SOX9 in Autoimmunity and Inflammation: A Janus-Faced Regulator in Disease Pathogenesis and Therapeutic Development
This article comprehensively examines the dual role of the transcription factor SOX9 in autoimmune and inflammatory disorders.
SOX9 in Autoimmunity and Inflammation: A Janus-Faced Regulator in Disease Pathogenesis and Therapeutic Development
Abstract
This article comprehensively examines the dual role of the transcription factor SOX9 in autoimmune and inflammatory disorders. Targeting researchers and drug development professionals, it synthesizes foundational knowledge of SOX9's structure and its context-dependent functions as both a driver of pathology and a mediator of tissue repair. The scope spans exploratory mechanisms in diseases like thyroid eye disease and osteoarthritis, methodological advances in targeting SOX9, strategies to navigate its complex biology, and comparative analyses validating its prognostic and therapeutic utility. The review aims to bridge molecular understanding with clinical translation, highlighting SOX9's emerging promise as a biomarker and therapeutic target.
The Dual Nature of SOX9: Unraveling Its Structure and Context-Dependent Roles in Immunity
The SOX9 (SRY-related HMG-box 9) protein is a transcription factor belonging to the SOX family, characterized by a conserved high-mobility group (HMG) box DNA-binding domain. As a pivotal regulator of diverse developmental processes, SOX9 functions as a master controller of chondrogenesis, male sex determination, gliogenesis, and numerous other differentiation pathways. In the context of autoimmune diseases and inflammatory disorders, SOX9 has emerged as a significant autoantigen and regulatory factor, with demonstrated roles in conditions such as autoimmune polyendocrine syndrome type I (APS I) and vitiligo [1] [2]. Understanding the precise architectural organization of SOX9—its functional domains, DNA-binding specificity, and regulatory mechanisms—provides critical insights for developing targeted therapeutic strategies for these conditions. This technical guide comprehensively details the protein architecture of SOX9, with particular emphasis on aspects relevant to immune dysregulation and inflammatory disease pathogenesis.
SOX9 Domain Architecture and Functional Organization
The functional capabilities of SOX9 are encoded within a modular domain structure that facilitates DNA binding, dimerization, transcriptional activation, and protein-protein interactions. The human SOX9 protein comprises 509 amino acids organized into several functionally distinct domains [3].
Table 1: Functional Domains of Human SOX9 Protein
| Domain Name | Position | Key Functions | Molecular Characteristics |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates SOX9 self-association | Critical for functional plasticity and partner interaction [4] |
| HMG Box | Central | DNA binding and bending; nuclear localization | Contains nuclear localization (NLS) and export (NES) signals; binds sequence (A/T)(A/T)CAA(A/T)G [4] [3] [5] |
| Transcriptional Activation Domain Middle (TAM) | Central | Transcriptional activation | Synergizes with TAC; interaction platform for cofactors [3] |
| Transcriptional Activation Domain C-terminal (TAC) | C-terminal | Primary transcriptional activation | Interacts with cofactors (e.g., Tip60); inhibits β-catenin in chondrogenesis [3] |
| PQA-rich Domain | C-terminal | Transcriptional enhancement | Proline/Glutamine/Alanine-rich; enhances transactivation potential [4] [3] |
The DIM domain enables SOX9 dimerization, which is essential for its transcriptional regulatory functions. The central HMG domain represents the core DNA-binding module that confers sequence-specific DNA recognition and bending. The transactivation domains (TAM and TAC) facilitate recruitment of transcriptional co-regulators, while the PQA domain provides additional transactivation capacity, particularly in mammalian systems [4] [3].
Evolutionary analyses reveal that the DIM and TAD domains exhibit higher tolerance for molecular changes (as indicated by elevated Ka/Ks ratios) compared to the HMG box, suggesting these domains contribute significantly to SOX9's functional plasticity and ability to undergo subfunctionalization, as observed in teleost duplicates Sox9a and Sox9b [4].
DNA-Binding Specificity and Mechanisms
The DNA-binding specificity of SOX9 is primarily determined by its HMG box domain, which recognizes and binds to specific DNA sequences through minor groove interactions.
Core Binding Motif and Flanking Sequences
Systematic analyses using random oligonucleotide selection assays have defined the optimal SOX9 binding sequence as AGAACAATGG [5]. This sequence contains the core SOX family binding element AACAAT, flanked by 5' AG and 3' GG nucleotides, which enhance binding specificity for SOX9.
Table 2: DNA-Binding Specificity of SOX9 HMG Domain
| Binding Element | Sequence | Relative Binding Affinity | Functional Significance |
|---|---|---|---|
| Optimal SOX9 Site | AGAACAATGG | Highest | Confirmed by EMSA, competition, dissociation studies [5] |
| Core SOX Element | AACAAT | Moderate | Common binding motif for SOX family proteins [5] |
| SRY Preference | Differing flanking nucleotides | Lower for SOX9 | Demonstrates specificity among SOX family members [5] |
The DNA-binding mechanism involves SOX9-induced DNA bending, which facilitates the assembly of enhanceosome complexes through recruitment of additional transcriptional co-regulators. This bending is achieved through intercalation of specific hydrophobic amino acid residues from the HMG domain into the DNA minor groove, creating a significant bend angle that promotes chromatin remodeling and transcriptional activation [4].
Transcriptional Regulation of Target Genes
Through its DNA-binding capability, SOX9 directly regulates numerous target genes involved in development and disease, including:
- Col2a1: Encodes type II collagen, essential for cartilage matrix [6]
- Aggrecan: Major proteoglycan in cartilage extracellular matrix [6]
- COL11A2: Fibrillar collagen component of cartilage [6]
- Hexokinase 1 (Hk1): Key glycolytic enzyme implicated in neuropathic pain [7]
The specificity of SOX9 for its target genes is further refined through cooperative interactions with partner transcription factors and contextual cellular cues.
SOX9 Regulation and Post-Translational Modifications
SOX9 activity is subject to complex regulatory controls, including transcriptional, post-translational, and epigenetic mechanisms. Phosphorylation represents a particularly significant regulatory mechanism with implications for disease pathogenesis.
Phosphorylation at Serine 181
Phosphorylation at serine 181 (S181) represents a critical regulatory switch controlling SOX9 function:
- Subcellular localization: Phosphorylation enhances nuclear translocation and DNA binding [7]
- Transcriptional activity: Phosphorylated SOX9 exhibits enhanced transactivation of target genes [8]
- Pathological implications: Elevated pSOX9 levels are observed in systemic sclerosis (SSc) fibroblasts and contribute to fibrotic processes [8]
In neuropathic pain models, nerve injury induces aberrant SOX9 phosphorylation, triggering increased transcription of hexokinase 1 (Hk1) and resulting in heightened glycolytic flux in astrocytes [7]. The resulting lactate overproduction promotes histone lactylation (H3K9la), which remodels chromatin to favor expression of pro-inflammatory and neurotoxic genes, ultimately establishing chronic pain states [7].
Transcriptional Regulation of SOX9 Expression
SOX9 expression is itself regulated at the transcriptional level, primarily through its promoter region which contains two functional CCAAT boxes (CCAAT-1 and CCAAT-2) that bind the CCAAT-binding factor (CBF/NF-Y) [6]. Mutation or deletion of these CCAAT boxes significantly diminishes SOX9 promoter activity, highlighting their essential role in SOX9 transcription [6].
Additional regulatory inputs include:
- Pro-inflammatory cytokines: IL-1β and TNF-α suppress SOX9 expression via NF-κB signaling [6] [9]
- Growth factors: FGFs upregulate SOX9 through MAP kinase pathways [6]
- NF-κB signaling: Directly binds SOX9 promoter to positively regulate expression in osteoarthritis [9]
SOX9 in Autoimmune and Inflammatory Disease Contexts
SOX9 as an Autoantigen
SOX9 functions as an autoantigen in autoimmune polyendocrine syndrome type I (APS I), with approximately 15% of APS I patients exhibiting immunoreactivity against SOX9 [1] [2]. Notably, among APS I patients with vitiligo, 63% show positive reactivity against SOX10 (a SOX9-related protein), and all SOX9-reactive patients also display SOX10 reactivity, suggesting shared epitopes between these SOX family members [1]. This autoantigen status positions SOX9 as a significant factor in autoimmune disease pathogenesis.
SOX9 in Fibrotic Disorders
In systemic sclerosis (SSc), phosphorylated SOX9 (pSOX9) contributes to the persistent activation of myofibroblasts, the effector cells responsible for excessive extracellular matrix deposition characteristic of fibrosis [8]. TGF-β potently stimulates pSOX9 levels, establishing a pro-fibrotic feedback loop that drives disease progression [8].
Experimental Analysis of SOX9 Function
Key Methodologies for SOX9 Investigation
Table 3: Essential Experimental Protocols for SOX9 Functional Analysis
| Method | Key Applications | Technical Considerations |
|---|---|---|
| Chromatin Immunoprecipitation (ChIP) | Identify direct SOX9 target genes; map binding sites | Use validated SOX9 antibodies; include negative control regions |
| Proximity Ligation Assay (PLA) | Detect protein-protein interactions in situ | Optimize antibody concentrations; include single-antibody controls [10] |
| RNA Immunoprecipitation (RIP) | Investigate SOX9-RNA interactions | Cross-linking methods preserve transient interactions [10] |
| Luciferase Reporter Assays | Measure SOX9 transcriptional activity | Include SOX-binding (SOX) and control (SAC) constructs [10] |
| Electrophoretic Mobility Shift Assay (EMSA) | Analyze DNA-binding specificity | Use purified HMG domain; include competition experiments [5] |
| Site-Directed Mutagenesis | Determine functional domain requirements | Target key residues (e.g., S181, W143R) [10] [4] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for SOX9 Investigation
| Reagent Category | Specific Examples | Applications and Functions |
|---|---|---|
| SOX9 Antibodies | Mouse monoclonal anti-SOX9 (Sigma-Aldrich); Rabbit anti-SOX9 (Merck) | Western blot, immunofluorescence, PLA, ChIP [10] |
| Expression Constructs | N-terminally FLAG-tagged wild-type SOX9 (pcDNA3); SOX9 mutants (K68E, R94H, W143R) | Functional domain analysis; structure-function studies [10] [4] |
| Reporter Systems | SOX-luciferase reporter (7× AACAAAG); Control SAC-luciferase | Transcriptional activity measurement [10] |
| SOX9 Mutants | DelDIM (dimerization deficient); MiniSOX9 | Domain functional analysis [10] [4] |
| Knockdown Approaches | SOX9-specific siRNAs | Functional validation; target gene identification [10] |
| Interaction Partner Antibodies | Anti-p54nrb, Anti-PSF, Anti-Y14, Anti-SAM68 | Co-immunoprecipitation; PLA for complex detection [10] |
SOX9-RNA Binding and Splicing Regulation
Beyond its canonical function as a transcription factor, SOX9 exhibits RNA-binding capacity and regulates alternative splicing of hundreds of genes independently of its transcriptional activity [10]. SOX9 associates with several RNA-binding proteins, including the core exon junction complex component Y14, and approximately half of SOX9 splicing targets require Y14 for regulation [10]. This moonlighting function expands the mechanistic repertoire of SOX9 in gene regulation.
SOX9 represents a multifunctional regulatory protein with complex domain architecture that facilitates its diverse roles in development, homeostasis, and disease. The modular organization of SOX9—comprising dimerization, DNA-binding, and transactivation domains—enables context-dependent functions through differential protein interactions and post-translational modifications. In autoimmune and inflammatory disease contexts, SOX9 operates as both an autoantigen and a pathogenic regulator, contributing to conditions including vitiligo, systemic sclerosis, and neuropathic pain through distinct molecular mechanisms. The experimental frameworks and reagent tools outlined in this guide provide foundational resources for advancing SOX9-focused research, with particular relevance for therapeutic development targeting SOX9 in immune-related pathologies.
SOX9 (SRY-Box Transcription Factor 9) is emerging as a critical transcription factor with remarkably dualistic functions in immune and inflammatory regulation. As a member of the SOX family characterized by a conserved high-mobility group (HMG) box DNA-binding domain, SOX9 plays essential roles in development, chondrogenesis, and stem cell maintenance [3] [11]. Recent research has illuminated its complex, context-dependent roles in immunological processes, where it can simultaneously drive pro-inflammatory pathways in certain environments while exerting protective, anti-inflammatory effects in others [3]. This dichotomous nature positions SOX9 as a "Janus-faced" regulator with significant implications for understanding autoimmune diseases, inflammatory disorders, and cancer immunology. The precise molecular mechanisms that determine SOX9's functional orientation remain a vibrant area of investigation, particularly within the broader context of autoimmune disease and inflammatory disorder research. This technical guide comprehensively examines the molecular basis for SOX9's dual immune functions, analyzes its roles in specific pathological contexts, and provides detailed experimental methodologies for researchers investigating this multifaceted regulator.
Structural Basis and Molecular Mechanisms of SOX9 Function
Protein Architecture and Functional Domains
The SOX9 protein contains several structurally and functionally distinct domains that enable its diverse regulatory capabilities. The N-terminal dimerization domain (DIM) facilitates protein-protein interactions, while the central HMG box domain mediates sequence-specific DNA binding, nuclear localization, and DNA bending [3]. This domain contains embedded nuclear localization (NLS) and nuclear export (NES) signals that enable nucleocytoplasmic shuttling [3]. The C-terminal region houses two transcriptional activation domains - a central transcriptional activation domain (TAM) and a C-terminal transcriptional activation domain (TAC) - which interact with various cofactors like Tip60 to enhance transcriptional activity [3]. Additionally, a proline/glutamine/alanine (PQA)-rich domain is essential for full transcriptional activation potential [3].
Table 1: Functional Domains of SOX9 Protein
| Domain | Position | Key Functions | Interacting Partners |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Protein-protein interactions, dimer formation | Other SOX9 molecules, transcription cofactors |
| HMG Box Domain | Central | DNA binding, nuclear localization, DNA bending | Specific DNA sequences (CCTTGAG), importin proteins |
| Transcriptional Activation Domain (TAM) | Central | Transcriptional activation | Transcriptional co-activators |
| Transcriptional Activation Domain (TAC) | C-terminal | Transcriptional activation, β-catenin inhibition | Tip60, β-catenin |
| PQA-rich Domain | C-terminal | Transcriptional activation | Transcriptional machinery components |
Key Signaling Pathways and Molecular Interactions
SOX9 participates in multiple signaling networks that contextualize its dual immune functions. In neuropathic pain, SOX9 transcriptionally regulates hexokinase 1 (HK1), catalyzing the rate-limiting first step of glycolysis [7]. Nerve injury induces abnormal SOX9 phosphorylation at serine 181, triggering aberrant HK1 activation and high-rate astrocytic glycolysis [7]. The resulting excessive lactate production remodels histone modifications via lactylation (H3K9la), promoting transcriptional activation of pro-inflammatory and neurotoxic genes [7]. This SOX9-HK1-H3K9la axis represents a crucial immunometabolic pathway in neuroinflammation.
In cartilage and inflammatory joint environments, SOX9 interacts with the NF-κB signaling pathway, which can positively regulate SOX9 expression by directly binding to its promoter region [9]. The NF-κB-SOX9 signaling axis contributes significantly to osteoarthritis pathogenesis, linking inflammation with cartilage homeostasis disruption [9]. Additionally, computational docking analyses reveal that pharmaceutical agents like Lopinavir/Ritonavir can interact with osteoarthritis-related targets including HIF-1α, SOX9, and IL-1β, suggesting modulation of hypoxic, inflammatory, and epigenetic pathways [12].
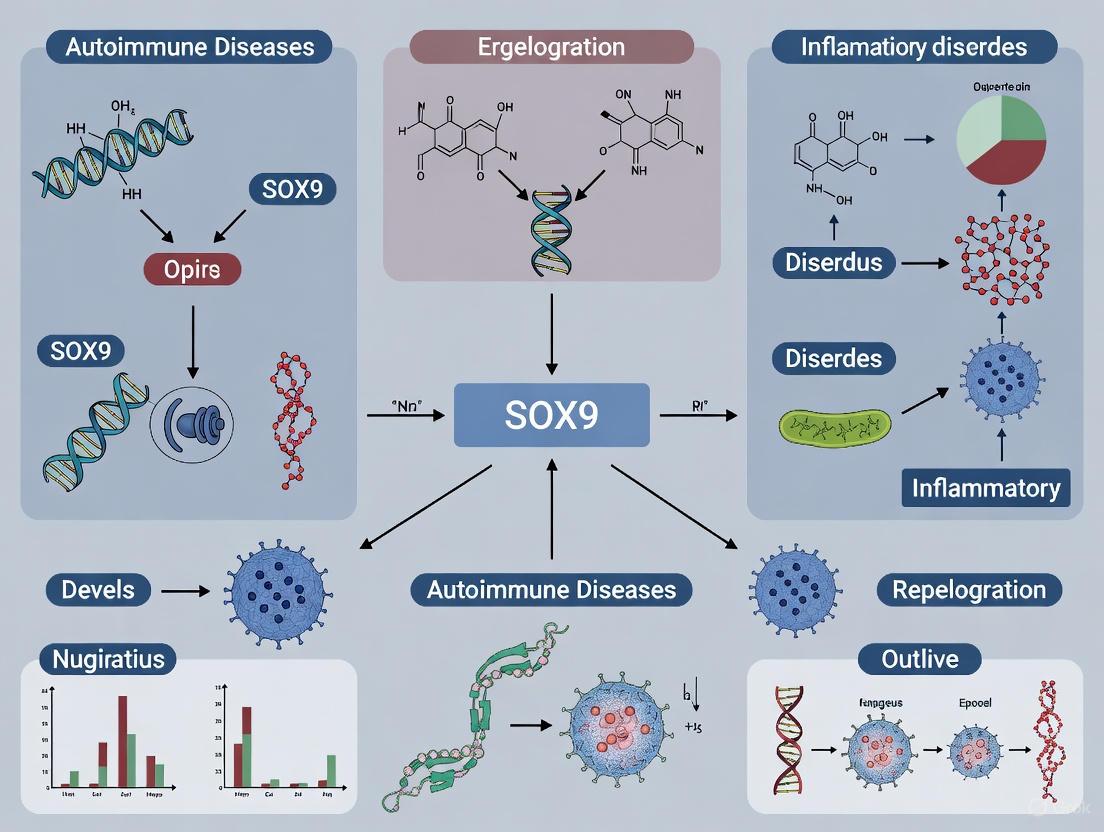
Figure 1: SOX9-Driven Pro-Inflammatory Pathway in Neuropathic Pain. This diagram illustrates the SOX9-HK1-H3K9la axis through which SOX9 activation promotes neuroinflammation following nerve injury.
Pro-Inflammatory Functions of SOX9
SOX9 in Neuroinflammation and Pain Pathogenesis
Single-cell RNA sequencing studies of dorsal spinal astrocytes in neuropathic pain models have revealed distinct astrocyte subpopulations with SOX9 playing a central role in driving pro-inflammatory phenotypes [7]. Following nerve injury, SOX9 phosphorylation triggers a metabolic shift toward heightened glycolysis through HK1 activation, resulting in lactate production and subsequent histone lactylation that promotes expression of pro-inflammatory and neurotoxic genes [7]. This mechanism drives the expansion of pathogenic astrocyte clusters (particularly Astro1) characterized by elevated expression of pro-inflammatory signaling molecules (NF-κB pathway components, Gstm1) and neurotoxic factors (C3, Cfb) [7]. These SOX9-driven neuroinflammatory astrocytes sustain central sensitization and chronic pain states even after peripheral injury resolution.
SOX9 in Tumor Immunosuppression
In cancer contexts, SOX9 frequently exhibits pro-tumorigenic and immunosuppressive functions. Bioinformatics analyses of tumor microenvironment data reveal that SOX9 overexpression negatively correlates with anti-tumor immune cell infiltration and function [3]. Specifically, SOX9 expression shows negative correlations with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while positively correlating with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. Furthermore, SOX9 overexpression negatively correlates with genes associated with the cytotoxic function of CD8+ T cells, NK cells, and M1 macrophages [3]. This immunomodulatory capacity enables SOX9 to facilitate tumor immune escape by creating an "immune desert" microenvironment that suppresses effective anti-tumor immunity [3].
Table 2: SOX9 Correlation with Immune Cell Infiltration in Cancer
| Immune Cell Type | Correlation with SOX9 Expression | Functional Consequences |
|---|---|---|
| B Cells | Negative | Reduced antibody production, impaired humoral immunity |
| Cytotoxic CD8+ T Cells | Negative | Diminished tumor cell killing capacity |
| NK Cells | Negative | Reduced innate immune surveillance |
| M1 Macrophages | Negative | Decreased pro-inflammatory, anti-tumor responses |
| Neutrophils | Positive | Increased immunosuppressive microenvironment |
| M2 Macrophages | Positive | Enhanced tissue repair, pro-tumor functions |
| Tregs | Positive | Suppressed effector T cell responses |
Protective and Anti-Inflammatory Functions of SOX9
SOX9 in Tissue Homeostasis and Resolution of Inflammation
In direct contrast to its pro-inflammatory roles, SOX9 demonstrates significant protective functions across multiple tissue contexts. In Alzheimer's disease research, boosting SOX9 expression in astrocytes enhanced clearance of amyloid-β plaques through increased phagocytic activity, effectively acting as a "vacuum cleaner" to remove toxic protein aggregates [13]. Importantly, in symptomatic Alzheimer's mouse models that already exhibited cognitive impairment and established plaque pathology, elevating SOX9 levels improved cognitive performance and reduced plaque burden over time [13]. This suggests SOX9 enhancement represents a natural, cell-based mechanism to combat neurodegenerative decline.
In dental pulp inflammation models, SOX9 acts as a critical maintainer of tissue homeostasis. Normal dental pulp tissue exhibits strong SOX9 expression (76.56% positive cells), which significantly decreases in inflamed pulp (16.40% positive cells) [14] [15]. SOX9 knockdown experiments demonstrate that reduced SOX9 expression inhibits type I collagen production, stimulates MMP2 and MMP13 enzymatic activities, and regulates IL-8 secretion [14]. Chromatin immunoprecipitation confirms SOX9 protein directly binds to MMP-1, MMP-13, and IL-8 gene promoters, with this binding reduced by TNF-α treatment [15]. These findings position SOX9 as a key regulator of extracellular matrix balance and inflammatory mediator production in tissue-specific contexts.
SOX9 in Cartilage Integrity and Joint Homeostasis
In osteoarthritis, SOX9 plays complex, context-dependent roles in maintaining cartilage integrity. While certain inflammatory conditions can exploit SOX9 activities for pathological outcomes, in joint homeostasis SOX9 serves as a "master regulator" of chondrocyte function [9] [16]. SOX9 is essential for chondrocyte differentiation and directly regulates expression of cartilage-specific genes and extracellular matrix components including collagen type II and aggrecan [16]. The transcription factor cooperates with SOX5 and SOX6 to maintain chondrocyte phenotype and cartilage structural integrity [16]. Research demonstrates elevated SOX9 mRNA expression in OA-affected articular cartilage compared to control tissue, suggesting a compensatory mechanism to counteract disease progression [16].
Figure 2: Context-Dependent Outcomes of SOX9 Modulation. This diagram illustrates how SOX9 enhancement produces protective effects in neurodegenerative contexts while SOX9 reduction promotes inflammatory responses in peripheral tissues.
Experimental Approaches and Research Methodologies
Detailed Protocol: Investigating SOX9 in Inflammatory Models
SOX9 Knockdown in Human Dental Pulp Cells (HDPCs) to Study Inflammatory Responses
Objective: To elucidate SOX9's role in regulating extracellular matrix balance, cytokine expression, and immune cell recruitment in inflammatory contexts.
Methodology:
- Cell Culture and Treatment: Maintain HDPCs in appropriate growth media. Treat cells with recombinant human TNF-α (10-50 ng/mL) or P. gingivalis lysate to induce inflammatory conditions.
- SOX9 Knockdown: Transfert HDPCs with SOX9-specific small interfering RNA (siRNA) using lipid-based transfection reagents. Include scrambled siRNA as negative control.
- Gene Expression Analysis:
- Extract total RNA using TRIzol reagent
- Perform quantitative PCR (qPCR) with SOX9-specific primers
- Analyze expression of extracellular matrix genes (COL1A1, MMP1, MMP2, MMP13) and inflammatory mediators (IL-8)
- Protein Analysis:
- Perform Western blotting to confirm SOX9 knockdown at protein level
- Use gelatin/collagen zymography to assess MMP enzymatic activity
- Cytokine Profiling:
- Analyze culture supernatants using antibody arrays to screen multiple cytokines
- Validate key findings with ELISA for IL-8 quantification
- Immune Cell Functional Assays:
- Condition media from SOX9-knockdown HDPCs and apply to THP-1 monocyte cultures
- Perform cell migration assays using transwell systems
- Assess cell attachment and phagocytic activity
- Chromatin Immunoprecipitation (ChIP):
- Crosslink proteins to DNA with formaldehyde
- Immunoprecipitate with SOX9-specific antibody
- Analyze bound DNA fragments for MMP-1, MMP-13, and IL-8 promoter regions
Expected Outcomes: Successful SOX9 knockdown should result in reduced type I collagen production, increased MMP2 and MMP13 activity, elevated IL-8 secretion, and enhanced monocyte recruitment and activation [14] [15].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Immunology Studies
| Reagent/Category | Specific Examples | Research Applications | Technical Notes |
|---|---|---|---|
| SOX9 Modulation | SOX9 siRNA, SOX9 overexpression plasmids, CRISPR/Cas9 SOX9 knockout systems | Gain/loss-of-function studies | Validate efficiency via qPCR and Western blot |
| Cell Culture Models | Human dental pulp cells (HDPCs), primary chondrocytes, astrocytes, cancer cell lines | Tissue-specific functional studies | Primary cells better reflect physiological responses |
| Inflammation Inducers | Recombinant human TNF-α, P. gingivalis lysate, LPS | Establishing inflammatory conditions | Optimize concentration and exposure time |
| Analysis Antibodies | Anti-SOX9 (ChIP-grade), anti-collagen I, anti-MMP2/13, anti-IL-8 | Protein detection, localization, ChIP | Verify antibody specificity for application |
| Molecular Biology Assays | qPCR primers for SOX9/target genes, gelatin/collagen zymography kits | Gene expression, enzymatic activity | Include proper controls for zymography |
| Animal Models | Spared nerve injury (SNI) rats, Alzheimer's mouse models, osteoarthritis models | In vivo validation | Choose model relevant to research question |
Research Implications and Therapeutic Perspectives
The dual nature of SOX9 as both pro-inflammatory and protective regulator presents both challenges and opportunities for therapeutic development. In cancer contexts, SOX9 inhibition may counteract immunosuppression and enhance anti-tumor immunity [3] [11]. Conversely, in neurodegenerative diseases like Alzheimer's, SOX9 enhancement could promote clearance of pathological protein aggregates [13]. In inflammatory joint diseases, the situation is particularly complex, as SOX9 contributes to both cartilage maintenance and pathological processes [12] [9] [16].
Drug development strategies must account for this context dependence. Computational analyses suggest existing pharmaceuticals like Lopinavir/Ritonavir can interact with the SOX9-HIF-1α-IL-1β network, potentially offering repurposing opportunities for osteoarthritis treatment [12]. Future research should focus on identifying the precise molecular switches that determine SOX9's functional orientation in specific tissues and disease states, potentially enabling development of context-specific therapeutics that can either inhibit or enhance SOX9 activity based on therapeutic need.
For researchers in autoimmune and inflammatory diseases, SOX9 represents a compelling target that integrates metabolic programming (glycolysis), epigenetic regulation (histone lactylation), and immune cell function—three pillars of modern immunology research. The experimental frameworks and technical resources provided in this guide offer foundational methodologies for advancing our understanding of this multifaceted transcription factor and harnessing its therapeutic potential.
The transcription factor SOX9 (SRY-box transcription factor 9) has emerged as a critical regulator of fibrotic processes across diverse organ systems and disease contexts. Originally identified for its fundamental role in developmental processes including chondrogenesis and sex determination, SOX9 is now recognized as a central mediator of pathological fibrosis—a common endpoint in chronic inflammatory and autoimmune diseases characterized by excessive extracellular matrix (ECM) deposition that leads to tissue scarring and organ dysfunction [17] [18]. This whitepaper synthesizes current mechanistic understanding of SOX9-driven fibrogenesis, with specific focus on its roles in thyroid eye disease (TED), schistosomiasis-induced liver fibrosis, and hepatic fibrosis, contextualized within the broader framework of autoimmune and inflammatory disorder research. The findings presented herein underscore SOX9's potential as a therapeutic target for antifibrotic interventions.
SOX9 Expression and Function in Fibrotic Diseases: Quantitative Evidence
Table 1: SOX9-Associated Fibrotic Markers Across Disease Contexts
| Disease Context | SOX9 Expression Change | Key Regulated ECM Components | Functional Consequences | Experimental Models |
|---|---|---|---|---|
| Thyroid Eye Disease | Significantly increased in TED orbital fibroblasts vs. healthy controls [19] | COL1, OPN, FN1, VIM [19] | Enhanced contraction, migration, proliferation, antiapoptotic ability of OFs [19] | Primary human OF cultures (TED: n=10; controls: n=6) [19] |
| Liver Fibrosis (General) | Upregulated in activated hepatic stellate cells [20] | OPN, GPNMB, FN1, SPARC, VIM [20] | Progressive ECM deposition, scarring, impaired liver function [20] | CCl4 and BDL mouse models; human patient serum [20] |
| Schistosomiasis-Associated Liver Fibrosis | Ectopically expressed in myofibroblasts within granuloma and hepatocytes [21] | Collagens, granuloma-associated ECM components [21] | Disorganized granuloma formation, diffuse liver injury [21] | S. mansoni-infected SOX9-deficient mice [21] |
| Tracheal Fibrosis | Upregulated in TGF-β1-treated tracheal fibroblasts [22] | MMP10, COL1, other ECM components via Wnt/β-catenin [22] | Fibroblast activation, proliferation, apoptosis resistance [22] | Rat tracheal fibroblast (RTF) models [22] |
Table 2: Quantitative Changes in SOX9-Regulated ECM Proteins in Liver Fibrosis Patient Serum
| SOX9 Target Protein | Change in Fibrosis | Performance as Biomarker | Key Findings |
|---|---|---|---|
| Osteopontin (OPN) | Significantly increased [20] | Superior to established clinical biomarkers for early-stage detection [20] | Directly regulated by SOX9; strongly correlates with fibrosis severity [20] |
| Vimentin (VIM) | Significantly increased [20] | Superior to established clinical biomarkers for early-stage detection [20] | Correlates with fibrosis severity; may be indirectly regulated by SOX9 [20] |
| Fibronectin (FN1) | Significantly increased [20] | Effective for fibrosis stratification [20] | Direct SOX9 target with conserved binding motifs [20] |
| Osteoactivin (GPNMB) | Significantly increased [20] | Effective for fibrosis stratification [20] | Contains conserved SOX9 binding motifs; confirmed by ChIP [20] |
| Osteonectin (SPARC) | Significantly increased [20] | Effective for fibrosis stratification [20] | Direct SOX9 target with conserved binding motifs [20] |
Disease-Specific Mechanistic Insights
Thyroid Eye Disease (TED)
In TED, an autoimmune disorder, SOX9 is significantly overexpressed in orbital fibroblasts (OFs) compared to healthy controls [19]. Mechanistically, SOX9 drives fibrotic pathogenesis through multiple pathways. It directly binds to the epidermal growth factor receptor (EGFR) promoter, activating the MAPK/ERK1/2 signaling pathway, which in turn promotes OF proliferation, differentiation, contractility, and migration [19]. SOX9 also transcriptionally regulates numerous extracellular matrix (ECM)-related genes, creating a profibrotic cellular environment. Experimental SOX9 knockdown ameliorates these effects, while its overexpression exacerbates the fibrotic phenotype [19].
Schistosomiasis-Associated Liver Fibrosis
During Schistosoma mansoni infection, SOX9 becomes ectopically expressed in hepatic myofibroblasts within egg granulomas and surrounding hepatocytes [21]. This expression is crucial for forming organized granulomatous barriers that contain toxic egg secretions. SOX9 deficiency results in significantly diminished granuloma size and disrupted ECM barrier formation, leading to more diffuse liver injury and altered immune responses characterized by pronounced eosinophilia and expansion of Ly6clo monocytes [21]. This demonstrates SOX9's critical role in balancing immune cell recruitment and fibrotic containment during parasitic infection.
Liver Fibrosis (General)
In hepatic fibrosis, SOX9 is upregulated in activated hepatic stellate cells (HSCs)—the primary fibrogenic cells in the liver [20]. Transcriptomic analyses reveal that approximately 30-37% of genes regulated by SOX9 in HSCs are ECM-related [20]. SOX9 directly transcriptionally activates multiple profibrotic factors including osteopontin (OPN), osteoactivin (GPNMB), fibronectin (FN1), osteonectin (SPARC), and vimentin (VIM) through conserved binding motifs in their promoter regions [20]. These SOX9-regulated proteins are significantly elevated in serum from patients with liver fibrosis and correlate with disease severity, suggesting their utility as biomarkers [20].
Core Signaling Pathways and Molecular Mechanisms
Figure 1: SOX9-Regulated Signaling Pathways in Fibrosis. SOX9 operates within a complex network of signaling pathways, including MAPK/ERK, Wnt/β-catenin, and metabolic pathways, to drive fibrotic processes through transcriptional regulation of ECM components and profibrotic factors.
