic Pathways
For research applications, PICADAR should be integrated within a comprehensive diagnostic algorithm:
Figure 2: PICADAR in PCD Diagnostic Pathway
Essential Research Reagents and Materials
Table 3: Research Reagent Solutions for PCD Diagnostic Studies
| Item | Function/Application | Specifications/Examples |
|---|---|---|
| Structured Data Collection Form | Standardized PICADAR parameter assessment | Customized proforma based on original validation study [4] |
| Nasal Nitric Oxide Analyzer | Complementary screening measurement | Niox Mino/Vero (Aerocrine AB) or CLD 88sp (ECO MEDICS) [17] [22] |
| High-Speed Video Microscopy | Ciliary beat pattern analysis | Keyence Motion Analyzer, Basler acA1300-200um camera [17] [22] |
| TEM Equipment | Ultrastructural ciliary analysis | Standard electron microscopy protocols [17] |
| Genetic Testing Platform | PCD gene mutation identification | Next-generation sequencing panels (e.g., 22-39 PCD genes) [17] [22] |
| Immunofluorescence Antibodies | Ciliary protein localization | Anti-DNAH5, Anti-GAS8 antibodies [22] |
Methodological Considerations for Research
- Population Selection: PICADAR validation specifically included patients with chronic wet cough; application to populations without this symptom is limited [17]
- Data Quality Control: Implement standardized training for interviewers to minimize assessment variability [4]
- Statistical Analysis: Utilize ROC curve analysis to assess tool performance; calculate sensitivity, specificity, and AUC values [17] [4]
- Multicenter Validation: Consider study design that enables external validation across different patient populations and clinical settings
The PICADAR questionnaire represents a validated, practical tool for identifying high-risk PCD patients in research settings. Its standardized administration and scoring system enables efficient triage for specialized diagnostic testing. While PICADAR demonstrates strong predictive performance, researchers should consider its limitations regarding patient selection and complement it with objective measures like nNO for enhanced accuracy. The continued validation of PICADAR across diverse populations will further establish its utility in advancing PCD research and clinical diagnostics.
In the diagnosis of primary ciliary dyskinesia (PCD), a rare genetic disorder affecting respiratory cilia function, the journey from initial patient assessment to definitive diagnosis presents significant challenges. Specialized diagnostic tests require expensive equipment and expert interpretation, creating barriers to accessibility [4]. In this context, the PICADAR (PrImary CiliARy DyskinesiA Rule) prediction tool emerges as a clinically valuable screening instrument that enables efficient patient prioritization for confirmatory testing through systematic data collection and score calculation [4].
This guide objectively evaluates PICADAR's performance against alternative diagnostic approaches, examining its sensitivity, specificity, and practical implementation within the research and clinical workflow for PCD diagnosis.
Quantitative Performance Comparison of PCD Diagnostic Methods
The following table summarizes the key performance metrics of PICADAR compared to other established diagnostic methods for PCD, based on validation studies.
Table 1: Performance Metrics of PCD Diagnostic Tools
| Diagnostic Method | Reported Sensitivity | Reported Specificity | Key Limitations |
|---|---|---|---|
| PICADAR Score | 0.90 (at cut-off ≥5) [4] | 0.75 (at cut-off ≥5) [4] | Relies on accurate patient history; performance may vary in non-validation populations. |
| Nasal Nitric Oxide (nNO) | Efficient for screening [4] | Efficient for screening [4] | Requires expensive equipment and trained technicians [4]. |
| Genetic Testing | Limited sensitivity as a standalone test [7] | High, but complex genetic etiology [7] | >50 associated genes; no single test has high sensitivity and specificity [7]. |
| High-Speed Video Microscopy Analysis (HSVA) | Used in composite diagnosis [4] | Used in composite diagnosis [4] | Requires specialist center and experienced scientists [4]. |
| Transmission Electron Microscopy (TEM) | Identifies ~70% of ultrastructural defects [4] | Used in composite diagnosis [4] | Invasive; requires specialized infrastructure and expertise [4]. |
Experimental Protocols and Validation Data
PICADAR Derivation and Validation Methodology
The PICADAR prediction tool was developed and validated through a multi-stage process:
- Study Population: The derivative group consisted of 641 consecutive patients with a definitive diagnostic outcome referred to the University Hospital Southampton (UHS) PCD diagnostic center between 2007 and 2013. A proforma was used to collect patient data through clinical interview prior to diagnostic testing [4].
- Validation Cohort: External validation was performed using a sample of 187 patients (93 PCD-positive, 94 PCD-negative) referred to the Royal Brompton Hospital (RBH). An equal number of positive and negative referrals were randomly selected from patients referred between 1983 and 2013 [4].
- Diagnostic Standard: A positive PCD diagnosis was typically based on a classic clinical history with at least two abnormal diagnostic tests, including hallmark TEM findings, hallmark ciliary beat pattern (CBP), or nasal nitric oxide (nNO) ≤30 nL·min⁻¹. In some cases, patients with a strong history were diagnosed based on a single definitive test [4].
- Statistical Analysis: Logistic regression analysis identified significant predictors from 27 potential variables. Model performance was assessed using Receiver Operating Characteristic (ROC) curve analysis, calculating the Area Under the Curve (AUC). The model was simplified into a practical scoring tool (PICADAR) where the score for each predictor corresponds to their regression coefficient rounded to the nearest integer [4].
PICADAR Score Calculation and Interpretation
The PICADAR tool is applied to patients with persistent wet cough and calculates a score based on seven clinical parameters obtained from patient history [4]. The following workflow illustrates the diagnostic pathway incorporating PICADAR:
Diagram 1: PICADAR Clinical Decision Workflow
Performance Metrics and Validation Outcomes
The PICADAR tool demonstrated strong predictive performance in both derivation and validation populations:
- Derivation Group (n=641): The AUC was 0.91, indicating excellent discriminatory power. At the recommended cut-off score of 5 points, sensitivity was 0.90 and specificity was 0.75 [4].
- Validation Group (n=187): The tool maintained strong performance with an AUC of 0.87, confirming its validity in an external population [4].
- Diagnostic Yield: In the derivation cohort, 75 patients (12%) were diagnosed with PCD, while 566 (88%) had a negative diagnosis [4].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key reagents and materials essential for conducting comprehensive PCD diagnostic research, including the evaluation of clinical prediction tools like PICADAR.
Table 2: Essential Research Reagents and Materials for PCD Diagnostic Studies
| Item Name | Function/Application in PCD Research |
|---|---|
| Clinical History Proforma | Standardized data collection tool for PICADAR parameters and other clinical features prior to diagnostic testing [4]. |
| Nasal Nitric Oxide (nNO) Analyzer | Measures nNO levels for screening; values ≤30 nL·min⁻¹ support PCD diagnosis [4]. |
| High-Speed Video Microscopy System | Analyzes ciliary beat pattern and frequency from nasal epithelial brush biopsies [4] [7]. |
| Transmission Electron Microscope | Evaluates ultrastructural defects in cilia (e.g., dynein arm defects, microtubule disorganization) [4] [7]. |
| Genetic Testing Panels | Identifies mutations in over 50 known PCD-associated genes (e.g., DNAH5, DNAI1, CCDC39, CCDC40) [7]. |
| Cell Culture Materials for ALI Culture | Re-differentiates ciliated epithelium for confirmatory ciliary functional analysis when initial results are inconclusive [4]. |
PICADAR represents a validated, cost-effective first-line tool for identifying patients at high probability of PCD who warrant further specialized testing. Its standardized approach to data collection from patient history and simple scoring calculation facilitates early diagnosis, particularly in settings with limited immediate access to complex diagnostic modalities. While PICADAR cannot replace definitive diagnostic tests, its integration into a structured diagnostic pathway enables more efficient resource allocation and accelerates the time to diagnosis for this rare genetic disorder.
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary function, leading to impaired mucociliary clearance with an estimated prevalence ranging from 1:10,000 to 1:40,000 [15] [9]. The diagnostic pathway for PCD presents significant challenges due to the nonspecific nature of its symptoms, which overlap with more common respiratory conditions like asthma, recurrent bronchitis, and cystic fibrosis [9]. This diagnostic complexity is compounded by the absence of a single "gold standard" test and the highly specialized nature of definitive PCD diagnostic testing, which requires expensive equipment and experienced scientists [15] [23]. Consequently, many patients experience diagnostic delays, with some reports indicating over 40 visits to medical professionals before receiving appropriate referral for PCD testing [9].
Within this challenging diagnostic landscape, clinical prediction tools have emerged as valuable assets for identifying patients who require specialist referral. The European Respiratory Society (ERS) guidelines acknowledge the utility of such tools, specifically recommending the PCD Rule (PICADAR) for assessing referral likelihood [6] [23]. This review critically examines the integration of PICADAR into referral pathways, evaluating its performance characteristics against alternative approaches, and exploring its role in facilitating appropriate patient flow from general practice to specialist PCD centers.
PICADAR: Structure, Application, and Performance
Tool Development and Predictive Parameters
PICADAR was developed through a prospective study of 641 consecutive patients referred for PCD testing to create a practical diagnostic predictive tool using readily available clinical information [15]. The tool applies specifically to patients with persistent wet cough and incorporates seven predictive parameters easily obtained through patient history and clinical interview [15].
Table 1: PICADAR Predictive Parameters and Scoring System
| Predictive Parameter | Score |
|---|---|
| Full-term gestation | 2 points |
| Neonatal chest symptoms | 2 points |
| Neonatal intensive care unit admission | 2 points |
| Chronic rhinitis | 1 point |
| Ear symptoms | 1 point |
| Situs inversus | 2 points |
| Congenital cardiac defect | 4 points |
The PICADAR score is calculated by summing the points for each present parameter, with total scores ranging from 0 to 14 [15]. The developers established a cut-off score of 5 points, at which the tool demonstrates optimal performance characteristics for identifying patients requiring specialist testing [15].
Performance Characteristics and Validation
The original validation study for PICADAR reported strong diagnostic performance metrics. At the recommended cut-off score of 5 points, the tool demonstrated a sensitivity of 0.90 and specificity of 0.75 [15]. The area under the curve (AUC) for the internally validated tool was 0.91, indicating excellent discriminative ability, while external validation in a second diagnostic center showed an AUC of 0.87, confirming good validity across different populations [15].
However, a 2025 study evaluating PICADAR in 269 genetically confirmed PCD patients revealed important limitations in sensitivity [6]. The overall sensitivity was 75%, significantly lower than originally reported, with particularly reduced sensitivity in specific patient subgroups: 61% in patients without laterality defects (situs solitus) and 59% in those without hallmark ultrastructural defects [6]. Notably, 7% of genetically confirmed PCD patients were ruled out by PICADAR's initial requirement for daily wet cough [6].
Table 2: PICADAR Performance Across Studies
| Study | Population | Sensitivity | Specificity | AUC | Limitations Identified |
|---|---|---|---|---|---|
| Behan et al. (2016) [15] | 641 referrals (75 PCD+) | 0.90 | 0.75 | 0.91 (internal) 0.87 (external) | - |
| Omran et al. (2025) [6] | 269 genetically confirmed PCD | 0.75 (overall) 0.61 (situs solitus) 0.59 (no hallmark defects) | - | - | Low sensitivity in specific subgroups; excludes patients without daily wet cough |
Comparative Analysis of PCD Diagnostic Prediction Tools
North American CDCF Criteria
The American Thoracic Society (ATS) guidelines utilize a different approach known as the North American Criteria Defined Clinical Features (NA-CDCF) [23]. This method relies on a four-point clinical symptoms score, requiring the presence of two of four specific clinical features to warrant referral for diagnostic testing [23]. While this approach provides good specificity (0.72), ensuring that diagnostic services primarily evaluate likely cases, it demonstrates insufficient sensitivity (0.80) for effective screening [23]. This performance gap means approximately 20% of genuine PCD patients would not be referred for testing and might never receive a correct diagnosis [23].
Performance Comparison and Clinical Implications
When directly compared, PICADAR demonstrates superior sensitivity (0.97 at a cutoff of 4 points) compared to the NA-CDCF approach, while maintaining reasonable specificity (0.48) [23]. This performance advantage makes PICADAR particularly valuable for minimizing false negatives in clinical practice, though at the cost of higher false positives than the NA-CDCF criteria [23].
The choice between these tools involves a fundamental trade-off in screening strategy. PICADAR's higher sensitivity makes it preferable for ensuring that potentially affected patients are not missed, while the NA-CDCF's higher specificity may be advantageous in settings with extremely limited specialist capacity [23]. Importantly, neither tool should be used in isolation for definitive diagnosis, but rather as part of a comprehensive diagnostic pathway that incorporates more specialized testing [6] [23].
Experimental Protocols and Diagnostic Pathways
Original PICADAR Derivation Methodology
The development of PICADAR followed a rigorous methodological approach [15]. Researchers analyzed data from 641 consecutive patients with definitive diagnostic outcomes from the University Hospital Southampton PCD diagnostic center (2007-2013) [15]. A standardized proforma was used to collect patient data through clinical interviews prior to diagnostic testing [15]. Potential predictors were restricted to information readily available in nonspecialist settings, with 27 initial variables evaluated using logistic regression analysis [15]. The final model was simplified into a practical scoring tool, with points corresponding to regression coefficients rounded to the nearest integer [15]. External validation was performed using data from 187 patients at the Royal Brompton Hospital [15].
Comprehensive PCD Diagnostic Pathway
The current ERS guidelines recommend a multi-test diagnostic pathway for PCD that incorporates clinical prediction tools as initial screening steps [9] [23]. The recommended diagnostic algorithm begins with clinical suspicion based on symptoms, followed by nasal nitric oxide (nNO) measurement, which typically shows extremely low levels in PCD patients [9] [23]. Subsequent testing includes high-speed video microscopy analysis (HSVA) to assess ciliary function and beat pattern, transmission electron microscopy (TEM) to evaluate ultrastructural defects, and genetic testing to identify mutations in over 45 known PCD-associated genes [9] [23] [24].
Diagram 1: Integrated PCD Diagnostic Pathway Incorporating PICADAR. This workflow illustrates the sequential diagnostic process from initial clinical suspicion through specialized testing.
Essential Research Reagents and Methodologies
Key Research Reagents for PCD Diagnostic Evaluation
Table 3: Essential Research Reagents for PCD Diagnostic Studies
| Reagent/Equipment | Primary Function | Application in PCD Research |
|---|---|---|
| Nasal nitric oxide (nNO) analyzer | Measures nasal nitric oxide concentration | Screening tool; nNO is typically extremely low in PCD patients [9] |
| High-speed video microscopy system | Records and analyzes ciliary beat frequency and pattern | Assessment of ciliary function and identification of characteristic dyskinetic patterns [23] |
| Transmission electron microscope | Visualizes ultrastructural defects in ciliary axoneme | Identification of hallmark defects in dynein arms, microtubule organization [9] |
| Antibodies for immunofluorescence (DNAH5, GAS8) | Labels specific ciliary proteins | Detection of protein localization defects; cheaper alternative to TEM [22] |
| Genetic sequencing panels | Identifies mutations in PCD-associated genes | Confirmation of diagnosis; over 45 known PCD genes [7] [24] |
| Nasal epithelial brush biopsy equipment | Obtains respiratory epithelial cells | Sample collection for HSVA, TEM, IF, and cell culture [22] |
Methodological Considerations for Tool Validation
Recent studies have highlighted important methodological considerations for validating PCD diagnostic tools. The 2025 sensitivity analysis of PICADAR utilized genetically confirmed PCD cases as the reference standard, providing a more rigorous evaluation than earlier studies that relied on composite diagnostic outcomes [6]. This approach revealed significant variations in sensitivity across different PCD genotypes and phenotypes, underscoring the importance of accounting for genetic heterogeneity in tool validation [6]. Additionally, the finding that 7% of genetically confirmed PCD patients did not report daily wet cough highlights a critical limitation in PICADAR's initial screening question [6].
International collaboration has emerged as a valuable strategy for enhancing diagnostic capabilities, particularly for limited-resource settings [22]. Such collaborations enable access to specialized techniques like immunofluorescence analysis, which can resolve diagnostically challenging cases with inconclusive genetic results [22]. These partnerships also facilitate the sharing of methodological expertise and validation of diagnostic approaches across diverse patient populations.
The integration of PICADAR into referral pathways for primary ciliary dyskinesia represents a significant advancement in identifying appropriate candidates for specialized diagnostic testing. While the tool demonstrates good overall accuracy and has been validated across multiple clinical settings, recent evidence reveals important limitations in its sensitivity, particularly for patients without laterality defects or those who lack hallmark ultrastructural defects on electron microscopy [6]. These findings underscore the necessity of using PICADAR as part of a comprehensive diagnostic strategy rather than as a standalone decision tool.
For researchers and clinicians developing referral pathways, the evidence suggests that PICADAR serves best as an initial screening instrument within a multi-test diagnostic algorithm. Its higher sensitivity compared to the North American CDCF criteria makes it preferable for minimizing false negatives, though clinical judgment remains essential, particularly for patients with strong clinical features who score below the PICADAR threshold [6] [23]. Future efforts should focus on refining predictive tools to better capture the full phenotypic spectrum of PCD, including patients with normal situs and those without classic ultrastructural defects, while international collaborations continue to enhance diagnostic capabilities across healthcare settings.
The PICADAR (Primary Ciliary Dyskinesia Rule) tool is a clinical prediction rule designed to identify patients with a high probability of Primary Ciliary Dyskinesia (PCD) before they undergo complex, specialized diagnostic testing [16] [15]. It was developed to address the challenge of PCD's nonspecific symptoms and the highly specialized nature of confirmatory tests [15]. The tool applies to patients with a persistent wet cough and incorporates seven readily available clinical parameters from a patient's history [16].
The scoring system is as follows, where each predictive parameter is assigned a specific point value [15]:
Table: The PICADAR Scoring System
| Predictive Parameter | Points Assigned |
|---|---|
| Full-term gestation (≥37 weeks) | 2 |
| Neonatal chest symptoms (within 1st month of life) | 2 |
| Admission to a neonatal intensive care unit | 1 |
| Chronic rhinitis (persisting for >3 months) | 1 |
| Ear symptoms (chronic otitis media or hearing loss) | 1 |
| Situs inversus | 4 |
| Congenital cardiac defect | 2 |
To use PICADAR, a clinician collects the patient's history for these seven items and sums the corresponding points to generate a total score. This score estimates the probability of a positive PCD diagnosis.
