SOX9 in Cancer Immunity: Mechanisms, Biomarker Potential, and Therapeutic Targeting of the Tumor Microenvironment
The transcription factor SOX9 is a pivotal, yet dualistic, regulator of the tumor immune microenvironment.
SOX9 in Cancer Immunity: Mechanisms, Biomarker Potential, and Therapeutic Targeting of the Tumor Microenvironment
Abstract
The transcription factor SOX9 is a pivotal, yet dualistic, regulator of the tumor immune microenvironment. This review synthesizes current evidence establishing that SOX9 drives immune evasion in multiple cancers—including lung adenocarcinoma, glioblastoma, and head and neck squamous cell carcinoma—by suppressing the infiltration and function of cytotoxic CD8+ T cells, NK cells, and dendritic cells, while often promoting immunosuppressive elements. We explore the foundational biology of SOX9, methodologies for its study and inhibition, strategies to overcome associated immunotherapy resistance, and its validation as a diagnostic and prognostic biomarker. For researchers and drug development professionals, this article underscores SOX9's emerging promise as a therapeutic target to reprogram the tumor microenvironment and overcome barriers in cancer immunotherapy.
The Dual Role of SOX9: Unraveling Its Foundational Biology in Cancer and Immune Evasion
The SRY-box transcription factor 9 (SOX9) is a master regulatory protein with a well-established role in embryonic development and cell fate determination. Recent research has increasingly framed SOX9 within the context of cancer research, particularly its profound influence on the tumor immune microenvironment [1]. SOX9 operates as a pioneer transcription factor, capable of binding to compacted chromatin and initiating large-scale transcriptional reprogramming [2]. This ability allows it to dictate cell identity, a function co-opted in various cancers to promote tumor progression and immune evasion. Its expression is frequently dysregulated in solid malignancies, where it correlates with poor prognosis, drug resistance, and the establishment of an "immune cold" tumor landscape [1] [3] [4]. Understanding the structural basis of SOX9's transcriptional activity is therefore paramount for developing novel diagnostic and therapeutic strategies in oncology.
Architectural Blueprint: The Functional Domains of SOX9
The human SOX9 protein comprises 509 amino acids and contains several functionally specialized domains that work in concert to regulate its transcriptional output [1] [5]. These domains orchestrate DNA binding, protein partnership, nuclear transport, and the recruitment of transcriptional co-regulators.
Table 1: Core Functional Domains of the SOX9 Protein
| Domain Name | Location (Amino Acids) | Primary Function | Key Interacting Partners/Motifs |
|---|---|---|---|
| Dimerization Domain (DIM) | N-Terminus | Facilitates homodimerization or heterodimerization with other SOXE proteins. | SOX9 itself, SOX8, SOX10 [1] [5] |
| HMG Box | Central | Confers sequence-specific DNA binding, induces DNA bending, and contains nuclear localization (NLS) and export (NES) signals [1]. | Recognizes consensus motif (A/TA/TCAAA/TG) [6] |
| Transactivation Domain Middle (TAM) | Central | Synergizes with TAC to enhance transcriptional potential [1] [5]. | Transcriptional co-activators |
| Transactivation Domain C-terminal (TAC) | C-Terminus | Critical for interaction with major transcriptional co-activators; essential for inhibiting β-catenin in chondrocytes [1] [5]. | CBP/p300, TIP60, MED12, WWP2 [7] [5] [8] |
| PQA-rich Domain | C-Terminus | A proline/glutamine/alanine-rich region necessary for full transactivation capability [1] [5]. | Enhances transcriptional activity |
The sequential arrangement and cooperative function of these domains enable SOX9 to perform its complex role as a transcriptional regulator. The diagram below illustrates the linear organization of these domains and their primary functional contributions.
Molecular Mechanisms: How Domain Structure Dictates Transcriptional Activity and Immune Regulation
The functional domains of SOX9 confer its transcriptional activity through a multi-step process involving DNA binding, partnership with other factors, and recruitment of epigenetic modifiers. In cancer, these mechanisms directly impact immune cell infiltration and anti-tumor immunity.
DNA Binding and Chromatin Remodeling
The HMG domain allows SOX9 to bind specific DNA sequences and function as a pioneer factor [2]. It accesses its cognate motifs, such as AGAACAATGG, even within closed chromatin regions. Upon binding, SOX9 induces DNA bending and initiates nucleosome displacement, thereby opening the chromatin landscape and making it accessible for other transcription factors and co-activators [2]. This pioneer activity is fundamental to its role in fate switching, both in development and in cancer, where it can activate a pro-tumorigenic transcriptional program.
Dimerization and Partner Factor Interactions
The Dimerization Domain (DIM) is critical for SOX9 function. SOX9 can form homodimers on palindromic DNA sequences, a requirement for the transactivation of cartilage-specific genes like COL2A1 [5]. Furthermore, SOX9 heterodimerizes with other SOXE family members (SOX8, SOX10), which can confer functional redundancy or specificity depending on the cellular context [6]. Beyond SOX partners, SOX9's transcriptional output is defined by its collaboration with context-specific partner factors (e.g., β-catenin, SF1), which determine whether it acts as an activator or a repressor of target genes [6].
Recruitment of Transcriptional Co-activators
The Transactivation Domains (TAM and TAC) are the primary interfaces for co-activator recruitment. The TAC domain, in particular, directly interacts with major epigenetic co-activators like CREB-binding protein (CBP) and its homolog p300 [7] [5] [8]. These co-activators possess histone acetyltransferase activity, which loosens chromatin structure and promotes gene transcription. The interaction between SOX9 and CBP/p300 is essential for the expression of chondrocyte-specific genes but is also a general mechanism for SOX9-driven transcription [7] [8]. In the context of cancer, this recruitment is key to establishing oncogenic gene expression programs.
A Mechanism of Fate Switching: Competition for Epigenetic Factors
A pivotal study revealed that SOX9's role in cell fate switching involves not only activating new genes but also silencing the previous cellular identity. As SOX9 binds to new enhancers and recruits co-activators like CBP/p300 and other chromatin modifiers (e.g., the SWI/SNF complex), it effectively sequesters a limited pool of these epigenetic factors [2]. This competition depletes co-activators from the enhancers of the cell's original gene expression program, leading to their silencing. This mechanism explains how SOX9 can efficiently suppress epithelial genes in epidermal stem cells while simultaneously activating a hair follicle stem cell program, a process directly relevant to the genesis of basal cell carcinoma [2].
SOX9 Domain Function in Immune Cell Infiltration and Cancer
The molecular functions of SOX9's domains directly enable its role in shaping the tumor immune microenvironment. Its activity as a transcriptional hub allows it to influence the expression of chemokines, cytokines, and other regulators that determine immune cell composition within tumors.
Creating an "Immune Cold" Tumor Microenvironment
In KRAS-mutant lung cancer, overexpression of SOX9 creates an "immune cold" condition, characterized by poor infiltration of cytotoxic immune cells. Research indicates that this is a primary mechanism through which SOX9 regulates tumor development [4]. The transcriptional networks activated by SOX9, dependent on its DNA-binding and co-activator recruitment capabilities, likely suppress the expression of key chemokines required for T-cell recruitment.
Correlation with Specific Immune Cell Populations
Bioinformatics analyses across multiple cancers reveal distinct correlations between SOX9 expression and immune cell infiltration. These patterns are summarized in the table below and are a direct consequence of SOX9's transcriptional regulatory function.
Table 2: Correlation of SOX9 Expression with Immune Cell Infiltration in Cancer
| Immune Cell Type | Correlation with SOX9 Expression | Context and Potential Impact |
|---|---|---|
| CD8+ T cells | Negative Correlation | Associated with impaired cytotoxic T cell function [1] [3]. |
| Neutrophils | Positive Correlation | Linked to pro-tumorigenic neutrophil states [1]. |
| Macrophages | Positive Correlation (M2) | Associated with M2-like, pro-tumorigenic macrophages [1]. |
| B cells & Plasma Cells | Negative Correlation | Suggests an impaired humoral anti-tumor response [1]. |
| NK Cells | Negative Correlation | Indicates reduced natural killer cell activity [1]. |
Mediating Resistance to Immunotherapy
A direct link between SOX9 and resistance to combination immunotherapy (anti-PD-1 + anti-LAG-3) was identified in head and neck squamous cell carcinoma (HNSCC) [9]. In this context, SOX9+ tumor cells were significantly enriched in treatment-resistant samples. Mechanistically, SOX9 was shown to directly transcriptionally activate Annexin A1 (Anxa1), which then bound to Formyl Peptide Receptor 1 (Fpr1) on neutrophils. This Anxa1-Fpr1 axis induced neutrophil apoptosis, preventing their accumulation in the tumor and subsequently impairing the infiltration and tumor-killing capacity of cytotoxic CD8+ T and γδ T cells [9]. This pathway illustrates how SOX9's core function as a transcription factor directly subverts anti-tumor immunity.
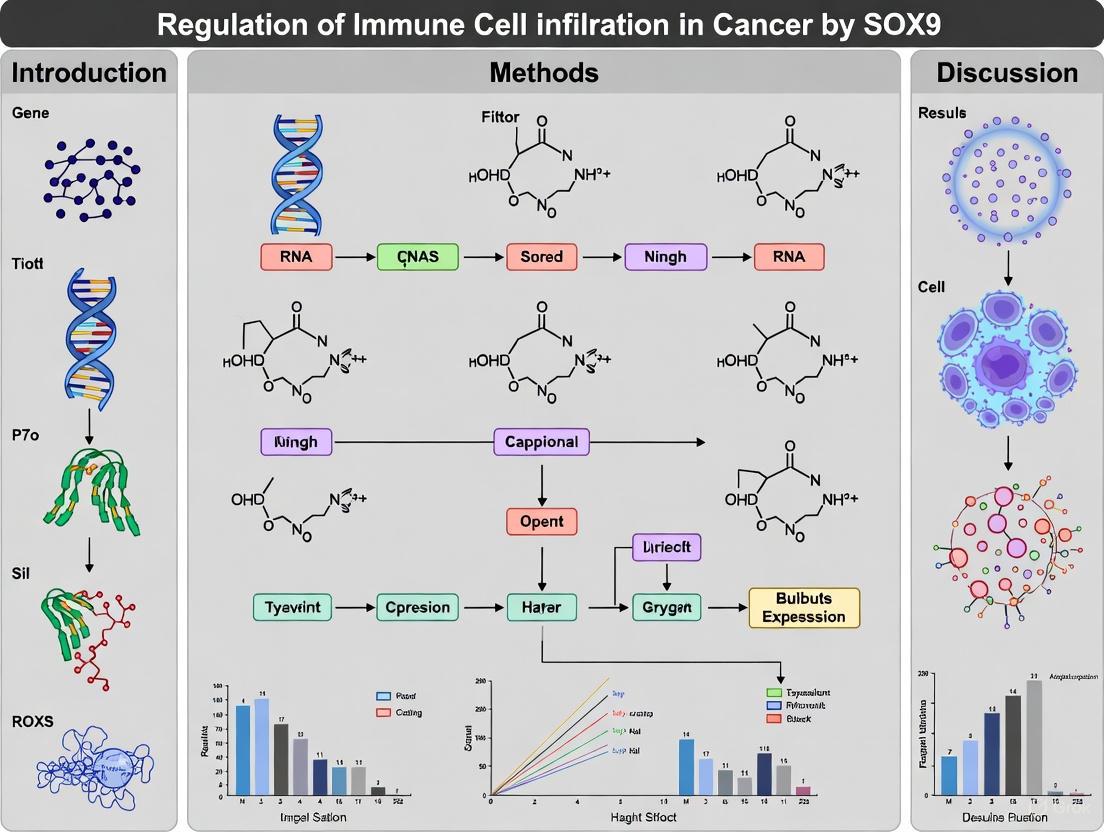
The following diagram synthesizes this mechanism, showing how SOX9's transcriptional activity leads to immunotherapy resistance.
Experimental Analysis of SOX9 Structure and Function
Key Experimental Workflows
Investigating SOX9 requires a multi-faceted approach to dissect its structure, function, and role in the tumor immune microenvironment. The following workflow outlines a comprehensive experimental strategy.
Detailed Methodologies for Key Assays
Chromatin Immunoprecipitation (ChIP) and CUT&RUN
Objective: To identify genomic regions where SOX9 directly binds and to assess co-activator recruitment (e.g., p300).
- Protocol (ChIP): Cells (e.g., chondrosarcoma line SW1353) are cross-linked with formaldehyde. Chromatin is sheared by sonication and immunoprecipitated using antibodies specific for SOX9, p300, or control IgG [7] [8]. Precipitated DNA is purified and analyzed via qPCR for specific loci or sequenced (ChIP-seq).
- Protocol (CUT&RUN): This is a more recent, high-sensitivity alternative. Permeabilized cells are incubated with a target antibody (e.g., anti-MYC for MYC-tagged SOX9) [2]. The pA-MNase enzyme is then recruited, which cleaves DNA around the antibody-binding site upon activation. The cleaved DNA fragments are extracted and sequenced, providing a high-resolution map of transcription factor binding with low background [2].
Promoter/Reporter Assays
Objective: To test the functional impact of specific SOX9 domains on transcriptional activation.
- Protocol: A reporter plasmid (e.g., luciferase) under the control of a SOX9-responsive promoter (e.g., from the COL2A1 gene) is co-transfected into cells along with plasmids expressing wild-type or mutant SOX9 (e.g., lacking the TAC domain) [7] [5] [8]. Co-transfection with co-activators like CBP/p300 can further enhance activity [7]. Luciferase activity is measured after 24-48 hours to quantify transcriptional output, directly linking domain structure to function.
Functional Validation in Cancer and Immunity
Objective: To establish the causal role of SOX9 in tumor growth and immune modulation.
- In Vitro Knockout/Knockdown: SOX9 expression is modulated in cancer cell lines (e.g., 22RV1, PC3, H1975) using siRNA, shRNA, or CRISPR-Cas9. Subsequent analyses measure changes in proliferation, invasion, and expression of immune factors [3].
- In Vivo Models:
- Transgenic Mice: Inducible, tissue-specific mouse models (e.g., Krt14-rtTA;TRE-Sox9) allow timed reactivation of SOX9 in adult epidermal stem cells, enabling the study of fate switching and tumor initiation (e.g., BCC) in the native tissue context [2].
- Xenograft Models: SOX9-modulated cancer cells are implanted into immunocompromised mice. Tumor growth is monitored, comparing control vs. SOX9-knockdown groups [3].
- Immunotherapy Resistance Models: C57BL/6 wild-type mice with 4NQO-induced HNSCC are treated with anti-PD-1 and anti-LAG-3. Resistant and sensitive tumors are analyzed using scRNA-seq to identify SOX9+ subpopulations, followed by validation in various transgenic models [9].
The Scientist's Toolkit: Key Research Reagents and Models
Table 3: Essential Research Tools for Studying SOX9
| Reagent / Model | Specification / Example | Primary Function in Research |
|---|---|---|
| SOX9 Antibodies | Validated for ChIP, CUT&RUN, Western Blot, IHC | Detecting SOX9 protein expression, localization, and chromatin binding. |
| Expression Plasmids | Wild-type and domain mutants (e.g., ΔTAC, ΔDIM) | Structure-function analysis in promoter/reporter assays. |
| Cell Lines | SW1353 (chondrosarcoma), 22RV1/PC3 (prostate), H1975 (lung) | In vitro models for manipulating SOX9 and studying its functional effects. |
| Mouse Models | Krt14-rtTA;TRE-Sox9 (inducible), 4NQO-induced HNSCC | In vivo validation of SOX9 in tumorigenesis, fate switching, and therapy resistance. |
| Small Molecule Inhibitors | Cordycepin (adenosine analog) | Tool for pharmacologically inhibiting SOX9 expression in cancer cells [3]. |
The transcriptional activity of SOX9, and by extension its powerful influence on tumor immune infiltration, is fundamentally rooted in its multi-domain protein structure. The HMG box provides the foundation for DNA binding and pioneer factor activity, the DIM domain enables complex formation, and the transactivation domains, particularly the TAC, serve as a critical platform for recruiting co-activators like CBP/p300. This recruitment is not only activating but also competitive, allowing SOX9 to orchestrate widespread epigenetic changes that define cell fate. In cancer, hijacking this mechanistic blueprint allows SOX9 to establish immunosuppressive microenvironments and drive resistance to immunotherapy. Therefore, targeting the interactions between SOX9's functional domains and its co-regulatory partners represents a promising, albeit challenging, frontier for novel cancer therapeutics.
SOX9 as a Master Regulator of Development and Its Hijacking in Carcinogenesis
The SRY-related HMG-box transcription factor 9 (SOX9) is a pivotal regulator of embryonic development, cell fate determination, and tissue homeostasis. This whitepaper examines the dual nature of SOX9 as both a master developmental regulator and a central player in carcinogenesis. We synthesize current understanding of how SOX9's normal developmental functions are co-opted during tumorigenesis, with particular emphasis on its emerging role in modulating immune cell infiltration and shaping the tumor microenvironment. The document provides a technical resource for researchers and drug development professionals, including comprehensive data synthesis, experimental protocols, and visualization of SOX9-mediated mechanisms in development and cancer.
SOX9 belongs to the SOX family of transcription factors, characterized by a highly conserved high-mobility group (HMG) DNA-binding domain. Initially identified for its crucial role in sex determination and chondrogenesis, SOX9 is now recognized as a master regulator of development in multiple organs including pancreas, liver, heart, lung, and kidney [10] [11]. Beyond development, accumulating evidence demonstrates that SOX9 is frequently dysregulated in cancer, where it promotes tumor initiation, progression, metastasis, and therapy resistance [12] [13]. SOX9 exhibits context-dependent dual functions—acting as both an oncogene and tumor suppressor—across diverse cancer types [12]. This whitepaper explores the molecular mechanisms through which SOX9 executes its developmental programs and how these same mechanisms are hijacked in carcinogenesis, with special focus on its emerging role as a regulator of immune cell infiltration in the tumor microenvironment.
Molecular Structure and Functional Domains of SOX9
The SOX9 protein contains several functionally specialized domains that enable its transcriptional regulatory activities:
- Dimerization Domain (DIM): Located ahead of the HMG box, facilitates protein-protein interactions [1]
- HMG Box Domain: Comprises three α-helices arranged in an L-shape that binds to specific DNA sequences (CCTTGAG) and contains embedded nuclear localization (NLS) and export (NES) signals [1] [14]
- Transcriptional Activation Domains: Two activation domains - TAM (central) and TAC (C-terminal) - that interact with cofactors to enhance transcriptional activity [1]
- PQA-Rich Domain: Proline/glutamine/alanine-rich region necessary for transcriptional activation [1]
The HMG domain enables DNA binding and bending, facilitating the assembly of enhanceosomes, while the transactivation domains recruit additional cofactors to regulate target gene expression [1] [11].
Figure 1: Domain organization of human SOX9 protein illustrating functional regions
SOX9 as a Master Regulator of Normal Development
Embryonic Development and Organogenesis
SOX9 plays indispensable roles in the development of multiple organ systems through its regulation of progenitor cell maintenance and differentiation:
Pancreatic Development: SOX9 maintains multipotent pancreatic progenitors, initiates endocrine differentiation, and maintains pancreatic ductal identity [10]. It interacts with Fgf and Notch signaling pathways to balance progenitor expansion and differentiation [10].
Chondrogenesis and Skeletal Development: SOX9 is expressed throughout chondrocyte differentiation, with particularly strong activity in proliferating and prehypertrophic chondrocytes [15]. It regulates cartilage matrix production and endochondral ossification [11].
Neural Development: SOX9 controls neural stem cell maintenance and Müller glial cell development in the retina [11].
Reproductive System Development: SOX9 is crucial for testis determination and male sex differentiation through its regulation of Sertoli cell differentiation [14].
Stem Cell Maintenance and Differentiation
SOX9 maintains stem/progenitor cell populations in multiple tissues, including breast, pancreas, and liver [16]. It coordinates with signaling pathways such as Wnt/β-catenin, Notch, and FGF to balance self-renewal and differentiation decisions [10] [14].
SOX9 Hijacking in Carcinogenesis
Mechanisms of SOX9 Dysregulation in Cancer
SOX9 expression is altered in cancer through multiple mechanisms:
Epigenetic Regulation: Aberrant DNA methylation of SOX9 promoter regions occurs in various cancers. Hypomethylation leads to SOX9 overexpression in bladder, colorectal, and other cancers [14].
Post-transcriptional Regulation: Multiple miRNAs regulate SOX9 expression, including miR-140, miR-215-5p, miR-613, and miR-101 [16] [11]. SOX9 also participates in feedback loops with long non-coding RNAs such as linc02095 [16].
Transcriptional Regulation: SOX9 expression is controlled by key signaling pathways often dysregulated in cancer, including Wnt/β-catenin, AKT, and EGFR-ERK pathways [14] [16].
SOX9's Oncogenic Functions
SOX9 drives multiple hallmarks of cancer through diverse molecular mechanisms:
Cell Survival and Apoptosis Evasion: SOX9 directly represses pro-apoptotic genes including tnfrsf1b, fadd, tnfrsf10a, tnfrsf10b, and ripk1 [17]. Knockout of SOX9 induces profound apoptosis in triple-negative breast cancer models [17].
Epithelial-Mesenchymal Transition and Metastasis: SOX9 promotes EMT by directly binding to promoters of EMT-regulating genes including vim, cldn1, ctnnb1, and zeb1 [17]. It enhances invasive capacity and metastatic dissemination in multiple cancer types [17] [14].
Stemness Maintenance: SOX9 maintains cancer stem cell populations by activating stemness-associated pathways and transcription factors including Bmi1 and Slug (SNAI2) [16]. It supports latent cancer cell survival and tumor-initiating capabilities [16].
Table 1: SOX9 Dysregulation Across Cancer Types
| Cancer Type | SOX9 Expression | Functional Role | Clinical Correlation |
|---|---|---|---|
| Triple-Negative Breast Cancer | Overexpressed | Essential for survival and metastasis; regulates apoptosis and EMT genes [17] | Poor prognosis; therapeutic target [17] [14] |
| Colorectal Cancer | Overexpressed | Promotes tumor progression; regulates Wnt signaling [1] | Correlates with immune cell infiltration patterns [1] |
| Glioblastoma | Overexpressed | Diagnostic and prognostic biomarker [18] | Better prognosis in lymphoid invasion subgroups; correlates with immune infiltration [18] |
| Liver Cancer | Overexpressed | Drives progression and therapy resistance [1] | Poor prognosis [11] |
| Lung Cancer | Overexpressed | Promotes invasion and drug resistance [1] | Correlates with tumor grading and survival [18] |
| Prostate Cancer | Overexpressed | Contributes to immune desert microenvironment [1] | Therapeutic target [11] |
SOX9 Regulation of Immune Cell Infiltration in Cancer
SOX9 as a Modulator of the Tumor Immune Microenvironment
SOX9 plays a complex, "double-edged sword" role in immunology, acting as both an promoter of immune escape and a facilitator of tissue repair [1]. Its expression correlates significantly with specific immune infiltration patterns across cancer types:
Immunosuppressive Microenvironment: In colorectal cancer, SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while positively correlating with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1].
Immune Desert Formation: In prostate cancer, SOX9 contributes to an "immune desert" microenvironment characterized by decreased effector immune cells (CD8+CXCR6+ T cells, activated neutrophils) and increased immunosuppressive cells (Tregs, M2 macrophages, anergic neutrophils) [1].
Immune Checkpoint Regulation: SOX9 expression correlates with immune checkpoint molecule expression in glioblastoma, indicating its involvement in immunosuppressive pathways [18].
Mechanisms of SOX9-Mediated Immune Evasion
SOX9 promotes tumor immune escape through multiple mechanisms:
Direct Immune Cell Regulation: SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), modulating lineage commitment of early thymic progenitors and influencing αβ T cell versus γδ T cell differentiation balance [1].
Latent Cell Survival: SOX9 and SOX2 maintain latent cancer cell survival and tumor-initiating capabilities under immunotolerant conditions, enabling immune evasion and metastatic dormancy [16].
Cytokine Signaling Modulation: Prostaglandin E2 (PGE2) activates SOX9 expression in progenitor cells, contributing to immunomodulation and tissue regeneration programs that can be co-opted in cancer [16].
Table 2: SOX9 Correlation with Immune Cell Infiltration in Cancer
| Immune Cell Type | Correlation with SOX9 | Cancer Context | Functional Consequences |
|---|---|---|---|
| CD8+ T cells | Negative correlation | Colorectal Cancer [1] | Reduced cytotoxic function |
| NK cells | Negative correlation | Multiple Cancers [1] | Impaired tumor cell killing |
| M1 Macrophages | Negative correlation | Multiple Cancers [1] | Reduced anti-tumor activity |
| M2 Macrophages | Positive correlation | Prostate Cancer [1] | Enhanced immunosuppression |
| Tregs | Positive correlation | Prostate Cancer [1] | Increased suppression of anti-tumor immunity |
| Neutrophils | Positive correlation | Colorectal Cancer [1] | Promotion of pro-tumor microenvironment |
| B cells | Negative correlation | Colorectal Cancer [1] | Diminished humoral immunity |
Figure 2: SOX9-mediated mechanisms of immune regulation in the tumor microenvironment
SOX9 as a Therapeutic Target and Biomarker
SOX9 in Therapy Resistance
SOX9 contributes significantly to treatment resistance through multiple mechanisms:
Chemotherapy Resistance: SOX9 confers resistance to various chemotherapeutic agents across cancer types. In gastric cancer, miR-613-mediated SOX9 downregulation increases sensitivity to cisplatin [11]. In breast cancer, SOX9 enhances endocrine therapy resistance through regulatory interactions with miRNAs [11].
Radiation Resistance: SOX9 expression is associated with radioresistance in multiple cancers, potentially through enhanced DNA damage repair and stem cell survival pathways [13].
Targeted Therapy Resistance: SOX9 promotes resistance to EGFR-tyrosine kinase inhibitors in lung cancer through Wnt/β-catenin pathway activation and EMT induction [11].
Therapeutic Targeting Strategies
Several approaches show promise for targeting SOX9 in cancer:
Direct SOX9 Inhibition: Preclinical studies demonstrate that SOX9 knockdown suppresses tumor growth and metastasis in triple-negative breast cancer models, providing rationale for SOX9 inhibitor development [17].
* miRNA-Based Approaches:* Restoration of SOX9-targeting miRNAs (e.g., miR-613, miR-190) represents a potential strategy to counteract SOX9-mediated therapy resistance [11].
Combination Therapies: Co-targeting SOX9 with standard therapies may overcome resistance mechanisms and improve treatment efficacy [13].
Table 3: SOX9 as a Prognostic Biomarker in Cancer
| Cancer Type | Prognostic Value | Clinical Utility |
|---|---|---|
| Colorectal Cancer | Poor prognosis [11] | Predicts relapse in stage II patients [11] |
| Glioma | Poor prognosis [11] | Independent prognostic factor for IDH-mutant cases [18] |
| Hepatocellular Carcinoma | Poor prognosis [11] | Correlation with progression features [11] |
| Non-Small Cell Lung Cancer | Poor prognosis [11] | Correlation with tumor grading [18] |
| Osteosarcoma | Poor prognosis [11] | Potential diagnostic and prognostic biomarker [11] |
| Pancreatic Ductal Adenocarcinoma | Poor prognosis [11] | Associated with chemoresistance [11] |
Experimental Approaches for SOX9 Research
Key Methodologies for SOX9 Investigation
Gene Expression Manipulation:
- siRNA/shRNA-mediated knockdown for functional studies [17]
- CRISPR/Cas9 knockout for comprehensive phenotypic analysis [17]
- Overexpression vectors for gain-of-function experiments
Molecular Interaction Mapping:
- Chromatin Immunoprecipitation (ChIP) assays to identify direct SOX9 target genes [17]
- CHIP-seq for genome-wide binding site identification [17]
- Protein-protein interaction studies (co-immunoprecipitation, yeast two-hybrid)
Transcriptomic Analyses:
- RNA-seq for identifying SOX9-regulated genes and pathways [18] [15]
- Single-cell RNA-seq to examine cell-type-specific SOX9 functions [1]
- Spatial transcriptomics to map SOX9 expression in tissue context [1]
Immune Microenvironment Characterization:
- Immune cell infiltration analysis using ssGSEA [18]
- ESTIMATE algorithm for tumor microenvironment assessment [18]
- Correlation analysis between SOX9 expression and immune checkpoint markers [18]
Research Reagent Solutions
Table 4: Essential Research Tools for SOX9 Investigation
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| SOX9 Antibodies | ChIP-grade anti-SOX9; IHC-validated clones | Protein detection, localization, chromatin binding studies | Validate for specific applications (WB, IHC, ChIP) |
| Gene Expression Modulators | SOX9-specific siRNA/shRNA; CRISPR guides; expression vectors | Functional studies of SOX9 loss/gain-of-function | Optimize delivery efficiency; control for off-target effects |
| OMICs Datasets | TCGA, GTEx, CCLE | Correlation analysis, expression profiling across cancers | Normalize across platforms; consider batch effects |
| Cell Line Models | TNBC lines (MDA-MB-231); patient-derived organoids | In vitro mechanistic studies | Authenticate regularly; monitor phenotypic stability |
| Animal Models | Conditional Sox9 knockout mice; xenograft models | In vivo functional validation | Consider genetic background; appropriate controls |
SOX9 represents a paradigm of developmental master regulators co-opted in carcinogenesis. Its pleiotropic functions in normal development—including progenitor cell maintenance, differentiation control, and tissue patterning—are systematically hijacked during tumorigenesis to drive cancer progression, metastasis, and therapy resistance. The emerging role of SOX9 as a regulator of immune cell infiltration and architect of immunosuppressive tumor microenvironments positions it as a compelling therapeutic target, particularly in the context of immunotherapy combinations.
Future research should prioritize the development of specific SOX9 inhibitors, elucidation of SOX9's role in therapy-induced immune changes, and comprehensive mapping of SOX9's immune-regulatory networks across cancer types. The integration of SOX9 targeting with existing immunotherapies represents a promising avenue for overcoming resistance and improving patient outcomes across multiple cancer types.
The SOX9 (SRY-box transcription factor 9) protein is a transcription factor with a highly conserved high-mobility group (HMG) box DNA-binding domain that recognizes the sequence CCTTGAG [1] [19]. This nuclear protein contains several functional domains organized from N- to C-terminus: a dimerization domain (DIM), the HMG box domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [1]. While SOX9 plays crucial roles in embryonic development, chondrogenesis, and stem cell regulation, its dysregulation has emerged as a significant oncogenic driver in numerous cancers [1] [19].
Beyond its established functions in tumor proliferation and metastasis, SOX9 has recently been identified as a master regulator of the tumor immune microenvironment [20] [21]. This whitepaper synthesizes current mechanistic insights into how SOX9 creates an immunosuppressive niche that fosters tumor immune evasion and resistance to immunotherapy. Understanding these mechanisms provides critical insights for developing novel therapeutic strategies to reverse immune suppression in SOX9-high tumors.
SOX9 as a Driver of Immune-Suppressive Tumor Microenvironments
Core Mechanisms of SOX9-Mediated Immune Evasion
SOX9 orchestrates a multifaceted immunosuppressive program through several interconnected mechanisms that collectively establish an 'immune-cold' tumor microenvironment (Table 1).
Table 1: Core Mechanisms of SOX9-Mediated Immune Suppression
| Mechanism | Key Findings | Experimental Evidence |
|---|---|---|
| Inhibition of Immune Cell Infiltration | Significantly reduces CD8+ T, NK, and dendritic cell infiltration | Flow cytometry, IHC in KrasG12D mouse LUAD; Analysis of TCGA datasets [20] |
| Collagen Deposition & Tumor Stiffness | Elevates collagen-related gene expression and increases collagen fibers | Histology, gene expression analysis in murine and human LUAD [20] |
| Immune Checkpoint Regulation | Upregulates B7x (B7-H4) immune checkpoint | Genetic screens in breast cancer models [21] |
| Stemness & Dormancy Programs | Promotes stem-like transcriptional state enabling immune evasion | RNA-seq, chromatin analysis in ovarian cancer and breast cancer models [19] [22] |
SOX9-Mediated Suppression of Cytotoxic Immunity
A primary mechanism through which SOX9 confers immune evasion is by functionally suppressing cytotoxic immune populations. In KrasG12D-driven lung adenocarcinoma (LUAD) models, SOX9 loss significantly increased infiltration of CD8+ T cells, natural killer (NK) cells, and dendritic cells (DCs) into tumors [20]. This effect was consistently observed across multiple cancer types, with bioinformatic analyses revealing that SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages [1]. These findings position SOX9 as a central regulator of cytotoxic immune exclusion.
SOX9 Modulation of the Physical Tumor Microenvironment
Extracellular Matrix Remodeling
Beyond direct effects on immune cell function, SOX9 significantly alters the physical properties of the tumor microenvironment. Research demonstrates that SOX9 elevates collagen-related gene expression and substantially increases collagen fiber deposition [20]. This extracellular matrix remodeling increases tumor stiffness, creating a physical barrier that impedes immune cell infiltration and activity. The proposed mechanism suggests that SOX9 increases tumor stiffness and inhibits tumor-infiltrating dendritic cells, thereby suppressing CD8+ T cell and NK cell infiltration and activity through both biochemical and biomechanical mechanisms [20].
