PICADAR Score Limitations: Assessing Diagnostic Sensitivity in PCD Patients with Situs Solitus
This article critically evaluates the PICADAR score, a clinical prediction tool for Primary Ciliary Dyskinesia (PCD), with a specific focus on its significantly reduced sensitivity in patients with situs solitus...
PICADAR Score Limitations: Assessing Diagnostic Sensitivity in PCD Patients with Situs Solitus
Abstract
This article critically evaluates the PICADAR score, a clinical prediction tool for Primary Ciliary Dyskinesia (PCD), with a specific focus on its significantly reduced sensitivity in patients with situs solitus (normal organ arrangement). Recent evidence from a 2025 study of 269 genetically confirmed PCD patients reveals an overall sensitivity of 75%, which drops to 61% in situs solitus cases compared to 95% in those with laterality defects. We explore the clinical and genetic factors underlying this performance gap, discuss implications for patient identification in research and drug development, and examine emerging diagnostic strategies to improve early detection of PCD across all phenotypic presentations.
Understanding PICADAR and the Situs Solitus Sensitivity Gap in PCD Diagnosis
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder inherited predominantly in an autosomal recessive manner, affecting the structure and function of motile cilia [1]. With an estimated prevalence ranging from 1:7,500 to 1:20,000 live births, PCD leads to impaired mucociliary clearance, resulting in recurrent respiratory tract infections, chronic rhinosinusitis, otitis media, bronchiectasis, and laterality defects [1] [2]. The diagnostic journey for PCD is fraught with challenges due to the absence of a single gold standard test, the genetic complexity involving more than 50 associated genes, and the significant phenotypic heterogeneity that characterizes the disease [1] [3]. This clinical and genetic variability often leads to delayed diagnosis, particularly in cases lacking classic features such as situs inversus [4] [2].
The PICADAR (Primary Ciliary Dyskinesia Rule) tool was developed to address these challenges by providing a clinical prediction rule to identify high-risk patients requiring specialized testing [5]. However, emerging research reveals critical limitations in its sensitivity, especially in patients with situs solitus (normal organ arrangement) and those without hallmark ultrastructural defects [4]. This technical analysis examines the clinical heterogeneity of PCD and evaluates the performance of diagnostic tools within the context of advancing diagnostic technologies.
Clinical Heterogeneity in PCD
The clinical presentation of PCD varies significantly among patients, influenced by the underlying genetic defect and the corresponding ultrastructural ciliary abnormality [1] [2].
Core Clinical Manifestations
- Neonatal Respiratory Distress: Over 80% of neonates with PCD experience respiratory symptoms within the first day of life, with term infants often requiring respiratory support despite the absence of lung immaturity [1].
- Chronic Respiratory Symptoms: Persistent daily wet cough beginning in infancy, chronic rhinitis, and recurrent lower respiratory tract infections are hallmark symptoms [1] [3].
- Otological Manifestations: Approximately 75-95% of patients experience recurrent otitis media, often leading to hearing impairment and frequently requiring interventions [1] [5].
- Laterality Defects: Approximately half of PCD patients exhibit situs inversus totalis, while 6-12% present with heterotaxy syndromes, which may be associated with complex congenital heart defects [1] [5].
Genetic and Ultrastructural Correlations
PCD exhibits extensive genetic heterogeneity, with mutations in more than 50 genes encoding various ciliary proteins [1]. Different genetic mutations lead to distinct ultrastructural defects that correlate with disease severity and clinical presentation:
Table 1: Genetic Mutations and Associated Ultrastructural Defects in PCD
| Ultrastructural Defect | Mutated Genes | Clinical Correlations |
|---|---|---|
| Outer Dynein Arm (ODA) defects | DNAH5, DNAI1, DNAI2, DNAL1, CCDC114, CCDC151, ARMC4 | Milder disease course; relatively preserved lung function in DNAH11 mutations [1] |
| ODA + Inner Dynein Arm (IDA) defects | DNAAF1-3, HEATR2, LRRC50, DYX1C1, ZMYND10, SPAG1 | Disrupted dynein arm assembly; combined functional impairment [1] |
| IDA defects + Microtubule Disorganization (MTD) | CCDC39, CCDC40 | More severe disease; pronounced bronchiectasis, poorer lung function [1] |
| Central Pair (CP) defects | HYDIN, RSPH9, RSPH4A | Abnormal swirling ciliary beating; no risk of situs inversus [1] |
Diagnostic Challenges in PCD
The diagnosis of PCD requires a multifaceted approach due to the absence of a single definitive test with high sensitivity and specificity [1]. This complexity is compounded by the phenomenon of secondary ciliary dyskinesia (SCD), where environmental factors such as respiratory infections or tobacco smoke cause temporary ciliary abnormalities that can mimic PCD [2] [6].
Diagnostic Modalities
Table 2: Diagnostic Methods for PCD Confirmation
| Diagnostic Method | Key Features | Limitations |
|---|---|---|
| Nasal Nitric Oxide (nNO) | Dramatically reduced levels (10-15% of normal) in most PCD patients [7] [3] | Difficult to measure in young children; requires specialized equipment and patient cooperation [7] [3] |
| High-Speed Video Microscopy Analysis (HSVA) | Evaluates ciliary beat pattern and frequency; abnormal patterns specific to PCD [1] [7] | Requires experienced personnel; subjective interpretation in borderline cases [7] |
| Transmission Electron Microscopy (TEM) | Considered gold standard; identifies ultrastructural defects [1] [8] | Invasive procedure; 30% of PCD cases have normal ultrastructure [7] [6] |
| Genetic Testing | Identifies mutations in >50 PCD-associated genes [1] [3] | Expensive; not all causative genes identified; variants of uncertain significance [1] |
Quantitative Analytical Approaches
Recent technological advances have introduced quantitative methods to improve diagnostic accuracy:
- Digital Ciliary Feature Counting: Software solutions enable standardized quantification of ciliary ultrastructure from TEM images, reducing human error and improving reproducibility [8] [6].
- Automated Ciliary Beat Pattern Analysis: Quantitative parameters such as "distance traveled by the cilium tip weighted by the percentage of beating ciliated edges" have demonstrated 96% sensitivity and 95% specificity in distinguishing PCD from non-PCD cases [7].
- PCD Quant Program: Automated analysis of ciliary ultrastructure that evaluates primary and secondary defects and analyzes mutual orientation of cilia in the ciliary border [6].
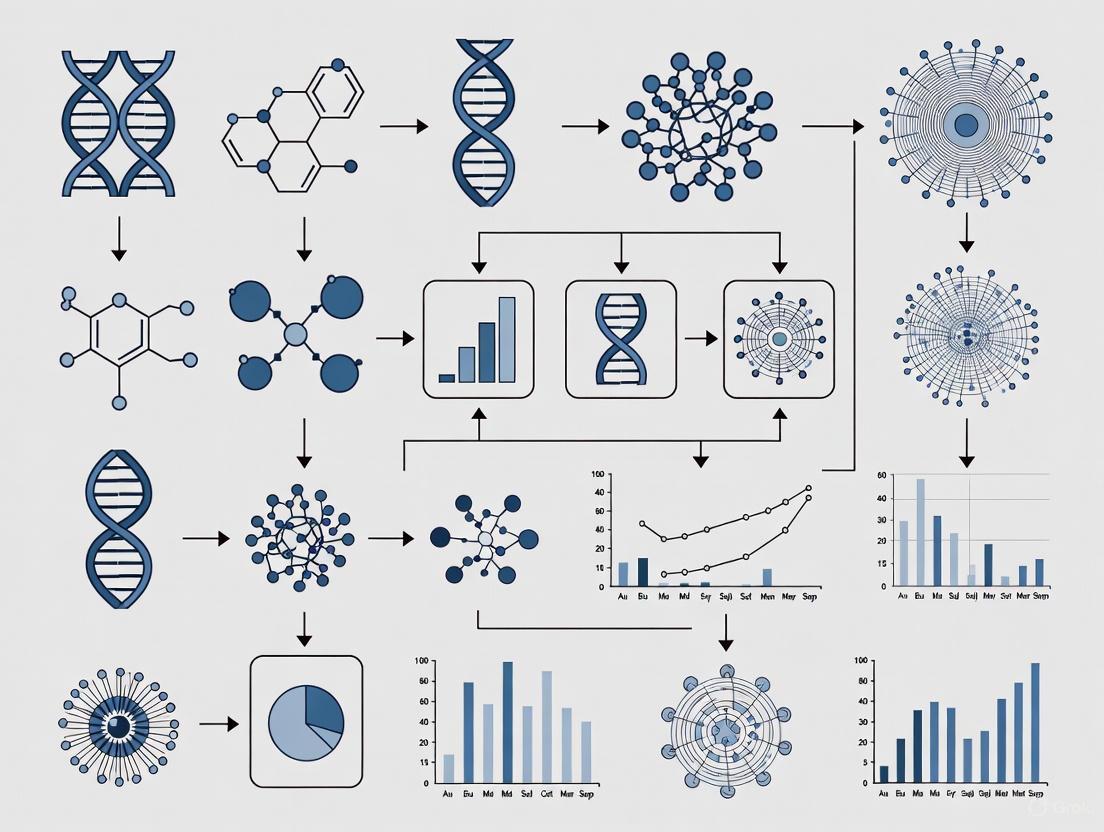
The following diagram illustrates the complex diagnostic pathway for PCD, highlighting the role of predictive tools like PICADAR within the overall workflow:
PICADAR Tool: Performance and Limitations in Situs Solitus
The PICADAR tool was developed to provide clinicians with a practical clinical prediction rule to identify patients requiring specialized PCD testing [5]. It consists of seven predictive parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care unit admission, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defects [9] [5].
Performance Characteristics
In initial validation studies, PICADAR demonstrated promising characteristics with a sensitivity of 0.90 and specificity of 0.75 at a cut-off score of 5 points, with area under the curve (AUC) values of 0.91 and 0.87 in internal and external validation, respectively [5].
However, recent research has revealed significant limitations in PICADAR's performance, particularly in specific patient subgroups:
Table 3: PICADAR Sensitivity Across Patient Subgroups
| Patient Subgroup | Sensitivity | Median PICADAR Score | Research Findings |
|---|---|---|---|
| Overall PCD Population | 75% | 7 (IQR: 5-9) | 7% of genetically confirmed PCD patients ruled out due to absence of daily wet cough [4] |
| Patients with Laterality Defects | 95% | 10 (IQR: 8-11) | Strong predictive value in classic PCD presentation [4] |
| Patients with Situs Solitus | 61% | 6 (IQR: 4-8) | Significantly reduced detection capability [4] |
| Patients without Hallmark Ultrastructural Defects | 59% | N/R | Limited identification of atypical PCD variants [4] |
Comparative Performance of Predictive Tools
Research comparing PICADAR with other predictive tools reveals important differences in their clinical utility:
Table 4: Comparison of PCD Predictive Tools
| Tool | Components | Advantages | Limitations |
|---|---|---|---|
| PICADAR | 7 parameters including laterality defects, neonatal symptoms, chronic rhinitis, ear symptoms [5] | Good overall accuracy in initial validation; simple scoring system [5] | Requires daily wet cough; lower sensitivity in situs solitus (61%); difficult to recall neonatal history in older patients [4] [3] |
| Clinical Index (CI) | 7-item questionnaire focusing on respiratory difficulties, rhinitis, pneumonia, bronchitis, otitis, nasal discharge, antibiotic use [3] | Does not require assessment of laterality or congenital heart defects; applicable without detailed neonatal history [3] | Less validated across diverse populations [3] |
| NA-CDCF | 4 criteria: laterality defects, unexplained neonatal respiratory distress, early-onset year-round nasal congestion, early-onset year-round wet cough [3] | Simple criteria; high specificity [3] | Lower sensitivity compared to other tools [3] |
A 2021 study demonstrated that the Clinical Index (CI) showed a larger area under the ROC curve compared to NA-CDCF, while no significant difference was found between PICADAR and NA-CDCF [3]. The combination of these clinical tools with nNO measurement further improved predictive power for all instruments [3].
Advanced Diagnostic Methodologies
Transmission Electron Microscopy Protocols
Standardized TEM analysis remains crucial for PCD diagnosis, with specific methodological requirements:
- Sample Preparation: Nasal brushings are fixed with 2.5% glutaraldehyde, post-fixed with osmium tetroxide, dehydrated in graded ethanol series, and embedded in araldite resin [8] [6].
- Sectioning and Imaging: Ultrathin sections (70-90 nm thickness) are cut, contrasted with uranyl acetate and lead citrate, and imaged at 25,000x magnification [8] [6].
- Quantitative Analysis: A minimum of 50 well-oriented ciliary cross-sections must be evaluated according to international consensus guidelines [8]. Defects are classified as:
- Class 1: Hallmark diagnostic defects (ODA defects, ODA+IDA defects, MTD+IDA defects)
- Class 2: Indicative of PCD diagnosis with other supporting evidence (central complex defects, microtubular disorganization with IDA present) [6].
High-Speed Video Microscopy Analysis
HSVA requires precise technical execution for reliable results:
- Sample Collection: Ciliated epithelium obtained via nasal brushing with 2-3 mm cytology brushes [7].
- Analysis Conditions: Examination within 3 hours at 37°C using an inverted microscope with oil immersion 100x objective [7].
- Recording Parameters: Digital recording at ≥355 frames per second, analyzing 20 distinct ciliated edges per sample [7].
- Quantitative Parameters: Includes ciliary beat frequency, beat pattern analysis, power stroke duration, recovery duration, and distance traveled by cilium tip per second [7].
The relationship between genetic defects, ultrastructural abnormalities, and functional consequences can be visualized as follows:
Research Reagent Solutions
Table 5: Essential Research Materials for PCD Diagnostic Investigations
| Reagent/Equipment | Application | Technical Function | Example Protocols |
|---|---|---|---|
| Glutaraldehyde (2.5%) | TEM sample fixation | Preserves ciliary ultrastructure by cross-linking proteins | Fixation overnight at 4°C [8] [6] |
| Osmium Tetroxide (1-2%) | TEM post-fixation | Stains and fixes lipid membranes for enhanced contrast | Incubation for 1 hour [8] [6] |
| Araldite Resin | TEM embedding | Provides stable matrix for ultrathin sectioning | Embedding at 65°C for 72 hours [8] |
| Uranyl Acetate & Lead Citrate | TEM contrasting | Heavy metal stains for electron density contrast | Staining for 7 and 5 minutes respectively [8] |
| Media 199/B1 BSA Medium | HSVA sample transport | Maintains ciliary viability and function post-collection | Examination within 3 hours at 37°C [7] |
| Niox Mino/Vero Analyzer | nNO measurement | Electrochemical detection of nasal nitric oxide | Aspiration at 5 mL·s⁻¹ via nasal olive [3] |
| Digital Ciliary Counters | TEM quantification | Standardized tallying of ciliary features | Automated Excel report generation [8] |
Primary Ciliary Dyskinesia presents significant diagnostic challenges due to its extensive clinical and genetic heterogeneity. While the PICADAR tool represents a valuable clinical prediction rule, its substantially reduced sensitivity in patients with situs solitus (61%) and those without hallmark ultrastructural defects (59%) limits its utility as a standalone screening method [4]. This performance gap highlights the critical need for continued refinement of predictive algorithms and the integration of multiple diagnostic approaches.
The future of PCD diagnosis lies in the development of more sophisticated predictive tools that incorporate quantitative analytical methods, genetic profiling, and standardized ultrastructural assessment. Such advances will be particularly crucial for identifying atypical PCD cases lacking classic features like laterality defects, ultimately reducing diagnostic delays and improving long-term patient outcomes through early intervention and specialized care.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary function, leading to impaired mucociliary clearance. Patients typically present with chronic respiratory symptoms beginning in early infancy, including persistent wet cough, recurrent chest infections, chronic rhinitis, and ear symptoms [5]. Approximately 50% of patients exhibit situs inversus, with 6%-12% having heterotaxic syndromes that may include complex congenital cardiac defects [5]. The diagnostic pathway for PCD is complex, requiring specialized equipment and expertise, creating significant barriers to timely diagnosis [5].
The PICADAR (PrImary CiliARy DyskinesiA Rule) score was developed to address this challenge by providing a simple, evidence-based clinical prediction tool. This tool helps identify symptomatic patients who should be referred for definitive PCD testing, potentially facilitating earlier diagnosis while conserving specialized diagnostic resources for high-probability cases [5].
Original Study Methodology
Study Population and Design
The original PICADAR development and validation study employed a two-center design [5]:
- Derivation Group: 641 consecutive patients referred to the University Hospital Southampton (UHS) PCD diagnostic center between 2007-2013
- Validation Group: 187 patients (93 PCD-positive, 94 PCD-negative) from Royal Brompton Hospital (RBH), selected to include similar numbers of positive and negative diagnoses
All participants had a definitive diagnostic outcome for PCD. Data collection utilized a standardized proforma completed by clinicians during clinical interviews prior to diagnostic testing [5].
Diagnostic Criteria for PCD
The diagnostic approach followed established UK guidelines requiring a typical clinical history plus at least two abnormal diagnostic tests [5]:
- "Hallmark" transmission electron microscopy (TEM) defects
- "Hallmark" ciliary beat pattern (CBP) abnormalities
- Nasal nitric oxide (nNO) ≤30 nL·min⁻¹
In cases with exceptionally strong clinical presentation (e.g., affected sibling, full clinical phenotype), diagnosis could be confirmed based on either hallmark TEM findings alone or repeated high-speed video microscopy analysis (HSVMA) consistent with PCD [5].
Statistical Analysis and Model Development
The analytical approach encompassed multiple stages [5]:
- Univariate Analysis: Compared characteristics of PCD-positive and PCD-negative referrals using t-tests, Mann-Whitney tests, chi-squared tests, or Fisher's exact tests as appropriate
- Predictor Selection: 27 potential clinical variables were evaluated for inclusion
- Model Development: Logistic regression with forward step-wise methods identified significant predictors
- Performance Assessment: Receiver operating characteristic (ROC) curve analysis evaluated discriminative ability
- Model Calibration: Hosmer-Lemeshow goodness-of-fit test assessed agreement between predicted probabilities and actual outcomes
The final model was simplified into a practical scoring tool (PICADAR) by rounding regression coefficients to the nearest integer [5].
The PICADAR Tool Parameters and Scoring
PICADAR applies specifically to patients with persistent wet cough and incorporates seven readily available clinical parameters [5]:
Table 1: PICADAR Scoring Parameters and Points
| Clinical Parameter | Points |
|---|---|
| Full-term gestation | 2 |
| Neonatal chest symptoms | 1 |
| Neonatal intensive care unit admission | 1 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 4 |
| Congenital cardiac defect | 2 |
Parameter Definitions
- Full-term gestation: ≥37 weeks gestation [5]
- Neonatal chest symptoms: Respiratory distress, tachypnea, or cough requiring medical attention during neonatal period [5]
- Neonatal intensive care admission: Any admission to special care baby unit [5]
- Chronic rhinitis: Persistent nasal symptoms lasting >3 months [5]
- Ear symptoms: Chronic serous otitis media, chronic ear perforation, or hearing loss [5]
- Situs inversus: Complete reversal of thoracic and abdominal organs [5]
- Congenital cardiac defect: Structural heart abnormalities present at birth [5]
Original Performance Metrics
The PICADAR score demonstrated strong performance characteristics in both derivation and validation populations [5]:
Table 2: PICADAR Performance Characteristics
| Metric | Derivation Group | Validation Group |
|---|---|---|
| Area Under Curve (AUC) | 0.91 | 0.87 |
| Recommended Cut-off Score | ≥5 points | ≥5 points |
| Sensitivity at Cut-off | 0.90 | Not specified |
| Specificity at Cut-off | 0.75 | Not specified |
| PCD Prevalence in Cohort | 12% (75/641) | 50% (93/187) |
The validation group differed from the derivation population in several respects: younger age (median 3 years vs. 9 years), higher proportion of non-white patients, and greater consanguinity prevalence [5].
Contemporary Research on PICADAR Limitations
Recent evidence has highlighted important limitations in PICADAR's sensitivity, particularly in specific PCD subpopulations.
A 2025 study analyzing 269 genetically confirmed PCD patients found PICADAR's overall sensitivity was 75% when applying the recommended ≥5 points threshold [4]. Performance varied substantially across clinical subgroups:
Table 3: PICADAR Sensitivity by Patient Subgroup
| Patient Subgroup | Sensitivity | Median Score |
|---|---|---|
| All Genetically Confirmed PCD | 75% (202/269) | 7 (IQR: 5-9) |
| With Laterality Defects | 95% | 10 (IQR: 8-11) |
| With Situs Solitus | 61% | 6 (IQR: 4-8) |
| With Hallmark Ultrastructural Defects | 83% | Not specified |
| Without Hallmark Ultrastructural Defects | 59% | Not specified |
Critically, 7% of genetically confirmed PCD patients were automatically excluded from PICADAR assessment due to absence of daily wet cough, a mandatory starting criterion [4]. This finding highlights a significant limitation in the tool's applicability to all PCD presentations.
A 2023 Korean multicenter study of 41 PCD patients further demonstrated real-world variability in PICADAR performance, with only 15 of 41 patients (37%) scoring above the 5-point threshold [10]. This suggests potential ethnic or geographic variations in PCD presentation that may affect tool performance.
Experimental Protocols for PICADAR Validation
Patient Recruitment and Data Collection
The original PICADAR validation protocol specified these key methodologies [5]:
- Consecutive Recruitment: All patients referred for PCD testing were considered for inclusion
- Prospective Data Collection: Clinical history proforma completed prior to diagnostic testing
- Blinding: Clinicians completing proformas were unaware of final diagnostic outcome
- Comprehensive Clinical Data: Included neonatal history, respiratory symptoms, otological symptoms, laterality abnormalities, and family history
Diagnostic Confirmation Protocol
The original study employed this rigorous diagnostic workflow:
Research Reagent Solutions
Table 4: Essential Research Materials for PCD Diagnostic Studies
| Reagent/Equipment | Function in PCD Diagnosis | Technical Specifications |
|---|---|---|
| Transmission Electron Microscope | Visualization of ciliary ultrastructural defects | High-resolution imaging of dynein arms, microtubule arrangement |
| High-Speed Video Microscopy System | Analysis of ciliary beat pattern and frequency | Capable of ≥500 frames per second capture |
| Nasal Nitric Oxide Analyzer | Measurement of nNO levels for screening | Chemiluminescence technology, cutoff ≤30 nL·min⁻¹ |
| Nasal Mucosal Biopsy Brush | Collection of ciliated epithelial cells | Flexible cytology brush for inferior turbinate sampling |
| Cell Culture Materials | Ciliary differentiation at air-liquid interface | DMEM/F-12 medium, fetal bovine serum, antibiotic-antimycotic |
The PICADAR score represents a clinically valuable prediction tool that successfully identifies high-probability PCD candidates using readily available clinical data. Its development through rigorous methodology and validation in independent populations supports its utility in resource-optimization for PCD diagnosis.
However, emerging evidence indicates significant limitations in sensitivity for patients with situs solitus (61%) and those without hallmark ultrastructural defects (59%) [4]. These findings underscore the critical need for complementary diagnostic approaches, particularly as genetic testing reveals broader phenotypic diversity in PCD. Future research should focus on refining predictive tools to capture the full spectrum of PCD presentation, especially for patients without classic laterality defects.
Primary Ciliary Dyskinesia (PCD) is a rare autosomal recessive disorder caused by mutations affecting motile cilia function, with an estimated prevalence of 1 in 16,000 individuals [11]. The clinical presentation of PCD encompasses a spectrum of laterality defects resulting from dysfunctional motile cilia during embryonic development, particularly at the embryonic node where they establish left-right asymmetry [12] [11]. This abnormal ciliary function during embryogenesis leads to random determination of organ positioning, resulting in either normal arrangement (situs solitus), complete mirror-image reversal (situs inversus totalis), or ambiguous arrangement (situs ambiguus) [13] [12]. Understanding this spectrum is crucial for researchers and clinicians, as the type of laterality defect influences diagnostic approaches, clinical management, and prognostic outcomes.
The historical recognition of the connection between laterality defects and respiratory disease dates to 1933, when Manes Kartagener described the triad of chronic sinusitis, bronchiectasis, and situs inversus totalis, subsequently termed Kartagener syndrome [12]. Contemporary research has revealed that approximately 50% of PCD patients exhibit situs inversus totalis, while another subset presents with situs ambiguus and heterotaxy syndromes [11]. The genetic basis of PCD involves mutations in over 50 genes encoding proteins essential for ciliary structure and function, with different genetic subtypes correlating with varying ultrastructural defects and clinical manifestations [12] [11].
Table 1: Classification of Laterality Patterns in PCD
| Laterality Category | Definition | Approximate Prevalence in PCD | Key Characteristics |
|---|---|---|---|
| Situs Solitus (SS) | Normal arrangement of thoracic and abdominal organs | 46.9% [11] | Normal asymmetry; left lung bilobed, right lung trilobed; left-sided cardiac apex and stomach |
| Situs Inversus Totalis (SI) | Complete mirror-image reversal of thoracic and abdominal organs | 41.0% [11] | Total reversal of organ positioning; generally not associated with congenital heart defects |
| Situs Ambiguus (SA) | Ambiguous arrangement with elements of both situs solitus and inversus | 12.1% [11] | Often associated with complex congenital heart disease and other malformations |
Diagnostic Challenges: PICADAR Tool and Situs Solitus Sensitivity
The PICADAR (PCD Inclusion Criteria And Diagnostic ARtificial intelligence) tool represents a clinical prediction rule developed to identify patients requiring specialized PCD testing [9]. This diagnostic predictive tool incorporates seven clinical parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care admission, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defects [9]. Each parameter is assigned a points value, with a recommended cutoff score of ≥5 points indicating high suspicion for PCD and warranting further diagnostic investigation [9]. While initially validated with promising accuracy (sensitivity 0.90, specificity 0.75), recent research has revealed significant limitations in its sensitivity, particularly for patients with situs solitus [4].
A critical evaluation of PICADAR in a genetically confirmed PCD cohort demonstrated an overall sensitivity of 75%, with stark contrasts between different patient subgroups [4]. The tool performed excellently in patients with laterality defects (95% sensitivity), but showed markedly reduced detection capability for patients with situs solitus (61% sensitivity) [4]. This substantial discrepancy highlights a critical diagnostic gap, as nearly half of all PCD patients present with situs solitus [11]. The tool's initial question about persistent daily wet cough further compounds this limitation, as 7% of genetically confirmed PCD patients reported no daily wet cough and would be automatically excluded from further evaluation using the standard PICADAR protocol [4].
Table 2: PICADAR Performance Across Situs Subgroups
| Patient Subgroup | Sensitivity | Median PICADAR Score | Implications for Diagnosis |
|---|---|---|---|
| All PCD Patients | 75% [4] | 7 (IQR: 5-9) [4] | 1 in 4 PCD patients missed |
| With Laterality Defects | 95% [4] | 10 (IQR: 8-11) [4] | Excellent detection capability |
| With Situs Solitus | 61% [4] | 6 (IQR: 4-8) [4] | Nearly 40% of cases potentially missed |
| With Hallmark Ultrastructural Defects | 83% [4] | N/R | Better detection than those without |
| Without Hallmark Ultrastructural Defects | 59% [4] | N/R | Over 40% of cases potentially missed |
The suboptimal performance of PICADAR in situs solitus patients has profound implications for PCD diagnosis and research. This population often experiences significant diagnostic delays due to the absence of the clinically obvious laterality defects that prompt earlier investigation [12]. Furthermore, the sensitivity limitations extend beyond situs status to include patients with specific ultrastructural defects, as those without hallmark electron microscopic abnormalities demonstrated only 59% sensitivity [4]. These findings underscore the necessity for improved predictive tools that can better identify PCD across the entire clinical spectrum, particularly for those without classic laterality defects.
Methodologies for Comprehensive PCD Diagnosis
Establishing a definitive PCD diagnosis requires a multifaceted approach combining clinical evaluation with specialized laboratory techniques. The following experimental protocols represent current gold-standard methodologies for PCD diagnosis and characterization, particularly relevant for research settings and clinical trials.
Nasal Nitric Oxide (nNO) Measurement Protocol
Nasal nitric oxide measurement serves as a valuable screening tool due to significantly reduced nNO levels in most PCD patients [11]. The standardized protocol involves:
- Equipment Setup: Chemiluminescence analyzers (CLD 88 series, NIOX Flex, or Sievers NOA 280i) calibrated according to manufacturer specifications [11].
- Participant Preparation: Avoidance of nasal manipulation, topical medications, and vigorous exercise for 24 hours prior to testing. Confirmation of no current upper respiratory infection [11].
