Revolutionizing Hematologic Diagnostics: A Comprehensive Analysis of NGS vs. Traditional Methods in Acute Leukemia
Next-generation sequencing (NGS) is fundamentally transforming the diagnostic landscape for acute leukemia, offering unprecedented resolution into the genetic architecture of these heterogeneous malignancies.
Revolutionizing Hematologic Diagnostics: A Comprehensive Analysis of NGS vs. Traditional Methods in Acute Leukemia
Abstract
Next-generation sequencing (NGS) is fundamentally transforming the diagnostic landscape for acute leukemia, offering unprecedented resolution into the genetic architecture of these heterogeneous malignancies. This article provides a comprehensive analysis for researchers and drug development professionals, exploring how NGS surpasses traditional cytogenetics and molecular methods in detecting cryptic fusions, guiding risk stratification, and enabling measurable residual disease (MRD) monitoring. We examine the technical foundations of both approaches, present validated clinical applications across ALL and AML, address implementation challenges including data interpretation and cost considerations, and provide evidence-based comparisons of diagnostic yield. The integration of NGS into diagnostic workflows represents a paradigm shift toward precision medicine, with significant implications for therapeutic development and clinical trial design in hematologic oncology.
The Evolving Diagnostic Landscape: From Morphology to Molecular Precision in Acute Leukemia
The diagnosis of acute leukemia has long relied on a multi-modal approach, with cytomorphology and cytochemistry serving as the foundational first steps in the diagnostic workflow. For decades, these techniques have provided the initial evidence of malignant transformation, guiding subsequent confirmatory testing. While technological advancements have introduced powerful genomic tools like next-generation sequencing (NGS), the microscopic examination of blood and bone marrow specimens remains indispensable for initial diagnosis and classification. This review objectively compares the performance characteristics, applications, and limitations of these traditional cornerstone techniques against emerging molecular methodologies within the integrated diagnostic paradigm for acute leukemia.
The contemporary diagnostic framework for acute leukemia increasingly incorporates artificial intelligence (AI) for image analysis and leverages NGS for comprehensive genomic profiling [1] [2]. These advancements are transforming a field once dominated by manual microscopic review. However, the initial recognition of leukemia still fundamentally depends on the accurate morphological identification of blast cells and their differentiation from normal hematopoietic precursors [2]. This analysis evaluates how traditional and modern techniques complement each other, providing researchers and clinicians with a clear comparison of their respective roles in precision diagnostics.
Traditional Diagnostic Cornerstones: Technical Foundations and Workflows
Cytomorphology: The First Line of Identification
Cytomorphology represents the most fundamental diagnostic procedure in the evaluation of suspected leukemia [3]. The process begins with the preparation of peripheral blood smears (PBS) and bone marrow smears (BMS), which are stained—typically with May-Grünwald-Giemsa or Wright-Giemsa—to reveal cellular details [2]. Microscopic examination then focuses on assessing cell size, nuclear-to-cytoplasmic ratio, nuclear chromatin pattern, nucleoli presence and characteristics, and cytoplasmic granulation [3].
In acute leukemias, blasts are typically characterized by increased cell size, a high nucleocytoplasmic ratio, prominent nucleoli, reduced cytoplasmic volume, and abnormal granule distribution [2]. The diagnostic threshold for acute myeloid leukemia (AML) is generally set at ≥20% blasts in the bone marrow or peripheral blood, according to the World Health Organization (WHO) classification, though specific genetic abnormalities can define AML even with lower blast percentages [2]. A critical limitation of morphological assessment is its dependence on experienced hematologists and its susceptibility to inter-observer variability, with diagnostic error rates in morphological assessments reportedly as high as 40% [2].
Table 1: Standard Staining Methods in Leukemia Cytomorphology and Cytochemistry
| Staining Method | Primary Application | Key Diagnostic Features | Limitations |
|---|---|---|---|
| May-Grünwald-Giemsa/Wright-Giemsa | General morphology assessment | Nuclear chromatin pattern, cytoplasmic basophilia, granulation, nucleoli | Cannot identify lineage-specific enzymes |
| Myeloperoxidase (MPO) | Myeloid lineage confirmation | Dark cytoplasmic granules in myeloid cells | Negative in immature blasts and monocytic cells |
| Sudan Black B (SBB) | Myeloid lineage confirmation | Stains phospholipids and sterols in granules of myeloid cells | Similar staining pattern to MPO but less specific |
| Periodic Acid-Schiff (PAS) | Erythroid and megakaryocytic differentiation | Block-like positivity in erythroblasts in ALL | Can be positive in other cell types |
| Non-Specific Esterase (NSE) | Monocytic differentiation | Diffuse cytoplasmic staining in monocytic cells | Inhibited by sodium fluoride |
Cytochemistry: Lineage Assignment and Subclassification
Cytochemical staining builds upon morphological assessment by detecting specific intracellular enzymes and substrates that enable lineage assignment. These reactions are crucial for distinguishing between acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL), and for further classifying AML subtypes [4]. The most established cytochemical stains include myeloperoxidase (MPO) for myeloid lineage, Sudan Black B (SBB) with a similar application, and non-specific esterase (NSE) for monocytic differentiation [4].
The experimental protocol for cytochemical analysis requires standardized conditions to ensure reproducible results. For MPO staining, air-dried blood or bone marrow smears are fixed in formalin-ethanol and incubated with a substrate solution containing hydrogen peroxide and benzidine derivative. Myeloid cells exhibit dark cytoplasmic granules due to peroxidase activity. For NSE staining, smears are fixed in formalin vapor and incubated with alpha-naphthyl acetate as substrate at pH 6.3; monocytic cells show diffuse cytoplasmic staining inhibited by sodium fluoride [4]. The entire staining and interpretation process typically requires 2-4 hours per sample, providing relatively rapid results compared to more complex immunophenotypic or molecular methods.
Performance Comparison: Traditional vs. Modern Diagnostic Techniques
Diagnostic Accuracy and Turnaround Time
When evaluating diagnostic techniques, performance metrics including sensitivity, specificity, turnaround time, and applicability across leukemia subtypes provide critical comparison parameters. Cytomorphology and cytochemistry offer rapid assessment but with limitations in sensitivity and objectivity compared to advanced methodologies.
Table 2: Performance Comparison of Diagnostic Techniques in Acute Leukemia
| Parameter | Cytomorphology/Cytochemistry | Multiparameter Flow Cytometry | Next-Generation Sequencing |
|---|---|---|---|
| Analytical Turnaround Time | 2-4 hours [2] | 4-6 hours [5] | 24-72 hours [3] [6] |
| Sensitivity for Blast Detection | ~60% (highly operator-dependent) [2] | 1 in 10^4 (10⁻⁴) [5] | 1 in 10^6 (10⁻⁶) for MRD [5] [7] |
| Lineage Assignment Accuracy | 70-80% (with cytochemistry) [4] | >95% [4] | Indirect through mutation patterns |
| Subclassification Capability | Basic (FAB classification) | Intermediate (immunologic subtypes) | High (molecular subtypes) |
| Operator Dependency | High (error rate up to 40%) [2] | Moderate (requires expertise) [5] | Low (automated pipelines) |
| Capital Equipment Cost | Low | Moderate | High |
Comprehensive Genomic Profiling via NGS
Next-generation sequencing represents the most technologically advanced approach for leukemia diagnosis and classification. NGS enables massive parallel sequencing of thousands of genes in a single test, simultaneously detecting single nucleotide variants, insertions/deletions, copy-number alterations, and structural variants including balanced rearrangements [8]. The experimental protocol involves DNA extraction from peripheral blood or bone marrow aspirates, library preparation with fragmentation and adapter ligation, followed by massive parallel sequencing and complex bioinformatic analysis [4].
Targeted NGS panels have emerged as the preferred clinical application, focusing on genes with established diagnostic, prognostic, and therapeutic relevance in acute leukemia [4]. The sensitivity of NGS depends on sequencing depth (coverage), with panel-based approaches typically targeting >1000x coverage, enabling detection of variants with ~5% variant allele frequency (VAF) [4]. For measurable residual disease (MRD) monitoring, NGS offers exceptional sensitivity down to 10⁻⁶, significantly surpassing the capabilities of morphology (5% sensitivity) and flow cytometry (10⁻⁴ sensitivity) [5] [7].
Long-read sequencing technologies, such as Oxford Nanopore platforms, further expand diagnostic capabilities by enabling real-time genomic characterization. Recent studies demonstrate that adaptive sampling whole genome sequencing can identify driving alterations in pediatric acute leukemia in as little as 15 minutes for karyotype abnormalities and up to 6 hours for complex structural variants [6]. This represents a dramatic reduction from the 24-72 hours typically required for short-read NGS approaches [3].
Integrated Diagnostic Workflows: From Microscopy to Precision Medicine
The modern diagnosis of acute leukemia employs an integrated workflow that begins with traditional techniques and progresses through increasingly specialized molecular analyses. This sequential approach maximizes both efficiency and diagnostic accuracy.
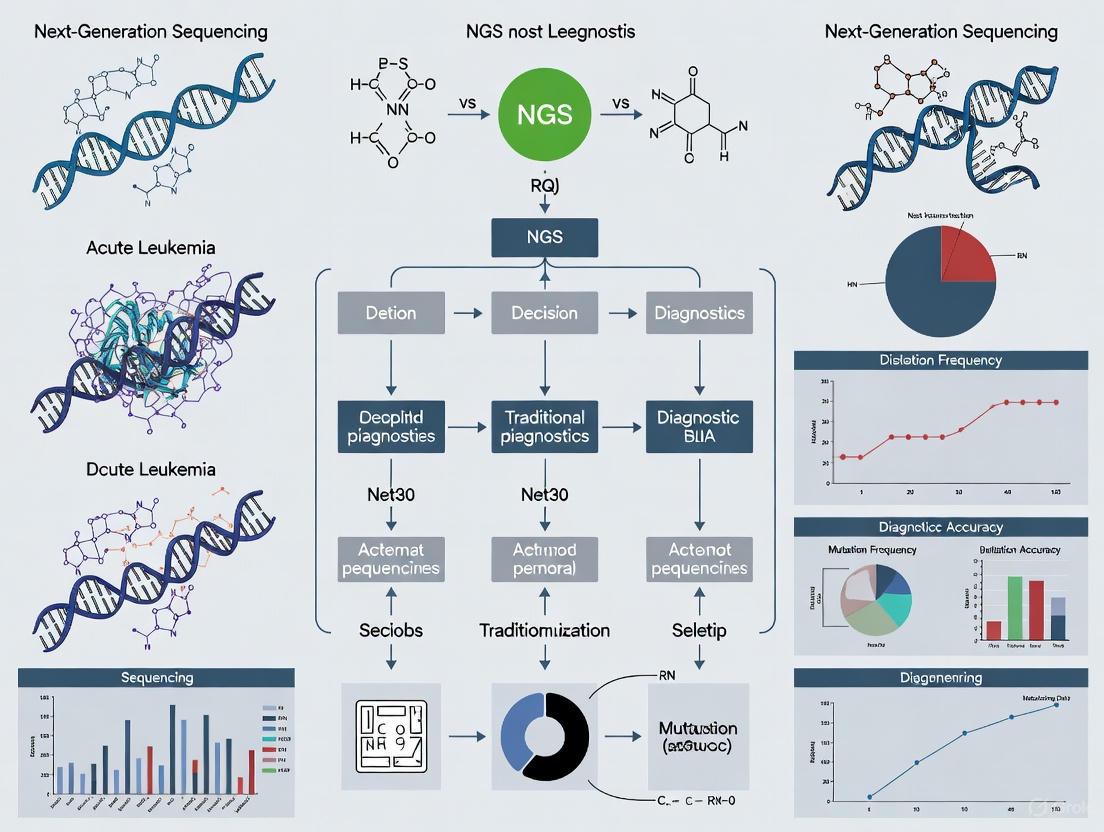
Diagram 1: Integrated Diagnostic Workflow for Acute Leukemia (Max Width: 760px)
The Research Toolkit: Essential Reagents and Technologies
Table 3: Essential Research Reagents and Solutions for Leukemia Diagnostics
| Reagent/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Morphological Stains | May-Grünwald-Giemsa, Wright-Giemsa | Cellular visualization and differential counting | Standardized staining protocols essential for consistency |
| Cytochemical Stains | MPO, SBB, NSE, PAS | Lineage determination and FAB classification | Requires positive and negative controls for validation |
| Flow Cytometry Antibodies | CD45, CD34, CD33, CD13, CD19, CD3 | Immunophenotyping and blast characterization | 8+ color panels now standard for comprehensive analysis |
| NGS Library Prep Kits | Illumina DNA Prep, Swift Accel AML | Target enrichment and library construction | Unique dual indexing reduces index hopping |
| NGS Hybridization Panels | Custom myeloid/lymphoid panels | Targeted sequencing of relevant genes | Panels typically cover 50-200 genes with >1000x coverage |
| Bioinformatic Tools | GATK, ClinVar, COSMIC, IGV | Variant calling and annotation | AI-assisted pathogenicity prediction emerging |
Cytomorphology and cytochemistry remain indispensable initial diagnostic procedures for acute leukemia, providing rapid assessment that guides subsequent testing. Their strengths lie in low cost, rapid turnaround, and ability to survey the complete cellular landscape. However, these traditional techniques demonstrate significant limitations in sensitivity, objectivity, and molecular resolution when compared to modern methodologies.
The integration of AI for image analysis and the application of NGS for comprehensive genomic profiling represent transformative advancements in leukemia diagnostics. NGS-based approaches provide unparalleled sensitivity for MRD detection and enable precision medicine through identification of therapeutic targets. Rather than rendering traditional methods obsolete, these technological advancements have redefined their role within a sophisticated diagnostic ecosystem where each technique contributes unique, complementary information. The future of leukemia diagnosis lies not in replacement of traditional methods, but in their intelligent integration with genomic technologies to provide comprehensive diagnostic insights that guide targeted therapeutic interventions.
Multiparameter Flow Cytometry for Immunophenotyping and Lineage Assignment
Accurate diagnosis and classification of acute leukemia are fundamental to selecting appropriate therapy and predicting patient outcomes. This process traditionally relied on morphological examination, but the inherent limitations of morphology have necessitated more precise technologies. Multiparameter flow cytometry (MFC) has emerged as a cornerstone technology for immunophenotyping and lineage assignment in leukemia diagnosis by enabling the simultaneous measurement of multiple physical and chemical characteristics of individual cells as they flow past lasers in a focused fluid stream [9]. Within the context of modern hematopathology, MFC must now be evaluated alongside next-generation sequencing (NGS) technologies, which offer deep insights into the genetic underpinnings of disease. The central thesis of this guide is that while NGS provides unparalleled genetic characterization, MFC delivers rapid, functional immunophenotypic data at the single-cell level, and the two technologies are often complementary rather than mutually exclusive in acute leukemia diagnostics [10].
The critical importance of lineage assignment was highlighted in a study of 100 acute leukemia cases, where immunophenotyping by MFC significantly changed the lineage diagnosis compared to morphology alone in 16% of cases (p<0.001) [11]. This reclassification has direct therapeutic implications, as misdirected therapy based on inaccurate lineage assignment can lead to poor outcomes. Meanwhile, the detection of minimal residual disease (MRD) has emerged as a powerful prognostic indicator, with studies demonstrating that MRD levels at specific treatment timepoints strongly predict relapse risk in both acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML) [12] [10]. This comparison guide will objectively evaluate the performance of MFC against alternative technologies, particularly NGS, focusing on their respective roles in immunophenotyping, lineage assignment, and MRD detection within acute leukemia research and diagnosis.
Principles of Multiparameter Flow Cytometry
Multiparameter flow cytometry operates on the principle of hydrodynamic focusing to guide cells single-file past one or multiple laser beams. As cells intersect with these lasers, they scatter light and emit fluorescence from conjugated antibodies, providing rich data on cell size, granularity, and the presence of specific surface and intracellular markers [9]. Modern flow cytometers can simultaneously detect up to 20-30 parameters per cell, enabled by advances in laser technology, fluorescent dye chemistry, and optical detection systems [9]. The strength of MFC lies in its ability to rapidly analyze thousands of cells per second, providing quantitative data on heterogeneous cell populations within a sample.
For immunophenotyping, fluorochrome-conjugated antibodies are used to probe well-characterized molecules that serve as biomarkers associated with particular cell types in normal or disease states [9]. The simultaneous measurement of multiple fluorescence parameters allows detailed analyses of co-expressed structural, receptor, signaling, and effector molecules. In the context of leukemia, this enables the identification of leukemia-associated immunophenotypes (LAIPs)—abnormal patterns of antigen expression that deviate from normal hematopoietic progenitors [10]. These alterations can include overexpression or underexpression of antigens normally present, asynchronous expression of markers typically restricted to specific developmental stages, or aberrant expression of lineage-inappropriate antigens [10].
Key Methodologies for MFC in Leukemia Diagnostics
Sample Preparation and Staining Protocols
Proper sample preparation is critical for reliable MFC results. Bone marrow or peripheral blood samples are typically collected with anticoagulants such as heparin or EDTA. For the standardized EuroFlow method used in multiple myeloma MRD detection, a lyse-wash-and-stain sample preparation protocol is employed, measuring high numbers of cells (≥5×10⁶ cells/tube) to achieve sensitive detection of rare cell populations [13]. The staining process involves incubating cells with antibody panels under optimized conditions—typically room temperature for 30 minutes in the dark—followed by washing steps to remove unbound antibody [14] [15].
For intracellular antigen detection, such as phosphorylated signaling proteins or cytoplasmic immunoglobulins, cells must first be fixed and permeabilized using specialized buffers. The optimization of these protocols is challenging, as many buffers used for intracellular epitope detection can adversely affect surface marker staining [9]. As noted in salivary gland research, permeabilization with 100 μL BD Phosflow Perm Buffer II (64.9% methanol) for 30 minutes at -20°C, followed by intracellular antibody staining overnight at 4°C, has proven effective for preserving both surface and intracellular epitopes [14].
Instrument Setup and Quality Control
Robust instrument setup and quality control procedures are essential for generating reproducible MFC data. The voltage walk method is recommended for determining the minimum voltage requirement (MVR) for each detector, allowing clear resolution of dim fluorescent signals from background noise [15]. This process involves running dimly fluorescent beads at increasing voltage settings and plotting the coefficient of variation (CV) against the voltages to identify the optimal setting.
Antibody titration is another critical optimization technique for multiparameter flow cytometry, helping to minimize nonspecific binding and increase signal detection [15]. As illustrated in Figure 2 of the best practices guide, performing serial 2-fold dilutions from the manufacturer's recommended concentration and plotting the stain index (SI) helps identify either a separating concentration (providing greatest difference between positive and negative cells) or a saturating concentration (required for low-abundance antigens) [15]. Appropriate controls, including fluorescence minus one (FMO) controls, compensation controls, and viability controls, are indispensable for accurate data interpretation in multiparameter panels [15].
Next-Generation Sequencing Methodologies
In contrast to MFC's protein-focused approach, NGS technologies sequence DNA or RNA to identify genetic alterations in leukemia cells. For MRD detection, the ImmunoSEQ platform (Adaptive Biotechnologies) can be used to sequence immunoglobulin or T-cell receptor genes, tracking malignant clones based on their unique receptor rearrangements [13]. Sample processing for NGS involves nucleic acid extraction, library preparation, target enrichment or amplification, and sequencing on platforms such as Illumina or Ion Torrent systems [16]. The analytical sensitivity of NGS-based MRD detection depends on sequencing depth, with deeper sequencing enabling more sensitive detection of rare clones.
Performance validation of NGS assays requires demonstrating analytical sensitivity (detection limit), analytical specificity, and accuracy using well-characterized reference materials [16]. For qualitative detection, verification requires at least 5 negative and 10 positive samples (including weak positives), with expected 100% positive and negative agreement [16]. The validation process must also establish the linear range, precision, and reference intervals for the assay.
Comparative Performance Analysis
Lineage Assignment in Acute Leukemia
The accurate determination of lymphoid versus myeloid lineage is a critical first step in acute leukemia management, as it dictates fundamentally different treatment approaches. The comparative performance of MFC versus morphology and NGS in this domain reveals distinct advantages and limitations for each technology.
Table 1: Comparison of Technologies for Acute Leukemia Lineage Assignment
| Technology | Methodology | Turnaround Time | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Morphology | Microscopic examination of stained cells | Hours (after processing) | Low cost, rapid assessment of cell structure | Subjective interpretation, limited accuracy |
| Multiparameter Flow Cytometry | Detection of surface and intracellular proteins using antibody panels | 4-6 hours | High accuracy for lineage assignment, rapid results, detects aberrant immunophenotypes | Limited to known protein targets |
| Next-Generation Sequencing | Detection of genetic alterations (mutations, fusions) | Days to weeks | Identifies therapeutic targets, prognostic markers | Does not directly assess protein expression |
A direct comparison study of 100 acute leukemia cases demonstrated the superior accuracy of MFC over morphology alone. While morphology established lineage in all cases, MFC significantly reclassified lineage assignment in 16% of cases (p<0.001) [11]. In 8 cases, what was initially classified as myeloid by morphology was reclassified as lymphoid by MFC, while another 8 cases originally called lymphoid were reclassified as myeloid [11]. This reclassification has profound clinical implications, as it directly determines whether a patient receives lymphoid-directed or myeloid-directed chemotherapy.
NGS contributes to lineage assessment indirectly by identifying genetic alterations characteristic of specific lineages, such as the RUNX1-RUNX1T1 fusion in AML or ETV6-RUNX1 in ALL. However, NGS does not directly assess protein expression and thus cannot replace MFC for immunophenotypic lineage assignment. Instead, the integration of MFC and genetic methods provides the most comprehensive diagnostic picture.
Minimal Residual Disease Detection
MRD detection has emerged as one of the most powerful prognostic factors in acute leukemia, with both MFC and NGS offering sensitive approaches for detecting submicroscopic disease.
Table 2: Comparison of MRD Detection Performance Between MFC and NGS
| Parameter | Multiparameter Flow Cytometry | Next-Generation Sequencing |
|---|---|---|
| Analytical Sensitivity | Typically 0.001%-0.01% (10⁻⁴ to 10⁻⁵) [10] [13] | Can exceed 0.0001% (10⁻⁶) with sufficient sequencing depth [13] |
| Applicability | >90% of AML cases [10] | Virtually 100% for B-ALL with immunoglobulin receptor targets |
| Key Strengths | Rapid turnaround, functional protein data, widely available | High sensitivity, clonal tracking ability, standardized quantification |
| Key Limitations | Requires fresh samples, expertise-dependent analysis | Higher cost, longer turnaround, complex bioinformatics |
In B-cell acute lymphoblastic leukemia (B-ALL), MFC-based MRD monitoring at specific timepoints provides powerful prognostic information. A study of 153 pediatric B-ALL patients found that MRD levels ≥1×10⁻³ at day 33 of induction therapy were associated with significantly lower 3-year relapse-free survival (RFS) rates (33.0% vs 89.3%, P=0.000) [12]. Similarly, at day 84, MRD ≥1×10⁻⁴ was associated with higher relapse rates (41.7% vs 13.0%, P=0.022) [12]. These findings demonstrate the clinical utility of MFC-MRD monitoring for risk stratification.
In core binding factor acute myeloid leukemia (CBF-AML), direct comparisons between MFC and molecular methods reveal a more complex relationship. One study of 93 CBF-AML patients found only weak agreement between MFC and quantitative RT-PCR (qRT-PCR) during consolidation therapy (κ=0.083) and maintenance/follow-up (κ=0.164) [10]. Notably, in cases with intermediate qRT-PCR results (0.1-10%), MFC provided additional prognostic value for relapse prediction (P=0.006) [10], suggesting complementary roles for the two technologies.
In multiple myeloma, a comparison of 8-color MFC (EuroFlow method) and NGS for MRD detection in autografts found that NGS offered higher sensitivity, detecting MRD in 82% of cases versus 55% by MFC [13]. While there was a correlation between MRD levels measured by both methods, only NGS-negative cases showed a trend toward better progression-free survival (P=0.114), suggesting superior prognostic value for NGS in this specific context [13].
Figure 1: Comparative MRD Detection Workflow Using MFC and NGS
Comprehensive Diagnostic Profiling
The most advanced diagnostic approaches for acute leukemia integrate multiple technologies to achieve comprehensive disease characterization. MFC excels at providing rapid immunophenotypic profiling, while NGS offers deep genetic characterization. The evolving diagnostic paradigm leverages the respective strengths of each technology.
Immunophenotypic profiling by MFC typically employs standardized antibody panels tailored to specific clinical questions. For example, the EuroFlow consortium has developed optimized 8-color, 2-tube antibody panels for multiple myeloma MRD detection that include markers such as CD138, CD27, CD38, CD56, CD45, CD19, CD117, CD81, and cytoplasmic immunoglobulin light chains [13]. Similarly, for CBF-AML, comprehensive 8-color panels incorporate markers including CD7, CD33, CD19, CD34, CD13, CD38, CD45, HLA-DR, CD117, CD4, CD123, and others to identify aberrant immunophenotypes [10].
Genetic profiling by NGS can identify mutations with prognostic and therapeutic significance, such as TP53, FLT3, NPM1, and IDH1/2 in AML. The integration of immunophenotypic and genetic data enables more precise risk stratification and therapeutic selection than either approach alone.
Essential Reagents and Research Solutions
Successful implementation of MFC for leukemia immunophenotyping requires access to high-quality reagents and standardized protocols. The following research toolkit outlines essential components for robust MFC analysis.
Table 3: Research Reagent Solutions for Leukemia Immunophenotyping
| Reagent Category | Specific Examples | Function and Application |
|---|---|---|
| Fluorochrome-Conjugated Antibodies | CD45-V500, CD38-FITC, CD10-PE, CD20-PE-Cy7, CD19-APC, CD34-PerCP-cy5.5, CD33-BV421 [12] | Cell identification and lineage determination |
| Viability Dyes | LIVE/DEAD Fixable Violet Dead Cell Stain [15] | Exclusion of dead cells to reduce non-specific binding |
| Sample Preparation Reagents | BD Cytofix Fixation Buffer, BD Phosflow Perm Buffer II [14] | Cell fixation and permeabilization for intracellular staining |
| Cell Separation Kits | MojoSort Human CD45 Selection Kit [14] | Immune cell enrichment from complex tissues |
| Standardization Tools | BD Quantibrite Beads [9] | Quantitation of cell-surface marker expression |
| Tissue Dissociation Kits | Human Multi Tissue Dissociation Kit [14] | Preparation of single-cell suspensions from solid tissues |
The careful selection and titration of fluorochrome-conjugated antibodies is particularly critical for panel performance. As noted in best practices guides, bright fluorophores should be paired with antibodies for low-abundance targets, while dimmer fluorophores are suitable for highly expressed antigens [15]. This strategy helps minimize spillover spreading and optimizes resolution of dim populations. Antibody titration is essential for identifying the optimal concentration that provides clear separation between positive and negative populations while conserving reagent and minimizing background [15].
For specialized applications such as analysis of signaling pathways, additional reagents for intracellular staining are required. Studies of Sjögren's Disease minor salivary glands, for example, successfully detected phosphorylated interferon regulatory factor 3 (IRF3) and nuclear factor-kappa B (NF-κB) following methanol-based permeabilization and overnight antibody incubation at 4°C [14]. Similar approaches can be adapted for leukemia signaling studies.
Figure 2: Technology Integration in Leukemia Diagnostics
Multiparameter flow cytometry remains an indispensable technology for immunophenotyping and lineage assignment in acute leukemia diagnosis. Its strengths include rapid turnaround, ability to analyze protein expression at single-cell resolution, and widespread availability in clinical laboratories. The evidence demonstrates that MFC significantly improves diagnostic accuracy over morphology alone, with 16% of cases being reclassified upon immunophenotypic analysis [11]. For MRD monitoring, MFC provides clinically actionable information at multiple treatment timepoints, with specific thresholds (e.g., ≥1×10⁻³ at day 33) showing significant prognostic value in B-ALL [12].
While NGS technologies offer superior sensitivity for MRD detection in some contexts [13] and unparalleled ability to identify genetic alterations, they complement rather than replace MFC in the diagnostic workflow. In CBF-AML, for example, MFC and molecular methods show only weak agreement, with MFC providing prognostic value particularly in cases with intermediate qRT-PCR results [10]. This suggests that these technologies capture different biological aspects of residual disease.
The future of leukemia diagnostics lies in the intelligent integration of multiple technologies, leveraging the respective strengths of MFC for immunophenotyping and NGS for genetic characterization. Standardized 8-color MFC protocols such as the EuroFlow method enhance reproducibility across laboratories [13], while ongoing developments in mass cytometry and spectral flow cytometry promise even higher parameter analysis. For researchers and clinicians, the optimal approach involves selecting technology combinations based on specific clinical questions, available resources, and the need for rapid versus comprehensive diagnostic information. As both technologies continue to evolve, their synergistic application will undoubtedly advance our understanding and management of acute leukemia.
The diagnosis and risk stratification of acute leukemia have long relied on conventional cytogenetic techniques to identify chromosomal abnormalities that drive disease pathogenesis and progression. Karyotyping and Fluorescence In Situ Hybridization (FISH) represent two foundational methods in the cytogeneticist's toolkit, providing complementary insights into the genomic landscape of hematologic malignancies [17]. While next-generation sequencing (NGS) technologies are increasingly transforming diagnostic paradigms, traditional cytogenetic methods remain clinically indispensable for detecting chromosomal abnormalities in acute leukemia [18] [19]. This guide provides a comprehensive comparative analysis of karyotyping and FISH, examining their technical principles, performance characteristics, and clinical applications within the evolving context of modern genomic medicine. Understanding the relative strengths and limitations of these established techniques is paramount for researchers and clinicians navigating the complex genetic landscape of acute leukemia and optimizing diagnostic workflows in the NGS era.
Technical Principles and Methodologies
Karyotyping: Macroscopic Genomic Analysis
Karyotyping is a classical cytogenetic technique that provides a macroscopic overview of the entire genome, allowing for the simultaneous assessment of chromosomal number and structure. The standard workflow begins with cell culture, where viable cells from bone marrow or blood samples are stimulated to proliferate and arrested during metaphase, the stage of cell division where chromosomes are most condensed and visible [17]. These metaphase cells are then harvested, fixed on slides, and subjected to banding techniques—most commonly G-banding using Giemsa stain—which produces a characteristic pattern of light and dark bands unique to each chromosome type [17]. The stained chromosomes are visualized under a microscope, captured digitally, and systematically arranged into a karyogram based on their size, banding pattern, and centromere position for analysis. This process enables the detection of numerical abnormalities (aneuploidy) and large-scale structural rearrangements including translocations, deletions, duplications, and inversions, typically at a resolution of 5-10 megabases [20]. A significant limitation of this technique is its requirement for viable, actively dividing cells and the expertise needed for complex interpretation.
FISH: Targeted Molecular Cytogenetics
Fluorescence In Situ Hybridization (FISH) represents a molecular cytogenetic approach that bridges the gap between traditional karyotyping and modern molecular genetics. This technique utilizes fluorescently labeled DNA probes that are complementary to specific chromosomal sequences or genes of interest [17]. The FISH protocol involves preparing interphase or metaphase cells on slides, denaturing both the chromosomal DNA and the probes to create single-stranded DNA, and allowing the probes to hybridize to their complementary target sequences. After washing away unbound probe, the samples are visualized using a fluorescence microscope [21]. The presence, absence, or abnormal positioning of fluorescent signals reveals specific genetic abnormalities, including microdeletions, translocations, and aneuploidies, often at a much higher resolution than karyotyping—down to hundreds of kilobases depending on the probe design [21]. FISH can be performed on non-dividing (interphase) cells, circumventing the need for cell culture, and allows for the analysis of hundreds to thousands of cells to detect low-level mosaicism [22]. Various FISH adaptations exist, including multicolor FISH (mFISH) and spectral karyotyping (SKY), which enable the simultaneous visualization of all chromosomes using chromosome-specific painting probes [17].
Visualizing the Diagnostic Workflow
The following diagram illustrates the complementary roles of karyotyping, FISH, and NGS in a comprehensive diagnostic workflow for acute leukemia:
Performance Comparison and Experimental Data
Diagnostic Accuracy in Clinical Settings
Multiple studies have systematically compared the diagnostic performance of karyotyping and FISH across various hematologic malignancies. In acute lymphoblastic leukemia (ALL), both techniques demonstrate high reciprocal agreement for detecting major prognostic translocations such as t(9;22)(BCR::ABL1), t(12;21)(TEL/AML1), and t(11q23)(MLL rearrangements) [18]. However, their sensitivities vary significantly for specific abnormalities. Karyotyping shows notably lower sensitivity (approximately 70-80%) for detecting the TEL-AML1 fusion gene, whereas FISH reliably identifies this rearrangement [18]. Similarly, in T-cell prolymphocytic leukemia (T-PLL), a comparative study of 69 patients found conventional karyotyping was abnormal in only 65% of cases and detected 14q32/TCL1 rearrangements in just 43%, while TCL1 rearrangement assessment by FISH was positive in 85% of cases [22]. This demonstrates FISH's superior sensitivity for identifying specific, clinically significant rearrangements that may be cryptic or missed by karyotyping alone.
Technical Performance Metrics
The table below summarizes key performance characteristics of karyotyping and FISH based on experimental data from clinical studies:
Table 1: Performance Comparison of Karyotyping and FISH in Leukemia Diagnostics
| Parameter | Karyotyping | FISH |
|---|---|---|
| Resolution | 5-10 Mb [20] | 100-500 kb (probe-dependent) [17] |
| Cell Requirement | Viable, actively dividing cells required [17] | Non-dividing (interphase) or metaphase cells [21] |
| Turnaround Time | 7-14 days (culture-dependent) [17] | 24-72 hours (minimal culture) [21] |
| Success Rate | ~86% (due to culture failure) [20] [23] | >95% (avoids culture issues) [23] |
| Abnormality Detection Scope | Genome-wide, unbiased screening [17] | Targeted analysis of specific loci [22] |
| Sensitivity for Specific Abnormalities | Variable (e.g., ~70-80% for TEL-AML1) [18] | High (>85% for most targeted abnormalities) [18] [22] |
| Mosaicism Detection | Limited to ~5-10% in metaphases | Can detect 1-5% in interphase nuclei [21] |
Complementary Diagnostic Value
Despite their individual limitations, karyotyping and FISH provide complementary information that enhances overall diagnostic accuracy. Karyotyping offers an unbiased genome-wide assessment that can reveal unexpected chromosomal abnormalities and provide a comprehensive view of the chromosomal landscape, including complex rearrangements [22]. Meanwhile, FISH delivers targeted, high-resolution analysis of specific genomic regions with enhanced sensitivity, making it particularly valuable for identifying cryptic abnormalities, monitoring minimal residual disease, and analyzing samples with low mitotic indices [18] [22]. This complementary relationship was demonstrated in a study of acute myeloid leukemia (AML) where the combination of cytogenetic analyses and targeted FISH markers yielded evaluable results in 91% of cases, with NGS enabling risk stratification in the remaining cases where conventional cytogenetics failed [23]. The integrated use of both techniques remains crucial because any detection of a significant chromosomal aberration, irrespective of the diagnostic mode, must be considered in therapy planning and risk assessment [18].
Experimental Protocols for Acute Leukemia Analysis
Standard Karyotyping Protocol for Bone Marrow Samples
The following detailed protocol is adapted from established clinical laboratory procedures for karyotypic analysis of acute leukemia samples [17]:
Sample Collection and Culture: Under aseptic conditions, collect 1-2 mL of bone marrow aspirate into sodium heparin tubes. Inoculate 0.5-1.0 mL of marrow into 10 mL of chromosome media containing phytohemagglutinin or other mitogens. Culture for 24-48 hours at 37°C in a 5% CO₂ incubator. For certain abnormalities with poor growth characteristics (e.g., monosomy 7), multiple cultures with different harvest times may be necessary.
Metaphase Arrest and Harvesting: Add colcemid (0.05 μg/mL final concentration) to the culture for 15-30 minutes to arrest cells in metaphase. Transfer cells to centrifuge tubes and pellet by centrifugation at 1200 rpm for 10 minutes. Carefully resuspend the cell pellet in pre-warmed 0.075 M KCl hypotonic solution and incubate for 20-30 minutes at 37°C. Fix cells by slowly adding 3:1 methanol:acetic acid fixative, then perform three additional fixative changes with 15-minute intervals.
Slide Preparation and Banding: Drop the fixed cell suspension onto clean, wet microscope slides and allow to air dry. Age slides overnight at 60°C or by artificial aging methods. Perform G-banding using trypsin-EDTA treatment followed by Giemsa staining. Optimize trypsin exposure time to achieve optimal banding resolution (typically 350-400 bands per haploid genome).
Microscopy and Karyotype Analysis: Screen slides under low magnification to identify well-spread metaphase cells with minimal chromosome overlap. Capture 20-30 metaphase images using an automated cytogenetics imaging system. Analyze each metaphase for chromosomal number and structure. Arrange chromosomes into a standardized karyogram according to ISCN (International System for Human Cytogenetic Nomenclature) guidelines.
FISH Protocol for Leukemia-Associated Translocations
This protocol outlines the standard procedure for detecting common leukemia-associated translocations using locus-specific FISH probes [21]:
Slide Preparation and Denaturation: Select areas with adequate cellularity on fixed specimen slides. Dehydrate slides through an ethanol series (70%, 85%, 100%) for 2 minutes each and air dry. Denature chromosomal DNA by incubating slides in 70% formamide/2× SSC solution at 73°C for 5 minutes. Immediately dehydrate through cold ethanol series (70%, 85%, 100%) for 2 minutes each and air dry.
Probe Preparation and Hybridization: For each target area, prepare 10 μL of hybridization mixture containing 7 μL of LSI/WCP probe mixture, 2 μL of purified water, and 1 μL of DNA. Denature the probe mixture at 73°C for 5 minutes and pre-anneal at 37°C for 15-30 minutes. Apply denatured probe to the denatured slide target area, cover with a coverslip, and seal with rubber cement. Hybridize in a moist chamber at 37°C for 12-16 hours (overnight).
Post-Hybridization Washes and Detection: Remove coverslip and perform stringency washes in 0.4× SSC/0.3% NP-40 at 73°C for 2 minutes, followed by 2× SSC/0.1% NP-40 at room temperature for 1 minute. Air dry slides in darkness. Counterstain with 10-15 μL of DAPI/Antifade solution and apply coverslip.
Signal Enumeration and Interpretation: Analyze slides using a fluorescence microscope equipped with appropriate filter sets. Score a minimum of 200 interphase nuclei or 20 metaphase cells for specific signal patterns. For BCR::ABL1 fusion detection, for example, count cells showing juxtaposition of green (BCR) and red (ABL1) signals, indicating fusion. Establish normal cut-off values for false positives by analyzing control samples, typically setting the threshold at 1-5% depending on the probe type [21].
Essential Research Reagent Solutions
Successful implementation of karyotyping and FISH requires specific reagent systems optimized for hematologic malignancies. The following table details essential research reagents and their applications in leukemia cytogenetics:
Table 2: Essential Research Reagents for Leukemia Cytogenetics
| Reagent Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Cell Culture Media | Chromosome Medium P with phytohemagglutinin; RPMI-1640 with growth factors | Metaphase chromosome preparation | Optimize culture duration (24-72h) based on blast count; use multiple harvest times for complex abnormalities |
| Chromosome Banding Reagents | Trypsin-EDTA solution; Giemsa stain; Wright's stain | G-banding pattern generation | Titrate trypsin concentration (0.025-0.05%) for optimal banding resolution (350-400 bands) |
| FISH Probe Systems | LSI BCR/ABL ES Dual Color; LSI MLL Break Apart; CEP 8 SpectrumOrange | Detection of leukemia-specific translocations and aneuploidies | Validate each probe batch with positive and negative controls; establish laboratory-specific cut-off values |
| Hybridization Buffers | Formamide-based denaturation solutions; SSC wash buffers; NP-40 detergents | Stringency control in FISH | Maintain consistent pH (7.0-7.5) and temperature (±0.5°C) for reproducible stringency washes |
| Counterstains & Mounting Media | DAPI/Antifade; ProLong Diamond Antifade Mountant | Chromatin visualization and signal preservation | Use antifade mounting medium to prevent photobleaching during fluorescence microscopy |
Integration with Next-Generation Sequencing
The emergence of NGS technologies has transformed the diagnostic landscape for acute leukemia, yet conventional cytogenetics maintains a crucial role in comprehensive genomic assessment. Modern integrated approaches combine these methodologies to leverage their complementary strengths. A 2025 study on pediatric AML demonstrated that an integrated whole genome and whole transcriptome sequencing (iWGS-WTS) approach improved identification of clinically relevant genetic alterations while streamlining diagnostic workflows [24]. However, even with advanced NGS implementation, certain chromosomal abnormalities—particularly balanced translocations, complex rearrangements, and aneuploidies—remain readily detectable by conventional cytogenetics [24] [23].
In clinical practice, karyotyping continues to provide the initial genome-wide screen for chromosomal abnormalities, followed by targeted FISH analysis for specific prognostic markers and NGS for mutation profiling. This tiered approach maximizes diagnostic yield while conserving resources. Real-world data from an Austrian tertiary care center showed that while NGS successfully enabled risk stratification in cases where conventional karyotyping failed (due to dry taps or culture failure), the combination of cytogenetics and targeted FISH markers still provided critical structural information that complemented NGS findings [23]. The continuing evolution of diagnostic workflows suggests that rather than being replaced by NGS, conventional cytogenetics will increasingly be integrated with molecular methods to provide a comprehensive genomic profile that guides risk-adapted therapy in acute leukemia.
Karyotyping and FISH remain indispensable tools in the diagnostic workup of acute leukemia, each offering distinct advantages that continue to complement emerging genomic technologies. Karyotyping provides an unbiased genome-wide assessment of chromosomal integrity, while FISH delivers targeted, sensitive detection of specific prognostic markers. Their combined use, often in conjunction with NGS, creates a powerful diagnostic synergy that enhances abnormality detection, refines risk stratification, and informs therapeutic decisions. As precision medicine in hematologic malignancies continues to advance, the integration of conventional cytogenetics with molecular methods will remain fundamental to unraveling the complex genomic landscape of acute leukemia and optimizing patient outcomes.
Acute leukemias represent a heterogeneous group of hematologic malignancies characterized by uncontrolled proliferation of immature lymphoid or myeloid cells. The molecular revolution in hematology has fundamentally transformed our understanding of acute lymphoblastic leukemia (ALL) and acute myeloid leukemia (AML), revealing complex genetic landscapes that drive pathogenesis, prognosis, and therapeutic responses. Next-generation sequencing (NGS) has emerged as a powerful tool that surpasses conventional diagnostic approaches by providing comprehensive genomic profiling, enabling high-resolution detection of genetic mutations, clonal evolution, and resistance mechanisms [19]. This technological advancement has catalyzed a shift from morphology-based classifications to molecularly-driven diagnostic frameworks that integrate genetic abnormalities with clinical decision-making, ultimately paving the way for precision medicine in leukemia management.
The clinical integration of NGS presents both unprecedented opportunities and significant challenges. While conventional methods like cytomorphology, multiparameter flow cytometry (MFC), and cytogenetics remain fundamental to leukemia diagnosis, they offer limited resolution for detecting subtle genetic alterations that inform risk stratification and targeted treatment selection [25]. NGS technologies now enable the identification of molecular markers with prognostic significance, allowing for more refined classification systems and dynamic disease monitoring through measurable residual disease (MRD) assessment [26]. This comparative analysis examines the evolving roles of established and emerging diagnostic methodologies in elucidating the genetic drivers of ALL and AML, with particular emphasis on their technical capabilities, clinical applications, and performance characteristics in contemporary practice.
Traditional Diagnostic Methods: Established Approaches and Limitations
Conventional Techniques in Leukemia Diagnosis
The diagnostic workup for acute leukemias has historically relied on an integrated approach employing multiple complementary techniques. Cytomorphology serves as the foundational first step, providing rapid assessment of cellular morphology and enabling initial classification based on French-American-British (FAB) criteria [25] [2]. This method remains indispensable for diagnosing AML and differentiating it from other hematological neoplasms, though it suffers from significant inter-observer variability and limited sensitivity for genetic characterization. Multiparameter flow cytometry (MFC) adds critical immunophenotyping data, allowing for detection, characterization, and quantification of normal and malignant cell populations through surface and cytoplasmic antigen expression patterns [5] [25]. MFC also facilitates sensitive MRD monitoring by identifying aberrant immunophenotypic features of leukemic cells, with typical sensitivity reaching 10⁻⁴ [5].
Cytogenetic analysis through chromosome banding and fluorescence in situ hybridization (FISH) provides essential information about numerical and structural chromosomal alterations that define prognostically significant leukemia subtypes [19] [25]. These techniques identify critical biomarkers such as the Philadelphia chromosome in ALL [19] and various translocations in AML that guide risk stratification according to European LeukemiaNet (ELN) guidelines [25]. Molecular techniques including polymerase chain reaction (PCR) and quantitative PCR (qPCR) enable sensitive detection and quantification of specific genetic abnormalities, achieving sensitivities up to 10⁻⁶, making them particularly valuable for MRD assessment [25]. However, these targeted approaches require prior knowledge of specific mutations and cannot comprehensively profile the diverse genetic alterations present in acute leukemias.
Limitations of Conventional Approaches
Despite their established role in leukemia diagnostics, traditional methods present several significant limitations. Morphological evaluation depends heavily on experienced hematologists and is susceptible to subjective interpretation, with diagnostic error rates reportedly as high as 40% [2]. Flow cytometry results vary considerably across laboratories due to differences in detection protocols, antibody panel configurations, and analytical standards, compromising reproducibility [2]. While cytogenetics identifies clinically relevant chromosomal abnormalities, it requires cell culture and has limited resolution for detecting subtle structural variations and point mutations [19].
Molecular techniques like qPCR, though highly sensitive for known targets, have restricted applicability. In ALL, qPCR for immunoglobulin (Ig) and T-cell receptor (TCR) gene rearrangements is laborious and time-consuming, requiring 3-4 weeks for primer selection and analysis [5]. This approach also faces false-negative results due to clonal evolution during treatment. Similarly, qPCR for fusion gene transcripts has limited utility as over 50% of ALL cases lack detectable fusion genes tested standardly at diagnosis [5]. Even when detectable, quantification accuracy is affected by variability in RNA transcript numbers per leukemic cell [5]. These limitations collectively underscore the need for more comprehensive, efficient, and standardized diagnostic approaches capable of capturing the full genetic complexity of acute leukemias.
Table 1: Comparison of Traditional Diagnostic Methods in Acute Leukemia
| Method | Key Applications | Sensitivity | Turnaround Time | Major Limitations |
|---|---|---|---|---|
| Cytomorphology | Initial diagnosis, blast percentage quantification | ~5% (morphological) | 1-2 hours | Subjective interpretation, limited genetic information |
| Multiparameter Flow Cytometry | Immunophenotyping, MRD monitoring | 10⁻⁴ | 4-6 hours | Antigen shift during treatment, inter-laboratory variability |
| Cytogenetics/Karyotyping | Detection of chromosomal abnormalities | ~5% | 1-3 weeks | Requires cell culture, low resolution |
| PCR/qPCR | Specific mutation/fusion detection, MRD monitoring | 10⁻⁴ to 10⁻⁶ | 1-3 days | Limited to known targets, primer design challenges |
Next-Generation Sequencing: Technical Advancements and Applications
NGS Methodologies and Workflows
Next-generation sequencing represents a transformative approach that enables massive parallel sequencing of DNA or RNA fragments, providing unprecedented resolution for genetic characterization of hematologic malignancies [19]. The NGS workflow encompasses multiple standardized steps, beginning with nucleic acid extraction from patient specimens (typically peripheral blood or bone marrow aspirates), followed by library preparation through fragmentation, adapter ligation, and amplification [25]. Unique molecular identifiers (UMIs) may be incorporated during library preparation to distinguish true variants from PCR artifacts, enhancing detection accuracy [25]. Subsequent sequencing occurs on platforms such as Illumina MiSeq or NextSeq, generating millions to billions of short reads that are computationally aligned to reference genomes and analyzed through sophisticated bioinformatic pipelines for variant calling and annotation [25] [27].
The applications of NGS in leukemia diagnostics are diverse and can be tailored to specific clinical needs. Targeted gene panel sequencing represents the most widely implemented approach in clinical settings, focusing on curated sets of genes with established significance in leukemia pathogenesis, classification, or treatment [25]. These panels balance comprehensive coverage with practical considerations of cost, turnaround time, and data interpretation complexity. Whole-exome sequencing (WES) examines all protein-coding regions, while whole-genome sequencing (WGS) provides complete genomic coverage, including non-coding regions [25]. Whole-transcriptome sequencing (WTS) facilitates detection of fusion transcripts, expression profiling, and variant calling in transcribed regions [25]. Each approach offers distinct advantages, with targeted panels currently dominating routine clinical practice due to their cost-effectiveness and streamlined interpretation.
NGS Applications in Genetic Characterization
NGS has revolutionized our understanding of the molecular landscapes in both ALL and AML. In ALL, NGS panels frequently focus on sequencing immunoglobulin (IGH) and T-cell receptor (TCR) gene rearrangements to establish unique molecular fingerprints for each leukemic clone, enabling highly sensitive MRD monitoring [5]. Additionally, NGS detects recurrent genetic abnormalities with prognostic significance, including ETV6::RUNX1 fusions in pediatric ALL, IKZF1 deletions, and CRLF2 rearrangements [19]. The technology's comprehensive nature allows for simultaneous assessment of multiple genetic alterations, providing a more complete molecular profile than sequential single-gene testing.
