SOX9: A Janus-Faced Regulator of Innate and Adaptive Immunity in Disease and Therapy
This review synthesizes current knowledge on the transcription factor SOX9, a pivotal but dualistic regulator of both innate and adaptive immune mechanisms.
SOX9: A Janus-Faced Regulator of Innate and Adaptive Immunity in Disease and Therapy
Abstract
This review synthesizes current knowledge on the transcription factor SOX9, a pivotal but dualistic regulator of both innate and adaptive immune mechanisms. We explore its foundational biology, from protein structure to its complex, context-dependent roles in immune cell development, tumor immunology, and inflammatory diseases. The article details methodological approaches for studying SOX9, addresses key challenges in therapeutic targeting, and provides a comparative analysis of its functions across different physiological systems. Aimed at researchers and drug development professionals, this work underscores SOX9's significant potential as a therapeutic target in cancer and immune-related pathologies, while outlining critical future research directions to harness its immunomodulatory power.
Unraveling the SOX9 Enigma: Structure, Expression, and Fundamental Immune Roles
The transcription factor SOX9 (SRY-related HMG box 9) serves as a pivotal regulator in embryonic development and organogenesis, with emerging roles in immunological processes. While initially characterized for its essential functions in chondrogenesis and sex determination, recent evidence positions SOX9 at the intersection of innate and adaptive immunity, influencing immune cell differentiation, tumor immune evasion, and inflammatory tissue responses [1] [2]. The multifaceted functionality of SOX9 across these diverse biological contexts is encoded within its distinct protein architecture. This review decodes the functional domains of SOX9—the HMG box, DIM, TAM, and TAC—elucidating how their coordinated actions underpin SOX9's mechanism in immunity and disease.
SOX9 Protein Domain Architecture
The human SOX9 protein comprises 509 amino acids with a modular structure consisting of several functionally specialized domains [3] [1] [4]. These domains work in concert to facilitate DNA binding, protein-protein interactions, and transcriptional regulation.
Table 1: Core Functional Domains of Human SOX9 Protein
| Domain | Position | Key Functions | Molecular Mechanisms |
|---|---|---|---|
| Dimerization (DIM) | N-terminal | Facilitates homo- and heterodimerization | Enables SOXE protein interactions via DIM-HMG box contacts [3] [4] |
| HMG Box | Central | Sequence-specific DNA binding and bending | Binds consensus motif AGAACAATGG; induces DNA bending via L-shaped complex [3] [1] |
| Transactivation Middle (TAM) | Central | Transcriptional activation | Synergizes with TAC; interacts with transcriptional co-activators [3] [1] |
| PQA-Rich | C-terminal | Enhances transactivation | Stabilizes SOX9; lacks autonomous transactivation capability [3] [4] |
| Transactivation C-terminal (TAC) | C-terminal | Primary transcriptional activation | Recruits MED12, CBP/p300, TIP60, WWP2; inhibits β-catenin [3] [1] |
The HMG Box: DNA Binding and Bending Domain
The High Mobility Group (HMG) box represents the defining feature of SOX proteins, facilitating sequence-specific DNA binding. This domain recognizes and binds to the consensus DNA sequence AGAACAATGG, with AACAAT forming the core binding element [3]. Upon binding, the HMG domain induces significant bending of the DNA helix by forming an L-shaped complex within the minor groove [2]. This bending is thought to facilitate the assembly of larger transcriptional complexes by bringing distal regulatory elements into closer proximity. The HMG domain also contains embedded nuclear localization signals (NLS) that direct SOX9 to the nucleus, essential for its function as a transcription factor [1].
The Dimerization Domain (DIM)
Located upstream of the HMG box, the DIM domain is characteristic of the SOXE subgroup (SOX8, SOX9, SOX10). This domain enables the formation of both homodimers and heterodimers with other SOXE proteins [3]. Dimerization occurs through selective interactions between the DIM domain of one molecule and the HMG box of another, rather than through DIM-DIM interactions [4]. This capacity for dimerization significantly expands the regulatory potential of SOX9, allowing for cooperative DNA binding and the regulation of distinct sets of target genes, which is particularly relevant in cell-type-specific immune responses [3].
Transactivation Domains: TAM and TAC
SOX9 possesses two transactivation domains that mediate interactions with the transcriptional machinery:
- TAM (Transactivation Domain in the Middle): Works synergistically with the TAC domain to activate tissue-specific genes, such as those in cartilage development [3] [1].
- TAC (C-terminal Transactivation Domain): Serves as the primary transactivation interface, directly recruiting co-activators including MED12 (a component of the mediator complex), CBP/p300 (histone acetyltransferases), TIP60, and WWP2 (an E3 ubiquitin ligase) [3]. The TAC domain is also critically involved in the inhibition of β-catenin signaling during cell differentiation processes [1].
The PQA-Rich Domain
The proline, glutamine, and alanine (PQA)-rich domain, while lacking autonomous transactivation capability, plays a supportive role in stabilizing the SOX9 protein and enhancing its transactivation potential in vitro [3] [4]. Its exact mechanistic role in immune functions remains an active area of investigation.
SOX9 in Innate and Adaptive Immunity Mechanisms
SOX9 exhibits a dual role in immunology, functioning as a "double-edged sword" in both innate and adaptive immunity [1]. Its expression and function within immune cells and the tissue microenvironment significantly influence disease outcomes.
SOX9 in Innate Immunity and Inflammation
Within the innate immune system, SOX9 contributes to tissue repair and inflammatory responses. In conditions like osteoarthritis, increased SOX9 levels help maintain macrophage function and contribute to cartilage formation and tissue regeneration [1]. Furthermore, SOX9 is implicated in the regulation of trained immunity—a functional state of innate immune cells characterized by epigenetic and metabolic reprogramming that allows for enhanced responses to secondary challenges. As hematopoietic stem and progenitor cells (HSPCs) serve as a cellular reservoir for trained immunity, the role of transcription factors like SOX9 in shaping these long-term responses warrants deeper exploration [5].
SOX9 in Adaptive Immunity and Cancer Immunomodulation
SOX9 plays a complex role in modulating adaptive immunity, particularly in the context of cancer. It influences T-cell lineage commitment, where it can cooperate with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a, Blk), thereby modulating the balance between αβ and γδ T-cell differentiation [1].
In the tumor microenvironment, SOX9 is a critical mediator of immune evasion. Bioinformatics analyses of data from The Cancer Genome Atlas reveal that SOX9 expression correlates negatively with the infiltration levels of B cells, resting mast cells, and monocytes [1]. Its overexpression in tumors like colorectal cancer negatively correlates with genes associated with the anti-tumor functions of CD8+ T cells and NK cells [1]. SOX9 also helps latent cancer cells maintain stemness and avoid immune surveillance in secondary sites, facilitating metastatic dormancy and outgrowth [6].
Table 2: SOX9-Mediated Immunomodulation in Disease Contexts
| Disease Context | Role in Immunity | Key Mechanisms & Correlations |
|---|---|---|
| Cancer (e.g., Colorectal, Prostate) | Promotes tumor immune escape | Negative correlation with CD8+ T cells, NK cells, M1 macrophages; creates "immune desert" microenvironment [1] |
| Osteoarthritis | Supports tissue repair | Maintains macrophage function; promotes cartilage formation and regeneration [1] |
| Lung & Liver Inflammation | Regulates immune response | Interacts with damage-associated molecular patterns (DAMPs) and acute-phase protein production [7] |
Experimental Analysis of SOX9 Function
The complex functions of SOX9 are dissected using a suite of molecular, cellular, and bioinformatic techniques. Key experimental workflows for studying its DNA binding, transcriptional activity, and dimerization are outlined below.
Analyzing DNA Binding and Transcriptional Regulation
Chromatin Immunoprecipitation (ChIP) is a cornerstone method for identifying direct genomic targets of SOX9. The protocol involves cross-linking SOX9 to its bound DNA in cells, shearing chromatin, immunoprecipitating SOX9-DNA complexes with a specific antibody, and then quantifying the associated DNA sequences via qPCR or sequencing (ChIP-seq) [4]. This method has been instrumental in mapping SOX9 binding to enhancers like the Testis-specific Enhancer of Sox9 (TES) and promoters of target genes such as COL2A1 and COL10A1 [2] [4].
The Dual-Luciferase Reporter Assay is used to validate the transcriptional activity of SOX9 on specific promoter or enhancer elements. A DNA fragment containing putative SOX9 binding sites is cloned upstream of a firefly luciferase gene. This reporter construct is co-transfected into cells along with a SOX9 expression plasmid. A second Renilla luciferase plasmid serves as a transfection control. The ratio of firefly to Renilla luminescence indicates the degree of SOX9-dependent transactivation, allowing researchers to quantify the functional impact of SOX9 mutations or partner interactions [4].
Investigating SOX9 Dimerization and Partner Interactions
The functional versatility of SOX9 is largely dictated by its partnership with other transcription factors. SOX9 generally requires cooperative binding with partner factors (e.g., SF1 in testis determination or SOX5/SOX6 in chondrogenesis) to specific composite DNA elements for full transcriptional activity [2]. These partnerships can determine whether SOX9 acts as a transcriptional activator or repressor. For instance, during hypertrophic chondrocyte maturation, a SOX9-Gli complex represses Col10a1 expression, whereas a SOX9-SOX5/6 complex activates Col2a1 [2].
Co-immunoprecipitation (Co-IP) is a key technique for validating these physical interactions. Cells are lysed, and an antibody against SOX9 or its putative partner is used to pull down the protein complex. The co-precipitated proteins are then separated by gel electrophoresis and detected via western blotting with specific antibodies, confirming direct protein-protein interactions [2].
The Scientist's Toolkit: Research Reagent Solutions
Advancing SOX9 research, particularly in immunology, relies on a standardized set of high-quality reagents and tools.
Table 3: Essential Research Reagents for SOX9 Investigation
| Research Reagent | Specific Example/Model | Function & Application |
|---|---|---|
| SOX9 Antibodies | ChIP-grade anti-SOX9 | Validated for Chromatin Immunoprecipitation to identify genomic binding sites [4] |
| SOX9 Reporter Cell Lines | C3H10T1/2 mesenchymal cell line | Model for studying FGF-mediated SOX9 regulation via MAPK pathway [4] |
| Gene Manipulation Tools | siRNA/shRNA for SOX9 knockdown | Functional studies to determine necessity of SOX9 in immune or cancer processes [6] |
| In Vivo Models | Tissue-specific Sox9 knockout mice | Determine cell-autonomous functions of SOX9 in development and disease [3] [2] |
| Bioinformatics Databases | The Cancer Genome Atlas (TCGA) | Analyze correlations between SOX9 expression and immune cell infiltration in tumors [1] |
| Guanosine-8-d-1 | Guanosine-8-d-1 Deuterated Standard|Supplier | Guanosine-8-d-1 is a stable isotope-labeled internal standard for precise bioanalytical research. This product is for Research Use Only. Not for human or veterinary use. |
| Butoconazole-d5 (nitrate) | Butoconazole-d5 (nitrate), MF:C19H18Cl3N3O3S, MW:479.8 g/mol | Chemical Reagent |
The functional domains of SOX9 constitute an integrated molecular machine that directs cell fate in development and orchestrates complex responses in immunity. The HMG box, DIM, TAM, and TAC domains provide SOX9 with the versatility to act as a key nodal point in transcriptional networks relevant to both innate and adaptive immunity. Future research should focus on delineating the cell-type-specific functions of SOX9 within different immune cell populations and understanding how its post-translational modifications fine-tune its activity in inflammatory and cancerous contexts. Given its pronounced role in tumor immune evasion and fibrosis, SOX9 represents a promising, albeit challenging, therapeutic target. The development of small molecules or biologics capable of selectively modulating specific SOX9 domains or its interactions with partner proteins could open new avenues for treating cancer and immune-related diseases.
The transcription factor SOX9, a member of the SRY-related HMG-box family, is increasingly recognized as a pivotal regulator of macrophage biology within the innate immune system. This whitepaper synthesizes current research demonstrating that SOX9 functions as a context-dependent, janus-faced modulator of macrophage polarization, inflammatory responses, and metabolic reprogramming. Evidence from oncology, hepatology, and osteoarthritis research reveals that SOX9 can drive both pro-inflammatory M1 and anti-inflammatory M2 macrophage phenotypes through distinct molecular mechanisms, including the Caspase 6/NR4A1/SOX9 signaling axis and modulation of the NF-κB/IL-17 pathway. The complex duality of SOX9 in macrophage regulation presents significant challenges and opportunities for therapeutic targeting in inflammatory diseases, cancer, and regenerative medicine. This technical guide comprehensively details the molecular mechanisms, experimental methodologies, and research tools essential for advancing the study of SOX9 in macrophage biology and innate immunity.
The SOX (SRY-related HMG-box) family of transcription factors represents highly conserved proteins characterized by a high-mobility group (HMG) box DNA-binding domain that facilitates DNA bending and chromatin remodeling [1] [8]. SOX9, a 509-amino acid polypeptide, contains several functionally critical domains: an N-terminal dimerization domain (DIM), the central HMG box domain, two transcriptional activation domains (TAM and TAC), and a C-terminal proline/glutamine/alanine (PQA)-rich domain [1]. While initially characterized for its essential roles in chondrogenesis, sex determination, and embryogenesis, SOX9 has emerged as a significant immunoregulator with particular importance in macrophage biology.
The innate immune system provides rapid, non-specific host defense through cellular components including macrophages, neutrophils, and monocytes, alongside acute-phase proteins and complement [1]. Macrophages, as central effectors of innate immunity, exhibit remarkable plasticity, polarizing into context-dependent functional states—most broadly categorized as pro-inflammatory M1 or anti-inflammatory M2 phenotypes—in response to microenvironmental signals [9] [10]. SOX9 sits at the interface of innate and adaptive immunity, modulating macrophage polarization and function while also influencing T cell development and differentiation [1]. This positioning makes SOX9 a critical factor in immune homeostasis, inflammatory disease progression, and tumor immunology.
Molecular Mechanisms of SOX9 in Macrophage Regulation
Signaling Pathways and Transcriptional Networks
SOX9 regulates macrophage function through several defined molecular pathways, demonstrating remarkable context-dependent behavior:
Caspase 6/NR4A1/SOX9 Inflammatory Axis: In ischemia/reperfusion-stressed fatty livers, Caspase 6 activation in macrophages (Kupffer cells) triggers downstream signaling involving nuclear receptor NR4A1 and SOX9 [11]. Macrophage NR4A1 co-localizes with SOX9 in the nucleus under inflammatory conditions, where SOX9 acts as a coactivator for NR4A1 to directly target S100A9 transcription [11]. This signaling cascade ultimately promotes NEK7/NLRP3-driven inflammasome activation and pyroptosis, establishing a pro-inflammatory macrophage phenotype.
NF-κB/IL-17 Pathway Modulation: In temporomandibular joint osteoarthritis (TMJOA), the soluble epoxide hydrolase inhibitor TPPU inhibits M1 macrophage polarization and subsequent cartilage degradation through a mechanism involving SOX9 upregulation [10]. RNA-seq analysis identified the NF-κB/IL-17 pathway as a key target, with SOX9 expression increasing in chondrocytes when co-cultured with TPPU-treated macrophages, suggesting SOX9 mediates cross-talk between macrophages and tissue cells in inflammatory contexts [10].
Metabolic Reprogramming Interface: While direct evidence of SOX9 regulating macrophage metabolism is still emerging, parallels exist with known metabolic regulators of macrophage polarization. For instance, ubiquitin-specific protease 7 (USP7) regulates M1 macrophage polarization through pyruvate kinase M2 (PKM2)-mediated metabolic reprogramming, favoring glycolysis [12]. Given SOX9's involvement in macrophage polarization, its potential role in immunometabolism represents a promising research frontier.
Table 1: SOX9-Associated Signaling Pathways in Macrophage Regulation
| Signaling Pathway | Cellular Context | Key Molecular Interactors | Macrophage Phenotype Outcome |
|---|---|---|---|
| Caspase 6/NR4A1/SOX9 | Hepatic IR Injury | S100A9, NEK7, NLRP3 | Pro-inflammatory (M1-like) |
| NF-κB/IL-17 | TMJ Osteoarthritis | TPPU, sEHi, COL2 | Transition from M1 to M2 |
| Metabolic Reprogramming | Inflammatory Stress | PKM2, Glycolytic Enzymes | Context-dependent (M1/M2) |
Duality in Macrophage Polarization
SOX9 exhibits remarkable functional plasticity in directing macrophage polarization, demonstrating opposing effects across different disease contexts:
Pro-inflammatory Functions: In fatty liver ischemia/reperfusion injury, the Caspase 6/NR4A1/SOX9 axis promotes a pro-inflammatory macrophage phenotype characterized by enhanced IL-1β, TNF-α, and CXCL-2 production, alongside NLRP3 inflammasome activation and pyroptosis [11]. SOX9 deficiency in this context attenuates liver damage, inflammatory cell infiltration, and proinflammatory mediator release [11].
Pro-regenerative Functions: In osteoarthritis models, SOX9 expression in chondrocytes increases when co-cultured with TPPU-treated macrophages that exhibit reduced M1 polarization [10]. This suggests SOX9 contributes to tissue repair responses associated with anti-inflammatory macrophage phenotypes. Similarly, in renal tissues of molly fish, SOX9 co-expression with Nrf2 in stem cells suggests a role in tissue repair and regeneration potentially influenced by macrophage-derived signals [13].
Experimental Models and Methodologies
In Vivo Model Systems
Murine Fatty Liver Ischemia/Reperfusion Model: This model establishes the role of macrophage SOX9 in sterile inflammation. Caspase 6-knockout (Caspase 6KO) mice generated via the CRISPR/Cas9 system undergo 60 minutes of hepatic ischemia followed by 6 hours of reperfusion [11]. Assessment includes serum ALT measurement, histopathological evaluation of liver architecture, immunofluorescence for macrophage markers (CD11b) and neutrophil activation, alongside quantification of proinflammatory factors and NLRP3 inflammasome components [11].
Unilateral Anterior Crossbite (UAC) TMJ Osteoarthritis Model: This model investigates SOX9 in macrophage-mediated joint degeneration. Mice receive metal tubes bonded to maxillary and mandibular incisors to create mechanical stress [10]. TPPU treatment (3 mg/kg via oral gavage every other day) tests therapeutic modulation of macrophage polarization. Outcomes include histological analysis of synovial inflammation and cartilage degradation (H&E, Safranin-O/Fast Green staining), immunohistochemistry for inflammatory markers (TNF-α, IL-1β) and chondrogenic indicators (SOX9, COL II) [10].
Severe Acute Pancreatitis (SAP) Model: This system explores metabolic regulation of macrophage polarization. SAP is induced in mice via six hourly intraperitoneal caerulein (50 μg/kg) injections followed by LPS (10 mg/kg) [12]. USP7 knockdown using AAV-sh-USP7 evaluates effects on macrophage polarization, with assessment of serum amylase/lipase, pancreatic histology, inflammatory cytokines, and metabolic profiling via Seahorse assay (ECAR, OCR) [12].
In Vitro Techniques
Macrophage-Chondrocyte Co-culture Systems: RAW264.7 macrophages and ATDC5 chondrogenic cells are co-cultured to investigate macrophage polarization effects on chondrogenesis [10]. Macrophages are stimulated with LPS/IFN-γ for M1 polarization or IL-4 for M2 polarization, with or without TPPU treatment. Chondrogenic differentiation is assessed via Alcian Blue staining and RT-qPCR for chondrogenic markers (SOX9, COL2) [10].
Metabolic Assays: Seahorse XF Analyzers measure extracellular acidification rates (ECAR) and oxygen consumption rates (OCR) to quantify glycolytic flux and oxidative phosphorylation in polarized macrophages [12]. These parameters define metabolic reprogramming associated with M1 (glycolysis) versus M2 (OXPHOS) phenotypes.
Molecular Interaction Studies: Co-immunoprecipitation (Co-IP) and ubiquitination assays determine protein-protein interactions and post-translational modifications, such as USP7-mediated deubiquitination of PKM2 in macrophage metabolic reprogramming [12]. Chromatin immunoprecipitation (ChIP) identifies direct transcriptional targets of SOX9 in macrophages.
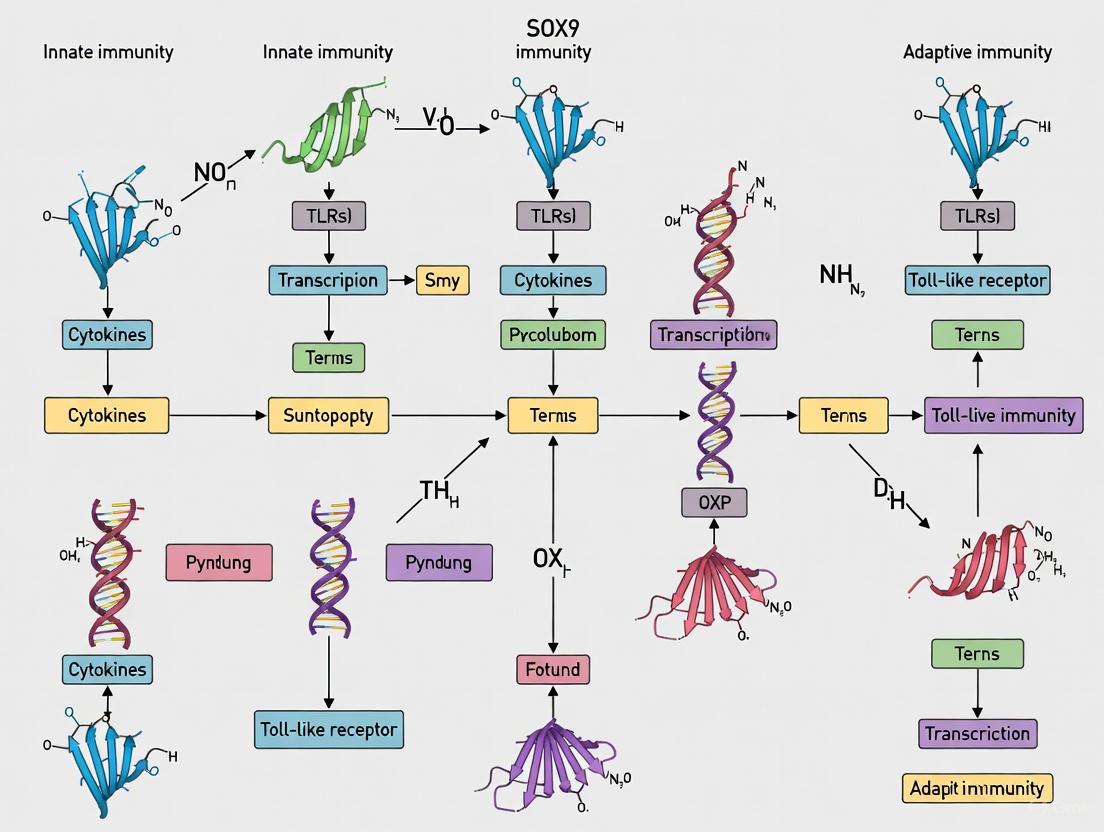
Figure 1: SOX9-Associated Signaling Pathways in Macrophage Polarization. SOX9 participates in multiple context-dependent pathways regulating macrophage polarization, promoting pro-inflammatory M1 phenotypes through the Caspase 6/NR4A1 axis while inhibitors like TPPU facilitate transitions toward anti-inflammatory M2 states via NF-κB/IL-17 modulation.
Research Reagent Solutions
Table 2: Essential Research Reagents for Investigating SOX9 in Macrophage Biology
| Reagent/Category | Specific Examples | Research Application | Key Findings Enabled |
|---|---|---|---|
| Animal Models | Caspase 6KO mice [11], UAC TMJOA model [10] | In vivo role of SOX9 in tissue-specific inflammation | SOX9 promotes inflammation in hepatic IR; supports repair in OA |
| Chemical Inhibitors/Activators | TPPU (sEHi) [10], Compound 3K (PKM2 inhibitor) [12] | Pathway modulation in macrophage polarization | TPPU inhibits M1 polarization via SOX9; PKM2 inhibition reverses USP7 effects |
| Cell Lines/Culture Systems | RAW264.7 macrophages, ATDC5 chondrocytes, primary Kupffer cells [10] [11] | In vitro mechanistic studies | SOX9 mediates macrophage-chondrocyte crosstalk in OA |
| Antibodies for Detection | Anti-SOX9, anti-CD68/Iba1 (macrophages), anti-NR4A1, anti-S100A9 [13] [11] | Cell phenotyping, protein localization | SOX9 co-localizes with NR4A1 in macrophage nuclei |
| Molecular Tools | AAV-sh-USP7, Caspase 6 siRNA, Co-IP assays [11] [12] | Mechanistic pathway analysis | SOX9 acts as NR4A1 coactivator; Caspase 6 regulates SOX9 expression |
Technical Protocols
Protocol: Assessing SOX9 in Macrophage Polarization In Vitro
Objective: Determine SOX9 expression dynamics during macrophage polarization and its functional consequences.
Materials:
- RAW264.7 macrophages or primary bone marrow-derived macrophages
- Polarization inducing agents: LPS (200 ng/mL) + IFN-γ (2.5 ng/mL) for M1; IL-4 (10 ng/mL) for M2
- TPPU (sEHi, 1-10 μM) for pathway inhibition
- RNA extraction kit, RT-qPCR reagents, Western blot materials
- SOX9, iNOS, Arg1, IL-1β, TNF-α antibodies
Procedure:
- Macrophage Culture: Seed RAW264.7 cells (2×10^5 cells/mL) in complete DMEM and allow to adhere for 4 hours.
- Polarization Induction: Treat cells with:
- M1 polarization: LPS (200 ng/mL) + IFN-γ (2.5 ng/mL) for 12-24 hours
- M2 polarization: IL-4 (10 ng/mL) for 12-24 hours
- Experimental groups: Include TPPU pre-treatment (1-10 μM, 2 hours prior to polarization inducers)
- Sample Collection:
- RNA Extraction: Harvest cells in TRIzol, extract RNA, synthesize cDNA
- Protein Extraction: Lyse cells in RIPA buffer with protease inhibitors
- SOX9 Expression Analysis:
- RT-qPCR: Use SOX9 primers (F: 5'-AGGAGACCGAGCGAGAC-3', R: 5'-CAGCGCCTTGAAGATAGC-3') with GAPDH normalization
- Western Blot: Separate proteins (30-50 μg) by SDS-PAGE, transfer to PVDF, incubate with anti-SOX9 (1:1000) and corresponding secondary antibodies
- Functional Assays:
- Cytokine Measurement: Collect conditioned media, analyze IL-1β, TNF-α, IL-10 via ELISA
- Phagocytosis Assay: Add fluorescent beads (1μm), incubate 2 hours, quantify internalization by flow cytometry
- Data Analysis: Normalize SOX9 expression to housekeeping genes/proteins, compare across polarization conditions ± TPPU (one-way ANOVA, p<0.05 significant).
Protocol: Evaluating the Caspase 6/NR4A1/SOX9 Axis in Macrophages
Objective: Characterize the functional interaction between Caspase 6, NR4A1, and SOX9 in macrophage inflammatory responses.
Materials:
- Caspase 6KO macrophages or Caspase 6 siRNA
- NR4A1 and SOX9 expression plasmids
- Co-immunoprecipitation kit
- ChIP assay reagents
- S100A9 ELISA kit
Procedure:
- Genetic Manipulation:
- Knockdown: Transfect macrophages with Caspase 6 siRNA (50 nM, 48 hours) using Lipofectamine 3000
- Overexpression: Co-transfect with NR4A1 and SOX9 expression plasmids (1-2 μg each, 48 hours)
- Stimulation: Activate transfected macrophages with LPS (200 ng/mL, 6 hours)
- Protein Interaction Analysis:
- Co-IP: Lyse cells in NP-40 buffer, incubate with anti-NR4A1 antibody (2 μg, overnight, 4°C), capture with Protein A/G beads, elute and immunoblot for SOX9
- Transcriptional Regulation:
- ChIP: Cross-link proteins to DNA (1% formaldehyde, 10 minutes), sonicate chromatin, immunoprecipitate with anti-NR4A1 or anti-SOX9, purify DNA, analyze S100A9 promoter region by qPCR
- Downstream Signaling:
- Measure S100A9 secretion by ELISA per manufacturer's instructions
- Analyze NLRP3 inflammasome components (NEK7, NLRP3, cleaved Caspase-1) by Western blot
- Data Interpretation: Correlate NR4A1-SOX9 interaction strength with S100A9 expression and inflammasome activation across experimental conditions.
Figure 2: Experimental Workflow for SOX9-Macrophage Studies. Comprehensive methodology for investigating SOX9 function in macrophage polarization, encompassing cellular models, genetic and pharmacological manipulations, multi-parameter analyses, and integrated data interpretation.
Discussion and Therapeutic Implications
SOX9 as a Context-Dependent Immunoregulator
SOX9 exemplifies the complexity of transcription factor biology in immune regulation, demonstrating strikingly divergent functions across tissue environments and disease states. In hepatic ischemia/reperfusion injury, SOX9 drives pro-inflammatory macrophage activation through the Caspase 6/NR4A1/SOX9 axis, promoting S100A9 expression and NLRP3 inflammasome-mediated pyroptosis [11]. Conversely, in osteoarthritis models, SOX9 appears protective, with its expression increased in chondrocytes co-cultured with TPPU-treated macrophages exhibiting reduced M1 polarization [10]. This functional duality positions SOX9 as a sophisticated regulator of immune homeostasis rather than a simplistic pro- or anti-inflammatory factor.
The therapeutic implications of SOX9's functional plasticity are substantial. In cancer contexts, SOX9 overexpression correlates with altered immune cell infiltration, including negative correlations with B cells, resting mast cells, and monocytes, but positive correlations with neutrophils, macrophages, and activated T cells [1]. These patterns suggest SOX9 contributes to immunosuppressive tumor microenvironments, making it a potential target for combination immunotherapy. In inflammatory and degenerative diseases, strategies to modulate SOX9 activity—such as sEH inhibition with TPPU—offer promise for redirecting macrophage polarization toward reparative phenotypes [10].
Future Research Directions
Several critical questions remain unanswered regarding SOX9's role in macrophage biology. The precise mechanisms governing SOX9's context-dependent effects—whether determined by post-translational modifications, interacting protein partners, or cellular microenvironment—require systematic investigation. Additionally, SOX9's potential role in macrophage metabolic reprogramming represents a promising research frontier, particularly given the established importance of metabolic shifts in macrophage polarization [12]. The development of macrophage-specific SOX9 knockout models would help delineate cell-autonomous versus non-autonomous functions, while single-cell RNA sequencing could reveal SOX9-associated macrophage subpopulations across tissues and disease states.
From a translational perspective, targeting SOX9 therapeutically will require strategies that account for its functional duality. Small molecule inhibitors, monoclonal antibodies, or gene therapy approaches could modulate SOX9 activity in a cell-type or context-specific manner. The successful application of TPPU in osteoarthritis models suggests pharmacological manipulation of upstream regulators may offer more nuanced control than direct SOX9 targeting [10]. As our understanding of SOX9 in macrophage biology continues to evolve, so too will opportunities for innovative immunotherapeutic interventions across oncology, autoimmunity, and regenerative medicine.
The SRY-related HMG-box 9 (SOX9) transcription factor is widely recognized for its fundamental roles in chondrogenesis, sex determination, and cell fate specification during embryonic development. However, emerging research has illuminated its significant and complex functions within the immune system, particularly in adaptive immunity. SOX9 operates as a dual-function regulator, acting as both an activator and repressor across diverse immune cell types and contributing to the regulation of numerous biological processes [1]. This review synthesizes current understanding of how SOX9 directly influences T-cell and B-cell lineage fate decisions, bridging developmental biology with immunology to provide insights for therapeutic targeting.
The adaptive immune system, characterized by its specificity and memory, relies on precise transcriptional programming to generate diverse lymphocytes capable of recognizing myriad antigens. SOX9 has recently emerged as a crucial modulator in this process, with demonstrated roles in the differentiation and regulation of various immune lineages [1]. Its expression and function in immune cells further complicate the already intricate landscape of immune development, positioning SOX9 as a pivotal factor at the intersection of innate and adaptive immunity research.
Molecular Characteristics of SOX9
Structural Domains and Functional Motifs
SOX9 encodes a 509 amino acid polypeptide containing several functionally critical domains organized from N- to C-terminus [1]:
- Dimerization domain (DIM): Facilitates protein-protein interactions
- HMG box domain: Mediates DNA binding and induces significant bending at consensus motifs
- Central transcriptional activation domain (TAM): Synergizes with TAC to augment transcriptional potential
- C-terminal transcriptional activation domain (TAC): Interacts with cofactors to enhance transcriptional activity
- Proline/glutamine/alanine (PQA)-rich domain: Necessary for transcriptional activation
The HMG domain deserves particular emphasis as it defines the SOX family and enables SOX9 to recognize specific DNA sequences (CCTTGAG), inducing structural bends that remodel chromatin architecture [1] [2]. This domain also contains embedded nuclear localization and export signals that facilitate nucleocytoplasmic shuttling [1].