Figure 1: SOX9-Mediated Extracellular Matrix Remodeling and Immune Suppression. SOX9 increases collagen deposition and tumor stiffness, creating a physical barrier that impairs immune cell infiltration and function.
Key Experimental Models and Methodologies
In Vivo Genetic Models
Several sophisticated genetic models have been instrumental in elucidating SOX9's immunomodulatory functions:
CRISPR/Cas9-Mediated Sox9 Knockout in KrasG12D LUAD: The pSECC CRISPR system was used to deliver Cre recombinase and Sox9-targeting guide RNAs (sgSox9.2-pSECC) via intratracheal instillation [20]. Control groups received tdTomato guide RNA (sgTom). Tumor burden and immune infiltration were analyzed at weeks 18, 24, and 30 post-delivery using histology, flow cytometry, and IHC.
Conditional Sox9 Knockout Mice: KrasLSL-G12D;Sox9flox/flox (KSf/f) mice were generated using Cre-LoxP technology [20]. Lenti-Cre was delivered intratracheally to activate KrasG12D expression and delete Sox9 simultaneously. Survival analysis, tumor grading, and immune profiling were performed at endpoint (380 days).
Inducible SOX9 Expression Systems: For breast cancer and skin cancer studies, Krt14-rtTA;TRE-Sox9 mice enabled doxycycline-inducible SOX9 expression in epithelial cells [2]. Tumor formation and immune profiling were conducted at multiple timepoints post-induction.
Organoid and Allograft Models
3D tumor organoid cultures derived from KrasG12D mouse lung tumors (mTC11, mTC14 cell lines) demonstrated that SOX9 overexpression significantly increased organoid size and cellularity [20]. Syngeneic allograft models using immunocompetent and immunocompromised mice revealed that SOX9-promoted tumor growth was significantly attenuated in immunodeficient hosts, indicating its immunomodulatory function depends on host immunity [20].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for Studying SOX9 in Tumor Immunity
| Reagent/Category | Specific Examples | Application & Function |
|---|---|---|
| Genetic Models | KrasLSL-G12D;Sox9flox/flox mice | Determine SOX9 loss-of-function effects in autochthonous tumors [20] |
| Krt14-rtTA;TRE-Sox9 mice | Inducible SOX9 expression for temporal control [2] | |
| Cell Lines | KrasG12D mouse lung tumor lines (mTC11, mTC14) | Organoid formation and allograft studies [20] |
| SOX9 Targeting | Sox9 guide RNAs (sgSox9.2) | CRISPR-mediated knockout [20] |
| Lentiviral SOX9 constructs | SOX9 overexpression studies [20] | |
| Analysis Tools | Anti-SOX9 antibodies | IHC, flow cytometry, Western blot [20] [18] |
| Immune cell markers (CD8, NK1.1, CD11c) | Flow cytometry and IHC for immune profiling [20] |
SOX9 in Cancer-Type Specific Contexts
Pan-Cancer Patterns
Analysis of SOX9 expression across 33 cancer types revealed it is significantly upregulated in 15 cancer types (including CESC, COAD, GBM, LIHC, LUAD, LUSC, PAAD) while being downregulated in only 2 cancers (SKCM, TGCT) [3]. This pan-cancer pattern underscores its broad oncogenic role while highlighting context-dependent functions.
Lung Adenocarcinoma
In LUAD, SOX9 is significantly upregulated in KRAS-mutant cases and drives tumor progression through immune suppression [20]. Patients with SOX9-high tumors show significantly shorter survival, and SOX9 expression correlates with reduced CD8+ T cell, NK cell, and dendritic cell infiltration [20].
Breast Cancer
In breast cancer, SOX9 triggers tumorigenesis by facilitating immune escape [3] [19]. A SOX9-B7x (B7-H4) axis safeguards dedifferentiated tumor cells from immune surveillance to drive breast cancer progression [21]. SOX9 also promotes stemness and maintains dormant cancer cells that evade immune detection [19].
Glioblastoma
In GBM, SOX9 expression correlates with immune cell infiltration and checkpoint expression, indicating its involvement in the immunosuppressive tumor microenvironment [18]. High SOX9 expression serves as a diagnostic and prognostic biomarker, particularly in IDH-mutant cases [18].
SOX9 as a Therapeutic Target
Current Therapeutic Investigations
Several strategic approaches are being explored to target SOX9-mediated immune suppression:
Small Molecule Inhibitors: Cordycepin (an adenosine analog) inhibits both protein and mRNA expression of SOX9 in a dose-dependent manner in cancer cell lines (22RV1, PC3, H1975), indicating its anticancer roles likely involve SOX9 inhibition [3].
Combination Immunotherapy: Given SOX9's role in establishing 'cold' tumors, combining SOX9 inhibition with immune checkpoint blockers represents a promising strategy. SOX9 loss synergizes with PD-L1/TMB for improved patient stratification [23].
Epigenetic Modulators: As SOX9 functions as a pioneer factor that competes for epigenetic regulators [2], targeting associated chromatin modifiers may disrupt its immunosuppressive program.
Technical Approaches for SOX9 Targeting
Figure 2: Strategic Approaches for Targeting SOX9-Mediated Immune Suppression. Multiple therapeutic strategies are being developed to inhibit SOX9 function or target its downstream immunosuppressive effectors.
SOX9 emerges as a master regulator of the tumor immune microenvironment, driving the formation of 'immune-cold' tumors through multiple integrated mechanisms. By suppressing cytotoxic immune cell infiltration, promoting extracellular matrix remodeling, upregulating immune checkpoints, and enforcing stemness programs, SOX9 creates a comprehensive immunosuppressive niche that facilitates tumor progression and therapy resistance.
The experimental frameworks and reagent tools outlined in this review provide a roadmap for continued investigation into SOX9-mediated immune evasion. As targeting SOX9 represents a promising strategy for reversing immune suppression across multiple cancer types, future work should focus on developing specific SOX9 inhibitors and rational combination therapies that convert 'cold' SOX9-high tumors into 'hot', immunoresponsive microenvironments.
Correlation Between SOX9 Expression and Specific Immune Cell Infiltration Patterns
The transcription factor SOX9 is increasingly recognized as a pivotal regulator within the tumor microenvironment (TME), where it demonstrates a profound capacity to modulate immune cell infiltration patterns across various cancer types. This whitepaper synthesizes current research elucidating the complex correlations between SOX9 expression levels and specific immune cell populations, including T lymphocytes, B cells, macrophages, and neutrophils. Through pan-cancer analyses and cancer-specific investigations, SOX9 emerges as a master regulator of immune evasion mechanisms, predominantly through the creation of immunosuppressive microenvironments. The findings summarized herein establish SOX9 as a compelling therapeutic target and prognostic biomarker in oncology, with significant implications for drug development and immunotherapeutic strategies.
SOX9 (SRY-box transcription factor 9) is a transcription factor belonging to the SOX protein family, characterized by a highly conserved high-mobility group (HMG) box domain that facilitates DNA binding and transcriptional regulation [24]. While initially studied for its crucial roles in embryonic development, chondrogenesis, and sex determination, SOX9 has more recently been identified as a significant contributor to cancer progression and immune regulation [1]. The protein contains several functional domains organized from N- to C-terminus: a dimerization domain (DIM), the HMG box domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [1].
In the context of cancer, SOX9 exhibits a dual nature, functioning as either an oncogene or tumor suppressor in a tissue-dependent manner [3]. Pan-cancer analyses reveal that SOX9 expression is significantly upregulated in fifteen cancer types, including glioblastoma (GBM), colorectal adenocarcinoma (COAD), liver hepatocellular carcinoma (LIHC), lung squamous cell carcinoma (LUSC), and pancreatic adenocarcinoma (PAAD), while being downregulated in only two cancers (skin cutaneous melanoma [SKCM] and testicular germ cell tumors [TGCT]) compared to matched healthy tissues [3]. Beyond its direct oncogenic functions, SOX9 has emerged as a key modulator of the tumor immune microenvironment, where it influences immune cell recruitment, differentiation, and function through complex regulatory networks [1].
Pan-Cancer Expression Patterns of SOX9 and Immune Infiltration
Comprehensive pan-cancer analyses have established that SOX9 expression significantly correlates with altered immune infiltration patterns across multiple cancer types. These correlations demonstrate considerable heterogeneity, reflecting the context-dependent nature of SOX9 function in different tumor microenvironments.
Table 1: SOX9 Expression Patterns and Correlation with Immune Infiltration Across Cancers
| Cancer Type | SOX9 Expression vs. Normal | Positive Correlation with Immune Infiltration | Negative Correlation with Immune Infiltration |
|---|---|---|---|
| Multiple Cancers (15 types) | Significantly increased [3] | Neutrophils, Macrophages, Activated mast cells [1] | B cells, Resting mast cells, Resting T cells, Monocytes [1] |
| Colorectal Cancer | Upregulated [3] | Activated T cells, Activated mast cells, Neutrophils [1] | B cells, Resting mast cells, Resting T cells, Monocytes, Plasma cells, Eosinophils [1] |
| Glioma/GBM | Upregulated [18] | Better prognosis in lymphoid invasion subgroups [18] | Correlated with immunosuppressive TME [18] |
| Liver Cancer | Upregulated [3] | Associated with glycolytic reprogramming [25] | CD8+ T cell function, NK cell function [1] |
| Melanoma | Significantly decreased [3] | (SOX9 acts as tumor suppressor) [3] | (SOX9 restoration inhibits tumorigenesis) [3] |
The prognostic implications of SOX9 expression further underscore its clinical relevance. High SOX9 expression is positively correlated with worst overall survival in lower grade glioma (LGG), cervical squamous cell carcinoma (CESC), and thymoma (THYM), suggesting its potential utility as a prognostic biomarker [3]. Interestingly, in glioblastoma, high SOX9 expression was remarkably associated with better prognosis in the lymphoid invasion subgroups, highlighting the complex, context-dependent relationship between SOX9 and immune responses [18].
Cancer-Type Specific Mechanisms and Relationships
Glioblastoma and Glioma
In glioblastoma, SOX9 is highly expressed and has been identified as a diagnostic and prognostic biomarker, particularly in isocitrate dehydrogenase (IDH)-mutant cases [18]. Its expression is closely correlated with immune infiltration and checkpoint expression, indicating its involvement in the immunosuppressive tumor microenvironment. Surprisingly, high SOX9 expression in GBM demonstrates a complex relationship with survival outcomes, showing association with better prognosis in specific lymphoid invasion subgroups, suggesting that the functional consequences of SOX9 expression may depend on the specific immune contexture within the TME [18].
Colorectal and Gastrointestinal Cancers
In colorectal cancer, SOX9 has been identified as a characteristic gene for early and late diagnosis, with its expression showing distinct correlations with various immune populations. The transcription factor negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while demonstrating positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1]. This pattern suggests that SOX9 contributes to an immune-evasion permissive microenvironment while simultaneously promoting pro-tumorigenic inflammatory responses.
Liver Cancers and Fibrosis
In hepatic fibrosis, a precancerous condition, SOX9 has been identified as one of six core glycolysis-related genes (GRGs) associated with disease progression, suggesting a connection between SOX9-mediated metabolic reprogramming and immune modulation [25]. Cluster analyses based on core GRGs revealed that patients with higher expression of these genes, including SOX9, exhibited significantly enhanced immune infiltration, particularly of adaptive immune cells, representing a mixed landscape of T cells, mast cells, and pro-fibrogenic cells distinct from innate immune-dominant profiles [25].
Lung Adenocarcinoma
Research has demonstrated that SOX9 suppresses the tumor microenvironment in lung adenocarcinoma and is mutually exclusive with various tumor immune checkpoints [18]. The infiltration of immune cells in lung adenocarcinoma is significantly influenced by multiple immune cell types, with high infiltration of all but Type 2 T helper (Th2) cells correlating with a favorable prognosis [26]. While the direct relationship between SOX9 and these infiltration patterns requires further investigation, the established role of SOX9 in LUAD progression suggests it contributes to the immunosuppressive landscape.
Experimental Models and Methodologies for Investigating SOX9-Immune Interactions
Bioinformatics and Computational Approaches
Multiple computational frameworks have been employed to decipher the relationship between SOX9 expression and immune infiltration patterns:
RNA Sequencing Data Analysis: SOX9 expression analysis typically begins with acquiring RNA-seq data from public repositories such as The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases [18]. Data preprocessing includes normalization of raw counts, batch effect correction using principal component analysis (PCA), and differential expression analysis with thresholds set at adjusted p-value < 0.05 and |log2FC| > 0.5-1 [25].
Immune Cell Infiltration Quantification: Infiltration levels of various immune cell types are commonly determined using several algorithms:
- CIBERSORT: Utilizes the LM22 signature matrix and 1,000 permutations to estimate immune cell proportions from bulk RNA-seq data [27].
- Single-sample Gene Set Enrichment Analysis (ssGSEA): Depends on integrated immune gene sets from published studies to determine immune cell infiltration [26].
- ESTIMATE Algorithm: Calculates immune and stromal scores to infer the presence of infiltrating cells [27].
Correlation Analysis: Statistical correlations between SOX9 expression and immune cell infiltration levels are typically evaluated using Spearman's rank correlation test, with significance thresholds set at p < 0.05 [18].
Functional Validation in Cellular Models
In vitro models are essential for validating bioinformatic predictions and elucidating mechanistic relationships:
Cell Culture Systems: Prostate cancer cells (22RV1, PC3) and lung cancer cells (H1975) have been employed to investigate SOX9-immune interactions. These cells are typically maintained in RPMI 1640 or DMEM medium supplemented with 10-15% fetal bovine serum and 1% penicillin/streptomycin at 37°C with 5% CO₂ [3].
SOX9 Modulation Experiments: Small molecule inhibitors, such as cordycepin (CD), have been used to inhibit SOX9 expression. Treatment protocols typically involve exposing cells to CD at final concentrations of 0, 10, 20, and 40 μM for 24 hours, followed by collection of protein and RNA for expression analysis [3].
Western Blot Analysis: Protein expression validation is performed through standard Western blot protocols. Cells are lysed in EBC buffer and 2×SDS loading buffer, followed by electrophoresis, transfer to PVDF membranes, and immunoblotting with SOX9-specific antibodies [3].
Gene Expression Analysis: Total RNA is extracted using standardized protocols (e.g., TRIzol method), followed by reverse transcription and quantitative PCR to monitor SOX9 mRNA expression levels [3].
Table 2: Essential Research Reagents for SOX9-Immune Infiltration Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Cell Lines | 22RV1, PC3, H1975 [3] | In vitro models for SOX9 functional studies |
| SOX9 Modulators | Cordycepin [3] | Small molecule inhibitor of SOX9 expression |
| Antibodies | Anti-SOX9 [3] | Protein detection via Western blot/IHC |
| Bioinformatics Tools | CIBERSORT, ESTIMATE [27] | Computational estimation of immune infiltration |
| Databases | TCGA, GTEx, HPA [18] | Sources of transcriptomic and proteomic data |
| Pathway Analysis Tools | ClusterProfiler, Metascape [18] | Functional enrichment analysis |
Molecular Mechanisms Underlying SOX9-Mediated Immune Regulation
SOX9 influences immune infiltration through multiple interconnected molecular pathways that collectively shape the tumor immune microenvironment.
Direct Transcriptional Regulation of Immune Factors
As a transcription factor, SOX9 directly binds to promoter regions of genes involved in immune cell recruitment and function. In thymoma, SOX9 expression is negatively correlated with target genes related to Th17 cell differentiation, primary immunodeficiency, PD-L1 expression, and the T-cell receptor signaling pathway, suggesting its involvement in immune dysregulation [3]. Through its HMG domain, SOX9 recognizes the CCTTGAG motif and regulates the expression of chemokines, cytokines, and immune checkpoint molecules that collectively determine the composition and functional state of immune infiltrates [3].
Metabolic Reprogramming of the Tumor Microenvironment
SOX9 has been identified as a core glycolysis-related gene in hepatic fibrosis, indicating its role in metabolic reprogramming that indirectly influences immune cell function [25]. The glycolytic switch in cancer cells and associated stromal components creates a metabolite-rich microenvironment that suppresses antitumor immunity while promoting the expansion of immunosuppressive cell populations, such as M2 macrophages and regulatory T cells [25].
Interaction with Key Signaling Pathways
SOX9 is a downstream effector and modulator of several embryonic signaling pathways, including TGFβ, WNT, BMP, IHH, NFκB, and HIF, all of which have established roles in immune regulation [28]. In chondrocytes, SOX9 transcriptional activity is modulated by anabolic factors (BMP7 and GREM1) and catabolic inhibitors (DKK1 and FRZb) [28]. These same pathways have parallel functions in immune cell differentiation and activation, positioning SOX9 as an integrative node between developmental signaling and immune responses in the TME.
Therapeutic Implications and Future Directions
The established correlation between SOX9 expression and immune infiltration patterns presents compelling therapeutic opportunities for cancer treatment.
SOX9 as a Therapeutic Target
Cordycepin (CD), an adenosine analog, has demonstrated the ability to inhibit both protein and mRNA expression of SOX9 in a dose-dependent manner in 22RV1, PC3, and H1975 cancer cells, indicating its potential as an anticancer agent that likely functions, at least partially, through SOX9 inhibition [3]. The development of more specific and potent SOX9 inhibitors represents a promising avenue for therapeutic intervention, particularly in cancers where SOX9 drives immunosuppression.
Immunotherapy Combinations
Given SOX9's association with immunosuppressive TMEs, targeting SOX9 may enhance the efficacy of existing immunotherapies, such as immune checkpoint inhibitors. SOX9 expression correlates with immune checkpoint expression in glioblastoma, suggesting that combined approaches might overcome resistance mechanisms [18]. Additionally, strategies focusing on SOX9-mediated metabolic reprogramming could normalize the metabolic microenvironment and restore antitumor immunity [25].
Biomarker Development and Patient Stratification
The consistent association between SOX9 expression patterns and specific immune infiltration signatures supports its development as a biomarker for patient stratification. In pancreatic ductal adenocarcinoma, patients can be classified into myeloid-enriched or adaptive-enriched tumor microenvironments, with myeloid enrichment associated with shorter overall survival [29]. Similar stratification approaches based on SOX9 expression and associated immune signatures could help identify patients most likely to benefit from specific therapeutic regimens.
SOX9 represents a critical regulatory node connecting tumor cell biology with immune responses in the tumor microenvironment. Through pan-cancer analyses and mechanistic studies, consistent patterns have emerged linking SOX9 expression with specific immune infiltration profiles, typically characterized by suppressed antitumor immunity and enhanced immunosuppressive populations. The molecular mechanisms underlying these correlations involve direct transcriptional regulation, metabolic reprogramming, and interactions with key signaling pathways. Further investigation into SOX9-immune interactions will advance our understanding of tumor immunology and provide novel therapeutic strategies for targeting the immune microenvironment in SOX9-driven cancers.
The SRY-related HMG-box 9 (SOX9) transcription factor represents a paradigm of functional duality in cancer biology. As a key developmental regulator involved in chondrogenesis, sex determination, and stem cell maintenance, SOX9 exhibits context-dependent roles that defy simple categorization [1] [30]. Emerging evidence positions SOX9 at the critical interface between tumor cells and the immune microenvironment, where it orchestrates complex transcriptional programs that can either suppress or promote tumorigenesis depending on cellular context [1]. This whitepaper synthesizes current understanding of SOX9's dualistic nature, with particular emphasis on its regulation of immune cell infiltration—a crucial determinant of therapeutic response and patient outcomes in multiple cancer types.
SOX9 belongs to the SOXE family of transcription factors, characterized by a conserved high-mobility group (HMG) box domain that facilitates DNA binding and nuclear localization [30]. The protein structure includes self-dimerization domains, the HMG domain, and transactivation domains that collectively enable SOX9 to regulate diverse transcriptional networks [1] [30]. Its functional complexity is further amplified through post-translational modifications, epigenetic regulation, and interactions with various signaling pathways, creating a multifaceted protein whose oncogenic or tumor-suppressive functions are dictated by specific cellular environments.
Molecular Architecture and Functional Domains of SOX9
The SOX9 protein contains several structurally and functionally distinct domains that enable its diverse biological activities. Understanding this molecular architecture is fundamental to deciphering its context-dependent functions in cancer.
Structural Domains and Their Functions
Table 1: Functional domains of the SOX9 protein
| Domain | Position | Primary Functions |
|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein-protein interactions and dimer formation |
| HMG Box | Central | DNA binding, nuclear localization, nucleocytoplasmic shuttling |
| Central Transcriptional Activation Domain (TAM) | Middle | Synergistic transcriptional activation with TAC |
| Proline/Glutamine/Alanine-rich Domain (PQA) | C-terminal | Transcriptional activation through unknown mechanisms |
| C-terminal Transcriptional Activation Domain (TAC) | C-terminal | Interacts with cofactors (e.g., Tip60), inhibits β-catenin |
The HMG domain serves dual roles, directing nuclear localization through embedded nuclear localization and export signals while facilitating sequence-specific DNA binding [1]. The C-terminal transcriptional activation domain (TAC) interacts with diverse cofactors such as Tip60 to enhance SOX9's transcriptional activity and is essential for β-catenin inhibition during cellular differentiation processes [1]. The central transcriptional activation domain (TAM) functions synergistically with TAC to augment SOX9's transcriptional potential, while the PQA-rich domain contributes to transcriptional activation through mechanisms that remain partially characterized [1].
Figure 1: SOX9 protein domain structure and primary functions. The HMG domain facilitates DNA binding and nuclear localization, while activation domains (TAM, TAC, PQA) enable transcriptional regulation through cofactor interactions.
Regulatory Mechanisms Controlling SOX9 Activity
SOX9 expression and function are regulated through multiple mechanisms that contribute to its context-dependent roles in cancer:
Transcriptional Regulation: SOX9 expression is controlled by epigenetic modifications including promoter methylation and histone acetylation. Hypermethylation of SOX9 promoter regions has been associated with silenced expression in specific cancer contexts [30].
Post-transcriptional Regulation: Non-coding RNAs, particularly microRNAs (miRNAs) and long non-coding RNAs (lncRNAs), significantly modulate SOX9 expression. For instance, miR-215-5p directly targets SOX9 and inhibits its expression in breast cancer models [19].
Post-translational Modifications: Phosphorylation at specific residues (e.g., serine 181) regulates SOX9 transcriptional activity and stability, creating interfaces with key signaling pathways such as AKT [19].
SOX9 as an Oncogene: Mechanisms and Immune Consequences
In most documented cancer contexts, SOX9 functions as a potent oncogene that drives tumor progression through multiple mechanisms while simultaneously shaping an immunosuppressive microenvironment.
Oncogenic Signaling Networks
Table 2: SOX9 as an oncogene across cancer types
| Cancer Type | Oncogenic Mechanisms | Impact on Immune Microenvironment |
|---|---|---|
| Lung Cancer | Accelerates KRAS-driven tumor formation; regulates stemness | Creates "immune cold" tumors; reduces immune cell infiltration [4] |
| Ovarian Cancer | Drives platinum resistance; reprograms cancer stem cells | Promotes immunoevasion; enriches stem-like transcriptional state [31] [32] |
| Breast Cancer | Promotes cell proliferation via AKT/SOX10 axis; regulates BCSC maintenance | Facilitates immune evasion of latent cancer cells [19] |
| Glioblastoma | Correlates with immune infiltration and checkpoint expression | Contributes to immunosuppressive TME; associated with specific immune subsets [33] [18] |
| Liver Cancer | Highly expressed in HCC tissues; promotes self-renewal | Associated with poor prognosis and altered immune landscape [30] |
In lung cancer, SOX9 overexpression accelerates KRAS-driven tumor formation and creates an "immune cold" microenvironment characterized by reduced immune cell infiltration [4]. This immune-evasion mechanism may explain why some KRAS-positive lung cancer patients exhibit poor responses to immunotherapy. SOX9 appears to actively suppress the infiltration and function of anti-tumor immune cells, though the precise molecular mediators remain under investigation.
In ovarian cancer, SOX9 drives platinum resistance through transcriptional reprogramming that establishes a stem-like state [32]. Northwestern Medicine researchers demonstrated that SOX9 is epigenetically upregulated in response to chemotherapy in ovarian cancer cell lines and patient samples [31]. Using CRISPR/Cas9 gene-editing, they established that SOX9 expression alone was sufficient to reprogram ovarian cancer cells into stem-like cancer cells that continuously self-renew, proliferate, and resist chemotherapy [31]. Single-cell RNA sequencing of primary patient tumors revealed a rare cluster of cells with high SOX9 expression and stem-like features, positioning SOX9 as a master regulator of this chemoresistant population [31].
SOX9-Mediated Regulation of Tumor Immune Microenvironment
SOX9 significantly influences the composition and function of immune cells within the tumor microenvironment through several established mechanisms:
Immune Cell Infiltration: Bioinformatics analyses of colorectal cancer data reveal that SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while positively correlating with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1].
Immune Checkpoint Regulation: In glioblastoma, SOX9 expression correlates with immune checkpoint expression and specific immune infiltration patterns, suggesting involvement in immunosuppressive pathway regulation [33] [18].
Latent Cancer Cell Survival: SOX9 and SOX2 help maintain dormant cancer cells in secondary metastatic sites by enabling evasion of immune surveillance under immunotolerant conditions [19].
Figure 2: SOX9 oncogenic functions in immune regulation. SOX9 overexpression promotes cancer stem cell properties and alters cytokine secretion, leading to reduced anti-tumor immunity and therapy resistance.
SOX9 as a Tumor Suppressor: ContextualExceptions
Despite its predominant oncogenic role, SOX9 demonstrates tumor-suppressive functions in specific cellular contexts, particularly in gastrointestinal malignancies.
Tumor Suppressive Mechanisms
In colon cancer, SOX9 acts as a tumor suppressor by inhibiting epithelial-mesenchymal transition (EMT) and suppressing SOX2 induction [34]. This tumor-suppressive activity contrasts sharply with its oncogenic functions in other cancer types and highlights the critical importance of cellular context in determining SOX9 activity. Mechanistic studies reveal that SOX9 suppresses tumor progression through constraint of pro-invasive transcriptional programs and stemness factors that would otherwise drive malignant progression.
Additional evidence supporting SOX9's tumor-suppressive role comes from studies of cervical cancer, where it transactivates p21WAF1/CIP1 and suppresses tumor growth [30]. In these contexts, SOX9 functions as a cell cycle regulator and differentiation promoter, opposing the proliferative and stem-like states it encourages in other malignancies.
Contextual Determinants of SOX9 Function
The factors that determine whether SOX9 functions as an oncogene or tumor suppressor include:
- Tissue of Origin: SOX9 exhibits tissue-specific functions rooted in its developmental roles
- Genetic Background: Mutational status of key pathways (e.g., Wnt/β-catenin, KRAS) influences SOX9 activity
- Epigenetic Landscape: Chromatin accessibility and methylation status dictate SOX9 transcriptional programs
- Cellular Differentiation State: SOX9 functions differently in stem versus differentiated cells
Experimental Approaches for Investigating SOX9 Function
Key Methodologies and Applications
Table 3: Experimental approaches for SOX9 functional analysis
| Methodology | Key Applications | Representative Findings |
|---|---|---|
| CRISPR/Cas9 Gene Editing | Functional knockout studies; gene activation | SOX9 ablation increases platinum sensitivity in ovarian cancer [32] |
| Single-cell RNA Sequencing | Tumor heterogeneity analysis; stem cell identification | Rare SOX9+ stem-like cell cluster identification in ovarian cancer [32] |
| Multiomics Integration | Transcriptomic and epigenomic profiling | SOX9 super-enhancer identification in chemoresistant cells [32] |
| Immune Cell Infiltration Analysis | Bioinformatics assessment of TME composition | SOX9 correlation with specific immune subsets in colorectal cancer [1] |
| Proteomic and Western Blotting | Protein expression validation | SOX9 upregulation confirmation in glioma tissues [33] [18] |
Research Reagent Solutions
Table 4: Essential research reagents for SOX9 investigation
| Reagent/Category | Specific Examples | Research Applications |
|---|---|---|
| Gene Editing Tools | CRISPR/Cas9 with SOX9-targeting sgRNA | Functional knockout studies; chemosensitivity assessment [32] |
| Expression Analysis | RNA-seq platforms; scRNA-seq | SOX9 expression profiling; transcriptional divergence measurement [32] |
| Protein Detection | Western blotting; immunohistochemistry | SOX9 protein level validation in clinical samples [33] [18] |
| Databases | TCGA; GTEx; LinkedOmics | Bioinformatics analysis of SOX9 in cancer cohorts [33] [18] |
| Cell Line Models | OVCAR4; Kuramochi; COV362 | In vitro chemoresistance studies [32] |
Therapeutic Implications and Future Directions
SOX9 as a Therapeutic Target
The context-dependent nature of SOX9 presents both challenges and opportunities for therapeutic targeting. Several strategic approaches have emerged:
Direct Targeting: Although transcription factors have traditionally been considered "undruggable," emerging strategies aim to develop small molecule inhibitors that disrupt SOX9-DNA or SOX9-cofactor interactions.
Epigenetic Modulation: Since SOX9 is epigenetically upregulated in chemoresistant cancers, epigenetic drugs such as DNA methyltransferase inhibitors or HDAC inhibitors may indirectly modulate SOX9 activity [30].
Combination Therapies: SOX9 inhibition may sensitize tumors to conventional chemotherapy, as demonstrated in ovarian cancer models where SOX9 ablation enhanced platinum sensitivity [32].
Immunotherapy Integration: In SOX9-high "immune cold" tumors, combining SOX9-targeted approaches with immunotherapies may overcome resistance mechanisms [4].
SOX9 as a Biomarker
SOX9 shows significant promise as a diagnostic, prognostic, and predictive biomarker across multiple cancer types:
Diagnostic Biomarker: SOX9 expression effectively distinguishes malignant from normal tissues in glioblastoma and other cancers [33] [18].
Prognostic Indicator: High SOX9 expression generally correlates with poor survival, though in specific contexts (such as IDH-mutant glioblastoma subgroups with lymphoid invasion) it associates with better prognosis [33] [18].
Predictive Biomarker: SOX9 levels may predict response to chemotherapy and immunotherapy, enabling treatment stratification [4] [32].
Figure 3: Clinical applications of SOX9 as a cancer biomarker. SOX9 expression analysis informs diagnosis, prognostic stratification, and prediction of therapy response across multiple cancer types.
SOX9 embodies the complexity of cancer biology, functioning as either an oncogene or tumor suppressor depending on cellular context. Its dualistic nature is particularly evident in its regulation of immune cell infiltration, where it can either foster an immunosuppressive microenvironment conducive to tumor progression or constraining malignant behavior in context-specific manners. The intricate relationship between SOX9 and the tumor immune microenvironment underscores its potential as both a therapeutic target and biomarker across multiple cancer types.
Future research directions should focus on elucidating the precise molecular determinants that dictate SOX9's functional outcomes, developing clinically viable targeting strategies, and validating SOX9's utility as a predictive biomarker for immunotherapy response. As these efforts advance, SOX9 will continue to provide critical insights into the fundamental mechanisms of cancer progression and treatment resistance while offering promising avenues for therapeutic intervention.
From Bench to Bedside: Analytical Methods and Therapeutic Targeting of SOX9
The SRY-box transcription factor 9 (SOX9) is a critical developmental regulator that has emerged as a significant oncogenic factor across diverse cancer types. Through advanced bioinformatics and multi-omics approaches, researchers have established that SOX9 expression is significantly upregulated in numerous malignancies and plays a pivotal role in regulating tumor immune microenvironments. This technical guide explores computational methodologies for analyzing SOX9 expression patterns, immune correlates, and clinical implications in pan-cancer datasets, providing researchers with standardized frameworks for investigating SOX9 as a potential diagnostic, prognostic, and therapeutic target.
SOX9 Expression Patterns Across Cancers
Pan-Cancer Expression Landscape
Comprehensive analyses of SOX9 expression across multiple cancer types reveal a consistent pattern of dysregulation. A recent pan-cancer study examining 33 different cancer types found that SOX9 expression was significantly increased in fifteen cancers compared to matched healthy tissues, including glioblastoma (GBM), colon adenocarcinoma (COAD), liver hepatocellular carcinoma (LIHC), lung squamous cell carcinoma (LUSC), and pancreatic adenocarcinoma (PAAD). Conversely, SOX9 expression was significantly decreased in only two cancer types: skin cutaneous melanoma (SKCM) and testicular germ cell tumors (TGCT) [3].
