SOX9: The Prototypical Janus-Faced Regulator in Immunity and Disease
The transcription factor SOX9 is a critical yet paradoxical regulator of the immune system, functioning as a double-edged sword in health and disease.
SOX9: The Prototypical Janus-Faced Regulator in Immunity and Disease
Abstract
The transcription factor SOX9 is a critical yet paradoxical regulator of the immune system, functioning as a double-edged sword in health and disease. This review synthesizes recent advances to explore SOX9's dual roles: it drives tumor immune escape by creating immunosuppressive microenvironments yet is essential for tissue repair and regeneration in inflammatory and fibrotic diseases. We cover SOX9's foundational biology, mechanisms of action in different immunological contexts, and the associated challenges for therapeutic targeting. By integrating findings from cancer, fibrosis, and infectious disease models, this article provides a framework for researchers and drug development professionals to navigate the complexities of SOX9, with the goal of informing the development of novel, context-specific immunotherapies.
Unraveling SOX9: Molecular Structure, Normal Immune Functions, and Dual Regulatory Roles
The transcription factor SOX9 (SRY-related HMG box 9) serves as a pivotal regulator across diverse biological processes, functioning as a master conductor of development, stem cell maintenance, and disease pathogenesis. Its haploinsufficiency causes campomelic dysplasia, a severe skeletal malformation syndrome often accompanied by 46,XY sex reversal [1] [2]. Beyond its established roles in embryogenesis, recent research has illuminated SOX9's function as a Janus-faced regulator in immunology, where it exhibits context-dependent dual roles—promoting tumor immune escape while facilitating tissue repair in inflammatory conditions [3]. Understanding the molecular architecture of SOX9, comprising its functional domains and key interacting partners, is fundamental to explaining its versatile functions and developing targeted therapeutic strategies for cancer and immune-related diseases.
Structural Domains of SOX9
The SOX9 protein is composed of several functionally specialized domains that orchestrate its DNA binding, dimerization, and transcriptional activities. The domain organization, consistent across multiple studies, is summarized in the table below.
Table 1: Functional Domains of the Human SOX9 Protein
| Domain Name | Position | Key Functions | Interacting Partners/Features |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates self-dimerization and heterodimerization with other SOXE proteins [4]. | Required for DNA binding and transactivation of cartilage-specific genes [5]. |
| HMG Box | Central | - Binds DNA at consensus motif (A/TA/TCAAA/TG) [1].- Induces DNA bending [5].- Contains nuclear localization (NLS) and export signals (NES) [3]. | Embedded NLS/NES enable nucleocytoplasmic shuttling [3]. |
| Transactivation Domain Middle (TAM) | Middle | Synergizes with TAC to augment transcriptional potential [3] [5]. | Interacts with co-activators to enhance transcriptional activity. |
| Transactivation Domain C-terminal (TAC) | C-terminal | Critical for transcriptional activation and inhibition of β-catenin [3] [5]. | Binds cofactors (MED12, CBP/p300, TIP60, WWP2) [5]. |
| PQA-Rich Domain | C-terminal | Enhances transactivation but lacks autonomous activity [3] [5]. | Proline/Glutamine/Alanine-rich region; unique to mammals [4]. |
The High Mobility Group (HMG) box is the defining DNA-binding domain, enabling SOX9 to recognize and bind to the specific consensus sequence (A/TA/TCAAA/TG) in the minor groove of DNA, inducing a significant bend of approximately 80° [1] [5]. This domain also contains embedded nuclear localization and export signals, facilitating its shuttling between the cytoplasm and nucleus [3].
Aft the HMG box lies the dimerization domain (DIM), which is crucial for the formation of SOX9 homodimers or heterodimers with other SOXE subgroup members like SOX8 and SOX10 [1] [4]. This dimerization is essential for the recognition of palindromic DNA sequences and the transactivation of key target genes, particularly during chondrogenesis [5].
The transcriptional activity of SOX9 is mediated by its transactivation domains, TAM (middle) and TAC (C-terminal). The TAC domain is particularly critical, as it interacts with renowned transcriptional co-activators such as CBP/p300, TIP60, and components of the mediator complex (e.g., MED12) to recruit the basal transcriptional machinery [5]. Furthermore, the TAC domain is required for the inhibition of β-catenin signaling during chondrocyte differentiation [3] [5]. The TAM and TAC domains function synergistically to activate gene expression [3]. Finally, the PQA-rich domain, while unable to activate transcription on its own, serves to enhance the transactivation capability of the other domains and appears to be a mammalian-specific feature [5] [4].
Figure 1: Functional Domain Architecture of SOX9. The diagram illustrates the modular structure of SOX9 and the primary functions associated with its core domains.
Post-Translational Regulation and Partner Interactions
SOX9's activity is not solely determined by its structure but is finely modulated by a complex network of post-translational modifications (PTMs) and protein-protein interactions. These regulatory mechanisms enable SOX9 to function appropriately across diverse cellular contexts.
Table 2: Key Regulatory Mechanisms of SOX9 Activity
| Regulatory Mechanism | Effect on SOX9 | Biological Context |
|---|---|---|
| Phosphorylation (by PKA) | Enhances DNA-binding affinity and promotes nuclear translocation [1]. | Testis development; neural crest delamination [1]. |
| SUMOylation | Can enhance or repress transcriptional activity; acts as a developmental switch [1]. | Chondrogenesis; inner ear vs. neural crest development in Xenopus [1]. |
| MicroRNA Regulation | Inhibits SOX9 expression at the post-transcriptional level [1]. | Lung development, chondrogenesis, neurogenesis [1]. |
| Ubiquitin-Proteasome Pathway | Degrades SOX9 protein, repressing its transcriptional activity [1]. | Hypertrophic chondrocytes [1]. |
A central theme in SOX9's function is its reliance on partner factors. SOX9 generally does not activate transcription in isolation; it requires cooperative binding with other transcription factors to specific composite DNA elements [1]. The functional outcome—activation or repression of a target gene—depends heavily on the specific partner factor recruited.
- Transcriptional Activation: A classic example is the activation of the Col2a1 gene in chondrocytes. This requires the cooperative binding of a SOX9 dimer alongside a dimer of SOX5 or SOX6 (SOXD proteins) to the enhancer region [1]. This partnership is fundamental to chondrogenesis and extracellular matrix deposition.
- Transcriptional Repression: Conversely, SOX9 can repress gene expression by recruiting different partners. During chondrocyte maturation, SOX9 partners with Gli proteins to repress Col10a1, a gene required for hypertrophy, thereby preventing premature maturation [1].
- Stepwise Progression in Development: Partner switching allows for the stepwise progression of developmental pathways. In male gonad development, the initial complex of SRY and SF1 activates SOX9 expression. The newly synthesized SOX9 protein then replaces SRY, partnering with SF1 to drive the subsequent stages of testis development, creating a self-perpetuating regulatory loop [1].
Figure 2: SOX9 Partner Factors Determine Transcriptional Outcome. SOX9 requires partner factors to regulate gene expression, leading to either activation or repression depending on the cellular context and the specific partner recruited.
SOX9 as a Janus-Faced Regulator in Immunology
The molecular architecture of SOX9 underpins its dual role in immunology, where it can function as both an oncogenic promoter of immune escape and a beneficial mediator of tissue repair.
SOX9 in Tumor Immune Evasion
In the tumor microenvironment, SOX9 is frequently overexpressed and facilitates immune escape through multiple mechanisms [3] [6]. Its ability to interact with diverse partners allows it to suppress anti-tumor immunity synergistically.
- T Cell Regulation: SOX9 overexpression in tumors correlates with reduced infiltration and function of cytotoxic CD8+ T cells. It can promote T cell exhaustion by upregulating immune checkpoint molecules like LAG3 and can impair T cell development by modulating RORC [6].
- NK Cell Evasion: SOX9 enables tumor cells to evade Natural Killer (NK) cell surveillance. In breast cancer models, SOX9 overexpression upregulates ligands like ULBP, which engage the NKG2D receptor on NK cells, potentially leading to receptor internalization and impaired NK cell function [6].
- Macrophage Polarization: SOX9 promotes polarization of tumor-associated macrophages (TAMs) towards the immunosuppressive M2 phenotype. In gastric cancer, SOX9 upregulates LIF, which drives M2 macrophage differentiation, creating an environment conducive to tumor growth [6].
- Myeloid-Derived Suppressor Cell (MDSC) Recruitment: In pancreatic cancer, the SOX9/CXCL5/CXCR2 axis is critical for recruiting polymorphonuclear MDSCs, which suppress T cell activity and accelerate tumor progression [6].
SOX9 in Tissue Repair and Inflammation
Conversely, in non-malignant inflammatory contexts, SOX9 plays a protective and reparative role, again leveraging its functional domains to regulate gene expression.
- Osteoarthritis (OA): In healthy cartilage, SOX9 is essential for producing collagen and aggrecan. It interacts with the NF-κB pathway and promotes macrophage polarization from the pro-inflammatory M1 to the anti-inflammatory M2 phenotype, helping to resolve inflammation [6].
- Lung and Kidney Repair: Following injury, SOX9 expression in type II alveolar epithelial cells (ATIIs) and renal epithelial cells (RECs) is crucial for tissue regeneration. It is stimulated by IL-4 from regulatory T cells (Tregs) and promotes repair by modulating macrophage activity and secreting reparative factors like complement C3 [6].
Experimental Toolkit for SOX9 Research
Studying the complex biology of SOX9 requires a multifaceted experimental approach. The table below outlines key reagents and methodologies used in the field.
Table 3: Research Reagent Solutions for SOX9 Investigation
| Reagent/Method | Function/Principle | Key Applications |
|---|---|---|
| siRNA / shRNA | Gene silencing via targeted mRNA degradation. | Functional validation; depleting SOX9 to study its role in cancer progression and drug resistance [6]. |
| CRISPR/Cas9 (Knockout) | Complete gene knockout via targeted DNA cleavage. | Establishing SOX9-essential roles in cell survival, differentiation, and tumorigenesis [6]. |
| CRISPR-dCas9 (Activation) | Targeted gene activation using a catalytically dead Cas9 fused to transactivators. | Upregulating SOX9 to study its therapeutic potential in tissue repair (e.g., osteoarthritis) [6]. |
| Chromatin Conformation Capture (4C/Hi-C) | Mapping long-range chromatin interactions and topological domains. | Identifying tissue-specific SOX9 enhancers located megabases away from the gene [7]. |
| Co-immunoprecipitation (Co-IP) | Identifying direct protein-protein interactions. | Discovering SOX9 partner factors (e.g., with Gli for repression, or SF1 in testis development) [1]. |
| Reporter Gene Assays | Measuring transcriptional activity on a specific promoter/enhancer. | Characterizing SOX9 transactivation domains and validating enhancer elements [1] [7]. |
Figure 3: Experimental Workflow for SOX9 Functional Studies. A logical flow of key methodologies used to dissect the expression, regulation, and diverse functions of SOX9, from initial genetic manipulation to final phenotypic validation.
The molecular architecture of SOX9, characterized by its modular functional domains, provides the foundation for its remarkable functional versatility. The HMG box, DIM, TAM, and TAC domains work in concert, with their activity precisely tuned by post-translational modifications and, most critically, by interactions with specific partner proteins. It is this very plasticity that allows SOX9 to function as a Janus-faced regulator, capable of driving pathogenic processes like tumor immune evasion and mediating beneficial outcomes such as tissue repair. Future research focused on resolving the structural details of SOX9-partner complexes and the tissue-specific determinants of its partner selection will be crucial. Such insights will pave the way for novel therapeutic strategies that can selectively inhibit SOX9's oncogenic functions or harness its regenerative potential, ultimately enabling more precise targeting in cancer and immune-related diseases.
SOX9 in Immune Cell Development and Homeostasis
The Sex-determining Region Y-related High-Mobility Group Box 9 (SOX9) protein, a member of the SOX family of transcription factors, operates as a critical regulatory node at the intersection of developmental biology, immunology, and cellular homeostasis. While extensively studied in chondrogenesis and sex determination, its functions in immune cell development and homeostasis have recently emerged as pivotal to understanding both physiological tissue maintenance and pathological immune dysregulation. SOX9 exhibits a Janus-faced character in immunological contexts, functioning as both an activator and repressor across diverse immune cell types and tissue environments [3]. This dual nature enables SOX9 to govern fundamental processes including thymic T-cell development, tumor immune escape, and the maintenance of stem cell niches that support immune cell populations. The protein's structural architecture, featuring a high-mobility group (HMG) box DNA-binding domain flanked by transcriptional activation and dimerization domains, permits sophisticated regulatory interactions with chromatin and transcriptional co-factors [3]. This review synthesizes current understanding of SOX9's multifaceted roles in immune cell development and homeostasis, with particular emphasis on its mechanistic actions in shaping immune cell identity, function, and tissue distribution.
Structural and Functional Domains of SOX9
The SOX9 protein encodes a 509 amino acid polypeptide with several functionally specialized domains that collectively determine its biological activity [8] [3]. The dimerization domain (DIM), located upstream of the HMG box, facilitates DNA-dependent dimerization, a critical feature for binding to palindromic DNA sequences and executing specific transcriptional programs [3] [9]. The central HMG box domain represents the defining structural motif of the SOX family, conferring sequence-specific DNA binding to ACAA/TG motifs while simultaneously enabling nucleocytoplasmic shuttling through embedded nuclear localization (NLS) and nuclear export signals (NES) [3]. Flanking the HMG box are two transcriptional activation domains: a central TAM domain and a C-terminal TAC domain, which operate synergistically to recruit co-activators and enhance transcriptional output [3]. The TAC domain specifically interacts with chromatin modifiers such as Tip60 and plays a crucial role in inhibiting β-catenin signaling during differentiation processes [3]. Finally, a proline/glutamine/alanine (PQA)-rich domain completes the C-terminal region and is indispensable for full transcriptional activation potential [3].
Table 1: Functional Domains of SOX9 Protein
| Domain | Position | Key Functions | Structural Features |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | DNA-dependent dimerization; enables binding to palindromic sequences | Mediates cooperative DNA binding |
| HMG Box Domain | Central | DNA binding to ACAA/TG motifs; nuclear import/export | Contains embedded NLS/NES signals; 79 amino acids |
| Transcriptional Activation Domain Middle (TAM) | Central | Synergistic transcriptional activation | Interacts with co-activators |
| Transcriptional Activation Domain C-terminal (TAC) | C-terminal | Recruitment of chromatin modifiers; β-catenin inhibition | Binds Tip60; essential for differentiation |
| PQA-rich Domain | C-terminal | Transcriptional activation | Proline/Glutamine/Alanine-rich region |
The functional significance of these domains is highlighted by the pathological consequences of their disruption. Mutations affecting SOX9, particularly those impairing dimerization capacity, are associated with Campomelic Dysplasia, a severe skeletal malformation syndrome often accompanied by XY sex reversal and congenital heart defects, underscoring the protein's fundamental role in multiple developmental pathways [9].
SOX9 in Immune Cell Development and Differentiation
T-Cell Development in the Thymus
SOX9 plays a nuanced role in thymic T-cell development, particularly influencing the lineage commitment of early thymic progenitors. During T-cell maturation, SOX9 cooperates with the transcription factor c-Maf to activate key genetic programs including Rorc and effector genes such as Il17a and Blk, thereby modulating the developmental balance between conventional αβ T cells and the more innate-like γδ T cell populations [3]. This regulatory function positions SOX9 as a determinant in the establishment of T-cell functional diversity. In thymoma, SOX9 expression demonstrates a negative correlation with genes associated with Th17 cell differentiation, primary immunodeficiency pathways, PD-L1 expression, and T-cell receptor signaling, suggesting its involvement in establishing appropriate thymic microenvironments for T-cell selection and maturation [8].
B-Cell Lymphomas
While SOX9 does not appear to play a significant role in normal B-cell development, it emerges as an important oncogenic driver in certain B-cell malignancies. In Diffuse Large B-cell Lymphoma (DLBCL), SOX9 becomes overexpressed and functions to promote cell proliferation, inhibit apoptosis, and facilitate cancer progression [3]. This pathological expression highlights the potential dysregulation of SOX9 in immune cell homeostasis and its context-dependent functions.
Innate Immune Cells and Tumor Microenvironment
Beyond adaptive immunity, SOX9 significantly influences innate immune cell populations and their positioning within tissue environments. Comprehensive bioinformatics analyses of tumor datasets reveal striking correlations between SOX9 expression patterns and immune cell infiltration landscapes [3]. In colorectal cancer, SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while demonstrating positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. Similarly, in breast cancer systems, SOX9 triggers tumorigenesis by facilitating the immune escape of tumor cells, in part through the establishment of an immunosuppressive microenvironment [8] [10].
Table 2: SOX9 Correlation with Immune Cell Infiltration in Cancer
| Cancer Type | Positive Correlation With | Negative Correlation With | Functional Consequences |
|---|---|---|---|
| Colorectal Cancer | Neutrophils, Macrophages, Activated mast cells, Naive/activated T cells | B cells, Resting mast cells, Resting T cells, Monocytes, Plasma cells, Eosinophils | Altered immune landscape; potential immunosuppression |
| Multiple Cancers (General) | Memory CD4+ T cells, M2 macrophages, Tregs | CD8+ T cells, NK cells, M1 macrophages | Immune evasion; impaired cytotoxic response |
| Breast Cancer | Immunosuppressive cells | Cytotoxic T cells | Immune escape facilitated through SOX9-B7x axis |
| Prostate Cancer | Tregs, M2 macrophages, Anergic neutrophils | CD8+ CXCR6+ T cells, Activated neutrophils | "Immune desert" microenvironment |
SOX9 in Cellular Homeostasis and Tissue Maintenance
Retinal and Corneal Homeostasis
In the adult mouse eye, SOX9 performs critical functions in maintaining retinal integrity and supporting limbal stem cell populations. Genetic ablation of SOX9 in adult mice triggers severe retinal degeneration characterized by loss of Müller glial cells and complete depletion of the photoreceptor layer [11]. SOX9 expression persists in multiple adult ocular cell types, including retinal pigmented epithelium cells, Müller glial cells, and the limbal and corneal basal epithelia, where it supports tissue homeostasis [11]. Through lineage tracing and single-cell RNA sequencing approaches, researchers have demonstrated that SOX9 marks a basal limbal stem cell population capable of generating long-lived clones that contribute to both stem cell maintenance and corneal epithelial homeostasis [11]. These findings establish SOX9 as essential for the maintenance of retinal integrity and proper limbal stem cell differentiation in the adult mammalian eye.
Stem Cell Maintenance and Differentiation
SOX9 operates as a key regulator of stem cell populations across multiple tissues. In skin epithelium, SOX9 functions as a pioneer transcription factor that can reprogram epidermal stem cells (EpdSCs) toward a hair follicle stem cell (HFSC) fate [12]. This fate switching involves SOX9 binding to closed chromatin regions at key hair follicle enhancers, where it recruits co-factors to initiate chromatin remodeling and transcriptional activation of hair follicle-specific genes [12]. Simultaneously, SOX9 indirectly silences epidermal genes by redistributing epigenetic factors away from epidermal enhancers [12]. This dual functionality demonstrates how SOX9 maintains tissue homeostasis by balancing stem cell differentiation pathways. Similarly, in the intestinal epithelium, SOX9 contributes to the maintenance of stem cell compartments, with its disruption leading to homeostatic imbalances [11].
Chromatin Remodeling and Pioneer Factor Activity
SOX9 exhibits bona fide pioneer factor activity, enabling it to bind cognate motifs in compacted chromatin and initiate epigenetic reprogramming. In epidermal stem cell systems, SOX9 binds to closed chromatin regions at W1 of induction, with increased accessibility at these binding sites emerging between W1 and W2, demonstrating its capacity to recognize and engage silent genomic regions [12]. Approximately 30% of SOX9 binding sites are situated within closed chromatin prior to its expression, and these sites subsequently display nucleosome displacement as evidenced by decreased histone H3 occupancy and reduced cleavage under targets and release using nuclease (CUT&RUN) fragment lengths [12].
In human umbilical vein endothelial cells (HUVECs), SOX9 overexpression drives endothelial-to-mesenchymal transition (EndMT) by opening chromatin at silent mesenchymal genes and depositing active histone modifications [9]. This reprogramming function is guided by SOX dimer motifs and enrichment of the histone variant H2A.Z, which may poise these regions for activation [9]. Interestingly, SOX9 chromatin binding is highly dynamic, potentially due to eviction by histone phosphorylation, yet the chromatin changes it initiates remain persistent [9]. This combination of dynamic binding and stable epigenetic alteration exemplifies how SOX9 can establish new cellular states during development and homeostasis.
SOX9 in Pathological Contexts
Cancer and Chemoresistance
SOX9 emerges as a significant driver of tumor progression and therapy resistance across multiple cancer types. Comprehensive pan-cancer analyses reveal that SOX9 expression is significantly upregulated in fifteen cancer types compared to matched healthy tissues, including CESC, COAD, ESCA, GBM, KIRP, LGG, LIHC, LUSC, OV, PAAD, READ, STAD, THYM, UCES, and UCS [8]. Conversely, SOX9 expression decreases in only two cancers (SKCM and TGCT), highlighting its predominantly oncogenic character across most malignancies [8].
In high-grade serous ovarian cancer (HGSOC), SOX9 plays a critical role in driving chemoresistance. Epigenetic upregulation of SOX9 occurs in response to platinum-based chemotherapy, and forced SOX9 expression alone is sufficient to induce a stem-like transcriptional state and significant platinum resistance in vivo [13]. Single-cell RNA sequencing of patient tumors before and after neoadjuvant chemotherapy reveals that SOX9 becomes consistently upregulated following treatment, and a rare cluster of SOX9-expressing cells in treatment-naive tumors shows enrichment for cancer stem cell markers and chemoresistance-associated stress gene modules [13] [14]. SOX9 expression in ovarian cancer correlates with increased transcriptional divergence—a metric of transcriptional plasticity and malleability that is amplified in stem cells and cancer stem cells—suggesting a mechanism by which SOX9 promotes adaptive resistance [13].
Immune Evasion Mechanisms
SOX9 contributes to immune evasion through multiple mechanisms. In breast cancer, SOX9 establishes an immunosuppressive microenvironment by upregulating the immune checkpoint molecule B7x (B7-H4/VTCN1), creating a protective shield for dedifferentiated tumor cells against immune surveillance [10]. This SOX9-B7x axis represents a crucial mechanism through which tumors escape immune destruction. Additionally, SOX9 expression in prostate cancer correlates with shifts in immune cell populations, including decreases in effector immune cells (CD8+CXCR6+ T cells and activated neutrophils) and increases in immunosuppressive cells (Tregs, M2 macrophages, and anergic neutrophils), ultimately generating an "immune desert" microenvironment that facilitates tumor progression [3].
Experimental Approaches and Methodologies
Key Experimental Protocols
Chromatin Accessibility and Binding Assays
Investigations of SOX9's pioneer factor activity employ sophisticated epigenomic techniques. CUT&RUN (Cleavage Under Targets and Release using Nuclease) sequencing enables high-resolution mapping of SOX9 binding sites across the genome [12]. This method utilizes micrococcal nuclease conjugated to antibodies specific to SOX9, cleaving DNA in proximity to binding sites and providing a sensitive alternative to traditional ChIP-seq. Assay for Transposase-Accessible Chromatin with high-throughput sequencing (ATAC-seq) simultaneously assesses chromatin accessibility dynamics during SOX9-mediated reprogramming [12]. The combination of these approaches allows researchers to temporally resolve SOX9 binding relative to chromatin opening events.
Lineage Tracing and Fate Mapping
To examine SOX9's role in stem cell populations, researchers employ inducible Cre/LoxP systems for lineage tracing. The CAGG-CreER recombinase system activated by tamoxifen administration enables temporal control of SOX9 deletion or expression in adult animals [11]. When combined with reporter alleles (e.g., Rosa26-lacZ or Rosa26-tdTomato), this approach permits fate mapping of SOX9-expressing cells and their progeny, revealing contributions to tissue maintenance and regeneration [11].
Single-Cell RNA Sequencing
Single-cell RNA sequencing (scRNA-seq) technologies enable dissection of SOX9's roles in heterogeneous cell populations. In ovarian cancer studies, scRNA-seq of patient tumors before and after chemotherapy treatment revealed population-level induction of SOX9 and its association with a stem-like transcriptional state [13]. Computational analysis of these datasets includes calculating transcriptional divergence (P50/P50 ratio) to measure transcriptional plasticity, which is elevated in SOX9-high cells [13].
Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 Investigations
| Reagent/Cell Line | Application | Key Features/Utility | Representative Studies |
|---|---|---|---|
| HUVECs (Human Umbilical Vein Endothelial Cells) | EndMT reprogramming studies | SOX9-induced mesenchymal transition; chromatin remodeling studies | [9] |
| OVCAR4, Kuramochi, COV362 | Ovarian cancer chemoresistance | Carboplatin-induced SOX9 upregulation; stem-like state formation | [13] |
| 22RV1, PC3, H1975 | Small molecule screening | Cordycepin dose-response studies; SOX9 inhibition assays | [8] |
| Krt14-rtTA;TRE-Sox9 mice | In vivo fate switching models | Inducible SOX9 expression in epidermal stem cells; BCC formation | [12] |
| CAGG-CreER;Sox9flox/flox mice | Adult tissue-specific knockout | Tamoxifen-inducible Sox9 deletion; retinal degeneration studies | [11] |
| Anti-SOX9 antibodies (R&D Systems AF3045) | Immunostaining, Western blot | Species-specific; validated for IHC and immunofluorescence | [9] |
| Cordycepin (adenosine analog) | SOX9 inhibition studies | Dose-dependent SOX9 downregulation; anticancer effects | [8] |
Concluding Perspectives
SOX9 emerges as a multifaceted regulator of immune cell development and homeostasis, operating through mechanisms that span transcriptional regulation, chromatin remodeling, and cellular reprogramming. Its Janus-faced character enables context-dependent functions in immune cell differentiation, stem cell maintenance, and tissue homeostasis. The pioneer factor activity of SOX9 allows it to initiate fate switching by opening new enhancer regions while simultaneously silencing previous cellular identities through competition for epigenetic co-factors. In pathological contexts, SOX9 drives cancer progression, chemoresistance, and immune evasion, highlighting its potential as both biomarker and therapeutic target. Future research directions should focus on developing small molecule inhibitors targeting SOX9 activity or its downstream effectors, particularly for overcoming chemotherapy resistance. Additionally, spatial omics technologies promise to illuminate SOX9's roles in organizing immune microenvironments in situ, potentially revealing new therapeutic opportunities for modulating immune responses in cancer, autoimmunity, and tissue regeneration contexts.