Regulatory Mechanisms
SOX9 activity is finely tuned through multiple regulatory layers:
- Post-translational modifications: Phosphorylation by protein kinase A enhances DNA-binding affinity and promotes nuclear translocation [2]. SUMOylation can either activate or repress SOX9-dependent transcription depending on cellular context [2].
- Partner factor interactions: SOX9 generally requires binding partners for transcriptional activity, with the resulting complex determining whether activation or repression occurs [2].
- Epigenetic regulation: SOX9 competes for epigenetic factors to remodel chromatin landscapes, functioning as a pioneer factor in fate switching [14].
Table 1: Key Functional Domains of SOX9 Protein
| Domain | Position | Primary Function | Mechanistic Insight |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein self-association | Enables cooperative DNA binding |
| HMG Box | Middle | DNA binding and bending | Recognizes (A/TA/TCAAA/TG) motif; induces nucleosome displacement |
| Transcriptional Activation Domain (TAM) | Middle | Transcriptional activation | Works synergistically with TAC domain |
| Transcriptional Activation Domain (TAC) | C-terminal | Transcriptional activation | Interacts with cofactors (e.g., Tip60); inhibits β-catenin |
| PQA-rich Domain | C-terminal | Transcriptional activation | Rich in proline, glutamine, alanine residues |
SOX9 in T-Cell Lineage Commitment
Regulation of T-Cell Development
SOX9 plays a context-dependent role in T-cell development, particularly influencing the balance between different T-cell subsets. During thymic development, SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes including Il17a and Blk [1]. This cooperation modulates the lineage commitment of early thymic progenitors, potentially influencing the critical balance between αβ T cell and γδ T cell differentiation [1].
The role of SOX9 extends beyond development to tumor immunology, where it significantly impacts the tumor microenvironment. SOX9 expression negatively correlates with genes associated with the function of CD8+ T cells and NK cells, while showing a positive correlation with memory CD4+ T cells [1]. This suggests SOX9 participates in shaping the functional capacity of T-cell populations in pathological conditions.
Mechanism of SOX9-Mediated Immunosuppression
In breast cancer models, SOX9 demonstrates a remarkable capacity for immune evasion by suppressing T-cell function. SOX9-expressing tumor cells significantly suppress proliferation of both CD8+ and CD4+ T cells compared to control cells [15]. Furthermore, in antigen-specific cytotoxicity assays, SOX9 overexpression significantly reduces T-cell-mediated killing, indicating that SOX9 enables tumor cells to resist immune attack [15].
The mechanistic basis for this immunosuppression involves SOX9-induced expression of the immune checkpoint B7x (B7-H4) through STAT3 activation and direct transcriptional regulation [15]. This pathway establishes a protective shield around dedifferentiated tumor cells, safeguarding them from immunosurveillance. The significance of this pathway is confirmed by the finding that T-cell depletion restores tumor progression in SOX9-deficient environments [15].
Figure 1: SOX9-B7x Axis in T-cell Suppression. SOX9 activates STAT3 and directly transcribes B7x, which inhibits T-cell receptor signaling, reducing T-cell proliferation and cytotoxicity.
SOX9 in B-Cell Biology and Pathology
B-Cell Development and Oncogenic Transformation
While SOX9 does not appear to play a significant role in normal B-cell development, it emerges as a potent oncogenic driver in certain B-cell malignancies. In Diffuse Large B-cell Lymphoma (DLBCL), SOX9 is overexpressed and functions as an oncogene by promoting cell proliferation, inhibiting apoptosis, and contributing to cancer progression [1].
This pathological expression contrasts with its minimal role in physiological B-cell development, suggesting that SOX9 may represent a therapeutic vulnerability in specific B-cell malignancies. The mechanisms through which SOX9 drives oncogenesis in B-cells likely involve its established roles in stem cell maintenance and proliferation control, though the precise pathways remain under investigation.
Experimental Approaches for Studying SOX9 in Immunity
Key Methodologies and Workflows
Investigating SOX9's role in immune regulation requires multidisciplinary approaches. Recent studies have utilized multiomics strategies combining chromatin accessibility assays, transcriptomic profiling, and proteomic analyses to dissect SOX9-mediated mechanisms [16] [14].
The fundamental workflow for establishing SOX9's immunoregulatory functions involves genetic manipulation followed by comprehensive immune phenotyping. Northwestern Medicine scientists employed CRISPR/Cas9 gene-editing to turn on the SOX9 gene in cancer cell lines, with subsequent transcriptome analysis revealing that SOX9 expression reprogrammed ovarian cancer cells into stem-like cancer cells with enhanced survival properties [16].
Figure 2: Experimental Workflow for SOX9 Immune Function Analysis. Key steps include genetic manipulation, multi-omics profiling, functional immune assays, and in vivo validation.
Essential Research Reagents and Tools
Table 2: Key Research Reagents for Studying SOX9 in Immune Contexts
| Reagent/Tool | Function/Application | Experimental Context |
|---|---|---|
| CRISPRa SOX9 activation | Enables controlled SOX9 overexpression | Study of SOX9 gain-of-function in tumor and immune cells [16] |
| Anti-CD3/CD28 antibodies | T-cell stimulation and expansion | T-cell proliferation and functional assays [15] |
| C3-TAg mouse model | Models basal-like breast cancer | In vivo study of SOX9 in tumor progression and immune evasion [15] |
| scRNA-seq | Single-cell transcriptomic profiling | Identification of rare SOX9+ stem-like cell populations [16] |
| CUT&RUN/ATAC-seq | Epigenetic and chromatin profiling | Mapping SOX9 binding sites and chromatin accessibility [14] |
| HLA-A2/NY-ESO-1 TCR | Antigen-specific T-cell cytotoxicity | Measurement of antigen-specific T-cell killing capacity [15] |
Therapeutic Implications and Future Directions
SOX9 as an Immunotherapeutic Target
The dual nature of SOX9 in immunity presents both challenges and opportunities for therapeutic intervention. In cancer contexts, SOX9 represents a promising target for overcoming immunosuppression. Studies demonstrate that targeting the SOX9-B7x axis inhibits tumor growth and activates antitumor immune responses, potentially overcoming resistance to anti-PD-L1 immunotherapy [15].
The finding that SOX9 is epigenetically upregulated in response to chemotherapy in ovarian cancer cell lines and patient samples further underscores its therapeutic relevance [16]. This SOX9 upregulation drives a stem-like phenotype associated with treatment resistance, suggesting that SOX9 inhibition could enhance conventional therapies.
Technical Considerations for SOX9-Targeted Approaches
Several strategic considerations emerge for targeting SOX9 therapeutically:
- Context-dependent effects: SOX9 has opposing roles in different biological processes, necessitating precise targeting to avoid disrupting its physiological functions in tissue homeostasis [1].
- Direct versus indirect targeting: Given the challenges of directly targeting transcription factors, potential strategies include interfering with SOX9-partner interactions or downstream effectors like B7x [15].
- Biomarker development: SOX9 expression shows promise as a biomarker for predicting therapeutic response and disease progression, particularly in cancers with stem-like features [16].
SOX9 has emerged as a critical regulator at the nexus of developmental biology and immunology, with demonstrated roles in T-cell polarization and B-cell malignancy. Its function as a pioneer transcription factor enables SOX9 to orchestrate broad transcriptional programs that influence immune cell fate and function. The recently elucidated SOX9-B7x axis represents a significant mechanism of immune evasion in cancer, highlighting the therapeutic potential of disrupting this pathway.
Future research should focus on delineating the context-specific determinants of SOX9 function in different immune subsets and developing sophisticated targeting strategies that leverage its dual role in immunity and tissue homeostasis. As our understanding of SOX9 in adaptive immunity deepens, so too will opportunities for innovative immunotherapeutic interventions across a spectrum of diseases.
{article}
The SOX9-Wnt/β-catenin Signaling Axis: A Core Crosstalk in Immune Regulation
The SOX9-Wnt/β-catenin signaling axis represents a fundamental regulatory circuit that governs critical cellular processes in both development and disease. Emerging evidence positions this crosstalk as a pivotal regulator at the nexus of immune cell function and tumor immunology. SOX9, a transcription factor with a context-dependent dual role, engages in sophisticated molecular dialogues with the canonical Wnt pathway to modulate immune cell differentiation, tumor immune evasion, and the establishment of immunosuppressive microenvironments. This whitepaper synthesizes current mechanistic insights, detailing how SOX9 directly binds β-catenin to promote its degradation, inhibits β-catenin/TCF transcriptional complexes, and orchestrates the expression of Wnt-related genes. Furthermore, we explore the axis's divergent impacts on innate and adaptive immunity, its role in shaping immune cell infiltration in malignancies, and its promising therapeutic potential. The complex, and sometimes contradictory, nature of this regulatory interplay underscores its significance as a master modulator of the immune response in physiological and pathological states.
The SRY-related HMG-box 9 (SOX9) protein is a multifaceted transcription factor belonging to the SOX family, characterized by a highly conserved High Mobility Group (HMG) box DNA-binding domain [1] [17]. Originally recognized for its non-redundant roles in chondrogenesis, sex determination, and stem cell maintenance, SOX9 is now increasingly implicated in the regulation of the immune system [1]. Its function is aptly described as "Janus-faced," acting as a double-edged sword in immunobiology [1]. On one hand, SOX9 can promote immune escape in cancer by impairing immune cell function; on the other, it contributes to tissue repair and regeneration by maintaining macrophage function [1].
The canonical Wnt/β-catenin signaling pathway is a highly conserved system that controls stem cell fate and is frequently dysregulated in cancer and immune-related diseases [17] [18]. The intricate cross-regulation between SOX9 and the Wnt pathway forms a critical signaling node that influences a broad spectrum of biological activities, from organ development to tumorigenesis [17] [18]. This whitepaper dissects the molecular mechanics of the SOX9-Wnt/β-catenin axis and frames its operational logic within the context of innate versus adaptive immunity, providing a foundational resource for researchers and drug development professionals aiming to target this pathway.
Molecular Mechanisms of the SOX9-Wnt/β-catenin Crosstalk
Structural Foundations of SOX9
The functional capabilities of SOX9 are dictated by its multi-domain structure. The key domains, from N- to C-terminus, include:
- Dimerization Domain (DIM): Facilitates the homologous dimerization of SOX9 proteins [1] [17].
- HMG Domain: Contains the DNA-binding motif, two nuclear localization signals (NLS), and one nuclear export signal (NES), enabling DNA binding and nucleocytoplasmic shuttling [1] [17] [18].
- Central Transcriptional Activation Domain (TAM): Functions synergistically with the C-terminal domain to augment transcriptional activity [1].
- C-terminal Transactivation Domain (TAC): Critical for interacting with coactivators and other transcription factors, including β-catenin [1] [17] [19].
- PQA-rich Domain: A proline/glutamine/alanine-rich motif that enhances the transactivation potency of the TAC domain [1] [17].
This modular architecture allows SOX9 to perform its diverse roles as a transcriptional regulator and a key interaction partner for signaling molecules like β-catenin.
Key Molecular Interactions with the Wnt Pathway
SOX9 primarily functions as an important antagonist of the canonical Wnt signaling pathway through several sophisticated, multi-tiered mechanisms [17] [18]. The following diagram synthesizes these core inhibitory mechanisms:
Diagram 1: SOX9 Inhibitory Mechanisms on Canonical Wnt Signaling. SOX9 antagonizes the Wnt/β-catenin pathway by promoting β-catenin degradation through multiple systems and by directly inhibiting the formation and function of the β-catenin/TCF transcriptional complex.
The mechanisms illustrated above can be categorized as follows:
Promotion of β-Catenin Degradation: SOX9 binds directly to β-catenin via its C-terminal TAC domain, leading to β-catenin degradation in a ubiquitination/proteasome-dependent manner [18] [20] [19]. The N-terminal region of SOX9, including the HMG domain, can recruit components of the β-catenin "destruction complex" (like GSK3β) into the nucleus, enhancing nuclear β-catenin phosphorylation and degradation [18] [20]. SOX9 can also induce β-catenin turnover via lysosomal degradation and through transcriptional activation of MAML2, a potent β-catenin antagonist [18].
Inhibition of β-Catenin/TCF Transcriptional Activity: The TAC domain of SOX9 competes with TCF/LEF factors for binding to the ARM repeats of β-catenin, thereby preventing the formation of a productive transcriptional complex [18] [19]. Furthermore, due to the structural similarity of their HMG domains, SOX9 can directly compete with TCF/LEF for binding to consensus DNA sequences on Wnt target genes [18].
Transcriptional Regulation of Wnt Pathway Components: ChIP-seq analyses reveal that SOX9 binds to enhancers of various Wnt signaling-related genes, acting as either a transcriptional activator or repressor depending on the cellular context and target gene [21]. For instance, in intestinal epithelial stem cells, SOX9 can activate repressors of the Wnt pathway, and its loss of function can lead to Wnt overactivation [21].
Table 1: Molecular Mechanisms of SOX9-Mediated Wnt Pathway Inhibition
| Mechanism Category | Specific Action | Functional Outcome | Key Supporting Domains |
|---|---|---|---|
| β-Catenin Degradation | Ubiquitin/Proteasome pathway [18] [19] | Reduced β-catenin protein stability | HMG domain, TAC domain [20] |
| Lysosomal breakdown [18] | Reduced β-catenin protein stability | Not fully specified | |
| Transcriptional activation of MAML2 [18] | Increased expression of β-catenin antagonist | Transcriptional activation domains | |
| Transcriptional Complex Disruption | Competitive binding to β-catenin [18] [19] | Inhibition of β-catenin/TCF complex formation | TAC domain |
| Competitive DNA binding [18] | Displacement of TCF/LEF from target genes | HMG domain | |
| Pathway Component Regulation | Activation of Wnt antagonists [21] | Enhanced intrinsic inhibition of Wnt signaling | Transcriptional activation domains |
The Axis in Innate and Adaptive Immunity
The SOX9-Wnt/β-catenin crosstalk exerts profound and distinct influences on the two arms of the immune system. Its role is highly context-dependent, contributing to both homeostatic immune function and pathological dysregulation.
Role in Innate Immunity
Within the innate immune system, SOX9 is crucial for the function of macrophages, which are key players in inflammation, tissue repair, and cancer. Increased levels of SOX9 help maintain macrophage function, contributing to cartilage formation and tissue regeneration [1]. Furthermore, Prostaglandin E2 (PGE2), a classic mediator of inflammation, has been shown to play a role in immunomodulation and tissue regeneration by activating SOX9 expression in endogenous renal progenitor cells, highlighting a link between inflammatory mediators and SOX9 in innate repair processes [22].
Role in Adaptive Immunity
The axis plays a more nuanced role in shaping the adaptive immune response, particularly within the tumor microenvironment.
- T Cell Development and Function: SOX9 participates in the differentiation of early thymic progenitors. It can cooperate with c-Maf to activate
Rorcand keyTγδ17effector genes (Il17a,Blk), thereby modulating the lineage commitment balance between αβ T cells and γδ T cells [1]. In cancer, bioinformatics analyses reveal that high SOX9 expression negatively correlates with genes associated with the function of CD8+ T cells and shows a positive correlation with memory CD4+ T cells [1]. - B Cell Lymphoma: While not significant in normal B cell development, SOX9 is overexpressed in certain B-cell lymphomas, such as Diffuse Large B-cell Lymphoma (DLBCL), where it acts as an oncogene by promoting proliferation and inhibiting apoptosis [1].
- Immune Evasion: SOX9 is a critical facilitator of immune evasion and cancer cell dormancy. SOX9, along with SOX2, sustains stemness in latent cancer cells, preserving their long-term survival and tumor-initiating capabilities while helping them avoid immune surveillance in secondary metastatic sites [22].
Table 2: Immune Correlates of SOX9 Expression in the Tumor Microenvironment
| Immune Parameter | Correlation with SOX9 Expression | Potential Immunological Impact |
|---|---|---|
| CD8+ T Cells | Negative correlation with CD8+ T cell function genes [1] | Impairment of cytotoxic T cell activity, promoting immune escape |
| Macrophages | Positive correlation with macrophage infiltration [1] | Potential shift towards pro-tumoral (M2) phenotypes |
| Memory CD4+ T Cells | Positive correlation [1] | Altered T helper cell response |
| Neutrophils | Positive correlation [1] | Potential for increased neutrophilic-driven inflammation |
| Immune Checkpoints | Correlated with expression in Glioblastoma [23] | Contribution to an immunosuppressive microenvironment |
Experimental Analysis and Research Toolkit
Investigating the SOX9-Wnt/β-catenin axis requires a combination of molecular, cellular, and bioinformatic techniques. The following workflow and toolkit outline standard approaches for probing this interaction.
Key Experimental Workflow
A typical experimental pipeline to validate and characterize the axis involves the following stages, which can be adapted based on the research question:
Diagram 2: Generalized Experimental Workflow. A sequential pipeline for investigating the SOX9-Wnt/β-catenin axis, from initial cellular manipulation to systems-level validation.
The Scientist's Toolkit: Essential Reagents and Assays
Table 3: Key Research Reagent Solutions for Investigating the SOX9-Wnt Axis
| Reagent / Assay | Primary Function | Example Application |
|---|---|---|
| Super-TOPFLASH Reporter | Reporter plasmid containing TCF/LEF binding sites to measure canonical Wnt/β-catenin transcriptional activity [20]. | Quantifying the inhibitory effect of SOX9 on Wnt pathway activity upon co-transfection. |
| Co-Immunoprecipitation (Co-IP) | Validates direct protein-protein interactions in cell lysates [20]. | Confirming physical interaction between SOX9 and β-catenin using anti-SOX9 or anti-β-catenin antibodies. |
| GST Pull-down Assay | Confirms direct binary protein interactions in a cell-free system [20]. | Using purified GST-β-catenin to pull down in vitro translated SOX9 protein fragments. |
| Chromatin Immunoprecipitation (ChIP) | Identifies genomic regions bound by a specific transcription factor [21]. | Mapping SOX9 binding sites on enhancers/promoters of Wnt pathway genes (e.g., Wnt4, Fzd8). |
| Adenoviral Vectors | Efficient delivery and overexpression or knockdown of genes in a wide range of cell types, including primary cells [20]. | Overexpressing wild-type or mutant SOX9 in primary chondrocytes or cancer cells to assess phenotypic effects. |
| Pathway Inhibitors | Chemical tools to perturb specific pathway components. | Using proteasome inhibitor (MG132) or lysosome inhibitor (NH4Cl) to determine the mechanism of SOX9-induced β-catenin degradation [20]. |
| ssGSEA/ESTIMATE Algorithms | Bioinformatics algorithms for quantifying immune cell infiltration from RNA-seq data [23]. | Correlating SOX9 expression levels with abundances of CD8+ T cells, macrophages, and other immune subsets in TCGA datasets. |
| Bromo-PEG4-PFP ester | Bromo-PEG4-PFP ester, MF:C17H20BrF5O6, MW:495.2 g/mol | Chemical Reagent |
| D-Idose-18O2 | D-Idose-18O2, MF:C6H12O6, MW:184.16 g/mol | Chemical Reagent |
Detailed Protocol: Luciferase Reporter Assay for SOX9-Mediated Wnt Inhibition
This protocol is adapted from methodologies used to demonstrate SOX9's antagonistic effect on Wnt signaling [20].
- Cell Seeding: Seed appropriate cell lines (e.g., HEK293, CHO, or relevant cancer cell lines) in 24-well plates the day before transfection to achieve 60-80% confluency.
- Plasmid Transfection: Transfect cells using a standard method (e.g., Lipofectamine PLUS). Each well should receive:
- Super-TOPFLASH or FOPFLASH plasmid (negative control): 400 ng.
- SOX9 expression plasmid or empty vector control: 100-500 ng (titrate for optimal effect).
- Renilla Luciferase plasmid (phRL-null): 10 ng for normalization of transfection efficiency.
- Keep the total DNA amount constant by supplementing with empty vector DNA.
- Stimulation (Optional): If studying endogenous pathway activation, treat cells with Wnt-conditioned media or a GSK3β inhibitor (e.g., CHIR99021) 24 hours post-transfection.
- Lysate Preparation: Harvest cells 48 hours post-transfection using passive lysis buffer.
- Luciferase Measurement: Measure Firefly and Renilla luciferase activities sequentially using a Dual-Luciferase Reporter Assay System on a luminometer.
- Data Analysis: Calculate the relative luciferase activity by normalizing Firefly luminescence to Renilla luminescence for each well. The results are typically presented as the average ± S.D. of the relative luciferase activity (TOPFLASH/FOPFLASH ratio) from at least three independent transfections. A significant decrease in the ratio in SOX9-expressing cells compared to the control indicates inhibition of Wnt/β-catenin signaling.
Therapeutic Implications and Future Directions
The potent regulatory function of the SOX9-Wnt/β-catenin axis in immune regulation and cancer progression makes it a compelling target for therapeutic intervention.
Diagnostic and Prognostic Value
SOX9 is highly expressed in numerous solid malignancies, including breast, lung, liver, and gastric cancers, where its levels often correlate with poor prognosis [22] [1]. However, its prognostic implication can be complex and context-dependent. For example, in glioblastoma (GBM), high SOX9 expression was remarkably associated with a better prognosis in specific patient subgroups, such as those with lymphoid invasion, and was identified as an independent prognostic factor for IDH-mutant cases [23]. SOX9 expression is also closely correlated with immune cell infiltration and the expression of immune checkpoints in GBM, indicating its involvement in shaping the immunosuppressive tumor microenvironment [23].
Targeting the Axis for Immuno-Oncology
Strategies to disrupt the SOX9-Wnt/β-catenin axis hold promise for overcoming chemotherapy resistance and improving cancer immunotherapy [22] [1]. Given the role of this axis in fostering an "immune desert" microenvironment—characterized by decreased effector T cells and increased immunosuppressive cells—its inhibition could potentially reverse immune evasion and sensitize tumors to existing immunotherapies [1]. This is particularly relevant for cancers like triple-negative breast cancer, where SOX9 is implicated in regulating cancer stem cells and therapy resistance [22]. Future efforts could focus on developing small molecule inhibitors that disrupt the SOX9-β-catenin protein interaction or leveraging epigenetic drugs to modulate SOX9 expression.
The SOX9-Wnt/β-catenin signaling axis constitutes a core regulatory circuit that exerts sophisticated control over immune cell differentiation, function, and tumor immunology. Through direct protein interactions, transcriptional regulation, and control of protein stability, this crosstalk maintains a delicate balance that influences both innate and adaptive immunity. Its deregulation contributes significantly to immune evasion, metastatic dormancy, and therapy resistance in cancer. While the "Janus-faced" nature of SOX9 presents a challenge for therapeutic targeting, it also underscores its biological significance. A deeper mechanistic understanding of this axis, particularly in specific immune cell subsets and tumor types, will be crucial for unlocking its full potential as a source of diagnostic biomarkers and novel therapeutic targets for cancer and immune-related diseases.
{/article}
The transcription factor SOX9, a member of the SRY-related HMG-box family, is emerging as a pivotal epigenetic landscaper in immune system regulation. This whitepaper synthesizes current evidence demonstrating how SOX9 governs chromatin dynamics to influence both innate and adaptive immunity. By functioning as a pioneer transcription factor, SOX9 directly remodels chromatin architecture, thereby controlling transcriptional programs in immune cells and contributing to pathological states including cancer immune evasion and autoimmune conditions. Understanding SOX9-mediated epigenetic reprogramming provides novel therapeutic opportunities for immune-mediated diseases through targeted chromatin remodeling.
SOX9 exhibits context-dependent dual functions across diverse immune cell types, acting as both an activator and repressor of immunological processes [1]. Its expression is frequently dysregulated in solid malignancies and inflammatory diseases, positioning it at the epicenter of immune homeostasis and dysregulation. The protein's structure contains several functionally critical domains: a dimerization domain (DIM), the High Mobility Group (HMG) box DNA-binding domain, and two transcriptional activation domains (TAM and TAC) that facilitate interactions with cofactors [1]. The HMG domain enables SOX9 to perform its pioneering functions through nucleocytoplasmic shuttling and DNA binding [1]. This structural complexity allows SOX9 to interface with epigenetic machinery to reshape the immune epigenetic landscape.
SOX9's Role in Innate versus Adaptive Immunity
SOX9 in Innate Immune Cells
Monocytes and macrophages exhibit significant SOX9-mediated epigenetic regulation in inflammatory disease contexts. In rheumatoid arthritis (RA), monocytes display a distinct "RA-associated chromatin dysregulation signature" characterized by specific patterns of chromatin accessibility at promoters and active enhancers [24]. These differentially accessible regions are highly enriched for cytokine and immune-associated pathways, including "bone inflammation disease" and "rheumatoid arthritis" ontologies [24]. This chromatin signature strongly correlates with serum C-reactive protein (CRP) levels, and in vitro experiments confirm that CRP induces this specific chromatin dysregulation in monocytes via the transcription factor FRA2 [24]. This establishes a direct link between inflammatory mediators and SOX9-influenced epigenetic states in innate immune cells.
SOX9 in Adaptive Immune Cells
In adaptive immunity, SOX9 plays specialized roles in lymphocyte development and function. During T cell development, SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating the lineage commitment of early thymic progenitors and potentially influencing the balance between αβ T cell and γδ T cell differentiation [1]. While SOX9 does not play a significant role in normal B cell development, it is overexpressed in certain B-cell lymphomas, such as Diffuse Large B-cell Lymphoma (DLBCL), where it acts as an oncogene by promoting cell proliferation, inhibiting apoptosis, and contributing to cancer progression [1]. This cell-type-specific functionality underscores SOX9's contextual epigenetic influence across immune cell lineages.
Table 1: SOX9 Functions Across Immune Cell Types
| Immune Cell Type | SOX9 Function | Epigenetic Impact | Disease Association |
|---|---|---|---|
| Monocytes/Macrophages | Chromatin dysregulation in response to inflammatory signals | Altered accessibility at inflammatory gene enhancers/promoters | Rheumatoid arthritis, Cancer immune evasion |
| T Cells | Modulation of Tγδ17 lineage commitment through Rorc activation | Remodeling of T-cell differentiation gene loci | Altered effector T-cell function |
| B Cells | Oncogenic transformation (minimal role in normal development) | Reprogramming of proliferation/apoptosis genes | B-cell lymphomas (e.g., DLBCL) |
| Tumor Microenvironment | Regulation of immune cell infiltration | Global changes in chromatin accessibility networks | Multiple solid tumors |
Molecular Mechanisms of SOX9-Mediated Chromatin Remodeling
Pioneer Factor Activity
SOX9 demonstrates bona fide pioneer factor capability by binding to cognate motifs within closed chromatin and initiating nucleosome displacement [14]. In epidermal stem cell reprogramming models, SOX9 binds to key hair follicle enhancers de novo, with nearly 30% of SOX9 binding sites situated within closed chromatin before activation [14]. This pioneering activity occurs before increases in chromatin accessibility, which subsequently emerges between 1-2 weeks after initial SOX9 binding [14]. During this process, SOX9-bound opening peaks display a time-dependent decrease in cleavage under targets and release using nuclease (CUT&RUN) fragment length, indicating nucleosome displacement – a hallmark of pioneer factor activity [14].
Chromatin Accessibility Remodeling
The temporal dynamics of SOX9-mediated chromatin opening reveal a sophisticated reprogramming mechanism. SOX9 induces global chromatin changes predominantly at distal enhancers rather than promoters [14]. Principal component analysis of chromatin accessibility during SOX9-driven reprogramming shows that early and late timepoints form distinct clusters, with intermediary timepoints (e.g., 2 weeks post-induction) representing a transitional chromatin state [14]. This indicates that SOX9 orchestrates a coordinated sequence of epigenetic events rather than simultaneous genome-wide changes.
Histone Modification Dynamics
SOX9 collaborates with histone-modifying enzymes to establish active chromatin states. The histone acetyltransferase P300 is significantly enriched at SOX9 enhancers, co-localizing with H3K27ac marks and SOX9 transcription factors [25]. P300-mediated H3K27 acetylation at enhancer regions (e-SR-A and e-ALDI) is crucial for SOX9 transcriptional activation [25]. Additionally, transcriptional activation of SOX9 is associated with selective deposition of active histone modifications (H3K4me3, H3K9ac, and H3K27ac) at its enhancer and promoter regions [25]. SOX9 also helps remove epigenetic signatures of transcriptional repression and establishes active-promoter and active-enhancer marks at cell-type-specific loci, though it is not absolutely required to initiate these changes in all contexts [26].
Competitive Redistribution of Epigenetic Regulators
A novel mechanism of SOX9-mediated repression involves competitive redistribution of epigenetic co-factors. As SOX9 binds and opens key enhancers de novo, it simultaneously recruits co-factors away from previous cell identity enhancers, which consequently become silenced [14]. This indirect silencing mechanism represents an efficient strategy for cell fate switching. When SOX9's ability to bind DNA is abrogated, it can still mediate silencing, but when it cannot bind chromatin remodelers, the fate switch fails altogether [14], highlighting the essential nature of these epigenetic interactions.
Diagram 1: SOX9-Mediated Chromatin Remodeling Pathway. This diagram illustrates the mechanistic process by which SOX9 accesses closed chromatin, recruits histone modifiers, opens new enhancer regions, and indirectly silences previous cell identity enhancers through competitive redistribution of epigenetic co-factors.
Experimental Approaches for Studying SOX9-Chromatin Interactions
Chromatin Accessibility Assessment Methods
Several high-throughput techniques enable genome-wide profiling of SOX9-mediated chromatin changes:
ATAC-seq (Assay for Transposase-Accessible Chromatin using sequencing) utilizes hyperactive Tn5 transposase to simultaneously fragment and tag accessible genomic regions with sequencing adapters [27]. This method provides a simplified approach to map genome-wide accessibility patterns with limited cell numbers, including single-cell applications [27]. The standard protocol involves: (1) cell lysis and nucleus isolation, (2) tagmentation reaction with Tn5 transposase, (3) DNA purification, and (4) library amplification and sequencing [27].
DNase-seq relies on the sensitivity of accessible regions to DNase I cleavage, followed by sequencing of cleaved ends [27]. This method identifies DNase hypersensitivity sites (DHSs) that primarily correspond to nucleosome-depleted regions [27].
MNase-seq uses micrococcal nuclease to digest unprotected DNA, revealing nucleosome positioning by sequencing the protected fragments [27].
FAIRE-seq (Formaldehyde-Assisted Isolation of Regulatory Elements) separates nucleosome-depleted DNA based on chromatin crosslinking and solubility properties [27].
Table 2: Chromatin Accessibility Profiling Techniques
| Method | Principle | Resolution | Advantages | Limitations |
|---|---|---|---|---|
| ATAC-seq | Hyperactive Tn5 transposase tags accessible DNA | Single-base | Low cell input, fast protocol, single-cell applications | Mitochondrial DNA contamination |
| DNase-seq | DNase I cleavage of accessible DNA | Single-base | Gold standard, well-established | High cell input, complex protocol |
| MNase-seq | MNase digestion of unprotected DNA | Nucleosome-level | Precise nucleosome positioning | Identifies inaccessible regions |
| FAIRE-seq | Differential crosslinking/solubility of open chromatin | 100-500 bp | No enzyme optimization needed | Lower resolution, high background |
Mapping SOX9-Chromatin Interactions
CUT&RUN (Cleavage Under Targets and Release Using Nuclease) enables precise mapping of transcription factor binding sites with excellent signal-to-noise ratio [14]. This method uses antibody-directed MNase cleavage to release protein-bound DNA fragments, followed by sequencing. For SOX9 binding studies, the protocol typically includes: (1) permeabilization of cells/nuclei, (2) antibody binding against SOX9, (3) protein A-MNase fusion protein recruitment, (4) calcium-activated cleavage, and (5) DNA extraction and sequencing [14].
ChIP-seq (Chromatin Immunoprecipitation with sequencing) provides an alternative approach to identify SOX9-bound genomic regions through crosslinking, immunoprecipitation with SOX9 antibodies, and sequencing of associated DNA [26].