Table 1: SOX9 Expression Patterns Across Selected Cancer Types
| Cancer Type | Expression Direction | Clinical Association | Prognostic Value |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly increased | IDH-mutant status association | Better prognosis in lymphoid invasion subgroups |
| Lung Adenocarcinoma | Significantly increased | Correlates with tumor grading | Poorer overall survival |
| Colon Adenocarcinoma | Significantly increased | Diagnostic biomarker potential | Shorter overall survival in high-expression cases |
| Breast Cancer | Significantly increased | Promotes immune evasion | Correlates with chemotherapy resistance |
| Skin Cutaneous Melanoma | Significantly decreased | Tumor suppressor potential | Inhibits tumorigenicity in model systems |
Analytical Approaches for SOX9 Expression Quantification
Standardized pipelines for SOX9 expression analysis typically incorporate data from multiple repositories:
- TCGA (The Cancer Genome Atlas): Provides RNA-seq data for SOX9 across various cancer types
- GTEx (Genotype-Tissue Expression): Offers normal tissue expression baselines
- CCLE (Cancer Cell Line Encyclopedia): Facilitates in vitro validation studies
Recommended analytical workflow includes:
- Data acquisition and normalization using TCGAbiolinks or similar packages
- Differential expression analysis with DESeq2 or limma packages
- Batch effect correction using ComBat or similar algorithms
- Validation through protein-level assessment via Human Protein Atlas [18] [3]
SOX9 Regulation of Immune Cell Infiltration
Mechanisms of Immune Microenvironment Modulation
SOX9 exhibits a complex, "Janus-faced" role in immune regulation, functioning as both an activator and repressor across different immune cell populations [1]. The transcription factor operates through several key mechanisms:
Direct Transcriptional Regulation: SOX9 recognizes the CCTTGAG motif along with other HMG-box class DNA-binding proteins, directly influencing expression of immune-related genes [3].
Stemness Maintenance: SOX9 helps maintain cancer stem cell properties, preserving long-term survival and tumor-initiating capabilities while promoting immune evasion [19].
Cytokine and Chemokine Modulation: SOX9 expression correlates with altered cytokine profiles in the tumor microenvironment, particularly affecting IL-6, IL-8, and CCL5 signaling [19].
Immune Cell-Type Specific Infiltration Patterns
Correlation analyses between SOX9 expression and immune cell infiltration reveal distinct patterns across cancer types:
Table 2: SOX9 Correlation with Immune Cell Infiltration in Selected Cancers
| Cancer Type | Positively Correlated Immune Cells | Negatively Correlated Immune Cells |
|---|---|---|
| Colorectal Cancer | Neutrophils, macrophages, activated mast cells, naive/activated T cells | B cells, resting mast cells, resting T cells, monocytes, plasma cells, eosinophils |
| Lung Adenocarcinoma | Memory CD4+ T cells | CD8+ T cells, NK cells, M1 macrophages |
| Glioblastoma | Multiple infiltrating immune populations (context-dependent) | Variable based on molecular subtype |
In glioblastoma, particularly in IDH-mutant cases, high SOX9 expression remarkably associates with better prognosis in lymphoid invasion subgroups, suggesting a complex relationship between SOX9-mediated immune infiltration and clinical outcomes [18] [33].
Computational Methodologies and Experimental Protocols
Immune Infiltration Analysis Workflows
The following diagram illustrates a standardized computational workflow for analyzing SOX9-associated immune infiltration:
Detailed Methodologies for Key Analyses
Immune Cell Infiltration Estimation
CIBERSORT Methodology:
- Input: Normalized gene expression matrix (TPM or FPKM)
- Signature matrix: LM22 (22 immune cell phenotypes)
- Permutations: 1000 for accurate p-value calculation
- Filtering: Samples with CIBERSORT p < 0.05 considered for further analysis
- Normalization: CIBERSORT outputs normalized to sum to 1 for cross-sample comparison [35]
ssGSEA Implementation:
- Algorithm: Single-sample Gene Set Enrichment Analysis
- Application: Quantification of 24 immune cell types using specific gene signatures
- Packages: GSVA package in R (version 1.34.0 or higher)
- Normalization: Standard score transformation for comparative analysis [18]
Differential Expression and Functional Enrichment
SOX9-Associated Gene Identification:
- Tool: LinkedOmics for co-expression analysis
- Statistical threshold: Adjusted p-value < 0.05
- Visualization: Heatmaps of top 35 positively/negatively correlated genes [18]
Functional Enrichment Pipeline:
- GO/KEGG Analysis: ClusterProfiler package in R
- Parameters: |logFC| > 2, adjusted p-value < 0.05
- Gene Set Enrichment Analysis (GSEA): 1000 permutations, FDR q-value < 0.25 [18]
Table 3: Key Research Reagent Solutions for SOX9 and Immune Infiltration Studies
| Reagent/Resource | Function | Example Application | Key Features |
|---|---|---|---|
| Cordycepin | Small molecule SOX9 inhibitor | Downregulates SOX9 mRNA and protein expression in dose-dependent manner | Adenosine analog; inhibits SOX9 in 22RV1, PC3, and H1975 cell lines at 10-40μM concentrations |
| CIBERSORT | Computational deconvolution algorithm | Estimates 22 immune cell type fractions from bulk tumor transcriptomes | Support vector regression-based; most accurate method for immune cell discrimination |
| ESTIMATE Algorithm | Tumor microenvironment scoring | Infer stromal and immune scores in tumor samples | Calculates stromal, immune, and estimate scores from gene expression data |
| Anti-SOX9 Antibodies | Protein-level detection and validation | Western blot, immunohistochemistry of tumor vs. normal tissues | Validation through Human Protein Atlas; specificity for 56kDa SOX9 protein |
| TCGAbiolinks R Package | Integrated TCGA data access | Retrieval and analysis of SOX9 expression across cancer types | Accesses clinical, genomic, and transcriptomic data from TCGA |
SOX9 in Therapeutic Context and Clinical Translation
SOX9 as a Therapeutic Target
Emerging evidence positions SOX9 as a promising therapeutic target in multiple cancer contexts:
Cordycepin Treatment: This adenosine analog demonstrates dose-dependent inhibition of SOX9 at both protein and mRNA levels in prostate cancer (22RV1, PC3) and lung cancer (H1975) cell lines, suggesting its anticancer roles may operate through SOX9 inhibition [3].
Immunotherapy Interactions: SOX9 expression correlates with immune checkpoint expression in glioblastoma, indicating its potential involvement in immunosuppressive tumor microenvironments and possible synergy with checkpoint blockade therapies [18].
Chemotherapy Resistance: In breast cancer models, SOX9 contributes to chemoresistance through multiple pathways, including regulation of stemness properties and interaction with long non-coding RNAs such as linc02095 [19].
Diagnostic and Prognostic Applications
The clinical utility of SOX9 extends to diagnostic and prognostic applications:
Diagnostic Biomarker: SOX9 demonstrates high specificity and sensitivity in distinguishing tumor from normal tissues in multiple cancer types, with ROC analysis supporting its diagnostic value [18] [36].
Prognostic Models: Incorporation of SOX9 into nomogram prognostic models, alongside other factors like IDH status in glioblastoma, provides robust prediction of patient outcomes [18] [33].
Molecular Subtyping: SOX9 expression patterns contribute to refined molecular classification of tumors, enabling more precise prognostic stratification and therapeutic selection [37].
The integration of bioinformatics and multi-omics approaches has firmly established SOX9 as a critical regulator of oncogenesis and immune microenvironment composition across diverse cancer types. Standardized computational pipelines for analyzing SOX9 expression and immune correlates have enabled researchers to uncover complex relationships between this transcription factor and tumor biology. Future research directions should focus on developing SOX9-targeted therapeutic strategies, validating its utility in clinical diagnostic applications, and further elucidating the mechanistic basis of its immunomodulatory functions. The continued refinement of multi-omics analytical frameworks will undoubtedly yield additional insights into SOX9's multifaceted roles in cancer biology and treatment response.
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) is a transcription factor with a demonstrated role in development, stemness, and cancer progression. Recent evidence has positioned SOX9 as a crucial regulator of the tumor immune microenvironment, influencing immune cell infiltration, differentiation, and function [1]. This whitepaper explores how advanced transcriptional profiling technologies, particularly single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics, are revolutionizing our understanding of SOX9's complex role in cancer immunology at unprecedented cellular resolution.
SOX9 exhibits a Janus-faced, or dualistic nature in immunobiology. It can function as a proto-oncogene in most cancers, promoting immune escape, while in certain contexts, it supports tissue repair and maintains macrophage function [1]. This duality, coupled with its significant heterogeneity of expression and function across different cell types within the tumor ecosystem, necessitates investigation at the single-cell level. Bulk sequencing approaches, which average gene expression across all cells in a sample, mask this critical cellular heterogeneity and context-dependent function. scRNA-seq and spatial transcriptomics overcome this limitation, enabling researchers to precisely dissect SOX9's cell-type-specific expression patterns, its correlation with immune cell states, and its spatial coordination within the tumor niche.
SOX9 in Cancer and Immune Regulation: A Dual-Faced Factor
The SOX9 protein contains several key functional domains that orchestrate its activity as a transcription factor. The High Mobility Group (HMG) box is the defining DNA-binding domain, which also facilitates nuclear localization. The protein also contains a dimerization domain (DIM), two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain essential for its transcriptional potential [1]. SOX9 is involved in a wide array of biological processes, from chondrogenesis and sex determination to the regulation of progenitor cell populations.
The Dual Role of SOX9 in Tumor Immunity
Evidence from pan-cancer analyses and specific cancer type studies reveals SOX9's complex and often contradictory roles.
SOX9 as an Oncogene and Immune Suppressor: SOX9 is frequently overexpressed in numerous solid malignancies, including colorectal, liver, lung, and breast cancers [1] [3]. Its expression levels often correlate positively with tumor occurrence, progression, and poor prognosis. From an immunological perspective, SOX9 can promote an immunosuppressive tumor microenvironment (TME). In colorectal cancer, SOX9 expression negatively correlates with the infiltration of B cells, resting mast cells, and monocytes, while positively correlating with neutrophils and macrophages [1]. Similarly, in breast cancer, SOX9 facilitates immune escape by sustaining the stemness of latent cancer cells, allowing them to evade immune surveillance and survive in metastatic sites [16].
SOX9 in Tissue Homeostasis and Macrophage Function: Conversely, SOX9 also has protective and regenerative functions. Increased SOX9 levels help maintain macrophage function and contribute to cartilage formation and tissue repair [1]. This highlights its role as a "double-edged sword" in immunology, where its functional outcome is highly context-dependent [1].
Pan-Cancer Expression and Prognostic Value: A comprehensive analysis of SOX9 across 33 cancer types found its expression was significantly upregulated in fifteen cancers (including COAD, LIHC, PAAD) and downregulated in only two (SKCM and TGCT) compared to healthy tissues [3]. This same study established that high SOX9 expression is positively correlated with the worst overall survival in cancers like LGG, CESC, and THYM, underscoring its value as a prognostic biomarker [3].
The table below summarizes the association between SOX9 expression and patient survival across various cancer types.
Table 1: Association of SOX9 Expression with Patient Overall Survival (OS) in Pan-Cancer Analysis
| Cancer Type | SOX9 Expression vs. Normal | Correlation with Overall Survival |
|---|---|---|
| LGG | Increased | Shorter OS |
| CESC | Increased | Shorter OS |
| THYM | Increased | Shorter OS |
| ACC | Not Specified | Longer OS |
| SKCM | Decreased | Not Specified |
| TGCT | Decreased | Not Specified |
Source: Adapted from [3]
Single-Cell and Spatial Transcriptomics: Deciphering SOX9-Mediated Immune Modulation
The application of scRNA-seq and spatial transcriptomics has been instrumental in moving beyond bulk tissue averages to precisely define SOX9's influence on specific cellular subsets within the TME.
Revealing SOX9-Associated Immune Cell Infiltration Patterns
scRNA-seq enables the deconvolution of the TME into its constituent cell types—cancer cells, immune cells, and stromal cells—and allows for the correlation of SOX9 expression with specific immune cell populations.
In prostate cancer, integrated single-cell and spatial transcriptomic analyses revealed that an immune "desert" microenvironment, characterized by decreased effector CD8+ T cells and increased immunosuppressive Tregs and M2 macrophages, is associated with a subpopulation of club cells exhibiting high SOX9 and low androgen receptor (AR) expression [1]. This suggests a mechanism by which SOX9 may indirectly shape an immunosuppressive niche.
In lung adenocarcinoma (LUAD), scRNA-seq of ground-glass nodules (GGN) and part-solid nodules (PSN) has identified distinct macrophage subsets, including CXCL9+ and TREM2+ tumor-associated macrophages (TAMs), whose abundances shift during invasion and metastasis. While not directly measuring SOX9 in macrophages, this study showcases the power of scRNA-seq to dissect the immune contexture that SOX9 is known to modulate [38].
Elucidating Cell-Specific Functions of SOX9
Beyond correlation, these technologies can pinpoint the cell types where SOX9 is active and what pathways it regulates.
A study on adult cerebral cortex astrocytes used patch-based single-cell transcriptomics after Cas9-mediated deletion of SOX9. This revealed that SOX9 deletion in astrocytes had non-cell-autonomous effects, specifically affecting surrounding microglia (brain-resident immune cells) [39]. This finding highlights that SOX9 function in one cell type can remotely influence the state of neighboring immune cells, a complex relationship difficult to uncover without single-cell resolution.
In the precancerous gastric niche, scRNA-seq and spatial transcriptomics have identified SOX9 as a key driver gene for intestinal metaplasia (IM), a pre-malignant condition [40]. SOX9 was found to mark gastric stem cells and modulate their division, a process required for malignant transformation. Spatial context was critical for understanding the expansion of this SOX9-positive progenitor population during early carcinogenesis.
The following diagram illustrates the core workflow of a single-cell RNA sequencing experiment, from tissue dissociation to data analysis, which enables the discovery of SOX9's cell-specific functions.
Spatial Transcriptomics: Mapping the SOX9 Niche
Spatial transcriptomics adds a crucial layer of information by preserving the geographical context of gene expression.
In pulmonary fibrosis, image-based spatial transcriptomics was used to map 1.6 million cells, characterizing distinct spatial niches and the dysregulation associated with disease [41]. While focused on a non-cancerous disease, this study exemplifies the methodology's power to localize specific cell types and states within a complex tissue architecture. Applying this to cancer allows researchers to identify whether SOX9-expressing cells cluster in specific regions—for example, the invasive front, perivascular niches, or areas of immune exclusion—and what other cells they interact with.
In pancreatic ductal adenocarcinoma (PDAC), scRNA-seq analysis of ductal cells across disease stages (I-IV) showed that SOX9 is a common marker of ductal identity [42]. As cancer progressed, these ductal cells underwent significant transcriptional shifts, downregulating programs related to normal biological functions and upregulating pathways for cell adhesion and cytokine production. This suggests that SOX9-positive cancer cells dynamically evolve their interaction with the TME during malignancy.
Experimental Framework: Profiling SOX9 with Single-Cell Resolution
This section outlines a detailed experimental protocol for investigating SOX9's role in the TME using scRNA-seq, drawing from established methodologies in the cited literature.
Key Research Reagent Solutions
The following table catalogues essential reagents and tools required for executing a typical scRNA-seq study focused on SOX9.
Table 2: Essential Research Reagents for scRNA-seq Analysis of SOX9
| Reagent / Tool | Function / Purpose | Example / Note |
|---|---|---|
| Single-Cell Platform | Partitions cells/nuclei into nanoliter droplets for barcoding | 10x Genomics Chromium Controller [43] [38] |
| Library Prep Kit | Constructs sequencing libraries from barcoded cDNA | Chromium Next GEM Single Cell 3' Reagent Kits [38] |
| Sequencing Platform | Generates high-throughput sequence data | Illumina NovaSeq [43] |
| Bioinformatic Tools | Processes raw data, performs normalization, clustering, and analysis | Seurat R package [38], CellRanger [38] |
| Reference Genome | Aligns sequencing reads to a reference | Human (GRCh38) or Mouse (GRCm39) genome assembly [38] |
| Cell Sorting Markers | For pre-enrichment of specific populations (optional) | Antibodies against EpCAM (epithelial cells), CD45 (immune cells) |
Detailed scRNA-seq Wet-Lab Protocol
Sample Acquisition and Single-Cell Suspension Preparation:
- Obtain fresh tumor tissues and adjacent normal tissues via surgical resection [38].
- Immediately place tissue in ice-cold, oxygenated transport medium (e.g., RPMI 1640) [38].
- Mechanically mince the tissue using a scalpel and dissociate into a single-cell suspension using a GentleMACS Dissociator with a validated enzyme cocktail (e.g., collagenase IV, dispase, DNase I) [38].
- Pass the cell suspension through a 30-70 μm cell strainer to remove debris and obtain a single-cell suspension.
- Perform manual counting with a hemocytometer and assess cell viability using Trypan Blue or similar dyes. Aim for >90% viability.
Single-Cell Barcoding and Library Preparation:
- Adjust the cell concentration to the optimal range for your platform (e.g., 700-1,200 cells/μL for 10x Genomics).
- Load the cell suspension, along with master mix and barcoded gel beads, onto a microfluidic chip (e.g., Chromium Next GEM Chip) to generate Gel Bead-In-Emulsions (GEMs) [38].
- Inside each GEM, cells are lysed, and released mRNA is barcoded with a Unique Molecular Identifier (UMI) and cell barcode during reverse transcription [38].
- Break the emulsions, recover barcoded cDNA, and amplify it via PCR.
- Fragment the amplified cDNA and add sequencing adapters (P5 and P7) to construct the final library [38].
- Quality control the library using a Bioanalyzer or TapeStation to confirm fragment size distribution.
Sequencing:
- Pool libraries if multiplexing and sequence on an appropriate Illumina platform (e.g., NovaSeq 6000) to a sufficient depth (e.g., 50,000 reads per cell) [43].
Computational Analysis Workflow
Primary Data Processing:
- Use
Cell Ranger count(10x Genomics) or a similar pipeline to demultiplex raw sequencing data, align reads to a reference genome (e.g., GRCh38), and generate a feature-barcode matrix [38].
- Use
Quality Control and Filtering:
- Import the matrix into R/Python using Seurat [38] or Scanpy.
- Filter out low-quality cells: typically, those with <500 unique genes detected, >25% mitochondrial reads (indicating apoptosis or stress), or high UMI counts potential doublets [38].
- Remove doublets computationally using tools like
DoubletFinder[38].
Normalization, Integration, and Clustering:
- Normalize the data using methods like
SCTransform(Seurat) or log-normalization. - Identify the top highly variable genes.
- Perform linear dimensionality reduction (Principal Component Analysis).
- Use Harmony or Seurat's integration to correct for batch effects between samples [38].
- Conduct non-linear dimensionality reduction for visualization (UMAP/t-SNE).
- Cluster cells using a graph-based clustering algorithm (e.g., Louvain) to identify distinct cell populations [38].
- Normalize the data using methods like
SOX9-Focused Analysis:
- Cell Type Annotation: Manually annotate clusters using canonical markers (e.g.,
PTPRC/CD45 for immune cells,EPCAMfor epithelial,COL1A1for fibroblasts) [43] [42]. - SOX9 Expression Assessment: Visualize
SOX9expression across UMAP clusters and across pre-defined cell types [42]. - Differential Expression: Identify genes co-expressed with
SOX9or differentially expressed inSOX9high vs. low subpopulations within a specific cell type. - Trajectory Inference: Use tools like Monocle2 [42] or PAGA to investigate whether
SOX9expression is associated with developmental lineages or state transitions (e.g., in ductal cells or T cells). - Cell-Cell Communication: Infer potential interactions between
SOX9+cells and immune cells using tools like CellChat or NicheNet [42].
- Cell Type Annotation: Manually annotate clusters using canonical markers (e.g.,
The following diagram synthesizes the key findings on how SOX9 expression in different cellular compartments of the tumor microenvironment influences immune cell function and infiltration, as revealed by single-cell studies.
The integration of single-cell and spatial transcriptomics has fundamentally advanced our comprehension of SOX9 from a mere marker of cell fate to a dynamic, context-dependent orchestrator of the tumor immune landscape. These technologies have been pivotal in uncovering SOX9's cell-type-specific functions, its role in shaping immunosuppressive niches, and its influence on intercellular communication within the TME.
Looking forward, several emerging areas hold promise for both research and therapeutic development. There is a pressing need to further elucidate the spatial coordination of SOX9+ niches using multi-omics approaches that combine scRNA-seq with spatial transcriptomics and proteomics. Furthermore, investigating the potential of SOX9 as a therapeutic target is a compelling frontier. For instance, the natural compound Cordycepin has been shown to inhibit SOX9 expression in a dose-dependent manner in cancer cell lines, suggesting a potential avenue for therapeutic intervention [3]. Finally, the translation of SOX9-related findings into clinical applications, such as using SOX9-based signatures for patient stratification or as biomarkers for immunotherapy response, represents a critical next step. The continued application of high-resolution transcriptional technologies will be indispensable in driving these efforts forward, ultimately contributing to improved cancer diagnostics and therapies.
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator in developmental biology, stem cell maintenance, and carcinogenesis. Recent investigations have progressively illuminated its significant role in modulating tumor immunology, particularly through the regulation of immune cell infiltration within the tumor microenvironment (TME). In the context of cancer research, SOX9 influences key processes including cancer initiation, progression, invasiveness, and metastasis [44]. Utilizing Genetically Engineered Mouse Models (GEMMs) in combination with the precision of CRISPR-Cas9 genome editing provides an unparalleled approach to dissect the complex functions of SOX9. This technical guide outlines the methodologies for validating SOX9 function in vivo, specifically framing its role within the thesis that SOX9 is a master regulator of immune cell infiltration in cancer, a mechanism with profound implications for therapeutic resistance and biomarker development [18] [9].
SOX9 in Cancer and Immune Regulation: The Rationale for In Vivo Study
SOX9 as a Diagnostic, Prognostic, and Immune Modulator
Recent pan-cancer analyses reveal that SOX9 is highly expressed in a range of malignant tissues, including glioblastoma (GBM) [18]. Its role, however, appears context-dependent. While often associated with adverse outcomes, high SOX9 expression in GBM was remarkably associated with a better prognosis in specific subgroups, such as those with lymphoid invasion [18]. Multivariate Cox regression analysis further identified high SOX9 expression as an independent prognostic factor for IDH-mutant glioblastoma [18]. Critically, correlation analyses indicate that SOX9 expression is significantly correlated with immune cell infiltration and the expression of immune checkpoints in GBM, suggesting its intimate involvement in shaping the immunosuppressive tumor microenvironment [18].
Uncovering the SOX9-Anxa1-Fpr1 Axis in Therapy Resistance
A seminal 2025 study in head and neck squamous cell carcinoma (HNSCC) provided a mechanistic link between SOX9 and immune evasion. Using single-cell RNA sequencing in a mouse model resistant to anti-LAG-3 plus anti-PD-1 combination therapy, researchers identified a significant enrichment of Sox9+ tumor cells [9]. The study elucidated that Sox9 directly regulates the expression of annexin A1 (Anxa1). This interaction initiates a critical immune-suppressive pathway: the Anxa1 protein mediates apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils via the Anxa1-Fpr1 axis. This process promotes mitochondrial fission and inhibits mitophagy, ultimately preventing the accumulation of neutrophils in tumor tissues [9]. The reduction of these Fpr1+ neutrophils subsequently impairs the infiltration and tumor-cell killing ability of cytotoxic CD8 T and γδT cells, establishing a robust mechanism for resistance to combination immunotherapy [9]. This axis was validated using various transgenic mouse models, underscoring the power of in vivo systems [9].
Table 1: Key Findings Linking SOX9 to Cancer Immune Regulation
| Cancer Type | SOX9-Related Finding | Impact on Immunity & Therapy | Source |
|---|---|---|---|
| Glioblastoma (GBM) | High expression correlated with immune infiltration and checkpoints | Modifies tumor microenvironment; prognostic in IDH-mutant subgroups | [18] |
| Head and Neck SCC | Enriched in anti-LAG-3/anti-PD-1 resistant tumors | Initiates Anxa1-Fpr1 axis, depletes neutrophils, impairs cytotoxic T cells | [9] |
| Various Cancers | Overexpressed, regulates stemness and metastasis | Influences cancer stem cell (CSC) populations and immune interactions | [44] |
Preclinical Model Systems for SOX9 Investigation
Genetically Engineered Mouse Models (GEMMs)
GEMMs allow for de novo tumorigenesis within a natural immune-proficient environment, making them indispensable for studying the complex interplay between tumor cells and the immune system [45]. For SOX9 research, several modeling strategies can be employed:
- Conditional Knockout/Knockin Models: Using Cre-loxP or similar systems to target Sox9 deletion or expression in specific cell types (e.g., epithelial cells) and at defined time points. This is crucial for isolating its function in particular stages of tumorigenesis or in specific cellular compartments within the TME.
- Inducible Expression Models: Models that allow for the controlled induction of Sox9 expression are valuable for defining its role in established tumors and during therapeutic interventions.
- Transgenic Models for Cell-Specific Targeting: The development of transgenic driver lines, as part of large-scale toolkits, enables the selective targeting and manipulation of specific cortical cell populations, a approach that can be adapted for tumor cell-specific studies [46].
CRISPR-Cas9 for Precision Genome Editing
The CRISPR-Cas system, particularly the Cas9 nuclease from Streptococcus pyogenes (SpCas9), has revolutionized genome editing due to its reliance on easily programmable guide RNAs (gRNAs) for target specificity [44] [47]. Its applications in studying SOX family genes, including SOX9, are extensive. The system's versatility and feasibility have made it the most suitable tool for discovering gene functions and generating appropriate cellular and animal models [44]. Key applications include:
- Gene Knockout: Disrupting the Sox9 gene or its regulatory elements to study loss-of-function phenotypes.
- Gene Knock-in: Introducing specific mutations or reporter genes (e.g., GFP) into the Sox9 locus for lineage tracing or functional studies.
- Epigenetic Modulation: Using nuclease-deficient Cas9 (dCas9) fused to transcriptional activators/repressors to manipulate Sox9 expression without altering the underlying DNA sequence [47].
Experimental Protocols: Validating SOX9 Function In Vivo
Protocol: Generating a Sox9-Specific Knockout GEMM using CRISPR-Cas9
This protocol details the creation of a conditional Sox9 knockout model to investigate its cell-autonomous role in tumor cells.
Objective: To generate a floxed Sox9 mouse model (Sox9fl/fl) for Cre-dependent deletion in specific cell types. Materials:
- gRNAs: Two gRNAs targeting sequences flanking the critical exon(s) of the Sox9 gene (e.g., the HMG domain).
- Cas9 Protein: Purified SpCas9 protein.
- Donor DNA: A single-stranded DNA oligonucleotide donor containing the loxP sites, homologous arms, and a selectable marker (if needed).
- Microinjection Setup: Equipment for zygote microinjection and embryo transfer.
Method:
- gRNA Design and Validation: Design two gRNAs with high on-target efficiency and low off-target risk. Validate cleavage efficiency in vitro using a T7E1 assay or next-generation sequencing.
- Ribonucleoprotein (RNP) Complex Formation: Complex the validated gRNAs with SpCas9 protein to form RNPs.
- Zygote Microinjection: Co-inject the RNP complexes and the donor DNA template into fertilized mouse zygotes. The non-viral RNP delivery method is preferred for its reduced off-target effects and minimal cellular toxicity [47].
- Embryo Transfer and Founder Identification: Transfer the injected zygotes into pseudopregnant female mice. Genotype the resulting offspring (founders) via PCR and sequencing to identify those with correct loxP site integration.
- Breeding and Expansion: Cross the positive founder mice with Flp deleter mice to remove any selection cassette, then breed to establish a stable Sox9fl/fl line. Cross this line with a cell-type-specific Cre driver line (e.g., Keratin14-Cre for epithelial cells) to achieve targeted Sox9 deletion.
Protocol: In Vivo Validation of the SOX9-Anxa1-Fpr1 Axis
This protocol leverages a resistant HNSCC mouse model to functionally validate the mechanism of therapy resistance mediated by SOX9.
Objective: To confirm that Sox9 in epithelial cells mediates resistance to dual immunotherapy via the Anxa1-Fpr1 axis on neutrophils. Materials:
- Mouse Model: 4-nitroquinoline 1-oxide (4NQO)-induced HNSCC model in C57BL/6 wild-type and transgenic mice.
- Therapeutics: Anti-PD-1 and anti-LAG-3 blocking antibodies.
- Transgenic Models: Sox9fl/fl;K14-Cre mice and Fpr1-/- mice.
- Analysis Tools: Equipment for scRNA-seq, flow cytometry, and immunohistochemistry.
Method:
- Model Establishment and Treatment: Induce HNSCC in WT, Sox9fl/fl;K14-Cre (epithelial-specific Sox9 KO), and Fpr1-/- mice using 4NQO water for 16 weeks followed by 8 weeks of normal water [9].
- Therapy Administration: Treat tumor-bearing mice with control IgG, anti-PD-1, anti-LAG-3, or the combination. Monitor tumor growth and classify mice as resistant or sensitive based on RECIST criteria [9].
- Single-Cell RNA Sequencing: Pool and process resistant, sensitive, and control tumor tissues into single-cell suspensions. Perform scRNA-seq to identify cell populations and transcriptional profiles, specifically characterizing Sox9+ epithelial cells and Fpr1+ neutrophils [9].
- Functional Validation:
- Genetic Rescue: Compare therapy response and immune cell infiltration in Sox9fl/fl;K14-Cre mice versus WT controls.
- Neutrophil Depletion/Ablation: Assess if the absence of the Fpr1 receptor in Fpr1-/- mice recapitulates the resistant phenotype in a Sox9-independent manner.
- Mechanistic Analysis: Use flow cytometry to quantify tumor-infiltrating CD8+ T, γδT, and Fpr1+ neutrophils. Perform IHC/IF for Anxa1, Sox9, and cleaved-caspase 3 in neutrophil populations to assess apoptosis. Evaluate mitochondrial fission and BNIP3 expression in isolated neutrophils via Western blot.
Data Analysis and Integration
- Immune Infiltration Analysis: Utilize bioinformatic packages like ssGSEA and ESTIMATE to correlate Sox9 expression levels with immune cell infiltration scores from RNA-seq data [18].
- Pathway Enrichment Analysis: Perform GO and KEGG enrichment analyses on differentially expressed genes between Sox9-high and Sox9-low tumors to identify impacted biological processes and pathways [18].
Table 2: Key Research Reagents and Models for SOX9 Studies
| Reagent / Model Type | Specific Example / System | Function in SOX9 Research |
|---|---|---|
| Genetically Engineered Mouse Model (GEMM) | Sox9fl/fl;K14-Cre | Enables cell-type-specific (e.g., epithelial) knockout of Sox9 to study cell-autonomous functions. |
| Immunocompetent Tumor Model | 4NQO-induced HNSCC [9] | Models de novo tumorigenesis in an intact immune system to study SOX9-immune interactions. |
| CRISPR-Cas9 System | RNP Complexes (Cas9 + gRNA) [47] | Allows for precise Sox9 gene knockout, knock-in, or epigenetic regulation in vivo and in vitro. |
| Viral Delivery Vector | Adeno-associated virus (AAV) [44] | Used to deliver CRISPR components or gene constructs; enhancer AAVs can target specific cell types [46]. |
| Specialized NCG Mouse Model | NCG-hIL15-FcγR-KO [48] | Advanced immunodeficient model for evaluating human immune cell (e.g., CAR-T, NK) engraftment and function. |
Visualizing the Core Mechanism and Workflow
The following diagrams illustrate the key molecular mechanism of SOX9-mediated resistance and the overarching experimental workflow for its validation.
Diagram Title: SOX9-Anxa1-Fpr1 Axis Drives Immunotherapy Resistance
Diagram Title: Experimental Workflow for Validating SOX9 Function
The integration of sophisticated GEMMs with the precision of CRISPR-Cas9 technology provides a powerful, multifaceted platform to validate the in vivo functions of SOX9. The recent discovery of its role in driving resistance to combination immunotherapy via the Anxa1-Fpr1 axis underscores its critical function as a regulator of the tumor immune microenvironment. The experimental protocols and resources detailed in this guide offer a robust roadmap for researchers to systematically decode the mechanisms by which SOX9 modulates immune cell infiltration, ultimately contributing to the development of novel biomarkers and therapeutic strategies that target SOX9 pathways to overcome cancer resistance.
The transcription factor SOX9 has emerged as a critical regulator in cancer progression and therapeutic resistance, particularly through its role in modulating immune cell infiltration within the tumor microenvironment. This technical review comprehensively evaluates the potential of cordycepin, a natural nucleoside analogue derived from Cordyceps militaris, as a pharmacological inhibitor of SOX9. We synthesize recent evidence demonstrating cordycepin's multi-faceted mechanism of action, including direct SOX9 suppression, disruption of SOX9-mediated signaling pathways, and consequent remodeling of the tumor immune landscape. The article provides detailed experimental protocols for investigating cordycepin's effects on SOX9 expression and activity, along with analytical frameworks for assessing subsequent impacts on cancer biology and antitumor immunity. This evaluation positions cordycepin as a promising template for developing novel SOX9-targeted therapies to overcome immune evasion in cancer.
SRY-box transcription factor 9 (SOX9) belongs to the SOX family of transcription factors characterized by a highly conserved high-mobility group (HMG) DNA-binding domain. Beyond its well-established roles in embryonic development, chondrogenesis, and sex determination, SOX9 has gained significant attention as a key player in oncogenesis [1]. SOX9 is frequently overexpressed in diverse malignancies including glioblastoma, colorectal cancer, liver cancer, lung cancer, and breast cancer, where its expression often correlates with advanced disease stage, therapeutic resistance, and poor prognosis [18] [1] [49].