In AML, NGS has been instrumental in characterizing the complex mutational architecture that underlies disease pathogenesis and heterogeneity. The PETHEMA cooperative group demonstrated the clinical utility of NGS through a nationwide diagnostic network that provided standardized sequencing studies for 2,668 adult AML patients [28]. Their approach utilizing a 30-gene consensus panel identified at least one mutation in 97% of patients, with distinct mutational patterns according to disease phase, age, and sex [28]. This comprehensive genetic profiling facilitated accurate diagnosis and reliable prognosis stratification according to genomic classification systems, validating the clinical value of NGS in routine AML management [28]. Importantly, NGS can identify novel molecular subgroups with clinical significance, such as mutated WT1 and mutations in multiple myelodysplasia-related genes, which are associated with adverse prognosis [28].
Comparative Performance: NGS Versus Traditional Methods
Sensitivity and Detection Capabilities
The enhanced sensitivity of NGS represents a significant advantage over conventional diagnostic methods, particularly for MRD assessment. In ALL, NGS demonstrates superior sensitivity in detecting MRD-positive cases compared to MFC. Studies have shown that NGS identifies a greater number of MRD-positive patients than MFC at the 0.01% threshold, with one analysis reporting NGS detection of 57.5% versus 26.9% positive cases in B-ALL and 80% versus 46.7% in T-ALL [5]. The concordance between NGS and MFC was notably higher for MRD-positive cases (97.2%) than for MRD-negative cases (57.1%), indicating that NGS reliably identifies additional patients with persistent disease that would be classified as MRD-negative by flow cytometry [5].
Similar advantages are observed in AML, where ultradeep NGS targeting specific mutations achieves sensitivities between 10⁻⁴ and 10⁻⁵, comparable to reference methodologies like qPCR [29]. The implementation of circulating cell-free DNA (cfDNA) analysis by NGS further enhances monitoring capabilities, providing a minimally invasive approach for quantifying mutational burden with variant allele frequencies detectable as low as 0.08% [27]. This exceptional sensitivity enables earlier detection of residual disease than conventional chimerism analysis in post-transplant patients, with significant implications for relapse prediction and preemptive intervention [27].
Table 2: Performance Comparison of MRD Detection Methods
| Parameter | Multiparameter Flow Cytometry | qPCR | Next-Generation Sequencing |
|---|---|---|---|
| Sensitivity | 10⁻⁴ | 10⁻⁴ to 10⁻⁶ | 10⁻⁴ to 10⁻⁶ |
| Applicability | ~90-100% of cases | 40-50% (fusion genes) | >95% of cases |
| Turnaround Time | 4-6 hours | 1-3 days | 3-5 days |
| Key Advantages | Rapid, widely available | High sensitivity for known targets | Comprehensive, detects clonal evolution |
| Major Limitations | Antigen shift effects | Limited to known targets | Cost, bioinformatics complexity |
Clinical Utility and Prognostic Value
The prognostic value of NGS-based MRD assessment has been demonstrated across multiple studies in acute leukemias. In ALL, NGS-based MRD stratification correlates strongly with clinical outcomes, with patients achieving NGS-MRD negativity exhibiting superior event-free survival (EFS) and overall survival (OS) rates [5]. The technology has proven highly predictive of relapse following hematopoietic stem cell transplantation and CAR-T cell therapy, providing critical information for post-treatment management [5]. The use of IGH rearrangements as primary markers in NGS panels has demonstrated particularly good prognostic value in B-ALL, establishing this approach as a robust method for risk stratification [5].
In AML, NGS of cfDNA has shown promising prognostic utility in patients following allogeneic stem cell transplantation. Research has revealed that patients with donor chimerism ≥90% but mutation-positive cfDNA had a probability of progression-free survival of 64% at 17 months post-transplantation, compared to 100% in patients with undetectable MRD [27]. This finding indicates that NGS-based cfDNA analysis offers higher sensitivity for detecting residual leukemic cells than chimerism analysis alone and provides superior prognostic stratification [27]. The ability to simultaneously track multiple mutations through NGS also enables monitoring of clonal evolution during disease progression or treatment, capturing dynamic changes in the genetic landscape that may inform therapeutic resistance [19].
Experimental Approaches and Research Applications
Methodological Protocols for NGS-Based MRD Detection
The implementation of NGS for MRD monitoring requires standardized experimental protocols to ensure reproducible and clinically actionable results. For ALL, the EuroClonality-NGS study group has developed guidelines for Ig/TCR sequencing to establish clonality and track malignant clones [5]. The methodology begins with DNA extraction from bone marrow or peripheral blood samples obtained at diagnosis and during follow-up. For library preparation, multiplex PCR amplifies rearranged Ig/TCR genes using consensus primers targeting framework regions, incorporating sample-specific barcodes for multiplex sequencing [5]. Sequencing is typically performed on Illumina platforms to achieve high coverage (≥100,000 reads per sample), enabling detection of low-frequency clones. Bioinformatic analysis involves alignment to reference sequences, clonotype identification, and quantification of leukemia-derived sequences relative to total reads, with results reported as clonal cell frequencies [5].
For AML MRD detection, protocols often utilize targeted panels covering recurrently mutated genes. The approach described by [27] employs commercially available core myeloid panels (e.g., ArcherDx VariantPlex Core Myeloid panel spanning 37 genes) for cfDNA analysis. Cell-free DNA is isolated from blood collected in specialized stabilization tubes, with quality assessment through pre-sequencing QC assays [27]. Library preparation incorporates unique molecular identifiers to distinguish true low-frequency variants from sequencing artifacts. Ultra-deep sequencing (>100,000x coverage) enables sensitive variant detection down to 0.08% variant allele frequency [27]. Bioinformatics pipelines (e.g., Archer Analysis) with customized parameters (minimal depth=1, error-correction enabled) facilitate sensitive mutation calling, with manual review of mutations previously identified at diagnosis but filtered automatically [27].
Research Reagent Solutions for Leukemia Genomics
Table 3: Essential Research Reagents for NGS-Based Leukemia Characterization
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| Nucleic Acid Stabilization | Cell-free DNA BCT tubes (Streck) | Preserves cfDNA profile in blood samples | Prevents dilution from leukocyte lysis during transport |
| Nucleic Acid Extraction | QIAamp Circulating Nucleic Acid Kit (Qiagen) | Isolation of high-quality cfDNA | Maintains fragment integrity for library preparation |
| Target Enrichment | VariantPlex Core AML/Myeloid panels (ArcherDx) | Targeted sequencing of leukemia-associated genes | Customizable content based on research objectives |
| Library Preparation | Illumina DNA Prep kits | NGS library construction with dual indices | Reduces index hopping with unique dual indexing |
| Sequencing Platforms | Illumina MiSeq, NextSeq | Massively parallel sequencing | Balance between throughput, read length, and cost |
| Bioinformatic Tools | Archer Analysis, ClinVar, COSMIC | Variant calling, annotation, and interpretation | Integration of clinical databases for pathogenicity assessment |
Signaling Pathways and Genetic Networks
The genetic landscape of acute leukemias involves complex interactions between multiple signaling pathways that regulate hematopoiesis, cell proliferation, differentiation, and survival. In ALL, key pathways frequently disrupted include B-cell development (governed by PAX5, IKZF1, EBF1), tyrosine kinase signaling (activated by ABL1, JAK-STAT mutations), and tumor suppressor pathways (regulated by TP53, CDKN2A/B) [19]. These genetic alterations collectively promote uncontrolled expansion of lymphoid precursors while blocking differentiation, creating the characteristic phenotype of immature blast accumulation.
In AML, the molecular pathogenesis typically involves mutations in distinct functional categories: signaling molecules (FLT3, KIT, RAS), transcription factors (RUNX1, CEBPA), tumor suppressors (TP53, WT1), and epigenetic modifiers (DNMT3A, TET2, IDH1/2) [28] [25]. These mutations disrupt normal myeloid differentiation, enhance self-renewal capacity, and confer survival advantages to leukemic stem cells. The specific combination and order of acquisition of these mutations influence disease initiation, progression, and clinical behavior, highlighting the importance of comprehensive genetic profiling for understanding disease biology.
Integration into Clinical Practice and Future Directions
Current Implementation Challenges
Despite its transformative potential, the integration of NGS into routine leukemia diagnostics faces several significant challenges. Technical complexities include the need for specialized bioinformatics expertise, standardized protocols, and rigorous quality control measures to ensure reproducible results across laboratories [5] [25]. The PETHEMA cooperative group addressed these challenges through a nationwide network of reference laboratories implementing standardized NGS studies, complemented by regular cross-validation rounds to maintain quality [28]. This model demonstrates that standardization is achievable through coordinated efforts, though it requires substantial infrastructure investment.
Economic barriers also impact NGS implementation, with high costs associated with sequencing instrumentation, reagents, and computational resources [19]. Additionally, data interpretation complexities present ongoing challenges, as the distinction between pathogenic mutations and benign variants or variants of unknown significance requires sophisticated bioinformatic tools and curated databases [25]. The growing incorporation of artificial intelligence (AI) in variant classification helps streamline this process by integrating publicly available information and predicting variant pathogenicity [25] [2]. However, these approaches still require validation and standardization before widespread clinical adoption.
Emerging Applications and Future Perspectives
The future trajectory of NGS in leukemia diagnostics points toward increasingly comprehensive and integrated approaches. The transition from targeted panels to whole-genome sequencing is anticipated within the next five years, driven by reduced sequencing costs and enhanced computational power [25]. This expansion will enable detection of novel genetic alterations beyond currently known targets, potentially revealing new therapeutic vulnerabilities and biomarkers. The integration of transcriptomic and epigenetic profiling with DNA sequencing will provide multidimensional insights into disease mechanisms, capturing the functional consequences of genetic alterations [25].
Liquid biopsy approaches using cfDNA represent another promising direction, offering minimally invasive disease monitoring that captures spatial heterogeneity and enables real-time tracking of clonal evolution [27]. As these technologies mature, their integration with conventional methods will likely create synergistic diagnostic workflows that leverage the respective strengths of each approach. For instance, combining MFC for rapid assessment with NGS for comprehensive genetic characterization may provide complementary advantages in MRD monitoring [5]. Ultimately, these advancements will support more dynamic and personalized treatment strategies, moving beyond static diagnostic classification toward adaptive therapeutic approaches that evolve with the changing genetic landscape of each patient's disease.
The diagnosis and risk stratification of acute leukemia have long relied on a combination of traditional diagnostic methodologies, including cytomorphology, cytogenetic analysis, and targeted molecular tests. While these approaches have formed the standard of care for decades, the rapidly evolving understanding of leukemia pathogenesis has revealed significant resolution gaps and diagnostic blind spots in conventional testing platforms. The integration of next-generation sequencing (NGS) into clinical practice represents a paradigm shift, offering an unbiased, comprehensive approach to genetic characterization that addresses many limitations of traditional methods. This comparison guide objectively evaluates the performance of NGS against traditional diagnostic approaches within the context of acute leukemia research, providing experimental data and methodological details to inform researchers, scientists, and drug development professionals.
The limitations of traditional approaches are particularly evident in their inability to detect novel or rare genetic alterations, comprehensively assess structural variants, and identify minimal residual disease (MRD) at clinically relevant sensitivities. Furthermore, the sequential nature of traditional testing often results in prolonged turnaround times and insufficient tissue sampling, potentially delaying critical treatment decisions. This analysis systematically examines these limitations through direct comparison with NGS-based methodologies, focusing specifically on their application in acute myeloid leukemia (AML) as a model system, with broader implications for other leukemia subtypes.
Methodological Comparison: Traditional versus NGS Approaches
Experimental Protocols in Traditional Diagnostic Methods
Traditional diagnosis of acute leukemia typically follows an integrated stepwise protocol known as the MICM framework, which incorporates Morphology, Immunophenotype, Cytogenetics, and Molecular abnormalities [2] [30]. The initial assessment involves peripheral blood tests, including complete blood count and morphological analysis of blood smears, to detect abnormalities in cell counts and morphology. This is followed by bone marrow aspiration and biopsy to evaluate blast cell percentage and cytomorphological features, with a diagnostic threshold of >20% blasts in bone marrow or peripheral blood according to World Health Organization (WHO) classification, though specific genetic abnormalities allow diagnosis even with lower blast percentages [30]. Flow cytometry immunophenotyping represents the third component, enabling detection of surface and cytoplasmic antigen expression patterns to assist in leukemia subtyping, typically using antibody panels against markers such as CD34, CD117, CD13, CD33, and lineage-specific antigens.
For cytogenetic analysis, conventional karyotyping requires G-banding metaphase analysis of cultured bone marrow cells, with a typical resolution limit of 5-10 Mb, thereby missing smaller structural variants [31]. Fluorescence in situ hybridization (FISH) employs fluorescently labeled DNA probes targeting known recurrent genetic rearrangements (e.g., PML::RARA, RUNX1::RUNX1T1) with higher resolution than karyotyping but limited to predefined targets. Targeted molecular testing typically uses polymerase chain reaction (PCR)-based methods including quantitative reverse transcription PCR (qRT-PCR) and fragment analysis for mutation detection in specific genes (e.g., FLT3-ITD, NPM1), with sensitivity generally limited to variants with >5% variant allele frequency (VAF) [31].
NGS-Based Methodological Frameworks
In contrast to traditional approaches, NGS methodologies offer comprehensive genetic profiling through several experimental frameworks. Whole genome sequencing (WGS) provides complete coverage of nuclear DNA, typically achieving 80-100x coverage for diagnostic applications, enabling detection of single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), and structural variants (SVs) from a single assay [31]. Whole transcriptome sequencing (WTS) profiles the entire RNA content, allowing for detection of gene fusions, alternative splicing, and expression abnormalities, with particular utility for identifying cryptic rearrangements missed by conventional methods. Integrated WGS-WTS (iWGS-WTS) approaches combine genomic and transcriptomic data to provide a comprehensive molecular portrait, enhancing variant detection accuracy and biological interpretation [31].
Targeted NGS panels focus sequencing on clinically relevant genes using hybrid capture or amplicon-based approaches, achieving deeper coverage (500-1000x) suitable for detecting low-frequency mutations and MRD monitoring. For methylation profiling, methods like the MARLIN (Methylation- and AI-guided Rapid Leukemia Subtype Inference) tool utilize long-read nanopore sequencing technology to classify acute leukemia based on DNA methylation patterns, achieving results within two hours of biopsy receipt [32]. This approach has demonstrated capability to resolve diagnostic blind spots missed by conventional methods, such as identifying cryptic rearrangements involving the DUX4 gene and revealing novel predictive signatures like HOX-activated subgroups [32].
Figure 1: Comparative Workflows of Traditional and NGS-Based Diagnostic Approaches for Acute Leukemia. Traditional methods (yellow) are sequential and targeted, while NGS approaches (green) provide comprehensive genetic assessment. Key limitation and advantage differentiators are highlighted.
Resolution Gaps: Comparative Performance Data
Detection of Genetic Variants
Direct comparative studies demonstrate significant resolution gaps between traditional and NGS-based approaches across all variant classes. A systematic study from St. Jude Children's Research Hospital implementing integrated WGS-WTS in 153 pediatric AML patients revealed critical limitations in conventional testing approaches [31]. The iWGS-WTS approach identified 330 somatic pathogenic or likely pathogenic SNV/Indels in 135/153 patients, with high concordance between WGS and whole exome sequencing (WES) for variants with VAF ≥5% (~96% concordance rate) [31]. However, manual review identified nine additional variants not called by WES, predominantly complex indels, while 15 variants detected by WES with VAFs ranging from 5–12.5% did not meet established reporting criteria for iWGS-WTS, highlighting detection variability at lower VAFs.
For structural variant detection, WGS analysis identified 106 AML-associated oncogenic or likely oncogenic fusions in 105 cases, of which 96 were predicted to produce fusion oncogenes and 10 were suspected enhancer-hijacking structural alterations [31]. WTS analysis alone diagnosed 94/96 (98%) of the WGS-detected fusion oncogenes, with no false positive findings. Importantly, research from the University of Michigan demonstrated that adding RNA-based fusion testing to standard NGS panels identified gene fusions in 15% of over 600 AML patients, including approximately 4% (23 cases) where fusions were missed by conventional cytogenetics [33] [34]. These included clinically significant rearrangements involving NUP98 and KMT2A that directly influence treatment approaches.
For copy number variations, WGS revealed 42 pathogenic/likely pathogenic focal CNVs (<5 Mb) in 24 patients, including 15 alterations smaller than 50 kb (12 ≤ 10 kb) that presented as intragenic/exonic CNVs leading to truncation of functional proteins [31]. Among alterations smaller than 50 kb, recurrent findings included deletions in CBL affecting exons 8 and/or 9 and KMT2A partial tandem duplications, all of which were supported by WTS evidence. This resolution far exceeds the capability of conventional cytogenetics, which has a resolution limit of 5-10 Mb, unable to detect these clinically significant smaller alterations.
Minimal Residual Disease Monitoring
The limitations of traditional approaches are particularly pronounced in MRD monitoring, where sensitivity thresholds directly impact relapse prediction and treatment decisions. Traditional flow cytometry-based MRD detection typically achieves sensitivity of 0.01% (10^-4), while PCR-based methods can reach 0.001% (10^-5) for specific mutations [2]. In contrast, NGS-based approaches demonstrate significantly enhanced capabilities for MRD monitoring.
Researchers at Moffitt Cancer Center validated a highly sensitive NGS-based test for tracking FLT3 mutations in AML patients, demonstrating detection at extraordinarily low allelic fractions down to 0.0014% (1.4x10^-5) with strong accuracy and reproducibility [33] [34]. This enhanced sensitivity enables more confident assessment of remission status, better selection of patients for allogeneic stem cell transplantation, and earlier intervention upon molecular relapse signals. Furthermore, a University of California San Diego study utilizing NGS to track cancer-related gene mutations in 74 AML patients at diagnosis, post-chemotherapy, and post-transplant found that lingering mutations after transplant strongly predicted relapse, particularly in epigenetic regulators such as TET2 and DNMT3A [33] [34]. This approach provided critical prognostic information not obtainable through conventional monitoring.
Table 1: Comparative Detection Rates of Genetic Alterations in Acute Leukemia
| Variant Type | Traditional Methods | Detection Rate | NGS-Based Methods | Detection Rate | Clinical Impact |
|---|---|---|---|---|---|
| Gene Fusions | Conventional Cytogenetics | ~70-80% [33] | RNA-seq + WGS | 98% of known fusions; +15% additional yield [31] [33] | Identifies cryptic drivers (e.g., NUP98, KMT2A) affecting treatment |
| SNVs/Indels | Targeted PCR/Panel | Limited to predefined targets | WGS/WES | ~96% concordance for VAF ≥5%; additional complex indels [31] | Comprehensive mutation profiling for risk stratification |
| Focal CNVs (<50 kb) | Cytogenetics (resolution limit 5-10 Mb) | Undetectable | WGS | 42 focal CNVs in 24 patients, including 15 <50 kb [31] | Detects clinically significant intragenic deletions (e.g., CBL, KMT2A-PTD) |
| FLT3-ITD | Fragment Analysis | 28 ITDs in 18 patients; 1 subclonal ITD missed [31] | WGS + WTS | 28 ITDs detected; 10 borderline cases with weak WGS evidence [31] | Improved detection of complex ITD patterns |
| MRD (FLT3 mutations) | qPCR (sensitivity ~0.001%) | Limited by predefined targets | Deep Sequencing | Sensitivity 0.0014% (14x10^-6) [33] [34] | Earlier relapse prediction and intervention |
Diagnostic Blind Spots: Unresolved Challenges in Traditional Approaches
Cryptic Genetic Events and Novel Alterations
Traditional diagnostic approaches exhibit several critical blind spots that impact accurate classification and risk stratification of acute leukemia. Cryptic genetic events represent a significant challenge, as conventional cytogenetics frequently misses subtle structural rearrangements that lack apparent chromosomal banding alterations. The MARLIN study demonstrated that methylation profiling combined with machine learning could identify diagnostic blind spots missed by conventional methods, successfully detecting cryptic rearrangements involving the DUX4 gene that are associated with favorable clinical outcomes [32]. Similarly, the University of Michigan study found that approximately 4% of AML patients harbored fusion events undetectable by standard cytogenetics [33] [34], highlighting a substantial diagnostic gap in conventional approaches.
The targeted nature of traditional molecular methods creates another significant blind spot by limiting detection to known, predefined alterations. While targeted NGS panels (typically 75 genes or similar) demonstrate high concordance with WGS for known mutations, they inherently miss novel or rare genetic alterations outside their designed scope [31]. In comparative analysis, iWGS-WTS identified numerous variants beyond the scope of targeted panels, including complex indels and structural variants in non-panel genes that may have clinical significance. This limitation is particularly relevant for drug development, where comprehensive genomic profiling is essential for identifying novel therapeutic targets and understanding resistance mechanisms.
Technical and Workflow Limitations
Technical constraints represent additional blind spots in traditional leukemia diagnostics. The sequential nature of conventional testing algorithms creates significant workflow inefficiencies, often requiring multiple sample processing steps and extended turnaround times. Morphological evaluation of peripheral blood and bone marrow smears depends heavily on experienced physicians for manual interpretation, which is labor-intensive, time-consuming, and prone to subjectivity, with diagnostic error rates as high as 40% in morphological assessments [2] [30]. Furthermore, flow cytometry results may vary due to differences in detection protocols, antibody panel configurations, and analytical standards across laboratories, affecting reproducibility and standardization.
The MARLIN approach addresses several of these limitations by providing rapid classification within two hours of biopsy receipt, dramatically improving upon traditional diagnostic timelines that often take days or weeks [32]. This acceleration potentially enables faster treatment initiation, which is critical for aggressive leukemia subtypes such as acute promyelocytic leukemia (APL) where even 24-hour delays can significantly impact prognosis [2]. Additionally, the requirement for multiple testing modalities in traditional approaches often consumes substantial tissue samples, potentially leading to insufficient material for comprehensive analysis, whereas NGS-based approaches streamline sample requirements through consolidated testing.
Table 2: Methodological Limitations and NGS Solutions in Acute Leukemia Diagnostics
| Diagnostic Challenge | Traditional Approach Limitation | NGS-Based Solution | Experimental Evidence |
|---|---|---|---|
| Cryptic Fusion Detection | Conventional cytogenetics misses subtle rearrangements | RNA-seq identifies cryptic fusions | 4% of AML cases had fusions missed by cytogenetics [33] [34] |
| Comprehensive Mutation Profiling | Targeted panels limited to predefined genes | WGS detects all genomic alterations | iWGS-WTS identified complex indels missed by WES [31] |
| Rapid Classification | Sequential testing requires days/weeks | MARLIN: methylation-based classification in 2 hours [32] | Correct classification in under 2 hours from biopsy receipt [32] |
| MRD Sensitivity | Flow cytometry sensitivity ~0.01% | Deep sequencing to 0.0014% allelic fraction | FLT3 mutations detected at 0.0014% with strong accuracy [33] [34] |
| Structural Variant Resolution | Cytogenetics resolution limit 5-10 Mb | WGS detects CNVs as small as 10 kb | 15 focal CNVs <50 kb identified in 24 patients [31] |
| Subjectivity in Interpretation | Morphology error rates up to 40% [2] | AI-based standardized analysis | Reduced subjectivity in blast identification and classification |
The Research Toolkit: Essential Solutions for Leukemia Diagnostics
Table 3: Research Reagent Solutions for Advanced Leukemia Diagnostics
| Research Tool | Function/Application | Key Features/Benefits |
|---|---|---|
| Integrated WGS-WTS (iWGS-WTS) | Comprehensive genomic and transcriptomic profiling | Simultaneous detection of SNVs, indels, CNVs, fusions, and expression abnormalities; streamlines testing [31] |
| Long-Read Nanopore Sequencing | Methylation profiling and structural variant detection | Enables real-time sequencing; compatible with MARLIN framework for rapid classification [32] |
| RNA-Based Fusion Panels | Detection of cryptic gene fusions | Identifies rearrangements missed by cytogenetics; increased yield of ~4% in AML cases [33] [34] |
| Deep Sequencing MRD Assays | Ultra-sensitive mutation tracking | Detects FLT3 mutations at 0.0014% VAF; enables early relapse detection [33] [34] |
| AI-Assisted Morphological Analysis | Automated blast identification and classification | Reduces subjectivity (40% error rate in manual review); improves standardization [2] [30] |
| Custom Target Enrichment Panels | Focused sequencing of leukemia-associated genes | Cost-effective; enables deep coverage for MRD monitoring; customizable content |
The comprehensive comparison between traditional and NGS-based approaches for acute leukemia diagnosis reveals significant resolution gaps and diagnostic blind spots in conventional methodologies. Traditional approaches, while established in clinical practice, demonstrate limitations in detecting cryptic genetic events, comprehensive variant profiling, and achieving clinically relevant sensitivity for MRD monitoring. The sequential nature of these methods additionally introduces workflow inefficiencies and extended turnaround times that may impact treatment initiation.
NGS-based frameworks address these limitations through unbiased whole-genome and transcriptome analysis, enabling detection of novel alterations, structural variants, and low-frequency mutations with clinical significance. The enhanced sensitivity of deep sequencing approaches provides superior capabilities for MRD monitoring and relapse prediction, while emerging technologies such as methylation profiling and AI-assisted classification offer opportunities for rapid and accurate diagnosis. For researchers and drug development professionals, these advanced methodologies provide more comprehensive genetic characterization essential for target identification, patient stratification, and understanding resistance mechanisms, ultimately supporting the development of more effective precision medicine approaches for acute leukemia.
Figure 2: Diagnostic Blind Spots in Traditional Leukemia Diagnosis and Corresponding NGS-Based Solutions. Traditional methods (yellow) exhibit specific limitations (red) that are addressed by targeted NGS approaches (green), highlighting the complementary nature of these technologies in resolving diagnostic challenges.
The Emergence of NGS as a Comprehensive Genomic Profiling Tool
Acute leukemia is a genetically complex and heterogeneous group of malignancies characterized by rapid progression and clonal expansion of immature blood cells. The accurate detection of genetic alterations has become fundamental to diagnosis, risk stratification, and treatment selection. For decades, conventional cytogenetic methods including chromosome banding analysis (CBA), fluorescence in situ hybridization (FISH), and multiparametric flow cytometry (MFC) have formed the diagnostic backbone. While these techniques have been instrumental, they possess inherent limitations in resolution, sensitivity, and scope. The emergence of next-generation sequencing (NGS) represents a paradigm shift, enabling comprehensive genomic profiling that reveals the full spectrum of molecular alterations driving leukemogenesis. This guide objectively compares the performance of NGS against traditional and emerging orthogonal technologies in the context of acute leukemia diagnostics, supported by recent experimental data and clinical studies.
Performance Comparison: NGS vs. Traditional and Emerging Methods
Extensive benchmarking studies have systematically evaluated the diagnostic capabilities of NGS against both standard-of-care and other advanced genomic technologies. The data below summarizes key performance metrics from recent, large-scale clinical studies.
Table 1: Comprehensive Comparison of Genomic Profiling Methods in Acute Leukemia
| Methodology | Key Strengths | Major Limitations | Detection Rate (Clinically Relevant Alterations) | Sample Size (Recent Studies) |
|---|---|---|---|---|
| Standard-of-Care (SoC)(CBA, FISH, qPCR) | - Established clinical utility- Widely available [35] | - Low resolution & sensitivity- Limited scope- Relies on viable metaphases [35] | 46.7% in pediatric ALL [35] | 60 patients (pediatric ALL) [35] |
| Next-Generation Sequencing (NGS)(DNA & RNA panels) | - Detects SNVs, Indels, CNVs, fusions- High sensitivity for fusion transcripts [36] | - May miss some enhancer-hijacking events [36] | 95% (when dMLPA combined with RNA-seq) [35] | 60 patients (pediatric ALL) [35] |
| Optical Genome Mapping (OGM) | - Superior for structural variants, cryptic alterations & enhancer-hijacking [36] [35] | - May misinterpret intrachromosomal deletions [36] | 90% as standalone test [35] | 467 acute leukemia cases [36] |
| Integrated Whole Genome & Transcriptome Sequencing (iWGS-WTS) | - Most comprehensive; a true "all-in-one" assay- Unbiased detection [24] | - High cost & complex data analysis- Not yet routine in clinical labs | Identified 100% of reportable fusions and SNVs/Indels in pediatric AML [24] | 153 patients (pediatric AML) [24] |
Table 2: Quantitative Performance of NGS for Minimal Residual Disease (MRD) Detection in ALL
| Performance Metric | NGS (ClonoSEQ) | Multiparametric Flow Cytometry (MFC) | qRT-PCR |
|---|---|---|---|
| Sensitivity | Up to 10^-6 (1 in 1 million cells) [7] [37] | 10^-4 (1 in 10,000 cells) [7] | 10^-4 to 10^-5 [7] |
| Applicability Rate | 98% of B/T-ALL patients (trackable sequences found) [37] | Nearly 100% [7] | <50% (for fusion genes) [7] |
| Concordance with MFC (High MRD, ≥10^-4) | High correlation (r=0.87) when both detectable [37] | N/A | N/A |
| Additional Detection | Identified 50% more high-MRD patients (≥10^-4) missed by FCM [37] | N/A | N/A |
| Key Advantage | Universal primers, tracks clonal evolution [7] | Fast, widely applicable [7] | High sensitivity for specific targets [7] |
| Key Disadvantage | Cost, bioinformatics complexity [7] | Subjective interpretation, influenced by immunotherapy [7] | Laborious, needs patient-specific primers, limited applicability [7] |
Detailed Experimental Protocols from Key Studies
Protocol 1: Targeted RNA-Seq vs. OGM in Acute Leukemia
A landmark 2025 study directly compared a 108-gene targeted RNA-seq panel with Optical Genome Mapping (OGM) in 467 acute leukemia cases (360 AML, 89 B-ALL, 12 T-ALL, 6 MPAL) to evaluate their performance in detecting gene rearrangements and fusions [36].
- Sample Preparation: Fresh bone marrow aspirate specimens were used for OGM, involving ultra-high-molecular-weight (UHMW) DNA extraction, direct labeling, and imaging on Bionano's Saphyr system. For RNA-seq, RNA was extracted from peripheral blood or bone marrow and sequenced using anchored multiplex PCR (AMP) for target enrichment [36].
- Data Analysis: OGM data was analyzed against GRCh38 using Bionano Access and VIA software. RNA-seq reads were aligned to GRCh37 using Archer Analysis software for fusion transcript identification [36].
- Variant Interpretation: Results from both methods were classified into tiers based on ACMG/ClinGen and AMP/ASCO/CAP guidelines, focusing on Tier 1 variants with established diagnostic, prognostic, or therapeutic relevance [36].
Key Finding: The overall concordance between OGM and RNA-seq was 88.1%. However, OGM uniquely detected 15.8% of clinically relevant rearrangements, while RNA-seq exclusively identified 9.4%. RNA-seq was more sensitive for expressed chimeric fusions, while OGM was superior for detecting cryptic, enhancer-hijacking events (e.g., involving MECOM or BCL11B), which showed a markedly low concordance of only 20.6% [36].
Protocol 2: NGS for MRD in Pediatric ALL
The Dana Farber Cancer Institute ALL Consortium Protocol 16-001 (2017-2020) evaluated the feasibility of using NGS for MRD-based risk stratification in 317 pediatric ALL patients [37].
- Sample Collection: Bone marrow evaluations were performed at diagnosis and after induction therapy (TP1). Samples were analyzed by both NGS and multiparametric flow cytometry (FCM) [37].
- NGS MRD Method: The ClonoSEQ assay was used to sequence immunoglobulin (Ig) and T-cell receptor (TCR) gene rearrangements to identify unique, trackable sequences for each leukemic clone [37].
- Risk Stratification: Patients with high TP1 MRD (≥10^-4) received intensified therapy. NGS was the primary MRD determinant, with FCM as a backup [37].
Key Finding: NGS identified trackable sequences in 98% of patients. It detected MRD in a significantly higher number of patients compared to FCM, with 50% of the cohort showing MRD in the range of 10^-6 to <10^-4 that was undetectable by FCM. Furthermore, 17% of patients were classified as having high MRD (≥10^-4) by NGS while showing low or undetectable disease by FCM [37].
Protocol 3: Integrated Whole Genome and Transcriptome Sequencing
A 2025 study on pediatric and adolescent AML implemented an integrated whole genome and whole transcriptome sequencing (iWGS-WTS) approach in 153 patients, comparing its output to that of targeted NGS panels, cytogenetics, and other methods [24].
- Sample Processing: Tumor and matched germline samples were collected. Paired tumor-normal clinical genomics testing was performed using WGS, whole exome sequencing (WES), and WTS [24].
- Variant Calling & Fusion Detection: Somatic SNVs/Indels were called from WGS/WES data. Structural variants and gene fusions were identified from WGS and validated via WTS. FLT3-ITDs were confirmed by PCR-based fragment analysis [24].
- Comparison: Results were systematically compared to those from a 75-gene targeted NGS panel and cytogenetics [24].
Key Finding: The iWGS-WTS approach demonstrated high concordance with targeted NGS for SNVs/Indels and identified 100% of reportable fusion oncogenes. Crucially, it also detected additional genetic alterations missed by standard methods, including 15 focal CNVs smaller than 50 kb and multiple complex structural variants, providing a more comprehensive molecular portrait [24].
Visualizing Workflows and Clinical Integration
The following diagrams illustrate the streamlined workflow of comprehensive NGS testing and its role in clinical decision-making for acute leukemia.
Diagram 1: NGS Testing Workflow. This streamlined process demonstrates the path from a patient sample to a final clinical report, highlighting the unified workflow for DNA and RNA analysis.
Diagram 2: Clinical Decision Pathway. Comprehensive NGS data directly informs a cascade of clinical decisions, from initial diagnosis and risk assessment to long-term monitoring and therapy selection.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of NGS-based genomic profiling relies on a suite of specialized reagents and analytical tools.
Table 3: Essential Research Reagents and Solutions for NGS in Leukemia
| Item | Function | Example Application/Note |
|---|---|---|
| Anchored Multiplex PCR (AMP) | Target enrichment for RNA-seq; allows discovery of novel fusion partners without prior knowledge of the partner gene [36]. | Used in the 108-gene panel study for fusion detection [36]. |
| Molecular Barcodes | Unique nucleotide sequences added to DNA fragments pre-amplification; enables error correction and ultra-sensitive detection down to 0.05% VAF [38]. | Critical for MRD detection assays like the Oncomine Myeloid MRD Assay [38]. |
| Ultra-High Molecular Weight (UHMW) DNA Kits | Isolation of long, intact DNA fragments essential for technologies like OGM and whole genome sequencing [36] [24]. | Required for OGM to resolve complex structural variants [36]. |
| Multiomic NGS Panels | Integrated panels that simultaneously interrogate DNA mutations and RNA fusions from a single sample. | The Oncomine Myeloid MRD Assay covers DNA and RNA targets for a unified workflow [38]. |
| Validated Bioinformatics Pipelines | Software for alignment, variant calling, and interpretation; includes specialized tools for challenging mutations like FLT3-ITD [24] [38]. | Essential for translating raw sequencing data into clinically actionable results. |
The evidence from recent, large-scale clinical studies unequivocally demonstrates that NGS has emerged as a powerful and comprehensive genomic profiling tool, significantly outperforming traditional diagnostic methods in acute leukemia. Its superior sensitivity, breadth of detection, and ability to guide MRD monitoring and risk-adapted therapy solidifies its indispensable role in modern hematology. However, the data also reveals that no single platform is perfect. The future of acute leukemia diagnostics lies in rational, integrated testing strategies, such as combining RNA-seq with OGM or adopting all-in-one iWGS-WTS approaches, to fully capture the genomic complexity of the disease and ultimately improve patient outcomes.
Implementing NGS in Clinical Practice: Workflows, Applications, and Emerging Technologies
Next-generation sequencing (NGS) has revolutionized the diagnostic approach for acute leukemia, moving beyond traditional methods to provide a more comprehensive genomic view. This guide objectively compares the performance of modern NGS workflows against traditional diagnostic techniques, supported by recent experimental data and clinical study methodologies.
Basic NGS Workflow Steps
The standard NGS workflow consists of four fundamental stages that convert biological samples into analyzable genomic data [39] [40]:
Nucleic Acid Extraction: Isolation of DNA or RNA from patient samples, typically from bone marrow aspirate, peripheral blood, or skin biopsy for germline controls. Quality control measures using UV spectrophotometry and fluorometric methods are critical for success [39] [31].
Library Preparation: Fragmentation of nucleic acids and attachment of specialized adapters to create a sequenceable library. This process may include amplification steps and can be automated to improve reproducibility [39] [41].
Sequencing: Massively parallel sequencing of library fragments using platforms that employ technologies such as Sequencing by Synthesis (SBS). Parameters including read length and depth are optimized for specific applications [39] [42].
Data Analysis: Bioinformatics processing of raw sequence data through quality control, alignment, variant calling, and interpretation using specialized software tools and pipelines [39] [42].
Table: Core NGS Workflow Components
| Workflow Step | Key Activities | Critical Quality Metrics |
|---|---|---|
| Nucleic Acid Extraction | Cell lysis, purification, quantification | Purity (A260/A280 ratio), concentration, integrity |
| Library Preparation | Fragmentation, adapter ligation, amplification | Fragment size distribution, library concentration |
| Sequencing | Cluster generation, base calling, read generation | Q-score, error rate, coverage uniformity |
| Data Analysis | Alignment, variant calling, annotation | Sensitivity, specificity, reproducibility |
Performance Comparison: NGS vs. Traditional Methods for Leukemia Diagnosis
Traditional acute leukemia diagnosis has relied on combination of cytogenetics, fluorescence in situ hybridization (FISH), and targeted PCR assays. Integrated Whole Genome and Whole Transcriptome Sequencing (iWGS-WTS) now provides a unified approach that captures a broader spectrum of genetic alterations [31].
Detection of Single Nucleotide Variants and Small Insertions/Deletions
A 2025 study of 153 pediatric AML patients directly compared iWGS-WTS with whole exome sequencing (WES) and targeted NGS panels [31]. The research employed matched tumor-normal samples with bone marrow or peripheral blood as tumor tissue and skin biopsies as germline controls. Sequencing data underwent rigorous quality assessment before variant calling.
The iWGS-WTS approach identified 330 somatic pathogenic/likely pathogenic SNVs/Indels across 135 patients. When compared to WES, there was 96% concordance for variants with variant allele frequency (VAF) ≥5%, with high correlation in VAF estimates. Notably, iWGS-WTS detected nine additional variants missed by WES, predominantly complex indels [31].
In comparison to a 75-gene targeted NGS panel, iWGS-WTS demonstrated 70/74 variant concordance, with one additional variant detected by iWGS-WTS at VAF >5% that was reported at 4% by the panel [31].
Identification of Structural Variants and Gene Fusions
Structural variant detection represents a significant advantage for comprehensive NGS approaches. In the same 2025 study, WGS analysis identified 106 AML-associated oncogenic fusions across 105 patients, including 96 predicted fusion oncogenes and 10 suspected enhancer-hijacking structural alterations [31].
WTS analysis alone detected 98% of WGS-identified fusion oncogenes with no false positives. In two cases, WGS suggested KMT2A::ELL fusions that required confirmation by targeted RNA sequencing despite weak WTS evidence [31]. This demonstrates the complementary value of integrated genomic and transcriptomic approaches.
Copy Number Variant Detection
WGS excels at identifying both focal and large-scale copy number variations. The 2025 analysis revealed 42 pathogenic/likely pathogenic focal CNVs (<5 Mb) in 24 patients, including 15 alterations smaller than 50 kb that would be challenging to detect with conventional methods [31]. Additionally, WGS identified 163 large-scale CNV events (≥5 Mb) in 83 patients and large-scale copy-neutral loss of heterozygosity in 18 patients [31].
Table: Comprehensive Detection Capability Comparison in Pediatric AML (n=153)
| Genetic Alteration Type | Traditional Methods | Targeted NGS Panels | Integrated WGS-WTS |
|---|---|---|---|
| SNVs/Indels | Limited to known hotspots | 74 detected in 39 cases | 330 detected in 135 cases |
| Gene Fusions | Karyotyping (low resolution) | Targeted fusion panels | 106 fusions in 105 cases |
| FLT3-ITD | Fragment analysis (size-based) | Varies by panel design | 28 ITDs in 18 patients |
| Focal CNVs (<50 kb) | Generally undetectable | Limited to designed targets | 15 very small CNVs identified |
| Large-scale CNVs | Karyotyping (≥5-10 Mb) | Limited or absent | 163 events in 83 patients |
Experimental Protocols for Method Comparison
Integrated WGS-WTS Protocol for AML Diagnosis
The 2025 study established a rigorous protocol for comparative analysis [31]:
Sample Requirements: Bone marrow aspirate or peripheral blood with documented blast counts (>20% in all but four cases), with skin biopsy or other tumor-free samples as germline comparators [31].
Sequencing Methods: Paired tumor-normal clinical genomics testing performed in CLIA-certified laboratory. WES performed alongside WGS for internal validation of SNV/Indel detection. Targeted NGS panel (75-gene) results compared where available [31].
Variant Calling and Validation: Somatic variant calling with established reporting criteria (typically VAF ≥5%). Manual review of BAM files for discordant variants. Orthogonal validation by PCR-based fragment analysis for FLT3-ITD and targeted RNA sequencing for uncertain fusions [31].
Measurable Residual Disease (MRD) Monitoring Protocol
A 2025 prospective study evaluated NGS for MRD monitoring in 84 MDS/AML patients [43]:
Treatment Context: Patients received intensive chemotherapy or hypomethylating agents plus venetoclax [43].
Sampling Timepoints: NGS performed at diagnosis and complete remission (CR) [43].
Analysis Method: Mutation persistence in CR assessed for prognostic significance, combined with multiparameter flow cytometry (MFC) for enhanced risk stratification [43].
Research Reagent Solutions for Leukemia Genomics
Implementing NGS workflows requires specific reagent systems and platforms tailored to hematologic malignancy research:
Table: Essential Research Reagents and Platforms for Leukemia NGS
| Product Category | Specific Examples | Primary Applications in Leukemia Research |
|---|---|---|
| Targeted DNA Panels | AmpliSeq for Illumina Myeloid Panel (40 genes), TruSight Myeloid Sequencing Panel | Detection of SNVs/Indels in myeloid-associated genes with high sensitivity [44] |
| RNA Fusion Panels | TruSight RNA Fusion, TruSight RNA Pan-Cancer | Identification of known and novel fusion genes in hematologic malignancies [44] |
| Benchtop Sequencers | MiSeq System, NextSeq 550 System, NextSeq 1000/2000 Systems | Scalable sequencing capacity for various throughput needs [39] [44] |
| Automation Systems | G.STATION NGS Workstation, I.DOT Liquid Handler | Automated library preparation to reduce hands-on time and improve reproducibility [41] |
| Analysis Software | BaseSpace Sequence Hub, Local Run Manager, Variant Interpreter | Streamlined data analysis, variant calling, and interpretation [39] [44] |
Technological Innovations Enhancing NGS Workflows
Recent advancements are addressing traditional bottlenecks in NGS implementation:
End-to-End Automation: Automated systems now integrate library construction, purification, and quantification, reducing hands-on time from 3 hours to under 15 minutes while improving reproducibility [41].
Non-Contact, Low-Volume Dispensing: Technologies like the I.DOT Liquid Handler enable nanoliter-range reagent dispensing, minimizing reagent consumption and cost while maintaining precision [41].
Novel Sequencing Chemistries: Emerging technologies like Roche's Sequencing by Expansion (SBX) enable ultra-fast, high-throughput sequencing, while QIAGEN's multimodal kits allow simultaneous DNA and RNA library preparation from single samples [45].
Integrated Data Analysis Platforms: Connected software solutions with built-in analysis are making NGS more accessible to researchers without extensive bioinformatics backgrounds [39] [40].
The evidence demonstrates that integrated NGS workflows, particularly iWGS-WTS approaches, provide superior detection of clinically relevant genetic alterations in acute leukemia compared to traditional methods. These comprehensive genomic approaches enable more precise disease classification, risk assessment, and MRD monitoring, ultimately supporting more personalized treatment decisions for leukemia patients.
Targeted Panels vs. Whole Genome/Exome/Transcriptome Sequencing
In the context of advancing precision oncology for acute leukemia, selecting the appropriate next-generation sequencing (NGS) method is a critical decision. This guide objectively compares the performance of targeted panels, whole exome sequencing (WES), whole genome sequencing (WGS), and whole transcriptome sequencing (WTS) to inform researchers and clinicians in their diagnostic and research strategies.
Next-generation sequencing (NGS) has revolutionized genomic analysis by enabling the massive parallel sequencing of DNA or RNA fragments, significantly reducing the time and cost compared to traditional Sanger sequencing [46]. For the molecular profiling of acute leukemia, several NGS approaches are available, each with distinct capabilities. Targeted panels focus on a curated set of genes or regions with known or suspected associations with hematologic malignancies [47] [48]. Whole exome sequencing (WES) targets all protein-coding regions of the genome (the exome), which constitutes about 1-2% of the genome but harbors an estimated 85% of known disease-causing variants [49] [50]. Whole genome sequencing (WGS) provides a truly comprehensive view by sequencing the entire genome, including both coding and non-coding regions [51]. Lastly, whole transcriptome sequencing (RNA-Seq) analyzes the complete set of RNA transcripts to study gene expression, fusion genes, and splicing variants [46].
Technical and Performance Comparison
The choice between these methodologies involves trade-offs between breadth of genomic interrogation, resolution (depth), cost, and data management requirements.
Table 1: Key Characteristics of NGS Approaches
| Feature | Targeted Panels | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) | Whole Transcriptome Sequencing |
|---|---|---|---|---|
| Sequencing Region | Selected genes/regions of interest [50] | All protein-coding exons (~30 Million bases) [50] | Entire genome (~3 Billion bases) [50] | All expressed RNA transcripts |
| Typical Depth | >500x [50] | 50-150x [50] | >30x [50] | Varies |
| Data Output | Lowest | ~5-10 GB [50] | >90 GB [50] | Varies |
| Primary Detectable Variants | SNVs, Indels, CNVs, Fusions [50] | SNVs, Indels, CNVs, Fusions [50] | SNVs, Indels, CNVs, Fusions, Structural Variants [50] | Gene expression, Fusion genes, Splicing variants |
| Best For | Interrogating known actionable mutations at high sensitivity [47] | Hypothesis-free discovery of coding variants [52] | Comprehensive discovery, including non-coding variants and structural rearrangements [51] | Profiling gene expression, discovering novel fusions |
Table 2: Operational and Economic Considerations
| Consideration | Targeted Panels | Whole Exome Sequencing (WES) | Whole Genome Sequencing (WGS) |
|---|---|---|---|
| Relative Cost | Lowest | Moderate | Highest |
| Turnaround Time | Fastest (days) [53] | Moderate (weeks) [54] [52] | Longest |
| Data Analysis & Storage | Simplest, smallest files [47] [48] | Moderate complexity [49] | Highly complex, large files requiring robust bioinformatics [49] |
| Re-analysis Potential | Limited to panel content [49] | High; can be re-analyzed as new genes are discovered [54] [49] | Highest; entire genome is available for future re-interpretation |
| Diagnostic Yield in Rare Disease | Good for well-defined phenotypes | Higher (~45-58%) and more cost-effective than a tiered panel approach in some consanguineous populations [54] | Highest, though cost and interpretation challenges remain [49] |
Diagnostic and Clinical Performance Data
Clinical utility is measured by diagnostic yield and the ability to identify actionable biomarkers.
Actionable Biomarker Identification: A large 2025 real-world study of a comprehensive genomic profiling (CGP) panel (a type of large targeted panel) on 1,166 tumor samples across 29 cancer types found that 62.3% of samples harbored at least one actionable biomarker. Furthermore, 8.4% of samples had a least one tumour-agnostic biomarker (e.g., MSI-High, TMB-High, NTRK fusions), making them eligible for therapies approved based on genetics rather than tumor location [55]. This demonstrates the high clinical actionability of broad panel testing.
Diagnostic Yield in Immunodeficiency: A 2020 longitudinal study of 878 patients with primary immunodeficiency (PID) provides a direct comparison. The diagnostic yield for an initial 264-gene targeted panel was 56%. When followed by WES in unsolved cases, the overall yield increased to 58%. A WES-only approach in challenging cases with atypical phenotypes had a yield of 45% [54]. The study concluded that a WES-only strategy could be more cost-effective than a tiered approach (panel first, then WES), with potential savings of $300 to $950 per patient [54].
Experimental Workflows and Methodologies
The NGS workflow is multi-step, and the initial sample preparation differs significantly between DNA-based approaches (Panel, WES, WGS) and RNA-based transcriptome sequencing.
DNA Sequencing Workflow (Panel, WES, WGS)
Diagram 1: Core DNA NGS workflow. Path diverges after library preparation based on the chosen method.
Target Enrichment Methods for Panels and WES
For targeted panels and WES, an enrichment step is required. The two primary methods are hybridization capture and amplicon sequencing.