Multi-Omics Integration Approaches
Advanced multimodal techniques now enable simultaneous detection of epigenetic modifications, chromatin states, and gene expression in the same sample at single-cell resolution [27]. Combining ATAC-seq with RNA-seq from the same cells allows direct correlation of SOX9-mediated accessibility changes with transcriptional outcomes. Integration with histone modification ChIP-seq data (H3K27ac, H3K4me3) further delineates the functional state of SOX9-targeted regulatory elements.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9-Chromatin Studies
| Reagent/Category | Specific Examples | Research Application | Function |
|---|---|---|---|
| SOX9 Antibodies | Anti-SOX9 (ChIP-grade), Anti-MYC (for tagged SOX9) | CUT&RUN, ChIP-seq, Immunofluorescence | SOX9 detection and localization |
| Chromatin Assay Kits | ATAC-seq Kit, ChIP-seq Kit, CUT&RUN Kit | Chromatin accessibility profiling, TF binding | Genome-wide mapping of open chromatin and SOX9 binding sites |
| Epigenetic Modulators | P300 inhibitors, Histone deacetylase inhibitors | Functional perturbation studies | Modify histone acetylation states to test SOX9 dependence |
| Cell Line Models | HGSOC lines (OVCAR4, Kuramochi, COV362), LCLs, Primary immune cells | In vitro and ex vivo studies | Model systems for SOX9 manipulation in relevant cellular contexts |
| Genetic Tools | CRISPR/Cas9 SOX9 KO, Doxycycline-inducible SOX9 expression, siRNA against P300 | Functional validation of SOX9 mechanisms | Targeted manipulation of SOX9 expression and function |
| Multi-omics Platforms | 10x Genomics Single Cell Multiome ATAC + Gene Expression | Integrated chromatin and transcriptome analysis | Simultaneous profiling of accessibility and gene expression |
| Fmoc-Thr(tBu)-OH-13C4,15N | Fmoc-Thr(tBu)-OH-13C4,15N, MF:C23H27NO5, MW:402.4 g/mol | Chemical Reagent | Bench Chemicals |
| Norethindrone Acetate-D8 | Norethindrone Acetate-d8 Deuterated Standard | Bench Chemicals |
SOX9 in Disease Pathogenesis and Therapeutic Implications
Cancer and Chemoresistance
In high-grade serous ovarian cancer (HGSOC), SOX9 is epigenetically upregulated following platinum-based chemotherapy and drives chemoresistance by reprogramming the transcriptional state of naive cells into a stem-like state [28]. This SOX9-mediated reprogramming induces significant chemoresistance in vivo and increases transcriptional divergence – a metric of transcriptional plasticity and stemness [28]. Single-cell analysis of patient tumors reveals that chemotherapy induces rapid population-level induction of SOX9 that enriches for this stem-like transcriptional state [28]. SOX9 ablation through CRISPR/Cas9 significantly increases platinum sensitivity in HGSOC models [28].
Immune Dysregulation
Chromatin accessibility variation in immune cells provides insights into SOX9's role in immune-mediated diseases [29]. Accessible chromatin regions in lymphoblastoid cell lines (LCLs) are significantly enriched for heritability of immune-mediated diseases, suggesting that SOX9-mediated accessibility changes in these regions contribute to disease pathogenesis [29]. In rheumatoid arthritis, the monocyte-specific chromatin accessibility signature strongly correlates with disease activity and CRP levels, indicating SOX9's potential role in perpetuating inflammatory circuits [24].
Therapeutic Targeting Opportunities
The mechanistic understanding of SOX9's epigenetic functions reveals several therapeutic intervention points:
- Direct SOX9 inhibition to prevent pioneer factor activity and chromatin remodeling
- Targeting SOX9-cofactor interactions (e.g., P300 inhibitors) to disrupt specific aspects of SOX9 function
- Epigenetic editing of SOX9-targeted enhancers to reverse pathological gene expression programs
- Small molecule disruptors of SOX9-DNA binding to prevent transcriptional reprogramming
SOX9 serves as a master epigenetic landscaper in immune cells, directly remodeling chromatin accessibility through its pioneer factor capabilities to influence both innate and adaptive immunity. By integrating inflammatory signals with chromatin remodeling activities, SOX9 establishes and maintains pathological states in cancer and autoimmune diseases. The continuing elucidation of SOX9-dependent epigenetic mechanisms will undoubtedly reveal novel therapeutic opportunities for modulating immune function in human disease through targeted epigenetic interventions. Future research should focus on developing cell-type-specific SOX9 modulators and exploring combination therapies that simultaneously target SOX9 and its collaborating epigenetic regulators.
From Bench to Bedside: Techniques and Translational Applications for SOX9 Research
The SRY-box transcription factor 9 (SOX9) is a pivotal regulatory protein with emerging significance in both innate and adaptive immunity, positioning it as a critical molecule in the interface between development, cancer, and immunology. As a transcription factor containing a high-mobility group (HMG) box DNA-binding domain, SOX9 recognizes the specific DNA sequence CCTTGAG and regulates numerous target genes involved in cell fate determination [30]. Recent research has illuminated SOX9's function as a janus-faced regulator in immunity, on one hand promoting immune escape in tumors by impairing immune cell function, while on the other hand maintaining macrophage function and contributing to tissue regeneration and repair [1]. This dual role makes precise profiling of SOX9 expression patterns essential for understanding its contributions to both pathological and physiological processes.
The clinical relevance of SOX9 spans diverse disease contexts, with particularly important implications for cancer biology. SOX9 is frequently overexpressed in various solid malignancies, where its expression levels positively correlate with tumor occurrence and progression [1]. In bone tumors, SOX9 overexpression correlates with tumor severity, grade, invasion features, poor response to therapy, and recurrence [31]. Similarly, in non-small cell lung cancer (NSCLC), SOX9 upregulation significantly correlates with histological stage and shorter patient survival time [32]. Beyond its established oncogenic roles, SOX9 also exhibits tumor-suppressor characteristics in specific contexts such as melanoma, highlighting its cell-type-dependent functions [33]. This complex expression profile across normal and diseased tissues necessitates robust detection methodologies including qPCR, Western blot, and immunohistochemistry to fully elucidate its functional contributions to disease pathogenesis and immunity.
SOX9 Expression Patterns Across Normal Tissues
Comprehensive mapping of SOX9 expression in normal tissues provides a essential baseline for interpreting its dysregulation in disease states. According to the Human Protein Atlas, SOX9 demonstrates widespread but specific expression across numerous tissue types, with particularly prominent presence in tissues of epithelial origin [34]. The protein exhibits a general nuclear expression pattern consistent with its function as a transcription factor, though cytoplasmic localization can occasionally be observed under specific conditions [30] [34].
Table 1: SOX9 Protein Expression in Normal Human Tissues Based on Immunohistochemistry
| Tissue Category | Specific Tissue | SOX9 Expression Pattern |
|---|---|---|
| Gastrointestinal Tract | Colon | Strong nuclear staining in crypt epithelial cells, especially at base |
| Small intestine | Strong nuclear staining in crypt epithelial cells | |
| Stomach | Moderate to strong nuclear staining in surface epithelial cells | |
| Liver | Moderate to strong nuclear staining in intrahepatic bile ducts | |
| Male Reproductive | Testis | Strong staining in Sertoli cells |
| Prostate | Strong positivity in basal cells | |
| Respiratory System | Respiratory epithelium | Moderate to strong positivity in most epithelial cells |
| Endocrine Tissues | Thyroid | Moderate to strong positivity of follicular cells |
| Skin | Epidermis | Weak to moderate nuclear staining in bottom 2/3 of squamous epithelium |
The RNA expression data from the Human Protein Atlas reveals that SOX9 displays a tissue-enhanced specificity pattern, with particularly high expression in salivary gland, and moderate expression across numerous other tissues [34]. SOX9 is part of a gene expression cluster designated "Brain & Liver - Signaling," which includes 153 genes with similar expression patterns primarily involved in signaling functions [34]. This normal expression profile reflects SOX9's fundamental roles in cellular differentiation, tissue development, and stem cell maintenance across multiple organ systems.
SOX9 in Diseased Tissues: Cancer and Beyond
Oncogenic Roles Across Cancer Types
SOX9 demonstrates significant overexpression in numerous cancer types, where it frequently contributes to aggressive disease phenotypes and poor clinical outcomes. In malignant bone tumors, SOX9 expression is remarkably elevated compared to tumor margin tissues, with malignant tumors showing higher expression than benign tumors [31]. Among specific bone cancer types, osteosarcoma exhibits the highest SOX9 expression levels, followed by Ewing sarcoma and chondrosarcoma [31]. This overexpression pattern extends to circulating SOX9 in peripheral blood mononuclear cells, suggesting its potential utility as a liquid biopsy marker [31].
In non-small cell lung cancer (NSCLC), SOX9 is upregulated at both mRNA and protein levels in cancer tissues compared to adjacent non-cancerous tissues [32]. Immunohistochemical analysis of 142 NSCLC biopsies revealed high SOX9 expression in 52.1% of cases, with upregulation significantly correlated with advanced histological stage and shorter survival time [32]. Multivariate analysis identified SOX9 upregulation as an independent prognostic indicator for NSCLC patient survival, highlighting its clinical relevance [32].
Table 2: SOX9 Dysregulation Across Human Cancers
| Cancer Type | SOX9 Expression Pattern | Clinical Correlations |
|---|---|---|
| Bone Tumors | Overexpressed in malignant vs benign tumors | Correlates with high grade, metastasis, recurrence, poor therapy response |
| Non-Small Cell Lung Cancer | Upregulated in tumor tissues | Associated with advanced stage, shorter survival, independent prognostic factor |
| Glioblastoma | Highly expressed in tumor tissues | Better prognosis in lymphoid invasion subgroups; diagnostic and prognostic biomarker |
| High-Grade Serous Ovarian Cancer | Chemotherapy-induced upregulation | Drives chemoresistance and stem-like transcriptional state |
| Triple-Negative Breast Cancer | SOX9-AS1 lncRNA overexpressed | High expression associated with favorable prognosis |
SOX9 in the Tumor Immune Microenvironment
The interplay between SOX9 and the tumor immune microenvironment represents a critical aspect of its oncogenic function, with distinct implications for both innate and adaptive immunity. SOX9 expression shows significant correlations with immune cell infiltration patterns across cancer types [1]. In colorectal cancer, SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1]. These patterns suggest SOX9 may contribute to establishing an immunosuppressive tumor microenvironment.
In the context of adaptive immunity, SOX9 participates in T cell development by cooperating with c-Maf to activate Rorc and key Tγδ17 effector genes, thereby modulating lineage commitment of early thymic progenitors and influencing the balance between αβ T cell and γδ T cell differentiation [1]. This regulatory function positions SOX9 as a significant factor in shaping the adaptive immune response within tumor contexts. The transcription factor also demonstrates relationships with immune checkpoint expression, further supporting its relevance to modern immunotherapy approaches [23].
Methodological Approaches for SOX9 Detection
Quantitative PCR (qPCR) Analysis
qPCR represents a fundamental methodology for quantifying SOX9 expression at the transcriptional level in both tissue and blood samples. The technique offers high sensitivity and specificity when optimized with appropriate primer designs and normalization strategies.
Recommended Protocol:
- Primer Design: Custom primers should flank exon-exon boundaries to minimize genomic DNA amplification. For human SOX9, effective primer sequences include:
- Forward: 5'-CGAAATCAACGAGAAACTGGAC-3'
- Reverse: 5'-ATTTAGCACACTGATCACACG-3'
- Probe: 5'-(FAM)CCATCATCCTCCACGCTTGCTCTG(TAMRA)-3' [32]
- RNA Extraction: Use TRIzol reagent followed by purification with PureLink RNA Mini Kit according to manufacturer's instructions [32].
- Reverse Transcription: Convert 1μg total RNA to cDNA using reverse transcriptase with oligo(dT) or random hexamers.
- qPCR Conditions: Perform reactions in triplicate with standard cycling conditions: 50°C for 2 min, 95°C for 10 min, followed by 40 cycles of 95°C for 15 sec and 60°C for 1 min [32].
- Normalization: Use housekeeping genes such as GAPDH with primers:
- Forward: 5'-GACTCATGACCACAGTCCATGC-3'
- Reverse: 5'-AGAGGCAGGGATGATGTTCTG-3'
- Probe: 5'-(FAM)CATCACTGCCACCCAGAAGACTGTG(TAMRA)-3' [32]
- Data Analysis: Calculate expression using the 2^(-ΔΔCt) method relative to control samples.
For circulating SOX9 detection, peripheral blood mononuclear cells (PBMCs) should be isolated from whole blood prior to RNA extraction. Studies have successfully employed this approach to identify elevated SOX9 in patient blood samples compared to healthy controls [31].
Western Blot Analysis
Western blotting provides protein-level confirmation of SOX9 expression, complementing transcriptional data from qPCR with information about protein size and post-translational modifications.
Standard Protocol:
- Protein Extraction: Harvest cells in RIPA buffer supplemented with protease inhibitors (e.g., PMSF). For tissues, homogenize samples prior to extraction [31] [32].
- Protein Quantification: Determine concentration using bicinchoninic acid (BCA) assay according to manufacturer's instructions [32].
- Electrophoresis: Separate 20-50μg total protein on 10% SDS-polyacrylamide gels [32].
- Membrane Transfer: Transfer to polyvinylidene difluoride (PVDF) membranes using standard wet or semi-dry transfer systems [31].
- Blocking: Incubate membrane with 5% non-fat dry milk in TBST for 1 hour at room temperature.
- Antibody Incubation:
- Detection: Use SuperSignal West Pico Chemiluminescent Substrate according to manufacturer's protocol [32].
- Loading Control: Strip and reprobe membrane with anti-actin mouse monoclonal antibody (1:2,000 dilution; Millipore) [32].
This protocol has successfully demonstrated elevated SOX9 protein levels in lung cancer cell lines compared to normal human pneumonocytes, confirming transcriptional upregulation observed in qPCR analyses [32].
Immunohistochemistry (IHC)
IHC provides spatial context for SOX9 expression within tissue architecture, allowing correlation of expression patterns with specific histological features and cell types.
Validated Protocol:
- Tissue Preparation: Use freshly cut paraffin-embedded sections (less than 10 days between cutting and staining) [30].
- Antigen Retrieval: Perform heat-induced epitope retrieval for 5 minutes in an autoclave at 121°C in pH 7.8 Target Retrieval Solution buffer [30].
- Primary Antibody: Apply anti-SOX9 antibody (e.g., MSVA-709R at 1:50 dilution) at 37°C for 60 minutes [30].
- Detection System: Use EnVision Kit (Dako, Agilent) according to manufacturer's directions for visualization [30].
- Counterstaining: Use hematoxylin for nuclear counterstaining.
- Controls: Include positive control (colon tissue with strong SOX9 immunostaining in epithelial cells of crypt base) and negative control (colon tissue with absent SOX9 in non-epithelial cell types) [30].
Alternative Protocol:
- Deparaffinization: Deparaffinize sections with xylenes and rehydrate through graded ethanol series.
- Antigen Retrieval: Submerge sections in EDTA antigenic retrieval buffer and microwave for antigen retrieval [32].
- Peroxidase Blocking: Treat with 3% hydrogen peroxide in methanol for 10 minutes.
- Blocking: Incubate in 1% bovine serum albumin for 30 minutes.
- Primary Antibody: Incubate with rabbit anti-SOX9 (1:50 dilution; Millipore) at 4°C overnight [32].
- Detection: Use biotinylated anti-rabbit secondary antibody (Zymed) followed by streptavidin-HRP and DAB development [32].
IHC analysis enables assessment of SOX9 subcellular localization (primarily nuclear) and correlation with pathological parameters, as demonstrated in studies linking SOX9 overexpression with advanced tumor stage and poor prognosis [32].
Research Reagent Solutions
Table 3: Essential Reagents for SOX9 Research
| Reagent Category | Specific Product | Application | Key Features |
|---|---|---|---|
| Antibodies | Recombinant Rabbit monoclonal MSVA-709R [30] | IHC | Reactivity: Human; Dilution: 1:50-1:75; Cellular localization: Nucleus |
| Rabbit Recombinant Monoclonal (Cat # 702016) [35] | WB, ICC/IF, ChIP | Reactivity: Human, Mouse; 100μg size | |
| Mouse Monoclonal (Cat # 14-9765-82) [35] | WB, IHC (P), ICC/IF, ChIP | Reactivity: Human, Mouse, Rat | |
| Rabbit Polyclonal (Cat # PA5-81966) [35] | WB, IHC (P), ICC/IF | Reactivity: Human, Mouse, Rat | |
| qPCR Assays | Custom primers and probes [32] | Gene expression analysis | Exon-spanning designs; FAM/TAMRA labeled probes |
| Positive Control Tissues | Colon tissue [30] | IHC control | Strong SOX9 staining in epithelial cells of crypt base |
| Bone tumor tissues [31] | Disease model | Elevated SOX9 expression in malignant cases |
SOX9 in Innate vs Adaptive Immunity: Mechanistic Insights
SOX9 in Innate Immune Regulation
Within the innate immune system, SOX9 exerts significant influence on macrophage function and polarization states. Increased levels of SOX9 help maintain macrophage function, contributing to cartilage formation, tissue regeneration, and repair processes [1]. This protective function positions SOX9 as a potential mediator in inflammatory conditions such as osteoarthritis, where it may promote tissue homeostasis and resolution of inflammation. The transcription factor's involvement in chondrogenesis and extracellular matrix organization further supports its role in tissue repair mechanisms central to innate immune responses.
In cancer contexts, SOX9 expression correlates with specific macrophage populations within the tumor microenvironment. In prostate cancer, single-cell RNA sequencing and spatial transcriptomics analyses reveal that SOX9 expression patterns associate with shifts in the immune landscape, including increases in immunosuppressive M2 macrophages (TAM Macro-2) [1]. These correlations suggest SOX9 may contribute to establishing an immunosuppressive niche favorable to tumor progression by influencing innate immune cell differentiation and function.
SOX9 in Adaptive Immune Regulation
SOX9 plays a multifaceted role in shaping adaptive immune responses, particularly through its effects on T cell development and differentiation. During T cell development in the thymus, SOX9 cooperates with transcription factor c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating the lineage commitment of early thymic progenitors and influencing the balance between αβ T cell and γδ T cell differentiation [1]. This developmental function underscores SOX9's importance in establishing proper T cell repertoire and function.
In cancer environments, SOX9 expression demonstrates significant correlations with T cell infiltration and function. Bioinformatic analyses indicate that SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells and shows positive correlation with memory CD4+ T cells [1]. These relationships may contribute to the "immune desert" phenomenon observed in some SOX9-high tumors, characterized by decreased effector immune cells and increased immunosuppressive populations [1]. The net effect of these SOX9-mediated immunomodulatory functions is often impaired anti-tumor immunity and promotion of immune escape mechanisms.
SOX9 as a Therapeutic Target
The strategic position of SOX9 at the intersection of cancer progression and immune regulation renders it an attractive therapeutic target for multiple disease contexts. Evidence from mechanistic studies indicates that SOX9 ablation enhances platinum sensitivity in high-grade serous ovarian cancer, with SOX9 knockout significantly increasing sensitivity to carboplatin treatment in colony formation assays [28]. This finding suggests that targeting SOX9 may overcome chemoresistance across multiple cancer types.
Small molecule compounds show promise for pharmacological targeting of SOX9 expression and function. The adenosine analog cordycepin inhibits both protein and mRNA expression of SOX9 in a dose-dependent manner in prostate cancer (22RV1, PC3) and lung cancer (H1975) cell lines, indicating its anticancer roles may operate partially through SOX9 inhibition [33]. This pharmacological approach demonstrates the feasibility of modulating SOX9 activity for therapeutic benefit.
From an immunological perspective, SOX9 represents a promising candidate for combination therapies with existing immunomodulatory approaches. SOX9 expression correlates with immune checkpoint expression in glioblastoma, suggesting potential synergistic effects between SOX9 inhibition and immune checkpoint blockade [23]. Additionally, the transcription factor's role in establishing immunosuppressive tumor microenvironments positions it as a target for normalizing antitumor immunity and enhancing response to immunotherapies.
Concluding Remarks
Comprehensive profiling of SOX9 expression through qPCR, Western blot, and IHC provides invaluable insights into its diverse roles in both normal physiology and disease pathogenesis, with particular relevance to immunological processes. The consistent demonstration of SOX9 overexpression across multiple cancer types, coupled with its association with aggressive clinical features and therapy resistance, underscores its importance as a biomarker and potential therapeutic target. The development of standardized, optimized protocols for SOX9 detection across different sample types will enhance reproducibility and comparability across studies.
Future research directions should focus on elucidating the context-dependent mechanisms through which SOX9 influences innate versus adaptive immune responses, with particular attention to its cell-type-specific functions. The paradoxical role of SOX9 as both an oncogene and tumor suppressor in different contexts warrants further investigation to identify the molecular determinants of these opposing functions. From a translational perspective, advancing SOX9-targeted therapeutic strategies, particularly in combination with existing modalities such as chemotherapy and immunotherapy, holds significant promise for improving outcomes across multiple disease states.
The SRY-box transcription factor 9 (SOX9) is a pivotal developmental regulator that has emerged as a significant player in both innate and adaptive immunity. As a transcription factor containing a high-mobility group (HMG) DNA-binding domain, SOX9 recognizes the specific sequence CCTTGAG and regulates diverse biological processes from chondrogenesis to cell fate determination [1] [6]. Recent evidence reveals that SOX9 exhibits context-dependent dual functions across diverse immune cell types, contributing to the regulation of numerous biological processes [1]. In cancer biology, SOX9 is frequently overexpressed in various solid malignancies, where its expression levels positively correlate with tumor occurrence and progression [1]. This technical guide provides comprehensive methodologies for manipulating SOX9 expression using siRNA knockdown and lentiviral overexpression systems, with particular emphasis on applications in immunological research.
SOX9 plays a significant role in immune cell development, participating in the differentiation and regulation of diverse immune lineages [1]. Regarding T cell development, SOX9 can cooperate with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating the lineage commitment of early thymic progenitors and potentially influencing the balance between αβ T cell and γδ T cell differentiation [1]. Within the B cell lineage, while SOX9 does not have a known significant role in normal B cell development, it is overexpressed in certain types of B-cell lymphomas, where it acts as an oncogene by promoting cell proliferation and inhibiting apoptosis [1]. These immunoregulatory functions make SOX9 an compelling target for functional genetic manipulation in immunological studies.
SOX9 Functional Domains and Signaling Pathways
Structural Organization of SOX9 Protein
The SOX9 protein contains several functionally distinct domains organized from N- to C-terminus [1]:
- Dimerization domain (DIM): Facilitates protein-protein interactions
- HMG box domain: Binds DNA in a sequence-specific manner and contains nuclear localization signals
- Central transcriptional activation domain (TAM): Synergistically enhances transcriptional activity
- C-terminal transcriptional activation domain (TAC): Interacts with cofactors to enhance transcriptional activity
- Proline/glutamine/alanine (PQA)-rich domain: Necessary for transcriptional activation
The HMG domain serves dual roles: it directs nuclear localization via embedded localization (NLS) and export (NES) signals, enabling nucleocytoplasmic shuttling, and facilitates DNA binding [1]. The C-terminal transcriptional activation domain (TAC) interacts with diverse cofactors, such as Tip60, to enhance SOX9's transcriptional activity and is also essential for β-catenin inhibition during chondrocyte differentiation [1].
SOX9 in Signaling Pathways Relevant to Immunity
SOX9 interacts with multiple signaling pathways that have significant implications for immune function and cancer biology. Mechanistic studies have revealed that SOX9 contributes to tamoxifen resistance by regulating ALDH1A3 expression and modulating Wnt signaling in breast cancer [36]. Additionally, long non-coding RNAs such as SOX9-AS1 resist triple-negative breast cancer senescence via regulating the Wnt signalling pathway [37]. The regulation of Wnt signaling by SOX9 creates important connections with immune cell function in the tumor microenvironment.
Table 1: Key Signaling Pathways Involving SOX9 with Immunological Relevance
| Pathway | SOX9 Function | Immunological Context | Experimental Evidence |
|---|---|---|---|
| Wnt/β-catenin | Regulates pathway activation; downstream target | Affects T cell differentiation and function | SOX9-AS1 knockdown facilitates senescence via Wnt in TNBC [37] |
| DNA Damage Repair | Binds promoters of DDR genes (SMARCA4, UIMC1, SLX4) | Impacts immune recognition of stressed cells | SOX9 enhances DNA repair in ovarian cancer [36] |
| Stemness Pathways | Maintains progenitor cell state | Influences immune evasion | SOX9 sustains latent cancer cell dormancy [6] |
| EMT Programs | Promotes epithelial-mesenchymal transition | Affects macrophage polarization and recruitment | SOX9 induces EMT in lung cancer via Wnt/β-catenin [38] |
siRNA-Mediated SOX9 Knockdown Methodology
siRNA Design and Validation
siRNA-mediated knockdown represents a powerful approach for transient SOX9 suppression in immune function studies. Effective siRNA targeting requires careful design and validation to ensure specificity and efficacy.
Target Sequence Selection: For rat Sox9 targeting (NCBI accession number NM080403), the RNA interference target sequence GAAGGAGAGCGAGGAAGAT has demonstrated efficacy [39]. This target was synthesized, annealed, and ligated into lentiviral vectors between AgeI and EcoRI restriction sites following the U6 promoter [39].
Control Design: A scrambled shRNA containing a nontargeting sequence (TTCTCCGAACGTGTCACGT) should be used as a negative control to account for off-target effects [39].
Validation Methods:
- Western blot analysis to confirm protein reduction
- RT-PCR to measure mRNA level decreases
- Functional assays to confirm phenotypic effects
Table 2: siRNA Sequences for SOX9 Knockdown
| Application | Target Sequence (5'-3') | Vector System | Efficacy Validation |
|---|---|---|---|
| Rat SOX9 KD | GAAGGAGAGCGAGGAAGAT | pLKD-CMV-Puro-U6-shRNA | >70% protein reduction [39] |
| Control | TTCTCCGAACGTGTCACGT | Same as above | No significant target reduction [39] |
| Human SOX9 KD | Custom designs based on transcript variant | siRNA oligo transfection | ABCA1 siRNA validation method [40] |
Experimental Workflow for siRNA Knockdown
The following diagram illustrates the complete workflow for SOX9 knockdown experiments:
Key Applications in Immune Research
SOX9 knockdown has revealed significant insights into its immunoregulatory functions:
Immune Evasion Mechanisms: Studies have demonstrated that SOX9 plays a crucial part in immune evasion by maintaining cancer cell stemness. Knocking down SOX9 expression can disrupt this immune evasion, potentially making cells more visible to immune surveillance [6].
Cellular Senescence and SASP: SOX9 knockdown facilitates tamoxifen-induced cellular senescence and the transcription of senescence-associated secretory phenotype (SASP) factors (IL-1α, IL-1β, IL-6 and IL-8) by resisting senescence-induced Wnt signal (GSK-3β/β-catenin) activation [37]. This has significant implications for both innate and adaptive immune responses to senescent cells.
Immune Cell Infiltration Analysis: Immune infiltration examination using CIBERSORT algorithms revealed that low SOX9 expression was accompanied by a high infiltration of naïve B cells, CD8+ T cells and γδ T cells, indicating that targeted inhibition of SOX9 can mobilize immune infiltration [37].
Lentiviral Overexpression Systems for SOX9
Lentiviral Vector Design and Construction
Lentiviral systems provide stable, long-term SOX9 overexpression, making them ideal for studying chronic immunological processes and cancer-immune interactions.
Vector Components:
- SOX9 Insert: Full-length human SOX9 cDNA (509 amino acids, NCBI reference)
- Promoter Selection: CMV promoter for strong constitutive expression
- Selection Markers: Puromycin resistance for stable cell line creation
- Regulatory Elements: WPRE for enhanced expression
Viral Production:
- Packaging System: Third-generation lentiviral packaging plasmids
- Transfection: HEK293T cells for viral production
- Concentration: Ultrafiltration or ultracentrifugation to achieve titers of 1×10^8 IU/mL or higher [39]
Experimental Workflow for Lentiviral Overexpression
The following diagram outlines the process for creating SOX9-overexpressing cells:
Key Applications in Immune Mechanism Research
SOX9 overexpression systems have revealed crucial mechanisms in immune function:
Therapy Resistance: Elevated expression of SOX9 contributes to olaparib resistance in ovarian cancer by enhancing DNA damage repair capabilities [36]. This has implications for how cancer cells evade immune-mediated destruction following genotoxic stress.
Stemness and Dormancy: SOX9 overexpression can maintain tumor-initiating capabilities and support long-term survival of latent cancer cells. Research shows that SOX9 works in concert with Slug (SNAI2) to encourage cancer cell proliferation and metastasis while potentially maintaining dormancy in metastatic sites [6].
Immune Modulation: SOX9 overexpression influences the tumor microenvironment by regulating interactions between cancer cells and stromal components. SOX9 expression correlates with altered immune cell infiltration patterns in various cancers, potentially creating an immunosuppressive microenvironment [1] [23].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for SOX9 Genetic Manipulation Studies
| Reagent Category | Specific Examples | Function/Application | Validation Considerations |
|---|---|---|---|
| SOX9 Antibodies | Anti-SOX9 (AB5535, Sigma) [36] | Western blot, IHC, immunofluorescence | Species reactivity, application-specific validation |
| siRNA Sequences | Target: GAAGGAGAGCGAGGAAGAT [39] | Transient knockdown | Off-target effects, efficiency confirmation |
| Lentiviral Vectors | pLKD-CMV-Puro-U6-shRNA [39] | Stable knockdown/overexpression | Titer verification, biosafety compliance |
| Cell Lines | MDA-MB-231, SKOV3, HEK293T [37] [36] | In vitro functional studies | Authentication, mycoplasma testing |
| Selection Agents | Puromycin [39] | Stable cell line creation | Dose optimization, kill curve analysis |
| qPCR Assays | SOX9-specific primers and probes | Expression quantification | Primer efficiency, reference gene selection |
| Culture Media | RPMI 1640, DMEM with 10% FBS [36] [41] | Cell maintenance and experiments | Serum batch consistency, supplementation |
| Chlorambucil-d8-1 | Chlorambucil-d8-1, MF:C14H19Cl2NO2, MW:312.3 g/mol | Chemical Reagent | Bench Chemicals |
| Lumiracoxib-d6 | Lumiracoxib-d6, MF:C15H13ClFNO2, MW:299.75 g/mol | Chemical Reagent | Bench Chemicals |
Technical Considerations and Troubleshooting
Optimization Parameters
Successful SOX9 manipulation requires careful optimization of several parameters:
Transfection Efficiency:
- For siRNA: Optimize lipid-based transfection reagents using fluorescent controls
- For lentivirus: Determine MOI (multiplicity of infection) using reporter viruses
- Cell density at time of transduction (typically 30-50% confluency)
Timing Considerations:
- siRNA effects: Peak knockdown at 48-72 hours post-transfection
- Lentiviral expression: Stable integration within 72-96 hours, selection begins after 24-48 hours
Validation Timeline:
- mRNA levels: Assess at 24-48 hours (siRNA) or 72+ hours (lentiviral)
- Protein levels: Assess at 48-72 hours (siRNA) or 96+ hours (lentiviral) due to protein half-life
Common Technical Challenges and Solutions
Table 4: Troubleshooting Guide for SOX9 Manipulation
| Problem | Potential Causes | Solutions | Preventive Measures |
|---|---|---|---|
| Low Knockdown Efficiency | Poor siRNA design, inefficient delivery | Validate multiple target sequences, optimize transfection reagents | Use published effective sequences, include positive controls |
| Cellular Toxicity | Off-target effects, excessive viral load | Titrate siRNA/virus concentration, use inducible systems | Perform kill curve analysis, test multiple MOIs |
| Inconsistent Results | Cell line drift, mycoplasma contamination | Authenticate cell lines, test for contamination | Regular monitoring, use early passage cells |
| Incomplete Validation | Antibody specificity, assay sensitivity | Use multiple validation methods, include proper controls | Validate antibodies in multiple applications, use digital PCR |
The strategic application of siRNA knockdown and lentiviral overexpression models for SOX9 manipulation provides powerful tools for deciphering its complex roles in immunological processes. These techniques have revealed SOX9's functions in immune cell differentiation, tumor immune evasion, therapy resistance, and microenvironment remodeling. The continuing refinement of these genetic manipulation approaches, including inducible systems and cell-type specific targeting, will further enhance our understanding of SOX9's dual roles in innate and adaptive immunity. As research progresses, these methodologies will prove invaluable for both basic immune mechanism studies and the development of SOX9-targeted therapeutic interventions.
The SOX9 transcription factor is increasingly recognized as a pivotal regulator of the tumor immune microenvironment, influencing cancer progression through complex interactions with both innate and adaptive immunity. This whitepaper provides a comprehensive technical guide for investigating SOX9-mediated immune cell infiltration using bioinformatics approaches, with emphasis on Single Sample Gene Set Enrichment Analysis (ssGSEA). We detail experimental methodologies, analytical frameworks, and visualization techniques to elucidate SOX9's dual roles in immunomodulation, offering researchers standardized protocols for quantifying immune infiltration patterns across cancer types. The integrated approaches outlined herein enable systematic characterization of SOX9's context-dependent functions, serving as essential tools for identifying potential immunotherapeutic targets in SOX9-driven malignancies.