Experimental Methodologies and Research Workflows
Table 3: Key Experimental Approaches for SOX9 Fibrosis Research
| Methodology | Key Applications | Technical Considerations | Representative Findings |
|---|---|---|---|
| Primary Cell Culture | Culture of orbital fibroblasts (TED), hepatic stellate cells (liver fibrosis), tracheal fibroblasts [19] [20] [22] | Use early passages (P3-P8); confirm phenotype; maintain from multiple donors [19] | TED-OFs show higher SOX9 vs. controls; enhanced contractility, proliferation [19] |
| SOX9 Modulation | siRNA knockdown; lentiviral overexpression; CRISPR/Cas9; transgenic models [19] [21] [22] | Confirm efficiency via qPCR/Western; use multiple targeting sequences [19] | SOX9 knockdown reduces ECM genes, contraction; overexpression promotes fibrosis [19] |
| Transcriptomic Analysis | RNA-seq; microarray; single-cell RNA-seq; ChIP-seq [19] [20] [7] | Multiple bioinformatics validation; pathway enrichment analysis; integration with ChIP [19] [20] | ~30% SOX9-regulated genes are ECM-related; identified EGFR, MMP10 as direct targets [19] [20] [22] |
| Chromatin Immunoprecipitation | Identify direct SOX9 target genes; mapping binding sites [19] [20] [22] | Validate antibody specificity; include positive/negative controls; qPCR validation [19] | SOX9 binds promoters of EGFR, OPN, GPNMB, FN1, SPARC [19] [20] |
| Animal Fibrosis Models | CCl4-induced liver fibrosis; bile duct ligation; schistosoma infection; tracheal injury [21] [20] [22] | Use inducible, cell-specific knockout models; monitor survival with global KO [21] | SOX9 deficiency reduces scarring, improves function; disrupts granuloma formation [21] [20] |
Figure 2: Experimental Workflow for SOX9 Fibrosis Research. Comprehensive approach integrating sample collection, genetic manipulation, multi-omics analysis, functional assays, and clinical validation to elucidate SOX9's role in fibrotic pathogenesis.
Table 4: Essential Research Reagents for SOX9 Fibrosis Investigations
| Reagent Category | Specific Examples | Research Applications | Key Considerations |
|---|---|---|---|
| SOX9 Modulation Tools | SOX9 siRNA/shRNA; SOX9 overexpression lentiviruses/adenoviruses; Cre-lox conditional KO models [19] [21] [22] | Gain/loss-of-function studies; target validation | Validate efficiency via qRT-PCR/Western; use multiple targeting sequences; control for off-target effects [19] |
| Cell Culture Models | Primary orbital fibroblasts (TED); hepatic stellate cells; tracheal fibroblasts; immortalized cell lines [19] [20] [22] | Disease-specific mechanistic studies; drug screening | Use early passages; confirm phenotype; maintain cells from multiple donors [19] |
| Antibodies | Anti-SOX9 (ChIP-grade); anti-phospho-SOX9 (S64, S181); anti-ECM proteins (COL1, OPN, FN1); anti-αSMA [19] [20] | Immunofluorescence; Western blot; IHC; ChIP | Verify specificity for application; species compatibility; validate phospho-specific antibodies [19] |
| Animal Models | Inducible SOX9 knockout mice; CCl4 liver fibrosis model; bile duct ligation; schistosoma infection; tracheal injury [21] [20] [22] | In vivo target validation; therapeutic testing | Consider temporal control with inducible systems; monitor animal welfare with global KO [21] |
| Analysis Kits/Assays | Collagen gel contraction assay; EdU proliferation kit; migration assay systems; ELISA for ECM proteins [19] [20] | Functional characterization; biomarker quantification | Standardize conditions across experiments; include appropriate controls [19] |
The accumulated evidence unequivocally establishes SOX9 as a master regulator of fibrotic pathogenesis across multiple disease contexts, including thyroid eye disease, schistosomiasis, and organ fibrosis. SOX9 drives fibrosis through conserved mechanisms involving transcriptional activation of ECM components, regulation of key signaling pathways (MAPK/ERK, Wnt/β-catenin), and modulation of cellular phenotypes including proliferation, contraction, and apoptosis resistance. The consistent finding that SOX9 ablation ameliorates fibrosis across diverse disease models highlights its potential as a promising therapeutic target. Future research should focus on developing cell-specific targeting strategies and small molecule inhibitors directed against SOX9 or its critical downstream effectors to combat fibrotic diseases.
SOX9, a master transcription factor, is indispensable for chondrogenesis and the maintenance of articular cartilage. Its precise regulation ensures a balance between anabolic processes, driven by extracellular matrix (ECM) components like type II collagen and aggrecan, and catabolic processes mediated by enzymes such as matrix metalloproteinase 13 (MMP13). Disruption of SOX9 homeostasis is a hallmark of osteoarthritis (OA), leading to progressive cartilage degradation. This whitepaper delves into the molecular mechanisms governing SOX9 expression and activity, highlighting its role as a pivotal node in the interplay between anabolic and catabolic signaling. Within the broader context of autoimmune and inflammatory disorders, understanding the dual-faced nature of SOX9 in tissue homeostasis and inflammation provides critical insights for developing targeted therapeutic strategies for OA and related conditions.
SOX9 is a member of the SRY-related high-mobility group (HMG) box family of transcription factors. In healthy articular cartilage, chondrocytes maintain tissue homeostasis by balancing the synthesis and breakdown of the ECM [23]. SOX9 is a central orchestrator of this equilibrium, directly transactivating genes for essential anabolic components including type II collagen (COL2A1) and aggrecan (ACAN) [24] [25]. It often functions in a trio with the related transcription factors SOX5 and SOX6 to activate the full repertoire of chondrocyte-specific genes [26] [25]. The persistence of chondrocytes and the maintenance of SOX9 activity are what distinguish articular cartilage from the cartilaginous templates that undergo endochondral ossification during skeletal development [23]. The loss of this homeostatic balance, frequently associated with decreased SOX9 function, is a fundamental driver of OA pathology [23] [24].
Molecular Regulation of SOX9
The expression and transcriptional activity of SOX9 are controlled through multiple intricate layers of regulation, ensuring precise spatial and temporal control over chondrocyte function.
Transcriptional and Post-Translational Control
SOX9 protein contains several critical functional domains: a dimerization domain (DIM), the HMG box DNA-binding domain, and two transcriptional activation domains (TAM and TAC) [3]. The HMG domain facilitates nuclear localization and DNA binding, while the TAC domain interacts with cofactors like Tip60 to enhance transcriptional activity [3]. SOX9 activity is significantly modulated by post-translational modifications (PTMs). Phosphorylation can influence its transactivation potential, and sumoylation targets SOX9 for proteasomal degradation [27]. Recent research underscores that SOX9 stability is a critical control point. The E3 ubiquitin ligase FBXW7 targets SOX9 for ubiquitination and degradation, a process that can be counteracted by the deubiquitinating enzyme USP28, which stabilizes the SOX9 protein [28].
Post-Transcriptional Regulation by RNA-Binding Proteins and microRNAs
RNA-binding proteins (RNABPs) are crucial post-transcriptional regulators of SOX9. The RNABP tristetraprolin (TTP) binds to adenine-uracil (AU)-rich elements in the 3' untranslated region (UTR) of SOX9 mRNA, promoting its decay. Knockdown of TTP results in increased SOX9 mRNA half-life and elevated protein expression [27]. Conversely, the RNABP HuR regulates catabolic factors like MMP13 [27]. MicroRNAs (miRNAs) represent another key regulatory layer. For instance, miRNA-145 directly inhibits SOX9 expression, while miRNA-140, whose expression is strengthened by the SOX trio, promotes chondrocyte proliferation [25]. This creates a complex network of checks and balances fine-tuning SOX9 levels.
SOX9 in Cartilage Anabolism and Catabolism
SOX9 sits at the fulcrum of cartilage homeostasis, directly promoting anabolic pathways while suppressing catabolic ones.
SOX9-Driven Anabolic Pathways
SOX9 is the primary factor driving the expression of the major structural components of the cartilage ECM. It binds to enhancer elements in genes such as COL2A1 and ACAN, dramatically upregulating their transcription [25]. This activity is essential for both cartilage development and its maintenance in adulthood. The cooperation between SOX9, SOX5, and SOX6 is particularly important for achieving high-level expression of these genes [26].
SOX9 Dysregulation and Catabolic Activation
In OA, the disruption of SOX9 homeostasis leads to a catabolic shift. Degradation of SOX9, driven by factors like metabolic stress, results in the diminished transcription of COL2A1 and ACAN [24]. Furthermore, SOX9 deficiency can lead to the epigenetic upregulation of major catabolic enzymes. For example, elevated fatty acid oxidation in chondrocytes leads to acetyl-CoA accumulation, which alters histone acetylation patterns and promotes the transcriptional activation of MMP13 and ADAMTS7, even as SOX9 itself is degraded [24]. This creates a vicious cycle of ECM destruction.
Table 1: SOX9 Target Genes in Cartilage Homeostasis
| Gene | Function | Effect of SOX9 | Role in Homeostasis |
|---|---|---|---|
| COL2A1 | Encodes Type II Collagen | Transcriptional Activation | Anabolic: Forms structural fibrillar network of cartilage |
| ACAN | Encodes Aggrecan | Transcriptional Activation | Anabolic: Provides osmotic resistance for load-bearing |
| MMP13 | Encrates Collagenase 3 | Indirect Repression | Catabolic: Degrades Type II collagen; repressed by SOX9 activity |
Metabolic Dysregulation and SOX9 in OA Pathogenesis
Emerging evidence positions OA as a metabolic disease, where lipid and energy metabolism directly impinge upon SOX9 function.
Lipid Stress and SOX9 Degradation
In obesity-related OA (ObOA), synovial fluid contains elevated levels of free fatty acids (FFAs) [24]. Chondrocytes uptake these FFAs, which then undergo mitochondrial fatty acid oxidation (FAO). This process yields acetyl-CoA, a key metabolic intermediate. Excessive acetyl-CoA accumulation leads to hyperacetylation and activation of the FAO enzyme HADHA, creating a feed-forward loop that further boosts FAO [24]. Crucially, elevated FAO reduces AMPK activity, which impairs SOX9 phosphorylation. This altered PTM status makes SOX9 more susceptible to ubiquitination and proteasomal degradation, thereby crippling anabolic functions [24].
Glycolysis and Epigenetic Remodeling
A parallel metabolic pathway, glycolysis, also interfaces with gene regulation in a SOX9-dependent manner. In neuropathic pain models (a different but related pathological state), aberrant SOX9 phosphorylation increases its nuclear translocation and transcriptional activation of hexokinase 1 (Hk1), the rate-limiting enzyme in glycolysis [7]. The resulting high glycolytic flux produces excessive lactate, which drives histone lactylation (H3K9la) on promoters of pro-inflammatory and neurotoxic genes, promoting a pathogenic cellular phenotype [7]. This illustrates a mechanism where SOX9 activity can, under specific pathological metabolic conditions, inadvertently fuel a catabolic state.
The diagram below illustrates the core regulatory network and pathological mechanisms of SOX9 in OA.
Experimental Approaches and Research Reagents
Investigating SOX9 requires a multifaceted approach, from in vitro cell culture to sophisticated molecular biology techniques.
Key Experimental Protocols
Protocol 1: Investigating RNABP Regulation of SOX9 mRNA Stability [27]
- Cell Culture: Use primary human articular chondrocytes (HACs) or SW1353 chondrosarcoma cells. Culture in DMEM with 10% FBS.
- Gene Knockdown: Transfect cells at 90-95% confluence with 10 pmol/cm² of siRNA targeting TTP, HuR, or a non-targeting control siRNA using Lipofectamine 2000.
- mRNA Decay Analysis: 24-48 hours post-transfection, treat cells with a transcriptional inhibitor like Actinomycin D. Harvest cells at time points (e.g., 0, 1, 2, 4, 8 hours).
- Analysis: Isolate total RNA, perform reverse transcription, and analyze SOX9 mRNA levels using RT-qPCR. Calculate half-life from the decay curve.
- Validation: Confirm protein knockdown and SOX9 protein level changes via western blotting.
Protocol 2: Modeling Lipid Stress and SOX9 Degradation [24]
- In Vitro Model: Treat primary mouse chondrocytes with free fatty acids (FFAs) or adipocyte-conditioned medium (adipo-CM) to mimic lipid stress.
- Assessment:
- ECM Deposition: Use 3D agarose culture or micromass co-culture, staining for proteoglycans (e.g., Alcian Blue) to visualize ECM reduction.
- Gene Expression: Extract RNA from treated chondrocytes and perform RT-qPCR for anabolic (SOX9, COL2A1, ACAN) and catabolic (MMP13) markers.
- Protein Analysis: Perform western blotting to monitor SOX9 protein levels and associated PTMs (e.g., phosphorylation, ubiquitination).
- In Vivo Model: Utilize a high-fat diet (HFD)-fed mouse model subjected to destabilization of the medial meniscus (DMM) to study metabolism-associated post-traumatic OA.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for SOX9 and Cartilage Homeostasis Research
| Reagent / Tool | Function/Application | Example Use |
|---|---|---|
| siRNA (TTP, HuR) | Post-transcriptional gene knockdown | Elucidating RNABP control of SOX9 mRNA stability [27] |
| Free Fatty Acids (FFAs) | Inducing metabolic stress in vitro | Modeling lipid-induced SOX9 degradation and catabolic shift [24] |
| Trimetazidine | FAO inhibitor, AMPK activator | Testing therapeutic intervention in OA models [24] |
| AZ1 (USP28 Inhibitor) | Induces SOX9 degradation via USP28 inhibition | Exploring SOX9 protein stabilization mechanisms [28] |
| Anti-SOX9 Antibody | Protein detection (Western Blot, IHC) | Quantifying SOX9 protein expression and localization [27] [28] |
| HFD-DMM Mouse Model | In vivo model of metabolism-associated OA | Studying SOX9 in a context of obesity and joint injury [24] |
Discussion and Therapeutic Implications
The central role of SOX9 in cartilage homeostasis makes it an attractive yet complex therapeutic target. Its dual nature—essential for anabolism but whose dysregulation can contribute to catabolism—requires nuanced intervention strategies. Simply overexpressing SOX9 may be insufficient if the pathological microenvironment, such as metabolic stress, remains unaddressed.
Promising therapeutic avenues emerging from recent research include:
- Targeting SOX9 Regulators: Inhibiting deubiquitinases like USP28 to promote SOX9 degradation could be explored in contexts where SOX9 is pathologically stabilized, such as in cancer [28]. Conversely, stabilizing SOX9 by targeting its upstream regulators (e.g., with the FAO inhibitor Trimetazidine) shows efficacy in preclinical OA models [24].
- Modulating Metabolic Pathways: Given the strong link between lipid/glucose metabolism and SOX9 stability/function, interventions that normalize chondrocyte metabolism hold great promise for restoring SOX9 homeostasis [7] [24].
- Epigenetic Therapies: Targeting the downstream epigenetic consequences of SOX9 dysregulation, such as specific histone lactylation or acetylation marks, could offer a way to suppress catabolic gene expression without directly manipulating SOX9 itself [24] [29].
In the broader context of autoimmune and inflammatory disorders, the immunomodulatory functions of SOX9, including its role in macrophage function and T-cell differentiation, suggest that insights from cartilage biology may have relevance for other inflammatory tissue-destructive diseases [3]. Future research must focus on achieving cell-type and context-specific modulation of SOX9 to halt disease progression and promote genuine cartilage regeneration.
The SRY-related HMG-box 9 (SOX9) transcription factor, a member of the evolutionarily conserved SOX family, has emerged as a critical regulator of tumor progression and immune modulation. Recent research reveals that SOX9 exhibits a dual, "Janus-faced" nature in immunology, functioning as a master orchestrator of the tumor microenvironment (TME) [3]. On one hand, SOX9 promotes tumor immune escape by creating an immunosuppressive niche; on the other hand, it contributes to tissue repair and regeneration in inflammatory contexts [3]. This paradoxical role positions SOX9 at the interface of cancer biology and immunology, offering promising therapeutic avenues for targeting the TME. The protein's functional complexity stems from its multi-domain structure, which includes a dimerization domain (DIM), the characteristic HMG box DNA-binding domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [3]. This structural composition enables SOX9 to interact with diverse cofactors and target genes, allowing it to regulate wide transcriptional programs that shape immune responses within the TME.
Structural Basis of SOX9 Function
The SOX9 protein contains several functionally specialized domains that enable its role as a transcriptional regulator. The high mobility group (HMG) box domain serves dual purposes: it facilitates DNA binding and contains nuclear localization and export signals that enable nucleocytoplasmic shuttling [3]. The C-terminal transcriptional activation domain (TAC) interacts with cofactors like Tip60 to enhance transcriptional activity and is essential for β-catenin inhibition during cell differentiation [3]. The central transcriptional activation domain (TAM) functions synergistically with TAC to augment SOX9's transcriptional potential. Ahead of the HMG box lies the dimerization domain (DIM), while the PQA-rich domain is necessary for transcriptional activation [3]. This modular structure allows SOX9 to integrate into multiple signaling networks and regulate diverse target genes involved in immune cell function and communication within the TME.
SOX9-Mediated Mechanisms of Immune Evasion
Suppression of Anti-Tumor Immune Cell Infiltration
SOX9 orchestrates a comprehensive immunosuppressive program within the TME by limiting the infiltration and function of cytotoxic immune cells. In KrasG12D-driven lung adenocarcinoma (LUAD) models, SOX9 expression significantly suppresses the recruitment of tumor-infiltrating CD8+ T cells, natural killer (NK) cells, and dendritic cells [30]. This exclusion of effector immune cells creates an "immune desert" microenvironment that facilitates tumor immune escape. The mechanisms underlying this exclusion involve SOX9-mediated elevation of collagen-related gene expression and substantial increases in collagen fibers, resulting in increased tumor stiffness that physically impedes immune cell infiltration [30]. Additionally, bioinformatics analyses of colorectal cancer data reveal that SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. These findings position SOX9 as a master regulator of the immune landscape across multiple cancer types.
Regulation of Immunosuppressive Cell Populations
Beyond excluding cytotoxic immune cells, SOX9 actively promotes the accumulation and function of immunosuppressive cell populations. Single-cell RNA sequencing and spatial transcriptomics analyses in prostate cancer patients demonstrate that SOX9 expression is associated with increased immunosuppressive cells, including regulatory T cells (Tregs) and M2 macrophages (TAM Macro-2), while decreasing effector immune cells such as CD8+CXCR6+ T cells [3]. This imbalance establishes an immunosuppressive milieu conducive to tumor progression. In liver cancer, SOX18 (a SOX family member related to SOX9) promotes the accumulation of Tregs and immunosuppressive tumor-associated macrophages (TAMs) by transactivating PD-L1 and CXCL12 [31]. Similarly, SOX12 increases intratumoral Treg infiltration and decreases CD8+ T-cell infiltration in liver cancer [31]. These findings across the SOX family highlight a conserved mechanism whereby SOX transcription factors shape the immunosuppressive landscape of the TME.
Metabolic Reprogramming of the Immune Microenvironment
Emerging evidence indicates that SOX9 drives immunometabolic reprogramming that sustains the immunosuppressive TME. In neuropathic pain models, which share features with cancer-associated inflammation, SOX9 transcriptionally regulates hexokinase 1 (Hk1), the enzyme that catalyzes the rate-limiting first step of glycolysis [7]. Nerve injury induces abnormal SOX9 phosphorylation, triggering aberrant Hk1 activation and high-rate astrocytic glycolysis [7]. The resulting excessive lactate production remodels histones of gene promoters via lactylation (H3K9la), promoting transcriptional modules of pro-inflammatory and neurotoxic genes while reducing beneficial cell populations [7]. This SOX9-Hk1-H3K9la axis represents a novel immunometabolic mechanism that may similarly operate in the TME to promote pathogenic cellular states and suppress anti-tumor immunity. The metabolic reprogramming driven by SOX9 creates a hostile environment for effector immune cells while supporting immunosuppressive populations that thrive in lactate-rich conditions.
Table 1: SO9-Mediated Effects on Immune Cell Populations in the Tumor Microenvironment
| Immune Cell Type | Effect of SOX9 | Mechanism | Cancer Type |
|---|---|---|---|
| CD8+ T cells | Suppresses infiltration and function | Increased collagen deposition and tumor stiffness; negative correlation with cytotoxic gene signatures | Lung adenocarcinoma, Colorectal cancer [3] [30] |
| Natural Killer (NK) cells | Suppresses infiltration | SOX9-driven physical barriers in TME; suppressed recruitment signals | Lung adenocarcinoma [30] |
| Dendritic cells | Suppresses infiltration and antigen presentation | Collagen-rich physical barriers; altered chemokine profiles | Lung adenocarcinoma [30] |
| Regulatory T cells (Tregs) | Promotes accumulation and function | Direct and indirect transcriptional regulation; potential PD-L1 transactivation | Prostate cancer, Liver cancer [3] [31] |
| M2 Macrophages | Promotes polarization and function | Complex cytokine and chemokine regulation; metabolic reprogramming | Prostate cancer, Multiple solid tumors [3] [31] |
| B cells | Suppresses infiltration | Altered chemotactic signals in TME | Colorectal cancer [3] |
SOX9 in Cancer Progression and Clinical Outcomes
Prognostic Significance Across Cancers
SOX9 overexpression is frequently associated with advanced disease stage and poor prognosis across multiple cancer types, reflecting its potent role in driving tumor progression and immune evasion. A meta-analysis of gastric cancer studies demonstrated that SOX9 expression significantly correlates with depth of invasion and advanced TNM stage [32]. Patients with high SOX9 expression exhibited significantly shorter 1-year, 3-year, and 5-year overall survival, establishing SOX9 as a potential prognostic biomarker [32]. In non-small cell lung cancer, patients with SOX9-high tumors show significantly shorter survival, while SOX9-low patients experience significantly longer survival [30]. Interrogation of The Cancer Genome Atlas data confirms this association, with SOX9 upregulation linked to poorer outcomes [30]. Interestingly, in glioblastoma, high SOX9 expression shows a complex relationship with prognosis, being remarkably associated with better prognosis in lymphoid invasion subgroups but serving as an independent prognostic factor for IDH-mutant cases [33]. These context-dependent associations highlight the tissue-specific functions of SOX9 and its integration with other molecular pathways in determining clinical outcomes.
Functional Role in Tumor Development
The functional importance of SOX9 in tumor development extends beyond correlation to direct causation. In KrasG12D-driven mouse lung adenocarcinoma models, loss of Sox9 significantly reduces lung tumor development, burden, and progression, contributing to significantly longer overall survival [30]. Sox9 knockout mice exhibited dramatically fewer high-grade tumors, with SOX9 being predominantly expressed in larger, proliferative, and high-grade tumors [30]. Similarly, in liver cancer models, deletion of the tumor suppressor Pten in SOX9+ cells induces their transformation, enabling them to give rise to mixed-lineage tumors manifesting features of both hepatocellular carcinoma and intrahepatic cholangiocarcinoma [34]. The tumorigenic potential of these transformed SOX9+ cells requires liver injury for activation, demonstrating how SOX9 interfaces with environmental cues to drive carcinogenesis [34]. These functional studies establish SOX9 not merely as a biomarker but as a bona fide driver of tumor development and progression across multiple cancer types.
Table 2: Clinical and Prognostic Significance of SOX9 in Human Cancers
| Cancer Type | Expression Pattern | Clinical Correlations | Prognostic Value |
|---|---|---|---|
| Gastric Cancer | Upregulated | Depth of invasion, TNM stage | Shorter 1-, 3-, and 5-year overall survival [32] |
| Lung Adenocarcinoma | Upregulated | Tumor grade, proliferation index | Shorter overall survival [30] |
| Glioblastoma | Upregulated | IDH mutation status, lymphoid invasion | Better prognosis in lymphoid invasion subgroups; independent prognostic factor in IDH-mutant cases [33] |
| Colorectal Cancer | Upregulated | Altered immune cell infiltration patterns | Associated with immunosuppressive TME [3] |
| Liver Cancer | Upregulated | Advanced tumor stage, higher tumor grade | Poorer recurrence-free and overall survival [34] |
| Breast Cancer | Upregulated | Tumor initiation, progression, stemness | Associated with basal-like subtype and poor outcomes [11] |
Experimental Models and Methodologies
In Vivo Cancer Models
Studies elucidating SOX9's role in immune regulation have employed sophisticated genetically engineered mouse models that enable precise manipulation of Sox9 expression in specific cellular contexts. The KrasLSL-G12D; Sox9flox/flox (KSf/f) model utilizes Cre-LoxP technology to achieve Sox9 knockout specifically in KrasG12D-driven tumor cells [30]. This approach demonstrates that Sox9 loss significantly reduces lung tumor burden and prolongs survival, with immunohistochemical analysis revealing decreased Ki67+ proliferating cells in SOX9- tumors [30]. Alternatively, the pSECC CRISPR-mediated genome editing system combines CRISPR and Cre recombinase to knockout Sox9 and activate KrasG12D simultaneously, confirming that Sox9 deletion decreases tumor number and burden while suppressing progression to high-grade tumors [30]. For lineage tracing studies, the PtenloxP/loxP; Sox9-CreERT+; R26RYFP model enables tamoxifen-inducible deletion of Pten in SOX9+ cells while labeling them with YFP [34]. This model revealed that transformed SOX9+ cells can give rise to mixed-lineage liver tumors, with all tumor cells expressing YFP, confirming their origin from SOX9+ cells [34]. These models provide powerful tools for dissecting SOX9's cell-autonomous and non-autonomous functions in tumor progression and immune modulation.
Immunological Assessment Techniques
Comprehensive immunological profiling in SOX9 studies employs multiple complementary techniques to characterize the immune microenvironment. Flow cytometry analysis of dissociated tumors enables quantification of immune cell populations, demonstrating SOX9-mediated suppression of CD8+ T cells, NK cells, and dendritic cells [30]. Gene expression analysis by RNA sequencing and RT-qPCR reveals SOX9-associated signatures related to collagen deposition, immune cell function, and metabolic pathways [3] [30]. Single-cell RNA sequencing (scRNA-seq) provides unprecedented resolution of cellular heterogeneity, as demonstrated in neuropathic pain models where scRNA-seq identified distinct astrocyte clusters and elucidated metabolic regulation of neuroinflammatory subsets [7]. Bioinformatic analysis of human cancer datasets, such as The Cancer Genome Atlas, enables correlation of SOX9 expression with immune signatures and patient outcomes [3] [32] [33]. Immunohistochemistry and immunofluorescence validate protein expression and localization, showing co-expression of hepatocyte and cholangiocyte markers in SOX9-derived liver tumors [34]. These multidisciplinary approaches collectively provide a comprehensive understanding of how SOX9 shapes the immunological landscape of tumors.
Diagram 1: SOX9 Mechanisms in Immune Evasion: This diagram illustrates the primary mechanisms through which SOX9 orchestrates tumor immune evasion, including direct immune suppression, metabolic reprogramming, creation of physical barriers, and promotion of pro-tumor inflammation.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating SOX9 in the Tumor Immune Microenvironment
| Reagent/Tool | Function/Application | Key Features | Representative Use |
|---|---|---|---|
| Sox9-floxed mice (Sox9flox/flox) | Conditional Sox9 knockout | Enables cell-type specific Sox9 deletion; compatible with Cre drivers | Studying Sox9 loss-of-function in specific cell populations [30] [34] |
| Sox9-CreERT+ mice | Inducible genetic targeting | Tamoxifen-inducible Cre expression in SOX9+ cells; enables lineage tracing | Fate mapping of SOX9+ cells and their progeny [34] |
| pSECC CRISPR system | In vivo genome editing | Combines CRISPR-mediated gene knockout with Cre-dependent oncogene activation | Simultaneous Sox9 knockout and KrasG12D activation in lung models [30] |
| R26RYFP reporter | Lineage tracing | Cre-dependent YFP expression; permanent labeling of targeted cells | Tracking SOX9+ cell fate in liver carcinogenesis [34] |
| Anti-SOX9 antibodies | IHC, IF, Western blot | Detection of SOX9 protein expression and localization | Assessing SOX9 expression in tumor tissues [30] [32] |
| scRNA-seq platforms | Cellular heterogeneity analysis | High-resolution transcriptomic profiling of individual cells | Identifying SOX9-associated cell clusters in TME [7] |
Therapeutic Implications and Future Directions
SOX9 as a Therapeutic Target
The compelling evidence for SOX9's role in driving immune evasion positions it as an attractive therapeutic target for cancer treatment. Several strategies emerge for targeting SOX9 therapeutically. Small molecule inhibitors that disrupt SOX9's transcriptional activity or its interactions with cofactors could potentially reverse its immunosuppressive programming [3]. Alternatively, targeting downstream effectors of SOX9, such as the SOX9-Hk1-H3K9la axis identified in neuropathic pain models, may provide more specific approaches to modulate SOX9 function without completely abrogating its physiological roles [7]. Given SOX9's role in promoting tumor stiffness and collagen deposition, combining SOX9-targeted approaches with anti-fibrotic agents may enhance immune cell infiltration and improve response to immunotherapy [30]. Additionally, the context-dependent functions of SOX9 suggest that patient stratification based on SOX9 expression patterns or activity signatures will be essential for developing effective SOX9-directed therapies. The dual nature of SOX9 in immunity necessitates careful therapeutic modulation rather than complete inhibition to avoid compromising its beneficial roles in tissue homeostasis and repair [3].
Integration with Immunotherapy
The immunosuppressive functions of SOX9 suggest that its inhibition could synergize with existing immunotherapies, particularly immune checkpoint inhibitors. SOX9-mediated suppression of CD8+ T cell and NK cell infiltration likely contributes to resistance against anti-PD-1/PD-L1 therapies [30]. Preclinical models demonstrate that SOX9 promotes an "immune desert" phenotype characterized by exclusion of cytotoxic immune cells, which is associated with poor response to checkpoint blockade [3] [30]. Therefore, combining SOX9 inhibition with immune checkpoint blockade may convert immune-excluded tumors into immune-inflamed ones, potentially expanding the proportion of patients who benefit from immunotherapy. Furthermore, the correlation between SOX9 expression and immune checkpoint molecules like PD-L1 in some cancer contexts suggests interconnected regulatory networks [31] [33]. Future studies should explore whether SOX9 directly regulates checkpoint molecule expression and whether SOX9 inhibition can enhance the efficacy of adoptive cell therapies, such as CAR-T cells, by improving their trafficking and persistence within tumors.
Diagram 2: SOX9-HK1 Immunometabolic Axis: This diagram outlines the SOX9-HK1 immunometabolic axis identified in neuropathic pain, demonstrating how SOX9 activation drives glycolytic reprogramming and epigenetic changes via lactate production, potentially mirroring mechanisms in the tumor microenvironment.
SOX9 emerges as a master orchestrator of the tumor immune microenvironment, integrating transcriptional control, metabolic reprogramming, and extracellular matrix remodeling to create an immunosuppressive niche that facilitates tumor progression. Its dual functions in immune regulation—promoting immunosuppressive cell populations while excluding cytotoxic effector cells—highlight its potential as both a prognostic biomarker and therapeutic target. The experimental models and methodologies reviewed provide robust tools for further dissecting SOX9's complex roles in cancer-immune interactions. As research continues to unravel the context-dependent functions of SOX9 across different cancer types and its integration with autoimmune and inflammatory pathways, targeting this multifaceted transcription factor may offer novel opportunities to overcome resistance to current immunotherapies and improve patient outcomes across multiple cancer types.
Targeting SOX9: From Molecular Pathways to Therapeutic Interventions
Gene therapy represents a transformative frontier for treating autoimmune and inflammatory disorders, aiming to address the underlying pathological mechanisms rather than merely alleviating symptoms. Within this landscape, adeno-associated virus (AAV)-mediated gene delivery has emerged as a promising vehicle for sustained therapeutic gene expression. This technical guide focuses on the coordinated delivery of two potent biological agents: Sex-determining region Y-box 9 (SOX9), a transcription factor critical for tissue homeostasis and repair, and Interleukin-1 Receptor Antagonist (IL-1Ra), a natural inhibitor of the key pro-inflammatory cytokine IL-1. The synergistic potential of SOX9 and IL-1Ra is particularly compelling within the context of chronic inflammatory diseases such as osteoarthritis and rheumatoid arthritis, where inflammation and tissue destruction are intertwined. This whitepaper provides an in-depth examination of the therapeutic rationale, experimental evidence, technical protocols, and clinical translation of AAV vectors engineered to co-deliver SOX9 and IL-1Ra, framed for an audience of researchers, scientists, and drug development professionals.
Therapeutic Rationale and Biological Mechanisms
The IL-1 Pathway and Rationale for IL-1Ra Gene Therapy
The interleukin-1 (IL-1) signaling pathway is a master regulator of inflammation and innate immunity. Its dysregulation is a pathogenic cornerstone of numerous chronic inflammatory diseases, including rheumatoid arthritis (RA) and osteoarthritis (OA) [35] [36]. IL-1α and IL-1β, the two primary agonists, initiate a potent pro-inflammatory cascade upon binding to the IL-1 receptor type 1 (IL-1R1). This triggers the recruitment of the myeloid differentiation primary response 88 (MyD88) adapter protein, leading to the activation of nuclear factor-kappa B (NF-κB) and mitogen-activated protein (MAP) kinase pathways, and ultimately the production of cytokines (e.g., IL-6, TNF), chemokines, and destructive enzymes [36].
