Preventing Overfitting in m6A-lncRNA Signatures: A Cross-Validation Guide for Robust Biomarker Development
This article provides a comprehensive framework for researchers and drug development professionals to construct and validate prognostic m6A-related lncRNA signatures while rigorously preventing overfitting.
Preventing Overfitting in m6A-lncRNA Signatures: A Cross-Validation Guide for Robust Biomarker Development
Abstract
This article provides a comprehensive framework for researchers and drug development professionals to construct and validate prognostic m6A-related lncRNA signatures while rigorously preventing overfitting. It covers the foundational biology of m6A and lncRNA interactions, practical methodologies for model construction using techniques like LASSO regression, advanced troubleshooting with interpretable machine learning, and robust validation strategies. By synthesizing current best practices from computational biology and clinical research, this guide aims to enhance the reproducibility, clinical translatability, and predictive power of m6A-lncRNA models in cancer research and therapeutic development.
The Biological Bridge: Understanding m6A and lncRNA Interactions in Cancer
FAQs: Core Concepts of m6A RNA Methylation
1. What is m6A RNA methylation and why is it important? N6-methyladenosine (m6A) is the most prevalent, abundant, and conserved internal chemical modification found in messenger RNAs (mRNAs) and various non-coding RNAs in eukaryotes [1] [2]. It is a dynamic and reversible process that regulates several facets of RNA metabolism, including RNA splicing, export, localization, translation, and stability [1] [3]. Due to its comprehensive roles in fundamental biological processes, m6A is crucial in embryonic development, cell fate determination, and a variety of physiological processes. Dysregulation of m6A is closely linked to cancer progression, metastasis, and drug resistance [2].
2. What are the core components of the m6A writer complex? The m6A modification is installed by a multi-component methyltransferase complex ("writer"). The core complex includes [1] [3] [4]:
- METTL3: The catalytic subunit that transfers the methyl group.
- METTL14: Serves as an essential RNA-binding scaffold, allosterically activating and enhancing METTL3's catalytic activity. It forms a stable heterodimer with METTL3.
- WTAP: A regulatory subunit that interacts with METTL3 and METTL14, facilitating their localization to nuclear speckles and modulating m6A levels, though it lacks catalytic activity itself. Other important adapter proteins include KIAA1429 (VIRMA), which guides region-selective methylation, particularly in the 3'UTR; RBM15/RBM15B, which recruits the complex to specific RNA sites; and ZC3H13, which is critical for the nuclear localization of the writer complex [1].
3. Which proteins serve as m6A erasers? The removal of m6A is performed by demethylases ("erasers"), making the modification reversible. The two known m6A erasers are [4] [2]:
- FTO (Fat mass and obesity-associated protein): The first m6A demethylase discovered. It preferentially demethylates m6Am, an m6A-related modification, but also acts on m6A.
- ALKBH5: The other major m6A demethylase, which plays critical roles in various biological processes and cancers. The activity and specificity of these erasers can be highly context-dependent, varying by cell type, subcellular localization, and external stimuli [3].
4. How do m6A reader proteins exert their functions? m6A reader proteins recognize and bind to m6A-modified RNAs, executing the functional outcomes of the modification. They contain various m6A-binding domains and can be categorized as follows [4]:
- YTH Domain Family: This is a major class of readers.
- YTHDF1: Promotes translation efficiency, often in cooperation with YTHDF3.
- YTHDF2: Regulates mRNA stability and degradation.
- YTHDF3: Assists in translation and decay.
- YTHDC1: Regulates alternative splicing in the nucleus.
- YTHDC2: Enhances translation efficiency and can decrease RNA abundance.
- Other Readers: These include:
- IGF2BPs (IGF2BP1/2/3): Promote the stability and storage of target mRNAs.
- HNRNPs (e.g., HNRNPC/G): Bind to m6A-modified RNAs and regulate their processing by facilitating structural changes in the RNA.
Troubleshooting Guides for m6A Research
Issue 1: Inconsistent m6A-seq/MeRIP-seq Results
| Potential Cause | Solution / Verification Step |
|---|---|
| Inadequate Immunoprecipitation (IP) Efficiency | Use knockout-validated antibodies for IP [4]. Include positive and negative control RNAs to verify IP specificity and efficiency. |
| RNA Degradation or Low Quality | Always use RNA with high integrity (RIN > 8). Perform all RNA handling and fragmentation steps on ice with RNase-free reagents. |
| Insufficient Input RNA | Ensure you are using the recommended amount of input RNA (typically 1-5 µg for total RNA). Pilot experiments can help determine the optimal input for your sample type. |
| Improper Normalization | Use spike-in RNAs (e.g., from other species) with known m6A status to control for technical variability during library preparation and sequencing [5]. |
| High Background Noise | Optimize washing stringency after IP. For single-nucleotide resolution, consider advanced methods like miCLIP, which can reduce background and map sites more precisely [4]. |
Issue 2: Overfitting in m6A-Related Prognostic Model Construction A common challenge in constructing prognostic signatures based on m6A-related lncRNAs is the risk of overfitting, where a model performs well on training data but poorly on independent validation data.
- Preventive Protocol: Rigorous Cross-Validation
- Data Splitting: Divide your entire dataset (e.g., from TCGA) randomly into a training set (e.g., 70%) and a hold-out test set (e.g., 30%). The test set should not be used until the final model evaluation.
- Feature Selection on Training Set: Within the training set only, use univariate Cox regression to identify m6A-related lncRNAs significantly associated with survival.
- LASSO Regression: Apply the LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression to the training set. LASSO penalizes the complexity of the model, forcing the coefficients of less important variables toward zero, thus preventing overfitting [6] [7]. The penalty parameter (λ) should be determined via tenfold cross-validation within the training set, typically choosing the λ value that gives the minimum partial likelihood deviance or the largest λ within one standard error of the minimum (the "1-SE" rule for a more parsimonious model).
- Model Validation: Apply the final model with the selected lncRNAs and their coefficients from the training set to the untouched test set. Evaluate its performance on the test set using Kaplan-Meier survival analysis and time-dependent Receiver Operating Characteristic (ROC) curves [6] [7].
- External Validation: For maximum robustness, validate the model on a completely independent cohort from a different source (e.g., GEO database) [8].
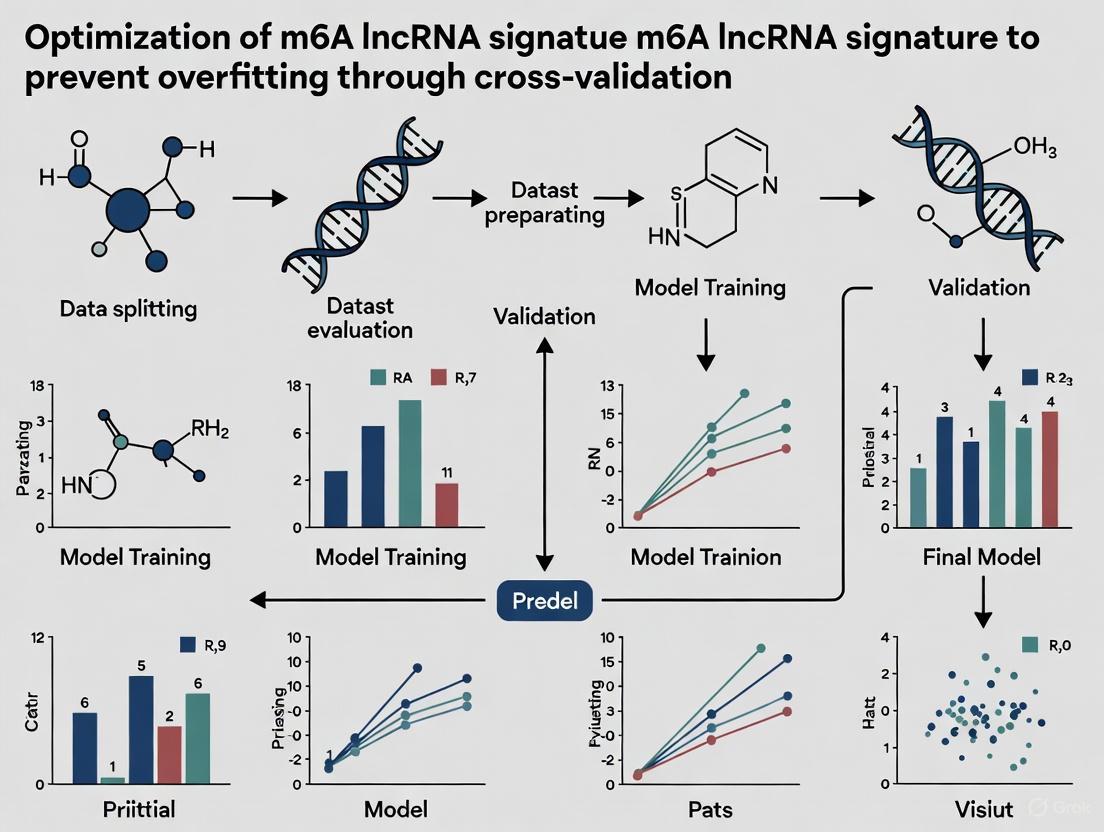
The following workflow outlines the key steps for building a robust prognostic model, integrating the cross-validation and feature selection methods described above to prevent overfitting.
Issue 3: Difficulty in Visualizing RNA Localization and Expression
- Solution A: Fluorescence In Situ Hybridization (FISH)
- Method: Use DNA or RNA probes complementary to your target RNA sequence, labeled with a fluorophore. This is highly sequence-specific and can be used to detect individual RNA strands in fixed cells [9].
- Troubleshooting: High background can be an issue. Consider derivatives like molecular beacons or Forced Intercalation (FIT) probes, which fluoresce only upon binding to the target, significantly reducing background signal [9].
- Solution B: MS2-MCP System for Live-Cell Imaging
- Method: Engineer the RNA of interest to include multiple MS2-binding sites (MBS). Co-express this with a GFP-fused MS2 coat protein (MCP). The GFP-MCP will bind to the MBS, allowing tracking of single mRNA molecules in living cells [9].
- Troubleshooting: Be aware that the large tag appendages might interfere with normal mRNA function or localization. Generating a transgenic organism for this can be time-consuming [9].
Research Reagent Solutions
The following table lists key reagents for studying m6A RNA methylation, drawing from validated research tools and methodologies.
| Reagent / Tool | Category | Primary Function / Application |
|---|---|---|
| METTL3 Antibody [4] | Writer | Immunoprecipitation (IP), Western Blot (WB), Immunohistochemistry (IHC) to study writer complex localization and expression. |
| ALKBH5 Antibody [4] | Eraser | WB, IHC to detect levels of the m6A demethylase. |
| YTHDF2 Antibody [4] | Reader | IP, WB, IHC, ICC/IF to investigate reader protein function and abundance. |
| m6A-Specific Antibody (e.g., ab151230) [4] | Detection | Core reagent for m6A mapping techniques (MeRIP-seq, miCLIP). |
| 5-Ethynyluridine (EU) [9] | Metabolic Labeling | Incorporates into newly transcribed RNA; can be visualized via click chemistry with a fluorophore for RNA dynamics studies. |
| LASSO Regression Model [6] [7] | Bioinformatics | Statistical method to prevent overfitting during prognostic signature construction by penalizing model complexity. |
| ssGSEA Algorithm [6] [7] | Bioinformatics | Used to evaluate immune cell infiltration and immune function scores in the tumor microenvironment based on m6A-related signatures. |
| Molecular Beacons / FIT Probes [9] | Imaging | Fluorescent probes for highly specific, low-background RNA visualization in live or fixed cells. |
m6A Regulators at a Glance
The table below provides a concise summary of the key proteins involved in m6A RNA methylation, highlighting their main components and functions.
| Regulator Type | Key Components | Primary Function |
|---|---|---|
| Writers | METTL3, METTL14, WTAP, KIAA1429 (VIRMA), RBM15/15B, ZC3H13 [1] [2] | Form a multi-protein complex that installs the m6A mark on RNA co-transcriptionally. METTL3 is the catalytic core. |
| Erasers | FTO, ALKBH5 [4] [2] | Enzymatically remove the m6A mark, enabling dynamic and reversible regulation of RNA methylation. |
| Readers | YTHDF1/2/3, YTHDC1/2, IGF2BP1/2/3, HNRNPC/G [4] [2] | Recognize and bind to m6A-modified RNAs, dictating the functional outcome (e.g., splicing, decay, translation). |
The following diagram illustrates the coordinated workflow of m6A methylation, from the installation of the mark by writers to its recognition by readers and removal by erasers, ultimately influencing the fate of the modified RNA.
Functional Roles of Long Non-Coding RNAs in Gene Regulation and Oncogenesis
Long non-coding RNAs (lncRNAs) are RNA molecules exceeding 200 nucleotides in length that lack protein-coding capacity. Once considered transcriptional "noise," they are now recognized as critical regulators of diverse cellular processes, with tissue-specific expression patterns particularly evident in tumors [10]. Their intricate involvement in tumorigenesis spans cancer initiation, progression, recurrence, metastasis, and chemotherapy resistance [10].
The functional significance of lncRNAs is profoundly influenced by post-transcriptional modifications, with N6-methyladenosine (m6A) emerging as a pivotal regulator. As the most common internal RNA modification in eukaryotes, m6A dynamically and reversibly fine-tunes RNA metabolism through writer (methyltransferases), eraser (demethylases), and reader (recognition proteins) proteins [11] [12]. This modification system significantly influences lncRNA generation, stability, and molecular interactions, creating a sophisticated regulatory layer in oncogenesis [13] [14].
Frequently Asked Questions (FAQs)
Q1: What fundamental roles do lncRNAs play in gene regulation and cancer development?
LncRNAs function through diverse mechanistic pathways to regulate gene expression. They can act as transcriptional regulators by modulating chromatin architecture and recruiting transcription factors, or influence post-transcriptional processes including RNA splicing, stability, and translation [10]. Through these mechanisms, lncRNAs impact critical cancer hallmarks such as uncoordinated cell proliferation, resistance to apoptosis, and metastatic potential [15]. Their expression patterns offer promising biomarkers for early cancer detection and prognosis, while their functional roles present opportunities for innovative therapeutic strategies [10].
Q2: How does m6A modification influence lncRNA function in cancer contexts?
m6A modification significantly impacts lncRNA stability, processing, and molecular interactions. For instance, METTL3-mediated m6A modification of lncRNA XIST suppresses colon cancer tumorigenicity and migration [11]. Similarly, YTHDF3 recognizes m6A-modified lncRNA GAS5, promoting its degradation and exacerbating colorectal cancer progression [16]. In bladder cancer, RBM15 and METTL3 synergistically promote m6A modification of specific lncRNAs, facilitating malignant progression [13]. These examples illustrate how m6A modifications can either promote or suppress tumorigenesis depending on the specific lncRNA and cellular context.
Q3: What practical strategies can prevent overfitting when developing m6A-related lncRNA prognostic signatures?
Robust prognostic model development requires careful statistical approaches. The following table summarizes key methodological considerations identified from multiple studies:
Table 1: Strategies for Preventing Overfitting in Prognostic Signature Development
| Method | Implementation | Study Example |
|---|---|---|
| LASSO Regression | Applies regularization to shrink coefficients and select most relevant features | Used in CRC [17], bladder cancer [13], and ovarian cancer [14] studies |
| Cross-Validation | Employ k-fold (typically 10-fold) validation during model training | Implemented in colon adenocarcinoma [11] and other cancer studies |
| Multi-Dataset Validation | Validate final model in independent patient cohorts from different sources | CRC models validated across 6 GEO datasets [18]; Ovarian cancer validated in GSE9891, GSE26193 [14] |
| External Experimental Validation | Confirm lncRNA expression in independent patient samples | CRC study validation in 55-patient in-house cohort [18]; Ovarian cancer validation in 60 clinical specimens [14] |
Q4: How can researchers identify authentic m6A-related lncRNAs for their studies?
Multiple complementary approaches can identify m6A-related lncRNAs. The most comprehensive strategy integrates:
- Co-expression Analysis: Calculate correlation coefficients between m6A regulators and lncRNAs (typically |R| > 0.4, p < 0.001) [11] [14]
- Database Mining: Utilize resources like M6A2Target documenting lncRNAs methylated or bound by m6A regulators [18]
- Experimental Evidence: Employ methylated RNA immunoprecipitation sequencing (MeRIP-seq) to confirm direct m6A modification
- Functional Impact Assessment: Evaluate expression changes following m6A regulator knockdown/overexpression [18]
Troubleshooting Common Experimental Challenges
Problem: Inconsistent prognostic signature performance across validation cohorts
Solution:
- Ensure consistent normalization methods across training and validation datasets
- Account for batch effects using algorithms like "Combat" when combining datasets [16]
- Verify that lncRNA detection probes are comparable across different platforms
- Consider biological variables including cancer subtypes, stages, and patient demographics that might affect signature performance
Problem: Difficulty distinguishing true m6A-related lncRNAs from incidental correlations
Solution:
- Apply stringent correlation thresholds (|R| > 0.4, p < 0.001) [11] [14]
- Require evidence from multiple identification methods (co-expression plus database or experimental support)
- Validate top candidates through experimental approaches such as RIP-qPCR or MeRIP-PCR
- Consider only lncRNAs with reasonable expression levels (e.g., median FPKM > 1) to ensure biological relevance [18]
Problem: Low predictive accuracy of m6A-lncRNA prognostic models
Solution:
- Incorporate clinical parameters with established prognostic value (e.g., pathologic stage) into nomograms [11]
- Consider integrating multiple RNA modification types (e.g., both m6A and m5C) for comprehensive signatures [16]
- Ensure proper feature selection through LASSO regression to eliminate redundant variables
- Validate time-dependent ROC curves at multiple intervals (1, 3, 5 years) to assess temporal performance [17]
Key Experimental Workflows
The development of robust m6A-related lncRNA signatures follows a systematic workflow that integrates bioinformatics analyses with experimental validation:
Diagram 1: m6A-LncRNA Signature Development Workflow
Research Reagent Solutions
Table 2: Essential Research Reagents for m6A-LncRNA Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| m6A Writers | METTL3, METTL14, METTL16, WTAP, RBM15/RBM15B, VIRMA, ZC3H13 | Methyltransferase enzymes that catalyze m6A modification [11] [13] |
| m6A Erasers | FTO, ALKBH5 | Demethylase enzymes that remove m6A modifications [11] [14] |
| m6A Readers | YTHDF1-3, YTHDC1-2, HNRNPC, HNRNPA2B1, IGF2BP1-3 | Recognition proteins that bind m6A-modified RNAs [18] [11] [14] |
| Data Resources | TCGA, GEO datasets (GSE17538, GSE39582, GSE9891, etc.) | Provide transcriptomic data and clinical information for analysis [18] [16] [14] |
| Analytical Tools | R packages: "limma", "DESeq2", "glmnet", "pRRophetic" | Differential expression, LASSO regression, drug sensitivity prediction [18] [11] |
Advanced Technical Considerations
Integrating Multi-Omics Data Advanced m6A-lncRNA studies increasingly integrate multiple data types. For example, investigating cross-talk between m6A- and m5C-related lncRNAs in colorectal cancer has revealed complex regulatory networks affecting tumor microenvironment and immunotherapy response [16]. Such integrated approaches provide more comprehensive insights into cancer mechanisms than single-modification analyses.
Tumor Microenvironment and Immunotherapy Applications m6A-related lncRNA signatures show promise in predicting immunotherapy responses. Studies have demonstrated that low-risk colorectal cancer patients based on m6A/m5C-related lncRNA profiles exhibit enhanced response to anti-PD-1/L1 immunotherapy [16]. Similarly, distinct risk groups show different sensitivities to various chemotherapeutic agents, enabling potential treatment stratification [11].
Functional Validation Approaches Beyond computational predictions, rigorous functional validation is essential. This includes:
- In vitro assays measuring proliferation, invasion, and migration following lncRNA modulation
- In vivo models such as the N-methyl-N-nitrosourea (MNU)-induced rat bladder carcinoma model [13]
- Mechanistic studies investigating specific pathways (e.g., METTL3/RBM15 synergistic promotion of bladder cancer progression) [13]
The investigation of m6A-modified lncRNAs represents a frontier in cancer research, offering insights into tumor biology and promising clinical applications. Robust signature development requires meticulous attention to statistical methods, particularly overfitting prevention through regularization and multi-cohort validation. As research progresses, integrating these molecular signatures with clinical parameters and therapeutic response data will be essential for realizing their potential in personalized cancer medicine.
Core Molecular Mechanisms: How does m6A directly regulate lncRNA function?
N6-methyladenosine (m6A) regulates long non-coding RNA (lncRNA) function and stability through a complex interplay between writer, reader, and eraser proteins. This modification represents a critical layer of post-transcriptional control that significantly influences lncRNA biology.
Reader-Protein Mediated Stability Control: The m6A reader protein HNRNPA2B1 directly binds to m6A-modified lncRNAs to enhance their stability. A key example is the lncRNA NORHA, where HNRNPA2B1 binding at multiple m6A sites (including A261, A441, and A919) stabilizes the transcript in sow granulosa cells (sGCs). This stabilization promotes sGC apoptosis by activating the NORHA-FoxO1 axis, which subsequently represses cytochrome P450 family 19 subfamily A member 1 (CYP19A1) expression and suppresses 17β-estradiol biosynthesis [19].
Reader-Dependent Functional Modulation: The m6A reader IGF2BP2 functions as a critical stabilizer for specific lncRNAs. In renal cell carcinoma (RCC), IGF2BP2, mediated by the methyltransferase METTL14, recognizes m6A modification sites on the lncRNA LHX1-DT and promotes its stability. This stabilized LHX1-DT then acts as a competing endogenous RNA (ceRNA) by sponging miR-590-5p, which in turn downregulates PDCD4, ultimately inhibiting RCC cell proliferation and invasion [20].
Writer-Mediated Regulation: The m6A methyltransferase complex, particularly METTL3, serves as a crucial mediator in lncRNA regulation. Research demonstrates that HNRNPA2B1 functions as a critical mediator of METTL3-dependent m6A modification, modulating NORHA expression and activity in cellular systems [19].
The following diagram illustrates these core regulatory pathways:
Experimental Protocols: Key Methodologies for Investigating m6A-lncRNA Interactions
Transcriptome-Wide m6A Site Mapping
Purpose: To identify specific m6A modification sites on lncRNAs at a transcriptome-wide scale [19].
Protocol:
- RNA Isolation and Fragmentation: Extract high-quality total RNA using TRIzol reagent. Fragment RNA to 100-150 nucleotides using RNA fragmentation buffer.
- Immunoprecipitation: Incubate fragmented RNA with anti-m6A antibody (5μg) and protein A/G magnetic beads in IP buffer (150mM NaCl, 10mM Tris-HCl, pH 7.4, 0.1% NP-40) for 2 hours at 4°C.
- Washing and Elution: Wash beads 3 times with IP buffer. Elute m6A-modified RNA using elution buffer (6.7mM N6-methyladenosine in IP buffer).