The SRY-related HMG-box transcription factor 9 (SOX9) plays critical roles in development, differentiation, and stem cell maintenance, with emerging evidence establishing its significance in immunoregulation across multiple cancer types. SOX9 exhibits a "Janus-faced" character in immunity, functioning as both an activator and repressor across diverse immune cell populations [1]. Within the tumor microenvironment, SOX9 operates at the interface of innate and adaptive immunity, influencing processes from macrophage polarization to T-cell function.
Innate immunity provides rapid, non-specific defense through components including macrophages, neutrophils, monocytes, dendritic cells, complement proteins, and cytokines [1]. Adaptive immunity delivers antigen-specific responses orchestrated by T and B lymphocytes, developing over days to weeks but generating immunological memory [1]. SOX9 modulates both arms through distinct mechanisms, contributing to its context-dependent pro-tumorigenic or anti-tumorigenic effects.
Bioinformatics approaches, particularly ssGSEA, have proven invaluable for deciphering SOX9's complex immunomodulatory functions by transforming gene expression profiles into immune enrichment scores that quantify the activity of specific biological processes within individual samples [42]. This technical guide outlines standardized methodologies for applying these powerful analytical techniques to investigate SOX9-mediated immune regulation, with emphasis on practical implementation for research and drug development.
SOX9 in Immunobiology: Mechanisms and Significance
Structural and Functional Domains of SOX9
The SOX9 protein contains several functionally specialized domains that enable its transcriptional regulatory capabilities:
- Dimerization Domain (DIM): Facilitates protein-protein interactions
- HMG Box Domain: Mediates DNA binding and nuclear localization through embedded nuclear localization (NLS) and export (NES) signals
- Transcriptional Activation Domains (TAM and TAC): Drive target gene transcription, with TAC particularly important for β-catenin inhibition during differentiation
- PQA-Rich Domain: Proline/glutamine/alanine-rich region necessary for transcriptional activation [1]
These structural elements enable SOX9 to recognize specific DNA motifs (CCTTGAG), interact with co-factors like Tip60, and regulate diverse transcriptional programs in both development and cancer [1] [41].
SOX9 in Immune Cell Regulation
SOX9 participates in the differentiation and function of multiple immune lineages through distinct mechanisms:
T-cell Development: SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), modulating lineage commitment of early thymic progenitors and influencing the balance between αβ T-cell and γδ T-cell differentiation [1].
B-cell Lymphomas: While having minimal known role in normal B-cell development, SOX9 is overexpressed in Diffuse Large B-cell Lymphoma (DLBCL), where it functions oncogenically by promoting proliferation and inhibiting apoptosis [1].
Myeloid Cells: SOX9 helps maintain macrophage function and contributes to cartilage formation, tissue regeneration, and repair, demonstrating its importance in innate immune regulation [1].
Tumor Microenvironment: SOX9 expression correlates with specific immune infiltration patterns across cancers, typically showing negative correlations with cytotoxic cells (CD8+ T cells, NK cells, M1 macrophages) while positively correlating with immunosuppressive populations (Tregs, M2 macrophages) in many contexts [1] [43].
Bioinformatics Approaches for Analyzing Immune Infiltration
Single Sample GSEA (ssGSEA) Fundamentals
ssGSEA extends traditional Gene Set Enrichment Analysis by calculating separate enrichment scores for each pairing of a sample and gene set, independent of phenotype labeling [42]. This transformation converts a sample's gene expression profile into a gene set enrichment profile representing the activity levels of biological processes and pathways.
Key Algorithmic Features:
- Input: Gene expression data (GCT format) and predefined gene sets
- Normalization: Options include rank, log.rank, and log normalization
- Weighting: Exponential weight (default: 0.75) applied in enrichment score calculation
- Output: Enrichment scores for each sample-gene set pairing [42]
The resulting enrichment scores represent the degree to which genes in a particular set are coordinately up- or down-regulated within a sample, enabling characterization of cell states in terms of biological process activity rather than individual gene expression [42].
ssGSEA Implementation for Immune Cell Infiltration
The ssGSEA projection methodology follows these key steps:
Figure 1: ssGSEA Workflow for Immune Cell Infiltration Analysis
Step 1: Data Preparation and Normalization
- Obtain gene expression data from tumor samples (RNA-seq or microarray)
- Format data according to GCT specification with genes as rows and samples as columns
- Perform appropriate normalization (rank recommended for ssGSEA) [42]
Step 2: Gene Set Selection
- Curate immune cell-specific gene signatures from reference databases (MSigDB, ImmPort)
- Define gene sets for specific immune populations (T-cells, B-cells, macrophages, etc.)
- Apply minimum gene set size filter (default: 10 genes) to ensure robustness [42] [44]
Step 3: ssGSEA Projection
- Calculate enrichment scores using the ssGSEA algorithm with default parameters
- Generate enrichment score matrix representing immune cell abundances
- The projection transforms expression data to pathway-level space [42]
Step 4: Correlation with SOX9 Expression
- Integrate SOX9 expression values with immune enrichment scores
- Perform correlation analysis (Spearman or Pearson based on distribution)
- Identify significant associations between SOX9 and specific immune populations [41] [45]
Experimental Protocols and Methodologies
Computational Analysis Pipeline for SOX9-Immune Interactions
A comprehensive SOX9 immunophenotyping analysis requires multiple bioinformatics approaches:
Differential Expression Analysis
- Use limma package (R/Bioconductor) for identifying differentially expressed genes
- Apply thresholds: |log2FC| > 1 and adjusted p-value < 0.05
- Compare SOX9-high vs SOX9-low samples or tumor vs normal tissues [46] [47]
Immune Infiltration Quantification
- Apply ssGSEA via GSVA package (version 1.34.0 or higher) using immune cell signatures
- Alternatively, use ESTIMATE algorithm for overall immune/stromal scores
- Validate with complementary methods (CIBERSORT, EPIC, MCP-counter) [45] [44]
Functional Enrichment Analysis
- Perform Gene Ontology (GO) and KEGG pathway analysis using clusterProfiler
- Conduct Gene Set Enrichment Analysis (GSEA) for pathway-level insights
- Utilize Metascape for integrated functional enrichment visualization [46] [45]
Statistical Analysis and Visualization
- Employ correlation analyses (Spearman's test) for SOX9-immune relationships
- Use Wilcoxon rank sum test for group comparisons
- Implement survival analysis (Kaplan-Meier, Cox regression) for clinical correlations [45]
Technical Validation Approaches
Wet-Lab Validation of Computational Findings
- RT-qPCR: Validate SOX9 expression and selected immune markers in patient samples (24 IDD tissues vs 12 normal disc tissues as reference) [46]
- Western Blotting: Confirm SOX9 protein levels using standardized protocols (EBC buffer lysis, PVDF membrane transfer) [41]
- Immunohistochemistry: Localize SOX9 expression and immune cell markers (CD8 for T-cells, CD68 for macrophages) in tissue sections [43]
Single-Cell RNA Sequencing Validation
- Process scRNA-seq data using Seurat package (resolution = 0.9 for clustering)
- Annotate cell types based on canonical markers
- Analyze SOX9 expression across immune and tumor cell populations [48]
Table 1: Key Research Reagent Solutions for SOX9-Immune Studies
| Reagent/Resource | Function/Application | Specifications/Alternatives |
|---|---|---|
| SOX9 Antibodies | IHC, WB for protein detection | Validation for specific applications required |
| Immune Cell Markers (CD3, CD8, CD68, CD20) | Immune population identification | Fluorophore-conjugated for flow cytometry |
| Gene Expression Databases (TCGA, GTEx, CCLE) | Reference datasets for validation | Processed RNA-seq data (FPKM/TPM) |
| Cell Lines (22RV1, PC3, H1975) | In vitro functional studies | Culture in RPMI 1640/DMEM + 10% FBS |
| Cordycepin | SOX9 inhibition studies | 10-40μM treatment for 24h [41] |
| ssGSEA Software (GenePattern, GSVA) | Immune infiltration analysis | R implementation available [42] |
SOX9 in Cancer Immunity: Key Findings and Signaling Pathways
Context-Dependent Immunomodulatory Functions
SOX9 demonstrates tissue-specific and cancer-type-dependent effects on immune regulation:
Lung Adenocarcinoma (LUAD)
- SOX9 suppresses infiltration of CD8+ T cells, natural killer cells, and dendritic cells
- Increases collagen-related gene expression and tumor stiffness, modulating physical properties of the microenvironment
- Creates an "immune desert" environment conducive to tumor progression [43]
Glioma/Glioblastoma
- High SOX9 expression correlates with immune infiltration patterns in specific subgroups
- Associates with better prognosis in lymphoid invasion subgroups (n=478, P<0.05)
- Correlates with immune checkpoint expression, indicating involvement in immunosuppressive microenvironment [45]
Pan-Cancer Patterns
- SOX9 upregulated in 15/33 cancer types (including COAD, LIHC, PAAD) and downregulated in only 2/33 (SKCM, TGCT)
- Expression negatively correlates with cytotoxic cells (CD8+ T cells, NK cells) in multiple cancers
- High expression associated with worse overall survival in LGG, CESC, THYM [41]
SOX9-Mediated Immunosuppressive Mechanisms
SOX9 promotes tumor immune evasion through multiple interconnected pathways:
Figure 2: SOX9-Mediated Immunosuppressive Signaling Network
Extracellular Matrix Remodeling
- SOX9 significantly elevates collagen-related gene expression
- Increases collagen fibers and tumor stiffness, creating physical barriers to immune infiltration
- Contributes to exclusion of cytotoxic immune cells from tumor islets [43]
Immune Cell Function Modulation
- Suppresses dendritic cell infiltration, impairing antigen presentation
- Reduces CD8+ T cell and NK cell abundance and activity
- Promotes immunosuppressive macrophage populations [43]
Checkpoint Pathway Regulation
- Correlates with expression of multiple immune checkpoints in glioma
- Associates with PD-L1 expression and T-cell receptor signaling pathways
- Contributes to T-cell exhaustion phenotypes [45]
Data Presentation and Analysis Frameworks
Quantitative Analysis of SOX9-Immune Correlations
Table 2: SOX9 Expression and Immune Infiltration Patterns Across Cancers
| Cancer Type | SOX9 Expression Trend | Key Immune Correlations | Clinical Impact |
|---|---|---|---|
| Lung Adenocarcinoma | Upregulated | Negative: CD8+ T cells, NK cells, DCsPositive: Collagen, Tregs | Worse survival (p=0.0039) [43] |
| Glioma | Upregulated | Context-dependent: Correlation with better prognosis in lymphoid invasion subgroup | Prognostic biomarker, especially in IDH-mutant cases [45] |
| Colorectal Cancer | Upregulated | Negative: B cells, resting mast cells, monocytesPositive: Neutrophils, macrophages, activated mast cells | Associated with progression [1] |
| Melanoma (SKCM) | Downregulated | Inverse pattern to upregulated cancers | Tumor suppressor role [41] |
| Thymoma | Upregulated | Negative correlation with Th17 genes, PD-L1, TCR signaling | Shorter overall survival [41] |
Methodological Considerations for Robust Analysis
Data Quality Control
- Verify RNA integrity (RIN >7 for sequencing applications)
- Implement batch effect correction (ComBat, Harmony) for multi-dataset analyses
- Ensure sufficient sample size (minimum n=10 per group for statistical power)
Analytical Validation
- Cross-validate ssGSEA results with multiple immune deconvolution methods
- Perform sensitivity analyses with different gene set collections
- Employ false discovery rate control for multiple comparisons
Technical Replication
- Include biological and technical replicates in experimental designs
- Validate findings in independent cohorts when possible
- Correlate mRNA and protein expression where feasible
The integrated bioinformatics and experimental approaches outlined in this technical guide provide a standardized framework for investigating SOX9-mediated immune cell infiltration across cancer types. The ssGSEA methodology offers particular utility for quantifying immune microenvironment composition and linking SOX9 expression patterns to functional immune states.
SOX9 emerges as a master regulator of tumor-immune interactions, operating through conserved mechanisms including extracellular matrix remodeling, immune cell exclusion, and functional suppression of cytotoxic populations. Its context-dependent roles in innate versus adaptive immunity highlight the importance of tissue-specific analyses and careful experimental design.
These standardized protocols enable systematic characterization of SOX9's immunomodulatory functions, supporting drug development efforts targeting the SOX9-immune axis across multiple cancer types. The analytical frameworks detailed herein facilitate biomarker discovery, patient stratification, and therapeutic response assessment in both preclinical and clinical contexts.
The SRY-Box Transcription Factor 9 (SOX9) is a high-mobility group (HMG) box transcription factor and a master regulator of cell fate decisions, stem/progenitor cell functions, and tissue development. Recent research has illuminated its complex, context-dependent roles within the immune system, influencing both innate and adaptive immunity through epigenetic reprogramming and transcriptional regulation [1]. SOX9 operates as a pioneer factor capable of binding condensed chromatin, initiating nucleosome displacement, and recruiting chromatin modifiers to enact large-scale transcriptional changes [49]. This capacity for chromatin remodeling positions SOX9 at the nexus of immune cell differentiation, tumor immune evasion, and inflammatory disease processes. This technical guide details the integrated application of Chromatin Immunoprecipitation (ChIP) and the Assay for Transposase-Accessible Chromatin using sequencing (ATAC-seq) to map SOX9 binding events and its consequent reshaping of the chromatin landscape, with a specific focus on immunological contexts.
Technical Foundations: ChIP-seq and ATAC-seq
Chromatin Immunoprecipitation Sequencing (ChIP-seq)
ChIP-seq identifies genome-wide binding sites for a specific protein, such as a transcription factor or histone modification. The protocol involves cross-linking proteins to DNA, chromatin fragmentation, immunoprecipitation with a target-specific antibody, and high-throughput sequencing of the purified DNA.
Key Experimental Protocol for SOX9 ChIP-seq:
- Cross-linking: Fix cells (e.g., cultured immune cells, cancer cell lines, or primary tissues) with formaldehyde to covalently link SOX9 to its DNA binding sites.
- Cell Lysis and Chromatin Shearing: Lyse cells and fragment chromatin via sonication to an average size of 200-500 bp.
- Immunoprecipitation: Incubate chromatin with a validated anti-SOX9 antibody. Use pre-immune IgG as a negative control. Capture antibody-chromatin complexes using protein A/G beads.
- Reversal of Cross-linking and Purification: Elute immunoprecipitated DNA, reverse cross-links, and treat with RNase and proteinase K. Purify DNA for library construction.
- Library Preparation and Sequencing: Prepare sequencing libraries from input (non-immunoprecipitated) and IP DNA for high-throughput sequencing.
Assay for Transposase-Accessible Chromatin using sequencing (ATAC-seq)
ATAC-seq probes genome-wide chromatin accessibility by leveraging a hyperactive Tn5 transposase. Tn5 simultaneously fragments and tags accessible DNA regions with sequencing adapters, which are then amplified and sequenced [27].
Key Experimental Protocol for ATAC-seq:
- Cell Preparation: Harvest and wash cells. Use a low number of viable cells (50,000-100,000 for bulk ATAC-seq; can be scaled down for single-cell assays). Critical step: maintain nuclear integrity.
- Transposition Reaction: Resuspend nuclei in a buffer containing the Tn5 transposase. Incubate to allow for tagmentation of open chromatin regions.
- DNA Purification: Purify tagmented DNA using a clean-up protocol.
- Library Amplification and Sequencing: Amplify purified DNA with PCR using primers compatible with the Tn5-loaded adapters. Sequence the resulting library.
Table 1: Core Research Reagent Solutions for SOX9 Chromatin Studies
| Reagent/Category | Specific Examples & Functions | Key Considerations |
|---|---|---|
| SOX9 Antibodies | Validated ChIP-grade antibodies for immunoprecipitation (e.g., anti-SOX9 [49]). | Specificity is paramount; validate via knockout cell controls. |
| Tn5 Transposase | Commercially available kits (Nextera-based) for ATAC-seq library prep [27] [50]. | Enzyme activity lot-to-lot consistency affects data quality. |
| Chromatin Shearing | Sonication devices (e.g., Bioruptor, Covaris) or enzymatic fragmentation kits. | Optimize for fragment size distribution; sonication avoids sequence bias. |
| Bioinformatics Tools | Peak Callers: MACS2 (for ChIP-seq), Gem (for ATAC-seq). ATAC-seq Specific: ENCODE ATAC-seq pipeline [50]. | Tool selection depends on data type (narrow vs. broad peaks). |
SOX9 in Innate and Adaptive Immunity: An Epigenetic Perspective
SOX9 as a Pioneer Factor in Chromatin Remodeling
SOX9's function as a pioneer factor is fundamental to its role in immune and cancer biology. It can bind to its cognate motifs within closed chromatin, subsequently initiating the opening of these regions. Temporal analyses show that SOX9 binding (W1) precedes the increase in chromatin accessibility (W2), a hallmark of pioneer activity [49]. Nearly 30% of SOX9 binding sites are in initially closed chromatin, and its binding leads to nucleosome displacement, as evidenced by loss of histone H3 signal and decreased fragment length in CUT&RUN assays [49]. This pioneering activity allows SOX9 to launch profound transcriptional reprogramming, diverting cell fate in both development and disease.
SOX9-Mediated Immunosuppression in Cancer
In basal-like breast cancer (BLBC), a SOX9-B7x axis safeguards dedifferentiated tumor cells from immune surveillance. SOX9 upregulates the immune checkpoint molecule B7x (B7-H4) via direct transcriptional regulation and STAT3 activation [15]. This mechanism is critical for establishing an "immune-cold" tumor microenvironment:
- Conditional knockout (cKO) of Sox9 in premalignant mouse lesions led to a massive accumulation of infiltrating CD3+ T cells, including both CD4+ and CD8+ subsets, and elevated levels of granzyme B+ and perforin+ cells [15].
- Functional Impact: Depleting T cells in Sox9-cKO mice restored the progression of stalled premalignant lesions to invasive carcinoma, demonstrating that SOX9-mediated immunosuppression is required for tumor progression [15].
- Human Relevance: In human breast cancer, SOX9 and B7x expression are correlated and associated with reduced CD8+ T cell infiltration [15]. SOX9 expression in human cancer cells directly suppresses the proliferation and cytotoxic function of human T cells in vitro [15].
SOX9 in Immune Cell Development and Function
SOX9 participates in the differentiation and regulation of diverse immune lineages:
- T cell development: SOX9 can cooperate with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a, Blk), modulating the lineage commitment of early thymic progenitors and influencing the balance between αβ and γδ T cell differentiation [1].
- B cell malignancies: While its role in normal B-cell development is less defined, SOX9 is overexpressed in Diffuse Large B-cell Lymphoma (DLBCL), where it acts as an oncogene by promoting proliferation and inhibiting apoptosis [1].
- Trained Immunity: Emerging evidence suggests that long-lived hematopoietic stem and progenitor cells (HSPCs) serve as a reservoir for innate immune memory, or "trained immunity," which is epigenetically encoded [5]. While not directly linked to SOX9 in the provided results, this paradigm highlights the importance of studying transcription factors like SOX9 in the epigenetic reprogramming of immune progenitors.
SOX9 in Metastatic Dormancy and Immune Evasion
In metastatic breast cancer, SOX9 is a critical mediator of cancer cell quiescence (dormancy). Retinoic acid (RA)-stimulated transcriptional memory, sustained by oncogenic enhancers, promotes quiescence in disseminated tumor cells (DTCs) through the upregulation of SOX9 [51]. This quiescent state, orchestrated by SOX9, increases the fitness of DTCs by supporting their escape from NK-mediated immune surveillance [51]. This illustrates a direct mechanism where SOX9-driven epigenetic programming facilitates evasion from innate immune cells.
Integrated Data Analysis and Visualization
Integrating ChIP-seq and ATAC-seq data is powerful for establishing a causal link between transcription factor binding and subsequent chromatin remodeling.
Workflow for Multi-Omics Integration
The following diagram illustrates the core workflow for integrating ChIP-seq and ATAC-seq data to define SOX9-driven regulatory networks, particularly in an immunological context.
Key Analytical Outputs
Table 2: Key Quantitative Outputs from Integrated SOX9 ChIP-seq/ATAC-seq Analyses
| Analytical Metric | Description | Biological Interpretation in Immune Context |
|---|---|---|
| SOX9 Peak Number | Genome-wide loci bound by SOX9. | Indicates the scale of the direct SOX9 regulon; can expand in disease states. |
| Peak Genomic Distribution | Percentage of peaks in promoters, enhancers, intergenic regions. | Enhancer binding suggests a key role in cell identity/immunity gene regulation. |
| Overlap of SOX9 Peaks with ATAC-seq Peaks | Percentage of SOX9 binding sites in open chromatin. | High overlap suggests binding at pre-established sites; lower overlap (e.g., 30% in closed chromatin) indicates pioneer activity [49]. |
| Differential SOX9 Binding | Changes in SOX9 occupancy between conditions (e.g., +/- cytokine). | Identifies context-specific gene targets, e.g., pathways activated in immunosuppression. |
| Differential Chromatin Accessibility | Changes in ATAC-seq peaks between conditions (e.g., SOX9 OE vs KO). | Reveals genome-wide chromatin remodeling consequences of SOX9 activity. |
| De Novo Motif Discovery | Identification of enriched DNA sequences under SOX9 peaks. | Confirms SOX9 binding motif; identifies co-binding factors (e.g., STAT3 in BLBC [15]). |
The integration of ChIP-seq and ATAC-seq provides a powerful, unbiased methodology to delineate the direct and indirect genomic functions of SOX9. As research continues to unravel the "Janus-faced" nature of SOX9 in immunology—promoting immune escape in cancer while contributing to tissue repair—these epigenetic mapping techniques will be indispensable. They offer a mechanistic bridge between SOX9's role as a pioneer transcription factor and its profound effects on innate and adaptive immune responses, ultimately illuminating new paths for therapeutic intervention in cancer and immune-related diseases.
The SOX9 transcription factor, a pivotal regulator of embryonic development and stem cell maintenance, has emerged as a critical oncoprotein and a promising target in cancer immunotherapy. This whitepaper delineates the dual role of SOX9 within innate and adaptive immunity mechanisms in the tumor microenvironment (TME). It synthesizes current evidence demonstrating how SOX9 drives tumor immune evasion by establishing an immunosuppressive TME, promoting T-cell exclusion, and fostering chemotherapy resistance. Comprehensive analysis of SOX9 expression across pan-cancers confirms its significant upregulation in numerous malignancies, correlating with poor prognosis. Furthermore, this review details the molecular pathways through which SOX9 orchestrates immune suppression, highlights emerging therapeutic strategies to target SOX9, and provides a standardized experimental framework for investigating SOX9 function in cancer immunology, offering researchers a foundational toolkit for advancing SOX9-targeted immunotherapies.
The SRY-related HMG-box 9 (SOX9) protein is a transcription factor with a well-established role in developmental processes, including chondrogenesis, sex determination, and organogenesis [1] [6]. Structurally, SOX9 contains several functional domains: a dimerization domain (DIM), a high-mobility group (HMG) box for DNA binding, and two transcriptional activation domains (TAM and TAC) [1]. Beyond development, SOX9 is frequently dysregulated in cancer, where it often acts as an oncogene by promoting cell proliferation, stemness, metastasis, and therapy resistance [52] [6] [43].
In the context of tumor immunology, SOX9 exhibits a "double-edged sword" nature, playing a complex and dual role in immunoregulation [1]. This whitepaper frames SOX9's function within the distinct yet interconnected realms of innate and adaptive immunity:
- Innate Immunity: SOX9 influences the function of innate immune cells, such as macrophages, and contributes to the maintenance of an immunosuppressive tumor microenvironment [1] [23].
- Adaptive Immunity: SOX9 directly impairs adaptive immune responses by suppressing T-cell infiltration and function, facilitating immune escape for dedifferentiated, stem-like tumor cells [1] [15].
This technical guide will explore the mechanisms by which SOX9 modulates these immune pathways, its potential as a biomarker and therapeutic target, and provide detailed methodologies for its study.
SOX9 as a Master Regulator of the Immunosuppressive Tumor Microenvironment
SOX9 drives the creation of an "immune-cold" tumor microenvironment, characterized by exclusion of cytotoxic T cells and enrichment of immunosuppressive elements. This role is crucial for protecting dedifferentiated, stem-like tumor cells from immune surveillance.
The SOX9-B7x Axis in T-cell Suppression
A seminal study identified a direct mechanistic link between SOX9 and the immune checkpoint molecule B7x (B7-H4/VTCN1) [15]. In basal-like breast cancer, SOX9 is upregulated in dedifferentiated tumor cells and is required for the progression of pre-malignant lesions to invasive carcinoma. This progression depends on SOX9's ability to suppress infiltrating T lymphocytes [15]. The molecular pathway involves:
- STAT3 Activation and Direct Transcription: SOX9 induces B7x expression through both direct transcriptional regulation and STAT3 activation.
- Protection from Immune Killing: B7x, expressed on the tumor cell surface, directly inhibits T-cell proliferation and cytokine production. Engineered SOX9-expressing tumor cells significantly suppress the proliferation of both CD8+ and CD4+ T cells and reduce antigen-specific T-cell-mediated killing in vitro [15].
- Clinical Correlation: In human breast cancer, high SOX9 and B7x expression are correlated and associated with reduced CD8+ T cell infiltration, confirming the clinical relevance of this axis [15].
The following diagram illustrates this key immunosuppressive pathway:
Diagram 1: The SOX9-B7x Immunosuppressive Axis. SOX9 upregulates the immune checkpoint B7x via STAT3 activation and direct gene transcription. B7x subsequently inhibits T-cell proliferation and function, leading to immune evasion.
Modulation of Immune Cell Infiltration
Beyond the B7x pathway, SOX9 expression broadly correlates with specific patterns of immune cell infiltration in the TME. Bioinformatics analyses of tumor datasets reveal that high SOX9 levels are associated with an immunosuppressive landscape [1] [23]. Key correlations include:
- Negative Correlation: SOX9 expression negatively correlates with the infiltration levels of cytotoxic CD8+ T cells, natural killer (NK) cells, and anti-tumor M1 macrophages [1] [43].
- Positive Correlation: SOX9 shows a positive correlation with immunosuppressive cells, such as M2 macrophages and regulatory T cells (Tregs) [1].
- Extracellular Matrix Remodeling: In lung adenocarcinoma, SOX9 significantly elevates collagen-related gene expression and increases collagen fiber deposition. This is proposed to increase tumor stiffness and form a physical barrier that inhibits the infiltration of dendritic cells, CD8+ T cells, and NK cells [43].
SOX9 as a Driver of Chemotherapy Resistance
A critical aspect of SOX9's role in cancer is its contribution to therapy failure. Research has established that SOX9 is epigenetically upregulated in ovarian cancer cells following chemotherapy treatment [52]. This upregulation promotes a phenotypic shift:
- Cancer Stem Cell Reprogramming: SOX9 expression reprograms ovarian cancer cells into stem-like cancer cells, also known as tumor-initiating cells. These cells continuously self-renew, proliferate, and are intrinsically resistant to chemotherapy [52].
- Clinical Evidence: Single-cell RNA sequencing of primary patient ovarian cancer tumors confirmed the presence of a rare cluster of cells with high SOX9 expression and stem-like features, underscoring its role as a master regulator of chemoresistance [52].
The mechanism of SOX9-driven chemoresistance is summarized below:
Diagram 2: SOX9-Mediated Chemoresistance. Chemotherapy treatment induces the epigenetic upregulation of SOX9. Elevated SOX9 drives the reprogramming of differentiated cancer cells into a stem-like, tumor-initiating state, which is a key mediator of resistance to treatment.
Pan-Cancer Expression and Prognostic Value of SOX9
Comprehensive genomic analyses have established SOX9 as a significant biomarker across multiple cancer types. A pan-cancer study analyzing 33 cancer types found SOX9 expression was significantly upregulated in fifteen cancers compared to matched healthy tissues, including glioblastoma (GBM), ovarian cancer (OV), lung squamous cell carcinoma (LUSC), colon adenocarcinoma (COAD), and liver hepatocellular carcinoma (LIHC) [41]. Conversely, SOX9 expression was decreased in only two cancers, skin cutaneous melanoma (SKCM) and testicular germ cell tumors (TGCT), indicating its role is context-dependent but predominantly oncogenic [41].
The prognostic value of SOX9 is starkly evident in survival analysis. For instance, in non-small cell lung cancer (NSCLC), patients with SOX9-high tumors have significantly shorter overall survival [43]. Furthermore, high SOX9 expression is positively correlated with worst overall survival in cancers like low-grade glioma (LGG) and cervical cancer (CESC), solidifying its utility as a prognostic marker [41].
Table 1: SOX9 Expression and Prognostic Significance in Selected Cancers
| Cancer Type | SOX9 Expression (vs. Normal) | Correlation with Prognosis | Key Immune Correlations |
|---|---|---|---|
| Ovarian Cancer | Significantly Upregulated [52] | Associated with chemoresistance [52] | Drives stem-like, immune-evasive cells [52] |
| Lung Adenocarcinoma | Significantly Upregulated [41] [43] | Shorter overall survival [43] | Suppresses CD8+ T, NK, and dendritic cell infiltration [43] |
| Basal-like Breast Cancer | Upregulated [15] | Promotes malignant progression [15] | Induces B7x, reduces CD8+ T cells [15] |
| Glioblastoma (GBM) | Significantly Upregulated [41] [23] | Varies by subtype and IDH status [23] | Correlated with immune infiltration and checkpoint expression [23] |
| Colorectal Cancer | Significantly Upregulated [41] | Poor prognosis [1] | Negative correlation with B cells and resting T cells [1] |
| Melanoma (SKCM) | Significantly Downregulated [41] | Tumor suppressor role [41] | Not applicable |
Experimental Toolkit for SOX9 Research
To facilitate research into SOX9, this section outlines key experimental models, methodologies, and reagents used in the cited studies.
Key Research Models and Reagents
Table 2: Essential Reagents and Models for SOX9-Focused Cancer Immunotherapy Research
| Category / Reagent | Specific Example | Application and Function | Reference |
|---|---|---|---|
| In Vivo Models | C3-TAg mouse model (BLBC); KrasLSL-G12D (LUAD) | Recapitulates human cancer progression for studying SOX9 in tumorigenesis and immune evasion. | [15] [43] |
| Genetic Manipulation | CRISPR/Cas9 (sgRNA: sgSox9.2); Cre-LoxP system | Achieves Sox9 knockout to study loss-of-function effects in vitro and in vivo. | [15] [43] |
| Ex Vivo Model | 3D Tumor Organoid Culture | Assesses SOX9-driven tumor cell growth and proliferation in a physiologically relevant context. | [43] |
| Immune Profiling | Flow Cytometry (CD3, CD4, CD8, CD45); IHC (Granzyme B, Ki67) | Quantifies tumor-infiltrating immune cell populations and cytotoxic activity. | [15] [43] |
| Small Molecule Inhibitor | Cordycepin (CD) | An adenosine analog that inhibits SOX9 mRNA and protein expression in a dose-dependent manner. | [41] |
| DPPI-3,4,5-P3-d62 (sodium) | DPPI-3,4,5-P3-d62 (sodium), MF:C41H78Na4O22P4, MW:1201.3 g/mol | Chemical Reagent | Bench Chemicals |
| Pazufloxacin-d4 | Pazufloxacin-d4, MF:C16H15FN2O4, MW:322.32 g/mol | Chemical Reagent | Bench Chemicals |
Detailed Experimental Protocol: Validating the SOX9-B7x Axis
The following protocol is adapted from the critical study by Liu et al. that established the SOX9-B7x pathway [15].
Objective: To determine if SOX9 expression in tumor cells directly suppresses T-cell function via B7x and to test the efficacy of B7x targeting.
Methodology:
In Vivo Model of Tumor Progression:
- Animals: Use immunocompetent mouse models (e.g., MMTV-iCre;Sox9Fl/Fl;C3-TAg for BLBC).
- Intervention: Compare tumor progression and immune infiltration in Sox9-WT vs. Sox9-cKO mice.
- Analysis:
- Histology/IHC: Analyze lymphocytic infiltrates in pre-malignant and malignant lesions using antibodies against CD3, CD4, CD8, and Granzyme B.
- Flow Cytometry: Perform spectral flow cytometry on dissociated tumors to quantify immune cell populations (CD45+, CD4+ T, CD8+ T, B cells, etc.).
T-cell Depletion Rescue Experiment:
- Intervention: Administer anti-CD4 and anti-CD8 depleting antibodies to Sox9-cKO mice.
- Outcome Measurement: Monitor and compare the onset of invasive tumors in depleted vs. isotype control mice. This confirms that T-cells are the mediators of the blocked tumor progression in Sox9-cKO animals.
In Vitro T-cell Functional Assays:
- Co-culture System:
- Engineeer SOX9-negative human breast cancer cells (e.g., MCF7ras) to overexpress SOX9 (SOX9-OE).
- Co-culture these cells with human CD4+ and CD8+ T cells isolated from PBMCs.