- Measurement Technique:
- For cooperative participants (typically >5 years): Measurements obtained during a 5-second plateau while exhaling through a resistor against closed velum. Reported values represent the mean of three maneuvers for each naris [11].
- For younger or uncooperative participants: Tidal breathing measurements, using the mean of the five highest tidal peaks from each naris [11].
- Interpretation Criteria: Velum closure nNO values <77 nL/min and tidal breathing nNO values <40 nL/min are considered indicative of PCD [11].
Transmission Electron Microscopy (TEM) Protocol
Ciliary ultrastructural analysis remains a cornerstone of PCD diagnosis, performed as follows:
- Sample Collection: Nasal epithelial biopsy obtained via brushing or curettage from the inferior turbinate or nasal floor [11].
- Sample Processing: Immediate fixation in glutaraldehyde followed by osmium tetroxide post-fixation, dehydration in graded ethanol series, and embedding in resin [11].
- Imaging and Analysis: Ultrathin sections (60-90nm) examined using transmission electron microscope (e.g., Zeiss EM900). Photomicrographs reviewed independently by multiple blinded observers [11].
- Defect Classification: Hallmark defects categorized as outer dynein arm (ODA) defects, inner dynein arm (IDA) defects, combined ODA+IDA defects, or central apparatus (CA) defects with microtubular disorganization [11].
Genetic Analysis Protocol
Genetic testing provides definitive diagnosis and is essential for understanding genotype-phenotype correlations:
- DNA Extraction: High-quality DNA isolated from blood or saliva samples using standardized extraction kits [11].
- Testing Approach:
- First-tier: Simultaneous DNA methylation analysis and oligo-SNP combination array (OSA) to identify 15q11.2-q13 deletions and uniparental disomy [14].
- Second-tier: DNA polymorphism testing for cases with abnormal methylation but no deletion detected [14].
- Targeted Gene Panels: Next-generation sequencing panels for known PCD-associated genes (DNAI1, DNAH5, DNAAF2, CCDC39, CCDC40, etc.) based on ultrastructural findings [11].
- Variant Interpretation: Sequence variants classified according to ACMG guidelines, with confirmation of biallelic mutations in trans configuration [11].
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Essential Research Materials for PCD Investigation
| Research Tool Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| nNO Measurement Systems | Eco Medics CLD 88 series, Aerocrine NIOX Flex, Sievers NOA 280i [11] | Quantitative assessment of nasal nitric oxide production as PCD screening tool | Requires standardized protocols and age-appropriate reference values |
| Electron Microscopy Equipment | Zeiss EM900 transmission electron microscope [11] | Ultrastructural analysis of ciliary axonemal defects | Expertise in sample preparation and interpretation essential; potential for secondary damage |
| Genetic Analysis Platforms | Oligo-SNP combination arrays, MS-MLPA, DNA methylation analysis, next-generation sequencing panels [14] [11] | Identification of PCD-causing mutations and determination of molecular etiology | Enables genotype-phenotype correlations; requires functional validation of novel variants |
| Cell Culture Models | Air-liquid interface (ALI) cultures of primary respiratory epithelial cells [11] | Functional ciliary assessment and personalized therapeutic testing | Maintains ciliated differentiation but requires specialized culture conditions |
| High-Speed Video Microscopy Analysis | Digital high-speed video systems with motion analysis software [11] | Quantitative assessment of ciliary beat frequency and pattern | Critical for functional confirmation; requires immediate analysis post-collection |
The research toolkit for PCD investigation has evolved significantly, enabling more precise characterization of the disorder's heterogeneous manifestations. Genetic analysis platforms now facilitate comprehensive mutation detection across multiple PCD-associated genes, with oligo-SNP combination arrays particularly valuable for detecting deletions and uniparental disomy [14]. Functional assessment tools, including high-speed video microscopy and cell culture models, provide critical insights into ciliary dynamics and enable personalized therapeutic testing [11]. The integration of these methodologies allows researchers to establish robust genotype-phenotype correlations, essential for understanding the spectrum of clinical presentations across different situs arrangements.
The spectrum of laterality defects in PCD represents a compelling model for understanding the complex relationship between genetic mutations, ciliary function, and embryonic development. The significant limitations of current diagnostic tools like PICADAR in identifying situs solitus cases underscore the pressing need for more sophisticated predictive algorithms that incorporate genetic, ultrastructural, and functional data beyond clinical features alone [4]. Future research should prioritize the development of next-generation diagnostic approaches that leverage multi-omics technologies and artificial intelligence to improve detection accuracy across all PCD subtypes.
From a therapeutic perspective, the varying clinical presentations between situs subgroups may necessitate tailored management strategies. The high prevalence of congenital heart disease in the situs ambiguus population (approximately 4.9% with complex cardiac defects) demands specialized cardiopulmonary management protocols [11]. Additionally, the relationship between specific genetic mutations and laterality outcomes offers opportunities for personalized medicine approaches in PCD. As novel therapies targeting specific molecular defects emerge, understanding how these interventions affect patients across the laterality spectrum will be crucial for optimizing therapeutic efficacy and improving long-term outcomes for all PCD patients.
Genetic Diversity and Ultrastructural Variations in PCD Pathophysiology
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous, inherited disorder resulting from impaired ciliary function, leading to chronic oto-sino-pulmonary disease, laterality defects, and infertility [1]. With over 50 identified causative genes, predominantly inherited in an autosomal recessive pattern, PCD exhibits remarkable genetic diversity that manifests in distinct ultrastructural ciliary defects and varied clinical phenotypes [1] [15]. This complex relationship between genotype, ciliary ultrastructure, and clinical presentation presents significant challenges for diagnosis and prognosis, necessitating a sophisticated, multimodal diagnostic approach [16]. Understanding these genotype-phenotype correlations is particularly crucial within the context of PICADAR (PrImary CiliARy DyskinesiA Rule) score application, especially regarding its sensitivity in patients with situs solitus (normal organ arrangement) compared to those with situs inversus [17] [18]. This technical review comprehensively examines the genetic landscape of PCD, its corresponding ultrastructural variations, and the implications for diagnostic strategies and future therapeutic development.
Genetic Landscape of PCD
Inheritance Patterns and Molecular Genetics
PCD is primarily an autosomal recessive disorder, though X-linked recessive forms (involving genes such as DNAAF6 and RPGR) and autosomal dominant forms (involving FOXJ1) have also been documented [19] [16]. The genetic landscape is characterized by extensive heterogeneity, with pathogenic variants in more than 50 genes accounting for approximately 60-70% of diagnosed cases [15] [16]. These genes encode proteins critical for the proper assembly, structure, and function of motile cilia. The axoneme, the core structural component of motile cilia, has a conserved "9+2" microtubule arrangement: nine peripheral microtubule doublets encircling a central pair of single microtubules [1] [16]. The peripheral doublets feature outer dynein arms (ODA) and inner dynein arms (IDA), which are molecular motors essential for ciliary beating. These structures are interconnected by nexin links and connected to the central pair by radial spokes [1].
Major Genetic Variants and Population-Specific Distributions
The distribution of PCD-causing genes varies significantly across different ethnic and geographic populations, influencing both clinical presentation and diagnostic strategies.
Table 1: Major PCD-Associated Genes and Their Ultrastructural Correlates
| Gene | Ultrastructural Defect | Protein Function | Population Notes |
|---|---|---|---|
| DNAH5 [1] | ODA Defect | Dynein Heavy Chain | Most common genetic cause in multiple populations [19] [18] [16] |
| DNAH11 [1] | Normal Ultrastructure | Dynein Heavy Chain | Associated with relatively preserved lung function [1] |
| RSPH1 [16] | Central Pair (CP) Defect | Radial Spoke Head | Associated with a severe phenotype in Spanish cohort [16] |
| CCDC39/CCDC40 [1] | IDA Defect + Microtubule Disorganization (MTD) | Nexin-Dynein Regulatory Complex | More severe disease course, early bronchiectasis [1] |
| HYDIN [1] | Central Pair (CP) Defect | Central Pair Projection Protein | No risk for situs inversus [1] |
| RSPH9/RSPH4A [1] | Central Pair (CP) Defect | Radial Spoke Protein | No risk for situs inversus [1] |
| DNAAF1-3, LRRC6 [1] | ODA + IDA Defect | Dynein Arm Assembly Factor | Defects in cytoplasmic assembly of dynein arms |
Table 2: Regional Variations in Common PCD Genes
| Region/Population | Common Genes | Key Findings |
|---|---|---|
| Central China [19] | DNAH5 (46.2%), DNAH11 (23.1%) | High male predominance; lower incidence of situs inversus (46.7%) |
| Southwest Saudi Arabia [18] | DNAH5 (17.9%), RSPH9 (14.3%), DNAI2 (14.3%) | High consanguinity; 64% had neonatal respiratory distress |
| Egypt [15] | Various (16 genes identified) | 91.9% consanguinity; ODA defects most common (32%) |
| Japan [17] | Not specified in abstract | Situs inversus in only 25% of patients, suggesting different major genes |
| Spain [16] | DNAH5, RSPH1, DNAH11 | RSPH1 associated with a severe phenotype, contrary to previous reports |
Ultrastructural Defects and Functional Impairments
The ultrastructural defects observed via transmission electron microscopy (TEM) provide a critical link between genetic mutations and clinical dysfunction. These defects are categorized into hallmark (class 1) and supportive (class 2) abnormalities [16].
- Outer Dynein Arm (ODA) Defects: Result from mutations in genes such as DNAH5, DNAI1, DNAI2, and CCDC114 [1]. These defects lead to absent or shortened ODAs, reducing ciliary beat frequency and often associated with a relatively milder disease course [1].
- Combined ODA and IDA Defects: Caused by mutations in dynein arm assembly factors (e.g., DNAAF1-3, LRRC6), leading to the absence of both motor complexes and severe ciliary immotility or profound hypomotility [1].
- Inner Dynein Arm (IDA) Defects with Microtubule Disorganization: Associated with mutations in CCDC39 and CCDC40, which disrupt the organization of the axonemal microtubules and radial spokes [1]. This results in a stiff, uncoordinated beating pattern and is correlated with a more severe clinical phenotype, including early-onset bronchiectasis [1].
- Central Apparatus Defects: Involve abnormalities of the central pair (CP) of microtubules or radial spokes, associated with mutations in HYDIN, RSPH9, RSPH4A, and RSPH1 [1] [16]. These defects cause an abnormal, swirling ciliary beat pattern rather than complete immotility. Notably, these defects do not cause laterality defects like situs inversus, as the embryonic nodal cilia lack a central pair [1].
Approximately 30% of PCD cases have normal ciliary ultrastructure despite clear functional and genetic evidence of disease, highlighting the limitations of TEM and the necessity for complementary diagnostic techniques [15] [16].
Diagnostic Approaches and Experimental Protocols
Multimodal Diagnostic Framework
No single test serves as a gold standard for PCD diagnosis. A combination of techniques is required to achieve a definitive diagnosis, as recommended by European and North American guidelines [1] [15] [16]. The following core methodologies form the basis of a comprehensive PCD diagnostic workup.
High-Speed Video Microscopy Analysis (HSVA)
Protocol [16]:
- Sample Collection: Ciliated nasal epithelial cells are obtained via nasal brushing and immediately placed in high-glucose DMEM supplemented with antibiotics.
- Imaging: Samples are observed at room temperature using a conventional microscope equipped with a high-speed video camera (e.g., Basler acA1300-200um), recording at a minimum of 120 frames per second under 63x magnification.
- Analysis: Recordings are analyzed using software like the Sisson-Ammons Video Analysis (SAVA) system. Ciliary beat pattern (CBP) and ciliary beat frequency (CBF) are assessed by at least two independent observers.
- Interpretation: Samples are classified as:
- Normal: Coordinated, metachronal wave movement.
- Immotile: Complete absence of movement.
- Dyskinetic: Abnormal, uncoordinated, or stiff beating patterns.
HSVA is highly sensitive but can be confounded by secondary ciliary dyskinesia due to infection or inflammation [16].
Transmission Electron Microscopy (TEM)
- Processing: Nasal brush biopsies or mucosal samples are fixed in glutaraldehyde, post-fixed in osmium tetroxide, dehydrated, and embedded in resin.
- Sectioning: Ultrathin sections (60-90 nm) are cut using an ultramicrotome and mounted on grids.
- Staining: Grids are stained with heavy metals (e.g., uranyl acetate and lead citrate) to enhance contrast.
- Imaging and Analysis: Samples are visualized under a transmission electron microscope. A minimum of 50-100 well-oriented ciliary cross-sections are examined for hallmark defects (e.g., absent ODAs, IDAs, or central apparatus defects) [16].
Genetic Analysis
- DNA Extraction: Genomic DNA is extracted from peripheral blood samples using standardized kits.
- Next-Generation Sequencing (NGS): The most common approach is using a targeted PCD gene panel or whole-exome sequencing (WES). Libraries are prepared (e.g., using Agilent SureSelect capture) and sequenced on platforms like Illumina or DNBSEQ-T7.
- Bioinformatic Analysis: Sequence reads are aligned to a reference genome (e.g., hg19). Variants are called and annotated using pipelines involving tools like BWA, Sentieon, and ANNOVAR.
- Variant Interpretation: Variants are filtered against population databases (e.g., gnomAD) and classified according to ACMG/AMP guidelines. Pathogenic and likely pathogenic variants in trans (on both alleles of a gene) confirm the diagnosis. Segregation analysis in family members can be performed for validation.
Immunofluorescence (IF) Analysis
Protocol [15]:
- Sample Preparation: Nasal brushing samples are smeared onto glass slides, fixed, and permeabilized.
- Antibody Staining: Slides are incubated with primary antibodies against specific ciliary proteins (e.g., monoclonal mouse anti-DNAH5, polyclonal rabbit anti-GAS8). Fluorescently labeled secondary antibodies are then applied.
- Imaging and Analysis: Samples are visualized using a fluorescence microscope. The absence or abnormal localization of the target protein, compared to healthy controls, confirms the pathogenicity of a genetic variant and the specific defect.
The logical workflow for diagnosis and the relationship between genetic defects and ciliary ultrastructure can be visualized as follows:
Diagram 1: Integrated Diagnostic Workflow for PCD. A multimodal approach is essential, combining clinical scores like PICADAR with functional (HSVA, nNO), structural (TEM), and molecular (Genetics, IF) tests to confirm a diagnosis.
Diagram 2: Genotype to Phenotype Correlation in PCD. Genetic mutations lead to specific protein defects, which manifest as distinct ultrastructural abnormalities. These defects cause characteristic ciliary dysfunction, ultimately driving the clinical disease presentation and informing the diagnostic pathway.
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Reagents and Materials for PCD Research
| Reagent/Material | Function/Application | Example Usage in Protocols |
|---|---|---|
| Nasal Brush Biopsy Kit | Collection of ciliated nasal epithelial cells | Sample collection for HSVA, TEM, and IF [15] [16] |
| High-Glucose DMEM with Antibiotics | Transport and short-term maintenance of cell viability | Preservation of ciliary function post-collection for HSVA [16] |
| Glutaraldehyde Fixative | Cross-linking and preservation of ultrastructure | Primary fixation of samples for TEM analysis [16] |
| Anti-Ciliary Protein Antibodies | Specific labeling of ciliary components | IF staining to confirm protein localization (e.g., anti-DNAH5) [15] |
| NGS Gene Panels (PCD-specific) | Targeted sequencing of known PCD genes | Genetic confirmation of diagnosis; identifies known and novel variants [19] [18] |
| DNA Extraction Kits | Isolation of high-quality genomic DNA | Preparation of DNA for genetic sequencing [19] [18] |
Implications for PICADAR Score and Situs Solitus
The PICADAR score is a validated clinical prediction tool that uses symptoms like neonatal respiratory distress, chronic cough, and situs inversus to identify patients at high risk for PCD [18]. However, the score's sensitivity is inherently influenced by population genetics. In populations where genes causing situs solitus (normal arrangement) are more prevalent, the PICADAR score's sensitivity may be reduced.
- Genetic Influence on Laterality: Defects in genes that disrupt the function of embryonic nodal cilia (which lack a central pair) cause randomization of left-right body asymmetry [1]. Consequently, patients with mutations in central apparatus genes (e.g., RSPH9, RSPH4A, HYDIN) almost exclusively have situs solitus [1].
- Regional Variations: The Japanese PCD cohort demonstrated a strikingly low rate of situs inversus (25%), directly challenging the classic teaching that 50% of PCD patients have this finding and indicating a different genetic background [17]. Similarly, a Chinese cohort reported a lower incidence of situs inversus (46.7%) [19].
- Impact on PICADAR: A study from Saudi Arabia confirmed that patients with PCD and situs inversus had a significantly higher median PICADAR score (11.5) than those with situs solitus (7.5) [18]. This demonstrates that in regions with a high prevalence of central apparatus or other situs solitus-associated gene mutations, reliance on the PICADAR score alone may miss a substantial number of patients.
Therefore, the genetic and ultrastructural diversity of PCD must be considered when applying clinical screening tools, underscoring the need for population-specific validation and a low threshold for advanced diagnostic testing even in patients with situs solitus.
The pathophysiology of PCD is defined by a profound genetic diversity that directly dictates the ultrastructural and functional pathology of motile cilia. A deep understanding of the correlations between specific genetic mutations (e.g., DNAH5, CCDC40, RSPH1), their resulting ultrastructural defects (e.g., ODA loss, microtubular disorganization), and the consequent clinical phenotypes is paramount for advancing the field. This knowledge is critical not only for refining diagnostic algorithms and interpreting tools like the PICADAR score in the context of situs solitus but also for paving the way for genotype-specific therapeutic interventions. Future research must focus on elucidating the remaining genetic causes of PCD, standardizing multimodal diagnostic protocols globally, and developing targeted treatments that address the underlying molecular defects in this complex and heterogeneous disease.
The Critical Role of Predictive Tools in PCD Research and Clinical Trials
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder affecting motile cilia, with an estimated prevalence of 1 in 7,554 to 1 in 40,000 individuals [20] [10]. This ciliopathy results in impaired mucociliary clearance, leading to chronic and progressive oto-sino-pulmonary disease, laterality defects, and infertility [1] [10]. The diagnostic journey for PCD patients is often protracted, with a median age of diagnosis at 5 years in the U.S., though this varies significantly across populations [21] [10]. Such delays occur despite the fact that over 80% of neonates with PCD require respiratory support within the first day of life and symptoms typically begin in infancy [1]. This diagnostic odyssey poses substantial challenges for clinical management and trial recruitment alike.
The complex genetic landscape of PCD, with mutations in over 50 identified genes, coupled with the absence of a single gold-standard diagnostic test, creates formidable barriers for timely identification and intervention [22] [1]. Diagnostic confirmation requires specialized testing available only at reference centers, including nasal nitric oxide measurement, high-speed video microscopy analysis, transmission electron microscopy, and genetic testing [5] [1] [10]. These resource-intensive modalities are inaccessible to many patients, contributing to significant underdiagnosis. It is estimated that while approximately 45,000 individuals in North America live with PCD, only about 1,000 have been diagnosed [20]. This stark diagnostic gap underscores the critical need for accessible predictive tools that can identify candidates for definitive testing and stratify disease risk and progression.
Established Clinical Prediction Tools: Performance and Limitations
PICADAR: Development and Validation
The Primary Ciliary Dyskinesia Rule (PICADAR) represents one of the first systematic attempts to create a practical clinical diagnostic tool for PCD. Developed by Behan et al. in 2016, this prediction rule was designed to guide non-specialists in identifying patients who warrant referral for specialized PCD testing [5]. The tool was derived from a study of 641 consecutive patients referred for PCD testing, of which 75 (12%) received a positive diagnosis. Through logistic regression analysis, seven readily obtainable clinical parameters were identified as predictive of PCD [5] [9].
The PICADAR tool applies specifically to patients with persistent wet cough and evaluates the following parameters:
- Full-term gestation
- Neonatal chest symptoms
- Neonatal intensive care unit admission
- Chronic rhinitis
- Chronic ear symptoms
- Situs inversus
- Congenital cardiac defect
In its original validation, PICADAR demonstrated a sensitivity of 0.90 and specificity of 0.75 at a cutoff score of 5 points, with an area under the curve (AUC) of 0.91 in the derivation cohort and 0.87 in an external validation cohort [5]. This performance suggested strong potential for clinical implementation as a screening tool.
Table 1: PICADAR Scoring System and Original Performance Metrics
| Parameter | Points | Original Sensitivity | Original Specificity |
|---|---|---|---|
| Full-term gestation | 1 | 0.90 | 0.75 |
| Neonatal chest symptoms | 1 | ||
| Neonatal intensive care admission | 1 | ||
| Chronic rhinitis | 1 | ||
| Chronic ear symptoms | 2 | ||
| Situs inversus | 2 | ||
| Congenital cardiac defect | 3 | ||
| Total Possible Score | 11 |
Contemporary Limitations and Phenotypic Challenges
Recent evidence has revealed significant limitations in PICADAR's performance across PCD subpopulations. A 2025 study by Omran et al. evaluating 269 genetically confirmed PCD patients found substantially lower overall sensitivity of 75% compared to the original validation [4]. Most notably, the tool demonstrated markedly reduced sensitivity in key subgroups: only 61% in patients with situs solitus (normal organ arrangement) and 59% in those without hallmark ultrastructural defects on electron microscopy [4].
A critical design limitation identified in the study is PICADAR's initial question about daily wet cough: 18 individuals (7%) in their genetically confirmed PCD cohort reported no daily wet cough and would have been automatically excluded from further evaluation according to the tool's algorithm [4]. This finding challenges the tool's fundamental assumption about universal symptom presentation.
The same study revealed that PICADAR performance varied significantly based on associated ciliary ultrastructure, with higher sensitivity in patients with hallmark defects (83%) compared to those without (59%) [4]. This structural heterogeneity corresponds with the extensive genetic diversity in PCD, where different genotypes manifest distinct ultrastructural defects and clinical phenotypes [1].
Table 2: Contemporary PICADAR Performance Across PCD Subgroups
| Patient Subgroup | Sensitivity | Median Score (IQR) | Study |
|---|---|---|---|
| Overall PCD population | 75% | 7 (5-9) | Omran et al., 2025 |
| With laterality defects | 95% | 10 (8-11) | Omran et al., 2025 |
| With situs solitus | 61% | 6 (4-8) | Omran et al., 2025 |
| With hallmark ultrastructural defects | 83% | - | Omran et al., 2025 |
| Without hallmark ultrastructural defects | 59% | - | Omran et al., 2025 |
| Korean PCD cohort (multicenter study) | 36.6% (≥5 points) | - | Ahn et al., 2023 |
These findings carry profound implications for clinical trials and research. The systematic under-identification of patients without classic laterality defects or specific ultrastructural abnormalities may introduce selection bias in study populations, potentially skewing trial results and limiting generalizability. Furthermore, the delayed diagnosis of these subpopulations may affect their response to interventions, particularly if earlier treatment might have altered disease progression.
Emerging Methodologies: Machine Learning and Genotype-Specific Tools
Machine Learning Approaches for PCD Screening
Novel machine learning (ML) approaches are emerging to address the limitations of rule-based clinical prediction tools. A 2025 feasibility study demonstrated the application of a random forest model to screen for PCD using data from the PCD Foundation Registry and a national claims database [20] [22]. This approach utilized diagnostic, procedural, and pharmaceutical codes associated with PCD to develop ML features for classification.
The study employed several technical innovations to overcome the challenges of rare disease screening:
- Privacy-preserving record linkage via tokenization to connect registry and claims data while maintaining patient confidentiality
- Feature engineering that captured temporal patterns in healthcare utilization, including:
- "PRESENCE" scoring for permanent conditions
- "COUNT" scoring for serious clinical events
- "COVERAGE" scoring for chronic conditions based on appearance across 2-week periods
- Addressing class imbalance through synthetic data augmentation and expanded case definitions
The model demonstrated promising performance characteristics suitable for screening applications. Using 82 confirmed PCD cases and 4,161 matched controls, the initial model achieved a sensitivity of 0.75-0.94 and positive predictive value (PPV) of 0.45-0.73 [22]. When expanded to include 319 patients with suggestive clinical codes (Q34.8+EM) and 8,214 controls, performance improved to sensitivity of 0.82-0.90 and PPV of 0.51-0.54 [20] [22]. When applied to a cohort of 1.32 million pediatric patients, the model identified 7,705 positive cases, corresponding to a prevalence of 1:7,554 that aligns with PCD epidemiological estimates [22].
Figure 1: Machine Learning Workflow for PCD Screening. This diagram illustrates the data sources, feature engineering approaches, and model development process for machine learning-based PCD identification.
Genotype-Specific Predictive and Prognostic Tools
Beyond screening and diagnosis, predictive tools are emerging for prognosis and disease management. The RSPH4A-PCDx (Predicted Capacity Decline Index), developed in 2025, represents a novel genotype-specific tool designed to predict lung function decline in patients with RSPH4A-associated PCD [21]. This tool was developed through retrospective analysis of a genetically homogeneous Puerto Rican cohort with the RSPH4A [c.921+3_6delAAGT] founder variant, which accounts for over 69% of PCD cases in this population [21].
The PCDx tool was developed using longitudinal spirometry data from 25 patients, generating 254 measurements. Analysis revealed a median annual FEV1 decline of -0.75% predicted, with significantly lower lung function at diagnosis in adults (median FEV1 48% predicted) compared to pediatric patients (median FEV1 71% predicted) [21]. The index estimates the age and time until a patient reaches the 30% FEV1 threshold, at which lung transplant referral is typically considered [21].
Table 3: RSPH4A-PCDx Development Cohort Characteristics
| Characteristic | Value |
|---|---|
| Patients (n) | 25 |
| Median age at diagnosis (years) | 20 |
| Median FEV1 at diagnosis (% predicted) | 55% |
| Median annual FEV1 decline (% predicted) | -0.75% |
| Pediatric patients (<21 years) | 44% |
| Adult patients (≥21 years) | 56% |
| Presence of bronchiectasis | 100% |
This approach highlights the potential for genotype-specific prediction tools in PCD, which may enable more personalized surveillance and intervention strategies. The development of similar tools for other common PCD genotypes, such as DNAH5 and DNAH11, could significantly enhance clinical management and trial stratification.
Experimental Protocols and Methodologies
Validation Studies for Clinical Prediction Tools
Robust validation of predictive tools requires methodologically sound approaches. The 2025 study by Omran et al. provides a template for contemporary validation of PCD prediction tools [4]. Their methodology included:
Patient Population:
- 269 individuals with genetically confirmed PCD
- Comprehensive subgroup analysis based on laterality defects and ultrastructural abnormalities
Statistical Analysis:
- Sensitivity calculation based on proportion of individuals scoring ≥5 points as recommended
- Median PICADAR scores with interquartile ranges (IQR) for subgroup comparisons
- Statistical significance testing using appropriate methods (p<0.0001 for key comparisons)
This validation approach highlights the importance of genetically confirmed cohorts and subgroup analyses to identify potential biases in tool performance.
Machine Learning Model Development
The ML approach for PCD screening employed a detailed technical workflow [22]:
Feature Engineering:
- Diagnostic, procedural, and pharmaceutical codes were mapped to 28 broad feature categories
- Three numerical scoring mechanisms were developed:
- PRESENCE: Binary scoring (1.0/0.0) for permanent conditions
- COUNT: Summation of serious clinical events
- COVERAGE: Number of 2-week periods with code appearances for chronic conditions
Model Training and Validation:
- Random forest classifier implementation
- 5-fold cross-validation to assess performance
- Multiple cohort definitions to address data limitations:
- Gold-standard cohort: 82 confirmed PCD cases from PCDFR
- Expanded cohort: 319 Q34.8+EM patients with suggestive clinical codes
- Synthetic data augmentation techniques to address class imbalance
This protocol demonstrates the adaptability required for rare disease screening, where limited confirmed cases necessitate innovative approaches to model development.