The transcription factor SOX9 exemplifies a "Janus-faced" regulator in human physiology, performing contrasting, context-dependent roles in oncogenic immune suppression and beneficial tissue repair. This review synthesizes current mechanistic insights into how SOX9 facilitates tumor immune escape by modulating the tumor microenvironment and inhibiting cytotoxic immune cell functions, while in parallel promoting tissue regeneration in conditions like osteoarthritis and intervertebral disc degeneration. We present quantitative analyses of SOX9's roles, detailed experimental methodologies for probing its functions, key signaling pathways, and essential research tools. Understanding these dual aspects is critical for developing targeted therapeutic strategies that inhibit SOX9's detrimental effects in cancer while harnessing its regenerative potential.
SOX9 (SRY-Box Transcription Factor 9), a member of the SOX family of transcription factors containing a highly conserved high-mobility group (HMG) box DNA-binding domain, is a pivotal developmental regulator with emerging roles in disease pathogenesis [3] [15]. The "Janus face" metaphor aptly describes its functional duality: in cancer, SOX9 frequently acts as an oncogene promoting tumor progression and immune evasion, whereas in tissue repair contexts, it drives regenerative processes including chondrogenesis and extracellular matrix (ECM) restoration [3]. This dichotomy presents both challenges and opportunities for therapeutic intervention. This technical review comprehensively examines the mechanistic basis of SOX9's dual functions, with particular emphasis on its immunological roles, to inform targeted drug discovery and development efforts.
SOX9 Structure and Functional Domains
The human SOX9 protein comprises 509 amino acids with several functionally critical domains organized from N- to C-terminus [3] [16]:
- Dimerization Domain (DIM): Facilitates formation of homo- and heterodimers with other SOXE proteins (SOX8, SOX10)
- HMG Box Domain: Bends target DNA into an L-shaped complex, enabling sequence-specific binding to the motif AGAACAATGG
- Transactivation Domain Middle (TAM): Synergistically enhances transcriptional activation
- P/Q/A-rich Domain: Proline/glutamine/alanine-rich region that stabilizes SOX9
- Transactivation Domain C-terminal (TAC): Interacts with cofactors like Tip60 to potentiate transcriptional activity
Table 1: SOX9 Protein Domains and Functional Characteristics
| Domain | Position | Key Functions | Structural Features |
|---|---|---|---|
| DIM | N-terminal | Dimerization with SOXE factors | Enables hetero-/homo-dimerization |
| HMG Box | Central | DNA binding, nuclear localization | L-shaped DNA bending, 79 amino acids |
| TAM | Middle | Transcriptional activation | Synergizes with TAC domain |
| P/Q/A | C-terminal | Protein stabilization | Proline/glutamine/alanine-rich |
| TAC | C-terminal | Co-factor interaction, β-catenin inhibition | Interacts with Tip60 |
Post-translational modifications, particularly phosphorylation at serine residues (S64, S181, S211), further regulate SOX9 activity, DNA binding affinity, and protein stability, adding another layer of control to its transcriptional functions [16].
The Suppressive Face: SOX9 in Tumor Immunity and Immune Evasion
SOX9-Mediated Modulation of Tumor Immune Microenvironment
In multiple cancer types, SOX9 overexpression creates an immunosuppressive tumor microenvironment (TME) that facilitates immune evasion. In KrasG12D-driven lung adenocarcinoma (LUAD) models, SOX9 depletion significantly reduced tumor burden and progression, with extended survival in Sox9-knockout mice [17]. Mechanistically, SOX9 suppresses infiltration and function of cytotoxic immune cells while promoting collagen deposition and tumor stiffness, physically impeding immune cell access [17].
Table 2: SOX9 Correlation with Immune Cell Infiltration in Cancer
| Immune Cell Type | Correlation with SOX9 | Functional Consequences | Cancer Types Studied |
|---|---|---|---|
| CD8+ T cells | Negative | Reduced cytotoxic function, decreased infiltration | Lung adenocarcinoma, Colorectal cancer |
| Natural Killer (NK) cells | Negative | Suppressed activity | Lung adenocarcinoma |
| Dendritic cells | Negative | Impaired antigen presentation | Lung adenocarcinoma |
| M1 Macrophages | Negative | Reduced anti-tumor response | Colorectal cancer |
| Neutrophils | Positive | Increased immunosuppressive subtypes | Lung adenocarcinoma |
| M2 Macrophages | Positive | Enhanced pro-tumor functions | Colorectal cancer |
| T-regulatory cells | Positive | Increased immunosuppression | Prostate cancer |
Bioinformatic analyses of TCGA data reveal SOX9 expression negatively correlates with genes associated with CD8+ T cell, NK cell, and M1 macrophage function, while showing positive correlation with immunosuppressive populations like Tregs and M2 macrophages [3]. In colorectal cancer, SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils [3]. Single-cell RNA sequencing in prostate cancer demonstrates that SOX9-enriched tumor regions exhibit an "immune desert" phenotype, characterized by decreased effector CD8+CXCR6+ T cells and increased immunosuppressive Tregs and M2 macrophages [3].
Molecular Mechanisms of SOX9-Driven Immune Evasion
SOX9 employs multiple molecular strategies to suppress anti-tumor immunity:
- Extracellular Matrix Remodeling: SOX9 significantly elevates collagen-related gene expression and increases collagen fibers, potentially creating a physical barrier to immune infiltration [17].
- Stemness Maintenance: SOX9 collaborates with SOX2 to maintain cancer stem cell properties, enabling long-term survival and immune evasion of dormant cancer cells at metastatic sites [18].
- Cytokine Signaling Modulation: SOX9 expression in cancer-associated fibroblasts and other stromal components alters cytokine secretion profiles toward immunosuppressive patterns [18].
- Checkpoint Regulation: While direct links to canonical checkpoints like PD-1/PD-L1 require further validation, SOX9's broad immunosuppressive effects position it as a potential regulator of immune checkpoint expression.
The Regenerative Face: SOX9 in Tissue Repair and Regeneration
SOX9 in Cartilage Regeneration and Osteoarthritis
In stark contrast to its oncogenic role, SOX9 is indispensable for cartilage development and repair. It regulates type II procollagen expression, essential for chondrocyte function and cartilage integrity [19]. Increased SOX9 levels help maintain macrophage function, contributing to cartilage formation and tissue regeneration in osteoarthritis (OA) [3]. SOX9 acts as a master transcription factor during chondrogenesis, directly activating crucial ECM genes including COL2A1, ACAN, and COMP [16].
SOX9 in Intervertebral Disc Regeneration
Recent innovative approaches have leveraged SOX9's regenerative potential for intervertebral disc (IVD) degeneration. CRISPR/Cas9-engineered tonsil-derived mesenchymal stromal cells (ToMSCs) with inducible SOX9 and TGFβ1 co-expression demonstrated superior chondrogenic differentiation and ECM restoration in rat degeneration models [19]. These dual-factor expressing cells significantly improved disc hydration (confirmed by MRI), enhanced aggrecan and type II collagen synthesis, and reduced inflammation compared to single-factor treatments [19].
SOX9 in Fibrosis Resolution and Tissue Homeostasis
SOX9 plays context-dependent roles in fibrotic processes across various organs. It promotes fibrosis in cardiac, liver, kidney, and pulmonary tissues through regulation of extracellular matrix component accumulation [16] [20]. However, in regenerative contexts, SOX9 appears critical for appropriate tissue repair and homeostasis restoration, particularly in epithelial tissues and cartilage, where it balances proliferation and differentiation [18].
Experimental Models and Methodologies for SOX9 Research
Genetic Manipulation Approaches
CRISPR/Cas9-Mediated Gene Editing: The Tet-off regulatory system combined with CRISPR/Cas9 enables precise integration of SOX9 transgenes into safe harbor loci (e.g., AAVS1). This allows controlled, inducible SOX9 expression in therapeutic cell types like ToMSCs [19].
Protocol: Generation of SOX9-Engineered ToMSCs
- Isplicate ToMSCs from tonsil tissue using collagenase type I/DNase I digestion and Ficoll-Paque density gradient centrifugation
- Design donor construct with SOX9 cDNA under Tet-off promoter control with P2A-linked TGFβ1
- Transfect with pAAVS1-puro-Tetoff-SOX9-TGFβ1-CAG-tTA-Advanced plasmid and Cas9/gRNA targeting AAVS1 locus
- Select with puromycin and validate integration via Western blot and qRT-PCR
- Induce SOX9/TGFβ1 expression via doxycycline withdrawal
Cre-LoxP and CRISPR in Vivo Models: For lung adenocarcinoma studies, intratracheal delivery of lenti-Cre to KrasLSL-G12D;Sox9flox/flox mice enables tissue-specific Sox9 knockout, while pSECC CRISPR/Cas9 systems allow concurrent KrasG12D activation and Sox9 knockout [17].
Functional Assays for SOX9 Activity
Tumor Organoid Culture: 3D organoid systems assess SOX9-driven proliferation using KrasG12D mouse lung tumor cells, with growth metrics and Ki67 immunohistochemistry quantifying proliferation [17].
Immune Cell Infiltration Analysis: Flow cytometry of dissociated tumors evaluates CD8+ T cell, NK cell, and dendritic cell populations in Sox9-proficient versus deficient microenvironments [17].
Chondrogenic Differentiation Assay: ToMSCs cultured in chondrogenic medium (StemPro Chondrogenesis Differentiation Kit) for 21 days, with Alcian blue staining quantifying proteoglycan deposition [19].
Signaling Pathways and Molecular Networks
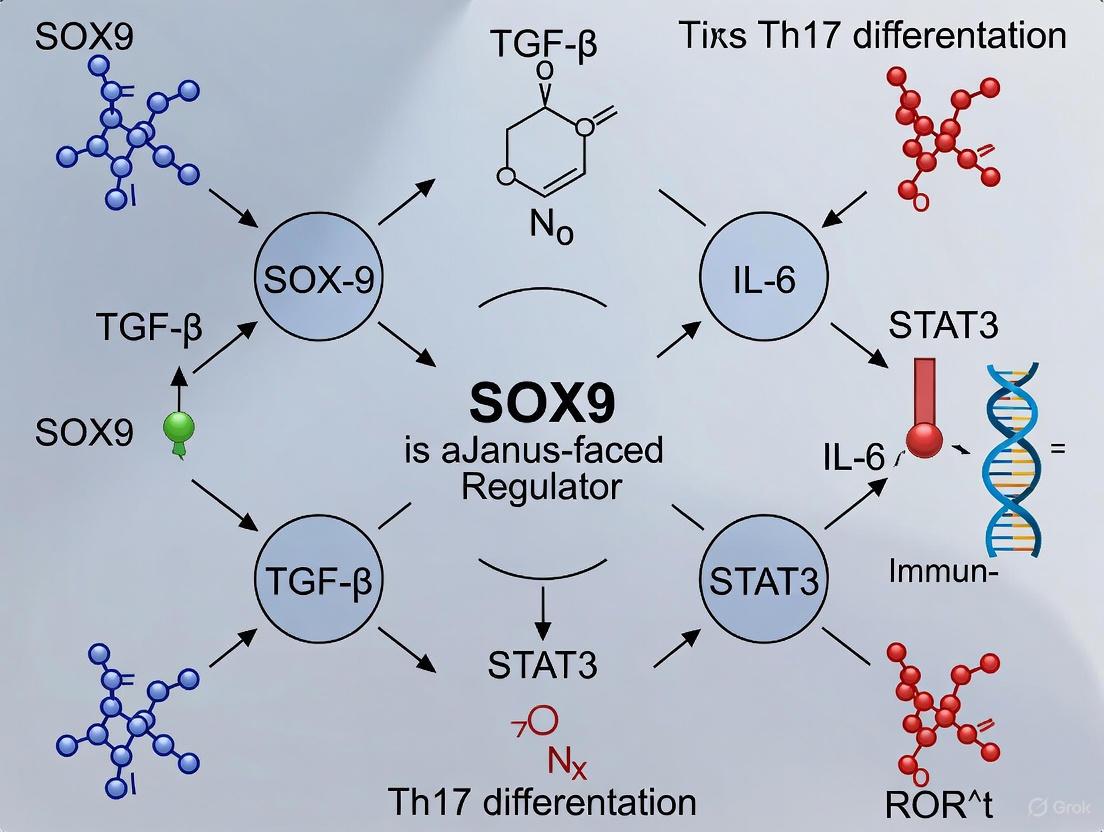
SOX9 Signaling Network in Cancer and Repair
Research Reagent Solutions
Table 3: Essential Research Tools for SOX9 Investigation
| Reagent/Cell Line | Application | Key Features | Source/Reference |
|---|---|---|---|
| KrasLSL-G12D;Sox9flox/flox mice | In vivo tumor modeling | Conditional Sox9 knockout in KRAS-driven cancer | [17] |
| ToMSCs (tonsil-derived MSC) | Regenerative therapy | High proliferative capacity, chondrogenic potential | [19] |
| pAAVS1-puro-Tetoff-SOX9-TGFβ1 | Inducible gene expression | Tet-off regulated SOX9/TGFβ1 co-expression | [19] |
| mTC11/mTC14 cells | 3D organoid culture | KrasG12D mouse lung tumor cells | [17] |
| StemPro Chondrogenesis Kit | Differentiation assay | Defined medium for chondrogenic differentiation | [19] |
Therapeutic Implications and Future Perspectives
The dual nature of SOX9 presents unique challenges for therapeutic targeting. In oncology, SOX9 inhibition strategies must spare its physiological functions in renewing tissues. Potential approaches include:
- Context-Specific Inhibitors: Develop modulators that selectively disrupt SOX9 interactions in tumor cells while preserving regenerative functions
- Combination Immunotherapies: Pair SOX9-targeting agents with immune checkpoint inhibitors to overcome multiple resistance mechanisms
- Regenerative Engineering: Harness SOX9's tissue-reparative functions with tightly regulated expression systems for degenerative diseases
The temporal control offered by Tet-off systems in CRISPR-engineered cells represents a promising safety strategy for clinical translation, minimizing risks of continuous SOX9 overexpression [19].
SOX9 embodies a true biological Janus factor, governing both pathological immune suppression in cancer and essential tissue repair processes. Its context-dependent functions necessitate sophisticated therapeutic approaches that can selectively modulate its activity based on disease setting. Future research should focus on delineating the precise molecular determinants of SOX9's functional switch and developing precision targeting strategies that can therapeutically exploit its dual nature.
Developmental Roles Informing Immunological Functions
The SRY (Sex-determining Region Y)-box 9 (SOX9) transcription factor represents a paradigm of functional versatility, executing essential roles in embryonic development that subsequently inform its complex, context-dependent functions within the immunological landscape. Initially characterized for its fundamental contributions to chondrogenesis, skeletal formation, and sex determination, SOX9 has emerged as a critical regulator of immune cell differentiation, tumor immunology, and inflammatory processes [3] [21]. This evolutionary conservation of developmental mechanisms redeployed in immunological contexts positions SOX9 as a quintessential "Janus-faced" regulator, capable of exerting both beneficial and detrimental effects depending on cellular context [3]. The transcription factor's capacity to regulate diverse biological processes stems from its sophisticated structural organization, which enables precise DNA binding, protein-protein interactions, and transcriptional activation of context-specific genetic programs. Understanding how SOX9's developmental blueprint informs its immunological functions provides critical insights for therapeutic targeting in cancer, autoimmune disorders, and inflammatory diseases.
Molecular Architecture and Functional Domains of SOX9
The SOX9 protein exhibits a modular architecture consisting of functionally specialized domains that orchestrate its transcriptional regulatory capabilities. These domains facilitate DNA recognition, protein dimerization, and transcriptional activation, enabling SOX9 to coordinate complex genetic programs in both developmental and immunological contexts.
Structural Organization and Functional Motifs
Table 1: Functional domains of the SOX9 protein
| Domain | Position | Primary Function | Biological Significance |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein self-association | Enables formation of transcriptionally active complexes |
| HMG Box | Central | DNA binding and nuclear localization | Recognizes specific DNA sequences (CCTTGAG); contains nuclear localization signal |
| Central Transcriptional Activation Domain (TAM) | Middle | Recruits co-activators | Synergistically enhances transcriptional potential |
| P/Q/A-rich Domain | C-terminal | Transcriptional activation | Proline/glutamine/alanine-rich region essential for transactivation |
| C-terminal Transcriptional Activation Domain (TAC) | C-terminal | Interacts with transcriptional cofactors | Binds Tip60; inhibits β-catenin during chondrocyte differentiation |
The High Mobility Group (HMG) box domain represents SOX9's central functional module, comprising an L-shaped arrangement of three α-helices that facilitates sequence-specific DNA binding to the consensus motif (A/T)(A/T)CAA(A/T)G [3] [15]. This domain contains embedded nuclear localization signals that direct SOX9 to its genomic targets while additionally enabling nucleocytoplasmic shuttling in response to specific cellular signals [3]. The C-terminal transcriptional activation domain (TAC) serves as a critical interface for protein-protein interactions, notably with the coactivator Tip60, thereby amplifying SOX9's transcriptional potency [3]. The synergistic operation between TAM and TAC domains enables SOX9 to activate transcription of target genes with remarkable specificity and efficiency across diverse cellular contexts.
Figure 1: Domain architecture of SOX9 protein illustrating functional regions and their primary activities
SOX9 in Embryonic Development: A Foundation for Immunological Functions
SOX9 executes fundamental roles in embryonic development that establish mechanistic precedents for its subsequent immunological activities. The transcription factor's involvement in cell fate determination, progenitor cell maintenance, and tissue morphogenesis during development provides a conceptual framework for understanding its functions in immune cell differentiation and tumor microenvironment regulation.
Chondrogenesis and Skeletal Development
During chondrocyte differentiation, SOX9 functions as a master regulatory transcription factor that directly activates expression of critical extracellular matrix components, including collagen type II alpha 1 chain (COL2A1) and collagen type XI alpha 2 chain (COL11A2) [21]. Genome-wide binding analyses using chromatin immunoprecipitation sequencing (ChIP-seq) have revealed that SOX9 preferentially binds to intronic and distal regulatory regions in developing limb buds, with a significant enrichment for palindromic SOX binding motifs that facilitate homodimer formation [21]. This binding pattern enables robust transcriptional activation of the chondrogenic program through cooperative interactions with enhancer elements. The conservation of SOX9 binding regions and target genes in chondrogenesis across vertebrate species, including mouse and chicken, underscores the evolutionary importance of this regulatory circuit [21]. The mechanistic paradigm of SOX9-mediated transcriptional activation of structural genes during chondrogenesis finds parallel in its ability to regulate extracellular matrix composition in pathological contexts, including fibrotic diseases and tumor stroma formation.
Gonadal Development and Sex Determination
In mammalian testis development, SOX9 expression is upregulated by SRY and promotes Sertoli cell differentiation, thereby directing male sexual development [21]. Comparative analyses of SOX9 binding patterns in developing gonads have revealed distinct organizational principles compared to chondrogenic contexts. In male gonads, SOX9 exhibits preferential binding to proximal upstream regions of target genes, with significantly fewer palindromic SOX motifs compared to limb bud development [21]. This context-dependent DNA binding behavior demonstrates SOX9's remarkable adaptability to different transcriptional environments. The regulatory relationship between SOX9 and anti-Müllerian hormone (AMH), which triggers Müllerian duct regression during male development, exemplifies SOX9's capacity to orchestrate complex morphogenetic events through direct transcriptional control [8] [21]. This developmental plasticity in regulating cell fate decisions establishes a precedent for SOX9's later involvement in immune cell differentiation and lineage commitment.
Experimental Approaches for SOX9 Functional Characterization
Elucidating SOX9's diverse biological roles requires sophisticated methodological approaches that capture its genomic interactions, transcriptional outputs, and functional consequences across developmental and immunological contexts.
Genomic Localization and Binding Site Analysis
Table 2: Key methodological approaches for SOX9 research
| Method | Application | Key Findings | Technical Considerations |
|---|---|---|---|
| Chromatin Immunoprecipitation Sequencing (ChIP-seq) | Genome-wide mapping of SOX9 binding sites | Cell type-specific binding patterns; enriched in intronic/distal regions in chondrocytes vs upstream regions in gonads | Antibody specificity critical; cross-linking conditions affect resolution |
| RNA Sequencing | Transcriptomic profiling of SOX9-dependent gene expression | Identification of SOX9 target genes; pathway enrichment analysis | Combine with ChIP-seq to distinguish direct vs indirect targets |
| Immunohistochemistry / Immunofluorescence | Spatial localization of SOX9 protein in tissues | Ectopic expression in fibrotic livers; tumor vs normal tissue distribution | Validates database findings at protein level; requires high-quality antibodies |
| Bioinformatics Analysis (GEPIA, HPA, TCGA) | Pan-cancer expression correlation and prognostic significance | SOX9 upregulated in 15/33 cancer types; prognostic value in LGG, CESC, THYM | Large sample sizes but potential batch effects between datasets |
| Cell Culture with Compound Treatment | Functional validation of SOX9 modulation | Cordycepin inhibits SOX9 expression in dose-dependent manner | Requires multiple cell lines; physiological relevance of concentrations |
Chromatin immunoprecipitation followed by sequencing (ChIP-seq) represents the gold standard for identifying genome-wide SOX9 binding sites. The standard protocol involves cross-linking proteins to DNA with formaldehyde, cell lysis, chromatin fragmentation by sonication to 200-500 bp fragments, immunoprecipitation with validated SOX9-specific antibodies, and library preparation for high-throughput sequencing [21]. Comparative ChIP-seq analyses between mouse and chicken embryonic tissues have revealed that SOX9 exhibits higher conservation of target genes and binding regions in chondrocytes compared to Sertoli cells, highlighting the tissue-specific evolution of its regulatory networks [21]. These findings underscore the importance of employing cross-species validation approaches when investigating SOX9's functional conservation.
Expression Analysis and Functional Validation
RNA sequencing coupled with computational analyses from databases such as The Cancer Genome Atlas (TCGA) and Genotype-Tissue Expression (GTEx) has enabled comprehensive profiling of SOX9 expression patterns across normal and pathological tissues [8] [22]. For functional validation, cancer cell lines (e.g., prostate cancer cells PC3 and 22RV1, lung cancer cell H1975) are cultured under standard conditions (RPMI 1640 or DMEM medium with 10-15% FBS at 37°C with 5% CO2) and treated with potential SOX9-modulating compounds such as cordycepin [8]. Western blot analysis following treatment involves cell lysis in EBC buffer, protein separation by SDS-PAGE, transfer to PVDF membranes, and immunodetection using SOX9-specific antibodies [8]. This integrated methodological approach enables rigorous characterization of SOX9's functional roles across biological contexts.
Figure 2: Experimental workflow for SOX9 genomic localization and functional characterization
SOX9 as a Regulator of Immune Function and Tumor Immunology
The mechanistic principles governing SOX9's developmental functions directly inform its multifaceted roles in immunological processes, particularly in the context of cancer immunology and inflammatory responses.
SOX9 in Cancer Immunobiology
Comprehensive pan-cancer analyses have revealed that SOX9 expression is significantly elevated in 15 of 33 cancer types, including glioblastoma (GBM), colon adenocarcinoma (COAD), liver hepatocellular carcinoma (LIHC), lung squamous cell carcinoma (LUSC), and pancreatic adenocarcinoma (PAAD) [8]. This overexpression pattern positions SOX9 primarily as an oncogenic driver across diverse malignancies. Importantly, SOX9 expression demonstrates significant correlation with immune cell infiltration patterns in the tumor microenvironment, exhibiting negative associations with cytotoxic immune cells (CD8+ T cells, NK cells, M1 macrophages) while showing positive correlations with immunosuppressive populations (Tregs, M2 macrophages, activated neutrophils) [3] [22]. These patterns collectively generate an "immune desert" microenvironment that facilitates tumor immune escape and represents a modern manifestation of SOX9's developmental capacity to orchestrate cellular microenvironments [3].
In specific contexts such as thymoma, SOX9 expression demonstrates negative correlation with genes associated with PD-L1 expression and T-cell receptor signaling pathways, suggesting its involvement in immune checkpoint regulation [8]. Additionally, SOX9 promotes immune evasion by maintaining cancer stem cell populations in a dormant state that avoids immune detection, particularly in metastatic contexts [23]. This capacity to regulate stemness properties represents a direct extension of SOX9's developmental function in maintaining progenitor cell populations, now co-opted to promote tumor survival in immunological contexts.
SOX9 in Inflammatory Responses and Tissue Repair
Beyond cancer, SOX9 plays critical roles in inflammatory processes and tissue repair mechanisms. During schistosomiasis infection, SOX9 becomes ectopically expressed in myofibroblasts within hepatic granulomas and surrounding hepatocytes, where it orchestrates extracellular matrix deposition to contain parasitic egg toxins [24]. In the absence of SOX9, granuloma structure becomes disrupted, leading to diffuse liver injury and altered immune cell recruitment, including expanded Ly6clo monocyte populations and exaggerated Type 2 inflammation with pronounced eosinophilia [24]. This demonstrates SOX9's essential role in containing inflammatory damage while simultaneously highlighting its potential contribution to pathological fibrosis.
In osteoarthritis, SOX9 expression contributes to maintaining macrophage function and promoting cartilage formation, underscoring its tissue-reparative capacities [3]. This dual functionality in both promoting and resolving inflammation exemplifies SOX9's Janus-faced character in immunological contexts, mirroring its developmental versatility in coordinating both anabolic and catabolic processes during morphogenesis.
Therapeutic Targeting and Research Reagents
The strategic targeting of SOX9 represents a promising therapeutic approach for cancer and immune-related disorders, leveraging insights from its developmental and immunological functions.
Research Reagent Solutions
Table 3: Essential research reagents for SOX9 investigation
| Reagent/Category | Specific Examples | Research Application | Function/Mechanism |
|---|---|---|---|
| Cell Lines | 22RV1, PC3, H1975 | In vitro functional studies | Prostate and lung cancer lines for SOX9 modulation experiments |
| Chemical Inhibitors | Cordycepin | SOX9 pathway inhibition | Adenosine analog; reduces SOX9 mRNA and protein expression |
| Databases | HPA, TCGA, GTEx, GEPIA | Expression analysis | SOX9 expression in normal/tumor tissues; prognostic correlation |
| Antibodies | SOX9 ChIP-grade | Immunodetection methods | Chromatin immunoprecipitation; immunohistochemistry |
| Animal Models | Sox9-deficient mice | In vivo functional validation | Global and tissue-specific knockout models |
Cordycepin (3'-deoxyadenosine), an adenosine analog derived from Cordyceps sinensis, has demonstrated significant capacity to inhibit SOX9 expression at both mRNA and protein levels in a dose-dependent manner in prostate cancer (22RV1, PC3) and lung cancer (H1975) cell lines [8]. Treatment protocols typically involve 24-hour exposure at concentrations ranging from 10-40 μM, followed by assessment of SOX9 expression changes via Western blot or quantitative RT-PCR [8]. For genomic studies, ChIP-grade SOX9 antibodies enable precise mapping of SOX9 binding sites, while validated immunohistochemistry antibodies facilitate spatial localization of SOX9 protein in tissue sections [8] [21]. The integration of data from public repositories including The Human Protein Atlas (HPA), The Cancer Genome Atlas (TCGA), and Gene Expression Profile Interaction Analysis (GEPIA) provides comprehensive expression datasets for SOX9 across normal and pathological contexts [8] [22].
