Revolutionizing Neuropharmacology: Advances in 3D Bioprinted Blood-Brain Barrier Models for Drug Discovery
The blood-brain barrier (BBB) represents a major challenge in developing therapeutics for central nervous system diseases.
Revolutionizing Neuropharmacology: Advances in 3D Bioprinted Blood-Brain Barrier Models for Drug Discovery
Abstract
The blood-brain barrier (BBB) represents a major challenge in developing therapeutics for central nervous system diseases. This article explores the transformative role of three-dimensional (3D) bioprinting in creating physiologically relevant in vitro BBB models. We examine the foundational anatomy of the BBB, methodological advances in bioprinting techniques and bioink design, strategies for overcoming technical challenges in model fabrication, and validation frameworks for assessing model performance. For researchers, scientists, and drug development professionals, these engineered BBB constructs offer unprecedented opportunities to study neurodegenerative disease mechanisms, enhance drug permeability prediction, and accelerate CNS drug development with greater human relevance than traditional 2D cultures or animal models.
The Blood-Brain Barrier Blueprint: Anatomy, Function, and Modeling Imperatives
The neurovascular unit (NVU) represents a functional multicellular complex that is critical for maintaining the sophisticated microenvironment of the central nervous system (CNS). At its core lies the blood-brain barrier (BBB), a highly selective interface that not only protects the brain from potentially harmful substances in the blood but also regulates the transport of nutrients and essential molecules [1] [2]. The BBB's exceptional properties are not intrinsic to a single cell type but emerge from the continuous, dynamic interplay between brain microvascular endothelial cells (BMECs), pericytes, and astrocytes [1] [3]. This tri-cellular relationship forms the fundamental biological basis for advanced in vitro modeling, particularly through 3D bioprinting technologies that seek to recapitulate human neurovascular physiology for drug development and disease modeling [4] [5].
The growing emphasis on developing physiologically relevant in vitro models stems from recognized limitations of traditional systems. While animal models have provided foundational knowledge, they cannot fully mimic the complexity of the human brain due to species-specific adaptations, including differences in gene expression patterns, lipid profiles, and the proportion and complexity of astrocytes [1]. Furthermore, conventional 2D in vitro models fail to replicate the crucial dimensionality, cell-ECM interactions, and mechanical cues present in the native neurovascular environment [4]. The integration of 3D bioprinting technologies addresses these limitations by enabling precise spatial organization of multiple cell types within biomimetic hydrogels, creating engineered tissue constructs with enhanced physiological relevance for studying BBB function and pathology [4] [5].
Core Cellular Components of the NVU
Brain Microvascular Endothelial Cells (BMECs)
BMECs constitute the primary physical barrier between the blood and brain parenchyma. Unlike peripheral endothelial cells, BMECs exhibit distinctive morphological, structural, and functional characteristics that underlie their barrier properties [1] [2]. These include continuous, complex tight junctions (TJs) that significantly limit paracellular flux, an absence of fenestrations, minimal pinocytic activity, and expression of specialized transport mechanisms [1]. The TJs are molecularly unique structures composed of various proteins including claudins, occludins, junctional adhesion molecules (JAMs), and accessory proteins that collectively form the "physical barrier" of the BBB [1] [2].
BMECs also express specific enzymes and transporters that facilitate efficient nutrient transport into the CNS while actively effluxing toxic metabolites [1]. These functional capabilities are not autonomously established but depend on continuous signaling interactions with neighboring pericytes and astrocytes [1] [3]. The BMECs' strategic position allows them to serve as the interface for molecular exchange between the vascular system and neural tissue, making them the primary determinant of BBB selectivity and a critical component in 3D bioprinted BBB models [4] [5].
Pericytes
Pericytes are mural cells embedded within the basement membrane that intimately surround the brain microvascular endothelium. These cells play multifaceted roles in BBB development, maintenance, and regulation [2] [3]. Through the secretion of signaling factors such as vascular endothelial growth factor and transforming growth factor-beta, pericytes dynamically regulate endothelial tight junction integrity and permeability [2]. They are also involved in critical vascular processes including angiogenesis, vascular maturation, and regulation of cerebral blood flow [2] [3].
Experimental evidence from 3D human BBB-on-chip models demonstrates that pericytes contribute significantly to neuroinflammatory responses. When stimulated with inflammatory triggers like tumor necrosis factor-alpha (TNF-α), the presence of pericytes results in distinct secretion profiles for cytokines such as interleukin-6 (IL-6) and granulocyte colony-stimulating factor (G-CSF) [3]. This highlights the active role of pericytes in neuroimmune regulation beyond their structural support functions. In 3D bioprinting applications, incorporating pericytes is essential for establishing proper barrier function and replicating the cellular crosstalk that maintains BBB integrity [4] [6].
Astrocytes
Astrocytes, the most abundant glial cells in the CNS, extend numerous end-feet processes that extensively cover the abluminal surface of brain capillaries. These end-feet formations create an almost continuous envelope around the microvasculature, facilitating bidirectional communication between vascular and neural compartments [1] [2]. Astrocytes promote endothelial cell differentiation and enhance tight junction stability through the release of soluble factors including brain-derived neurotrophic factor [2]. They also indirectly regulate nutrient transport efficiency by sensing and responding to metabolic demands within the brain parenchyma [2].
Human brains possess a higher proportion and complexity of neocortical astrocytes compared to rodent brains, underscoring the importance of human-cell-based models for translational research [1]. Astrocytes exhibit numerous receptors involved in innate immunity and, when activated, secrete soluble factors mediating both innate and adaptive immune responses [3]. In engineered 3D BBB models, the inclusion of astrocytes is crucial for replicating the neurovascular interface, as they provide essential cues for BMEC differentiation and barrier function while contributing to the neuroinflammatory responses observed in pathological conditions [3] [6].
Table 1: Quantitative Characteristics of Human Brain Microvasculature and Cellular Components
| Parameter | Value | Significance |
|---|---|---|
| Total microvessel length | ~600 km | Extensive surface area for blood-brain exchange [7] |
| Microvessel density | ~500 m/cm³ | High vascularization meets metabolic demands [7] |
| Neuron density scaling | ∝ V⁻¹⁄⁶ | Inverse relationship with brain volume across species [7] |
| Capillary diameter | 7-10 μm | Smaller than peripheral capillaries [7] |
| Intercapillary distance | ~40 μm | Ensures oxygen diffusion to all neurons [7] |
| Neuron-to-capillary distance | 10-20 μm | Optimized for nutrient/waste exchange [7] |
Cell-Cell Signaling and Functional Integration
The functional integrity of the BBB emerges from sophisticated cell-cell signaling between BMECs, pericytes, and astrocytes. This signaling occurs through both direct contact and paracrine mechanisms, creating a dynamic regulatory network that maintains CNS homeostasis [3] [6]. Several evolutionarily conserved signaling pathways have been identified as crucial for BBB development and function, including Wnt/β-catenin, retinoic acid, and sonic hedgehog pathways [6]. Recent research has revealed that the endothelial transmembrane receptor Unc5B and its ligand netrin-1 regulate BBB integrity by maintaining Wnt/β-catenin signaling [6].
In neuroinflammatory conditions, the distinct contributions of each cell type become particularly evident. When exposed to inflammatory triggers such as TNF-α, the cellular components of the NVU respond with cell-type-specific cytokine secretion patterns [3]. Studies using 3D human BBB-on-chip models have demonstrated that the presence of astrocytes or pericytes significantly influences the secretion profiles of G-CSF and IL-6, with response levels significantly greater than those observed in static Transwell co-culture systems [3]. This highlights the importance of physiologically relevant models for studying neurovascular inflammation and cell-type-specific contributions to disease processes.
Diagram 1: NVU signaling and inflammation response pathways.
3D Bioprinting Strategies for NVU Modeling
3D bioprinting has emerged as a powerful biofabrication technology for creating sophisticated in vitro models of the NVU that better replicate the human brain's cellular composition, microenvironment, and architecture [1] [4]. Unlike traditional 2D models or self-assembled organoids, 3D bioprinting offers precise control over tissue architecture and matrix properties while maintaining good cell viability [4]. This precision is particularly valuable for modeling complex structures like the NVU, where the spatial arrangement of different cell types directly influences functionality [4] [5].
The fundamental approach to bioprinting NVU models involves depositing cell-laden hydrogels (bioinks) in predefined patterns to recreate the hierarchical structure of brain tissue [1] [4]. These biofabrication strategies can be categorized based on whether cellular components are seeded onto constructs after device fabrication or encapsulated in biomaterials during the fabrication process [4]. The cell-encapsulating approach enables superior control over cell number and positioning, resulting in better reproducibility, and allows cells to encounter ECM cues from all directions, resembling their physiological state [4]. Common bioprinting modalities include extrusion-based, inkjet, and stereolithographic systems, each with distinct advantages for specific aspects of NVU modeling [4].
Advanced 3D-bioprinted BBB models incorporate multiple cell types (BMECs, pericytes, and astrocytes) within a vascular-like architecture, often using collagen gels or other biomimetic hydrogels as the supporting matrix [3]. These models can better replicate the cylindrical geometry of brain microvessels and incorporate relevant mechanical cues compared to rigid ECM substrates used in conventional models [3]. The ability to create reproducible, personalized models makes 3D bioprinting especially suitable for modeling diseases with high interpatient heterogeneity, such as glioblastoma [4].
Table 2: Advanced 3D Bioprinting Models of the NVU/BBB
| Model Type | Key Features | Advantages | Reference |
|---|---|---|---|
| 3D BBB-on-a-chip | Cylindrical collagen gel with hollow lumen; Primary human BMECs, pericytes, astrocytes | Permits analysis of individual cell type contributions; Enhanced neuroinflammatory responses | [3] |
| 3D-bioprinted GBM/BBB | Patient-derived cells; Controlled spatial organization in hydrogels | Reproducible, personalized models for high heterogeneity diseases | [4] |
| Microfluidic BBB models | Integration of fluid flow and shear stress; Real-time permeability monitoring | Dynamic conditions better mimic physiology; Suitable for drug transport studies | [8] [9] |
Experimental Protocols for NVU Modeling
3D Human BBB-on-Chip Fabrication
This protocol outlines the methodology for creating a microengineered 3D model of the human BBB within a microfluidic chip, adapted from Herland et al. [3]. The model recapitulates key features of the neurovascular unit, including a cylindrical vascular structure, relevant cellular components, and physiological flow conditions.
Materials and Reagents:
- Primary human brain microvascular endothelial cells (hBMVECs)
- Primary human brain pericytes
- Primary human astrocytes
- Collagen type I solution
- Sylgard 184 polydimethylsiloxane (PDMS)
- Microfluidic channel molds (1 mm width × 1 mm height × 20 mm length)
- CSC complete medium
- Astrocyte medium
- Attachment factor
Procedure:
Microfluidic Device Fabrication:
- Produce microfluidic devices using soft lithography with PDMS.
- Pour degassed 10:1 base:crosslinking PDMS mix onto the mold.
- Crosslink at 80°C for 18 hours.
- Punch inlets and outlets of 1.5 mm diameter in the molded PDMS.
- Bond the device to a 100 μm layer of spin-coated PDMS using oxygen plasma treatment (50 W for 20 seconds).
- Bake at 80°C for 18 hours to strengthen bonding.
Collagen Gel Preparation and Loading:
- Prepare collagen solution according to manufacturer's instructions.
- Inject collagen solution into the microfluidic channel and allow polymerization at 37°C.
- Create a central hollow lumen within the collagen gel using a needle or similar implement.
Cell Seeding and Culture:
- Culture hBMVECs on the inner surface of the collagen gel lumen.
- For co-culture models, seed primary human brain pericytes beneath the endothelium or primary human brain astrocytes within the surrounding collagen gel.
- Initiate medium flow through the lumen after cell attachment.
- Maintain cells with appropriate media (CSC complete medium for hBMVECs and pericytes, Astrocyte medium for astrocytes).
- Culture for 5-7 days to establish mature barrier function before experimentation.
Barrier Function Assessment:
- Measure transendothelial electrical resistance (TEER) using microelectrodes.
- Perform permeability assays with fluorescent tracers (e.g., FITC-dextran).
- Assess tight junction localization via immunostaining for ZO-1, occludin, and claudin-5.
Inflammatory Stimulation and Cytokine Analysis
This protocol describes the methodology for evaluating neuroinflammatory responses in 3D BBB models, enabling the identification of distinct contributions from astrocytes and pericytes [3].
Materials and Reagents:
- Recombinant human TNF-α
- Cell culture media appropriate for the BBB model
- Multiplex cytokine assay kits (e.g., for G-CSF, IL-6)
- Collection tubes for conditioned media
Procedure:
Inflammatory Stimulation:
- Replace culture media with fresh media containing TNF-α (recommended starting concentration: 10-100 ng/mL).
- Include control conditions without TNF-α stimulation.
- Incubate for 6-24 hours depending on experimental objectives.
Conditioned Media Collection:
- Collect conditioned media from each experimental condition at designated time points.
- Centrifuge media to remove cellular debris (1000 × g, 10 minutes).
- Aliquot and store supernatants at -80°C until analysis.
Cytokine Measurement:
- Quantify cytokine levels (G-CSF, IL-6) using multiplex bead-based immunoassays or ELISA according to manufacturer protocols.
- Normalize cytokine concentrations to total protein content or cell number.
- Compare secretion profiles between different cellular configurations (endothelium alone, endothelium with pericytes, endothelium with astrocytes).
Data Analysis:
- Perform statistical analysis to identify significant differences in cytokine secretion between conditions.
- Relate cytokine profiles to barrier function measurements from parallel experiments.
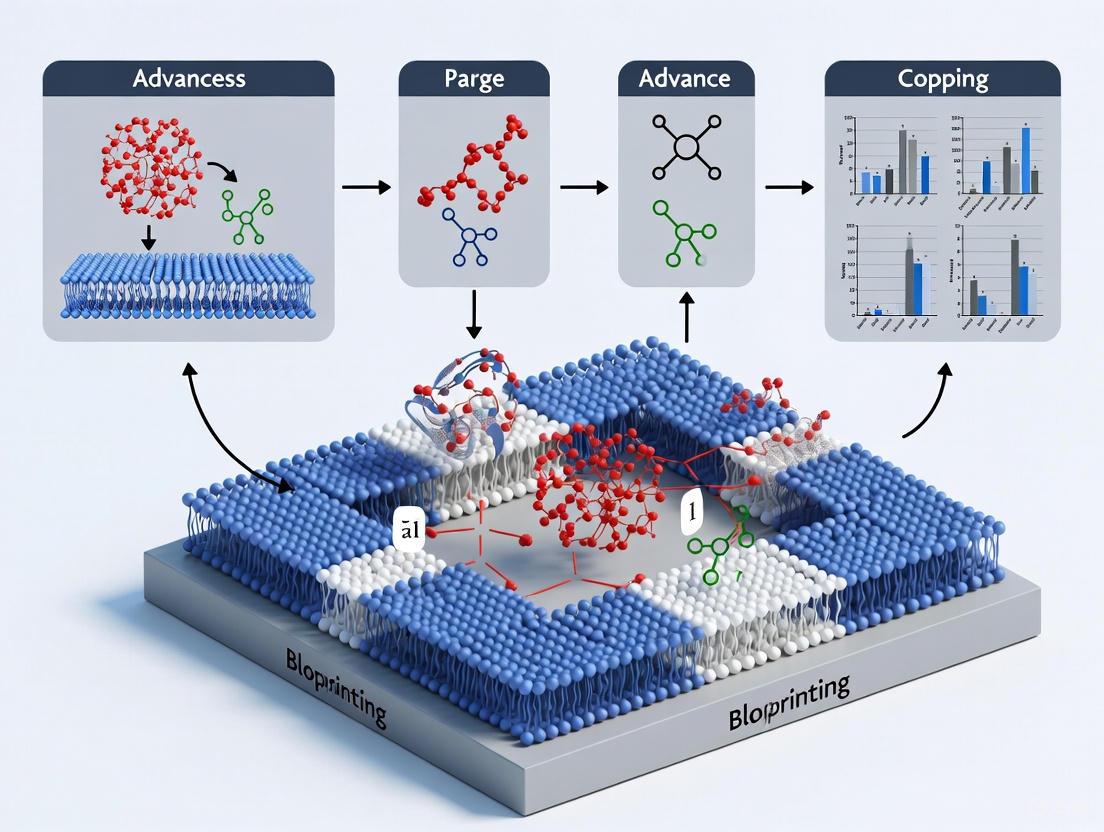
Diagram 2: 3D BBB model fabrication and analysis workflow.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for 3D NVU Modeling
| Reagent/Material | Function/Application | Specific Examples |
|---|---|---|
| Primary Human BMVECs | Core barrier-forming endothelial cells | Human brain microvascular endothelial cells (hBMVECs) from cortical origin [3] |
| Primary Human Pericytes | Vascular support and barrier regulation | Human brain pericytes from cortical origin [3] |
| Primary Human Astrocytes | Glial support and barrier induction | Human astrocytes of cortical origin [3] |
| Collagen Type I | Natural hydrogel for 3D matrix support | Cylindrical collagen gel containing central hollow lumen [3] |
| PDMS | Microfluidic device fabrication | Sylgard 184 polydimethylsiloxane [3] |
| TNF-α | Pro-inflammatory stimulus for barrier challenge | Recombinant human TNF-α for neuroinflammatory studies [3] |
| Cytokine Assays | Quantification of inflammatory responses | Multiplex assays for G-CSF, IL-6 measurement [3] |
The cellular architecture of the neurovascular unit, comprising BMECs, pericytes, and astrocytes, represents a highly integrated system whose functionality emerges from sophisticated intercellular crosstalk. Understanding this tri-cellular relationship is fundamental to advancing 3D bioprinting technologies for creating physiologically relevant BBB models. These advanced models demonstrate superior performance in recapitulating human neurovascular physiology, particularly in complex processes such as neuroinflammation where the distinct contributions of individual cell types become evident [3].
The continued refinement of 3D-bioprinted NVU models holds significant promise for transforming neuroscience research and drug development. By incorporating patient-derived cells and controlling spatial organization within biomimetic hydrogels, these models offer unprecedented opportunities for studying disease mechanisms, screening neurotherapeutics, and developing personalized medicine approaches for neurological disorders [4] [5]. As bioprinting technologies evolve to better replicate the dynamic mechanical and biochemical microenvironment of the native neurovascular unit, they will increasingly bridge the gap between conventional in vitro models and in vivo physiology, accelerating the development of effective therapies for CNS disorders.
The blood-brain barrier (BBB) is a highly selective, dynamic interface that separates the central nervous system (CNS) from the systemic circulation, maintaining the precise microenvironment required for neural function and protecting the brain from blood-borne pathogens and toxins [10] [11]. This barrier function primarily resides at the level of the endothelial cells lining cerebral microvessels, which are uniquely characterized by robust, continuous tight junctions that eliminate the paracellular space between adjacent cells [12] [11]. These junctional complexes are more than just physical seals; they are dynamic structures that regulate paracellular permeability, help maintain cellular polarity, and contribute to signaling pathways that control proliferation and differentiation [12].
The integrity of the BBB is critically dependent on the molecular composition of tight junctions, whose key transmembrane proteins include occludin, claudins, and junctional adhesion molecules (JAMs) [12] [13]. These proteins are connected to the actin cytoskeleton via intracellular scaffold proteins, such as zonula occludens (ZO)-1 and ZO-2, forming a supramolecular complex that is essential for barrier properties [12] [14]. Dysregulation of these proteins is a hallmark of BBB breakdown in numerous neurological conditions, including ischemic stroke, multiple sclerosis, and neurodegenerative diseases, and also presents a major challenge for the delivery of therapeutics to the CNS [15] [14] [11].
Recent advances in 3D bioprinting are revolutionizing the study of these proteins by enabling the creation of sophisticated, physiologically relevant human BBB models [16] [10] [13]. These in vitro platforms incorporate multiple cell types, perfusable flow, and customized extracellular matrices, providing unprecedented opportunities to investigate tight junction biology, model neurological diseases, and screen for drugs designed to modulate barrier permeability [16] [13]. This whitepaper provides an in-depth technical review of the core tight junction proteins—occludin, claudins, and JAMs—and details their critical role in barrier integrity within the context of modern 3D bioprinting research.
Structural and Functional Anatomy of Tight Junctions
The Supramolecular Complex of the Tight Junction
Tight junctions (TJs) form an apical belt-like network of protein strands between neighboring endothelial and epithelial cells, creating the primary seal that limits the paracellular diffusion of solutes, ions, and cells [12]. Ultrastructurally, these strands appear in freeze-fracture electron micrographs as closely spaced particles with a diameter of approximately 10 nm [12]. The TJ is not a simple static seal but a dynamic, multi-protein complex composed of transmembrane proteins, cytoplasmic plaque proteins, and their links to the cytoskeleton.
The figure below illustrates the organization of this supramolecular complex and its critical role in maintaining the blood-brain barrier.
- Transmembrane Proteins: The core sealing function is provided by the claudin family, which polymerizes to form the primary paracellular seal [12]. Occludin contributes to the regulation of solute diffusion and TJ dynamics, while JAMs are involved in the initial establishment of cell-cell contacts and leukocyte transmigration [12] [13].
- Scaffold Proteins and Cytoskeletal Linkage: Intracellularly, the zonula occludens (ZO) proteins, particularly ZO-1 and ZO-2, serve as critical plaque proteins [12] [14]. They contain multiple protein-binding domains, including PDZ domains, which allow them to simultaneously bind the cytoplasmic tails of claudins, occludin, and JAMs, and connect the entire complex to the actin cytoskeleton [12]. This linkage is vital for both the structural stability of the TJ and its ability to rapidly respond to extracellular and intracellular signals.
Core Tight Junction Proteins: Composition and Properties
The functional properties of the TJ are determined by the specific composition and stoichiometry of its transmembrane proteins. The table below summarizes the key characteristics of the major TJ protein families.
Table 1: Core Tight Junction Transmembrane Proteins
| Protein Family | Key Members at BBB | Gene (Human) | Molecular Weight | Primary Function | Structural Features |
|---|---|---|---|---|---|
| Claudins [12] [11] | Claudin-5, -3, -1 | CLDN5 (Chr. 22) | 20-29 kDa | Primary seal formation; determines paracellular charge and size selectivity [12]. | - 4 transmembrane domains- Two extracellular loops (ECL1 & ECL2)- N- and C-terminal cytoplasmic tails- PDZ-binding motif on C-terminus [11]. |
| Occludin [12] [14] | Occludin | OCLN | ~65 kDa | Regulates paracellular diffusion and TJ stability; signaling functions [14]. | - 4 transmembrane domains- Two extracellular loops- C-terminal cytoplasmic tail binds ZO proteins. |
| JAMs [12] [13] | JAM-A (JAM-1) | F11R | ~32 kDa | Cell adhesion; leukocyte transmigration; early TJ assembly [13]. | - Single transmembrane domain- Two extracellular Ig-like domains- PDZ-binding motif on C-terminus. |
In-Depth Analysis of Key Tight Junction Proteins
Claudins: The Architects of Paracellular Selectivity
The claudin family, with its 27 known members, forms the backbone of tight junction strands and is the principal determinant of paracellular permeability properties [12] [17]. These ~20-29 kDa proteins contain four transmembrane domains, two extracellular loops (ECL1 and ECL2), and intracellular N- and C-terminal tails. The first extracellular loop (ECL1) is particularly critical for the barrier function, containing a consensus sequence with two cysteine residues that form a disulfide bridge, which is essential for the sealing function [12] [11]. The second extracellular loop (ECL2) is involved in strand formation via trans-interactions between claudins on adjacent cells [11]. Most claudins possess a C-terminal PDZ-binding motif that facilitates interaction with scaffold proteins like ZO-1 [12].
Claudin-5 is the most abundant and best-studied claudin at the BBB. Its mRNA levels are approximately 600 times higher than those of other claudins found at the barrier, such as claudin-1, -3, and -12 [11]. It is often termed the "gatekeeper" of the BBB, and its deletion in mouse models leads to a selective increase in permeability to small molecules (<800 Da) while the barrier remains intact against larger molecules [11]. Its expression is regulated by signals from other cells in the neurovascular unit, notably Sonic Hedgehog (SHH) secreted from astrocytes [11].
Other claudins present at the BBB include claudin-3, which also contributes to barrier tightness, and claudin-1 [13] [11]. The specific combination and density of different claudin types determine the overall permeability and ion selectivity of the paracellular pathway.
Table 2: Functional Roles of Selected Claudin Family Members
| Claudin | Primary Tissue/Barrier Expression | Paracellular Function | Relevance to BBB & Disease |
|---|---|---|---|
| Claudin-5 [12] [11] | Brain endothelial cells (BBB) | Forms a tight seal against small molecules [11]. | Critical for BBB integrity; downregulation implicated in stroke, MS, and psychiatric disorders [11]. |
| Claudin-1 [12] [17] | Skin, liver, BBB | Maintains tight junction integrity. | Downregulation increases BBB permeability and may facilitate tumor cell invasion [17]. |
| Claudin-3 [13] [11] | Brain endothelial cells, epithelia | Contributes to tight junction formation. | Expressed at the BBB; role in barrier function is an active area of research [13]. |
| Claudin-11 [12] | Oligodendrocytes, Sertoli cells | Forms electrical seal in myelin; blood-testis barrier. | Not a BBB component, but critical for CNS insulation. |
Occludin: A Key Regulatory Protein
Occludin was the first transmembrane protein identified in TJs. While not essential for the initial formation of TJ strands, it plays a crucial modulatory role in barrier function. In vitro studies have long suggested its importance in regulating paracellular diffusion of solutes and TJ stability [14].
Recent in vivo evidence using occludin-deficient mice subjected to ischemic stroke has solidified its critical role. These mice exhibited:
- Continuously impaired neurological function compared to wild-type mice.
- Increased BBB permeability in both acute and chronic phases after stroke, as measured by leakage of Evans blue and fluorescent tracers.
- Larger infarct volumes and higher post-stroke mortality.
- Reduced expression of claudin-5 and ZO-1, suggesting occludin is necessary for maintaining the full expression of other key TJ components [14].
This study demonstrates that occludin plays a vital role in the pathophysiology of stroke, modulating BBB integrity and long-term neurological outcome.
Junctional Adhesion Molecules (JAMs): Multifunctional Adhesion Proteins
JAMs are immunoglobulin superfamily proteins that localize to tight junctions and are involved in a diverse set of functions. They contribute to the early stages of TJ assembly by promoting homophilic trans-interactions between adjacent endothelial cells [12] [13]. Beyond their structural role, JAMs are critically involved in regulating the transmigration of leukocytes across the endothelium during inflammatory responses [12]. For example, JAM-1 is essential for BBB integrity and is implicated in the inflammatory processes of diseases like multiple sclerosis [13].
Tight Junction Dysfunction in Neurological Pathologies
Dysregulation of tight junction proteins is a common pathogenic mechanism in a wide array of neurological disorders, leading to BBB breakdown and subsequent neuronal damage.
- Ischemic Stroke: Following cerebral ischemia, a biphasic opening of the BBB occurs, with permeability peaks at 3h and 72h after reperfusion [15]. This correlates with a significant decrease in the mRNA and protein expression of claudin-5, occludin, and ZO-1, as well as a redistribution of these proteins away from the cell borders [15] [14]. The protein kinase C delta (PKCδ) pathway has been implicated in this TJ disruption [15].
- Neurodegenerative Diseases (NDDs): BBB dysfunction is an early hallmark of Alzheimer's disease (AD) and Parkinson's disease (PD) [10] [13]. In AD, impaired clearance of amyloid-beta (Aβ) and disruption of TJ proteins contribute to disease progression [13]. Similarly, in PD, BBB breakdown may allow entry of neurotoxins and inflammatory mediators that exacerbate the pathology linked to misfolded alpha-synuclein [13].
- Neuroinflammation (e.g., Multiple Sclerosis): In experimental autoimmune encephalomyelitis (EAE), a model for MS, 3D imaging reveals a heterogeneous and fragmented loss of claudin-5 staining, particularly in venules, which are the primary sites of leukocyte extravasation [18]. This focal disruption of TJs is a key step in allowing immune cells to invade the CNS.
- Brain Metastases: Tumor cells from cancers such as lung cancer, breast cancer, and melanoma must breach the BBB to form metastatic lesions in the brain. They achieve this by altering the expression of TJ proteins, particularly claudin-5, thereby increasing BBB permeability and facilitating their transmigration [19] [17].
3D Bioprinting for Advanced BBB Modeling
Two-dimensional (2D) Transwell cultures have been the workhorse of in vitro BBB modeling but fail to recapitulate the spatial geometry, fluid shear stress, and complex cell-cell interactions of the native neurovascular unit [16] [10]. 3D bioprinting has emerged as a powerful technology to overcome these limitations by creating customizable, physiologically relevant human BBB models.
Key Design Considerations for 3D Bioprinted BBB Models
To create a mini-BBB that accurately mimics in vivo function, several key parameters must be addressed:
- Cellular Composition: The model must incorporate the three key cell types of the neurovascular unit: brain microvascular endothelial cells (BMECs), pericytes, and astrocytes [10] [13]. The inclusion of all three enhances TJ formation and barrier tightness.
- Perfusable Flow and Shear Stress: Incorporating dynamic flow is critical to apply physiological shear stress (5–23 dyn/cm²), which influences endothelial cell alignment, morphology, and upregulation of TJ proteins [13].
- Physiological Parameters: The model should strive to replicate in vivo metrics, including capillary-like diameters of 7–10 μm and trans-endothelial electrical resistance (TEER) values ranging from 1,500 to 8,000 Ω·cm² [13].
Experimental Workflow for 3D Bioprinting a Human BBB Model
The following diagram outlines a generalized protocol for creating and validating a 3D bioprinted BBB model, integrating key steps from recent research.
Detailed Experimental Protocol: Bioprinting a Vascularized BBB Model for TBI Research
Based on a study by Galpayage Dona et al. (2021) that used a CELLINK LUMEN X DLP bioprinter, the following protocol can be adapted to model Tight Junction disruption in Traumatic Brain Injury (TBI) [16].
Objective: To create a 3D vascularized BBB model and subject it to a stretch injury (TBI model) to study subsequent TJ disruption and barrier dysfunction.
Materials and Reagents: Table 3: Research Reagent Solutions for 3D BBB Bioprinting
| Item | Function/Description | Example/Source |
|---|---|---|
| PEGDA PhotoInk [16] | Synthetic hydrogel polymer; provides structural integrity and tunable mechanical properties. | CELLINK (Note: Specific product lines updated) |
| GelMA PhotoInk [16] | Methacrylated gelatin; provides natural cell-adhesion motifs within the hydrogel matrix. | CELLINK (Note: Specific product lines updated) |
| Primary Human Brain Microvascular Endothelial Cells (HBMECs) [16] | The core cell type forming the barrier; primary cells are preferred for physiological relevance. | Commercial cell vendors |
| DL-based 3D Bioprinter [16] | High-resolution printer for crosslinking photosensitive bioinks into complex 3D microfluidic scaffolds. | e.g., CELLINK LUMEN X |
| Perfusion System [16] | Mimics blood flow; provides shear stress critical for endothelial cell function and TJ formation. | Custom or commercial microfluidic systems |
| Antibodies for Immunostaining [18] | For visualizing and quantifying TJ proteins (e.g., anti-Claudin-5, anti-Occludin, anti-ZO-1). | Multiple commercial suppliers |
Methodology:
- Bioink Preparation and Bioprinting: Prepare a combination of PEGDA and GelMA PhotoInks. Using the DLP bioprinter, fabricate a 3D cube containing a network of microchannels with diameters ranging from 100 to 300 microns, based on a pre-designed CAD file [16].
- Cell Seeding and Culture: On day 1 post-printing, seed primary human brain microvascular endothelial cells (HBMECs) into the lumens of the bioprinted scaffold. Allow the cells to adhere and form a confluent, endothelialized monolayer over 5-7 days of culture [16].
- Barrier Maturation and Validation: Connect the endothelialized scaffold to a perfusion apparatus to introduce physiological flow. Validate barrier integrity at day 7 by measuring the permeability to fluorescent tracers (e.g., dextran) that should be blocked by an intact BBB, and/or by immunostaining for claudin-5 and occludin to confirm proper TJ formation [16].
- TBI Induction via Stretch Injury: On day 7, apply a controlled tensile strain to the 3D model using a stretching device to simulate a traumatic brain injury [16].
- Post-Injury Analysis:
- Permeability Assay: Post-injury, re-perfuse with dextran to quantify any increase in permeability, indicating BBB dysfunction.
- TJ Protein Analysis: Fix the model at various time points post-injury and perform immunofluorescence staining for claudin-5, occludin, and ZO-1. Use 3D imaging and analysis software to quantify changes in protein expression, density, and localization [18].
Quantitative Analysis of TJ Proteins in 3D Models
Advanced 3D imaging and quantification techniques are essential for accurately assessing TJ integrity in complex models. A study by Paul et al. (2013) demonstrated a method for 3D contour-based segmentation of spinal cord microvessels to quantify junctional claudin-5 density [18]. The workflow involves:
- Acquiring confocal z-stacks of thick (e.g., 60µm) tissue sections or 3D models immunostained for claudin-5 and a vascular marker (e.g., Laminin).
- Using software (e.g., Imaris) to create an individual contour for each confocal z-slice by tracing the vessel of interest.
- Merging the individual contours into a single 3D contour surface, which is used to isolate the microvessel and estimate its surface area.
- Creating an isosurface for the claudin-5 signal within the contoured volume to calculate the number of voxels and their intensity, providing a measure of claudin-5 density [18].
This approach allows researchers to move beyond qualitative assessments and obtain precise, quantitative data on TJ protein expression in specific vascular segments under normal and pathological conditions.
The tight junction proteins occludin, claudins, and JAMs form a sophisticated complex that is fundamental to the integrity and function of the blood-brain barrier. A deep understanding of their structure, interactions, and regulation is crucial for elucidating the pathogenesis of a wide spectrum of neurological diseases and for developing strategies to enhance drug delivery to the CNS. The advent of 3D bioprinting technology marks a significant leap forward, providing researchers with powerful, human-relevant models to study these proteins in a physiologically authentic context. These advanced in vitro systems enable the dissection of molecular mechanisms underlying TJ disruption in disease, the screening of therapeutics designed to restore barrier function, and the generation of personalized models for precision medicine. As bioprinting resolution, bioink fidelity, and functional validation continue to improve, these 3D-bioprinted BBB models are poised to become an indispensable tool in translational neuroscience research.