Table 4: Key Research Reagents and Resources for PCD Predictive Tool Development
| Resource | Function/Application | Specifications/Considerations |
|---|---|---|
| Clinical Data Proformas | Standardized collection of patient history and symptoms | Should include PICADAR parameters, neonatal history, laterality status [5] |
| Genetic Confirmation Panel | Gold-standard diagnosis for validation studies | Must cover >50 known PCD genes; whole-exome sequencing recommended [1] [10] |
| Transmission Electron Microscopy | Ultrastructural analysis for phenotype-genotype correlation | Identifies ODA, IDA, MTD, CP defects; requires specialist interpretation [1] [10] |
| High-Speed Video Microscopy | Ciliary beat pattern and frequency analysis | Specialized equipment; requires culture to exclude secondary effects [1] |
| Nasal Nitric Oxide Measurement | Functional screening modality | nNO ≤30 nL·min−1 suggestive of PCD; requires patient cooperation [5] [1] |
| Claims Data Mapping | Feature development for ML approaches | Requires ICD-10, CPT code mapping to PCD features; temporal analysis essential [20] [22] |
| Privacy-Preserving Record Linkage | Connecting registry and claims data | Tokenization methods enable cross-dataset analysis while protecting privacy [22] |
Implications for Clinical Trial Design and Therapeutic Development
The evolution of predictive tools in PCD carries profound implications for clinical trial design and therapeutic development. Accurate phenotyping and genotyping become paramount in this genetically heterogeneous disorder, where treatment responses may vary significantly across genetic subtypes.
The integration of genotype-specific prognostic tools, such as the RSPH4A-PCDx, enables more sophisticated trial stratification and endpoint selection [21]. Rather than relying solely on universal inclusion criteria, trials can target specific genetic subgroups with higher rates of progression, potentially increasing statistical power with smaller sample sizes. Furthermore, these tools facilitate enrichment strategies by identifying patients most likely to experience meaningful decline during trial periods.
For clinical implementation, a sequential screening approach may optimize resource utilization while maximizing case identification. This might begin with broad application of ML screening to electronic health records or claims data, followed by clinical rule application (with awareness of limitations in subpopulations), and culminating in specialist referral for definitive diagnostic testing [4] [20] [22].
Figure 2: Integrated Diagnostic and Trial Recruitment Pathway for PCD. This flowchart illustrates a comprehensive approach to patient identification, diagnosis, and stratification for clinical trials.
The development and validation of predictive tools for PCD have evolved substantially from initial clinical rule-based systems to sophisticated ML approaches and genotype-specific prognostic indices. While PICADAR represented an important advancement in standardized clinical assessment, its limitations in specific subpopulations highlight the necessity for more nuanced approaches [4]. The integration of machine learning methodologies offers promising avenues for population-level screening, particularly important for a rare disease with significant diagnostic delays [20] [22].
Future tool development must address several critical challenges. First, the creation of validated electronic health record phenotypes will enable more efficient case identification across healthcare systems. Second, international collaboration is essential to develop diverse training datasets that capture the full spectrum of PCD genotypes and phenotypes across ethnic populations. Third, the development of dynamic prediction models that incorporate longitudinal clinical data may provide more accurate prognostication than static tools.
For the clinical trial ecosystem, these advanced predictive tools offer the potential to transform patient recruitment, stratification, and endpoint selection. By precisely identifying at-risk populations and predicting disease trajectories, researchers can design more efficient trials with enriched populations likely to demonstrate treatment effects. Furthermore, genotype-specific tools enable targeted therapeutic development aligned with precision medicine approaches.
As PCD research advances, predictive tools will undoubtedly play an increasingly central role in connecting patients with evolving therapeutic opportunities, ultimately reducing the diagnostic odyssey and improving long-term outcomes for this complex genetic disorder.
Implementing PICADAR: Scoring Methodology and Clinical Application Guidelines
The PICADAR (PrImary CiliARy DyskinesiA Rule) algorithm represents a significant advancement in the clinical identification of patients with primary ciliary dyskinesia (PCD), a rare genetic disorder affecting motile cilia. This diagnostic predictive tool utilizes seven readily obtainable clinical parameters to estimate the probability of PCD before employing complex, expensive diagnostic testing. While demonstrating strong overall performance, emerging research reveals substantial limitations in PICADAR's sensitivity for PCD patients with situs solitus (normal organ arrangement), highlighting critical considerations for researchers and clinicians in drug development and diagnostic innovation. This technical guide comprehensively examines PICADAR's foundational development, algorithmic structure, validation metrics, and specific performance characteristics across different phenotypic presentations.
Primary ciliary dyskinesia is an autosomal recessive genetic disorder characterized by abnormal ciliary structure and function, leading to impaired mucociliary clearance. Clinical manifestations typically include chronic wet cough beginning in infancy, persistent rhinitis, recurrent otitis media, and lower respiratory tract infections that often progress to bronchiectasis [5]. A hallmark feature involves laterality defects, with approximately 50% of patients exhibiting situs inversus totalis (complete mirror-image reversal of thoracic and abdominal organs) and 6-12% presenting with heterotaxy syndromes that may include complex congenital heart defects [5] [23]. The estimated prevalence ranges from 1:2,000 to 1:40,000 live births, though true prevalence is challenging to determine due to diagnostic limitations and underrecognition [5].
Definitive PCD diagnosis presents substantial challenges, as no single gold standard test exists. European guidelines recommend confirmation in specialized centers using a combination of diagnostic approaches, including transmission electron microscopy (TEM) of ciliary ultrastructure, high-speed video microscopy analysis (HSVMA) of ciliary beat pattern and frequency, and nasal nitric oxide (nNO) measurement [5]. These methodologies require expensive equipment, specialized expertise, and are typically available only at tertiary care centers. The complexity of current diagnostic pathways often results in delayed diagnosis, with one European survey demonstrating median diagnostic delays from symptom onset to confirmation exceeding five years [5]. This diagnostic delay underscores the critical need for effective screening tools to identify appropriate candidates for specialized testing.
Development and Validation of the PICADAR Algorithm
Study Population and Design
The PICADAR algorithm was developed through a prospective study of 641 consecutive patients referred for PCD testing to the University Hospital Southampton (UHS) diagnostic center between 2007-2013 [9] [5]. All participants underwent comprehensive diagnostic evaluation, with 75 patients (12%) receiving a definitive PCD diagnosis and 566 (88%) excluded from diagnosis. The cohort included patients aged 0-79 years (median 9 years), with 44% male participants [5]. External validation was performed using a sample of 187 patients (93 PCD-positive, 94 PCD-negative) from the Royal Brompton Hospital (RBH), with this cohort being significantly younger (median 3 years) and including more participants from consanguineous backgrounds, reflecting different population characteristics [5].
PCD diagnosis in both centers followed standardized UK criteria, typically requiring a characteristic clinical history with at least two abnormal diagnostic tests: hallmark ultrastructural defects on transmission electron microscopy, characteristic ciliary beat pattern abnormalities on high-speed video microscopy analysis, and/or low nasal nitric oxide (nNO ≤30 nL·min⁻¹) [5]. In rare cases with exceptionally strong clinical presentation (e.g., affected sibling, classic phenotype), diagnosis was confirmed based on a single definitive test result.
Predictive Parameter Selection and Model Development
The research team identified 27 potential predictor variables from information readily available in non-specialist clinical settings. Through systematic analysis using logistic regression with forward step-wise methods, seven parameters demonstrated statistically significant predictive value for PCD diagnosis [9] [5]. The final model was simplified into a practical scoring tool (PICADAR) by rounding regression coefficients to the nearest integer, creating an easily calculable point-based system.
Table 1: The Seven Predictive Parameters of the PICADAR Algorithm
| Predictive Parameter | Description | Points |
|---|---|---|
| Full-term gestation | Born at or beyond 37 weeks gestation | 2 |
| Neonatal chest symptoms | Respiratory distress or symptoms requiring medical attention in the neonatal period | 2 |
| Neonatal intensive care admission | Admission to NICU or special care baby unit | 1 |
| Chronic rhinitis | Persistent, year-round nasal congestion lasting >3 months | 1 |
| Ear symptoms | Chronic otitis media, recurrent ear infections, or hearing problems | 1 |
| Situs inversus | Mirror-image reversal of thoracic and abdominal organs | 2 |
| Congenital cardiac defect | Any structural heart defect present at birth | 2 |
The PICADAR tool applies specifically to patients with persistent wet cough, which serves as an entry criterion rather than a scored parameter [9]. Each parameter contributes independently to the total score, which ranges from 0 to 11 points.
Algorithm Performance and Validation
The PICADAR algorithm demonstrated strong discriminatory power in both internal and external validation. Receiver operating characteristic (ROC) curve analysis showed an area under the curve (AUC) of 0.91 in the derivation cohort and 0.87 in the external validation cohort, indicating good to excellent diagnostic accuracy [9] [5]. At the recommended cutoff score of ≥5 points, the tool achieved a sensitivity of 0.90 and specificity of 0.75, effectively identifying most true PCD cases while minimizing unnecessary referrals [9].
Table 2: PICADAR Performance Metrics Across Validation Studies
| Performance Measure | Derivation Cohort (n=641) | External Validation Cohort (n=187) |
|---|---|---|
| Area Under Curve (AUC) | 0.91 | 0.87 |
| Sensitivity at cutoff ≥5 | 0.90 | 0.86 |
| Specificity at cutoff ≥5 | 0.75 | 0.73 |
| Positive Predictive Value | Not reported | Not reported |
| Negative Predictive Value | Not reported | Not reported |
The positive predictive value of PICADAR increases substantially with higher scores. Patients scoring ≥5 points have an 11.1% probability of PCD diagnosis, while those scoring ≥10 points exceed 90% probability [24]. This graduated risk assessment allows clinicians to prioritize referrals based on score severity.
The Scientist's Toolkit: Essential Research Reagents and Methodologies
Table 3: Key Research Reagents and Materials for PCD Diagnostic Research
| Reagent/Equipment | Function in PCD Research | Application Example |
|---|---|---|
| Transmission Electron Microscope | Visualization of ciliary ultrastructural defects | Identification of outer dynein arm defects in PCD patients [5] |
| High-speed Video Microscope | Analysis of ciliary beat pattern and frequency | Distinguishing primary from secondary ciliary dyskinesia [5] |
| Nasal Nitric Oxide Analyzer | Measurement of nNO levels as screening tool | Confirming low nNO (<30 nL·min⁻¹) in PCD patients [5] |
| Whole Exome Sequencing Platforms | Genetic characterization of PCD patients | Identification of pathogenic variants in PCD-associated genes [18] |
| Air-Liquid Interface Cell Culture System | Ciliary differentiation and regeneration | Obtaining ciliated epithelium free of secondary damage [5] |
| PCD Gene Panels | Targeted genetic analysis | Comprehensive screening of >50 known PCD-associated genes [23] |
Critical Analysis of PICADAR Sensitivity in Situs Solitus Populations
Emerging Evidence of Sensitivity Limitations
Recent research has revealed significant limitations in PICADAR's sensitivity, particularly for PCD patients with situs solitus (normal organ arrangement). A 2025 study by Omran et al. evaluated PICADAR performance in 269 genetically confirmed PCD patients and found substantially lower sensitivity than originally reported [4]. Critically, 18 individuals (7%) with confirmed PCD reported no daily wet cough, automatically ruling out PCD according to PICADAR's initial screening question [4].
The overall sensitivity in this genetically confirmed cohort was 75%, significantly lower than the 90% reported in the original derivation study [4]. When stratified by laterality status, the tool demonstrated dramatically different performance: 95% sensitivity in patients with laterality defects (situs inversus or heterotaxy) compared to only 61% sensitivity in those with situs solitus (p<0.0001) [4]. This finding highlights a critical weakness in PICADAR's ability to identify nearly 40% of PCD patients with normal organ arrangement.
Impact of Ciliary Ultrastructure on Test Performance
Further stratification by ciliary ultrastructure revealed additional performance variations. The Omran et al. study demonstrated higher PICADAR sensitivity in patients with hallmark ultrastructural defects (83%) compared to those without such defects (59%, p<0.0001) [4]. This finding correlates with genetic subtypes, as certain PCD genotypes are associated with normal ciliary ultrastructure yet still cause significant clinical disease.
Supporting evidence comes from a Japanese cohort study that found only 25% of PCD patients exhibited situs inversus, substantially lower than the approximately 50% typically reported in Western populations [17]. This difference reflects variations in prevalent genetic mutations across ethnic groups and further complicates PICADAR's application in diverse populations. The mean PICADAR score in this Japanese cohort was 7.3 points (range 3-14), with significantly higher scores in patients with situs inversus compared to those with situs solitus [17].
Implications for Research and Clinical Practice
The substantially reduced sensitivity of PICADAR in situs solitus populations has profound implications for PCD research and clinical practice. First, reliance on PICADAR alone may systematically exclude specific PCD subtypes from research cohorts, creating selection bias that impacts the understanding of disease spectrum and natural history. Second, the tool's limitations necessitate supplementary screening approaches, particularly in populations with high rates of consanguinity or specific genetic backgrounds [18].
These findings underscore the importance of context-specific tool application. In populations with frequent laterality defects, PICADAR performs excellently, while in groups with predominant situs solitus, such as the Japanese cohort where only 25% show situs inversus, the tool's utility diminishes considerably [17]. Researchers must therefore consider local epidemiology and genetic patterns when implementing PICADAR in study protocols.
The PICADAR algorithm represents an important innovation in PCD diagnostics, providing a validated, cost-effective method for identifying high-probability candidates for specialized testing. Its seven-parameter structure enables rapid assessment in routine clinical settings, potentially reducing diagnostic delays. However, emerging evidence of significantly reduced sensitivity in situs solitus patients (61%) and those without hallmark ultrastructural defects (59%) necessitates cautious application and supplementary diagnostic approaches [4].
Future research should focus on refining predictive algorithms to better capture the full PCD phenotypic spectrum, particularly through incorporation of genetic data and improved understanding of genotype-phenotype correlations. Enhanced screening tools must address the substantial proportion of PCD patients presenting without classic laterality defects or with atypical clinical features. For drug development professionals and researchers, these limitations highlight the critical importance of comprehensive phenotyping in clinical trials and the potential for selection bias in study populations identified solely through PICADAR screening.
As PCD genetics continues to evolve, with over 50 causative genes currently identified [18], integration of genetic markers with clinical prediction rules may yield next-generation algorithms with improved sensitivity across all PCD subtypes. Until then, PICADAR remains a valuable but imperfect tool that requires informed application within its demonstrated limitations, particularly for situs solitus patients who constitute nearly half of all PCD cases.
The Primary Ciliary Dyskinesia Rule (PICADAR) represents a significant advancement in the identification of patients requiring specialized diagnostic evaluation for Primary Ciliary Dyskinesia (PCD). This in-depth technical guide examines the critical role of daily wet cough as an essential prerequisite within the PICADAR framework, with particular focus on its implications for test sensitivity in patients with situs solitus (normal organ arrangement). Evidence indicates that while PICADAR demonstrates strong overall performance, its dependency on persistent wet cough creates substantial blind spots in specific PCD subpopulations, particularly those without laterality defects. Recent validation studies reveal concerning sensitivity gaps, with rates dropping to approximately 61% in situs solitus patients compared to 95% in those with situs inversus. This analysis provides researchers and drug development professionals with comprehensive methodological frameworks, quantitative performance data, and emerging approaches to address these limitations in both clinical and research settings.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder affecting approximately 1 in 10,000 to 1 in 20,000 live births, characterized by impaired ciliary structure and function [25]. The clinical presentation typically involves chronic upper and lower respiratory tract manifestations, with daily wet cough representing a cardinal symptom due to defective mucociliary clearance [5]. The diagnostic pathway for PCD remains challenging due to the heterogeneity of genetic causes (mutations in more than 50 identified genes), the technical complexity of confirmatory tests (transmission electron microscopy, high-speed video microscopy, genetic testing), and the requirement for specialized equipment and expertise [26].
The PICADAR tool was developed to address the critical need for effective patient stratification prior to intensive diagnostic investigation [5] [9]. This clinical prediction rule leverages seven readily obtainable clinical parameters to estimate the probability of PCD, thereby guiding appropriate referral to specialized centers. The tool's operational framework fundamentally depends on the presence of persistent wet cough as an entry criterion for assessment, establishing this symptom as a gatekeeper for further evaluation [4]. This prerequisite, while clinically justified by the pathophysiology of PCD, introduces significant implications for the tool's sensitivity across phenotypic variants of the disease, particularly in research contexts focused on situs solitus populations.
Within the broader thesis context of PICADAR score sensitivity research in situs solitus, understanding this foundational requirement is essential. The tool's architecture inherently privileges certain PCD phenotypes while potentially overlooking others, creating methodological considerations for both clinical implementation and research design in therapeutic development.
The Centrality of Daily Wet Cough in PICADAR
Pathophysiological Basis for Cough as a Prerequisite
The persistent daily wet cough requirement in PICADAR assessment is grounded in the fundamental pathophysiology of PCD. Motile cilia throughout the respiratory tract are responsible for mucociliary clearance, a primary defense mechanism that removes mucus, debris, and pathogens from the airways [5]. In PCD, ciliary dysfunction results in the accumulation of secretions, leading to the characteristic chronic wet cough as the body's compensatory mechanism to clear airways [25]. This symptom represents a direct clinical manifestation of the underlying molecular defect, making it a logical cornerstone for screening.
From a clinical epidemiology perspective, wet cough demonstrates exceptionally high sensitivity for PCD, though with limited specificity as it occurs in many other respiratory conditions [25]. The European Respiratory Society guidelines explicitly note that a persistent wet cough is always found in PCD patients, typically accompanied by one or more additional features including persistent rhinitis, chronic middle ear disease, neonatal respiratory distress, or laterality defects [25]. This universal presence establishes wet cough as a necessary, though not sufficient, criterion for case identification.
Operational Role in the PICADAR Algorithm
Within the PICADAR algorithm, the presence of daily wet cough functions as a binary gatekeeper that determines eligibility for further scoring [4]. Patients without this symptom are automatically considered negative for PCD according to the tool's protocol, regardless of other clinical features that might suggest the disease. This operational characteristic has profound implications for test sensitivity, particularly in atypical presentations or mild phenotypes.
Recent research evaluating 269 genetically confirmed PCD patients revealed that approximately 7% (18 individuals) reported no daily wet cough and would have been incorrectly excluded from further assessment by PICADAR's current structure [4]. This finding challenges the assumption that all PCD manifestations include this symptom and highlights a significant limitation in the tool's architecture, especially relevant for research focused on expanding the recognized phenotypic spectrum of PCD.
Table: Impact of Daily Wet Cough Prerequisite in Genetically Confirmed PCD Population
| Study Population | Total PCD Cases | Cases Without Daily Wet Cough | Percentage Excluded | Clinical Implications |
|---|---|---|---|---|
| Genetically confirmed PCD cohort [4] | 269 | 18 | 7% | False negatives due to algorithmic structure |
PICADAR Scoring System and Quantitative Assessment
Scoring Parameters and Values
The PICADAR tool incorporates seven predictive parameters derived from multivariable logistic regression analysis of clinical features in patients referred for PCD testing [5] [9]. Each parameter is assigned an integer value based on its regression coefficient, with the total score determining the probability of PCD and corresponding referral recommendations.
Table: PICADAR Scoring Parameters and Point Values
| Parameter | Point Value | Clinical Definition | Pathophysiological Basis |
|---|---|---|---|
| Full-term gestation | 2 | Born at or after 37 weeks gestation | Distinguishes from prematurity-related respiratory symptoms |
| Neonatal chest symptoms | 2 | Respiratory distress, tachypnea, or requirement for oxygen in term neonate | Reflects initial impairment of mucociliary clearance after birth |
| Neonatal intensive care admission | 1 | Requirement for NICU care in term infant | Indicates severity of neonatal respiratory compromise |
| Chronic rhinitis | 1 | Daily nasal congestion/rhinorrhea persisting >3 months | Upper airway ciliary dysfunction |
| Ear symptoms | 1 | Chronic otitis media, effusion, or hearing impairment | Eustachian tube ciliary dysfunction |
| Situs inversus | 4 | Complete mirror-image arrangement of thoracic/abdominal organs | Embryonic nodal ciliary dysfunction during development |
| Congenital cardiac defect | 3 | Structural heart abnormality confirmed by echocardiography | Associated with heterotaxy syndromes from nodal ciliary defects |
Performance Characteristics and Interpretation
The PICADAR score demonstrates robust overall performance characteristics in its initial validation study involving 641 consecutive referrals, with 75 (12%) positive PCD diagnoses [5]. The tool's discriminatory power was quantified using receiver operating characteristic (ROC) curve analysis, showing excellent performance in both internal and external validation cohorts.
Table: PICADAR Performance Characteristics from Validation Studies
| Performance Metric | Derivation Cohort (n=641) | External Validation Cohort (n=157) | Clinical Utility |
|---|---|---|---|
| Area Under Curve (AUC) | 0.91 | 0.87 | Excellent discrimination |
| Optimal Cut-off Score | ≥5 points | ≥5 points | Standard referral threshold |
| Sensitivity at Cut-off | 0.90 | 0.86 | Identifies majority of true cases |
| Specificity at Cut-off | 0.75 | 0.73 | Reduces unnecessary referrals |
| Positive Cases | 75 (12%) | 80 (51%) | Different prevalence between cohorts |
Score interpretation follows a tiered probability structure: patients scoring below 5 points have low PCD probability and typically do not require specialist referral; those scoring 5-10 points have intermediate probability (approximately 11.1% at ≥5 points) and should be referred for further testing; while patients scoring above 10 points demonstrate high probability (>90%) of PCD [24]. This stratified approach enables efficient resource allocation in specialized diagnostic centers.
Experimental Methodologies for PICADAR Validation
Original Validation Study Design
The original PICADAR validation employed a prospective consecutive cohort design with external validation, following rigorous methodology for clinical prediction rules [5]. The study population comprised 641 consecutive patients referred to the University Hospital Southampton PCD diagnostic center between 2007-2013, with a definitive diagnostic outcome established through reference standard testing.
Data Collection Protocol: A standardized proforma was completed by clinicians during face-to-face interviews prior to diagnostic testing. Collected data included demographic information, gestational age, neonatal history (NICU admission, respiratory symptoms), respiratory symptoms (chronic cough, rhinitis), otological history, laterality abnormalities, cardiac defects, and family history. Data was coded using a standardized system (yes=0, no=1, missing=99) to ensure consistency [5].
Statistical Analysis: Logistic regression analysis identified significant predictors from 27 candidate variables. Model performance was assessed through ROC curve analysis, with discrimination considered good if AUC >0.8. The Hosmer-Lemeshow goodness-of-fit test evaluated calibration, with p<0.05 indicating poor agreement between predicted probabilities and actual outcomes. Multiple imputation addressed potential biases from missing data [5].
Diagnostic Reference Standard: PCD diagnosis was confirmed using a composite reference standard including: (1) hallmark transmission electron microscopy defects, (2) characteristic ciliary beat pattern abnormalities on high-speed video microscopy, (3) nasal nitric oxide levels ≤30 nL·min⁻¹, or (4) strong clinical phenotype with at least one abnormal test [5]. This comprehensive approach accommodated the absence of a single gold standard test for PCD.
Recent Validation Methodologies
Recent studies have employed genetic confirmation as the reference standard to reassess PICADAR performance, reflecting evolving diagnostic standards. A 2025 study analyzed 269 genetically confirmed PCD patients, calculating PICADAR scores retrospectively based on comprehensive clinical data [4].
Genetic Testing Protocol: Next-generation sequencing was performed using targeted gene panels encompassing known PCD-associated genes (39 genes in one protocol). Additional investigation for extensive intragenic rearrangements in common genes (DNAH5, DNAI1) employed MLPA (Multiplex Ligation-dependent Probe Amplification) with SALSA MLPA Probemix [26]. This comprehensive genetic analysis provided a robust reference standard.
Subgroup Analysis: Pre-specified subgroup analyses examined PICADAR performance according to (1) laterality status (situs solitus versus situs inversus/heterotaxy) and (2) associated ciliary ultrastructure (hallmark defects versus normal ultrastructure) [4]. These analyses specifically addressed the tool's performance across clinically important PCD subpopulations.
Handling of Missing Data: For adult populations, historical neonatal data was carefully documented from available medical records and parental recall, with sensitivity analyses conducted to assess potential biases from incomplete historical information [5].
Critical Analysis of Sensitivity in Situs Solitus Populations
Quantitative Sensitivity Deficits
Recent evidence reveals substantial limitations in PICADAR's sensitivity for PCD patients with situs solitus (normal organ arrangement). In a cohort of 269 genetically confirmed PCD patients, the overall sensitivity of PICADAR (using the recommended ≥5 cut-off) was 75%, significantly lower than originally reported [4]. This performance deficit was markedly exaggerated when stratified by laterality status.
Table: PICADAR Sensitivity Stratified by Laterality and Ultrastructure
| Patient Subgroup | Sensitivity (%) | Median PICADAR Score (IQR) | Statistical Significance | Clinical Implications |
|---|---|---|---|---|
| Overall PCD population [4] | 75% | 7 (5-9) | Reference | Substantial false negatives |
| Laterality defects [4] | 95% | 10 (8-11) | p<0.0001 | Excellent performance |
| Situs solitus [4] | 61% | 6 (4-8) | p<0.0001 | Concerning false negative rate |
| Hallmark ultrastructural defects [4] | 83% | Not reported | p<0.0001 | Moderate performance |
| Normal ultrastructure [4] | 59% | Not reported | p<0.0001 | Poor performance |
The data demonstrates that PICADAR's performance is heavily dependent on laterality status, with a 34-percentage-point sensitivity difference between patients with and without laterality defects. This dependency creates a significant blind spot in identifying PCD patients with normal organ arrangement, who represent approximately half of all PCD cases [4].
Methodological Implications for Research
The sensitivity limitations in situs solitus populations have profound implications for research design and interpretation:
Selection Bias in Study Populations: Research relying solely on PICADAR for patient identification will systematically underrepresent situs solitus cases, potentially skewing genotype-phenotype correlations and therapeutic trial populations.
Diagnostic Delay Considerations: The median PICADAR score of 6 in situs solitus patients places them near the referral threshold of 5, suggesting these patients may present with subtler clinical features and experience longer diagnostic journeys [4].
Ultrastructural Correlations: The significantly lower sensitivity in patients with normal ciliary ultrastructure (59%) highlights particular challenges in diagnosing PCD subtypes without hallmark electron microscopy findings [4]. These patients often have mutations in genes not associated with classic ultrastructural defects.
Alternative Diagnostic Approaches and Adjunctive Tools
Complementary Predictive Instruments
Research has identified several alternative and complementary predictive tools that may address PICADAR's limitations in situs solitus populations:
Clinical Index (CI): This seven-item questionnaire demonstrates potential advantages over PICADAR by not requiring assessment of laterality or congenital heart defects for basic evaluation [26]. In a comparative study of 1401 patients, CI showed larger area under the ROC curve than the North American criteria (NA-CDCF), though direct comparison with PICADAR was limited by the latter's wet cough prerequisite [26].
North American Criteria (NA-CDCF): This tool defines four clinical criteria: laterality defects, unexplained neonatal respiratory distress, early-onset year-round nasal congestion, and early-onset year-round wet cough [26]. While demonstrating similar performance to PICADAR in some validations, it shares limitations in situs solitus populations due to the weighting of laterality defects.
Nasal Nitric Oxide (nNO) Integration: Measurement of nNO significantly enhances the predictive power of all clinical tools. When combined with PICADAR, nNO improves both sensitivity and specificity, potentially mitigating some limitations in situs solitus identification [26]. nNO measurement serves as a valuable objective adjunct, particularly for patients with intermediate clinical scores.
Advanced Diagnostic Protocols
For research requiring comprehensive PCD case identification, particularly encompassing situs solitus cases, multimodal diagnostic protocols are essential:
Extended Genetic Testing: Next-generation sequencing panels encompassing all known PCD genes (currently >50 genes) provide a definitive diagnostic approach, though availability may be limited to specialized centers [26]. This method is particularly crucial for patients with normal ultrastructure and situs solitus.
Cell Culture and Re-differentiation: For cases with inconclusive initial testing, airway epithelial cell cultures that restore ciliated epithelium after differentiation at air-liquid interface can eliminate secondary ciliary dyskinesia and provide more reliable functional and structural analysis [5] [26].
Immunofluorescence Microscopy: This emerging technique detects abnormalities in ciliary protein localization, complementing TEM by identifying defects in cases with normal ultrastructure [25]. The method shows promise for identifying specific PCD subtypes that may be missed by conventional approaches.
