Standardizing Lipidomic Protocols for Clinical Samples: A Roadmap from Bench to Bedside
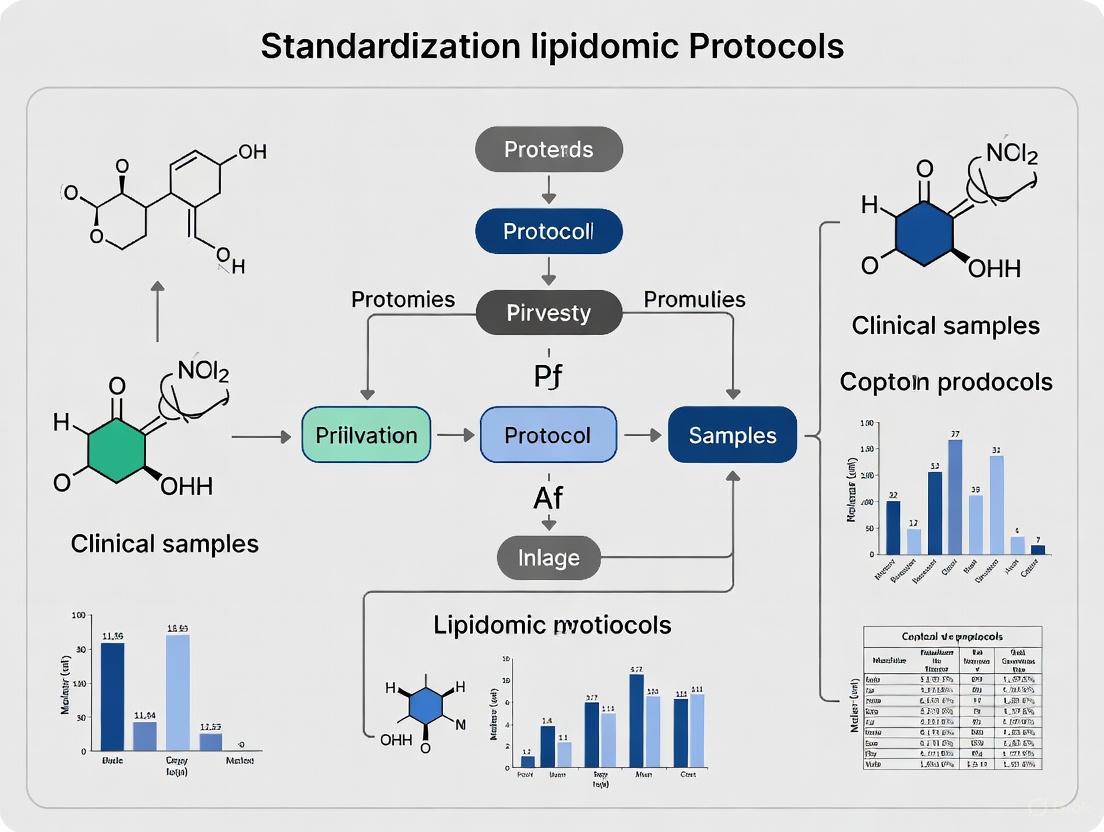
This article provides a comprehensive guide for researchers and drug development professionals on standardizing lipidomic protocols for clinical samples.
Standardizing Lipidomic Protocols for Clinical Samples: A Roadmap from Bench to Bedside
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on standardizing lipidomic protocols for clinical samples. It explores the foundational importance of pre-analytical standardization for reliable biomarker discovery, details methodological strategies from sample collection to data acquisition, addresses key troubleshooting and data analysis challenges, and establishes frameworks for analytical validation and cross-platform reproducibility. By synthesizing the latest evidence and guidelines, this review aims to bridge the gap between foundational lipid research and robust clinical application, ultimately enhancing the translational potential of lipid-based biomarkers in precision medicine.
The Critical Role of Standardization in Clinical Lipidomics
Why Pre-analytical Standardization is Non-negotiable for Reliable Biomarkers
Core Concepts: The Impact of Pre-analytical Variables
What is the pre-analytical phase and why is it a major source of error?
The pre-analytical phase encompasses all processes from test selection and patient preparation to sample collection, handling, transport, and storage before analysis [1]. This phase is the most error-prone part of the total testing process, contributing to 46% to 68.2% of all laboratory errors [2]. For metabolomics and lipidomics, pre-analytical issues account for up to 80% of laboratory testing errors [3]. Because many pre-analytical tasks occur outside the controlled laboratory environment, they present a significant challenge for ensuring reproducible and accurate biomarker data [4].
How do pre-analytical errors specifically affect lipidomics and metabolomics results?
Lipids and metabolites exhibit a wide range of stabilities ex vivo. Prolonged exposure of whole blood to room temperature allows continued metabolic activity in blood cells, altering the concentrations of sensitive species [5]. For example, in EDTA whole blood:
- After 24 hours at 21°C, 325 lipid species remained stable, but significant instabilities were detected for fatty acids (FA), lysophosphatidylethanolamine (LPE), and lysophosphatidylcholine (LPC) [5].
- After 48 hours at room temperature, more than 30% of 1012 tested metabolites showed significant changes, with nucleotides, energy-related metabolites, peptides, and carbohydrates being most affected [3].
These ex vivo distortions can lead to the misinterpretation of data, the pursuit of false biomarker candidates, and reduced inter-laboratory comparability [6].
Troubleshooting Guides
Problem: Unstable Lipidomics Results in Multi-Center Studies
| Potential Cause | Investigation Steps | Corrective & Preventive Actions |
|---|---|---|
| Variable whole blood handling times [5] | Audit SOPs at all collection sites. Track time from draw to centrifugation for a sample batch. | Standardize a maximum hold time (e.g., 4 hours) and implement immediate cooling of whole blood tubes on ice water or at 4°C [6] [3]. |
| Inconsistent whole blood holding temperatures [5] [3] | Review temperature logs during transport and storage. | Provide all sites with standardized cool packs or portable refrigerated boxes. Mandate permanent cooling of whole blood before processing [5]. |
| Use of different anticoagulants [7] | Confirm the anticoagulant used in all samples. Check for chemical interferences in MS data (e.g., formate clusters). | Harmonize the type of blood collection tube across the entire study. For metabolomics, heparin is often recommended, but consistency is paramount [7]. |
Experimental Protocol: Evaluating Lipid Stability in Whole Blood
- Objective: To determine the stability of your lipid species of interest under different pre-analytical conditions.
- Methodology:
- Collect blood from ≥5 healthy volunteers into standardized K3EDTA tubes [5].
- Immediately aliquot whole blood and expose aliquots to different conditions (e.g., 0.5h, 1h, 2h, 4h, 24h) at 4°C, 21°C (RT), and 30°C [5].
- After each time point, centrifuge samples at 4°C (e.g., 3,100 g for 7 min) to obtain plasma [5].
- Store all plasma aliquots at -80°C until batch analysis.
- Perform lipid extraction using a validated method (e.g., MTBE/methanol/water) [5] and analyze via UHPLC-high resolution mass spectrometry.
- Data Analysis: Use fold-change analysis to compare lipid concentrations at each time/temperature point against the baseline (time 0) sample. Lipids with a significant fold-change (e.g., >±20%) are considered unstable under that condition [6].
Problem: High Rate of Sample Rejection or Hemolysis
| Potential Cause | Investigation Steps | Corrective & Preventive Actions |
|---|---|---|
| Improper phlebotomy technique [8] | Observe collection technique. Check if samples are drawn from IV lines. | Implement training for phlebotomists and clinical staff. Draw blood from the opposite arm of an IV infusion [2]. |
| Incorrect sample mixing [2] | Check for clots in anticoagulant tubes. Interview staff on mixing practices. | Educate on the need for gentle inversion (e.g., 8-10 times) immediately after collection. |
| Prolonged tourniquet application [8] | Time tourniquet application during draws. | Enforce a tourniquet time of less than 60 seconds. |
Problem: Degradation of Metabolites During Sample Processing
| Potential Cause | Investigation Steps | Corrective & Preventive Actions |
|---|---|---|
| Delayed centrifugation [3] [7] | Audit the time from sample collection to plasma separation. | Centrifuge within 2 hours of collection for most metabolites. For maximum stability, process immediately on ice or at 4°C [3]. |
| Inconsistent clotting time for serum [7] | Record the exact clotting time for serum samples. | Standardize clotting time (e.g., 30-60 minutes) at room temperature [7]. |
| Multiple freeze-thaw cycles [7] | Review sample storage logs and freeze-thaw history. | Aliquot samples into single-use portions before initial freezing. Strictly limit freeze-thaw cycles. |
Frequently Asked Questions (FAQs)
General Principles
Q1: What are the most critical steps to control immediately after blood collection? The most critical steps are temperature and time until centrifugation [5] [3]. Whole blood should be cooled immediately (on ice water or at 4°C) and plasma should be separated from cells within a defined, short time frame, ideally within 2 hours [3]. This step is more critical than the handling of plasma/serum itself, as the billions of cells in whole blood remain metabolically active and can rapidly alter the concentration of labile lipids and metabolites [5].
Q2: Should I use plasma or serum for my lipidomics study? Both are acceptable, but plasma is generally recommended for better standardization [3]. The clotting process for serum generation introduces variability (clotting time) and can lead to the release of lipids and metabolites from platelets. Plasma generation is faster and easier to standardize. Crucially, you must be consistent throughout your study and clearly report which matrix was used [7].
Q3: How many freeze-thaw cycles can my samples tolerate? Freeze-thaw cycles should be minimized as much as possible. The stability of individual lipids and metabolites varies, but repeated cycling increases the risk of degradation. The best practice is to aliquot samples before the first freezing to avoid any freeze-thaw cycles for future analyses [7].
Sample Collection & Handling
Q4: Which anticoagulant should I use for plasma lipidomics? K3EDTA and heparin are common choices. However, the anticoagulant can affect the results for specific metabolites. For instance, sodium citrate interferes with the measurement of citric acid [7]. Test the tubes beforehand for interferences. The key is to use the same type of tube throughout your entire study [3] [7].
Q5: My samples were left at room temperature for 6 hours before processing. Can I still use them? It depends on your analytes of interest. While many lipid species are stable for 24 hours at 21°C, a significant number are not [5]. For a broad, untargeted analysis, this delay would likely introduce major artifacts. You should check your data against stability lists from studies like [5] or use quality control markers (e.g., a rise in lysolipids) to flag potentially compromised samples. For future experiments, this scenario should be avoided.
Q6: How does hemolysis affect lipidomics results? Hemolysis releases intracellular contents, including metabolites and enzymes, into the plasma or serum. Intracellular metabolite concentrations can be over 10 times higher than extracellular levels, leading to significant increases in many measured concentrations [7]. Hemolyzed samples should be noted during preparation, and their data should be interpreted with extreme caution or the sample excluded.
Storage & Analysis
Q7: What is the best long-term storage temperature for lipidomics samples? -80°C is the standard for long-term storage of plasma and serum samples for lipidomics and metabolomics studies. Even at -80°C, some metabolites may degrade over very long periods (years), so monitoring sample quality over time is advised [7].
Q8: How can I check if my samples have undergone pre-analytical degradation? Incorporate Quality Control (QC) samples during your analysis. A QC sample can be a pooled sample from all individuals that is analyzed repeatedly throughout the sequence. Drift in the signal of specific lipids in the QC sample can indicate analytical issues. Furthermore, research has identified potential QC markers for pre-analytical artifacts, such as specific lysophospholipids that increase with prolonged whole blood contact [5]. Monitoring these can help assess sample quality.
Essential Data & Protocols
Stability of Lipid Classes in Whole Blood
The following table summarizes quantitative data on lipid stability in EDTA whole blood, based on a study of 417 lipid species [5]. This can guide the urgency of processing for your target lipids.
| Lipid Class / Category | Key Stability Findings in Whole Blood | Recommendation for Max Hold Time (at RT) |
|---|---|---|
| Robust Lipids (e.g., many PC, SM, CE species) | 325 species stable for 24h at 21°C; 288 species stable for 24h at 30°C. | ≤ 24 hours [5] |
| Sensitive Lipids (e.g., FA, LPE, LPC) | Most significant instabilities detected in these classes. | Process as quickly as possible (within 2h) [5] |
| Oxylipins | No alterations beyond 20% variance for up to 4h at 20°C. | ≤ 4 hours [3] |
| General Metabolome (non-targeted) | ~10% of metabolite features changed significantly within 120 min at RT. | ≤ 2 hours (with immediate cooling strongly advised) [3] |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function & Importance in Pre-analytical Standardization |
|---|---|
| K3EDTA Blood Collection Tubes | Preferred anticoagulant for plasma preparation in many lipidomics studies; prevents clotting by chelating calcium. Consistency in tube type is critical [6] [5]. |
| Pre-chilled Cool Packs / Ice Water Bath | Essential for immediate cooling of whole blood tubes after draw. Slows down cellular metabolism ex vivo, preserving the profile of unstable lipids and metabolites [6] [3]. |
| Timer | To accurately track and record the time from blood draw to centrifugation. This is a key variable that must be standardized and documented [5]. |
| Refrigerated Centrifuge | Allows for centrifugation at 4°C, further stabilizing the sample during processing by reducing enzymatic activity [5]. |
| Cryogenic Vials (Pre-labeled) | For aliquoting plasma/serum after centrifugation. Using pre-labeled vials saves time and reduces the risk of sample mix-ups. Aliquoting avoids repeated freeze-thaw cycles [7]. |
| Standard Operating Procedure (SOP) | A detailed, written protocol for every step from patient preparation to final storage. This is the most important tool to ensure consistency across personnel and sites [3]. |
Workflow Diagrams
Sample Journey from Blood Draw to Analysis
Decision Tree for Sample Usability
Foundational Knowledge: Lipid Classification and Functions
Lipids are a diverse group of hydrophobic or amphipathic molecules, insoluble in water but soluble in organic solvents, that are essential for all known forms of life [9] [10]. The LIPID MAPS classification system, a widely accepted framework in lipidomics research, categorizes lipids into eight main categories based on their chemical structures and biosynthetic pathways [11] [10].
Table 1: Lipid Categories, Structures, and Primary Biological Functions
| Lipid Category | Core Structure | Key Subclasses | Primary Biological Functions |
|---|---|---|---|
| Fatty Acyls (FA) [10] | Carboxylic acid with hydrocarbon chain [12] | Fatty acids, Eicosanoids, Prostaglandins [10] | Energy source, inflammatory signaling, pain/fever mediation [13] |
| Glycerolipids (GL) [10] | Glycerol backbone with fatty acyl chains [12] | Mono-, Di-, Triacylglycerols [10] | Long-term energy storage, thermal insulation [12] [13] |
| Glycerophospholipids (GP) [10] | Glycerol, two fatty acids, phosphate headgroup [12] | Phosphatidylcholine (PC), Phosphatidylethanolamine (PE), Phosphatidylinositol (PI) [10] | Primary structural component of cell membranes, cell signaling, metabolic precursors [12] [13] |
| Sphingolipids (SP) [10] | Sphingoid base backbone [10] | Ceramides (Cer), Sphingomyelins, Gangliosides [12] [10] | Membrane structural components, powerful signaling molecules regulating inflammation and cell death [12] [14] |
| Sterol Lipids (ST) [11] | Four fused hydrocarbon rings [12] | Cholesterol, Steroid hormones [12] | Membrane fluidity, precursor to bile acids, vitamin D, and steroid hormones [12] [13] |
| Prenol Lipids (PR) [11] | Isoprene subunits [10] | Fat-soluble vitamins (A, D, E, K), Polyprenols [10] [13] | Enzyme activation, antioxidant function, molecular transport across membranes [13] |
| Saccharolipids (SL) [11] | Fatty acids linked to sugar backbones [10] | Acylated glucosamine precursors [10] | Membrane components in some microorganisms [10] |
| Polyketides (PK) [11] | Condensation of ketoacyl subunits [10] | Various macrocycles and polyethers [10] | Often have antimicrobial or pharmacological activity [10] |
The diagram below illustrates the hierarchical relationship of this classification system and the primary biological functions of the main lipid categories.
Methodologies in Lipidomics: A Technical Comparison
Lipidomics, the large-scale study of lipid molecular species and their biological functions, relies on advanced analytical technologies [11]. The choice of methodology is critical and depends on the research question, with a fundamental divide between targeted and untargeted approaches.
Table 2: Core Lipidomics Methodologies and Their Characteristics
| Methodology | Description | Key Applications | Key Advantages | Key Limitations |
|---|---|---|---|---|
| Untargeted Lipidomics [11] | Global profiling to detect & quantify all measurable lipids in a sample. | Biomarker discovery, novel pathway identification, comprehensive phenotyping [11]. | Hypothesis-generating; broad coverage of lipid species [11]. | Limited sensitivity for low-abundance lipids; requires complex data processing; lower reproducibility [11] [15]. |
| Targeted Lipidomics [11] | Precise quantification of a predefined set of lipids. | Validation of biomarkers, clinical assays, focused pathway analysis [16]. | High sensitivity, specificity, and reproducibility; ideal for clinical translation [11] [16]. | Limited to known lipids; requires prior knowledge [11]. |
| Pseudotargeted Lipidomics [11] | Combines wide coverage of untargeted with precision of targeted. | Bridging discovery and validation phases [11]. | Improved reproducibility and coverage compared to untargeted [11]. | More complex method development [11]. |
| NMR Spectroscopy [16] | Quantifies lipids based on magnetic properties in a magnetic field. | High-throughput clinical lipoprotein subclass analysis (e.g., LipoProfile) [16]. | High reproducibility, non-destructive, minimal sample prep [16]. | Lower sensitivity and lipidomic coverage compared to MS [16]. |
FAQs and Troubleshooting for Lipidomics Research
Q1: Our lipid identifications lack reproducibility between software platforms. What are the primary causes and solutions?
A: Inconsistent identifications across different lipidomics software are a major, yet underappreciated, challenge. A 2024 study found that two popular platforms, MS DIAL and Lipostar, showed only 14.0% identification agreement from identical LC-MS spectra using default settings. Even with fragmentation (MS2) data, agreement only rose to 36.1% [15].
- Primary Causes: Discrepancies stem from the use of different lipid spectral libraries (e.g., LipidBlast vs. LipidMAPS), varying peak alignment algorithms, and insufficient use of retention time information. Co-elution of lipids can also lead to incorrect MS2 spectral assignments [15].
- Solutions:
- Mandatory Manual Curation: Do not rely solely on automated "top-hit" identifications. Visually inspect spectra for quality and plausibility [15].
- Cross-Platform Validation: Process your data with more than one software platform to identify conflicting annotations.
- Utilize MS2 Data: Always strive to acquire and use fragmentation data to confirm identifications.