Therapeutic Implications and Future Directions
The compelling correlation between SOX9 expression and poor prognosis across multiple cancer types, coupled with its fundamental roles in therapy resistance mechanisms, positions SOX9 as an attractive therapeutic target [25] [15]. Future therapeutic strategies may include direct SOX9 inhibitors, degrader molecules, or approaches targeting critical downstream effectors in SOX9-dependent pathways. Additionally, the integration of SOX9 expression biomarkers into diagnostic and prognostic algorithms holds significant promise for patient stratification and treatment selection [22] [26]. However, the therapeutic targeting of SOX9 must account for its crucial physiological functions in tissue homeostasis and repair, necessitating strategies that achieve context-specific modulation rather than complete inhibition [3]. The ongoing characterization of SOX9's dual roles in immunology will continue to inform the development of sophisticated targeting approaches that leverage its developmental legacy for therapeutic benefit in cancer and immune-related diseases.
Investigating SOX9: Techniques, Models, and Therapeutic Targeting Strategies
The transcription factor SOX9 (SRY-box transcription factor 9) exemplifies functional duality, or "Janus-faced" activity, within biological systems. It plays critically divergent roles across physiological and pathological contexts, functioning as both a master regulator of development and a pivotal influencer of disease progression. In immunology, SOX9 demonstrates remarkable duality: it can promote immune escape in malignancies by impairing immune cell function, yet in other contexts, increased SOX9 levels help maintain macrophage function and contribute to tissue regeneration and repair [3]. Resolving these context-dependent functions requires advanced analytical tools capable of dissecting cellular heterogeneity and spatial context. Single-cell RNA sequencing (scRNA-seq) and spatial transcriptomics have emerged as transformative technologies in this pursuit, enabling researchers to delineate the complex regulatory networks and cellular interactions governed by SOX9 with unprecedented resolution [27] [28]. This technical guide explores how these methodologies are revolutionizing SOX9 research within immunological contexts, providing detailed experimental frameworks and analytical workflows for researchers investigating this multifunctional transcription factor.
Methodological Foundations: Core Technologies and Workflows
Single-Cell RNA Sequencing (scRNA-seq) for SOX9+ Cell Characterization
scRNA-seq enables comprehensive profiling of SOX9-expressing cellular subsets and their transcriptional identities within complex tissues. The standard workflow involves:
Cell Isolation and Preparation: Fresh tissue samples are dissociated into single-cell suspensions using enzymatic and mechanical methods. For bone tissues, which present particular challenges due to the rigid matrix, optimized protocols incorporating collagenase digestion are essential [29]. Cell viability should exceed 80% as determined by 7-aminoactinomycin D (7AAD) staining and fluorescence-activated cell sorting (FACS) [28].
Library Preparation and Sequencing: Single-cell libraries are typically prepared using platform-specific kits (e.g., 10x Genomics Chromium System) targeting 3'-end transcripts. Sequencing depth should aim for 50,000-100,000 reads per cell using paired-end sequencing on Illumina platforms [27] [28].
Quality Control and Preprocessing: Raw sequencing data is processed through alignment pipelines (e.g., Cell Ranger) followed by quality control metrics in R/Python environments. Cells with fewer than 200 genes or high mitochondrial content (>20%) should be filtered out. Normalization is performed using methods like SCTransform in Seurat to correct for technical variation [27].
Downstream Analysis: Processed data undergoes dimensionality reduction (PCA, UMAP), clustering, and cell type annotation using canonical markers. SOX9-expressing populations can be further analyzed for differential expression, trajectory inference (using Monocle3), and regulatory network analysis to identify SOX9-associated pathways [28] [1].
Table 1: Key scRNA-seq Analysis Packages for SOX9 Research
| Package | Primary Function | Application in SOX9 Research |
|---|---|---|
| Seurat | Single-cell data integration, clustering, and visualization | Identification of SOX9+ cell populations and their molecular signatures [27] |
| Monocle | Trajectory inference and pseudotemporal ordering | Mapping differentiation trajectories of SOX9+ progenitor cells [27] [28] |
| CellChat | Cell-cell communication analysis | Inference of SOX9-mediated signaling pathways [27] |
| inferCNV | Copy number variation analysis | Distinguishing malignant from non-malignant SOX9+ epithelial cells [28] |
Spatial Transcriptomics for Contextualizing SOX9 Expression
Spatial transcriptomics preserves the architectural context of SOX9 expression, enabling correlation of transcriptional data with histological positioning. Two primary platforms are utilized:
Visium Spatial Gene Expression System (10x Genomics): This whole-transcriptome approach captures RNA from tissue sections mounted on patterned arrays. For calcified tissues like bone, optimal decalcification using Morse's solution for 20 hours at room temperature significantly improves RNA quality while preserving tissue architecture [27]. The protocol involves:
- Tissue fixation in 4% paraformaldehyde (PFA) overnight at 4°C
- Decalcification in Morse's solution
- Paraffin embedding and sectioning (6-μm thickness)
- H&E staining and imaging
- Tissue permeabilization and cDNA synthesis on the array
- Library preparation and sequencing
Image-Based In Situ Sequencing (Xenium Platform): This targeted approach enables subcellular resolution for a predefined gene panel (typically 300-500 genes). The methodology includes:
- Fresh frozen or FFPE tissue sectioning
- Hybridization of gene-specific probes
- Sequential rounds of fluorescence imaging
- Automated cell segmentation based on nuclear staining
- Transcript assignment to cellular compartments [30]
Spatial Data Analysis: Processed data is analyzed using Space Ranger pipelines followed by integration with Seurat for spatial clustering. The CARD package enables spatial deconvolution to estimate cell-type proportions within each spot. CellChat can be applied to identify spatially restricted receptor-ligand interactions involving SOX9+ cells [27] [30].
Figure 1: Integrated Workflow for Spatial Transcriptomics in SOX9 Research
Integrated Analytical Approaches for SOX9 Research
Resolving SOX9+ Cellular Niches and Interactions
The integration of scRNA-seq and spatial transcriptomics enables comprehensive mapping of SOX9+ cellular niches and their functional interactions:
Niche Identification: Combined analysis can identify SOX9+ cells within specific tissue microenvironments. In gastric cancer research, this approach revealed cancer stem cells (CSCs) with high SOX9 expression interacting with inflammatory cancer-associated fibroblasts (iCAFs) and immunosuppressive macrophages to construct a protumorigenic niche [28]. Graph neural networks (e.g., GraphSAGE) can identify transcript-based niches agnostic of cell assignment, followed by Gaussian mixture models to cluster transcriptional microenvironments [30].
Cell-Cell Communication Analysis: Tools like CellChat leverage ligand-receptor databases to infer communication probabilities between SOX9+ cells and neighboring populations. In bone fracture healing, this analysis revealed how SOX9+ mesenchymal progenitor cells recruit macrophages via specific signaling pathways during early healing phases [27]. In gastric cancer, iCAFs were found to enhance tumor stemness by upregulating SOX9 through amphiregulin (AREG) signaling [28].
Trajectory Analysis and Pseudotime Ordering: RNA velocity and pseudotime analysis can reconstruct differentiation trajectories of SOX9+ cells. In gastric cancer, these analyses illuminated the transition from mature gastric chief cells to SOX9-high CSCs, identifying key transcriptional regulators along this transdifferentiation path [28].
Table 2: SOX9 Context-Dependent Functions Revealed by Advanced Transcriptomics
| Biological Context | SOX9 Function | Key Interacting Cells/Pathways | Experimental Evidence |
|---|---|---|---|
| Bone Fracture Healing | Activation of mesenchymal progenitor cells; chondrogenesis | Recruitment of macrophages; differentiation to osteogenic cells [27] | Spatial transcriptomics of mouse femur fracture model (Days 0, 5, 15) [27] |
| Gastric Cancer | Maintenance of cancer stem cell phenotype; promotion of drug resistance | Interaction with iCAFs via AREG-ERBB2 axis; immunosuppressive T cells and macrophages [28] | scRNA-seq (28 samples) + spatial transcriptomics (4 GC samples) [28] |
| Pulmonary Fibrosis | Epithelial dysregulation in distal lung remodeling | Association with aberrant basaloid cells and activated fibroblasts [30] | Image-based spatial transcriptomics (1.6M cells from 35 lungs) [30] |
| Melanoma | Tumor suppression; inhibition of tumorigenicity | Restoration of retinoic acid sensitivity; PGD2-mediated upregulation [8] | Pan-cancer analysis of SOX9 expression across 33 cancer types [8] |
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents for SOX9 Transcriptomics Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Tissue Processing | Morse's Solution | Decalcification of bone tissues for RNA preservation [27] |
| 4% Paraformaldehyde (PFA) | Tissue fixation preserving RNA integrity [27] | |
| Single-Cell Platforms | 10x Genomics Chromium | Single-cell partitioning and barcoding [27] [28] |
| Visium Spatial Gene Expression | Spatial transcriptomics for FFPE tissues [27] | |
| Spatial Transcriptomics | Visium CytAssist Spatial Gene Expression for FFPE | Targeted spatial transcriptomics [27] |
| Xenium In Situ Gene Expression | Subcellular resolution spatial transcriptomics [30] | |
| Analysis Packages | Seurat v5 | Single-cell data integration and clustering [27] [30] |
| Monocle | Trajectory inference and pseudotemporal ordering [27] | |
| CellChat | Cell-cell communication analysis [27] | |
| CARD | Spatial deconvolution of transcriptomic data [27] |
Signaling Pathways and Molecular Networks
SOX9 participates in diverse signaling pathways that maintain its Janus-faced functionality across tissue contexts. Integrated transcriptomic analyses have elucidated these networks:
Figure 2: SOX9 Regulatory Networks and Functional Outcomes
Therapeutic Implications and Future Directions
The resolution afforded by single-cell and spatial transcriptomics in SOX9 research has significant implications for therapeutic development:
Target Identification: Integrated analyses have identified promising targets upstream and downstream of SOX9, including the AREG-ERBB2 axis in gastric cancer and WNT signaling components across multiple malignancies [28] [1]. Small molecule inhibitors targeting these pathways represent promising therapeutic avenues.
Biomarker Discovery: SOX9 expression patterns and associated gene signatures show prognostic value across cancer types. High SOX9 expression correlates with worsened overall survival in LGG, CESC, and THYM, suggesting utility as a prognostic biomarker [8]. Single-cell analyses further enable identification of SOX9-associated cellular states predictive of treatment response.
Therapeutic Modulation: Compound screening has identified agents capable of modulating SOX9 expression, including cordycepin, which inhibits SOX9 expression in a dose-dependent manner in prostate and lung cancer cell lines [8]. Similar approaches could yield additional candidates for targeting SOX9-driven pathologies.
Niche-Directed Therapies: Spatial transcriptomics enables development of therapies targeting specific SOX9+ cellular niches rather than individual cell types. In gastric cancer, this might involve disrupting the CSC-iCAF immunosuppressive niche through combinatorial approaches [28].
As these technologies continue to evolve, they will further illuminate the complex duality of SOX9 in immunological contexts, enabling more precise therapeutic interventions that account for its context-dependent functions across tissue homeostasis, regeneration, and disease.
The transcription factor SOX9 exemplifies a "Janus-faced regulator" in immunology, playing paradoxical, context-dependent roles in both promoting and suppressing disease pathways [3]. It is frequently overexpressed in solid malignancies, where it facilitates tumor immune escape, yet it also contributes to tissue repair and maintenance of macrophage function in inflammatory conditions [3]. Resolving these dual functions requires sophisticated in vivo model systems that can replicate the complexity of the immune microenvironment. Genetic models, ranging from conventional knock-out (KO) mice to conditionally targeted and disease-specific strains, provide the essential tools for dissecting these mechanisms, enabling the precise functional validation necessary for diagnostic and therapeutic development [31] [32].
This technical guide details the deployment of these models in SOX9 research, with a focus on methodological execution. It provides a framework for selecting and implementing models that can effectively capture SOX9's dual role in immunological processes, from cancer to tissue damage and repair.
Core Genetic Model Technologies and Methodologies
The investigation of SOX9 in vivo relies on a suite of genetic engineering technologies, each with specific applications and methodological considerations for immunology research.
Conventional and Conditional Gene Targeting
Single-gene knock-out and knock-in models represent a foundational approach. Knock-out mice are generated by inactivating the Sox9 gene to study loss-of-function phenotypes, while knock-in models insert a transgene (e.g., a fluorescent reporter or a mutant allele) into a specific locus to track expression or model genetic variations [31].
Key Experimental Protocol: Generating a SOX9 Knock-Out Mouse Model
- Vector Construction: A targeting vector is designed for the murine Sox9 locus, replacing critical exons (e.g., the HMG-box domain) with a positive selection marker, such as the neomycin resistance (Neoᵣ) gene. The vector includes homologous arms for recombination.
- Embryonic Stem (ES) Cell Culture and Transfection: Mouse ES cells are cultured and electroporated with the linearized targeting vector.
- Selection and Screening: ES cells are selected with G418 (neomycin). Surviving clones are screened via Southern blotting or long-range PCR to identify homologous recombination events.
- Blastocyst Injection and Breeding: Correctly targeted ES cells are injected into mouse blastocysts, which are then implanted into pseudopregnant foster mothers. The resulting chimeric offspring are bred with wild-type mice to achieve germline transmission of the mutated Sox9 allele [31].
A significant limitation of constitutive KO is that complete Sox9 deletion is embryonically lethal due to its vital role in development [3]. Conditional gene modification systems overcome this hurdle.
Key Experimental Protocol: Inducing Tissue-Specific SOX9 Deletion
- Cre/loxP System: This system uses two mouse lines [31]:
- "Floxed" SOX9 line (Sox9ᶠˡᵒˣ) : The Sox9 allele is flanked by loxP sites.
- Cre Recombinase line: Expresses Cre under a tissue-specific promoter (e.g., Lck-Cre for T-cells, LysM-Cre for myeloid cells) or an inducible promoter (e.g., Cre-ERᵀ², activated by tamoxifen).
- Crossbreeding and Genotyping: The Sox9ᶠˡᵒˣ and Cre lines are crossbred. Offspring carrying both Sox9ᶠˡᵒˣ and Cre are identified by PCR genotyping.
- Phenotypic Analysis: For inducible models, tamoxifen is administered to adult mice to activate Cre-ERᵀ², triggering SOX9 deletion in specific cell types at a defined time, thus allowing study of its role in adult physiology and disease.
Transgenesis and Large-Scale Mutation Screens
Transgenesis involves the addition of foreign genetic material—such as a human SOX9 cDNA driven by a constitutive or immune-cell-specific promoter—to the mouse genome. This is used to model SOX9 overexpression phenotypes, particularly its oncogenic roles [31]. For non-directed, discovery-based research, large-scale mutation screens using chemicals like N-ethyl-N-nitrosourea (ENU) or X-rays can generate random mutations, followed by phenotypic screening to identify novel genes and pathways involved in SOX9-related biology [31].
Application of Models in Disease-Specific SOX9 Studies
The selection of an appropriate animal model is dictated by the specific disease context under investigation, as SOX9's function is highly tissue- and microenvironment-dependent.
Cancer and the Tumor Immune Microenvironment
SOX9 is highly expressed in numerous cancers, including glioblastoma (GBM), liver, lung, and breast cancer, where it promotes tumor proliferation, metastasis, and chemoresistance [3] [22] [33]. In the tumor microenvironment (TME), SOX9 expression correlates strongly with specific patterns of immune cell infiltration.
Table 1: SOX9 Correlation with Immune Cell Infiltration in Human Cancers (based on transcriptomic data from TCGA etc.)
| Cancer Type | Positive Correlation With | Negative Correlation With |
|---|---|---|
| Colorectal Cancer (CRC) | Neutrophils, Macrophages, Activated Mast cells [3] | B cells, Resting Mast cells, Resting T cells, Monocytes [3] |
| Glioblastoma (GBM) | Better prognosis in lymphoid invasion subgroups; linked to immunosuppressive TME [22] | CD8+ T cell function, NK cell function, M1 macrophages [3] |
| Prostate Cancer (PCa) | Immunosuppressive cells (Tregs, M2 Macrophages) [3] | Effector immune cells (CD8+CXCR6+ T cells) [3] |
Experimental Workflow: Studying SOX9 in a Glioblastoma Immune Context The following diagram outlines a typical workflow for using a genetically engineered mouse model to study SOX9's role in GBM.
Inflammatory Diseases and Tissue Repair
In contrast to its pro-tumorigenic role, SOX9 is essential for tissue repair and integrity in inflammatory disease settings. A definitive study used a schistosomiasis model of liver damage to demonstrate that SOX9 is ectopically expressed in myofibroblasts within the hepatic granuloma and surrounding hepatocytes [34].
Key Experimental Protocol: SOX9 in Schistosomiasis-Induced Liver Damage
- Disease Model Induction: Wild-type (WT) and SOX9-deficient mice are percutaneously infected with Schistosoma mansoni cercariae.
- Granuloma Analysis: After 8-12 weeks, livers are harvested. Granuloma size and integrity are quantified from histological sections (H&E stain). The extracellular matrix (ECM) barrier is assessed (Trichrome stain).
- Immune Phenotyping: Hepatic leukocytes are isolated and analyzed by flow cytometry. SOX9 deficiency results in increased neutrophils and Ly6Cˡᵒ monocytes, and exaggerated Type 2 inflammation (eosinophilia) [34].
- Conclusion: SOX9 is critical for forming an intact ECM barrier around eggs; its loss leads to diffuse liver injury and an dysregulated immune response [34].
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Reagents for SOX9 In Vivo Research
| Reagent / Model | Function/Description | Key Application in SOX9 Research |
|---|---|---|
| Cre-loxP System | Enables cell-type-specific gene deletion ("floxed" allele) or activation. | To dissect SOX9 function in specific immune lineages (e.g., T-cells, macrophages) without embryonic lethality [31]. |
| Conditional KO (cKO) Mice | Mice with "floxed" Sox9 allele crossed with Cre-driver lines. | Core model for establishing cell-autonomous functions of SOX9 in vivo. |
| Tamoxifen | Inducer of Cre-ERᵀ² activity. | Allows temporal control of SOX9 deletion in adult animals, e.g., after disease initiation. |
| Syngeneic Tumor Cells | Cancer cell lines derived from the same genetic background as the host mouse. | Used in transplantation models (e.g., GBM) to study SOX9's role in tumor-immune interactions in an immunocompetent host [22]. |
| Schistosoma mansoni | Parasite used to model granulomatous liver disease. | To study SOX9's pro-repair and immunomodulatory functions in a chronic inflammatory setting [34]. |
| Cordycepin | Adenosine analog, small molecule inhibitor. | Shown to inhibit SOX9 mRNA and protein expression in cancer cell lines; a potential therapeutic agent [33]. |
The path to harnessing the therapeutic potential of the Janus-faced SOX9 protein lies in the sophisticated use of in vivo genetic models. From conventional KOs that reveal fundamental biology to conditional and disease-specific models that dissect context-dependent roles in cancer and inflammation, these tools are indispensable. The integration of detailed molecular protocols with robust in vivo phenotypic data is paramount for translating findings into novel immunotherapeutic strategies for cancer and immune-related diseases. Future efforts will likely focus on developing more refined models to further unravel the complex interplay between SOX9 and the immune system.
The transcription factor SOX9 (SRY-Box Transcription Factor 9) represents a paradigm of functional duality in biological systems. As a janus-faced regulator, SOX9 plays critical yet opposing roles in both physiological homeostasis and pathological processes, presenting unique challenges and opportunities for therapeutic intervention [3]. While indispensable for normal development, chondrogenesis, and tissue repair, SOX9 is frequently re-expressed in multiple cancer types, where it drives tumor initiation, progression, metastasis, and therapy resistance [3] [35]. This dichotomy is particularly evident in immunology, where SOX9 both promotes immune escape in cancer contexts and maintains macrophage function for tissue regeneration and repair [3]. The molecular basis of SOX9's dual functionality stems from its complex regulation, context-dependent expression, and integration with diverse signaling pathways. This technical guide comprehensively examines current strategies for targeting SOX9, with particular emphasis on degradation approaches and inhibitory modalities, while providing detailed methodological frameworks for researchers pursuing SOX9-directed therapeutics.
SOX9 Structure, Function, and Regulatory Mechanisms
Structural Organization and Functional Domains
SOX9 protein comprises several functionally specialized domains that orchestrate its transcriptional activity (Table 1). The high mobility group (HMG) box facilitates sequence-specific DNA binding to the consensus sequence CCTTGAG and mediates nuclear localization through embedded nuclear localization signals (NLS) [3] [23]. Flanking this central DNA-binding domain are additional functional regions: an N-terminal dimerization domain (DIM), a central transcriptional activation domain (TAM), and a C-terminal transcriptional activation domain (TAC) rich in proline, glutamine, and alanine (PQA) residues [3]. The TAC domain is particularly crucial as it interacts with co-factors like Tip60 to enhance SOX9's transcriptional potency and inhibits β-catenin during chondrocyte differentiation [3].
Table 1: Key Functional Domains of SOX9 Protein
| Domain | Position | Primary Function | Molecular Interactions |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Protein-protein interaction | Facilitates SOX9 dimerization |
| HMG Box | Central | DNA binding, Nuclear import | Binds DNA consensus CCTTGAG |
| Central Transcriptional Activation Domain (TAM) | Middle | Transcriptional activation | Synergizes with TAC domain |
| C-terminal Transcriptional Activation Domain (TAC) | C-terminal | Transcriptional activation, Co-factor recruitment | Interacts with Tip60, inhibits β-catenin |
| PQA-rich Domain | C-terminal | Transcriptional activation | Proline/Glutamine/Alanine-rich region |
Regulatory Mechanisms Controlling SOX9 Stability and Activity
SOX9 protein levels are tightly regulated through multiple mechanisms, with the ubiquitin-proteasome system (UPS) serving as a primary pathway for post-translational control. SOX9 undergoes polyubiquitination mediated by the E3 ubiquitin ligase SCFFBW7 (Skp1/Cul1/F-box), which recognizes a conserved GSK3-phosphorylated motif (Thr236-Thr240) on SOX9 [36]. This modification targets SOX9 for proteasomal degradation, effectively limiting its cellular abundance [36] [37]. Specific mutations, such as K398A in human SOX9, disrupt this ubiquitination process and significantly enhance SOX9 protein stability [37]. Additionally, SOX9 stability is modulated by PI3K/AKT/mTOR signaling through GSK3 inhibition, while cooperation with SNAI2 further regulates SOX9 protein turnover [36]. These regulatory circuits establish precise control over SOX9 expression and function, with their dysruption contributing to various pathologies.
SOX9 as a Therapeutic Target in Disease
Oncogenic Roles of SOX9 Across Cancer Types
SOX9 exhibits frequent overexpression in diverse malignancies, where it functions as a potent oncogene driving multiple hallmarks of cancer. In medulloblastoma, SOX9 promotes metastatic dissemination and confers resistance to cisplatin chemotherapy, with elevated SOX9 levels correlating with poor patient outcomes [36]. Similarly, in non-small cell lung cancer (NSCLC), SOX9 expression associates with poor overall survival and invasive histopathology, particularly in papillary adenocarcinoma subtypes [35]. Interestingly, SOX9 demonstrates histopathology-selective functions in NSCLC, promoting papillary adenocarcinoma progression while suppressing metastasis in squamous cell carcinomas [35]. In breast cancer, SOX9 drives tumor initiation and progression through multiple mechanisms, including regulation of the cell cycle, cooperation with Slug (SNAI2) to promote proliferation and metastasis, and participation in positive feedback loops with long non-coding RNAs [23]. SOX9 also contributes significantly to osteosarcoma pathogenesis, where it is overexpressed in high-grade, metastatic, and recurrent tumors and regulates cancer stem cell populations [38].
SOX9 in Immunomodulation and Tissue Homeostasis
Beyond its oncogenic functions, SOX9 plays crucial roles in immune regulation and tissue maintenance. SOX9 contributes to the formation of an "immune desert" microenvironment in prostate cancer by shifting the balance from effector immune cells (CD8+ CXCR6+ T cells) to immunosuppressive populations (Tregs, M2 macrophages) [3]. In latency-competent cancer cells, SOX9 helps maintain dormancy and enables immune evasion by sustaining cellular stemness [23]. Paradoxically, in non-pathological contexts, SOX9 supports macrophage function and facilitates cartilage formation, tissue regeneration, and repair processes [3]. In metabolic contexts, SOX9 overexpression protects against hepatic lipid accumulation in MASH (metabolic dysfunction-associated steatohepatitis) through AMPK pathway activation, highlighting its protective functions in metabolic disease [39]. In pancreatic beta cells, SOX9 regulates alternative splicing of genes critical for insulin secretion, with its depletion leading to glucose intolerance and disrupted beta cell function [40].
Targeting SOX9: Degradation Strategies and Inhibitory Approaches
Exploiting the Ubiquitin-Proteasome System for SOX9 Degradation
The most strategically advanced approach for targeting SOX9 involves leveraging endogenous protein quality control mechanisms to direct its degradation (Table 2). The SCFFBW7 ubiquitin ligase complex serves as the primary physiological regulator of SOX9 turnover, recognizing SOX9 through a conserved degron motif (Thr236-Thr240) that requires prior phosphorylation by GSK3β [36]. In cancers with FBW7 mutations or downregulation, this regulatory axis is disrupted, leading to SOX9 accumulation and enhanced malignancy [36]. Therapeutic strategies can restore SOX9 degradation through GSK3 stimulation via PI3K/AKT/mTOR pathway inhibition, which promotes SOX9 phosphorylation and subsequent FBW7-mediated ubiquitination [36]. Combination treatments employing PI3K/AKT/mTOR inhibitors with cisplatin demonstrate synthetic lethality in medulloblastoma models, effectively re-sensitizing tumors to chemotherapy [36].