- Library Preparation and Sequencing: Construct libraries using the eluted RNA with standard kits. Sequence on Illumina platform (150bp paired-end).
- Bioinformatic Analysis: Map reads to reference genome. Call m6A peaks using specialized software (e.g., exomePeak, MeTPeak). Validate specific sites through motif analysis.
RNA Immunoprecipitation (RIP) for Reader-lncRNA Binding
Purpose: To validate direct binding between m6A reader proteins and specific lncRNAs [19] [20].
Protocol:
- Cell Lysis: Lyse cells in RIP lysis buffer (150mM KCl, 25mM Tris pH 7.4, 5mM EDTA, 0.5mM DTT, 0.5% NP-40) supplemented with protease inhibitors and RNase inhibitors.
- Antibody Binding: Incubate 5μg of target antibody (e.g., anti-HNRNPA2B1, anti-IGF2BP2) or control IgG with protein A/G magnetic beads for 30 minutes at room temperature.
- Immunoprecipitation: Incubate antibody-bound beads with cell lysate (containing 500μg total protein) for 4 hours at 4°C with rotation.
- Washing: Wash beads 5 times with RIP wash buffer.
- RNA Extraction: Isolate bound RNA using TRIzol LS reagent. Treat with DNase I to remove genomic DNA contamination.
- Analysis: Analyze target lncRNA enrichment by RT-qPCR or RNA sequencing.
Luciferase Reporter Assays for Functional Validation
Purpose: To investigate how m6A modifications affect lncRNA function and interaction networks [20].
Protocol:
- Vector Construction: Clone wild-type and m6A site-mutant lncRNA sequences into psiCHECK-2 vector downstream of Renilla luciferase gene.
- Cell Transfection: Seed 293T or relevant cell line in 24-well plates. Transfect with 500ng of reporter construct using lipofectamine 3000.
- Dual-Luciferase Assay: After 48 hours, harvest cells and measure Firefly and Renilla luciferase activities using Dual-Luciferase Reporter Assay System.
- Data Analysis: Normalize Renilla luciferase activity to Firefly luciferase activity. Compare relative luciferase activity between wild-type and mutant constructs.
Troubleshooting Common Experimental Challenges
FAQ: Addressing Specific Technical Issues
Q: Why do I observe high background in my m6A-RIP experiments? A: High background often results from antibody nonspecificity or insufficient washing. Titrate your anti-m6A antibody to determine optimal concentration (typically 2-5μg). Increase wash stringency by adding high-salt washes (300mM NaCl). Include proper controls: IgG control, RNA input control, and beads-only control. Validate antibody specificity with synthetic m6A-modified and unmodified RNA oligos [19].
Q: How can I distinguish direct stabilization effects from indirect transcriptional regulation? A: Perform transcriptional inhibition assays using actinomycin D (2-5μg/mL) at multiple time points (0, 2, 4, 8 hours) after reader protein knockdown/overexpression. Measure lncRNA half-life by RT-qPCR. Combine with m6A site mutation in luciferase reporter constructs to confirm direct effects [19] [20].
Q: What approaches can validate functional outcomes of specific m6A-lncRNA axes? A: Employ multiple complementary approaches: (1) CRISPR/Cas9-mediated m6A site editing; (2) Reader protein knockdown via siRNA/shRNA; (3) Rescue experiments with wild-type and m6A site-mutant lncRNAs; (4) Functional assays relevant to your biological context (e.g., apoptosis, proliferation, migration) [19] [20].
Troubleshooting Guide for Common Problems
Table: Troubleshooting m6A-lncRNA Experiments
| Problem | Potential Causes | Solutions |
|---|---|---|
| Poor RIP enrichment | Inadequate antibody specificity | Validate antibody with positive controls; try different lots |
| Insufficient crosslinking | Optimize UV crosslinking time (typically 150-400 mJ/cm²) | |
| RNA degradation | Use fresh RNase inhibitors; work on ice | |
| Inconsistent luciferase results | m6A site context missing | Include longer genomic fragments (>500bp) around sites |
| Transfection efficiency | Normalize with co-transfected control; use stable lines | |
| Cell-type specific effects | Verify reader/writer expression in your cell model | |
| High variability in RNA stability assays | Uneven actinomycin D treatment | Pre-warm media; use fresh stock solutions |
| Inaccurate time points | Strictly adhere to collection times; technical replicates | |
| Poor separation in risk models | Overfitting | Implement cross-validation; use multiple datasets |
| Biological heterogeneity | Increase sample size; validate with orthogonal methods |
Research Reagent Solutions: Essential Tools for m6A-lncRNA Studies
Table: Key Research Reagents for m6A-lncRNA Investigations
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| m6A Writers | METTL3/METTL14 expression plasmids | Gain-of-function studies; rescue experiments |
| m6A Erasers | FTO, ALKBH5 inhibitors (e.g., FB23, IOX3) | Increase m6A levels; assess modification effects |
| m6A Readers | HNRNPA2B1, IGF2BP2 antibodies | RIP assays; Western blot; immunohistochemistry |
| Validation Tools | Anti-m6A antibodies (Abcam, Synaptic Systems) | meRIP; dot blot; immunofluorescence |
| Luciferase reporter vectors (psiCHECK-2) | Functional validation of m6A sites | |
| Critical Assays | Actinomycin D | RNA stability/half-life measurements |
| Ribosome profiling kits | Translation efficiency assessment | |
| Bioinformatic Tools | exomePeak, MeTPeak | m6A peak calling from sequencing data |
| SRAMP | m6A site prediction in lncRNAs |
Preventing Overfitting in m6A-lncRNA Signature Development
The development of prognostic signatures based on m6A-related lncRNAs requires rigorous methodological approaches to prevent overfitting and ensure clinical applicability.
Cross-Validation Strategies: Implement multiple validation cycles using independent datasets. For example, in pancreatic ductal adenocarcinoma research, signatures developed in TCGA datasets were validated in independent ICGC cohorts [21]. Similarly, colorectal cancer prognostic models were validated through both internal cross-validation and temporal validation (1, 3, and 5-year predictions) [17].
Statistical Regularization Methods: Employ least absolute shrinkage and selection operator (LASSO) Cox regression to minimize overfitting risk. This approach penalizes model complexity while selecting the most informative m6A-related lncRNAs for prognostic signatures [17] [21]. The optimal penalty parameter should be estimated through tenfold cross-validation.
Clinical Applicability Assessment: Enhance model robustness by developing nomograms that integrate the m6A-lncRNA signature with conventional clinical parameters. These nomograms should demonstrate superior predictive accuracy compared to both the signature alone and traditional staging systems, as demonstrated in PDAC research [21].
The following diagram illustrates a robust workflow for developing validated m6A-lncRNA signatures:
Advanced Technical Considerations: Ribosome Association and Its Implications
Recent evidence reveals unexpected complexity in lncRNA regulation, particularly regarding ribosome association and its impact on stability:
Ribosome Engagement Effects: Ribosome association can either stabilize or destabilize lncRNAs through competing mechanisms. Protection from nucleases can increase stability, while ribosome-associated decay pathways (e.g., nonsense-mediated decay) may promote degradation. Ribosome profiling studies show that up to 70% of cytosolic lncRNAs interact with ribosomes in human cell lines, suggesting this is a widespread phenomenon [22].
Translation Coupling: The relationship between translation efficiency and RNA stability, partly explained by codon optimality, may extend to certain lncRNAs. In humans, codons with G or C at the third position (GC3) associate with increased transcript stability, while those with A or U at the third position (AU3) typically reduce stability [22].
Experimental Implications: When investigating lncRNA stability, consider potential ribosome association through ribosome profiling or polysome fractionation. The interaction between translation and lncRNA decay offers broad implications for RNA biology and provides new insights into lncRNA regulation in both cellular and disease contexts [22].
Frequently Asked Questions (FAQs)
Q1: What are the core components of the m6A modification machinery that interact with lncRNAs? The m6A modification process is governed by three classes of proteins often called "writers," "erasers," and "readers." Writers, such as the METTL3-METTL14-WTAP complex, VIRMA, and RBM15, install the m6A modification. Erasers, including FTO and ALKBH5, remove the modification. Readers, such as YTHDF1-3, YTHDC1-2, and IGF2BP1-3, recognize the m6A marks and determine the functional outcome on the target lncRNA, influencing its stability, splicing, transport, and translation [23] [24].
Q2: How can I prevent overfitting when building a prognostic m6A-related lncRNA signature? The most robust method to prevent overfitting is to employ the least absolute shrinkage and selection operator (LASSO) Cox regression analysis combined with 10-fold cross-validation. This statistical approach penalizes the complexity of the model, forcing it to select only the lncRNAs with the strongest prognostic power, thereby reducing the risk of modeling noise. This methodology has been successfully implemented in multiple studies to construct reliable multi-lncRNA signatures [17] [11] [14].
Q3: What is a common workflow for identifying and validating m6A-related lncRNA signatures? A standard, validated workflow consists of the following stages [11] [14]:
- Data Acquisition: Obtain RNA-seq data and clinical information from public repositories like The Cancer Genome Atlas (TCGA).
- lncRNA Identification: Filter and extract the expression profiles of known lncRNAs.
- Correlation Analysis: Identify m6A-related lncRNAs by calculating correlation coefficients (e.g., Spearman or Pearson) between the expression of established m6A regulators and all lncRNAs.
- Prognostic Screening: Use univariate Cox regression to select lncRNAs significantly associated with patient survival.
- Signature Construction: Apply LASSO Cox regression to refine the lncRNA list and build a multi-lncRNA prognostic model.
- Model Validation: Validate the model's performance in an internal test set and, if possible, in independent external datasets (e.g., from GEO). Evaluate using Kaplan-Meier survival analysis and time-dependent Receiver Operating Characteristic (ROC) curves.
Q4: Our lab identified an m6A-related lncRNA associated with drug resistance. What are the first steps to validate its functional role? Initial functional validation typically involves gain-of-function and loss-of-function experiments in relevant cell line models. Knockdown of the lncRNA using siRNAs or shRNAs in resistant cell lines is performed to see if it restores drug sensitivity. Conversely, overexpressing the lncRNA in sensitive cell lines can test if it confers resistance. The core mechanistic step is to determine if this function is dependent on m6A modification by knocking down key "writer" or "eraser" proteins (e.g., METTL3, FTO) and assessing if the lncRNA's effect is abolished [24].
Q5: How can an m6A-lncRNA signature inform treatment selection, particularly for immunotherapy? Risk scores derived from m6A-lncRNA signatures have been shown to correlate with the tumor immune microenvironment. Studies in colorectal and colon cancer have found that low-risk patients often exhibit stronger immune cell infiltration and higher expression of immune checkpoints like PD-1 and CTLA-4, suggesting they might be better candidates for immunotherapy. Furthermore, these models can predict sensitivity to specific chemotherapeutic and targeted drugs, helping to guide personalized therapy selection [17] [11].
Troubleshooting Guides
Issue 1: Poor Performance or Lack of Generalization in the Prognostic Model
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Overfitting | The model performs well on the training data but poorly on the validation/test data. | Apply LASSO regression with 10-fold cross-validation during model construction. Ensure the number of lncRNAs in the signature is small relative to the number of patient samples [11]. |
| Batch Effects | Significant performance drop when applying the model to an external dataset from a different source. | Use batch effect correction algorithms (e.g., ComBat) when integrating datasets. Validate the model in multiple independent cohorts to ensure robustness [14]. |
| Incorrect Risk Stratification | The Kaplan-Meier curve does not show a significant separation between high- and low-risk groups. | Re-evaluate the correlation and Cox regression thresholds. Use the median risk score from the training set as the cutoff for the test set, do not recalculate the median in the test set [17] [14]. |
Issue 2: Difficulty in Establishing a Mechanistic Link Between an m6A-Modified lncRNA and Drug Resistance
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Unclear m6A dependency | Knocking down the lncRNA has an effect, but it's unknown if m6A modification regulates this effect. | Perform MeRIP-qPCR or RIP-qPCR to confirm the lncRNA directly binds to m6A writers/readers. Modulate m6A levels (e.g., knock down METTL3/FTO) and see if the lncRNA's stability and function change [24]. |
| Complex ceRNA Networks | The lncRNA may act as a sponge for multiple miRNAs, making it difficult to pinpoint the key pathway. | Construct a competing endogenous RNA (ceRNA) network bioinformatically. Validate key miRNA interactions using luciferase reporter assays. Focus on downstream pathways known to be involved in drug resistance (e.g., PI3K/AKT) [24] [14]. |
| Inadequate Cell Model | Using a drug-sensitive cell line to study resistance mechanisms. | Generate isogenic drug-resistant cell lines by long-term culture in low doses of the therapeutic agent (e.g., tyrosine kinase inhibitors). This models the development of clinical resistance [24]. |
Quantitative Evidence of m6A-lncRNA Axes in Cancer
The table below summarizes key evidence from recent studies documenting the role of specific m6A-lncRNA axes in cancer progression and therapy resistance.
| Cancer Type | m6A Regulator | lncRNA | Functional Role & Mechanism | Clinical/Experimental Evidence | Ref |
|---|---|---|---|---|---|
| Colorectal Cancer | Not Specified | LINC00543 | Part of an 8-lncRNA prognostic signature; linked to immune function, particularly type I interferon response. | AUC of prognostic model: 0.753 (1-year), 0.682 (3-year), 0.706 (5-year). High-risk group had poorer prognosis. | [17] |
| Colon Adenocarcinoma | Multiple | 12-lncRNA Signature | Risk model predicts prognosis, immunotherapy response, and drug sensitivity. | Model was an independent prognostic factor. Low-risk group showed more sensitivity to Afatinib, Metformin and better response to immunotherapy. | [11] |
| Ovarian Cancer | Multiple | 7-lncRNA Signature | Predicts patient prognosis; a related ceRNA network suggests mechanistic involvement in OC progression. | Validated in TCGA and two independent GEO datasets (GSE9891, GSE26193) and 60 clinical specimens. | [14] |
| Chronic Myeloid Leukemia | FTO | SENCR, PROX1-AS1, LINC00892 | FTO-mediated m6A hypomethylation stabilizes these lncRNAs, promoting TKI resistance via PI3K signaling (e.g., ITGA2, F2R). | Upregulated in TKI-resistant patients. Knockdown restored TKI sensitivity. PI3K inhibitor (Alpelisib) eradicated resistant cells in vivo. | [24] |
Experimental Protocols
Protocol 1: Constructing an m6A-Related lncRNA Prognostic Signature
This protocol is adapted from established methodologies used in multiple cancer studies [11] [14].
Data Collection:
- Download RNA sequencing (RNA-seq) data and corresponding clinical data (e.g., survival time, survival status, pathologic stage) for your cancer of interest from TCGA.
- Extract the expression matrix of a predefined set of m6A regulators (Writers: METTL3, METTL14, WTAP, etc.; Erasers: FTO, ALKBH5; Readers: YTHDF1-3, IGF2BP1-3, etc.).
Identification of m6A-Related lncRNAs:
- From the RNA-seq data, filter and extract the expression profile of all long non-coding RNAs.
- Perform correlation analysis (e.g., Pearson or Spearman) between each m6A regulator and each lncRNA across all tumor samples.
- Identify m6A-related lncRNAs using a strict threshold (commonly |correlation coefficient| > 0.4 and p-value < 0.001).
Prognostic Model Construction:
- Randomly divide the patient cohort into a training set (e.g., 70%) and a test set (e.g., 30%).
- On the training set, perform univariate Cox regression analysis on the m6A-related lncRNAs to identify those significantly associated with overall survival (p < 0.05).
- Subject the significant lncRNAs to LASSO Cox regression analysis with 10-fold cross-validation to select the most robust predictors and prevent overfitting.
- Use the results of the LASSO analysis to perform multivariate Cox regression to assign a coefficient to each selected lncRNA.
- Calculate the risk score for each patient using the formula:
Risk Score = ∑(Expr_lncRNA_i * Coef_lncRNA_i).
Model Validation:
- Apply the risk score formula to the test set and the entire TCGA cohort.
- Classify patients into high-risk and low-risk groups based on the median risk score from the training set.
- Use Kaplan-Meier survival analysis with the log-rank test to evaluate the difference in survival between the two groups.
- Assess the predictive accuracy of the model using time-dependent ROC curve analysis for 1, 3, and 5-year overall survival.
Protocol 2: Validating the Functional Role of an m6A-Modified lncRNA in Drug Resistance
This protocol is based on mechanistic studies in leukemia and other cancers [23] [24].
Establish Resistant Cell Lines:
- Generate TKI-resistant (e.g., imatinib, nilotinib) or other drug-resistant cell lines by chronically exposing sensitive parental cells (e.g., K562) to increasing concentrations of the drug over 8-10 weeks.
Confirm m6A Modification and Dependency:
- MeRIP-qPCR: Use an anti-m6A antibody to immunoprecipitate methylated RNA and detect the specific enrichment of your target lncRNA in the pull-down fraction compared to the input via qPCR.
- Functional Dependency: Knock down m6A erasers (e.g., FTO, ALKBH5) or writers (e.g., METTL3) in the resistant cells using siRNAs or shRNAs. Measure the expression and half-life of the target lncRNA via qPCR after transcriptional inhibition (e.g., Actinomycin D assay). If the lncRNA is stabilized by m6A erasure, FTO knockdown should decrease its stability.
Functional Rescue Experiments:
- Knock down the target lncRNA (e.g., SENCR, PROX1-AS1) in the resistant cell lines using specific shRNAs.
- Perform in vitro drug sensitivity assays (e.g., CCK-8, CellTiter-Glo) to measure the IC50 of the therapeutic drug. Successful knockdown should significantly lower the IC50, indicating re-sensitization.
- Rescue the phenotype by overexpressing a wild-type lncRNA construct and, as a control, an m6A site-mutant lncRNA construct. If the function is m6A-dependent, the mutant should not fully rescue the resistance.
Identify Downstream Pathway:
- Use RNA-seq or qPCR arrays after lncRNA knockdown to identify differentially expressed genes.
- Perform pathway enrichment analysis (e.g., KEGG, GO) to find activated signaling pathways (e.g., PI3K/AKT).
- Validate in vivo using a xenograft mouse model. Treat mice engrafted with resistant cells with a pathway-specific inhibitor (e.g., PI3K inhibitor Alpelisib) and monitor tumor growth and survival.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function/Brief Explanation | Example Usage |
|---|---|---|
| TCGA & GEO Databases | Primary sources for high-throughput transcriptomic data and clinical information needed to discover and validate lncRNA signatures. | Used as the training and validation cohorts in nearly all cited studies [17] [11] [14]. |
| LASSO Cox Regression | A statistical method that performs both variable selection and regularization to enhance prediction accuracy and interpretability of the prognostic model. | Core algorithm for constructing the multi-lncRNA signatures while preventing overfitting [11] [14]. |
| shRNAs/siRNAs | Synthetic RNA molecules used for targeted knockdown of specific genes (e.g., lncRNAs, FTO, METTL3) in loss-of-function studies. | Used to knock down lncRNAs (SENCR, PROX1-AS1) and FTO to validate their functional role in TKI resistance [24]. |
| m6A Immunoprecipitation (MeRIP) | Technique that uses an anti-m6A antibody to pull down methylated RNA fragments, allowing for the identification and validation of m6A-modified transcripts like lncRNAs. | Essential for confirming the direct m6A modification on lncRNAs of interest (e.g., via MeRIP-qPCR) [24]. |
| TIDE Algorithm / Immunophenoscore (IPS) | Computational tools to predict tumor immune dysfunction and exclusion (TIDE) or quantify the immunogenicity of a tumor (IPS), correlating risk scores with immunotherapy response. | Used to predict which patient risk groups are more likely to respond to anti-PD-1/CTLA-4 immunotherapy [11]. |
| pRRophetic R Package | A computational tool that uses gene expression data to predict the chemosensitivity of tumor samples to a wide array of compounds based on the GDSC database. | Used to estimate IC50 values for drugs like Afatinib, Doxorubicin, and Olaparib in different risk groups [11]. |
Signaling Pathway and Workflow Diagrams
Diagram 1: FTO-lncRNA-PI3K Axis in Drug Resistance
Diagram Title: FTO-lncRNA-PI3K Axis in TKI Resistance
Diagram 2: m6A-lncRNA Signature Development Workflow
Diagram Title: m6A-lncRNA Signature Development Workflow
N6-methyladenosine (m6A) RNA modification represents the most prevalent internal chemical alteration in eukaryotic mRNA and non-coding RNA, functioning as a reversible and dynamic regulator that critically influences RNA splicing, stability, export, translation, and degradation [25] [26]. This modification process is orchestrated by three classes of regulatory proteins: methyltransferases ("writers" such as METTL3, METTL14, and WTAP), demethylases ("erasers" including FTO and ALKBH5), and binding proteins ("readers" like YTHDF1-3 and IGF2BP1-3) that interpret the m6A marks [27] [11]. Long non-coding RNAs (lncRNAs) are transcripts exceeding 200 nucleotides without protein-coding capacity that regulate gene expression at epigenetic, transcriptional, and post-transcriptional levels [26]. The intersection of these fields has revealed that m6A modifications significantly influence lncRNA function, and conversely, lncRNAs can regulate m6A modifications, creating a complex regulatory network with profound implications for cancer biology [6] [28].
The integration of m6A and lncRNA research has opened new avenues for prognostic biomarker development across multiple cancer types. m6A-related lncRNA signatures have demonstrated remarkable predictive power for patient survival outcomes, tumor progression, and therapeutic responses [21] [11] [29]. These signatures typically comprise multiple m6A-related lncRNAs identified through comprehensive bioinformatics analyses of large cancer datasets, particularly from The Cancer Genome Atlas (TCGA), followed by experimental validation [27] [6] [30]. The prognostic utility of these signatures stems from their ability to capture critical aspects of tumor behavior, including immune microenvironment composition, metastatic potential, and drug resistance mechanisms, providing a more comprehensive prognostic picture than single biomarkers [25] [21].
Key Research Reagent Solutions
Table 1: Essential Research Reagents for m6A-lncRNA Investigations
| Reagent Category | Specific Examples | Research Application |
|---|---|---|
| m6A Regulator Antibodies | Anti-METTL3, Anti-METTL14, Anti-ALKBH5, Anti-YTHDF1 | Immunohistochemistry validation of m6A regulator expression in tumor tissues [6] |
| Cell Culture Reagents | DMEM with 10% FBS, penicillin-streptomycin | Maintenance of cancer cell lines (e.g., 143B osteosarcoma, HCT116 colon cancer) for functional studies [25] [28] |
| RNA Isolation & qRT-PCR Kits | Trizol RNA extraction, cDNA synthesis kits, SYBR Green Master Mix | Validation of lncRNA expression in patient tissues and cell lines [6] [28] [29] |
| Cell Proliferation Assays | Cell Counting Kit-8 (CCK-8) | Functional assessment of lncRNA effects on cancer cell growth [28] [29] |
| siRNA/shRNA Constructs | siRNA targeting UBA6-AS1, LINC00528 | Knockdown studies to investigate lncRNA functional mechanisms [28] [31] |
Experimental Protocols for Signature Development and Validation
Bioinformatics Identification of m6A-related lncRNAs
The standard workflow begins with data acquisition from TCGA and other databases such as GEO or ICGC, containing RNA-seq data and clinical information for specific cancer types [27] [21] [30]. Following data preprocessing and normalization, researchers identify m6A-related lncRNAs through co-expression analysis between known m6A regulators and all annotated lncRNAs. The typical parameters include a Pearson correlation coefficient >0.4 and p-value <0.001 [25] [26] [31]. For example, in a colon adenocarcinoma study, this approach identified 1,573 m6A-related lncRNAs from 14,142 annotated lncRNAs [28]. Univariate Cox regression analysis then screens these lncRNAs to identify those significantly associated with overall survival (p < 0.05), typically reducing the candidate pool to 5-30 prognostic lncRNAs [11] [30].