The blood-brain barrier (BBB) is a highly selective, multi-component interface that rigorously controls molecular exchange between the bloodstream and the central nervous system (CNS). This dynamic barrier is formed by brain capillary endothelial cells (BCECs) whose maturation and function depend on intricate interactions with astrocytes, pericytes, and neurons, collectively forming the neurovascular unit (NVU) [20] [10]. The BBB's primary function is to maintain brain homeostasis by protecting neural tissue from neurotoxic plasma components, blood cells, and pathogens while ensuring optimal neuronal function [13]. For researchers developing CNS therapeutics, the BBB presents a formidable delivery challenge, as it selectively restricts the passage of most pharmaceutical agents [20] [21].
Understanding the specialized transport mechanisms that govern molecular transit across the BBB is crucial for advancing neurological drug development. These pathways can be broadly categorized into three principal systems: solute carriers (SLCs) for facilitated transport of small molecules, receptor-mediated transcytosis (RMT) for macromolecule delivery, and ATP-binding cassette (ABC) efflux pumps that actively exclude xenobiotics [20] [22] [23]. The emergence of sophisticated 3D bioprinted BBB models now provides unprecedented opportunities to study these transport mechanisms in physiologically relevant human systems, offering insights that could accelerate the development of CNS-targeted therapies [13] [24].
Solute Carrier (SLC) Transport Systems
Solute carriers represent a large superfamily of membrane transport proteins that facilitate the movement of essential nutrients, ions, and metabolites across the BBB. These transporters are crucial for maintaining the nutritional and metabolic balance required for proper brain function. The SLC superfamily includes 244 genes expressed in brain microvessels, encompassing transporters for glucose (slc2a1), lactate (slc16a1), cationic amino acids (slc7a1), and neutral amino acids (slc7a5) [25].
Mechanism and Classification of SLC Transporters
SLC transporters primarily operate through facilitated diffusion or secondary active transport mechanisms. Facilitated diffusion involves the passive movement of substrates down their concentration gradients without energy expenditure, while secondary active transport couples substrate movement to ion gradients (typically Na+) to drive accumulation against concentration gradients [22] [25]. These transporters can be further categorized based on their membrane polarization within brain endothelial cells, with distinct transporters strategically localized to either the luminal (blood-facing) or abluminal (brain-facing) membranes to enable vectorial transport of substrates [25].
A key feature of many SLC transporters is their exchange mechanism, where the influx of one substrate is coupled to the efflux of another. For instance, the large neutral amino acid transporter LAT1 (SLC7A5) facilitates the uptake of essential amino acids into the brain in exchange for intracellular glutamine [25]. This antiport system enables the brain to acquire dietary essential amino acids that cannot be synthesized internally while simultaneously eliminating potentially neurotoxic metabolites.
Major SLC Transporter Families at the BBB
Table 1: Key SLC Transporters at the Blood-Brain Barrier
| Transporter Family | Representative Members | Substrates | Transport Mechanism | Localization |
|---|---|---|---|---|
| Amino Acid Transporters | LAT1 (SLC7A5/SLC3A2) | Large neutral AAs (phenylalanine, leucine) | Facilitated diffusion (antiport) | Luminal & abluminal |
| CAT1 (SLC7A1) | Cationic AAs (arginine, lysine) | Facilitated diffusion | Primarily luminal | |
| EAAT1-3 (SLC1A1-3) | Acidic AAs (glutamate, aspartate) | Na+-dependent symport | Primarily abluminal | |
| Carbohydrate Transporters | GLUT1 (SLC2A1) | Glucose, galactose | Facilitated diffusion | Luminal & abluminal |
| Monocarboxylate Transporters | MCT1 (SLC16A1) | Lactate, pyruvate, ketone bodies | H+-coupled symport | Luminal & abluminal |
| Organic Anion/Cation Transporters | OATP1A2 (SLCO1A2) | Organic anions, steroids | Na+-independent exchange | Luminal |
| OCTN2 (SLC22A5) | Carnitine, organic cations | Na+-dependent symport | Luminal |
The amino acid transporters represent one of the most diverse and critical SLC groups at the BBB. The concentration of amino acids in brain extracellular fluid is approximately tenfold lower than in plasma, with glutamine being the exception [25]. This gradient is tightly regulated by polarized AA transporters distributed across both membranes of endothelial cells. For example, sodium-independent transporters (Systems L and y+) are located on both luminal and abluminal membranes and mediate bidirectional AA transport, while sodium-dependent transporters (Systems A, ASC, N, and X-AG) are predominantly located on the abluminal membrane and actively pump AAs from brain to blood [25].
The glucose transporter GLUT1 (SLC2A1) is particularly abundant at the BBB and is responsible for supplying glucose to meet the brain's high metabolic demands. GLUT1 facilitates the bidirectional transport of glucose down its concentration gradient, with expression levels approximately three times higher on the abluminal side compared to the luminal side, potentially reflecting the brain's priority for glucose uptake over export [10].
Diagram 1: SLC-mediated amino acid transport across the BBB. Sodium-independent transporters (red) facilitate bidirectional exchange, while sodium-dependent transporters (blue) actively clear neurotoxic metabolites from the brain.
Receptor-Mediated Transcytosis (RMT)
Receptor-mediated transcytosis is a vesicular transport pathway that enables the selective movement of macromolecules across the BBB. This process represents a promising route for delivering therapeutic biologics, including proteins, antibodies, and nanoparticle drug carriers, to the CNS [21] [26]. RMT begins with the specific binding of a ligand to its cognate receptor on the luminal surface of brain endothelial cells, triggering clathrin-coated pit formation, followed by endocytosis, vesicular trafficking through various intracellular compartments, and eventual exocytosis at the abluminal membrane [21].
Key RMT Receptors at the BBB
Several receptors have been identified as mediators of transcytosis at the BBB, each with distinct expression patterns, ligand specificities, and transport capacities. A comprehensive transcriptomics study comparing RMT receptor expression in mouse and human brain microvessels revealed significant species differences that must be considered when translating preclinical findings [26].
Table 2: Major RMT Receptors at the Blood-Brain Barrier
| Receptor | Primary Ligands | Species Expression Pattern | Relative Abundance | Therapeutic Applications |
|---|---|---|---|---|
| Transferrin Receptor (TfR) | Transferrin, iron | Higher in mouse vs. human BMV | High in both species | Historical "prototypical" target for RMT |
| Insulin Receptor (INSR) | Insulin | Enriched in human BMV vs. brain and lung | Moderate | Clinical trials for antibody-mediated delivery |
| Insulin-like Growth Factor 1 Receptor (IGF1R) | IGF-1 | Enriched in mouse BMV vs. periphery | Moderate | Potential target for antibody shuttles |
| Low-density Lipoprotein Receptor (LDLR) | ApoE, ApoB | Similar expression across tissues | High | Angiopep-2 platform (LRP1 ligand) |
| LRP1 | Multiple ligands | Similar expression across tissues | High | Angiopep-2 platform in clinical trials |
| LRP8 | ApoE, thrombospondin | Enriched in mouse BMV vs. periphery | Low | Potential specialized transport |
| Leptin Receptor (LEPR) | Leptin | Not enriched in BMV | Moderate | Natural transport system for leptin |
The transferrin receptor (TfR) has served as the prototype RMT receptor for decades and has been extensively exploited for brain delivery of therapeutic antibodies and nanoparticles [26]. However, recent studies have revealed challenges with TfR-targeting approaches, including fast systemic clearance, on-target toxicity against TfR-rich reticulocytes, and limited transport efficiency in primates [26]. These limitations have prompted the exploration of alternative RMT receptors.
The insulin receptor (INSR) has emerged as a promising target for RMT-mediated brain delivery, particularly in humans where it shows enrichment in brain microvessels compared to both brain parenchyma and peripheral tissues like lung [26]. This expression profile is ideal for therapeutic targeting, as it may enable extended systemic half-life, reduced peripheral toxicity, and efficient brain delivery. Anti-human INSR antibodies are currently being evaluated in clinical trials for CNS drug delivery [26].
RMT Mechanisms and Intracellular Trafficking
The RMT process involves a carefully orchestrated sequence of intracellular events. After ligand binding, the receptor-ligand complex is internalized via clathrin-coated vesicles, which subsequently lose their clathrin coat and acidify to form early endosomes [21]. The acidic environment of the compartment of uncoupling receptor and ligand (CURL) promotes dissociation of the ligand from the receptor, allowing the receptor to recycle back to the plasma membrane while the ligand proceeds through the transcytotic pathway [22] [21].
The intracellular fate of RMT cargo is influenced by multiple factors, including receptor affinity, binding site occupancy, and the specific signaling pathways activated upon receptor engagement. Some receptors, like TfR, undergo constitutive recycling regardless of ligand occupancy, while others may require specific activation or display regulated trafficking patterns [26]. Understanding these subtleties is crucial for engineering effective RMT-based delivery systems that can successfully navigate the complex intracellular environment of brain endothelial cells.
ABC Efflux Pumps
ATP-binding cassette (ABC) transporters constitute a major defense mechanism at the BBB that actively restricts the brain penetration of xenobiotics and contributes to multidrug resistance in neurological disorders and brain cancers [20] [23]. These primary active transporters utilize energy derived from ATP hydrolysis to pump substrates against their concentration gradients, effectively limiting their accumulation in the CNS.
Major ABC Transporters at the BBB
The ABC superfamily encompasses 48 distinct transporters categorized into seven families (ABCA-ABCG), with several members playing critical roles in BBB function [20]. The most extensively studied and clinically relevant ABC transporter at the BBB is P-glycoprotein (P-gp/ABCB1), a 170 kDa transmembrane glycoprotein that recognizes an extraordinarily diverse array of structurally unrelated compounds [20] [23].
Table 3: ABC Efflux Transporters at the Blood-Brain Barrier
| Transporter | Gene | Substrates | Localization | Clinical Significance |
|---|---|---|---|---|
| P-glycoprotein | ABCB1 (MDR1) | Diverse chemotherapeutic agents, opioids, HIV protease inhibitors | Luminal membrane | Major determinant of CNS drug penetration; contributes to pharmacoresistance in epilepsy and brain tumors |
| Breast Cancer Resistance Protein | ABCG2 (BCRP) | Tyrosine kinase inhibitors, flavinoids, statins | Luminal membrane | Limits brain penetration of chemotherapeutics; works synergistically with P-gp |
| Multidrug Resistance Proteins | ABCC1 (MRP1) | Conjugated metabolites, antivirals, antibiotics | Luminal & abluminal membranes | Contributes to drug resistance in epilepsy; effluxes β-amyloid peptides |
| ABCC2 (MRP2) | Glucuronide and glutathione conjugates | Luminal membrane | Upregulated in refractory epilepsy | |
| ABCC4 (MRP4) | Nucleoside analogs, oseltamivir | Luminal membrane | Limits CNS penetration of antiviral drugs |
P-gp is strategically localized primarily on the luminal membrane of brain capillary endothelial cells, where it efficiently extrudes substrates back into the bloodstream, preventing their CNS entry [23]. Immunogold cytochemistry studies have revealed that P-gp density is approximately 1.4-fold higher at the abluminal compared to the luminal membrane, suggesting a potential additional role in directing substances toward brain interstitial fluid [23]. The functional importance of P-gp is dramatically illustrated in mdr1a/mdr1b knockout mice, which display significantly increased brain penetration of P-gp substrates like ivermectin, resulting in neurotoxicity at normally subtherapeutic doses [23].
Breast cancer resistance protein (BCRP/ABCG2) often works synergistically with P-gp, exhibiting overlapping substrate specificities and creating a formidable cooperative barrier function [23]. The multidrug resistance proteins (MRPs/ABCC) transport a diverse array of organic anions, including drug conjugates (e.g., glucuronide, glutathione) and various anticancer and antiviral agents [20]. MRP4 is particularly notable for its role in limiting the brain penetration of oseltamivir, the active metabolite of the influenza drug Tamiflu [20].
Regulation and Inhibition of ABC Transporters
The expression and function of ABC transporters are influenced by various factors, including inflammatory mediators, oxidative stress, and drug interactions. Several pharmacological inhibitors have been developed to block ABC transporter function, including verapamil, cyclosporine A, and valspodar for P-gp [23]. However, clinical trials combining these inhibitors with CNS drugs have largely failed due to dose-limiting toxicities resulting from simultaneously increased penetration into non-CNS tissues, where P-gp also serves protective functions [23].
More recent strategies have focused on developing specific and potent third-generation inhibitors like tariquidar and elacridar, which show improved efficacy and safety profiles [23]. Alternatively, rather than systemic inhibition, some approaches aim to temporarily disrupt BBB efflux transport through localized delivery or prodrug designs that bypass recognition by ABC transporters altogether.
3D Bioprinted BBB Models for Transport Studies
Advanced in vitro BBB models created through 3D bioprinting technologies represent a transformative approach for studying transport mechanisms and screening CNS drug candidates. These models overcome critical limitations of traditional 2D systems and animal models by recapitulating the multicellular architecture, dynamic flow conditions, and cell-matrix interactions of the human NVU [13] [24].
Key Design Considerations for 3D Bioprinted BBB Models
Physiologically relevant BBB models must incorporate several critical design elements to accurately mimic in vivo barrier function and transport properties. The inclusion of all three key BBB cell types—brain microvascular endothelial cells (BMECs), astrocytes, and pericytes—is essential for achieving appropriate tight junction formation and barrier tightness [13]. Cellular composition can be derived from various sources, including primary cells, immortalized cell lines, and induced pluripotent stem cells (iPSCs), with iPSCs showing particular promise for generating patient-specific models [13].
The incorporation of dynamic, perfusable flow is another critical factor, as physiological shear stress (typically 5-23 dyn/cm² in human brain capillaries) significantly influences endothelial cell alignment, morphology, and tight junction protein expression [13]. Furthermore, 3D-bioprinted models must replicate key physical parameters of brain capillaries, including diameters of 7-10 μm and trans-endothelial electrical resistance (TEER) values ranging from 1,500 to 8,000 Ω·cm² to match in vivo measurements [13].
Experimental Protocols for Transport Studies in 3D-Bioprinted BBB
Model Fabrication Using Digital Light Processing (DLP): Recent advances in DLP-based bioprinting enable the creation of complex, perfusable vascular networks with tunable topology and selective functionalization with bioactive peptides [24]. The protocol typically involves:
- Preparing a photocrosslinkable bioink containing gelatin methacrylate (GelMA) and polyethylene glycol diacrylate (PEGDA)
- Functionalizing with specific peptide motifs (RGD, IKVAV, HAVDI) to mediate endothelial cell attachment and coverage
- Printing the 3D channel architecture using DLP with precise spatial control
- Seeding endothelial cells into the luminal channels and astrocytes in the surrounding hydrogel
- Establishing physiological flow conditions using perfusion systems [24]
Barrier Integrity Assessment: TEER measurement remains the gold standard for evaluating barrier integrity in 3D-bioprinted models. Advanced systems incorporate real-time TEER monitoring electrodes directly within the perfusion chips to enable continuous assessment without disrupting the culture environment [13]. Additionally, the localization and expression of tight junction proteins (ZO-1, occludin, claudin-5) are routinely evaluated using immunofluorescence and confocal microscopy [24].
Permeability and Transport Studies: The permeability of test compounds across 3D-bioprinted BBB models is typically quantified using fluorescent or radiolabeled tracers with known permeability profiles. The apparent permeability coefficient (Papp) is calculated using the formula: Papp = (dQ/dt)/(A × C₀), where dQ/dt is the transport rate, A is the surface area, and C₀ is the initial concentration [13]. Specific transport pathways can be characterized using inhibitors of particular mechanisms: phloretin for GLUT1, AMD3100 for CXCR4-mediated transport, and Ko143 for BCRP efflux [10].
Diagram 2: Experimental workflow for 3D-bioprinted BBB model development and transport studies, highlighting key validation and application stages.
The Researcher's Toolkit: Essential Reagents and Materials
Table 4: Essential Research Reagents for BBB Transport Studies
| Reagent/Material | Function/Application | Example Specifications |
|---|---|---|
| Photocrosslinkable Bioinks | 3D scaffold fabrication | GelMA (5-15% w/v), PEGDA, peptide-functionalized hydrogels |
| Bioactive Peptides | Functionalization of hydrogels | RGD (cell adhesion), IKVAV (neurite outgrowth), HAVDI (cell-cell adhesion) |
| Primary Cells/iPSCs | BBB cellular components | Brain microvascular endothelial cells, astrocytes, pericytes |
| TEER Measurement System | Barrier integrity assessment | Epithelial voltohmmeter, integrated electrodes |
| Tight Junction Markers | Immunofluorescence validation | Anti-ZO-1, anti-claudin-5, anti-occludin antibodies |
| Transport Inhibitors | Mechanistic transport studies | Phloretin (GLUT1), Ko143 (BCRP), Verapamil (P-gp) |
| Permeability Tracers | Barrier function assessment | Sodium fluorescein (376 Da), Dextran (4-70 kDa) |
| Cytokine Cocktails | Disease modeling | TNF-α, IL-6, IL-1β for neuroinflammation studies |
The sophisticated transport systems of the BBB—solute carriers, receptor-mediated transcytosis, and ABC efflux pumps—collectively maintain CNS homeostasis while presenting formidable challenges for therapeutic delivery. Advances in 3D bioprinting have revolutionized our ability to model these transport mechanisms in physiologically relevant human systems, enabling more predictive screening of CNS drug candidates and investigation of disease-specific barrier alterations. These technologies allow researchers to dissect the complex interplay between transport pathways while maintaining the multicellular architecture and hemodynamic forces critical to BBB function. As 3D bioprinting methodologies continue to evolve, they promise to accelerate the development of novel strategies for overcoming the BBB and treating neurological disorders with enhanced precision and efficacy.
The blood-brain barrier (BBB) is a highly selective, dynamic interface that separates the circulating blood from the central nervous system (CNS), playing a dual role in protecting the brain from potentially toxic substances while regulating the transport of essential nutrients and metabolites [27] [28]. This sophisticated biological barrier is composed of brain microvascular endothelial cells (BMECs) interconnected by tight junctions (TJs), which are supported by pericytes, astrocytes, and the basement membrane in a specialized structure known as the neurovascular unit (NVU) [27] [29]. The BBB's impeccable barrier function, characterized by transendothelial electrical resistance (TEER) values reaching 1500-8000 Ω·cm² in humans, presents a formidable challenge for drug delivery to the CNS, with more than 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics failing to cross this protective interface [27] [30]. Understanding and modeling the BBB is therefore crucial for developing treatments for the increasing burden of CNS disorders, which represent one of the leading causes of global disability and mortality [29].
The pursuit of effective CNS therapies has been hampered by the limitations of traditional models used in preclinical research. For decades, scientists have relied primarily on two-dimensional (2D) in vitro cultures and animal models to study BBB function and screen potential therapeutics. However, these conventional approaches often fail to recapitulate the structural complexity and physiological functions of the human BBB, leading to unreliable predictions of drug efficacy and safety in humans [28] [29]. This review comprehensively examines the technical and physiological shortcomings of these traditional models within the context of advancing 3D bioprinting technologies for BBB modeling, highlighting how emerging biofabrication strategies offer promising solutions to overcome these limitations.
Fundamental Shortcomings of Two-Dimensional (2D) In Vitro Models
Structural and Physiological Limitations
Two-dimensional monolayer cultures, particularly the widely used Transwell system, represent the most basic approach to modeling the BBB in vitro. In this setup, endothelial cells are cultured on porous membranes, sometimes in co-culture with other NVU cells placed in the lower chamber. While these models offer simplicity, cost-effectiveness, and scalability for high-throughput screening, they suffer from significant limitations in replicating the physiological BBB environment [13] [28].
The most notable shortcoming of 2D models is their inability to mimic the cylindrical geometry of human brain capillaries, which typically range from 7-10 μm in diameter in the human brain [31]. This geometrical disparity profoundly affects cell morphology, polarity, and cell-cell interactions. In vivo, BMECs experience curvature that influences their behavior, with human BMECs resisting elongation and alignment in response to curvature—a potential evolutionary adaptation to reduce paracellular transport [31]. In flat 2D cultures, this natural curvature is absent, resulting in abnormal cell spreading and functionality.
Furthermore, 2D static models fail to incorporate hemodynamic forces, particularly the shear stress generated by blood flow. In human brain capillaries, endothelial cells experience wall shear stress ranging from 20-40 dyne/cm² in capillaries to 1-4 dyne/cm² in post-capillary venules [31]. This mechanical stimulation is crucial for maintaining BBB integrity, as it regulates the expression of tight junction proteins and transporters. The absence of these critical biomechanical cues in 2D models results in aberrant gene expression, reduced junctional tightness, and altered transporter activity compared to the in vivo BBB [13].
Simplified Cellular Microenvironment and Junctionality
The oversimplified cellular composition of most 2D models represents another significant limitation. While the BBB functions as a multicellular system, basic Transwell models typically utilize only endothelial cells, neglecting essential interactions with pericytes, astrocytes, and neurons that are critical for barrier induction and maintenance [27] [13]. Even when implemented in co-culture systems, the spatial organization of these supporting cells does not recapitulate their natural anatomical positions relative to the endothelial cells.
This simplified microenvironment leads to deficient tight junction formation and functionality. While 2D models develop some junctional complexity, their TJ networks are structurally and functionally inferior to those in the physiological BBB. The TEER values achieved in 2D models rarely exceed 1000 Ω·cm², significantly lower than the 1500-8000 Ω·cm² measured in humans [31]. Similarly, the expression of key tight junction proteins like claudin-5, occludin, and ZO-1 is often reduced or improperly localized in 2D cultures compared to the in vivo setting [27].
Table 1: Quantitative Comparison of Key BBB Parameters Between 2D Models and Human In Vivo Conditions
| Parameter | 2D In Vitro Models | Human In Vivo BBB |
|---|---|---|
| TEER (Ω·cm²) | Typically 130-857 [27], rarely >1000 | 1500-8000 [31] |
| Vessel Geometry | Flat monolayer | Cylindrical, 7-10 μm diameter capillaries [31] |
| Shear Stress | Absent (static) or non-physiological (flow systems) | 20-40 dyne/cm² (capillaries) [31] |
| Cellular Interactions | Limited contact in co-culture | Direct physical contact in neurovascular unit |
| TJ Protein Expression | Reduced claudin-5, occludin expression | Fully developed junctional complexes |
| Efflux Transporter Activity | Often diminished or aberrant | Fully functional P-gp, BCRP, MRP-1 |
The functional expression of transporters is also compromised in 2D models. Critical efflux transporters such as P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP) often exhibit altered expression levels and activity compared to in vivo conditions [27]. This transporter dysfunction significantly impacts drug permeability assessments, potentially leading to false positives in CNS drug screening campaigns. Additionally, receptor-mediated transcytosis systems—increasingly exploited for therapeutic delivery—are frequently inadequately represented in simplified 2D systems [28].
Critical Species Differences and Translational Limitations of Animal Models
Molecular and Functional Disparities
Animal models have long been considered the gold standard for preclinical BBB and CNS drug development studies. However, significant species differences between animal models and humans profoundly limit their predictive value and translational potential. These interspecies variations manifest at multiple levels, from molecular expression patterns to functional barrier properties.
Critical differences exist in the expression and functionality of transport systems at the BBB. For instance, Jamieson et al. reported that humans have 1.85-fold higher expression of BCRP and 2.33-fold lower expression of P-glycoprotein compared to mice [27]. Such divergence in key efflux transporters can dramatically alter the brain penetration profiles of their substrate drugs, leading to misleading predictions about human pharmacokinetics. Similarly, species differences in the expression of tight junction proteins and receptors further complicate the extrapolation of animal data to human clinical settings [27] [29].
The variability in transporter expression profiles across species significantly impacts drug development. A comparative analysis of membrane transporter proteins revealed substantial differences between humans and common preclinical species like rats, mice, and non-human primates [32]. These molecular disparities contribute to the high failure rate of CNS drugs in clinical trials, as compounds that show promising penetration in animal models may exhibit completely different distribution characteristics in humans due to differences in transporter affinity, density, or activity.
Inadequate Disease Modeling and Technical Limitations
Animal models frequently fail to recapitulate human pathophysiology of neurological disorders. The complex, multifactorial nature of conditions like Alzheimer's disease, Parkinson's disease, and glioblastoma involves intricate interactions between genetic predisposition, environmental factors, and aging processes that are challenging to model accurately in animals [33] [30]. Additionally, many neurological disorders exhibit species-specific manifestations that further limit the translational relevance of animal studies.
From a technical perspective, animal models present challenges for real-time monitoring and mechanistic studies. The complex physiology of living animals and difficulties in experimental procedures limit the ability to perform detailed, real-time measurements of analyte distribution and barrier function [29]. While advanced imaging techniques have been developed to study BBB dysfunction in animal models, the translation of these methods into clinical applications remains slow [34].
Table 2: Limitations of Animal Models in BBB Research and Drug Development
| Limitation Category | Specific Examples | Impact on Research |
|---|---|---|
| Molecular Differences | 1.85-fold higher BCRP in humans vs. mice [27]; Different TJ protein expression patterns | Altered drug permeability predictions; Poor translation to human responses |
| Functional Variations | Differences in efflux transporter activity; Species-specific metabolic pathways | Misleading pharmacokinetic and pharmacodynamic data |
| Disease Modeling | Inability to fully recapitulate human neurodegenerative diseases; Species-specific pathophysiology | Limited understanding of disease mechanisms; Poor predictive value for therapeutic efficacy |
| Technical Challenges | Difficult real-time monitoring; Complex surgical procedures; Ethical constraints | Limited mechanistic insights; Reduced experimental throughput |
| Resource Considerations | High costs; Time-consuming protocols; Specialized facilities required | Limited accessibility; Reduced scalability for screening |
Perhaps the most compelling evidence of the limitations of animal models comes from clinical translation statistics. Reports indicate that more than 80% of drugs shown to be effective in animal models eventually fail in human clinical trials [29]. This staggering attrition rate underscores the critical need for more human-relevant models that can better predict therapeutic outcomes in patients.
The Promise of 3D Bioprinting for Next-Generation BBB Modeling
In response to the limitations of traditional models, researchers have developed increasingly sophisticated three-dimensional (3D) in vitro models that better recapitulate the structural and functional complexity of the human BBB. Among these advanced approaches, 3D bioprinting has emerged as a particularly promising technology for creating physiologically relevant BBB models [13] [33].
3D bioprinting enables the precise spatial organization of multiple cell types within a biomimetic extracellular matrix, allowing for the creation of complex tissue architectures that closely resemble the native neurovascular unit. This capability addresses a fundamental limitation of 2D models by permitting the appropriate 3D arrangement of endothelial cells, pericytes, and astrocytes relative to one another [13] [30]. Furthermore, 3D bioprinting facilitates the incorporation of perfusable vascular networks that can be subjected to physiological shear stress, thereby restoring this critical biomechanical cue missing from traditional static cultures [16].
The technology also enables the creation of patient-specific models through the use of human-induced pluripotent stem cells (hiPSCs). These patient-derived cells can be differentiated into the various cellular components of the NVU, providing a powerful platform for studying personalized therapeutic responses and disease-specific BBB pathologies [32] [30]. This approach is particularly valuable for neurodegenerative disease research, where BBB dysfunction is increasingly recognized as a contributing factor to disease pathogenesis [13] [30].
Diagram 1: Evolutionary progression from traditional models to 3D bioprinted BBB platforms, highlighting key advantages of the bioprinting approach.
Essential Research Reagents and Materials for Advanced BBB Modeling
The development of physiologically relevant 3D BBB models requires specialized materials and reagents to replicate the native brain microenvironment. The table below outlines key components used in advanced BBB model systems, particularly 3D bioprinting approaches.
Table 3: Essential Research Reagents and Materials for 3D Bioprinted BBB Models
| Category | Specific Examples | Function and Importance |
|---|---|---|
| Bioinks | PEGDA, GelMA, Hyaluronic acid, Fibrin | Provide tunable 3D microenvironment with appropriate mechanical properties (2-4 kPa) matching brain tissue [30] [16] |
| Cellular Components | hiPSC-derived BMECs, Pericytes, Astrocytes, Neural stem cells | Enable species-matched, patient-specific modeling of neurovascular unit [13] [32] |
| Basement Membrane Proteins | Collagen IV, Laminin, Fibronectin, Heparan sulfate proteoglycans | Recreate native basement membrane composition for proper cell-matrix interactions [31] |
| Perfusion Systems | Microfluidic chips, Tubing networks, Peristaltic pumps | Introduce physiological shear stress (5-23 dyne/cm²) and nutrient delivery [13] [31] |
| Characterization Tools | TEER measurement electrodes, Tracer molecules (dextran), Confocal microscopy | Assess barrier integrity, permeability, and 3D structure non-invasively [16] [31] |
The limitations of traditional 2D cultures and animal models in BBB research are substantial and multifaceted. Two-dimensional models fail to recapitulate the structural complexity, physiological shear stress, and proper cellular interactions of the native neurovascular unit, while animal models are hampered by significant species differences that limit their translational predictive value. These shortcomings have contributed to the high failure rate of CNS therapeutics in clinical development, highlighting the critical need for more human-relevant models.
Advanced 3D bioprinting technologies represent a promising paradigm shift in BBB modeling, offering unprecedented capabilities to create physiologically relevant human-specific platforms with appropriate geometry, mechanical cues, and multicellular complexity. By addressing the fundamental limitations of traditional approaches, 3D bioprinted BBB models have the potential to accelerate CNS drug discovery, improve translational predictability, and advance our understanding of BBB function in health and disease. As these biofabrication technologies continue to evolve, they are poised to become indispensable tools in the quest to develop effective therapies for neurological disorders.
The blood-brain barrier (BBB) represents a critical frontier in the understanding and treatment of neurodegenerative diseases (NDDs). This complex multicellular structure, once viewed primarily as a static protective shield, is now recognized as a dynamically impaired interface in conditions like Alzheimer's disease (AD) and Parkinson's disease (PD). BBB dysfunction is not merely a secondary consequence but may constitute an early pathogenic event that initiates and amplifies neurodegenerative processes [35] [36]. The growing burden of NDDs on global healthcare systems, with approximately 15% of the global population affected, has intensified research focus on the BBB as both a contributor to disease pathology and a potential therapeutic target [13] [37]. Current data reveals that BBB breakdown can significantly impact neuronal and synaptic function, influencing neurodegenerative processes through multiple interconnected mechanisms including impaired clearance of toxic metabolites, neuroinflammation, and disrupted cerebral homeostasis [35] [36].
The clinical imperative to understand BBB dysfunction stems from its dual role in NDDs: its pathological contribution to disease progression and its formidable obstruction to CNS-targeted therapies. With over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics failing to cross the BBB, developing strategies to either protect BBB integrity or leverage its transport mechanisms represents one of the most significant challenges in modern neurology and drug development [2]. This review examines the cellular and molecular underpinnings of BBB dysfunction in neurodegeneration, explores advanced 3D bioprinting approaches for modeling these pathological changes, and discusses emerging therapeutic strategies targeting the BBB in NDDs.
Molecular and Cellular Mechanisms of BBB Dysfunction
Structural and Functional Components of the Neurovascular Unit
The BBB functions as a highly specialized vascular interface primarily formed by brain microvascular endothelial cells (BMECs) that exhibit unique properties distinguishing them from peripheral endothelial cells. These BMECs are characterized by continuous tight junctions (TJs), minimal transcytosis rates, and expression of specialized transport systems that collectively maintain CNS homeostasis [13] [36]. The TJs comprise transmembrane proteins including occludin, claudins (particularly claudin-3 and claudin-5), and junctional adhesion molecules (JAMs), which are linked to the actin cytoskeleton via cytoplasmic scaffolding proteins such as ZO-1 [13]. These junctional complexes create a high-resistance barrier with transendothelial electrical resistance (TEER) values ranging from 1,500 to 8,000 Ω·cm² in physiological conditions [13].
Beyond the endothelial layer, the BBB incorporates other critical cellular components within the neurovascular unit (NVU). Pericytes are embedded within the vascular basement membrane and play essential roles in regulating BBB permeability, stabilizing vascular structure, and coordinating clearance of toxic metabolites [10] [36]. Astrocytes extend end-feet processes that envelop cerebral microvessels, contributing to BBB integrity through the release of trophic factors and regulation of water and ion homeostasis via aquaporin-4 channels [10]. The basement membrane, composed of collagen IV, laminin, nidogen, and other glycoproteins, provides structural support and biochemical cues that influence BBB cellular behavior [13] [10].
Table 1: Cellular Components of the Neurovascular Unit and Their Functions
| Cell Type | Location | Primary Functions |
|---|---|---|
| Brain Microvascular Endothelial Cells (BMECs) | Lumen of cerebral capillaries | Form tight junctions; express transport systems; regulate molecular passage |
| Pericytes | Embedded in vascular basement membrane | Regulate permeability; stabilize vasculature; clear toxins; coordinate immune response |
| Astrocytes | Parenchymal side with end-feet enveloping vessels | Release trophic factors; regulate water/ion homeostasis; modulate blood flow |
| Neurons | Adjacent to neurovascular unit | Regulate cerebral blood flow via neurovascular coupling |
Transport Mechanisms Across the BBB
The BBB regulates molecular transit through multiple specialized transport pathways that become compromised in neurodegenerative states. Paracellular transport of polar solutes is severely restricted under physiological conditions by TJ complexes but may become aberrantly permeable in NDDs due to junctional protein disruption [10]. Transcellular transport mechanisms include: (1) carrier-mediated transport (CMT) of essential nutrients such as glucose (via GLUT1) and amino acids (via LAT1); (2) receptor-mediated transcytosis (RMT) of larger molecules including transferrin and lipoproteins; (3) adsorptive-mediated transcytosis (AMT) utilizing charge interactions; and (4) active efflux transport via ATP-binding cassette (ABC) transporters like P-glycoprotein (P-gp) that expel neurotoxins and therapeutic drugs [10] [36] [2]. The proper functioning of these transport systems is crucial for brain health, as they ensure adequate nutrient delivery while preventing accumulation of toxic metabolites.
Pathological Mechanisms in Neurodegenerative Diseases
BBB dysfunction manifests across multiple NDDs through shared and distinct pathological mechanisms. In Alzheimer's disease, BBB impairment involves impaired clearance of amyloid-β (Aβ) peptides, partly due to reduced expression of efflux transporters at the BBB [13] [36]. The lipoprotein receptor LRP1, which normally mediates Aβ clearance from brain to blood, shows decreased expression, while the receptor for advanced glycation end products (RAGE), which facilitates Aβ influx into the brain, demonstrates increased expression [10] [36]. This imbalance promotes Aβ accumulation and contributes to neurovascular uncoupling, ultimately leading to regional cerebral blood flow deficits [36].