Diagnostic Performance and Interpretation of Scores
The performance of the PICADAR score was validated in both a derivation group and an external validation group, demonstrating good accuracy [16] [15]. The table below summarizes the key performance metrics for the established cut-off score.
Table: Diagnostic Performance of the PICADAR Tool
| Metric | Result (Cut-off Score of 5) |
|---|---|
| Sensitivity | 0.90 (90%) |
| Specificity | 0.75 (75%) |
| Area Under the Curve (AUC) - Internal Validation | 0.91 |
| Area Under the Curve (AUC) - External Validation | 0.87 |
A cut-off score of 5 points is recommended for clinical use, providing an optimal balance between sensitivity and specificity [15]. At this threshold:
- A score of <5 points indicates a low probability of PCD. The tool correctly identifies 75% of patients without the disease (specificity) [15].
- A score of ≥5 points indicates a high probability of PCD. The tool successfully identifies 90% of patients who have the disease (sensitivity) and should be referred for specialized diagnostic testing [16] [15].
Experimental Protocol for PICADAR Validation
The development and validation of the PICADAR tool followed a rigorous methodological process, as detailed in the original study [15].
Study Population and Data Collection
- Derivation Group: Data was collected from 641 consecutive patients referred to the University Hospital Southampton (UHS) PCD diagnostic center. A definitive diagnostic outcome was established for all patients, with 75 (12%) diagnosed as PCD-positive [15].
- Validation Group: The tool was externally validated using a sample of 187 patients from the Royal Brompton Hospital (RBH), comprising 93 PCD-positive and 94 PCD-negative individuals [15].
- A standardized proforma was used to collect patient data through a clinical interview prior to any diagnostic testing, ensuring the predictors were based solely on history [15].
Diagnostic Testing (Reference Standard)
A positive PCD diagnosis was confirmed using a combination of highly specialized tests, which served as the reference standard against which PICADAR was measured. The diagnostic criteria typically required a classic clinical history plus abnormalities in at least two of the following tests [15]:
- "Hallmark" Ultrastructural Defects on Transmission Electron Microscopy (TEM)
- "Hallmark" Ciliary Beat Pattern (CBP) analyzed by high-speed video microscopy
- Low Nasal Nitric Oxide (nNO) (≤30 nL·min⁻¹)
In some cases, patients with a very strong clinical history (e.g., an affected sibling) were diagnosed based on a single, definitive abnormal test result [15].
Statistical Analysis and Model Development
- Univariate Analysis: Potential predictor variables were first analyzed individually to compare their frequency in PCD-positive versus PCD-negative patients using t-tests, Chi-squared tests, or Fisher's exact tests as appropriate [15].
- Logistic Regression: Significant predictors from the univariate analysis were entered into a forward step-wise logistic regression model. This identified the seven independent predictors that constitute the final PICADAR tool [15].
- Performance Assessment: The model's ability to discriminate between PCD and non-PCD cases was evaluated using Receiver Operating Characteristic (ROC) curve analysis, reporting the Area Under the Curve (AUC). Calibration (agreement between predicted and observed outcomes) was assessed with the Hosmer-Lemeshow goodness-of-fit test [15].
Clinical Workflow and Application
The following diagram illustrates the clinical decision pathway for a patient with a persistent wet cough, from initial history-taking to specialist referral based on the PICADAR score.
The Scientist's Toolkit: Essential Reagents and Materials for PCD Diagnostics
The definitive diagnosis of PCD relies on specialized techniques available at reference centers. The following table lists key reagents, materials, and equipment essential for the experimental protocols cited in the PICADAR validation study and contemporary PCD diagnostics [7] [15].
Table: Key Research Reagent Solutions for PCD Diagnostics
| Item | Function/Application in PCD Diagnosis |
|---|---|
| Transmission Electron Microscope (TEM) | Used to visualize the ultrastructural defects in cilia (e.g., absent dynein arms, microtubule disorganization) [7]. |
| High-Speed Video Microscope (HSVMA) | Captures and analyzes ciliary beat patterns and frequency to identify abnormal motility characteristic of PCD [15]. |
| Nasal Nitric Oxide (nNO) Analyzer | Measures nNO concentration, which is characteristically very low in most PCD patients, serving as a efficient screening tool [15]. |
| Genetic Testing Panels | Identify mutations in over 50 known PCD-associated genes (e.g., DNAH5, DNAI1, CCDC39, CCDC40) for genetic confirmation [7]. |
| Cell Culture Media (for Air-Liquid Interface Culture) | Used to re-differentiate ciliated epithelial cells from biopsy samples, helping to rule out secondary ciliary dyskinesia caused by infection or inflammation [15]. |
| Antibodies for Immunofluorescence (IF) | Target specific ciliary proteins (e.g., DNAH5, GAS8) to detect their absence or mislocalization, aiding in genetic-specific diagnoses [7]. |
Operational Considerations in Multicenter and International Settings
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder caused by impaired ciliary function, leading to chronic respiratory infections, otitis media, bronchiectasis, and in approximately half of cases, laterality defects such as situs inversus [7]. The estimated prevalence ranges from 1:7,500 to 1:20,000 live births, though underdiagnosis is common due to diagnostic challenges [7]. No single gold standard test exists for PCD diagnosis, with current approaches requiring specialized testing including nasal nitric oxide (nNO) measurement, high-speed video microscopy analysis (HSVA), transmission electron microscopy (TEM), and genetic testing [7]. These tests demand expensive equipment, technical expertise, and are typically available only at specialized centers, creating significant barriers to timely diagnosis, particularly in resource-limited settings [4].
The PICADAR (PrImary CiliARy DyskinesiA Rule) prediction tool was developed to help identify patients with high probability of PCD who should be referred for specialized diagnostic testing [4]. This tool utilizes clinical features readily obtainable from patient history to estimate PCD likelihood. Understanding its operational characteristics in diverse clinical settings is essential for optimizing diagnostic pathways, especially in multicenter and international contexts where patient populations, healthcare resources, and clinical expertise may vary substantially.
PICADAR Tool: Components and Scoring Methodology
Original Validation and Scoring System
The PICADAR tool was originally developed and validated in a UK population, with its derivation published in 2016 [4]. The tool applies specifically to patients with persistent wet cough and assesses seven clinical parameters:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care unit admission
- Chronic rhinitis
- Ear symptoms (chronic otitis media with hearing impairment)
- Situs inversus
- Congenital cardiac defect
Each parameter is assigned a point value based on its regression coefficient, with the total score determining the probability of PCD [4]. In the original validation study, a cut-off score of ≥5 points demonstrated a sensitivity of 0.90 and specificity of 0.75 for predicting PCD, with an area under the curve (AUC) of 0.91 in the derivation cohort and 0.87 in the external validation cohort [4].
Table 1: PICADAR Scoring System and Original Performance Metrics
| Clinical Parameter | Points Assigned |
|---|---|
| Full-term gestation | 1 point |
| Neonatal chest symptoms | 1 point |
| Neonatal intensive care unit admission | 2 points |
| Chronic rhinitis | 1 point |
| Ear symptoms | 1 point |
| Situs inversus | 2 points |
| Congenital cardiac defect | 3 points |
| Total Possible Score | 11 points |
Table 2: Original PICADAR Performance Characteristics (2016 Study)
| Metric | Derivation Cohort | External Validation Cohort |
|---|---|---|
| Sample Size | 641 patients (75 PCD-positive) | 187 patients (93 PCD-positive) |
| Recommended Cut-off | ≥5 points | ≥5 points |
| Sensitivity | 0.90 | Not specified |
| Specificity | 0.75 | Not specified |
| Area Under Curve (AUC) | 0.91 | 0.87 |
Experimental Protocol for PICADAR Assessment
The methodology for applying and validating PICADAR follows a standardized protocol:
Patient Population: The tool is designed for patients with persistent wet cough referred for PCD evaluation. The original derivation cohort included 641 consecutive patients with definitive diagnostic outcomes from a single center [4].
Data Collection: Clinical history is obtained through a structured proforma completed by clinicians during patient interviews prior to diagnostic testing. Information collected includes neonatal history, respiratory symptoms, laterality defects, and cardiac anomalies [4].
Diagnostic Confirmation: PCD diagnosis is confirmed using a combination of tests including "hallmark" TEM defects, characteristic ciliary beat pattern abnormalities on HSVA, low nNO levels (≤30 nL·min⁻¹), or in cases with strong clinical phenotype, a single definitive test may suffice [4].
Statistical Analysis: Logistic regression analysis identifies significant predictors, with points assigned based on regression coefficients. Receiver operating characteristic (ROC) curve analysis determines optimal cut-off scores, and external validation assesses generalizability to different populations [4].
Contemporary Evidence on PICADAR Performance
Recent Multicenter Evaluation (2025 Study)
A 2025 multicenter study evaluated PICADAR's performance in 269 individuals with genetically confirmed PCD, revealing significant limitations not apparent in the original validation [6]. This study found that 18 individuals (7%) with confirmed PCD reported no daily wet cough, automatically ruling out PCD according to PICADAR's initial screening question [6]. The overall sensitivity was 75%, substantially lower than the original 90% reported in the 2016 study [6] [4].
Table 3: Contemporary PICADAR Performance Metrics (2025 Study)
| Patient Subgroup | Sample Size | Median PICADAR Score | Sensitivity |
|---|---|---|---|
| Overall Population | 269 | 7 (IQR: 5-9) | 75% |
| With Laterality Defects | Not specified | 10 (IQR: 8-11) | 95% |
| With Situs Solitus (normal arrangement) | Not specified | 6 (IQR: 4-8) | 61% |
| With Hallmark Ultrastructural Defects | Not specified | Not specified | 83% |
| Without Hallmark Ultrastructural Defects | Not specified | Not specified | 59% |
Operational Limitations in Diverse Settings
The 2025 study identified critical operational limitations with significant implications for multicenter and international use:
Dependence on Laterality Defects: PICADAR demonstrates substantially higher sensitivity in patients with laterality defects (95%) compared to those with situs solitus (61%) [6]. This creates diagnostic disparity, as approximately half of PCD patients have normal body arrangement [7].
Influence of Ultrastructural Defects: Sensitivity varies significantly based on underlying ciliary ultrastructure, with higher sensitivity in patients with hallmark defects (83%) versus those without (59%) [6]. This is operationally significant given the genetic heterogeneity of PCD, with over 50 associated genes encoding various ciliary components [7].
Exclusion of Atypical Presentations: The initial screening question regarding daily wet cough automatically excludes approximately 7% of genetically confirmed PCD cases [6], creating a fundamental limitation in case detection.
The following diagram illustrates the PICADAR assessment workflow and its impact on diagnostic decision-making:
Comparison with Alternative Diagnostic Approaches
Diagnostic Modalities for PCD
PCD diagnosis requires a multifaceted approach due to the absence of a single gold standard test. The following table outlines key diagnostic methods and their operational characteristics:
Table 4: Comparison of PCD Diagnostic Modalities
| Diagnostic Method | Operational Principle | Sensitivity | Specificity | Specialized Requirements |
|---|---|---|---|---|
| Nasal Nitric Oxide (nNO) | Measures low nNO levels in PCD | High (but varies) | High | Expired gas analyzer, trained technician, cooperative patient |
| High-Speed Video Microscopy (HSVA) | Analyzes ciliary beat pattern and frequency | High (in expert hands) | High | Specialized microscope, expert interpretation, cell culture capability |
| Transmission Electron Microscopy (TEM) | Identifies ultrastructural ciliary defects | ~70% (misses non-ultrastructural forms) | High | Electron microscope, expert preparation/interpretation |
| Genetic Testing | Identifies mutations in >50 PCD-associated genes | >70% and increasing | High | Genetic sequencing platform, bioinformatics expertise, variant interpretation |
| Immunofluorescence (IF) | Detects absence of ciliary proteins | Depends on antibodies used | High | Specific antibodies, fluorescence microscope |
Integrated Diagnostic Pathways
Contemporary PCD diagnosis employs a sequential, multimodal approach. The following diagram illustrates a comprehensive diagnostic pathway incorporating PICADAR and other modalities:
Research Reagent Solutions for PCD Diagnostic Investigations
Specialized reagents and materials are essential for conducting PCD diagnostic tests. The following table outlines key resources required for establishing PCD diagnostic capabilities:
Table 5: Essential Research Reagents for PCD Diagnostic Studies
| Reagent/Material | Primary Application | Technical Function | Operational Considerations |
|---|---|---|---|
| Nasal Epithelial Brush | HSVA, TEM, cell culture | Obtains ciliated epithelium | Must be cytology brush; requires proper technique to avoid bleeding |
| Cell Culture Media | Ex vivo ciliary differentiation | Supports epithelial cell growth and ciliogenesis | Requires air-liquid interface culture system for proper differentiation |
| Electron Microscopy Fixatives | TEM ultrastructural analysis | Preserves ciliary microstructure | Glutaraldehyde-based fixatives; requires careful handling and processing |
| Antibody Panels for Immunofluorescence | Protein localization | Detects absence of specific ciliary proteins | Target selection based on genetic results (e.g., DNAH5, DNAI1) |
| Genetic Sequencing Panels | Genetic diagnosis | Identifies mutations in PCD-associated genes | Should include >40 known PCD genes; requires variant interpretation expertise |
| nNO Analyzer | nNO measurement | Measures nasal nitric oxide concentration | Requires chemiluminescence analyzer; patient cooperation essential |
Operational Implications for Multicenter and International Implementation
Considerations for Resource-Variable Settings
The implementation of PICADAR and subsequent diagnostic pathways requires careful consideration of local resources and expertise:
Population Heterogeneity: The 2025 validation study revealed that PICADAR performance varies significantly across patient subgroups [6]. Implementation in populations with different genetic backgrounds or disease manifestations may yield different performance characteristics than originally reported.
Infrastructure Requirements: While PICADAR itself requires only clinical assessment, subsequent diagnostic tests have substantial infrastructure needs. nNO measurement requires expensive analyzers and trained technicians [4], while TEM and HSVA demand specialized equipment and expert interpretation [7].
Diagnostic Network Models: European guidelines recommend a network approach with satellite screening centers accessing specialist diagnostic facilities [4]. PICADAR can serve as an initial triage tool in such networks, but its limitations must be recognized within the diagnostic algorithm.
Recommendations for Future Implementation
Based on contemporary evidence, the following operational recommendations emerge:
Contextual Application: PICADAR should not be used as the sole determinant for initiating PCD diagnostic work-up, particularly in populations with high rates of situs solitus or non-hallmark ultrastructural defects [6].
Complementary Tools: Alternative predictive tools are needed, particularly for PCD patients with normal body arrangement and normal ciliary ultrastructure [6]. These might incorporate additional clinical features or genetic information.
Quality Assurance: Multicenter implementation requires standardized training in PICADAR assessment and systematic auditing of its performance across different settings to monitor real-world effectiveness.
The evolving understanding of PICADAR's limitations highlights the importance of continuous validation of diagnostic tools across diverse clinical settings and patient populations to ensure equitable access to accurate PCD diagnosis.
Limitations and Performance Gaps in Real-World Application
The diagnosis of Primary Ciliary Dyskinesia (PCD) presents substantial challenges due to the heterogeneity of clinical manifestations and the absence of a single gold standard diagnostic test [11]. In this complex diagnostic landscape, clinical prediction tools have emerged as essential instruments for identifying patients who should be referred for specialized testing. Among these, the Primary Ciliary DyskinesiA Rule (PICADAR) has gained prominence and has been incorporated into European Respiratory Society (ERS) guidelines as a recommended screening instrument [11] [23]. However, recent evidence highlights a critical limitation in its design: the mandatory requirement of a persistent daily wet cough as an initial screening gatekeeper. This analysis examines how this prerequisite creates a significant source of false negatives, particularly in specific patient subgroups and populations, potentially delaying accurate diagnosis and appropriate management.
Performance Comparison of PCD Diagnostic Tools
Quantitative Performance Metrics
Extensive validation studies have revealed considerable variation in the sensitivity and specificity of PICADAR compared to other predictive instruments. The following table summarizes the comparative performance of available diagnostic prediction tools.
Table 1: Performance Characteristics of PCD Diagnostic Prediction Tools
| Tool Name | Reported Sensitivity | Reported Specificity | Area Under Curve (AUC) | Key Limitations |
|---|---|---|---|---|
| PICADAR (Original Validation) [15] | 0.90 | 0.75 | 0.91 (internal), 0.87 (external) | Requires persistent wet cough; lower sensitivity in situs solitus patients |
| PICADAR (Recent Multicenter Study) [6] | 0.75 (overall), 0.61 (situs solitus only) | N/R | N/R | Excludes patients without daily wet cough (7% of genetically confirmed PCD) |
| Clinical Index (CI) [17] | Comparable to PICADAR | Comparable to PICADAR | Larger than NA-CDCF (p=0.005) | Does not require assessment of laterality or cardiac defects |
| NA-CDCF [17] | Lower than PICADAR in some validations | Lower than PICADAR in some validations | No difference from PICADAR (p=0.093) | Requires multiple clinical features |
Impact of the Daily Wet Cough Requirement
The foundational requirement of PICADAR is that patients must present with a persistent daily wet cough to proceed with further scoring. Recent evidence demonstrates this design creates a fundamental flaw in sensitivity:
Direct Exclusion of Confirmed PCD Cases: A 2025 multicenter evaluation demonstrated that 7% of genetically confirmed PCD patients were excluded from PICADAR assessment because they did not report a daily wet cough [6]. These patients would automatically be ruled negative for PCD despite having a genetically confirmed diagnosis.
Variable Presentation Across Populations: The clinical presentation of PCD shows significant geographical variation. A Japanese study of 67 PCD patients found that only 25% had situs inversus, contrary to the approximately 50% typically reported in Western populations [8]. This suggests that the predictive value of specific clinical features, including cough characteristics, may vary across ethnic groups and genotypes.
Analysis of Diagnostic Accuracy Across Subgroups
Stratified Performance Metrics
The performance of PICADAR varies substantially across different patient subgroups, particularly when stratified by the presence of laterality defects and ultrastructural characteristics.