Prognostic Signature Construction Using LASSO Regression
To prevent overfitting—a critical concern in multi-gene signature development—researchers employ Least Absolute Shrinkation and Selection Operator (LASSO) Cox regression analysis [27] [11]. This technique penalizes the magnitude of regression coefficients, effectively reducing the number of lncRNAs in the final model while maintaining predictive power. The process involves 10-fold cross-validation to determine the optimal penalty parameter (λ) at the minimum partial likelihood deviance [21] [29]. A risk score formula is then generated: Risk score = (β1 × Exp1) + (β2 × Exp2) + ... + (βn × Expn), where β represents the regression coefficient and Exp represents the expression level of each included lncRNA [11] [29]. Patients are stratified into high-risk and low-risk groups using the median risk score as cutoff, and Kaplan-Meier analysis with log-rank testing validates the signature's prognostic value [6] [21].
Diagram 1: Comprehensive Workflow for Developing m6A-lncRNA Prognostic Signatures
Immune Microenvironment and Drug Sensitivity Analysis
The tumor immune microenvironment evaluation represents a crucial validation step for m6A-lncRNA signatures. Researchers employ multiple algorithms to assess immune characteristics, including ESTIMATE for calculating stromal, immune, and ESTIMATE scores [25] [26], CIBERSORT for quantifying 22 types of immune cell infiltration [25] [27], and single-sample GSEA (ssGSEA) for evaluating immune function and pathway activity [21] [29]. Additionally, the Tumor Immune Dysfunction and Exclusion (TIDE) algorithm predicts immunotherapy response, while tumor mutation burden (TMB) calculations offer complementary immunogenicity metrics [28] [29]. For drug sensitivity assessment, researchers utilize the R package "pRRophetic" to predict half-maximal inhibitory concentration (IC50) values for various chemotherapeutic agents based on the GDSC database, identifying potential therapeutic vulnerabilities associated with specific risk groups [21] [11] [29].
Technical FAQs and Troubleshooting Guides
Signature Development and Validation
Q1: What correlation thresholds are appropriate for identifying genuine m6A-related lncRNAs?
A: Most studies employ absolute Pearson correlation coefficients >0.4 with statistical significance (p < 0.001) [25] [26] [31]. However, when working with larger sample sizes, stricter thresholds (>0.5) may reduce false positives. For smaller datasets (n < 100), a threshold of >0.3 may be acceptable if supported by additional evidence from databases like M6A2Target that document validated m6A-lncRNA interactions [30]. Always perform sensitivity analyses to ensure results are robust across different threshold values.
Q2: How can we prevent overfitting when constructing multi-lncRNA signatures?
A: Implement multiple safeguards: (1) Utilize LASSO regression with 10-fold cross-validation to penalize model complexity [27] [21]; (2) Split datasets into training (typically 50-70%) and testing cohorts before model development [28] [29]; (3) Validate signatures in completely independent external cohorts from GEO or ICGC databases [21] [30]; (4) Apply bootstrapping methods (1000+ resamples) to assess model stability [27]; (5) Ensure the events-per-variable ratio exceeds 10, preferably including 10-15 outcome events per lncRNA in the signature [11].
Experimental Validation Challenges
Q3: What approaches effectively validate the functional roles of signature lncRNAs?
A: Employ a multi-method validation strategy: (1) Confirm differential expression in patient tissues versus normal controls using qRT-PCR [30] [28]; (2) Perform loss-of-function experiments using siRNA or shRNA knockdown in relevant cancer cell lines [28] [31]; (3) Assess phenotypic effects through functional assays (CCK-8 for proliferation, transwell for migration/invasion) [28] [29]; (4) Investigate molecular mechanisms via RNA immunoprecipitation to confirm m6A regulator interactions [25]; (5) Validate clinical relevance through immunohistochemistry of paired m6A regulators [6].
Q4: How do we address discrepancies between bioinformatics predictions and experimental results?
A: First, verify data quality and normalization methods in bioinformatics analyses. Second, ensure cell line models appropriately represent the cancer type studied. Third, consider tissue-specific and context-dependent functions of lncRNAs that may not be captured in vitro. Fourth, examine potential compensation mechanisms in knockout models that might mask phenotypes. Fifth, validate key bioinformatics predictions (e.g., immune cell infiltration) using orthogonal methods such as flow cytometry or multiplex immunohistochemistry on patient samples [25] [26].
Table 2: Performance of m6A-lncRNA Signatures Across Various Cancers
| Cancer Type | Number of lncRNAs in Signature | Predictive Performance (AUC) | Key Clinical Associations |
|---|---|---|---|
| Osteosarcoma [25] | 6 | 1-year AUC: 0.70-0.80 | Immune score, tumor purity, monocyte infiltration |
| Early-Stage Colorectal Cancer [27] | 5 | 3-year AUC: 0.754 (test cohort) | Response to camptothecin and cisplatin |
| Breast Cancer [6] | 6 | 3-year AUC: 0.70-0.85 | M2 macrophage infiltration, immune status |
| Pancreatic Ductal Adenocarcinoma [21] | 9 | 3-year AUC: 0.65-0.75 | Somatic mutations, immunocyte infiltration, chemosensitivity |
| Colon Adenocarcinoma [11] | 12 | 3-year AUC: 0.70-0.80 | Pathologic stage, immunotherapy response |
| Laryngeal Carcinoma [31] | 4 | 1-year AUC: 0.65-0.75 | Smoking status, immune microenvironment |
Integration with Clinical Practice and Therapeutic Development
The transition of m6A-lncRNA signatures from research tools to clinical applications requires addressing several methodological considerations. First, standardization of analytical protocols across institutions is essential, particularly for RNA extraction, library preparation, and normalization procedures in transcriptomic analyses [30] [28]. Second, the development of cost-effective targeted assays measuring only signature lncRNAs (rather than whole transcriptome sequencing) would enhance clinical feasibility. Third, establishing universal risk score cutoffs through multi-institutional consortia would improve reproducibility [21] [29].
For therapeutic development, m6A-lncRNA signatures offer two major advantages: they identify novel therapeutic targets and enable patient stratification for treatment selection [11] [28]. For instance, in colon adenocarcinoma, the lncRNA UBA6-AS1 was identified as a functional oncogene that promotes cell proliferation, representing a potential therapeutic target [28]. Similarly, in osteosarcoma, AC004812.2 was characterized as a protective factor that inhibits cancer cell proliferation and regulates m6A readers IGF2BP1 and YTHDF1 [25]. Beyond targeting specific lncRNAs, these signatures can guide treatment selection by predicting response to chemotherapy, immunotherapy, and targeted therapies [27] [11].
Diagram 2: Clinical Applications of m6A-lncRNA Signatures in Precision Oncology
The emerging evidence suggests that m6A-lncRNA signatures not only predict patient outcomes but also reflect fundamental biological processes driving cancer progression. Their association with tumor immune microenvironments [25] [26], cellular metabolism [11], and drug resistance mechanisms [21] [29] positions these signatures as valuable tools for advancing personalized cancer medicine. As validation studies accumulate and technological advances reduce implementation costs, m6A-lncRNA signatures are poised to become integral components of cancer diagnostics and therapeutic development pipelines.
Building Your Signature: A Step-by-Step Guide to Model Construction with Built-In Regularization
Frequently Asked Questions (FAQs)
Q1: What are the main challenges when downloading TCGA data for multi-omics analysis, and how can I overcome them?
The primary challenges include complex file naming conventions with 36-character opaque file IDs, difficulty linking disparate data types to individual case IDs, and the need to use multiple tools for a complete workflow. The TCGADownloadHelper pipeline addresses these by providing a streamlined approach that uses the GDC portal's cart system for file selection and the GDC Data Transfer Tool for downloads, while automatically replacing cryptic file names with human-readable case IDs using the GDC Sample Sheet [32] [33].
Q2: How can I ensure my m6A-related lncRNA prognostic model doesn't overfit the data?
Multiple strategies exist to prevent overfitting. Employ LASSO Cox regression analysis with 10-fold cross-validation to identify lncRNAs most correlated with overall survival while penalizing model complexity [11]. Additionally, validate your model in independent testing cohorts and use the median risk score from the training set to stratify patients in validation sets [11]. For robust performance assessment, calculate time-dependent ROC curves for 1-, 3-, and 5-year survival predictions [17].
Q3: What preprocessing steps are critical for GEO data before analysis?
For microarray data from GEO, essential preprocessing includes data aggregation, standardization, and quality control. Use the default 90th percentile normalization method for data preprocessing. When selecting differentially expressed genes, apply thresholds such as ≥2 and ≤-2 fold change with Benjamini-Hochberg corrected p-value of 0.05 to ensure statistical significance while controlling for false discoveries [34].
Q4: How can I integrate data from both TCGA and GEO databases effectively?
Successful integration requires careful batch effect removal between datasets. Apply algorithms like the 'ComBat' algorithm from the sva R package to eliminate potential batch effects between different datasets. Ensure consistent gene annotation using resources like GENCODE and perform differential expression analysis with standardized thresholds (e.g., \|log2FC\|>1 and adjusted p-value<0.05) across all datasets [35] [36].
Troubleshooting Guides
Issue 1: Difficulty Managing TCGA Data Structure
Problem: Researchers struggle with TCGA's complex folder structure and cryptic filenames, making it difficult to correlate multi-modal data for individual patients [32] [33].
Solution: Table: TCGA Data Types and File Formats
| Data Type | File Formats | Analysis Pipelines | Common Challenges |
|---|---|---|---|
| Whole-Genome Sequencing | BAM (alignments), VCF (variants) | BWA, CaVEMan, Pindel, BRASS | Large file sizes, complex variant calling outputs |
| RNA Sequencing | BAM, count files | STAR, Arriba | Linking expression to clinical outcomes |
| DNA Methylation | IDAT, processed matrices | Minfi, SeSAMe | Normalization, batch effects |
| Clinical Data | XML, TSV | Custom parsing | Inconsistent formatting across cancer types |
Implementation Steps:
- Install TCGADownloadHelper from GitHub and set up the conda environment using the provided yaml file [32]
- Create the required folder structure with subdirectories for clinicaldata, manifests, and samplesheets_prior
- Download your cart file (manifest), sample sheet, and clinical metadata from the GDC portal
- Configure the data/config.yaml file with your specific directory locations and file names
- Execute the pipeline to download data and automatically reorganize files with human-readable case IDs [32] [33]
Issue 2: Preventing Overfitting in Prognostic Signature Development
Problem: Models with too many features perform well on training data but poorly on validation data, limiting clinical utility [17] [11].
Solution: Table: Overfitting Prevention Techniques for Signature Development
| Technique | Implementation | Key Parameters | Validation Approach |
|---|---|---|---|
| LASSO Regression | glmnet package in R | Regularization parameter λ via 10-fold cross-validation | Monitor deviance vs lambda plot |
| Feature Selection | Univariate Cox PH regression + multivariate analysis | p<0.01 for initial screening | Consistency across training/test splits |
| Risk Stratification | Median risk score threshold | Cohort-specific median calculation | Kaplan-Meier analysis in validation sets |
| Performance Assessment | Time-dependent ROC curves | 1-, 3-, 5-year AUC values | Calibration plots, decision curve analysis |
Implementation Steps:
- Identify m6A-related lncRNAs through Spearman's correlation analysis (absolute correlation coefficient > 0.4 and p < 0.001) [11]
- Apply univariate Cox proportional hazards regression to identify prognostic lncRNAs (p < 0.05)
- Use LASSO Cox regression with 10-fold cross-validation to construct the final model with minimal features
- Calculate risk scores using the formula: Risk score = Σ(Coefi * Expi) where Coef represents regression coefficient and Exp represents expression level [11]
- Validate using independent datasets and assess clinical utility with decision curve analysis [35]
Issue 3: Handling GEO Data with Different Platforms and Normalization Methods
Problem: Inconsistent preprocessing of GEO data leads to irreproducible differential expression results [34] [35].
Solution:
Implementation Steps:
- Download raw data from GEO accession pages and note the platform used (e.g., GPL26963 for lncRNA arrays) [34]
- For microarray data, use Agilent Feature Extraction or appropriate platform-specific tools for data aggregation and normalization
- Apply 90th percentile normalization method for lncRNA array data [34]
- Use the "limma" package in R for differential expression analysis with thresholds of \|log2FC\|>1 and adjusted p<0.05 [35]
- Perform functional enrichment analysis using clusterProfiler for GO and KEGG pathways [35]
Experimental Protocols for Validation
Protocol 1: Experimental Validation of lncRNA Expression
Purpose: Validate computational predictions of key lncRNAs using patient samples [36].
Materials:
- TRIzol reagent for RNA extraction
- NanoDrop spectrophotometer for RNA quantification
- HiScript III RT SuperMix kit for cDNA synthesis
- ChamQ Universal SYBR qPCR Master Mix
- Primers for target lncRNAs (e.g., LINC01615, AC007998.3) [36]
Methods:
- Collect CRC tumor tissues and matched adjacent normal tissues (ensure proper ethical approval)
- Extract total RNA using TRIzol reagent following manufacturer's protocol
- Measure RNA concentration and quality using NanoDrop
- Synthesize cDNA using reverse transcription kit
- Perform qPCR reactions with gene-specific primers and SYBR Green master mix
- Calculate relative expression using the 2−ΔΔCt method with GAPDH as reference gene
- Analyze differences using two-sided Wilcoxon's rank-sum test [36]
Protocol 2: Construction and Validation of Nomograms
Purpose: Develop clinically applicable tools for survival prediction [35].
Methods:
- Identify independent prognostic factors through univariate and multivariate Cox regression analyses
- Develop the nomogram using the rms package in R, integrating the risk model with clinical factors like pathologic stage
- Validate temporal discrimination via time-dependent ROC curves with AUC quantification
- Assess prediction accuracy using calibration curves
- Evaluate clinical utility through decision curve analysis to determine net benefit [35]
Workflow Diagrams
Data Integration and Analysis Workflow
m6A-LncRNA Signature Development Process
Research Reagent Solutions
Table: Essential Research Reagents and Materials
| Reagent/Material | Function/Purpose | Example Sources/Products |
|---|---|---|
| TRIzol Reagent | Total RNA extraction from tissues | Thermo Fisher Scientific [35] [37] |
| Agilent lncRNA Microarray | lncRNA expression profiling | Agilent-085982 Arraystar human lncRNA V5 microarray [34] |
| HiScript III RT SuperMix | cDNA synthesis from RNA | Vazyme Biotech [36] |
| ChamQ SYBR qPCR Master Mix | Quantitative PCR reactions | Vazyme Biotech [36] |
| GDC Data Transfer Tool | TCGA data download | NCI Genomic Data Commons [32] [33] |
| CIBERSORTx Algorithm | Immune cell infiltration estimation | CIBERSORTx web portal [35] [36] |
Frequently Asked Questions (FAQs)
Q1: What are the primary methods for identifying m6A-related lncRNAs from transcriptomic data? The most common method involves correlation analysis between lncRNA expression profiles and known m6A regulators using large-scale datasets like TCGA. Researchers typically calculate Spearman or Pearson correlation coefficients between lncRNAs and m6A regulators (writers, erasers, and readers), then apply statistical thresholds to identify significant associations. Studies often use an absolute correlation coefficient > 0.3-0.4 with a p-value < 0.05 as selection criteria [38] [39] [30].
Q2: What correlation thresholds are typically used to define m6A-related lncRNAs? Research protocols commonly employ the following thresholds:
Table: Standard Correlation Thresholds for m6A-lncRNA Identification
| Application | Correlation Coefficient | P-value | Reference |
|---|---|---|---|
| Initial screening | >0.2 or <-0.2 | <0.05 | [30] |
| Standard identification | >0.3 | <0.05 | [39] |
| Stringent selection | >0.4 | <0.05 | [38] |
Q3: How can I validate that my identified m6A-related lncRNAs are functionally significant? Beyond computational identification, experimental validation is crucial. This includes:
- Knockdown experiments: Assessing functional impact on proliferation, invasion, migration, and apoptosis in cancer cell lines (e.g., A549 for lung cancer) [38]
- Drug resistance assays: Evaluating impact on chemoresistance (e.g., cisplatin resistance) [38]
- Mechanistic studies: Examining effects on epithelial-mesenchymal transition (EMT) and key signaling pathways [38]
Q4: What are the common pitfalls in m6A-lncRNA signature development and how can I avoid them? Common issues include:
- Overfitting: When using multiple lncRNAs for prognostic signatures, employ LASSO Cox regression analysis to select the most relevant features [40] [30]
- Lack of validation: Always validate findings in independent cohorts (e.g., GEO datasets) [30]
- Insufficient statistical power: Ensure adequate sample sizes through power calculations
Troubleshooting Guides
Problem: Poor Correlation Between m6A Regulators and Candidate lncRNAs
Potential Causes and Solutions:
Insufficient data quality
- Solution: Verify RNA sequencing quality metrics and normalize expression data properly
- Check: Ensure adequate read depth and mapping quality for both coding and non-coding transcripts
Inappropriate correlation method
- Solution: Use Spearman correlation for non-normally distributed data rather than Pearson correlation
- Alternative: Apply weighted co-expression network analysis (WGCNA) for more robust association detection [40]
Tissue-specific effects
- Solution: Consider that m6A-lncRNA relationships may be tissue-specific; verify findings in context-appropriate datasets [41]
Problem: Prognostic Signature Performs Poorly in Validation Cohorts
Validation Strategy Table:
Table: Validation Approaches for m6A-lncRNA Signatures
| Validation Type | Method | Purpose | Acceptance Criteria |
|---|---|---|---|
| Internal validation | Bootstrap resampling or cross-validation | Assess model stability | Consistency index >0.7 |
| External validation | Independent datasets (e.g., GEO) | Generalizability | AUC >0.65 in external sets |
| Clinical validation | Association with clinicopathological features | Clinical relevance | Significant correlation with known prognostic factors |
| Experimental validation | Functional assays in cell lines/animal models | Biological relevance | Reproducible phenotypic effects |
Implementation Steps:
- Perform LASSO regression to reduce overfitting [30]
- Apply time-dependent ROC analysis to assess predictive accuracy [38]
- Construct nomograms combining your signature with clinical parameters [38] [40]
- Validate in at least 2-3 independent cohorts with sufficient sample size (>100 patients) [30]
Problem: Uncertain Functional Significance of Identified m6A-related lncRNAs
Experimental Workflow:
Key Experimental Considerations:
- Use appropriate cell lines relevant to your tissue of interest (e.g., A549 for lung cancer, patient-derived cells when possible) [38]
- Include both normal and cancer cells for comparison where feasible [38]
- Assess multiple functional endpoints (proliferation, invasion, migration, apoptosis, drug resistance) [38]
- Examine effects on relevant signaling pathways through gene set enrichment analysis (GSEA) [38]
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for m6A-lncRNA Research
| Reagent Type | Specific Examples | Function/Application |
|---|---|---|
| m6A Regulator Targets | METTL3/METTL14 antibodies, FTO/ALKBH5 inhibitors | Writer/eraser manipulation and detection |
| Cell Lines | A549 (lung), patient-derived glioblastoma cells | Functional validation in disease-relevant models [38] [41] |
| Analysis Tools | CIBERSORT, DESeq2, glmnet, survival R packages | Immune infiltration, differential expression, LASSO regression, survival analysis [38] [30] |
| Validation Reagents | siRNA/shRNA constructs, cisplatin chemotherapy | Functional assessment and drug resistance evaluation [38] |
| Sequencing Methods | MeRIP-seq, miCLIP, direct RNA sequencing | m6A modification mapping at various resolutions [42] [43] |
Experimental Protocols
Protocol 1: Identification of m6A-Related lncRNAs from TCGA Data
Data Acquisition
Expression Correlation Analysis
- Calculate Spearman correlation coefficients between all lncRNAs and m6A regulators
- Apply filtration threshold (absolute correlation coefficient >0.3, p-value <0.05)
- Identify m6A-related lncRNAs meeting these criteria [39]
Survival Analysis
- Perform univariate Cox regression analysis to identify prognostic m6A-related lncRNAs
- Use significant lncRNAs in multivariate Cox regression to establish risk scores [38]
Protocol 2: Functional Validation of m6A-Related lncRNAs
Expression Validation
Functional Assays
- Transfert appropriate cell lines with siRNA or shRNA targeting candidate lncRNAs
- Assess proliferation (MTT assay), invasion (Transwell), migration (wound healing)
- Evaluate apoptosis (Annexin V staining) and drug sensitivity (e.g., to cisplatin) [38]
This technical support guide provides comprehensive methodologies for identifying, validating, and troubleshooting m6A-related lncRNA research, with specific emphasis on preventing overfitting through appropriate statistical methods and validation frameworks.
In high-dimensional biological research, such as the development of m6A-related lncRNA signatures for cancer prognosis, the number of predictor variables (genes, lncRNAs) often far exceeds the number of observations (patient samples). This n << p scenario makes conventional statistical methods prone to overfitting, where models perform well on training data but fail to generalize to new datasets. LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression addresses this challenge by performing automatic variable selection while simultaneously preventing overfitting through regularization. This technical guide provides troubleshooting and methodological support for researchers implementing LASSO Cox regression in their genomic signature development workflows.
Frequently Asked Questions (FAQs)
Q1: What is the primary advantage of using LASSO Cox regression for high-dimensional survival data?
LASSO Cox regression combines the Cox proportional hazards model with L1 regularization to perform automatic variable selection in survival analysis. Its key advantages include:
- Automatic Variable Selection: Shrinks coefficients of less important variables to exactly zero, effectively selecting only the most relevant features [44].
- Handles High-Dimensional Data: Functions effectively even when the number of variables approaches or exceeds the sample size (p ≥ n) [44] [45].
- Prevents Overfitting: Regularization through penalty parameters improves model generalizability to new data [46].
- Clinical Interpretability: Produces sparse models with selected key variables, facilitating biological interpretation [44].
Q2: Why does my LASSO Cox model select zero variables, and how can I address this?
A model selecting zero variables indicates that at the chosen lambda value, all coefficients are shrunk to zero. This commonly occurs when:
- Insufficient Predictive Signal: Your predictor variables may not contain meaningful information about the survival outcome [47].
- Overly Stringent Lambda: The penalty parameter λ may be too large, forcing all coefficients to zero [46].