In Parkinson's disease, BBB dysfunction permits increased entry of neurotoxicants from the circulation and reduces clearance of accumulated α-synuclein aggregates [13]. Neuroinflammatory signaling induces TJ disruption through pro-inflammatory cytokines such as TNF-α and IL-1β, which downregulate claudin-5 and occludin expression [13] [38]. Additionally, ABC transporter dysfunction may limit the efflux of α-synuclein, further promoting its accumulation [13].
The following diagram illustrates the key molecular mechanisms of BBB dysfunction in neurodegenerative diseases:
Diagram 1: Molecular mechanisms of BBB dysfunction in neurodegenerative diseases. Neurodegenerative processes trigger multiple BBB dysfunction mechanisms including tight junction disassembly, neuroinflammation, cerebral blood flow disruption, transport system dysfunction, and pericyte degeneration. These mechanisms collectively contribute to pathological consequences such as amyloid-β accumulation, α-synuclein aggregation, oxidative stress, and immune cell infiltration.
3D Bioprinting Strategies for Modeling the BBB in Neurodegeneration
Advanced Bioprinting Technologies and Bioink Development
Traditional in vitro BBB models, particularly 2D Transwell systems, have limitations in replicating the physiological complexity of the human BBB, including its 3D architecture, cellular interactions, and dynamic flow conditions [13]. To address these limitations, 3D bioprinting has emerged as a powerful technology for generating spatially organized, customizable, and physiologically relevant BBB constructs. Key bioprinting approaches include extrusion-based bioprinting, inkjet bioprinting, and stereolithography, each offering distinct advantages for BBB modeling [13] [39].
A critical advancement in this field has been the development of specialized bioinks that provide appropriate microenvironments for BBB cells. Recently, researchers created a cerebrovascular-specific bioink using decellularized extracellular matrix (CBVdECM) derived from porcine brain and blood vessels [38]. This bioink promotes the spontaneous self-assembly of a dual-layered structure when printed with human brain microvascular endothelial cells (HBMECs) and human brain vascular pericytes (HBVPs), closely mimicking the native BBB architecture [38]. The CBVdECM bioink supports the formation and organization of tight junction proteins typically absent in conventional 2D models, enabling more accurate modeling of neuroinflammatory mechanisms in NDDs [38].
Table 2: Key Research Reagent Solutions for BBB Bioprinting and Modeling
| Reagent/Cell Type | Function/Application | Key Features |
|---|---|---|
| Cerebrovascular-specific bioink (CBVdECM) | Provides physiological microenvironment for BBB cells | Derived from porcine brain/blood vessels; promotes self-assembly of dual-layered structures |
| Human Brain Microvascular Endothelial Cells (HBMECs) | Form the endothelial barrier component | Express tight junctions; respond to shear stress; key for barrier integrity |
| Human Brain Vascular Pericytes (HBVPs) | Recapitulate pericyte-endothelial interactions | Regulate barrier function; stabilize vasculature; embedded in basement membrane |
| Decellularized Extracellular Matrix (dECM) | Biomaterial scaffolding for 3D constructs | Retains tissue-specific biochemical cues; enhances physiological relevance |
| Tight Junction Markers (claudin-5, occludin, ZO-1) | Assess barrier integrity in models | Indicators of proper BBB formation; disrupted in neurodegenerative conditions |
Integrated Workflow for Creating 3D Bioprinted BBB Models
The process of developing functional 3D bioprinted BBB models involves multiple coordinated stages from design to validation. The following diagram outlines this comprehensive workflow:
Diagram 2: Workflow for creating 3D bioprinted BBB models. The process begins with model design and bioink formulation, proceeds through cell sourcing, bioprinting, maturation under dynamic flow conditions, validation using functional assays, and culminates in disease modeling and therapeutic testing. Key methodological components for each stage are indicated with dashed connections.
Experimental Protocols for BBB Model Characterization
Protocol 1: TEER Measurement and Permeability Assessment
Objective: Quantify barrier integrity of 3D bioprinted BBB models.
- TEER Measurement:
- Use specialized electrodes designed for 3D constructs
- Measure impedance across the endothelial barrier daily
- Calculate TEER values (Ω·cm²) by subtracting background and multiplying by membrane area
- Validate against physiological benchmarks (1,500-8,000 Ω·cm²) [13]
- Permeability Assay:
- Apply fluorescent tracers of varying molecular weights (e.g., sodium fluorescein (376 Da), dextran conjugates (3-70 kDa))
- Sample from both luminal and abluminal compartments at timed intervals
- Calculate permeability coefficients (Papp) using standard formulas
- Compare values to in vivo measurements for validation [13] [10]
Protocol 2: Immunofluorescence Analysis of Tight Junction Proteins
Objective: Visualize and quantify tight junction organization in bioprinted BBB models.
- Fixation and Sectioning:
- Fix constructs in 4% paraformaldehyde for 30 minutes at 4°C
- Cryosection at 10-20μm thickness or prepare whole mounts for imaging
Immunostaining:
- Permeabilize with 0.1% Triton X-100 for 10 minutes
- Block with 5% normal serum for 1 hour
- Incubate with primary antibodies against claudin-5, occludin, and ZO-1 overnight at 4°C
- Apply fluorescent secondary antibodies for 2 hours at room temperature
- Counterstain nuclei with DAPI and image using confocal microscopy [13] [38]
Image Analysis:
- Quantify junctional continuity using line intensity profiling
- Assess protein localization at cell boundaries
- Compare organization between healthy and disease-state models
Therapeutic Implications and Future Directions
BBB-Targeted Therapeutic Strategies
The growing understanding of BBB dysfunction in NDDs has catalyzed the development of novel therapeutic strategies aimed at either restoring barrier integrity or leveraging BBB transport mechanisms for drug delivery. BBB preservation approaches focus on protecting TJ integrity, reducing neuroinflammation, and supporting pericyte function to maintain barrier stability [35] [36]. Experimental interventions include targeting pro-inflammatory signaling pathways, enhancing clearance of neurotoxic proteins, and promoting vascular stability through trophic support.
For CNS drug delivery, receptor-mediated transcytosis (RMT) has emerged as a promising platform for transporting therapeutics across the BBB. Major pharmaceutical companies are increasingly investing in RMT-based platforms targeting receptors such as transferrin receptor (TfR1), insulin-like growth factor 1 receptor (IGF1R), and CD98hc [40]. These platforms conjugate therapeutic molecules to antibodies targeting these receptors, effectively "shuttling" drugs across the endothelial barrier. Notably, Roche's Trontinemab, a TfR1-targeting anti-Aβ antibody, has demonstrated impressive clinical results with 91% of patients achieving amyloid clearance within 28 weeks at the highest dose, validating this approach [40].
Table 3: BBB-Targeted Therapeutic Platforms in Development
| Platform/Strategy | Mechanism | Therapeutic Modality | Development Status |
|---|---|---|---|
| Brainshuttle (Roche) | TfR1-mediated transcytosis | Anti-Aβ antibody (Trontinemab) | Clinical trials (91% amyloid clearance at 28 weeks) |
| Dual ATV (Denali) | TfR1 & CD98hc targeting | Antibody, ASO, siRNA | Preclinical/Clinical development |
| Grabody-B (ABL Bio) | IGF1R targeting | Antibody, ASO, siRNA | Partnership with GSK for AD/PD |
| JUST-AAV (JCR Pharma) | TfR1-mediated transcytosis | AAV gene therapy | Licensed by AstraZeneca's Alexion |
| CBVdECM Bioprinting | Physiological BBB modeling | Drug screening platform | Research phase (POSTECH/Seoul National) |
Future Perspectives in BBB Research and Therapeutics
The field of BBB research in neurodegeneration is rapidly evolving, with several promising directions emerging. The integration of advanced 3D bioprinting with microfluidic systems creates opportunities for developing more sophisticated human BBB models that incorporate fluid flow and shear stress, better mimicking physiological conditions [13] [41]. These systems can be further enhanced through the incorporation of patient-derived cells to create personalized models that reflect individual disease characteristics and therapeutic responses [10] [38].
Future research priorities should include the development of standardized validation protocols for BBB models, establishment of correlations between in vitro measures and clinical outcomes, and creation of integrated models that incorporate additional CNS cell types including neurons, microglia, and oligodendrocytes to better recapitulate the neurovascular unit in its entirety [13] [38]. From a therapeutic perspective, combining BBB-protective strategies with enhanced drug delivery systems holds promise for addressing both the barrier dysfunction itself and the underlying neurodegenerative pathology.
BBB dysfunction represents a critical clinical imperative in neurodegenerative diseases, contributing to disease pathogenesis through multiple interconnected mechanisms and presenting a formidable challenge to therapeutic development. Advanced 3D bioprinting technologies now enable the creation of increasingly sophisticated human BBB models that recapitulate key aspects of neurodegeneration, providing powerful platforms for investigating disease mechanisms and screening potential therapeutics. The convergence of these model systems with innovative BBB-targeted drug delivery approaches, particularly RMT-based platforms, offers renewed hope for effectively treating neurodegenerative disorders. As these technologies continue to evolve and integrate, they hold the potential to transform our approach to understanding and treating BBB dysfunction in NDDs, ultimately improving outcomes for patients facing these devastating conditions.
Fabricating the Barrier: Bioprinting Techniques, Bioinks, and Functional Applications
Three-dimensional (3D) bioprinting has emerged as a transformative technology in tissue engineering and regenerative medicine, enabling the precise fabrication of complex, cell-laden constructs. By adapting principles from additive manufacturing, bioprinting allows for the layer-by-layer deposition of bioinks—combinations of living cells, biomaterials, and bioactive molecules—to create tissue mimics with spatially controlled architectures. Within the specific context of blood-brain barrier (BBB) modeling, the choice of bioprinting technique is paramount, as it directly impacts the ability to replicate the barrier's intricate cellular organization, perfusable vascular networks, and physiological function [13] [4]. The BBB is a complex multicellular structure essential for maintaining central nervous system homeostasis, and its dysfunction is a key feature of many neurodegenerative diseases [13] [30]. This guide provides a detailed technical examination of the three core bioprinting modalities—extrusion, inkjet, and laser-assisted—focusing on their mechanisms, comparative advantages, and critical application in developing advanced, physiologically relevant BBB models for drug development and disease research.
Core Bioprinting Technologies
The three primary bioprinting modalities differ fundamentally in their actuation mechanisms, which dictates their suitability for specific applications in BBB modeling. The following table provides a quantitative comparison of their key characteristics.
Table 1: Comparative Analysis of Core Bioprinting Modalities
| Parameter | Extrusion-Based | Inkjet-Based | Laser-Assisted |
|---|---|---|---|
| Mechanism | Pneumatic or mechanical (piston/screw) dispensing [4] | Thermal or piezoelectric droplet ejection [4] | Laser-induced forward transfer (LIFT) [42] [43] |
| Resolution | 100 - 1000 μm [4] | 50 - 300 μm [4] | ~20 μm [43] |
| Cell Viability | 40% - 95%+ [4] | >85% [4] | >95% [42] |
| Viscosity Range | High (30 - 6x10⁷ mPa•s) [4] | Low (3.5 - 12 mPa•s) [4] | Wide, nozzle-free (1 - 300 mPa•s) [42] [43] |
| Print Speed | Slow to Medium | Fast | Slow to Medium |
| Key Advantage for BBB | Strongest modality for creating perfusable, multi-layer vascular channels [44] | High throughput for rapid screening of bioink formulations [4] | Superior resolution for patterning delicate neural cells and complex geometries [42] [45] |
| Primary Limitation | Shear stress on cells can impact viability [4] | Limited by bioink viscosity, clogging [4] | Complexity and cost of laser setup [45] [43] |
Extrusion-Based Bioprinting
Extrusion bioprinting operates by continuously depositing filaments of bioink through a micronozzle under pneumatic or mechanical pressure [4]. Its capacity to handle high-viscosity bioinks, including those laden with high cell densities or supportive hydrogels, makes it indispensable for creating the robust, 3D structures required in tissue engineering.
A key advancement for BBB modeling is coaxial extrusion, which utilizes a concentric nozzle to fabricate hollow, tubular structures in a single step. A seminal application of this technique involved the fabrication of a three-layer vascular structure mimicking the BBB. In this process, a photocurable bioink in the inner layer and a photoinitiator in the outer layer diffuse at the interface. Upon UV exposure, a crosslinked hollow tube is formed, which can subsequently be seeded with endothelial cells to create a perfusable barrier [44]. This model has demonstrated excellent perfusion capacity and the critical barrier function of blocking macromolecular drugs while allowing small molecules to pass, making it a promising candidate for neuroprotective drug screening [44].
Inkjet-Based Bioprinting
Inkjet bioprinting functions like an office printer, utilizing thermal or piezoelectric actuators to generate picoliter-to-nanoliter droplets of bioink in a drop-on-demand manner [4]. The thermal mechanism employs a heating element to create a vapor bubble that expels a droplet, while the piezoelectric mechanism uses a crystal's deformation to generate acoustic pressure waves. Both methods enable high-speed, non-contact printing, which is advantageous for high-throughput applications.
However, its utility is constrained by bioink viscosity, as high-viscosity fluids cannot be easily ejected, and risks of nozzle clogging necessitate careful bioink formulation [4]. While less commonly used for creating the dense, volumetric structures of the BBB itself, its speed and precision make it valuable for patterning specific cell types or proteins onto pre-formed structures to enhance biological functionality.
Laser-Assisted Bioprinting
Laser-assisted bioprinting (LAB) is a nozzle-free technique that operates on the principle of Laser-Induced Forward Transfer (LIFT) [42] [43]. A typical setup consists of a pulsed laser source, a "ribbon" coated with a thin layer of laser-absorbing material (often gold or titanium) and a layer of bioink, and a receiving substrate. When the laser pulse is focused on the absorbing layer, it generates a high-pressure vapor bubble that propels a tiny droplet of the bioink from the ribbon onto the substrate below [45] [43]. This orifice-free nature eliminates shear stress-related cell damage and clogging, resulting in exceptionally high cell viability (>95%) [42]. Furthermore, it can accommodate a wide range of bioink viscosities, providing significant formulation flexibility [43].
Its high resolution (up to ~20 μm), which is sufficient for single-cell patterning, is particularly beneficial for BBB models that require precise spatial organization of different neural and vascular cell types, such as recreating the neurovascular unit with neurons, astrocytes, and endothelial cells [42] [45]. Techniques like Laser Induced Side Transfer (LIST) have been successfully used to print delicate primary neurons, a cell type critical for advanced neural tissue models [45].
Application in Blood-Brain Barrier Modeling
The ultimate goal in BBB bioprinting is to recapitulate the neurovascular unit (NVU), which comprises brain microvascular endothelial cells (BMECs), pericytes, and astrocytes, all interacting within a relevant extracellular matrix (ECM) [13]. A physiologically relevant model must incorporate all three cell types to enhance the formation of tight junctions (TJs) and barrier tightness, which is critical for accurate disease modeling and drug transport studies [13]. Key metrics for validation include Trans-Endothelial Electrical Resistance (TEER), which should approach in vivo values of 1,500–8,000 Ω·cm², and permeability assays [13].
Table 2: Essential Research Reagents for Bioprinting a Blood-Brain Barrier Model
| Reagent Category | Specific Examples | Function in the BBB Model |
|---|---|---|
| Cells | Brain Microvascular Endothelial Cells (BMECs), Pericytes, Astrocytes [13] | Recapitulate the core cellular components of the neurovascular unit. BMECs form the barrier, supported by pericytes and astrocytes. |
| Bioink Polymers | Gelatin methacrylate (GelMA), Hyaluronic acid, Fibrin, Collagen [4] [30] | Form the hydrogel scaffold that mimics the brain's extracellular matrix, providing structural support and biochemical cues. |
| Crosslinkers | Photoinitiators (e.g., LAP, Irgacure 2959) for UV light [44] | Induce gelation of the bioink to stabilize the 3D printed structure post-deposition. |
| Culture Media | Endothelial cell growth media, Astrocyte media | Provide cell-type-specific nutrients and factors to maintain co-culture viability and function. |
| Barrier Integrity Assays | TEER electrodes, Fluorescent tracers (e.g., dextran) [13] | Quantitatively evaluate the formation and functionality of the endothelial barrier. |
Extrusion bioprinting, particularly coaxial methods, excels at creating the foundational vascular structure. The perfusable channels it produces allow for the application of physiological shear stress (5–23 dyn/cm²), a mechanical cue known to influence endothelial cell alignment, morphology, and upregulation of TJ proteins like claudin-5 and occludin, which are fundamental to barrier integrity [13] [44]. Once a vascular channel is established, laser-assisted bioprinting can be employed to precisely pattern astrocytes and pericytes in the surrounding "brain parenchyma" compartment with high spatial resolution, thereby mimicking the native anatomical relationships [42]. This multi-modal approach combines the strengths of different printing technologies to achieve a more holistic and functional BBB model.
Diagram: Integrated Workflow for Bioprinting a BBB Model. This workflow illustrates a multi-modal strategy, leveraging coaxial extrusion for vascular structures and laser-assisted printing for precise cell patterning, followed by maturation under flow.
Detailed Experimental Protocol: Coaxial Bioprinting of a BBB Model
The following protocol details the methodology for fabricating a three-layer vascular structure with BBB function, as cited in the literature [44]. This serves as a concrete example of how extrusion bioprinting is applied in practice.
Pre-Printing Preparation
- Bioink Formulation: Prepare a photocurable bioink, such as Gelatin Methacrylate (GelMA). The bioink should be sterilized and maintained at 4°C to prevent premature gelation.
- Cell Culture and Harvesting: Expand and culture the necessary cells, typically human brain microvascular endothelial cells (HBMECs). Harvest the cells at ~90% confluency using standard trypsinization methods. Centrifuge and resuspend the cell pellet in the prepared bioink at a desired concentration (e.g., 5-10 million cells/mL). Keep the cell-laden bioink on ice.
- Printer Setup: Install and calibrate a coaxial printhead on the bioprinter. The inner nozzle typically dispenses the cell-laden photocurable bioink, while the outer nozzle dispenses a solution containing a photoinitiator. Load the bioinks into their respective syringes, ensuring no air bubbles are present.
Printing Process
- Set Printing Parameters: Adjust pneumatic pressures or volumetric flow rates for both the inner and outer flows to achieve a stable, continuous hollow filament. Optimize the print speed to match the extrusion rate.
- Fabricate the Tubular Structure: Direct the printer to extrude the coaxial filament into the desired 3D pattern (e.g., a straight tube or simple lattice) onto a receiving substrate.
- In-Situ Crosslinking: Simultaneously expose the extruding filament to a UV light source (e.g., 365 nm wavelength) positioned at the printhead. The photoinitiator from the outer layer diffuses into the inner layer, causing crosslinking specifically at the interface and forming a solid hollow tube.
- Post-Printing Rinsing: After printing the complete structure, gently perfuse the lumen of the channel with cell culture medium to remove any uncrosslinked bioink material from the interior.
Post-Printing Culture and Analysis
- Perfusion Culture: Connect the bioprinted structure to a microfluidic perfusion system or a bioreactor. Begin perfusing the lumen with endothelial cell growth medium at a low flow rate, gradually increasing to a physiological shear stress.
- Barrier Function Assessment:
- TEER Measurement: Insert microelectrodes into the perfusion system to periodically measure Trans-Endothelial Electrical Resistance. A rising TEER value indicates the formation of tight junctions and a functional barrier.
- Permeability Assay: Introduce fluorescently tagged molecules of different sizes (e.g., 4 kDa and 70 kDa dextran) into the perfusate. Collect samples from the "brain" side compartment and quantify the fluorescence to calculate the apparent permeability coefficient (Papp). A functional BBB will show low permeability to large molecules.
- Immunostaining: After the experiment, fix the construct and immunostain for key tight junction proteins (e.g., ZO-1, Claudin-5) to visualize the integrity and maturity of the endothelial barrier.
The selection of an appropriate bioprinting modality is a critical determinant in the successful engineering of a physiologically relevant blood-brain barrier model. Extrusion bioprinting stands out for fabricating the robust, perfusable vascular channels that form the model's foundation. Inkjet printing offers speed for specific patterning and screening tasks, while laser-assisted bioprinting provides unparalleled resolution for arranging delicate neural cells. The future of BBB modeling lies not in relying on a single technology, but in the strategic integration of these complementary modalities. This multi-modal approach, combined with advances in bioinks and bioreactor culture, is paving the way for highly predictive human-specific models. These advanced constructs hold the potential to dramatically accelerate the development of therapeutics for neurodegenerative diseases by providing a more reliable and human-relevant platform for drug screening and mechanistic studies.
In the evolving field of 3D bioprinting for blood-brain barrier (BBB) modeling, bioink formulation serves as the foundational element that determines the success of fabricated constructs. Bioinks are defined as a solution of a biomaterial or mixture of several biomaterials in hydrogel form, usually encapsulating desired cell types, used for creating tissue constructs [46]. These materials can be cross-linked or stabilized during or immediately after bioprinting to generate the final shape, structure, and architecture of the designed construct [46]. For BBB modeling specifically, bioinks must replicate the unique multicellular environment and specialized functions of the neurovascular unit (NVU), which includes brain microvascular endothelial cells (BMECs), pericytes, and astrocytes [10] [13].
The growing burden of neurodegenerative diseases affecting approximately 15% of the global population has intensified the need for accurate BBB models to study pathogenesis and evaluate CNS-targeted therapies [13]. A critical factor in NDD pathogenesis is BBB dysfunction, which may precede and contribute to neuronal degeneration by allowing entry of neurotoxic plasma components, inflammatory mediators, and immune cells into the CNS [13]. The market size for 3D bioprinting was $2.13 billion in 2022 and is expected to grow to $8.3 billion by 2030, with a compound annual growth rate of 18.51%, reflecting the increasing importance of this field [47].
An ideal bioink for BBB modeling must meet several critical requirements: possess proper mechanical, rheological, and biological properties of the target tissues; provide a supportive microenvironment for cell viability and function; enable the formation of tight junctions between endothelial cells; and permit the necessary cell-cell interactions that regulate BBB permeability [46] [13]. The following sections provide a comprehensive technical analysis of natural, synthetic, and hybrid polymer strategies for bioink formulation tailored specifically for BBB modeling applications.
Natural Polymer-Based Bioinks
Natural polymers derived from biological sources offer inherent biocompatibility and bioactivity that make them attractive for BBB modeling. These materials typically contain cell-adhesive motifs and enzymatic cleavage sites that support cell migration, proliferation, and differentiation.
Gelatin Methacryloyl (GelMA)
GelMA has emerged as one of the most widely used natural polymer-based bioinks for BBB modeling due to its tunable mechanical properties and presence of arginine-glycine-aspartic acid (RGD) cell adhesion motifs. Research demonstrates that GelMA PhotoInk has been successfully employed in combination with PEGDA to create 3D microfluidic scaffolds of the brain's microvessels with diameters ranging from 100 to 300 microns [16]. The resulting 3D cubes of microvessels were connected to a perfusion apparatus to mimic blood flowing through microvessels, enabling the culture of both fetal and adult brain microvascular endothelial cells that formed fully endothelialized vasculature after a few days [16].
Table 1: Natural Polymer Bioinks for BBB Modeling
| Bioink Type | Key Advantages | Limitations | BBB-Specific Applications |
|---|---|---|---|
| GelMA | Contains RGD adhesion motifs; tunable mechanical properties; enzymatically degradable | Limited mechanical strength; batch-to-batch variability | Microvascular scaffold fabrication; co-culture systems with endothelial cells and astrocytes [16] |
| Decellularized ECM (dECM) | Tissue-specific biochemical composition; preserves native ECM components | Complex processing; potential immunogenicity; variable mechanical properties | Cerebrovascular-specific bioink from brain and blood vessel dECM for tubular vascular models [48] |
| Collagen Type I | Major component of native basement membrane; promotes cell adhesion | Low viscosity; slow gelation at physiological conditions | Coating culture surfaces for hBMVECs and pericytes [49] [50] |
| Hyaluronic Acid | Native component of brain ECM; modifiable with adhesive peptides | Poor mechanical properties; lacks cell adhesion sites | Thiol-modified versions used in hydrogel mixtures for BBB models [49] |
Decellularized Extracellular Matrix (dECM)
dECM bioinks derived from brain and blood vessels offer significant advantages for BBB modeling by preserving tissue-specific biochemical compositions. Researchers have developed a cerebrovascular-specific bioink using decellularized extracellular matrix (CBVdECM) derived from the brain and blood vessels of pigs [48]. This bioink, when combined with human brain microvascular endothelial cells and human brain vascular pericytes, enabled the creation of a tubular vascular model that closely resembled the architecture of biological blood vessels, with self-assembled inner and outer vascular walls [48]. The tissue-specific signaling motifs present in dECM bioinks enhance the expression of tight junction proteins and other specialized BBB functions.
Experimental Protocol: GelMA Hydrogel Preparation for BBB Modeling
Materials Required:
- GelMA polymer (CELLINK GelMA PhotoInk or equivalent)
- Photoinitiator (Lithium phenyl-2,4,6-trimethylbenzoylphosphinate, LAP)
- Phosphate-buffered saline (PBS)
- Primary human brain microvascular endothelial cells (hBMVECs)
- Astrocytes and pericytes
- UV light source (wavelength 320-400 nm, intensity 5-20 mW/cm²)
Methodology:
- Prepare 5-15% (w/v) GelMA solution in PBS containing 0.5-1% (w/v) LAP photoinitiator.
- Sterilize the solution by passing through a 0.22 μm filter under laminar flow hood.
- Mix hBMVECs with the GelMA solution at a density of 5-10 × 10^6 cells/mL.
- For co-culture systems, sequentially or simultaneously incorporate astrocytes and pericytes at ratios reflecting native NVU (typically 1:0.2:0.5 endothelial:pericyte:astrocyte).
- Load the cell-laden bioink into a digital light processing (DLP) bioprinter cartridge.
- Bioprint using UV light at 365 nm wavelength with intensity of 10-15 mW/cm² for 10-60 seconds exposure time depending on layer thickness and bioink concentration.
- Culture the bioprinted constructs in endothelial growth media (EGM-2 MV BulletKit) supplemented with relevant growth factors.
- Implement perfusion through the vascular lumens within 24 hours post-printing to stimulate barrier genesis [49] [50].
Synthetic Polymer-Based Bioinks
Synthetic polymers offer precise control over mechanical properties, degradation rates, and chemical functionality, making them valuable components in bioinks for BBB modeling where structural integrity and reproducibility are critical.
Polyethylene Glycol Diacrylate (PEGDA)
PEGDA has become a cornerstone synthetic polymer for BBB modeling due to its tunable mechanical properties, biocompatibility, and ability to be functionalized with adhesion peptides. Research demonstrates that PEGDA PhotoInk is frequently combined with natural polymers like GelMA to create hybrid bioinks for BBB models [16]. The Temple University research team utilized Volumetric's PEGDA PhotoInk with molecular weights varying between 200-500 Da to fine-tune the mechanical properties of their bioprinted BBB constructs [49] [50]. The non-adhesive nature of pure PEGDA necessitates functionalization with cell-adhesive peptides (e.g., RGD, YIGSR) to support endothelial cell attachment and spreading, which are essential for forming continuous endothelial layers in BBB models.
Table 2: Synthetic Polymer Bioinks for BBB Modeling
| Bioink Type | Key Advantages | Limitations | Modification Strategies |
|---|---|---|---|
| PEGDA | Precise control over mechanical properties; highly reproducible; tunable degradation | Lacks cell adhesion sites; requires functionalization | Incorporation of RGD, IKVAV, or YIGSR peptides; blending with natural polymers [49] [16] |
| PEGDA-GelMA Hybrids | Balanced mechanical and biological properties; customizable viscosity | Optimization required for component ratios | Typically 5-10% PEGDA with 5-15% GelMA; adjusted based on molecular weights [16] |
Experimental Protocol: PEGDA Functionalization and Bioprinting
Materials Required:
- PEGDA (molecular weight 200-500 Da)
- Photoinitiator (Irgacure 2959 or LAP)
- Cell-adhesive peptides (RGD, IKVAV, YIGSR)
- Acrylate-PEG-NHS for peptide conjugation
- Triethanolamine (co-initiator)
- Vascular endothelial growth factor (VEGF)
Functionalization Methodology:
- Dissolve PEGDA in 50 mM HEPES buffer (pH 7.4) at 10% (w/v) concentration.
- Add Acrylate-PEG-NHS (5 mM final concentration) to the PEGDA solution.
- Incorporate cell-adhesive peptides (RGD, 2 mM final concentration) and mix for 2 hours at 4°C.
- Dialyze the functionalized PEGDA against deionized water for 24 hours to remove unreacted peptides.
- Lyophilize the functionalized PEGDA and store at -20°C until use.
Bioprinting Protocol:
- Reconstitute functionalized PEGDA at 10-20% (w/v) in culture-grade PBS.
- Add photoinitiator (0.5% w/v LAP) and filter sterilize.
- Mix with hBMVECs at 5-10 × 10^6 cells/mL concentration.
- For DLP bioprinting, use UV exposure (365 nm, 5-15 mW/cm²) for 10-30 seconds per layer.
- Post-printing, cure constructs with additional UV exposure (365 nm, 10 mW/cm²) for 60 seconds.
- Transfer to perfusion bioreactor system within 24 hours for continuous medium flow (shear stress 5-20 dyn/cm²) [49] [50].
Hybrid Polymer Strategies
Hybrid bioinks that combine natural and synthetic polymers have emerged as the most promising approach for BBB modeling, offering a balance between the bioactivity of natural materials and the mechanical tunability of synthetic polymers.
PEGDA-GelMA Composite Bioinks
The combination of PEGDA and GelMA has been successfully implemented in multiple BBB modeling studies. Researchers at Temple University utilized a combination of PEGDA PhotoInk and GelMA PhotoInk to bioprint 3D microfluidic scaffolds that supported the formation of endothelialized vasculature with diameters between 150-350 μm [49] [50]. This hybrid approach allowed independent tuning of mechanical properties through the PEGDA component while maintaining critical cell-matrix interactions through the GelMA component. The optimal formulation supported the culture of both fetal and adult brain microvascular endothelial cells, with fully endothelialized vasculature observed within days of perfusion culture [16].
Design Considerations for Hybrid Bioinks in BBB Modeling
When formulating hybrid bioinks for BBB applications, several key parameters must be optimized:
Mechanical Properties: The storage modulus (G') of the bioink should typically range from 100-5000 Pa to mimic brain tissue stiffness while maintaining printability. The complex viscosity should be between 10-50 Pa·s for extrusion-based printing and 1-10 Pa·s for DLP printing.
Degradation Kinetics: Hybrid bioinks should demonstrate controlled degradation that allows endothelial cell migration and capillary formation while maintaining structural integrity during the maturation phase (typically 7-14 days).
Permeability Characteristics: The porosity and pore size of crosslinked hydrogels should initially restrict cellular infiltration (∼5-20 μm) but permit sequentiated remodeling by encapsulated cells to form capillary networks.
Table 3: Optimization Parameters for Hybrid Bioinks in BBB Modeling
| Parameter | Target Range | Measurement Technique | Impact on BBB Function |
|---|---|---|---|
| Storage Modulus (G') | 0.5-5 kPa | Rheometry | Influences endothelial cell spreading and tight junction formation |
| Mesh Size | 5-20 nm | Mathematical modeling from swelling ratios | Controls diffusion of nutrients and therapeutic compounds |
| Degradation Time | 7-28 days | Mass loss measurement | Should match tissue formation timeline |
| Contact Angle | 30-60° | Goniometry | Affects protein adsorption and cell adhesion |
| Permeability Coefficient | 1-5 × 10^-6 cm/s | Fluorescent dextran diffusion | Should approach in vivo BBB values (~10^-7 cm/s) with cellular components |
Diagram 1: Bioink Design Strategy for BBB Models. This workflow illustrates the integrated approach combining natural and synthetic polymers to achieve optimal bioink properties for blood-brain barrier modeling.
The Scientist's Toolkit: Essential Reagents for BBB Bioink Research
Table 4: Research Reagent Solutions for BBB Bioink Development
| Reagent/Category | Specific Examples | Function in BBB Bioink Formulation |
|---|---|---|
| Base Polymers | GelMA PhotoInk, PEGDA PhotoInk (200, 500 MW), PEGDA Start PhotoInk | Structural backbone of bioink; determines mechanical properties and printability [49] [16] |
| Photoinitiators | Lithium phenyl-2,4,6-trimethylbenzoylphosphinate (LAP), Irgacure 2959 | Enable light-based crosslinking of bioinks during bioprinting process [49] |
| ECM Components | Collagen I, Fibronectin, Matrigel, Thiol-Modified Hyaluronan/Heparin | Enhance bioactivity; promote cell adhesion and barrier function [49] [50] |
| Cell Culture Media | EGM-2 MV BulletKit, Advanced DMEM/F12 | Support viability and proliferation of BBB-specific cell types [49] [50] |
| Characterization Reagents | CellTracker dyes, Hoechst 33342, antibodies to ZO-1, claudin-5, occludin | Enable assessment of barrier integrity and cellular organization [49] [50] |
The development of advanced bioink formulations specifically designed for BBB modeling represents a critical frontier in neurological research and drug development. The integration of natural polymers providing biological cues with synthetic polymers offering mechanical precision has enabled the creation of increasingly sophisticated BBB models that better recapitulate the human neurovascular unit. As these technologies continue to evolve, future directions will likely include the development of patient-specific bioinks derived from induced pluripotent stem cells, dynamic bioinks with spatially patterned biochemical cues, and multi-material bioprinting strategies that can replicate the complex anatomical relationships of the complete neurovascular unit. These advances will accelerate drug discovery for neurological disorders and enhance our understanding of BBB pathophysiology in neurodegenerative diseases.
Diagram 2: Integrated Workflow for BBB Bioink Development. This diagram outlines the key decision points and considerations in developing functional in vitro BBB models, highlighting the interconnected relationships between material selection, cell source, and fabrication techniques.