Table: Essential Research Reagent Solutions for Comprehensive PCD Diagnosis
| Reagent/Technology | Primary Application | Research Utility | Technical Considerations |
|---|---|---|---|
| Next-generation sequencing panels | Genetic confirmation | Identifies mutations in >50 PCD-associated genes | Requires bioinformatics expertise for variant interpretation |
| Transmission Electron Microscopy reagents | Ultrastructural analysis | Identifies hallmark ciliary defects | Technically demanding, requires experienced personnel |
| High-speed video microscopy systems | Ciliary function analysis | Quantifies ciliary beat frequency and pattern | Specialized equipment, requires standardization |
| Nasal nitric oxide analyzers | Screening measurement | Non-invasive objective measure | Age-dependent values, technical standardization required |
| Air-liquid interface culture media | Ciliary culture | Eliminates secondary dyskinesia | 4-6 week differentiation period, technical complexity |
| Immunofluorescence antibodies | Protein localization | Detects defects with normal ultrastructure | Limited commercial availability for some ciliary proteins |
The daily wet cough prerequisite in PICADAR assessment represents both a pathophysiologically justified cornerstone and a significant limitation for comprehensive PCD identification, particularly in situs solitus populations. While the tool demonstrates excellent performance characteristics in classic PCD presentations with laterality defects (95% sensitivity), its utility diminishes substantially in patients with normal organ arrangement (61% sensitivity) and those without hallmark ultrastructural defects (59% sensitivity) [4].
For researchers and drug development professionals, these limitations necessitate methodological adaptations:
Supplementary Case Identification: Research protocols must incorporate additional screening methods beyond PICADAR, particularly genetic screening of at-risk populations regardless of cough status or laterality.
Phenotypic Spectrum Expansion: The 7% of genetically confirmed PCD patients without daily wet cough represent an important population for understanding the full phenotypic expression of ciliopathies [4].
Tool Refinement: Development of modified predictive tools that maintain PICADAR's advantages while reducing dependence on laterality features represents an important research direction.
The essential prerequisite of daily wet cough in PICADAR creates a critical methodological consideration for research design, particularly in studies focused on expanding the recognized phenotypic spectrum of PCD or developing targeted therapies for specific genetic subtypes. Future validation studies should prioritize prospective designs in genetically confirmed populations, with explicit attention to performance across clinically relevant subgroups, to optimize case identification and overcome the current sensitivity limitations in situs solitus patients.
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal ciliary function, leading to impaired mucociliary clearance. The diagnosis is challenging due to non-specific symptoms and the requirement for highly specialized, expensive testing available only at specialized centers [5] [1]. The PICADAR (PrImary CiliARy DyskinesiA Rule) score was developed as a clinical prediction rule to identify patients with persistent wet cough who require referral for definitive PCD testing [5]. This validated tool utilizes seven readily available clinical parameters to estimate probability of PCD, thereby facilitating early diagnosis while preventing overburdening of specialized diagnostic services [5] [3].
Within PCD diagnostics, approximately half of patients exhibit situs inversus (complete reversal of thoracic and abdominal organs), while others have situs solitus (normal organ arrangement) or heterotaxy (ambiguous organ arrangement) [5] [1]. Research focused on PICADAR's performance in situs solitus patients is particularly valuable, as these cases present greater diagnostic challenge due to the absence of this classic clinical sign. Understanding cut-off values and their corresponding probability estimations across different patient populations ensures appropriate application of this predictive tool in both research and clinical settings.
PICADAR Scoring Parameters and Calculation
The PICADAR score applies to patients with persistent wet cough and incorporates seven clinical parameters obtained through patient history [5]. Each parameter contributes a specific point value to the total score, with weights determined through logistic regression analysis of the original derivation cohort [5].
Table 1: PICADAR Scoring Parameters and Point Values
| Clinical Parameter | Point Value |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms | 2 |
| Neonatal intensive care unit admission | 2 |
| Chronic rhinitis | 1 |
| Ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital heart defect | 2 |
Calculation involves summing points for all parameters present in the patient's history. The resulting total score ranges from 0 to 11 points, with higher scores indicating greater probability of PCD [5]. For research applications, particularly in situs solitus populations, it is important to note that these patients cannot contribute points for situs inversus, thus their maximum possible score is 9 rather than 11.
Cut-off Values and Diagnostic Performance
Established Cut-off Values and Performance Metrics
The foundational PICADAR validation study established a cut-off value of 5 points as optimal for discriminating between PCD-positive and PCD-negative cases [5]. At this threshold, the tool demonstrated high sensitivity with acceptable specificity in the original derivation cohort.
Table 2: PICADAR Performance at Established Cut-off Values
| Cut-off Score | Sensitivity | Specificity | Population | AUC |
|---|---|---|---|---|
| ≥5 points | 0.90 | 0.75 | Derivation (n=641) | 0.91 |
| ≥5 points | - | - | Validation (n=187) | 0.87 |
The area under the receiver operating characteristic curve (AUC) was 0.91 in the internal validation and 0.87 in the external validation cohort, indicating good to excellent discriminatory performance [5]. These validation studies confirmed PICADAR as a robust prediction tool ready for implementation in respiratory centers referring to PCD specialty centers.
Comparative Performance with Other Predictive Tools
Subsequent validation studies have compared PICADAR against other predictive instruments, including the Clinical Index (CI) and North American Criteria Defined Clinical Features (NA-CDCF). A 2021 study evaluating all three tools in 1,401 patients found PICADAR and NA-CDCF demonstrated similar performance, while CI potentially outperformed both in certain metrics [3].
Notably, PICADAR could not be calculated in 6.1% of patients (86/1401) due to the absence of chronic wet cough, highlighting an important limitation for its universal application [3]. For the situs solitus subpopulation, the absence of points for situs inversus necessarily lowers the total score, potentially affecting test sensitivity in this cohort and warranting population-specific validation.
Experimental Protocols for PICADAR Validation
Original Derivation and Validation Methodology
The original PICADAR derivation and validation followed a rigorous methodological protocol [5]:
Study Population: The derivation group included 641 consecutive patients with definitive diagnostic outcomes from the University Hospital Southampton PCD diagnostic center (2007-2013). The validation group included 187 patients (93 PCD-positive, 94 PCD-negative) from Royal Brompton Hospital [5].
Data Collection: Researchers collected data using a standardized proforma completed by clinicians during clinical interviews prior to diagnostic testing. Parameters included gestational age, neonatal respiratory symptoms, neonatal intensive care admission, chronic rhinitis, ear symptoms, situs abnormalities, and congenital heart defects [5].
Diagnostic Reference Standard: PCD diagnosis was confirmed using a combination of methods including transmission electron microscopy (TEM), ciliary beat pattern (CBP) analysis, nasal nitric oxide measurement (nNO ≤30 nL·min⁻¹), and clinical phenotype in accordance with contemporary guidelines [5].
Statistical Analysis: Logistic regression identified significant predictors, with regression coefficients rounded to integers to create the scoring system. Performance was assessed using receiver operating characteristic (ROC) curve analysis, with AUC values interpreted as moderate (0.6-0.8) or good (>0.8) [5].
Contemporary Validation Approaches
Recent studies have employed enhanced methodological approaches:
Extended Diagnostic Criteria: Later validations incorporate expanded genetic testing panels, high-speed video microscopy analysis (HSVM), and immunofluorescence staining, reflecting evolving diagnostic standards [27] [3].
Multicenter Designs: Contemporary studies utilize larger, multinational cohorts to enhance generalizability and assess cross-population performance [3].
Comparative Analyses: Modern protocols often include head-to-head comparisons of multiple prediction tools (PICADAR, CI, NA-CDCF) to guide clinical implementation [3].
Integrated Biomarkers: Some study designs evaluate the incremental value of combining PICADAR with nNO measurement, demonstrating enhanced predictive performance when used in combination [3].
Research Reagent Solutions for PCD Diagnostic Studies
Table 3: Essential Research Reagents and Materials for PCD Diagnostic Studies
| Reagent/Material | Application in PCD Research | Specific Examples |
|---|---|---|
| Primary Antibodies | Immunofluorescence staining for ciliary protein localization | Mouse anti-DNAH5 [27]; Rabbit anti-GAS8 [27] |
| Secondary Antibodies | Detection of primary antibodies in IF protocols | Goat Anti-mouse Alexa Fluor 488; Anti-rabbit Alexa Fluor 546 [27] |
| Cell Culture Media | Maintenance of respiratory epithelial cells | RPMI 1640 Medium [27] |
| Fixation Reagents | Preservation of cellular structure for microscopy | 4% paraformaldehyde [27] |
| Permeabilization Agents | Antibody penetration for intracellular staining | 0.2% Triton X-100 [27] |
| Nuclear Stains | Cell identification in microscopy | Hoechst 33342 [27] |
| Nasal Nitric Oxide Analyzers | nNO measurement as PCD screening tool | CLD 88sp NO analyzer (ECO MEDICS) [27]; Niox Mino/Vero [3] |
PICADAR Application in Research and Clinical Decision-Making
Implementation in Situs Solitus Research
For research focused specifically on situs solitus PCD cases, PICADAR application requires special methodological considerations. The absence of points for situs inversus means researchers should:
- Calculate expected score ranges specific to the situs solitus population (maximum 9 points versus 11 in mixed populations)
- Validate population-specific cut-off values that may differ from the general PCD population
- Consider adjusted probability estimations that account for the different score distribution
- Report situs status explicitly in all research findings to facilitate interpretation
Recent studies demonstrate that PICADAR remains a valuable tool in situs solitus research, with cases scoring ≥5 points on remaining parameters still showing high probability of PCD diagnosis [27]. One study reported that all patients with abnormal immunofluorescence findings had PICADAR scores of 6 or above despite situs solitus status [27].
Integration with Contemporary Diagnostic Pathways
The diagnostic workflow for PCD has evolved since PICADAR's development, now incorporating more advanced genetic and imaging technologies. The following diagram illustrates how PICADAR integrates into a modern diagnostic pathway for PCD, with special consideration for situs solitus cases:
Diagram 1: PICADAR in PCD Diagnostic Pathway (Max Width: 760px)
Interpretation of Probability Estimations
The original PICADAR study established that scores ≥5 points correspond with high PCD probability, but subsequent research enables more nuanced interpretation:
Low Probability (Scores 0-4): Unlikely to have PCD; consider alternative diagnoses such as cystic fibrosis, immune deficiencies, or chronic aspiration [5] [3].
Intermediate Probability (Scores 5-7): Moderate to high probability warranting comprehensive PCD evaluation; in situs solitus patients, scores in this range should trigger specialist referral despite absence of laterality defects [5] [27].
High Probability (Scores 8-11): Very high probability of PCD; should receive expedited specialist referral and comprehensive diagnostic testing [5].
For research purposes, particularly in drug development studies targeting PCD subpopulations, these probability estimations help ensure appropriate patient stratification and cohort selection. The integration of PICADAR with nNO measurement further enhances predictive power, with one study demonstrating significant improvement in sensitivity and specificity when both tools are used in combination [3].
The PICADAR score represents a validated, clinically practical tool for predicting PCD probability in patients with persistent wet cough. The established cut-off of ≥5 points provides optimal sensitivity (0.90) and specificity (0.75) in general PCD populations, though application in situs solitus research requires consideration of the modified scoring range. Through proper understanding of cut-off values, probability estimations, and implementation protocols, researchers can effectively utilize PICADAR to advance PCD diagnostics and therapeutics, particularly for the more diagnostically challenging situs solitus patient population.
Data Collection Best Practices for Research Settings
Data collection serves as the foundational pillar of scientific research, determining the reliability, validity, and ultimate success of research outcomes. In specialized research contexts such as investigating the sensitivity of the PICADAR score for situs solitus, implementing robust data collection methodologies becomes particularly critical. The PICADAR (Prediction of Independent Contractions of the Diaphragm and Accessory Respiratory muscles) score is a clinical tool used to predict successful extubation in intensive care patients, and researching its sensitivity in normal anatomical arrangements (situs solitus) requires exceptionally precise data collection frameworks [28].
According to Forrester Research's The State of Data Quality 2023, data quality remains a top challenge for many organizations, highlighting the importance of implementing systematic approaches to data acquisition [28]. The selection of appropriate data collection techniques directly influences the accuracy of insights gained, making methodological rigor non-negotiable in clinical research settings where diagnostic tool validation is concerned [28]. This technical guide provides comprehensive methodologies and best practices for collecting research data that meets stringent scientific and regulatory standards.
Data Collection Methodology Classification
Research data collection methods broadly fall into three categories: qualitative, quantitative, and mixed-methods approaches. Each category offers distinct advantages and is suited to different research objectives within clinical and scientific investigations.
Qualitative Data Collection Techniques
Qualitative methods focus on non-numerical, descriptive data that provides depth and context to research questions. These techniques are particularly valuable in exploratory research or when seeking to understand experiences, behaviors, and perceptions [28].
Table 1: Qualitative Data Collection Methods
| Method | Key Characteristics | Research Applications | Considerations |
|---|---|---|---|
| Structured Interviews | Pre-determined questions, consistent across respondents [28] | Assessing standardized patient experiences, validating specific aspects of PICADAR scoring | Ensures data comparability but limits exploration of unexpected responses |
| Semi-structured Interviews | Core set of questions with flexibility for follow-up [28] | In-depth exploration of clinician reasoning behind PICADAR assessments | Balances structure with ability to probe emerging themes |
| Unstructured Interviews | Conversation-like flow without strict question framework [28] | Exploratory research on novel aspects of respiratory assessment | Provides rich, detailed data but challenging to analyze systematically |
| Focus Groups | Small group discussions (6-10 participants) with a moderator [28] | Understanding group dynamics in clinical assessment, generating new ideas | Groupthink may influence responses; skilled moderator required |
| Participant Observation | Researcher actively engages with the environment being studied [28] | Studying clinical workflows in ICU settings where PICADAR is applied | Provides contextual understanding but may introduce researcher bias |
| Non-participant Observation | Researcher observes without involvement [28] | Objective documentation of respiratory assessment practices | Maintains objectivity but may miss contextual nuances |
| Document & Record Analysis | Systematic study of pre-existing documents and records [28] | Analysis of medical records, clinical trial data, historical assessments | Cost-effective but requires careful authentication of sources |
Quantitative Data Collection Techniques
Quantitative methods emphasize numerical data that can be statistically analyzed to identify patterns, correlations, or causal relationships. These approaches are essential for validating clinical tools like the PICADAR score through empirical evidence [28].
Table 2: Quantitative Data Collection Methods
| Method | Data Type | Research Applications | Advantages/Limitations |
|---|---|---|---|
| Surveys & Questionnaires | Closed-ended questions, Likert scales, multiple-choice [28] | Collecting standardized patient data, symptom frequency, demographic information | Efficient for large samples; potential for bias if questions are leading |
| Structured Interviews & Checklists | Fixed set of questions with consistent delivery [28] | Systematic assessment of respiratory parameters across multiple patients | Standardized data collection; less flexible than semi-structured approaches |
| Physiological/Biometric Measures | Heart rate, respiratory rate, blood pressure, etc. [28] | Objective measurement of physiological parameters relevant to extubation outcomes | Highly accurate but requires specialized equipment and expertise |
| Web/Online Data Collection | Web surveys, server logs, online forms [28] | Multi-center trial data collection, patient-reported outcome measures | Scalable and cost-effective; potential sampling bias if digital access varies |
| Transaction Tracking | Purchase data, usage logs, interaction records [29] | Monitoring medical device utilization, resource allocation patterns | Provides behavioral data but may raise privacy concerns |
| IoT and Sensor Data Collection | Real-time physical world data from connected devices [29] | Continuous monitoring of patient vital signs, environmental factors in clinical settings | Automated, continuous data collection; requires technical infrastructure |
| API Data Integration | Automated data exchange between software systems [29] | Combining electronic health record data with research databases | Real-time data synchronization; requires technical expertise to implement |
Mixed-Methods and Triangulation Approaches
Mixed-methods research combines qualitative and quantitative techniques to provide a comprehensive understanding of research problems that cannot be fully addressed by either approach alone. Triangulation uses multiple data sources or methods to cross-verify findings and ensure research validity [28]. For PICADAR score sensitivity research, this might involve combining statistical analysis of patient outcomes with qualitative interviews with clinicians about their assessment experiences, providing both numerical evidence and contextual understanding [28].
Data Quality Assurance Framework
Ensuring data quality requires systematic implementation of validation processes, governance standards, and continuous monitoring throughout the research lifecycle.
Data Validation and Quality Checks
Implementing robust data validation involves establishing systematic processes to verify information at the point of entry and throughout its lifecycle. This prevents "garbage in, garbage out" scenarios where flawed data compromises research outcomes [30].
Practical Implementation Strategies:
- Field-Level Validation: Implement rules in data collection forms to verify format and completeness (e.g., ensuring numerical ranges for physiological measurements fall within plausible limits) [30]
- Automated Post-Collection Cleaning: Utilize tools that detect duplicates, standardize fields, and flag incomplete records for manual review [30]
- Data Quality KPIs: Establish and monitor key metrics such as completion rate, accuracy percentage, and duplicate records to identify systemic issues [30]
Standardized Collection Methods and Formats
Adopting standardized protocols, templates, and data formats across all research touchpoints ensures consistency and interoperability. This approach eliminates ambiguity, reduces data cleaning time, and creates analysis-ready datasets [30].
Standardization Framework:
- Data Dictionary: Develop a central document defining every data field, including name, format, and accepted values [30]
- Field Validation Rules: Implement formatting requirements in data capture tools (e.g., specific patterns for patient identifiers) [30]
- Industry Standards: Utilize established standards like ISO 8601 for dates and ISO 3166 for country codes to maintain consistency [30]
Data Source Credibility and Verification
Establishing source credibility involves authenticating data origins, implementing verification mechanisms, and continuously monitoring source quality. This process transforms simple data accumulation into a curated repository of high-quality research intelligence [30].
Verification Protocol:
- Source Registry: Document every data source, including origin, data type provided, and quality rating [30]
- Data Lineage Tracking: Implement tools to map data flow from source to destination, enabling rapid identification of quality issues [30]
- Cross-Reference Validation: Compare data from different sources to identify inconsistencies (e.g., cross-referencing clinical assessments with laboratory results) [30]
Ethical and Regulatory Compliance
Research data collection must adhere to ethical principles and regulatory requirements, particularly in clinical contexts involving human subjects.
Informed Consent and Privacy Compliance
Obtaining explicit, informed consent from research participants and strictly adhering to privacy regulations represents both an ethical imperative and legal requirement. The FDA's Patient-Focused Drug Development guidance series emphasizes systematic approaches to collecting robust and meaningful patient input while maintaining ethical standards [31].
Informed Consent Framework:
- Clear Language: Avoid legal jargon in consent forms; clearly explain what data is collected, how it will be used, and with whom it will be shared [30]
- Granular Choices: Provide separate opt-in options for different types of data use and communication [30]
- Privacy by Design: Integrate privacy considerations into research technology from the outset, including security measures and access controls [30]
- Consent Records: Maintain secure, auditable records of when and how each participant provided consent [30]
Regulatory Alignment in Clinical Research
Regulatory agencies including the FDA, EMA, and others have established specific guidelines for data collection in clinical research contexts. The FDA's Patient-Focused Drug Development Guidance Series provides comprehensive methodological guidance for collecting and submitting patient experience data for medical product development and regulatory decision-making [31] [32].
Table 3: Regulatory Guidance Overview
| Regulatory Body | Guidance Focus | Key Requirements | Relevance to PICADAR Research |
|---|---|---|---|
| FDA PFDD Guidance 1 | Collecting comprehensive and representative input [31] | Sampling methods, defining target population, development of sampling strategy | Ensures appropriate patient selection for sensitivity studies |
| FDA PFDD Guidance 2 | Methods for eliciting information from patients [31] | Best practices in qualitative research, interview guides, survey question selection | Guides development of structured assessment protocols |
| FDA PFDD Guidance 3 | Selecting, developing, or modifying clinical outcome assessments [32] | Fit-for-purpose clinical outcome assessments for measuring patient-important outcomes | Directly relevant to PICADAR as a clinical assessment tool |
| ICH E6(R3) | Good Clinical Practice standards [33] [34] | Data integrity, traceability, risk-based approaches to clinical trials | Ensures research meets international ethical and quality standards |
Implementation Protocols
Successful implementation of data collection frameworks requires meticulous planning, appropriate tool selection, and systematic execution.
Defining Data Collection Objectives
Establishing clear, focused objectives represents the critical first step in research data collection. Well-defined goals ensure every data point serves a distinct purpose and contributes directly to research outcomes [30].
Objective-Setting Protocol:
- SMART Goals: Create Specific, Measurable, Achievable, Relevant, and Time-bound objectives that anchor the data strategy [30]
- Stakeholder Alignment: Conduct collaborative sessions with all research team members to define success metrics and required data [30]
- Documentation: Create a shared document outlining each data collection goal and its alignment with broader research questions [30]
Sampling Framework and Bias Mitigation
Collecting data that accurately represents the target population requires methodological techniques to minimize systematic errors and ensure valid, generalizable conclusions [30].
Bias Mitigation Strategies:
- Representative Sampling: Implement sampling methods that ensure all relevant patient subgroups are appropriately included in PICADAR sensitivity research [30]
- Blinded Data Collection: When feasible, ensure data collectors are blinded to research hypotheses to prevent unconscious influence on data collection [30]
- Cross-Validation: Use multiple assessment methods or raters to verify key observations and measurements [30]
Technology and Tool Selection
Choosing appropriate data collection technologies requires alignment with research objectives, regulatory requirements, and practical implementation constraints.
The Scientist's Toolkit: Essential Research Materials
| Item Category | Specific Examples | Function in Research | PICADAR Application Examples |
|---|---|---|---|
| Electronic Data Capture (EDC) Systems | REDCap, Medidata Rave, Oracle Clinical [35] | Secure, compliant data collection and management | Structured collection of patient assessment data across multiple sites |
| Clinical Outcome Assessments (COAs) | Patient-reported outcome measures, clinician-reported outcomes [32] | Standardized measurement of patient health status | PICADAR score assessment forms, extubation outcome measures |
| Biometric Sensors | Wearable heart rate monitors, pulse oximeters, respiratory rate sensors [28] [29] | Continuous, objective physiological data collection | Monitoring patient vital signs pre- and post-extubation |
| Data Validation Tools | Field validation rules, automated quality checks, duplicate detection [30] | Ensuring data accuracy, completeness, and consistency | Real-time validation of PICADAR score component entries |
| Privacy and Consent Management | Secure consent documentation, access controls, audit trails [30] | Maintaining participant privacy and regulatory compliance | Managing patient consent for respiratory assessment data collection |
| API Integration Platforms | MuleSoft, Dell Boomi, custom integration solutions [29] | Connecting disparate data systems for comprehensive datasets | Combining electronic health record data with research databases |
Implementing rigorous data collection practices is fundamental to producing valid, reliable, and regulatory-compliant research outcomes. For specialized clinical research such as investigating PICADAR score sensitivity in situs solitus, methodological precision becomes particularly critical. By adopting systematic approaches to data collection—including appropriate methodology selection, robust quality assurance, ethical compliance, and careful implementation—researchers can ensure their findings withstand scientific scrutiny and contribute meaningfully to clinical knowledge. The framework presented in this guide provides a comprehensive foundation for designing and executing data collection protocols that meet the highest standards of research excellence.
Integrating PICADAR with Other Diagnostic Modalities in Research Protocols
The PICADAR (PrImary Ciliary DyskinesiA Rule) tool represents a significant advancement in the initial screening and referral pathway for Primary Ciliary Dyskinesia (PCD), a rare genetic disorder characterized by abnormal ciliary function leading to chronic respiratory symptoms. This diagnostic predictive tool was specifically developed to identify patients requiring specialized PCD testing through the assessment of seven readily available clinical parameters. The development of PICADAR addressed a critical clinical need: PCD diagnostic tests are highly specialized, requiring expensive equipment and experienced scientists, while the symptoms of PCD are nonspecific, making guidance on whom to refer for testing particularly valuable for clinicians [5].
Within the context of modern PCD research protocols, PICADAR serves as an essential clinical decision rule that enables more efficient patient stratification prior to undertaking complex diagnostic investigations. The tool's integration with other diagnostic modalities has become increasingly important as research advances our understanding of PCD heterogeneity, particularly regarding its variable sensitivity across different patient subgroups, including those with situs solitus (normal organ arrangement) versus those with situs inversus (mirror-image organ arrangement) [36]. This technical guide examines the evidence-based approaches for incorporating PICADAR within comprehensive PCD diagnostic frameworks, with specific attention to methodological considerations for research applications.
PICADAR: Core Components and Performance Characteristics
The PICADAR Scoring System
The PICADAR tool operates through a straightforward scoring system based on seven clinical parameters that can be readily obtained through patient history. The tool applies specifically to patients with persistent wet cough, which serves as an initial screening criterion [5]. The predictive parameters and their corresponding point values are detailed in Table 1.
Table 1: PICADAR Scoring Parameters and Values
| Clinical Parameter | Point Value |
|---|---|
| Full-term gestation | 1 point |
| Neonatal chest symptoms | 2 points |
| Neonatal intensive care unit admission | 2 points |
| Chronic rhinitis | 1 point |
| Chronic ear symptoms | 1 point |
| Situs inversus | 4 points |
| Congenital cardiac defect | 2 points |
The total PICADAR score ranges from 0 to 13 points, with the originally recommended cut-off score of ≥5 points indicating a high probability of PCD and warranting referral for specialized testing [5]. In the initial validation study, this cut-off demonstrated a sensitivity of 0.90 and specificity of 0.75, with an area under the curve (AUC) of 0.91 in the derivation group and 0.87 in the external validation group [5].
Performance Characteristics Across Patient Subgroups
Recent research has revealed crucial limitations in PICADAR's performance, particularly when applied to specific PCD patient subgroups. A 2025 study by Schramm et al. examining 269 genetically confirmed PCD cases found substantially different sensitivity profiles based on the presence or absence of laterality defects [36]. The overall sensitivity of PICADAR in this cohort was 75%, significantly lower than originally reported [36].
Table 2: PICADAR Performance Stratified by Laterality and Ultrastructural Defects
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) | Statistical Significance |
|---|---|---|---|
| All PCD patients (n=269) | 75% | 7 (5-9) | Reference |
| Patients with laterality defects | 95% | 10 (8-11) | p<0.0001 |
| Patients with situs solitus | 61% | 6 (4-8) | p<0.0001 |
| Patients with hallmark ultrastructural defects | 83% | Not reported | p<0.0001 |
| Patients without hallmark ultrastructural defects | 59% | Not reported | p<0.0001 |
The same study identified that 7% (18/269) of genetically confirmed PCD patients reported no daily wet cough, which would have automatically excluded them from PICADAR assessment according to the tool's initial question, representing a significant limitation in case identification [36]. This finding highlights the critical importance of considering PICADAR as part of a broader diagnostic strategy rather than relying on it as a standalone screening tool, particularly in research protocols focused on PCD patients with normal body composition.
Integration with Established Diagnostic Modalities
Complementary Diagnostic Framework
The European Respiratory Society (ERS) guidelines recommend a multifaceted approach to PCD diagnosis, with PICADAR serving as one component within a sequential diagnostic protocol. The integration framework leverages the respective strengths of each modality while mitigating their individual limitations, as illustrated below:
This integrated framework demonstrates how PICADAR serves as an initial stratification tool within a comprehensive diagnostic pathway. The sequential approach optimizes resource utilization by directing the most complex and expensive testing toward patients with the highest pre-test probability of PCD, while maintaining sensitivity through the inclusion of multiple confirmatory modalities.
Nasal Nitric Oxide (nNO) and PICADAR Synergy
Nasal nitric oxide measurement serves as a key secondary screening tool following positive PICADAR assessment. nNO has established utility as a PCD screening measure, with levels typically ≤30 nL·min⁻¹ in confirmed cases [5] [37]. The combination of PICADAR and nNO creates a powerful screening sequence:
- Protocol Implementation: Patients with PICADAR scores ≥5 undergo nNO measurement using standardized chemiluminescence analyzers with velum closure techniques.
- Complementary Value: While PICADAR identifies clinical phenotypes suggestive of PCD, nNO provides objective physiological evidence of ciliary dysfunction.
- Research Considerations: Recent evidence indicates that some PCD genetic variants show discrepancies with nNO measurements, highlighting the importance of not relying exclusively on this modality [37].
The diagnostic workflow incorporating both PICADAR and nNO can be summarized as follows:
Research Protocol Methodologies
Experimental Design for PICADAR Validation Studies
Research protocols evaluating PICADAR's performance should incorporate specific methodological standards to ensure valid and generalizable results. Based on the original derivation and recent validation studies, the following experimental framework is recommended:
Table 3: Key Methodological Components for PICADAR Research Protocols
| Protocol Component | Specifications | Rationale |
|---|---|---|
| Study Population | Consecutive patients referred for PCD testing with definitive diagnostic outcomes | Minimizes selection bias and provides real-world performance data |
| Sample Size | Minimum 100 participants per center to ensure adequate power for subgroup analyses | Enables stratification by laterality defects, age, and genetic variants |
| Data Collection | Standardized proforma completed by clinicians prior to diagnostic testing | Eliminates diagnostic review bias and ensures blinded assessment |
| PICADAR Application | Strict adherence to the seven predefined parameters with consistent scoring | Maintains standardization across different research settings |
| Reference Standard | Genetic confirmation and/or combination of hallmark TEM defects and abnormal ciliary beat pattern | Provides definitive diagnosis for sensitivity/specificity calculations |
| Statistical Analysis | Receiver operating characteristic (ROC) curve analysis with area under curve (AUC) calculation | Quantifies discriminatory performance and enables comparison with other tools |
The original PICADAR derivation study analyzed data from 641 consecutive patients, with 75 (12%) diagnosed with PCD, while the recent 2025 validation study included 269 genetically confirmed PCD cases, demonstrating the importance of adequate sample sizes for meaningful subgroup analyses [5] [36].
