SOX9 in the Tumor Immune Microenvironment: A Double-Edged Sword in Cancer Progression and Therapy
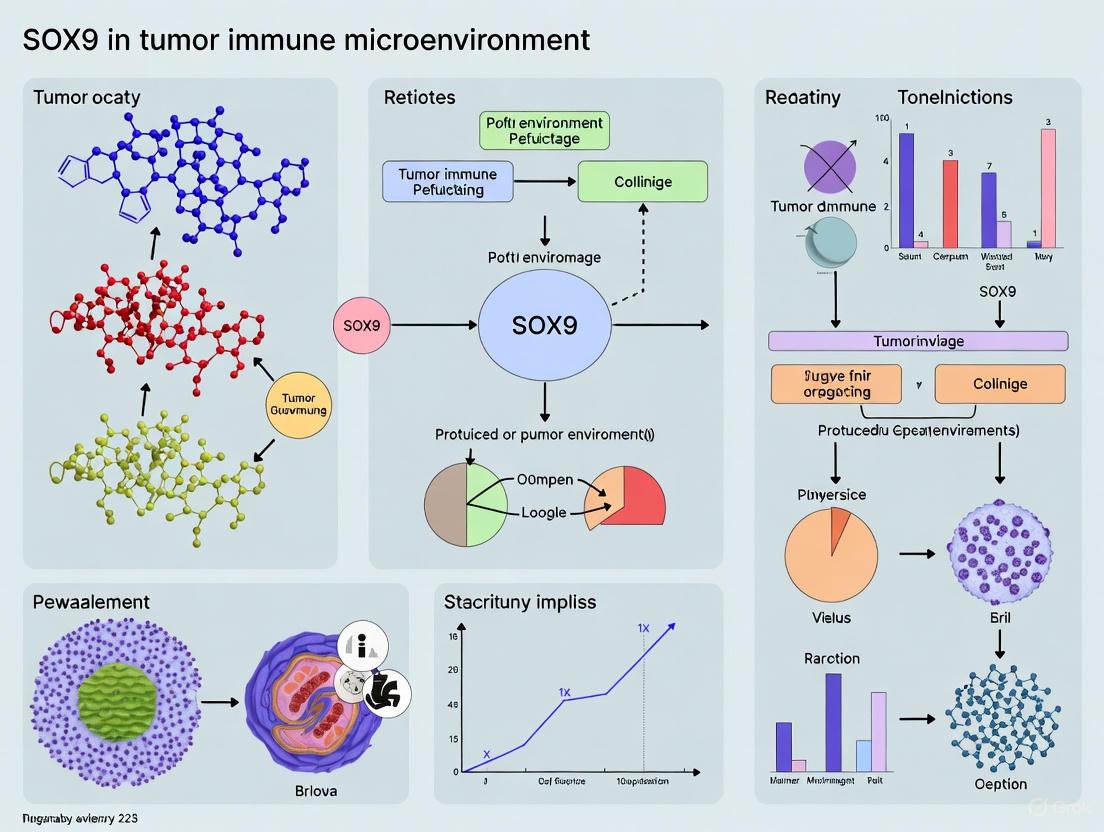
This article synthesizes current knowledge on the transcription factor SOX9, a pivotal yet dualistic regulator within the tumor immune microenvironment (TIME).
SOX9 in the Tumor Immune Microenvironment: A Double-Edged Sword in Cancer Progression and Therapy
Abstract
This article synthesizes current knowledge on the transcription factor SOX9, a pivotal yet dualistic regulator within the tumor immune microenvironment (TIME). We explore its foundational biology, from its structure and pioneer factor function to its complex role in modulating immune cell infiltration, fostering an immunosuppressive milieu, and driving immune evasion across various cancers. Methodologically, we detail how SOX9 is investigated—from bioinformatics analyses of clinical datasets to functional studies—and evaluate its emerging promise as a therapeutic target and prognostic biomarker. The content also addresses the challenges in targeting SOX9, including its cell-context-dependent functions and role in drug resistance, while validating its clinical relevance through correlation with patient outcomes and immune checkpoint expression. This resource is tailored for researchers, scientists, and drug development professionals seeking to understand and therapeutically exploit SOX9's multifaceted functions in oncology.
The Dual Nature of SOX9: From Pioneer Factor to Immune Modulator
SOX9 Protein Structure and Functional Domains
The SOX9 (SRY-related HMG-box 9) protein is a transcription factor belonging to the SOXE subgroup of the SOX family, playing critical roles in embryonic development, cell differentiation, and tissue homeostasis [1] [2]. In recent years, SOX9 has emerged as a significant regulator in cancer biology, particularly within the tumor immune microenvironment, where it exhibits complex, context-dependent functions [3] [4]. Understanding its structural architecture and functional domains provides essential insights for developing targeted cancer therapies. This technical guide comprehensively details SOX9 protein structure, domain functionality, and experimental methodologies for investigating its role in tumor immunology.
Protein Domain Architecture
The human SOX9 protein comprises 509 amino acids with multiple functionally specialized domains organized linearly from N- to C-terminus [3] [1]. These domains mediate DNA binding, protein-protein interactions, nuclear localization, and transcriptional activation.
Table 1: SOX9 Functional Domains and Characteristics
| Domain Name | Position (Amino Acids) | Key Functions | Structural Features |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal (ahead of HMG box) | Facilitates SOX9 homodimerization and heterodimerization with SOXE proteins | Required for DNA binding and transactivation of specific target genes [3] [1] |
| HMG Box Domain | Central region | Sequence-specific DNA binding, nuclear localization, DNA bending | Contains nuclear localization (NLS) and export (NES) signals; recognizes consensus sequence CCTTGAG [3] [5] [2] |
| Central Transcriptional Activation Domain (TAM) | Middle region | Synergizes with TAC to enhance transcriptional potential | Interacts with transcriptional co-activators and basal transcriptional machinery [3] [1] |
| PQA-Rich Domain | C-terminal region | Enhances transactivation capability | Proline/glutamine/alanine-rich region; lacks autonomous transactivation [3] [1] |
| C-terminal Transcriptional Activation Domain (TAC) | C-terminus | Primary transcriptional activation | Binds cofactors (Tip60, CBP/p300, MED12, WWP2); inhibits β-catenin during chondrocyte differentiation [3] [1] |
Table 2: SOX9 Post-Translational Modifications and Regulatory Mechanisms
| Modification Type | Site/Region | Functional Consequences | Biological Context |
|---|---|---|---|
| Phosphorylation | PKA phosphorylation site | Modulates transcriptional activity | Cell signaling integration [5] |
| Protein-Protein Interactions | Multiple domains | Beta-catenin binding, protein kinase A binding, mediator complex interactions | Alters transcriptional specificity and chromatin remodeling [1] [5] |
Structural Basis for SOX9 Function in Tumor Immunology
SOX9's domain structure enables its multifunctional capabilities in both developmental processes and cancer pathophysiology, particularly within the tumor immune microenvironment. The HMG domain facilitates sequence-specific DNA binding to the consensus motif AGAACAATGG, with AACAAT forming the core binding element [1]. This DNA binding induces structural bending of approximately 70-85 degrees, altering chromatin architecture and accessibility for additional transcriptional regulators [2].
The dimerization domain enables SOX9 to form homodimers on palindromic composite DNA motifs separated by 3-5 nucleotides, particularly in cancer and chondrocyte contexts [1]. SOXE protein heterodimerization occurs through DIM domain interaction with the HMG box of partner proteins, expanding regulatory complexity in tumor cells [1].
Transcriptional activation domains TAM and TAC recruit distinct coactivator complexes: TAC physically interacts with MED12, CBP/p300, TIP60, and WWP2, enhancing transcriptional activity through chromatin modifications [1]. The PQA-rich domain, while lacking autonomous transactivation capability, significantly enhances SOX9's capacity to transactivate reporter plasmids with tandemly repeated SOX9 binding sites [1].
SOX9 in Tumor Immune Microenvironment Regulation
SOX9 plays a dual role in immunomodulation, functioning as both an oncogene and tissue repair regulator [3]. In cancer contexts, SOX9 promotes immunosuppression through multiple mechanisms mediated by its structural domains:
Immune Cell Infiltration Modulation
Bioinformatics analyses of TCGA data reveal SOX9 expression correlates significantly with altered immune cell infiltration patterns across multiple cancer types [3]. In colorectal cancer, SOX9 negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while positively correlating with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. Single-cell RNA sequencing in prostate cancer demonstrates SOX9+ tumor cells associate with an "immune desert" microenvironment characterized by decreased CD8+CXCR6+ T cells and increased immunosuppressive Tregs and M2 macrophages [3].
Cancer Stem Cell Maintenance and Immune Evasion
The structural plasticity of SOX9 enables its function as a pioneer factor that can remodel chromatin architecture, facilitating transcriptional reprogramming toward stem-like states [6]. In high-grade serous ovarian cancer, chemotherapy-induced SOX9 upregulation drives acquisition of chemoresistance through a cancer stem cell (CSC)-like state [6]. SOX9 maintains tumor cells in a stem-like, dormant state that evades immune surveillance by impairing immune cell function and promoting long-term survival in metastatic sites [3] [4].
Signaling Pathway Integration in Tumor Immunity
SOX9 interacts with multiple signaling pathways crucial for tumor-immune crosstalk. In cervical cancer, SOX9 transcriptionally activates PLOD3, which promotes oncogenesis through the IL-6/JAK/STAT3 pathway, creating an immunosuppressive microenvironment [7]. The TAC domain's ability to inhibit β-catenin demonstrates SOX9's intersection with Wnt signaling, a pathway increasingly recognized for its immunomodulatory functions in cancer [3] [1].
SOX9 Signaling in Tumor Immunity
Experimental Methodologies for SOX9 Research
SOX9 Expression Modulation and Functional Assays
CRISPR/Cas9-Mediated SOX9 Knockout
- Protocol: Design sgRNAs targeting SOX9 exon regions. Transfect HGSOC cell lines (OVCAR4, Kuramochi, COV362) with Cas9-sgRNA ribonucleoprotein complexes using lipofection. Validate knockout via Western blot and functional assays [6].
- Application: SOX9 ablation significantly increases platinum sensitivity measured by colony formation assays (2-tailed Student's t-test, P = 0.0025) [6].
Epigenetic Modulation of SOX9 Expression
- Protocol: Treat cancer cells with epigenetic modulators (HDAC inhibitors, DNA methyltransferase inhibitors) to assess SOX9 super-enhancer commissioning. Combine with chromatin immunoprecipitation (ChIP) for H3K27ac to identify resistant state-specific regulatory elements [6].
- Application: Demonstrates nongenetic mechanisms of SOX9 upregulation in chemoresistant cells, independent of genetic mutations [6].
SOX9 Transcriptional Activity Assessment
Chromatin Immunoprecipitation Sequencing (ChIP-seq)
- Protocol: Crosslink cells with formaldehyde, sonicate chromatin, immunoprecipitate with SOX9-specific antibodies. Sequence bound DNA fragments and analyze for SOX9 binding motifs and target genes [6].
- Application: Identifies SOX9 direct targets in cancer cells, including PLOD3 in cervical cancer and stemness-associated genes in ovarian cancer [6] [7].
Single-Cell Multiomic Profiling
- Protocol: Perform simultaneous RNA sequencing and ATAC sequencing on individual cells from patient tumors before and after chemotherapy. Analyze SOX9 expression correlation with chromatin accessibility and transcriptional divergence [6].
- Application: Reveals SOX9-mediated transcriptional reprogramming in rare cell subpopulations driving chemoresistance [6].
SOX9-Protein Interaction Mapping
Co-Immunoprecipitation and Mass Spectrometry
- Protocol: Lyse cells in non-denaturing buffer, incubate with SOX9 antibody, precipitate with protein A/G beads. Analyze bound proteins via liquid chromatography-mass spectrometry (LC-MS/MS) [1].
- Application: Identifies SOX9 interaction partners including β-catenin, WWP2, and mediator complex subunits, elucidating mechanisms of context-dependent SOX9 function [1].
Table 3: Key Research Reagent Solutions for SOX9 Investigation
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| SOX9 Modulation Tools | CRISPR/Cas9 KO, SOX9-targeting sgRNAs, SOX9 expression vectors | Gain/loss-of-function studies | Functional validation in cancer models [6] |
| SOX9 Detection Reagents | SOX9 antibodies (ChIP-grade, IF/IHC-validated), SOX9-IRES-tdTomato reporter | Protein localization, expression quantification | Lineage tracing, expression analysis [6] [8] |
| Cell Line Models | HGSOC lines (OVCAR4, Kuramochi), prostate cancer lines, patient-derived organoids | Disease modeling, therapeutic testing | Chemoresistance, immune evasion studies [3] [6] |
| Pathway Modulators | JAK inhibitors (Ruxolitinib), STAT3 inhibitors, BMP2, TGFβ3 | Signaling pathway dissection | Mechanistic studies of SOX9 function [6] [7] |
| Analytical Platforms | scRNA-seq, ATAC-seq, ChIP-seq, RNA-seq | Multiomics profiling | Transcriptional network analysis [6] |
SOX9-Targeted Therapeutic Strategies
The structural and functional insights into SOX9 domains provide rationale for therapeutic targeting in cancer immunotherapy. Several strategic approaches are under investigation:
Direct SOX9 Inhibition
Targeting the HMG domain to disrupt DNA binding presents a direct approach but faces challenges due to structural similarities across SOX family members. Small molecules interfering with SOX9 dimerization or cofactor recruitment offer alternative strategies [3].
SOX9 Pathway Modulation
Inhibition of SOX9-upregulated pathways provides indirect targeting opportunities. In cervical cancer, targeting the downstream SOX9/PLOD3/IL-6/JAK/STAT3 axis suppresses multiple malignant phenotypes [7]. Combination therapies targeting both SOX9 and immune checkpoints may overcome SOX9-mediated immunosuppression [3] [9].
SOX9-Based Diagnostic and Prognostic Applications
In glioblastoma, SOX9 expression serves as a diagnostic and prognostic biomarker, particularly in IDH-mutant cases [9]. SOX9-based gene signatures enable robust nomogram models for patient stratification and treatment planning [9].
SOX9 Therapeutic Targeting Approaches
SOX9 represents a structurally complex transcription factor with multifaceted functions in tumor immunology. Its domain architecture enables DNA binding, protein interactions, and transcriptional regulation that collectively influence immune cell infiltration, cancer stemness, and therapy resistance. Comprehensive understanding of SOX9 structure-function relationships provides the foundation for developing targeted interventions to disrupt its pro-tumorigenic activities while preserving its tissue-reparative functions. Future research should focus on isoform-specific targeting, context-dependent function manipulation, and combination strategies with immunotherapies to overcome SOX9-mediated immune evasion in cancer.
SOX9 as a Pioneer Transcription Factor in Cell Fate Reprogramming
SOX9, a member of the SRY-related HMG-box transcription factor family, has emerged as a critical regulator in cell fate determination and a pivotal player within the tumor immune microenvironment. This whitepaper synthesizes current research elucidating SOX9's function as a pioneer transcription factor, its mechanistic roles in oncogenesis and immune modulation, and its promise as a therapeutic target. We provide a detailed analysis of SOX9's context-dependent functions, which range from sustaining stemness and promoting immune evasion to facilitating tissue repair. This guide consolidates quantitative data, experimental methodologies, and molecular pathways for researchers and drug development professionals working at the intersection of transcriptional regulation and cancer immunology.
The SOX (SRY-related HMG-box) family of transcription factors are pivotal nuclear proteins characterized by a highly conserved High Mobility Group (HMG) box domain that facilitates DNA binding [3] [9]. Transcription factor SOX-9 recognizes the specific DNA sequence CCTTGAG and is a master regulator of developmental processes, including chondrogenesis, sex determination, and neural crest cell development [2]. Beyond its developmental roles, SOX9 is frequently dysregulated in numerous solid malignancies. Its expression is significantly upregulated in cancers such as colorectal, liver, lung, breast, and pancreatic cancer, where it often correlates with poor prognosis, drug resistance, and metastatic progression [3] [10] [11]. Conversely, in certain contexts like melanoma and specific gynecological cancers, SOX9 can act as a tumor suppressor, highlighting its complex, context-dependent nature [11] [12]. Recently, SOX9 has been identified as a key modulator of the tumor immune microenvironment (TIME), where it influences immune cell infiltration, function, and checkpoint expression, thereby shaping anti-tumor immunity [3] [9] [13].
SOX9 as a Pioneer Transcription Factor: Mechanisms and Evidence
Pioneer transcription factors are defined by their ability to bind to compacted chromatin, initiate chromatin remodeling, and promote an epigenetic landscape permissive for gene activation. Growing evidence positions SOX9 within this functional category.
Molecular Structure and DNA Binding Dynamics
SOX9's structure underpins its potential pioneer activity. Key functional domains include [3]:
- HMG Box: The evolutionarily conserved DNA-binding domain.
- Dimerization Domain (DIM): Enables protein-protein interactions.
- Transcriptional Activation Domains (TAM and TAC): Located in the middle and C-terminal regions, respectively, they recruit co-activators like Tip60 to enhance transcriptional output.
Crucially, live-cell studies in chondrocytes have revealed that approximately 50% of cellular SOX9 is bound to DNA at any given time, with a remarkably short half-time of residence of about 14 seconds [2]. This highly dynamic yet pervasive chromatin interaction is a hallmark of pioneer factor activity, allowing SOX9 to scan the genome and maintain regulatory element accessibility.
Chromatin Accessibility and Dosage Sensitivity
Recent research utilizing a degradation tag (dTAG) system to precisely titrate SOX9 levels in human embryonic stem cell-derived cranial neural crest cells (CNCCs) provides direct evidence of its role in chromatin regulation [14]. Assay for Transposase-Accessible Chromatin with sequencing (ATAC-seq) under varying SOX9 concentrations demonstrated that most SOX9-dependent regulatory elements (REs) are buffered against small dosage reductions. However, a subset of REs, particularly those directly and primarily regulated by SOX9, exhibited heightened sensitivity to SOX9 dosage. These sensitive REs were enriched near genes critical for chondrogenesis and craniofacial development, indicating that SOX9 dosage directly controls key developmental pathways by modulating chromatin architecture [14].
Table 1: Key Structural Domains of SOX9 Protein
| Domain Name | Location | Primary Function |
|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein-protein interaction and dimerization |
| HMG Box | Central | DNA binding, nuclear localization, and nucleocytoplasmic shuttling |
| Central Transcriptional Activation Domain (TAM) | Middle | Synergizes with TAC to augment transcriptional potential |
| C-terminal Transcriptional Activation Domain (TAC) | C-terminal | Interacts with cofactors (e.g., Tip60); inhibits β-catenin |
| PQA-rich Domain | C-terminal | Necessary for transcriptional activation |
The following diagram illustrates the dynamic interplay between SOX9 dosage and its functional outcomes on chromatin and gene expression:
SOX9 in the Tumor Immune Microenvironment
SOX9 orchestrates a complex interplay between tumor cells and the immune system, functioning as a "double-edged sword" [3]. Its role is multifaceted, influencing immune cell differentiation, recruitment, and function.
Regulation of Immune Cell Differentiation and Infiltration
- T-cell Development: SOX9 cooperates with transcription factor c-Maf to activate
Rorcand key effector genes likeIl17aandBlk, thereby modulating the lineage commitment of early thymic progenitors towards γδ T cells and Tγδ17 cells [3]. - B-cell Lymphoma: While not crucial for normal B-cell development, SOX9 is overexpressed in Diffuse Large B-cell Lymphoma (DLBCL), where it acts as an oncogene by promoting proliferation and inhibiting apoptosis [3].
- Immune Cell Infiltration: Bioinformatics analyses of TCGA data reveal that SOX9 expression correlates with specific immune infiltration patterns. In colorectal cancer, high SOX9 negatively correlates with B cells, resting mast cells, and monocytes, but positively correlates with neutrophils, macrophages, and naive/activated T cells [3]. Similarly, in breast cancer, SOX9 expression is associated with an immunosuppressive microenvironment [10].
Orchestration of Immune Evasion
SOX9 drives immune escape through several non-mutually exclusive mechanisms:
- Sustaining Cellular Stemness: SOX9, along with SOX2, is crucial for maintaining the long-term survival and tumor-initiating capacity of latent cancer cells by sustaining stemness, enabling them to remain dormant in metastatic sites and evade immune surveillance [10].
- Regulating Immune Checkpoints:
- In melanoma, SOX9 indirectly regulates CEACAM1, a homophilic immune checkpoint protein that protects tumor cells from T-cell-mediated killing. Knockdown of SOX9 leads to CEACAM1 up-regulation and increased resistance to T-cell cytotoxicity [15] [12].
- In breast cancer, a SOX9-B7x (B7-H4/VTCN1) axis safeguards dedifferentiated tumor cells from immune surveillance. SOX9 directly promotes the expression of the immune checkpoint B7x, which in turn inhibits the activity of tumor-infiltrating lymphocytes, facilitating cancer progression [13].
- Creating an "Immune Desert": In prostate cancer, SOX9 contributes to an "immune desert" microenvironment by promoting a shift where immunosuppressive cells (Tregs, M2 macrophages) are increased, and effector immune cells (CD8+ T cells) are decreased [3].
Table 2: SOX9-Mediated Regulation of Immune Checkpoints and Ligands
| Immune Modulator | Cancer Type | Regulation by SOX9 | Functional Outcome |
|---|---|---|---|
| CEACAM1 | Melanoma | Indirect transcriptional downregulation | SOX9 knockdown increases CEACAM1, leading to T-cell resistance [15] [12] |
| B7x (B7-H4/VTCN1) | Breast Cancer | Direct transcriptional upregulation | Inhibits tumor-infiltrating lymphocyte function, driving immune escape [13] |
| PD-L1 | Thymoma | Expression negatively correlated | Suggests potential interplay with key checkpoint pathways [9] |
The pathway below summarizes the key mechanisms by which SOX9 modulates the tumor immune microenvironment:
Experimental Models and Research Toolkit
Studying SOX9 requires robust models and reagents to dissect its complex functions. Below are key methodologies and tools derived from recent literature.
Key Experimental Workflow: Precise Modulation of SOX9 Dosage
The dTAG system represents a state-of-the-art method for precisely controlling protein levels in cells, as applied to SOX9 in human CNCCs [14].
Detailed Protocol:
- Cell Line Engineering:
- Use a selection-free genome editing method (e.g., CRISPR-Cas9) in human embryonic stem cells (hESCs) to introduce a FKBP12F36V–mNeonGreen–V5 tag at the C-terminus of the endogenous SOX9 gene.
- The FKBP12F36V tag is a degradation tag (dTAG), mNeonGreen serves as a fluorescent proxy for SOX9 levels, and V5 allows for biochemical detection.
- Differentiate the tagged hESCs into cranial neural crest cells (CNCCs) using established protocols.
SOX9 Titration and Treatment:
- Treat SOX9-tagged CNCCs with a dilution series of the heterobifunctional molecule dTAGV-1.
- dTAGV-1 binds the FKBP12F36V tag and recruits the endogenous ubiquitin-proteasome system, leading to targeted degradation of SOX9.
- Typical treatment: Incubate cells with dTAGV-1 concentrations ranging from 0.5 nM to 500 nM for 24-48 hours to achieve a gradient of SOX9 protein levels.
Downstream Analysis:
- Flow Cytometry: Use mNeonGreen fluorescence to quantify SOX9 protein levels at the single-cell level.
- ATAC-seq: Perform on cells across the SOX9 dosage range to map changes in chromatin accessibility.
- RNA-seq: Analyze transcriptomic changes to identify dosage-sensitive genes.
- Functional Assays: Subject cells to differentiation assays (e.g., chondrogenesis) to link SOX9 dosage to phenotypic outcomes.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents for Investigating SOX9 Function
| Reagent / Tool | Function/Application | Example Use Case |
|---|---|---|
| dTAGV-1 Molecule | Induces degradation of FKBP12F36V-tagged SOX9 | Precise titration of SOX9 protein levels in tagged cell lines [14] |
| SOX9-specific siRNA/siRNA | Knocks down endogenous SOX9 expression | Functional validation of SOX9 in immune resistance (e.g., CEACAM1 studies) [15] |
| Recombinant Adenovirus (Ad/GFP-SOX9) | Overexpression of SOX9 | Investigating SOX9's role in keratinocyte proliferation and differentiation [16] |
| Anti-CEACAM1 blocking mAb | Functional blocking of CEACAM1 immune checkpoint | Restoring T-cell mediated killing in melanoma models [12] |
| Cordycepin (CD) | Small molecule inhibitor of SOX9 expression | Testing anti-cancer effects via SOX9 inhibition in prostate and lung cancer cells [11] |
Therapeutic Targeting and Future Directions
The dual role of SOX9 in tumorigenesis and immunity presents both a challenge and an opportunity for therapeutic intervention.
- SOX9 as a Biomarker: High SOX9 expression shows diagnostic and prognostic value in multiple cancers, including glioma and breast cancer [9] [10]. It can stratify patients based on immune infiltration patterns and potential response to therapy.
- Small Molecule Inhibition: The natural compound Cordycepin inhibits both SOX9 protein and mRNA expression in a dose-dependent manner in prostate (22RV1, PC3) and lung (H1975) cancer cells, demonstrating the feasibility of targeting SOX9 pharmacologically [11].
- Immunomodulatory Strategies: Combining SOX9-modulating agents with existing immunotherapies (e.g., anti-PD-1/PD-L1) is a promising avenue. For instance, targeting the SOX9-B7x axis could sensitize breast tumors to immune attack [13].
- Challenge of Context-Dependency: A major hurdle is SOX9's tissue and disease-specific roles. In melanoma, where SOX9 can act as a tumor suppressor, therapeutic inhibition would be counterproductive [11] [12]. Future work must focus on defining context-specific SOX9 networks and identifying safe therapeutic windows.
SOX9 exemplifies the modern paradigm of a pioneer transcription factor, directly shaping the chromatin landscape to control cell fate and influence the surrounding microenvironment. Its integral role in orchestrating an immunosuppressive niche by regulating checkpoint expression, immune cell infiltration, and cancer cell stemness solidifies its position as a high-value target for oncological research. While challenges remain due to its context-dependent functionality, the continued development of precise experimental models and therapeutic agents, as detailed in this guide, provides a clear pathway for harnessing the biology of SOX9 to advance cancer treatment, particularly in the realm of combination immunotherapies.
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) is an evolutionarily conserved transcription factor that has emerged as a critical, yet paradoxical, regulator within the tumor immune microenvironment (TIME). Initially recognized for its fundamental roles in embryonic development, chondrogenesis, and sex determination, SOX9 is frequently dysregulated across diverse cancer types [3]. Contemporary research has illuminated its function as a janus-faced regulator in immunology, capable of exerting both pro-tumorigenic and anti-tumorigenic effects depending on cellular context [3]. This duality presents a significant challenge and opportunity for therapeutic development. Within the complex ecosystem of the TIME, SOX9 modulates key processes including immune cell infiltration, differentiation of immunosuppressive cells, and the expression of immune checkpoint molecules [3] [4]. Its expression in both tumor cells and stromal components, such as endothelial cells, underscores its multifaceted role in shaping an immunosuppressive landscape that facilitates tumor progression and metastasis [17]. This whitepaper synthesizes current mechanistic insights into SOX9's dualistic functions, providing a technical framework for researchers navigating its potential as a therapeutic target.
Structural and Functional Basis of SOX9
Molecular Architecture
The functional capacity of SOX9 is encoded within its distinct protein domains, which facilitate DNA binding, nuclear localization, and transcriptional regulation.
- Dimerization Domain (DIM): Located ahead of the HMG box, this domain facilitates protein-protein interactions and dimer formation [3].
- HMG Box Domain: This evolutionarily conserved, approximately 79-amino acid domain is responsible for DNA binding. It recognizes the specific DNA sequence CCTTGAG and induces DNA bending, thereby altering chromatin architecture and modulating transcriptional activity [3] [10]. Embedded within this domain are nuclear localization signals (NLS) and nuclear export signals (NES) that enable nucleocytoplasmic shuttling [3].
- Transcriptional Activation Domains (TAM and TAC): The central (TAM) and C-terminal (TAC) transcriptional activation domains are crucial for SOX9's transactivation potential. The TAC domain interacts with cofactors like Tip60 to enhance transcriptional activity and is essential for inhibiting β-catenin during chondrocyte differentiation [3].
- PQA-Rich Domain: This proline/glutamine/alanine-rich domain is necessary for full transcriptional activation [3].
Table 1: Functional Domains of the SOX9 Protein
| Domain | Location | Primary Function |
|---|---|---|
| Dimerization (DIM) | N-terminal | Facilitates protein-protein interaction and dimerization |
| HMG Box | Central | DNA binding, sequence-specific recognition (CCTTGAG), DNA bending, nuclear import/export |
| Transcriptional Activation Middle (TAM) | Central | Synergizes with TAC to augment transcriptional potential |
| Transcriptional Activation C-terminal (TAC) | C-terminal | Interacts with co-factors (e.g., Tip60), inhibits β-catenin |
| PQA-Rich Domain | C-terminal | Necessary for transcriptional activation |
DOT Visualization: SOX9 Protein Domain Structure
Diagram 1: SOX9 protein domain architecture.
The Immunosuppressive Face of SOX9 in Cancer
Orchestrating an Immunosuppressive Tumor Microenvironment
In many cancers, SOX9 acts as a potent oncogene by fostering an immunosuppressive TIME. This is achieved through several interconnected mechanisms:
- Inhibition of Cytotoxic Immune Cell Infiltration: Bioinformatic analyses of colorectal cancer data reveal that high SOX9 expression negatively correlates with the infiltration levels of B cells, resting mast cells, monocytes, plasma cells, and eosinophils [3]. Furthermore, SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells and NK cells [3]. In liver cancer, the related family member SOX12 increases intratumoral Treg infiltration and decreases CD8+ T-cell infiltration [4].
- Promotion of Immunosuppressive Cell Populations: SOX9 expression shows positive correlations with neutrophils, macrophages, and activated mast cells [3]. In breast cancer, a SOX9-B7x (B7-H4/VTCN1) axis has been identified, which safeguards dedifferentiated tumor cells from immune surveillance by suppressing tumor-infiltrating lymphocytes [13].
- Mediation of Therapy Resistance: A critical mechanism of resistance to anti-LAG-3 plus anti-PD-1 combination therapy in head and neck squamous cell carcinoma (HNSCC) is mediated by SOX9+ tumor cells. These cells interact with Fpr1+ neutrophils via the ANXA1-FPR1 axis, which promotes mitochondrial fission and inhibits mitophagy by downregulating BNIP3 expression. This prevents neutrophil accumulation, ultimately impairing the infiltration and cytotoxic capacity of CD8+ T and γδT cells [18].
Table 2: Correlations Between SOX9 Expression and Immune Cell Infiltration in Cancer
| Immune Cell Type | Correlation with High SOX9 | Functional Consequence |
|---|---|---|
| CD8+ T cells | Negative [3] | Reduced cytotoxic cell killing |
| NK cells | Negative [3] | Impaired innate immune surveillance |
| M1 Macrophages | Negative [3] | Loss of anti-tumor macrophage activity |
| Neutrophils | Positive [3] | Increased immunosuppressive environment |
| Macrophages (M2/TAMs) | Positive [3] | Promotion of tumor growth and angiogenesis |
| Tregs | Positive (via SOX12) [4] | Suppression of effector T cell function |
| B cells & Plasma cells | Negative [3] | Diminished humoral immune response |
DOT Visualization: SOX9 in Immunosuppression and Therapy Resistance
Diagram 2: SOX9-mediated immunosuppression and therapy resistance pathways.
The Immune-Permissive Face of SOX9 in Homeostasis and Disease
Contrasting its pro-tumorigenic role, SOX9 also exhibits immune-permissive and tissue-reparative functions, highlighting its context-dependent nature.
- Maintenance of Macrophage Function: Increased levels of SOX9 help maintain macrophage function, contributing to cartilage formation, tissue regeneration, and repair [3]. This is particularly relevant in inflammatory diseases like osteoarthritis (OA) [3].
- Role in T-cell Development: During T-cell development, SOX9 can cooperate with c-Maf to activate Rorc and key Tγδ17 effector genes (such as Il17a and Blk). This modulates the lineage commitment of early thymic progenitors, potentially influencing the balance between αβ T cell and γδ T cell differentiation [3].
- Association with Improved Prognosis in Specific Contexts: Surprisingly, in glioblastoma (GBM), high SOX9 expression was remarkably associated with a better prognosis in the lymphoid invasion subgroups and was identified as an independent prognostic factor for IDH-mutant cases [9] [19]. This underscores the cancer subtype-specific functions of SOX9.
SOX9 in the Stromal Compartment: shaping the Vascular Niche
The role of SOX9 extends beyond tumor cells to critical stromal components, notably the tumor vasculature.
- Expression in Tumor Endothelial Cells: SOX9 is upregulated in tumor-associated endothelial cells in both mouse models and human cancers (e.g., melanoma, lung, colorectal, breast, and ovarian cancers) [17]. This expression is predominantly localized to tip and venous endothelial cells, including high endothelial venules (HEVs) [17].
- Driver of Immature Vasculature: In melanoma models, endothelial-specific conditional knockout of Sox9 resulted in a significant reduction in total endothelial cells, tumor size, and lung metastases. Despite fewer vessels, the remaining vasculature exhibited increased pericyte coverage and maturity, which reduced hypoxia (decreased GLUT1 and HIF1α) [17].
- Reversal of Immune Exclusion: The "normalization" of tumor vessels upon endothelial SOX9 deletion led to a dramatic increase in CD4 and CD8 T cell infiltration into the tumor core, effectively reshaping the TIME from immune-depleted to immune-infiltrated [17].
DOT Visualization: Endothelial SOX9 in Tumor Vascular Immune Crosstalk
Diagram 3: SOX9's role in tumor vessel function and immune access.