SOX9 contributes to tumor progression through multiple mechanisms: promoting vascularization, driving proliferation, enhancing metastatic potential, conferring resistance to apoptosis, and critically, modulating the tumor immune microenvironment [1]. Bioinformatic analyses of tumor datasets reveal that SOX9 expression significantly correlates with altered immune cell infiltration patterns, typically characterized by suppressed antitumor immunity and enhanced immunosuppressive cell populations [18] [1]. Specifically, SOX9 overexpression negatively correlates with cytotoxic CD8+ T cells, NK cells, and M1 macrophages while positively associating with immunosuppressive elements such as Tregs and M2 macrophages [1]. This capacity to shape an "immune desert" microenvironment makes SOX9 an attractive target for cancer immunotherapy [1].
Cordycepin as a Pharmacological Inhibitor of SOX9
Source and Chemical Properties
Cordycepin (3'-deoxyadenosine) is a natural nucleoside analogue isolated from the medicinal fungus Cordyceps militaris [50] [51]. Structurally, cordycepin differs from adenosine by the absence of a hydroxyl group at the 3' position of the ribose ring [51]. This minor structural modification enables cordycepin to interfere with various biochemical processes, including RNA synthesis, polyadenylation, and purine metabolism, through molecular mimicry [50] [51]. After cellular uptake, cordycepin undergoes phosphorylation to form cordycepin triphosphate, which can be erroneously incorporated into RNA chains, leading to premature transcription termination [51].
Direct Evidence for SOX9 Suppression
Recent studies have demonstrated that cordycepin directly suppresses SOX9 expression at both transcriptional and translational levels:
- Dose-dependent suppression: Treatment of cancer cell lines (22RV1, PC3, and H1975) with cordycepin resulted in significant reduction of both SOX9 mRNA and protein expression in a concentration-dependent manner [49].
- Pan-cancer relevance: Comprehensive analysis confirms SOX9 overexpression in 15 of 33 cancer types, highlighting the broad therapeutic potential of cordycepin-mediated SOX9 suppression [49].
- Mechanistic insights: Cordycepin appears to target SOX9 through multiple pathways, including inhibition of the Wnt/β-catenin signaling axis which is directly regulated by SOX9 [52] [53].
Table 1: Experimental Evidence for Cordycepin-Mediated SOX9 Suppression
| Cancer Model | Cordycepin Concentration | Exposure Time | Observed Effects on SOX9 | Reference |
|---|---|---|---|---|
| Prostate cancer (22RV1, PC3 cells) | 100-400 μM | 24 hours | Dose-dependent decrease in both mRNA and protein levels | [49] |
| Lung cancer (H1975 cells) | 100-400 μM | 24 hours | Dose-dependent decrease in both mRNA and protein levels | [49] |
| Diabetic liver fibrosis model | 5-20 mg/kg (in vivo) | 16 weeks | Inhibition of SOX9-mediated Wnt/β-catenin signal axis | [52] |
| Hepatic stellate cells (LX-2) | 12.5-50 μM | 24-48 hours | Suppressed SOX9 expression and nuclear β-catenin translocation | [52] |
Molecular Mechanisms of Action
Cordycepin modulates SOX9 activity and expression through several interconnected molecular pathways:
As illustrated in Figure 1, cordycepin targets SOX9 through both direct suppression and pathway modulation. A key mechanism involves disruption of the SOX9-Wnt/β-catenin positive feedback loop. SOX9 promotes β-catenin nuclear translocation and activates Wnt signaling, which in turn further stimulates SOX9 expression [52] [53]. Cordycepin interferes with this cycle by inhibiting β-catenin nuclear translocation and downstream Wnt signaling activity [52].
Immunomodulatory Consequences of SOX9 Suppression
Remodeling the Tumor Immune Microenvironment
SOX9 suppression by cordycepin triggers significant changes in the tumor immune landscape, potentially reversing immune evasion mechanisms employed by cancer cells:
- Enhanced immune cell cytotoxicity: Cordycepin treatment significantly enhances T-cell mediated killing of cancer cells in co-culture models. This effect is attributed to reduced PD-L1 expression on tumor cells and enhanced immune recognition [54] [55].
- Immune checkpoint regulation: Cordycepin targets the ubiquitin E3 ligase HRD1, promoting PD-L1 degradation through the ubiquitin-proteasome pathway. This mechanism synergizes with immune checkpoint inhibitors [54].
- NK cell activation: Cordycepin upregulates NKG2D ligand expression on cancer cells while simultaneously enhancing NKG2D receptor expression on natural killer (NK) cells, facilitating improved immune recognition and elimination [55].
- Cytokine modulation: Cordyceps militaris extract (containing cordycepin) stimulates production of immunostimulatory cytokines including IL-2, IL-6, and IL-10, further enhancing antitumor immunity [55].
Table 2: Immunomodulatory Effects of Cordycepin in Cancer Models
| Immune Parameter | Experimental System | Cordycepin Effect | Functional Outcome | Reference |
|---|---|---|---|---|
| PD-L1 expression | Colorectal cancer cells (HCT116, RKO) | Downregulation via HRD1-mediated degradation | Enhanced T-cell cytotoxicity | [54] |
| NKG2D ligands | Breast and hepatocellular carcinoma cells | Significant upregulation | Improved NK cell recognition | [55] |
| Immune cell cytotoxicity | Co-culture models (T cells + cancer cells) | 40-60% increase in cancer cell death | Enhanced tumor cell elimination | [54] [55] |
| Cytokine production | Immune cell cultures | Increased IL-2, IL-6, IL-10 | Enhanced immune activation | [55] |
| HLA-ABC expression | Cancer cell lines | Decreased expression | Reduced antigen presentation inhibition | [55] |
Impact on Immune Cell Infiltration Patterns
The correlation between SOX9 expression and immune cell infiltration has been extensively documented through bioinformatic analyses of tumor datasets:
- Negative correlations: High SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, monocytes, plasma cells, and eosinophils in colorectal cancer [1].
- Positive correlations: SOX9 shows positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells in specific cancer contexts [1].
- Therapeutic reversal: Cordycepin-mediated SOX9 suppression potentially reverses these patterns, though direct experimental validation requires further investigation.
Experimental Approaches for Evaluating Cordycepin
In Vitro Assessment Protocols
Cell Culture and Treatment Conditions
- Cell lines: Prostate cancer (22RV1, PC3), lung cancer (H1975), colorectal cancer (HCT116, RKO), hepatic stellate cells (LX-2), and other relevant models [52] [54] [49].
- Culture conditions: Maintain cells in appropriate media (RPMI 1640 or DMEM) supplemented with 10% FBS at 37°C with 5% CO₂ [49].
- Cordycepin treatment: Prepare cordycepin stock solution in suitable solvent (DMSO or water). Treatment concentrations typically range from 12.5-400 μM for 24-48 hours, depending on cell type and assay [52] [49].
SOX9 Expression Analysis
- qRT-PCR for mRNA quantification:
- Extract total RNA using TRIzol reagent
- Synthesize cDNA using reverse transcriptase
- Perform qPCR with SOX9-specific primers (forward: 5'-AGGAGAGCGAGCTGAGCAA-3', reverse: 5'-TGGTACTTGTAGTCCGGGTGGT-3')
- Normalize to housekeeping genes (GAPDH or β-actin) [49]
- Western blotting for protein quantification:
- Lyse cells in RIPA buffer with protease inhibitors
- Separate proteins (20-30 μg) by SDS-PAGE
- Transfer to PVDF membrane, block with 5% non-fat milk
- Incubate with anti-SOX9 primary antibody (1:1000) overnight at 4°C
- Incubate with HRP-conjugated secondary antibody (1:5000)
- Detect using ECL substrate and quantify band intensity [52] [49]
Functional Assays
- Cell viability: CCK-8 assay with 5×10³ cells/well, cordycepin treatment for 24h, measure absorbance at 450nm [54] [55].
- Immune cell cytotoxicity: Co-culture cancer cells with Jurkat cells overexpressing PD-1, assess tumor cell survival via crystal violet staining [54].
- Migration and invasion: Transwell assays with/without Matrigel coating, cordycepin treatment for 48h, count migrated/invaded cells [56].
In Vivo Evaluation Models
Diabetic Liver Fibrosis Model [52] [53]
- Animals: C57BL/6J mice (6-8 weeks old)
- Model induction: High-fat diet for 8 weeks + streptozotocin (STZ) injection (40 mg/kg for 3 consecutive days)
- Cordycepin treatment: 5-20 mg/kg administered orally for 16 weeks
- Endpoint analyses: Blood glucose monitoring, liver function tests (ALT, AST), histopathological examination (H&E, Masson's trichrome staining), SOX9 and Wnt pathway component analysis by immunohistochemistry
Subcutaneous Tumor Model [54]
- Animals: Female C57BL/6J mice (6-8 weeks old)
- Model establishment: Subcutaneous injection of MC38 colorectal cancer cells (5×10⁵ cells/mouse)
- Cordycepin treatment: 25-50 mg/kg daily via intraperitoneal injection
- Endpoint analyses: Tumor volume measurement, immunohistochemistry for SOX9 and PD-L1, immune cell infiltration analysis by flow cytometry
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating Cordycepin-Mediated SOX9 Suppression
| Reagent Category | Specific Examples | Application/Function | Reference |
|---|---|---|---|
| Cell lines | 22RV1, PC3, H1975, HCT116, RKO, LX-2 | In vitro models for SOX9 expression and drug response studies | [52] [54] [49] |
| Antibodies | Anti-SOX9, Anti-β-catenin, Anti-PD-L1 | Protein detection via Western blot, IHC, and flow cytometry | [52] [54] |
| Assay kits | CCK-8, EdU, Caspase-3/7 | Assessment of cell viability, proliferation, and apoptosis | [54] [55] |
| Animal models | HFD/STZ-induced diabetic mice, MC38 subcutaneous tumor model | In vivo evaluation of efficacy and mechanisms | [52] [54] |
| Molecular biology reagents | siRNA targeting SOX9 and β-catenin, lipofectamine transfection reagent | Mechanistic studies through gene knockdown | [52] |
Therapeutic Implications and Combination Strategies
The strategic inhibition of SOX9 by cordycepin presents several promising therapeutic applications:
Overcoming Chemoresistance SOX9 contributes to therapy resistance in multiple cancers, including temozolomide resistance in glioblastoma [56]. Cordycepin-mediated SOX9 suppression potentially reverses this resistance, as demonstrated by the synergistic effects observed when combining super-enhancer inhibitors with conventional chemotherapeutics [56].
Immunotherapy Synergy Cordycepin's dual action on SOX9 suppression and PD-L1 degradation creates favorable conditions for enhanced response to immune checkpoint inhibitors [54]. Preclinical data shows cordycepin exhibits potential synergistic therapeutic effects when combined with anti-CTLA-4 antibodies [54].
Metabolic Modulation In diabetic liver fibrosis models, cordycepin ameliorates hyperglycemia-induced liver dysfunction and fibrotic lesions through SOX9/Wnt/β-catenin pathway inhibition [52] [53]. This suggests applications in cancer-associated metabolic disorders.
Cordycepin represents a promising natural product template for developing SOX9-targeted therapies in cancer. Its multi-mechanistic approach—simultaneously suppressing SOX9 expression, disrupting associated signaling pathways, and modulating immune responses—positions it as a unique therapeutic candidate. The experimental protocols outlined herein provide robust frameworks for investigating cordycepin's effects in various cancer models, with particular relevance to overcoming immune evasion.
Future research should prioritize structure-activity relationship studies to develop cordycepin analogs with improved bioavailability and potency [51], combination strategies with existing immunotherapies [54], and validation in patient-derived organoid models and clinical trials. Furthermore, the relationship between SOX9 suppression and subsequent changes in immune cell infiltration requires detailed characterization using single-cell RNA sequencing and spatial transcriptomics approaches. As the field advances, cordycepin and its derivatives hold significant potential as targeted agents for disrupting SOX9-mediated immunosuppression in cancer.
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) transcription factor has emerged as a critical regulator in both embryonic development and cancer pathogenesis. Recent evidence has positioned SOX9 as a central node in the tumor ecosystem, influencing not only cancer cell-intrinsic processes like proliferation, stemness, and metastasis but alsoextensively remodeling the tumor immune microenvironment [57] [1]. This dual function makes SOX9 a promising predictive biomarker for patient stratification, particularly in the context of immunotherapy and targeted treatment approaches. The transcription factor operates as a "double-edged sword" in immunology, capable of both promoting immune escape through impairment of immune cell function and contributing to tissue maintenance and repair in different contexts [1]. This comprehensive review synthesizes current understanding of SOX9 as a predictive biomarker, with emphasis on its role in regulating immune cell infiltration, and provides technical guidance for its implementation in research and clinical applications.
SOX9 Expression Patterns Across Human Cancers
SOX9 demonstrates remarkably consistent overexpression patterns across diverse human malignancies. A comprehensive pan-cancer analysis revealed that SOX9 expression was significantly increased in fifteen different cancer types, including glioblastoma (GBM), colorectal cancer (COAD), esophageal cancer (ESCA), liver cancer (LIHC), lung squamous cell carcinoma (LUSC), ovarian cancer (OV), pancreatic cancer (PAAD), and stomach cancer (STAD), among others [3]. In contrast, SOX9 expression was significantly decreased in only two cancer types: skin cutaneous melanoma (SKCM) and testicular germ cell tumors (TGCT) [3]. This pattern suggests that SOX9 predominantly functions as a proto-oncogene across most human solid tumors.
Table 1: SOX9 Expression Patterns and Prognostic Value Across Selected Cancers
| Cancer Type | Expression Pattern | Prognostic Value | Correlation with Immune Features |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly upregulated [33] [18] | Better prognosis in lymphoid invasion subgroups; independent prognostic factor for IDH-mutant cases [33] | Correlated with immune cell infiltration and checkpoint expression [33] |
| Bone Tumors | Higher in malignant vs. benign tumors; highest in osteosarcoma [58] | Associated with high grade, metastasis, recurrence, poor therapy response [58] | Circulating SOX9 detectable in peripheral blood [58] |
| Liver Cancer (HCC) | Overexpressed in tumor tissues [57] | Poor disease-free and overall survival [57] | Regulates CSCs stemness via Frizzled-7 [57] |
| Colorectal Cancer | Significantly upregulated [3] [59] | Poor overall survival [59] | Negative correlation with B cells, resting mast cells, resting T cells; positive with neutrophils, macrophages [1] |
| Breast Cancer | Overexpressed in tumor tissues [57] [59] | Poor overall survival [57] [59] | SOX9-AS1 lncRNA inhibits immune infiltration [60] |
| Prostate Cancer | Overexpressed in tumor tissues [61] [59] | Poor relapse-free and overall survival [57] | Creates "immune desert" microenvironment; decreases CD8+ T cells, increases Tregs [1] |
The prognostic significance of SOX9 overexpression has been validated through systematic meta-analysis encompassing 3,307 patients across 17 studies, which confirmed that high SOX9 expression predicts unfavorable overall survival (HR: 1.66, 95% CI: 1.36-2.02) and disease-free survival (HR: 3.54, 95% CI: 2.29-5.47) in multivariate analysis [59]. Furthermore, pooled odds ratios indicated that SOX9 overexpression significantly correlates with aggressive clinicopathological features including large tumor size, lymph node metastasis, distant metastasis, and advanced clinical stage [59].
SOX9 as a Regulator of Tumor Immune Microenvironment
Mechanisms of Immune Modulation
SOX9 exerts profound effects on the tumor immune microenvironment through multiple interconnected mechanisms. It directly influences immune cell differentiation and function, particularly in T-cell development, where it cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating lineage commitment of early thymic progenitors [1]. This fundamental role in immune cell programming extends to the tumor context, where SOX9 actively shapes an immunosuppressive niche.
In the tumor ecosystem, SOX9 expression demonstrates consistent negative correlation with antitumor immune components while recruiting or activating immunosuppressive elements. In colorectal cancer, SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, but positively correlates with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1]. Similarly, in multiple cancer types, SOX9 overexpression negatively correlates with genes associated with the cytotoxic function of CD8+ T cells, NK cells, and M1 macrophages, while showing a positive correlation with memory CD4+ T cells [1].
Table 2: SOX9-Associated Immune Alterations in the Tumor Microenvironment
| Immune Component | Direction of Correlation | Functional Consequences |
|---|---|---|
| CD8+ T cells | Negative [1] | Reduced cytotoxic T-cell activity and tumor cell killing |
| NK cells | Negative [1] | Diminished innate immune surveillance |
| M1 Macrophages | Negative [1] | Decreased antitumor inflammatory responses |
| B cells | Negative [1] | Impaired humoral immunity |
| Tregs | Positive [1] | Enhanced immunosuppressive environment |
| M2 Macrophages | Positive [1] | Promotion of tissue remodeling and angiogenesis |
| Neutrophils | Positive [1] | Increased inflammatory support for tumor growth |
The emerging role of SOX9-related long noncoding RNAs adds another layer of immunoregulatory complexity. In triple-negative breast cancer, SOX9-AS1 overexpression has been shown to inhibit immune infiltration, particularly reducing populations of naïve B cells, CD8+ T cells, and γδ T cells [60]. This lncRNA-mediated mechanism represents an additional pathway through which the SOX9 axis suppresses antitumor immunity.
Impact on Immune Checkpoints and Therapeutic Resistance
SOX9 expression closely correlates with immune checkpoint expression patterns in various cancers. In glioblastoma, SOX9 expression significantly correlates with the expression of multiple immune checkpoints, indicating its involvement in establishing an immunosuppressive tumor microenvironment [33] [18]. This relationship positions SOX9 as a potential biomarker for predicting response to immune checkpoint inhibitors and for developing combination therapies that simultaneously target SOX9 signaling and immune checkpoints.
The transcription factor also contributes substantially to therapy resistance through multiple mechanisms. SOX9 has been demonstrated to confer resistance to conventional chemotherapeutics, targeted therapies, and radiotherapy across various cancer types [61]. In non-small cell lung cancer, SOX9 promotes resistance to EGFR-tyrosine kinase inhibitors by regulating β-catenin and epithelial-to-mesenchymal transition [61]. Similarly, in breast cancer, SOX9 expression has been linked to endocrine therapy resistance, while in hepatocellular carcinoma, it contributes to sorafenib resistance through regulation of cancer stem cell phenotypes [61].
Technical Guide: Experimental Approaches for SOX9 Analysis
Expression Analysis Methodologies
RNA Sequencing and Bioinformatics Analysis RNA-seq data from public databases such as The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) provide foundational resources for SOX9 expression analysis. The standard analytical workflow involves:
- Data acquisition of HTSeq-FPKM or HTSeq-Count data from TCGA repository [33] [18]
- Differential expression analysis using DESeq2 R package with thresholds of |logFC| > 2 and adjusted p-value < 0.05 [33]
- Functional enrichment analysis via GO/KEGG using ClusterProfiler package [33] [18]
- Gene Set Enrichment Analysis (GSEA) to elucidate functional and pathway differences between SOX9 high- and low-expression groups [33]
Protein Level Detection Techniques
- Immunohistochemistry (IHC): Formalin-fixed paraffin-embedded tissue sections are stained using SOX9 antibodies (commonly from Santa Cruz, Millipore, or Abcam) [58] [59]. Evaluation typically uses percentage scoring (PS) or immunoreactive score (IRS) systems.
- Western Blotting: Protein extracts from tumor tissues or cell lines are separated by SDS-PAGE, transferred to PVDF membranes, and probed with anti-SOX9 antibodies [58] [3]. This provides quantitative protein expression data.
- Immunofluorescence: Allows subcellular localization of SOX9 and co-localization studies with immune markers [3].
Circulating SOX9 Detection For liquid biopsy applications, SOX9 mRNA expression can be measured in peripheral blood mononuclear cells (PBMCs) using:
- RNA extraction from PBMCs followed by reverse transcription
- Quantitative real-time PCR with SYBR Green or TaqMan chemistry [58]
- Normalization to housekeeping genes (GAPDH, ACTB)
Immune Infiltration Analysis
Comprehensive assessment of SOX9-related immune infiltration involves multiple computational and experimental approaches:
Computational Deconvolution Methods
- ssGSEA (single-sample Gene Set Enrichment Analysis): Implemented through the GSVA package in R to estimate immune cell abundance from bulk RNA-seq data [33] [18]
- ESTIMATE Algorithm: Calculates immune and stromal scores to infer tumor purity [33]
- CIBERSORT: Deconvolutes transcriptomic data to quantify 22 immune cell subtypes [60]
- TIMER Database: Provides precomputed immune infiltration levels for TCGA samples
Experimental Validation Techniques
- Flow Cytometry: Surface and intracellular staining for immune cell markers (CD3, CD4, CD8, CD19, CD56, CD68, etc.) in tumor dissociates
- Immunofluorescence Multiplexing: Simultaneous detection of SOX9 and immune markers in tissue sections
- Spatial Transcriptomics: Mapping SOX9 expression patterns in relation to immune cell locations within tumor architecture [1]
Research Reagent Solutions for SOX9 Studies
Table 3: Essential Research Reagents for SOX9 Biomarker Investigation
| Reagent Category | Specific Examples | Application Notes |
|---|---|---|
| SOX9 Antibodies | Santa Cruz (sc-166505), Millipore (AB5535), Abcam (ab185966) | Validation for specific applications required; differences in performance for IHC vs. WB [59] |
| Cell Lines | 22RV1 (prostate cancer), PC3 (prostate cancer), H1975 (lung cancer), MDA-MB-231 (breast cancer) | Context-dependent SOX9 expression; baseline characterization essential [3] |
| Small Molecule Inhibitors | Cordycepin (adenosine analog) | Dose-dependent SOX9 inhibition; 10-40 μM range in cancer cells [3] |
| siRNA/shRNA | SOX9-specific silencing constructs | Validation of knockdown efficiency at both mRNA and protein levels critical |
| ELISA Kits | Human SOX9 ELISA kits | Serum/plasma detection; requires pre-analytical validation |
| PCR Assays | TaqMan Gene Expression Assays (SOX9: Hs00165814_m1) | Standardized quantification; normalisation to reference genes essential |
SOX9-Based Patient Stratification Framework
Diagnostic and Prognostic Integration
The development of SOX9-based patient stratification models requires integration of multiple data types. In glioblastoma, a robust nomogram prognostic model incorporating SOX9, OR4K2, and IDH status has demonstrated clinical utility for individualized prediction of overall survival [33] [18]. Similar approaches have been validated in liver fibrosis, where a panel of SOX9-regulated extracellular matrix proteins (OPN, GPNMB, FN1, SPARC, VIM) in patient serum correlates with disease severity and outperforms established clinical biomarkers for detecting early stages [62].
For circulating SOX9 detection, studies in bone cancer patients have demonstrated significantly elevated SOX9 expression in PBMCs from patients with malignant bone tumors compared to healthy individuals, with further elevation in patients with high-grade, metastatic, and recurrent tumors [58]. This circulating detection approach offers potential for minimally invasive monitoring and early detection.
Therapeutic Implications and Targeting Strategies
The strategic targeting of SOX9 encompasses multiple approaches:
- Direct transcriptional inhibition: Small molecules like cordycepin have demonstrated dose-dependent suppression of SOX9 expression in prostate and lung cancer cells [3]
- Post-transcriptional regulation: miRNA-based approaches (miR-101, miR-613, miR-490-3p) that target SOX9 mRNA [61]
- Combination with immunotherapy: Simultaneous targeting of SOX9 and immune checkpoints to reverse immunosuppression
- Therapeutic monitoring: Serial assessment of SOX9 expression and SOX9-regulated proteins as pharmacodynamic biomarkers
The integration of SOX9 status into therapeutic decision-making requires consideration of cancer type, molecular context, and immune microenvironment composition. For instance, in IDH-mutant glioblastomas, SOX9 expression serves as an independent prognostic factor [33], while in prostate cancer, SOX9 expression patterns may indicate lineage plasticity and treatment resistance [1].
SOX9 represents a promising predictive biomarker that integrates tumor-intrinsic signaling with immune microenvironment regulation. Its consistent overexpression across multiple cancer types, association with aggressive clinicopathological features, and demonstrable role in shaping immunosuppressive environments position SOX9 as a valuable tool for patient stratification. The ongoing development of standardized detection methodologies, computational frameworks for immune context analysis, and therapeutic targeting approaches will accelerate the clinical translation of SOX9-based stratification. Future research directions should focus on validating SOX9 in prospective clinical trials, developing standardized circulating biomarker assays, and exploring combination therapies that concurrently target SOX9 signaling and immune escape mechanisms.
Overcoming Hurdles: SOX9-Driven Resistance to Immunotherapy and Combination Strategies
Mechanisms of SOX9-Mediated Resistance to Anti-PD-1 and Anti-LAG-3 Therapy
The combination of anti-PD-1 and anti-LAG-3 immune checkpoint inhibitors (ICIs) represents a significant advancement in cancer immunotherapy, showing superior efficacy compared to monotherapies in treating various malignancies. However, a substantial proportion of patients develop resistance to this combination therapy. Recent research has identified the transcription factor SRY (sex determining region Y)-box 9 (SOX9) as a pivotal regulator of resistance mechanisms in head and neck squamous cell carcinoma (HNSCC) and other cancer types [9] [63]. This whitepaper delineates the molecular mechanisms by which SOX9 orchestrates an immunosuppressive tumor microenvironment (TME) and provides detailed experimental methodologies for investigating these resistance pathways, framed within the broader context of SOX9 regulation of immune cell infiltration in cancer research.
Core Mechanism: SOX9-Driven Immunosuppressive Axis
The SOX9-ANXA1-FPR1 Signaling Cascade
Recent findings demonstrate that SOX9 mediates resistance to anti-PD-1 and anti-LAG-3 combination therapy through a precisely regulated molecular cascade:
SOX9 Upregulation in Resistant Tumors: Single-cell RNA sequencing (scRNA-seq) analyses of HNSCC mouse models revealed significant enrichment of SOX9+ tumor cells in samples resistant to anti-LAG-3 plus anti-PD-1 therapy [9]. These SOX9+ tumor cells constituted distinct subclusters (designated E-resi1 and E-resi2) that were predominantly present in resistant tumors [9].
Transcriptional Regulation of ANXA1: SOX9 directly binds to and regulates the expression of annexin A1 (Anxa1), a protein involved in apoptosis and inflammatory responses [9] [63]. Chromatin immunoprecipitation (ChIP) assays confirmed direct promoter binding of SOX9 to Anxa1 regulatory regions.
Neutrophil Apoptosis via FPR1: The ANXA1 protein secreted by SOX9+ tumor cells interacts with formyl peptide receptor 1 (Fpr1) expressed on neutrophils [9]. This ANXA1-FPR1 axis induces a signaling cascade that promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (Bnip3) expression, ultimately triggering apoptosis in Fpr1+ neutrophils [9] [63].
Immune Cell Exclusion: The reduction of Fpr1+ neutrophils impairs the infiltration and cytotoxic activity of CD8+ T cells and γδT cells within the TME, creating an "immune desert" and enabling tumor immune escape [9] [1].
Table 1: Key Components of the SOX9-Mediated Resistance Pathway
| Component | Full Name | Function in Resistance Pathway | Experimental Evidence |
|---|---|---|---|
| SOX9 | SRY-box transcription factor 9 | Master regulator; initiates resistance pathway by transcriptionally activating ANXA1 | scRNA-seq, transgenic mouse models, ChIP [9] |
| ANXA1 | Annexin A1 | Mediates apoptosis of Fpr1+ neutrophils | KO/KD models, antibody blockade [9] [63] |
| FPR1 | Formyl peptide receptor 1 | Neutrophil surface receptor for ANXA1; mediates apoptotic signaling | Flow cytometry, transgenic models [9] |
| BNIP3 | BCL2/adenovirus E1B 19kDa interacting protein 3 | Regulates mitophagy; downregulated by ANXA1-FPR1 signaling | Western blot, qPCR [9] |
| Cd8 T cells | Cytotoxic T lymphocytes | Impaired infiltration and killing capacity in resistant TME | Flow cytometry, immunohistochemistry [9] |
| γδT cells | Gamma delta T cells | Reduced tumor infiltration in resistant microenvironment | scRNA-seq, immune profiling [9] |
SOX9 as a Regulator of Immune Cell Infiltration
Beyond the specific ANXA1-FPR1 axis, SOX9 exhibits broader regulation of immune cell infiltration across cancer types:
Correlation with Immunosuppressive Microenvironments: Bioinformatics analyses of human cancer datasets reveal that SOX9 overexpression negatively correlates with genes associated with CD8+ T cell function, NK cell activity, and M1 macrophage polarization [1]. Conversely, SOX9 shows positive correlation with immunosuppressive cell populations, including M2 macrophages and regulatory T cells (Tregs) in certain contexts [1].
Dual Role in Different Cancers: While SOX9 primarily acts as an oncogene in most cancers (including HNSCC, colorectal, and lung cancers), it can function as a tumor suppressor in specific contexts such as melanoma [3]. This duality underscores the context-dependent nature of SOX9 immunoregulation.
Association with Clinical Outcomes: High SOX9 expression correlates with poor overall survival in multiple cancer types, including low-grade glioma (LGG), cervical squamous cell carcinoma (CESC), and thymoma (THYM) [3], highlighting its clinical significance as a prognostic biomarker and potential therapeutic target.
Experimental Models & Methodologies
In Vivo Modeling of Therapy Resistance
HNSCC Mouse Model Establishment Protocol [9]:
Carcinogen Induction:
- Utilize 8-12 week old C57BL/6 wild-type (WT) mice
- Administer 4-nitroquinoline 1-oxide (4NQO) in drinking water (100 μg/mL) for 16 weeks
- Replace with normal water for additional 8 weeks to permit HNSCC development
Therapy Administration:
- Randomize tumor-bearing mice into four treatment groups (n=7-10/group):
- Control IgG
- Anti-PD-1 monotherapy
- Anti-LAG-3 monotherapy
- Anti-LAG-3 + anti-PD-1 combination therapy
- Administer treatments via intraperitoneal injection every 4 days
- Monitor tumor size every 4 days from initial treatment
- Randomize tumor-bearing mice into four treatment groups (n=7-10/group):
Resistance Classification:
- Apply Response Evaluation Criteria in Solid Tumors (RECIST)
- Classify as "resistant" if tumor volume increases >20% from baseline 14 days post-treatment initiation
- Approximately 42.9% of animals typically develop resistance [9]
Validation Techniques:
- Magnetic Resonance Imaging (MRI): Monitor tumor growth processes in live animals
- Histopathological Analysis: H&E staining of tongue tissues for advanced tumor phenotypes
- Immunohistochemistry (IHC): Assess cell proliferation (Ki67) and apoptosis (cleaved-Caspase3)
Diagram Title: Experimental Workflow for SOX9 Resistance Mechanism Investigation
Single-Cell RNA Sequencing Protocol
Comprehensive Immune Cell Profiling Workflow [9]:
Sample Preparation:
- Pool tumor tissues from three mice per experimental group
- Digest tissues into single-cell suspensions using collagenase/hyaluronidase cocktail
- Split suspensions into two technical replicates for library construction
scRNA-seq Processing:
- Use 10X Genomics platform for library preparation
- Sequence to depth of >50,000 reads per cell
- Target cell recovery: >4,500 cells per sample
Bioinformatic Analysis:
- Quality Control: Filter cells with >10% mitochondrial reads or <200 detected genes
- Cell Type Identification: Use canonical markers:
- Epithelial cells: Krt14, Krt5, Krt6a
- Immune cells: Ptprc, Cd74, Cd3g
- Fibroblasts: Col1a1, Col3a1, Apod
- Endothelial cells: Flt1, Pecam1, Eng
- Malignant Cell Identification: Apply CopyKAT algorithm to distinguish aneuploid tumor cells
- Differential Expression: Identify SOX9+ subpopulations using Seurat
Validation Experiments:
- Flow Cytometry: Confirm immune cell population changes (CD8+ T cells, γδT cells, neutrophils)
- IHC/IF: Verify protein-level expression of SOX9, ANXA1, and FPR1
- Functional Assays: Assess neutrophil apoptosis via TUNEL staining
Table 2: Key Research Reagent Solutions for SOX9 Resistance Studies
| Reagent/Cell Line | Specific Type/Model | Experimental Function | Research Context |
|---|---|---|---|
| Mouse Model | C57BL/6 WT with 4NQO-induced HNSCC | In vivo therapy response and resistance modeling | Primary resistance model [9] |
| Transgenic Models | SOX9 knockout/overexpression models | Validate causal role of SOX9 in resistance | Mechanism confirmation [9] |
| Cancer Cell Lines | 22RV1, PC3, H1975 | In vitro SOX9 manipulation and signaling studies | Cordycepin testing [3] |
| SOX9 Inhibitor | Cordycepin (adenosine analog) | Small molecule inhibition of SOX9 expression | Therapeutic intervention studies [3] |
| Antibodies | Anti-PD-1, Anti-LAG-3, Anti-ANXA1 | Immune checkpoint blockade and pathway inhibition | Therapy and mechanism blockade [9] [64] |
| scRNA-seq Platform | 10X Genomics with Cell Ranger | Single-cell transcriptomic profiling | Tumor microenvironment characterization [9] |
The SOX9 Immunoregulatory Network
Molecular Regulation of SOX9
SOX9 expression and activity are regulated through multiple mechanisms that contribute to its role in therapy resistance:
Transcriptional Regulation: SOX9 expression is controlled by promoter methylation status and enhancer activation in cancer cells. Hypomethylation of the SOX9 promoter correlates with increased expression in multiple cancer types [1].