Table 2: PICADAR Performance Stratified by Patient Characteristics
| Patient Subgroup | Median PICADAR Score (IQR) | Sensitivity | Key Findings |
|---|---|---|---|
| All Genetically Confirmed PCD [6] | 7 (5-9) | 75% | 18/269 (7%) excluded upfront due to no daily wet cough |
| PCD with Laterality Defects [6] | 10 (8-11) | 95% | Significantly higher scores and sensitivity |
| PCD with Situs Solitus [6] | 6 (4-8) | 61% | Substantially reduced detection capability |
| PCD with Hallmark Ultrastructural Defects [6] | N/R | 83% | Better detection compared to non-hallmark defects |
| PCD without Hallmark Ultrastructural Defects [6] | N/R | 59% | Poor sensitivity for genetically confirmed cases |
Comparative Tool Performance in Clinical Practice
A 2021 study comparing the feasibility and performance of three predictive tools (CI, PICADAR, and NA-CDCF) in 1,401 patients referred for PCD testing revealed important practical considerations:
- PICADAR could not be assessed in 6.1% of patients (86/1401) specifically due to the absence of chronic wet cough [17].
- The Clinical Index (CI) demonstrated potential advantages as it does not require assessment of laterality or congenital heart defects, making it applicable to a broader patient population [17].
- The study confirmed that nasal nitric oxide (nNO) measurement significantly improved the predictive power of all three clinical tools when used in combination [17].
Experimental Protocols and Methodologies
Original PICADAR Derivation and Validation
The original PICADAR tool was developed through a standardized methodological approach:
- Derivation Cohort: 641 consecutive patients with definitive diagnostic outcomes from the University Hospital Southampton PCD diagnostic center (2007-2013) [15].
- Validation Cohort: 187 patients (93 PCD-positive, 94 PCD-negative) from Royal Brompton Hospital to externally validate the score [15].
- Predictor Variables: Seven predictive parameters were identified: full-term gestation, neonatal chest symptoms, neonatal intensive care admittance, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defect [15].
- Statistical Analysis: Logistic regression was used to develop the prediction tool, with performance tested by receiver operating characteristic (ROC) curve analyses [15].
Recent Sensitivity Analysis Protocol
The 2025 multicenter evaluation employed rigorous methodology to assess PICADAR's limitations:
- Study Population: 269 individuals with genetically confirmed PCD, providing a definitive gold standard [6].
- Assessment Method: PICADAR scores were calculated retrospectively based on clinical data, with particular attention to the initial daily wet cough requirement [6].
- Stratified Analysis: Subgroups were analyzed based on the presence of laterality defects and predicted hallmark ultrastructural defects [6].
- Outcome Measures: The primary outcome was sensitivity, defined as the proportion of genetically confirmed PCD patients scoring ≥5 points as recommended [6].
Diagnostic Pathways and Workflows
PICADAR Application Workflow
The following diagram illustrates the standard PICADAR application pathway and its limitations:
Enhanced Diagnostic Pathway Integrating nNO
Combining clinical prediction tools with objective testing improves overall diagnostic accuracy:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials and Methods for PCD Diagnostic Research
| Tool/Reagent | Primary Function | Application in PCD Diagnostics |
|---|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Measures nasal nitric oxide concentration | Screening tool; significantly lower levels in most PCD patients [17] [11] |
| High-Speed Video Microscopy (HSVA) | Analyzes ciliary beat frequency and pattern | Functional assessment of ciliary motion; detects dyskinetic patterns [11] [23] |
| Transmission Electron Microscopy (TEM) | Visualizes ciliary ultrastructure | Identifies hallmark structural defects in ciliary axoneme [15] [11] |
| Genetic Sequencing Panels | Identifies mutations in PCD-associated genes | Confirmatory testing; over 50 known PCD genes [17] |
| Air-Liquid Interface (ALI) Culture | Cell culture technique for ciliary differentiation | Reduces secondary dyskinesia; improves diagnostic accuracy [11] |
| Immunofluorescence (IF) Labeling | Detects ciliary protein localization | Identifies protein mislocalization in specific genetic defects [11] |
The PICADAR tool represents an important advancement in standardizing the referral process for PCD diagnosis, but its mandatory daily wet cough requirement creates a significant source of false negatives that affects particular patient subgroups disproportionately. The 7% of genetically confirmed PCD patients who do not present with daily wet cough are systematically excluded from further evaluation [6]. Furthermore, the tool demonstrates substantially reduced sensitivity in patients with situs solitus (61%) and those without hallmark ultrastructural defects (59%) [6]. These limitations highlight the necessity for a more nuanced diagnostic approach that incorporates multiple prediction tools and objective testing measures such as nNO measurement. Future diagnostic algorithms should prioritize flexibility and recognize the diverse clinical presentations of PCD across different genetic backgrounds and populations, particularly as our understanding of genotype-phenotype correlations continues to evolve.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary structure and function, leading to impaired mucociliary clearance. The diagnostic pathway for PCD is complex, requiring specialized testing available only at tertiary referral centers. In this context, the PICADAR (PrImary CiliARy DyskinesiA Rule) score emerges as a crucial clinical prediction tool designed to identify high-risk patients requiring definitive diagnostic testing. This objective comparison guide evaluates the performance of PICADAR against other predictive instruments, with particular focus on how laterality defects and ultrastructural phenotypes introduce variability in its sensitivity and specificity. Understanding these performance characteristics is essential for researchers, scientists, and drug development professionals working to optimize PCD diagnosis and develop targeted therapies.
Comparative Analysis of PCD Predictive Tools
Several clinical prediction tools have been developed to guide PCD referral patterns. The PICADAR score, initially derived and validated in a UK population, incorporates seven clinical parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care admittance, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defect [15]. Each parameter contributes to a cumulative score that predicts the probability of PCD, with a cutoff score of 5 points demonstrating a sensitivity of 0.90 and specificity of 0.75 in the original derivation cohort [15].
The Clinical Index (CI) represents an alternative approach with a simplified seven-item questionnaire that does not require assessment of laterality or congenital heart defects, making it potentially applicable to a broader patient population [17]. Meanwhile, the North American Criteria Defined Clinical Features (NA-CDCF) focuses on four key features: laterality defects, unexplained neonatal respiratory distress syndrome, early-onset year-round nasal congestion, and early-onset year-round wet cough [17].
Performance Metrics Across Different Populations
Table 1: Performance Characteristics of PCD Predictive Tools
| Predictive Tool | Study Population | Sample Size (PCD+/Total) | AUC | Sensitivity | Specificity | Key Limitations |
|---|---|---|---|---|---|---|
| PICADAR | UK (Derivation) [15] | 75/641 | 0.91 | 0.90 | 0.75 | Requires persistent wet cough; cannot assess in ~6% of referrals |
| PICADAR | External Validation [15] | 93/187 | 0.87 | - | - | Performance varies with population characteristics |
| PICADAR | Japanese Cohort [8] | 67/67 | - | - | - | Lower prevalence of situs inversus (25%) reduces predictive value |
| Clinical Index (CI) | Czech Cohort [17] | 67/1401 | >PICADAR* | - | - | Does not require laterality assessment; applicable to broader population |
| NA-CDCF | Czech Cohort [17] | 67/1401 | - | - | Limited validation across diverse populations |
*The study demonstrated that AUC for CI was statistically larger than for NA-CDCF (p=0.005), while AUC for PICADAR and NA-CDCF did not significantly differ (p=0.093) [17].
Enhancement with Nasal Nitric Oxide Testing
The combination of clinical prediction tools with nasal nitric oxide (nNO) measurement significantly improves diagnostic accuracy. As demonstrated in a prospective study of 142 consecutive referrals, the combination of PICADAR with nNO at a threshold of 100 nl/min achieved perfect sensitivity (1.00) for identifying PCD-positive patients [25]. This combined approach offers a powerful screening strategy before proceeding to more invasive and expensive confirmatory testing.
Table 2: Performance of PICADAR with nNO at Different Thresholds
| Screening Method | nNO Threshold (nl/min) | Sensitivity | Specificity | False Positives | False Negatives |
|---|---|---|---|---|---|
| PICADAR alone [25] | N/A | 0.88 | 0.95 | 6 | 4 |
| nNO alone [25] | 30 | 0.91 | 0.95 | 6 | 3 |
| nNO alone [25] | 77 | 0.94 | 0.82 | 20 | 2 |
| nNO alone [25] | 100 | 1.00 | 0.73 | 30 | 0 |
| PICADAR + nNO [25] | 30 | 0.94 | 0.89 | 12 | 2 |
| PICADAR + nNO [25] | 77 | 0.94 | 0.78 | 25 | 2 |
| PICADAR + nNO [25] | 100 | 1.00 | 0.70 | 33 | 0 |
Impact of Laterality Defects on PICADAR Performance
Genetic and Population Variability in Laterality Defects
The performance of PICADAR is particularly influenced by the prevalence of laterality defects in different populations. Traditional teaching suggests that approximately 50% of PCD patients exhibit situs inversus, but recent evidence reveals significant ethnic and genetic variability. In a Japanese cohort of 67 PCD patients, only 25% presented with situs inversus, a substantially lower proportion than observed in European populations [8]. This discrepancy stems from differences in the major disease-causing genes across ethnic groups.
The PICADAR score assigns significant weight to laterality defects, with situs inversus contributing 2 points and congenital cardiac defects contributing 1 point toward the total score [15]. In populations with a lower prevalence of these features, such as the Japanese cohort, the predictive value of PICADAR may be consequently reduced. Researchers must consider this geographic and genetic variability when implementing PICADAR in different settings or conducting multinational clinical trials.
Consequences for Sensitivity and Specificity
The variable prevalence of laterality defects introduces corresponding variability in PICADAR's sensitivity and specificity across populations. In populations with high prevalence of situs inversus, PICADAR demonstrates strong discriminatory power with an area under the curve (AUC) of 0.91 in internal validation and 0.87 in external validation [15]. However, in populations with lower prevalence of laterality defects, the tool's ability to discriminate between PCD-positive and PCD-negative cases may be compromised.
This population-specific performance presents particular challenges for drug development professionals designing inclusion criteria for clinical trials. Over-reliance on PICADAR in populations where laterality defects are less common may lead to exclusion of eligible PCD patients with atypical presentations, potentially limiting trial generalizability and recruitment efficiency.
Methodological Protocols for PCD Diagnostic Prediction
PICADAR Original Study Methodology
The development and validation of PICADAR followed rigorous methodological standards. The original derivation study analyzed data from 641 consecutive patients with definitive diagnostic outcomes from the University Hospital Southampton PCD diagnostic center (2007-2013) [15]. A standardized proforma was used to collect patient data through clinical interview prior to diagnostic testing, ensuring unbiased assessment of predictive parameters.
Diagnostic confirmation followed contemporary guidelines, requiring a typical clinical history with at least two abnormal diagnostic tests, including "hallmark" transmission electron microscopy (TEM) findings, "hallmark" ciliary beat pattern (CBP), or nasal nitric oxide (nNO) ≤30 nL·min⁻¹ [15]. In cases with strong clinical phenotype or family history, diagnosis could be established based on either hallmark TEM or repeated high-speed video microscopy analysis consistent with PCD.
Statistical analysis employed logistic regression to identify significant predictors, with model performance assessed through receiver operating characteristic (ROC) curve analysis and calculation of the area under the curve (AUC). The final model was simplified into a practical points-based scoring system (PICADAR) and externally validated in a second diagnostic center [15].
Comparative Study Methodology
A more recent comparative study evaluated PICADAR alongside the Clinical Index (CI) and NA-CDCF in an unselected cohort of 1401 patients referred for PCD diagnostics [17]. This study employed a comprehensive diagnostic approach including nNO measurement in patients older than 3 years, high-speed video microscopy (HSVM), transmission electron microscopy (TEM), and genetic testing using next-generation sequencing of a 39-gene PCD panel [17].
The study design allowed for direct comparison of the predictive characteristics of the three tools using ROC curve analysis. Statistical comparisons of the AUC values employed established methods to determine significant differences in predictive power between instruments. This robust methodological approach provides high-quality evidence for tool selection in clinical and research settings.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for PCD Diagnostic Studies
| Reagent/Equipment | Specific Function | Application in PCD Research |
|---|---|---|
| Nasal Nitric Oxide Analyzer (Niox Mino/Vero) | Measures nasal NO concentration electrochemically | PCD screening; levels <30 nL/min highly suggestive of PCD [17] |
| High-Speed Video Microscopy System | Visualizes and records ciliary beat frequency and pattern | Assessment of ciliary function; identification of characteristic beat patterns [17] |
| Transmission Electron Microscope | Ultrastructural visualization of ciliary axoneme | Identification of definitive ultrastructural defects in cilia [15] |
| Next-Generation Sequencing Panel | Genetic analysis of PCD-associated genes | Confirmation of disease-causing mutations; genotype-phenotype correlations [17] |
| Cell Culture Materials | Air-liquid interface culture systems | Differentiation of primary versus secondary ciliary dyskinesia [15] |
Diagnostic Pathway and Genetic Influences
The following diagram illustrates the role of PICADAR within the broader PCD diagnostic pathway and how genetic variations influence clinical presentation:
PCD Diagnostic Pathway
PICADAR Scoring Methodology
The calculation of PICADAR scores follows a specific points system based on clinical parameters:
PICADAR Scoring System
Discussion and Research Implications
The variable sensitivity of PICADAR in relation to laterality defects and ultrastructural phenotypes has significant implications for research and clinical practice. The tool demonstrates strong performance in populations with typical PCD presentations including situs inversus, but its effectiveness diminishes in populations where laterality defects are less common, such as in Japanese patients [8]. This variability underscores the importance of population-specific validation and potential adjustment of cutoff scores or weighting parameters based on local genetic and clinical characteristics.
For drug development professionals, these findings highlight the necessity of implementing comprehensive diagnostic strategies that do not overly rely on single predictive instruments. The combination of clinical prediction tools like PICADAR with nNO measurement provides enhanced sensitivity [25], potentially reducing the risk of excluding eligible patients from clinical trials based on atypical presentations. Furthermore, researchers should consider the genetic heterogeneity of PCD across different ethnic groups when designing multinational trials, as the performance of screening tools may vary significantly between populations.
Future research directions should focus on developing population-specific adjustments to existing prediction tools, exploring the integration of genetic markers into clinical prediction algorithms, and validating modified approaches across diverse patient cohorts. Such efforts will enhance the early and accurate identification of PCD patients, facilitating timely intervention and appropriate recruitment for clinical trials of emerging therapies.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder impairing mucociliary clearance and leading to chronic otosinopulmonary disease [4]. Diagnosis remains challenging due to the genetic complexity and absence of a single gold-standard test [26] [27]. The PrImary CiliARy DyskinesiA Rule (PICADAR) was developed as a clinical prediction tool to identify patients needing specialized testing, using seven easily obtainable clinical parameters [4]. While its initial validation showed promise, this analysis examines its performance specifically in genetically confirmed PCD populations, a cohort critical for understanding its real-world diagnostic accuracy.
PICADAR Tool Composition and Scoring
The PICADAR tool is designed for patients with persistent wet cough and assesses seven clinical parameters obtained through patient history [4]. Each parameter is assigned a points value based on its regression coefficient, with the total score determining the probability of PCD.
Table 1: PICADAR Predictive Parameters and Scoring System
| Predictive Parameter | Points Value |
|---|---|
| Full-term gestation | 1.5 |
| Neonatal chest symptoms | 2.0 |
| Neonatal intensive care unit admission | 2.0 |
| Chronic rhinitis | 1.5 |
| Ear symptoms | 1.5 |
| Situs inversus | 2.0 |
| Congenital cardiac defect | 4.0 |
In the original validation study, a cut-off score of 5 points demonstrated a sensitivity of 0.90 and specificity of 0.75 for predicting PCD, with an area under the curve (AUC) of 0.91 in the derivation group and 0.87 in the external validation group [4]. The tool's initial performance established it as a potentially valuable screening instrument for general respiratory specialists.
Performance in Genetically Confirmed PCD Populations
Recent evidence from a 2025 study reveals significant limitations in PICADAR's performance when applied to genetically confirmed PCD populations [5]. This multicenter evaluation of 269 individuals with genetically confirmed PCD found substantially reduced sensitivity compared to original validation studies.
Table 2: PICADAR Performance in Genetically Confirmed PCD Population
| Performance Measure | Original Validation [4] | Genetically Confirmed PCD [5] |
|---|---|---|
| Overall Sensitivity | 90% | 75% |
| Sensitivity in Situs Solitus | Not specified | 61% |
| Sensitivity with Laterality Defects | Not specified | 95% |
| Sensitivity with Hallmark Ultrastructural Defects | Not specified | 83% |
| Sensitivity without Hallmark Ultrastructural Defects | Not specified | 59% |
| Patients Excluded for No Daily Wet Cough | Not applicable | 7% (18/269) |
The study identified that 18 individuals (7%) with genetically confirmed PCD reported no daily wet cough, automatically ruling out PCD according to PICADAR's initial screening question [5]. The median PICADAR score in the genetically confirmed cohort was 7 (IQR: 5-9), with dramatically different performance across subgroups based on clinical presentation.
Comparative Analysis of Diagnostic Testing Modalities
PCD diagnosis typically employs a multi-test approach due to the absence of a gold standard [26] [27]. Understanding PICADAR's role requires comparison with other diagnostic methods.
Table 3: Comparison of PCD Diagnostic Testing Modalities
| Diagnostic Method | Sensitivity | Specificity | Limitations |
|---|---|---|---|
| PICADAR (Genetic Cohort) | 75% [5] | 75% (original) [4] | Limited sensitivity in situs solitus (61%) [5] |
| High-Speed Video Microscopy Analysis (HSVMA) | 100% [26] | 93% [26] | Requires significant expertise; may need repeated sampling [26] |
| Transmission Electron Microscopy (TEM) | ~79% (21% false negative) [26] | 100% [26] | Misses PCD with normal ultrastructure [26] |
| Nasal Nitric Oxide (nNO) | 91% [26] | 96% [26] | Misses ~10% of cases; requires expensive equipment [26] |
| Genetic Testing | Varies by gene panel | High for identified mutations | Expanding gene discovery; not all mutations identified [27] |
The European Respiratory Society (ERS) and American Thoracic Society (ATS) have developed different diagnostic algorithms, which can lead to contradictory diagnoses in approximately 15% of patients [27]. This highlights the complexity of PCD diagnosis and the need for improved screening tools.