- Data-Driven Outlier Detection: Implement machine learning-based quality control steps, such as support vector machine regression, to flag potential false positives [15].
Q2: What are the critical pre-analytical factors to control when collecting clinical samples for lipidomic analysis?
A: Pre-analytical variability is a major obstacle to standardizing clinical lipidomics.
- Fasting State: For plasma/serum lipidomics, a 12-hour fasting period is essential to allow for the clearance of dietary chylomicrons, which otherwise dominate the lipid profile and mask endogenous signals [12].
- Standardized Sampling: Use specialized blood collection tubes that prevent lipid oxidation (e.g., containing butylated hydroxytoluene (BHT)) [14]. Standardize the time of day for collection to account for diurnal rhythms.
- Sample Processing and Storage: Ensure consistent processing protocols (e.g., centrifugation speed and time to separate plasma/serum). Snap-freeze samples in liquid nitrogen and store at -80°C to preserve lipid integrity [17].
Q3: Which lipid classes are currently showing the highest translational potential as clinical biomarkers?
A: While many lipids are under investigation, two classes stand out for their strong clinical evidence:
- Sphingolipids, specifically Ceramides: Certain ceramide species are powerful predictors of cardiovascular death. A clinically available assay (CERT2 score) that combines ceramides with phosphatidylcholines has been validated across large cohorts and licensed to major diagnostic companies for predicting cardiovascular risk [16] [14].
- Phospholipids: Specific phosphatidylcholine (PC) species are integral to the aforementioned CERT2 score. Furthermore, a ratio of phosphatidylinositol (36:2) to PC (38:4) has been identified as a potential biomarker for predicting which patients will benefit from statin treatment [16].
The diagram below summarizes a generalized workflow for a lipidomics study, highlighting key steps where the issues from the FAQs commonly arise.
Detailed Experimental Protocol: Serum Lipidomics for Biomarker Discovery
The following protocol is adapted from current best practices for untargeted lipidomic profiling of human serum, a common workflow in clinical research [17].
Objective: To comprehensively profile lipid species from human serum for the discovery of disease biomarkers.
Materials & Reagents:
- Serum Samples (collected after 12-hour fast, stored at -80°C)
- Internal Standards (ISTDs): A mixture of deuterated or otherwise isotopically labeled lipids (e.g., Avanti EquiSPLASH LIPIDOMIX) covering multiple lipid classes is essential for quantification [15].
- Extraction Solvents: Chilled methanol, methyl-tert-butyl ether (MTBE) or chloroform, with 0.01% BHT to prevent oxidation [15].
- LC-MS Solvents: LC-MS grade water, acetonitrile, isopropanol, supplemented with 10 mM ammonium formate/acetate for mobile phase additives [17] [15].
Procedure:
- Sample Preparation:
- Thaw serum samples on ice.
- Pipette a precise volume (e.g., 10 µL) of serum into a glass tube.
- Add a known amount of the ISTD mixture to every sample, quality control (QC) pool, and blank. This corrects for variability in extraction and ionization.
- Vortex thoroughly.
Lipid Extraction (MTBE/Methanol Method):
- Add a volume of methanol (e.g., 225 µL) to the serum, vortex.
- Add a larger volume of MTBE (e.g., 750 µL), vortex and shake for 10 minutes at room temperature.
- Add volumes of water and/or water:methanol mixture (e.g., 188 µL) to induce phase separation. Centrifuge.
- The upper organic (MTBE) layer, containing the lipids, is collected and evaporated to dryness under a gentle stream of nitrogen gas.
- Reconstitute the dried lipid extract in a suitable solvent mix (e.g., 9:1 isopropanol:acetonitrile) for LC-MS analysis [15].
LC-MS Analysis:
- Chromatography: Use a reversed-phase C18 column (e.g., 50-100mm length, sub-2µm particle size) maintained at a controlled temperature (e.g., 45-55°C). Employ a binary gradient from a polar (A: acetonitrile/water 60:40) to a non-polar solvent (B: isopropanol/acetonitrile 90:10) over a 10-20 minute run time [15].
- Mass Spectrometry: Acquire data in both positive and negative ionization modes using data-dependent acquisition (DDA) or data-independent acquisition (DIA) on a high-resolution mass spectrometer (e.g., Q-TOF). This ensures broad lipid coverage. MS2 fragmentation spectra are crucial for identification [11] [15].
Data Processing and Analysis:
- Process raw data using software (e.g., MS DIAL, Lipostar, XCMS) for peak picking, alignment, and identification against databases (e.g., LipidMAPS, LipidBlast).
- Crucially, perform manual curation of identifications as outlined in FAQ #1 [15].
- Export a normalized data matrix (lipid species vs. abundance) for statistical and bioinformatic analysis, including multivariate statistics and machine learning for biomarker model development [16].
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Reagents and Materials for Clinical Lipidomics
| Reagent/Material | Function | Example Product / Note |
|---|---|---|
| Deuterated Internal Standards | Corrects for losses during extraction and ion suppression/enhancement during MS analysis; enables absolute quantification [15]. | Avanti EquiSPLASH LIPIDOMIX; a mixture covering multiple lipid classes. |
| Antioxidants | Prevents oxidation of unsaturated lipids during extraction and storage, which can generate artifacts [15]. | Butylated Hydroxytoluene (BHT), added to extraction solvents at ~0.01%. |
| LC-MS Grade Solvents | Minimizes background noise and ion suppression, ensuring high-quality chromatographic separation and mass spec detection. | Water, acetonitrile, isopropanol, methanol, chloroform/MTBE. |
| Stable Isotope-Labeled Standards | Used in targeted assays as internal standards for specific lipid species or pathways. | e.g., Deuterated Ceramide (d18:1/17:0) for quantifying specific ceramides [16]. |
| Standard Reference Materials (SRM) | Provides a benchmark for instrument performance, method validation, and inter-laboratory comparison [16]. | National Institute of Standards and Technology (NIST) Standard Reference Materials. |
| Specialized Blood Collection Tubes | Stabilizes the lipidome at the moment of collection, reducing pre-analytical variability. | Tubes with specific preservatives for metabolomics/lipidomics (e.g., with BHT or other stabilizers) [14]. |
In clinical lipidomics, the integrity of research data is heavily dependent on the biological fidelity of samples before they ever reach the mass spectrometer. The pre-analytical phase—encompassing sample collection, processing, and storage—introduces significant vulnerabilities that can distort the native lipid profile. Lipids are particularly sensitive to enzymatic degradation, oxidation, and chemical modification when exposed to suboptimal handling conditions. Recognizing and standardizing these pre-analytical procedures is therefore a critical prerequisite for ensuring reliable measurement of metabolites and lipids in LC-MS-based clinical research [18]. This technical support center provides troubleshooting guidance and validated protocols to help researchers identify, mitigate, and correct for these ex vivo vulnerabilities, supporting the broader goal of standardizing lipidomic protocols for clinical samples.
Quantitative Impact of Pre-Analytical Variables
Understanding the specific impact of different handling conditions is the first step in troubleshooting. The following table summarizes how key variables quantitatively affect major lipid classes, based on controlled studies.
Table 1: Impact of Sample Handling Conditions on Major Lipid Classes
| Pre-Analytical Variable | Affected Lipid Classes | Nature of Distortion | Documented Magnitude of Change |
|---|---|---|---|
| Delayed Processing (at Room Temperature) | Lysophosphatidylcholines (LPC), Phosphatidylcholines (PC), Free Fatty Acids [18] | Increase in lysolipids (e.g., LPC, LPE) and free fatty acids due to enzymatic activity (e.g., phospholipases) [18] | Significant alterations reported; specific compound classes show high sensitivity to processing delays [18]. |
| Inappropriate Freezing/Thawing | Phospholipids, Sphingolipids [18] [19] | Phase separation, membrane disruption, and accelerated hydrolysis [18] | Multiple freeze-thaw cycles lead to progressive degradation; single cycles can be detrimental for certain species [18]. |
| Collection Tube Anticoagulant (e.g., K3EDTA vs. Heparin) | Multiple classes including Sphingomyelins, Ether-linked Phospholipids [18] [19] | Altered enzymatic activity and chemical stability; ion chelation can affect metal-dependent processes [18] | Profound differences in lipid profiles observed; K3EDTA plasma is often standardized for clinical research [18]. |
| Ex Vivo Oxidation (due to prolonged RT exposure) | Polyunsaturated Fatty Acids (PUFAs), Phospholipids containing PUFAs [18] | Formation of oxidized lipid species and hydroperoxides, loss of native unsaturated lipids [18] | Can be mitigated by antioxidants like BHT; otherwise, rapid and significant for vulnerable species [18]. |
Troubleshooting Common Pre-Analytical Artifacts
This section addresses specific issues users might encounter, providing diagnostic steps and corrective actions.
Problem 1: Inconsistent Lysophospholipid Levels Between Sample Batches
- Question: "Why are my LPC and LPE levels highly variable across samples collected on different days, even from the same subject?"
- Background: Lysophospholipids are signaling lipids generated by the hydrolysis of phospholipids. Their levels are highly sensitive to pre-analytical enzymatic activity.
- Diagnosis:
- Check the time between blood draw and plasma separation. Prolonged contact with blood cells at room temperature is a primary cause.
- Verify the temperature during this interval. Enzymatic activity is temperature-dependent.
- Review the centrifugation protocol. Inconsistent g-force or time can lead to variable cell removal.
- Solution:
- Standardize the plasma processing time. The "clip-to-freezer" time should be minimized and consistent (e.g., consistently within 30 minutes) [18].
- Process all samples at a standardized temperature (e.g., 4°C) to slow enzymatic degradation.
- Ensure consistent centrifugation conditions (e.g., 2000 × g for 10 minutes at 4°C) across all samples.
Problem 2: Appearance of "Ghost Peaks" or High Baseline in Chromatograms
- Question: "My LC-MS chromatograms show unexpected peaks and a noisy baseline, interfering with quantitation. What could be causing this?"
- Background: Ghost peaks and baseline anomalies often stem from chemical contaminants introduced during sample handling or from the degradation of samples during storage [20].
- Diagnosis:
- Run a blank injection (solvent only). If ghost peaks persist, the contamination is from the mobile phase, solvents, or the LC system itself [20].
- If blanks are clean, the issue is likely in the sample. Check:
- Leaching from plasticware: Certain lipids can adsorb to or leach from specific types of tubes.
- Sample carryover in the autosampler.
- Degradation during storage, leading to new, oxidized lipid species.
- Solution:
- Use high-purity, MS-grade solvents and additives for both mobile phase and sample preparation.
- Use low-adsorption, certified tubes for sample storage.
- Implement rigorous autosampler washing protocols.
- Store samples at -80°C and avoid repeated freeze-thaw cycles. Use single-use aliquots.
Problem 3: Shifts in Retention Time or Poor Peak Shape
- Question: "My lipid peaks are tailing or their retention times are drifting, making alignment and identification difficult."
- Background: While often related to the LC-MS instrument itself (e.g., column degradation, pump issues), pre-analytical factors can also be the root cause [20].
- Diagnosis:
- Check the sample matrix. An over-abundance of proteins or salts from inefficient protein precipitation can foul the LC column.
- Inspect for non-volatile contaminants in the sample that can accumulate on the column head.
- Review the sample reconstitution solvent. Mismatched solvent strength can cause peak broadening.
- Solution:
- Optimize and validate the protein precipitation step to ensure efficiency and reproducibility.
- Ensure samples are properly centrifuged after preparation to remove any particulate matter before injection.
- Reconstitute the final extract in a solvent that matches the initial mobile phase composition.
Standardized Experimental Protocols for Robust Lipidomics
To ensure reproducibility, follow these detailed methodologies for key stages of sample processing.
Protocol 1: Standardized Blood Collection and Plasma Processing for Lipidomics
Objective: To obtain plasma with lipid profiles that closely reflect the in vivo state by minimizing ex vivo alterations.
Reagents & Materials:
- K3EDTA vacuum blood collection tubes (validated for low lipid absorption) [18]
- Pre-chilled centrifuge capable of maintaining 4°C
- Polypropylene cryovials (low-adsorption)
- Liquid nitrogen or -80°C freezer
- Phosphate-Buffered Saline (PBS)
- Antioxidant (e.g., 2,6-di-tert-butyl-4-methylphenol, BHT) [18]
Workflow:
- Collection: Perform venipuncture using K3EDTA tubes. Invert gently to mix.
- Immediate Transfer: Place tubes in a pre-chilled rack (4°C) or ice-water slurry immediately after draw.
- Prompt Processing: Centrifuge within 30 minutes of collection at 2000 × g for 10 minutes at 4°C [18].
- Careful Aliquotting: Using a pipette, carefully transfer the upper plasma layer to pre-labeled cryovials, avoiding the buffy coat and platelet layer.
- Rapid Freezing: Flash-freeze aliquots in liquid nitrogen or place directly in a -80°C freezer. Record the exact freeze time.
- Storage: Store samples at -80°C until analysis. Avoid freeze-thaw cycles.
The following diagram illustrates the critical control points in this workflow to prevent a cascade of ex vivo degradation.
Protocol 2: Quality Control and Batch Monitoring
Objective: To monitor analytical performance and ensure data quality across different sample batches.
Reagents & Materials:
- Stable Isotope Labeled Internal Standards (IS) for key lipid classes [19]
- National Institute of Standards and Technology (NIST) plasma reference material [19]
- Quality Control (QC) pool created from a small aliquot of all study samples
Workflow:
- Internal Standard Addition: Add a mixture of stable isotope-labeled lipid internal standards to every sample at the beginning of extraction to correct for losses during preparation and instrument variability [19].
- QC Sample Preparation: Create a large, homogeneous pool of human plasma from a subset of samples or a commercial source. Aliquot and store at -80°C.
- Batch Analysis Design: Include multiple replicates of the NIST plasma and the study-specific QC pool dispersed evenly throughout the sample sequence in each batch.
- Performance Monitoring: Track the retention time stability, peak area of key lipids in the QC samples, and internal standard response across all runs. A between-batch reproducibility (coefficient of variation) of <15% (and ideally <10%, as demonstrated in large studies) is a common target [19].
The Scientist's Toolkit: Essential Research Reagents
The following table details key materials required for implementing robust clinical lipidomic protocols.
Table 2: Essential Reagents and Materials for Clinical Lipidomics
| Item | Function & Importance | Key Considerations |
|---|---|---|
| K3EDTA Tubes | Preferred anticoagulant for plasma collection in lipidomics. Prevents coagulation by chelating calcium. | Standardized use minimizes inter-study variability. Shown to yield more consistent lipid profiles compared to heparin [18] [19]. |
| Stable Isotope Internal Standards | Synthetic lipids with heavy isotopes (e.g., ^13C, ^2H) added to each sample prior to extraction. | Corrects for matrix effects, recovery variations, and instrument sensitivity drift. Essential for precise quantification [19]. |
| Antioxidants (e.g., BHT) | Added during sample processing to inhibit ex vivo oxidation of unsaturated lipids. | Crucial for preserving the native state of polyunsaturated fatty acids and preventing the formation of oxidation artifacts [18]. |
| MS-Grade Solvents | High-purity solvents (ACN, MeOH, MTBE, etc.) for lipid extraction and LC-MS analysis. | Minimizes chemical noise, background interference, and injector/column contamination, which is a common source of ghost peaks and high baseline [20]. |
| NIST SRM 1950 | Standard Reference Material for human plasma. | Used as a quality control to monitor method performance and ensure inter-laboratory comparability [19]. |
Welcome to the Lipidomics Technical Support Center. This resource is designed to help researchers, scientists, and drug development professionals navigate the specific challenges of implementing data-driven lipidomics protocols with clinical samples. A core challenge in the field is the balance between analytical rigor, which is essential for reproducible biomarker discovery, and clinical feasibility, which dictates the practical application of these methods in healthcare settings.
A primary source of technical difficulty is the lack of standardization across platforms and laboratories [21]. This guide provides targeted troubleshooting advice, frequently asked questions (FAQs), and detailed protocols to help you overcome these hurdles and generate high-quality, clinically relevant lipidomic data.
Troubleshooting Guides
Guide 1: Addressing Inconsistent Lipid Identifications Between Software Platforms
Problem: Users obtain different lipid identification results when processing the same LC-MS spectral data with different software platforms (e.g., MS DIAL vs. Lipostar), leading to irreproducible biomarker discovery [22].
Symptoms:
- Low overlap in identified lipid species when the same raw data file is processed with two different software tools.
- Putative lipid biomarkers cannot be validated across different laboratory sites or in meta-analyses.
Diagnosis and Solutions:
| Step | Action | Rationale and Expected Outcome |
|---|---|---|
| 1. Cross-Platform Verification | Process identical LC-MS spectra in at least two open-access platforms (e.g., MS DIAL, Lipostar) and compare outputs. | A case study showed only 14.0% identification agreement using default settings with MS1 data and 36.1% with MS2 spectra [22]. This step highlights the scale of the problem. |
| 2. Mandatory Manual Curation | Manually inspect the MS2 fragmentation spectra for putative lipid identifications, especially for key biomarkers. | This is the most critical step for reducing false positives caused by co-elution of closely related lipids or limitations in library matching algorithms [22]. |
| 3. Multi-Mode LC-MS Validation | Collect and compare data from both positive and negative ionization modes for the same sample. | A lipid identified with high confidence in both modes is more likely to be a correct annotation. This adds a layer of verification [22]. |
| 4. Data-Driven Outlier Detection | Apply a machine learning-based quality control step, such as Support Vector Machine (SVM) regression with leave-one-out cross-validation, to retention time data. | This can help flag lipid identifications that are outliers from predicted retention behavior, indicating potential false positives for further manual review [22]. |
Guide 2: Managing Missing Values in Lipidomics Datasets
Problem: Lipid concentration tables contain a significant number of missing values (NA, NaN), complicating statistical analysis and biological interpretation [23].
Symptoms:
- Many lipid species have concentration values missing in a non-random pattern across sample groups.
- Statistical software fails or produces biased results during multivariate analysis.
Diagnosis and Solutions:
| Step | Action | Rationale and Expected Outcome |
|---|---|---|
| 1. Investigate the Cause | Before imputation, investigate why values are missing. Is it due to low abundance (common in clinical samples), peak picking errors, or alignment issues? | Correctly classifying the type of missing data—Missing Completely at Random (MCAR), Missing at Random (MAR), or Missing Not at Random (MNAR)—is essential for choosing the right imputation strategy [23]. |
| 2. Pre-filter the Data | Remove lipid species where the number of missing values exceeds a defined threshold (e.g., >35% of samples) [23]. | This simplifies the dataset and avoids imputing data for lipids that are effectively undetected in your experiment. |
| 3. Select an Imputation Method | Choose an imputation method based on the nature of your missing data. | k-Nearest Neighbors (kNN) : Often recommended for MCAR and MNAR data in shotgun lipidomics [23]. Random Forest : Performs well for MCAR/MAR data in LC/MS metabolomics [23]. Half-minimum (hm) : Imputing with a percentage of the lowest measured concentration is a common and effective method for MNAR data (e.g., values below the limit of detection) [23]. |
Frequently Asked Questions (FAQs)
FAQ 1: What are the two most critical types of lipids for health and how do they impact clinical biomarker discovery?