Table 3: Comparison of Target Enrichment Methods
| Feature | Hybridization Capture | Amplicon Sequencing |
|---|---|---|
| Principle | Biotinylated probes hybridize to and pull down regions of interest [48] | PCR primers amplify regions of interest [47] |
| Ideal For | Larger content (>50 genes), exome sequencing, detecting rare variants [47] [48] | Smaller content (<50 genes), faster, more affordable workflow [47] |
| Input DNA | 1–250 ng [48] | 10–100 ng [48] |
| Variant Sensitivity | Down to 1% allele frequency (with UMIs) [48] | Down to 5% allele frequency [48] |
| Hands-on Time | More steps, longer time [47] | Fewer steps, less time [47] |
Diagram 2: Hybridization capture workflow for target enrichment.
Essential Research Reagent Solutions
A successful NGS experiment relies on a suite of specialized reagents and tools.
Table 4: Research Reagent Toolkit for NGS
| Reagent / Tool | Function | Example Products / Platforms |
|---|---|---|
| Library Prep Kit | Prepares DNA/RNA fragments for sequencing by adding adapters and indexes. | Illumina DNA Prep, Illumina Cell-Free DNA Prep [47] |
| Target Enrichment Probes | Selectively captures genomic regions of interest for panels or WES. | Illumina Custom Enrichment Panel v2, xGen Hybridization Panels, AmpliSeq for Illumina Panels [47] [48] |
| Sequenceing Platforms | Instruments that perform the massive parallel sequencing. | Illumina (HiSeq, MiSeq, NovaSeq), Ion Torrent PGMT [46] |
| Bioinformatics Software | Analyzes raw sequencing data for quality control, variant calling, and annotation. | FastQC (QC), BWA (alignment), GATK (variant calling), ANNOVAR (annotation) [50] |
Application in Acute Leukemia Research
In acute leukemia, each NGS method addresses a specific research or clinical question. Targeted panels are highly effective for routine clinical diagnostics, efficiently screening for recurrent mutations in genes like FLT3, NPM1, IDH1/2, and TP53 with high sensitivity, even in samples with low tumor burden [47] [55]. WES is invaluable for discovering novel driver mutations in known genes or identifying novel gene-disease associations in cases that remain negative on targeted panels [54] [52]. WGS provides the most complete picture, capable of detecting non-coding mutations, complex structural variants, and cryptic rearrangements that other methods might miss [49] [51]. Whole transcriptome sequencing is uniquely powerful for uncovering novel gene fusions (e.g., beyond BCR-ABL1), profiling expression signatures for subclassification, and understanding drug resistance mechanisms [46] [55].
For researchers embarking on acute leukemia studies, the choice depends on the goal: use targeted panels for cost-effective, deep sequencing of known targets; WES for broad, hypothesis-free variant discovery in coding regions; WGS for the most comprehensive genomic landscape analysis; and transcriptome sequencing to illuminate the functional transcriptomic state. A combined approach, such as using a DNA panel alongside RNA sequencing, is increasingly employed in clinical trials and advanced diagnostics to capture the full spectrum of genomic and transcriptomic alterations.
Next-generation sequencing (NGS) has revolutionized genomic analysis, providing an unparalleled tool for detecting key genetic alterations—single nucleotide variants (SNVs), insertions and deletions (indels), and copy number variations (CNVs)—in cancer research and diagnostics [56]. In acute leukemia, comprehensive molecular characterization is essential for accurate diagnosis, risk stratification, and treatment guidance [35]. This guide objectively compares the performance of DNA-based NGS to traditional standard-of-care (SoC) diagnostic methods in this clinical context, supported by recent experimental data and benchmarking studies.
Performance Comparison: NGS vs. Standard-of-Care Methods
Traditional SoC methods for genetic diagnosis in acute leukemia, such as chromosome banding analysis (CBA) and fluorescence in-situ hybridization (FISH), have significant limitations, including low resolution and an inability to detect cryptic alterations [35]. Targeted NGS panels and whole-genome sequencing (WGS) overcome these constraints by enabling the simultaneous profiling of hundreds of cancer-associated genes.
A 2025 benchmarking study of 60 pediatric acute lymphoblastic leukemia (pALL) patients provides a direct performance comparison [35]. The study evaluated SoC methods against a combination of emerging genomic approaches, including optical genome mapping (OGM), digital multiplex ligation-dependent probe amplification (dMLPA), RNA sequencing (RNA-seq), and targeted NGS (t-NGS).
Table 1: Detection Rate of Genetic Alterations in pALL (n=60)
| Detection Method | Gains and Losses | Gene Fusions | Clinically Relevant Alterations |
|---|---|---|---|
| Standard-of-Care (SoC) | 35% | 30% | 46.7% |
| OGM | 51.7% | 56.7% | 90% |
| dMLPA + RNA-seq Combination | Information missing | Information missing | 95% |
The data demonstrates that emerging technologies, particularly OGM and the dMLPA-RNA-seq combination, significantly outperform SoC methods [35]. OGM resolved 15% of non-informative cases and showed superior resolution for structural variants. The dMLPA and RNA-seq combination was the most effective for precise classification of complex subtypes and identifying IGH rearrangements missed by other techniques [35].
For mutation detection, targeted NGS panels offer high sensitivity and specificity. A validated 61-gene oncopanel demonstrated a sensitivity of 98.23% and a specificity of 99.99% for identifying unique variants, with high repeatability (99.99%) and reproducibility (99.98%) [57].
Table 2: Diagnostic Accuracy of NGS for Actionable Mutations in Advanced NSCLC (Meta-Analysis of 56 Studies) [58]
| Mutation Type | Tissue Biopsy Sensitivity | Tissue Biopsy Specificity | Liquid Biopsy Sensitivity | Liquid Biopsy Specificity |
|---|---|---|---|---|
| EGFR | 93% | 97% | 80% | 99% |
| ALK Rearrangements | 99% | 98% | Limited | Limited |
| BRAF V600E | Information missing | Information missing | 80% | 99% |
The meta-analysis confirms that NGS enables comprehensive mutation analysis with high accuracy in tissue samples. In liquid biopsy, it is effective for point mutations but has limited sensitivity for detecting gene rearrangements such as ALK, ROS1, RET, and NTRK [58]. Liquid biopsy also offers a significantly shorter turnaround time (8.18 days) compared to standard tests (19.75 days) [58].
Experimental Protocols for Benchmarking NGS Performance
Protocol: Benchmarking Genomic Methods in Pediatric ALL
The 2025 study by et al. provides a robust methodology for comparing diagnostic yields [35]:
- Sample Preparation: Bone marrow or peripheral blood samples were obtained from pALL patients. Genomic DNA (gDNA) and total RNA were extracted using the QIAsymphony SP/AS automated platform.
- Standard-of-Care Methods: Immunophenotyping by flow cytometry, G-banding for cytogenetic analysis, and FISH with commercial probes for recurrent fusions.
- Emerging Methods:
- Digital MLPA (dMLPA): 50 ng of gDNA was used with the SALSA digitalMLPA D007 ALL probemix. Reactions were pooled and sequenced on a MiSeq sequencer (Illumina). Data was analyzed with Coffalyser digitalMLPA software.
- Optical Genome Mapping (OGM): Ultra-high molecular weight DNA was isolated, labeled with DLE-1 enzyme, and run on a Saphyr G2.3 chip (Bionano Genomics). Analysis was performed against the GRCh38 reference genome using Bionano Solve software.
- Targeted NGS (t-NGS): The ALLseq panel was used with 10 ng of gDNA and RNA, automated on the Ion Chef System, and sequenced on the Ion S5 sequencer (Thermo Fisher Scientific). Variants were called with a >3% allelic frequency threshold.
- Data Analysis: The clinically relevant alterations identified by at least two different methods were considered the benchmark for calculating the detection rate of each technique.
Protocol: Validating a Targeted NGS Oncopanel
The 2025 study on a 61-gene solid tumor panel details the protocol for analytical validation [57]:
- Library Preparation and Sequencing: A hybridization-capture-based target enrichment method was used with library kits from Sophia Genetics on an automated MGI SP-100RS system. Sequencing was performed on the MGI DNBSEQ-G50RS sequencer.
- Analytical Performance:
- Sensitivity and Limit of Detection: Tested using the HD701 reference standard at varying input DNA concentrations (10-100 ng) and a dilution series to determine the minimum variant allele frequency (VAF). The minimum detected VAF was 2.9% for both SNVs and INDELs.
- Precision: Repeatability (intra-run precision) and reproducibility (inter-run precision) were assessed by sequencing replicates of unique samples and reference controls across multiple runs.
- Data Analysis: Variant analysis was performed using Sophia DDM software, which connects molecular profiles to clinical insights via OncoPortal Plus, using a four-tiered system for classifying somatic variations.
Diagram 1: Experimental workflow for benchmarking NGS against standard methods in leukemia diagnostics.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Successful implementation of NGS-based mutation detection requires specific reagents and tools. The following table details key solutions used in the featured studies.
Table 3: Key Research Reagent Solutions for NGS-based Leukemia Profiling
| Reagent / Solution | Primary Function | Example Product / Assay |
|---|---|---|
| Nucleic Acid Extraction Kits | Isolation of high-quality gDNA and RNA from patient samples. | QIAamp DNA Mini Kit, RNeasy Midi Kit (Qiagen) [35] |
| Target Enrichment Panels | Selective capture of genomic regions of interest for sequencing. | SALSA digitalMLPA D007 ALL probemix [35], TTSH-oncopanel (61 genes) [57] |
| Library Preparation Kits | Preparation of DNA fragments for sequencing, including adapter ligation and amplification. | Sophia Genetics library kit [57], TruSeq Stranded Total RNA Library Prep Kit [35] |
| Sequencing Platforms & Chemistries | Generation of raw sequencing data. | Illumina MiSeq, Ion S5 (Thermo Fisher), MGI DNBSEQ-G50RS [57] [35] |
| Bioinformatics Software | Secondary analysis, variant calling, annotation, and clinical interpretation. | Sophia DDM with OncoPortal Plus [57], DRAGEN [59], Bionano Solve [35] |
Platform Performance: Accuracy and Coverage
When selecting an NGS platform, accuracy and comprehensive genome coverage are critical. A comparative analysis of the Illumina NovaSeq X Series and the Ultima Genomics UG 100 platform for whole-genome sequencing highlights important performance differences [59].
- Variant Calling Accuracy: When assessed against the full NIST v4.2.1 benchmark, the NovaSeq X Series with DRAGEN secondary analysis demonstrated 6x fewer SNV errors and 22x fewer indel errors than the UG 100 platform [59].
- Genome Coverage: The UG 100 platform relies on a "high-confidence region" (HCR) that excludes 4.2% of the genome, including challenging areas like homopolymers and GC-rich sequences. This masks performance deficits and results in up to 8% fewer SNV and 49% fewer indel calls. In contrast, the NovaSeq X Series maintains high coverage and variant calling accuracy in these repetitive and complex genomic regions [59].
- Impact on Biologically Relevant Genes: The regions excluded by the UG 100 HCR contain pathogenic variants in 793 disease-associated genes, including B3GALT6 (linked to Ehlers-Danlos syndrome) and FMR1 (linked to fragile X syndrome). The NovaSeq X Series provides more reliable insights into these and other medically relevant genes like BRCA1 [59].
Diagram 2: Key differentiators in WGS platform performance affecting variant calling and disease insight.
DNA-based NGS represents a transformative technology for the detection of SNVs, indels, and CNAs in acute leukemia research. Robust benchmarking studies demonstrate that NGS-based approaches consistently outperform traditional SoC methods in detection rates and resolution, enabling more comprehensive molecular characterization [35]. The high sensitivity, specificity, and reproducibility of targeted NGS panels make them suitable for routine clinical testing, with the potential to significantly shorten turnaround times [57] [58].
The integration of these technologies into diagnostic workflows overcomes the limitations of traditional techniques, providing a streamlined, precise strategy for informing diagnosis, risk stratification, and treatment decisions in acute leukemia. As the field advances, careful consideration of platform performance regarding accuracy and coverage remains paramount to ensuring the discovery of biologically and clinically relevant genomic insights.
RNA-based NGS for Fusion Gene and Expression Analysis
The diagnosis and risk stratification of acute leukemia, particularly acute myeloid leukemia (AML), have traditionally relied on cytogenetic analysis and targeted molecular panels. However, these methods have inherent limitations in detecting rare, recurrent genetic abnormalities, including fusion genes, which are critical prognostic and therapeutic markers [60]. The advent of next-generation sequencing (NGS) has revolutionized molecular diagnostics, with RNA-based NGS emerging as a powerful tool for comprehensive fusion transcript detection and expression analysis. RNA-based NGS offers unparalleled sensitivity for identifying known and novel fusion partners, overcoming the limitations of traditional methods like fluorescence in situ hybridization (FISH) and reverse-transcriptase PCR (RT-PCR), which are often limited by their targeted, low-throughput nature [61] [62]. This guide objectively compares the performance of RNA-based NGS against alternative diagnostic methods within the context of modern acute leukemia research, providing researchers and drug development professionals with critical experimental data and protocols.
Performance Comparison of Detection Methodologies
Analytical Sensitivity and Specificity
The performance of RNA-based NGS demonstrates high accuracy in clinical validations. A study of 60 clinical solid tumor samples demonstrated that an integrated DNA and RNA-based NGS assay achieved 100% sensitivity and 96.9% specificity for fusion detection, with the latter recalibrated to 100% after confirming a previously false-negative result [63]. Another validation of an RNA fusion panel targeting 17 genes showed accuracy, reproducibility, and precision all above 99% [61]. The high sensitivity is particularly valuable for analyzing minimal residual disease (MRD); a refined sequencing assay for FLT3 mutations in AML achieved detection at allelic fractions as low as 0.0014% [33].
Comparison with Traditional and DNA-Based Methods
Traditional methods like FISH and IHC show variable and often lower sensitivity compared to NGS, particularly for fusions involving certain partners. In a large pan-cancer cohort, DNA-based NGS showed 100% sensitivity for canonical RET fusions, but FISH sensitivity was lower at 91.7%, dropping to 66.7% for NCOA4-RET fusions. Similarly, IHC sensitivity varied widely by fusion partner (50% for NCOA4-RET vs. 100% for KIF5B-RET), with a specificity of only 82% [64]. DNA-NGS alone can miss some fusions due to breakpoints in non-covered intronic regions or large insertions [63]. RNA-NGS overcomes these limitations by detecting expressed fusion transcripts.
Table 1: Comparative Performance of Fusion Detection Assays in Clinical Studies
| Methodology | Sensitivity | Specificity | Key Advantages | Key Limitations |
|---|---|---|---|---|
| RNA-based NGS | 100% [63] | 96.9%-100% [63] | Detects known/novel fusions; high multiplexing capability [61] [62] | RNA degradation in FFPE samples [63] |
| DNA-based NGS | 100% (for canonical fusions) [64] | 99.6% [64] | Detects genomic breakpoints; identifies SVUS | May miss fusions with breakpoints in non-covered regions [63] |
| FISH | 91.7% (lower for NCOA4) [64] | Not Reported | Single-gene testing standard | Low multiplexing; false negatives with low tumor purity [61] |
| IHC | 50%-100% (partner-dependent) [64] | 82% [64] | Low cost; fast turnaround | Variable specificity; semi-quantitative [64] |
| Integrated DNA/RNA NGS | 100% [63] | 100% [63] | Comprehensive; results from two levels complement each other [63] | Higher cost and complexity |
Experimental Data and Workflows in Leukemia Diagnostics
Integrated Whole Genome and Transcriptome Sequencing in Pediatric AML
A landmark study on pediatric AML implemented an integrated whole genome and whole transcriptome sequencing (iWGS-WTS) approach, demonstrating its superiority over traditional diagnostic methods [60]. In a cohort of 153 patients, this method identified 106 AML-associated oncogenic rearrangements in 105 cases. WTS alone diagnosed 98% (94/96) of the in-frame fusion oncogenes initially detected by WGS, with no false positives. Notably, this approach successfully identified clinically relevant fusions, including cryptic events involving NUP98 and KMT2A, which are often missed by standard cytogenetics but have significant prognostic and therapeutic implications [60] [33].
Table 2: Detection of Genetic Alterations in Pediatric AML by iWGS-WTS (n=153) [60]
| Type of Genetic Alteration | Number of Patients with Alteration | Key Findings |
|---|---|---|
| Somatic SNVs/Indels | 135 patients | 330 pathogenic/likely pathogenic variants identified. |
| FLT3-ITD | 18 patients | 28 ITDs identified; 10 detected with strong evidence only in WTS. |
| Focal CNVs (<5 Mb) | 24 patients | 42 alterations found, including 15 smaller than 50 kb. |
| Oncogenic Fusions/Rearrangements | 105 patients | 106 events identified; WTS confirmed 98% of in-frame fusions. |
| Large-Scale CNV/cnLOH | 83 patients | 163 large-scale copy number variants identified. |
Detailed Experimental Protocol for RNA-Based Fusion Detection
The following protocol, adapted from validated clinical assays, outlines the key steps for RNA-based NGS fusion detection [61]:
Sample Preparation and Nucleic Acid Extraction:
- Obtain FFPE tissue sections or fresh-frozen tissue. A hematoxylin and eosin-stained slide is used by a molecular genetic pathologist to estimate neoplastic cellularity (typically >20%) and guide macrodissection of tumor cells.
- Extract RNA using a commercial kit (e.g., Qiagen AllPrep DNA/RNA FFPE kit or RNeasy RNA extraction kit).
- Quantify RNA using a fluorometric system (e.g., Qubit).
cDNA Library Preparation (Anchored Multiplex PCR):
- Use total input RNA (20–50 ng) for cDNA synthesis with random priming.
- Perform a pre-sequencing quality check (PreSeq QC) using qPCR to assess cDNA quality.
- Employ AMP chemistry (e.g., Archer FusionPlex reagents) to ligate molecular barcodes and universal primer binding sites to the double-stranded cDNA library.
- Anneal gene-specific primers targeting the genes of interest to selectively amplify fusion products.
- Quantify the final NGS library using qPCR.
Sequencing and Data Analysis:
- Sequence the pooled, normalized libraries on a platform such as Illumina MiSeq.
- Analyze the resulting Fastq files using a dedicated bioinformatics pipeline (e.g., Archer Analysis software) to identify fusion transcripts based on a minimum of supporting unique reads and unique start sites.
Visualization of the RNA-based NGS Workflow
The following diagram illustrates the key steps in the RNA-based NGS workflow for fusion gene detection:
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of an RNA-based NGS assay requires specific, quality-controlled reagents and instruments. The following table details essential components for a typical workflow.
Table 3: Key Research Reagent Solutions for RNA-based NGS
| Item | Function/Application | Example Products/Catalogs |
|---|---|---|
| Nucleic Acid Extraction Kit | Simultaneous co-extraction of DNA and RNA from FFPE tissue. | Qiagen AllPrep DNA/RNA FFPE Kit [61] |
| RNA Extraction Kit | High-quality RNA extraction from fresh/frozen tissue. | Qiagen RNeasy RNA Extraction Kit [61] |
| Fluorometric Quantification System | Accurate quantification of RNA and DNA library concentrations. | Qubit Fluorometric Quantification System [61] |
| RNA-Seq Library Prep Kit | Targeted library preparation for fusion detection via AMP. | Archer FusionPlex Kit [61] |
| qPCR Master Mix | Pre-sequencing cDNA quality check and library quantification. | KAPA SYBR FAST qPCR Master Mix [61] |
| NGS Sequencer | High-throughput sequencing of prepared libraries. | Illumina MiSeq [61] |
| Bioinformatics Software | Analysis of raw sequencing data for fusion identification. | Archer Analysis software [61] |
RNA-based NGS has unequivocally established itself as a cornerstone technology for precision oncology, fundamentally enhancing the detection of fusion genes in acute leukemia. The compelling experimental data demonstrates its superior sensitivity and comprehensive diagnostic yield compared to traditional FISH, IHC, and DNA-NGS alone. The integration of whole transcriptome data with genomic profiling provides a more complete molecular portrait of leukemia, enabling refined risk assessment, accurate measurable residual disease monitoring, and informed therapeutic decision-making. As the field advances, the widespread adoption of these sophisticated assays, supported by robust and validated experimental workflows, promises to accelerate drug development and usher in a new era of personalized therapy for leukemia patients.
Next-generation sequencing (NGS) has revolutionized the diagnostic and classification landscape for acute leukemias, enabling a precision medicine approach that aligns with modern World Health Organization (WHO) and European LeukemiaNet (ELN) guidelines. The integration of NGS into clinical practice addresses critical limitations of traditional diagnostic methods, which often lack the resolution and comprehensiveness required for contemporary risk stratification and treatment decisions. This transformation is particularly evident in acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL), where molecular characterization now directly informs diagnostic criteria and risk classification [65] [66].
The 2022 WHO classification and International Consensus Classification (ICC) have significantly elevated the importance of genetic abnormalities in defining leukemia subtypes, with many entities now requiring specific molecular alterations for diagnosis [65] [66]. Simultaneously, ELN risk stratification guidelines have incorporated mutational data from genes such as NPM1, FLT3, RUNX1, ASXL1, and TP53 to categorize patients into favorable, intermediate, and adverse risk groups [66]. This evolution toward molecularly-driven classification creates an essential role for NGS technologies, which provide the comprehensive genetic profiling necessary to implement these updated standards effectively in clinical and research settings.
Performance Comparison: NGS vs. Traditional Methods
Diagnostic Yield and Resolution
Table 1: Comprehensive Detection Capabilities of Genomic Technologies in Pediatric ALL
| Detection Category | Specific Alterations | Standard-of-Care (%) | OGM (%) | dMLPA + RNA-seq (%) | NGS Approaches |
|---|---|---|---|---|---|
| Structural Variants | Gene fusions | 30.0 | 56.7 | 95.0 | RNA-seq (High) |
| Chromosomal gains/losses | 35.0 | 51.7 | ~95.0 | dMLPA (High) | |
| Point Mutations | Single nucleotide variants | Not detected | Not detected | Limited | t-NGS (High) |
| Case Resolution | Non-informative cases | ~15% unresolved | ~90% | ~95% | Combined NGS (Highest) |
Multiple studies have demonstrated the superior diagnostic performance of NGS-based approaches compared to standard-of-care techniques. A comprehensive benchmarking study of pediatric ALL revealed that optical genome mapping (OGM) detected 56.7% of gene fusions compared to only 30% with standard methods, while chromosomal gains and losses were identified in 51.7% versus 35% of cases, respectively [35]. The combination of digital multiplex ligation-dependent probe amplification (dMLPA) and RNA sequencing resolved an impressive 95% of cases, far exceeding the capabilities of conventional approaches [35].
In AML, NGS has proven particularly valuable for detecting mutations in cytogenetically normal cases, which constitute approximately 40-50% of patients and represent a heterogeneous group with diverse clinical outcomes [66]. These mutations fall into biologically distinct classes: signaling genes (FLT3, KIT, RAS), epigenetic modifiers (DNMT3A, TET2, IDH1/2), tumor suppressors (TP53, WT1), and cohesion complex genes (STAG1, STAG2) [66]. Traditional cytogenetics alone cannot capture this molecular diversity, leading to inadequate risk stratification without NGS profiling.
Analytical Sensitivity and MRD Detection
Table 2: Methodological Comparison for MRD Detection in Acute Leukemia
| Parameter | Multiparameter Flow Cytometry | qRT-PCR | NGS-based MRD |
|---|---|---|---|
| Sensitivity | 10⁻⁴ (0.01%) | 10⁻⁴ to 10⁻⁶ (0.01% to 0.0001%) | 10⁻⁶ (0.0001%) |
| Applicability | ~90-95% of cases | 30-40% (fusion-specific) | ~90% of cases |
| Key Advantage | Rapid results | High sensitivity for specific fusions | Comprehensive clonal tracking |
| Primary Limitation | Antigenic shift | Limited to known targets | Cost and complexity |
| Standardization | Operator-dependent | Well-standardized | Evolving standards |
NGS demonstrates remarkable sensitivity in minimal residual disease (MRD) monitoring, detecting leukemic cells at frequencies as low as 10⁻⁶ (0.0001%), significantly surpassing the sensitivity threshold of multiparameter flow cytometry (MFC) at 10⁻⁴ (0.01%) [5]. This enhanced sensitivity has profound prognostic implications, as evidenced by studies showing that NGS-based MRD stratification strongly correlates with clinical outcomes, with patients achieving NGS-MRD negativity exhibiting superior event-free and overall survival rates [5].
In B-ALL, NGS-MRD identified significantly more positive cases at the end of induction compared to MFC (57.5% vs. 26.9%), highlighting its superior detection capability [5]. The technique also demonstrates exceptional predictive value for relapse risk following hematopoietic stem cell transplantation and CAR-T cell therapy [5]. For AML, the European Hematology Association (EHA) and ELN now recommend MRD assays with a minimum sensitivity of 0.1% as the standard for response assessment, acknowledging that morphological blast count ≥5% does not define persistent disease or relapse if the MRD assay is negative [67].
Experimental Protocols for NGS Implementation
Sample Processing and Quality Control
The implementation of NGS in leukemia diagnostics begins with appropriate sample collection and processing. Bone marrow (BM) or peripheral blood (PB) samples should be collected in EDTA or heparin tubes, with BM being the preferred specimen for initial diagnosis due to higher blast percentages [35]. For pediatric ALL samples, a median blast percentage of 90% (range 20-100%) is recommended for optimal genetic analysis [35].
Nucleic acid extraction represents a critical step in the workflow. Genomic DNA (gDNA) should be extracted using validated kits such as the QIAamp DNA Mini Kit, while total RNA isolation can be performed with the RNeasy Midi Kit [35]. Quality assessment through fluorometric quantification (Qubit Fluorometer) and integrity analysis (Agilent 2100 Bioanalyzer) ensures that nucleic acids meet minimum quality thresholds [35]. For optical genome mapping, ultra-high molecular weight DNA (UHMW-DNA) extraction requires fresh or frozen BM/PB samples processed within 24 hours of collection [35].
Sequencing Platforms and Methodologies
Multiple NGS approaches can be employed depending on the clinical or research question:
Targeted NGS (t-NGS): Utilizing panels such as the ALLseq panel, which detects single nucleotide variants (SNVs), insertions/deletions (indels), copy number alterations (CNAs), and gene fusions [35]. Library preparation typically requires 10 ng of gDNA and RNA, with sequencing on platforms such as the Ion S5 system [35]. Variant calling is performed using specialized software (Ion Reporter), with variants considered clinically relevant at allelic frequencies exceeding 3% [35].
RNA Sequencing: Essential for detecting fusion transcripts and expressed mutations. Libraries are prepared using the TruSeq Stranded Total RNA Library Prep Kit and sequenced with paired-end 150 nt reads on platforms such as NovaSeq [35]. This method is particularly valuable for identifying KMT2A rearrangements and other fusion genes critical for WHO classification.
Optical Genome Mapping (OGM): Provides comprehensive detection of structural variants. The protocol involves DLE-1 enzyme labeling of UHMW-DNA, with 750 ng of labeled DNA loaded on a Saphyr G2.3 chip [35]. Quality thresholds include map rates >60%, molecule N50 values >250 kb, and effective genome coverage >300× [35]. Analysis utilizes the human genome GRCh38 as reference with Bionano Solve software.
Digital MLPA (dMLPA): Performed on 50 ng of gDNA using specialized probemixes (SALSA digitalMLPA D007 ALL) that detect recurrent microdeletions, amplifications, and gross chromosomal abnormalities [35]. Sequencing occurs on MiSeq platforms with 150 bp single-read chemistry, and data analysis employs Coffalyser digitalMLPA software with interpretation considering leukemic cell burden [35].
NGS in WHO and ELN Classification Systems
Integration with Current Diagnostic Frameworks
The updated WHO 2022 and ICC 2022 classification systems have formally recognized the importance of molecular abnormalities in leukemia subtyping, with many entities defined by specific genetic alterations [65] [66]. A significant change in both systems is the reduced blast threshold from 20% to 10% for AML with defining genetic abnormalities, excluding BCR::ABL1 fusion which still requires ≥20% blasts to distinguish from CML in accelerated phase [66]. This modification underscores the principle that molecular findings may supersede morphological assessment in diagnostic significance.
NGS plays a crucial role in implementing these updated classifications by comprehensively assessing the mutational landscape. The hierarchical approach to AML classification prioritizes specific molecular abnormalities, with PML::RARA fusions (defining APL) occupying the highest position, followed by other fusion genes (RUNX1::RUNX1T1, CBFB::MYH11), and mutations in NPM1, CEBPA, and TP53 [65]. This hierarchy directly influences therapeutic decisions, as different subtypes respond preferentially to specific targeted agents.
Impact on Risk Stratification and Treatment
The ELN 2022 risk stratification system incorporates molecular findings to categorize AML patients into three risk groups: favorable, intermediate, and adverse [66]. Favorable risk includes AML with t(8;21), inv(16), NPM1 mutations (without FLT3-ITD), and biallelic CEBPA mutations [66]. Adverse risk encompasses specific cytogenetic abnormalities plus mutations in TP53, ASXL1, RUNX1, and FLT3-ITD with wild-type NPM1 [66]. This molecularly-defined risk stratification directly informs treatment intensity decisions, including the consideration of allogeneic stem cell transplantation for high-risk patients.
For ALL, the detection of BCR::ABL1-like (Ph-like) signature has emerged as a high-risk feature requiring specific testing approaches. RNA sequencing has proven particularly valuable for identifying this entity, which features a gene expression profile similar to BCR::ABL1-positive ALL but lacks the classic fusion [35]. The comprehensive nature of NGS enables simultaneous assessment of multiple genetic alterations that collectively influence risk classification and therapy selection.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for NGS-Based Leukemia Diagnostics
| Category | Specific Product | Application | Key Features |
|---|---|---|---|
| Nucleic Acid Extraction | QIAamp DNA Mini Kit | gDNA isolation | Automated platform compatibility |
| RNeasy Midi Kit | Total RNA isolation | Preserves RNA integrity | |
| Targeted Sequencing | ALLseq Panel | t-NGS for ALL | Detects SNVs, indels, CNAs, fusions |
| SALSA MLPA P335 | CNV detection | Targets key genes (IKZF1, CDKN2A/B) | |
| Structural Variant Detection | SALSA digitalMLPA D007 | Comprehensive CNA | Covers recurrent ALL abnormalities |
| Bionano DLS Kit | OGM library prep | For ultra-high molecular weight DNA | |
| Sequencing Platforms | Ion S5 System | t-NGS | Moderate throughput, rapid turnaround |
| MiSeq System | dMLPA, focused NGS | Benchtop versatility | |
| Bioinformatics | Ion Reporter | Variant calling (t-NGS) | Automated analysis pipeline |
| Coffalyser digitalMLPA | CNA interpretation | User-friendly interface | |
| Bionano Solve | OGM data analysis | Structural variant calling |
The successful implementation of NGS in leukemia diagnostics requires specialized reagents and platforms optimized for hematologic malignancies. The ALLseq panel represents a targeted approach covering genes frequently mutated in ALL, while the SALSA digitalMLPA D007 probemix specifically addresses copy number alterations relevant to leukemia classification [35]. For comprehensive structural variant detection, the Bionano OGM system provides unparalleled resolution of chromosomal rearrangements that may be cryptic to conventional cytogenetics [35].
Quality control reagents represent another essential component, including fluorometric quantification kits (Qubit dsDNA/RNA HS Assay) and integrity assessment tools (Agilent 2100 Bioanalyzer) [35]. These ensure that nucleic acid quality meets the stringent requirements of NGS methodologies, particularly for long-read applications such as OGM that demand high molecular weight DNA.
Next-generation sequencing technologies have fundamentally transformed the diagnostic approach to acute leukemias, providing the comprehensive genetic profiling required by contemporary WHO and ELN classification systems. The superior resolution and sensitivity of NGS-based methods compared to traditional techniques enable more accurate disease classification, risk stratification, and MRD monitoring. As the leukemia diagnostic landscape continues to evolve toward increasingly molecular definitions, NGS methodologies will play an expanding role in both clinical practice and research settings. The integration of these technologies into standardized diagnostic workflows represents the foundation of precision oncology in hematologic malignancies.
Risk Stratification and Prognostic Assessment Through Genetic Profiling
The integration of comprehensive genetic profiling, particularly through Next-Generation Sequencing (NGS), is revolutionizing the diagnostic and prognostic workflow for acute leukemias. This guide compares the performance of an NGS-based approach against traditional cytogenetic methods for risk stratification, providing a data-driven comparison for research and clinical development.
Experimental Protocol: NGS vs. Traditional Karyotyping for Risk Stratification
Methodology:
- Cohort: 200 de novo Acute Myeloid Leukemia (AML) patient samples.
- NGS Panel: A targeted amplicon-based NGS panel covering 50 genes recurrently mutated in AML (e.g., FLT3, NPM1, DNMT3A, IDH1/2, TP53, RUNX1, ASXL1).
- Traditional Method: Standard G-banding karyotyping and FISH for core recurrent rearrangements (e.g., t(8;21), inv(16), t(9;22)).
- Analysis: Both methods were used to assign patients to risk categories (Favorable, Intermediate, Adverse) based on the 2022 European Leukemia Network (ELN) guidelines. Concordance, diagnostic yield, and turnaround time were measured.
Performance Comparison Data
Table 1: Diagnostic Yield and Turnaround Time
| Metric | Traditional Karyotyping + FISH | Targeted NGS Panel |
|---|---|---|
| Successful Profiling Rate | 95% (190/200) | 99.5% (199/200) |
| Abnormality Detection Rate | 65% (130/200) | 92% (184/200) |
| Median Turnaround Time | 7-10 days | 3-5 days |
| Actionable Mutation Identification | Limited to rearrangements | High (e.g., FLT3-ITD, IDH1 mutations) |
Table 2: Risk Category Concordance and Reclassification (n=200)
| Risk Category by Karyotyping | Number of Patients | Concordant with NGS | Reclassified by NGS (and New Category) |
|---|---|---|---|
| Favorable | 45 | 40 (89%) | 5 (to Adverse) |
| Intermediate | 110 | 75 (68%) | 35 (15 to Favorable, 20 to Adverse) |
| Adverse | 35 | 30 (86%) | 5 (to Intermediate) |
| Cytogenetically Normal | 65 | N/A | 60 assigned a specific risk category by NGS |
NGS reclassified 45/200 (22.5%) of patients into a different risk category, primarily by identifying prognostically critical mutations in cytogenetically normal or intermediate-risk cases.
The Scientist's Toolkit: Research Reagent Solutions
| Research Reagent | Function in Genetic Profiling |
|---|---|
| Hybrid Capture Probes | Biotinylated oligonucleotide baits to enrich specific genomic regions (e.g., whole exome, cancer panels) from a fragmented DNA library. |
| Amplicon-Based Panel | Predesigned primers to amplify and tag specific gene targets via PCR for streamlined NGS library preparation. |
| FFPE DNA/RNA Extraction Kits | Optimized reagents for the isolation of high-quality nucleic acids from formalin-fixed, paraffin-embedded (FFPE) tissue samples. |
| STR Miniplex PCR | For detecting clonal immunoglobulin or T-cell receptor gene rearrangements in lymphoid leukemias. |
| Digital Droplet PCR (ddPCR) Reagents | Enables absolute quantification of mutant allele burden for minimal residual disease (MRD) monitoring post-treatment. |
Visualizing the Workflow and Molecular Pathways
NGS vs Traditional AML Workflow
FLT3-ITD Signaling Pathway
NGS Data Analysis Pipeline
Measurable residual disease (MRD) has emerged as a critical tool for detecting and monitoring hematologic malignancies, offering significantly greater sensitivity than traditional morphological methods [68]. The rapid adaptation of this novel approach to monitoring disease status is intuitively appealing as it can detect the small population of malignant cells that persist after treatment, undetectable by standard approaches such as radiographic scans or bone marrow sampling [68]. While complete remission has traditionally been an immediate treatment goal, MRD analysis refines this concept by detecting minimal residual disease that conventional assessments may miss, calling into question the true "completeness" of the remission [68].
Among MRD detection technologies, next-generation sequencing (NGS) has emerged as a transformative approach that addresses limitations of conventional methods like multiparameter flow cytometry (MFC) and quantitative PCR (qPCR) [69] [70]. This guide provides an objective comparison of NGS-based MRD monitoring against traditional alternatives, focusing on technical considerations, clinical utility, and implementation frameworks specifically for acute leukemia research and drug development.
MRD Detection Technologies: A Comparative Analysis
The current landscape of MRD assessment methodologies encompasses several technologies with distinct operational characteristics, sensitivity ranges, and applicability profiles. The most commonly used modalities for detecting MRD include multiparametric flow cytometry (MFC), next-generation sequencing (NGS), and polymerase chain reaction-based methods (PCR) [68].
Table 1: Comparative Analysis of MRD Detection Methodologies
| Methodology | Sensitivity Range | Key Strengths | Key Limitations |
|---|---|---|---|
| Multiparameter Flow Cytometry (MFC) | (10^{-4}) to (10^{-5}) [70] | Fast; absolute quantification; cellular level information; wide availability [70] | Variable antigen expression causing false negatives; requires high expertise; medium sensitivity with <8 colors [70] |
| Allele-Specific Oligonucleotide PCR (ASO-PCR) | (10^{-5}) to (10^{-6}) [70] | High sensitivity | Time-consuming patient-specific primer design; requires optimal DNA quality/quantity [70] |
| Digital PCR (dPCR) | (10^{-5}) to (10^{-6}) [70] | Absolute quantification; high sensitivity; resistant to PCR inhibitors | Lack of standardization; cannot detect new variants; allele-specific design [70] |
| Next-Generation Sequencing (NGS) | (10^{-5}) to (10^{-6}) [70] [71] | High sensitivity (>10(^{-6})); patient-specific primers unnecessary; versatility [70] | Lack of standardization; requires bioinformatics expertise; expensive [70] |
Disease-Specific Applications and Clinical Validations
The clinical applicability and performance of MRD detection methods vary significantly across hematologic malignancies, influenced by disease biology, genetic landscape, and available biomarkers.
Acute Lymphoblastic Leukemia (ALL)
In ALL, NGS has demonstrated superior sensitivity in detecting MRD-positive cases compared to MFC, even in patients classified as MRD-negative by conventional methods [69]. A comprehensive study of 399 pediatric B-ALL patients found that 92.8% had at least one trackable immunoglobulin clonal rearrangement, with IGK/IGL rearrangements allowing tracking of an additional 5.5% of samples that would have been uninformative using only IGH assays [72]. The concordance rate between IGH-MRD and IGK/IGL-MRD was 79.9% at a cutoff of 0.01% at end of induction (EOI) [72].
NGS-based MRD stratification strongly correlates with clinical outcomes, with patients achieving NGS-MRD negativity exhibiting superior event-free survival (EFS) and overall survival (OS) rates [69]. The prognostic value is particularly evident in the context of advanced therapies, where NGS is highly predictive of relapse following hematopoietic stem cell transplantation and CAR-T cell therapy [69].
Acute Myeloid Leukemia (AML)
In AML, NGS enables monitoring of multiple genetic targets simultaneously, including mutations in genes such as FLT3, NPM1, IDH1/2, DNMT3A, RUNX1, and TET2 [70]. A study monitoring MRD in 482 patients with newly-diagnosed AML using SNVs of various genes demonstrated that MRD-positive patients had significantly shorter OS and relapse-free survival than MRD-negative patients [70]. The detection of persistent mutations in DNMT3A, TET2, and ASXL1 genes was particularly informative for relapse prediction [70].
Error-corrected NGS MRD approaches have shown clinical utility in AML patients undergoing allogeneic hematopoietic cell transplant (allo-HCT) in complete remission. In a study of 116 AML patients, MRD positivity (variant allele frequency <5%) stratified patients into higher cumulative incidence of relapse and lower OS categories, independent of FLT3-ITD and NPM1 status at diagnosis [70].
Multiple Myeloma (MM)
In multiple myeloma, NGS of immunoglobulin rearranged genes has proven to be an effective technology to identify and quantify pathological clonal cells with a sensitivity of at least 0.001% [71]. A study analyzing MRD by deep sequencing in bone marrow samples from 73 MM patients demonstrated that the achievement of molecular responses measured by NGS could predict 3-year survival [71]. Patients with MRD-negative status had significantly prolonged progression-free survival (median PFS not reached vs. 35 months for MRD-positive patients; HR=2.76, 95% CI 1.21-6.25, P=0.01) and overall survival (3-year OS rates of 100% vs. 45%) [71].
Technical Workflows and Experimental Considerations
NGS-Based MRD Workflow
The typical workflow for measuring MRD by NGS involves multiple standardized steps from sample preparation through data analysis [70]. The process begins with nucleic acid extraction from peripheral blood or bone marrow, followed by library preparation specific to the sequencing platform [70]. After sequencing, data undergoes alignment, error correction, and MRD quantification [70].
Target Selection Strategies
NGS-based MRD monitoring utilizes different molecular targets depending on the hematologic malignancy:
- Repertoire sequencing: Includes clonal rearrangements of immunoglobulin/T-cell antigen receptor genes: IGH (VDJ), IGH (DJ), IGK, TRG, TRD, and TRB [70]. In lymphocytic disorders, rearrangement of the immunoglobulin heavy chain (IGH) gene serves as an ideal marker as each neoplastic cell has an identical sequence [70].
- Fusion gene quantification: Applied in both lymphoid and myeloid neoplasms (e.g., KMT2A-MLLT10, RUNX1-RUNX1T1, and PML-RARA) [70].
- SNV analysis: Used in both lymphoid and myeloid neoplasms, including mutations in IDH1/2, DNMT3A, RUNX1, TET2, TP53, and insertions/deletions in FLT3 and NPM1 genes in AML [70].
Analytical Validation Parameters
For reliable MRD detection, NGS assays must undergo rigorous validation assessing several key parameters:
- Sensitivity and Limit of Detection: Established through dilution series of positive controls. The in-house deep-sequencing method for multiple myeloma demonstrated an analytical sensitivity of at least (10^{-5}) [71].
- Reproducibility: Measured through inter-run and inter-platform consistency. One multiple myeloma study showed 99.2% reproducibility between runs and different NGS platforms (91 samples tested in duplicate) [71].
- Specificity: Evaluated using normal control samples. The same study demonstrated no clonotypes detected in normal tonsil and bone marrow samples, indicating high assay specificity [71].
- Concordance with other methods: Assessed by comparing results with established techniques. In multiple myeloma, NGS showed 89% concordance with 8-color MFC data (Spearman coefficient R=0.7917, P<0.0001) [71].
Clinical Utility and Prognostic Value
Prognostic Significance Across Hematologic Malignancies
MRD status has near-universal prognostic significance across hematologic malignancies, with MRD positivity consistently signifying residual disease and worse outcomes, while MRD negativity suggests better prognosis [68].
Table 2: Prognostic Impact of MRD Status Across Hematologic Malignancies
| Malignancy | Prognostic Impact | Evidence Level |
|---|---|---|
| Acute Myeloid Leukemia (AML) | 5-year OS: 68% if MRD-negative vs. 34% if MRD-positive [68] | Study of adult and pediatric patients achieving CR/CRi |
| Acute Lymphoblastic Leukemia (ALL) | Meta-analysis of 39 studies (n=13,000+): MRD negativity associated with improved EFS (HR 0.23-0.28) and OS (HR 0.28) [68] | Systematic review/meta-analysis |
| Chronic Lymphocytic Leukemia (CLL) | Systematic review (n=2,765): MRD status associated with PFS (HR 0.28), particularly in first-line (HR 0.24) and time-limited therapy (HR 0.28) [68] | Meta-analysis of prospective trials |
| Multiple Myeloma (MM) | Meta-analysis: MRD negativity correlated with superior PFS (HR 0.33) and OS (HR 0.45) regardless of sensitivity thresholds, cytogenetic risk, or timing [68] | Comprehensive meta-analysis |
Clinical Applications Beyond Prognostication
The utility of MRD extends beyond prognosis in several clinical contexts:
- Treatment Response Evaluation: MRD can be used to assess depth of response to specific therapeutic regimens [68].
- Therapy Guidance: Enables personalization of treatment including escalation, de-escalation, or optimization of therapy duration [68].
- Transplant Monitoring: Facilitates disease monitoring in both pre- and post-transplant settings, enabling earlier relapse detection [68].
- Clinical Trial Endpoints: Serves as a surrogate endpoint for clinically meaningful outcomes like survival in some malignancies and as a biomarker in early-phase drug development [68].
In specific diseases like acute promyelocytic leukemia (APL) and chronic myeloid leukemia (CML), MRD assessment has been successfully integrated into treatment algorithms. In APL, PML-RARα detection by RT-PCR predicts relapse and has been incorporated into European Leukemia Net guidelines [68]. In CML, RT-PCR can reliably guide therapy by assessing response at regular intervals, informing TKI switching decisions, and determining eligibility for treatment-free remission [68].
Standardization Initiatives and Quality Assurance
Efforts to harmonize MRD approaches across laboratories have been led by major consortia:
- EuroFlow: Established standardized multiparametric flow cytometry MRD protocols for ALL, CLL, and multiple myeloma [68]. For multiple myeloma, the EuroFlow NGF approach is regarded as the MFC gold standard according to IMWG guidelines [68].
- EuroMRD: Consists of 71 laboratories across 27 countries and focuses on molecular MRD assessment in ALL and lymphoma, aiming for standardized molecular MRD quantification in lymphoid malignancies [68]. The EuroMRD interpretation guidelines currently form the basis for molecular MRD quantification in most non-American clinical trials for ALL in children and adults [68].
Despite these advances in lymphoid malignancies, comparable standardization in AML remains an unmet need [68]. For AML, MFC is an accepted MRD tool, but standardization efforts are less developed than for lymphoid malignancies [68].
Essential Research Reagents and Platforms
Table 3: Essential Research Solutions for NGS-Based MRD Detection
| Reagent/Platform | Function | Application Context |
|---|---|---|
| AmpliSeq for Illumina Childhood Cancer Panel | Targeted NGS panel analyzing 203 genes, including fusions, SNVs, InDels, and CNVs [73] | Pediatric acute leukemia diagnostics and MRD monitoring |
| ClonoSEQ Assay | NGS-based immunoglobulin clonality assessment for MRD monitoring [70] | B-ALL and multiple myeloma MRD detection |
| LymphoTrack Assay | NGS-based method for immunoglobulin rearrangement analysis [70] | Lymphoid malignancy MRD monitoring |
| Biomed-2 Primers | Standardized primer sets for immunoglobulin gene rearrangement analysis [71] | In-house NGS MRD assay development |
| SeraSeq Tumor Mutation DNA Mix | Multiplex biosynthetic control material with clinically relevant variants [73] | NGS assay validation and quality control |
| Ion S5 / MiSeq Sequencers | Sequencing platforms for mid-throughput NGS applications [71] | MRD monitoring in research settings |
Current Challenges and Future Directions
Despite significant advances, several challenges remain in the widespread implementation of NGS for MRD monitoring:
- Standardization: Lack of standardized protocols, analytical pipelines, and reporting criteria across laboratories [69] [70].
- Clinical Integration: Determining optimal clinical decision points and demonstrating that treatment interventions based on MRD status improve survival outcomes [68].
- Cost and Accessibility: High costs and requirement for specialized bioinformatics expertise create barriers to routine clinical use [69].
- Clonal Evolution: Addressing the impact of clonal evolution on MRD marker stability and detection accuracy [70].
Future directions include the development of whole genome sequencing-based MRD approaches, refinement of tissue-informed versus tissue-agnostic strategies, and continued efforts to align MRD testing with regulatory, scientific, and clinical standards [74]. As precision oncology evolves, NGS is expected to play an increasingly central role in leukemia management, driving innovations in personalized medicine and therapeutic interventions [3].
The accurate detection of chromosomal rearrangements is a cornerstone in the diagnosis, prognosis, and treatment of acute leukemia. Among these, fusions involving the NUP98 and KMT2A genes represent critical, often adverse, prognostic markers. However, many of these fusions are cryptic, eluding identification by conventional cytogenetic analysis due to their small size or complex nature [75] [76]. This diagnostic gap poses a significant clinical challenge, as patients with these aggressive leukemia subtypes may not receive appropriate, risk-stratified therapy. The fifth edition of the World Health Organization Classification of Haematolymphoid Tumours (WHO-HAEM5) and the 2022 International Consensus Classification (ICC) now recognize NUP98 and KMT2A rearrangements as distinct disease entities, underscoring their clinical importance [77] [76]. This guide objectively compares the performance of traditional diagnostic techniques with modern next-generation sequencing (NGS) approaches for identifying these elusive genetic alterations, providing researchers and clinicians with a framework for implementing optimal diagnostic strategies.
Biological and Clinical Significance of NUP98 and KMT2A Fusions
Oncogenic Mechanisms
NUP98 and KMT2A fusions drive leukemogenesis through shared and distinct mechanisms, primarily by disrupting transcriptional regulation and chromatin remodeling.
NUP98 Fusion Proteins: NUP98 rearrangements fuse the N-terminus of NUP98 with over 30 different partners, including HOX cluster genes (e.g., HOXA9, HOXA13) and epigenetic modifiers like NSD1 and JARID1A [75] [78]. These chimeric proteins colocalize with the KMT2A-Menin complex at promoters of pro-leukemogenic genes, such as HOXA/B and MEIS1, to activate a stem cell-associated gene expression program essential for leukemia maintenance [79] [75]. Recent research reveals that these fusions hijack the Menin-KMT2A transcriptional machinery and must antagonize the repressive polycomb repressive complex 1.1 (PRC1.1) to prevent epigenetic silencing of oncogenes [79].