Experimental Protocols for PCD Diagnostic Evaluation
Genetic Confirmation Protocol
The 2025 PICADAR validation study employed comprehensive genetic testing to establish a definitive PCD diagnosis [5]. The methodology included:
- Study Population: 269 individuals with genetically confirmed PCD from multicenter cohorts
- Genetic Analysis: Comprehensive genetic testing identifying biallelic pathogenic mutations in known PCD-associated genes
- PICADAR Assessment: Retrospective application of PICADAR tool through clinical record review
- Statistical Analysis: Sensitivity calculation based on proportion of individuals scoring ≥5 points; subgroup analyses for laterality defects and ultrastructural defects using appropriate statistical tests with significance at p<0.05
Diagnostic Testing Protocol
The foundational study on PCD diagnostic testing accuracy provides the methodology for evaluating individual diagnostic modalities [26]:
- Participants: 654 consecutive patients referred for PCD diagnostics
- Testing Methods: Simultaneous application of nNO, HSVMA, and TEM
- nNO Measurement: Using chemiluminescence analyzer (NIOX Flex) with cut-off of ≤30 nL·min⁻¹ during breath-hold
- HSVMA Protocol: Nasal brush biopsy with recording of ciliary epithelium at 500 fps; assessment of ciliary beat pattern and frequency
- TEM Analysis: Examination of ≥100 cilia in transverse section at ×60,000 magnification
- Diagnostic Confirmation: Multidisciplinary team review considering all clinical and diagnostic data
Diagnostic Pathway and Performance Relationships
The following diagram illustrates the diagnostic pathway for PCD and how PICADAR fits into the overall process, particularly highlighting its performance limitations in genetically confirmed populations:
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for PCD Diagnostic Studies
| Reagent/Equipment | Function/Application | Example Specifications |
|---|---|---|
| Nasal Nitric Oxide Analyzer | Measures nNO concentration for screening | Chemiluminescence analyzer (e.g., NIOX Flex), aspiration at 0.3 L·min⁻¹ during breath-hold [26] |
| High-Speed Video Microscope | Analyzes ciliary beat pattern and frequency | Inverted microscope with high-speed camera (≥500 fps), e.g., Olympus IX73 with FLIR 3.2 MP Mono camera [27] |
| Transmission Electron Microscope | Evaluates ciliary ultrastructure | High-resolution TEM capable of ×60,000 magnification for axonemal structure assessment [26] |
| Air-Liquid Interface (ALI) Culture System | Differentiates primary from secondary ciliary dyskinesia | Cell culture system allowing ciliary differentiation after nasal brushing [26] [27] |
| Genetic Sequencing Platform | Identifies pathogenic mutations in PCD-associated genes | Next-generation sequencing with comprehensive PCD gene panels (∼50 known genes) [27] |
| Immunofluorescence Staining Reagents | Detects missing ciliary proteins | Antibodies against DNAH5, GAS8, RSPH9, and other ciliary proteins [27] |
PICADAR represents a valuable initial screening tool for PCD, particularly in settings with limited access to specialized equipment. However, its significantly reduced sensitivity in genetically confirmed populations—especially those with situs solitus (61%) or without hallmark ultrastructural defects (59%)—highlight critical limitations [5]. These findings emphasize that PICADAR should not be used as the sole determinant for referring patients for specialized PCD testing. Clinicians should maintain a low threshold for specialist referral for patients with strong clinical features of PCD despite low PICADAR scores, particularly given that 7% of genetically confirmed PCD patients lack the requisite daily wet cough [5]. Future development of predictive tools must account for the evolving understanding of PCD genetics and phenotypes to improve detection of atypical cases.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder impairing motile cilia function, leading to chronic otosinopulmonary disease, laterality defects, and infertility [28]. Diagnosis remains challenging due to the absence of a single gold standard test, often requiring a combination of complex investigations [11]. The Primary Ciliary Dyskinesia Rule (PICADAR) is a clinical predictive tool recommended by the European Respiratory Society (ERS) to identify patients needing specialized PCD testing [11] [15]. It uses a scoring system based on clinical features such as daily wet cough, neonatal respiratory symptoms, situs abnormalities, and chronic ear or nasal issues [28]. A score of ≥5 points suggests a high likelihood of PCD and warrants further investigation [15].
While PICADAR demonstrates good diagnostic performance in broad PCD populations, its sensitivity is not uniform across all patient subgroups. Recent evidence reveals significant limitations in its ability to identify patients with specific clinical and ultrastructural characteristics, namely those with situs solitus (normal organ arrangement) and those with normal ciliary ultrastructure [5]. This analysis objectively compares PICADAR's performance using recent experimental data to delineate these high-risk subgroups, providing researchers and clinicians with critical insights for diagnostic protocol refinement.
Performance Analysis of PICADAR Across Subgroups
A 2025 study by Schramm et al. evaluated PICADAR's sensitivity in a large cohort of 269 genetically confirmed PCD patients, providing the most robust data for subgroup analysis [5]. The findings demonstrate that PICADAR's performance is highly variable and dependent on specific patient characteristics.
Table 1: Overall Sensitivity of PICADAR in Genetically Confirmed PCD (n=269)
| Metric | Value |
|---|---|
| Overall Sensitivity | 75% (202/269) |
| Median PICADAR Score | 7 points (IQR: 5 – 9) |
| Patients Excluded by Initial "No Daily Wet Cough" Response | 7% (18/269) |
The Situs Solitus Subgroup
The most significant performance gap was observed between patients with and without laterality defects. The presence of situs inversus or heterotaxy is a high-point item in the PICADAR score, making its absence a critical factor in missed diagnoses [5].
Table 2: PICADAR Performance Stratified by Laterality
| Subgroup | Sensitivity | Median PICADAR Score (IQR) | Statistical Significance |
|---|---|---|---|
| All Individuals with Laterality Defects | 95% | 10 (IQR 8-11) | p < 0.0001 |
| Individuals with Situs Solitus | 61% | 6 (IQR 4-8) |
This 34-percentage-point difference in sensitivity highlights that nearly 40% of PCD patients with normal organ arrangement would not be referred for further testing based on the PICADAR threshold [5]. This is particularly concerning given that the prevalence of situs inversus in some populations, such as Japanese PCD patients, can be as low as 25%, underscoring the potential for widespread under-identification in such cohorts [8].
The Normal Ultrastructure Subgroup
PICADAR's performance was further stratified by whether a patient's genotype was predicted to cause hallmark defects in ciliary ultrastructure, detectable via Transmission Electron Microscopy (TEM). Approximately 30% of PCD patients have normal ciliary ultrastructure [28], and this subgroup is also at high risk of being missed.
Table 3: PICADAR Performance Stratified by Predicted Ciliary Ultrastructure
| Subgroup | Sensitivity | Median PICADAR Score (IQR) | Statistical Significance |
|---|---|---|---|
| With Hallmark Ultrastructural Defects | 83% | 8 (IQR 6-10) | p < 0.0001 |
| Without Hallmark Ultrastructural Defects | 59% | 6 (IQR 4-8) |
The 24-percentage-point sensitivity drop in patients without hallmark ultrastructural defects indicates that PICADAR is significantly less effective in identifying patients with specific genetic variants that preserve normal ciliary anatomy [5]. This is a critical limitation, as these patients require genetic testing or other specialized methods for diagnosis.
Experimental Protocols and Methodologies
Understanding the experimental design behind this data is crucial for evaluating its validity and applicability.
Cohort Study by Schramm et al. (2025)
The primary data cited in this analysis originates from a multi-center study designed to evaluate PICADAR's sensitivity in a genetically confirmed PCD population [5] [29].
- Study Population: 269 individuals with a genetically confirmed PCD diagnosis from the University Hospital Münster, Germany, and the University of Copenhagen, Denmark [5].
- Data Collection: PICADAR scores were assessed by pulmonary teams during patient consultations. For children, legal guardians provided answers. Data was extracted from the international ERN LUNG PCD registry [29].
- PICADAR Administration: The tool was applied as described by Behan et al. [15]. The initial question regarding a "daily wet cough starting in early childhood" served as a gatekeeper; a negative response terminated the assessment with a score of 0 [5] [29].
- Subgroup Analysis: The cohort was divided based on the presence of laterality defects (situs inversus/heterotaxy vs. situs solitus) and based on genotypes predictive of hallmark ultrastructural defects on TEM [5].
- Statistical Analysis: Sensitivity was calculated as the proportion of individuals scoring ≥5 points. The Mann-Whitney U test was used to compare PICADAR scores between subgroups [5].
Original PICADAR Derivation and Validation
The benchmark for PICADAR's expected performance comes from its original development study [15].
- Study Population (Derivation): 641 consecutive patients referred for PCD testing at University Hospital Southampton (UHS), of which 75 (12%) were PCD-positive. Diagnosis was based on a typical clinical history and at least two abnormal tests (e.g., hallmark TEM, hallmark ciliary beat pattern, or low nNO) [15].
- Study Population (Validation): 187 patients from Royal Brompton Hospital (RBH), with an equal number of PCD-positive (n=93) and PCD-negative (n=94) referrals randomly selected [15].
- Model Development: 27 potential clinical variables were analyzed. Significant predictors were identified using logistic regression, and the model was simplified into a practical scoring tool (PICADAR) [15].
- Performance Metrics: The model's discriminative ability was tested using Receiver Operating Characteristic (ROC) curve analysis, reporting Area Under the Curve (AUC), sensitivity, and specificity [15].
The following workflow diagram illustrates the diagnostic pathway and the points where high-risk subgroups may be missed.
The Scientist's Toolkit: Research Reagent Solutions
For researchers investigating PCD diagnostics and pathophysiology, the following key materials and methods are essential.
Table 4: Key Reagents and Methods for PCD Diagnostic Research
| Research Tool | Primary Function in PCD Research |
|---|---|
| Genetic Sequencing Panels | Targeted investigation of >50 known PCD genes to confirm diagnosis and establish genotype-phenotype correlations [30]. |
| Transmission Electron Microscopy (TEM) | Visualization of ciliary ultrastructure to identify hallmark defects (e.g., absent outer/inner dynein arms) in approximately 70% of PCD cases [11] [28]. |
| High-Speed Video Microscopy Analysis (HSVA) | Functional assessment of ciliary beat frequency and, critically, ciliary beat pattern, which is essential for diagnosis [11]. |
| Nasal Nitric Oxide (nNO) Measurement | A highly sensitive screening test in cooperative children (>6 years) and adults; low nNO levels support a PCD diagnosis [11] [28]. |
| Air-Liquid Interface (ALI) Cell Culture | A method to re-differentiate and culture ciliated epithelial cells, used to differentiate primary from secondary ciliary dyskinesia and improve diagnostic accuracy of HSVA [11]. |
| Immunofluorescence (IF) Microscopy | Detection of missing or mislocalized ciliary proteins, serving as a proxy for genetic defects and aiding in diagnosis, especially in cases with normal ultrastructure [11] [30]. |
The quantitative data and experimental evidence confirm that PICADAR has major limitations in identifying PCD in patients with situs solitus and those with normal ciliary ultrastructure, with sensitivities plummeting to approximately 60% in these subgroups. This performance gap is likely attributable to the original derivation cohort's reliance on diagnostic methods (TEM, HSVA) that are less effective at identifying PCD variants that preserve normal ciliary structure and function [5] [29]. Consequently, reliance on PICADAR as a primary triage tool systematically biases referrals against these specific patient populations.
For clinical practice, this mandates caution in using PICADAR as the sole factor for estimating PCD likelihood. A strong clinical history should prompt further investigation even with a low PICADAR score [11]. For the research community, these findings highlight an urgent need to develop and validate novel predictive tools or to refine existing algorithms to better capture the full genetic and phenotypic spectrum of PCD, particularly for high-risk subgroups currently falling through the diagnostic net.
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary function, leading to impaired mucociliary clearance. Patients typically present with chronic wet cough, recurrent respiratory infections, chronic rhinosinusitis, and otitis media, with approximately half exhibiting laterality defects such as situs inversus [15] [7]. The diagnostic journey for PCD is challenging due to the nonspecific nature of its symptoms and the requirement for highly specialized, expensive confirmatory testing available only at specialized centers [15]. In response to these challenges, the PrImary CiliARy DyskinesiA Rule (PICADAR) was developed as a clinical prediction tool to identify patients with a high probability of PCD before proceeding to complex diagnostic testing [15] [16].
PICADAR represents a strategic approach to mitigating risk in the PCD diagnostic process—specifically, the risk of delayed diagnosis versus the risk of overburdening specialized services. For researchers and clinicians, understanding the performance characteristics, appropriate applications, and limitations of PICADAR is essential for optimizing diagnostic pathways. This guide provides a comprehensive, evidence-based comparison of PICADAR's performance against alternative approaches, equipping drug development professionals and scientists with the data needed to make informed decisions in both clinical and research settings.
PICADAR: Original Validation and Performance
Tool Development and Methodology
The PICADAR tool was developed through a rigorous methodology to ensure its predictive validity [15]. Researchers analyzed data from 641 consecutive patients referred for PCD testing at the University Hospital Southampton (UHS) between 2007 and 2013. Using logistic regression analysis of 27 potential clinical variables, they identified seven key predictors readily available from patient history to create a practical scoring system.
The resulting PICADAR tool applies specifically to patients with persistent wet cough and incorporates these seven predictive parameters:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care unit admission
- Chronic rhinitis
- Chronic ear symptoms
- Situs inversus
- Congenital cardiac defect
Each parameter contributes a specific point value to a total score, which correlates with the probability of a PCD diagnosis [15]. The tool was subsequently externally validated using a sample of 187 patients from the Royal Brompton Hospital (RBH), demonstrating its robustness across different patient populations.
Original Performance Metrics
In its original validation study, PICADAR demonstrated strong performance characteristics [15] [16]. Of the 641 referrals in the derivation group, 75 (12%) were ultimately diagnosed with PCD. The tool showed excellent discriminatory power, with an area under the receiver operating characteristic curve (AUC) of 0.91 upon internal validation and 0.87 upon external validation.
Table 1: Original Performance Metrics of PICADAR
| Metric | Derivation Cohort | Validation Cohort |
|---|---|---|
| Sample Size | 641 patients | 187 patients |
| PCD Prevalence | 12% (75 patients) | 50% (93 patients) |
| Optimal Cut-off Score | 5 points | 5 points |
| Sensitivity | 0.90 | Not specified |
| Specificity | 0.75 | Not specified |
| Area Under Curve (AUC) | 0.91 | 0.87 |
The validation cohort was selectively enriched with PCD-positive cases (50% prevalence compared to 12% in the derivation cohort) to better assess tool performance across the disease spectrum [15]. At the recommended cut-off score of 5 points, PICADAR achieved a sensitivity of 0.90 and specificity of 0.75, indicating a strong ability to correctly identify patients with PCD while filtering out a substantial proportion of those without the condition.
Limitations and Contemporary Performance Evidence
Emerging Evidence on Sensitivity Limitations
Recent research has raised important considerations regarding PICADAR's sensitivity, particularly in specific PCD subpopulations. A 2025 study by Schramm et al. evaluated PICADAR's performance in 269 individuals with genetically confirmed PCD, providing critical insights into its real-world applicability [6] [5].
The study revealed an overall sensitivity of 75% (202/269), notably lower than the 90% reported in the original validation study. Alarmingly, 18 individuals (7%) with genetically confirmed PCD reported no daily wet cough, which would have automatically excluded them from PICADAR assessment according to the tool's initial screening question [6].
Table 2: Contemporary Performance Data Across PCD Subpopulations
| Patient Subgroup | Sample Size | Median PICADAR Score (IQR) | Sensitivity |
|---|---|---|---|
| Overall Genetically Confirmed PCD | 269 | 7 (5-9) | 75% |
| With Laterality Defects | Not specified | 10 (8-11) | 95% |
| With Situs Solitus (normal arrangement) | Not specified | 6 (4-8) | 61% |
| With Hallmark Ultrastructural Defects | Not specified | Not specified | 83% |
| Without Hallmark Ultrastructural Defects | Not specified | Not specified | 59% |
These findings highlight significant variability in PICADAR's performance across different phenotypic expressions of PCD. The tool demonstrates excellent sensitivity in patients with laterality defects (95%) but substantially lower sensitivity in those with situs solitus (61%) or without hallmark ultrastructural defects (59%) [6].
Geographical and Genetic Considerations
Further limitations emerge when considering geographical and genetic variations in PCD presentation. A Japanese study of 67 PCD patients found that only 25% exhibited situs inversus—markedly lower than the approximately 50% typically reported in other populations [8]. This discrepancy reflects differences in the major disease-causing genes across ethnic groups, particularly the lower prevalence of DNAH11 mutations in Japanese patients.
This geographical variation has direct implications for PICADAR's performance, as situs inversus is a high-point value parameter in the scoring system. The Japanese cohort had a mean PICADAR score of 7.3 points (range: 3-14), indicating that the tool remained applicable in this population, albeit with potentially altered performance characteristics due to the different phenotypic spectrum [8].
Experimental Protocols and Methodologies
Original PICADAR Validation Protocol
The original PICADAR validation followed a rigorous methodological protocol [15]. Researchers collected data using a standardized proforma completed by clinicians during patient interviews prior to diagnostic testing. The diagnostic outcome for PCD was determined using contemporary UK standards, typically requiring a characteristic clinical history plus at least two abnormal specialized tests: hallmark transmission electron microscopy (TEM) findings, hallmark ciliary beat pattern (CBP) abnormalities, or low nasal nitric oxide (nNO ≤30 nL·min⁻¹).
Statistical analysis involved logistic regression to identify significant predictors, with model performance assessed through receiver operating characteristic (ROC) curve analysis and the Hosmer-Lemeshow goodness-of-fit test. The final tool was derived by rounding regression coefficients to the nearest integer to create a practical scoring system. External validation employed similar protocols at a different specialist center, ensuring generalizability across settings.
Contemporary Sensitivity Analysis Protocol
The 2025 sensitivity study followed a distinct protocol focused on genetically confirmed PCD cases [6] [5]. Researchers evaluated 269 individuals with genetically proven PCD, calculating PICADAR scores based on retrospective clinical data. Sensitivity was determined by the proportion of patients scoring ≥5 points, the recommended threshold for suspecting PCD.
Subgroup analyses examined the impact of two key factors:
- Laterality defects: Comparing patients with situs inversus/heterotaxy versus situs solitus
- Ultrastructural defects: Comparing patients with predicted hallmark defects (e.g., outer dynein arm defects) versus those without
Statistical comparisons used appropriate tests (e.g., Mann-Whitney U for score distributions, Chi-square for sensitivity comparisons) with significance set at p<0.05. This protocol design allowed for stratified assessment of PICADAR's performance across clinically relevant subpopulations.
Decision Framework: Application Guidelines
Based on the cumulative evidence, the following decision framework outlines when to use PICADAR and when to consider alternatives.