While many lipids are important, two classes have a major impact on health and are central to clinical biomarker research:
- Phospholipids: These are the structural foundation of all cell membranes. Their composition influences membrane fluidity and how cells respond to hormones and medications. Abnormalities can appear years before clinical symptoms of metabolic disorders [14].
- Sphingolipids (particularly ceramides): These function as powerful signaling molecules that regulate inflammation, cell death, and metabolism. Elevated ceramide levels are a strong predictor of cardiovascular events, often outperforming traditional cholesterol measurements [14].
FAQ 2: Our clinical lipidomics data is very complex. What are the best practices for statistical processing and visualization?
For robust and reproducible analysis, a solid core of freely available tools in R or Python is recommended [23].
- Data Preparation: Handle missing values as described in the troubleshooting guide above. Normalize data to remove unwanted technical variation (e.g., batch effects) using quality control (QC) samples.
- Statistical Analysis: Use both univariate (e.g., student's t-test, ANOVA) and multivariate methods (e.g., Principal Component Analysis - PCA). PCA is excellent for visualizing overall data structure and identifying outliers [24] [23].
- Visualization: Create standard plots like volcano plots (to visualize significance vs. fold-change) and heatmaps (to show clustering of samples and lipids) [23]. These tools help identify statistically significant trends and biologically relevant differences.
FAQ 3: What is the core difference between untargeted and targeted lipidomics workflows, and when should I use each?
The choice of workflow is fundamental to experimental design.
- Untargeted Lipidomics (Discovery): The goal is to comprehensively profile as many lipids as possible without prior hypothesis. It is used for hypothesis generation and biomarker discovery. This typically involves LC-MS workflows to separate complex mixtures, or shotgun workflows for rapid profiling [24] [25].
- Targeted Lipidomics (Validation): This method focuses on accurate identification and absolute quantification of a predefined set of lipids. It is hypothesis-driven and used to validate findings from untargeted studies on a larger cohort [25].
FAQ 4: How can I visually diagnose problems in my LC-MS/MS method to improve data quality?
The open-source platform DO-MS (Data-driven Optimization of MS) is designed for this purpose [26].
- It interactively visualizes data from all levels of a bottom-up LC-MS/MS analysis (e.g., from MaxQuant output).
- You can diagnose specific issues like poor sampling of elution peak apexes, MS2-level co-isolation, or contamination.
- By using DO-MS to optimize parameters, one study achieved a 370% increase in the efficient delivery of ions for MS2 analysis [26].
Experimental Protocol Tables
Table 1: Standardized LC-MS Lipidomics Protocol for Clinical Serum/Plasma Samples
This protocol provides a foundational workflow for robust lipid analysis of common clinical samples [22] [24] [25].
| Step | Parameter | Specification | Technical Notes |
|---|---|---|---|
| 1. Sample Prep | Lipid Extraction | Modified Folch (Chloroform: Methanol, 2:1) or MTBE method. | Include a cocktail of deuterated internal standards (e.g., Avanti EquiSPLASH) added before extraction to monitor recovery and enable quantification [22] [21]. |
| 2. LC Separation | Column | Reversed-Phase (e.g., C18 or C30). | C30 columns offer superior separation for lipid isomers [24]. |
| Mobile Phase | (A) Water/Acetonitrile; (B) Isopropanol/Acetonitrile. Both with 10mM Ammonium Formate [22]. | Additive promotes positive ion formation. | |
| 3. MS Analysis | Ionization | Electrospray Ionization (ESI). | Soft ionization for intact lipid molecules. |
| Mode | Data-Dependent Acquisition (DDA). | Acquires MS1 spectra followed by MS2 fragmentation of the most abundant ions. | |
| Polarity | Switch between Positive and Negative mode in separate runs. | Essential for comprehensive coverage of different lipid classes [22] [24]. | |
| 4. Data Processing | Software | MS DIAL, Lipostar, or commercial platforms. | Always perform manual curation of top lipid identifications using MS2 spectra [22]. |
| Database | LipidBlast, LipidMAPS. | Use consistent library versions for project-long reproducibility. |
Table 2: Key Research Reagent Solutions for Lipidomics
This table details essential materials and their critical functions in ensuring accurate and reproducible lipidomics data [22] [21].
| Reagent / Material | Function | Application Note |
|---|---|---|
| Deuterated Lipid Internal Standards | - Correct for loss during extraction.- Monitor ionization efficiency.- Enable absolute quantification. | Chemically pure, synthetic standards (e.g., from Avanti Polar Lipids) are optimal. A mixture covering multiple lipid classes (e.g., Avanti EquiSPLASH) is recommended [22] [21]. |
| Quality Control (QC) Sample | - Monitor instrument stability over the run.- Assess technical variability and batch effects. | Typically a pool of a small aliquot of all biological samples analyzed. Run QCs repeatedly throughout the sequence [23]. |
| Standard Reference Material (SRM) | - Benchmark laboratory performance.- Cross-lab standardization. | For plasma/serum, NIST SRM 1950 is a commonly used reference material with consensus concentrations for many metabolites and lipids [23]. |
| Specialized Solvents | - High-purity, LC-MS grade solvents (e.g., Chloroform, Methanol, Isopropanol). | Minimize background noise and ion suppression. Use solvents with low UV absorbance and without plasticizers or antioxidants that interfere with MS. |
Lipidomics Workflow and Data Analysis Diagrams
Lipidomics Clinical Sample Workflow
Data Analysis & Troubleshooting Pathway
Implementing Robust Lipidomics Workflows: From Sample to Data
Core Concepts in Pre-analytical Lipidomics
Why Pre-analytical Phase is Critical: The pre-analytical phase encompasses all steps from patient preparation to the point where the sample is ready for analysis. Studies indicate that 46% to 68% of errors in laboratory testing occur in this phase, making it the most error-prone part of the workflow [27]. For lipidomics, the inherent chemical complexity and susceptibility of lipids to degradation mean that inappropriate sampling techniques, storage temperatures, and handling protocols can result in the degradation of complex lipids and the generation of oxidized or hydrolyzed artifacts [28]. Adhering to standardized pre-analytical practices is therefore fundamental for ensuring data quality, reproducibility, and the validity of biological conclusions.
Frequently Asked Questions & Troubleshooting
Q1: Our lipidomics data shows unexpectedly high levels of lysophospholipids. What could be causing this during sample handling?
Unexpectedly high levels of lysophospholipids are a common pre-analytical artifact. The primary causes and solutions are:
- Cause: Improper Sample Storage Temperature. Leaving plasma or serum samples at room temperature for extended periods leads to the enzymatic breakdown of phospholipids. Phospholipase A2 (PLA2) activity increases, hydrolyzing the sn-2 ester bond of phosphatidylcholines (PC) and phosphatidylethanolamines (PE), generating lysophosphatidylcholines (LPC) and lysophosphatidylethanolamines (LPE) [29] [30].
- Solution: Process samples as quickly as possible after collection. If immediate processing is not possible, flash-freeze samples and store them at -80 °C to quench enzymatic activity. Avoid repeated freeze-thaw cycles [29] [30] [28].
- Cause: Acidic Extraction Conditions. While acidic conditions can improve the extraction efficiency of anionic lipids, using excessively high acid concentrations or prolonged extraction times can promote non-enzymatic hydrolysis of ester bonds, artificially inflating lysophospholipid levels [30].
- Solution: If using an acidic extraction protocol, strictly control the acid concentration and extraction time as defined during method validation [30].
Q2: We are observing significant lipid oxidation in our samples. How can we prevent this?
Lipid oxidation, particularly for polyunsaturated fatty acids (PUFA), is a major concern. Prevention requires a multi-step approach:
- Cause: Exposure to Oxygen and Free Radicals. Auto-oxidation is a free radical chain reaction that is accelerated by the presence of oxygen and metal ions [28].
- Solution: Add antioxidants like butylated hydroxytoluene (BHT) to the extraction solvents to quench free radicals [29] [28]. After preparation, store lipid extracts in airtight containers with an inert gas headspace (e.g., nitrogen) to minimize oxygen exposure.
- Cause: Exposure to Light and Heat. Photooxidation and thermally induced decomposition can generate peroxides and other secondary oxidation products [28].
- Solution: Perform extraction and handling steps under dimmed light or amber glass vials where possible. Keep samples on ice or in the cold whenever feasible. Store lipid extracts at -20 °C or lower in organic solvents with antioxidants [28].
Q3: What is the single most important step to ensure correct patient sample identification?
The most critical step is positive patient identification at the bedside using at least two permanent identifiers.
- Procedure: Confirm the patient's identity by checking their identification wristband and asking the patient to state their full name and date of birth. This must be cross-referenced with the specimen labels and request form [27] [31].
- Pitfall to Avoid: Never pre-label specimen tubes before collection, as this dramatically increases the risk of the wrong sample being placed into a pre-labeled tube [31]. Label the tube in the presence of the patient after venipuncture.
Standardized Protocols for Lipidomic Samples
Blood Collection and Initial Handling
The foundation of a reliable lipidomic analysis is proper blood collection.
- Fasting Status: For routine lipid profiling (cholesterol, triglycerides), fasting is no longer universally recommended as postprandial changes are often clinically insignificant. However, follow the specific requirements of your study protocol [27].
- Anticoagulants: Use the anticoagulant specified by your validated method. Be aware that calcium-chelating anticoagulants like EDTA and citrate can affect calcium-dependent lipid formation or degradation ex vivo [29].
- Order of Draw: Adhere to a strict order of draw to prevent cross-contamination between tubes. A typical sequence is: 1. Blood culture tubes, 2. Sodium citrate, 3. Serum gel tubes, 4. Lithium heparin, 5. EDTA tubes [27].
- Avoiding Haemolysis: Minimize tourniquet time, use an appropriately sized needle, and avoid transferring blood through a needle. Gently invert tubes to mix; never shake them, as haemolysis can alter analyte concentrations [27].
Sample Homogenization Techniques
Homogenization is critical for tissues and cells to ensure lipids from all compartments are equally accessible.
- Shear-Force Grinding: Using a Potter-Elvehjem homogenizer or ULTRA-TURRAX in a cold solvent is a frequently used method [30].
- Cryogenic Crushing: For frozen tissues, crushing the material under liquid nitrogen using a pestle and mortar is effective. Be aware that frozen tissue may contain ice, which can distort results if normalized by frozen weight [30].
- Cell Disruption: Cells can be effectively disrupted using a pebble mill with beads or a nitrogen cavitation bomb, the latter of which avoids shear stress on biomolecules [30].
Lipid Extraction Methodologies
The choice of extraction method impacts the recovery of different lipid classes. The table below summarizes common techniques.
Table 1: Comparison of Common Lipid Extraction Methods
| Method | Solvent System | Key Advantages | Key Limitations | Best For |
|---|---|---|---|---|
| Folch / Bligh & Dyer [30] | Chlorform/Methanol/Water | Considered the "gold standard"; high efficiency for many lipids. | Uses hazardous chloroform; lower phase is organic, making pipetting less convenient. | Broad-range lipidomics. |
| MTBE [30] | MTBE/Methanol/Water | Less toxic than chloroform; upper phase is organic, simplifying pipetting. Comparable efficiency to Folch. | May be less efficient for saturated fatty acids and plasmalogens [30]. | High-throughput, safer laboratory environment. |
| BUME [30] | Butanol/Methanol & Heptane/Ethyl Acetate | Designed for full automation in 96-well plates; avoids chloroform. | Requires specific solvent systems. | Automated, high-throughput screening. |
| Protein Precipitation (One-step) [29] [30] | e.g., Isopropanol, Methanol, Acetonitrile | Fast, robust; higher efficiency for very polar lipids (e.g., S1P, LPC) [30]. | Extracts more non-lipid compounds, increasing ion suppression and instrument contamination. | Rapid preparation for specific, polar lipid targets. |
Lipid Degradation Pathways
The following diagram illustrates the primary pathways of lipid degradation that can occur during poor sample handling, leading to analytical artifacts.
The Scientist's Toolkit: Essential Research Reagents
This table details key reagents used in the pre-analytical phase to maintain lipid stability and integrity.
Table 2: Essential Reagents for Pre-analytical Lipidomics
| Reagent / Material | Function / Purpose | Specific Examples & Notes |
|---|---|---|
| Antioxidants [29] [28] | Quench free radicals to prevent lipid oxidation. | Butylated Hydroxytoluene (BHT) is commonly added to extraction solvents. |
| Protease Inhibitor Cocktails [29] | Stabilize proteinaceous factors; crucial when also measuring obesity-associated hormones (leptin, adiponectin). | Added to serum/plasma to prevent hormone degradation. |
| Chloroform [30] | Organic solvent for liquid-liquid extraction. | Used in Folch and Bligh & Dyer methods. Hazardous; requires careful handling. |
| Methyl tert-Butyl Ether (MTBE) [30] | Less hazardous alternative to chloroform for liquid-liquid extraction. | Organic phase forms the upper layer, simplifying pipetting. |
| Internal Standards (IS) [29] | Correct for variability in extraction efficiency and instrument response. | Stable isotope-labeled analogs of target lipids should be added as early as possible in the protocol. |
| Acid (e.g., Formic Acid) [30] | Improve extraction efficiency of anionic lipids. | Must be used with strict control of concentration and time to avoid hydrolysis artifacts. |
In clinical lipidomics, the choice of analytical strategy is a fundamental decision that directly impacts the quality, reliability, and interpretability of your data. Whether your goal is hypothesis generation or rigorous validation, no single approach fits all research questions. This guide provides a detailed comparison of targeted, untargeted, and pseudo-targeted lipidomics strategies to help you select and optimize the right methodology for your clinical samples, supporting the broader standardization of lipidomic protocols in clinical research.
Core Strategy Comparison: Key Technical Specifications
The table below summarizes the primary technical characteristics of the three main lipidomics approaches to guide your initial selection.
| Feature | Untargeted Lipidomics | Targeted Lipidomics | Pseudo-targeted Lipidomics |
|---|---|---|---|
| Primary Goal | Comprehensive, hypothesis-generating exploration of all measurable lipids [32] [25] | Precise, accurate quantification of a predefined set of lipids [32] [33] | Combines broad coverage with improved quantification accuracy [32] |
| Analytical Focus | Global lipid profiling; discovery of novel biomarkers [32] | Validation of candidate biomarkers; absolute quantification [32] [25] | High-coverage lipid profiling and structural characterization [34] |
| Data Acquisition | DDA, DIA, IDA on HRMS (Q-TOF, Orbitrap) [32] | MRM/PRM on UPLC-QQQ MS or TQ MS [32] [33] | Integrated workflow from untargeted to targeted, sometimes with derivatization (e.g., PB reaction) [32] [34] |
| Throughput | Medium (longer chromatographic runs) | High (shorter, optimized runs) | Medium to High |
| Key Clinical Application | Biomarker discovery; pathophysiological mechanism investigation [32] [25] | Diagnostic biomarker validation; therapeutic monitoring [32] [33] | Comprehensive profiling and precise structural elucidation of complex samples [34] |
Frequently Asked Questions & Troubleshooting Guides
Study Design and Strategy Selection
Q: How do I choose the right strategy for my clinical research question?
A: Follow this decision workflow to align your research objective with the appropriate lipidomics strategy.
Troubleshooting Guide:
- Problem: Discovery study yields too many insignificant lipid hits.
- Solution: Ensure adequate sample size and statistical power during the design phase. For case-control studies, preliminary power analysis is crucial [35].
- Problem: Targeted assay lacks coverage for unexpected but biologically relevant lipids.
- Solution: Consider a pseudo-targeted approach, which uses information from initial untargeted analyses to ensure high coverage and quantitative accuracy [32].
Sample Preparation and Lipid Extraction
Q: Which lipid extraction method should I use for my clinical sample type to ensure optimal recovery and reproducibility?
A: The optimal extraction protocol depends heavily on your sample matrix and the lipid classes of interest. The table below summarizes validated methods for common clinical sample types.
| Sample Type | Recommended Extraction Method(s) | Key Considerations |
|---|---|---|
| Plasma/Serum | Folch (Chloroform/Methanol) | Considered a "gold standard" for efficacy and reproducibility [36]. |
| Plasma/Serum | BUME (Butanol/Methanol) | Effective alternative to Folch; more amenable to automation [36]. |
| Liver / Intestine | MMC (Methanol/MTBE/Chloroform) or BUME | These methods are more favored for these specific tissues [36]. |
| Brain Tissue | Folch (Chloroform/Methanol) | Optimum for efficacy and reproducibility [36]. High in cholesterol and sphingolipids [25]. |
| Cultured Cells | Folch or MTBE (Methanol/MTBE) | MTBE offers ease of use (organic top layer) [36]. |
| General Use | MTBE (Methanol/MTBE) | Chloroform-free; organic phase is top layer, simplifying collection [36]. |
Troubleshooting Guide:
- Problem: Poor reproducibility and high technical variation in lipid recovery.
- Solution: Avoid monophasic methods like IPA and EE, which have shown poor reproducibility for many tissues [36]. Always add stable isotope-labeled internal standards (SIL-ISTDs) prior to extraction to correct for losses and matrix effects [33] [36].
- Problem: Low recovery of specific lipid classes (e.g., LysoPLs, Sphingolipids).
- Solution: The MTBE method can show significantly lower recoveries for lysophospholipids and sphingosines. This can be compensated for by the use of class-specific SIL-ISTDs [36].
Data Quality and Analytical Robustness
Q: How can I monitor and ensure data quality throughout my lipidomics workflow?
A: Implement a comprehensive quality control (QC) framework. Key steps include:
- Use Pooled QC (PQC) Samples: Create a pooled sample from all study samples and analyze it repeatedly throughout the batch to monitor instrument stability [37].
- Use Surrogate QC (sQC): Commercial reference plasma can be evaluated as a long-term reference and surrogate QC to assess analytical variation [37].
- Incorporate Extraction Quality Controls (EQCs): Use EQCs to monitor variability introduced during the sample preparation stage, effectively helping to mitigate batch effects [35].
Troubleshooting Guide:
- Problem: Batch effects are obscuring biological signals.
- Solution: Randomize sample analysis order and intersperse pooled QC samples throughout the run. Apply batch effect correction algorithms (e.g., Wave) during data pre-processing [35].