The body's natural counterbalance to this pathway is the Interleukin-1 Receptor Antagonist (IL-1Ra), a secreted protein that competes with IL-1α and IL-1β for binding to IL-1R1 without initiating signal transduction. In many chronic inflammatory diseases, the balance between IL-1 and IL-1Ra is skewed towards inflammation. Traditional protein-based therapies with recombinant IL-1Ra (e.g., anakinra) are limited by short half-lives, necessitating frequent injections and failing to maintain effective joint concentrations [37]. AAV-mediated gene therapy surmounts this hurdle by enabling long-term, local production of IL-1Ra within the joint, thereby re-establishing the physiological anti-inflammatory balance [38] [35].
SOX9: A Master Regulator of Homeostasis and Repair
SOX9 is a transcription factor belonging to the SRY-related high-mobility group (HMG)-box family. It is a critical specifier and regulator in multiple biological processes, including chondrogenesis, glial cell function, and male sex determination [7] [39] [40]. Its role in maintaining tissue homeostasis and mitigating inflammatory responses is of particular therapeutic interest.
In the context of inflammatory joint disease, SOX9 is essential for chondrocyte health and cartilage matrix synthesis. It directly regulates the expression of key cartilage-specific extracellular matrix (ECM) components, such as type II collagen (COL2A1) and aggrecan. Furthermore, evidence suggests SOX9 exerts anti-inflammatory effects. Inhibition of SOX9 in dental pulp cells was shown to promote a pro-inflammatory state, increasing production of IL-8 and enhancing matrix metalloproteinase (MMP) activity, which leads to ECM degradation [14]. Conversely, boosting SOX9 in astrocytes promotes a protective phenotype, enhancing their phagocytic capacity to clear amyloid-β plaques in Alzheimer's disease models [13]. In neuropathic pain, aberrant SOX9 phosphorylation drives a metabolic shift towards glycolysis in a deleterious astrocyte subset, fueling neuroinflammation [7]. Thus, SOX9's function is highly context-dependent, but its targeted delivery can promote an anti-inflammatory, pro-regenerative state.
Table 1: Key Biological Functions of SOX9 and IL-1Ra
| Therapeutic Agent | Primary Function | Role in Inflammatory Disease | Consequence of Deficiency/Dysregulation |
|---|---|---|---|
| IL-1Ra | Natural antagonist of IL-1R1 | Blocks IL-1-driven inflammation and tissue destruction | Unchecked IL-1 signaling; chronic inflammation; cartilage degradation [35] [36] |
| SOX9 | Transcription factor; master regulator of cartilage and glial function | Promotes cartilage matrix synthesis; maintains tissue homeostasis; can inhibit inflammatory responses | Reduced matrix synthesis; increased MMP activity; emergence of pathogenic cell states [38] [14] [7] |
Preclinical and Clinical Evidence
Efficacy of Co-delivery in Osteoarthritis Models
Recent preclinical studies provide compelling evidence for the superior efficacy of co-delivering SOX9 and IL-1Ra compared to either treatment alone. A 2025 study investigated this combination in surgically induced osteoarthritis animal models (rats and rabbits) using a single-stranded AAV (scAAV) vector [38].
Key findings from this study are summarized in the table below:
Table 2: Summary of Efficacy Outcomes from AAV-Mediated SOX9 and IL-1Ra Co-delivery in Preclinical OA Models [38]
| Model System | Treatment | Key Efficacy Outcomes |
|---|---|---|
| MMT/ACLT-induced KOA (Rat) | scAAV-oIL-1Ra | Improved gait (increased footprint area & pressure); reduced subchondral bone lesions; significantly reduced cartilage wear and pathological scores. |
| MMT-induced KOA (Rabbit) | scAAV-oIL-1Ra | Improved weight-bearing symmetry (indicating pain relief) after 8 weeks; decreased Kellgren-Lawrence (K-L) scores on X-ray; reduced cartilage loss and pathology scores. |
| ACLT+MMT-induced KOA (Rat) | scAAV-oIL-1Ra + SOX9 | Significantly alleviated subchondral bone lesions, cartilage destruction, and synovial inflammation. Demonstrated superior efficacy versus single treatments. |
The study concluded that the combination therapy not only inhibited IL-1-mediated inflammatory signaling but also promoted cartilage homeostasis and repair, suggesting strong clinical potential [38].
Advanced IL-1Ra Gene Therapy Constructs
Innovations in vector design are enhancing the safety and specificity of IL-1Ra therapy. One advanced approach involves the use of an inflammation-inducible promoter to control the expression of a secreted human IL-1Ra (sIL-1Ra). This system, delivered via a recombinant AAV (rAAV), is designed to mimic the body's natural feedback mechanism by "turning on" sIL-1Ra production specifically in the presence of pro-inflammatory cytokines and bone morphogenic proteins (BMPs) enriched in inflamed joints [35].
In a mouse model of rheumatoid arthritis, this inducible sIL-1Ra was remarkably more effective than a constitutively expressed version in ameliorating inflammatory arthritis. Treated mice showed significant reductions in circulating immune cells, expression of inflammatory genes, joint swelling, and bone destruction. Furthermore, a single systemic administration of this rAAV-sIL-1Ra vector almost completely reversed spontaneous inflammatory arthritis and skeletal abnormalities in IL-1Ra-deficient mice, modeling the human DIRA syndrome [35]. This highlights the potential of pathophysiology-responsive gene regulation for treating chronic inflammatory diseases.
Clinical Trial Landscape
The translation of AAV-mediated gene therapy for joint disease is underway, though the clinical landscape is still nascent. Pacira BioSciences is advancing a notable candidate, PCRX-201 (enekinragene inzadenovec), an intra-articular gene therapy for osteoarthritis of the knee designed to boost local production of IL-1Ra [41].
PCRX-201 incorporates an inducible promoter and is based on a proprietary high-capacity adenovirus (HCAd) vector platform, which offers advantages over traditional AAV, including a larger transgene capacity and potential for re-dosing [41]. The ongoing two-part, multicenter Phase 2 ASCEND study is evaluating the safety and efficacy of PCRX-201. The company reported continued durable and clinically meaningful improvements in knee pain, stiffness, and function through three years post-administration, with a well-tolerated safety profile [41]. PCRX-201 has received Regenerative Medicine Advanced Therapy (RMAT) designation from the U.S. FDA, underscoring its potential.
Table 3: Overview of Selected Clinical Trials for Joint Disease Gene Therapy
| Therapeutic Candidate / Identifier | Vector / Gene | Indication | Sponsor | Key Design Features / Status |
|---|---|---|---|---|
| PCRX-201 (ASCEND study) | HCAd / IL-1Ra | Osteoarthritis of the Knee | Pacira BioSciences | Inflammation-inducible promoter; Phase 2 ongoing; RMAT designation [41]. |
| NCT02790723 | AAV2.5 / IL-1Ra | Knee Osteoarthritis | Mayo Clinic | Phase I/II trial assessing safety, tolerability, and effects on pain and function [37]. |
| ICM-203 (NCT05454566) | AAV5.2 / Nkx3.2 | Knee Osteoarthritis | ICM Co., Ltd. | Encodes a transcription factor involved in chondrocyte activity; interim results show mixed outcomes [37]. |
| NCT03445715 | AAV5 / sTNFR1 | Rheumatoid Arthritis (Wrist) | Arthrogen | Delivers soluble TNF receptor to block TNF-α; one of several trials for RA [37]. |
Technical and Methodological Guide
Experimental Protocol for Preclinical OA Model Validation
The following detailed methodology is adapted from the 2025 co-delivery study, providing a robust framework for validating AAV-SOX9/IL-1Ra efficacy [38].
1. Vector Construction and Preparation:
- Therapeutic Genes: Clone full-length cDNA for the species-specific IL-1Ra and SOX9 genes.
- Vector Backbone: Utilize a single-stranded AAV (scAAV) backbone (e.g., scAAV2) to enable rapid transgene expression. The use of a self-complementary genome is optional but enhances kinetics.
- Promoter Selection: Employ a strong, ubiquitous promoter such as CAG (hybrid CMV early enhancer/chicken β-actin) or a synthetic, inflammation-inducible promoter (e.g., based on NF-κB response elements) for context-specific expression [35].
- Virus Production: Package the recombinant genome into the desired AAV capsid (e.g., AAV2, AAV5, or a engineered capsid with tropism for synovium and chondrocytes) using a standard triple-transfection method in HEK293 cells. Purify via iodixanol gradient ultracentrifugation or affinity chromatography, and titrate via digital droplet PCR to determine genome copies (GC)/mL.
2. Animal Model Induction and Dosing:
- Osteoarthritis Model: Induce knee osteoarthritis (KOA) in Sprague-Dawley rats (or other relevant species) using the medial meniscal tear (MMT) model alone or in combination with anterior cruciate ligament transection (ACLT). This surgically induces instability, leading to progressive cartilage degradation.
- Group Allocation: Randomize animals into groups (e.g., n=8-12): (1) Sham-operated control, (2) Disease model + saline, (3) Disease model + scAAV-IL-1Ra, (4) Disease model + scAAV-SOX9, (5) Disease model + scAAV-IL-1Ra-SOX9 (co-delivery).
- Administration: Administer a single intra-articular injection of the AAV construct (e.g., 50 μL containing 1x10^11 - 1x10^12 total GC) into the knee joint cavity 1-2 weeks post-surgery to allow disease establishment.
3. Outcome Assessment and Endpoints:
- Functional and Pain-Related Behaviors: Quantify weekly from baseline to endpoint (e.g., 8-12 weeks post-injection).
- Gait Analysis: Use a dynamic pressure walkway to measure footprint area and weight-bearing distribution (asymmetry indicates pain).
- Weight-Bearing: Measure spontaneous weight-bearing on the affected limb using an incapacitance tester.
- Radiological and Histological Analysis: At study termination, collect knee joints for analysis.
- X-ray/Micro-CT: Score subchondral bone lesions and joint space narrowing using a standardized system like the Kellgren-Lawrence (K-L) grade.
- Histopathology: Process, section, and stain joints with Safranin-O/Fast Green and Hematoxylin & Eosin (H&E). Score cartilage degradation, synovitis, and overall joint pathology using the Osteoarthritis Research Society International (OARSI) scoring system or Mankin's score by blinded evaluators.
- Molecular Analysis: Isulate protein and RNA from cartilage/synovial tissue.
- qPCR/Western Blot: Quantify expression of SOX9, IL-1Ra, inflammatory markers (IL-1β, IL-6, TNF), matrix genes (COL2A1, aggrecan), and catabolic enzymes (MMP-13, ADAMTS-5).
- ELISA: Measure levels of IL-1Ra and inflammatory cytokines in synovial fluid or conditioned media.
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Research Reagents for AAV-SOX9/IL-1Ra Investigations
| Reagent / Resource | Function and Application | Examples / Notes |
|---|---|---|
| AAV Serotypes | Determines tissue tropism and transduction efficiency. | AAV2, AAV5: Common in early trials for synovium/chondrocytes [37]. AAV8, AAVDJ: For systemic delivery. Engineered capsids for enhanced joint targeting. |
| Inducible Promoters | Enables context-specific, inflammation-responsive transgene expression. | Promoters responsive to NF-κB or STAT signaling pathways [35]. |
| Animal OA Models | Preclinical in vivo validation of therapeutic efficacy. | MMT, ACLT, or MMT/ACLT combined models in rats or rabbits [38]. Chemical induction (e.g., mono-iodoacetate) is an alternative. |
| Behavioral Assay Equipment | Quantifies functional pain relief and motor improvement. | Dynamic pressure-sensitive walkway (e.g., CatWalk), incapacitance tester [38]. |
| Histopathology Stains & Scoring Systems | Evaluates cartilage integrity, proteoglycan content, and synovial inflammation. | Safranin-O/Fast Green (proteoglycan), H&E (cellular structure). OARSI scoring system for standardized assessment [38]. |
| Molecular Assays | Validates transgene expression and analyzes downstream molecular effects. | qPCR for gene expression, Western Blot/ELISA for protein quantification, chromatin immunoprecipitation (ChIP) for SOX9 binding studies [14]. |
Signaling Pathway and Experimental Workflow Visualization
The following DOT language scripts generate diagrams illustrating the core mechanistic pathway and the experimental workflow. They are designed with high color contrast for clarity.
Diagram 1: Mechanism of AAV-SOX9/IL-1Ra Action in an Inflamed Joint This diagram illustrates how the co-delivery therapy counteracts disease mechanisms at both the extracellular (IL-1Ra) and intracellular (SOX9) levels.
Diagram 2: Preclinical Experimental Workflow for AAV-SOX9/IL-1Ra Validation This flowchart outlines the key stages of a standard in vivo efficacy study, from model establishment to final analysis.
Challenges and Future Directions
Despite the promising preclinical and early clinical data, several hurdles remain for the widespread clinical adoption of AAV-mediated SOX9/IL-1Ra therapy.
- AAV Delivery Barriers: Intra-articular delivery faces challenges related to transduction efficiency in dense cartilage tissue and the synovial lining. The joint environment contains proteoglycans and other extracellular matrix components that can impede vector diffusion. Furthermore, the presence of preexisting humoral immunity to certain AAV serotypes in a significant portion of the population can neutralize the vector before it can transduce target cells [37].
- Immunogenicity and Safety: While AAV is less immunogenic than other viral vectors, the capsid and transgene product can still elicit host cellular and immune responses, potentially limiting re-dosing and long-term expression. Strategies to mitigate this include capsid engineering to evade pre-existing immunity and the use of tissue-specific or inducible promoters to minimize off-target expression [37].
- Vector Capacity and Cost: The packaging capacity of standard AAV (~4.7 kb) is a constraint for delivering multiple large genes or complex regulatory circuits. While the HCAd platform used for PCRX-201 addresses this, its long-term immunogenicity profile is still being characterized [41]. Manufacturing complexity also leads to high costs, posing challenges for commercial viability [37].
Future research should focus on developing novel engineered AAV capsids with enhanced tropism for joint tissues, optimizing inflammation-responsive promoters for finer control of transgene expression, and establishing reliable biodistribution and safety profiles in large animal models. The synergistic potential of SOX9 and IL-1Ra represents a paradigm shift from symptomatic relief to disease modification, holding immense promise for revolutionizing the treatment of debilitating autoimmune and inflammatory disorders.
Cordycepin (3'-deoxyadenosine), a primary bioactive compound derived from Cordyceps species, has emerged as a potent small-molecule inhibitor of the transcription factor SOX9. This whitepaper details the mechanistic basis and experimental evidence for cordycepin-mediated SOX9 suppression, framing its therapeutic potential within the context of SOX9's pivotal role in autoimmune diseases and inflammatory disorders. We consolidate quantitative data on cordycepin's efficacy across cancer cell lines, provide detailed methodologies for key validation experiments, and delineate the associated signaling pathways. Given SOX9's established function in promoting fibroblast activation, tissue fibrosis, and immune dysregulation—key drivers of autoimmune pathology—targeted inhibition via cordycepin represents a promising strategic avenue for therapeutic intervention.
The SRY-related HMG-box 9 (SOX9) protein is a transcription factor with a defining High Mobility Group (HMG) box DNA-binding domain. It orchestrates diverse biological processes, including cell fate determination, organ development, and immune regulation [3]. Beyond its well-characterized roles in development and cancer, SOX9 is increasingly recognized as a central regulator in inflammatory and fibrotic processes [17].
- Dual Role in Immunity: SOX9 exhibits a "double-edged sword" function in immunology. It can promote tumor immune escape by impairing immune cell function, yet it also helps maintain macrophage function critical for tissue repair and cartilage formation [3].
- Driver of Fibrosis: SOX9 is a key transcriptional regulator in organ fibrosis, contributing to pathological extracellular matrix (ECM) accumulation in the heart, liver, kidney, and lungs. Its expression is frequently upregulated by profibrotic cytokines like TGF-β [17].
- Role in Autoimmune Pathology: In the autoimmune context of Thyroid Eye Disease (TED), SOX9 is significantly overexpressed in orbital fibroblasts (OFs). It activates these cells via the MAPK/ERK1/2 signaling pathway, promoting proliferation, differentiation, and ECM production—key events in orbital fibrosis [19].
The compelling association between elevated SOX9 and disease pathogenesis makes the discovery of effective suppressors a research priority.
Cordycepin as a SOX9 Suppressor: Quantitative Evidence
Cordycepin, an adenosine analog, demonstrates a direct and dose-dependent inhibitory effect on SOX9 expression. Key quantitative evidence from pan-cancer analyses and in vitro studies is summarized in the table below.
Table 1: Quantitative Evidence for Cordycepin-Mediated SOX9 Suppression
| Cancer Cell Line / Context | Experimental Treatment | Effect on SOX9 Protein/mRNA | Correlated Anticancer Effects |
|---|---|---|---|
| Prostate Cancer (22RV1 cells) [42] | Cordycepin (0, 10, 20, 40 µM for 24h) | Inhibition in a dose-dependent manner | Inhibition of tumorigenicity [42] |
| Prostate Cancer (PC3 cells) [42] | Cordycepin (0, 10, 20, 40 µM for 24h) | Inhibition in a dose-dependent manner | Inhibition of tumorigenicity [42] |
| Lung Cancer (H1975 cells) [42] | Cordycepin (0, 10, 20, 40 µM for 24h) | Inhibition in a dose-dependent manner | Inhibition of tumorigenicity [42] |
| Pan-Cancer Analysis [42] | N/A (Bioinformatic correlation) | SOX9 significantly upregulated in 15 of 33 cancer types | High SOX9 correlated with worst overall survival in LGG, CESC, THYM |
These findings establish cordycepin as a consistent suppressor of SOX9 expression across multiple cell types, providing a mechanistic rationale for its documented anticancer roles [42].
Experimental Protocols for Validating SOX9 Inhibition
To empirically validate the effect of cordycepin on SOX9, the following detailed methodologies can be employed.
Cell Culture and Cordycepin Treatment Protocol
This protocol is adapted from studies demonstrating successful SOX9 suppression [42].
- Cell Lines: Utilize relevant cancer cell lines (e.g., 22RV1, PC3, H1975) or disease-specific primary cells (e.g., Orbital Fibroblasts from TED patients [19]).
- Culture Conditions:
- Maintain cells in RPMI 1640 or DMEM medium supplemented with 10-15% Fetal Bovine Serum (FBS) and 1% penicillin/streptomycin at 37°C in a 5% CO₂ humidified incubator.
- Cordycepin Treatment:
- Prepare a stock solution of cordycepin in an appropriate solvent (e.g., DMSO or water) and dilute to working concentrations in culture medium.
- Seed cells in 12-well plates. Upon reaching 70-80% confluence, treat with cordycepin at a range of concentrations (e.g., 0, 10, 20, 40 µM) for 24 hours. Include a vehicle control.
Western Blotting for SOX9 Protein Expression
This protocol enables quantification of SOX9 protein levels post-treatment [42].
- Protein Extraction: Post-treatment, lyse cells using RIPA buffer supplemented with protease and phosphatase inhibitors. Determine protein concentration with a BCA assay.
- Gel Electrophoresis and Transfer: Load equal amounts of protein (20-40 µg) onto an SDS-polyacrylamide gel. After electrophoresis, transfer proteins to a PVDF membrane.
- Immunoblotting:
- Block the membrane with 5% non-fat milk in TBST.
- Incubate with primary antibodies against SOX9 and a loading control (e.g., β-Actin) overnight at 4°C.
- Incubate with appropriate horseradish peroxidase (HRP)-conjugated secondary antibodies.
- Visualize bands using an enhanced chemiluminescence (ECL) detection system and analyze band density.
RT-PCR for SOX9 mRNA Expression
This protocol assesses transcriptional inhibition of SOX9 [42].
- RNA Extraction: Isolate total RNA from treated cells using TRIzol reagent or a commercial RNA purification kit.
- cDNA Synthesis: Reverse transcribe 2 µg of RNA into cDNA using M-MLV reverse transcriptase.
- Quantitative PCR (qPCR):
- Perform qPCR using SYBR Green master mix and gene-specific primers for SOX9 and a housekeeping gene (e.g., GAPDH).
- Calculate relative gene expression using the 2^–ΔΔCT method.
Mechanistic Insights: Cordycepin's Action on SOX9 and Related Pathways
Cordycepin's suppression of SOX9 is situated within a broader anti-inflammatory and antifibrotic mechanism. The compound concurrently inhibits key signaling pathways that interact with SOX9 activity.
Table 2: Cordycepin's Multifaceted Mechanisms of Action
| Mechanism of Action | Observed Effect | Biological Consequence |
|---|---|---|
| SOX9 Suppression [42] | Dose-dependent downregulation of SOX9 mRNA and protein. | Reduction of SOX9-driven oncogenic & profibrotic programs. |
| MAPK/ERK Pathway Inhibition [43] | Suppression of LPS-induced phosphorylation of ERK1/2, p38, and JNK. | Attenuation of pro-inflammatory signaling and cell activation. |
| NF-κB Pathway Inhibition [43] | Inhibition of IκB-α degradation and nuclear translocation of NF-κB/p65. | Reduced transcription of pro-inflammatory genes (TNF-α, IL-1β, iNOS, COX-2). |
| TLR4 Signaling Disruption [43] | Inhibition of LPS binding to macrophages and reduced TLR4/MyD88 expression. | Blunted initiation of innate immune responses. |
The interplay between these pathways and SOX9 activation can be visualized in the following diagram. Cordycepin exerts its effects at multiple nodes, with SOX9 suppression being a key outcome.
Diagram: Cordycepin inhibits SOX9 and pro-fibrotic signaling. Cordycepin suppresses SOX9 expression and activity while concurrently inhibiting the MAPK and NF-κB pathways, thereby disrupting key drivers of inflammation and fibrosis.
The Scientist's Toolkit: Essential Research Reagents
The following table catalogues critical reagents for investigating SOX9 biology and cordycepin's effects.
Table 3: Research Reagent Solutions for SOX9 and Cordycepin Studies
| Reagent / Resource | Function & Application | Example Use Case |
|---|---|---|
| Cordycepin (3'-deoxyadenosine) | Small molecule inhibitor; core compound for SOX9 suppression studies. | In vitro treatment of cell lines to assess SOX9 downregulation and functional effects [42]. |
| Anti-SOX9 Antibody | Detection and quantification of SOX9 protein levels via Western Blot, IF, IHC. | Validate SOX9 knockdown or overexpression; measure protein levels after cordycepin treatment [19]. |
| Primary Orbital Fibroblasts (OFs) | Disease-relevant primary cells for modeling fibrotic mechanisms. | Study SOX9's role in TED and test anti-fibrotic efficacy of cordycepin [19]. |
| siRNA targeting SOX9 | Genetic knockdown tool to validate SOX9-specific phenotypes. | Confirm that SOX9 inhibition is responsible for observed effects (e.g., reduced contraction, ECM gene expression) [19]. |
| Phospho-Specific Antibodies (p-ERK, p-p38) | Interrogation of MAPK pathway activity downstream of SOX9 or cordycepin. | Mechanistic studies to link SOX9 activity or cordycepin treatment to MAPK signaling modulation [19] [43]. |
The evidence consolidates cordycepin's role as a potent, dose-dependent suppressor of SOX9. Its ability to simultaneously dampen the MAPK and NF-κB pathways creates a powerful polypharmacological profile, disrupting the core inflammatory and fibrotic circuits in which SOX9 is embedded. Given SOX9's well-documented overexpression in autoimmune fibrotic conditions like Thyroid Eye Disease, targeted inhibition with cordycepin presents a compelling therapeutic strategy.
Future work should focus on:
- Elucidating the precise molecular mechanism by which cordycepin regulates SOX9 transcription or protein stability.
- Validating the efficacy of cordycepin in in vivo models of autoimmune and fibrotic diseases.
- Exploring the potential of cordycepin-based therapies or more potent derivatives for clinical translation in managing SOX9-driven pathologies.
The NF-κB/SOX9 signaling axis represents a critical regulatory pathway in inflammatory disorders and autoimmune diseases. This technical review examines the mechanistic role of rosmarinic acid (RosA), a natural polyphenolic compound, in modulating this pathway. We present comprehensive experimental data demonstrating RosA's dual functionality in suppressing NF-κB-mediated inflammation while simultaneously promoting SOX9-driven cartilage regeneration. Through systematic analysis of in vitro, ex vivo, and in vivo studies, this whitepaper establishes RosA as a promising therapeutic candidate for targeting the NF-κB/SOX9 axis in osteoarthritis and related inflammatory conditions, providing researchers with detailed methodological frameworks for further investigation.
The nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) and SRY-Box Transcription Factor 9 (SOX9) form an integrated signaling network that maintains tissue homeostasis under physiological conditions but becomes dysregulated in inflammatory and autoimmune pathologies. NF-κB is a ubiquitously expressed transcription factor that regulates numerous genes involved in inflammation, immunity, cell proliferation, and apoptosis [44]. The canonical NF-κB pathway is activated by various stimuli, including pro-inflammatory cytokines like IL-1β, leading to IκB kinase (IKK)-mediated phosphorylation and degradation of IκB proteins, which allows NF-κB dimers (typically p65/p50) to translocate to the nucleus and activate target genes [44] [45].
SOX9, a high-mobility group box transcription factor, serves as the "master regulator" of chondrogenesis and is essential for chondrocyte differentiation, cartilage development, and extracellular matrix (ECM) production [44] [3]. In osteoarthritis (OA) and related inflammatory joint disorders, pro-inflammatory cytokines activate NF-κB signaling, which subsequently suppresses SOX9 expression and transcriptional activity, creating an imbalance between catabolic and anabolic processes in articular cartilage [46] [44]. This NF-κB/SOX9 imbalance results in elevated expression of matrix-degrading enzymes (MMPs, ADAMTS) and decreased production of essential ECM components like type II collagen and aggrecan, ultimately driving cartilage destruction [46] [47].
Rosmarinic Acid: Source, Chemistry, and Bioavailability
Rosmarinic acid (RosA) is a water-soluble phenolic compound and an ester of caffeic acid and 3,4-dihydroxyphenyllactic acid (molecular formula: C18H16O8) that was first isolated from rosemary (Rosmarinus officinalis L.) in 1958 [48]. It is abundantly present in plants of the Lamiaceae family (including rosemary, oregano, basil, sage, and mint) and the Boraginaceae family [46] [48]. RosA's chemical structure features two catechol moieties, which confer potent antioxidant activity through free radical scavenging and enhance its solubility and stability [46].
Table 1: Bioavailability and Metabolic Profile of Rosmarinic Acid
| Parameter | Details | Experimental Evidence |
|---|---|---|
| Absorption | Partially metabolized to caffeic acid and coumaric acid in the rat body | [48] |
| Bioavailability | Water-soluble with approximately 90% secretion efficacy in infusions | [48] |
| Potential Daily Intake | Approximately 110 mg daily (∼1.6 mg/kg for 70 kg adult) from dietary sources | [48] |
| Therapeutic Doses (Preclinical) | 10-100 μM (in vitro); 5-50 mg/kg (in vivo rodent studies) | [46] [47] [48] |
| Mechanisms of Action | Direct antioxidant activity; Modulation of inflammatory signaling pathways; Induction of glutathione biosynthesis | [48] |
Beyond its well-documented antioxidant and antimicrobial properties, RosA has demonstrated significant anti-inflammatory effects across various disease models, including arthritis, colitis, and atopic dermatitis [47]. Its therapeutic potential stems from its ability to modulate multiple signaling pathways, particularly the NF-κB pathway, and influence the expression of key transcription factors like SOX9 [46].
Mechanistic Insights: Rosmarinic Acid Modulation of the NF-κB/SOX9 Axis
Suppression of NF-κB-Mediated Inflammation
RosA exerts potent anti-inflammatory effects primarily through suppression of the NF-κB signaling pathway. In vitro studies using IL-1β-stimulated chondrocytes demonstrate that RosA treatment significantly reduces phosphorylation and degradation of IκB protein, thereby preventing nuclear translocation of the NF-κB p65 subunit [46]. Immunocytochemistry analysis confirmed decreased p65 translocation to the nucleus in RosA-treated chondrocytes compared to IL-1β-stimulated controls [46]. This inhibition of NF-κB activation translates to downstream reduction in expression of catabolic factors central to OA pathogenesis.
Table 2: Effect of Rosmarinic Acid on Catabolic Factors in IL-1β-Stimulated Chondrocytes
| Catabolic Factor | Function in OA Pathogenesis | Effect of RosA Treatment | Experimental Method |
|---|---|---|---|
| MMP-3 | Degrades ECM components including proteoglycans | Significant reduction | RT-PCR, Western blot [46] |
| MMP-13 | Primary collagenase degrading type II collagen | Significant reduction | RT-PCR, Western blot [46] |
| COX-2 | Induces prostaglandin E2 synthesis, mediating pain and inflammation | Significant reduction | ELISA, Western blot [46] |
| ADAMTS-4 | Aggrecanase responsible for aggrecan degradation | Significant reduction | RT-PCR [47] |
| ADAMTS-5 | Aggrecanase responsible for aggrecan degradation | Significant reduction | RT-PCR [47] |
The molecular mechanisms of RosA's anti-inflammatory effects also involve suppression of the MAPK signaling pathway in immune cells. In LPS-stimulated RAW 264.7 macrophages, rosmarinosin A (a dimeric phenylpropanoid derived from RosA) reduced production of nitric oxide (NO) and prostaglandin E2 (PGE2) through modulation of iNOS and COX-2 expression, respectively [49]. This was associated with inhibited phosphorylation of JNK, ERK, and p38 MAP kinases, indicating broad-spectrum anti-inflammatory activity across multiple signaling pathways [49].
Promotion of SOX9-Mediated Cartilage Regeneration
Beyond suppressing catabolic processes, RosA directly enhances anabolic processes in cartilage through upregulation of SOX9 and its target genes. SOX9 is the master transcription factor for chondrogenesis that directly regulates expression of essential ECM components including type II collagen (Col2a1) and aggrecan (Acan) [46] [44]. Research has established that NF-κB can positively regulate SOX9 expression by directly binding to its promoter region, creating a complex regulatory relationship in inflammatory conditions [44] [50].
In vitro analyses demonstrate that RosA treatment promotes SOX9 expression in chondrocytes, even under inflammatory conditions induced by IL-1β [46]. This effect was consistently observed across multiple experimental systems:
Table 3: Effect of Rosmarinic Acid on Anabolic Factors in Cartilage
| Anabolic Factor | Function in Cartilage Homeostasis | Effect of RosA Treatment | Experimental Context |
|---|---|---|---|
| SOX9 | Master regulator of chondrogenesis; transcription factor for COL2A1 and ACAN | Promoted expression | In vitro, ex vivo, in vivo [46] |
| Col2a1 | Primary collagen type in articular cartilage | Induced expression | In vitro, ex vivo, in vivo [46] |
| Acan | Major proteoglycan in cartilage ECM | Induced expression | In vitro, ex vivo, in vivo [46] |
Ex vivo experiments using cartilage explants confirmed these findings, with RosA protecting against sulfated proteoglycan erosion triggered by IL-1β, as demonstrated by alcian blue staining [46]. Furthermore, immunohistochemical analysis of cartilage tissues from animal models revealed enhanced SOX9, Col2a1, and Acan expression following RosA treatment [46].
The relationship between NF-κB and SOX9 represents a complex regulatory loop in inflammatory conditions. While NF-κB activation generally suppresses SOX9 expression in established inflammation, evidence suggests that NF-κB can directly bind to the SOX9 promoter and positively regulate its expression under specific contexts, particularly during development and tissue repair [44] [50]. RosA appears to modulate this relationship by suppressing the inflammatory arm of NF-κB signaling while permitting or potentially enhancing its regulatory functions related to SOX9 expression.
Diagram 1: Rosmarinic Acid Modulation of the NF-κB/SOX9 Signaling Axis in Chondrocytes. RosA suppresses NF-κB activation by inhibiting IκBα phosphorylation and p65 nuclear translocation, thereby reducing catabolic factor expression. Simultaneously, RosA promotes SOX9 expression and enhances ECM synthesis, rebalancing cartilage homeostasis.