Diagram 1: PCD Diagnostic Decision Pathway Incorporating PICADAR
When to Use PICADAR
PICADAR is most appropriate in these clinical scenarios:
- Initial Triage: As a first-line screening tool for patients with persistent wet cough to determine need for specialist referral [15]
- High-Prevalence Settings: In populations with typical PCD presentations, particularly those with laterality defects where sensitivity exceeds 90% [6]
- Resource-Limited Contexts: When access to nNO measurement or other screening tools is limited, as it relies solely on clinical history [15]
- Research Screening: For identifying potential PCD cohorts in epidemiological studies or clinical trial recruitment [15] [6]
When to Seek Alternatives
Consider alternative approaches or proceed directly to specialist testing when:
- High Clinical Suspicion with Low PICADAR Score: Particularly in patients with strong family history, consanguinity, or typical symptoms but low PICADAR scores [6] [5]
- Atypical Presentations: Patients without daily wet cough (7% of genetically confirmed PCD cases) or with situs solitus and normal ultrastructure [6]
- Specific Ethnic Populations: Groups with known different genotypic/phenotypic patterns, such as Japanese populations with low situs inversus prevalence [8]
- Access to Advanced Screening: When nNO measurement is available, which may offer higher sensitivity across PCD subtypes [15] [7]
Alternative Diagnostic Approaches
Comparison of PCD Diagnostic Methods
Table 3: Comparison of PCD Diagnostic and Screening Methods
| Method | Sensitivity | Specificity | Advantages | Limitations |
|---|---|---|---|---|
| PICADAR | 75-90% [15] [6] | 75% [15] | Quick, inexpensive, no equipment | Lower sensitivity in situs solitus [6] |
| Nasal NO (nNO) | ~90% (varies) [15] [7] | ~90% [15] [7] | Well-validated, quantitative | Requires expensive equipment, trained technicians [15] |
| Genetic Testing | >90% (expanding) [7] | ~100% [7] | Definitive diagnosis, prognostic value | Cost, variants of unknown significance, >50 genes [7] |
| High-Speed Video Microscopy | ~90% [7] | ~90% [7] | Direct functional assessment | Specialist centers only, secondary dyskinesia confounds [7] |
| Transmission Electron Microscopy | ~70% [15] [7] | ~95% [7] | Gold standard for ultrastructure | Misses normal ultrastructure forms, technical expertise [15] [7] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for PCD Diagnostic Development
| Reagent/Technology | Primary Function | Application in PCD Research |
|---|---|---|
| Transmission Electron Microscope | Visualize ciliary ultrastructure | Identify hallmark defects (ODA, IDA, MTD) [7] |
| High-Speed Video Microscope | Analyze ciliary beat pattern and frequency | Assess ciliary motility defects [15] [7] |
| Nasal Nitric Oxide Analyzer | Measure nNO concentration | Screening tool (low nNO suggests PCD) [15] [7] |
| Next-Generation Sequencing Panels | Detect mutations in >50 PCD genes | Genetic confirmation, genotype-phenotype correlation [6] [7] |
| Cell Culture Systems (ALI) | Differentiate respiratory epithelial cells | Obtain ciliated epithelium for functional testing [15] |
| Immunofluorescence Assays | Localize specific ciliary proteins | Confirm absence/mislocalization of proteins [7] |
PICADAR remains a valuable tool in the initial assessment of patients with suspected PCD, particularly for triaging referrals to specialized centers. Its strength lies in utilizing readily available clinical information without requiring specialized equipment or technical expertise. However, emerging evidence demonstrates significant limitations in its sensitivity, especially for patients without laterality defects or those with specific genetic subtypes that preserve normal ciliary ultrastructure.
For researchers and clinicians, a strategic approach to PCD diagnosis should incorporate PICADAR as one component of a comprehensive diagnostic pathway rather than relying on it as a standalone decision tool. In cases of high clinical suspicion despite low PICADAR scores, or in populations with known atypical presentations, proceeding directly to advanced testing including nNO measurement and genetic analysis is warranted. Future development of more sensitive prediction tools that incorporate genetic and molecular markers may help address the current limitations and improve diagnostic accuracy across the diverse spectrum of PCD presentations.
Comparative Evaluation and Emerging Alternatives in PCD Screening
Primary ciliary dyskinesia (PCD) is a rare genetic disorder characterized by impaired mucociliary clearance due to defects in the structure and function of motile cilia. The diagnostic pathway for PCD is complex, with no single definitive test, often requiring a combination of specialized investigations such as nasal nitric oxide (nNO) measurement, high-speed video microscopy (HSVM), transmission electron microscopy (TEM), and genetic analysis [17] [15]. These tests are technologically demanding and typically available only at specialized tertiary centers, creating a critical need for effective predictive clinical tools to identify high-risk patients who should be referred for comprehensive diagnostic workup [17] [31].
Several clinical prediction tools have been developed to address this need, including the PICADAR (PrImary CiliARy DyskinesiA Rule), NA-CDCF (North America Criteria Defined Clinical Features), CI (Clinical Index), and the newer CInew13 score [17] [15] [32]. Each tool utilizes different clinical parameters and scoring systems to estimate the probability of PCD. This article provides a comprehensive head-to-head comparison of these four predictive instruments, evaluating their diagnostic performance, methodological requirements, and practical applicability within the context of PCD diagnostic research. The analysis is based primarily on a 2021 large-scale comparative study that directly evaluated all these tools in a cohort of 1,401 patients suspected of having PCD [17] [32] [31].
Tool Design and Methodological Approaches
Fundamental Design Philosophies
The four predictive tools exhibit distinct design philosophies in their approach to identifying PCD susceptibility. PICADAR was specifically developed for patients with persistent wet cough and incorporates seven predictive parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care unit (NICU) admission, situs inversus, congenital cardiac defect, chronic rhinitis, and ear symptoms [15] [16]. Its development involved logistic regression analysis of 641 consecutive referrals, with external validation in an independent cohort [15]. The tool assigns weighted points to each parameter, with a recommended referral cutoff score of ≥5 points demonstrating 90% sensitivity and 75% specificity in derivation studies [15].
In contrast, the Clinical Index (CI) employs a simpler, unweighted 7-item questionnaire focusing on respiratory symptoms: significant respiratory difficulties after birth; rhinitis or excessive mucus production in the first 2 months of life; pneumonia; three or more bronchitis episodes; chronic secretoric otitis or >3 acute otitis episodes; year-round nasal discharge or obstruction; and antibiotic treatment for acute upper respiratory infections more than three times [17]. Each affirmative response scores one point, with higher scores indicating greater PCD probability. Unlike PICADAR, CI does not require assessment of laterality defects or congenital heart defects, potentially simplifying its application in primary care settings [17].
The NA-CDCF tool takes a minimalist approach, defining just four clinical criteria: laterality defects, unexplained neonatal respiratory distress syndrome (RDS), early-onset year-round nasal congestion, and early-onset year-round wet cough [17]. This tool emerged from North American clinical criteria and emphasizes cardinal features of PCD without complex scoring systems.
The CInew13 represents a comprehensive approach that incorporates all signs and symptoms present in the CI, PICADAR, and NA-CDCF tools [17]. This integrated instrument was developed to potentially capture the broadest spectrum of PCD manifestations, though its practical utility requires further validation.
Table 1: Core Components of PCD Predictive Tools
| Assessment Component | PICADAR | Clinical Index | NA-CDCF | CInew13 |
|---|---|---|---|---|
| Neonatal Symptoms | Neonatal chest symptoms, NICU admission | Respiratory difficulties after birth | Unexplained neonatal RDS | Comprehensive inclusion |
| Laterality Defects | Situs inversus | Not included | Laterality defects | Included |
| Cardiac Defects | Congenital heart defect | Not included | Not included | Included |
| Respiratory History | Considered via other parameters | Pneumonia, recurrent bronchitis | Early-onset wet cough | Comprehensive inclusion |
| Upper Airway Symptoms | Chronic rhinitis | Year-round nasal discharge/obstruction | Early-onset year-round nasal congestion | Comprehensive inclusion |
| Otologic Symptoms | Ear symptoms | Chronic/recurrent otitis | Not included | Included |
| Infectious History | Not directly included | Recurrent antibiotic use | Not included | Included |
| Gestational Age | Full-term gestation | Not included | Not included | Included |
Key Methodological Protocols
The 2021 comparative study that serves as the primary source for this analysis employed rigorous methodological standards [17] [31]. The research involved 1,401 patients with suspected PCD referred to a tertiary center for HSVM testing between January 2012 and December 2020. PCD was definitively diagnosed in 67 patients (4.8%) using a combination of diagnostic methods including TEM, genetic testing, and clinical judgment following ERS guidelines [17].
The diagnostic protocol included:
- nNO measurement using an electrochemical analyzer (Niox Mino or Niox Vero) with a standard protocol based on 2005 ATS/ERS recommendations [17] [31].
- HSVM analysis using the Keyence Motion Analyzer Microscope VW-6000/5000 to assess ciliary beat frequency and pattern [17].
- TEM examination of nasal brushings or endobronchial biopsy samples processed according to established laboratory protocols [17].
- Genetic testing using next-generation sequencing with a panel of 39 PCD genes and MLPA analysis for DNAH5 and DNAI1 genes [17].
For each patient, CI, PICADAR, and NA-CDCF scores were calculated based on clinical data retrieved from medical records. The predictive characteristics of each tool were analyzed using receiver operating characteristics (ROC) curves, with areas under the curve (AUC) compared using DeLong's test [17] [31].
The following diagram illustrates the experimental workflow for tool comparison:
Diagram 1: Experimental Workflow for Tool Comparison. The diagram illustrates the sequential process from patient enrollment through data collection, diagnostic confirmation, and statistical analysis used in the comparative study [17] [31].
Performance Metrics and Comparative Analysis
Diagnostic Accuracy and Statistical Performance
The 2021 comparative study provided direct head-to-head comparison of the four predictive tools in the same patient population, enabling robust statistical analysis of their relative performance [17] [31]. All tools demonstrated significantly higher scores in the PCD group compared to non-PCD patients (p < 0.001), confirming their general utility in discriminating PCD cases.
The Clinical Index (CI) achieved the largest area under the ROC curve (AUC), which was statistically superior to NA-CDCF (p = 0.005) [17] [32]. While CI also showed a larger AUC than PICADAR, this difference did not reach statistical significance in all comparisons. The PICADAR and NA-CDCF tools demonstrated comparable AUC values (p = 0.093) [17]. The comprehensive CInew13 tool, which incorporates elements from all other instruments, showed promising performance but requires further validation in diverse populations [17].
Table 2: Performance Metrics of PCD Predictive Tools
| Predictive Tool | AUC | Optimal Cut-off | Sensitivity | Specificity | Key Strengths | Key Limitations |
|---|---|---|---|---|---|---|
| PICADAR | 0.87-0.91 (external validation) [15] | ≥5 points | 0.90 [15] | 0.75 [15] | Externally validated, good sensitivity | Requires chronic wet cough, cannot assess 6.1% without this symptom [17] |
| Clinical Index (CI) | Largest in 2021 study [17] | Not specified | Not specified | Not specified | No need for laterality or cardiac assessment, applicable to broader population | Limited external validation compared to PICADAR |
| NA-CDCF | Smaller than CI (p=0.005) [17] | Not specified | Not specified | Not specified | Simple, minimal criteria | Lower discriminative power than other tools |
| CInew13 | Promising, requires further validation [17] | Not specified | Not specified | Not specified | Comprehensive, includes all symptoms from other tools | Complex, may be less practical for rapid screening |
Impact of nNO Measurement on Predictive Power
An important secondary finding from the comparative study was the significant enhancement of predictive power when each clinical tool was combined with nasal nitric oxide (nNO) measurement [17] [31]. nNO measurement was performed in 569 patients older than 3 years using standardized protocols with electrochemical analyzers [17].
The integration of nNO with each predictive tool resulted in:
- Improved sensitivity and specificity for all three main instruments (CI, PICADAR, and NA-CDCF)
- Enhanced discrimination between PCD and non-PCD cases
- Strengthened predictive characteristics beyond clinical criteria alone [17]
This finding underscores the complementary role of objective physiological testing alongside clinical prediction rules in the PCD diagnostic pathway. The combination approach may be particularly valuable in borderline cases where clinical scores alone provide indeterminate results.
Practical Implementation and Research Applications
Clinical Utility and Application Challenges
Each predictive tool presents distinct advantages and limitations in clinical and research settings. PICADAR demonstrated high sensitivity (90%) in its derivation study, making it valuable for minimizing false negatives [15]. However, a significant limitation emerged in the comparative study, where it could not be assessed in 6.1% of patients (86 individuals) due to the absence of chronic wet cough, a mandatory criterion for PICADAR application [17]. This restriction may limit its utility in populations where chronic wet cough is not a predominant feature.
The Clinical Index showed particular strengths in its broader applicability, as it does not require assessment of laterality defects or congenital heart defects [17]. This makes CI potentially more practical in primary care settings where access to specialized cardiac imaging or detailed laterality assessment may be limited. The simpler scoring system (one point per clinical feature) also enhances its usability for rapid screening.
The NA-CDCF, with its minimal criteria, offers the advantage of rapid application but appears to have lower discriminative power based on the smaller AUC compared to CI [17]. This tool may be most useful as an initial quick screening instrument rather than a comprehensive predictive tool.
Ethnic and Geographical Considerations
Research suggests that the performance of PCD predictive tools may vary across different ethnic and geographical populations. A Japanese study of 67 PCD patients found that only 25% exhibited situs inversus, substantially lower than the approximately 50% typically reported in Western populations [8]. This difference reflects variations in the distribution of causative genes across ethnic groups.
This geographical variation has important implications for tool selection and interpretation:
- Tools heavily weighted toward laterality defects (like PICADAR) may have reduced sensitivity in Asian populations
- The general rule that "situs inversus is observed in approximately 50% of PCD patients" cannot be universally applied [8]
- Population-specific validation or adjustment of cutoff scores may be necessary for optimal performance across diverse ethnic groups
The Scientist's Toolkit: Essential Research Reagents and Technologies
Table 3: Essential Research Materials for PCD Diagnostic Studies
| Research Tool | Primary Function | Application in PCD Diagnostics |
|---|---|---|
| Electrochemical nNO Analyzer (Niox Mino/Vero) | Measure nasal nitric oxide concentrations | Screening tool; low nNO supports PCD diagnosis [17] [31] |
| High-Speed Video Microscopy Systems (Keyence Motion Analyzer) | Analyze ciliary beat frequency and pattern | Assess ciliary motility; characteristic patterns suggest PCD [17] |
| Transmission Electron Microscope | Visualize ciliary ultrastructure | Identify structural defects in ciliary apparatus [17] |
| Next-Generation Sequencing Platforms | Genetic analysis of PCD-associated genes | Identify pathogenic mutations in >50 known PCD genes [17] |
| MLPA Reagents (SALSA MLPA Probemix) | Detect extensive intragenic rearrangements | Identify large deletions in DNAH5 and DNAI1 genes [17] |
The following diagram illustrates the integration of predictive tools within the broader PCD diagnostic pathway:
Diagram 2: PCD Diagnostic Pathway with Predictive Tool Integration. This diagram shows how clinical prediction tools fit within the sequential diagnostic workflow for PCD, from initial suspicion through confirmatory testing [17] [31].
The comparative analysis of PICADAR, NA-CDCF, Clinical Index, and CInew13 reveals distinct performance characteristics and practical considerations for each tool. The Clinical Index demonstrated superior discriminative power in direct comparison, with a larger AUC than NA-CDCF and comparable performance to PICADAR, while offering broader applicability without the need for assessment of laterality defects or congenital heart anomalies [17].
PICADAR remains a valuable tool with robust external validation, particularly in populations where chronic wet cough is a consistent feature [15]. However, its limitation in patients without this symptom (6.1% of the cohort) somewhat restricts its application [17]. The NA-CDCF tool, while simple to apply, showed lower discriminative power than CI in the comparative study [17].
A critical finding across all studies is the enhanced predictive power achieved when clinical tools are combined with nNO measurement [17] [31]. This synergistic approach leverages both clinical features and objective physiological measurement, potentially offering the highest diagnostic accuracy.
For researchers and clinicians, tool selection should consider the specific clinical context, population characteristics, and available resources. The emerging evidence of significant ethnic variation in PCD manifestations further underscores the need for population-specific validation of these predictive instruments [8]. Future research should focus on refining these tools, establishing population-adjusted cutoff scores, and exploring the integration of genetic markers into clinical prediction algorithms.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder impairing motile cilia function, leading to chronic respiratory infections, fertility issues, and in approximately half of patients, laterality defects such as situs inversus [7]. The PICADAR (PrImary CiliARy DyskinesiA Rule) score is a clinical prediction tool recommended by the European Respiratory Society (ERS) to guide the initial assessment of PCD likelihood before advanced testing [6]. Unlike complex laboratory investigations, PICADAR uses a simple set of clinical criteria to determine whether a patient should be referred for definitive PCD diagnostics. However, as its use expands globally, recent validation studies have raised critical questions about its real-world performance across diverse patient populations and genetic subtypes. This analysis synthesizes evidence from recent investigations to objectively evaluate PICADAR's sensitivity, identify its limitations, and compare its performance against emerging diagnostic approaches, providing researchers and clinicians with evidence-based guidance for implementation.
Performance Analysis of PICADAR
Recent validation studies demonstrate that PICADAR's performance varies significantly across different patient subgroups, with overall sensitivity substantially lower than initially reported. A 2025 study by Omran et al. evaluating 269 genetically confirmed PCD patients found the tool has critical limitations in real-world application [6].
Table 1: Overall Performance of PICADAR in Genetically Confirmed PCD (n=269)
| Metric | Value | Details |
|---|---|---|
| Overall Sensitivity | 75% (202/269) | Proportion scoring ≥5 points (recommended threshold) |
| Median Score | 7 points | IQR: 5-9 |
| Major Limitation | 7% (18/269) | Patients with no daily wet cough automatically ruled out |
| Key Finding | Subgroup variation | Sensitivity significantly differs by laterality and ultrastructural defects |
The finding that 7% of genetically confirmed PCD patients were automatically excluded for lacking daily wet cough highlights a fundamental flaw in the tool's initial screening logic [6]. This subgroup of patients would be missed entirely under current PICADAR protocols, potentially delaying diagnosis and treatment initiation.
Subgroup Performance Variations
Stratified analysis reveals PICADAR's performance is heavily influenced by specific patient characteristics, particularly the presence of laterality defects and hallmark ultrastructural abnormalities.