Post-Translational Modifications (PTMs):
- Acetylation and SUMOylation: Promote nuclear translocation of SOX9, enhancing its transcriptional activity [65]
- Phosphorylation: Modulates DNA binding affinity and protein stability
- Ubiquitination: Regulates SOX9 protein degradation and turnover
Non-Coding RNA Regulation:
- miRNAs: Multiple miRNAs (e.g., miR-101, miR-145, miR-214) directly target SOX9 3'UTR to suppress its expression
- lncRNAs: Several long non-coding RNAs (e.g., HOTAIR, MALAT1) regulate SOX9 expression through competitive endogenous RNA (ceRNA) mechanisms [1]
SOX9 in the Broader Immune Context
SOX9 interacts with multiple immune components beyond the ANXA1-FPR1 axis:
T Cell Development: SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), modulating lineage commitment of early thymic progenitors and influencing the balance between αβ T cell and γδ T cell differentiation [1].
Myeloid Cell Regulation: In addition to neutrophils, SOX9 expression influences macrophage polarization and function. High SOX9 levels in tumors correlate with increased M2-like macrophage signatures, associated with immunosuppression [1].
Cytokine and Chemokine Modulation: SOX9 regulates the expression of various chemokines that control immune cell trafficking, including CXCL12 and CCL5, further shaping the immune landscape of tumors [65].
Diagram Title: SOX9 Immunoregulatory Network in Therapy Resistance
Therapeutic Implications & Future Directions
Targeting the SOX9 Pathway
Several strategic approaches show promise for overcoming SOX9-mediated therapy resistance:
Direct SOX9 Inhibition:
- Cordycepin: This adenosine analog inhibits both protein and mRNA expression of SOX9 in a dose-dependent manner in cancer cell lines (22RV1, PC3, H1975) [3]. Treatment with 10-40 μM cordycepin for 24 hours significantly reduces SOX9 expression.
- Small Molecule Development: High-throughput screening approaches are identifying compounds that disrupt SOX9 DNA-binding or protein-protein interactions.
ANXA1-FPR1 Axis Targeting:
- ANXA1 Neutralization: Monoclonal antibodies against ANXA1 block its interaction with FPR1 on neutrophils
- FPR1 Antagonists: Small molecule inhibitors of FPR1 prevent ANXA1-mediated neutrophil apoptosis
Combination Immunotherapy:
- Rational combination strategies that target SOX9 signaling alongside immune checkpoint blockade
- Sequential therapy approaches to precondition the TME before ICI administration
Biomarker Development
SOX9 represents a promising biomarker for predicting therapy response and patient stratification:
Predictive Value: High SOX9 expression in tumors may identify patients less likely to respond to anti-PD-1/anti-LAG-3 combination therapy [4]. Assessment of SOX9 expression status could guide therapeutic decisions between different immunotherapy regimens.
Measurement Platforms:
- IHC Assays: Robust clinical-grade IHC assays for SOX9 protein detection
- Liquid Biopsies: Circulating tumor cell SOX9 expression as a non-invasive monitoring approach
- Multiplexed Spatial Transcriptomics: Simultaneous assessment of SOX9 expression and immune cell infiltration within tumor regions
SOX9 has emerged as a central regulator of resistance to anti-PD-1 and anti-LAG-3 combination immunotherapy through its role in shaping an immunosuppressive tumor microenvironment. The elucidated SOX9-ANXA1-FPR1 pathway provides both explanatory power for clinical resistance patterns and actionable targets for therapeutic intervention. Future research directions should focus on validating these mechanisms in human tumors, developing clinical-grade SOX9 detection assays, and advancing combination strategies that counteract SOX9-mediated immunosuppression. Integration of SOX9 status into immunotherapy treatment algorithms holds significant promise for personalizing cancer immunotherapy and overcoming treatment resistance.
The regulation of immune cell infiltration into the tumor microenvironment (TME) is a cornerstone of cancer biology and a critical determinant of the efficacy of immunotherapies. Within this context, the transcription factor SRY (sex determining region Y)-box 9 (SOX9) has emerged as a pivotal, though double-edged, regulator. While essential for developmental processes and tissue homeostasis, SOX9 is frequently overexpressed in various solid malignancies, where its expression levels positively correlate with tumor occurrence and progression [1]. SOX9 helps tumor cells maintain a stem-like state and is significantly implicated in chemoresistance and malignant potential [1] [66]. A key aspect of its oncogenic function is its ability to shape an immunosuppressive TME. Bioinformatics analyses reveal that SOX9 expression negatively correlates with the infiltration levels of cytotoxic immune cells, such as CD8+ T cells and NK cells, while often showing a positive correlation with immunosuppressive populations like neutrophils and macrophages [1]. This manipulation of the immune landscape facilitates immune evasion, a major challenge in oncology that allows tumors to evade surveillance and destruction [67]. This whitepaper delves into a specific and potent mechanism of SOX9-driven immune evasion: its regulation of the Annexin A1-Formyl Peptide Receptor 1 (ANXA1-FPR1) axis to induce neutrophil apoptosis, thereby impairing anti-tumor immunity and driving resistance to combination immunotherapy.
Molecular Mechanism of the SOX9-ANXA1-FPR1 Pathway
The molecular pathway connecting SOX9 to neutrophil apoptosis and immune evasion has been elucidated through sophisticated in vivo modeling and single-cell analyses. The core mechanism can be broken down into a series of distinct, sequential steps, as illustrated in the diagram below and detailed thereafter.
Diagram 1: The SOX9-ANXA1-FPR1 Signaling Axis in Therapy Resistance. This diagram illustrates the sequential molecular and cellular events, from SOX9 upregulation in tumor cells to the establishment of a therapy-resistant tumor microenvironment.
- SOX9 Upregulation in Resistant Tumors: The pathway is initiated by the significant enrichment of Sox9+ tumor cells in samples resistant to anti-LAG-3 and anti-PD-1 combination therapy, as identified by single-cell RNA sequencing (scRNA-seq) in a head and neck squamous cell carcinoma (HNSCC) mouse model [9].
- Transcriptional Regulation of ANXA1 by SOX9: The transcription factor SOX9 directly binds to regulatory elements and activates the transcription of the ANXA1 gene [9]. This leads to the overexpression and secretion of the ANXA1 protein into the TME.
- ANXA1-FPR1 Interaction and Neutrophil Apoptosis: The secreted ANXA1 protein acts as an external signal, binding to Formyl Peptide Receptor 1 (FPR1) on the surface of neutrophils [9]. This ligand-receptor interaction triggers an intracellular signaling cascade within the neutrophil that promotes mitochondrial fission and, critically, inhibits mitophagy (the selective autophagy of damaged mitochondria) by downregulating the expression of BCL2/adenovirus E1B interacting protein 3 (Bnip3) [9]. The disruption in mitochondrial homeostasis and energy balance ultimately forces the neutrophil into apoptosis.
- Cellular Consequences in the Tumor Microenvironment: The ANXA1-FPR1-mediated induction of apoptosis in Fpr1+ neutrophils prevents their accumulation within tumor tissues [9]. This reduction of neutrophils in the TME is not a bystander effect; it directly impairs the infiltration and tumor-cell killing ability of cytotoxic CD8+ T cells and γδT cells [9]. The loss of this coordinated immune attack renders the combination immunotherapy ineffective, leading to the outgrowth of treatment-resistant tumors.
Key Experimental Data and Evidence
The existence and significance of the SOX9-ANXA1-FPR1 axis are supported by robust in vivo data. The following tables summarize the key quantitative findings and experimental models that validate this pathway.
Table 1: In Vivo Therapeutic Response and Cellular Proportions in HNSCC Mouse Model
| Experimental Group | Therapy Response Rate | Proportion of Immune Cells in TME (scRNA-seq) | Key Phenotypic Observations |
|---|---|---|---|
| Combination Therapy-Sensitive | 57.1% (8/14 animals) | Dramatically increased | Partial reduction in tumor progression; almost complete tumor eradication; decreased Ki67 (cell proliferation); greatly elevated cleaved-Caspase3 (apoptosis) [9]. |
| Combination Therapy-Resistant | 42.9% (6/14 animals) | Comparable to control | Tumors grew >20% larger; advanced tumor phenotype; high Ki67; low cleaved-Caspase3 [9]. |
| Control (IgG) | N/A | Baseline (lowest) | Progressive tumor growth [9]. |
Table 2: Validation Using Transgenic Mouse Models
| Experimental Model / Intervention | Key Finding | Mechanistic Insight |
|---|---|---|
| Sox9 transgenic overexpression | Confirmed mediation of resistance | Elevated Sox9 in epithelial cells initiates the cascade [9]. |
| Anxa1 knockout (KO) models | Reversed neutrophil apoptosis | Validated Anxa1 as the critical secreted effector [9]. |
| Fpr1 knockout (KO) models | Abrogated neutrophil apoptosis and restored therapy sensitivity | Confirmed Fpr1 as the necessary receptor on neutrophils for the pathway's function [9]. |
| Anti-ANXA1 Therapeutic Antibody (MDX-124) | Inhibited cancer cell growth in vitro and in vivo [68] | Provides proof-of-concept for targeting this axis therapeutically. |
Detailed Experimental Protocols
To enable researchers to replicate and build upon these findings, this section outlines the core methodologies used to investigate this pathway.
Establishing a Mouse Model for Combination Therapy Resistance
- Animal Model: C57BL/6 wild-type mice.
- Tumor Induction: HNSCC is induced by administering 4-nitroquinoline 1-oxide (4NQO) in drinking water for 16 weeks, followed by 8 weeks of normal water [9].
- Treatment Groups: Mice with established tumors are randomized into four groups receiving: control IgG, anti-PD-1 monotherapy, anti-LAG-3 monotherapy, or anti-LAG-3 plus anti-PD-1 combination therapy [9].
- Response Monitoring: Tumor size is assessed every 4 days. According to RECIST-like criteria, tumors growing more than 20% larger than their original size 14 days post-initial treatment are classified as resistant, while those showing reduction are classified as sensitive [9].
- Validation: Tumor progression is monitored via magnetic resonance imaging (MRI), and post-treatment tissues are analyzed through histopathology (H&E staining) and immunohistochemistry for markers like Ki67 (proliferation) and cleaved-Caspase3 (apoptosis) [9].
Single-Cell RNA Sequencing (scRNA-seq) for Cellular Deconvolution
- Sample Preparation: Pooled tumor tissues from resistant, sensitive, and control groups are digested into single-cell suspensions [9].
- Library Construction and Sequencing: Single-cell libraries are constructed using a standard platform (e.g., 10x Genomics) and sequenced.
- Data Analysis:
- Quality Control: Filter out low-quality cells, doublets, and high mitochondrial content cells.
- Clustering and Annotation: Unsupervised clustering is performed, and major cell types (epithelial, immune, fibroblast, endothelial) are annotated using canonical markers (e.g., Krt14/Krt5 for epithelial cells; Ptprc/Cd3g for immune cells) [9].
- Malignant Cell Identification: Tools like CopyKAT are used on the epithelial cell cluster to distinguish aneuploid malignant cells from non-malignant epithelial cells [9].
- Subcluster Analysis: Malignant cells are re-clustered to identify therapy-resistant (e.g., E-resi1, E-resi2) and therapy-sensitive (E-sens) subpopulations [9].
- Differential Expression: Identify differentially expressed genes (e.g., Sox9, Anxa1) in resistant versus sensitive subclusters.
Validating the ANXA1-FPR1 Functional Interaction
- Genetic Validation: Utilize Sox9, Anxa1, and Fpr1 transgenic or knockout mouse models in the 4NQO-HNSCC therapeutic setup. The core finding is that ablation of Anxa1 or Fpr1 rescues neutrophil apoptosis and restores sensitivity to combination therapy, confirming their essential role [9].
- In Vitro Neutrophil Apoptosis Assay:
- Neutrophil Isolation: Isolate primary neutrophils from mouse bone marrow or human donor blood using density gradient centrifugation.
- Co-culture: Co-culture neutrophils with conditioned media from SOX9-high tumor cells or recombinant ANXA1 protein. Include controls with FPR1/Fpr1 antagonists or neutralizing antibodies.
- Apoptosis Measurement: After 12-24 hours, assess apoptosis using Annexin V / Propidium Iodide (PI) staining followed by flow cytometry [68]. Annexin V+/PI- cells indicate early apoptosis, while Annexin V+/PI+ indicate late apoptosis/necrosis.
- Mechanistic Profiling: To investigate the mitochondrial dysfunction, assess key parameters such as:
- Mitochondrial Membrane Potential (ΔΨm): Using JC-1 or TMRM dyes and flow cytometry.
- Reactive Oxygen Species (ROS): Using CellROX or MitoSOX dyes.
- BNIP3 Expression: Quantify via qPCR or western blot from treated neutrophils [9].
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential Reagents for Investigating the SOX9-ANXA1-FPR1 Axis
| Reagent / Tool | Function / Application | Example & Notes |
|---|---|---|
| 4NQO-Induced HNSCC Model | In vivo model for studying HNSCC pathogenesis and therapy resistance [9]. | C57BL/6 mice; mimics human HNSCC progression and immune context. |
| Anti-PD-1 & Anti-LAG-3 Antibodies | To establish combination immunotherapy resistance model in vivo [9]. | Relatlimab (anti-LAG-3) and Nivolumab (anti-PD-1) are clinical counterparts. |
| scRNA-seq Platform | To deconvolute tumor heterogeneity and identify resistant cell subpopulations [9]. | 10x Genomics Chromium platform is widely used. |
| CopyKAT Algorithm | Computational tool to identify aneuploid malignant cells from scRNA-seq data [9]. | Critical for accurately defining tumor-specific subclusters. |
| Sox9/Anxa1/Fpr1 Genetically Modified Mice | For functional validation of each component of the pathway in vivo [9]. | KO models are used to confirm necessity; transgenic models confirm sufficiency. |
| Recombinant ANXA1 Protein & Anti-ANXA1 mAb | To exogenously manipulate the ANXA1-FPR1 axis in vitro and in vivo. | MDX-124 is a humanized therapeutic anti-ANXA1 antibody that inhibits cancer growth [68]. |
| FPR1 Antagonists | To pharmacologically block the ANXA1-FPR1 interaction in vitro. | Useful for mechanistic studies in neutrophil co-culture assays. |
| Annexin V Apoptosis Kit | Gold-standard for detecting phosphatidylserine externalization during apoptosis [68]. | Used with flow cytometry to quantify neutrophil apoptosis. |
| Mitochondrial Dyes (JC-1, TMRM, MitoSOX) | To assess mitochondrial health, including membrane potential and ROS production [9]. | Key for validating the mitochondrial fission and mitophagy inhibition phenotype. |
The discovery that the SOX9-ANXA1-FPR1 axis mediates resistance to combined immune checkpoint blockade represents a significant advance in our understanding of cancer immune evasion. This pathway highlights how a tumor cell-intrinsic transcription factor can orchestrate a complex paracrine signaling circuit to eliminate a key component of the anti-tumor immune response. Targeting this axis presents a promising therapeutic strategy to overcome resistance. The development of MDX-124, a humanized monoclonal antibody against ANXA1, which inhibits cancer cell growth in vitro and in vivo by disrupting its interaction with FPR1/2 and arresting the cell cycle, provides a compelling proof-of-concept [68]. Future efforts should focus on developing potent FPR1-specific antagonists and identifying patient populations with high SOX9/ANXA1 activity who would most benefit from such combinatorial approaches. Integrating these strategies with existing immunotherapies holds the potential to re-sensitize resistant tumors and improve long-term patient outcomes.
The transcription factor SOX9, a member of the SRY-related HMG-box family, has emerged as a critical regulator in cancer biology, particularly through its role in remodeling the tumor extracellular matrix (ECM). This whitepaper delineates the mechanistic pathways through which SOX9 directly promotes collagen deposition and creates a physical barrier that impedes immune cell infiltration into tumors. We detail how SOX9 drives desmoplasia—the excessive accumulation of collagen-rich ECM—and fosters an immunosuppressive tumor microenvironment (TME) that facilitates immune evasion. The document provides a comprehensive technical guide, including summarized quantitative data, detailed experimental protocols for key methodologies, and visualizations of core signaling pathways, serving as a resource for researchers and drug development professionals targeting the SOX9-ECM axis in oncology.
SOX9 is a pivotal transcription factor with well-established roles in embryonic development, chondrogenesis, and cell fate determination [19] [2]. In cancer, SOX9 is frequently overexpressed and functions as a potent oncogene across diverse malignancies, including breast, lung, and gastrointestinal cancers [19] [1]. Its oncogenic portfolio extends beyond promoting proliferation and metastasis to include the active remodeling of the TME. A key aspect of this remodeling is the deregulation of collagen, the core structural component of the ECM. Collagen heterogeneity, dictated by the expression of various collagen subtypes and their organizational status, is now recognized as a master regulator of the anti-tumor immune response [69]. Excessive collagen deposition and cross-linking increase stromal density, creating a physical barrier that restricts immune cell access to cancer cells and establishes an immunosuppressive niche. This whitepaper synthesizes current evidence positioning SOX9 as a direct transcriptional driver of this collagen-rich, immune-excluded TME, framing it within the broader thesis of SOX9 as a central regulator of immune cell infiltration in cancer.
Molecular Mechanisms: How SOX9 Drives Collagen Deposition and ECM Remodeling
SOX9 regulates the collagen-rich ECM through multiple, interconnected molecular pathways. Its function as a pioneer factor and its direct transcriptional control over collagen genes establish a pro-fibrotic program that shapes the TME.
SOX9 as a Pioneer Factor in Chromatin Remodeling
A fundamental mechanism by which SOX9 reprograms cell fate and ECM composition is through its function as a pioneer transcription factor. SOX9 possesses the unique ability to bind its cognate DNA motifs in closed, compacted chromatin, initiating a cascade of epigenetic remodeling that activates silent genes.
- Evidence from Engineered Models: In vivo studies using inducible SOX9 expression in adult epidermal stem cells demonstrated that SOX9 binds to key enhancer regions while they are still in a closed chromatin state (as determined by ATAC-seq). This binding occurs prior to observable increases in chromatin accessibility and is followed by nucleosome displacement, a hallmark of pioneer activity [2].
- Mechanism of Action: Upon binding, SOX9 recruits histone-modifying enzymes and members of the SWI/SNF chromatin remodeling complex. This recruitment leads to the deposition of active histone modifications (e.g., H3K27ac) and the opening of chromatin, thereby activating transcription of mesenchymal and ECM-related genes [2] [70]. This pioneer function is particularly critical during endothelial-to-mesenchymal transition (EndMT), a process that contributes fibroblasts and ECM to the stroma. During EndMT, SOX9 binding at silent chromatin regions guides the opening of chromatin and is directed by the presence of SOX dimer motifs and the histone variant H2A.Z [70].
Direct Transcriptional Regulation of Collagen Genes
The most direct link between SOX9 and collagen matrix deposition is its established role as a direct transcriptional regulator of the type II collagen gene (COL2A1).
- Foundational Discovery: Seminal work published in Nature Genetics demonstrated that SOX9 protein binds specifically to conserved sequences within the first intron of the COL2A1 gene. Mutating these SOX9-binding sequences abolished chondrocyte-specific expression of a COL2A1-driven reporter in transgenic mice. Furthermore, ectopic expression of SOX9 was sufficient to trans-activate both a COL2A1 reporter and the endogenous Col2a1 gene [71] [72].
- Implication for Cancer: While this regulation was first identified in chondrogenesis, the fundamental mechanism holds true in oncogenic contexts. The direct activation of major collagen genes like COL2A1 by SOX9 provides a clear pathway for the increased collagen deposition observed in SOX9-high tumors.
Induction of Pro-Fibrotic Cellular Transitions
SOX9 is a master regulator of cellular transitions that directly contribute fibroblasts and collagen-producing cells to the TME.
- Endothelial-to-Mesenchymal Transition (EndMT): SOX9 expression is sufficient to reprogram human umbilical vein endothelial cells (HUVECs) into a mesenchymal fate. This transition is characterized by a loss of endothelial markers (e.g., CD31) and a gain of mesenchymal markers (e.g., Vimentin, Periostin) [70]. Genome-wide mapping confirmed that SOX9 opens chromatin at silent mesenchymal genes during this process. Cells undergoing EndMT become a source of ECM components, including collagen, within the TME.
- Interaction with Cancer-Associated Fibroblasts (CAFs): The tumor stroma is replete with CAFs, which are prolific producers of collagen. SOX9 expression in cancer cells can drive the recruitment and activation of CAFs. Communication between cancer cells and fibroblasts in the TME encourages cancer cell heterogeneity and increases drug resistance [19]. Activated CAFs, in turn, further exacerbate collagen deposition, creating a feed-forward loop of stromal desmoplasia.
The table below summarizes the key molecular mechanisms by which SOX9 drives ECM remodeling.
Table 1: Molecular Mechanisms of SOX9 in ECM Remodeling
| Mechanism | Molecular Action | Experimental Evidence | Outcome in TME |
|---|---|---|---|
| Pioneer Factor Activity | Binds closed chromatin; recruits histone modifiers & SWI/SNF complex to open chromatin. | CUT&RUN and ATAC-seq in murine EpdSCs; chromatin landscape analysis in HUVECs [2] [70]. | De novo activation of mesenchymal and ECM gene enhancers. |
| Direct Collagen Regulation | Binds specific enhancer sequences in intron 1 of the COL2A1 gene to activate transcription. | EMSA, transgenic mouse reporter assays, ectopic SOX9 expression [71] [72]. | Increased synthesis and deposition of type II collagen. |
| Induction of EndMT | Reprograms endothelial cells to mesenchymal fate; downregulates CD31, upregulates VIM, POSTN. | RNA-seq, immunostaining, migration assays in SOX9-overexpressing HUVECs [70]. | Generation of collagen-producing mesenchymal cells from the endothelium. |
Consequences for the Immune Microenvironment
The SOX9-driven accumulation of a collagen-rich ECM has profound implications for the anti-tumor immune response, primarily by establishing a physical and biochemical barrier to immunity.
Creating a Physical Barrier to Immune Cell Infiltration
The dense, cross-linked network of collagen fibers significantly increases the physical stiffness of the tumor stroma. This creates a biomechanical barrier that physically impedes the trafficking and intratumoral infiltration of cytotoxic immune cells, such as CD8+ T cells and Natural Killer (NK) cells [69]. Tumors characterized by this phenomenon are often classified as "immune-cold" or excluded, where immune cells are present at the tumor margin but cannot penetrate the core. This barrier effect directly protects cancer cells from immune-mediated killing.
Shaping an Immunosuppressive Cellular Milieu
Beyond the physical barrier, the SOX9-shaped TME actively suppresses immune function by altering the composition of tumor-infiltrating immune cells.
- Bioinformatic Correlations: Pan-cancer analyses reveal that high SOX9 expression correlates with altered immune cell infiltration. It is often negatively correlated with the presence and function of CD8+ T cells and NK cells, and positively correlated with the accumulation of immunosuppressive cells, including regulatory T cells (Tregs) and M2-like tumor-associated macrophages (TAMs) [1].
- Mechanistic Insights: SOX9 contributes to immune evasion by helping latent cancer cells maintain a stem-like, dormant state and avoid immune surveillance [19] [66]. This dormancy allows cancer cells to persist in secondary sites for extended periods. Furthermore, the collagen-rich ECM itself can recruit and polarize macrophages towards an immunosuppressive M2 phenotype, further cementing an immune-resistant TME [69].
Table 2: SOX9-Driven Immune Consequences in the TME
| Immune Parameter | Effect of High SOX9 | Supporting Evidence |
|---|---|---|
| Cytotoxic CD8+ T Cells | ↓ Infiltration and function | Negative correlation with CD8+ T cell gene signatures; impaired tumor cell killing [66] [1]. |
| Regulatory T Cells (Tregs) | ↑ Infiltration and activity | Positive correlation with Treg abundance; recruitment to the TME [66] [1]. |
| Macrophage Polarity | Shift to M2 (immunosuppressive) phenotype | Correlation with M2 TAMs; collagenous ECM promotes M2 polarization [69] [1]. |
| Overall Immune Status | Promotion of "immune-cold" or excluded phenotype | Association with collagen deposition, barrier formation, and immune cell exclusion [69]. |
Experimental Approaches and Methodologies
This section provides detailed protocols for key experiments used to investigate the relationship between SOX9, collagen ECM, and immune evasion.
Assessing SOX9-Driven Chromatin Remodeling (ATAC-seq)
Objective: To map genome-wide changes in chromatin accessibility following SOX9 induction. Workflow:
- Cell Preparation: Use a controlled system (e.g., Doxycycline-inducible SOX9 expression in relevant cell lines). Harvest cells at multiple time points (e.g., 0, 1, 2 weeks post-induction) in biological replicates.
- Nuclei Isolation & Tagmentation: Lyse cells and isolate nuclei. Treat nuclei with the hyperactive Tn5 transposase, which simultaneously fragments and adaptor-tags accessible genomic regions.
- Library Preparation & Sequencing: Purify the tagmented DNA and amplify it with barcoded primers to create a sequencing library. Pool libraries and perform high-throughput sequencing (e.g., Illumina).
- Bioinformatic Analysis:
- Alignment: Map sequenced reads to the reference genome (e.g., GRCh37/hg19).
- Peak Calling: Identify regions of significant chromatin accessibility (peaks) using tools like MACS2.
- Differential Analysis: Compare peaks across time points to identify regions that become more or less accessible upon SOX9 expression.
- Motif & Annotation: Analyze sequences within dynamic peaks for enrichment of SOX family binding motifs and annotate peaks to genomic features (promoters, enhancers).
Evaluating Collagen Deposition and Organization (Histology)
Objective: To visualize and quantify collagen fiber content and architecture in SOX9-high versus control tumors. Workflow:
- Tissue Preparation: Fix tumor tissue samples in formalin and embed in paraffin (FFPE). Section tissues at 4-5 µm thickness.
- Picrosirius Red Staining:
- Deparaffinize and rehydrate sections through a graded alcohol series.
- Incubate sections in 0.1% Sirius Red in saturated picric acid for 60 minutes.
- Rinse briefly in acidified water and dehydrate rapidly through alcohols and xylene.
- Mount with a resinous mounting medium.
- Imaging and Analysis:
- Brightfield Microscopy: Image sections to assess total collagen area (stained red).
- Polarized Light Microscopy: Image the same sections under polarized light. Thick, tightly packed collagen fibers (e.g., mature, cross-linked) appear orange/red, while thinner, less organized fibers appear green. This provides information on collagen maturity and organization.
- Quantification: Use image analysis software (e.g., ImageJ/Fiji) to calculate the percentage of area stained for collagen and the ratio of red-to-green fiber signals.
In Vitro EndMT Induction and Functional Assay
Objective: To demonstrate SOX9's capacity to drive EndMT and enhance the migratory, matrix-producing phenotype of endothelial cells. Workflow:
- Cell Culture & Transduction: Culture Human Umbilical Vein Endothelial Cells (HUVECs) in complete Medium 200. Transduce cells with a lentivirus carrying SOX9-GFP or an empty vector-GFP control. Use a viral titer that achieves >95% transduction efficiency (confirmed by GFP fluorescence).
- Validation of EndMT:
- RNA-seq: 72 hours post-transduction, extract total RNA (e.g., using TRIzol). Prepare libraries and sequence. Align reads to the reference genome and perform differential expression analysis to confirm downregulation of endothelial genes (PECAM1, CDH5) and upregulation of mesenchymal genes (VIM, SNAI2, COL1A1, COL2A1).
- Immunostaining: Fix transduced cells and co-stain for endothelial (e.g., ERG) and mesenchymal (e.g., VIM, POSTN) markers. Confirm loss of endothelial and gain of mesenchymal protein expression via confocal microscopy.
- Functional Migration Assay (Transwell):
- Seed 15,000 transduced HUVECs in the upper chamber of a 5 µm polycarbonate transwell insert.
- After 24 hours, remove non-migratory cells from the upper chamber with a cotton swab.
- Fix the membrane, stain with DAPI, and image the lower side of the membrane.
- Count the number of migrated nuclei per field of view. SOX9-overexpressing cells are expected to show significantly increased migratory capacity [70].
The Scientist's Toolkit: Key Research Reagents
The following table lists essential reagents and tools for investigating SOX9's role in ECM and immune modulation.
Table 3: Essential Research Reagents for SOX9-ECM Studies
| Reagent / Tool | Specific Example | Function & Application |
|---|---|---|
| Inducible SOX9 System | Doxycycline-inducible SOX9 expression vector (e.g., pLVX-TetOne-SOX9). | Allows controlled, temporal induction of SOX9 to study direct early and late effects on chromatin and gene expression. |
| SOX9 Antibodies | Goat anti-SOX9 (R&D Systems, AF3045); Rabbit monoclonal anti-SOX9 (e.g., MilliporeSigma, AB5535). | For Chromatin Immunoprecipitation (ChIP/CUT&RUN), Western Blotting, and Immunofluorescence. |
| Endothelial Cell Model | Primary Human Umbilical Vein Endothelial Cells (HUVECs, e.g., Thermo Fisher, C0035C). | Gold-standard in vitro model for studying Endothelial-to-Mesenchymal Transition (EndMT). |
| Collagen Staining Kits | Picrosirius Red Stain Kit (e.g., Abcam, ab150681). | Histological staining for visualization and quantification of collagen fibers in tissue sections. |
| Mouse Models | Krt14-rtTA; TRE-Sox9 (for skin/EpdSC studies); Endothelial-specific Cre-driven SOX9 overexpression. | In vivo models to study SOX9's role in ECM remodeling and immune evasion in a physiological TME context. |
Visualizing the Core Pathway: SOX9 to Immune Exclusion
The following diagram, generated using Graphviz DOT language, illustrates the sequential pathway through which SOX9 activity in a tumor cell leads to the creation of an immune-excluded tumor microenvironment.
Diagram Title: SOX9 Drives Immune Exclusion via ECM Remodeling
The evidence consolidates SOX9 as a master regulator of the collagen-rich extracellular matrix, acting through direct gene transcription, pioneer factor-mediated chromatin remodeling, and the induction of pro-fibrotic cellular transitions. This activity directly contributes to the formation of a physical barrier that restricts immune cell infiltration and fosters an immunosuppressive microenvironment, enabling cancer immune evasion. Targeting the SOX9-ECM axis therefore presents a compelling therapeutic strategy to convert "immune-cold" tumors into "immune-hot" ones, potentially overcoming resistance to existing immunotherapies. Future efforts should focus on developing specific SOX9 inhibitors, disrupting its interaction with chromatin remodeling complexes, or employing stromal-depleting agents in combination with immune checkpoint blockade in SOX9-high malignancies.
The transcription factor SOX9 has emerged as a pivotal regulator of tumor progression and immune evasion across multiple cancer types. This whitepaper synthesizes current research demonstrating how SOX9 modulates the tumor immune microenvironment through regulation of immune cell infiltration and checkpoint protein expression. We present a comprehensive analysis of the molecular mechanisms underlying SOX9-mediated immunosuppression, with particular emphasis on its recently characterized relationship with the B7x immune checkpoint pathway. Experimental data and methodologies are provided to support the development of combined therapeutic approaches targeting SOX9 alongside established immune checkpoint inhibitors. The synthesized evidence positions SOX9 as a promising therapeutic target whose inhibition may enhance response rates to existing immunotherapies and overcome resistance mechanisms in poorly immunogenic tumors.
SOX9 (SRY-box transcription factor 9) is a transcription factor with diverse roles in embryonic development, cell differentiation, and stem cell maintenance. Recent evidence has established its significance in cancer biology, where it frequently functions as a key driver of tumor progression [3]. Beyond its established roles in promoting tumor growth and metastasis, SOX9 has recently been identified as a critical mediator of immunosuppression within the tumor microenvironment (TME) [73]. This function positions SOX9 as an attractive target for combination immunotherapy approaches.
In the context of cancer, SOX9 expression is significantly upregulated in numerous malignancies including glioblastoma (GBM), colorectal cancer, liver cancer, and basal-like breast cancer [33] [3]. This elevated expression correlates with advanced disease stage and poorer prognosis in several cancer types, though its prognostic implications can be context-dependent [33]. Mechanistically, SOX9 promotes the dedifferentiation of tumor cells toward stem-like states characterized by enhanced plasticity, treatment resistance, and immune evasion capabilities [73]. This review focuses specifically on the mechanisms through which SOX9 regulates immune cell infiltration and checkpoint expression, and how targeting these pathways may synergize with immune checkpoint blockade (ICB) therapy.
SOX9 Regulation of Immune Cell Infiltration and Checkpoint Expression
Correlative Evidence from Pan-Cancer Analyses
Comprehensive pan-cancer analyses reveal that SOX9 expression significantly correlates with altered immune landscapes across multiple tumor types. In glioblastoma, high SOX9 expression is associated with specific patterns of immune cell infiltration and checkpoint molecule expression [33] [18]. Transcriptomic analyses of GBM samples demonstrate that SOX9 expression positively correlates with immunosuppressive signaling pathways and specific immune checkpoint genes [18]. Surprisingly, in certain GBM subtypes characterized by lymphoid invasion, high SOX9 expression was associated with better prognosis, suggesting complex, context-dependent immunomodulatory functions [33].