Experimental Models and Methodologies for Investigating SOX9
Key Experimental Workflows
Cut-edge research into SOX9's role in the TIME employs sophisticated in vivo models and high-resolution molecular techniques.
In Vivo Therapy Resistance Models:
- Model Induction: Head and neck squamous cell carcinoma (HNSCC) is induced in C57BL/6 wild-type mice by administering 4-nitroquinoline 1-oxide (4NQO) in drinking water for 16 weeks, followed by normal water for 8 weeks [18].
- Treatment Protocol: Mice with established tumors are randomly assigned to control IgG, anti-PD-1, anti-LAG-3, or anti-LAG-3 plus anti-PD-1 combination therapy groups [18].
- Resistance Classification: Tumors growing >20% larger than original size 14 days post-treatment are classified as resistant based on RECIST criteria [18].
- Downstream Analysis: Resistant and sensitive tumors are subjected to single-cell RNA sequencing (scRNA-seq) and histological analysis (e.g., Ki67, cleaved-Caspase3) to identify key cellular and molecular players like SOX9+ tumor cells and the ANXA1-FPR1 axis [18].
Endothelial-Specific Knockout Models:
- Genetic Tool: Sox9fl/fl/Cdh5CreERt2/Rosa-YFP mice allow for tamoxifen-inducible, endothelial-specific deletion of Sox9, with lineage tracing via YFP [17].
- Tumor Inoculation: Melanoma cells (e.g., B16-F0, HcMel12) are inoculated intradermally after Sox9 deletion is induced [17].
- Phenotypic Analysis: Tumors are analyzed for size, metastasis, vessel density (CD31+ immunostaining), pericyte coverage (maturity), hypoxia markers (GLUT1, HIF1α), and immune cell infiltration (flow cytometry, immunostaining) [17].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Reagents and Models for SOX9 and TIME Research
| Reagent / Model | Function / Application | Key Findings Enabled |
|---|---|---|
| Sox9fl/fl/Cdh5CreERt2 mice | Endothelial-specific, inducible Sox9 knockout | Links endothelial SOX9 to vessel maturity, hypoxia, and T-cell infiltration [17]. |
| 4NQO-induced HNSCC mouse model | Immunocompetent model of oral carcinogenesis | Identified SOX9+/ANXA1+ tumor cells in anti-LAG-3/PD-1 resistance [18]. |
| Single-cell RNA Sequencing (scRNA-seq) | High-resolution transcriptomic profiling of TME | Revealed SOX9-enriched epithelial subclusters in resistant tumors [18]. |
| Anti-LAG-3 + Anti-PD-1 Antibodies | Immune checkpoint blockade combination therapy | Uncovers mechanisms of acquired resistance in the TME [18]. |
| Cdh5-CreER RosaYFP mice | Genetic lineage tracing of endothelial cells | Confirmed SOX9 protein expression in tumor endothelial cells [17]. |
| Human Melanoma Conditioned Media | In vitro mimic of tumor-endothelial crosstalk | Showed tumor-derived factors upregulate SOX9 in ECFCs, enhancing progenitor self-renewal [17]. |
SOX9 embodies the complexity of the tumor immune microenvironment, functioning as a master regulator whose influence varies dramatically based on cellular origin, tumor type, and disease stage. Its immunosuppressive actions—mediated through the impairment of cytotoxic cells, recruitment of immunosuppressive populations, and direct contribution to therapy resistance—make it a compelling therapeutic target in oncology [3] [18]. Conversely, its role in fostering a normalized vascular niche and its context-dependent association with improved prognosis caution against a one-size-fits-all therapeutic approach [9] [19] [17].
Future research must focus on dissecting the precise molecular switches that determine SOX9's dualistic function. Targeting specific SOX9-dependent pathways—such as the ANXA1-FPR1 axis in neutrophils or the B7x immune checkpoint in breast cancer—rather than SOX9 itself, may offer a more precise strategy to block its pro-tumorigenic functions while preserving its homeostatic roles [18] [13]. Furthermore, combining SOX9 pathway inhibitors with existing immunotherapies, such as immune checkpoint blockade, represents a promising avenue to overcome resistance and improve patient outcomes. As a central node in the TIME network, SOX9 continues to offer profound insights into the mechanics of immune evasion and activation.
SOX9-Mediated Regulation of Key Immune Cell Populations (T cells, Macrophages, Neutrophils)
The transcription factor SOX9, a member of the SRY-related high-mobility group (HMG) box family, is widely recognized for its fundamental roles in embryonic development, cell fate determination, and tissue homeostasis [20] [21]. In recent years, its significance has extended to the field of immunology and oncology, where it acts as a pivotal regulator within the tumor immune microenvironment (TIME). SOX9 exhibits a complex, "double-edged sword" nature in immunobiology: it can promote immune escape in cancer contexts yet also contribute to tissue maintenance and repair in inflammatory conditions [3]. This whitepaper synthesizes current mechanistic insights into how SOX9 directly and indirectly regulates the function and activity of key immune cell populations—T cells, macrophages, and neutrophils—thereby shaping anti-tumor immunity and influencing therapeutic outcomes. Understanding these interactions is critical for developing novel immunotherapeutic strategies targeting the SOX9 pathway.
SOX9 Structure and Functional Domains
The functional versatility of SOX9 is underpinned by its multi-domain structure. SOX9 encodes a 509-amino acid protein characterized by several key domains [3] [20]:
- Dimerization Domain (DIM): Located ahead of the HMG box, facilitates protein-protein interactions.
- HMG Box Domain: The defining, evolutionarily conserved DNA-binding motif that recognizes the specific DNA sequence (A/TA/TCAAA/TG). It contains embedded nuclear localization (NLS) and nuclear export (NES) signals, enabling nucleocytoplasmic shuttling [3] [21].
- Transcriptional Activation Domains: SOX9 possesses two activation domains: a central (TAM) and a C-terminal (TAC) domain, which interact with cofactors like Tip60 to potentiate transcriptional activity [3].
- PQA-Rich Domain: A proline, glutamine, and alanine-rich region necessary for full transcriptional activation [3].
SOX9's activity is further modulated by various post-transcriptional modifications, including phosphorylation by Protein Kinase A (PKA), which enhances its DNA-binding affinity and nuclear translocation, and SUMOylation, which can context-dependently either enhance or repress its transcriptional activity [20]. The regulation of SOX9 expression and function is a complex process involving transcriptional control, epigenetic modifications, and post-transcriptional regulation by non-coding RNAs [3].
Regulation of T Cells by SOX9
Direct and Indirect Mechanisms of T Cell Suppression
SOX9 influences T cell biology through both direct regulation of T cell development and indirect mechanisms that suppress cytotoxic function within the TIME.
- Lineage Commitment and γδ T Cell Modulation: During early T cell development in the thymus, SOX9 cooperates with the transcription factor c-Maf to activate
Rorcand key effector genes likeIl17aandBlk. This activity modulates the lineage commitment of early thymic progenitors, potentially influencing the balance between αβ and γδ T cell differentiation, particularly favoring Tγδ17 cells [3]. - Impairment of Cytotoxic T Cell Infiltration and Function: In established tumors, SOX9 plays a major role in suppressing CD8+ T cell-mediated immunity. Bioinformatics analyses of clinical tumor samples (e.g., from The Cancer Genome Atlas) reveal that SOX9 overexpression negatively correlates with genes associated with CD8+ T cell function [3]. Furthermore, in a head and neck squamous cell carcinoma (HNSCC) model, SOX9+ tumor cells were significantly enriched in tumors resistant to combined anti-PD-1 and anti-LAG-3 immunotherapy. The mechanism involves SOX9-driven suppression of neutrophil recruitment, which subsequently impairs the infiltration and tumor-killing capacity of cytotoxic CD8+ T cells and γδT cells, creating an "immune desert" microenvironment [18].
- Immune Checkpoint Regulation: In breast cancer, a novel SOX9-B7x (B7-H4/VTCN1) axis has been identified. SOX9 directly safeguards dedifferentiated, stem-like tumor cells from immune surveillance by upregulating the immune checkpoint molecule B7x, which inhibits T cell activation. This axis represents a direct mechanism through which SOX9+ tumor cells evade T cell-mediated killing [13].
Quantitative Data on SOX9 and T Cell Correlations
Table 1: Correlation between SOX9 expression and T cell parameters in human cancers
| Cancer Type | Correlation with CD8+ T Cell Function | Correlation with CD4+ T Cell Subsets | Clinical/Experimental Context | Source |
|---|---|---|---|---|
| Colorectal Cancer | Negative correlation | Positive correlation with naive/activated T cells; Negative with resting T cells | Bioinformatic analysis of TCGA data | [3] |
| Pan-Cancer (various) | Negative correlation with associated genes | Positive correlation with memory CD4+ T cells | Bioinformatic analysis | [3] |
| Head & Neck SCC | Reduced infiltration and killing capacity | Not specified | Resistance to anti-PD-1 + anti-LAG-3 therapy | [18] |
| Breast Cancer | Inhibition of activation via B7x upregulation | Not specified | Protection of dedifferentiated tumor cells | [13] |
Regulation of Macrophages by SOX9
SOX9 as a Mediator of Tumor-Associated Macrophage (TAM) Function
The interaction between SOX9 and macrophages is bidirectional and plays a critical role in promoting tumor progression and metastasis.
- TAM-Derived TGF-β Induces SOX9: In non-small cell lung cancer (NSCLC), tumor-associated macrophages (TAMs), which predominantly exhibit an immunosuppressive M2 phenotype, secrete high levels of Transforming Growth Factor-beta (TGF-β). This TGF-β acts on cancer cells to upregulate SOX9 expression via the C-jun/SMAD3 signaling pathway [22].
- SOX9-Dependent Epithelial-Mesenchymal Transition (EMT): The TGF-β-induced upregulation of SOX9 in tumor cells drives the epithelial-to-mesenchymal transition (EMT), a key process in metastasis. This is characterized by loss of E-cadherin and gain of vimentin. Knockdown of SOX9 inhibits this TGF-β-mediated EMT, confirming SOX9's essential role in this pathway [22].
- Clinical Correlations and Prognosis: Immunohistochemical analyses of human NSCLC tissues show a positive correlation between the density of CD163+ TAMs and SOX9 expression in tumor cells. Patients with high co-expression of both CD163 and SOX9 experience significantly shorter overall and disease-free survival compared to those with low expression of either marker alone, underscoring the clinical relevance of this axis [22].
The Dual Role of SOX9 in Macrophage Biology
While SOX9 in tumor cells is co-opted by TAMs to drive malignancy, it also has a protective role in macrophage biology in certain contexts. Increased levels of SOX9 help maintain macrophage function, contributing to tissue regeneration and repair, such as in cartilage formation and wound healing [3]. This highlights the context-dependent nature of SOX9's functions.
Regulation of Neutrophils by SOX9
A Novel SOX9-ANXA1 Axis in Immunotherapy Resistance
Recent research has uncovered a critical pathway by which SOX9 regulates neutrophil activity to drive resistance to combination immunotherapy.
- SOX9-Driven ANXA1 Expression: In HNSCC models resistant to anti-PD-1 plus anti-LAG-3 therapy, SOX9+ tumor cells are enriched and directly regulate the expression of Annexin A1 (ANXA1) [18].
- ANXA1-FPR1 Axis Induces Neutrophil Apoptosis: The ANXA1 protein secreted by SOX9-high tumor cells binds to its receptor, Formyl Peptide Receptor 1 (Fpr1), on neutrophils. This interaction triggers a signaling cascade within neutrophils that promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (BNIP3), ultimately leading to neutrophil apoptosis [18].
- Suppression of Anti-Tumor Immunity: The depletion of Fpr1+ neutrophils via this axis prevents their accumulation in tumor tissues. Since neutrophils can play a role in recruiting and activating cytotoxic lymphocytes, their loss impairs the infiltration and tumor-cell killing ability of CD8+ T and γδT cells, thereby driving therapy resistance [18].
Correlative Data on SOX9 and Neutrophils
Table 2: Observed relationships between SOX9 and neutrophils in cancer
| Cancer Type | Correlation with Neutrophils | Proposed Mechanism | Outcome | Source |
|---|---|---|---|---|
| Colorectal Cancer | Positive correlation with neutrophil infiltration | Not fully elucidated | Potential promotion of pro-tumor microenvironment | [3] |
| Head & Neck SCC | Negative correlation with Fpr1+ neutrophil accumulation | SOX9-ANXA1-FPR1 axis inducing apoptosis | Resistance to anti-PD-1 + anti-LAG-3 therapy | [18] |
Visualizing Key SOX9-Immune Signaling Pathways
SOX9 in TAM-Driven Tumor Metastasis
This diagram illustrates the signaling pathway by which Tumor-Associated Macrophages (TAMs) promote cancer metastasis through SOX9.
SOX9-ANXA1 Axis in Therapy Resistance
This diagram outlines the mechanism by which SOX9-expressing tumor cells drive immunotherapy resistance by inducing neutrophil apoptosis.
Experimental Protocols for Key Studies
Protocol 1: Investigating the TAM-TGFβ-SOX9-EMT Axis
This protocol is derived from the study linking TAMs, TGF-β, SOX9, and EMT in lung cancer [22].
Key Research Reagents:
- Cell Lines: Human monocytic THP-1 cells (for macrophage differentiation), human lung adenocarcinoma cells (A549, H1299).
- Cytokines: Recombinant human TGF-β, TGF-β receptor inhibitor.
- Antibodies: For Western Blot (SOX9, E-cadherin, Vimentin), for Immunofluorescence/Immunohistochemistry (CD163 for TAMs, SOX9).
- shRNA: SOX9-targeting shRNA for knockdown experiments.
Methodology:
- TAM Generation: Differentiate THP-1 monocytes into macrophages using Phorbol 12-myristate 13-acetate (PMA).
- Conditioned Media/Co-culture: Culture A549 or H1299 cells with either (a) supernatant from TAM cultures or (b) directly with TAMs in a transwell system. Include controls with recombinant TGF-β and a condition with TGF-β receptor inhibitor.
- Functional Assays:
- Proliferation: MTT assay after 48 hours of treatment.
- Migration/Invasion: Transwell migration and Matrigel invasion assays post-co-culture.
- Molecular Analysis:
- Protein Level: Western Blot to analyze changes in SOX9, E-cadherin, and vimentin.
- Gene Expression: qRT-PCR to quantify SOX9, EMT marker mRNA.
- Pathway Analysis: Western Blot for phospho-SMAD3 and c-Jun to confirm pathway activation.
- SOX9 Knockdown: Transduce cancer cells with SOX9-shRNA lentivirus and repeat co-culture/functional assays to confirm dependency.
Protocol 2: Elucidating the SOX9-ANXA1-FPR1 Axis in Therapy Resistance
This protocol is based on the 2025 study exploring resistance to anti-LAG-3 plus anti-PD-1 therapy in HNSCC [18].
Key Research Reagents:
- Mouse Model: 4-nitroquinoline 1-oxide (4NQO)-induced HNSCC in C57BL/6 wild-type and transgenic mice (e.g., Sox9 conditional KO, Fpr1 KO).
- Therapeutic Antibodies: Anti-PD-1, Anti-LAG-3.
- Single-Cell RNA Sequencing: Platform for transcriptomic profiling (e.g., 10x Genomics).
- Flow Cytometry Antibodies: For immune cell phenotyping (CD45, CD3, CD8, γδTCR, Ly6G for neutrophils, FPR1).
Methodology:
- Tumor Induction & Treatment: Induce HNSCC in mice via 4NQO-water. Randomize tumor-bearing mice into control and combination therapy (anti-PD-1 + anti-LAG-3) groups.
- Resistance Phenotyping: Monitor tumor growth via caliper measurements and MRI. Classify mice as "resistant" or "sensitive" based on RECIST criteria.
- Single-Cell RNA Sequencing:
- Pool and digest resistant and sensitive tumor tissues into single-cell suspensions.
- Perform scRNA-seq library preparation and sequencing.
- Perform bioinformatic analysis (cell clustering, differential expression, trajectory inference) to identify SOX9+ epithelial subclusters and ANXA1 expression.
- Mechanistic Validation:
- In Vivo: Utilize Sox9-epithelial specific knockout mice or Fpr1 knockout mice in the 4NQO/therapy model to validate the axis.
- Ex Vivo: Co-culture Sox9-high tumor cells with bone marrow-derived neutrophils. Assess neutrophil apoptosis (e.g., by flow cytometry for Annexin V) and BNIP3 expression.
- Immunophenotyping: By flow cytometry, quantify the infiltration of Fpr1+ neutrophils, CD8+ T cells, and γδT cells in tumors from different treatment groups and genotypes.
The Scientist's Toolkit: Key Research Reagents
Table 3: Essential reagents for studying SOX9 in the immune microenvironment
| Reagent Category | Specific Example | Function/Application | Key Findings Enabled |
|---|---|---|---|
| Cell Lines | THP-1 (human monocytes) | Differentiate into macrophages for TAM co-culture studies | Demonstrated TAM-secreted TGF-β induces SOX9 and EMT [22] |
| A549, H1299 (lung cancer) | Models for studying SOX9 function in EMT and invasion | ||
| Cytokines & Inhibitors | Recombinant TGF-β | Directly activate TGF-β signaling to study SOX9 upregulation | Validated SOX9 as a key downstream effector of TGF-β [22] |
| TGF-β Receptor Inhibitor | Block TGF-β signaling to confirm pathway specificity | ||
| Genetic Tools | SOX9-targeting shRNA/siRNA | Knockdown SOX9 expression to test functional necessity | Confirmed SOX9 is essential for TGF-β-mediated EMT and metastasis [22] |
| Sox9-floxed & Fpr1-KO mice | Genetically manipulate target genes in specific cell types in vivo | Established causal role of SOX9-ANXA1-FPR1 axis in therapy resistance [18] | |
| Antibodies for IHC/IF | Anti-CD163 | Marker for M2-like Tumor-Associated Macrophages (TAMs) | Showed positive correlation between TAM density and SOX9 expression in human NSCLC [22] |
| Anti-SOX9 | Detect SOX9 protein expression and localization | ||
| Therapeutic Antibodies | Anti-PD-1 + Anti-LAG-3 | Combination immunotherapy to model clinical treatment | Uncovered SOX9-mediated resistance mechanism in HNSCC [18] |
| Analysis Platforms | Single-Cell RNA Sequencing | Unbiased profiling of tumor and immune cell populations | Identified enriched SOX9+ tumor subcluster in resistant tumors [18] |
Mechanisms of SOX9 in Tumor Immune Evasion and Sustaining Stemness
The transcription factor SOX9 (SRY-Box Transcription Factor 9) is increasingly recognized as a pivotal regulator in cancer biology, functioning at the critical intersection of tumor immune evasion and stemness maintenance. As a member of the SOX family of transcription factors, SOX9 plays essential roles in embryonic development, cell differentiation, and tissue homeostasis [3] [23]. In cancer, however, SOX9 becomes dysregulated, contributing to multiple malignant processes. This whitepaper synthesizes current mechanistic understanding of how SOX9 facilitates the formation of an immunosuppressive tumor microenvironment and sustains a stem-like state in cancer cells, thereby promoting therapeutic resistance and disease progression. The dual functionality of SOX9 in these processes positions it as a compelling therapeutic target in oncology, particularly for aggressive malignancies characterized by high levels of cellular plasticity and immune evasion [3] [4].
Structural and Functional Characteristics of SOX9
Molecular Architecture
SOX9 protein contains several functionally distinct domains that enable its diverse roles in transcriptional regulation. The N-terminal dimerization domain (DIM) facilitates protein-protein interactions, while the central High Mobility Group (HMG) box domain mediates DNA binding and nuclear localization [3]. This HMG domain recognizes the specific DNA sequence CCTTGAG and can bind to compacted chromatin, exhibiting characteristics of a pioneer factor [24]. The C-terminal region contains two transcriptional activation domains (TAM and TAC) and a proline/glutamine/alanine (PQA)-rich domain, which are essential for SOX9's transactivation potential through interactions with various cofactors [3].
SOX9 as a Pioneer Factor
Recent research has established SOX9 as a bona fide pioneer transcription factor capable of binding to its cognate motifs in closed chromatin and initiating chromatin remodeling [24]. Through engineered mouse models, studies have demonstrated that SOX9 can bind to closed chromatin regions in epidermal stem cells, with nearly 30% of its binding sites located in inaccessible chromatin prior to SOX9 expression [24]. Following binding, SOX9 recruits histone and chromatin modifiers that displace nucleosomes, leading to increased chromatin accessibility at key enhancer regions and enabling fate switching from epidermal to hair follicle stem cells [24]. This pioneer function is mechanistically crucial for SOX9's ability to drive transcriptional reprogramming toward stem-like states in cancer cells.
SOX9 in Sustaining Cancer Stemness
Mechanisms of Stemness Regulation
Cancer stem cells (CSCs) represent a subpopulation of tumor cells with enhanced self-renewal capacity, differentiation potential, and therapeutic resistance [25]. SOX9 contributes to the maintenance and emergence of CSCs through multiple interconnected mechanisms:
Transcriptional Reprogramming: SOX9 drives a stem-like transcriptional state by globally altering the epigenetic landscape and gene expression profile of cancer cells [6]. In high-grade serous ovarian cancer (HGSOC), SOX9 expression induces significant transcriptional divergence, defined as the ratio of expression between highly expressed and lowly expressed genes (P50/P50), which is characteristic of stem cells with enhanced plasticity [6].
Chemotherapy-Induced Stemness: Platinum-based chemotherapy actively induces SOX9 expression, creating a feed-forward loop that enriches for CSC-like populations [6]. Single-cell RNA sequencing of HGSOC patient samples before and after neoadjuvant chemotherapy revealed consistent SOX9 upregulation in post-treatment cancer cells, with significant increase observed in 8 of 11 patients [6].
Pioneer Factor Activity: As a pioneer factor, SOX9 competes for epigenetic factors to switch stem cell fates [24]. When reactivated in adult epidermal stem cells, SOX9 binds to closed chromatin at hair follicle stem cell enhancers, recruits chromatin remodelers to open these regions, and simultaneously redistributes co-factors away from epidermal enhancers, effectively silencing the original cellular identity [24].
Table 1: SOX9-Mediated Stemness Mechanisms Across Cancer Types
| Cancer Type | Stemness Mechanism | Functional Outcome | Experimental Evidence |
|---|---|---|---|
| Ovarian Cancer | Chemotherapy-induced SOX9 upregulation | Platinum resistance, CSC enrichment | scRNA-seq of patient tumors pre/post chemotherapy [6] |
| Breast Cancer | Positive feedback with linc02095; AKT-SOX9-SOX10 axis | Tumor initiation, basal-like BC progression | Gene expression analysis, promoter studies [23] |
| Multiple Solid Tumors | Transcriptional reprogramming to stem-like state | Increased tumor initiation capacity | In vivo tumor formation assays [6] [25] |
| Skin Carcinogenesis | Pioneer factor-mediated fate switching | Transition from epidermal to neoplastic stem cells | Lineage tracing, chromatin analysis [24] |
Signaling Pathways in SOX9-Mediated Stemness
SOX9 intersects with multiple signaling pathways that converge on stemness maintenance:
Wnt/β-catenin Signaling: The TAC domain of SOX9 inhibits β-catenin during chondrocyte differentiation, suggesting similar regulatory interactions in cancer contexts [3].
AKT Signaling: In triple-negative breast cancer, SOX9 serves as an AKT substrate and regulates SOX10 transcription, creating a pro-stemness signaling axis [23].
Epigenetic Modulator Recruitment: SOX9 directly interacts with histone deacetylases (HDACs) and chromatin remodeling complexes to alter transcriptional programs fundamental to stem cell identity [23] [24].
SOX9 in Tumor Immune Evasion
Mechanisms of Immune Suppression
SOX9 employs multiple strategies to help cancer cells evade immune detection and elimination:
Immune Cell Exclusion and Dysfunction: Bioinformatics analyses of colorectal cancer data reveal that SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils [3]. Conversely, SOX9 shows positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells, suggesting specific reshaping of the immune landscape [3].
Impairment of Anti-Tumor Immunity: SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with memory CD4+ T cells [3]. In prostate cancer, SOX9 expression contributes to an "immune desert" microenvironment characterized by decreased effector immune cells (CD8+CXCR6+ T cells) and increased immunosuppressive cells (Tregs, M2 macrophages) [3].
Dormancy and Immune Evasion: SOX9 helps maintain cancer cells in a dormant state, allowing them to evade immune surveillance in secondary metastatic sites [23]. This dormancy mechanism enables long-term survival of disseminated cancer cells under immunotolerant conditions [23].
Table 2: SOX9-Mediated Immune Evasion Mechanisms
| Immune Evasion Mechanism | Functional Consequence | Experimental Support |
|---|---|---|
| Altered immune cell infiltration | Creation of immunosuppressive microenvironment | Correlation analysis with TCGA data [3] |
| Inhibition of effector immune cells | Reduced CD8+ T cell and NK cell function | Gene expression correlation analysis [3] |
| Promotion of dormant state | Escape from immune surveillance in metastasis | In vivo models of latent cancer cells [23] |
| Induction of stem-like properties | Resistance to T-cell mediated killing | CSC-immune cell interaction studies [25] |
SOX9 and the Immunosuppressive Niche
Within the tumor microenvironment, SOX9 contributes to the formation and maintenance of an immunosuppressive niche through several mechanisms. Cancer stem cells, whose properties are reinforced by SOX9, actively secrete immunosuppressive cytokines that attract regulatory immune cells such as myeloid-derived suppressor cells (MDSCs) and Tregs [25]. Furthermore, SOX9-expressing cells can downregulate major histocompatibility complex (MHC) molecules, reducing antigen presentation and thereby limiting T-cell recognition and activation [25]. In the specific context of glioma, high SOX9 expression correlates significantly with immune cell infiltration and checkpoint expression, indicating its involvement in establishing an immunosuppressive tumor microenvironment [9].
Experimental Models and Methodologies
Key Research Protocols
Investigating SOX9 in Chemoresistance
Experimental Objective: To determine SOX9's role in platinum resistance in high-grade serous ovarian cancer (HGSOC) [6].
Methodology Details:
- Cell Line Models: Multiple HGSOC cell lines (OVCAR4, Kuramochi, COV362) treated with carboplatin at clinically relevant concentrations.
- SOX9 Modulation: CRISPR/Cas9-mediated knockout of SOX9 using specific sgRNAs; epigenetic upregulation of endogenous SOX9 loci.
- Functional Assays: Colony formation assays to assess platinum sensitivity; Incucyte live-cell imaging for growth kinetics.
- Transcriptional Analysis: Bulk and single-cell RNA sequencing to profile transcriptional changes; measurement of transcriptional divergence (P50/P50 ratio).
- In Vivo Validation: Xenograft models to assess tumor formation capacity and chemoresistance.
Key Findings: SOX9 knockout significantly increased platinum sensitivity (p=0.0025), while its overexpression induced chemoresistance and enriched for stem-like subpopulations in vivo [6].
SOX9 Pioneer Function Analysis
Experimental Objective: To characterize SOX9's pioneer factor activity in cell fate switching [24].
Methodology Details:
- Mouse Engineering: Generated Krt14-rtTA;TRE-Sox9 mice enabling inducible SOX9 expression in adult epidermal stem cells.
- Temporal Monitoring: Tracked phenotypic changes weekly post-doxycycline induction over 12 weeks.
- Epigenetic Profiling: CUT&RUN sequencing for SOX9 chromatin binding; ATAC-seq for chromatin accessibility; RNA-seq for transcriptomic dynamics.
- Proteomic Analysis: Identification of SOX9-interacting chromatin modifiers.
- Functional Validation: Engraftment studies on immunocompromised mice to assess later-stage reprogramming.
Key Findings: SOX9 bound to closed chromatin (30% of binding sites) before nucleosome displacement and chromatin opening; simultaneously recruited co-factors away from original enhancers, enabling fate switching [24].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Studying SOX9 Function
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| SOX9 Modulation | CRISPR/Cas9 with SOX9 sgRNAs; Doxycycline-inducible SOX9 constructs | Functional studies | SOX9 knockout/overexpression to assess phenotypic consequences |
| Lineage Tracing | Krt14-rtTA; TRE-Sox9 mouse model | In vivo fate mapping | Inducible SOX9 expression in specific cell populations |
| Chromatin Analysis | CUT&RUN sequencing; ATAC-seq | Epigenetic profiling | Mapping SOX9 binding and chromatin accessibility dynamics |
| Single-Cell Profiling | scRNA-seq (10X Genomics) | Cellular heterogeneity assessment | Identifying SOX9+ subpopulations and associated signatures |
| Cell Sorting | FACS with stem cell markers (CD44, CD133) | CSC isolation | Purification of stem-like populations for downstream analysis |
| Spatial Analysis | Spatial transcriptomics; Multiplex immunofluorescence | Tissue context preservation | Mapping SOX9 expression within tumor immune microenvironment |
Visualizing SOX9 Mechanisms
SOX9 in Stemness and Immune Evasion
Diagram 1: SOX9 multimodal mechanisms in cancer stemness and immune evasion.
Experimental Workflow for SOX9 Chemoresistance Studies
Diagram 2: Experimental workflow for SOX9 chemoresistance studies.
Clinical Implications and Therapeutic Opportunities
The mechanistic insights into SOX9 function in tumor immune evasion and stemness maintenance reveal several promising therapeutic avenues. SOX9 represents a potential target to overcome chemoresistance, particularly in aggressive malignancies like HGSOC where its expression is induced by platinum-based chemotherapy [6]. Combining SOX9-targeting approaches with immune checkpoint inhibitors may help counteract the immunosuppressive microenvironment fostered by SOX9-expressing tumors [4]. Additionally, interventions that disrupt SOX9's pioneer factor activity or its interactions with chromatin modifiers could potentially block the transcriptional reprogramming that underlies cancer stemness [24].
The context-dependent nature of SOX9 function - notably its different roles across cancer types - necessitates careful therapeutic development. In glioma, for instance, high SOX9 expression surprisingly associates with better prognosis in specific molecular subgroups, highlighting the importance of patient stratification [9]. Ongoing efforts to develop small molecule inhibitors targeting SOX9-DNA interactions or SOX9-cofactor complexes show promise for ultimately translating these mechanistic insights into clinical applications.
SOX9 emerges as a master regulator at the nexus of cancer stemness and immune evasion, employing its pioneer factor capabilities to orchestrate transcriptional programs that sustain stem-like states while simultaneously creating an immunosuppressive tumor microenvironment. Through multimodal mechanisms including transcriptional reprogramming, epigenetic modification, and alteration of immune cell composition and function, SOX9 promotes therapeutic resistance and disease progression across multiple cancer types. Future research focusing on contextual determinants of SOX9 function and development of targeted interventions holds significant promise for improving outcomes in aggressive malignancies characterized by SOX9 dysregulation.
Investigating SOX9: From Bench to Bedside Tools and Strategies
The tumor immune microenvironment (TIME) plays a critical role in cancer progression and therapeutic response, with transcription factors emerging as key regulators of this complex ecosystem. Among these, SOX9 (SRY-related HMG-box 9) has garnered significant attention as both a diagnostic and prognostic biomarker across various malignancies. This technical guide outlines comprehensive bioinformatics methodologies for investigating SOX9 expression patterns and their correlation with immune infiltration using publicly available genomic datasets, particularly The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases. The analytical frameworks presented herein provide researchers with standardized approaches to elucidate SOX9's multifaceted role in shaping the immunosuppressive landscape of tumors, enabling deeper mechanistic insights and potential therapeutic targeting strategies.
SOX9 Expression Analysis in Pan-Cancer Context
Data Acquisition and Processing
The initial phase of SOX9 analysis involves systematic data acquisition from coordinated database resources. The following repositories provide essential genomic data:
- TCGA Data Portal: Primary source for cancer transcriptome data (HTSeq-FPKM and HTSeq-Count formats)
- GTEx Portal: Normal tissue transcriptome references for comparative analysis
- Human Protein Atlas: Validation of transcriptomic findings at protein level
- cBioPortal: Integrated genomics including mutation and copy number variations
Standardized data processing should include uniform normalization across datasets, batch effect correction, and log2 transformation of expression values to ensure comparability between malignant and normal tissue profiles [9] [11].
Pan-Cancer SOX9 Expression Patterns
Comprehensive analysis across multiple cancer types reveals distinct SOX9 expression patterns that underscore its context-dependent oncogenic functions. The table below summarizes SOX9 dysregulation across representative malignancies:
Table 1: SOX9 Expression Patterns Across Various Cancers
| Cancer Type | SOX9 Expression | Prognostic Association | Immune Correlation |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly upregulated | Better prognosis in lymphoid invasion subgroups | Correlated with immune checkpoint expression |
| Low-Grade Glioma (LGG) | Significantly upregulated | Shorter overall survival | Associated with immunosuppressive microenvironment |
| Colorectal Cancer | Upregulated | Poorer prognosis | Negative correlation with B cells, resting mast cells |
| Liver Cancer | Upregulated | Shorter overall survival | Positive correlation with neutrophils, macrophages |
| Ovarian Cancer | Chemotherapy-induced | Shorter overall survival | Enriched in stem-like chemoresistant cells |
| Skin Melanoma | Downregulated | Tumor suppressor role | Context-dependent immune effects |
| Testicular Cancer | Downregulated | Varied prognosis | Limited characterization |
SOX9 demonstrates significant upregulation in 15 of 33 analyzed cancer types, including GBM, COAD, LGG, LIHC, OV, and PAAD, positioning it primarily as an oncogenic driver in most malignancies. Conversely, only SKCM and TGCT show significant SOX9 downregulation, suggesting tissue-specific tumor suppressor functions [11]. Notably, in glioblastoma, high SOX9 expression shows a surprising association with better prognosis in specific patient subgroups, particularly those with lymphoid invasion, highlighting the context-dependent nature of its function [9].