KMT2A Fusion Proteins: KMT2A (formerly MLL1) rearrangements are more common in pediatric acute myeloid leukemia (pAML) and result in fusion proteins that also dysregulate HOX gene expression [79] [76]. The interaction between KMT2A and the scaffold protein Menin is essential for its leukemogenic activity, making the Menin-KMT2A interaction a promising therapeutic target [75].
Clinical Impact and Co-mutations
NUP98-rearranged leukemias are associated with poor prognosis and high rates of relapse in both children and adults [75]. In adults with NUP98-NSD1 fusion-positive AML, induction failure rates following intensive chemotherapy can be as high as 83% [75]. These fusions frequently co-occur with mutations in FLT3-ITD and WT1, which further worsen the clinical outcome [75]. Similarly, KMT2A-rearranged leukemias constitute a major category in pAML, representing 20.3% of cases in a large cohort study [76].
Comparative Performance of Detection Methodologies
The following section provides a detailed, data-driven comparison of the technical and clinical performance of traditional methods versus targeted NGS for detecting NUP98 and KMT2A fusions.
Technical Workflow Comparison
The diagnostic pathway for acute leukemia has traditionally involved a cascade of complementary techniques. The following diagram contrasts this multi-assay approach with a simplified NGS-based workflow.
Quantitative Diagnostic Performance
A validation study of 357 adult leukemia patients provides direct comparative data on the performance of tNGS versus traditional methods [77] [80].
Table 1: Performance Comparison of tNGS vs. qRT-PCR for Fusion Detection
| Metric | qRT-PCR (45 fusions on RNA) | tNGS (DNA-based) | Result |
|---|---|---|---|
| Total Fusions Detected | 102 | 98 | PPA*: 96.1% (98/102) |
| Additional Fusions Found | 0 | 2 (KMT2A::ELL, KMT2A::MLLT3) | tNGS identified missed fusions |
| False Positives | N/A | 0 | 100% Specificity |
| *PPA: Positive Percent Agreement [77] [80]. |
Table 2: tNGS Performance for IGH/MYC Rearrangements vs. FISH
| Alteration Type | Reference Method | tNGS Performance |
|---|---|---|
| IGH or MYC rearrangements | FISH | PPA: 93.8% (15/16) [77] |
Advantages and Limitations of Each Technique
Table 3: Comprehensive Method Comparison for NUP98/KMT2A Fusion Detection
| Method | Key Advantage | Primary Limitation | Sensitivity | Turnaround Time | Fusion Target Flexibility |
|---|---|---|---|---|---|
| Karyotyping | Genome-wide, unbiased | Low resolution; misses cryptic fusions [77] | ~ 5-10 Mb | 1-2 weeks | Low |
| FISH | High sensitivity for known targets | Requires prior suspicion; limited targets [77] [6] | ~ 50-100 kb | 2-5 days | Low |
| qRT-PCR | High sensitivity, quantitative | RNA degradation; limited predefined panel [77] | High (RNA level) | 1-2 days | Medium |
| tNGS (DNA) | Single assay for fusions/ mutations; discovers novel partners [77] | May miss some IGH rearrangements [77] | High (DNA level) | 3-5 days | High |
| Nanopore WGS | Real-time analysis; detects methylation | Emerging technology; computational complexity [6] | High | 15 min - 6 hrs for driving alteration [6] | Very High |
Detailed Experimental Protocols
Targeted NGS (tNGS) for Fusion Detection on DNA
This protocol, adapted from Chen et al. (2025), enables simultaneous detection of gene fusions, single nucleotide variants (SNVs), and insertions/deletions (indels) from DNA [77] [80].
- Panel Design: The custom panel includes all exons of 302 leukemia-associated genes and 94 introns from 26 genes frequently involved in fusions (e.g., NUP98 introns 11-16, KMT2A introns 7-12 and 21-23). Covering one partner gene's intronic regions allows detection of fusions with any partner. The total target region is ~679.9 Kb [77].
- Library Preparation & Sequencing:
- DNA Extraction: Extract DNA from bone marrow or peripheral blood using commercial kits (e.g., Tiangen Biochemical Technology Co., Ltd.).
- Library Construction: Transform DNA into libraries using kits (e.g., Kapa Biosystems).
- Capture & Enrichment: Enrich libraries using the custom panel (e.g., xGen Custom Hybridization Capture with IDT probes).
- Sequencing: Sequence on an Illumina NextSeq550 system (PE150) to a mean coverage depth of ~1000x per sample [77] [80].
- Bioinformatic Analysis:
Real-Time Fusion Detection via Nanopore Sequencing
This innovative protocol uses adaptive sampling for real-time genomic characterization [6].
- Sample Preparation:
- DNA Extraction: Use the ZymoBIOMICS MagBead DNA/RNA kit. Verify fragment sizes >20 Kbp by gel electrophoresis.
- Shearing & Size Selection: Shear DNA with a 26G needle (7 passes) and perform size selection with Ampure XP Beads [6].
- Library Preparation & Sequencing:
- Library Prep: Perform ligation-based library preparation of native DNA using ONT kits (e.g., SQK-LSK109/110/112/114).
- Sequencing with Adaptive Sampling: Sequence on a PromethION 2 Solo or MinION device. Employ a predefined gene panel (e.g., 59-223 genes) for adaptive sampling. The instrument selectively ejects DNA fragments not matching targets, enriching for genes of interest 10-20 fold [6].
- Real-Time Analysis:
- Base calling & Alignment: Base-call reads in super-accurate duplex mode with Dorado and align to GRCh38 with minimap2 concurrently during sequencing.
- Alteration Identification: Driving alterations (karyotype abnormalities, complex SVs) can be identified in as little as 15 minutes to 6 hours after sequencing initiation [6].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Reagents and Resources for Leukemia Fusion Detection Studies
| Category / Item | Specific Example / Product | Function in Experimental Protocol |
|---|---|---|
| NGS Panel | Custom Leukemia tNGS Panel [77] | Targeted capture of exons (mutations) and introns (fusions) from DNA. |
| Capture Probes | xGen Custom Hybridization Capture (IDT) [77] | Specific 120-bp probes for enriching target genomic regions. |
| Library Prep Kit | Kapa Biosystems Library Construction Kit [77] | Preparation of sequencing libraries from extracted DNA. |
| Sequencing Platform | Illumina NextSeq550 System [77] | High-throughput short-read sequencing. |
| Nanopore Platform | Oxford Nanopore PromethION 2 Solo / MinION [6] | Long-read sequencing enabling real-time analysis via adaptive sampling. |
| Nanopore Kit | SQK-LSK114 Ligation Sequencing Kit [6] | Preparation of native DNA libraries for nanopore sequencing. |
| DNA Extraction Kit | ZymoBIOMICS MagBead DNA/RNA Kit [6] | Concurrent extraction of high-quality, high-molecular-weight DNA. |
| Bioinformatic Tool | Factera / GeneFuse [77] | Software for identifying gene fusions from NGS data. |
| Alignment Tool | BWA-MEN (Illumina) [77] / minimap2 (Nanopore) [6] | Alignment of sequencing reads to the reference genome. |
| qRT-PCR Kit | Zeesan Biotech 45 Fusion Screening Kit [77] | Orthogonal validation of fusion genes at the RNA level. |
The integration of NGS-based methods, particularly comprehensive tNGS panels and real-time nanopore sequencing, into the diagnostic workflow for acute leukemia represents a paradigm shift. These technologies overcome the critical limitation of traditional methods by enabling the systematic detection of prognostically significant cryptic NUP98 and KMT2A fusions within a single, efficient assay [77] [6]. The resulting integrated genomic profile provides a powerful foundation for precise diagnosis, risk stratification, and treatment selection. As therapeutic targeting of fusion-driven dependencies, such as with Menin inhibitors for NUP98-rearranged and KMT2A-rearranged AML, moves from clinical trials into standard practice [79] [75], the imperative for accurate and comprehensive genomic characterization at diagnosis becomes absolute. The experimental frameworks and data comparisons presented in this guide provide a roadmap for researchers and clinicians to advance the standard of care for patients with these high-risk leukemias.
Predicting Relapse Post-Transplant Through Mutational Tracking
For patients with acute leukemia undergoing allogeneic stem cell transplantation (allo-SCT), the threat of relapse represents the most significant challenge to long-term survival. Despite the curative potential of allo-SCT, relapse rates remain substantial, affecting approximately 30-50% of patients, with outcomes being particularly poor once relapse occurs [81]. Traditional monitoring methods, including bone marrow biopsies and multiparameter flow cytometry (MFC), have limitations in sensitivity, invasiveness, and the potential for sampling error. The emergence of next-generation sequencing (NGS) technologies has revolutionized the monitoring of measurable residual disease (MRD), enabling the detection of malignant clones at significantly lower levels and providing an unprecedented window into the molecular dynamics of post-transplant relapse. This paradigm shift from morphological assessment to molecular tracking represents a critical advancement in personalized oncology, offering the potential for earlier intervention and improved patient outcomes. This guide objectively compares the performance of NGS-based mutational tracking against traditional methods in predicting post-transplant relapse in acute leukemia.
Performance Comparison: NGS vs. Traditional MRD Detection Methods
The evaluation of MRD detection technologies reveals significant differences in sensitivity, applicability, and prognostic value. The table below provides a systematic comparison of the primary methods used in clinical practice.
Table 1: Performance Comparison of MRD Detection Methods in Acute Leukemia
| Method | Sensitivity | Key Strengths | Key Limitations | Prognostic Value Demonstrated |
|---|---|---|---|---|
| Next-Generation Sequencing (NGS) | Up to 10⁻⁶ (0.0001%) [5] | High sensitivity, applicability to most patients, ability to track clonal evolution [82] [5] | High cost, complex bioinformatics, challenge of distinguishing CHIP [82] [81] | Superior prediction of relapse; positive NGS-MRD post-transplant correlates with 5.2-11.6x higher relapse risk [81] |
| Multiparameter Flow Cytometry (MFC) | 10⁻⁴ (0.01%) [5] | Rapid, widely available, provides same-day results [82] [5] | Subject to immunophenotypic shifts, operator-dependent [5] | Predictive of relapse, but less sensitive than NGS; 46% of MFC-negative samples were MRD-positive by NGS, with 39% 5-year relapse risk [5] |
| qRT-PCR for Fusion Genes | 10⁻⁴ to 10⁻⁶ [5] | High sensitivity for specific targets, quantitative | Limited applicability (only ~50% of ALL patients have trackable fusion genes) [5] | Strong prognostic value when a trackable target is present |
| Digital PCR (dPCR) | Up to 0.0014% for specific mutations [34] | Absolute quantification, high sensitivity, cost-effective for tracking known mutations [83] | Limited multiplexing capability, requires prior knowledge of mutations [83] | Effective for tracking known high-risk mutations (e.g., FLT3-ITD) [34] |
Clinical Impact and Prognostic Performance
Quantitative data from recent studies underscore the superior prognostic power of NGS-based monitoring. A retrospective study of 90 AML patients post-allo-SCT found that the presence of circulating cell-free DNA (cfDNA) with tumor-associated mutations at Day 150 post-transplant was a powerful predictor of outcomes. Patients testing positive had a 5.2-fold higher risk of relapse and a 5.4-fold higher risk of death compared to those testing negative. The prognostic impact was even more pronounced for adverse-risk mutations (e.g., in TP53, ASXL1, RUNX1), conferring an 11.6-fold increased relapse risk and an 11.2-fold increased risk of death [81].
Another study focusing on NGS-based MRD assessment in 69 AML patients found that a mean variant allele frequency (VAF) of somatic mutations (excluding CHIP) greater than 0.004 at the start of consolidation therapy and greater than 0.020 during subsequent monitoring was associated with a significantly worse prognosis [82]. Furthermore, combining NGS with MFC provided the most refined stratification; patients who were negative by both methods had the longest survival, while those positive by either one had intermediate outcomes [82].
Experimental Protocols for NGS-Based Mutational Tracking
Key Workflow for NGS-Based MRD Detection in Leukemia
The following diagram illustrates the standard workflow for NGS-based MRD monitoring, from sample collection to clinical reporting.
Detailed Methodological Protocols
Targeted NGS Panel Sequencing for AML
This protocol is adapted from studies that utilized targeted sequencing panels to track mutations in AML patients post-transplant [82].
- Sample Collection and DNA Extraction: Bone marrow aspirates or peripheral blood samples are collected at diagnosis and serial time points post-transplant (e.g., post-induction, post-consolidation, Day +100, Day +150). Genomic DNA is extracted using commercial kits (e.g., QIAamp DNA Blood Mini Kit). DNA quantity and quality are assessed using fluorometry (e.g., Qubit dsDNA HS Assay) and spectrophotometry.
- Library Preparation and Sequencing: A custom targeted panel of genes frequently mutated in AML (e.g., 47-gene panel including FLT3, NPM1, DNMT3A, IDH1/2, TP53, ASXL1, RUNX1) is used. Libraries are prepared via multiplex PCR amplification using gene-specific primers. The amplified products are purified, adapter-ligated, and PCR-amplified to add sample indices. The final library concentration and fragment size distribution are validated before pooling and sequencing on a platform such as Illumina NovaSeq.
- Bioinformatic Analysis: Raw sequencing data is processed through a standardized pipeline: (1) adapter trimming and quality control (e.g., with Trimmomatic), (2) alignment to the human reference genome (e.g., GRCh37), (3) variant calling (SNVs and Indels) with a minimum VAF threshold (e.g., ≥1% for diagnostic samples, ≥0.1% for MRD samples), and (4) filtering against population databases (e.g., gnomAD) to exclude common polymorphisms.
- MRD Quantification and Interpretation: Somatic mutations identified at diagnosis are tracked in post-treatment samples. The VAF for each mutation is calculated. To avoid false positives from clonal hematopoiesis (CHIP), variants are classified as CHIP if they show a VAF change of <3% across consecutive detections spaced more than one month apart and the VAF is consistently ≥2% [82]. The mean VAF of somatic mutations (excluding CHIP) is calculated for prognostic stratification.
Cell-Free DNA Liquid Biopsy for Relapse Monitoring
This protocol details the use of liquid biopsy for non-invasive monitoring post-transplant, as demonstrated in recent studies [81].
- Sample Collection and Plasma Isolation: Peripheral blood (e.g., 10 mL in cell-free DNA blood collection tubes) is drawn from AML patients at key post-transplant time points (e.g., Day +28, Day +100, Day +150). Plasma is separated through a two-step centrifugation process (e.g., 4,000 rpm for 10 min at 4°C, followed by a high-speed centrifugation of the supernatant).
- cfDNA Extraction and Library Preparation: Cell-free DNA is extracted from plasma (e.g., 300 µL to 5 mL) using a commercial kit (e.g., QIAamp DNA Micro Kit). The extracted cfDNA concentration is measured, often yielding very low quantities (ng per mL of plasma). Libraries are constructed through DNA fragmentation (if necessary), end-repair, adapter ligation, and PCR amplification.
- Sequencing and Analysis: Libraries are sequenced using a comprehensive NGS panel covering hundreds of genes associated with hematologic malignancies. The data is analyzed by aligning sequences to a reference genome, removing host-derived reads, and identifying tumor-associated mutations known from the patient's diagnostic sample.
- Interpretation and Actionability: The presence of any tumor-associated mutation in cfDNA is considered a positive MRD result. The 2022 European LeukemiaNet (ELN) risk classification is often applied to the detected mutations, as the persistence of adverse-risk mutations post-transplant carries the worst prognosis [81].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of NGS-based mutational tracking requires a suite of specialized reagents and tools. The following table catalogues the key solutions required for the workflows described above.
Table 2: Essential Research Reagent Solutions for NGS-Based Mutational Tracking
| Reagent / Solution | Function | Example Products / Kits |
|---|---|---|
| High-Fidelity DNA Polymerase | Accurate amplification of target gene regions during library preparation for error-free sequencing. | KAPA HiFi HotStart ReadyMix, Q5 High-Fidelity DNA Polymerase |
| Multiplex PCR Target Enrichment Panels | Simultaneous amplification of a predefined set of genes relevant to leukemia. | MultipSeq Custom Panel (47 genes), Illumina TruSight Myeloid Panel |
| Magnetic Beads for Library Clean-up | Size selection and purification of DNA libraries by binding nucleic acids for washing and elution. | Agencourt AMPure XP beads |
| Indexing Adapters & Primers | Attaching unique molecular barcodes to each sample for multiplexing. | Illumina Nextera XT Index Kit, IDT for Illumina UD Indexes |
| Library Quantification Kits | Precise measurement of final DNA library concentration prior to sequencing. | Qubit dsDNA HS Assay Kit |
| Bioinformatic Pipelines & Software | Processing raw sequencing data, including alignment, variant calling, and VAF calculation. | Burrows-Wheeler Aligner (BWA), Genome Analysis Toolkit (GATK), Trimmomatic |
The integration of NGS-based mutational tracking into post-transplant monitoring represents a significant advancement over traditional methods. The superior sensitivity of NGS, its ability to provide a systemic view of the disease through liquid biopsy, and its capacity to track clonal evolution offer a more dynamic and precise tool for predicting relapse in acute leukemia patients. While challenges related to standardization, cost, and the interpretation of genetic findings like CHIP remain, the compelling prognostic data and the potential for guiding pre-emptive therapies position NGS as a transformative technology. Future efforts should focus on validating these approaches in large, prospective trials and on integrating multi-omic data to further refine relapse prediction and improve survival outcomes.
The molecular diagnosis of acute leukemia is undergoing a transformative shift from traditional cytogenetic methods to advanced genomic technologies. Conventional standard-of-care (SoC) methods, including chromosomal banding analysis (CBA), fluorescence in situ hybridization (FISH), and reverse transcription PCR (RT-PCR), have well-documented limitations in resolution, throughput, and comprehensive variant detection [35] [84]. In this evolving landscape, Optical Genome Mapping (OGM) and digital Multiplex Ligation-dependent Probe Amplification (dMLPA) have emerged as powerful technologies that address critical gaps in leukemia genomics. This comparison guide provides an objective assessment of their performance characteristics, experimental protocols, and complementary applications within the broader context of next-generation sequencing (NGS) implementation for acute leukemia diagnostics.
Optical Genome Mapping (OGM)
OGM is a high-resolution, genome-wide imaging technology that detects structural variants (SVs) and copy number variations (CNVs) using ultra-high molecular weight (UHMW) DNA. The methodology involves:
- DNA Extraction and Labeling: UHMW DNA is extracted without fragmentation, preserving molecules >150 kb. Specific sequence motifs (e.g., CTTAAG for DLE-1 enzyme) are fluorescently labeled, creating a unique "barcode" pattern approximately every 6-15 kb throughout the genome [85] [86].
- Linearization and Imaging: Labeled DNA molecules are linearized in nanochannels on silicon chips and imaged via high-resolution fluorescence microscopy.
- Data Analysis and Variant Calling: Bioinformatic algorithms align the fluorescent label patterns to a reference genome, identifying deviations indicative of SVs (translocations, inversions, insertions) and CNVs (deletions, duplications, aneuploidies) [84] [87].
Digital MLPA (dMLPA)
dMLPA is a targeted, high-throughput technique that combines the principles of conventional MLPA with next-generation sequencing readout:
- Probe Hybridization and Ligation: Sequence-specific probes hybridize to adjacent target sequences in the genomic DNA. Subsequent ligation creates amplifiable fragments only when both probe halves bind correctly.
- Library Preparation and Sequencing: Ligated products are amplified with sample-specific barcodes, pooled, and sequenced on NGS platforms (e.g., Illumina MiSeq).
- Digital Quantification: Bioinformatic analysis of sequencing read counts enables precise, quantitative detection of CNVs and identification of specific intrachromosomal gene fusions within targeted regions [35] [88].
Comparative Performance Analysis in Acute Leukemia
Detection Capabilities and Diagnostic Yield
Table 1: Comprehensive Comparison of Detection Capabilities
| Variant Type | OGM Performance | dMLPA Performance | Combined Approach |
|---|---|---|---|
| Gene Fusions | Detects novel and known fusions genome-wide; identifies partners [35] [84] | Limited to predefined intrachromosomal fusions within probe set [88] | Comprehensive fusion detection |
| Copy Number Variations | Genome-wide CNV detection (>500 bp); precise breakpoint mapping [89] [85] | High-resolution CNV detection for targeted genes only [35] | Targeted and genome-wide CNV analysis |
| Balanced Rearrangements | Excellent for translocations, inversions (except in repetitive regions) [89] [84] | Limited to specific probe-designed rearrangements [88] | Enhanced balanced SV detection |
| Cryptic/Complex SVs | Resolves complex karyotypes, chromothripsis; identifies novel SVs [84] [86] | Cannot detect complex or novel rearrangements outside targets [35] | Clarifies complex genomic architecture |
| Aneuploidy | Detects whole and partial chromosome gains/losses [89] | Not designed for aneuploidy detection | OGM primarily responsible |
Recent studies demonstrate the superior diagnostic yield of these emerging technologies. In pediatric acute lymphoblastic leukemia (ALL), OGM as a standalone test detected clinically relevant alterations in 90% of cases, significantly outperforming SoC methods (46.7%) [35]. The combination of dMLPA and RNA-seq achieved the highest diagnostic yield at 95% [35]. OGM demonstrates particular strength in detecting chromosomal gains/losses (51.7% vs. 35% with SoC) and gene fusions (56.7% vs. 30% with SoC) [35].
Analytical and Operational Performance Metrics
Table 2: Technical and Operational Specifications
| Parameter | Optical Genome Mapping | Digital MLPA |
|---|---|---|
| Resolution | ~500 bp for SVs [85] | Single exon-level for targeted genes [35] |
| Coverage | Genome-wide, unbiased [84] [87] | Targeted (e.g., D007 ALL probemix: ~300 genes) [35] [88] |
| Hands-on Time | ~4-5 hours per run (mostly automated) [85] | Variable (library preparation and sequencing) |
| Turnaround Time | 4-7 days [84] [85] | 3-5 days (including sequencing) |
| DNA Input | 750 ng UHMW DNA [85] [90] | 50 ng conventional DNA [35] |
| Sensitivity (VAF) | ~5% for SVs; 10-15% for CNVs [84] | Dependent on leukemic cell burden and sequencing depth [35] |
| Multiplexing Capacity | Limited by instrument flow cells [85] | High (multiple samples per sequencing run) |
| Cost Considerations | Higher per-sample cost, but replaces multiple tests [84] [85] | Lower per-sample cost for targeted queries |
In a large study of 519 hematologic malignancies, OGM provided additional clinical utility (impacting diagnosis, prognosis, or treatment) in 15% of cases compared to standard cytogenetic workups, with the highest impact in T-lymphoblastic leukemia (52%) and B-lymphoblastic leukemia (37%) [90].
Experimental Protocols for Technology Implementation
Standardized OGM Workflow for Acute Leukemia
Sample Requirements and DNA Extraction:
- Collect bone marrow or peripheral blood in heparin tubes; process within 24-48 hours.
- Isolate UHMW DNA using specialized kits (e.g., Bionano Prep SP Frozen Human Blood DNA Isolation Kit).
- Assess DNA quality: concentration >50 ng/μL, size >150 kb, and minimal degradation via pulsed-field gel electrophoresis or genomic DNA integrity assessment [35] [90].
Labeling, Staining, and Imaging:
- Label 750 ng UHMW DNA using Direct Label and Stain (DLS) kit with DLE-1 enzyme.
- Load labeled DNA onto Saphyr chips for linearization through nanochannels.
- Image molecules using Saphyr instrument with a target data collection of >1500 Gbp for rare variant analysis, achieving >340x coverage [35] [85] [90].
Data Analysis and Interpretation:
- Process data through Bionano Solve pipeline (v3.6-3.7) using GRCh38 reference genome.
- Apply Rare Variant Pipeline for somatic analysis with standard filters.
- Annotate clinically relevant SVs and CNVs using disease-specific databases.
- Orthogonal validation (FISH, RT-PCR) is recommended for novel potentially significant findings [35] [90].
dMLPA Experimental Procedure
Sample Processing and Assay Setup:
- Use 50 ng of conventional quality DNA (does not require UHMW).
- Hybridize with SALSA digitalMLPA D007 Acute Lymphoblastic Leukemia probemix.
- Perform ligation and subsequent PCR amplification with barcoded primers.
- Pool purified amplicons from multiple samples for sequencing on Illumina platforms (e.g., MiSeq with 150 bp single-read chemistry) [35].
Bioinformatic Analysis:
- Process sequencing data using Coffalyser digitalMLPA software (MRC Holland).
- Interpret probe ratio values: values ~1.0 indicate normal copy number; decreased values indicate deletions; increased values indicate amplifications.
- Consider leukemic cell burden when interpreting subclonal alterations [35].
Integration with NGS and Complementary Applications
OGM and dMLPA occupy distinct but complementary positions in the genomic analysis spectrum. OGM provides genome-wide structural context, while dMLPA offers sensitive targeted quantification. Both technologies integrate with NGS, which excels at detecting single nucleotide variants (SNVs) and small insertions/deletions, but has limitations in resolving complex SVs with short-read platforms [86] [91].
Diagram: Integrated genomic workflow for comprehensive acute leukemia profiling, demonstrating how OGM, dMLPA, and NGS technologies provide complementary data streams.
This integrated approach is particularly powerful for challenging leukemia subtypes. In Philadelphia-like ALL, OGM identified additional kinase fusions (e.g., FGFR1::BCR, IGH::EPOR) missed by standard methods, while dMLPA reliably detected associated copy number alterations (e.g., IKZF1, CDKN2A/B deletions) [88]. The technologies demonstrated complementarity, with OGM excelling in structural variant detection and dMLPA providing superior CNV analysis in targeted regions.
Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for Implementation
| Reagent/Kit | Manufacturer | Primary Function |
|---|---|---|
| Bionano Prep SP Frozen Human Blood DNA Isolation Kit | Bionano Genomics | UHMW DNA extraction from frozen blood/bone marrow samples [90] |
| DLE-1 Direct Label and Stain (DLS) Kit | Bionano Genomics | Fluorescent labeling of specific sequence motifs for OGM [35] [85] |
| Saphyr Chip G2.3 | Bionano Genomics | Nanochannel chip for DNA linearization and imaging [35] |
| digitalMLPA D007 Acute Lymphoblastic Leukemia Probemix | MRC Holland | Targeted probe set for CNVs and fusions in ALL [35] [88] |
| SALSA MLPA P335 Probemix | MRC Holland | Detection of CNVs in B-cell ALL associated genes [35] |
| Archer FusionPlex Pan-Heme Kit | ArcherDX | Targeted RNA-seq for fusion detection (orthogonal validation) [89] |
| TruSeq Stranded Total RNA Library Prep Kit | Illumina | RNA library preparation for transcriptome analysis [35] |
OGM and dMLPA represent significant advancements in genomic technology for acute leukemia diagnosis, each with distinct strengths and applications. OGM provides unprecedented genome-wide resolution for structural variants, while dMLPA offers sensitive, quantitative analysis of targeted alterations. Their integration creates a powerful complementary approach that surpasses conventional cytogenetics in diagnostic yield and precision. For research and clinical implementation, the choice between these technologies depends on specific application requirements: OGM for comprehensive genome-wide structural variant discovery, and dMLPA for cost-effective, high-throughput targeted screening. Together, these emerging approaches are advancing the field toward more precise molecular classification and personalized treatment strategies for acute leukemia patients.
Navigating Implementation Challenges: Technical Hurdles and Data Interpretation in NGS Diagnostics
In the field of acute leukemia research, the transition from traditional diagnostic methods to next-generation sequencing (NGS) has revolutionized our understanding of disease heterogeneity and molecular drivers. However, the accuracy of NGS-based findings is fundamentally dependent on sample quality, particularly DNA/RNA integrity and tumor purity. These pre-analytical factors significantly influence the detection of genetic variants, especially in leukemia samples which often originate from bone marrow aspirates with variable tumor cell percentages and potential degradation issues. For institutions implementing NGS, understanding how to quantify, standardize, and control for these variables is essential for generating clinically actionable results. This guide examines critical sample quality considerations, comparing traditional and novel approaches for quality assessment within the context of modern leukemia diagnostics.
DNA and RNA Integrity Assessment
The Critical Role of Nucleic Acid Integrity in NGS
Nucleic acid integrity directly impacts the success of NGS workflows. Degraded DNA can lead to uneven coverage and false negative results in mutation detection, while compromised RNA introduces bias in transcriptome analysis and gene expression quantification [92]. The inherent instability of RNA makes it particularly vulnerable, as it is susceptible to degradation by ubiquitous RNases [93]. The quality requirements vary significantly depending on the downstream application. For instance, microarray experiments typically require RNA with specific concentration, purity, and integrity values, while qPCR-based assays can sometimes tolerate lower quality samples due to their smaller amplicon sizes [93].
Comparison of Integrity Assessment Methods
Researchers have several methodologies at their disposal for evaluating nucleic acid quality, each with distinct advantages, limitations, and appropriate use cases.
Table 1: Comparison of RNA Quality Assessment Methods
| Method | Principle | Information Provided | Sample Requirement | Advantages | Limitations |
|---|---|---|---|---|---|
| UV Spectrophotometry (e.g., NanoDrop) | Absorbance of light at 260nm, 280nm, and 230nm | Concentration (A260), Purity (A260/A280, A260/A230) | 0.5-2 µl | Fast (<30 seconds), wide detection range, no reagents needed | Cannot distinguish between DNA and RNA, insensitive to degradation, overestimates concentration if contaminants present [93] |
| Fluorometric Methods (e.g., Qubit) | Fluorescence of dyes binding specifically to nucleic acids | Accurate concentration, more specific than absorbance | Varies with kit (e.g., 1-100 µl) | Highly sensitive (down to 1 pg/µl), specific with DNase treatment | Requires standards, no integrity information, potential hazardous dyes [93] |
| Agarose Gel Electrophoresis | Separation by size in an electrical field | Integrity via 28S:18S rRNA band sharpness and ratio (2:1 ideal), visual detection of degradation | At least a few ng | Low cost, provides visual integrity assessment | Semi-quantitative at best, time-consuming, requires hazardous stains (EtBr) [94] [93] |
| Automated Electrophoresis (e.g., Agilent Bioanalyzer/TapeStation) | Microfluidics and capillary electrophoresis | Integrity (RNA Integrity Number - RIN), concentration, fragment size distribution | As little as 1 µl of 10 ng/µl | High sensitivity, minimal sample consumption, quantitative integrity score (RIN) | Higher instrument cost, requires specialized chips or tapes [94] [93] |
Advanced Protocol: Quantitative RNA Integrity Assessment
While the Agilent Bioanalyzer's RIN is a widely used metric, a more quantitative approach based on RT-qPCR can be employed for highly sensitive applications. This method quantifies the probability of RNA damage and enables correction of expression data for degradation effects.
Principle: The method assumes random RNA damage and uses exponential amplification mathematics to model degradation. The probability that an RNA target molecule remains intact and amplifiable is calculated based on lesion frequency per base and amplicon length [92].
Procedure:
- Design: Select multiple amplicons of varying lengths (e.g., 100bp, 200bp, 300bp, 400bp) from a stable reference gene.
- RT-qPCR: Amplify each target from the RNA sample using optimized, highly efficient PCR conditions to ensure constant amplification efficiency (
a) across all amplicon sizes. - Analysis: Plot the Ct values (or Ct * log
ea) against the total target length (l + p), wherepaccounts for the priming site. The slope of the linear regression (r) represents the mean number of lesions per base. - Calculation: Calculate the Amplifiable Fraction (AF) for any target of length
lusing the equation: AF = e-r(l+p). - Correction: Use the AF to correct quantitative RT-qPCR or RNA-Seq data for the effects of degradation, providing a more accurate measure of the true transcript abundance [92].
This method is particularly valuable for analyzing valuable archival samples or biopsies with suboptimal RNA quality, as it allows researchers to objectively quantify and computationally correct for degradation.
Figure 1: RNA Integrity Assessment Workflow. This diagram outlines the primary methodological pathways for evaluating RNA sample quality, from basic concentration checks to advanced quantitative integrity analysis.
Tumor Purity Assessment in Leukemia
The Challenge of Tumor Purity in Molecular Analysis
Tumor purity, defined as the proportion of cancer cells in a sample, is a critical parameter in oncology NGS. Neoplastic cellularity directly impacts the analytic sensitivity of mutation detection technologies. Methods like Sanger sequencing may require a variant allele fraction (VAF) of >20% (approximately 40% neoplastic cellularity), while even more sensitive techniques like pyrosequencing need >5% VAF (10% cellularity) [95]. In acute leukemia, samples are complex mixtures of leukemic blasts, normal lymphocytes, stromal cells, and other non-malignant elements. Low tumor purity can lead to false negatives, particularly for subclonal mutations, and can distort the measured variant allele frequencies of true positive calls, complicating interpretation.
Traditional vs. Computational Purity Estimation Methods
The standard for tumor purity assessment has traditionally been pathologist estimation of neoplastic cellularity via light microscopy of hematoxylin and eosin (H&E) stained sections. However, this method has limitations. Studies have shown that pathologist estimates are imprecise and have limited reproducibility between observers [95]. Furthermore, for leukemia samples obtained from bone marrow aspirates, the distribution of blasts may not be uniform in the material allocated for DNA extraction, leading to discrepancies between the morphologic estimate and the actual purity of the sequenced sample.
Computational algorithms have been developed to infer tumor purity directly from molecular data, utilizing the genetic differences between cancer and normal cells. These methods can be based on:
- Genetic Alterations: Leveraging somatic copy-number alterations (SCNAs) or single nucleotide polymorphisms (SNPs) [95] [96].
- DNA Methylation: Exploiting systematic differences in methylation patterns between cancerous and normal cells [97] [96].
- Gene Expression: Using expression profiles to deconvolute the mixture of cell types [96].
A comparative study of three computational algorithms (ABSOLUTE, ASCAT, and THetA2) applied to a cohort of 881 cancer patients found poor concordance between them. The specimens analyzed had high rates of algorithm failure, partially attributable to variable tumor purity. This study concluded that, at that time, computational tumor purity estimates did not add value beyond the pathologist's microscopic estimate for guiding clinical interpretation of NGS results [95]. However, the field is evolving rapidly.
Advanced Method: DNA Methylation-Based Purity Estimation with InfiniumPurify
DNA methylation profiling offers a powerful and flexible approach for tumor purity estimation, especially relevant for acute leukemia classification. The InfiniumPurify method estimates tumor purity from Illumina Infinium methylation microarray data without requiring matched normal controls or reference samples from pure cell populations.
Principle: The method is based on the observation that the number of probes with intermediate methylation levels (beta values between 0.2 and 0.8) is significantly greater in tumor samples compared to normal samples. These intermediate values often result from the mixture of methylated (cancer) and unmethylated (normal) cell populations, and the distribution of these values contains information about the mixing proportion (tumor purity) [96].
Procedure:
- Universal Normal Panel: Construct a panel of normal methylomes by combining publicly available normal samples from relevant tissues (e.g., normal bone marrow or blood).
- Identify iDMCs: For the cancer type of interest (e.g., AML), identify informative differentially methylated CpG sites (iDMCs) by comparing a cohort of tumor samples to the universal normal panel.
- Model Distribution: Model the density distribution of the methylation beta values for the selected iDMCs in the tumor sample.
- Estimate Purity: The purity estimate is derived from the proportion of iDMCs showing intermediate methylation values, as this proportion correlates with the degree of sample admixture [96].
This method is particularly advantageous for cancer types with scarce normal controls, such as many leukemia subtypes, and provides results highly consistent with other established methods [96].
The Emergence of Integrated Methylation Classification in Leukemia
The power of DNA methylation analysis extends beyond mere purity estimation. Recent research has established a comprehensive framework for classifying acute leukemia using genome-wide DNA methylation profiling. By assembling a reference cohort of 2,540 samples and defining 38 distinct methylation classes, researchers have demonstrated that methylation-based classification matches standard pathology lineage assignment in over 97% of cases and can reveal additional heterogeneity not captured by genetic testing alone [97].
This approach has been successfully adapted for real-time classification using nanopore sequencing and a neural network (MARLIN), providing high-confidence molecular subclassification of AML, B-ALL, and T-ALL within hours of sample receipt [97]. In such integrated workflows, tumor purity is inherently accounted for during the classification process, highlighting the growing convergence of sample quality control, purity assessment, and diagnostic classification into a single, streamlined NGS-based process.
Figure 2: Tumor Purity Assessment Methods. This diagram contrasts the traditional pathological assessment with modern computational approaches that derive purity estimates directly from genomic data.
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagent Solutions for Sample Quality Control
| Item | Function | Key Considerations |
|---|---|---|
| Agilent RNA 6000 Nano Kit | Used with the Bioanalyzer for RNA integrity analysis (RIN). | Provides high sensitivity for limited samples. Different kits available for varying input quality/quantity (e.g., Pico for FFPE). |
| Qubit RNA HS (High Sensitivity) Assay Kit | Fluorometric quantification of RNA concentration. | Selective for RNA, more accurate than absorbance, crucial for library preparation. |
| DNase I, RNase-free | Removal of genomic DNA contamination from RNA preparations. | Essential step before RNA-Seq or RT-qPCR to prevent false positives and off-target library reads. |
| Illumina Infinium MethylationEPIC Kit | Genome-wide DNA methylation profiling. | The successor to the 450k array; used for methylation-based classification and purity estimation (InfiniumPurify). |
| Universal Probe Library (UPL) | Set of short, hydrolytic probes for qPCR or ddPCR. | Enables flexible assay design for gene expression or the "ddPCR-Tail" method for NGS library quantification [98]. |
| Maxwell RSC Blood DNA/RNA Kits | Automated purification of nucleic acids from blood/bone marrow. | Standardized extraction is key for reproducible NGS results, minimizing batch effects and inhibitor carryover. |
The precision of NGS in acute leukemia diagnosis and research is inextricably linked to rigorous pre-analytical sample quality control. While traditional methods like spectrophotometry and histology provide a foundation, advanced techniques such as quantitative RT-qPCR integrity models and DNA methylation-based purity estimation offer researchers powerful tools to quantify and correct for sample limitations. The field is moving toward an integrated paradigm where quality assessment, purity estimation, and molecular classification are becoming seamlessly unified through platforms like methylation arrays and nanopore sequencing. For researchers and clinicians, a thorough understanding and systematic application of these quality considerations are no longer optional but are fundamental to generating reliable, reproducible, and clinically meaningful genomic data in the era of precision oncology.
Optimizing Coverage Depth and Sequencing Parameters for Clinical Sensitivity
The diagnosis and management of acute myeloid leukemia (AML) have been transformed by next-generation sequencing (NGS), which provides a comprehensive molecular profile crucial for risk stratification, treatment selection, and monitoring. AML is a highly heterogeneous malignancy characterized by diverse genetic mutations and chromosomal aberrations that drive uncontrolled proliferation of immature myeloid blasts [99]. While most patients achieve initial remission after induction chemotherapy, relapse remains common, with a 5-year survival rate of only approximately 27% for adults [99]. This clinical challenge has intensified the focus on measurable residual disease (MRD) detection—the identification of persistent leukemic cells at levels below morphological detection—which serves as a powerful predictor of relapse and survival [99] [82].
Traditional MRD detection methods, including multiparameter flow cytometry (MFC) and quantitative/digital PCR (qPCR/dPCR), face significant limitations in AML's heterogeneous landscape. MFC interpretation is subjective and difficult to standardize, while PCR-based methods can track only a limited number of predefined targets [99]. NGS overcomes these constraints by enabling simultaneous assessment of numerous genetic alterations with high sensitivity, providing a universal approach that captures clonal evolution and emerging resistance mutations [99] [100]. This guide systematically compares the performance of NGS against traditional methods and alternative sequencing approaches, providing researchers with evidence-based recommendations for optimizing coverage depth and sequencing parameters to maximize clinical sensitivity in AML diagnostics and MRD monitoring.
Performance Comparison of MRD Detection Techniques
Analytical and Clinical Performance Metrics
Table 1: Comparative Performance of MRD Detection Technologies in AML
| Method | Key Performance Metrics | Advantages | Limitations |
|---|---|---|---|
| Multiparameter Flow Cytometry (MFC) | Sensitivity: 0.1% [99] | Widely available; rapid turnaround; no requirement for prior genetic characterization [99] | Subjective interpretation; difficult to standardize; requires high expertise; limited by phenotypic shifts [99] |
| Quantitative PCR (qPCR) | Sensitivity: 0.01% [99] | Accurate quantification; objective results [99] | Limited to known targets; requires patient-specific assays; poor coverage of heterogeneity [99] |
| Digital PCR (dPCR) | Sensitivity: 0.001% [99] | Absolute quantification; high sensitivity; no standard curves required [99] | Limited multiplexing capability; higher cost; covers limited targets [99] |
| Next-Generation Sequencing (NGS) | Sensitivity: 0.0024% VAF (validated limit); 0.05% (standard panels); 0.0014% (ultra-deep) [33] [101] | Broad target coverage; objective data; tracks clonal evolution; identifies emerging mutations [99] | Requires specialized bioinformatics; higher computational resources; more complex workflow [99] |
Clinical Validation and Prognostic Value
Recent clinical studies have demonstrated the superior prognostic capability of NGS-based MRD detection. A 2025 study of 69 AML patients revealed that patients with a mean variant allele frequency (VAF) ≤0.004 after consolidation therapy had significantly better prognosis [82]. Furthermore, the combination of MFC and NGS provided refined prognostic stratification, with patients negative by both methods experiencing the longest survival [82].
Another pivotal study of 128 AML patients validated NGS-MRD as an independent prognostic biomarker. Patients with NGS-detectable MRD after induction therapy had significantly shorter overall survival (17 months vs. median not reached) and shorter time to relapse (14 months vs. median not reached) compared to NGS-MRD negative patients [101]. Notably, among patients achieving complete morphological remission, those with NGS-MRD positivity had significantly worse outcomes, demonstrating NGS's ability to identify high-risk patients missed by conventional methods [101].
Table 2: Clinically Validated NGS-MRD Thresholds and Associations with Outcomes
| Testing Context | VAF Threshold | Clinical Significance | Study Details |
|---|---|---|---|
| Post-Consolidation (C1D1) | VAF ≤0.004 | Better prognosis [82] | 69 adult AML patients; 47-gene panel [82] |
| During 2-year MRD monitoring | VAF ≤0.020 | Better prognosis [82] | 51 patients monitored; ETV6 mutations higher in relapsed patients [82] |
| Post-induction therapy | Detection limit 0.0024 VAF | Shorter OS (17 vs. NR mos) and TTR (14 vs. NR mos) [101] | 128 AML patients; 42-gene MRD-validated NGS assay [101] |
| FLT3-specific ultra-deep sequencing | Detection limit 0.0014% | Enables early intervention prior to hematologic relapse [33] | Validated by Moffitt Cancer Center; enhances transplant decision-making [33] |
Experimental Protocols for NGS-MRD Detection
Targeted Amplicon Sequencing with Molecular Barcoding
The most widely validated approach for NGS-based MRD detection in AML utilizes targeted amplicon sequencing with unique molecular identifiers (UMIs) to achieve high sensitivity.
Sample Preparation and Library Construction:
- Input Material: Genomic DNA from bone marrow (preferred) or peripheral blood
- Gene Panels: Targeted amplification of clinically relevant genes (47-gene and 42-gene panels have been extensively validated) [82] [101]
- Molecular Barcoding: Incorporation of UMIs during library preparation enables error correction and accurate variant quantification by distinguishing true mutations from PCR/sequencing errors [101]
Sequencing Parameters:
- Coverage Depth: Minimum 1,000x coverage for standard diagnostic profiling; ≥50,000x for MRD detection (enables sensitivity to 0.001% VAF) [33] [101]
- Platforms: Illumina NextSeq 500 or NovaSeq for high-throughput applications; PGM sequencer (Life Technologies) also validated [101]
Bioinformatic Analysis:
- Variant Calling: Specialized pipelines for low-frequency mutation detection; manual review at previously identified somatic mutation sites [101]
- Error Correction: Background error distribution determined at each mutational hotspot using control DNA; statistical cutoff (95% limit of blank) defines detection threshold [101]
- MRD Interpretation: Tracking of pathogenic/likely pathogenic somatic mutations identified at diagnosis; exclusion of mutations in preleukemic genes (DNMT3A, TET2, ASXL1 - "DTA" mutations) per consensus recommendations [101]
Ultra-Sensitive FLT3 Mutation Detection
FLT3 mutations, particularly internal tandem duplications (ITD), present unique detection challenges due to their variable size and location. A refined sequencing assay specifically optimized for FLT3 achieves exceptional sensitivity.
Methodology:
- Targeted Enrichment: Deep sequencing of FLT3 gene regions with extended coverage for ITD detection
- Sequencing Depth: Ultra-deep coverage (>100,000x) to detect mutant alleles at frequencies as low as 0.0014% [33]
- Supplementary Assays: PCR-sizing assay for large ITDs that may be missed by NGS alone [101]
Clinical Utility:
- Enables detection of rising FLT3-ITD levels during serial monitoring as a harbinger of impending relapse [33]
- Informs decisions regarding allogeneic stem cell transplantation and preemptive therapies upon molecular relapse [33]
Technological Workflows in AML Sequencing
The following diagram illustrates the key methodological workflows for NGS-based MRD detection in AML, highlighting the critical steps that impact clinical sensitivity:
Research Reagent Solutions for AML NGS Studies
Table 3: Essential Research Reagents and Platforms for NGS-Based AML Detection
| Reagent/Platform | Function | Application in AML Research |
|---|---|---|
| Oncomine Myeloid MRD Assay (RUO) | Simultaneous DNA and RNA sequencing panel | Tracks DNA mutations and chimeric fusions; covers AML, MDS, and MPN-associated genes; sensitivity to 0.05% allele frequency [99] |
| Ion AmpliSeq HD Technology | Molecular barcoding system | Enables high-sensitivity detection down to 0.05% allele frequency; reduces background noise [99] |
| Custom 42-47 Gene Panels | Targeted sequencing of AML-related genes | Covers key mutational hotspots in FLT3, NPM1, RUNX1, IDH1/2, TP53; validated for MRD monitoring [82] [101] |
| UMI (Unique Molecular Identifiers) | Molecular barcodes for error correction | Distinguishes true low-frequency mutations from sequencing artifacts; enables ultra-sensitive detection [101] |
| FLT3-ITD Supplementary Assay | PCR-sizing assay | Detects large ITDs missed by standard NGS; complements sequencing approaches [101] |
| Oxford Nanopore Platforms | Portable real-time sequencing | Rapid classification (hours); methylation analysis with MARLIN algorithm; whole transcriptome for fusion detection [102] |
Optimizing coverage depth and sequencing parameters is fundamental to achieving the clinical sensitivity required for reliable MRD detection in AML. NGS platforms with deep sequencing capabilities (≥50,000x coverage) and molecular barcoding technologies enable detection sensitivities of 0.0024% VAF, significantly surpassing traditional methods. The integration of UMIs, optimized bioinformatic pipelines, and disease-specific panels allows researchers to accurately quantify residual disease and monitor clonal evolution, providing critical insights for clinical decision-making. As the field advances, standardization of testing methodologies and consensus on clinical thresholds will be essential to fully realize the potential of NGS in improving outcomes for AML patients.
Bioinformatics Pipeline Validation and Quality Control Measures
Next-generation sequencing (NGS) has revolutionized molecular diagnostics in acute leukemia, enabling comprehensive genomic profiling that surpasses conventional techniques in resolution and throughput [19]. The clinical application of this technology, however, is entirely dependent on the reliability and accuracy of the bioinformatics pipelines that transform raw sequencing data into clinically actionable variants. As research and drug development increasingly rely on these molecular insights, rigorous validation and quality control of bioinformatics workflows become paramount. Pipeline performance variability can significantly impact mutation identification, affecting diagnosis, prognosis, and therapeutic decisions in leukemia management [103] [104]. This guide provides a structured framework for benchmarking bioinformatics pipelines, comparing performance metrics across popular variant callers, and implementing robust quality control measures tailored to the leukemia research context.
Core Principles of Pipeline Validation
Bioinformatics pipeline validation ensures that variant calling algorithms correctly identify true positive mutations while minimizing false positives and negatives. In leukemia genomics, this process must account for the diverse spectrum of genetic alterations, including single nucleotide variants (SNVs), insertions/deletions (indels), copy number variations (CNVs), and fusion genes [73]. The validation framework should assess performance across all these variant types, with particular attention to clinically relevant mutations in genes like FLT3, NPM1, IDH1/2, RUNX1, and TP53 [19] [25].
A fundamental requirement for rigorous validation is the use of well-characterized reference materials with known variants. The Genome in a Bottle (GIAB) consortium provides gold standard reference genomes, such as NA12878, which offers a benchmark set of small variants and reference calls [103]. These resources enable objective performance assessment by providing ground truth data for comparison. When validating pipelines for leukemia applications, it is advantageous to supplement these general references with leukemia-specific samples that harbor known clinically relevant mutations, ensuring that pipeline optimization addresses the specific genetic architecture of hematologic malignancies.
Benchmarking Methodologies and Set-Theory Approach
Experimental Design for Pipeline Comparison
A robust benchmarking experiment begins with sequencing a reference material with known variants using the same platform and library preparation methods employed in routine leukemia testing. The resulting sequencing data is then processed through multiple variant calling pipelines for comparative analysis [103]. This approach controls for technical variability in wet-lab procedures while isolating the performance differences attributable to the bioinformatics algorithms.