Experimental Validation: Methodological Frameworks
In Vitro Assessment Protocols
Primary Chondrocyte Isolation and Culture
- Source: Articular chondrocytes isolated from 5-day-old ICR mice tibial plateaus and femoral condyles [46]
- Digestion Protocol: Enzymatic digestion with 0.2% type II collagenase in DMEM medium [46]
- Culture Conditions: Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10% fetal bovine serum (FBS) and 1% antibiotic solution at 37°C with 5% CO₂ [46]
- Treatment Protocol: Chondrocytes treated simultaneously with IL-1β (1 ng/mL) and RosA at concentrations of 10, 50, and 100 μM for 24 hours [46]
Cytotoxicity Analysis
- Assay Kit: EZ-Cytox Cell Viability Assay Kit (DoGenBio, Seoul, Korea) [46]
- Cell Seeding Density: 9 × 10³ cells per well in 96-well plates [46]
- Incubation Period: 48 hours before treatment [46]
- RosA Concentration Range: 50, 100, and 200 μM for 24 hours in serum-free DMEM [46]
- Detection Method: WST-1 solution mixed with DMEM (1:100 v/v), incubated for 3 hours in dark, absorbance measured at 450 nm using microplate reader [46]
Molecular Analysis Techniques
- Gene Expression: RT-PCR and qRT-PCR analysis of catabolic (MMP-3, MMP-13, COX-2) and anabolic (SOX9, Col2a1, Acan) factors [46]
- Protein Expression: Western blotting for NF-κB pathway components (p65, p-p65, IκBα) and cartilage markers [46]
- Cytokine Measurement: ELISA for prostaglandin E2 (PGE2) and inflammatory cytokines [46]
- NF-κB Localization: Immunocytochemistry (ICC) for p65 nuclear translocation using specific antibodies [46]
Ex Vivo and In Vivo Models
Cartilage Explant Culture
- Source: Femur and tibia cartilage explants from 5-day-old ICR mice [46]
- Culture Conditions: DMEM supplemented with 10% FBS, IL-1β, and RosA for 72 hours [46]
- Histological Analysis: Alcian blue staining for sulfated proteoglycan content [46]
- Protein Localization: Immunohistochemistry (IHC) for catabolic and anabolic factors [46]
In Vivo Osteoarthritis Model
- Animal Model: Destabilization of the medial meniscus (DMM)-induced OA in male C57BL/6 mice (18-20 g) [46]
- Histological Assessment: Safranin-O staining for cartilage destruction evaluation [46]
- Grading System: Osteoarthritis Research Society International (OARSI) scoring for cartilage degradation [46]
- Immunohistochemistry: Quantification of catabolic and anabolic factors in mice knee joints [46]
Diagram 2: Comprehensive Experimental Workflow for Evaluating Rosmarinic Acid Effects. The multi-stage approach validates RosA mechanisms from cellular to whole-animal levels, ensuring comprehensive assessment of its impact on the NF-κB/SOX9 axis.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for Investigating RosA Effects on NF-κB/SOX9 Axis
| Reagent/Category | Specific Examples | Function/Application | Source/Reference |
|---|---|---|---|
| RosA Sources | Sigma-Aldrich (St. Louis, MO, USA); Natural plant extracts (rosemary, oregano, basil) | Experimental treatment; dissolved in 100% ethanol | [46] |
| Inflammatory Stimuli | Recombinant IL-1β proteins (Gen Script, Piscataway, NJ, USA); LPS | Induction of inflammatory response in cellular and tissue models | [46] [49] |
| Cell Culture Models | Primary mouse articular chondrocytes; RAW 264.7 macrophages | In vitro assessment of anti-inflammatory and chondroprotective effects | [46] [49] |
| Viability Assays | EZ-Cytox Cell Viability Assay Kit; MTT assay | Determination of non-cytotoxic concentrations of RosA | [46] [49] |
| Molecular Biology Kits | RT-PCR; qRT-PCR; Western blotting; ELISA | Analysis of gene and protein expression of catabolic and anabolic factors | [46] |
| Histological Stains | Safranin-O; Alcian blue | Assessment of proteoglycan content and cartilage integrity | [46] |
| Antibodies | Anti-p65; Anti-p-p65; Anti-IκBα; Anti-SOX9; Anti-Col2a1; Anti-MMP-13 | Immunocytochemistry, immunohistochemistry, and Western blot analysis | [46] |
| Animal Models | DMM-induced OA mouse model (C57BL/6) | In vivo validation of chondroprotective effects | [46] |
Therapeutic Implications and Future Research Directions
The dual functionality of RosA in simultaneously suppressing NF-κB-driven inflammation and promoting SOX9-mediated cartilage regeneration positions it as a promising therapeutic candidate for osteoarthritis and related inflammatory joint disorders. Current OA management primarily relies on NSAIDs that merely alleviate symptoms without addressing underlying cartilage degeneration and may cause significant adverse effects [46] [47]. RosA represents a disease-modifying approach that targets fundamental pathological processes.
Future research should focus on several key areas:
- Delivery Optimization: Developing advanced delivery systems to enhance RosA bioavailability and joint targeting
- Combination Therapies: Exploring synergistic effects of RosA with other bioactive compounds or conventional therapeutics
- Clinical Translation: Conducting well-designed clinical trials to establish efficacy and optimal dosing in human populations
- Broader Applications: Investigating RosA's potential in other SOX9-related inflammatory and autoimmune conditions
The comprehensive mechanistic data and experimental protocols presented in this review provide researchers with the necessary framework to advance these investigations and fully exploit the therapeutic potential of rosmarinic acid in modulating the NF-κB/SOX9 axis.
The crosstalk between MAPK/ERK, EGFR, and NF-κB signaling pathways constitutes a critical regulatory axis in autoimmune and inflammatory disorders, with the transcription factor SOX9 emerging as a key molecular integrator. This whitepaper synthesizes current research demonstrating how these pathways converge to regulate SOX9 expression and activity, driving pathological processes including fibrosis, chronic inflammation, and tissue remodeling. We provide a technical analysis of the underlying mechanisms, summarize quantitative findings from key studies, and present detailed experimental methodologies for investigating this crosstalk. The comprehensive synthesis aims to equip researchers with the tools and knowledge necessary to develop targeted therapeutic strategies for SOX9-mediated autoimmune diseases.
SOX9 (SRY-box transcription factor 9) is a multifunctional transcription factor belonging to the SOX family, characterized by an evolutionarily conserved High Mobility Group (HMG) box DNA-binding domain. While crucial for embryonic development, chondrogenesis, and organogenesis, SOX9 has recently emerged as a pivotal regulator in pathological processes across various autoimmune and inflammatory disorders. Its expression is quiescent in many adult tissues but rapidly induced by injury, inflammation, and oncogenic signals [3] [51]. The positioning of SOX9 at the convergence point of multiple signaling pathways enables it to function as an integrator of pro-fibrotic and inflammatory signals, making it a molecule of significant interest in therapeutic development.
The EGFR-MAPK/ERK-NF-κB signaling axis represents a core regulatory network controlling SOX9 expression and activity. This whitepaper examines the molecular architecture of this crosstalk, detailing how extracellular signals are transmitted through these pathways to modulate SOX9-driven transcriptional programs in disease states. Understanding this sophisticated regulatory network provides critical insights for targeting SOX9 therapeutically in conditions ranging from thyroid eye disease and organ fibrosis to osteoarthritis.
Molecular Architecture of SOX9
Structural Domains and Functional Motifs
The human SOX9 protein comprises 509 amino acids with several functionally distinct domains organized from N- to C-terminus [3] [17]:
- Dimerization Domain (DIM): Located upstream of the HMG domain, facilitates formation of homo- and heterodimers with other SOXE transcription factors (SOX8 and SOX10).
- HMG Box Domain: Evolutionarily conserved DNA-binding motif that recognizes specific DNA sequences (AGAACAATGG), bending DNA into an L-shaped complex to alter gene expression.
- Transcriptional Activation Domains: Two activation domains - TAM (central) and TAC (C-terminal) - interact with cofactors to enhance transcriptional activity.
- PQA-Rich Domain: Proline/glutamine/alanine-rich region that stabilizes SOX9 and enhances transactivation capabilities.
Post-Translational Modifications and Regulation
SOX9 activity is precisely regulated through various post-translational modifications [17]:
- Phosphorylation: ERK1/2 phosphorylates SOX9 at S64 and S181, enhancing nuclear localization and transcriptional activity. PKA-mediated phosphorylation at these same residues promotes nuclear import during gonadal development.
- Epigenetic Regulation: DNA methylation of the SOX9 promoter varies by tissue context, with hypermethylation observed in certain cancers and hypomethylation maintaining expression in others. Histone modifications including H3K9 and H3K27 trimethylation also regulate SOX9 accessibility.
Pathway Crosstalk: EGFR, MAPK/ERK, and NF-κB Signaling Convergence on SOX9
EGFR-MAPK/ERK-SOX9 Signaling Axis
The EGFR-MAPK/ERK pathway serves as a primary upstream regulator of SOX9 expression and function. Upon EGFR activation by ligands including EGF, TGF-α, and HB-EGF, the receptor undergoes dimerization and autophosphorylation, initiating a downstream signaling cascade through RAS-RAF-MEK-ERK [51] [52]. Phosphorylated ERK1/2 then modulates SOX9 through multiple mechanisms:
- Transcriptional Regulation: ERK signaling induces SOX9 gene expression, as demonstrated in urothelial carcinoma where EGFR-ERK activation led to significant SOX9 upregulation [51].
- Post-translational Modification: ERK1/2 directly phosphorylates SOX9 at serine residues 64 and 181, enhancing its nuclear localization and transcriptional activity [17].
- Feedback Amplification: SOX9 can transcriptionally activate EGFR expression, creating a positive feedback loop that sustains pathway activity, as observed in thyroid eye disease orbital fibroblasts [19].
Table 1: Experimental Evidence for EGFR-ERK-SOX9 Axis in Disease Models
| Disease Context | Experimental Findings | Functional Consequences | Citation |
|---|---|---|---|
| Thyroid Eye Disease | SOX9 binding to EGFR promoter confirmed by ChIP-qPCR; ERK inhibition reduced SOX9 effects | Increased fibroblast activation, contraction, and anti-apoptotic ability | [19] |
| Pancreatic Cancer | EGF stimulation induced SOX9-dependent TSPAN8 expression; EGFR inhibition blocked this effect | Enhanced cancer cell invasion and metastasis | [53] |
| Urothelial Carcinoma | EGFR/ERK blockade suppressed constitutive SOX9 upregulation in cancer cells | Promoted cell migration and invasion in vitro | [51] |
| Ovarian Function | ERK1/2 phosphorylation regulated SOX9/FOXL2 ratio in granulosa cells | Shift from estradiol to progesterone production | [54] |
NF-κB-SOX9 Signaling Interrelationship
The NF-κB pathway directly regulates SOX9 transcription while also functioning as a downstream mediator of its effects. In osteoarthritis, NF-κB directly binds to the SOX9 promoter region to activate its expression, creating a pro-inflammatory feedback loop [9]. This NF-κB-SOX9 axis promotes the expression of extracellular matrix components and inflammatory mediators that drive disease progression. The relationship appears bidirectional, with SOX9 potentially influencing NF-κB activity, though the precise mechanisms require further elucidation.
Integrated Crosstalk Model
The signaling integration between these pathways creates a sophisticated regulatory network:
- Parallel Activation: Common upstream stimuli (e.g., inflammatory cytokines, tissue injury) simultaneously activate EGFR, MAPK/ERK, and NF-κB pathways.
- Sequential Signaling: EGFR activation initiates MAPK/ERK signaling, which modulates SOX9 activity, while NF-κB independently regulates SOX9 expression.
- Feedback Loops: SOX9 amplifies its own expression by transcriptionally regulating EGFR, creating a positive feedback loop that sustains pathway activity in chronic conditions.
- Context-Dependent Outcomes: The functional consequences of this crosstalk vary by tissue context, contributing to fibrosis, inflammation, or tissue remodeling depending on the cellular environment.
Figure 1: Integrated Crosstalk of MAPK/ERK, EGFR, and NF-κB Pathways Regulating SOX9 in Autoimmune and Inflammatory Disorders
SOX9 in Autoimmune and Inflammatory Disorders: Mechanistic Insights
Fibrotic Disorders
SOX9 serves as a master regulator of organ fibrosis through its ability to drive extracellular matrix production and fibroblast activation [17]:
- Thyroid Eye Disease: Orbital fibroblasts exhibit significantly elevated SOX9 expression, which promotes contraction, anti-apoptotic ability, and extracellular matrix gene expression through the MAPK/ERK pathway [19].
- Cardiac, Pulmonary, and Renal Fibrosis: SOX9 is upregulated across multiple fibrotic conditions, where it stimulates pathological ECM component production and maintains myofibroblast activation states.
- Hepatic Fibrosis: SOX9 contributes to liver fibrosis progression by regulating the expression of collagen and other matrix components in hepatic stellate cells.
The persistence of SOX9 expression in chronic injury settings disrupts normal tissue repair processes, leading to excessive scar formation and organ dysfunction.
Inflammatory Joint Diseases
In osteoarthritis, SOX9 exhibits a complex dual role - essential for chondrocyte homeostasis but contributing to pathology when dysregulated [3] [9]. The NF-κB-SOX9 signaling axis promotes catabolic processes in chondrocytes, driving the expression of matrix-degrading enzymes and inflammatory mediators. This creates a vicious cycle where inflammation stimulates SOX9 expression, which further perpetuates inflammatory responses.
Cancer and Inflammation
SOX9 is highly expressed in various solid malignancies, where it promotes tumor immune evasion by creating an "immune desert" microenvironment [3]. SOX9 expression negatively correlates with cytotoxic CD8+ T cell infiltration while positively correlating with immunosuppressive Tregs and M2 macrophages. This immunomodulatory function highlights how SOX9 can suppress adaptive immune responses in chronic inflammatory settings.
Table 2: Quantitative Findings on SOX9 Dysregulation in Disease Contexts
| Disease Context | SOX9 Expression Change | Key Signaling Pathways Involved | Functional Measurements |
|---|---|---|---|
| Thyroid Eye Disease | Significant increase in mRNA and protein in OFs | EGFR-MAPK/ERK-SOX9 | Increased contraction, proliferation, ECM gene expression |
| Osteoarthritis | Context-dependent regulation | NF-κB-SOX9 | Cartilage degradation, synovial inflammation |
| Pancreatic Cancer | Upregulated in response to EGF | EGFR-ERK-SOX9-TSPAN8 | Enhanced invasion and metastasis |
| Urothelial Carcinoma | Constitutively upregulated in invasive cancers | EGFR-ERK-SOX9 | Increased migration and invasion |
| Organ Fibrosis | Elevated across multiple organs | TGF-β-SOX9 with MAPK cooperation | Excessive ECM accumulation |
Experimental Approaches for Investigating Pathway Crosstalk
Core Methodologies for Pathway Analysis
SOX9 Expression and Localization Analysis
- Immunohistochemistry/Fluorescence: Tissue sections or cultured cells are fixed, permeabilized, and incubated with anti-SOX9 antibodies followed by fluorophore-conjugated secondary antibodies. Confocal microscopy visualizes SOX9 localization and expression levels [19].
- Western Blotting: Protein lysates from treated cells are separated by SDS-PAGE, transferred to membranes, and probed with phospho-specific and total antibodies against SOX9, ERK, EGFR, and NF-κB components [19] [54].
- qRT-PCR: RNA extracted from tissues or cells is reverse transcribed and analyzed using SYBR Green-based quantitative PCR with primers specific for SOX9 and target genes [19].
Pathway Modulation Techniques
- Pharmacological Inhibition:
- EGFR inhibitors: Erlotinib (10-20 μM)
- MEK/ERK inhibitors: U0126 (10-50 μM), PD98059 (50 μM)
- NF-κB inhibitors: BAY-11-7082 (5-10 μM)
- Genetic Manipulation:
- siRNA/shRNA-mediated knockdown of SOX9, EGFR, or NF-κB components
- Lentiviral overexpression of SOX9 or constitutive active pathway components
- Stimuli and Induction:
- EGF treatment (10-50 ng/mL) to activate EGFR pathway
- Inflammatory cytokines (TNF-α, IL-1β) to activate NF-κB
- Tissue injury models (e.g., cyclophosphamide-induced bladder injury) [51]
Functional Assays
- Cell Migration and Invasion: Transwell assays with Matrigel coating for invasion assessment [51] [53].
- Proliferation Assays: EdU incorporation or MTT assays to measure cell growth [19].
- Fibroblast Contraction: Collagen gel contraction assays to assess contractile ability [19].
- Protein-DNA Interactions: Chromatin immunoprecipitation (ChIP) to verify direct SOX9 binding to target gene promoters [19].
Technical Considerations and Optimization
Successful experimental investigation of this crosstalk requires:
- Time-Course Analyses: Pathway activation and SOX9 induction occur at different timepoints, requiring careful temporal mapping.
- Combinatorial Approaches: Simultaneous pathway inhibition to establish hierarchy and redundancy in signaling.
- Cell Type-Specific Responses: Primary cells from disease contexts (e.g., orbital fibroblasts from TED patients) may respond differently than established cell lines.
- Validation in Multiple Models: Findings from in vitro systems should be confirmed in animal models and human tissue specimens.
Figure 2: Experimental Workflow for Investigating EGFR-ERK-NF-κB-SOX9 Signaling Crosstalk
Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9-Pathway Investigations
| Reagent Category | Specific Examples | Application Context | Key Findings Enabled |
|---|---|---|---|
| EGFR Inhibitors | Erlotinib (10-20 μM) | Urothelial carcinoma, pancreatic cancer | Blocked constitutive SOX9 upregulation in cancer cells [51] [53] |
| MEK/ERK Inhibitors | U0126 (10 μM), PD98059 (50 μM) | Thyroid eye disease, ovarian function | Inhibited SOX9-induced fibroblast activation; regulated steroidogenesis [19] [54] |
| SOX9 Modulation | siRNA/shRNA knockdown, Lentiviral overexpression | Multiple disease contexts | Established necessity and sufficiency of SOX9 in fibrosis and invasion [19] [53] |
| SOX9 Antibodies | Chemicon #AB5535 | Immunoblotting, IHC, IF | Detected SOX9 upregulation in injury and disease contexts [51] [19] |
| Pathway Activation | EGF (10-50 ng/mL), HB-EGF (10-50 ng/mL) | Pancreatic cancer, urothelial injury | Induced SOX9 expression and downstream target genes [51] [53] |
Therapeutic Targeting Strategies
Current Intervention Approaches
The EGFR-MAPK/ERK-NF-κB-SOX9 axis presents multiple targeting opportunities:
- Receptor-Level Inhibition: EGFR-targeted therapies (erlotinib, gefitinib) already exist for cancer and could be repurposed for autoimmune conditions with SOX9 dysregulation.
- Kinase Inhibition: MEK inhibitors in clinical development could address pathological SOX9 activation downstream of multiple stimuli.
- SOX9-Directed Therapeutics: Direct targeting of SOX9 remains challenging but could involve interference with DNA binding, dimerization, or cofactor interactions.
- Combination Approaches: Simultaneous pathway targeting may overcome compensatory mechanisms and feedback loops.
Preclinical Evidence
Studies in thyroid eye disease demonstrate that SOX9/EGFR targeting suppresses orbital fibroblast activation, suggesting therapeutic potential [19]. In pancreatic cancer, the EGF-SOX9-TSPAN8 cascade has been identified as a promising intervention point [53]. The conserved nature of this signaling network across conditions suggests that successful targeting strategies could have broad applications.
The crosstalk between MAPK/ERK, EGFR, and NF-κB pathways converges on SOX9 to drive critical pathological processes in autoimmune and inflammatory disorders. SOX9 functions as a dynamic regulatory hub that integrates multiple signaling inputs to coordinate transcriptional programs governing fibrosis, inflammation, and tissue remodeling. The experimental frameworks and technical approaches outlined in this whitepaper provide researchers with validated methodologies for investigating this complex signaling network.
Future research should prioritize:
- Development of SOX9-specific targeting strategies
- Elucidation of cell-type-specific functions of SOX9 in disease contexts
- Exploration of epigenetic regulation within this signaling network
- Investigation of temporal dynamics in pathway crosstalk
- Validation of therapeutic interventions in advanced disease models
The strategic modulation of this integrated signaling axis holds significant promise for innovative therapeutic approaches in SOX9-mediated autoimmune and inflammatory diseases.
The transcription factor SOX9 (SRY-box 9) has emerged as a critical regulator in autoimmune diseases and inflammatory disorders, exhibiting complex, context-dependent functions that position it as a promising therapeutic target. SOX9 plays a dual role in immunology, functioning as a "double-edged sword" that can either promote pathological processes or facilitate tissue repair depending on the cellular environment [3]. This janus-faced character is particularly evident in its interactions with immune components—on one hand, SOX9 promotes tumor immune escape by impairing immune cell function, while on the other hand, it helps maintain macrophage function and contributes to cartilage formation, tissue regeneration, and repair [3]. Understanding these multifaceted roles provides the foundation for developing targeted RNA-based interventions that can precisely modulate SOX9 activity in specific pathological contexts.
Recent advances in single-cell RNA sequencing (scRNA-seq) have revolutionized our understanding of SOX9's role in inflammatory diseases at cellular resolution. This technology enables researchers to investigate cellular heterogeneity and identify distinct cellular subpopulations contributing to disease pathogenesis [55]. In neuropathic pain models, scRNA-seq has revealed how SOX9 regulates the emergence of neuroinflammatory astrocyte subsets through metabolic reprogramming [7]. Similarly, in osteoarthritis, single-cell analyses have identified distinct chondrocyte populations with varying SOX9 expression patterns correlated with disease progression [56]. These insights are critical for designing cell-type-specific therapeutic approaches that target SOX9 in precisely defined pathological cell populations while sparing beneficial cellular functions.
RNA-Based Therapeutic Platforms for SOX9 Modulation
Platform Diversity and Mechanisms of Action
RNA-based technologies represent a versatile class of therapeutics with significant potential for modulating SOX9 in inflammatory diseases. These platforms leverage different mechanisms to achieve targeted gene regulation at the transcriptional and post-transcriptional levels, each offering distinct advantages for specific therapeutic applications. The major RNA-based therapeutic platforms include:
Table 1: RNA-Based Therapeutic Platforms for SOX9 Modulation
| Platform | Mechanism of Action | Key Advantages | Therapeutic Applications for SOX9 |
|---|---|---|---|
| mRNA | Encodes functional SOX9 protein for supplementation | Sustained protein expression; No nuclear entry required | Cartilage regeneration; Neuroprotective astrocyte activation [57] [13] |
| siRNA | Silences specific genes through RNA interference | High specificity; Reversible effect | Downregulation of pathogenic SOX9 signaling pathways [57] |
| circRNA | Circular RNA for prolonged protein expression | Superior stability; Low immunogenicity | Sustained SOX5/SOX9 expression in osteoarthritis [58] |
| CRISPR-Cas9/gRNA | Precise gene editing or transcriptional regulation | Permanent modification; Versatile targeting | Sox9 activation and RelA inhibition in engineered MSCs [56] |
| miRNA/anti-miRNA | Regulates networks of genes through endogenous pathways | Multi-gene regulation; Natural mechanism | Fine-tuning of SOX9-related signaling networks [57] |
Delivery Systems and Chemical Modifications
Effective delivery of RNA therapeutics requires sophisticated carrier systems to overcome biological barriers. Lipid nanoparticles (LNPs) have been widely used for mRNA delivery but can trigger inflammatory responses in joint applications [59]. Alternative delivery systems include polyplex nanomicelles with polyethylene glycol (PEG) surfaces that minimize inflammatory reactions, making them particularly suitable for sensitive tissues like articular cartilage [59]. Additionally, polymeric micelles based on PEO and PPO copolymers have demonstrated efficacy in delivering genetic material encoding SOX9 to human articular chondrocytes, even in the presence of osteoarthritis-associated inflammatory cytokines [60].
Chemical modifications of RNA are crucial for enhancing stability, delivery, and safety profiles. Common modifications include 2′-O-methyl (2′OMe) and 2′-fluoro (2′F) substitutions at the ribose ring, which confer resistance to endonuclease degradation [57]. Phosphate linkage modifications through phosphorothioation improve nuclease resistance and plasma protein binding, while base modifications can reduce immunogenicity [57]. These engineered modifications are particularly important for therapeutics targeting SOX9 in inflammatory environments, where excessive immune activation could exacerbate disease pathology.
Combinatorial Approaches for Enhanced Efficacy
Synergistic Target Selection
Combinatorial RNA-based therapies that simultaneously modulate multiple targets in SOX9-related pathways have demonstrated superior efficacy compared to single-target approaches. A prominent example combines SOX9 activation with RelA (NF-κB) inhibition using CRISPR-dCas9 technology [56]. This dual approach enhances the chondrogenic potential of mesenchymal stromal cells (MSCs) while concurrently dampening inflammatory responses, addressing both the anabolic and inflammatory components of osteoarthritis [56]. The synergistic effect arises from SOX9's role as a master regulator of chondrogenesis and RelA's position as a primary mediator of inflammation, creating a balanced therapeutic outcome that single-target interventions cannot achieve.
Another combinatorial strategy employs dual mRNA therapy combining interleukin-1 receptor antagonist (IL-1Ra) with RUNX1, a transcription factor critical for chondrogenesis [59]. This approach recognizes that while RUNX1 is essential for maintaining cartilage homeostasis, effective control of joint inflammation is required for its full therapeutic activity. The combination produces synergistic benefits, with IL-1Ra mitigating inflammation and protecting chondrocyte viability, thereby enabling RUNX1 to manifest its chondroprotective functions more effectively [59]. This rationale could be extended to SOX9-based therapies, where combining SOX9 modulation with anti-inflammatory agents may enhance regenerative outcomes.
Multi-Platform Delivery Strategies
Advanced combinatorial approaches leverage multiple RNA platforms simultaneously to achieve sophisticated regulation of SOX9 networks. For instance, circRNA-based protein replacement can be combined with siRNA-mediated pathway inhibition to simultaneously boost beneficial SOX9 functions while suppressing pathological processes. In a proof-of-concept study, circRNA-mediated supplementation of SOX5, a downstream effector of SOX9, effectively mitigated osteoarthritis progression in male mice [58]. This protein replacement approach could be combined with siRNA targeting catabolic enzymes like MMP13 or ADAMTS5 to simultaneously promote anabolic processes while inhibiting matrix degradation.
The integration of CRISPR-based transcriptional activation with conventional mRNA supplementation represents another promising combinatorial strategy. CRISPR-dCas9 systems can be designed to achieve fine-tuned, endogenous SOX9 activation that captures different transcription isoforms and retains the gene's potential to be regulated by intrinsic signaling factors [56]. This can be supplemented with exogenous mRNA encoding modified SOX9 variants with enhanced stability or activity, creating a multi-level approach that maximizes therapeutic SOX9 signaling while maintaining natural regulatory mechanisms.
Experimental Protocols and Methodologies
CRISPR-Mediated SOX9 Activation and RelA Inhibition
The simultaneous activation of SOX9 and inhibition of RelA using CRISPR-dCas9 technology represents a sophisticated approach for enhancing the therapeutic properties of mesenchymal stromal cells (MSCs). The following protocol outlines the key methodological steps:
Vector Construction and Delivery:
- Construct lentiviral vectors expressing dSpCas9-VP64 (for CRISPR activation) and dSaCas9-KRAB (for CRISPR interference) [56]
- Design and clone guide RNA sequences targeting Sox9 promoter regions (e.g., Sox9-2: CGGGTTGGGTGACGAGACAGG; Sox9-3: ACTTACACACTCGGACGTCCC) and RelA promoter regions (e.g., RelA-1: CCGAAATCCCCTAAAAACAGA; RelA-3: TGCTCCCGCGGAGGCCAGTGA) [56]
- Transduce bone marrow-derived MSCs with both vectors simultaneously using appropriate viral titers
- Implement selection protocols using antibiotics (e.g., puromycin) to obtain stable cell lines
In Vitro Validation:
- Perform quantitative PCR to verify Sox9 upregulation and RelA downregulation at mRNA level
- Conduct immunoblotting to confirm corresponding protein expression changes
- Assess chondrogenic differentiation capacity in pellet cultures using chondrogenic medium supplemented with TGF-β3 for 21-28 days
- Analyze extracellular matrix production through Alcian blue staining for proteoglycans and immunostaining for type II collagen
- Evaluate immunomodulatory potential by measuring secretion of anti-inflammatory factors (e.g., IL-10, TGF-β) and inhibition of T-cell proliferation in co-culture assays
In Vivo Application:
- Administer engineered MSCs (~10^5 cells) via intra-articular injection in murine osteoarthritis models (e.g., destabilization of medial meniscus)
- Monitor cell persistence and tissue distribution using in vivo imaging or histological tracking
- Assess therapeutic outcomes through pain behavior tests, histological scoring (OARSI system), and analysis of cartilage degradation biomarkers
Diagram Title: CRISPR Engineering of MSCs for Osteoarthritis
circRNA-Based Protein Replacement Therapy
Circular RNA-based protein replacement represents an innovative approach for sustaining SOX9 activity in diseased tissues. The following protocol details ivcRNA production and application:
ivcRNA Synthesis and Validation:
- Clone SOX9 coding sequence into pSP73 vector containing T7 promoter and 120 bp poly A/T sequence [58]
- Perform in vitro transcription using T7 RNA polymerase with unmodified ribonucleoside triphosphates
- Circulate linear RNA transcripts using permuted intron-exon sequences or ribozyme-based methods
- Purify ivcRNA using RNeasy Mini Kit and assess quality via Bioanalyzer
- Validate translation efficiency in chondrocyte cell lines using Western blot for SOX9
Formulation and Delivery:
- Complex ivcRNA with delivery vehicle (e.g., polyplex nanomicelles at N/P ratio of 3) [59]
- Characterize nanoparticle size (100-200 nm) and polydispersity index using dynamic light scattering
- Administer via intra-articular injection (e.g., 10 μg ivcRNA in 50 μL volume) in OA models
- Assess protein expression duration using luciferase reporter ivcRNA and in vivo imaging
Functional Assessment:
- Evaluate cartilage protection through histology (Safranin O/Fast Green staining)
- Quantify OARSI scores and cartilage thickness measurements
- Analyze anabolic (COL2, aggrecan) and catabolic (MMP13, ADAMTS5) marker expression
- Assess pain behavior through mechanical allodynia and weight-bearing tests
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for SOX9 and RNA Therapeutics Research
| Reagent/Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Delivery Systems | PEG-PAsp(TET) nanomicelles [59], PF68/T908 polymeric micelles [60], Lipid nanoparticles | RNA therapeutic encapsulation and delivery | Nanomicelles reduce inflammatory responses compared to LNPs in joints [59] |
| Vector Systems | dSpCas9-VP64 [56], dSaCas9-KRAB [56], rAAV-FLAG-hsox9 [60] | CRISPR activation/interference and gene overexpression | rAAV vectors mainly remain episomal, reducing insertional mutagenesis risk [60] |
| Cell Culture Models | Primary human OA chondrocytes [60], Bone marrow stromal cells (BMSCs) [56], Astrocyte cultures | In vitro screening and mechanism studies | Human OA chondrocytes require ethical approval and special culture conditions [60] |
| Animal Models | DMM surgery model [56] [58], MIA-induced OA [59], SNI neuropathic pain model [7] | Preclinical efficacy assessment | MIA model produces rapid inflammation, DMM mimics post-traumatic OA [58] [59] |
| Analytical Tools | scRNA-seq platforms [55], OARSI scoring system [56], Raman spectroscopy [59] | Outcome assessment and mechanism elucidation | scRNA-seq reveals cellular heterogeneity but requires specialized bioinformatics [55] |
Signaling Pathways and Molecular Mechanisms
SOX9 in Immunometabolic Regulation
Recent research has elucidated a novel SOX9-hexokinase 1-glycolysis axis that drives pathogenic processes in neuroinflammatory conditions. In neuropathic pain, nerve injury induces abnormal SOX9 phosphorylation at site 181, triggering enhanced nuclear translocation and transcriptional activation of hexokinase 1 (Hk1), the enzyme catalyzing the first irreversible step of glycolysis [7]. The resulting heightened glycolytic flux produces excessive lactate, which remodels histones through H3K9 lactylation, promoting transcriptional activation of pro-inflammatory and neurotoxic genes in specific astrocyte subpopulations [7]. This immunometabolic pathway represents a promising target for RNA-based interventions, where anti-miRNAs or siRNA could disrupt the SOX9-Hk1 interaction or inhibit downstream lactylation-mediated gene expression.
Diagram Title: SOX9-HK1 Immunometabolic Pathway in Neuroinflammation
Cross-Disease Significance of SOX9 Pathways
The therapeutic relevance of SOX9 extends across multiple disease contexts, revealing both conserved and specialized functions. In Alzheimer's disease, SOX9 enhancement in astrocytes promotes phagocytic clearance of amyloid-β plaques, with elevated SOX9 expression triggering astrocytes to "vacuum" pathological protein aggregates [13]. This protective function positions SOX9 as a potential target for RNA-based therapies in neurodegenerative proteinopathies. In osteoarthritis, SOX9 works in concert with other transcription factors like RUNX1 to maintain chondrocyte homeostasis, with its deficiency leading to impaired extracellular matrix organization and accelerated disease progression [58]. The conservation of SOX9's protective roles across these diverse conditions suggests that RNA therapeutics developed for one indication may have relevant applications in others, particularly when targeting specific cell types like chondrocytes or astrocytes.
The emerging strategies in RNA-based therapies and combinatorial treatments centered on SOX9 modulation represent a paradigm shift in approaching autoimmune diseases and inflammatory disorders. The versatility of RNA platforms—from mRNA supplementation to CRISPR-mediated gene regulation—enables unprecedented precision in targeting SOX9's context-dependent functions. Future developments will likely focus on cell-type-specific delivery systems that can direct SOX9-modulating therapeutics to precise cellular subpopulations identified through single-cell transcriptomics, thereby maximizing therapeutic efficacy while minimizing off-target effects.
The integration of artificial intelligence and machine learning with multi-omics data holds particular promise for advancing SOX9-targeted therapies [55]. These approaches can help model the complex regulatory networks controlled by SOX9 and predict optimal combinatorial strategies for specific patient endotypes. Additionally, continued innovation in RNA chemistry and delivery systems will address current limitations in stability, immunogenicity, and tissue-specific targeting. As these technologies mature, SOX9-focused RNA therapeutics have the potential to transition from preclinical success to clinical application, offering new hope for patients with currently intractable autoimmune and inflammatory diseases.
Navigating Complexities: Challenges in SOX9-Targeted Therapy and Diagnostic Development
The transcription factor SOX9 (SRY-related HMG-box 9) represents a critical regulatory node in numerous physiological and pathological processes, presenting a complex paradox for therapeutic targeting. As a key developmental regulator, SOX9 maintains essential functions in tissue homeostasis, cartilage formation, and cell fate determination. However, in disease contexts, SOX9 becomes dysregulated, driving pathogenesis through mechanisms ranging from cancer stem cell expansion to fibrotic progression and neuroinflammation. This technical guide examines the context-dependent duality of SOX9 functions and provides strategic frameworks for leveraging its beneficial roles while suppressing its pathogenic activities, with particular emphasis on applications in autoimmune and inflammatory disease research. The molecular basis of SOX9's functional duality stems from its complex interactions with cell-type specific partners, post-translational modifications, and epigenetic landscapes that determine its transcriptional output across different tissue environments and disease states.