- Suboptimal Evaluation Metric: Using classification error as the cross-validation metric can be problematic for survival data [47].
Troubleshooting Steps:
- Verify Variable Standardization: LASSO requires standardized predictors; ensure you're using the default
standardize = TRUEinglmnet[47]. - Adjust Cross-Validation Metric: Switch from
type.measure = "class"totype.measure = "deviance"or use AUC-based metrics [47]. - Explore Lambda Values: Examine the full cross-validation results using
plot(cv.modelfitted)to identify where the error curve minimizes. - Check Event Frequency: Ensure you have adequate events (at least 5-10 events per candidate predictor) for reliable estimation [44].
Q3: How does cross-validation work in LASSO Cox regression, and why is it crucial?
Cross-validation (CV) is essential for determining the optimal regularization parameter (λ) and estimating model performance without overfitting. The process involves:
- K-Fold Cross-Validation: Data is partitioned into k subsets (typically k=10), with each subset serving as a validation set while the remaining k-1 subsets are used for training [44] [46].
- Lambda Selection: CV identifies the λ value that minimizes prediction error (lambda.min) or the most parsimonious model within one standard error of the minimum (lambda.1se) [44].
- Performance Estimation: The outer CV loop provides an unbiased estimate of how the model will perform on new, unseen data [45].
For high-dimensional genomic studies, nested (double) cross-validation is recommended, where an inner loop selects features and an outer loop estimates performance, providing more reliable generalizability estimates [45].
Q4: What are the key differences between LASSO Cox and traditional Cox regression?
Table: Comparison between LASSO Cox and Traditional Cox Regression
| Feature | LASSO Cox Regression | Traditional Cox Regression |
|---|---|---|
| Variable Selection | Automatic via L1 penalty | Manual or stepwise selection |
| High-Dimensional Data | Handles p >> n scenarios | Fails when p ≥ n |
| Coefficient Estimation | Shrinks coefficients toward zero | Maximum likelihood estimation |
| Overfitting Risk | Reduced via regularization | High in high-dimensional settings |
| Model Interpretation | Sparse, parsimonious models | All variables retained in final model |
| Implementation | Requires tuning parameter (λ) selection | No tuning parameters needed |
Q5: How should I preprocess my data before applying LASSO Cox regression?
Proper data preprocessing is critical for reliable LASSO Cox results:
- Standardization: Ensure all predictor variables are standardized to have mean = 0 and variance = 1 before analysis, as LASSO is sensitive to variable scales [44] [46].
- Missing Data: Implement appropriate missing data handling (imputation or complete-case analysis) based on the missingness mechanism and proportion.
- Outlier Detection: Identify and address extreme outliers that might disproportionately influence results.
- Censoring Assurance: Verify that censoring is non-informative and appropriately documented in your survival data.
Troubleshooting Common Experimental Issues
Problem 1: Unstable Feature Selection Across Samples
Symptoms: Different subsets of your data yield different selected features, indicating instability in the model.
Solutions:
- Implement repeated nested cross-validation to aggregate feature importance across multiple runs [45].
- Use the
lambda.1seinstead oflambda.minfor more conservative feature selection [44]. - Apply stability selection methods or bootstrap aggregation to identify consistently selected features.
- Consider the SurvRank algorithm, which weights features according to their performance across CV folds [45].
Problem 2: Poor Model Performance on Validation Data
Symptoms: Your model shows good discrimination on training data (high C-index) but performs poorly on test data.
Solutions:
- Re-evaluate your predictor variables for biological relevance and measurement quality.
- Ensure strict separation between training and test sets during model development.
- Reduce the number of candidate predictors through pre-filtering using univariate methods.
- Check for systematic differences between your training and validation cohorts.
- Consider whether your sample size provides adequate power for the number of predictors.
Problem 3: Inappropriate Handling of Correlated Predictors
Symptoms: LASSO arbitrarily selects one variable from a group of correlated predictors, potentially missing biologically important features.
Solutions:
- Conduct correlation analysis among predictors before model building.
- Consider using Elastic Net (alpha between 0 and 1) if retaining correlated features is biologically justified.
- Apply domain knowledge to guide the selection when correlations reflect biological redundancy.
- Use cluster-based feature selection to group correlated variables before LASSO application.
Experimental Protocols
Protocol 1: Basic LASSO Cox Regression Implementation
This protocol outlines the standard workflow for implementing LASSO Cox regression in R using the glmnet package.
Materials and Software:
- R statistical environment (version 4.0 or higher)
glmnetpackage for LASSO implementationsurvivalpackage for data handling- High-dimensional dataset with survival outcomes
Procedure:
- Data Preparation:
Model Fitting with Cross-Validation:
Model Evaluation and Interpretation:
Protocol 2: Nested Cross-Validation for Unbiased Performance Estimation
This advanced protocol provides a framework for nested cross-validation, which delivers more realistic performance estimates for high-dimensional settings.
Procedure:
- Define Outer and Inner Loops:
- Outer loop: 5-10 folds for performance estimation
- Inner loop: 5-10 folds for parameter tuning
- Implementation:
Research Reagent Solutions
Table: Essential Computational Tools for LASSO Cox Regression in m6A-lncRNA Research
| Tool/Resource | Function | Application Context |
|---|---|---|
| glmnet R Package | Implementation of LASSO for various models | Primary tool for fitting LASSO Cox models [44] |
| TCGA Database | Source of cancer genomic and clinical data | Obtaining lncRNA expression and survival data [17] [11] [29] |
| GDSC Database | Drug sensitivity and response data | Predicting therapeutic response based on risk groups [11] [29] |
| TIDE Algorithm | Immunotherapy response prediction | Evaluating potential immunotherapy efficacy [11] [29] |
| SurvRank R Package | Feature ranking for survival data | Complementary approach for feature selection [45] |
| GENCODE | Reference lncRNA annotation | Accurate identification and annotation of lncRNAs [29] |
Workflow Visualization
LASSO Cox Regression Workflow for m6A-lncRNA Signature Development
Troubleshooting Common LASSO Cox Regression Issues
LASSO Cox regression represents a powerful approach for developing parsimonious prognostic signatures from high-dimensional m6A-related lncRNA data while mitigating overfitting risks. Successful implementation requires careful attention to data preprocessing, appropriate cross-validation strategies, and thorough validation. By following the troubleshooting guidelines and experimental protocols outlined in this technical guide, researchers can enhance the reliability and clinical applicability of their genomic signature research.
Frequently Asked Questions (FAQs)
1. What is the fundamental formula for calculating a patient's risk score in a prognostic model?
The risk score is typically a linear combination of the expression levels of signature genes (e.g., m6A-related lncRNAs), each weighted by their regression coefficient. The formula is:
Risk Score = Σ (Coefficient_i * Expression_i) [11]
In this equation, Coefficient_i is the regression coefficient derived from multivariate analysis (like LASSO Cox regression) for each lncRNA, and Expression_i is the measured expression level of that lncRNA in a patient's sample [11].
2. Why is it critical to use cross-validation when building a risk model? Cross-validation is essential for preventing overfitting, which occurs when a model is too complex and learns the noise in the training data instead of the underlying pattern. This leads to poor performance on new, unseen data [48]. By resampling the data and averaging the results, cross-validation provides a more reliable estimate of how the model will perform in practice [48].
3. What is the standard method for determining the optimal cut-off value to stratify patients into high-risk and low-risk groups? A common and robust method is to use the median risk score from the training cohort as the cut-off value [11]. All patients with a risk score above the median are classified as high-risk, and those below are classified as low-risk. This binary classification is then validated using Kaplan-Meier survival analysis and log-rank tests to confirm a statistically significant difference in survival between the two groups [11].
4. My risk model performs well on the training data but poorly on the validation data. What could be the cause? This is a classic sign of overfitting [48]. Potential causes and solutions include:
- Insufficient Feature Selection: The model may be based on too many variables. Consider using regularization techniques like LASSO regression to penalize and eliminate less important features [11].
- Inadequate Validation: The model needs to be rigorously tested on a completely independent validation dataset [11].
- Data Leakage: Ensure that no information from the validation set was used during the model training or feature selection process.
5. How can I visually assess the performance and accuracy of my prognostic model? Two key visual tools are:
- Kaplan-Meier Survival Curves: Show the proportion of patients surviving over time for the high-risk and low-risk groups. A clear separation between the curves indicates the model's prognostic power [17] [11].
- Receiver Operating Characteristic (ROC) Curves: Plot the model's true positive rate against the false positive rate. The Area Under the Curve (AUC) value quantifies the model's accuracy; an AUC of 0.5 is no better than chance, while 1.0 represents perfect prediction [17] [11].
Troubleshooting Guides
Problem: The prognostic signature is too complex with too many lncRNAs.
- Potential Cause: The initial feature selection was not stringent enough, including lncRNAs with weak predictive power.
- Solution: Apply LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression analysis. This method shrinks the coefficients of less important variables to zero, effectively performing feature selection and yielding a more parsimonious model [11].
- Protocol:
- Input the candidate prognostic lncRNAs identified from univariate Cox analysis into a LASSO Cox regression model.
- Perform 10-fold cross-validation to select the optimal penalty parameter (lambda) that minimizes the cross-validation error [11].
- The lncRNAs with non-zero coefficients from this model are retained for the final risk signature.
Problem: The risk score cut-off does not yield statistically significant survival differences.
- Potential Cause: The distribution of risk scores may be skewed, making the median an ineffective separator. The chosen cut-off may not be optimal for your specific dataset.
- Solution: Use a more data-driven approach to find the cut-off that maximizes the survival difference between groups. The "surv_cutpoint" function from the R package
survminercan be used to determine the most statistically significant cut-point based on log-rank test statistics. - Protocol:
- Apply the
surv_cutpointfunction to your training cohort's risk scores and corresponding survival data. - The function will output the optimal cut-point value.
- Classify patients using this new value.
- Validate the separation using Kaplan-Meier analysis on the validation cohort.
- Apply the
Problem: The model's performance is unstable across different data splits.
- Potential Cause: High variance in performance estimates, often due to a small sample size or a single, non-representative train-test split.
- Solution: Replace the simple holdout validation method with k-fold cross-validation [48].
- Protocol:
- Randomly split the entire dataset into k equal-sized folds (commonly k=5 or k=10) [48].
- For each unique fold:
- Treat the fold as a validation set.
- Train the model on the remaining k-1 folds.
- Calculate the performance metric (e.g., AUC) on the held-out fold.
- The final model performance is the average of the k performance scores. This provides a more robust and reliable estimate [48].
Experimental Protocols & Data Presentation
Table 1: Core Components of an m6A-Related lncRNA Risk Model
| Component | Description | Example from Literature |
|---|---|---|
| Data Source | Public repository for genomic and clinical data. | The Cancer Genome Atlas (TCGA) - COAD dataset [11]. |
| Signature Genes | Final set of lncRNAs used in the model. | A 12-lncRNA signature [11] or an 8-lncRNA signature [17]. |
| Risk Formula | Mathematical equation to compute the score. | Risk Score = Σ (Coefficienti * Expressioni) [11]. |
| Cut-off Method | Threshold for risk group stratification. | Median risk score of the training cohort [11]. |
| Validation Metrics | Statistical measures to assess performance. | Kaplan-Meier analysis with log-rank test; ROC analysis with AUC (1-, 3-, 5-year) [17] [11]. |
| Multivariate Analysis | Method to confirm the model is an independent prognostic factor. | Cox proportional hazards regression including clinical variables like age and stage [11]. |
Table 2: Key Reagent Solutions for Model Construction
| Research Reagent / Resource | Function in the Experiment |
|---|---|
| TCGA Database | Provides the essential high-throughput RNA sequencing data and corresponding clinical information (survival time, status, stage) for model development and validation [17] [11]. |
| R Software | The primary computational environment for statistical analysis, including data preprocessing, survival analysis, LASSO regression, and visualization [49]. |
| LASSO Cox Regression | A statistical algorithm used to build the risk model by selecting the most predictive lncRNAs from a larger pool while preventing overfitting [11]. |
| Cross-Validation (e.g., 10-fold) | A resampling procedure used during model building (especially with LASSO) to tune parameters and ensure the model generalizes well to unseen data [48] [11]. |
| Gene Set Enrichment Analysis (GSEA) | A computational method to interpret the biological meaning of the risk model by identifying signaling pathways and functions enriched in the high-risk group [11]. |
Protocol: Constructing and Validating the Risk Model
- Data Acquisition and Preprocessing:
- Download RNA-seq data and clinical data for your disease of interest (e.g., Colon Adenocarcinoma) from TCGA [11].
- Annotate lncRNAs and extract the expression of m6A-related genes.
- Identification of m6A-Related lncRNAs:
- Perform correlation analysis (e.g., Spearman) between m6A genes and all lncRNAs.
- Identify lncRNAs with a significant correlation (e.g., |R| > 0.4, p < 0.001) as m6A-related lncRNAs [11].
- Prognostic Signature Construction:
- Perform univariate Cox regression on the m6A-related lncRNAs in the training cohort to identify those significantly associated with overall survival (p < 0.05) [11].
- Input the significant lncRNAs into a LASSO Cox regression analysis to shrink the list and build a robust model. Use 10-fold cross-validation to select the best lambda value [11].
- Construct the final model and calculate the risk score for each patient using the defined formula.
- Determination of Cut-off Value and Stratification:
- Calculate the median risk score in the training cohort [11].
- Use this median to classify patients in both training and validation cohorts into high- and low-risk groups.
- Model Validation:
- Perform Kaplan-Meier survival analysis with a log-rank test to evaluate the significance of survival difference between the two risk groups in both cohorts [17] [11].
- Use time-dependent ROC curve analysis to assess the model's predictive accuracy for 1, 3, and 5-year survival and report the AUC values [17] [11].
- Conduct univariate and multivariate Cox regression analyses to determine if the risk score is an independent prognostic factor compared to clinical variables like age and stage [11].
Workflow and Relationship Visualizations
Risk Model Development Workflow
Overfitting Prevention Strategy
Frequently Asked Questions
Q1: My Kaplan-Meier curves show a clear separation between high-risk and low-risk groups, but my multivariate Cox regression is not significant. What could be the cause? This discrepancy often arises from overfitting or issues with model generalizability. A visually significant Kaplan-Meier split may not hold when controlling for other clinical variables. First, ensure your risk groups were defined on a training set and validated on a separate test set, as significant splits can occur by chance, especially with small sample sizes. Second, check for multicollinearity between your m6A-lncRNA signature and other covariates (e.g., pathologic stage); high correlation can make independent prognostic value difficult to detect. Finally, verify that the proportional hazards assumption holds for your Cox model, as violations can lead to non-significant results [50] [14].
Q2: What are the best practices for using ROC analysis with time-to-event data to avoid misleading results? Standard ROC analysis ignores time, which can be misleading for survival outcomes. Use time-dependent ROC curves that account for when events occur. The Incident/Dynamic (I/D) definition is often most appropriate for prognostic biomarkers: it measures the ability of a baseline marker (like an m6A-lncRNA signature) to distinguish between individuals who experience an event at a specific time (cases) and those who are event-free at that time (controls). This provides a more accurate assessment of prognostic performance over the study period than a single, static ROC curve. Always report AUC values at pre-specified, clinically relevant time points (e.g., 1, 3, and 5 years) [51].
Q3: How can I validate that my m6A-lncRNA signature is clinically relevant and not just statistically significant? Statistical significance is only the first step. Follow the established framework for biomarker validity:
- Analytical Validity: Prove your assay for measuring the lncRNA signature is accurate, precise, and reproducible across different labs and reagent batches.
- Clinical Validity: Demonstrate that the signature consistently predicts clinical outcomes (like overall survival) in multiple, independent patient cohorts.
- Clinical Utility: Provide evidence that using the signature leads to better treatment decisions or improved patient outcomes, which is crucial for clinical adoption and regulatory approval [52] [53].
Q4: My model performs well on internal validation but poorly on an external dataset from a different patient population. How can I address this? Poor external validation often signals overfitting or a lack of generalizability. To address this:
- Increase Cohort Diversity: Ensure your training data encompasses the demographic and clinical variability (e.g., age, cancer stage, ethnicity) your model will encounter in the real world.
- Use Robust Feature Selection: Employ regularized methods like LASSO Cox regression during model building to reduce the number of lncRNAs in your signature and minimize the retention of noise-specific features.
- Incorprising Biological Insight: Prioritize lncRNAs with known biological roles in m6A modification or your cancer of interest, as these are more likely to be consistently relevant across populations [52] [16] [14].
Experimental Protocols for Key Analyses
Protocol 1: Constructing an m6A-Related lncRNA Prognostic Signature
This methodology is adapted from established studies in ovarian and colon cancer [11] [14].
1. Data Acquisition and Preprocessing
- Source RNA-seq data and corresponding clinical data (survival time, survival status, and pathologic stage) from public repositories like The Cancer Genome Atlas (TCGA).
- Extract the expression profiles of known m6A regulators (writers, erasers, readers) and all lncRNAs.
- Randomly split the patient cohort into a training set (e.g., 70%) and a test set (e.g., 30%).
2. Identification of m6A-Related lncRNAs
- Perform correlation analysis (e.g., Pearson or Spearman) between the expression of each m6A regulator and each lncRNA.
- Identify m6A-related lncRNAs using a strict correlation threshold (e.g., |R| > 0.4 and p < 0.001).
3. Univariate Cox Regression Analysis
- Fit a univariate Cox model for each m6A-related lncRNA with overall survival as the endpoint.
- Retain lncRNAs with a significant p-value (e.g., p < 0.05) for further analysis.
4. Signature Construction via LASSO Cox Regression
- To prevent overfitting, apply LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression to the prognostic lncRNAs from the previous step on the training set.
- Use 10-fold cross-validation to identify the optimal penalty parameter (lambda) that minimizes the cross-validation error.
- The final model will include a subset of lncRNAs with non-zero coefficients. The risk score for each patient is calculated using the formula: Risk Score = (CoefficientlncRNA1 × ExpressionlncRNA1) + (CoefficientlncRNA2 × ExpressionlncRNA2) + ...
5. Model Validation
- Apply the formula to the test set. Split patients into high-risk and low-risk groups based on the median risk score from the training set.
- Use Kaplan-Meier survival analysis and the log-rank test to assess the significance of the survival difference between the two groups in both the training and test sets.
Protocol 2: Time-Dependent ROC Curve Analysis
This protocol is based on methods for analyzing censored survival data [51].
1. Define the Context
- Choose the definition of sensitivity and specificity that fits your research question. For a prognostic m6A-lncRNA signature, the Incident/Dynamic (I/D) definition is often used:
- Sensitivity (Incident): Probability that a patient who dies at time t has a high-risk score.
- Specificity (Dynamic): Probability that a patient who survives beyond time t has a low-risk score.
2. Calculate AUC at Specific Time Points
- Use statistical software (e.g., the
timeROCpackage in R) to calculate the time-dependent AUC. - Specify key time points for evaluation based on clinical relevance (e.g., 1, 3, and 5 years).
3. Interpret the Results
- The AUC(t) represents the probability that a randomly selected patient who experiences the event at time t (case) has a higher risk score than a randomly selected patient who is event-free at time t (control).
- An AUC(t) of 0.5 indicates no predictive discrimination, while 1.0 indicates perfect discrimination.
Performance Data from Literature
The following table summarizes key performance metrics from recent studies employing similar methodologies for biomarker development in oncology.
| Study Focus / Cancer Type | Model Type | Key Performance Metrics | Validation Approach |
|---|---|---|---|
| Breast Cancer Recuriction [50] | LightGBM (ML) | AUC = 92% (Recurrence Prediction) | External validation with data from Baheya Foundation |
| Breast Cancer Recuriction [50] | Cox Regression (Survival) | C-index = 0.837 | Internal validation |
| m6A-lncRNA in Colorectal Cancer [17] | 8-lncRNA Signature | AUC: 0.753 (1-y), 0.682 (3-y), 0.706 (5-y) | Internal validation via TCGA dataset |
| m6A-lncRNA in Ovarian Cancer [14] | 7-lncRNA Signature | Significant Kaplan-Meier split (p < 0.05), Independent prognostic factor in multivariate analysis | Validation in two external GEO datasets (GSE9891, GSE26193) and 60 local clinical specimens |
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Resource | Function in Experiment | Key Considerations |
|---|---|---|
| TCGA/ GEO Datasets | Primary source of standardized RNA-seq data and clinical information for model training and initial validation. | Ensure datasets have sufficient sample size, follow-up time, and relevant clinical annotations for your cancer type. |
| LASSO Cox Regression | A feature selection and regularization technique that constructs a parsimonious model to reduce overfitting. | The choice of the penalty parameter (lambda) is critical; it is typically determined via cross-validation. |
| Time-Dependent ROC Analysis | Evaluates the discrimination accuracy of a prognostic model at specific time points for time-to-event data. | More appropriate than standard ROC for survival outcomes. The "I/D" definition is recommended for prognostic studies. |
| Nomogram | A graphical tool that integrates the lncRNA signature with clinical factors (e.g., stage) to provide an individualized probability of an outcome. | Enhances clinical applicability by providing an easy-to-use visual aid for risk estimation [17] [11]. |
| External Validation Cohort | A completely independent dataset used to test the generalizability of the model, often from a different institution or geographic region. | The gold standard for proving that a model is not overfit. Examples: GEO datasets, Baheya Foundation data [50] [14]. |
Analytical Workflow Diagram
The diagram below visualizes the complete workflow for developing and validating an m6A-lncRNA prognostic signature, highlighting key steps to prevent overfitting.
Figure 1: Workflow for m6A-lncRNA Signature Development and Validation. The process begins with data collection and proceeds through rigorous statistical modeling (green). The initial performance assessment (blue) employs multiple methods, followed by critical internal and external validation steps (red) to ensure model robustness and prevent overfitting.
Beyond Basic CV: Advanced Strategies for Model Robustness and Interpretability
Frequently Asked Questions (FAQs)
1. What is the primary cause of overfitting in m6A-lncRNA prognostic models, and how can I detect it? Overfitting typically occurs when a model is too complex relative to the amount of available training data, causing it to memorize noise rather than learn generalizable biological patterns. Key indicators include:
- Performance Discrepancy: High accuracy on your training dataset but significantly poorer performance (e.g., lower AUC in ROC analysis) on an independent validation set or test cohort [6] [29].
- Feature Over-reliance: The model's predictive power is dependent on a very small number of omics features (e.g., 1-2 lncRNAs) without robust biological correlation, which often fails to validate in external datasets [54].
2. My model performs well in cross-validation but fails in clinical samples. What multi-omics validation strategies should I prioritize? This is a classic sign of a model that hasn't been sufficiently validated. Beyond standard cross-validation, you should:
- Integrate Functional Validation: Use qRT-PCR on a separate set of clinical samples (e.g., from your institution's biobank) to confirm the expression trends of the lncRNAs in your signature [6] [29].
- Correlate with m6A Regulator Expression: Perform immunohistochemistry or Western Blot on matched tissue samples to verify that the protein levels of key m6A "writers" (e.g., METTL3, METTL14) or "erasers" (e.g., FTO) are consistent with your computational predictions [6] [55].