- Stimulate T-cells with anti-CD3/CD28 antibodies.
- Readouts:
- Proliferation Assay: Measure T-cell proliferation via CFSE dilution or similar method.
- Cytotoxicity Assay: For antigen-specific killing, transduce CD8+ T cells with a lentiviral vector expressing a known TCR (e.g., NY-ESO-1 specific). Co-culture with HLA-matched SOX9-OE and control tumor cells and measure specific lysis.
- Co-culture System:
Therapeutic Intervention:
- In Vivo Treatment: Treat established tumors in SOX9-high models with a blocking anti-B7x antibody, alone and in combination with anti-PD-L1.
- Outcome Measurement: Assess tumor growth, survival, and re-analyze the tumor immune microenvironment via flow cytometry to validate the target.
SOX9 has been unequivocally identified as a master regulator of tumor progression, functioning as a critical node linking cancer cell dedifferentiation, chemoresistance, and immunosuppression. Its role in suppressing both innate and adaptive anti-tumor immunity, primarily through mechanisms like the induction of the B7x checkpoint and modulation of the collagen-rich extracellular matrix, makes it a compelling therapeutic target.
Future research should focus on:
- Developing Direct SOX9 Inhibitors: While challenging, targeting transcription factors directly with small molecules or protein-degraders is an area of active exploration. The dTAG system used for precise modulation of SOX9 levels in developmental models provides a promising methodological framework [53].
- Combination Therapies: Targeting SOX9 downstream pathways, such as B7x, in combination with existing immunotherapies (e.g., anti-PD-1/PD-L1) represents a near-term strategy to overcome resistance in "immune-cold" tumors [15].
- Biomarker Development: Validating SOX9 expression levels and activity signatures as predictive biomarkers for patient stratification will be crucial for the success of SOX9-targeted therapies.
In conclusion, the therapeutic exploration of SOX9 holds significant promise for breaking theå£åž’ of therapy resistance and immune evasion in oncology, potentially offering new hope for patients with aggressive and treatment-refractory cancers.
Navigating Complexities: Challenges and Refinements in SOX9 Immunobiology
The transcription factor SOX9 (SRY-Box Transcription Factor 9) represents a paradigm of functional duality in biological systems. As a key member of the SOX family of transcription factors, it contains a highly conserved high-mobility group (HMG) box DNA-binding domain that enables recognition of specific DNA sequences and regulation of diverse transcriptional programs [1] [22]. Recent research has illuminated SOX9's complex, context-dependent roles—functioning as both a potent oncogene and a crucial tissue-protective factor [1]. This dual nature is particularly evident within immunological contexts, where SOX9 operates at the intersection of innate and adaptive immunity, influencing disease progression through multiple mechanisms.
SOX9's functional complexity stems from its sophisticated protein structure, which includes several specialized domains: a dimerization domain (DIM), the HMG box domain responsible for DNA binding and nuclear localization, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [1]. This structural configuration allows SOX9 to interact with diverse cofactors and target genes, enabling its participation in seemingly contradictory biological processes. In cancer biology, SOX9 is frequently overexpressed across various solid malignancies and is significantly implicated in tumor chemoresistance and malignant potential [1] [28]. Conversely, in tissue homeostasis and repair, SOX9 is indispensable for maintaining macrophage function, facilitating cartilage formation, and promoting tissue regeneration and repair [1] [54].
This technical review comprehensively examines the molecular mechanisms underlying SOX9's dual roles, with particular emphasis on its functions within innate and adaptive immunity. We integrate recent advances in understanding SOX9's signaling networks, provide detailed experimental protocols for studying its functions, and visualize key signaling pathways to assist researchers in navigating this complex field.
Structural Basis for SOX9 Functional Diversity
SOX9's capacity to fulfill diverse biological roles is fundamentally rooted in its multi-domain architecture. The HMG box domain serves dual functions: it facilitates specific DNA binding to the consensus sequence CCTTGAG while also containing embedded nuclear localization (NLS) and nuclear export (NES) signals that enable dynamic nucleocytoplasmic shuttling [1] [22]. The C-terminal transcriptional activation domain (TAC) mediates critical interactions with cofactors such as Tip60, while the central transcriptional activation domain (TAM) functions synergistically with TAC to augment SOX9's transcriptional potential [1]. The PQA-rich domain is essential for full transcriptional activation capacity, though its precise mechanistic contributions remain under investigation.
Table 1: Functional Domains of SOX9 Protein
| Domain | Position | Key Functions | Interacting Partners |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein-protein interactions | Other SOX proteins, co-factors |
| HMG Box Domain | Central | DNA binding, nuclear localization/export | Specific DNA sequences, importin/exportin |
| Transcriptional Activation Domain Middle (TAM) | Central | Transcriptional activation | Transcriptional co-activators |
| Transcriptional Activation Domain C-terminal (TAC) | C-terminal | Transcriptional activation, β-catenin inhibition | Tip60, β-catenin |
| PQA-rich Domain | C-terminal | Transcriptional activation | Unknown |
SOX9 exhibits complex expression patterns across tissues and cell types. According to the Human Protein Atlas, SOX9 demonstrates tissue-enhanced expression in salivary gland and shows cell type-enriched expression in cholangiocytes, pituitary gland undifferentiated cells, prostate basal glandular cells, Sertoli cells, and thyroid glandular cells [55]. Notably, SOX9 is not detected in immune cells under normal conditions, suggesting its immunomodulatory functions may be context-dependent or restricted to specific pathological conditions [55].
SOX9 in Oncogenesis: Mechanisms and Immune Modulation
SOX9 as a Driver of Tumor Progression
SOX9 functions as a potent oncogene across numerous cancer types, including liver cancer, lung cancer, breast cancer, gastric cancer, and glioblastoma [1] [22] [23]. Its pro-tumorigenic activities encompass multiple hallmarks of cancer, with particularly significant roles in promoting tumor proliferation, metastasis, chemotherapy resistance, and stemness maintenance. In high-grade serous ovarian cancer (HGSOC), SOX9 drives chemoresistance by reprogramming the transcriptional state of naive cells into a stem-like state [28]. Epigenetic upregulation of SOX9 is sufficient to induce significant platinum resistance in vivo, and SOX9 expression is consistently upregulated in patient tumors following platinum-based chemotherapy [28].
The molecular mechanisms through which SOX9 promotes tumor progression involve complex signaling networks. In cervical cancer, SOX9 transcriptionally activates PLOD3, which subsequently promotes cancer progression via the IL-6/JAK/STAT3 pathway [56]. This SOX9/PLOD3/IL-6/JAK/STAT3 axis drives multiple malignant phenotypes including proliferation, apoptosis resistance, migration, and invasion [56]. Similarly, in breast cancer, SOX9 interacts with long non-coding RNA linc02095 to create a positive feedback loop that promotes cell growth and tumor progression [22]. SOX9 also accelerates AKT-dependent tumor growth by regulating SOX10 expression through direct binding to the SOX10 promoter [22].
SOX9 in Tumor Microenvironment and Immune Evasion
A critical aspect of SOX9's pro-tumorigenic function involves its profound impact on the tumor immune microenvironment. Bioinformatics analyses of data from The Cancer Genome Atlas reveal that SOX9 expression strongly correlates with specific patterns of immune cell infiltration [1]. In colorectal cancer, SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1].
SOX9 plays a particularly important role in immune evasion mechanisms. Malladi et al. first demonstrated that SOX9 is crucial for immune evasion, observing that latent cancer cells with high SOX9 expression could maintain long-term survival and tumor-initiating capabilities while remaining dormant in secondary metastatic sites and avoiding immune surveillance [22]. In prostate cancer, SOX9 contributes to the formation of an "immune desert" microenvironment that promotes tumor immune escape by driving a shift in the immune landscape that decreases effector immune cells while increasing immunosuppressive cells [1].
Table 2: SOX9 Correlation with Immune Cell Infiltration in Cancer
| Immune Cell Type | Correlation with SOX9 | Functional Consequences |
|---|---|---|
| CD8+ T cells | Negative | Impaired cytotoxic function |
| NK cells | Negative | Reduced tumor cell killing |
| M1 macrophages | Negative | Decreased anti-tumor immunity |
| Memory CD4+ T cells | Positive | Potential immune regulation |
| Neutrophils | Positive | Pro-tumorigenic inflammation |
| M2 macrophages | Positive | Immunosuppressive microenvironment |
| Tregs | Positive | Suppressed anti-tumor immunity |
Diagram 1: SOX9-Driven Pro-Tumorigenic Signaling and Immune Evasion Pathways. SOX9 activates multiple oncogenic pathways including the PLOD3/IL-6/JAK/STAT3 axis while simultaneously modulating the tumor immune microenvironment to promote immunosuppression.
Tissue-Protective Functions of SOX9 in Regeneration and Repair
SOX9 in Liver Regeneration and Repair
In stark contrast to its pro-tumorigenic roles, SOX9 fulfills essential tissue-protective functions in various organ systems, particularly in the liver. Following partial hepatectomy, mature hepatocytes undergo conversion to Sox9+HNF4α+ hybrid hepatocytes (HybHPs) that play critical roles in liver regeneration [54]. These bipotential cells demonstrate high regenerative capacity and can repopulate the liver after chronic hepatocyte injury. Mechanistically, the LPS/NF-κB pathway activates Bcl3, which forms a complex with YAP1, leading to YAP1 deubiquitination and nuclear translocation, ultimately resulting in SOX9 upregulation and mature hepatocyte conversion [54].
The functional significance of SOX9 in liver regeneration has been definitively established through loss-of-function experiments. Knockdown of SOX9 expression suppresses hepatocyte proliferation and blocks the recovery of lost hepatic tissue following partial hepatectomy [54]. This highlights the non-redundant role of SOX9 in orchestrating regenerative responses in mammalian tissues.
SOX9 in Ocular Homeostasis and Retinal Protection
SOX9 plays equally critical protective roles in maintaining ocular integrity. In the adult mouse eye, SOX9 expression persists in multiple cell types including retinal pigmented epithelium cells, Müller glial cells, and limbal and corneal basal epithelia [57]. Induced deletion of SOX9 in adult mice triggers severe retinal degeneration characterized by loss of Müller glial cells and complete depletion of the photoreceptor layer [57]. This demonstrates SOX9's essential role in maintaining retinal structure and function.
Additionally, SOX9 serves crucial functions in limbal stem cell biology. Single-cell RNA sequencing combined with SOX9 lineage tracing has revealed that SOX9 is expressed in a basal limbal stem cell population capable of forming two distinct types of long-lived cell clones involved in stem cell maintenance and homeostasis [57]. Mosaic analysis confirms that SOX9 is essential for proper limbal stem cell differentiation, underscoring its fundamental role in corneal epithelial maintenance and repair.
SOX9 in Fibrosis Resolution and Tissue Remodeling
Emerging evidence indicates that SOX9 participates in organ fibrosis affecting cardiac, liver, kidney, and pulmonary tissues [58]. While fibrosis represents a common endpoint in chronic inflammatory diseases characterized by excessive extracellular matrix accumulation, SOX9 appears to play complex roles in this process. In mammalian kidneys, SOX9 functions as a "switch" that links regeneration to fibrosis at the single-cell level [58]. This positioning suggests SOX9 represents a potential antifibrotic treatment target, though its precise functions likely vary across tissue contexts and disease stages.
Experimental Approaches for Studying SOX9 Function
In Vitro and Cell-Based Assays
Investigation of SOX9 function employs diverse methodological approaches. Gene manipulation techniques include CRISPR/Cas9-mediated knockout using SOX9-targeting sgRNAs, with efficacy confirmed through colony formation assays demonstrating significantly increased sensitivity to carboplatin treatment in SOX9-depleted cells [28]. RNA interference approaches utilizing shRNAs targeting SOX9 and YAP1, delivered via viral vectors such as pDKD-CMV-eGFP-U6-shRNA constructs, enable efficient gene silencing [54]. For gain-of-function studies, plasmid vectors including plvx-IRES-puro-flag-mbcl3 for Bcl3 overexpression and pAdeno-MCMV-Yap1-HIS-IRES-EGFP for YAP1 overexpression have been successfully employed [54].
Gene expression analysis typically involves RNA extraction using RNeasy Mini kits, reverse transcription with Bestar qPCR RT kits, and real-time PCR performed with SYBR PrimeScript RT-PCR kits [54]. Protein analysis by western blotting utilizes specific antibodies against SOX9, HNF4α, TERT, E-Cadherin, and Vimentin, among others [54]. Subcellular localization studies employ NE-PER Nuclear and Cytoplasmic Extraction kits followed by western blotting with appropriate antibodies [54].
In Vivo Models and Therapeutic Assessment
Multiple murine models facilitate investigation of SOX9 function in physiological contexts. Partial hepatectomy (PHx) models demonstrate SOX9's role in liver regeneration, with liver-to-body-weight ratios calculated to assess regenerative capacity [54]. Chimeric Fah−/− mice repopulated with wild-type hepatocytes enable study of hepatocyte conversion and expansion [54]. For tissue-specific gene deletion, tamoxifen-inducible CAGG-CreER systems combined with conditional Sox9flox/flox alleles allow temporal control of Sox9 ablation in adult animals [57].
Therapeutic assessment approaches include Kaplan-Meier overall survival analysis using databases such as GEPIA2 and Kaplan-Meier Plotter [56]. Immune cell infiltration analysis employs ssGSEA and ESTIMATE algorithms applied to RNA sequencing data [23]. Drug sensitivity assays, particularly to platinum-based chemotherapeutics, evaluate SOX9's role in chemoresistance using colony formation assays and Incucyte live-cell imaging systems [28].
Table 3: Essential Research Reagents for SOX9 Investigation
| Reagent/Category | Specific Examples | Research Applications |
|---|---|---|
| Expression Vectors | pDKD-CMV-eGFP-U6-shRNA-SOX9, plvx-IRES-puro-flag-mbcl3, pAdeno-MCMV-Yap1-3Flag-IRES2-EGFP | Gene overexpression and silencing |
| Antibodies | Anti-SOX9, Anti-HNF4α, Anti-E-Cadherin, Anti-Vimentin | Protein detection and localization |
| Cell Lines | HEK293T, AML12, OVCAR4, Kuramochi, COV362, HeLa | In vitro mechanistic studies |
| Animal Models | C57BL/6, TLR4−/−, Bcl3−/−, Fah−/−, CAGG-CreER;Sox9flox/flox | In vivo functional validation |
| Analysis Kits | RNeasy Mini Kit, Bestar qPCR RT Kit, SYBR PrimeScript RT-PCR Kit, NE-PER Extraction Kit | Molecular analysis |
Strategic Pathways for Therapeutic Targeting of SOX9
The dual nature of SOX9 function presents both challenges and opportunities for therapeutic development. Several strategic approaches emerge from recent research findings. Small molecule inhibitors targeting the SOX9/PLOD3/IL-6/JAK/STAT3 axis show promise in cervical cancer models, potentially disrupting multiple malignant phenotypes simultaneously [56]. Epigenetic modulators represent another attractive approach, given that epigenetic upregulation of SOX9 is sufficient to induce chemoresistance in HGSOC [28]. Targeting SOX9-mediated stemness pathways may provide opportunities to overcome chemotherapy resistance across multiple cancer types.
For tissue-protective applications, strategies to enhance SOX9-mediated regeneration while minimizing oncogenic risk are needed. In liver regeneration, modulation of the LPS/Bcl3/YAP1/SOX9 pathway could potentially enhance regenerative capacity without promoting tumorigenesis [54]. Similarly, in ocular diseases, SOX9 manipulation might maintain retinal integrity and support limbal stem cell function [57]. The context-dependent nature of SOX9 function necessitates careful therapeutic windows to achieve desired outcomes without adverse effects.
Diagram 2: SOX9-Mediated Tissue Protective Pathways and Assessment Methods. SOX9 activation through the LPS/Bcl3/YAP1 axis promotes tissue regeneration, which can be evaluated through multiple experimental approaches including histology, single-cell RNA sequencing, lineage tracing, and functional assays.
Concluding Perspectives and Future Directions
The dualistic nature of SOX9 presents both challenges and opportunities for therapeutic development. Future research should prioritize understanding the contextual determinants that dictate SOX9's functional outcomes—specifically, what molecular and microenvironmental factors direct SOX9 toward pro-tumorigenic versus tissue-protective programs. Single-cell multi-omics approaches will be particularly valuable for elucidating the heterogeneous functions of SOX9 across different cellular subpopulations within complex tissues.
From a translational perspective, the development of context-specific SOX9 modulators represents a promising frontier. Such agents would ideally inhibit SOX9's pro-tumorigenic functions while preserving or enhancing its tissue-protective capacities. The integration of SOX9 expression and activity biomarkers into diagnostic and prognostic algorithms may also enable better patient stratification and treatment selection. Furthermore, combining SOX9-targeted approaches with established immunotherapies could potentially overcome resistance mechanisms and improve outcomes in refractory malignancies.
As our understanding of SOX9's complex biology continues to evolve, this transcription factor increasingly emerges as a master regulator at the intersection of multiple critical pathways in health and disease. The strategic resolution of SOX9's functional duality will undoubtedly yield significant advances in both oncological and regenerative medicine.
The transcription factor SOX9 exhibits profound context-dependent functionality, acting as a potent oncogene in numerous cancers while serving as a master regulator of cartilage homeostasis in osteoarthritis (OA). This whitepaper explores the dual nature of SOX9 within innate and adaptive immunity mechanisms, synthesizing recent findings from cancer and OA research. We analyze the contrasting molecular mechanisms governing SOX9 activity across these pathological states, provide detailed experimental protocols for investigating its context-dependent functions, and propose strategic approaches for therapeutic targeting. The insights presented herein aim to guide researchers and drug development professionals in navigating the complexities of SOX9 biology for targeted therapeutic interventions.
SOX9 (SRY-Box Transcription Factor 9) is a high-mobility group (HMG) box transcription factor that plays critical yet contradictory roles in human pathophysiology. In cancer biology, SOX9 is frequently overexpressed and functions as an oncogene driving tumor progression, stemness, and immune evasion [1] [6]. Conversely, in osteoarthritis, SOX9 serves as a master regulator of chondrogenesis whose preservation and activation represent promising therapeutic strategies [59] [60]. This paradoxical behavior presents both challenges and opportunities for therapeutic development. Understanding the mechanisms underlying these context-dependent effects is essential for developing targeted interventions that can selectively inhibit SOX9's pathogenic functions in cancer while preserving or enhancing its protective roles in joint homeostasis.
SOX9 Structure and Functional Domains
SOX9 contains several functionally critical domains organized from N- to C-terminus: a dimerization domain (DIM), the HMG box domain responsible for DNA binding and nuclear localization, a central transcriptional activation domain (TAM), a C-terminal transcriptional activation domain (TAC), and a proline/glutamine/alanine (PQA)-rich domain [1]. The HMG domain facilitates DNA binding and nucleocytoplasmic shuttling via embedded nuclear localization (NLS) and nuclear export (NES) signals, while the TAC domain interacts with cofactors like Tip60 to enhance transcriptional activity [1]. These structural elements enable SOX9 to function as a transcriptional regulator across diverse biological contexts.
Table 1: SOX9 Protein Domains and Functions
| Domain | Position | Key Functions |
|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein-protein interactions |
| HMG Box Domain | Central | DNA binding, nuclear localization, nuclear export |
| Transcriptional Activation Domain (TAM) | Central | Synergizes with TAC to enhance transcriptional potential |
| Transcriptional Activation Domain (TAC) | C-terminal | Interacts with cofactors (e.g., Tip60); inhibits β-catenin during chondrocyte differentiation |
| PQA-Rich Domain | C-terminal | Necessary for transcriptional activation |
SOX9 in Cancer: Mechanisms of Oncogenesis and Immune Evasion
SOX9 as an Oncogenic Driver
SOX9 is highly expressed in various solid malignancies, including liver, lung, breast, gastric, and ovarian cancers, where its expression levels positively correlate with tumor occurrence, progression, and poor prognosis [1] [28] [6]. In high-grade serous ovarian cancer (HGSOC), SOX9 is epigenetically upregulated following platinum-based chemotherapy, inducing a stem-like transcriptional state and significant chemoresistance [28]. SOX9 ablation increases platinum sensitivity, while its overexpression promotes drug tolerance through transcriptional reprogramming [28]. Similarly, in breast cancer, SOX9 promotes tumor initiation and progression through multiple pathways, including regulation of the cell cycle, interaction with HDAC9 to control mitosis, and formation of positive feedback loops with long non-coding RNAs [6].
SOX9 in Tumor Immune Microenvironment Regulation
SOX9 plays a multifaceted role in shaping the tumor immune microenvironment to facilitate immune evasion. Bioinformatics analyses reveal that SOX9 expression correlates with specific patterns of immune cell infiltration. In colorectal cancer, SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1]. SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with memory CD4+ T cells [1]. Through these mechanisms, SOX9 contributes to the creation of an "immune desert" microenvironment that promotes tumor immune escape [1].
Table 2: SOX9 in Cancer vs. Osteoarthritis: Functional Dichotomy
| Parameter | Cancer Context | Osteoarthritis Context |
|---|---|---|
| Expression Level | Frequently overexpressed [1] [6] | Reduced or dysfunctional activity [61] |
| Primary Role | Oncogene promoting progression [28] [6] | Master chondrogenic regulator [59] |
| Immune Modulation | Promotes immunosuppression and immune evasion [1] [8] | Maintains macrophage function for tissue repair [1] |
| Cellular State | Induces stem-like, chemoresistant state [28] | Promotes chondrocyte differentiation and ECM synthesis [59] |
| Therapeutic Goal | Inhibition or downregulation [1] | Activation or preservation [59] [60] |
SOX9 in Osteoarthritis: Mechanisms of Cartilage Homeostasis and Repair
SOX9 as Master Chondrogenic Regulator
In articular cartilage, SOX9 serves as the "master regulator" of chondrocytes, maintaining chondrocyte phenotype and cartilage homeostasis by triggering expression of critical extracellular matrix (ECM) components including type II collagen (COL2A1) and aggrecan (ACAN) [59] [61]. SOX9 transcriptional activity is significantly amplified through synergistic interactions with SOX5 and SOX6, forming the "SOX trio" that acts in concert at cartilage-specific enhancers [59]. SOX9 deficiency results in proteoglycan loss in healthy cartilage and exacerbates post-trauma cartilage erosion, highlighting its essential role in cartilage integrity [61].
Metabolic Regulation of SOX9 in OA
Recent research has revealed that altered lipid metabolism in chondrocytes significantly impacts SOX9 stability and function. In obesity-associated OA, enhanced fatty acid oxidation (FAO) leads to acetyl-CoA accumulation, which reduces AMPK activity, impairs SOX9 phosphorylation, and ultimately promotes its ubiquitination-mediated degradation [61]. This metabolic regulation represents a crucial link between obesity and OA progression, independent of mechanical loading. Cartilage-targeted delivery of the FAO inhibitor trimetazidine, which also activates AMPK, demonstrates superior efficacy in mouse models of metabolism-associated post-traumatic OA [61].
Experimental Models and Methodologies
Investigating SOX9 in Cancer Models
Chemoresistance Studies in HGSOC:
- Cell Lines: HGSOC cell lines (OVCAR4, Kuramochi, COV362) treated with carboplatin [28]
- SOX9 Modulation: CRISPR/Cas9 knockout for loss-of-function; epigenetic upregulation for gain-of-function studies [28]
- Assays: Colony formation assays to assess chemosensitivity; Incucyte live-cell imaging for growth kinetics; single-cell RNA sequencing of patient tumors pre- and post-neoadjuvant chemotherapy [28]
- Transcriptional Analysis: Measurement of transcriptional divergence (P50/P50 ratio) as a metric for transcriptional plasticity and stemness [28]
Immune Microenvironment Analysis:
- Bioinformatics: Integration of whole exome and RNA sequencing data from TCGA to correlate SOX9 expression with immune cell infiltration patterns [1]
- Single-cell RNA Sequencing: Analysis of immune cell populations and their functional states in SOX9-high versus SOX9-low tumors [1]
Investigating SOX9 in Osteoarthritis Models
LNP-mediated mRNA Delivery:
- Formulation: Systematic development of lipid nanoparticles (LNPs) with varying ratios of ionizable lipid (SM-102), cholesterol, DSPC, and DMG-PEG2000 [59]
- mRNA Payload: Co-delivery of SOX5 and SOX9 mRNAs for synergistic enhancement of chondrogenesis [59]
- In Vivo Model: ACLT-induced osteoarthritis rat model with intra-articular LNP injections [59]
- Outcome Measures: Histological assessment of cartilage degradation, quantification of ECM components (COL2A1, ACAN), inflammation markers (TNF-α, IL-1β, IL-6) [59]
CRISPR-dCas9 Mediated Gene Regulation:
- Engineering Approach: Simultaneous Sox9 activation and RelA inhibition using dSpCas9-VP64 (activation) and dSaCas9-KRAB (repression) systems [60]
- Cell Therapy: Intraarticular injection of engineered mesenchymal stromal cells (MSCs) in surgical mouse OA model [60]
- Assessment: Cartilage degradation scoring, pain behavior measurements, immunohistochemistry for cartilage markers, analysis of cell survival in joint tissues [60]
Diagram 1: Context-Dependent SOX9 Regulation
Strategic Approaches for Context-Specific Therapeutic Targeting
Cancer: SOX9 Inhibition Strategies
The oncogenic functions of SOX9 make it an attractive therapeutic target in cancer. Potential strategies include:
- Epigenetic Modulation: Targeting super-enhancers and epigenetic regulators that control SOX9 expression [28]
- Transcriptional Interference: Disrupting SOX9-mediated transcriptional networks that maintain stemness and chemoresistance [28]
- Immune Microenvironment Reprogramming: Combining SOX9 inhibition with immunotherapies to reverse immune suppression [1] [8]
Osteoarthritis: SOX9 Preservation and Activation
Therapeutic approaches for OA focus on preserving or enhancing SOX9 function:
- LNP-mediated mRNA Delivery: Co-delivery of SOX5 and SOX9 mRNAs to synergistically enhance chondrogenesis and counteract senescence [59]
- CRISPR-dCas9 Activation: Precise upregulation of endogenous SOX9 combined with inhibition of inflammatory pathways (e.g., RelA/NF-κB) [60]
- Metabolic Modulation: Targeting fatty acid oxidation with inhibitors like trimetazidine to prevent SOX9 degradation [61]
- SOX9 Stabilization: Developing approaches to enhance SOX9 phosphorylation and prevent ubiquitin-mediated degradation [61]
Table 3: Research Reagent Solutions for SOX9 Studies
| Reagent/Tool | Application | Function | Source/Model |
|---|---|---|---|
| LNP Formulations | mRNA delivery to chondrocytes | Co-delivery of SOX5/SOX9 mRNAs for cartilage regeneration | [59] |
| dSpCas9-VP64/dSaCas9-KRAB | CRISPRa/i gene regulation | Simultaneous Sox9 activation and RelA inhibition | [60] |
| HGSOC Cell Lines | Cancer chemoresistance studies | OVCAR4, Kuramochi, COV362 for SOX9 functional assays | [28] |
| ACLT Rat Model | OA therapeutic testing | Surgical model for evaluating SOX9-based therapies | [59] |
| HFD-DMM Mouse Model | Metabolism-associated OA | Combines high-fat diet with surgical OA induction | [61] |
The context-dependent functions of SOX9 present both challenges and opportunities for therapeutic development. In cancer, SOX9 drives pathogenesis through promoting stemness, chemoresistance, and immune evasion, making it a valuable therapeutic target. Conversely, in osteoarthritis, SOX9 is essential for cartilage homeostasis, and its preservation or activation represents a promising therapeutic strategy. Future research should focus on understanding the precise molecular mechanisms that determine SOX9's context-specific functions, including post-translational modifications, protein interaction partners, and epigenetic regulation. The development of sophisticated delivery systems, such as optimized LNPs and CRISPR-dCas9 platforms, provides powerful tools for targeting SOX9 in a context-appropriate manner. By leveraging these advanced technologies and deepening our understanding of SOX9 biology, researchers can develop targeted interventions that selectively modulate SOX9 function for therapeutic benefit across diverse disease contexts.
The transcription factor SOX9 is a critical regulator in development, stem cell maintenance, and disease pathogenesis, with emerging dual roles in both innate and adaptive immunity. Its expression pattern is complex—maintaining tissue homeostasis in some contexts while driving pathological processes in others, including cancer, fibrosis, and neurodegeneration. This technical guide addresses common methodological pitfalls in SOX9 research, providing optimized protocols for specific detection and functional analysis. We emphasize approaches that distinguish SOX9's context-dependent functions across immune regulation and tissue-specific pathologies, enabling more accurate mechanistic studies and therapeutic development.
SOX9 (SRY-Box Transcription Factor 9) exhibits context-dependent dual functions across biological systems. In immunology, SOX9 acts as a "double-edged sword," capable of both promoting immune escape in tumors and contributing to tissue repair and regeneration in inflammatory conditions [1]. Its expression in stromal cells and influence on immune cell infiltration creates complex regulatory networks in the tumor microenvironment [1] [23]. Beyond immunity, SOX9 maintains retinal integrity, prevents neurodegeneration, regulates adipogenesis, and drives fibrosis through extracellular matrix production [57] [62] [63]. This functional diversity necessitates highly specific detection methods and carefully controlled functional assays to accurately characterize SOX9's multifaceted roles in health and disease.
Technical Challenges in SOX9 Detection
Accurate SOX9 detection faces several challenges: antibody specificity across model systems, temporal expression dynamics, post-translational modifications, and subcellular localization. SOX9 undergoes nucleocytoplasmic shuttling, with phosphorylation at specific sites (e.g., S181) altering its transcriptional activity and nuclear localization [1] [64]. Furthermore, SOX9 exists in distinct functional states across cell types—from stem cell populations in the limbus to reactive astrocytes in neurodegenerative contexts—requiring validation methods that account for this heterogeneity [57] [65].
Antibody Validation and Selection
Comprehensive antibody validation is essential for specific SOX9 detection. The table below outlines key validation parameters for SOX9 antibodies:
Table 1: Antibody Validation Parameters for SOX9 Detection
| Validation Method | Experimental Approach | Expected Outcome |
|---|---|---|
| Knockout/Knockdown Validation | siRNA/shRNA-mediated Sox9 depletion in target cells | >80% reduction in signal in Western blot/ICC compared to control |
| Cross-Reactivity Testing | Western blot against recombinant SOX8, SOX10 proteins | No detectable binding to other SOXE family members |
| Epitope Mapping | Peptide competition assays using immunizing peptide | Dose-dependent reduction in signal with peptide pre-incubation |
| Tissue Specificity | IHC on Sox9-knockout tissue sections | Absence of staining in knockout tissues |
Method-Specific Optimization
Immunohistochemistry (IHC) Protocol
- Tissue Preparation: Fixation in 4% PFA for 24 hours maximum to prevent epitope masking
- Antigen Retrieval: Citrate buffer (pH 6.0) with 20-minute steam heating for nuclear SOX9 detection
- Blocking: 5% normal goat serum + 2% BSA + 0.1% Triton X-100 for 1 hour
- Primary Antibody: Rabbit anti-SOX9 (1:500) incubation at 4°C overnight
- Validation Controls: Include tissues with known SOX9 expression (e.g., cartilage, limbal stem cells) and negative controls (Sox9-deficient tissues) [57]
Western Blotting Protocol
- Nuclear Extraction: Prepare separate nuclear and cytoplasmic fractions to detect subcellular localization
- Gel Electrophoresis: 10% SDS-PAGE with extended run time (2 hours at 100V) for clear separation at ~65kDa
- Transfer: Wet transfer at 4°C for 2 hours at 100V
- Blocking: 5% non-fat milk in TBST for 1 hour
- Detection: ECL with multiple exposure times to ensure linear detection range
SOX9 Functional Assays in Disease Contexts
Functional analysis of SOX9 requires carefully controlled assays that account for its diverse roles across pathological contexts.
