PICADAR in PCD Diagnosis: A Critical Appraisal for Researchers and Drug Developers
This article provides a comprehensive analysis of the PICADAR (PrImary CiliARy DyskinesiA Rule) tool within the modern Primary Ciliary Dyskinesia (PCD) diagnostic workflow.
PICADAR in PCD Diagnosis: A Critical Appraisal for Researchers and Drug Developers
Abstract
This article provides a comprehensive analysis of the PICADAR (PrImary CiliARy DyskinesiA Rule) tool within the modern Primary Ciliary Dyskinesia (PCD) diagnostic workflow. Aimed at researchers, scientists, and drug development professionals, it explores the tool's foundational principles, methodological application, and growing evidence of its limitations, particularly in genetically diverse populations without classic hallmark symptoms. We synthesize recent validation studies, compare PICADAR's performance against other diagnostic modalities, and discuss the critical implications for patient stratification in clinical trials and the development of next-generation diagnostic strategies.
Understanding PICADAR: Origins, Principles, and Its Role in PCD Diagnostic Pathways
The PrImary CiliAry DyskinesiA Rule (PICADAR) is a validated clinical prediction tool designed to identify patients requiring specialized testing for Primary Ciliary Dyskinesia (PCD) [1]. This tool addresses a critical diagnostic challenge in PCD management, as the condition presents with nonspecific symptoms that overlap with other respiratory diseases, while definitive diagnostic tests are highly specialized, expensive, and limited to specialized centers [2]. PICADAR enables clinicians in nonspecialist settings to systematically assess symptomatic patients using readily available clinical history, facilitating appropriate referral to specialist PCD diagnostic centers [1] [2].
Developed and validated through multicenter research, PICADAR represents a simple diagnostic clinical prediction rule with good accuracy and validity, ready for implementation in respiratory centers referring to PCD specialty clinics [1]. Its application within a comprehensive PCD diagnostic workflow helps optimize resource allocation while promoting early diagnosis, which is crucial for implementing appropriate management strategies that can improve long-term respiratory outcomes [2] [3].
The Seven Predictive Parameters of PICADAR
PICADAR incorporates seven clinical parameters derived from patient history that collectively predict the probability of PCD. The tool applies specifically to patients with persistent wet cough and evaluates factors primarily from the neonatal period and early childhood [1] [2]. Each parameter contributes to a total score that determines referral recommendation.
Table 1: The Seven Predictive Parameters of PICADAR
| Parameter | Description | Clinical Assessment |
|---|---|---|
| Full-term gestation | Birth at or beyond 37 weeks gestation | Documented gestational age at birth |
| Neonatal chest symptoms | Respiratory distress, tachypnea, or cough in the neonatal period | Medical record review or parental recall |
| Neonatal intensive care unit admission | Requirement for special care baby unit admission after birth | Medical record confirmation |
| Chronic rhinitis | Persistent nasal congestion/discharge lasting >3 months | Patient history and clinical evaluation |
| Ear symptoms | Chronic otitis media, hearing impairment, or tympanostomy tubes | Clinical history and otologic examination |
| Situs inversus | Complete reversal of thoracic and abdominal organs | Clinical examination, echocardiogram, or radiologic confirmation |
| Congenital cardiac defect | Structural heart abnormality present at birth | Echocardiogram and cardiology evaluation |
These parameters were identified through logistic regression analysis of consecutive patients referred for PCD testing, with each parameter demonstrating independent predictive value for PCD diagnosis [1]. The parameters reflect the multisystem nature of PCD, encompassing neonatal respiratory adaptation, chronic upper and lower respiratory manifestations, and laterality defects associated with embryonic nodal cilia dysfunction [2] [3].
Scoring System and Diagnostic Performance
The PICADAR scoring system assigns points to each parameter based on their regression coefficients, with the total score determining the probability of PCD and corresponding referral recommendation.
Table 2: PICADAR Scoring System and Interpretation
| Parameter | Score Value |
|---|---|
| Full-term gestation | 2 points |
| Neonatal chest symptoms | 2 points |
| Neonatal intensive care unit admission | 1 point |
| Chronic rhinitis | 1 point |
| Ear symptoms | 1 point |
| Situs inversus | 2 points |
| Congenital cardiac defect | 2 points |
| Total Possible Score | 11 points |
Table 3: Diagnostic Performance of PICADAR
| Metric | Derivation Cohort | Validation Cohort |
|---|---|---|
| Number of patients | 641 | 187 |
| PCD prevalence | 12% (75/641) | 50% (93/187) |
| Recommended cut-off | ≥5 points | ≥5 points |
| Sensitivity | 0.90 | Not specified |
| Specificity | 0.75 | Not specified |
| Area Under Curve (AUC) | 0.91 | 0.87 |
The original validation study demonstrated that at the recommended cut-off score of 5 points, PICADAR achieved a sensitivity of 0.90 and specificity of 0.75, with an area under the receiver operating characteristic curve of 0.91 upon internal validation and 0.87 upon external validation in a separate patient cohort [1]. This indicates good discriminatory power for identifying patients with a high probability of PCD who warrant specialized diagnostic testing.
Research Reagent Solutions for PCD Diagnostic Studies
Table 4: Essential Research Materials for PCD Diagnostic Investigations
| Reagent/Material | Application in PCD Research | Experimental Function |
|---|---|---|
| Transmission Electron Microscopy (TEM) | Ciliary ultrastructure analysis | Identifies hallmark defects in dynein arms (ODA/IDA), microtubule organization, and central apparatus [3] [4] |
| High-speed Video Microscopy Analysis (HSVA) | Ciliary beat pattern assessment | Detects abnormal ciliary motility patterns characteristic of PCD [3] |
| Nasal Nitric Oxide (nNO) measurement | Screening and diagnostic testing | Measures reduced nNO levels (<30 nL·min⁻¹) associated with PCD [2] [3] |
| Genetic testing panels | Molecular diagnosis | Identifies mutations in >50 known PCD-associated genes [3] [4] |
| Immunofluorescence staining | Protein localization in cilia | Detects absence or mislocalization of ciliary proteins resulting from genetic defects [3] |
| Cell culture materials | Ciliary function studies | Supports air-liquid interface culture for ciliary differentiation and repeated functional testing [2] |
Implementation Protocol for PICADAR in Research Settings
Patient Eligibility Assessment
- Inclusion Criteria: Patients with persistent wet cough (>3 months) presenting to respiratory or ENT services [1]
- Exclusion Criteria: Patients without chronic respiratory symptoms or with established alternative diagnoses explaining respiratory symptoms
Data Collection Methodology
- Gestational age verification through birth records or parental recall
- Neonatal history documentation including respiratory symptoms and NICU admission
- Chronic symptom assessment evaluating rhinitis and ear symptoms duration and characteristics
- Laterality evaluation via clinical examination and imaging records
- Cardiac defect screening through echocardiography reports or clinical history
Scoring and Interpretation Protocol
- Calculate total PICADAR score by summing points for each positive parameter
- Apply cut-off score of ≥5 points to identify high-probability PCD cases
- Refer patients meeting cut-off for specialized PCD testing
- Document sensitivity and specificity within specific research populations
Limitations and Contemporary Research Perspectives
Recent evidence has highlighted important limitations of PICADAR that researchers must consider when implementing this tool. A 2025 study by Schramm et al. demonstrated significantly variable sensitivity based on patient characteristics [5].
The overall sensitivity of PICADAR was 75% in a genetically confirmed PCD cohort, with notably lower sensitivity in specific subgroups [5]:
- 95% sensitivity in patients with laterality defects
- 61% sensitivity in patients with situs solitus (normal organ arrangement)
- 83% sensitivity in patients with hallmark ultrastructural defects
- 59% sensitivity in patients without hallmark ultrastructural defects
Critically, PICADAR automatically classifies patients without daily wet cough as negative for PCD, which excluded 7% of genetically confirmed PCD cases in recent studies [5]. This limitation underscores that PICADAR should not be used as the sole determinant for PCD diagnosis but rather as one component within a comprehensive diagnostic workflow that includes advanced testing modalities [5] [3].
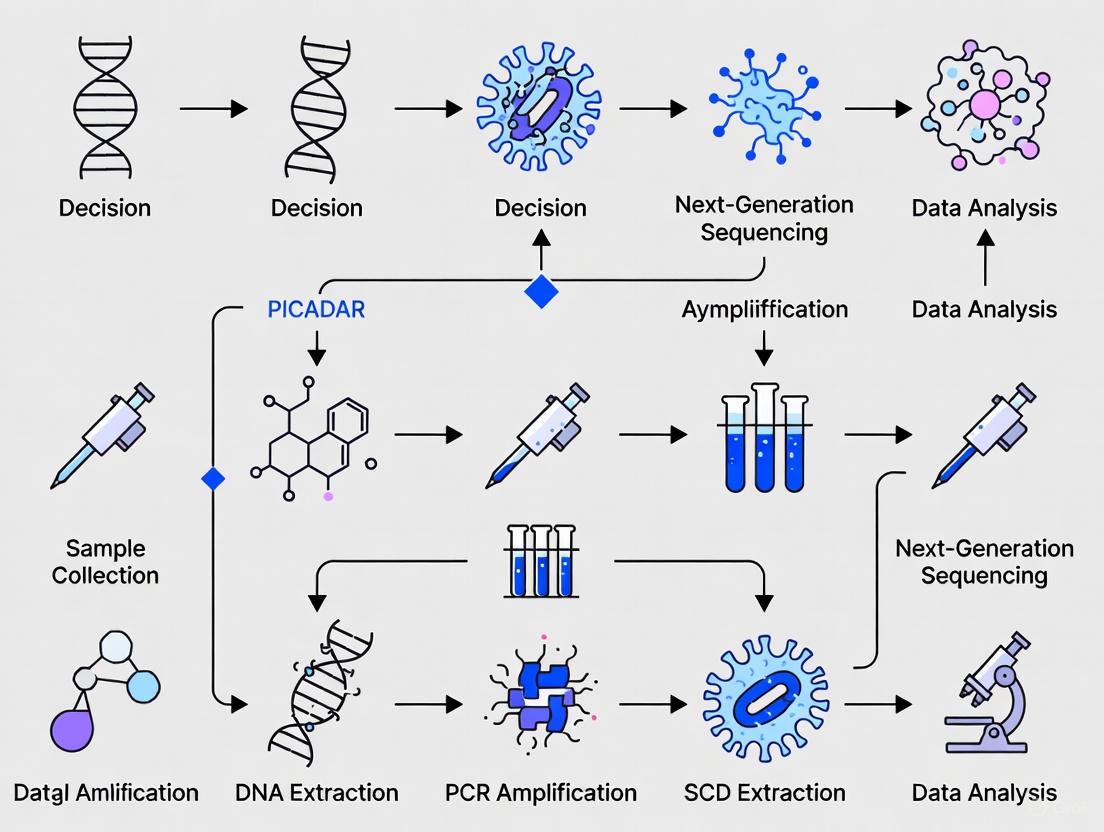
PICADAR Clinical Decision Pathway
Integration with Contemporary PCD Diagnostic Workflows
Modern PCD diagnosis requires a multimodal approach, with PICADAR serving as an initial screening tool rather than a definitive diagnostic test [3]. The European Respiratory Society guidelines recommend comprehensive testing including nasal nitric oxide measurement, high-speed video microscopy analysis, transmission electron microscopy, and genetic testing for definitive diagnosis [3] [4].
Research implementation of PICADAR should account for its variable performance across different patient populations and PCD genotypes. The tool demonstrates higher sensitivity in classic PCD presentations with laterality defects and hallmark ultrastructural abnormalities, but may miss cases with normal organ arrangement or preserved ciliary ultrastructure [5]. This underscores the importance of developing complementary prediction tools that address the limitations of PICADAR, particularly for patients with normal body symmetry and ultrastructure [5].
When incorporated as part of a systematic diagnostic protocol, PICADAR provides valuable clinical stratification that can optimize resource allocation in PCD diagnostic services while ensuring that patients with suggestive clinical features receive appropriate multidisciplinary care [3].
The Diagnostic Challenge of PCD and the Need for Screening Tools
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder of motile cilia function, with an estimated prevalence ranging from 1:7,500 to 1:20,000 live births [3] [6]. This autosomal recessive condition arises from mutations in more than 50 known genes encoding proteins essential for proper ciliary structure and function, leading to impaired mucociliary clearance and subsequent recurrent respiratory tract infections, chronic rhinosinusitis, otitis media, bronchiectasis, and laterality defects in approximately half of patients [3] [7]. The clinical presentation of PCD is notoriously nonspecific, overlapping significantly with other common respiratory conditions such as cystic fibrosis, primary immunodeficiencies, and recurrent viral illnesses, creating substantial diagnostic challenges [6].
The absence of a single gold-standard diagnostic test complicates PCD diagnosis, necessitating a multifaceted approach that may include nasal nitric oxide (nNO) measurement, high-speed video microscopy analysis (HSVA), transmission electron microscopy (TEM), genetic testing, and immunofluorescence staining [3] [8]. Each of these specialized tests has limitations in sensitivity, specificity, and accessibility, often requiring expensive equipment and experienced personnel not readily available outside specialized centers [2] [9]. This diagnostic complexity, combined with low disease awareness, frequently leads to substantial diagnostic delays, during which progressive lung damage may occur [3] [8]. Consequently, developing and implementing efficient screening tools to identify patients who require definitive diagnostic testing represents a critical priority in PCD research and clinical care [2] [9].
Current Diagnostic Landscape and the Role of Screening Tools
Established Diagnostic Methods for PCD
The diagnosis of PCD relies on a combination of specialized tests, each with distinct strengths and limitations. According to current guidelines, definitive diagnosis typically requires either identification of biallelic pathogenic mutations in a PCD-associated gene or demonstration of specific ciliary ultrastructural defects by electron microscopy [3] [8]. Nasal nitric oxide (nNO) measurement has emerged as a valuable screening test, with most PCD patients exhibiting significantly low nNO levels (<77 nL/min), though this method has reduced sensitivity in certain populations such as children under 5 years and patients with specific genetic mutations [6]. High-speed video microscopy analysis (HSVA) enables direct assessment of ciliary beat frequency and pattern, providing functional information but requiring considerable expertise for interpretation [3]. Transmission electron microscopy (TEM) remains a cornerstone of PCD diagnosis, allowing visualization of characteristic ultrastructural defects in the ciliary axoneme, including outer dynein arm (ODA) deficiencies, inner dynein arm (IDA) defects, and microtubular disorganization [3]. Immunofluorescence staining using antibodies against ciliary proteins offers a complementary approach, particularly valuable when genetic testing identifies variants of uncertain significance or when TEM appears normal despite strong clinical suspicion [3] [8].
Table 1: Established Diagnostic Methods for Primary Ciliary Dyskinesia
| Method | Principle | Key Strengths | Major Limitations |
|---|---|---|---|
| Nasal Nitric Oxide (nNO) | Measures levels of nasal nitric oxide, typically low in PCD | Non-invasive, excellent screening tool (high sensitivity) | Reduced sensitivity in young children, specific genetic subtypes; requires patient cooperation |
| Genetic Testing | Identifies mutations in >50 known PCD-associated genes | Definitive diagnosis, enables genetic counseling | 5-10% of cases have no identified mutation; variants of uncertain significance |
| Transmission Electron Microscopy (TEM) | Visualizes ciliary ultrastructural defects | Historical gold standard, identifies specific defect categories | 30% of PCD cases have normal ultrastructure; requires tissue processing expertise |
| High-Speed Video Microscopy Analysis (HSVA) | Analyzes ciliary beat pattern and frequency | Assesses functional impairment; can detect subtle defects | Requires significant expertise; secondary dyskinesia from infection can confound results |
| Immunofluorescence (IF) | Stains ciliary proteins with fluorescent antibodies | Can detect mislocalization of proteins | Limited availability; not standardized across centers |
Clinical Screening Tools and Their Performance
In response to the diagnostic challenges in PCD, several clinical screening tools have been developed to identify patients at high risk who should be referred for specialized testing. The most widely studied among these is PICADAR (PrImary CiliARy DyskinesiA Rule), a clinical prediction rule derived and validated in multiple populations [2]. PICADAR utilizes seven clinical parameters readily obtained from patient history to calculate a score predicting the probability of PCD. External validation studies have demonstrated good discriminative ability, with an area under the curve (AUC) of 0.87 in one validation cohort [2]. The North American Criteria Defined Clinical Features (NA-CDCF), endorsed by the American Thoracic Society, represent another screening approach consisting of four key clinical features shown in Table 2 [6]. These criteria were developed through retrospective analysis of patients referred to PCD centers and have been incorporated into clinical guidelines.
Recent research, however, has highlighted important limitations of these screening tools. A 2025 study by Omran et al. found that PICADAR has variable sensitivity depending on patient characteristics, with significantly lower sensitivity in patients without laterality defects (61%) and those without hallmark ultrastructural defects (59%) compared to those with these features (95% and 83%, respectively) [10]. This finding is clinically important as it suggests that reliance on PICADAR alone may miss a substantial proportion of PCD cases, particularly those with milder or atypical presentations. Additionally, the same study noted that approximately 7% of genetically confirmed PCD patients do not report the persistent daily wet cough that serves as an initial gatekeeping question in the PICADAR algorithm, automatically ruling them out despite having confirmed disease [10].