Table 2: Experimentally Validated Approaches for Targeting SOX9
| Therapeutic Approach | Molecular Mechanism | Experimental Context | Outcome |
|---|---|---|---|
| PI3K/AKT/mTOR Inhibition | Activates GSK3, enhancing FBW7-mediated SOX9 degradation | Medulloblastoma cells | Re-sensitization to cisplatin; reduced metastasis |
| FBW7 Reactivation | Restores SOX9 ubiquitination and proteasomal degradation | Medulloblastoma with FBW7 deficiency | Decreased SOX9 protein levels; suppressed malignancy |
| SOX9-Degron Targeting | Direct engagement of SOX9 degron by small molecules | Multiple cancer types (preclinical) | Promotes SOX9 degradation |
| AMPK Pathway Activation | SOX9-mediated metabolic regulation | MASH models | Reduced hepatic lipid accumulation; improved steatohepatitis |
| SOX9-SNAI2 Disruption | Interferes with SOX9-SNAI2 functional cooperation | Breast cancer models | Reduced stemness and tumor-initiating capacity |
Indirect Targeting of SOX9 Through Pathway Modulation
While direct SOX9 inhibitors remain under development, indirect targeting of SOX9-regulatory pathways represents a viable alternative strategy. In MASH, SOX9 overexpression activates AMPK signaling, thereby ameliorating hepatic lipid accumulation and inflammation [39]. This suggests that SOX9 itself could be harnessed therapeutically in metabolic diseases. In breast cancer, targeting the SOX9-miR-215-5p axis suppresses SOX9 expression and inhibits proliferation, migration, and invasion [23]. Similarly, disruption of SOX9-Bmi1 interaction or SOX9-HDAC9 signaling impairs breast cancer cell proliferation [23]. In osteosarcoma, melatonin treatment downregulates SOX9-mediated signaling pathways and inhibits cancer stem cell populations [38]. These approaches demonstrate the viability of modulating SOX9 activity through its regulatory networks rather than direct targeting.
Experimental Protocols for SOX9-Targeted Therapeutic Development
Assessing SOX9 Degradation via Ubiquitin-Proteasome Pathway
Objective: To evaluate candidate compounds for their ability to promote SOX9 degradation through the ubiquitin-proteasome system.
Materials:
- Cell lines endogenously expressing SOX9 (e.g., medulloblastoma, breast cancer, or osteosarcoma lines)
- Proteasome inhibitors (MG132, lactacystin)
- PI3K/AKT/mTOR pathway inhibitors (e.g., PI3K inhibitors: LY294002; AKT inhibitors: MK-2206; mTOR inhibitors: rapamycin)
- Cycloheximide (protein synthesis inhibitor)
- Antibodies: anti-SOX9, anti-ubiquitin, anti-FBW7, anti-phospho-GSK3β, anti-GSK3β
- Plasmid constructs: wild-type SOX9, SOX9-T236A/T240A (phospho-dead mutant), SOX9-K398A (ubiquitination-resistant mutant)
Methodology:
- Treatment and Inhibition: Culture cells and treat with candidate compounds in the presence or absence of proteasome inhibitors (10 μM MG132 or 10 μM lactacystin) for 4-16 hours.
- Protein Synthesis Block: For protein stability assays, treat cells with 100 μg/mL cycloheximide to block new protein synthesis and harvest at time points (0, 30, 60, 120, 240 min) post-treatment.
- Pathway Modulation: To test GSK3β involvement, pre-treat cells with PI3K/AKT/mTOR inhibitors for 2 hours before compound addition.
- Western Blot Analysis: Lyse cells in RIPA buffer containing protease and phosphatase inhibitors. Separate proteins by SDS-PAGE, transfer to PVDF membranes, and probe with anti-SOX9 antibody. Use β-actin as loading control.
- Immunoprecipitation: For ubiquitination assays, immunoprecipitate SOX9 from MG132-treated cell lysates using anti-SOX9 antibody, then immunoblot with anti-ubiquitin antibody to detect polyubiquitinated SOX9.
- Quantitative Analysis: Determine SOX9 protein half-life by densitometric analysis of western blots from cycloheximide chase experiments.
Data Interpretation: Compounds that reduce SOX9 protein levels in a proteasome-inhibitor-reversible manner likely promote SOX9 degradation via the ubiquitin-proteasome pathway. Enhanced SOX9-ubiquitination confirms direct engagement of the degradation machinery.
Functional Validation of SOX9 Targeting in Cancer Stem Cell Populations
Objective: To assess the efficacy of SOX9-targeting approaches on cancer stem cell (CSC) properties and tumor-initiating capacity.
Materials:
- Primary tumor cells or established cancer cell lines with defined CSC subpopulations
- Sphere-forming medium (serum-free DMEM/F12 supplemented with B27, EGF, bFGF)
- Flow cytometry antibodies for CSC markers (CD44, CD133, CD117)
- Limiting dilution transplantation assay components (immunocompromised mice)
- SOX9 knockdown or overexpression constructs
Methodology:
- Sphere Formation Assay: Seed single-cell suspensions in ultra-low attachment plates with sphere-forming medium. Treat with SOX9-targeting compounds or vehicle control for 7-14 days, refreshing medium and compounds every 3-4 days.
- Flow Cytometric Analysis: Harvest cells, stain with CSC surface markers, and analyze by flow cytometry to quantify CSC frequency after treatment.
- Limiting Dilution Transplantation: Serially dilute treated and untreated cells, transplant subcutaneously or orthotopically into immunocompromised mice (NOD/SCID/IL2Rγ-/-). Monitor tumor formation for 8-16 weeks.
- Extreme Limiting Dilution Analysis (ELDA): Use ELDA software to calculate CSC frequency from transplantation data.
- Secondary Transplantation: Isploy cells from primary tumors and transplant into secondary recipients to assess self-renewal capacity.
Data Interpretation: Effective SOX9 targeting should reduce sphere-forming efficiency, decrease CSC marker expression, and diminish tumor-initiating frequency in transplantation assays. The CSC frequency reduction provides a quantitative measure of compound efficacy against the tumor-initiating cell population.
Diagram 1: SOX9 Targeted Degradation via Ubiquitin-Proteasome System and Functional Outcomes. This diagram illustrates the molecular pathway for targeted SOX9 degradation and the resulting anti-tumor effects.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9-Targeted Investigations
| Reagent Category | Specific Examples | Research Application | Technical Considerations |
|---|---|---|---|
| SOX9 Modulators | PI3K/AKT/mTOR inhibitors (LY294002, MK-2206, rapamycin) | Activate GSK3 to promote SOX9 degradation | Confirm reduced SOX9 protein via western blot |
| Proteasome inhibitors (MG132, lactacystin) | Stabilize SOX9 to study degradation mechanisms | Use at 10-20 μM for 4-16 hours | |
| Molecular Tools | SOX9 phospho-mutants (T236A/T240A) | Study degradation-resistant SOX9 | Abolishes FBW7 recognition |
| SOX9 ubiquitination-mutant (K398A) | Examine ubiquitination-independent stabilization | Increases SOX9 half-life | |
| FBW7 wild-type and mutant constructs | Investigate SOX9-ubiquitin ligase interaction | Arg465, Arg479, Arg505 critical for SOX9 binding | |
| Detection Reagents | Anti-SOX9 antibodies (multiple clones) | Immunodetection in various applications | Validation essential due to specificity issues |
| CSC marker antibodies (CD44, CD133, CD117) | Flow cytometric analysis of stem cell populations | Combination markers improve specificity | |
| Cell Culture Models | Medulloblastoma stem-like cells | Study SOX9 in therapy resistance | Culture in stem cell conditions |
| Patient-derived organoids | Physiologically relevant SOX9 modeling | Preserves tumor microenvironment | |
| SOX9-knockdown/knockout lines | Determine SOX9-specific phenotypes | Use inducible systems for essential functions |
The therapeutic targeting of SOX9 represents a promising but complex frontier in precision oncology and disease treatment. The functional duality of SOX9 necessitates context-dependent approaches, with degradation strategies showing particular promise in oncology applications where SOX9 drives tumor progression [3] [36] [35]. The well-characterized ubiquitin-proteasome pathway for SOX9 regulation provides multiple entry points for therapeutic intervention, from enhancing GSK3-mediated phosphorylation to restoring FBW7 function [36] [37]. Future directions should focus on developing direct SOX9 degraders using proteolysis-targeting chimera (PROTAC) technology, which could leverage the endogenous ubiquitin-proteasome system for precise SOX9 elimination. Additionally, the tissue-specific functions of SOX9 underscore the importance of therapeutic windows that exploit differential SOX9 dependency between normal and pathological tissues [35]. As our understanding of SOX9's janus-faced biology deepens, particularly its immunomodulatory roles, increasingly sophisticated targeting strategies will emerge, offering new avenues for therapeutic intervention across the spectrum of human disease.
Leveraging SOX9 as a Predictive Biomarker for Immunotherapy
The transcription factor SOX9 (SRY-related HMG-box 9) has emerged as a critical regulator of tumor biology with complex, context-dependent roles in immunotherapy response. This technical review synthesizes current evidence establishing SOX9 as a janus-faced immunomodulator and predictive biomarker. We examine the mechanistic basis for SOX9-mediated immunotherapy resistance through regulation of immune cell infiltration, checkpoint expression, and neutrophil apoptosis, while also considering its paradoxical protective roles in specific contexts. Comprehensive experimental methodologies for SOX9 detection and functional characterization are detailed, alongside a curated research toolkit for investigating SOX9 in immuno-oncology. The data presented support the clinical translation of SOX9 assessment for patient stratification and combination therapy development.
SOX9, a transcription factor containing a highly conserved high-mobility group (HMG) domain, plays dual roles in tumor immunology, functioning as both an oncogenic driver and tumor suppressor depending on cellular context [3] [8]. This janus-faced character is particularly evident in immunotherapy responses, where SOX9 can either promote or inhibit antitumor immunity through distinct molecular pathways. The SOX9 protein contains several functional domains organized from N- to C-terminus: a dimerization domain (DIM), the HMG box domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [3]. While SOX9 is crucial for normal developmental processes including chondrogenesis and organogenesis, its dysregulation is frequently observed in multiple cancers and significantly impacts tumor-immune interactions.
Table 1: SOX9 Expression Patterns Across Cancers
| Cancer Type | SOX9 Expression | Correlation with Prognosis | Immune Correlates |
|---|---|---|---|
| Glioblastoma (GBM) | Significantly upregulated [26] [22] | Better prognosis in lymphoid invasion subgroups [26] | Correlated with immune cell infiltration and checkpoint expression [26] |
| Head and Neck Squamous Cell Carcinoma (HNSCC) | Enriched in therapy-resistant tumors [41] | Associated with resistance to anti-LAG-3 + anti-PD-1 [41] | Mediates neutrophil apoptosis via ANXA1-FPR1 axis [41] |
| Hepatocellular Carcinoma (HCC) | Overexpressed [42] [15] | Shorter RFS and OS; sorafenib resistance [42] | Promotes immunosuppressive TME [42] |
| Lung Adenocarcinoma (LUAD) | Upregulated [15] | Poorer overall survival [15] | Mutually exclusive with various immune checkpoints [26] |
| Melanoma | Downregulated [8] | Tumor suppressor role [8] | Not well characterized |
Molecular Mechanisms of SOX9 in Immunotherapy Response
SOX9 in Immune Evasion and Resistance
SOX9 promotes immunotherapy resistance through multiple interconnected mechanisms. In head and neck squamous cell carcinoma (HNSCC), single-cell RNA sequencing of tumors resistant to anti-LAG-3 plus anti-PD-1 combination therapy revealed significant enrichment of SOX9+ tumor cells [41]. These cells mediate resistance through a sophisticated mechanism wherein SOX9 directly regulates annexin A1 (ANXA1) expression, which subsequently binds to formyl peptide receptor 1 (Fpr1) on neutrophils. This ANXA1-FPR1 axis promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (Bnip3) expression, ultimately inducing neutrophil apoptosis and preventing neutrophil accumulation in tumor tissues [41]. The reduction of Fpr1+ neutrophils impairs the infiltration and cytotoxic capacity of CD8+ T and γδT cells within the tumor microenvironment, facilitating immune escape.
SOX9 and Immune Cell Infiltration
The relationship between SOX9 expression and immune cell infiltration varies across cancer types but follows recognizable patterns. In glioblastoma, high SOX9 expression correlates significantly with immune infiltration patterns and checkpoint expression, particularly in isocitrate dehydrogenase (IDH)-mutant cases [26] [22]. Bioinformatic analyses of colorectal cancer demonstrate that SOX9 expression negatively correlates with infiltration levels of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. Similarly, in other solid tumors, SOX9 overexpression typically negatively correlates with genes associated with the function of CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with memory CD4+ T cells [3]. These patterns collectively suggest that SOX9 contributes to an immunosuppressive tumor microenvironment that favors tumor progression and therapy resistance.
Context-Dependent Protective Functions
Paradoxically, SOX9 can also function as a favorable prognostic indicator in specific contexts. In glioblastoma, high SOX9 expression was remarkably associated with better prognosis in lymphoid invasion subgroups in a sample of 478 cases (P < 0.05) [26]. Furthermore, high expression of SOX9 was an independent prognostic factor for IDH-mutant glioblastoma in Cox regression analysis [26] [22]. This demonstrates the janus-faced nature of SOX9 in immuno-oncology, where its prognostic and predictive value is highly dependent on tumor type, molecular context, and immune microenvironment composition.
Diagnostic and Prognostic Applications
SOX9 as a Predictive Biomarker
The predictive capacity of SOX9 for immunotherapy response is supported by multiple clinical and preclinical studies. In hepatocellular carcinoma (HCC), patients with SOX9-positive tumors had significantly shorter recurrence-free survival (RFS) and overall survival (OS) compared to SOX9-negative patients, highlighting its prognostic value [42]. SOX9 status also predicts response to sorafenib in HCC, with SOX9-positive tumors demonstrating enhanced resistance mechanisms [42]. Pan-cancer analyses reveal that SOX9 expression is significantly increased in fifteen cancer types, including GBM, COAD, LIHC, LUAD, and PAAD, but significantly decreased in only two cancers (SKCM and TGCT) compared with matched healthy tissues, suggesting that SOX9 expression is upregulated in most cancer types (15/33) as a proto-oncogene [8].
Table 2: Prognostic Value of SOX9 Across Cancers
| Cancer Type | Prognostic Significance | Statistical Measures | Clinical Implications |
|---|---|---|---|
| Glioblastoma | Independent prognostic factor for IDH-mutant cases [26] | P < 0.05 in lymphoid invasion subgroups (n=478) [26] | Better prognosis in specific immune contexts |
| Hepatocellular Carcinoma | Shorter RFS and OS [42] | Significant in survival analysis [42] | Predictive of sorafenib resistance |
| Head and Neck Cancer | Resistance to anti-LAG-3 + anti-PD-1 [41] | 42.9% of animals resistant in vivo [41] | Biomarker for combo immunotherapy resistance |
| Lung Adenocarcinoma | Poorer overall survival [15] | Significant correlation with tumor grading [15] | Potential target for combination therapy |
| Thymoma | Short overall survival [8] | Correlated with worst OS [8] | Diagnostic and prognostic marker |
Novel Detection Methodologies
Advanced technologies are emerging for SOX9 detection, including non-invasive imaging approaches. A deep reinforcement learning (DRL) model has been developed to preoperatively and non-invasively predict SOX9 expression from CT images in HCC patients [42]. This model achieved an area under the curve (AUC) of 91.00% (95% confidence interval: 88.64-93.15%), outperforming conventional deep learning methods by over 10% [42]. The model incorporates reinforcement learning to guide attention toward regions closely associated with SOX9 expression while using only preoperative contrast-enhanced CT images, effectively reducing background noise interference and significantly improving prediction accuracy.
Experimental Protocols for SOX9 Investigation
Gene Expression Analysis
SOX9 Expression Profiling in Pan-Cancers:
- Data Sources: Utilize TCGA (The Cancer Genome Atlas) and GTEx (Genotype-Tissue Expression) databases for RNA-seq data of SOX9 expression [26] [22]. Access data through the TCGA repository (https://portal.gdc.cancer.gov/repository) and GTEx portal (https://gtexportal.org/).
- Processing: Download HTSeq-FPKM and HTSeq-Count data for samples of interest. Process using DESeq2 R package for differential expression analysis with threshold of |log fold change (logFC)| >2 and adjusted P-value (adj P-value) <0.05 [26].
- Validation: Confirm protein-level expression using western blotting of tumor tissues and adjacent normal tissues. Utilize Human Protein Atlas (HPA) (https://www.proteinatlas.org/) for transcriptomic and protein expression validation [22] [8].
- Functional Enrichment: Perform GO/KEGG analysis using ClusteProfiler package in R (version 3.14.3) with threshold of adjusted P-value <0.05 and FDR q-value <0.25 [26]. Use Metascape (https://metascape.org) for visualization of enriched biological processes, cellular components, molecular functions and KEGG pathway terms [22].
Immune Correlation Analysis
SOX9 and Immune Infiltration Assessment:
- Methodology: Apply ssGSEA (single-sample Gene Set Enrichment Analysis) and ESTIMATE algorithms using GSVA package (version 1.34.0) in R for immune infiltration correlation analysis of SOX9 [26] [22].
- Statistical Analysis: Evaluate significance using Spearman's test for correlation analyses. Use Wilcoxon rank sum test to analyze correlation between SOX9 expression and immune checkpoint expression in cancer samples [26].
- Single-Cell Analysis: For resistance mechanisms, perform single-cell RNA sequencing on resistant versus sensitive tumor tissues. Process using standard 10x Genomics pipeline. Identify malignant cells using CopyKAT algorithm to distinguish aneuploid tumor cell subpopulations [41].
- Pathway Analysis: Conduct gene set enrichment analysis (GSEA) to elucidate functional and pathway differences between high- and low-SOX9 expression groups. Permutate gene set 1,000 times for each analysis [26].
In Vivo Therapeutic Validation
Animal Model for Immunotherapy Resistance:
- Model Generation: Induce HNSCC in C57BL/6 wild-type mice by feeding with 4-nitroquinoline 1-oxide (4NQO) water for 16 weeks, followed by normal water for another 8 weeks [41].
- Treatment Protocol: Administer anti-LAG-3 (relatlimab) and anti-PD-1 (nivolumab) antibodies to tumor-bearing mice. Assess every 4 days from initial treatment.
- Resistance Classification: Define resistant tumors as those growing more than 20% larger in size compared to original size 14 days after initial treatment, according to RECIST criteria [41].
- Validation: Utilize magnetic resonance imaging (MRI) to monitor tumor growth processes. Confirm resistance mechanisms through various transgenic mouse models and immunohistochemical analysis of Ki67 and cleaved-Caspase3 [41].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 Investigation
| Reagent/Category | Specific Examples | Function/Application | Experimental Notes |
|---|---|---|---|
| SOX9 Detection Antibodies | Anti-SOX9 for IHC, IF, Western blot [43] | Protein localization and quantification | Validate knockout efficiency; co-localize with EpCAM for BEC-specific staining [43] |
| Immune Cell Markers | Anti-EpCAM (BECs), CD8, CD4, Fpr1 (neutrophils) [43] [41] | Immune cell identification and quantification | Use for co-localization studies and immune infiltration analysis |
| Apoptosis Assays | Cleaved caspase-3 staining [41] | Detection of apoptotic cells | Critical for evaluating neutrophil apoptosis in resistance models |
| Animal Models | Sox9-floxed mice (Albumin-Cre), 4NQO-induced HNSCC model [43] [41] | In vivo functional studies | Confirm recombination efficiency; monitor for cyst development in aged models [43] |
| Therapeutic Antibodies | Anti-PD-1, anti-LAG-3 [41] | Immunotherapy treatment studies | Use combination therapy to evaluate resistance mechanisms |
| Computational Tools | DESeq2, GSVA, ClusteProfiler R packages [26] | Bioinformatics analysis | Implement reinforcement learning for CT image analysis [42] |
| Pathway Modulators | Activin A inhibitors, Cordycepin [43] [8] | Mechanistic studies | Cordycepin inhibits SOX9 in dose-dependent manner [8] |
SOX9 represents a promising yet complex predictive biomarker for immunotherapy response, characterized by its janus-faced functionality in different tumor contexts. The mechanistic insights into SOX9-mediated therapy resistance, particularly through the ANXA1-FPR1 neutrophil axis in HNSCC, provide compelling rationale for its clinical development as a biomarker. The emergence of novel detection methodologies, including non-invasive deep learning approaches for SOX9 assessment from standard CT images, offers exciting opportunities for clinical translation.
Future research should focus on validating SOX9 cutoff values for patient stratification across different cancer types, developing standardized detection assays, and exploring SOX9-targeted combination therapies to overcome immunotherapy resistance. The integration of SOX9 status with existing biomarkers such as PD-L1 expression, tumor mutational burden, and immune cell infiltration signatures will likely enhance predictive accuracy. As our understanding of SOX9's dual roles in tumor immunology continues to evolve, this transcription factor promises to become an increasingly valuable component of precision immuno-oncology.
Navigating SOX9 Complexity: Context-Dependent Effects and Therapeutic Challenges
The transcription factor SOX9 (SRY-related HMG-box 9) exemplifies the paradigm of context-dependent functionality in biological systems. As a pivotal regulator with dualistic functions, SOX9 demonstrates remarkable capacity to drive both reparative regeneration and pathological fibrosis across diverse organ systems. This dichotomous nature presents a significant challenge for therapeutic targeting, as SOX9 operates within a delicate balance influenced by cellular microenvironment, injury context, and signaling dynamics. Emerging evidence positions SOX9 as a master regulator of cell fate whose activity must be precisely tuned to achieve therapeutic benefit without adverse pathological consequences. In organ systems ranging from kidney and liver to retina and pancreas, SOX9 activation can promote either functional tissue restoration or progressive scar formation, depending on the duration, intensity, and spatial organization of its expression [44] [45]. Understanding the molecular determinants of these divergent outcomes represents a critical frontier in molecular immunology and regenerative medicine, with profound implications for drug development targeting fibrotic disorders, degenerative diseases, and cancer.
SOX9 in Organ Fibrosis: Mechanisms and Pathways
Pro-Fibrotic Roles Across Organ Systems
SOX9 drives fibrosis through multiple conserved mechanisms involving extracellular matrix (ECM) remodeling, fibroblast activation, and epithelial-mesenchymal crosstalk. The pro-fibrotic functions of SOX9 manifest across virtually all major organ systems, with particularly well-characterized roles in kidney, liver, lung, and tracheal fibrosis [44] [46].
In renal fibrosis, SOX9 activation in injured proximal tubular epithelial cells serves as a key determinant of progressive scarring. Following acute kidney injury, a dynamic SOX9/CDH6 switch governs the transition from regeneration to fibrosis at the single-cell level. Tubular lineages that successfully regenerate epithelia demonstrate transient SOX9 activation (SOX9on-off), whereas lineages with unrestored apicobasolateral polarity maintain persistent SOX9 activity (SOX9on-on) and acquire Cadherin-6 (CDH6) expression [45]. These SOX9on-on CDH6pos cells generate single-cell WNT activity that drives a fibroproliferative response in adjacent fibroblasts, effectively orchestrating the transition from acute injury to chronic kidney disease [45]. This mechanism has been validated in human transplanted kidneys, confirming its clinical relevance.
In tracheal fibrosis, SOX9 drives fibroblast activation and ECM deposition through direct regulation of matrix metalloproteinase MMP10 via the Wnt/β-catenin signaling pathway [46]. Experimental manipulation demonstrates that SOX9 overexpression activates fibroblasts and promotes ECM deposition, while SOX9 silencing inhibits cell proliferation, migration, and ECM deposition, induces G2 arrest, and increases apoptosis in tracheal fibroblast cells [46]. The identification of this SOX9–MMP10–ECM biosynthesis axis reveals a direct mechanistic link between SOX9 and matrix remodeling in fibrotic contexts.
Table 1: SOX9-Mediated Fibrotic Pathways Across Organ Systems
| Organ System | Key Fibrotic Mechanisms | Signaling Pathways | Functional Outcomes |
|---|---|---|---|
| Kidney | SOX9on-on/CDH6+ cell state persistence; Single-cell WNT signaling to fibroblasts | Wnt/β-catenin | AKI to CKD progression; Tubular atrophy; Interstitial fibrosis |
| Liver | Hepatic stellate cell activation; ECM component upregulation | TGF-β; MAPK | Cirrhosis; Portal hypertension; Liver failure |
| Lung | Fibroblast-to-myofibroblast transition; Collagen deposition | TGF-β/Smad; ERK1/2 | Pulmonary fibrosis; Impaired gas exchange |
| Trachea | SOX9-MMP10-ECM biosynthesis axis; Fibroblast proliferation | Wnt/β-catenin; TGF-β | Tracheal stenosis; Airway obstruction |
| Heart | Cardiac fibroblast activation; Excessive collagen production | TGF-β; PKA | Myocardial stiffness; Diastolic dysfunction |
Molecular Regulation of SOX9 Activity
SOX9 function is regulated through multiple molecular mechanisms including post-translational modifications, epigenetic regulation, and intricate cross-talk with key signaling pathways. The canonical Wnt/β-catenin pathway exhibits particularly complex bidirectional regulation with SOX9, creating context-dependent feedback loops that influence both developmental and pathological processes [47].
SOX9 can antagonize Wnt signaling through several mechanisms: (1) promoting ubiquitination/proteasome-dependent degradation of β-catenin via direct binding with its C-terminus; (2) inducing lysosomal breakdown of β-catenin; (3) activating mastermind-like transcriptional coactivator 2 (MAML2)-related β-catenin turnover; and (4) reducing nuclear translocation of β-catenin [47]. Additionally, SOX9 competes with TCF/LEF factors for binding to β-catenin's ARM repeats, thereby preventing formation of the β-catenin-TCF/LEF complex and inhibiting transcription of Wnt target genes [47].
Post-translational modifications significantly modulate SOX9 activity. Phosphorylation at serine residues S64 and S181 by extracellular signal-regulated kinases 1 and 2 (ERK1/2) or cAMP-dependent protein kinase A (PKA) enhances SOX9's nuclear localization and transcriptional activity [44]. Epigenetic regulation through DNA methylation of the SOX9 promoter represents another key control mechanism, with differential methylation patterns observed in various cancers and pathological states [44].
Table 2: SOX9 Expression and Functional Regulation by Signaling Pathways
| Regulatory Signal | Pathway | Effect on SOX9 | Biological Context |
|---|---|---|---|
| TSH | cAMP/PKA/CREB | Transcriptional upregulation | Thyroid differentiation and function |
| TGF-β | Smad3 | Inhibition of TSH-induced expression | Thyroid follicular cells |
| FGF | MAPK | Increased mRNA expression | Mesenchymal cells and chondrocytes |
| IL-1β | NF-κB | Decreased promoter activity | Inflammation |
| Sublytic C5b-9 | ERK1/2 | Phosphorylation at S64, S181 | Cell injury and complement activation |
| β-catenin | Wnt | Mutual antagonism | Stem cell homeostasis; Cancer |
SOX9 in Tissue Regeneration and Repair
Regenerative Functions in Adult Tissues
Beyond its pro-fibrotic roles, SOX9 serves critical functions in tissue homeostasis, stem cell maintenance, and regenerative repair across multiple organ systems. In the adult mouse eye, SOX9 is essential for preventing retinal degeneration and maintaining limbal stem cell function. Conditional deletion of SOX9 in adult mice triggers severe retinal degeneration characterized by loss of Müller glial cells and complete depletion of the photoreceptor layer [48] [11]. Additionally, SOX9 expression in a basal limbal stem cell population is required for generating long-lived clones that maintain corneal epithelial homeostasis, with mosaic analysis confirming that SOX9 is essential for proper limbal stem cell differentiation [11].