The blood-brain barrier (BBB) is not a static interface but a dynamic system where mechanical forces, particularly fluid shear stress, play a fundamental role in maintaining barrier integrity and function. Fluid shear stress, the frictional force exerted by blood flow on endothelial cells, is a critical physiological cue that regulates BBB phenotype through mechanotransduction pathways [49]. In vivo, brain microvascular endothelial cells experience shear stress ranging between 5 and 23 dyn/cm² [13] [28], which promotes the formation of tight junctions and enhances barrier properties—a process known as barriergenesis [49]. Traditional static 3D bioprinted BBB models lack these critical hemodynamic forces, resulting in less mature barriers with reduced physiological relevance. This technical guide examines current methodologies for incorporating dynamic flow and shear stress simulation into 3D bioprinted BBB models, providing researchers with practical frameworks for creating more physiologically accurate neurovascular constructs for drug development and disease modeling.
Fundamental Design Principles for Flow-Based BBB Systems
Key Cellular Components and Architectural Considerations
Recapitulating the human BBB requires careful consideration of both cellular composition and structural organization. The essential cellular elements include:
- Brain Microvascular Endothelial Cells (BMECs): Form the primary barrier, connected by complex tight junctions (TJs) comprising occludin, claudins (particularly claudin-5), and junctional adhesion molecules (JAMs) [13] [28]. These TJ proteins are upregulated under appropriate shear stress conditions.
- Pericytes: Embedded within the basement membrane, pericytes regulate BBB permeability by modulating TJ protein expression and providing vascular stability [13] [10].
- Astrocytes: Their end-feet processes envelop the vascular tube and contribute to BBB integrity through the release of soluble factors and direct contact [10].
The basal lamina provides structural support through extracellular matrix (ECM) components including collagen IV, laminin, nidogen, and perlecan [13]. The ideal 3D bioprinted construct should replicate the cylindrical geometry of human brain capillaries, which typically range from 7-10 μm in diameter [13], though bioprinted constructs often feature larger diameters of 150-350 μm due to current technical limitations [49].
Biomechanical Principles of Shear Stress in Microvasculature
Shear stress (τ) in cylindrical vessels can be calculated using the simplified equation:
τ = (4μQ)/(πr³)
Where μ is fluid viscosity, Q is volumetric flow rate, and r is the vessel radius. This relationship demonstrates the profound influence of vessel diameter on shear stress levels, highlighting the importance of precise dimensional control in bioprinted constructs. The application of physiological shear stress:
- Induces polarization of BMECs and upregulates tight and adherens junction proteins [49]
- Enhances barrier integrity as measured by trans-epithelial electrical resistance (TEER), with physiological values ranging from 1,500 to 8,000 Ω·cm² [13]
- Activates mechanotransduction pathways that influence gene expression and cellular homeostasis [49]
Table 1: Target Parameters for Physiologically Relevant BBB Models
| Parameter | Target Range | Physiological Significance |
|---|---|---|
| Shear Stress | 5-23 dyn/cm² | Induces barriergenesis, enhances TJ formation [13] [49] |
| Capillary Diameter | 7-10 μm (native); 150-350 μm (engineered) | Influences shear stress magnitude, nutrient transport [13] [49] |
| TEER | 1,500-8,000 Ω·cm² | Indicator of barrier integrity and tight junction formation [13] |
| Flow Rate | Variable (to achieve target shear stress) | Determines nutrient delivery and waste removal [49] |
Implementation Strategies for Dynamic Flow Systems
Bioprinting Techniques for Vascular Network Fabrication
Multiple bioprinting modalities can be employed to create the complex 3D architectures required for perfusable vascular networks:
- Microextrusion Bioprinting: The most common technique utilizing pneumatic or mechanical (piston/screw-driven) systems to deposit bioinks in continuous filaments [51] [52]. While capable of creating large-scale constructs with structural integrity, this method has relatively low resolution (~100 μm) and can impose high shear stress on cells during extrusion [51].
- Digital Light Processing (DLP): A vat photopolymerization technique that uses projected light patterns to crosslink photosensitive bioinks in a layer-by-layer fashion [49]. This approach enables high-resolution fabrication of complex vascular networks with branching geometries and controlled internal diameters.
- Stereolithography (SLA): Similar to DLP but uses a focused laser beam for higher resolution patterning of photopolymerizable hydrogels [52].
For BBB modeling, DLP-based bioprinting offers significant advantages for creating the intricate, perfusable vascular networks needed to replicate the unique morphology of brain capillaries [49]. The methodology typically involves printing acellular hydrogel constructs with embedded lumens that are subsequently endothelialized and perfused.
Perfusion Systems and Flow Control
Implementing controlled flow requires integration of bioprinted constructs with perfusion systems. The following components are essential:
- Peristaltic or syringe pumps for precise flow control
- Compliant tubing with minimal gas permeability
- Pressure sensors to monitor system integrity
- Sterile reservoirs for culture medium
- Bubble traps to prevent embolization of microvessels
A critical consideration is the gradual acceleration of flow rates to allow for endothelial adaptation. Research protocols typically initiate perfusion at low flow rates (generating ~1-2 dyn/cm² shear stress) and gradually increase to physiological levels over 3-7 days [49]. This gradual conditioning promotes proper endothelial alignment and junction formation without causing cell detachment or apoptosis.
Table 2: Experimental Parameters for Microextrusion Bioprinting of Vascular Constructs
| Parameter | Typical Range | Impact on Construct Viability |
|---|---|---|
| Nozzle Diameter | 22G (≈410 μm) to 27G (≈210 μm) | Smaller diameters increase resolution but also shear stress [52] |
| Printing Pressure | 15-30 kPa (pneumatic) | Excessive pressure compromises cell viability [52] |
| Bioink Viscosity | 1-30 mPa·s (inkjet); 30-6×10⁷ mPa·s (extrusion) | Higher viscosity improves shape fidelity but requires higher extrusion pressure [51] [53] |
| Printing Temperature | 4-37°C (depending on crosslinking mechanism) | Affects bioink viscosity and gelation kinetics [53] |
| Shear Stress During Extrusion | <10 kPa (for viability >80%) | Critical for maintaining cell viability post-printing [52] |
Experimental Protocol: Fabricating a Perfusable 3D BBB Model
Materials and Bioink Formulation
Essential Research Reagent Solutions:
- Base Hydrogel: Polyethylene glycol diacrylate (PEGDA) or Gelatin methacryloyl (GelMA) provide tunable mechanical properties and photopolymerizability [49]
- ECM Components: Collagen I (50 μg/mL for coating), fibronectin, hyaluronan/heparin mixture to mimic native basement membrane [49]
- Cell Culture Media: Endothelial growth medium (EGM-2 MV) for BMECs, specialized media for astrocytes and pericytes [49]
- Primary Human Cells: Brain microvascular endothelial cells (hBMVECs), pericytes, and astrocytes in co-culture [49]
- Characterization Reagents: Immunofluorescence antibodies for ZO-1, claudin-5, occludin, CD31; fluorescent tracers for permeability assays (e.g., dextran conjugates) [49]
Step-by-Step Biopabrication Workflow
Diagram 1: 3D Bioprinting Workflow for BBB Model
In Silico Design: Create digital models of vascular networks with branching topologies and diameters of 150-350 μm using CAD software (e.g., Fusion 360) [49].
DLP Bioprinting: Fabricate acellular hydrogel constructs using photosensitive bioinks such as PEGDA or GelMA. The Lumen X bioprinter or similar systems can create complex 3D cytoarchitectural arrangements [49].
Lumen Cellularization:
- Condition luminal surfaces with collagen I (50 μg/mL) and fibronectin
- Introduce primary human brain microvascular endothelial cells (hBMVECs) at density of 1-2×10⁶ cells/mL
- Allow 24-48 hours for endothelial attachment under static conditions [49]
Pericyte and Astrocyte Incorporation:
- Seed pericytes within the surrounding matrix during bioink preparation
- Seed astrocytes on the abluminal surface after endothelialization [49]
Perfusion Conditioning:
- Connect construct to perfusion system with careful bubble removal
- Initiate flow at low shear stress (1-2 dyn/cm²) for 24 hours
- Gradually increase to 5-20 dyn/cm² over 5-7 days [49]
Characterization and Validation Methods
Barrier Integrity Assessment
- Transendothelial Electrical Resistance (TEER): Use specialized electrode systems designed for 3D constructs. Target values: >1,500 Ω·cm² for physiological relevance [13].
- Permeability Assays: Measure flux of molecular tracers (e.g., 4-70 kDa fluorescent dextran) across the barrier. Calculate permeability coefficient (Papp) and compare to established models [49].
- Immunofluorescence Staining: Validate TJ protein expression (ZO-1, claudin-5, occludin) and cellular organization. Proper shear stress conditioning should demonstrate continuous, well-localized TJ proteins [49].
Functional Transport Studies
- Receptor-Mediated Transcytosis: Assess transport of ligands for transferrin receptor (TfR), insulin receptor (IR), or low-density lipoprotein receptor-related protein 1 (LRP-1) [28].
- Efflux Transporter Activity: Evaluate P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP) function using specific substrates and inhibitors [28].
- Solute Carrier Transport: Characterize nutrient transport via GLUT1 (glucose), LAT1 (amino acids), and other specialized transporters [10].
Mechanotransduction Pathways in BBB Endothelium
The application of physiological shear stress activates several key signaling pathways that regulate BBB function:
Diagram 2: BBB Mechanotransduction Pathways
The diagram illustrates how mechanical forces are converted into biochemical signals that drive BBB maturation. Key elements include:
- Mechanosensors: Piezo1 channels, integrins, and VE-cadherin complexes detect shear stress
- Signaling Pathways: PI3K/Akt, MAPK, and KLF2/4 transcription factors are activated
- Functional Outcomes: Enhanced tight junction formation, cell polarization, and efflux transporter expression collectively contribute to barrier integrity
Technical Challenges and Future Directions
Despite significant advances, several challenges remain in perfecting dynamic flow systems for 3D bioprinted BBB models:
- Nozzle Optimization: Standard 3D printing nozzles may improve flow rates and reduce dispensing pressure compared to conical tips, but require further optimization for cellular viability [52].
- Vascular Complexity: Current bioprinting approaches struggle to replicate the hierarchical branching and size reduction (to ~7-10 μm) of native brain capillaries [13].
- Long-Term Stability: Maintaining barrier function beyond 7-10 days remains challenging, requiring improved bioink formulations and conditioning protocols.
- Shear Stress Gradients: Realistic models should incorporate physiological shear stress gradients rather than uniform flow profiles.
Future developments will likely focus on multi-material bioprinting to better replicate the layered structure of the neurovascular unit, and integration of sensors for real-time monitoring of barrier function during perfusion studies [9]. As these technologies mature, they will enable more predictive models for drug permeability testing and disease modeling.
The incorporation of dynamic flow and physiological shear stress simulation represents a critical advancement in 3D bioprinted BBB models, transforming them from static cellular aggregates to responsive, physiologically relevant systems. By implementing the methodologies outlined in this guide—including appropriate bioprinting techniques, gradual perfusion conditioning, and comprehensive validation—researchers can create sophisticated neurovascular models that more accurately replicate the human BBB. These advanced systems will significantly enhance our ability to study neurological diseases, screen neurotherapeutics, and develop personalized medicine approaches for disorders involving BBB dysfunction.
The blood-brain barrier (BBB) is a specialized structure fundamental to maintaining the homeostasis of the central nervous system (CNS) by tightly regulating the exchange of molecules between the bloodstream and the brain parenchyma [54] [55]. Its dysfunction is implicated in a wide range of neurological disorders, including Alzheimer's disease (AD) and Parkinson's disease (PD) [54] [13]. The BBB's core physiological unit, the neurovascular unit (NVU), is composed of brain microvascular endothelial cells (BMECs), pericytes, and astrocytes, which work in concert to maintain barrier integrity and function [55] [13]. Traditional in vitro models, particularly monocultures, fail to recapitulate the complex cellular crosstalk of the native NVU, leading to poor translational outcomes in drug development [54] [13].
Multicellular co-culture systems address this limitation by incorporating the key cellular components of the NVU, thereby providing enhanced physiological relevance. These systems enable researchers to study the individual contributions of each cell type to the overall BBB function while maintaining their paracrine and juxtacrine signaling [54]. This is crucial for elucidating disease mechanisms and for the reliable assessment of drug permeability and neurotoxicity. The integration of co-culture systems within advanced platforms like 3D bioprinting and dynamic microfluidic devices represents a significant leap forward in creating human-relevant models for CNS research and therapy development [33] [13].
Core Components of a Physiologically Relevant BBB Co-Culture
Cellular Composition of the Neurovascular Unit
A physiologically relevant BBB co-culture must integrate the three primary cell types of the NVU, each playing a distinct and critical role.
- Brain Microvascular Endothelial Cells (BMECs): BMECs form the physical barrier itself. They are characterized by continuous tight junctions (composed of proteins like claudin-5, occludin, and ZO-1) that severely restrict paracellular flux, and low rates of transcytosis [13]. These features are essential for creating the high electrical resistance that defines a functional BBB. In vitro, the integrity of the BMEC layer is often quantified by measuring the Transendothelial Electrical Resistance (TEER), with physiologically relevant models aiming for values between 1,500 and 8,000 Ω·cm² [13].
- Pericytes (PC): Pericytes are embedded within the basement membrane and encircle the endothelial cells. They are vital for regulating BBB permeability by modulating the expression of tight junction proteins in BMECs, thereby directly influencing barrier tightness and vascular stability [54] [13]. The inclusion of pericytes in co-culture systems has been shown to be essential for maintaining in vivo-like BBB properties [54].
- Astrocytes (AC): Astrocytes are glial cells that extend their end-feet processes, which envelop the brain's blood vessels. Through the release of soluble factors and direct physical contact, astrocytes contribute to the induction and maintenance of the barrier phenotype in BMECs [54] [13]. They also help maintain CNS homeostasis and respond to injury.
The Extracellular Matrix (ECM) and Dynamic Flow
Beyond cellular composition, the microenvironment is a critical determinant of barrier function.
- The Extracellular Matrix (ECM): The BBB ECM provides not only structural support but also essential biochemical cues. It is primarily composed of collagen IV, laminin, nidogen, and fibronectin, creating a unique basement membrane that supports NVU function [13]. In 3D bioprinted models, hydrogels combining alginate and gelatin have been successfully used as bioinks to mimic this natural ECM [56].
- Dynamic Flow: The incorporation of perfusable flow is a key design consideration for advanced co-culture systems [13]. Laminar flow generates shear stress on the endothelial surface, a mechanical stimulus reported to be between 5 and 23 dyn/cm² in human brain capillaries [13]. This shear stress promotes cell alignment, influences morphology, and upregulates the expression of tight junction proteins, all of which are essential for achieving a mature, functional barrier in vitro [54] [13].
Experimental Platforms and Protocols for BBB Co-Culture
Platform 1: The Kirkstall Quasi Vivo Dynamic Co-culture System
This system allows multiple cell types to be cultured in interconnected chambers under continuous flow, enabling communication through shared medium without direct cell-cell contact.
Key Experimental Protocol [54]:
- Cell Seeding: Culture human primary brain endothelial cells (HBECs), pericytes (HBVPs), and astrocytes (HAs) on appropriate scaffolds (e.g., coated coverslips) within separate but interconnected chambers of the QV500 system.
- Medium Formulation: Develop and use an "improved medium" capable of supporting all three cell types simultaneously.
- Flow Rate Optimization: Determine the optimal flow rate that sustains all cell types. For primary human cells, a flow rate of 50 µl/min, generating a wall shear stress of 2 × 10⁻⁶ Pa (2 × 10⁻⁵ dynes cm⁻²), was found to be optimal. Higher flow rates (e.g., 300 µl/min) were tolerated by HBECs but led to the death of astrocytes and pericytes.
- Validation & Experimentation: Confirm cell phenotypes via immunocytochemistry (e.g., CD31 for HBECs, α-actin for HBVPs, GFAP for HAs). The system can then be used for toxicity screening, such as treating the co-culture with amyloid-beta 25-35 peptide (Aβ25-35) to model Alzheimer's disease pathology.
Quantitative Parameters:
| Parameter | Value / Specification | Application / Note |
|---|---|---|
| Flow Rate | 50 µl/min | Optimal for primary human BBB cells [54] |
| Shear Stress | 2 x 10⁻⁶ Pa (2 x 10⁻⁵ dynes cm⁻²) | Corresponds to 50 µl/min flow [54] |
| HBEC Viability | ~140.5% of static control | After 72h under flow in triplicate culture [54] |
| Aβ25-35 Treatment | 20 µM | Used for proof-of-concept toxicity study [54] |
Platform 2: hiPSC-Derived BMEC and Microglia Co-culture in Transwell
This protocol outlines a simplified serum-free co-culture system using hiPSC-derived cells to incorporate a microglial component, which is key for modeling neuroinflammation.
- Key Experimental Protocol [55]:
- BMEC Differentiation: Differentiate hiPSCs into BMECs over 12 days using a specified induction and specification medium under hypoxic conditions (5% O₂) to enforce an endothelial phenotype.
- Microglia Differentiation: Generate hiPSC-derived microglia via embryoid body formation and subsequent maturation in a specialized microglia differentiation medium for 10 days.
- Co-culture Assembly: Seed the differentiated BMECs onto collagen IV/fibronectin-coated Transwell filters. Introduce the hiPSC-derived microglia to the system using a serum-free medium that does not compromise the barrier integrity.
- Functional Assessment: Monitor barrier integrity by regularly measuring TEER. An LPS challenge can be used to induce a neuroinflammatory response, characterized by a drop in TEER and secretion of pro-inflammatory cytokines.
Platform 3: 3D Bioprinting of the BBB
3D bioprinting offers unparalleled spatial control for creating complex, architecturally accurate BBB models.
- Key Experimental Strategy [13] [56]:
- Bioprinting Technique Selection: Utilize techniques such as extrusion-based bioprinting.
- Bioink Formulation: Employ composite hydrogels like alginate-gelatin or an Aqueous Two-Phase Printing (ATPP) system to create a liquid-phase microstructure that supports the co-culture of multiple cell types within a 3D ECM-like matrix [56].
- Design and Fabrication: Print a 3D construct that spatially organizes BMECs, pericytes, and astrocytes to mimic the anatomical arrangement of the native NVU. The design should include perfusable channels to introduce dynamic flow.
- Maturation and Testing: Culture the printed construct under dynamic flow conditions to promote barrier maturation. Assess functionality through TEER measurements, permeability assays (e.g., using fluorescent tracers), and immunostaining of tight junction proteins.
The Scientist's Toolkit: Essential Reagents and Materials
Table: Key Research Reagent Solutions for BBB Co-culture Models
| Item | Function / Application | Example in Context |
|---|---|---|
| hiPSC Lines | Patient-specific source for deriving all human NVU cell types, enabling disease modeling. | BIONi010-C line for microglia differentiation; hiPSSFC086 for BMEC differentiation [55]. |
| Specialized Growth Media | Formulated to support the simultaneous growth of multiple cell types without compromising their individual phenotypes or barrier properties. | "Improved medium" for primary tri-culture [54]; serum-free medium for hiPSC BMEC-microglia co-culture [55]. |
| ECM Coating Reagents | Provide the biochemical and structural cues of the basement membrane to support cell adhesion, growth, and function. | Collagen IV & Fibronectin for coating Transwells [55]; GFR Matrigel for hiPSC culture [55]. |
| Hydrogel Bioinks | Serve as the 3D scaffold in bioprinting, mimicking the native extracellular matrix. | Alginate/Gelatin composites [56]; Aqueous Two-Phase Printing (ATPP) systems [56]. |
| Phenotyping Antibodies | Essential for validating cell identity and morphology in the co-culture via immunocytochemistry. | Anti-CD31 (Endothelial cells), Anti-α-actin (Pericytes), Anti-GFAP (Astrocytes) [54]. |
| Tight Junction Markers | Used to assess barrier integrity and maturation at a molecular level. | Antibodies against ZO-1, Occludin, Claudin-5 [54] [13]. |
| Cytokines & Inducers | Used to differentiate cells from hiPSCs or to induce pathological states like neuroinflammation. | rhBMP4, rhVEGF, rhSCF for microglia progenitors; LPS to trigger inflammation [55]. |
Quantitative Assessment of BBB Co-culture Models
Evaluating the success of a multicellular BBB construct relies on quantifying key functional metrics that report on barrier integrity and cell viability.
Table: Key Quantitative Metrics for Assessing BBB Co-culture Models
| Metric | Target / Physiological Range | Measurement Technique | Significance |
|---|---|---|---|
| Transendothelial ElectricalResistance (TEER) | 1,500 - 8,000 Ω·cm² [13] | EVOM volt/ohm meter with STX2 electrode [55] | Gold standard for non-invasively assessing tight junction formation and barrier integrity. |
| Cell Viability | >100% relative to static control (e.g., 140.5% for HBECs under flow) [54] | MTT assay [54] | Indicates the health of the culture under dynamic conditions and in response to toxic insults. |
| Wall Shear Stress | 5 - 23 dyn/cm² (in vivo target)2 x 10⁻⁵ dynes cm⁻² (in vitro model) [54] [13] | Calculated based on flow rate, viscosity, and channel geometry. | Critical mechanical stimulus for promoting a mature endothelial phenotype. |
| Capillary Diameter | 7 - 10 μm (in vivo) [13] | High-resolution imaging and fabrication. | A key physical parameter for bioprinted models to mimic in vivo geometry. |
Multicellular co-culture systems are indispensable tools for creating physiologically relevant models of the blood-brain barrier. By integrating the core cellular components of the neurovascular unit—BMECs, pericytes, and astrocytes—and incorporating critical microenvironmental cues like dynamic flow and a biomimetic ECM, these systems bridge the gap between simple monocultures and complex in vivo physiology. The experimental platforms and detailed protocols outlined here provide a framework for researchers to investigate BBB function, dysfunction in neurodegenerative diseases, and central nervous system drug delivery with greater accuracy and predictive power. As the field advances, the convergence of patient-specific hiPSCs with sophisticated 3D bioprinting technologies will further enhance the precision and translational value of these multicellular constructs, ultimately accelerating the development of effective therapies for neurological disorders.
The blood-brain barrier (BBB) represents one of the most significant challenges in central nervous system (CNS) drug discovery, excluding over 98% of small-molecule drugs and nearly 100% of large-molecule therapeutics from reaching their intended targets [2]. This high rate of attrition in neurotherapeutic development has created an urgent need for more predictive in vitro models that can accurately simulate human BBB physiology. Traditional two-dimensional (2D) models and animal systems have demonstrated limited translational relevance, failing to fully recapitulate the complex cellular interactions, shear stress, and three-dimensional architecture of the human neurovascular unit [13] [4]. In response to these limitations, 3D bioprinting has emerged as a transformative technology for engineering physiologically relevant BBB models that bridge the gap between conventional in vitro screens and clinical outcomes.
Advanced 3D bioprinting techniques enable the precise spatial arrangement of all major BBB cellular components—brain microvascular endothelial cells (BMECs), pericytes, and astrocytes—within a tunable extracellular matrix (ECM) that mimics the native brain microenvironment [13] [49]. These models incorporate crucial physiological parameters such as tubular vascular structures, physiological shear stress, and cell-ECM interactions that are essential for establishing authentic barrier properties, including the formation of complex tight junctions and functional transport systems [57] [49]. This technical guide explores the application of 3D bioprinted BBB models as next-generation platforms for permeability screening and toxicity assessment, providing detailed methodologies, experimental protocols, and analytical frameworks to accelerate CNS drug discovery.
Fundamentals of 3D Bioprinted BBB Models
Key Cellular Components and Architecture
Physiologically relevant BBB models require the incorporation of the complete neurovascular unit to achieve native-like barrier function. The core cellular composition includes:
Brain Microvascular Endothelial Cells (BMECs): These cells form the primary barrier through complex tight junctions comprising proteins such as claudin-5, occludin, and JAM-1, which significantly restrict paracellular transport [13]. BMECs also express specialized transport systems including efflux pumps (P-glycoprotein, BCRP) and receptor-mediated transporters (Transferrin receptor, LRP1) [57].
Pericytes: Embedded within the basement membrane, pericytes play a critical role in regulating BBB permeability by modulating the expression of tight junction proteins in endothelial cells and providing vascular stability [13] [58]. In advanced 3D models, pericytes form a surrounding layer outside the endothelial lining, creating a dual-layered structure that closely resembles actual blood vessels [58].
Astrocytes: Their end-feet processes envelop the blood vessels and contribute to BBB integrity through the release of soluble factors that promote endothelial cell differentiation and tight junction stability [2]. Astrocytes are typically embedded in the surrounding bioink matrix in 3D bioprinted constructs [57].
The extracellular matrix composition is equally critical for authentic BBB function. Decellularized extracellular matrix (dECM) from porcine brain and blood vessels has been successfully used to create cerebrovascular-specific bioinks that promote the spontaneous self-assembly of dual-layered vascular structures and enhance barrier properties [58].
3D Bioprinting Techniques for BBB Modeling
Several bioprinting technologies have been adapted for BBB model fabrication, each offering distinct advantages:
Extrusion-Based Bioprinting: This method utilizes pneumatic or piston-driven systems to deposit cell-laden bioinks in a layer-by-layer fashion. While capable of handling high-viscosity materials, it imposes significant shear stress on cells, potentially affecting viability [59]. Nozzle size, pressure, and printing speed must be carefully optimized to balance structural fidelity with cell health.
Stereolithography (SLA) and Digital Light Processing (DLP): These vat polymerization techniques use light to crosslink photocrosslinkable bioinks with high resolution and reproducibility [49]. DLP-based bioprinting has been successfully employed to create complex, perfusable vascular networks with diameters ranging from 150-350 μm, comparable to human brain capillaries [49]. A key advantage is the ability to generate branching vascular networks with relevant cytoarchitecture and multicellular arrangement.
Projection Stereolithography: This emerging technique represents one of the most advanced approaches for fabricating perfusable BBB models, enabling the patterning of complex vessel geometries and precise arrangement of multiple cell populations [57].
Table 1: Comparison of 3D Bioprinting Techniques for BBB Models
| Bioprinting Technique | Resolution | Speed | Cell Viability | Key Advantages | Limitations |
|---|---|---|---|---|---|
| Extrusion-Based | 100-500 μm | Medium | Medium (~40-80%) [59] | Handles high viscosity materials; multi-material capability | High shear stress; limited resolution |
| Stereolithography (SLA) | 25-100 μm | Slow | High (>85%) [59] | High resolution; smooth surfaces | Limited material choices; potential UV damage |
| Digital Light Processing (DLP) | 10-50 μm | Fast | High (>90%) [49] | Fast printing; high resolution; excellent for vascular networks | Material limitations; requires photocrosslinkable bioinks |
| Projection Stereolithography | 10-100 μm | Fast | High (>90%) [57] | Complex geometries; precise cell patterning; perfusable vessels | Specialized equipment; protocol complexity |
Permeability Screening Using 3D Bioprinted BBB Models
Model Fabrication for Permeability Studies
The following protocol outlines the steps for creating a perfusable 3D bioprinted BBB model suitable for high-quality permeability screening:
Bioink Preparation: Prepare a hydrogel bioink combining PEGDA (polyethylene glycol diacrylate) with gelatin methacryloyl (GelMA) or cerebrovascular-specific dECM bioink [58] [49]. Incorporate primary human astrocytes (50,000 cells/mL) and pericytes (25,000 cells/mL) directly into the bioink mixture.
Vascular Template Printing: Utilize DLP bioprinting to fabricate a cylindrical vascular network template (diameter: 200-300 μm) within the astrocyte-pericyte-laden hydrogel matrix. Employ STL files of 3D cytoarchitectural arrangements designed using Fusion 360 or Blender software [49].
Endothelialization: Seed primary human brain microvascular endothelial cells (hBMVECs, 1-2×10^6 cells/mL) into the lumen of the printed vascular channel and allow for adhesion (4-6 hours) [49].
Perfusion Culture: Connect the bioprinted construct to a perfusion system and circulate endothelial growth medium (EGM-2MV supplemented with ECGS and heparin) at a physiological shear stress of 5-20 dyn/cm² for 7-10 days to facilitate barrier maturation [49].
Barrier Validation: Confirm the formation of continuous tight junctions via immunostaining for ZO-1, claudin-5, and occludin before initiating permeability studies [57].
Quantitative Permeability Assessment Protocol
The integrity and functionality of the bioprinted BBB model can be quantified using established permeability tracers:
Tracer Preparation: Prepare working solutions of fluorescent permeability tracers (10 μg/mL sodium fluorescein, 10 μg/mL FITC-dextran series) in Hanks' Balanced Salt Solution (HBSS) [57].
Perfusion Setup: Connect the bioprinted BBB model to a perfusion system and circulate the tracer solution through the vascular lumen at physiological shear stress (5-20 dyn/cm²).
Sample Collection: Collect samples from the abluminal (brain) compartment at 10, 20, 30, 45, and 60-minute time points.
Quantification: Measure fluorescence using a microplate reader (excitation/emission: 485/535 nm for fluorescein) and calculate the apparent permeability coefficient (P_app) using the following equation:
Papp = (dC/dt) × (V/(A × Clum))
Where dC/dt is the change in abluminal concentration over time, V is the abluminal volume, A is the surface area of the vessel, and C_lum is the constant luminal concentration.
Validation Benchmarking: Compare obtained P_app values against established physiological ranges and published values for known CNS-permeable and impermeable compounds.
Table 2: Permeability Coefficients of Reference Compounds in 3D Bioprinted BBB Models
| Compound | Molecular Weight (Da) | P_app (×10⁻⁶ cm/s) in 3D Bioprinted Model | P_app (×10⁻⁶ cm/s) in Human BBB | Transport Mechanism |
|---|---|---|---|---|
| Sodium Fluorescein | 376 | 1.5 - 3.0 [57] | 0.5 - 2.5 [57] | Paracellular (low) |
| Caffeine | 194 | 35 - 45 [2] | 40 - 50 [2] | Transcellular passive diffusion |
| Sucrose | 342 | 0.8 - 1.5 [57] | 0.5 - 1.2 [57] | Paracellular marker |
| Diazepam | 285 | 25 - 35 [2] | 20 - 30 [2] | Transcellular passive diffusion |
| FITC-Dextran 4kDa | 4,000 | 0.5 - 1.2 [57] | 0.3 - 0.8 [57] | Paracellular (intermediate) |
| FITC-Dextran 40kDa | 40,000 | 0.1 - 0.3 [57] | <0.1 [57] | Paracellular (high) |
Assessment of Transport Mechanisms
Beyond basic permeability screening, 3D bioprinted BBB models enable detailed investigation of specific transport pathways:
Passive Diffusion Screening: Evaluate transcellular passive diffusion using lipophilic compounds with molecular weight <500 Da and LogP>2 [2]. The model should demonstrate superior discrimination compared to 2D systems due to more authentic tight junction formation.
Efflux Transporter Activity: Assess P-glycoprotein (P-gp) and BCRP functionality through directional transport studies with known substrates (e.g., digoxin, loperamide) with and without specific inhibitors (verapamil, Ko143) [57]. Immunostaining confirms transporter localization and expression.
Receptor-Mediated Transcytosis (RMT): Investigate potential for biologic drug delivery using ligands targeting transferrin receptor (TfR) or insulin receptor [2]. Quantify uptake and transcytosis using fluorescently-labeled ligands.
Carrier-Mediated Transport (CMT): Evaluate nutrient transporter (GLUT1, LAT1) functionality using competitive assays with prototype substrates (glucose, L-DOPA) [2].
Toxicity Assessment Using 3D Bioprinted BBB Models
Multiparametric Toxicity Screening Protocol
3D bioprinted BBB models enable comprehensive toxicity assessment through multiple analytical endpoints:
Barrier Integrity Assessment:
- Real-time TEER Monitoring: Incorporate embedded electrodes for continuous transendothelial electrical resistance measurement. Physiological TEER values should range from 1,500-8,000 Ω·cm² [13].
- Paracellular Permeability Tracking: Use sodium fluorescein (376 Da) as a small molecule tracer to assess tight junction integrity following compound exposure.
Cell Viability Analysis:
- Live/Dead Staining: Perform viability assays using Calcein-AM (live cells) and propidium iodide (dead cells) after 24-hour compound exposure.
- Lactate Dehydrogenase (LDH) Release: Quantify LDH in the culture medium as a marker of cytotoxicity using commercial assay kits.
Inflammatory Response Profiling:
- Cytokine Secretion Analysis: Measure IL-6, IL-1β, and TNF-α release via ELISA following 24-hour compound exposure.
- Adhesion Molecule Expression: Quantify VCAM-1 and ICAM-1 surface expression via immunostaining after inflammatory stimulus (e.g., TNF-α, IL-1β) [58].
Functional Assessment:
- Efflux Transporter Activity: Evaluate P-gp and BCRP function using fluorescent substrates (rhodamine 123, Hoechst 33342) with and without test compounds.
- Tight Junction Integrity: Analyze ZO-1, claudin-5, and occludin organization via confocal microscopy and image analysis.
Neuroinflammatory Modeling
The protocol below details how to model neuroinflammatory responses in 3D bioprinted BBB models:
Inflammatory Challenge: Expose the bioprinted BBB model to inflammatory cytokines (TNF-α and IL-1β at 10-50 ng/mL for 6-24 hours) to simulate neuroinflammatory conditions associated with neurodegenerative diseases [58].
Permeability Changes: Measure the increase in permeability to FITC-dextran (4 kDa) following inflammatory challenge. Well-differentiated models typically show a 2-4 fold increase in permeability under inflammatory conditions.
Tight Junction Rearrangement: Visualize and quantify the discontinuous organization and internalization of tight junction proteins (ZO-1, claudin-5) using immunostaining and confocal microscopy.
Adhesion Molecule Upregulation: Assess increased expression of ICAM-1 and VCAM-1 on endothelial cells, which promotes immune cell adhesion and trafficking.