- Problem: Inaccurate quantification in untargeted lipidomics.
- Solution: For relative quantification in untargeted workflows, use class-specific internal standards. For absolute quantification, transition to a targeted MRM method, which provides higher accuracy and reproducibility [32] [33].
Essential Research Reagent Solutions
A successful lipidomics study relies on high-quality reagents and standards. The following table lists essential materials for setting up a robust clinical lipidomics workflow.
| Reagent / Material | Function / Application | Technical Notes |
|---|---|---|
| Stable Isotope-Labeled Internal Standards (SIL-ISTDs) | Correct for extraction efficiency, ionization suppression, and instrument variability; enable absolute quantification. | Critical: Add as early as possible in the workflow (prior to extraction). Use a mixture covering all lipid classes of interest [33] [36]. |
| LC-MS Grade Solvents | Lipid extraction, mobile phase preparation. | Use high-purity solvents (e.g., Methanol, Chloroform, Isopropanol, MTBE) to minimize background noise and ion suppression [36]. |
| Solid Phase Extraction (SPE) Plates | Clean-up of lipid extracts; fractionation of lipid classes. | Useful for removing interfering compounds in complex samples (e.g., plasma) prior to MS analysis. |
| Pooled Quality Control (PQC) Material | Monitoring instrument stability and data quality throughout the analytical batch. | Prepare from a pool of all study samples or use a commercial surrogate QC (sQC) [37] [35]. |
| Chromatography Columns | Separation of complex lipid mixtures. | C18 columns are standard for reversed-phase LC-MS lipidomics. |
| Mass Spectrometers | Lipid detection, identification, and quantification. | Q-TOF / Orbitrap: For untargeted discovery [32]. Triple Quadrupole (TQ/UPLC-QQQ): For targeted quantification (MRM) [32] [33]. |
Standardizing lipidomic protocols for clinical samples requires a clear understanding of the strengths and limitations of each analytical strategy. The path to robust, reproducible data involves selecting the right approach for your biological question, employing a rigorously tested and well-controlled sample preparation protocol, and implementing a comprehensive QC system from sample collection to data processing. By adhering to these guidelines, researchers can generate high-quality, reliable lipidomic data that advances our understanding of disease mechanisms and accelerates biomarker discovery.
Frequently Asked Questions (FAQs)
1. How can I protect my LC-MS system from contamination when analyzing complex clinical lipidomic samples? Contamination can lead to signal suppression and increased instrument maintenance. To mitigate this:
- Use a Divert Valve: Install a valve between the HPLC and MS to direct only the peaks of interest into the mass spectrometer, diverting the solvent front and high organic wash portions of the gradient away from the ion source [38].
- Implement Robust Sample Preparation: For complex clinical matrices like plasma or serum, simple filtration may be insufficient. Techniques like solid-phase extraction (SPE) are often necessary to remove dissolved contaminants and endogenous matrix components that can foul the system [38].
2. What are the critical considerations for preparing mobile phases in LC-MS lipidomics? Mobile phase composition is crucial for robust ionization and preventing source contamination.
- Use Volatile Additives: Always use volatile buffers and acids, such as ammonium formate, ammonium acetate, or formic acid. Avoid non-volatile additives like phosphate buffers, as they will contaminate the ion source [38].
- Ensure High Purity: Use LC-MS grade solvents and additives of the highest possible purity to reduce chemical noise [39].
- Start with Low Concentrations: A good starting point is 10 mM for buffers or 0.05% (v/v) for acids. A general principle is: "If a little bit works, a little bit less probably works better" [38].
3. What is the first thing I should do when my LC-MS results seem abnormal? Your first step should be to run a benchmarking method [38]. This method consists of five replicate injections of a standard compound like reserpine on a method known to be working. If the benchmark performs as expected, the problem lies with your specific method or sample preparation. If the benchmark fails, the issue is likely with the instrument itself, guiding your troubleshooting efforts efficiently [38].
4. How often should I vent my mass spectrometer? You should avoid venting the instrument too frequently [38]. Mass spectrometers are most reliable when kept under stable vacuum. Venting increases wear and tear, with the turbo pump being particularly vulnerable. The rush of atmospheric air when re-establishing vacuum places significant strain on the turbo vanes and bearings, accelerating wear [38].
Troubleshooting Guides
Guide 1: Solving Common Chromatographic Peak Problems
The following table outlines symptoms, potential causes, and solutions for issues with peak shape, which are critical for accurate identification and quantification in lipidomics.
Table 1: Troubleshooting Guide for Chromatographic Peak Anomalies
| Symptom | Potential Cause | Recommended Solution |
|---|---|---|
| Peak Tailing | Column overloading | Dilute the sample or decrease the injection volume [39]. |
| Contamination | Prepare fresh mobile phase, flush or replace the column, and use a matched guard column [39]. | |
| Interactions with active silanol sites | Add a volatile buffer (e.g., 10 mM ammonium formate) to your mobile phase to block active sites [39]. | |
| Peak Fronting | Sample solvent stronger than mobile phase | Dilute the sample in a solvent that matches (or is weaker than) the initial mobile phase composition [39]. |
| Column contamination or degradation | Flush the column following the manufacturer's procedure or replace it if regeneration fails [39]. | |
| Peak Splitting | Sample solvent incompatibility | Ensure the sample is dissolved in the same solvent composition (or weaker) as the initial mobile phase [39]. |
| Poor tubing connections | Check and ensure all tubing and ferrules are fully seated in the column and system ports [39]. | |
| Broad Peaks | Flow rate too low | Increase the mobile phase flow rate within method limits [39]. |
| Column temperature too low | Raise the column temperature [39]. | |
| Excessive extra-column volume | Use shorter tubing with a smaller internal diameter to minimize peak dispersion [39]. | |
| Decreased Sensitivity | Sample adsorption or system issues | For initial injections, condition the system with preliminary sample injections. For general loss, check for calculation errors, leaks, or incorrect injection volumes [39]. |
| Analyze a known standard. If the response is low, the issue is instrument-related; if normal, the problem is in sample preparation [39]. |
Guide 2: Addressing Baseline and System Pressure Issues
An unstable baseline or abnormal system pressure can indicate underlying problems.
Table 2: Troubleshooting Guide for Baseline and Pressure Issues
| Symptom | Pattern | Potential Cause | Recommended Solution |
|---|---|---|---|
| Erratic Baseline | Irregular, noisy signal | Air bubble in the flow cell or a system leak | Purge the system with fresh mobile phase and check all fittings for leaks [39]. |
| UV detector lamp or flow cell failure | Change the detector lamp or clean/replace the flow cell [39]. | ||
| Cyclical Baseline | Regular, repeating pattern | Pump piston or seal issues | Perform routine maintenance on the pump, including replacing seals and pistons [39]. |
| High Backpressure | Sustained increase | Clogged frit or guard column | Replace the guard column. If pressure remains high, the analytical column may be clogged and require flushing or replacement [39]. |
| Blocked inline filter or tubing | Check and clean or replace the system’s inline filter and capillary tubing [39]. |
Workflow and Logic Diagrams
Troubleshooting Logic
Method Development & Optimization
Research Reagent Solutions
Table 3: Essential Reagents and Materials for Clinical Lipidomics LC-MS
| Reagent/Material | Function in LC-MS Workflow | Technical Notes for Lipidomics |
|---|---|---|
| LC-MS Grade Solvents | Provides low background signal; reduces ion source contamination. | Essential for high-sensitivity detection of low-abundance lipids. |
| Ammonium Formate/Acetate | Volatile buffer salts for controlling mobile phase pH. | Promotes stable ionization; 10 mM is a standard starting concentration [38] [39]. |
| Formic Acid | Volatile acidic additive to promote positive ionization. | A good alternative to TFA, which can cause significant signal suppression [38]. |
| Solid-Phase Extraction Kits | Clean-up and pre-concentration of lipid samples from complex matrices. | Critical for removing phospholipids and other interferents from clinical samples [38]. |
| Guard Column | Protects the analytical column from contaminants and particulates. | Should match the stationary phase of the analytical column; requires regular replacement [39]. |
| Divert Valve | Directs HPLC flow to waste or MS. | Preserves ion source by diverting non-analyte portions of the run (e.g., solvent front) [38]. |
Frequently Asked Questions (FAQs)
FAQ 1: Why can't I use a single solvent system for all my sample types? Different biological matrices have varying compositions of polar and non-polar metabolites, as well as different physical properties. For instance, plasma and liver tissue require distinct optimization strategies. A biphasic CHCl₃/MeOH/H₂O method is suitable for polar and lipid extraction from plasma after NMR-based metabolomics analysis. In contrast, for liver tissue, a two-step extraction involving CHCl₃/MeOH followed by MeOH/H₂O is recommended due to its complex structure and lipid diversity [40].
FAQ 2: What is the impact of using multiple analytical platforms on my limited sample? Using multiple platforms (e.g., NMR and various UHPLC-MS setups) provides a more unbiased and comprehensive metabolic profile. The challenge of limited sample material is addressed by developing sequential extraction protocols that allow for multi-platform analysis from a single sample. This approach enables polar metabolite profiling via NMR and UHPLC-MS, and lipidomics from the resuspended dried lipid extract [40].
FAQ 3: How critical is standardized nomenclature for my lipidomics data? Standardized nomenclature is crucial for data reproducibility, sharing, and comparative analysis. Inconsistent naming is a significant source of confusion. It is recommended to use the LIPID MAPS classification system and shorthand notation, which have been widely adopted by journals and repositories to ensure clarity and enable meta-analyses across different studies [41] [42].
FAQ 4: Where should I deposit my lipidomics data? Large lipidomics datasets should be deposited in recognized repositories to support future data mining and integration. Recommended repositories include the Metabolomics Workbench and MetaboLights. Using these resources with the LIPID MAPS nomenclature facilitates data standardization and reuse in systems biology [41].
Troubleshooting Guides
Issue 1: Poor Recovery of Both Polar and Non-Polar Metabolites
Problem: The extraction protocol fails to efficiently isolate a broad range of metabolites, leading to low coverage.
Solution: Implement an optimized, sequential extraction protocol tailored to your sample type.
- For Plasma Samples: Use a biphasic CHCl₃/MeOH/H₂O system. This method is optimal in terms of the number of annotated metabolites, reproducibility, and sample conservation. It allows for sequential analysis of the same sample [40].
- For Liver or Other Tissues: Employ a two-step extraction.
- First, extract with CHCl₃/MeOH for lipids.
- Follow with MeOH/H₂O for polar metabolites. The dried lipid extract can be resuspended for lipidomics, while the polar extract can be used for further untargeted profiling [40].
Issue 2: Inconsistent Lipid Identification and Nomenclature
Problem: Lipid names are inconsistent across datasets, hampering comparison with other studies.
Solution: Adhere to international standards for lipid identification and reporting [41] [42].
- Use LIPID MAPS: Apply the LIPID MAPS classification system and the updated shorthand notation for reporting lipid structures.
- Match Authentic Standards: For targeted assays, confirm that the retention time of lipids in your biological samples matches that of synthetic standards to avoid misidentifying isomers.
- Report Level of Identification: Clearly state the level of structural detail confirmed by your mass spectrometric data (e.g., based on accurate mass, retention time, or MS/MS fragmentation).
- Follow Reporting Guidelines: Consult the guidelines developed by the Lipidomics Standard Initiative (LSI) for major lipidomics workflows [43].
Issue 3: Challenges in Quantitative Accuracy
Problem: Quantitative results vary due to methodological inconsistencies.
Solution: Implement rigorous quantitative practices [41].
- Use Internal Standards: Utilize stable isotope-labeled internal standards for absolute quantitation where possible. For relative quantitation, ensure the experimental series is well-controlled.
- Chromatographic Resolution: Ensure peaks are properly resolved. For targeted methods, chromatographic peaks should be Gaussian-shaped with a signal-to-noise ratio of at least 5:1 for quantification, and have 6-10 data points across the peak.
- Validate with Raw Data: Perform limit of detection (LOD) and limit of quantitation (LOQ) determinations using raw, unsmoothed data. Manually inspect raw data chromatograms to verify software-generated assignments.
Experimental Protocols for Clinical Samples
Optimized Sequential Extraction for Multi-Platform Analysis
This protocol enables NMR-based metabolomics and UHPLC-MS-based lipidomics from a single sample of plasma or liver tissue [40].
Protocol for Plasma
- Sample Preparation: Start with a single plasma sample.
- NMR Analysis: First, analyze the native or minimally prepared sample using
¹H NMR. - Biphasic Extraction: Following NMR, subject the sample to a biphasic extraction using CHCl₃/MeOH/H₂O.
- Phase Separation: Separate the polar (aqueous) and non-polar (organic) phases.
- Multi-Platform Analysis:
- Analyze the polar phase for metabolomics using UHPLC-Q-Orbitrap MS.
- Analyze the non-polar phase for lipidomics using UHPLC-QqQ MS.
Protocol for Liver Tissue
- Sample Preparation: Start with a single liver tissue sample.
- NMR Analysis: Begin with
¹H NMRanalysis. - Two-Step Sequential Extraction:
- Step 1 (Lipid-rich fraction): Extract with CHCl₃/MeOH. Resuspend the dried extract for lipidomics analysis (e.g., via UHPLC-MS).
- Step 2 (Polar metabolite fraction): Subsequently, extract the residue with MeOH/H₂O. Use this polar extract for further untargeted metabolomics by UHPLC-Q-Orbitrap MS.
Table 1: Comparison of optimized extraction methods for plasma and liver tissue.
| Sample Type | Recommended Method | Key Advantages | Sequential Analysis Order |
|---|---|---|---|
| Plasma | Biphasic CHCl₃/MeOH/H₂O | Comprehensive coverage of polar and lipid metabolites; high reproducibility; sample-conserving [40]. | 1. NMR → 2. Polar & Lipid UHPLC-MS |
| Liver Tissue | Two-step: CHCl₃/MeOH followed by MeOH/H₂O | Effective for complex tissue; allows separate, in-depth analysis of lipid and polar fractions [40]. | 1. NMR → 2. Lipidomics (from 1st extract) → 3. Metabolomics (from 2nd extract) |
Key Data Reporting Standards
Adhering to community-developed guidelines is essential for the quality and reproducibility of lipidomics data in clinical research [41].
Table 2: Essential guidelines for reporting lipidomics data.
| Aspect | Minimum Reporting Standard | Example/Additional Detail |
|---|---|---|
| Nomenclature | Use LIPID MAPS classification and shorthand notation [42]. | e.g., PC(16:0_18:1) for a glycerophosphocholine. |
| Authentic Standards | Confirm retention time matches synthetic standards for positive identification [41]. | Critical for discriminating between lipid isomers. |
| Peak Quality | Report signal-to-noise, data points across a peak, and provide raw chromatograms [41]. | S/N ≥5:1 for LOQ; 6-10 data points per peak. |
| Quantitation | Specify whether absolute or relative; describe internal standards used [41]. | Stable isotope dilution is the gold standard for absolute quantitation. |
| Data Deposition | Deposit in recognized repositories (e.g., Metabolomics Workbench) [41]. | Use LIPID MAPS nomenclature upon deposition. |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key reagents, standards, and software for robust lipidomics.
| Item | Function / Purpose |
|---|---|
| Chloroform (CHCl₃) & Methanol (MeOH) | Primary solvents for biphasic extraction, effectively separating polar and non-polar metabolites [40]. |
| Synthetic Lipid Standards | Authentic chemical standards for validating lipid identification and retention time, and for quantitative calibration [41]. |
| Stable Isotope-Labeled Internal Standards | Added to samples for correcting losses during preparation and enabling absolute quantitation via mass spectrometry [41]. |
| LIPID MAPS Database | The primary curated resource for lipid structures, classification, nomenclature, and mass spectrometric data [42]. |
| Lipid Data Analyzer (LDA) | Open-source software for automated processing and quantification of lipidomic MS data [41]. |
| Metabolomics Workbench | A public repository for depositing, sharing, and discovering metabolomics and lipidomics data [41]. |
Workflow and Relationship Diagrams
Optimized Lipidomics Workflow
Lipid Identification & Reporting Standards
Overcoming Analytical Challenges and Data Complexity
Troubleshooting Guides
Guide 1: Identifying Your Missing Data Mechanism
Q: How do I determine if my missing lipidomics data is MCAR, MAR, or MNAR? A: Correctly identifying the nature of your missing data is the most critical step in choosing the right imputation strategy. Misdiagnosis can lead to significant bias in your results.
- MCAR (Missing Completely at Random): The fact that a value is missing is unrelated to any observed or unobserved variables. For example, a sample is lost due to a tube breakage or a data entry error.
- MAR (Missing at Random): The probability of a value being missing may depend on other observed variables, but not on the unobserved (missing) value itself. For instance, the likelihood of a lipid species being missing may be higher in samples with a lower total lipid concentration (an observed value).
- MNAR (Missing Not at Random): The probability of a value being missing depends on the value itself. This is common in lipidomics when lipid concentrations fall below the instrument's limit of detection. The value is missing precisely because it is too low to be detected [44] [45].
Guide 2: Selecting an Imputation Algorithm
Q: Which imputation method should I use for my dataset? A: The choice of imputation method is highly dependent on the missing data mechanism and the specific characteristics of your lipidomics dataset. The table below summarizes recommendations based on recent methodological studies.
Table 1: Imputation Method Recommendations for Lipidomics Data
| Method | Best For | Key Advantages | Key Limitations | Citation |
|---|---|---|---|---|
| k-nearest neighbor (knn-TN, knn-CR) | All types, especially MNAR | Effective independent of missingness type; handles low-abundance lipids | Requires similar correlation structure in data | [44] [45] |
| Half-Minimum (HM) | MNAR (values below detection) | Simple, intuitive for limit-of-detection data | Can underestimate variance; poor for MCAR/MAR | [44] |
| Random Forest | MCAR, MAR | Robust non-parametric method | Less suitable for MNAR data | [44] [46] |
| Mean Imputation | MCAR | Simple, fast | Can distort distributions and correlations | [44] |
| Predictive Mean Matching (PMM) | MCAR, MAR | Preserves data distribution | Computationally intensive | [46] |
| Complete Case Analysis | MCAR with few missing values | Simple | Inefficient; biased if not MCAR | [47] |
Experimental Protocol: Implementing k-nearest neighbor (knn) Imputation
- Data Preprocessing: Log-transform your lipid concentration data to approximate a normal distribution.
- Method Selection: Choose either:
knn-TN(Truncated Normal): Assumes a truncated normal distribution, suitable for MNAR data.knn-CR(Correlation-based): Uses correlation structure between lipids, effective for all missingness types [45].