In pancreatic beta cells, SOX9 maintains functional integrity through a novel mechanism involving regulation of alternative splicing. SOX9 depletion disrupts splicing patterns and reduces expression of protein-coding splice variants of serine-rich splicing factor SRSF5, leading to impaired insulin secretion without affecting beta cell identity markers [49]. This represents a non-canonical function for SOX9 beyond its established role as a transcription factor, expanding its functional repertoire in cellular homeostasis.
The thyroid gland demonstrates SOX9's role in maintaining differentiated function, where it is regulated by crosstalk between TSH, TGFβ, and thyroid transcription factors. TSH stimulates SOX9 expression via the cAMP/PKA pathway through CREB binding to a CRE site in the SOX9 promoter, while TGFβ signals through Smad proteins to inhibit TSH-induced SOX9 transcription [50]. SOX9 subsequently increases transcriptional activation of Pax8 and Foxe1 promoters, establishing its position within the thyroid transcription factor network [50].
The SOX9 Switch: Regeneration Versus Fibrosis
The decision between regenerative and fibrotic outcomes hinges on a dynamic SOX9 activity switch that senses epithelial repair status. Following kidney injury, SOX9 activation in damaged proximal tubular epithelial cells initiates a repair program. Successful regeneration is characterized by transient SOX9 activation (SOX9on-off), with silencing occurring upon restoration of apicobasolateral polarity [45]. In contrast, persistently injured epithelia maintain SOX9 activity (SOX9on-on) and acquire CDH6 expression, adopting a reprogrammed cell state that generates paracrine WNT signals to stimulate adjacent fibroblasts [45].
This single-cell decision mechanism explains the spatial heterogeneity of fibrosis observed within the same injured tissue microenvironment. The SOX9on-on CDH6pos cell state represents a "sensor" of epithelial repair status, with its activity determining whether regeneration occurs with or without fibrosis. Similar dynamics are observed across injury models, including ischemia-reperfusion injury and rhabdomyolysis-induced AKI, confirming the generalizability of this mechanism [45].
Experimental Approaches and Methodologies
Key Experimental Models and Workflows
Investigation of SOX9's context-dependent functions employs sophisticated genetic models and single-cell technologies. Lineage tracing approaches using Sox9IRES-CreERT2/+: R26RtdT/+ animals enable fate mapping of injury-induced SOX9+ cells, allowing precise tracking of their progeny and identification of divergent regenerative and fibrotic lineages [45]. This model system, combined with bilateral ischemia reperfusion injury, has been instrumental in elucidating the SOX9/CDH6 switch mechanism in kidney fibrosis.
For retinal studies, tamoxifen-inducible Cre/LoxP systems with CAGG-CreERT recombinase and conditional Sox9flox/flox alleles enable temporal control of SOX9 deletion in adult mice, bypassing developmental requirements and specifically addressing SOX9's role in tissue maintenance [48] [11]. This approach revealed SOX9's essential function in preventing retinal degeneration and maintaining Müller glial cells.
In cancer research, multiomics approaches combining bulk and single-cell sequencing with epigenetic modulation have identified SOX9 as a key chemo-induced driver of chemoresistance in high-grade serous ovarian cancer [13]. SOX9 upregulation induces a stem-like transcriptional state and significant platinum resistance, demonstrating its role in cancer cell plasticity and therapy resistance.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating SOX9 Function
| Reagent/Tool | Function/Application | Experimental Utility |
|---|---|---|
| Sox9IRES-CreERT2/+: R26RtdT/+ mice | Lineage tracing of SOX9+ cells | Fate mapping of injury-induced SOX9 lineages; Identification of SOX9on-off vs SOX9on-on trajectories |
| Conditional Sox9flox/flox alleles | Tissue-specific and temporal SOX9 deletion | Dissection of SOX9 function in specific cell types and adult tissues without developmental compensation |
| CAGG-CreERT recombinase | Ubiquitous inducible Cre activity | Widespread SOX9 deletion in adult tissues; Analysis of SOX9 requirements in tissue homeostasis |
| Ad-SOX9 (SOX9 overexpression adenovirus) | SOX9 gain-of-function | Investigation of SOX9 effects on fibroblast activation, ECM deposition, and target gene regulation |
| SOX9-targeting siRNA/shRNA | SOX9 loss-of-function | Analysis of SOX9 requirement in specific cell types; Identification of SOX9-dependent processes |
| SOX9-Luc promoter constructs | Reporter assays | Analysis of SOX9 transcriptional regulation; Identification of signaling pathways controlling SOX9 expression |
| Anti-SOX9 antibodies (validated) | Immunodetection | Protein localization and expression analysis across tissues and cell types |
| scRNA-seq platforms | Single-cell transcriptomics | Identification of SOX9+ cell states; Characterization of heterogeneous SOX9 lineages |
Signaling Pathways and Molecular Interactions
Diagram 1: SOX9 Regulation and Context-Dependent Functional Outcomes. SOX9 integrates multiple external signals through specific signaling pathways, resulting in context-dependent outcomes including tissue regeneration, fibrosis, or cancer progression. The antagonistic relationship with Wnt/β-catenin signaling creates important regulatory feedback. PTMs = Post-Translational Modifications.
Therapeutic Implications and Future Directions
The dualistic nature of SOX9 presents both challenges and opportunities for therapeutic intervention. Successful targeting will require context-specific strategies that consider temporal dynamics, cellular microenvironment, and organ-specific functions. Several promising approaches emerge from current research:
First, modulating the duration rather than complete inhibition of SOX9 activity may yield superior outcomes. Therapeutic strategies that promote the SOX9on-off transition in injured tissues could enhance regeneration while preventing fibrosis, essentially "harnessing" SOX9's reparative capacity without triggering pathological scarring [45]. Small molecule inhibitors that disrupt SOX9 interactions with fibrotic mediators while preserving its regenerative functions represent an attractive drug development avenue.
Second, targeting SOX9 downstream effectors rather than SOX9 itself may provide greater specificity. In tracheal fibrosis, the SOX9–MMP10–ECM biosynthesis axis offers multiple potential intervention points [46]. Similarly, in renal fibrosis, disrupting the paracrine WNT signaling from SOX9on-on CDH6pos cells to fibroblasts could prevent fibrosis while preserving epithelial repair mechanisms [45].
Third, SOX9-based diagnostic and prognostic applications are emerging, particularly in oncology. In glioblastoma, SOX9 expression serves as a diagnostic and prognostic indicator, with high expression associated with distinct molecular subtypes and immune infiltration patterns [26]. Similarly, in ovarian cancer, SOX9 expression correlates with chemoresistance and poor survival, suggesting its potential as a biomarker for treatment selection [13].
Future research should prioritize elucidating the epigenetic and post-translational control mechanisms that determine SOX9's context-dependent functions, developing more precise tools for temporal and spatial control of SOX9 activity, and validating therapeutic concepts in human model systems. The integration of single-cell multi-omics across diverse injury and disease contexts will further refine our understanding of SOX9's Janus-faced biology and accelerate translation to clinical applications.
The transcription factor SOX9 (SRY-box transcription factor 9) exemplifies a paradigm of functional duality in immunology and cancer biology, acting as a true "Janus-faced" regulator. While critically required for normal development, organogenesis, and tissue homeostasis, SOX9 becomes dysregulated in numerous malignancies, where it can exert either oncogenic or tumor-suppressive effects depending on tissue context [3] [51]. This review focuses on its emerging role as a master regulator of the tumor immune microenvironment, particularly its capacity to drive the formation of "immune cold" tumors—characterized by minimal T cell infiltration and poor response to immunotherapy.
SOX9's structural composition underpins its functional complexity. The protein contains several functional domains: a dimerization domain (DIM), the high mobility group (HMG) box DNA-binding domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [3]. The HMG domain facilitates nuclear localization and sequence-specific DNA binding, while the transcriptional activation domains interact with various cofactors to regulate target gene expression. This modular structure enables SOX9 to participate in diverse transcriptional programs across different biological contexts.
In the landscape of cancer immunology, SOX9 has emerged as a key mediator of immunosuppression. Pan-cancer analyses reveal that SOX9 is significantly upregulated in 15 of 33 cancer types, including cervical (CESC), colorectal (COAD), lung (LUAD), and liver (LIHC) cancers, where its expression often correlates with poor survival outcomes [8]. Conversely, SOX9 demonstrates tumor-suppressive functions in specific contexts such as melanoma and certain cervical cancers [52] [8]. This review will dissect the mechanisms through which SOX9 creates immunosuppressive tumor microenvironments and outline strategic approaches to counteract its immunosuppressive functions, with the goal of converting immune cold tumors into immune hot, therapy-responsive lesions.
Mechanisms of SOX9-Mediated Immunosuppression
Regulation of Immune Cell Infiltration and Function
SOX9 orchestrates a comprehensive immunosuppressive program primarily through modulating immune cell infiltration and functional states within the tumor microenvironment. In lung adenocarcinoma (LUAD), SOX9 expression creates an "immune cold" condition by significantly reducing the infiltration and anti-tumor activity of critical immune populations, including CD8+ T cells, natural killer (NK) cells, and dendritic cells [17] [53]. This exclusion of cytotoxic lymphocytes establishes a permissive environment for tumor growth and metastasis.
The mechanisms underlying this immune cell exclusion involve SOX9-mediated regulation of the extracellular matrix. Research demonstrates that SOX9 significantly elevates collagen-related gene expression and increases collagen fiber deposition in tumors [17]. This enhanced stromal fibrosis creates a physical barrier that imped immune cell penetration into the tumor core. Additionally, SOX9 suppresses the expression of chemokines and other recruitment signals necessary for effective immune trafficking, further contributing to the immune cold phenotype.
Beyond physical exclusion, SOX9 actively manipulates immune cell functionality. Transcriptional analyses reveal that SOX9 overexpression negatively correlates with genes associated with the effector functions of CD8+ T cells, NK cells, and M1 macrophages [3]. In head and neck squamous cell carcinoma (HNSCC) models, SOX9+ tumor cells drive resistance to combined anti-LAG-3 and anti-PD-1 immunotherapy by regulating the annexin A1 (Anxa1)/formyl peptide receptor 1 (Fpr1) axis [54]. This pathway mediates apoptosis of Fpr1+ neutrophils, which in turn impairs the infiltration and tumor-killing capacity of cytotoxic CD8+ T and γδ T cells within the tumor microenvironment.
Table 1: SO9-Mediated Effects on Different Immune Cell Populations
| Immune Cell Type | Effect of SOX9 | Proposed Mechanism | Functional Consequence |
|---|---|---|---|
| CD8+ T Cells | Reduced infiltration & function | Collagen deposition; Chemokine suppression | Impaired tumor cell killing |
| Natural Killer (NK) Cells | Suppressed activity | Inhibition of activation signals | Reduced innate anti-tumor immunity |
| Dendritic Cells | Decreased abundance & function | Altered differentiation | Impaired antigen presentation |
| Neutrophils | Increased apoptosis (Fpr1+) | ANXA1-FPR1 axis activation | Loss of cytotoxic lymphocyte support |
| Macrophages | Polarization toward M2 phenotype | Transcriptional reprogramming | Immunosuppressive TME |
Induction of Immunosuppressive Signaling Pathways
SOX9 engages multiple molecular pathways to establish immunosuppression, with recent research illuminating the ANXA1-FPR1 axis as a critical mechanism in therapy resistance. In HNSCC models resistant to anti-LAG3 plus anti-PD1 combination therapy, SOX9 directly regulates the expression of annexin A1 (ANXA1), which subsequently binds to formyl peptide receptor 1 (FPR1) on neutrophils [54]. This interaction promotes mitochondrial fission and inhibits mitophagy by downregulating BCL2/adenovirus E1B interacting protein 3 (BNIP3) expression, ultimately leading to neutrophil apoptosis. The reduction of FPR1+ neutrophils diminishes the cytotoxic activity of CD8+ T and γδT cells, enabling tumors to evade immune destruction.
Simultaneously, SOX9 contributes to the maintenance of cancer stem cell (CSC) properties, which are intrinsically associated with immune evasion. CSCs characterized by high SOX9 expression can manipulate their microenvironment by releasing immunosuppressive cytokines that attract regulatory immune cells such as myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs) [55]. Furthermore, SOX9+ CSCs often exhibit reduced major histocompatibility complex (MHC) molecule expression, limiting their visibility to the adaptive immune system and facilitating immune escape.
Diagram 1: SOX9-Driven Immunosuppressive Pathways. This diagram illustrates the key molecular mechanisms through which SOX9 creates an immune cold tumor microenvironment, including the ANXA1-FPR1 axis leading to neutrophil apoptosis and collagen-mediated T-cell exclusion.
Experimental Models: Elucidating SOX9 Function in Immunosuppression
In Vivo Models and Key Findings
Animal models have been instrumental in defining SOX9's role in tumor immunity and immunotherapy resistance. In KRAS-driven lung adenocarcinoma models, Sox9 knockout significantly delayed tumor formation and progression while prolonging overall survival [17]. Strikingly, the pro-tumor effects of SOX9 were significantly attenuated in immunocompromised mice compared to syngeneic immunocompetent hosts, indicating that SOX9-driven tumor growth is partially dependent on its immunomodulatory functions [17].
Transgenic mouse models have further illuminated SOX9's role in therapy resistance. In HNSCC models, Sox9+ tumor cells were significantly enriched in tumors resistant to anti-LAG-3 plus anti-PD-1 combination therapy [54]. Utilizing various transgenic models, researchers demonstrated that ablation of the Anxa1-Fpr1 axis could restore therapeutic efficacy, providing direct mechanistic insight into SOX9-mediated immunotherapy resistance.
Xenograft studies using cervical cancer cell lines have reinforced the context-dependent nature of SOX9 function. SOX9 overexpression in SiHa and C33A cervical carcinoma cells inhibited tumor growth, whereas SOX9 silencing in HeLa cells promoted tumor formation [52]. These findings highlight the tissue-specific duality of SOX9 function and underscore the importance of context-dependent investigation.
Table 2: Key In Vivo Findings on SOX9 in Tumor Immunity
| Cancer Type | Model System | Key Findings | Reference |
|---|---|---|---|
| Lung Adenocarcinoma | KrasG12D; Sox9 knockout mice | Sox9 loss reduced tumor burden, suppressed progression, increased immune cell infiltration | [17] |
| Head & Neck SCC | Immunocompetent mouse model | Sox9+ cells enriched in anti-LAG3/PD-1 resistant tumors via ANXA1-FPR1 axis | [54] |
| Cervical Cancer | Xenograft (SiHa, C33A, HeLa) | Context-dependent effects: tumor suppressor in some lines, promoter in others | [52] |
| Multiple Cancers | Syngeneic vs. immunocompromised hosts | SOX9 tumor-promoting effects diminished in immunodeficient mice | [17] |
Methodological Approaches for Investigating SOX9 Function
Genetic Manipulation of SOX9 Expression
CRISPR/Cas9-Mediated Knockout: For in vivo Sox9 knockout in the KrasG12D-driven LUAD model, researchers employed a pSECC CRISPR system combining Cre recombinase with guide RNAs targeting Sox9 [17]. The experimental workflow involved:
- Design and validation of three guide RNAs targeting mouse Sox9
- Intratracheal delivery of sgSox9.2-pSECC or control sgTom-pSECC
- Tumor monitoring at 18, 24, and 30 weeks post-infection
- Assessment of tumor number, burden, and grade distribution This approach demonstrated that Sox9 knockout significantly reduced both tumor number and burden while suppressing progression to high-grade lesions.
Lentiviral Overexpression and Knockdown: Gain-of-function and loss-of-function studies in cell lines typically utilize lentiviral systems:
- Overexpression: Full-length human SOX9 cDNA cloned into lentiviral expression vectors, followed by transduction and selection
- Knockdown: shRNA constructs targeting specific SOX9 sequences or siRNA for transient knockdown For example, in cervical cancer studies, SOX9 was stably overexpressed in SiHa and C33A cells (low endogenous SOX9) and knocked down in HeLa cells (high endogenous SOX9) [52]. Functional assays included growth curves, MTT assays, and cell cycle analysis by FACS, revealing that SOX9 inhibited proliferation by blocking G1/S transition through p21 transactivation.
Immune Monitoring and Characterization
Comprehensive immune profiling is essential for evaluating SOX9's immunomodulatory effects. Standardized approaches include:
- Flow Cytometry: Quantification of immune cell populations (CD45+ leukocytes, CD3+ T cells, CD8+ cytotoxic T cells, CD4+ helper T cells, NK cells, neutrophils, macrophages) in dissociated tumors
- Immunohistochemistry/Iimmunofluorescence: Spatial analysis of SOX9 expression alongside immune markers (CD8, CD4, NKp46, IBA1 for macrophages) and functional markers (Ki67 for proliferation)
- Cytokine/Chemokine Profiling: Multiplex ELISA or Luminex assays to quantify soluble mediators in tumor homogenates or conditioned media
- RNA Sequencing: Bulk and single-cell transcriptomics to identify SOX9-regulated genes and pathways in tumor and stromal compartments
Therapeutic Strategies to Counteract SOX9-Mediated Immunosuppression
Direct and Indirect SOX9 Targeting Approaches
Small Molecule Inhibitors
While direct targeting of transcription factors remains challenging, several indirect strategies show promise. Cordycepin, an adenosine analog derived from Cordyceps sinensis, demonstrates dose-dependent inhibition of SOX9 expression in prostate cancer (22RV1, PC3) and lung cancer (H1975) cell lines [8]. Treatment with 10-40 μM cordycepin for 24 hours significantly reduced both SOX9 protein and mRNA levels, suggesting its potential as a SOX9-targeting therapeutic. The molecular mechanisms likely involve modulation of the AMPK signaling pathway, although precise molecular targets require further elucidation.
Immunotherapy Combinations
Strategic immunotherapy combinations may overcome SOX9-mediated resistance. Although SOX9+ tumors resist anti-LAG-3 plus anti-PD-1 therapy, targeting the downstream ANXA1-FPR1 axis could restore sensitivity [54]. Potential approaches include:
- ANXA1-neutralizing antibodies to prevent neutrophil apoptosis
- FPR1 antagonists to maintain protective neutrophil populations
- BNIP3 inducers to counteract SOX9-mediated mitophagy inhibition
Additionally, therapies targeting cancer stem cells may eliminate the SOX9+ subpopulation responsible for therapy resistance and immune evasion. Development of CSC-directed CAR-T cells or dendritic cell vaccines could complement existing immunotherapies to address tumor heterogeneity and plasticity.
Biomarker Development and Patient Stratification
The development of robust SOX9 biomarkers is crucial for patient selection and therapeutic monitoring. Potential applications include:
- Immunohistochemical staining for SOX9 protein in tumor biopsies to identify high-risk patients
- Gene expression signatures reflecting SOX9 activity and associated immunosuppressive pathways
- Liquid biopsy approaches detecting SOX9+ circulating tumor cells or SOX9-related gene expression patterns
Retrospective analysis of immunotherapy trial datasets should evaluate whether SOX9 expression predicts resistance to immune checkpoint inhibitors, potentially guiding treatment selection [53]. Patients with SOX9-high tumors might benefit from SOX9-directed therapies alongside standard immunotherapies.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating SOX9 in Cancer Immunology
| Reagent Category | Specific Examples | Application/Function | Research Context |
|---|---|---|---|
| Cell Lines | SiHa, C33A (cervical cancer, low SOX9); HeLa (cervical cancer, high SOX9); mTC11, mTC14 (KrasG12D mouse LUAD) | In vitro modeling of SOX9 gain/loss-of-function | [52] [17] |
| Animal Models | KrasLSL-G12D; Sox9flox/flox GEMM; Immunocompetent HNSCC models; Syngeneic graft models | In vivo study of SOX9 in tumor immunity and therapy response | [17] [54] |
| Genetic Tools | pSECC CRISPR/Cas9 system (sgSox9); Lentiviral Cre; SOX9 overexpression constructs; SOX9 shRNA/siRNA | Precise genetic manipulation of SOX9 expression | [52] [17] |
| Antibodies | Anti-SOX9 (IHC, WB, flow); Anti-Ki67 (proliferation); Anti-CD8, CD4, NKp46 (immune cell staining) | Detection and quantification of SOX9 and immune markers | [52] [17] |
| Small Molecules | Cordycepin (SOX9 inhibitor); Potential ANXA1-FPR1 axis modulators | Pharmacological targeting of SOX9 pathway | [8] [54] |
SOX9 represents a pivotal node in the network of tumor-immune interactions, serving as both a key driver of immunosuppression and a promising therapeutic target. Its Janus-faced nature across different cancer types underscores the complexity of its biological functions and the need for context-specific therapeutic approaches. The mechanistic insights gained from recent studies—particularly regarding SOX9's role in regulating immune cell infiltration, function, and therapy resistance—provide a solid foundation for developing novel combinatorial strategies.
Future research should prioritize the identification of direct SOX9 inhibitors through high-throughput compound screening and structure-based drug design. Additionally, clinical validation of SOX9 as a predictive biomarker for immunotherapy response could enable better patient stratification. The development of therapies targeting SOX9-positive cancer stem cells may be particularly important for preventing tumor recurrence and addressing therapeutic resistance.
As our understanding of SOX9's immunoregulatory functions deepens, so too will our ability to therapeutically modulate this pathway to overcome immunosuppression in cold tumors. By integrating SOX9-targeting approaches with established immunotherapies, we may ultimately convert immune cold tumors into immune hot, therapy-responsive lesions, significantly improving outcomes for cancer patients.
Addressing Technical Hurdles in Targeting Transcription Factors
The transcription factor SOX9 exemplifies the "Janus-faced" regulatory paradox prevalent in immunology and cancer biology. It functions as a critical cell fate determiner during development and a stem cell regulator in adult tissues, yet its dysregulation is implicated in fibrosis, cancer progression, and immune evasion [1]. This dual nature creates significant technical challenges for therapeutic targeting. While SOX9 inhibition may counteract tumor immune escape, it could simultaneously disrupt its essential tissue-reparative functions, such as cartilage formation and macrophage-mediated repair [3]. This review dissects the specific technical hurdles in targeting SOX9 and outlines advanced methodological frameworks to overcome them, providing a strategic guide for researchers and drug development professionals working at the intersection of transcription factor biology and immunology.
Molecular Characterization of SOX9
Structural Domains and Functional Motifs
SOX9 contains several functionally critical domains that represent potential targeting interfaces but also contribute to its technical elusiveness. The High Mobility Group (HMG) box domain facilitates DNA binding and nuclear localization via embedded nuclear localization (NLS) and export (NES) signals [3]. Flanking this are a dimerization domain (DIM) and two transcriptional activation domains—one central (TAM) and one at the C-terminus (TAC) [3]. The C-terminal TAC interacts with cofactors like Tip60 to enhance transcriptional activity and is essential for β-catenin inhibition during chondrocyte differentiation [3]. A proline/glutamine/alanine (PQA)-rich domain is also necessary for transcriptional activation [3].
Table 1: Key Functional Domains of SOX9 Protein
| Domain | Position | Key Functions | Targeting Challenges |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates self-dimerization and partner factor interaction | Protein-protein interface is large and often lacks deep pockets for small molecules |
| HMG Box | Central | DNA binding, nuclear localization, sequence-specific recognition | Direct DNA binding inhibition risks genomic instability and off-target effects |
| Central Transcriptional Activation Domain (TAM) | Middle | Synergizes with TAC to augment transcriptional potential | Intrinsically disordered region difficult to target with conventional compounds |
| C-terminal Transcriptional Activation Domain (TAC) | C-terminal | Interacts with cofactors (Tip60), inhibits β-catenin | Context-dependent cofactor recruitment complicates predictable inhibition |
| PQA-rich Domain | C-terminal | Transcriptional activation | Redundant functions within SoxE subgroup complicate specific targeting |
Context-Dependent Regulation and Activity
SOX9 exhibits remarkable functional plasticity governed by post-transcriptional modifications and partner factor interactions. Phosphorylation by protein kinase A (PKA) enhances its DNA-binding affinity and drives nuclear translocation [1]. SUMOylation exerts context-dependent effects, sometimes enhancing (e.g., on Col2a1 reporter) and other times repressing SOX9 transcriptional activity [1]. The ubiquitin-proteasome pathway degrades SOX9 in hypertrophic chondrocytes, adding another regulatory layer [1]. MicroRNAs including those active in lung development, chondrogenesis, and neurogenesis further fine-tune SOX9 expression [1]. Critically, SOX9 generally requires partnership with other transcription factors (e.g., Sf1 in gonad development) to form functional complexes that recognize composite DNA elements, with the specific partner determining whether SOX9 activates or represses target genes [1].
Technical Hurdles in SOX9 Targeting
Functional Redundancy and Specificity Challenges
A primary technical obstacle stems from functional redundancy within the SOX family, particularly the SoxE subgroup (SOX8, SOX9, SOX10). Knockout studies reveal that single SOX9 deletion often produces milder phenotypes than double or triple SoxE mutants, indicating substantial functional overlap [1]. For instance, while individual Sox9 or Sox10 deletion preserves oligodendrocyte formation, their combined deletion causes widespread apoptosis [1]. This redundancy complicates therapeutic targeting, as inhibiting SOX9 alone may yield limited efficacy due to compensation by SOX8 or SOX10. However, the temporal and quantitative expression differences between subgroup members create windows of opportunity for specific targeting [1].
Direct Targeting Limitations
The structural characteristics of SOX9 present fundamental pharmacological challenges. The DNA-binding HMG domain engages in extensive protein-DNA interfaces that are notoriously difficult to disrupt with small molecules without affecting global genomic integrity. Protein-protein interactions involving SOX9, particularly with partner factors, occur across large, relatively flat surfaces that typically lack deep pockets for high-affinity small-molecule binding [1]. Furthermore, SOX9's transcriptional activation domains often exist as intrinsically disordered regions, defying conventional structure-based drug design approaches that require well-defined binding pockets.
Dual Immunological Roles Complicate Therapeutic Strategy
SOX9 exhibits clinically challenging "Janus-faced" behavior in immunomodulation. In cancer contexts, SOX9 promotes immune escape by impairing immune cell function—it negatively correlates with infiltration of B cells, CD8+ T cells, NK cells, and M1 macrophages while positively correlating with neutrophils, M2 macrophages, and Tregs [3]. This establishes SOX9 as a potential immunosuppressive target. Conversely, SOX9 maintains macrophage function supporting cartilage formation, tissue regeneration, and repair [3]. This duality creates a significant therapeutic dilemma: systemic SOX9 inhibition might counteract tumor immune evasion but simultaneously compromise tissue homeostasis and repair mechanisms, particularly in cartilage and stem cell niches.