Table 2: PICADAR Sensitivity Across Patient Subgroups
| Subgroup | Sensitivity | Median Score | Statistical Significance |
|---|---|---|---|
| With Laterality Defects | 95% | 10 (IQR: 8-11) | p < 0.0001 |
| With Situs Solitus (normal arrangement) | 61% | 6 (IQR: 4-8) | |
| With Hallmark Ultrastructural Defects | 83% | Not reported | p < 0.0001 |
| Without Hallmark Ultrastructural Defects | 59% | Not reported |
The dramatically higher sensitivity in patients with laterality defects (95% vs. 61%) indicates PICADAR is optimized for the classic PCD presentation but performs poorly in patients with normal organ arrangement [6]. This has significant implications for diagnostic protocols, particularly in populations where laterality defects are less common, such as in Japan where only 25% of PCD patients present with situs inversus [8].
Comparative Diagnostic Approaches
International Diagnostic Algorithms
The absence of a single gold standard test for PCD has led to different diagnostic approaches, which yield conflicting results in a substantial number of cases [27].
Table 3: Comparison of International PCD Diagnostic Guidelines
| Guideline/Algorithm | Key Components | Diagnostic Categories | Strengths |
|---|---|---|---|
| European Respiratory Society (ERS) | nNO, HSVM, TEM, Genetics | 1. PCD positive2. PCD highly likely3. PCD highly unlikely4. Inconclusive | Comprehensive multi-method approach |
| American Thoracic Society (ATS) | nNO as primary, Genetic panel, TEM | 1. PCD diagnosed2. PCD not diagnosed | Focus on accessible initial test (nNO) |
| PCD-UNIBE Algorithm | Adds IF and ALI cell culture to ERS | Same as ERS | Enhanced structural protein analysis |
A direct clinical comparison of these algorithms found disagreement in 15% of cases (8/54 patients), with the ATS algorithm diagnosing more patients positive than the ERS algorithm in this cohort [27]. This discordance underscores the need for an internationally harmonized diagnostic approach.
Comprehensive Diagnostic Workflows
Specialized PCD centers have developed integrated workflows that combine multiple complementary techniques to overcome the limitations of individual methods. The following diagram illustrates a comprehensive diagnostic pathway that incorporates both traditional and advanced techniques:
This comprehensive approach proved essential in a study of 100 patients, where no single method could diagnose all 17 confirmed PCD cases: HSVM was diagnostic in 12, IF in 14, TEM in 5, and genetics in 11 cases [33]. The integration of ALI cell culture was particularly valuable for differentiating primary from secondary ciliary defects.
Emerging and Specialized Techniques
Immunofluorescence (IF) analysis has emerged as a powerful complementary technique, particularly for cases with normal ultrastructure but clear clinical symptoms. In a collaborative study between Turkish and German centers, IF analysis of DNAH5 and GAS8 proteins in respiratory epithelial cells provided critical diagnostic information for patients with inconclusive genetic results [22]. This approach identified specific protein localization defects that guided subsequent genetic testing, leading to confirmed diagnoses. The value of international collaboration for accessing specialized techniques like IF is particularly important for limited-resource countries [22].
Experimental Protocols and Methodologies
PICADAR Validation Study Design
The recent validation study by Omran et al. followed a rigorous methodological protocol to assess PICADAR's real-world performance [6]:
- Population: 269 individuals with genetically confirmed PCD, ensuring an objective diagnostic standard
- PICADAR Application: Retrospective calculation of PICADAR scores based on comprehensive medical record review
- Statistical Analysis: Sensitivity calculation based on the proportion of patients scoring ≥5 points (the recommended threshold); subgroup analyses based on laterality defects and ultrastructural abnormalities; statistical significance testing using appropriate methods (p<0.0001 for key comparisons)
- Limitation Assessment: Specific evaluation of patients excluded by the "no daily wet cough" criterion
This protocol represents a robust validation approach using genetically confirmed cases as the reference standard, providing high-quality evidence for PICADAR's real-world performance.
High-Speed Video Microscopy (HSVM) Analysis
HSVM serves as a cornerstone functional assessment in PCD diagnostics, with standardized protocols implemented at specialized centers [27] [33]:
- Sample Collection: Nasal epithelial cells obtained via brush biopsy using interdental brushes
- Preparation: Cells suspended in culture medium (RPMI) and placed in sealed imaging chambers
- Imaging: Recorded on inverted microscopes with high-speed cameras (300 frames per second, 640×480 pixels)
- Analysis Parameters:
- Ciliary beating pattern (CBP)
- Beating frequency (CBF)
- Coordination of cilia movement
- Particle transport capability
- Quality Control: Analysis of both fresh samples and ALI cell cultures to exclude secondary dyskinesia
The PCD-UNIBE center enhanced this protocol with custom-developed "Cilialyzer" software for standardized analysis [33].
Immunofluorescence (IF) Staining Protocol
The IF protocol used in the Turkish-German collaborative study exemplifies how specialized techniques can resolve diagnostically challenging cases [22]:
- Sample Preparation: Nasal brush cells fixed in 4% paraformaldehyde, permeabilized with 0.2% Triton X-100
- Antibody Incubation:
- Primary antibodies: Anti-DNAH5 (ODA protein) and anti-GAS8 (nexin-dynein regulatory complex)
- Secondary antibodies: Alexa Fluor-conjugated (488 for DNAH5, 546 for GAS8)
- Nuclear counterstain: Hoechst 33342
- Imaging: High-resolution fluorescence microscopy using structured illumination (ApoTome.2)
- Analysis: Assessment of protein presence and localization within the ciliary axoneme
This protocol successfully identified five patients with specific defects (DNAH5 absence, abnormal distribution, or ciliogenesis defects) among 19 genetically inconclusive cases [22].
Essential Research Reagents and Materials
The complex diagnostic workflow for PCD requires specialized reagents and equipment. The following table details key solutions and materials essential for conducting PCD diagnostics and research.
Table 4: Research Reagent Solutions for PCD Diagnostics
| Reagent/Material | Specific Examples | Research Application | Function in PCD Diagnostics |
|---|---|---|---|
| Cell Culture Media | PneumaCult Media Kits (Stemcell Technologies) | ALI cell culture | Supports differentiation of ciliated respiratory epithelium |
| Primary Antibodies | Mouse anti-DNAH5, Rabbit anti-GAS8 (HPA041311) | Immunofluorescence | Detects outer dynein arm and nexin-dynein regulatory complex proteins |
| Secondary Antibodies | Goat Anti-mouse Alexa Fluor 488, Anti-rabbit Alexa Fluor 546 | Immunofluorescence | Fluorescent detection of primary antibody binding |
| Imaging Chambers | Grace Bio-Labs CoverWell | HSVM | Provides controlled environment for ciliary motion analysis |
| Nitric Oxide Analyzers | CLD 88sp (ECO MEDICS) | nNO measurement | Quantifies nasal nitric oxide for screening |
| High-Speed Cameras | FLIR 3.2 MP Mono Grasshopper3 | HSVM | Captures rapid ciliary beating (300 fps) |
| Genetic Testing Panels | Targeted PCD gene panels (22+ genes) | Genetic analysis | Identifies pathogenic variants in PCD-associated genes |
These specialized reagents enable the comprehensive multi-method approach required for accurate PCD diagnosis, with each component addressing specific diagnostic challenges in this heterogeneous disorder.
Recent validation studies provide compelling evidence that PICADAR serves as a useful but limited tool for initial PCD assessment. With 75% overall sensitivity that drops to approximately 60% in patients without laterality defects or hallmark ultrastructural abnormalities, it cannot function as a standalone screening method [6]. The tool's fundamental structure—particularly the automatic exclusion of patients without daily wet cough—represents a significant vulnerability in its design. The optimal diagnostic approach combines multiple complementary techniques in a structured algorithm, as no single method achieves perfect sensitivity [27] [33]. Future efforts should focus on developing more inclusive clinical prediction tools that account for the full phenotypic spectrum of PCD, particularly in populations with different genetic profiles and lower rates of laterality defects [8]. For drug development professionals and researchers, these findings underscore the necessity of implementing comprehensive diagnostic protocols rather than relying on simplified clinical scores alone.
The Receiver Operating Characteristic (ROC) curve is a fundamental statistical tool used to evaluate the diagnostic performance of classification models, particularly in scenarios where test results are presented as continuous or ordinal variables rather than dichotomous outcomes [34]. Originally developed during World War II for analyzing signals on radar screens, ROC analysis was later adopted in psychology and has since become a cornerstone method in medical research, bioinformatics, and machine learning [34]. The method provides a comprehensive framework for assessing how well a diagnostic test, biomarker, or predictive model can distinguish between two defined states, such as diseased versus non-diseased or positive versus negative cases.
In clinical practice and research, ROC analysis addresses a critical challenge: determining the optimal cut-off value for a continuous test result to classify subjects accurately [35]. This process enables researchers and clinicians to balance the competing priorities of sensitivity (correctly identifying true positives) and specificity (correctly identifying true negatives) across the entire range of possible test values [36]. The visual nature of the ROC curve facilitates intuitive understanding of a test's discriminatory power, while the quantitative metric of the Area Under the Curve (AUC) provides a single numerical summary of overall performance [37].
The application of ROC analysis has grown exponentially in recent decades. In nephrology research alone, the use of ROC curves quadrupled from 307 papers in 2003-2013 to 1,332 papers in 2013-2023 [35]. This expansion reflects the increasing importance of rigorous evaluation for novel biomarkers, diagnostic tools, and predictive models across biomedical research and drug development.
Theoretical Foundations
Key Diagnostic Accuracy Metrics
Understanding ROC analysis requires familiarity with the fundamental metrics of diagnostic test performance. These metrics derive from a 2x2 contingency table that cross-tabulates the true condition of subjects (as determined by a gold standard test) with the results of the index test being evaluated [36].
Sensitivity (also called the True Positive Rate) measures the proportion of actually diseased individuals who are correctly identified by the test. It is calculated as True Positives divided by the sum of True Positives and False Negatives [35] [36]. High sensitivity is crucial when the cost of missing a disease is high, such as in screening for serious conditions.
Specificity measures the proportion of actually disease-free individuals who are correctly identified by the test. It is calculated as True Negatives divided by the sum of True Negatives and False Positives [35] [36]. Specificity becomes particularly important when false positives would lead to invasive, expensive, or risky follow-up procedures.
Positive Predictive Value (PPV) represents the probability that a subject with a positive test result truly has the disease, while Negative Predictive Value (NPV) represents the probability that a subject with a negative test result truly does not have the disease [35]. Unlike sensitivity and specificity, PPV and NPV are influenced by disease prevalence in the population.
Table 1: Fundamental Diagnostic Accuracy Metrics
| Metric | Calculation | Interpretation |
|---|---|---|
| Sensitivity | True Positives / (True Positives + False Negatives) | Ability to correctly identify diseased individuals |
| Specificity | True Negatives / (True Negatives + False Positives) | Ability to correctly identify disease-free individuals |
| Positive Predictive Value | True Positives / (True Positives + False Positives) | Probability disease is present when test is positive |
| Negative Predictive Value | True Negatives / (True Negatives + False Negatives) | Probability disease is absent when test is negative |
| Accuracy | (True Positives + True Negatives) / Total Cases | Overall correctness of the test |
The relationship between sensitivity and specificity is inherently inverse; as sensitivity increases, specificity typically decreases, and vice versa [34]. This trade-off forms the foundational concept that ROC analysis leverages to evaluate test performance across all possible decision thresholds.
The ROC Curve Construction
An ROC curve graphically represents the relationship between sensitivity and specificity across all possible cut-off values for a diagnostic test [34]. The curve is constructed by plotting the True Positive Rate (sensitivity) on the y-axis against the False Positive Rate (1 - specificity) on the x-axis for each possible threshold value of the test [35] [38].
The process begins with collecting continuous test results from subjects with known disease status (determined by a gold standard reference) [36]. For each possible test value that could serve as a cut-off, a 2x2 table is created, and the corresponding sensitivity and 1-specificity values are calculated [34]. These coordinate points are then plotted on the graph, and their connection forms the ROC curve [35].
The position of points along the curve reflects different decision thresholds. Points in the lower-left corner represent strict criteria that minimize false positives but may miss true positives (high specificity, low sensitivity). Points in the upper-right corner represent lenient criteria that capture most true positives but include more false positives (high sensitivity, low specificity) [34]. The ideal operating point depends on the clinical context and the relative consequences of false positives versus false negatives.
Diagram 1: ROC Curve Construction Workflow. This diagram illustrates the step-by-step process of creating an ROC curve from continuous test data, including determination of true disease status, calculation of performance metrics across thresholds, and final curve generation.
Interpreting the ROC Curve
Visual Interpretation and AUC
The ROC curve provides immediate visual insights into a test's discriminatory ability. A curve that closely follows the left-hand border and then the top border of the ROC space indicates excellent diagnostic performance [38]. Conversely, a curve that lies close to the 45-degree diagonal line suggests that the test performs no better than chance [35] [37].
The diagonal line from the bottom-left to top-right corners represents the ROC curve of a test with no discriminatory value, where the true positive rate equals the false positive rate at all thresholds [35] [38]. This line has an Area Under the Curve (AUC) of 0.5, equivalent to random guessing. The perfect test with 100% sensitivity and 100% specificity would yield an ROC curve that passes through the top-left corner, with an AUC of 1.0 [35].
The Area Under the Curve (AUC) serves as a single numeric summary of the test's overall discriminatory performance [37]. Also known as the c-statistic (concordance statistic), the AUC represents the probability that a randomly selected diseased individual will have a higher test value than a randomly selected non-diseased individual [38]. This interpretation highlights the AUC as a measure of how well the test separates the two groups.
Table 2: AUC Value Interpretation Guidelines
| AUC Value Range | Interpretation | Clinical Utility |
|---|---|---|
| 0.9 - 1.0 | Excellent discrimination | High clinical utility |
| 0.8 - 0.9 | Considerable/good discrimination | Clinically useful |
| 0.7 - 0.8 | Fair discrimination | Moderate clinical utility |
| 0.6 - 0.7 | Poor discrimination | Limited clinical utility |
| 0.5 - 0.6 | Fail/no discrimination | No clinical utility |
AUC values above 0.80 are generally considered clinically useful, while values below 0.80 indicate limited clinical utility, even if they are statistically significant [37]. However, AUC interpretation should also consider the confidence interval around the estimate. A narrow confidence interval indicates greater precision in the AUC estimate, while a wide interval suggests uncertainty about the true discriminatory performance [37].
Types of ROC Curves
ROC curves can be generated using different statistical approaches, each with distinct advantages and limitations. The two primary methods are nonparametric (empirical) and parametric ROC curves [34].
Nonparametric ROC curves do not assume any specific distribution for the test results in the diseased and non-diseased populations [34]. This method plots the actual observed sensitivity and 1-specificity values for each possible threshold, resulting in a characteristic jagged or staircase appearance [34]. The nonparametric approach is widely used because it requires no distributional assumptions and provides unbiased estimates of sensitivity and specificity [34].
Parametric ROC curves assume that the test results follow specific probability distributions (typically normal distributions) in the diseased and non-diseased groups [34]. This method produces smooth curves that allow comparison at any sensitivity and specificity value, not just the observed thresholds [34]. However, parametric methods may produce improper ROC curves if the data violate distributional assumptions, and the curves do not necessarily pass through all observed points [34].
Table 3: Comparison of ROC Curve Types
| Characteristic | Nonparametric ROC Curve | Parametric ROC Curve |
|---|---|---|
| Distribution Assumption | No distributional assumptions | Assumes normal distribution |
| Curve Appearance | Jagged, staircase pattern | Smooth curve |
| Data Utilization | Uses all observed data | May discard actual data points |
| Computational Complexity | Simple computation | Complex computation |
| Comparison Flexibility | Only at observed values | At any sensitivity/specificity |
A third category, semiparametric ROC curves, attempts to overcome the limitations of both approaches by providing smooth curves without requiring strict distributional assumptions. However, this method is not widely implemented in statistical software and is less commonly used in medical research [34].
Practical Applications and Methodologies
Determining Optimal Cut-off Values
One of the most valuable applications of ROC analysis in research and clinical practice is identifying the optimal cut-off value that maximizes a test's discriminatory performance [35]. Several statistical methods exist for this purpose, each with distinct advantages depending on the clinical context and relative importance of sensitivity versus specificity.
The Youden Index (J) is the most commonly used method for determining the optimal cut-off point [37]. Calculated as J = sensitivity + specificity - 1, the Youden Index identifies the threshold that maximizes the sum of sensitivity and specificity [37]. This approach implicitly assigns equal weight to false positives and false negatives, making it appropriate when the consequences of both error types are similar.
Alternative methods include:
- Distance to corner: Minimizes the Euclidean distance to the top-left corner (0,1) of the ROC plot
- Cost analysis: Incorporates explicit costs or utilities associated with correct and incorrect classifications
- Diagnostic odds ratio maximization: Selects the threshold that maximizes the odds of positive test results in diseased versus non-diseased subjects
The choice of method should align with the clinical context. In screening tests for serious diseases where missing cases has severe consequences, a threshold favoring high sensitivity may be preferred. Conversely, for confirmatory tests where false positives lead to invasive procedures, a threshold favoring high specificity might be more appropriate [36].
Diagram 2: Optimal Cut-off Selection Methodology. This workflow illustrates the process for determining the optimal diagnostic threshold, including statistical methods and clinical considerations that influence final threshold selection.
Experimental Protocols for ROC Analysis
Proper experimental design is crucial for generating valid ROC analysis results. The STARD (Standards for Reporting of Diagnostic Accuracy) statement provides a comprehensive framework for conducting and reporting diagnostic accuracy studies, including those utilizing ROC analysis [36]. The following protocol outlines key methodological considerations:
Subject Recruitment and Reference Standard
- Enroll a consecutive series of patients in whom the target condition is suspected [36]
- Apply the same reference standard (gold standard) diagnostic method to all participants [36]
- Ensure blinded interpretation of index test and reference standard results to avoid verification bias
Sample Size Considerations
- Conduct power analysis prior to study initiation
- Include sufficient numbers of both diseased and non-diseased subjects
- Account for expected AUC values and precision requirements in sample size calculations [37]
Data Collection and Analysis
- Measure the index test quantitatively across its continuous range
- Document all potential cut-off values and their corresponding sensitivity and specificity
- Calculate the AUC with 95% confidence intervals using appropriate statistical methods [37]
- For multiple tests, perform statistical comparison of ROC curves using methods such as the DeLong test [37] [39]
Validation Procedures
- Validate optimal cut-off values in an independent population to avoid overfitting [35]
- Report all measures of diagnostic accuracy, including likelihood ratios and predictive values [37]
- Provide ROC curves in publications to allow visual assessment of test performance [39]
This methodological framework ensures that ROC analysis results are reliable, reproducible, and clinically applicable. Adherence to established standards like STARD enhances the quality and interpretability of diagnostic accuracy studies [36].