Integration with Genetic and Genomic Approaches
Advanced research protocols should incorporate genetic testing as both a validation tool and a means of understanding phenotypic-genotypic correlations in PICADAR performance. The following methodological approach is recommended:
Candidate Selection: Patients with PICADAR scores ≥5 should undergo next-generation sequencing PCD gene panels, while those with scores <5 but strong clinical suspicion should also be considered for genetic testing to identify false negatives.
Stratified Analysis: Genetic results should be correlated with PICADAR scores to identify specific genotypes associated with lower scores, particularly in situs solitus patients.
Functional Validation: For novel genetic variants identified, functional studies including ciliary waveform analysis and immunofluorescence imaging should be performed to confirm pathogenicity.
Recent research indicates that PICADAR demonstrates higher sensitivity in individuals with hallmark ultrastructural defects (83%) compared to those without (59%), highlighting the relationship between ciliary ultrastructure and clinical presentation [36]. This stratification is particularly relevant for genetic research, as specific genetic variants correspond to distinct ultrastructural phenotypes.
Advanced Technical Considerations
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for PCD Diagnostic Studies
| Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| Nasal Epithelial Cell Brushes | Collection of ciliated epithelium for functional and structural analysis | Medical-grade cytology brushes, diameter 2-3mm, single-use sterilized |
| Electron Microscopy Fixatives | Preservation of ciliary ultrastructure for TEM analysis | Glutaraldehyde (2.5%-3.0%) in cacodylate buffer (0.1M, pH 7.4) |
| High-Speed Video Microscopy Equipment | Analysis of ciliary beat pattern and frequency | Capable of ≥500 frames per second with minimum 100x magnification |
| nNO Analyzers | Measurement of nasal nitric oxide for screening | Chemiluminescence analyzers with automated aspiration systems |
| PCD Gene Panels | Genetic confirmation and variant identification | Next-generation sequencing panels covering ≥35 known PCD-associated genes |
| Cell Culture Media | Ciliary differentiation at air-liquid interface | DMEM/Ham's F12 with required growth factors and differentiation supplements |
Emerging Diagnostic Technologies and Research Applications
The PCD diagnostic landscape continues to evolve with several emerging technologies offering potential for enhanced integration with clinical prediction tools like PICADAR:
Exhaled Breath Condensate Analysis: This non-invasive method shows promise as a future diagnostic tool, potentially providing biochemical markers of ciliary dysfunction [37].
Advanced Genetic Techniques: Whole exome and genome sequencing are increasingly identifying novel PCD genetic variants, particularly in patients with atypical presentations that may score lower on PICADAR [37].
Therapeutic Monitoring Applications: As new treatments including azithromycin maintenance therapy and gene therapies emerge, PICADAR may have utility in identifying candidates for early intervention and monitoring treatment responses [37] [38].
Research protocols should incorporate provisions for biospecimen banking (DNA, respiratory epithelial cells) to enable future studies correlating PICADAR scores with emerging biomarkers and genetic discoveries.
The integration of PICADAR within comprehensive PCD research protocols represents a strategic approach to patient stratification that optimizes resource utilization while maintaining diagnostic sensitivity. The tool's particular value lies in its ability to identify classic PCD phenotypes, though recent evidence confirms significant limitations in detecting non-classical presentations, especially in patients with situs solitus and normal ciliary ultrastructure.
Future research directions should focus on refining predictive algorithms to improve sensitivity across all PCD subgroups, potentially through the development of modified scoring systems or PICADAR-based decision trees that incorporate additional clinical parameters. The ongoing validation of PICADAR across diverse populations and its integration with emerging diagnostic technologies will continue to enhance its research utility and clinical application in the evolving landscape of PCD diagnosis and management.
Identifying PICADAR Limitations and Optimization Strategies for Situs Solitus Cases
The Primary Ciliary Dyskinesia Rule (PICADAR) is a diagnostic predictive tool recommended by the European Respiratory Society (ERS) to identify patients who should undergo definitive testing for Primary Ciliary Dyskinesia (PCD) [39]. PCD is a genetically heterogeneous respiratory ciliopathy characterized by reduced mucociliary clearance, leading to chronic wet cough, rhinitis, middle ear disease, and laterality defects such as situs inversus in approximately 50% of patients [39]. In the absence of a single gold standard diagnostic test, robust predictive tools are essential for appropriate patient referral within complex diagnostic pathways. However, recent evidence reveals that PICADAR's performance is not uniform across all PCD patient subgroups, exhibiting a significant sensitivity gap between patients with normal body situs (situs solitus) and those with laterality defects [4] [36]. This whitepaper quantifies this gap, analyzes its implications for research and clinical practice, and details the experimental protocols used to uncover it.
Core Quantitative Findings: A Pronounced Sensitivity Gap
A 2025 study by Schramm et al. evaluated PICADAR's sensitivity in a cohort of 269 individuals with genetically confirmed PCD [4] [36]. The findings demonstrate a stark contrast in the tool's ability to correctly identify PCD based on the presence or absence of a laterality defect.
Table 1: PICADAR Sensitivity in Genetically Confirmed PCD Patients
| Patient Subgroup | Number of Patients | Median PICADAR Score (IQR) | Sensitivity |
|---|---|---|---|
| Overall Cohort | 269 | 7 (IQR: 5 – 9) | 75% (202/269) |
| With Laterality Defects | Not Specified | 10 (IQR: 8 - 11) | 95% |
| With Situs Solitus | Not Specified | 6 (IQR: 4 - 8) | 61% |
The statistical difference between the sensitivity in the two groups was highly significant (p < 0.0001) [4] [36]. This indicates that nearly all PCD patients with laterality defects are correctly flagged by PICADAR, whereas about 4 in 10 PCD patients with normal organ arrangement (situs solitus) would be missed.
Further stratification by the associated ciliary ultrastructure, a key pathological feature in PCD, revealed another dimension to this performance gap.
Table 2: PICADAR Sensitivity Stratified by Ciliary Ultrastructure
| Ciliary Ultrastructure | Sensitivity |
|---|---|
| Hallmark Ultrastructural Defects | 83% |
| Absent Hallmark Ultrastructural Defects | 59% |
The sensitivity was significantly higher (p < 0.0001) in patients with hallmark defects on transmission electron microscopy compared to those without [4] [36]. This subgroup, often lacking both laterality defects and classic ultrastructural findings, represents a major diagnostic challenge where PICADAR's utility is most limited.
Experimental Protocol: Uncovering the Sensitivity Gap
The critical findings on PICADAR's variable sensitivity were generated through a rigorous retrospective cohort study design [4] [36]. The methodology provides a template for validating diagnostic prediction tools.
Study Population and Data Collection
- Cohort: The study included 269 individuals with a genetically confirmed diagnosis of PCD, establishing an unambiguous reference standard [4] [36].
- Data Extraction: Researchers collected data on the specific clinical features required to calculate the PICADAR score. This includes the initial gatekeeper question—"daily wet cough"—and the seven subsequent questions related to neonatal respiratory symptoms, situs anomalies, congenital cardiac defects, and chronic ear/nose symptoms [4].
PICADAR Scoring and Analysis
- Score Calculation: A PICADAR score was calculated for each participant based on their clinical history. Per the tool's protocol, individuals reporting no daily wet cough were automatically considered negative for PCD [4] [36].
- Sensitivity Analysis: The primary analysis calculated test sensitivity as the proportion of the genetically confirmed PCD cohort that scored ≥5 points, the recommended cut-off for triggering formal PCD testing [4] [36].
- Subgroup Analysis: The cohort was stratified into subgroups based on the presence of laterality defects (e.g., situs inversus) or situs solitus, and again by the presence or absence of hallmark ciliary ultrastructural defects. Sensitivity was recalculated for each subgroup [4] [36].
- Statistical Testing: A p-value of <0.0001 was calculated to determine the statistical significance of the sensitivity differences observed between the situs solitus and laterality defects subgroups, confirming the gap is not due to chance [4] [36].
Figure 1: Experimental workflow for PICADAR sensitivity analysis. The pathway shows how genetically confirmed PCD patients are classified by the PICADAR tool, leading to True Positive and False Negative outcomes.
The Scientist's Toolkit: Research Reagent Solutions
Research into PCD diagnostics relies on a suite of specialized techniques and reagents to confirm the disease and understand its pathophysiology.
Table 3: Essential Reagents and Materials for PCD Diagnostic Research
| Research Tool | Primary Function in PCD Research |
|---|---|
| Genetic Confirmation Panels | Next-generation sequencing panels targeting over 50 known PCD genes to establish a definitive molecular diagnosis, serving as the gold standard in genetic studies [4] [36]. |
| Transmission Electron Microscopy (TEM) | Used to visualize the ciliary ultrastructure (e.g., outer/inner dynein arms, nexin links) in nasal or bronchial biopsy samples. Identifies hallmark defects but can yield normal results in up to 30% of PCD cases [39]. |
| High-Speed Video Microscopy Analysis (HSVA) | Captures ciliary beat frequency and pattern from fresh clinical samples. Abnormal beat patterns are indicative of ciliary dysfunction. Often requires culture at an air-liquid interface (ALI) to differentiate primary from secondary defects [39]. |
| Nasal Nitric Oxide (nNO) Measurement | A functional screening test where low nNO levels (e.g., <77 nL/min in children over 6) are highly suggestive of PCD. Typically measured by chemiluminescence analyzer with velum closure [39]. |
| Immunofluorescence (IF) Assays | Uses antibodies against specific ciliary proteins (e.g., DNAH5, DNALI1) to detect the mislocalization or absence of these proteins in patient cilia, which can correlate with genetic and ultrastructural findings [39]. |
Implications for Research and Drug Development
The identified sensitivity gap has profound implications beyond clinical diagnosis, directly impacting therapeutic development.
- Patient Recruitment for Clinical Trials: Heavy reliance on PICADAR for trial screening could lead to the systematic exclusion of up to 39% of the potential PCD patient population—those with situs solitus [4] [36]. This enriches the trial cohort with a specific PCD subpopulation (those with laterality defects), potentially limiting the generalizability of trial results and leading to therapies that are less effective for the broader PCD community.
- Biomarker and Endpoint Development: The findings underscore that PCD is not a single entity but a spectrum of diseases with varying genetic causes and clinical presentations. Tools like PICADAR that are weighted towards specific features (e.g., laterality defects) may inadvertently define the disease based on these features. Researchers must ensure that novel biomarkers and clinical endpoints are validated across all PCD subgroups, including the situs solitus and ultrastructurally normal populations.
- Need for Next-Generation Predictive Tools: The limited sensitivity of PICADAR in key subgroups signals a clear need for the development and validation of more sophisticated predictive tools [4] [36]. These could incorporate genetic data, expanded clinical features, or results from initial nNO screening to improve overall sensitivity and ensure all PCD patients are identified for entry into the diagnostic and therapeutic pipeline.
Figure 2: Impact of PICADAR sensitivity gap on drug development. The diagram illustrates how reliance on PICADAR for clinical trial screening can create a biased cohort and the necessary steps to mitigate this issue.
The quantification of PICADAR's sensitivity—61% in situs solitus versus 95% with laterality defects—provides critical, actionable data for the PCD research and drug development community [4] [36]. This performance chasm demonstrates that while PICADAR is a useful initial tool, it is an imperfect gatekeeper. Its application without recognition of its limitations risks missing a large segment of the PCD population, potentially skewing clinical trial results and hampering the development of universally effective therapies. Future efforts must be directed toward creating and validating more inclusive diagnostic algorithms that maintain high sensitivity across the entire phenotypic spectrum of PCD. For drug development professionals, a thorough understanding of this sensitivity gap is essential for designing robust, inclusive, and generalizable clinical trials.
The Primary Ciliary Dyskinesia Rule (PICADAR) is a clinical prediction tool recommended by the European Respiratory Society to identify patients requiring specialized testing for Primary Ciliary Dyskinesia (PCD). Recent research reveals its diagnostic sensitivity is heavily dependent on underlying ciliary ultrastructure, demonstrating 83% sensitivity in patients with hallmark ultrastructural defects compared to just 59% sensitivity in those without these defects. This technical analysis examines the profound impact of ciliary ultrastructure on PICADAR performance, providing methodologies, analytical frameworks, and clinical implications for researchers and drug development professionals working on PCD diagnostics and therapeutics.
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous disorder affecting approximately 1 in 10,000-20,000 live births, characterized by abnormal ciliary structure and function leading to chronic oto-sino-pulmonary disease [25]. The diagnostic pathway for PCD is complex, requiring specialized testing available only at reference centers. To address this challenge, the PICADAR tool was developed as a simple clinical prediction rule using seven readily available clinical parameters to identify patients needing specialist referral [5].
While initial validation studies reported PICADAR sensitivity of 0.90 and specificity of 0.75 at a cutoff score of 5 points [5], emerging evidence indicates its performance varies substantially across PCD subpopulations. Recent research examining 269 genetically confirmed PCD patients reveals that ciliary ultrastructure significantly influences PICADAR's diagnostic accuracy, with sensitivity dropping markedly in patients lacking hallmark ultrastructural defects [4] [40]. This technical guide explores this critical performance discrepancy within the context of advancing PCD diagnostic research.
PICADAR Tool Composition and Application
Clinical Parameters and Scoring
The PICADAR tool applies to patients with persistent wet cough and assesses seven predictive parameters, with scores assigned based on regression coefficients rounded to the nearest integer [5]:
Table 1: PICADAR Scoring Parameters
| Clinical Parameter | Score |
|---|---|
| Full-term gestation | 1 point |
| Neonatal chest symptoms | 1 point |
| Neonatal intensive care admission | 2 points |
| Chronic rhinitis | 1 point |
| Chronic ear symptoms | 1 point |
| Situs inversus | 4 points |
| Congenital cardiac defect | 2 points |
The total PICADAR score ranges from 0-12 points, with the originally recommended cutoff of ≥5 points indicating high PCD probability and warranting specialist referral [5]. The tool was designed for use by general respiratory and ENT specialists to improve appropriate referrals to specialized PCD diagnostic centers.
Diagnostic Performance in Initial Validation
In the original derivation and validation study, PICADAR demonstrated excellent diagnostic characteristics:
Table 2: Initial PICADAR Validation Performance
| Metric | Derivation Group (n=641) | Validation Group (n=187) |
|---|---|---|
| Area Under Curve (AUC) | 0.91 | 0.87 |
| Sensitivity (at ≥5 points) | 0.90 | - |
| Specificity (at ≥5 points) | 0.75 | - |
| PCD Prevalence | 12% | 50% (by design) |
The original study concluded that PICADAR represented "a simple diagnostic clinical prediction rule with good accuracy and validity" ready for implementation in respiratory centers referring to PCD specialty centers [5].
Ciliary Ultrastructure Classification in PCD
Consensus Guidelines for TEM Analysis
Transmission Electron Microscopy (TEM) remains a cornerstone of PCD diagnosis, with international consensus guidelines standardizing the classification of ciliary ultrastructural defects [41]. The guidelines categorize findings as follows:
Class 1: Hallmark Defects - Confirmatory for PCD when present in >50% of transverse ciliary sections:
- Outer Dynein Arm (ODA) defects
- Combined Outer and Inner Dynein Arm (ODA+IDA) defects
- Microtubular disorganization with inner dynein arm loss
Class 2: Probable Defects - Require confirmation by additional PCD testing modalities:
- ODA+IDA defects in 25%-50% of cilia
- Central complex defects
- Few or no cilia with mis-located basal bodies
The diagnostic sensitivity of TEM alone never exceeds 70% since approximately 30% of genetically-confirmed PCD patients have normal ciliary ultrastructure [41]. This fundamental limitation directly impacts the performance of clinical prediction tools like PICADAR.
Ultrastructural Defects and Genotypic Correlations
Different genetic mutations in PCD result in distinct ultrastructural phenotypes. For example:
- DNAH5 and DNAI1 mutations typically cause isolated ODA defects
- CCDC39 and CCDC40 mutations cause microtubular disorganization with IDA loss
- DNAH11 mutations and HYDIN defects typically present with normal ultrastructure [42]
The distribution of these genetic subtypes within a study population significantly influences the observed performance characteristics of clinical prediction tools.
Differential Sensitivity Analysis: Methodology and Findings
Study Population and Analytical Approach
A 2025 study analyzed 269 individuals with genetically confirmed PCD to evaluate PICADAR's sensitivity across ultrastructural subgroups [4] [40]. The methodological approach included:
Inclusion Criteria: Genetically confirmed PCD diagnosis regardless of clinical presentation or ultrastructural phenotype
PICADAR Application: Standardized calculation of scores based on medical record review, applying the established ≥5 point cutoff for positive screening
Stratified Analysis: Subgroup comparison based on:
- Presence or absence of laterality defects (situs inversus totalis vs. situs solitus)
- TEM classification (hallmark defects vs. normal ultrastructure or non-hallmark defects)
Statistical Analysis: Sensitivity calculations with 95% confidence intervals, median scores with interquartile ranges (IQR), and comparative analyses using appropriate statistical tests
Key Findings: The Ultrastructure Impact
The study revealed striking differences in PICADAR performance based on ultrastructural category:
Table 3: PICADAR Sensitivity by Ultrastructural Category
| Patient Subgroup | n | Median PICADAR Score [IQR] | Sensitivity (%) |
|---|---|---|---|
| Overall Population | 269 | 7 [5-9] | 75% |
| Hallmark Ultrastructural Defects | - | - | 83% |
| Non-Hallmark Ultrastructural Features | - | - | 59% |
| Laterality Defects (Situs Inversus) | - | 10 [8-11] | 95% |
| Situs Solitus (Normal Laterality) | - | 6 [4-8] | 61% |
The 24-percentage-point difference in sensitivity between hallmark and non-hallmark groups (83% vs. 59%) highlights a critical diagnostic gap [4] [40]. Furthermore, the study found that 7% (18/269) of genetically confirmed PCD patients reported no daily wet cough, automatically ruling out PCD according to PICADAR's initial screening question [4].
Experimental Protocols for Ultrastructure-Based Diagnostic Validation
Patient Recruitment and Phenotyping
Robust validation of PCD diagnostic tools requires meticulous patient characterization:
Inclusion Criteria:
- Genetically confirmed PCD through comprehensive genetic testing (either targeted gene panels or whole exome sequencing)
- Age >5 years to ensure symptom development
- Informed consent for detailed clinical data collection
Clinical Data Collection:
- Standardized questionnaire covering all PICADAR parameters
- Verification of medical records for neonatal history and congenital anomalies
- Systematic documentation of respiratory and otological symptoms
- High-resolution imaging for bronchiectasis assessment
Ethical Considerations: Study approval by institutional review boards, with particular attention to genetic data protection and pediatric assent procedures.
TEM Processing and Analysis Protocol
Standardized TEM methodology is essential for consistent ultrastructural classification:
Sample Collection:
- Nasal brush biopsies from inferior turbinate under direct visualization
- Immediate placement in 2.5% glutaraldehyde in 0.1M cacodylate buffer (pH 7.4)
- Processing within 2 hours of collection
Sample Processing:
- Post-fixation in 1% osmium tetroxide for 1 hour
- Dehydration through graded ethanol series (10%-100%)
- Resin infiltration and embedding in Agar Scientific low viscosity resin
- Polymerization at 70°C for 24 hours
Ultramicrotomy and Imaging:
- Sectioning at 70nm thickness using Leica EM UC6 ultramicrotome
- Double staining with uranyl acetate and Reynold's lead citrate
- Imaging at 120kV using FEI Tecnai Spirit TEM
- Minimum 50 ciliary cross-sections analyzed per patient
Classification Criteria:
- Hallmark defects: >50% cilia showing ODA, ODA+IDA, or specific microtubular defects
- Normal ultrastructure: <10% cilia with any defect
- Secondary defects: Documented but not considered diagnostic without clinical correlation
PICADAR Scoring and Statistical Analysis
Standardized application of PICADAR and appropriate statistical methods:
Blinded Assessment:
- PICADAR scoring performed independently by two clinicians
- Discrepancies resolved by third reviewer
- Scorers blinded to TEM and genetic results
Statistical Analysis:
- Sensitivity, specificity, positive and negative predictive values calculated
- 95% confidence intervals using exact binomial methods
- Median scores with interquartile ranges for non-normal distributions
- Subgroup comparisons using Chi-square or Fisher's exact tests for categorical data
- Statistical significance defined as p<0.05
Sample Size Justification:
- Minimum 250 participants to detect 15% sensitivity difference with 80% power
- Oversampling of rare subgroups (normal ultrastructure, situs solitus)
Visualization of Diagnostic Pathways and Relationships
Diagram 1: PICADAR Diagnostic Pathway with Sensitivity Limitations
Diagram 2: Ultrastructural Impact on PICADAR Sensitivity
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Materials for PCD Diagnostic Studies
| Category | Specific Item/Technique | Research Application | Key Considerations |
|---|---|---|---|
| Clinical Assessment Tools | PICADAR questionnaire | Standardized clinical phenotyping | Validate translation if multilingual cohorts |
| TEM Processing | Glutaraldehyde (2.5% in cacodylate buffer) | Primary fixation of ciliary structure | EM-grade, fresh preparation essential |
| TEM Processing | Osmium tetroxide (1%) | Secondary fixation for membrane contrast | Highly toxic, requires fume hood |
| TEM Processing | Agar Scientific LV Resin | Embedding for ultrastructural preservation | Low viscosity improves infiltration |
| Genetic Analysis | Targeted PCD gene panels (>30 genes) | Genetic confirmation of diagnosis | Coverage of major PCD genes essential |
| Ciliary Function | High-speed video microscopy | Ciliary beat frequency/pattern analysis | Requires specialized equipment, expertise |
| Cell Culture | Air-liquid interface (ALI) culture | Ciliary differentiation, secondary change reversal | 4-6 week differentiation period required |
Discussion and Research Implications
The substantial difference in PICADAR sensitivity between patients with and without hallmark ultrastructural defects (83% vs. 59%) has profound implications for PCD research and clinical practice. This discrepancy likely reflects fundamental differences in phenotypic expression across PCD genetic subtypes.
Pathophysiological Basis for Performance Variation
The superior PICADAR performance in hallmark defect populations stems from several factors:
- Stronger phenotype association: ODA defects correlate with more severe ciliary dysfunction and earlier symptom presentation
- Higher situs inversus prevalence: Certain ultrastructural defects (particularly ODA defects) more frequently affect nodal cilia during embryogenesis, resulting in laterality defects that contribute substantially to PICADAR scores [4]
- Earlier diagnosis: More dramatic clinical presentations prompt earlier specialist referral and diagnosis
Conversely, PCD patients with normal ultrastructure or subtle defects often present with milder respiratory symptoms, less frequent neonatal respiratory distress, and lower rates of situs inversus, resulting in lower PICADAR scores and reduced sensitivity [42].
Implications for Diagnostic Algorithm Development
These findings necessitate a reevaluation of PCD diagnostic pathways, particularly for resource-limited settings where TEM may be the only specialized test available [41]. The European Respiratory Society guidelines appropriately recommend further testing in cases with strong clinical suspicion despite normal ultrastructure [39], but implementation remains challenging.
Future diagnostic algorithms should incorporate:
- Ultrastructure-aware interpretation of clinical prediction tools
- Lower PICADAR thresholds for subpopulations with normal ultrastructure
- Expanded genetic testing for cases with discordant clinical and ultrastructural findings
- Novel biomarker development for ultrastructurally normal PCD variants
The differential sensitivity of PICADAR based on ciliary ultrastructure represents a critical consideration for researchers, clinicians, and drug developers working in PCD. While PICADAR remains a valuable screening tool, its limited sensitivity (59%) in patients without hallmark ultrastructural defects necessitates supplementary approaches for comprehensive case identification. Future research should focus on developing ultrastructure-specific screening algorithms and validating novel biomarkers to ensure all PCD patients receive accurate, timely diagnoses regardless of their underlying structural phenotype.
The Primary Ciliary Dyskinesia Rule (PICADAR) is a validated diagnostic predictive tool recommended by the European Respiratory Society to determine the likelihood of a Primary Ciliary Dyskinesia (PCD) diagnosis and guide subsequent testing [4]. This eight-item clinical score evaluates factors including gestational age, situs status, congenital heart disease, and early-onset respiratory symptoms to identify patients requiring definitive PCD diagnostic testing [4]. Its algorithm begins with a critical initial question: the presence of a daily wet cough starting in infancy [4].
Recent research reveals a significant limitation in this foundational criterion. A 2025 genetic study demonstrated that approximately 7% of genetically confirmed PCD patients did not report this symptom, leading to their automatic exclusion from further PICADAR evaluation and potential diagnostic delay [4]. This technical analysis examines the sensitivity limitations of the PICADAR tool, with particular focus on its performance across patient subgroups with normal organ arrangement (situs solitus) and those with atypical ciliary ultrastructure, providing crucial insights for researchers and drug development professionals working to improve diagnostic protocols.
Quantitative Analysis of PICADAR Sensitivity
A comprehensive 2025 genetic study by Omran et al. evaluated the sensitivity of the PICADAR tool in a cohort of 269 individuals with genetically confirmed PCD [4]. The findings revealed substantial variations in test performance based on clinical and structural phenotypes.
Table 1: PICADAR Sensitivity in Genetically Confirmed PCD (n=269)
| Patient Subgroup | Number of Patients | Median PICADAR Score (IQR) | Sensitivity (%) |
|---|---|---|---|
| Overall Cohort | 269 | 7 (5–9) | 75% (202/269) |
| Patients without daily wet cough | 18 | N/A (Ruleed out) | 0% (Excluded) |
| With Laterality Defects | Information missing | 10 (8–11) | 95% |
| With Situs Solitus (normal arrangement) | Information missing | 6 (4–8) | 61% |
| With Hallmark Ultrastructural Defects | Information missing | Information missing | 83% |
| Without Hallmark Ultrastructural Defects | Information missing | Information missing | 59% |
The data demonstrates that the absence of a daily wet cough led to the immediate exclusion of 18 patients (7%) from further PICADAR assessment, despite subsequent genetic confirmation of PCD [4]. Furthermore, sensitivity dropped precipitously to 61% in patients with situs solitus and to 59% in those lacking hallmark ultrastructural defects on transmission electron microscopy [4]. This confirms that the tool's utility is significantly diminished for PCD populations with normal body composition or normal ciliary ultrastructure.
Materials and Methods: Experimental Protocols for PCD Diagnostic Research
To ensure reproducibility and validate these findings, the following detailed methodologies are provided for key experiments cited in this analysis.
Patient Cohort Identification and Genetic Confirmation
The foundational study employed a rigorous protocol for patient recruitment and genetic verification [4] [43].
- Patient Recruitment: A retrospective, multi-center analysis was conducted, enrolling individuals with a clinically or genetically suspected PCD diagnosis. The cohort included 269 genetically confirmed patients to establish a definitive phenotype-genotype correlation [4].
- Inclusion Criteria: Diagnosis was based on the presence of biallelic pathogenic variants in a known PCD-associated gene, as per international guidelines [43].
- Genetic Testing Method: Whole Exome Sequencing (WES) was performed. Genomic DNA was extracted using a QIAamp Blood Midi Kit (QIAGEN). The amplified DNA was captured using the GenCap WES capture kit, sequencing whole exons and 20 bp of flanking intronic regions on the DNBSEQ (DNBSEQ-T7) platform with 150 bp paired-end reads. Bioinformatic analysis mapped clean reads to the UCSC hg19 reference genome using BWA software. SNP and InDel variants were detected using Sentieon software and annotated with ANNOVAR against multiple databases (1000 genome, ESP6500, dbSNP, EXAC, HGMD). Pathogenicity was assessed according to ACMG guidelines, with verification via Sanger sequencing on an ABI3730xl sequencer [43].
PICADAR Application and Sensitivity Analysis
The methodology for applying the PICADAR tool and calculating its sensitivity was clearly defined [4].