Table 1: SOX9 Expression Patterns Across Cancer Types
| Cancer Type | SOX9 Expression vs. Normal | Correlation with Immune Infiltration | Prognostic Association |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly increased [33] [3] | Correlated with specific immune subsets and checkpoint expression [33] | Context-dependent; better prognosis in lymphoid invasion subgroups [33] |
| Breast Cancer (Basal-like) | Increased [73] | Reduced CD8+ T cell infiltration [73] | Shorter overall survival [73] |
| Lung Adenocarcinoma | Increased [33] | Suppressive tumor microenvironment [33] | Poorer overall survival [33] |
| Thymoma | Increased [3] | Negative correlation with Th17 differentiation genes [3] | Shorter overall survival [3] |
| Skin Cutaneous Melanoma | Decreased [3] | Not specified | Tumor suppressor role [3] |
Mechanistic Insights: The SOX9-B7x Immunosuppressive Axis
Recent research has elucidated a direct mechanistic link between SOX9 and immune checkpoint regulation. In basal-like breast cancer, SOX9 directly regulates the expression of B7x (also known as B7-H4 or VTCN1), an immune checkpoint molecule that inhibits T-cell activation and cytotoxicity [73]. This SOX9-B7x axis protects dedifferentiated tumor cells from immune surveillance and is essential for progression from pre-malignant lesions to invasive carcinoma [73].
The molecular pathway involves SOX9-mediated transcriptional activation of B7x through STAT3 signaling and direct binding to the B7x promoter region [73]. In mouse models of breast cancer, SOX9-mediated immunosuppression was required for tumor progression, and B7x targeting inhibited tumor growth and overcame resistance to anti-PD-L1 therapy [73]. This pathway establishes SOX9 as an upstream regulator of a non-redundant immunosuppressive mechanism that complements established PD-1/PD-L1 and CTLA-4 axes.
Figure 1: SOX9-B7x Immunosuppressive Axis. SOX9 activates STAT3 signaling and directly binds the B7x promoter to transcriptionally upregulate this immune checkpoint molecule, leading to T-cell suppression and immune evasion.
Experimental Models and Methodologies for SOX9-Immune Axis Investigation
In Vitro and In Vivo Models
The investigation of SOX9's role in immune regulation employs diverse experimental models. In vitro studies utilize cancer cell lines (e.g., prostate cancer cells 22RV1 and PC3, lung cancer cell H1975) to assess SOX9 expression and function [3]. These models allow for genetic manipulation (overexpression, knockdown, knockout) and subsequent analysis of downstream effects on immune-related gene expression.
In vivo, immunocompetent mouse models of breast cancer have been instrumental in establishing the SOX9-B7x axis [73]. These models demonstrate that SOX9-mediated immunosuppression is required for progression from in situ tumors to invasive carcinoma, and enable evaluation of therapeutic interventions targeting this pathway [73]. Orthotopic transplantation models and genetically engineered mouse models (GEMMs) that recapitulate spontaneous tumor development provide complementary insights into the temporal dynamics of SOX9-mediated immune evasion.
Analytical and Molecular Techniques
Comprehensive molecular profiling techniques are essential for characterizing SOX9-dependent immunomodulatory mechanisms:
RNA Sequencing: Bulk and single-cell RNA sequencing of tumor samples with high versus low SOX9 expression identifies differentially expressed genes and immune signatures [33] [18]. The DESeq2 R package is commonly used for differential expression analysis [33].
Immune Infiltration Analysis: Computational methods like ssGSEA (single-sample Gene Set Enrichment Analysis) and the ESTIMATE algorithm quantify immune cell infiltration from transcriptomic data and correlate these patterns with SOX9 expression [33] [18].
Functional Enrichment Analysis: GO (Gene Ontology) and KEGG (Kyoto Encyclopedia of Genes and Genomes) analyses identify biological processes and pathways enriched in SOX9-high tumors [33] [18]. Gene Set Enrichment Analysis (GSEA) reveals pathway-level differences between SOX9 expression groups.
Protein-Protein Interaction Networks: STRING database analysis and Cytoscape visualization identify functional protein networks associated with SOX9-mediated immune regulation [33].
Table 2: Key Experimental Methodologies for SOX9-Immune Axis Investigation
| Method Category | Specific Techniques | Key Applications | References |
|---|---|---|---|
| Transcriptomic Analysis | RNA-seq (TCGA, GTEx databases), scRNA-seq, GSEA | Identify SOX9-correlated genes and pathways, immune signatures | [33] [18] |
| Computational Immunology | ssGSEA, ESTIMATE, CIBERSORT, TIMER | Quantify immune cell infiltration, correlate with SOX9 expression | [33] [18] |
| Pathway Analysis | GO, KEGG, Metascape, PPI networks | Elucidate biological processes and pathways regulated by SOX9 | [33] [18] |
| Genetic Manipulation | siRNA/shRNA knockdown, CRISPR/Cas9 knockout, overexpression vectors | Establish causal relationships between SOX9 and immune phenotypes | [3] [73] |
| Preclinical Models | Syngeneic grafts, GEMMs, patient-derived xenografts | Evaluate SOX9 function in immune-competent contexts | [73] |
Therapeutic Targeting Strategies: Combining SOX9 Inhibition with Immune Checkpoint Blockade
SOX9-Targeted Therapeutic Approaches
Several strategies have emerged for therapeutic targeting of SOX9:
Small Molecule Inhibitors: Cordycepin (an adenosine analog) demonstrates dose-dependent inhibition of SOX9 expression in cancer cell lines (22RV1, PC3, H1975), suggesting its potential as a SOX9-targeting agent [3]. High-throughput screening approaches may identify additional compounds that modulate SOX9 activity or expression.
Gene Targeting Approaches: RNA interference (siRNA, shRNA) and CRISPR/Cas9-mediated knockout of SOX9 reduce tumor growth and reverse immunosuppressive phenotypes in experimental models [73].
Transcriptional and Post-translational Regulation: Strategies targeting SOX9 transcription, protein stability, or interaction with co-factors represent emerging approaches that require further development.
Rationale for Combination with Immune Checkpoint Inhibitors
The mechanistic relationship between SOX9 and immune checkpoint expression provides a strong rationale for combination therapy. Preclinical evidence demonstrates that B7x targeting inhibits tumor growth and overcomes resistance to anti-PD-L1 therapy in advanced tumors [73]. Given that SOX9 transcriptionally regulates B7x, SOX9 inhibition may similarly sensitize tumors to established checkpoint inhibitors.
Combination strategies may be particularly effective in poorly immunogenic "cold" tumors, where SOX9-mediated dedifferentiation contributes to immune exclusion. By simultaneously targeting SOX9 and immune checkpoints, these approaches may promote T-cell infiltration while reversing checkpoint-mediated T-cell exhaustion, creating a more favorable tumor immune microenvironment.
Figure 2: SOX9 Inhibition Synergizes with Immune Checkpoint Blockade. SOX9 targeting reduces B7x expression, relieving T-cell suppression, while immune checkpoint inhibitors further enhance T-cell function, resulting in combined antitumor effects.
Biomarker-Driven Patient Selection
The successful clinical translation of SOX9-targeted combination therapies will require biomarker-driven patient selection strategies. Potential predictive biomarkers include:
SOX9 Expression Levels: Tumors with high SOX9 expression may derive greatest benefit from SOX9-targeted therapies.
B7x/H4 Expression: Given the direct regulatory relationship, B7x expression may serve as a pharmacodynamic marker of SOX9 pathway activity.
Immune Gene Signatures: Transcriptomic signatures reflecting SOX9-mediated immunosuppression may identify patients most likely to respond to combination therapy.
IDH Mutation Status: In glioblastoma, SOX9 represents an independent prognostic factor specifically in IDH-mutant cases, suggesting mutation-specific therapeutic implications [33].
Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating SOX9 and Immune Checkpoints
| Reagent Category | Specific Examples | Research Application | Key Functions |
|---|---|---|---|
| Cell Lines | 22RV1, PC3, H1975, patient-derived organoids | In vitro mechanistic studies | Model SOX9 expression and signaling across cancer types [3] |
| Genetic Tools | SOX9 siRNA/shRNA, CRISPR/Cas9 KO systems, SOX9 expression vectors | Genetic manipulation | Establish causal relationships through loss/gain-of-function studies [3] [73] |
| Antibodies | Anti-SOX9, anti-B7x/B7-H4, anti-PD-L1, anti-CD8 | Immunohistochemistry, Western blot, flow cytometry | Detect protein expression, immune cell infiltration [73] |
| Small Molecules | Cordycepin, STAT3 inhibitors | Pharmacological inhibition | Modulate SOX9 expression and signaling pathways [3] |
| Databases | TCGA, GTEx, HPA, cBioPortal | Bioinformatic analysis | Access transcriptomic, proteomic, and clinical data [33] [3] |
The emerging role of SOX9 as a regulator of tumor immune evasion opens promising avenues for combination immunotherapy. The recently elucidated SOX9-B7x axis provides a mechanistic foundation for rational combination strategies that simultaneously target SOX9 and established immune checkpoints. Preclinical evidence supports the therapeutic potential of this approach, particularly in poorly immunogenic tumors characterized by SOX9-mediated immunosuppression.
Future research should focus on developing more specific and potent SOX9 inhibitors, validating predictive biomarkers for patient selection, and designing clinical trials that test the synergy between SOX9-targeted agents and immune checkpoint blockade. As our understanding of SOX9's immunoregulatory functions continues to evolve, targeting this pathway may represent a crucial strategy for expanding the efficacy of cancer immunotherapy to broader patient populations.
Addressing the Challenges of Directly Targeting a Transcription Factor
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator in cancer biology, particularly through its function in modulating immune cell infiltration within the tumor microenvironment. As a member of the SOX family of transcriptional regulators, SOX9 contains a highly conserved high-mobility group (HMG) domain that enables DNA binding and recognition of the specific sequence CCTTGAG [3] [1] [49]. This 509-amino acid protein plays fundamental roles in embryonic development, chondrogenesis, and stem cell maintenance, but its dysregulation has been strongly implicated in tumorigenesis across multiple cancer types [1] [16]. SOX9 is frequently overexpressed in various malignancies including glioblastoma (GBM), colorectal cancer, lung cancer, breast cancer, and ovarian cancer, where it drives tumor initiation, progression, and therapeutic resistance [33] [32] [16]. Beyond its cell-autonomous oncogenic functions, SOX9 has recently been identified as a key modulator of the tumor immune microenvironment, influencing immune cell infiltration and function to foster an immunosuppressive niche that supports tumor progression and immune evasion [33] [1].
Despite its clear importance in cancer pathogenesis and immunomodulation, directly targeting SOX9 with conventional therapeutic approaches presents substantial challenges. As a nuclear transcription factor, SOX9 lacks enzymatic activity or easily targetable binding pockets, making conventional small-molecule inhibition strategies particularly difficult [2]. Furthermore, SOX9 operates as a pioneer transcription factor capable of binding to compacted chromatin and initiating large-scale transcriptional reprogramming, a function that involves complex protein-protein interactions and epigenetic modifications that are challenging to disrupt pharmacologically [2]. This whitepaper examines the multifaceted challenges in directly targeting SOX9, analyzes its role in regulating immune cell infiltration in cancer, and explores innovative experimental and therapeutic strategies to overcome these barriers in drug development.
Molecular Structure and Function of SOX9
Structural Domains and Functional Motifs
SOX9 protein contains several critically important functional domains that mediate its diverse biological activities. The N-terminal dimerization domain (DIM) facilitates protein-protein interactions, while the central HMG box domain enables sequence-specific DNA binding and nuclear localization through embedded nuclear localization signals (NLS) [1]. The protein contains two transcriptional activation domains—a central transcriptional activation domain (TAM) and a C-terminal transcriptional activation domain (TAC)—that work synergistically to enhance SOX9's transcriptional potential [1]. Additionally, a proline/glutamine/alanine (PQA)-rich domain is essential for full transcriptional activation capability. Each of these domains presents potential targeting opportunities but also contributes to the complexity of disrupting SOX9 function.
SOX9 as a Pioneer Transcription Factor
Recent research has established SOX9 as a bona fide pioneer transcription factor capable of binding to its cognate motifs within closed chromatin regions and initiating chromatin remodeling [2]. Through sophisticated genetic engineering and epigenetic profiling, studies have demonstrated that SOX9 can bind to approximately 30% of its target sites in closed chromatin before initiating nucleosome displacement and chromatin opening [2]. This pioneer function enables SOX9 to initiate large-scale transcriptional reprogramming events that drive cell fate transitions, including the conversion of normal cells to malignant states and the acquisition of therapy-resistant phenotypes.
Table 1: Key Functional Domains of SOX9 Protein
| Domain | Position | Primary Function | Targeting Challenges |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein-protein interactions | Shallow interaction surfaces |
| HMG Box Domain | Central | DNA binding, nuclear localization | High affinity for DNA, difficult to disrupt |
| Transcriptional Activation Domain (TAM) | Middle | Transcriptional activation | Intrinsically disordered region |
| Transcriptional Activation Domain (TAC) | C-terminal | Transcriptional activation, β-catenin inhibition | Multiple co-factor interactions |
| PQA-rich Domain | C-terminal | Transcriptional activation | Structural instability |
SOX9 in Cancer Immunomodulation: Mechanisms and Evidence
Regulation of Immune Cell Infiltration
SOX9 expression demonstrates complex correlations with specific immune cell populations within the tumor microenvironment across different cancer types. Comprehensive bioinformatics analyses of tumor sequencing data from The Cancer Genome Atlas and other resources have revealed that SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils in colorectal cancer [1]. Conversely, SOX9 shows positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1]. In glioblastoma, SOX9 expression is closely correlated with immune cell infiltration and expression of critical immune checkpoints, indicating its involvement in establishing an immunosuppressive tumor microenvironment [33] [18].
Single-cell RNA sequencing and spatial transcriptomics analyses in prostate cancer have demonstrated that SOX9 expression is associated with significant shifts in the immune landscape, including decreases in effector immune cells such as CD8+CXCR6+ T cells and activated neutrophils, while immunosuppressive cells including Tregs and M2 macrophages (TAM Macro-2) are increased [1]. This imbalance ultimately creates an "immune desert" microenvironment that facilitates tumor immune escape. Additionally, in breast cancer, SOX9 has been shown to trigger tumorigenesis by facilitating the immune escape of tumor cells, further supporting its role in modulating anti-tumor immunity [49].
Impact on Immune Checkpoints and T-cell Function
SOX9 expression influences the expression of critical immune checkpoint molecules that regulate T-cell function and anti-tumor immunity. Research has revealed that SOX9 expression in thymoma negatively correlates with genes related to PD-L1 expression and T-cell receptor signaling pathways [49]. Additionally, studies in lung adenocarcinoma have found that SOX9 suppresses the tumor microenvironment and shows mutual exclusivity with various tumor immune checkpoints [33]. These findings suggest that SOX9 may participate in immune evasion through modulation of checkpoint molecule expression.
The downregulation of SOX9 has been associated with reduced T-cell cytotoxicity, indicating its importance in maintaining T-cell function [49]. Furthermore, SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), thereby modulating lineage commitment of early thymic progenitors and influencing the balance between αβ T cell and γδ T cell differentiation [1]. This complex regulation of T-cell development and function highlights the multifaceted mechanisms through which SOX9 influences adaptive immunity.
Table 2: SOX9 Correlation with Immune Cell Infiltration Across Cancers
| Immune Cell Type | Correlation with SOX9 | Cancer Types Studied | Functional Consequences |
|---|---|---|---|
| CD8+ T cells | Negative | Prostate, Breast | Reduced cytotoxic activity |
| Tregs | Positive | Prostate | Enhanced immunosuppression |
| M2 Macrophages | Positive | Prostate, Colorectal | Immune suppression, tissue remodeling |
| B cells | Negative | Colorectal | Diminished humoral immunity |
| Neutrophils | Positive | Colorectal, Prostate | Increased inflammation |
| NK cells | Negative | Multiple | Reduced innate immunity |
Experimental Approaches for Studying SOX9 Function
Multi-Omics Profiling and Bioinformatics Analysis
Comprehensive analysis of SOX9 expression patterns and function requires integration of multiple experimental approaches. RNA sequencing data from resources such as The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases provide essential transcriptomic information [33] [18]. Functional enrichment analysis of SOX9-correlated genes can be performed using Gene Ontology (GO), Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis, and Gene Set Enrichment Analysis (GSEA) [33]. Protein-protein interaction networks can be predicted using the STRING database and visualized with Cytoscape, while chromatin accessibility and binding sites can be assessed through ATAC-seq and CUT&RUN sequencing [33] [2].
For immune-specific analyses, the ssGSEA package and ESTIMATE package in the GSVA package enable detailed immuno-infiltration correlation analysis of SOX9 [33]. These computational approaches can be complemented with experimental validation using Western blotting, immunohistochemistry, and immunofluorescence to confirm protein-level expression and localization [3] [49].
Genetic and Epigenetic Manipulation
CRISPR/Cas9-mediated knockout of SOX9 has demonstrated increased sensitivity to carboplatin treatment in high-grade serous ovarian cancer (HGSOC) cell lines, as measured by colony formation assays [32]. Inducible expression systems, such as tetracycline-responsive SOX9 expression in engineered mouse models, enable temporal control over SOX9 activation and facilitate analysis of its reprogramming capabilities in adult tissue stem cells [2].
Epigenetic modulation approaches include targeting SOX9-associated super-enhancers that are commissioned specifically in therapy-resistant cells [32]. Small molecule inhibitors such as cordycepin (an adenosine analog) have shown efficacy in reducing both protein and mRNA expression of SOX9 in a dose-dependent manner in prostate cancer cell lines (22RV1, PC3) and lung cancer cells (H1975) [3] [49].
Figure 1: Experimental Workflow for SOX9 Functional Analysis
Challenges in Directly Targeting SOX9
Molecular and Structural Barriers
The direct targeting of SOX9 faces significant molecular challenges due to its structural characteristics and mode of action. As a transcription factor, SOX9 primarily functions through protein-DNA and protein-protein interactions that involve large, relatively flat surfaces with low druggability [2]. Unlike enzymes with well-defined active pockets, SOX9 lacks deep binding cavities that can be readily targeted with small molecules. The HMG domain, responsible for DNA binding, exhibits high affinity for specific DNA sequences, making competitive inhibition particularly challenging without disrupting essential genetic programs in normal tissues.
SOX9's function as a pioneer transcription factor adds additional complexity to targeting strategies. Its ability to bind nucleosomal DNA in compacted chromatin and recruit chromatin remodeling complexes represents a dynamic process that is difficult to disrupt with conventional therapeutics [2]. The temporal progression of SOX9-mediated reprogramming—beginning with chromatin binding, followed by recruitment of co-factors, nucleosome displacement, and eventual transcriptional activation—creates multiple potential intervention points but requires precise temporal control that is challenging to achieve pharmacologically.
Context-Dependent Functions and Therapeutic Window
SOX9 exhibits context-dependent dual functions across different biological systems and cancer types, creating significant challenges for therapeutic targeting. While SOX9 typically functions as an oncogene in most cancers, promoting tumor progression and immune evasion, it can act as a tumor suppressor in specific contexts such as melanoma [3] [49]. This dual nature raises concerns about potential adverse effects when targeting SOX9 systemically. Furthermore, SOX9 plays essential roles in normal tissue homeostasis, including chondrogenesis, testicular development, and maintenance of progenitor cell populations in various organs [1] [16]. Disruption of these physiological functions could lead to unacceptable toxicities, narrowing the therapeutic window for SOX9-directed therapies.
The complex role of SOX9 in immune regulation further complicates targeting strategies. While SOX9 promotes immunosuppression in the tumor microenvironment, it also contributes to maintaining macrophage function and supporting tissue regeneration and repair processes [1]. This "double-edged sword" characteristic of SOX9 in immunology means that systemic inhibition might inadvertently compromise beneficial immune functions or tissue repair mechanisms.
Figure 2: SOX9-Mediated Immunosuppression Pathways
Alternative Targeting Strategies and Research Tools
Indirect Targeting Approaches
Given the challenges of direct SOX9 inhibition, several indirect targeting strategies have emerged as promising alternatives. Epigenetic modulation represents a viable approach, as demonstrated by the identification of SOX9 as a resistant state-specific, super-enhancer-regulated transcription factor in high-grade serous ovarian cancer [32]. Targeting these regulatory elements or the epigenetic writers, readers, and erasers that control SOX9 expression and activity may provide more tractable intervention points. Small molecule inhibitors such as cordycepin have shown efficacy in reducing SOX9 expression in cancer cell lines, suggesting potential for pharmacological intervention [3] [49].
Another indirect approach focuses on disrupting critical downstream pathways and effectors of SOX9-mediated oncogenesis. Research has revealed that SOX9 regulates downstream transcription factors that drive tumorigenesis, including oncogenic transcriptional regulators that chart the path to cancers typified by constitutive SOX9 expression [2]. Targeting these downstream effectors may enable more specific disruption of SOX9's oncogenic functions while preserving its physiological roles. Additionally, targeting SOX9-regulated immune mediators may allow for selective disruption of its immunomodulatory functions without directly inhibiting SOX9 itself.
Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 Investigation
| Reagent/Category | Specific Examples | Function/Application | Key Considerations |
|---|---|---|---|
| Cell Line Models | OVCAR4, Kuramochi, COV362 (ovarian); PC3, 22RV1 (prostate); H1975 (lung) | In vitro functional studies | Context-dependent SOX9 expression and function |
| Animal Models | Krt14-rtTA;TRE-Sox9 mice; Xenograft models | In vivo tumorigenesis and therapy studies | Inducible systems enable temporal control |
| Genetic Tools | CRISPR/Cas9 KO; siRNA/shRNA; Inducible expression systems | Functional validation | Confirm efficiency and specificity |
| Antibodies | Anti-SOX9 (Western, IHC, IF); Anti-MYC epitope | Detection and quantification | Validate specificity for applications |
| Small Molecules | Cordycepin; Carboplatin | Therapeutic mechanism studies | Dose optimization required |
| Omics Databases | TCGA; GTEx; HPA; cBioPortal | Bioinformatics analysis | Multi-dataset validation recommended |
The transcription factor SOX9 presents a compelling but challenging therapeutic target in cancer, particularly due to its critical role in regulating immune cell infiltration and establishing immunosuppressive tumor microenvironments. While direct targeting approaches face significant hurdles due to SOX9's structural characteristics and complex biological functions, integrated research strategies combining multi-omics profiling, sophisticated genetic models, and indirect targeting methods offer promising paths forward. The development of context-specific interventions that leverage our growing understanding of SOX9's immunomodulatory functions may enable more precise therapeutic approaches that disrupt its oncogenic activities while preserving essential physiological functions. As research continues to elucidate the nuanced mechanisms of SOX9 in cancer immunity, new opportunities will likely emerge for overcoming the challenges of targeting this pivotal transcription factor.
Clinical Translation and Pan-Cancer Analysis: Validating SOX9 as a Biomarker and Target
The transcription factor SOX9, a member of the SRY-related HMG-box family, has emerged as a critical regulator in cancer progression and a promising prognostic biomarker across multiple malignancies. This whitepaper synthesizes current evidence establishing the correlation between SOX9 overexpression and poor survival outcomes in lung cancer, glioma, and other solid tumors. Beyond its prognostic utility, we examine SOX9's functional role in regulating immune cell infiltration within the tumor microenvironment, highlighting mechanisms through which SOX9 facilitates immune evasion. Through comprehensive analysis of molecular pathways, clinical validation studies, and experimental methodologies, this review provides researchers and drug development professionals with a technical framework for targeting SOX9 in cancer therapeutics. The findings underscore SOX9's potential not only as a biomarker but as a central node in cancer pathogenesis through its dual functions in promoting tumor progression and suppressing anti-tumor immunity.
SOX9 (SRY-related high mobility group-box 9) is a transcription factor with diverse roles in embryonic development, cell fate determination, and tissue homeostasis. Its gene maps to chromosome 17q24.3 and encodes a 509-amino acid protein containing a highly conserved HMG (high-mobility group box) DNA-binding domain that recognizes the specific motif CCTTGAG [3]. While initially characterized for its crucial functions in chondrogenesis, sex determination, and organogenesis, SOX9 has more recently been implicated as a significant contributor to oncogenesis across diverse tissue types.
The context-dependent nature of SOX9 in cancer is noteworthy. In most carcinomas, including lung, breast, and gastrointestinal malignancies, SOX9 acts as a proto-oncogene that drives tumor initiation, progression, and therapeutic resistance [3]. However, in specific malignancies such as melanoma and certain cervical and bladder cancers, SOX9 demonstrates tumor-suppressive properties, highlighting the tissue-specific complexity of its functions [3] [20]. This paradoxical behavior necessitates careful investigation of SOX9 within specific cancer contexts.
Emerging evidence has illuminated SOX9's role in modulating the tumor immune microenvironment, positioning it as a key regulator of immune cell infiltration and function. SOX9 appears to facilitate immune evasion through multiple mechanisms, including suppression of dendritic cell activity, inhibition of CD8+ T cell and natural killer cell infiltration, and regulation of immune checkpoint molecules [20] [18]. This immune-regulatory function, combined with its direct oncogenic activities, establishes SOX9 as a compelling therapeutic target and prognostic indicator in modern cancer research.
SOX9 Overexpression as a Prognostic Indicator Across Cancers
Comprehensive analyses across multiple cancer types have consistently demonstrated that elevated SOX9 expression correlates with aggressive disease features and diminished survival outcomes. The table below summarizes key prognostic associations of SOX9 overexpression in major cancer types.
Table 1: Prognostic Significance of SOX9 Overexpression Across Cancers
| Cancer Type | Prognostic Association | Statistical Significance | Sample Size | References |
|---|---|---|---|---|
| Non-Small Cell Lung Cancer (NSCLC) | Shorter overall survival | P < 0.001 | 142 patients | [74] |
| Lung Adenocarcinoma (LUAD) | Shorter overall survival | P = 0.0039 | TCGA dataset | [20] |
| Glioblastoma (GBM) | Better prognosis in lymphoid invasion subgroups | P < 0.05 | 478 cases | [18] [33] [75] |
| Multiple Cancers (Pan-Cancer) | Shorter OS in LGG, CESC, THYM; Longer OS in ACC | Variable by cancer type | 10,535 samples (TCGA) | [3] |
| Hepatitis C-induced Liver Fibrosis | Unfavorable outcomes in early-stage fibrosis | Not specified | 216 biopsy samples | [76] [77] |
Lung Cancer
In non-small cell lung cancer (NSCLC), SOX9 demonstrates significant prognostic utility. A 2012 clinical study of 142 NSCLC patients revealed that SOX9 was upregulated in 52.1% (74/142) of cases, with high expression significantly correlated with advanced histological stage (P = 0.017) and shorter survival time (P < 0.001) [74]. Multivariate analysis confirmed SOX9 upregulation as an independent prognostic indicator for NSCLC patient survival, establishing its clinical value beyond conventional parameters.
In lung adenocarcinoma (LUAD), interrogation of The Cancer Genome Atlas (TCGA) dataset confirmed that patients with SOX9-high tumors (top 20% of samples) experienced significantly shorter survival (P = 0.0039) compared to those with SOX9-low expression [20]. This finding aligns with functional studies demonstrating that SOX9 promotes EGFR-TKI resistance through activation of β-catenin and induction of epithelial-to-mesenchymal transition (EMT), thereby facilitating therapeutic escape and disease progression [78].
Glioma
In glioblastoma (GBM), the most common and aggressive primary brain tumor in adults, SOX9 expression demonstrates complex prognostic implications. While generally associated with poor outcomes, high SOX9 expression shows a surprising correlation with better prognosis in specific molecular subgroups, particularly among patients with lymphoid invasion (P < 0.05) [18] [33]. This paradoxical relationship underscores the context-dependent nature of SOX9 in neuro-oncology.
Further analysis reveals that SOX9 serves as an independent prognostic factor for IDH (isocitrate dehydrogenase)-mutant gliomas, enabling more refined patient stratification within this molecularly defined subset [18] [75]. The incorporation of SOX9 expression into nomogram prognostic models has enhanced predictive accuracy for glioblastoma outcomes, facilitating more personalized clinical management.
Other Cancers
Pan-cancer analyses examining SOX9 expression across 33 cancer types have revealed that SOX9 is significantly upregulated in fifteen malignancies, including CESC, COAD, ESCA, GBM, KIRP, LGG, LIHC, LUSC, OV, PAAD, READ, STAD, THYM, UCES, and UCS, while being downregulated in only two cancers (SKCM and TGCT) compared to matched healthy tissues [3]. This pattern establishes SOX9 as primarily oncogenic across most human cancers.
In hepatitis C-induced liver fibrosis, elevated SOX9 expression correlates with unfavorable outcomes in early-stage disease, identifying it as a potential biomarker for progressive liver disease and hepatocarcinogenesis risk [76]. The association between SOX9 and hepatic stellate cell activation further underscores its role in precancerous fibrotic conditions.
Molecular Mechanisms of SOX9 in Cancer Progression
SOX9 drives tumor progression through diverse molecular mechanisms that vary by cellular context but share common themes across cancer types. The diagram below illustrates key signaling pathways through which SOX9 promotes oncogenesis.
Figure 1: SOX9-Driven Oncogenic Signaling Pathways. SOX9 is transcriptionally induced by multiple oncogenic signals (EGFR, KRAS, NOTCH, TGF-β) and promotes tumor progression through regulation of downstream processes including EMT, β-catenin signaling, cancer stemness, proliferation, and tumor microenvironment (TME) remodeling, ultimately leading to therapeutic resistance.
Regulation of Cell Proliferation and Tumor Growth
In KrasG12D-driven lung adenocarcinoma models, Sox9 knockout significantly reduces tumor development, burden, and progression, contributing to substantially longer overall survival [20]. Specifically, loss of Sox9 function decreased both tumor number (P = 0.018) and burden (P = 0.029), while suppressing progression to high-grade tumors. Only one grade 3 tumor was observed in Sox9 knockout lungs compared to twelve grade 3 tumors in controls [20]. This pronounced effect on tumor grade distribution highlights SOX9's critical role in disease advancement.
Mechanistically, SOX9 enhances tumor cell proliferation, as demonstrated by significantly higher percentages of Ki67-positive cells in SOX9+ tumors (P = 0.00092) [20]. Three-dimensional tumor organoid cultures confirmed that SOX9 overexpression increases organoid size and cellularity, establishing its direct growth-promoting effects in controlled experimental systems.
Therapeutic Resistance Mechanisms
SOX9 drives resistance to targeted therapies in multiple cancer types. In lung cancer, SOX9 promotes epidermal growth factor receptor-tyrosine kinase inhibitor (EGFR-TKI) resistance through β-catenin activation and induction of epithelial-to-mesenchymal transition (EMT) [78]. This mechanism enables tumor cells to bypass EGFR dependency, a common resistance pathway in lung adenocarcinoma management.
The relationship between SOX9 and EMT extends beyond lung cancer, representing a fundamental resistance mechanism across carcinomas. SOX9 regulates expression of EMT markers, modifying promoter activities of β-catenin and facilitating the transition to a mesenchymal, invasive phenotype associated with therapeutic escape [78]. This plasticity mechanism represents a significant clinical challenge that SOX9 inhibition might potentially overcome.
SOX9 Regulation of Immune Cell Infiltration in the Tumor Microenvironment
A pivotal aspect of SOX9's oncogenic function involves its regulation of the tumor immune microenvironment, creating an immunosuppressive niche that facilitates cancer progression. The diagram below illustrates how SOX9 modulates immune cell infiltration to suppress anti-tumor immunity.
Figure 2: SOX9 Regulation of Tumor Immune Microenvironment. SOX9 creates an immunosuppressive niche by increasing collagen production and physical barrier formation, suppressing dendritic cell (DC) infiltration, inhibiting CD8+ T cell and natural killer (NK) cell recruitment, and modulating immune checkpoint expression, collectively facilitating immune evasion.
Modulation of Immune Cell Infiltration
In KrasG12D-driven lung adenocarcinoma, SOX9 suppresses infiltration of critical anti-tumor immune populations, including CD8+ T cells, natural killer (NK) cells, and dendritic cells (DCs) [20]. This coordinated suppression of multiple immune lineages creates a permissive environment for tumor growth. Comparative studies in immunocompromised versus immunocompetent mice revealed that SOX9-promoted tumor growth was significantly attenuated in immunodeficient hosts, confirming the essential role of immune modulation in SOX9's oncogenic function [20].
The mechanisms underlying SOX9-mediated immune exclusion involve substantial elevation of collagen-related gene expression and increased collagen fiber deposition within the tumor microenvironment [20]. This extracellular matrix remodeling increases tumor stiffness and creates physical barriers to immune cell penetration, particularly affecting dendritic cell infiltration which subsequently impairs CD8+ T cell and NK cell recruitment and activation.
Immune Checkpoint Regulation
In glioblastoma, SOX9 expression correlates significantly with immune checkpoint expression and immune cell infiltration patterns [18] [33]. This relationship positions SOX9 within the immunosuppressive network of GBM, potentially influencing response to immune checkpoint inhibitors. Similar associations between SOX9 and immune checkpoint molecules have been observed in lung adenocarcinoma, where SOX9 appears mutually exclusive with various tumor immune checkpoints [18].