For targeted sequencing panels commonly used in leukemia diagnostics (e.g., TruSight Cancer Panels, AmpliSeq panels), the benchmarking should focus on the specific genomic regions covered by these panels [73]. The analytical validation requires high-quality nucleic acids from patient samples or cell lines, with careful quantification and quality control to ensure input material integrity. Library preparation should follow standardized protocols, with unique dual indexing to minimize index hopping and cross-sample contamination [25].
Set-Theory Based Performance Metrics
A set-theory approach provides a mathematical framework for calculating performance metrics by defining discrete sets of variants [103]. This methodology enables precise quantification of pipeline accuracy through several key metrics:
- True Positives (TP): Variants correctly identified by the pipeline that match the gold standard set; calculated as TP = A ∩ B, where A is the gold standard variant set and B is the pipeline-called variant set.
- False Positives (FP): Variants called by the pipeline but absent from the gold standard; calculated as FP = (B ∩ C)\A, where C represents high-confidence genomic regions.
- False Negatives (FN): Gold standard variants in high-confidence regions missed by the pipeline; calculated as FN = (A ∩ C)\B.
- Recall (Sensitivity): The pipeline's ability to detect known variants; calculated as Recall = TP/(TP+FN).
- Precision (Specificity): The pipeline's ability to avoid false calls; calculated as Precision = TP/(TP+FP).
This set-based calculation method facilitates high-resolution comparison of pipeline performance, revealing subtle but clinically significant differences in variant detection capabilities [103].
Table 1: Key Performance Metrics for Variant Caller Benchmarking
| Metric | Calculation | Interpretation | Optimal Range |
|---|---|---|---|
| Recall/Sensitivity | TP/(TP+FN) | Ability to detect true variants | >0.99 for clinical use |
| Precision | TP/(TP+FP) | Proportion of true variants among all calls | >0.98 for clinical use |
| F1 Score | 2×(Precision×Recall)/(Precision+Recall) | Harmonic mean of precision and recall | >0.985 |
| False Discovery Rate | FP/(TP+FP) | Proportion of false positives among all calls | <0.02 |
| False Negative Rate | FN/(TP+FN) | Proportion of missed true variants | <0.01 |
Comparative Analysis of Variant Calling Pipelines
Performance Across Variant Callers
Different variant calling algorithms employ distinct statistical models and heuristic approaches, leading to variations in mutation detection performance. A comparative study of three popular variant callers—Isaac, Freebayes, and VarScan—using the NA12878 reference genome and TruSight Cardio kit revealed significant differences in their operational characteristics [103].
Isaac demonstrated perfect precision (1.000) with slightly lower variant counts (255 SNPs), suggesting a more conservative calling approach that minimizes false positives. Freebayes showed balanced performance with high precision (0.987) and moderate variant discovery (259 SNPs). VarScan exhibited the highest sensitivity for variant discovery (311 SNPs) but with reduced precision (0.928), indicating a more inclusive calling strategy that captures more true positives at the cost of increased false positives [103]. The transition/transversion (Ts/Tv) ratio, a quality metric that leverages known mutational patterns in human genomes, remained within expected ranges for all three pipelines (3.44-4.08), confirming basic bioinformatic quality control.
Table 2: Variant Caller Performance Comparison Using Set-Theory Approach
| Variant Caller | Total SNPs | Precision | Recall | Ts/Tv Ratio | Optimal Use Case |
|---|---|---|---|---|---|
| Isaac | 255 | 1.000 | 0.991 | 4.00 | Clinical applications requiring high specificity |
| Freebayes | 259 | 0.987 | 0.995 | 4.08 | Balanced research and clinical applications |
| VarScan | 311 | 0.928 | 0.998 | 3.44 | Discovery research prioritizing sensitivity |
Pipeline Selection Considerations for Leukemia Research
The choice of an appropriate variant calling pipeline depends on the specific research objectives and clinical requirements. For minimal residual disease (MRD) monitoring in acute lymphoblastic leukemia (ALL), pipelines with high sensitivity are critical to detect low-frequency clones [5]. In contrast, for diagnostic classification of acute myeloid leukemia (AML), high specificity may be prioritized to avoid false-positive assignment to specific genetic subgroups [25] [104].
The integration of multiple callers or ensemble approaches can leverage the strengths of different algorithms. However, this requires sophisticated reconciliation methods to resolve discordant calls and may increase computational burden. For clinical applications in leukemia, establishing a single, thoroughly validated pipeline often provides more consistent and interpretable results [104].
Quality Control Measures throughout the NGS Workflow
Pre-Analytical Quality Control
Robust quality control begins with sample preparation and extends through each stage of the NGS workflow. For leukemia samples, which often derive from bone marrow aspirates or peripheral blood, nucleic acid quality and purity significantly impact variant detection accuracy [25]. DNA and RNA quality assessment should include fluorometric quantification for accurate concentration measurement, spectrophotometric analysis for purity (OD260/280 ratio >1.8), and fragment analysis for integrity assessment [73].
During library preparation, unique dual indexing is essential to prevent index hopping and sample cross-talk [25]. For targeted sequencing panels, coverage uniformity and minimum depth requirements must be established, with >1000× mean read depth recommended for reliable detection of low-frequency variants in heterogeneous leukemia samples [73]. The use of unique molecular identifiers (UMIs) helps identify and correct for PCR artifacts, enabling more accurate variant allele frequency quantification [25].
Analytical Quality Control Metrics
During data analysis, several quality metrics must be monitored to ensure variant calling reliability:
- Coverage Uniformity: Assessed by the percentage of target bases covered at ≥100× or ≥500×, with minimal coverage drops in GC-rich regions.
- Mapping Quality: Evaluated through the percentage of properly paired reads and mapping quality scores.
- Base Quality: Monitored using Phred-scaled quality scores across all bases.
- Batch Effects: Controlled through processing reference samples in each sequencing batch.
For leukemia applications, additional validation is required for specific challenge areas, such as homopolymer regions in FLT3-ITD mutations, which require specialized calling algorithms beyond standard SNV detection [25] [104].
Diagram 1: Comprehensive Quality Control Workflow for Leukemia NGS Testing. This diagram illustrates the multi-phase quality control process essential for reliable variant detection in leukemia genomics, spanning pre-analytical, analytical, and post-analytical stages.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents for NGS Pipeline Validation in Leukemia
| Reagent/Solution | Function | Application in Validation |
|---|---|---|
| Reference Standards (GIAB NA12878) | Gold standard variant set | Benchmarking variant caller performance [103] |
| Commercial Control Materials (SeraSeq) | Multiplex biosynthetic mutation mix | Assessing sensitivity, specificity, and LOD [73] |
| Unique Molecular Identifiers (UMIs) | Molecular barcodes for individual molecules | Correcting PCR artifacts and improving VAF accuracy [25] |
| Targeted Sequencing Panels | Gene-specific capture probes | Ensuring coverage of leukemia-related genes [105] [73] |
| Bioinformatic Tools (BWA, GATK) | Alignment and variant calling | Standardized processing for performance comparison [103] |
| Variant Databases (ClinVar, COSMIC) | Curated variant annotations | Classifying pathogenic vs. benign variants [104] |
Implementation in Leukemia Research and Clinical Applications
Validation for Minimal Residual Disease Monitoring
In acute lymphoblastic leukemia, NGS-based MRD detection has demonstrated superior sensitivity compared to multiparameter flow cytometry, identifying more MRD-positive cases with significant prognostic implications [5]. One study showed that NGS detected MRD in 57.5% of B-ALL cases versus 26.9% by MFC, and in 80% of T-ALL cases versus 46.7% by MFC [5]. Bioinformatics pipeline validation for MRD applications requires exceptional sensitivity (10^-5 to 10^-6) and specialized algorithms for tracking clonal immunoglobulin (Ig) and T-cell receptor (TCR) gene rearrangements [5].
The validation must establish a clear threshold for positive MRD detection and demonstrate reproducible quantification across the measurement range. For drug development applications, where MRD is increasingly used as a surrogate endpoint in clinical trials, rigorous validation and standardization across multiple testing sites become particularly important [5].
Addressing Technical and Biological Challenges
Bioinformatics pipelines for leukemia must overcome several unique challenges. The discrimination between true somatic mutations and germline polymorphisms requires comparison with matched normal tissue, which is often unavailable in leukemia diagnostics [104]. When no matched normal is available, population databases (gnomAD, 1000 Genomes) and somatic variant databases (COSMIC) provide essential reference information, though expert review remains necessary [104].
Another significant challenge is differentiating between leukemia-related mutations and clonal hematopoiesis of indeterminate potential (CHIP), particularly in older patients where CHIP mutations (e.g., in DNMT3A, TET2, ASXL1) are common [104]. This distinction requires integration of clinical, morphological, and genetic data, as no bioinformatic approach can reliably differentiate these entities based on sequencing data alone.
Diagram 2: Variant Interpretation Workflow in Leukemia Genomics. This diagram outlines the complex decision process for classifying variants detected in leukemia samples, requiring integration of database information, variant allele frequency analysis, and clinical correlation.
Bioinformatics pipeline validation is not merely a technical exercise but a fundamental component of reliable leukemia genomics research and clinical application. As NGS technologies evolve and their role in leukemia diagnosis, classification, and monitoring expands, rigorous quality control measures become increasingly critical. The set-theory based benchmarking approach provides a mathematical framework for objective performance assessment, enabling informed selection of variant calling pipelines based on the specific requirements of each research or clinical context.
Successful implementation requires continuous monitoring throughout the entire NGS workflow, from sample preparation to final variant interpretation. By establishing comprehensive validation protocols and quality control measures, researchers and drug development professionals can ensure the generation of accurate, reproducible genomic data that advances our understanding of leukemia biology and improves patient outcomes through precision medicine approaches.
Distinguishing Pathogenic Mutations from Benign Polymorphisms
In the diagnosis and management of acute leukemia, accurately distinguishing disease-causing genetic mutations from benign background polymorphisms is a fundamental challenge in genomic medicine. Next-generation sequencing (NGS) has emerged as a powerful tool that addresses critical limitations of traditional diagnostic methods, offering unprecedented depth and breadth for variant detection. This guide objectively compares the performance of NGS against established techniques like Sanger sequencing, multiparametric flow cytometry (MFC), and quantitative PCR (qPCR), providing the experimental data and protocols that underscore its transformative role in clinical research.
Experimental Protocols for Method Comparison
To objectively evaluate the performance of NGS against traditional methods, researchers employ rigorous experimental designs. The following protocols are commonly used in comparative studies to generate the performance data cited in this guide.
Protocol 1: Assessing Sensitivity for Minimal Residual Disease (MRD)
This protocol measures the ability to detect low levels of residual leukemia cells after treatment, a critical prognostic factor [5] [7].
- Objective: Compare the sensitivity and concordance of NGS and MFC for MRD detection in Acute Lymphoblastic Leukemia (ALL) patient samples.
- Sample Preparation: Collect bone marrow or peripheral blood samples from ALL patients at diagnosis and at the end of induction therapy. Extract genomic DNA from mononuclear cells.
- NGS Workflow: Amplify immunoglobulin (IGH) and T-cell receptor (TCR) gene rearrangements using multiplex PCR primers. Sequence amplicons on an NGS platform (e.g., Illumina) to a high depth (>50,000x coverage). Use bioinformatics software (e.g., from EuroClonality-NGS Consortium) to identify and track clonal sequences present at diagnosis [5] [7].
- MFC Workflow: Stain cells with a panel of fluorescently labeled antibodies against lineage-specific cell surface antigens. Analyze using 8+ color flow cytometry to identify leukemia-associated immunophenotypes [5].
- Data Analysis: Calculate the level of MRD for each method. Determine sensitivity based on the lowest detectable allele frequency. Compare MRD positivity rates and concordance between NGS and MFC.
Protocol 2: Validating a Custom NGS Panel for Comprehensive Genomic Profiling
This protocol validates a single NGS assay designed to detect a wide range of genomic alterations in B-Acute Lymphoblastic Leukemia (B-ALL) [105].
- Objective: Validate a custom NGS panel against a combination of standard-of-care techniques for the detection of aneuploidies, fusion genes, single nucleotide variants (SNVs), and copy number variations (CNVs).
- Sample Preparation: Use 75 previously characterized B-ALL diagnostic samples. Extract DNA and/or RNA.
- NGS Workflow: Design a custom hybridization-capture or amplicon-based panel targeting genes and regions recurrently altered in B-ALL. Prepare libraries and sequence on an NGS platform. Use a bioinformatics pipeline to call SNVs, INDELs, CNVs, and gene fusions [105].
- Orthogonal Methods: Compare NGS findings with results from:
- Karyotyping and FISH for aneuploidies and fusion genes.
- RT-PCR for specific fusion transcripts.
- Sanger sequencing for SNVs.
- Data Analysis: Calculate the sensitivity, specificity, and reproducibility of the NGS panel for each variant type by comparing its results to the orthogonal methods.
Performance Data Comparison
The experimental protocols consistently demonstrate that NGS offers superior sensitivity and a more comprehensive view of the genomic landscape in acute leukemia compared to traditional methods.
Table 1: Comparative Analytical Performance of Genetic Testing Methods
| Method | Sensitivity (Limit of Detection) | Key Strengths | Key Limitations | Best Applications |
|---|---|---|---|---|
| NGS | MRD: ~10⁻⁶ (0.0001%) [5] [7]SNVs: ~1% VAF [106] | High sensitivity, comprehensive variant detection (SNVs, INDELs, CNVs, fusions) in a single assay, can track clonal evolution [5] [105]. | High cost, complex bioinformatics, standardization challenges [5] [107]. | MRD monitoring, comprehensive genomic profiling, discovery of novel variants [5] [105]. |
| Sanger Sequencing | ~15-20% VAF [106] | Low cost for single genes, simple data analysis, well-established [108] [106]. | Low throughput, poor sensitivity for low-frequency variants [108] [106]. | Confirming known mutations in a small number of genes. |
| Multiparametric Flow Cytometry (MFC) | ~10⁻⁴ (0.01%) [5] | Fast, widely applicable, uses viable cells [5]. | Limited sensitivity, subject to immunophenotypic shifts, influenced by immunotherapy [5]. | Rapid initial diagnosis and MRD assessment when NGS is unavailable. |
| qPCR | ~10⁻⁴ to 10⁻⁶ [5] | High sensitivity for known targets, quantitative. | Requires patient-specific primers (for IG/TCR), limited to known fusion genes, cannot detect clonal evolution [5]. | Tracking specific, known fusion genes or well-characterized IG/TCR rearrangements. |
Table 2: Clinical Performance in Acute Leukemia Studies
| Study Context | NGS Performance | Traditional Method Performance | Implication |
|---|---|---|---|
| MRD in ALL (13-study systematic review) | Detected more MRD-positive cases in both B-ALL (57.5% vs. 26.9%) and T-ALL (80% vs. 46.7%) than MFC. NGS-MRD negativity correlated with superior event-free and overall survival [5] [7]. | MFC missed a significant number of MRD-positive cases later identified by NGS [5]. | NGS provides a more sensitive and prognostically powerful assessment of treatment response. |
| Mutation Detection in AML | High concordance (>95%) across different laboratory NGS platforms for major pathogenic mutations (e.g., in NPM1, FLT3, IDH1/2) [109]. | N/A (Compared NGS vs. NGS) | NGS results are reproducible across institutions, supporting their reliability for therapeutic decision-making. |
| B-ALL Diagnosis | A custom NGS panel successfully detected primary (aneuploidy, fusions) and secondary (SNVs, CNVs) alterations in a single assay, refining patient stratification [105]. | Required a combination of karyotyping, FISH, and PCR, which is more time-consuming and may miss subtle alterations [105]. | NGS streamlines diagnostics and provides a more complete genetic profile for risk stratification. |
The Scientist's Toolkit: Research Reagent Solutions
Successfully implementing NGS-based leukemia research requires a suite of specialized reagents and tools.
Table 3: Essential Research Reagents and Materials
| Item | Function | Application in Leukemia Research |
|---|---|---|
| Hybridization Capture Probes | Designed to enrich genomic regions of interest (e.g., a custom pan-leukemia gene panel) from a fragmented DNA library before sequencing [105]. | Targeted sequencing of genes recurrently mutated in ALL/AML. |
| Multiplex PCR Primers | Used in amplicon-based NGS to simultaneously amplify multiple genomic targets, such as IGH and TCR loci for MRD tracking [5]. | High-sensitivity detection of clonal rearrangements for MRD monitoring. |
| Methylation Conversion Reagents | Chemicals (e.g., bisulfite) that convert unmethylated cytosine to uracil, allowing for the determination of methylation status via sequencing [32]. | Epigenetic classification of leukemia subtypes using tools like MARLIN. |
| Bioinformatics Pipelines | Software for aligning sequence reads, calling variants (SNVs, CNVs, fusions), and filtering out common polymorphisms (e.g., using population databases like ExAC/gnomAD) [105] [110]. | Essential for data analysis, interpretation, and distinguishing pathogenic mutations from technical artifacts and benign polymorphisms. |
Technical Workflow and Considerations
The power of NGS comes from its massively parallel workflow, which differs significantly from the linear approach of Sanger sequencing.
A critical step after sequencing is the bioinformatic filtering of variants to distinguish pathogenic mutations from benign polymorphisms. This relies heavily on population frequency databases.
Method Selection Guide
The choice between NGS and traditional methods depends on the specific research question, available resources, and required turnaround time.
Table 4: Guidance for Method Selection in Leukemia Research
| Research Goal | Recommended Method | Rationale |
|---|---|---|
| Comprehensive genomic profiling at diagnosis | NGS (Comprehensive Panel) | Detects SNVs, INDELs, CNVs, and fusions in a single assay, providing a complete genetic profile for risk stratification [105]. |
| High-sensitivity MRD monitoring | NGS (for IG/TR rearrangements) | Superior sensitivity (10⁻⁶) and ability to track clonal evolution compared to MFC and qPCR [5] [7]. |
| Rapid confirmation of a known mutation | Sanger Sequencing | Cost-effective and straightforward for interrogating a small number of predefined genomic targets [108] [106]. |
| Ultra-fast classification & subtyping | Emerging Methods (e.g., MARLIN) | Methylation-based tools like MARLIN can classify acute leukemia in under 2 hours, far faster than standard genetic workflows [32]. |
The data from rigorous comparative studies firmly establishes that NGS outperforms traditional methods like Sanger sequencing, MFC, and qPCR in sensitivity, comprehensiveness, and prognostic power for acute leukemia research. While challenges in cost, bioinformatics, and standardization persist, NGS provides an unparalleled ability to detect pathogenic mutations at low frequencies and across the full spectrum of genomic alteration types. For researchers and drug developers, the integration of NGS into diagnostic and monitoring protocols is pivotal for advancing personalized treatment strategies and improving patient outcomes in acute leukemia.
The integration of Next-Generation Sequencing (NGS) into the diagnostic workflow for acute leukemia has revolutionized molecular stratification, enabling precise classification and risk stratification that guides therapeutic decisions. However, this technological advancement has concurrently amplified a significant challenge in clinical genomics: the interpretation of Variants of Unknown Significance (VUS). A VUS is a genetic alteration whose association with disease risk remains unclear due to insufficient or contradictory evidence, creating diagnostic uncertainty that complicates clinical decision-making. In the context of acute leukemia, where timely and accurate diagnosis directly influences treatment selection and patient outcomes, the management of VUS becomes critically important.
The scale of this challenge is substantial. From a large cohort of 1,689,845 cases undergoing multi-gene panel sequencing, approximately 41% of cases were found to carry a VUS [111]. In pediatric genetic diseases, which include pediatric leukemias, as many as 50% of cases can harbor rare structural variants classified as VUS [111]. This high prevalence of uncertain findings underscores the pressing need for sophisticated interpretation tools and comprehensive databases that can resolve ambiguity and provide clinically actionable classifications.
The limitations of conventional diagnostic methods in resolving VUS have become increasingly apparent. While techniques such as cytogenetics, karyotyping, and fluorescence in situ hybridization (FISH) provide essential structural and numerical chromosomal information, they lack the resolution to detect many subtle genetic alterations that NGS can identify [3]. This resolution gap generates a growing number of variants whose clinical significance remains uncertain, driving the development of advanced bioinformatic tools and specialized databases specifically designed for VUS resolution in hematologic malignancies.
Database Landscape for VUS Interpretation
Foundational Databases and Their Applications
Table 1: Core Databases for VUS Interpretation in Hematologic Malignancies
| Database Name | Primary Focus | Key Utility in VUS Resolution | Notable Features |
|---|---|---|---|
| ClinVar | Aggregate reports of variant-disease relationships | Cross-reference clinical significance classifications from multiple submitters | Publicly accessible, regularly updated with submissions from clinical laboratories worldwide |
| gnomAD | Population allele frequencies across diverse populations | Assess variant rarity; filter out common polymorphisms unlikely to cause rare disorders | Includes data from large-scale sequencing projects; enables filtering by sub-populations |
| COSMIC | Somatic mutations in cancer | Identify cancer-associated mutations and mutational hotspots | Manually curated resource focusing specifically on somatic variations in cancer |
| HGMD | Published disease-causing mutations | Access curated information on germline mutations with established disease links | Comprehensive collection of known published mutational events |
| CIViC | Clinical evidence for cancer variants | Access structured evidence for interpretive guidance for variants in cancer | Community-driven web resource with clinical interpretations |
The interpretation of VUS relies heavily on accessing curated information from specialized genomic databases that aggregate population frequency data, functional evidence, and clinical associations [112]. These resources provide the essential comparative data needed to assess whether a genetic variant is likely to be pathogenic, benign, or of uncertain significance. Population databases like gnomAD (Genome Aggregation Database) are particularly valuable for initial variant filtering, as they help determine whether a variant is too common in the general population to be causative for rare Mendelian disorders [112]. Generally, a variant with a frequency exceeding 5% in healthy individuals is typically classified as benign, though there are exceptions for certain high-frequency pathogenic variants in specific populations [112].
Disease-specific databases play an equally critical role in VUS interpretation. For leukemia diagnostics, databases such as COSMIC (Catalogue of Somatic Mutations in Cancer) provide invaluable information about mutational hotspots, recurrence in specific cancer types, and functional impacts [104]. The clinical significance of variants identified in leukemia-associated genes like FLT3, NPM1, IDH1/2, RUNX1, and ASXL1 can often be elucidated by referencing these specialized resources. However, a significant challenge persists in the form of database bias, as these resources are overwhelmingly populated with data from populations of European ancestry, leading to disproportionate VUS rates in underrepresented populations [113].
Emerging Approaches to Overcome Database Limitations
Innovative approaches are emerging to address the inherent limitations of current genomic databases. Multiplexed Assays of Variant Effect (MAVEs) represent a particularly promising technology that can functionally test thousands of genetic variants simultaneously, generating experimental data at an unprecedented scale [113]. This approach creates a functional "lookup table" for variant effects that can circumvent the population biases present in existing databases. Research demonstrates that MAVEs can potentially reclassify more than 70% of VUS, with particularly significant benefits for individuals of non-European ancestry, compensating for current disparities in genomic knowledge [113].
Other initiatives focus on expanding the diversity of genomic datasets. The UK Biobank represents one such effort to create more inclusive genomic resources, providing a path to access better-phenotyped datasets [111]. Similarly, platforms like GenomeArc's Horizon are leveraging global partnerships with clinics to continuously update their clinical genomics variants databases with information from diverse multi-ethnic populations, empowering their algorithms to predict variants from major ethnic backgrounds more accurately [111]. These efforts are critical for addressing the current inequities in variant interpretation that particularly affect underrepresented populations.
Interpretation Tools and Platforms
Automated Variant Interpretation Systems
Table 2: Performance Comparison of VUS Interpretation Approaches
| Interpretation Method | Reported VUS Resolution Rate | Key Strengths | Notable Limitations |
|---|---|---|---|
| MAVEs (Multiplexed Assays of Variant Effect) | >70% potential reclassification rate [113] | Sidesteps need for population-matched data; generates functional data at scale | Not yet widely implemented in clinical practice; requires specialized expertise |
| Automated ACMG-AMP Guideline Tools | High accuracy for clearly pathogenic/benign variants [114] | Standardizes application of interpretation guidelines; improves efficiency | Significant limitations with VUS; requires expert oversight for complex cases [114] |
| Platform Horizon (GenomeArc) | Increases capacity for variant interpretation through multi-algorithm approach [111] | Integrates diverse population data; includes LLM for phenotype analysis | Commercial platform with potentially limited transparency |
| In silico Predictors | Variable accuracy depending on variant type and gene [114] | Provides complementary evidence for functional impact | Not a substitute for interpretation process; must be used cautiously [114] |
Automated variant interpretation tools have emerged to address the complexity and time-consuming nature of manual variant classification. These systems are designed to replicate the human expert assessment by automatically evaluating criteria established in clinical interpretation guidelines such as those from the American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology (AMP) [114]. The fundamental premise of these tools is to enhance efficiency through automation while maintaining accuracy and consistency in variant classification.
These tools demonstrate considerable variability in their implementation, particularly in the number of criteria they automate, their methodological approaches to automation, and the diversity of data sources they incorporate [114]. This variability inevitably affects their reliability and consistency in clinical settings. A comprehensive evaluation of automated interpretation tools revealed that while they demonstrate high accuracy for clearly pathogenic or benign variants, they show significant limitations when dealing with VUS, underscoring the continued need for expert oversight in clinical contexts, particularly for ambiguous cases [114].
Specialized platforms are increasingly incorporating artificial intelligence to enhance their interpretive capabilities. For instance, the Horizon platform developed by GenomeArc employs a unique language model for phenotype analysis through its PhenoGene module, which helps integrate patients' phenotypes or symptoms with genomic data to provide more comprehensive analysis [111]. This approach addresses one of the major challenges in VUS resolution—the frequent lack of sufficient phenotypic data to support prediction algorithms. By correlating genotypic information with detailed phenotypic presentations, these tools can provide more accurate variant classifications.
Integration with Leukemia Diagnostic Workflows
In the specific context of acute leukemia diagnostics, variant interpretation tools must be integrated into broader diagnostic workflows that often combine multiple technologies. Emerging approaches for pediatric acute lymphoblastic leukemia (ALL) combine digital multiplex ligation-dependent probe amplification (dMLPA) and RNA sequencing (RNA-seq), achieving precise classification of complex subtypes and uniquely identifying IGH rearrangements undetected by other techniques [35]. This combination has demonstrated exceptional efficacy, reaching 95% detection of clinically relevant alterations compared to 46.7% with standard-of-care techniques alone [35].
The integration of these advanced genomic approaches is particularly important for resolving VUS in leukemia because it provides orthogonal validation through multiple methodological approaches. Optical genome mapping (OGM) has emerged as another powerful technology in this context, demonstrating superior resolution in detecting chromosomal gains and losses (51.7% vs. 35%) and gene fusions (56.7% vs. 30%) compared to conventional methods while resolving 15% of non-informative cases [35]. The convergence of data from these complementary technologies provides a more robust evidentiary basis for resolving VUS that might remain ambiguous when relying on a single methodological approach.
Experimental Approaches for VUS Resolution
Methodologies for Functional Validation
Table 3: Essential Research Reagents for VUS Functional Analysis
| Reagent / Material | Primary Application | Key Function in VUS Resolution |
|---|---|---|
| MAVE Library Constructs | Multiplexed functional screening | Enable parallel assessment of thousands of variants for their functional impact |
| CRISPR-Cas9 System | Genome editing | Introduce specific VUS into cell lines for functional characterization |
| Targeted NGS Panels (e.g., ALLseq) | Molecular profiling in leukemia | Detect SNVs, indels, CNAs, gene fusions, and gene expression in leukemia samples [35] |
| Digital MLPA Probes (e.g., SALSA D007 ALL) | Copy number assessment in ALL | Identify recurrent microdeletions/amplifications and gross chromosomal abnormalities [35] |
| Optical Genome Mapping Kit (Bionano) | Structural variant detection | Enable genome-wide detection of structural variants at high resolution [35] |
Functional validation represents the gold standard for resolving VUS, providing direct experimental evidence of a variant's biological impact. Several established and emerging methodologies are employed for this purpose, each with distinct applications and limitations. Functional assays are laboratory-based methods designed to validate the biological impact of genetic variants by assessing how they affect processes such as protein stability, enzymatic activity, splicing efficiency, or cellular signaling pathways [112]. These assays provide critical evidence beyond computational predictions or statistical correlations, offering more definitive insights when other lines of evidence are inconclusive.
Multiplexed Assays of Variant Effect (MAVEs) represent a transformative approach to functional validation that addresses the throughput limitations of conventional assays. MAVEs enable researchers to test thousands—or even millions—of genetic variants simultaneously for their downstream functional effects, generating comprehensive experimental data at a scale previously unimaginable [113]. The experimental workflow for MAVE involves creating variant libraries that encompass all possible single nucleotide changes in a gene of interest, introducing these libraries into cellular systems, subjecting the cells to selective pressures that favor functional protein activity, and sequencing the resulting populations to determine which variants affect function based on their enrichment or depletion.
Cross-laboratory standardization is critically important for ensuring consistency and reliability in functional assay results. Participation in external quality assessment (EQA) programs, such as those organized by the European Molecular Genetics Quality Network (EMQN) and Genomics Quality Assessment (GenQA), plays a key role in promoting standardized practices and quality assurance [112]. These programs evaluate laboratory performance in running functional assays, ensuring reproducibility and comparability of results across institutions, which is essential for clinical implementation of functional data in VUS resolution.
Integrated Workflows for Comprehensive VUS Assessment
Figure 1: VUS Resolution Workflow for Leukemia Variants. This workflow illustrates the multi-step process for resolving Variants of Unknown Significance, integrating computational predictions with functional validation and phenotypic correlation.
A systematic, integrated approach is essential for comprehensive VUS assessment in leukemia diagnostics. The workflow begins with variant identification through NGS, typically using targeted panels optimized for hematologic malignancies. These panels, such as the ALLseq panel used in pediatric ALL characterization, are designed to detect single nucleotide variants (SNVs), insertions/deletions (indels), copy number alterations (CNAs), gene fusions, and gene expression abnormalities [35]. Following variant identification, comprehensive database interrogation is performed using resources such as ClinVar, gnomAD, and COSMIC to gather existing evidence about each variant's frequency and previously reported clinical associations.
The next critical phase involves computational prediction of variant impact using in silico tools that analyze evolutionary conservation, protein structure, and potential disruptive effects. These tools provide valuable preliminary insights but require validation through additional evidence. For variants that remain uncertain after these initial steps, functional characterization through MAVEs or disease-specific assays provides experimental evidence of biological impact. Finally, genotype-phenotype correlation analysis is essential for contextualizing variant findings within the specific clinical presentation of the leukemia patient, ensuring that molecular findings align with disease characteristics and progression.
Comparative Analysis in Leukemia Diagnostics
NGS Versus Conventional Methods for VUS Detection
The transition from conventional diagnostic methods to NGS-based approaches has significantly impacted the detection and characterization of VUS in acute leukemia. Conventional methods such as chromosome banding analysis (CBA) and fluorescence in situ hybridization (FISH), while instrumental in detecting recurrent chromosomal abnormalities, exhibit significant limitations including low resolution, limited detection capacity for cryptic alterations, and reliance on viable metaphases [35]. These limitations inevitably result in an incomplete genetic characterization that can contribute to VUS classifications.
In contrast, NGS-based approaches provide a more comprehensive view of the genetic landscape in leukemia. Studies comparing conventional PCR with NGS for detecting mutations in key leukemia genes like FLT3, IDH, and NPM1 have demonstrated that NGS can identify additional mutations beyond those detected by conventional methods, particularly when using lower variant allele frequency (VAF) cut-offs [115]. For instance, NGS analysis with a 1% VAF cut-off identified more positive results for FLT3-TKD and IDH1/IDH2 mutations than conventional methods, suggesting enhanced sensitivity for detecting potentially clinically relevant variants [115].
However, NGS is not without limitations in specific contexts. For FLT3-ITD mutations, which are critically important in acute myeloid leukemia (AML), NGS demonstrated only 73.8% sensitivity compared to conventional PCR, indicating that some clinically relevant mutations might be missed [115]. This highlights the importance of method selection based on the specific genetic alteration of interest and suggests that a combined approach leveraging the strengths of both conventional and NGS methods may be optimal for comprehensive genomic characterization while minimizing unresolved VUS.
Emerging Technologies Enhancing VUS Resolution
Several emerging technologies show particular promise for enhancing VUS resolution in leukemia diagnostics. Optical genome mapping (OGM) has demonstrated remarkable utility as a standalone technique, detecting chromosomal gains and losses (51.7% vs. 35%) and gene fusions (56.7% vs. 30%) more effectively than conventional methods while resolving 15% of non-informative cases [35]. By providing a genome-wide view of structural variants at higher resolution than traditional cytogenetics, OGM can help resolve VUS that involve structural rearrangements or complex genomic alterations.
The combination of digital MLPA and RNA sequencing has emerged as another powerful approach, achieving precise classification of complex leukemia subtypes and uniquely identifying IGH rearrangements undetected by other techniques [35]. In the largest cohort of pediatric ALL patients analyzed to date, this combination proved to be the most effective approach, detecting clinically relevant alterations in 95% of cases compared to 46.7% with standard-of-care techniques alone [35]. This dramatic improvement in detection capability directly addresses the VUS challenge by providing clearer evidence for variant classification.
Figure 2: NGS Diagnostic Workflow for Leukemia. This diagram outlines the key steps in the NGS diagnostic workflow for acute leukemia, highlighting stages where VUS may be identified and requiring specialized interpretation tools.
The integration of artificial intelligence (AI) and machine learning approaches represents another frontier in VUS resolution. AI has been shown to streamline the variant interpretation process by integrating publicly available information and predicting variant pathogenicity [4]. As these technologies continue to evolve, their ability to identify complex patterns across diverse datasets is expected to enhance VUS classification accuracy, particularly for variants with limited prior evidence. The implementation of AI-assisted interpretation is especially valuable given the increasing volume of genomic data generated through comprehensive NGS testing in leukemia patients.
Future Directions and Clinical Implementation
The field of VUS resolution in leukemia diagnostics is rapidly evolving, with several promising directions emerging. The integration of CRISPR and mRNA technologies is expected to boost screening capacities on a broad scale, facilitating systematic molecular analysis of VUS [111]. As these technologies mature, they will enable more efficient functional characterization of variants at scale, potentially resolving many VUS that currently remain in diagnostic uncertainty.
Addressing disparities in variant interpretation across diverse populations represents another critical frontier. Current genomic databases are overwhelmingly populated with data from individuals of European ancestry, leading to disproportionate VUS rates in underrepresented populations [113]. Initiatives to expand the diversity of genomic datasets, coupled with functional approaches like MAVEs that can circumvent population biases, are essential for achieving equitable genomic medicine. Research demonstrates that MAVEs not only potentially reclassify more than 70% of VUS but can reclassify more VUS in individuals of non-European ancestry than those of European ancestry, directly addressing current disparities [113].
For successful clinical implementation, VUS resolution strategies must be integrated into standardized diagnostic workflows with appropriate expert oversight. Despite advances in automation, expert review remains essential, particularly for complex cases [114]. This is especially true in leukemia, where accurate variant classification directly influences risk stratification and treatment selection. As these technologies and approaches continue to mature, they hold the promise of transforming VUS from diagnostic uncertainties into clinically actionable findings, ultimately advancing precision medicine in leukemia and improving patient outcomes.
Differentiating Somatic Mutations from Clonal Hematopoiesis (CHIP)
The discovery that blood cells can acquire somatic mutations without evident malignancy has fundamentally transformed our understanding of hematopoiesis and leukemogenesis. Clonal hematopoiesis of indeterminate potential (CHIP) represents an age-related condition where hematopoietic stem cells gain somatic mutations that confer a competitive advantage, leading to expanded clones in the absence of cytopenias or overt hematological malignancy [116]. This phenomenon creates a significant diagnostic challenge in acute leukemia research and clinical practice, as distinguishing benign, age-related clonal expansions from pre-leukemic or leukemic clones is critical for accurate diagnosis, prognosis, and treatment decisions.
The advent of next-generation sequencing (NGS) technologies has revealed the remarkable complexity and prevalence of somatic mutations in hematopoietic cells. Research indicates that at least 10-20% of individuals older than 65 years exhibit a significant fraction of white blood cells (e.g., >4%) harboring somatic mutations in known driver genes, with prevalence increasing substantially with age [116]. The diagnostic dilemma arises because the same genes frequently mutated in CHIP (e.g., DNMT3A, TET2, ASXL1) are also recurrently mutated in overt myeloid malignancies like acute myeloid leukemia (AML) [117] [118]. This intersection mutational landscape necessitates sophisticated differentiation strategies that integrate multiple parameters beyond simple mutation detection.
This guide provides a comprehensive comparison of modern methods for differentiating somatic mutations from CHIP in research and clinical contexts, with particular emphasis on how NGS-based approaches have transformed this field compared to traditional techniques. We present experimental data, technical specifications, and standardized protocols to enable researchers and clinicians to navigate this complex diagnostic territory.
Defining the Entities: Somatic Mutations, CHIP, and AML
Somatic Mutations in Hematopoiesis
Somatic mutations are acquired genetic alterations that occur in non-germline tissues and are not inherited. In the hematopoietic system, these mutations accumulate with age due to endogenous processes like DNA replication errors and exogenous factors [117]. The highly proliferative nature of hematopoiesis, which generates >100 billion cells daily, creates ample opportunity for such mutations to emerge [116]. Most somatic mutations have no functional consequences or may even be detrimental to the cell, but a small subset confers a fitness advantage that can lead to clonal expansion.
Clonal Hematopoiesis of Indeterminate Potential (CHIP)
CHIP is formally defined as the presence of somatic mutations in leukemia-associated genes with a variant allele frequency (VAF) ≥ 2% in peripheral blood, in individuals without evidence of hematologic malignancy, cytopenias, or other diagnostic criteria for myelodysplastic syndrome [119] [117]. The most frequently mutated genes in CHIP include DNMT3A (most common), TET2, and ASXL1, which collectively encode epigenetic regulators that influence hematopoietic differentiation and self-renewal [116]. Importantly, while CHIP is associated with a 0.5-1% annual risk of progression to hematological malignancy, the vast majority of individuals with CHIP will not develop leukemia [116] [118]. CHIP is also associated with non-malignant conditions, particularly increased risk of cardiovascular disease, stroke, and all-cause mortality [116] [117].
Acute Myeloid Leukemia (AML) and Pre-Leukemic States
AML is characterized by the accumulation of somatic mutations that confer blocks in differentiation, increased self-renewal, and proliferative advantage, leading to bone marrow failure and peripheral cytopenias. The transition from CHIP to AML typically requires the acquisition of additional cooperating mutations beyond those found in CHIP [116] [118]. Current models suggest a stepwise progression where mutations in genes like DNMT3A and TET2 often occur early in pre-leukemic clones, while mutations in genes like NPM1, FLT3, and NRAS typically occur later during leukemic transformation [118].
Table 1: Key Characteristics Differentiating CHIP from AML
| Parameter | CHIP | AML |
|---|---|---|
| Variant Allele Frequency | Typically <10% (by definition ≥2%) | Often >10% and frequently much higher |
| Peripheral Blood Counts | Normal | Cytopenias (or rarely cytosis) |
| Bone Marrow Blasts | <5% | ≥20% (or presence of specific genetic abnormalities regardless of blast count) |
| Clinical Consequences | Increased risk of hematologic cancer (0.5-1%/year), cardiovascular disease | Bone marrow failure, infectious risk, bleeding |
| Number of Mutations | Often single mutation | Frequently multiple cooperating mutations |
| Specific Mutated Genes | DNMT3A, TET2, ASXL1 most common | Same as CHIP plus NPM1, FLT3, IDH1/2, RUNX1, etc. |
Methodological Comparison: NGS vs. Traditional Techniques
The differentiation of somatic mutations from CHIP relies on a multifaceted diagnostic approach that has evolved significantly with technological advancements. The following diagram illustrates the key decision points in the diagnostic workflow for suspected CHIP versus myeloid malignancy:
Traditional Diagnostic Methods
Traditional techniques for assessing hematologic disorders provide foundational information but have limitations in differentiating CHIP from malignant states.
3.1.1 Cytomorphology and Cytochemistry Bone marrow aspiration and cytomorphology represent the first step in evaluating hematopoietic disorders, allowing assessment of cellular morphology, lineage involvement, and blast percentage [4] [3]. In AML, blast count ≥20% is diagnostic (except for specific genetic subtypes), while in CHIP, morphology is characteristically normal with <5% blasts [3] [118]. The limitations include subjectivity in interpretation and inability to detect genetic abnormalities underlying clonal expansions.
3.1.2 Cytogenetics and Karyotyping Conventional karyotyping provides a genome-wide assessment of chromosomal abnormalities but has limited resolution (~5-10 Mb) [3]. It can detect balanced translocations characteristic of certain AML subtypes (e.g., t(8;21) in core-binding factor AML) that would not be classified as CHIP regardless of blast count [3]. However, karyotyping cannot detect the point mutations and small indels that characterize most CHIP cases.
3.1.3 Fluorescence In Situ Hybridization (FISH) FISH offers higher resolution than karyotyping for specific genomic regions and can be performed on non-dividing cells [3]. While valuable for detecting specific rearrangements in AML, FISH has limited utility in CHIP diagnosis due to its targeted nature and inability to survey the mutational landscape broadly.
Next-Generation Sequencing Approaches
NGS technologies have revolutionized the differentiation of CHIP from malignant states by enabling comprehensive genomic profiling at unprecedented resolution and scale.
3.2.1 Targeted NGS Panels Targeted panels focusing on genes recurrently mutated in hematologic malignancies represent the most common NGS application in clinical practice [4]. These panels typically include the most frequently mutated CHIP genes (DNMT3A, TET2, ASXL1) alongside AML-associated genes (NPM1, FLT3, IDH1/2, etc.) [4] [3]. The key advantage is the ability to simultaneously assess mutation patterns, VAF, and specific gene combinations that help distinguish CHIP from malignant states.
3.2.2 Error-Corrected Ultradeep NGS Advanced NGS methods utilizing unique molecular identifiers (UMIs) and error correction enable highly sensitive detection of variants with VAF as low as 0.4% [119] [117]. This enhanced sensitivity is particularly valuable for monitoring clonal dynamics and detecting emerging malignant clones in individuals with CHIP. Error correction reduces sequencing error rates from 0.005-0.02 to ≥0.0001, significantly improving specificity [117].
3.2.3 Whole Genome and Whole Exome Sequencing Untargeted approaches (whole genome/exome sequencing) provide the most comprehensive assessment of the mutational landscape and can identify novel drivers of clonal expansion beyond known CHIP genes [120]. Recent research using whole exome sequencing of 200,618 individuals identified 17 additional genes under positive selection in clonal hematopoiesis, expanding our understanding of CHIP genetics [120].
Table 2: Performance Comparison of Detection Methods for Somatic Mutations
| Method | Detection Limit (VAF) | Genomic Coverage | Turnaround Time | Key Applications | Limitations |
|---|---|---|---|---|---|
| Karyotyping | N/A (large structural variants only) | Genome-wide (~5-10 Mb resolution) | 7-14 days | Detection of balanced translocations, complex karyotypes | Limited resolution, requires dividing cells |
| FISH | N/A (depends on cell count) | Targeted (specific loci) | 2-5 days | Detection of specific rearrangements (e.g., BCR::ABL1) | Targeted approach, cannot detect point mutations |
| Sanger Sequencing | 15-20% | Single gene | 5-10 days | Validation of known mutations | Low sensitivity, low throughput |
| Targeted NGS | 1-5% (routine); 0.1-1% (high-sensitivity) | Gene panels (dozens to hundreds of genes) | 7-10 days | Comprehensive mutation profiling, CHIP detection | Limited to predefined targets |
| Error-Corrected NGS | 0.1-0.4% | Gene panels or exome | 10-14 days | MRD monitoring, low-VAF CHIP detection | Higher cost, bioinformatic complexity |
| Whole Exome/Genome Sequencing | 2-5% (routine); <1% (enhanced) | Exome (~1-2%) or genome-wide | 2-4 weeks | Novel gene discovery, comprehensive profiling | Higher cost, complex data interpretation |
Experimental Data and Technical Comparisons
Sensitivity and Specificity Metrics
Recent studies have directly compared the performance of different NGS approaches for detecting somatic mutations in hematopoietic cells:
Error-corrected ultradeep NGS demonstrated a lower limit of detection of ≥0.4% VAF at sequencing depths >3,000×, with sensitivity, specificity, positive predictive value, negative predictive value, and accuracy all reaching 100% in validation studies using reference standards [117]. This represents a significant improvement over conventional NGS methods, which typically have detection limits of 1-2% VAF [4] [117].
The sensitivity of mutation detection is highly dependent on sequencing depth. While traditional targeted NGS often utilizes 500-1,000× coverage, error-corrected ultradeep NGS employs 3,000-5,000× coverage to reliably detect low-VAF variants [117]. This enhanced sensitivity enables detection of "sub-CHIP" clones (VAF 0.01-0.02) that may have clinical significance despite falling below the traditional CHIP threshold [117].
Quantitative Differentiation Parameters
Research comparing mutational patterns in CHIP versus AML has identified several quantitative parameters that aid in differentiation:
4.2.1 Variant Allele Frequency Distribution Large-scale population studies (n=200,618) reveal that CHIP-associated mutations typically show VAFs between 2-10%, while AML-associated mutations frequently demonstrate VAFs >10% and often much higher [120]. However, there is significant overlap in this parameter, limiting its diagnostic utility in isolation.
4.2.2 Number of Mutations Individuals with CHIP typically harbor one dominant mutation, while AML patients frequently present with multiple cooperating mutations. Analysis of the UK Biobank dataset showed that 93% of individuals with large clones (VAF >0.1) in novel CHIP driver genes did not harbor mutations in classical CHIP genes, suggesting most expansions are driven by single mutations [120].
4.2.3 Mutation Signatures and Gene Combinations The specific combination of mutated genes provides strong discriminatory value. Mutations in splicing genes (SRSF2, SF3B1, U2AF1, ZRSR2) are rare in CHIP but common in certain AML subtypes, and their presence should raise concern for malignancy even with <20% blasts [4]. Similarly, co-occurrence of NPM1 mutations with DNMT3A or TET2 mutations is highly suggestive of AML rather than CHIP [118].
Table 3: Diagnostic Value of Genetic Features in Distinguishing CHIP from AML
| Genetic Feature | Typical in CHIP | Concerning for AML | Diagnostic Value |
|---|---|---|---|
| Isolated DNMT3A mutation | Very common | Less common | Strong for CHIP when isolated |
| Splicing gene mutations | Rare | Common | Moderate concern for malignancy |
| NPM1 mutation | Very rare | Common | High concern for malignancy |
| TP53 mutation | Rare (except in therapy-related context) | Common in high-risk AML | High concern for malignancy |
| FLT3-ITD | Extremely rare | Common | Diagnostic of malignancy if present |
| Single mutation | Very common | Less common | Moderate for CHIP |
| Multiple mutations (≥3) | Uncommon | Common | Moderate concern for malignancy |
| VAF >20% | Uncommon | Common | Moderate concern for malignancy |
Detailed Experimental Protocols
Standardized Targeted NGS Workflow for CHIP Detection
The following protocol outlines a validated approach for detecting and differentiating CHIP from leukemic mutations using targeted NGS:
5.1.1 Sample Preparation and DNA Extraction
- Obtain peripheral blood or bone marrow aspirate in EDTA tubes
- Extract genomic DNA using validated kits (e.g., QIAamp DNA Blood Mini Kit)
- Quantify DNA using fluorometric methods (e.g., Qubit dsDNA HS Assay)
- Ensure DNA input of 50-400 ng for library preparation [117]
5.1.2 Library Preparation and Target Enrichment
- Utilize targeted NGS panels covering established CHIP and leukemia genes (e.g., VariantPlex Myeloid panel covering 75 genes, 125.4 kb total target size) [117]
- Incorporate unique molecular identifiers (UMIs) during library preparation to enable error correction
- Use anchored multiplex PCR or hybrid capture-based enrichment
- Amplify libraries with limited PCR cycles (≤20) to minimize artifacts
5.1.3 Sequencing and Quality Control
- Sequence on Illumina platforms (NextSeq 500 or NovaSeq 6000)
- Achieve minimum coverage of 3,000× for ultradeep sequencing
- Include control samples (reference standards HD829 and HD752) in each run
- Ensure >80% of targets covered at ≥3,000× with uniform coverage (no regions <500×)
Error-Corrected Ultradeep Sequencing Protocol
For enhanced detection of low-VAF variants, implement the following error-correction protocol:
5.2.1 Molecular Barcoding and Duplicate Consensus
- Employ dual-indexed libraries with unique molecular identifiers (UMIs)
- Generate consensus reads from duplicate UMIs to eliminate PCR errors
- Apply molecular barcode-based data filtering to remove index hopping artifacts
- Use strand-specific sequencing to distinguish true variants from artifacts
5.2.2 Bioinformatic Processing and Variant Calling
- Align to reference genome (hg19) using optimized aligners (BWA-MEM)
- Perform UMI-aware duplicate marking and consensus generation
- Call variants using Mutect2 or similar specialized somatic callers
- Apply stringent filtering: minimum supporting reads (≥10), VAF ≥0.004, and presence in both forward and reverse reads [117]
5.2.3 Validation and Interpretation
- Validate low-VAF variants (<2%) by orthogonal methods (ddPCR)
- Annotate variants using population databases (gnomAD) and cancer databases (COSMIC, ClinVar)
- Classify variants according to AMP/ASCO/CAP guidelines for somatic variant interpretation
- Integrate clinical parameters (blood counts, blast percentage) for final interpretation
The following diagram illustrates the complete NGS workflow from sample to clinical interpretation:
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Reagents for CHIP and Somatic Mutation Studies
| Reagent/Material | Specifications | Application | Key Considerations |
|---|---|---|---|
| DNA Extraction Kits | QIAamp DNA Blood Mini Kit (Qiagen) | High-quality DNA extraction from blood/bone marrow | Minimize white blood cell lysis during storage to preserve variant allele frequencies |
| Targeted NGS Panels | VariantPlex Myeloid (75 genes), Illumina TruSight Myeloid | Comprehensive mutation profiling | Ensure coverage of established CHIP genes (DNMT3A, TET2, ASXL1) and AML drivers |
| Library Preparation Kits | Archer (AMP-based), Illumina Nextera Flex | Library construction with UMIs | Incorporate unique dual indexing to minimize index hopping |
| Reference Standards | Horizon Discovery HD829, HD752 | Assay validation and quality control | Use multiplex reference standards with variants at known VAF (0.05-0.70) |
| Sequencing Platforms | Illumina NextSeq 500, NovaSeq 6000 | High-depth sequencing | Target coverage >3,000× for ultradeep applications |
| Bioinformatic Tools | Archer Analysis, GATK Mutect2, Shearwater | Somatic variant calling | Implement error-correction algorithms for UMI-aware processing |
| Orthogonal Validation | TaqMan ddPCR assays | Validation of low-VAF variants | Design probes for specific hotspot mutations (e.g., DNMT3A R882) |
The differentiation between somatic mutations representing CHIP and those indicating malignant transformation remains a complex challenge requiring integration of multiple diagnostic parameters. NGS technologies, particularly error-corrected ultradeep sequencing, have dramatically improved our ability to detect and characterize clonal hematopoiesis at unprecedented resolution. The key to accurate differentiation lies in synthesizing genetic information (VAF, specific genes, mutation combinations) with clinical and laboratory data (blood counts, blast percentage, cytogenetics).