Experimental Frameworks for SOX9 Research
Mapping Regulated Target Genes
Accurately identifying direct regulatory targets represents a foundational challenge in SOX9 research. The ART-TF (Atlas of Regulated Target Genes) methodology combines ChIP-seq binding data with gene expression changes following TF perturbation to delineate "regulated target genes" [56]. This approach distinguishes genuine regulatory relationships from non-functional binding events, with statistical methods like the Expected Proportion of False Positives (EPFP) threshold controlling for false positives [56].
Table 2: Experimental Approaches for Identifying SOX9 Target Genes
| Method | Principle | Key Output | Advantages | Limitations |
|---|---|---|---|---|
| ChIP-seq | Immunoprecipitation of crosslinked chromatin with SOX9 antibodies | Genome-wide binding sites | Identifies direct physical binding; high resolution | Does not distinguish functional from non-functional binding |
| Perturbation RNA-seq | RNA sequencing after SOX9 knockout/knockdown | Differentially expressed genes following SOX9 manipulation | Reveals functional consequences of SOX9 loss | Indirect effects and compensatory mechanisms may confound results |
| Motif Analysis | Bioinformatics scanning for SOX9 consensus binding motifs | Predicted binding sites based on sequence | Can predict binding potential genome-wide | High false positive rate; does not reflect cellular context |
| Integrated Approach (ART-TF) | Combines ChIP-seq and perturbation data | Statistically validated regulated target genes | Controlled false positive rate; identifies functional binding | Computationally intensive; requires multiple datasets |
The integration of promoter and enhancer binding information significantly enhances target gene identification. Most human TFs (82.1%) regulate targets primarily via enhancer binding, with repression more frequently mediated through promoter binding than activation [56]. Analyzing enhancer-promoter loops is particularly important for strong activator and repressor TFs like SOX9.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagent Solutions for SOX9 Investigation
| Reagent Category | Specific Examples | Experimental Function | Considerations |
|---|---|---|---|
| ChIP-grade Antibodies | Validated SOX9 antibodies for chromatin immunoprecipitation | Mapping genome-wide SOX9 binding sites | Specificity validation critical through knockout controls |
| Perturbation Tools | CRISPR/Cas9 guides, siRNA/shRNA constructs, inducible expression systems | Manipulating SOX9 expression levels | Inducible systems allow temporal control to study immediate effects |
| Bioinformatics Databases | TFTG, ART-TF, CistromeDB, KnockTF, TRRUST | Accessing curated SOX9 target genes and regulatory networks | TFTG integrates multiple identification strategies [57] |
| Pathway Reporters | Col2a1, Col10a1 reporter constructs | Monitoring SOX9 transcriptional activity | Context-dependent responses require multiple reporter systems |
| Animal Models | Tissue-specific Sox9 knockout mice, campomelic dysplasia models | Studying SOX9 function in development and disease | Functional redundancy may require compound SoxE knockouts |
Visualization of SOX9 Regulatory Networks
SOX9 Regulatory Network and Modulation
Strategic Approaches for Therapeutic Targeting
Indirect Pathway Modulation
Given the direct targeting challenges, strategic indirect modulation of SOX9 activity offers promising alternatives. Targeting upstream regulators or downstream effectors in SOX9-associated signaling pathways provides pharmacological leverage. Key upstream pathways include Hedgehog (Hh), which upregulates SOX9 to generate chondrogenic precursors, and Wnt/β-catenin, which interacts with SOX9 in complex, context-dependent manners [1]. In intestinal stem cells, Wnt upregulates SOX9 for proliferation and Paneth cell differentiation, while in other contexts SOX9 inhibits β-catenin transcription [1]. Protein kinase A (PKA) activation represents another indirect strategy, as PKA phosphorylates SOX9 to enhance its DNA-binding affinity and nuclear translocation [1].
Context-Specific Intervention Strategies
Leveraging tissue- and disease-specific SOX9 interactions enables more precise targeting approaches. In cancer immunotherapy applications, targeting SOX9's role in establishing immunosuppressive tumor microenvironments could complement existing immunotherapies. Research shows SOX9 overexpression negatively correlates with genes associated with CD8+ T cell, NK cell, and M1 macrophage function while positively correlating with immunosuppressive cell populations [3]. Computational approaches integrating whole exome and RNA sequencing data can identify SOX9-associated immune signatures specific to cancer types, enabling development of combination therapies that simultaneously target SOX9 and its coordinated immune evasion mechanisms [3].
Epigenetic and Chromatin-Based Targeting
Exploiting the chromatin landscape of SOX9-regulated genes offers another strategic avenue. SOX9 frequently operates through enhancer and super-enhancer elements, particularly in stem cell populations [56]. Targeting components of these regulatory complexes or the epigenetic writers/readers that establish activating chromatin marks could disrupt SOX9-mediated transcription more selectively than direct SOX9 inhibition. The development of BET bromodomain inhibitors and other chromatin-modifying drugs provides precedent for this approach, which could be adapted specifically for SOX9-dependent transcriptional programs in disease contexts.
The technical hurdles in targeting SOX9 reflect broader challenges in transcription factor therapeutics—functional redundancy, difficult binding interfaces, and contextual functional duality. Overcoming these obstacles requires integrated experimental strategies that combine precise genomic mapping, functional validation, and systems-level understanding of SOX9's immunomodulatory networks. The most promising paths forward involve indirect modulation of SOX9 activity through upstream regulators, partner factors, or chromatin environments, coupled with context-specific delivery approaches that leverage tissue- and disease-specific expression patterns. As methodological advances continue to unravel the complexities of SOX9 regulation and function, the strategic integration of multidisciplinary approaches will be essential for translating our growing mechanistic understanding into targeted therapeutic interventions that safely exploit the Janus-faced nature of this pivotal transcription factor.
Optimizing Therapeutic Windows to Minimize Disruption of Physiological Repair
The transcription factor SOX9 (SRY-Box Transcription Factor 9) exemplifies a fundamental challenge in targeted therapy: its simultaneous regulation of both pathological processes and essential physiological repair mechanisms. As a janus-faced regulator, SOX9 exhibits context-dependent dual functions—acting as both an activator and repressor across diverse immune cell types and tissue environments [3]. This biological duality creates a critical therapeutic imperative: interventions must selectively target SOX9's disease-driving functions while preserving its reparative roles. In cancer, SOX9 is frequently overexpressed and promotes tumor immune escape by impairing immune cell function, making it a valuable therapeutic target [3]. Conversely, in tissue repair contexts, SOX9 helps maintain macrophage function and contributes to cartilage formation, tissue regeneration, and repair [3]. This technical guide examines strategies to optimize therapeutic windows when targeting SOX9, with methodologies designed to maximize efficacy while minimizing disruption of its physiological repair functions.
SOX9 Biology: Mechanisms of Dual Functionality
Structural and Functional Domains
The SOX9 protein contains several functionally specialized domains that enable its diverse biological roles. As illustrated below, these include a dimerization domain (DIM), the high mobility group (HMG) box DNA-binding domain, two transcriptional activation domains (TAM and TAC), and a proline/glutamine/alanine (PQA)-rich domain [3]. The HMG domain facilitates both DNA binding and nuclear localization through embedded nuclear localization and export signals [3]. The C-terminal transcriptional activation domain (TAC) interacts with cofactors like Tip60 to enhance SOX9's transcriptional activity and is essential for β-catenin inhibition during chondrocyte differentiation [3].
SOX9 as a Pioneer Factor in Fate Switching
Recent research has revealed SOX9's function as a pioneer transcription factor capable of binding cognate motifs in closed chromatin and initiating cell fate switches [58]. This pioneer activity enables SOX9 to reprogram transcriptional landscapes by simultaneously activating new genetic programs while silencing previous cellular identities. In skin epithelium, SOX9 binding to closed chromatin at hair follicle stem cell enhancers recruits histone and chromatin modifiers to remodel and open chromatin for transcription [58]. Concurrently, SOX9 redistributes co-factors away from epidermal stem cell enhancers, thereby silencing the previous cellular identity [58]. This competitive mechanism for epigenetic factors represents a fundamental aspect of SOX9's function that must be considered when designing therapeutic interventions.
Disease Contexts: SOX9's Dual Roles in Pathology and Repair
Cancer: Immune Modulation and Escape
In oncology, SOX9 exhibits predominantly pro-tumorigenic activities across multiple cancer types. It is highly expressed in various solid malignancies including liver cancer, lung cancer, breast cancer, and gastric cancer, where its expression levels positively correlate with tumor occurrence and progression [3]. SOX9 contributes to key oncogenic processes including vascularization, drug resistance, tumor proliferation, metastasis, and apoptosis evasion [3]. Through its interactions with the tumor microenvironment, SOX9 facilitates immunosuppression by negatively correlating with anti-tumor immune cells like CD8+ T cells, NK cells, and M1 macrophages, while showing positive correlation with immunosuppressive cell populations [3]. In high-grade serous ovarian cancer, SOX9 drives chemoresistance by reprogramming the transcriptional state of naive cells into a stem-like state [13].
Table 1: SOX9 in Cancer: Pathological vs. Protective Functions
| Cancer Type | Pathological Role of SOX9 | Therapeutic Implications | Reference |
|---|---|---|---|
| Colorectal Cancer | Promotes proliferation, migration, invasion; regulates β-catenin, cyclin D1, c-Myc | siRNA knockdown inhibits tumor growth | [59] |
| Breast Cancer | Drives basal-like breast cancer; promotes immune evasion; maintains stemness | Potential target for combination therapy | [23] |
| Glioblastoma | Highly expressed; correlation with immune infiltration and checkpoints | Diagnostic and prognostic biomarker | [22] |
| Ovarian Cancer | Drives platinum resistance; induces stem-like transcriptional state | Target for overcoming chemoresistance | [13] |
| Prostate Cancer | Overexpression promotes tumor growth; knockdown represses growth | Oncogenic dependency | [8] |
Repair Processes: Tissue Homeostasis and Regeneration
In contrast to its pro-tumorigenic roles, SOX9 performs essential functions in tissue maintenance and repair across multiple organ systems. In osteoarthritis, SOX9 plays a central role in cartilage homeostasis by orchestrating the expression of key extracellular matrix components such as type II collagen (COL II) and aggrecan (ACAN) [60]. The synergistic action of SOX9 with SOX5 and SOX6 (the "SOX trio") markedly enhances anabolic signaling, promoting synthesis of critical cartilage ECM components [60]. During schistosomiasis-induced liver damage, SOX9 is essential for myofibroblast-driven hepatic granuloma integrity and parenchymal repair [34]. In the absence of SOX9, granuloma size is significantly diminished, and mice fail to produce a robust ECM barrier around eggs, resulting in more diffuse liver injury [24].
Table 2: SOX9 in Physiological Repair and Regeneration
| Biological Context | Repair Function of SOX9 | Consequences of SOX9 Disruption | Reference |
|---|---|---|---|
| Cartilage Homeostasis | Orchestrates COL2 and aggrecan expression; chondrocyte differentiation | Cartilage degradation; impaired joint function | [60] |
| Liver Repair (Schistosomiasis) | Maintains granuloma integrity; coordinates ECM barrier | Diffuse liver injury; scattered immune cells | [34] [24] |
| Hair Follicle Development | Fate switching from epidermal to hair follicle stem cells | impaired hair follicle morphogenesis | [58] |
| Hepatic Progenitor Cells | Marker for hepatic stem/progenitor cell populations | Disrupted liver regeneration | [3] |
Therapeutic Strategies: Targeting SOX9 with Precision
Delivery Platforms for Spatiotemporal Control
Advanced delivery systems enable precise targeting of SOX9 modulation to specific tissues and cell types, potentially preserving its physiological functions elsewhere. Lipid nanoparticles (LNPs) have emerged as a leading platform for nucleic acid delivery, effectively encapsulating and protecting mRNA or siRNA payloads while enhancing cellular internalization [60] [59]. For osteoarthritis treatment, optimized LNP-mediated delivery of SOX5 and SOX9 mRNAs into chondrocytes demonstrated efficient cartilage regeneration with minimal off-target effects [60]. In colorectal cancer, cRGDfK peptide-modified LNPs enabled targeted delivery of SOX9 siRNA to tumor cells, significantly inhibiting proliferation, migration, and invasion while demonstrating favorable safety profiles [59].
Expression Modulation Techniques
Different disease contexts require either enhancement or suppression of SOX9 activity, necessitating diverse molecular approaches:
SOX9 Enhancement Strategies: For degenerative conditions like osteoarthritis, LNP-mediated delivery of SOX9 mRNA combined with SOX5 mRNA creates a synergistic effect that enhances anabolic signaling and promotes synthesis of cartilage ECM components [60]. This approach demonstrates the importance of context-specific co-factors in achieving therapeutic efficacy.
SOX9 Suppression Approaches: In oncology contexts, multiple platforms enable SOX9 inhibition. Small interfering RNA (siRNA) systems targeting SOX9 effectively silence expression and downstream oncogenic pathways [59]. Small molecule inhibitors like cordycepin demonstrate dose-dependent inhibition of SOX9 expression in cancer cell lines, suggesting potential for pharmacological intervention [8].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for SOX9 Investigation
| Reagent / Tool | Function / Application | Key Features / Considerations | Reference |
|---|---|---|---|
| SOX9 siRNA-LNPs | Gene silencing in vitro and in vivo | cRGDfK modification enhances tumor targeting; ~160nm size | [59] |
| SOX5/SOX9 mRNA-LNPs | Protein replacement therapy | Synergistic enhancement of cartilage regeneration | [60] |
| Cordycepin | Small molecule SOX9 inhibitor | Dose-dependent SOX9 suppression; natural compound | [8] |
| Anti-SOX9 Antibodies | Detection, quantification, localization | Critical for IHC, WB; validate specificity | [60] [24] |
| CRISPR/Cas9 SOX9 KO | Genetic ablation studies | Confirms SOX9 necessity; controls for off-target effects | [13] |
Experimental Protocols: Assessing Efficacy and Safety
In Vitro Models for Therapeutic Window Determination
Protocol 1: Senescent Chondrocyte Model for Cartilage Repair
- Cell Source: Primary human chondrocytes or chondrocyte cell lines
- Senescence Induction: Treat with H₂O₂ (100-500µM) or IL-1β (10ng/mL) for 48 hours
- Therapeutic Intervention: Transfert with SOX5/SOX9 mRNA-LNPs (0.1-1.0µg/mL)
- Outcome Measures: SA-β-galactosidase activity, COL2A1 and ACAN expression (qRT-PCR, Western blot), MMP-13 and ADAMTS-5 expression, cell proliferation (CCK-8)
- Therapeutic Index Calculation: Ratio of ECM synthesis enhancement to inflammatory mediator reduction [60]
Protocol 2: Cancer Stem Cell Enrichment for Oncology Applications
- Cell Culture: HGSOC lines (OVCAR4, Kuramochi, COV362) or CRC lines (HCT-116, Caco-2)
- Platinum Treatment: Carboplatin (IC50 concentration) for 72 hours to induce SOX9
- Therapeutic Intervention: SiSOX9-LNPs (10-100nM) or cordycepin (10-40µM)
- Outcome Measures: Colony formation assay, tumor spheroid formation, SOX9 and stemness markers (SOX2, OCT4), chemoresistance genes
- Safety Assessment: Primary cell toxicity (hepatocytes, chondrocytes) at therapeutic concentrations [59] [13]
In Vivo Models for Contextual Efficacy
Protocol 3: ACLT-Induced Osteoarthritis Rat Model
- Animal Model: Sprague-Dawley rats (250-300g) with anterior cruciate ligament transection
- Therapeutic Dosing: Intra-articular injection of SOX5/SOX9 mRNA-LNPs (10-50µg) biweekly for 8 weeks
- Outcome Measures: OARSI histopathology scoring, synovitis evaluation, mechanical allodynia, gait analysis, ECM component quantification
- Safety Endpoints: Systemic inflammation markers, off-target SOX9 expression in non-articular tissues [60]
Protocol 4: Schistosoma mansoni Liver Granuloma Model
- Infection Model: SOX9-deficient and wild-type mice infected with S. mansoni cercariae
- Assessment Timeline: Analyze at 7, 14, 28, 56 days post-infection
- Outcome Measures: Granuloma size and organization, collagen deposition (picrosirius red), immune cell profiling (neutrophils, monocytes, eosinophils), hepatocyte injury markers
- Therapeutic Window Indicator: Ratio of granuloma integrity preservation to fibrotic progression [24]
Pathway Visualization: SOX9 Modulation Strategies
The diagram below illustrates the strategic approach to modulating SOX9 activity within specific therapeutic contexts, highlighting key decision points for optimizing the therapeutic window.
Optimizing therapeutic windows when targeting the dual-faced regulator SOX9 requires a multidimensional approach that considers context-specific biology, spatiotemporal control, and comprehensive safety monitoring. The most promising strategies leverage advanced delivery platforms like LNPs to restrict SOX9 modulation to target tissues while preserving its physiological functions in healthy tissues. For degenerative conditions, synergistic approaches (e.g., SOX5/SOX9 combination) enhance therapeutic efficacy at lower doses, while in oncology, precise suppression mechanisms (siRNA, small molecules) can selectively target pathological SOX9 functions. Future directions should focus on smart delivery systems with micro-environment responsiveness, personalized dosing regimens based on SOX9 expression biomarkers, and combination therapies that address compensatory mechanisms. Through careful application of these principles, researchers can develop SOX9-targeted therapies that effectively treat disease while minimizing disruption to essential physiological repair processes.
Validating SOX9's Roles: Cross-Disease Analysis and Biomarker Potential
The transcription factor SOX9 is a master developmental regulator frequently re-expressed in diverse pathological contexts, functioning as a quintessential Janus-faced molecule with opposing, context-dependent roles. This whitepaper provides a systematic comparison of SOX9's functions across cancer, fibrotic, and infectious disease models, synthesizing current research to elucidate its complex mechanisms. We detail how SOX9 drives tumor progression in non-small cell lung cancer (NSCLC) while suppressing metastasis in squamous subtypes, promotes extracellular matrix (ECM) deposition in fibrotic diseases, and orchestrates protective granuloma formation in schistosomiasis. Through integrated analysis of experimental data, methodological protocols, and signaling pathways, this review establishes SOX9 as a pleiotropic regulator whose therapeutic targeting requires precise disease-specific understanding, offering researchers a comprehensive technical resource for navigating its dualistic nature in pathophysiology and therapeutic development.
SOX9 (SRY-box 9) is a member of the SOX family of transcription factors, characterized by an evolutionarily conserved high-mobility group (HMG) box DNA-binding domain. This 509-amino acid protein functions as a key developmental regulator involved in chondrogenesis, sex determination, and organogenesis [3] [61]. Beyond development, SOX9 is frequently re-expressed in various pathological states, demonstrating remarkable functional duality across different disease contexts. The protein contains several functionally critical domains: an N-terminal dimerization domain (DIM), the central HMG box responsible for DNA binding and nuclear localization, a central transcriptional activation domain (TAM), a C-terminal transcriptional activation domain (TAC), and a proline/glutamine/alanine (PQA)-rich domain essential for transcriptional activation [3]. As a pioneer transcription factor, SOX9 can bind to compacted chromatin, initiate nucleosome displacement, and recruit epigenetic modifiers to remodel the chromatin landscape, thereby enabling cell fate transitions [58]. This fundamental capacity underpins its diverse roles across pathological contexts, where it can function either as an oncogene or tumor suppressor in cancer, a pro-fibrotic driver, or an organizer of host defense in infectious disease.
SOX9 in Cancer Models
Context-Dependent Roles in Tumor Progression
In cancer, SOX9 predominantly exhibits oncogenic properties, with overexpression documented across numerous malignancies including lung, liver, breast, gastric, and colorectal cancers [3] [61]. Its expression frequently correlates with advanced disease stage, metastatic progression, chemoresistance, and poor survival outcomes. However, research reveals significant context-dependent duality in its functions, particularly evident in lung cancer models.
Table 1: SOX9 in Cancer Pathology - Key Experimental Findings
| Cancer Type | Model System | Primary Finding | Molecular Mechanisms | Pathological Impact |
|---|---|---|---|---|
| Non-Small Cell Lung Cancer (Papillary) | KrasG12D;Lkb1fl/fl mice | SOX9 deletion disrupts tumor growth [35] | Required for progression of surfactant protein C-expressing progenitor cells [35] | Promoter of papillary adenocarcinoma progression |
| Non-Small Cell Lung Cancer (Squamous) | KrasG12D;Lkb1fl/fl mice | SOX9 loss enhances metastasis [35] | Altered collagen IV deposition in basement membrane [35] | Metastasis-suppressing role in squamous histotype |
| Basal Cell Carcinoma | Inducible SOX9 mouse model (Krt14-rtTA;TRE-Sox9) | SOX9 activation reprograms epidermal stem cells [58] | Pioneer factor activity; chromatin remodeling; redistribution of epigenetic co-factors [58] | Drives tumorigenesis through fate switching |
| Multiple Solid Tumors | Human cancer samples & cell lines | Correlates with immune suppression [3] | Reduced CD8+ T cell infiltration; altered macrophage polarization; immune checkpoint regulation [3] | Promotes tumor immune escape |
Key Experimental Protocols in Cancer Models
Genetic Deletion in Murine NSCLC Models:
- Animal Model: KrasG12D;Lkb1fl/fl mice crossed with Sox9flox mice (B6.129S7-Sox9tm2Crm/J) [35].
- Tumor Initiation: Intranasal infection with progenitor cell-directed Ad5-Cre viruses to induce lung-specific recombination.
- Genotyping: Protocol 29713 from Jackson Laboratory for SOX9 genotyping.
- Tissue Processing: Lungs harvested, processed, embedded in paraffin, sectioned at 4μm thickness.
- Histopathology & IHC: H&E staining for histotype classification; immunohistochemistry for SOX9, Ki-67, pAKT, pERK with antigen retrieval (10mM sodium citrate, pH 6.0); BrightVision poly-HRP detection system.
- Image Analysis: Whole-slide scanning (PANNORAMIC 250); ROI-specific analysis using Spa-R software and ImageJ/Fiji; CellProfiler for nuclear quantification [35].
Inducible SOX9 Reprogramming Model:
- Transgenic System: Krt14-rtTA;TRE-Sox9 mice with MYC-tagged SOX9 [58].
- Induction Protocol: Doxycycline administration in drinking water to activate SOX9 expression in epidermal stem cells.
- Time Course Analysis: Monitoring at weekly intervals for up to 12 weeks.
- Transcriptomic Profiling: RNA-seq on FACS-purified epidermal stem cells at multiple timepoints.
- Epigenetic Analysis: CUT&RUN sequencing for SOX9 binding; ATAC-seq for chromatin accessibility [58].
SOX9 in Fibrotic Disease Models
Pro-fibrotic Functions Across Organ Systems
SOX9 demonstrates consistent pro-fibrotic activity across multiple organ systems, driving pathological scarring through direct regulation of extracellular matrix (ECM) components and fibroblast activation. Its expression in fibrotic contexts is induced by mechanosensitive signaling and inflammatory cytokines.
Table 2: SOX9 in Fibrotic Pathology - Key Experimental Findings
| Disease Model | Model System | Primary Finding | Molecular Mechanisms | Functional Outcome |
|---|---|---|---|---|
| Idiopathic Pulmonary Fibrosis | Human IPF samples; TGF-α & bleomycin mouse models | SOX9 upregulated via MAPK/PI3K & Wilms' tumor 1 [62] | Regulates FMT, migration, survival, ECM production [62] | Fibroblast activation & collagen deposition |
| Liver Fibrosis | CCl₄ & BDL models; SOX9-null mice | SOX9 loss reduces scarring, improves function [63] | Direct transcriptional regulation of ECM targets: OPN, FN1, SPARC, VIM, GPNMB [63] | Core regulator of fibrotic ECM deposition |
| Liver Fibrosis (Patient Correlation) | Human serum samples (Metavir staging) | SOX9 targets correlate with fibrosis severity [63] | OPN & VIM superior to established biomarkers for early detection [63] | Diagnostic & prognostic potential |
Key Experimental Protocols in Fibrosis Models
Liver Fibrosis Models & Serum Biomarker Analysis:
- Fibrosis Induction: Carbon tetrachloride (CCl₄) injection or bile duct ligation (BDL) in control (Sox9fl/fl; RosaCreER−/−) and SOX9-deficient (Sox9fl/fl; RosaCreER+/−) mice [63].
- Histological Assessment: Picrosirius red staining for collagen; IHC for SOX9, α-SMA, and ECM targets.
- HSC Culture & SOX9 Depletion: Activated rat hepatic stellate cells transfected with SOX9 siRNA; transcriptome analysis via microarray.
- Chromatin Immunoprecipitation: SOX9 antibody ChIP to verify direct binding to ECM gene promoters.
- Patient Serum Analysis: ELISA-based immunoassays for SOX9-regulated ECM proteins (OPN, VIM, SPARC, GPNMB, FN1) in well-phenotyped chronic hepatitis C cohort [63].
* Pulmonary Fibrosis Models:*
- In Vivo Models: TGF-α-induced pulmonary fibrosis and bleomycin-induced models.
- Fibroblast-Specific Deletion: Conditional SOX9 knockout in fibroblasts demonstrating attenuated collagen deposition and improved lung function [62].
- Myofibroblast Overexpression: SOX9 overexpression augmenting fibroblast activation and pulmonary fibrosis [62].
- Mechanistic Studies: MAPK/PI3K inhibition experiments to establish signaling pathways regulating SOX9 upregulation [62].
SOX9 in Infectious Disease Models
Role in Host Defense and Pathological Containment
In infectious contexts, SOX9 plays a critical role in organizing host protective responses, particularly in containment strategies during parasitic infections. Research in schistosomiasis models reveals its essential function in granuloma formation and integrity.
Table 3: SOX9 in Infectious Disease Pathology - Key Experimental Findings
| Infection Model | Model System | Primary Finding | Molecular Mechanisms | Pathological Outcome |
|---|---|---|---|---|
| Schistosomiasis (S. mansoni) | Global SOX9-deficient mice | SOX9 essential for granuloma integrity [34] [24] | ECM barrier formation around eggs; immune cell recruitment regulation [34] [24] | Containment of liver damage |
| Schistosomiasis Immunology | SOX9-deficient infected mice | Altered hepatic immune profiles [34] | Increased neutrophils & monocytes; exaggerated Type 2 inflammation; pronounced eosinophilia [34] | Disrupted immune coordination |
Key Experimental Protocols in Infectious Models
Schistosomiasis Infection Model:
- Parasite Infection: Schistosoma mansoni infection in global SOX9-deficient and control mice [24].