The functional connection between SOX9 and immune evasion is further supported by research in breast cancer, where a SOX9-B7x axis safeguards dedifferentiated tumor cells from immune surveillance to drive disease progression [21]. B7x (B7-H4) is an inhibitory immune checkpoint molecule that limits T cell activation, connecting SOX9 to direct regulation of immune inhibitory pathways.
Context-Dependent Immune Regulation
The immune-regulatory functions of SOX9 demonstrate context-dependent characteristics across cancer types. In thymoma, SOX9 expression negatively correlates with genes involved in Th17 cell differentiation, primary immunodeficiency, PD-L1 expression, and T-cell receptor signaling pathways [3]. This suggests tissue-specific mechanisms of immune dysregulation.
Conversely, in breast cancer, SOX9 triggers tumorigenesis by facilitating immune escape of tumor cells through distinct mechanisms [3]. This tissue-specific variability in SOX9 immune functions underscores the complexity of targeting SOX9 therapeutically and necessitates careful evaluation within each cancer context.
Experimental Methodologies for SOX9 Research
Detection and Quantification Methods
Accurate measurement of SOX9 expression at both RNA and protein levels is essential for prognostic validation. The table below outlines key experimental approaches for SOX9 detection and their applications in cancer research.
Table 2: Experimental Methods for SOX9 Detection and Functional Analysis
| Method Category | Specific Techniques | Key Applications | Representative Findings |
|---|---|---|---|
| mRNA Expression Analysis | Real-time RT-PCR, RNA Sequencing | Quantify SOX9 transcript levels in tissues and cell lines | Elevated SOX9 mRNA in NSCLC tissues vs. adjacent normal tissues [74] |
| Protein Detection | Western Blotting, Immunohistochemistry (IHC) | Determine SOX9 protein expression and localization | High SOX9 protein in 74/142 (52.1%) NSCLC biopsies [74] |
| Spatial Analysis | Immunofluorescence, IHC on tissue microarrays | Correlate SOX9 expression with tumor grade and location | SOX9 mainly expressed in larger, proliferative, high-grade tumors [20] |
| Functional Genomics | CRISPR/Cas9 knockout, siRNA/shRNA knockdown | Assess SOX9 loss-of-function effects | Sox9 knockout reduces KrasG12D-driven tumor burden [20] |
| In Vitro Modeling | 3D tumor organoid cultures | Study SOX9 in tissue-relevant contexts | SOX9 increases organoid size and cell number [20] |
| Immune Analysis | Flow cytometry, ssGSEA, CIBERSORT | Characterize immune cell infiltration | SOX9 suppresses CD8+ T, NK, and dendritic cell infiltration [20] [18] |
In Vivo and In Vitro Models
Genetically engineered mouse models (GEMMs) have proven invaluable for establishing the causal role of SOX9 in tumor progression. The KrasLSL-G12D;Sox9flox/flox (KSf/f) model demonstrated that Sox9 knockout significantly extends survival (P = 0.0012) and reduces lung tumor burden (P = 0.011) compared to controls [20]. These models provide physiological relevant systems for evaluating SOX9 targeting strategies.
Three-dimensional organoid cultures recapitulate tissue architecture and cell-cell interactions, offering a robust platform for studying SOX9 function in vitro. In KrasG12D mouse lung tumor cell lines, SOX9 overexpression significantly increased organoid size and cellularity, confirming its direct growth-promoting effects independent of systemic influences [20].
Bioinformatics and Computational Approaches
Leveraging public databases like The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) enables comprehensive analysis of SOX9 expression patterns across malignancies [18] [3]. Differential gene expression analysis, gene set enrichment analysis (GSEA), and immune deconvolution algorithms provide insights into SOX9-associated signaling pathways and immune profiles.
Prognostic model development incorporating SOX9 expression has shown enhanced predictive accuracy. In glioblastoma, nomogram models integrating SOX9, OR4K2, and IDH status improve outcome prediction [18] [75]. Similarly, in hepatitis C-induced liver fibrosis, models based on nine SOX9-related differentially expressed genes outperform conventional APRI and FIB4 indicators [76].
Table 3: Key Research Reagents for SOX9 Investigation
| Reagent/Resource | Specific Examples | Application | Technical Notes |
|---|---|---|---|
| SOX9 Antibodies | Anti-SOX9 rabbit monoclonal (IHC), anti-SOX9 for Western blot | Protein detection and localization | Validate species reactivity; optimal dilution varies by application |
| Cell Line Models | A549, NCI-H522 (lung cancer); PC3, 22RV1 (prostate); H1975 (NSCLC) | In vitro functional studies | Confirm SOX9 expression baseline; use authenticated lines |
| Animal Models | KrasLSL-G12D;Sox9flox/flox mice; Immunocompromised vs syngeneic hosts | In vivo tumorigenesis and therapy studies | Consider immune status for immunotherapy applications |
| CRISPR Systems | sgRNA targeting Sox9 (e.g., sgSox9.2-pSECC) | Genetic knockout | Use multiple guides to control for off-target effects |
| Databases | TCGA, GTEx, cBioPortal, Human Protein Atlas | Bioinformatics analysis | Leverage multi-omics data for comprehensive analysis |
| Small Molecule Inhibitors | Cordycepin (adenosine analog) | SOX9 pathway modulation | Dose-dependent SOX9 inhibition observed (10-40 μM) [3] |
Key Technical Considerations
When investigating SOX9, several technical considerations ensure reliable results. For immunohistochemical analysis, careful antibody validation is essential, with attention to nuclear localization pattern expected for this transcription factor. In functional studies, employing both gain-of-function (overexpression) and loss-of-function (CRISPR, siRNA) approaches provides complementary evidence for SOX9's roles.
The selection of appropriate model systems should consider the biological context, with 3D organoid cultures often providing more physiologically relevant data than conventional 2D cultures, particularly for evaluating tumor-immune interactions [20]. For immune microenvironment studies, comparison between immunocompetent and immunodeficient models helps delineate direct tumor cell-intrinsic effects from immune-mediated mechanisms.
The cumulative evidence firmly establishes SOX9 overexpression as a significant prognostic indicator across multiple cancer types, with particularly strong validation in lung cancer and glioma. Its association with aggressive disease features, therapeutic resistance, and poor survival outcomes underscores its clinical relevance as a biomarker. Beyond prognostic utility, SOX9 emerges as a central regulator of the tumor immune microenvironment, orchestrating an immunosuppressive niche through modulation of collagen deposition, immune cell infiltration, and potentially immune checkpoint expression.
Future research directions should focus on elucidating the precise molecular mechanisms through which SOX9 regulates immune cell function, particularly its effects on dendritic cell biology and T cell activation. The development of specific SOX9 inhibitors represents a promising therapeutic frontier, with natural compounds like cordycepin demonstrating preliminary efficacy in suppressing SOX9 expression [3]. Additionally, integrating SOX9 assessment into clinical trial designs could stratify patients most likely to benefit from SOX9-targeted approaches or immune checkpoint inhibitors.
The dual function of SOX9 in driving both intrinsic tumor progression and immune evasion positions it as a compelling target for combination therapies. Simultaneously targeting SOX9 and immune checkpoints might overcome resistance mechanisms that limit current immunotherapies. As our understanding of SOX9's context-dependent functions deepens, the translation of these findings into clinical applications holds significant promise for improving outcomes across multiple cancer types.
The SRY-box transcription factor 9 (SOX9) is a pivotal regulator of embryonic development, cell differentiation, and stem cell maintenance. In cancer, SOX9 exhibits a dual nature, functioning as either a proto-oncogene or tumor suppressor in a context-dependent manner. This technical review synthesizes evidence from pan-cancer analyses demonstrating that SOX9 is significantly upregulated in the majority of 15+ cancer types, where it promotes tumorigenesis through the maintenance of stemness, regulation of immune cell infiltration, and induction of chemoresistance. We provide comprehensive quantitative data on SOX9 expression patterns across malignancies, detailed experimental methodologies for investigating its function, and visualization of its central role in modulating the tumor immune microenvironment. The collective evidence positions SOX9 as a promising diagnostic and prognostic biomarker and an emerging therapeutic target in oncology.
SOX9 (SRY-box transcription factor 9) is a transcription factor belonging to the SOX family of proteins characterized by a highly conserved high-mobility group (HMG) box DNA-binding domain [66] [79]. This domain enables SOX9 to recognize the specific DNA sequence CCTTGAG, leading to DNA bending and altered chromatin organization that modulates transcriptional activity [80] [79]. Beyond its well-established roles in chondrogenesis, sex determination, and embryonic development, SOX9 has emerged as a critical player in oncogenesis with complex, context-dependent functions [1] [16].
Comprehensive pan-cancer analyses reveal that SOX9 expression is significantly elevated in fifteen different cancer types compared to their matched healthy tissues, including cervical squamous cell carcinoma (CESC), colon adenocarcinoma (COAD), esophageal carcinoma (ESCA), glioblastoma (GBM), kidney renal papillary cell carcinoma (KIRP), brain lower grade glioma (LGG), liver hepatocellular carcinoma (LIHC), lung squamous cell carcinoma (LUSC), ovarian cancer (OV), pancreatic adenocarcinoma (PAAD), rectum adenocarcinoma (READ), stomach adenocarcinoma (STAD), thymoma (THYM), uterine carcinosarcoma (UCS), and uterine corpus endometrial carcinoma (UCES) [80] [3]. In contrast, SOX9 expression is significantly decreased in only two malignancies: skin cutaneous melanoma (SKCM) and testicular germ cell tumors (TGCT) [80] [3]. This expression pattern suggests SOX9 primarily functions as a proto-oncogene in most cancer types, while exhibiting tumor suppressor properties in specific contexts [80].
Pan-Cancer SOX9 Expression and Prognostic Significance
Large-scale transcriptomic and proteomic analyses across multiple cancer types have established distinct patterns of SOX9 expression with significant clinical implications. The table below summarizes SOX9 expression and its prognostic value across various malignancies.
Table 1: SOX9 Expression and Prognostic Significance Across Cancers
| Cancer Type | SOX9 Expression vs. Normal | Prognostic Association | Clinical Implications |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly increased [80] | Better prognosis in lymphoid invasion subgroups [33] | Independent prognostic factor for IDH-mutant cases [33] |
| Liver Hepatocellular Carcinoma (LIHC) | Significantly increased [80] | Poor survival (HR=2.103) [81] | Negative prognostic factor validated in multiple cohorts [81] |
| Lower Grade Glioma (LGG) | Significantly increased [80] | Short overall survival [80] | Prognostic marker for worst outcomes [80] |
| Thymoma (THYM) | Significantly increased [80] | Short overall survival [80] | Correlates with immune dysregulation [80] |
| Breast Cancer | Frequently overexpressed [16] | Widespread negative prognostic significance [81] | Driver of basal-like subtype [16] |
| Ovarian Cancer | Significantly increased [80] | Negative prognostic factor [81] | Shorter survival after platinum therapy [32] |
| Lung Cancer | Significantly increased in LUSC [80] | Negative prognostic factor [81] | Correlates with tumor grade and survival [33] |
| Skin Cutaneous Melanoma (SKCM) | Significantly decreased [80] | Tumor suppressor role [80] | Inhibits tumorigenicity in models [80] |
The prognostic impact of SOX9 extends beyond individual cancer types, with validation studies across large patient cohorts (breast cancer n=3,951; ovarian cancer n=1,306; lung cancer n=1,926; gastric cancer n=876) consistently demonstrating that high SOX9 expression serves as a negative prognostic factor [81]. Multivariate analysis in hepatocellular carcinoma confirms SOX9 as an independent prognostic marker even after adjustment for other clinicopathological factors (HR=2.103, 95%CI=1.064-4.156, p=0.021) [81].
SOX9 Regulation of Immune Cell Infiltration in the Tumor Microenvironment
A key mechanism through which SOX9 influences cancer progression is by modulating the tumor immune microenvironment. SOX9 expression correlates significantly with specific immune infiltration patterns across multiple cancer types, contributing to an immunosuppressive milieu that facilitates immune evasion.
Table 2: SOX9 Correlation with Immune Cell Infiltration Across Cancers
| Cancer Type | Positive Correlation | Negative Correlation | Immune Evasion Mechanisms |
|---|---|---|---|
| Colorectal Cancer | Neutrophils, Macrophages, Activated mast cells, Naive/activated T cells [1] | B cells, Resting mast cells, Resting T cells, Monocytes, Plasma cells, Eosinophils [1] | Creates "immune desert" microenvironment [1] |
| Prostate Cancer | Tregs, M2 macrophages (TAM Macro-2), Anergic neutrophils [1] | CD8+CXCR6+ T cells, Activated neutrophils [1] | Androgen deprivation enriches SOX9+ club cells [1] |
| Liver Cancer | Regulatory T-cell (Treg) infiltration [66] | CD8+ T-cell infiltration [66] | SOX12 increases Tregs and decreases CD8+ T cells [66] |
| Multiple Cancers | PD-L1 expression, Immunosuppressive cells [66] | CD8+ T cell activity, Antigen presentation [66] | Impairs immune cell function [1] |
The following diagram illustrates how SOX9 orchestrates tumor immune evasion through multiple interconnected mechanisms:
SOX9-Mediated Mechanisms of Immune Evasion
Beyond the mechanisms illustrated above, SOX9 contributes to cancer immune evasion by enabling tumor cell dormancy and maintaining stemness. Research indicates that SOX2 and SOX9 are crucial for latent cancer cells to remain dormant in secondary metastatic sites and avoid immune surveillance under immunotolerant conditions [16]. In breast cancer, SOX9 triggers tumorigenesis by facilitating the immune escape of tumor cells [3], while in thymoma, SOX9 expression negatively correlates with genes related to Th17 cell differentiation, primary immunodeficiency, PD-L1 expression, and T-cell receptor signaling pathways [3].
SOX9 in Cancer Stemness and Therapeutic Resistance
SOX9 plays a pivotal role in maintaining cancer stem cells (CSCs) and promoting therapy resistance across multiple cancer types. In high-grade serous ovarian cancer (HGSOC), SOX9 is epigenetically upregulated following platinum-based chemotherapy and is sufficient to induce chemoresistance [32]. Mechanistically, SOX9 increases transcriptional divergence, reprogramming naive cells into a stem-like state characterized by enhanced plasticity and drug tolerance [32].
The following diagram illustrates the experimental workflow for investigating SOX9-mediated chemoresistance, as demonstrated in ovarian cancer studies:
Experimental Workflow for SOX9 in Chemoresistance
Functional studies demonstrate that SOX9 knockout significantly increases sensitivity to carboplatin treatment in HGSOC cell lines (p=0.0025) [32]. Longitudinal single-cell RNA-Seq analysis of patient tumors before and after neoadjuvant chemotherapy confirms that SOX9 is consistently upregulated in post-treatment cancer cells across the majority of patients (8 of 11), supporting its role in clinical chemoresistance [32]. In hepatocellular carcinoma, SOX9 expression is associated with stem cell features in all tested cell lines (p<0.05), and reduced SOX9 expression decreases the growth of liver cancer cells (p<0.05) [81].
Experimental Models and Research Reagent Solutions
Investigating SOX9 function in cancer requires well-characterized experimental models and reagents. The following table details key research tools and their applications in SOX9 studies:
Table 3: Essential Research Reagents and Experimental Models for SOX9 Studies
| Reagent/Model | Specifications | Application | Key Findings |
|---|---|---|---|
| Cell Lines | Prostate: 22RV1, PC3Lung: H1975Liver: HepG2, Hep3BBreast: MCF7, BT474, SUM159Ovarian: OVCAR4, Kuramochi, COV362 [3] [32] [81] | Functional assays, drug testing, mechanistic studies | SOX9 KD reduces cancer cell growth; stem cell models [3] [81] |
| SOX9 Antibody | Polyclonal rabbit anti-human SOX9 (ab76997, Abcam) [81] | Immunohistochemistry, Western blot | Semi-quantitative scoring of SOX9+ tumor cells [81] |
| CRISPR/Cas9 | SOX9-targeting sgRNA [32] | Gene knockout studies | Increased platinum sensitivity in HGSOC [32] |
| Cordycepin | Adenosine analog from Cordyceps sinensis [3] | Small molecule inhibition | Inhibits SOX9 mRNA and protein dose-dependently [3] |
| siRNA | SOX9-specific siRNA [81] | Transient knockdown | Reduces liver cancer cell growth (p<0.05) [81] |
Detailed Experimental Protocol: SOX9 Inhibition with Cordycepin
The following methodology outlines the approach for investigating SOX9 inhibition using cordycepin in cancer cell lines:
Cell Culture and Treatment:
- Prostate cancer cells (PC3 and 22RV1) and lung cancer cells (H1975) are maintained in appropriate media (RPMI 1640 for PC3 and H1975; DMEM for 22RV1) supplemented with 10-15% fetal bovine serum and 1% penicillin/streptomycin [3].
- Cells are cultured in a 37°C incubator with 5% CO₂ and inoculated in 12-well plates for experiments [3].
- Cordycepin is dissolved and treated at final concentrations of 0, 10, 20, and 40 µM for 24 hours [3].
Protein and RNA Analysis:
- After treatment, cells are lysed using EBC buffer and 2×SDS loading buffer to collect proteins [3].
- Protein samples are boiled at 100°C for 5 minutes and electrophoresed using the Bio-Rad Mini PROTEAN Tetra System [3].
- Proteins are transferred to PVDF membranes under ice bath conditions [3].
- For RNA analysis, total RNA is extracted by reverse transcription following established protocols [3].
This experimental approach has demonstrated that cordycepin inhibits both protein and mRNA expression of SOX9 in a dose-dependent manner in 22RV1, PC3, and H1975 cells, indicating its anticancer roles likely occur through SOX9 inhibition [3].
SOX9 emerges as a master regulator of oncogenesis across diverse cancer types, functioning through the maintenance of cancer stemness, induction of therapeutic resistance, and profound modulation of the tumor immune microenvironment. The consistent pattern of SOX9 overexpression in the majority of cancers, coupled with its strong association with poor clinical outcomes, positions SOX9 as a valuable diagnostic and prognostic biomarker in precision oncology.
Therapeutic targeting of SOX9 represents a promising avenue for cancer treatment. Evidence that cordycepin inhibits SOX9 expression in a dose-dependent manner provides a foundation for developing novel SOX9-targeted therapies [3]. Furthermore, the role of SOX9 in mediating chemoresistance suggests that SOX9 inhibition could potentially re-sensitize resistant tumors to conventional chemotherapeutic agents [32]. Future research should focus on developing more specific and potent SOX9 inhibitors, validating their efficacy in preclinical models, and identifying patient selection biomarkers for SOX9-targeted therapies.
Given the complex dual nature of SOX9 in both promoting immune evasion while also contributing to tissue repair processes, therapeutic strategies must carefully balance efficacy with potential toxicities. Nevertheless, the comprehensive evidence across multiple cancer types solidifies SOX9 as a compelling therapeutic target worthy of continued investigation in cancer drug development.
The interaction between the transcription factor SOX9 and the immune checkpoint protein PD-L1 represents a complex and crucial regulatory axis within the tumor microenvironment. This technical review synthesizes current evidence demonstrating that SOX9 operates as a master regulator of immune checkpoint expression, predominantly through indirect transcriptional mechanisms and modulation of immune cell infiltration. Accumulating data from pan-cancer analyses, single-cell sequencing studies, and functional genetic experiments reveal that SOX9 expression correlates with an immunosuppressive tumor microenvironment characterized by altered PD-L1 expression patterns, impaired cytotoxic T-cell function, and recruitment of immunosuppressive cell populations. This comprehensive analysis delineates the molecular pathways connecting SOX9 to PD-L1 regulation and provides detailed methodological frameworks for investigating this relationship, offering valuable insights for researchers developing novel immunotherapeutic strategies.
SRY-box transcription factor 9 (SOX9) is a high-mobility group (HMG) box transcription factor with established roles in development, cell fate determination, and differentiation. Beyond its developmental functions, SOX9 has emerged as a significant oncogenic regulator across diverse cancer types, including thymic epithelial tumors, glioblastoma, melanoma, and various carcinomas [82] [3] [18]. Structurally, SOX9 contains several functional domains: an N-terminal dimerization domain (DIM), the central HMG box DNA-binding domain, and C-terminal transcriptional activation domains (TAM and TAC) that facilitate interactions with co-regulators [1]. The position of SOX9 at the intersection of tumor progression and immune regulation has garnered substantial research interest, particularly regarding its influence on immune checkpoint pathways, including the PD-1/PD-L1 axis.
The programmed death-ligand 1 (PD-L1)/PD-1 pathway represents a critical immune checkpoint that suppresses T-cell-mediated antitumor immunity. Tumor cell-intrinsic expression of PD-L1 can be either constitutive (PD-L1CON) or induced by inflammatory signals (PD-L1IND), particularly interferon-gamma (IFN-γ) [83]. Understanding the molecular drivers of PD-L1 expression is essential for optimizing checkpoint immunotherapy. Emerging evidence positions SOX9 as a key upstream regulator that shapes the immune landscape through both direct transcriptional mechanisms and indirect effects on immune cell composition, creating a microenvironment conducive to immune evasion [82] [1] [9]. This review systematically examines the relationship between SOX9 and PD-L1 expression, detailing the underlying molecular mechanisms, experimental approaches for investigation, and therapeutic implications.
Molecular Mechanisms Connecting SOX9 to PD-L1 Regulation
Direct Transcriptional Regulation and Pathway Interactions
The relationship between SOX9 and PD-L1 expression operates through multiple interconnected biological pathways. While direct binding of SOX9 to the PD-L1 promoter remains to be conclusively demonstrated, substantial evidence indicates that SOX9 influences PD-L1 through intermediate transcriptional networks and signaling pathways:
Transcriptional Reprogramming: In melanoma, constitutive PD-L1 expression (PD-L1CON) is associated with extensive transcriptomic reprogramming characterized by dedifferentiation and activation of innate inflammatory pathways, including IFN and TNF signaling [83]. While SOX9's role in this specific context requires further elucidation, it participates in similar reprogramming events in other malignancies.
Negative Correlation with PD-L1 Pathway Genes: Bioinformatics analysis of thymoma samples from The Cancer Genome Atlas (TCGA) revealed a significant negative correlation between SOX9 expression and genes involved in PD-L1 expression and PD-1 checkpoint pathways [82]. This suggests SOX9 may suppress certain aspects of checkpoint signaling while potentially enhancing others in a context-dependent manner.
Tuft Cell Phenotype Association: In thymic epithelial tumors, high SOX9 expression correlates positively with POU2F3 and TRPM5, master regulators of tuft cells [82]. This phenotypic switch may indirectly influence PD-L1 expression through alterations in tumor cell differentiation states.
Table 1: SOX9 Correlation with Immune Checkpoint Pathways Across Cancer Types
| Cancer Type | Correlation with PD-L1 | Proposed Mechanism | Functional Outcome |
|---|---|---|---|
| Thymic Epithelial Tumors | Negative correlation with PD-L1 pathway genes | Transcriptional suppression of PD-L1 related signaling | Immune dysregulation |
| Head and Neck Squamous Cell Carcinoma | Indirect via ANXA1/FPR1 axis | SOX9-induced ANXA1 promotes neutrophil apoptosis | Resistance to anti-PD-1/anti-LAG-3 therapy |
| Melanoma | Context-dependent | Association with dedifferentiated state | Potential modulation of PD-L1CON expression |
| Colorectal Cancer | Not directly specified | Negative correlation with resting T-cells and monocytes | Altered immune infiltration landscape |
SOX9-Mediated Modulation of the Immune Microenvironment
SOX9 significantly influences PD-L1 expression indirectly through profound effects on immune cell infiltration and composition within the tumor microenvironment:
Promotion of Immunosuppressive Cell Populations: In thymoma, high SOX9 expression is associated with significant domination of M2 macrophages, which exhibit immunosuppressive properties and can potentially express PD-L1 [82]. Similarly, in prostate cancer models, SOX9 expression correlates with increased immunosuppressive cells including Tregs and M2 macrophages, creating an "immune desert" microenvironment [1].
Inhibition of Cytotoxic Immune Cells: SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells and NK cells [1]. This impairment of cytotoxic immunity may reduce IFN-γ production, consequently affecting inducible PD-L1 expression.
Neutrophil Regulation via ANXA1-FPR1 Axis: Recent research in head and neck squamous cell carcinoma (HNSCC) revealed that SOX9+ tumor cells directly regulate annexin A1 (ANXA1) expression, which mediates apoptosis of formyl peptide receptor 1 (FPR1)+ neutrophils through the ANXA1-FPR1 axis [9]. This pathway inhibits neutrophil accumulation in tumors, ultimately impairing infiltration and cytotoxic function of CD8+ T and γδT cells.
The following diagram illustrates the core molecular and cellular pathways through which SOX9 influences PD-L1 expression and immune checkpoint function:
Diagram 1: SOX9-PD-L1 Regulatory Axis. This diagram illustrates the direct and indirect mechanisms through which SOX9 influences PD-L1 expression and contributes to immunotherapy resistance.
Experimental Approaches for Investigating SOX9-PD-L1 Relationships
Bioinformatics and Transcriptomic Analysis Protocols
Comprehensive bioinformatics approaches have been essential for elucidating the relationship between SOX9 and PD-L1:
Differential Gene Expression Analysis:
- Tool Implementation: Utilize R software with the limma package to identify differentially expressed genes (DEGs) between high and low SOX9 expression groups [82].
- Threshold Parameters: Apply |log2(fold-change)| > 2 and adjusted p-value < 0.05 as significance thresholds [82].
- Data Sources: TCGA datasets provide standardized gene expression data across multiple cancer types, including thymoma (108 cases) and thymic carcinoma (11 cases) [82].
Gene Set Enrichment Analysis (GSEA):
- Software: Use GSEA software (version 4.0.3) from the Broad Institute to generate heat-maps of the top 100 DEGs [82].
- Pathway Mapping: Identify genes positively and negatively associated with SOX9 expression and map them to known signaling pathways including proteoglycans in cancer, cell adhesion molecules, extracellular matrix-receptor interaction, and TGF-β signaling pathways [82].
Immune Infiltration Analysis:
- Algorithm Application: Employ the Tumor Immune Estimation Resource (TIMER) database for systematic analysis of immune infiltration levels [82].
- Cell Type Quantification: Use single-sample GSEA (ssGSEA) and ESTIMATE algorithms to quantify immune cell subsets and overall immune scores in tumors with varying SOX9 expression [18].
Table 2: Key Research Reagents and Experimental Resources
| Reagent/Resource | Specification | Application | Example Source |
|---|---|---|---|
| Anti-SOX9 Antibody | Polyclonal rabbit anti-SOX9 (AB5535; Sigma-Aldrich) at 1:100 dilution | Immunohistochemistry staining of SOX9 in tumor tissues | [82] |
| PD-L1 Detection | PE anti-human CD274/PD-L1 (Biolegend, catalog# 329706) | Flow cytometry analysis of PD-L1 surface expression | [83] |
| Cell Lines | PD-L1CON (MM127, MM595, COLO239F) and PD-L1IND (NZM12, NZM15, WM115) melanoma lines | In vitro models of constitutive vs inducible PD-L1 expression | [83] |
| Animal Model | 4NQO-induced HNSCC mouse model (C57BL/6 background) | In vivo studies of therapy resistance mechanisms | [9] |
| Software | R package with limma, ClusterProfiler, ggplot2 | Bioinformatics analysis of gene expression data | [82] [18] |
Functional Validation Methodologies
Robust experimental validation is required to confirm bioinformatic predictions of SOX9-PD-L1 relationships:
Immunohistochemistry and Staining Evaluation:
- Protocol: Perform heat-induced antigen retrieval with 0.01 M sodium citrate buffer (pH=6.0) at 98°C for 10 minutes [82].
- Staining Quantification: Score SOX9 immunostaining semi-quantitatively based on intensity (0-3 scale) and proportion of positive tumor cell nuclei (0-3 scale) [82].
- Threshold Definition: Define high SOX9 expression as final immunostaining scores >3 (product of intensity and proportion scores) [82].
Flow Cytometry for PD-L1 Expression:
- Cell Preparation: Process tumor tissues through mechanical dissociation and 70μm filtration to obtain single-cell suspensions [84].
- Staining Protocol: Use fixable viability stains (e.g., FVS450) to exclude dead cells, followed by surface staining with anti-PD-L1 antibodies [83].
- Gating Strategy: Apply fluorescence minus one (FMO) and isotype controls to establish appropriate gating boundaries [84].
- Analysis Parameters: For melanoma cell lines, define PD-L1CON as MFI >10,000 and PD-L1IND as MFI <500 after background subtraction [83].
Single-Cell RNA Sequencing:
- Sample Preparation: Pool tumor tissues from multiple mice (typically n=3 per condition) and digest into single-cell suspensions [9].
- Quality Control: Filter cells based on standard QC parameters (mitochondrial DNA percentage, number of features) [9].
- Cell Type Identification: Use canonical markers to identify major cell types: epithelial cells (Krt14, Krt5, Krt6a), fibroblasts (Col1a1, Col3a1), endothelial cells (Flt1, Pecam1), and immune cells (Ptprc, Cd3g) [9].
- Malignant Cell Identification: Apply CopyKAT algorithm to distinguish aneuploid tumor cells from non-malignant epithelial cells [9].
The following diagram outlines a comprehensive experimental workflow for investigating SOX9 and PD-L1 relationships:
Diagram 2: Experimental Workflow for SOX9/PD-L1 Research. This workflow outlines key methodological approaches from sample collection through data integration.
Therapeutic Implications and Future Directions
The relationship between SOX9 and PD-L1 has significant implications for cancer immunotherapy development and patient stratification:
Predictive Biomarker Potential: Pan-cancer analyses indicate that high SOX9 expression correlates with shortened overall survival in LGG, CESC, and THYM, suggesting its utility as a prognostic biomarker [3] [49]. The inverse relationship between SOX9 and PD-L1 pathway genes in thymomas may inform response predictions to PD-1/PD-L1 inhibitors [82].
Resistance Mechanisms: In HNSCC, Sox9+ tumor cell enrichment mediates resistance to anti-LAG-3 plus anti-PD-1 combination therapy through the ANXA1-FPR1 axis and subsequent impairment of neutrophil accumulation [9]. Targeting this axis may overcome resistance to combination immunotherapy.
Pharmacological Targeting: Cordycepin (CD), an adenosine analog, inhibits both protein and mRNA expression of SOX9 in a dose-dependent manner in cancer cell lines (22RV1, PC3, and H1975) [3] [49]. This SOX9 inhibition represents a promising strategy to counteract SOX9-mediated immunosuppression.
Context-Dependent Considerations: The functional consequences of SOX9 expression appear cancer-type specific. In melanoma, SOX9 expression is typically decreased compared to normal skin, and its upregulation inhibits tumorigenesis in experimental models [3] [49]. This contrasts with most other cancers where SOX9 acts as an oncogene, highlighting the importance of context-specific investigations.
Future research should prioritize the development of SOX9-targeted therapeutic approaches, validation of SOX9 as a predictive biomarker for immunotherapy response, and elaboration of the precise molecular mechanisms through which SOX9 regulates PD-L1 expression in different cancer types. The integration of SOX9 modulation with existing immune checkpoint inhibitors represents a promising avenue for overcoming current limitations in cancer immunotherapy.
The translation of preclinical discoveries into clinically actionable insights represents a critical challenge in oncology. This validation process is particularly crucial for understanding transcription factors like SOX9 (SRY-related HMG-box 9), which has emerged as a master regulator of immune cell infiltration within the tumor microenvironment (TME). SOX9, a transcription factor containing a highly conserved high-mobility group (HMG) box domain, recognizes specific DNA sequences and plays essential roles in embryonic development, cell differentiation, and tissue homeostasis [1] [33]. Recent evidence has positioned SOX9 as a janus-faced regulator in cancer immunology, demonstrating context-dependent roles across various malignancies [1]. This technical guide examines the methodologies and analytical frameworks for validating SOX9-mediated immune regulation using human biospecimens, providing researchers with standardized approaches to bridge preclinical findings and clinical application.
SOX9 Expression Patterns Across Human Cancers: Diagnostic and Prognostic Significance
Comprehensive analysis of SOX9 expression across human malignancies reveals distinct patterns with significant implications for tumor immunity and patient outcomes. Evidence from The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases demonstrates that SOX9 is frequently dysregulated in multiple cancer types [3].
Table 1: SOX9 Expression Patterns and Clinical Correlations in Human Cancers
| Cancer Type | SOX9 Expression Pattern | Correlation with Prognosis | Immune Context |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly upregulated | Better prognosis in lymphoid invasion subgroups | Correlated with immune checkpoint expression |
| Colorectal Cancer | Highly expressed | Associated with poor prognosis | Negative correlation with B cells, resting T cells; positive with neutrophils, macrophages |
| Lung Adenocarcinoma | Upregulated | Shorter overall survival | Mutually exclusive with various immune checkpoints |
| Melanoma (SKCM) | Significantly decreased | Inhibits tumorigenicity when expressed | Contributes to retinoic acid sensitivity |
| Testicular Germ Cell Tumors (TGCT) | Significantly decreased | Not fully characterized | Limited evidence |
| Cervical Cancer | Upregulated | Promotes malignant phenotypes | Activates IL-6/JAK/STAT3 pathway |
Analysis of 33 cancer types from TCGA revealed that SOX9 expression was significantly increased in 15 cancer types (including CESC, COAD, ESCA, GBM, KIRP, LGG, LIHC, LUSC, OV, PAAD, READ, STAD, THYM, UCES, and UCS) while significantly decreased in only two cancers (SKCM and TGCT) compared with matched healthy tissues [3]. This pan-cancer expression pattern suggests SOX9 primarily functions as a proto-oncogene in most cancer contexts, though it can act as a tumor suppressor in specific malignancies like melanoma [3].