Table 2: Clinical Screening Tools for Primary Ciliary Dyskinesia
| Screening Tool | Components | Performance Characteristics | Target Population |
|---|---|---|---|
| PICADAR | Seven parameters: full-term gestation, neonatal chest symptoms, NICU admission, chronic rhinitis, ear symptoms, situs inversus, congenital cardiac defect | Sensitivity: 90%, Specificity: 75% at cutoff ≥5 points; AUC: 0.87 in validation cohort [2] | Patients with persistent wet cough; validated in specialist referral populations |
| North American CDCF | Four features: term neonate with unexplained respiratory distress, daily wet cough beginning ≤6 months, daily nasal congestion beginning ≤6 months, organ laterality defect [6] | Developed from retrospective analysis of PCD center referrals; incorporated into ATS guidelines | Children with chronic otitis media or rhinosinusitis with early onset |
| Combined Clinical Screening | PICADAR questions plus nNO measurement | In one study, identified patients for referral but did not yield new PCD diagnoses in small cohort [6] | Patients in tertiary otolaryngology clinics with chronic upper airway disease |
PICADAR: A Detailed Analysis of the Primary Ciliary Dyskinesia Rule
Development and Validation of PICADAR
The PICADAR tool was developed through a systematic process aimed at creating a practical clinical prediction rule to identify patients with a high probability of PCD who warrant specialized testing. The derivation study analyzed 641 consecutive patients referred for PCD testing at the University Hospital Southampton between 2007 and 2013, of whom 75 (12%) received a definitive PCD diagnosis [2]. Researchers collected data on 27 potential predictor variables and used logistic regression analysis to identify the seven most predictive clinical features readily available in non-specialist settings. The tool was subsequently validated in an external population of 187 patients from the Royal Brompton Hospital, demonstrating good discriminative ability with an area under the ROC curve of 0.87 in the validation cohort [2].
PICADAR is specifically designed for patients with persistent wet cough, which serves as an initial screening question. The tool assigns points based on the presence or absence of seven clinical features, with total scores ranging from 0 to 12 points. The recommended cutoff score of ≥5 points provides a sensitivity of 0.90 and specificity of 0.75 for PCD diagnosis in the derivation cohort [2]. The specific parameters and their assigned point values are detailed in Table 3, providing clinicians with a simple scoring system that can be quickly calculated during routine clinical encounters.
Table 3: PICADAR Scoring System and Point Allocation
| Clinical Parameter | Point Value |
|---|---|
| Full-term gestation (>37 weeks) | 2 |
| Neonatal chest symptoms (requiring medical intervention) | 2 |
| Admission to neonatal intensive care unit | 1 |
| Chronic rhinitis (persisting >3 months) | 1 |
| Persistent ear symptoms/serial otitis media | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 3 |
| Total Possible Score | 12 |
Limitations and Contextual Considerations for PICADAR
While PICADAR represents a valuable contribution to PCD screening, recent evidence has highlighted important limitations that clinicians and researchers must consider. A 2025 study by Omran et al. evaluating PICADAR in 269 genetically confirmed PCD patients found an overall sensitivity of 75%, substantially lower than the 90% reported in the original derivation study [10]. This discrepancy may reflect differences in study populations, with the validation study including a broader spectrum of PCD genotypes and phenotypes. The analysis revealed particularly concerning deficits in sensitivity among specific patient subgroups: only 61% for patients with situs solitus (normal organ arrangement) and 59% for those without hallmark ultrastructural defects on electron microscopy [10].
These findings suggest that PICADAR's performance is highly dependent on patient characteristics, with significantly better identification of PCD patients who present with classic features such as laterality defects or characteristic ultrastructural abnormalities. The tool's initial gatekeeping question regarding the presence of daily wet cough may also inadvertently exclude approximately 7% of genuine PCD cases who do not report this symptom [10]. This limitation is particularly relevant for adult patients or those with milder disease manifestations. Therefore, while PICADAR serves as a useful screening tool, it should not be used as the sole determinant for deciding whether to initiate a PCD diagnostic workup, particularly in patients with suggestive but atypical clinical presentations [10]. Clinical judgment remains essential, and the tool should be considered as an adjunct to rather than a replacement for comprehensive clinical assessment.
Experimental Protocols for PCD Diagnostic Evaluation
Protocol for PICADAR Implementation and Validation Studies
The implementation of PICADAR in clinical or research settings requires systematic approach to ensure consistent and accurate application. The following protocol outlines the standardized methodology for administering and validating the PICADAR tool:
Patient Population Definition:
- Include patients with persistent wet cough (>3 months duration) who are being evaluated for possible PCD
- Exclude patients with previously confirmed diagnoses of cystic fibrosis, primary immunodeficiency, or other known causes of chronic cough
Data Collection Procedure:
- Conduct structured clinical interviews using a standardized data collection form
- Verify neonatal history through review of medical records when available
- Document the presence or absence of each PICADAR parameter as defined in Table 3
- Specifically ascertain gestational age, as premature birth (<37 weeks) excludes points for full-term gestation and affects scoring for neonatal respiratory symptoms
Scoring and Interpretation:
- Calculate total PICADAR score by summing points for all positive parameters
- Apply the recommended cutoff score of ≥5 points to identify high-probability patients for referral to specialized PCD testing
- Document any missing data elements and consider their potential impact on score accuracy
Validation Methodology:
- Compare PICADAR scores against definitive diagnostic outcomes (genetic confirmation or definitive TEM findings)
- Calculate sensitivity, specificity, positive predictive value, and negative predictive value in the specific population being studied
- Perform subgroup analyses to assess performance across different patient demographics and clinical presentations
This protocol ensures consistent application of the PICADAR tool and facilitates comparison of results across different clinical settings and patient populations.
Protocol for Nasal Nitric Oxide Measurement in PCD Screening
Nasal nitric oxide (nNO) measurement serves as an important objective screening test for PCD, with most patients exhibiting characteristically low levels. The following protocol outlines the standardized procedure for nNO measurement based on American Thoracic Society operational guidelines:
Equipment Setup:
- Utilize a chemiluminescence nitric oxide analyzer (e.g., Eco Physics CLD 88 SP) with appropriate calibration
- Set sampling flow rate to 0.32 L/min with atmospheric NO measurements recorded before each test
- Ensure availability of appropriate nasal olive or nozzle for secure nasal connection
Patient Preparation:
- Exclude patients with acute respiratory infections within the preceding 4 weeks
- Instruct patients to avoid caffeine, food, and tobacco for at least one hour prior to testing
- Ask patients to gently clear nasal passages of obstructive mucus if possible
Testing Procedure:
- For cooperative children (typically >5 years) and adults: employ breath-holding technique with exhalation against resistance
- For younger or less cooperative children: utilize tidal breathing method without breath-holding
- Obtain measurements from both nares when possible, with at least two measurements per nostril
- Record the mean of plateau values as the final nNO value
Interpretation and Quality Control:
- Consider nNO values <77 nL/min as suggestive of PCD and warranting further investigation
- Repeat testing in 4-6 weeks for patients with initially low nNO to confirm persistence of low values
- Exclude technically inadequate measurements (e.g., unstable plateau, leak around nasal olive)
This standardized protocol ensures reliable nNO measurements that can be compared across different testing sessions and clinical centers.
Research Gaps and Future Directions in PCD Screening and Diagnosis
Despite advances in PCD diagnosis, significant research gaps remain that limit our ability to identify all affected individuals promptly and accurately. Current priorities for PCD research, as identified through a mixed-methods study involving specialists from 15 countries, include improving diagnostic approaches, understanding disease prevalence and natural history, characterizing phenotypic variability, developing better disease monitoring tools, establishing effective treatment strategies, and defining appropriate endpoints for clinical trials [9]. The limited awareness of PCD among healthcare professionals and difficulties securing research funding were consistently identified as major barriers to progress, with more than one-third of researchers reporting undertaking predominantly unfunded research [9].
The BEAT-PCD (Better Experimental Approaches to Treat Primary Ciliary Dyskinesia) Clinical Research Collaboration represents a major international effort to address these challenges through a structured framework of work packages focused on diagnostic improvement, clinical trial development, patient engagement, and data resource expansion [7]. This collaborative network aims to standardize diagnostic practices across centers, particularly for tests such as high-speed video microscopy and immunofluorescence where interpretation criteria remain variable [7]. Future directions in PCD screening may include the development of next-generation predictive tools that incorporate genetic risk scores, biomarker profiles, and quantitative ciliary function parameters to improve sensitivity across the diverse PCD phenotypic spectrum. Additionally, efforts to increase disease awareness among primary care physicians, pediatricians, and otolaryngologists through targeted educational initiatives may help reduce diagnostic delays and ensure appropriate referral of at-risk patients for specialized testing.
Table 4: Essential Research Reagents and Resources for PCD Diagnostic Studies
| Category | Specific Resource | Application in PCD Research |
|---|---|---|
| Genetic Analysis | Targeted next-generation sequencing panels for >50 PCD-associated genes (e.g., DNAH5, DNAH11, CCDC39, CCDC40) [3] | Comprehensive mutation screening; genotype-phenotype correlations |
| Cell Culture Models | Air-liquid interface (ALI) culture systems for respiratory epithelial cells | Differentiation of ciliated epithelium; functional assessment after culture |
| Antibodies for Immunofluorescence | Antibodies against dynein arm proteins (DNAH5, DNAI1), radial spoke proteins (RSPH1, RSPH4A), central apparatus proteins (HYDIN) [3] | Protein localization; assessment of ciliary assembly defects |
| Electron Microscopy Reagents | Glutaraldehyde, osmium tetroxide, uranyl acetate, lead citrate | Ultrastructural analysis of ciliary axoneme |
| nNO Measurement Equipment | Chemiluminescence nitric oxide analyzer (e.g., Eco Physics CLD 88 SP) with nasal interface | Objective screening measurement; diagnostic support |
| High-Speed Video Microscopy | High-speed camera (>500 frames/second) with phase-contrast microscope | Ciliary beat frequency and pattern analysis |
| Clinical Data Collection Tools | Standardized clinical history forms (e.g., FOLLOW-PCD), PICADAR calculator | Systematic phenotyping; clinical prediction rule application |
This toolkit represents essential resources for conducting comprehensive PCD diagnostic research, enabling investigators to implement the multi-test diagnostic approach necessary for accurate PCD diagnosis and characterization. The integration of these resources within collaborative research networks such as BEAT-PCD facilitates standardization and comparison of results across different research centers and clinical sites [7].
The diagnosis of Primary Ciliary Dyskinesia (PCD) is challenging due to the non-specific nature of its symptoms and the requirement for highly specialized, expensive diagnostic tests available only at specialized centers [2]. To guide non-specialists in identifying patients who require referral for definitive testing, Behan et al. (2016) developed and validated a diagnostic prediction tool named PICADAR (PrImary CiliARy DyskinesiA Rule) [2] [1]. This application note details the original validation of PICADAR, focusing on its sensitivity and specificity within the derivation cohorts, and provides a framework for its use in a PCD diagnostic workflow.
The primary objective of the original study was to create a practical clinical tool using easily obtainable patient history information to predict the probability of PCD before specialized testing [2]. The tool was designed to be used in patients with a persistent wet cough.
- Derivation Cohort: The model was developed using data from 641 consecutive patients referred to the University Hospital Southampton (UHS) PCD diagnostic center. Of these, 75 (12%) received a positive PCD diagnosis [2].
- Validation Cohort: The tool was externally validated using a sample of 187 patients from the Royal Brompton Hospital (RBH), selected to include similar numbers of positive and negative diagnoses [2].
The predictive performance of PICADAR in the original derivation and validation studies is summarized in the table below.
Table 1: Performance Metrics of PICADAR in Original Cohorts
| Cohort | Number of Subjects (PCD+/Total) | Area Under the Curve (AUC) | Sensitivity | Specificity | Recommended Cut-off Score |
|---|---|---|---|---|---|
| Derivation (UHS) | 75 / 641 | 0.91 | 0.90 | 0.75 | 5 points |
| External Validation (RBH) | 93 / 187 | 0.87 | Not explicitly stated | Not explicitly stated | 5 points |
The PICADAR score is calculated from seven clinical parameters, each assigned a specific point value. The total score determines the probability of a PCD diagnosis.
Table 2: The PICADAR Scoring System
| Predictive Parameter | Points Assigned |
|---|---|
| Situs Inversus | 2 |
| Congenital Cardiac Defect | 2 |
| Full-Term Gestation (≥37 weeks) | 1 |
| Neonatal Chest Symptoms (before 1 month of age) | 1 |
| Admission to Neonatal Intensive Care Unit (NICU) | 1 |
| Chronic Rhinitis (persisting for ≥3 months) | 1 |
| Ear Symptoms (chronic otitis media or >3 episodes of acute otitis media) | 1 |
Experimental Protocols from Original Validation
Patient Recruitment and Data Collection
- Study Population: The derivation group consisted of 641 consecutive patients with a definitive diagnostic outcome referred to the UHS diagnostic center between 2007 and 2013 [2].
- Data Collection: A proforma was used to collect patient data through a clinical interview conducted by a clinician prior to any diagnostic testing for PCD. This ensured the predictive tool was based solely on information available in a non-specialist setting [2].
- Variables: Data collected included patient demographics, neonatal history (gestational age, NICU admission, respiratory symptoms), and clinical features (laterality defects, congenital heart defects, chronic rhinitis, ear symptoms, chronic wet cough) [2].
Diagnostic Testing Protocol (Reference Standard)
The diagnosis of PCD was confirmed using a combination of specialized tests, as per UK guidelines at the time [2] [1]:
- A positive diagnosis was typically based on a characteristic clinical history plus at least two abnormal diagnostic tests.
- Key diagnostic tests included:
- "Hallmark" Transmission Electron Microscopy (TEM) defects.
- "Hallmark" Ciliary Beat Pattern (CBP) observed using high-speed video microscopy analysis (HSVMA).
- Low Nasal Nitric Oxide (nNO) measurement (≤30 nL·min⁻¹).
- In cases with a very strong clinical phenotype (e.g., sibling with PCD, classic triad of symptoms), a diagnosis could be made based on a single hallmark TEM or repeated HSVMA result [2].
Statistical Analysis and Model Development
- Variable Selection: Twenty-seven potential predictor variables were initially identified. Their individual significance for predicting a PCD diagnosis was assessed using chi-squared tests, Fisher's exact tests, t-tests, or Mann-Whitney tests as appropriate [2].
- Logistic Regression: Significant predictors from the univariate analysis were entered into a logistic regression model using forward step-wise methods to identify the most parsimonious set of predictive variables [2].
- Tool Creation: The regression coefficients from the final logistic model were rounded to the nearest integer to create a practical points-based scoring system (PICADAR) [2].
- Performance Evaluation: The model's discriminative ability was assessed using Receiver Operating Characteristic (ROC) curve analysis, and the Area Under the Curve (AUC) was calculated. Calibration was evaluated using the Hosmer-Lemeshow goodness-of-fit test [2].
- Validation: The performance of the PICADAR score was tested internally and externally on the RBH validation cohort using ROC curve analysis [2].
PICADAR Diagnostic Workflow
The following diagram illustrates the logical workflow for using PICADAR in a diagnostic pathway for PCD.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for PCD Diagnostic Research
| Item / Technique | Function in PCD Diagnosis / Research |
|---|---|
| High-Speed Video Microscopy (HSVMA) | To visualize and analyze ciliary beat pattern and frequency, identifying characteristic dyskinetic or immotile patterns [2] [11]. |
| Transmission Electron Microscopy (TEM) | To examine the ultrastructure of ciliary axonemes for hallmark defects (e.g., outer/inner dynein arm loss) [2] [11]. |
| Nasal Nitric Oxide (nNO) Measurement | To measure nNO levels, which are characteristically very low in most PCD patients, serving as a useful screening test [2] [11]. |
| Genetic Sequencing (Next-Generation Panels) | To identify disease-causing mutations in over 50 known PCD-related genes, providing genetic confirmation [11]. |
| Cell Culture (Air-Liquid Interface) | To differentiate primary from secondary ciliary dyskinesia by re-growing ciliated epithelium in a controlled environment, freeing cilia from inflammatory damage [2]. |
Critical Analysis and Subsequent Validation
While the original validation demonstrated good accuracy, subsequent independent studies have highlighted important limitations, particularly regarding the tool's sensitivity.
- Sensitivity in Specific Subgroups: A 2025 study by Omran et al. found the overall sensitivity of PICADAR (cut-off ≥5) in a genetically confirmed cohort was 75%, significantly lower than the original derivation [10]. The sensitivity was notably higher in individuals with laterality defects (95%) compared to those with normal situs (situs solitus, 61%) [10].
- Dependence on Ciliary Ultrastructure: The same study reported higher sensitivity in patients with hallmark ultrastructural defects (83%) versus those without (59%) [10].
- Exclusion of Patients: PICADAR cannot be applied to the estimated 7% of PCD patients who do not have a daily wet cough, as this is a prerequisite for using the tool [10].
- Comparison with Other Tools: A 2021 study found that while PICADAR performed well, an alternative Clinical Index (CI) demonstrated a larger AUC and may be a feasible predictive tool that outperforms PICADAR in some settings [11].