SOX9 Structure and Functional Domains
The human SOX9 protein comprises 509 amino acids with several functionally critical domains that enable its diverse regulatory capabilities. Understanding these domains is essential for designing targeted interventions.
Table 1: Functional Domains of SOX9 Protein
| Domain | Position | Key Functions | Therapeutic Significance |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates SOXE protein homo/heterodimer formation | Target for disrupting pathogenic protein complexes |
| HMG Box | Central | DNA-binding, nuclear localization, DNA bending | Core DNA recognition domain with limited targetability |
| TAM (Transactivation Domain Middle) | Central | Transcriptional activation, cofactor recruitment | Potential site for enhancing beneficial transactivation |
| PQA-rich Domain | Central | Protein stabilization, enhances transactivation | Modulator of protein stability and activity |
| TAC (Transactivation Domain C-terminal) | C-terminal | Transcriptional activation, β-catenin inhibition | Critical domain for context-specific cofactor interactions |
The HMG box domain facilitates sequence-specific DNA binding to the consensus motif (A/T)(A/T)CAA(A/T)G, while the transactivation domains (TAM and TAC) mediate interactions with coregulators including Tip60 and other chromatin-modifying complexes [3]. Post-translational modifications, particularly phosphorylation at serine residues S64, S181, and S211, regulate SOX9 nuclear localization and transcriptional activity [17]. These structural features represent potential nodes for therapeutic intervention to modulate SOX9 activity in a context-dependent manner.
Figure 1: SOX9 Functional Domains and Modification Sites. The diagram illustrates key structural domains and post-translational modification sites that regulate SOX9 activity. Targeting these domains represents potential therapeutic strategies.
Context-Dependent Roles of SOX9 in Disease Pathogenesis
SOX9 exhibits remarkably divergent functions across different disease contexts, necessitating precise understanding of its role in specific pathological environments.
Beneficial Roles: Tissue Protection and Repair
In neurodegenerative and joint homeostasis contexts, SOX9 activation demonstrates protective functions:
Alzheimer's Disease: SOX9 overexpression in astrocytes enhances phagocytic clearance of amyloid-β plaques, reduces plaque burden, and preserves cognitive function in mouse models. Astrocytes with elevated SOX9 show increased structural complexity and plaque-clearing activity, functioning like "vacuum cleaners" to remove toxic protein aggregates [61].
Osteoarthritis: SOX9 serves as the "master regulator" of chondrogenesis, maintaining chondrocyte phenotype and cartilage homeostasis. CRISPR-mediated Sox9 activation in mesenchymal stromal cells (MSCs) enhances chondrogenic potential and attenuates cartilage degradation in murine OA models [56].
Tissue Repair: SOX9 contributes to resolution of inflammation and tissue regeneration by maintaining macrophage function and regulating extracellular matrix balance. It inhibits production of destructive matrix metalloproteinases (MMP2, MMP13) and regulates IL-8 production in dental pulp models [14].
Pathogenic Roles: Disease Progression and Therapy Resistance
In contrast, SOX9 drives pathogenesis in multiple disease contexts:
Cancer: SOX9 is highly expressed in various malignancies (ovarian, liver, lung, breast, gastric cancers) where it promotes chemoresistance, stem-like transcriptional states, and tumor progression. In high-grade serous ovarian cancer (HGSOC), SOX9 induction following platinum chemotherapy drives a stem-like population with significant chemoresistance [62] [63].
Neuropathic Pain: Nerve injury-induced SOX9 phosphorylation triggers aberrant hexokinase 1 (Hk1) activation, driving high-rate glycolysis in specific astrocyte subpopulations. This metabolic reprogramming promotes pro-inflammatory and neurotoxic gene programs through lactate-mediated histone lactylation (H3K9la), ultimately causing chronic pain states [7].
Organ Fibrosis: SOX9 promotes fibrosis in cardiac, hepatic, renal, and pulmonary tissues through excessive extracellular matrix deposition. It serves as a key regulator in the pathological fibrotic process that leads to organ dysfunction [17].
Immune Regulation: SOX9 exhibits dual roles in immunity, acting as a "double-edged sword" by promoting immune escape in tumors while maintaining macrophage function for tissue repair in inflammatory conditions [3].
Table 2: Context-Dependent SOX9 Functions in Disease
| Disease Context | SOX9 Role | Key Mechanisms | Therapeutic Implications |
|---|---|---|---|
| Alzheimer's Disease | Beneficial | Enhances astrocyte phagocytosis of Aβ plaques | SOX9 activation may slow cognitive decline |
| Osteoarthritis | Beneficial | Maintains chondrocyte phenotype, cartilage homeostasis | CRISPRa of SOX9 in MSCs promotes joint repair |
| Neuropathic Pain | Pathogenic | Drives glycolytic switching in astrocytes via Hk1 regulation | Inhibiting SOX9-Hk1 axis relieves pain |
| Ovarian Cancer | Pathogenic | Induces stem-like state, chemoresistance | SOX9 ablation sensitizes to platinum therapy |
| Organ Fibrosis | Pathogenic | Promotes ECM deposition across multiple tissues | SOX9 inhibition may slow fibrotic progression |
Experimental Approaches for SOX9 Functional Analysis
Targeted SOX9 Modulation Techniques
Advanced genetic and epigenetic tools enable precise manipulation of SOX9 activity:
CRISPR-dCas9 Systems for SOX9 Regulation: The CRISPR-dCas9 platform allows fine-tuning of SOX9 expression without permanent genomic alterations. The system utilizes:
- CRISPRa (activation): dSpCas9-VP64 fusion protein targeted to Sox9 promoter regions via specific guide RNAs (Sox9-1 to Sox9-5) for transcriptional activation [56]
- CRISPRi (interference): dSaCas9-KRAB fusion for targeted transcriptional repression [56]
- Dual regulation: Simultaneous Sox9 activation and RelA inhibition to enhance chondrogenic potential while suppressing inflammatory responses [56]
Guide RNA Selection for SOX9 Targeting: Effective sgRNAs for Sox9 activation include:
- Sox9-1: GAGCTAGCCGTGATTGGCCCG (PAM: AGG, position: -74)
- Sox9-2: CGGGTTGGGTGACGAGACAGG (PAM: AGG, position: -167)
- Sox9-3: ACTTACACACTCGGACGTCCC (PAM: GGG, position: -276)
- Sox9-4: TGGACCGGATTTTGGAAGGG (PAM: GGG, position: -124)
- Sox9-5: AGGGAGGGGAGCTCAGCCAG (PAM: AGG, position: -198) [56]
Analytical Methods for SOX9 Functional Assessment
Comprehensive multi-omics approaches enable detailed characterization of SOX9 activities:
Single-Cell RNA Sequencing (scRNA-seq): scRNA-seq reveals SOX9-associated cell subpopulations and transcriptional states:
- Identification of neuroinflammatory astrocyte subtypes in neuropathic pain [7]
- Analysis of SOX9-induced stem-like clusters in chemoresistant ovarian cancer [62]
- Characterization of chondrocyte subtypes in osteoarthritis models [56]
Chromatin Analysis Techniques:
- Chromatin Immunoprecipitation (ChIP): Maps SOX9 binding to target gene promoters (MMP-1, MMP-13, IL-8, Hk1) [14] [7]
- ATAC-seq: Assesses chromatin accessibility changes following SOX9 manipulation
- H3K9la lactylation profiling: Identifies metabolic-epigenetic coupling in neuropathic pain [7]
Functional Assays:
- Phagocytosis assays: Quantify amyloid-β clearance in SOX9-modulated astrocytes [61]
- Glycolytic rate analysis: Measures extracellular acidification in SOX9-Hk1 modulated cells [7]
- Colony formation assays: Assess chemoresistance in SOX9-modified cancer cells [62]
- Behavioral tests: Evaluate pain sensitivity in neuropathic pain models [7]
Figure 2: Experimental Workflow for SOX9 Functional Analysis. The diagram outlines integrated approaches for modulating and analyzing SOX9 functions across different disease contexts.
Strategic Framework for Targeting SOX9
Disease-Selective Intervention Strategies
Successful targeting of SOX9 requires context-dependent approaches that consider its dual functions:
For Neurodegenerative Conditions (Beneficial Role Enhancement):
- SOX9 Activation: Utilize CRISPRa systems with Sox9-targeting gRNAs (Sox9-2, Sox9-3) to enhance astrocyte phagocytic function [61] [56]
- Stabilization Approaches: Develop small molecules that enhance SOX9 nuclear localization or protein stability through modulation of phosphorylation sites (S64, S181) [17]
- Combination Therapy: Pair SOX9 enhancement with anti-inflammatory agents to maximize beneficial effects while minimizing potential pro-inflammatory consequences
For Cancer and Fibrotic Diseases (Pathogenic Role Suppression):
- SOX9 Inhibition: Implement CRISPRi with RelA-1 to RelA-5 gRNAs to suppress SOX9-mediated stemness and chemoresistance [56] [62]
- Epigenetic Modulation: Target SOX9 super-enhancers or utilize EZH2-mediated methylation to reduce SOX9 expression in malignancies [17]
- Pathway Interruption: Develop inhibitors targeting SOX9 downstream effectors (Hk1 in neuropathic pain) rather than SOX9 itself to maintain physiological functions [7]
For Autoimmune and Inflammatory Contexts:
- Precision Modulation: Utilize cell-type specific delivery systems to modulate SOX9 in target tissues while sparing beneficial functions
- Dimerization Disruption: Develop peptide inhibitors that interfere with SOX9 partnership with inflammatory transcription factors
- Post-translational Targeting: Modulate phosphorylation states to direct SOX9 toward beneficial transcriptional programs
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Investigation
| Reagent/Cell Model | Application | Key Features | Experimental Use |
|---|---|---|---|
| CRISPR-dCas9-VP64 System | SOX9 activation | dSpCas9-VP64 fusion with Sox9-targeting gRNAs | Transcriptional activation of endogenous SOX9 [56] |
| CRISPR-dSaCas9-KRAB System | SOX9 interference | dSaCas9-KRAB fusion with RelA-targeting gRNAs | Transcriptional repression with minimal off-target effects [56] |
| Alzheimer's Mouse Models | Neurodegenerative research | APP/PS1 models with amyloid pathology | Testing SOX9-enhanced plaque clearance [61] |
| Spared Nerve Injury (SNI) Rat Model | Neuropathic pain studies | Chronic pain with astrocyte reactivity | SOX9-Hk1-glycolysis pathway analysis [7] |
| Patient-Derived Ovarian Cancer Cells | Chemoresistance modeling | Platinum-sensitive and resistant lines | SOX9 stem-like state analysis [62] |
| Primary Chondrocytes/MSCs | Cartilage research | Human or murine primary cells | Chondrogenic differentiation studies [56] |
| SOX9 Phospho-Specific Antibodies | Post-translational analysis | S64, S181, S211 phosphorylation sites | Assessing SOX9 activation state [7] [17] |
The strategic targeting of SOX9 represents a promising but complex therapeutic frontier, particularly for autoimmune and inflammatory disorders where context-dependent outcomes are paramount. Future efforts should focus on developing precision modulation approaches that can selectively enhance beneficial SOX9 functions in tissue protection and repair while suppressing its pathogenic roles in fibrosis, cancer progression, and chronic inflammation. The integration of advanced delivery systems, cell-type specific targeting, and sophisticated molecular tools will be essential to successfully navigate the SOX9 paradox and translate these strategies into effective therapies for diverse disease contexts.
The SRY-Box Transcription Factor 9 (SOX9) has emerged as a critical developmental regulator with multifaceted roles in disease pathogenesis, particularly in cancer, inflammatory disorders, and autoimmune conditions. As a transcription factor containing a high-mobility group (HMG) domain, SOX9 recognizes the specific DNA sequence CCTTGAG and regulates diverse cellular processes including cell fate determination, stemness maintenance, and extracellular matrix (ECM) composition [64] [11]. Its expression is regulated through complex mechanisms including post-translational modifications (phosphorylation, SUMOylation), microRNAs, and the ubiquitin-proteasome pathway [64]. Despite its promise as a biomarker and therapeutic target, SOX9 presents significant challenges due to its remarkable heterogeneity across disease contexts, patient populations, and even cellular subpopulations within the same tissue. This technical guide examines the sources and implications of SOX9 heterogeneity, providing frameworks for researchers and drug development professionals to navigate these complexities in autoimmune and inflammatory disease research.
SOX9 Expression Heterogeneity: Quantitative Evidence Across Pathologies
SOX9 demonstrates dramatic expression variability across different disease types, stages, and cellular compartments. The table below summarizes key quantitative findings from recent studies:
Table 1: Heterogeneous SOX9 Expression Patterns Across Pathological Conditions
| Disease Context | Expression Pattern | Correlation with Clinical Parameters | Study Details |
|---|---|---|---|
| Malignant Bone Tumors | Remarkable overexpression in tumor vs. margin tissues (p < 0.0001); Higher in malignant vs. benign tumors (p < 0.0001) | Correlated with tumor severity, grade, invasion, poor therapy response, and recurrence [65] | 150 bone tumor tissues, 150 tumor margins, 150 patient blood samples [65] |
| High-Grade Serous Ovarian Cancer (HGSOC) | Significant upregulation following platinum-based chemotherapy; Top quartile SOX9 expression associated with shorter overall survival (HR = 1.33; log-rank P = 0.017) [62] | Driven by epigenetic upregulation; induces stem-like transcriptional state and chemoresistance [62] | Single-cell RNA-Seq of 11 patient tumors before/after chemotherapy; 51,786 cells total [62] |
| Liver Fibrosis | Prevalence in patient biopsies predicts progression to cirrhosis; Regulates >30% of ECM-related genes in hepatic stellate cells [20] | SOX9-regulated ECM proteins (OPN, VIM, SPARC, GPNMB, FN1) correlate with fibrosis severity in serum [20] | Transcriptomic analysis of Sox9-abrogated myofibroblasts; patient serum cohort (n=50) [20] |
| Neuropathic Pain | Aberrant phosphorylation at site 181 in spinal astrocytes; Triggers HK1 activation and glycolytic shift [7] | Drives emergence of neuroinflammatory astrocyte subsets (Astro1); Reduces beneficial populations (Astro3) [7] | Single-cell RNA-seq of dorsal horn astrocytes in rat neuropathic pain model [7] |
| Glioblastoma | Highly expressed in tumor tissues; Paradoxically associated with better prognosis in lymphoid invasion subgroups [33] | Independent prognostic factor for IDH-mutant cases; Correlates with immune infiltration and checkpoint expression [33] | RNA-seq data from TCGA and GTEx databases; 478 cases [33] |
This expression heterogeneity extends beyond disease type to encompass temporal dynamics, cellular compartmentalization, and patient-specific factors. In ovarian cancer, SOX9 expression is rapidly induced within 72 hours of platinum treatment [62], while in neuropathic pain, chronic phases feature stable SOX9-mediated transcriptional programs in specific astrocyte subpopulations [7].
Molecular Mechanisms Underlying SOX9 Heterogeneity
Context-Dependent Transcriptional Regulation
SOX9 exhibits remarkable functional plasticity based on cellular context, achieved through several mechanisms:
Partner Factor Interactions: SOX9 requires partnership with tissue-specific co-factors for transcriptional specificity. In chondrogenesis, SOX9 dimers recruit SOX5/6 dimers to activate Col2a1, while during hypertrophic chondrocyte maturation, SOX9 recruits Gli proteins to repress Col10a1 [64]. This partner factor availability creates tissue-specific activity profiles.
Post-Translational Modifications: Phosphorylation by protein kinase A enhances SOX9 DNA-binding affinity and nuclear translocation [64]. SUMOylation differentially regulates SOX9 activity—enhancing transcriptional activity on the Col2a1 reporter in some contexts while compromising it in others [64].
Epigenetic Regulation: In ovarian cancer, SOX9 is regulated through resistant state-specific super-enhancers that are commissioned during chemoresistance development [62]. This epigenetic reprogramming creates stable expression states that persist through cell divisions.
Metabolic Regulation and Signaling Cross-Talk
Recent work reveals sophisticated metabolic regulation of SOX9 activity. In neuropathic pain, nerve injury induces abnormal SOX9 phosphorylation, triggering aberrant hexokinase 1 (HK1) activation and heightened astrocytic glycolysis [7]. The resulting lactate production remodels histone modifications via lactylation (H3K9la), promoting pro-inflammatory and neurotoxic gene modules [7]. This places SOX9 at the nexus of metabolic and transcriptional reprogramming in disease states.
Table 2: SOX9-Regulated Signaling Pathways Across Disease Contexts
| Signaling Pathway | Disease Context | Functional Outcome | Mechanistic Insight |
|---|---|---|---|
| Hedgehog Signaling | Liver fibrosis, Chondrogenesis | Upregulates SOX9 for progenitor generation and maturation [64] | Sonic hedgehog (Shh) upregulates SOX9 in chondrogenic precursors; Indian hedgehog (Ihh) regulates chondrocyte maturation [64] |
| Wnt/β-catenin | Intestinal homeostasis, Cancer | Context-dependent pro/anti-tumor effects [64] [11] | Sox9 interacts with β-catenin to inhibit its transcription; Upregulated for intestinal stem cell proliferation [64] |
| AKT Signaling | Breast cancer | Promotes AKT-dependent tumor growth [11] | SOX9 is AKT substrate at serine 181; regulates SOX10 promoter during transcription [11] |
| Fibrotic Signaling | Liver fibrosis, OA | ECM deposition and tissue scarring [3] [20] | SOX9 activated by profibrotic factors in hepatic stellate cells; regulates multiple ECM components [20] |
Technical Approaches for Resolving SOX9 Heterogeneity
Single-Cell Resolution Technologies
Bulk tissue analysis obscures critical SOX9 expression patterns in cellular subpopulations. Single-cell RNA sequencing (scRNA-seq) has revealed previously unappreciated heterogeneity:
In neuropathic pain, scRNA-seq of dorsal spinal cord identified 5 distinct astrocyte subpopulations with divergent SOX9 expression patterns and functional associations [7]. The pro-inflammatory Astro1 subpopulation expanded during pain development and showed high SOX9-driven glycolytic activation, while homeostatic Astro3 populations diminished [7].
In ovarian cancer, single-cell analysis of 51,786 cells from patient tumors before and after chemotherapy revealed that SOX9 upregulation occurred consistently in post-chemotherapy cells, with significant increase in 8 of 11 patients [62]. This approach enabled quantification of SOX9-associated transcriptional divergence, a metric of cellular plasticity.
Spatial Profiling and Microenvironmental Context
Spatial transcriptomics and multiplexed immunohistochemistry preserve architectural context that is crucial for interpreting SOX9 heterogeneity:
In prostate cancer, spatial transcriptomics revealed immune landscape shifts characterized by decreased effector immune cells and increased immunosuppressive populations, creating an "immune desert" microenvironment [3]. SOX9 expression patterns were linked to specific cellular neighborhoods with distinct clinical implications.
For bone tumors, simultaneous assessment of local (tissue) and circulating (PBMC) SOX9 provided a more comprehensive biomarker profile than either measure alone [65]. Malignant bone tumors showed higher SOX9 expression compared to benign tumors, with osteosarcoma exhibiting the highest levels [65].
Experimental Protocols for SOX9 Functional Analysis
Table 3: Research Reagent Solutions for SOX9 Investigation
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| Gene Ablation Systems | CRISPR/Cas9 with SOX9-targeting sgRNA; siRNA-mediated knockdown | Establish causal relationships between SOX9 and functional outcomes [62] | SOX9 knockout increased platinum sensitivity in HGSOC lines [62] |
| Chromatin Analysis | Chromatin Immunoprecipitation (ChIP) with SOX9 antibody | Identify direct transcriptional targets; map binding sites [20] | Confirmed SOX9 binding to promoters of OPN, GPNMB, FN1, SPARC in HSCs [20] |
| Animal Models | Sox9-floxed mice (Sox9fl/fl; RosaCreER+/−); Nerve injury models | In vivo validation of SOX9 function in disease pathogenesis [7] [20] | Sox9-loss reduced fibrosis and ECM targets in CCl4 and BDL models [20] |
| Expression Analysis | scRNA-seq; ELISA for SOX9-regulated proteins (OPN, VIM) | Quantify SOX9 expression and downstream effects at single-cell resolution [62] [20] | Identified rare SOX9-expressing cell clusters in primary tumors [62] |
Detailed Protocol: SOX9 Chromatin Immunoprecipitation (ChIP) Based on methodology from liver fibrosis studies [20]:
- Crosslink proteins to DNA in cultured hepatic stellate cells or tissue samples using 1% formaldehyde for 10 minutes at room temperature.
- Quench cross-linking with 125mM glycine for 5 minutes.
- Lyse cells and sonicate chromatin to shear DNA to 200-500bp fragments.
- Immunoprecipitate with validated SOX9 antibody overnight at 4°C. Include species-matched IgG control.
- Capture antibody-chromatin complexes using protein A/G beads.
- Reverse crosslinks, purify DNA, and analyze target enrichment via qPCR with primers for conserved SOX9 binding motifs identified in promoters of genes of interest (e.g., OPN, GPNMB, FN1, SPARC).
Detailed Protocol: Single-Cell RNA Sequencing Analysis Adapted from neuropathic pain and ovarian cancer studies [62] [7]:
- Tissue dissociation to single-cell suspension with viability >80%.
- Single-cell partitioning and barcoding using 10X Genomics platform.
- cDNA synthesis, amplification, and library preparation following manufacturer protocols.
- Sequencing on Illumina platform to target depth of 50,000 reads/cell.
- Data processing using Seurat or similar pipeline: quality control, normalization, integration.
- Unsupervised clustering and cluster annotation using canonical cell type markers.
- SOX9 expression analysis across clusters, conditions, and pseudotime trajectories.
- Transcriptional divergence calculation: P50/P50 = sum of top 50% expressed genes / sum of bottom 50% expressed genes [62].
SOX9 in Autoimmune and Inflammatory Disorders: Special Considerations
While much SOX9 research has focused on cancer, its role in immunoregulation presents compelling implications for autoimmune and inflammatory diseases:
Dual Immunological Role: SOX9 functions as a "double-edged sword" in immunity [3]. It can promote immune escape in cancer by impairing immune cell function, yet also help maintain macrophage function for tissue repair and regeneration [3]. This duality necessitates careful contextual interpretation.
Extracellular Matrix Remodeling: In liver fibrosis, SOX9 regulates over 30% of ECM-related genes in hepatic stellate cells [20]. The SOX9-dependent matrisome components (OPN, GPNMB, FN1, SPARC, VIM) are detectable in serum and correlate with disease severity, suggesting utility as minimally invasive biomarkers [20].
Neuroinflammation Modulation: In neuropathic pain, SOX9 drives metabolic reprogramming of astrocytes toward a pro-inflammatory, neurotoxic phenotype [7]. Targeted modulation of the SOX9-HK1-H3K9la axis specifically dampens neuroinflammatory subsets while preserving beneficial populations, suggesting precise therapeutic targeting strategies [7].
Visualizing SOX9 Regulatory Networks
The following diagram illustrates the core molecular network through which SOX9 influences disease heterogeneity, integrating mechanisms highlighted across multiple studies:
SOX9 Regulatory Network Determining Functional Heterogeneity
The experimental workflow for resolving SOX9 heterogeneity integrates multiple technologies as shown below:
Experimental Workflow for Resolving SOX9 Heterogeneity
Overcoming SOX9 heterogeneity challenges requires a multidimensional approach:
Contextual Interpretation: SOX9 expression must be interpreted within specific pathological, cellular, and temporal contexts. The same expression level may have divergent implications in different diseases or even different stages of the same disease.
Compartmental Analysis: Simultaneous assessment of local (tissue) and circulating (serum, PBMC) SOX9 provides complementary information, as demonstrated in bone cancer [65] and liver fibrosis [20].
Single-Resolution Profiling: Bulk tissue analysis obscures critical subpopulation dynamics. Technologies like scRNA-seq and spatial transcriptomics are essential for resolving cell-type-specific SOX9 functions.
Functional Biomarker Panels: Rather than relying on SOX9 alone, developing panels of SOX9-regulated targets (e.g., OPN, VIM, SPARC for fibrosis) provides more robust clinical correlates [20].
The heterogeneity of SOX9 expression across diseases and patients represents both a challenge and an opportunity. By employing sophisticated resolution strategies and contextual interpretation, researchers can harness this plasticity for improved patient stratification, disease monitoring, and targeted therapeutic development in autoimmune and inflammatory disorders.
Optimizing Delivery Systems for Tissue-Specific Targeting and Sustained Expression
The SRY-box transcription factor 9 (SOX9) is emerging as a critical regulatory node in the pathogenesis of autoimmune and inflammatory disorders, presenting both a compelling therapeutic target and a significant delivery challenge. Recent research has illuminated its complex, context-dependent functions—acting as a "double-edged sword" in immunology [3]. In certain disease contexts, such as Thyroid Eye Disease (TED), SOX9 is significantly overexpressed in orbital fibroblasts, where it activates pathogenic processes via the MAPK/ERK1/2 signaling pathway and promotes fibrosis through epidermal growth factor receptor (EGFR) regulation [19]. Conversely, in Alzheimer's disease models, boosting SOX9 in astrocytes enhances the clearance of toxic amyloid plaques and preserves cognitive function, suggesting protective roles in neurodegenerative conditions [13]. This functional duality necessitates precisely controlled delivery systems that can target specific tissues while avoiding off-target effects.
The development of effective delivery strategies for SOX9 modulation requires overcoming multiple biological barriers. Therapeutic agents must reach specific cell types within affected tissues, achieve sufficient intracellular concentrations, and maintain therapeutic activity over clinically relevant durations. This technical guide examines current approaches for optimizing tissue-specific targeting and sustained expression of SOX9-directed therapies, with particular emphasis on applications in autoimmune and inflammatory disease research. By addressing these delivery challenges, researchers can better harness SOX9's therapeutic potential while mitigating potential adverse effects associated with its pleiotropic functions.
SOX9 Biology and Pathological Relevance
Molecular Structure and Function
SOX9 is a member of the SRY-related high-mobility group (HMG) box transcription factor family, encoding a 509 amino acid polypeptide with several functionally distinct domains [3]. The protein contains an N-terminal dimerization domain (DIM), a central HMG box DNA-binding domain, two transcriptional activation domains (TAM and TAC), and a C-terminal proline/glutamine/alanine (PQA)-rich domain. The HMG domain facilitates nuclear localization and specific DNA binding, while the transcriptional activation domains interact with various cofactors to regulate gene expression. This modular structure enables SOX9 to participate in diverse transcriptional programs across different tissue contexts.
Tissue Expression Patterns
SOX9 demonstrates a tissue-enhanced expression pattern, with particularly notable presence in salivary gland, brain, liver, and various connective tissues according to the Human Protein Atlas [66]. Its expression is specifically elevated in pathological contexts; for instance, SOX9 mRNA and protein levels are significantly higher in orbital fibroblasts from TED patients compared to healthy controls [19]. This tissue- and disease-specific expression pattern creates both opportunities and challenges for targeted therapeutic interventions, as delivery systems must distinguish between pathological and physiological expression contexts.
SOX9 in Disease Mechanisms
In autoimmune and inflammatory conditions, SOX9 contributes to pathogenesis through multiple mechanisms. In TED, SOX9 overexpression activates orbital fibroblasts, promoting their transformation, migration, proliferation, and enhancing their contractile and anti-apoptotic capabilities [19]. SOX9 directly binds to the EGFR promoter and activates the MAPK/ERK1/2 signaling pathway, establishing a pro-fibrotic cascade. Transcriptomic analyses reveal that SOX9 regulates extracellular matrix-related genes, further reinforcing its role in tissue remodeling and fibrosis. Understanding these mechanisms is essential for designing targeted delivery systems that can effectively interrupt pathogenic signaling while preserving beneficial SOX9 functions in other tissues.
Current Experimental Models and Methodologies
In Vitro Models for SOX9 Research
Table 1: Key In Vitro Models for SOX9 Delivery Studies
| Model System | Application | Key Readouts | Considerations |
|---|---|---|---|
| Primary Orbital Fibroblasts (TED patients) | Fibrosis mechanisms, SOX9 pathway analysis | Contractility, proliferation, ECM gene expression, phosphorylation signaling | Maintains disease-specific phenotype; limited expansion capacity |
| Astrocyte Cultures | Neuroinflammatory modeling, plaque clearance studies | Phagocytosis assays, cytokine secretion, morphological changes | Relevant for CNS-targeted delivery testing |
| Chondrocyte Cultures | Developmental studies, cartilage regeneration | Chondrogenic markers, matrix production, differentiation status | Useful for regenerative applications |
| Mesenchymal Stem Cells (MSCs) | Cell-based delivery, differentiation studies | Multilineage differentiation, immunomodulatory factors, migration assays | Potential as delivery vehicles for SOX9 modulators |
Primary cell cultures represent a cornerstone in SOX9 research, particularly for investigating disease-specific mechanisms. The isolation and culture of orbital fibroblasts from TED patients follows established protocols: tissue samples are cut into 1-2 mm³ pieces and transferred to culture plates, allowing fibroblasts to migrate out [19]. Cells between passages 3-8 with good viability are recommended for experiments to maintain phenotypic stability. For SOX9 manipulation, researchers typically employ either knockdown approaches using small interfering RNA (siRNA) or overexpression through lentivirus transduction. These in vitro systems enable precise assessment of SOX9's functional roles through various assays including collagen gel contraction for fibroblast contractility, EdU incorporation for proliferation, and transcriptomic analysis via RNA sequencing.
In Vivo Models for Delivery System Validation
Animal models provide critical platforms for evaluating the efficacy and specificity of SOX9-targeted delivery systems. In Alzheimer's disease research, mouse models that have already developed cognitive impairment and amyloid plaques offer particularly relevant systems for testing therapeutic interventions, as they more closely mimic the clinical scenario in human patients [13]. In these models, researchers can monitor cognitive performance over extended periods (e.g., six months) using behavioral tests such as novel object recognition and spatial memory tasks, while post-mortem analysis quantifies plaque accumulation and astrocyte activation. For fibrosis-focused studies, models that develop progressive tissue fibrosis can be employed to assess the impact of SOX9 modulation on extracellular matrix deposition and tissue remodeling. These in vivo systems enable researchers to evaluate both the therapeutic efficacy and potential off-target effects of SOX9-directed therapies, providing critical preclinical data for delivery system optimization.
Delivery Strategies for SOX9 Modulation
Nucleic Acid-Based Approaches
Gene therapy approaches for SOX9 modulation primarily utilize either knockdown strategies with siRNA or overexpression systems with plasmid DNA or viral vectors. For SOX9 suppression, siRNA sequences targeting specific SOX9 transcripts can be designed and delivered via lipid nanoparticles or other non-viral vectors. Experimental protocols typically involve transfection of siRNA oligonucleotides (e.g., 20-50 nM concentration) using appropriate transfection reagents, with efficacy confirmed by qRT-PCR and Western blotting 48-72 hours post-transfection [19]. For SOX9 enhancement, lentiviral vectors encoding the SOX9 coding sequence under control of tissue-specific promoters enable sustained expression. Lentiviral transduction protocols generally involve viral particle incubation with target cells at appropriate multiplicities of infection (MOI), often with polybrene enhancement (e.g., 4-8 μg/mL), followed by antibiotic selection if stable integration is desired. The choice between knockdown and overexpression strategies depends on the pathological context—SOX9 inhibition may be beneficial in fibrotic conditions like TED, while enhancement could be therapeutic in neurodegenerative contexts like Alzheimer's disease.
Cell-Based Delivery Systems
Mesenchymal stem cells (MSCs) represent promising delivery vehicles for SOX9 modulation, particularly given their innate tropism for inflamed tissues and immunomodulatory properties [67]. MSC-based delivery systems can be engineered to express SOX9 modulators (either enhancing or inhibiting factors) through genetic modification prior to administration. The therapeutic protocol involves isolating MSCs from appropriate sources (bone marrow, adipose tissue, or umbilical cord), expanding them in culture under defined conditions, genetically modifying them to express the desired SOX9 regulator, and administering them systemically or locally to target tissues. These cells naturally home to sites of inflammation and can release therapeutic factors through paracrine mechanisms. MSCs offer particular advantages for delivery to privileged sites or across biological barriers that challenge conventional nanoparticle or viral approaches. Additionally, MSCs can be pre-conditioned to enhance their survival, homing capacity, and therapeutic factor production before administration.
Targeting Strategies for Tissue Specificity
Leveraging Tissue-Specific Enhancers and Promoters
The SOX9 gene locus contains multiple tissue-specific enhancers that direct its expression in particular cell types, including chondrocytes, Sertoli cells, and cranial neural crest cells [68]. This natural regulatory architecture provides valuable insights for designing targeted delivery systems. Research comparing SOX9 binding patterns in different tissues reveals that in limb buds, SOX9 preferentially binds to intronic and distal regions, while in male gonads, it more frequently associates with proximal upstream regions of genes [69]. These tissue-specific binding patterns correlate with distinct motif preferences—SOX palindromic repeats are more common in limb bud binding regions compared to male gonad targets. Delivery systems can exploit these natural regulatory elements by incorporating tissue-specific promoters or enhancers in genetic constructs to restrict SOX9 modulator expression to desired tissues. For example, constructs using cartilage-specific promoters could target SOX9 modulation to joint tissues while avoiding off-target effects in other organs.