In glioblastoma, SOX9 overexpression shows unique prognostic significance. Contrary to patterns in other cancers, high SOX9 expression in GBM is remarkably associated with better prognosis in lymphoid invasion subgroups, highlighting the context-dependent nature of SOX9 function [33] [18]. Furthermore, high SOX9 expression serves as an independent prognostic factor for IDH-mutant glioblastoma in Cox regression analysis, emphasizing its clinical relevance in molecularly defined subgroups [33].
Methodological Framework: Analyzing SOX9-Mediated Immune Infiltration in Clinical Biospecimens
Transcriptomic Analysis of SOX9 Expression and Immune Correlates
The validation of SOX9-related findings in clinical samples requires a multi-dimensional approach to transcriptomic analysis:
RNA Sequencing Data Processing: Begin with HTSeq-Count or FPKM data from TCGA or GEO repositories. For differential expression analysis, utilize the DESeq2 R package with thresholds set at \|log2Fold Change\| > 1 and adjusted p-value < 0.05 [33] [85]. Normalize microarray data using the limma package with similar thresholds [86].
Co-expression Network Analysis: Implement Weighted Gene Co-expression Network Analysis (WGCNA) to identify gene modules correlated with SOX9 expression patterns. Set the scale-free fit index (R²) > 0.85 and mean connectivity near zero to determine the optimal soft threshold power (β) for network construction [85].
Immune Infiltration Quantification: Apply the ssGSEA algorithm from the GSVA package to compute enrichment scores for immune cell populations [33] [86]. Alternatively, utilize the CIBERSORT method to deconvolute transcriptomic expression matrices and estimate abundances of 22 immune cell types [87]. The xCell algorithm provides additional resolution for analyzing 64 immune and stromal cell populations [86].
Table 2: Key Computational Tools for SOX9 Immune Infiltration Analysis
| Tool/Package | Primary Function | Application Context |
|---|---|---|
| DESeq2 (R) | Differential expression analysis | RNA-seq count data |
| limma (R) | Differential expression analysis | Microarray data |
| WGCNA (R) | Co-expression network analysis | Identifying correlated gene modules |
| ssGSEA/GSVA (R) | Gene set variation analysis | Immune cell enrichment scoring |
| CIBERSORT | Deconvolution algorithm | Estimating immune cell fractions |
| xCell | Cell type enrichment analysis | Immune and stromal cell quantification |
| LinkedOmics | Multi-omics data analysis | Identifying SOX9-correlated genes |
| Metascape | Functional enrichment | Pathway and process enrichment |
Functional Validation of SOX9 in Immune Regulation
Beyond correlative analyses, functional validation is essential to establish causal relationships:
SOX9 Pathway Manipulation: In cervical cancer models, small interfering RNA (siRNA)-mediated SOX9 knockdown demonstrated significant suppression of malignant phenotypes, including reduced proliferation, increased apoptosis, and decreased migration/invasion capabilities [88]. Similar approaches in prostate cancer (PC3, 22RV1) and lung cancer (H1975) cell lines confirmed SOX9's functional role in tumor progression [3].
Pharmacological Inhibition Studies: The adenosine analog cordycepin has shown dose-dependent inhibition of both SOX9 protein and mRNA expression in 22RV1, PC3, and H1975 cells, suggesting its potential as a therapeutic agent targeting SOX9 pathways [3].
Immune Checkpoint Correlation Analysis: Evaluate relationships between SOX9 expression and immune checkpoint molecules (PD-1, PD-L1, CTLA-4) using Spearman's correlation tests on transcriptomic data [33]. In glioblastoma, SOX9 expression shows significant correlation with multiple immune checkpoints, indicating its involvement in immunosuppressive networks [33].
Analytical Workflows: From Data to Biological Insight
Diagram 1: SOX9 Immune Infiltration Analysis Workflow
SOX9-Mediated Mechanisms of Immune Regulation in the Tumor Microenvironment
SOX9 influences antitumor immunity through multiple interconnected mechanisms that shape the immunosuppressive tumor microenvironment:
Direct Modulation of Immune Cell Infiltration
Analyses of clinical biospecimens reveal that SOX9 expression significantly correlates with altered immune cell infiltration patterns across cancer types. In colorectal cancer, SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [1]. Similarly, in prostate cancer, SOX9 expression contributes to an "immune desert" microenvironment characterized by decreased effector immune cells (CD8+CXCR6+ T cells and activated neutrophils) and increased immunosuppressive cells (Tregs, M2 macrophages, and anergic neutrophils) [1].
Regulation of Immune Checkpoint Pathways
SOX9 interacts with key immune checkpoint pathways to facilitate immune evasion. Research indicates that SOX9 expression in thymoma negatively correlates with genes related to PD-L1 expression and T-cell receptor signaling pathways [66]. In breast cancer, SOX9 triggers tumorigenesis by facilitating the immune escape of tumor cells, potentially through checkpoint regulation [3]. These findings position SOX9 within the broader network of immune checkpoint regulation, suggesting its potential as a target for combination immunotherapy approaches.
Inflammatory Pathway Activation
The SOX9/PLOD3/IL-6/JAK/STAT3 axis represents a critical mechanism through which SOX9 promotes tumor progression and immune modulation in cervical cancer [88]. This pathway activation creates a pro-tumorigenic inflammatory milieu that supports cancer cell survival and dampens effective antitumor immunity. In melanoma models, SOX9 expression restoration increased sensitivity to retinoic acid, demonstrating its role in therapeutic response modulation [3].
Diagram 2: SOX9-Mediated Immunosuppressive Mechanisms
Table 3: Research Reagent Solutions for SOX9 Immune Function Studies
| Reagent/Resource | Function/Application | Specifications & Examples |
|---|---|---|
| SOX9 Antibodies | Immunodetection and quantification | Western blot, IHC, IF; Validate specificity with knockout controls |
| siRNA/shSOX9 Constructs | SOX9 knockdown studies | Sequence-verified constructs with appropriate scramble controls |
| TCGA/GTEx Datasets | Transcriptomic reference data | Processed RNA-seq data with clinical annotations |
| GEO Datasets | Validation cohorts | Independent patient cohorts with expression data |
| Cordycepin | Small molecule SOX9 inhibitor | Dose range: 10-40 μM; 24-hour treatment [3] |
| Cell Line Models | Functional validation | Prostate: 22RV1, PC3; Lung: H1975; Cervical: HeLa [3] [88] |
| Immune Cell Signature Panels | Deconvolution analysis | Curated gene sets for specific immune populations |
| Animal Models | In vivo validation | Xenograft models with humanized immune systems |
Interpretation and Clinical Translation Framework
Context-Dependent Analysis of SOX9 Functions
The dual nature of SOX9 as both oncogene and tumor suppressor necessitates careful interpretation of results within specific pathological contexts. In most carcinomas (including colorectal, gastric, liver, and lung cancers), SOX9 acts predominantly as an oncogene, promoting tumor progression and immune evasion [1] [3]. However, in glioblastoma, high SOX9 expression correlates with better prognosis in specific molecular subgroups, particularly those with lymphoid invasion [33] [18]. This context-dependent functionality underscores the importance of disease-specific validation when extrapolating SOX9-related findings.
Biomarker Development and Validation
The robust association between SOX9 expression and clinical outcomes supports its development as a diagnostic and prognostic biomarker. In glioblastoma, SOX9-based gene signatures contribute to nomogram models that effectively predict patient outcomes [33]. For clinical translation, researchers should:
- Validate assay conditions using clinical biospecimens with known outcomes
- Establish standardized scoring systems for SOX9 expression in different sample types (FFPE, frozen tissue, liquid biopsies)
- Define context-specific cutoff values for SOX9 expression levels correlated with clinical outcomes
- Integrate SOX9 assessment with established markers (e.g., IDH status in glioma) for improved stratification
Therapeutic Targeting Considerations
The transcriptional regulation of immune pathways positions SOX9 as an attractive therapeutic target. Preclinical evidence demonstrates that cordycepin inhibits SOX9 expression in a dose-dependent manner, suggesting the feasibility of pharmacological targeting [3]. For therapeutic development, researchers should prioritize:
- Identification of SOX9-dependent vulnerabilities in specific cancer subtypes
- Development of targeted degradation approaches for SOX9 protein
- Exploration of combination strategies with immune checkpoint inhibitors
- Assessment of therapeutic windows based on SOX9's roles in normal tissue homeostasis
The integration of clinical biospecimen analysis with sophisticated computational methods provides an essential framework for validating SOX9's multifaceted roles in regulating tumor immune infiltration. As research progresses, standardized methodologies for assessing SOX9 expression and its immunomodulatory functions will enhance reproducibility across studies. The context-dependent nature of SOX9 activity necessitates disease-specific validation, while its position within critical immune regulatory networks offers promising avenues for therapeutic intervention. Through rigorous application of the approaches outlined in this technical guide, researchers can effectively translate preclinical findings on SOX9 into clinically relevant insights that advance cancer diagnosis, prognosis, and treatment.
The SRY-related HMG-box (SOX) family of transcription factors plays crucial roles in embryonic development, cell differentiation, and stem cell maintenance [66]. Among these members, SOX9 has emerged as a particularly significant regulator in cancer biology, where its dysregulation contributes significantly to tumorigenesis, progression, and therapeutic resistance. Recent advances have illuminated its unique function within the SOX family in orchestrating tumor immune evasion—a process by which cancer cells avoid detection and elimination by the host immune system [66] [1]. This review provides a comprehensive analysis of SOX9's distinct mechanisms in modulating immune cell infiltration and function within the tumor microenvironment (TME), framing these findings within the broader context of SOX family biology to highlight the specialized role of SOX9 as a master regulator of the immunosuppressive niche.
Unlike other SOX members that may have more limited or context-dependent immune functions, SOX9 demonstrates a remarkable capacity to simultaneously influence multiple aspects of the cancer-immune dialogue. It functions as a "double-edged sword" in immunology, playing complex and sometimes contradictory roles across different biological contexts [1]. In cancer, however, it predominantly acts as an immunosuppressive factor by creating what researchers have termed an "immune cold" environment—characterized by poor infiltration and function of anti-tumor immune cells [4]. This capacity positions SOX9 as a critical node in the immune evasion network and an promising therapeutic target for overcoming resistance to current immunotherapies.
Structural and Functional Distinctions of SOX9 Within the SOX Family
Comparative Structural Organization of SOX Proteins
The SOX family proteins share a highly conserved high-mobility group (HMG) box domain comprising approximately 79 amino acids that enables DNA binding and bending, subsequently altering chromatin organization to modulate gene transcription [66]. However, SOX9 possesses several distinctive structural features that contribute to its unique functional capabilities. The SOX9 protein contains multiple functional domains organized from N- to C-terminus: a dimerization domain (DIM), the defining HMG box domain, and two transcriptional activation domains—one central (TAM) and one at the C-terminus (TAC)—along with a proline/glutamine/alanine (PQA)-rich domain [1].
The HMG domain serves dual roles, directing nuclear localization through embedded nuclear localization signals (NLS) and facilitating DNA binding [1]. The C-terminal transcriptional activation domain (TAC) interacts with diverse cofactors such as Tip60 to enhance SOX9's transcriptional activity and is essential for β-catenin inhibition during cellular differentiation processes [1]. These structural specializations enable SOX9 to function as a potent transcriptional regulator with broader target gene networks compared to many other SOX family members.
SOX9's Distinct Immune Regulatory Profile Within the SOX Family
While multiple SOX family members have been implicated in immune regulation, SOX9 demonstrates a particularly broad and potent influence on the tumor immune microenvironment. The table below provides a comparative overview of key SOX family members and their documented roles in immune evasion:
Table 1: Comparative Roles of SOX Family Members in Cancer Immune Evasion
| SOX Member | Role in Immune Evasion | Key Mechanisms | Cancer Contexts |
|---|---|---|---|
| SOX9 | Creates "immune cold" tumors; induces immunosuppression | Recruits Tregs and M2 macrophages; upregulates PD-L1; decreases CD8+ T cell and NK cell infiltration | Lung, breast, ovarian, glioblastoma [1] [18] [4] |
| SOX2 | Promotes immune evasion | Upregulates PD-L1; enhances Treg recruitment; alleviates JAK-STAT pathway | Multiple solid tumors [66] |
| SOX4 | Inhibits protective immunity | Suppresses innate and adaptive immune pathways | Various cancers [66] |
| SOX11 | Creates immunosuppressive microenvironment | Increases Treg infiltration; downregulates antigen processing and presentation | Various cancers [66] |
| SOX12 | Modifies T-cell infiltration | Increases Tregs; decreases CD8+ T-cells | Liver cancer [66] |
| SOX17 | Prevents anti-tumor T cell responses | Inhibits IFNγ sensing and response | Various cancers [66] |
| SOX18 | Promotes immunosuppressive milieu | Transactivates PD-L1 and CXCL12; recruits Tregs and TAMs | Liver cancer [66] |
This comparative analysis reveals SOX9's unique capacity to simultaneously regulate multiple immunosuppressive cell populations and immune checkpoint molecules, positioning it as a master regulator of the immunosuppressive tumor microenvironment.
Molecular Mechanisms of SOX9-Mediated Immune Evasion
Regulation of Immune Cell Infiltration and Function
SOX9 exerts profound effects on the composition and functional state of immune cells within the tumor microenvironment through several interconnected mechanisms:
Modulation of T-cell Populations: SOX9 expression negatively correlates with genes associated with the function of CD8+ T cells and shows a positive correlation with memory CD4+ T cells [1]. In prostate cancer, SOX9 expression is associated with an "immune desert" microenvironment characterized by decreased effector immune cells (including CD8+CXCR6+ T cells) and increased immunosuppressive cells (including Tregs) [1]. This reshaping of the T-cell landscape effectively cripples the adaptive anti-tumor immune response.
Control of Myeloid Cell Compartment: SOX9 expression demonstrates a positive correlation with neutrophils and macrophages, particularly the M2-polarized tumor-associated macrophages (TAMs) that possess immunosuppressive properties [1] [18]. In glioblastoma, SOX9 expression closely correlates with specific patterns of immune cell infiltration, contributing to the immunosuppressive character of the TME [18].
Creation of an "Immune Cold" Environment: Research in KRAS-mutant lung cancer demonstrates that SOX9 overexpression creates "immune cold" conditions where the immune system fails to adequately control tumor growth [4]. Knocking out SOX9 delayed tumor formation, while its overexpression accelerated tumorigenesis, primarily through profound effects on immune cell infiltration [4].
The following diagram illustrates the core signaling pathway through which SOX9 orchestrates immune evasion:
Figure 1: SOX9-Mediated Immune Evasion Pathway. SOX9 expression drives the formation of an "immune cold" tumor microenvironment through multiple coordinated mechanisms that suppress effector immune cells while expanding immunosuppressive populations.
Regulation of Immune Checkpoint Molecules
Beyond its effects on immune cell populations, SOX9 directly and indirectly regulates the expression of critical immune checkpoint molecules that facilitate immune evasion:
PD-L1 Transactivation: SOX9 has been demonstrated to transactivate PD-L1, a key immune checkpoint protein that inhibits T-cell function upon binding to its receptor PD-1 [66]. This upregulation creates a primary mechanism of adaptive immune resistance.
Correlation with Multiple Checkpoints: In glioblastoma, SOX9 expression shows significant correlation with various immune checkpoints, suggesting its broader role in regulating the immune checkpoint landscape [18]. This multi-checkpoint regulation may contribute to the resistance patterns observed in SOX9-high tumors.
Induction of Stemness and Plasticity
A particularly insidious mechanism through which SOX9 promotes immune evasion is by enhancing cancer stem cell (CSC) properties and transcriptional plasticity:
Chemotherapy-Induced SOX9 Upregulation: In high-grade serous ovarian cancer (HGSOC), chemotherapy treatment results in rapid population-level induction of SOX9 that enriches for a stem-like transcriptional state [32]. This SOX9-high subpopulation demonstrates significant chemoresistance in vivo.
Transcriptional Reprogramming: SOX9 increases transcriptional divergence, reprogramming the transcriptional state of naive cells into a stem-like state [32]. This enhanced plasticity allows cancer cells to better adapt to therapeutic pressures and immune surveillance.
Maintenance of Dormancy: SOX9 helps maintain latent cancer cells in a dormant state within secondary metastatic sites, enabling them to avoid immune monitoring under immunotolerant conditions [19]. This dormancy represents a profound form of immune evasion that facilitates long-term metastatic recurrence.
Quantitative Evidence: Correlating SOX9 Expression with Immune Parameters Across Cancers
The impact of SOX9 on the tumor immune microenvironment is substantiated by comprehensive transcriptomic analyses across multiple cancer types. The table below summarizes key quantitative relationships between SOX9 expression and immune parameters:
Table 2: SOX9 Correlation with Immune Parameters Across Cancer Types
| Cancer Type | Immeregent Parameter | Correlation with SOX9 | Clinical/Prognostic Impact |
|---|---|---|---|
| Colorectal Cancer | B cells, resting mast cells, monocytes | Negative | Not specified [1] |
| Colorectal Cancer | Neutrophils, macrophages, activated mast cells | Positive | Not specified [1] |
| Multiple Cancers | CD8+ T cell function, NK cell function | Negative | Poor response to immunotherapy [1] [4] |
| Multiple Cancers | Memory CD4+ T cells | Positive | Immunosuppressive microenvironment [1] |
| Prostate Cancer | CD8+CXCR6+ T cells | Negative | "Immune desert" formation [1] |
| Prostate Cancer | Tregs, M2 macrophages | Positive | Therapy resistance [1] |
| Glioblastoma | Immune checkpoint molecules | Positive | Immunosuppressive TME [18] |
| Glioblastoma | Specific immune infiltration patterns | Significant correlation | Prognostic value [18] |
| Ovarian Cancer | Stem-like transcriptional state | Positive | Platinum resistance [32] |
These consistent patterns across diverse cancer types underscore the fundamental role of SOX9 in shaping immunosuppressive microenvironments and highlight its potential as both a predictive biomarker and therapeutic target.
Experimental Approaches for Investigating SOX9 in Immune Evasion
Methodologies for Assessing SOX9-Immune Interactions
Research into SOX9's role in immune evasion employs sophisticated methodological approaches that combine molecular manipulation with comprehensive immune profiling:
Immune Cell Infiltration Analysis: The ssGSEA package and ESTIMATE algorithm in the GSVA package are used for immuno-infiltration correlation analysis of SOX9, with statistical significance evaluated by Spearman's test [18] [33]. This computational approach allows researchers to quantify the relationship between SOX9 expression levels and specific immune cell populations in large patient cohorts.
Single-Cell RNA Sequencing (scRNA-Seq): Longitudinal scRNA-Seq of patient tumors before and after chemotherapy has revealed that SOX9 is consistently upregulated in post-treatment cancer cells, providing direct evidence of therapy-induced SOX9-mediated immune adaptation [32].
Spatial Transcriptomics: In prostate cancer research, combined single-cell RNA sequencing and spatial transcriptomics have identified SOX9-enriched subpopulations and their association with shifted immune landscapes characterized by decreased effector cells and increased immunosuppressive populations [1].
The following workflow diagram outlines a comprehensive experimental approach for studying SOX9 in immune evasion:
Figure 2: Experimental Workflow for SOX9-Immune Evasion Research. A multi-modal approach combining genetic manipulation, advanced omics technologies, and functional validation to decipher SOX9's role in shaping the tumor immune microenvironment.
Essential Research Reagents and Tools
The investigation of SOX9 in immune contexts requires specialized research tools and reagents, summarized in the table below:
Table 3: Essential Research Reagents for Studying SOX9 in Immune Evasion
| Reagent/Tool | Category | Specific Examples | Research Application |
|---|---|---|---|
| SOX9 Modulators | Genetic Tools | CRISPR/Cas9 KO, siRNA, overexpression vectors | Functional validation of SOX9 in immune regulation [32] |
| Immune Profiling Tools | Antibody Panels | Flow cytometry antibodies for T cells, Tregs, macrophages, neutrophils | Quantification of immune cell populations [1] [18] |
| Transcriptomic Platforms | Analysis Platforms | scRNA-Seq, spatial transcriptomics, RNA-Seq | Comprehensive immune microenvironment analysis [1] [32] |
| Computational Algorithms | Bioinformatics Tools | ssGSEA, ESTIMATE, CIBERSORT | Deconvolution of immune cell infiltration [18] [33] |
| Animal Models | In Vivo Systems | Immunocompetent mouse models, PDX models | Study of SOX9-immune interactions in physiologic context [4] |
| Therapeutic Inhibitors | Chemical Tools | USP28 inhibitors (AZ1) | Targeting SOX9 protein stability [89] |
Therapeutic Implications and Future Directions
SOX9 as a Therapeutic Target in Immuno-Oncology
The central role of SOX9 in coordinating immune evasion programs makes it an attractive therapeutic target for overcoming resistance to current immunotherapies:
Biomarker Potential: SOX9 shows promise as a predictive biomarker for immunotherapy response. In lung cancer, patients with high SOX9 expression may be less likely to respond to immune checkpoint inhibitors, suggesting that SOX9 assessment could guide treatment selection [4].
Overcoming Chemoresistance: In ovarian cancer, SOX9 upregulation following platinum-based chemotherapy induces a stem-like transcriptional state associated with chemoresistance [32]. Targeting SOX9 or its regulatory pathways may prevent or reverse this adaptive resistance mechanism.
Protein Stability Modulation: Recent research has identified that the deubiquitinating enzyme USP28 stabilizes SOX9 protein by inhibiting its FBXW7-mediated ubiquitination and degradation [89]. The USP28-specific inhibitor AZ1 reduces SOX9 protein stability and increases sensitivity to PARP inhibitors in ovarian cancer models, suggesting a viable therapeutic strategy [89].
Integration with Current Immunotherapies
Future therapeutic development should focus on rational combinations that target SOX9-dependent resistance mechanisms while leveraging existing immunotherapies:
Sequencing Considerations: The dynamic regulation of SOX9 in response to therapy suggests that timing of SOX9-targeted interventions may be critical. Preemptive targeting might prevent the development of resistant, SOX9-high subpopulations.
Patient Stratification: Assessment of SOX9 expression levels and activity could help identify patient subgroups most likely to benefit from specific combination therapies, particularly those with "immune cold" tumors that typically respond poorly to checkpoint inhibition alone.
Microenvironment Reprogramming: Rather than direct SOX9 inhibition, which may be challenging due to its transcription factor nature, alternative approaches focusing on reprogramming the SOX9-shaped microenvironment may offer more immediately viable therapeutic avenues.
SOX9 occupies a unique position within the SOX family as a master regulator of the immunosuppressive tumor microenvironment. Through its coordinated effects on multiple immune cell populations, checkpoint molecules, and cancer cell intrinsic properties including stemness and plasticity, SOX9 drives the formation of "immune cold" tumors that resist current immunotherapies. Its consistent association with therapy resistance across cancer types, coupled with emerging strategies to target its regulatory networks, positions SOX9 as both a valuable biomarker and promising therapeutic target in the ongoing effort to overcome immune evasion in cancer. Future research should focus on elucidating the complete spectrum of SOX9-regulated immune pathways and developing clinically viable strategies to disrupt these pathways for therapeutic benefit.
Conclusion
SOX9 emerges as a central, master regulator of the immunosuppressive tumor microenvironment, functioning as a critical barrier to effective anti-tumor immunity and a key driver of resistance to checkpoint immunotherapy. Its influence, mediated through mechanisms like the ANXA1-FPR1 axis, suppression of cytotoxic cell infiltration, and remodeling of the extracellular matrix, underscores its potential as both a powerful prognostic biomarker and a compelling therapeutic target. Future research must focus on developing clinically viable strategies to inhibit SOX9 activity or its downstream effectors. Combining these novel approaches with existing immunotherapies represents a promising frontier for overcoming treatment resistance and improving outcomes for cancer patients, particularly those with SOX9-high tumors.
References
- 1. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 2. The pioneer factor SOX9 competes for epigenetic factors to ... [https://www.nature.com/articles/s41556-023-01184-y]
- 3. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 4. Studying the Role of Sox9 in Lung Cancer [https://news.cuanschutz.edu/cancer-center/sox9-in-lung-cancer]
- 5. SOX9 in organogenesis: shared and unique transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482574/]
- 6. The versatile functions of Sox9 in development, stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4326072/]
- 7. Transcriptional co-activators CREB-binding protein and ... [https://pubmed.ncbi.nlm.nih.gov/12732631/]
- 8. Transcriptional Co-activators CREB-binding Protein and ... [https://www.sciencedirect.com/science/article/pii/S0021925820846900]
- 9. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://www.nature.com/articles/s41467-025-59050-4]
- 10. Sox9: a master regulator of the pancreatic program [https://pubmed.ncbi.nlm.nih.gov/25148367/]
- 11. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/pii/S1359644622002136]
- 12. SOX9: An emerging driving factor from cancer progression ... [https://pubmed.ncbi.nlm.nih.gov/33524528/]
- 13. SOX9 as an emerging target for anticancer drugs and a ... [https://pubmed.ncbi.nlm.nih.gov/35636723/]
- 14. SOX9: The master regulator of cell fate in breast cancer [https://www.sciencedirect.com/science/article/abs/pii/S0006295219304885]
- 15. Sox9 Functions as a Master Regulator of Antler Growth ... [https://pubmed.ncbi.nlm.nih.gov/29185790/]
- 16. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 17. SOX9 Is Essential for Triple-Negative Breast Cancer Cell ... [https://pubmed.ncbi.nlm.nih.gov/32661114/]
- 18. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 19. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 20. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 21. A SOX9-B7x axis safeguards dedifferentiated tumor cells ... [https://www.sciencedirect.com/science/article/pii/S1534580723005518]
- 22. SOX9 drives a stem-like transcriptional state and platinum ... [https://www.jci.org/articles/view/186467]
- 23. 9p21 loss confers a cold tumor immune microenvironment ... [https://www.nature.com/articles/s41467-021-25894-9]
- 24. SOX9 - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/sox9]
- 25. Identification of glycolysis-related clusters and immune cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12626809/]
- 26. Pan-Cancer Analysis of Immune Cell Infiltration Identifies a ... [https://pubmed.ncbi.nlm.nih.gov/32714316/]
- 27. The Immune Cell Infiltration Patterns and Characterization ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2022.852708/full]
- 28. Dissecting SOX9 dynamics reveals its differential regulation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11649970/]
- 29. Distinct immune cell infiltration patterns in pancreatic ductal ... [https://www.nature.com/articles/s41467-024-55424-2]
- 30. SOX9: An emerging driving factor from cancer progression ... [https://www.sciencedirect.com/science/article/abs/pii/S0304419X21000160]
- 31. Transcription Factor Drives Chemotherapy Resistance in ... [https://news.feinberg.northwestern.edu/2025/10/30/transcription-factor-drives-chemotherapy-resistance-in-ovarian-cancer/]
- 32. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 33. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 34. SOX9 suppresses colon cancer via inhibiting epithelial ... [https://www.jci.org/articles/view/184115]
- 35. Immune cell infiltration as a biomarker for the diagnosis and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6426802/]
- 36. Analysis of immune infiltration in basal cell carcinoma ... [https://link.springer.com/article/10.1007/s12672-025-02621-0]
- 37. Integrative multiomics analysis reveals the subtypes and key ... [https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-025-06725-7]
- 38. Single-cell RNA sequencing reveals immune ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-024-02177-7]
- 39. Single Cell Deletion of the Transcription Factors Trps1 and ... [https://pubmed.ncbi.nlm.nih.gov/39610085/]
- 40. Single-cell RNA sequencing to map tumor heterogeneity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11399521/]
- 41. Spatial transcriptomics identifies molecular niche ... [https://www.nature.com/articles/s41588-025-02080-x]
- 42. Single-cell transcriptomics analysis reveals dynamic ... [https://www.nature.com/articles/s41598-025-86950-8]
- 43. Single-cell RNA-seq enables comprehensive tumour and ... [https://www.nature.com/articles/ncomms15081]
- 44. Editing SOX Genes by CRISPR-Cas - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC8583549/]
- 45. Preclinical models of soft tissue sarcomas [https://www.sciencedirect.com/science/article/pii/S1040842825000095]
- 46. A suite of enhancer AAVs and transgenic mouse lines for ... [https://www.sciencedirect.com/science/article/pii/S0092867425005136]
- 47. Genome editing of immune cells using CRISPR/Cas9 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7851445/]
- 48. AACR 2025_GemPharmatech [https://en.gempharmatech.com/content/details100645_5778465.html]
- 49. Comprehensive analysis, immune, and cordycepin ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1149986/full]
- 50. Pharmacological and therapeutic potential of Cordyceps with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3909570/]
- 51. Structural and pharmacological insights into cordycepin for ... [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2024.1367820/full]
- 52. Cordycepin alleviates diabetes mellitus-associated hepatic ... [https://pubmed.ncbi.nlm.nih.gov/39260158/]
- 53. Cordycepin alleviates diabetes mellitus-associated hepatic ... [https://www.sciencedirect.com/science/article/abs/pii/S004520682400717X]
- 54. Cordycepin Targets HRD1 to Promote Cancer Cell PD‐L1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12531455/]
- 55. Enhancing cancer immunotherapy using cordycepin and ... [https://www.nature.com/articles/s41598-024-72833-x]
- 56. Super-enhancer inhibitors THZ2 and JQ1 reverse ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366492/]
- 57. SOX9 Stem-Cell Factor: Clinical and Functional Relevance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463569/]
- 58. The local and circulating SOX9 as a potential biomarker for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7292907/]
- 59. Upregulated SOX9 expression indicates worse prognosis ... [https://www.oncotarget.com/article/22635/text/]
- 60. Immunosuppressive SOX9‐AS1 Resists Triple‐Negative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11569622/]
- 61. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002136]
- 62. SOX9 regulated matrix proteins are increased in patients ... [https://www.nature.com/articles/s41598-018-36037-4]
- 63. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://pubmed.ncbi.nlm.nih.gov/40295483/]
- 64. Understanding LAG-3 Signaling - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC8156499/]
- 65. SOX on tumors, a comfort or a constraint? [https://www.nature.com/articles/s41420-024-01834-6]
- 66. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 67. Immune evasion in cancer: mechanisms and cutting-edge ... [https://www.nature.com/articles/s41392-025-02280-1]
- 68. A therapeutic antibody targeting annexin-A1 inhibits cancer ... [https://www.nature.com/articles/s41388-023-02919-9]
- 69. Collagen heterogeneity: a barrier and bridge driving tumor ... [https://pubmed.ncbi.nlm.nih.gov/40921908/]
- 70. SOX9 reprograms endothelial cells by altering the chromatin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9410909/]
- 71. SOX9 directly regulates the type-II collagen gene [https://pubmed.ncbi.nlm.nih.gov/9171829/]
- 72. SOX9 directly regulates the type-ll collagen gene [https://www.nature.com/articles/ng0697-174]
- 73. A SOX -B7x axis safeguards dedifferentiated tumor 9 from... cells [https://pubmed.ncbi.nlm.nih.gov/37963469/]
- 74. Clinical significance of SOX9 in human non-small cell lung ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3313873/]
- 75. High expression of SOX9 is a diagnostic and prognostic ... [https://pubmed.ncbi.nlm.nih.gov/40692865/]
- 76. Identification of SOX9-related prognostic DEGs and a ... [https://pubmed.ncbi.nlm.nih.gov/39622395/]
- 77. Identification of SOX9-related prognostic DEGs and a ... [https://www.sciencedirect.com/science/article/pii/S037811192401014X]
- 78. SOX9 promotes epidermal growth factor receptor-tyrosine ... [https://www.sciencedirect.com/science/article/abs/pii/S0024320521005944]
- 79. protein SOX summary - The Human Protein Atlas 9 expression [https://www.proteinatlas.org/ENSG00000125398-SOX9]
- 80. Comprehensive analysis, immune, and cordycepin regulation for... [https://pubmed.ncbi.nlm.nih.gov/37020558/]
- 81. is a proliferation and stem cell factor in... | PLOS One SOX 9 [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0187814]
- 82. Diagnostic and Prognostic Significances of SOX9 in Thymic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8580949/]
- 83. Transcriptional Reprogramming and Constitutive PD-L1 ... [https://www.mdpi.com/2072-6694/13/17/4250]
- 84. PPARγ inhibition boosts efficacy of PD-L1 Checkpoint ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7097912/]
- 85. Identification and validation of biomarkers, construction ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1559422/full]
- 86. Exploration of effective biomarkers and infiltrating immune ... [https://www.nature.com/articles/s41598-025-18589-4]
- 87. Diagnostic biomarkers and immune infiltration profiles ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12060493/]
- 88. Oncogenic role of PLOD3 mediated by SOX9 through IL-6/ ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656825006655]
- 89. USP28 promotes PARP inhibitor resistance by enhancing ... [https://www.nature.com/articles/s41419-025-07647-4]