- PICADAR Scoring: The PICADAR tool was applied to all 269 patients based on their clinical records. The initial filter question regarding "daily wet cough" was strictly enforced. Patients without this symptom were scored as negative and excluded from further scoring.
- Sensitivity Calculation: For patients reporting a daily wet cough, the remaining seven PICADAR questions were scored. The proportion of patients scoring ≥5 points (the recommended threshold for initiating PCD diagnostic work-up) was calculated to determine overall sensitivity.
- Stratified Analysis: Subgroup analyses were performed to examine sensitivity based on the presence or absence of laterality defects (situs inversus totalis or heterotaxy) and the presence or absence of hallmark ciliary ultrastructural defects (e.g., outer dynein arm defects) as determined by transmission electron microscopy (TEM). A p-value of <0.05 was considered statistically significant [4].
Research Reagent Solutions for PCD Diagnostics
The following table details key reagents, platforms, and software essential for conducting genetic and functional research in PCD.
Table 2: Essential Research Tools for PCD Diagnostic Studies
| Item Name | Specific Function/Use Case | Key Details/Alternatives |
|---|---|---|
| QIAamp Blood Midi Kit (QIAGEN) | Genomic DNA extraction from patient blood samples. | Ensures high-quality, high-molecular-weight DNA for sequencing. |
| GenCap WES Capture Kit | Target enrichment for whole exome sequencing. | Covers exonic regions and flanking sequences for variant discovery. |
| DNBSEQ-T7 Platform | High-throughput next-generation sequencing. | Provides 150 bp paired-end reads for comprehensive coverage. |
| BWA (Burrows-Wheeler Aligner) | Mapping sequenced reads to a reference genome (hg19). | Critical first step in the bioinformatic pipeline for alignment. |
| ANNOVAR Software | Functional annotation of genetic variants. | Annotates with population frequency and predictive scores (SIFT, PolyPhen-2). |
| ABI3730xl Sequencer | Sanger sequencing for variant validation and segregation analysis. | Gold standard for confirming variants identified by NGS. |
| Nakulen Breath Analyzer (Sunvou-CA2122) | Measuring nasal Nitric Oxide (nNO) levels. | Low nNO is a supportive screening test for PCD [43]. |
PICADAR Workflow and Its Diagnostic Gap
The following diagram illustrates the standard PICADAR assessment pathway and highlights the critical point where a subset of genetically confirmed PCD patients is excluded.
Impact of Clinical and Ultrastructural Phenotypes on PICADAR Performance
The sensitivity of the PICADAR tool is highly dependent on patient phenotype. The following diagram maps the relationship between key patient characteristics and the corresponding performance of the diagnostic tool.
This phenotypic stratification reveals a critical diagnostic blind spot. The reliance on classic symptoms like daily wet cough and laterality defects fails to capture patients with normal organ arrangement (situs solitus) or those with normal ciliary ultrastructure, despite genetic confirmation of disease [4] [17]. Epidemiological studies in Japan corroborate this, showing only 25% of PCD patients had situs inversus, challenging the traditional 50% statistic and highlighting ethnic variations in genotype-phenotype correlations that further complicate PICADAR's universal application [17].
The finding that 7% of genetically confirmed PCD patients are excluded at the first step of the PICADAR algorithm due to the absence of a daily wet cough represents a significant vulnerability in the current diagnostic pathway [4]. This omission, compounded by the tool's substantially reduced sensitivity in patients with situs solitus (61%) or non-hallmark ultrastructural defects (59%), underscores an urgent need for refined predictive models [4]. For the research and drug development community, these findings are paramount. Reliance on a tool with these specific limitations risks systematically excluding a subset of PCD patients from clinical trials and targeted therapeutic interventions, such as the investigational mRNA-based therapy RCT1100 for DNAI1-related PCD [44]. Future efforts must focus on developing next-generation diagnostic algorithms that incorporate genetic and molecular data from the outset, ensuring all PCD patients are identified early and eligible for emerging, genotype-specific treatments.
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder characterized by abnormal motile cilia function, leading to chronic oto-sino-pulmonary disease, laterality defects, and subfertility [45]. With over 50 identified causative genes and no single gold-standard diagnostic test, the diagnosis of PCD remains challenging in clinical practice [46] [45]. The PrImary CiliARy DyskinesiA Rule (PICADAR) represents a clinical prediction tool developed to identify symptomatic patients requiring specialized PCD testing [5]. However, the sensitivity of this tool, particularly in patients with situs solitus (normal organ arrangement), can be influenced by both the specific genetic variants present and the ethnic background of the patient [18]. This technical review synthesizes evidence from international populations to examine the critical interplay between ethnicity, genotype, and the performance of clinical diagnostic tools like PICADAR, providing researchers and drug development professionals with essential insights for designing targeted studies and therapies.
The PICADAR Tool: Foundation and Application in PCD Diagnosis
Development and Standard Application
The PICADAR tool was developed to address the need for a practical, evidence-based method to identify patients with a high probability of PCD prior to specialized, invasive, and costly confirmatory testing [5]. Derived from a large prospective population, it utilizes seven easily obtainable clinical parameters from a patient's history. Its development was a significant advancement, as it provided a standardized approach for general respiratory specialists to determine whom to refer for complex PCD diagnostics, which often require expensive equipment and expert interpretation [5] [39].
Table 1: The PICADAR Scoring Criteria and Point Values
| Predictive Parameter | Criteria for Point Assignment | Points |
|---|---|---|
| Gestational Age at Birth | Full-term gestation (≥37 weeks) | 2 |
| Neonatal Chest Symptoms | Presence at term (e.g., respiratory distress) | 2 |
| Neonatal Intensive Care Admission | Admission at term for respiratory symptoms | 1 |
| Chronic Rhinitis | Persistent, perennial rhinitis | 1 |
| Chronic Ear Symptoms | Chronic otitis media, hearing loss, or perforation | 1 |
| Situs Inversus | Confirmed situs inversus totalis | 2 |
| Congenital Cardiac Defect | Any confirmed congenital heart defect | 1 |
In the original validation study, a PICADAR score of ≥5 points demonstrated a sensitivity of 0.90 and specificity of 0.75 for predicting a positive PCD diagnosis, with an area under the curve (AUC) of 0.91 upon internal validation and 0.87 upon external validation [5]. This performance confirmed its utility as a robust screening tool in diverse clinical settings.
Detailed Experimental Protocol for PICADAR Application
For researchers employing PICADAR in clinical studies, adherence to a standardized protocol is critical for data consistency.
1. Patient Interview and Data Collection: A structured proforma should be used to collect data from the patient or caregiver prior to any definitive diagnostic testing for PCD [5]. The interviewer must be trained to ask specific, non-leading questions.
- Full-term gestation: Confirm birth at or after 37 weeks of gestation.
- Neonatal chest symptoms: Inquire specifically about respiratory distress, tachypnea, or requirement for supplemental oxygen at term.
- Neonatal intensive care unit admission: Document if the admission was specifically for respiratory concerns at term.
- Chronic rhinitis: Define as persistent, year-round nasal congestion or rhinorrhea, beginning in the first year of life and lasting for more than 3 months annually.
- Chronic ear symptoms: Document a history of recurrent otitis media, chronic serous otitis ("glue ear"), tympanostomy tube placement, or hearing loss.
- Situs inversus: Confirm via imaging reports (e.g., chest radiograph or abdominal ultrasonography).
- Congenital cardiac defect: Confirm via echocardiography report or medical records.
2. Scoring and Interpretation: Points are assigned as detailed in Table 1. The total score is calculated, and patients are stratified into risk categories. In research contexts, the original cut-off of ≥5 points is commonly used to define "high suspicion" for PCD [5]. However, studies have shown that this cut-off may need adjustment in specific populations, particularly those with a high prevalence of situs solitus [18].
Ethnic Variations in PCD Genotypes
The genetic landscape of PCD is not uniform across global populations. Specific ethnic groups demonstrate distinct prevalences of pathogenic variants, which directly influences disease presentation and the efficacy of phenotype-based diagnostic tools.
Regional Genetic Spectra
Table 2: Predominant PCD Genetic Variants in Selected International Populations
| Population | Most Prevalent Gene(s) | Key Genetic Findings | Reported Situs Inversus Prevalence |
|---|---|---|---|
| Chinese | DNAH5 | c.8383C>T is a common mutated variant, rare in other ethnicities [46]. | 50% (Kartagener Syndrome) [46] |
| Southwest Saudi Arabian | DNAH5, RSPH9, DNAI2, LRRC56 | DNAH5 represented 17.9% of cases; diverse genetic profile with multiple less common genes [18]. | Not explicitly stated, but present in cohort [18] |
| Korean | DNAH5, DNAAF1 | DNAH5 and DNAAF1 had the highest mutation rates; rare genotypes (RPGR, HYDIN, NME5) also identified [10]. | Not explicitly stated |
| European (General) | Multiple, including CCDC39, CCDC40, DNAH5 | Over 50 genes identified; ~20-30% of patients have no identified genetic cause [45]. | 40-50% [45] |
The implications of these genetic differences are profound. For instance, variants in genes like RSPH9 and HYDIN are associated with central apparatus defects and patients almost universally have situs solitus [18] [10]. Consequently, in populations where these genotypes are more common, a greater proportion of PCD patients will present with situs solitus, directly impacting the sensitivity of the PICADAR tool, which assigns significant weight to situs inversus.
The Critical Interplay: Genotype, Situs Status, and PICADAR Sensitivity
Evidence of Reduced PICADAR Sensitivity in Situs Solitus
A 2023 cross-sectional study from Southwest Saudi Arabia provided direct, quantitative evidence of how situs status affects PICADAR scores [18]. In this cohort, the median PICADAR score in patients with PCD and situs inversus was 11.5 (Q1: 10, Q3: 12.5), which was significantly higher than the median score of 7.5 (Q1: 5.8, Q3: 8) in patients with PCD and situs solitus (U = 10.5; p < 0.001) [18]. This finding is critical because it demonstrates that a substantial subset of PCD patients—those with situs solitus—systematically achieve lower PICADAR scores. If the standard cut-off of 5 is used, some of these patients may fall below the threshold for referral, potentially delaying diagnosis.
This phenomenon is genetically mediated. The establishment of left-right body asymmetry in embryogenesis depends on motile cilia function at the embryonic node [45]. Pathogenic variants in certain genes (e.g., DNAH5, DNAI1) are frequently associated with randomization of lateralization, leading to a ~50% chance of situs inversus. In contrast, variants in other genes, particularly those causing central pair apparatus defects (e.g., RSPH9, RSPH4A, HYDIN), are almost exclusively associated with situs solitus [18] [10] [45]. Therefore, the prevalence of these "situs solitus-associated" genotypes within an ethnic population will directly determine the proportion of PCD patients without laterality defects and, consequently, the overall sensitivity of the PICADAR tool for that population.
Figure 1: Logical Relationship Between Genotype, Situs Status, and PICADAR-Led Diagnosis. The pathway shows how a patient's specific PCD genotype ultimately influences the diagnostic outcome through its effect on situs status and the resulting PICADAR score.
Methodologies for Comprehensive PCD Diagnosis in Research
Integrated Diagnostic Workflow
Given the limitations of any single test, a combination of diagnostic modalities is essential for robust PCD confirmation in research settings, especially in populations with genotypic diversity.
Figure 2: A Consensus-Based Diagnostic Workflow for PCD Research. This algorithm, adapted from international guidelines, illustrates a multi-modal approach. Notably, the pathway allows for genetic testing in cases with a strong clinical history even if the initial PICADAR score is not indicative, acknowledging the tool's reduced sensitivity in situs solitus cases [39] [18].
Detailed Experimental Protocol for Genetic Analysis via Whole-Exome Sequencing (WES)
Genetic testing has become a cornerstone for confirming PCD, especially when functional tests are inconclusive or unavailable [46] [18]. The following protocol details the WES methodology as used in recent international studies.
1. DNA Extraction and Quality Control:
- Collect whole blood samples in EDTA tubes from probands and, for trio analysis, from biological parents.
- Extract genomic DNA using a commercial extraction kit (e.g., PerkinElmer Chemagic DNA CS200 kit).
- Quantify DNA using a fluorescence-based method (e.g., PicoGreen reagent) and ensure purity (A260/A280 ratio ~1.8). A minimum of 1 μg of input DNA is typically required [18].
2. Library Preparation and Exome Capture:
- Fragment the genomic DNA by sonication or enzymatic digestion to a target size of 150-200 bp.
- Perform end-repair, adenylation, and ligation of sequencing adapters to create the library.
- Enrich the exonic regions by hybridizing the library to a biotinylated oligonucleotide bait panel (e.g., Agilent SureSelect Clinical Research Exome v3 or SureSelect Human All Exon V6) [18] [10].
- Capture the hybridized fragments using streptavidin-coated magnetic beads and wash away non-specific binding.
3. Sequencing and Bioinformatic Analysis:
- Amplify the captured library and perform paired-end sequencing (e.g., 2x150 bp) on a high-throughput platform (e.g., Illumina NovaSeq 6000 or HiSeq 2500) [18] [10].
- Map the raw sequence reads to a reference genome (e.g., hg19/GRCh37) using aligners like the Burrows-Wheeler Aligner (BWA).
- Perform variant calling (single nucleotide variants, indels) using tools like GATK. Annotate variants using SnpEff.
- Filtering Strategy: Prioritize variants in a pre-defined list of known PCD-associated genes. Focus on loss-of-function variants (nonsense, frameshift, splice-site) and missense variants predicted to be damaging by in silico tools. Filter based on population frequency (e.g., <1% in gnomAD) and segregate according to the expected inheritance model (typically autosomal recessive or X-linked) [18]. Confirm compound heterozygosity or homozygosity in trans.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for PCD Investigation
| Item | Function/Application in PCD Research |
|---|---|
| Agilent SureSelect Exome Capture Kits | Target enrichment for whole-exome sequencing to identify pathogenic variants in over 50 known PCD genes [18]. |
| Illumina Sequencing Platforms (e.g., NovaSeq 6000) | High-throughput next-generation sequencing to generate the raw data for genetic analysis [18] [10]. |
| Transmission Electron Microscope (TEM) | Visualization of ciliary ultrastructural defects (e.g., outer/inner dynein arm absence, central pair defects) in nasal or bronchial biopsy samples [46] [47] [10]. |
| Chemiluminescence Nitric Oxide Analyzer | Measurement of nasal nitric oxide (nNO) levels, which are characteristically low in most PCD patients, serving as a sensitive screening tool [39]. |
| High-Speed Video Microscope | Analysis of ciliary beat frequency and pattern from fresh ciliated epithelial samples, a key functional diagnostic test [39]. |
| Air-Liquid Interface (ALI) Culture Media | Culture of respiratory epithelial cells to regenerate cilia and eliminate secondary dyskinesia, improving the diagnostic accuracy of HSVA and TEM [39]. |
The diagnosis of Primary Ciliary Dyskinesia is a complex puzzle where pieces of clinical presentation, genetic makeup, and ethnic background must be carefully assembled. Evidence from international populations consistently shows that the PICADAR tool's performance is intrinsically linked to the local genetic spectrum, with significantly lower scores in patients with situs solitus, a phenotype strongly associated with specific genotypes like RSPH9 and HYDIN [18] [10]. For researchers and drug developers, these findings are paramount. They underscore the necessity of:
- Validating clinical prediction tools like PICADAR within specific ethnic cohorts before deployment.
- Employing a multi-modal diagnostic protocol that integrates genetic testing to capture the full genotypic diversity of PCD, especially in cases with atypical presentation (e.g., situs solitus and low PICADAR scores).
- Considering ethnic and genotypic prevalence when designing patient recruitment strategies for clinical trials, to ensure enrolled cohorts accurately represent the target population and to enable the development of genotype-specific therapies. A one-size-fits-all approach to PCD diagnosis is untenable; precision medicine, informed by ethnic and genotypic considerations, is the path forward.
Supplemental Screening Approaches for Enhanced Case Identification
Primary Ciliary Dyskinesia (PCD) is a rare, genetically heterogeneous motile ciliopathy characterized by chronic oto-sino-pulmonary disease. Accurate diagnosis is critical for managing long-term complications, but remains challenging due to the disease's phenotypic diversity. The PICADAR (PCD Rule) score is a diagnostic predictive tool recommended by the European Respiratory Society (ERS) to assess the likelihood of PCD prior to definitive testing. However, recent evidence reveals significant limitations in its sensitivity, particularly in specific patient subgroups. This creates an pressing need for supplemental screening approaches that can enhance case identification, especially for patients falsely ruled out by PICADAR. This technical guide examines the performance limitations of PICADAR and details validated supplemental screening methodologies to improve diagnostic sensitivity within the context of advancing PICADAR score situs solitus sensitivity research.
Research demonstrates that PICADAR's overall sensitivity in a genetically confirmed PCD population is approximately 75%, meaning one-quarter of true PCD cases are missed. The tool's performance is markedly worse in two key subgroups: individuals with situs solitus (normal organ arrangement), where sensitivity drops to 61%, and those with absent hallmark ultrastructural defects on transmission electron microscopy, where sensitivity is only 59% [4]. This deficiency stems from PICADAR's initial question which automatically rules out PCD in individuals without daily wet cough—a feature absent in 7% of genetically confirmed cases [4]. For researchers and drug development professionals, understanding these limitations is essential for designing robust patient identification strategies in clinical trials and translational research programs.
Quantitative Analysis of PICADAR Performance and Supplemental Methods
PICADAR Performance Characteristics Across PCD Subpopulations
Table 1: PICADAR Sensitivity Analysis in Genetically Confirmed PCD Cohorts (n=269)
| Patient Subgroup | Sample Size | Median PICADAR Score (IQR) | Sensitivity (%) | Statistical Significance (p-value) |
|---|---|---|---|---|
| Overall PCD Population | 269 | 7 (5-9) | 75 | Reference |
| With Laterality Defects | Not specified | 10 (8-11) | 95 | <0.0001 |
| With Situs Solitus (normal arrangement) | Not specified | 6 (4-8) | 61 | <0.0001 |
| With Hallmark Ultrastructural Defects | Not specified | Not specified | 83 | <0.0001 |
| Without Hallmark Ultrastructural Defects | Not specified | Not specified | 59 | <0.0001 |
| Without Daily Wet Cough | 18 (7%) | Not applicable (ruled out) | 0 | Not applicable |
Comparative Performance of Supplemental Screening Modalities
Table 2: Supplemental Screening Modalities for Enhanced PCD Case Identification
| Screening Method | Technical Principle | Target Population | Estimated Incremental Detection Yield | Advantages | Limitations |
|---|---|---|---|---|---|
| Nasal Nitric Oxide (nNO) Measurement | Chemiluminescence analysis of nasal nitric oxide levels | Patients with situs solitus or absent hallmark defects | High (complements genetic testing) | Non-invasive, rapid, high negative predictive value | Requires specialized equipment, cooperation, affected by acute infection |
| Genetic Testing (Next-Generation Sequencing Panels) | Identification of pathogenic variants in >40 known PCD genes | All suspected PCD cases, especially PICADAR-negative | 5.3 per 1000 screens (based on ultrasound analogy) | Comprehensive, definitive diagnosis, enables genetic counseling | May identify variants of uncertain significance, expensive |
| Transmission Electron Microscopy (TEM) | Ultrastructural analysis of ciliary axoneme | Patients with normal situs or atypical presentation | Identifies 59% of PICADAR-missed cases | Visual confirmation of defects, establishes phenotype-genotype correlation | Invasive (biopsy required), specialized expertise needed, normal result doesn't exclude PCD |
| High-Speed Video Microscopy Analysis (HSVA) | Digital analysis of ciliary beat frequency and pattern | Suspected PCD with normal nNO/TEM | 2.5-4.0 per 1000 screens (based on ultrasound analogy) | Functional assessment, can detect subtle motility defects | Limited availability, requires fresh tissue, specialized analysis |
Experimental Protocols for Supplemental Screening Methodologies
Protocol 1: Nasal Nitric Oxide Measurement Procedure
Purpose: To measure nasal nitric oxide production as a non-invasive screening test for PCD, characterized by very low nNO levels.
Materials and Equipment:
- Chemiluminescence nitric oxide analyzer
- Nasal olive or nasal cavity catheter
- Saline for nasal lavage (if required)
- Nose clips for velum closure
- Calibration gases for analyzer
Methodology:
- Patient preparation: Exclude patients with current acute respiratory infection or nasal polyps which may affect results.
- Instrument calibration: Perform daily calibration according to manufacturer specifications using certified calibration gases.
- Sampling technique: Insert nasal olive securely into one nostril while occluding the other nostril.
- Velum closure: Patient performs breath-hold maneuver against closed glottis or says "k" repeatedly to maintain velopharyngeal closure.
- Measurement: Sample nasal air at constant flow rate (typically 3 mL/s) until stable plateau is achieved (usually 30-45 seconds).
- Repetition: Repeat measurement in contralateral nostril and calculate mean value.
- Interpretation: nNO values <77 nL/min in children or <100 nL/min in adults strongly suggest PCD and warrant further investigation.
Validation Parameters:
- Intra-individual coefficient of variation: <10% between measurements
- Minimum acceptable plateau duration: 30 seconds of stable reading
- Quality control: Daily calibration verification with known standard concentrations
Protocol 2: Genetic Testing Methodology for PCD
Purpose: To identify pathogenic mutations in known PCD-associated genes using next-generation sequencing.
Materials and Equipment:
- DNA extraction kit (blood or saliva)
- Next-generation sequencing platform
- PCD gene panel (minimum 40 genes including DNAH5, DNAH11, DNAI1, CCDC39, CCDC40, RSPH1, etc.)
- Bioinformatics analysis pipeline
- Sanger sequencing reagents for confirmation
Methodology:
- Sample collection: Collect peripheral blood in EDTA tubes or saliva using appropriate collection kits.
- DNA extraction: Isolate genomic DNA using standardized extraction protocols, quantifying yield and purity.
- Library preparation: Fragment DNA and attach sequencing adapters using commercial library preparation kits.
- Target enrichment: Hybridize library to PCD-specific gene panel probes or use amplicon-based approach.
- Sequencing: Perform massively parallel sequencing on NGS platform (Illumina recommended).
- Bioinformatics analysis:
- Map reads to reference genome (GRCh38)
- Variant calling and annotation
- Filter against population databases (gnomAD, 1000 Genomes)
- Pathogenicity prediction using in silico tools (SIFT, PolyPhen-2, CADD)
- Validation: Confirm pathogenic variants using Sanger sequencing.
- Interpretation: Classify variants according to ACMG guidelines and correlate with clinical phenotype.
Quality Control Measures:
- Minimum sequencing depth: 50x for all target regions
- Coverage uniformity: >95% of target bases at 20x coverage
- Positive control variants when available
- Blinded analysis of known samples for proficiency testing
Protocol 3: Transmission Electron Microscopy Protocol
Purpose: To visualize ciliary ultrastructure and identify hallmark defects associated with PCD.
Materials and Equipment:
- Bronchoscopy equipment for nasal or bronchial biopsy
- Glutaraldehyde fixative (2.5-3% in cacodylate buffer)
- Osmium tetroxide post-fixation solution
- Epoxy resin for embedding
- Ultramicrotome
- Transmission electron microscope
- Uranyl acetate and lead citrate for staining
Methodology:
- Biopsy collection: Obtain 3-4 ciliated epithelial samples from inferior nasal turbinate or bronchial mucosa.
- Immediate fixation: Place tissue immediately in cold glutaraldehyde fixative for 24 hours.
- Post-fixation: Transfer to 1% osmium tetroxide for 1 hour.
- Dehydration: Serial ethanol dehydration (50%, 70%, 90%, 100%).
- Embedding: Infiltrate with propylene oxide and embed in epoxy resin.
- Sectioning: Cut semi-thin sections (1μm) for orientation, then ultra-thin sections (70-90nm) for TEM.
- Staining: Contrast sections with uranyl acetate and lead citrate.
- Microscopy: Examine at 60-80kV, capturing multiple cross-sections of cilia.
- Analysis: Evaluate 50-100 ciliary cross-sections for:
- Outer dynein arm presence and morphology
- Inner dynein arm presence and morphology
- Microtubular organization (9+2 pattern)
- Central apparatus defects
- Other structural abnormalities
Interpretation Criteria:
- Normal: Regular 9+2 microtubule arrangement with complete inner and outer dynein arms
- Hallmark defect: Absence or substantial shortening of outer dynein arms ± inner dynein arms
- Suggestive defect: Isolated inner dynein arm defects or microtubular disorganization
- Inconclusive: Technical artifacts or insufficient number of evaluable cilia
Visualizations of Diagnostic Pathways and Methodologies
PCD Diagnostic Pathway Incorporating Supplemental Screening
Method Comparison Experiment Workflow for Diagnostic Validation
Research Reagent Solutions for PCD Diagnostic Investigations
Table 3: Essential Research Reagents and Materials for PCD Diagnostic Studies
| Reagent/Material | Specific Application | Function/Utility | Technical Notes |
|---|---|---|---|
| Chemiluminescence NO Analyzer | Nasal nitric oxide measurement | Quantifies low nNO levels characteristic of PCD | Requires calibration gases; velum closure technique critical |
| Next-Generation Sequencing Panels | Genetic testing for PCD | Simultaneous analysis of >40 known PCD genes | Comprehensive panels should include recent gene discoveries |
| Glutaraldehyde Fixative (2.5-3%) | TEM specimen preparation | Preserves ciliary ultrastructure for electron microscopy | Must be cold and used immediately after biopsy collection |
| Anti-DNAH5 Antibodies | Immunofluorescence staining | Identifies outer dynein arm protein defects | Correlates with TEM findings; useful for specific genetic subtypes |
| Anti-DNAI1 Antibodies | Immunofluorescence staining | Detects outer dynein arm intermediate chain defects | Complementary to genetic testing for certain PCD forms |
| High-Speed Video Microscopy System | Ciliary functional analysis | Quantifies ciliary beat frequency and pattern | Requires fresh, unfixed tissue; specialized analysis software |
| Cell Culture Media for Air-Liquid Interface | Ciliated epithelial cell culture | Generates differentiated ciliated epithelium from biopsies | Enables repeat testing without additional biopsies |
| Whole-Exome/Genome Sequencing Reagents | Novel gene discovery | Identifies new PCD-associated genes in unsolved cases | Research tool for cases negative on standard panels |
The limitations of PICADAR, particularly its substantially reduced sensitivity in patients with situs solitus and those without hallmark ultrastructural defects, necessitate a multifaceted approach to PCD diagnosis. No single test provides perfect sensitivity and specificity, but an integrated sequential approach combining nasal nitric oxide measurement, genetic testing, and specialized ciliary structural and functional analyses can significantly enhance case identification beyond what PICADAR alone can achieve. For researchers and drug development professionals, understanding these complementary diagnostic methodologies is essential for accurate patient stratification in clinical trials and the development of targeted therapies. Future directions should focus on refining diagnostic algorithms through the incorporation of emerging technologies such as whole-genome sequencing and advanced ciliary functional assessments, with the goal of achieving near-universal diagnostic sensitivity regardless of phenotypic presentation or underlying genetic cause.
Evidence-Based Validation: Comparing PICADAR Performance with Emerging Diagnostic Tools
This whitepaper presents a critical analysis of a 2025 validation study assessing the sensitivity of the Primary Ciliary Dyskinesia Rule (PICADAR) diagnostic tool in a large cohort of 269 genetically confirmed Primary Ciliary Dyskinesia (PCD) patients. The study reveals significant limitations in PICADAR's sensitivity, particularly in patients with situs solitus (normal organ arrangement) and those without hallmark ultrastructural ciliary defects. Overall sensitivity was 75%, but this dropped markedly to 61% in patients with situs solitus compared to 95% in those with laterality defects. These findings challenge the universal application of PICADAR as a standalone screening tool and underscore the necessity for more sophisticated diagnostic approaches, including machine learning algorithms and expanded genetic testing, to improve early detection of this underdiagnosed rare disease.
Primary Ciliary Dyskinesia (PCD) is a rare, progressive genetic disorder affecting motile cilia function, leading to impaired mucociliary clearance with clinical manifestations including chronic oto-sino-pulmonary infections, bronchiectasis, and laterality defects [48] [15]. With an estimated prevalence of at least 1 in 7,554, PCD remains significantly underdiagnosed due to phenotypic overlap with common respiratory diseases and lack of specific ICD codes [48] [49]. Diagnostic delays are common, often extending into later childhood or adulthood, preventing timely interventions that could mitigate long-term respiratory damage [48].
The PICADAR (PCD Rule) tool was developed as a clinical predictive instrument to identify patients requiring specialized PCD testing. Recommended by the European Respiratory Society (ERS), PICADAR uses seven clinical questions to generate a score estimating PCD likelihood [36]. However, despite its endorsement in diagnostic guidelines, comprehensive validation studies have been limited.