- Time Course Analysis: Monitoring SOX9 expression patterns throughout infection duration (up to 56 days).
- Histological Analysis: IHC for SOX9 localization (cholangiocytes, hepatocytes, HSCs); α-SMA for myofibroblasts; picrosirius red for collagen; CK19/HNF4α for cell type identification.
- Immune Phenotyping: Flow cytometry of hepatic immune cells; quantification of neutrophil, monocyte, eosinophil, and CD4+ T cell populations [24].
- Granuloma Assessment: Size measurement; structural integrity scoring; ECM barrier evaluation.
Comparative Signaling Pathways and Molecular Mechanisms
SOX9 executes its diverse pathological functions through context-specific signaling networks and molecular interactions. The diagrams below illustrate key pathway mechanisms in cancer and fibrotic disease contexts.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for SOX9 Investigation
| Reagent Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Animal Models | KrasG12D;Lkb1fl/fl; Sox9flox mice (B6.129S7-Sox9tm2Crm/J) [35] | Cancer histotype-specific studies | Enables tissue-specific & temporal SOX9 deletion |
| Krt14-rtTA;TRE-Sox9 inducible mice [58] | Cell fate switching & reprogramming studies | MYC-tag allows SOX9 tracking; doxycycline-controlled | |
| Global & fibroblast-specific SOX9 KO [62] [24] | Fibrosis & infection studies | Assess cell-type specific functions in pathophysiology | |
| Cell Lines | Activated hepatic stellate cells [63] | Fibrosis mechanism screening | Primary cells best mimic in vivo activation state |
| NSCLC cell lines with histotype origins [35] | Cancer pathway analysis | Context-dependent responses require multiple lines | |
| Antibodies | Anti-SOX9 (validated for IHC, ChIP) [35] [63] | Protein localization & quantification | Species-specific validation critical |
| Anti-α-SMA, Collagen I/IV [35] [63] | Fibrosis & ECM assessment | Standard myofibroblast & scarring markers | |
| Anti-Ki-67, pERK, pAKT [35] | Proliferation & signaling analysis | Phospho-specific require careful tissue handling | |
| Molecular Tools | SOX9 siRNA/shRNA [62] [63] | Acute knockdown studies | Multiple sequences recommended for specificity |
| SOX9-CRISPR/Cas9 [3] | Stable knockout generation | Off-target effects require careful controls | |
| SOX9-CRISPR-dCas9 [3] | Targeted transcriptional activation | Epigenetic context influences efficacy | |
| Analytical Kits | ELISA for OPN, VIM, FN1, SPARC [63] | Serum biomarker quantification | Coefficient of variation <10% for reliability |
| ATAC-seq kit [58] | Chromatin accessibility profiling | Fresh tissue or properly frozen samples essential | |
| CUT&RUN kit [58] | Transcription factor binding | Superior to ChIP-seq for low-input samples |
SOX9 emerges as a master regulatory node across pathological contexts, demonstrating remarkable functional duality that reflects its fundamental role as a cell fate regulator. In cancer, it drives progression in papillary lung adenocarcinoma while restraining metastasis in squamous subtypes. In fibrosis, it consistently promotes ECM deposition and tissue scarring across organ systems. In infectious disease, it orchestrates protective granuloma formation to contain pathogen-induced damage. This functional pleiotropy presents both challenges and opportunities for therapeutic targeting. Successful intervention strategies will require precise context-specific understanding, careful cell-type targeting, and sophisticated delivery systems to either inhibit or enhance SOX9 function based on pathological context. Future research should prioritize mapping the complete SOX9 interactome across different diseases, developing more sophisticated disease-specific targeting approaches, and advancing clinical translation of SOX9-modulating strategies that leverage its Janus-faced nature for therapeutic benefit.
Correlating SOX9 Expression with Clinical Outcomes and Treatment Resistance
The SRY-Box Transcription Factor 9 (SOX9) is a high-mobility group box transcription factor that plays crucial roles in embryonic development, stem cell maintenance, and cell fate determination. Beyond its developmental functions, SOX9 has emerged as a critical regulator in cancer pathogenesis, influencing tumor initiation, progression, and therapeutic response. This whitepaper synthesizes current evidence establishing SOX9 as a significant biomarker and mediator of clinical outcomes and treatment resistance across diverse malignancies. Framed within the context of SOX9's Janus-faced nature in immunology and cancer biology, this review provides a comprehensive analysis of its dual roles, molecular mechanisms, and therapeutic implications for researchers and drug development professionals.
SOX9 Expression Correlates with Poor Clinical Outcomes Across Cancers
Accumulating evidence from multiple cancer types demonstrates that elevated SOX9 expression frequently correlates with aggressive disease features and poor clinical outcomes. The table below summarizes key findings regarding SOX9's prognostic significance across various malignancies:
Table 1: SOX9 Expression and Clinical Correlations in Human Cancers
| Cancer Type | Expression Pattern | Clinical Correlation | Prognostic Significance |
|---|---|---|---|
| High-Grade Serous Ovarian Cancer | Upregulated in tumors vs. normal fallopian tube epithelium; induced by platinum chemotherapy | Shorter overall survival for patients in top SOX9 expression quartile (HR=1.33) [13] | Negative prognostic indicator |
| Glioblastoma (GBM) | Highly expressed in tumor tissues | Association with IDH-mutant status; correlated with immune infiltration [22] [26] | Context-dependent: better prognosis in lymphoid invasion subgroups |
| Bone Cancer | Overexpressed in malignant vs. benign tumors; elevated in circulating PBMCs | Higher expression in metastatic, recurrent tumors and poor therapy responders [64] | Positive correlation with tumor severity and malignancy |
| Gastric Cancer | Frequently overexpressed | Correlation with tumor grade, progression, and chemoresistance [65] [66] | Poor survival in multiple patient cohorts |
| Breast Cancer | Overexpressed across subtypes | Association with basal-like subtype, proliferation, and stemness [23] | Correlated with aggressive features and treatment resistance |
Analysis of The Cancer Genome Atlas data reveals SOX9 expression is significantly higher in high-grade serous ovarian cancer (HGSOC) tissues compared to normal fallopian tube epithelium, with important clinical implications [13]. In an integrated microarray database of ovarian cancer patients, those in the top quartile of SOX9 expression following platinum treatment had significantly shorter overall survival probability compared to those in the bottom quartile (hazard ratio = 1.33; log-rank P = 0.017) [13]. Similarly, in bone cancer, SOX9 overexpression is associated with high-grade, metastatic, and recurrent tumors, as well as those with poor response to therapy [64].
The context-dependent nature of SOX9's prognostic significance is particularly evident in glioblastoma, where high SOX9 expression shows a surprising association with better prognosis in specific subgroups, particularly those with lymphoid invasion [22] [26]. This duality underscores SOX9's Janus-faced regulatory nature and highlights the importance of considering tumor-specific contexts when evaluating its clinical significance.
SOX9 as a Key Driver of Treatment Resistance
Platinum-Based Chemotherapy Resistance
Recent studies have established SOX9 as a critical mediator of resistance to platinum-based chemotherapy in multiple cancer types. In high-grade serous ovarian cancer, SOX9 expression is epigenetically upregulated in response to carboplatin treatment, with significant induction observed at both RNA and protein levels within 72 hours of exposure [13]. This chemotherapy-induced SOX9 upregulation is recapitulated in primary patient tumors, with single-cell RNA sequencing of longitudinal samples from 11 HGSOC patients revealing consistent SOX9 upregulation following neoadjuvant platinum/taxane chemotherapy [13]. Functional studies demonstrate that SOX9 ablation significantly increases sensitivity to carboplatin treatment, while its overexpression induces robust chemoresistance both in vitro and in vivo [13] [14].
The resistance mechanisms involve SOX9-mediated transcriptional reprogramming toward a stem-like state. Through single-cell multiomic profiling, researchers have identified that SOX9 expression increases transcriptional divergence, representing a metric of transcriptional plasticity that enables cancer cells to adapt to therapeutic stress [13]. This reprogramming generates a stem-like subpopulation enriched for chemoresistance-associated stress gene modules, with SOX9 acting as a master regulator of these cancer stem cells [13] [14].
Molecular Mechanisms of SOX9-Mediated Resistance
Several distinct molecular pathways have been identified through which SOX9 drives treatment resistance:
Table 2: Molecular Mechanisms of SOX9-Mediated Treatment Resistance
| Mechanism | Pathway Components | Functional Outcome | Cancer Context |
|---|---|---|---|
| Transcriptional Reprogramming | Super-enhancer commissioning; Transcriptional divergence increase | Stem-like state transition; Enhanced plasticity | Ovarian Cancer [13] |
| Epigenetic Signaling Axis | CDK1/DNMT1/miR-145/SOX9/BCL-xL | Apoptosis evasion; Cisplatin resistance | Gastric Cancer [66] |
| Cell Cycle Regulation | SOX9/BMI1/p21CIP axis | Senescence evasion; Enhanced proliferation | Gastric Cancer, Glioblastoma, Pancreatic Cancer [65] |
| Anti-apoptotic Signaling | Direct BCL-xL transcriptional activation | Apoptosis suppression; Chemoresistance | Gastric Cancer [66] |
In gastric cancer, a detailed CDK1-SOX9-BCL-xL signaling axis has been elucidated as a key mediator of cisplatin resistance. CDK1 regulates SOX9 through an miR-145-dependent epigenetic mechanism: CDK1-mediated phosphorylation activates DNMT1, driving methylation-dependent silencing of miR-145, thereby relieving miR-145's repression of SOX9 [66]. Subsequently, SOX9 directly transcriptionally upregulates the anti-apoptotic protein BCL-xL, enabling evasion of cisplatin-induced apoptosis [66]. Pharmacological inhibition of CDK1 using dinaciclib disrupts this pathway and resensitizes resistant models to cisplatin, demonstrating the therapeutic potential of targeting this axis [66].
Additionally, the SOX9-BMI1-p21CIP axis represents a conserved mechanism across gastric cancer, glioblastoma, and pancreatic adenocarcinoma [65]. SOX9 positively regulates the transcriptional repressor BMI1, which in turn represses the tumor suppressor p21CIP, leading to enhanced proliferation and senescence evasion [65]. This pathway operates in differentiated tumor bulk cells, indicating SOX9's role extends beyond cancer stem cell regulation to broader tumor progression mechanisms.
Diagram 1: SOX9-Driven Molecular Pathways in Treatment Resistance. This diagram illustrates the key molecular mechanisms through which SOX9 promotes treatment resistance, including the CDK1-SOX9-BCL-xL axis and the SOX9-BMI1-p21CIP pathway.
Methodologies for Investigating SOX9 in Cancer
Experimental Approaches for SOX9 Functional Characterization
A multidisciplinary approach combining computational analyses with experimental validation has proven essential for elucidating SOX9's roles in cancer progression and treatment resistance. The following experimental protocols represent key methodologies employed in recent studies:
Multiomics Profiling of SOX9-Mediated Transcriptional Reprogramming
- Single-Cell RNA Sequencing: Utilize 10x Genomics platform for single-cell capture and library preparation. Sequence on Illumina platforms with minimum depth of 50,000 reads per cell. Process data using Cell Ranger pipeline followed by Seurat or Scanpy for dimensional reduction, clustering, and differential expression analysis [13].
- Bulk RNA Sequencing: Extract total RNA using TRIzol reagent with quality control (RIN > 8.0). Prepare libraries using poly-A selection and strand-specific protocols. Sequence to depth of 30-50 million reads per sample. Analyze differential expression using DESeq2 or edgeR packages [13] [22].
- Chromatin Immunoprecipitation (ChIP): Crosslink cells with 1% formaldehyde for 10 minutes. Sonicate chromatin to 200-500 bp fragments. Immunoprecipitate with validated SOX9 antibody. Sequence libraries on Illumina platform and analyze peaks using MACS2 with appropriate controls [66].
- Data Integration: Employ tools like ArchR or Signac for single-cell multiome data integration. Identify differentially accessible regions and transcription factor motif enrichment.
Functional Validation of SOX9 in Chemoresistance
- CRISPR/Cas9-Mediated Gene Editing: Design sgRNAs targeting SOX9 coding sequence. Transduce cells with lentiCRISPRv2 constructs. Validate knockout via Western blot and Sanger sequencing. Perform competition assays to assess fitness effects [13] [14].
- Inducible SOX9 Expression Systems: Utilize lentiviral Tet-On systems for doxycycline-inducible SOX9 expression. Titrate doxycycline concentration for optimal induction with minimal leakiness. Validate expression kinetics via time-course Western blotting [13].
- Chemosensitivity Assays: Treat SOX9-modified cells with serial dilutions of chemotherapeutic agents (e.g., carboplatin, cisplatin). Assess viability using CellTiter-Glo or colony formation assays after 72-hour treatment. Calculate IC50 values using four-parameter logistic regression [13] [66].
- Patient-Derived Models: Establish patient-derived organoids (PDOs) and xenografts (PDXs) from fresh tumor tissue. Maintain in defined matrices with optimized media formulations. Validate SOX9 expression in models compared to original tumors via IHC and qRT-PCR [66].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Investigation
| Reagent Category | Specific Examples | Application | Considerations |
|---|---|---|---|
| SOX9 Antibodies | Rabbit monoclonal [EPR14335-78] (Abcam); Mouse monoclonal [2Q3378] (Invitrogen) | Western blot, IHC, ChIP | Validate specificity using KO controls; optimal dilution varies by application |
| Cell Line Models | OVCAR4 (ovarian); Kuramochi (ovarian); AGS (gastric); U251 (glioblastoma) | In vitro functional studies | Authenticate via STR profiling; monitor mycoplasma contamination regularly |
| Animal Models | Patient-derived xenografts; Tff1 knockout mice; Cdk1 conditional knockout mice | In vivo therapeutic studies | Implement tamoxifen induction for conditional models; monitor tumor volume 3x/week |
| Pharmacologic Inhibitors | Dinaciclib (CDK1 inhibitor); Cisplatin; Carboplatin | Pathway targeting and chemoresistance studies | Optimize dosing through MTD studies; consider combination therapy approaches |
| qRT-PCR Assays | TaqMan Gene Expression Assays (SOX9: Hs00165814_m1); SYBR Green with validated primers | Gene expression quantification | Normalize to multiple housekeeping genes; verify primer efficiency (90-110%) |
SOX9 in the Tumor Immune Microenvironment
The Janus-faced nature of SOX9 is particularly evident in its complex interactions with the tumor immune microenvironment. SOX9 expression demonstrates significant correlations with immune cell infiltration patterns across cancer types. In colorectal cancer, SOX9 expression negatively correlates with infiltration of B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils, while showing positive correlations with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]. Similarly, in prostate cancer, SOX9 expression is associated with an "immune desert" microenvironment characterized by decreased effector immune cells (CD8+CXCR6+ T cells and activated neutrophils) and increased immunosuppressive cells (Tregs, M2 macrophages, and anergic neutrophils) [3].
SOX9 plays a direct role in immune evasion mechanisms. Studies have shown that SOX9, along with SOX2, is crucial for maintaining latent cancer cells in a dormant state at secondary metastatic sites while avoiding immune surveillance under immunotolerant conditions [23]. This immune evasion capability contributes to the persistence of minimal residual disease following therapy and eventual tumor recurrence.
The paradoxical, context-dependent functions of SOX9 extend to its immunomodulatory roles. While generally associated with immunosuppressive microenvironments in epithelial cancers, in glioblastoma, high SOX9 expression shows association with better prognosis in specific immunological contexts, particularly in tumors with lymphoid invasion [22] [26]. This duality underscores the importance of considering tumor-type specific interactions when evaluating SOX9 as a potential therapeutic target.
Therapeutic Implications and Future Directions
The compelling evidence linking SOX9 expression to treatment resistance across multiple cancer types positions it as an attractive therapeutic target. Several strategic approaches emerge for targeting SOX9-mediated resistance pathways:
Direct SOX9 Targeting
- Small Molecule Inhibitors: Development of compounds that interfere with SOX9 DNA binding or protein-protein interactions. High-throughput screening of compound libraries using SOX9-responsive reporter systems can identify potential inhibitors.
- Transcriptional Suppression: Utilizing epigenetic modifiers to modulate SOX9 expression through its regulatory super-enhancers. BET bromodomain inhibitors show potential in downregulating super-enhancer driven oncogenes including SOX9.
- Protein Degradation: Proteolysis-targeting chimeras (PROTACs) designed to direct SOX9 for ubiquitin-mediated degradation represent an emerging strategy.
Pathway-Targeted Approaches
- CDK1 Inhibition: Pharmacological CDK1 inhibition using dinaciclib has demonstrated efficacy in disrupting the CDK1-SOX9-BCL-xL axis and resensitizing gastric cancer models to cisplatin [66]. This approach has advanced to preclinical testing in patient-derived xenograft models.
- Combination Therapies: Rational combination strategies that concurrently target SOX9 upstream regulators and downstream effectors may prevent compensatory resistance mechanisms. For example, combining CDK1 inhibitors with BCL-xL antagonists may yield synergistic effects in gastric cancer.
- Immunotherapy Combinations: Given SOX9's role in shaping the immunosuppressive tumor microenvironment, combining SOX9-targeted approaches with immune checkpoint inhibitors may overcome resistance to current immunotherapies.
Biomarker Development
- Circulating SOX9 Detection: The identification of SOX9 in peripheral blood mononuclear cells of bone cancer patients suggests potential for liquid biopsy applications [64]. Developing robust assays for circulating SOX9 detection could enable monitoring of treatment response and early detection of recurrence.
- SOX9 Activity Signatures: Beyond expression levels, developing gene expression signatures that reflect SOX9 transcriptional activity may provide more accurate predictive biomarkers for patient stratification.
SOX9 represents a pivotal node in the molecular networks governing treatment resistance and cancer progression. Its consistent association with poor clinical outcomes across diverse malignancies, coupled with its functional role in driving chemoresistance through multiple molecular mechanisms, underscores its significance as a biomarker and therapeutic target. The Janus-faced nature of SOX9 regulation, particularly evident in its context-dependent immune interactions, highlights the complexity of targeting this multifunctional transcription factor.
Future research directions should focus on elucidating the determinants of SOX9's context-specific functions, developing clinically viable targeting strategies, and validating SOX9-based biomarkers for patient stratification. As our understanding of SOX9's molecular functions continues to expand, so too will opportunities for translating this knowledge into improved therapeutic outcomes for cancer patients facing treatment-resistant disease.
Validation of Downstream Effectors and Regulatory Networks
The transcription factor SOX9 (SRY-related HMG-box 9) exemplifies a molecular "Janus face" in immunology and cancer biology, displaying context-dependent dual functions that critically influence disease progression and therapeutic outcomes [3]. As a key member of the SOX family of transcription factors, SOX9 contains a highly conserved high mobility group (HMG) domain that facilitates DNA binding and nuclear localization [3] [22]. This structural organization enables SOX9 to function as both an activator and repressor across diverse biological processes, maintaining a delicate balance between pathological and protective immunological functions [3]. In cancer, SOX9 frequently acts as an oncogene, promoting tumor immune escape by impairing immune cell function, while in inflammatory and tissue repair contexts, it helps maintain macrophage function and contributes to cartilage formation, tissue regeneration, and repair [3]. This technical guide provides comprehensive methodologies and frameworks for validating SOX9's downstream effectors and regulatory networks, with particular emphasis on its immunomodulatory functions relevant to drug development.
SOX9 Structure and Functional Domains
SOX9 encodes a 509 amino acid polypeptide containing several functionally critical domains organized from N- to C-terminus [3]. Understanding these domains is essential for designing experiments to investigate SOX9's regulatory networks:
- Dimerization Domain (DIM): Facilitates protein-protein interactions and complex formation
- HMG Box Domain: Serves dual roles in nuclear localization (via embedded NLS/NES signals) and sequence-specific DNA binding
- Transcriptional Activation Domains: Comprise a central activation domain (TAM) and C-terminal domain (TAC) that interact with cofactors to enhance transcriptional activity
- PQA-rich Domain: Proline/glutamine/alanine-rich region necessary for transcriptional activation
The HMG and transcriptional activation domains are primarily responsible for SOX9's core functions, with the C-terminal TAC domain specifically interacting with diverse cofactors like Tip60 to enhance SOX9's transcriptional activity and inhibit β-catenin during chondrocyte differentiation [3].
Table 1: SOX9 Protein Domains and Functional Characteristics
| Domain | Position | Key Functions | Interacting Partners |
|---|---|---|---|
| Dimerization Domain (DIM) | N-terminal | Facilitates protein complex formation | Unknown specific partners |
| HMG Box | Central | DNA binding, nuclear localization/export | DNA sequences, nuclear transport machinery |
| Transcriptional Activation Domain (TAM) | Middle | Synergistic transcriptional activation | Transcriptional co-activators |
| Transcriptional Activation Domain (TAC) | C-terminal | Primary transcriptional activation, β-catenin inhibition | Tip60, β-catenin |
| PQA-rich Domain | C-terminal | Transcriptional activation | Transcriptional machinery |
Methodologies for Mapping SOX9 Regulatory Networks
Precise Modulation of SOX9 Dosage Using dTAG System
Understanding SOX9 dosage effects is critical given its haploinsufficiency associations in human disorders. The degradation tag (dTAG) system enables precise modulation of SOX9 levels to study dose-dependent effects on regulatory networks [67].
Experimental Protocol:
- Cell Model Establishment: Generate SOX9-tagged human embryonic stem cells (hESCs) using selection-free genome editing to introduce FKBP12-F36V–mNeonGreen–V5 tag at the SOX9 carboxy terminus
- Differentiation: Differentiate SOX9-tagged hESCs into cranial neural crest cells (CNCCs) using established protocols yielding molecularly homogeneous populations
- Dosage Titration: Treat SOX9-tagged CNCCs with dTAGV-1 dilution series (typically 10-fold dilutions) for 24-48 hours to achieve graduated SOX9 concentrations
- Validation: Quantify SOX9 levels via fluorescence (mNeonGreen) and immunoblotting (V5 epitope) to confirm uniform dosage effects across cell populations
Key Applications:
- Chromatin accessibility profiling via ATAC-seq at multiple SOX9 dosages
- Identification of buffered versus sensitive regulatory elements (REs)
- Gene expression dose-response relationships using RNA-seq
- Correlation of RE sensitivity with phenotypic outcomes
Identifying SOX9-Dependent Regulatory Elements
Chromatin accessibility mapping following SOX9 dosage modulation reveals distinct classes of regulatory elements with varying sensitivity to transcription factor levels [67].
ATAC-seq Protocol for SOX9 RE Identification:
- Cell Preparation: Harvest SOX9-tagged CNCCs at six distinct SOX9 dosages achieved by dTAGV-1 titration
- Library Preparation: Perform ATAC-seq using standard protocols with appropriate controls (WT CNCCs treated with DMSO or high-dose dTAGV-1)
- Bioinformatic Analysis:
- Peak calling to identify ~150,000 reproducible candidate REs
- Principal component analysis to visualize SOX9 dosage effects
- Pairwise comparisons between reduced SOX9 dosages and full dosage
- Nonlinear modeling of RE responses using Hill equation
- RE Classification: Categorize REs as buffered (minimal accessibility changes until substantial SOX9 reduction) or sensitive (accessibility correlated with SOX9 dosage)
Key Findings from SOX9 RE Mapping:
- Most SOX9-dependent REs are buffered against small dosage decreases
- REs directly and primarily regulated by SOX9 show heightened dosage sensitivity
- Sensitive REs are enriched near genes affecting chondrogenesis and craniofacial development
- Buffering leads to robust, nonlinear dosage-to-phenotype relationships
Validating SOX9-Driven Gene Regulatory Networks
SOX9 participates in cooperative regulatory networks with other transcription factors to control cell fate decisions and maintain tissue identity [68].
Experimental Approaches:
- Cooperative Binding Assays:
- Chromatin immunoprecipitation (ChIP) for SOX9 and partner TFs (e.g., Pdx1)
- Sequential ChIP to confirm co-occupancy at shared regulatory sequences
- motif analysis to identify composite DNA binding sites
Functional Validation of Network Components:
- CRISPRi/a-mediated perturbation of network nodes
- Reporter assays with wild-type and mutated RE sequences
- Differentiation assays to assess lineage specification effects
Cross-species Conservation Analysis:
- Comparative genomics to identify evolutionarily conserved network architectures
- Validation in animal models (e.g., mouse knockout systems)
Table 2: Experimentally Validated SOX9 Regulatory Networks
| Biological Context | Key Network Partners | Regulatory Targets | Functional Outcome |
|---|---|---|---|
| Pancreatic Development | Pdx1 [68] | Intestinal fate determinants (Cdx2) | Repression of intestinal lineage choice |
| Intestinal Epithelium | β-catenin/TCF4 [69] [70] | CDX2, MUC2 | Maintenance of progenitor phenotype |
| Chondrogenesis | β-catenin [3] | Col2a1, Aggrecan | Cartilage matrix production |
| Beta Cell Function | SRSF5 [40] | Alternative splicing targets | Regulation of insulin secretion |
SOX9 in Immune Regulation and Tumor Microenvironment
Methodologies for Assessing SOX9-Mediated Immune Modulation
SOX9 significantly influences tumor immune cell infiltration, making it crucial to validate its immunomodulatory networks in cancer contexts [3] [22].
Comprehensive Immune Profiling Protocol:
- Bioinformatic Analysis of Immune Infiltration:
- Integrate whole exome and RNA sequencing data from TCGA and other databases
- Calculate correlation between SOX9 expression and immune cell signatures
- Perform single-cell RNA sequencing and spatial transcriptomics in relevant cancer models
Functional Immune Cell Assays:
- Co-culture systems with SOX9-modulated cancer cells and immune cells
- Flow cytometry analysis of immune cell activation markers
- Cytokine profiling via multiplex assays
- Migration/invasion assays to assess chemotactic effects
In Vivo Validation:
- Syngeneic tumor models with SOX9-modulated cancer cells
- Immune cell depletion studies to identify critical effector populations
- Analysis of tumor-infiltrating lymphocytes via flow cytometry
Key SOX9-Immune Correlations:
- Negative correlation with B cells, resting mast cells, resting T cells, monocytes, plasma cells, and eosinophils [3]
- Positive correlation with neutrophils, macrophages, activated mast cells, and naive/activated T cells [3]
- Negative association with CD8+ T cell, NK cell, and M1 macrophage function genes [3]
- Positive correlation with memory CD4+ T cells [3]
Analyzing SOX9 in the Adaptive Immune Response
Beyond innate immunity, SOX9 plays significant roles in adaptive immune cell development and function [3].