Gain/Loss-of-Function Approaches
Table 2: SOX9 Modulation Approaches Across Disease Models
| Disease Context | Approach | Key Readouts | Technical Considerations |
|---|---|---|---|
| Neurodegeneration (Alzheimer's) | Sox9 overexpression in astrocytes | Amyloid-β plaque clearance, cognitive function tests (object recognition) | Use tamoxifen-inducible systems in already-impaired models [65] [66] |
| Liver Fibrosis | siRNA-mediated Sox9 knockdown in hepatic stellate cells | ECM protein levels (OPN, VIM, FN1), collagen deposition, serum biomarkers | Validate knockdown efficiency in primary HSCs; monitor multiple ECM targets [63] |
| Cancer (Glioblastoma, Breast) | CRISPRa/i for Sox9 modulation | Stemness markers, chemoresistance, immune cell infiltration profiles | Account for heterogeneous tumor cell populations; single-cell analysis recommended [22] [23] |
| Neuropathic Pain | Phospho-mutant Sox9 (S181A) expression | Glycolytic flux (HK1 activity), lactate production, H3K9la modification | Monitor astrocyte subtype transitions via scRNA-seq [64] |
Assessing SOX9-Mediated Immune Modulation
SOX9 regulates immune cell infiltration and function in both innate and adaptive immunity. The following protocol assesses SOX9-dependent immunomodulation:
Co-culture Assay for Immune Cell Infiltration:
- Setup: Establish co-cultures of SOX9-modulated cancer cells (e.g., glioblastoma, breast cancer) with peripheral blood mononuclear cells (PBMCs) in Transwell systems
- Conditioned Media: Collect media from SOX9-high and SOX9-low cells for cytokine profiling
- Flow Cytometry Panel: Analyze immune cell populations using CD45 (pan-immune), CD3 (T-cells), CD19 (B-cells), CD14 (monocytes), CD56 (NK cells), and CD11b (myeloid cells)
- Functional Assays: Measure T-cell proliferation (CFSE dilution), macrophage polarization (CD206 vs. HLA-DR), and cytokine production (IL-10, TGF-β, IFN-γ) [1] [23]
SOX9 Signaling Networks: Visualization and Analysis
SOX9 participates in complex signaling networks that vary by cellular context. The following diagrams illustrate key SOX9-regulated pathways in different pathological conditions.
Figure 1: SOX9-HK1-glycolysis axis in neuropathic pain. SOX9 phosphorylation upregulates HK1, increasing glycolysis and lactate production, which promotes histone lactylation (H3K9la) and neuroinflammatory astrocyte programming [64].
Figure 2: SOX9 regulates ECM production in liver fibrosis. SOX9 is induced in activated hepatic stellate cells (HSCs), transcriptionally activating ECM genes whose protein products contribute to fibrosis and serve as serum biomarkers [63].
Table 3: Key Research Reagents for SOX9 Investigations
| Reagent Type | Specific Examples | Application Notes |
|---|---|---|
| Validated Antibodies | Rabbit anti-SOX9 (Millipore AB5535), Mouse anti-SOX9 (Santa Cruz sc-166505) | Validate species cross-reactivity; optimal for IHC, WB, ChIP [57] [63] |
| Cell Models | Primary hepatic stellate cells, Limbal stem cells, Astrocyte cultures, Patient-derived organoids | Maintain appropriate differentiation status; confirm SOX9 expression baseline [57] [63] |
| Animal Models | Sox9-floxed mice (Sox9flox/flox), Inducible Cre systems (CAGG-CreER), Alzheimer's model mice (APP/PS1) | Control induction timing; monitor mosaic recombination [57] [65] |
| Critical Assays | ChIP-qPCR (ECM gene promoters), scRNA-seq (astrocyte heterogeneity), Seahorse (glycolytic flux) | Include appropriate normalization controls [64] [63] |
| Pathway Modulators | Rho/Rac1 inhibitors (CT04), HK1 activators/inhibitors, Lactylation modifiers | Verify specificity through rescue experiments [62] [64] |
Addressing technical pitfalls in SOX9 detection and functional analysis requires standardized validation approaches, context-specific assay design, and integrative analysis of SOX9's diverse functions. The methods outlined in this guide provide a framework for generating reproducible, mechanistically insightful data on SOX9's roles in immunity and disease. As research continues to elucidate SOX9's complex regulatory networks, these rigorous technical approaches will be essential for developing targeted therapies that modulate SOX9 activity in specific pathological contexts.
The transcription factor SRY-related HMG-box 9 (SOX9) presents a compelling therapeutic target across multiple disease domains, including cancer, neurodegenerative disorders, and inflammatory conditions. However, its diverse physiological roles across different tissue types create significant challenges for therapeutic targeting, primarily due to the risk of on-target, off-tissue toxicity. SOX9 exhibits a complex, dualistic nature in biological systems—it functions as both an oncogene promoting tumor immune evasion and a protective factor maintaining tissue homeostasis and repair [1]. This dichotomy is particularly evident in its functions within innate versus adaptive immunity, where SOX9 modulates macrophage function in tissue regeneration while simultaneously impairing immune cell function to facilitate cancer immune escape [1].
The clinical imperative for cell-type specific targeting strategies stems from SOX9's multifaceted roles. In cancer, SOX9 is frequently overexpressed in various solid malignancies including liver cancer, lung cancer, breast cancer, and gastric cancer, where its expression levels positively correlate with tumor occurrence and progression [1]. In glioblastoma, SOX9 expression serves as a diagnostic and prognostic biomarker, with its expression closely correlated with immune infiltration and checkpoint expression [23]. Conversely, in neurological contexts, SOX9 plays protective roles—recent research demonstrates that boosting SOX9 in astrocytes helps clear amyloid plaques in Alzheimer's disease models and preserves cognitive function [67] [65]. Similarly, in neuropathic pain, SOX9 drives astrocyte-mediated neuroinflammation through metabolic reprogramming [68]. This diverse functional profile necessitates sophisticated targeting approaches that can precisely engage SOX9 in pathological contexts while sparing its physiological functions.
SOX9 Contextual Biology: Innate vs. Adaptive Immunity Mechanisms
Structural and Functional Basis of SOX9 Pleiotropy
SOX9 encodes a 509 amino acid polypeptide containing several functionally critical domains: an N-terminal dimerization domain (DIM), the central HMG box DNA-binding domain, two transcriptional activation domains (TAM and TAC), and a C-terminal proline/glutamine/alanine (PQA)-rich domain [1]. The HMG domain facilitates both DNA binding and nuclear localization through embedded nuclear localization (NLS) and nuclear export (NES) signals, enabling nucleocytoplasmic shuttling [1]. The C-terminal transcriptional activation domain (TAC) interacts with various cofactors including Tip60 to enhance SOX9's transcriptional activity, while TAM functions synergistically with TAC to augment transcriptional potential [1]. This modular structure enables context-dependent protein interactions and functions that vary by cell type and physiological state.
SOX9 in Innate Immunity and Tissue Homeostasis
Within innate immunity, SOX9 exhibits predominantly protective functions, particularly in tissue maintenance and repair. In the central nervous system, SOX9 regulates astrocyte function in multiple disease contexts. In Alzheimer's disease models, SOX9 overexpression in astrocytes promotes Aβ plaque phagocytosis through enhanced cleaning activity, effectively clearing plaques from the brain and preserving cognitive function [67] [65]. This protective function is particularly notable because boosting SOX9 was beneficial even in mice that had already developed cognitive impairment and amyloid plaques, suggesting potential therapeutic relevance for symptomatic Alzheimer's disease [65].
In neuropathic pain conditions, SOX9 plays a more complex role in spinal cord astrocytes. Nerve injury induces abnormal SOX9 phosphorylation, triggering aberrant hexokinase 1 (Hk1) activation that drives high-rate astrocytic glycolysis [68]. The resulting excessive lactate production remodels histone modifications via lactylation (H3K9la), promoting transcriptional modules of pro-inflammatory and neurotoxic genes that ultimately cause neuropathic pain [68]. This pathway illustrates how SOX9's metabolic regulation in innate immune glial cells can drive pathological processes.
Single-cell RNA sequencing analyses of dorsal spinal astrocytes in neuropathic pain have identified distinct astrocyte subpopulations with SOX9-associated pathogenic signatures. The most expanded subpopulation (Astro1) during neuropathic pain development exhibits gene expression patterns associated with pathogenic astrocyte activities, including pro-inflammatory signaling and neurotoxic genes [68]. These findings highlight the importance of targeting specific pathological astrocyte subpopulations to avoid disrupting beneficial astrocyte functions.
SOX9 in Adaptive Immunity and Cancer Immunobiology
Within adaptive immunity, SOX9 modulates T-cell development and function, participating in the differentiation and regulation of diverse immune lineages. SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating the lineage commitment of early thymic progenitors and potentially influencing the balance between αβ T-cell and γδ T-cell differentiation [1]. This function positions SOX9 as a regulator of T-cell fate decisions during development.
In cancer biology, SOX9 emerges as a potent driver of tumor immune evasion through multiple mechanisms. Extensive bioinformatics analyses indicate strong associations between SOX9 expression and altered immune cell infiltration within tumor microenvironments [1]. In colorectal cancer, SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1]. Similarly, in various cancers, SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with memory CD4+ T cells [1].
Table 1: SOX9-Mediated Immune Evasion Mechanisms in Cancer
| Mechanism | Functional Consequence | Therapeutic Implications |
|---|---|---|
| Altered immune cell infiltration | Reduced CD8+ T cell and NK cell activity; Increased immunosuppressive cells | Combination therapies with immune checkpoint inhibitors |
| Metabolic reprogramming | Enhanced glycolysis supporting immune suppression | Metabolic inhibitors with SOX9-targeted approaches |
| Stem-like state induction | Chemoresistance and immune evasion | Differentiation therapy combined with SOX9 inhibition |
| Checkpoint regulation | Potential PD-L1 modulation | Dual targeting of SOX9 and immune checkpoints |
In ovarian cancer, SOX9 drives chemoresistance through induction of a stem-like transcriptional state. SOX9 expression is significantly induced by platinum treatment in high-grade serous ovarian cancer (HGSOC), and its epigenetic upregulation is sufficient to induce chemoresistance in multiple HGSOC lines [28]. Single-cell analysis demonstrates that chemotherapy treatment results in rapid population-level induction of SOX9 that enriches for a stem-like transcriptional state, establishing SOX9 as a critical regulator of early steps of transcriptional reprogramming that lead to chemoresistance [28].
Quantitative Analysis of SOX9 Expression and Function Across Tissues
Comprehensive analysis of SOX9 expression patterns and their functional consequences reveals critical considerations for cell-type specific targeting. The table below summarizes key quantitative relationships between SOX9 expression levels and functional outcomes across different tissue and disease contexts.
Table 2: SOX9 Expression-Outcome Relationships Across Tissue Contexts
| Tissue/Cell Type | Expression Level | Functional Outcome | Therapeutic Opportunity |
|---|---|---|---|
| Alzheimer's astrocytes | Increased | Enhanced plaque clearance, cognitive preservation | Sox9 activation |
| Neuropathic pain astrocytes | Increased | Glycolytic activation, neuroinflammation, pain | Sox9 pathway inhibition |
| Ovarian cancer cells | Chemotherapy-induced | Stem-like state, chemoresistance | Sox9 inhibition with chemotherapy |
| Colorectal cancer | Overexpressed | Altered immune infiltration, immune evasion | Sox9 inhibition with immunotherapy |
| Glioblastoma | Highly expressed | Prognostic biomarker, immune suppression | Context-dependent modulation |
The prognostic significance of SOX9 varies considerably by tissue context. In ovarian cancer, patients in the top quartile of SOX9 expression following platinum treatment had significantly shorter overall survival probability than patients in the bottom quartile (hazard ratio = 1.33; log-rank P = 0.017) [28]. Conversely, in glioblastoma, high SOX9 expression was remarkably associated with better prognosis in the lymphoid invasion subgroups [23]. This context-dependent relationship underscores the importance of tissue-specific understanding when developing targeting strategies.
Cell-Type Specific Targeting Strategies: Methodological Approaches
Transcriptional Targeting Methodologies
Transcriptional targeting strategies leverage cell-type specific promoter elements to restrict SOX9 modulation to particular cellular contexts. The following experimental protocol outlines the key methodological approach for developing transcriptional targeting systems:
Protocol 1: Cell-Type Specific Promoter Validation for SOX9 Targeting
- Identify candidate promoters from single-cell RNA sequencing datasets specific to target cell populations (e.g., astrocyte-specific GFAP promoter, cancer-specific SOX9 auto-regulatory elements)
- Clone candidate promoters upstream of reporter genes (e.g., GFP, luciferase) in lentiviral or AAV vectors
- Validate specificity in mixed cell culture systems using flow cytometry and immunocytochemistry
- Assess silencing potential in non-target cell types using qRT-PCR and Western blot
- Test in vivo specificity using transgenic reporter models or xenotransplantation models
- Evaluate long-term stability of expression patterns in relevant disease models
Recent single-cell transcriptomic analyses have identified specific astrocyte subpopulations with distinct SOX9-associated pathogenic signatures, providing potential promoter elements for targeting neuropathic pain-associated astrocytes while sparing homeostatic astrocyte functions [68]. Similarly, in cancer, chemotherapy-induced SOX9 expression provides opportunities for therapy-responsive transcriptional targeting systems [28].
Post-Translational Modification Targeting
Post-translational modifications of SOX9 offer additional layers of cell-type specific regulation. In neuropathic pain, nerve damage induces abnormal phosphorylation of SOX9 at site 181, leading to increased nuclear translocation with abnormally high transcriptional activation of Hk1 [68]. This phosphorylation-specific activation mechanism provides a potential targeting opportunity limited to pathological states.
Protocol 2: Phosphorylation-State Specific SOX9 Targeting
- Generate phospho-specific SOX9 antibodies targeting phosphorylation site 181
- Validate antibody specificity using phosphorylation-deficient (S181A) and phosphomimetic (S181D) SOX9 mutants
- Conjugate with therapeutic modalities including PROTAC degraders, nanoparticle delivery systems, or imaging agents
- Test binding specificity in cell-free systems using peptide arrays
- Evaluate functional targeting in primary astrocyte cultures under inflammatory conditions
- Assess in vivo efficacy in neuropathic pain models using behavioral and biochemical readouts
Epigenetic Targeting Approaches
Epigenetic regulation of SOX9 provides another avenue for cell-type specific modulation. In ovarian cancer, SOX9 expression is regulated through resistant state-specific super-enhancers that are commissioned specifically in chemotherapy-resistant cells [28]. These epigenetic control elements can be leveraged for targeted intervention.
Protocol 3: Epigenetic Editing of SOX9 Locus
- Map cell-type specific enhancer elements using ATAC-seq and H3K27ac ChIP-seq in target versus non-target cells
- Design engineered zinc finger or CRISPR/dCas9 systems with transcriptional effector domains (KRAB for repression, VP64 for activation)
- Incorporate cell-type specific targeting moieties including nanobodies or peptide ligands on lipid nanoparticles
- Validate epigenetic modifications using ChIP-qPCR for specific histone modifications
- Assess transcriptional outcomes using single-cell RNA sequencing
- Evaluate functional consequences in disease-relevant functional assays
Experimental Validation: Signaling Pathways and Workflows
The diagram below illustrates the core SOX9 signaling pathway across different cellular contexts, highlighting potential intervention points for cell-type specific targeting:
The experimental workflow for validating cell-type specific targeting strategies involves multiple validation steps as illustrated below:
Research Reagent Solutions for SOX9 Targeting
Table 3: Essential Research Reagents for SOX9 Cell-Type Specific Targeting
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Cell-type specific promoters | GFAP (astrocytes), CD44 (cancer stem cells), SOX9 auto-regulatory elements | Restrict transgenic expression to target cells | Promoter size constraints, silencing potential |
| Phospho-specific antibodies | Anti-SOX9 pS181, Pan-SOX9 antibodies | Detect post-translational modifications in specific cell states | Cross-reactivity validation, application-specific validation |
| Epigenetic editors | dCas9-KRAB, dCas9-VP64, zinc finger repressors | Cell-type specific SOX9 modulation | Off-target epigenetic effects, delivery efficiency |
| Animal models | SOX9 reporter mice, SOX9 conditional knockout, Disease-specific models (Alzheimer's, neuropathic pain, cancer) | In vivo validation of targeting strategies | Species-specific differences, disease model relevance |
| Single-cell analysis tools | scRNA-seq, ATAC-seq, CITE-seq | Target identification and validation | Computational infrastructure, sample processing protocols |
The development of cell-type specific targeting strategies for SOX9 represents a critical frontier in therapeutic development across neurological disorders, cancer, and inflammatory diseases. The divergent roles of SOX9 in innate versus adaptive immunity—from promoting neuroinflammation in pain states to enabling tissue repair in neurodegeneration—necessitate precisely calibrated interventions that can modulate SOX9 activity in specific cellular contexts while avoiding on-target, off-tissue toxicity.
Future directions should focus on leveraging emerging single-cell multi-omics datasets to identify increasingly refined cell-type specific regulatory elements, developing smart delivery systems that respond to disease-specific microenvironments, and creating combinatorial approaches that target SOX9 in concert with complementary pathways. The successful clinical translation of SOX9-targeted therapies will depend on this sophisticated targeting approach, ensuring that therapeutic benefits are achieved without disrupting SOX9's essential physiological functions across diverse tissue contexts.
The emerging concept of "trained immunity" reveals that innate immune cells can build long-term inflammatory memory, challenging the traditional dichotomy between innate and adaptive immunity. Central to this phenomenon is the metabolic and epigenetic reprogramming of both hematopoietic progenitors and tissue-resident stem cells. This review elucidates the pivotal role of the transcription factor SOX9 as a key regulator bridging this process. We explore how SOX9, functioning as a pioneer factor, orchestrates a stem-like transcriptional state by remodeling the epigenome, thereby conferring sustained inflammatory phenotypes. The mechanistic insights provided herein, framed within the broader context of SOX9 in immunity, offer a foundation for novel therapeutic strategies in cancer, chronic inflammatory diseases, and regenerative medicine.
The immune system's ability to remember past encounters extends beyond the antigen-specific memory of B and T lymphocytes. Trained immunity, a de facto innate immune memory, enables innate immune cells and their progenitors to mount a heightened response upon re-exposure to a stimulus [69]. This memory is underpinned by epigenetic reprogramming and metabolic shifts in hematopoietic stem and progenitor cells (HSPCs), leading to altered responses in their myeloid progeny—a process termed central trained immunity [69]. Concurrently, self-renewing, tissue-resident cells like macrophages and astrocytes can undergo peripheral trained immunity [69]. The SOX family of transcription factors, particularly SOX9, has emerged as a critical node in regulating cell fate and stemness. Recent evidence positions SOX9 at the intersection of trained immunity and stem cell biology, where it drives long-term transcriptional reprogramming, influencing disease outcomes from cancer to neuroinflammation [1] [14] [64].
SOX9 Biology and Its Dual Role in Immunity
SOX9 is a member of the SRY-related HMG-box (SOX) family of transcription factors. Its protein structure includes a high-mobility group (HMG) box domain for DNA binding, a dimerization domain (DIM), and two transcriptional activation domains (TAM and TAC) [1]. As a pioneer factor, SOX9 can bind to compacted chromatin, initiate nucleosome displacement, and open chromatin for subsequent transcriptional activation [14].
In immunity, SOX9 exhibits a complex, context-dependent "double-edged sword" function [1]. It is crucial for maintaining macrophage function and promoting tissue repair [1]. Conversely, in cancer, SOX9 is frequently overexpressed and drives immune evasion by impairing immune cell function, contributing to an immunosuppressive microenvironment [1] [8]. Its role is not limited to adaptive immunity; it is a significant regulator of innate immune mechanisms and the emergent phenotypes of trained immunity.
Table 1: SOX9 Expression and Role in Different Tissues and Pathologies
| Tissue/Pathology | SOX9 Expression/Role | Functional Outcome | Reference |
|---|---|---|---|
| Hair Follicle Development | Pioneer factor activity | Reprograms epidermal stem cells to hair follicle stem cell fate | [14] |
| High-Grade Serous Ovarian Cancer | Chemotherapy-induced upregulation | Drives chemoresistance and a stem-like transcriptional state | [28] |
| Neuropathic Pain | Phosphorylation-induced activation in astrocytes | Triggers aberrant glycolysis and neuroinflammatory astrocyte subsets | [64] |
| Breast Cancer | Sustained expression in dedifferentiated cells | Promotes immune evasion via the B7x immune checkpoint | [70] |
| Liver | Expressed in Sox9+ periportal cells | Cell source for in vivo reprogramming to insulin-secreting cells | [71] |
Molecular Mechanisms: SOX9 as an Epigenetic and Metabolic Switch
SOX9 governs long-term cell reprogramming through two interconnected mechanisms: direct epigenetic remodeling and metabolic regulation.
Pioneer Factor Activity and Competitive Epigenetic Remodeling
In skin epidermis, SOX9 binding to closed chromatin at hair follicle-specific enhancers is a critical first step in fate switching. This binding recruits histone and chromatin modifiers, leading to nucleosome displacement and chromatin opening at pro-differentiation genes [14]. Simultaneously, SOX9 indirectly silences the previous cell identity by competing for and sequestering a limited pool of essential epigenetic co-factors (e.g., histone acetyltransferases, chromatin remodelers) away from the epidermal stem cell enhancers [14]. This competition model explains how a single pioneer factor can simultaneously activate one genetic program while repressing another.
Metabolic Reprogramming via the SOX9-HK1 Axis
In a model of neuropathic pain, nerve injury triggers phosphorylation of SOX9, enhancing its nuclear translocation and transcriptional activation of hexokinase 1 (HK1), the enzyme catalyzing the first irreversible step of glycolysis [64]. This leads to a high glycolytic flux and excessive lactate production. Lactate, in turn, serves as a precursor for histone lactylation (H3K9la), a novel epigenetic mark that promotes the transcription of pro-inflammatory and neurotoxic genes in a specific astrocyte subset (Astro1), driving chronic pain [64]. This axis directly links SOX9-driven metabolic changes to epigenetic reprogramming and long-lasting inflammatory memory in the central nervous system.
Experimental Protocols for Investigating SOX9-Mediated Reprogramming
Inducing and Tracking SOX9-Mediated Fate SwitchingIn Vivo
- Animal Model: Use transgenic mice where a MYC-epitope-tagged Sox9 transgene is controlled by a tetracycline-responsive element (TRE-Sox9) and crossed with a line expressing the reverse tetracycline-controlled transactivator (rtTA) under a tissue-specific promoter (e.g., Krt14-rtTA for epidermal stem cells) [14].
- Induction Protocol: Administer doxycycline (DOX) in the chow or drinking water to induce SOX9 expression. Monitor mice weekly for morphological changes [14].
- Lineage Tracing: For fate mapping, cross with Sox9-CreERT2 and reporter mice (e.g., Rosa26-loxP-STOP-loxP-tdTomato) to track the progeny of SOX9+ cells [71].
- Tissue Analysis: Harvest tissues at defined timepoints (e.g., Week 1, 2, 6, 12) post-induction for:
Profiling the Epigenetic and Transcriptional Landscape
- CUT&RUN (Cleavage Under Targets & Release Using Nuclease): Perform on FACS-sorted cells using a SOX9 antibody to map SOX9 genomic binding sites temporally. This method is suitable for low cell numbers and provides high-resolution transcription factor binding data [14].
- ATAC-seq (Assay for Transposase-Accessible Chromatin with sequencing): Apply to the same cell populations to assess global changes in chromatin accessibility throughout the reprogramming process [14].
- scRNA-seq (Single-Cell RNA Sequencing): Profile heterogeneous tissues (e.g., spinal cord in neuropathic pain models) to identify distinct cellular clusters and analyze SOX9 expression and its target genes across subpopulations [28] [64].
- ChIP-seq (Chromatin Immunoprecipitation with sequencing): For histone modifications (e.g., H3K27ac, H3K4me3, H3K9la) to link SOX9 activity to specific epigenetic marks [64].
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Studying SOX9 in Reprogramming and Immunity
| Reagent / Tool | Function / Application | Key Experimental Use |
|---|---|---|
| Krt14-rtTA; TRE-Sox9 Mice | Inducible, tissue-specific SOX9 expression in vivo | Model for studying SOX9-induced cell fate switching and tumorigenesis in epidermal stem cells [14] |
| CRISPR/Cas9 with SOX9 sgRNA | Targeted knockout of SOX9 | Functional validation of SOX9 necessity in chemoresistance and other phenotypes [28] |
| Anti-SOX9 Antibody | Immunodetection and chromatin immunoprecipitation | Used for immunofluorescence, Western blot, and CUT&RUN/ChIP-seq to visualize protein and map binding sites [14] |
| scRNA-seq Platform (10x Genomics) | Single-cell transcriptomic profiling | Unraveling cellular heterogeneity and identifying SOX9-expressing subpopulations in tissues [28] [64] |
| Glycolytic Rate Assay | Measurement of glycolytic flux (ECAR) | Functional assessment of the SOX9-HK1 axis in modulating cellular metabolism [64] |
SOX9 in Disease and Therapeutic Implications
The role of SOX9 in inflammatory memory and stem cell reprogramming has profound implications for human disease.
- Cancer and Chemoresistance: In high-grade serous ovarian cancer (HGSOC), platinum-based chemotherapy induces SOX9 expression. SOX9 is sufficient to drive a stem-like transcriptional state and confer significant platinum resistance [28]. Single-cell analysis of patient tumors confirms that SOX9 is upregulated post-chemotherapy, enriching for a stem-like, chemoresistant population [28].
- Neuroinflammatory Disease: In neuropathic pain, the SOX9-HK1-H3K9la axis establishes a maladaptive, long-lasting inflammatory memory in spinal cord astrocytes. Targeted modulation of this axis specifically dampens neuroinflammatory astrocyte subsets, promoting long-lasting pain relief, highlighting its therapeutic potential [64].
- Immune Evasion: In breast cancer, SOX9 safeguards dedifferentiated, stem-like tumor cells from immune surveillance by upregulating the immune checkpoint molecule B7x (B7-H4/VTCN1), creating an "immune desert" microenvironment [70]. This connects SOX9-driven stemness directly to the suppression of anti-tumor immunity.
SOX9 is a master regulator that deciphers and encodes inflammatory memory into long-term stem cell reprogramming. Through its dual capacity as a metabolic sensor and pioneer factor, it orchestrates widespread epigenetic changes that lock cells into sustained pro-inflammatory or stem-like states. This underpins its critical role in pathologies ranging from chronic pain to cancer chemoresistance. Future research should focus on:
- Identifying the specific co-factors SOX9 competes for in different cell types.
- Developing strategies to disrupt the SOX9-HK1-lactylation axis in neuroinflammation.
- Designing therapeutic interventions that selectively target SOX9-driven stemness without compromising its vital roles in tissue homeostasis and repair.
Understanding the precise mechanisms of SOX9-mediated reprogramming will unlock novel immunotherapeutic and regenerative medicine approaches aimed at erasing maladaptive inflammatory memory.
SOX9 in Cross-Tissue Perspective: Validating Roles from Cancer to Inflammation
The transcription factor SOX9 (SRY-related HMG-box 9) plays complex, context-dependent roles across multiple cancer types, functioning as both an oncogene and tumor suppressor through its regulation of cancer stemness, therapeutic resistance, and immune modulation. This whitepaper provides a comprehensive analysis of SOX9's differential functions in glioblastoma, breast, and gastrointestinal cancers, with particular emphasis on its intersecting roles in innate and adaptive immunity. By integrating recent molecular findings, experimental protocols, and pathway visualizations, we aim to establish a foundational framework for developing SOX9-targeted therapeutic strategies. The evidence demonstrates that SOX9 operates as a key regulatory node at the crossroads of tumorigenesis and immune evasion, making it a promising target for precision oncology approaches.
SOX9 Expression and Prognostic Significance Across Cancers
SOX9 exhibits markedly different expression patterns and clinical correlations across cancer types, reflecting its context-dependent biological functions. Table 1 summarizes the comparative oncology of SOX9 across the malignancies discussed in this review.
Table 1: Comparative Oncology of SOX9 Across Cancer Types
| Cancer Type | SOX9 Expression | Prognostic Significance | Primary Functions | Immune Correlations |
|---|---|---|---|---|
| Glioblastoma | Highly expressed [45] [23] | Better prognosis in IDH-mutant cases [45] | Diagnostic biomarker, immune infiltration regulation | Correlated with immune checkpoint expression and immunosuppressive TME [45] |
| Breast Cancer | Frequently overexpressed [6] | Driver of basal-like subtype and endocrine resistance [6] [72] | Tumor initiation, proliferation, metastasis | Promotes immune evasion by sustaining cancer stemness [6] |
| Gastric Cancer | Overexpressed, associated with chemoresistance [73] | Poor survival in chemoresistant cases [73] | Chemotherapy resistance, anti-apoptotic signaling | Limited direct evidence in search results |
| Colon Cancer | Reduced or absent in aggressive subsets [74] | Tumor suppressor; low SOX9 predicts poor survival [74] | Inhibits EMT and tumor progression | Limited direct evidence in search results |
Molecular Mechanisms and Signaling Pathways
SOX9 in Glioblastoma
In glioblastoma, SOX9 emerges as a significant diagnostic and prognostic biomarker, particularly in IDH-mutant cases [45]. Analysis of RNA sequencing data from TCGA and GTEx databases reveals that high SOX9 expression correlates strongly with immune cell infiltration and checkpoint expression, indicating its involvement in shaping the immunosuppressive tumor microenvironment [45] [23]. Surprisingly, in contrast to other cancers, high SOX9 expression in GBM is associated with better prognosis in specific molecular subgroups, especially those with lymphoid invasion [45].
The transcriptional network regulated by SOX9 in GBM involves 126 differentially significant genes, with 29 upregulated and 97 downregulated, suggesting a complex regulatory landscape [45]. Functional enrichment analyses indicate that these genes participate in critical cancer pathways including cell cycle regulation, signaling pathways, and immune response modulation.
Figure 1: SOX9 Regulatory Network in Glioblastoma. SOX9 expression correlates with immune infiltration and checkpoint expression in the tumor microenvironment (TME), with prognostic implications particularly significant in IDH-mutant cases.
SOX9 in Breast Cancer
In breast cancer, SOX9 demonstrates potent oncogenic functions, driving tumor initiation, proliferation, and therapy resistance through multiple molecular mechanisms [6]. SOX9 is significantly upregulated in basal-like breast cancer and serves as a determinant of ER-negative luminal stem/progenitor cells [6]. It creates a positive feedback loop with long non-coding RNA linc02095, mutually reinforcing each other's expression to promote tumor progression [6].
A critical mechanism of SOX9-mediated therapeutic resistance occurs in hormone receptor-positive breast cancers, where tamoxifen treatment promotes the formation of a RUNX2-ER complex that alters the ER cistrome and facilitates SOX9 upregulation [72]. This SOX9 induction is sufficient to drive resistance to both tamoxifen and estrogen deprivation therapies [72]. Additionally, SOX9 accelerates AKT-dependent tumor growth by regulating SOX10 expression and directly interacts with polycomb group protein Bmi1 to suppress tumor suppressor pathways [6].
Figure 2: SOX9-Mediated Therapeutic Resistance in Breast Cancer. Tamoxifen promotes RUNX2-ER complex formation leading to SOX9 upregulation, which drives stemness, metastasis, and therapy resistance through a positive feedback loop with linc02095.
SOX9 in Gastrointestinal Cancers
The role of SOX9 in gastrointestinal cancers demonstrates striking tissue-specific heterogeneity, functioning as an oncogene in gastric cancer while exhibiting tumor suppressor activity in colorectal cancer.
In gastric cancer, SOX9 overexpression drives chemoresistance through a well-characterized CDK1-SOX9-BCL-xL axis [73]. CDK1 regulates SOX9 through a miR-145-dependent epigenetic mechanism: CDK1-mediated phosphorylation activates DNMT1, which drives methylation-dependent silencing of miR-145, thereby relieving miR-145's repression of SOX9 [73]. The transcriptionally active SOX9 then directly upregulates BCL-xL, an anti-apoptotic protein that enables evasion of cisplatin-induced cell death [73].
In colorectal cancer, SOX9 exhibits tumor suppressor characteristics, contrasting with its oncogenic functions in other tissues [74]. Combined inactivation of SOX9 and APC results in more invasive tumors compared to APC inactivation alone, suggesting that SOX9 loss promotes tumor progression [74]. This invasive phenotype is enabled through epithelial-mesenchymal transition (EMT), allowing normally stationary colon cells to migrate and invade surrounding tissues [74]. Clinical data from nearly 400 patients in the TCGA database confirm that approximately 20% of colorectal cancers have low or absent SOX9 levels, with these patients experiencing lower overall survival [74].
SOX9 at the Intersection of Innate and Adaptive Immunity
SOX9 plays a complex, dual role in immunoregulation, functioning as a "double-edged sword" in both innate and adaptive immunity within the tumor microenvironment [1]. Its immunomodulatory functions have significant implications for cancer progression and therapeutic response.
Innate Immune Regulation
SOX9 significantly influences innate immune cells within the TME, particularly tumor-associated macrophages (TAMs) and neutrophils. Bioinformatics analyses reveal that SOX9 expression negatively correlates with genes associated with M1 macrophage function while showing positive correlation with M2-like polarization [1]. In colorectal cancer, SOX9 expression negatively correlates with infiltration levels of resting mast cells, monocytes, and eosinophils, but positively correlates with neutrophils and activated mast cells [1]. This cellular composition favors an immunosuppressive environment that facilitates tumor progression.