The original validation of PICADAR established it as a simple, non-invasive tool with good sensitivity (0.90) and specificity (0.75) in its derivation cohort for identifying patients with a persistent wet cough who require specialist referral for PCD testing [2]. Its strength lies in using readily available clinical data. However, researchers and clinicians must be aware of its limitations, particularly its reduced sensitivity in patients with situs solitus or without hallmark ultrastructural defects [10]. Therefore, PICADAR should be used as an initial risk-stratification tool within a broader diagnostic workflow and not as the sole criterion for deciding whether to initiate a PCD diagnostic work-up.
The diagnosis of Primary Ciliary Dyskinesia (PCD) presents significant challenges due to the heterogeneity of its clinical presentation and the limitations of any single diagnostic test. Symptoms of PCD are nonspecific, and guidance on whom to refer for specialized testing has historically been limited [2]. Diagnostic tests for PCD are highly specialised, requiring expensive equipment and experienced scientists, creating barriers to timely diagnosis [2]. This diagnostic complexity has necessitated the development of clinical prediction tools and standardized international guidelines to identify patients requiring comprehensive testing and to harmonize diagnostic approaches across centers.
The recent unification of European Respiratory Society (ERS) and American Thoracic Society (ATS) guidelines represents a significant advancement in the field, creating universal standards for PCD diagnosis [12] [13]. These guidelines formally recognize the importance of clinical prediction tools like PICADAR (PrImary CiliARy DyskinesiA Rule) for identifying high-risk patients who should be referred for specialized diagnostic testing [13]. This document examines the integration of PICADAR into international guidelines and provides detailed protocols for its implementation within the PCD diagnostic workflow.
ERS/ATS Unified Guideline Recommendations on Diagnostic Testing
The 2024 joint ERS and ATS guidelines represent a harmonized international approach to PCD diagnosis, replacing previous separate guidelines from each organization [13]. These evidence-based guidelines were developed using GRADE methodology and provide clear recommendations on diagnostic testing strategies.
Table 1: ERS/ATS 2024 Guideline Recommendations for PCD Diagnostic Tests
| Diagnostic Test | Recommendation Strength | Certainty of Evidence | Key Considerations |
|---|---|---|---|
| Nasal Nitric Oxide (nNO) with velum closure | Strong | Moderate | Not suitable as standalone test; requires specialized equipment |
| High-Speed Video Microscopy Analysis (HSVM) | Strong | Very Low | Only test that directly visualizes ciliary dyskinesia; should be performed in specialist centers |
| Immunofluorescence (IF) staining | Strong | High | Batch-to-batch variability requires experienced laboratories; useful for genetic variants of unknown significance |
| Transmission Electron Microscopy (TEM) | Reference standard | High | Combined with genetic testing as reference standard for diagnosis |
| Genetic Testing | Reference standard | High | Encouraged due to implications for management; identifies ~60-70% of cases |
The guidelines emphasize that no single test has 100% specificity and sensitivity, which necessitates the use of multiple tests in the diagnostic approach [13]. A key recommendation states that no single adjunct test is suitable as a standalone to diagnose PCD, and no single adjunct or reference test is suitable to exclude PCD [12]. The pretest probability based on symptoms should be considered when interpreting results, highlighting the importance of clinical prediction tools like PICADAR in the initial assessment of patients [12].
PICADAR: Validation and Performance Metrics
The PICADAR tool was developed specifically to address the challenge of identifying appropriate patients for referral to specialist PCD centers. It utilizes seven easily obtainable clinical parameters to calculate a probability score for PCD [2] [1].
Table 2: PICADAR Scoring System and Parameters
| Parameter | Score |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 2 |
| Total Possible Score | 11 |
PICADAR applies specifically to patients with persistent wet cough and has demonstrated robust performance characteristics in validation studies [2]. The tool showed sensitivity of 0.90 and specificity of 0.75 at a cut-off score of 5 points in the original derivation study [1]. The area under the curve (AUC) for the internally validated tool was 0.91, with external validation showing an AUC of 0.87 [2]. These performance metrics indicate good accuracy and validity for identifying patients who require specialist testing.
Recent comparative studies have evaluated PICADAR against other predictive tools. A 2021 study comparing PICADAR with a Clinical Index (CI) and North American criteria (NA-CDCF) found that all three tools showed significantly higher scores in PCD patients compared to non-PCD patients [14]. The study noted that PICADAR could not be assessed in 6.1% of patients without chronic wet cough, highlighting an important limitation in its application [14].
Detailed Protocol: Implementing PICADAR in Research Settings
Patient Eligibility and Data Collection
The PICADAR tool is designed for patients with persistent wet cough who are suspected of having PCD. Researchers should implement the following standardized protocol:
Inclusion Criteria: Patients with chronic wet cough (>3 months) requiring further investigation for potential PCD. Age should be documented, though PICADAR has been validated across age groups.
Data Collection Method: A structured clinical interview should be conducted prior to diagnostic testing. A standardized proforma is recommended to ensure consistent data collection across sites [2].
Parameter Definitions:
- Full-term gestation: Defined as ≥37 weeks gestational age [2]
- Neonatal chest symptoms: Unexplained respiratory distress in term neonates, including tachypnea, requiring supplemental oxygen, or radiographic changes [15] [16]
- Neonatal intensive care admission: Admission to NICU for respiratory support in a term neonate [2]
- Chronic rhinitis: Daily, year-round nasal congestion evident in the first years of life [16]
- Ear symptoms: Recurrent otitis media or persistent glue ear [2] [16]
- Situs inversus: Complete mirror-image arrangement of thoracic and abdominal organs [15]
- Congenital cardiac defect: Structural heart abnormalities, particularly associated with heterotaxy [2] [15]
Scoring and Interpretation Protocol
Score Calculation: Sum points for all present parameters (Table 2).
Interpretation Guidelines:
Integration with nNO: When available, nNO measurement can further improve predictive power. A study demonstrated that combining nNO with clinical prediction tools enhanced sensitivity and specificity [14].
Diagnostic Workflow Integration
The following workflow diagram illustrates the integration of PICADAR within the comprehensive PCD diagnostic pathway as recommended by international guidelines:
Cost-Effectiveness and Algorithm Performance
Economic considerations support the use of PICADAR as a gatekeeping tool for more expensive diagnostic testing. A 2019 cost-effectiveness analysis compared three diagnostic algorithms for PCD [17].
Table 3: Diagnostic Algorithm Performance and Cost-Effectiveness
| Diagnostic Algorithm | *PCD Patients Identified | Mean Annual Cost (€) | Cost-Effectiveness Notes |
|---|---|---|---|
| nNO + HSVM in sequence | 274/320 | €136,000 | Dominated nNO + TEM (less costly and more effective) |
| nNO + TEM in sequence | 198/320 | €150,000 | Less effective than sequential nNO + HSVM |
| nNO/HSVM in parallel + confirmatory TEM | 313/320 | €209,000 | ICE ratio: €2.1K per additional PCD patient identified |
| Expected PCD patients in initial population of 1000 referrals: 320 |
The analysis demonstrated that the diagnostic algorithm with parallel testing (nNO/HSVM+TEM) outperformed algorithms with tests in sequence, identifying more PCD patients at a reasonable incremental cost [17]. Using PICADAR to select high-probability patients for these comprehensive diagnostic pathways optimizes resource utilization in healthcare systems.
Research Reagent Solutions and Essential Materials
Table 4: Essential Research Materials for PCD Diagnostic Implementation
| Reagent/Equipment | Function/Application | Implementation Notes |
|---|---|---|
| Chemiluminescence NO Analyzer | Measurement of nasal nitric oxide (nNO) | Stationary analyzer for velum closure technique; cost approximately €40,000 [17] |
| High-Speed Video Microscope | Analysis of ciliary beat frequency and pattern | Requires camera capable of ≥500 frames/second; specialist operation needed [15] |
| Transmission Electron Microscope | Visualization of ciliary ultrastructure | Requires chemical fixation and specialized staining protocols [15] |
| Nasal Brushing Tools | Collection of respiratory epithelial cells | Sterile cytology brushes for inferior nasal turbinate sampling [17] |
| Immunofluorescence Antibodies | Detection of specific ciliary protein localization | Batch-to-batch variability requires quality control; useful for genetic variants of unknown significance [13] |
| Next-Generation Sequencing Platform | Genetic analysis of >40 known PCD genes | Identifies ~60-70% of PCD cases; whole-exome sequencing for unresolved cases [15] [18] |
| Cell Culture Materials | Air-liquid interface culture for ciliary function analysis | Used to differentiate primary from secondary ciliary dyskinesia [2] |
The integration of PICADAR into international guidelines represents a significant advancement in standardizing the approach to PCD diagnosis. The ERS/ATS guidelines provide a clear framework for utilizing this clinical prediction tool alongside specialized diagnostic tests to improve early detection of PCD. The implementation of PICADAR in referral pathways enhances the efficiency of specialist center utilization and promotes earlier diagnosis, which is crucial for implementing appropriate management strategies before irreversible lung damage occurs [17].
Future developments in PCD diagnosis will likely include the refinement of predictive tools through the incorporation of genetic and biomarker data, potentially enhancing their accuracy further. As genetic testing becomes more comprehensive and accessible, integration of genetic data with clinical prediction rules may facilitate even earlier diagnosis. The ongoing international collaboration through networks such as ERN-LUNG and the continued validation of diagnostic protocols across diverse populations will be essential to optimize PCD diagnosis and management globally [15].
Implementing PICADAR: A Step-by-Step Guide to Calculation and Clinical Application
Within the diagnostic pathway for Primary Ciliary Dyskinesia (PCD), the presence of a daily wet cough is the essential, non-negotiable clinical entry criterion. This persistent symptom, beginning in infancy or early childhood, reflects the core pathophysiology of PCD: impaired mucociliary clearance leading to chronic mucus retention and recurrent respiratory infections [1] [3]. For researchers and clinicians developing efficient diagnostic workflows, this single feature serves as the critical first filter, identifying the patient population in whom further investigation with tools like the PICADAR (PrImary CiliAry DyskinesiA Rule) score is justified. This application note details the role of this prerequisite and provides standardized protocols for the implementation and validation of the PICADAR tool within a research setting focused on PCD.
The PICADAR Prediction Tool
The PICADAR tool is a clinical prediction rule developed to identify patients with a high probability of having PCD after they have been preselected based on the key symptom of a persistent wet cough [1] [2]. It quantifies this probability by assigning points for seven readily ascertainable clinical features.
Scoring Parameters and Point Values
Table 1: The PICADAR Scoring Criteria [1] [2]
| Predictive Parameter | Score Value |
|---|---|
| Full-term gestation (≥37 weeks) | 2 points |
| Neonatal chest symptoms (e.g., cough, tachypnea) | 2 points |
| Admission to a neonatal intensive care unit (NICU) | 1 point |
| Chronic rhinitis (persisting >3 months) | 1 point |
| Chronic ear or hearing symptoms (persisting >3 months) | 1 point |
| Situs inversus (confirmed radiologically) | 2 points |
| Congenital cardiac defect | 2 points |
The total PICADAR score is the sum of the points for each applicable parameter. The tool's performance characteristics are summarized below.
Table 2: Performance Characteristics of the PICADAR Tool [1] [2] [19]
| Metric | Performance (Cut-off ≥5 points) | Notes |
|---|---|---|
| Sensitivity | 0.90 | Correctly identifies 90% of true PCD cases |
| Specificity | 0.75 | Correctly excludes 75% of non-PCD cases |
| Area Under the Curve (AUC) | 0.91 (Internal Validation) | Indicates excellent diagnostic accuracy |
| 0.87 (External Validation) | Confirms robust generalizability | |
| Modified PICADAR (Adult Study) | Score ≥2 points: Sensitivity 1.00, Specificity 0.89 | Adapted for adult bronchiectasis populations [19] |
Experimental Protocols
Protocol 1: Application of the PICADAR Score in a Research Cohort
This protocol standardizes the process of calculating the PICADAR score for subjects enrolled in a PCD diagnostic study.
- Subject Identification: Recruit patients with a definitive diagnostic outcome (PCD-positive or PCD-negative) based on reference standard tests (e.g., transmission electron microscopy, genetic testing, high-speed video microscopy) [2] [3].
- Data Collection: Collect clinical history data via a structured proforma prior to knowledge of the diagnostic outcome. The following data points must be ascertained:
- Gestational age at birth.
- Neonatal respiratory history, including specific chest symptoms and any admission to a NICU.
- Chronicity of upper airway symptoms, specifically rhinitis and ear/hearing problems, defined as persisting for more than three months.
- Laterality status (situs solitus, situs inversus, or heterotaxy) via radiological report.
- Presence of any congenital cardiac defect via medical record.
- Score Calculation: For each subject, apply the criteria in Table 1 to calculate a total PICADAR score.
- Data Analysis: Determine the sensitivity and specificity of various score cut-offs (e.g., ≥5 points) using the definitive diagnosis as the reference standard. Generate a Receiver Operating Characteristic (ROC) curve and calculate the Area Under the Curve (AUC) to assess overall discriminative ability [1] [2].
Protocol 2: Correlative Analysis with Nasal Nitric Oxide (nNO) Measurement
This protocol outlines a methodology for evaluating PICADAR in conjunction with nNO, a known screening biomarker for PCD.
- Subject Population: Enroll a cohort of patients with bronchiectasis or chronic wet cough of unknown etiology.
- Parallel Testing: Perform both PICADAR scoring (Protocol 1) and nNO measurement on all subjects during a clinically stable state, absent of acute pulmonary exacerbations [19].
- nNO Measurement: Measure nNO concentration using a chemiluminescence analyzer according to international standards (e.g., velum closure technique, constant flow rate). Record the value in nL/min [19] [3].
- Data Integration and Analysis:
- Compare mean nNO levels between PICADAR-high (e.g., ≥5) and PICADAR-low (<5) groups using appropriate statistical tests (e.g., t-test).
- Establish the optimal diagnostic nNO cut-off value for your cohort using ROC analysis (e.g., 77 nL/min as reported in prior studies) [19].
- Evaluate the sensitivity and specificity of a sequential screening algorithm where PICADAR is applied first, followed by nNO measurement in high-scoring individuals.
Diagnostic Workflow Visualization
The following diagram illustrates the logical workflow for integrating the daily wet cough prerequisite and the PICADAR tool into a comprehensive PCD diagnostic pathway for research.
PCD Diagnostic Research Workflow
Research Reagent Solutions
The following table details key materials and methodologies essential for research into PCD diagnostics, extending beyond the clinical PICADAR score.
Table 3: Essential Research Materials and Methods for PCD Investigation
| Item / Method | Function in PCD Research | Application Note |
|---|---|---|
| Nasal Nitric Oxide (nNO) Analyzer | Measures low nNO levels, a hallmark screening biomarker for PCD. | Chemiluminescence devices are standard. Requires strict protocol adherence during stable state [19] [3]. |
| High-Speed Video Microscopy (HSVA) | Analyzes ciliary beat pattern and frequency from nasal brush biopsies. | Identifies characteristic dysfunctional motility. Requires expert analysis to distinguish from secondary dyskinesia [2] [3]. |
| Transmission Electron Microscopy (TEM) | Visualizes ultrastructural defects in ciliary axonemes (e.g., absent dynein arms). | Considered a definitive test, but ~30% of PCD cases have normal ultrastructure [2] [18] [3]. |
| Next-Generation Sequencing (NGS) Panels | Identifies pathogenic variants in >50 known PCD-causing genes. | Crucial for genetic diagnosis and correlating genotype with phenotype. Detects mutations in cases with normal TEM [18] [3]. |
| Air-Liquid Interface (ALI) Cell Culture | Differentiates nasal or bronchial epithelial cells to regenerate ciliated epithelium in vitro. | Used to re-differentiate cilia after biopsy, allowing for repeated functional and structural testing without repeated patient sampling [2]. |
The integration of the daily wet cough as a mandatory prerequisite, followed by the systematic application of the PICADAR score, creates a robust and efficient first tier in the PCD diagnostic research pipeline. This structured approach optimally enriches study cohorts for patients with a high pre-test probability of PCD, thereby maximizing the yield and cost-effectiveness of subsequent, more complex and expensive confirmatory tests. Standardizing this protocol, as outlined in this document, ensures reproducibility and facilitates meaningful comparisons across research studies, ultimately accelerating progress in understanding and treating this rare genetic disease.
The PICADAR prediction tool is a clinically validated, quantitative instrument designed to identify patients with a high probability of Primary Ciliary Dyskinesia for onward referral to specialist diagnostic centers [1]. Early and accurate diagnosis of PCD is critical for implementing appropriate management strategies to preserve lung function, yet the nonspecific nature of its symptoms often leads to diagnostic delays [3] [8]. PICADAR addresses this challenge by providing physicians with a simple, evidence-based rule that utilizes seven readily obtainable clinical parameters from patient history [2]. This application note details the implementation, scoring, and integration of the PICADAR tool within a comprehensive PCD diagnostic workflow for research and clinical professionals.
The PICADAR Scoring System: Criteria and Point Values
The PICADAR tool is applied to patients presenting with a persistent wet cough. It assesses seven clinical parameters, each assigned a specific point value based on multivariate logistic regression analysis [2]. The total score determines the probability of PCD and the need for specialist testing.