Antibody and Ligand-Based Targeting
Surface functionalization of delivery vehicles with targeting ligands enables active tissue- and cell-specific delivery. While the search results don't provide explicit examples of targeted delivery systems for SOX9 modulators, the general principle involves conjugating nanoparticles, viral vectors, or other carriers with antibodies, peptides, or other ligands that recognize molecules preferentially expressed on target cells. In the context of autoimmune and inflammatory conditions, potential targeting moieties could include antibodies against fibroblast activation protein (FAP) for fibrotic tissues, or ligands for receptors upregulated on activated immune cells. The targeting strategy should be validated using in vitro binding assays with relevant cell types (e.g., TED orbital fibroblasts versus healthy controls) before progressing to in vivo efficacy studies. Targeting specificity can be quantified through comparative delivery experiments, measuring the accumulation of therapeutic agents in target versus non-target tissues and assessing functional outcomes in both compartments.
Characterization and Validation of Delivery Systems
Analytical Methods for Delivery Assessment
Table 2: Key Methodologies for Characterizing SOX9-Targeted Delivery Systems
| Method Category | Specific Techniques | Parameters Measured | Technical Considerations |
|---|---|---|---|
| Molecular Confirmation | qRT-PCR, Western Blot, RNA-seq | SOX9 expression levels, pathway activation, target gene regulation | Use multiple validation methods; time-course studies recommended |
| Cellular Uptake and Localization | Immunofluorescence, FACS, IHC | Cellular internalization, subcellular localization, tissue distribution | Quantify across multiple cell types; assess functional correlation |
| Spatial Analysis | MESA framework, CODEX, spatial transcriptomics | Tissue architecture, cellular neighborhoods, spatial expression patterns | Requires specialized computational tools; preserves tissue context |
| Functional Assays | Collagen contraction, EdU proliferation, phagocytosis | Pathophysiological processes, cellular behaviors, therapeutic efficacy | Link molecular changes to functional outcomes; disease-relevant readouts |
Comprehensive characterization of SOX9-targeted delivery systems requires multi-level validation from molecular to functional endpoints. At the molecular level, SOX9 expression modulation should be confirmed using quantitative RT-PCR for mRNA levels and Western blotting for protein expression [19]. The 2−ΔΔCT method is standard for qRT-PCR analysis, with GAPDH typically serving as the endogenous control. For Western blotting, radioimmunoprecipitation assay (RIPA) buffer supplemented with protease and phosphatase inhibitors is recommended for protein extraction, with equal protein loading confirmed through bicinchoninic acid (BCA) protein assays. Beyond confirming SOX9 level changes, researchers should assess downstream pathway activation—for example, phosphorylated ERK1/2 levels in fibrosis models or amyloid phagocytosis in neurodegenerative contexts. Chromatin immunoprecipitation followed by qPCR (ChIP-qPCR) can directly verify SOX9 binding to putative target genes such as EGFR, providing mechanistic validation.
Advanced Spatial Analysis Frameworks
The MESA (multiomics and ecological spatial analysis) framework represents a cutting-edge approach for quantitatively characterizing tissue states and delivery system effects [70]. This method adapts ecological diversity metrics to analyze spatial omics data, enabling researchers to systematically evaluate cellular organization and interactions within tissues. The MESA pipeline involves integrating spatial omics data with single-cell datasets from the same tissue type and disease condition, matching cells across modalities to create enriched multiomics profiles. The framework then characterizes local cellular neighborhoods and identifies conserved patterns using k-means clustering. MESA introduces several quantitative metrics including the Multiscale Diversity Index (MDI) to evaluate diversity variations across spatial scales, Global Diversity Index (GDI) to assess whether patches of similar diversity are spatially adjacent, and Local Diversity Index (LDI) to identify high- and low-diversity "hot spots." Applying this analytical approach to SOX9-targeted therapy development could reveal how delivery systems alter tissue microenvironments at multiple scales, potentially identifying previously unrecognized spatial structures and key cell populations linked to disease states and therapeutic outcomes.
Research Reagent Solutions
Essential Experimental Tools
Table 3: Key Research Reagents for SOX9-Targeted Delivery Studies
| Reagent Category | Specific Examples | Primary Applications | Technical Notes |
|---|---|---|---|
| SOX9 Modulation | siRNA oligonucleotides, lentiviral SOX9 constructs, CRISPR/Cas9 systems | SOX9 knockdown/overexpression, gene editing | Validate specificity; include appropriate controls |
| Detection Antibodies | Anti-SOX9, anti-pERK1/2, anti-EGFR, ECM protein antibodies | Immunofluorescence, Western blot, IHC, flow cytometry | Verify species reactivity; optimize concentrations |
| Cell Culture Reagents | Primary cell media, transfection reagents, selection antibiotics | Maintenance and genetic manipulation of target cells | Use low-passage primary cells; optimize transfection |
| Functional Assay Kits | Collagen gel contraction, EdU proliferation, phagocytosis kits | Assessing cellular functional responses | Standardize assay conditions across experiments |
| Spatial Analysis Platforms | CODEX, CosMx SMI, RNAscope systems | Tissue context preservation, spatial expression mapping | Requires specialized instrumentation and analysis |
Selecting appropriate research reagents is critical for successful development and evaluation of SOX9-targeted delivery systems. For SOX9 detection, validated antibodies against specific SOX9 epitopes are essential for techniques including immunofluorescence, Western blotting, and immunohistochemistry. For genetic manipulation, siRNA sequences should be designed to target specific SOX9 transcript regions and validated for efficacy and specificity through dose-response studies. Lentiviral constructs for SOX9 overexpression should incorporate appropriate regulatory elements and selection markers for stable cell line generation. Functional assay kits must be selected based on disease relevance—for fibrotic conditions like TED, collagen gel contraction assays measure fibroblast contractility, while EdU incorporation assays quantify proliferation rates. For neurodegenerative applications, phagocytosis assays assess amyloid clearance capacity. When establishing new methodologies, researchers should systematically optimize reagent concentrations, incubation times, and detection parameters using appropriate controls to ensure robust and reproducible results.
Signaling Pathways and Experimental Workflows
SOX9 in Fibrotic Signaling
SOX9 Profibrotic Signaling Pathway
The diagram illustrates the key signaling pathway through which SOX9 promotes fibrosis in conditions like Thyroid Eye Disease. TGF-β accumulation serves as the crucial initiating step, upregulating SOX9 expression [19]. SOX9 then directly binds to the epidermal growth factor receptor (EGFR) promoter, activating its expression. Both SOX9 and EGFR contribute to the activation of the MAPK/ERK1/2 signaling pathway, which ultimately drives the fibrotic response characterized by excessive extracellular matrix deposition, fibroblast proliferation, and tissue remodeling. This pathway represents a potential interception point for targeted therapies aiming to disrupt SOX9-mediated fibrotic processes in autoimmune conditions.
Experimental Workflow for Delivery System Evaluation
Delivery System Evaluation Workflow
This workflow outlines a comprehensive approach for developing and validating SOX9-targeted delivery systems. The process begins with delivery system design, incorporating tissue-specific targeting elements and SOX9 modulators. In the in vitro phase, systems are tested in relevant cellular models (e.g., primary orbital fibroblasts for TED applications), assessing molecular endpoints (SOX9 expression, pathway activation) and functional outcomes (proliferation, contractility, ECM production). Promising candidates advance to in vivo evaluation in disease-relevant animal models, with careful monitoring of therapeutic effects and potential off-target impacts. Spatial analysis techniques like MESA provide detailed characterization of tissue-level effects, generating data that feeds back into delivery system refinement. This iterative process continues until optimal performance characteristics are achieved.
The development of optimized delivery systems for tissue-specific SOX9 targeting represents a frontier in therapeutic intervention for autoimmune and inflammatory disorders. The functional duality of SOX9—pathogenic in fibrotic conditions yet protective in neurodegenerative contexts—demands exquisite precision in delivery approaches. Current strategies leveraging nucleic acid technologies, viral vectors, and cell-based systems show promise but require further refinement to achieve true tissue specificity and sustained expression control. The integration of advanced analytical frameworks like MESA, which adapt ecological principles to spatial omics analysis, provides unprecedented resolution for evaluating how delivery systems alter tissue microenvironments. As these technologies mature, researchers will be better equipped to design SOX9-targeted therapies that maximize therapeutic benefit while minimizing off-target effects, ultimately translating this promising biological target into effective clinical interventions for complex inflammatory diseases.
Mitigating Off-Target Effects in SOX9 Signaling Pathway Modulation
The transcription factor SOX9 (SRY-related HMG-box 9) plays a critical role in developmental processes, stem cell maintenance, and tissue homeostasis. Recent evidence has positioned SOX9 as a significant regulator in immune cell development and function, with direct implications for autoimmune and inflammatory disorders [3]. SOX9 exhibits context-dependent dual functions—acting as both an activator and repressor—across diverse immune cell types, thereby contributing to the regulation of numerous biological processes [3]. In rheumatoid arthritis (RA), for instance, SOX9 expression is associated with cartilage protection and repair mechanisms, yet its dysregulation can contribute to pathogenic processes in the synovial microenvironment [3]. Similarly, in systemic lupus erythematosus (SLE), SOX9-mediated pathways interact with immune checkpoint molecules, suggesting its potential as a therapeutic target [71]. Given this nuanced role, precise modulation of SOX9 signaling has emerged as a promising therapeutic strategy, though it presents significant challenges regarding specificity and off-target effects.
SOX9 Biology and Signaling Cross-Talk
Molecular Structure and Functional Domains
SOX9 is a member of the SOXE transcription factor family, characterized by several functionally critical domains that represent potential intervention points:
- HMG Domain: A highly conserved high-mobility group (HMG) box domain facilitates DNA binding to the consensus sequence (A/TA/TCAAA/TG), inducing significant DNA bending. This domain contains nuclear localization signals (NLS) and a nuclear export signal (NES) that regulate nucleocytoplasmic shuttling [64] [3].
- Dimerization Domain (DIM): Located ahead of the HMG box, this domain enables SOX9 self-dimerization or heterodimerization with partner transcription factors [3].
- Transactivation Domains: SOX9 contains two transcriptional activation domains—a central domain (TAM) and a C-terminal domain (TAC)—that interact with co-activators to enhance transcriptional activity [3].
- PQA-Rich Domain: A proline, glutamine, and alanine-rich region necessary for full transcriptional activation potential [3].
Key Signaling Pathway Interactions
SOX9 participates in complex cross-regulatory networks with critical signaling pathways, particularly the canonical Wnt/β-catenin pathway. This intricate relationship represents both an opportunity for therapeutic intervention and a potential source of off-target effects:
Diagram: SOX9-Wnt/β-catenin Cross-Regulation. SOX9 inhibits the canonical Wnt pathway by promoting β-catenin degradation and competing with TCF/LEF factors [72].
The molecular mechanisms of SOX9-mediated inhibition of canonical Wnt signaling include [72]:
- β-catenin degradation: SOX9 directly binds β-catenin via its C-terminus, promoting ubiquitination and proteasomal degradation
- Complex disruption: SOX9 inhibits β-catenin/TCF complex formation through competitive binding
- Antagonist activation: SOX9 transcriptionally activates Wnt pathway antagonists
- Nuclear translocation: SOX9 reduces nuclear β-catenin levels through sequestration and re-localization
Off-Target Effects: Mechanisms and Risks in SOX9 Modulation
Pathway Cross-Talk and Compensatory Mechanisms
The interconnected nature of signaling pathways presents significant challenges for specific SOX9 modulation:
Hedgehog Signaling Interdependence: Sonic hedgehog (Shh) upregulates SOX9 to generate chondrogenic precursors, while Indian hedgehog (Ihh) upregulates SOX9 for proliferation and maturation of chondrocytes [64]. Disruption of SOX9 can therefore inadvertently affect hedgehog-mediated processes.
Feedback Loops in Wnt/SOX9 Axis: The SOX9-Wnt/β-catenin relationship forms a precise balance maintained through mutual antagonism. Artificial disruption of SOX9 can release this inhibition, causing uncontrolled Wnt pathway activation with consequences including [73] [72]:
- Fibrotic responses in multiple tissues
- Enhanced stem cell proliferation and differentiation defects
- Tumorigenic transformation in susceptible microenvironments
Immune Cell Dysregulation
As SOX9 plays distinct roles in various immune cell populations, non-specific modulation can disrupt immune homeostasis:
Table 1: SOX9 Functions in Immune Cells and Associated Off-Target Risks
| Immune Cell Type | Normal SOX9 Function | Off-Target Consequences |
|---|---|---|
| Macrophages | Maintains function; contributes to cartilage formation and tissue repair [3] | Altered polarization; impaired tissue repair; exacerbated inflammation |
| T Cells | Cooperates with c-Maf to activate Rorc and modulate αβ vs. γδ T cell balance [3] | Disrupted T cell development; altered inflammatory responses |
| B Cells | Not significant in normal development; overexpressed in B-cell lymphomas [3] | Unintended effects in B-cell populations during targeted therapies |
SOX9 Pleiotropy in Tissue Homeostasis
SOX9 exhibits diverse functions across tissues, creating potential for unintended consequences:
- Chondrogenesis: SOX9 activates ECM genes (Col2a1, Col9a1, Aggrecan) and directly represses Col10a1 during hypertrophy [64]
- Epithelial Differentiation: In lung development, SOX9 regulates branch morphogenesis and maintains adult airway distal progenitor cells [73]
- Organ Fibrosis: SOX9 is upregulated in liver fibrosis downstream of Hedgehog signaling, modulating osteopontin expression [64]
Strategic Framework for Mitigating Off-Target Effects
Targeting Specificity in CRISPR-Cas9 Approaches
CRISPR-based gene editing represents a powerful approach for SOX9 modulation but requires careful optimization to minimize off-target effects:
Table 2: Strategies to Enhance CRISPR-Cas9 Specificity for SOX9 Targeting
| Strategy | Mechanism | Application to SOX9 |
|---|---|---|
| sgRNA Optimization | Improved guide RNA design reduces off-target binding | Target SOX9 functional domains with high-specificity sgRNAs |
| High-Fidelity Cas Variants | Engineered Cas9 with reduced off-target activity (eSpCas9, SpCas9-HF1) [74] [75] | Use for precise SOX9 gene editing with minimal unintended cleavage |
| CRISPR Nickase | Cas9 nickase creates single-strand breaks, reducing off-target mutations [75] | Pair nickases for SOX9 editing while decreasing off-target effects |
| Prime Editing | Search-and-replace editing without double-strand breaks [75] | Precisely modify SOX9 sequences without inducing DNA damage response |
| RNP Delivery | Ribonucleoprotein complex delivery reduces prolonged Cas9 expression [74] | Transient SOX9 targeting with limited off-target exposure |
Experimental Protocol: In Vitro Assessment of CRISPR Off-Target Effects [74] [76]
- Guide RNA Design: Design sgRNAs targeting SOX9 functional domains using algorithm-based tools (CRISPOR, Cas-OFFinder) with strict specificity scoring
- Specificity Validation: Employ biased (targeted) and unbiased (genome-wide) off-target detection methods:
- Biased Detection: Cas-OFFinder, CCTop to predict potential off-target sites
- Unbiased Detection: GUIDE-seq, CIRCLE-seq for genome-wide off-target identification
- Cell Transfection: Deliver CRISPR components via RNP electroporation into target cells
- Off-Target Assessment:
- Deep sequencing of predicted off-target loci
- RNA-seq to evaluate transcriptomic-wide effects
- Functional validation of potential off-target hits
- Specificity Quantification: Calculate off-target ratio (off-target read counts/on-target read counts)
Small Molecule Inhibitors and Biological Therapeutics
Small molecule approaches targeting SOX9 require precise compound design to avoid pathway cross-talk:
Experimental Protocol: High-Content Screening for SOX9 Inhibitor Specificity
- Reporter System Development:
- Generate SOX9-responsive luciferase reporter cell lines (SOX9-Luc)
- Create parallel reporter systems for Wnt, Hedgehog, and other related pathways
- Compound Screening:
- Primary screen: SOX9-Luc activity inhibition
- Counter-screens: Pathway-specific reporters to identify non-selective compounds
- Specificity Profiling:
- Transcriptomic analysis (RNA-seq) after compound treatment
- Assessment of known SOX9 target genes (Col2a1, Agcan) versus unrelated pathway genes
- Validation:
- Chromatin immunoprecipitation (ChIP) to confirm direct SOX9 target disruption
- Functional assays in SOX9-dependent cellular models
Spatial and Temporal Control of SOX9 Modulation
Restricting SOX9 modulation to specific cellular contexts and timeframes significantly reduces off-target effects:
Diagram: Spatial-Temporal Control Strategy. A sequential approach to restrict SOX9 modulation to specific contexts [73] [72].
Implementation Strategies:
- Cell-Type Specific Promoters: Drive SOX9-modulating constructs with tissue-specific promoters (e.g., COL2A1 for chondrocytes, SPC for alveolar cells)
- Microrna Response Elements: Incorporate miR-122 or other tissue-specific miRNA targets to restrict expression to desired cell types
- Inducible Systems: Utilize tetracycline- or rapamycin-inducible expression systems for temporal control
- Ligand-Targeted Delivery: Conjugate SOX9 modulators with antibodies or ligands targeting cell surface markers overexpressed in diseased tissues
Validation and Detection Methodologies
Comprehensive Off-Target Assessment
Rigorous validation requires orthogonal methods to detect both anticipated and unanticipated off-target effects:
Genomic and Epigenomic Approaches:
- Whole Genome Sequencing: Identify large structural variations and unexpected editing events
- ATAC-Seq: Assess chromatin accessibility changes at potential off-target loci
- ChIP-Seq: Evaluate SOX9 binding genome-wide and confirm specific targeting
- DNA Methylation Analysis: Detect epigenetic changes resulting from off-target effects
Functional and Phenotypic Assays:
- Multiplexed Functional Screens: Evaluate potential off-target hits in parallel using pooled screening approaches
- High-Content Imaging: Assess morphological changes indicative of pathway dysregulation
- Cellular Profiling: Comprehensive flow cytometry panels to evaluate immune cell populations
- Cytokine Secretion Analysis: Multiplex cytokine arrays to detect inflammatory signatures
In Vivo Validation Models
Experimental Protocol: Preclinical Specificity Assessment [73]
- Animal Model Selection: Utilize tissue-specific SOX9 reporter mice coupled with disease-relevant models (e.g., collagen-induced arthritis for autoimmune applications)
- Biodistribution Analysis: Quantitative PCR of target and off-target tissues following therapeutic administration
- Functional Assessment:
- Histopathological evaluation of major organs
- Serum biomarkers for tissue damage (ALT, AST, creatinine)
- Behavioral and physiological monitoring
- Long-Term Follow-Up: Extended observation to detect delayed off-target effects
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents for SOX9 Research with Specificity Controls
| Reagent Category | Specific Examples | Application and Specificity Considerations |
|---|---|---|
| CRISPR Tools | SOX9-specific sgRNAs, High-fidelity Cas9 variants, CRISPRi/a systems [76] | Prioritize sgRNAs with high GuideScan specificity scores; include multiple sgRNAs per target with different off-target profiles |
| Small Molecule Modulators | Experimental SOX9 inhibitors (research-grade), Wnt pathway modulators as controls [72] | Include pathway-specific controls to distinguish direct vs. indirect effects; use multiple chemotypes to confirm target engagement |
| Antibodies | Anti-SOX9 (ChIP-grade), Anti-β-catenin, Phospho-specific antibodies for pathway analysis [64] | Validate antibodies for specific applications (IHC vs. WB vs. ChIP); include isotype controls |
| Cell Lines | SOX9 reporter lines, SOX9 knockout lines, Inducible expression systems [73] | Use matched control lines (e.g., wild-type vs. knockout); employ multiple cell models to confirm generalizability |
| Animal Models | Tissue-specific SOX9 knockout mice, SOX9 reporter strains, Disease models with SOX9 involvement [73] | Include littermate controls; consider temporal control systems (Cre-ERT2) to developmental effects |
Precise modulation of the SOX9 signaling pathway represents a promising therapeutic approach for autoimmune and inflammatory disorders, but requires sophisticated strategies to minimize off-target effects. Successful implementation will depend on: (1) comprehensive understanding of SOX9's contextual functions in specific tissue and immune cell populations; (2) application of high-specificity targeting approaches including optimized CRISPR systems and tissue-restricted delivery; and (3) rigorous validation using orthogonal methods to detect both anticipated and unanticipated off-target effects. As these technologies mature, the research community will be better positioned to harness the therapeutic potential of SOX9 modulation while minimizing risks associated with off-target activities, ultimately enabling more effective treatments for autoimmune diseases with improved safety profiles.
The transcription factor SOX9 presents a compelling yet challenging therapeutic target for autoimmune and inflammatory disorders. Its biological function is inherently context-dependent, acting as a master regulator of tissue repair while simultaneously driving pathological processes in fibrosis and cancer. This duality, coupled with significant limitations in existing preclinical models, creates substantial hurdles in therapeutic development. Successful clinical translation requires a multifaceted strategy that integrates advanced disease modeling, rigorous biomarker identification, and innovative clinical trial designs to safely exploit the therapeutic potential of SOX9 modulation.
SOX9 (SRY-related High-Mobility Group Box 9) is a transcription factor with a complex dual role in immunological processes. It is crucial for developmental biology, cartilage formation, and stem cell maintenance, but its dysregulation is implicated in various disease states. In the context of autoimmune and inflammatory disorders, SOX9 exhibits a "double-edged sword" characteristic [3]. On one hand, it promotes tissue regeneration and maintains macrophage function; on the other, its inhibition can exacerbate inflammatory responses, as demonstrated in dental pulp models where SOX9 knockdown promoted immune activation and matrix degradation [14]. This paradoxical nature necessitates precise therapeutic targeting strategies to inhibit detrimental functions while preserving beneficial roles—a fundamental challenge in SOX9-focused drug development.
SOX9 Biology and Signaling Pathways: Relevance to Disease
Structural and Functional Domains
The SOX9 protein contains several functionally critical domains that represent potential intervention points for therapeutic modulation [3] [17]:
- HMG Box Domain: A conserved DNA-binding motif that recognizes specific sequences (AGAACAATGG), bends DNA, and facilitates transcription of target genes.
- Dimerization Domain (DIM): Enables SOX9 to form homodimers or heterodimers with related SOXE family members (SOX8, SOX10), enhancing DNA binding selectivity.
- Transactivation Domains (TAM and TAC): Regions that interact with co-activators to potentiate gene transcription, with TAC particularly important for inhibiting β-catenin during differentiation.
- PQA-Rich Domain: A proline/glutamine/alanine-rich region that stabilizes SOX9 and enhances its transactivation potential.
Key Regulatory Mechanisms
SOX9 expression and activity are controlled through multiple layers of regulation, each presenting opportunities and challenges for therapeutic intervention:
- Transcriptional Regulation: Fibroblast growth factors, CREB1, and CEBPB transcription factors regulate SOX9 promoter activity, while enhancer elements like TES/TESCO control tissue-specific expression [17].
- Epigenetic Modifications: DNA methylation and histone modifications significantly influence SOX9 expression patterns. In osteoarthritis, increased H3K9 and H3K27 trimethylation at SOX9 promoters reduces its expression [17].
- Post-Translational Modifications: Phosphorylation at serine residues (S64, S181) by PKA and ERK1/2 regulates SOX9 nuclear localization and transcriptional activity [17].
- RNA Modifications: m5C and m6A RNA methylation in the 3'UTR of SOX9 mRNA, mediated by Nsun4 and Mettl3 respectively, co-regulate SOX9 translation during chondrogenic differentiation—a mechanism potentially relevant to inflammatory tissue repair [77].
Preclinical Model Limitations in SOX9 Research
The translation of SOX9 biology into clinical applications faces significant challenges due to inherent limitations in existing preclinical model systems.
Table 1: Key Limitations of Preclinical Models in SOX9 Research
| Model System | Key Limitations | Specific SOX9 Research Challenges |
|---|---|---|
| 2D Cell Cultures | Lack tissue architecture and mechanical cues; oversimplified cellular interactions | Failed to replicate the complex SOX9 regulatory network present in native tissue environments; unable to model immune cell crosstalk |
| Conventional Animal Models | Species-specific differences in immune system and SOX9 regulation; artificial disease induction | Limited translation of SOX9's role in human autoimmune conditions; cannot fully recapitulate human disease heterogeneity |
| Xenograft Models | Lack human immune components; stromal mismatch | Inadequate for studying SOX9 in tumor-immune interactions [3]; cannot model SOX9 effects on human immune cell function |
| Genetic Models | Often incomplete representation of human disease pathophysiology | May not capture the nuanced, context-dependent functions of SOX9 across different tissues and disease stages |
Specific SOX9 Modeling Challenges
The context-dependent functionality of SOX9 presents unique challenges that conventional models struggle to address:
- Dual Role Complexity: SOX9 exhibits opposing functions across different physiological contexts. In fibrosis, SOX9 promotes extracellular matrix deposition in cardiac, hepatic, pulmonary, and renal tissues [17], while in inflammatory joint diseases, its anti-inflammatory and pro-regenerative functions are beneficial [3] [14]. Current models poorly capture these opposing functions within integrated physiological systems.
- Immune Modulation: SOX9 regulates multiple immune cell populations, including γδ T-cell differentiation through Rorc activation [3] and modulation of macrophage function. The species-specific differences in immune system composition and function limit translation from animal models.
- Stromal-Immune Interactions: SOX9 expression in fibroblasts regulates both fibrosis and inflammation, as demonstrated in cardiac models where fibroblast-specific SOX9 inactivation reduced both collagen deposition and inflammatory markers [78]. Conventional models often fail to recapitulate the complexity of these stromal-immune interactions.
Strategic Framework for Successful Clinical Translation
Overcoming the hurdles in SOX9 therapeutic development requires a comprehensive, integrated approach from bench to bedside.
Advanced Preclinical Models and Validation
Implementing more physiologically relevant model systems is crucial for derisking SOX9-targeted therapies:
- Humanized Mouse Models: Incorporating human immune systems or patient-derived xenografts better models SOX9's immunomodulatory functions and enables evaluation of human-specific therapeutic agents.
- 3D Organoid and Co-culture Systems: These models preserve tissue architecture and cellular interactions, allowing for more accurate assessment of SOX9's role in stromal-immune crosstalk and tissue remodeling.
- Patient-Derived Model Systems: As demonstrated in oncology research, patient-derived xenograft models can improve predictive accuracy for drug response [79]. Applying this approach to autoimmune diseases could enhance translation of SOX9 modulators.
Biomarker-Driven Clinical Development
The successful clinical translation of SOX9-targeted therapies requires robust biomarker strategies to identify responsive patient populations and monitor target engagement:
Table 2: Essential Biomarker Classes for SOX9-Targeted Therapy Development
| Biomarker Class | Purpose | Specific Examples/Approaches |
|---|---|---|
| Patient Selection Biomarkers | Identify patients most likely to respond to SOX9-targeted therapy | SOX9 expression levels in affected tissues; SOX9 autoantibodies in autoimmune polyendocrine syndrome [2]; genetic polymorphisms in SOX9 regulatory regions |
| Target Engagement Biomarkers | Verify that therapeutic agent modulates intended SOX9 pathway | Downstream gene expression signatures (collagen type II, aggrecan) [77] [80]; SOX9 phosphorylation status; imaging of SOX9-related tissue changes |
| Pharmacodynamic Biomarkers | Monitor biological response to SOX9-targeted intervention | Extracellular matrix turnover markers; inflammatory cytokines (IL-8) [14]; immune cell infiltration patterns |
| Resistance Biomarkers | Identify mechanisms of adaptive or innate resistance | Alternative pathway activation; SOX9 regulatory RNA expression; epigenetic modifications at SOX9 locus |
Clinical Trial Design Considerations
Innovative trial designs can accelerate the development of SOX9-targeted therapies while managing risks:
- Adaptive Trial Designs: Allow for modification of ongoing trials based on accumulating data, enabling more efficient evaluation of SOX9 modulators in different autoimmune indications.
- Biomarker-Enriched Enrollment: Strategically select patients based on SOX9 pathway activity or related biomarkers, increasing the likelihood of detecting clinical efficacy.
- Combination Therapy Approaches: Given SOX9's integration with multiple signaling pathways, rational combination strategies may enhance efficacy and overcome resistance mechanisms.
Experimental Approaches and Methodologies
Comprehensive characterization of SOX9 function and therapeutic potential requires integrated methodological approaches.
Core Experimental Workflows
The diagram below illustrates a generalized workflow for evaluating SOX9-targeted therapies from preclinical validation to clinical assessment:
Key Signaling Pathways in SOX9 Regulation
SOX9 integrates signals from multiple pathways that are relevant to autoimmune and inflammatory diseases:
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Investigation
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Genetic Manipulation Tools | SOX9 siRNA/shRNA; CRISPR/Cas9 systems; SOX9 overexpression vectors | Gain/loss-of-function studies to elucidate SOX9 roles in disease processes |
| Detection Antibodies | Anti-SOX9 (specific to HMG domain); phospho-specific SOX9 antibodies; collagen type II antibodies | Protein localization, expression quantification, and modification status assessment |
| Cell Culture Models | Primary chondrocytes; mesenchymal stem cells (BMSCs, hUC-MSCs); fibroblast lineages | Differentiation studies, tissue repair modeling, and fibrotic pathway analysis |
| Animal Models | Tissue-specific SOX9 knockout mice; fibrosis induction models (cardiac, hepatic, pulmonary) | In vivo validation of SOX9 function in disease pathophysiology and therapeutic testing |
| Specialized Assay Kits | Chromatin immunoprecipitation (ChIP); RNA immunoprecipitation; extracellular matrix degradation assays | Direct target identification; SOX9-RNA interaction mapping; matrix remodeling assessment |
The journey from bench to bedside for SOX9-targeted therapies requires careful navigation of its biological complexity and the limitations of current preclinical systems. The context-dependent functionality of SOX9—playing roles in both tissue protection and pathology—demands sophisticated therapeutic approaches that can achieve precise modulation rather than simple inhibition or activation. Success will depend on implementing advanced model systems, developing robust biomarker strategies, and designing innovative clinical trials that account for patient heterogeneity and disease context. As our understanding of SOX9's multifaceted roles in autoimmune and inflammatory disorders deepens, so too does the potential for transformative therapies that leverage its unique position at the intersection of tissue repair and immune regulation.
Validating SOX9: Prognostic Value, Cross-Disease Analysis, and Target Prioritization
The SRY-related HMG-box transcription factor 9 (SOX9) is a nuclear transcription factor belonging to the SOX protein family, characterized by a highly conserved high-mobility group (HMG) domain that encodes a 79-amino-acid DNA-binding domain. This domain enables SOX9 to recognize specific DNA sequences and regulate transcriptional activity [71]. The SOX9 gene maps to chromosome 17q24.3 and encodes a 509-amino-acid polypeptide with a molecular mass of approximately 56 kDa [42]. The protein structure contains several functional domains organized from N- to C-terminus: a dimerization domain (DIM), the HMG box domain, two transcriptional activation domains (a central TAM and C-terminal TAC), and a proline/glutamine/alanine (PQA)-rich domain [3]. The HMG domain facilitates DNA binding and contains nuclear localization and export signals, while the transcriptional activation domains interact with cofactors to enhance gene regulation.
SOX9 plays crucial roles in embryonic development, including chondrogenesis, sex determination, and organogenesis [3]. In recent years, research has revealed that SOX9 is dysregulated in numerous pathological conditions, including various cancers, autoimmune disorders, and inflammatory diseases. Its dual functionality as both an oncogene and tumor suppressor, depending on cellular context, alongside its emerging roles in immunomodulation, makes it a compelling subject for biomarker development [42] [3]. This technical review comprehensively evaluates SOX9 as a diagnostic and prognostic biomarker across multiple disease contexts, with particular emphasis on its validation in pan-cancer analyses and its relevance to autoimmune and inflammatory disease research.
SOX9 as a Diagnostic Biomarker: Pan-Cancer Evidence
Comprehensive pan-cancer analyses reveal that SOX9 expression is significantly elevated across multiple cancer types compared to matched normal tissues. Evidence from The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases demonstrates that SOX9 expression is significantly increased in fifteen cancer types: CESC, COAD, ESCA, GBM, KIRP, LGG, LIHC, LUSC, OV, PAAD, READ, STAD, THYM, UCES, and UCS [42]. In contrast, SOX9 expression is decreased in only two cancers: SKCM and TGCT. This pattern suggests that SOX9 primarily functions as a proto-oncogene in most cancer contexts.
Table 1: SOX9 Expression Across Selected Malignancies
| Cancer Type | SOX9 Expression Pattern | Clinical Correlation | Sample Size (Where Specified) |
|---|---|---|---|
| Glioblastoma (GBM) | Significant upregulation | Associated with IDH-mutant status | 478 cases [71] |
| Bone Tumors | Significant upregulation in malignant vs. benign | Correlates with tumor severity, grade, and metastasis | 150 tumor tissues [65] |
| Intrahepatic Cholangiocarcinoma (iCCA) | Significant upregulation | Shorter survival, chemoresistance | 59 patients [81] |
| Pancreatic Ductal Adenocarcinoma (PDAC) | Significant upregulation | Correlates with metastasis and poor survival | 87 patients [53] |
| Breast Cancer | Significant upregulation | Driver of basal-like subtype, proliferation, and therapy resistance | Multiple cell line studies [11] |
The diagnostic potential of SOX9 extends beyond tissue expression to circulating biomarkers. A 2020 study detected remarkable overexpression of SOX9 in peripheral blood mononuclear cells (PBMCs) from patients with malignant and benign bone tumors compared to healthy controls [65]. This circulating SOX9 expression was significantly upregulated in patients with high-grade, metastatic, and recurrent tumors, suggesting its potential as a non-invasive diagnostic biomarker.