Adaptive Immune Regulation
In the adaptive immune compartment, SOX9 expression demonstrates strong negative correlation with genes associated with CD8+ T cell and NK cell function [1]. This suggests that SOX9 contributes to the creation of an "immune desert" microenvironment characterized by diminished effector T cell infiltration and function. Additionally, SOX9 plays a direct role in T-cell development by cooperating with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating lineage commitment of early thymic progenitors and influencing the balance between αβ T cell and γδ T cell differentiation [1].
Immune Evasion Mechanisms
A critical mechanism of SOX9-mediated immune evasion involves maintaining cancer cell stemness and dormancy. Research demonstrates that SOX9, along with SOX2, is crucial for latent cancer cells to remain dormant in secondary metastatic sites and avoid immune surveillance under immunotolerant conditions [6]. This capacity to sustain stemness properties enables long-term survival of cancer cells while evading immune detection. Furthermore, SOX9 expression in prostate cancer contributes to an immunosuppressive niche, particularly in response to androgen deprivation therapy, which enriches a subpopulation of club cells characterized by high SOX9 and low AR expression, further weakening anti-tumor immune responses [1].
Experimental Models and Methodologies
Key Experimental Models for SOX9 Research
In Vitro Models:
- Patient-derived tumoroids from gastric cancer PDX models for chemoresistance studies [73]
- Tamoxifen-resistant (TAMR) breast cancer cell lines derived from MCF7 cells under long-term estrogen-deprived (LTED) conditions [72]
- Cisplatin-resistant gastric cancer cell lines (AGS, MKN28, MKN45) for chemoresistance mechanism investigation [73]
In Vivo Models:
- Patient-derived xenograft (PDX) models for evaluating therapeutic responses [73]
- Conditional knockout mouse models (Krt19CreERT/Cdk1flox/flox) for studying CDK1-SOX9 axis [73]
- Tff1 knockout mouse models for gastric cancer studies [73]
- Combined SOX9 and APC inactivation models for colorectal cancer research [74]
Core Methodological Approaches
Table 2: Essential Methodologies for SOX9 Cancer Research
| Method Category | Specific Techniques | Key Applications | Technical Considerations |
|---|---|---|---|
| Transcriptomic Analysis | RNA-sequencing from TCGA/GTEx [45], DESeq2 for DEG analysis [45], GSEA [45] | SOX9 expression profiling, differential gene expression, pathway enrichment | Adjust for multiple testing; FDR < 0.25 for GSEA significance [45] |
| Epigenetic Analysis | Chromatin Immunoprecipitation (ChIP) [73], DNA methylation analysis [73] | Transcription factor binding, DNA methylation status of miR-145 promoter | Quality control with positive/negative controls essential |
| Protein Analysis | Western blotting [73], Immunohistochemistry [73], Immunofluorescence [73] | Protein expression validation, subcellular localization, clinical correlation | Multiple antibody validation recommended |
| Functional Assays | siRNA knockdown [73], Boyden chamber migration [72], Radius assay [72] | Mechanistic studies, migration/invasion assessment, functional validation | Include rescue experiments for specificity |
| Computational Biology | PPI network analysis (STRING) [45], GO/KEGG enrichment [45], Immune infiltration estimation (ssGSEA) [45] | Pathway analysis, network modeling, immune contexture evaluation | Use multiple algorithms for validation |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Investigation
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| Cell Lines | MCF7 TAMR models [72], AGS/MKN28/MKN45 gastric lines [73] | In vitro mechanism studies, drug screening | Authenticate with STR profiling; monitor mycoplasma [73] |
| Animal Models | Krt19CreERT/Cdk1flox/flox mice [73], Tff1-/- models [73], PDX models [73] | In vivo validation, therapeutic testing | Tamoxifen induction for conditional KO [73] |
| Antibodies | SOX9 IHC/IF antibodies [73], CDK1 antibodies [73] | Protein detection, localization, quantification | Optimize dilution for specific applications |
| Chemical Inhibitors | Dinaciclib (CDK1 inhibitor) [73], Cisplatin [73] | Pathway targeting, chemoresistance studies | Dose optimization critical for in vivo use [73] |
| siRNA/shRNA | ON-TARGETplus human siSOX9 [73], siCDK1 [73] | Genetic knockdown, functional validation | Include multiple targets to rule off-target effects |
| Analysis Tools | R packages (DESeq2, ggplot2, ClusteProfiler) [45], STRING database [45], Metascape [45] | Bioinformatics, statistical analysis, visualization | Reproducible code implementation essential |
Therapeutic Implications and Future Directions
The contrasting roles of SOX9 across cancer types present both challenges and opportunities for therapeutic development. In cancers where SOX9 functions as an oncogene (breast, gastric), targeted inhibition strategies show promise, particularly in combination with conventional therapies. For instance, in gastric cancer, CDK1 inhibition using dinaciclib disrupts the CDK1-SOX9-BCL-xL axis and resensitizes resistant models to cisplatin [73]. In PDX models, combining dinaciclib with cisplatin synergistically reduced tumor volume and extended survival compared to monotherapies [73].
In contexts where SOX9 exhibits tumor suppressor activity (colorectal), restoration of SOX9 function or targeting downstream effectors represents a potential strategy. The discovery that SOX9 inactivation promotes tumor progression through EMT in colorectal cancer suggests that interventions preventing EMT may benefit patients with SOX9-low tumors [74].
From an immunological perspective, targeting SOX9 represents a promising approach to modulate the immunosuppressive tumor microenvironment. Given its correlation with immune checkpoint expression and immune cell infiltration patterns [45] [1], SOX9 inhibition may synergize with immune checkpoint blockers to convert "immune desert" or immunosuppressive microenvironments into immunologically active ones.
Future research directions should include:
- Development of tissue-specific SOX9 modulators to account for its context-dependent functions
- Combinatorial strategies targeting SOX9 together with immune checkpoints or conventional therapies
- Advanced patient stratification based on SOX9 expression patterns and immune contexture
- Investigation of SOX9 regulation in cancer stem cell populations and its role in therapeutic resistance
The complex, dual nature of SOX9 in both tumorigenesis and immunoregulation underscores its importance as a multifaceted therapeutic target in precision oncology.
The transcription factor SOX9 (SRY-related high-mobility group box 9) plays complex, context-dependent roles in inflammatory pathologies. As a key regulator of development and tissue homeostasis, SOX9 exhibits strikingly divergent functions in different inflammatory environments. This whitepaper examines its contrasting roles in osteoarthritis (OA), where it primarily functions as a protective, anabolic factor, and in dental pulp inflammation, where it appears to suppress immune responses. These opposing functions highlight the intricate balance SOX9 maintains within innate and adaptive immune mechanisms and present both challenges and opportunities for therapeutic targeting. Understanding SOX9's dichotomous nature is essential for developing context-specific treatments for inflammatory diseases.
SOX9 Structure and Fundamental Roles in Immunity
SOX9 is a 509-amino acid polypeptide containing several functionally critical domains: an N-terminal dimerization domain (DIM), the central high-mobility group (HMG) box DNA-binding domain, and two transcriptional activation domains (TAM and TAC) at the middle and C-terminal regions, followed by a proline/glutamine/alanine (PQA)-rich domain [1]. The HMG domain facilitates nuclear localization and DNA binding, while the activation domains interact with various cofactors to regulate transcriptional activity [1].
Within immune regulation, SOX9 demonstrates fascinating dualities. It modulates T-cell development by cooperating with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), influencing the balance between αβ and γδ T-cell differentiation [1]. While not crucial for normal B-cell development, SOX9 is overexpressed in certain B-cell lymphomas, acting as an oncogene by promoting proliferation and inhibiting apoptosis [1]. This context-dependent functionality makes SOX9 a "double-edged sword" in immunology, capable of both promoting and suppressing inflammatory responses depending on the cellular environment.
SOX9 in Osteoarthritis: Protective Roles and Anabolic Functions
SOX9 as Master Chondrogenic Regulator
In osteoarthritis, SOX9 serves as the "master regulator" of chondrocytes, maintaining chondrocyte phenotype and cartilage homeostasis [75]. It directly activates transcription of essential extracellular matrix (ECM) components including type II collagen (COL2A1) and aggrecan (ACAN) [61]. SOX9 deficiency results in proteoglycan loss in healthy cartilage and exacerbates post-trauma cartilage erosion [61], establishing its fundamental protective role in joint health.
Molecular Mechanisms of SOX9 Dysregulation in OA
Multiple molecular mechanisms contribute to SOX9 dysregulation in OA pathogenesis, with recent research highlighting several key pathways:
Table 1: Mechanisms of SOX9 Dysregulation in Osteoarthritis
| Mechanism | Pathway Components | Effect on SOX9 | Functional Outcome |
|---|---|---|---|
| Fatty Acid Oxidation (FAO) | Altered lipid metabolism, acetyl-CoA accumulation, reduced AMPK activity [61] | Impaired phosphorylation, ubiquitination-mediated degradation [61] | Reduced ECM synthesis, increased catabolic enzymes |
| NF-κB Signaling | NF-κB binding to SOX9 promoter [75] | Positive regulation of expression [75] | Chondrocyte formation and development |
| Post-Translational Modifications | Acetylation, ubiquitination modifications [76] | Altered stability and transcriptional activity [76] | Disrupted cartilage homeostasis |
| Epigenetic Regulation | Fatty acid-derived acetyl-CoA [61] | Altered transcriptional activity | MMP13 and ADAMTS7 activation |
Recent findings demonstrate that obesity-associated OA features enhanced chondrocyte fatty acid oxidation (FAO), leading to acetyl-CoA accumulation that reduces AMPK activity, impairs SOX9 phosphorylation, and promotes its ubiquitin-mediated degradation [61]. This metabolic dysregulation creates a catabolic shift in joint homeostasis.
SOX9-Targeted Therapeutic Strategies for OA
Several promising therapeutic approaches aim to preserve or restore SOX9 function in OA:
- FAO Inhibition: Cartilage-targeted delivery of trimetazidine, an FAO inhibitor and AMPK activator, demonstrates superior efficacy in mouse models of post-traumatic OA [61].
- Stem Cell-Derived Vesicles: Dental pulp stem cell-derived intracellular vesicles (DPSC-IVs) and extracellular vesicles (DPSC-EVs) promote cartilage matrix regeneration and suppress ECM degradation in temporomandibular joint osteoarthritis (TMJ-OA) [77].
- Signaling Pathway Modulation: Regulation of WNT, Nrf2/ARE, and NF-κB signaling pathways that interact with SOX9 [76].
- Physical Therapies: Shockwave therapy and acupuncture that may indirectly influence SOX9 activity [76].
Figure 1: SOX9 Regulatory Pathways in Osteoarthritis. SOX9 sits at the crossroads of protective (blue) and pathological (red) pathways in OA, with therapeutic interventions (green) targeting these mechanisms.
SOX9 in Dental Pulp Inflammation: Immune-Suppressive Roles
SOX9 Downregulation in Pulpitis
In contrast to its protective role in OA, SOX9 exhibits strong anti-inflammatory functions in dental pulp that are suppressed during infection. Immunohistochemistry reveals significantly higher SOX9 protein expression in normal dental pulp nuclei (76.56% positive) compared to inflamed pulp tissue (16.40% positive) [78]. mRNA expression follows the same pattern, with substantial reduction in inflamed pulp [78]. This suppression is mediated by bacterial pathogens and inflammatory cytokines like TNF-α, which downregulates SOX9 expression in human dental pulp cells (HDPCs) [78] [79].
Mechanisms of SOX9-Mediated Immune Regulation
SOX9 knockdown experiments reveal its multi-faceted role in regulating pulp immunity through several mechanisms:
Table 2: SOX9 Functions in Dental Pulp Inflammation
| Process | Effect of SOX9 Knockdown | Experimental Evidence |
|---|---|---|
| Extracellular Matrix Balance | Inhibits type I collagen production; stimulates MMP2 and MMP13 enzymatic activities [78] | Gelatin/collagen zymography, Western blot [78] |
| Cytokine Signaling | Regulates IL-8 production [78] | Antibody arrays, chromatin immunoprecipitation [78] |
| Immune Cell Function | Suppresses monocyte maturation, migration, attachment, and phagocytosis [78] | THP-1 cell migration, attachment, and phagocytosis assays [78] |
| Transcriptional Regulation | Reduced SOX9 binding to MMP1, MMP13, and IL-8 gene promoters after TNF-α treatment [78] | Chromatin immunoprecipitation (ChIP) [79] |
Chromatin immunoprecipitation studies demonstrate that TNF-α treatment reduces SOX9 binding to matrix metalloproteinase (MMP-1, MMP-13) and IL-8 gene promoters [78] [79], providing a direct mechanism for SOX9-mediated inflammatory regulation.
NF-κB-MMP12 Inflammatory Axis
In pulpitis, LPS-stimulated human dental pulp stem cells (hDPSCs) activate NF-κB signaling, which drives transcription of matrix metalloproteinase 12 (MMP12) [80]. This NF-κB→MMP12 cascade amplifies inflammatory responses independently of SOX9 regulation, representing a parallel inflammatory pathway in dental pulp [80].
Figure 2: SOX9 Inflammatory Regulation in Dental Pulp. SOX9 maintains homeostasis in normal pulp (blue) but is suppressed during infection (red), while parallel NF-κB pathways (yellow) drive inflammation independently.
Direct Comparison: Contrasting SOX9 Functions
The divergent roles of SOX9 in these two inflammatory contexts highlight its context-dependent functionality:
Table 3: SOX9 Functional Comparison in Osteoarthritis vs. Dental Pulp Inflammation
| Parameter | Osteoarthritis | Dental Pulp Inflammation |
|---|---|---|
| SOX9 Expression | Maintained or targeted for degradation [61] | Significantly downregulated [78] |
| Primary Role | Protective, anabolic [75] [61] | Immune suppressive [78] |
| ECM Regulation | Promotes COL2A1 and aggrecan synthesis [61] | Maintains type I collagen, inhibits MMPs [78] |
| Inflammatory Mediators | Suppresses MMP13, ADAMTS7 [61] | Regulates IL-8, modulates monocyte function [78] |
| Therapeutic Goal | Preserve or enhance SOX9 function [76] | Potential context-dependent modulation |
| Key Regulators | FAO, AMPK, NF-κB [61] [75] | TNF-α, bacterial pathogens [78] |
| Immune Context | Primarily innate immunity in joint tissue [1] | Innate and adaptive immune cell regulation [78] |
Experimental Approaches for SOX9 Research
Key Methodologies
Investigating SOX9's dual roles requires specialized experimental approaches:
- SOX9 Knockdown: MISSION esiRNA targeting human SOX9 effectively knocks down expression in human dental pulp cells (HDPCs) for functional studies [79].
- Chromatin Immunoprecipitation (ChIP): Identifies direct SOX9 binding to promoters of target genes like MMP1, MMP13, and IL-8 [78] [79].
- Inflammation Models: IL-1β-stimulated chondrocytes for OA studies [77]; LPS-stimulated hDPSCs or P. gingivalis/TNF-α-treated pulp cells for pulpitis models [78] [80].
- Functional Assays: Gelatin/collagen zymography for MMP activity [78]; Transwell migration, attachment, and phagocytosis assays for immune cell function [78].
The Researcher's Toolkit
Table 4: Essential Research Reagents for SOX9 Inflammation Studies
| Reagent/Cell Type | Application | Key Function |
|---|---|---|
| Human Dental Pulp Cells (HDPCs) | Pulp inflammation studies [78] [79] | Model SOX9 regulation in pulp tissue |
| Primary Chondrocytes | OA mechanism studies [61] | Study SOX9 in cartilage homeostasis |
| MISSION esiRNA (SOX9) | SOX9 knockdown [79] | Investigate SOX9 loss-of-function |
| THP-1 Monocyte Cell Line | Immune response assays [78] | Study monocyte function modulation |
| Recombinant TNF-α | Inflammation induction [78] | Model inflammatory SOX9 downregulation |
| IL-1β | Chondrocyte catabolism induction [77] | Stimulate OA-like conditions |
| LPS | NF-κB pathway activation [80] | Model bacterial-induced inflammation |
| Trimetazidine | FAO inhibition studies [61] | Test metabolic OA interventions |
SOX9 embodies the complexity of transcription factor biology in inflammatory diseases, functioning as either protector or suppressor depending on tissue context. In osteoarthritis, SOX9 maintenance represents a promising therapeutic strategy to preserve cartilage integrity, while in dental pulp inflammation, its anti-inflammatory properties suggest potential for modulating immune responses. Future research should explore the upstream regulators that determine SOX9's contextual functions and develop tissue-specific delivery systems for SOX9-modulating therapies. Understanding how SOX9 integrates innate and adaptive immune signaling will be crucial for developing next-generation immunomodulatory treatments that leverage its unique dual nature across inflammatory disease spectra.
The transcription factor SOX9, a key regulator of developmental processes and stem cell maintenance, has emerged as a critical oncogenic driver in multiple cancers. Recent investigations reveal a novel and pivotal function for SOX9 in orchestrating tumor immune evasion by regulating immune checkpoint expression and fostering an immune-suppressive tumor microenvironment (TME). This whitepaper synthesizes evidence establishing SOX9 as a master regulator of tumor cell dedifferentiation and a direct mediator of TME "desertification"—a state characterized by markedly reduced T lymphocyte infiltration. We delineate the mechanistic pathway through which SOX9 induces the expression of the non-classical immune checkpoint B7x (B7-H4), thereby suppressing T cell function and facilitating immune escape. Furthermore, we explore the interplay between the SOX9-B7x axis and canonical checkpoints like PD-1/PD-L1, discussing implications for combination immunotherapy resistance. The provided experimental protocols and research toolkit aim to equip scientists with methodologies to further investigate SOX9-mediated immunomodulation and advance targeted therapeutic strategies.
SOX9 is a member of the SRY-related high-mobility group (HMG) box transcription factor family, essential for cell fate determination, chondrogenesis, and organogenesis. In cancer, SOX9 is frequently overexpressed and promotes tumor initiation, progression, and therapy resistance by conferring stem-like properties upon tumor cells [1] [6]. Beyond its established role in tumorigenesis, SOX9 operates as a crucial nexus between tumor cell dedifferentiation and immune evasion. It functions as a pioneer factor, capable of binding closed chromatin and reprogramming the epigenetic landscape to drive transcriptional programs that simultaneously enforce a dedifferentiated, multipotent state and suppress anti-tumor immunity [14]. This dual capacity positions SOX9 as a central player in shaping the TME, particularly in driving its transition to an immune-"cold" or "desertified" state, which is refractory to current immune checkpoint blockade therapies.
Molecular Mechanisms of SOX9-Driven Immune Evasion
Direct Transcriptional Regulation of Immune Checkpoints
A primary mechanism of SOX9-mediated immunosuppression is the direct transcriptional upregulation of the immune checkpoint ligand B7x (B7-H4, VTCN1). In basal-like breast cancer (BLBC) models, SOX9 was shown to induce B7x expression through two distinct pathways:
- STAT3 Activation: SOX9 activates Signal Transducer and Activator of Transcription 3 (STAT3), a known regulator of various immunosuppressive genes.
- Direct Promoter Binding: SOX9 directly binds to the promoter region of the gene encoding B7x, acting as a transcription factor to drive its expression [15].
B7x is a potent inhibitor of T cell proliferation, cell cycle progression, and cytokine production (e.g., IL-2). Its specific upregulation in SOX9-high, dedifferentiated tumor cells protects them from T cell-mediated killing, thereby safeguarding the tumor-initiating cell pool [15] [81]. This SOX9-B7x axis is a dedifferentiation-associated immunosuppression pathway critical for malignant progression.
Induction of a Broadly Immunosuppressive Tumor Microenvironment
SOX9 orchestrates a comprehensive remodeling of the TME to favor immune escape. Key aspects of this remodeling include:
- T Cell Exclusion: Conditional knockout of Sox9 in premalignant murine breast lesions resulted in a massive accumulation of infiltrating CD3+ T cells, including both CD4+ and CD8+ subsets, along with elevated levels of granzyme B+ and perforin+ cytotoxic cells. This indicates that epithelial SOX9 is both necessary and sufficient to limit T lymphocyte recruitment and/or survival in nascent tumors [15].
- Altered Immune Cell Infiltration: Bioinformatics analyses of human cancer datasets (e.g., TCGA) reveal that high SOX9 expression correlates negatively with the infiltration of cytotoxic CD8+ T cells and NK cells. Conversely, it can be positively associated with immunosuppressive cell types, such as M2 macrophages and regulatory T cells (Tregs), contributing to the "immune desert" phenotype [1] [43].
- Extracellular Matrix (ECM) Remodeling: In lung adenocarcinoma, SOX9 significantly elevates the expression of collagen-related genes and increases the deposition of collagen fibers. This SOX9-driven increase in tumor stiffness is proposed to act as a physical barrier that inhibits the infiltration of dendritic cells, CD8+ T cells, and NK cells, further exacerbating the immune-cold TME [43].
Table 1: SOX9-Mediated Effects on Tumor-Infiltrating Immune Cells
| Immune Cell Type | Effect of High SOX9 | Functional Consequence |
|---|---|---|
| CD8+ Cytotoxic T Cells | ↓ Infiltration, ↓ Function | Reduced tumor cell killing |
| CD4+ T Helper Cells | ↓ Infiltration (Certain Subsets) | Impaired adaptive immune response |
| Natural Killer (NK) Cells | ↓ Infiltration, ↓ Activity | Loss of innate anti-tumor cytotoxicity |
| M1 Macrophages | ↓ Associated Gene Signature | Attenuated pro-inflammatory response |
| M2 Macrophages / TAMs | ↑ Infiltration (In some contexts) | Promotion of immunosuppression & tissue repair |
| Dendritic Cells (DCs) | ↓ Infiltration | Impaired antigen presentation & T cell priming |
The following diagram illustrates the core signaling pathway by which SOX9 promotes an immune-suppressive tumor microenvironment.
Diagram 1: SOX9-Driven Immunosuppressive Signaling Pathway. SOX9 promotes an immune-cold TME via B7x upregulation and ECM remodeling.
The SOX9-B7x Axis and Canonical Checkpoints: PD-1/PD-L1 and CTLA-4
While SOX9 directly regulates B7x, its relationship with the canonical checkpoints PD-1/PD-L1 and CTLA-4 is more nuanced and context-dependent.
- Distinct but Complementary Role to PD-1/PD-L1: In triple-negative breast cancer (TNBC), high B7x expression in tumor cells is associated with an immune-cold TME, whereas high PD-L1 is linked to an immunoreactive microenvironment [15]. This suggests that the SOX9-B7x pathway may represent a parallel, and potentially dominant, immune evasion mechanism in tumors that do not respond to anti-PD-1/PD-L1 therapy.
- Overcoming Anti-PD-L1 Resistance: The therapeutic potential of targeting the SOX9-B7x axis is highlighted by experiments in advanced mouse tumor models, where B7x targeting not only inhibited tumor growth on its own but also overcame resistance to anti-PD-L1 immunotherapy [15]. This positions the SOX9-B7x pathway as a promising candidate for combination therapy.
- Broad Checkpoint Regulation in Cancer Stem Cells: Cancer stem cells (CSCs), which are often enriched following SOX9 activation, display a wide array of immunoregulatory checkpoints on their surface. These include not only B7x but also B7-H3, VISTA, and HHLA2, which collectively contribute to resistance against anti-PD-1, anti-PD-L1, and anti-CTLA-4 therapies [81].
Table 2: Comparison of Immune Checkpoint Pathways in SOX9-High Tumors
| Feature | SOX9-B7x Axis | PD-1/PD-L1 Pathway | CTLA-4 Pathway |
|---|---|---|---|
| Primary Regulator | SOX9 (Transcription factor in tumor cell) | Inflammatory signals (e.g., IFN-γ) in TME | T cell activation |
| Key Ligand | B7x (B7-H4) | PD-L1 (B7-H1) | B7-1 / B7-2 (CD80/CD86) |
| Key Receptor | Not fully elucidated (putative on T cells) | PD-1 (on T cells) | CTLA-4 (on T cells) |
| Mechanism of Action | Inhibits T cell proliferation & cytokine production | Induces T cell exhaustion & apoptosis | Attenuates early T cell activation |
| Association with TME | Immune-cold / desertified | Can be present in both immune-hot and -cold | Lymph node & early TME |
| Therapeutic Implication | Emerging target to overcome anti-PD-1 resistance | Established target in multiple cancers | Established target (e.g., melanoma) |
Experimental Protocols for Investigating SOX9-Immune Checkpoint Interactions
Protocol: Validating the SOX9-B7x AxisIn Vivo
Objective: To determine the requirement of SOX9 for B7x expression and immune evasion during early tumorigenesis in vivo.
Materials:
- Mouse Model: C3-TAg mouse model of basal-like breast cancer [15].
- Genetic Manipulation: MMTV-iCre;Sox9Fl/Fl;C3-TAg mice (Sox9-cKO) and Sox9Fl/Fl;C3-TAg controls (WT).
- Antibodies: Anti-CD4 (clone GK1.5), Anti-CD8α (clone 2.43) for T cell depletion; Isotype controls.
Methodology:
- Tissue Collection: Harvest mammary glands from Sox9-cKO and WT mice at ~4 months of age when mammary intraepithelial neoplasia (MIN) develops.
- Immune Phenotyping:
- Flow Cytometry: Generate single-cell suspensions from mammary glands. Stain with fluorescently labeled antibodies against CD45, CD3, CD4, CD8, and B220. Analyze using spectral flow cytometry to quantify immune cell populations [15].
- Immunohistochemistry (IHC): Section mammary tissues. Perform IHC staining for CD3, CD8, Granzyme B, and Perform to visualize and quantify T cell infiltration and activation.
- Molecular Analysis:
- IHC/Immunofluorescence: Co-stain for SOX9 and B7x on serial tissue sections to assess correlation of protein expression.
- STAT3 Pathway Analysis: Perform Western blot or IHC for phosphorylated STAT3 (p-STAT3) on tissue lysates/sections.
- Functional Validation (T cell Depletion):
- Administer anti-CD4 and anti-CD8 depleting antibodies (or isotype control) to Sox9-cKO;C3-TAg mice intraperitoneally every 5 days for 2 months, starting at 3 months of age.
- Monitor for tumor onset and progression. Analyze resulting tumors for SOX9 expression to confirm origin from Sox9-null cells [15].
Protocol: Assessing SOX9-Mediated Suppression of Human T Cell FunctionIn Vitro
Objective: To test the direct impact of tumor cell-SOX9 on the proliferation and cytotoxic function of human T cells.
Materials:
- Cell Lines: SOX9-negative MCF7ras or HCC1937 (TNBC) human breast cancer cells.
- Genetic Manipulation: Lentiviral vectors for SOX9 overexpression (SOX9-OE) and empty vector control (EV).
- Human Immune Cells: Peripheral blood mononuclear cells (PBMCs) from healthy donors.
- Antigen-Specific T Cells: Engineered CD8+ T cells transduced with a lentiviral vector expressing an NY-ESO-1-specific T cell receptor (TCR) [15].
Methodology:
- T Cell Proliferation Assay:
- Isolate CD4+ and CD8+ T cells from human PBMCs.
- Co-culture control (EV) or SOX9-OE tumor cells with T cells in the presence of anti-CD3/CD28 stimulation.
- After 3-5 days, measure T cell proliferation using flow cytometry-based assays (e.g., CFSE dilution or Ki67 staining) [15].
- Antigen-Specific Cytotoxicity Assay:
- Co-culture control (EV) or SOX9-OE MCF7ras cells (which express NY-ESO-1 and HLA-A2) with NY-ESO-1 TCR-engineered CD8+ T cells.
- After 24-48 hours, quantify tumor cell killing using real-time cell death assays (e.g., IncuCyte caspase-3/7 reagent) or by measuring the release of lactate dehydrogenase (LDH) [15].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Studying SOX9 and Immune Checkpoints
| Reagent / Tool | Specific Example | Function & Application |
|---|---|---|
| Mouse Models | C3-TAg (BLBC); KrasLSL-G12D (LUAD) | Study SOX9 function in immunocompetent, autochthonous tumor contexts [15] [43]. |
| Conditional KO | MMTV-iCre;Sox9Fl/Fl | Enables tissue-specific deletion of Sox9 to study its necessity in tumor epithelium [15]. |
| SOX9 Expression | Inducible TRE-Sox9; Krt14-rtTA | Allows temporal control of SOX9 overexpression in specific cell types (e.g., epidermal stem cells) [14]. |
| Immune Cell Depleting Antibodies | Anti-CD4 (clone GK1.5); Anti-CD8α (clone 2.43) | Functionally validate the role of specific T cell subsets in controlling SOX9-deficient tumors [15]. |
| Flow Cytometry Panels | Antibodies against CD45, CD3, CD4, CD8, CD19, NK1.1, etc. | Comprehensive immune profiling of the tumor microenvironment [15] [43]. |
| Lentiviral Vectors | SOX9-OE; shSOX9; NY-ESO-1 TCR | Genetically manipulate SOX9 expression in tumor cells or engineer antigen-specific T cells [15]. |
| Critical Assays | Co-culture + CFSE proliferation; Cytotoxicity (LDH/IncuCyte) | Quantify the functional impact of SOX9 on T cell activity in vitro [15]. |
SOX9 is a master regulatory node that integrates control over tumor cell differentiation status with the capacity to sculpt a profoundly immunosuppressive TME. Its role in directly transactivating the B7x checkpoint and promoting T cell exclusion provides a mechanistic explanation for the immune-cold phenotype observed in SOX9-high cancers like BLBC and LUAD. The demonstrated ability of B7x blockade to overcome resistance to anti-PD-L1 therapy underscores the translational significance of this axis.
Future research should focus on:
- Identifying the B7x Receptor: The definitive receptor for B7x remains elusive; its identification is critical for fully understanding the pathway and developing receptor-blocking therapies.
- Exploring Epigenetic Co-factors: How SOX9, as a pioneer factor, competes for and redistributes epigenetic modifiers to simultaneously activate immunosuppressive programs and silence pro-inflammatory genes warrants deeper investigation [14].
- Developing SOX9-Targeted Therapies: Directly targeting transcription factors is notoriously challenging. Alternative strategies include exploiting synthetic lethality in SOX9-high tumors, developing protein degradation platforms (PROTACs), or identifying and targeting key downstream effector genes like B7x. In conclusion, correlating SOX9 with immune checkpoint regulation provides a robust framework for understanding and therapeutically targeting the immune-cold TME. Incorporating SOX9 and B7x status into biomarker panels could better stratify patients for existing immunotherapies and inform the development of novel combination regimens.
The transcription factor SRY-box transcription factor 9 (SOX9) is a well-established master regulator of embryonic development, cell-fate decisions, and differentiation in various tissues [82]. Beyond its developmental roles, SOX9 is increasingly implicated in the pathogenesis of numerous cancers, where it influences tumor initiation, metastasis, and drug resistance [82] [28]. Its function has been extensively studied in epithelial cell lineages across various malignancies, including lung adenocarcinoma, ovarian cancer, and glioblastoma [83] [28] [45]. However, its expression pattern and functional role within the immune compartment—specifically in myeloid and lymphoid cell subsets—remain a critical area of investigation. This whitepaper synthesizes current evidence to clarify SOX9 expression in immune cells and frames these findings within the broader thesis of SOX9's distinct roles in innate versus adaptive immunity. A precise understanding of its cell-type-specific expression is fundamental to deciphering its impact on the tumor immune microenvironment and its potential as a therapeutic target.
Single-Cell RNA Sequencing Evidence on SOX9 Expression in Immune Cells
Large-scale single-cell RNA sequencing (scRNA-seq) atlases provide the most direct evidence for evaluating gene expression across diverse cell types. Analysis of data from the Human Protein Atlas, which incorporates scRNA-seq data from normal tissues, offers a definitive conclusion regarding SOX9 expression in immune cells.
Table 1: SOX9 Expression Profile Based on Single-Cell Transcriptomics
| Data Source | Immune Cell Specificity | Specificity Category | Key Findings |
|---|---|---|---|
| Human Protein Atlas (scRNA-seq from normal tissues) [84] | Not detected | Not detected in immune cells | SOX9 mRNA is not detected in immune cell types; specificity is classified as "Not detected in immune cells". |
| Cell type enhanced (non-immune) | Secretory epithelial cells | Expression is enhanced in specific non-immune cell types, including ductal cells, gastric glandular cells, and prostatic club cells. |
This data indicates that SOX9 is not a marker for myeloid or lymphoid lineages and its primary functions, as derived from its expression pattern, are not intrinsic to immune cell biology. Therefore, the documented profound influence of SOX9 on the tumor immune microenvironment is likely an indirect effect, mediated through its expression in cancer or other stromal cells.
SOX9-Mediated Immunomodulation in the Tumor Microenvironment
Although SOX9 is not expressed in immune cells themselves, its activity in cancer cells sculpts the immune landscape of tumors, influencing both innate and adaptive anti-tumor responses. The mechanisms of this crosstalk are multifaceted and critical for understanding therapy resistance.