Therapeutic Testing: Evaluate potential protective compounds by pre-treating for 2-6 hours before inflammatory challenge and assessing the preservation of barrier function.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for 3D Bioprinted BBB Models
| Category | Reagent/Material | Specification/Example | Function | Key Considerations |
|---|---|---|---|---|
| Bioink Components | PEGDA PhotoInk | MW: 200-500 Da [49] | Primary hydrogel matrix provides structural integrity | Adjust molecular weight for permeability and mechanical properties |
| GelMA PhotoInk | 5-15% w/v [49] | Adds cell adhesion motifs and tunable mechanical properties | Concentration affects stiffness and degradation rate | |
| Cerebrovascular dECM | Porcine brain and vessel-derived [58] | Tissue-specific ECM promoting BBB differentiation | Enhances spontaneous cell self-organization | |
| Hyaluronan/Heparin | Thiol-modified [49] | Mimics brain ECM composition; supports signaling | Concentration affects hydrogel viscosity and printability | |
| Cells | hBMVECs | Primary human, passage <8 [49] | Forms endothelial barrier with tight junctions | Low passage maintains proper junctional protein expression |
| Pericytes | Primary human, passage <8 [49] | Regulates barrier function and vessel stability | Co-localizes with endothelial cells in dual-layer structure | |
| Astrocytes | Primary human, passage <10 [49] | Enhances barrier properties via end-feet contacts | Embed in surrounding matrix for physiological positioning | |
| Culture Reagents | EGM-2MV BulletKit | With supplements [49] | Endothelial growth medium with specific factors | Essential for maintaining endothelial phenotype |
| Endothelial Cell Growth Supplement | 30-50 μg/mL [49] | Promotes endothelial cell proliferation and function | Critical for long-term culture stability | |
| Heparin | 1 mg/mL [49] | Potentiates growth factor activity | Enhances endothelial cell function and barrier properties | |
| Characterization Tools | Anti-ZO-1 Antibody | Mouse anti-human, 1:200 [49] | Tight junction protein visualization | Pattern indicates barrier maturity and integrity |
| Anti-Claudin-5 Antibody | Rabbit anti-human, 1:100 [49] | Key tight junction protein specific to BBB | Reduction correlates with increased permeability | |
| Anti-P-gp Antibody | Mouse anti-human, 1:200 [57] | Efflux transporter localization and expression | Confirms functional transporter expression | |
| Permeability Tracers | Sodium Fluorescein | 376 Da, 10 μg/mL [57] | Small molecule paracellular permeability marker | Baseline barrier integrity assessment |
| FITC-Dextran Series | 4, 10, 40 kDa [57] | Size-dependent permeability assessment | Molecular weight cut-off profiling |
3D bioprinting represents a paradigm shift in BBB modeling for drug discovery applications, offering unprecedented physiological relevance through precise spatial control of cellular organization, incorporation of physiological flow conditions, and tissue-specific extracellular matrix environments. These advanced models demonstrate superior predictive capability for both permeability screening and toxicity assessment compared to traditional 2D systems. The protocols and methodologies outlined in this technical guide provide researchers with comprehensive frameworks for implementing 3D bioprinted BBB models in preclinical drug development workflows.
Future directions in the field include the integration of additional cell types (microglia, neurons) to create more comprehensive neurovascular unit models, incorporation of patient-derived cells for personalized medicine applications, implementation of sensor technologies for real-time monitoring of barrier function, and development of higher throughput screening platforms [58] [9]. As these technologies continue to mature, 3D bioprinted BBB models are poised to significantly improve the predictability of CNS drug development, potentially reducing late-stage attrition rates and accelerating the delivery of effective neurotherapeutics to patients.
Overcoming Technical Hurdles: Optimization Strategies for Robust BBB Models
The development of bioinks represents one of the most significant challenges in the advancement of 3D bioprinting, particularly for sophisticated applications such as blood-brain barrier (BBB) modeling. Bioinks must simultaneously satisfy three competing requirements: printability (the ability to be accurately deposited into complex 3D structures), cytocompatibility (the capacity to support cell viability and function), and mechanical properties (appropriate structural integrity and stability). This trilemma poses a substantial technical hurdle for researchers developing in vitro BBB models for neurodegenerative disease research and drug development [13] [60].
The pursuit of a bioink that optimally balances these properties has become a central focus in tissue engineering. As the field moves toward more complex tissue constructs, the limitations of existing bioinks become increasingly apparent. For BBB modeling specifically, the bioink must facilitate the creation of perfusable vascular networks with appropriate barrier function while supporting the viability and function of multiple cell types, including brain microvascular endothelial cells, pericytes, and astrocytes [13] [10]. This technical guide examines the fundamental challenges in bioink development and provides a comprehensive framework for achieving this critical balance, with specific application to the advancement of BBB research.
Defining the Core Bioink Properties
Printability: From Rheology to Structural Fidelity
Printability refers to a bioink's ability to be processed through a bioprinter and maintain the intended structural architecture post-printing. This property is predominantly governed by the bioink's rheological behavior and gelation kinetics [60] [61].
The rheological properties of bioinks are crucial for determining their performance during the printing process. A key characteristic is shear-thinning behavior, where viscosity decreases under shear stress during extrusion and rapidly recovers once deposited. This property prevents excessive shear stress on encapsulated cells while maintaining structural fidelity after deposition [60]. Additionally, the viscosity of bioink formulations must be tunable to accommodate different printing technologies. For instance, droplet-based bioprinters typically require viscosities around 10 mPa·s, while extrusion-based systems need significantly higher viscosities ranging from 30 to 6×10⁷ mPa·s [60].
Gelation kinetics similarly play a critical role in printability. Bioinks with appropriately timed gelation mechanisms—whether thermal, ionic, or photochemical—enable rapid stabilization of deposited filaments. Research has demonstrated that bioinks with prolonged gelation times tend to result in poorer printability due to insufficient structural support during the printing process [61].
Cytocompatibility: Preserving Cellular Viability and Function
Cytocompatibility encompasses not only initial cell viability post-printing but also the long-term support of cellular functions, including proliferation, differentiation, and tissue-specific functionality. For BBB models, this extends to the formation of tight junctions and the expression of appropriate transporters [13] [10].
Multiple factors influence cytocompatibility, including the biocompatibility of base materials, degradation products, and the shear stresses experienced during printing. Studies have shown that cell viability can exhibit an exponential relationship with induced shear stress during extrusion, emphasizing the need to carefully control printing parameters [61]. Additionally, the biochemical composition of bioinks must provide appropriate cell adhesion motifs and signaling cues to support specific cellular functions. For BBB models, this includes facilitating the formation of tight junctions between endothelial cells and supporting astrocyte end-feet interactions [10].
The long-term maintenance of cytocompatibility requires that bioinks permit nutrient diffusion, metabolic waste removal, and, in some cases, vascularization to support tissue maturation. For barrier tissues like the BBB, the bioink must also enable the establishment of appropriate polarity and transport properties [13].
Mechanical Properties: Mimicking Native Tissue Environments
Mechanical properties encompass the structural stability, stiffness, and degradation behavior of the printed construct. These characteristics must align with the native tissue being modeled—for the BBB, this involves matching the mechanical microenvironment of brain tissue and cerebral vasculature [13] [24].
The elastic modulus (stiffness) of the bioink significantly influences cellular behavior through mechanotransduction pathways. For neural tissues, including the BBB, lower stiffness values typically in the range of 0.1-1 kPa are often desirable to mimic the native brain microenvironment [24]. However, the bioink must also provide sufficient structural integrity to maintain perfusable lumens under physiological flow conditions.
The degradation rate of the bioink must be carefully balanced with tissue maturation. If the material degrades too quickly, the structural integrity may be lost before the cells have deposited sufficient extracellular matrix. Conversely, if degradation is too slow, it may impede tissue remodeling and integration [60]. For long-term BBB models, maintaining mechanical stability for several weeks is often necessary to allow for full barrier maturation [13].
Table 1: Key Bioink Properties and Their Technical Specifications for BBB Modeling
| Property | Technical Requirements | Measurement Methods | Target Values for BBB Models |
|---|---|---|---|
| Printability | Shear-thinning behavior, appropriate viscosity, rapid gelation | Rheometry, filament collapse tests, printability assessment | Viscosity: 30-6×10⁷ mPa·s (extrusion-based); Fiber diameter consistency >90% [60] [61] |
| Cytocompatibility | Support cell viability, function, and barrier formation | Live/dead assay, immunofluorescence, TEER measurement | Cell viability >85%; TEER: 1,500-8,000 Ω·cm² [13] [61] |
| Mechanical Properties | Appropriate stiffness, structural integrity, degradation rate | Compression testing, dynamic mechanical analysis, swelling tests | Elastic modulus: 0.1-1 kPa; Stability >21 days [62] [24] |
Quantitative Analysis of Bioink Properties
The relationship between bioink composition and its resulting properties can be quantitatively characterized to guide formulation design. Recent studies have provided specific data on how material combinations affect key parameters.
Rheological analysis reveals how composition affects flow behavior. For example, a study optimizing alginate (Alg), carboxymethyl cellulose (CMC), and gelatin methacrylate (GelMA) blends identified 4% Alg–10% CMC–GelMA (at 8%, 12%, and 16% concentrations) as optimal formulations. These compositions demonstrated appropriate shear-thinning behavior and gelation properties conducive to printing [62].
The mechanical performance of bioinks can be precisely tuned through material selection and crosslinking strategies. In the aforementioned Alg-CMC-GelMA system, the dual crosslinking approach (UV curing plus CaCl₂ ionic crosslinking) produced scaffolds with variable stiffness suitable for gradient tissue regeneration. These constructs maintained long-term mechanical stability for up to 21 days, with the 4% Alg–10% CMC–16% GelMA formulation exhibiting superior mechanical performance and enhanced cell proliferation [62].
Table 2: Experimental Data for Alginate-CMC-GelMA Bioink Formulations [62]
| Composition (Alg-CMC-GelMA) | Printability Score | Cell Viability (%) | Compressive Modulus (kPa) | Stability Duration (days) |
|---|---|---|---|---|
| 4%-10%-8% | 0.82 | 87.3 | 12.5 ± 1.2 | 21 |
| 4%-10%-12% | 0.85 | 89.1 | 15.8 ± 1.5 | 21 |
| 4%-10%-16% | 0.88 | 91.5 | 18.3 ± 1.7 | 21 |
The optimization of printing parameters significantly influences the resulting cellular viability. Research with embryonic stem cells demonstrated that viability increases with higher printing temperatures and lower gelatin concentrations, revealing an exponential relationship between cell viability and induced shear stress during printing [61].
Experimental Protocols for Bioink Evaluation
Protocol 1: Rheological and Printability Assessment
A comprehensive protocol for evaluating bioink printability involves sequential rheological tests and printing assessments:
Rheological Characterization:
- Perform viscosity measurements under steady-state shear conditions across a shear rate range of 0.1 to 100 s⁻¹
- Conduct oscillatory frequency sweeps (0.1-10 Hz) at constant strain to characterize viscoelastic properties
- Perform time-dependent recovery tests to assess self-healing behavior [62]
Printability Assessment:
- Utilize a semi-quantitative method to evaluate printed filament morphology
- Print grid structures and characterize fiber diameter uniformity and pore regularity
- Quantify the printability value (P) using dimensional analysis of printed filaments [61]
Gelation Kinetics:
- Monitor storage (G') and loss (G") moduli over time after triggering gelation
- Determine gelation time as the point where G' surpasses G"
- For photopolymerizable inks, measure the time to achieve gelation under UV exposure [62]
Protocol 2: Cytocompatibility and Barrier Function Assessment
For BBB-specific bioinks, functional assessment of barrier properties is essential:
Cell Viability Analysis:
- Encapsulate cells at appropriate density (typically 1-10 million cells/mL)
- Assess viability at 24, 48, and 72 hours post-printing using live/dead staining
- Quantify metabolic activity using AlamarBlue or MTT assays [61]
Barrier Integrity Assessment:
Immunofluorescence and Imaging:
Material Strategies for Balancing Bioink Properties
Hybrid and Composite Bioinks
The combination of multiple materials in hybrid bioinks has emerged as a powerful strategy to balance competing requirements. Natural polymers like alginate and gelatin provide biocompatibility and cell interaction sites, while synthetic components or modified natural polymers offer tunable mechanical properties and printability [62] [60].
Alginate-gelatin systems leverage the rapid ionic crosslinking of alginate with the thermoresponsive behavior of gelatin. This combination allows for temperature-controlled printing followed by stabilization through calcium-mediated crosslinking. The addition of GelMA introduces the capability for secondary UV crosslinking, enabling the creation of more complex structures with enhanced mechanical properties [62].
For BBB models specifically, incorporating matrix components that mimic the native basement membrane (e.g., collagen IV, laminin, fibronectin) can enhance barrier function. These can be integrated into bioinks as full proteins or through bioactive peptides (e.g., RGD, IKVAV) that promote specific cellular interactions [10] [24].
Functional Modification and Bioactive Signaling
Advanced bioink strategies incorporate bioactive signals to direct cellular behavior and tissue maturation. For BBB models, this includes:
- Peptide functionalization with sequences derived from extracellular matrix proteins or cell-cell adhesion molecules
- Controlled release of growth factors that promote endothelial barrier formation and maintenance
- Gene-activated bioinks that provide genetic instructions to encapsulated cells [63]
Research has demonstrated that specific peptide motifs can significantly influence endothelialization and tight junction formation. In one study, HAVDI and IKVAV peptides lined channels exhibited significantly greater endothelialization and increased ZO-1 localization to cell-cell junctions compared to other motifs [24].
Diagram 1: Bioink Development Workflow - This diagram illustrates the iterative process of bioink design, from material selection through property optimization to final application.
Application to Blood-Brain Barrier Modeling
Specialized Requirements for BBB Bioinks
The creation of functional in vitro BBB models imposes specific requirements on bioink design beyond general tissue engineering applications. These include:
- Support for multiple cell types in spatially defined arrangements, including endothelial cells, pericytes, and astrocytes
- Formation of tight junctions with appropriate localization of proteins such as ZO-1, occludin, and claudin-5
- Regulation of permeability to mimic the selective transport properties of the native BBB
- Response to fluid shear stress through incorporation of perfusable channels [13] [10]
The cellular composition of BBB models is critical for achieving physiological functionality. Incorporating all three key BBB cell types—brain microvascular endothelial cells, astrocytes, and pericytes—enhances tight junction formation and barrier tightness, enabling more accurate replication of BBB anatomical and functional complexity [13].
Advanced Bioprinting Strategies for BBB Models
Advanced bioprinting technologies enable the creation of complex BBB models with perfusable vascular networks. Digital light processing (DLP) printing allows for the creation of channels with complex topologies that can be functionalized with specific peptide motifs in different regions [24] [50].
A key advancement in BBB model development is the incorporation of dynamic flow to simulate capillary blood flow and associated shear stress. Physiological shear stress in human brain capillaries ranges between 5 and 23 dyn/cm², and this mechanical stimulus influences cell alignment, morphology, and upregulation of tight junction proteins [13].
Diagram 2: From Native BBB to Bioprinted Model - This diagram illustrates the translation of native BBB anatomy and functionality into design requirements for bioinks used in 3D bioprinted models.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Reagents for Bioink Development and BBB Modeling
| Category | Specific Materials | Function/Application | Key References |
|---|---|---|---|
| Natural Polymers | Alginate, Gelatin methacrylate (GelMA), Carboxymethyl cellulose (CMC), Collagen, Hyaluronic acid | Provide biocompatibility, cell adhesion motifs, and tunable physical properties | [62] [60] |
| Synthetic Polymers | Poly(ethylene glycol) diacrylate (PEGDA), Polycaprolactone (PCL) | Offer controllable mechanical properties, degradation rates, and photopolymerizability | [63] [50] |
| Crosslinking Agents | Calcium chloride (CaCl₂), UV initiators (LAP, Irgacure 2959), Enzymatic crosslinkers (e.g., transglutaminase) | Enable stabilization of printed structures through ionic, covalent, or enzymatic mechanisms | [62] [50] |
| Bioactive Peptides | RGD, IKVAV, HAVDI, YIGSR | Promote specific cell-matrix interactions and enhance cellular function | [24] |
| Cells for BBB Models | Brain microvascular endothelial cells (BMECs), Pericytes, Astrocytes | Recapitulate cellular complexity of the neurovascular unit | [13] [10] |
| Characterization Reagents | Live/Dead viability assays, antibodies against tight junction proteins (ZO-1, occludin, claudin-5), TEER measurement systems | Assess bioink performance, barrier formation, and functionality | [13] [50] |
The development of bioinks that successfully balance printability, cytocompatibility, and mechanical properties remains a significant challenge, but continued advances in material science and biofabrication technologies are steadily addressing these limitations. For BBB modeling in particular, the emergence of multi-material bioprinting systems, increasingly sophisticated bioactive functionalization strategies, and improved understanding of BBB biology are enabling the creation of more physiologically relevant models.
Future directions in bioink development for BBB applications include the creation of patient-specific models using induced pluripotent stem cell-derived neural cells, the incorporation of immune cell components to better model neuroinflammatory conditions, and the development of dynamic bioinks that can evolve their properties in response to environmental cues or external triggers. As these technologies mature, they will undoubtedly accelerate both fundamental neuroscience research and the development of novel therapeutics for neurodegenerative diseases.
Transendothelial Electrical Resistance (TEER) is a gold-standard, quantitative metric for evaluating the integrity and functional tightness of in vitro blood-brain barrier (BBB) models [64]. It directly measures the restriction of paracellular ion movement, serving as a sensitive indicator of tight junction formation and quality. In the context of three-dimensional (3D) bioprinted BBB models, achieving physiological TEER values—which range from 1,500 to 8,000 Ω·cm² in vivo—is a significant benchmark for model validation and a prerequisite for meaningful drug transport and disease studies [13] [64]. Unlike traditional 2D Transwell systems, 3D bioprinting offers unprecedented control over cellular spatial organization, extracellular matrix (ECM) biochemistry, and dynamic flow conditions, all of which are levers that can be manipulated to enhance barrier tightness. This technical guide synthesizes current strategies for optimizing these parameters to achieve robust, physiologically relevant TEER in 3D-bioprinted BBB constructs, providing a vital resource for advancing neuroscience research and therapeutic development.
Physiological Benchmarks and Key Design Considerations
The foundational step in engineering a superior BBB model is understanding the benchmark of native barrier function and the key elements that influence it.
- Physiological TEER Benchmark: A physiologically relevant in vitro BBB model should aim for a TEER value between 1,500 and 8,000 Ω·cm², reflecting the tightness of the human BBB in vivo [13] [64].
- Key Design Considerations for 3D Models: To reach this benchmark, 3D-bioprinted models must incorporate several critical design features that go beyond conventional cultures.
- Multicellular Composition: The BBB is not solely an endothelial structure. Including all key cell types—brain microvascular endothelial cells (BMECs), pericytes, and astrocytes—is essential for inducing and maintaining high TEER through synergistic interactions [13] [28].
- Dynamic Perfusion: The endothelial lumen in vivo is subjected to constant shear stress from blood flow, a critical mechanical cue that upregulates tight junction protein expression. Bioprinted constructs should incorporate perfusable flow, with target shear stress levels between 5 and 23 dyn/cm² to mimic human brain capillary conditions [13].
- Geometric Fidelity: High-resolution bioprinting is required to create vascular channels with diameters of 7–10 μm, replicating the scale of true brain capillaries and supporting proper endothelial cell function [13].
Table 1: Key Cell Types and Their Roles in the Neurovascular Unit
| Cell Type | Primary Function in BBB | Impact on TEER and Barrier Integrity |
|---|---|---|
| Brain Microvascular Endothelial Cells (BMECs) | Form the primary physical barrier; express tight junction proteins [28]. | Directly responsible for generating TEER. The quality and maturity of tight junctions determine the baseline resistance. |
| Pericytes | Embedded within the basement membrane; regulate vascular stability and BBB permeability [13]. | Modulate the expression of tight junction proteins in BMECs (e.g., claudin-5), thereby enhancing barrier tightness [13]. |
| Astrocytes | Envelop blood vessels with end-feet processes; maintain CNS homeostasis [13]. | Contribute to the induction and regulation of BBB permeability through secreted factors and physical interactions [13]. |
Strategic Pillars for Enhancing TEER in 3D-Bioprinted Models
Achieving high TEER requires a multi-faceted approach that addresses the cellular, biochemical, and biophysical environment simultaneously.
Biomaterial and Bioink Engineering
The bioink serves as the synthetic extracellular matrix (ECM), providing both structural support and biochemical cues to the encapsulated cells.
- Incorporation of Bioactive Peptides: Functionalizing hydrogels with specific peptide motifs that mediate cell-matrix interactions is a powerful strategy. Recent research using Digital Light Processing (DLP) bioprinting has demonstrated that peptides like IKVAV (laminin-derived) and HAVDI (cadherin-derived) significantly enhance endothelial coverage and promote the localization of the tight junction protein ZO-1 to cell-cell junctions compared to traditional RGD peptides [24].
- Mimicking Native BBB ECM: The BBB's basement membrane has a unique composition, primarily consisting of collagen IV, laminin, nidogen, and perlecan, while notably lacking hyaluronic acid [13]. Bioinks formulated to recapitulate this specific biochemical environment provide more authentic cues for barrier maturation.
- Spatial Functionalization: A major advantage of advanced bioprinting is the ability to spatially pattern different bioactive cues. For instance, one peptide (e.g., HAVDI) can be "clicked" into the vascular channel walls to support endothelial cells, while a different peptide (e.g., RGD) is present in the surrounding bulk hydrogel to facilitate astrocyte attachment, creating a more physiologically relevant co-culture system [24].
Integration of Dynamic Perfusion
Static culture conditions fail to provide the critical mechanical stimulation required for full BBB differentiation.
- Mechanotransduction and Tight Junction Upregulation: Laminar shear stress from perfusion activates signaling pathways in BMECs that lead to the increased expression and reorganization of tight junction proteins, including occludin, claudin-5, and ZO-1, directly resulting in higher TEER measurements [13] [9].
- System Design for Bioprinted Constructs: Perfusion can be achieved by connecting the luminal inlet and outlet of the bioprinted vascular channel to a pump system, enabling continuous or intermittent flow of culture medium [16]. This transforms the model from a static structure to a dynamic "BBB-on-a-chip."
Advanced Fabrication and Process Control
The precision of the fabrication process itself is crucial for generating consistent, high-quality barriers.
- High-Resolution Bioprinting: Light-based bioprinting techniques, such as DLP, offer the XY resolution down to 50 μm and Z precision down to 5 μm required to create the complex, thin-walled 3D microfluidic scaffolds that mimic in vivo topology [16] [24].
- Intelligent Process Monitoring: Emerging techniques focus on integrating AI-based image analysis to perform layer-by-layer comparison of the printed construct with the intended digital design. This allows for real-time identification of defects (e.g., over- or under-deposition of bio-ink) and adaptive correction of printing parameters, ensuring greater inter-tissue reproducibility and structural fidelity, which are foundational for reliable TEER [65].
Experimental Workflow and Protocol for TEER Measurement
A standardized protocol is essential for the accurate and consistent assessment of TEER in 3D-bioprinted BBB models. The following workflow outlines the key steps from model fabrication to functional validation.
Detailed Protocol for TEER Measurement
This protocol assumes a perfusable, 3D-bioprinted BBB construct has been created and matured in culture.
Pre-measurement Calibration:
- Calibrate the TEER measurement instrument (e.g., epithelial voltohmmeter or integrated electrodes) according to the manufacturer's instructions [64].
- If using a custom system, ensure the stability and known impedance of reference resistors.
Measurement Setup:
- For constructs with integrated electrodes, switch the system to measurement mode [64].
- For constructs without integrated electrodes, carefully insert Ag/AgCl or similarly compatible electrodes into the luminal (blood) and abluminal (brain) compartments, ensuring they are sterile and do not damage the endothelial layer.
- Maintain the system at a constant temperature of 37°C throughout the measurement, as TEER is temperature-sensitive [64].
Data Acquisition:
- Apply a low-voltage, alternating current (AC) signal across the endothelial layer. The specific frequency may vary by system but is often in the range of 10-1000 Hz [64].
- Measure the resulting impedance or resistance. Many modern systems will provide a direct resistance readout in ohms (Ω).
Data Normalization:
- To enable comparison across different model geometries, the raw resistance value (in Ω) must be normalized. Multiply the measured resistance by the effective surface area of the barrier (in cm²).
- Calculation:
TEER (Ω·cm²) = Measured Resistance (Ω) × Surface Area (cm²). - For 3D tubular structures, the surface area can be calculated based on the diameter and length of the perfusable channel [64].
Validation and Interpretation:
- Compare the calculated TEER value to the physiological benchmark of 1,500-8,000 Ω·cm².
- Always measure the TEER of a cell-free scaffold and subtract this value from the measurement of the cellularized construct to account for the intrinsic resistance of the biomaterial itself.
- Correlate TEER data with diffusive solute permeability assays (e.g., using sodium fluorescein or FITC-dextran) for a comprehensive assessment of barrier function [66] [64].
The Scientist's Toolkit: Essential Reagents and Materials
Table 2: Key Research Reagents and Materials for 3D-Bioprinted BBB Models
| Item/Category | Specific Examples | Function and Application |
|---|---|---|
| Bioinks & Hydrogels | PEGDA, GelMA, collagen-based hydrogels [16] [24]. | Form the printable 3D scaffold that provides mechanical support and biochemical cues. |
| Bioactive Peptides | RGD, IKVAV, HAVDI [24]. | Functionalize hydrogels to promote specific cell adhesion, spreading, and tight junction formation. |
| Key Cell Sources | Primary human BMECs, hiPSC-derived BMECs/astrocytes/pericytes, immortalized lines (bEnd.3, HCMEC/D3) [13] [66]. | Populate the model to form the neurovascular unit. Cell source critically impacts barrier performance. |
| TEER Measurement | Epithelial voltohmmeter (e.g., EVOM2), custom Ag/AgCl electrodes, integrated microelectrodes [64]. | Enable non-invasive, real-time quantification of barrier integrity and tightness. |
| Permeability Tracers | Sodium fluorescein (376 Da), FITC-dextran (e.g., 70 kDa) [66]. | Used in transport assays to functionally validate barrier selectivity in conjunction with TEER. |
| Tight Junction Markers | Antibodies against ZO-1, occludin, claudin-5 [13] [24]. | Enable immunofluorescence staining and imaging to visually confirm the presence and morphology of tight junctions. |
Achieving physiological TEER in 3D-bioprinted blood-brain barrier models is a complex but attainable goal that hinges on a holistic integration of cellular biology, materials science, and precision engineering. By strategically designing bioinks with bioactive components, incorporating physiological perfusion, and leveraging high-resolution, controlled fabrication processes, researchers can create advanced in vitro barriers that truly mimic the tightness and functionality of the human BBB. As these strategies continue to evolve and become more standardized, they will profoundly accelerate the pace of CNS drug discovery and our understanding of neurological disease mechanisms.
The creation of lifelike microcapillary networks represents one of the most significant challenges in advancing 3D bioprinting for blood-brain barrier (BBB) modeling. Functional vasculature is not merely a structural component but a biological necessity for maintaining tissue viability and enabling realistic drug permeability studies. In the context of neurodegenerative disease research and therapeutic development, the absence of perfusable microvascular networks in traditional models has severely limited their predictive capability and physiological relevance [13]. The emergence of sophisticated 3D bioprinting technologies has revolutionized this landscape by offering unprecedented control over the spatial arrangement of multiple cell types and extracellular matrix components, thereby enabling the fabrication of complex, hierarchical vascular structures that closely mimic native physiology [67].
The critical importance of vascularization becomes evident when considering the fundamental biological constraint known as the diffusion limit—approximately 100-200 micrometers—beyond which cells suffer from hypoxia, nutrient deficiency, and waste accumulation [68]. This limitation poses a substantial barrier to engineering tissue constructs of therapeutically relevant sizes. Furthermore, the blood-brain barrier itself exemplifies the functional sophistication of cerebral microvasculature, characterized by specialized brain microvascular endothelial cells (BMECs) interconnected by complex tight junctions and supported by pericytes, astrocytes, and surrounding extracellular matrix [13] [10]. Recapitulating this neurovascular unit in vitro requires not only anatomical accuracy but also functional proficiency in selective permeability, transporter expression, and response to physiological and pathological stimuli.
Fundamental Design Principles for Microcapillary Networks
Structural and Functional Characteristics of Native Microvasculature
Functional multiscale microvasculature is inherently challenging to biofabricate due to three defining characteristics that must be simultaneously recreated: (1) a hollow, endothelialized lumen; (2) a hierarchically branched network topology; and (3) a complex signaling environment that dynamically regulates vascular function [69]. The hierarchical organization spans from larger arterioles (40-300 μm diameter) to capillaries (7-10 μm diameter in the brain) and post-capillary venules (10-100 μm diameter), each with distinct structural and functional attributes [69] [70].
The neurovascular unit of the BBB exemplifies this structural complexity, where brain microvascular endothelial cells form continuous junctional complexes with low rates of transcytosis, distinguishing them from peripheral endothelial cells [13] [10]. These are embedded within a specialized basement membrane and intimately associated with pericytes and astrocytic end-feet, creating a sophisticated multicellular interface that regulates molecular exchange between blood and brain parenchyma [10]. The recreation of this architecture necessitates careful consideration of cellular composition, spatial organization, and biomechanical cues.
Table 1: Key Physiological Parameters for Biomimetic BBB Microvasculature
| Parameter | Physiological Range | Significance |
|---|---|---|
| Vessel Diameter | Capillaries: 7-10 μm [13] | Determines flow resistance, wall shear stress, and capillary bed density |
| Trans-Endothelial Electrical Resistance (TEER) | 1,500 - 8,000 Ω·cm² [13] | Indicator of barrier tightness and junctional complexity |
| Wall Shear Stress | 5-23 dyn/cm² [13] | Mechanical stimulus regulating endothelial alignment, morphology, and junctional protein expression |
| Cellular Composition | BMECs, pericytes, astrocytes [13] | Essential for recapitulating neurovascular unit function |
Biomechanical and Biochemical Signaling Cues
The biomechanical environment plays a crucial role in vascular development and function. Physiological shear stress (5-23 dyn/cm² in human brain capillaries) influences endothelial cell alignment, morphology, and upregulation of tight junction proteins, all essential for barrier integrity [13]. Furthermore, the basement membrane composition of cerebral microvessels differs significantly from other tissues, lacking hyaluronic acid and consisting primarily of collagen IV, laminin, nidogen, perlecan, and fibronectin [13]. These components provide both structural support and biochemical cues that influence BBB cellular behavior and barrier function.
The signaling milieu represents another critical design consideration, with specific growth factors, cytokines, and matrix-bound ligands guiding vasculogenesis, angiogenesis, and barrier maturation. Vascular endothelial growth factor (VEGF) and sphingosine-1-phosphate (S1P) have been identified as particularly important in stimulating vascular network formation, especially when co-cultured with supporting cells such as fibroblasts or pericytes [68]. The establishment of appropriate cell-cell signaling through direct contact (e.g., peg-and-socket connections between endothelial cells and pericytes) and paracrine factors further enhances barrier properties and promotes vascular stability [10].
Figure 1: Fundamental design principles for engineering biomimetic microvascular networks, highlighting the essential structural, cellular, and signaling components that must be recapitulated from native physiology.
3D Bioprinting Strategies for Vascular Network Fabrication
Extrusion-Based Bioprinting Techniques
Extrusion-based bioprinting (EBB) has emerged as a particularly accessible and adaptable technology for vascular network fabrication, capable of depositing cell-laden bioinks in precise spatial patterns [69]. This approach leverages pneumatic or mechanical pressure to extrude bioinks through nozzles, allowing for the creation of complex 3D structures layer by layer. The development of free-form reversible embedding of suspended hydrogels (FRESH) has significantly advanced EBB capabilities by enabling the extrusion of low-viscosity bioinks within a support bath that provides temporary mechanical restraint until crosslinking is complete [71]. This technique has expanded the repertoire of bioinks suitable for creating delicate vascular structures with high resolution and cell viability.
Several specific EBB methodologies have been developed to address the unique challenges of vascular lumen formation:
Sacrificial Printing: This approach involves printing a fugitive ink (typically gelatin, carbohydrate glass, or Pluronic F127) that is subsequently encapsulated within a structural bioink and removed through melting, dissolution, or enzymatic degradation to create hollow channels [69]. This technique enables the fabrication of complex, branched vascular networks with geometrical control, although the resolution is typically limited to channels >100 μm in diameter [69].
Coaxial Printing: Utilizing concentric nozzles, this technique allows for the simultaneous extrusion of different materials, enabling direct fabrication of hollow, endothelialized tubes in a single step [67]. The inner core can consist of a temporary filler material or crosslinking solution, while the outer shell contains the structural bioink and cells. This method has been successfully employed to create multi-layered vascular constructs resembling native vessel architecture [67].
In-Bath Printing: By extruding bioinks directly into a yield-stress support bath (typically gelatin or carbomer microparticles), this technique enables the stabilization of printed filaments without immediate crosslinking, facilitating the creation of complex 3D structures that would otherwise collapse under gravity [71]. This approach is particularly valuable for generating intricate microvascular networks with branching topologies.
Complementary Vascularization Approaches
While extrusion-based bioprinting establishes the foundational vasculature, complementary techniques are often employed to achieve the full hierarchical complexity of microvascular networks:
Vascular Templating: This method involves inserting cylindrical objects (microneedles, wires) into hydrogels then removing them to create channels that are subsequently endothelialized [70]. While suitable for creating large linear vessels (60-700 μm), this technique is limited in generating branched networks and smaller capillary-sized structures [70].
Self-Assembly: Leveraging the innate morphogenetic capabilities of endothelial cells, this approach utilizes biological stimuli (VEGF, S1P) to induce the spontaneous formation of capillary networks through vasculogenesis or angiogenic sprouting from pre-formed vessels [69] [68]. When combined with bioprinted mesoscale channels, this strategy can bridge the critical resolution gap between engineered vessels and functional capillaries [69].
Table 2: Comparison of Vascular Fabrication Techniques for BBB Models
| Technique | Resolution Range | Key Advantages | Limitations |
|---|---|---|---|
| Sacrificial Printing | 100-1000 μm [69] | Complex geometries, branching networks | Limited resolution, post-processing required |
| Coaxial Printing | 200-2000 μm [67] | Direct hollow tube formation, multi-layered walls | Limited complexity, relatively large diameters |
| Vascular Templating | 60-700 μm [70] | Simple cylindrical channels, high fidelity | Primarily linear structures, no branching |
| Self-Assembly | 5-50 μm [69] | True capillary formation, biological fidelity | Limited spatial control, reproducibility challenges |
Integrated Experimental Workflow for Vascularized BBB Models
The fabrication of perfusable microcapillary networks for BBB modeling requires a methodical, multi-stage approach that integrates various bioprinting and tissue engineering strategies. The following workflow outlines a comprehensive protocol for generating hierarchical vascular networks within 3D bioprinted constructs.
Phase 1: Foundation Fabrication Using Sacrificial Molding
The initial phase establishes the mesoscale vascular foundation that will later serve as the perfusion conduit for the entire network [71]:
Scaffold Design: Create a 3D computer model of the desired vascular scaffold shape using CAD software, typically featuring a cylindrical structure with an inner diameter of 0.9 mm, outer diameter of 2 mm, and height of 18 mm, supplemented with radial fenestrations (0.22 mm diameter) to facilitate anastomosis with surrounding capillaries [71].