Table 1: The Seven Clinical Criteria of the PICADAR Tool
| Clinical Criterion | Description | Point Value |
|---|---|---|
| Full-Term Gestation | Gestational age ≥37 weeks at birth [2]. | 2 |
| Neonatal Chest Symptoms | Respiratory distress or other chest symptoms present at birth [1] [2]. | 2 |
| Neonatal Intensive Care Admission | Requirement for admission to a special care baby unit after birth [1] [2]. | 1 |
| Chronic Rhinitis | Persistent, daily nasal congestion lasting >3 months, beginning in infancy [1] [8]. | 1 |
| Ear Symptoms | History of recurrent otitis media or persistent glue ear [1] [8]. | 1 |
| Situs Inversus | Complete mirror-image transposition of the thoracic and abdominal organs [20] [1]. | 4 |
| Congenital Cardiac Defect | Presence of any congenital heart abnormality [1] [2]. | 2 |
Interpretation of Scores and Diagnostic Performance
The points for all applicable criteria are summed to generate a total PICADAR score. The tool's performance characteristics, validated in a derivation group of 641 patients, are as follows [2]:
Table 2: PICADAR Performance Metrics
| Metric | Score ≥5 Points | Area Under the Curve (AUC) |
|---|---|---|
| Sensitivity | 0.90 (90%) | 0.91 (Internal Validation) |
| Specificity | 0.75 (75%) | 0.87 (External Validation) |
A cut-off score of 5 points or higher is recommended to refer a patient for definitive PCD testing, providing an optimal balance between sensitivity and specificity [2]. It is crucial to note that the tool's sensitivity is significantly higher in patients with laterality defects (95%) compared to those with normal organ arrangement (situs solitus, 61%) [10].
Experimental Protocol for PICADAR Assessment
Materials and Equipment
- Patient medical history records.
- Structured data collection form (electronic or paper).
- Clinical interview space.
Step-by-Step Procedural Guide
- Patient Identification: Apply the tool only to patients with a history of a persistent, daily wet cough [1].
- Data Collection: Conduct a structured clinical interview or review the patient's medical records to ascertain the presence or absence of each of the seven PICADAR criteria.
- Scoring: Assign points for each positive criterion as detailed in Table 1.
- Calculation and Action:
- Calculate the total score.
- If the score is ≥5, the patient has a high probability of PCD and should be referred to a specialist PCD center for confirmatory testing [2].
- If the score is <5, PCD is less likely, but clinical judgment should prevail, especially in cases with strong suggestive features but no laterality defect [10].
Integration into the PCD Diagnostic Workflow
The PICADAR tool serves as a critical initial gatekeeper in a multi-step PCD diagnostic pathway. The following diagram illustrates its role in the broader clinical and research workflow, from symptom presentation to confirmed diagnosis.
Research Reagent Solutions for PCD Diagnostics
Following a positive PICADAR screen, specialist centers employ a range of advanced techniques for confirmatory diagnosis. The table below outlines key reagents and materials used in these foundational diagnostic methods.
Table 3: Essential Research Reagents for PCD Confirmatory Testing
| Reagent / Material | Primary Function in PCD Diagnostics | Associated Technique |
|---|---|---|
| Antibodies for Ciliary Proteins | Immunofluorescence staining to visualize and localize specific ciliary proteins (e.g., DNAH5, GAS8) [3]. | Immunofluorescence Microscopy (IF) |
| Electron Microscopy Reagents | Processing nasal or bronchial biopsies to analyze the ultrastructural anatomy of cilia (e.g., ODA, IDA, CP defects) [3] [8]. | Transmission Electron Microscopy (TEM) |
| Genetic Panels | Targeted sequencing of >50 known PCD-causing genes (e.g., DNAH5, DNAI1, CCDC39, CCDC40) to identify biallelic pathogenic mutations [3] [8]. | Genetic Testing |
| Cell Culture Media | Air-liquid interface (ALI) culture of ciliated epithelial cells to differentiate primary from secondary ciliary dyskinesia [2]. | Cell Culture & High-Speed Videomicroscopy (HSVA) |
The PICADAR tool provides a standardized, evidence-based method for risk-stratifying patients for PCD. Its strength lies in using simple clinical data, making it accessible for use in non-specialist settings to streamline referral pathways [1] [2]. For the research scientist, PICADAR offers a validated phenotype stratification tool for cohort studies and clinical trials.
A critical consideration is the tool's limited sensitivity in specific subpopulations, particularly individuals with situs solitus (normal organ arrangement) or those with PCD caused by genetic mutations that do not produce hallmark ultrastructural defects on TEM [10]. Therefore, PICADAR should be a guide, not a replacement, for clinical judgment. A negative score in a patient with a strong clinical phenotype should not preclude further investigation.
In conclusion, integrating the PICADAR tool at the front lines of clinical suspicion for PCD, followed by a multi-modal diagnostic protocol at specialist centers, represents the current optimal pathway for achieving a timely and accurate diagnosis, thereby enabling early intervention and improved long-term patient outcomes.
The Primary Ciliary CiliAry DyskinesiA Rule (PICADAR) is a clinical prediction tool designed to identify patients requiring specialized testing for Primary Ciliary Dyskinesia (PCD) [2]. This diagnostic predictive tool was developed to address the challenge posed by the nonspecific nature of PCD symptoms and the highly specialized, expensive nature of definitive diagnostic tests [2] [21]. PICADAR enables healthcare providers and researchers to quantify the pre-test probability of PCD using clinical history alone, providing a evidence-based approach for patient referral to specialized centers [2] [21].
The tool applies specifically to patients presenting with persistent wet cough and incorporates seven readily obtainable clinical parameters from patient history [2]. The derivation and validation of the PICADAR score represented a significant advancement in standardizing the referral pathway for PCD diagnosis, offering a practical solution for clinical and research settings where access to specialized equipment like nasal nitric oxide (nNO) measurement or transmission electron microscopy (TEM) may be limited [2] [21].
Establishing the Diagnostic Cut-off Point (≥5)
Original Derivation and Validation
The diagnostic cut-off point of ≥5 points for PICADAR was established through rigorous statistical analysis during its original development and validation study. The researchers utilized logistic regression analysis on a derivation cohort of 641 consecutively referred patients to identify significant predictors and develop a simplified practical prediction tool [2].
Table 1: PICADAR Scoring System and Point Allocation
| Predictive Parameter | Points Assigned |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 2 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 4 |
| Maximum Possible Score | 13 |
The performance of the PICADAR score at the ≥5 cut-off was tested using receiver operating characteristic (ROC) curve analyses. In the derivation group, the tool demonstrated a sensitivity of 0.90 and specificity of 0.75, with an area under the curve (AUC) of 0.91 [2]. The tool was subsequently externally validated in a second diagnostic center, where it maintained good discriminative ability with an AUC of 0.87 [2]. This robust validation process confirmed that a score of ≥5 points provided the optimal balance between identifying true positive cases while minimizing false negatives, a critical consideration for a rare disease where missed diagnosis can have significant clinical consequences.
Performance Characteristics and Recent Evidence
While the original validation demonstrated strong performance characteristics, recent studies have provided additional insights into the real-world performance of the PICADAR score, particularly regarding its sensitivity across different PCD subpopulations.
Table 2: Performance Characteristics of PICADAR at ≥5 Cut-off
| Study Population | Sensitivity | Specificity | Area Under Curve (AUC) | Sample Size |
|---|---|---|---|---|
| Original Derivation Cohort | 90% | 75% | 0.91 | 641 (75 PCD-positive) |
| External Validation Cohort | Not specified | Not specified | 0.87 | 187 (93 PCD-positive) |
| Genetically Confirmed PCD (2025) | 75% | Not specified | Not specified | 269 PCD-positive |
A 2025 study assessing PICADAR's performance in 269 individuals with genetically confirmed PCD revealed an overall sensitivity of 75% at the ≥5 cut-off point, lower than the original derivation cohort [5] [10]. This study further identified significant variations in sensitivity based on clinical presentation: sensitivity was substantially higher in individuals with laterality defects (95%) compared to those with situs solitus (normal organ arrangement, 61%) [5] [10]. Similarly, sensitivity differed based on ultrastructural defects, with higher sensitivity in individuals with hallmark defects (83%) versus those without (59%) [5] [10].
Critically, this recent research highlighted that 7% (18/269) of genetically confirmed PCD patients reported no daily wet cough and would have been ruled out according to PICADAR's initial screening question [5] [10]. These findings underscore the importance of recognizing the limitations of the ≥5 cut-off point, particularly for patients with normal body composition or normal ciliary ultrastructure who may present with atypical symptoms.
Experimental Protocol for PICADAR Application
Patient Eligibility and Data Collection
The PICADAR score should be applied to patients with persistent wet cough lasting more than 3 months [2]. Data collection should occur through structured clinical interview prior to any specialized PCD diagnostic testing. The following protocol ensures standardized application:
Initial Screening: Confirm the presence of persistent wet cough. If absent, note that PICADAR does not apply, though PCD may still be possible in rare cases [5] [10].
Clinical History Assessment: Systematically assess for the seven predictive parameters through directed questioning and review of medical records:
- Full-term gestation: Defined as ≥37 weeks gestation
- Neonatal chest symptoms: Respiratory distress, tachypnea, or requirement for oxygen supplementation in the neonatal period (first 28 days of life)
- Neonatal intensive care admission: Any admission to neonatal intensive care unit specifically for respiratory concerns
- Chronic rhinitis: Nasal congestion or rhinorrhea persisting for >3 months
- Ear symptoms: Chronic otitis media with effusion ('glue ear') or recurrent acute otitis media
- Situs inversus: Radiologically confirmed complete mirror-image arrangement of thoracic and abdominal organs
- Congenital cardiac defect: Any structural heart defect confirmed by echocardiography
Scoring Application: Assign points for each positive parameter according to Table 1 and calculate the total PICADAR score.
Interpretation and Referral Decision
The following diagnostic workflow should be applied for score interpretation and subsequent management decisions:
Research Reagent Solutions for PCD Diagnostic Workflow
The following table details essential materials and methodologies used in the comprehensive PCD diagnostic workflow following PICADAR screening.
Table 3: Research Reagent Solutions for PCD Diagnostic Confirmation
| Reagent/Equipment | Function in PCD Diagnosis | Protocol Specifications |
|---|---|---|
| Stationary Chemiluminescence NO Analyzer | Measures nasal nitric oxide (nNO) levels for screening | Velum closure technique required; cut-off value ≤30 nL·min⁻¹ highly suggestive of PCD [21] |
| High-Speed Video Microscopy System | Records ciliary beat frequency and pattern from nasal brushings | Sample collected after 4-6 weeks infection-free; requires air-liquid interface culture for accuracy [21] |
| Transmission Electron Microscope | Identifies hallmark ciliary ultrastructural defects | Technically demanding; requires experienced personnel for interpretation [21] |
| Genetic Testing Panel | Confirms PCD-causing mutations in >30 known genes | Not recommended as initial test; used for confirmation or inconclusive cases [21] |
Critical Analysis of the ≥5 Cut-off Point in Research Context
The established PICADAR cut-off point of ≥5 represents a calculated balance between sensitivity and specificity, but requires nuanced interpretation in both clinical and research settings. The original validation demonstrated that this threshold successfully identified 90% of true PCD cases while correctly excluding 75% of non-PCD patients [2]. However, emerging evidence suggests that this performance is not uniform across all PCD subtypes.
Researchers should particularly note the reduced sensitivity (61%) in patients with situs solitus and the complete exclusion of PCD patients without daily wet cough (representing 7% of genetically confirmed cases) [5] [10]. These limitations highlight critical gaps in our current phenotypic understanding of PCD and suggest that the pathobiological mechanisms underlying laterality defects and cough presentation may involve distinct genetic and functional pathways.
For drug development professionals and clinical trial designers, these limitations have practical implications. Using PICADAR as a sole enrichment strategy for patient recruitment may systematically exclude important PCD subpopulations, particularly those with normal body composition or specific genetic variants associated with normal ultrastructure. Future research should focus on developing complementary tools that enhance sensitivity for these currently under-recognized patient groups, potentially incorporating genetic markers or novel functional assessments to create a more comprehensive diagnostic approach.
Application Note: PICADAR in PCD Diagnostic Workflow Research
Background and Rationale
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary function, leading to chronic oto-sino-pulmonary disease [2]. Diagnostic testing for PCD is complex, requiring specialized equipment and expertise available only at specialist centers [2]. The PICADAR (PrImary CiliARy DyskinesiA Rule) tool was developed to provide a evidence-based method for identifying patients who should be referred for definitive PCD testing [2] [1]. This application note details the integration of PICADAR into patient referral pathways, framed within broader research on optimizing PCD diagnostic workflows.
Recent evidence has highlighted important limitations in PICADAR's sensitivity, particularly in specific patient subgroups [5]. This necessitates a refined application protocol that accounts for these limitations while maintaining the tool's utility in triaging patients. The workflow described herein aims to standardize referral processes while identifying areas for further predictive tool development.
Performance Characteristics and Limitations
Table 1: PICADAR Performance Characteristics from Validation Studies
| Study Parameter | Original Validation (Behan et al. 2016) | Recent Assessment (Schramm et al. 2025) |
|---|---|---|
| Study Population | 641 referrals, 75 PCD-positive [2] | 269 genetically confirmed PCD individuals [5] |
| Overall Sensitivity | 0.90 (at cut-off ≥5 points) [2] | 0.75 [5] |
| Specificity | 0.75 (at cut-off ≥5 points) [2] | Not reported |
| Area Under Curve (AUC) | 0.91 (internal), 0.87 (external) [2] | Not reported |
| Key Limitation | Not fully assessed in genetically confirmed cohort [2] | 7% of PCD patients excluded for no daily wet cough; lower sensitivity in situs solitus (61%) and non-hallmark ultrastructure (59%) [5] |
Experimental Protocols
Protocol 1: PICADAR Data Collection and Scoring
Purpose: To standardize the collection of clinical history and calculation of PICADAR score for PCD risk assessment.
Patient Population: Patients with persistent wet cough from birth or early infancy, for whom PCD is a clinical consideration [2].
Materials Required:
- Clinical history questionnaire
- PICADAR scoring sheet
Methodology:
- Confirm Persistent Wet Cough: Establish the presence of a persistent wet cough since birth or early infancy. Patients without this symptom are not eligible for PICADAR assessment and should be referred based on strong clinical suspicion alone, given recent data [5].
- Collect Clinical History: Interview the patient and/or caregiver to ascertain the seven predictive parameters [2]:
- Full-term gestation (≥37 weeks)
- Neonatal chest symptoms (within first 4 weeks of life)
- Admission to neonatal intensive care unit (within first 4 weeks)
- Chronic rhinitis (>3 months duration)
- Chronic ear or hearing symptoms (>3 months)
- Situs inversus (radiologically confirmed)
- Congenital cardiac defect (echocardiographically confirmed)
- Score Calculation: Assign points for each positive parameter as shown in Table 2.
- Interpretation: Sum the points to obtain the total PICADAR score.
Table 2: PICADAR Scoring Criteria [2]
| Predictive Parameter | Points |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care admission | 2 |
| Chronic rhinitis | 1 |
| Chronic ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 4 |
Protocol 2: Diagnostic Pathway Integration and Validation
Purpose: To implement and validate PICADAR within a referral network to specialist PCD centers.
Materials Required:
- Access to electronic health records
- Standardized referral forms
- Diagnostic testing capabilities (nNO, HSVM, TEM, genetic testing)
Methodology:
- Pathway Implementation:
- Train referring clinicians in PICADAR application
- Establish a standardized referral process from secondary to tertiary care
- Implement electronic referral forms with embedded PICADAR calculator
- Referral Triage:
- Score ≥5: High probability; expedited referral for diagnostic testing
- Score <5 but strong clinical suspicion: Standard referral, considering recent sensitivity data [5]
- No daily wet cough but strong clinical features (e.g., neonatal distress, laterality defect): Direct referral, bypassing PICADAR [5]
- Diagnostic Confirmation:
- Conduct comprehensive testing at specialist center per ERS guidelines [2]
- Compare PICADAR scores with definitive diagnostic outcomes
- Quality Assurance:
- Monitor sensitivity and specificity within local population
- Stratify performance by patient subgroups (laterality status, ultrastructural defect)
- Refine local referral thresholds based on audit data
Workflow Visualization
PCD Diagnostic Referral Pathway
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for PCD Diagnostic Workflow Research
| Research Tool | Function/Application in PCD Research |
|---|---|
| Clinical History Proforma | Standardized questionnaire for collecting PICADAR parameters; ensures consistent data acquisition across study sites [2]. |
| High-Speed Video Microscopy (HSVM) | Captures ciliary beat pattern and frequency; key diagnostic tool for functional ciliary assessment [2]. |
| Transmission Electron Microscopy (TEM) | Visualizes ciliary ultrastructure; identifies hallmark defects (e.g., outer dynein arm缺失) [2]. |
| Nasal Nitric Oxide (nNO) Measurement | Non-invasive screening tool; low nNO (<30 nL/min) supports PCD diagnosis [2]. |
| Genetic Testing Panels | Identifies pathogenic variants in >45 known PCD genes; provides definitive diagnosis, especially in cases with normal ultrastructure [5]. |
| Air-Liquid Interface (ALI) Cell Culture | Differentiates primary ciliated cells; used to eliminate secondary ciliary dyskinesia and re-test inconclusive cases [2]. |
| Immunofluorescence Microscopy | Detects specific protein localization defects in ciliary structure; complementary to TEM analysis [2]. |
Navigating PICADAR's Limitations: Identifying At-Risk Populations and Diagnostic Gaps
This application note details a critical performance limitation of the Primary Ciliary Dyskinesia Rule (PICADAR), a diagnostic predictive tool for Primary Ciliary Dyskinesia (PCD). Recent validation studies reveal that PICADAR's sensitivity is substantially lower in patients with situs solitus (normal organ arrangement) compared to those with situs inversus (mirror-image organ arrangement). For researchers and clinicians utilizing this tool in PCD diagnostic workflows, awareness of this disparity is paramount to avoid false-negative results and ensure at-risk populations are correctly identified for further testing.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous motile ciliopathy characterized by neonatal respiratory distress, chronic upper and lower respiratory tract infections, subfertility, and laterality defects [22]. The estimated prevalence is between 1:7,500 to 1:30,000, though under-diagnosis remains a significant challenge [22]. Laterality defects, which include situs inversus totalis (mirror-image organ arrangement) and heterotaxy, occur in approximately half of all PCD patients due to dysfunction of motile embryonic nodal cilia [23] [22]. The presence of situs inversus is a highly specific, though not sensitive, indicator of PCD.