Methodological Framework for Immune Infiltration Analysis
Computational Approaches for Immune Deconvolution
Several algorithmically distinct methods enable quantitative assessment of immune cell infiltration from bulk tumor transcriptomes:
Table 2: Computational Methods for Immune Infiltration Analysis
| Method | Algorithm Type | Key Outputs | Applicable Packages |
|---|---|---|---|
| ssGSEA | Gene set enrichment | Immune cell enrichment scores | GSVA R package (v1.34.0) |
| ESTIMATE | Stromal/immune signature scoring | Immune/stromal/estimate scores | ESTIMATE R package |
| TIMER2.0 | Deconvolution-based | Immune cell abundance fractions | TIMER2.0 web tool |
| CIBERSORT | Deconvolution with support vector regression | Relative immune cell proportions | CIBERSORT web portal |
| EPIC | Deconvolution with constrained regression | Immune and cancer cell fractions | EPIC R package |
The ssGSEA and ESTIMATE algorithms implemented through the GSVA R package provide robust frameworks for quantifying overall immune infiltration levels, while platform-specific tools like TIMER2.0 enable cancer-type-specific immune cell abundance estimation [9]. For SOX9-focused analyses, correlation with specific immune subsets, particularly cytotoxic T cells, Tregs, and tumor-associated macrophages, yields the most biologically relevant insights into its immunomodulatory functions [4] [3].
Immune Checkpoint Correlation Analysis
Beyond cellular infiltration, SOX9's potential role in immune evasion can be assessed through correlation with established immune checkpoint molecules. Standard analytical workflows should incorporate:
- Expression correlation analysis between SOX9 and checkpoint genes (PD-L1, CTLA-4, LAG-3, TIGIT)
- Differential expression testing (Wilcoxon rank-sum test) of checkpoints between SOX9-high and SOX9-low groups
- Multivariate regression adjusting for tumor purity and overall immune infiltration
In glioblastoma, SOX9 expression demonstrates significant correlation with multiple immune checkpoints, suggesting its potential involvement in establishing an immunosuppressive niche [9].
Experimental Protocols and Workflows
Core Bioinformatics Workflow for SOX9-Immune Analysis
The following diagram illustrates the integrated analytical pipeline for comprehensive SOX9-immune interaction profiling:
Differential Gene Expression Analysis Protocol
Software Requirements: R (v4.0+), DESeq2 (v1.30+), limma (v3.46+), ggplot2 (v3.3.6)
Step-by-Step Protocol:
Data Preprocessing
- Download HTSeq-Count data for target cancer type from TCGA
- Filter low-count genes (<10 counts across 90% of samples)
- Normalize using DESeq2's median of ratios method or limma's voom transformation
Differential Expression Analysis
- Define sample groups (SOX9-high vs SOX9-low based on median expression)
- Implement DESeq2 pipeline for RNA-Seq data:
- Apply significance thresholds: |logFC| > 1, adjusted p-value < 0.05
- Generate visualization outputs: volcano plots, heatmaps
Validation Analysis
Immune Correlation Analysis Protocol
Software Requirements: GSVA (v1.38+), ESTIMATE (v1.0+), ggplot2 (v3.3.6)
Step-by-Step Protocol:
Immune Infiltration Scoring
- Calculate ssGSEA enrichment scores for immune cell signatures:
- Compute ESTIMATE scores for tumor microenvironment assessment:
Correlation Analysis
- Calculate Spearman correlation coefficients between SOX9 expression and immune scores
- Perform subgroup stratification based on SOX9 expression tertiles
- Apply multiple testing correction (Benjamini-Hochberg FDR < 0.25)
Statistical Validation
Advanced Analytical Approaches
Functional Enrichment Analysis Pipeline
Following identification of SOX9-correlated genes, functional enrichment analysis elucidates potential biological mechanisms:
Software Requirements: clusterProfiler (v4.0+), Metascape, Enrichr
Implementation Protocol:
Gene Set Preparation
- Extract significant SOX9-correlated genes (FDR < 0.05)
- Separate into up- and down-regulated gene lists
Multi-Ontology Enrichment
- Execute Gene Ontology (GO) analysis for Biological Process, Cellular Component, Molecular Function
- Perform KEGG pathway enrichment for signaling pathway identification
- Conduct GSEA for predefined molecular signatures
Protein-Protein Interaction Network Construction
Prognostic Model Development
Integrating SOX9 into clinical prognostic models enables translational applications:
Software Requirements: rms (v6.2+), glmnet (v4.1+), survival (v3.2+)
Implementation Protocol:
Feature Selection
- Apply LASSO Cox regression to identify non-zero coefficients
- Select optimal lambda through 10-fold cross-validation
- Incorporate clinical variables (IDH status, stage, grade)
Nomogram Construction
- Develop multivariate Cox proportional hazards model
- Generate nomogram for individualized survival prediction
- Validate through calibration plots and concordance index (C-index) [9]
Table 3: Essential Research Reagents and Computational Tools for SOX9-Immune Analyses
| Resource Type | Specific Tool/Reagent | Application Purpose | Key Features |
|---|---|---|---|
| Bioinformatics Packages | DESeq2 R package | Differential expression analysis | Negative binomial distribution, shrinkage estimation |
| GSVA R package | Immune infiltration analysis | Gene set variation analysis, single-sample scoring | |
| clusterProfiler R package | Functional enrichment | GO, KEGG, GSEA in unified framework | |
| Database Resources | TCGA Data Portal | Cancer genomics data | Multi-omics data for 33 cancer types |
| GTEx Portal | Normal tissue reference | RNA-seq from 54 non-diseased tissue sites | |
| Human Protein Atlas | Protein expression validation | Immunohistochemistry-based tissue mapping | |
| Experimental Reagents | Cordycepin (CD) | SOX9 expression modulation | Adenosine analog, dose-dependent SOX9 inhibition |
| Anti-SOX9 antibodies | Protein validation | Western blot, IHC validation (HPA standards) | |
| Cell Line Models | 22RV1, PC3, H1975 | In vitro functional validation | SOX9-responsive cancer cell lines |
Interpretation and Translational Applications
Contextualizing SOX9's Dual Immunological Roles
Analysis of SOX9 within the tumor immune microenvironment reveals its Janus-faced character in cancer immunology. In most carcinomas, SOX9 exhibits immunosuppressive functions through multiple mechanisms: regulation of immune checkpoint expression, recruitment of pro-tumor immune cells, and creation of an "immune desert" microenvironment. However, in specific contexts such as thymoma, SOX9 demonstrates immune-stimulatory associations, including negative correlation with PD-L1 expression and T-cell receptor signaling pathways [3]. This contextual duality necessitates careful interpretation of SOX9-immune correlations within specific cancer types and microenvironments.
Therapeutic Implications and Target Validation
The consistent association between SOX9 and chemotherapy resistance across multiple cancer types, particularly in high-grade serous ovarian cancer where it drives a stem-like transcriptional state, positions SOX9 as a promising therapeutic target [6] [26]. Small molecule inhibitors such as cordycepin demonstrate dose-dependent SOX9 suppression in prostate and lung cancer models, validating its pharmacological tractability [11]. Furthermore, SOX9's correlation with immune checkpoint expression suggests potential for combination strategies integrating SOX9 pathway inhibition with existing immunotherapies.
This technical guide provides comprehensive bioinformatics frameworks for investigating SOX9 expression and immune correlations in cancer. The standardized workflows enable reproducible analysis across cancer types, while the integrated multi-omics approaches facilitate deeper mechanistic insights into SOX9's regulation of the tumor immune microenvironment. As research continues to elucidate SOX9's complex roles in immune evasion and therapy resistance, these analytical protocols will support the development of SOX9-targeted therapeutic strategies and biomarker-based patient stratification approaches.
The transcription factor SOX9 is a critical regulator of diverse biological processes, and its dysregulation is increasingly implicated in the formation and function of the tumor immune microenvironment (TIME). SOX9 exhibits a complex, "double-edged sword" role in immunology; it can promote tumor immune escape by impairing immune cell function, yet in other contexts, it helps maintain macrophage function and contributes to tissue repair [3]. Understanding the precise mechanisms by which SOX9 exerts these effects requires techniques that can map its interactions with the genome and its role in reshaping chromatin architecture. Functional genomics assays, primarily Chromatin Immunoprecipitation followed by sequencing (ChIP-seq) and the Assay for Transposase-Accessible Chromatin using sequencing (ATAC-seq), are indispensable tools for this purpose. This technical guide details the application of these assays to study SOX9 in the context of the TIME, providing validated protocols, data analysis workflows, and interpretive frameworks for researchers and drug development professionals.
SOX9 Functional Assays in Tumor Immunology
The Role of SOX9 in the Tumor Immune Microenvironment
SOX9's influence on the TIME is multifaceted. Bioinformatic analyses of clinical datasets reveal that SOX9 expression levels correlate significantly with specific patterns of immune cell infiltration. For instance, in colorectal cancer, high SOX9 expression is negatively correlated with the infiltration of B cells, resting mast cells, and monocytes, but positively correlated with neutrophils, macrophages, and activated mast cells [3]. Furthermore, SOX9 overexpression is linked to impaired function of CD8+ T cells and natural killer (NK) cells, key mediators of anti-tumor immunity [3]. A critical mechanism by which SOX9 fosters an immunosuppressive environment is through the promotion of an "immune desert" phenotype, as observed in prostate cancer, where SOX9-high tumor cells are associated with a landscape depleted of effector immune cells and enriched in immunosuppressive regulatory T cells (Tregs) and M2 macrophages [3]. These findings underscore the necessity of employing ChIP-seq and ATAC-seq to delineate the direct transcriptional programs through which SOX9 orchestrates these changes.
ChIP-seq for Direct Mapping of SOX9 Binding
ChIP-seq is the gold-standard method for identifying the genomic locations where a transcription factor like SOX9 directly binds DNA. The workflow (detailed in Section 4.1) involves cross-linking SOX9 to DNA, shearing chromatin, immunoprecipitating SOX9-DNA complexes with a specific antibody, and sequencing the bound DNA fragments. This yields a genome-wide map of SOX9 binding sites, which can be integrated with transcriptomic data to link direct binding to target gene regulation. In the context of cancer and immunity, SOX9 ChIP-seq can identify its binding sites in the regulatory elements of genes that control immune cell recruitment, function, and differentiation.
ATAC-seq for Profiling SOX9-Driven Chromatin Remodeling
ATAC-seq provides a powerful, rapid method for profiling genome-wide chromatin accessibility. It uses a hyperactive Tn5 transposase to simultaneously cut and tag open chromatin regions with sequencing adapters [27]. Because transcription factor binding influences local chromatin accessibility, ATAC-seq can reveal the functional impact of SOX9 activity. Its application is particularly relevant for studying SOX9's dosage-sensitive effects. Recent studies using precise modulation of SOX9 levels in human facial progenitor cells have demonstrated that most SOX9-dependent regulatory elements are buffered against small dosage decreases, but a subset of primarily regulated elements shows heightened sensitivity [14]. This principle is directly applicable to cancer biology, where SOX9 copy number alterations or changes in upstream signaling could similarly lead to selective, dosage-sensitive changes in the chromatin landscape of tumor and immune cells, thereby reshaping the TIME.
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogues essential reagents and their functions for successfully executing SOX9-focused ChIP-seq and ATAC-seq studies.
Table 1: Key Research Reagents for SOX9 ChIP-seq and ATAC-seq Studies
| Reagent / Tool | Function / Application | Technical Notes |
|---|---|---|
| SOX9 Antibody (ChIP-grade) | Immunoprecipitation of SOX9-DNA complexes in ChIP-seq. | Critical for success; must be validated for specificity and efficacy in ChIP assays. |
| dTAG System (FKBP12F⁶³⁶V) | Precise, rapid degradation of tagged SOX9 protein to study dosage effects [14]. | Enables titration of SOX9 levels to model haploinsufficiency or overexpression. |
| Hyperactive Tn5 Transposase | Enzyme for tagmentation in ATAC-seq; inserts adapters into open chromatin [27]. | The core reagent of the ATAC-seq assay. |
| MACS2 / MACS3 / Genrich | Software for peak calling from ChIP-seq and ATAC-seq data [28] [27]. | Genrich has a dedicated ATAC-seq mode. MACS2 is a widely used alternative. |
| HOMER | Toolkit for motif discovery and functional annotation of genomic regions [28]. | Identifies SOX9 binding motifs and annotates peaks to genomic features. |
| Bowtie2 | Aligns sequencing reads to a reference genome [28] [29]. | Standard for high-speed and memory-efficient alignment. |
| ENCODE Blacklisted Regions | A curated list of genomic regions prone to artifactual signals [28]. | Peaks in these regions should be filtered out to improve data quality. |
Experimental Protocols for Core Assays
ChIP-seq Protocol for SOX9 Binding Site Identification
This protocol outlines the key steps for mapping SOX9-DNA interactions.
Diagram 1: ChIP-seq workflow for SOX9 binding site identification.
- Cell Fixation and Lysis: Treat cells (e.g., cancer cell lines, primary immune cells) with 1% formaldehyde for 10 minutes at room temperature to cross-link proteins to DNA. Quench with glycine. Harvest cells and lyse using an appropriate lysis buffer.
- Chromatin Shearing: Sonicate cross-linked chromatin to shear DNA into fragments of 200–500 bp. This can be achieved using a sonicator (e.g., Covaris or Bioruptor). Verify fragment size using agarose gel electrophoresis or a Bioanalyzer.
- Immunoprecipitation: Pre-clear the sheared chromatin with Protein A/G beads. Incubate the chromatin supernatant with a high-specificity anti-SOX9 antibody overnight at 4°C. The following day, add Protein A/G beads to capture the antibody-bound complexes. Wash the beads stringently with low-salt, high-salt, and LiCl wash buffers to remove non-specifically bound DNA.
- Elution and Reverse Cross-linking: Elute the immunoprecipitated complexes from the beads using an elution buffer (e.g., 1% SDS, 100mM NaHCO3). Reverse the cross-links by incubating with NaCl at 65°C for several hours or overnight.
- DNA Purification and Library Prep: Treat with RNase A and Proteinase K. Purify the DNA using a PCR purification kit or phenol-chloroform extraction. This DNA is used to construct a sequencing library with standard methods, which is then quantified and sequenced on an Illumina platform.
ATAC-seq Protocol for Chromatin Accessibility Profiling
This protocol, based on established pipelines, is optimized for profiling chromatin accessibility in SOX9-relevant models [28] [27].
Diagram 2: ATAC-seq workflow for chromatin accessibility profiling.
- Nuclei Preparation: Harvest 50,000–100,000 cells and lyse them with a cold lysis buffer (e.g., 10 mM Tris-Cl pH 7.4, 10 mM NaCl, 3 mM MgCl2, 0.1% IGEPAL CA-630) to isolate nuclei. Immediately pellet the nuclei and resuspend them in a transposase reaction mix.
- Tagmentation Reaction: Incubate the nuclei with the Tn5 transposase (commercially available, e.g., from Illumina) at 37°C for 30 minutes. This step simultaneously fragments accessible DNA and adds sequencing adapters.
- DNA Purification: Purify the tagmented DNA using a MinElute PCR Purification Kit or SPRI beads.
- Library Amplification: Amplify the purified DNA via PCR using 1x NEBnext PCR master mix and indexing primers. Determine the optimal number of PCR cycles using a qPCR side reaction to avoid over-amplification.
- Library Clean-up and QC: Purify the final library using SPRI beads. Assess library quality and fragment size distribution using a Bioanalyzer or TapeStation. A successful ATAC-seq library shows a characteristic periodicity corresponding to nucleosome-free, mononucleosome, and dinucleosome fragments.
- Sequencing: Sequence the library on an Illumina platform (typically paired-end sequencing).
Data Analysis and Quality Control
Quality Control Metrics and Thresholds
Rigorous quality control (QC) is essential for generating reliable data. The following table summarizes key QC metrics for ATAC-seq and ChIP-seq, based on ENCODE guidelines and modern protocols [28].
Table 2: Essential Quality Control Metrics for ChIP-seq and ATAC-seq Data
| Metric | Recommended Threshold | Assay | Rationale |
|---|---|---|---|
| Total Reads | > 50 million (25M for PE) | ATAC-seq | Ensures sufficient coverage for peak calling [28]. |
| Filtered Reads | > 10 million | ATAC-seq | Indicates enough high-quality, mappable fragments [28]. |
| Alignment Rate | > 80% | Both | Confirms efficient mapping to the reference genome. |
| FRiP Score | > 0.3 (or > 0.2 acceptable) | Both | Measures enrichment; fraction of reads in peaks. |
| Non-Redundant Fraction (NRF) | > 0.8 | Both | Indicates low levels of PCR duplicates. |
| TSS Enrichment | > 10% in promoter-TSS | ATAC-seq | Confirms expected enrichment at transcription start sites [28]. |
| Peak Number per Sample | > 50,000 | ATAC-seq | Indicates a robust accessibility profile [28]. |
Computational Analysis Workflows
A standardized analysis pipeline ensures reproducibility.
Pre-processing and Alignment:
- Quality Control: Assess raw read quality with FastQC.
- Adapter Trimming: Remove adapters and low-quality bases using fastp or Cutadapt [28].
- Alignment: Map reads to the appropriate reference genome (e.g., hg38) using Bowtie 2. For ATAC-seq, remove reads mapping to mitochondrial DNA [28] [29].
- Post-alignment Processing: Filter alignments to remove duplicates and reads overlapping ENCODE blacklisted regions using Picard or samtools [28].
Peak Calling:
Downstream Analysis:
- Differential Analysis: For ATAC-seq, identify Differential Accessibility Regions (DARs) between conditions (e.g., high vs. low SOX9) using tools like DiffBind [29].
- Motif Analysis: Use HOMER to perform de novo motif discovery and known motif enrichment analysis within SOX9 peaks to identify its binding motif and co-factor partnerships [28].
- Peak Annotation: Annotate peaks to genomic features (promoters, introns, enhancers) using ChIPseeker or HOMER [29].
- Data Integration: Correlate SOX9 binding (ChIP-seq) or chromatin accessibility changes (ATAC-seq) with differential gene expression (RNA-seq) to build a direct regulatory model [29].
Interpreting SOX9 Functional Genomics Data in TIME
Linking Molecular Data to Immunological Phenotypes
The ultimate goal of these assays is to derive mechanistic insights into SOX9's role in the TIME. For example, if SOX9 ChIP-seq in cancer cells reveals binding to the promoter of a chemokine gene, and ATAC-seq shows that SOX9 knockdown reduces accessibility at that locus, it suggests SOX9 directly regulates that chemokine. This finding can then be linked to in vitro or in vivo data showing that SOX9 expression correlates with the recruitment of specific immune cell populations [3]. Furthermore, the concept of dosage sensitivity is crucial. SOX9-dependent regulatory elements (REs) display varying sensitivity to SOX9 levels; some are buffered against small changes, while others, often those with direct, primary regulation, are highly sensitive [14]. In cancer, this could mean that modest changes in SOX9 levels, potentially induced by therapy or microenvironmental signals, could disproportionately alter the expression of a key set of immune-modulatory genes, thereby reprogramming the TIME.
Application in Therapeutic Development
Identifying the direct transcriptional targets of SOX9 in the tumor and stromal compartments opens avenues for therapeutic intervention. The SOX9-driven transcriptional network represents a potential target for small molecules or gene therapies. Moreover, combining SOX9-targeting strategies with immunotherapies (e.g., immune checkpoint blockers) could be a powerful synergistic approach. For instance, inhibiting SOX9 might reverse its suppression of CD8+ T cell and NK cell function, thereby making "immune desert" tumors more susceptible to checkpoint inhibition [3] [10]. The functional genomics assays described here are the foundational tools for identifying these synergistic nodes and guiding rational combination therapies.
SOX9 as a Diagnostic and Prognostic Biomarker in Cancers like Glioblastoma and Breast Cancer
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator in cancer biology, functioning as both a diagnostic and prognostic biomarker across multiple malignancies. This technical review synthesizes current evidence establishing SOX9 as a pivotal player in tumor pathogenesis, with particular focus on its roles in glioblastoma (GBM) and breast cancer. We examine the molecular mechanisms through which SOX9 influences cancer cell proliferation, stemness, chemotherapy resistance, and immunomodulation within the tumor microenvironment. The analysis incorporates recent findings from multi-omics studies, functional genetic screens, and clinical correlative analyses that position SOX9 at the intersection of tumor cell intrinsic programming and immune evasion mechanisms. This comprehensive assessment validates SOX9 as a promising therapeutic target and biomarker with growing clinical relevance in oncology.
SOX9 belongs to the SOX family of transcription factors characterized by a highly conserved high-mobility group (HMG) domain that facilitates DNA binding and transcriptional regulation [9]. Initially recognized for its crucial roles in embryonic development, chondrogenesis, and sex determination, SOX9 is now established as a significant contributor to oncogenesis across diverse tissue types [10] [3]. The protein structure includes several functional domains: an N-terminal dimerization domain (DIM), the central HMG box domain responsible for DNA binding, two transcriptional activation domains (TAM and TAC), and a C-terminal proline/glutamine/alanine-rich domain [3].
In cancer contexts, SOX9 demonstrates context-dependent dual functions, acting as both an oncogene and tumor suppressor in a tissue-specific manner [3]. However, in most carcinomas, including GBM and breast cancer, SOX9 functions predominantly as an oncoprotein, driving tumor initiation, progression, stemness maintenance, and therapy resistance [9] [10] [30]. SOX9 expression is frequently elevated in malignant tissues compared to corresponding normal tissues, with its overexpression correlating with advanced disease stage and poor clinical outcomes [9] [30]. Beyond its cell-autonomous functions, emerging evidence highlights SOX9's significant role in shaping the tumor immune microenvironment, thereby influencing response to immunotherapies and contributing to therapeutic resistance [3] [18].
Molecular Mechanisms of SOX9 in Oncogenesis
SOX9 regulates multiple hallmarks of cancer through intricate molecular mechanisms that vary across cancer types. Its transcriptional activity coordinates diverse signaling pathways that collectively drive malignant progression.
Regulation of Cancer Stemness and Differentiation
SOX9 serves as a master regulator of cancer stemness across multiple malignancies. In high-grade serous ovarian cancer, SOX9 expression reprogrammed cancer cells into stem-like tumor-initiating cells characterized by continuous self-renewal and proliferation capacity [26]. Mechanistically, SOX9 cooperates with Slug (SNAI2) to promote breast cancer cell proliferation and metastasis while maintaining stem cell properties [10]. In glioblastoma, SOX9 maintains stemness through regulation of key developmental pathways that are co-opted during oncogenesis [9].
Signaling Pathway Integration
SOX9 intersects with multiple oncogenic signaling cascades. It activates the polycomb group protein Bmi1 promoter, whose overexpression suppresses the tumor suppressor Ink4a/Arf loci [10]. In breast cancer, SOX9 accelerates AKT-dependent tumor growth by regulating SOX10, with SOX9 identified as an AKT substrate at the serine 181 consensus site [10]. The transcription factor also mediates oncogenic transformation in breast cancer by regulating transforming growth factor β and Wnt/β-catenin signaling pathways [10] [30].
Epigenetic and Post-transcriptional Regulation
SOX9 expression and activity are modulated through various epigenetic mechanisms. DNA methylation status of the SOX9 promoter region is dysregulated in several tumor types, contributing to its aberrant expression [30]. Additionally, SOX9 is regulated at the post-transcriptional level by multiple miRNAs, including miR-215-5p in breast cancer, where miR-215-5p overexpression inhibits proliferation, migration, and invasion by targeting SOX9 [10]. The long non-coding RNA linc02095 creates a positive feedback loop with SOX9, mutually regulating each other's expression to promote breast cancer cell growth and tumor progression [10].
Table 1: Key Molecular Functions of SOX9 in Cancer Pathogenesis
| Molecular Function | Mechanism | Cancer Context |
|---|---|---|
| Stemness Maintenance | Reprograms cancer cells to stem-like state; cooperates with Slug | Ovarian cancer, Breast cancer [26] [10] |
| Cell Cycle Progression | Promotes G1/S transition; regulates cyclins and CDKs | Multiple solid tumors [10] |
| Therapy Resistance | Upregulated in response to chemotherapy; promotes survival | Ovarian cancer, GBM [26] [9] |
| Immune Evasion | Modulates immune cell infiltration; regulates checkpoint expression | GBM, HNSCC [9] [18] |
| Metastasis | Enhances migratory and invasive capabilities | Breast cancer, Lung adenocarcinoma [10] [9] |
SOX9 as a Diagnostic Biomarker
SOX9 demonstrates significant utility as a diagnostic biomarker across multiple cancer types, with its expression patterns distinguishing malignant from normal tissues and correlating with specific molecular subtypes.
Expression Patterns in Malignant Versus Normal Tissues
Comprehensive analyses of SOX9 expression reveal consistent overexpression in tumor tissues compared to their normal counterparts. In glioblastoma, SOX9 is highly expressed in malignant tissues compared to adjacent normal brain tissue, with protein-level validation confirming this differential expression [9] [19]. Pan-cancer RNA-seq data from TCGA and GTEx databases establish SOX9 overexpression across a spectrum of malignant tumors, including GBM, breast cancer, lung cancer, liver cancer, and pancreatic cancer [9] [3]. This consistent overexpression pattern positions SOX9 as a valuable diagnostic marker with potential application across multiple solid tumors.
Diagnostic Performance in Specific Cancers
In glioblastoma, receiver operating characteristic (ROC) analysis demonstrates that SOX9 expression effectively discriminates between tumor and normal tissues, supporting its predictive value for GBM diagnosis [9] [19]. For breast cancer, SOX9 expression differs according to molecular subtypes, with particularly high expression in basal-like/triple-negative breast cancer, where it functions as a driver of tumor development [10] [30]. The diagnostic accuracy of SOX9 is further enhanced when evaluated in combination with specific genetic alterations, such as IDH mutation status in glioma [9].
SOX9 as a Prognostic Biomarker
The prognostic significance of SOX9 has been extensively investigated across multiple cancer types, with consistent correlations between its expression levels and clinical outcomes.
Prognostic Value in Glioblastoma
In glioblastoma, SOX9 expression carries significant prognostic implications, though its relationship to survival outcomes demonstrates context-dependent patterns. Surprisingly, high SOX9 expression was remarkably associated with better prognosis in the lymphoid invasion subgroups in a sample of 478 cases [9] [19]. Furthermore, high expression of SOX9 was an independent prognostic factor for IDH-mutant cases in Cox regression analysis [9]. SOX9 expression was incorporated into a nomogram prognostic model alongside OR4K2 and IDH status, demonstrating robust predictive accuracy for patient outcomes [9] [19].
Prognostic Significance in Breast Cancer
In breast cancer, SOX9 overexpression generally correlates with poor prognosis parameters. SOX9 is significantly upregulated during the initial stages of tumor development and serves as a driver of basal-like breast cancer progression [10]. Clinical evidence demonstrates that breast cancer tumor tissues overexpress SOX9, whereas normal tissues show very low expression, with this overexpression pattern correlating with aggressive disease features [30]. The prognostic impact of SOX9 in breast cancer is modulated by molecular subtype, with particularly strong prognostic significance in triple-negative and basal-like subtypes [10] [30].
Pan-Cancer Prognostic Implications
Across multiple cancer types, SOX9 expression consistently associates with adverse clinicopathological features and survival outcomes. In lung adenocarcinoma, SOX9 upregulation significantly correlates with tumor grading and poorer overall survival rates [9]. Similarly, in ovarian cancer, high SOX9 expression defines a subpopulation of stem-like cells that contribute to platinum resistance and disease recurrence [26]. The consistent prognostic value across diverse malignancies underscores SOX9's fundamental role in driving aggressive tumor behavior.
Table 2: Prognostic Significance of SOX9 Across Cancer Types
| Cancer Type | Prognostic Significance | Associated Clinical Features |
|---|---|---|
| Glioblastoma | Better prognosis in lymphoid invasion subgroups; independent prognostic factor for IDH-mutant | IDH mutation status, lymphoid invasion [9] [19] |
| Breast Cancer | Poor prognosis in most studies; driver of basal-like subtype | Basal-like phenotype, triple-negative status [10] [30] |
| Ovarian Cancer | Associated with platinum resistance and poor outcomes | Chemoresistance, stem-like phenotype [26] |
| Lung Adenocarcinoma | Correlates with poorer overall survival | Advanced tumor grading [9] |
| Head and Neck Cancer | Mediates resistance to combination immunotherapy | Anti-PD-1/LAG-3 therapy resistance [18] |
SOX9 in the Tumor Immune Microenvironment
SOX9 plays a multifaceted role in shaping the tumor immune microenvironment, functioning as a critical nexus between cancer cell-intrinsic signaling and immune evasion mechanisms.
Regulation of Immune Cell Infiltration
SOX9 expression correlates with specific immune infiltration patterns across cancer types. In glioblastoma, correlation analysis indicated SOX9 expression was correlated with immune cell infiltration and expression of immune checkpoints [9] [19]. Bioinformatic analyses of colorectal cancer demonstrate that SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. These patterns suggest SOX9 contributes to an immunosuppressive microenvironment that facilitates immune escape.
Modulation of Immune Checkpoint Expression
SOX9 directly influences the expression of immune checkpoint molecules. Research in lung adenocarcinoma found that SOX9 suppresses the tumor microenvironment and is mutually exclusive with various tumor immune checkpoints [9]. In head and neck squamous cell carcinoma (HNSCC), SOX9+ tumor cells mediate resistance to anti-LAG-3 plus anti-PD-1 combination therapy through interaction with Fpr1+ neutrophils [18]. This modulation of checkpoint expression represents a mechanism through which SOX9-expressing tumors evade immune surveillance.
Mechanisms of Therapy Resistance
SOX9 contributes to resistance against immunotherapies through distinct molecular mechanisms. Single-cell RNA sequencing of HNSCC resistant to anti-LAG-3 plus anti-PD-1 therapy revealed significant enrichment of Sox9+ tumor cells [18]. Mechanistically, SOX9 directly regulates annexin A1 (Anxa1) expression, mediating apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils through the Anxa1-Fpr1 axis [18]. This pathway promotes mitochondrial fission, inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (Bnip3) expression, and ultimately prevents neutrophil accumulation in tumor tissues [18]. The reduction of Fpr1+ neutrophils impairs the infiltration and tumor cell-killing ability of cytotoxic CD8 T and γδT cells within the tumor microenvironment, thereby driving resistance to combination therapy [18].
Figure 1: SOX9-Mediated Immunotherapy Resistance Mechanism. SOX9+ tumor cells drive resistance to anti-PD-1/LAG-3 therapy by regulating ANXA1 expression, which engages FPR1 on neutrophils to induce mitochondrial dysfunction and apoptosis, ultimately reducing cytotoxic T cell activity in the tumor microenvironment [18].
Experimental Models and Methodologies
The investigation of SOX9 in cancer biology employs diverse experimental approaches that elucidate its functional roles and clinical relevance.
Genomic and Transcriptomic Analyses
Comprehensive genomic and transcriptomic datasets have been instrumental in characterizing SOX9's roles across cancers. The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases provide RNA sequencing data for analyzing SOX9 expression and identifying differentially expressed genes [9] [19]. Functional enrichment analysis of SOX9-correlated genes utilizes GO/KEGG, Gene Set Enrichment Analysis (GSEA), and protein-protein interaction (PPI) network construction [9]. Single-cell RNA sequencing (scRNA-seq) enables resolution of SOX9 expression at cellular resolution, identifying rare subpopulations with stem-like features in patient tumors [26] [18].
Functional Genetic Screening
Genetic screening approaches have proven powerful in identifying SOX9's functional contributions to cancer pathogenesis. CRISPR/Cas9 gene-editing demonstrates that SOX9 activation reprogrammed ovarian cancer cells into stem-like tumor-initiating cells [26]. Perturb-Seq studies, combining CRISPR perturbations with single-cell RNA sequencing, identify genes including CYP19A1 that interact with SOX9 networks in glioblastoma radiotherapy response [31]. These functional genomics approaches establish causal relationships between SOX9 expression and cancer phenotypes like chemoresistance.
Clinical Correlation Studies
Clinical correlative analyses establish connections between SOX9 expression patterns and patient outcomes. Kaplan-Meier and Cox regression analyses assess the clinical significance of SOX9 in glioblastoma and other cancers [9] [19]. Immunohistochemical validation using tumor microarrays confirms SOX9 protein expression in clinical samples and correlates it with clinicopathological parameters [26]. Nomogram prognostic models incorporate SOX9 alongside other molecular features to predict patient survival [9].
Table 3: Key Experimental Approaches for SOX9 Research
| Methodology | Application | Key Insights |
|---|---|---|
| TCGA/GTEx Bioinformatic Analysis | Pan-cancer expression profiling | SOX9 overexpression across malignancies [9] [19] |
| scRNA-seq | Tumor heterogeneity mapping | Rare SOX9+ stem-like subpopulations [26] [18] |
| CRISPR/Cas9 Screening | Functional genetic validation | SOX9 drives stemness and chemoresistance [26] |
| Immune Cell Infiltration Analysis | Tumor microenvironment characterization | SOX9 correlates with immunosuppressive landscapes [9] [3] |
| Prognostic Modeling (Nomogram) | Clinical outcome prediction | SOX9 enhances prognostic accuracy with other biomarkers [9] |
Therapeutic Implications and Future Directions
The established roles of SOX9 in cancer pathogenesis position it as an attractive therapeutic target with particular relevance for treatment-resistant disease.
SOX9 as a Therapeutic Target
SOX9 represents a promising therapeutic target based on its central role in driving stemness, therapy resistance, and immune evasion. In ovarian cancer, SOX9 inhibition could potentially reverse platinum resistance by targeting the stem-like cell population [26]. For breast cancer, targeting SOX9 may improve therapeutic efficacy, particularly in basal-like subtypes where it serves as a key driver [10] [30]. In glioblastoma, SOX9's correlation with immune infiltration and checkpoint expression suggests potential for combination immunotherapies [9]. The development of small molecule inhibitors or strategies to target downstream SOX9 effectors could prevent the acquired chemoresistance mediated by SOX9-dependent reprogramming [26].