- Utilize Public Multi-omics Data: Validate your findings in independent, multi-omics cohorts from databases like TCGA, CPTAC, or DriverDBv4, which contain linked genomic, transcriptomic, and proteomic data [54].
3. How can I address class imbalance in my dataset when building a risk stratification model? Class imbalance, where one outcome (e.g., "high-risk") is underrepresented, can severely bias your model. Techniques to mitigate this include:
- Resampling Techniques: Apply algorithms like SMOTE (Synthetic Minority Over-sampling Technique) to generate synthetic samples for the underrepresented class, creating a more balanced dataset for training [56].
- Algorithmic Approaches: Use ensemble methods like Random Forest, which can be more robust to class imbalance. Some studies have successfully combined RF with SMOTE (RF-SMOTE) for improved prediction of underrepresented classes [56].
- Validation with Balanced Metrics: Rely on metrics like AUC-ROC and precision-recall curves instead of overall accuracy, which can be misleading with imbalanced data [56].
4. What are the best practices for selecting features for a final, clinically interpretable model? Avoid relying on a single feature selection method. A robust pipeline should be multi-staged:
- Start with Univariate Analysis: Use univariate Cox regression to identify lncRNAs with a significant initial association with patient survival [29].
- Apply Regularization: Employ LASSO (Least Absolute Shrinkage and Selection Operator) Cox regression to penalize model complexity and reduce the number of features, thus mitigating overfitting [6] [29].
- Finalize with Multivariate Analysis: Incorporate the LASSO-selected features into a multivariate Cox regression model to confirm their independent prognostic value while accounting for other clinical variables [29].
Troubleshooting Guides
Issue: Poor Generalization of Prognostic Signature to External Datasets
Problem: A 6-m6A-lncRNA signature developed from TCGA breast cancer data shows excellent predictive power (5-year AUC >0.85) in the training cohort but fails (AUC <0.6) when applied to data from a different sequencing center.
Solution: Implement a Multi-Technique Validation Workflow
Re-run Feature Selection with Stability Analysis:
- Action: Instead of a single LASSO run, perform 1000 bootstrap iterations of the LASSO regression on your training data.
- Check: Calculate the frequency with which each lncRNA is selected across all iterations. Retain only features with a selection frequency >80%. This ensures your signature is stable and not dependent on a random subset of the data.
Employ Multiple Resampling Validation Techniques:
- Action: Beyond simple train-test splits, use both 10-fold cross-validation and repeated hold-out validation.
- Check: Compare the distribution of performance metrics (e.g., C-index, AUC) across all validation folds. A wide variation suggests high model variance and instability, indicating a need for simpler model.
Conduct Biological Plausibility Checks via Multi-Omics Integration:
- Action: Correlate the expression of your signature's lncRNAs with the expression of established m6A regulators (writers/erasers/readers) in a public multi-omics database.
- Check: If your m6A-related lncRNA signature shows no correlation with the core m6A machinery, its biological premise is weak. This step helps filter out computationally derived but biologically meaningless models [6] [54].
The following workflow integrates these techniques into a cohesive strategy for building a robust model.
Issue: Model Performance is Skewed by Dominant But Biologically Irrelevant Features
Problem: Your risk model is overwhelmingly driven by a single, highly variable lncRNA. While it boosts training accuracy, it masks the contribution of other features and is not reproducible.
Solution: Mitigate Feature Dominance and Validate Biologically
Apply Data Preprocessing and Balanced Feature Engineering:
- Action: Normalize your lncRNA expression data (e.g., using TPM or FPKM) and consider log-transformation to reduce the impact of extreme outliers. For datasets with imbalanced outcomes, use SMOTE to create a synthetic balanced training set [56].
Utilize Interpretable Machine Learning (IML) for Debugging:
- Action: After training, use SHAP (SHapley Additive exPlanations) analysis to quantify the contribution of each lncRNA to every individual prediction.
- Check: If a single lncRNA has an outsized and consistent SHAP value across most high-risk predictions, it is a dominant feature. Investigate if this lncRNA has a known biological link to m6A modification; if not, it may be an artifact.
Incorporate Experimental Validation Early:
- Action: Before finalizing the model, use qRT-PCR to measure the expression of the dominant lncRNA and a few others from your signature in a small set of cell lines (e.g., normal vs. cancerous) [29].
- Check: If the qRT-PCR results do not corroborate the sequencing data's expression trend for the key lncRNA, this is a major red flag regarding the feature's reliability and should prompt a re-evaluation of the feature set.
The diagram below outlines this multi-faceted debugging process.
Research Reagent Solutions
The following table details key materials and their functions for experimental validation of m6A-lncRNA signatures, as cited in the literature.
| Research Reagent | Primary Function / Application | Key Consideration / Rationale |
|---|---|---|
| SYBR Green Master Mix [6] [29] | For quantitative RT-PCR (qRT-PCR) validation of lncRNA expression levels in cell lines or patient tissues. | Enables precise, cost-effective quantification of the specific lncRNAs identified in your computational signature. |
| Primary Antibodies (e.g., anti-METTL3, anti-METTL14) [6] [55] | For immunohistochemistry (IHC) to visualize and quantify protein expression of m6A regulators in tissue sections. | Provides spatial protein-level evidence to correlate with your lncRNA signature's risk groups (e.g., high-risk vs. low-risk). |
| DAB Peroxidase Substrate Kit [6] | Used with IHC for chromogenic detection of antibody binding, allowing visualization under a microscope. | A critical component for generating the visible stain that is quantified in IHC analysis of m6A regulator proteins. |
| Trizol Reagent [6] | For high-quality total RNA extraction from tissue or cell samples, preserving the integrity of lncRNAs. | High-quality, intact RNA is a prerequisite for accurate downstream qRT-PCR validation of lncRNA signatures. |
| 1st Strand cDNA Synthesis Kit [6] | Reverse transcribes extracted RNA into stable cDNA for subsequent qRT-PCR amplification. | Essential first step in the qRT-PCR workflow, converting the RNA of interest (including lncRNAs) into a DNA template. |
Data Presentation: m6A-lncRNA Signature Case Studies
The table below summarizes quantitative data from published studies that successfully developed m6A-lncRNA prognostic signatures, highlighting their methodology and validation techniques to prevent overfitting.
| Cancer Type | No. of lncRNAs in Final Signature | Key Validation Techniques Used | Reported Performance (e.g., 5-yr AUC) | Reference |
|---|---|---|---|---|
| Breast Cancer | 6 (e.g., Z68871.1, OTUD6B-AS1, EGOT) | Cox regression, Kaplan-Meier, ROC, PCA, GSEA, immune status analysis, in vitro assay [6]. | "Excellent independent prognostic factor"; validated with clinical samples [6]. | [6] |
| Pancreatic Adenocarcinoma | 4 | LASSO-Cox, ROC curve (2,3,5-yr OS), ssGSEA, TIDE, TMB, qPCR on cell lines, drug sensitivity (CCK8) assay [29]. | Reasonably predicted 2-, 3-, and 5-year OS; validated with qPCR and drug response [29]. | [29] |
Core Experimental Protocols
Protocol 1: In vitro Validation of m6A-lncRNA Signature Using qRT-PCR
Purpose: To experimentally confirm the expression levels of lncRNAs identified in a computational signature using pancreatic adenocarcinoma cell lines [29].
Methodology:
- Cell Culture: Maintain relevant PDAC cell lines (e.g., AsPC-1, PANC-1) and a normal pancreatic cell line under standard conditions.
- RNA Extraction: Extract total RNA from cells using Trizol reagent according to the manufacturer's protocol. Assess RNA purity and concentration using a spectrophotometer.
- cDNA Synthesis: Reverse transcribe 1 µg of total RNA into cDNA using a 1st Strand cDNA Synthesis Kit with random hexamers.
- Quantitative PCR: Prepare duplicate reactions using SYBR Green Master Mix and gene-specific primers for the target lncRNAs. Perform amplification on a real-time PCR system using the following cycling conditions:
- Hold Stage: 95°C for 5 minutes.
- PCR Stage (40 cycles): 95°C for 15 seconds (denaturation) followed by 60°C for 1 minute (annealing/extension).
- Melt Curve Stage: 95°C for 15 seconds, 60°C for 1 minute, 95°C for 15 seconds.
- Data Analysis: Calculate relative gene expression using the 2^(-ΔΔCt) method, normalizing to a stable endogenous control (e.g., GAPDH) and relative to the normal control cell line.
Protocol 2: Validation of m6A Regulator Expression via Immunohistochemistry
Purpose: To validate the protein expression of m6A regulators (e.g., METTL3) in breast cancer tissue sections and correlate it with the high-risk and low-risk groups defined by the lncRNA signature [6].
Methodology:
- Tissue Preparation: Obtain formalin-fixed, paraffin-embedded (FFPE) breast cancer tissue sections from patients classified into high-risk and low-risk groups.
- Deparaffinization and Rehydration: Bake slides at 60°C, then deparaffinize in xylene and rehydrate through a graded alcohol series (100%, 95%, 70%) to water.
- Antigen Retrieval: Perform heat-induced epitope retrieval by heating slides in citrate buffer (pH 6.0) using a pressure cooker or microwave.
- Immunostaining:
- Block endogenous peroxidase activity with 3% hydrogen peroxide.
- Block nonspecific binding with 5% normal goat serum for 1 hour at room temperature.
- Incubate sections with primary antibody against human METTL3 (e.g., 1:100 dilution) overnight at 4°C.
- Wash and incubate with an HRP-conjugated secondary antibody for 1 hour at room temperature.
- Visualization and Counterstaining: Develop the signal using a DAB Peroxidase Substrate Kit, which produces a brown precipitate. Counterstain the nuclei with Hematoxylin.
- Imaging and Scoring: Capture digital images using a light microscope. Score the staining intensity and percentage of positive tumor cells in a blinded manner. Compare the METTL3 protein expression scores between the high-risk and low-risk patient groups.
In the field of bioinformatics and computational biology, developing robust molecular signatures—such as those based on m6A-related long non-coding RNAs (lncRNAs)—is critical for prognostic prediction and therapeutic discovery. A significant challenge in this endeavor is model overfitting, where a model performs well on training data but fails to generalize to unseen data [57]. Cross-validation (CV) provides a powerful set of techniques to combat this issue, offering more reliable estimates of a model's true performance on independent data [48] [57]. For researchers constructing m6A-lncRNA prognostic signatures, a proper validation strategy is not an afterthought but a fundamental component of a credible analysis pipeline. This guide delves into three essential cross-validation methods, providing troubleshooting and protocols tailored to the context of m6A-lncRNA research.
Understanding Core Cross-Validation Methods
k-Fold Cross-Validation
Summary: k-Fold Cross-Validation is a fundamental resampling technique used to assess a model's generalizability. It works by partitioning the dataset into 'k' equal-sized folds. The model is trained on k-1 folds and tested on the remaining fold. This process is repeated k times, with each fold serving as the test set exactly once [48]. The final performance metric is the average of the results from all k iterations.
Table 1: k-Fold Cross-Validation Process (k=5 Example)
| Iteration | Training Set Observations | Testing Set Observations |
|---|---|---|
| 1 | [5-24] | [0-4] |
| 2 | [0-4, 10-24] | [5-9] |
| 3 | [0-9, 15-24] | [10-14] |
| 4 | [0-14, 20-24] | [15-19] |
| 5 | [0-19] | [20-24] |
Experimental Protocol for m6A-lncRNA Signature Development:
- Prepare Your Dataset: Begin with your complete matrix of m6A-related lncRNA expression data (rows: patient samples, columns: lncRNAs) and the corresponding clinical survival data.
- Initialize k-Fold Object: Use a library like scikit-learn's
KFoldto define the number of folds (e.g.,n_splits=5or10). Settingshuffle=Truewith arandom_stateensures reproducibility [48]. - Iterate and Validate: For each train-test split generated by the k-fold object:
- Subset your expression and clinical data into training and test sets.
- On the training set, perform your entire model construction workflow (e.g., feature selection using LASSO Cox regression and model fitting).
- Use the fitted model to calculate risk scores for the patients in the test set.
- Evaluate the prognostic performance on the test set using a metric of your choice, such as the C-index or AUC for time-dependent ROC curves.
- Aggregate Results: Collect the performance metric from each iteration. The mean performance across all k folds provides a robust estimate of your signature's predictive accuracy [48].
Stratified k-Fold Cross-Validation
Summary: Stratified k-Fold Cross-Validation is an enhancement of the standard k-fold method designed specifically for classification problems and, crucially, for imbalanced datasets. It ensures that each fold preserves the same percentage of samples for each class as the complete dataset [58] [59]. This is vital in medical research where outcome events (e.g., death vs. survival) are often unevenly distributed.
Problem with Random Splitting: In a binary classification dataset with 100 samples (80 Class 0, 20 Class 1), a random 80:20 split could potentially allocate all 20 Class 1 samples to the test set. A model trained on such data would never learn to classify Class 1, leading to a misleadingly high accuracy that reflects only the majority class [59].
Experimental Protocol for Binary Clinical Outcomes:
- Define Outcome: Identify your binary classification outcome, such as "5-year survival" (e.g., survived vs. deceased).
- Initialize Stratified k-Fold: Use scikit-learn's
StratifiedKFoldobject. The stratification is performed based on the class labels (y). - Stratified Iteration: The splitting process is identical to standard k-fold, but the
StratifiedKFold.split(X, y)method automatically ensures the class distribution in each fold mirrors the overall distribution [59]. - Model Training & Evaluation: Train and evaluate your classifier (e.g., a logistic regression model predicting survival) within this stratified loop.
Table 2: Standard k-Fold vs. Stratified k-Fold for Imbalanced Data
| Feature | Standard k-Fold | Stratified k-Fold |
|---|---|---|
| Class Distribution | Random; can be uneven across folds. | Preserved; each fold reflects overall class proportions. |
| Risk for Imbalanced Data | High risk of non-representative folds and biased performance estimates. | Mitigates bias by ensuring minority class representation in all folds. |
| Best Use Case | Regression tasks or balanced classification. | Classification tasks, especially with imbalanced classes. |
Nested Cross-Validation
Summary: Nested Cross-Validation is an advanced technique used when you need to perform both hyperparameter tuning and model evaluation. It consists of two layers of loops: an inner loop for tuning the model and an outer loop for evaluating the tuned model's performance. This strict separation prevents data leakage and an optimistic bias in performance estimation, as the test set in the outer loop is completely untouched during the model selection process [60] [57] [61].
Why it's Crucial for Signature Development: When building an m6A-lncRNA signature, you likely tune parameters (e.g., the penalty in LASSO Cox regression). If you use the same data to both tune this parameter and evaluate the final model, you "tune to the test set," and the performance will not generalize [57]. Nested CV provides an unbiased estimate of how your entire model-building procedure (including tuning) will perform on unseen data.
Experimental Protocol for Hyperparameter Tuning:
- Define Loops: Set up an outer loop (e.g., 5-fold) and an inner loop (e.g., 5-fold). The outer loop splits the data into training and test sets. The inner loop splits the outer training set into further training and validation sets.
- Outer Loop Iteration: For each outer split, the outer training set is used for model selection.
- Inner Loop Tuning: On the outer training set, perform k-fold CV (the inner loop) with a grid search (e.g.,
GridSearchCV) to find the best hyperparameters. The model is trained on the inner training folds and validated on the inner validation fold. - Final Training and Testing: Train a new model on the entire outer training set using the best hyperparameters found in the inner loop. Evaluate this final model on the held-out outer test set.
- Repeat and Aggregate: Repeat for all outer folds. The average performance on the outer test sets is an unbiased estimate of your model's generalization error [60].
Troubleshooting Guides & FAQs
Frequently Asked Questions
Table 3: Frequently Asked Questions on Cross-Validation
| Question | Answer |
|---|---|
| How do I interpret varying scores across k-folds? | Some variation is normal. High variance (e.g., Fold 1: 90%, Fold 2: 60%) suggests your model is sensitive to the specific data it's trained on, possibly due to a small dataset, outliers, or hidden data subclasses. The mean provides the best estimate, but a large standard deviation warrants caution [48] [57]. |
| My dataset is small. Should I use LOOCV (Leave-One-Out CV) or k-fold? | While LOOCV (k=n) uses maximum data for training and has low bias, it is computationally expensive and can produce high-variance estimates, especially with outliers [48]. For small datasets, a common and recommended practice is to use stratified k-fold with a high k (like k=5 or k=10) to balance bias and variance [48] [62]. |
| How does nested CV prevent data leakage? | Nested CV strictly separates the data used to select a model's hyperparameters (inner loop) from the data used to evaluate its final performance (outer loop). This prevents information from the "test" set from leaking back into the training and tuning process, a common cause of over-optimistic results [60] [57]. |
| Can I use k-fold for time-series data? | Standard k-fold is inappropriate for time-series data due to temporal dependencies. Instead, use specialized methods like forward-chaining (e.g., TimeSeriesSplit in scikit-learn) where the model is always trained on past data and tested on future data. |
| What is a key pitfall when using a single train/test split? | A single split can be highly non-representative, especially with small or imbalanced datasets. The performance can vary drastically based on a single, fortunate (or unfortunate) split, leading to an unreliable performance estimate [57] [59]. Cross-validation averages over multiple splits to provide a more stable and reliable estimate. |
Common Error Messages and Solutions
Problem:
ValueError: The least populated class in y has only 1 member, which is too few. The minimum number of groups for any class cannot be less than 2.- Cause: You are attempting stratified k-fold on a dataset where one of the classes has a very small number of samples (fewer than the number of folds, k).
- Solution: Consider using a stratified shuffle split, reducing the number of folds (
n_splits), or applying synthetic oversampling techniques (like SMOTE) with caution, ensuring the oversampling is applied only to the training folds within the CV loop to prevent data leakage.
Problem: Model performance is excellent during cross-validation but drops significantly on a truly external validation cohort.
- Cause 1: Data Leakage. Preprocessing (e.g., normalization, imputation) was applied to the entire dataset before splitting into training and test folds. The test folds thus contained information from the training data.
- Solution 1: Use a
Pipelinein scikit-learn to encapsulate all preprocessing and modeling steps. This ensures thatfit_transformis only applied to the training fold, andtransformis applied to the test fold within each CV iteration [60]. - Cause 2: Dataset Shift. The external cohort has a different underlying distribution (e.g., different sequencing platform, patient population, or sample collection protocol).
- Solution 2: Perform thorough exploratory data analysis to compare distributions between development and validation cohorts. Use domain adaptation techniques or ensure your training data is more representative of the target population.
Table 4: Key Resources for m6A-lncRNA Signature Development and Validation
| Resource / Solution | Function / Description | Application in m6A-lncRNA Research |
|---|---|---|
| TCGA & GTEx Databases | Public repositories providing RNA-seq data and clinical information for various cancers and normal tissues. | Primary source for acquiring lncRNA expression data and corresponding patient survival information for model development [63] [29]. |
| Scikit-learn Library | A comprehensive Python library for machine learning, providing implementations for k-fold, stratified k-fold, grid search, and pipelines. | Used to implement the entire cross-validation workflow, from data splitting to model training and evaluation [48] [60] [59]. |
| LASSO Cox Regression | A regularized survival analysis method that performs both variable selection and model fitting. | The core algorithm for selecting the most prognostic m6A-related lncRNAs and constructing the risk score signature while preventing overfitting [63] [29]. |
| Computational Pipeline | A scripted workflow (e.g., in Python or R) that chains data preprocessing, feature selection, and model validation. | Ensures reproducibility and prevents data leakage by automating the cross-validation process [60]. |
| GENCODE Annotation | A comprehensive reference of human lncRNA genes and their genomic coordinates. | Used to accurately annotate and filter lncRNAs from raw RNA-seq data downloaded from TCGA [29]. |
| SRAMP Database | A tool for predicting m6A modification sites on RNA sequences. | Can be used to computationally validate the potential m6A modification sites on identified prognostic lncRNAs [29]. |
Troubleshooting Guides & FAQs
How do I prevent overfitting when constructing an m6A-related lncRNA prognostic signature?
Problem: The prognostic model performs well on training data but fails to generalize to external validation cohorts, indicating potential overfitting.
Solution: Implement rigorous cross-validation and regularization techniques during model construction.
- Apply LASSO Cox Regression: This method performs both variable selection and regularization to enhance model generalizability. The tuning parameter (λ) should be determined via 10-fold cross-validation to prevent overfitting [11] [17] [14].
- Utilize Multiple Validation Cohorts: Validate the signature in independent datasets from sources like GEO (Gene Expression Omnibus) to ensure robustness [14].
- Conduct Clinicopathological Stratified Analysis: Test the model's performance across different patient subgroups to verify consistent predictive ability [64].
Example Protocol:
- Randomly divide your TCGA dataset into training and test sets (typically 2:1 ratio) [64]
- Perform 10-fold cross-validation on the training set to identify optimal λ in LASSO regression [11]
- Apply the model with selected λ to the test set
- Validate in external datasets (e.g., GSE9891, GSE26193 for ovarian cancer) [14]
- Perform subgroup analyses based on clinical characteristics
What statistical methods ensure the identified m6A-related lncRNAs are truly prognostic?
Problem: Uncertainty about whether identified lncRNAs genuinely associate with patient survival rather than representing random associations.
Solution: Implement a multi-step statistical filtering process with appropriate significance thresholds.
- Employ Univariate Cox Regression: Initially screen all m6A-related lncRNAs using univariate Cox analysis with a significance threshold of p < 0.05 [11] [14].
- Apply Multivariate Cox Regression: For the final model construction, use multivariate Cox regression to calculate risk scores based on the expression levels and regression coefficients of selected lncRNAs [14].
- Use Correlation Analysis: Identify m6A-related lncRNAs through Pearson or Spearman correlation analysis with |correlation coefficient| > 0.4 and p < 0.001 [11] [16] [14].
Risk Score Formula: The risk score for each patient should be calculated using: Risk score = Σ(Coefi * Expri) where Coefi represents the regression coefficient from multivariate Cox analysis and Expri represents the expression level of each lncRNA [11] [14].
How can I validate the functional mechanisms of m6A-related lncRNAs in the laboratory?
Problem: Computational predictions of m6A modification on specific lncRNAs require experimental validation.
Solution: Implement established molecular biology techniques to confirm m6A modifications and functional impacts.
- Perform MeRIP-qPCR (Methylated RNA Immunoprecipitation followed by qPCR): This technique specifically validates m6A modification on candidate lncRNAs using m6A-specific antibodies [65].
- Conduct Functional Assays: Implement in vitro experiments including CCK-8 assays for proliferation, transwell assays for migration/invasion, and colony formation assays [65].
- Validate in Animal Models: Use xenograft models to confirm tumor growth effects observed in cellular models [65].
Detailed MeRIP-qPCR Protocol:
- Fragment RNA to 100-500 nucleotides using RNA fragmentation reagent
- Incubate with m6A-specific antibody conjugated to magnetic beads
- Wash beads extensively to remove non-specifically bound RNA
- Elute m6A-modified RNA using competitive elution with m6A nucleotide
- Reverse transcribe and quantify target lncRNA using qPCR
- Normalize results to input RNA controls [65]
What approaches help connect computational findings to clinical applications?