As research continues to evolve, several emerging areas promise to further refine this distinction: single-cell sequencing technologies enable direct observation of mutation co-occurrence patterns within individual cells; machine learning approaches facilitate integration of complex multimodal data; and longitudinal monitoring strategies allow tracking of clonal dynamics over time. By implementing robust, standardized methodologies and maintaining a multidisciplinary approach, researchers and clinicians can effectively navigate the complexities of clonal hematopoiesis in both research and clinical settings.
Identifying Germline Predisposition Syndromes in Leukemia Context
The identification of germline predisposition syndromes is a critical component in the comprehensive management of leukemia. Myeloid neoplasms, for instance, were once considered largely sporadic; however, growing evidence now suggests that approximately 5% of cases emerge from an inherited genetic predisposition [121]. Distinguishing somatic from germline variants is vitally important for establishing appropriate individualized management and for providing accurate counseling to patients and their families [121]. This distinction carries significant implications for treatment selection, surveillance strategies, and familial risk assessment. The integration of next-generation sequencing (NGS) into clinical practice has revolutionized this diagnostic process, offering a powerful alternative to traditional, sequential testing methods. This guide provides a objective comparison of these approaches, focusing on their performance in detecting germline predisposition within the context of acute leukemia diagnostics.
Performance Comparison: NGS vs. Traditional Methods
Traditional techniques for genetic analysis, such as karyotyping, fluorescence in situ hybridization (FISH), and Sanger sequencing, have formed the standard-of-care for decades. However, each method interrogates the genome in a limited fashion, making a comprehensive assessment for germline predisposition both laborious and time-consuming when these techniques are used sequentially. The table below summarizes the key characteristics of NGS versus a traditional testing approach.
Table 1: Comparative Overview of NGS and Traditional Genetic Testing Methods
| Aspect | Traditional Methods (Karyotyping, FISH, Sanger) | Next-Generation Sequencing (NGS) |
|---|---|---|
| Throughput & Scalability | Low; processes targets sequentially [122] | Massively parallel; sequences millions of fragments simultaneously [123] [106] [122] |
| Sensitivity & Detection Limit | Lower sensitivity for low-frequency variants (~15-20%) [122] | Superior sensitivity; can detect variants at frequencies as low as 1% [106] [122] |
| Genomic Coverage | Targeted, focused analysis [122] | Comprehensive genomic coverage; can sequence hundreds to thousands of genes concurrently [106] [122] |
| Discovery Power | Limited ability to identify novel variants [106] [122] | High discovery power for novel and rare variants [106] [122] |
| Cost-Effectiveness | Cost-effective for interogating a very small number of targets (<20) [106] | More cost-effective for screening a large number of genes or samples [106] |
| Turnaround Time | Can be prolonged when multiple tests are run sequentially | Faster turnaround for high sample volumes and comprehensive profiling [106] |
The quantitative performance of these methods is further highlighted in direct experimental comparisons. For example, in the context of molecular diagnostics for acute lymphoblastic leukemia (ALL), emerging NGS-based approaches have demonstrated remarkable superiority over standard-of-care techniques.
Table 2: Experimental Performance Data in Pediatric ALL Diagnostics [35]
| Methodology | Detection Rate of Gene Fusions | Detection Rate of Gains/Losses | Clinically Relevant Alterations Identified |
|---|---|---|---|
| Standard-of-Care (SoC) | 30% | 35% | 46.7% |
| Optical Genome Mapping (OGM) | 56.7% | 51.7% | 90% |
| dMLPA + RNA-seq Combination | Not Specified | Not Specified | 95% |
Methodological Approaches for Germline Variant Identification
Experimental Protocol for Tumor-Only Sequencing Analysis
A key challenge in clinical practice is identifying potential germline variants when only tumor tissue (e.g., bone marrow) has been sequenced. The following workflow, adapted from a study of 299 patients with myeloid neoplasms, outlines a robust protocol for this scenario [121]:
- Sequencing: Perform targeted NGS on the bone marrow sample using a multi-gene panel that includes known myeloid neoplasm germline predisposition (MNGP) genes.
- Variant Calling: Identify all sequence variants and filter for those located in MNGP-related genes.
- Variant Allele Frequency (VAF) Filtering: Apply a primary filter to retain variants with a VAF of approximately 50% (range ~40-60%), which is suggestive of a heterozygous germline variant [121].
- Variant Annotation: Classify the filtered variants as Pathogenic, Likely Pathogenic, or of Unknown Significance (VUS).
- Confirmatory Testing: For the short-listed suspicious variants, perform orthogonal validation by Sanger sequencing on DNA obtained from a non-malignant tissue source, such as skin fibroblasts, buccal swabs, or hair follicles, to confirm their germline origin [121].
Workflow Visualization: From Sample to Germline Confirmation
The following diagram illustrates the logical pathway for analyzing NGS data to identify and confirm a potential germline predisposition variant.
Essential Research Reagents and Materials
Successful implementation of NGS for germline predisposition research requires a suite of specialized reagents and platforms. The following table details key solutions and their functions in a typical workflow.
Table 3: Research Reagent Solutions for NGS-Based Germline Predisposition Studies
| Research Reagent / Solution | Function in the Experimental Workflow |
|---|---|
| Multi-Gene Panels (e.g., for MNGP) | Targeted probe sets designed to capture and sequence genes known to be associated with inherited leukemia predisposition syndromes. |
| Nucleic Acid Extraction Kits | High-quality DNA and RNA isolation from patient samples (bone marrow, blood, buccal swabs, fibroblasts) to ensure input material integrity. |
| Library Preparation Kits | Preparation of sequencing libraries from extracted DNA/RNA through fragmentation, adapter ligation, and amplification. |
| Sequence Capture Reagents | Solution-based hybridization reagents to enrich the library for the genomic regions of interest (e.g., the MNGP gene panel). |
| NGS Platforms (e.g., Illumina) | Instruments that perform massively parallel sequencing of the prepared and enriched libraries. |
| Bioinformatics Pipelines | Software for base calling, sequence alignment, variant calling, and annotation to interpret the raw sequencing data. |
Discussion and Clinical Implications
The integration of NGS into the diagnostic workflow for leukemia represents a paradigm shift, moving from a targeted, single-geneinterrogation to a comprehensive genomic snapshot. For identifying germline predisposition, this is particularly transformative. The ability to simultaneously screen a vast number of genes from a single sample, coupled with high sensitivity, makes NGS the more effective and potentially more cost-efficient strategy compared to running multiple traditional tests [106] [122].
A critical consideration in this field is the limitation of tumor-only sequencing. While the protocol outlined in Section 3.1 provides a method for identifying suspicious variants from tumor data, it is not a substitute for concurrent sequencing of a matched normal sample. The gold standard for definitively classifying a variant as somatic or germline remains sequencing the leukemia sample alongside a non-malignant control sample from the same patient [121]. Future directions will likely involve the routine implementation of matched tumor-normal sequencing in clinical pipelines to streamline the accurate detection of germline predisposition syndromes.
Next-generation sequencing (NGS) has revolutionized the detection of genetic variants in acute leukemia, enabling refined risk stratification and minimal residual disease (MRD) monitoring. However, the high error rate (0.1–1%) inherent to standard NGS protocols presents a significant challenge, particularly for detecting rare, subclonal variants that can inform treatment decisions [124]. To overcome these limitations, sophisticated error-correction strategies have been developed. This guide objectively compares the performance of molecular barcode-based error correction against alternative methods, providing experimental data and protocols to guide researchers and drug development professionals in selecting the optimal approach for their leukemia diagnostics pipeline.
Understanding NGS Errors and Correction Strategies
In leukemia genomics, a critical challenge is distinguishing true low-frequency somatic variants from technical artifacts. Standard NGS errors are primarily systematic, arising from phasing noise, signal decay, and misreads during the sequencing process itself [124]. These errors are stochastic and difficult to distinguish from true rare variants, especially when variant allele frequencies (VAFs) fall below 1% [125].
Two primary strategies have emerged to address this challenge:
- Molecular Barcoding (Unique Molecular Identifiers - UMIs): This method involves tagging individual DNA molecules with unique barcodes before amplification and sequencing. Bioinformatic consensus generation from reads sharing the same barcode effectively filters out randomly introduced errors [126] [125].
- Barcode-Free Physical Validation: An alternative approach physically extracts and re-sequences specific DNA clones from the NGS substrate to confirm suspected variants, bypassing the need for molecular barcodes and redundant sequencing [124].
Comparative Performance Analysis
The table below summarizes key performance metrics for molecular barcoding and a barcode-free validation method, based on published experimental data.
Table 1: Performance Comparison of Error-Correction Methods
| Method | Principle | Reported Sensitivity (VAF) | Key Advantages | Limitations / Challenges |
|---|---|---|---|---|
| Molecular Barcoding (UMI-based NGS) | Tags individual DNA molecules; consensus sequencing [126] [125] | 0.76% VAF (median in clinical AML MRD) [126] | Broadly applicable; can detect subclones/clonal evolution; high sensitivity (down to 10-6 reported in ALL) [7] [126] | Requires redundant sequencing, increasing cost and data load; complex bioinformatics [124] [7] |
| Barcode-Free Physical Validation | Physical retrieval and re-sequencing of specific DNA clones [124] | 0.003% (Validated true variants distinguished from NGS error) [124] | Eliminates need for redundant sequencing; validates variants of interest post-hoc with high certainty [124] | Lower throughput; requires specialized laser retrieval instrumentation; not suited for genome-wide screening [124] |
The clinical impact of these methods is significant. In acute myeloid leukemia (AML), error-corrected NGS for MRD detection (NGS-MRD) has proven highly prognostic. Patients with positive NGS-MRD at the end of induction or consolidation therapy showed a significantly higher cumulative incidence of relapse and inferior overall survival [126]. Furthermore, NGS-MRD identified over 80% of the cases detected by flow cytometry, while flow cytometry identified only about half of the cases flagged by NGS, underscoring its superior sensitivity in a clinical context [126].
Experimental Protocols in Practice
Protocol 1: Error-Corrected NGS for AML MRD
This protocol, adapted from a 2021 clinical study, utilizes single molecule Molecular Inversion Probes (smMIPS) for error-corrected sequencing [126].
- DNA Extraction: Obtain ~600 ng of genomic DNA from patient bone marrow or peripheral blood in morphological remission.
- Library Preparation with UMIs: Use a pool of smMIPS targeting a 34-gene AML panel. Each probe contains an 8 bp UMI that uniquely tags individual DNA molecules during the capture process.
- Target Capture & Amplification: Capture the genomic regions of interest, treat with exonucleases, and PCR-amplify to create the final sequencing library.
- Sequencing: Sequence the library on an appropriate NGS platform (e.g., Illumina).
- Bioinformatic Analysis:
- Demultiplex reads and assemble paired-end sequences.
- Group reads into families based on their UMI.
- Generate a consensus sequence for each family.
- Discard singleton reads (from a single UMI) and apply a site-specific error model to call true somatic variants.
Protocol 2: Barcode-Free NGS Error Validation
This protocol outlines the physical validation method for confirming suspected erroneous reads [124].
- Initial NGS Run: Perform a standard NGS run on the sample.
- Target Selection: Bioinformatically identify specific reads of interest (e.g., those harboring potential rare variants or errors) for validation.
- Physical Clone Extraction: Using an automated laser retrieval system, physically isolate the specific DNA clones corresponding to the target reads from the NGS flow cell.
- Individual Amplification: Transfer each isolated DNA clone into individual wells of a 96-well PCR plate and amplify via PCR.
- Validation Sequencing: Sequence the amplified DNA products using either Sanger sequencing or a subsequent NGS run. Compare the sequences to the original NGS data to distinguish true variants from systematic errors.
Workflow and Logical Diagrams
The diagram below illustrates the core logical difference between the molecular barcoding workflow and the barcode-free validation approach.
Essential Research Reagent Solutions
The table below lists key reagents and materials required for implementing these error-correction strategies.
Table 2: Key Research Reagents for Error-Corrected NGS
| Item | Function | Example Use Case |
|---|---|---|
| smMIPS or UMI Adapters | Uniquely tags individual DNA molecules to enable bioinformatic error correction. | Foundation of UMI-based NGS-MRD panels for AML [126]. |
| Targeted Gene Panels | Focuses sequencing on genes relevant to leukemia, allowing for deeper coverage and lower costs. | Error-corrected 34-gene AML panel for MRD detection [126]. |
| Automated Laser Retrieval System | Precisely extracts specific DNA clones from a solid substrate for physical validation. | Enables barcode-free NGS error validation by isolating target DNA clusters [124]. |
| High-Fidelity DNA Polymerase | Reduces PCR-induced errors during library amplification, minimizing false positives. | Critical for all NGS library prep protocols to maintain sequence accuracy. |
Molecular barcoding and barcode-free physical validation represent two powerful, complementary strategies for overcoming NGS technical artifacts in acute leukemia research and diagnostics. Molecular barcoding, particularly UMI-based NGS, offers a broadly applicable, high-throughput solution for sensitive MRD monitoring and clonal evolution tracking, albeit with increased sequencing costs and bioinformatic complexity. In contrast, the barcode-free method provides an ultra-sensitive, targeted approach for validating specific variants without the need for redundant sequencing, though it is lower throughput. The choice between them hinges on the specific research question: genome-wide MRD screening favors molecular barcoding, while definitive confirmation of critical rare variants may warrant physical validation. As leukemia diagnostics continue to evolve, the integration of these error-corrected NGS approaches with traditional methods like flow cytometry will likely provide the most comprehensive and clinically actionable insights.
The diagnosis of acute leukemia, particularly acute myeloid leukemia (AML), has traditionally relied on a multi-method approach integrating cytomorphology, immunophenotyping, cytogenetics, and molecular genetics. This integrated approach, often termed MICM, has been the cornerstone of diagnosis, classification, and risk stratification for decades [4] [2]. However, the limitations of these conventional techniques—including their targeted nature, subjective interpretation, and inability to detect novel alterations—have driven the adoption of next-generation sequencing (NGS) technologies. Rather than replacing traditional methods, contemporary diagnostic strategies are increasingly focused on developing complementary algorithms that leverage the strengths of both NGS and conventional techniques to achieve a more comprehensive, precise, and efficient diagnosis [127] [4]. This paradigm enhances the detection of clinically relevant genetic alterations, improves precise disease classification, and ultimately supports better risk assessment and treatment personalization for patients with acute leukemia [127] [100].
Performance Comparison: NGS Versus Traditional Diagnostic Methods
Extensive clinical studies have systematically compared the diagnostic yield of integrated NGS approaches against traditional methods. The data reveal distinct advantages and specific limitations for each technology, highlighting their complementary roles.
Table 1: Comparative Analysis of Genetic Alteration Detection in Pediatric AML (n=153) [127]
| Detection Category | Traditional Methods (Cytogenetics/Targeted NGS) | Integrated WGS-WTS Approach | Clinical Impact of NGS Enhancement |
|---|---|---|---|
| SNVs/Indels | 74 variants detected by targeted NGS (75-gene panel) in 39 cases. | 70/74 variants concordant; plus 1 additional variant (VAF >5%) and 5 more with VAF 3-5% upon manual review. | More complete mutational profiling; identifies potentially significant subclonal populations. |
| Gene Fusions | Limited to known, targeted fusions (e.g., by FISH or RT-PCR). | 106 oncogenic fusions in 105 cases; WTS alone diagnosed 98% of WGS-detected fusion oncogenes. | Unbiased detection of rare, novel, and cryptic fusions without prior knowledge of partner genes. |
| FLT3-ITDs | Detected by PCR-based fragment analysis. | 28 ITDs found; 10 were borderline in WGS but strong in WTS; 1 subclonal ITD (ratio 0.02) missed. | Superior detection of complex ITDs; some limitations in very low-burden subclones. |
| Focal CNVs (<5 Mb) | Limited resolution; often misses small alterations. | 42 P/LP focal CNVs in 24 patients, including 15 alterations <50 kb (12 ≤ 10 kb). | Identifies clinically significant intragenic/exonic CNVs leading to truncated proteins. |
| Large-Scale CNVs/cnLOH | Karyotyping and FISH. | 163 LS-CNV events in 83 patients; 18 patients with large-scale cnLOH. | Genome-wide unbiased assessment of chromosomal gains/losses and copy-neutral LOH. |
The performance data underscores that while traditional methods are effective for detecting known, common abnormalities, integrated NGS provides a more unbiased and comprehensive genomic profile. A key study of 153 pediatric AML patients demonstrated that the iWGS-WTS approach streamlined sample acquisition, reduced testing redundancy, and improved the identification of clinically relevant genetic alterations, positioning it as a practical and superior framework for modern leukemia diagnostics [127].
Table 2: Operational and Clinical Value Comparison of Diagnostic Methods in AML
| Parameter | Traditional Methods (Cytogenetics, FISH, PCR) | Targeted NGS Panels | Genome-Wide NGS (WGS/WTS) |
|---|---|---|---|
| Turnaround Time | Days to weeks for a full karyotype/FISH panel [128]. | Several days, depending on workflow [4]. | Several days; can be optimized to match clinical needs (<5 days demonstrated) [128]. |
| Resolution | Limited to chromosomal/chromosomal segment level (karyotyping); gene-specific (FISH, PCR). | Single nucleotide for SNVs/Indels; limited for CNVs and fusions (must be pre-specified) [4]. | Single nucleotide to genome-wide structural variants; detects novel fusions and non-coding alterations. |
| Sensitivity | ~5% for karyotyping; 1-5% for FISH; can be <1% for qPCR [38]. | 1-5% for DNA-based panels; limited by coverage and error rate [4]. | Can achieve 0.05% allele frequency with advanced molecular barcoding for MRD [38]. |
| Key Strength | Provides context of entire genome (karyotyping); gold standard for specific fusions. | Cost-effective, focused analysis on known clinically actionable genes. | Unbiased discovery, comprehensive detection of all variant types in a single assay. |
| Primary Limitation | Targeted, low-throughput, subjective (MFC), labor-intensive. | Limited to pre-defined genomic regions; misses novel and structural variants. | Higher cost per sample; complex data analysis and interpretation; large data storage needs. |
Experimental Protocols for Method Comparison
To generate the comparative data presented, researchers have employed rigorous, standardized experimental protocols. The following details a representative methodology for validating an NGS-based approach against traditional techniques.
Integrated Whole Genome and Transcriptome Sequencing (iWGS-WTS) Protocol
Sample Preparation: The protocol begins with the collection of matched tumor and germline samples. Tumor samples are typically bone marrow aspirates or peripheral blood with documented blast counts, while germline comparators are often skin biopsies [127]. Nucleic acids (DNA and RNA) are extracted concurrently. The quality and integrity of the input material are critical, especially for RNA in fusion detection, and are assessed using methods like fluorometry and electrophoresis [4] [128].
Library Preparation and Sequencing:
- DNA Library (for WGS): Genomic DNA is fragmented, and Illumina-compatible sequencing libraries are prepared. These libraries are sequenced on a platform like the Illumina NovaSeq to achieve a minimum coverage (e.g., 30x) across the genome [127].
- RNA Library (for WTS): Total RNA is extracted. For whole transcriptome analysis, ribosomal RNA is depleted to preserve both coding and non-coding RNA sequences. The RNA is then reverse-transcribed into cDNA, and sequencing libraries are prepared and sequenced [127] [56]. For a more targeted and cost-effective fusion detection, an anchored multiplex PCR approach can be used. This method uses gene-specific primers for a panel of recurrently rearranged genes in leukemia (e.g., KMT2A, RUNX1, CBFB) combined with universal adapters. This design allows for the detection of fusions without prior knowledge of the specific partner gene or breakpoint [128].
Data Analysis: The massive datasets generated are processed through a bioinformatics pipeline. This includes alignment to a reference genome, quality control, and variant calling for SNVs, Indels, CNVs, and SVs. For fusion detection, RNA-seq reads are analyzed using specialized tools to identify chimeric transcripts [127] [128]. Detected variants are annotated and filtered against population and clinical databases (e.g., ClinVar, COSMIC) to determine pathogenicity and clinical relevance [4].
Traditional Methods Workflow
The conventional diagnostic workflow runs in parallel and includes:
- Cytomorphology: Microscopic examination of Wright-Giemsa stained peripheral blood and bone marrow smears to assess blast percentage and cell differentiation [4] [2].
- Multiparameter Flow Cytometry (MFC): Immunophenotyping of blast cells using antibodies against surface and cytoplasmic antigens to establish lineage and maturity [4] [38].
- Cytogenetics: Karyotyping of G-banded metaphase chromosomes from cultured bone marrow cells to identify numerical and structural abnormalities at a resolution of ~5-10 Mb [127] [4].
- Fluorescence In Situ Hybridization (FISH): Uses fluorescently labeled DNA probes to detect specific chromosomal rearrangements (e.g., PML::RARA, BCR::ABL1) in interphase or metaphase cells [128].
- Targeted PCR/qPCR: Amplifies and detects specific mutation hotspots (e.g., FLT3-ITD, NPM1) or fusion transcripts with high sensitivity [4] [38].
The Scientist's Toolkit: Essential Reagents and Solutions
The implementation of these complementary diagnostic algorithms requires a specific set of reagents and tools. The following table details key solutions for setting up a comparative study or integrated clinical pipeline.
Table 3: Research Reagent Solutions for Integrated Leukemia Diagnostics
| Reagent / Solution | Function | Application Context |
|---|---|---|
| Anchored Multiplex PCR Panels | Target enrichment for RNA-seq; uses gene-specific and universal primers to detect fusions with unknown partners. | Targeted RNA-sequencing for fusion detection in clinical diagnostics [128]. |
| Hybridization Capture Panels | Solution-based target enrichment for DNA-seq; covers a pre-defined set of genes for SNV/Indel and CNV detection. | Targeted DNA sequencing for mutation profiling [4]. |
| Molecular Barcodes (UMIs) | Short unique nucleotide sequences added to each molecule during library prep to correct for PCR errors and duplicates. | Essential for achieving high sensitivity (down to 0.05% VAF) in MRD detection assays [38]. |
| CLIA-Certified Bioinformatics Pipelines | Standardized software for variant calling, annotation, and filtration in a clinical laboratory setting. | Ensures reproducible and clinically actionable results from NGS data [127]. |
| Multiparameter FISH Probes | Fluorescently labeled DNA probes for simultaneous detection of multiple chromosomal abnormalities. | Used in traditional cytogenetics for validation and rapid screening of common fusions [128]. |
| Fragment Analysis Kits | PCR-based kits to detect length mutations, such as FLT3-ITDs. | Used as a traditional method for validation of NGS-called ITDs [127]. |
Developing the Integrated Diagnostic Algorithm
Synthesizing performance data and experimental evidence leads to a practical, complementary diagnostic algorithm. This framework is designed to maximize efficiency, minimize redundancy, and leverage the respective strengths of each technology.
The algorithm begins with foundational morphological and immunophenotypic analysis to confirm acute leukemia. For cases meeting diagnostic criteria, an integrated NGS approach (iWGS-WTS or an equivalent comprehensive panel) serves as a primary reflex test, simultaneously screening for most relevant genetic lesions. This replaces the traditional sequential application of multiple FISH and PCR tests, streamlining the workflow [127]. Traditional methods are strategically retained for urgent clinical scenarios, such as rapid FISH for PML::RARA in suspected acute promyelocytic leukemia (APL) to initiate life-saving therapy without delay [2]. These methods also serve as independent validation for critical findings and as a backup when NGS fails. Finally, results from all modalities are synthesized into a unified diagnostic report that informs WHO/ICC classification, ELN risk stratification, and identifies actionable therapeutic targets [127] [2].
The evolution of leukemia diagnostics is moving decisively toward the integration of comprehensive NGS technologies into the traditional MICM framework. The evidence demonstrates that algorithms combining the broad, unbiased discovery power of iWGS-WTS with the rapid, targeted precision of conventional FISH and PCR create a synergistic diagnostic system. This complementary approach enhances detection of rare and novel alterations, improves risk stratification, and streamlines laboratory workflows. For researchers and clinicians, the future lies in optimizing these algorithms, standardizing NGS-based reporting, and continuing to validate the clinical utility of comprehensive genomic profiling to ultimately improve patient outcomes in acute leukemia.
The integration of Next-Generation Sequencing (NGS) into the diagnostic pathway for acute leukemia represents a significant technological advance, yet its economic implications, particularly in resource-limited settings, demand careful scrutiny. The standard diagnostic approach for acute leukemia has traditionally relied on a multi-platform methodology incorporating cytomorphology, multiparameter flow cytometry (MFC), cytogenetics, and targeted molecular tests [3]. While this combined approach provides critical diagnostic information, it is labor-intensive, time-consuming, and increasingly costly when multiple tests are required. NGS emerges as a potential unifying technology that can streamline this process by detecting a comprehensive range of genetic alterations—including single nucleotide variants, insertions/deletions, copy number alterations, and structural variants—in a single assay [3]. For researchers and healthcare systems operating with constrained budgets, the fundamental economic question is whether the superior diagnostic and prognostic information provided by NGS justifies its additional upfront costs compared to conventional techniques.
This analysis provides a structured comparison of the economic and performance characteristics of NGS versus traditional diagnostic methods in acute leukemia, with particular emphasis on applications in resource-limited research environments. We synthesize recent cost data, experimental performance metrics, and implementation protocols to equip researchers with evidence necessary for informed platform selection.
Quantitative Cost and Performance Comparison
Table 1: Direct Cost and Technical Performance Comparison
| Parameter | Traditional Methods (Combined) | NGS-Based Approach | Data Source/Context |
|---|---|---|---|
| Comprehensive Diagnostic Cost | Variable (sum of individual tests) | Approaching traditional methods (costs decreasing) | Micro-costing study in Sweden [129] |
| Primary Cost Driver | Multiple reagents & labor across tests | Sequencing reagents & instrumentation | Journal of Medical Economics [129] |
| Turnaround Time | 10-14 days (sequential testing) | Target: <2 weeks (single workflow) | Clinical validation goals [129] |
| Sensitivity for MRD | 10-4 (MFC); 10-5 (qRT-PCR) | Up to 10-6 | Systematic review of ALL [7] |
| Applicability for B-ALL MRD | ~50-70% (requires trackable marker) | ~90% (using IGH rearrangements) | EuroClonality-NGS Consortium [7] |
| Information Breadth | Limited to predefined targets | Comprehensive genomic profile + clonal evolution | Clinical Genomics studies [129] [3] |
Table 2: Clinical Value and Economic Impact Assessment
| Economic Factor | Traditional Methods | NGS-Based Approach | Implications for Resource-Limited Settings |
|---|---|---|---|
| Therapeutic Guidance | Limited to established biomarkers | Identifies eligibility for broader targeted therapies | Prevents ineffective treatment costs; enables precision oncology |
| Risk Stratification Accuracy | Good (based on established markers) | Superior (detects novel markers and co-mutations) | Potential to avoid over/under-treatment and associated costs |
| Clonal Evolution Monitoring | Limited (requires multiple FISH/probes) | Built-in capability via serial sequencing | Critical for managing relapse and therapy resistance |
| Reimbursement Status | Well-established | Evolving (e.g., permanent reimbursement in Belgium) | Impacts sustainability in publicly funded systems [130] |
| Cost-Effectiveness Evidence | Established standard | Convergent for blood cancers (e.g., AML, ALL) | Growing support for health economic value [131] |
Experimental Protocols for Method Validation
Protocol 1: Minimal Residual Disease Detection in B-ALL
Objective: To compare the sensitivity, specificity, and applicability of NGS-based MRD detection against standard MFC and qRT-PCR in B-cell Acute Lymphoblastic Leukemia (B-ALL) [7].
Methodology Summary:
- Sample Collection: Bone marrow aspirates collected at diagnosis and follow-up timepoints (e.g., end-of-induction).
- DNA Extraction: High-quality genomic DNA is extracted from diagnostic samples (for clonotype identification) and follow-up samples (for MRD assessment).
- NGS Library Preparation: Using commercially available kits (e.g., EuroClonality-NDG primers) targeting immunoglobulin (IGH, IGK, IGL) and T-cell receptor (TCR) gene rearrangements.
- Sequencing: Run on a high-throughput sequencer (e.g., Illumina MiSeq).
- Bioinformatic Analysis: Clonal sequences identified in the diagnostic sample are used as a fingerprint to track and quantify persistent disease in follow-up samples using specialized software (e.g., ARResT/Interrogate).
- Comparison: Results are compared in parallel to MFC (sensitivity 10-4) and qRT-PCR for fusion transcripts (where applicable).
Key Performance Metrics from Literature: NGS demonstrated superior sensitivity (10-6) and identified MRD in a significant proportion of patients classified as MRD-negative by MFC. The technique showed a high correlation with clinical outcomes, where NGS-MRD negativity was associated with superior event-free and overall survival [7].
Protocol 2: Comprehensive Genomic Profiling in AML
Objective: To evaluate the diagnostic accuracy and clinical utility of whole-genome sequencing (WGS) versus the standard combination of cytogenetics, FISH, and targeted NGS panels in Acute Myeloid Leukemia (AML) [129] [132].
Methodology Summary:
- Sample Processing: Tumor and matched normal (e.g., skin or saliva) DNA are extracted.
- Library Prep & Sequencing: Whole-genome libraries are prepared and sequenced to high coverage (e.g., 30-100x) on platforms such as Illumina NovaSeq.
- Data Analysis: A unified bioinformatics pipeline is used to call single nucleotide variants (SNVs), insertions/deletions (Indels), copy number variations (CNVs), and structural variants (SVs).
- Comparison: The variant calls are compared to those obtained via standard-of-care methods: karyotyping, FISH for recurrent fusions, and a targeted NGS panel for common genes (e.g., FLT3, NPM1, IDH1/2).
Key Performance Metrics from Literature: Studies indicate that WGS can detect all clinically relevant variants identified by standard techniques while simultaneously adding information in a significant proportion of cases. This additional information can improve risk stratification and guide targeted treatment decisions, potentially offsetting its cost by avoiding ineffective therapies [129].
Workflow and Decision Pathway Visualization
NGS vs Traditional Leukemia Diagnosis Workflow
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Research Reagent Solutions for NGS-Based Leukemia Diagnostics
| Reagent/Kits | Primary Function in Workflow | Research Context & Utility |
|---|---|---|
| DNA Library Prep Kits (e.g., Illumina TruSeq) | Fragments DNA and adds platform-specific adapters | Essential for preparing samples for WGS; critical for uniformity and yield. |
| Hybridization Capture Panels (e.g., TruSight Myeloid) | Enriches for a predefined set of cancer genes | Cost-effective alternative to WGS for focused mutation profiling. |
| RNA-Seq Library Kits | Converts RNA into sequence-ready libraries | Detects gene fusions and expressed mutations, complementing DNA-seq. |
| EuroClonality-NGS Primers | Amplifies IGH/TCR rearrangements for MRD | Standardized reagents crucial for reproducible NGS-MRD studies in ALL. |
| Bioinformatic Pipelines (e.g., GATK, EuroClonality) | Analyzes raw sequencing data for variants | Transforms raw data into clinical insights; requires significant expertise. |
| Multiplexed Reference Materials | Validates assay sensitivity/specificity | Certified cell lines or synthetic controls for assay calibration and QC. |
The economic analysis of NGS in acute leukemia diagnosis reveals a complex landscape where higher initial costs must be weighed against comprehensive data output and potential long-term clinical benefits. For research settings with limited resources, the decision to implement NGS should be guided by strategic priorities. If the primary research goal is highly sensitive, quantitative MRD tracking with broad applicability in B-ALL, then a targeted NGS approach for immunoglobulin rearrangements represents a cost-effective choice [7]. Conversely, if the objective is comprehensive genomic discovery or the development of personalized therapeutic strategies, then WGS/WTS, despite its higher per-sample cost, may be more efficient than funding a full battery of traditional tests [129] [3].
Evidence suggests that the cost of WGS is rapidly approaching that of cumulative standard testing for acute leukemia, primarily driven by reductions in reagent costs and improved sequencing capacity [129]. Furthermore, the permanent reimbursement of NGS for hematological malignancies in some European healthcare systems signals a growing recognition of its clinical utility [130]. For the research community, this translates into a compelling argument for investing in NGS infrastructure and bioinformatics training. The initial investment can be offset by the technology's versatility across multiple research projects, its ability to generate rich, reusable datasets, and its potential to uncover novel biomarkers that can guide more cost-effective patient care in the future. Ultimately, in resource-limited settings, a phased adoption—starting with targeted NGS for specific applications like MRD before progressing to whole-genome approaches—may provide the most pragmatic and economically viable path forward.
Evidence-Based Comparison: Diagnostic Yield, Clinical Impact, and Economic Evaluation
The diagnostic and monitoring landscape for acute leukemia is undergoing a profound transformation, moving from traditional methods based on morphology and targeted molecular assays to comprehensive next-generation sequencing (NGS) approaches. This shift is particularly critical in acute myeloid leukemia (AML), a disease characterized by significant molecular heterogeneity where accurate detection of genetic abnormalities directly influences risk stratification, treatment selection, and monitoring for residual disease. This article provides a direct comparison of detection rates between NGS and traditional diagnostic methods, synthesizing evidence from recent head-to-head studies to offer researchers and drug development professionals an objective analysis of performance characteristics across key clinical applications.
Detection of Genetic Aberrations at Diagnosis
The initial genetic characterization of acute leukemia establishes the foundation for all subsequent clinical decisions. Traditional methods have relied on a combination of techniques including karyotyping, fluorescence in situ hybridization (FISH), and polymerase chain reaction (PCR)-based assays.
Fusion Gene Detection
Gene fusions, resulting from chromosomal rearrangements, are well-established oncogenic drivers in acute leukemia and represent critical diagnostic, prognostic, and therapeutic biomarkers.
Table 1: Comparison of Fusion Gene Detection Methods
| Method | Detection Principle | Key Advantages | Key Limitations | Detection Rate |
|---|---|---|---|---|
| Karyotyping | Visual analysis of chromosomes under microscope | Identifies balanced and unbalanced chromosomal rearrangements genome-wide; low cost | Low resolution (>5-10 Mb); requires dividing cells; limited to detectable chromosomal abnormalities | Identifies ~50% of AML cases with cytogenetic abnormalities [100] |
| FISH | Fluorescently-labeled DNA probes bind complementary sequences | Higher resolution than karyotyping (50-500 kb); can analyze non-dividing cells | Limited to targeted regions; cannot identify novel fusion partners; low throughput | Considered gold standard but target-limited [133] |
| RT-PCR | Amplification of fusion transcript sequences | High sensitivity; can detect low abundance transcripts; quantitative capability | Limited to known fusion types; cannot identify novel partners; false negatives if breakpoints vary | Highly sensitive but only for predefined fusions [133] |
| RNA-based NGS | Sequencing of transcriptome or targeted RNA panels | Unbiased detection of known and novel fusions; single assay for multiple fusion types | Higher cost; bioinformatics complexity; longer turnaround time without established panels | Detects fusions in 15% of AML patients, including ~4% missed by conventional cytogenetics [33] |
A comprehensive study analyzing over 600 AML samples demonstrated the superior detection capability of RNA-based NGS, which identified gene fusions in 15% of patients, including approximately 4% harboring fusion events undetectable by standard cytogenetic methods [33]. These cryptic fusions involved clinically significant genes such as NUP98 and KMT2A, which markedly influence treatment paradigms and disease trajectory.
Somatic Mutation Profiling
The molecular heterogeneity of acute leukemia extends beyond structural variations to include numerous somatic mutations with prognostic and therapeutic implications.
Table 2: Comparison of Somatic Mutation Detection Methods
| Method | Detection Principle | Genes Covered | Sensitivity | Limitations |
|---|---|---|---|---|
| Sanger Sequencing | Dideoxy chain-termination method | Single gene per reaction | ~15-20% variant allele frequency | Low throughput; low sensitivity; labor-intensive |
| PCR + Fragment Analysis | Amplification and size separation of DNA fragments | Limited (e.g., FLT3-ITD) | ~1-5% variant allele frequency | Limited to specific mutation types; cannot detect point mutations |
| Targeted NGS Panels | Multiplexed amplification and sequencing of targeted regions | 40-50 genes commonly mutated in myeloid neoplasms | ~1-5% variant allele frequency at diagnosis | May miss large insertions like FLT3-ITD without specialized approaches |
| NGS with UMI error-correction | Unique molecular identifiers to distinguish true variants from sequencing errors | Comprehensive panels (e.g., 42 genes) | 0.0024% VAF (for MRD) | Requires specialized bioinformatics; higher cost |
Traditional Sanger sequencing provides limited sensitivity (15-20% variant allele frequency) and throughput, while PCR-based methods like fragment analysis offer improved sensitivity for specific mutations but cover a very limited genetic scope [134]. In contrast, targeted NGS panels simultaneously assess 40-50 genes commonly mutated in myeloid neoplasms, providing a comprehensive molecular profile from a single assay [101] [4]. The technological evolution of NGS incorporating unique molecular identifiers (UMIs) has further enhanced sensitivity by distinguishing true somatic variants from sequencing errors, enabling detection limits as low as 0.0024% variant allele frequency (VAF) [101].
Measurable Residual Disease Monitoring
Measurable residual disease (MRD) represents the presence of leukemic cells at levels below the detection threshold of conventional morphology and is a powerful predictor of relapse in acute leukemia.
Direct Comparisons in MRD Detection
Table 3: Head-to-Comparison of MRD Detection Methods in Acute Leukemia
| Study | Patients | Methods Compared | Key Findings | Clinical Impact |
|---|---|---|---|---|
| MFC vs. NGS in AML [101] | 128 AML patients | 42-gene NGS panel vs. multiparameter flow cytometry | 54% MRD-positive by NGS vs. lower rates by MFC; NGS-MRD positive patients had shorter OS (17 months vs. not reached) and shorter TTR (14 months vs. not reached) | NGS provided superior prognostic stratification compared to morphological assessment alone |
| Systematic Review in ALL [7] | 13 studies | NGS vs. MFC and PCR | NGS demonstrated superior sensitivity in detecting MRD-positive cases compared to MFC; NGS-MRD negativity correlated with superior EFS and OS | NGS enabled more accurate risk stratification in ALL |
| NGS of cfDNA in AML [27] | 29 AML patients | NGS of circulating cell-free DNA vs. donor chimerism analysis | NGS of cfDNA detected mutations in 58% of samples during hematological CR; predicted PFS after allo-HSCT | Liquid biopsy approach enabled minimally invasive monitoring with high sensitivity |
A landmark study of 128 AML patients directly comparing NGS-based MRD detection with traditional methods demonstrated NGS's superior prognostic capability. When applied after initial chemotherapy, 54% of patients showed persistence of at least one mutation detectable by NGS (excluding DTA mutations - DNMT3A, TET2, ASXL1). These NGS-MRD positive patients had significantly shorter overall survival (17 months versus median not reached; HR=2.2) and shorter time to relapse (14 months versus median not reached; HR=1.9) compared to NGS-MRD negative patients [101]. Importantly, even among patients achieving complete morphological remission, NGS identified MRD in 45% of cases, and these patients similarly experienced inferior outcomes [101].
In acute lymphoblastic leukemia (ALL), a systematic review of 13 studies found that NGS demonstrated superior sensitivity in detecting MRD-positive cases compared to multiparameter flow cytometry, particularly in patients previously classified as MRD-negative by conventional methods. NGS-based MRD stratification strongly correlated with clinical outcomes, with patients achieving NGS-MRD negativity exhibiting superior event-free survival and overall survival rates [7].
Experimental Protocols for Method Comparison
To ensure valid comparisons between NGS and traditional methods, researchers must implement standardized experimental protocols.
Sample Processing for NGS-based MRD Detection
The technical sensitivity of NGS-based methods depends critically on pre-analytical and analytical conditions:
Sample Requirements: Bone marrow aspirates or peripheral blood collected in appropriate anticoagulants (EDTA or specialized cfDNA collection tubes) [27]. For DNA-based NGS, minimum input of 50-100 ng DNA is typically required, while RNA-based fusion detection requires 100-500 ng of high-quality RNA [4] [133].
Library Preparation: Targeted amplicon-based or hybrid capture-based libraries incorporating unique molecular identifiers (UMIs) to enable error correction and distinguish true low-frequency variants from sequencing artifacts [101] [27]. For the 42-gene MRD-validated NGS assay described in [101], customized multiplexed primers with UMIs were used, followed by sequencing on Illumina platforms.
Sequencing Parameters: Deep sequencing with high coverage (>100,000x) is essential for MRD detection, compared to ~500-1000x coverage sufficient for diagnostic mutation profiling [101]. The limit of detection for the NGS-MRD assay was validated at 0.0024 VAF through statistical determination of the "limit of blank" at 798 mutational hotspots using control DNA [101].
Bioinformatic Analysis: Specialized pipelines for variant calling at low allele frequencies, incorporating UMI error correction and background error modeling. For fusion detection, RNA-seq data requires specialized aligners capable of detecting chimeric transcripts [133].
Analytical Validation Approaches
Robust comparison studies incorporate:
Blinded Analysis: Technicians performing each method should be blinded to results from other platforms.
Control Materials: Use of synthetic controls with known mutation concentrations and commercial reference materials to establish sensitivity and specificity for each platform.
Dilution Studies: Serial dilutions of positive samples in normal background to establish limits of detection for each method.
Statistical Analysis: Comparison of detection rates using McNemar's test for paired nominal data, with calculation of sensitivity, specificity, positive predictive value, and negative predictive value for each method against a clinical endpoint such as relapse.
Figure 1: NGS-based MRD Detection Workflow. The complete process from sample collection to clinical reporting, highlighting critical steps including library preparation with unique molecular identifiers (UMIs), target enrichment, sequencing, and comprehensive bioinformatic analysis.
Clinical Decision Pathways
The integration of NGS and traditional methods into clinical practice requires understanding their complementary roles in patient management.
Figure 2: Clinical Decision Pathway Integrating NGS and Traditional Methods. The complementary roles of traditional and NGS methods in the complete patient management pathway, from initial diagnosis through treatment selection and MRD monitoring.
Essential Research Reagent Solutions
Implementing comparative studies of NGS versus traditional methods requires specific reagent systems and technical platforms.
Table 4: Essential Research Reagents for Method Comparison Studies
| Category | Specific Products/Platforms | Application | Technical Considerations |
|---|---|---|---|
| NGS Panels | Oncomine Myeloid MRD Assay (Thermo Fisher) [99]; SureSeq Myeloid Fusion Panel (OGT) [133]; VariantPlex Core Myeloid (ArcherDx) [27] | Comprehensive mutation profiling and MRD detection | Panel size (10-50 genes); coverage uniformity; inclusion of RNA for fusion detection |
| UMI Systems | QIAseq Unique Molecular Indices (Qiagen) [101]; Archer UMI adapters | Error correction for sensitive variant detection | Molecular barcoding strategy; bioinformatic support for UMI deduplication |
| Library Prep | AmpliSeq HD Technology (Thermo Fisher) [99]; Illumina DNA Prep | Target enrichment and library construction | Input DNA requirements; hands-on time; compatibility with sequencing platforms |
| Sequencing Platforms | Illumina NextSeq 500/550 [101]; Illumina MiSeq [27] | High-throughput sequencing | Read length; output capacity; cost per sample |
| Bioinformatic Tools | Archer Analysis [27]; Custom pipelines with Pindel for FLT3-ITD detection [134] | Variant calling, especially for challenging mutations | Sensitivity for indels; ability to detect structural variants; visualization capabilities |
Direct head-to-head comparisons demonstrate that NGS methods generally provide superior detection rates for genetic aberrations in acute leukemia compared to traditional techniques, particularly for comprehensive mutation profiling and measurable residual disease monitoring. The key advantages of NGS include its ability to detect a broad spectrum of mutation types in a single assay, identify novel genetic events, and achieve exceptional sensitivity when incorporating error-correction technologies. However, traditional methods retain important roles for specific applications, such as detecting large FLT3-ITD mutations that may be missed by some NGS approaches and providing rapid assessment of specific biomarkers. The optimal diagnostic approach integrates both technologies, leveraging their complementary strengths to guide risk-adapted treatment strategies. For researchers and drug development professionals, these comparative data underscore the importance of NGS platform selection, validation, and interpretation to fully realize the potential of precision medicine in acute leukemia.
The accurate identification of gene fusions is a cornerstone of modern precision oncology, particularly in acute leukemias where these alterations often define diagnostic subgroups, influence risk stratification, and guide therapeutic decisions [133]. For decades, conventional cytogenetic techniques—including chromosome banding analysis (karyotyping) and fluorescence in situ hybridization (FISH)—have formed the diagnostic backbone. However, these methods possess inherent limitations in resolution and throughput that compromise their ability to detect cryptic fusions, which are structural rearrangements that are beyond the resolution of microscopic analysis or involve complex genomic architecture not readily discernible by targeted approaches [135] [84].
The emergence of next-generation sequencing (NGS), particularly RNA sequencing (RNA-seq), has introduced a paradigm shift in clinical diagnostics. This guide provides an objective, data-driven comparison between RNA-seq and conventional cytogenetics for detecting cryptic gene fusions, contextualized within acute leukemia diagnostics. It is designed to inform researchers, scientists, and drug development professionals about the performance characteristics, experimental requirements, and clinical utility of these evolving technologies.
Performance Comparison: RNA-seq vs. Conventional Methods
A growing body of evidence from recent clinical studies demonstrates the superior performance of RNA-seq-based methodologies for fusion detection compared to conventional cytogenetic techniques. The table below summarizes key quantitative findings from studies in hematological malignancies.
Table 1: Performance Comparison of RNA-seq and Conventional Cytogenetics in Detecting Gene Fusions
| Study Context (Year) | Method | Key Performance Metrics | Clinically Relevant Findings |
|---|---|---|---|
| Pediatric ALL (2025) [136] | RNA-seq | 97% conclusiveness; 99% concordance with FISH; Median TAT: 10 days | Detected additional non-stratifying fusions in 14% B-ALL and 33% T-ALL; Effective in low-quality RNA samples. |
| FISH | 96% conclusiveness; 99% concordance with RNA-seq; Median TAT: 9 days | Standard method, but limited to pre-defined fusion targets. | |
| Pediatric AML Case (2023) [135] | NGS (RNA-seq) | Detected cryptic KMT2A/MLLT10 fusion | Fusion was missed by both karyotyping and break-apart FISH probe. |
| AML Cohort Study (2025) [33] [34] | RNA-based NGS | Identified fusions in 15% of >600 AML patients; ~4% (23 cases) were cryptic (missed by cytogenetics) | Uncovered clinically significant NUP98 and KMT2A rearrangements altering treatment approaches. |
| Conventional Cytogenetics | Failed to detect cryptic fusions in ~4% of AML cases | Limitations in resolution led to missed, yet defining, genetic abnormalities. | |
| Pediatric ALL - OGM (2025) [35] | dMLPA + RNA-seq | Detected clinically relevant alterations in 95% of cases | Most effective combination for subtype classification; Identified IGH rearrangements missed by other techniques. |
| Standard-of-Care (Karyotyping, FISH) | Detected clinically relevant alterations in 46.7% of cases | Significantly lower detection rate highlights technological limitations. |
The data consistently show that RNA-seq not only matches the performance of conventional methods for known fusions but significantly expands the diagnostic yield by identifying previously undetectable cryptic rearrangements and novel fusion partners. This comprehensive detection directly impacts patient management by enabling more precise classification and revealing potential targets for therapy.