Mold Fabrication: Design and 3D print a sacrificial mold using a water-soluble filament such as butene-diol vinyl alcohol copolymer (BVOH) via fused deposition modeling with a layer height of 0.1 mm [71].
Polymer Solution Preparation: Prepare a 1:1 mixture of poly-L-lactic-acid (PLLA) and polylactic-co-glycolic-acid (PLGA) in 1,4-dioxane (70 mg/mL each) by dissolving overnight at 70°C with continuous mixing [71].
Mold Filling and Processing: Fill the BVOH molds with the polymer solution using positive displacement pipettes, followed by centrifugation at 100 × g for 2 minutes to ensure complete filling. Freeze at -80°C for at least 30 minutes, then lyophilize overnight to remove solvent [71].
Mold Removal and Scaffold Recovery: Dissolve the sacrificial BVOH mold in deionized water baths under gentle stirring, replacing water as it becomes cloudy until complete mold dissolution, then air-dry the resulting vascular scaffolds [71].
Scaffold Coating: Disinfect scaffolds in 70% ethanol for 30 minutes, wash with PBS, then coat with human fibronectin (50 μg/mL in PBS) by incubation at 37°C for 60 minutes to promote endothelial cell adhesion [71].
Phase 2: Microvascular Network Bioprinting
This phase involves the creation of the capillary network using advanced bioprinting techniques:
Bioink Formulation: Prepare a cerebrovascular-specific bioink using decellularized extracellular matrix (dECM) derived from brain tissue and blood vessels, which provides tissue-specific biochemical cues [58]. Alternatively, recombinant human collagen methacrylate (rhCollMA) can be neutralized with phosphate buffer and diluted to 10 mg/mL concentration, then combined with a porogen-photoinitiator solution [71].
Cell Preparation: Isolate and expand relevant cell types, typically human brain microvascular endothelial cells (HBMECs), human brain vascular pericytes (HBVPs), and potentially astrocytes. For the vascular component, suspend endothelial cells at high density (5-20 × 10^6 cells/mL) in the bioink [58] [71].
FRESH Bioprinting: Employ a support bath (typically gelatin microparticles or carbomer) to enable the extrusion of low-viscosity bioinks. Print the cellularized bioink into the support bath using a 22G-27G nozzle (200-400 μm inner diameter) at pressures of 15-25 psi, maintaining temperature control (4-10°C for collagen-based inks) [71].
Crosslinking and Support Removal: Photo-crosslink methacrylated bioinks using UV light (365 nm, 5-15 mW/cm² for 30-60 seconds) or initiate thermal gelation as appropriate for the specific bioink chemistry. Gently remove the support bath through dissolution or washing after crosslinking is complete [71].
Phase 3: Network Maturation and Perfusion
The final phase focuses on establishing functional connections and enhancing network maturity:
Anastomosis Induction: Culture the bioprinted microvasculature in proximity to the mesoscale vascular scaffold to promote spontaneous connection between the two networks via angiogenic sprouting or vasculogenesis [69] [71].
Perfusion Establishment: Connect the vascular scaffold to a perfusion system, initially employing low flow rates (0.1-1 mL/h) to establish luminal patency, then gradually increasing to physiological shear stress levels (5-23 dyn/cm²) over 3-7 days [13] [69].
Maturation Conditioning: Culture under continuous perfusion with appropriate medium supplements (VEGF, S1P, forskolin) for 7-14 days to enhance barrier properties and network stability [69].
Figure 2: Integrated experimental workflow for fabricating vascularized BBB models, showing the sequential phases from foundation fabrication to functional maturation.
The Scientist's Toolkit: Essential Research Reagents and Materials
The successful implementation of vascularized BBB models requires careful selection of materials, cells, and characterization tools. The following table summarizes key components essential for establishing robust, physiologically relevant microcapillary networks.
Table 3: Essential Research Reagents for Vascularized BBB Models
| Category | Specific Examples | Function and Application |
|---|---|---|
| Bioink Materials | Recombinant collagen-methacrylate (rhCollMA) [71], Cerebrovascular dECM [58], Fibrin, Gelatin methacryloyl (GelMA) | Provide structural support and biochemical cues for cell proliferation, differentiation, and network formation |
| Sacrificial Materials | BVOH filament [71], Gelatin, Carbohydrate glass, Pluronic F127 | Create hollow lumens and channels that are subsequently removed to establish perfusable networks |
| Cell Sources | HBMECs [58], iPSC-derived BMECs [70], Brain vascular pericytes [58], Astrocytes | Recapitulate cellular complexity of neurovascular unit; patient-specific iPSCs enable personalized disease modeling |
| Signaling Molecules | VEGF [68], S1P [68], bFGF [68], TNF-α, IL-1β [58] | Induce angiogenesis, regulate barrier properties, model inflammatory responses |
| Characterization Tools | TEER measurement systems [13], Immunofluorescence (claudin-5, ZO-1, CD31) [68], Permeability assays (dextrans, drugs) [13] | Assess barrier integrity, junctional protein expression, and functional transport properties |
Applications in BBB Modeling and Neurodegenerative Disease Research
The development of vascularized, perfusable microcapillary networks has profound implications for BBB modeling and neurodegenerative disease research. These advanced platforms enable more physiologically relevant investigation of disease mechanisms and therapeutic interventions.
Neurodegenerative Disease Modeling
BBB dysfunction is increasingly recognized as an early pathological feature in neurodegenerative diseases including Alzheimer's disease (AD), Parkinson's disease (PD), Huntington's disease, and amyotrophic lateral sclerosis [10]. Vascularized BBB models facilitate the study of specific disease processes, such as the accumulation of amyloid-β (Aβ) in AD and misfolded alpha-synuclein in PD, in the context of a functioning neurovascular unit [13]. These models have demonstrated particular utility in investigating neuroinflammatory mechanisms, with researchers successfully replicating BBB permeability changes and inflammatory responses following exposure to inflammation-inducing substances such as TNF-α and IL-1β [58].
Drug Discovery and Development
The pharmaceutical industry faces significant challenges in CNS drug development, with poor BBB penetration being a major contributor to high attrition rates. Vascularized BBB models offer a sophisticated platform for predicting drug permeability and assessing transporter-mediated efflux in a human-specific context [13] [10]. These models enable high-throughput screening of candidate compounds, evaluation of nanoparticle delivery systems, and investigation of strategies to enhance BBB penetration for therapeutic agents [9]. Furthermore, the integration of patient-derived cells enables personalized medicine approaches, allowing for the prediction of individual patient responses to specific therapeutic regimens [10].
The creation of lifelike microcapillary networks through advanced 3D bioprinting strategies represents a transformative advancement in blood-brain barrier modeling. By integrating multiple fabrication techniques—including sacrificial printing, coaxial extrusion, and self-assembly—researchers can now engineer hierarchical vascular networks that closely mimic native physiology in both structure and function. These developments have profound implications for understanding neurodegenerative disease mechanisms, screening therapeutic compounds, and developing personalized medicine approaches. As bioprinting technologies continue to evolve with improvements in resolution, speed, and biomaterial options, we anticipate further refinement of these vascularized models, ultimately enabling more predictive and clinically relevant studies of BBB function and dysfunction.
Long-Term Model Stability and Functional Maintenance
The adoption of three-dimensional (3D) bioprinted blood-brain barrier (BBB) models is transforming neuroscience research and central nervous system (CNS) drug development. These advanced in vitro systems offer a physiologically relevant platform that surpasses the limitations of traditional two-dimensional (2D) Transwell cultures and animal models [13] [72]. However, a significant challenge that remains is ensuring the long-term stability and functional maintenance of these sophisticated constructs. For a bioprinted BBB model to be truly useful in prolonged studies, such as chronic disease modeling or extended drug efficacy and toxicity testing, it must reliably mimic in vivo barrier properties over weeks, not just days. This technical guide outlines the core principles, quantitative assessment methods, and detailed experimental protocols essential for achieving and verifying long-term stability in 3D bioprinted BBB models, providing researchers with a framework for generating robust and reproducible data.
Core Design Principles for Long-Term Stability
The long-term viability of a 3D bioprinted BBB model hinges on its initial design and fabrication. Several key principles must be addressed to create a foundation for sustained functionality.
- 2.1 Physiological Cellular Composition and Co-culture: A fully functional BBB is not composed of endothelial cells alone. It is a multicellular structure where brain microvascular endothelial cells (BMECs), pericytes, and astrocytes interact synergistically to induce and maintain barrier tightness [13] [73]. Incorporating all three cell types in the bioprinting process is crucial. Pericytes regulate BBB permeability by modulating the expression of tight junction proteins in BMECs, while astrocytic end-feet provide critical signals that support barrier integrity [13]. Long-term stability requires that these cellular interactions are supported by the model's design.
- 2.2 Dynamic Perfusable Flow: The inclusion of a perfusable flow system that generates physiological shear stress (reported to be between 5 and 23 dyn/cm² in human brain capillaries) is not an optional enhancement but a necessity for long-term culture [13]. This mechanical stimulus promotes endothelial cell health, directs cell alignment, and upregulates the expression of tight junction proteins, all of which are essential for a stable, functional barrier over time [13]. Static models inevitably deteriorate due to the lack of these critical biomechanical cues.
- 2.3 Biomimetic Hydrogel and Scaffold Design: The bioink and overall scaffold must provide a biomimetic extracellular matrix (ECM). The BBB ECM consists primarily of collagen IV, laminin, nidogen, and fibronectin, providing both structural support and essential biochemical cues [13]. Bioinks should be designed to mimic this native environment. Furthermore, the use of self-healing hydrogels can be advantageous, as they allow for high-resolution printing and support the fusion of cellular spheroids into high-cell-density microtissues, which more accurately recapitulate organotypic conditions and can enhance model longevity [74].
Quantitative Metrics for Stability and Function
To longitudinally track a model's health and functionality, researchers must employ a suite of quantitative assays. The key parameters to monitor are summarized in Table 1 below.
Table 1: Key Quantitative Metrics for Long-Term BBB Model Assessment
| Metric | Description | Target In Vivo / Physiologically Relevant Values | Measurement Techniques |
|---|---|---|---|
| Barrier Integrity | |||
| Trans-Endothelial Electrical Resistance (TEER) | Measures the electrical resistance across the endothelial layer, directly indicating tight junction formation and integrity. | 1,500 - 8,000 Ω·cm² [13] | Voltmeter/EVOM; Electrode arrays integrated into microfluidic systems. |
| Apparent Permeability (Papp) | Quantifies the passive diffusion of molecular tracers across the barrier. | Low permeability to small molecules and proteins [72] | Fluorescence or LC-MS/MS analysis of tracer molecules (e.g., sucrose, dextrans, sodium fluorescein). |
| Tight Junction Expression | Presence and localization of key proteins that form the physical barrier. | High expression of claudin-5, occludin, JAM-1 [13] | Immunofluorescence staining; Western Blot; qPCR. |
| Cellular Viability | Percentage of living cells within the 3D construct over time. | >90% [74] | Live/Dead assays (e.g., calcein-AM/ethidium homodimer); alamarBlue metabolic activity tests [75]. |
| Functional Transport | Activity of efflux transporters like P-glycoprotein (P-gp). | Active, ATP-dependent efflux [72] | Rhodamine 123 accumulation/efflux assays with and without inhibitors (e.g., verapamil). |
Detailed Experimental Protocols for Longitudinal Assessment
This section provides detailed methodologies for key experiments cited in this guide, enabling researchers to systematically evaluate model stability.
4.1 Protocol: Measuring Trans-Endothelial Electrical Resistance (TEER) in a Bioprinted BBB Model
- Purpose: To non-invasively and quantitatively monitor the integrity of the barrier formed by brain microvascular endothelial cells in real-time throughout the culture period.
- Materials: Bioprinted BBB construct in a compatible housing (e.g., Transwell insert or microfluidic chip), voltohmmeter with "chopstick" or integrated electrodes, cell culture medium pre-warmed to 37°C.
- Procedure:
- Calibration: Calibrate the voltohmmeter according to the manufacturer's instructions using a blank (cell-free) construct filled with culture medium.
- Measurement: Aspirate the medium from both the apical ("blood") and basolateral ("brain") compartments. Gently replace with fresh pre-warmed medium to ensure consistent ion concentrations.
- Sterilize the electrodes with 70% ethanol and allow them to air dry. Carefully place the electrodes into the apical and basolateral compartments, ensuring they do not touch the bioprinted tissue itself.
- Record the resistance value (in Ω) from the meter. Repeat the measurement at three distinct locations across the construct surface to account for heterogeneity.
- Calculate the average resistance and subtract the average value obtained from a blank (cell-free) construct.
- Multiply the corrected resistance by the effective surface area of the bioprinted barrier (in cm²) to obtain the TEER value in Ω·cm².
- Longitudinal Tracking: Perform this measurement every 2-3 days. A stable or increasing TEER value over time indicates good barrier formation and maintenance. A sudden drop suggests loss of barrier integrity, potentially due to contamination, toxicity, or cell death.
4.2 Protocol: Immunofluorescence Staining for Tight Junction Proteins
- Purpose: To visually confirm the presence, localization, and continuity of tight junction proteins in the bioprinted model at specific time points.
- Materials: Bioprinted BBB constructs, 4% paraformaldehyde (PFA), phosphate-buffered saline (PBS), permeabilization buffer (e.g., 0.1% Triton X-100 in PBS), blocking buffer (e.g., 1% BSA in PBS), primary antibodies (e.g., anti-claudin-5, anti-occludin), fluorescently conjugated secondary antibodies, DAPI stain, mounting medium.
- Procedure:
- Fixation: Gently wash the construct with PBS and fix with 4% PFA for 15-20 minutes at room temperature.
- Permeabilization and Blocking: Wash with PBS, then permeabilize with 0.1% Triton X-100 for 10-15 minutes. Wash again and incubate with blocking buffer for 1 hour to prevent non-specific antibody binding.
- Primary Antibody Incubation: Incubate the construct with the primary antibody diluted in blocking buffer overnight at 4°C.
- Secondary Antibody Incubation: Wash thoroughly with PBS to remove unbound primary antibody, then incubate with the fluorescent secondary antibody (e.g., Alexa Fluor 488 donkey anti-rabbit) diluted in blocking buffer for 1-2 hours at room temperature, protected from light.
- Counterstaining and Mounting: Wash again and counterstain with DAPI to label cell nuclei. Carefully mount the construct on a glass slide using an antifade mounting medium [75].
- Imaging: Image using a confocal microscope. Analyze the images for continuous, belt-like staining at the cell-cell borders of endothelial cells, which indicates proper tight junction assembly.
4.3 Protocol: Permeability (Papp) Assay
- Purpose: To functionally assess the barrier's selectivity and its ability to restrict the paracellular passage of molecules.
- Materials: Bioprinted BBB construct, permeability tracer (e.g., 10 kDa FITC-dextran), transport buffer (e.g., HBSS), fluorescence plate reader or LC-MS/MS.
- Procedure:
- Preparation: Pre-warm all solutions to 37°C. Gently wash the construct with transport buffer.
- Dosing: Add the tracer molecule to the apical ("blood") compartment.
- Sampling: At a predetermined time (e.g., 30, 60, 90, 120 minutes), sample a small volume (e.g., 50-100 µL) from the basolateral ("brain") compartment. Immediately replace the sampled volume with fresh, pre-warmed transport buffer to maintain hydrostatic pressure.
- Analysis: Measure the fluorescence or concentration of the tracer in the basolateral samples using a plate reader or LC-MS/MS.
- Calculation: Calculate the apparent permeability (Papp) using the formula: ( P{app} = (dQ/dt) / (A \times C0) ) where ( dQ/dt ) is the steady-state flux rate of the tracer (mol/s), ( A ) is the surface area of the barrier (cm²), and ( C_0 ) is the initial tracer concentration in the donor compartment (mol/mL). A low, stable Papp value over time confirms a tight, functional barrier.
Visualization of Workflows and Relationships
The following diagrams, generated using Graphviz DOT language, illustrate the core experimental workflow and the critical functional relationships within the BBB.
Diagram 1: Workflow for establishing and maintaining a long-term 3D bioprinted BBB model, highlighting the cyclical nature of functional assessment.
Diagram 2: Key functional relationships within the BBB neurovascular unit that underpin long-term model stability.
The Scientist's Toolkit: Essential Research Reagents
Successful fabrication and maintenance of a stable, bioprinted BBB model require a carefully selected set of reagents and materials. Table 2 details the core components of the research toolkit.
Table 2: Essential Research Reagents and Materials for 3D Bioprinted BBB Models
| Category | Item | Function / Purpose | Example / Notes |
|---|---|---|---|
| Cells | Brain Microvascular Endothelial Cells (BMECs) | Forms the primary barrier; expresses tight junctions and transporters. | iPSC-derived cells offer a human-relevant, scalable source [13] [73]. |
| Pericytes | Regulates BBB permeability and provides vascular stability [13]. | Primary human pericytes or iPSC-derived. | |
| Astrocytes | Provides inductive signals for barrier formation via end-feet processes [13]. | Primary human astrocytes or iPSC-derived. | |
| Bioink & Scaffold | Gelatin Methacryloyl (GelMA) | A common photocrosslinkable hydrogel providing a tunable, cell-friendly ECM-like environment [76] [75]. | Often combined with other polymers; concentration affects stiffness. |
| Hyaluronic Acid (HA) Derivatives | Component of native ECM; can be modified to create self-healing, shear-thinning hydrogels for advanced bioprinting [74]. | Useful for spheroid-based bioprinting approaches. | |
| Photoinitiator (e.g., Irgacure, LAP) | Initiates crosslinking of the bioink upon exposure to UV or visible light, solidifying the printed structure [76] [75]. | LAP is preferred for cell viability due to lower cytotoxicity and use of visible light. | |
| Cell Culture | Specialized Growth Media | Supports the growth and maintenance of specific cell types within the co-culture. | e.g., Endothelial Cell Growth Medium, Neurobasal Medium for astrocytes [75]. |
| Growth Factors & Supplements | Promotes cell proliferation, differentiation, and barrier maturation. | e.g., VEGF, EGF, FGF, B-27 Supplement, N-2 Supplement [75]. | |
| Assessment | TEER Measurement System | For quantitative, non-invasive tracking of barrier integrity. | e.g., voltohmmeter with custom electrodes for chip designs. |
| Permeability Tracers | Molecules used to functionally assess barrier tightness. | e.g., FITC-dextran (4-70 kDa), sodium fluorescein (376 Da) [72]. | |
| Antibodies for Staining | For visualizing key proteins to confirm model phenotype. | Anti-claudin-5, anti-occludin, anti-CD31 (endothelial marker) [75]. |
Achieving long-term stability in 3D bioprinted BBB models is a multifaceted endeavor that hinges on a principled design, meticulous fabrication, and rigorous longitudinal assessment. By adhering to the core tenets of physiological cellular composition, dynamic perfusion, and biomimetic matrix design, and by employing the quantitative metrics and detailed protocols outlined in this guide, researchers can create highly reliable and robust models. These advanced tools will profoundly impact the study of neurological diseases and accelerate the development of therapeutics capable of crossing the most formidable barrier in the human body.
Scalability and Reproducibility for High-Throughput Screening Applications
The blood-brain barrier (BBB) represents a critical challenge in central nervous system (CNS) drug development, with more than a billion people affected by neurological disorders worldwide and few effective therapeutic options available [49]. Traditional two-dimensional (2D) static models and animal studies have proven insufficient for predicting human clinical outcomes, creating a significant translational gap in pharmaceutical research [28] [49]. The emergence of three-dimensional (3D) bioprinted BBB models offers promising solutions to these challenges by recreating the physiological cytoarchitecture and multicellular arrangement of the human neurovascular unit [70] [49]. However, for these advanced models to effectively impact drug discovery pipelines, they must overcome two fundamental constraints: scalability for high-throughput screening (HTS) applications and reproducibility for reliable data generation across experiments and laboratories [77] [13]. This technical guide examines current advancements and methodologies in 3D bioprinted BBB models that address these critical requirements, providing researchers with frameworks for implementing these systems within drug development workflows.
Technological Foundations for Scalable BBB Models
Integration with Standardized Screening Platforms
A significant advancement in scalable BBB modeling comes from the development of organ-on-chip (OOC) platforms specifically designed for high-throughput applications. The AKITA platform exemplifies this approach with its standard 96-well and 384-well plate layouts that ensure compatibility with existing laboratory automation and high-throughput data collection systems [77]. This standardization addresses a major limitation of early microfluidic systems, which featured non-standardized designs that complicated automated liquid handling and data analysis. The platform incorporates integrated trans-epithelial electrical resistance (TEER) sensors that enable rapid, repeated, and non-invasive monitoring of barrier integrity throughout experiments, providing quantitative quality control metrics essential for reliable screening data [77]. Similarly, recent innovations in high-throughput transcriptomic screening technologies, such as MERCURIUS DRUG-seq, allow for the assessment of thousands of compounds using 384-well plate formats while generating data-rich, transcriptome-wide outputs [78]. These systems maintain the physiological relevance of 3D BBB models while achieving the throughput requirements of early drug discovery stages.
Advanced Bioprinting Methodologies for Reproducibility
Light-based bioprinting technologies, including digital light processing (DLP), have emerged as powerful tools for creating highly reproducible 3D BBB constructs [49]. These systems utilize computer-aided design (CAD) models to generate consistent 3D cytoarchitectural arrangements with vessel diameters ranging from 150-350μm, though higher-resolution systems can approach the 7-10μm diameter of human brain capillaries [49] [13]. The process begins with in silico design of vascular networks using software such as Fusion 360 and Blender, which are then exported as STL files to bioprinters like the Lumen X [49]. This digital workflow ensures precise geometric control across multiple fabrications, significantly enhancing inter-experiment reproducibility compared to manual fabrication methods. Additionally, the use of cross-linkable photo-bioinks including polyethylene glycol diacrylate (PEGDA) and gelatin methacryloyl (GelMA) provides consistent mechanical and chemical properties that support robust cellular maturation and barrier function [49]. These bioinks can be customized with bioactive components such as collagen I, fibronectin, and hyaluronan-heparin mixtures to better mimic the native BBB extracellular matrix environment [49].
Quantitative Performance Metrics of Scalable Systems
Table 1: Performance Metrics of Scalable BBB Platforms
| Platform Type | Throughput Capacity | Key Reproducibility Features | Barrier Integrity Metrics | Reference |
|---|---|---|---|---|
| Standardized OOC (AKITA) | 96-384 well format | Integrated TEER, standardized design | Continuous TEER monitoring (1500-8000 Ω·cm²) | [77] |
| 3D Bioprinted Constructs | Medium throughput (4-24 chips/run) | CAD-controlled geometry, standardized bioinks | Permeability assays, TJ protein expression | [49] [13] |
| High-throughput Transcriptomics | 384-well format | Automated library prep, bulk RNA barcoding | Gene expression profiling of BBB markers | [78] |
| Microfluidic HTS Platforms | 10,000-100,000 compounds/day | Automation-compatible assay designs | Fluorescent tracer permeability | [79] [78] |
Table 2: Comparison of Fabrication Techniques for Scalable BBB Models
| Fabrication Method | Scalability Potential | Reproducibility Challenges | Typical Applications | Reference |
|---|---|---|---|---|
| 3D Bioprinting (DLP) | Medium-High (parallel fabrication) | Excellent (digital design control) | Drug discovery, disease modeling | [49] [13] |
| 3D Templating | Low-Medium (manual intensive) | Moderate (channel consistency) | Basic permeability studies | [70] |
| Self-assembling Networks | Low (biological variability) | Poor (uncontrolled formation) | Developmental biology studies | [70] |
| Standardized Microfluidics | High (mass production) | Excellent (injection molding) | High-throughput screening | [77] |
Experimental Protocols for Reproducible BBB Model Generation
Protocol 1: Scalable 3D Bioprinting of BBB Constructs
The following methodology outlines the steps for generating reproducible, perfusable 3D BBB models suitable for screening applications [49]:
Step 1: In Silico Design – Create 3D vascular network designs using CAD software (e.g., Fusion 360, Blender) with channel diameters of 150-350μm and branching geometries that mimic cerebral microvasculature. Export designs as STL files for bioprinting.
Step 2: Bioink Preparation – Prepare PEGDA-GelMA composite bioinks supplemented with 0.1% (w/v) photoinitiator. For enhanced biological activity, supplement with 50μg/mL collagen I, 25μg/mL fibronectin, and 0.5% (w/v) thiol-modified hyaluronan/heparin mixture.
Step 3: Bioprinting Parameters – Utilize DLP bioprinting with exposure parameters optimized for the specific bioink formulation (typically 10-20mW/cm² at 365-405nm wavelength with 10-30 second exposure times per layer).
Step 4: Cellularization – Seed primary human brain microvascular endothelial cells (hBMVECs) at a density of 5-10×10⁶ cells/mL into the printed lumens. Allow 4-6 hours for attachment before initiating perfusion.
Step 5: Perfusion Culture – Connect constructs to perfusion bioreactors or pump systems generating physiological shear stress of 5-23 dyn/cm². Culture for 7-14 days with continuous media perfusion to achieve barrier maturation.
Step 6: Quality Control – Validate endothelialization through viability staining (e.g., Calcein-AM) and confirm barrier integrity via TEER measurements (>1500 Ω·cm²) or fluorescent tracer permeability (e.g., 10kDa dextran).
Protocol 2: High-Throughput Screening Workflow Using Standardized OOC
For drug permeability screening applications, the following protocol enables efficient testing of compound libraries [77]:
Step 1: Platform Preparation – Acquire standardized AKITA plates or similar 96/384-well formatted OOC devices. Pre-coat microfluidic channels with 50μg/mL collagen IV and 10μg/mL fibronectin for 2 hours at 37°C.
Step 2: Cell Seeding – Prepare co-cultures of hBMVECs (2.5×10⁵ cells/mL), human pericytes (1×10⁵ cells/mL), and human astrocytes (1×10⁵ cells/mL) in appropriate ratios. Seed endothelial cells in the vascular channel and supporting cells in the brain compartment using automated liquid handlers.
Step 3: Barrier Maturation – Culture platforms under continuous perfusion (5-20 dyn/cm² shear stress) for 5-7 days. Monitor TEER values daily using integrated electrodes until stable values >1500 Ω·cm² are achieved.
Step 4: Compound Library Application – Introduce test compounds (typically 1-100μM in DMSO concentration) to the vascular channel using automated pipetting systems. Include quality control standards (e.g., high permeability markers, low permeability references) in each plate.
Step 5: Permeability Quantification – Sample the brain compartment at designated timepoints (e.g., 1, 2, 4, 8 hours) for LC-MS/MS analysis or use in-line fluorescent detection for tracer molecules.
Step 6: Data Analysis – Calculate apparent permeability coefficients (Papp) and normalize to control compounds. Apply quality filters based on TEER maintenance throughout experiments.
Diagram 1: 3D Bioprinting Workflow for Reproducible BBB Models
Research Reagent Solutions for BBB HTS Applications
Table 3: Essential Research Reagents for Scalable BBB Model Development
| Reagent Category | Specific Examples | Function | Application Notes | Reference |
|---|---|---|---|---|
| Bioink Materials | PEGDA, GelMA, PEGDA Start PhotoInk | Structural scaffold providing 3D environment | Adjust mechanical properties via molecular weight; GelMA enhances cell adhesion | [49] |
| ECM Components | Collagen I, Fibronectin, Matrigel, Hyaluronan-Heparin | Mimic native basement membrane composition | Critical for barrier maturation; concentration affects permeability | [49] |
| Cell Culture Media | EGM-2 MV BulletKit, Advanced DMEM/F12 | Support viability of BBB cell types | Supplement with ECGS, heparin, FBS for endothelial cells | [49] |
| Barrier Integrity Assays | TEER electrodes, Fluorescent tracers (e.g., 10kDa dextran), TJ protein antibodies | Quantify barrier function and tight junction formation | Integrated TEER enables continuous monitoring | [77] [13] |
| Imaging Reagents | CellTracker dyes, Hoechst 33342, Phalloidin, ZO-1 antibodies | Visualize cellular organization and junction proteins | Essential for quality control pre-screening | [49] |
Implementation Challenges and Future Directions
Despite significant advances, several challenges remain in achieving optimal scalability and reproducibility in 3D bioprinted BBB models. Cell sourcing consistency represents a critical factor, with variations between primary cell isolates and induced pluripotent stem cell (iPSC)-differentiated endothelial cells potentially introducing inter-experiment variability [13]. Furthermore, the complexity of data analysis from high-content screening approaches, particularly image-based assays and transcriptomic datasets, creates bottlenecks in screening workflows that require advanced computational solutions [78]. Future developments are likely to focus on increased automation throughout the fabrication and screening pipeline, standardized quality control metrics beyond TEER measurements, and the integration of patient-derived cells for personalized medicine applications [77] [13]. The convergence of these technologies with machine learning approaches for data analysis will further enhance the predictive power of these models, ultimately accelerating CNS drug development and improving outcomes for patients with neurological disorders.
Diagram 2: Integrated HTS Workflow for 3D BBB Models
Benchmarking Bioprinted BBB Models: Validation Metrics and Comparative Analysis
Functional validation is a critical step in the development of physiologically relevant in vitro blood-brain barrier (BBB) models. For 3D bioprinted BBB constructs, demonstrating barrier integrity and function through quantitative measures is essential for establishing model credibility and ensuring reliable experimental outcomes in drug discovery and disease modeling. The complex cellular architecture achieved through advanced bioprinting must be matched by functional performance that recapitulates the selective permeability of the native neurovascular unit [49] [9].
This technical guide details the core methodologies for validating 3D bioprinted BBB models, focusing on three principal techniques: Transendothelial Electrical Resistance (TEER) measurement, permeability assays, and tracer studies. The integration of these complementary approaches provides a comprehensive assessment of barrier integrity, forming the foundation for their application in predictive toxicology and therapeutic development for neurological disorders [28] [80].
Transendothelial Electrical Resistance (TEER) Measurement
Principles and Significance
TEER is a gold-standard, non-invasive quantitative technique that measures the integrity and tightness of the endothelial barrier by quantifying the electrical resistance across the cell layer. This resistance is primarily generated by the complex network of tight junction proteins (e.g., claudin-5, occludin, ZO-1) that seal the paracellular pathway between brain microvascular endothelial cells (BMECs) [81] [28]. In vivo, the BBB exhibits high electrical resistance, with values ranging from 1,500 to 8,000 Ω·cm² in various species, reflecting its exceptional tightness [13]. Therefore, a high TEER value in an in vitro model is a key indicator of a well-differentiated, functional BBB.
Measurement Methodologies and Platforms
The implementation of TEER measurement varies significantly between traditional and advanced platforms. The table below compares the primary approaches used in BBB modeling.
Table 1: Comparison of TEER Measurement Systems for BBB Models
| System Type | Measurement Principle | Key Advantages | Key Limitations | Compatibility with 3D Bioprinting |
|---|---|---|---|---|
| Traditional / Transwell | Epithelial Voltohmmeter with "chopstick" electrodes [81]. | - Simple operation- Widely accessible- Low cost | - Low spatial resolution- Poor current density uniformity- Electrode positioning variability affects results [81] | Low |
| Integrated Microfluidic / OOC | Electrodes (e.g., ITO-Pt) permanently integrated into the chip design, often in a 4-electrode configuration [81]. | - Real-time, continuous monitoring- High-resolution data- Excellent current density uniformity- Enables simultaneous live imaging [81] | - Complex fabrication- Higher initial cost- Device-specific calibration | High |
For 3D bioprinted models, integration with microfluidic organ-on-a-chip (OOC) platforms is the most advanced approach. These systems allow for real-time TEER monitoring under physiological flow conditions, which is crucial for assessing barrier maturation and its dynamic response to stimuli [81]. For instance, a human-cell-based BBB platform with integrated transparent electrodes was able to detect a rapid decrease in TEER following an oxygen-glucose deprivation (OGD) insult, an event that occurred before observable morphological changes in the endothelial cells [81].
Experimental Protocol for Integrated TEER Measurement
Materials:
- BBB-on-a-Chip device with integrated TEER electrodes (e.g., ITO/Pt) [81].
- TEER measurement unit or impedance analyzer.
- Cell culture medium (pre-warmed to 37°C).
- Sterile conditions (e.g., biosafety cabinet).
Procedure:
- Baseline Measurement: After seeding endothelial cells in the device, initiate periodic TEER measurements. A culture period of 4-7 days is typically required to establish a mature barrier with a stable, high TEER value [81] [80].
- System Setup: Place the device in the measurement station, ensuring electrical connections are secure. Maintain the device at 37°C during measurement to ensure physiological relevance.
- Measurement: Activate the impedance analyzer. Integrated systems often allow for automated, periodic measurements without disturbing the culture.
- Data Normalization: Record the impedance value. Subtract the resistance of a cell-free device (blank control) and multiply the result by the effective surface area of the barrier (A) to calculate TEER in Ω·cm² [81].
- Validation Threshold: Models are generally considered to have a viable barrier when TEER values exceed 150 Ω·cm², though advanced systems aiming for greater physiological relevance target values in the thousands [80].
Figure 1: Workflow for Real-Time TEER Monitoring in a Bioprinted BBB-on-a-Chip Model.
Permeability Assays
Principles and Significance
Permeability assays quantitatively evaluate the passive and active transport of molecules across the BBB, providing a direct functional readout of its selectivity. While TEER measures ionic flux, permeability assays assess the passage of specific, pharmaceutically relevant molecules. The apparent permeability coefficient (P_app), calculated from these assays, is a critical parameter for predicting the brain penetration potential of drug candidates [80]. A robust 3D BBB model should effectively restrict the passage of hydrophilic molecules while allowing the transport of small lipophilic compounds.
Standard Tracer Molecules and Controls
A panel of control compounds with well-established permeability profiles is used to validate and benchmark the performance of a BBB model.