The PICADAR (PrImary CiliARy DyskinesiA Rule) tool was developed to help identify patients requiring definitive PCD testing [1] [2]. It is a clinical prediction rule based on seven readily obtainable patient history parameters. Its development aimed to address the challenge of PCD's non-specific symptoms and the complexity of confirmatory tests, which require specialized equipment and expertise [2]. The tool's performance, however, is now shown to be heavily influenced by the patient's situs status.
Performance Analysis: Quantifying the Situs Solitus Sensitivity Gap
A 2025 study by Schramm et al. directly evaluated the sensitivity of PICADAR in a cohort of 269 individuals with genetically confirmed PCD [5]. The findings reveal a stark contrast in the tool's ability to correctly identify PCD patients based on their organ arrangement.
Table 1: PICADAR Sensitivity by Situs Status and Ultrastructure
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) | Statistical Significance (p-value) |
|---|---|---|---|
| Overall Cohort (n=269) | 75% (202/269) | 7 (5 – 9) | (Reference) |
| With Laterality Defects | 95% | 10 (8 – 11) | <0.0001 |
| With Situs Solitus (n=61%) | 61% | 6 (4 – 8) | <0.0001* |
| With Hallmark Ultrastructural Defects | 83% | Not Reported | <0.0001 |
| Without Hallmark Ultrastructural Defects | 59% | Not Reported | <0.0001* |
Note: IQR = Interquartile Range; * denotes p-value compared to group with laterality defects.
The data demonstrates a critical sensitivity gap of 34 percentage points between patients with laterality defects and those with situs solitus [5]. This means that in a population of genetically confirmed PCD patients, PICADAR would fail to identify nearly 4 out of 10 individuals with normally arranged organs. Furthermore, sensitivity is further reduced in patients who lack hallmark ciliary ultrastructural defects on transmission electron microscopy, a known PCD subgroup [5].
The original 2016 validation study for PICADAR reported a overall sensitivity of 0.90 and specificity of 0.75 for a cut-off score of 5 points [1] [2]. It is important to note that this high sensitivity was likely influenced by the composition of the study population. The recent 2025 study underscores that these performance metrics cannot be generalized, particularly to the situs solitus PCD population [5].
Table 2: Comparison of PICADAR Performance Metrics
| Study | Population | Reported Sensitivity | Reported Specificity | Key Limitation Identified |
|---|---|---|---|---|
| Behan et al. (2016) [1] [2] | 641 consecutive referrals | 0.90 | 0.75 | Population composition bias; performance not stratified by situs. |
| Schramm et al. (2025) [5] | 269 genetically confirmed PCD | 0.75 (Overall) | Not Reported | Quantifies severely limited sensitivity in situs solitus patients (0.61). |
Experimental Protocols
Protocol 1: PICADAR Score Calculation and Interpretation
The PICADAR tool is designed for patients with a persistent wet cough. The following protocol details its application and interpretation, with special consideration for the situs solitus gap.
1. Patient History Takedown: Collect the following seven clinical parameters from the patient's medical history or direct interview [1] [2]:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care unit (NICU) admission
- Chronic rhinitis
- Chronic ear symptoms
- Situs inversus
- Congenital cardiac defect
2. Score Assignment: Assign points for each parameter as defined in the original tool [1] [2]. The points for each feature are weighted based on their predictive strength.
3. Total Score Calculation: Sum the points from all seven parameters to obtain the total PICADAR score.
4. Interpretation and Referral Decision:
- Score ≥ 5 Points: According to the original validation, this score indicates a high probability of PCD and warrants referral for definitive diagnostic testing [1] [2].
- Critical Consideration for Scores < 5: A low score does not rule out PCD. Due to the tool's low sensitivity in situs solitus patients (61%), a strong clinical history of persistent wet cough from infancy, chronic rhinitis, and chronic otitis media should override a low PICADAR score and still trigger referral for specialist evaluation and testing [5] [24].
Protocol 2: Comprehensive PCD Diagnostic Workflow for At-Risk Patients
Given PICADAR's limitations, the following diagnostic protocol, aligned with European Respiratory Society (ERS) guidelines, is recommended for patients with a clinical history suggestive of PCD, regardless of their PICADAR score [24].
Diagram 1: PCD Diagnostic Workflow integrating PICADAR with confirmatory tests. A strong clinical history should trigger referral even with a low PICADAR score, especially in situs solitus.
1. Initial Clinical Assessment & PICADAR Screening:
- Take a detailed clinical history, including the seven PICADAR parameters.
- Calculate the PICADAR score.
- Decision Point: Proceed with further testing if PICADAR score is ≥5 OR if the clinical history is strongly suggestive (e.g., daily wet cough from infancy, unexplained neonatal respiratory distress in a term infant, persistent rhinitis, bronchiectasis) even with a low score [24].
2. Initial Specialist Investigation: Nasal Nitric Oxide (nNO):
- Procedure: Measure nNO levels, preferably using a chemiluminescence analyzer with a velum closure technique in patients over 6 years old. Tidal breathing is used for children under 6 [24].
- Interpretation: Abnormally low nNO is a strong indicator of PCD and mandates further confirmatory testing. Note: A normal nNO does not exclude PCD, and patients with a strong clinical phenotype should still be referred for further testing [24].
3. Confirmatory Diagnostic Testing in a Specialist Centre: Definitive diagnosis requires a combination of tests, as no single test is 100% sensitive and specific [24]. The following are conducted at specialized PCD diagnostic centers:
- High-Speed Video Microscopy Analysis (HSVMA): Assesses ciliary beat frequency and, critically, ciliary beat pattern. Beat pattern analysis is more specific than frequency alone [24]. To improve diagnostic accuracy and control for secondary dyskinesia, this analysis should be repeated after ciliary culture at an air-liquid interface (ALI) [24].
- Transmission Electron Microscopy (TEM): Analyzes ciliary ultrastructure for hallmark defects (e.g., absent outer/inner dynein arms). The presence of a hallmark defect is confirmatory, but normal ultrastructure does not rule out PCD [24].
- Genetic Testing: Identifies pathogenic variants in one of the over 50 known PCD-causing genes. This is becoming an increasingly integral part of the diagnostic pathway [22] [24].
- Immunofluorescence (IF): Uses antibodies to detect the absence or mislocalization of ciliary proteins, which can indicate specific genetic defects [24].
The Scientist's Toolkit: Research Reagent Solutions
For research into PCD pathophysiology and the development of novel diagnostics, the following tools and reagents are essential.
Table 3: Key Research Reagents and Materials for PCD Investigation
| Research Tool / Reagent | Primary Function in PCD Research | Application Context |
|---|---|---|
| Transmission Electron Microscopy (TEM) | Visualization of ciliary axonemal ultrastructure (e.g., dynein arms, microtubule defects) [24]. | Gold-standard for identifying hallmark structural defects; used for diagnostic validation and phenotype-genotype correlation. |
| High-Speed Video Cameras | Recording ciliary motion for subsequent analysis of beat frequency and pattern [24]. | Core component of HSVMA; enables functional assessment of ciliary motility. |
| Air-Liquid Interface (ALI) Culture Systems | Differentiating and culturing respiratory epithelial cells to regenerate ciliated epithelium [24]. | Critical for obtaining cilia free from secondary inflammatory damage, improving diagnostic specificity of HSVMA and TEM. |
| PCD Gene Panels (NGS) | Targeted sequencing of known PCD-associated genes [22] [24]. | Efficient genetic screening for pathogenic variants; essential for genetic confirmation and expanding genotype-phenotype understanding. |
| Immunofluorescence (IF) Antibodies | Specific labeling of ciliary proteins (e.g., DNAH5, DNAI1, GAS8) [24]. | Detects protein mislocalization/absence; useful for diagnosing PCD cases with normal ultrastructure and for functional validation of genetic findings. |
| Chemiluminescence Nitric Oxide Analyzers | Precise measurement of low nasal nitric oxide (nNO) levels [24]. | Standard equipment for nNO measurement, a key screening test for PCD. |
The data unequivocally demonstrates that PICADAR should not be used as a standalone rule-out tool for PCD, particularly in the patient cohort with normally arranged organs [5]. Its reliance on clinical features like situs inversus, which is absent in all situs solitus patients, inherently creates a performance bias that systematically overlooks a large subset of the PCD population.
For researchers designing clinical trials or epidemiological studies, this sensitivity gap poses a significant risk of population bias if PICADAR is used as a primary screening tool. For clinicians, over-reliance on a low PICADAR score in a symptomatic patient with situs solitus could lead to tragic diagnostic delays, allowing progressive lung damage to occur.
Conclusion: PICADAR serves as a useful initial checklist to raise clinical suspicion. However, its application must be contextualized within its documented limitations. A definitive PCD diagnostic workflow must be driven by a combination of strong clinical phenotype—especially a persistent wet cough beginning in infancy—and advanced specialized testing, rather than a PICADAR score alone. Future research must focus on developing and validating more sensitive predictive tools that perform robustly across all PCD subpopulations, irrespective of situs status.
This application note details a critical limitation in the current Primary Ciliary Dyskinesia (PCD) diagnostic workflow: the reduced predictive accuracy of the PICADAR clinical tool in genetically confirmed PCD patients who have normal ciliary ultrastructure. As PCD is a genetically heterogeneous disorder involving over 50 identified genes, a significant subset of patients presents without the classic "hallmark" ultrastructural defects traditionally associated with the condition. Recent evidence demonstrates that the PICADAR score, which is recommended by European Respiratory Society (ERS) guidelines to determine pre-test probability for PCD, exhibits substantially lower sensitivity in these genetically complex cases. This technical brief provides quantitative validation of these limitations and proposes modified experimental and diagnostic protocols to enhance detection accuracy within research and clinical settings, ensuring comprehensive patient capture for therapeutic development pipelines.
Quantitative Analysis of PICADAR Performance
The PICADAR tool employs an initial screening question regarding daily wet cough since early childhood, followed by seven additional weighted questions. A score ≥5 suggests a high probability of PCD and warrants further diagnostic testing [25]. However, its performance varies dramatically across genetic subtypes.
Table 1: Sensitivity of PICADAR Based on Clinical and Ultrastructural Features
| Patient Subgroup | Sensitivity (%) | Median PICADAR Score (IQR) | p-value vs. Reference Group |
|---|---|---|---|
| Overall PCD Cohort (n=269) | 75 (202/269) | 7 (5 – 9) | - |
| With Laterality Defects (e.g., Situs Inversus) | 95 | 10 (8 – 11) | <0.0001 |
| With Situs Solitus (normal organ arrangement) | 61 | 6 (4 – 8) | (Reference) |
| With Hallmark Ultrastructural Defects (on TEM) | 83 | - | <0.0001 |
| Without Hallmark Ultrastructural Defects (normal TEM) | 59 | - | (Reference) |
Data derived from a multicenter study of 269 genetically confirmed PCD patients [25] [10]. IQR: Interquartile Range; TEM: Transmission Electron Microscopy.
A critical finding is that 7% (18/269) of genetically confirmed PCD patients were automatically ruled out by the initial PICADAR question due to the absence of a daily wet cough, preventing them from proceeding to the full questionnaire [25]. The data in Table 1 establish that the tool's sensitivity is significantly compromised in key patient subgroups, particularly those with situs solitus and those with mutations that result in normal ciliary ultrastructure.
Genetic Basis and Ultrastructural Correlation
PCD genetics directly explain the observed limitations in clinical prediction tools. The disease follows predominantly autosomal recessive inheritance, with mutations in over 50 genes affecting ciliary assembly, structure, and function [3].
Table 2: Common PCD Genetic Variants and Their Associated Ultrastructural Phenotypes
| Gene | Ultrastructural Defect (by TEM) | Key Clinical/Functional Characteristics |
|---|---|---|
| DNAH5, DNAI1, DNAI2 | Outer Dynein Arm (ODA) Defect | Associated with laterality defects; relatively milder lung disease [3]. |
| CCDC39, CCDC40 | Combined Inner Dynein Arm (IDA) Defect & Microtubule Disorganization (MTD) | More severe disease course; earlier onset bronchiectasis [3] [26]. |
| DNAH11 | Normal Ultrastructure | Abnormal ciliary motility despite normal TEM appearance; associated with situs inversus but preserved lung function [3]. |
| HYDIN | Normal Ultrastructure | Defect affects central pair projection; abnormal, swirling ciliary beat pattern [3]. |
| RSPH9, RSPH4A | Normal Ultrastructure (or Central Pair Defects) | No increased risk of situs inversus (nodal cilia lack central pair) [3]. |
Genes associated with normal ciliary ultrastructure (e.g., DNAH11, HYDIN) account for a substantial proportion of PCD cases. The clinical presentation of patients with these genotypes often lacks the high-point features in the PICADAR score, such as laterality defects, leading to lower scores and false-negative screening results [25] [3]. Furthermore, recent research on CCDC39 and CCDC40 reveals that their protein products form a critical scaffold for assembling other ciliary proteins; their absence leads not only to ciliary dysfunction but also to a cell fate shift in some airway epithelial cells from ciliated to mucus-producing, potentially altering clinical manifestations [26].
Experimental Protocol: Validating Predictive Tools in Genetically-Defined Cohorts
Objective
To quantitatively evaluate the sensitivity and specificity of the PICADAR clinical prediction tool across genetically defined subgroups of PCD patients, with a focus on those with normal ciliary ultrastructure.
Materials and Reagents
Table 3: Research Reagent Solutions for PCD Diagnostic Validation
| Item | Function in Protocol | Example/Note |
|---|---|---|
| PICADAR Questionnaire | Standardized clinical data collection | Administered to patients/guardians; prerequisite: "daily wet cough" [25]. |
| Genetic DNA Sample | Gold-standard genetic confirmation | From whole blood or saliva. |
| Whole Exome Sequencing (WES) Kit | Identification of pathogenic variants in >50 PCD genes | e.g., GenCap WES capture kit [27]. |
| Nasal Nitric Oxide (nNO) Analyzer | Low nNO is a supportive diagnostic finding | e.g., Nakulen breath analyzer (Sunvou-CA2122 model) [27]. |
| Transmission Electron Microscope (TEM) | Assessment of ciliary ultrastructure | Identifies hallmark defects (ODA, IDA, MTD). |
| High-Speed Video Microscopy (HSVA) | Functional analysis of ciliary beat pattern and frequency | Essential for diagnosing PCD with normal ultrastructure. |
| Immunofluorescence (IF) Antibody Panel | Assessment of ciliary protein localization | Detects absence/mislocalization of specific proteins (e.g., DNAH5). |
Step-by-Step Methodology
- Patient Cohort Recruitment: Recruit a minimum of 50 genetically confirmed PCD patients, ensuring representation across key genotypic groups: a) genes causing hallmark ultrastructural defects (e.g., DNAH5), and b) genes causing normal ultrastructure (e.g., DNAH11, HYDIN). Obtain informed consent and ethical approval [25] [27].
- PICADAR Administration: A trained pulmonary team administers the PICADAR questionnaire to patients or their legal guardians. Record all answers and calculate the total score. A score of ≥5 is considered positive [25].
- Genetic Confirmation (Reference Standard):
- Extract genomic DNA using a commercial kit (e.g., QIAamp Blood Midi Kit).
- Perform Whole Exome Sequencing using a platform like DNBSEQ (DNBSEQ-T7).
- Map sequences to a human reference genome (e.g., UCSC hg19) and annotate variants using software like ANNOVAR.
- Classify variants according to ACMG/AMP guidelines [25] [27].
- Ultrastructural and Functional Phenotyping:
- Data Analysis:
- Calculate the sensitivity of PICADAR (score ≥5) for the overall cohort and for each genetic/ultrastructural subgroup.
- Use Mann-Whitney-U tests to compare PICADAR score distributions between groups (e.g., situs solitus vs. laterality defects).
- Employ Fisher's exact test to assess associations between PICADAR results and genetic subgroups [25].
PCD Diagnostic Workflow & PICADAR Gaps
Modified Diagnostic Pathway Integrating Genetic Understanding
Given the established limitations of PICADAR, a modified diagnostic pathway is recommended for research and clinical practice to ensure all PCD patients are identified.
Enhanced PCD Diagnostic Pathway
This enhanced pathway acknowledges that a low PICADAR score cannot reliably exclude PCD, particularly in cases with normal ultrastructure genetics. It promotes the earlier use of genetic testing, as encouraged by recent ERS/ATS guidelines [12], to resolve diagnostically challenging cases.