Comparative Performance Assessment
ROC Analysis in Research Applications
ROC analysis serves multiple critical functions in research settings, particularly in the evaluation and comparison of diagnostic modalities. Understanding these applications enables researchers to design more robust studies and interpret findings more accurately.
Diagnostic Performance Evaluation: ROC analysis allows comprehensive assessment of a single test's ability to distinguish between diseased and non-diseased individuals [35]. For example, Zhou et al. used ROC analysis to evaluate the diagnostic performance of asprosin for metabolic syndrome in hemodialysis patients, finding an AUC of 72.5% (95% CI: 63.9-81.1) with optimal cut-off at 369.85 ng/mL (sensitivity 82.4%, specificity 51.8%) [35]. This application helps determine whether novel biomarkers have sufficient discriminatory power for clinical use.
Prognostic Prediction: Beyond diagnostic applications, ROC analysis evaluates the predictive value of biomarkers for future outcomes [35]. Rodrigues et al. investigated the urea-to-albumin ratio (UAR) for predicting mortality in critically ill COVID-19 patients using ROC analysis [35]. This prognostic application supports risk stratification and clinical decision-making.
Test Comparison: ROC analysis enables direct comparison of two or more diagnostic tests on the same population [34]. The DeLong test provides a statistical method for comparing AUC values between tests, determining whether observed differences in discriminatory performance are statistically significant [37] [39]. This application is particularly valuable when evaluating new tests against established standards or comparing multiple candidate biomarkers.
Multivariable Model Assessment: In machine learning and predictive modeling, ROC analysis evaluates the performance of complex models that incorporate multiple variables [34] [38]. The AUC provides a standardized metric for comparing different modeling approaches and selecting the most effective predictive algorithm.
Research Reagent Solutions
Table 4: Essential Research Materials for ROC Analysis Studies
| Research Material | Function/Application | Considerations |
|---|---|---|
| Gold Standard Reference Test | Definitive diagnosis for classification | Must have established accuracy; ethical considerations |
| Index Test Materials | Experimental diagnostic method | Standardized protocols; quantitative measurement |
| Statistical Software | ROC curve generation and analysis | Capabilities for AUC comparison, confidence intervals |
| Biological Samples | Biomarker measurement and validation | Appropriate storage conditions; sample stability |
| Clinical Data Collection Forms | Standardized data capture | Include all relevant clinical variables and outcomes |
Advanced Considerations
Methodological Limitations and Alternatives
While ROC analysis is a powerful and widely used method, researchers should recognize its limitations and consider complementary approaches when appropriate. Understanding these constraints ensures proper application and interpretation of ROC analysis results.
ROC curves do not directly display the specific cut-off values along the curve, making it challenging to associate particular threshold values with specific points on the curve [34]. Additionally, the visual appearance of ROC curves can be affected by sample size, with smaller samples producing jagged curves regardless of the analytical method used [34].
The AUC, while useful as a summary measure, can occasionally be misleading. A classifier with high AUC may perform worse in clinically relevant regions than another classifier with lower overall AUC [38]. This limitation has prompted development of alternative approaches:
Partial AUC: Focuses on specific regions of the ROC curve that are clinically relevant, such as high-sensitivity or high-specificity ranges [34]. This approach is valuable when only certain portions of the ROC space are meaningful for clinical decision-making.
Decision Curve Analysis: Evaluates the clinical utility of diagnostic tests by incorporating clinical consequences and patient preferences into the assessment [38]. This method goes beyond pure discrimination to consider how tests impact clinical decisions.
Precision-Recall Curves: Particularly useful when dealing with imbalanced datasets where one class is much rarer than the other. Unlike ROC curves, precision-recall curves remain informative when class distributions are skewed.
Despite these limitations, ROC analysis remains the standard method for evaluating diagnostic test discrimination when appropriate gold standards are available and the research question focuses on distinguishing between two clearly defined states.
Implementation Tools and Technical Protocols
Multiple statistical tools and software packages facilitate ROC analysis implementation, ranging from specialized applications to general statistical programming environments. The choice of tool depends on study complexity, analytical requirements, and researcher proficiency.
Specialized Web Tools: Web-based applications like the tools referenced in Kim and Hwang (2020) provide user-friendly interfaces for basic ROC analysis [39]. These tools typically allow data input, ROC curve generation, AUC calculation with confidence intervals, and cut-off optimization using methods like the Youden Index [39]. They are particularly suitable for researchers without advanced statistical training.
Statistical Software Packages: Comprehensive statistical programs including R, SPSS, SAS, and Stata offer extensive ROC analysis capabilities. These platforms support advanced analyses such as comparison of multiple ROC curves, partial AUC calculation, and sophisticated visualization options. The R language, in particular, has numerous packages dedicated to ROC analysis (e.g., pROC, ROCR) that provide extensive functionality for complex analytical needs.
Study Design and Reporting Guidelines: Proper implementation of ROC analysis requires adherence to methodological standards throughout the research process. The STARD (Standards for Reporting of Diagnostic Accuracy) statement provides a 25-item checklist and flow diagram to ensure comprehensive reporting of diagnostic accuracy studies [36]. Following these guidelines enhances study quality, reproducibility, and clinical applicability.
Regardless of the analytical tool selected, validation of findings in independent populations remains essential for establishing the generalizability of ROC analysis results [35]. This step is particularly crucial when determining optimal cut-off values for clinical application, as it mitigates the risk of overfitting to the derivation dataset.
In the field of rare genetic disorders, the definition of a diagnostic "gold standard" is undergoing a fundamental transformation. Genetic testing, powered by next-generation sequencing (NGS) and advanced bioinformatics, is progressively reshaping validation paradigms that have relied on traditional clinical and functional assessments. This shift is particularly evident in complex heterogeneous conditions like primary ciliary dyskinesia (PCD), where the limitations of existing diagnostic tools are becoming increasingly apparent. PCD, a rare inherited disease affecting motile cilia, involves mutations in more than 50 genes with diverse ultrastructural and functional consequences [7]. The growing integration of genetic validation is not merely supplementing but actively redefining diagnostic pathways, offering unprecedented precision while introducing new complexities.
The trajectory of this evolution reflects broader trends across medical genetics. Where diagnostic criteria once prioritized clinical features and specialized testing like transmission electron microscopy (TEM) and high-speed video microscopy analysis (HSVA), genetic testing now provides a fundamental validation layer. This transition is fueled by technological advancements that have made genetic analysis more comprehensive and accessible. In 2025, genetic testing has crossed the chasm into mainstream medical practice, growing in volume and application scope across predictive diagnostics, pharmacogenomics, and direct-to-consumer markets [40]. The integration of artificial intelligence and machine learning algorithms has further accelerated this shift, enabling researchers to identify novel disease-associated genes and improve variant classification at scale [41]. Within this context, the reevaluation of established diagnostic tools like PICADAR against genetically confirmed cases provides a crucial case study in how genetic validation is recalibrating diagnostic standards.
Comparative Analysis of PCD Diagnostic Methods
Performance Metrics of Current Diagnostic Tools
The diagnostic pathway for primary ciliary dyskinesia has traditionally employed a multifaceted approach incorporating clinical prediction tools, functional assessments, ultrastructural analysis, and genetic testing. Each method offers distinct advantages and limitations in sensitivity, specificity, and operational requirements, creating a complex diagnostic ecosystem where genetic confirmation increasingly serves as the definitive arbiter.
Table 1: Comparative Performance of Primary Diagnostic Methods for PCD
| Diagnostic Method | Principle | Reported Sensitivity | Reported Specificity | Key Limitations |
|---|---|---|---|---|
| PICADAR (Clinical Score) | 7-item clinical predictive tool | 75% (overall); 61% (situs solitus); 95% (laterality defects) [5] | ~48% (at ≥5 cutoff) [23] | Misses patients without daily wet cough; lower sensitivity in key subgroups |
| Nasal Nitric Oxide (nNO) | Measurement of nasal nitric oxide production | Limited; false negatives common (e.g., CCDC103, DNAH9, RSPH1 mutations) [23] | High when abnormal | Requires patient cooperation; unavailable in many centers |
| High-Speed Video Microscopy Analysis (HSVA) | Evaluation of ciliary beat pattern and frequency | High for specific ultrastructural defects | High when abnormal | Requires specialized expertise; limited availability |
| Transmission Electron Microscopy (TEM) | Ultrastructural assessment of ciliary components | 70-80% (misses normal ultrastructure cases) [7] [23] | High when abnormal | Resource-intensive; cannot detect all PCD genotypes |
| Genetic Testing | Identification of mutations in >50 PCD-associated genes | >90% for known genes [7] | High for pathogenic variants | Variants of uncertain significance; may miss novel genes |
The performance data reveal critical insights into the evolving diagnostic landscape. The PICADAR tool, while recommended by European Respiratory Society guidelines, demonstrates notably variable sensitivity depending on patient presentation. Recent research involving 269 genetically confirmed PCD patients found PICADAR missed 25% of cases overall, with significantly worse performance (39% missed) in patients with normal organ placement (situs solitus) [5]. This limitation stems from the tool's initial question about daily wet cough; individuals without this symptom are automatically ruled out, despite 7% of genetically confirmed PCD patients not reporting daily wet cough [5]. These findings underscore the risks of relying solely on clinical prediction tools, particularly for patients with atypical presentations or milder respiratory symptoms.
The complementary roles of functional, ultrastructural, and genetic testing create a diagnostic ecosystem where these modalities increasingly validate one another. HSVA maintains particular value for detecting PCD cases with normal ultrastructure (e.g., DNAH11 mutations) where TEM results appear normal [23]. Similarly, genetic testing provides definitive diagnosis in cases with ambiguous functional or ultrastructural findings, but has its own limitations regarding variants of uncertain significance [23]. The evolving standard thus emphasizes a integrated approach where genetic evidence serves as the definitive validation layer when available and conclusive.
Genetic Testing's Expanding Role in Diagnostic Confirmation
The growing primacy of genetic testing in PCD diagnosis reflects both technical advancements and the recognized limitations of traditional methods. The genetic heterogeneity of PCD continues to expand, with more than 40-50 identified causative genes and ongoing discovery of new disease-associated loci [7]. Different genetic profiles correlate with specific ultrastructural defects and clinical manifestations, creating complex genotype-phenotype relationships that influence diagnostic strategies.
Table 2: Major PCD Genetic Groups and Their Characteristics
| Genetic Category | Representative Genes | Ultrastructural Defect | Clinical Notes |
|---|---|---|---|
| Outer Dynein Arm Defects | DNAH5, DNAI1, DNAI2, DNAL1 | ODA defects | Milder disease course [7] |
| Outer + Inner Dynein Arm Defects | DNAAF1-3, LRRC50, DYX1C1 | ODA + IDA defects | Impaired dynein assembly |
| Inner Dynein Arm Defects | CCDC39, CCDC40 | IDA + microtubule disorganization | More severe disease; poorer lung function [7] |
| Central Apparatus Defects | RSPH9, RSPH4A, HYDIN | Central pair defects | No laterality defects risk [7] |
The comprehensive nature of modern genetic testing approaches enables detection across this diverse genetic spectrum. Next-generation sequencing technologies, particularly whole exome and genome sequencing, have demonstrated superior diagnostic utility compared to targeted gene panels for complex conditions [41]. Research showcasing these capabilities includes studies of over 62,000 individuals with autism, which have identified core gene sets and genetic correlations with related conditions [41]. The demonstrated accuracy of NGS-based copy number variant detection compared to chromosomal microarrays further reinforces its central diagnostic role [41].
The validation paradigm is further advanced through long-read sequencing technologies, which address limitations of short-read NGS in detecting structural variants and resolving complex genomic regions. Recent clinical validations demonstrate long-read sequencing's strong potential for improving diagnostics through accurate detection of repeat expansions and resolution of difficult-to-sequence regions [41]. As these technologies become more accessible, they promise to expand the spectrum of genetically resolvable cases, particularly for patients with strong clinical suspicion but inconclusive results from initial genetic testing.
Experimental Protocols and Methodologies
PICADAR Validation Study Design
Recent research evaluating PICADAR's performance exemplifies the critical role of genetic confirmation in validating diagnostic tools. This multi-center study employed a rigorous methodology to assess the clinical prediction rule against a genetically confirmed cohort [5].
Patient Cohort and Eligibility Criteria: The study enrolled 269 individuals with genetically confirmed PCD from specialized centers in Germany and Denmark. Inclusion required definitive genetic diagnosis through identification of biallelic pathogenic mutations in known PCD genes, establishing a confirmed reference standard against which PICADAR's performance was measured. This genetically validated cohort included patients with diverse genetic subtypes and clinical presentations, enabling subgroup analyses based on laterality defects and ultrastructural characteristics.
PICADAR Application Protocol: Researchers applied the PICADAR tool according to its standard seven-item scoring system, which assesses clinical features including neonatal respiratory symptoms, laterality defects, chronic respiratory symptoms, and otologic history. The protocol maintained strict adherence to the original PICADAR development criteria, with specific attention to the initial gatekeeping question regarding daily wet cough since infancy [5].
Statistical Analysis Plan: Sensitivity calculations focused on the proportion of genetically confirmed PCD patients scoring above the recommended PICADAR cutoff (≥5 points). Researchers performed stratified analyses to evaluate performance differences between key subgroups, particularly comparing patients with laterality defects (situs inversus or heterotaxy) against those with normal situs (situs solitus). Additional stratification examined performance variation between patients with hallmark ultrastructural defects versus those with normal ciliary ultrastructure [5].
This methodological approach, using genetic confirmation as the validation anchor, provides a robust framework for evaluating clinical prediction tools. The results demonstrated PICADAR's limited sensitivity, particularly in patients without laterality defects (61% sensitivity) and those without hallmark ultrastructural defects (59% sensitivity) [5]. These findings highlight the critical importance of genetic validation in revealing limitations not apparent during initial tool development.
Comprehensive Genetic Testing Workflow
The evolving genetic testing paradigm for disorders like PCD employs a sophisticated multi-layered approach that maximizes diagnostic yield while addressing the technical challenges of genomic analysis.
Sample Processing and Sequencing Phase:
- DNA Extraction: High-quality genomic DNA isolation from patient blood or saliva samples using standardized extraction kits.
- Library Preparation: Fragmentation and adapter ligation appropriate for the sequencing platform, with target enrichment if employing exome sequencing.
- Next-Generation Sequencing: High-throughput sequencing using platforms such as Illumina NovaSeq X or Oxford Nanopore technologies, with choice between whole genome, exome, or targeted approaches based on clinical indication [42].
- Quality Control: Assessment of read quality, coverage depth, and contamination metrics before proceeding to analysis.
Bioinformatic Analysis Pipeline:
- Alignment and Variant Calling: Mapping of sequence reads to reference genome (GRCh38) using optimized aligners, followed by variant identification across diverse variant types (SNVs, indels, CNVs).
- Variant Annotation and Filtering: Functional annotation of variants using population frequency databases (gnomAD), in silico prediction tools, and disease-specific databases (ClinVar).
- Variant Prioritization: Application of phenotype-aware algorithms and artificial intelligence tools to identify candidate pathogenic variants [41] [42].
- Copy Number Variant Analysis: Specialized detection of exon-level deletions/duplications from sequencing data, with demonstrated high concordance to chromosomal microarrays [41].
Validation and Interpretation Phase:
- Orthogonal Confirmation: Sanger sequencing or other methods for validating pathogenic variants in clinically reported genes.
- Segregation Analysis: Family studies when available to assess co-segregation of variants with phenotype.
- Genotype-Phenotype Correlation: Assessment of variant compatibility with clinical and ultrastructural findings [23].
- Reporting: Generation of clinical reports documenting pathogenic variants, with attention to variants of uncertain significance and their potential implications.
This comprehensive workflow demonstrates how modern genetic testing integrates multiple technological approaches to maximize diagnostic sensitivity while maintaining specificity. The incorporation of artificial intelligence and machine learning tools has further enhanced variant classification accuracy and accelerated novel gene discovery, with advanced techniques now identifying de novo variants with high accuracy in high-throughput diagnostic laboratories [41].
Figure 1: Comprehensive Genetic Testing Workflow for Diagnostic Validation. The integrated process spans sample processing, bioinformatic analysis, and clinical interpretation, enhanced by next-generation sequencing platforms, AI-powered classification tools, and comprehensive annotation databases.
Technological Innovations Driving Paradigm Shift
Next-Generation Sequencing and AI Integration
The transformation of genetic testing from a specialized tool to a central diagnostic validator has been catalyzed by revolutionary advances in sequencing technologies and computational analysis. Next-generation sequencing platforms have dramatically reduced the cost and time required for comprehensive genetic analysis while simultaneously improving accuracy and throughput. Illumina's NovaSeq X platform exemplifies this progress, enabling large-scale whole genome sequencing projects that were previously impractical in clinical settings [42]. The parallel emergence of long-read sequencing technologies from Oxford Nanopore and PacBio addresses historical limitations in detecting structural variants and resolving complex genomic regions, with recent clinical validations demonstrating strong potential for improved diagnosis in critically ill newborns [41].
The integration of artificial intelligence and machine learning has created a synergistic effect, amplifying the diagnostic power of genomic data. AI algorithms now systematically analyze massive genomic datasets, identifying patterns and associations that escape conventional detection methods. Tools like Google's DeepVariant employ deep learning to achieve superior variant calling accuracy compared to traditional methods [42]. At the clinical research level, advanced machine learning techniques are accelerating novel gene discovery and streamlining variant classification at scale. GeneDx's implementation of these approaches demonstrates how AI can extract meaningful diagnostic insights from the vast genomic datasets generated by NGS platforms [41]. This convergence of sequencing technologies and intelligent analysis represents a fundamental shift in diagnostic capabilities, enabling the genetic validation paradigm that is reshaping diagnostic standards for PCD and other genetic disorders.