SOX9 as a Predictive Biomarker
SOX9 shows significant potential as a predictive biomarker for therapy response and resistance. In head and neck cancer, SOX9 enrichment identifies tumors resistant to anti-LAG-3 plus anti-PD-1 combination therapy [18]. Assessment of SOX9 expression could guide patient selection for specific treatment regimens, potentially avoiding ineffective therapies in SOX9-high tumors. The integration of SOX9 status with existing biomarkers like IDH mutation in glioma or molecular subtypes in breast cancer could refine prognostic stratification and therapeutic decision-making [9] [30].
Research Reagent Solutions
The investigation of SOX9 requires specialized research tools and methodologies essential for advancing both basic and translational research.
Table 4: Essential Research Reagents for SOX9 Investigation
| Research Tool | Specific Examples | Research Application |
|---|---|---|
| Genomic Databases | TCGA, GTEx, LinkedOmics | SOX9 expression analysis across cancers [9] [19] |
| Genetic Screening | CRISPR/Cas9, CRISPRi, RNAi | Functional validation of SOX9 roles [26] [31] |
| Single-Cell Technologies | scRNA-seq, CopyKAT | Tumor heterogeneity and subpopulation analysis [18] |
| Immune Analysis | ssGSEA, ESTIMATE algorithm | Immune infiltration correlation studies [9] [3] |
| Animal Models | 4NQO-induced HNSCC, transgenic mice | Therapy resistance mechanisms [18] |
SOX9 has established itself as a significant diagnostic and prognostic biomarker with crucial functions in cancer pathogenesis, particularly in glioblastoma and breast cancer. Its roles in maintaining cancer stemness, driving therapy resistance, and shaping the immunosuppressive tumor microenvironment position SOX9 at the nexus of key oncogenic processes. The development of SOX9-targeted therapeutic strategies and its integration into multimodal biomarker panels represent promising avenues for improving outcomes in treatment-resistant cancers. Future research should focus on elucidating the context-dependent mechanisms of SOX9 regulation, developing specific SOX9 inhibitors, and validating its predictive value in prospective clinical trials.
The SRY-box transcription factor 9 (SOX9) has emerged as a critical regulatory node in cancer biology, exerting profound influence over tumor progression, therapy resistance, and the formation of the immunosuppressive tumor microenvironment (TME). As a transcription factor with a conserved High Mobility Group (HMG) box DNA-binding domain, SOX9 recognizes the CCTTGAG motif to regulate gene expression programs governing cell fate determination, stemness, and differentiation [3] [32]. In the context of cancer, SOX9 frequently undergoes dysregulation, functioning as a master regulator of tumorigenesis across diverse malignancies including breast, ovarian, colorectal, and liver cancers [3] [10] [26]. Beyond its established roles in promoting cancer cell proliferation, invasion, and chemoresistance, recent investigations have illuminated the complex immunomodulatory functions of SOX9 within the TME [3] [10]. This multifaceted involvement positions SOX9 as an attractive therapeutic target for disrupting the pathogenic circuits that sustain cancer progression and immune evasion.
The therapeutic targeting of transcription factors like SOX9 has historically presented significant challenges due to their inherent structural characteristics and nuclear localization. However, growing understanding of SOX9's regulatory networks and the identification of natural compounds with SOX9-modulatory activity have opened promising avenues for therapeutic intervention. Among these, cordycepin (COR), a natural nucleoside analog derived from Cordyceps militaris, has demonstrated notable potential to inhibit SOX9 expression and activity, thereby disrupting SOX9-mediated oncogenic signaling and immune modulation [33] [11]. This technical review comprehensively examines the mechanistic basis for targeting SOX9 in cancer, with particular emphasis on cordycepin as a prototype small molecule inhibitor, and provides detailed experimental frameworks for evaluating SOX9 inhibition in the context of tumor immunology.
SOX9 Structure, Function, and Oncogenic Mechanisms
Structural Organization and Functional Domains
The human SOX9 protein comprises 509 amino acids with several functionally specialized domains that orchestrate its transcriptional activity [3] [32]. The N-terminal dimerization domain (DIM) facilitates the formation of homodimers and heterodimers with other SOXE subgroup members (SOX8 and SOX10), enabling cooperative DNA binding [32]. The central HMG box domain mediates sequence-specific DNA binding, bending the DNA helix to facilitate transcriptional complex assembly [3]. This domain contains embedded nuclear localization (NLS) and nuclear export (NES) signals that govern SOX9's nucleocytoplasmic shuttling [3]. The C-terminal region houses two transcriptional activation domains (TAM and TAC) that interact with co-activators such as Tip60 to potentiate gene expression [3] [32]. Additionally, a proline/glutamine/alanine (PQA)-rich domain contributes to transcriptional activation without intrinsic transactivation capability [32].
SOX9 Dysregulation in Human Cancers
SOX9 overexpression is a recurrent feature across multiple cancer types, where it drives oncogenic transformation and disease progression through diverse mechanisms. Comprehensive pan-cancer analyses reveal that SOX9 expression is significantly elevated in fifteen different cancer types, including colorectal (COAD), liver (LIHC), ovarian (OV), breast (BRCA), and lung (LUSC) carcinomas, while being decreased in only two cancer types (skin cutaneous melanoma and testicular germ cell tumors) [11]. This expression pattern underscores SOX9's predominant role as a proto-oncogene in most malignancy contexts. Critically, elevated SOX9 expression frequently correlates with poor clinical outcomes, serving as a prognostic biomarker for reduced overall survival in cancers such as low-grade glioma (LGG), cervical squamous cell carcinoma (CESC), and thymoma (THYM) [11].
Table 1: SOX9 Dysregulation Across Human Cancers
| Cancer Type | SOX9 Expression | Functional Role | Clinical Correlation |
|---|---|---|---|
| Colorectal (COAD) | Significantly increased | Oncogene | Promotes proliferation, immune evasion |
| Liver (LIHC) | Significantly increased | Oncogene | Drives fibrosis, tumor progression |
| Ovarian (OV) | Significantly increased | Oncogene | Chemotherapy resistance, stemness |
| Breast (BRCA) | Significantly increased | Oncogene | Immune evasion, metastasis |
| Lung (LUSC) | Significantly increased | Oncogene | Poor prognosis |
| Skin Melanoma (SKCM) | Significantly decreased | Tumor suppressor | Inhibits tumorigenesis when expressed |
SOX9-Mediated Therapy Resistance
A particularly challenging aspect of SOX9 biology in oncology is its prominent role in mediating resistance to conventional and targeted therapies. In high-grade serous ovarian cancer, SOX9 is epigenetically upregulated following chemotherapy, driving the emergence of a stem-like cell population with enhanced self-renewal capacity and chemoresistance [26]. Similarly, in breast cancer, SOX9 contributes to tamoxifen resistance by regulating ALDH1A3 expression and modulating Wnt signaling pathways [34]. Recent mechanistic studies have elucidated that SOX9 also promotes PARP inhibitor resistance in ovarian cancer by enhancing DNA damage repair through transcriptional regulation of key DNA repair genes including SMARCA4, UIMC1, and SLX4 [34]. This central role in therapy resistance underscores the critical need for effective SOX9-targeting strategies to overcome treatment failure in advanced cancers.
SOX9 in Tumor Immunity and the Microenvironment
Regulation of Immune Cell Infiltration and Function
SOX9 exerts multifaceted effects on immune cell populations within the TME, shaping an immunosuppressive landscape that facilitates tumor immune evasion. Bioinformatics analyses of colorectal cancer samples reveal that elevated SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. Specifically, SOX9 overexpression demonstrates negative correlation with genes associated with the cytotoxic function of CD8+ T cells, NK cells, and M1 macrophages, while exhibiting positive correlation with memory CD4+ T cells [3]. These findings suggest that SOX9 orchestrates broad changes in immune cell composition and functional states within the TME, potentially through regulation of chemokine networks or immune cell recruitment pathways.
Immune Evasion Mechanisms
At the cellular level, SOX9 contributes critically to immune evasion by promoting the survival and persistence of tumor-initiating cells with stem-like properties. Studies have demonstrated that SOX2 and SOX9 work cooperatively to maintain cancer cell stemness, preserving the long-term survival and tumor-initiating capacity of latent cancer cells [10]. Under immunotolerant conditions, these transcription factors enable dormant cancer cells to persist in secondary metastatic sites while evading immune surveillance [10]. Furthermore, SOX9 influences immune checkpoint regulation, with evidence suggesting associations between SOX9 expression and pathways involved in PD-L1 expression and T-cell receptor signaling in thymoma [11]. These immunomodulatory functions position SOX9 as a key regulator of the immune-tolerant niche that supports cancer progression and metastasis.
Stromal Interactions and Angiogenesis
Beyond direct effects on immune cells, SOX9 modulates the broader TME through interactions with stromal components and regulation of angiogenesis. SOX9 expression in cancer cells facilitates communication with cancer-associated fibroblasts (CAFs), tumor-associated macrophages (TAMs), and endothelial cells, fostering a pro-tumorigenic microenvironment [10]. In breast cancer, these interactions promote heterogeneity and multidrug resistance through cytokine secretion and extracellular matrix remodeling [10]. Additionally, SOX9 has a established relationship with tumor vascularization, further supporting the development of a nutrient-rich, immunosuppressive TME [3]. The pleiotropic effects of SOX9 on diverse cellular components of the TME highlight its central position as a regulator of the tumor ecosystem.
Cordycepin as a Prototype Small Molecule Inhibitor of SOX9
Chemical Properties and Source
Cordycepin (3'-deoxyadenosine) is a natural nucleoside analog isolated from the traditional medicinal fungus Cordyceps militaris [33] [35] [36]. Structurally, cordycepin differs from adenosine by the absence of a hydroxyl group at the 3' position of the ribose moiety, a modification that confers unique biological activities including anti-inflammatory, anti-tumor, and immunomodulatory properties [36] [11]. In Cordyceps militaris extracts, cordycepin is typically present alongside other bioactive compounds such as pentostatin, adenosine, cordycepic acid, polysaccharides, and proteins, with quantitative analyses revealing approximately 21.50 mg of cordycepin per 1 gram of ethanolic extract [36].
Direct SOX9 Inhibitory Effects
Experimental evidence demonstrates that cordycepin directly suppresses SOX9 expression at both transcriptional and protein levels. In prostate cancer (22RV1, PC3) and lung cancer (H1975) cell lines, cordycepin treatment inhibited both protein and mRNA expressions of SOX9 in a dose-dependent manner [11]. This SOX9 suppression contributes to cordycepin's broader anticancer effects, including inhibition of cancer cell migration and invasion [11]. In the context of diabetes-associated hepatic fibrosis, cordycepin was shown to significantly inhibit SOX9 expression in vivo and in vitro, thereby attenuating activation of the profibrotic Wnt/β-catenin signaling axis [33]. Mechanistic studies in hepatic stellate cell models revealed that SOX9 knockdown potentiated the inhibitory effects of cordycepin on Wnt3a and β-catenin expression, confirming SOX9 involvement in cordycepin's mechanism of action [33].
Impact on Immune Checkpoint Regulation
Beyond direct SOX9 inhibition, cordycepin modulates immune checkpoint molecules to enhance antitumor immunity. Research in colorectal cancer models demonstrates that cordycepin specifically targets the ubiquitin E3 ligase HRD1, promoting PD-L1 degradation through the ubiquitin-proteasome pathway [35]. This mechanism effectively reduces both total and membrane-associated PD-L1 protein levels in cancer cells, restoring T cell-mediated cytotoxicity against tumor cells [35]. The dual capacity to simultaneously inhibit SOX9 and promote PD-L1 degradation positions cordycepin as a multifaceted immunomodulatory agent capable of reversing key immune evasion mechanisms in the TME.
Immunogenic Modulation of Cancer Cells
Cordycepin further enhances antitumor immunity by modifying the surface antigen profile of cancer cells to increase their susceptibility to immune effector cells. Treatment of breast cancer (MCF-7, MDA-MB-231) and hepatocellular carcinoma (Huh-7, SNU-449) cell lines with cordycepin or Cordyceps militaris ethanolic extract (Cm-EE) significantly increased expression of NKG2D ligands and death receptors (FasR, DR4, DR5) while decreasing HLA-ABC-positive cells [36]. These changes create a more immunogenic phenotype that enhances recognition and elimination by immune effector cells. Functional co-culture experiments confirmed that cordycepin pre-treatment significantly enhanced the cytotoxic killing of cancer cells by immune effector populations, validating the functional consequences of these immunogenic modifications [36].
Table 2: Multifaceted Mechanisms of Cordycepin in Cancer and Immunomodulation
| Mechanistic Category | Specific Effect | Experimental Evidence |
|---|---|---|
| SOX9 Inhibition | Dose-dependent reduction of SOX9 mRNA and protein | Prostate cancer cells (22RV1, PC3), lung cancer cells (H1975) [11] |
| Wnt/β-catenin Pathway Suppression | Inhibition of SOX9-mediated Wnt/β-catenin signaling | Diabetic hepatic fibrosis models [33] |
| Immune Checkpoint Regulation | HRD1-mediated PD-L1 degradation via ubiquitin-proteasome pathway | Colorectal cancer cells (HCT116, RKO) [35] |
| Surface Antigen Modulation | Increased NKG2D ligands and death receptors; decreased HLA-ABC | Breast cancer, hepatocellular carcinoma cells [36] |
| Immune Cell Function Enhancement | Increased NKG2D receptor and Trail expression on NK cells | CD3-negative effector immune cells [36] |
| Cytokine Modulation | Stimulated IL-2, IL-6, and IL-10 production | Cordyceps militaris extract in immune cells [36] |
Experimental Framework for Evaluating SOX9 Inhibition
In Vitro Assessment of SOX9 Expression and Function
Cell Culture and Treatment Conditions: Prostate cancer cells (PC3, 22RV1) and lung cancer cells (H1975) are maintained in standard culture conditions (RPMI 1640 or DMEM medium with 10% FBS, 37°C, 5% CO2) [11]. Cordycepin is dissolved in appropriate vehicle (typically DMSO or water) and administered at varying concentrations (0-40 μM) for 24 hours to assess dose-dependent effects [11]. For SOX9 stabilization studies, ovarian cancer cells (SKOV3, UWB1.289) can be treated with the USP28 inhibitor AZ1 (1-5 μM) alone or in combination with PARP inhibitors like olaparib to evaluate effects on SOX9 protein stability [34].
Western Blot Analysis for SOX9 Protein Expression: Following treatment, cells are lysed using RIPA buffer supplemented with protease inhibitors [11] [34]. Protein concentrations are determined by BCA assay, and 20-40 μg of total protein lysate is separated by SDS-PAGE (8-15% gels) and transferred to PVDF membranes [34]. Membranes are incubated with anti-SOX9 antibody (1:1000 dilution) followed by appropriate HRP-conjugated secondary antibodies (1:5000 dilution) [34]. Band visualization is performed using enhanced chemiluminescence, with quantification relative to loading controls (β-actin) via densitometric analysis [11].
Quantitative RT-PCR for SOX9 Transcript Levels: Total RNA is extracted using standard methodologies (TRIzol or commercial kits) and reverse transcribed to cDNA [11]. qPCR is performed using SOX9-specific primers with the following typical cycling conditions: 95°C for 10 minutes, followed by 40 cycles of 95°C for 15 seconds and 60°C for 1 minute [11]. Expression levels are normalized to housekeeping genes (GAPDH, β-actin) and analyzed using the 2^(-ΔΔCt) method to determine fold changes in SOX9 mRNA expression relative to control treatments.
Functional Assays for Immune Modulation
Immune Cell Cytotoxicity Co-culture Assays: Cancer cells are pre-treated with cordycepin (100 μM) or Cm-EE (100 μg/mL) for 24 hours, then co-cultured with immune effector cells (PD-1-overexpressing Jurkat T cells, NK cells, or peripheral blood mononuclear cells) at varying effector-to-target ratios [35] [36]. After 24-48 hours of co-culture, cancer cell cytotoxicity is quantified using crystal violet staining, lactate dehydrogenase release assays, or flow cytometry-based apoptosis detection (Annexin V/PI staining) [35] [36]. Specific immune cell populations can be characterized by surface marker staining (CD3 for T cells, CD56 for NK cells) followed by flow cytometric analysis.
Surface Immune Marker Analysis: Following cordycepin treatment, cancer cells are harvested and stained with fluorochrome-conjugated antibodies against PD-L1, HLA-ABC, NKG2D ligands (MICA/B), death receptors (FasR, DR4, DR5), and appropriate isotype controls [35] [36]. Samples are analyzed by flow cytometry, with median fluorescence intensity and percentage of positive cells quantified relative to untreated controls. For immune checkpoint studies, internalization assays can be performed using pH-sensitive antibodies to track PD-L1 trafficking [35].
Cytokine Profiling: Supernatants from cordycepin-treated immune cells or co-culture systems are collected and analyzed for cytokine secretion profiles using ELISA or multiplex bead-based arrays [36]. Key cytokines to monitor include IL-2, IL-6, IL-10, IL-12, IFN-γ, and TNF-α, which provide insight into Th1/Th2 polarization and overall immune activation status [36].
Diagram: SOX9 Regulatory Network and Cordycepin Mechanism of Action
In Vivo Therapeutic Efficacy Models
Subcutaneous Tumor Models: For evaluating cordycepin efficacy in vivo, MC38 colorectal cancer cells or other relevant syngeneic models are injected subcutaneously into immunocompetent mice (C57BL/6J) [35]. Once tumors reach measurable size (50-100 mm³), mice are randomized into treatment groups receiving cordycepin (25-50 mg/kg) via intraperitoneal or oral administration, either as monotherapy or in combination with immune checkpoint inhibitors (anti-CTLA-4, anti-PD-1) [35]. Tumor dimensions are measured regularly by caliper, with volume calculated as (length × width²)/2. Animals are monitored for overall health, weight change, and signs of toxicity throughout the study period.
Immune Monitoring in Tumor Tissue: Following sacrifice, tumors are harvested for comprehensive immune analysis. Single-cell suspensions are prepared by mechanical dissociation and enzymatic digestion (collagenase/hyaluronidase) for flow cytometric immunophenotyping of tumor-infiltrating lymphocytes (CD8+, CD4+, Tregs), myeloid cells (macrophages, dendritic cells), and NK cells [3] [36]. Intracellular cytokine staining (IFN-γ, TNF-α) following ex vivo stimulation provides functional assessment of immune activation. For spatial analysis of immune cell distribution, formalin-fixed paraffin-embedded sections can be subjected to multiplex immunohistochemistry using validated antibody panels against immune cell markers and SOX9 [3].
SOX9 Expression Analysis in Tumor Tissue: Tumor samples are processed for SOX9 detection by immunohistochemistry using validated anti-SOX9 antibodies [11]. Staining intensity and percentage of positive cells are scored by pathologists blinded to treatment groups. Alternatively, SOX9 mRNA levels can be quantified in snap-frozen tumor tissues by RNA extraction followed by qRT-PCR analysis [11]. Correlation analyses between SOX9 expression levels, immune cell infiltration, and treatment response provide insights into potential biomarkers for cordycepin sensitivity.
Research Reagent Solutions for SOX9 Studies
Table 3: Essential Research Reagents for SOX9-Targeted Investigations
| Reagent Category | Specific Examples | Application Purpose | Technical Notes |
|---|---|---|---|
| SOX9 Detection Antibodies | Rabbit anti-SOX9 (Abcam ab5535), Mouse anti-SOX9 (Sigma AB5535) | Western blot, IHC, immunofluorescence | Validate specificity with SOX9-knockdown controls |
| SOX9 Modulation Tools | CRISPR/Cas9 KO plasmids, siRNA/shRNA constructs | SOX9 loss-of-function studies | Multiple sequences recommended to control for off-target effects |
| SOX9 Activity Reporters | SOX9-responsive luciferase constructs (e.g., with CCTTGAG repeats) | Screening for SOX9 inhibitors | Include mutant response elements as controls |
| Cordycepin Formulations | Cordycepin (>98% purity), Cordyceps militaris extracts | SOX9 inhibition studies | Consider pharmacokinetic optimization for in vivo use |
| USP28 Inhibitors | AZ1 compound (Selleck S8904) | SOX9 stabilization studies | Use at 1-5 μM concentration in cell-based assays |
| Pathway Inhibitors | XAV939 (Wnt inhibitor), Olaparib (PARPi) | Combination studies with SOX9 targeting | Assess synergistic effects with cordycepin |
| Immune Checkpoint Reagents | Anti-PD-1, anti-PD-L1, anti-CTLA-4 antibodies | Combination immunotherapy studies | Multiple clone options available for murine and human systems |
The strategic targeting of SOX9 represents a promising therapeutic approach for disrupting the pathogenic circuits that sustain cancer progression and immune evasion. Cordycepin, as a natural product-derived small molecule, demonstrates multifaceted capacity to inhibit SOX9 expression and activity while concurrently modulating critical immune checkpoints like PD-L1. The experimental frameworks outlined herein provide standardized methodologies for evaluating SOX9 inhibition across preclinical models, with particular emphasis on immunological readouts that reflect the complex interplay between SOX9 activity and antitumor immunity.
Future research directions should prioritize the development of more potent and selective SOX9 inhibitors through structure-based drug design and high-throughput screening approaches. Additionally, combination strategies integrating SOX9 inhibition with established immunotherapies (immune checkpoint blockers, CAR-T cells) warrant systematic investigation to identify synergistic treatment regimens. The advancement of SOX9-focused therapeutic strategies holds significant potential to overcome key mechanisms of therapy resistance and immune evasion, ultimately contributing to improved outcomes for cancer patients across multiple malignancy types.
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator in cancer biology, extending beyond its well-characterized roles in embryonic development and chondrogenesis. Recent research has illuminated its significant contributions to tumor progression and therapeutic resistance across diverse cancer types [37]. As a pivotal component of the tumor immune microenvironment, SOX9 operates as a molecular hub integrating multiple signaling pathways that confer adaptive advantages to cancer cells under therapeutic pressure. This whitepaper synthesizes current mechanistic understanding of SOX9-mediated drug resistance, with particular emphasis on its function within the immunosuppressive tumor landscape. We provide a comprehensive technical resource for researchers and drug development professionals, integrating quantitative data summaries, experimental methodologies, and visual schematics of the underlying molecular networks. The complex duality of SOX9 function—acting as either an oncogene or tumor suppressor in a context-dependent manner—underscores the necessity for precise mechanistic dissection to develop effective therapeutic strategies that target SOX9-related resistance pathways [3].
Molecular Mechanisms of SOX9-Mediated Drug Resistance
Regulation of SOX9 Expression and Stability
SOX9 protein levels and transcriptional activity are tightly regulated through multiple mechanisms that become co-opted in drug-resistant cancers. Understanding these regulatory networks is fundamental to developing targeted interventions.
Transcriptional and Post-translational Control: SOX9 expression is regulated by microRNAs (miRNAs), methylation, phosphorylation, and acetylation processes [37]. The deubiquitinating enzyme USP28 has been identified as a novel interacting partner that stabilizes SOX9 protein by inhibiting its FBXW7-mediated ubiquitination and degradation [34]. This stabilization pathway is particularly important in ovarian cancer, where USP28-mediated SOX9 upregulation contributes to PARP inhibitor resistance.
Experimental Evidence: In ovarian cancer models, Co-IP and mass spectrometry assays demonstrated direct binding between USP28 and SOX9 [34]. Treatment with the USP28-specific inhibitor AZ1 reduced SOX9 protein stability and sensitized ovarian cancer cells to olaparib, confirming the therapeutic relevance of this regulatory axis [34].
Stemness Maintenance and Epithelial-Mesenchymal Transition
SOX9 drives critical phenotypic transitions that enable therapeutic escape through the acquisition of stem-like properties and enhanced plasticity.
Cancer Stem Cell (CSC) Regulation: SOX9 has been broadly studied in the field of cancer stem cells (CSCs) and epithelial-mesenchymal transition (EMT) [37]. In high-grade serous ovarian cancer (HGSOC), SOX9 maintains a stem-like transcriptional state associated with platinum resistance [38]. Mechanistically, SOX9 activates key stemness-associated pathways and represses differentiation markers, creating a cellular state refractory to conventional chemotherapy.
EMT Program Activation: Similar to its developmental functions, SOX9 regulates EMT in cancer through activation of transcription factors like Slug (SNAI2) [39]. In breast cancer, SOX9 works in concert with Slug to promote cancer cell proliferation and metastasis [10]. This transition to a mesenchymal state is coupled with enhanced invasive capacity and therapeutic resistance.
Table 1: SOX9-Mediated Resistance Mechanisms Across Cancer Types
| Cancer Type | Resistance Mechanism | Key Effectors | Therapeutic Context |
|---|---|---|---|
| Ovarian Cancer | Enhanced DNA damage repair | SMARCA4, UIMC1, SLX4 | PARP inhibitor (Olaparib) [34] |
| Ovarian Cancer | Stemness maintenance | ALDH1, Wnt signaling | Platinum-based therapy [38] |
| Breast Cancer | Immune evasion | SOX2/SOX9 axis | Dormancy and metastatic escape [10] |
| Liver Cancer | Lineage plasticity | YAP1, NRAS | Combined HCC-CCA tumors [40] |
| Multiple Cancers | ABC transporter upregulation | ABCB1, ABCG2 | Chemotherapy [37] |
DNA Damage Repair Enhancement
A central mechanism of SOX9-mediated resistance involves the enhancement of DNA repair capacity, particularly in response to genotoxic therapies.
DDR Gene Regulation: Chromatin immunoprecipitation sequencing (ChIP-Seq) in ovarian cancer cells revealed that SOX9 binds to promoters of key DNA damage repair (DDR) genes including SMARCA4, UIMC1, and SLX4 [34]. This direct transcriptional regulation enhances homologous recombination and other DNA repair pathways, effectively neutralizing DNA-damaging agents and PARP inhibitors.
Functional Validation: Depletion of SOX9 in ovarian cancer models resulted in sustained DNA damage markers (γH2AX foci) and increased apoptosis following olaparib treatment, confirming its functional role in DDR [34]. This mechanistic insight provides rationale for targeting SOX9 in combination with PARP inhibitors.
Figure 1: USP28-SOX9 Regulatory Axis in PARPi Resistance. USP28 stabilizes SOX9 by counteracting FBXW7-mediated ubiquitination. SOX9 transcriptionally activates DNA damage repair (DDR) genes, leading to PARP inhibitor resistance.
SOX9 in the Tumor Immune Microenvironment
Immunomodulatory Functions
SOX9 exhibits complex, context-dependent roles in immune regulation that significantly impact therapeutic responses. Its function as a "double-edged sword" in immunology reflects its dual capacity to both promote and suppress immune activity depending on the cellular context [3].
Immune Cell Infiltration Patterns: Bioinformatics analyses of colorectal cancer data reveal distinct correlations between SOX9 expression and immune cell infiltration. SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3].
CD8+ T Cell Function Suppression: In multiple cancer types, SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with memory CD4+ T cells [3]. This immunosuppressive orientation creates a microenvironment conducive to tumor progression and therapy resistance.
Immune Evasion in Metastatic Dormancy: SOX9 plays a crucial role in immune evasion by maintaining cancer cell dormancy and stemness. Research has demonstrated that latent cancer cells exhibit high SOX2 and SOX9 expression, which preserves their long-term survival and tumor-initiating capabilities while avoiding immune surveillance in secondary metastatic sites [10].
Context-Dependent Dual Roles
The paradoxical functions of SOX9 in different cancer types and developmental contexts highlight its complex relationship with immune regulation:
Pro-regenerative Functions: In non-malignant contexts, SOX9 helps maintain macrophage function, contributing to cartilage formation, tissue regeneration, and repair [3]. This pro-regenerative capacity becomes co-opted in the tumor microenvironment to support cancer cell survival and expansion.
Lineage-Dependent Effects: In prostate cancer, single-cell RNA sequencing analyses revealed that androgen deprivation therapy (ADT) enriches a subpopulation of club cells characterized by high SOX9 and low AR expression, contributing to an "immune desert" microenvironment that promotes tumor immune escape [3].
Figure 2: Dual Immunological Roles of SOX9. SOX9 exhibits context-dependent functions, simultaneously promoting immune suppression in cancer while supporting protective immune functions in tissue repair and regeneration.
Table 2: SOX9 Correlation with Immune Parameters in Cancer
| Immune Parameter | Correlation with SOX9 | Functional Consequence | Cancer Types Studied |
|---|---|---|---|
| CD8+ T cell function | Negative [3] | Impaired cytotoxic response | Multiple solid tumors |
| NK cell activity | Negative [3] | Reduced innate immune surveillance | Multiple solid tumors |
| M1 macrophages | Negative [3] | Attenuated anti-tumor immunity | Multiple solid tumors |
| B cell infiltration | Negative [3] | Diminished humoral response | Colorectal cancer |
| Neutrophils | Positive [3] | Potential N2 polarization | Colorectal cancer |
| Macrophages | Positive [3] | M2-like TAM differentiation | Colorectal cancer |
| Tregs | Context-dependent | Immune suppression | Prostate cancer [3] |
Experimental Models and Methodologies
Key Experimental Approaches
The investigation of SOX9 in drug resistance employs diverse methodological approaches that enable mechanistic dissection of its multifaceted functions.
Genetic Manipulation Models: The context-dependent functions of SOX9 have been elucidated through sophisticated genetic models. In combined hepatocellular-cholangiocarcinoma (cHCC-CCA), liver-specific developmental Sox9 elimination using Alb-Cre;Sox9flox/flox (LKO) and CRISPR/Cas9-based tumor-specific acute Sox9 elimination (CKO) revealed contrasting responses depending on the genetic context and oncogenic drivers (Akt-YAP1 vs. Akt-NRAS) [40]. These models demonstrate that SOX9 elimination may hold promise as a therapeutic approach for a subset of cHCC-CCA, highlighting the importance of context-specific strategies.
Therapeutic Resistance Models: PARPi-resistant ovarian cancer cell lines (e.g., SKOV3/Ola) generated through continuous exposure to increasing olaparib concentrations have been instrumental in identifying SOX9 upregulation as a consistent feature of acquired resistance [34]. These models facilitate the discovery of resistance mechanisms and testing of combination therapies.
Analytical Techniques
Advanced molecular techniques have provided unprecedented insights into SOX9 function at transcriptional, protein, and genomic levels.
Chromatin Immunoprecipitation Sequencing (ChIP-Seq): ChIP-Seq analysis in ovarian cancer cells revealed genome-wide SOX9 binding sites, identifying direct targets including DDR genes (SMARCA4, UIMC1, SLX4) [34]. This approach provides comprehensive mapping of SOX9 transcriptional networks.
Protein Interaction Studies: Co-immunoprecipitation (Co-IP) assays combined with mass spectrometry identified USP28 as a novel SOX9 interacting partner [34]. For Co-IP experiments, cells are lysed and proteins incubated with specific antibodies or IgG control overnight, followed by protein A/G magnetic bead pulldown, washing, and western blot analysis.
Ubiquitination Assays: To demonstrate USP28-mediated stabilization of SOX9, ubiquitination assays were performed in HEK293T cells co-transfected with SOX9, FBXW7, and USP28 constructs, treated with MG132 proteasome inhibitor, followed by SOX9 immunoprecipitation and ubiquitin western blotting [34].
Therapeutic Targeting Strategies
Direct and Indirect Targeting Approaches
Several strategic approaches have emerged for countering SOX9-mediated therapy resistance.
USP28 Inhibition: The identification of USP28 as a key SOX9 stabilizer provides a promising indirect targeting strategy. The USP28-specific inhibitor AZ1 reduces SOX9 protein stability and increases PARPi sensitivity in ovarian cancer models [34]. This combination approach targets the SOX9 stabilization machinery rather than SOX9 itself.
Transcriptional Network Disruption: Small molecules that interfere with SOX9 DNA binding or transcriptional cofactor recruitment represent an attractive but challenging approach. Current efforts focus on downstream effectors rather than direct SOX9 inhibition.
Immunotherapy Combinations: Given SOX9's role in creating immunosuppressive microenvironments, combining SOX9 pathway inhibition with immune checkpoint blockers (anti-PD-1/PD-L1, anti-CTLA-4) may provide synergistic benefits [3]. This approach potentially reverses SOX9-mediated T-cell dysfunction while activating anti-tumor immunity.
Context-Dependent Therapeutic Considerations
The dual nature of SOX9 function necessitates careful therapeutic stratification:
Cancer-Type Specificity: SOX9 acts as a proto-oncogene in most contexts but can function as a tumor suppressor in specific cancer types [37]. Comprehensive biomarker assessment is essential before targeting SOX9 therapeutically.
Lineage Plasticity Management: In liver cancer models, Sox9 elimination prevents YAP1-mediated cholangiocarcinoma formation while stimulating poorly differentiated HCC proliferation [40]. This paradoxical effect underscores the need for detailed understanding of SOX9's lineage-specific functions.
Therapeutic Window Optimization: The essential roles of SOX9 in non-malignant tissue homeostasis (e.g., cartilage maintenance, tissue repair) require careful therapeutic window determination to avoid on-target toxicities [3] [41].