In glioblastoma, SOX9 expression demonstrates significant diagnostic utility. Receiver operating characteristic (ROC) analysis confirmed its predictive value for GBM diagnosis, with high expression remarkably associated with better prognosis in specific molecular subgroups [71]. This context-dependent diagnostic and prognostic value underscores the importance of patient stratification when evaluating SOX9 as a biomarker.
Prognostic Significance of SOX9 Across Cancers
SOX9 expression shows strong correlations with clinical outcomes across multiple malignancies, though its prognostic impact varies by cancer type and context.
Table 2: Prognostic Value of SOX9 in Different Cancers
| Cancer Type | Prognostic Association | Statistical Significance | Additional Factors |
|---|---|---|---|
| Glioblastoma (GBM) | Better prognosis in lymphoid invasion subgroups | P < 0.05 | Independent prognostic factor for IDH-mutant [71] |
| Low-Grade Glioma (LGG) | Shorter overall survival | Significant | Positive correlation with worst OS [42] |
| Intrahepatic Cholangiocarcinoma (iCCA) | Shorter survival time | Significant | Median survival: 62 vs. 22 months (low vs. high SOX9) with chemotherapy [81] |
| Cervical Cancer (CESC) | Shorter overall survival | Significant | Positive correlation with worst OS [42] |
| Thymoma (THYM) | Shorter overall survival | Significant | Positive correlation with worst OS [42] |
| Adrenocortical Carcinoma (ACC) | Longer overall survival | Significant | Negative correlation with worst OS [42] |
| Pancreatic Ductal Adenocarcinoma (PDAC) | Poor survival | P = 0.002 | Correlates with tumor stage and metastasis [53] |
In intrahepatic cholangiocarcinoma, patients with high SOX9 expression had significantly shorter survival times than those with low expression. For patients receiving chemotherapy, the median survival time was 62 months for low SOX9 expressers compared to only 22 months for high expressers [81]. Multivariate analysis confirmed SOX9 as an independent prognostic factor, highlighting its clinical utility for patient stratification.
The prognostic value of SOX9 often extends beyond simple expression levels to include specific gene signatures. In glioblastoma, researchers developed a prognostic model incorporating SOX9, OR4K2, and IDH status into a nomogram that demonstrated robust predictive accuracy [71]. Such integrated models represent the next generation of SOX9-based prognostic tools.
SOX9 in Immune Regulation and Tumor Microenvironment
SOX9 plays a complex, dual role in immunology, functioning as a "double-edged sword" in immune regulation [3]. On one hand, it promotes immune escape by impairing immune cell function, making it a potential therapeutic target in cancer. On the other hand, increased SOX9 levels help maintain macrophage function, contributing to cartilage formation, tissue regeneration, and repair.
In the tumor microenvironment, SOX9 expression correlates significantly with immune cell infiltration patterns. In glioblastoma, correlation analysis indicated that SOX9 expression was associated with immune cell infiltration and expression of immune checkpoints [71]. Bioinformatic analyses of colorectal cancer revealed that SOX9 expression negatively correlated with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, but positively correlated with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3].
SOX9 contributes to tumor immune evasion through multiple mechanisms. Research has demonstrated that SOX2 and SOX9 are crucial for latent cancer cells to remain dormant in secondary metastatic sites and avoid immune monitoring under immunotolerant conditions [11]. In breast cancer progression, SOX9 triggers tumorigenesis by facilitating the immune escape of tumor cells [42]. Additionally, SOX9 expression in thymoma was negatively correlated with genes related to Th17 cell differentiation, primary immunodeficiency, PD-L1 expression, and T-cell receptor signaling pathways [42].
SOX9 in Autoimmune and Inflammatory Disorders
Beyond cancer, SOX9 plays significant roles in autoimmune and inflammatory conditions. In autoimmune polyendocrine syndrome type I, SOX9 has been identified as a vitiligo autoantigen, highlighting its involvement in autoimmune pathogenesis [2]. This autoantigen status suggests that SOX9 may contribute to the loss of immune tolerance in specific autoimmune contexts.
In osteoarthritis, SOX9 functions as a "master regulator" of chondrocytes and maintains chondrocyte phenotype and cartilage homeostasis [9]. The nuclear factor-κB (NF-κB) signaling pathway positively regulates SOX9 expression by directly binding to its promoter region, forming a NF-κB-SOX9 signaling axis that significantly influences disease progression [9]. This pathway represents a critical link between inflammation and tissue homeostasis in joint disorders.
The role of SOX9 in tissue repair and regeneration further extends its relevance to inflammatory conditions. Increased SOX9 levels help maintain macrophage function and contribute to cartilage formation, tissue regeneration, and repair processes [3]. This dual functionality in both promoting and resolving inflammation exemplifies the "Janus-faced" nature of SOX9 in immunity and tissue homeostasis.
SOX9-Targeted Therapeutic Strategies and Experimental Models
Therapeutic Targeting Approaches
Several strategies have emerged for targeting SOX9 in cancer and other diseases:
Small Molecule Inhibitors: Cordycepin (CD), an adenosine analog, inhibits both protein and mRNA expression of SOX9 in a dose-dependent manner in 22RV1, PC3, and H1975 cancer cells, indicating its anticancer roles likely via SOX9 inhibition [42]. This natural compound represents a promising starting point for SOX9-targeted therapy development.
EGFR-Tyrosine Kinase Inhibitors: In pancreatic cancer, increased SOX9 and TSPAN8 levels were downregulated in vitro by EGFR tyrosine kinase inhibitors [53]. This approach targets the EGF-SOX9-TSPAN8 signaling cascade that drives PDAC invasion and metastasis.
Chemotherapy Response Modulation: In intrahepatic cholangiocarcinoma, SOX9 knockdown significantly inhibited gemcitabine-induced phosphorylation of checkpoint kinase 1 and suppressed the expression of multidrug resistance genes [81]. Targeting SOX9 may therefore reverse chemoresistance in specific cancer contexts.
Experimental Models and Methodologies
In Vivo Metastasis Models: In pancreatic cancer research, SW1990 cells with or without HA-TSPAN8 expression were injected into athymic nude mice via intrasplenic injection to construct a liver metastasis model. Cells expressing HA-TSPAN8 (regulated by SOX9) showed strong metastatic ability and shortened survival times [53].
Gene Silencing Approaches: RNA interference techniques using siRNA targeting human SOX9 effectively knocked down SOX9 expression in various cancer cell lines. SOX9 depletion markedly increased gemcitabine-induced apoptosis in CCA cells and inhibited invasion and migration capabilities in multiple cancer models [81] [53].
Protein Detection Methods: Immunohistochemistry staining for SOX9 typically uses semi-quantitative scoring systems based on the intensity and proportion of positive tumor cell nuclei. Formalin-fixed, paraffin-embedded specimens are deparaffinized, and antigen retrieval is performed before incubation with anti-SOX9 antibodies [81].
The Scientist's Toolkit: Essential Research Reagents and Methods
Table 3: Key Research Reagents and Experimental Tools for SOX9 Studies
| Reagent/Assay | Specific Example | Application and Function | Reference |
|---|---|---|---|
| Anti-SOX9 Antibodies | Polyclonal rabbit anti-SOX9 antibody (HPA001758; Sigma-Aldrich) | Immunohistochemistry for SOX9 protein detection in tissue specimens | [81] |
| Cell Line Models | Prostate cancer cells (22RV1, PC3), Lung cancer cell (H1975) | In vitro studies of SOX9 function and inhibition | [42] |
| Gene Silencing Reagents | siRNA targeting human SOX9 (M-021507-00, Dharmacon) | RNA interference to knock down SOX9 expression | [81] |
| Small Molecule Inhibitors | Cordycepin (Chengdu Must Bio-Technology) | Inhibits SOX9 expression in cancer cells | [42] |
| Animal Metastasis Models | Athymic nude mice with intrasplenic injection | In vivo assessment of SOX9-mediated metastasis | [53] |
| Database Resources | Human Protein Atlas (HPA), TCGA, GTEx, GEPIA2 | Bioinformatics analysis of SOX9 expression | [71] [42] |
| Protein Analysis | Western blot with cell lysis in EBC buffer | Detection of SOX9 protein expression levels | [42] |
SOX9 has emerged as a clinically significant diagnostic and prognostic biomarker across multiple cancer types, with additional relevance in autoimmune and inflammatory disorders. Its validated overexpression in numerous malignancies, association with clinical outcomes, and central role in therapeutic response underscore its translational potential. The development of circulating SOX9 detection methods further enhances its utility as a non-invasive biomarker.
Future research directions should focus on standardizing SOX9 detection and quantification methods across platforms, validating cut-off values for clinical stratification, and developing targeted therapeutic strategies that modulate SOX9 activity or expression. The integration of SOX9 biomarkers with other molecular features in multivariate models will likely enhance their predictive power. Furthermore, exploring the dual immunomodulatory functions of SOX9 in both cancer and autoimmune contexts may reveal novel therapeutic opportunities for immune-mediated diseases.
As evidence continues to accumulate, SOX9 is positioned to transition from a research biomarker to a clinically implemented tool for patient stratification, treatment selection, and monitoring across a spectrum of diseases.
Comparative Analysis of SOX9 Expression and Function Across Autoimmune, Inflammatory, and Neoplastic Diseases
The transcription factor SOX9 is a pivotal regulator of diverse biological processes, with context-dependent roles that significantly influence disease pathogenesis. This whitepaper provides a comparative analysis of SOX9's expression patterns, molecular mechanisms, and functional impacts across autoimmune, inflammatory, and neoplastic conditions. In neurodegenerative and neuroinflammatory diseases, SOX9 often exhibits protective functions, such as promoting clearance of toxic aggregates. In contrast, its role in cancer is predominantly oncogenic, driving processes like chemoresistance and stemness. The dual nature of SOX9 in immunobiology—acting as both a promoter of tissue repair and a facilitator of immune escape—makes it a complex but promising therapeutic target. This review synthesizes recent findings to outline key pathways, experimental methodologies, and potential therapeutic strategies targeting SOX9, providing a resource for researchers and drug development professionals.
SOX9 (SRY-box 9) is a transcription factor belonging to the SOX family, characterized by a highly conserved High Mobility Group (HMG) box DNA-binding domain [3] [17]. It is a critical effector in embryonic development, cell differentiation, and tissue homeostasis. Recent research has underscored its significance in a wide spectrum of human diseases. However, its function is not monolithic; it operates as a "Janus-faced regulator," with its impact being highly dependent on the disease context and cellular environment [3]. This review systematically dissects the dual roles of SOX9, comparing its protective mechanisms in inflammatory and autoimmune contexts with its pathogenic drivers in oncology, and explores the ensuing implications for targeted therapies.
SOX9 in Inflammatory and Autoimmune Diseases
Neuroinflammatory and Neurodegenerative Diseases
In the central nervous system (CNS), SOX9 expression in astrocytes has been linked to beneficial outcomes in models of Alzheimer's disease (AD) and neuropathic pain.
Alzheimer's Disease: In mouse models of AD that had already developed cognitive impairment and amyloid-β (Aβ) plaques, targeted overexpression of SOX9 in astrocytes led to a significant reduction in plaque burden and preservation of memory and cognitive function [61] [82]. Mechanistically, elevated SOX9 enhanced the phagocytic capability of astrocytes, effectively acting as a "vacuum cleaner" for Aβ plaques. This process was found to be dependent on the upregulation of the phagocytic receptor MEGF10 [82].
Neuropathic Pain (NeP): In a rat model of neuropathic pain, nerve injury-induced phosphorylation of SOX9 at serine 181 triggered a pathogenic cascade [7]. Phosphorylated SOX9 transcriptionally activated Hexokinase 1 (Hk1), the rate-limiting enzyme in glycolysis. This led to heightened glycolytic flux in specific astrocyte subpopulations, excessive lactate production, and subsequent histone lactylation (H3K9la). This epigenetic remodeling promoted the transcription of pro-inflammatory and neurotoxic genes, ultimately driving chronic pain. Targeted modulation of the SOX9-Hk1-H3K9la axis provided long-lasting pain relief [7].
Table 1: SOX9 in Inflammatory and Autoimmune Diseases
| Disease Context | Expression Pattern | Primary Function | Key Molecular Mechanism | Overall Pathogenic/Protective Role |
|---|---|---|---|---|
| Alzheimer's Disease [61] [82] | Overexpression in astrocytes | Enhances amyloid-β plaque clearance | SOX9 ↑ → MEGF10 ↑ → Aβ phagocytosis ↑ | Protective |
| Neuropathic Pain [7] | Aberrant activation & phosphorylation in spinal astrocytes | Drives neuroinflammation and central sensitization | p-SOX9 ↑ → HK1 ↑ → Glycolysis/Lactate ↑ → H3K9la ↑ → Pro-inflammatory genes ↑ | Pathogenic |
| General Immunology [3] | Context-dependent in immune cells | Regulates immune cell differentiation and function; can impair anti-tumor immunity | Modulation of T-cell (e.g., Rorc) and B-cell functions; correlation with immune cell infiltration | Dual (Janus-faced) |
A Putative Role in Systemic Autoimmunity
While the search results primarily detail SOX9's role in CNS inflammation, its function as an immunomodulator suggests relevance in systemic autoimmune diseases. SOX9 is involved in T-cell development, particularly in modulating the balance between αβ and γδ T-cell lineages by cooperating with c-Maf to activate Rorc and key Tγδ17 effector genes like Il17a [3]. Furthermore, its expression correlates with patterns of immune cell infiltration in cancers, indicating a capacity to shape the immune microenvironment [3] [33]. This immunomodulatory potential positions SOX9 as a molecule of interest in conditions like rheumatoid arthritis and lupus, though direct evidence from these disease contexts is an area for future investigation.
SOX9 in Neoplastic Diseases
In oncology, SOX9 is frequently overexpressed and is widely associated with tumor progression, metastasis, and poor prognosis across various cancer types, including ovarian cancer, glioblastoma, and others [62] [3] [33].
Ovarian Cancer: SOX9 is a critical driver of chemoresistance in high-grade serous ovarian cancer (HGSOC). Chemotherapy (e.g., carboplatin) epigenetically upregulates SOX9 [62] [83]. SOX9 expression, in turn, reprograms the transcriptional state of naive cancer cells, inducing a stem-like, drug-tolerant state. These SOX9-high cancer stem cells (CSCs) exhibit enhanced self-renewal capacity and are enriched in post-chemotherapy patient samples, contributing to disease relapse [62]. Ablating SOX9 significantly increases platinum sensitivity [62].
Glioblastoma (GBM): SOX9 is highly expressed in GBM and serves as a diagnostic and prognostic biomarker [33] [84]. Its high expression is an independent prognostic factor for IDH-mutant glioma and is closely correlated with an immunosuppressive tumor microenvironment, characterized by specific patterns of immune cell infiltration and immune checkpoint expression [33].
Table 2: SOX9 in Neoplastic Diseases
| Disease Context | Expression Pattern | Primary Function | Key Molecular Mechanism | Prognostic Association |
|---|---|---|---|---|
| Ovarian Cancer [62] [83] | Chemotherapy-induced upregulation | Drives chemoresistance and stemness | SOX9 ↑ → Transcriptional reprogramming → Stem-like CSC state ↑ | Shorter overall survival |
| Glioblastoma (GBM) [33] [84] | High expression | Promotes tumor progression, modulates immune microenvironment | Correlation with immune infiltration and checkpoint expression | Diagnostic biomarker; independent prognostic factor in IDH-mutant cases |
| Pan-Cancer [3] | Frequently overexpressed | Promotes proliferation, metastasis, and immune evasion | Interaction with various signaling pathways (e.g., Wnt/β-catenin); negative correlation with CD8+ T cell function | Poor prognosis in multiple cancers (e.g., lung adenocarcinoma) |
Comparative Analysis: The Dual Nature of SOX9
The contrasting roles of SOX9 highlight its context-dependent functionality. The table below provides a direct comparison of its attributes across disease categories.
Table 3: Comparative Analysis of SOX9's Roles
| Feature | Inflammatory/Autoimmune Context | Neoplastic Context |
|---|---|---|
| Primary Role | Often protective (e.g., AD) or context-specific driver (e.g., NeP) | Predominantly oncogenic and pro-tumorigenic |
| Key Cellular Process | Regulation of astrocyte phagocytosis; immunomodulation; metabolic reprogramming | Maintenance of cancer stem cells; transcriptional reprogramming for chemoresistance |
| Therapeutic Goal | Agonism: Enhance protective function (e.g., in AD) [61] | Antagonism: Inhibit oncogenic function to overcome resistance [62] [83] |
| Impact on Microenvironment | Can promote resolution of pathology (plaque clearance) [82] | Creates an immunosuppressive niche conducive to tumor growth [33] |
| Molecular Pathways | MEGF10, Glycolysis/HK1, Histone Lactylation [7] [82] | Super-enhancer driven expression, Stemness pathways [62] |
Core Experimental Protocols for Investigating SOX9
This section outlines key methodologies used in the cited research to elucidate SOX9's function.
Protocol: Evaluating SOX9's Role in Alzheimer's Disease Models
- Objective: To determine the effect of astrocytic SOX9 overexpression on amyloid-β pathology and cognitive function in symptomatic AD mice [61] [82].
- Experimental Workflow:
- Animal Model: Use transgenic AD mouse models (e.g., APP/PS1) that have already developed amyloid plaques and cognitive deficits.
- Genetic Manipulation: Employ viral vectors (e.g., AAV) with an astrocyte-specific promoter (e.g., GFAP) to overexpress Sox9 or a control gene in the hippocampus.
- Behavioral Testing: Conduct cognitive assays at multiple time points over a long-term period (e.g., 6 months). Standard tests include:
- Novel Object Recognition Test: Assesses episodic memory.
- Morris Water Maze or Radial Arm Water Maze: Evaluates spatial learning and memory.
- Tissue Collection and Analysis:
- Histology: Process brain sections for immunohistochemistry.
- Plaque Quantification: Stain with Aβ-specific antibodies (e.g., 6E10) and use image analysis software to quantify plaque load and morphology.
- Astrocyte Analysis: Co-stain with astrocyte markers (e.g., GFAP, S100β) and phagocytosis markers (e.g., CD68, MEGF10) to assess astrocyte activation and phagocytic activity.
- Mechanistic Validation: Use co-immunoprecipitation or Western blotting to confirm upregulation of downstream effectors like MEGF10 [82].
Protocol: Targeting SOX9-Driven Chemoresistance in Ovarian Cancer
- Objective: To establish SOX9 as a driver of chemoresistance and identify SOX9-high cancer stem cells [62].
- Experimental Workflow:
- In Vitro Models:
- Cell Lines: Use established HGSOC cell lines (e.g., OVCAR4, Kuramochi).
- Chemotherapy Treatment: Treat cells with carboplatin and monitor SOX9 expression via qRT-PCR and Western blot over time (e.g., 72 hours).
- Genetic Perturbation: Perform CRISPR/Cas9-mediated knockout of SOX9 or epigenetic activation of its endogenous locus.
- Functional Assays:
- Colony Formation Assay: Measure clonogenic survival post-chemotherapy in SOX9-knockout vs. control cells.
- Stemness Assays: Evaluate sphere-forming capacity in ultra-low attachment plates.
- Analysis of Patient Samples:
- Longitudinal scRNA-seq: Analyze publicly available datasets from HGSOC patients pre- and post-neoadjuvant chemotherapy (NACT). Identify epithelial cancer cells and compare SOX9 expression and transcriptional divergence.
- Tumor Microarrays: Validate SOX9 protein levels and localization in a larger cohort of patient samples, correlating with clinical outcomes.
- In Vivo Validation:
- Use xenograft models to test the effect of SOX9 modulation on tumor growth and response to carboplatin treatment in vivo.
- In Vitro Models:
The Scientist's Toolkit: Key Research Reagents
Table 4: Essential Reagents for SOX9 Research
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| AAV-GFAP-SOX9 | Enables cell-type-specific (astrocyte) overexpression of SOX9 in vivo. | Investigating SOX9's therapeutic potential in Alzheimer's mouse models [61]. |
| CRISPR/Cas9 SOX9 KO | Allows for precise genetic ablation of SOX9 to study loss-of-function phenotypes. | Establishing the necessity of SOX9 for chemoresistance in ovarian cancer cells [62]. |
| scRNA-seq & Multiomics | Profiles transcriptomes of individual cells; integrates with epigenetic data. | Identifying rare SOX9-high stem-like cells in tumors; analyzing global transcriptional reprogramming [7] [62]. |
| Phospho-Specific SOX9 (S181) Antibody | Detects the active, phosphorylated form of SOX9. | Uncovering the role of p-SOX9 in neuropathic pain pathogenesis [7]. |
| Anti-MEGF10 Antibody | Labels and validates expression of the key SOX9 downstream phagocytic receptor. | Mechanistic validation of the SOX9-MEGF10 pathway in astrocyte-mediated plaque clearance [82]. |
Signaling Pathway Visualizations
SOX9 in Neuropathic Pain Pathway
SOX9-Driven Neuropathic Pain Pathway
SOX9 in Alzheimer's Disease and Cancer
Contrasting SOX9 Functions in Alzheimer's vs. Cancer
SOX9 emerges as a master regulator whose functional output is critically determined by the disease context. In Alzheimer's disease, harnessing its ability to activate protective mechanisms like phagocytosis presents a novel therapeutic avenue. Conversely, in cancer, inhibiting SOX9 or its downstream effectors holds the potential to counteract chemoresistance and improve patient outcomes. The major challenge and future direction lie in developing context-specific strategies to safely modulate SOX9 activity. Promising approaches include the development of small molecule inhibitors that disrupt SOX9's interaction with co-factors, epigenetic drugs to prevent its aberrant induction, and cell-type-specific delivery systems for gene therapy. A deeper understanding of the post-translational modifications and partner proteins that dictate SOX9's functional specificity will be essential for translating these insights into effective, targeted therapies for a wide range of human diseases.
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator at the intersection of development, cancer, and immunology. Recent research has illuminated its complex, dual role in immune regulation—acting as a "double-edged sword" in various pathological contexts [85]. On one hand, SOX9 promotes tumor progression and immune escape in multiple cancers; on the other hand, it contributes to tissue maintenance and repair processes [85]. This review examines the correlation between SOX9 expression, immune cell infiltration, and immune checkpoint expression, with particular focus on glioblastoma (GBM) and other malignancies, providing insights relevant to both oncology and autoimmune disease research.
Molecular Structure and Immunological Functions of SOX9
Structural Domains and Functional Motifs
SOX9 encodes a 509 amino acid polypeptide containing several functionally critical domains [85]. The N-terminal dimerization domain (DIM) facilitates protein-protein interactions, while the central High Mobility Group (HMG) box domain enables sequence-specific DNA binding and contains embedded nuclear localization (NLS) and nuclear export (NES) signals that govern nucleocytoplasmic shuttling [85]. The C-terminal region contains two transcriptional activation domains—TAM (central) and TAC (C-terminal)—that interact with cofactors like Tip60 to enhance transcriptional activity [85]. A proline/glutamine/alanine (PQA)-rich domain completes the structure and is essential for transcriptional activation [85].
SOX9 in Immune Cell Development and Function
SOX9 plays significant roles in immune cell differentiation and regulation. During T-cell development, SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating the lineage commitment of early thymic progenitors and influencing the balance between αβ and γδ T-cell differentiation [85]. While SOX9 has no well-defined role in normal B-cell development, it is overexpressed in certain B-cell lymphomas, such as Diffuse Large B-cell Lymphoma (DLBCL), where it acts as an oncogene by promoting proliferation and inhibiting apoptosis [85].
Table 1: SOX9 Expression Patterns Across Cancers
| Cancer Type | SOX9 Expression | Correlation with Prognosis | Immune Correlations |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly increased [42] [71] | Better prognosis in lymphoid invasion subgroups [71] | Correlated with immune cell infiltration and checkpoint expression [71] |
| Low-Grade Glioma (LGG) | Significantly increased [42] | Shortened overall survival [42] | Not specified |
| THYM (Thymoma) | Significantly increased [42] | Shortened overall survival [42] | Negatively correlated with Th17 genes and PD-L1 pathway [42] |
| CESC (Cervical cancer) | Significantly increased [42] | Shortened overall survival [42] | Not specified |
| COAD (Colon adenocarcinoma) | Significantly increased [42] | Not specified | Negative correlation with B cells, resting mast cells, monocytes [85] |
| SKCM (Skin Cutaneous Melanoma) | Significantly decreased [42] | Not specified | Tumor suppressor role identified [42] |
| TGCT (Testicular germ cell tumors) | Significantly decreased [42] | Not specified | Not specified |
SOX9 in Cancer: Mechanisms and Immune Interactions
SOX9 and Tumor Immune Cell Infiltration
Extensive bioinformatics analyses demonstrate strong associations between SOX9 expression and immune cell infiltration patterns across cancers. In colorectal cancer (CRC), SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [85]. Similarly, in pan-cancer analyses, SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with memory CD4+ T cells [85].
In prostate cancer, single-cell RNA sequencing and spatial transcriptomics reveal that androgen deprivation therapy enriches a subpopulation of club cells characterized by high SOX9 and low androgen receptor expression, contributing to an "immune desert" microenvironment that promotes tumor immune escape [85]. This population is associated with decreased effector immune cells (CD8+CXCR6+ T cells and activated neutrophils) and increased immunosuppressive cells (Tregs and M2 macrophages) [85].
Regulatory Mechanisms of SOX9 in Cancer
SOX9 expression and activity are regulated through multiple mechanisms in cancer. Transcriptional regulation involves changes in epigenetic modifications including methylation and acetylation [85]. Post-transcriptional regulation primarily involves non-coding RNAs, particularly miRNAs and lncRNAs [85]. SOX9 operates as a downstream target of several embryonic signaling pathways and has documented relationships with vascularization, drug resistance, tumor proliferation, metastasis, and apoptosis [85].
SOX9 in Glioblastoma: Diagnostic and Prognostic Significance
SOX9 Expression Patterns in GBM
In glioblastoma, SOX9 is highly expressed and represents a significant diagnostic and prognostic biomarker [71]. Analysis of RNA sequencing data from The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases confirms SOX9 overexpression in GBM tissues compared to normal brain tissue [71]. Surprisingly, in contrast to many other cancers, high SOX9 expression in GBM is remarkably associated with better prognosis in lymphoid invasion subgroups [71]. Furthermore, high SOX9 expression serves as an independent prognostic factor for IDH-mutant glioblastomas in Cox regression analysis [71].
SOX9 and Immune Infiltration in GBM Microenvironment
SOX9 expression in GBM shows significant correlation with immune cell infiltration and checkpoint expression, indicating its involvement in the immunosuppressive tumor microenvironment [71]. Comprehensive analysis reveals that SOX9 expression correlates with specific immune cell populations and contributes to the immunosuppressive landscape characteristic of GBM.
Table 2: Key Immune Checkpoints in Glioblastoma Microenvironment
| Immune Checkpoint | Primary Expression in GBM | Functional Role | Therapeutic Status |
|---|---|---|---|
| VISTA | Microglia and MDM [86] | Potential mechanism for evading immune system attacks [86] | Potential novel target |
| TIM-3 | Microglia and MDM [86] | Co-inhibitory molecule [86] | Under investigation |
| PSGL-1 | Microglia and MDM [86] | Acidic pH-selective receptor of VISTA [86] | Potential target |
| VSIG-3 | Neoplastic cells and oligodendrocytes [86] | Ligand of VISTA [86] | Potential target |
| PD-1/PD-L1 | Limited expression [86] | Traditional checkpoint; limited in GBM [86] | Clinical trials unsuccessful |
| CTLA-4 | Limited expression [86] | Traditional checkpoint; limited in GBM [86] | Clinical trials unsuccessful |
The Immunosuppressive GBM Microenvironment and Checkpoint Expression
GBM as an Immunologically "Cold" Tumor
Glioblastoma creates a highly immunosuppressive microenvironment through multiple mechanisms. GBM has a low tumor mutational burden, reducing potential neoantigens available for immune recognition [87]. The tumor expresses indoleamine 2,3-dioxygenase (IDO), which converts tryptophan to kynurenines, inducing T-cell apoptosis and increasing immunosuppressive programming [87]. GBM also drives systemic T-cell lymphopenia through loss of sphingosine-1-phosphate receptor 1 from T-cell surfaces, resulting in T-cell sequestration in bone marrow [87]. Additionally, GBM generates high levels of soluble immunosuppressive mediators including TGF-β, IL-10, IL-7, and prostaglandin E2, which suppress effector T-cell activity [87].
Novel Checkpoint Expression in GBM
Single-nucleus RNA sequencing and spatial transcriptomic analyses of untreated GBM samples reveal distinctive patterns of immune checkpoint expression that differ from conventional checkpoints. While PD-1, PD-L1, CTLA-4, LAG-3 and TIGIT show limited expression in GBM [86], alternative checkpoints including TIM-3, VISTA, PSGL-1, and VSIG-3 demonstrate prominent expression [86]. These checkpoints are primarily expressed in microglia and monocyte-derived macrophages, with VSIG-3 (the VISTA ligand) mainly expressed in neoplastic cells and oligodendrocytes [86].
Interactions between specific neoplastic cell subpopulations and immune cells are particularly significant. "Neoplastic cells_6"—a subpopulation identified through single-cell analysis that expresses high levels of invasion and proliferation-related genes (PTTG1, CCNB1, CENPF, MKi67, TOP2A)—shows markedly altered ligand-receptor interactions with microglia, suggesting a potential mechanism for evading immune attacks [86]. The VISTA/VSIG3 signaling pathway appears to play a crucial role in these GBM immune interactions [86].
Experimental Approaches and Methodologies
Technical Approaches for Analyzing SOX9 and Immune Interactions
Comprehensive analysis of SOX9 in immune regulation employs multiple advanced methodologies. RNA sequencing data from TCGA and GTEx databases provide transcriptomic profiles across cancers [42] [71]. Single-nucleus RNA sequencing (snRNA-seq) enables resolution of cellular heterogeneity within tumors, particularly valuable in GBM [86]. Spatial transcriptomics (ST) combines histological imaging with transcriptomic data, retaining positional information for mRNA distribution in tissue sections [86]. Multimodal intersection analysis (MIA) integrates snRNA-seq and ST datasets to reconstruct cellular interaction networks [86]. Immune cell infiltration analysis utilizes computational approaches like ssGSEA (single-sample Gene Set Enrichment Analysis) and ESTIMATE algorithm to infer immune cell abundances from bulk transcriptomic data [71].
Diagram 1: Experimental workflow for analyzing SOX9-immune interactions in cancer. The approach integrates multiple omics technologies to connect molecular findings with therapeutic applications.
Table 3: Essential Research Resources for SOX9-Immune Investigations
| Resource Type | Specific Examples | Application and Function |
|---|---|---|
| Databases | TCGA (cancer.gov), GTEx (gtexportal.org), HPA (proteinatlas.org) | Source of transcriptomic and proteomic data for normal and tumor tissues |
| Analytical Tools | GEPIA2, cBioPortal, LinkedOmics | Analysis of gene expression, mutations, survival correlations, and associated pathways |
| Cell Line Models | 22RV1 (prostate cancer), PC3 (prostate cancer), H1975 (lung cancer) | In vitro models for SOX9 perturbation studies and therapeutic testing |
| Experimental Reagents | Cordycepin (adenosine analog) | Small molecule inhibitor of SOX9 expression for mechanistic studies |
| Computational Methods | ssGSEA, ESTIMATE, CellPhoneDB | Analysis of immune cell infiltration and cell-cell communication networks |
| Sequencing Technologies | 10X Genomics snRNA-seq, Spatial Transcriptomics | Resolution of cellular heterogeneity and spatial organization in tumor microenvironment |
SOX9-Targeted Therapeutic Strategies
Modulation of SOX9 Expression and Activity
Research has identified several approaches to target SOX9 therapeutically. The natural compound cordycepin (an adenosine analog) inhibits both protein and mRNA expression of SOX9 in a dose-dependent manner in prostate cancer (22RV1, PC3) and lung cancer (H1975) cell lines, demonstrating its potential as an anticancer agent working through SOX9 inhibition [42]. Given the role of SOX9 in maintaining the immunosuppressive tumor microenvironment, combination strategies targeting SOX9 along with immune checkpoints represent a promising avenue. The identification of novel immune checkpoints in GBM—including VISTA, TIM-3, PSGL-1, and VSIG-3—provides potential combination targets for therapy [86].
Clinical Translation and Challenges
Despite promising preclinical findings, therapeutic targeting of SOX9 in GBM and other cancers faces challenges. Clinical trials of immune checkpoint inhibitors in GBM have been largely disappointing to date [87]. The CheckMate 143, 498, and 548 trials investigating nivolumab (anti-PD-1) in both newly diagnosed and recurrent GBM failed to demonstrate significant survival benefits compared to standard therapies [87]. This lack of efficacy highlights the need for better understanding of GBM immunology and more sophisticated combination approaches that may include SOX9 modulation.
Diagram 2: SOX9-HK1 immunometabolic pathway in neuroinflammation. This pathway, identified in neuropathic pain models, demonstrates how SOX9 drives inflammatory responses through metabolic reprogramming, with potential relevance to glioma microenvironment.
SOX9 represents a critical node connecting tumor biology, immune regulation, and metabolic reprogramming. Its correlation with specific immune infiltration patterns and checkpoint expression highlights its potential as both a biomarker and therapeutic target. The dual nature of SOX9 function—promoting immunosuppression in most cancers while potentially playing protective roles in specific GBM contexts—underscores the importance of context-dependent investigation.