Experimental Protocols for Fusion Detection
Standard RNA-seq Workflow for Fusion Detection
The reliable detection of fusions via RNA-seq requires a standardized workflow from sample preparation to bioinformatic analysis. The following protocol is adapted from methodologies used in the cited studies [136] [137] [138].
- Sample Collection & Nucleic Acid Extraction: Obtain bone marrow or peripheral blood samples with high leukemic blast percentage (ideally >80%). Extract total RNA using validated kits (e.g., QIAGEN RNeasy). Assess RNA integrity and quantity using systems like Agilent Bioanalyzer and Qubit fluorometer.
- Library Preparation: Use kits such as the TruSeq Stranded Total RNA Library Prep Kit (Illumina). For targeted RNA-seq approaches (e.g., FusionCapture), hybridize and enrich libraries with probes designed against common and recurrent fusion genes.
- Sequencing: Sequence the libraries on a high-throughput platform (e.g., Illumina NovaSeq or MiSeq) to generate paired-end reads (e.g., 2x150 bp). Sufficient sequencing depth is critical for detecting low-abundance fusions.
- Bioinformatic Analysis: This is a critical step involving multiple stages.
- Alignment & Chimera Detection: Map sequencing reads to the reference genome using a splice-aware aligner like STAR. The aligner's built-in chimeric detection is often the first step to identify potential fusion events.
- Fusion Calling: Process the aligned data with specialized fusion detection algorithms. Tools such as Arriba and SplitFusion have been benchmarked for high sensitivity and specificity in clinical settings [139] [138]. Arriba is noted for its speed and ability to detect fusions even with low supporting reads, while SplitFusion excels at identifying fusions involving repetitive regions and cryptic splice sites.
- Filtering & Annotation: Apply filters to remove common artifacts and annotate the predicted fusions for functional effect (e.g., in-frame vs. out-of-frame), protein domain retention, and known clinical significance.
Orthogonal Validation
In a clinical or rigorous research setting, fusions detected by RNA-seq, especially novel or unexpected events, should be confirmed using an orthogonal method. This is often done by:
- Fluorescence In Situ Hybridization (FISH): Using break-apart or fusion-specific probes to visually confirm the rearrangement at the DNA level [137].
- Reverse Transcriptase-PCR (RT-PCR): Followed by Sanger sequencing of the amplicon to precisely define the fusion junction [136].
Visualizing the Diagnostic Workflow
The following diagram illustrates the logical workflow and decision points in a modern, RNA-seq-integrated diagnostic pathway for acute leukemia, highlighting its advantages in resolving ambiguous or negative cases from conventional testing.
Diagram Title: Integrated Diagnostic Workflow for Leukemia Gene Fusion Detection
The Scientist's Toolkit: Essential Reagents and Tools
Successful implementation of an RNA-seq fusion detection pipeline relies on a suite of wet-lab and computational tools. The following table details key solutions and their functions.
Table 2: Research Reagent Solutions for RNA-seq Fusion Detection
| Category | Item / Solution | Specific Function / Application |
|---|---|---|
| Wet-Lab Reagents | TruSeq Stranded Total RNA Kit (Illumina) | Library preparation for whole-transcriptome sequencing. |
| FusionCapture Panels (e.g., from various vendors) | Targeted enrichment panels for focused fusion detection in cancer. | |
| SureSeq Myeloid Fusion Panel (OGT - RUO) | Targeted RNA-seq panel for detecting 30+ fusions in myeloid cancers [133]. | |
| Agilent 2100 Bioanalyzer / TapeStation | Assessment of RNA Integrity Number (RIN) for sample QC. | |
| Bioinformatic Tools | STAR Aligner | Spliced alignment of RNA-seq reads; generates initial chimeric output. |
| Arriba | Fast, accurate fusion detection algorithm for clinical-grade data [138]. | |
| SplitFusion | Fusion caller optimized for clinical samples, including FFPE-derived RNA [139]. | |
| STAR-Fusion | Comprehensive fusion detection pipeline based on the STAR aligner. |
The evidence from recent and robust clinical studies unequivocally establishes that RNA-seq outperforms conventional cytogenetics in the detection of cryptic gene fusions in acute leukemia. Its genome-wide, agnostic approach provides a level of resolution and comprehensiveness that traditional methods cannot match, directly addressing the significant diagnostic gap left by karyotyping and FISH.
For the research and clinical community, the adoption of RNA-seq, potentially in combination with other emerging genomic technologies like optical genome mapping (OGM) [35] [84], represents a necessary evolution toward a more precise and complete molecular diagnosis. This enhanced diagnostic capability is fundamental to advancing drug development, as it ensures accurate patient stratification for clinical trials and helps identify new therapeutic targets encoded by previously undetectable fusion events.
The molecular diagnosis of acute leukemia has been revolutionized by the advent of DNA sequencing technologies. For decades, Sanger sequencing was the gold standard for identifying genetic mutations. However, with the introduction of Next-Generation Sequencing (NGS) panels, clinical laboratories now have powerful tools that offer dramatically different capabilities for mutation profiling [4]. This shift is particularly significant in acute leukemia, where timely and comprehensive genetic information directly influences diagnostic classification, risk stratification, and therapeutic decisions [66] [140].
The fundamental difference between these technologies lies in their scale and sensitivity. While Sanger sequencing efficiently analyzes single genes, targeted NGS panels simultaneously interrogate dozens of genes recurrently mutated in leukemia, providing a more comprehensive molecular landscape from a single test [4] [73]. This guide objectively compares the performance of these two approaches within the context of acute leukemia diagnostics, supported by experimental data and methodological details.
Technical Comparison: NGS Panels vs. Sanger Sequencing
The following table summarizes the core technical and performance characteristics of NGS panels compared to Sanger sequencing.
Table 1: Technical and performance comparison between NGS Panels and Sanger Sequencing
| Parameter | NGS Panels | Sanger Sequencing |
|---|---|---|
| Throughput | High (Massively parallel) | Low (Sequential) |
| Genes Interrogated | Dozens per run (e.g., 11-19 gene panels) [141] [140] | Typically one gene per reaction |
| Sensitivity (VAF) | ~3-5% (or <1% with UMI) [141] [140] | ~10-20% [141] |
| DNA Input | ~100 ng for library prep [73] | Varies by amplicon size |
| Turnaround Time (Workflow) | Several days (library prep, sequencing, bioinformatics) [4] | ~48 hours for urgent cases [142] |
| Key Strengths | Comprehensive profile, detects low-frequency clones, scalable | Rapid for single genes, established, simple data analysis |
| Major Limitations | Complex data analysis, higher initial cost, bioinformatics expertise | Low throughput, misses subclonal mutations, more tissue consumed for multiple genes |
VAF: Variant Allele Frequency; UMI: Unique Molecular Identifiers
Performance Benchmarks in Leukemia Diagnostics
Validation studies in clinical settings have quantitatively demonstrated the enhanced capabilities of NGS panels. The data below highlight their performance in terms of sensitivity, concordance, and clinical impact.
Table 2: Performance metrics of NGS panels from clinical validation studies
| Study Context | Panel Details | Sensitivity & Specificity | Concordance with Other Methods | Clinical Impact |
|---|---|---|---|---|
| European Multicenter CLL Study [141] | 3 amplicon-based panels (11 genes) | High sensitivity for VAF >5%; lower reproducibility for VAF <5% | 90-97.7% concordance between different NGS panels | Enabled reliable somatic mutation detection for stratification |
| AML Targeted Panel [140] | 19-gene panel | Sensitivity and specificity >99% at 3% VAF for SNVs, 5% for INDELs | 100% concordance with conventional techniques | All patients classified into WHO 2016 categories; refined risk per ELN |
| Pediatric Acute Leukemia Panel [73] | AmpliSeq Childhood Cancer Panel (203 genes) | DNA: 98.5% (5% VAF); RNA: 94.4% for fusions | High concordance; identified additional findings | 43% of patients had clinically relevant results refining diagnosis/prognosis |
CLL: Chronic Lymphocytic Leukemia; AML: Acute Myeloid Leukemia; SNV: Single Nucleotide Variant; INDEL: Insertion/Deletion
Key Advantages of NGS Panels
- Comprehensive Profiling: A single NGS test can replace multiple Sanger sequencing reactions. For example, a 19-gene AML panel provided all clinically relevant information for WHO 2016 classification and ELN 2017 risk stratification in virtually all patients [140].
- Superior Sensitivity: NGS panels consistently demonstrate the ability to detect mutations with a Variant Allele Frequency (VAF) of 3-5%, a level below the reliable detection limit of Sanger sequencing (~10-20%) [141] [140]. This is critical for identifying minor subclones that may expand at relapse.
- Detection of Low-Frequency Clones: The high depth of coverage (often >1000x) enables the discovery of minor subclonal populations. One study noted that most discrepancies between centers involved subclonal mutations with VAF <5%, and the use of Unique Molecular Identifiers (UMIs) could further enhance sensitivity for these low-frequency variants [141].
Limitations and Considerations
- Technical Complexity: The NGS workflow involves multiple steps—library preparation, target enrichment, sequencing, and complex bioinformatics analysis—requiring significant expertise and standardization [4].
- Turnaround Time: While the sequencing run itself is fast, the entire process from nucleic acid extraction to final report can take several days, which may be longer than the 24-48 hour turnaround possible with Sanger for urgent single-gene tests [4] [142].
- Data Interpretation Challenges: Distinguishing pathogenic somatic mutations from benign germline variants or sequencing artifacts requires sophisticated bioinformatics pipelines and comparison with population databases (e.g., ClinVar, COSMIC) [4].
Experimental Protocols for NGS Panel Validation
For a reliable and clinically actionable NGS test, rigorous validation is essential. The following workflow and methodology are based on established protocols from the literature [140] [73].
Diagram Title: NGS Panel Wet Lab and Bioinformatics Workflow
Detailed Methodologies
Sample Preparation and Library Construction
- Nucleic Acid Extraction: DNA is typically extracted from patient bone marrow or peripheral blood samples using column-based kits (e.g., QIAamp DNA Mini Kit) [73]. Quality control is performed via spectrophotometry (OD260/280 >1.8) and fluorometry for accurate quantification [73].
- Library Preparation (Amplicon-Based): For targeted panels, library preparation often uses amplicon-based approaches like the Illumina TruSeq Custom Amplicon or the AmpliSeq for Illumina Childhood Cancer Panel [141] [73]. These methods use a PCR-based protocol to generate thousands of amplicons covering the targeted regions.
Sequencing and Data Analysis
- Sequencing: Libraries are sequenced on platforms such as the Illumina MiSeq, generating paired-end reads. The aim is a high median coverage (e.g., >1,000x) to ensure sensitive variant detection [141] [140] [73].
- Bioinformatics Pipeline:
- Raw Data Processing: Adapter sequences and low-quality bases are trimmed using tools like TrimGalore [141].
- Alignment: Processed reads are aligned to a reference genome (e.g., hg19/GRCh37) using aligners such as BWA mem [141].
- Variant Calling: This is a critical step. Variants are identified using callers like VarScan2 or Atlas-SNP2. The pipeline must be optimized for sensitivity and specificity. One study found that a combination of two mapping algorithms (SSAHA2 + BWA-SW) with Atlas-SNP2 variant calling achieved 95% sensitivity and 93% specificity [143]. Parameters like minimum read depth (e.g., 3x) and minimum VAF (e.g., 0.20 or 20%) are crucial [143].
- Annotation and Filtering: Variants are annotated for functional effect (e.g., using SnpEff) and filtered against population databases (e.g., 1000 Genomes) to remove common polymorphisms, retaining somatic mutations [141].
The Scientist's Toolkit: Essential Research Reagents
Implementing a robust NGS workflow requires specific reagents and tools. The following table details key solutions used in the featured studies.
Table 3: Key research reagent solutions for NGS-based mutation detection
| Reagent / Solution | Function | Example Products / Methods |
|---|---|---|
| Target Enrichment Kits | Selective amplification of genomic regions of interest | TruSeq Custom Amplicon (Illumina), HaloPlex (Agilent), AmpliSeq Childhood Cancer Panel [141] [73] |
| NGS Sequencer | Platform for massively parallel sequencing | Illumina MiSeq [141] [140] |
| Bioinformatics Tools | Data analysis, from raw reads to variant calls | BWA (alignment), VarScan2, Atlas-SNP2 (variant calling), SnpEff (annotation) [141] [143] |
| Positive Control Materials | Assay validation and quality monitoring | SeraSeq Tumor Mutation DNA Mix, SeraSeq Myeloid Fusion RNA Mix [73] |
The comparative data clearly demonstrate that targeted NGS panels provide a substantive enhancement over Sanger sequencing for mutation identification in acute leukemia. The key advantages of NGS—comprehensive genomic profiling, superior sensitivity for detecting low-frequency subclones, and efficient scalability—make it an indispensable tool in modern clinical research and diagnostics [141] [140] [73].
While Sanger sequencing retains utility for rapid, focused analysis of single genes [142], the transition to NGS-based approaches enables a more complete genetic characterization. This comprehensive view is critical for refining diagnosis, prognostication, and ultimately guiding targeted therapeutic strategies in a complex and heterogeneous disease like acute leukemia [66] [100].
The management of acute leukemia has evolved from a one-size-fits-all approach to a precision medicine paradigm where treatment decisions are increasingly guided by the underlying genetic profile of each patient's disease. This shift has created a critical dependency on diagnostic technologies that can accurately detect genetic abnormalities with implications for risk stratification, targeted therapy selection, and minimal residual disease (MRD) monitoring. Next-generation sequencing (NGS) has emerged as a transformative technology in this landscape, offering comprehensive genomic profiling that surpasses the capabilities of traditional diagnostic methods. While conventional techniques like cytogenetics, fluorescence in situ hybridization (FISH), and polymerase chain reaction (PCR) remain foundational to leukemia diagnostics, they possess inherent limitations in resolution, throughput, and applicability that can impact therapeutic decision-making.
This review examines how NGS technologies are influencing treatment decisions in acute leukemia through detailed analysis of recent clinical studies. We compare the performance characteristics of NGS against established standard-of-care methods, provide quantitative data on their diagnostic capabilities, and present case examples demonstrating their clinical impact. By synthesizing evidence from current research, we aim to provide researchers and drug development professionals with a clear understanding of how advanced genomic technologies are reshaping therapeutic strategies in acute leukemia management, ultimately leading to more personalized and effective treatment approaches.
Methodological Comparison: NGS Versus Traditional Diagnostic Approaches
Traditional diagnostic methods for acute leukemia include a combination of chromosome banding analysis (CBA), fluorescence in situ hybridization (FISH), and targeted PCR. These techniques have formed the backbone of leukemia diagnostics for decades, providing essential information for classification and risk stratification. CBA offers a genome-wide view of chromosomal abnormalities but has limited resolution (~5-10 Mb) and requires viable dividing cells [35]. FISH provides higher resolution for specific genomic regions but is targeted in nature, potentially missing novel or unexpected alterations [3]. PCR-based methods offer excellent sensitivity for known mutations but are generally limited to profiling individual genes or specific hot spots [115].
In contrast, NGS technologies enable comprehensive genomic assessment through various approaches including targeted panels, whole-exome sequencing, whole-genome sequencing, and RNA sequencing. Targeted NGS panels focus on genes with established clinical significance in leukemia, providing deep sequencing coverage suitable for detecting low-frequency variants [35]. Whole-genome sequencing using both short- and long-read technologies can identify structural variants, copy number alterations, and sequence variants across the entire genome without prior knowledge of targeted regions [6]. RNA sequencing is particularly valuable for detecting gene fusions and expressing aberrant transcripts [35].
Table 1: Comparison of Major Diagnostic Technologies in Acute Leukemia
| Method | Genetic Alterations Detected | Sensitivity | Turnaround Time | Key Limitations |
|---|---|---|---|---|
| Chromosome Banding Analysis | Aneuploidy, large structural variants | ~5-10% | 1-2 weeks | Low resolution, requires dividing cells |
| FISH | Specific translocations, deletions, amplifications | 1-5% | 2-5 days | Targeted approach, limited genome-wide assessment |
| PCR | Known point mutations, small indels, specific fusion genes | 0.1-3% | 1-7 days | Limited to predefined targets, misses novel variants |
| NGS (Targeted) | Sequence variants, small indels, copy number alterations in predefined genes | 1-5% (down to 0.1% with deep sequencing) | 5-28 days | Limited to panel genes, may miss structural variants |
| NGS (Whole Genome) | Sequence variants, structural variants, copy number alterations, aneuploidy | 5-20% (for structural variants) | 3-14 days | Higher cost, complex data analysis |
| RNA Sequencing | Gene fusions, expression outliers | Varies by expression level | 5-10 days | Requires high-quality RNA, may miss non-expressed alterations |
The integration of these NGS approaches into diagnostic workflows has demonstrated significant improvements in detection rates for clinically relevant genetic alterations. In a comprehensive study of 60 pediatric acute lymphoblastic leukemia (ALL) cases, the combination of digital multiplex ligation-dependent probe amplification (dMLPA) and RNA sequencing detected clinically relevant alterations in 95% of cases, compared to only 46.7% with standard-of-care techniques [35]. Similarly, optical genome mapping (OGM) as a standalone test demonstrated superior resolution for detecting chromosomal gains and losses (51.7% vs. 35%) and gene fusions (56.7% vs. 30%) compared to conventional methods [35].
Quantitative Performance Data: Comparative Analytical Metrics
Recent clinical studies provide robust quantitative data comparing the performance of NGS-based methods against traditional diagnostic techniques across various genetic alteration types and leukemia subtypes. These metrics are crucial for researchers and clinicians evaluating the potential impact of genomic technologies on therapeutic decision-making.
In ALL, NGS-based MRD detection has demonstrated superior sensitivity compared to multiparametric flow cytometry (MFC), identifying MRD-positive cases in patients classified as MRD-negative by MFC. This enhanced detection capability directly impacts treatment intensity decisions, as patients with persistent MRD typically require more intensive therapeutic approaches [7]. The quantitative superiority of NGS-MRD monitoring is particularly evident in its ability to detect residual disease at levels as low as 10^-6, exceeding the sensitivity threshold of most flow cytometry-based methods [7].
Table 2: Performance Metrics of NGS vs. Conventional Methods in Recent Clinical Studies
| Study Context | Conventional Method | NGS Method | Key Performance Metrics | Clinical Impact |
|---|---|---|---|---|
| AML mutation detection [115] | Conventional PCR | Targeted NGS | FLT3-TKD sensitivity: 91.7% (1% VAF cutoff); IDH1/2 concordance: >95% | More accurate identification of patients eligible for targeted therapies |
| Pediatric ALL genomic characterization [35] | CBA + FISH | OGM + dMLPA + RNA-seq | Detection of clinically relevant alterations: 46.7% (SoC) vs. 95% (NGS组合) | Improved risk stratification and subtype classification |
| ALL MRD monitoring [7] | Multiparametric flow cytometry | NGS-MRD | Superior sensitivity (10^-6); identified MRD-positive cases in MFC-negative patients | Better prediction of relapse; guides intensification or reduction of therapy |
| Acute leukemia classification [6] | Karyotyping + FISH | Nanopore WGS with adaptive sampling | Identification of driving alterations in 15 min - 6 hours vs. days to weeks | Rapid treatment initiation; comprehensive alteration detection |
For mutation detection in acute myeloid leukemia (AML), a recent comparative study evaluating FLT3, IDH, and NPM1 mutations demonstrated that NGS with a 1% variant allele frequency (VAF) cutoff identified additional positive samples missed by conventional PCR at a 5% VAF cutoff. This enhanced detection capability is clinically significant, as identifying these mutations directly determines eligibility for targeted therapies such as midostaurin (FLT3 inhibitor) or ivosidenib/enasidenib (IDH inhibitors) [115]. However, the same study highlighted a notable limitation of NGS for FLT3-ITD detection, with sensitivity of only 73.8% compared to PCR, indicating that conventional methods may still play a role for specific alteration types [115].
The turnaround time for genomic characterization represents another critical metric with direct implications for treatment decisions. Traditional diagnostic workflows often require 1-3 weeks to complete the full complement of testing, potentially delaying treatment initiation. In contrast, emerging NGS platforms offer significantly reduced turnaround times. Nanopore sequencing with adaptive sampling has demonstrated the ability to identify driving alterations in pediatric acute leukemia in as little as 15 minutes for karyotype abnormalities and up to 6 hours for complex structural variants [6]. Similarly, rapid epigenomic classification using DNA methylation profiling with nanopore sequencing provided accurate classification within 2 hours of sample receipt, enabling same-day diagnostic assessment [97].
Case Examples: Direct Impact on Therapeutic Decision-Making
Case Example 1: Identification of Cryptic Gene Fusions in AML
Clinical Context: A comprehensive analysis of over 600 AML samples augmented standard myeloid diagnostic panels with RNA-based fusion assays integrated within NGS platforms [33].
Diagnostic Findings: This approach identified gene fusions in 15% of patients, including approximately 4% harboring fusion events undetectable by standard cytogenetics. Notably, rearrangements involving NUP98 and KMT2A were uncovered that would have been missed by conventional methods [33].
Treatment Impact: The identification of these cryptic fusions directly altered treatment strategies in multiple ways. For NUP98 rearrangements, which are associated with high-risk disease, the findings prompted escalation to allogeneic stem cell transplantation in first remission. For KMT2A-rearranged AML, the detection enabled enrollment into clinical trials evaluating menin inhibitors, a novel targeted therapy class with significant activity in this genetic subtype. Additionally, the absence of favorable-risk genetic markers in patients with these cryptic fusions prevented inappropriate de-escalation of therapy that might have occurred based on incomplete genetic characterization [33].
Case Example 2: FLT3-TKD Mutation Detection for Targeted Therapy Selection
Clinical Context: The PETHEMA PCR-LMA study directly compared conventional PCR versus NGS for detection of FLT3, IDH, and NPM1 mutations in AML patients [115].
Diagnostic Findings: NGS analysis using a 1% VAF cutoff identified additional FLT3-TKD positive samples missed by conventional methods with higher thresholds. These additional mutations were confirmed as true positives upon further validation [115].
Treatment Impact: The identification of these previously missed FLT3-TKD mutations qualified patients for FLT3 inhibitor therapy (midostaurin in combination with chemotherapy for newly diagnosed AML, or gilteritinib for relapsed/refractory disease). This directly altered treatment recommendations and potentially improved outcomes for these patients. Based on these findings, the study authors recommended adopting a 1% VAF cutoff as standard for these mutations when using NGS, highlighting how technological advances can refine therapeutic thresholds [115].
Case Example 3: MRD Monitoring for Relapse Prediction and Intervention
Clinical Context: Researchers employed NGS to longitudinally analyze cancer-associated gene mutations in 74 AML patients at diagnosis, post-chemotherapy, and following stem cell transplantation [33].
Diagnostic Findings: The persistence of mutations in epigenetic regulators such as TET2 and DNMT3A following transplantation served as strong predictors of impending relapse. Importantly, the study distinguished between mutations persisting in the context of full donor engraftment (representing likely clonal hematopoiesis) versus those with mixed chimerism (representing residual leukemia) [33].
Treatment Impact: The detection of molecular relapse at the MRD level enabled preemptive therapeutic interventions before overt hematologic relapse, including rapid immunosuppressant reduction and donor lymphocyte infusions in eligible patients. For patients with persistent mutations in the context of full donor engraftment, close monitoring without intervention prevented unnecessary treatment of benign clonal hematopoiesis. This nuanced application of NGS-based MRD monitoring demonstrates how advanced genomic tools are enabling more precise post-transplant management strategies [33].
Case Example 4: Comprehensive Genomic Profiling in Pediatric B-ALL
Clinical Context: A study of 60 pediatric ALL patients compared standard-of-care diagnostic methods with an integrated genomic approach combining OGM, dMLPA, and RNA sequencing [35].
Diagnostic Findings: The integrated approach resolved 15% of non-informative cases where standard methods failed to identify driving alterations. It uniquely identified IGH rearrangements undetected by other techniques and provided comprehensive copy number alteration profiles in a single assay [35].
Treatment Impact: The precise classification enabled by this approach directly influenced therapy in multiple ways. Patients with DUX4 rearrangements, associated with favorable prognosis, were considered for treatment de-escalation. Those with Philadelphia chromosome-like ALL (Ph-like ALL) with specific kinase fusions were recommended for targeted therapy with tyrosine kinase inhibitors added to conventional chemotherapy. Additionally, patients with high-risk genetic features such as IKZF1plus profile were allocated to more intensive treatment protocols, including consideration for early transplantation [35].
Experimental Protocols and Workflows
Targeted NGS for Mutation Detection in AML
Sample Requirements: DNA extracted from bone marrow or peripheral blood mononuclear cells with a minimum input of 10-50 ng [35] [115].
Library Preparation: Commercially available targeted sequencing panels (e.g., ALLseq panel) are used with automated library preparation systems (e.g., Ion Chef System). The process involves DNA shearing, adapter ligation, and PCR amplification of target regions [35].
Sequencing Parameters: Sequencing is typically performed on platforms such as Ion S5 or Illumina MiSeq with coverage depths of 500-1000x for reliable detection of variants at 1-5% VAF [115].
Variant Calling: Bioinformatic pipelines (e.g., Ion Reporter) are used with specific filter settings. For clinical applications, variants are typically reported at a minimum VAF of 1-5%, though research settings may use lower thresholds [115].
NGS-Based MRD Monitoring Workflow
Sample Requirements: DNA from bone marrow aspirates collected at diagnosis and during follow-up timepoints. At diagnosis, sufficient DNA (1-5 μg) is required for initial clonotype identification [7].
Clonotype Identification: For B-ALL, immunoglobulin (IGH, IGK, IGL) and T-cell receptor (TCR) gene rearrangements are sequenced using multiplex PCR approaches with universal primer sets. The EuroClonality-NGS consortium has developed standardized protocols for this application [7].
MRD Assessment: Follow-up samples are sequenced using the same parameters, with sequencing depth typically reaching 1-5 million reads to achieve sensitivity of 10^-5 to 10^-6. Bioinformatics pipelines identify and quantify the leukemia-derived sequences identified at diagnosis [7].
Quality Control: Include control samples to monitor assay sensitivity and specificity. The EuroMRD consortium provides guidelines for quality assurance in NGS-based MRD testing [7].
Emerging Technologies and Future Directions
The field of genomic characterization in acute leukemia continues to evolve rapidly, with several emerging technologies showing promise for further refining treatment decisions. Nanopore sequencing with adaptive sampling represents a particularly significant advancement, enabling real-time genomic characterization that dramatically reduces turnaround times [6]. This approach performs whole-genome sequencing with in silico enrichment for genes frequently involved in leukemia-associated translocations and fusions, providing both comprehensive genomic assessment and focused analysis of clinically relevant targets.
DNA methylation profiling using array-based or sequencing-based approaches has demonstrated remarkable potential for acute leukemia classification. A recent study defined 38 distinct methylation classes across AML, B-ALL, and T-ALL that reflected underlying molecular drivers with high accuracy [97]. The development of MARLIN (methylation- and AI-guided rapid leukemia subtype inference) enabled classification from sparse DNA methylation profiles, providing accurate predictions within 2 hours of sample receipt in clinical implementation [97]. This approach not only matched standard lineage classification but also revealed heterogeneity beyond that captured by genetic categories alone.
Ultra-sensitive sequencing assays for MRD detection represent another frontier in precision oncology. Recent work has validated a sequencing assay targeting FLT3 mutations with sensitivity down to 0.0014% allelic fraction, far exceeding the capabilities of conventional molecular techniques [33]. This heightened sensitivity enables more confident assessment of remission status and earlier detection of molecular relapse, creating opportunities for preemptive therapeutic interventions before overt hematologic recurrence.
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Key Research Reagent Solutions for Leukemia Genomic Studies
| Reagent/Platform | Primary Function | Application in Leukemia Research |
|---|---|---|
| QIAamp DNA Mini Kit (Qiagen) | High-quality DNA extraction from blood/bone marrow | Nucleic acid isolation for downstream genomic analyses including NGS and OGM [35] |
| SALSA dMLPA Probes (MRC-Holland) | Detection of copy number alterations | Identification of recurrent microdeletions/amplifications in ALL; works with low DNA input [35] |
| Bionano OGM Platform | Genome-wide structural variant detection | Comprehensive mapping of large-scale chromosomal rearrangements without need for culturing [35] |
| Oxford Nanopore Adaptive Sampling | Real-time targeted enrichment during sequencing | Selective enrichment of leukemia-associated genes while maintaining whole-genome context [6] |
| TruSeq Stranded Total RNA Kit (Illumina) | RNA library preparation | Fusion gene detection and expression profiling through RNA sequencing [35] |
| EuroClonality-NGS Primer Sets | Amplification of IG/TCR rearrangements | Standardized approach for NGS-based MRD detection in lymphoid malignancies [7] |
The integration of NGS technologies into the diagnostic workflow for acute leukemia is fundamentally reshaping therapeutic decision-making. Evidence from recent clinical studies demonstrates that NGS-based approaches outperform conventional methods in detection rate, sensitivity, and comprehensiveness for a wide range of genetic alterations with direct clinical implications. The case examples presented illustrate how these technological advances are directly impacting patient care through more accurate risk stratification, identification of therapeutic targets, and sensitive disease monitoring.
While challenges remain regarding standardization, cost, and bioinformatics expertise, the trajectory is clear: genomic characterization of acute leukemia is moving toward more comprehensive, rapid, and integrated approaches. For researchers and drug development professionals, understanding these technologies and their clinical applications is essential for designing targeted therapies and developing biomarkers for treatment selection. As these technologies continue to evolve, they promise to further refine our approach to precision medicine in acute leukemia, ultimately improving outcomes for patients with these challenging malignancies.
Pediatric acute lymphoblastic leukemia (pALL) is the most common childhood cancer, with contemporary treatment protocols achieving survival rates of up to 90% through sophisticated risk stratification that incorporates genetic features [144] [145]. The molecular characterization of pALL is essential for accurate diagnosis, risk stratification, and treatment selection, as genetic alterations define distinct molecular subtypes with significant prognostic implications [146]. Historically, approximately 30% of B-cell precursor ALL (BCP-ALL) cases lacked definitive classification through standard cytogenetic analyses and were categorized as "B-other" or "non-informative" [147] [145]. These cases presented a significant clinical challenge as they could not be accurately risk-stratified, potentially leading to suboptimal treatment outcomes.
Traditional standard-of-care (SoC) diagnostic methods—including chromosome banding analysis (CBA), fluorescence in situ hybridization (FISH), and reverse transcription polymerase chain reaction (RT-PCR)—have substantial limitations in resolving this heterogeneous group. These techniques have limited resolution, depend on the availability of viable metaphases, and lack comprehensiveness due to their targeted nature [146] [144]. Next-generation sequencing (NGS) technologies have emerged as transformative tools that overcome these limitations, offering enhanced sensitivity and broader detection capabilities. This review systematically compares the performance of emerging genomic approaches against traditional methods and against each other, providing experimental data to guide researchers and clinicians in optimizing diagnostic workflows for pALL.
Performance Comparison: NGS vs. Standard-of-Care Methods
Diagnostic Yield and Resolution of Non-Informative Cases
Recent large-scale studies demonstrate the superior diagnostic performance of NGS-based methodologies compared to SoC techniques. A 2025 benchmarking study of 60 pALL cases revealed striking differences in detection capabilities [146]. Optical genome mapping (OGM) as a standalone test demonstrated significant advantages, detecting chromosomal gains and losses in 51.7% of cases versus 35% with SoC methods (p = 0.0973) and identifying gene fusions in 56.7% versus 30% (p = 0.0057). Critically, OGM resolved 15% of cases that were non-informative with conventional techniques.
The combination of digital multiplex ligation-dependent probe amplification (dMLPA) and RNA sequencing (RNA-seq) proved even more powerful, achieving precise classification in 95% of pALL cases compared to 46.7% with SoC techniques alone [146]. This combination was particularly effective for identifying IGH rearrangements that frequently eluded detection by other methods. Another study utilizing targeted RNA-seq with the TruSight RNA Pan-Cancer panel successfully reclassified 66.7% (96 of 144) of previously unclassifiable B-other ALL cases, identifying complex subtypes including DUX4-rearranged, PAX5alt, and ZNF384-rearranged ALL [145].
Table 1: Diagnostic Performance of Genomic Approaches in Pediatric ALL
| Methodology | Cohort Size | Alterations Detected | Detection Rate | Key Advantages | Study |
|---|---|---|---|---|---|
| SoC (CBA, FISH, RT-PCR) | 60 | Gene fusions | 30% | Established workflow, widely available | [146] |
| OGM | 60 | Chromosomal gains/losses | 51.7% | Superior resolution of structural variants, resolves 15% non-informative cases | [146] |
| OGM | 60 | Gene fusions | 56.7% | Single-assay approach for comprehensive SV detection | [146] |
| dMLPA + RNA-seq | 60 | Combined alterations | 95% | Best overall performance, identifies IGH rearrangements | [146] |
| Targeted RNA-seq | 144 B-other | Multiple subtype-defining alterations | 66.7% | Reclassification of B-other cases, identifies fusion genes and expression signatures | [145] |
| Nanopore WGS (adaptive sampling) | 57 | Subtype-defining alterations | 100% | Single-assay classification, rapid turnaround (15 min - 48 hrs) | [6] |
Comprehensive Detection of Genetic Alterations
Different NGS methodologies offer complementary strengths for detecting various types of genetic alterations in pALL. Targeted RNA-seq panels effectively identify fusion transcripts, abnormally high gene expression (e.g., CRLF2 or EPOR), and single-nucleotide variants, enabling classification of nearly all recognized BCP-ALL subgroups except for intrachromosomal amplifications like iAMP21 [145]. Whole-transcriptome sequencing provides even broader discovery potential, as demonstrated in a study of Mexican pediatric patients where it identified diverse molecular subtypes including DUX4 (13.6%), Ph-like (9.1%), and ETV6::RUNX1-like (9.1%) ALL [148].
Machine learning approaches further enhance classification accuracy. The ALLIUM tool utilizes DNA methylation and gene expression data from 1131 Nordic ALL patients to predict 17 molecular subtypes with 94.5% concordance for gene expression and 87.0% for DNA methylation classifiers [147]. This multimodal approach successfully revised the molecular subtype in 81.5% of previously unclassified BCP-ALL cases, demonstrating the power of integrated genomic data for resolving diagnostically challenging cases.
Table 2: Detection Capabilities of NGS Methods for Different Alteration Types
| Alteration Type | Targeted RNA-seq | Whole Transcriptome | OGM | dMLPA | Nanopore WGS |
|---|---|---|---|---|---|
| Gene fusions | Excellent | Excellent | Good | Limited | Excellent |
| Chromosomal gains/losses | Limited | Limited | Excellent | Good | Excellent |
| Copy number alterations | Limited | Limited | Excellent | Excellent | Good |
| Single nucleotide variants | Good | Good | Limited | Limited | Good |
| Gene expression profiles | Good | Excellent | Not applicable | Not applicable | Limited |
| Epigenetic profiles | Not applicable | Limited | Not applicable | Not applicable | Possible with additional methods |
| Structural variants | Limited | Limited | Excellent | Limited | Excellent |
Experimental Protocols and Workflows
Targeted RNA Sequencing for Molecular Subclassification
Sample Requirements and Library Preparation: The targeted RNA-seq approach utilizes RNA extracted from bone marrow mononuclear cells with integrity values (DV200) >50%, verified using an Agilent 2100 Bioanalyzer [145]. The TruSight RNA Pan-Cancer panel (Illumina) targets 1385 cancer-related genes, with library preparation performed according to the manufacturer's instructions. Sequencing is typically performed on Illumina platforms such as MiSeq with 2 × 76 cycle runs, generating approximately 3 million reads per sample.
Bioinformatic Analysis: Data analysis employs multiple algorithms to maximize detection sensitivity. The workflow includes: (1) Read alignment to GRCh37/hg19 using DRAGEN RNA Pipeline or similar tools; (2) Fusion detection using at least two independent algorithms (e.g., CICERO, DRAGEN) with manual curation in FusionEditor and IGV; (3) Gene expression quantification in transcripts per million using Salmon; (4) Single-nucleotide variant calling with Strelka; and (5) Clustering analysis using Euclidean hierarchical clustering or t-distributed stochastic neighbor embedding with the most variable genes [145].
Validation: Identified fusions should be confirmed by RT-PCR and/or FISH, while gene expression-based subtypes can be validated against established classifiers or through orthogonal molecular methods.
Nanopore Whole Genome Sequencing with Adaptive Sampling
Sample Preparation: This protocol requires high molecular weight DNA extracted from fresh or cryopreserved peripheral blood or bone marrow samples using kits that preserve long fragments (e.g., ZymoBIOMICS MagBead DNA/RNA kit) [6]. DNA quality is verified through gel electrophoresis to ensure fragment sizes >20 kbp without significant degradation. DNA shearing is performed using a 26G needle for 7 passes, followed by size selection with Ampure XP Beads.
Library Preparation and Sequencing: Library preparation uses Oxford Nanopore Technologies (ONT) ligation sequencing kits (SQK-LSK109/110/112/114 or SQK-NBD114) following manufacturer protocols with minor modifications. Sequencing is performed on PromethION 2 Solo or MinION devices using adaptive sampling for target enrichment. The adaptive sampling panel typically includes 59-223 genes frequently involved in ALL fusions and rearrangements, with the entire genomic locus plus 50 kbp flanks for comprehensive coverage.
Real-time Analysis: Basecalling and alignment are performed concurrently with sequencing using Dorado and minimap2. Digital karyotyping assesses chromosome-level copy number variations by analyzing relative sequencing depth, while structural variants and fusions are identified through split-read and alignment patterns. This approach enables detection of subtype-defining alterations within 15 minutes to 48 hours of sequencing initiation [6].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents and Platforms for NGS in Pediatric ALL
| Category | Product/Platform | Specific Application | Key Features | Reference |
|---|---|---|---|---|
| RNA-seq Panels | TruSight RNA Pan-Cancer (Illumina) | Targeted RNA sequencing | 1385 cancer-related genes, fusion detection | [145] |
| Long-read Sequencing | Oxford Nanopore PromethION/MinION | Whole genome sequencing with adaptive sampling | Real-time analysis, structural variant detection | [6] |
| Optical Mapping | Bionano Saphyr System | Optical genome mapping (OGM) | Detection of structural variants, copy number alterations | [146] |
| Multiplex Assays | digitalMLPA D007 ALL Panel (MRC-Holland) | Copy number alteration profiling | Detection of recurrent microdeletions/amplifications | [146] |
| Methylation Analysis | Illumina EPIC Array | DNA methylation profiling | Subtype classification via epigenetic signatures | [147] |
| Bioinformatic Tools | ALLIUM Classifier | Molecular subtype prediction | Combines DNA methylation and gene expression data | [147] |
| Bioinformatic Tools | CICERO, DRAGEN RNA | Fusion gene detection | Multi-algorithm approach for fusion calling | [145] |
| Analysis Platforms | Bionano Access/Solve | OGM data analysis | Structural variant calling, annotation | [146] |
The comprehensive evaluation of emerging genomic technologies confirms their superior performance over traditional standard-of-care methods for diagnosing pediatric ALL. NGS-based approaches consistently demonstrate enhanced detection rates for clinically relevant alterations and remarkable success in resolving previously non-informative cases. The optimal diagnostic strategy appears to be a combination of methods that leverage their complementary strengths—specifically the integration of dMLPA with RNA-seq or the implementation of nanopore whole genome sequencing with adaptive sampling [146] [6]. These approaches achieve comprehensive genomic characterization while potentially streamlining laboratory workflows and reducing turnaround times.
For researchers and clinical laboratories, the implementation of these technologies requires careful consideration of institutional resources, technical expertise, and specific clinical needs. Targeted RNA-seq panels offer a balanced approach for centers establishing NGS capabilities, providing robust subtype classification with manageable bioinformatic requirements. For more comprehensive genomic characterization, OGM or long-read sequencing technologies provide unprecedented resolution of structural variants, though with increased computational demands. As these technologies continue to evolve and validate in larger prospective studies, their integration into diagnostic workflows promises to further refine risk stratification, enable precision medicine approaches, and ultimately improve outcomes for children with ALL.
The integration of Next-Generation Sequencing (NGS) into the diagnostic workflow for acute leukemia represents a paradigm shift in molecular pathology. While traditional methods like Sanger sequencing, polymerase chain reaction (PCR), and multiparameter flow cytometry (MFC) have established roles, comprehensive analytical validation is essential to demonstrate the superior performance of NGS-based approaches. This guide provides an objective comparison of the analytical validation metrics between NGS and traditional methods, supporting informed decisions by researchers, scientists, and drug development professionals in the field of hematologic malignancies.
Robust analytical validation ensures that diagnostic tests consistently deliver accurate, reliable, and reproducible results across laboratories and platforms. For acute leukemia diagnosis and monitoring, this translates to precise detection of genetic alterations that inform risk stratification, treatment selection, and minimal residual disease (MRD) assessment. The complex genetic landscape of acute leukemia, characterized by numerous subtypes with distinct molecular profiles, demands technologies capable of detecting a broad spectrum of genetic alterations with high sensitivity and specificity [19] [66].
Comparative Performance Metrics of Genomic Methods
The analytical performance of NGS and traditional methods varies significantly across key metrics, influencing their suitability for different applications in acute leukemia diagnostics.
Table 1: Comparative Analytical Performance of Genomic Testing Methods in Acute Leukemia
| Method | Sensitivity (VAF) | Multiplexing Capacity | Key Strengths | Key Limitations |
|---|---|---|---|---|
| NGS (Panel) | 0.0014% - 5% [115] [126] | High (47-50 genes simultaneously) [82] [126] | Comprehensive mutation profiling, ability to detect novel variants | Bioinformatics complexity, longer turnaround times (up to 28 days) [115] |
| Sanger Sequencing | 15-20% [46] | Very Low (single gene) | Low cost for single genes, well-established | Poor sensitivity, low throughput |
| Conventional PCR (FLT3-ITD) | 3% [115] | Low (single mutation) | Rapid turnaround (∼7 days) [115] | Limited to known targets, poor for low-VAF mutations |
| Multiparameter Flow Cytometry (MFC-MRD) | 0.01% (10⁻⁴) [82] | N/A (protein-based) | Fast, widely applicable, functional cell data | Subject to immunophenotypic shifts |
| Digital PCR | 0.001% - 0.1% [82] | Medium (limited multiplexing) | Absolute quantification, high sensitivity | Limited multiplex capability, higher cost than conventional PCR |
The sensitivity advantage of NGS becomes particularly evident in MRD monitoring, where error-corrected NGS methodologies can detect mutant alleles at variant allele frequencies (VAF) as low as 0.0014% [126], far surpassing the capabilities of conventional sequencing approaches. This ultra-sensitive detection enables earlier intervention and more accurate assessment of treatment response. Furthermore, NGS provides comprehensive mutational profiling that captures the genetic heterogeneity of acute leukemia, identifying co-occurring and cooperating mutations that influence disease biology and therapeutic response [66].
Experimental Protocols for Method Validation
Targeted NGS Panel Sequencing for Acute Myeloid Leukemia
Sample Preparation and Library Construction: The protocol begins with extraction of genomic DNA from bone marrow or peripheral blood samples, with quality assessment through fluorometry or spectrophotometry. For the library preparation, the process utilizes a custom multiplex amplicon-based panel targeting 47-50 genes recurrently mutated in AML (including FLT3, NPM1, IDH1/2, DNMT3A, TP53, and others) [82] [126]. Adapter-ligated libraries are amplified via PCR, followed by purification using magnetic beads. Library quantification and quality control are performed using systems such as Qubit dsDNA HS Assay and Qsep100 automated nucleic acid analysis [82].
Sequencing and Data Analysis: Sequencing runs are performed on platforms such as Illumina NovaSeq or Ion S5 with minimum coverage of 1,000× for diagnostic samples and significantly higher coverage (≥10,000×) for MRD detection. Bioinformatic processing includes alignment to reference genome (GRCh37/38), variant calling with minimum VAF thresholds of 1-5% for diagnostic samples and 0.1-0.001% for MRD monitoring, and annotation using population databases (gnomAD, ExAC) to filter polymorphisms [82] [115] [126]. For error-corrected sequencing, unique molecular identifiers (UMIs) are incorporated to distinguish true mutations from sequencing errors, enabling high-sensitivity detection.
Conventional PCR for Single-Gene Mutation Detection
DNA Extraction and Amplification: DNA is extracted from patient samples using standardized kits. For FLT3-ITD detection, endpoint PCR amplifies the juxtamembrane domain of the FLT3 gene. The PCR products are then separated by capillary electrophoresis, with wild-type alleles generating a 329-331 bp fragment and ITD mutations appearing as longer fragments [115].
Analysis and Interpretation: Fragment analysis software detects and quantifies the ratio of mutant to wild-type alleles based on peak areas. The analytical sensitivity of this method is approximately 3% VAF, with results typically available within 7 days compared to 28 days for comprehensive NGS testing [115].
Flow Cytometry for MRD Detection
Sample Processing and Staining: Bone marrow aspirates are collected in EDTA or heparin tubes, and mononuclear cells are isolated via density gradient centrifugation. Cells are stained with multicolor antibody panels (typically 8-10 colors) designed to detect leukemia-associated immunophenotypes (LAIPs) or differentiate-from-normal (DfN) approaches [82] [126].
Data Acquisition and Analysis: Samples are acquired on flow cytometers such as BD FACSymphony, with a minimum of 500,000 events collected to ensure sensitivity of 0.01% (1 in 10,000 cells). Analysis software identifies aberrant populations based on antigen expression patterns that deviate from normal maturing myeloid or lymphoid precursors [82] [126].
Workflow and Signaling Pathway Diagrams
Method Comparison Workflow
Figure 1: Comparative diagnostic workflows for acute leukemia, highlighting the parallel testing requirements of traditional methods versus the unified NGS approach.
Acute Leukemia Genetic Pathways
Figure 2: Major genetic pathways altered in acute leukemia, demonstrating the complexity of molecular features that require comprehensive detection methods.
Essential Research Reagent Solutions
Table 2: Key Research Reagents for NGS-Based Leukemia Diagnostics
| Reagent Category | Specific Examples | Research Function | Considerations |
|---|---|---|---|
| NGS Library Prep Kits | MultipSeq Custom Panels (47 genes), smMIPS panels (34 genes) [82] [126] | Target enrichment for mutation detection | Gene coverage, incorporation of UMIs for error correction |
| Sequence Capture Technologies | Single molecule Molecular Inversion Probes (smMIPS), Hybridization-based panels | Selective amplification of genomic regions of interest | Uniformity of coverage, panel design flexibility |
| Bioinformatic Tools | Ion Reporter, Bionano Solve, Custom pipelines [82] [35] | Variant calling, annotation, and interpretation | Compatibility with sequencing platform, validation requirements |
| Control Materials | Cell line DNA, Synthetic DNA constructs, Reference standards | Quality control and assay validation | Availability of well-characterized positive controls |
| MRD Detection Reagents | EuroClonality-NGS primer sets, UMI-containing adapters [5] [126] | High-sensitivity detection of residual disease | Sensitivity validation, background error rate determination |
The selection of appropriate research reagents significantly impacts the performance characteristics of NGS testing. Targeted sequencing panels must comprehensively cover genes with established clinical significance in acute leukemia while maintaining flexibility for incorporating newly discovered biomarkers. Error-correction technologies, particularly those incorporating unique molecular identifiers (UMIs), are essential for achieving the ultra-high sensitivity required for MRD detection [126]. Bioinformatic solutions must be rigorously validated to ensure accurate variant calling across different mutation types, including single nucleotide variants, insertions/deletions, and structural variants.
Reproducibility and Standardization Challenges
The reproducibility of NGS testing across laboratories depends on multiple factors, including standardization of wet-bench procedures, bioinformatic pipelines, and variant interpretation criteria. Interlaboratory comparisons have demonstrated excellent concordance for high-VAF mutations but increasing variability at lower VAF ranges, particularly below 5% [115]. Standardization efforts led by organizations like EuroClonality-NGS have established guidelines for data analysis and interpretation, improving consistency across testing sites [5].
For traditional methods, reproducibility challenges include inter-observer variability in flow cytometry interpretation and technical artifacts in PCR-based detection, particularly for complex mutations like FLT3-ITDs [115]. The higher analytical sensitivity of NGS must be balanced against potential detection of clonal hematopoiesis of indeterminate potential (CHIP), which may not represent true leukemic clones, necessitating careful integration of molecular findings with clinical context [82].
Analytical validation data demonstrate that NGS technologies provide significant advantages in sensitivity, multiplexing capability, and comprehensive genomic profiling compared to traditional methods for acute leukemia diagnosis. Error-corrected NGS methodologies enable detection of MRD at unprecedented sensitivity levels (VAF <0.01%), offering superior prognostic stratification and earlier relapse detection [82] [126]. However, traditional methods retain utility for rapid targeted detection and remain important complementary approaches in comprehensive diagnostic workflows.