- Parameter Tuning: Determine the optimal number of neighbors (k) via cross-validation. A common starting point is k=5 or k=10.
- Implementation: Use available R packages (e.g.,
imputeorVIM) or Python libraries (e.g.,scikit-learnorfancyimpute). - Validation: Assess imputation quality using metrics like Normalized Root Mean Square Error (NRMSE) if ground truth is available [44].
Guide 3: Advanced Data Harmonization
Q: How can I integrate lipidomics datasets from different platforms or with different resolutions? A: Dataset harmonization is a common challenge. A predictive framework using elastic-net models can impute unmeasured lipid species from a lower-resolution dataset into a higher-resolution one [48].
Experimental Protocol: Dataset Harmonization via Predictive Modeling
- Designate Datasets: Identify your high-resolution dataset (reference) and lower-resolution dataset (target).
- Align Nomenclature: Map lipid species between datasets. A lipid in the target dataset may correspond to a composite of several isomeric species in the reference dataset [48].
- Check Concordance: Calculate partial correlation vectors for shared lipids. Remove lipids with discordant association patterns between datasets (e.g., those with distances >2.5 Median Absolute Deviations from the median) [48].
- Build Models: For each lipid to be imputed, construct an elastic-net prediction model using the remaining lipids as predictors in the reference dataset.
- Impute and Validate: Apply the models to the target dataset to predict unmeasured lipids. Validate imputations using an independent, comprehensively profiled cohort if available [48].
Frequently Asked Questions (FAQs)
Q: Is it ever acceptable to use zero imputation for missing lipid values? A: Generally, no. The consensus from recent studies is that zero imputation consistently gives poor results. It is not a biologically plausible value for most lipid concentrations and can severely bias downstream analyses [44].
Q: What is the maximum proportion of missing values that can be reliably imputed? A: There is no universal cutoff, but performance degrades as the proportion of missing values increases. One study noted that when the proportion of missing values is small (e.g., <10%), most methods perform reasonably well. With a higher proportion of missing values (e.g., >20%-30%), the choice of method becomes critical, and even the best methods may struggle, especially if the data is MNAR and the sample size is small [47] [44].
Q: How does multiple imputation by chained equations (MICE) handle different variable types? A: MICE is flexible and can handle mixed data types (continuous and categorical) by specifying different subroutines (e.g., predictive mean matching for continuous variables, logistic regression for binary variables). Subroutines like classification and regression trees (CART) and random forests can handle both types without specification [46].
Q: Why is standardization important in lipidomics, and what efforts are underway? A: Standardization is crucial to reduce inter-laboratory variation and establish consensus concentrations for lipids, which is a prerequisite for translating findings into clinical practice. Landmark initiatives like the Ceramide Ring Trial, involving 34 laboratories across 19 countries, aim to set new benchmarks by establishing reference values for clinically relevant lipids like ceramides using standardized protocols and authentic standards [49].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials for Standardized Lipidomics Research
| Reagent / Material | Function & Application | Example / Specification |
|---|---|---|
| NIST SRM 1950 | Standard Reference Material of metabolites in human plasma; used for quality control and inter-laboratory standardization [49]. | National Institute of Standards and Technology |
| Authentic Ceramide Standards | Precisely quantified chemical standards used for calibration and quantification of endogenous ceramide levels [49]. | Avanti Polar Lipids |
| Specialized Solvent Systems | Mobile phase for chromatographic separation of lipid species in mass spectrometry [48]. | e.g., IPA/ACN or THF-based systems |
| Plasma Quality Control (PQC) Samples | Pooled plasma samples run alongside experimental samples to monitor assay performance and reproducibility over time [48]. | In-house or commercial pools |
| Lipid Nanoparticles (LNPs) | Specialized delivery systems enabling precise targeting of medications in lipid-based therapies; a key tool in translational research [14]. | Various formulations |
Frequently Asked Questions (FAQs)
1. What is the primary goal of normalization in lipidomics? The main goal is to reduce unwanted technical variation arising from factors like sample preparation, instrumental noise, and batch effects, while preserving the biological variation of interest. This is crucial for making accurate biological inferences from the data [50] [51].
2. Why is removing unwanted variation particularly important for clinical samples? Clinical samples are highly susceptible to pre-analytical variations. Factors like sample storage temperature and duration can cause ex vivo distortions in the concentrations of many lipids and metabolites, which can compromise the reliability of potential biomarkers if not properly standardized and normalized [6].
3. Can I use a single internal standard for normalizing my lipidomics data? The use of a single internal standard is generally discouraged, as it can lead to highly variable normalized values. Recent literature demonstrates that using multiple internal standards is a more adequate practice for effectively removing unwanted variation [50].
4. How do I choose between different normalization methods? The choice depends on your data structure and the goals of your analysis. Key considerations include [50] [51]:
- The type of analysis: Is it supervised (e.g., identifying differentially abundant lipids between known groups) or unsupervised (e.g., clustering, correlation analysis)?
- Data characteristics: The performance of a normalization method can depend on the underlying data structure.
- Assumptions of the method: Ensure the method's assumptions, such as the "self-averaging" property in scaling methods, are valid for your dataset. It is recommended to evaluate the method's effectiveness based on metrics like the consistency of Quality Control (QC) samples and the preservation of expected biological variance [50] [51].
5. What are some common pitfalls in data normalization? A major pitfall is the selection of an inappropriate normalization method, which can inadvertently mask genuine biological signals or introduce biases, leading to inaccurate findings. This is especially critical in time-course experiments, where normalization must not distort the underlying longitudinal data structure [51].
Troubleshooting Guides
Problem 1: Poor Separation of Groups in Multivariate Analysis After Normalization
Symptoms: Principal Component Analysis (PCA) or other clustering methods show poor separation between sample groups (e.g., disease vs. control) that you expect to be different.
Diagnosis: The chosen normalization method may be too aggressive and is potentially removing some of the biological variation of interest along with the technical noise [51].
Solution:
- Re-evaluate your method: Compare the results using different normalization techniques. For lipidomics, methods like Probabilistic Quotient Normalization (PQN) and LOESS normalization using QC samples (LOESSQC) have been identified as top performers in recent multi-omics studies [51].
- Check QC samples: Assess the consistency of your QC samples before and after normalization. A good method should improve the clustering of QCs, indicating reduced technical variation [50] [51].
- Use a data-driven approach: Apply a framework that evaluates how normalization affects the variance explained by your factors of interest (e.g., treatment, time). The method should preserve or enhance this biological variance while reducing residual noise [51].
Problem 2: Persistent Batch Effects in the Data
Symptoms: Samples cluster by processing batch or injection date instead of by biological group in multivariate analysis.
Diagnosis: Standard scaling normalization methods (e.g., Total Ion Current) are insufficient to correct for strong batch effects or signal drift over time [50].
Solution:
- Utilize Quality Control Samples: Employ normalization methods that explicitly use pooled QC samples to model and correct for systematic errors. The SERRF (Systematical Error Removal using Random Forest) method is a machine learning approach designed for this purpose, though it should be used with caution as it may overfit in some cases [51].
- Consider Advanced Methods: Methods like RUV (Remove Unwanted Variation) that use quality control metabolites or internal standards can be very effective for accommodating both observed and unobserved unwanted variation, including batch effects [50].
- Standardize pre-analytics: Ensure meticulous pre-analytical sample handling to minimize the introduction of batch effects at the source. Follow standardized protocols for sample storage temperature and duration [6].
Symptoms: After normalization, the time-dependent trajectory of lipids appears flattened or distorted.
Diagnosis: The normalization method is not suitable for time-course data and is removing the time-related biological variance that you are trying to study [51].
Solution:
- Select temporal-study-appropriate methods: Choose methods known to perform well in time-course designs. Studies have shown that PQN and LOESSQC are robust choices as they effectively reduce technical variation without masking time-related variance [51].
- Avoid over-fitting methods: Be cautious with complex algorithms that might learn and remove the temporal patterns in your data. Assess if the variance explained by the time factor is preserved after normalization [51].
- Validate findings: Cross-validate the temporal patterns you discover with other analytical techniques or experimental validations.
Experimental Protocols for Normalization Assessment
Protocol: Evaluating Normalization Methods for Robust Lipidomics
Objective: To identify the most robust normalization method for a given clinical lipidomics dataset by assessing improvement in QC consistency and preservation of biological variance.
Materials:
- Raw lipid abundance data matrix
- Metadata file specifying sample groups, batches, and time points (if applicable)
- R or Python statistical environment
- Relevant software packages (e.g.,
limmain R)
Methodology:
- Data Preparation: Pre-process your raw data (peak picking, alignment, imputation of missing values) to obtain a complete data matrix [51].
- Apply Multiple Normalization Methods: Apply a panel of normalization methods to the same dataset. A recommended panel for lipidomics includes:
- Evaluate Performance Metrics:
- QC Consistency: Calculate the relative standard deviation (RSD) or coefficient of variation (CV) for each lipid feature in the QC samples before and after normalization. A successful method will significantly reduce the median RSD of QCs [51].
- Biological Variance Preservation: Perform PCA or ANOVA on the normalized data. A good method should increase the separation between predefined biological groups (e.g., treatment vs. control) or preserve the proportion of variance explained by a time factor in temporal studies [51].
- Visual Inspection: Create PCA scores plots to visually check for the removal of technical artifacts (tight QC clustering) and enhanced separation of biological groups.
The workflow for this evaluation protocol is summarized in the following diagram:
Protocol: Standardizing Pre-analytical Sample Handling for Plasma/Serum Lipidomics
Objective: To establish a standardized protocol for collecting and handling blood-based clinical samples to minimize ex vivo distortions of lipids prior to LC-MS analysis.
Materials:
- K3EDTA blood collection tubes
- Pre-chilled centrifuge
- Ice-water bath (for "freezing temperature" processing)
- Cryogenic vials
- -80°C freezer
Methodology [6]:
- Blood Collection: Draw blood into K3EDTA tubes.
- Plasma Separation: Centrifuge tubes at recommended g-force and time (e.g., 2,000 g for 10 minutes) at 4°C.
- Aliquoting: Immediately aliquot the plasma supernatant into cryovials.
- Storage: Flash-freeze aliquots in a mixture of dry ice and ethanol or directly in a -80°C freezer. Avoid intermediate storage at room temperature or -20°C.
- Stability Assessment: For novel biomarkers, conduct stability tests by exposing replicate samples to different storage temperatures and durations. Analyze using a fold-change approach to determine analyte-specific vulnerabilities.
The table below summarizes key normalization methods, their mechanisms, and their applicability to help you select an appropriate technique.
| Method | Mechanism | Pros | Cons | Best For |
|---|---|---|---|---|
| Total Ion Current (TIC) [50] | Scales each sample to the total sum of all feature intensities. | Simple, fast. | Relies on "self-averaging" assumption (total intensity is constant), which often fails [50]. | Initial data exploration; not recommended as a primary method for lipidomics. |
| Median Normalization [50] [51] | Scales each sample to the median intensity of all features. | Robust to very high-intensity outliers. | Still makes a global scaling assumption; may not correct for complex biases. | Datasets with strong outliers; proteomics [51]. |
| Probabilistic Quotient Normalization (PQN) [51] | Estimates a sample-specific dilution factor based on the ratio of feature intensities to a reference spectrum (e.g., median QC sample). | Accounts for overall concentration differences; does not assume a normal distribution. | Requires a reliable reference. | Metabolomics and Lipidomics; temporal studies; considered a top-performing method [51]. |
| LOESS (QC-Based) [51] | Fits a local regression model to the QC data based on injection order to correct for signal drift. | Effectively corrects for non-linear signal drift over time. | Requires a sufficient number of QC samples injected throughout the run. | Datasets with significant run-order drift; Lipidomics and Metabolomics [51]. |
| Quantile Normalization [51] | Forces the distribution of feature intensities to be identical across all samples. | Creates a very stable data structure. | Makes a strong assumption that the overall distribution is the same, which can remove biological variance [51]. | Not generally recommended for lipidomics if biological changes are global. |
| SERRF [51] | A machine learning method (Random Forest) that uses feature correlations in QC samples to model and correct systematic errors. | Powerful for correcting complex, non-linear batch effects and injection order artifacts. | Risk of overfitting and inadvertently removing biological variance [51]. | Complex batch effect correction when other methods fail; use with caution. |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table lists key materials required for robust lipidomics workflows, from sample collection to data normalization.
| Item | Function / Purpose | Example / Key Consideration |
|---|---|---|
| K3EDTA Plasma Tubes [6] | Standardized blood collection to prevent coagulation and provide a matrix for lipid analysis. | Preferred over serum for certain lipid classes to minimize ex vivo changes during clot formation. |
| Pooled Quality Control (QC) Sample [50] [51] | A representative sample used to monitor and correct for technical variation throughout the analytical run. | Created by mixing a small aliquot of every biological sample in the study. Injected repeatedly throughout the sequence. |
| Multiple Internal Standards [50] | Chemically similar compounds added to each sample to correct for losses during preparation and variation in instrument response. | Use a cocktail of stable isotope-labeled lipids covering different lipid classes (e.g., LPC, PC, TG, Ceramides). Avoids the pitfalls of a single standard [50]. |
| Dual-Column LC-MS System [52] | Expands metabolite coverage by combining orthogonal separation chemistries (e.g., Reversed-Phase and HILIC) in a single workflow. | Ensures comprehensive analysis of both polar and non-polar lipids, reducing analytical blind spots [52]. |
| Pre-chilled Centrifuge [6] | Rapid processing of blood samples at controlled, low temperatures. | Critical for pre-analytical standardization to prevent degradation of unstable lipids. |
Troubleshooting Guide: Resolving Common Software Inconsistencies
FAQ 1: Why do different lipidomics software platforms (like MS DIAL and Lipostar) provide different identifications when processing my identical LC-MS data?
This is a fundamental reproducibility challenge in the lipidomics field. When identical liquid chromatography-mass spectrometry (LC-MS) spectral data are processed by different software platforms, the identification results can vary significantly due to differences in their underlying algorithms, lipid libraries, and processing parameters [22].
Recommended Solution:
- Mandatory Manual Curation: Do not rely solely on automated "top hit" identifications. Visually inspect the spectra, including MS1 and MS2 data, for all putative lipid identifications [22].
- Cross-Platform Validation: Process your data with more than one software tool if possible. Identifications confirmed by multiple platforms have higher confidence [22].
- Utilize MS2 Data: While not infallible, using fragmentation (MS2) spectra significantly improves identification agreement compared to MS1-only data [22] [53].
FAQ 2: What are the main technical causes for these software discrepancies?
The discrepancies arise from several steps in the data processing workflow [22]:
- Different Lipid Libraries: Platforms may use different built-in databases (e.g., LipidBlast, LipidMAPS, ALEX123), which have varying levels of coverage and curation [22].
- Spectral Alignment Methodologies: Algorithms for peak alignment and retention time adjustment are often opaque to the user and can vary, leading to different feature lists [22].
- Inconsistent Use of Retention Time: Many software tools do not fully leverage retention time (tR) as a key parameter for improving identifications [22].
- Co-elution and Co-fragmentation: In complex samples, closely related lipids may elute simultaneously, leading to mixed MS2 spectra that are interpreted differently by each software [22].
FAQ 3: How can I improve the confidence of my lipid identifications in a clinical sample context?
Improving confidence is critical for translating lipidomic findings into clinically relevant biomarkers [11].
- Multi-Mode LC-MS Validation: Validate identifications across both positive and negative LC-MS ionization modes [22] [53].
- Data-Driven Quality Control: Supplement manual curation with statistical and machine learning-based outlier detection to flag potential false positives. One demonstrated method uses support vector machine (SVM) regression with leave-one-out cross-validation (LOOCV) to predict retention time and identify outliers [22].
- Follow Standards Initiatives: Adhere to the guidelines set by the Lipidomics Standards Initiative (LSI) for quality controls and minimum reporting information where available [22].
Quantitative Data on Software Reproducibility
The table below summarizes key findings from a cross-platform comparison study, highlighting the scale of the reproducibility challenge.
Table 1: Summary of Lipid Identification Agreement Between MS DIAL and Lipostar Software Platforms
| Comparison Metric | MS1 Data (Agreement) | MS2 Data (Agreement) | Key Takeaway |
|---|---|---|---|
| Overall Identification Match | 14.0% | 36.1% | Using fragmentation data (MS2) more than doubles reproducibility, but consensus remains low [22] [53]. |
| Required Conditions for a "Match" | Lipid formula, class, and aligned retention time (within 5 seconds) had to be identical to be considered in agreement [22]. |
Detailed Experimental Protocol for a Cross-Platform Validation Experiment
The following methodology is adapted from a published case study that quantified the reproducibility gap between MS DIAL and Lipostar [22]. This protocol can be used as a template for performing your own software benchmarking.
1. Sample Preparation and LC-MS Analysis
- Biological Sample: Use a standardized lipid extract. The cited study used a lipid extraction from the PANC-1 human pancreatic adenocarcinoma cell line.
- Extraction Method: Perform a modified Folch extraction using a chilled methanol/chloroform solution (1:2 v/v), supplemented with an antioxidant like 0.01% butylated hydroxytoluene (BHT) to prevent oxidation.
- Internal Standard: Add a quantitative MS internal standard mixture (e.g., Avanti EquiSPLASH LIPIDOMIX) to the final extract for quality control.
- LC-MS Instrumentation: Use a UPLC system coupled to a high-resolution mass spectrometer (e.g., ZenoTOF 7600).
- Chromatography:
- Column: Luna Omega Polar C18 column.
- Flow Rate: 8 µL/min.
- Mobile Phase: A) 60:40 Acetonitrile/Water; B) 85:10:5 Isopropanol/Water/Acetonitrile. Both supplemented with 10 mM ammonium formate and 0.1% formic acid.
- Gradient: 40% B to 99% B over 5 minutes, hold at 99% B for 5 minutes, then re-equilibrate.
- Mass Spectrometry: Operate in data-dependent acquisition (DDA) mode to collect both MS1 and MS2 spectra. The specific method should be optimized for your instrument.
2. Data Processing in Multiple Software Platforms
- Software Selection: Process the identical set of raw spectral data files in the software platforms you wish to compare (e.g., MS DIAL v4.9 and Lipostar v2.1.4).
- Parameter Settings: Configure the software settings to be as similar as possible. Use default libraries if your aim is to test typical out-of-the-box performance.
- Output: Generate a list of putative lipid identifications from each platform, including the chemical formula, lipid class, retention time, and MS/MS match status.
3. Data Comparison and Analysis
- Alignment of Identifications: Compare the two output datasets to find overlapping and unique annotations.
- Match Criteria: Define a strict set of rules for what constitutes an agreement. The cited study required: 1) identical lipid formula, 2) identical lipid class, and 3) aligned retention time consistent within a 5-second window [22].