Figure 3: Therapeutic Targeting Strategies for SOX9-Mediated Resistance. Connecting specific SOX9-driven resistance mechanisms with corresponding targeted approaches and rational combination strategies.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Investigating SOX9 in Drug Resistance
| Reagent Category | Specific Examples | Application/Function | Experimental Context |
|---|---|---|---|
| Cell Lines | SKOV3/Ola (PARPi-resistant) [34] | Resistance mechanism studies | Ovarian cancer PARPi resistance |
| Akt-YAP1; Akt-NRAS cHCC-CCA models [40] | Lineage plasticity studies | Liver cancer plasticity | |
| Antibodies | Anti-SOX9 (AB5535, Sigma) [34] | Western blot, IHC, IP | SOX9 protein detection |
| Anti-γH2AX (ab81299, Abcam) [34] | DNA damage quantification | DDR functional assays | |
| Anti-USP28 (17707-1-AP, Proteintech) [34] | Protein interaction studies | USP28-SOX9 axis | |
| Anti-FBXW7 (ab192328, Abcam) [34] | Ubiquitination mechanism | SOX9 degradation studies | |
| Chemical Inhibitors | AZ1 (USP28 inhibitor) [34] | SOX9 destabilization | Combination with PARPi |
| Olaparib (PARPi) [34] | DDR pathway inhibition | Ovarian cancer models | |
| MG132 (proteasome inhibitor) [34] | Protein stabilization assays | Ubiquitination studies | |
| Expression Vectors | Flag-SOX9 constructs [34] | SOX9 overexpression studies | Functional rescue experiments |
| shRNA/SiRNA against SOX9 [34] | SOX9 knockdown | Loss-of-function studies | |
| Animal Models | Alb-Cre;Sox9flox/flox (LKO) [40] | Developmental SOX9 deletion | Liver cancer models |
| OPN-CreERT2; Sox9 iKO [40] | Inducible SOX9 deletion | Therapeutic efficacy studies |
SOX9 represents a critical node in the complex network of cancer drug resistance, integrating signals from multiple pathways to confer adaptive advantages to cancer cells. Its multifaceted functions—spanning stemness maintenance, DNA damage repair enhancement, immune modulation, and lineage plasticity—establish SOX9 as a high-value therapeutic target. The recent identification of specific regulatory mechanisms, particularly the USP28-SOX9 stabilization axis, provides promising avenues for targeted intervention. However, the context-dependent duality of SOX9 function necessitates sophisticated patient stratification and biomarker development. Future research directions should prioritize the development of direct SOX9 inhibitors, validation of combination strategies in advanced preclinical models, and comprehensive analysis of SOX9 immune-modulatory functions across cancer types. As our understanding of SOX9 biology continues to evolve, so too will opportunities to disrupt the resistance pathways it controls, potentially restoring therapeutic sensitivity across multiple cancer types.
Navigating the Complexities: Challenges in Targeting SOX9 for Immunotherapy
The SRY-related HMG-box 9 (SOX9) transcription factor represents a paradigm of functional duality in cancer biology, operating as either an oncogene or tumor suppressor in a context-dependent manner. As a key regulator of embryonic development, cell differentiation, and stem cell maintenance, SOX9 plays complex and often contradictory roles in tumorigenesis [42]. This transcription factor is frequently overexpressed in diverse solid malignancies, where its expression levels positively correlate with tumor occurrence, progression, and poor prognosis [3]. However, emerging evidence reveals that SOX9 can also function as a tumor suppressor in specific contexts, creating significant challenges for therapeutic targeting [43]. Understanding the mechanisms that govern SOX9's dual functions is critical for advancing SOX9-based therapeutic strategies, particularly within the framework of tumor immune microenvironment research.
The functional paradox of SOX9 extends to its role in modulating the tumor immune microenvironment (TIME), where it exhibits "Janus-faced" characteristics by both promoting and suppressing anti-tumor immunity [3]. This review synthesizes current understanding of SOX9's context-dependent functions, with particular emphasis on its mechanisms of action within the immune landscape of tumors. We provide a comprehensive analysis of experimental approaches for investigating SOX9 function, detailed signaling pathways, and resource tools for researchers exploring SOX9 as a therapeutic target in cancer.
SOX9 in Oncogenesis: Mechanisms and Immune Evasion
Oncogenic Functions Across Cancer Types
SOX9 demonstrates consistent oncogenic properties across numerous cancer types, where it drives key hallmarks of cancer through multiple molecular mechanisms. In lung adenocarcinoma (LUAD), SOX9 is significantly upregulated in KRAS-mutant tumors and drives tumor progression through enhanced cell proliferation and suppression of anti-tumor immunity [43]. Genetic knockout studies in KrasG12D-driven mouse models revealed that Sox9 loss significantly reduces lung tumor development, burden, and progression, contributing to substantially longer overall survival [43]. Similarly, in breast cancer, SOX9 regulates tumor initiation, proliferation, and chemotherapy resistance through multiple pathways, including interactions with long non-coding RNAs and key signaling pathways [10].
Table 1: SOX9 as an Oncogene in Various Cancers
| Cancer Type | Oncogenic Mechanism | Impact on TIME | Experimental Evidence |
|---|---|---|---|
| Lung Adenocarcinoma | Drives KRAS-induced tumor progression; increases collagen deposition | Suppresses CD8+ T, NK, and dendritic cell infiltration | CRISPR/Cas9 knockout in GEMMs; organoid models [43] |
| Breast Cancer | Promotes tumor initiation, proliferation, and stemness; regulates SOX10 via AKT | Facilitates immune evasion by maintaining cancer cell dormancy | Cell line studies; expression analysis [10] |
| Colorectal Cancer | Overexpressed and correlates with altered immune infiltration | Negative correlation with B cells, resting mast cells, and resting T cells | Bioinformatics analysis of TCGA data [3] |
| Head and Neck SCC | Regulates ANXA1 expression to mediate neutrophil apoptosis | Reduces Fpr1+ neutrophils and impairs cytotoxic cell function | scRNA-seq in mouse models; transgenic validation [18] |
| Glioblastoma | Highly expressed and correlates with immune infiltration patterns | Associated with immunosuppressive microenvironment | RNA-seq from TCGA/GTEx; immune correlation analysis [9] |
Mechanisms of Immune Modulation
SOX9 employs diverse strategies to suppress anti-tumor immunity and facilitate immune evasion. In lung adenocarcinoma, SOX9 suppresses immune cell infiltration by functionally impairing tumor-associated CD8+ T cells, natural killer cells, and dendritic cells [43]. Mechanistically, SOX9 significantly elevates collagen-related gene expression and increases collagen fiber deposition, potentially creating a physical barrier to immune cell infiltration [43]. This remodeling of the extracellular matrix represents a novel mechanism through which SOX9 modulates the TIME.
In head and neck squamous cell carcinoma (HNSCC), SOX9 mediates resistance to combined anti-LAG-3 and anti-PD-1 immunotherapy through a distinct pathway. SOX9 directly regulates the expression of annexin A1 (Anxa1), which induces apoptosis of formyl peptide receptor 1 (Fpr1)+ neutrophils via the Anxa1-Fpr1 axis [18]. This pathway promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (Bnip3) expression, ultimately preventing neutrophil accumulation in tumor tissues. The reduction of Fpr1+ neutrophils impairs the infiltration and tumor cell-killing capacity of cytotoxic CD8+ T and γδT cells within the TIME, thereby driving resistance to combination immunotherapy [18].
Tumor Suppressor Functions: ContextualExceptions
Tissue-Specific Tumor Suppressive Mechanisms
Despite its predominant oncogenic role, SOX9 exhibits tumor suppressor activity in specific contexts, including melanoma, cervical, and bladder cancers [43]. The mechanisms underlying these contradictory functions remain incompletely understood but appear to involve tissue-specific signaling networks and cellular contexts. In some systems, SOX9 has demonstrated anti-proliferative effects, such as in T47D breast cancer cell lines where it contributes to G0/G1 cell cycle arrest [10]. The retinoid acid pathway can induce SOX9 expression, which subsequently upregulates the transcription inhibitor HES-1, supporting a potential tumor-suppressive function in certain molecular contexts [10].
Table 2: SOX9 as a Tumor Suppressor in Specific Contexts
| Cancer Type | Tumor Suppressor Mechanism | Impact on TIME | Experimental Evidence |
|---|---|---|---|
| Melanoma | Not fully characterized | Limited data | Clinical observation [43] |
| Cervical Cancer | Not fully characterized | Limited data | Clinical observation [43] |
| Bladder Cancer | Not fully characterized | Limited data | Clinical observation [43] |
| Breast Cancer (context-dependent) | Mediates G0/G1 cell cycle arrest; induces HES-1 expression | Not characterized | T47D and MCF-7 cell line studies [10] |
Determinants of Functional Duality
The contextual factors that determine whether SOX9 functions as an oncogene or tumor suppressor remain an active area of investigation. Potential determinants include:
- Cellular lineage and differentiation status: SOX9's role varies across tissue types, likely reflecting its normal physiological functions in specific organs [42]
- Genetic background and mutational status: SOX9 exhibits stronger oncogenic activity in KRAS-mutant lung cancers [43]
- Microenvironmental cues: Signaling molecules from the tumor microenvironment, such as TGF-β and BMPs, can modulate SOX9 activity [44]
- Post-translational modifications: Acetylation and SUMOylation regulate SOX9's subcellular localization and function [42]
- Interaction with co-factors: SOX9's transcriptional activity depends on partnership with tissue-specific co-factors that may determine target gene specificity [3]
Experimental Models and Methodologies
In Vivo Models for SOX9 Functional Studies
Several sophisticated mouse models have been developed to investigate SOX9 function in cancer progression and therapy response:
KrasG12D-driven lung adenocarcinoma models: Both CRISPR/Cas9 and Cre-LoxP gene knockout approaches have been employed to demonstrate that Sox9 loss significantly reduces lung tumor development, burden, and progression [43]. The KrasLSL-G12D;Sox9flox/flox (KSf/f) genetically engineered mouse model shows significantly longer survival compared to controls, with reduced progression to high-grade tumors [43].
4-nitroquinoline 1-oxide (4NQO)-induced HNSCC model: This immunocompetent model has been instrumental in identifying SOX9-mediated resistance to anti-LAG-3 plus anti-PD-1 combination therapy [18]. Mice with similar tumor lesions are randomly divided into treatment groups and assessed every 4 days from initial treatment, with resistant tumors defined as those growing more than 20% larger than original size within 14 days according to RECIST criteria [18].
Tumor organoid and allograft models: 3D tumor organoid culture systems combined with allograft transplantation in syngeneic C57BL/6J mice demonstrate that SOX9-driven tumor growth is significantly attenuated in immunocompromised versus immunocompetent mice, highlighting the importance of immune mechanisms in SOX9 oncogenic function [43].
Analytical Approaches for TIME Studies
Comprehensive profiling of the tumor immune microenvironment requires multiple complementary approaches:
Single-cell RNA sequencing (scRNA-seq): This technology has revealed significant enrichment of Sox9+ tumor cells in immunotherapy-resistant HNSCC samples [18]. Standard workflow includes tissue digestion into single-cell suspensions, library construction, quality control filtering, and cell type identification using canonical markers (e.g., Krt14/Krt5 for epithelial cells, Ptprc/Cd3g for immune cells) [18].
Immune cell infiltration analysis: The ssGSEA package and ESTIMATE algorithm in the GSVA package enable quantitative assessment of immune cell infiltration from bulk RNA-seq data [9] [19]. These tools allow correlation of SOX9 expression with specific immune cell populations.
Flow cytometry and immunohistochemistry: Validation of computational findings requires direct measurement of immune cell populations using fluorochrome-conjugated antibodies for cell surface markers (e.g., CD8, CD4, NK1.1) and intracellular staining for functional markers (e.g., Ki67, cleaved Caspase-3) [18] [43].
SOX9-Mediated Signaling Pathways in TIME Regulation
Diagram 1: SOX9 signaling pathways in immune regulation. SOX9 drives immune suppression through multiple mechanisms including ANXA1-FPR1 mediated neutrophil apoptosis, collagen deposition creating physical barriers, and maintenance of cancer cell dormancy. Contextual factors including genetic background, tissue context, post-translational modifications (PTM), and microenvironmental cues determine SOX9's functional outcomes.
Research Reagent Solutions Toolkit
Table 3: Essential Research Reagents for SOX9 and TIME Studies
| Reagent/Category | Specific Examples | Application/Function | Key Considerations |
|---|---|---|---|
| Mouse Models | KrasLSL-G12D;Sox9flox/flox (KSf/f); 4NQO-induced HNSCC model | In vivo studies of SOX9 function in tumor progression and therapy response | Syngeneic models preserve intact immune system for TIME studies [43] |
| Cell Models | KrasG12D mouse lung tumor lines (mTC11, mTC14); 3D organoid cultures | In vitro mechanistic studies and drug screening | 3D organoids better recapitulate tumor architecture and signaling [43] |
| Genetic Tools | pSECC CRISPR/Cas9 system; Cre-LoxP conditional knockout; sgRNAs targeting Sox9 | Precise genetic manipulation of SOX9 | Multiple sgRNAs recommended to control for off-target effects [43] |
| Antibodies for IHC/Flow | Anti-SOX9, Anti-Ki67, Anti-cleaved Caspase-3, CD8, CD4, NK1.1, FPR1 | Phenotypic characterization and immune profiling | Validate antibodies for specific applications and species [18] [43] |
| scRNA-seq Platforms | 10X Genomics; inDrops | High-resolution analysis of tumor and immune cell heterogeneity | Include sample multiplexing to control for batch effects [18] |
| Bioinformatics Tools | CopyKAT; Seurat; GSVA/ssGSEA; ESTIMATE | Computational analysis of SOX9 expression and immune correlations | Apply multiple algorithms to confirm key findings [9] [18] |
SOX9 represents a compelling therapeutic target in oncology due to its central role in regulating tumor progression and the immune microenvironment. However, its context-dependent functions pose significant challenges for therapeutic development. Future research should prioritize several key areas:
First, a more comprehensive understanding of the determinants governing SOX9's functional duality is needed. This includes systematic investigation of how tissue-specific co-factors, post-translational modifications, and microenvironmental signals dictate whether SOX9 acts as an oncogene or tumor suppressor. Second, the development of SOX9-targeted therapies must account for its complex roles in both tumor cells and immune cells within the TIME. Strategies to inhibit SOX9's immunosuppressive functions while preserving potential tumor-suppressive activities will require sophisticated targeting approaches. Third, reliable biomarkers for predicting SOX9 function in individual patients and tumors must be established to enable patient stratification for SOX9-directed therapies.
Overcoming these challenges will require integrated approaches combining sophisticated genetic models, multi-omics profiling, and functional immune assays. As our understanding of SOX9's context-dependent functions deepens, so too will our ability to harness this knowledge for therapeutic benefit in cancer treatment.
Overcoming SOX9-Mediated Chemoresistance in Solid Tumors
The transcription factor SOX9 (SRY-Box Transcription Factor 9) has emerged as a critical regulator of chemoresistance across multiple solid tumors, functioning primarily through its influence on the tumor immune microenvironment (TIME). Originally recognized for its roles in embryonic development and chondrogenesis, SOX9 is frequently overexpressed in malignancies including ovarian, breast, glioblastoma, and head and neck cancers [3] [10]. Its expression is associated with poor prognosis, advanced tumor staging, and therapeutic resistance [19] [9]. SOX9 mediates chemoresistance through dual mechanisms: intrinsically, by reprogramming cancer cells into a stem-like, drug-tolerant state, and extrinsically, by sculpting an immunosuppressive TIME that protects tumors from immune clearance [6] [18]. This whitepaper synthesizes recent advances in understanding SOX9-driven resistance mechanisms and outlines experimental approaches and therapeutic strategies for targeting SOX9 to overcome chemoresistance in solid tumors.
Molecular Mechanisms of SOX9-Mediated Chemoresistance
SOX9-Driven Transcriptional Reprogramming and Stemness
SOX9 orchestrates a transcriptional program that promotes cancer stem cell (CSC) properties, a primary mechanism of chemoresistance. In high-grade serous ovarian cancer (HGSOC), SOX9 is epigenetically upregulated following platinum-based chemotherapy, inducing a stem-like transcriptional state [6]. This reprogramming is characterized by increased transcriptional divergence, a metric reflecting enhanced transcriptional plasticity that enables adaptation to therapeutic stress [6]. Mechanistically, SOX9-expressing cells show enrichment for CSC markers and chemoresistance-associated stress gene modules. Experimental induction of SOX9 is sufficient to drive chemoresistance in vivo, establishing its causal role in this process [6] [26].
SOX9 in DNA Damage Repair and PARP Inhibitor Resistance
Beyond conventional chemotherapy, SOX9 contributes to resistance against targeted therapies like PARP inhibitors (PARPi) in ovarian cancer. SOX9 regulates the expression of key DNA damage repair (DDR) genes, including SMARCA4, UIMC1, and SLX4 [34]. The deubiquitinating enzyme USP28 stabilizes SOX9 protein by inhibiting its FBXW7-mediated ubiquitination and degradation. This USP28-SOX9 axis enhances DDR capacity, conferring PARPi resistance. Accordingly, USP28 inhibition with AZ1 destabilizes SOX9 and resensitizes ovarian cancer cells to olaparib [34].
SOX9-Mediated Immunosuppression in the Tumor Microenvironment
SOX9 promotes an immunosuppressive TIME through multiple mechanisms. In head and neck squamous cell carcinoma (HNSCC), SOX9+ tumor cells drive resistance to combined anti-PD-1 and anti-LAG-3 immunotherapy by regulating neutrophil function [18]. SOX9 directly transactivates annexin A1 (Anxa1), which engages formyl peptide receptor 1 (Fpr1) on neutrophils. This Anxa1-Fpr1 axis promotes mitochondrial fission and inhibits mitophagy by downregulating BNIP3, ultimately inducing neutrophil apoptosis and reducing their tumor infiltration [18]. The loss of neutrophils impairs cytotoxic CD8+ T cell and γδ T cell recruitment and function, creating an "immune desert" microenvironment conducive to therapy resistance [18]. Furthermore, SOX9 expression correlates with altered immune cell infiltration in glioblastoma, influencing immune checkpoint expression and contributing to an immunosuppressive niche [19] [9].
Table 1: SOX9-Mediated Chemoresistance Mechanisms Across Solid Tumors
| Cancer Type | Resistance Mechanism | Key Effectors | Therapeutic Context |
|---|---|---|---|
| Ovarian Cancer | Transcriptional reprogramming to stem-like state | Increased transcriptional divergence, CSC enrichment | Platinum-based chemotherapy [6] |
| Ovarian Cancer | Enhanced DNA damage repair | USP28 stabilization, SMARCA4, UIMC1, SLX4 | PARP inhibitor resistance [34] |
| Head and Neck Cancer | Immunosuppression via neutrophil modulation | Anxa1-Fpr1 axis, BNIP3 downregulation | Anti-PD-1 + anti-LAG-3 therapy [18] |
| Breast Cancer | Stemness maintenance, Immune evasion | SOX2/SOX9 cooperation, ALDH1A3 regulation | Chemotherapy, Targeted therapy [10] |
| Glioblastoma | Immune cell infiltration alterations | Immune checkpoint correlation | Immunotherapy [19] [9] |
Experimental Approaches for Investigating SOX9 in Chemoresistance
Single-Cell Multi-Omics for Dissecting SOX9 Functions
Single-cell RNA sequencing (scRNA-seq) enables the identification and characterization of rare SOX9+ subpopulations in tumors. The following workflow outlines key steps:
- Tumor Dissociation: Generate single-cell suspensions from patient-derived xenografts or primary tumors using enzymatic digestion (e.g., collagenase/hyaluronidase) [18].
- Cell Viability Assessment: Ensure >90% viability via trypan blue exclusion before library preparation.
- scRNA-seq Library Preparation: Use 10x Genomics platform for droplet-based partitioning and barcoding. Incorporate cell hashing for sample multiplexing [6] [18].
- Bioinformatic Analysis:
- Quality Control: Filter cells based on unique molecular counts, mitochondrial gene percentage, and doublet detection.
- Clustering and Annotation: Perform dimensionality reduction (PCA, UMAP) and cluster identification. Annotate cell types using canonical markers (e.g., EPCAM for epithelial cells, PTPRC for immune cells) [18].
- SOX9+ Subpopulation Analysis: Extract epithelial cells and use CopyKAT to distinguish malignant from non-malignant cells. Identify SOX9+ clusters and perform differential expression analysis [18].
- Trajectory Inference: Apply pseudotime algorithms (Monocle, PAGA) to reconstruct differentiation trajectories and position SOX9+ cells within hierarchies [6].
This approach revealed that SOX9+ tumor cells are enriched in HNSCC resistant to anti-PD-1/anti-LAG-3 therapy and in HGSOC after platinum chemotherapy [6] [18].
Epigenetic Modulation of SOX9 Expression
CRISPR-based epigenetic editing tools enable precise manipulation of SOX9 expression to establish causal relationships:
- CRISPR Activation (CRISPRa):
- Design sgRNAs targeting the SOX9 promoter or upstream enhancer regions.
- Transduce cells with lentiviral vectors encoding dCas9-VP64 (activator) and MS2-p65-HSF1 (synergistic activator modules).
- Select with puromycin (2 µg/mL) for 72 hours and validate SOX9 upregulation via qRT-PCR and western blot [6].
- Super-Enhancer Mapping:
- Perform H3K27ac ChIP-seq in chemoresistant vs. sensitive cell lines to identify resistant state-specific super-enhancers.
- Validate SOX9 as a super-enhancer target gene through chromatin interaction analysis (Hi-C or ChIA-PET) [6].
- Functional Validation:
- Assess chemoresistance via colony formation assays following SOX9 epigenetic activation.
- Evaluate stemness properties using tumorsphere formation assays and CSC marker expression (CD44, CD133) [6].
In Vivo Modeling of SOX9-Mediated Resistance
Genetically engineered mouse models (GEMMs) and patient-derived xenografts (PDXs) are crucial for validating SOX9 function:
- Therapy Resistance Models:
- Genetic Manipulation in vivo:
- Generate conditional Sox9 knockout mice (Sox9 fl/fl) crossed with tissue-specific Cre drivers (e.g., K14-Cre for epithelial cells).
- Alternatively, transduce PDXs with doxycycline-inducible SOX9 shRNAs via lentiviral injection to achieve temporal control [18].
- Immune Monitoring:
- Analyze tumor-infiltrating lymphocytes and neutrophils by flow cytometry (CD45+CD3+CD8+ for cytotoxic T cells, CD45+Ly6G+ for neutrophils) and immunohistochemistry (cleaved caspase-3 for apoptosis, Ki-67 for proliferation) [18].
Visualization of SOX9 Signaling Networks
SOX9 Stabilization and DNA Damage Repair Pathway
Diagram Title: SOX9 Stabilization in PARPi Resistance
SOX9-Mediated Immune Evasion Mechanism
Diagram Title: SOX9-Driven Immune Evasion Pathway
Therapeutic Strategies for Targeting SOX9-Mediated Resistance
Direct and Indirect SOX9 Targeting Approaches
Several strategic approaches have emerged for countering SOX9-mediated resistance:
- USP28 Inhibition: Small molecule inhibitors like AZ1 disrupt USP28-mediated SOX9 stabilization, promoting its proteasomal degradation. Combining AZ1 with PARPis significantly resensitizes ovarian cancer cells to olaparib in vitro and in vivo [34].
- Epigenetic Modulation: Targeting SOX9-associated super-enhancers with bromodomain inhibitors (e.g., JQ1) downregulates SOX9 expression and reverses the stem-like, chemoresistant phenotype in HGSOC [6].
- Immunotherapy Combinations: Neutralizing the SOX9-Anxa1-Fpr1 axis with Anxa1 blocking antibodies restores neutrophil accumulation and enhances cytotoxic T cell infiltration, overcoming resistance to immune checkpoint blockade in HNSCC [18].
- Transcriptional Inhibition: Developing small molecules that interfere with SOX9 DNA binding or co-factor interactions represents an emerging strategy, though this approach remains in preclinical development.
Table 2: Experimental Models for Studying SOX9-Mediated Resistance
| Experimental Model | Key Applications | Readouts | References |
|---|---|---|---|
| HGSOC Xenografts with Inducible SOX9 | Validate SOX9 sufficiency for chemoresistance | Tumor growth, Platinum sensitivity, CSC marker expression | [6] |
| 4NQO HNSCC Mouse Model | Study SOX9 in immunotherapy resistance | Tumor volume, Immune cell infiltration (CyTOF), Survival | [18] |
| Patient-Derived Organoids | High-throughput drug screening | Viability, Apoptosis, Gene expression profiling | [6] [34] |
| GEMM with Conditional Sox9 Knockout | Establish SOX9 necessity in resistance | Response to therapy, Lineage tracing, Tumor initiation | [18] |
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating SOX9 Function
| Reagent/Cell Line | Specific Type/Model | Research Application | Key Findings Enabled |
|---|---|---|---|
| HGSOC Cell Lines | OVCAR4, Kuramochi, COV362 | In vitro chemoresistance models | SOX9 induction post-platinum treatment [6] |
| PARPi-Resistant Line | SKOV3/Ola | PARPi resistance mechanisms | SOX9 correlation with PARPi resistance [34] |
| SOX9 Antibodies | AB5535 (Sigma) | Western blot, IHC, Co-IP | SOX9 protein expression validation [34] |
| CRISPR Tools | SOX9-targeting sgRNA, dCas9-VP64 | SOX9 knockout and activation | Causal role of SOX9 in resistance [6] |
| Mouse Models | 4NQO-induced HNSCC, Sox9 fl/fl | In vivo therapy response testing | SOX9 role in immunotherapy resistance [18] |
| USP28 Inhibitor | AZ1 | Target validation studies | SOX9 destabilization strategy [34] |
SOX9 represents a central node in the molecular network governing chemoresistance in solid tumors, functioning through integrated mechanisms involving stemness programming, DNA repair enhancement, and immunosuppression. Targeting SOX9 directly or its regulatory axis (e.g., USP28-SOX9) presents a promising therapeutic strategy to overcome resistance to chemotherapy, targeted therapy, and immunotherapy. Future research should focus on developing clinical-grade SOX9 inhibitors, validating SOX9 as a predictive biomarker in clinical trials, and exploring rational combination therapies that simultaneously target SOX9 and its downstream effectors. A comprehensive understanding of SOX9's context-specific functions in different tumor types will be essential for translating these findings into improved patient outcomes.
The tumor immune microenvironment (TIME) is a critical determinant of cancer progression and therapeutic response. A key orchestrator of immunosuppression within the TIME is the transcription factor SOX9. This whitepaper delineates the mechanistic role of SOX9 in driving tumor immune evasion through the direct and indirect regulation of immunosuppressive cells, notably regulatory T cells (Tregs) and M2-polarized macrophages. We synthesize current evidence that positions SOX9 as a pivotal regulator of an immunosuppressive feedback loop, provide structured quantitative data and experimental protocols for its study, and discuss the therapeutic potential of targeting the SOX9 axis to recalibrate the TIME for improved anticancer immunity.
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) is a transcription factor well-known for its roles in embryonic development, chondrogenesis, and stem cell maintenance [3]. Beyond these physiological functions, SOX9 is frequently overexpressed in diverse solid malignancies, including liver, lung, breast, and gastric cancers, where its expression levels positively correlate with tumor occurrence, progression, and poor prognosis [3]. SOX9 contributes to tumorigenesis by regulating key processes such as vascularization, drug resistance, proliferation, metastasis, and apoptosis [3].
Emerging research has unveiled a complex and dual role for SOX9 in immunology, characterizing it as a "double-edged sword" or a "Janus-faced" regulator [3]. In the context of cancer, SOX9 promotes immune escape by impairing the function of antitumor immune cells. Conversely, in certain inflammatory and tissue repair contexts, SOX9 helps maintain macrophage function and contributes to regeneration [3]. This whitepaper focuses on the pro-tumoral facet of SOX9, specifically its capacity to foster an immunosuppressive TIME by modulating Tregs and M2 macrophages, thereby creating a formidable barrier to effective anticancer immunity and immunotherapy.
SOX9: Structure, Regulation, and Immunological Function
Protein Structure and Functional Domains
SOX9 is a 509-amino acid polypeptide member of the SRY-related HMG box protein family. Its functional domains, organized from N- to C-terminus, include [3]:
- Dimerization Domain (DIM): Facilitates protein-protein interactions.
- HMG Box Domain: The defining DNA-binding motif that enables sequence-specific DNA binding and induces DNA bending. This domain also contains nuclear localization (NLS) and export (NES) signals, enabling nucleocytoplasmic shuttling.
- Central Transcriptional Activation Domain (TAM): Works synergistically with other domains to augment transcriptional potential.
- Proline/Glutamine/Alanine (PQA)-rich Domain: Essential for transcriptional activation.
- C-terminal Transcriptional Activation Domain (TAC): Interacts with co-factors (e.g., Tip60) to enhance transcriptional activity and is involved in inhibiting β-catenin signaling during differentiation.
Mechanisms of SOX9 Regulation in Cancer
The expression and activity of SOX9 in cancer are tightly controlled through multiple layers of regulation:
- Transcriptional Regulation: Involves changes in epigenetic alterations such as promoter methylation and histone acetylation [3].
- Post-transcriptional Regulation: Primarily involves non-coding RNAs, including miRNAs and lncRNAs, which can target SOX9 mRNA for degradation or inhibit its translation [3].
- Post-translational Regulation: Protein stability is a key control point. For instance, the E3 ubiquitin ligase FBXW7 targets SOX9 for ubiquitination and degradation. Conversely, the deubiquitinating enzyme USP28 stabilizes SOX9 by removing ubiquitin chains, and elevated USP28 expression contributes to therapy resistance by enhancing SOX9-mediated DNA damage repair in ovarian cancer [34].
SOX9 in Immune Cell Development and Differentiation
SOX9 plays a context-dependent role in immune cell lineage commitment:
- T-cells: SOX9 can cooperate with c-Maf to activate
Rorcand key Tγδ17 effector genes (Il17a,Blk), thereby modulating the balance between αβ and γδ T cell differentiation in the thymus [3]. - B-cells: While not crucial for normal B-cell development, SOX9 acts as an oncogene in Diffuse Large B-cell Lymphoma (DLBCL), promoting proliferation and inhibiting apoptosis [3].
SOX9 as a Master Regulator of Tumor-Promoting Immunosuppression
SOX9 fosters an immunosuppressive TIME through two primary, interconnected mechanisms: shaping immune cell infiltration and directly regulating key immunosuppressive cell populations.
SOX9 and Immune Cell Infiltration
Bioinformatics analyses of large-scale tumor datasets, such as The Cancer Genome Atlas (TCGA), reveal a strong association between SOX9 expression and altered immune cell infiltration. The table below summarizes correlations observed in cancers like colorectal cancer (CRC) [3].
Table 1: Correlation between SOX9 Expression and Immune Cell Infiltration in Cancer
| Immune Cell Type | Correlation with SOX9 | Functional Implication in TIME |
|---|---|---|
| B cells | Negative | Diminished humoral immunity |
| Resting Mast cells | Negative | Loss of potential pro-inflammatory actors |
| Monocytes | Negative | Reduced precursor pool for dendritic cells |
| Plasma cells | Negative | Impaired antibody production |
| CD8+ T cells | Negative (functionally) | Weakened cytotoxic killing of tumor cells [3] |
| NK cells | Negative (functionally) | Reduced innate immune surveillance [3] |
| Neutrophils | Positive | Potential enrichment of pro-tumoral N2 subsets |
| Macrophages | Positive | Enrichment of M2-like Tumor-Associated Macrophages (TAMs) |
| Activated Mast cells | Positive | Potential promotion of angiogenesis and tissue remodeling |
| Naive/Activated CD4+ T cells | Positive | Altered helper T cell responses |
These data indicate that high SOX9 expression is linked to an "immune desert" or functionally excluded TIME, characterized by a depletion of cytotoxic lymphocytes and an enrichment of myeloid cells with immunosuppressive potential [3].
Directing Immunosuppressive Cell Fate and Function
The SOX family, including SOX9, is directly implicated in cancer immune evasion by regulating antigen presentation, shaping the immunosuppressive milieu, and controlling immune checkpoint molecules like PD-L1 [4]. SOX9 contributes significantly to this paradigm.
SOX9 and Regulatory T cells (Tregs)
Tregs are a subset of CD4+ T cells defined by the expression of the transcription factor Foxp3. They are critical for maintaining self-tolerance but in cancer, they suppress antitumor immunity, hindering immunosurveillance and promoting tumor progression [45]. Tregs utilize multiple suppressive mechanisms, including the production of inhibitory cytokines (IL-10, TGF-β, IL-35), consumption of IL-2, and expression of inhibitory receptors like CTLA-4 [46].
Evidence points to a role for SOX9 in promoting a Treg-favorable environment. In prostate cancer, single-cell RNA sequencing has revealed that therapy can enrich a cell subpopulation characterized by high SOX9 and low androgen receptor (AR). This shift in the cellular landscape is associated with an increase in immunosuppressive Tregs and a concomitant decrease in effector immune cells like CD8+ T cells, ultimately creating an "immune desert" microenvironment [3].
SOX9 and M2 Macrophages
Macrophages are plastic cells that can be polarized into different functional phenotypes in response to environmental signals. The classically activated M1-like macrophages are pro-inflammatory and possess antitumor activity, while the alternatively activated M2-like macrophages are anti-inflammatory, promote tissue repair, and contribute to immunosuppression, angiogenesis, and metastasis in cancer [47] [48]. Tumor-associated macrophages (TAMs) often exhibit an M2-like phenotype.
SOX9 expression in the tumor compartment is associated with a shift towards M2 macrophage dominance. Bioinformatic analyses show that SOX9 overexpression negatively correlates with genes associated with M1 macrophage function, while showing a positive correlation with immunosuppressive M2 macrophages [3]. This suggests that SOX9-expressing tumor cells either recruit or educate macrophages towards an M2-like, pro-tumoral state.
The following diagram illustrates the core immunosuppressive network orchestrated by SOX9 in the tumor immune microenvironment.
SOX9-Driven Immunosuppressive Network in Tumors
Experimental Approaches for Investigating the SOX9-Treg-M2 Axis
To empirically dissect the mechanisms outlined above, researchers can employ the following detailed methodologies.