This analysis examines a seminal 2025 study by Schramm et al. that evaluated PICADAR's performance in 269 genetically confirmed PCD cases, with particular focus on its efficacy in patients with situs solitus within the broader context of PICADAR score situs solitus sensitivity research. The findings have profound implications for diagnostic protocols and early intervention strategies.
Methodology of the 2025 Validation Study
Study Population and Design
The 2025 investigation employed a retrospective cohort design analyzing 269 individuals with genetically confirmed PCD [36]. Genetic confirmation served as the diagnostic gold standard, eliminating potential misclassification bias present in earlier studies relying solely on ultrastructural defects.
Inclusion Criteria:
- Genetically confirmed PCD diagnosis
- Comprehensive clinical data for PICADAR scoring
Exclusion Criteria:
- Incomplete clinical records
- Inconclusive genetic results
PICADAR Assessment Protocol
The PICADAR tool was applied according to standard clinical protocols [36] [17]:
Initial Screening Question: Participants were first assessed for the presence of daily wet cough. Individuals without this symptom were automatically rated negative for PCD according to standard PICADAR interpretation.
Scoring System Application: For patients reporting daily wet cough, seven clinical components were evaluated:
- Neonatal respiratory symptoms
- Presence of congenital heart defects
- Situs inversus totalis
- Situs ambiguus/heterotaxia
- Persistent perennial rhinitis
- Persistent perennial otitis media
- Chest symptoms
- Score Interpretation: A threshold of ≥5 points was used to determine positive PCD likelihood, as recommended in standard PICADAR guidelines.
Subgroup Analysis
To investigate phenotypic variability, researchers conducted stratified analyses based on:
Laterality Status: Patients were categorized as having:
- Situs inversus (complete mirror-image organ arrangement)
- Situs ambiguus (heterotaxia)
- Situs solitus (normal organ arrangement)
Ultrastructural Defects: Patients were grouped by predicted ciliary ultrastructure:
- Hallmark defects (outer dynein arm, combined outer and inner dynein arm defects, microtubular disorganization)
- Non-hallmark defects (normal ultrastructure or other abnormalities)
Statistical Analysis
Statistical analyses included:
- Sensitivity calculation (proportion of true positives correctly identified)
- Descriptive statistics (median, interquartile range) for PICADAR scores
- Comparative analyses using appropriate statistical tests (e.g., chi-square for sensitivity comparisons)
- A significance threshold of p < 0.05 was applied
Results and Quantitative Analysis
The 2025 cohort study demonstrated significant limitations in PICADAR's overall diagnostic sensitivity:
Table 1: Overall PICADAR Performance in 269 Genetically Confirmed PCD Patients
| Metric | Value | Interpretation |
|---|---|---|
| Overall Sensitivity | 75% (202/269) | Identifies only 3 of 4 true PCD cases |
| Median PICADAR Score | 7 points (IQR: 5-9) | Majority score above diagnostic threshold |
| Cases Missed (False Negatives) | 67 patients | PICADAR would not refer for confirmatory testing |
| Cases Excluded by Initial Question | 18 patients (7%) | No daily wet cough, ruled out prior to scoring |
The median PICADAR score of 7 points (IQR: 5-9) indicates most genetically confirmed patients scored above the recommended threshold, yet a substantial proportion (25%) fell below the cutoff point [36].
Impact of Laterality Defects on Sensitivity
Subgroup analysis revealed dramatic differences in PICADAR performance based on laterality status:
Table 2: PICADAR Sensitivity Stratified by Laterality Status
| Laterality Subgroup | Sensitivity | Median Score | Statistical Significance |
|---|---|---|---|
| All Laterality Defects | 95% | 10 points (IQR: 8-11) | Reference |
| Situs Solitus Only | 61% | 6 points (IQR: 4-8) | p < 0.0001 |
The profoundly lower sensitivity (61%) in situs solitus patients highlights a critical weakness in case identification for this population, who lack this recognizable clinical feature [36].
Influence of Ultrastructural Defects
Further stratification by ciliary ultrastructure revealed additional limitations:
Table 3: PICADAR Performance by Ciliary Ultrastructure
| Ultrastructural Category | Sensitivity | Clinical Implication |
|---|---|---|
| Hallmark Ultrastructural Defects | 83% | Better identification of classic PCD variants |
| Non-Hallmark Ultrastructural Defects | 59% | Poor detection of genetically confirmed cases with normal EM |
The significantly lower sensitivity (59%) in patients without hallmark ultrastructural defects (p < 0.0001) indicates PICADAR disproportionately misses patients with specific genetic subtypes that manifest normal or non-diagnostic electron microscopy [36].
Discussion
Clinical Implications for Situs Solitus Patients
The profoundly reduced PICADAR sensitivity (61%) in situs solitus patients represents the most significant finding with direct clinical implications. These patients already experience diagnostic delays due to the absence of the clinically apparent laterality defects that often trigger PCD investigation. The heavy weighting of situs abnormalities in the PICADAR scoring system (2 points for situs inversus, 1 point for heterotaxia) inherently disadvantages situs solitus patients, who constitute approximately 75% of the Japanese PCD population and substantial proportions elsewhere [17].
This sensitivity deficit is particularly concerning given that certain genetic subtypes of PCD, including those involving DNAH9 mutations, frequently present with situs solitus and subtle respiratory symptoms that may not trigger PICADAR screening [50]. These patients often endure years of misdiagnosis as asthma or chronic bronchitis before receiving accurate diagnosis.
Integration with Emerging Diagnostic Technologies
The limitations identified in this 2025 validation study underscore the necessity for complementary diagnostic approaches:
Machine Learning Screening Models: Recent research demonstrates the feasibility of machine learning algorithms for PCD screening using claims data. Random forest models trained on composite claims data have shown promising performance (sensitivity 0.82-0.90, PPV 0.51-0.54) suitable for population screening [48] [49]. These models utilize diagnostic, procedural, and pharmaceutical codes across broad feature categories including airway symptoms, congenital malformations, ear and nose conditions, and specific procedures.
Advanced Genetic Testing: Next-generation sequencing panels identifying pathogenic variants in over 50 PCD-related genes have become increasingly crucial, especially for patients with non-diagnostic PICADAR scores or normal ciliary ultrastructure [15]. Genetic testing confirmed PCD diagnosis in 50.7% of clinically suspected Egyptian cases, with defects distributed across outer dynein arms (32%), central pair (19%), radial spokes (16%), and ciliogenesis (14%) [15].
Nasal Nitric Oxide (nNO) Measurement: nNO remains a valuable screening tool, with extremely low concentrations (e.g., 44 ppb) providing strong diagnostic indicators even in genetically confirmed cases with subtle clinical presentations [50].
Geographical and Ethnic Considerations
The performance of clinical prediction tools like PICADAR must be contextualized within geographical and ethnic populations. The 2025 Japanese clinical analysis revealed situs inversus in only 25% of PCD patients, substantially lower than the approximately 50% reported in other populations [17]. This divergence reflects differences in predominant causative genes across ethnic groups, necessitating population-specific diagnostic approaches.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Materials for PCD Diagnostic Studies
| Reagent/Resource | Function/Application | Example Use Case |
|---|---|---|
| PCD Multigene NGS Panel | Simultaneous analysis of >50 PCD-related genes | Genetic confirmation of diagnosis [15] |
| Anti-DNAH5 Antibodies | Immunofluorescence detection of outer dynein arm defects | Validation of pathogenic DNAH5 variants [15] |
| Anti-GAS8 Antibodies | Immunofluorescence analysis of nexin-dynein regulatory complexes | Confirmation of GAS8-related PCD variants [15] |
| Electron Microscopy | Ultrastructural assessment of ciliary defects | Identification of hallmark defects (ODA, IDA) [50] |
| Nasal Nitric Oxide Analyzer | Measurement of nasal NO concentration (chemiluminescence) | Non-invasive screening (PCD: <77 nL/min) [50] |
| High-Speed Video Microscopy | Analysis of ciliary beat patterns and frequency | Functional assessment of ciliary motility [50] |
Visualizations
PICADAR Clinical Decision Pathway
PICADAR Sensitivity by Patient Subgroups
The 2025 cohort analysis of 269 genetically confirmed PCD patients provides compelling evidence that PICADAR has significant limitations as a standalone screening tool, particularly for patients with situs solitus and those without hallmark ultrastructural defects. The substantially reduced sensitivity in these subgroups (61% and 59%, respectively) necessitates a paradigm shift in PCD diagnostic approaches.
Future directions should integrate multiple complementary strategies:
- Development of population-specific clinical prediction tools accounting for ethnic variations in common genetic variants
- Implementation of machine learning algorithms for scalable screening using electronic health record data
- Adoption of expanded genetic testing panels for patients with suggestive clinical features regardless of PICADAR scores
- Standardization of nNO testing across clinical centers as a non-invasive screening modality
These findings reinforce that while clinical prediction rules like PICADAR provide valuable frameworks, overreliance on any single tool risks perpetuating diagnostic delays in this genetically and phenotypically heterogeneous disease. A multimodal diagnostic approach is essential to improve early detection and clinical outcomes for all PCD patients, particularly those with subtler presentations lacking classic features like situs inversus.
In medical research and clinical practice, diagnostic tests are essential tools for determining the presence or absence of a disease. The performance of these tests is quantitatively assessed using key metrics, primarily sensitivity and specificity, which are intrinsic properties of a test and prevalence-independent [51] [52]. These metrics, along with positive and negative predictive values, provide a comprehensive framework for evaluating a test's clinical utility [53]. Understanding these concepts is fundamental for researchers and clinicians to accurately interpret test results, make informed diagnostic decisions, and evaluate new diagnostic technologies.
This guide explores these core metrics in detail, using the PICADAR (PrImary Ciliary Dyskinesia Rule) score as a case study to illustrate their application and limitations in a real-world research context, particularly focusing on its performance in patient subgroups such as those with situs solitus (normal organ arrangement) [4].
Core Definitions and Calculations
Sensitivity and Specificity
Sensitivity, also known as the true positive rate, measures a test's ability to correctly identify individuals who have the disease [51] [52]. It is defined as the proportion of truly diseased individuals who test positive. A highly sensitive test is crucial for "ruling out" a disease when the result is negative, as it minimizes false negatives [52]. This is particularly important when the consequences of missing a disease are severe, or the treatment is highly effective and low-risk.
Specificity, or the true negative rate, measures a test's ability to correctly identify individuals who do not have the disease [51] [52]. It is defined as the proportion of truly non-diseased individuals who test negative. A highly specific test is valuable for "ruling in" a disease when the result is positive, as it minimizes false positives [52]. This is critical when a positive test leads to further invasive testing, significant expense, or patient anxiety.
The mathematical formulas for these metrics are derived from a 2x2 contingency table, which cross-tabulates the test results (positive or negative) with the true disease status (present or absent) [51].
Table 1: 2x2 Contingency Table for Diagnostic Test Evaluation
| Disease Present | Disease Absent | |
|---|---|---|
| Test Positive | True Positive (A) | False Positive (B) |
| Test Negative | False Negative (C) | True Negative (D) |
Based on this table:
Predictive Values and Likelihood Ratios
While sensitivity and specificity are stable test characteristics, Predictive Values are highly dependent on the prevalence of the disease in the population being tested [51].
- Positive Predictive Value (PPV): The probability that a subject with a positive test result truly has the disease. PPV = A / (A + B) [51].
- Negative Predictive Value (NPV): The probability that a subject with a negative test result truly does not have the disease. NPV = D / (C + D) [51].
Likelihood Ratios (LRs) provide another measure of diagnostic accuracy that is not influenced by disease prevalence [51].
- Positive Likelihood Ratio (LR+): How much more likely a positive test result is in a diseased person compared to a non-diseased person. LR+ = Sensitivity / (1 - Specificity) [51].
- Negative Likelihood Ratio (LR-): How much more likely a negative test result is in a diseased person compared to a non-diseased person. LR- = (1 - Sensitivity) / Specificity [51].
Diagram 1: Diagnostic Test Outcome Pathways
The PICADAR Score: A Case Study in Diagnostic Performance
Tool Development and Original Performance
The PICADAR score is a clinical prediction rule designed to identify patients with a high probability of Primary Ciliary Dyskinesia (PCD) for referral to specialized diagnostic testing [5]. PCD is a rare genetic disorder affecting motile cilia, leading to chronic respiratory symptoms. Its diagnosis requires complex, expensive tests, making a simple screening tool highly valuable [5].
PICADAR was developed using logistic regression on data from 641 consecutively referred patients. It consists of seven readily obtainable clinical parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care admittance, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defect [5]. In its original validation study, a cut-off score of 5 points demonstrated a sensitivity of 0.90 and a specificity of 0.75, with an area under the receiver operating characteristic (ROC) curve of 0.91, indicating good overall accuracy [5].
Table 2: Original PICADAR Score Validation Performance (Derivation Group)
| Metric | Performance | Population |
|---|---|---|
| Sensitivity | 0.90 | 641 referrals (75 PCD-positive) |
| Specificity | 0.75 | 641 referrals (566 PCD-negative) |
| Area Under Curve (AUC) | 0.91 | Internal validation |
| AUC | 0.87 | External validation (n=187) |
Recent Findings on Performance Variability
A 2025 study critically evaluated PICADAR's performance in a cohort of 269 individuals with genetically confirmed PCD, providing a robust assessment of its real-world sensitivity [4]. The study revealed significant limitations.
The overall sensitivity of PICADAR was 75% (202/269), meaning it missed 25% of true PCD cases [4]. Furthermore, 18 individuals (7%) were ruled out for PCD based on the initial PICADAR question alone (absence of a daily wet cough), despite having a confirmed genetic diagnosis [4]. This highlights a critical flaw in the tool's initial screening logic.
Most notably, the study stratified sensitivity by patient characteristics, uncovering substantial performance disparities:
Table 3: Stratified Sensitivity of PICADAR in Genetically Confirmed PCD (2025 Study)
| Patient Subgroup | Sensitivity | Median Score (IQR) |
|---|---|---|
| Overall (n=269) | 75% | 7 (5 - 9) |
| With Laterality Defects | 95% | 10 (8 - 11) |
| With Situs Solitus | 61% | 6 (4 - 8) |
| With Hallmark Ultrastructural Defects | 83% | Not Reported |
| Without Hallmark Ultrastructural Defects | 59% | Not Reported |
The data demonstrates that PICADAR's sensitivity is significantly higher in patients with laterality defects (95%) compared to those with situs solitus (61%) [4]. This finding is critical for researchers and clinicians, as it indicates that PICADAR may be inadequate as a standalone tool for estimating the likelihood of PCD in patients with normal organ arrangement, potentially leading to under-diagnosis in this subgroup [4].
Experimental Protocols for Metric Evaluation
Protocol for Validating a Diagnostic Tool
The following protocol outlines the key steps for evaluating a diagnostic test's performance, based on methodologies used in the cited PICADAR studies [4] [5].
- Define Study Population: Recruit a consecutive or random sample of patients from the intended use population for the test. The population should reflect the spectrum of disease severity and confounding conditions encountered in clinical practice.
- Apply Reference Standard: Administer the best available method (the reference standard) to all study participants to definitively determine the presence or absence of the target condition. In PCD research, this may include genetic testing, transmission electron microscopy, and high-speed video microscopy [4] [5].
- Administer Index Test: Apply the new diagnostic tool (e.g., the PICADAR score) to all participants. This should be performed independently, and ideally blinded, from the reference standard to avoid bias.
- Construct 2x2 Table: Tally the results by cross-classifying the outcomes of the index test and the reference standard for all subjects.
- Calculate Performance Metrics: Use the formulas in Section 2.1 to compute sensitivity, specificity, PPV, and NPV.
- Perform Subgroup Analysis: Stratify the study population by key clinical variables (e.g., presence of situs solitus vs. laterality defects) to assess the consistency of test performance across different patient groups [4].
- Statistical Analysis: Generate a Receiver Operating Characteristic (ROC) curve to visualize the trade-off between sensitivity and specificity at different cut-off points and calculate the Area Under the Curve (AUC) as a measure of overall discriminative ability [5].
Protocol for Assessing Clinical Impact
- Simulate Clinical Scenarios: Apply the test's performance metrics (sensitivity, specificity) to populations with different disease prevalences to model the expected number of false positives and false negatives.
- Calculate Predictive Values: Determine the PPV and NPV for each specific clinical setting based on the local prevalence of the disease [51].
- Evaluate Health Outcomes: Design studies to assess how the implementation of the test affects patient management, time to diagnosis, treatment efficacy, and overall health outcomes.
Essential Research Reagents and Materials
The evaluation of diagnostic tests like the PICADAR score relies on a foundation of well-defined materials and patient data.
Table 4: Essential Research Materials for Diagnostic Test Evaluation
| Item | Function in Research Context |
|---|---|
| Validated Reference Standard | The best available method (e.g., genetic sequencing, composite diagnostic criteria) to establish true disease status against which the new test is compared [4] [5]. |
| Structured Clinical Data Proforma | A standardized form used to collect patient history and clinical parameters consistently across all study participants, ensuring data uniformity [5]. |
| Biostatistical Software (e.g., SPSS, R) | Software used for performing logistic regression, generating ROC curves, calculating AUC, and computing sensitivity, specificity, and predictive values with confidence intervals [5]. |
| Characterized Patient Biobank | A collection of biological samples (e.g., DNA, ciliary biopsies) from patients with and without the disease, essential for validating genetic and cellular tests [4]. |
Visualization of the Sensitivity-Specificity Relationship
A fundamental principle in diagnostic testing is the inverse relationship between sensitivity and specificity; as one increases, the other typically decreases [51] [52]. This trade-off is governed by the selected test cut-off point. The ROC curve is the standard graphical method for visualizing this relationship across all possible cut-offs, helping researchers select an optimal balance for their specific clinical context [5].
Diagram 2: Test Cut-off and Metric Trade-offs
PICADAR vs. Nasal Nitric Oxide Testing in Different Patient Subgroups
Primary ciliary dyskinesia (PCD) is a rare, genetically heterogeneous disorder caused by impaired structure and/or function of motile cilia, leading to chronic oto-sino-pulmonary disease, laterality defects, and infertility. The diagnostic pathway for PCD is complex, requiring specialized testing available only at reference centers. Within this pathway, effective screening tools are crucial for identifying high-risk patients who warrant definitive diagnostic testing. The PICADAR score (PrImary CiliAry DyskinesiA Rule) and nasal nitric oxide (nNO) measurement represent two fundamental screening approaches. This whitepaper provides a technical analysis of their performance, with a specific focus on their varying efficacy across different patient subgroups, particularly those with situs solitus (normal organ arrangement). This focus is critical for ongoing research, as diminished sensitivity in this population can lead to significant underdiagnosis and delays in initiating appropriate management.
PICADAR: A Clinical Prediction Rule
The PICADAR tool is a diagnostic prediction rule developed to identify patients with a high probability of PCD using easily obtainable clinical history. It was designed for use in patients with a persistent wet cough [5].
Experimental Protocol & Methodology: The original derivation study analyzed data from 641 consecutive patients referred for PCD testing [5]. A clinical history proforma was completed prior to diagnostic testing. Logistic regression analysis was used to identify the most predictive clinical features from 27 potential variables. The resulting tool consists of seven predictive parameters, each assigned a point value based on its regression coefficient [5].
Table 1: The PICADAR Scoring System
| Predictive Parameter | Points |
|---|---|
| Full-term gestation | 1 |
| Neonatal chest symptoms (at term) | 1 |
| Admission to neonatal intensive care unit | 1 |
| Chronic rhinitis | 1 |
| Chronic ear symptoms | 1 |
| Situs inversus | 2 |
| Congenital cardiac defect | 2 |
| Total Possible Score | 9 |
A score of ≥5 points is recommended as the cut-off for referring a patient for definitive PCD testing, providing a sensitivity of 0.90 and a specificity of 0.75 in the original derivation cohort [5].
Nasal Nitric Oxide Measurement
Nasal nitric oxide (nNO) is a well-established biomarker for PCD. Patients with PCD typically have markedly low nNO levels compared to healthy controls and most patients with other respiratory conditions such as cystic fibrosis or asthma.
Experimental Protocol & Methodology: nNO measurement is performed using an electrochemical analyzer according to standardized protocols, such as those from the American Thoracic Society/European Respiratory Society [3]. The technique involves aspirating nasal air from one nostril while the patient exhales against resistance to close the velum, preventing contamination from lower airway NO. A sampling flow rate of 5 mL·s⁻¹ is commonly used, and results are expressed in parts per billion (ppb) or nL/min [54] [3]. A value of ≤77 nL/min has been identified as a highly discriminative cut-off for screening adults with bronchiectasis for PCD, while other protocols use a cut-off of ≤30 nL·min⁻¹ [54] [5].
Comparative Performance Analysis
The performance of PICADAR and nNO is not uniform; it varies significantly based on the patient population and the presence of specific clinical and ultrastructural features. The following table summarizes key performance metrics from recent studies.
Table 2: Performance Metrics of PICADAR vs. nNO Across Studies
| Study / Tool | Study Population | Sensitivity | Specificity | AUC | Key Findings |
|---|---|---|---|---|---|
| Behan et al. (2016) [5] | 641 referrals with chronic wet cough | 0.90 (score ≥5) | 0.75 (score ≥5) | 0.91 (derivation) | Original validation showed high accuracy. |
| Rademacher et al. (2017) [54] | 185 adults with bronchiectasis | - | - | - | nNO ≤77 nL/min best differentiated PCD from non-PCD. |
| Schramm et al. (2025) [4] [36] | 269 genetically confirmed PCD | 0.75 (overall) | - | - | Critical limitation revealed. |
| Pohunek et al. (2021) [3] | 1401 unselected referrals | - | - | 0.87 (PICADAR) | nNO further improved the predictive power of all clinical tools. |
The Critical Limitation of PICADAR in Situs Solitus Subgroups
Recent research has critically evaluated the real-world sensitivity of PICADAR, revealing substantial limitations in specific patient subgroups. A 2025 study by Schramm et al. evaluated PICADAR in 269 individuals with genetically confirmed PCD [4] [36].
The findings were striking:
- Overall Sensitivity: The overall sensitivity of PICADAR (using a ≥5 cut-off) was only 75%, meaning one in four genetically confirmed PCD patients would have been missed by the tool [4] [36].
- Situs Solitus vs. Laterality Defects: The sensitivity dropped dramatically to 61% in PCD patients with situs solitus. In contrast, it was significantly higher (95%) in patients with laterality defects (situs inversus or heterotaxy) [4] [36]. This is because the tool assigns 2 points each for situs inversus and congenital heart defects, making a high score much more likely in patients with these features.
- Impact of Ultrastructure: Sensitivity was also lower in patients without hallmark ultrastructural defects on transmission electron microscopy (TEM) (59%) compared to those with such defects (83%) [4] [36]. Many of these patients with normal ultrastructure have mutations in genes like DNAH11 and present with situs solitus.
Furthermore, the tool's initial requirement for a daily wet cough automatically rules out PCD in individuals without this symptom, which accounted for 7% of the genetically confirmed cohort in the 2025 study [4] [36].
Performance of nNO and Combined Approaches
nNO measurement serves as a highly effective screening tool. In a study of adults with bronchiectasis, mean nNO was significantly lower in the PCD group (25 nL/min) compared to the non-PCD group (227 nL/min) [54]. While nNO is a robust physiological biomarker, its measurement requires expensive equipment and trained technicians, which may not be available in non-specialist settings [5].
Research indicates that combining clinical prediction tools with nNO measurement enhances screening efficacy. A 2021 study demonstrated that nNO further improved the predictive power of PICADAR and other clinical indices [3]. This suggests an integrated screening algorithm, where a high PICADAR score or a low nNO measurement triggers a referral for definitive testing, may be the most effective strategy to capture a broader range of PCD phenotypes.
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key reagents and equipment essential for conducting research and diagnostics in the field of PCD screening and confirmation.
Table 3: Key Research Reagent Solutions for PCD Investigation
| Reagent / Equipment | Function / Application | Exemplar Use Case |
|---|---|---|
| Electrochemical nNO Analyzer (e.g., Niox Vero) | Measures nasal nitric oxide concentration for PCD screening. | Standardized measurement of nNO levels using tidal breathing or velum closure techniques [3]. |
| High-Speed Video Microscopy (HSVM) System | Analyzes ciliary beat frequency and pattern from nasal brush biopsies. | Differentiating between primary and secondary ciliary dyskinesia; identifying characteristic abnormal beat patterns [3] [1]. |
| Transmission Electron Microscope (TEM) | Visualizes ultrastructural defects in ciliary axonemes. | Identifying hallmark defects (e.g., absent outer dynein arms) in ciliary cross-sections for diagnostic confirmation [47] [1]. |
| Next-Generation Sequencing (NGS) Gene Panels | Detects mutations in over 50 known PCD-associated genes. | Genetic confirmation of diagnosis, especially in cases with normal nNO or equivocal HSVM/TEM results [3] [1]. |
| Cell Culture Media for Air-Liquid Interface (ALI) Culture | Differentiates respiratory epithelial cells and regenerates cilia. | Removing secondary ciliary dyskinesia in vitro for more accurate HSVM and TEM analysis [5]. |
Integrated Diagnostic Workflow
The following diagram illustrates a proposed diagnostic workflow that integrates both PICADAR and nNO, accounting for the limitations in situs solitus patients. This algorithm emphasizes the need for complementary testing to maximize sensitivity.
Discussion and Future Directions
The evidence clearly demonstrates that while PICADAR is a valuable and simple tool, its reliance on clinical features like laterality defects renders it a less sensitive predictor for PCD patients with situs solitus. This is a critical consideration for drug development and clinical research, as enrolling a representative patient population requires screening tools that do not systematically exclude a substantial portion of the PCD spectrum. The markedly reduced sensitivity of 61% in this subgroup is a major caveat that researchers must account for in study design and patient recruitment strategies [4] [36].
nNO measurement, as an objective biomarker, is less susceptible to this particular bias and serves as a powerful complementary screen. However, its limited accessibility due to cost and technical requirements remains a barrier. Future research should focus on the development and validation of next-generation predictive tools that incorporate genetic and proteomic data to improve sensitivity across all PCD subgroups, especially those with situs solitus and normal ciliary ultrastructure. Furthermore, exploring the cost-effectiveness of different screening algorithms, including the universal application of nNO in high-prevalence settings like bronchiectasis clinics, is warranted.
For the research community, it is imperative to not rely solely on PICADAR for patient selection or epidemiological studies. A multifaceted screening approach, a low threshold for definitive testing in patients with suggestive symptoms despite a low PICADAR score, and the development of more inclusive predictive models are essential steps toward improving the diagnosis and management of all individuals with PCD.
The development of robust biomarkers is a cornerstone of precision medicine, enabling disease detection, patient stratification, and prediction of treatment response. Within this landscape, genetic testing has emerged as a powerful validation benchmark, providing an objective measure against which the performance of other diagnostic and predictive tools can be rigorously assessed. This is particularly evident in complex genetic disorders like primary ciliary dyskinesia (PCD), where the limitations of clinical prediction tools become apparent without genetic confirmation.
The PICADAR score (PrImary CiliARy DyskinesiA Rule) represents a case study in the necessity of genetic validation. Originally developed as a clinical tool to identify patients requiring specialized PCD testing, PICADAR demonstrated promising initial validation with reported sensitivity of 0.90 and specificity of 0.75 at a cut-off score of 5 points [9]. However, recent evidence reveals significant limitations in its performance, particularly in patient subgroups without classic laterality defects [4]. This underscores the essential role of genetically confirmed diagnoses as a benchmark for evaluating and refining clinical prediction tools.
The integration of genomic biomarkers—defined as DNA or RNA characteristics that indicate normal biological processes, pathogenic processes, or responses to interventions—provides a foundational framework for validating clinical tools [55]. This technical guide explores the critical implications of using genetic testing as a validation benchmark, with specific applications in PCD research and broader biomarker development.
Biomarker Classifications and Validation Frameworks
Biomarker Categories in Medical Research
Biomarkers serve distinct functions across the medical research continuum, from risk assessment to treatment monitoring. Regulatory agencies including the FDA and EMA have established standardized definitions for biomarker categories [56]:
- Diagnostic biomarkers confirm the presence or absence of a disease or disease subtype.
- Prognostic biomarkers predict the natural history of a disease regardless of therapy.
- Predictive biomarkers identify individuals more likely to respond to a specific therapeutic intervention.
- Susceptibility/Risk biomarkers identify the potential for developing a disease in asymptomatic individuals.