Problem: Difficulty translating computational signatures into clinically useful tools.
Solution: Develop integrated clinical prediction tools and assess therapeutic implications.
- Construct Nomograms: Combine the genetic signature with clinical parameters like pathologic stage to create quantitative prognostic tools [11] [17].
- Analyze Therapeutic Implications: Investigate how risk groups correlate with drug sensitivity using IC50 values from databases like GDSC (Genomics of Drug Sensitivity in Cancer) [11].
- Evaluate Immunotherapy Response: Assess immune checkpoint expression and use algorithms like TIDE to predict immunotherapy response across risk groups [11] [16].
Nomogram Development Steps:
- Identify independent prognostic factors through multivariate Cox regression
- Assign point values to each factor based on regression coefficients
- Create a scoring system that sums points across factors
- Correlate total points with predicted survival probabilities
- Validate nomogram accuracy using calibration plots [11]
Experimental Protocols & Methodologies
Core Bioinformatics Pipeline for m6A-Related lncRNA Signature Development
Data Acquisition and Preprocessing:
- Download RNA-seq data and clinical information from TCGA (https://portal.gdc.cancer.gov/)
- Annotate lncRNAs using GTF files from Ensembl (http://asia.ensembl.org/index.html)
- Normalize expression data using TPM or FPKM values
- Merge multiple datasets using batch effect correction algorithms like "ComBat" when necessary [16] [64]
Identification of m6A-Related lncRNAs:
- Compile list of established m6A regulators (writers, erasers, readers) from literature [11]
- Calculate correlation coefficients between m6A regulators and all lncRNAs
- Apply filtering criteria: |correlation coefficient| > 0.4 and p < 0.001 [16] [14]
- Visualize relationships using cytoscope software [14]
Prognostic Model Construction:
- Perform univariate Cox regression to identify prognostic m6A-related lncRNAs (p < 0.05)
- Apply LASSO Cox regression for feature selection and to prevent overfitting
- Use 10-fold cross-validation to determine optimal penalty parameter λ [11]
- Calculate risk scores using multivariate Cox regression coefficients
- Divide patients into high- and low-risk groups using median risk score or X-tile determined cutoff [64]
Model Validation:
- Test prognostic performance in training, testing, and external validation cohorts
- Generate Kaplan-Meier survival curves and calculate log-rank p-values
- Assess predictive accuracy using time-dependent ROC curves at 1, 3, and 5 years [17] [14]
- Perform multivariate Cox analysis adjusting for clinical covariates to demonstrate independence
Functional Validation Experimental Protocol
Cell Culture and Transfection:
- Maintain glioma cell lines (e.g., HS683, T98G) in appropriate media with 10% FBS
- Transfect with siRNA or overexpression vectors using lipofectamine-based methods
- Include appropriate negative controls (scrambled siRNA, empty vector) [65]
Proliferation and Colony Formation Assays:
- Perform CCK-8 assays: seed 2,000 cells/well, measure absorbance at 450nm at 0, 24, 48, 72 hours
- Conduct colony formation assays: seed 500 cells/well, stain with crystal violet after 14 days, count colonies >50 cells [65]
Migration and Invasion Assays:
- Use transwell chambers with 8μm pores
- For invasion assays, coat membranes with Matrigel (1:8 dilution)
- Seed 5×10⁴ cells in serum-free media in upper chamber
- Incubate for 24-48 hours, fix with methanol, stain with crystal violet, count cells in five random fields [65]
m6A Modification Validation:
- Perform MeRIP-qPCR as described in troubleshooting section
- Use specific antibodies against m6A for immunoprecipitation
- Include input and IgG controls for normalization [65]
Animal Studies:
- Use 4-6 week old nude mice (n=5 per group)
- Subcutaneously inject 5×10⁶ transfected cells per mouse
- Measure tumor dimensions every 5 days using calipers
- Calculate tumor volume using formula: V = (length × width²)/2
- Euthanize mice after 4-5 weeks, harvest and weigh tumors [65]
Research Reagent Solutions
| Reagent/Tool | Function | Application Example |
|---|---|---|
| TCGA Database | Provides RNA-seq data and clinical information | Source for lncRNA expression and survival data [11] [64] |
| GDSC Database | Contains drug sensitivity data | Predicting chemotherapeutic response in risk groups [11] |
| CIBERSORT | Deconvolutes immune cell fractions from RNA-seq data | Analyzing tumor immune microenvironment [16] [64] |
| ESTIMATE Algorithm | Calculates stromal and immune scores | Characterizing tumor microenvironment [64] |
| m6A-Specific Antibodies | Immunoprecipitation of m6A-modified RNAs | MeRIP-qPCR validation of m6A modifications [65] |
| LASSO Regression | Regularized feature selection for high-dimensional data | Constructing prognostic signatures without overfitting [11] [17] |
| TIDE Algorithm | Models tumor immune evasion | Predicting immunotherapy response [11] |
Computational Workflow Diagram
m6A-lncRNA Functional Mechanism Diagram
Table 1: m6A-lncRNA Signature Performance Metrics Across Studies
| Cancer Type | Signature Size | AUC (1-year) | AUC (3-year) | Validation Cohort | Independent Prognostic |
|---|---|---|---|---|---|
| Colon Adenocarcinoma [11] | 12 lncRNAs | Not specified | Not specified | Internal test set | Yes (p < 0.05) |
| Colorectal Cancer [17] | 8 lncRNAs | 0.753 | 0.682 | Internal validation | Yes |
| Hepatocellular Carcinoma [64] | 9 lncRNAs | Not specified | Not specified | Training (n=226) & validation (n=116) | Yes |
| Ovarian Cancer [14] | 7 lncRNAs | Not specified | Not specified | GSE9891 (n=285), GSE26193 (n=107) | Yes |
Table 2: Statistical Thresholds for m6A-lncRNA Identification
| Analysis Step | Statistical Method | Threshold Criteria | Purpose | ||
|---|---|---|---|---|---|
| lncRNA Identification | Pearson/Spearman correlation | r | > 0.4, p < 0.001 [11] [16] | Define m6A-related lncRNAs | |
| Prognostic Screening | Univariate Cox regression | p < 0.05 [11] [14] | Initial prognostic lncRNA selection | ||
| Feature Selection | LASSO Cox regression | Minimum λ with 10-fold CV [11] | Prevent overfitting, select optimal features | ||
| Final Model | Multivariate Cox regression | Risk score = Σ(Coefi × Expri) [14] | Calculate individual patient risk | ||
| Group Stratification | X-tile software/median cutoff | Optimal cutoff determination [64] | Define high/low risk groups |
Frequently Asked Questions
Q1: My m6A-lncRNA prognostic model achieves 95% accuracy, yet fails to identify actual cancer cases. What is wrong?
This is a classic sign of class imbalance, often described as "fool's gold" in data mining [66]. When one class (e.g., non-cancer samples) significantly outnumbers another (e.g., cancer cases), models become biased toward the majority class. Your model likely achieves high accuracy by simply predicting "non-cancer" for all samples while failing to detect the medically critical minority class [67] [68]. In such cases, accuracy becomes a misleading metric, and you should prioritize recall, F1-score, or PR-AUC instead [67] [69].
Q2: When developing an m6A-lncRNA signature, should I apply SMOTE to the entire dataset before cross-validation?
No, this constitutes data leakage and will lead to overoptimistic, unreliable results [67]. You should only apply resampling techniques like SMOTE to the training folds within your cross-validation process, keeping the test folds completely untouched and representative of the original data distribution [67]. Modifying your test data with synthetic samples invalidates your evaluation.
Q3: For tree-based models predicting lncRNA-disease associations, what imbalance approach works best?
For tree-based models like XGBoost, LightGBM, or Random Forest, class weighting is generally more effective than data modification techniques like SMOTE [67]. Tree models can naturally handle imbalance by adjusting how they split data. Using built-in parameters like scale_pos_weight in XGBoost or class_weight='balanced' in scikit-learn is recommended, as SMOTE can create redundant synthetic points that don't provide new information for these algorithms [67] [70].
Q4: What evaluation metrics should I prioritize for highly imbalanced m6A-lncRNA data?
Avoid accuracy. Instead, use a combination of these metrics:
- Precision-Recall Curve (PR-AUC): Particularly informative for severe imbalance [67] [69]
- F1-Score: Balances precision and recall [68] [69]
- Recall: Critical for ensuring you capture minority class instances [67]
- Confusion Matrix: Provides granular view of performance across classes [67] [69]
- Matthews Correlation Coefficient (MCC): Robust for imbalanced datasets [69]
Troubleshooting Guides
Problem: Model Bias Toward Majority Class
Symptoms: High accuracy but poor minority class recall; consistent majority class predictions; failed clinical validation despite good benchmark performance [67] [66].
Solutions:
Stratified Data Splitting
Always use stratified splitting to maintain class proportions in training and test sets [67].
Algorithm-Specific Solutions
For Tree Models (XGBoost, LightGBM):
For Linear Models & Neural Networks:
SMOTE works well for these algorithms but avoid for tree models [67].
Threshold Tuning
Instead of default 0.5, choose optimal threshold based on precision-recall tradeoff [67].
Problem: Overfitting on Minority Class
Symptoms: Good training performance but poor testing; excessive focus on minority noise samples; declining majority class performance.
Solutions:
Advanced Sampling Techniques
Ensemble Methods
Regularization Strategies
Technical Reference: Data Imbalance Techniques
Table 1: Comparison of Data-Level Techniques for Handling Class Imbalance
| Technique | Mechanism | Best For | Advantages | Limitations |
|---|---|---|---|---|
| Random Oversampling | Duplicates minority samples [68] | Small datasets, quick prototyping | Simple implementation, no data loss | High overfitting risk [68] |
| SMOTE | Creates synthetic minority samples [67] [68] | Linear models, SVM, neural networks [67] | Generates new patterns, reduces overfitting vs random oversampling | Can create unrealistic samples; poor for tree models [67] |
| Random Undersampling | Removes majority samples [67] [68] | Large datasets, computational efficiency | Faster training, reduces bias | Loses potentially useful information [67] |
| Cluster-Based Sampling | Applies clustering before sampling [69] | Complex, multi-subtype minority classes | Preserves cluster structure, generates representative samples | Computationally intensive |
| SMOTE Variants (K-Means SMOTE, SVM-SMOTE) | Focuses sampling on critical areas [69] | Datasets with noisy samples or clear decision boundaries | Targets hard-to-learn regions, cleaner samples | Parameter sensitive, complex implementation |
Table 2: Algorithm-Specific Solutions for Class Imbalance
| Algorithm Category | Preferred Technique | Implementation | Considerations |
|---|---|---|---|
| Tree Models (XGBoost, LightGBM, Random Forest) | Class weights [67] | scale_pos_weight (XGBoost), class_weight='balanced' (sklearn) |
More effective than SMOTE for trees [67] |
| Linear Models (Logistic Regression, SVM) | SMOTE or class weights [67] | SMOTE() + standard training |
Both approaches effective |
| Deep Learning | Focal Loss [67] [69] or weighted loss | FocalLoss(alpha=0.25, gamma=2) |
Handles extreme imbalance; focuses on hard examples |
| Ensemble Methods | Hybrid approaches [69] | SMOTEBoost, RUSBoost [69] | Combines benefits of multiple techniques |
Experimental Protocols for m6A-lncRNA Research
Protocol 1: Building Robust m6A-lncRNA Prognostic Signatures
Background: m6A-related lncRNA prognostic models frequently suffer from imbalance due to rare disease subtypes or limited event occurrences [17] [11] [14].
Materials:
- Data Source: TCGA (The Cancer Genome Atlas) database [17] [11] [14]
- m6A Regulators: 23 recognized m6A regulators (writers, erasers, readers) [11] [14]
- LncRNA Identification: Pearson correlation analysis (|R| > 0.4, p < 0.001) to identify m6A-related lncRNAs [11] [14] [16]
Methodology:
Data Preparation & Splitting
- Obtain RNA-seq data and clinical information from TCGA
- Identify m6A-related lncRNAs via correlation analysis
- Apply stratified splitting to maintain event rates in training/test sets [67]
Feature Selection with Imbalance Awareness
Model Validation with Appropriate Metrics
Protocol 2: Cross-Validation Strategies for Imbalanced Data
Standard k-fold CV Problem: Random splitting may create folds with zero minority samples [70].
Recommended Approach: Stratified k-fold CV maintaining class proportions [67] [70]. For lncRNA-disease association prediction, employ pair-wise or leave-one-out cross-validation specific to linkage prediction tasks [70].
Research Reagent Solutions
Table 3: Essential Resources for m6A-lncRNA Imbalance Research
| Resource Type | Specific Tool/Database | Purpose | Application Notes |
|---|---|---|---|
| Data Sources | TCGA (The Cancer Genome Atlas) [17] [11] [14] | Primary molecular and clinical data | Standardized processing essential |
| Validation Datasets | GEO (Gene Expression Omnibus) [14] [16] | Independent validation cohorts | Batch effect correction required [16] |
| m6A Regulators | 23-gene set (METTL3, METTL14, WTAP, FTO, ALKBH5, YTHDF1-3, etc.) [11] [14] | Define m6A-related lncRNAs | Consistent regulator set enables cross-study comparison |
| LncRNA Databases | lncRNADisease v2.0 [70], MNDR v2.0 [70] | Experimentally validated LDAs | Ground truth for model evaluation |
| Software Tools | LDA-GARB [70], SDLDA, LDNFSGB, LDAenDL [70] | Specialized LDA prediction | Handle imbalance via noise-robust gradient boosting [70] |
| Programming Environments | R (survival, glmnet), Python (scikit-learn, imbalanced-learn) [17] [70] | Implementation of analysis | Stratified sampling functions critical |
Workflow Visualization
Diagram 1: Comprehensive workflow for addressing data imbalance in m6A-lncRNA research, emphasizing technique selection based on algorithm type and rigorous validation protocols.
Diagram 2: Diagnostic and solution framework for identifying and addressing data imbalance issues in m6A-lncRNA signature development.
Core Reproducibility Principles FAQ
What is reproducible research, and why is it critical for computational biology? Reproducible research can be independently recreated from the same data and the same code used by the original team [71]. In the context of optimizing m6A-related lncRNA signatures, this transparency is a minimum condition for findings to be believable and trustworthy, allowing others to validate prognostic models and their clinical applicability [17] [11] [71].
Our team uses custom scripts for analysis. How can we ensure someone else can run our code in the future?
Making your code available is the first step, but avoiding "dependency hell" is crucial [71]. Clearly record all dependencies with version numbers. Use environment management tools like renv for R to create an isolated, project-specific environment that can be easily deleted and re-created, which is far more efficient than debugging future failures [72] [71].
What is the single most important document for a reusable research project? A README file is the most critical piece of project-level documentation. It introduces the project, explains how to set up the code, and guides others on how to reuse your materials. It is usually the first thing a user or collaborator sees in your project [71].
Troubleshooting Common Experimental & Computational Issues
We are getting poor duplicate precision and inappropriately high values in our ELISA data. What could be the cause? This is a classic symptom of contamination. Your ELISA kits are highly sensitive and can be contaminated by concentrated sources of the analyte (e.g., cell culture media, upstream samples) present in the lab environment [73].
- Solution: Do not perform assays in areas where concentrated forms of cell culture media or sera are used. Clean all work surfaces and equipment beforehand. Use pipette tips with aerosol barrier filters and avoid talking or breathing over an uncovered microtiter plate [73].
When we re-run our model training script on a different machine, we get different results, even with the same code. How can we fix this? This indicates that your computational environment is not reproducible.
- Solution: Implement data versioning. Using a system like lakeFS, you can take a commit of your data repository each time your data changes. To reproduce a specific model training run, your code can then read data from a path that includes the unique, immutable
commit_idgenerated for that run, guaranteeing identical input data [74].
The ROC curve accuracy of our m6A-lncRNA prognostic model is lower on new validation datasets. How can we prevent this overfitting? Your feature selection and model building process must incorporate robust statistical techniques designed to prevent overfitting.
- Solution: When constructing your m6A-related lncRNA signature, use the least absolute shrinkage and selection operator (LASSO) Cox regression for feature selection. This method penalizes the complexity of the model, selecting only the lncRNAs most correlated with survival outcomes. Always perform 10-fold cross-validation during this process to prevent overfitting and ensure your model generalizes well to new data [17] [11] [14].
Key Research Reagent Solutions
The table below details essential materials and their functions in developing m6A-lncRNA prognostic signatures, based on cited experimental protocols.
Table 1: Essential Research Reagents and Resources for m6A-lncRNA Signature Development
| Item | Function / Explanation |
|---|---|
| TCGA/CEO Data | Primary source of high-throughput RNA sequencing data and clinical information for model construction and validation [17] [11] [16]. |
| m6A Regulator List | A predefined set of known writers, erasers, and readers (e.g., METTL3, FTO, YTHDF1) used to identify m6A-related lncRNAs via correlation analysis [11] [16] [14]. |
| LASSO Cox Regression | A statistical method used to reduce the number of prognostic lncRNAs in the model, thereby preventing overfitting and building a more robust risk signature [17] [11] [14]. |
| Risk Score Formula | A linear combination of the expression levels of selected lncRNAs weighted by their regression coefficients. Used to stratify patients into high- and low-risk groups [11] [14]. |
| Nomogram | A graphical tool that combines the risk model with clinical factors (like pathologic stage) to provide a quantitative, clinically applicable method for predicting individual patient prognosis [17] [11]. |
Experimental Protocols & Workflows
Detailed Methodology: Constructing an m6A-Related lncRNA Prognostic Signature
The following workflow is standardized from multiple studies on m6A-lncRNA signatures in cancer [17] [11] [16].
Data Acquisition and Preparation:
- Download RNA sequencing data (in FPKM or TPM format) and corresponding clinical data (overall survival time, status, pathologic stage, etc.) for a cancer cohort (e.g., TCGA-COAD).
- Extract the expression data of known m6A regulators and all lncRNAs from the dataset.
Identification of m6A-Related lncRNAs:
Prognostic lncRNA Screening and Model Construction:
- Perform univariate Cox regression analysis on the m6A-related lncRNAs to identify those significantly associated with overall survival (p < 0.05).
- Input the significant lncRNAs into a LASSO Cox regression analysis to further reduce dimensionality and select the most potent predictors.
- Perform 10-fold cross-validation during the LASSO analysis to select the optimal penalty parameter (lambda) and prevent overfitting.
- Use the selected lncRNAs to build a multivariate Cox proportional hazards model. The output is a risk score formula:
Risk score = ∑(Coef_i * Expr_i), whereCoef_iis the regression coefficient andExpr_iis the expression level of each lncRNA [11] [14].
Model Validation and Application:
- Calculate the risk score for each patient and stratify them into high- and low-risk groups using the median risk score as a cutoff.
- Validate the model's performance using Kaplan-Meier survival analysis and time-dependent receiver operating characteristic (ROC) curves.
- Test the model as an independent prognostic factor via univariate and multivariate Cox regression analyses that include clinical variables like age and stage.
- Construct a nomogram that integrates the risk score and key clinical factors to predict 1-, 3-, and 5-year survival probabilities [17] [11].
Workflow for m6A-lncRNA Signature Development
Visualization: Model Validation and Clinical Translation Logic
The following diagram outlines the logical flow from model construction to its clinical application, showing how overfitting prevention is central to creating a reliable tool.
Logic Flow from Model Construction to Clinical Application
From Model to Clinic: Rigorous Validation and Benchmarking for Clinical Translation
Frequently Asked Questions (FAQs)
Q1: Why is independent cohort validation absolutely essential for an m6A-related lncRNA signature? Independent cohort validation tests your signature on completely separate datasets that were not used during model development. This process confirms that your signature can reliably predict patient outcomes beyond the original training data, verifying that it has learned true biological patterns rather than dataset-specific noise. Without this critical step, there is a high risk that your signature is overfitted and will perform poorly in real-world clinical applications [18] [14].
Q2: What are the main sources for independent validation cohorts? Researchers typically use these key sources:
- International Cancer Genome Consortium (ICGC) databases [21]
- Gene Expression Omnibus (GEO) repository datasets [18] [14]
- In-house clinical cohorts collected from your institution [18] [30]
- Multi-institutional collaborations pooling resources
Q3: How many validation cohorts should I use for a robust study? While no fixed rule exists, studies with strong validation typically use multiple independent cohorts. For example, one study validated their m6A-lncRNA signature for colorectal cancer across six different GEO datasets totaling 1,077 patients, plus an additional in-house cohort of 55 patients [18] [30]. This multi-cohort approach dramatically strengthens the credibility of your findings.
Q4: What statistical metrics demonstrate successful validation? Successful validation requires consistent performance across these key metrics:
- Significant survival separation in Kaplan-Meier analysis (log-rank p < 0.05)
- Stable time-dependent AUC values (typically >0.6 for 1-, 3-, 5-year survival)
- Independent prognostic value in multivariate Cox regression (p < 0.05)
Q5: My signature performs well on training data but poorly on validation cohorts. What went wrong? This classic overfitting problem can stem from several issues:
- Insufficient feature selection during model development
- Technical batch effects between different sequencing platforms
- Inadequate sample size in the training phase
- Clinical heterogeneity between patient populations Address this by returning to feature selection, applying combat batch correction, or collecting more training samples.
Troubleshooting Guides
Problem: Signature Fails to Validate in External Cohorts
Symptoms:
- Non-significant p-values (>0.05) in survival analysis of external cohorts
- Dramatic drop in AUC values (e.g., from 0.8 to 0.55)
- Hazard ratio confidence intervals crossing 1.0
Solution:
- Check cohort compatibility: Ensure similar inclusion criteria, cancer stages, and treatment histories
- Apply batch effect correction: Use ComBat or other normalization methods to address platform differences
- Revisit feature selection: Return to LASSO Cox regression to eliminate redundant lncRNAs
- Adjust risk score calculation: Verify the formula application matches your original method
Problem: Inconsistent Risk Group Separation
Symptoms:
- Poor separation of Kaplan-Meier curves
- Overlapping risk groups in PCA visualization
- Non-significant log-rank test results
Solution:
- Optimize cutoff selection: Test percentiles (median, quartiles) or maximally selected rank statistics
- Validate stratification in subgroups: Test performance within specific clinical stages
- Verify expression normalization: Ensure consistent processing of RNA-seq data
Experimental Protocols
Protocol 1: Multi-Cohort Validation Strategy
Objective: To validate m6A-related lncRNA signature across multiple independent datasets
Materials:
- Established risk score formula from discovery phase
- Independent cohort datasets (GEO, ICGC, or institutional)
- Statistical software (R recommended)
Procedure:
- Data Preprocessing
- Download and normalize expression matrices from validation cohorts
- Extract the specific lncRNAs included in your signature
- Annotate clinical endpoints (overall survival/progression-free survival)
Risk Score Calculation
- Apply your established formula:
Risk score = Σ(coefficient_i × expression_i) - Example from colorectal cancer research:
m6A-LncScore = 0.32*SLCO4A1-AS1 + 0.41*MELTF-AS1 + 0.44*SH3PXD2A-AS1 + 0.39*H19 + 0.48*PCAT6[18]
- Apply your established formula:
Patient Stratification
- Apply the original training cohort cutoff OR optimize for the new cohort
- Classify patients into high-risk and low-risk groups
Statistical Validation
- Perform Kaplan-Meier survival analysis with log-rank test
- Calculate time-dependent ROC curves (1, 3, 5 years)
- Conduct univariate and multivariate Cox regression
Clinical Utility Assessment
Expected Outcomes: Consistent prognostic separation with statistically significant hazard ratios across all validation cohorts.