Protocol: Assessing SOX9-Mediated Transcriptional Regulation of DDR Genes
This protocol is adapted from research demonstrating SOX9's role in PARP inhibitor resistance in ovarian cancer [34].
- Objective: To identify and validate direct transcriptional targets of SOX9 involved in DNA damage repair (DDR) and other pathways.
- Materials:
- Ovarian cancer cell lines (e.g., SKOV3, UWB1.289) and their PARPi-resistant derivatives.
- SOX9-specific siRNA or shRNA for knockdown; SOX9 overexpression plasmid.
- Antibodies: Anti-SOX9, Anti-H3K27ac, Normal Rabbit IgG.
- PARP inhibitor (e.g., Olaparib), USP28 inhibitor (AZ1).
- CUT&RUN Assay Kit.
- qPCR reagents and primers for target genes (e.g.,
SMARCA4,UIMC1,SLX4).
- Methodology:
- Cell Treatment: Treat parental and resistant cells with Olaparib ± AZ1 for 24 hours.
- SOX9 Perturbation: Knock down or overexpress SOX9 in your cell model of choice.
- CUT&RUN Assay: a. Harvest ~500,000 cells per condition. b. Permeabilize cells and incubate with anti-SOX9 antibody or IgG control. c. Add pA-MNase enzyme, activate with Ca²⁺ to cleave DNA at antibody-bound sites. d. Extract and purify the released DNA fragments. e. Prepare libraries for next-generation sequencing (CUT&RUN-Seq).
- Data Analysis: Map sequencing reads to the reference genome. Call peaks (SOX9 binding sites) and annotate them to gene promoters. Integrate with H3K27ac ChIP-Seq data to identify active enhancers and super-enhancers associated with SOX9.
- Target Validation: Perform qRT-PCR and Western Blot on candidate target genes (e.g.,
SMARCA4,UIMC1,SLX4) from the CUT&RUN data to confirm SOX9-dependent regulation.
- Expected Outcome: Identification of direct SOX9 target genes in DDR and other pathways, providing a mechanistic link between SOX9 and therapy resistance.
Protocol: Evaluating the Impact of SOX9 on Macrophage Polarization
This protocol uses a conditioned medium approach to study tumor cell-macrophage crosstalk.
- Objective: To determine if SOX9 expression in tumor cells influences the polarization of macrophages towards an M1 or M2 phenotype.
- Materials:
- Tumor cell lines with SOX9 knockdown/overexpression and their respective controls.
- Human monocyte cell line (e.g., THP-1) or primary human monocytes.
- Phorbol 12-myristate 13-acetate (PMA) to differentiate THP-1 into macrophages.
- ELISA kits or Luminex assays for cytokines (IL-10, TGF-β, IL-12, TNF-α).
- Flow cytometry antibodies: CD68 (pan-macrophage), CD86 (M1 marker), CD206 (M2 marker), CD163 (M2 marker).
- Methodology:
- Generate Conditioned Medium (CM): Culture SOX9-modulated and control tumor cells in serum-free medium for 48 hours. Collect the supernatant, centrifuge, and filter-sterilize to obtain CM.
- Differentiate and Polarize Macrophages: Differentiate THP-1 monocytes into M0 macrophages using PMA. Wash the cells and then treat them for 48 hours with:
- Standard M1-polarizing cytokines (IFN-γ + LPS).
- Standard M2-polarizing cytokines (IL-4 + IL-13).
- 50% Tumor Cell CM mixed with 50% fresh culture medium.
- Phenotype Analysis: a. Flow Cytometry: Harvest macrophages and stain for M1 (CD86) and M2 (CD206, CD163) surface markers. Analyze the mean fluorescence intensity (MFI) and percentage of positive cells. b. Cytokine Secretion: Measure the secretion of M1-associated (TNF-α, IL-12) and M2-associated (IL-10, TGF-β) cytokines in the culture supernatant using ELISA.
- Functional Assays: Co-culture polarized macrophages with autologous or allogeneic T cells to assess their capacity to suppress T cell proliferation (e.g., using CFSE dilution assays).
- Expected Outcome: CM from SOX9-high tumor cells should promote a macrophage phenotype with higher M2 marker expression, increased IL-10/TGF-β secretion, and greater T cell suppressive capacity compared to CM from SOX9-low cells.
The Scientist's Toolkit: Key Research Reagents
The following table compiles essential reagents for investigating the SOX9-Treg-M2 macrophage axis, as derived from the cited experimental approaches.
Table 2: Essential Research Reagents for SOX9 and Immunosuppression Studies
| Reagent / Tool | Category | Primary Function in Research | Example Application |
|---|---|---|---|
| SOX9 shRNA/siRNA | Genetic Tool | Knocks down SOX9 expression to study loss-of-function phenotypes. | Determine necessity of SOX9 for Treg recruitment/M2 polarization [3] [34]. |
| SOX9 Expression Plasmid | Genetic Tool | Overexpresses SOX9 to study gain-of-function phenotypes. | Investigate sufficiency of SOX9 in driving immune gene signatures [34]. |
| Anti-SOX9 Antibody | Immunological Tool | Detects SOX9 protein (Western Blot, IHC); used for CUT&RUN/ChIP. | Identify SOX9 expression in tumor tissues; map genomic binding sites [34]. |
| USP28 Inhibitor (AZ1) | Small Molecule Inhibitor | Blocks USP28 activity, promoting SOX9 degradation. | Sensitize tumor cells to PARP inhibitors; reduce SOX9 protein levels [34]. |
| Super-Enhancer Inhibitors (THZ2, JQ1) | Small Molecule Inhibitor | Targets transcriptional machinery at super-enhancers to downregulate SE-driven oncogenes like SOX9. | Reverse chemotherapy resistance in glioblastoma and other cancers [49]. |
| Anti-CD206 (MMR) / Anti-CD163 | Flow Cytometry Antibodies | Identifies M2-like macrophages via surface marker staining. | Phenotype macrophages after co-culture with SOX9-high tumor cells [47] [48]. |
| Anti-Foxp3 Antibody | Flow Cytometry Antibodies | Intracellular staining for definitive identification of Tregs. | Quantify Treg infiltration in SOX9-modulated tumor models [45] [46]. |
| Recombinant IL-4 / IL-13 | Polarizing Cytokines | In vitro polarization of naive macrophages towards an M2 phenotype. | Generate positive control M2 macrophages for functional assays [47] [50]. |
Therapeutic Targeting of the SOX9 Pathway
The strategic inhibition of SOX9 represents a promising avenue to disrupt the immunosuppressive feedback loop in the TIME. Current investigative strategies include:
- Targeting SOX9 Stability: The USP28-SOX9 axis is a druggable vulnerability. Using the USP28-specific inhibitor AZ1 to promote SOX9 degradation has been shown to impair DNA damage repair and re-sensitize ovarian cancer cells to PARP inhibitors [34]. This approach could similarly be tested to reverse SOX9-mediated immunosuppression.
- Targeting Transcriptional Dependencies: SOX9 expression can be driven by super-enhancers in certain cancers. Inhibitors of super-enhancer machinery, such as the CDK7 inhibitor THZ2 and the BRD4 inhibitor JQ1, have demonstrated efficacy in suppressing SOX9 expression and reversing chemoresistance in glioblastoma models [49]. This strategy aims to shut down the oncogenic and immunomodulatory program at its source.
- Combination Immunotherapy: Based on the mechanistic evidence, a rational therapeutic approach would combine SOX9 pathway inhibitors with existing immunotherapies. For example, a USP28 inhibitor (to degrade SOX9) could be paired with an anti-PD-1 antibody. The former would remodel the TIME by reducing Treg and M2 macrophage suppression, while the latter would directly reinvigorate the exposed cytotoxic T cells, potentially leading to synergistic antitumor activity.
The workflow for developing such a combination therapy, from target identification to in vivo validation, is outlined below.
SOX9-Targeted Therapy Development Workflow
SOX9 emerges as a central, master regulatory node in establishing and maintaining an immunosuppressive TIME. Through its ability to alter immune cell infiltration, promote the expansion and function of Tregs and M2 macrophages, and drive therapy resistance, SOX9 creates a formidable barrier to effective anticancer immunity. A deep, mechanistic understanding of the SOX9-Treg-M2 macrophage axis is paramount for advancing immune-oncology. The experimental frameworks and research tools detailed herein provide a roadmap for investigators to further dissect this complex biology. Ultimately, translating these insights into targeted therapies, particularly in rational combination with immunotherapy, holds significant promise for overcoming immunosuppression and improving outcomes for cancer patients.
Strategies to Counteract SOX9's Role in Metastatic Latency and Immune Evasion
SOX9: A Janus-Faced Regulator in the Tumor Immune Microenvironment
The SRY-Box Transcription Factor 9 (SOX9) has emerged as a critical transcriptional regulator with paradoxical functions in cancer progression and metastasis. Within the context of the tumor immune microenvironment (TIME), SOX9 operates as a "double-edged sword," playing key yet opposing roles in different biological contexts [3]. On one hand, it promotes tumor immune evasion and maintains metastatic latency, while on the other, it contributes to tissue regeneration and repair processes [3]. This dual nature makes SOX9 a challenging but promising therapeutic target.
SOX9 is frequently overexpressed in diverse solid malignancies, including colorectal, breast, lung, and prostate cancers, where its expression levels positively correlate with tumor occurrence, progression, and poor prognosis [3] [23] [51]. Structurally, SOX9 contains several functional domains: an N-terminal dimerization domain (DIM), a central High Mobility Group (HMG) box DNA-binding domain, and transcriptional activation domains (TAM and TAC) at the C-terminus [3]. The HMG domain facilitates nuclear localization and DNA binding, while the transactivation domains interact with cofactors to regulate transcriptional activity.
In the broader context of TIME research, SOX9 represents a nodal point connecting cancer stemness, immune modulation, and metastatic progression. Its ability to shape an immunosuppressive microenvironment while maintaining dormant disseminated tumor cells positions SOX9 as a master regulator of the metastatic cascade [52]. Understanding and counteracting SOX9-mediated mechanisms therefore represents a crucial frontier in oncology research and therapeutic development.
Molecular Mechanisms of SOX9 in Metastatic Latency
Orchestrating Cellular Dormancy
The concept of metastatic latency describes the prolonged dormant state wherein disseminated cancer cells survive in secondary organs without proliferating, eventually leading to metastasis after extended periods [52]. SOX9 plays a fundamental role in establishing and maintaining this latent state through multiple interconnected mechanisms:
Stemness Programming: SOX9 confers stem cell-like characteristics to latency-competent cancer (LCC) cells, maintaining their tumor-initiating potential during extended dormant periods [52]. In colorectal cancer models, SOX9 levels are significantly higher in metastatic (SW620) compared to primary (SW480) cells derived from the same patient, with elevated SOX9 expression correlating with enhanced self-renewal capacity and tumorsphere formation [53].
Cell Cycle Regulation: LCC cells exhibit a pronounced propensity to enter quiescence. Experiments with 5-ethynyl-2´-deoxyuridine (EdU) labeling demonstrated that approximately 60% of LCC cells retained EdU after 14 days in mouse models, compared to only 15-25% of parental populations, indicating reduced proliferation [52]. Three months post-inoculation, approximately 90% of LCC cells in distant organs were negative for the proliferation marker Ki-67 [52].
WNT Pathway Inhibition: SOX9-positive LCC cells actively self-impose a slow-cycling state through autocrine production of the WNT inhibitor DKK1 [52]. This creates a self-sustaining regulatory loop where SOX9 expression maintains a stem-like state while simultaneously enforcing quiescence through WNT suppression.
Table 1: Experimental Evidence for SOX9 in Metastatic Latency
| Experimental Model | Key Findings | Molecular Mechanisms | Citation |
|---|---|---|---|
| H2087-LCC1/LCC2 (lung cancer) and HCC1954-LCC1 (breast cancer) cell lines | Isolated latency-competent cells with extended dormant periods in mice; >90% of cells remained as single cells or small clusters for months | SOX2/SOX9-dependent stemness; DKK1-mediated WNT inhibition; slow-cycling state | [52] |
| SW480/SW620 paired cell lines (colorectal cancer) | SOX9 levels higher in metastatic SW620 vs. primary SW480; correlated with self-renewal capacity | Enhanced tumorsphere formation; regulation of BMI1, CD133; phosphorylation at S64, S181 | [53] |
| In vivo mouse models | LCC cells showed rounded morphology after transient capillary spreading; associated with vasculature | Reduced proliferation (Ki-67 negative); maintained tumor-initiating capacity; organ-specific localization | [52] |
Signaling Pathways Governing SOX9-Mediated Dormancy
The maintenance of dormant SOX9-positive cells involves complex signaling interactions with the tissue microenvironment:
Dormancy Signaling Pathways Regulated by SOX9
The balance between ERK and p38 MAPK signaling serves as a critical switch for cellular dormancy, with SOX9 operating within this regulatory framework [44]. Additional microenvironmental factors including TGF-β, BMP-7, and all-trans retinoic acid (atRA) from bone marrow stromal cells further reinforce the dormant state through SOX9-mediated programming [44].
SOX9-Mediated Immune Evasion Mechanisms
Shaping an Immunosuppressive Microenvironment
SOX9 employs multiple strategies to suppress anti-tumor immunity and create a favorable microenvironment for dormant cell survival:
Immune Cell Exclusion and Dysfunction: Bioinformatics analyses of colorectal cancer data reveal that SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, monocytes, plasma cells, and eosinophils [3]. SOX9 overexpression negatively regulates genes associated with CD8+ T cell function, NK cells, and M1 macrophages, while showing positive correlation with immunosuppressive memory CD4+ T cells [3].
Innate Immune Evasion: Through DKK1-mediated WNT inhibition and subsequent slow-cycling state, SOX9-positive LCC cells achieve broad downregulation of ULBP ligands for NK cells, effectively evading NK cell-mediated clearance [52]. This represents a novel mechanism where quiescence itself provides immune protection.
Checkpoint Regulation: SOX9 contributes to the upregulation of immune checkpoint molecules, including PD-L1, in melanoma and other cancers [4]. This creates a direct mechanism for T cell exhaustion within the SOX9-modified tumor microenvironment.
Table 2: SOX9-Mediated Immune Evasion Mechanisms Across Cancer Types
| Immune Mechanism | Effect on TIME | Experimental Evidence | Therapeutic Implications |
|---|---|---|---|
| NK Cell Evasion | Downregulation of NK cell activating ligands | LCC cells show reduced ULBP ligand expression; resistant to NK-mediated killing | Combination strategies to activate NK cells |
| T Cell Dysfunction | Reduced CD8+ T cell infiltration and function | Negative correlation with CD8+ T cell genes; positive correlation with Tregs | Immune checkpoint inhibitors with SOX9 targeting |
| Macrophage Polarization | Promotion of M2-like immunosuppressive phenotypes | Correlation with M2 macrophage signatures; reduced M1-associated genes | Macrophage repolarization strategies |
| Myeloid Recruitment | Increased immunosuppressive myeloid cells | Association with TAMs and MDSCs in tumor models | Targeting chemokine pathways |
Vascular-Mediated Immune Exclusion
Recent research has uncovered SOX9's role in tumor vasculature, contributing to immune exclusion:
SOX9 in Vascular-Mediated Immune Evasion
Endothelial-specific SOX9 deletion in mouse melanoma models resulted in more mature vessels with increased pericyte coverage, reduced hypoxia, and dramatic increases in CD4+ and CD8+ T cell infiltration into tumor centers [17]. This demonstrates SOX9's role in orchestrating vascular-mediated immune exclusion independent of its cancer cell-autonomous functions.
Experimental Models and Research Tools
Key Methodologies for Studying SOX9 Function
Several experimental approaches have been instrumental in characterizing SOX9's role in metastatic latency and immune evasion:
Latency-Competent Cancer (LCC) Cell Isolation: The seminal study by Malladi et al. (2016) established a methodology for isolating LCC cells through in vivo selection in immunocompromised mice [52]. H2087 (stage I lung adenocarcinoma) and HCC1954 (stage IIA HER2+ breast tumor) cells were transduced with GFP-luciferase reporters, intracardially injected into Foxn1nu mice, and dormant cells were recovered from organs of mice that remained metastasis-free for 3 months [52].
Tumorsphere Formation Assays: These assays measure self-renewal capacity as a proxy for stemness. SOX9 overexpression in SW480 colorectal cancer cells generated 4-fold greater primary tumorspheres and 2.5-fold higher secondary tumorsphere formation compared to controls [53].
In Vivo Lineage Tracing: Endothelial-specific Sox9 knockout mice (Sox9fl/fl/Cdh5CreERt2/Rosa-YFP) enabled precise tracking of SOX9 function in tumor vasculature, revealing its critical role in vessel maturation and immune cell recruitment [17].
Phosphorylation Mutant Studies: Investigation of SOX9 post-translational modifications using S64A and S181A phosphorylation site mutants demonstrated the importance of these residues for SOX9's full functional activity in promoting stemness and invasion [53].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Functional Studies
| Reagent/Cell Line | Application | Key Features | Experimental Use |
|---|---|---|---|
| H2087-LCC1/LCC2 | Latency modeling | Derived from stage I lung adenocarcinoma; dormant in vivo | Studying mechanistic basis of metastatic latency |
| SW480/SW620 pair | Metastasis progression | Isogenic primary/metastatic pair from same patient | Comparing SOX9 expression and function across progression |
| Sox9fl/fl/Cdh5CreER mice | Endothelial-specific knockout | Tamoxifen-inducible SOX9 deletion in endothelium | Studying SOX9 role in tumor vasculature and immune exclusion |
| Phospho-mutant SOX9 (S64A, S181A) | Post-translational modification studies | Disrupted phosphorylation sites | Elucidating signaling regulation of SOX9 activity |
| Anti-SOX9 antibodies | Detection and quantification | Specific for SOX9 protein in IHC, IF, WB | Assessing SOX9 expression in tissues and cells |
| DKK1 inhibitors | WNT pathway modulation | Counteract SOX9-mediated WNT suppression | Testing dormancy reversal strategies |
Therapeutic Strategies to Counteract SOX9
Direct and Indirect Targeting Approaches
Several strategic approaches have emerged to counteract SOX9-mediated metastatic latency and immune evasion:
mTOR Inhibition: Rapamycin treatment inhibits SOX9-mediated self-renewal and tumor growth in colorectal cancer models [53]. The inhibition appears to be SOX9-dependent, suggesting particular efficacy against SOX9-driven malignancies.
Epigenetic Modulators: As SOX9 operates within enhancer-mediated transcriptional networks, targeting enhancer dysfunction represents a promising approach [54]. Bromodomain and extra-terminal (BET) inhibitors, histone deacetylase (HDAC) inhibitors, and other epigenetic drugs may disrupt SOX9-mediated transcriptional programs.
SOX9 Degradation Strategies: Targeted protein degradation approaches, including proteolysis-targeting chimeras (PROTACs), offer potential for direct SOX9 elimination [51]. While still in early development, this approach could circumvent the challenges of transcription factor druggability.
Combination Immunotherapy: Based on the mechanism of SOX9-mediated immune exclusion, combining SOX9-targeted approaches with immune checkpoint inhibitors may yield synergistic effects [3] [17]. Preclinical models demonstrate that SOX9 ablation enhances T cell infiltration, potentially creating a more favorable environment for checkpoint inhibitor efficacy.
Preclinical Evidence for Therapeutic Interventions
Therapeutic Targeting of SOX9-Driven Phenotypes
The complex nature of SOX9 signaling necessitates multi-faceted therapeutic approaches. Rapamycin has demonstrated efficacy in preclinical models of colorectal cancer, where it inhibits SOX9-dependent self-renewal and tumor growth [53]. Emerging evidence also supports combination strategies that simultaneously target SOX9 signaling and its downstream immunological consequences.
SOX9 represents a critical nexus point in the regulation of metastatic latency and immune evasion within the tumor microenvironment. Its dual functions in maintaining cancer stemness while shaping an immunosuppressive niche make it a challenging yet promising therapeutic target. Future research directions should focus on several key areas:
First, the development of specific SOX9 inhibitors or degraders remains a paramount goal. While current strategies indirectly target SOX9 function through mTOR inhibition or epigenetic modulation, direct targeting would provide a more precise therapeutic tool. Second, understanding the contextual determinants of SOX9's dual functions may reveal opportunities for selectively inhibiting its pro-tumorigenic while preserving its tissue-regenerative capacities. Finally, biomarker-driven clinical trials are needed to identify patient populations most likely to benefit from SOX9-targeted therapies, particularly those with evidence of SOX9-mediated immune exclusion or dormant disseminated disease.
As technical capabilities in single-cell analysis, spatial transcriptomics, and epigenetic profiling continue to advance, our understanding of SOX9's multifaceted roles in cancer progression will undoubtedly deepen. The integration of SOX9-targeted approaches with established and emerging immunotherapies represents a promising frontier in oncology, with potential to meaningfully impact metastatic disease outcomes.
The SRY-related HMG-box transcription factor 9 (SOX9) represents a critical therapeutic target in oncology, though its targeting presents a significant biological challenge due to its functional duality. As a key regulator of developmental processes, SOX9 plays essential roles in chondrogenesis, neural crest development, and tissue homeostasis, while simultaneously functioning as a potent oncogene in numerous malignancies [3]. This paradox is particularly evident in its immunomodulatory functions, where SOX9 promotes tumor immune escape yet maintains macrophage function for tissue repair and regeneration [3]. The transcription factor achieves this functional diversity through complex regulatory mechanisms, including direct transcriptional activation, partnership with co-factors, and unexpectedly, through direct roles in alternative splicing of hundreds of genes independent of its transcriptional activity [55]. This technical guide examines the molecular basis of SOX9's dual functions within the tumor immune microenvironment and provides a framework for developing therapeutic strategies that selectively inhibit its oncogenic functions while preserving its tissue-reparative roles, with particular emphasis on quantitative dosing parameters and experimental approaches for defining the therapeutic window.
SOX9 Structure-Function Relationships and Regulatory Mechanisms
Functional Domains and Their Roles
SOX9 contains several structurally and functionally distinct domains that mediate its diverse biological activities. Understanding these domains is crucial for designing targeted therapeutic interventions.
Table 1: SOX9 Functional Domains and Their Characteristics
| Domain | Position | Key Functions | Therapeutic Significance |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein-protein interactions | Potential target for disrupting oncogenic complexes |
| HMG Box | Central | DNA binding, nuclear localization, chromatin bending | Core DNA-binding function; difficult to target directly |
| Transcriptional Activation Domain (TAM) | Middle | Synergistic transcriptional activation | Could be disrupted to modulate specific gene programs |
| Transcriptional Activation Domain (TAC) | C-terminal | Interacts with co-factors (e.g., Tip60), inhibits β-catenin | Domain-specific targeting may separate pathological vs. physiological functions |
| PQA-rich Domain | C-terminal | Transcriptional activation | Functional significance still being elucidated |
The HMG domain serves dual roles: it directs nuclear localization via embedded nuclear localization and export signals, enabling nucleocytoplasmic shuttling, and facilitates DNA binding through minor groove interactions [3]. The C-terminal transcriptional activation domain (TAC) interacts with diverse cofactors, such as Tip60, to enhance SOX9's transcriptional activity and is essential for β-catenin inhibition during chondrocyte differentiation [3]. The central transcriptional activation domain (TAM) functions synergistically with TAC to augment SOX9's transcriptional potential [3].
Multi-Level Regulatory Mechanisms
SOX9 exhibits complex regulation across transcriptional, post-transcriptional, and post-translational levels:
Transcriptional Regulation: SOX9 expression is controlled by epigenetic modifications including promoter methylation and histone acetylation [3]. These modifications create cell-type-specific expression patterns that could be exploited for selective targeting.
Post-transcriptional Regulation: SOX9 is modulated by various non-coding RNAs, including miRNAs (e.g., miR-215-5p in breast cancer) and long non-coding RNAs (e.g., linc02095) that create feedback loops to fine-tune SOX9 expression levels [10].
Novel Splicing Function: Beyond its transcriptional roles, SOX9 regulates alternative splicing of hundreds of genes without affecting their expression levels [55]. This splicing function is uncoupled from its transcriptional activity through specific mutants and occurs through SOX9's association with RNA-binding proteins, particularly the exon junction complex component Y14 [55]. This moonlighting function significantly expands SOX9's regulatory potential and represents a previously overlooked aspect of its biology with therapeutic implications.
SOX9 in the Tumor Immune Microenvironment: Mechanisms and Therapeutic Implications
SOX9-Mediated Immunosuppressive Networks
SOX9 orchestrates a profoundly immunosuppressive microenvironment through multiple interconnected mechanisms that facilitate immune escape across various cancer types.
Table 2: SOX9-Mediated Effects on Immune Cell Populations in the Tumor Microenvironment
| Immune Cell Type | Effect of SOX9 | Functional Consequences | Documented In |
|---|---|---|---|
| CD8+ T cells | Negative correlation with functional genes | Impaired cytotoxic T cell activity | Colorectal Cancer [3] |
| NK cells | Negative correlation with functional genes | Reduced innate immune surveillance | Colorectal Cancer [3] |
| M1 Macrophages | Negative correlation | Diminished anti-tumor immunity | Colorectal Cancer [3] |
| Tregs | Positive correlation | Enhanced immunosuppression | Prostate Cancer [3] |
| M2 Macrophages (TAMs) | Positive correlation | Increased pro-tumor polarization | Prostate Cancer [3] |
| Neutrophils | Shift to immunosuppressive anergic phenotype | Creation of "immune desert" microenvironment | Prostate Cancer [3] |
The immunomodulatory functions of SOX9 extend beyond mere correlation to direct causal relationships. In breast cancer, SOX9 and SOX2 collaboratively maintain cancer stem cell populations in a dormant, immunoevasive state, enabling long-term survival and metastatic potential [10]. Similarly, in prostate cancer, androgen deprivation therapy enriches a subpopulation of club cells characterized by high SOX9 and low androgen receptor expression, indirectly weakening anti-tumor immunity and contributing to an "immune desert" phenotype [3]. These findings position SOX9 as a master regulator of the immunosuppressive niche.
SOX9 in Tissue Repair and Regeneration
Paradoxically, while SOX9 drives immune evasion in tumors, it simultaneously plays critical roles in physiological tissue repair and regeneration. This duality presents the central challenge for therapeutic targeting. In tissue repair contexts, SOX9 contributes to macrophage functional maintenance, cartilage formation, and overall tissue regeneration [3]. During the regenerative cascade, SOX9 responds to damage-associated molecular patterns (DAMPs) released from injured tissues, which activate pattern recognition receptors and downstream NF-κB signaling [56]. This signaling initiates a repair program involving stem cell recruitment, proliferation, and differentiation – processes in which SOX9 is intimately involved [56]. The transcription factor is particularly important in chondrogenesis and extracellular matrix remodeling, essential components of tissue repair across multiple organ systems.
Quantitative Dosage Sensitivity: Defining the Therapeutic Window
Experimental Approaches for Measuring SOX9 Dosage Effects
Precise modulation of transcription factor levels is essential for understanding dosage-sensitive phenomena. The degradation tag (dTAG) system represents a cutting-edge methodology for titrating SOX9 levels in physiologically relevant models:
dTAG System Protocol for SOX9 Dosage Titration:
- Cell Line Engineering: Introduce FKBP12-F36V–mNeonGreen–V5 tag at the SOX9 carboxy terminus in human embryonic stem cells (hESCs) using selection-free genome editing [14].
- Differentiation: Differentiate SOX9-tagged hESCs into cranial neural crest cells (CNCCs) using established protocols that yield molecularly homogeneous populations [14].
- Dosage Titration: Treat SOX9-tagged CNCCs with a dTAGV-1 dilution series (typically spanning 0.5-500 nM) for 24-48 hours to achieve distinct, reproducible SOX9 concentrations [14].
- Validation: Quantify SOX9 levels via single-cell fluorescence measurements confirming unimodal distribution shifts correlating with dTAGV-1 concentration [14].
- Phenotypic Assessment: Apply ATAC-seq, RNA-seq, and functional chondrogenesis assays across the dosage spectrum to identify sensitive versus buffered responses [14].
This approach enables researchers to model the effects of SOX9 reduction at trait-relevant ranges, mirroring the dosage alterations observed in human genetic variation and haploinsufficiency disorders.
Dosage Sensitivity Landscapes
Quantitative studies reveal that most SOX9-dependent regulatory elements exhibit buffered responses to small dosage reductions, while a subset shows heightened sensitivity:
Key Findings on SOX9 Dosage Sensitivity:
- Regulatory elements directly and primarily regulated by SOX9 demonstrate heightened sensitivity to dosage changes [14].
- Sensitive elements and genes preferentially affect functional chondrogenesis and are associated with craniofacial shape variation [14].
- Nonlinear dosage-to-phenotype relationships predominate, with specific phenotypes showing differential sensitivity [14].
- Even 10-13% reduction in Sox9 mRNA levels produces reproducible morphological changes in murine models, indicating exquisite sensitivity of certain developmental programs [14].
These findings suggest that therapeutic strategies must account for tissue-specific and process-specific dosage sensitivities, as global SOX9 inhibition would likely disrupt both sensitive pathological processes and essential physiological functions.
Experimental Framework for Evaluating SOX9-Targeted Therapies
Research Reagent Solutions for SOX9 Investigation
Table 3: Essential Research Reagents for SOX9 Functional Studies
| Reagent/Category | Specific Examples | Function/Application | Experimental Context |
|---|---|---|---|
| SOX9 Modulation Systems | dTAG-SOX9 (FKBP12-F36V–mNeonGreen–V5) | Precise protein level titration | Dosage-response studies [14] |
| SOX9 Mutants | DelDIM, K68E, R94H, W143R, MiniSOX9 | Uncoupled transcriptional and splicing functions | Mechanistic studies [55] |
| Splicing Assay Tools | ZDHHC16 minigene | Monitoring alternative splicing patterns | Splicing function analysis [55] |
| RNA-Binding Protein Antibodies | Anti-Y14, anti-p54nrb/NONO, anti-PSF, anti-SAM68 | Protein-protein interaction studies | Splicing complex analysis [55] |
| Proximity Ligation Assay | Duolink green kit | Detecting protein associations <40nm apart | Protein complex validation [55] |
Key Methodological Approaches
Proximity Ligation Assay (PLA) for SOX9-Protein Interactions:
- Fix cells with 4% paraformaldehyde for 10 minutes, then permeabilize with PBS/Triton 1% [55].
- Block with PBS/BSA 5% for 45 minutes at room temperature [55].
- Incubate with primary antibodies against SOX9 and potential partners for 1 hour [55].
- Use species-specific secondary antibodies conjugated to PLA probes, followed by ligation and amplification steps [55].
- Mount with ProLong Gold antifade medium with Hoechst and analyze fluorescence via wide-field microscopy [55].
Alternative Splicing Analysis Pipeline:
- Perform SOX9 knockdown via siRNA (50 nM, 72 hours) or titrated degradation in DLD-1 or HEK293T cells [55].
- Extract total RNA using RNeasy Plus Mini Kit with DNase treatment [55].
- Convert 1-2 μg RNA to cDNA using SuperScript III reverse transcriptase (50°C for 1 hour) [55].
- Perform PCR or quantitative RT-PCR with primers designed to flank alternative exons [55].
- Analyze splicing changes via gel electrophoresis or sequencing approaches [55].
Strategic Pathways for Therapeutic Development
Conceptual Framework for Selective SOX9 Modulation
The following diagram illustrates the core strategic approach for optimizing SOX9 therapeutic windows:
Targeting SOX9-Associated Splicing Machinery
The discovery of SOX9's splicing regulation function opens alternative therapeutic avenues. Rather than direct SOX9 inhibition, targeting its interactions with splicing components may provide greater selectivity:
Key Splicing-Related Targets:
- Y14 (EJC component): Critical mediator of SOX9-dependent splicing regulation; approximately half of SOX9 splicing targets require Y14 [55].
- p54nrb/NONO: Previously identified SOX9 partner in tissue-specific splicing regulation [55].
- SAM68: RNA-binding protein that associates with SOX9 in splicing complexes [55].
Therapeutic disruption of these specific protein-protein interactions could potentially uncouple SOX9's pathological splicing programs from its essential transcriptional functions, creating a more favorable therapeutic index.
The path to clinically viable SOX9-targeted therapies requires sophisticated approaches that acknowledge the transcription factor's functional complexity and dosage sensitivity. Successful strategies will likely involve context-dependent inhibition, domain-specific targeting, careful dosage titration, and combination approaches that leverage synthetic lethal interactions. The emerging understanding of SOX9's splicing functions provides additional avenues for selective intervention. As techniques for precise TF modulation continue to advance, the therapeutic window for SOX9 inhibition will become increasingly defined, offering promise for targeting this master regulator across multiple cancer types while preserving its essential tissue-repair functions.
Clinical and Pan-Cancer Validation of SOX9's Role in the TIME
The SRY-box transcription factor 9 (SOX9) is a pivotal nuclear transcription factor with a highly conserved high-mobility group (HMG) box domain that recognizes specific DNA sequences and regulates gene expression [9]. Initially recognized for its crucial roles in embryonic development, chondrogenesis, and sex determination, SOX9 has emerged as a significant player in oncogenesis [3] [11]. This whitepaper synthesizes evidence from a comprehensive pan-cancer analysis of SOX9 expression patterns and their intricate relationships with tumor immune microenvironments, providing a technical resource for researchers and therapeutic developers.
SOX9 exemplifies a "JANUS-faced" regulator in cancer biology, operating with context-dependent duality—functioning as both an oncogene and tumor suppressor across different malignancies [3]. Beyond its cell-autonomous functions in proliferation and metastasis, SOX9 has emerged as a potent modulator of the tumor immune landscape, influencing immune cell infiltration, checkpoint expression, and ultimately, response to immunotherapy [3] [13]. This analysis delineates the pan-cancer expression profile of SOX9, deciphers its immune correlates, and presents standardized methodological frameworks for investigating SOX9 in cancer immunology.