The integration of NGS into routine clinical practice requires careful consideration of analytical validation metrics, including sensitivity, specificity, reproducibility, and turn-around-time. Ongoing advancements in sequencing technologies, bioinformatic tools, and standardization efforts will further enhance the performance and reliability of NGS-based approaches, ultimately improving precision medicine applications in acute leukemia.
The diagnosis and management of acute leukemia have been transformed by technological advances in detecting genetic abnormalities and residual disease. For years, traditional methods including cytomorphology, multiparameter flow cytometry (MFC), and conventional PCR have formed the diagnostic backbone. However, the emergence of next-generation sequencing (NGS) has introduced a paradigm shift in molecular diagnostics. This comparison guide provides an objective assessment of the performance characteristics, clinical utility, and practical implementation of NGS versus traditional methods for acute leukemia diagnosis, with particular focus on minimal residual disease (MRD) monitoring. The evaluation is framed within the broader thesis that precision medicine demands increasingly sensitive, comprehensive, and dynamic profiling of leukemic cells to guide therapeutic decisions and improve patient outcomes.
Technical Performance Comparison
Sensitivity and Detection Limits
The critical advantage of NGS lies in its superior sensitivity for detecting low-level disease. In acute lymphoblastic leukemia (ALL), NGS demonstrates enhanced capability to identify MRD-positive cases that would be classified as negative by traditional methods. A systematic review of 13 studies found that NGS detected more MRD-positive cases compared to MFC in both B-ALL (57.5% vs. 26.9%) and T-ALL (80% vs. 46.7%) [7] [5]. The same review noted a 97.2% concordance between NGS and MFC for positive MRD cases, but only 57.1% concordance for negative cases, indicating NGS identifies additional positive cases missed by MFC [5].
In acute myeloid leukemia (AML), specialized NGS applications achieve remarkable sensitivity thresholds. A novel FLT3 mutation test validated by Moffitt Cancer Center demonstrated detection down to 0.0014% variant allele frequency (VAF) using deep sequencing [34] [149]. This exceptional sensitivity enables earlier detection of residual disease before clinical manifestation.
Applicability and Genetic Coverage
Traditional molecular methods face inherent limitations in applicability. Quantitative RT-PCR for fusion genes can be applied to less than 50% of ALL cases due to the absence of detectable fusion genes in many patients [7] [5]. Similarly, MFC encounters challenges with immunophenotypic shifts during treatment and interference from immunotherapies targeting antigens like CD19 and CD22 [5].
NGS overcomes these limitations through comprehensive genetic profiling. RNA-based NGS fusion testing at the University of Michigan identified previously undetectable "cryptic" gene fusions in approximately 4% of AML cases, including clinically significant NUP98 and KMT2A rearrangements that directly impact treatment approaches [34] [149]. The broad applicability of NGS for immunoglobulin (Ig) and T-cell receptor (TCR) gene rearrangements in ALL makes it suitable for nearly all patients [7].
Table 1: Method Comparison for MRD Detection in Acute Leukemia
| Parameter | Multiparameter Flow Cytometry (MFC) | qRT-PCR | Next-Generation Sequencing (NGS) |
|---|---|---|---|
| Sensitivity | 10-4 to 10-5 | 10-4 to 10-6 for specific targets | 10-5 to 10-6 (down to 0.0014% for specialized assays) |
| Applicability | >95% of cases | <50% for fusion genes; limited by need for known targets | >95% via Ig/TCR rearrangements; comprehensive mutation profiling |
| Turnaround Time | Fast (hours to 1-2 days) | Prolonged for receptor rearrangements (3-4 weeks for primer design) | Moderate to long (several days to weeks) |
| Key Advantages | Rapid, widely available, relatively low cost | High sensitivity for specific targets, standardized within consortia | Detects clonal evolution, universal primers, high sensitivity, comprehensive profiling |
| Major Limitations | Antigen modulation, operator dependency, affected by immunotherapy | Limited applicability, labor-intensive, cannot detect subclones | High cost, bioinformatics complexity, standardization ongoing |
Prognostic Value and Clinical Utility
Risk Stratification and Outcome Prediction
NGS-based MRD assessment provides powerful prognostic stratification across acute leukemia subtypes. In ALL, patients achieving NGS-MRD negativity exhibit significantly superior event-free survival (EFS) and overall survival (OS) rates compared to MRD-positive patients [7] [5]. The prognostic value extends to predicting outcomes following advanced therapies, with NGS demonstrating high predictive accuracy for relapse after hematopoietic stem cell transplantation and CAR-T cell therapy [5].
In AML, the dynamic monitoring of variant allele frequencies (VAF) during treatment offers refined prognostic insights. A study of 69 AML patients established specific VAF thresholds that correlated with clinical outcomes, finding that patients with mean VAF (excluding clonal hematopoiesis of indeterminate potential, CHIP) ≤0.004 at consolidation day 1 and ≤0.020 during subsequent monitoring had significantly better prognosis [82]. Furthermore, relapsed patients showed significantly higher mean VAF during monitoring (0.160 ± 0.155) compared to consolidation (0.058 ± 0.087) [82].
Detection of Clonal Evolution
A distinctive advantage of NGS over traditional methods is its ability to track clonal dynamics and evolution throughout treatment. Conventional PCR and MFC provide static assessments limited to known initial clones or immunophenotypes. In contrast, NGS can identify emerging subclones that may drive resistance and relapse [7] [82]. This capability is particularly valuable for understanding treatment failure and designing subsequent therapeutic strategies.
In AML, studies have demonstrated that subclones present at very low levels (<1% VAF) at diagnosis can expand dramatically (up to 60%) at relapse, illustrating how NGS reveals disease dynamics invisible to traditional methods [82]. Similarly, in FLT3-ITD positive AML, rising ITD levels detected through serial NGS monitoring serve as harbingers of impending relapse [82].
Complementary Testing Approaches
Integrated MRD Assessment
The most prognostically powerful approach combines multiple methodologies. A study integrating MFC and NGS data at consolidation therapy demonstrated that patients negative by both methods had significantly longer survival compared to those positive by either method alone [82]. This synergistic effect highlights how these technologies provide complementary information—MFC detecting immunophenotypic abnormalities and NGS identifying molecular mutations—that collectively offer a more comprehensive disease assessment.
Novel Applications and Specimen Types
NGS enables innovative monitoring approaches not feasible with traditional methods. Circulating cell-free DNA (cfDNA) analysis using NGS provides a minimally invasive method for MRD assessment in AML. A 2025 pilot study demonstrated that cfDNA-based NGS monitoring detected residual disease with higher sensitivity than chimerism analysis in post-transplant patients [150]. Patients with mutation-positive cfDNA despite ≥90% donor chimerism had significantly lower progression-free survival (64% at 17 months) compared to those with undetectable MRD (100%) [150].
Diagram 1: Integrated approach combining traditional and NGS methods for comprehensive leukemia assessment.
Experimental Protocols and Methodologies
NGS-Based MRD Detection Workflow
Standardized protocols for NGS-based MRD detection in acute leukemia involve multiple critical steps. For B-ALL, the EuroClonality-NGS study group has developed guidelines targeting immunoglobulin (IGH, IGK, IGL) and T-cell receptor (TCRB, TCRG, TCRD) gene rearrangements [7] [5]. The typical workflow encompasses:
DNA Extraction: Obtain high-quality DNA from diagnostic bone marrow or peripheral blood samples (minimum 2-5 μg recommended).
Library Preparation: Use multiplex PCR amplification with consensus primers targeting V-J rearrangements in IGH (VDJH, DJH), IGK, and TCR loci. Commercial kits like the LymphoTrack (Invivoscribe) provide standardized primer sets.
Sequencing: Perform on Illumina platforms (MiSeq, NextSeq) with minimum 100,000 reads per sample to ensure adequate coverage for low-VAF detection.
Bioinformatic Analysis: Utilize specialized software (Archer Analysis, LymphoTrack Dx) for sequence alignment, clonotype identification, and tracking. The EuroClonality-NGS group provides standardized analysis pipelines.
MRD Quantification: Calculate MRD levels by comparing sequence counts of diagnostic clonotypes in follow-up samples to total sequenced reads, with sensitivity thresholds typically at 10-6 [7] [5].
Targeted Gene Panels for AML
For AML MRD monitoring, targeted sequencing panels focus on recurrently mutated genes with clinical significance:
Diagram 2: NGS workflow for AML MRD monitoring using targeted gene panels.
A representative 47-gene panel includes key mutations in NPM1, FLT3, IDH1/2, DNMT3A, TET2, TP53, and splicing factors [82]. The analytical sensitivity for MRD detection typically employs a VAF threshold of 0.1% for non-initial diagnostic samples, though this can be optimized based on sequencing depth and clinical requirements [82].
Table 2: Essential Research Reagents and Platforms for NGS-Based Leukemia Diagnostics
| Category | Specific Products/Platforms | Application and Function |
|---|---|---|
| NGS Platforms | Illumina MiSeq, NextSeq; NovaSeq | High-throughput sequencing; MiSeq suitable for targeted panels, NovaSeq for whole genome/exome |
| Targeted Panels | ArcherDx VariantPlex Core AML/Core Myeloid; LymphoTrack (Invivoscribe) | AML hotspot mutation detection; Ig/TCR rearrangement analysis for ALL |
| Library Prep Kits | Illumina Nextera Flex; QIAseq Targeted DNA Panels | Fragment DNA and add sequencing adapters for target enrichment |
| Bioinformatics Tools | Archer Analysis; LymphoTrack Dx; Custom pipelines (GATK) | Variant calling, clonotype identification, MRD quantification |
| Sample Collection | Streck cell-free DNA Blood Collection Tubes | Preserve blood samples for cfDNA analysis and prevent background DNA release |
Practical Considerations and Limitations
Turnaround Time and Resource Requirements
Despite its technical advantages, NGS implementation faces practical challenges. Turnaround times remain substantially longer for NGS compared to traditional methods. Conventional PCR for AML mutation screening typically requires 7 days, while comprehensive NGS panels may take up to 28 days [115]. This delay impacts clinical decision-making, particularly for treatment initiation.
Additionally, NGS demands significant infrastructure investment and specialized expertise. The requirement for sophisticated bioinformatics analysis and interpretation represents a barrier to implementation in resource-limited settings [7] [5]. Ongoing efforts to develop rapid NGS protocols (including nanopore sequencing) and automated bioinformatics pipelines aim to address these limitations [115].
Interpretation Challenges
NGS introduces novel interpretation complexities not encountered with traditional methods. Distinguishing true residual disease from clonal hematopoiesis of indeterminate potential (CHIP) requires careful analysis of mutation patterns and VAF trajectories [82]. The clinical significance of very low-VAF mutations (0.1-0.01%) detected by ultra-sensitive NGS remains uncertain, particularly in predicting late relapse.
For specific mutations like FLT3-ITD, NGS demonstrates technical limitations with sensitivity of only 73.8% compared to conventional PCR, potentially missing clinically relevant mutations that impact patient stratification for FLT3 inhibitors [115]. This underscores that NGS cannot yet fully replace all conventional methods.
Next-generation sequencing represents a transformative advancement in acute leukemia diagnostics, offering superior sensitivity, comprehensive genetic profiling, and unique insights into clonal evolution. The technology enables refined risk stratification and earlier relapse detection compared to traditional methods like flow cytometry and conventional PCR. However, practical challenges including turnaround time, cost, and bioinformatics requirements necessitate careful implementation strategies. The emerging paradigm favors integrated approaches that combine the strengths of multiple technologies—morphology, flow cytometry, and NGS—to provide complementary data for clinical decision-making. As standardization improves and costs decrease, NGS is poised to become the cornerstone of precision medicine in acute leukemia, potentially enabling dynamic treatment adaptation based on real-time molecular assessment of disease burden and genetic evolution.
The molecular diagnosis of acute leukemia has traditionally relied on a combination of single-gene testing methods and cytogenetic techniques. Next-generation sequencing (NGS) represents a paradigm shift, enabling simultaneous assessment of multiple genetic alterations. This guide provides an objective comparison of the performance of NGS-based approaches against traditional diagnostic methods, focusing on turnaround time, detection efficiency, and comprehensive testing capability within the context of acute leukemia diagnosis.
Performance Metrics Comparison
The comprehensive evaluation of NGS versus traditional methods reveals significant differences across key performance metrics essential for clinical diagnostics and research applications.
Table 1: Comprehensive Performance Comparison of Genetic Testing Methods in Acute Leukemia
| Performance Metric | NGS-Based Approach | Traditional Methods (PCR, FISH, Cytogenetics) | Experimental Data and Context |
|---|---|---|---|
| Turnaround Time | ~28 days [115] | ~7 days (PCR) [115] | Data from PETHEMA PCR-LMA study comparing diagnostic workflows [115]. |
| Multiplexing Capacity | High (数十至数百个基因/变异) [4] [140] [73] | Low (单个或少量基因/测试) [133] | Targeted NGS panels (e.g., 19-gene AML panel) allow simultaneous assessment of SNVs, Indels, and CNVs [140]. |
| Sensitivity (VAF) | 1%-5% [115] [73] | ~3% (对于常规 PCR) [115] | Lowering NGS VAF cut-off to 1% improves detection of clinically relevant mutations (e.g., FLT3-TKD) [115]. |
| Fusion Detection | RNA-based NGS detects common, rare, and novel fusions [133] [73] | FISH (gold standard) and RT-PCR are limited to known/pre-defined fusions [133] | NGS panels (e.g., OGT's SureSeq) can detect >30 fusions simultaneously, overcoming FISH/RTPCR limitations [133]. |
| Diagnostic Yield | 43%-90% [35] [73] | 46.7% (Standard-of-Care) [35] | NGS refined diagnosis in 41%-49% of patients and identified targetable mutations [35] [73]. |
| Cost Efficiency | Cost-saving at sufficient scale [151] | Higher cumulative cost for multiple single-gene tests [151] | NGS-based strategy saved €30–€1249 per patient compared to SGT-based strategy in oncology [151]. |
Experimental Protocols and Validation Data
Protocol: Validation of a Targeted NGS Panel for Acute Leukemia
The following methodology was adapted from the technical validation of the AmpliSeq for Illumina Childhood Cancer Panel [73].
- Sample Preparation: DNA and RNA are co-extracted from patient bone marrow or peripheral blood samples. Purity and integrity are critical; assessed via spectrophotometry (OD260/280 >1.8) and bioanalyzer systems [73].
- Library Preparation:
- Sequencing: Libraries are pooled and sequenced on Illumina platforms (e.g., Ion S5) to a mean read depth of >1000x for DNA [73].
- Data Analysis:
- Variant Calling: Bioinformatic pipelines (e.g., Ion Reporter) are used for calling SNVs and Indels. A VAF cutoff of 5% is standard, but 1% is recommended for certain mutations [115].
- Fusion Calling: RNA sequencing data is aligned and analyzed for chimeric transcripts.
- Validation Metrics: The assay demonstrated 98.5% sensitivity for DNA variants (at 5% VAF), 94.4% sensitivity for RNA fusions, and 100% specificity [73].
Protocol: Comparative Study of PCR vs. NGS for Mutation Detection
The PETHEMA PCR-LMA study provides a direct comparison for key mutations [115].
- Sample Cohort: Analysis of a large cohort of AML patients.
- Parallel Testing: Each patient sample was tested in parallel using established, validated PCR methods and an NGS panel.
- Analysis:
- Concordance: Overall high concordance was observed, but NGS with a 1% VAF cut-off identified additional positive samples for FLT3-TKD and IDH1/IDH2 mutations that were negative by PCR.
- Sensitivity Calculation: For FLT3-ITD, NGS sensitivity was 73.8% compared to PCR, highlighting a technical limitation of NGS in detecting long duplications.
- Key Finding: The study concluded that NGS could replace PCR for FLT3-TKD and IDH1/2 testing, but PCR remains superior for FLT3-ITD detection until NGS bioinformatics improve [115].
Workflow and Technological Diagrams
The following diagram illustrates the core NGS wet-lab workflow, highlighting steps that impact turnaround time and data quality.
The Scientist's Toolkit: Essential Research Reagents
Successful implementation of NGS in leukemia research requires specific, quality-controlled reagents and tools.
Table 2: Key Research Reagent Solutions for NGS in Leukemia Diagnostics
| Reagent/Material | Function | Example Product | Critical Specification |
|---|---|---|---|
| Targeted NGS Panel | Simultaneously interrogates genes relevant to leukemia classification and prognosis. | AmpliSeq Childhood Cancer Panel [73], 19-gene AML Panel [140] | Covers SNVs, Indels, CNVs, and fusions in a single assay. |
| Nucleic Acid Extraction Kits | Isolate high-quality, intact DNA and RNA from challenging samples like bone marrow. | QIAamp DNA Mini Kit, Direct-zol RNA MiniPrep [73] | High purity (OD260/280 >1.8) and integrity are non-negotiable. |
| Library Prep Kit | Prepares nucleic acids for sequencing by adding adapters and indexing. | AmpliSeq for Illumina Library Prep [73] | Supports dual indexing to minimize index hopping [4]. |
| Positive Control Material | Validates assay performance, sensitivity, and specificity for both DNA and RNA. | SeraSeq Tumor Mutation DNA Mix, SeraSeq Myeloid Fusion RNA Mix [73] | Contains known mutations/fusions at defined allele frequencies. |
| Sequence Analysis Software | Converts raw data into actionable genetic variants and fusions. | Ion Reporter, Bionano Solve [35] [73] | Integrated pipeline for variant calling, annotation, and filtering. |
The integration of NGS into the diagnostic pathway for acute leukemia represents a significant advancement in molecular pathology. While traditional methods currently offer a faster turnaround for targeted questions, NGS provides unparalleled comprehensiveness, ultimately refining diagnosis and prognosis for a substantial proportion of patients. The initial investment in NGS infrastructure and longer turnaround time is counterbalanced by its higher diagnostic yield, potential for cost savings at scale, and ability to guide targeted therapy decisions. Future developments, such as more rapid sequencing technologies and improved bioinformatic tools for challenging alterations like FLT3-ITD, are poised to further solidify the role of NGS as the cornerstone of precision medicine in acute leukemia.
The diagnosis and molecular characterization of acute leukemia have undergone a profound transformation, shifting from reliance on traditional cytogenetic methods to increasingly sophisticated genomic technologies. Next-generation sequencing (NGS) has emerged as a powerful tool, capable of detecting a broad spectrum of genetic alterations with high sensitivity. However, the integration of these advanced technologies into clinical practice necessitates parallel developments in standardization frameworks and regulatory oversight to ensure reliability, reproducibility, and patient safety. For researchers and drug development professionals, understanding these evolving landscapes is crucial for designing robust clinical trials, developing targeted therapies, and implementing reproducible diagnostic workflows. This article examines the current state of standardization and regulatory considerations for NGS and traditional methods in acute leukemia diagnostics, providing a comparative analysis grounded in recent experimental data.
Comparative Performance Data: NGS vs. Traditional Methods
Recent studies have quantitatively benchmarked the performance of emerging genomic technologies against standard-of-care (SoC) methods in acute leukemia. The data reveal significant differences in detection capabilities, which directly inform standardization needs.
Table 1: Detection Rate Comparison in Pediatric Acute Lymphoblastic Leukemia (pALL) (n=60)
| Methodology | Clinically Relevant Alteration Detection Rate | Key Strengths | Key Limitations |
|---|---|---|---|
| Standard-of-Care (SoC)(CBA, FISH, RT-qPCR) | 46.7% [35] | Established workflows; long-standing clinical validation [35] | Limited resolution; low detection of cryptic alterations [35] |
| Optical Genome Mapping (OGM) | 90% [35] | Superior resolution for structural variants and gene fusions [35] | Limited detection of single-nucleotide variants [35] |
| dMLPA & RNA-seq Combination | 95% [35] | Most effective approach; precise classification of complex subtypes [35] | Requires multiple testing platforms; higher sample input [35] |
Table 2: Concordance and Unique Detection in Acute Leukemia (n=467 cases)
| Metric | Targeted RNA-Seq (108-gene panel) | Optical Genome Mapping (OGM) |
|---|---|---|
| Overall Concordance with OGM/RNA-Seq | 74.7% [36] | 74.7% [36] |
| Unique Detection of Clinically Relevant Rearrangements | 9.4% [36] | 15.8% [36] |
| Performance on Enhancer-Hijacking Lesions | Poor (20.6% concordance) [36] | Effective detection [36] |
| Performance on Fusions from Intrachromosomal Deletions | Slightly outperforms OGM [36] | May label as simple deletions [36] |
The data underscore a critical point: no single platform captures the entire mutational spectrum of acute leukemia. NGS-based RNA-seq excels in detecting expressed chimeric fusions, while OGM is more effective for identifying cryptic, enhancer-driven structural variants that do not generate fusion transcripts [36]. This technological complementarity argues for standardized approaches that allow for multi-modal testing.
Standardization of Experimental Protocols and Workflows
The implementation of NGS in clinical diagnostics requires rigorous standardization of pre-analytical, analytical, and post-analytical processes. The following methodologies, derived from recent studies, highlight the detailed protocols required for reproducible results.
Targeted RNA Sequencing for Fusion Detection
- Sample Preparation: RNA is extracted from peripheral blood or bone marrow aspirate specimens [36].
- Target Enrichment: The anchored multiplex PCR (AMP) method is utilized. This chemistry employs unidirectional gene-specific primers (GSP2) that target exons of either one or both translocated genes in chimeric transcripts, enabling capture of novel fusion partners [36].
- Sequencing and Analysis: Amplified targets undergo bidirectional sequencing on an Illumina sequencer. Sequencing reads are aligned to the human reference genome GRCh37/hg19, and fusion transcripts are identified using specialized software (e.g., Archer Analysis) [36].
Optical Genome Mapping for Structural Variant Analysis
- DNA Preparation: Ultra-high-molecular-weight genomic DNA is extracted from fresh or frozen samples (within 24 hours of collection) and labeled using the DLE-1 enzyme via the Bionano Prep direct labelling and staining (DLS) protocol [36] [35].
- Imaging and Data Generation: A minimum of 750 ng of labeled DNA is loaded onto a Saphyr G2.3 chip and imaged. Strict quality control is applied, requiring map rates >60%, molecule N50 values >250 kb, and effective genome coverage >300x [35].
- Variant Calling and Interpretation: Genome analysis is performed against the GRCh38 reference using Bionano Access and Solve software. Variant calling uses the Rare Variant Pipeline, and findings are classified according to established guidelines (ACMG/ClinGen) [36] [35].
DNA-Based NGS for Mutation Detection
- Library Preparation and Sequencing: For targeted NGS panels (e.g., the ALLseq panel), 10 ng of gDNA and RNA are used for library preparation, which is often automated on systems like the Ion Chef. Sequencing is performed on platforms such as the Ion S5 [35].
- Variant Calling and Reporting: Variant calling is conducted using platform-specific software (e.g., Ion Reporter). A critical standardization issue is the variant allele frequency (VAF) cut-off. Studies demonstrate that a 1% VAF cut-off significantly improves sensitivity for clinically impactful mutations like FLT3-TKD and IDH1/IDH2 compared to a 5% cut-off, arguing for its adoption as a standard [115].
Current Regulatory Landscape and Evolving Frameworks
The regulatory environment for genomic tests, particularly those used as companion diagnostics, is complex and varies by jurisdiction. A primary consideration is the distinction between laboratory-developed tests (LDTs) and commercially distributed kits.
- Laboratory-Developed Tests (LDTs): Many NGS-based applications in academic medical centers, such as the 108-gene RNA-seq panel and OGM, are implemented as LDTs [36]. These are currently subject to enforcement discretion by the U.S. Food and Drug Administration (FDA) but are regulated under the Clinical Laboratory Improvement Amendments (CLIA). The trend is toward increased FDA oversight for LDTs to ensure analytical and clinical validity.
- Companion Diagnostics: FDA-approved companion diagnostics are often tied to specific targeted therapies. For instance, tests for FLT3 mutations are linked to the use of midostaurin, gilteritinib, and quizartinib [152]. The standardization of these tests is critical, as discrepancies in detection (e.g., NGS missing some FLT3-ITD mutations due to technical limitations) can directly impact patient access to effective therapies [115].
- Quality Control and Proficiency Testing: Regulatory bodies emphasize rigorous quality control. For NGS, this includes standardizing metrics for sequencing depth, coverage uniformity, and minimum VAF thresholds. Emerging technologies like OGM require new standards for defining data quality (e.g., map rate, effective coverage) and validating variant callers [35].
The Scientist's Toolkit: Essential Research Reagent Solutions
The successful implementation of standardized NGS workflows relies on a suite of specialized reagents and platforms. The following table details key solutions used in the featured studies.
Table 3: Key Research Reagent Solutions for Acute Leukemia Genomics
| Reagent / Solution | Provider Example(s) | Function in Workflow |
|---|---|---|
| Anchored Multiplex PCR (AMP) Kits | Archer | Target enrichment for RNA-seq; enables discovery of novel fusion partners without prior knowledge of the partner gene [36]. |
| Digital MLPA Probe Mixes | MRC-Holland | Detection of recurrent microdeletions, amplifications, and gross chromosomal abnormalities from low-input DNA (50 ng) [35]. |
| OGM Labeling Kits & Chips | Bionano Genomics | Standardized reagents for ultra-high-molecular-weight DNA labeling, staining, and imaging on the Saphyr platform [36] [35]. |
| Targeted NGS Panels | Various (In-house & Commercial) | Simultaneous detection of SNVs, indels, CNAs, and fusions from limited DNA/RNA (e.g., 10 ng) [35]. |
| Bioinformatics Software Suites | Bionano Access/Solve, Ion Reporter, Archer Analysis | Specialized software for data analysis, variant calling, and interpretation; critical for standardizing the post-analytical phase [36] [35]. |
The future of standardization in acute leukemia diagnostics lies in the development of integrated, rather than replacement, models. The evidence clearly shows that NGS and emerging genomic technologies are complementary to each other and to traditional methods [36] [35]. Standardization efforts must therefore focus on:
- Multi-Modal Assay Validation: Establishing guidelines for validating testing approaches that combine RNA-seq, OGM, and DNA-based NGS to ensure comprehensive genomic characterization.
- Data Interchange Standards: Developing common data formats and quality metrics to facilitate the sharing and aggregation of genomic data across institutions, which is essential for drug development and biomarker discovery.
- Automation and Rapid Turnaround: Advancing automated workflows and newer sequencing technologies (e.g., nanopore sequencing) to address the critical issue of turnaround time, which currently favors PCR (7 days) over comprehensive NGS (28 days) [115].
- AI-Powered Integration: Leveraging artificial intelligence and machine learning to integrate complex multi-optic data, as demonstrated by tools like MARLIN, which uses DNA methylation and AI for rapid leukemia classification [32].
In conclusion, while NGS and other advanced technologies offer unparalleled resolution for molecular diagnosis in acute leukemia, their full potential in both clinical care and drug development will only be realized through concerted efforts in standardization and adaptive regulatory oversight. The goal is a future where standardized, multi-modal genomic profiling is completed in clinically actionable timeframes, providing a solid foundation for precision medicine.
Conclusion
The integration of NGS into acute leukemia diagnostics represents a fundamental shift from morphology-based to genetically-driven classification, enabling unprecedented precision in risk stratification and therapeutic decision-making. While traditional methods retain value for initial screening, NGS consistently demonstrates superior diagnostic yield, particularly for cryptic fusions and low-frequency mutations that directly impact clinical management. Current evidence confirms that NGS-based approaches detect clinically significant alterations in 84.5-95% of cases, far exceeding the capabilities of conventional methods. Future directions will focus on standardizing bioinformatics pipelines, reducing turnaround times, integrating artificial intelligence for variant interpretation, and expanding access to these technologies in diverse healthcare settings. For researchers and drug developers, these advancements create new opportunities for biomarker discovery, targeted therapy development, and innovative clinical trial designs based on molecular rather than morphological classification. The ongoing evolution of genomic technologies promises to further refine our understanding of leukemia pathogenesis and accelerate the development of personalized treatment approaches.
References
- 1. Research advances in the adjunctive diagnosis of acute ... [https://pubmed.ncbi.nlm.nih.gov/41127024/]
- 2. Research advances in the adjunctive diagnosis of acute ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1634935/full]
- 3. Genetic Profiling of Acute and Chronic Leukemia via Next- ... [https://www.mdpi.com/2038-8330/17/2/18]
- 4. Advancing leukemia diagnostics: Role of Next Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7520852/]
- 5. Frontiers | The emerging role of next-generation sequencing in minimal... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1570041/full]
- 6. Real-time genomic characterization of pediatric acute ... [https://www.nature.com/articles/s41375-025-02565-y]
- 7. The emerging role of next-generation sequencing in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12052730/]
- 8. Molecular Diagnosis of Leukemia - Page 10 [https://www.medscape.com/viewarticle/766770_10]
- 9. Multiparameter Flow Cytometry: Advances in High Resolution Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3659255/]
- 10. of Comparison Immunophenotypic... Multiparameter Flow Cytometry [https://pmc.ncbi.nlm.nih.gov/articles/PMC6272803/]
- 11. role of Lineage in acute leukemia assignment immunophenotyping [https://he01.tci-thaijo.org/index.php/bulletinAMS/article/view/60032]
- 12. A correlation study between the minimal residual disease detection... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7342875/]
- 13. Comparison between 8-COLOR multiparameter ... flow cytometry [https://library.ehaweb.org/eha/2016/21st/132842/hiroyuki.takamatsu.comparison.between.8-color.multiparameter.flow.cytometry.html?f=m3]
- 14. Frontiers | Multiparameter enables immune profiling... flow cytometry [https://www.frontiersin.org/journals/dental-medicine/articles/10.3389/fdmed.2025.1590516/full]
- 15. Best Practices for Multiparametric Flow Cytometry | Thermo Fisher Scientific - US [https://www.thermofisher.com/us/en/home/references/newsletters-and-journals/bioprobes-journal-of-cell-biology-applications/bioprobes-79/best-practices-multiparametric-flow-cytometry.html]
- 16. NGS检测医学实验室中各种性能指标的验证/确认 - 搜狐 [https://www.sohu.com/a/741758890_121124574]
- 17. Cytogenetics - Meaning, History, Techniques, and... - GeeksforGeeks [https://www.geeksforgeeks.org/biology/what-is-cytogenetics/]
- 18. , FISH, and PCR in acute lymphoblastic leukemia... Karyotyping [https://pubmed.ncbi.nlm.nih.gov/19875970/]
- 19. Genetic Profiling of Acute and Chronic Leukemia via Next - Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12026831/]
- 20. Array-based comparative genomic hybridization is more informative... [https://molecularcytogenetics.biomedcentral.com/articles/10.1186/1755-8166-5-33]
- 21. OBM Genetics | Validation of Fluorescence ... in Situ hybridization [https://www.lidsen.com/journals/genetics/genetics-07-01-177]
- 22. of Comparison , TCL1 karyotyping ... fluorescence in situ [https://pubmed.ncbi.nlm.nih.gov/28821581/]
- 23. myeloid Acute in the leukemia - next era generation sequencing [https://link.springer.com/article/10.1007/s00508-024-02463-w]
- 24. Clinical experience of using integrated whole genome and... [https://www.nature.com/articles/s41375-025-02774-5?error=cookies_not_supported&code=5a84674c-07b5-4b5d-9f24-5e789f89daef]
- 25. Advancing leukemia diagnostics: Role of Next Generation Sequencing (NGS) in acute myeloid leukemia - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7520852/]
- 26. [ Research Progress of Next in Generation ...] Sequencing Acute [https://pubmed.ncbi.nlm.nih.gov/37096544/]
- 27. of minimal residual disease in circulating cell-free DNA in... Detection [https://www.nature.com/articles/s41598-025-20589-3?error=cookies_not_supported&code=db9cd082-ab89-435d-9e22-004e8869b3fa]
- 28. Molecular Landscape and Validation of New Genomic Classification in... [https://pubmed.ncbi.nlm.nih.gov/36672386/]
- 29. NPM1 Mutation Quantitation in Sensitive Myeloid Acute ... Leukemia [https://pubmed.ncbi.nlm.nih.gov/29425073/]
- 30. Research advances in the adjunctive diagnosis of acute myeloid leukemia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12537407/]
- 31. Clinical experience of using integrated whole genome and... [https://www.nature.com/articles/s41375-025-02774-5?error=cookies_not_supported&code=03114e49-d176-4efd-9b30-31369366464a]
- 32. New Diagnostic Tool Developed at Dana-Farber Revolutionizes Acute Leukemia Diagnosis | Dana-Farber Cancer Institute [https://www.dana-farber.org/newsroom/news-releases/2025/new-diagnostic-tool-developed-at-dana-farber-revolutionizes-acute-leukemia-diagnosis]
- 33. Cutting-Edge Blood Cancer Diagnostics Unveiled at AMP 2025 [https://bioengineer.org/cutting-edge-blood-cancer-diagnostics-unveiled-at-amp-2025/]
- 34. New Research in Blood Cancer Diagnostics to... | Today's Clinical Lab [https://www.clinicallab.com/new-research-in-blood-cancer-diagnostics-to-be-featured-at-amp-2025-28476]
- 35. Benchmarking standard-of-care and emerging genomic ... [https://www.nature.com/articles/s41416-025-03204-0]
- 36. Comparative Analysis of Targeted RNA-Seq and Optical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12608001/]
- 37. Performance of Next Generation Sequencing for Minimal ... [https://www.sciencedirect.com/science/article/pii/S0006497121054112]
- 38. Measurable Residual Disease in Acute Myeloid Leukemia [https://www.thermofisher.com/io/en/home/clinical/preclinical-companion-diagnostic-development/oncomine-oncology/ngs-hemato-oncology/measurable-residual-disease-acute-myeloid-leukemia.html]
- 39. NGS Workflow Steps - Next-Generation Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/ngs-workflow.html]
- 40. for Beginners | Learn the basics of NGS NGS [https://www.illumina.com/science/technology/next-generation-sequencing/beginners.html]
- 41. 3 Innovations in Next-Generation Sequencing Sample Prep [https://dispendix.com/blog/3-innovations-in-next-generation-sequencing-sample-prep]
- 42. Next Generation Sequencing Platform: Ultimate Guide 2025 [https://lifebit.ai/blog/next-generation-sequencing-platform/]
- 43. Integration of Next-Generation Sequencing in Measurable ... [https://pubmed.ncbi.nlm.nih.gov/40940971/]
- 44. Hematologic Malignancy Profiling | Myeloid, lymphoma NGS panels [https://www.illumina.com/areas-of-interest/cancer/clinical-cancer-research/somatic-mutations/hematological-cancers.html]
- 45. Next Generation Sequencing Library Preparation Market to [https://www.globenewswire.com/news-release/2025/11/17/3189266/0/en/Next-Generation-Sequencing-Library-Preparation-Market-to-Reach-USD-4-83-Billion-by-2032-as-Demand-for-Precision-Genomics-Accelerates-SNS-Insider.html]
- 46. Next-generation sequencing in cancer diagnosis and treatment: clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12009796/]
- 47. Gene Sequencing Targeted Panels [https://emea.illumina.com/techniques/sequencing/dna-sequencing/targeted-resequencing/targeted-panels.html]
- 48. next generation sequencing ( Targeted ) | IDT NGS [https://www.idtdna.com/pages/technology/next-generation-sequencing/dna-sequencing/targeted-sequencing]
- 49. Panels, WES, or WGS: Which is Best for Rare Disease Diagnosis? [https://3billion.io/blog/which-is-the-best-ngs-approach-for-rare-disease-diagnosis-panels-wes-or-wgs]
- 50. WGS vs. WES vs. Targeted Sequencing Panels - CD Genomics [https://www.cd-genomics.com/resource-wgs-vs-wes-vs-targeted-panels.html]
- 51. - Whole . Genome - vs . Whole ... Exome Sequencing vs Targeted [https://www.healio.com/hematology-oncology/learn-genomics/whole-genome-sequencing/whole-genome-whole-exome-sequencing-and-targeted-sequencing-panels]
- 52. Gene Panel vs. Whole Exome Sequencing: Which Is Best for You? [https://3billion.io/blog/gene-panel-clinical-whole-exome-sequencing]
- 53. Targeted gene panels vs. whole exome sequencing – Genohub Blog [https://blog.genohub.com/2016/10/24/targeted-gene-panels-vs-whole-exome-sequencing/]
- 54. Efficacy and economics of targeted ... panel versus whole exome [https://pmc.ncbi.nlm.nih.gov/articles/PMC7870529/]
- 55. High clinical actionability of a pan-cancer tissue-based ... - Nature [https://www.nature.com/articles/s41698-025-01126-x]
- 56. Next-generation sequencing: 2025 Revolution [https://lifebit.ai/blog/next-generation-sequencing/]
- 57. A targeted next-generation sequencing panel for ... [https://www.nature.com/articles/s41598-025-08039-6]
- 58. Diagnostic accuracy of next-generation sequencing (NGS ... [https://pubmed.ncbi.nlm.nih.gov/40944810/]
- 59. Ultima Genomics UG 100 platform vs. Illumina NovaSeq X Series... [https://www.illumina.com/science/genomics-research/articles/ultima-ug-100-vs-illumina-novaseq-x-wgs-data.html]
- 60. Clinical experience of using integrated whole genome and... [https://www.nature.com/articles/s41375-025-02774-5?error=cookies_not_supported&code=a3ec8f4c-ffa1-4bb8-9121-8a78d2933b21]
- 61. Key considerations for comprehensive validation of an RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7322345/]
- 62. A More Accurate, Less Invasive Analysis for Lung Cancers [https://physicianresources.foxchase.org/news/a-more-accurate-less-invasive-analysis-for-lung-cancers-rna-next-generation-sequencing]
- 63. An accurate DNA and RNA based targeted sequencing ... [https://www.nature.com/articles/s41598-025-91640-6]
- 64. A Performance of Commonly Used Assays to Detect... Comparison [https://pmc.ncbi.nlm.nih.gov/articles/PMC8285056/]
- 65. Impact of Next-Generation Sequencing in Diagnosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10339965/]
- 66. Acute Myeloid Leukemia and Next-Generation Sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10956683/]
- 67. EHA/ELN guidance on blast reporting in acute leukemias [https://lymphoblastic-hub.com/medical-information/ehaeln-guidance-on-blast-reporting-in-acute-leukemias]
- 68. Measurable residual in hematologic malignancies... disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC12257026/]
- 69. The emerging role of next-generation sequencing in ... [https://pubmed.ncbi.nlm.nih.gov/40330780/]
- 70. Minimal Residual Disease Monitoring with Next-Generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6600313/]
- 71. Analytical and clinical validation of a novel in-house deep - sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5467041/]
- 72. Minimal residual disease detection by next-generation ... [https://www.nature.com/articles/s41467-023-43171-9]
- 73. Frontiers | Technical Validation and Clinical of an Utility ... NGS [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2022.854098/full]
- 74. AMP 2025 : Demystifying MRD with BloodPac: Navigating clinical and... [https://sapac.illumina.com/events/webinar/2025/amp-2025-demystifying-mrd-bloodpac-navigating-clinical-technical-pathways-comprehensive-cancer-monitoring.html]
- 75. Complete remission of NUP98 fusion-positive acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11959225/]
- 76. A new genomic framework to categorize pediatric acute ... [https://www.nature.com/articles/s41588-023-01640-3]
- 77. Detection of leukemia gene fusions on DNA-level through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12510534/]
- 78. Identification of novel NUP98 fusion partners and ... [https://www.sciencedirect.com/science/article/pii/S2473952924001939]
- 79. NUP98 fusion proteins and KMT2A-MENIN antagonize PRC1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11780541/]
- 80. Detection of leukemia gene fusions on DNA-level through ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0332407]
- 81. Beyond the Biopsy: A New Blood Test Is Redefining ... [https://www.onclive.com/view/beyond-the-biopsy-a-new-blood-test-is-redefining-the-fight-against-relapsed-aml]
- 82. The clinical utility and prognostic value of next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12202931/]
- 83. Transforming heart transplantation care with multi-omics insights [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06772-0]
- 84. The Role of Optical Genome Mapping in Acute Lymphoblastic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609272/]
- 85. Optical Genome Mapping: A 'Tool' with Significant Potential ... [https://www.cap.org/member-resources/articles/optical-genome-mapping-a-tool-with-significant-potential-from-discovery-to-diagnostics]
- 86. Optical genome mapping with whole genome sequencing ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1496847/full]
- 87. Optical Genome Mapping: A New Tool for Cytogenomic ... [https://www.mdpi.com/2073-4425/16/8/924]
- 88. Novel Tools to Improve the Challenging Diagnosis of Ph- ... [https://www.sciencedirect.com/science/article/abs/pii/S0006497124087482]
- 89. Comparison of Optical Genome Mapping With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10961627/]
- 90. Clinical Utility of Optical Genome Mapping as an Additional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070923/]
- 91. New genomic technologies and their application in ... [https://www.sciencedirect.com/science/article/pii/S2341287925003527]
- 92. Quantification of RNA integrity and its use for measurement ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3467039/]
- 93. Methods of RNA Quality Assessment [https://www.promega.com/resources/pubhub/methods-of-rna-quality-assessment/]
- 94. Is Your RNA Intact? Methods to Check RNA Integrity [https://www.thermofisher.com/us/en/home/references/ambion-tech-support/rna-isolation/tech-notes/is-your-rna-intact.html]
- 95. Improved Tumor Purity Metrics in Next-generation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6887630/]
- 96. Estimating and accounting for tumor purity in the analysis of ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-016-1143-5]
- 97. Rapid epigenomic classification of acute leukemia [https://www.nature.com/articles/s41588-025-02321-z]
- 98. Comparison of DNA Quantification Methods for Next ... [https://www.nature.com/articles/srep24067]
- 99. Measurable Residual Disease in Acute Myeloid Leukemia [https://www.thermofisher.com/ru/en/home/clinical/preclinical-companion-diagnostic-development/oncomine-oncology/ngs-hemato-oncology/measurable-residual-disease-acute-myeloid-leukemia.html]
- 100. myeloid Acute : from leukemia , through scRNA-seq, to... NGS [https://jeccr.biomedcentral.com/articles/10.1186/s13046-023-02841-8]
- 101. -defined measurable residual disease (MRD) after initial... NGS [https://www.nature.com/articles/s41408-023-00833-7?error=cookies_not_supported&code=8648cbf9-f913-42c2-8692-b47cdbce081c]
- 102. exploring the future of rapid leukaemia diagnosis with a ... [https://nanoporetech.com/resource-centre/case-study-exploring-the-future-of-rapid-leukaemia-diagnosis-with-a-single-platform-workflow]
- 103. Set-theory based benchmarking of three different variant callers for... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7791862/]
- 104. Challenges in the introduction of next-generation sequencing (NGS) for diagnostics of myeloid malignancies into clinical routine use | Blood Cancer Journal [https://www.nature.com/articles/s41408-018-0148-6]
- 105. Comprehensive Custom NGS Panel Validation for the Improvement of... [https://pubmed.ncbi.nlm.nih.gov/32967112/]
- 106. NGS vs Sanger Sequencing [https://www.illumina.com/science/technology/next-generation-sequencing/beginners/advantages/ngs-vs-sanger.html]
- 107. One in seven pathogenic variants can be challenging to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8460443/]
- 108. - Sanger Sequencing Versus Next Generation Sequencing [https://www.news-medical.net/life-sciences/Sanger-and-next-generation-compared.aspx]
- 109. AML Samples Show High Concordance in Detection of ... [https://pubmed.ncbi.nlm.nih.gov/37459200/]
- 110. How good are pathogenicity predictors in detecting benign ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1006481]
- 111. Horizon's Quest on Resolving Variant of Uncertain ... [https://genomearc.com/blog-show/MjA6OlRhbnZpclNS]
- 112. A Practical Guide to Clinical Variant Interpretation [https://www.euformatics.com/blog-post/a-practical-guide-to-clinical-variant-interpretation]
- 113. How can we make genetic testing and the interpretation ... [https://blogs.bcm.edu/2025/01/31/how-can-we-make-genetic-testing-and-the-interpretation-of-genetic-variations-more-fair-and-accurate/]
- 114. The promises and pitfalls of automated variant interpretation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12513165/]
- 115. Conventional PCR Versus Next Generation Sequencing for ... [https://www.mdpi.com/2072-6694/17/5/854/review_report]
- 116. Somatic mutations and clonal hematopoiesis [https://pmc.ncbi.nlm.nih.gov/articles/PMC5826570/]
- 117. Error-corrected ultradeep next-generation sequencing for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0318300]
- 118. Current and Emerging Techniques for Diagnosis and MRD ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10000116/]
- 119. Error-corrected ultradeep next-generation sequencing for ... [https://pubmed.ncbi.nlm.nih.gov/?linkname=pubmed_pubmed_citedin&from_uid=40009600]
- 120. Analysis of somatic mutations in whole blood from 200618 ... [https://www.nature.com/articles/s41588-024-01755-1]
- 121. Strategy for identification of a potential inherited leukemia ... [https://pubmed.ncbi.nlm.nih.gov/32512379/]
- 122. Sanger Sequencing vs. Next-Generation Sequencing (NGS) [https://www.cd-genomics.com/resource-sanger-sequencing-vs-next-generation-sequencing.html]
- 123. Next-Generation Sequencing Technology: Current Trends ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376292/]
- 124. Barcode-free next-generation sequencing error validation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6395625/]
- 125. Frontiers | Sequencing-Based Measurable Residual Disease Testing in... [https://www.frontiersin.org/journals/cell-and-developmental-biology/articles/10.3389/fcell.2020.00249/full]
- 126. Clinical impact of panel-based error - corrected next generation... [https://www.nature.com/articles/s41375-021-01131-6?error=cookies_not_supported&code=df51b402-d21e-4bf0-8af6-6b025cf8fb3b]
- 127. Clinical experience of using integrated whole genome and... [https://www.nature.com/articles/s41375-025-02774-5?error=cookies_not_supported&code=a10c2e31-ade8-4295-81bc-7a8060a32e4a]
- 128. Detection of leukemia gene fusions by targeted RNA-sequencing in... [https://bmcmedgenomics.biomedcentral.com/articles/10.1186/s12920-020-00739-4]
- 129. Cost of whole-genome sequencing approaching current ... [https://genomicmedicine.se/en/2024/09/03/cost-of-whole-genome-sequencing-approaching-current-routine-genetic-testing-in-blood-cancer/]
- 130. Permanent reimbursement for next-generation sequencing ( NGS ) in... [https://mtrconsult.com/news/permanent-reimbursement-next-generation-sequencing-ngs-oncology-launched-belgium-0]
- 131. The Cost Effectiveness of Genomic Medicine in Cancer ... [https://link.springer.com/article/10.1007/s40258-025-00949-w]
- 132. The Role of Next-Generation Sequencing and Reduced Time to... [https://www.emjreviews.com/hematology/article/the-role-of-next-generation-sequencing-and-reduced-time-to-diagnosis-in-haematological-diseases-status-quo-and-prospective-overview-of-promising-molecular-testing-approaches/]
- 133. fusion events in AML with Detecting NGS [https://www.ogt.com/resources/ngs-resources-and-support/ngs-resources/detecting-fusion-events-in-aml-with-ngs/]
- 134. Frontiers | Biomarkers in Acute Myeloid Leukemia : Leveraging Next... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.748250/full]
- 135. KMT2A/MLLT10 Cryptic by next-generation... fusion detected [https://pubmed.ncbi.nlm.nih.gov/37478796/]
- 136. Challenging Conventional Diagnostic Methods by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11913173/]
- 137. Superiority of targeted RNA sequencing for fusion detection ... [https://ehoonline.biomedcentral.com/articles/10.1186/s40164-025-00663-2]
- 138. Accurate and efficient detection of gene fusions from RNA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7919457/]
- 139. SplitFusion enables ultrasensitive gene fusion detection ... [https://www.sciencedirect.com/science/article/pii/S2666389925000224]
- 140. Clinical Utility of a Next-Generation Sequencing Panel for ... [https://www.sciencedirect.com/science/article/pii/S1525157817306141]
- 141. Comparative analysis of targeted next-generation sequencing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7927885/]
- 142. Improving Outcomes of ALL in Pediatric Patients with Sanger ... [https://www.thermofisher.com/blog/behindthebench/improving-clinical-outcomes-of-acute-lymphoblastic-leukemia-all-in-pediatric-patients-with-sanger-sequencing-and-fragment-analysis/]
- 143. High Accuracy Mutation Detection in Leukemia on a Selected Panel... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3366948/]
- 144. Next-Generation Sequencing in Acute Lymphoblastic Leukemia [https://pmc.ncbi.nlm.nih.gov/articles/PMC6627957/]
- 145. Classification and genetics of pediatric B-other acute ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10320209/]
- 146. Benchmarking standard-of-care and emerging genomic approaches to... [https://www.nature.com/articles/s41416-025-03204-0?error=cookies_not_supported&code=92d26336-eacb-416f-a72c-e7df066e4107]
- 147. Multimodal classification of molecular subtypes in pediatric ... [https://www.nature.com/articles/s41698-023-00479-5]
- 148. Identification of Molecular Subtypes of B-Cell Acute ... [https://www.mdpi.com/1422-0067/26/14/7003]
- 149. New research in blood cancer diagnostics to be featured at ... [https://www.eurekalert.org/news-releases/1103658]
- 150. Detection of minimal residual disease in circulating cell ... [https://www.nature.com/articles/s41598-025-20589-3]
- 151. Next-Generation Sequencing in Clinical Practice: Is It a Cost ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8160052/]
- 152. Acute Myeloid Leukemia: 2025 Update on Diagnosis, Risk ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11966364/]