Implications for Research and Therapeutic Development
For researchers and drug development professionals, these findings have significant implications:
- Patient Cohort Definition: Clinical trials for novel therapeutics (e.g., gene therapies like RCT1100, an investigational mRNA-based therapeutic for DNAI1-related PCD [28]) must not rely solely on PICADAR for patient recruitment. Genotypic stratification is essential to avoid excluding eligible patients.
- Diagnostic Protocol Standardization: Multicenter research consortia should adopt the modified diagnostic pathway that integrates genetic testing alongside traditional functional assays to ensure comprehensive and accurate patient identification.
- * Biomarker Development:* There is a pressing need to discover and validate new clinical or molecular biomarkers that are independent of ultrastructural phenotype to improve pre-test probability assessment and disease monitoring.
The integration of a sophisticated genetic understanding into the PCD diagnostic workflow is no longer optional but a necessity for accurate patient identification, natural history studies, and the successful development of targeted genetic therapies.
The Primary Ciliary Dyskinesia Rule (PICADAR) is a clinical predictive tool developed to identify patients with high suspicion of primary ciliary dyskinesia (PCD) for referral to specialist diagnostic centers [1] [2]. While initial validation studies reported promising accuracy, its application in real-world clinical practice and research settings faces significant challenges, particularly concerning data availability and the limitations of retrospective assessment [5] [29] [14]. This document outlines these challenges within the context of PCD diagnostic workflow research, providing structured data, experimental protocols, and visual guides to aid researchers and drug development professionals in critically evaluating and applying the PICADAR tool.
Quantitative Performance Data in Research Cohorts
The performance of PICADAR varies significantly across different study populations and settings. The table below summarizes key quantitative findings from recent validation studies, highlighting the tool's sensitivity and the impact of specific patient phenotypes.
Table 1: Performance Metrics of PICADAR in Selected Research Studies
| Study Cohort | Sample Size (PCD+/Total) | PICADAR Cut-off | Reported Sensitivity | Key Limitations / Subgroup Analysis |
|---|---|---|---|---|
| Original Derivation (Behan et al., 2016) [1] [2] | 75 / 641 | ≥ 5 | 0.90 | Derived in a pre-selected cohort referred for testing; excludes patients without persistent wet cough. |
| Genetically Confirmed PCD Cohort (Schramm et al., 2025) [5] | 269 / 269 | ≥ 5 | 0.75 | 7% of PCD patients excluded for lacking daily wet cough. Sensitivity was 0.95 with laterality defects vs. 0.61 with situs solitus (normal organ arrangement). |
| Unselected Referral Cohort (Pohunek et al., 2021) [14] | 67 / 1401 | N/A | N/A | PICADAR could not be calculated for 6.1% of referred patients due to the absence of a chronic wet cough. Area Under the Curve (AUC) was 0.87. |
| Brazilian Tertiary Center (de C. Teixeira et al., 2022) [29] | N/A | N/A | N/A | Highlighted the tool's complexity and variable availability of required historical data in a resource-limited setting. |
Experimental Protocols for PICADAR Assessment
For researchers aiming to validate or apply PICADAR in diagnostic studies, adherence to a standardized protocol is crucial for ensuring consistent and comparable results.
Protocol: Calculation of the PICADAR Score
Objective: To systematically calculate a PICADAR score for a patient with suspected PCD to determine the need for referral for definitive diagnostic testing [1] [2].
Materials and Reagents:
- Patient clinical history record.
- PICADAR scoring sheet (physical or digital).
Methodology:
- Initial Screening Question: Confirm the presence of a persistent wet cough. If absent, the tool designates the patient as PCD-negative [5].
- Data Collection: For patients with a persistent wet cough, collect data on the seven predictive parameters listed below. Points are assigned for each positive finding.
- Score Calculation: Sum the points from all applicable parameters to obtain the total PICADAR score.
Table 2: PICADAR Scoring Parameters and Point Allocation
| Predictive Parameter | Clinical Definition | Point Allocation |
|---|---|---|
| Situs Inversus | Complete transposition of thoracic and abdominal organs confirmed by imaging (e.g., chest X-ray). | +2 |
| Congenital Cardiac Defect | Any structural heart defect present at birth, confirmed by echocardiography. | +2 |
| Full-Term Gestation | Birth at or after 37 weeks of gestation. | +1 |
| Neonatal Chest Symptoms | Unexplained respiratory distress or a requirement for respiratory support in a term neonate. | +1 |
| Neonatal Intensive Care Unit Admission | Admission to NICU for respiratory symptoms as a term neonate. | +1 |
| Chronic Rhinitis | Persistent, year-round nasal congestion or rhinorrhea, lasting >3 months, starting in the first year of life. | +1 |
| Ear and Hearing Symptoms | Chronic otitis media, recurrent acute otitis media, or serous otitis media with hearing loss. | +1 |
Interpretation: A total score of ≥ 5 points is recommended by the original developers as the threshold for referring a patient for further PCD diagnostic testing [1] [2] [21].
Protocol: Retrospective Validation of PICADAR
Objective: To assess the real-world diagnostic accuracy of PICADAR using retrospectively collected data from a PCD diagnostic center.
Materials and Reagents:
- Anonymized patient datasets including clinical history, PICADAR parameters, and definitive PCD diagnosis outcomes (e.g., genetic, TEM confirmation).
- Statistical analysis software (e.g., R, SPSS).
Methodology:
- Cohort Definition: Define the study population, including all patients referred for PCD testing over a specific period with a conclusive diagnostic outcome [14].
- Data Abstraction: Retrospectively extract the seven PICADAR parameters from patient clinical records. Document any missing data points [5] [29].
- Score Assignment: Calculate the PICADAR score for each patient where possible.
- Outcome Correlation: Compare the PICADAR score against the definitive PCD diagnosis (the reference standard).
- Statistical Analysis:
- Calculate sensitivity, specificity, and positive/negative predictive values.
- Generate a Receiver Operating Characteristic (ROC) curve and calculate the Area Under the Curve (AUC) [14].
- Perform subgroup analyses based on the presence of laterality defects or specific ultrastructural/genetic findings [5].
Visual Workflow: PICADAR in the PCD Diagnostic Pathway
The following diagram illustrates the role of PICADAR within the broader PCD diagnostic workflow and the specific challenges related to data availability.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing studies involving PICADAR and PCD diagnostics, the following table details essential materials and their functions.
Table 3: Essential Reagents and Materials for PCD Diagnostic Workflow Research
| Item / Assay | Function in Research Context | Application Notes |
|---|---|---|
| Structured Clinical Data Form | Standardizes the collection of patient history for the 7 PICADAR parameters. | Critical for ensuring consistent, retrospective data abstraction from electronic health records [14]. |
| Nasal Nitric Oxide (nNO) Analyzer | Measures nNO concentration; low nNO is a supportive screening test for PCD. | Used to validate and improve the predictive power of PICADAR. Not a standalone diagnostic [21] [14]. |
| High-Speed Video Microscopy (HSVA) | Records ciliary beat frequency and pattern from nasal brush biopsies. | A key diagnostic test. Requires patient to be free of acute respiratory infection for 4-6 weeks [29] [21]. |
| Transmission Electron Microscopy (TEM) | Visualizes ultrastructural defects in ciliary axonemes (e.g., absent dynein arms). | Considered a hallmark diagnostic test. Requires specialized expertise and processing protocols [5] [29] [21]. |
| Next-Generation Sequencing (NGS) Panel | Identifies pathogenic variants in over 50 known PCD-related genes. | Used for genetic confirmation. Increasingly important for patients with atypical ultrastructure or inconclusive other tests [5] [29] [21]. |
| Cell Culture Materials | Allows for re-differentiation of ciliated epithelium at an air-liquid interface (ALI). | Used to rule out secondary, transient ciliary dyskinesia and confirm primary defects [2] [21]. |
The PICADAR (PrImary CiliARy DyskinesiA Rule) score is a validated clinical prediction tool designed to identify patients who should be referred for specialized testing for Primary Ciliary Dyskinesia (PCD). It utilizes seven easily obtainable clinical parameters to calculate a score that ranges from 0 to 12, with a recommended cut-off of ≥5 points to proceed with diagnostic testing [2] [1]. This tool was developed to address the challenge of PCD's nonspecific symptoms and the highly specialized nature of definitive diagnostic tests [2].
However, emerging evidence indicates that strict adherence to the PICADAR cut-off can lead to missed diagnoses, particularly in specific patient subgroups [5] [25]. This document outlines the evidence-based mitigation strategies and protocols for researchers and clinicians to identify when a low PICADAR score should be overridden in favor of advanced testing, ensuring improved diagnostic sensitivity within the PCD diagnostic workflow.
Performance Data and Identified Limitations
Understanding the quantitative performance and specific limitations of the PICADAR score is fundamental to developing effective override strategies.
Established Performance Characteristics
The initial validation studies for PICADAR demonstrated strong performance in the derivation and initial validation cohorts, as summarized in Table 1 [2].
Table 1: Originally Reported Performance of PICADAR (Cut-off ≥5)
| Metric | Derivation Cohort (n=641) | Validation Cohort (n=187) |
|---|---|---|
| Sensitivity | 0.90 | Not explicitly reported |
| Specificity | 0.75 | Not explicitly reported |
| Area Under the Curve (AUC) | 0.91 | 0.87 |
Emerging Evidence on Limitations
A recent 2025 study evaluating PICADAR in a genetically confirmed PCD cohort (n=269) revealed critical limitations, demonstrating that the tool's sensitivity is not uniform across all PCD populations [5] [25]. The overall sensitivity was 75%, meaning one in four genetically confirmed PCD patients would have been missed using the standard cut-off [5].
Table 2: Sensitivity of PICADAR in a Genetically Confirmed PCD Cohort (2025 Data)
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| Overall PCD Cohort | 75% (202/269) | 7 (5 - 9) |
| With Laterality Defects | 95% | 10 (8 - 11) |
| With Situs Solitus (normal arrangement) | 61% | 6 (4 - 8) |
| With Predicted Hallmark Ultrastructural Defects | 83% | Not reported |
| Without Hallmark Ultrastructural Defects | 59% | Not reported |
Furthermore, the study found that 7% (18/269) of genetically confirmed PCD patients did not report a daily wet cough, which is a mandatory prerequisite for even completing the PICADAR questionnaire. These patients would have automatically been assigned a score of 0 and ruled out [5].
Override Criteria and Clinical Scenarios
Based on the synthesized evidence, advanced PCD testing is strongly recommended in the following scenarios, even in the context of a low PICADAR score (<5).
Override Scenario 1: Patients with Strong Clinical Phenotype butSitus Solitus
A PICADAR score below 5 should be overridden for patients with a compelling clinical history of PCD but with situs solitus (normal organ arrangement). The data shows that the sensitivity of PICADAR drops to 61% in this subgroup, as they do not receive the points allocated for situs inversus or congenital heart defects [5] [25]. A persistent wet cough combined with other classic features like unexplained neonatal respiratory distress in a term infant, persistent rhinitis, or chronic middle ear disease warrants further investigation [30] [21].
Override Scenario 2: Suspicion of Genetic Variants with Normal Ultrastructure
Proceed with advanced testing if there is clinical suspicion of a PCD-causing variant associated with normal ciliary ultrastructure. The 2025 study showed that the sensitivity of PICADAR was only 59% in patients without hallmark ultrastructural defects on transmission electron microscopy (TEM) [5]. With over 50 known PCD-causing genes, many of which (e.g., DNAH11, HYDIN) result in normal TEM findings, genetic testing becomes crucial in this context [25] [12].
Override Scenario 3: Atypical Presentations or Missing Key Symptoms
Override a low score for patients with an otherwise unexplained chronic respiratory phenotype who lack one of the cardinal PICADAR features. This includes:
- Patients without a daily wet cough: As 7% of genetically confirmed PCD cases lack this symptom, other indicators like early-onset bronchiectasis, chronic rhinosinusitis, or recurrent otitis media should trigger evaluation [5] [30].
- Patients with a strong family history: A first-degree family history of PCD or a history of recurrent respiratory infections should lower the threshold for testing [21].
Experimental and Diagnostic Protocols
This section details the methodologies for the key experiments and diagnostic tests cited in the literature and recommended for use after an override decision.
Protocol: PICADAR Score Calculation
The PICADAR tool is calculated as follows for any patient with a persistent daily wet cough starting in early childhood [2] [1].
Table 3: PICADAR Scoring System
| Predictive Parameter | Score |
|---|---|
| Full-term gestation (≥37 weeks) | 2 |
| Neonatal chest symptoms (within 1st month) | 2 |
| Admitted to neonatal intensive care unit | 1 |
| Chronic rhinitis (persisting >3 months) | 1 |
| Chronic ear symptoms/surgery | 1 |
| Situs Inversus Totalis | 4 |
| Congenital Cardiac Defect | 2 |
| Total Possible Score | 12 |
Procedure:
- Confirm the patient has a persistent daily wet cough that began in early childhood. If not, the score is 0.
- For each of the seven parameters, gather information through patient interview and medical record review.
- Assign the corresponding points for each "yes" answer.
- Sum the points to achieve the total PICADAR score.
Protocol: Advanced PCD Diagnostic Testing Pathway
Upon deciding to override a low PICADAR score, a sequential diagnostic pathway is recommended, in line with ERS/ATS guidelines [12].
Procedure:
Nasal Nitric Oxide (nNO) Measurement:
- Function: A screening test; low nNO is highly suggestive of PCD but not diagnostic by itself [12] [21].
- Methodology: Measured using a chemiluminescence analyzer with a velum closure technique. Consistently low nNO production (e.g., ≤30 nL·min⁻¹) strongly supports proceeding with further testing [2] [21].
High-Speed Video Microscopy Analysis (HSVA):
- Function: To assess ciliary beat frequency (CBF) and, more importantly, ciliary beat pattern (CBP) [12] [21].
- Methodology:
- A nasal epithelial biopsy is obtained via brushing.
- Ciliated cells are recorded at high frame rates (≥500 frames per second).
- The CBP is analyzed by experienced personnel for dyskinetic patterns (e.g., stiff, circular, or uncoordinated beating).
- To control for secondary ciliary dyskinesia due to infection, a second biopsy after 4-6 weeks or ciliogenesis culture (air-liquid interface culture) can be performed [2] [21].
Transmission Electron Microscopy (TEM):
- Function: To identify hallmark ultrastructural defects in cilia (e.g., outer dynein arm defects, inner dynein arm defects, microtubular disorganization) [12] [21].
- Methodology:
- Ciliated epithelial samples are fixed in glutaraldehyde.
- Samples are processed, sectioned, and stained for visualization under the electron microscope.
- A minimum of 100 well-oriented ciliary cross-sections are analyzed by an experienced microscopist [21].
Genetic Testing:
The Scientist's Toolkit: Research Reagent Solutions
The following table details key materials and reagents essential for conducting the advanced PCD diagnostic tests described in the protocols.
Table 4: Essential Research Reagents and Materials for PCD Diagnostics
| Item | Function/Application | Key Details & Considerations |
|---|---|---|
| Chemiluminescence NO Analyzer | Measures nasal nitric oxide (nNO) production rate. | Stationary analyzer used with velum closure technique; low nNO is a key PCD indicator [21]. |
| High-Speed Video Camera | Records ciliary beat frequency and pattern for HSVA. | Requires high frame rates (≥500 fps) and high resolution to capture ciliary motion dynamics [21]. |
| Transmission Electron Microscope | Visualizes ciliary ultrastructure to identify hallmark defects. | Used to analyze dynein arms, microtubules, and other core ciliary structures; requires expert interpretation [12] [21]. |
| Next-Generation Sequencing (NGS) Platform | Identifies pathogenic variants in PCD-associated genes. | Targeted panels, whole-exome, or whole-genome sequencing are used for genetic diagnosis [25] [12]. |
| Air-Liquid Interface (ALI) Culture Media | Regrows ciliated epithelium from biopsy samples. | Used to differentiate primary from secondary ciliary dyskinesia by allowing ciliogenesis in a controlled environment [2] [21]. |
| Glutaraldehyde Fixative | Preserves ciliary ultrastructure for TEM analysis. | Provides rapid and stable fixation of ciliary components to prevent artifactual changes [21]. |
PICADAR Under the Microscope: Comparative Performance and Validation in Genetically-Confirmed Cohorts
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous recessive disorder affecting motile cilia, leading to chronic respiratory symptoms, rhinosinusitis, hearing impairment, and organ laterality defects in approximately 50% of patients [31]. The PCD Rule (PICADAR) is a diagnostic predictive tool recommended by the European Respiratory Society (ERS) to estimate the probability of a PCD diagnosis and guide subsequent testing [5] [32]. However, its performance requires rigorous validation in large, genetically-confirmed populations to establish its reliability in clinical and research workflows. This application note synthesizes recent evidence on PICADAR's validity, providing structured data, experimental protocols, and analytical frameworks for researchers and drug development professionals.
Quantitative Validation of PICADAR Performance
A 2025 study by Schramm et al. evaluated the sensitivity of PICADAR in a cohort of 269 individuals with genetically confirmed PCD [5]. This represents a significant validation effort in a substantial, genetically-defined population. The core function of PICADAR is to use an initial question about daily wet cough; individuals without this symptom are ruled negative for PCD. For those with daily wet cough, it evaluates seven clinical criteria to generate a score [5].