Table 2: Standard Compounds for BBB Permeability Assay Validation
| Compound | Category | Known BBB Permeability | Primary Transport Mechanism | Function in Assay |
|---|---|---|---|---|
| Atenolol | Small Molecule | Low / Negligible [80] | Paracellular (restricted) | Negative Control |
| Caffeine | Small Molecule | High [80] | Transcellular passive diffusion | Positive Control |
| Propranolol | Small Molecule | High | Transcellular passive diffusion | Positive Control |
| Chlorpromazine | Small Molecule | High | Transcellular passive diffusion | Positive Control |
| 3 kDa Dextran | Large Molecule (Fluorescently-tagged) | Low / Negligible [80] | Paracellular (restricted) | Integrity Tracer |
| Gefitinib | Drug (EGFR inhibitor) | Moderate (P-gp substrate) [80] | Active Efflux | Drug Transport Model |
| Osimertinib | Drug (EGFR inhibitor) | High [80] | Passive Diffusion | Drug Transport Model |
Experimental Protocol for Permeability Assessment
Materials:
- 3D bioprinted BBB model (e.g., in a microfluidic device or transwell).
- Test and control compounds (e.g., from Table 2).
- Analytical instrument for quantification (e.g., LC-MS/MS for small molecules, plate reader for fluorescent tracers) [80].
- Sampling equipment (e.g., multi-channel pipettes).
Procedure:
- Model Preparation: Culture the bioprinted BBB model for 4-7 days until a stable, high TEER is established, confirming barrier maturity [80].
- Compound Application: Add the test and control compounds to the "blood" (luminal) compartment at a defined concentration (e.g., 1 µM for drug molecules) [80].
- Incubation: Allow the compounds to permeate for a set time (e.g., 24 hours). For kinetic studies, multiple shorter time points can be used [80].
- Sample Collection: At the endpoint, collect medium from the "brain" (abluminal) compartment.
- Quantification: Analyze the concentration of the compound in the abluminal sample using LC-MS/MS for drugs or a plate reader for fluorescent dextrans [80].
- Data Analysis: Calculate the Papp (in cm/s) using the formula:
- Papp = (dQ/dt) / (A × C₀)
- Where dQ/dt is the steady-state flux of the compound, A is the surface area of the barrier, and C₀ is the initial concentration in the donor compartment.
Figure 2: Logic of a Quantitative Permeability Assay for BBB Model Validation.
Tracer Studies
Principles and Applications
Tracer studies utilize detectable molecules (e.g., fluorescently-labeled or radiolabeled) to visualize and quantify molecular passage across the BBB. While closely related to permeability assays, tracer studies often provide additional spatial information, allowing researchers to visualize the route of transport (paracellular vs. transcellular) and identify localized barrier defects [80]. A classic application is the use of fluorescent dextran conjugates of different sizes to assess pore functionality and paracellular integrity.
Key Tracer Molecules and Their Uses
Table 3: Common Tracers for Functional BBB Studies
| Tracer Molecule | Size / Type | Primary Application | Interpretation of Results |
|---|---|---|---|
| Fluorescein Isothiocyanate (FITC)-Dextran | 4 kDa - 70 kDa | Assessment of paracellular integrity [80]. | Low permeability indicates intact tight junctions. Increased flux indicates barrier disruption. |
| Sodium Fluorescein | 376 Da | Small molecule permeability tracer. | Similar to FITC-dextran but for smaller molecules. |
| Evans Blue-Albumin | ~67 kDa (Albumin) | Visual assessment of gross barrier leakage, often in vivo. | Blue staining in brain tissue indicates significant barrier breakdown. |
| Receptor-Specific Ligands (e.g., Transferrin) | Protein | Study of Receptor-Mediated Transcytosis (RMT) [28] [80]. | Specific, saturable transport indicates functional RMT pathways. |
Experimental Protocol for Tracer Studies
Materials:
- 3D bioprinted BBB model.
- Fluorescent tracer (e.g., FITC-dextran, 3 kDa is common).
- Confocal microscope or high-content imaging system.
- Phosphate-Buffered Saline (PBS).
Procedure:
- Preparation: Rinse the luminal and abluminal compartments with pre-warmed PBS to remove residual medium.
- Tracer Application: Add the fluorescent tracer solution to the luminal compartment. A cell-free control (scaffold without cells) should be run in parallel to account for background tracer diffusion through the membrane and hydrogel [80].
- Incubation: Incubate for a defined period (e.g., 30-120 minutes). The duration should be optimized to be within the linear range of tracer accumulation.
- Termination and Fixation: Remove the tracer solution and rinse the compartments thoroughly with PBS to stop the reaction. Fix the model with 4% Paraformaldehyde (PFA) if subsequent immunostaining is planned.
- Imaging and Analysis:
- Quantitative: Collect medium from the abluminal compartment and measure fluorescence intensity with a plate reader to calculate P_app, as in Section 3.3.
- Qualitative/Spatial: Image the entire construct using confocal microscopy. Z-stack imaging can reconstruct the 3D path of the tracer, revealing if it is confined to the vascular channel or has penetrated into the surrounding "brain" compartment containing astrocytes and pericytes [49].
The Scientist's Toolkit: Key Research Reagent Solutions
Successful functional validation of 3D bioprinted BBB models relies on a suite of specialized reagents and tools. The table below details essential components for establishing and assessing these advanced in vitro systems.
Table 4: Essential Research Reagents and Tools for 3D Bioprinted BBB Validation
| Category | Item | Function and Application | Examples / Specifications |
|---|---|---|---|
| Cells | Primary Human Brain Microvascular Endothelial Cells (hBMVECs) | Form the core barrier layer; require co-culture for full functionality [49] [80]. | Isolated from tissue; express key tight junction proteins and transporters. |
| Primary Human Pericytes & Astrocytes | Critical supporting cells of the NVU; induce and maintain BBB properties in endothelial cells [81] [49] [80]. | Embedded in 3D hydrogel matrix (brain compartment). | |
| Bioinks & Scaffolds | Hydrogel Matrices | Provide the 3D structural support and biochemical microenvironment for cell growth [49] [4]. | Collagen I, Fibrin, GelMA, PEG-based hydrogels [49] [70]. |
| Validation Assays | TEER Measurement System | Quantifies real-time barrier integrity [81]. | Integrated electrodes in OOC platforms are superior for 3D models [81]. |
| Permeability Control Panel | Benchmarks model performance against known standards [80]. | Atenolol (low Papp), Caffeine (high Papp), 3kDa Dextran (integrity tracer) [80]. | |
| Fluorescent Tracers | Visualizes and quantifies barrier leak and transport pathways [80]. | FITC-Dextran (e.g., 3 kDa, 10 kDa, 70 kDa). | |
| Analytical Instruments | LC-MS/MS System | Gold-standard for sensitive and specific quantification of small molecule drug permeability [80]. | e.g., Agilent 1100 LC coupled with a SCIEX QTRAP [80]. |
| Confocal Microscope | Enables high-resolution 3D imaging of barrier structure and tracer localization [81] [49]. | For imaging tight junctions (ZO-1) and tracer penetration. |
Integrated Application in Advanced BBB Modeling
The true power of these validation techniques is realized when they are applied in concert within advanced, perfusable 3D bioprinted systems. These next-generation models move beyond static Transwells by incorporating physiological flow, which applies shear stress (typically 5-23 dyn/cm² for human brain capillaries) that is critical for inducing and maintaining BBB phenotype, including the upregulation of tight junction proteins and efflux transporters [49] [13].
Furthermore, the field is advancing towards the integration of optical and electrophysiological biosensors directly into microfluidic BBB systems. This allows for real-time monitoring of barrier status and the dynamics of drug interactions, providing a multiparametric analytical platform that far surpasses the capabilities of endpoint assays alone [9]. By employing TEER, permeability assays, and tracer studies as interdependent validation pillars, researchers can robustly qualify their 3D bioprinted BBB models, ensuring they serve as reliable and predictive tools for unraveling the complexities of the human neurovascular unit and accelerating CNS drug development.
The blood-brain barrier (BBB) is a highly selective interface critical for maintaining central nervous system (CNS) homeostasis. Its core architectural feature is the tight junction (TJ), a complex protein network that seals the paracellular space between brain microvascular endothelial cells (BMECs) [28] [82]. TJs strictly regulate the passage of ions, molecules, and immune cells from the bloodstream into the brain parenchyma [83]. A detailed molecular characterization of TJ proteins—their expression, localization, and interactions—is fundamental to understanding CNS health and disease.
Recent advancements in 3D bioprinting are revolutionizing this field. Traditional two-dimensional (2D) models fail to fully recapitulate the physiological architecture, fluid dynamics, and cell-cell interactions of the human BBB [9] [13]. Sophisticated 3D-bioprinted BBB models now enable the generation of spatially organized, perfusable vascular constructs that accurately mimic the native neurovascular unit (NVU) [13] [38]. These biomimetic platforms provide unprecedented tools for elucidating the molecular dynamics of TJ complexes in both health and disease, thereby accelerating drug discovery and therapeutic development for neurodegenerative diseases, brain tumors, and other CNS pathologies [9] [13] [4].
Molecular Architecture of Tight Junctions
Tight junctions are dynamic structures composed of transmembrane proteins, cytoplasmic scaffolding proteins, and signaling molecules that collectively form a selective paracellular barrier [82]. Table 1 summarizes the core protein components of the BBB TJs, their molecular functions, and key localization features.
Table 1: Core Protein Components of Blood-Brain Barrier Tight Junctions
| Protein Category | Protein Name | Molecular Function | Localization & Features |
|---|---|---|---|
| Transmembrane | Claudin-5 | Primary seal-forming protein; determines paracellular charge and size selectivity [84] [82]. | Predominant claudin in BBB; forms continuous TJ strands [84]. |
| Claudin-3 | Seal-forming protein; contributes to barrier integrity [82]. | BBB-enriched; loss associated with pathological breakdown [82]. | |
| Occludin | Regulatory protein; involved in TJ stability and redox sensing [82]. | Tetraspan protein; its oligomerization is redox-sensitive [82]. | |
| JAM-A (JAM-1) | Adhesion and signaling; facilitates TJ assembly and cell polarity [85] [82]. | Immunoglobulin-like protein; recruits polarity complexes [85]. | |
| Scaffolding | ZO-1, ZO-2, ZO-3 | Cytoplasmic plaque proteins; link transmembrane proteins to actin cytoskeleton [82]. | PDZ-domain proteins essential for clustering TJ proteins at the cell membrane [86] [82]. |
The functional integrity of TJs is maintained through continuous remodeling, governed by transcriptional regulation, post-translational modifications (e.g., phosphorylation), and interactions with the actomyosin cytoskeleton [82]. Furthermore, TJs exist in two distinct spatial configurations: bicellular TJs (bTJs), found at the contact of two cells, and tricellular TJs (tTJs), more complex structures found at the contact of three cells, which are sealed by specific proteins like tricellulin and angulins [84].
3D Bioprinting for Advanced BBB Modeling
The pursuit of physiological relevance in BBB modeling has driven the evolution from simple 2D cultures to advanced 3D systems. Two-dimensional Transwell models, while useful, lack spatial organization, physiological flow, and proper cell-ECM interactions, leading to an underdeveloped, "leaky" barrier phenotype [13] [28]. In contrast, 3D bioprinting enables the fabrication of customized, multicellular constructs that closely mimic the native NVU.
Key Bioprinting Strategies and Design Considerations
Several 3D bioprinting technologies are employed to create BBB models, primarily relying on extrusion-based methods to pattern bioinks—hydrogels containing living cells and biomolecules [13]. The design of a physiologically relevant, 3D-bioprinted BBB model requires careful consideration of multiple factors, as outlined in the workflow below.
A pivotal advancement in bioink development is the use of tissue-specific decellularized extracellular matrix (dECM). For instance, a recent study utilized a cerebrovascular-specific bioink (CBVdECM) derived from porcine brain and blood vessels [38]. When bioprinted with human brain microvascular endothelial cells (HBMECs) and human brain vascular pericytes (HBVPs), these cells self-assembled into a dual-layered structure that closely resembles the architecture of native cerebral blood vessels and promotes the formation of well-organized TJs [38].
Experimental Protocols for TJ Characterization
Characterizing TJ expression and localization in 3D-bioprinted models requires a multifaceted experimental approach. The following protocols are essential for a comprehensive molecular assessment.
Immunofluorescence Confocal Microscopy
This protocol visualizes the spatial distribution and organization of TJ proteins within the bioprinted construct.
- Fixation: Perfuse the bioprinted BBB construct with 4% paraformaldehyde (PFA) in PBS for 30 minutes at room temperature.
- Permeabilization and Blocking: Treat the construct with 0.3% Triton X-100 in PBS containing 5% normal goat serum for 1 hour to permeabilize membranes and block non-specific binding.
- Primary Antibody Incubation: Incubate with primary antibodies against TJ proteins (e.g., mouse anti-claudin-5, rabbit anti-ZO-1) diluted in blocking buffer overnight at 4°C.
- Secondary Antibody Incubation: Wash and incubate with fluorophore-conjugated secondary antibodies (e.g., Alexa Fluor 488 goat anti-mouse, Alexa Fluor 555 goat anti-rabbit) for 2 hours at room temperature, protected from light.
- Imaging and Analysis: Mount the construct and image using a confocal laser scanning microscope. Analyze images for protein localization at cell borders and the formation of continuous, belt-like structures indicative of mature TJs [38].
Transepithelial/Transendothelial Electrical Resistance (TEER) Measurement
TEER is a gold-standard, quantitative, non-invasive technique for assessing the functional integrity and tightness of the TJ barrier in real-time [13] [84].
- Setup: Integrate electrodes into the perfusion chamber of the bioprinted BBB model. Ensure electrodes make contact with the luminal (blood) and abluminal (brain) compartments.
- Measurement: Use a voltohmmeter or EVOM meter to apply an alternating current and measure the electrical resistance across the endothelial barrier.
- Calculation: Subtract the resistance of a blank construct (without cells) and the resistance of the membrane/support from the total measured resistance. Multiply this value by the surface area of the barrier (in cm²) to obtain the TEER value in the standard unit of Ω·cm².
- Interpretation: Monitor TEER values over time. A high TEER value (approaching the in vivo range of 1,500-8,000 Ω·cm²) indicates well-formed, functional TJs, while a drop in TEER suggests barrier disruption [13] [84].
Paracellular Permeability Assay
This assay quantitatively evaluates the barrier's functional competence by measuring the flux of tracer molecules across the bioprinted BBB.
- Tracer Selection: Choose fluorescent or radiolabeled tracers of varying sizes (e.g., 4 kDa FITC-dextran for small molecule passage, 70 kDa TRITC-dextran for larger molecules) to assess size-selective permeability.
- Perfusion and Sampling: Add the tracer to the luminal (inflow) compartment. Continuously perfuse the system at a physiological flow rate to generate relevant shear stress.
- Sample Collection: Collect samples from the abluminal (outflow) compartment at regular intervals over a defined period (e.g., 60-120 minutes).
- Quantification: Measure the concentration of the tracer in the abluminal samples using a fluorometer or scintillation counter. Calculate the Apparent Permeability Coefficient (Papp) using the formula:
Papp = (dQ/dt) / (A * C₀), wheredQ/dtis the steady-state flux rate,Ais the surface area of the barrier, andC₀is the initial tracer concentration in the luminal compartment [13]. A lower Papp value indicates a tighter barrier.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents for TJ Characterization in 3D BBB Models
| Reagent / Material | Function / Application | Specific Example |
|---|---|---|
| Cerebrovascular dECM Bioink | Provides a biomimetic microenvironment supporting TJ formation and BBB-specific function [38]. | CBVdECM (from porcine brain/blood vessels) [38]. |
| Primary Antibodies | Target-specific detection and visualization of TJ proteins via immunofluorescence. | Anti-Claudin-5, Anti-ZO-1, Anti-Occludin [38] [82]. |
| TEER Measurement System | Real-time, quantitative functional assessment of barrier integrity [13] [84]. | Integrated electrode systems for microfluidic chips or custom constructs. |
| Fluorescent Tracers | Quantitative functional assessment of paracellular permeability [13]. | FITC- or TRITC-conjugated dextrans (e.g., 4 kDa, 70 kDa). |
| Cytokines & Inducers | Modeling inflammatory pathways that disrupt TJs and increase permeability. | TNF-α, IL-1β [38]. |
Pathophysiological Applications and Therapeutic Insights
Dysregulation of TJ proteins is a hallmark of numerous CNS pathologies. In neurodegenerative diseases like Alzheimer's disease (AD) and Parkinson's disease (PD), BBB dysfunction, characterized by disrupted TJs and downregulation of claudin-5, may precede and contribute to neuronal degeneration by allowing neurotoxic plasma components into the CNS [13]. In glioblastoma (GBM), the loss of claudin-3 is associated with BBB breakdown, and the tumor's immunosuppressive microenvironment hinders drug delivery [4] [82].
3D-bioprinted BBB models are uniquely positioned to investigate these mechanisms and develop therapeutics. They enable the study of TJ modulation for drug delivery, such as the transient and size-selective opening of the BBB using claudin-5-specific siRNA [84]. Furthermore, they serve as high-throughput platforms for screening drugs designed to exploit receptor-mediated transcytosis (e.g., targeting TfR or LRP-1) to bypass TJs altogether and shuttle therapeutics into the brain [28].
The molecular characterization of tight junction protein expression and localization is fundamental to understanding the BBB in health and disease. The advent of 3D bioprinting has provided a transformative toolkit, enabling the creation of physiologically relevant human BBB models that recapitulate the complex architecture and dynamics of the neurovascular unit. These advanced models, characterized using robust experimental protocols for imaging and functional analysis, offer unprecedented insights into TJ biology. They are poised to dramatically accelerate the discovery of novel therapeutic strategies for a wide range of neurological disorders by providing a more predictive platform for drug screening and disease modeling.
The blood-brain barrier (BBB) is a highly selective, dynamic interface that precisely controls molecular exchange between the circulatory system and the central nervous system (CNS). This regulation is critical for maintaining brain homeostasis and presents a major challenge for delivering therapeutics to the brain [87]. Understanding the BBB's transport functions—including uptake, efflux, and receptor-mediated transcytosis (RMT)—is therefore fundamental to neuroscience research and drug development [88].
Advanced in vitro models, particularly those utilizing three-dimensional (3D) bioprinting, are revolutionizing our ability to study these transport mechanisms. Unlike traditional 2D models, 3D-bioprinted BBB constructs can recapitulate the multicellular architecture, geometry, and hemodynamic forces of the human neurovascular unit [13] [9]. This technical guide provides a comprehensive overview of the core methodologies for assessing transport function within these advanced model systems, framing them within the context of a broader thesis on 3D bioprinting for BBB modeling.
The Blood-Brain Barrier and Its Transport Mechanisms
Anatomical and Cellular Composition
The BBB is not a single entity but a complex multicellular structure within the neurovascular unit. Its core components include:
- Brain Microvascular Endothelial Cells (BMECs): These cells form the physical barrier, characterized by continuous tight junctions that significantly reduce paracellular permeability [13] [87]. They exhibit low rates of transcytosis compared to peripheral endothelial cells.
- Pericytes: Embedded within the capillary basement membrane, pericytes are essential for regulating BBB permeability, maintaining vascular stability, and coordinating angiogenic processes [13] [87].
- Astrocytes: Their end-feet processes envelop over 99% of the abluminal surface of brain capillaries. They contribute to BBB integrity and facilitate communication between neurons and the vasculature [13] [87].
The barrier function is further reinforced by tight junctions comprising proteins such as occludin, claudins (notably claudin-3 and claudin-5), and junctional adhesion molecules (JAMs) [13] [21]. The combined effect is a transendothelial electrical resistance (TEER) ranging from 1,500 to 8,000 Ω·cm² in vivo, a key metric for evaluating the integrity of in vitro BBB models [13].
Substances cross the BBB via several distinct pathways, illustrated in the following diagram and described in detail below.
The primary transport mechanisms across the BBB include:
- Paracellular Transport: The passive diffusion of substances between adjacent endothelial cells. This pathway is severely restricted under healthy conditions by tight junctions and is generally limited to small, hydrophilic molecules [21].
- Transcellular Transport: The movement of substances through the endothelial cell itself. This encompasses several specific mechanisms:
- Passive Diffusion: Small (<400-500 Da), lipophilic molecules can diffuse freely across the cell membrane [21] [87].
- Carrier-Mediated Transport (CMT): Specific solute carrier (SLC) transporters facilitate the uptake of essential nutrients, such as glucose (via GLUT1) and large neutral amino acids (via LAT1) [88] [21].
- Receptor-Mediated Transcytosis (RMT): Large molecules, including proteins and peptides, are transported via vesicular trafficking upon binding to specific receptors on the endothelial cell surface (e.g., transferrin receptor, insulin receptor) [21].
- Adsorptive-Mediated Transcytosis (AMT): An charge-dependent process where cationic substances interact with the negatively charged cell membrane, triggering vesicle formation and transcellular transport [21].
- Active Efflux Transport: ATP-binding cassette (ABC) transporters, such as P-glycoprotein (P-gp) and Breast Cancer Resistance Protein (BCRP), use energy to pump xenobiotics, toxins, and some drugs out of the endothelial cell back into the bloodstream, actively protecting the brain [88] [21].
Quantitative Assessment of Transport Function
A critical step in validating 3D-bioprinted BBB models is the quantitative assessment of their transport properties. The following parameters provide a comprehensive functional profile.
Table 1: Key Quantitative Parameters for BBB Transport Assessment
| Parameter | Description | Physiological Range (In Vivo) | Common Assessment Methods |
|---|---|---|---|
| Transendothelial Electrical Resistance (TEER) | Measures the integrity of tight junctions and paracellular pathway integrity. | 1,500 - 8,000 Ω·cm² [13] | Voltmeter/EVOM; Impedance Spectroscopy |
| Apparent Permeability (Papp) | Quantifies the rate of a compound's passage across the barrier. | Compound-dependent | Flux studies with tracer molecules (e.g., sucrose, inulin) |
| Solute Flux | Direct measurement of a molecule's movement across the barrier over time. | Compound-dependent | Fluorescent or radiolabeled tracers; LC-MS/MS |
| Efflux Transport Ratio | Indicates the activity and directionality of efflux transporters like P-gp. | >2 suggests active efflux [88] | Bidirectional transport assay (A-to-B vs. B-to-A) |
Tracer Molecules for Permeability Studies
Using validated tracer molecules with known transport pathways is essential for characterizing model functionality.
Table 2: Standard Tracer Molecules for BBB Permeability Assessment
| Tracer Molecule | Molecular Weight (Da) | Primary Transport Pathway | Use Case and Interpretation |
|---|---|---|---|
| Sodium Fluorescein | 376 | Paracellular / Passive Transcellular | A small molecule tracer; high permeability indicates compromised tight junctions. |
| Lucifer Yellow | 457 | Paracellular | A hydrophilic dye; used to assess paracellular integrity. |
| [³H]-Sucrose | 342 | Paracellular | A radiolabeled, metabolically inert sugar; a standard for paracellular leakage. |
| [¹⁴C]-Inulin | ~5,000 | Paracellular | A larger polysaccharide; used to detect larger pore formation or significant barrier disruption. |
Experimental Protocols for Transport Studies
The following protocols are adapted for 3D-bioprinted or microfluidic BBB models, which incorporate dynamic flow to simulate physiological shear stress (5-23 dyn/cm²) [13].
Protocol 1: Bidirectional Transport Assay to Evaluate Uptake and Efflux
Purpose: To distinguish between passive permeability and active efflux/influx transport. Key Reagents: Test compound, specific transporter inhibitors (e.g., Verapamil for P-gp [88]), Hanks' Balanced Salt Solution (HBSS).
- Model Preparation: Culture the 3D-bioprinted BBB model under physiological flow conditions until a high TEER value (>150 Ω·cm² for many in vitro models) is achieved.
- Buffer Equilibration: Wash both the luminal (blood) and abluminal (brain) compartments with pre-warmed transport buffer (e.g., HBSS, pH 7.4).
- Bidirectional Dosing:
- A-to-B (Apical-to-Basolateral) Direction: Add the test compound to the luminal compartment. Sample from the abluminal compartment at regular time intervals (e.g., 15, 30, 60, 120 min).
- B-to-A (Basolateral-to-Apical) Direction: Add the test compound to the abluminal compartment. Sample from the luminal compartment at the same time intervals.
- Inhibitor Studies: Repeat the assay in the presence of a specific transporter inhibitor added to both compartments.
- Sample Analysis: Quantify compound concentration in samples using HPLC, LC-MS/MS, or scintillation counting for radiolabeled compounds.
- Data Analysis:
- Calculate the apparent permeability (Papp) in both directions.
- Determine the Efflux Ratio (ER): ER = Papp (B-to-A) / Papp (A-to-B).
- An ER >> 2 indicates active efflux. A significant reduction in ER in the presence of an inhibitor confirms the involvement of a specific efflux transporter [88].
Protocol 2: Evaluating Receptor-Mediated Transcytosis (RMT)
Purpose: To quantify and characterize the transcellular transport of large molecules via specific receptors. Key Reagents: Ligand of interest (e.g., transferrin), fluorescently or radio-labeled ligand, excess unlabeled ligand (for competition), receptor-blocking antibody.
- Pre-incubation: Pre-treat the model with a blocking antibody or an excess of unlabeled ligand for 30-60 minutes to saturate the target receptor.
- Dosing: Apply a physiological concentration of the labeled ligand to the luminal compartment. Include a non-blocked control.
- Sampling: Collect samples from the abluminal compartment over time (e.g., every 30 minutes for up to 4 hours) while maintaining physiological flow.
- Analysis: Quantify the labeled ligand in the abluminal samples.
- Data Interpretation: Significantly reduced transport in the blocked condition compared to the control confirms RMT. The transport rate (e.g., in pmol/min/cm²) can be calculated from the slope of the cumulative transport vs. time curve. The workflow for this assessment is detailed below.
The Scientist's Toolkit: Research Reagent Solutions
Successful assessment of BBB transport requires a suite of specialized reagents and tools.
Table 3: Essential Research Reagents for BBB Transport Studies
| Reagent / Tool Category | Specific Examples | Function and Application |
|---|---|---|
| Cell Sources | Primary human BMECs, induced pluripotent stem cell (iPSC)-derived BMECs, immortalized cell lines (hCMEC/D3). | Form the core barrier structure. iPSC-derived cells are increasingly used for patient-specific models [13]. |
| Bioink Matrices | Fibrin, Collagen I, Hyaluronic acid (HA), Laminin-enriched gels. | Provide the 3D extracellular matrix (ECM) environment that supports cell viability and function [13]. |
| Tight Junction Markers | Antibodies against Claudin-5, Occludin, ZO-1. | Immunostaining and Western Blot to confirm the structural integrity of the BBB. |
| ABC Transporter Substrates & Inhibitors | Substrates: Digoxin (P-gp), Mitoxantrone (BCRP).Inhibitors: Verapamil, Elacridar (P-gp); Ko143 (BCRP) [88]. | Pharmacological tools to characterize and quantify efflux transporter activity in bidirectional assays. |
| RMT Ligands & Probes | Ligands: Transferrin, Anti-Transferrin Receptor Antibody.Probes: Alexa Fluor 488-conjugated Transferrin. | To study and quantify the RMT pathway; used for model validation and targeted drug delivery research [21]. |
| Permeability Tracers | Sodium Fluorescein, Lucifer Yellow, [³H]-Sucrose. | Validate barrier tightness and measure paracellular permeability. |
The accurate assessment of uptake, efflux, and receptor-mediated transcytosis is paramount for validating the physiological relevance of 3D-bioprinted BBB models. The quantitative parameters and detailed experimental protocols outlined in this guide provide a framework for rigorous functional characterization. As 3D bioprinting technologies continue to advance, offering greater control over geometry, cellular composition, and integration with biosensors [13] [9], these transport assays will become even more critical. They will enable researchers to not only create more faithful replicas of the human BBB but also to leverage these models for more predictive drug screening and to gain deeper insights into the role of barrier dysfunction in neurodegenerative diseases.
Comparative Analysis Against Microfluidic Platforms and Organoid Systems
The blood-brain barrier (BBB) is a highly selective, semi-permeable interface that separates the circulating blood from the brain's extracellular fluid, maintaining the delicate microenvironment required for proper neural function [9] [28]. Its complex cellular architecture, comprising brain microvascular endothelial cells (BMECs), pericytes, and astrocytes, creates a formidable challenge for drug delivery and neurological disease research [13] [10]. Traditional two-dimensional (2D) in vitro models and animal systems have proven insufficient for accurately recapitulating human BBB physiology, driving the development of advanced three-dimensional (3D) models [28].
Among these advancements, 3D bioprinting has emerged as a transformative technology that enables the creation of spatially organized, customizable, and physiologically relevant BBB constructs [13]. This review provides a comparative analysis of 3D bioprinted BBB models against two other prominent advanced platforms—microfluidic systems and brain organoids—within the context of a broader thesis on advances in 3D bioprinting for BBB modeling. By examining the technical capabilities, physiological relevance, and research applications of each platform, we aim to guide researchers and drug development professionals in selecting appropriate models for specific neuroscience applications.
Technological Platforms for BBB Modeling
3D Bioprinting Systems
Three-dimensional bioprinting employs additive manufacturing principles to create spatially controlled, multicellular BBB constructs with defined architecture. This approach typically utilizes bioinks—hydrogel materials incorporating living cells and biomolecules—to build complex 3D structures layer by layer [13]. Key bioprinting techniques include extrusion-based, inkjet, and laser-assisted printing, each offering distinct advantages for BBB modeling.
The principal advantage of 3D bioprinting lies in its precise control over spatial organization, allowing researchers to recreate the natural geometry of brain capillaries (typically 7-10 μm in diameter) and establish physiological cell-cell interactions [13]. This technology enables the incorporation of multiple cell types (BMECs, pericytes, astrocytes) in defined spatial arrangements that mimic the native neurovascular unit. Furthermore, 3D bioprinting facilitates the creation of perfusable vascular channels that can be subjected to physiological flow conditions, enhancing barrier functionality through the application of appropriate shear stress (0.1-6.0 dyn/cm²) [89].
Microfluidic Platforms (BBB-on-Chip)
Microfluidic technology, often referred to as "BBB-on-a-chip," utilizes micron-scale channels fabricated from materials such as polydimethylsiloxane (PDMS), polymethyl methacrylate (PMMA), glass, or silicon-based substrates to create controlled microenvironmental conditions [9] [90]. These platforms typically feature a sandwich configuration, parallel layouts, or three-position tubular structures with integrated porous membranes that separate fluid compartments representing blood and brain sides [90].
Microfluidic systems excel at replicating the dynamic flow conditions and mechanical forces experienced by the BBB in vivo. Through precise manipulation of fluid dynamics, these platforms can generate physiological shear stress (ranging from 5-23 dyn/cm² in human brain capillaries) and establish chemical gradients with high spatiotemporal resolution [13] [90]. The laminar flow characteristics at low Reynolds numbers in microchannels enable smooth, predictable fluid movement without turbulence, allowing accurate simulation of blood flow effects on endothelial cell behavior [90]. Recent advanced designs incorporate four-channel configurations that simultaneously model both the BBB and blood-cerebrospinal fluid barrier (BCSFB), more accurately representing the brain's complete barrier system [89].
Brain Organoid Systems
Brain organoids are self-organizing, three-dimensional structures derived from human pluripotent stem cells (hPSCs), including embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs) [91]. These models recapitulate key aspects of human brain development and organization through processes of self-assembly and differentiation, generating tissue that resembles the developing human brain with remarkable accuracy.
While not exclusively modeling the BBB, brain organoids can incorporate vascular components and barrier properties when co-cultured with endothelial cells or patterned toward specific brain regions [91]. Their principal strength lies in reproducing human-specific neurodevelopmental processes and complex cellular interactions within a 3D microenvironment. However, organoids often lack the controlled vascular perfusion and fluid dynamics critical for authentic BBB function, and they may develop with limited reproducibility and high variability in size and cellular composition [91].
Table 1: Comparative Analysis of BBB Modeling Platforms
| Parameter | 3D Bioprinting | Microfluidic Platforms | Brain Organoids |
|---|---|---|---|
| Spatial Control | High (precise deposition) | Moderate (channel geometry) | Low (self-organization) |
| Throughput | Moderate | Low to moderate | High (for screening) |
| Flow Integration | Possible with design | Excellent (inherent capability) | Limited |
| Shear Stress Control | Yes (0.1-6.0 dyn/cm²) | Yes (5-23 dyn/cm²) | No |
| Physiological TEER (Ω·cm²) | 1,500-8,000 | 1,500-8,000 | Variable/Low |
| Multicellular Complexity | High (programmed) | Moderate to high | High (emergent) |
| Reproducibility | High | Moderate to high | Low to moderate |
| Scalability | Moderate | Low to moderate | High |
| Fabrication Complexity | High | Moderate to high | Low |
| Cost | High | Moderate | Low to moderate |
Functional Assessment and Validation Methodologies
Barrier Integrity Assessment
A critical validation parameter for any BBB model is the demonstration of competent barrier function, typically measured through trans-endothelial electrical resistance (TEER). Physiologically relevant models should achieve TEER values ranging from 1,500 to 8,000 Ω·cm², mirroring in vivo measurements [13]. Microfluidic systems often incorporate embedded electrodes for real-time TEER monitoring, while 3D bioprinted models may require specialized sensor integration or endpoint measurements [90].
Permeability assays using tracer molecules (e.g., sodium fluorescein, dextrans) or model drugs provide functional assessment of paracellular and transcellular transport. These experiments measure the apparent permeability coefficient (Papp) across the barrier, with lower values indicating tighter barrier function [9]. Immunostaining and Western blot analysis of tight junction proteins (claudin-5, occludin, ZO-1) provide molecular validation of barrier integrity, with proper localization at cell boundaries confirming functional junction formation [13] [28].
Transport Mechanism Studies
Comprehensive BBB models must recapitulate the specialized transport systems of the native BBB, including solute carrier (SLC) transporters for nutrient uptake (e.g., GLUT1 for glucose), receptor-mediated transcytosis (RMT) for larger molecules, and ATP-binding cassette (ABC) efflux transporters (e.g., P-glycoprotein, BCRP) that actively remove substrates from the brain [28] [10].
Transport studies typically involve measuring the flux of specific substrates in the presence and absence of inhibitors. For example, Rhodamine 123 accumulation assays can assess P-gp efflux activity, while receptor-mediated transport can be evaluated using ligands targeting the transferrin receptor (TfR) or low-density lipoprotein receptor-related protein 1 (LRP-1) [28]. These experiments provide critical information about a model's capability to simulate the complex transport dynamics of the human BBB.