T Cell Development Assays:
- Mechanistic Studies:
- Chromatin conformation analysis in early thymic progenitors
- Reporter assays for Rorc, Il17a, and Blk genes
- CRISPR-based perturbation of SOX9 binding sites in T cell effector genes
- Functional Validation:
- In vitro T cell differentiation systems with SOX9 modulation
- Intracellular cytokine staining for IL-17 and other effector molecules
- Assessment of γδ versus αβ T cell lineage commitment
B Cell Malignancy Studies:
- SOX9 overexpression models in B-cell lymphomas (e.g., DLBCL)
- Functional assays for proliferation, apoptosis, and drug resistance
- Identification of direct SOX9 target genes in malignant B cells
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for SOX9 Network Validation
| Reagent/Tool | Specific Example | Application | Technical Notes |
|---|---|---|---|
| SOX9 Modulation System | dTAG (FKBP12-F36V–mNeonGreen–V5) [67] | Precise SOX9 dosage control | Enables 6+ distinct SOX9 concentrations; minimal off-target effects |
| Cell Models | hESC-derived CNCCs [67] | Craniofacial development studies | Molecularly homogeneous populations |
| Animal Models | Ins-Cre;Sox9fl/fl [40] | Beta cell function studies | Enables embryonic deletion in insulin-positive cells |
| Animal Models | MIP-CreERT;Sox9-/- [40] | Adult beta cell studies | Tamoxifen-inducible system for adult stage deletion |
| Bioinformatic Tools | LinkedOmics [22] | Correlation network analysis | Identifies positively/negatively correlated genes |
| Pathway Analysis | Metascape [22] | Functional enrichment | GO, KEGG, and protein-protein interaction networks |
| Immune Analysis | ssGSEA/ESTIMATE [22] | Immune cell infiltration | Quantifies tumor immune microenvironment composition |
| Chromatin Profiling | ATAC-seq [67] | Regulatory element mapping | Identifies SOX9-dependent REs and dosage sensitivity |
Concluding Perspectives: Therapeutic Implications
The validation of SOX9 downstream effectors and regulatory networks reveals compelling therapeutic opportunities, particularly given its Janus-faced nature in immunological contexts. SOX9 represents a promising therapeutic candidate for cancer and immune-related diseases, with distinct strategies required based on disease context [3]. In oncology, SOX9 inhibition may counteract its tumor-promoting functions, particularly its role in creating "immune desert" microenvironments through suppression of effector immune cells [3]. Conversely, in inflammatory diseases and tissue injury, SOX9 enhancement could promote its beneficial roles in macrophage function maintenance and tissue repair [3] [34]. The dosage sensitivity of specific SOX9-regulated pathways suggests that fine-tuned modulation rather than complete inhibition may be necessary for therapeutic success, particularly given the buffered nature of many SOX9-dependent regulatory elements [67]. Future validation studies should prioritize context-specific network analyses and the development of sophisticated dosage modulation strategies to leverage SOX9's dual immunological functions for therapeutic benefit.
Benchmarking SOX9 Against Other Immunomodulatory Transcription Factors
The SOX9 transcription factor exemplifies a "Janus-faced" regulator in immunology, demonstrating context-dependent roles in both promoting and suppressing immune responses. This review provides a comprehensive technical benchmarking of SOX9 against related transcription factors, examining its unique structural domains, DNA-binding preferences, and immunomodulatory functions. We analyze SOX9's dualistic behavior through quantitative comparative analyses, detailed experimental methodologies, and visualization of core signaling pathways. The findings highlight SOX9's potential as a therapeutic target in cancer and inflammatory diseases, emphasizing its distinct mechanisms of action within the immune landscape. This systematic evaluation aims to equip researchers and drug development professionals with refined tools and frameworks for investigating SOX9's complex immunoregulatory functions.
Transcription factors orchestrate immune cell development, differentiation, and function through complex genomic interactions. Among these, SOX9 (SRY-box 9) has emerged as a particularly versatile regulator with demonstrated roles in chondrogenesis, stem cell maintenance, and cancer biology [1]. Recent evidence positions SOX9 as a pivotal Janus-faced immunomodulator capable of both promoting and suppressing immune activity depending on cellular context [3]. This dual nature complicates therapeutic targeting while simultaneously offering potential for context-specific interventions.
This technical review provides a systematic benchmarking of SOX9 against related immunomodulatory transcription factors, with particular emphasis on its structural characteristics, genomic binding patterns, and functional outcomes in immune regulation. We integrate quantitative comparative data, detailed experimental protocols, and visual representations of SOX9's signaling networks to establish a comprehensive resource for researchers investigating this multifunctional protein. The analysis specifically focuses on SOX9's roles in shaping anti-tumor immunity and regulating immune cell infiltration, highlighting its emerging importance in cancer immunotherapy and inflammatory disease management.
Structural and Functional Benchmarking
Molecular Architecture and DNA Recognition Motifs
SOX9 belongs to the SOXE subgroup of transcription factors, characterized by several conserved functional domains that dictate its DNA-binding specificity and transcriptional activity. The protein structure includes an N-terminal dimerization domain (DIM), a central high mobility group (HMG) box responsible for DNA binding, and transcriptional activation domains (TAM and TAC) at the C-terminus [1] [3]. This configuration enables SOX9 to recognize specific DNA sequences—primarily (A/T)(A/T)CAA(A/T)G—while facilitating protein-protein interactions that modulate its transcriptional output [21].
Table 1: Structural Domains of SOX9 and Their Functions
| Domain | Position | Primary Function | Binding Partners |
|---|---|---|---|
| Dimerization (DIM) | N-terminal | Facilitates protein self-association and heterodimerization | SOX5, SOX6, other SOXE members |
| HMG Box | Central | DNA binding and bending; nuclear localization | Specific DNA sequences (A/T)(A/T)CAA(A/T)G |
| Transcriptional Activation (TAM) | Middle | Synergistic transactivation with TAC | Tip60, other co-activators |
| Transcriptional Activation (TAC) | C-terminal | Primary transactivation domain; inhibits β-catenin | β-catenin, various transcriptional co-regulators |
| PQA-rich domain | C-terminal | Modulates transcriptional activation | Various chromatin modifiers |
Comparative analyses reveal that SOX9 exhibits distinct DNA-binding preferences across different cell types. In chondrocytes, SOX9 frequently binds to palindromic SOX motifs within intronic and distal enhancer regions, often forming homodimers or partnering with SOX5/SOX6 to activate cartilage-specific genes [21] [71]. In Sertoli cells, however, SOX9 shows preferential binding to proximal upstream regions with fewer palindromic arrangements, suggesting alternative partner interactions [21]. This cell type-specific binding behavior underscores SOX9's functional adaptability and contextual regulation.
SOX9 as a Context-Dependent Immunomodulator
SOX9 demonstrates remarkable functional plasticity in immune regulation, operating as either an immunostimulatory or immunosuppressive factor depending on the pathophysiological context. In cancer settings, SOX9 frequently exhibits immunosuppressive properties by shaping a tumor microenvironment conducive to immune escape. Studies in lung adenocarcinoma demonstrate that SOX9 suppresses infiltration of CD8+ T cells, natural killer (NK) cells, and dendritic cells, thereby inhibiting anti-tumor immunity [72]. Similarly, bioinformatic analyses of colorectal cancer reveal negative correlations between SOX9 expression and infiltration of B cells, resting mast cells, and monocytes [3].
Conversely, in tissue repair and homeostasis contexts, SOX9 displays immunoprotective functions. Increased SOX9 levels help maintain macrophage function and contribute to cartilage formation and tissue regeneration [3]. This functional duality establishes SOX9 as a molecular switch whose activity must be precisely regulated to maintain immune homeostasis, with significant implications for therapeutic targeting across different disease states.
Table 2: SOX9's Dual Roles in Different Pathophysiological Contexts
| Context | Immunomodulatory Role | Mechanisms | Outcome |
|---|---|---|---|
| Lung Adenocarcinoma | Immunosuppressive | Suppresses CD8+ T, NK, and dendritic cell infiltration; increases collagen deposition | Enhanced tumor progression and immune escape [72] |
| Colorectal Cancer | Immunosuppressive | Negative correlation with B cells, resting mast cells, monocytes; positive correlation with neutrophils, macrophages | Creates permissive tumor microenvironment [3] |
| Tissue Regeneration | Immunoprotective | Maintains macrophage function; promotes cartilage formation | Supports tissue repair and homeostasis [3] |
| Latent Metastasis | Immunosuppressive | Sustains cancer cell stemness; enables immune evasion | Maintains dormant cancer cells in secondary sites [18] |
Comparative Genomic Landscape
Cell Type-Specific DNA Binding Patterns
Chromatin immunoprecipitation sequencing (ChIP-seq) analyses reveal striking differences in SOX9 genomic binding between tissue types, providing mechanistic insights into its context-specific functions. Comparative studies in mouse and chicken models demonstrate that SOX9 binding sites in chondrocytes are predominantly located in intronic and distal regions (32.4% upstream vs. 67.6% other genomic regions), frequently associating with super-enhancers that drive expression of cartilage-specific genes [21] [71]. In contrast, Sertoli cells exhibit preferential SOX9 binding to proximal upstream regions (51.9% upstream vs. 48.1% other regions), with fewer palindromic SOX motifs [21].
These binding patterns correlate with evolutionary conservation, with chondrocyte SOX9 targets showing higher cross-species preservation compared to Sertoli cell targets [21]. This suggests that SOX9's role in chondrogenesis represents a more ancient, conserved function, while its activities in gonadal development may be more lineage-specific. The tissue-specific binding patterns highlight SOX9's adaptability and its ability to collaborate with different partner factors to execute context-appropriate transcriptional programs.
Transcriptional Programs and Partner Interactions
SOX9 executes distinct transcriptional programs through collaboration with different partner factors. In chondrogenesis, SOX9 forms complexes with SOX5 and SOX6 to activate cartilage-specific extracellular matrix genes including COL2A1, ACAN, and COL11A2 [71]. This cooperative interaction enhances SOX9 DNA binding and transcriptional activation through a mechanism known as the chondrogenic trio. Genome-wide studies reveal that SOX9 and SOX5/SOX6 co-occupy thousands of genomic sites, preferentially binding to super-enhancers that control chondrocyte identity genes [71].
In immune contexts, SOX9 partners with different factors to modulate immunological outcomes. During T cell development, SOX9 cooperates with c-Maf to activate Rorc and key Tγδ17 effector genes (Il17a and Blk), influencing lineage commitment of early thymic progenitors [3]. In cancer settings, SOX9 interacts with β-catenin and SLUG to promote epithelial-mesenchymal transition and cancer stem cell properties [18] [72]. This partner flexibility enables SOX9 to participate in diverse regulatory networks, contributing to its functional pleiotropy in different biological contexts.
Experimental Methodologies
Chromatin Immunoprecipitation Sequencing (ChIP-seq)
Purpose: To identify genome-wide binding sites of SOX9 and characterize its transcriptional networks in different cellular contexts.
Detailed Protocol:
- Cell Preparation: Crosslink proteins to DNA in developing limb buds or male gonads using 1% formaldehyde for 10 minutes at room temperature. Quench crosslinking with 125mM glycine.
- Cell Lysis and Chromatin Shearing: Lyse cells in SDS lysis buffer and sonicate chromatin to fragments of 200-500 bp using a focused ultrasonicator. Verify fragment size by agarose gel electrophoresis.
- Immunoprecipitation: Incubate chromatin with validated anti-SOX9 antibody (e.g., Millipore AB5535) overnight at 4°C. Use protein A/G magnetic beads for capture. Include matched IgG controls for background subtraction.
- Washing and Elution: Wash beads sequentially with low salt, high salt, LiCl, and TE buffers. Elute complexes with elution buffer (1% SDS, 0.1M NaHCO3) and reverse crosslinks at 65°C overnight.
- Library Preparation and Sequencing: Purify DNA, end-repair, adenylate 3' ends, and ligate Illumina adapters. Amplify libraries by 12-15 PCR cycles and validate quality by Bioanalyzer. Sequence on Illumina platform (≥20 million reads/sample).
- Data Analysis: Align sequences to reference genome (e.g., mm10) using Bowtie2. Call peaks with MACS2 with FDR < 0.05. Annotate peaks to genomic features with HOMER. Identify motifs de novo using MEME-ChIP.
Technical Considerations: Cell type-specific binding patterns require analysis in pure cell populations. For heterogeneous tissues, fluorescence-activated cell sorting (FACS) is recommended prior to crosslinking. Antibody validation through knockout controls is essential for specificity confirmation [21] [71].
Deep Learning-Based SOX9 Expression Prediction
Purpose: To non-invasively predict SOX9 expression status from CT images using deep reinforcement learning (DRL).
Detailed Protocol:
- Data Collection: Acquire preoperative contrast-enhanced CT images from hepatocellular carcinoma (HCC) patients with corresponding SOX9 immunohistochemistry validation.
- Image Preprocessing: Standardize image intensity, resample to isotropic resolution, and apply data augmentation (rotation, flipping, intensity variations).
- Model Architecture: Implement a DRL framework with:
- Classification Module: Residual network (ResNet) with integrated self-attention mechanism for long-range feature modeling.
- Reinforcement Learning Agent: Generator with encoder-decoder architecture to produce weight matrices highlighting SOX9-relevant regions.
- Training Procedure: Train the model to minimize cross-entropy loss while the RL agent maximizes reward based on classification accuracy. Use adaptive moment estimation (Adam) optimizer with learning rate 1×10^-4.
- Validation: Assess model performance using area under the curve (AUC), precision-recall metrics, and survival analysis correlation with SOX9 status.
Applications: This approach achieved 91.00% AUC in predicting SOX9 expression from CT images, significantly outperforming conventional deep learning methods. The model successfully identified SOX9-positive HCC patients with shorter recurrence-free and overall survival, enabling non-invasive prognostic stratification [42].
Table 3: Research Reagent Solutions for SOX9 Investigation
| Reagent/Category | Specific Examples | Function/Application | Technical Considerations |
|---|---|---|---|
| SOX9 Antibodies | Millipore AB5535, Abcam ab185966 | Chromatin IP, immunohistochemistry, Western blot | Validate specificity with knockout controls; species compatibility |
| Cell Line Models | RCS chondrosarcoma, HEK-293, COS-7 | In vitro mechanistic studies | Verify SOX9 expression and functionality in chosen model |
| Animal Models | Sox9-floxed mice, KrasG12D-driven LUAD | In vivo functional validation | Consider temporal control (Cre-ERt2) for developmental studies |
| Sequencing Kits | TruSeq Stranded Total RNA Kit, ChIP-seq kits | Transcriptomic and epigenomic profiling | Optimize for input material; include appropriate controls |
| Bioinformatics Tools | MACS2, HOMER, MEME-ChIP, DESeq2 | Data analysis and interpretation | Adjust parameters for specific experimental designs |
Signaling Networks and Immunomodulatory Mechanisms
SOX9 in Cancer-Immune Signaling
SOX9 operates within complex signaling networks that bridge tumor progression and immune regulation. In lung adenocarcinoma driven by oncogenic KRAS, SOX9 emerges as a critical mediator of tumor progression and immune suppression. Mechanistic studies demonstrate that SOX9 deletion in KrasG12D-driven models significantly reduces tumor burden and prolongs survival, with attenuated effects in immunocompromised mice, highlighting its immunomodulatory functions [72].
SOX9 executes its immunosuppressive effects through multiple interconnected mechanisms. It directly suppresses infiltration of cytotoxic CD8+ T cells, natural killer cells, and dendritic cells while promoting collagen deposition and extracellular matrix remodeling. This creates a physical barrier to immune cell penetration and establishes an "immune desert" microenvironment [3] [72]. Additionally, SOX9 expression correlates with upregulation of immune checkpoint molecules and recruitment of immunosuppressive cell populations, including M2 macrophages and T regulatory cells.
Regulatory Circuits in Development and Disease
Beyond its cancer-related functions, SOX9 participates in essential regulatory circuits during development and tissue homeostasis. In chondrogenesis, SOX9 forms self-reinforcing transcriptional loops with SOX5 and SOX6 to maintain the chondrocyte differentiation program [71]. This regulatory triad controls the expression of essentially all major cartilage-specific extracellular matrix components while simultaneously repressing hypertrophic and osteogenic markers.
In immune development, SOX9 contributes to lineage decisions in early thymic progenitors, particularly in the balance between αβ and γδ T cell differentiation [3]. This function involves collaboration with c-Maf to activate key effector genes in Tγδ17 cells. The context-dependent nature of these regulatory circuits—whether promoting differentiation in development or suppression in cancer—highlights the importance of cellular microenvironment in determining SOX9's functional outcomes.
Therapeutic Implications and Targeting Strategies
The Janus-faced nature of SOX9 in immunity presents both challenges and opportunities for therapeutic intervention. In cancer contexts, SOX9 inhibition represents a promising strategy to counteract immune suppression and enhance anti-tumor immunity. Experimental approaches include:
- Direct Transcriptional Inhibition: Small molecules that disrupt SOX9 DNA binding or partner interactions.
- Post-translational Regulation: Modulation of SOX9 stability through ubiquitin-proteasome pathways.
- Epigenetic Modulation: Alteration of SOX9 expression through histone modification or DNA methylation.
- Non-coding RNA Strategies: Utilization of miRNAs or lncRNAs that regulate SOX9 expression or activity.
Conversely, in tissue repair and regenerative contexts, SOX9 activation may promote beneficial immune responses and support functional restoration. This dual potential necessitates context-specific therapeutic approaches and careful assessment of SOX9 status before intervention.
Advanced detection methods, including the deep learning-based CT analysis previously described, enable non-invasive assessment of SOX9 status, facilitating patient stratification for targeted therapies [42]. Additionally, combination approaches that simultaneously target SOX9 and immune checkpoints may synergize to overcome resistance mechanisms in cancer immunotherapy.
This technical benchmarking establishes SOX9 as a multifaceted immunomodulatory transcription factor with distinct characteristics that set it apart from other immune regulators. Its unique structural domains, cell type-specific DNA binding patterns, and context-dependent functional outcomes position SOX9 as a master regulator at the interface of development, cancer, and immunity. The experimental frameworks and analytical approaches detailed herein provide robust methodologies for further investigation of SOX9's complex biology.
Moving forward, key challenges include deciphering the molecular determinants of SOX9's functional duality and developing strategies to selectively target its pathological functions while preserving its physiological roles. The continued elucidation of SOX9's immunomodulatory networks will undoubtedly yield novel insights and therapeutic opportunities for cancer and immune-related diseases.
Conclusion
SOX9 emerges as a central, context-dependent orchestrator of immunity, whose therapeutic manipulation holds immense promise but requires a nuanced, precision-based approach. The key takeaway is that successfully targeting the 'bad' SOX9 that drives cancer progression and fibrosis, while sparing or even enhancing the 'good' SOX9 essential for tissue integrity and repair, represents the primary challenge and opportunity. Future research must focus on delineating the precise molecular switches that determine SOX9's functional output, developing cell-type-specific delivery systems, and validating its use as a robust biomarker for patient stratification in clinical trials. Overcoming these hurdles will unlock novel combinatorial immunotherapies and antifibrotic treatments, fundamentally advancing biomedical and clinical research for a range of devastating diseases.
References
- 1. The versatile functions of Sox9 in development, stem cells ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4326072/]
- 2. SOX9 - an overview [https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/sox9]
- 3. SOX9: a novel janus-faced regulator in immunity and its ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/full]
- 4. Dimerization and Transactivation Domains as Candidates for ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0156199]
- 5. SOX9 in organogenesis: shared and unique transcriptional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9482574/]
- 6. https://www.frontiersin.org/journals/molecular-biosciences/ ... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1700812/xml]
- 7. SOX9 chromatin folding domains correlate with its real ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5403132/]
- 8. Comprehensive analysis, immune, and cordycepin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10067558/]
- 9. SOX9 reprograms endothelial cells by altering the chromatin ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9410909/]
- 10. A SOX9-B7x axis safeguards dedifferentiated tumor cells ... [https://www.sciencedirect.com/science/article/pii/S1534580723005518]
- 11. Sox9 prevents retinal degeneration and is required for ... [https://elifesciences.org/articles/102337]
- 12. The pioneer factor SOX9 competes for epigenetic factors to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10415178/]
- 13. SOX9 drives a stem-like transcriptional state and platinum ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483608/]
- 14. Transcription Factor Drives Chemotherapy Resistance in ... [https://news.feinberg.northwestern.edu/2025/10/30/transcription-factor-drives-chemotherapy-resistance-in-ovarian-cancer/]
- 15. SOX9 as an emerging target for anticancer drugs and a ... [https://www.sciencedirect.com/science/article/abs/pii/S1359644622002136]
- 16. SOX9: a key transcriptional regulator in organ fibrosis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1507282/full]
- 17. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11809655/]
- 18. SOX9: an important factor in regulating breast cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360010/]
- 19. Enhanced disc regeneration through CRISPR/Cas9-mediated ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465725/]
- 20. SOX9: a key transcriptional regulator in organ fibrosis [https://pubmed.ncbi.nlm.nih.gov/39974732/]
- 21. Comparative analysis demonstrates cell type-specific ... [https://www.nature.com/articles/s41598-019-48979-4]
- 22. High expression of SOX9 is a diagnostic and prognostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12277172/]
- 23. SOX9: an important factor in regulating breast cancer [https://eurjmedres.biomedcentral.com/articles/10.1186/s40001-025-02730-0]
- 24. SOX9 plays an essential role in myofibroblast driven hepatic ... [https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1012928]
- 25. SOX9 as an emerging target for anticancer drugs and a ... [https://pubmed.ncbi.nlm.nih.gov/35636723/]
- 26. High expression of SOX9 is a diagnostic and prognostic ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1531937/full]
- 27. Integrating spatial and single-cell transcriptomics to ... [https://www.nature.com/articles/s42003-025-08316-0]
- 28. Dissecting the Spatial and Single‐Cell Transcriptomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12079437/]
- 29. Single-cell transcriptomics shaping the future of orthopedics [https://pmc.ncbi.nlm.nih.gov/articles/PMC12158553/]
- 30. Spatial transcriptomics identifies molecular niche ... [https://www.nature.com/articles/s41588-025-02080-x]
- 31. The Use of Animal Models in Studying Genetic Disease [http://www.nature.com/scitable/topicpage/the-use-of-animal-models-in-studying-855]
- 32. Evaluation of Five Mammalian Models for Human Disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10452283/]
- 33. Comprehensive analysis, immune, and cordycepin ... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2023.1149986/full]
- 34. SOX9 plays an essential role in myofibroblast driven ... [https://pubmed.ncbi.nlm.nih.gov/40489560/]
- 35. SOX9 has distinct roles in the formation and progression of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11497254/]
- 36. Targeting SOX9 for degradation to inhibit chemoresistance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5286959/]
- 37. The transcription factor Sox9 is degraded by the ubiquitin ... [https://www.sciencedirect.com/science/article/abs/pii/S0945053X04001246]
- 38. : A potential regulator of cancer stem cells in osteosarcoma - PMC Sox 9 [https://pmc.ncbi.nlm.nih.gov/articles/PMC11229887/]
- 39. overexpression protects against lipid accumulation in MASH via... SOX 9 [https://www.news-medical.net/news/20250117/SOX9-overexpression-protects-against-lipid-accumulation-in-MASH-via-AMPK-activation.aspx]
- 40. Sox9 regulates alternative splicing and pancreatic beta cell ... [https://www.nature.com/articles/s41467-023-44384-8]
- 41. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://www.nature.com/articles/s41467-025-59050-4]
- 42. Deep Reinforcement Learning for CT-Based Non-Invasive ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110404/]
- 43. Sox9 inhibits Activin A to promote biliary maturation and ... [https://www.nature.com/articles/s41467-025-56813-x]
- 44. SOX9: a key transcriptional regulator in organ fibrosis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11835943/]
- 45. SOX9 switch links regeneration to fibrosis at the single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11345873/]
- 46. Profibrotic role of the SOX9–MMP10–ECM biosynthesis ... [https://www.sciencedirect.com/science/article/pii/S2352304223003100]
- 47. Cross-regulation between SOX9 and the canonical Wnt ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10469848/]
- 48. Sox9 prevents retinal degeneration and is required for ... [https://elifesciences.org/reviewed-preprints/102337]
- 49. Sox9 regulates alternative splicing and pancreatic beta cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10796970/]
- 50. Sox9 is involved in the thyroid differentiation program and ... [https://www.nature.com/articles/s41598-022-06004-1]
- 51. SOX on tumors, a comfort or a constraint? - Nature [https://www.nature.com/articles/s41420-024-01834-6]
- 52. SOX9, a potential tumor suppressor in cervical cancer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4653037/]
- 53. Studying the Role of Sox9 in Lung Cancer [https://news.cuanschutz.edu/cancer-center/sox9-in-lung-cancer]
- 54. Resistance to anti-LAG-3 plus anti-PD-1 therapy in head ... [https://pubmed.ncbi.nlm.nih.gov/40295483/]
- 55. Cancer Stem Cells Connecting to Immunotherapy [https://www.mdpi.com/2072-6694/17/13/2100]
- 56. Atlas of regulated target genes of transcription factors (ART-TF ... [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-022-04924-3]
- 57. TFTG: A comprehensive database for human transcription ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11068477/]
- 58. The pioneer factor SOX9 competes for epigenetic factors to ... [https://www.nature.com/articles/s41556-023-01184-y]
- 59. SOX9 siRNA Loaded Lipid Nanoparticles Actively Targeted ... [https://www.sciencedirect.com/org/science/article/pii/S1543839225003496]
- 60. Optimized Lipid Nanoparticle-Mediated mRNA Co-Delivery of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12554278/]
- 61. SOX9 Stem-Cell Factor: Clinical and Functional Relevance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6463569/]
- 62. Dysregulated overexpression of Sox9 induces fibroblast ... [https://pubmed.ncbi.nlm.nih.gov/34520400/]
- 63. SOX9 regulated matrix proteins are increased in patients ... [https://www.nature.com/articles/s41598-018-36037-4]
- 64. The local and circulating SOX9 as a potential biomarker for ... [https://pubmed.ncbi.nlm.nih.gov/32551218/]
- 65. SOX9 promotes tumor progression through the axis BMI1- ... [https://www.nature.com/articles/s41598-019-57047-w]
- 66. CDK1 drives SOX9-mediated chemotherapeutic resistance in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12506374/]
- 67. Precise modulation of transcription factor levels identifies ... [https://www.nature.com/articles/s41588-023-01366-2]
- 68. A Gene Regulatory Network Cooperatively Controlled by ... [https://www.sciencedirect.com/science/article/pii/S2211124715010074]
- 69. SOX9 is an intestine crypt transcription factor, is regulated by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2172132/]
- 70. cell proliferation and is required for Paneth cell... Sox 9 regulates [https://pubmed.ncbi.nlm.nih.gov/17698607/]
- 71. The transcription factors SOX9 and SOX5/SOX6 cooperate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4787819/]
- 72. SOX9 drives KRAS-induced lung adenocarcinoma ... [https://www.nature.com/articles/s41388-023-02715-5]