Table 1: Overall Performance of PICADAR in a Genetically-Confirmed Cohort (n=269)
| Performance Metric | Result |
|---|---|
| Total Genetically Confirmed PCD Patients | 269 |
| Patients Ruled Out (No Daily Wet Cough) | 18 (7%) |
| Median PICADAR Score (IQR) | 7 (5 – 9) |
| Overall Sensitivity (Score ≥5) | 75% (202/269) |
Source: Schramm et al., 2025 [5]
Stratified Analysis by Clinical Subgroups
The sensitivity of PICADAR was not uniform across all subpopulations. Performance varied significantly based on the presence of laterality defects and hallmark ultrastructural defects, which are associated with specific genetic etiologies [5].
Table 2: Stratified Sensitivity Analysis of PICADAR
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| All Patients | 75% | 7 (5 – 9) |
| With Laterality Defects | 95% | 10 (8 – 11) |
| With Situs Solitus (normal arrangement) | 61% | 6 (4 – 8) |
| With Hallmark Ultrastructural Defects | 83% | Not Reported |
| Without Hallmark Ultrastructural Defects | 59% | Not Reported |
Source: Schramm et al., 2025 [5]
Experimental Protocols for PCD Diagnostic Validation
Protocol 1: PICADAR Validation in a Genetically-Confirmed Cohort
This protocol outlines the methodology used to validate the PICADAR tool, as employed in the seminal 2025 study [5].
1. Patient Cohort Selection:
- Inclusion Criteria: Recruit individuals with a confirmed PCD diagnosis based on the presence of biallelic pathogenic mutations in a known PCD-associated gene. Genetic analysis should follow established guidelines [31].
- Exclusion Criteria: Individuals with an incomplete genetic work-up or those with only a single pathogenic variant without confirmation of a second mutation in trans should be excluded to ensure a pure phenotype-genotype correlation.
2. Data Collection:
- Collect retrospective clinical data for each participant based on the seven criteria of the PICADAR tool:
- Gestational age at birth
- Presence of neonatal chest symptoms
- Presence of neonatal intensive care unit (NICU) admission
- Presence of persistent perennial rhinitis
- History of chronic ear symptoms
- History of chest symptoms in the absence of cold
- Presence of organ laterality defects [5]
- The presence of "daily wet cough" is used as the initial gatekeeper question.
- Collect retrospective clinical data for each participant based on the seven criteria of the PICADAR tool:
3. PICADAR Scoring:
- Assign points for each positive criterion according to the predefined PICADAR algorithm.
- Calculate a total score for each participant. A score of ≥5 points is considered to suggest a "high probability" for PCD, as per the tool's recommendation.
4. Data Analysis:
- Primary Outcome - Sensitivity: Calculate the sensitivity of the tool as the proportion of genetically-confirmed PCD patients who had a PICADAR score of ≥5.
- Stratified Analysis: Perform subgroup analyses to determine sensitivity in patients with and without laterality defects, and with and without hallmark ciliary ultrastructural defects on transmission electron microscopy (TEM).
Protocol 2: Comprehensive PCD Diagnostic Workflow with Integrated PICADAR
This protocol, adapted from the PCD-UNIBE center in Switzerland, describes a holistic diagnostic approach in which PICADAR can be utilized as an initial triage step [33].
1. Initial Clinical Assessment and Triage:
- Apply the PICADAR tool to patients with a clinical suspicion of PCD (e.g., those with at least two of the four key clinical features: year-round daily wet cough, year-round daily nasal congestion, neonatal respiratory distress at term birth, or organ laterality defects) [34].
- Patients with a high PICADAR score (e.g., ≥5) proceed to definitive diagnostic testing.
2. Definitive Diagnostic Testing:
- Nasal Brushing: Obtain nasal epithelial cells (NECs) from both nostrils using interdental brushes [33].
- Cell Culture: Culture primary NECs using air-liquid interface (ALI) protocols to regenerate ciliated epithelium. This step is critical for clearing secondary ciliary dyskinesia due to infection and improves diagnostic clarity [33].
- High-Speed Video Microscopy Analysis (HSVM): Analyze ciliary beating pattern (CBP) and frequency (CBF) of cultured cells using an inverted bright-field microscope and custom software (e.g., "Cilialyzer") [33].
- Immunofluorescence (IF) Staining: Label and assess key structural proteins of the ciliary axoneme (e.g., DNAH5, GAS8, RSPH9) to detect specific defects [33].
3. Confirmatory and Phenotyping Tests (Selected Cases):
- Transmission Electron Microscopy (TEM): Perform ultrastructural analysis on ciliary cross-sections to identify hallmark defects (e.g., absent outer/inner dynein arms) [33] [31].
- Genetic Testing: Conduct next-generation sequencing (e.g., whole-exome sequencing) with a panel of known PCD-associated genes to identify biallelic pathogenic variants [34] [33] [31].
4. Interdisciplinary Confirmation:
- Hold interdisciplinary meetings with pulmonologists and diagnostic specialists to review all findings (clinical, HSVM, IF, TEM, genetic) and confirm the final diagnosis [33].
The following workflow diagram illustrates this comprehensive diagnostic pathway, showing the role of PICADAR as an initial step.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for Comprehensive PCD Diagnostic Research
| Research Reagent / Material | Function in PCD Diagnostics |
|---|---|
| Interdental Brushes | Minimally invasive collection of nasal epithelial cells (NECs) for primary culture and analysis [33]. |
| PneumaCult Media Kits | Specialized culture media for the differentiation of primary NECs at the air-liquid interface (ALI) to generate ciliated epithelium [33]. |
| Inverted Bright-Field Microscope | Core equipment for high-speed video microscopy (HSVM) to visualize and record ciliary motility [33]. |
| Custom HSVM Analysis Software (e.g., Cilialyzer) | Software for quantitative analysis of ciliary beat frequency (CBF) and pattern (CBP) from video recordings [33]. |
| Antibodies for Axonemal Proteins (e.g., DNAH5, GAS8, RSPH9) | Key reagents for immunofluorescence (IF) staining to detect the absence or mislocalization of specific ciliary structural proteins [33]. |
| Transmission Electron Microscope | High-resolution imaging of ciliary ultrastructure (e.g., dynein arms, radial spokes) to identify hallmark defects [33] [31]. |
| Next-Generation Sequencing Panels | Genetic testing solutions targeting all known PCD-associated genes to identify pathogenic variants and confirm diagnosis [34] [31]. |
Recent validation in a large, genetically-confirmed cohort demonstrates that while PICADAR is a useful initial triage tool, its overall sensitivity of 75% is suboptimal for a standalone rule-in test, potentially missing one in four true PCD cases [5]. Its performance is significantly worse in patients with situs solitus (61% sensitivity) and those without hallmark ultrastructural defects (59% sensitivity) [5]. Therefore, for research and drug development purposes, a positive PICADAR score should be considered an entry point into a comprehensive diagnostic workflow—not a definitive diagnosis. This workflow must integrate advanced techniques like ALI cell culture, HSVM, IF, TEM, and extended genetic testing to achieve an accurate and phenotyped diagnosis, which is crucial for patient stratification in clinical trials and the development of genotype-specific therapies [34] [33].
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary function, leading to chronic oto-sino-pulmonary disease, laterality defects, and infertility [35] [36]. The diagnostic pathway is complex, requiring specialized, expensive tests like transmission electron microscopy (TEM), genetic sequencing, and nasal nitric oxide (nNO) measurement, which are not universally accessible [35] [36] [37]. This creates a pressing need for effective, evidence-based clinical prediction tools to identify high-probability patients for confirmatory testing. This Application Note provides a comparative analysis of the PICADAR tool and the ATS Clinical Screening Questionnaire (ATS-CSQ), framing them within a robust diagnostic workflow for researchers and drug development professionals.
Quantitative Performance Comparison of Predictive Tools
The following tables summarize the key performance metrics and operational characteristics of the two primary predictive tools.
Table 1: Performance Characteristics of PCD Predictive Tools
| Feature | PICADAR (PrImary CiliAry DyskinesiA Rule) | ATS Clinical Screening Questionnaire (ATS-CSQ) |
|---|---|---|
| Original Reported Sensitivity | 90% [36] | Data from search results is insufficient for a direct comparison. |
| Original Reported Specificity | 75% [36] | Data from search results is insufficient for a direct comparison. |
| Validated Cut-off Score | ≥5 points [36] | Not specified in available search results. |
| Recent Sensitivity Data | 75% overall; 95% with laterality defects vs. 61% with situs solitus [10] [5] | Not re-evaluated in the provided search results. |
| Key Limitation | Low sensitivity in patients without laterality defects or hallmark ultrastructural defects [10] [5] | Information is lacking in the provided search results. |
Table 2: Clinical Parameters and Scoring System for PICADAR Scoring applies to patients with persistent wet cough. A score ≥5 indicates high PCD probability [36].
| Predictive Parameter | Score |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms ever | 2 |
| Admission to a neonatal intensive care unit | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms (chronic otitis media or serous otitis) | 1 |
| Situs Inversus | 4 |
| Congenital cardiac defect | 2 |
Experimental Protocols for Tool Application and Validation
Protocol 1: Implementing the PICADAR Tool
Principle: PICADAR is a diagnostic prediction rule that uses seven easily obtainable clinical parameters from patient history to calculate a score estimating the probability of PCD [36].
Materials:
- Patient clinical history form.
- PICADAR scoring sheet (see Table 2).
Procedure:
- Patient Identification: Apply the tool to patients with a history of persistent wet cough [36].
- Data Collection: Through clinical interview or record review, ascertain the presence or absence of the seven parameters:
- Full-term gestation (≥37 weeks).
- History of neonatal chest symptoms.
- Admission to a neonatal intensive care unit.
- Presence of chronic rhinitis (>3 months).
- History of chronic ear symptoms (otitis media, serous otitis).
- Presence of situs inversus (confirmed by imaging).
- Diagnosis of a congenital cardiac defect.
- Scoring: Assign points for each positive parameter as detailed in Table 2.
- Interpretation: A total score of 5 or higher is recommended to identify patients at high risk for PCD who should be referred for definitive diagnostic testing [36].
Protocol 2: Integrating Predictive Tools into a Diagnostic Workflow
Principle: Predictive tools are screening instruments and must be integrated into a comprehensive diagnostic pathway. The following workflow, based on current literature, outlines this process from initial suspicion to confirmation.
Materials:
- Clinical screening questionnaire (PICADAR or ATS-CSQ).
- Access to specialist PCD diagnostic center.
- Diagnostic equipment for nNO, TEM, High-Speed Video Microscopy Analysis (HSVMA), and genetic testing.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Reagents and Materials for PCD Diagnostic Research
| Item | Function/Application in PCD Research |
|---|---|
| Nasal Epithelial Brush | Collects ciliated epithelial cell samples from the inferior turbinate for TEM and cell culture [35] [37]. |
| Glutaraldehyde (3%) | Primary fixative for ciliary ultrastructure preservation prior to TEM processing [35] [37]. |
| TEM with BEAT-PCD Criteria | Gold standard for visualizing hallmark ciliary ultrastructural defects (e.g., ODA/IDA loss) [35] [37]. |
| High-Speed Video Microscope | Captures and analyzes ciliary beat pattern (CBP) and frequency for functional assessment [36]. |
| Next-Generation Sequencing (NGS) Panel | Targeted genetic screening for pathogenic variants in over 50 known PCD-related genes [35]. |
| Saccharin Fragment (1mm) | Used in the saccharin transit time test, a low-cost screening tool for mucociliary clearance function [37]. |
Discussion & Strategic Application in Research
The quantitative data reveals a critical nuance in PICADAR's application. While its original validation showed high sensitivity (90%) [36], recent studies on genetically confirmed cohorts demonstrate significantly lower sensitivity (75% overall), particularly in subpopulations without laterality defects (61%) or hallmark ultrastructural defects (59%) [10] [5]. This indicates that PICADAR is an excellent tool for identifying classic PCD phenotypes but may fail to detect a substantial portion of patients with atypical presentations or normal ultrastructure.
For research and drug development, this has profound implications. Protocol Design: Relying solely on PICADAR for patient enrollment in clinical trials may systematically exclude a genetically distinct subset of the PCD population, leading to biased trial results. Diagnostic Strategy: A combination of tools, including low-cost functional tests like the saccharin test [37], is recommended to cast a wider net before committing to expensive confirmatory testing. The proposed diagnostic workflow (Section 3.2) provides a robust framework for ensuring comprehensive patient identification and characterization, which is fundamental for advancing therapeutic development and personalized medicine in PCD.
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder affecting motile cilia, leading to chronic otosinopulmonary disease, organ laterality defects, and reduced fertility [1] [2]. The diagnostic pathway for PCD is complex, with no single gold standard test, requiring a combination of specialized investigations available primarily at expert centers [38] [34]. This diagnostic challenge is compounded by the non-specific nature of PCD symptoms, which overlap with more common respiratory conditions [1]. The PICADAR score (PrImary CiliAry DyskinesiA Rule) has emerged as a validated clinical prediction tool designed to identify patients with persistent wet cough who warrant further specialized testing [1] [2]. This application note delineates the integral role of PICADAR within the multimodal PCD diagnostic framework, detailing its synergistic relationship with established tests including nasal nitric oxide (nNO), high-speed video microscopy (HSVM), transmission electron microscopy (TEM), and genetic analysis. We provide structured data and standardized protocols to guide its application in research and clinical practice, framing this within a broader thesis on optimizing PCD diagnostic workflows.
The PICADAR Tool: Composition and Performance
PICADAR is a symptom-based prediction rule derived and externally validated in consecutive patients referred for PCD testing [1] [2]. Its development involved logistic regression analysis of clinical data readily obtainable from patient history, resulting in a simple scoring system.
Table 1: The PICADAR Scoring System [1] [2]
| Predictive Parameter | Points |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Chronic ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 2 |
| Total Possible Score | 11 |
Table 2: Diagnostic Performance of PICADAR [1] [39]
| Metric | Derivation Cohort (n=641) | External Validation Cohort |
|---|---|---|
| Positive PCD Diagnoses | 75 (12%) | 93/187 (50%) |
| Recommended Cut-off Score | ≥ 5 points | ≥ 5 points |
| Sensitivity | 0.90 | - |
| Specificity | 0.75 | - |
| Area Under the Curve (AUC) | 0.91 | 0.87 |
The tool demonstrates good accuracy and validity for identifying patients at high risk for PCD. A modified version for adults with bronchiectasis, focusing on situs inversus, neonatal respiratory distress, congenital cardiac defect, chronic rhinosinusitis, and chronic ear symptoms, also showed discriminative value, with a score of ≥2 points yielding a sensitivity of 1.00 and specificity of 0.89 in one cohort [39].
The Multimodal Diagnostic Ecosystem for PCD
Specialized diagnostic tests for PCD each have distinct strengths and limitations, as summarized in the table below. PICADAR functions as the initial gatekeeper, triaging patients into this resource-intensive pathway.
Table 3: Key Diagnostic Modalities in the PCD Workflow [40] [34] [41]
| Diagnostic Method | Primary Function | Key Strength | Key Limitation |
|---|---|---|---|
| PICADAR | Clinical prediction rule; patient triage | Simple, quick, low-cost; uses readily available clinical history | Does not confirm diagnosis; performance may vary in adults |
| Nasal Nitric Oxide (nNO) | Screening / Diagnosis | Non-invasive; high sensitivity & specificity in cooperative patients ≥5 yrs | Requires specialized equipment; false negatives with upper respiratory infections |
| High-Speed Video Microscopy (HSVM) | Functional analysis of cilia | Assesses ciliary beat pattern and frequency | Requires significant expertise; lack of standardization across centers |
| Transmission Electron Microscopy (TEM) | Structural analysis of cilia | Identifies hallmark ultrastructural defects (e.g., ODA/IDA absence) | Invasive; ~30% of PCD cases have normal ultrastructure |
| Genetic Testing | Molecular diagnosis | Confirms diagnosis; enables genetic counseling | ~20% false-negative rate with extended panels; variants of unknown significance |
| Immunofluorescence (IF) | Protein localization | Cheaper/faster than TEM; can confirm pathogenicity of genetic variants | Limited availability; requires specialized antibodies and expertise |
The diagnostic workflow typically begins with clinical suspicion, followed by application of PICADAR, and then proceeds through a sequence of specialized tests. International guidelines from the ERS and ATS recommend that diagnostic testing should be initiated in patients with at least two of the following key clinical features: year-round daily wet cough, year-round daily nasal congestion, neonatal respiratory distress despite term birth, or organ laterality defects [34].
Figure 1: Proposed Diagnostic Workflow Integrating PICADAR. CBP: Ciliary Beat Pattern.
Synergistic Workflows: PICADAR and Objective Diagnostic Tests
PICADAR and Nasal Nitric Oxide (nNO)
nNO measurement is a well-established screening tool, with levels markedly reduced in most PCD patients [39] [34]. The two modalities function sequentially: PICADAR first identifies high-risk patients, who then undergo nNO testing. A study in adults with bronchiectasis found that combining a modified PICADAR score with nNO provided a cheap and effective screening algorithm [39]. In that cohort, the mean nNO was significantly lower in the PCD group (25 nL/min) compared to the non-PCD group (227 nL/min), and a cut-off of 77 nL/min best differentiated the groups [39].