- Calculate Agreement: The percentage agreement is calculated as the number of matching identifications divided by the total number of unique identifications across both platforms.
4. Post-Software Quality Control
- Retention Time Prediction with SVM/LOOCV:
- Assumption: Lipids of the same class elute in a predictable order based on their physicochemical properties.
- Method: Use a support vector machine (SVM) regression model with leave-one-out cross-validation (LOOCV) to predict the retention time of each putatively identified lipid based on its class and structure.
- Action: Identify lipids whose experimentally observed retention time is a significant outlier from the model's prediction. These are high-priority candidates for manual review and are likely false positives [22].
The following diagram illustrates the logical workflow and decision points for this quality control process.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Reagents and Software for Lipidomics Reproducibility Research
| Item Name | Function / Purpose | Example / Specification |
|---|---|---|
| Quantitative MS Internal Standard | Corrects for variability in extraction and ionization; enables quantification. | Avanti EquiSPLASH LIPIDOMIX (a mixture of deuterated lipids) [22]. |
| Antioxidant Additive | Prevents oxidation of unsaturated lipids during extraction and analysis. | 0.01% Butylated Hydroxytoluene (BHT) [22]. |
| LC-MS Grade Solvents | Ensures high purity for mobile phases to minimize background noise and ion suppression. | Acetonitrile, Isopropanol, Water, Chloroform, Methanol with 10 mM Ammonium Formate [22]. |
| Reverse-Phase UPLC Column | Separates a wide range of lipid classes by hydrophobicity prior to MS injection. | Polar C18 column (e.g., Luna Omega 3 µm, 50 x 0.3 mm) [22]. |
| Lipidomics Software Platforms | Used for automated peak picking, alignment, and identification from raw LC-MS data. | MS DIAL, Lipostar, LipidSearch, LipidMatch Suite [22] [54] [55]. |
| Lipid Structure Database | Reference library for matching accurate mass and MS/MS spectra. | LipidMAPS, LipidBlast [22] [56]. |
| High-Resolution Mass Spectrometer | Provides the accurate mass measurements essential for distinguishing between lipid species. | Instruments like ZenoTOF, Orbitrap, or Q-TOF [22] [57]. |
Visualization of the Lipid Identification Confidence Workflow
The following diagram maps the path from raw data to high-confidence lipid identification, integrating the key steps needed to overcome software inconsistencies.
Essential Tools for Statistical Analysis and Visualization in R and Python
Frequently Asked Questions (FAQs)
Q1: What are the most recommended R and Python libraries for creating publication-quality graphics from lipidomics data?
For R, ggplot2 is considered the gold standard for creating elegant and highly customizable static plots, making it ideal for publication-ready graphics [58]. For Python, Seaborn simplifies the creation of statistically oriented visualizations like violin plots and heatmaps with aesthetically pleasing defaults, while Matplotlib provides foundational control for creating publication-quality static visualizations [59] [60] [61].
Q2: How can I create interactive dashboards for exploring clinical lipidomics data?
In Python, Plotly specializes in creating interactive, web-based visualizations and dashboards that support zooming, panning, and hovering over data points [59] [60] [61]. Bokeh is another powerful Python library focused on building high-performance, web-ready interactive visualizations, even supporting real-time streaming data [59] [61]. In R, Leaflet allows for the creation of interactive maps for spatial data exploration [58].
Q3: My dataset has many missing values. What are the best practices for handling them before statistical analysis?
Missing values are common in lipidomics and metabolomics datasets and should be handled appropriately before analysis. Common strategies include:
- Filtering: Remove lipids or metabolites with a high percentage of missing values (e.g., >35%) [23].
- Imputation: Use methods like
k-nearest neighbors (kNN)orrandom forestto impute missing values that are Missing Completely at Random (MCAR) or Missing at Random (MAR). For values Missing Not at Random (MNAR), often due to being below the detection limit, imputation with a constant value (e.g., a percentage of the lowest concentration) can be appropriate [23].
Q4: What specialized tools are available in Python for processing raw mass spectrometry data from clinical samples?
pyOpenMS is an open-source Python library specifically designed for mass spectrometry, providing functionality for file handling, signal processing, quantitative analysis, and identification analysis for proteomics and metabolomics data [62].
Troubleshooting Guides
Issue 1: Inconsistent Lipid Quantification Due to Pre-analytical Sample Handling
Problem: Measured concentrations of lipids and metabolites are distorted, leading to unreliable data. This is often due to ex vivo degradation during sample collection and processing [6].
Solution: Implement standardized pre-analytical protocols. Research indicates that the stability of analytes varies, but meticulous processing is crucial for many lipids. Based on empirical data, consider these recommendations [6]:
- Use Appropriate Collection Tubes: Use K3EDTA whole-blood collection tubes.
- Control Storage Temperature: For short-term storage, keep plasma samples on ice or in ice water (Freezing Temperature, FT).
- Limit Storage Period: Minimize the intermediate storage period of plasma samples before final processing and analysis.
- Follow Data-Driven Protocols: Adopt specific, data-driven sample-handling protocols that balance the stability of the maximum number of analytes with practical feasibility in a clinical setting.
Issue 2: Common Data Preparation Errors in Statistical Processing
Problem: Statistical analysis yields misleading results due to improper data preparation, such as incorrect handling of missing values or skipped normalization.
Solution: Follow a standardized data preparation workflow before conducting any statistical tests or creating visualizations. The diagram below outlines the key steps and logical decisions involved in preparing a lipidomics dataset for analysis.
Issue 3: Visualization Fails to Reveal Biologically Relevant Patterns
Problem: Standard plots do not effectively communicate the statistically significant trends or biological relationships in the complex lipidomics data.
Solution: Select visualization types that are matched to the specific question you are asking of your data. The table below summarizes recommended visualizations for common analytical goals in lipidomics.
| Analytical Goal | Recommended Visualization Type | Example Libraries |
|---|---|---|
| Identify significantly altered lipids | Volcano plot [23] | R: ggplot2; Python: Matplotlib, Seaborn |
| Compare distributions across groups | Annotated box plots [23] | R: ggplot2; Python: Seaborn |
| Visualize correlations between lipids | Heatmap [23] [60] | R: ggplot2; Python: Seaborn |
| Reduce dimensionality & find clusters | PCA plot [23] | R: ggplot2; Python: Matplotlib, Seaborn |
| Group lipids based on common characteristics | Lipid maps, Fatty acyl chain plots [23] | R: ggplot2; Python: Matplotlib |
Issue 4: Choosing Between R and Python for Lipidomics Data Analysis
Problem: Uncertainty about whether to use R or Python for a lipidomics project, leading to delays in analysis.
Solution: The choice depends on your team's expertise and project needs. Both languages have powerful, evolving ecosystems. Below is a comparison of key packages for specific tasks to help you decide.
| Task | Recommended R Packages | Recommended Python Libraries |
|---|---|---|
| Primary Statistical Visualization | ggplot2 (static, publication-quality) [58] |
Seaborn (statistical, built on Matplotlib) [60] [61] |
| Interactive Visualization & Dashboards | Leaflet (interactive maps) [58], plotly (interactive charts) [63] |
Plotly (interactive, web-based) [59] [61], Bokeh (web-ready, real-time) [59] [61] |
| Data Wrangling & Workflow | targets (scalable, reproducible pipelines) [64], dplyr [58] |
pandas [60] |
| Mass Spectrometry Data Processing | - | pyOpenMS (proteomics & metabolomics) [62] |
| 3D & Specialized Visualizations | RGL (interactive 3D) [58], Rayrender (photorealistic 3D) [58] |
Matplotlib (foundational 2D/3D) [61], Plotly (3D) [61] |
Experimental Protocols & Workflows
Standardized Workflow for Statistical Processing and Visualization
For robust and reproducible analysis, follow a structured workflow from raw data to insight. The following diagram outlines a complete, standardized protocol for processing and visualizing lipidomics data.
Research Reagent Solutions for Lipidomics
The following table details essential materials and computational "reagents" (software tools) critical for ensuring reliable lipidomics analysis.
| Item/Tool Name | Function / Purpose |
|---|---|
| K3EDTA Plasma Tubes | Standardized blood collection tubes for pre-analytical sample preparation [6]. |
| Quality Control (QC) Samples | Pooled samples from all biological samples or commercial standards (e.g., NIST SRM 1950) used to monitor technical variability and for data normalization [23]. |
pyOpenMS (Python) |
Processes raw mass spectrometry data; handles file conversion, signal processing, and quantitative analysis [62]. |
ggplot2 (R) / Seaborn (Python) |
Core visualization libraries for creating descriptive statistics, annotated box plots, and other publication-quality graphics [23] [58] [60]. |
k-nearest neighbors (kNN) Algorithm |
A commonly recommended method for imputing missing values (MCAR, MAR) in lipidomics and metabolomics data matrices [23]. |
Ensuring Reproducibility and Translational Validity
FAQs: Addressing Core Challenges in Lipid Identification
Why is there a reproducibility crisis in lipidomics biomarker identification, and how can it be addressed? A significant reproducibility gap exists because different lipidomics software platforms can produce inconsistent results from identical spectral data. A 2024 study processing the same LC-MS data with MS DIAL and Lipostar found only 14.0% identification agreement using default settings. Even when using fragmentation (MS2) data, agreement only reached 36.1% [22] [53]. To address this, the lipidomics community has established the Lipidomics Standards Initiative (LSI), which creates guidelines for major lipidomics workflows, including sample collection, storage, data deconvolution, and reporting [43]. Essential steps to improve reproducibility include:
- Manual Curation: Visually inspecting spectra and software outputs is non-negotiable for reducing false positives [22].
- Multi-Mode Validation: Validating identifications across both positive and negative LC-MS modes [22] [53].
- Data-Driven QC: Employing machine learning and outlier detection methods to flag potentially erroneous identifications [22].
What are the most common sources of false positive identifications? The primary technical challenges leading to false positives are:
- Co-elution: When multiple lipids elute from the chromatography column simultaneously, leading to mixed fragmentation spectra and misidentification [22].
- Closely Related Lipids: Isobaric lipids or lipids with very similar structures can be difficult for software to distinguish confidently [22].
- Inconsistent Libraries: Different software platforms often use different lipid libraries (e.g., LipidBlast, LipidMAPS), which can lead to conflicting identifications [22] [65].
- Limited Use of Retention Time (tR): Many software tools do not fully exploit the rich information provided by chromatographic retention time, unlike in proteomics where it is more routinely integrated with machine learning [22].
Which software tools are recommended for lipidomics data analysis? The choice of software depends on the specific task. LIPID MAPS provides an interactive portal to guide users toward appropriate open-access tools for different aspects of data processing [65]. Key tools and their functions are listed in the table below.
Table: Key Lipidomics Software and Databases
| Tool Name | Primary Function | Key Feature |
|---|---|---|
| MS DIAL [22] [65] | Untargeted Lipidomics | Comprehensive software for data processing, lipid identification, and quantification. |
| Lipostar [22] [65] | Untargeted Lipidomics | Platform for LC-MS/MS lipidomics data processing and identification. |
| LIPID MAPS [66] [65] | Lipid Database | Centralized, curated database of lipid structures and associated data. |
| BioPAN [66] | Pathway Analysis | Web-based tool to explore lipid metabolic pathways and predict gene activity. |
| LipidLynxX [66] | Data Annotation & Conversion | Cross-matches and converts various lipid annotations to support data integration. |
| LipidFinder [66] | Peak Filtering | Distinguishes lipid-like features from contaminants and noise in LC-MS data. |
Experimental Protocols for Benchmarking and Quality Control
Protocol: Cross-Platform Software Consistency Check
This protocol allows you to benchmark the consistency of lipid identifications from different software packages using your own data.
1. Sample Preparation and LC-MS Analysis:
- Sample: Use a well-defined sample, such as a lipid extract from a human cell line (e.g., PANC-1 pancreatic adenocarcinoma cells) [22].
- Extraction: Perform a modified Folch extraction using a chilled methanol/chloroform solution (e.g., 1:2 v/v) with an antioxidant like BHT to prevent oxidation [22].
- Internal Standard: Add a quantitative internal standard mixture (e.g., Avanti EquiSPLASH LIPIDOMIX) for quality control [22].
- LC-MS Instrumentation: Analyze the sample using a UPLC system coupled to a high-resolution mass spectrometer (e.g., ZenoToF 7600) [22].
- Chromatography: Use a reversed-phase column (e.g., Luna Omega C18) with a binary gradient of acetonitrile/water and isopropanol/water/acetonitrile, both supplemented with 10 mM ammonium formate and 0.1% formic acid [22].
2. Data Processing:
- Export your raw LC-MS data files.
- Process the same set of files independently through at least two different lipidomics platforms (e.g., MS DIAL and Lipostar) using their default settings and libraries to start [22].
3. Data Comparison and Analysis:
- Export the lists of putative lipid identifications from each software.
- Compare the outputs. For this analysis, consider identifications to be in agreement only if they meet all of the following criteria:
- The molecular formula is identical.
- The lipid class is identical.
- The aligned retention time is consistent (e.g., within a 5-second window) [22].
- Calculate the percentage overlap. The low agreement rate you will likely find underscores the necessity of manual curation.
Protocol: Data-Driven Outlier Detection for Quality Control
This protocol uses a machine learning approach to identify potential false positive identifications from your software's output.
1. Data Preparation:
- From your lipidomics software output, create a data table (.csv file) containing the following for each putative lipid identification:
- Chemical formula of the parent molecule
- Lipid class
- Experimental retention time (tR)
- MS1 and MS2 status [22]
- Exclude lipids with a retention time below 1 minute, as these are considered to have no column retention and thus no useful chromatographic information [22].
2. Model Training and Prediction:
- Use a Support Vector Machine (SVM) regression algorithm combined with Leave-One-Out Cross-Validation (LOOCV).
- The model is trained to predict the expected retention time for a lipid based on its chemical properties (inferred from its identity). A lipid with an experimentally measured retention time that is a significant outlier from its model-predicted value may be a false positive and should be flagged for manual review [22].
- This process can be implemented in programming environments like R or Python and does not require high-performance computing clusters [22].
Workflow Visualization: Manual Curation and Data QC
The following diagram illustrates the integrated workflow of software-based identification and essential manual curation steps to ensure high-confidence lipid annotations.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Materials for Reproducible Lipidomics
| Reagent / Material | Function / Application | Example from Literature |
|---|---|---|
| Avanti EquiSPLASH LIPIDOMIX | Quantitative internal standard for MS; a mixture of deuterated lipids added before extraction for normalization and quality control. | Added at 16 ng/mL to PANC-1 cell lipid extract [22]. |
| Butylated Hydroxytoluene (BHT) | Antioxidant added to lipid extraction solvents to prevent lipid oxidation during sample preparation. | Supplemented at 0.01% in methanol/chloroform extraction solution [22]. |
| Luna Omega C18 Column | Reversed-phase UPLC column for separating a wide range of lipid molecules prior to mass spectrometry. | 3 µm polar C18, 50 × 0.3 mm; used for microflow separation [22]. |
| Ammonium Formate / Formic Acid | Mobile phase additives in LC-MS; enhance ionization efficiency and help control pH for robust and sensitive detection. | Added to both eluents A and B at 10 mM and 0.1% respectively [22]. |
| MS DIAL & Lipostar Software | Open-access software platforms for untargeted lipidomics data processing, identification, and quantification. | Used for cross-platform comparison study [22] [65]. |
Frequently Asked Questions (FAQs): Core Concepts and Troubleshooting
FAQ 1: What are the primary sources of irreproducibility in lipidomic data when correlating with clinical phenotypes, and how can they be mitigated?
Irreproducibility primarily stems from biological variability, lipid structural diversity, inconsistent sample processing, and a critical lack of standardized procedures [11]. A significant, often overlooked source is the inconsistency between lipidomics software platforms. When processing identical LC-MS spectral data, different software platforms can yield dramatically different results; one study found only 14.0% identification agreement using default settings, which improved to just 36.1% even when using more reliable MS2 fragmentation data [22].
- Mitigation Strategies:
- Manual Curation: Essential for reducing false positives, especially for closely related lipids and co-elution issues [22].
- Cross-Platform Validation: Validate key lipid identifications across more than one software platform [22].
- Standardized Protocols: Adopt the guidelines from the Lipidomics Standards Initiative (LSI) for quality control and reporting [22].
- Data-Driven QC: Employ machine learning-based outlier detection to flag potentially false positive identifications [22].
FAQ 2: How do I choose between targeted and untargeted lipidomics for a clinical phenotype correlation study?
The choice depends on the study's hypothesis and goals [67] [57].
- Untargeted Lipidomics is a discovery-oriented approach that aims to profile all detectable lipids in a sample without prior bias. It is ideal for hypothesis generation, discovering novel lipid biomarkers, and when the lipid species of interest are not known in advance. However, it may be limited by dynamic range and requires sophisticated data processing [11] [57].
- Targeted Lipidomics focuses on the precise identification and quantification of a predefined set of lipid species. It is used for hypothesis-driven research, validating biomarkers from untargeted studies, and achieving high sensitivity and accuracy for specific lipid classes or pathways known to be relevant to a clinical phenotype [67] [57].
FAQ 3: What are the key challenges in detecting and quantifying lipids in complex matrices like plasma?
Plasma presents several unique challenges [57]:
- Ion Suppression/Enhancement: The presence of numerous interfering compounds (proteins, salts, other metabolites) can suppress or enhance the ionization of target lipids, complicating accurate quantification.
- Wide Dynamic Range: Lipids in plasma can exist at concentrations ranging from picomolar to millimolar, requiring highly sensitive techniques to capture low-abundance species without being overwhelmed by abundant ones.
- Isobaric Interference: Many lipids, especially within the same class, have identical or nearly identical molecular weights, making them difficult to distinguish by mass alone [57].
- Mitigation Strategies involve rigorous sample preparation (e.g., solid-phase extraction), the use of high-resolution mass spectrometry to differentiate exact masses, and coupling with chromatography to separate lipids by retention time [67] [57].
FAQ 4: Which lipid classes have the most significant impact on health and are frequently correlated with clinical phenotypes?
While all lipids play roles, two major categories are frequently highlighted in clinical studies [14]:
- Phospholipids: As the structural foundation of all cell membranes, their composition directly impacts cellular function, fluidity, and signaling. Abnormalities in phospholipids can precede the development of conditions like insulin resistance by several years [14].
- Sphingolipids (particularly Ceramides): These function as powerful signaling molecules regulating inflammation, cell death, and metabolism. Elevated ceramide levels are strong predictors of cardiovascular events and correlate strongly with insulin resistance. Ceramide risk scores now often outperform traditional cholesterol measurements in predicting heart attack risk [14].