SOX9 and Innate Immune Evasion
The interaction between SOX9+ tumor cells and innate immune cells is a key mechanism of immune evasion. Research in lung cancer metastasis reveals that cancer cells exhibiting a SOX9-driven regenerative program display SOX9-dependent resistance to Natural Killer (NK) cells [83]. This resistance mechanism allows metastatic cells to escape NK cell-mediated killing, a crucial arm of the innate immune system. Furthermore, a study on head and neck squamous cell carcinoma (HNSCC) identified a novel SOX9-mediated immunosuppressive axis. SOX9 in tumor cells directly regulates the expression of Annexin A1 (Anxa1). This protein then interacts with Formyl Peptide Receptor 1 (Fpr1) on neutrophils, inducing apoptosis in these innate immune cells by promoting mitochondrial fission and inhibiting mitophagy. The subsequent reduction of Fpr1+ neutrophils in the tumor microenvironment impairs the anti-tumor immune response [85].
Table 2: SOX9 in Shaping the Immune Microenvironment Across Cancers
| Cancer Type | SOX9 Expression Context | Immune Interplay & Mechanism | Functional Outcome |
|---|---|---|---|
| Lung Adenocarcinoma [83] | Metastatic cancer cells | Confers resistance to NK cell-mediated killing. | Enables metastatic outbreak and immune evasion. |
| Head and Neck SCC [85] | Epithelial tumor cells | Upregulates Anxa1, which binds Fpr1 on neutrophils, causing their apoptosis. | Reduces neutrophil accumulation, impairing cytotoxic T cell function and driving therapy resistance. |
| Thymic Epithelial Tumors [82] | Tumor cells | High SOX9 expression correlates with an immunosuppressive microenvironment dominated by M2 macrophages. | Associated with unfavorable clinical outcomes. |
| Glioblastoma [45] | Tumor cells | Expression correlates with immune cell infiltration and checkpoint expression. | Contributes to an immunosuppressive microenvironment. |
SOX9 and Adaptive Immune Regulation
SOX9 also significantly influences the adaptive immune landscape. In thymic epithelial tumors (TETs), bioinformatics analysis has shown that high SOX9 expression is associated with the suppression of T-cell related pathways. Genes negatively associated with SOX9 expression were mapped to pathways including the T cell receptor signaling pathway, Th17 cell differentiation, and the PD-1 checkpoint pathway [82]. This suggests that SOX9 activity in tumor cells can create an immune "cold" microenvironment, hindering the activation and function of adaptive immune cells. The aforementioned HNSCC study further demonstrates that the SOX9-Anxa1 axis, by depleting neutrophils, subsequently impairs the infiltration and tumor-killing capacity of cytotoxic CD8 T cells and γδ T cells, leading to resistance against combined anti-PD-1 and anti-LAG-3 immunotherapy [85].
Experimental Protocols for Single-Cell Validation
For researchers aiming to validate SOX9 expression and its functional interactions, the following detailed methodologies, drawn from cited studies, provide a robust technical foundation.
Single-Cell RNA Sequencing (scRNA-seq) Workflow
The core protocol for profiling SOX9 expression and the immune microenvironment at single-cell resolution involves the following key steps, as implemented in recent studies [83] [85]:
- Single-Cell Suspension Preparation: Freshly resected human or mouse tumor tissues are dissociated into single-cell suspensions using enzymatic digestion (e.g., collagenase, dispase) and mechanical disruption.
- Cell Viability and Quality Control: The viability of the single-cell suspension is assessed using metrics like trypan blue exclusion or fluorescence-based viability dyes. Libraries with low viability or complexity are filtered out.
- Droplet-Based scRNA-seq Library Preparation: Single-cell suspensions are loaded into a microfluidic device (e.g., 10x Genomics) where individual cells are encapsulated in droplets with barcoded beads. Within each droplet, reverse transcription occurs, labeling each transcript with a unique cellular barcode and a unique molecular identifier (UMI). Libraries are then constructed and sequenced.
- Bioinformatic Analysis:
- Data Preprocessing: Raw sequencing data is processed using tools like
Cell Rangerto align reads to a reference genome and generate a feature-barcode matrix. - Quality Control and Filtering: Cells with an unusually high or low number of detected genes and a high percentage of mitochondrial reads are filtered out.
- Clustering and Cell Type Annotation: Dimensionality reduction (e.g., PCA, UMAP) is performed, and cells are clustered using graph-based algorithms (e.g., Phenograph, Seurat). Cell types are annotated based on the expression of canonical markers (e.g.,
PTPRCfor immune cells,CD3D/CD3Efor T cells,KRTgenes for epithelial cells). - SOX9 Expression Analysis: SOX9 expression is visualized on UMAP plots and its expression levels are quantified across the annotated cell clusters to determine its presence in immune versus non-immune populations.
- Data Preprocessing: Raw sequencing data is processed using tools like
Functional Validation via Genetic Perturbation
To establish causality in the SOX9-Anxa1-Fpr1 axis, as demonstrated in the HNSCC study, the following genetic and molecular approaches are critical [85]:
- In Vivo Transgenic Mouse Models: Utilize inducible, cell-type-specific Cre-driver lines (e.g.,
Krt14-rtTA;TRE-Sox9for epithelial-specific SOX9 expression) to manipulate SOX9 in a controlled manner. - CRISPR/Cas9-Mediated Knockout: To ablate SOX9 function, use CRISPR/Cas9 technology. Transduce tumor cells with lentivirus carrying SOX9-targeting sgRNA and Cas9. Validate knockout efficiency via Western blot and quantitative RT-PCR.
- Rescue Experiments: To confirm the specificity of the SOX9-Anxa1 pathway, perform rescue experiments in SOX9-knockout cells by re-introducing Anxa1 and assessing whether it restores the observed phenotype (e.g., neutrophil apoptosis).
- Chromatin Immunoprecipitation (ChIP): To test if SOX9 directly regulates Anxa1 transcription, perform ChIP assays. Cross-link SOX9 to DNA in tumor cells, immunoprecipitate with an anti-SOX9 antibody, and quantify the enrichment of the ANXA1 promoter region by qPCR.
Diagram 1: A logical workflow for experimentally validating the indirect immunomodulatory role of SOX9, based on findings from the literature.
The Scientist's Toolkit: Key Research Reagents and Solutions
The following table details essential materials and reagents, derived from the cited studies, for investigating SOX9 in the context of immunity.
Table 3: Research Reagent Solutions for SOX9-Immune Axis Studies
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Krt14-rtTA; TRE-Sox9 Mouse Model [14] | Enables inducible, epithelial-specific SOX9 expression in vivo. | Studying the causal role of SOX9 in tumor cells on immune microenvironment remodeling. |
| Anti-SOX9 Antibody [82] | Detects SOX9 protein expression via immunohistochemistry (IHC) or immunofluorescence (IF). | Validating SOX9 nuclear expression in tumor cells and confirming its absence in immune cells. |
| CRISPR/Cas9 with SOX9 sgRNA [28] | Mediates genetic knockout of SOX9 to study loss-of-function phenotypes. | Determining the necessity of SOX9 for conferring resistance to NK cell killing [83]. |
| Anti-Anxa1 / Anti-Fpr1 Neutralizing Antibodies [85] | Blocks the interaction between tumor-derived Anxa1 and Fpr1 on neutrophils. | Testing the functional role of the SOX9-Anxa1-Fpr1 axis in neutrophil apoptosis and therapy resistance. |
| Anti-PD-1 / Anti-LAG-3 Antibodies [85] | Immune checkpoint blockade for in vivo therapy studies. | Modeling and overcoming SOX9-mediated resistance to combination immunotherapy. |
| Droplet-Based scRNA-seq Kit (10x Genomics) [83] | Profiles transcriptomes of thousands of single cells from a heterogeneous sample. | Unbiased identification of SOX9+ tumor cell clusters and associated immune cell states. |
The consensus from single-cell transcriptomic data is clear: SOX9 is not expressed in myeloid or lymphoid cells. Its significant impact on innate and adaptive immunity is therefore an indirect, non-cell-autonomous effect. SOX9 operates as a master regulatory pioneer factor within cancer and epithelial cells, reprogramming their transcriptional state and secretome to sculpt an immunosuppressive tumor microenvironment [14]. Key mechanisms include inducing resistance to NK cells, activating the Anxa1-Fpr1 axis to deplete tumoricidal neutrophils, and suppressing T cell signaling pathways.
Future research should focus on targeting these SOX9-mediated immunomodulatory pathways. Strategies could involve inhibiting the SOX9-Anxa1-Fpr1 axis to restore neutrophil and cytotoxic T cell function, potentially overcoming resistance to existing immunotherapies. A deeper understanding of how the SOX9-driven secretome disables immune surveillance will be crucial for developing novel combination treatments aimed at restoring anti-tumor immunity.
Mendelian Randomization (MR) has emerged as a powerful methodological framework for strengthening causal inference in observational biomedical research. By leveraging genetic variants as instrumental variables, MR helps disentangle true causal relationships from confounding factors and reverse causation biases that often plague epidemiological studies. This whitepaper provides an in-depth technical examination of MR methodologies, with particular emphasis on applications in immunology and the study of transcription factors like SOX9. We detail experimental protocols, analytical frameworks, and recent advances including single-cell MR approaches that are revolutionizing our understanding of immune mechanisms in disease pathogenesis. The integration of MR evidence with functional genomic data offers a robust paradigm for identifying and validating novel therapeutic targets.
Mendelian Randomization constitutes a special application of instrumental variable analysis that uses genetic variants as proxies for modifiable exposures to assess causal relationships with health outcomes. The foundation of MR rests on three core assumptions, often termed the "IV assumptions": (1) the genetic variant must be robustly associated with the exposure of interest; (2) the variant must not be associated with confounding factors; and (3) the variant must influence the outcome only through the exposure, not via alternative pathways (pleiotropy). The random assortment of genetic alleles during meiosis essentially mimics a randomized experiment, thereby reducing susceptibility to confounding factors that typically complicate observational studies.
Recent methodological advances have significantly expanded MR applications in complex disease research. Two-sample MR, which uses summary statistics from separate genome-wide association studies (GWAS) for exposure and outcome, has dramatically increased statistical power and scope. Meanwhile, the integration of MR with molecular quantitative trait loci (QTL) data—particularly expression QTLs (eQTLs) and protein QTLs (pQTLs)—has enabled researchers to bridge the gap between genetic associations and biological mechanisms. These approaches are particularly valuable in immunology, where complex feedback mechanisms and cellular heterogeneity have traditionally challenged causal inference.
Methodological Foundations of Mendelian Randomization
Core Assumptions and Statistical Framework
The validity of any MR analysis depends on satisfying three fundamental assumptions, each with specific statistical tests for verification:
Relevance Assumption: Genetic instruments must strongly predict the exposure. This is typically assessed using F-statistics, with values >10 indicating sufficient instrument strength to avoid weak instrument bias. For single genetic variants, the F-statistic is calculated as F = (R²(n-2))/(1-R²), where R² represents the proportion of variance in the exposure explained by the variant.
Independence Assumption: Genetic instruments must be independent of confounders. This can be evaluated through systematic searches of phenotype databases and assessment of genetic correlations with potential confounding traits.
Exclusion Restriction: Genetic instruments must affect the outcome only through the exposure, not via alternative pathways. This assumption is challenged by horizontal pleiotropy, which can be detected using methods like MR-Egger regression and the MR-PRESSO global test.
Table 1: Key MR Analysis Methods and Their Applications
| Method | Underlying Principle | Strengths | Limitations |
|---|---|---|---|
| Inverse Variance Weighted (IVW) | Combines ratio estimates using inverse-variance weighting | Most statistically efficient when all variants are valid | Highly sensitive to directional pleiotropy |
| MR-Egger | Allows for balanced pleiotropy through regression with intercept | Provides bias-corrected estimates even with invalid instruments | Lower statistical power and sensitivity to outlier variants |
| Weighted Median | Provides consistent estimate if >50% of weight comes from valid instruments | Robust to invalid instruments when majority are valid | Requires at least 50% valid instruments for consistent estimation |
| MR-PRESSO | Detects and removes outliers showing significant horizontal pleiotropy | Identifies and corrects for pleiotropic outliers | Requires at least 50% valid instruments after outlier removal |
Advanced MR Designs and Applications
Two-sample MR has become the standard approach, utilizing GWAS summary statistics from different studies for exposure and outcome traits. This design offers substantial advantages in power and feasibility compared to single-sample MR that requires individual-level data. A recent two-sample MR investigation of circulating inflammatory proteins and osteoarthritis identified several putative causal relationships, including protective effects of urokinase-type plasminogen activator and adenosine deaminase, and risk-increasing effects of fractalkine and hepatocyte growth factor [86].
Multivariable MR extends the framework to address correlated exposures, enabling estimation of direct effects of one exposure while accounting for others. This is particularly valuable in immunology where cytokines and immune markers often exist in tightly regulated networks.
Non-linear MR methods have been developed to characterize potential threshold effects or U-shaped relationships, moving beyond the standard linearity assumption that has traditionally dominated MR analyses.
Single-Cell Mendelian Randomization: A Technical Deep Dive
Methodology and Workflow
Single-cell MR represents a cutting-edge advancement that integrates single-cell expression quantitative trait loci (sc-eQTLs) with GWAS data to identify cell-type-specific causal mechanisms. The fundamental workflow comprises several distinct stages:
Instrument Selection: Genetic variants are identified from sc-eQTL datasets (e.g., OneK1K), typically using a significance threshold of p < 0.005 for cis-eQTLs associated with eGenes. Independent instruments are obtained through linkage disequilibrium (LD) clumping with a stringent r² cutoff of 0.01.
Outcome Association: The selected genetic instruments are then proxied against disease outcome GWAS summary statistics. Recent applications have utilized COVID-19 outcomes from the COVID-19 Host Genetic Initiative (Round 7) [87].
Causal Estimation: For eGenes with a single eQTL, the Wald ratio method is applied. For genes with multiple conditionally independent eQTLs, a generalized inverse variance weighted (gIVW) approach that accounts for correlation between nearby eQTLs is implemented.
Validation and Colocalization: Additional analyses including Bayesian colocalization, LD checks, and host-pathogen protein-protein interaction predictions are performed to validate putative causal genes.
Single-cell MR Analysis Workflow
Application in COVID-19 Research
A landmark single-cell MR study analyzed 26,597 sc-eQTLs representing 16,597 genes across 14 peripheral blood immune cells against four COVID-19 outcomes [87]. This investigation identified 132 putative causal genes, with 58 representing novel associations not previously reported. Notably, 145 (73%) gene-COVID-19 pairs demonstrated effects in only one immune cell type, highlighting the extensive cell-type specificity of immune-mediated mechanisms. The study further integrated MR findings with drug trial information to develop a tiered system that prioritized 37 drug targets for COVID-19 intervention.
Table 2: Single-cell MR Findings in COVID-19 (Selected Examples)
| Gene | Key Immune Cell Type | MR Association | Novelty | Therapeutic Potential |
|---|---|---|---|---|
| NCR3 | Natural Killer cells | Severe COVID-19 | Known | Targeted drug in cancer clinical trials |
| IFNAR2 | Monocytes/Macrophages | SARS-CoV-2 infection | Known | Interferon signaling pathway |
| OAS1 | Endothelial cells | COVID-19 susceptibility | Known | Antiviral mechanism |
| 58 genes | Various | Various COVID-19 outcomes | Novel | Multiple candidate targets |
The pathway analyses revealed that putative causal genes were enriched in natural killer (NK) cell recruiting pathways but de-enriched in NK cells themselves, suggesting complex regulatory networks. Furthermore, a deep learning model predicted that 107 (81%) of the putative causal genes, including 41 novel genes, physically interact with SARS-CoV-2 proteins, providing mechanistic insights into host-virus interactions [87].
SOX9 in Innate and Adaptive Immunity: Genetic Evidence
SOX9 Structure and Dual Roles in Immunity
SOX9 (SRY-related HMG Box 9) is a transcription factor containing several functionally distinct domains: an N-terminal dimerization domain (DIM), a central high mobility group (HMG) box DNA-binding domain, two transcriptional activation domains (TAM and TAC), and a C-terminal proline/glutamine/alanine-rich domain [1]. The HMG domain facilitates both DNA binding and nuclear localization through embedded nuclear localization and export signals.
In immune regulation, SOX9 exhibits context-dependent dual functions, acting as what has been termed a "janus-faced regulator" [1]. In cancer biology, SOX9 frequently promotes tumor immune escape by impairing immune cell function, while in tissue repair contexts, it helps maintain macrophage function and contributes to cartilage formation and regeneration.
Genetic Evidence for SOX9's Immunological Functions
MR and related genetic approaches have provided compelling evidence for SOX9's causal roles in immune-related pathologies:
In Gastrointestinal Cancers: Integrated analysis of GWAS data with expression QTLs (eQTLs) and methylation QTLs (mQTLs) using summary-data-based Mendelian randomization (SMR) has revealed immune-mediated mechanisms in gastrointestinal carcinogenesis [48]. Although SOX9 was not specifically identified in this SMR analysis, the established overexpression of SOX9 in gastric, liver, and other gastrointestinal cancers suggests it operates within these immune-cancer networks.
In Neuroinflammation: Recent research has identified SOX9 as a critical regulator of neuroinflammatory astrocyte subtypes in neuropathic pain [64]. Nerve injury induces abnormal phosphorylation of SOX9, triggering aberrant transcriptional activation of hexokinase 1 (Hk1), which drives high-rate glycolysis in astrocytes. The resulting excessive lactate production remodels histone modifications via lactylation (H3K9la), promoting pro-inflammatory and neurotoxic gene expression programs.
In Pancreatic Beta Cell Function: SOX9 depletion in beta cells disrupts alternative splicing, leading to accumulation of non-functional isoforms of genes critical for beta cell function [88]. This represents a non-canonical role for SOX9 beyond its transcription factor function, highlighting the diverse mechanisms through which it influences cellular physiology and potentially immune-endocrine interactions.
SOX9 Domain Structure and Immune Functions
Experimental Protocols for MR-Informed Mechanistic Studies
Protocol 1: Functional Validation of Putative Causal Genes
Purpose: To experimentally validate MR-identified candidate genes in disease-relevant cellular models.
Materials and Methods:
- Cell Lines: Primary human cells or appropriate cell line models (e.g., iPSC-derived immune cells)
- Gene Modulation: CRISPR-Cas9 for knockout, siRNA/shRNA for knockdown, or expression vectors for overexpression
- Functional Assays: Transcriptomic analysis (RNA-seq), protein quantification (Western blot, ELISA), and disease-relevant phenotypic assays
Procedure:
- Prioritize candidate genes from MR analysis based on strength of genetic evidence and potential therapeutic relevance.
- Design and validate gene modulation tools (sgRNAs for CRISPR, siRNA sequences, or expression constructs).
- Transduce/transfect target cells using appropriate methods (lentiviral transduction, lipofectamine, or electroporation).
- Confirm efficient gene modulation using qRT-PCR and/or Western blot.
- Assess functional consequences using disease-relevant assays (e.g., cytokine production, cell migration, phagocytosis).
- Perform transcriptomic/proteomic profiling to identify downstream pathways.
This approach was successfully employed in validating the role of PLOD3 as a SOX9-regulated oncogene in cervical cancer, where SOX9 was shown to directly bind the PLOD3 promoter to activate its transcription, ultimately driving cancer progression through the IL-6/JAK/STAT3 pathway [89].
Protocol 2: Single-Cell RNA Sequencing for Cellular Heterogeneity
Purpose: To characterize cell-type-specific effects of genetic perturbations identified through MR.
Materials and Methods:
- Tissue Samples: Freshly isolated tissues or cultured cells from relevant model systems
- Single-Cell Platform: 10X Genomics Chromium system or similar platform
- Bioinformatic Tools: Seurat, Scanpy, or similar packages for scRNA-seq analysis
Procedure:
- Prepare single-cell suspensions with viability >85%.
- Perform single-cell partitioning and barcoding using appropriate platform.
- Conduct library preparation and sequencing to sufficient depth (>20,000 reads/cell).
- Process raw sequencing data through alignment, quality control, and normalization.
- Identify cell clusters using unsupervised clustering approaches.
- Annotate cell types using established marker genes.
- Perform differential expression analysis between conditions.
- Conduct trajectory analysis or cell-cell communication inference if applicable.
This protocol enabled the identification of distinct astrocyte subpopulations in neuropathic pain, including the discovery that pathogenic Astro1 subpopulations exhibit heightened glycolytic activation driven by SOX9-mediated regulation of Hk1 [64].
Table 3: Research Reagent Solutions for MR-Informed Mechanistic Studies
| Reagent Category | Specific Examples | Key Applications | Technical Considerations |
|---|---|---|---|
| Gene Modulation | CRISPR-Cas9, siRNA, shRNA, overexpression vectors | Functional validation of candidate genes | Efficiency optimization; control for off-target effects |
| Single-Cell Platforms | 10X Genomics, Drop-seq, inDrops | Cellular heterogeneity analysis | Cell viability critical; sample multiplexing recommended |
| Epigenomic Profiling | ATAC-seq, ChIP-seq, CUT&RUN | Regulatory mechanism elucidation | Cell number requirements; antibody validation |
| Spatial Transcriptomics | 10X Visium, Slide-seq, MERFISH | Tissue context preservation | Resolution trade-offs; cost considerations |
Integration of MR with Other Omics Technologies
The causal inference from MR studies gains substantial biological context when integrated with complementary omics approaches. Transcriptomic integration enables identification of differentially expressed genes in disease states, as demonstrated in osteoarthritis research where MR findings were combined with transcriptomic analysis of inflammatory proteins [86]. Epigenomic profiling provides insights into regulatory mechanisms, exemplified by studies of SOX9 dosage effects on chromatin accessibility [53]. Proteomic measurements allow direct quantification of protein abundances, bridging the gap between genetic variation and physiological function.
A particularly powerful framework emerges from the sequential application of these technologies: (1) MR establishes causal directions between molecular traits and disease; (2) transcriptomic/epigenomic profiling identifies dysregulated pathways; (3) experimental models validate mechanistic hypotheses; and (4) single-cell technologies resolve cellular heterogeneity. This integrated approach is advancing the characterization of SOX9's dual roles in immunity, where it can function either promotively or protectively depending on cellular context and disease state [1].
Mendelian Randomization represents a mature methodological framework for causal inference in disease biology, with recent single-cell extensions offering unprecedented resolution into cell-type-specific mechanisms. The integration of MR evidence with functional genomics has proven particularly valuable in complex fields like immunology, where it has helped characterize the context-dependent functions of regulators like SOX9. Future methodological developments will likely focus on addressing more complex causal questions, including: mediation analyses to delineate causal pathways; interaction models to identify context-dependent effects; and multi-omic integration to bridge molecular layers. As GWAS sample sizes continue to grow and single-cell QTL resources expand, MR approaches will play an increasingly central role in translating genetic discoveries into biological insights and therapeutic opportunities.
Conclusion
SOX9 emerges as a master regulatory node, intricately weaving through both innate and adaptive immune pathways with profound implications for health and disease. Its Janus-faced nature—promoting immune evasion in cancer while supporting tissue repair in inflammation—presents both a challenge and an opportunity for therapeutic intervention. Future research must prioritize the development of context-specific modulators of SOX9 activity, deepen our understanding of its role in establishing 'inflammatory memory' in stem cells, and validate its utility as a predictive biomarker in immuno-oncology. Successfully harnessing the dualistic power of SOX9 will be pivotal in advancing next-generation immunotherapies and regenerative medicine strategies.
References
- 1. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 2. The versatile functions of Sox9 in development, stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4326072/]
- 3. SOX9 in organogenesis: shared and unique transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482574/]
- 4. SOX9: a key transcriptional regulator in organ fibrosis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1507282/full]
- 5. Hematopoietic stem and progenitor cells as a reservoir for ... [https://elifesciences.org/articles/106610]
- 6. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 7. Inflammation and immunity in liver homeostasis and disease [https://www.nature.com/articles/s41423-025-01313-7]
- 8. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 9. The crosstalk among macrophages, chondrocytes and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512754/]
- 10. Targeted soluble epoxide hydrolase inhibits M1 macrophage ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-07003-2]
- 11. Caspase 6/NR4A1/SOX9 signaling axis regulates hepatic ... [https://www.nature.com/articles/s41420-023-01396-z]
- 12. Ubiquitin-specific protease 7 regulates macrophage ... [https://www.nature.com/articles/s41419-025-08081-2]
- 13. Immune cell diversity and regenerative markers reveal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12267737/]
- 14. The pioneer factor SOX9 competes for epigenetic factors to ... [https://www.nature.com/articles/s41556-023-01184-y]
- 15. A SOX9-B7x axis safeguards dedifferentiated tumor cells from immune surveillance to drive breast cancer progression - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842074/]
- 16. Transcription Factor Drives Chemotherapy Resistance in ... [https://news.feinberg.northwestern.edu/2025/10/30/transcription-factor-drives-chemotherapy-resistance-in-ovarian-cancer/]
- 17. Cross-regulation between SOX9 and the canonical Wnt ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2023.1250530/full]
- 18. Cross-regulation between SOX9 and the canonical Wnt ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10469848/]
- 19. Interactions between Sox9 and β-catenin control chondrocyte ... [https://genesdev.cshlp.org/content/18/9/1072]
- 20. Sox9 Inhibits Wnt Signaling by Promoting β-Catenin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2631972/]
- 21. Sox9 transcriptionally regulates Wnt signaling in intestinal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5345140/]
- 22. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 23. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 24. Chromatin accessibility landscapes of immune cells in ... [https://bmcbiol.biomedcentral.com/articles/10.1186/s12915-021-01011-6]
- 25. Epigenetic control of SOX9 gene by the histone ... [https://www.sciencedirect.com/science/article/pii/S2405844024092041]
- 26. SOX9 is dispensable for the initiation of epigenetic remodeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6078338/]
- 27. Chromatin accessibility: biological functions, molecular ... [https://www.nature.com/articles/s41392-024-02030-9]
- 28. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 29. Chromatin accessibility variation provides insights into ... [https://elifesciences.org/reviewed-preprints/98289v2]
- 30. SOX9 (MSVA-709R) [https://ms-validatedantibodies.com/product/sox9-msva-709r/]
- 31. The local and circulating SOX9 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292907/]
- 32. Clinical significance of SOX9 in human non-small cell lung ... [https://jeccr.biomedcentral.com/articles/10.1186/1756-9966-31-18]
- 33. Comprehensive analysis, immune, and cordycepin ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1149986/full]
- 34. Tissue expression of SOX9 - Summary [https://www.proteinatlas.org/ENSG00000125398-SOX9/tissue]
- 35. Anti-SOX9 Antibodies | Invitrogen [https://www.thermofisher.com/antibody/primary/target/sox9]
- 36. USP28 promotes PARP inhibitor resistance by enhancing ... [https://www.nature.com/articles/s41419-025-07647-4]
- 37. Immunosuppressive SOX9â€AS1 Resists Tripleâ€Negative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11569622/]
- 38. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002136]
- 39. Lentivirus vector-mediated knockdown of Sox9 shows ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6857779/]
- 40. Using siRNA Technique to Generate Transgenic Animals ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1618682/]
- 41. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 42. ssGSEAProjection (v4) [https://www.genepattern.org/modules/docs/ssGSEAProjection/4/]
- 43. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 44. ssGSEA score-based Ras dependency indexes derived ... [https://www.nature.com/articles/s41598-020-66986-8]
- 45. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 46. Identification of novel gene signatures and immune cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10380950/]
- 47. Analysis of immune infiltration in basal cell carcinoma ... [https://link.springer.com/article/10.1007/s12672-025-02621-0]
- 48. The relationship between innate/adaptive immunity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11177483/]
- 49. The pioneer factor SOX9 competes for epigenetic factors to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10415178/]
- 50. Review and Evaluate the Bioinformatics Analysis Strategies of ... [https://pubmed.ncbi.nlm.nih.gov/39255248/]
- 51. Oncogenic enhancers prime quiescent metastatic cells to ... [https://www.nature.com/articles/s41467-024-46524-0]
- 52. Targeting SOX9 May Help Overcome Ovarian Cancer ... [https://breakthroughsforphysicians.nm.org/obgyn-research-article-transcription-factor-ovarian-cancer]
- 53. Precise modulation of transcription factor levels identifies ... [https://www.nature.com/articles/s41588-023-01366-2]
- 54. LPS/Bcl3/YAP1 signaling promotes Sox +HNF4α+... 9 [https://www.nature.com/articles/s41419-022-04715-x?error=cookies_not_supported&code=9feb51e3-d085-4161-a51a-d203c1bdb018]
- 55. protein expression summary - The Human Protein Atlas SOX 9 [https://www.proteinatlas.org/ENSG00000125398-SOX9]
- 56. Oncogenic role of PLOD3 mediated by SOX9 through IL-6/ ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656825006655]
- 57. Sox9 prevents retinal degeneration and is required for ... [https://elifesciences.org/articles/102337]
- 58. SOX9: a key transcriptional regulator in organ fibrosis [https://pubmed.ncbi.nlm.nih.gov/39974732/]
- 59. Optimized Lipid Nanoparticle-Mediated mRNA Co-Delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554278/]
- 60. CRISPR-mediated Sox9 activation and RelA inhibition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11405173/]
- 61. Chondrocyte fatty acid oxidation drives osteoarthritis via ... [https://www.nature.com/articles/s41467-025-60037-4]
- 62. CTHRC1 Expression Results in Secretion-Mediated, SOX9 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898434/]
- 63. SOX9 regulated matrix proteins are increased in patients ... [https://www.nature.com/articles/s41598-018-36037-4]
- 64. Sox9 regulation of hexokinase 1 controls ... [https://www.nature.com/articles/s41467-025-65092-5]
- 65. Scientists Find a Way to Help the Brain Clear Alzheimer's ... [https://scitechdaily.com/scientists-find-a-way-to-help-the-brain-clear-alzheimers-plaques-naturally/]
- 66. Astrocyte-driven approach shows potential to reverse ... [https://www.news-medical.net/news/20251121/Astrocyte-driven-approach-shows-potential-to-reverse-cognitive-decline-in-Alzheimere28099s.aspx]
- 67. Boosting one protein helps the brain protect itself from ... [https://www.sciencedaily.com/releases/2025/11/251123085550.htm]
- 68. Sox9 regulation of hexokinase 1 controls neuroinflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639169/]
- 69. Trained immunity : induction of an inflammatory in disease memory [https://www.nature.com/articles/s41422-025-01171-y?error=cookies_not_supported&code=8c5bbc52-f22f-466d-bab0-f0171b78c6bb]
- 70. A SOX9-B7x axis safeguards dedifferentiated tumor cells ... [https://www.sciencedirect.com/science/article/pii/S1534580723005518]
- 71. In vivo reprogramming of Sox + 9 in the liver to insulin-secreting... cells [https://pubmed.ncbi.nlm.nih.gov/22949652/]
- 72. Embryonic transcription factor SOX9 drives breast cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5465894/]
- 73. CDK1 drives SOX9-mediated chemotherapeutic resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506374/]
- 74. Researchers identify roles of key genes in colon cancer ... [https://oncologynews.com.au/latest-news/researchers-identify-roles-of-key-genes-in-colon-cancer-development/]
- 75. The role of NF-κB-SOX9 signalling pathway in osteoarthritis [https://www.sciencedirect.com/science/article/pii/S2405844024132227]
- 76. Therapeutic potential of SOX family transcription factors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789227/]
- 77. Dental Pulp Stem Cell-Derived Intracellular Vesicles Promote ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12637053/]
- 78. Inhibition of SOX9 Promotes Inflammatory and Immune ... [https://www.sciencedirect.com/science/article/abs/pii/S0099239918300785]
- 79. Inhibition of SOX9 Promotes Inflammatory and Immune ... [https://www.merckmillipore.com/VE/es/tech-docs/paper/1014445]
- 80. Molecular mechanism of NF-κB-mediated transcriptional ... [https://www.sciencedirect.com/science/article/abs/pii/S134900792500088X]
- 81. Alternative immune checkpoints in immunoregulatory ... [https://www.sciencedirect.com/science/article/pii/S2405844023103793]
- 82. Diagnostic and Prognostic Significances of SOX9 in Thymic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8580949/]
- 83. Regenerative lineages and immune-mediated pruning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7021003/]
- 84. Single cell type - SOX9 [https://www.proteinatlas.org/ENSG00000125398-SOX9/single+cell]
- 85. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://www.nature.com/articles/s41467-025-59050-4]
- 86. The Causal Effects Between Circulating Inflammatory Proteins ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12236367/]
- 87. Single-cell transcriptome-wide Mendelian randomization and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11867302/]
- 88. Sox9 regulates alternative splicing and pancreatic beta cell ... [https://www.nature.com/articles/s41467-023-44384-8]
- 89. Oncogenic role of PLOD3 mediated by SOX9 through IL-6/ ... [https://pubmed.ncbi.nlm.nih.gov/41242365/]