Multi-Omics Integration and Functional Validation
The evolving validation paradigm extends beyond genomic sequencing alone to incorporate multi-omics integration, providing a more comprehensive understanding of genetic findings and their functional consequences. This approach combines genomics with transcriptomics, proteomics, metabolomics, and epigenomics to establish connections between genetic variants and their molecular phenotypes [42]. In the PCD diagnostic context, this might include transcriptome sequencing to validate the impact of splice-site variants or proteomic analysis to confirm absent ciliary proteins predicted by genetic results.
Functional genomics approaches further strengthen the validation framework by experimentally testing the pathogenicity of genetic variants. CRISPR-based technologies enable precise manipulation of candidate variants in cellular models, allowing researchers to assess their functional impact on ciliary structure and function [42]. High-throughput CRISPR screens can systematically identify genetic interactions and validate novel disease genes, providing mechanistic insights that support variant interpretation. These functional validation strategies are particularly valuable for assessing variants of uncertain significance, which represent a persistent challenge in clinical genetic testing [23].
The GeneDx Infinity platform exemplifies how large-scale genomic data is being leveraged to enhance diagnostic precision and drive discovery. By aggregating and analyzing extensive exome and genome sequencing datasets, this approach enables improved gene-disease curation, enhanced variant detection for complex conditions, and identification of novel disease-associated genes [41]. The demonstrated high concordance between NGS-based copy number variant detection and traditional chromosomal microarrays further reinforces the comprehensive nature of modern genetic analysis, reducing the need for multiple testing modalities [41].
Essential Research Reagent Solutions
The implementation of robust genetic validation protocols requires specialized research reagents and platforms that ensure analytical validity and reproducibility. The following solutions represent critical components for laboratories establishing genetic testing for diagnostic validation.
Table 3: Essential Research Reagents for Genetic Validation Studies
| Reagent Category | Specific Examples | Primary Function | Application Notes |
|---|---|---|---|
| NGS Library Prep Kits | Illumina DNA Prep | Fragmentation, adapter ligation, sample indexing | Critical for high-quality sequencing libraries; choice impacts coverage uniformity |
| Target Enrichment Systems | Illumina Exome Panel, IDT xGen | Target capture for exome/panel sequencing | Impact on coverage of disease-relevant genes; crucial for PCD gene panels |
| Sequencing Platforms | Illumina NovaSeq X, Oxford Nanopore | High-throughput DNA sequencing | Platform choice balances read length, accuracy, and throughput requirements |
| Variant Annotation Databases | gnomAD, ClinVar, VEP | Population frequency and pathogenicity annotation | Essential for variant filtering and interpretation |
| AI-Based Analysis Tools | DeepVariant, GEM AI | Variant calling and prioritization | Improve accuracy over traditional methods; enable phenotype-free analysis |
| CRISPR Screening Systems | Pooled lentiviral libraries | High-throughput functional validation | Identify critical genes; validate novel disease associations |
| Sanger Sequencing Reagents | BigDye Terminator | Orthogonal variant confirmation | Gold standard for clinical validation of reported variants |
| Bioinformatic Pipelines | GATK, Snakemake | Automated variant detection | Standardized analysis ensures reproducibility across studies |
These research reagents collectively enable the end-to-end genetic testing workflow, from sample preparation through final variant confirmation. The selection of appropriate reagents significantly impacts assay performance, particularly for challenging genomic regions relevant to PCD diagnosis. Genes such as DNAH11, HYDIN, and CCDC39 present specific technical challenges that may require optimized enrichment conditions or long-read sequencing approaches for comprehensive assessment [7]. The growing availability of long-read sequencing reagents from PacBio and Oxford Nanopore provides particularly valuable solutions for resolving complex structural variants and repetitive regions that challenge short-read technologies [41].
Quality control metrics throughout the testing process ensure reagent performance and analytical validity. The implementation of multiplexed sequencing approaches requires careful titration of indexing reagents to prevent sample cross-talk and ensure balanced representation. Similarly, enrichment-based methods require validation of off-target rates and coverage uniformity across PCD-associated genes. These quality assurance measures ensure that genetic testing provides the reliable results necessary for diagnostic validation, particularly when confirming or excluding PCD in patients with ambiguous functional or ultrastructural findings.
Implications for Research and Therapeutic Development
Redefining Diagnostic Pathways and Clinical Trials
The integration of comprehensive genetic testing into diagnostic paradigms is fundamentally reshaping patient stratification and therapeutic development. In PCD, the precise genetic characterization enabled by NGS and multi-omics approaches facilitates molecular subtyping that correlates with disease severity, progression patterns, and therapeutic responses. Patients with mutations in CCDC39 and CCDC40 genes, for instance, experience more severe disease courses and earlier development of bronchiectasis compared to those with outer dynein arm defects [7]. These stratification insights directly inform clinical trial design, enabling enrichment of patient populations most likely to demonstrate treatment benefits.
The evolving diagnostic standard is also accelerating therapeutic development through improved patient recruitment and biomarker validation. Genetic testing provides unambiguous inclusion criteria for trials of novel therapies, including gene-based treatments that target specific molecular defects. The ongoing research into gene and mRNA therapies for PCD leverages genetic diagnoses to identify patients most likely to benefit from mutation-specific interventions [7]. Similarly, the validation of liquid biopsy approaches for monitoring treatment response creates opportunities for less invasive assessment of therapeutic efficacy [43]. These advances collectively demonstrate how genetic validation is transforming not only diagnostic pathways but the entire therapeutic development continuum.
Future Directions and Emerging Applications
The trajectory of genetic testing suggests continued evolution of diagnostic validation paradigms through several emerging applications. Genomic newborn screening represents a particularly promising frontier, with projects like the GUARDIAN study demonstrating feasibility and diagnostic utility in large newborn cohorts [41]. The implementation of such screening could dramatically shorten the diagnostic odyssey for PCD patients, enabling early intervention before irreversible lung damage occurs.
The integration of real-world data (RWD) with genetic findings creates new opportunities for validating gene-disease relationships and understanding phenotypic spectra. As noted in recent industry analysis, "The future of clinical research lies in integrating real-world data (RWD) with clinical trial data to accelerate innovation" [44]. This approach enables continuous evidence generation across the patient lifecycle, potentially transforming clinical research from a separate process into an integrated component of patient care.
Emerging gene editing technologies further expand the diagnostic validation toolkit through functional assessment of genetic variants. Base editing and prime editing represent refined CRISPR tools that enable more precise genetic modifications, allowing researchers to model specific patient variants and assess their functional consequences [42]. These technologies not only facilitate variant interpretation but also create pathways for future therapeutic interventions that address the fundamental genetic defects in PCD and other rare diseases.
The continuing discovery of novel PCD-associated genes underscores the importance of maintaining flexible diagnostic approaches that incorporate emerging genetic evidence. Recent discoveries such as LRRC56 expand the genetic spectrum of PCD while highlighting the limitations of current genetic testing panels [7]. This dynamic landscape necessitates diagnostic protocols that can accommodate new genetic knowledge while maintaining rigorous standards for variant interpretation and clinical correlation. As genetic testing continues to evolve, its role as the definitive validator in diagnostic paradigms seems certain to expand, ultimately leading to more precise, personalized approaches to PCD diagnosis and management.
The Primary Ciliary Dyskinesia Rule (PICADAR), a clinical prediction tool for identifying patients who require definitive PCD testing, demonstrates significant limitations in recent validation studies. While its overall sensitivity was originally reported at 90%, newer research reveals this drops to approximately 75% in genetically confirmed PCD populations, with particularly poor performance (61% sensitivity) in patients without laterality defects. This analysis compares PICADAR's performance against current diagnostic standards and outlines the essential components for developing improved predictive tools through integrated genetic, clinical, and technological approaches.
Performance Benchmark: PICADAR's Established Metrics vs. Contemporary Validation
Table 1: Comparative Performance Metrics of PICADAR
| Evaluation Metric | Original Validation (2016) [15] | Recent Genetic Validation (2025) [5] [6] | Notable Performance Gaps |
|---|---|---|---|
| Overall Sensitivity | 90% | 75% | 15% decrease in real-world performance |
| Overall Specificity | 75% | Data not fully quantified | Specificity remains crucial for screening |
| AUC (Derivation) | 0.91 | Not reported | Original discrimination was excellent |
| AUC (Validation) | 0.87 | Not reported | Good external validation initially |
| Sensitivity in Situs Solitus | Not stratified | 61% | Major gap for patients with normal organ arrangement |
| Sensitivity with Hallmark Ultrastructural Defects | Not stratified | 83% | Better identification of classic phenotypes |
| Sensitivity without Hallmark Defects | Not stratified | 59% | Poor identification of non-classical presentations |
Experimental Protocols: Methodologies for Validation and Deficit Identification
Recent Sensitivity Analysis Protocol
Recent research evaluating PICADAR's limitations employed a rigorous methodological framework [5] [6]:
- Population: 269 individuals with genetically confirmed PCD, providing a definitive diagnostic standard
- PICADAR Application: Calculated scores based on seven predictive parameters:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care admission
- Chronic rhinitis
- Ear symptoms
- Situs inversus
- Congenital cardiac defect
- Scoring Threshold: Applied the recommended cut-off of ≥5 points for positive prediction
- Subgroup Analyses: Stratified by:
- Laterality defects (situs inversus/heterotaxy vs. situs solitus)
- Predicted hallmark ultrastructural ciliary defects
- Statistical Analysis: Calculated sensitivity across subgroups with comparative analysis (p<0.0001)
Original Development Methodology
The original PICADAR derivation followed this experimental design [15]:
- Derivation Cohort: 641 consecutive referrals to a PCD diagnostic center (2007-2013)
- External Validation: 187 patients from a second specialist center
- Predictor Selection: 27 potential variables narrowed to 7 significant predictors via logistic regression
- Diagnostic Standard: Composite outcome including hallmark transmission electron microscopy defects, characteristic ciliary beat pattern, and low nasal nitric oxide (nNO ≤30 nL·min⁻¹)
- Analysis: Receiver operating characteristic (ROC) curves to determine optimal cut-points
Pathway Analysis: Diagnostic Challenges and Future Solutions
The following diagram illustrates the identified limitations of the current predictive model and the integrated approach required for next-generation tools:
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 2: Essential Research Materials and Methodologies for PCD Predictive Tool Development
| Category | Specific Tool/Technique | Research Application | Key Considerations |
|---|---|---|---|
| Genetic Analysis | Next-generation sequencing panels [30] | Identifies mutations in >50 known PCD genes | Covers ~90% of known cases but limited by VUS interpretations |
| Ciliary Ultrastructure | Transmission electron microscopy (TEM) [7] | Identifies hallmark defects (ODA, IDA, MTD) | Missing 30% of PCD cases with normal ultrastructure |
| Functional Analysis | High-speed video microscopy analysis (HSVA) [7] | Evaluates ciliary beat pattern and frequency | Requires specialized expertise and equipment |
| Biomarker Measurement | Nasal nitric oxide (nNO) [7] [15] | Screening with nNO ≤30 nL·min⁻¹ | Technically demanding but efficient screening measure |
| Clinical Data Standardization | Structured patient history instruments [15] | Captures consistent phenotypic data | Essential for valid predictive model development |
| Computational Infrastructure | Machine learning algorithms [45] | Integrates multimodal data for prediction | Enables pattern recognition beyond linear models |
Future Directions: Integrating Multimodal Data Streams
The path toward next-generation predictive tools requires systematic integration of diverse data modalities while addressing PICADAR's documented limitations. Promising approaches include:
Genetic Integration: Incorporating known genotype-phenotype relationships, such as the association of CCDC39, CCDC40, and CCNO mutations with more severe disease, while recognizing that DNAH11 variants often present with milder phenotypes and preserved lung function [30]. This enables risk-stratified prediction models.
Advanced Imaging Analytics: Applying computational methods to high-speed video microscopy of ciliary function could extract subtle motion patterns indistinguishable to the human eye, creating quantitative biomarkers for specific genetic subtypes.
Multivariate Risk Modeling: Developing weighted algorithms that incorporate genetic risk scores, quantitative imaging features, and expanded clinical features beyond the current seven PICADAR parameters, potentially including respiratory support duration in neonates or specific infection patterns.
The future of PCD prediction lies in integrated diagnostic platforms that combine accessible clinical screening with rapidly advancing genetic and cellular diagnostics, ultimately enabling earlier identification and personalized management for all PCD patients regardless of their phenotypic presentation.
Conclusion
The PICADAR tool represents an important but imperfect step in streamlining PCD diagnosis. While it offers a simple, cost-effective screening method with good specificity, recent evidence underscores its major limitation: highly variable and often suboptimal sensitivity, particularly in patients without classic laterality defects or with normal ciliary ultrastructure. This performance gap can lead to missed diagnoses and delayed management. For biomedical researchers and clinicians, this analysis highlights that PICADAR should not be used in isolation. Its application must be contextual, understanding that a negative result does not rule out PCD in many cases. The future of PCD screening lies in developing more robust, genetically-informed tools or combinatorial approaches that maintain high specificity while achieving universally high sensitivity across all PCD genotypes and phenotypes, ultimately ensuring no patient is left undiagnosed.
References
- 1. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 2. Sensitivity, Specificity, and Predictive Values: Foundations, ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2017.00307/full]
- 3. Behavior of test specificity under an imperfect gold standard [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-025-02603-4]
- 4. PICADAR: a diagnostic predictive tool for primary ciliary ... [https://publications.ersnet.org/content/erj/47/4/1103]
- 5. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1]
- 6. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1691758/full]
- 7. Primary Ciliary Dyskinesia—Current Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525432/]
- 8. Analysis of the clinical features of Japanese patients with ... [https://www.sciencedirect.com/science/article/pii/S0385814621002248]
- 9. Clinical care for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC9489029/]
- 10. Challenges in Diagnosing Primary Ciliary Dyskinesia in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9324289/]
- 11. ERS Task Force guideline for the diagnosis of primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6054534/]
- 12. Accuracy of diagnostic testing in primary ciliary dyskinesia [https://publications.ersnet.org/content/erj/47/3/837]
- 13. Prevalence of primary ciliary dyskinesia in consecutive ... [https://www.nature.com/articles/pr2016263]
- 14. Diagnosing PCD [https://www.pcdfoundation.org/diagnosis/]
- 15. a diagnostic predictive tool for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819882/]
- 16. a diagnostic predictive tool for primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/26917608/]
- 17. Evaluation of a Clinical Index as a Predictive Tool for Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232329/]
- 18. Limitations of PICADAR as a diagnostic predictive tool for primary ... [https://labs.sciety.org/articles/by?article_doi=10.1101/2025.09.22.25336363]
- 19. Primary Ciliary Dyskinesia-Current Diagnostic and ... [https://pubmed.ncbi.nlm.nih.gov/41095888/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=pubmed-2&utm_content=1jg5TR3me1-BQfhrMRJvmReZR3Yaul4LWYrUgQB7CNp36u0YV8&fc=20230905104847&ff=20251110063826&v=2.18.0.post22+67771e2]
- 20. [PDF] PICADAR : a diagnostic predictive tool for... | Semantic Scholar [https://www.semanticscholar.org/paper/PICADAR%3A-a-diagnostic-predictive-tool-for-primary-Behan-Dimitrov/6a07baf86d1b4853db031cd999d7c7f804482cea]
- 21. in thesis and dissertation Questionnaire administration [https://www.projectguru.in/questionnaire-administration/]
- 22. Empowering limited-resource countries: collaborating with ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1547152/full]
- 23. The Controversies and Difficulties of Diagnosing Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6938149/]
- 24. Primary Ciliary Dyskinesia : Seminars in Respiratory & Critical ... [https://www.ovid.com/journals/srccm/fulltext/10.1055/s-0041-1730919~primary-ciliary-dyskinesia]
- 25. Effective patient selection for PCD diagnostics; the PICADAR ... [https://publications.ersnet.org/content/erj/48/suppl60/PA3124]
- 26. Accuracy of diagnostic testing in primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4771621/]
- 27. Diagnosis of primary ciliary dyskinesia: discrepancy according ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8558472/]
- 28. Primary Ciliary Dyskinesia - GeneReviews® - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK1122/]
- 29. 2025.09.22.25336363.source.xml [https://www.medrxiv.org/content/medrxiv/early/2025/09/23/2025.09.22.25336363.source.xml]
- 30. Primary Ciliary Dyskinesia: Integrating Genetics into ... [https://link.springer.com/article/10.1007/s13665-023-00332-x]
- 31. Evaluation of a Clinical Index as a Predictive Tool for ... [https://www.mdpi.com/2075-4418/11/6/1088]
- 32. Evaluation of a Clinical Index as a Predictive Tool for ... [https://pubmed.ncbi.nlm.nih.gov/34198708/]
- 33. A Comprehensive Approach for the Diagnosis of Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8466881/]
- 34. Receiver operating characteristic curve: overview and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8831439/]
- 35. ROC curve analysis: a useful statistic multi-tool in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11266376/]
- 36. sensitivity and specificity, ROC analysis, STARD statement [https://acutecaretesting.org/en/articles/diagnostic-accuracy--part-1brbasic-concepts-sensitivity-and-specificity-roc-analysis-stard-statement]
- 37. A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 38. What is a ROC Curve and How to Interpret It [https://www.displayr.com/what-is-a-roc-curve-how-to-interpret-it/]
- 39. Drawing Guidelines for Receiver Operating Characteristic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7308134/]
- 40. Genetic Testing Market Research Report 2025-2030 [https://www.globenewswire.com/news-release/2025/11/03/3179162/28124/en/Genetic-Testing-Market-Research-Report-2025-2030-Advances-in-Genomics-Aging-Populations-Pharmacogenomics-Oncology-Liquid-Biopsies-Fertility-Testing-and-Rising-DTC-Adoption-Driving-.html]
- 41. Release Details - Investor Relations - GeneDx, LLC [https://ir.genedx.com/news-releases/news-release-details/genedx-showcase-pioneering-research-findings-american-society]
- 42. 2025 and Beyond: The Future of Genomic Data Analysis ... [https://blog.crownbio.com/2025-and-beyond-the-future-of-genomic-data-analysis-and-innovations-in-genomics-services]
- 43. Genetic Testing in 2025: Trends, Insights & Future Forecasts [https://lifecode.life/genetic-testing-trends-2025/]
- 44. How genetic validation is transforming biotech industry in 2025 [https://www.drugdiscoverytrends.com/biotech-in-2025-precision-medicine-smarter-investments-and-more-emphasis-on-rwd-in-clinical-trials/]
- 45. A new framework to predict and visualize technology ... [https://www.sciencedirect.com/science/article/pii/S0040162524007583]