Protocol 2: Handling Technical Batch Effects
Objective: To minimize non-biological technical variations between cohorts
Procedure:
- Identify Batch Sources: Document sequencing platforms, protocols, and institutions
- Apply Correction Methods: Use ComBat, limma, or SVA packages in R
- Validate Correction: Demonstrate improved cohort integration via PCA plots
Performance Comparison Across Studies
The table below summarizes validation outcomes from published m6A-related lncRNA studies:
| Cancer Type | Training Cohort | Validation Cohorts | Key Validation Results | Reference |
|---|---|---|---|---|
| Colorectal Cancer | TCGA (n=622) | Six GEO datasets (n=1,077) + in-house (n=55) | Consistent PFS prediction across all cohorts; AUC maintained 0.65-0.75 | [18] |
| Pancreatic Ductal Adenocarcinoma | TCGA (n=170) | ICGC (n=82) | Significant OS separation (p<0.05); AUC 0.72 at 1 year | [21] |
| Ovarian Cancer | TCGA (n=379) | Two GEO datasets + in-house (n=60) | Poor prognosis accurately predicted (p<0.001); signature independent prognostic factor | [14] |
| Gastric Cancer | TCGA (n=375) | Internal validation | AUC 0.879 for OS prediction; immune infiltration differences confirmed | [75] |
| Lung Adenocarcinoma | TCGA (n=480) | Internal validation | OS significantly stratified (p<0.05); independent prognostic value confirmed | [38] |
The Scientist's Toolkit
Research Reagent Solutions
| Reagent/Tool | Function | Example Use Case | |
|---|---|---|---|
| TCGA Database | Discovery cohort source | Initial signature development and training | [38] [76] |
| GEO Datasets | Independent validation cohorts | Multi-cohort validation strategy | [18] [14] |
| CIBERSORT | Immune cell infiltration analysis | Mechanistic insights into signature function | [38] [76] |
| pRRophetic R Package | Drug sensitivity prediction | Translational application of signature | [21] [11] |
| ESTIMATE Algorithm | Tumor microenvironment scoring | Understanding immune contexture | [76] [21] |
| M6A2Target Database | m6A regulator-target interactions | Functional validation of m6A relationships | [18] |
Experimental Workflow Visualization
Validation Metrics Visualization
Successful independent validation requires meticulous attention to cohort selection, statistical rigor, and clinical relevance. By implementing these protocols and troubleshooting guides, researchers can develop m6A-related lncRNA signatures with genuine translational potential rather than statistical artifacts. The multi-cohort approach demonstrated in recent publications provides a robust framework for establishing prognostic tools that may eventually guide clinical decision-making.
Frequently Asked Questions (FAQs) on Nomogram Development and Validation
Q1: What are the key steps to prevent overfitting when building a prognostic model based on an m6A-lncRNA signature?
A1: Preventing overfitting requires a combination of robust feature selection and validation techniques. Key steps include:
- Employ Regularized Regression: Use the Least Absolute Shrinkage and Selection Operator (LASSO) regression to penalize the number of features in your model. This method shrinks the coefficients of less important variables to zero, effectively selecting only the most predictive m6A-related lncRNAs [77] [30] [78].
- Implement Cross-Validation: During the LASSO analysis, use 10-fold cross-validation to determine the optimal value for the tuning parameter (lambda). This process ensures the model's generalizability by repeatedly partitioning the dataset into training and validation folds [77].
- Conduct Multivariate Analysis: Finally, subject the lncRNAs selected by LASSO to a multivariate Cox regression analysis. This confirms their status as independent prognostic factors and provides the coefficients used to calculate the final risk score [30] [78].
Q2: How is the performance of a newly developed nomogram rigorously validated?
A2: Rigorous validation involves multiple steps and should be performed on both a training and an independent validation cohort.
- Discrimination: Evaluate how well the model separates patients with different outcomes using the Area Under the Receiver Operating Characteristic Curve (AUC). AUC values range from 0.5 (no discrimination) to 1.0 (perfect discrimination). A study on rheumatoid arthritis reported an AUC of 0.904 in its validation cohort, indicating excellent discrimination [79].
- Calibration: Assess the agreement between predicted probabilities and actual observed outcomes. This is typically done with a calibration plot. A plot that closely follows the 45-degree line indicates good calibration [79] [80].
- Clinical Utility: Use Decision Curve Analysis (DCA) to evaluate whether using the nomogram for clinical decisions would provide a net benefit compared to standard staging systems or other existing models [79] [80].
Q3: What are the essential components of a prognostic study's methodology section for a nomogram?
A3: A well-documented methodology should clearly describe the following:
- Data Source and Cohorts: Specify the public databases (e.g., TCGA, GEO) or institutional cohorts used. Clearly define how patients were allocated into training and validation sets (e.g., a 7:3 ratio) [77] [80].
- Variable Selection: Detail the process for identifying prognostic factors, which often involves univariate Cox regression followed by multivariate Cox regression [79] [80].
- Model Construction and Visualization: Describe the statistical software (e.g., R with the
rmspackage) used to build the nomogram, which visually represents the multivariate model [80] [30]. - Validation Metrics: Report the C-index, AUC values for specific time points (e.g., 1, 3, 5 years), and results from calibration and DCA [80].
Experimental Protocols for Key Analyses
Protocol 1: Developing an m6A/m5C-Related lncRNA Signature
This protocol outlines the process for identifying a prognostic lncRNA signature, as applied in studies on lung adenocarcinoma (LUAD) and colorectal cancer (CRC) [77] [16] [30].
1. Data Acquisition and Preprocessing:
- Obtain transcriptome data (e.g., FPKM or TPM values) and corresponding clinical data from databases like TCGA and GEO.
- Filter and normalize the data. For GEO datasets, use algorithms like "ComBat" to remove batch effects when combining multiple cohorts [16] [78].
2. Identify m6A/m5C-Related lncRNAs:
- Compile a list of known m6A and m5C regulators (writers, erasers, readers) from literature [16] [78].
- Perform a co-expression analysis (e.g., Pearson correlation) between the expression of all lncRNAs and the m6A/m5C regulators.
- Define m6A/m5C-related lncRNAs as those with a correlation coefficient |R| > 0.4 and a p-value < 0.001 [16].
3. Construct the Prognostic Signature:
- Perform univariate Cox regression on the m6A/m5C-related lncRNAs to identify candidates associated with overall survival (OS) or progression-free survival (PFS).
- Input the significant lncRNAs into a LASSO Cox regression analysis to reduce overfitting and select the most robust features.
- Build the final risk model using the lncRNAs retained by LASSO. The risk score is calculated using the formula:
Risk Score = (Expression of lncRNA1 × Coefficient1) + (Expression of lncRNA2 × Coefficient2) + ...[30] [78].
4. Validate the Signature:
- Divide patients into high-risk and low-risk groups based on the median risk score.
- Use Kaplan-Meier survival analysis with the log-rank test to compare survival outcomes between the two groups in both training and external validation cohorts [77] [30].
Protocol 2: Building and Validating a Prognostic Nomogram
This protocol is based on methodologies used in developing nomograms for rheumatoid arthritis and rectal cancer [79] [80].
1. Identify Independent Prognostic Factors:
- In the training cohort, perform univariate Cox regression to screen variables (clinical and molecular) associated with survival.
- Include significant variables from the univariate analysis in a multivariate Cox regression to identify independent prognostic factors.
2. Construct the Nomogram:
- Using R software and packages like
rms, build a nomogram that incorporates all independent prognostic factors identified in the multivariate analysis. Each factor is assigned a points scale, and the total points correspond to a probability of survival at specific time points (e.g., 1, 3, and 5 years) [80].
3. Validate the Nomogram:
- Discrimination: Calculate the C-index and plot time-dependent ROC curves to assess the model's ability to predict outcomes. A C-index of 0.721 indicates good predictive accuracy [80].
- Calibration: Generate calibration curves by plotting the nomogram-predicted survival probabilities against the actual observed survival rates. A curve close to the 45-degree line indicates good agreement [79] [80].
- Clinical Utility: Perform Decision Curve Analysis (DCA) to quantify the net clinical benefit of the nomogram across different threshold probabilities, comparing it to existing staging systems [79].
Visualization of Workflows and Relationships
Diagram: m6A-lncRNA Signature Development Workflow
Diagram: Nomogram Validation Process
Research Reagent Solutions
The table below lists key computational and data resources essential for building and validating prognostic models in cancer research.
| Resource Name | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| TCGA Database [77] [78] | Genomic Database | Provides comprehensive multi-omics data (e.g., RNA-seq) and clinical information for various cancer types. | Served as the primary training cohort for developing an m5C/m6A-related signature in LUAD [77] [78]. |
| GEO Database [77] [30] | Genomic Repository | A public repository of functional genomics data sets, used for independent validation of prognostic models. | Used to validate an m6A-related lncRNA signature across six independent CRC cohorts (GSE17538, GSE39582, etc.) [30]. |
| ConsensusClusterPlus [78] | R Package | Performs unsupervised clustering to identify distinct molecular subtypes based on gene expression patterns. | Used to identify m6A modification patterns in LUAD by clustering samples based on 21 m6A regulators [81] [78]. |
| glmnet [77] [78] | R Package | Fits LASSO regression models for feature selection, which is critical for preventing model overfitting. | Applied to shrink the number of prognostic lncRNAs and construct a parsimonious risk model [77] [78]. |
| GSVA / ssGSEA [77] [78] | Computational Algorithm | Evaluates the enrichment of specific gene sets (e.g., immune cells, pathways) in individual tumor samples. | Used to characterize the tumor microenvironment (TME) and analyze infiltrating immune cells in different risk groups [77] [78]. |
The following table consolidates key performance metrics from recent studies on prognostic model development, highlighting the utility of nomograms and molecular signatures.
| Study / Disease Focus | Model Type | Key Prognostic Factors | Training Cohort Performance (C-index/AUC) | Validation Cohort Performance (C-index/AUC) |
|---|---|---|---|---|
| Rheumatoid Arthritis (Mortality) [79] | Prognostic Nomogram | Age, Heart Failure, SIRI | AUC: 0.852 | AUC: 0.904 |
| Stages I-III Rectal Cancer [80] | PNI-Incorporated Nomogram | PNI, pTNM stage, Pre-/Post-op CEA, IBL | C-index: 0.7211-yr AUC: 0.855 | 1-yr AUC: 0.952 |
| Colorectal Cancer (PFS) [30] | m6A-LncRNA Signature | 5 m6A-related lncRNAs (e.g., SLCO4A1-AS1, H19) | Predictive for PFS in 622 TCGA patients | Validated in 1,077 patients from 6 GEO datasets |
A technical support guide for computational biologists
Troubleshooting Guide: Resolving Common Analysis Hurdles
FAQ 1: My m6A-lncRNA risk model performs well on the training data but fails on the validation set. What might be causing this overfitting?
Answer: This typically occurs when your model learns dataset-specific noise instead of biologically generalizable patterns. Implement these proven strategies:
- Apply LASSO Regression: Use Least Absolute Shrinkage and Selection Operator (LASSO) Cox regression to penalize model complexity and select only the most prognostic features [63] [29] [21].
- Implement Cross-Validation: Perform ten-fold cross-validation during model training to ensure your model's robustness. This technique repeatedly partitions your training data into subsets to validate parameters and prevent overfitting [63] [29].
- Validate Externally: Test your final model on a completely independent cohort from a different database (e.g., validate a TCGA model on an ICGC dataset) to confirm its general applicability [21].
FAQ 2: How can I functionally validate that my m6A-related lncRNA signature is genuinely linked to the tumor immune microenvironment?
Answer: Beyond standard survival analysis, deploy these multi-angle computational validations:
- Immune Infiltration Quantification: Use the CIBERSORT or ESTIMATE algorithms on your transcriptome data to calculate the relative fractions of 22 immune cell types or overall stromal/immune scores [82] [83] [84]. High-risk scores from your signature should correlate with immunosuppressive landscapes.
- Checkpoint Inhibitor Association: Examine the expression of established immune checkpoint genes (e.g., PD-1, PD-L1, CTLA-4). Signatures associated with immune evasion often show coordinated upregulation of these checkpoints [83] [21].
- TMB & MSI Correlation Analysis: Calculate TMB from somatic mutation data and obtain MSI status. Correlate these values with risk scores; positive correlations often indicate a signature reflective of tumor immunogenicity [82] [84].
FAQ 3: What are the essential data and quality control steps before constructing a signature?
Answer: A robust pipeline starts with meticulous data preparation:
- Data Sourcing: Obtain RNA-seq data, somatic mutation data, and complete clinical information from authoritative sources like TCGA and GTEx [63] [29] [84].
- LncRNA Identification: Use a reliable annotation file (e.g., from GENCODE) to accurately distinguish lncRNAs from messenger RNAs in the transcriptome data [63] [29].
- Filtering for Relevance: Identify m6A-related lncRNAs through co-expression analysis with known m6A regulators, using stringent cutoffs (e.g., |correlation coefficient| > 0.4 and p < 0.001) [63] [21].
- Clinical Data Curation: Ensure your patient cohort has adequate follow-up time (e.g., exclude patients with less than 30 days of follow-up) to avoid bias in survival analysis [21].
Experimental Protocols for Key Analyses
Protocol 1: Constructing an m6A-Related lncRNA Prognostic Signature
This protocol outlines the core methodology for building a robust risk model [63] [29] [21].
- Univariate Cox Analysis: Screen all m6A-related lncRNAs to identify those with a significant individual association with overall survival (P < 0.05).
- LASSO-Penalized Cox Regression: Apply LASSO to the significant lncRNAs from step 1. This step shrinks coefficients of less contributory genes to zero, selecting a parsimonious set of features and mitigating overfitting.
- Multivariate Cox Regression: Perform a final multivariate Cox analysis on the LASSO-selected genes to determine their independent prognostic value and calculate their regression coefficients (β).
- Calculate Risk Score: For each patient, compute a risk score using the formula: Risk score = (β~gene1~ × Exp~gene1~) + (β~gene2~ × Exp~gene2~) + ... + (β~geneN~ × Exp~geneN~) where Exp represents the expression level of each lncRNA in the signature.
- Stratify Patients: Divide patients into high-risk and low-risk groups using the median risk score from the training cohort as the cutoff point.
Protocol 2: Analyzing Correlation with Tumor Mutation Burden (TMB) and Immune Infiltration
This protocol describes how to link your signature to key tumor biological features [82] [84].
- TMB Calculation: Process somatic mutation data (e.g., from TCGA "MuTect2" files). TMB is defined as the total number of somatic mutations per megabase (Mb) of the exome genome.
- Group Stratification by TMB: Divide your tumor samples into high- and low-TMB groups, typically using the median TMB value or a published threshold (e.g., 20 mutations/Mb) [84].
- Immune Infiltration Analysis: Use the CIBERSORT deconvolution algorithm on gene expression data (with LM22 signature gene set) to estimate the proportional abundance of 22 immune cell types for each sample. Retain only results with a CIBERSORT p-value < 0.05 for accuracy [82] [84].
- Statistical Correlation: Compare immune cell infiltration levels between high- and low-TMB groups using the Wilcoxon rank-sum test. Correlate patient risk scores with both TMB values and the infiltration levels of specific immune cells (e.g., CD8+ T cells, macrophages) using Spearman's correlation.
Data Presentation: Quantitative Findings in Tumor Biology
Table 1: Reported Immune Cell Infiltration Differences in High-TMB vs. Low-TMB Colon Adenocarcinoma (COAD) Data derived from CIBERSORT analysis of TCGA cohorts, showing significantly higher infiltration of specific immune cells in high-TMB environments [82] [84].
| Immune Cell Type | Infiltration in High-TMB Group | Infiltration in Low-TMB Group | P-Value | Citation |
|---|---|---|---|---|
| CD8+ T cells | ↑ Higher | ↓ Lower | < 0.05 | [82] [84] |
| Activated Memory CD4+ T cells | ↑ Higher | ↓ Lower | < 0.05 | [82] |
| Activated NK cells | ↑ Higher | ↓ Lower | < 0.05 | [82] [84] |
| M1 Macrophages | ↑ Higher | ↓ Lower | < 0.05 | [82] [84] |
| T Follicular Helper cells | ↑ Higher | ↓ Lower | < 0.05 | [84] |
Table 2: Essential Research Reagent Solutions for m6A-lncRNA and TMB Analysis A curated list of key computational tools and databases for conducting the analyses described in this guide.
| Item Name | Function / Application | Brief Explanation | Citation |
|---|---|---|---|
| CIBERSORT Algorithm | Quantifying immune cell infiltration from transcriptome data. | A deconvolution algorithm that uses a reference gene signature (LM22) to estimate the proportion of 22 immune cell types in a mixed tissue. | [82] [83] [84] |
| maftools R Package | Analyzing and visualizing somatic mutation data. | Processes mutation annotation format (MAF) files to calculate TMB, visualize mutation landscapes, and identify mutated genes. | [82] [29] [84] |
| ImmPort Database | Sourcing immune-related genes for functional analysis. | A repository of curated genes involved in immune system processes, used to identify immune-related differentially expressed genes. | [83] [84] |
| GDSC Database | Predicting chemotherapeutic drug sensitivity. | Provides drug sensitivity data (IC50) from cancer cell lines, used to predict a patient's likely response to various drugs based on their transcriptomic profile. | [63] [29] [21] |
| TIDE Algorithm | Predicting immunotherapy response. | Models tumor immune evasion to predict which patients are likely to respond to immune checkpoint blockade therapy. | [63] [29] |
Visualizing Analytical Workflows and Relationships
The following diagrams, generated with Graphviz, illustrate the core workflows and biological relationships discussed in this guide.
Diagram 1: m6A-lncRNA Signature Development and Validation Pipeline
Diagram 2: Linking Molecular Signatures to Tumor Biology
FAQ: Model Performance and Benchmarking
Q: How do existing m6A-related lncRNA signatures typically perform on independent validation datasets?
A: Performance varies by cancer type, but well-constructed signatures generally show strong predictive capability. In colorectal cancer, a 5-lncRNA signature (SLCO4A1-AS1, MELTF-AS1, SH3PXD2A-AS1, H19, PCAT6) demonstrated robust performance when validated across six independent datasets (GSE17538, GSE39582, GSE33113, GSE31595, GSE29621, and GSE17536) comprising 1,077 patients, showing better performance than three previously established lncRNA signatures for predicting progression-free survival [30]. Similarly, in lung adenocarcinoma, an 8-lncRNA signature (m6ARLSig) effectively stratified patients into distinct risk groups with significantly different overall survival outcomes [38].
Q: What are the key metrics used to evaluate signature performance in published studies?
A: Researchers typically employ multiple statistical measures to comprehensively evaluate signature performance. These include:
- Time-dependent Receiver Operating Characteristic (ROC) curves and Area Under Curve (AUC) values to assess predictive accuracy
- Kaplan-Meier survival analysis with log-rank tests to compare survival between risk groups
- Univariate and multivariate Cox regression analyses to determine independent prognostic value
- Calibration curves to evaluate the agreement between predicted and observed outcomes
- Principal Component Analysis (PCA) to visualize patient stratification [30] [38]
Q: How can I assess whether my m6A-lncRNA signature is overfitting to the training data?
A: Several strategies can help identify and prevent overfitting:
- Perform k-fold cross-validation during model development (commonly 10-fold)
- Validate the signature on completely independent external datasets from different institutions or platforms
- Compare performance metrics between training and validation cohorts - significant performance drops suggest overfitting
- Use regularization techniques like LASSO Cox regression during feature selection to penalize complexity
- Ensure the number of events (patients with outcomes) adequately exceeds the number of features in your signature [30] [16]
Troubleshooting Experimental Protocols
Q: My m6A-lncRNA signature fails to validate in external datasets. What could be going wrong?
A: Several factors could contribute to poor external validation:
- Batch effects: Different sequencing platforms or laboratory protocols can introduce technical variation. Use combat algorithms or other batch correction methods before analysis [16].
- Cohort heterogeneity: Patient populations may differ in clinical characteristics, treatment history, or cancer subtypes. Perform subgroup analysis to identify where the signature works best.
- Platform compatibility: Ensure lncRNA annotation is consistent across datasets. Use standardized annotation files like Gencode.v34 and verify probe mapping for array data [30].
- Sample size inadequacy: Validation cohorts may be underpowered to detect the signature effect. Conduct power analysis before validation.
Solution: Reanalyze the validation dataset with strict uniform processing pipelines. Perform consensus clustering to identify molecular subtypes that might respond differently to the signature.
Q: The prognostic performance of my signature differs significantly between cancer types. Is this expected?
A: Yes, this is commonly observed and reflects cancer-type specificity of m6A mechanisms. For example:
- In colorectal cancer, m6A-related lncRNAs strongly predict progression-free survival [30]
- In gliomas, m6A lncRNA profiles differ between glioblastoma and low-grade glioma but showed limited prognostic value in one study [85]
- The biological context of m6A regulation varies across tissues, affecting signature portability
Solution: Develop cancer-type specific signatures rather than attempting pan-cancer applications. Validate the molecular mechanisms in cell lines or animal models specific to each cancer type.