Future research should focus on elucidating the precise molecular mechanisms through which SOX9 regulates immune cell functions and checkpoint expression, developing more specific SOX9-targeting agents, and designing sophisticated combination therapies that simultaneously target SOX9 and associated immune checkpoints. The integration of single-cell and spatial transcriptomic approaches will be essential for understanding the cellular heterogeneity of SOX9-expressing populations within tumor ecosystems. As these mechanisms are further clarified, targeting SOX9 may yield novel therapeutic opportunities not only in oncology but potentially in autoimmune and inflammatory disorders where immune dysregulation plays a central role.
The transcription factor SOX9 is a critical regulator in development and disease, acting as a pivotal node in cellular signaling networks. In the context of autoimmune and inflammatory disorders, understanding its regulatory mechanisms is essential for developing targeted therapies. This guide provides a technical roadmap for validating key downstream effectors of SOX9, with particular emphasis on its intersection with Epidermal Growth Factor Receptor (EGFR) signaling—a pathway increasingly implicated in immune cell function and tissue inflammation. We present integrated experimental data, standardized methodologies, and visualization tools to accelerate research in this complex field, enabling researchers to decipher the SOX9-EGFR axis with precision.
Quantitative Data Synthesis of SOX9 and EGFR Interactions
The relationship between SOX9 and EGFR signaling is context-dependent, with evidence of both regulatory and cooperative interactions across different physiological systems. The table below synthesizes key quantitative findings from recent studies that illuminate these complex relationships.
Table 1: Experimental Data on SOX9 and EGFR Pathway Interactions
| Experimental Context | Key Finding | Measurement Technique | Quantitative Result | Biological Implication |
|---|---|---|---|---|
| IVDD Model (NPCs) [88] | EGFR regulates JAK1 expression | IHC, in vivo validation with EGFR inactivation | JAK1 expression elevated under stress; unchanged with Gefitinib pretreatment | EGFR contributes to NPC degeneration via JAK1 upregulation |
| Bone Fracture Healing (Rat Model) [89] | Gefitinib (EGFR inhibitor) modulates SOX9 | Micro-CT, biomechanical testing, WB | Improved bone callus formation & quality; SOX9 overexpression reduced benefits | EGFR inhibition enhances healing by countering SOX9-driven metabolic reprogramming |
| Neuropathic Pain (Rat Model) [7] | SOX9 transcriptionally regulates Hk1 | scRNA-seq, metabolic flux analysis, ChIP | Aberrant Sox9 phosphorylation triggers Hk1 activation for high-rate glycolysis | SOX9-Hk1-lactylation axis controls deleterious astrocyte subsets |
| Colorectal Cancer [90] | JAK2/STAT3 pathway regulates SOX9 | UPLC-MS, qPCR, western blot | WMW suppresses stemness via JAK2/STAT3/SOX9 axis | SOX9 is a downstream effector of JAK2/STAT3 signaling |
These findings establish SOX9 as a critical effector downstream of multiple signaling pathways, including EGFR and JAK/STAT, across diverse disease models. The consistent theme across these studies is that SOX9 operates as an integrator of extracellular signals to control cellular metabolic and transcriptional programs in pathological states.
Experimental Protocols for Validating SOX9 Downstream Effectors
Single-Cell RNA Sequencing for Cellular Heterogeneity and Target Identification
Purpose: To identify novel SOX9-regulated cell subpopulations and candidate effector genes within complex tissues, such as those affected by autoimmune and inflammatory processes [88].
Detailed Workflow:
- Sample Preparation: Isolate cells from target tissue (e.g., dorsal spinal cord, nucleus pulposus, synovial fluid) from both diseased and control models.
- Single-Cell Suspension: Process tissues into single-cell suspensions using enzymatic digestion (e.g., collagenase/DNase mix) and mechanical dissociation. Filter through a 40μm strainer and assess viability (>80% required).
- Library Preparation & Sequencing: Use platform-specific kits (e.g., 10x Genomics) for barcoding, reverse transcription, and cDNA amplification. Sequence on an Illumina platform to a minimum depth of 50,000 reads per cell.
- Computational Analysis:
- Quality Control: Filter cells with high mitochondrial gene percentage (>20%) or low unique gene counts using Seurat package (v4.0.3+) [88].
- Dimensionality Reduction: Perform PCA on the top 2,000 highly variable genes. Use harmony algorithm to correct for batch effects [88].
- Clustering & Annotation: Cluster cells using graph-based methods (e.g., FindClusters in Seurat) and visualize with t-SNE or UMAP. Identify cluster markers using Wilcoxon rank-sum test with Bonferroni correction [88].
- Pseudotime Analysis: Utilize Monocle2 (v2.14.0) to reconstruct cellular trajectories and identify genes with significant dynamic changes along pseudotime using a likelihood ratio test [88].
Functional Validation of SOX9-Regulated Pathways
Purpose: To establish causal relationships between SOX9 and identified target genes or pathways using both pharmacological and genetic approaches.
Detailed Workflow:
- In Vitro Perturbation:
- Pharmacological Inhibition: Treat primary cells or cell lines with EGFR inhibitor Gefitinib (10μM) [88] [89] or JAK/STAT inhibitors for specified durations under inflammatory conditions (e.g., oxidative stress).
- Genetic Manipulation: Perform SOX9 overexpression using lentiviral constructs and knockdown via siRNA or CRISPR/Cas9 to directly test gene regulation.
- Metabolic Profiling: Using a Seahorse Analyzer, measure real-time extracellular acidification rate (ECAR) for glycolysis and oxygen consumption rate (OCR) for oxidative phosphorylation in cells with modulated SOX9 expression [89].
- Pathway Analysis:
- Western Blotting: Confirm protein-level changes in SOX9, p-EGFR, JAK1/2, STAT3, and HK1. Use GAPDH/β-actin as loading controls.
- Quantitative PCR (qPCR): Validate transcriptional changes in candidate target genes (e.g., HK1, collagen matrix genes) using SYBR Green protocols with 18S as housekeeping gene.
- Chromatin Immunoprecipitation (ChIP): Validate direct SOX9 binding to promoter regions of target genes like HK1 using validated SOX9 antibodies and normalizing to input DNA [7].
Signaling Pathway and Experimental Workflow Visualizations
The following diagrams, generated using Graphviz DOT language, illustrate the core signaling relationships and experimental approaches for validating SOX9 downstream effectors.
SOX9 EGFR JAK STAT Signaling Axis
Experimental Validation Workflow
The Scientist's Toolkit: Essential Research Reagents
The following table compiles key reagents and their applications for studying SOX9 and its downstream effectors, as evidenced in recent literature.
Table 2: Key Research Reagents for SOX9 and EGFR Pathway Studies
| Reagent / Tool | Primary Function | Application Example | Key Experimental Outcome |
|---|---|---|---|
| Gefitinib [88] [89] | EGFR Tyrosine Kinase Inhibitor | Bone fracture healing models; NPC degeneration studies | Inhibits EGFR signaling, attenuates JAK1 upregulation, modulates SOX9 activity |
| scRNA-seq [88] [7] | Cellular heterogeneity mapping | Identify astrocyte & NPC subpopulations in disease | Revealed pathogenic Astro1 subpopulation and Fib-NPC cluster expressing high EGFR |
| Seahorse Analyzer [89] | Real-time metabolic flux analysis | Measure OCR and ECAR in periosteal stem cells | Showed Gefitinib enhanced OXPHOS and FAO, counteracting SOX9 effects |
| SOX9 Antibodies [7] [89] | Protein detection & localization | IHC, Western Blot, ChIP | Confirmed SOX9 upregulation and nuclear localization in disease states |
| SOX9 Lentiviral Constructs [89] | Genetic overexpression | Bone fracture model | SOX9 overexpression reduced benefits of EGFR inhibition |
| UPLC-MS [90] | Compound identification & quantification | Analyze herbal formula WMW components | Identified 60 compounds; linked JAK2/STAT3 inhibition to SOX9 downregulation |
The rigorous validation of downstream effectors within the SOX9 regulatory network, particularly its intersection with EGFR signaling, provides critical insights for understanding the molecular pathogenesis of autoimmune and inflammatory diseases. The integrated approach presented here—combining high-resolution single-cell technologies, functional pharmacological and genetic perturbations, and mechanistic metabolic studies—offers a robust framework for target discovery and validation. As research in this area advances, the continued refinement of these methodologies will be essential for translating mechanistic understanding into novel therapeutic strategies that target the SOX9-EGFR axis in inflammatory disorders.
The SOX family of transcription factors represents a promising class of therapeutic targets in oncology and inflammatory diseases. Among these members, SOX9 has emerged as a particularly compelling candidate for drug development due to its dual functionality in tumor progression and immune regulation, frequent overexpression in diverse malignancies, and central role in therapy resistance mechanisms. This technical review provides a comprehensive comparative assessment of SOX9 against other SOX family members, integrating quantitative expression data, functional analyses, and therapeutic potential evaluation. We present structured experimental frameworks for investigating SOX9 function and targeting, along with visualization of key signaling pathways. The analysis substantiates the prioritization of SOX9 in drug development pipelines based on its multifaceted roles in cancer stemness, immune evasion, and microenvironment remodeling, positioning it as a high-value target for next-generation therapeutics.
The SOX (SRY-related HMG-box) family comprises approximately 20 transcription factors characterized by a highly conserved high-mobility group (HMG) DNA-binding domain that recognizes the specific sequence (A/T)(A/T)CAA(A/T)G [31] [91]. These proteins are classified into groups A-H based on domain structure similarity and functional characteristics [31]. SOX9 belongs to the SOXE subgroup (along with SOX8 and SOX10), which shares conserved functional domains beyond the HMG box that mediate transcriptional activation, protein-protein interactions, and post-translational regulation [3] [91].
While multiple SOX members have been implicated in pathological processes, SOX9 demonstrates distinctive characteristics that warrant particular attention in drug development. It functions as a master regulator of development in multiple tissue systems including cartilage, testes, heart valves, and neural crest derivatives [91]. In pathological contexts, SOX9 is frequently overexpressed across diverse solid tumors and contributes critically to multiple hallmarks of cancer through mechanisms distinct from other SOX family members [3] [92].
Comparative Analysis of SOX Family Members in Human Diseases
Expression Patterns and Functional Roles
Table 1: Comparative Analysis of Key SOX Family Members in Human Pathology
| SOX Member | Physiological Functions | Role in Cancer | Expression Pattern in Tumors | Therapeutic Potential |
|---|---|---|---|---|
| SOX9 | Chondrogenesis, sex determination, neural stem cell maintenance, organ development [3] [91] | Promotes tumor proliferation, metastasis, chemoresistance, stemness, and immune evasion [3] [62] [28] | Frequently overexpressed in multiple solid tumors (liver, lung, breast, ovarian, prostate) [3] [62] [92] | High (direct target, biomarker, immunotherapy candidate) [93] |
| SOX2 | Pluripotency maintenance, self-renewal of embryonic stem cells [31] | Promotes tumorigenesis, chemoresistance, stemness [92] [31] | Upregulated in various cancers [92] | Moderate (challenging due to essential stem cell functions) |
| SOX4 | Lymphocyte differentiation, neurogenesis, cardiovascular development [31] | Oncogenic in multiple cancers; regulates EMT [92] [31] | Overexpressed in various malignancies [92] | Moderate |
| SOX17 | Cardiovascular development, endoderm formation [31] [91] | Tumor suppressor in gastrointestinal cancers; regulates Wnt signaling [31] | Frequently downregulated in colorectal, gastric cancers [31] | Low (tumor suppressor, difficult to target therapeutically) |
| SOX18 | Vascular and lymphatic development [31] [91] | Promotes angiogenesis, lymphangiogenesis, and metastasis [92] [31] | Upregulated in various cancers [92] | Moderate (angiogenesis-specific applications) |
Quantitative Assessment of SOX9 in Human Cancers
Table 2: SOX9 Expression and Clinical Correlations Across Malignancies
| Cancer Type | SOX9 Expression Level | Clinical Correlation | Functional Role | Reference |
|---|---|---|---|---|
| High-Grade Serous Ovarian Cancer | Significantly elevated compared to normal fallopian tube epithelium (p<0.05) [62] | Top quartile SOX9 expression associated with shorter overall survival (HR=1.33; log-rank P=0.017) [62] | Drives platinum resistance, stem-like transcriptional state [62] | [62] |
| Glioblastoma (GBM) | Highly expressed in tumor tissues [71] | Better prognosis in lymphoid invasion subgroups (P<0.05); independent prognostic factor for IDH-mutant cases [71] | Correlates with immune cell infiltration and checkpoint expression [71] | [71] |
| Multiple Solid Tumors | Frequently overexpressed (liver, lung, breast, gastric) [3] | Correlates with poor prognosis, drug resistance, malignant potential [3] [92] | Promotes immune escape, tumor proliferation, metastasis [3] | [3] [92] |
| Triple-Negative Breast Cancer | Significant upregulation in early tumor formation [93] | Associated with disease progression and therapy resistance [93] | Maintains stem-like state, promotes aggression [93] | [93] |
SOX9-Specific Mechanisms in Pathobiology and Therapeutic Resistance
SOX9 in Cancer Stemness and Chemoresistance
SOX9 drives chemoresistance through multiple interconnected mechanisms. In high-grade serous ovarian cancer, SOX9 expression is epigenetically upregulated following platinum-based chemotherapy, inducing a stem-like transcriptional state associated with drug tolerance [62]. Single-cell RNA sequencing of patient tumors before and after neoadjuvant chemotherapy demonstrated consistent SOX9 upregulation in post-treatment cancer cells (Wilcoxon's paired P=0.032), with increased expression in 8 of 11 patients [62]. Mechanistically, SOX9 increases transcriptional divergence—a metric of transcriptional plasticity amplified in cancer stem cells—reprogramming naive cells toward a chemoresistant phenotype [62].
In ovarian cancer resistance to PARP inhibitors, SOX9 contributes to DNA damage repair capability through a deubiquitination-mediated stabilization mechanism. The deubiquitinating enzyme USP28 inhibits FBXW7-mediated SOX9 degradation, leading to SOX9 accumulation [28]. Chromatin immunoprecipitation sequencing revealed that SOX9 binds promoters of key DNA damage repair genes (SMARCA4, UIMC1, and SLX4), enhancing repair capacity and therapeutic resistance [28].
Figure 1: SOX9-Driven Therapeutic Resistance Mechanisms and Intervention Strategies. SOX9 promotes resistance to carboplatin and PARP inhibitors through multiple pathways, including stabilization via USP28 and transcriptional activation of DNA damage repair genes. Therapeutic interventions targeting this axis are shown in green.
SOX9 in Immune Regulation and Microenvironment Remodeling
SOX9 exhibits a dual role in immune regulation, functioning as both an activator and repressor across different immune contexts—characterized as a "double-edged sword" in immunity [3]. In cancer settings, SOX9 promotes immunosuppression through multiple mechanisms. Bioinformatics analyses of colorectal cancer datasets reveal that SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3].
In glioblastoma, SOX9 expression demonstrates complex relationships with the immune microenvironment. While generally associated with immunosuppression, high SOX9 expression correlates with better prognosis in specific lymphoid invasion subgroups, suggesting context-dependent functions [71]. SOX9 expression in GBM significantly correlates with immune cell infiltration and checkpoint expression, indicating involvement in establishing immunosuppressive niches [71].
Beyond oncology, SOX9 contributes to neuroinflammation in neuropathic pain through metabolic reprogramming of astrocytes. Nerve injury induces abnormal SOX9 phosphorylation, triggering transcriptional activation of hexokinase 1 (Hk1) and heightened glycolytic flux in specific astrocyte subpopulations [94]. The resulting lactate production remodels histone modifications via lactylation (H3K9la), promoting pro-inflammatory and neurotoxic gene expression programs that drive pain pathogenesis [94].
Experimental Frameworks for SOX9 Investigation
Core Methodologies for SOX9 Functional Characterization
Table 3: Essential Experimental Approaches for SOX9 Research
| Methodology | Application in SOX9 Research | Key Technical Considerations | Representative Findings |
|---|---|---|---|
| CRISPR/Cas9 Gene Editing | SOX9 knockout to assess functional necessity [62] | Use multiple sgRNAs to control for off-target effects; validate with Western blot [62] | SOX9 ablation increases platinum sensitivity in ovarian cancer cells (p=0.0025) [62] |
| Single-Cell RNA Sequencing | Analysis of SOX9 expression heterogeneity in tumor ecosystems [62] [94] | Include patient-matched pre- and post-treatment samples; utilize computational pipelines for trajectory analysis [62] | Identification of rare SOX9+ stem-like cells in primary tumors; chemotherapy-induced SOX9 upregulation [62] |
| Chromatin Immunoprecipitation Sequencing (ChIP-Seq) | Genome-wide mapping of SOX9 binding sites [28] | Optimize antibody specificity; include input DNA controls; integrate with RNA-seq data | SOX9 binds promoters of DDR genes (SMARCA4, UIMC1, SLX4) in ovarian cancer [28] |
| Molecular Docking and Dynamics Simulations | Vaccine design and small-molecule inhibitor development [93] | Utilize refined 3D structures; validate with molecular dynamics simulations | Multi-epitope vaccine targeting SOX9 shows favorable interactions with TLR2/TLR4 [93] |
| Co-Immunoprecipitation and Protein Stability Assays | Investigation of SOX9 protein-protein interactions and turnover [28] | Use reciprocal co-IP; combine with cycloheximide chase assays to measure half-life | USP28 stabilizes SOX9 by counteracting FBXW7-mediated ubiquitination [28] |
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Reagents for SOX9-Targeted Research
| Reagent Category | Specific Examples | Research Application | Functional Outcome |
|---|---|---|---|
| SOX9-Targeting sgRNAs | CRISPR/Cas9 guides for SOX9 knockout [62] | Functional validation of SOX9 necessity | Increased platinum sensitivity in HGSOC models [62] |
| USP28 Inhibitors | AZ1 [28] | Targeting SOX9 protein stability | Reduces SOX9 stability, sensitizes to PARP inhibition [28] |
| SOX9 Antibodies | Validation-grade antibodies for Western blot, ChIP [28] | Protein detection, localization, and chromatin binding studies | Identification of SOX9-DNA interactions; protein expression quantification [28] |
| Multi-Epitope Peptide Vaccines | SOX9-targeting vaccine constructs with L7/L12 adjuvant [93] | Immunotherapeutic approach for SOX9+ cancers | Induces SOX9-specific cellular and humoral immune responses [93] |
| Platinum Chemotherapeutics | Carboplatin [62] | Induction of SOX9 expression and resistance studies | Rapid SOX9 upregulation within 72 hours in HGSOC lines [62] |
Therapeutic Targeting Strategies for SOX9
Direct and Indirect Targeting Approaches
Several innovative strategies have emerged for therapeutic targeting of SOX9 in cancer and inflammatory diseases:
Immunotherapeutic Approaches: A novel multi-epitope peptide vaccine targeting SOX9 has been designed for triple-negative breast cancer. This vaccine incorporates B-cell, helper T lymphocyte (HTL), and cytotoxic T lymphocyte (CTL) epitopes with high antigenicity, non-toxicity, and non-allergenicity, linked with appropriate spacers and fused to the 50S ribosomal protein L7/L12 adjuvant [93]. In silico analyses predict strong cellular and humoral immune responses, with favorable interactions with Toll-like receptors TLR2 and TLR4 [93]. This approach circumvents the challenge of intracellular SOX9 localization that limits antibody-based therapies.
Small-Molecule Inhibition: While direct small-molecule inhibition of transcription factors remains challenging, targeting SOX9-regulatory proteins represents a promising alternative. The USP28-specific inhibitor AZ1 reduces SOX9 protein stability by promoting FBXW7-mediated ubiquitination and degradation, thereby sensitizing ovarian cancer cells to PARP inhibitors [28]. This combinatorial approach demonstrates the potential of targeting SOX9 stability regulators to overcome therapy resistance.
Metabolic Pathway Modulation: In neuropathic pain, targeting the SOX9-Hk1-glycolysis axis provides therapeutic benefit. Inhibition of SOX9-mediated hexokinase 1 activation dampens neuroinflammatory astrocyte subsets without affecting beneficial populations, resulting in long-lasting pain relief in preclinical models [94]. This approach demonstrates the potential of context-dependent SOX9 modulation in non-oncological indications.
Figure 2: SOX9 Pathological Functions and Corresponding Therapeutic Strategies. SOX9 drives multiple pathological processes across indications, with emerging targeted approaches shown in green.
Clinical Translation Considerations
The transition of SOX9-targeting therapies to clinical application requires careful consideration of several factors. Safety evaluation must address potential on-target toxicities given SOX9's roles in normal tissue homeostasis, particularly in cartilage, testes, and neural crest-derived tissues [93] [91]. The multi-epitope vaccine approach aims to minimize autoimmune reactions through careful epitope selection and exclusion of sequences with high homology to human proteins [93].
Patient stratification biomarkers will be essential for successful SOX9-targeted therapy development. SOX9 expression levels, subcellular localization, and post-translational modification status may identify patients most likely to benefit from SOX9-directed treatments [71] [28]. In glioblastoma, SOX9 demonstrates particular prognostic significance in IDH-mutant cases, highlighting the importance of genetic context [71].
Therapeutic efficacy may be enhanced through rational combination strategies. Preclinical evidence supports combining SOX9-targeting approaches with conventional chemotherapy, PARP inhibitors, or immunotherapy to overcome resistance mechanisms [62] [28]. The temporal dynamics of SOX9 induction following therapy suggest optimized scheduling may be critical for combination regimens [62].
SOX9 represents a premier target within the SOX transcription factor family for therapeutic development based on its multifaceted roles in pathogenesis, frequent dysregulation in human diseases, and susceptibility to multiple targeting strategies. The comparative assessment presented herein substantiates the prioritization of SOX9 in drug development pipelines based on several key characteristics: (1) its dual functionality in both tumor cell-intrinsic processes and immune microenvironment regulation; (2) its central role in therapy resistance mechanisms across diverse cancer types; (3) its demonstrated susceptibility to targeting through both direct and indirect approaches; and (4) its context-dependent functions that enable therapeutic window exploitation.
Future research directions should address several critical knowledge gaps. First, the contradictory roles SOX9 exhibits in different tumor types and microenvironments require deeper mechanistic understanding to enable context-specific therapeutic applications. Second, the development of direct SOX9 small-molecule inhibitors remains a substantial challenge that merits continued investment in structural biology and screening approaches. Third, the translational potential of SOX9-targeting vaccines requires comprehensive preclinical validation and safety assessment. Finally, the integration of SOX9-targeting approaches with established and emerging therapeutic modalities warrants systematic investigation to maximize clinical benefit.
The accumulating evidence positions SOX9 as a compelling therapeutic target worthy of prioritized development efforts. The experimental frameworks and strategic considerations outlined in this review provide a roadmap for advancing SOX9-targeted therapies toward clinical application, with potential to address significant unmet needs in oncology and inflammatory diseases.
Conclusion
SOX9 emerges as a master regulatory node with profound yet complex influence over immune responses, fibrosis, and tissue repair. Its Janus-faced nature necessitates a nuanced, context-aware approach for therapeutic targeting. Future research must prioritize the development of strategies that selectively inhibit its pathogenic functions in fibrotic and autoimmune contexts while preserving or enhancing its reparative roles in cartilage and tissue homeostasis. Advancing tissue-specific delivery systems, understanding its intricate crosstalk with key signaling pathways like NF-κB and MAPK/ERK, and validating its utility as a non-invasive biomarker are critical next steps. Successfully harnessing SOX9 holds immense potential for pioneering next-generation therapies for a spectrum of autoimmune, inflammatory, and fibrotic diseases.
References
- 1. The transcription factors SOX9 and SOX10 are vitiligo ... [https://pubmed.ncbi.nlm.nih.gov/11423552/]
- 2. The Transcription Factors SOX9 and SOX10 Are Vitiligo ... [https://www.sciencedirect.com/science/article/pii/S0021925819587968]
- 3. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 4. Dimerization and Transactivation Domains as Candidates for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0156199]
- 5. The DNA-binding specificity of SOX9 and other SOX proteins [https://pmc.ncbi.nlm.nih.gov/articles/PMC148324/]
- 6. Regulation of the human Sox9 promoter by the CCAAT ... [https://www.sciencedirect.com/science/article/abs/pii/S0945053X05000417]
- 7. Sox9 regulation of hexokinase 1 controls ... [https://www.nature.com/articles/s41467-025-65092-5]
- 8. Role of Phosporylated SOX9 in Systemic Sclerosis ... [https://grantome.com/grant/NIH/R21-AR070409-01A1]
- 9. The role of NF-κB-SOX9 signalling pathway in osteoarthritis [https://www.sciencedirect.com/science/article/pii/S2405844024132227]
- 10. SOX9 has distinct regulatory roles in alternative splicing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158501/]
- 11. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 12. in vitro and in silico exploration of the HIF-1α/SOX9/IL-1β ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255043/]
- 13. Boosting one protein helps the brain protect itself from ... [http://www.sciencedaily.com/releases/2025/11/251123085550.htm]
- 14. Inhibition of SOX9 Promotes Inflammatory and Immune ... [https://pubmed.ncbi.nlm.nih.gov/29571909/]
- 15. Inhibition of SOX9 Promotes Inflammatory and Immune ... [https://www.sciencedirect.com/science/article/abs/pii/S0099239918300785]
- 16. The Expression Level of SOX Family Transcription Factors' ... [https://www.mdpi.com/2077-0383/14/4/1176]
- 17. SOX9: a key transcriptional regulator in organ fibrosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11835943/]
- 18. Frontiers | SOX : a key transcriptional regulator in organ 9 fibrosis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1507282/full]
- 19. Induces Orbital Fibroblast Activation in SOX ... 9 Thyroid Eye Disease [https://pmc.ncbi.nlm.nih.gov/articles/PMC10866156/]
- 20. SOX9 regulated matrix proteins are increased in patients ... [https://www.nature.com/articles/s41598-018-36037-4]
- 21. SOX9 plays an essential role in myofibroblast driven hepatic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12148231/]
- 22. Profibrotic role of the SOX –MMP10–ECM biosynthesis axis in the... 9 [https://www.sciopen.com/article/10.1016/j.gendis.2023.06.012]
- 23. Cartilage Homeostasis and Osteoarthritis [https://pubmed.ncbi.nlm.nih.gov/35682994/]
- 24. Chondrocyte fatty acid oxidation drives osteoarthritis via ... [https://www.nature.com/articles/s41467-025-60037-4]
- 25. Regulation and function of SOX9 during cartilage ... [https://www.sciencedirect.com/science/article/abs/pii/S1044579X20300961]
- 26. The Expression Level of SOX Family Transcription Factors ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11856735/]
- 27. RNA binding proteins regulate anabolic and catabolic gene ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4917896/]
- 28. USP28 promotes PARP inhibitor resistance by enhancing ... [https://www.nature.com/articles/s41419-025-07647-4]
- 29. Epigenetic Regulation of Chondrocyte Catabolism and ... [https://www.sciencedirect.com/science/article/pii/S1016847823054778]
- 30. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 31. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 32. The Clinicopathological and Prognostic Significance of ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.668946/full]
- 33. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 34. Transformation of SOX9+ cells by Pten deletion synergizes ... [https://www.nature.com/articles/s41598-021-90958-1]
- 35. Nature-inspired IL-1 targeted therapy to treat chronic ... [https://pubmed.ncbi.nlm.nih.gov/40931517/]
- 36. IL-1 and IL-1ra are key regulators of the inflammatory ... [https://www.nature.com/articles/s41590-022-01160-y]
- 37. Navigating the Hurdles of Intra-Articular AAV Gene Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC12564301/]
- 38. Co-delivery of IL-1Ra and SOX9 via AAV inhibits ... [https://pubmed.ncbi.nlm.nih.gov/39833570/]
- 39. Diverse functions of SOX9 in liver development and ... [https://www.sciencedirect.com/science/article/pii/S2352304223002532]
- 40. Gene therapy for disorders of sex development [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1661127/full]
- 41. Release details [https://investor.pacira.com/news-releases/news-release-details/pacira-biosciences-concludes-patient-enrollment-part-phase-2]
- 42. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 43. Anti-inflammatory effects of cordycepin in lipopolysaccharide ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4206205/]
- 44. The role of NF-κB-SOX9 signalling pathway in osteoarthritis [https://pmc.ncbi.nlm.nih.gov/articles/PMC11419907/]
- 45. Role and mechanisms of the NF-ĸB signaling pathway in ... [https://www.sciencedirect.com/science/article/pii/S0753332222009027]
- 46. Rosmarinic acid promotes cartilage regeneration through ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11497390/]
- 47. A Review of the Anti-Inflammatory Effects of Rosmarinic ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2020.00153/full]
- 48. Therapeutic Potential of Rosmarinic Acid [https://www.mdpi.com/2076-3417/9/15/3139]
- 49. Rosmarinosin A Inhibits Inflammatory Response in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12472359/]
- 50. Epigenetic regulation of SOX9 by the NF-κB signaling ... [https://pubmed.ncbi.nlm.nih.gov/23592398/]
- 51. An EGFR-ERK-SOX9 signaling cascade Links Urothelial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3107391/]
- 52. EGFR in Cancer: Signaling Mechanisms, Drugs, and ... [https://www.mdpi.com/2072-6694/13/11/2748]
- 53. SOX9 is a critical regulator of TSPAN8-mediated ... [https://www.nature.com/articles/s41388-021-01864-9]
- 54. ERK1/2-SOX9/FOXL2 axis regulates ovarian ... [https://www.life-science-alliance.org/content/6/10/e202302100]
- 55. Clinical application of single‐cell RNA sequencing in disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12576031/]
- 56. CRISPR-mediated Sox9 activation and RelA inhibition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11405173/]
- 57. Engineering approaches for RNA-based and cell- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11129836/]
- 58. Circular RNA-based protein replacement therapy mitigates ... [https://www.nature.com/articles/s41467-025-63343-z]
- 59. mRNA-Based Combination Therapy for Inflammation ... [https://www.mdpi.com/1999-4923/17/10/1254]
- 60. Therapeutic Delivery of rAAV sox9 via Polymeric Micelles ... [https://www.mdpi.com/2079-4991/10/6/1238]
- 61. Boosting one protein helps the brain protect itself from ... [https://www.sciencedaily.com/releases/2025/11/251123085550.htm]
- 62. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 63. SOX9 drives a stem-like transcriptional state and platinum ... [https://www.jci.org/articles/view/186467]
- 64. The versatile functions of Sox9 in development, stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4326072/]
- 65. The local and circulating SOX9 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292907/]
- 66. Tissue expression of SOX9 - Summary [https://www.proteinatlas.org/ENSG00000125398-SOX9/tissue]
- 67. Mesenchymal stem cells in treating human diseases [https://www.nature.com/articles/s41392-025-02313-9]
- 68. SOX9: A genomic view of tissue specific expression and ... [https://pubmed.ncbi.nlm.nih.gov/28323209/]
- 69. Comparative analysis demonstrates cell type-specific ... [https://www.nature.com/articles/s41598-019-48979-4]
- 70. Quantitative characterization of tissue states using ... [https://www.nature.com/articles/s41588-025-02119-z]
- 71. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 72. Cross-regulation between SOX9 and the canonical Wnt ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2023.1250530/full]
- 73. Role of Sox9 in BPD and its effects on the Wnt/β-catenin ... [https://www.nature.com/articles/s41420-023-01795-2]
- 74. Latest Developed Strategies to Minimize the Off-Target ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7407193/]
- 75. Recent Advancements in Reducing the Off-Target Effect of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10802171/]
- 76. Mitigation of off-target toxicity in CRISPR-Cas9 screens for ... [https://www.nature.com/articles/s41467-019-11955-7]
- 77. Nsun4 and Mettl3 mediated translational reprogramming of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9133052/]
- 78. JCI Insight - Inactivation of Sox in fibroblasts reduces cardiac fibrosis... 9 [https://insight.jci.org/articles/view/126721]
- 79. From Bench to Bedside: Lessons Learned in Translating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3787906/]
- 80. Co-regulation of Sox9 and TGFβ1 transcription factors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10063891/]
- 81. SOX9 expression decreases survival of patients with ... [https://www.nature.com/articles/s41416-018-0338-9]
- 82. Astrocytic Sox9 overexpression in Alzheimer's disease mouse ... [https://pubmed.ncbi.nlm.nih.gov/41272323/]
- 83. Transcription Factor Drives Chemotherapy Resistance in ... [https://news.feinberg.northwestern.edu/2025/10/30/transcription-factor-drives-chemotherapy-resistance-in-ovarian-cancer/]
- 84. High expression of SOX9 is a diagnostic and prognostic ... [https://pubmed.ncbi.nlm.nih.gov/40692865/]
- 85. SOX9: A Novel Janus-Faced Regulator in Immunity and Its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/abstract]
- 86. Co-expression of immune checkpoints in glioblastoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11021796/]
- 87. Immune Checkpoint Inhibitors and Glioblastoma: A Review on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11075475/]
- 88. Identification of Potential Targets for EGFR-Regulated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12415117/]
- 89. Gefitinib Facilitates Bone Fracture Healing via Inhibition of ... [https://iv.iiarjournals.org/content/39/3/1394]
- 90. Wu Mei Wan suppresses colorectal cancer stemness by ... [https://www.sciencedirect.com/science/article/abs/pii/S0378874124012972]
- 91. SOX on tumors, a comfort or a constraint? [https://www.nature.com/articles/s41420-024-01834-6]
- 92. The role of SOX family members in solid tumours and ... [https://www.sciencedirect.com/science/article/pii/S1044579X1830141X]
- 93. Targeting SOX9: designing a novel vaccine against triple- ... [https://www.nature.com/articles/s41598-025-25499-y]
- 94. Sox9 regulation of hexokinase 1 controls neuroinflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639169/]