Table 2: Key Transport Systems to Validate in BBB Models
| Transport Mechanism | Key Components | Representative Substrates | Assessment Methods |
|---|---|---|---|
| Paracellular Diffusion | Tight junction proteins (claudin-5, occludin) | Sodium fluorescein, Lucifer yellow | Permeability coefficient, TEER |
| Carrier-Mediated Transport | GLUT1, LAT1, MCT1 | Glucose, large neutral amino acids | Competitive inhibition assays |
| Receptor-Mediated Transcytosis | TfR, IR, LRP-1 | Transferrin, insulin, angiopep-2 | Ligand conjugation, receptor blocking |
| Efflux Transport | P-gp, BCRP, MRP4 | Rhodamine 123, ivermectin | Accumulation assays with inhibitors |
| Adsorptive Transcytosis | Cationic molecules | Cationized albumin | Charge-based inhibition |
Experimental Protocols for BBB Model Evaluation
Protocol 1: TEER Measurement in Microfluidic Platforms
Principle: Transepithelial electrical resistance (TEER) quantifies barrier integrity by measuring electrical resistance across the cellular layer, reflecting the tightness of tight junctions.
Materials:
- Microfluidic BBB chip with integrated electrodes
- Voltmeter/EVOM instrument
- Cell culture medium at 37°C
- Sterile technique supplies
Procedure:
- Sterilize electrode surfaces with 70% ethanol and rinse with PBS.
- Pre-warm culture medium to 37°C and maintain throughout measurement.
- Position electrodes in the apical and basolateral reservoirs/channels.
- Apply alternating current (typically < 100 μA) and measure voltage.
- Calculate TEER using the formula: TEER (Ω·cm²) = (Rtotal - Rblank) × A, where Rtotal is measured resistance, Rblank is resistance without cells, and A is the effective membrane area.
- Perform measurements at consistent time points (e.g., daily) for temporal profiling.
Troubleshooting:
- Ensure stable temperature during measurement to prevent fluctuations.
- Account for channel geometry in resistance calculations for microfluidic systems.
- Validate with positive (high TEER) and negative (disrupted junctions) controls [13] [90].
Protocol 2: Permeability Assessment in 3D Bioprinted Constructs
Principle: The apparent permeability coefficient (Papp) quantifies the rate of molecule translocation across the BBB model, evaluating barrier selectivity.
Materials:
- 3D bioprinted BBB construct in perfusion system
- Tracer molecules (e.g., 4 kDa FITC-dextran, sodium fluorescein)
- Collection plates and multi-well plates
- Fluorescence plate reader or HPLC
- Peristaltic pump for flow control
Procedure:
- Prepare tracer solution in transport buffer at working concentration.
- Apply tracer to the "blood" (luminal) compartment of the construct.
- Collect samples from the "brain" (abluminal) compartment at timed intervals (e.g., 15, 30, 60, 90, 120 minutes).
- Measure tracer concentration in collected samples using appropriate detection methods.
- Calculate apparent permeability: Papp (cm/s) = (dQ/dt) / (A × C₀), where dQ/dt is the transport rate, A is the surface area, and C₀ is the initial donor concentration.
- Normalize values to control conditions and compare to established benchmarks.
Troubleshooting:
- Maintain physiological flow rates (shear stress 0.1-6.0 dyn/cm²) during assay.
- Confirm linearity of transport over time points.
- Include integrity markers to confirm barrier viability throughout experiment [13] [89].
Protocol 3: Immunofluorescence Analysis of Tight Junctions
Principle: Visualization and quantification of tight junction proteins confirms proper formation and localization of critical barrier components.
Materials:
- Cultured BBB model on appropriate substrate
- Fixative (4% paraformaldehyde)
- Permeabilization buffer (0.1-0.25% Triton X-100)
- Blocking solution (1-5% BSA or serum)
- Primary antibodies (anti-claudin-5, anti-occludin, anti-ZO-1)
- Fluorescently-labeled secondary antibodies
- Nuclear stain (DAPI, Hoechst)
- Mounting medium
- Confocal microscope
Procedure:
- Fix cells with 4% PFA for 15 minutes at room temperature.
- Permeabilize with 0.1% Triton X-100 for 5-10 minutes.
- Block with 1-5% BSA for 30-60 minutes to reduce nonspecific binding.
- Incubate with primary antibodies (diluted in blocking solution) overnight at 4°C.
- Wash 3× with PBS over 30 minutes.
- Incubate with fluorescent secondary antibodies for 1-2 hours at room temperature, protected from light.
- Counterstain nuclei with DAPI for 5 minutes.
- Mount samples and image using confocal microscopy.
- Analyze images for continuous, linear staining at cell boundaries.
Troubleshooting:
- Optimize antibody concentrations for specific model systems.
- Include no-primary-antibody controls to assess background fluorescence.
- Use consistent imaging parameters across experimental conditions for quantitative comparisons [13] [28].
Signaling Pathways in BBB Development and Dysfunction
The formation and maintenance of the BBB involves complex signaling pathways between cellular components of the neurovascular unit. The following diagram illustrates key signaling interactions in BBB physiology and pathology:
Diagram 1: Signaling Pathways in BBB Regulation. This diagram illustrates key molecular interactions between cellular components of the neurovascular unit in healthy and diseased states. Note the shift from stabilizing signals (Wnt/β-catenin, TGF-β) in homeostasis to disruptive pathways (NF-κB, VEGF) in pathology.
Research Applications and Disease Modeling
Neurodegenerative Disease Studies
BBB dysfunction is increasingly recognized as a critical component in neurodegenerative diseases, including Alzheimer's disease (AD) and Parkinson's disease (PD). Advanced BBB models enable investigation of disease-specific pathological processes, such as impaired amyloid-β clearance in AD and α-synuclein propagation in PD [13] [90].
Microfluidic platforms excel in modeling the spatiotemporal dynamics of neurodegenerative processes, allowing researchers to recreate chemical gradients of inflammatory mediators (e.g., TNF-α, IL-6) that activate the NF-κB signaling pathway in endothelial cells, leading to tight junction degradation [90]. These systems can simulate the "vicious cycle" of neurovascular uncoupling, where BBB disruption facilitates infiltration of peripheral inflammatory factors and neurotoxins, further exacerbating neuroinflammation and pathological protein aggregation [90].
3D bioprinted BBB models offer unique advantages for studying cell-type-specific contributions to neurodegeneration through precise spatial patterning of different neural and vascular cells. These models can incorporate patient-derived cells to create personalized platforms for investigating individual disease mechanisms and treatment responses [13].
Drug Delivery and Permeability Screening
All three platform types have significant applications in pharmaceutical research for evaluating CNS drug candidate permeability and optimizing delivery strategies. Microfluidic systems enable real-time monitoring of drug transport and barrier integrity under physiological flow conditions, providing more predictive data than static models [9] [92].
BBB-on-chip platforms have been employed to study receptor-mediated transcytosis (RMT) pathways for enhanced brain delivery of therapeutics. For example, models incorporating the transferrin receptor (TfR), insulin receptor (IR), and low-density lipoprotein receptor-related protein 1 (LRP-1) enable evaluation of targeted delivery systems, such as Angiopep-2-modified nanoparticles for improved brain penetration [28].
Three-dimensional bioprinted models facilitate medium-to-high throughput screening of compound libraries by enabling parallel fabrication of standardized BBB constructs. These systems can incorporate relevant cell sources (including patient-specific iPSC-derived cells) and physiological barrier properties, potentially improving the translational predictiveness of preclinical screening [13].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for BBB Modeling
| Reagent Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Cell Sources | iPSC-derived BMECs, primary human BMECs, immortalized cell lines (hCMEC/D3) | Barrier formation | iPSCs enable patient-specific models; primary cells maintain native characteristics |
| Bioink Materials | Collagen, fibrin, hyaluronic acid, gelatin methacryloyl (GelMA) | 3D scaffold provision | Mimic brain ECM mechanics (0.2-0.5 kPa stiffness); support cell viability and function |
| Barrier Inducers | glucocorticoids, cAMP agonists, Wnt/β-catenin pathway activators | Enhance TJ formation | Improve TEER values and reduce permeability |
| TJ Markers | Anti-claudin-5, anti-occludin, anti-ZO-1 antibodies | Barrier integrity assessment | Validate proper localization at cell boundaries via immunofluorescence |
| Transport Substrates | Sodium fluorescein, FITC-dextrans, Rhodamine 123 | Permeability and efflux studies | Vary molecular weight for size-selective permeability assessment |
| Cytokine Reagents | TNF-α, IL-6, IL-1β | Inflammation modeling | Reproduce neuroinflammatory conditions in neurodegeneration |
| ECM Proteins | Collagen IV, laminin, fibronectin | Basement membrane reconstitution | Provide structural support and biochemical cues for barrier function |
Integrated Workflow for BBB Model Development
The process of developing, validating, and applying advanced BBB models follows a logical progression from platform selection to experimental implementation. The following diagram outlines this comprehensive workflow:
Diagram 2: Integrated Workflow for BBB Model Development. This diagram outlines the systematic process from platform selection through experimental application, highlighting key options and methods at each stage.
The comparative analysis of 3D bioprinting against microfluidic platforms and organoid systems for BBB modeling reveals distinct advantages and limitations for each approach. Microfluidic BBB-on-chip platforms excel in replicating dynamic flow conditions and enabling real-time monitoring of barrier function, making them ideal for permeability studies and drug transport analysis. Brain organoids offer unparalleled recapitulation of human neurodevelopment and complex cellular interactions but face challenges in vascular integration and reproducibility. Three-dimensional bioprinting emerges as a promising intermediate, providing precise spatial control and customization while accommodating perfusion capabilities.
For the broader thesis on advances in 3D bioprinting for BBB modeling, this analysis positions bioprinting as a technology with significant potential for creating standardized, physiologically relevant models that bridge the gap between the physiological accuracy of microfluidic systems and the biological complexity of organoids. Future developments in bioink formulation, resolution enhancement, and sensor integration will likely expand the capabilities of 3D bioprinted BBB models, potentially enabling more predictive preclinical screening and personalized medicine approaches for neurological disorders.
The optimal choice of platform ultimately depends on specific research objectives, with each technology offering unique capabilities for advancing our understanding of BBB function and dysfunction in health and disease.
The blood-brain barrier (BBB) represents a formidable challenge in neurological drug development, preventing over 98% of small-molecule therapeutics from reaching the central nervous system in effective concentrations [93]. Predictive validation—the process of establishing a definitive correlation between model predictions and clinical outcomes—has therefore become the cornerstone of reliable BBB modeling. For research focused on advancing 3D bioprinting for BBB modeling, demonstrating a strong correlation with in vivo human data is not merely beneficial but essential for establishing translational relevance.
The field is moving from traditional 2D Transwell systems and animal models, which often fail to fully recapitulate human BBB physiology, toward more sophisticated 3D bioprinted models [13] [30]. These advanced models aim to replicate the intricate cellular composition and dynamic flow conditions of the human neurovascular unit. However, their ultimate value in drug development and disease modeling hinges on rigorous validation against clinical data. This guide details the experimental protocols, key metrics, and analytical frameworks necessary to establish this critical correlation, thereby enabling the development of highly predictive 3D-bioprinted BBB models for neurodegenerative disease research and therapeutic development.
Foundational Principles of BBB Permeability and Validation
Key Physicochemical and Biological Determinants of Permeability
The permeability of the BBB is governed by a combination of physicochemical properties of the compound and the biological features of the barrier itself. Passive diffusion, the primary transport mechanism for many small molecules, is largely a function of lipophilicity (often measured as LogP) and molecular size [93]. However, the native BBB is far more complex, featuring active transport mechanisms via influx and efflux transporters that are selective for specific molecules like hormones and proteins [93].
From a biological perspective, the BBB's core cellular components—brain microvascular endothelial cells (BMECs), pericytes, and astrocytes—collectively generate tight junctions (TJ) that severely restrict paracellular diffusion [13]. The TJ proteins, particularly claudin-5 and occludin, are fundamental to barrier integrity; their reduced expression is directly linked to increased permeability [13]. Furthermore, the extracellular matrix (ECM) of the BBB, comprising collagen IV, laminin, and nidogen, provides distinct biochemical and structural cues that influence cellular behavior and barrier function [13]. A predictive model must therefore account for both the compound's properties and the barrier's biological complexity.
Establishing a Correlation Framework: In Vitro, In Vivo, and Clinical Endpoints
The core of predictive validation lies in creating a quantitative link between model-derived measurements and in vivo or clinical endpoints. The most common validation pathway involves a two-step correlation process.
- In Vitro to In Vivo Correlation: This first establishes a relationship between a measurable output from the bioprinted model (e.g., effective permeability, ( Pe )) and an in vivo permeability metric. A seminal feasibility study demonstrated a remarkably strong correlation (( R^2 = 0.96 )) between the in vitro ( Pe ) of eight drugs measured in a human cell-based tri-culture BBB model and their in vivo ( Pe ) (denoted ( Q{ECF} )) estimated from human clinical data using CNS physiologically based pharmacokinetic (CNS-PBPK) modeling [94].
- In Vivo to Clinical Outcome Correlation: The second step links the in vivo permeability to actual clinical efficacy or toxicity outcomes. While this is complex and multifactorial, the ability to accurately predict brain concentrations via PBPK modeling is a critical intermediary step towards understanding dose-exposure-response relationships in patients [94].
Experimental Protocols for Model Validation
Protocol 1: Permeability Assay in 3D-Bioprinted BBB Models
This protocol details the measurement of effective permeability (( P_e )), a fundamental quantitative metric for validation.
Materials & Reagents:
- 3D-Bioprinted BBB Construct: A model typically consisting of a lumen structure lined with BMECs, supported by pericytes and astrocytes, embedded within a collagen IV-rich hydrogel (e.g., 2% w/v Porcine Brain Lipid in dodecane) [95] [13].
- Test Compounds: A diverse validation set of chemicals with known in vivo permeability, spanning a range of lipophilicities and molecular weights. This should include low, medium, and high-permeability compounds.
- Transport Buffer: PBS (pH 7.4) containing 1% DMSO as a solvent [95].
- Analytical Instrumentation: HPLC-MS/MS for quantitative analysis of compound concentrations.
Workflow:
- Pre-assay Preparation: Equilibrate the bioprinted BBB model in the transport buffer. Measure the trans-endothelial electrical resistance (TEER) to ensure barrier integrity meets a pre-defined threshold (target: 1500-8000 Ω·cm² for physiological relevance) [13].
- Compound Application: Introduce the test compound at a known concentration to the "blood" (apical) compartment of the bioprinted model.
- Incubation: Allow permeation to occur under dynamic flow conditions (shear stress of 5-23 dyn/cm²) for a set period (e.g., 30 minutes to several hours, optimized for compound stability) [95] [13].
- Sample Collection: At designated time points, collect samples from the "brain" (basolateral) compartment.
- Quantitative Analysis: Use HPLC-MS/MS to determine the concentration of the test compound that has permeated to the basolateral side.
- Permeability Calculation: Calculate the effective permeability (( Pe )) using the following equation, where ( dQ/dt ) is the steady-state flux, ( A ) is the surface area of the barrier, and ( C0 ) is the initial donor concentration [95]. ( Pe = \frac{dQ/dt}{A \times C0} )
Protocol 2: In Vitro-In Vivo Correlation (IVIVC) Analysis
This protocol describes how to formally correlate the in vitro permeability data with in vivo data.
Materials & Reagents:
- In vitro ( P_e ) values for the validation compound set from Protocol 1.
- In vivo permeability data (( Q_{ECF} )) for the same compounds, obtained from the literature or derived from human clinical data via CNS-PBPK modeling [94].
Workflow:
- Data Compilation: Create a dataset pairing the in vitro ( Pe ) value for each compound with its corresponding in vivo ( Q{ECF} ) value.
- Regression Analysis: Perform a linear regression analysis with in vitro ( Pe ) as the independent variable and in vivo ( Q{ECF} ) as the dependent variable.
- Correlation Assessment: Calculate the coefficient of determination (( R^2 )) to quantify the strength of the correlation. A value close to 1.0 indicates a strong predictive relationship, as demonstrated in the feasibility study [94].
Quantitative Data and Performance Metrics
The table below consolidates quantitative data from recent studies focusing on the correlation between in vitro models and in vivo or clinical permeability data.
Table 1: Performance Metrics of BBB Permeability Models and Validation Studies
| Study Focus / Model Type | Key Metric | Performance / Outcome | Dataset Size | Reference |
|---|---|---|---|---|
| IVIVC Feasibility (hiBBB model) | Correlation (R²) between in vitro ( Pe ) and in vivo ( Q{ECF} ) | R² = 0.96 | 8 drugs | [94] |
| PAMPA-BBB Predictive Model | Model fit (R²) for measured vs. predicted ( P_e ) | R² = 0.71 | 106 compounds | [95] |
| Machine Learning Ensemble (EnsembleBBB) | Predictive Accuracy (External Validation) | Accuracy: 95%, AUC: 0.92 | 7,807 molecules | [93] |
| Human CNS-PBPK Modeling | Application | Predicts brain drug concentration profiles in humans using in vitro permeability as input. | N/A | [94] |
Critical Performance Benchmarks for 3D-Bioprinted BBB Models
For a 3D-bioprinted model to be considered physiologically relevant, it should strive to meet the following benchmarks derived from in vivo human physiology:
Table 2: Key Physiological Benchmarks for a Predictive 3D-Bioprinted BBB Model
| Parameter | Target (In Vivo Human) | Relevance for Predictive Validation | |
|---|---|---|---|
| TEER | 1,500 - 8,000 Ω·cm² | Indicates tight junction formation and barrier integrity. | [13] |
| Shear Stress | 5 - 23 dyn/cm² | Mechanical stimulus that influences cell alignment and TJ protein expression. | [13] |
| Capillary Diameter | 7 - 10 μm | Structural feature that must be replicated for physiological relevance. | [13] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for 3D-Bioprinted BBB Model Development and Validation
| Research Reagent | Function in BBB Modeling | Technical Specification / Example | |
|---|---|---|---|
| Bioink | Forms the scaffold for 3D cell structure; provides mechanical support and biochemical cues. | Shear-thinning hydrogels (e.g., gelatin-based); Young's modulus of 2–4 kPa to match brain tissue. | [30] |
| Porcine Brain Lipids (PBL) | Creates an artificial membrane that mimics the lipid composition of the brain endothelium for permeability screening. | 2% (w/v) in dodecane for PAMPA-BBB assays. | [95] |
| Cellular Components | Recapitulates the multicellular complexity of the neurovascular unit. | Co-culture of Brain Microvascular Endothelial Cells (BMECs), Pericytes, and Astrocytes. | [13] |
| Tight Junction Staining Antibodies | Visualize and quantify the expression and localization of key TJ proteins, validating barrier integrity. | Antibodies against Claudin-5, Occludin, and JAM-1. | [13] |
Visualizing the Predictive Validation Workflow
Diagram: Predictive Validation Pathway for 3D-Bioprinted BBB Models
The following diagram outlines the logical workflow and key decision points for establishing predictive validation of a 3D-bioprinted BBB model, integrating both computational and experimental approaches.
The path to robust predictive validation of 3D-bioprinted BBB models is anchored in the rigorous quantitative correlation of in vitro permeability data with in vivo human outcomes. The demonstrated feasibility of achieving a high correlation (R² = 0.96) provides a compelling benchmark for the field [94]. The integration of these validated models with CNS-PBPK modeling and machine learning approaches represents the most promising strategy to transform drug development for neurological diseases [94] [96] [93]. As 3D bioprinting technologies advance, improving the resolution, reproducibility, and long-term stability of these constructs, their predictive power will only increase. This progress will ultimately accelerate the development of effective therapeutics for neurodegenerative diseases by providing a more reliable, human-relevant platform for preclinical testing.
Conclusion
3D bioprinting has emerged as a powerful platform for creating physiologically relevant blood-brain barrier models that bridge critical gaps between traditional 2D cultures, animal models, and human physiology. These advanced constructs recapitulate key aspects of BBB cellular architecture, tight junction complexity, and transport functionality, providing unprecedented opportunities for studying neurodegenerative disease mechanisms and accelerating CNS drug development. Future directions focus on integrating patient-specific iPSCs for personalized medicine applications, incorporating immune cell components and glymphatic system dynamics, leveraging AI for bioink optimization and predictive modeling, and advancing toward clinical validation through prospective studies comparing model predictions with human pharmacokinetic data. As these technologies mature, 3D bioprinted BBB models are poised to transform neuropharmacology by providing more predictive, human-relevant platforms for therapeutic development.
References
- 1. and human artificial Astrocytes - blood - PMC brain barrier models [https://pmc.ncbi.nlm.nih.gov/articles/PMC9519155/]
- 2. Frontiers | Strategies for delivering drugs across the blood-brain barrier for the treatment of neurodegenerative diseases [https://www.frontiersin.org/journals/drug-delivery/articles/10.3389/fddev.2025.1644633/full]
- 3. Distinct Contributions of Astrocytes and Pericytes to... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0150360]
- 4. Biomaterials and 3 Strategies to Model Glioblastoma and... D Bioprinting [https://pmc.ncbi.nlm.nih.gov/articles/PMC7854518/]
- 5. Modern Methods and Materials for Modeling Tissue and... Brain [https://elib.sfu-kras.ru/handle/2311/145138]
- 6. Cutting-edge advances in modeling the blood–brain barrier and tools for its reversible permeabilization for enhanced drug delivery into the brain - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10373415/]
- 7. Frontiers | The blood - brain : an engineering perspective barrier [https://www.frontiersin.org/journals/neuroengineering/articles/10.3389/fneng.2013.00007/full]
- 8. Recent advances in blood-brain barrier-on-a-chip models - PubMed [https://pubmed.ncbi.nlm.nih.gov/40127880/]
- 9. Recent advances in 3D models for multiparametric blood–brain barrier detection in microfluidic systems - Journal of Materials Chemistry B (RSC Publishing) DOI:10.1039/D4TB02499K [https://pubs.rsc.org/en/content/articlehtml/2025/tb/d4tb02499k]
- 10. Human mini-blood–brain barrier models for biomedical neuroscience research: a review | Biomaterials Research | Full Text [https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-022-00332-z]
- 11. -5: gatekeeper of neurological function | Fluids and Claudin of... Barriers [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-019-0123-z]
- 12. The Basic Requirement of Tight in Junction - Proteins ... Blood Brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC11172262/]
- 13. Frontiers | Advances in 3D Bioprinting for Modeling the Blood-Brain Barrier in Neurodegenerative Diseases [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1703403/abstract]
- 14. The tight junction protein occludin modulates blood–brain barrier integrity and neurological function after ischemic stroke in mice | Scientific Reports [https://www.nature.com/articles/s41598-023-29894-1]
- 15. Specific role of tight junction proteins claudin-5, occludin, and ZO-1 of the blood-brain barrier in a focal cerebral ischemic insult - PubMed [https://pubmed.ncbi.nlm.nih.gov/21318404/]
- 16. 3D Bioprinting Blood Brain Barrier and Traumatic Brain Injuries - CELLINK [https://www.cellink.com/customer-spotlight/bioprinting-of-vascularized-model-of-blood-brain-barrier-for-traumatic-brain-injury/]
- 17. Research progress on the role of Claudin family proteins in mediating blood-brain barrier selective permeability in tumor metastasis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12082546/]
- 18. Studying Blood - Brain in Barrier - Oxford... Tight Junction Proteins 3 D [https://imaris.oxinst.com/learning/view/article/studying-blood-brain-barrier-tight-junction-proteins-in-3d]
- 19. The role of claudin‑5 in blood‑brain barrier (BBB) and ... [https://www.spandidos-publications.com/10.3892/mmr.2013.1875]
- 20. - Blood machineries and targeted therapy of... brain barrier transport [https://pmc.ncbi.nlm.nih.gov/articles/PMC5326671/]
- 21. Frontiers | Transcytosis to Cross the Blood , New... Brain Barrier [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2018.01019/full]
- 22. Transport at the Blood Brain Barrier (BBB) | Davis and Ronaldson Laboratories [https://davislab.med.arizona.edu/transport-blood-brain-barrier-bbb]
- 23. Transport Mechanisms at the Blood–Brain Barrier and in Cellular Compartments of the Neurovascular Unit: Focus on CNS Delivery of Small Molecule Drugs [https://www.mdpi.com/1999-4923/14/7/1501]
- 24. A 3D-printed blood-brain barrier model with tunable topology and cell-matrix interactions - PubMed [https://pubmed.ncbi.nlm.nih.gov/37820611/]
- 25. Frontiers | Transport of Amino Acids Across the Blood-Brain Barrier [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2020.00973/full]
- 26. Differential expression of receptors - mediating ... receptor mediated [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-020-00209-0]
- 27. Current Status of In Vitro Models of the Blood-Brain Barrier - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9440157/]
- 28. Frontiers | 3D in vitro blood – brain models: recent advances... barrier [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1637602/full]
- 29. Experimental Models of In Vitro Blood–Brain Barrier for CNS Drug Delivery: An Evolutionary Perspective [https://www.mdpi.com/1422-0067/24/3/2710]
- 30. The rise of 3D bioprinting advancements in modeling neurodegenerative diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12177659/]
- 31. Benchmarking in vitro tissue-engineered blood – brain models barrier [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-018-0117-2]
- 32. Construction and Functional Evaluation of 2 and... | SpringerLink D [https://link.springer.com/chapter/10.1007/978-981-97-9495-9_14]
- 33. Biomaterials and 3D Bioprinting Strategies to Model Glioblastoma and the Blood-Brain Barrier - PubMed [https://pubmed.ncbi.nlm.nih.gov/33326131/]
- 34. Imaging blood-brain barrier dysfunction in animal disease models - PubMed [https://pubmed.ncbi.nlm.nih.gov/23134491/]
- 35. The blood-brain barrier as a treatment target for neurodegenerative disorders - PubMed [https://pubmed.ncbi.nlm.nih.gov/40096820/]
- 36. Cellular and molecular mechanisms of the blood–brain barrier... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11264766/]
- 37. The Expanding Burden of Neurodegenerative Diseases: An Unmet Medical and Social Need - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12339136/]
- 38. Self-assembling cerebral blood vessels: A breakthrough... | ScienceDaily [https://www.sciencedaily.com/releases/2025/02/250203203358.htm]
- 39. 3D bioprinting and its innovative approach for biomedical applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9790048/]
- 40. A New Frontier in CNS Drug Development: Overcoming the BBB Bottleneck with Humanized Mouse Models [https://www.cyagen.com/cyagen-lab-notes/cns-bbb-models]
- 41. Recent advances in 3 for multiparametric D – models ... blood brain [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d4tb02499k]
- 42. Laser-based bioprinting for multilayer cell patterning in tissue engineering and cancer research - PubMed [https://pubmed.ncbi.nlm.nih.gov/34223612/]
- 43. Design considerations of bioinks for laser bioprinting technique towards tissue regenerative applications - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S240588662200015X]
- 44. Coaxial bioprinting of a three-layer vascular structure exhibiting... [https://pubmed.ncbi.nlm.nih.gov/39787741/]
- 45. LIST: A Newly Developed Laser-assisted Cell Bioprinting Technology - PubMed [https://pubmed.ncbi.nlm.nih.gov/36313198/]
- 46. for Bioinks : an overview 3 D bioprinting [https://pubmed.ncbi.nlm.nih.gov/29492503/]
- 47. Engineering considerations in the design of tissue specific bioink for... [https://pubs.rsc.org/en/content/articlehtml/2025/bm/d4bm01192a]
- 48. Recent Bioprinting and Bioink Innovations- BioTechniques [https://www.biotechniques.com/bioengineering-biophysics/bioprinting-and-bioinks-the-latest-innovations-in-building-synthetic-biological-structures/]
- 49. A Next-Generation 3 Tissue-Engineered D of the Human Model ... Brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC10376721/]
- 50. A Next-Generation 3D Tissue-Engineered Model of the Human Brain Microvasculature to Study the Blood-Brain Barrier [https://www.mdpi.com/2306-5354/10/7/817]
- 51. Frontiers | 3 at the Frontier of Regenerative Medicine... D Bioprinting [https://www.frontiersin.org/journals/medical-technology/articles/10.3389/fmedt.2020.607648/full]
- 52. Computational simulation -based comparative analysis of standard... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10261129/]
- 53. Advances in 3 for regenerative medicine applications... D bioprinting [https://pmc.ncbi.nlm.nih.gov/articles/PMC11153344/]
- 54. A novel dynamic multicellular - co for studying... culture system [https://www.nature.com/articles/s41598-018-26480-8?error=cookies_not_supported&code=d2cef96a-65ad-48fe-a459-4448ecbad91b]
- 55. Generation of an hiPSC-Derived Co - Culture to Assess the... System [https://pmc.ncbi.nlm.nih.gov/articles/PMC8834542/]
- 56. Fabrication of Hydrogel Microchannels Using Aqueous Two-Phase... [https://link.springer.com/article/10.1007/s13206-023-00110-6]
- 57. Development of a 3D printed perfusable in vitro blood–brain barrier model for use as a scalable screening tool - Biomaterials Science (RSC Publishing) [https://pubs.rsc.org/en/content/articlelanding/2024/bm/d4bm00663a]
- 58. Innovative 3 - D model enhances understanding of... blood brain barrier [https://www.news-medical.net/news/20250203/Innovative-3D-blood-brain-barrier-model-enhances-understanding-of-neuroinflammation.aspx]
- 59. A review on cell damage, viability, and functionality during 3D bioprinting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9756521/]
- 60. Recent trends in bioinks for 3D printing | Biomaterials Research [https://biomaterialsres.biomedcentral.com/articles/10.1186/s40824-018-0122-1]
- 61. Effect of bioink on properties and cell viability for... printability [https://pubmed.ncbi.nlm.nih.gov/27634915/]
- 62. A comprehensive protocol for hydrogel-based bioink design: balancing... [https://pubs.rsc.org/en/content/articlelanding/2025/tb/d5tb00737b]
- 63. Advances in bioink-based 3D printed scaffolds: optimizing biocompatibility and mechanical properties for bone regeneration - Biomaterials Science (RSC Publishing) [https://pubs.rsc.org/en/content/articlelanding/2025/bm/d4bm01606h/unauth]
- 64. Transepithelial/Transendothelial Electrical Resistance ( TEER ) to... [https://link.springer.com/protocol/10.1007/978-1-4939-8946-1_6]
- 65. New 3 may improve production of engineered... D bioprinting technique [https://news.mit.edu/2025/new-3d-bioprinting-technique-may-improve-production-engineered-tissue-0917]
- 66. Quantification of In Vitro Blood-Brain Barrier Permeability - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12208173/]
- 67. Frontiers | 3D Bioprinting-Based Vascularized Tissue Models Mimicking Tissue-Specific Architecture and Pathophysiology for in vitro Studies [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.685507/full]
- 68. Bioprinting in Vascularization Strategies - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6305822/]
- 69. microvasculature: progressing from structure to function... Bioprinted [https://pmc.ncbi.nlm.nih.gov/articles/PMC8988885/]
- 70. Frontiers | The Use of Tissue Engineering to Fabricate Perfusable 3D Brain Microvessels in vitro [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2021.715431/full]
- 71. Fabrication of Engineered Vascular Flaps Using 3 Printing... D [https://app.jove.com/t/63920/fabrication-engineered-vascular-flaps-using-3d-printing]
- 72. In vitro Models of the Blood–Brain Barrier: Tools in Translational Medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8757867/]
- 73. in vitro 3 - D : recent blood and their... brain barrier models advances [https://pubmed.ncbi.nlm.nih.gov/41126959/]
- 74. of high cell-density heterogeneous tissue 3 ... D bioprinting models [https://www.nature.com/articles/s41467-021-21029-2?error=cookies_not_supported&code=17088cb6-abf9-494e-9421-9b301e9e6b9f]
- 75. for Protocol of a 3 in vitro D of neuroblastoma... bioprinting 3 D model [https://pmc.ncbi.nlm.nih.gov/articles/PMC12008580/]
- 76. Leveraging 3 and Photon-Counting Computed... D Bioprinting [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842604/]
- 77. and standardized organ-on-chip platform with TEER... Highly scalable [https://pubmed.ncbi.nlm.nih.gov/38346163/]
- 78. Maximizing Drug Discovery with High - Throughput and High-Content... [https://alitheagenomics.com/blog/maximizing-drug-discovery-with-high-throughput-and-high-content-screening]
- 79. sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology... [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/high-throughput-screening]
- 80. In Vitro Blood Brain Barrier Permeability Assessment [https://visikol.com/services/in-vitro/blood-brain-barrier/]
- 81. In Vitro 3 ‐ D ‐ Blood Model for Investigating Brain Insults... Barrier Barrier [https://pmc.ncbi.nlm.nih.gov/articles/PMC10104638/]
- 82. at the blood brain barrier: physiological architecture... Tight junctions [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/2045-8118-9-23]
- 83. Tight junction proteins - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0079610702000378]
- 84. Modulating Bioprobes for Drug Delivery System to the... Tight Junction [https://pmc.ncbi.nlm.nih.gov/articles/PMC7767277/]
- 85. Structural Features of Tight-Junction Proteins [https://www.mdpi.com/1422-0067/20/23/6020]
- 86. Molecular characterization of the tight junction protein ZO-1 in MDCK cells - PubMed [https://pubmed.ncbi.nlm.nih.gov/10094817/]
- 87. A blood – brain overview on structure, function, impairment, and... barrier [https://fluidsbarrierscns.biomedcentral.com/articles/10.1186/s12987-020-00230-3]
- 88. at the Transport – Mechanisms and in Cellular... Blood Brain Barrier [https://pmc.ncbi.nlm.nih.gov/articles/PMC9324459/]
- 89. A four-channel microfluidic of the model – blood and... brain [https://mnsl-journal.springeropen.com/articles/10.1186/s40486-024-00219-9]
- 90. Frontiers | Regulation of BBB function and pathological evolution of PD... [https://www.frontiersin.org/journals/aging-neuroscience/articles/10.3389/fnagi.2025.1599509/full]
- 91. Frontiers | Brain organoid model systems of neurodegenerative diseases: recent progress and future prospects [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1604435/full]
- 92. Implementation of blood - brain on barrier chip: Recent... microfluidic [https://pubmed.ncbi.nlm.nih.gov/37004842/]
- 93. Machine Learning in Drug Development for Neurological Diseases: A Review of Blood Brain Barrier Permeability Prediction Models - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11949286/]
- 94. In Vitro- In of Vivo - Correlation Permeability of... Blood Brain Barrier [https://pubmed.ncbi.nlm.nih.gov/35288803/]
- 95. Frontiers | Developing a predictive for model - blood - brain ... barrier [https://www.frontiersin.org/journals/toxicology/articles/10.3389/ftox.2025.1535112/full]
- 96. Machine learning based dynamic consensus model for predicting blood-brain barrier permeability - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0010482523004493]