SOX9 Overexpression Patterns Across Cancers
Comprehensive analysis of transcriptomic data from The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) databases reveals that SOX9 expression is significantly dysregulated across numerous cancer types [11]. The expression pattern demonstrates striking cancer-type specificity, with predominant overexpression in the majority of malignancies.
Table 1: SOX9 Expression Patterns Across Selected Cancers
| Cancer Type | SOX9 Expression Pattern | Prognostic Association |
|---|---|---|
| Glioblastoma (GBM) | Significantly upregulated [9] [11] [19] | Better prognosis in lymphoid invasion subgroups [9] [19] |
| Low-Grade Glioma (LGG) | Significantly upregulated [11] | Shorter overall survival [11] |
| Colorectal Cancer (COAD/READ) | Significantly upregulated [11] | Not specified in search results |
| Lung Squamous Cell Carcinoma (LUSC) | Significantly upregulated [11] | Not specified in search results |
| Liver Hepatocellular Carcinoma (LIHC) | Significantly upregulated [11] | Not specified in search results |
| Pancreatic Adenocarcinoma (PAAD) | Significantly upregulated [11] | Not specified in search results |
| Stomach Adenocarcinoma (STAD) | Significantly upregulated [11] | Not specified in search results |
| Cervical Cancer (CESC) | Significantly upregulated [11] | Shorter overall survival [11] |
| Thymoma (THYM) | Significantly upregulated [11] | Shorter overall survival [11] |
| Skin Cutaneous Melanoma (SKCM) | Significantly downregulated [11] | Tumor suppressor role [11] |
| Testicular Germ Cell Tumors (TGCT) | Significantly downregulated [11] | Not specified in search results |
Analysis of 33 cancer types demonstrated that SOX9 expression was significantly increased in 15 cancers (including GBM, COAD, LUSC, LIHC, PAAD, and STAD) while being significantly decreased in only two cancers (SKCM and TGCT) compared with matched healthy tissues [11]. This establishes SOX9 as a proto-oncogene in most cancer types. The prognostic significance of SOX9 expression also varies by cancer type, with high expression correlating with shorter overall survival in LGG, CESC, and THYM, but surprisingly with better prognosis in specific GBM subgroups characterized by lymphoid invasion [9] [11] [19].
SOX9 as a Regulator of Tumor Immune Microenvironment
Correlations with Immune Cell Infiltration
SOX9 expression demonstrates consistent and cancer-type-specific correlations with immune cell infiltration patterns, profoundly influencing the cellular composition of the tumor immune microenvironment.
Table 2: SOX9 Correlation with Immune Cell Infiltration Across Cancers
| Cancer Type | Positive Correlation with Immune Infiltration | Negative Correlation with Immune Infiltration |
|---|---|---|
| Colorectal Cancer | Neutrophils, macrophages, activated mast cells, naive/activated T cells [3] | B cells, resting mast cells, resting T cells, monocytes, plasma cells, eosinophils [3] |
| Multiple Cancers (general pattern) | Immunosuppressive cells: Tregs, M2 macrophages [3] | Cytotoxic cells: CD8+ T cell function, NK cells, M1 macrophages [3] |
| Breast Cancer | Dedifferentiated tumor cells, immune evasion [13] | Tumor-infiltrating lymphocytes, immune surveillance [13] |
In the colorectal cancer tumor microenvironment, SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, but positively correlates with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. Similarly, in multiple cancer types, SOX9 overexpression negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing a positive correlation with memory CD4+ T cells [3]. These patterns suggest that SOX9 contributes to an immunosuppressive microenvironment that may facilitate immune escape.
Regulation of Immune Checkpoints
SOX9 expression is closely correlated with immune checkpoint expression in various cancers. In glioblastoma, correlation analysis indicated SOX9 expression was correlated with expression of immune checkpoints, indicating its involvement in the immunosuppressive tumor microenvironment [9] [19]. A SOX9-B7x (B7-H4/VTCN1) axis has been identified that safeguards dedifferentiated tumor cells from immune surveillance to drive breast cancer progression [13]. This mechanism represents a direct link between SOX9-mediated cancer cell dedifferentiation and immune evasion through checkpoint regulation.
In lung adenocarcinoma, SOX9 suppresses the tumor microenvironment and is mutually exclusive with various tumor immune checkpoints [9] [19]. Additionally, in thymoma, SOX9 expression was negatively correlated with target genes related to PD-L1 expression and T-cell receptor signaling pathways, suggesting that SOX9 may be associated with immune dysregulation [11].
Molecular Mechanisms and Signaling Pathways
SOX9 regulates tumor immune evasion through multiple interconnected mechanisms. In breast cancer, SOX9 and long non-coding RNA linc02095 create positive feedback that encourages cell growth and tumor progression by regulating each other's expression [10]. SOX9 directly interacts with and activates the polycomb group protein Bmi1 promoter, whose overexpression suppresses the activity of the tumor suppressor InK4a/Arf loci [10].
The transcriptional and post-transcriptional regulation of SOX9 activity involves two primary categories. Transcriptional regulation includes changes in epigenetic alterations like methylation and acetylation, while post-transcriptional regulation primarily involves biological activities mediated by miRNA and lncRNA [3]. For instance, in colorectal cancer, the immune-related lnc-SOX9-4 promotes cancer progression via suppression of YBX1 poly-ubiquitination and degradation [57].
SOX9 Immune Regulation Network: This diagram illustrates the multifaceted role of SOX9 in regulating immune checkpoints, modulating immune cell populations, and activating molecular pathways that contribute to tumor immune evasion.
Experimental Protocols and Methodologies
Comprehensive SOX9 Expression Analysis
Data Acquisition and Preprocessing:
- Data Sources: Obtain RNA-seq data from TCGA (https://portal.gdc.cancer.gov/) and GTEx (https://gtexportal.org/) databases. For protein-level validation, utilize the Human Protein Atlas (HPA) (https://www.proteinatlas.org/) [9] [19].
- Data Formats: Download HTSeq-FPKM and HTSeq-Count data of cancer samples from TCGA repository for uniform processing [9] [19].
- Normalization: Apply appropriate normalization methods to account for technical variability between datasets (e.g., TPM, FPKM) [11].
Differential Expression Analysis:
- Software Implementation: Use DESeq2 R package to compare expression data between tumor and normal tissues, or between SOX9 high- and low-expression groups (typically using a cut-off value of 50%) to identify differentially expressed genes (DEGs) [9] [19].
- Visualization: Employ R package ggplot2 (version 3.3.6) to generate volcano plots of the results, with thresholds set at |log fold change (logFC)| >2 and adjusted P-value (adj P-value) <0.05 [9] [19].
Functional Enrichment Analysis:
- Pathway Analysis: Implement Gene Ontology (GO) functional analysis and Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway analysis using the ClusterProfiler package in R [9] [19].
- Gene Set Enrichment Analysis (GSEA): Use ClusterProfiler (version 3.14.3) for GSEA to elucidate functional and pathway differences between SOX9 high- and low-expression groups. Perform 1,000 permutations for each analysis, with adjusted P-value <0.05 and FDR q-value <0.25 considered statistically significant [9] [19].
SOX9 Analysis Workflow: This diagram outlines the comprehensive experimental workflow for analyzing SOX9 expression patterns and immune correlations, from data acquisition through immune infiltration analysis.
Immune Infiltration and Checkpoint Analysis
Immune Cell Infiltration Quantification:
- Methodology: Use the ssGSEA package and ESTIMATE package in the GSVA package (version 1.34.0) for immuno-infiltration correlation analysis of SOX9 [9] [19].
- Statistical Testing: Evaluate the statistical significance of differences by Spearman's test. Use Wilcoxon rank sum test to analyze the correlation between SOX9 expression and immune checkpoint expression [9] [19].
Protein-Protein Interaction (PPI) Network Construction:
- Network Prediction: Predict PPI networks of DEGs using the STRING database with an interaction score threshold of 0.4 as the cut-off criterion [9] [19].
- Visualization and Analysis: Map PPI networks using Cytoscape (version 3.7.1) and identify significant modules using MCODE (version 1.6.1) with selection criteria: MCODE scores >5, degree cut-off = 2, node score cut-off = 0.2, Max depth = 100, and k-score = 2 [9] [19].
In Vitro Validation Experiments
Cell Culture and Treatment:
- Cell Lines: Utilize relevant cancer cell lines (e.g., prostate cancer cells PC3 and 22RV1, lung cancer cell H1975) cultured in appropriate media (RPMI 1640 or DMEM) with 10-15% fetal bovine serum at 37°C with 5% CO₂ [11].
- Compound Treatment: For SOX9 inhibition studies, use compounds such as Cordycepin (CD), an adenosine analog, at concentrations of 0, 10, 20, and 40 µM for 24 hours [11].
Molecular Analysis:
- Western Blotting: Lyse cells in EBC buffer and 2×SDS loading buffer, separate proteins by electrophoresis, transfer to PVDF membrane, and detect SOX9 using specific antibodies [11].
- RNA Analysis: Extract total RNA and perform reverse transcription followed by quantitative PCR to measure SOX9 mRNA expression [11].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Bioinformatics Tools | TCGA Portal, GTEx Portal, HPA, GEPIA2, cBioPortal, LinkedOmics, Metascape | Data acquisition, expression analysis, and functional enrichment [9] [11] [19] |
| Statistical Software | R packages: DESeq2, ggplot2, ClusterProfiler, GSVA, ssGSEA, ESTIMATE | Differential expression, visualization, pathway analysis, immune infiltration quantification [9] [19] |
| Network Analysis | STRING database, Cytoscape, MCODE | PPI network construction and module identification [9] [19] |
| Experimental Compounds | Cordycepin (CD) | Small molecule inhibitor of SOX9 expression; used at 0-40 µM concentrations [11] |
| Cell Lines | 22RV1, PC3 (prostate cancer), H1975 (lung cancer) | In vitro models for SOX9 functional validation and therapeutic testing [11] |
| Molecular Biology | Western blot reagents, qRT-PCR reagents, specific antibodies | Protein and mRNA expression analysis of SOX9 and downstream targets [11] |
Therapeutic Implications and Future Directions
The strategic targeting of SOX9 presents promising therapeutic opportunities for cancer treatment. Cordycepin (CD), an adenosine analog, has demonstrated dose-dependent inhibition of both SOX9 protein and mRNA expressions in 22RV1, PC3, and H1975 cancer cells, indicating its anticancer roles likely operate via SOX9 inhibition [11]. The development of more specific SOX9 inhibitors represents an emerging frontier in oncology drug discovery.
The strong association between SOX9 and immune checkpoint expression, particularly the SOX9-B7x axis, suggests that SOX9 inhibition could synergize with existing immunotherapies [13]. By reversing SOX9-mediated immunosuppression, combination therapies may overcome resistance mechanisms and expand the population of patients benefiting from immune checkpoint blockade.
Furthermore, the prognostic significance of SOX9 expression in multiple cancers positions it as a potential biomarker for patient stratification and treatment selection [9] [11]. The integration of SOX9 expression data with mutational status (e.g., IDH-mutant in glioma) and immune profiles may enable more precise prognostic models and personalized therapeutic approaches [9] [19]. Future research should focus on developing clinically viable SOX9-targeting strategies and validating SOX9 as a companion diagnostic in prospective clinical trials.
Correlation of SOX9 Expression with Immune Checkpoint Molecules (e.g., PD-L1)
The transcription factor SOX9 is increasingly recognized as a pivotal regulator of the tumor immune microenvironment. This whitepaper synthesizes current evidence establishing that SOX9 expression is significantly correlated with the regulation of key immune checkpoint molecules and the formation of an immunosuppressive tumor microenvironment. Through direct and indirect mechanisms, SOX9 influences the expression of PD-1/PD-L1, modulates immune cell infiltration, and contributes to resistance against checkpoint immunotherapy across various cancer types. Understanding these correlations is crucial for developing novel therapeutic strategies to overcome immune resistance in SOX9-high malignancies.
The SOX9 (SRY-related HMG-box 9) transcription factor, known for its role in embryonic development and cell fate determination, has emerged as a critical oncoprotein in numerous cancers. Recent research has illuminated its complex functions within the tumor immune microenvironment (TIME), particularly its correlation with immune checkpoint molecules that regulate anti-tumor immunity [19] [3]. Immune checkpoints like PD-1/PD-L1 are crucial pathways that tumors co-opt to evade immune destruction, and checkpoint inhibitors have revolutionized cancer treatment. However, response rates vary significantly, driving the search for biomarkers and resistance mechanisms. SOX9 represents a key node in this landscape, functioning as a "double-edged sword" with context-dependent roles that either promote or suppress immune activity [3]. This technical review examines the molecular basis of SOX9's correlation with immune checkpoints, its impact on immunotherapy efficacy, and provides detailed methodologies for investigating these relationships.
Molecular Mechanisms of SOX9-Mediated Immune Checkpoint Regulation
SOX9 regulates immune checkpoint expression through multiple interconnected molecular pathways. Its function is highly context-dependent, varying across different cancer types.
Direct Transcriptional Networks and Indirect Pathways
In thymic epithelial tumors (TETs), bioinformatics analyses of patient data from The Cancer Genome Atlas (TCGA) revealed that high SOX9 expression is negatively associated with genes in the PD-1 checkpoint pathway [58]. This suggests that SOX9 may function as a negative regulator of this critical immune evasion system in certain malignancies. The correlation was identified through differential gene expression analysis, where genes negatively associated with SOX9 were mapped to the PD-1 checkpoint pathway in cancer using KEGG pathway enrichment.
In contrast, a 2025 study on head and neck squamous cell carcinoma (HNSCC) identified a distinct SOX9-mediated resistance pathway. Single-cell RNA sequencing of tumors resistant to anti-LAG-3 plus anti-PD-1 therapy revealed significant enrichment of SOX9+ tumor cells. The study mechanistically demonstrated that SOX9 directly regulates the expression of annexin A1 (AnxA1). This SOX9-AnxA1 axis subsequently mediates apoptosis of Fpr1+ neutrophils through mitochondrial dysfunction, preventing neutrophil accumulation and ultimately impairing the infiltration and cytotoxic capacity of CD8+ T and γδT cells within the tumor microenvironment [18].
In melanoma, SOX9 exhibits a contrasting relationship with the immune checkpoint CEACAM1. Knockdown of endogenous SOX9 results in CEACAM1 up-regulation at both mRNA and protein levels, while its overexpression has the opposite effect. Luciferase reporter assays determined that SOX9 controls CEACAM1 expression at the transcriptional level, but indirectly. Further investigation localized the SOX9-controlled region to the proximal 200bp of the CEACAM1 promoter and identified Sp1 and ETS1 as the primary transcription factors mediating this effect. Co-immunoprecipitation confirmed a physical interaction between SOX9 and Sp1 in melanoma cells, while SOX9 knockdown downregulated ETS1 [12]. This SOX9-CEACAM1 axis functionally renders melanoma cells resistant to T-cell-mediated killing [12].
Pan-Cancer Patterns of SOX9 Expression and Immune Correlation
A comprehensive pan-cancer analysis of SOX9 expression across 33 cancer types revealed that SOX9 is significantly upregulated in 15 cancers (including GBM, LIHC, LUSC, PAAD, and THYM) compared to matched healthy tissues [11]. This analysis, utilizing data from TCGA and GTEx, established SOX9 as a frequently overexpressed oncogene. Furthermore, this study and others have consistently found that SOX9 expression correlates with immune cell infiltration patterns. The correlation is often characterized by reduced infiltration of cytotoxic immune cells such as CD8+ T cells and NK cells, and an increase in immunosuppressive cell populations like M2 macrophages [3] [58] [11].
Table 1: Correlation of SOX9 with Immune Checkpoints and Infiltration Across Cancers
| Cancer Type | Correlated Immune Checkpoints | Correlated Immune Cells | Prognostic Value |
|---|---|---|---|
| Glioblastoma (GBM) | Correlated with immune checkpoint expression [19] [9] | Associated with immune cell infiltration and immunosuppressive microenvironment [19] [59] | Better prognosis in lymphoid invasion subgroups; independent prognostic factor in IDH-mutant cases [19] [9] |
| Lung Adenocarcinoma (LUAD) | Mutually exclusive with various immune checkpoints [19] [60] | Suppresses CD8+ T, NK, and dendritic cell infiltration [60] [61] | Contributes to poor survival; creates "immune cold" tumors [60] [61] |
| Thymic Epithelial Tumors (TETs) | Negative association with PD-1 checkpoint pathway genes [58] | M2 macrophage dominance in high SOX9 group [58] | High expression indicates unfavorable clinical outcome [58] |
| Head and Neck SCC (HNSCC) | Mediates resistance to anti-PD-1 + anti-LAG-3 therapy [18] | Reduces Fpr1+ neutrophils, impairing CD8+ T and γδT cell infiltration [18] | Enriched in therapy-resistant tumors [18] |
| Melanoma (SKCM) | Indirect negative regulation of CEACAM1 [12] | SOX9 knockdown increases T-cell resistance [12] | Acts as a tumor suppressor; low SOX9 promotes immune resistance [11] [12] |
SOX9 as a Determinant of Immunotherapy Response
The correlation between SOX9 and immune checkpoints extends functionally to influencing response to immunotherapy. In KRAS-driven lung adenocarcinoma, SOX9 overexpression creates an "immune cold" tumor microenvironment, characterized by reduced immune cell infiltration. This effect explains why some patients with this mutation respond poorly to immunotherapy. Animal model studies demonstrated that Sox9 knockout significantly delayed tumor formation and improved survival, with the tumor-promoting effect of SOX9 being significantly attenuated in immunocompromised mice compared to syngeneic mice, highlighting its immune-dependent mechanism [60] [61].
In the HNSCC mouse model, SOX9+ tumor cells were significantly enriched in tumors resistant to combination therapy with anti-LAG-3 and anti-PD-1 antibodies. This resistance was mediated through the SOX9-AnxA1-Fpr1 axis, which prevented the accumulation of neutrophils that are crucial for supporting cytotoxic T-cell function. This mechanism comprehensively explains how SOX9-expressing tumor cells can drive resistance to combination immune checkpoint blockade [18].
Table 2: Experimental Models Demonstrating SOX9 in Therapy Resistance
| Experimental System | Treatment | Key Findings | Molecular Mechanism |
|---|---|---|---|
| KrasG12D-driven LUAD Mouse Model [60] | Not specified | Sox9 loss reduced tumor burden and prolonged survival. Effect was attenuated in immunodeficient mice. | SOX9 suppresses infiltration and activity of CD8+ T, NK, and dendritic cells. Increases collagen fibers and tumor stiffness. |
| 4NQO-induced HNSCC Mouse Model [18] | Anti-LAG-3 + Anti-PD-1 | 42.9% of animals were resistant. Resistant tumors showed significant enrichment of Sox9+ tumor cells. | SOX9 transcriptionally upregulates AnxA1, inducing apoptosis of Fpr1+ neutrophils via mitochondrial fission, reducing cytotoxic T-cell infiltration. |
| Melanoma Cell Cultures (e.g., 526mel, 624mel) [12] | T-cell mediated killing in co-culture | SOX9 knockdown rendered melanoma cells more resistant to T-cell killing. | SOX9 knockdown indirectly upregulates CEACAM1 expression, a known mediator of T-cell inhibition. |
Essential Research Protocols for Investigating SOX9-Immune Checkpoint Axis
For researchers aiming to validate and explore the SOX9-immune checkpoint relationship, the following methodologies, derived from the cited literature, provide a robust experimental framework.
Bioinformatics Interrogation of SOX9 Correlations
Purpose: To identify correlations between SOX9 expression, immune checkpoint genes, and immune cell infiltration in human cancer datasets [19] [58] [11].
Workflow:
- Data Acquisition: Download RNA-seq data (HTSeq-Counts or FPKM) for your cancer of interest from public repositories like TCGA (https://portal.gdc.cancer.gov/) and normal tissue data from GTEx (https://gtexportal.org/).
- Differential Expression Analysis: Using R and the
DESeq2orlimmapackages, compare gene expression profiles between tumors with high and low SOX9 expression (dichotomized by median expression). Genes with \|log2(fold-change)\| > 2 and adjusted p-value < 0.05 are considered significant DEGs. - Functional Enrichment Analysis: Perform GO and KEGG pathway analysis on the DEGs using the
clusterProfilerR package. This will reveal if immune checkpoint pathways (e.g., "PD-1 checkpoint pathway in cancer") are enriched. - Immune Infiltration Estimation: Utilize the
GSVAR package withssGSEAor theESTIMATEalgorithm to quantify the abundance of various immune cell types (e.g., CD8+ T cells, neutrophils, M2 macrophages) from the tumor transcriptome data. - Correlation Analysis: Conduct Spearman's correlation tests between the SOX9 expression vector and the expression vectors of key immune checkpoint genes (e.g., PD-L1, LAG-3, CEACAM1) and the estimated immune cell infiltration scores.
Functional Validation of SOX9 in Immune Regulation
Purpose: To mechanistically validate the role of SOX9 in regulating immune checkpoints and modulating T-cell cytotoxicity [18] [12].
Workflow:
- SOX9 Modulation: Knock down or overexpress SOX9 in relevant cancer cell lines using CRISPR/Cas9, siRNA, or plasmid transfection.
- Checkpoint Expression Analysis:
- qPCR: Quantify mRNA levels of SOX9 and target immune checkpoints (e.g., ANXA1, CEACAM1).
- Western Blot / Flow Cytometry: Validate changes at the protein level.
- Promoter Reporter Assays: To test for direct transcriptional regulation, clone the promoter region of the target immune checkpoint gene (e.g., a ~1900bp region upstream of the ANXA1 or CEACAM1 ATG start codon) into a luciferase reporter vector. Co-transfect with SOX9 expression vector or control and measure luciferase activity.
- Co-culture T-cell Killing Assay:
- Co-culture SOX9-modulated cancer cells with activated peripheral blood mononuclear cells (PBMCs) or tumor-infiltrating lymphocytes (TILs).
- Measure cancer cell cytotoxicity using assays like real-time cell analysis, lactate dehydrogenase (LDH) release, or flow cytometry-based apoptosis staining (Annexin V/propidium iodide).
Visualizing Key Molecular Pathways
The following diagram illustrates the core signaling pathway by which SOX9 promotes an immunosuppressive microenvironment and confers resistance to combination immunotherapy, as identified in HNSCC [18].
Diagram Title: SOX9-ANXA1-FPR1 Axis in Immunotherapy Resistance
The Scientist's Toolkit: Key Research Reagents
The following table compiles essential reagents and resources for experimental investigation of SOX9 and immune checkpoints, as cited in the literature.
Table 3: Essential Research Reagents for SOX9-Immune Checkpoint Studies
| Reagent / Resource | Specifications & Function | Example Application |
|---|---|---|
| Anti-SOX9 Antibody | Polyclonal rabbit anti-SOX9 (e.g., AB5535; Sigma-Aldrich), dilution 1:100 for IHC. Used to detect nuclear SOX9 expression in formalin-fixed paraffin-embedded (FFPE) tissues [58]. | Immunohistochemical staining and scoring of patient tumor samples. |
| SOX9 Modulating Constructs | siRNA for knockdown; pCMV or pCDH vectors with full-length SOX9 cDNA for overexpression. Essential for gain/loss-of-function studies in cell lines [12]. | Mechanistic validation of SOX9's role in regulating checkpoint molecule expression. |
| Luciferase Reporter Vectors | Vectors containing cloned promoter sequences of immune checkpoint genes (e.g., ~1900bp CEACAM1 or ANXA1 promoter). Measures transcriptional activity and regulation [12]. | Determining if SOX9 directly or indirectly regulates a target gene's promoter. |
| Cordycepin (CD) | An adenosine analog (small molecule). Inhibits SOX9 mRNA and protein expression in a dose-dependent manner (e.g., 10-40 µM for 24h) in cancer cell lines [11]. | Exploring SOX9 as a druggable target; testing phenotypic effects of SOX9 inhibition. |
| Flow Cytometry Antibodies | Fluorochrome-conjugated antibodies against CEACAM1, PD-L1, ANXA1, Fpr1, and immune cell markers (CD45, CD3, CD8, CD56, etc.). | Quantifying protein expression on cell surfaces and profiling immune cell populations. |
| In Vivo Immunotherapy Models | C57BL/6 wild-type and transgenic mice (e.g., 4NQO-induced HNSCC model; KrasG12D-driven LUAD model). Treated with anti-PD-1, anti-LAG-3, or combination antibodies [60] [18]. | Studying SOX9's role in therapy resistance and tumor-immune system interactions in vivo. |
The evidence conclusively demonstrates a significant correlation between SOX9 expression and the regulation of immune checkpoint molecules across multiple cancer types. SOX9 operates through diverse mechanisms—including direct transcriptional control, intermediary proteins like ANXA1, and the regulation of co-factors like Sp1/ETS1—to foster an immunosuppressive microenvironment and drive resistance to immune checkpoint blockade therapy. Given that SOX9 itself is a transcription factor and is notoriously difficult to target directly with small molecules, future therapeutic strategies should focus on targeting its downstream effectors, such as the ANXA1-FPR1 axis, or identifying synergistic drug combinations that can reverse the SOX9-mediated immunosuppressive program. Integrating SOX9 expression and its associated gene signatures as biomarkers in clinical trials holds immediate promise for stratifying patients most likely to benefit from specific immunotherapy regimens.
The SOX9 (SRY-related HMG-box 9) transcription factor, a member of the SOXE subgroup of SOX proteins, is increasingly recognized as a pivotal regulator in both embryonic development and cancer biology. While its roles in chondrogenesis and male gonad determination are well-established, recent evidence has illuminated its significance in tumorigenesis across diverse cancer types [62]. SOX9 maintains stem and progenitor cells in tissues with high turnover and is crucial for postnatal injury repair [62]. In cancer, SOX9 frequently exhibits deregulated expression, influencing critical oncogenic processes including cancer stem-like cell (CSC) maintenance, epithelial-mesenchymal transition (EMT), metastasis, and therapy resistance [62] [63]. This review provides a comprehensive analysis of SOX9's context-dependent functions across glioblastoma (GBM), breast cancer, melanoma, and other malignancies, with particular emphasis on its emerging role in shaping the tumor immune microenvironment.
Clinical and Prognostic Significance of SOX9 Across Cancers
SOX9 expression demonstrates remarkable tissue-specific patterns with significant prognostic implications across different malignancies. The table below summarizes its clinical relevance in various cancer types.
Table 1: Clinical and Prognostic Significance of SOX9 in Human Cancers
| Cancer Type | Expression Status | Clinical/Prognostic Correlation | References |
|---|---|---|---|
| Hepatocellular Carcinoma | Overexpression | Poor prognosis, poor disease-free survival, poor overall survival | [62] |
| Breast Cancer | Overexpression | Promotes proliferation, tumorigenesis, metastasis; poor overall survival | [62] [10] |
| Glioblastoma (GBM) | Overexpression | Better prognosis in lymphoid invasion subgroups; independent prognostic factor for IDH-mutant cases | [19] |
| Prostate Cancer | Overexpression | Promotes cell proliferation, apoptosis resistance; high clinical stage; poor relapse-free and overall survival | [62] |
| Prostate Cancer | Downregulation | Promotes metastasis; advanced clinical stage; associated with ERG-positive tumors | [62] |
| Oral Squamous Cell Carcinoma | High SOX9 with low SOX2 | Worse overall survival; independent prognosticator | [64] |
| Melanoma | Dose-dependent | Low: anti-metastatic; High: pro-metastatic | [65] |
| Pancreatic Cancer | Overexpression | Promotes chemoresistance; prognostic marker | [62] [63] |
| Ovarian Cancer | Overexpression with HIF-2α | Induces TUBB3 expression; poor overall survival | [62] |
| Colorectal Cancer | Overexpression | Promotes cell proliferation, senescence inhibition, chemoresistance | [62] |
Analysis of The Cancer Genome Atlas (TCGA) data reveals that SOX9 alterations occur in approximately 1.2% of cancer samples (572 of 46,601 unique samples), with missense substitutions being the most frequent mutation type (38.81%) [62]. Copy number variations gain was reported in 108 unique samples and overexpression was present in 509 samples [62]. The context-dependent nature of SOX9 is particularly evident in cancers like prostate cancer and melanoma, where it can exhibit seemingly contradictory functions based on cellular context and expression levels [62] [65].
Molecular Mechanisms of SOX9 in Cancer Pathogenesis
Regulation of Cancer Stemness and Cell Proliferation
SOX9 plays a fundamental role in maintaining cancer stem-like cells (CSCs), a subpopulation responsible for tumor initiation, metastasis, and therapy resistance. In breast cancer, SOX9 is a key determinant of ER-negative luminal stem/progenitor cells and drives basal-like breast cancer development [10]. SOX9 maintains stemness by interacting with polycomb group protein Bmi1, whose overexpression suppresses tumor suppressor Ink4a/Arf sites [10]. Furthermore, SOX9 collaborates with Slug (SNAI2) to promote breast cancer cell proliferation and metastasis [10]. The regulation between SOX9 and long non-coding RNAs creates positive feedback loops that reinforce stemness properties, as demonstrated by the SOX9-linc02095 axis in breast cancer [10].
Interaction with Key Signaling Pathways
SOX9 intersects with multiple oncogenic signaling pathways in a context-dependent manner:
- Wnt/β-catenin pathway: SOX9 exhibits complex bidirectional regulation within this pathway. In hepatocellular carcinoma, SOX9 activates canonical Wnt/β-catenin signaling through Frizzled-7, endowing stemness features [62]. In breast cancer, SOX9 directly regulates Low Density Lipoprotein Receptor-related Protein 6 (LRP6) and T-cell Factor 4 (TCF4) expression, thereby modulating Wnt/β-catenin activation [66].
- TGF-β pathway: SOX9 is both regulated by and contributes to TGF-β signaling. In pancreatic cancer, SOX9 participates in TGF-β-mediated EMT and metastasis [63].
- Other pathways: SOX9 also interacts with Sonic Hedgehog (SHH), Notch, MAPK/ERK, and NF-κB pathways, creating a complex regulatory network that influences cancer progression [63].
Figure 1: SOX9 in Cancer Signaling Networks
Dose-Dependent Metastatic Fate Determination
The functional outcome of SOX9 expression is critically dependent on its expression levels, particularly evident in melanoma. SOX9 exhibits a dose-dependent effect on metastatic behavior [65]. At moderate expression levels, SOX9 demonstrates anti-metastatic properties, reducing melanoma growth and migratory capacity partly through elevated expression of cyclin-dependent kinase inhibitor p21 [65]. Conversely, high SOX9 expression levels, comparable to those detected in malignant melanoma specimens, promote metastatic progression by modulating matrix metalloproteinases and regulating mesenchymal migration through NEDD9-mediated focal adhesion dynamics and Rho GTPase signaling [65]. This dose-dependent duality reconciles previous contradictory findings regarding SOX9's role in melanoma progression.
SOX9 in the Tumor Immune Microenvironment
Regulation of Immune Evasion and Dormancy
SOX9 contributes significantly to cancer immune evasion, a crucial mechanism enabling tumor progression. SOX9 helps tumor cells maintain a stem-like state and evade innate immunity by remaining dormant for extended periods [4]. Research has demonstrated that latent cancer cells with high SOX9 expression can persist in secondary metastatic sites while avoiding immune surveillance under immunotolerant conditions [10]. This immune evasion capability positions SOX9 as a key facilitator of metastatic dormancy and subsequent recurrence.
Modulation of Immune Cell Infiltration and Checkpoints
In glioblastoma, SOX9 expression correlates significantly with immune cell infiltration and checkpoint expression [19]. High SOX9 expression is associated with an immunosuppressive tumor microenvironment, characterized by altered infiltration of various immune cells and regulation of immune checkpoint molecules [19]. Similar patterns are observed in other malignancies, where SOX9 contributes to the establishment of an immune-suppressive niche that facilitates tumor progression and resistance to immunotherapy.
Figure 2: SOX9-Mediated Immunosuppressive Mechanisms
Experimental Approaches for SOX9 Functional Analysis
Key Methodologies for Investigating SOX9 in Cancer
Research on SOX9 employs diverse experimental approaches to elucidate its functions in different cancer contexts:
Gene Expression Manipulation: Lentiviral transduction systems for SOX9 overexpression and shRNA-mediated knockdown are widely utilized. Specific SOX10 shRNA (5'-GACTTCGGCAACGTGGACATT-3') and SOX9 targeting approaches have been effectively employed in melanoma models [65]. For pancreatic cancer studies, transient transfection with SOX9-specific siRNA results in approximately 20-fold suppression of SOX9 protein expression [63].
Functional Assays: Standardized assays include AlamarBlue for cell proliferation, transwell invasion assays, colony formation assays, and tail vein injection models for metastasis assessment [65]. Live cell imaging monitors dynamics of melanoma migratory behavior, while RHOA and RAC1 activation assays measure Rho GTPase activity [65].
Transcriptomic Analysis: Full-transcriptome RNA sequencing following SOX9 knockdown reveals pathway alterations. Molecular pathway enrichment analysis using Gene Ontology, Reactome, and GSEA identifies processes regulated by SOX9 [63].
Clinical Correlation Studies: Immunohistochemistry on tissue microarrays with semi-automatic digital pathology scoring determines protein expression patterns across patient cohorts [64]. Correlation with clinical parameters and survival analysis establishes prognostic significance.