Performance Benchmarking Tables
Table 1: Published m6A-Related lncRNA Signatures and Their Performance Metrics
| Cancer Type | Signature Size | Key lncRNAs | Training Cohort | Validation Performance | Clinical Application |
|---|---|---|---|---|---|
| Colorectal Cancer [30] | 5 | SLCO4A1-AS1, MELTF-AS1, SH3PXD2A-AS1, H19, PCAT6 | TCGA (n=622) | Validated in 6 GEO datasets (n=1,077); Better than existing lncRNA signatures | Predicts progression-free survival; Independent prognostic factor |
| Lung Adenocarcinoma [38] | 8 | AL606489.1, COLCA1, others | TCGA-LUAD (n=480) | Significant survival difference between risk groups (p<0.05); Independent prognostic factor | Predicts overall survival; Associated with immune infiltration and drug response |
| Cervical Cancer [86] | 6 | AC016065.1, AC096992.2, AC119427.1, AC133644.1, AL121944.1, FOXD1_AS1 | TCGA-CESC + GTEx (n=393) | High prognostic prediction performance; Validated in clinical samples | Forecasts prognosis and treatment response; Linked to immunotherapy response |
| Esophageal Squamous Cell Carcinoma [39] | 10 | Not specified | TCGA-ESCC (n=81) | Good independent prediction in validation datasets; Stratifies patients into risk groups | Predicts survival outcomes; Characterizes immune landscape; Assesses immunotherapy response |
Table 2: Model Validation Approaches in m6A-lncRNA Studies
| Validation Method | Implementation | Advantages | Limitations |
|---|---|---|---|
| Internal Validation [30] [38] | K-fold cross-validation; Bootstrap resampling | Efficient use of available data; Reduces overfitting | May not capture between-dataset variability |
| External Validation [30] [16] | Applying signature to completely independent datasets from different sources | Tests generalizability; Gold standard for validation | Resource-intensive; Requires compatible datasets |
| Clinical Validation [30] [86] | Testing signature in prospectively collected cohorts or clinical samples | Assesses real-world performance; Closer to clinical application | Time-consuming and expensive |
| Biological Validation [38] [20] | Functional experiments in cell lines or animal models | Confirms biological relevance; Mechanistic insights | Does not directly test prognostic performance |
Experimental Workflow and Signaling Pathways
Validation Workflow for m6A-lncRNA Signatures
m6A-lncRNA Regulatory Axis in Cancer
Research Reagent Solutions
Table 3: Essential Research Materials and Databases for m6A-lncRNA Studies
| Resource Type | Specific Examples | Function/Purpose | Reference |
|---|---|---|---|
| Data Sources | TCGA (The Cancer Genome Atlas) | Provides RNA-seq data and clinical information for multiple cancer types | [30] [38] |
| GEO (Gene Expression Omnibus) | Source of independent validation datasets | [30] [16] | |
| m6A Regulator Databases | M6A2Target | Database of m6A-target interactions | [30] |
| FerrDB v2 | Database of ferroptosis-related genes | [86] | |
| LncRNA Annotation | Gencode.v34 | Standardized lncRNA annotation | [30] |
| lncATLAS, lncSLdb | LncRNA subcellular localization | [39] | |
| Analysis Tools/Packages | DESeq2 (R package) | Differential expression analysis | [30] |
| glmnet (R package) | LASSO Cox regression for feature selection | [30] [38] | |
| ConsensusClusterPlus (R package) | Unsupervised clustering for molecular subtyping | [16] [86] | |
| CIBERSORT | Immune cell infiltration analysis | [38] [16] | |
| Experimental Validation | Direct RNA long-read sequencing | m6A modification profiling at single-base resolution | [85] |
| Methylated RNA immunoprecipitation (MeRIP) | m6A modification detection | [42] [20] | |
| Quantitative RT-PCR | Validation of lncRNA expression in clinical samples | [30] [86] |
Functional validation of hub long non-coding RNAs (lncRNAs) is a critical step in transitioning from computational predictions to understanding their biological role in cancer and other diseases. This process confirms whether a candidate lncRNA actively participates in disease mechanisms such as tumor progression, immune response, or therapeutic resistance. The most established validation workflow progresses from in vitro cellular experiments to in vivo animal models, with techniques including gene knockdown/overexpression, phenotypic assays, and mechanistic investigations [87] [88] [29].
A properly validated lncRNA not only confirms the reliability of your original computational signature but also provides crucial evidence for its potential as a biomarker or therapeutic target [89] [90]. The following sections detail the core methodologies, complete with troubleshooting guides and essential reagents to support your research.
Core Experimental Workflow: A Visual Guide
The functional validation of a hub lncRNA follows a logical, multi-stage pathway. The diagram below outlines the key phases from initial cellular manipulation to final mechanistic insight.
Detailed Methodologies & Troubleshooting
Gene Expression Modulation
The first experimental step is to alter the expression level of your hub lncRNA in a relevant cellular model to observe subsequent effects.
Table 1: Primary Methods for lncRNA Expression Modulation
| Method | Key Function | Typical Efficiency | Duration of Effect |
|---|---|---|---|
| siRNA/shRNA | Knocks down expression by targeting mature lncRNA transcript [87] | 60-80% knockdown | Transient (5-7 days) |
| CRISPRi | Interferes with transcription by targeting lncRNA promoter [90] | 70-90% knockdown | Sustained (weeks) |
| ASO (Antisense Oligonucleotides) | Binds to lncRNA and induces degradation by RNase H [91] | 70-90% knockdown | Transient to sustained |
| Plasmid/Viral Vectors | Drives overexpression of full-length lncRNA [88] | 10-100 fold increase | Stable (with selection) |
FAQ: Why is my knockdown efficiency low even with high-quality reagents?
- Problem: Inefficient transfection is a common cause.
- Solution:
- Optimize Transfection: Use a fluorescently-labeled negative control siRNA to visually assess and optimize transfection efficiency under your microscope.
- Validate Assay: Ensure your qRT-PCR primers are designed to span an exon-exon junction (if applicable) or are specific to the spliced form of the lncRNA to avoid amplifying genomic DNA.
- Time Course: Perform a time-course experiment to find the peak knockdown time, which is typically 48-72 hours post-transfection.
FAQ: How can I confirm that my overexpression construct is functioning correctly?
- Problem: Unsure if transfected construct is being transcribed.
- Solution:
- Tag Your lncRNA: Use a vector that allows for a tag (like a MS2 stem-loop) to be incorporated into the transcript. This enables direct detection of the overexpressed lncRNA via its tag.
- qRT-PCR with Specific Primers: Design qPCR primers that are specific to the vector backbone or a unique sequence tag added to the lncRNA, ensuring you are detecting the exogenous transcript and not the endogenous one.
Phenotypic Screening Assays
After modulating lncRNA expression, the next step is to quantify changes in cellular behavior. The diagram below maps common phenotypic assays to the biological processes they probe.
Table 2: Key Phenotypic Assays and Protocols
| Phenotype | Core Assay | Detailed Protocol Summary | Key Output Measurement |
|---|---|---|---|
| Proliferation & Viability | CCK-8 Assay [29] | Seed cells in 96-well plate. Add CCK-8 reagent. Incubate 1-4 hours. Measure absorbance at 450nm. | OD450 value over time; IC50 for drug studies. |
| Clonogenic Survival | Colony Formation [88] | Seed a low density of cells. Culture for 1-3 weeks with media changes. Fix with methanol, stain with crystal violet. | Number and size of stained colonies. |
| Cell Death | Flow Cytometry (Annexin V/PI) [87] | Harvest cells, stain with Annexin V-FITC and Propidium Iodide (PI). Analyze by flow cytometry within 1 hour. | % of cells in early (Annexin V+/PI-) and late (Annexin V+/PI+) apoptosis. |
| Migration & Invasion | Transwell Assay | Seed cells in serum-free media in upper chamber (with Matrigel for invasion). Place complete media in lower chamber as chemoattractant. Incubate 24-48 hours. Stain and count cells that migrated through membrane. | Number of cells per field that migrated/invaded. |
FAQ: My negative control cells show high background migration in the Transwell assay.
- Problem: High background migration.
- Solution:
- Serum Starve: Ensure the cells in the upper chamber are properly serum-starved (e.g., 12-24 hours) to minimize basal migration.
- Check FBS: Use a batch of FBS that has been tested for its efficacy as a chemoattractant. The concentration in the lower chamber is typically 10-20%.
- Shorten Incubation: Reduce the incubation time to prevent excessive migration of control cells.
FAQ: The standard CCK-8 assay shows high variance between replicates for my slow-growing cells.
- Problem: High variance in viability assays.
- Solution:
- Normalize Cell Number: Precisely normalize the cell number at the seeding step using an automated cell counter.
- Extend Incubation: For slow-growing cells, extend the culture time before adding the CCK-8 reagent to increase the signal-to-noise ratio.
- Alternative Assays: Consider using more sensitive assays like ATP-based luminescence (e.g., CellTiter-Glo), which can be more robust for low cell numbers.
In Vivo Animal Models
In vivo experiments are crucial for validating lncRNA function within a complex tissue microenvironment.
Standard Protocol: Subcutaneous Xenograft Model [87]
- Cell Preparation: Harvest your control or lncRNA-knockdown/overexpression cells and resuspend them in a 1:1 mixture of PBS and Matrigel.
- Inoculation: Subcutaneously inject the cell suspension (e.g., 1-5 million cells per site) into the flanks of immunodeficient mice (e.g., BALB/c nude or NOD/SCID).
- Tumor Monitoring: Measure tumor dimensions with calipers 2-3 times per week. Calculate tumor volume using the formula: Volume = (Length × Width²) / 2.
- Endpoint Analysis: After 4-6 weeks, or when tumor size reaches the ethical limit, euthanize the mice. Harvest and weigh the tumors. A portion of the tumor should be snap-frozen for RNA/protein analysis, and another portion fixed for immunohistochemistry (IHC).
FAQ: We observed a significant difference in tumor growth in vivo, but how do we link this directly to the lncRNA and the tumor microenvironment?
- Problem: Difficulty connecting phenotype to mechanism in vivo.
- Solution:
- Confirm Expression: Isolate RNA from the harvested tumors and confirm by qRT-PCR that the lncRNA expression level (knockdown or overexpression) was maintained in vivo.
- Analyze Proliferation/Apoptosis: Perform IHC on tumor sections for markers like Ki-67 (proliferation) and Cleaved Caspase-3 (apoptosis) to quantify the cellular effects.
- Profile Immune Infiltration: As demonstrated in the MYOSLID study, use IHC or flow cytometry to analyze immune cells (e.g., CD4+ and CD8+ T cells) in the tumor, which can reveal effects on the immune microenvironment [87].
Mechanistic Investigation
Understanding the molecular mechanism of a hub lncRNA is the final step in functional validation.
Common Approaches:
- Subcellular Localization: Determine if the lncRNA is nuclear or cytoplasmic using RNA Fluorescence In Situ Hybridization (RNA-FISH) or fractionation followed by qRT-PCR. This provides critical clues about its function [90].
- Identifying Interaction Partners:
- RNA Immunoprecipitation (RIP): Uses antibodies to pull down proteins and identifies associated lncRNAs.
- ChIRP-MS / RAP-MS: Uses biotinylated antisense oligonucleotides to pull down the lncRNA and its direct protein partners, which are then identified by Mass Spectrometry (MS) [90].
- Luciferase Reporter Assays: If a lncRNA is suspected to sponge a miRNA (ceRNA mechanism), a reporter gene containing the putative miRNA binding site can be used to validate the interaction.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagent Solutions for lncRNA Functional Validation
| Reagent / Solution | Primary Function | Examples & Notes |
|---|---|---|
| Biotinylated Oligos | Pull down lncRNAs and their direct binding partners for mechanistic studies (e.g., ChIRP-MS) [90]. | Design ~20-25 nt antisense DNA oligos tiling along the full lncRNA sequence. |
| MS2/MS2 BP | Tag lncRNAs for localization, purification, or live-cell imaging. | MS2 stem-loops are inserted into the lncRNA expression vector; MS2 Coat Protein (MCP) is fused to GFP (for imaging) or a purification tag. |
| Specific Antibodies | Validate protein interactions and analyze phenotypic effects in cells and tissues. | Essential for RIP (e.g., anti-EZH2, anti-H3K27me3), Western Blot, and IHC (e.g., anti-Ki-67, anti-CD4, anti-CD8) [87] [90]. |
| qRT-PCR Kits | Quantitatively measure lncRNA expression levels after modulation and in tissues. | Select kits with high sensitivity for potentially low-abundance lncRNAs. Always normalize to stable housekeeping genes (e.g., GAPDH, ACTB). |
| Cell Viability Assays | Measure changes in proliferation and metabolic activity post-knockdown/overexpression. | CCK-8 [29], MTT, or CellTiter-Glo (luminescent, higher sensitivity). |
| siRNA/shRNA Libraries | Knock down lncRNA expression for initial functional screening. | Purchase pre-designed pools targeting your lncRNA from reputable vendors. Always include non-targeting scrambled controls. |
Conclusion
The development of a robust m6A-lncRNA signature is a multi-stage process that hinges on the rigorous application of overfitting prevention strategies from the outset. A successful model seamlessly integrates biological understanding with computational rigor, employing advanced cross-validation and interpretable machine learning to ensure its findings are both statistically sound and biologically plausible. Future directions should focus on the integration of single-cell m6A mapping data, the development of cross-species applicable models, and the application of these signatures for predicting immunotherapy responses. Ultimately, a meticulously validated m6A-lncRNA signature holds immense potential not only as a prognostic tool but also for illuminating novel therapeutic targets, thereby bridging the gap between computational discovery and clinical application in precision oncology.
References
- 1. writers, erasers, readers and functions in RNA metabolism [https://www.nature.com/articles/s41422-018-0040-8]
- 2. Role of m6A writers, erasers and readers in cancer [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-022-00298-7]
- 3. Where, when and how: context-dependent functions of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6527355/]
- 4. m6A writers, erasers, readers and their functions [https://www.abcam.com/en-us/technical-resources/pathways/m6a-functions-and-distribution]
- 5. Visualization methods for differential expression analysis [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-019-2968-1]
- 6. Identification and Validation of m -Related 6 as... A lncRNA Signature [https://pmc.ncbi.nlm.nih.gov/articles/PMC8555664/]
- 7. Identification of a novel m -related lncRNAs 6 and... A signature [https://link.springer.com/article/10.1186/s12885-024-11885-8?]
- 8. Frontiers | Cross -Talk Between m - and m5C-Related lncRNAs to... 6 A [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2022.740960/full]
- 9. Current techniques for visualizing RNA in cells - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4850879/]
- 10. Unveiling the Role of LncRNAs in Tumorigenesis [https://www.sciencedirect.com/science/article/pii/S305078712500085X]
- 11. Identification of an m6A-Related Long Noncoding RNA ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2022.910749/full]
- 12. Cross-Talk between N6-Methyladenosine and Their ... [https://www.mdpi.com/1422-0067/24/2/1665]
- 13. Enhancing m6A modification of lncRNA through METTL3 ... [https://www.sciencedirect.com/science/article/pii/S2405844024041963]
- 14. Identification and validation of a seven m6A-related lncRNAs ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-022-09591-4]
- 15. The Primary Role of Noncoding RNA in the Pathogenesis of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294578/]
- 16. Cross-Talk Between m6A- and m5C-Related lncRNAs to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8957790/]
- 17. Identification and Validation of a m6A-Related Long ... [https://pubmed.ncbi.nlm.nih.gov/39868645/]
- 18. Identification and Validation of an m6A-Related LncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9407446/]
- 19. HNRNPA2B1-mediated m modification enhances 6 NORHA... A lncRNA [https://www.zoores.ac.cn/article/doi/10.24272/j.issn.2095-8137.2024.378]
- 20. m6A reader IGF2BP2-stabilized lncRNA LHX1-DT inhibits ... [https://www.nature.com/articles/s41698-025-00958-x]
- 21. Prognostic signature based on m6A-related lncRNAs to ... [https://www.nature.com/articles/s41598-022-07112-8]
- 22. The impact of ribosome association on lncRNA stability [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599250/]
- 23. m6A Modification in Non-Coding RNA: The Role in Cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8564146/]
- 24. The RNA N6-methyladenosine methylome coordinates ... [https://www.nature.com/articles/s41419-025-08045-6]
- 25. N6-Methyladenosine-Related lncRNAs Are Potential ... [https://pubmed.ncbi.nlm.nih.gov/35186011/]
- 26. N6-Methyladenosine-Related lncRNAs Are Potential ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.805607/full]
- 27. Prognostic Value of N6-Methyladenosine-Related lncRNAs ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8546174/]
- 28. m6A-related lncRNAs are potential biomarkers for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9472555/]
- 29. Identification of a novel m6A-related lncRNAs signature and ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-11885-8]
- 30. Identification and Validation of an m6A-Related LncRNA ... [https://www.por-journal.com/journals/pathology-and-oncology-research/articles/10.3389/pore.2022.1610536/full]
- 31. Identification and validation of N6-methyladenosine (m6A) [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2023.1292164/full]
- 32. TCGADownloadHelper: simplifying TCGA data extraction ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1569290/full]
- 33. TCGADownloadHelper: simplifying TCGA data extraction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12081331/]
- 34. GSE213115 - GEO Accession viewer - NIH [https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE213115]
- 35. based on GEO and TCGA databases [https://pmc.ncbi.nlm.nih.gov/articles/PMC12094959/]
- 36. Identification of progression related LncRNAs in colorectal ... [https://www.nature.com/articles/s41598-025-02096-7]
- 37. Differential expression analysis of lncRNA and mRNA in ... [https://www.frontiersin.org/journals/veterinary-science/articles/10.3389/fvets.2025.1614599/full]
- 38. Development of a Prognostic m6A-Related lncRNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12495916/]
- 39. Identification of m6A/m5C-related lncRNA signature for ... [https://www.nature.com/articles/s41598-024-58743-y]
- 40. Comprehensive analysis of N6-methylandenosine ... [https://www.sciencedirect.com/science/article/pii/S2162253121003103]
- 41. m6A-lncRNA landscape highlights reduced levels of m6A ... [https://molmed.biomedcentral.com/articles/10.1186/s10020-025-01254-x]
- 42. m6A RNA Modification: Technologies Behind Future Anti ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12566448/]
- 43. m6A Modification in Coding and Non-coding RNAs: Roles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7141420/]
- 44. Lasso-Cox Regression for Variable Selection in Survival ... [https://www.serdarbalci.com/jsurvival/articles/09-lassocox-comprehensive.html]
- 45. Unbiased Prediction and Feature Selection in High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4827277/]
- 46. Chapter 54 Supervised Statistical Learning Using Lasso ... [https://rforhr.com/lassoregression.html]
- 47. Why does my Lasso regression show that the lowest error is ... [https://stats.stackexchange.com/questions/259872/why-does-my-lasso-regression-show-that-the-lowest-error-is-achieved-with-0-varia]
- 48. Cross Validation in Machine Learning [https://www.geeksforgeeks.org/machine-learning/cross-validation-machine-learning/]
- 49. Tutorial: development of an online risk calculator platform [https://pmc.ncbi.nlm.nih.gov/articles/PMC5879507/]
- 50. Leveraging survival analysis and machine learning for ... [https://www.nature.com/articles/s41598-025-87622-3]
- 51. Time-dependent ROC curve analysis in medical research [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-017-0332-6]
- 52. Biomarker Validation Guide 2025: Discovery to FDA Approval [https://www.motif.bio/blog/biomarker-discovery-validation-guide-2025]
- 53. Biomarker Validation: Avoiding Misleading Results [https://www.fiosgenomics.com/biomarker-validation-avoiding-misleading-results/]
- 54. Multi-omics strategies for biomarker discovery and application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638490/]
- 55. Targeting m6A methylation for early diagnosis and precision ... [https://cancerci.biomedcentral.com/articles/10.1186/s12935-025-03923-7]
- 56. A review of machine learning methods for imbalanced data ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc00270b]
- 57. A Guide to Cross-Validation for Artificial Intelligence in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10388213/]
- 58. A Comprehensive Guide to Stratified K-Fold Cross ... [https://medium.com/@juanc.olamendy/a-comprehensive-guide-to-stratified-k-fold-cross-validation-for-unbalanced-data-014691060f17]
- 59. Stratified K Fold Cross Validation [https://www.geeksforgeeks.org/machine-learning/stratified-k-fold-cross-validation/]
- 60. A Guide to Nested Cross-Validation with Code Step by Step [https://medium.com/@cd_24/a-guide-to-nested-cross-validation-with-code-step-by-step-6a8ad06d5af2]
- 61. A step by step guide to Nested Cross-Validation [https://www.analyticsvidhya.com/blog/2021/03/a-step-by-step-guide-to-nested-cross-validation/]
- 62. Practical Considerations and Applied Examples of Cross ... [https://ai.jmir.org/2023/1/e49023]
- 63. Identification of an m6A-Related Long Noncoding RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9326028/]
- 64. Identification and Validation of a Prognostic Prediction ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2021.784553/full]
- 65. The m6A modification of LncRNA LINC00200 regulated by ... [https://celldiv.biomedcentral.com/articles/10.1186/s13008-025-00155-z]
- 66. 4 Techniques to Handle Imbalanced Datasets [https://www.knime.com/blog/4-techniques-handle-imbalanced-datasets]
- 67. ⭐ Class Imbalance in Machine Learning — The Complete ... [https://medium.com/@dewasheesh.rana/class-imbalance-in-machine-learning-the-complete-2025-guide-with-code-math-visuals-best-731edc76fd1c]
- 68. How to Handle Imbalanced Data? [https://www.analyticsvidhya.com/blog/2021/06/5-techniques-to-handle-imbalanced-data-for-a-classification-problem/]
- 69. Imbalanced Data | Peter Lorenz - GitHub Pages [https://lorenz-peter.github.io/blog/2025/imbalanced-data/]
- 70. Predicting lncRNA and disease associations with graph ... [https://www.nature.com/articles/s41598-025-03269-0]
- 71. How to make your code reproducible? [https://odissei-data.nl/2025/10/03/how-to-make-your-code-reproducible/]
- 72. Advanced R: R for Reproducibility: Good Practices [https://bham-carpentries.github.io/2025-03-11-r-advanced/02-good-practices.html]
- 73. Troubleshooting & FAQs [https://www.cygnustechnologies.com/resources/guidelines?srsltid=AfmBOopHQfPx9fH-KVAfbkoJgwK74dwbUKHDvOloMTLrLbtgmmjCttQE]
- 74. Data Reproducibility and other Data Lake Best Practices [https://lakefs.io/blog/reproducibility/]
- 75. A new risk model based on a 11-m6A-related lncRNA ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-021-09062-2]
- 76. N6-Methyladenosine-Related lncRNA Signature Predicts ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8472391/]
- 77. RNA methylated long non-coding RNAs as potential ... [https://link.springer.com/article/10.1007/s12672-025-02693-y]
- 78. Identification of a novel m5C/m6A-related gene signature ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.990623/full]
- 79. Development and validation of a prognostic nomogram for ... [https://pubmed.ncbi.nlm.nih.gov/40313943/]
- 80. A prognostic nutritional index-based nomogram for ... [https://www.frontiersin.org/journals/nutrition/articles/10.3389/fnut.2025.1680287/full]
- 81. Link between m6A modification and infiltration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10903232/]
- 82. Correlations Between Tumor Mutation Burden and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7921807/]
- 83. Immune Infiltration in Gastric Cancer Microenvironment ... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2021.762029/full]
- 84. Exploration of the relationship between tumor mutation ... [https://www.medsci.org/v18p0685.htm]
- 85. m6A-lncRNA landscape highlights reduced levels of m6A ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085027/]
- 86. Development of a m6A- and ferroptosis-related LncRNA ... [https://bmccancer.biomedcentral.com/articles/10.1186/s12885-025-13974-8]
- 87. Identification and Validation of the lncRNA MYOSLID as a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9496742/]
- 88. Establishment and validation of lncRNA-related prognostic ... [https://www.sciencedirect.com/science/article/pii/S0888754323000654]
- 89. Discovery and Validation of Clinically Relevant Long Non- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9405614/]
- 90. Approaches for Identifying LncRNA-Associated Proteins ... [https://www.mdpi.com/2813-3137/3/3/27]
- 91. Identification, functional prediction, and key lncRNA ... [https://www.nature.com/articles/s41598-020-57451-7]