- Pharmacodynamic/Response biomarkers demonstrate that a biological response has occurred in an individual who has been exposed to a medical product.
- Monitoring biomarkers are measured serially to assess disease status or medical product exposure.
Essential Validation Criteria for Clinical Biomarkers
For any biomarker to achieve clinical utility, it must undergo rigorous validation across three critical domains [57]:
- Analytical Validity: The biomarker's ability to accurately and reliably measure the target molecule or characteristic, assessed through sensitivity, specificity, precision, and accuracy.
- Clinical Validity: The biomarker's ability to identify or predict the presence or absence of a specific disease or condition in a clinical population.
- Clinical Utility: The practical value of the biomarker for informing clinical decision-making, improving patient outcomes, and providing benefit over existing approaches.
Genetic testing, particularly for monogenic disorders, often serves as a reference method against which other biomarkers are evaluated for clinical validity, as it provides a definitive diagnosis against which performance metrics can be calculated.
PICADAR Performance: A Case Study in Genetic Validation
Original Validation and Recent Evidence
The PICADAR tool was developed to address the challenge of identifying PCD patients among those referred with suggestive symptoms. Its seven clinical parameters—full-term gestation, neonatal chest symptoms, neonatal intensive care admittance, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defect—were derived from logistic regression analysis of consecutively referred patients [9]. The tool's initial validation showed promising results:
Table 1: Original PICADAR Validation Performance [9]
| Validation Cohort | Area Under Curve (AUC) | Sensitivity | Specificity |
|---|---|---|---|
| Internal Validation | 0.91 | 0.90 | 0.75 |
| External Validation | 0.87 | Not reported | Not reported |
However, when evaluated against genetically confirmed PCD diagnoses, significant limitations emerged. A 2025 study examining 269 individuals with genetically confirmed PCD revealed that PICADAR missed a substantial proportion of cases, particularly those without classic PCD features [4]:
Table 2: PICADAR Performance in Genetically Confirmed PCD Patients [4]
| Patient Subgroup | Sensitivity | Median PICADAR Score (IQR) |
|---|---|---|
| Overall PCD Population | 75% | 7 (5-9) |
| PCD with Laterality Defects | 95% | 10 (8-11) |
| PCD with Situs Solitus (normal) | 61% | 6 (4-8) |
| PCD with Hallmark Ultrastructural Defects | 83% | Not reported |
| PCD without Hallmark Ultrastructural Defects | 59% | Not reported |
The study further identified that 7% of genetically confirmed PCD patients reported no daily wet cough, which would have automatically excluded them from PICADAR evaluation according to its initial screening question [4]. This demonstrates how clinical prediction rules may systematically exclude phenotypic variants that can only be identified through genetic testing.
Ethnic and Genotypic Variations in PCD Presentation
The performance of clinical prediction tools like PICADAR is further complicated by ethnic and genotypic variations in disease presentation. A Japanese study of 67 PCD patients found that only 25% presented with situs inversus, contrasting sharply with the approximately 50% rate typically reported in Western populations [17]. This discrepancy reflects differences in the major disease-causing genes across ethnic groups and highlights the risk of applying population-specific clinical tools without genetic validation.
Genetic Testing as a Validation Benchmark: Methodological Approaches
Experimental Protocol for Biomarker Validation Against Genetic Standards
The use of genetic testing as a validation benchmark requires systematic approaches to ensure robust and reproducible results. The following protocol outlines key methodological considerations:
1. Study Population Selection:
- Consecutive patient recruitment from relevant clinical settings to avoid selection bias
- Inclusion of broad phenotypic spectrum, including atypical presentations
- Prospective design with pre-specified analysis plans to minimize data-driven findings
- Adequate sample size with power calculations based on expected genetic prevalence
2. Reference Standard Definition:
- Application of established genetic diagnostic criteria for the target condition
- Comprehensive genetic testing using next-generation sequencing panels or whole exome sequencing
- Inclusion of copy number variant analysis where clinically relevant
- Functional validation of genetic variants of uncertain significance
3. Biomarker Performance Assessment:
- Calculation of sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV)
- Receiver operating characteristic (ROC) analysis with area under the curve (AUC) determination
- Stratified analysis across clinically relevant subgroups (e.g., by ethnicity, age, clinical features)
- Assessment of inter-rater reliability for subjective biomarker components
4. Statistical Considerations:
- Control for multiple comparisons when evaluating multiple biomarkers
- Internal validation through bootstrapping or cross-validation techniques
- External validation in independent cohorts to assess generalizability
- Adjustment for potential confounders through multivariate analysis
Workflow for Genetic Validation of Clinical Biomarkers
The following diagram illustrates the integrated workflow for validating clinical biomarkers against genetic testing benchmarks:
Implications for Biomarker Development and Refinement
Enhancing Predictive Models Through Genetic Insights
Genetic validation provides critical insights for refining clinical prediction tools in several key areas:
Identification of Phenotypic Variants: Genetic testing reveals disease-associated variants across the phenotypic spectrum, including mild or atypical presentations that may be missed by clinical criteria alone. The discovery that 7% of genetically confirmed PCD patients lack daily wet cough exemplifies how genetic benchmarks can identify systematic exclusions in clinical tools [4].
Population-Specific Adaptations: Ethnic variations in genetic architecture necessitate population-specific adjustments to clinical prediction tools. The significantly lower rate of situs inversus in Japanese PCD patients (25% versus ~50% in Western populations) demonstrates how genetic insights can guide tool modification for different ethnic groups [17].
Integration of Multi-Omics Data: Advanced biomarker development increasingly incorporates multi-omics approaches—integrating genomic, transcriptomic, proteomic, and metabolomic data—to create comprehensive biomarker signatures [57]. Genetic testing provides the foundational layer upon which these multi-dimensional models are built.
Advanced Analytical Approaches for Biomarker Development
The integration of machine learning and artificial intelligence with genetic validation has revolutionized biomarker development:
Feature Selection Optimization: Genetic validation enables the identification of the most informative clinical parameters for prediction models. In PCD, the stark difference in PICADAR performance between patients with and without laterality defects (95% versus 61% sensitivity) highlights the need for feature weighting adjustments based on genetic subpopulations [4].
Model Training and Validation: Genetic confirmation provides the reference standard for training machine learning algorithms. Recent approaches have utilized multiple algorithms—including lasso regression, random forests, support vector machines, and gradient boosting—with genetic confirmation as the outcome variable [58]. One study demonstrated that random forest algorithms achieved 0.97 accuracy in external validation when trained against genetically confirmed cases [58].
Continuous Model Refinement: Genetic testing enables ongoing refinement of clinical prediction tools as new gene-disease associations are discovered and phenotypic spectra are expanded.
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful development and validation of biomarkers against genetic benchmarks requires specialized research reagents and methodologies:
Table 3: Essential Research Reagents and Platforms for Biomarker Validation
| Category | Specific Tools/Platforms | Research Application |
|---|---|---|
| Genetic Analysis | Next-generation sequencing panels, Whole exome sequencing, SNP microarrays, CRISPR-based functional assays | Comprehensive mutation detection, variant identification, functional validation of genetic findings |
| Transcriptomic Profiling | RNA sequencing, Single-cell RNA sequencing, Microarrays, Quantitative RT-PCR | Gene expression analysis, identification of expression signatures, cellular heterogeneity assessment |
| Proteomic Analysis | Mass spectrometry, Immunofluorescence, Western blot, ELISA, Multiplex immunoassays | Protein expression and localization, post-translational modifications, pathway activation assessment |
| Cellular Models | Patient-derived organoids, Air-liquid interface (ALI) cultures, Primary cell cultures, Immortalized cell lines | Functional characterization of genetic variants, drug screening, disease modeling |
| Bioinformatics | AI and machine learning algorithms, Multi-omics integration platforms, Statistical analysis packages, Data visualization tools | Pattern recognition, biomarker signature development, predictive model building |
Emerging Technologies and Approaches
The field of biomarker development is rapidly evolving, with several promising technologies enhancing the integration of genetic validation:
Liquid Biopsies and Circulating Biomarkers: Non-invasive approaches for detecting circulating tumor DNA (ctDNA) and other circulating biomarkers are transforming cancer diagnostics and monitoring [57]. Similar approaches are being explored for genetic disorders through the detection of cell-free DNA.
Digital Biomarkers and Wearable Technology: Devices such as smartwatches and biosensors enable continuous monitoring of physiological parameters, providing real-world data that can be correlated with genetic predispositions [59].
Artificial Intelligence and Machine Learning: AI algorithms are increasingly employed to identify complex patterns in multi-omics data, predict disease risk based on genetic and clinical variables, and optimize biomarker panels for specific clinical contexts [57].
Genetic testing provides an essential validation benchmark for biomarker development, offering a definitive reference standard that enables rigorous assessment of clinical prediction tools. The case of PICADAR in PCD diagnosis illustrates both the utility and limitations of clinical prediction rules when evaluated against genetic confirmation. The significantly reduced sensitivity of PICADAR in patients with situs solitus (61%) versus those with laterality defects (95%) underscores the critical importance of genetic testing for validating and refining clinical tools across diverse patient populations [4].
As biomarker science advances, the integration of genetic testing with multi-omics approaches, advanced analytical methods, and innovative technologies will enable the development of more precise, personalized, and clinically useful biomarkers. This integration is essential for advancing precision medicine and ensuring that diagnostic and predictive tools perform reliably across all patient subgroups.
Primary ciliary dyskinesia (PCD) is a genetically heterogeneous disorder affecting motile cilia, with an estimated incidence of 1 in 7,500 births. This rare genetic disease demonstrates significant clinical heterogeneity and overlaps with other respiratory conditions like cystic fibrosis, creating substantial diagnostic challenges. The current diagnostic pathway for PCD relies on specialized tests including measurement of low nasal nitric oxide (nNO), high-speed video microscopy (HSVM) to assess ciliary beat pattern and frequency, transmission electron microscopy (TEM) to evaluate ciliary ultrastructure, and genetic testing [60]. Unfortunately, these diagnostic methods remain inaccessible to many patients due to their specialized nature, required expertise, and high costs. This diagnostic complexity has fueled interest in developing more accessible and accurate predictive models, beginning with clinical prediction tools like PICADAR.
The PICADAR tool (Primary Ciliary Dyskinesia Rule) was developed to identify patients requiring specialized PCD testing. This clinical prediction rule incorporates seven readily obtainable clinical parameters: full-term gestation, neonatal chest symptoms, neonatal intensive care admittance, chronic rhinitis, ear symptoms, situs inversus, and congenital cardiac defect [9]. While initially demonstrating promising sensitivity (0.90) and specificity (0.75) at a cut-off score of 5 points in its derivation study, recent evidence has revealed significant limitations in its performance across diverse patient populations [36] [4]. This whitepaper explores these limitations and outlines the development of next-generation predictive models that integrate genetic, molecular, and advanced computational approaches to overcome current diagnostic challenges.
Limitations of Current Predictive Tools
Sensitivity Concerns in Genetically Confirmed PCD Populations
Recent evidence has emerged questioning PICADAR's performance in real-world clinical settings, particularly its sensitivity in detecting PCD across different patient subgroups. A 2025 study by Schramm et al. evaluated PICADAR's sensitivity in 269 individuals with genetically confirmed PCD, revealing critical limitations [36] [4]. The findings demonstrated that PICADAR missed a significant proportion of PCD cases, with an overall sensitivity of 75% (202/269). Perhaps most notably, the tool performed particularly poorly in specific patient subgroups, failing to identify PCD in individuals without the classic laterality defects or hallmark ultrastructural defects [36].
Table 1: PICADAR Sensitivity in Genetically Confirmed PCD Populations
| Patient Subgroup | Sensitivity | Median PICADAR Score | Statistical Significance |
|---|---|---|---|
| Overall PCD Population | 75% (202/269) | 7 (IQR: 5-9) | Reference |
| With Laterality Defects | 95% | 10 (IQR: 8-11) | p < 0.0001 |
| With Situs Solitus (normal arrangement) | 61% | 6 (IQR: 4-8) | p < 0.0001 |
| With Hallmark Ultrastructural Defects | 83% | Not reported | p < 0.0001 |
| Without Hallmark Ultrastructural Defects | 59% | Not reported | p < 0.0001 |
A critical design limitation of PICADAR is its initial screening question about daily wet cough. The tool automatically excludes patients without this symptom from further evaluation. The study found that 18 individuals (7%) with genetically confirmed PCD reported no daily wet cough and would have been ruled out according to PICADAR's algorithm [36]. This finding challenges the fundamental structure of the prediction rule and highlights the clinical diversity of PCD presentation.
Geographical and Genetic Variability
Further complicating the picture is the emerging evidence of geographical variations in PCD presentation and genetic underpinnings. A Japanese study of 67 PCD patients found that situs inversus was present in only 25% of cases, significantly lower than the approximately 50% typically reported in other populations [17]. This discrepancy was attributed to differences in the major disease-causing genes within the Japanese population. The mean PICADAR score in this cohort was 7.3 points (range: 3-14), with only two cases having congenital cardiac anomalies [17]. These findings suggest that prediction models based predominantly on Western populations may not generalize well to other ethnic groups, necessitating population-specific adjustments or entirely new approaches.
Emerging Technologies for Next-Generation Prediction Models
Advanced Genetic Sequencing Approaches
The integration of comprehensive genetic testing represents a fundamental shift in PCD diagnostics. Current genetic testing approaches, primarily using targeted gene panels or whole exome sequencing, identify biallelic mutations in one of the over 50 known PCD genes in approximately 70% of clinically diagnosed cases [60]. This diagnostic gap highlights the need for more comprehensive genetic approaches that can detect complex structural variants and novel genetic mechanisms.
Whole genome sequencing (WGS) has emerged as a powerful tool to address these limitations. A 2024 study demonstrated WGS's ability to identify structural variants in known PCD genes (DNAH5, DNAAF4, DNAH11) that would be missed by conventional testing [60]. The study reported three large deletions ranging from 3 to 13 kb, for which WGS precisely identified breakpoints, permitting confirmation by Sanger sequencing [60]. Additionally, WGS enabled the identification of a de novo variant in a novel PCD gene, TUBB4B, expanding the understanding of PCD genetics beyond traditional autosomal recessive inheritance patterns [60].
Table 2: Performance of Genetic Testing Modalities in PCD Diagnosis
| Genetic Testing Method | Diagnostic Yield | Key Advantages | Limitations |
|---|---|---|---|
| Targeted Gene Panels | ~70% | Cost-effective for known genes; familiar interpretation | Limited to pre-defined gene sets; misses structural variants |
| Whole Exome Sequencing | ~70-75% | Broad coverage of coding regions; can identify novel genes | Misses non-coding and structural variants |
| Whole Genome Sequencing | Potentially higher (exact % TBD) | Detects structural variants, non-coding variants; comprehensive | Higher cost; complex data interpretation; storage requirements |
| Bioassay Platforms | Complementary to genetic testing | Functional assessment of pathway disruption; measures biological activity | Does not identify specific genetic defects |
WGS offers several distinct advantages for next-generation PCD prediction models: it provides unbiased genome coverage beyond the exons of currently known PCD genes, simultaneously detects single nucleotide variants, small insertion-deletions (indels), and complicated structural variants, and facilitates the discovery of novel PCD genes and inheritance patterns, as demonstrated by the identification of a de novo variant in TUBB4B [60].
Functional Assays and Biomarker Discovery
Beyond genetic sequencing, functional assays that measure the biological activity of dioxin-like compounds offer another innovative approach to understanding pathway disruptions in PCD. The DR-EcoScreen bioassay represents a promising methodology that measures biological equivalency (BEQ) levels in serum samples [61]. This bioassay system utilizes a mouse hepatoma Hepa1c1c7 cell line and offers significant practical advantages, requiring only a trace amount of sample (as little as 0.5 mL of serum) while providing sufficiently high recovery for exposure assessment [61].
The DR-EcoScreen platform demonstrated strong correlation with WHO toxic equivalent (WHO-TEQ) levels measured by instrumental methods in studies of Vietnamese men exposed to dioxins from Agent Orange [61]. The difference in fat-based BEQ levels between exposed and unexposed men was more pronounced than for crude BEQ levels, with a strong correlation between fat-based BEQ and WHO-TEQ levels [61]. While not directly developed for PCD, this assay principle could be adapted to measure functional pathway activity relevant to ciliary function.
Other emerging biomarker approaches include:
- Circulating microRNAs: Studies in other fields have identified specific miRNAs (e.g., miR-21, miR-16, miR-877) with high diagnostic accuracy for various conditions [62].
- Volatile Organic Compounds (VOCs): Analysis of VOC profiles in exhaled breath, feces, and skin sebum represents a non-invasive approach that could be explored for PCD [63].
- Liquid Biopsy Technologies: When combined with CRISPR/Cas systems, these enable sensitive detection of tumor-specific biomarkers that could be adapted for PCD markers [62].
Integrated Multi-Omics Prediction Model Framework
Architecture of Next-Generation Prediction Systems
The limitations of single-modality approaches like PICADAR highlight the necessity for integrated systems that combine multiple data types. Next-generation prediction models for PCD should incorporate clinical parameters, genetic data, functional assay results, and biomarker profiles into a unified diagnostic framework. This multi-layered approach can compensate for the limitations of individual components and provide a more comprehensive assessment of PCD likelihood.
A proposed integrated model would include:
Enhanced Clinical Scoring: Retaining valuable elements of PICADAR while modifying problematic components, particularly the initial daily wet cough requirement that excludes 7% of genuine PCD cases [36]. Additional clinical elements such as detailed family history, response to previous treatments, and quantitative imaging findings could enhance predictive value.
Genetic Risk Score: Incorporating results from whole genome sequencing, including both sequence variants and structural variants, weighted by their known association strength with PCD. Polygenic risk scores could be developed to account for the complex genetics of PCD.
Functional Pathway Assessment: Utilizing adapted bioassay platforms like DR-EcoScreen to measure biological pathway activity relevant to ciliary function [61]. These functional readouts provide validation for genetic findings and may detect abnormalities in cases with normal genetic testing.
Molecular Biomarker Panel: Integrating measurements of specific miRNAs, proteins, or volatile organic compounds associated with ciliary dysfunction into the prediction algorithm.
Validation Framework and Performance Metrics
Rigorous validation of next-generation prediction models requires large, diverse cohorts that include patients across the spectrum of PCD presentations. Particular attention should be paid to including adequate representation of patients with situs solitus and without hallmark ultrastructural defects, as these groups are most likely to be missed by current tools [36] [4]. Validation metrics should extend beyond overall accuracy to include subgroup-specific performance, clinical utility measures, and cost-effectiveness analyses.
Model performance should be benchmarked against the established limitations of PICADAR, with a target of achieving at least 90% sensitivity across all major PCD subgroups, including those with situs solitus (where PICADAR achieves only 61% sensitivity) and those without hallmark ultrastructural defects (where PICADAR achieves only 59% sensitivity) [36] [4].
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for PCD Diagnostic Development
| Research Tool | Function/Application | Key Features | Representative Use |
|---|---|---|---|
| DR-EcoScreen Cell Line | Mouse hepatoma Hepa1c1c7 cells for bioassay | Measures biological equivalency (BEQ); requires small sample volume (0.5 mL serum) | Functional assessment of pathway activity in serum samples [61] |
| Whole Genome Sequencing Platform | Comprehensive genetic analysis | Detects SNVs, indels, structural variants; unbiased genome coverage | Identification of complex structural variants in PCD genes [60] |
| CRISPR/Cas Systems | Gene editing and detection | Precise genome modification; highly specific nucleic acid detection | Potential application in liquid biopsy platforms for biomarker detection [62] |
| High-Speed Video Microscopy | Ciliary function analysis | Visualizes ciliary beat pattern and frequency | Reference standard for ciliary functional assessment [60] |
| Transmission Electron Microscopy | Ciliary ultrastructure examination | Nanoscale visualization of ciliary anatomy | Identification of hallmark ultrastructural defects [60] |
| Nasal Nitric Oxide Analyzer | nNO measurement as PCD screening | Markedly reduced nNO in PCD patients | Non-invasive screening modality [60] |
The development of next-generation predictive models for PCD represents an urgent clinical need, driven by the documented limitations of current tools like PICADAR, particularly their poor performance in specific patient subgroups. The integration of comprehensive genetic data from whole genome sequencing, functional assessments from adapted bioassay platforms, and innovative biomarker profiling offers a path toward more accurate and inclusive prediction models. These advanced systems must be rigorously validated across diverse populations and clinical settings to ensure they address the known geographical and genetic variabilities in PCD presentation. Through the strategic integration of multiple technological approaches, the field can move beyond the limitations of current clinical prediction rules and toward a more precise, inclusive, and accurate diagnostic future for primary ciliary dyskinesia.
Conclusion
The PICADAR score serves as an important but imperfect tool for identifying PCD patients, with significantly compromised sensitivity (61%) in the substantial subgroup of patients with situs solitus. This limitation is particularly pronounced in cases without hallmark ultrastructural defects (59% sensitivity) and varies across genetic and ethnic populations. For researchers and drug development professionals, these findings underscore the necessity of using PICADAR with caution and supplementing it with advanced diagnostic methods, particularly when recruiting patients for clinical trials where missing situs solitus cases could substantially impact study validity and generalizability. Future research must focus on developing more inclusive predictive tools that account for the full genetic and phenotypic spectrum of PCD, ultimately enabling earlier diagnosis and more targeted therapeutic development for all patient populations.
References
- 1. Primary Ciliary Dyskinesia—Current Diagnostic and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12525432/]
- 2. Primary Ciliary Dyskinesia: An Update on New Diagnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4062113/]
- 3. Evaluation of a Clinical Index as a Predictive Tool for Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232329/]
- 4. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1691758/full]
- 5. a diagnostic predictive tool for primary ciliary dyskinesia [https://pmc.ncbi.nlm.nih.gov/articles/PMC4819882/]
- 6. Quantitative Assessment of Ciliary Ultrastructure with the Use ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8394936/]
- 7. Quantitative analysis of ciliary beating in primary ciliary ... [https://ojrd.biomedcentral.com/articles/10.1186/1750-1172-7-78]
- 8. Ciliary Feature Counter: A program for the Quantitative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7459509/]
- 9. a diagnostic predictive tool for primary ciliary dyskinesia [https://pubmed.ncbi.nlm.nih.gov/26917608/]
- 10. Clinical Manifestations and Genotype of Primary Ciliary ... [https://e-aair.org/DOIx.php?id=10.4168/aair.2023.15.6.757]
- 11. Laterality Defects Other Than Situs Inversus Totalis in Primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4219335/]
- 12. Human Laterality Disorders: Pathogenesis, Clinical ... [https://www.sciencedirect.com/science/article/abs/pii/S0002962921001907]
- 13. Situs Inversus Totalis: A Clinical Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8901252/]
- 14. Prader-Willi Syndrome - GeneReviews® - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK1330/]
- 15. Clinical, phenotype and genotype correlations in primary ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1641739/full]
- 16. Clinical, Genetic, Morphological and Functional Correlations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12578735/]
- 17. Analysis of the clinical features of Japanese patients with ... [https://www.sciencedirect.com/science/article/pii/S0385814621002248]
- 18. Clinical and Genetic Characterization of Patients with ... [https://www.mdpi.com/2227-9067/10/10/1684]
- 19. Clinical features and genetic spectrum of children with primary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12202327/]
- 20. Feasibility of Machine Learning Analysis for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12047924/]
- 21. RSPH4A-PCDx: An Index to Predict Lung Function Decline in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12382859/]
- 22. Feasibility of machine learning analysis for the identification of ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-025-03966-z]
- 23. Which side are they on? Diagnosing primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10646753/]
- 24. a diagnostic predictive tool for primary ciliary dyskinesia [https://www.academia.edu/55769744/PICADAR_a_diagnostic_predictive_tool_for_primary_ciliary_dyskinesia]
- 25. Guidelines for the diagnosis of primary ciliary dyskinesia [https://www.waidid.org/publications/guidelines-for-the-diagnosis-of-primary-ciliary-dyskinesia]
- 26. Evaluation of a Clinical Index as a Predictive Tool for ... [https://www.mdpi.com/2075-4418/11/6/1088]
- 27. Empowering limited-resource countries: collaborating with ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1547152/full]
- 28. Top Data Collection Techniques: Best Practices for 2025 ... [https://www.ovaledge.com/blog/data-collection-techniques?hs_amp=true]
- 29. 10 Interesting Data Collection Techniques & Methods For ... [https://airbyte.com/data-engineering-resources/data-collection-techniques]
- 30. 10 Best Practices for Data Collection in 2025 [https://add-to-calendar-pro.com/articles/best-practices-for-data-collection]
- 31. Patient-Focused Drug Development Guidance Series [https://www.fda.gov/drugs/development-approval-process-drugs/fda-patient-focused-drug-development-guidance-series-enhancing-incorporation-patients-voice-medical]
- 32. Patient-Focused Drug Development: Selecting, ... [https://www.federalregister.gov/documents/2025/11/18/2025-20153/patient-focused-drug-development-selecting-developing-or-modifying-fit-for-purpose-clinical-outcome]
- 33. Regulatory Updates, September 2025 [https://www.caidya.com/resources/regulatory-updates-sept-2025/]
- 34. 10 Clinical Trial Regulatory Changes Coming in 2025 [https://en.ennov.com/blog/clinical-blog/trial-regulatory-changes-coming-2025/]
- 35. 3 Steps to Optimize Data Collection and Analysis in 2025 [https://statetechmagazine.com/article/2024/12/3-steps-optimize-data-collection-and-analysis-2025]
- 36. Limitations of PICADAR as a diagnostic predictive tool for ... [https://www.medrxiv.org/content/10.1101/2025.09.22.25336363v1]
- 37. Primary ciliary dyskinesia: A review [https://www.sciencedirect.com/science/article/pii/S2950008725000420]
- 38. Clinical developments experts have their eye on in 2025 [https://www.drugdiscoverynews.com/clinical-developments-experts-have-their-eye-on-in-2025-16196]
- 39. ERS Task Force guideline for the diagnosis of primary ciliary ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6054534/]
- 40. Limitations of PICADAR as a diagnostic predictive tool for primary ... [https://labs.sciety.org/articles/by?article_doi=10.1101/2025.09.22.25336363]
- 41. Ultrastructure for the diagnosis of primary ciliary dyskinesia in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10461090/]
- 42. Transmission electron microscopy study of suspected ... [https://www.nature.com/articles/s41598-022-06370-w]
- 43. Clinical features and genetic spectrum of children with ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1526675/full]
- 44. Primary Ciliary Dyskinesia [https://recodetx.com/pcd/]
- 45. Primary Ciliary Dyskinesia - GeneReviews® - NCBI Bookshelf [https://www.ncbi.nlm.nih.gov/books/NBK1122/]
- 46. Clinical characteristics and genetic spectrum of 26 individuals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8252271/]
- 47. Prevalence of primary ciliary dyskinesia in consecutive ... [https://www.nature.com/articles/pr2016263]
- 48. Feasibility of machine learning analysis for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12522419/]
- 49. Feasibility of Machine Learning Analysis for the ... [https://www.medrxiv.org/content/10.1101/2025.04.18.25326065v1]
- 50. A pediatric case of productive cough caused by novel ... [https://www.nature.com/articles/s41439-020-00134-6]
- 51. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 52. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 53. Reporting Results from Studies Evaluating Diagnostic Tests [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/statistical-guidance-reporting-results-studies-evaluating-diagnostic-tests-guidance-industry-and-fda]
- 54. Nasal Nitric Oxide Measurement and a Modified PICADAR ... [https://pubmed.ncbi.nlm.nih.gov/28783864/]
- 55. Genetic tests and genomic biomarkers - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC2781197/]
- 56. Discovery and validation of biomarkers to aid the ... [https://www.nature.com/articles/s41582-020-0362-2]
- 57. Unveiling the Essential Criteria for Validating Clinical ... [https://oxfordglobal.com/precision-medicine/resources/validating-clinical-biomarkers]
- 58. Development and validation of a biomarker-based ... [https://www.sciencedirect.com/science/article/pii/S2405844024174749]
- 59. Preclinical vs. Clinical Biomarkers: Understanding Their ... [https://blog.crownbio.com/preclinical-vs-clinical-biomarkers-understanding-their-distinct-roles-in-drug-development]
- 60. Whole genome sequencing enhances molecular diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11600997/]
- 61. Bioassay Using the DR-EcoScreen System to Measure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12197712/]
- 62. The Role of Liquid Biopsy and CRISPR/Cas Systems in ... [https://pubmed.ncbi.nlm.nih.gov/40647454/]
- 63. Volatile Organic Compounds (VOCs) in ... [https://www.mdpi.com/1420-3049/30/19/4028]