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagents for SOX9 Investigation
| Reagent/Cell Line | Application | Function/Relevance | Sources |
|---|---|---|---|
| Anti-SOX9 (3C10) monoclonal antibody | Immunohistochemistry, Western blot | SOX9 protein detection in formalin-fixed tissues | [64] |
| A375M, UACC-457, UACC-827, UACC-903 melanoma cells | In vitro melanoma studies | Panel of melanoma cell lines for functional studies | [65] |
| PANC-1, COLO357 pancreatic cells | Pancreatic cancer research | Primary and metastatic pancreatic cancer models | [63] |
| Lentiviral pWPI-SOX9 vector | SOX9 overexpression | Ectopic SOX9 expression in target cells | [65] |
| pLKO.1-shSOX10 construct | SOX10 knockdown | Investigate SOX9/SOX10 functional relationships | [65] |
| Tissue Microarrays (TMAs) | High-throughput tissue analysis | Simultaneous analysis of multiple patient samples | [64] |
Therapeutic Implications and Future Directions
The pivotal role of SOX9 in cancer stemness, metastasis, and immune evasion positions it as an attractive therapeutic target. Several strategic approaches emerge from current research:
Direct SOX9 Targeting: Development of small molecule inhibitors disrupting SOX9 DNA binding or protein-protein interactions represents a promising avenue. The structural characterization of SOX9's HMG and dimerization domains provides a foundation for rational drug design.
Pathway-Specific Interventions: Given SOX9's integration into multiple signaling networks, targeting SOX9-regulated pathways such as Wnt/β-catenin or TGF-β might provide indirect means of modulating SOX9 activity.
Immunotherapy Combinations: Since SOX9 contributes to immune evasion, combining SOX9-targeted approaches with immune checkpoint inhibitors may yield synergistic effects, particularly in immunologically "cold" tumors.
Context-Dependent Therapeutic Strategies: The dose-dependent and cancer-type-specific functions of SOX9 necessitate precise patient stratification and careful consideration of therapeutic contexts.
Future research should focus on elucidating the precise structural basis of SOX9's function, developing clinically viable targeting strategies, and understanding the dynamics of SOX9 expression and function throughout tumor evolution and therapeutic intervention.
SOX9 emerges as a multifaceted regulator in cancer biology, demonstrating context-dependent roles across different malignancies. Its involvement in cancer stemness, metastatic progression, therapy resistance, and immune modulation underscores its significance as a biomarker and therapeutic target. The complex, dose-dependent functions of SOX9, particularly its ability to shape the tumor immune microenvironment, highlight the need for sophisticated targeting approaches. As research continues to unravel the molecular intricacies of SOX9 function, the translation of these insights into clinical applications holds promise for improving outcomes across multiple cancer types.
The transcription factor SOX9 has emerged as a critical player in oncogenesis and tumor progression. Recent evidence solidifies its role not merely as a companion biomarker but as an independent prognostic factor across multiple cancer types. This whitepaper synthesizes clinical validation data from glioblastoma, gastric cancer, head and neck squamous cell carcinoma, and cervical cancer, establishing SOX9's significant association with overall survival, tumor invasion, therapy resistance, and key clinical parameters. Furthermore, we delineate SOX9's function within the tumor immune microenvironment, revealing its Janus-faced immunomodulatory capabilities that both suppress anti-tumor immunity and promote immune evasion, thereby positioning SOX9 as a compelling therapeutic target in oncology.
SOX9 (SRY-box transcription factor 9) belongs to the SOX family of transcription factors characterized by a highly conserved high-mobility group (HMG) DNA-binding domain. This nuclear transcription factor plays crucial roles in embryonic development, chondrogenesis, and stem cell maintenance. In recent years, SOX9 has been identified as a significant contributor to tumor pathogenesis across diverse cancer types. The protein contains several functional domains: a dimerization domain (DIM), the HMG box domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain, with the HMG and transcriptional activation domains primarily responsible for its core functions [3].
Beyond its established roles in tumor proliferation and metastasis, SOX9 operates as a pivotal regulator within the tumor immune microenvironment. It exhibits context-dependent dual functions—acting as both an activator and repressor across diverse immune cell types— thereby modulating numerous biological processes [3]. SOX9 expression correlates significantly with immune cell infiltration patterns and contributes to immunosuppression through various mechanisms, including regulation of immune checkpoint expression and interaction with infiltrating immune cells [19] [3]. This whitepaper consolidates clinical evidence validating SOX9 as an independent prognostic factor while exploring its multifaceted functions within the tumor immune landscape.
Clinical Validation of SOX9 as an Independent Prognostic Factor
Comprehensive clinical studies across multiple cancer types have validated SOX9 as an independent prognostic factor, with its expression significantly correlating with key clinicopathological parameters and survival outcomes.
Table 1: SOX9 as a Prognostic Indicator Across Cancers
| Cancer Type | Prognostic Significance | Key Clinical Correlations | Statistical Evidence |
|---|---|---|---|
| Glioblastoma (GBM) | Better prognosis in lymphoid invasion subgroups; Independent prognostic factor for IDH-mutant cases | Associated with immune infiltration and checkpoint expression | P < 0.05 in 478 cases [19] |
| Gastric Cancer | Shorter overall survival | Depth of invasion (OR=0.348), TNM stage (OR=0.428) | 1-year OS (OR=1.507, p=0.002); 3-year OS (OR=1.482, p=0.000); 5-year OS (OR=1.487, p=0.001) [67] |
| Cervical Cancer | Poor overall survival | PLOD3-mediated oncogenesis via IL-6/JAK/STAT3 pathway | p = 0.033 [7] |
| Head and Neck Squamous Cell Carcinoma | Resistance to anti-LAG-3 + anti-PD-1 therapy | Mediates immunosuppression via ANXA1-FPR1 axis on neutrophils | 42.9% of animals resistant to combination therapy [18] |
Multivariate Cox regression analyses from these studies confirm that SOX9 maintains independent prognostic value even when controlling for conventional clinicopathological parameters. In glioblastoma, high SOX9 expression emerged as an independent prognostic factor specifically in IDH-mutant cases [19]. The gastric cancer meta-analysis, encompassing 3,060 patients across 11 studies, demonstrated that SOX9 expression was significantly associated with both depth of invasion and advanced TNM stage, further strengthening its prognostic utility [67].
SOX9 in the Tumor Immune Microenvironment
Immunomodulatory Functions of SOX9
SOX9 plays a complex, dual role in immunomodulation, acting as a "double-edged sword" in the tumor immune microenvironment [3]. On one hand, it promotes immune escape by impairing immune cell function, making it a potential therapeutic target in cancer. On the other hand, increased SOX9 levels help maintain macrophage function, contributing to tissue regeneration and repair [3].
In the context of breast cancer, SOX9 plays a crucial role in immune evasion. Studies have revealed that SOX9, in conjunction with SOX2, helps maintain latent cancer cells in a dormant state at secondary metastatic sites while enabling them to avoid immune surveillance under immunotolerant conditions [10]. Additionally, a SOX9-B7x (VTCN1) axis has been identified in breast cancer, which safeguards dedifferentiated tumor cells from immune surveillance to drive cancer progression [13].
SOX9 and Immune Cell Infiltration
The relationship between SOX9 expression and immune cell infiltration patterns has been characterized through comprehensive bioinformatics analyses and experimental validation:
Table 2: SOX9 Correlation with Immune Cell Infiltration
| Immune Cell Type | Correlation with SOX9 | Functional Consequence |
|---|---|---|
| CD8+ T cells | Negative correlation | Reduced cytotoxic function [3] |
| NK cells | Negative correlation | Impaired tumor cell killing [3] |
| M1 Macrophages | Negative correlation | Diminished anti-tumor response [3] |
| Neutrophils | Positive correlation via ANXA1-FPR1 axis | Promoted mitochondrial fission, inhibited mitophagy, prevented accumulation [18] |
| B cells, resting mast cells, resting T cells | Negative correlation | Reduced anti-tumor immunity [3] |
| Memory CD4+ T cells | Positive correlation | Potential role in immune regulation [3] |
In head and neck squamous cell carcinoma, SOX9 mediates resistance to combination immunotherapy (anti-LAG-3 plus anti-PD-1) through a sophisticated mechanism involving tumor-neutrophil interactions. SOX9 directly regulates the expression of annexin A1 (ANXA1), which mediates apoptosis of formyl peptide receptor 1 (FPR1)+ neutrophils through the ANXA1-FPR1 axis. This interaction promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (BNIP3) expression, ultimately preventing neutrophil accumulation in tumor tissues. The reduction of FPR1+ neutrophils impairs the infiltration and tumor cell-killing ability of cytotoxic CD8+ T and γδT cells within the tumor microenvironment, thereby driving resistance to combination therapy [18].
SOX9 and Immune Checkpoints
In glioblastoma, SOX9 expression closely correlates with the expression of immune checkpoints, indicating its involvement in the immunosuppressive tumor microenvironment [19]. This relationship positions SOX9 as a potential regulator of immune exhaustion pathways and suggests its targeting might synergize with existing immune checkpoint inhibitors.
SOX9-Mediated Immunosuppression Pathway: This diagram illustrates the molecular mechanism by which SOX9 expression induces resistance to combination immunotherapy (anti-LAG-3 + anti-PD-1) in head and neck squamous cell carcinoma, primarily through neutrophil-mediated effects on cytotoxic T cells [18].
Experimental Protocols for SOX9 Prognostic Validation
Bioinformatic Analysis of SOX9 Expression and Prognostic Significance
Purpose: To validate SOX9 as an independent prognostic factor using publicly available cancer genomics datasets.
Materials and Reagents:
- RNA-seq data from TCGA (e.g., GBM, STAD, CESC projects)
- Normal tissue RNA-seq data from GTEx database
- Clinical follow-up data for survival analysis
- R statistical environment with specialized packages
Methodology:
- Data Acquisition: Download HTSeq-FPKM and HTSeq-Count data for relevant cancer types from TCGA data portal. Obtain matched normal tissue data from GTEx.
- Differential Expression Analysis: Utilize DESeq2 R package to compare SOX9 expression between tumor and normal tissues, applying threshold of |logFC| >2 and adjusted p-value <0.05.
- Survival Analysis: Implement Kaplan-Meier analysis with log-rank test to compare overall survival between high and low SOX9 expression groups.
- Multivariate Cox Regression: Assess independent prognostic value of SOX9 while controlling for clinicopathological variables including age, stage, and molecular subtypes.
- Immune Correlation Analysis: Use ssGSEA and ESTIMATE packages to analyze correlation between SOX9 expression and immune cell infiltration scores.
Validation: For gastric cancer, a meta-analysis approach combining 11 studies with 3,060 patients demonstrated significant correlation between SOX9 expression and depth of invasion (OR=0.348, 95% CI=0.247-0.489, p=0.000) and TNM stage (OR=0.428, 95% CI=0.308-0.595, p=0.000) [67].
Functional Validation of SOX9 in Therapy Resistance
Purpose: To experimentally validate SOX9's role in mediating resistance to combination immunotherapy.
Materials and Reagents:
- C57BL/6 wild-type mice
- 4-nitroquinoline 1-oxide (4NQO) for HNSCC induction
- Anti-PD-1 and anti-LAG-3 antibodies
- Single-cell RNA sequencing platform
- Transgenic mouse models for validation
Methodology:
- HNSCC Mouse Model: Administer 4NQO in drinking water for 16 weeks followed by normal water for 8 weeks to induce HNSCC.
- Treatment Groups: Randomize mice with similar tumor sizes into four groups: control IgG, anti-PD-1 monotherapy, anti-LAG-3 monotherapy, and anti-LAG-3 plus anti-PD-1 combination therapy.
- Resistance Assessment: Monitor tumor size every 4 days; classify tumors growing >20% from original size after 14 days as resistant per RECIST criteria.
- scRNA-seq Analysis: Pool tumor tissues from three mice per group, digest into single-cell suspensions, and perform scRNA-seq.
- Mechanistic Validation: Utilize various transgenic mouse models to confirm SOX9-ANXA1-FPR1 axis in mediating neutrophil apoptosis and subsequent T-cell dysfunction.
Key Findings: This approach identified that 42.9% of animals (6 out of 14) were resistant to combination therapy, with significant enrichment of SOX9+ tumor cells in resistant samples [18].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Research Reagents for SOX9 Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Bioinformatic Tools | TCGA/GTEx datasets, DESeq2 R package, ESTIMATE algorithm, LinkedOmics | Analysis of SOX9 expression, prognostic significance, and immune correlations [19] |
| Experimental Models | 4NQO-induced HNSCC mouse model, Transgenic mice (Sox9 conditional knockout) | Functional validation of SOX9 in therapy resistance and immune modulation [18] |
| Therapeutic Antibodies | Anti-PD-1, Anti-LAG-3 | Assessing SOX9 role in immunotherapy resistance [18] |
| Molecular Biology Reagents | scRNA-seq platform, Western blot reagents, IHC antibodies | Detection of SOX9 expression and downstream targets at protein level [19] [67] |
The cumulative evidence from multiple cancer types firmly establishes SOX9 as an independent prognostic factor with significant clinical relevance. Its dual role in direct tumor promotion and modulation of the immune microenvironment positions SOX9 as a promising therapeutic target. The mechanistic insights into SOX9-mediated therapy resistance, particularly through the newly identified SOX9-ANXA1-FPR1 axis in HNSCC, provide novel opportunities for combination therapies that could overcome current limitations of immunotherapy.
Future clinical validation efforts should focus on standardizing SOX9 assessment methods, defining optimal cutoff values for clinical stratification, and developing targeted approaches to disrupt SOX9-mediated immunosuppression. The integration of SOX9 status into clinical decision-making could potentially identify patient subgroups that might benefit from specific therapeutic strategies, ultimately advancing the field toward more personalized cancer management.
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical, albeit complex, regulator within the tumor immune microenvironment (TIME). Functioning as a "double-edged sword" in immunology, SOX9 demonstrates context-dependent roles that significantly influence cancer progression and therapeutic response [3]. On one hand, it can promote immune escape by impairing immune cell function; on the other, it contributes to maintaining macrophage function and tissue repair mechanisms [3]. Its frequent overexpression in diverse solid malignancies, including glioma, colorectal, breast, ovarian, and gastric cancers, is strongly correlated with tumor occurrence, progression, and particularly, the development of therapy resistance [3] [6] [9]. This dualistic nature, coupled with its significant association with immune cell infiltration patterns, positions SOX9 as a powerful biomarker for prognostic modeling. The integration of SOX9 expression data into multivariable statistical models, specifically nomograms, provides a promising approach for refining outcome prediction in oncology. These integrative models translate complex molecular and immunological data into practical, quantitative tools for stratifying patient risk and predicting therapeutic efficacy, thereby addressing a critical need in the era of personalized cancer therapy.
SOX9 in Oncogenesis and The Tumor Immune Microenvironment
Molecular Structure and Key Functional Domains
SOX9 is a 509-amino acid polypeptide member of the SOX family, characterized by several functionally critical domains. The High Mobility Group (HMG) box domain is responsible for DNA binding and contains embedded nuclear localization (NLS) and export (NES) signals, facilitating nucleocytoplasmic shuttling [3]. Flanking this are the N-terminal dimerization domain (DIM), two transcriptional activation domains—a central TAM and a C-terminal TAC—and a proline/glutamine/alanine (PQA)-rich domain essential for full transcriptional activity. The TAC domain is particularly crucial as it interacts with cofactors like Tip60 and inhibits β-catenin during chondrocyte differentiation, hinting at its broader regulatory potential in cancer signaling pathways [3].
Mechanisms of SOX9 in Tumor Immune Regulation
SOX9 influences the TIME through multiple interconnected mechanisms, primarily by modulating immune cell infiltration and function. Extensive bioinformatics analyses across cancers reveal that SOX9 expression exhibits distinct correlations with various immune cell populations. Key findings include:
- A strong negative correlation with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils [3].
- A significant positive correlation with neutrophils, macrophages, and activated mast cells [3].
- In specific contexts, SOX9 overexpression negatively correlates with genes associated with the anti-tumor functions of CD8+ T cells, NK cells, and M1 macrophages, while showing a positive correlation with memory CD4+ T cells [3].
In prostate cancer, single-cell RNA sequencing has revealed that SOX9 contributes to an "immune desert" microenvironment, characterized by a decrease in effector immune cells (e.g., CD8+CXCR6+ T cells) and an increase in immunosuppressive cells (e.g., Tregs, M2 macrophages) [3]. Furthermore, SOX9 plays a vital role in immune evasion by sustaining the stemness of latent cancer cells, enabling their long-term survival and capacity to avoid immune surveillance in metastatic sites [10]. Beyond direct immune modulation, SOX9 is a key driver of epigenetic reprogramming that induces a stem-like transcriptional state, contributing significantly to chemoresistance in cancers like high-grade serous ovarian cancer (HGSOC) [6].
Table 1: Correlation of SOX9 Expression with Immune Cell Infiltration in Solid Tumors
| Immune Cell Type | Correlation with SOX9 | Biological and Clinical Implications |
|---|---|---|
| CD8+ T cells | Negative | Impairment of cytotoxic anti-tumor response, immune escape |
| M1 Macrophages | Negative | Reduction in anti-tumor immune signaling |
| Neutrophils | Positive | Association with pro-tumorigenic, immunosuppressive environments |
| M2 Macrophages | Positive | Promotion of tumor growth, tissue remodeling, and immunosuppression |
| Memory CD4+ T cells | Positive | Context-dependent role requiring further functional validation |
| B cells | Negative | Attenuation of humoral anti-tumor immunity |
A Technical Framework for SOX9-Based Prognostic Nomograms
Core Principles of Nomogram Development
A nomogram is a graphical calculating device that transforms complex statistical regression models into a simple, user-friendly interface for individual probability estimation. Constructing a robust SOX9-based nomogram involves a multi-step process that integrates molecular data, clinical variables, and survival outcomes. The core principle is to create a multivariable Cox regression model where SOX9 expression (often dichotomized into high/low based on an optimal cut-off value) is included alongside other significant prognostic factors. Each variable is assigned a point contribution on a scale, and the sum of these points corresponds to a probability of a specific clinical outcome, such as overall survival (OS) or progression-free survival (PFS), at a given time point.
A Case Study in Glioblastoma (GBM)
A 2025 study provides a validated blueprint for building a SOX9-integrated nomogram in GBM [9] [19]. The researchers utilized RNA sequencing data from public repositories like The Cancer Genome Atlas (TCGA) and the Genotype-Tissue Expression (GTEx) database to analyze SOX9 expression and identify differentially expressed genes (DEGs) [9] [19]. The subsequent model building followed a rigorous statistical workflow:
- Variable Selection via LASSO Regression: To prevent overfitting and select the most potent predictors from a high-dimensional dataset, the Least Absolute Shrinkage and Selection Operator (LASSO) method was applied. This technique shrinks the coefficients of less important variables to zero, effectively performing variable selection. In the GBM study, this process screened out four non-zero coefficient genes that satisfied the lambda.min criterion [9].
- Multivariable Cox Regression Analysis: The selected variables, including SOX9 expression, were then subjected to multivariable Cox regression to identify independent prognostic factors. The analysis confirmed that high SOX9 expression, along with OR4K2 and IDH mutation status, were significant independent prognostic factors [9].
- Nomogram Construction and Validation: The final nomogram incorporated SOX9, OR4K2, and IDH status to individualize the prediction of OS [9]. The model's discrimination was evaluated using the Concordance Index (C-index), and its predictive accuracy was further assessed and compared against individual factors using Receiver Operating Characteristic (ROC) curve analysis. Calibration plots were used to graphically compare nomogram-predicted probabilities against observed outcomes [9].
Table 2: Essential Statistical and Computational Tools for Nomogram Development
| Tool/Method | Function in Nomogram Development | Application Example |
|---|---|---|
| LASSO Regression | Penalized regression technique for variable selection in high-dimensional data. | Screening for non-zero coefficient genes (e.g., OR4K2) from a pool of differentially expressed genes to include in the model [9]. |
| Multivariable Cox Model | Models the relationship between multiple predictor variables and survival time. | Determining the independent prognostic weight of SOX9, OR4K2, and IDH status in GBM [9]. |
| Concordance Index (C-index) | Measures the model's discrimination power; the probability that a randomly selected patient who had an event sooner had a higher risk score. | Used to determine the discrimination of the GBM nomogram (bootstrap resampling for validation) [9]. |
| ROC Analysis | Evaluates the diagnostic/prognostic accuracy of a model by plotting sensitivity vs. 1-specificity. | Comparing the predictive accuracy of the nomogram against separate prognostic factors [9]. |
| Kaplan-Meier Analysis | Non-parametric statistic used to estimate the survival function from lifetime data. | Initially establishing the association between high SOX9 expression and better prognosis in specific GBM subgroups (e.g., lymphoid invasion) [9]. |
Diagram 1: A generalized workflow for developing and validating a SOX9-based prognostic nomogram, integrating transcriptomic and clinical data.
Experimental Protocols for Validating SOX9 Function
In Vitro Functional Validation of SOX9 in Chemoresistance
Understanding the mechanistic role of SOX9 is crucial for justifying its inclusion in prognostic models. The following protocol, derived from a study on ovarian cancer, outlines key steps for validating SOX9's role in chemoresistance [6]:
Objective: To determine the necessity and sufficiency of SOX9 in conferring platinum resistance in High-Grade Serous Ovarian Cancer (HGSOC) cell lines.
Materials:
- Cell Lines: HGSOC lines (e.g., OVCAR4, Kuramochi, COV362).
- Reagents: Carboplatin, CRISPR/Cas9 system with SOX9-targeting sgRNA, lentiviral vectors for SOX9 overexpression, antibodies for Western blot (anti-SOX9, anti-β-Actin), cell viability assay kits (e.g., MTT, CellTiter-Glo), colony formation assay reagents.
Methodology:
- Chemotherapy Induction: Treat HGSOC cell lines with a clinically relevant dose of carboplatin (e.g., IC50 concentration) for 72 hours. Analyze SOX9 expression at both RNA (qRT-PCR) and protein (Western blot) levels to confirm acute induction [6].
- Genetic Knockout (Necessity Test):
- Use CRISPR/Cas9 with a SOX9-targeting sgRNA to generate SOX9-knockout populations in HGSOC lines.
- Treat parental and SOX9-knockout cells with a range of carboplatin concentrations.
- Assess platinum sensitivity using a colony formation assay, the gold standard for measuring long-term cell survival and proliferative capacity after genotoxic stress. The expected result is a significant increase in sensitivity (reduced colony formation) in knockout cells [6].
- Ectopic Overexpression (Sufficiency Test):
- Epigenetically upregulate SOX9 in sensitive HGSOC lines using lentiviral vectors or inducible systems.
- Perform in vivo tumorigenesis assays in mouse models (e.g., xenografts) to demonstrate that SOX9 overexpression is sufficient to induce significant chemoresistance and enrich for a stem-like transcriptional state in a living organism [6].
- Downstream Transcriptional Analysis: Utilize single-cell RNA-Seq (scRNA-Seq) on naive and SOX9-overexpressing tumors to demonstrate that SOX9 increases transcriptional divergence (a metric for transcriptional plasticity and stemness), reprogramming naive cells into a stem-like, chemoresistant state [6].
Protocol for Correlating SOX9 with Immune Checkpoints
Objective: To analyze the correlation between SOX9 expression and immune checkpoint molecules in a tumor cohort.
Materials:
- Dataset: RNA-seq data from a cancer cohort (e.g., TCGA-GBM).
- Software/R Packages: R package
GSVA(for single-sample GSEA),ESTIMATEpackage (for immune/stromal scoring),ggplot2for visualization.
Methodology:
- Immune Infiltration Estimation: Use the
GSVApackage to calculate enrichment scores for 24 immune cell types based on a predefined gene signature. Alternatively, use theESTIMATEalgorithm to generate immune, stromal, and estimate scores for each tumor sample [9]. - Immune Checkpoint Expression: Extract mRNA expression data (e.g., TPM, FPKM) for key immune checkpoint genes, such as PD-1, PD-L1, CTLA-4, LAG3, and others.
- Statistical Correlation: Perform Spearman's rank correlation analysis between the continuous variable of SOX9 expression and the expression levels of each immune checkpoint gene. Visualize the results using scatter plots or heatmaps.
- Group Comparison: Divide the cohort into SOX9-high and SOX9-low groups based on a median split or optimal cut-off. Use the Wilcoxon rank-sum test to compare the expression levels of immune checkpoints between these two groups [9]. A significant result suggests a potential link between SOX9 and an immunosuppressive microenvironment.
Table 3: Essential Research Tools for SOX9 and Tumor Microenvironment Studies
| Reagent/Resource | Function and Application | Specific Examples / Catalog Numbers |
|---|---|---|
| SOX9 Antibodies | Detection and quantification of SOX9 protein levels via Western Blot, IHC, and IF. | Validated antibodies for IHC (e.g., Abcam ab185966); for Western Blot (e.g., Cell Signaling Tech #82630). |
| CRISPR/Cas9 System | For genetic knockout of SOX9 to study its necessity in tumor progression and therapy resistance. | SOX9-targeting sgRNA (e.g., Horizon Genomics Edit-R system). |
| Lentiviral SOX9 Constructs | For stable and inducible overexpression of SOX9 to test its sufficiency in driving malignancy. | Lentiviral SOX9 ORF clone (e.g., from VectorBuilder). |
| Platinum Chemotherapeutics | Inducing SOX9 expression and testing chemoresistance in vitro and in vivo. | Carboplatin, Cisplatin (e.g., Selleckchem S1215, S1166). |
| scRNA-Seq Platforms | Profiling transcriptional heterogeneity and identifying SOX9-expressing stem-like subpopulations. | 10x Genomics Chromium Single Cell Gene Expression solution. |
| R Packages (GSVA, ESTIMATE) | Computational deconvolution of tumor transcriptomes to infer immune cell infiltration. | Bioconductor packages: GSVA, ESTIMATE. |
| Public Data Repositories | Source of transcriptomic, clinical, and mutation data for biomarker discovery and validation. | TCGA (cancergenome.nih.gov), GEO (ncbi.nlm.nih.gov/geo). |
The integration of SOX9 into prognostic nomograms represents a significant advancement in translating a complex biological regulator into a clinically actionable tool. The evidence confirms that SOX9 is more than a mere proliferation marker; it is a central node in a network governing stemness, chemoresistance, and immune suppression. The successful application of a SOX9-based model in GBM, which integrated immune context and IDH status, demonstrates the power of this integrative approach [9]. Future efforts must focus on standardizing SOX9 measurement (e.g., using immunohistochemistry cut-offs or RNA-seq thresholds) and validating these models in prospective, multi-institutional clinical trials. Furthermore, given SOX9's role as a master regulator of transcription, the development of targeted therapies, such as small molecule inhibitors or degrader molecules, could provide a synergistic therapeutic strategy. By combining SOX9-targeting agents with existing chemotherapy and immunotherapy, and using SOX9-based nomograms to select the patients most likely to benefit, we can move closer to a future of truly personalized and effective cancer medicine.
Conclusion
SOX9 emerges as a master regulator at the intersection of cancer biology and immunology, wielding significant influence over the tumor immune microenvironment. Its dualistic functions—promoting immune evasion while supporting tissue repair—underscore the complexity of targeting it therapeutically. Validation across pan-cancer data solidifies its role as a robust prognostic biomarker and a key contributor to an immunosuppressive landscape. Future research must focus on deciphering the context-dependent mechanisms governing SOX9's actions and developing sophisticated targeting strategies that inhibit its pro-tumorigenic and immunosuppressive functions without compromising its beneficial roles. Success in this endeavor promises to unlock novel, effective immunotherapeutic strategies for a range of aggressive cancers.
References
- 1. SOX9 in organogenesis: shared and unique transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482574/]
- 2. Sox9 [https://en.wikipedia.org/wiki/SOX9]
- 3. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 4. Role of the SOX family in cancer immune evasion [https://pmc.ncbi.nlm.nih.gov/articles/PMC11789896/]
- 5. SOX9 [Human] - GeneGlobe - QIAGEN [https://geneglobe.qiagen.com/us/knowledge/gene/ENSG00000125398]
- 6. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 7. Oncogenic role of PLOD3 mediated by SOX9 through IL-6/ ... [https://www.sciencedirect.com/science/article/abs/pii/S0898656825006655]
- 8. Recapitulation of endochondral ossification by hPSC- ... [https://www.nature.com/articles/s41467-025-58122-9]
- 9. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 10. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 11. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 12. indirectly regulates CEACAM1 expression and SOX ... 9 immune [https://www.oncotarget.com/article/7379/text/]
- 13. A SOX9-B7x axis safeguards dedifferentiated tumor cells ... [https://www.sciencedirect.com/science/article/pii/S1534580723005518]
- 14. Precise modulation of transcription factor levels identifies ... [https://www.nature.com/articles/s41588-023-01366-2]
- 15. indirectly regulates CEACAM1 expression and SOX ... 9 immune [https://pubmed.ncbi.nlm.nih.gov/26885752/]
- 16. Expression and Functional Role of Sox in Human... | PLOS One 9 [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0054355]
- 17. reactivation in cancer vessels shapes the... | SOX Square 9 Research [https://www.researchsquare.com/article/rs-5457583/v1]
- 18. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://www.nature.com/articles/s41467-025-59050-4]
- 19. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 20. The versatile functions of Sox9 in development, stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4326072/]
- 21. Diverse functions of SOX9 in liver development and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10958229/]
- 22. Tumor-associated macrophages promote tumor metastasis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5725132/]
- 23. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 24. The pioneer factor SOX9 competes for epigenetic factors to ... [https://www.nature.com/articles/s41556-023-01184-y]
- 25. Cancer Stem Cells Connecting to Immunotherapy [https://www.mdpi.com/2072-6694/17/13/2100]
- 26. Transcription Factor Drives Chemotherapy Resistance in ... [https://news.feinberg.northwestern.edu/2025/10/30/transcription-factor-drives-chemotherapy-resistance-in-ovarian-cancer/]
- 27. ATAC-seq — Epigenomics Workshop 2025 1 documentation [https://nbis-workshop-epigenomics.readthedocs.io/en/latest/content/tutorials/ATACseq/lab-atacseq-bulk.html]
- 28. ATAC-seq methods for consensus peak generation to ... [https://www.protocols.io/view/atac-seq-methods-for-consensus-peak-generation-to-daea2bae.html]
- 29. Combining ATAC-seq and RNA-seq reveals key genes for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12057259/]
- 30. SOX9: The master regulator of cell fate in breast cancer [https://www.sciencedirect.com/science/article/abs/pii/S0006295219304885]
- 31. Defining treatment-resistant brain cancer: Genetic ... [https://www.nature.com/articles/s41417-025-00980-y]
- 32. SOX9: a key transcriptional regulator in organ fibrosis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1507282/full]
- 33. Cordycepin alleviates diabetes mellitus-associated hepatic ... [https://pubmed.ncbi.nlm.nih.gov/39260158/]
- 34. USP28 promotes PARP inhibitor resistance by enhancing ... [https://www.nature.com/articles/s41419-025-07647-4]
- 35. Cordycepin Targets HRD1 to Promote Cancer Cell PD‐L1 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12531455/]
- 36. Enhancing cancer immunotherapy using cordycepin and ... [https://www.nature.com/articles/s41598-024-72833-x]
- 37. SOX9: An emerging driving factor from cancer progression ... [https://pubmed.ncbi.nlm.nih.gov/33524528/]
- 38. SOX9 drives a stem-like transcriptional state and platinum ... [https://www.jci.org/articles/view/186467]
- 39. Transcription Factor Sox9 - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/transcription-factor-sox9]
- 40. Context-Dependent Distinct Roles of SOX9 in Combined ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11394107/]
- 41. Co-regulation of Sox9 and TGFβ1 transcription factors in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10063891/]
- 42. SOX on tumors, a comfort or a constraint? [https://www.nature.com/articles/s41420-024-01834-6]
- 43. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 44. Cancer cell dormancy: An update to 2025 [https://bmrat.org/index.php/BMRAT/article/view/994]
- 45. Regulatory T cells in cancer immunosuppression [https://www.nature.com/articles/s41571-019-0175-7]
- 46. Mechanisms underlying immunosuppression by regulatory ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2024.1328193/full]
- 47. Macrophage polarization: an important role in inflammatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11039887/]
- 48. Macrophages in immunoregulation and therapeutics [https://www.nature.com/articles/s41392-023-01452-1]
- 49. Super-enhancer inhibitors THZ2 and JQ1 reverse ... [https://pubmed.ncbi.nlm.nih.gov/40843352/]
- 50. Immunosuppressive Functions of M2 Macrophages Derived ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7286967/]
- 51. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002136]
- 52. Metastatic Latency and Immune Evasion Through Autocrine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4808520/]
- 53. SOX9-regulated cell plasticity in colorectal metastasis is ... [https://www.nature.com/articles/srep32350]
- 54. Enhancer reprogramming: critical roles in cancer and ... [https://www.nature.com/articles/s41420-025-02366-3]
- 55. SOX9 has distinct regulatory roles in alternative splicing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6158501/]
- 56. The regenerative journey: exploring stem cell roles from injury ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12502613/]
- 57. Promotion of colorectal cancer progression by immune- ... [https://www.sciencedirect.com/science/article/pii/S0898656823002681]
- 58. Diagnostic and Prognostic Significances of SOX9 in ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.708735/full]
- 59. High expression of SOX9 is a diagnostic and prognostic ... [https://pubmed.ncbi.nlm.nih.gov/40692865/]
- 60. SOX9 drives KRAS-induced lung adenocarcinoma ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/37258742/]
- 61. Studying the Role of Sox9 in Lung Cancer [https://news.cuanschutz.edu/cancer-center/sox9-in-lung-cancer]
- 62. SOX9 Stem-Cell Factor: Clinical and Functional Relevance in Cancer - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6463569/]
- 63. Deciphering of SOX9 Functions in Pancreatic Cancer Cells [https://www.mdpi.com/1422-0067/26/6/2652]
- 64. Expression analysis of SOX2 and SOX9 in patients with oral squamous cell carcinoma - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11717967/]
- 65. SOX9 is a dose-dependent metastatic fate determinant in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6330758/]
- 66. SOX9 Regulates Low Density Lipoprotein Receptor-related ... [https://www.sciencedirect.com/science/article/pii/S0021925820435380]
- 67. The Clinicopathological and Prognostic Significance of ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2021.668946/full]