Troubleshooting Guides: Addressing Specific Experimental Issues
Problem 1: Low Agreement in Lipid Identifications Across Software or Laboratories
| Observation | Potential Cause | Solution |
|---|---|---|
| Low overlap of identified lipid species when the same dataset is processed by different software (e.g., MS DIAL vs. Lipostar) or in an inter-laboratory comparison. | Use of different default identification algorithms, spectral alignment methodologies, and lipid libraries (e.g., LipidBlast vs. LipidMAPS) [22]. | 1. Mandatory Manual Curation: Manually inspect MS2 spectra for top biomarker candidates [22].2. Utilize Retention Time: Use retention time (tR) as an additional confirmation parameter during validation [22].3. Standardize Settings: Align software settings and lipid libraries across the project where possible. |
Problem 2: Batch Effects in Large-Scale Lipidomics Studies
| Observation | Potential Cause | Solution |
|---|---|---|
| Clustering of samples by batch run date rather than by biological group in multivariate statistics (e.g., PCA). | Technical variability introduced from running samples in multiple LC-MS batches over time. This is a major limitation as batch sizes are typically small (48-96 samples) compared to large cohorts [68]. | 1. Study Design: Distribute samples from all experimental groups across all batches [68].2. Quality Control (QC) Samples: Inject a pooled QC sample repeatedly throughout the sequence to monitor instrument stability and for post-acquisition normalization [68].3. Internal Standards: Add isotope-labeled internal standards as early as possible in sample preparation to correct for technical biases [68]. |
Problem 3: Difficulty Distinguishing Lipid Isomers and Isobars
| Observation | Potential Cause | Solution |
|---|---|---|
| Inability to separate lipids with the same mass but different structures (e.g., sn-position of fatty acyl chains, double bond position). | Limitations of standard LC-MS setups in resolving structurally similar lipids that have identical mass-to-charge ratios [57]. | 1. Advanced Chromatography: Optimize LC conditions for better separation [57].2. Ion Mobility Mass Spectrometry (IM-MS): Implement IM-MS, which adds a separation dimension based on the ion's shape, size, and charge (Collision Cross-Section, CCS), to separate isomeric lipids [57].3. Advanced Fragmentation: Use specialized MS/MS techniques that reveal double bond and sn-positions [57]. |
Experimental Protocols & Workflows
Standardized Workflow for Untargeted Lipidomics of Clinical Plasma Samples
The following diagram illustrates the end-to-end workflow for obtaining lipidomic data from clinical plasma samples, from initial collection to final data output.
Detailed Protocol Steps:
Sample Preparation:
- Collection: Collect fasting blood samples in tubes containing anticoagulants (e.g., EDTA). To prevent lipid oxidation, consider adding antioxidants like butylated hydroxytoluene (BHT) [22].
- Storage: Flash-freeze plasma immediately and store at -80°C to prevent lipid degradation [67].
- Extraction: Perform lipid extraction using a validated method like the modified Folch (chloroform:methanol) or MTBE method. The most critical step is the early addition of isotope-labeled internal standards to correct for losses during preparation and analysis [68].
- Quality Control (QC): Create a pooled QC sample by combining a small aliquot of every sample in the study [68].
Data Acquisition:
- Chromatography: Use reversed-phase or HILIC chromatography to separate lipid classes. A typical C18 or C8 column is used with a gradient elution [68].
- Mass Spectrometry: Acquire data using a high-resolution mass spectrometer (e.g., Q-TOF). Data should be acquired in both positive and negative ion modes to maximize lipid coverage [57] [68].
- QC Injection: The pooled QC sample is injected at the beginning to condition the column and then repeatedly throughout the analytical sequence (e.g., after every 10 experimental samples) to monitor instrument performance and reproducibility [68].
Data Preprocessing:
- Conversion: Convert vendor-specific raw data files to an open format like mzXML using tools like ProteoWizard [68].
- Peak Picking: Use software like XCMS [68] or MS DIAL [22] for peak detection, alignment across samples, and retention time correction.
- Filtering: Remove peaks present in blank samples and impute any missing values using methods like k-nearest neighbors (kNN) [67].
Data Analysis and Integration:
- Statistics: Perform univariate (t-tests, ANOVA) and multivariate (PCA, PLS-DA) analyses to identify lipids differentially abundant between clinical phenotype groups [67].
- Identification: Identify lipids by matching accurate mass and MS/MS spectra against databases like LIPID MAPS [69] [67]. Manual curation of MS2 spectra is essential for confident identification [22].
- Pathway Analysis: Use tools like LipidSig or KEGG to map significant lipids onto biological pathways [67].
- Correlation with Phenotypes: Statistically correlate lipid abundance levels with quantitative clinical traits (e.g., lung function, BMI, lab values) to establish trans-omic relationships [70].
Protocol for Clinical Trans-Omics Correlation Analysis
This protocol outlines the steps for integrating identified lipid signatures with clinical phenome data [70].
- Define Clinical Phenomes: Collect and digitize a comprehensive set of clinical data. This can include:
- Anthropometrics: Body Mass Index (BMI), weight, height.
- Medical History: Smoking status, dust exposure history, disease complications.
- Laboratory Tests: pH, lipid panels, other blood biomarkers.
- Organ Function: Lung function tests (FEV1, FVC) [70].
- Generate Lipidomic Matrix: From the lipidomics workflow, create a data matrix where rows are samples, columns are lipid species, and values are normalized concentrations.
- Perform Integrative Statistics: Use correlation analyses (e.g., Spearman correlation) or more advanced multivariate models (e.g., Expression Quantitative Trait Locus (eQTL)-like models) to find significant associations between specific lipids and clinical variables [70].
- Visualize and Interpret: Create heatmaps or network diagrams to visualize the "trans-omic" network, showing how specific clinical features are connected to multiple lipids and vice versa [70].
Lipid-Phenotype Correlations: Key Quantitative Findings
The table below summarizes examples of specific lipid classes that have been quantitatively correlated with clinical phenotypes in recent studies.
| Lipid Class | Change Direction | Clinical Phenotype Correlation | Quantitative Finding (Fold-Change/Correlation) | Citation |
|---|---|---|---|---|
| Phosphatidylethanolamines (PE) | Upregulated | Pneumoconiosis (vs. Healthy) | Significantly increased (> 1.5-fold) [70] | |
| Phosphatidylcholines (PC) | Downregulated | Pneumoconiosis (vs. Healthy) | Significantly decreased (< 0.67-fold) [70] | |
| Ceramides (Cer) | Upregulated | Cardiovascular Risk | Ceramide risk score outperforms traditional cholesterol in predicting heart attack risk [14] | |
| Sphingomyelins (SM) | Inversely Correlated | Lung Function (FEV1) in COPD | Inversely correlated with FEV1 / FVC ratio [70] | |
| Phosphatidylcholines (PC) | Altered | PKU Phenotypes | Variation in polyunsaturated PC species observed across PKU phenotypes [71] |
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function | Example/Note |
|---|---|---|
| Isotope-Labeled Internal Standards | Critical for accurate quantification; corrects for losses during sample preparation and analysis variability. | Avanti EquiSPLASH LIPIDOMIX [22]. Should be added as early as possible in extraction [68]. |
| Chloroform-Methanol Mix | Organic solvents for liquid-liquid extraction of lipids from biological matrices (e.g., Folch method). | Standard for lipid extraction; use high-purity HPLC/MS grade [22] [67]. |
| Butylated Hydroxytoluene (BHT) | Antioxidant added during extraction to prevent oxidation of unsaturated lipids. | Added to extraction solvent at ~0.01% [22]. |
| Pooled Quality Control (QC) Sample | A homogeneous sample used to monitor instrument stability and reproducibility throughout the long LC-MS sequence. | Created from an aliquot of every sample in the study [68]. |
| High-Performance LC Columns | Separate complex lipid mixtures prior to mass spectrometry detection. | Reversed-Phase (e.g., C18, C8) or HILIC columns are common choices [68]. |
| Standard Reference Lipid Libraries | Databases for identifying lipids based on accurate mass and fragmentation patterns. | LIPID MAPS is a comprehensive, curated resource [69] [67]. |
Future Directions: The Role of Artificial Intelligence and Single-Cell Analysis
The field is rapidly evolving with new technologies that address current limitations.
- Artificial Intelligence (AI): Machine learning models are being used to improve lipid identification. For example, MS2Lipid has demonstrated up to 97.4% accuracy in predicting lipid subclasses from MS2 spectra [11]. AI also powers multi-omics aging clocks that integrate lipidomics with other data types to predict biological age and disease risk [72].
- Single-Cell Lipidomics: Advanced mass spectrometry techniques (Orbitrap, FT-ICR) and mass spectrometry imaging (MALDI-MSI, SIMS) are now enabling lipid profiling at the single-cell level. This reveals cellular heterogeneity in lipid metabolism that is obscured in bulk tissue analysis, offering unprecedented insights into cell-specific roles in disease and development [69].
Frequently Asked Questions (FAQs)
FAQ 1: Why is pre-analytical sample handling so critical in lipidomics, and which analytes are most vulnerable? Pre-analytical sample handling is a major source of ex vivo distortions for many lipids and metabolites. If not standardized, it can render samples unsuitable for reliable clinical diagnosis by altering analyte concentrations. Several lipids and lipid mediators are particularly prone to instability, including various lysophospholipids (LPA, LPC, LPE, LPG, LPI) and endocannabinoids (AEA, 1-AG, 2-AG) [6].
FAQ 2: What is the core difference between validating an AI tool for drug development and validating a lipidomic method? While both require rigorous evidence, AI validation in drug development demands prospective clinical evaluation and randomized controlled trials (RCTs) to prove impact on clinical decision-making and patient outcomes [73]. Lipidomic method validation focuses on analytical performance metrics like reproducibility, accuracy, and linear dynamic range across sample batches [74]. The common imperative is generating robust, real-world evidence to build trust and ensure reliability.
FAQ 3: My lipidomic dataset shows batch effects. How can this be addressed in the experimental design phase? Batch effects are a key limitation in LC-MS experiments. To mitigate them, distribute your samples among batches so that groups for comparison are present within the same batch. Crucially, avoid confounding your primary factor of interest with the batch covariate or the measurement order. Using stratified randomization and including quality control (QC) samples in each batch are essential practices [68].
FAQ 4: What are the consequences of deploying an AI-enabled medical device without adequate clinical validation? Devices cleared via pathways like the FDA's 510(k) that lack clinical evaluation are associated with a higher risk of recalls, often due to diagnostic or measurement errors. A significant proportion of recalls occur within the first year of authorization, which can undermine confidence in the technology among clinicians and patients [75].
Troubleshooting Guides
Issue 1: Unstable Analyte Measurements in Plasma Samples
Problem: Measurements for certain lipids or metabolites show high variability, suspected to be due to improper sample handling between collection and processing.
Solution: Implement a standardized pre-analytical protocol based on the stability profile of your target analytes. Below are data-driven recommendations [6]:
| Protocol Stringency | Storage Temperature | Maximum Storage Time | Recommended Use Case |
|---|---|---|---|
| Most Stringent | Freezing in ice water (FT) | 2 hours | Maximizes analyte integrity for unstable species (e.g., LPA, endocannabinoids) |
| Standard | Room Temperature (RT) | 2 hours | Suitable for a broad range of stable metabolites and lipids |
| Less Stringent | Room Temperature (RT) | 24 hours | Feasible for many stable analytes; justifies less strict handling |
Step-by-step Resolution:
- Identify: Review your analyte list against stability data. The fold change (FC) is a key metric for stability; a significant FC indicates vulnerability [6].
- Classify: Categorize your key analytes as "stable" or "unstable" based on published stability profiles from resources like [6].
- Select: Choose the most feasible protocol from the table above that ensures the integrity of your most critical, unstable analytes.
- Document and Adhere: Document the chosen protocol and ensure all personnel strictly adhere to it for every sample to ensure consistency.
Issue 2: Poor Data Quality in Untargeted Lipidomics LC-MS Workflow
Problem: The acquired LC-MS data has low signal-to-noise ratio, poor peak alignment, or persistent batch effects, complicating data analysis and interpretation.
Solution: Follow a standardized workflow for data acquisition and processing, incorporating quality controls at every stage.
Resolution Workflow:
Key Steps Explained:
- Internal Standards: Add isotope-labeled internal standards to the extraction buffer as early as possible to normalize for experimental biases [68].
- Batch Design: Use stratified randomization to distribute your samples across processing batches. This is vital to prevent the batch effect from obscuring or mimicking your biological signal of interest [68].
- Quality Control (QC): Inject pooled QC samples repeatedly throughout the sequence—for column conditioning, after every batch of samples, and after the run—to monitor instrument stability [68].
- Data Conversion & Import: Convert raw data to the open mzXML format. When importing into analysis tools like the xcms R package, organize your files in a folder structure that reflects your experimental design, as this can be used for initial sample grouping and peak alignment [68].
Issue 3: Insufficient Analytical Validation for Lipidomic Method
Problem: A developed lipidomics method lacks the necessary validation to be considered reliable for clinical research or to convince reviewers of its robustness.
Solution: Systematically validate all key analytical performance criteria as per established guidelines. The following table outlines the essential parameters to evaluate and report [74].
| Validation Criterion | Description & Best Practice |
|---|---|
| Reproducibility | Measure within-batch and from batch-to-batch. Must be analyzed using real samples (pooled or individual), not just standard mixtures. |
| Accuracy | Assess within-batch and from batch-to-batch. Must be tested in the sample matrix (e.g., plasma) at different concentration levels. |
| Limit of Detection | Determine the lowest amount of an analyte that can be reliably detected. |
| Linear Dynamic Range | Establish the concentration range over which the instrument response is linear. |
| Sample Carry Over | Evaluate if a measurement is affected by the previous sample. |
| Stability | Test analyte stability under various pre-analytical conditions (e.g., storage time, temperature). |
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and their functions for a reliable untargeted lipidomics workflow, based on the cited methodologies [68].
| Item | Function & Importance |
|---|---|
| K3EDTA Blood Collection Tubes | Standardized blood collection; anticoagulant prevents clotting, ensuring plasma consistency for pre-analytical studies [6]. |
| Isotope-Labeled Internal Standards | Added to samples pre-extraction to correct for losses during processing, matrix effects, and instrument variability [68]. |
| Stratified Randomization Plan | A statistical plan for assigning samples to processing batches to minimize bias and confound batch effects with the primary study variable [68]. |
| Pooled Quality Control (QC) Sample | A homogenized mix of all study samples; run repeatedly throughout the LC-MS sequence to monitor and correct for instrumental drift [68]. |
| Blank Samples | Samples without biological material (e.g., empty tube); processed alongside real samples to identify and filter out peaks from contamination [68]. |
| Reversed-Phase LC Column (e.g., C8) | The core of chromatographic separation; separates complex lipid mixtures by hydrophobicity prior to mass spectrometry detection [68]. |
| xcms R Software Package | A widely used, open-source tool for the processing, peak detection, alignment, and statistical analysis of untargeted LC-MS data [68]. |
Personalized medicine has evolved beyond genomics, with lipid-based strategies emerging as a powerful complement to traditional gene-based approaches. While genetics dominated personalized medicine for years, lipids now provide more actionable, real-time insights into metabolic health, inflammation status, and disease risk [14]. The healthcare landscape of 2025 has shifted dramatically toward lipid-focused personalized medicine, with the personalized medicine market growing to $426.82 billion in 2025, significantly driven by lipid-based approaches [14].
This technical support center provides standardized protocols and troubleshooting guides for researchers navigating both fields. Lipid profiles reflect current physiological states and can predict disease onset 3-5 years earlier than genetic markers alone, offering a critical window for intervention [14]. Meanwhile, gene-based methods provide essential information about inherent predispositions. Understanding both approaches enables researchers to develop more comprehensive diagnostic and therapeutic strategies.
Comparative Effectiveness Data
Quantitative Outcomes Comparison
Table 1: Direct Comparison of Lipid-Based vs. Gene-Based Personalized Medicine Outcomes
| Performance Metric | Lipid-Based Approach | Gene-Based Approach | Clinical Context |
|---|---|---|---|
| Cardiovascular Event Reduction | 37% reduction [14] | 19% reduction [14] | LIPID-HEART trial (2024) vs. gene-based risk assessments |
| Metabolic Syndrome Improvement | 43% greater improvement in insulin sensitivity [14] | Baseline comparison | RESPOND trial (2024) after six months |
| Inflammatory Marker Reduction | 27% greater reduction [14] | Baseline comparison | RESPOND trial (2024) after six months |
| Treatment Success Rates | 67% increase [14] | 31% improvement [14] | When examined before symptoms appeared |
| Alzheimer's Progression | 28% slower cognitive decline [14] | Limited success | BRAIN-LIPID study with custom lipid supplements |
| Cost-Effectiveness | ~$3,200 per QALY gained [14] | ~$12,700 per QALY gained [14] | 2025 healthcare economics analysis |
Clinical Application Profiles
Table 2: Application-Specific Performance of Lipid-Based and Gene-Based Approaches
| Clinical Application | Optimal Approach | Key Advantages | Limitations |
|---|---|---|---|
| Cardiovascular Prevention | Lipid-based | Ceramide risk scores outperform traditional cholesterol measurements [14] | Genetic markers show lower predictive accuracy [14] |
| Neurodegenerative Disorders | Lipid-based | Addresses specific membrane lipid abnormalities [14] | Genetic approaches prove difficult to modify [14] |
| Cancer Treatment | Lipid-based | LNP-delivered drugs reduce side effects by 40% [14] | Conventional chemotherapy less targeted |
| Therapeutic Delivery | Lipid-based | LNP market projected to reach $38.04B by 2034 [14] | Viral vectors risk insertional mutagenesis [76] |
| Long-term Genetic Conditions | Gene-based | Viral vectors enable permanent gene expression [76] | LNPs typically deliver transient RNA [76] |
| Precision Tissue Targeting | Gene-based | Viral vectors excel at specific tissue targeting [76] | LNP targeting capabilities still developing [76] |
Lipidomics Experimental Workflow
The following diagram illustrates the standardized lipidomics workflow for clinical samples, from collection to data interpretation:
Critical Pre-Analytical Considerations
Sample Collection & Handling:
- Blood Sampling: Collect fasting samples in specialized tubes that prevent lipid oxidation [14]. Use K3EDTA whole-blood collection tubes as they've been validated for lipid stability studies [6].
- Storage Temperature: Intermediate storage temperature significantly affects analyte concentrations. Implement strict temperature control immediately after collection [6].
- Processing Time: Many lipids are prone to ex vivo distortions. Process samples within 2 hours of collection for optimal lipid preservation [6].