PICADAR and Genetic Testing
Genetic testing is a cornerstone of PCD diagnosis, with extended panels identifying biallelic pathogenic variants in a known PCD gene in a significant proportion of cases [40] [34]. PICADAR serves as a valuable pre-genetic screening tool. Research demonstrates that patients with higher PICADAR scores are more likely to have positive genetic or immunofluorescence confirmation. One study reported that all patients with abnormal immunofluorescence findings (indicative of PCD) had a PICADAR score of 6 or above [40].
PICADAR within Integrated Diagnostic Algorithms
Cost-effectiveness analyses inform the structure of optimal diagnostic pathways. One simulation study compared three algorithms and found that a parallel testing approach (nNO and HSVM simultaneously, with TEM for confirmation in discordant cases) identified the most PCD patients (313 out of 320) but was also the most costly [17]. The sequential algorithm of nNO followed by HSVM was less costly and more effective than nNO followed by TEM [17]. In all these models, PICADAR is implicitly the critical first step that determines entry into the pathway, ensuring efficient use of resources.
Experimental Protocols
Protocol 1: Application of the PICADAR Tool
Objective: To standardize the calculation of the PICADAR score for triaging patients with suspected PCD. Materials: Patient medical record or structured clinical interview form. Procedure:
- Confirm the patient has a history of persistent wet cough.
- For each of the seven parameters in Table 1, ascertain the patient's history:
- Full-term gestation: Was the infant born at ≥37 weeks gestation?
- Neonatal chest symptoms: Did the infant require >24 hours of oxygen, had tachypnoea, or a chest radiograph abnormality in the first month of life?
- Neonatal intensive care admission: Was the infant admitted to a neonatal unit for any reason?
- Chronic rhinitis: Has the patient had perennial nasal congestion/rhinorrhoea for >3 months?
- Ear symptoms: History of recurrent otitis media or glue ear.
- Situs inversus: Confirmed by imaging (e.g., chest X-ray, abdominal ultrasound).
- Congenital cardiac defect: Confirmed by echocardiography.
- Assign the corresponding points for each "yes" answer.
- Sum the points to obtain the total PICADAR score. Interpretation: A score of ≥5 points indicates a high probability of PCD and warrants referral to a specialist center for further investigation [1] [2].
Protocol 2: High-Speed Video Microscopy Analysis
Objective: To assess ciliary function by evaluating ciliary beat frequency (CBF) and pattern (CBP). Materials: Nasal brush cytology, RPMI 1640 culture medium, inverted phase-contrast microscope with high-speed digital camera, Sisson-Ammons Video Analysis (SAVA) software, heater plate. Procedure [40]:
- Sample Collection: Obtain nasal epithelial cells from the inferior turbinate using a cytobrush under direct vision. Avoid topical anesthesia if possible.
- Sample Handling: Immediately place the sample in pre-warmed culture medium (RPMI 1640). Analyze within 24 hours.
- Microscopy Setup: Place a drop of cell suspension on a glass slide. Position on a heater plate maintained at 37°C on the microscope stage.
- Video Acquisition: Using an inverted microscope with a ×40 objective and a high-speed camera, record digital videos at a frame rate of 120–150 frames per second for durations of one minute with 15-second intervals.
- Analysis: Use SAVA software to quantitatively measure CBF. Qualitatively assess CBP from top and side views in real-time and slow-motion replay. Look for patterns such as immotility, stiff, flickering, or circular beats. Interpretation: A hallmark CBP is diagnostic for PCD. Note that secondary ciliary dyskinesia from infection can cause transient abnormalities, and cell culture may be required for confirmation [34].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Materials for PCD Diagnostic Investigations
| Item | Specific Example | Research Function |
|---|---|---|
| Anti-DNAH5 Antibody | Mouse monoclonal anti-DNAH5 [40] | Labels outer dynein arm protein for immunofluorescence (IF) analysis of ciliary axoneme. |
| Anti-GAS8 Antibody | Polyclonal rabbit anti-GAS8 (HPA041311) [40] | Labels nexin-dynein regulatory complex (N-DRC) protein for IF analysis. |
| Secondary Antibodies for IF | Goat Anti-mouse Alexa Fluor 488, Anti-rabbit Alexa Fluor 546 [40] | Fluorescently-labeled antibodies for detection of primary antibodies in IF. |
| Cell Culture Medium | RPMI 1640 Medium [40] | For transport and short-term maintenance of respiratory epithelial cells post-biopsy. |
| Nasal Brush for Biopsy | Cytobrush Plus (Medscand Medical) [40] | Standardized tool for obtaining ciliated epithelial cell samples from nasal turbinate. |
| Chemiluminescence NO Analyzer | CLD 88sp (ECO MEDICS AG) [40] | Gold-standard device for measuring nasal nitric oxide (nNO) concentrations. |
| High-Speed Video Camera | Basler acA1300-200um [40] | Captures high-frame-rate videos for ciliary beat analysis via HSVM. |
PICADAR is a foundational component of the modern PCD diagnostic ecosystem, providing an evidence-based, cost-effective method for identifying patients who require further specialized testing. Its integration with nNO, HSVM, TEM, and genetic testing creates a synergistic workflow that improves diagnostic efficiency and accuracy. Future research should focus on the development and validation of age-specific and population-specific modifications of the score, its integration with emerging techniques like immunofluorescence, and the implementation of the entire diagnostic pathway in resource-limited settings through international collaboration. As the genetic and molecular understanding of PCD expands, the role of clinical prediction tools like PICADAR will remain vital for ensuring timely diagnosis and access to appropriate care.
Application Note: Performance Evaluation of the PICADAR Tool
The Primary Ciliary Dyskinesia Rule (PICADAR) is a diagnostic predictive tool designed to identify patients requiring specialized testing for Primary Ciliary Dyskinesia (PCD). It utilizes seven clinical parameters readily obtained from patient history and is intended for use in patients with a persistent wet cough [2].
Table 1: Original PICADAR Validation Performance (2016) [2]
| Metric | Derivation Cohort (n=641) | External Validation Cohort (n=187) |
|---|---|---|
| Prevalence of PCD | 12% (75/641) | 51% (93/187) |
| Area Under the Curve (AUC) | 0.91 | 0.87 |
| Sensitivity (at score ≥5) | 0.90 | Not specified |
| Specificity (at score ≥5) | 0.75 | Not specified |
Table 2: Recent Sensitivity Analysis in a Genetically Confirmed Cohort (2025) [25]
| Patient Subgroup | Sample Size (n=269) | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|---|
| Overall Cohort | 269 | 75% (202/269) | 7 (5 – 9) |
| With Laterality Defects | Not specified | 95% | 10 (8 – 11) |
| With Situs Solitus (normal arrangement) | Not specified | 61% | 6 (4 – 8) |
| With Hallmark Ultrastructural Defects | Not specified | 83% | Not specified |
| Without Hallmark Ultrastructural Defects | Not specified | 59% | Not specified |
Note: 7% (18/269) of genetically confirmed PCD patients were excluded from scoring because they did not report a daily wet cough, an automatic exclusion criterion in PICADAR [25].
Operational and Economic Implications
The core economic argument for PICADAR lies in its role as an initial triage filter. Specialized PCD diagnostic tests are highly complex, requiring expensive equipment (e.g., transmission electron microscopy, high-speed video microscopy) and experienced scientists, making them scarce and costly resources [2]. By providing a quick, low-cost initial assessment, PICADAR aims to streamline referrals to these specialized centers.
However, this efficiency must be balanced against the cost of missed diagnoses. The 2025 data indicates that the tool's sensitivity is significantly lower than initially reported, particularly in key patient subgroups [25]. An over-reliance on PICADAR for triage could lead to:
- Delayed Diagnosis and Treatment: Particularly in the estimated 39% of patients with situs solitus and genetically confirmed PCD who score below the cutoff [25].
- Long-Term Health Costs: Untreated PCD leads to progressive lung damage and bronchiectasis, resulting in higher healthcare utilization over time [2].
- Inequitable Care: Performance variability across phenotypes may lead to disparities in diagnosis access for patients without classic symptoms like situs inversus.
Experimental Protocols
Protocol for Administering the PICADAR Tool
Objective: To standardize the collection of clinical history for calculating the PICADAR score to identify patients at high risk for PCD.
Patient Eligibility: The tool is applicable to patients with a persistent, daily wet cough that began in early childhood [2] [25].
Procedure:
- Initial Screening Question: Confirm the presence of a "daily wet cough that started in early childhood."
- If the answer is "No," the PICADAR score is 0, and the tool recommends against further PCD testing [25].
- If the answer is "Yes," proceed to the seven questions below.
- Data Collection: Ask the patient or their guardian the following questions and assign the corresponding points [2].
Table 3: PICADAR Scoring System [2]
| # | Clinical Parameter | Answer | Points |
|---|---|---|---|
| 1 | Full-term gestation? | Yes | 2 |
| No | 0 | ||
| 2 | Neonatal chest symptoms? | Yes | 2 |
| No | 0 | ||
| 3 | Admitted to neonatal intensive care unit? | Yes | 1 |
| No | 0 | ||
| 4 | Chronic rhinitis? | Yes | 1 |
| No | 0 | ||
| 5 | Ear symptoms? | Yes | 1 |
| No | 0 | ||
| 6 | Situs inversus? | Yes | 4 |
| No | 0 | ||
| 7 | Congenital cardiac defect? | Yes | 2 |
| No | 0 |
- Score Calculation and Interpretation:
- Sum the points from all seven questions. The total score ranges from 0 to 12.
- A score of 5 or more suggests a high probability of PCD, and further diagnostic testing at a specialist center is recommended [2].
- A score below 5 indicates a lower probability, but clinical judgment should prevail, especially in light of recent sensitivity data [25].
Protocol for Validating PICADAR in a Research Cohort
Objective: To evaluate the real-world sensitivity and specificity of the PICADAR tool against a genetically confirmed PCD diagnosis.
Study Population:
- Inclusion: Patients with a PCD diagnosis confirmed by genetic testing identifying biallelic, hemizygous, or mono-allelic disease-causing variants [25].
- Exclusion: Patients with an incomplete clinical history needed to calculate the PICADAR score.
Data Collection:
- Retrieve or collect responses to the eight PICADAR questions (initial wet cough screen + seven scored items) for all study participants.
- For any unanswered questions (e.g., unknown gestational age), assume "No"/"Full-term" as default, as per the original protocol [25].
- Calculate the PICADAR score for each participant.
Statistical Analysis:
- Sensitivity Calculation: Determine the proportion of genetically confirmed PCD patients who have a PICADAR score ≥5 [25].
- Sensitivity = (Number of PCD patients with score ≥5) / (Total number of PCD patients screened)
- Subgroup Analysis: Stratify the cohort and calculate sensitivity for key subgroups:
- Patients with laterality defects (e.g., situs inversus) vs. situs solitus.
- Patients with genetic variants associated with hallmark ultrastructural defects on transmission electron microscopy (TEM) vs. those without [25].
- Statistical Testing: Use Mann-Whitney U tests to compare the distribution of PICADAR scores between subgroups. Use Fisher's exact test to assess the association between PICADAR results (positive/negative) and subgroup membership [25].
Diagnostic Workflow Visualization
PICADAR Clinical Triage Workflow
PICADAR Sensitivity Across Subgroups
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials for PCD Diagnostic Research
| Item / Reagent | Function in PCD Research | Application Note |
|---|---|---|
| PICADAR Questionnaire | A clinical prediction rule to triage patients for further PCD testing. | Serves as a low-cost, initial screening tool. Its limitations in sensitivity, especially in patients without laterality defects, must be considered [25]. |
| Nasal Nitric Oxide (nNO) Measurement | A non-invasive screening test; low nNO production is strongly associated with PCD. | Used as a key diagnostic test in specialist centers. Recommended in combination with other tests for a definitive diagnosis [2]. |
| High-Speed Video Microscopy Analysis (HSVA) | Allows direct visualization of ciliary beat pattern and frequency. | Used to identify characteristic abnormal ciliary beat patterns associated with PCD. Requires experienced scientists for analysis [2]. |
| Transmission Electron Microscopy (TEM) | Evaluates the ultrastructural anatomy of cilia (e.g., absence of dynein arms). | Considered a hallmark diagnostic test, but ~30% of genetically confirmed PCD patients have normal ultrastructure [2] [25]. |
| Genetic Testing | Identifies pathogenic variants in over 50 known PCD-associated genes. | The definitive confirmatory test. Crucial for diagnosing patients with normal ciliary ultrastructure and for understanding genotype-phenotype correlations [25]. |
Conclusion
PICADAR remains a valuable but imperfect tool for triaging patients suspected of PCD. While it demonstrates high sensitivity in classic phenotypes with laterality defects, recent evidence from genetically-confirmed cohorts reveals significant limitations, particularly in patients with situs solitus or normal ciliary ultrastructure, where sensitivity can drop to nearly 60%. This has profound implications for research and drug development, as these underrepresented populations may be systematically excluded from studies if reliance on PICADAR is absolute. The future of PCD diagnosis lies in developing more inclusive predictive models, leveraging genetic insights, and adopting a multimodal diagnostic approach where no single test is definitive. For clinical trials and therapeutic development, rigorous patient identification strategies must extend beyond PICADAR to ensure enrollment of the full PCD phenotypic spectrum.
References
- 1. a diagnostic predictive tool for primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/26917608/]
- 2. a diagnostic predictive tool for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819882/]
- 3. Primary Ciliary Dyskinesia—Current Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525432/]
- 4. Clinical Manifestations and Genotype of Primary Ciliary ... [https://e-aair.org/DOIx.php?id=10.4168/aair.2023.15.6.757]
- 5. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1]
- 6. Implementation of a screening tool for primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8021076/]
- 7. The BEAT-PCD (Better Experimental Approaches to Treat ... [https://publications.ersnet.org/content/erj/57/2/2004601]
- 8. Diagnosing PCD [https://www.pcdfoundation.org/diagnosis/]
- 9. Priorities and barriers for research related to primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11440378/]
- 10. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1691758/full]
- 11. Evaluation of a Clinical Index as a Predictive Tool for Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232329/]
- 12. European Respiratory Society and American Thoracic ... [https://pubmed.ncbi.nlm.nih.gov/41005984/]
- 13. ERS and ATS unite for universal PCD diagnosis guideline [https://thelimbic.com/respiratory/ers-and-ats-unite-for-universal-pcd-diagnosis-guideline/]
- 14. Evaluation of a Clinical Index as a Predictive Tool for ... [https://www.mdpi.com/2075-4418/11/6/1088]
- 15. Clinical care for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC9489029/]
- 16. Primary Ciliary Dyskinesia: An Update on Clinical Aspects ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2017.00135/full]
- 17. Cost-effectiveness analysis of three algorithms for diagnosing ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-019-1116-3]
- 18. Practical guide for the diagnosis and management of ... [https://www.sciencedirect.com/science/article/pii/S0385814624000166]
- 19. Thieme E-Journals - Pneumologie / Full Text [https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0043-111909?device=desktop]
- 20. Situs Inversus Totalis: A Clinical Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8901252/]
- 21. Guidelines for the diagnosis of primary ciliary dyskinesia [https://www.waidid.org/publications/guidelines-for-the-diagnosis-of-primary-ciliary-dyskinesia]
- 22. Primary Ciliary Dyskinesia: A Clinical Review [https://www.mdpi.com/2073-4409/13/11/974]
- 23. Structural Heart Issues in Dextrocardia: Situs Type Matters [https://pmc.ncbi.nlm.nih.gov/articles/PMC7993426/]
- 24. ERS Task Force guideline for the diagnosis of primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6054534/]
- 25. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1.full-text]
- 26. Genetic analysis explains rare disease severity, points to ... [https://source.washu.edu/2025/03/genetic-analysis-explains-rare-disease-severity-points-to-possible-treatment/]
- 27. Clinical features and genetic spectrum of children with ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1526675/full]
- 28. Primary Ciliary Dyskinesia [https://recodetx.com/pcd/]
- 29. Challenges in Diagnosing Primary Ciliary Dyskinesia in a ... [https://www.mdpi.com/2073-4425/13/7/1252]
- 30. Primary ciliary dyskinesia: A review [https://www.sciencedirect.com/science/article/pii/S2950008725000420]
- 31. Analysis of Clinical Characteristics and Gene Variants ... [https://brieflands.com/journals/ijp/articles/132964]
- 32. Primary Ciliary Dyskinesia [https://www.jpediatricacademy.com/index.php/jpa/article/view/64]
- 33. A Comprehensive Approach for the Diagnosis of Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8466881/]
- 34. Summary for Clinicians: Diagnosis of Primary Ciliary Dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC7336768/]
- 35. Challenges in Diagnosing Primary Ciliary Dyskinesia in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9324289/]
- 36. PICADAR: a diagnostic predictive tool for primary ciliary ... [https://publications.ersnet.org/content/erj/47/4/1103]
- 37. Cross-sectional evaluation of the saccharin transit time test for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10181835/]
- 38. New Diagnostic Methods and Treatment Recommendations in Primary... [https://jpediatricacademy.com/index.php/jpa/article/view/64]
- 39. Thieme E-Journals - Pneumologie / Full Text [https://www.thieme-connect.com/products/ejournals/html/10.1055/s-0043-111909]
- 40. Frontiers | Empowering limited-resource countries: collaborating with... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1547152/full]
- 41. Transmission electron microscopy study of suspected primary ciliary... [https://www.nature.com/articles/s41598-022-06370-w?error=cookies_not_supported&code=5c04da08-483b-4f2e-a001-3563ccba7806]