Lipid Extraction Methods:
- Modified Bligh & Dyer: Chloroform/methanol/H₂O (1:1:0.9, v/v/v) for small tissue samples (<50 mg). Total lipids collect in chloroform phase [77].
- MTBE Method: Methyl tert-butyl ether/methanol/water (5:1.5:1.45, v/v/v). MTBE forms top layer, facilitating automation [77].
- BUME Method: Butanol/methanol (3:1, v/v) with heptane/ethyl acetate (3:1, v/v) and 1% acetic acid. Reduces water-soluble contaminants [77].
Essential Research Reagent Solutions
Table 3: Critical Reagents for Lipidomics and Genomics Research
| Reagent/Category | Function & Application | Technical Specifications |
|---|---|---|
| Internal Standards (IS) | Normalization for extraction efficiency, ion suppression, instrument variation [77] [68] | Isotope-labeled (deuterated, 13C) lipids matching target analytes; add early in extraction |
| Lipid Extraction Solvents | Efficient recovery of lipid species from biological matrices [77] [78] | HPLC-grade chloroform, methanol, MTBE; include antioxidant preservatives (BHT) for oxidizable lipids |
| Chromatography Columns | Separation of lipid classes prior to MS analysis [68] [57] | Reversed-Phase BEH C8 or C18 columns (e.g., Waters Acquity); guard columns to extend lifespan |
| Mass Spectrometry Ionization Reagents | Enhance ionization efficiency for different lipid classes [77] [57] | Ammonium formate/acetate for mobile phase modifiers; matrix compounds for MALDI (e.g., DHB) |
| Quality Control Materials | Monitor instrument performance and data quality across batches [6] [68] | Pooled quality control (QC) samples from study matrix; commercial quality control materials |
| Sample Preservation Solutions | Prevent ex vivo degradation of labile lipids during processing [6] | Protease/phosphatase inhibitors; antioxidant cocktails (e.g., BHT); chelating agents (EDTA) |
Troubleshooting Guides & FAQs
Pre-Analytical Challenges
Q: Our lipidomics results show high variability between technical replicates. Which pre-analytical factors should we investigate first? A: Focus on these critical factors:
- Sample Handling Temperature: Many lipids degrade rapidly at room temperature. Keep samples in ice water (0-4°C) during processing. Validate storage conditions for your specific lipid panels [6].
- Processing Time Consistency: Standardize the time between collection and freezing. For unstable lipids like lysophospholipids and lipid mediators, process within 2 hours [6].
- Internal Standard Addition: Add isotope-labeled internal standards immediately upon sample collection to correct for ex vivo degradation [68].
Q: How do we select the appropriate lipid extraction method for different sample types? A: Selection criteria include:
- Modified Bligh & Dyer: Ideal for small tissue samples (<50 mg) but requires chloroform handling [77].
- MTBE Method: Better for automation as MTBE forms the top layer, eliminating bottom phase collection issues [77].
- BUME Method: Superior for reducing water-soluble contaminants but challenging for evaporation due to butanol [77].
- Always validate recovery rates for your lipid classes of interest using spiked standards.
Analytical Method Challenges
Q: How do we optimize LC-MS/MS parameters for different lipid classes? A: Implement a systematic optimization approach:
- Ionization Mode Selection: Use positive ion mode for phospholipids (e.g., phosphatidylcholine, sphingomyelin) and negative mode for acidic lipids (e.g., fatty acids, phosphatidylserine) [57].
- Collision Energy Optimization: Fine-tune collision energies for each lipid class. Phosphatidylcholine requires different fragmentation energy than ceramides [57].
- Chromatography Conditions: Optimize mobile phase composition (acetonitrile, isopropanol, methanol ratios) and gradient elution to separate isobaric lipids [68] [57].
Q: Our method struggles with distinguishing lipids with similar molecular weights. What advanced techniques can help? A: Implement these solutions:
- High-Resolution Mass Spectrometry: Use instruments with resolution >75,000 at m/z 800 to resolve mass differences [77] [57].
- Ion Mobility Separation: Adds collision cross-section (CCS) values as an additional identifier, effectively separating isomeric lipids [57].
- Advanced Fragmentation Techniques: Use MS/MS with specific precursor ion scans (PIS) and neutral loss scans (NLS) to isolate class-specific fragments [77].
Q: We observe significant batch effects in our large-scale lipidomics study. How can we minimize this? A: Implement these strategies:
- Stratified Randomization: Distribute samples across batches based on key covariates (age, sex, group) to avoid confounding [68].
- Quality Control Placement: Inject pooled QC samples every 10-12 samples to monitor drift [68].
- Blank Samples: Include extraction blanks after every 23rd sample to monitor contamination [68].
- Internal Standard Normalization: Use multiple IS classes covering different lipid types to correct for batch effects [77] [68].
Data Analysis & Interpretation Challenges
Q: How do we handle the complex data processing requirements of untargeted lipidomics? A: Follow this standardized workflow:
- Data Conversion: Convert raw files to mzXML format using ProteoWizard for platform-independent processing [68].
- Peak Alignment: Use XCMS software with appropriate parameters to align peaks across samples [68].
- Lipid Annotation: Leverage fragmentation patterns and retention time alignment against standards [68] [57].
- Data Normalization: Apply multiple normalization steps including internal standards, quality control-based correction, and batch effect removal [68].
Methodological Standardization Protocols
Lipid Profiling for Clinical Samples
Comprehensive Lipid Extraction Protocol:
- Sample Preparation: Homogenize tissue samples in PBS (1:5 w/v) or aliquot 100 μL plasma/serum [78].
- Internal Standard Addition: Add 10 μL of SPLASH LIPIDOMIX or equivalent deuterated lipid mixture [77] [68].
- Extraction: Add 1 mL MTBE:methanol (5:1.5 v/v), vortex 10 min, incubate 1 hour at 4°C [77].
- Phase Separation: Add 250 μL water, centrifuge 10 min at 14,000×g, collect upper organic phase [77].
- Drying & Reconstitution: Dry under nitrogen, reconstitute in 100 μL isopropanol:acetonitrile:water (2:1:1 v/v) [78].
LC-MS/MS Analysis Conditions:
- Column: Waters Acquity UPLC BEH C8 (1.7 μm, 2.1×100 mm) with VanGuard pre-column [68].
- Mobile Phase: A) water:acetonitrile (4:6) with 10mM ammonium formate; B) isopropanol:acetonitrile (9:1) with 10mM ammonium formate [68].
- Gradient: 0-3 min 30% B, 3-15 min 30-100% B, 15-18 min 100% B, 18-25 min 30% B [68].
- MS Settings: ESI positive/negative switching, mass range 200-1200 m/z, collision energies optimized per lipid class [57].
Quality Assurance Framework
Pre-Analytical Quality Metrics:
- Sample Integrity: Document time-from-collection-to-freezing (<2 hours for optimal lipid preservation) [6].
- Hemolysis Index: Record for plasma samples as hemolysis affects lipid profiles [6].
- Storage Consistency: Maintain consistent storage at -80°C without freeze-thaw cycles [6].
Analytical Quality Controls:
- System Suitability: Test with standard lipid mixture before sample runs [68].
- Process Blanks: Monitor contamination in each extraction batch [68].
- Pooled QCs: Assess technical precision and normalize batch effects [68].
Lipid-based and gene-based personalized medicine offer complementary strengths. Lipid profiling provides real-time physiological snapshots with superior modifiability and faster response times, while genomics reveals inherent predispositions for long-term risk assessment [14].
Implementation Recommendations:
- For Preventive Medicine: Implement lipid-first assessment protocols leveraging their 3-5 year earlier disease prediction capability [14].
- For Therapeutic Monitoring: Utilize lipid profiles for treatment response assessment due to their dynamic nature and rapid modification timeline [14].
- For Genetic Disorders: Combine approaches using gene-based diagnosis with lipid-focused management of metabolic manifestations [14] [79].
Standardized lipidomic protocols must address pre-analytical variables as they significantly impact analytical reliability [6]. Implementing the troubleshooting guides and standardized workflows presented here will enhance reproducibility and clinical translation of lipid-based personalized medicine approaches.
Conclusion
Standardizing lipidomic protocols for clinical samples is no longer an optional refinement but a fundamental requirement for translating lipid biomarkers into reliable clinical tools. The path forward requires interdisciplinary collaboration to establish universally accepted protocols, improve software consistency, and conduct large-scale validation studies. Future success will depend on integrating artificial intelligence and machine learning with robust standardized workflows, ultimately enabling lipidomics to fulfill its promise in precision medicine for early diagnosis, personalized treatment strategies, and improved patient outcomes across a spectrum of diseases.
References
- 1. Preanalytical Errors in Clinical Laboratory Testing at a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10981510/]
- 2. Challenges in Preanalytical Phase of Laboratory Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC7109505/]
- 3. From bedside to bench—practical considerations to avoid ... [https://link.springer.com/article/10.1007/s00216-021-03450-0]
- 4. Taking Aim at Pre-analytical Errors [https://www.clinicallab.com/taking-aim-at-pre-analytical-errors-23640]
- 5. Ex vivo instability of lipids in whole blood: preanalytical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10208886/]
- 6. Pre-analytical sample handling standardization for reliable ... [https://pubmed.ncbi.nlm.nih.gov/36872954/]
- 7. Importance of pre-analytics for metabolomics studies [https://biocrates.com/importance-of-pre-analytics-for-metabolomics-studies/]
- 8. THE PREANALYTICAL ERRORS: A CONTINUOUS… [https://ascls.org/the-preanalytical-errors/]
- 9. Lipid | Definition, Structure, Examples, Functions, Types, & ... [https://www.britannica.com/science/lipid]
- 10. Lipid Classification System [https://lipidmaps.org/index.php/resources/education/classification]
- 11. Exploring lipidomics in biomarker discovery [https://www.sciencedirect.com/science/article/abs/pii/S0009898125005777]
- 12. Biochemistry, Lipids - StatPearls - NCBI Bookshelf - NIH [https://www.ncbi.nlm.nih.gov/books/NBK525952/]
- 13. Lipid Biological Functions [https://www.news-medical.net/life-sciences/Lipid-Biological-Functions.aspx]
- 14. Up-to-Date Look at Lipids Role in Precision Health (2025) [https://www.laboratoriosrubio.com/en/lipidomics-precision-health/]
- 15. Challenges in Lipidomics Biomarker Identification [https://www.mdpi.com/2218-1989/14/8/461]
- 16. Clinical lipidomics: realizing the potential of lipid profiling - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8528718/]
- 17. A protocol for investigating lipidomic dysregulation and ... [https://www.sciencedirect.com/science/article/pii/S2666166722000053]
- 18. Pre-analytical sample handling standardization for reliable ... [https://www.sciencedirect.com/science/article/pii/S2667145X23000093]
- 19. Clinical lipidomics reveals high individuality and sex ... [https://www.sciencedirect.com/science/article/pii/S0022227525000409]
- 20. Essentials of LC Troubleshooting, Part 4: What is Going On ... [https://www.chromatographyonline.com/view/essentials-of-lc-troubleshooting-part-4-what-is-going-on-with-the-baseline-]
- 21. Lipidomics in biomedical research: chance and challenges [https://www.ddw-online.com/lipidomics-in-biomedical-research-chance-and-challenges-12719-202108/]
- 22. Challenges in Lipidomics Biomarker Identification [https://pmc.ncbi.nlm.nih.gov/articles/PMC11356033/]
- 23. Best practices and tools in R and Python for statistical ... [https://www.nature.com/articles/s41467-025-63751-1]
- 24. Lipidomics Workflows [https://www.thermofisher.com/us/en/home/industrial/mass-spectrometry/mass-spectrometry-learning-center/mass-spectrometry-applications-area/metabolomics-mass-spectrometry/lipidomics-workflows.html]
- 25. Glial Biologist's Guide to Mass Spectrometry‐Based Lipidomics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11784846/]
- 26. Data-Driven Optimization of Mass Spectrometry Methods [https://pmc.ncbi.nlm.nih.gov/articles/PMC6737531/]
- 27. Preparation for blood tests: what can go wrong before the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12377977/]
- 28. A Review of Efforts to Improve Lipid Stability during Sample ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7725844/]
- 29. Sample Preparation Methods for Lipidomics Approaches ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7696154/]
- 30. Lipidomics from sample preparation to data analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC7118050/]
- 31. Errors with specimen and sample collection process [https://stateclaims.ie/learning-events/errors-with-specimen-and-sample-collection-process]
- 32. The strategic role of lipidomics in biomarker identification and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483926/]
- 33. Advancements in Mass Spectrometry-Based Targeted ... [https://www.mdpi.com/1420-3049/29/24/5934]
- 34. Pseudotargeted Lipidomics Strategy Enabling ... [https://www.purspec.com/pseudotargeted-lipidomics-strategy-enabling-comprehensive-profiling-and-precise-lipid-structural-elucidation-of-polyunsaturated-lipid-rich-echium-oil/]
- 35. Enhancing statistical power and data reliability in Lipidomics [https://www.sciencedirect.com/science/article/abs/pii/S0026265X25026943]
- 36. Evaluation of Lipid Extraction Protocols for Untargeted ... [https://www.mdpi.com/2218-1989/13/9/1002]
- 37. Analytical quality control in targeted lipidomics [https://www.sciencedirect.com/science/article/pii/S0003267025006191]
- 38. How to Avoid Problems in LC–MS [https://www.chromatographyonline.com/view/how-avoid-problems-lc-ms-0]
- 39. Effective LC Troubleshooting: Symptom-Based Strategies ... [https://www.restek.com/articles/effective-lc-troubleshooting-symptom-based-strategies-and-solutions?srsltid=AfmBOopyiCjcKb1wKEGeN_aJkTwQ57irxxPG3fndaAfGvyTutDPxn1dx]
- 40. Sample preparation optimization for metabolomics and ... [https://pubmed.ncbi.nlm.nih.gov/41075457/]
- 41. Steps Toward Minimal Reporting Standards for Lipidomics ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8376269/]
- 42. Update on LIPID MAPS classification, nomenclature, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7707175/]
- 43. Lipidomics Standard Initiative [https://lipidomicstandards.org/]
- 44. How To Deal With Missing Lipidomics Values [https://www.technologynetworks.com/proteomics/articles/how-to-deal-with-missing-lipidomics-values-386159]
- 45. Imputation of missing values in lipidomic datasets [https://pubmed.ncbi.nlm.nih.gov/38602226/]
- 46. A comparison of various imputation algorithms for missing data [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0319784]
- 47. Comparison of methods to handle missing values in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12107930/]
- 48. Imputation of plasma lipid species to facilitate integration ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10879118/]
- 49. Study sets new standards for lipidomics in cardiovascular ... [https://www.news-medical.net/news/20241012/Study-sets-new-standards-for-lipidomics-in-cardiovascular-disease-research.aspx]
- 50. Statistical methods for handling unwanted variation in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4544854/]
- 51. Evaluation of normalization strategies for mass spectrometry ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12214035/]
- 52. Advances in Dual-Column Chromatography for ... [https://www.sciencedirect.com/science/article/pii/S2772391725000647]
- 53. Challenges in Lipidomics Biomarker Identification [https://pubmed.ncbi.nlm.nih.gov/39195557/]
- 54. LipidSearch Software Support [https://www.thermofisher.com/us/en/home/technical-resources/technical-reference-library/mass-spectrometry-support-center/liquid-chromatography-mass-spectrometry-software-support/lipidsearch-software-support.html]
- 55. LipidMatch Suite [https://innovativeomics.com/software/lipidmatch-suite]
- 56. Mass Spectrometry Analysis Tools [https://lipidmaps.org/resources/tools?page=external]
- 57. Lipidomics Methodology FAQ [https://www.metwarebio.com/lipidomics-methodology-faq/]
- 58. Top 10 R Packages for Data Visualization in 2025 [https://vinova.sg/top-10-r-packages-for-data-visualization-in-2025/]
- 59. Top Python Data Visualization Libraries of 2025 [https://open-data-analytics.medium.com/top-python-data-visualization-libraries-of-2025-a28ec518dfae]
- 60. Five Python Data Visualization Examples (2025 Guide) [https://www.anaconda.com/topics/data-visualization-examples]
- 61. Top 10 Python Data Visualization Libraries in 2025 [https://reflex.dev/blog/2025-01-27-top-10-data-visualization-libraries/]
- 62. Summary — pyOpenMS 3.4.0dev documentation [https://pyopenms.readthedocs.io/]
- 63. The best R packages for data visualization [https://r-graph-gallery.com/best-dataviz-packages.html]
- 64. 10 Cutting-Edge R Tools Every Data Scientist Should ... [https://medium.com/data-science-collective/title-10-cutting-edge-r-tools-every-data-scientist-should-know-in-2025-85bd7a73dcb5]
- 65. Guiding the choice of informatics software and tools for ... [https://www.nature.com/articles/s41592-022-01710-0]
- 66. Lipid Analysis Software [https://www.lipidmaps.org/resources/tools/lm_software]
- 67. Steps Required to Interpret Lipidomics Data [https://www.metwarebio.com/how-to-interpret-lipidomics-data-a-step-by-step-guide/]
- 68. The Hitchhiker's Guide to Untargeted Lipidomics Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC8624948/]
- 69. Unravelling lipid heterogeneity: Advances in single-cell ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12270072/]
- 70. Novel lipidomes profile and clinical phenotype identified in ... [https://jhpn.biomedcentral.com/articles/10.1186/s41043-023-00400-7]
- 71. Metabolomics and Lipidomics Explore Phenotype-Specific ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12346085/]
- 72. Phenome-Wide Multi-Omics Integration Uncovers Distinct ... [https://arxiv.org/html/2510.12384v2]
- 73. AI in Drug Development: Clinical Validation and ... [https://globalforum.diaglobal.org/issue/june-2025/ai-in-drug-development-clinical-validation-and-regulatory-innovation-are-dual-imperatives/]
- 74. Method Validation – lipidomicstandards.org [https://lipidomicstandards.org/method-validation/]
- 75. Keep an Eye on Clinical Validation Gaps in AI-Enabled ... [https://www.aha.org/aha-center-health-innovation-market-scan/2025-09-16-keep-eye-clinical-validation-gaps-ai-enabled-medical-devices]
- 76. Lipid Nanoparticles vs. Viral Vectors: A Comparison for ... [https://www.helixbiotech.com/post/lipid-nanoparticles-vs-viral-vectors-a-comparison-for-gene-therapy]
- 77. Lipidomics: Techniques, applications, and outcomes ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5085849/]
- 78. Lipidomics Methods and Protocols [https://www.lipidmaps.org/resources/protocols/index.php]
- 79. Personalized Dietary Recommendations Based on Lipid ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8979208/]